- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support

What Is Problem-Solving Therapy?
Arlin Cuncic, MA, is the author of The Anxiety Workbook and founder of the website About Social Anxiety. She has a Master's degree in clinical psychology.
:max_bytes(150000):strip_icc():format(webp)/ArlinCuncic_1000-21af8749d2144aa0b0491c29319591c4.jpg)
Daniel B. Block, MD, is an award-winning, board-certified psychiatrist who operates a private practice in Pennsylvania.
:max_bytes(150000):strip_icc():format(webp)/block-8924ca72ff94426d940e8f7e639e3942.jpg)
Verywell / Madelyn Goodnight
Problem-Solving Therapy Techniques
How effective is problem-solving therapy, things to consider, how to get started.
Problem-solving therapy is a brief intervention that provides people with the tools they need to identify and solve problems that arise from big and small life stressors. It aims to improve your overall quality of life and reduce the negative impact of psychological and physical illness.
Problem-solving therapy can be used to treat depression , among other conditions. It can be administered by a doctor or mental health professional and may be combined with other treatment approaches.
At a Glance
Problem-solving therapy is a short-term treatment used to help people who are experiencing depression, stress, PTSD, self-harm, suicidal ideation, and other mental health problems develop the tools they need to deal with challenges. This approach teaches people to identify problems, generate solutions, and implement those solutions. Let's take a closer look at how problem-solving therapy can help people be more resilient and adaptive in the face of stress.
Problem-solving therapy is based on a model that takes into account the importance of real-life problem-solving. In other words, the key to managing the impact of stressful life events is to know how to address issues as they arise. Problem-solving therapy is very practical in its approach and is only concerned with the present, rather than delving into your past.
This form of therapy can take place one-on-one or in a group format and may be offered in person or online via telehealth . Sessions can be anywhere from 30 minutes to two hours long.
Key Components
There are two major components that make up the problem-solving therapy framework:
- Applying a positive problem-solving orientation to your life
- Using problem-solving skills
A positive problem-solving orientation means viewing things in an optimistic light, embracing self-efficacy , and accepting the idea that problems are a normal part of life. Problem-solving skills are behaviors that you can rely on to help you navigate conflict, even during times of stress. This includes skills like:
- Knowing how to identify a problem
- Defining the problem in a helpful way
- Trying to understand the problem more deeply
- Setting goals related to the problem
- Generating alternative, creative solutions to the problem
- Choosing the best course of action
- Implementing the choice you have made
- Evaluating the outcome to determine next steps
Problem-solving therapy is all about training you to become adaptive in your life so that you will start to see problems as challenges to be solved instead of insurmountable obstacles. It also means that you will recognize the action that is required to engage in effective problem-solving techniques.
Planful Problem-Solving
One problem-solving technique, called planful problem-solving, involves following a series of steps to fix issues in a healthy, constructive way:
- Problem definition and formulation : This step involves identifying the real-life problem that needs to be solved and formulating it in a way that allows you to generate potential solutions.
- Generation of alternative solutions : This stage involves coming up with various potential solutions to the problem at hand. The goal in this step is to brainstorm options to creatively address the life stressor in ways that you may not have previously considered.
- Decision-making strategies : This stage involves discussing different strategies for making decisions as well as identifying obstacles that may get in the way of solving the problem at hand.
- Solution implementation and verification : This stage involves implementing a chosen solution and then verifying whether it was effective in addressing the problem.
Other Techniques
Other techniques your therapist may go over include:
- Problem-solving multitasking , which helps you learn to think clearly and solve problems effectively even during times of stress
- Stop, slow down, think, and act (SSTA) , which is meant to encourage you to become more emotionally mindful when faced with conflict
- Healthy thinking and imagery , which teaches you how to embrace more positive self-talk while problem-solving
What Problem-Solving Therapy Can Help With
Problem-solving therapy addresses life stress issues and focuses on helping you find solutions to concrete issues. This approach can be applied to problems associated with various psychological and physiological symptoms.
Mental Health Issues
Problem-solving therapy may help address mental health issues, like:
- Chronic stress due to accumulating minor issues
- Complications associated with traumatic brain injury (TBI)
- Emotional distress
- Post-traumatic stress disorder (PTSD)
- Problems associated with a chronic disease like cancer, heart disease, or diabetes
- Self-harm and feelings of hopelessness
- Substance use
- Suicidal ideation
Specific Life Challenges
This form of therapy is also helpful for dealing with specific life problems, such as:
- Death of a loved one
- Dissatisfaction at work
- Everyday life stressors
- Family problems
- Financial difficulties
- Relationship conflicts
Your doctor or mental healthcare professional will be able to advise whether problem-solving therapy could be helpful for your particular issue. In general, if you are struggling with specific, concrete problems that you are having trouble finding solutions for, problem-solving therapy could be helpful for you.
Benefits of Problem-Solving Therapy
The skills learned in problem-solving therapy can be helpful for managing all areas of your life. These can include:
- Being able to identify which stressors trigger your negative emotions (e.g., sadness, anger)
- Confidence that you can handle problems that you face
- Having a systematic approach on how to deal with life's problems
- Having a toolbox of strategies to solve the issues you face
- Increased confidence to find creative solutions
- Knowing how to identify which barriers will impede your progress
- Knowing how to manage emotions when they arise
- Reduced avoidance and increased action-taking
- The ability to accept life problems that can't be solved
- The ability to make effective decisions
- The development of patience (realizing that not all problems have a "quick fix")
Problem-solving therapy can help people feel more empowered to deal with the problems they face in their lives. Rather than feeling overwhelmed when stressors begin to take a toll, this therapy introduces new coping skills that can boost self-efficacy and resilience .
Other Types of Therapy
Other similar types of therapy include cognitive-behavioral therapy (CBT) and solution-focused brief therapy (SFBT) . While these therapies work to change thinking and behaviors, they work a bit differently. Both CBT and SFBT are less structured than problem-solving therapy and may focus on broader issues. CBT focuses on identifying and changing maladaptive thoughts, and SFBT works to help people look for solutions and build self-efficacy based on strengths.
This form of therapy was initially developed to help people combat stress through effective problem-solving, and it was later adapted to address clinical depression specifically. Today, much of the research on problem-solving therapy deals with its effectiveness in treating depression.
Problem-solving therapy has been shown to help depression in:
- Older adults
- People coping with serious illnesses like cancer
Problem-solving therapy also appears to be effective as a brief treatment for depression, offering benefits in as little as six to eight sessions with a therapist or another healthcare professional. This may make it a good option for someone unable to commit to a lengthier treatment for depression.
Problem-solving therapy is not a good fit for everyone. It may not be effective at addressing issues that don't have clear solutions, like seeking meaning or purpose in life. Problem-solving therapy is also intended to treat specific problems, not general habits or thought patterns .
In general, it's also important to remember that problem-solving therapy is not a primary treatment for mental disorders. If you are living with the symptoms of a serious mental illness such as bipolar disorder or schizophrenia , you may need additional treatment with evidence-based approaches for your particular concern.
Problem-solving therapy is best aimed at someone who has a mental or physical issue that is being treated separately, but who also has life issues that go along with that problem that has yet to be addressed.
For example, it could help if you can't clean your house or pay your bills because of your depression, or if a cancer diagnosis is interfering with your quality of life.
Your doctor may be able to recommend therapists in your area who utilize this approach, or they may offer it themselves as part of their practice. You can also search for a problem-solving therapist with help from the American Psychological Association’s (APA) Society of Clinical Psychology .
If receiving problem-solving therapy from a doctor or mental healthcare professional is not an option for you, you could also consider implementing it as a self-help strategy using a workbook designed to help you learn problem-solving skills on your own.
During your first session, your therapist may spend some time explaining their process and approach. They may ask you to identify the problem you’re currently facing, and they’ll likely discuss your goals for therapy .
Keep In Mind
Problem-solving therapy may be a short-term intervention that's focused on solving a specific issue in your life. If you need further help with something more pervasive, it can also become a longer-term treatment option.
Get Help Now
We've tried, tested, and written unbiased reviews of the best online therapy programs including Talkspace, BetterHelp, and ReGain. Find out which option is the best for you.
Shang P, Cao X, You S, Feng X, Li N, Jia Y. Problem-solving therapy for major depressive disorders in older adults: an updated systematic review and meta-analysis of randomized controlled trials . Aging Clin Exp Res . 2021;33(6):1465-1475. doi:10.1007/s40520-020-01672-3
Cuijpers P, Wit L de, Kleiboer A, Karyotaki E, Ebert DD. Problem-solving therapy for adult depression: An updated meta-analysis . Eur Psychiatry . 2018;48(1):27-37. doi:10.1016/j.eurpsy.2017.11.006
Nezu AM, Nezu CM, D'Zurilla TJ. Problem-Solving Therapy: A Treatment Manual . New York; 2013. doi:10.1891/9780826109415.0001
Owens D, Wright-Hughes A, Graham L, et al. Problem-solving therapy rather than treatment as usual for adults after self-harm: a pragmatic, feasibility, randomised controlled trial (the MIDSHIPS trial) . Pilot Feasibility Stud . 2020;6:119. doi:10.1186/s40814-020-00668-0
Sorsdahl K, Stein DJ, Corrigall J, et al. The efficacy of a blended motivational interviewing and problem solving therapy intervention to reduce substance use among patients presenting for emergency services in South Africa: A randomized controlled trial . Subst Abuse Treat Prev Policy . 2015;10(1):46. doi:doi.org/10.1186/s13011-015-0042-1
Margolis SA, Osborne P, Gonzalez JS. Problem solving . In: Gellman MD, ed. Encyclopedia of Behavioral Medicine . Springer International Publishing; 2020:1745-1747. doi:10.1007/978-3-030-39903-0_208
Kirkham JG, Choi N, Seitz DP. Meta-analysis of problem solving therapy for the treatment of major depressive disorder in older adults . Int J Geriatr Psychiatry . 2016;31(5):526-535. doi:10.1002/gps.4358
Garand L, Rinaldo DE, Alberth MM, et al. Effects of problem solving therapy on mental health outcomes in family caregivers of persons with a new diagnosis of mild cognitive impairment or early dementia: A randomized controlled trial . Am J Geriatr Psychiatry . 2014;22(8):771-781. doi:10.1016/j.jagp.2013.07.007
Noyes K, Zapf AL, Depner RM, et al. Problem-solving skills training in adult cancer survivors: Bright IDEAS-AC pilot study . Cancer Treat Res Commun . 2022;31:100552. doi:10.1016/j.ctarc.2022.100552
Albert SM, King J, Anderson S, et al. Depression agency-based collaborative: effect of problem-solving therapy on risk of common mental disorders in older adults with home care needs . The American Journal of Geriatric Psychiatry . 2019;27(6):619-624. doi:10.1016/j.jagp.2019.01.002
By Arlin Cuncic, MA Arlin Cuncic, MA, is the author of The Anxiety Workbook and founder of the website About Social Anxiety. She has a Master's degree in clinical psychology.

Cognitive Behavioral Therapy
Solving problems the cognitive-behavioral way, problem solving is another part of behavioral therapy..
Posted February 2, 2022 | Reviewed by Ekua Hagan
- What Is Cognitive Behavioral Therapy?
- Find a therapist who practices CBT
- Problem-solving is one technique used on the behavioral side of cognitive-behavioral therapy.
- The problem-solving technique is an iterative, five-step process that requires one to identify the problem and test different solutions.
- The technique differs from ad-hoc problem-solving in its suspension of judgment and evaluation of each solution.
As I have mentioned in previous posts, cognitive behavioral therapy is more than challenging negative, automatic thoughts. There is a whole behavioral piece of this therapy that focuses on what people do and how to change their actions to support their mental health. In this post, I’ll talk about the problem-solving technique from cognitive behavioral therapy and what makes it unique.
The problem-solving technique
While there are many different variations of this technique, I am going to describe the version I typically use, and which includes the main components of the technique:
The first step is to clearly define the problem. Sometimes, this includes answering a series of questions to make sure the problem is described in detail. Sometimes, the client is able to define the problem pretty clearly on their own. Sometimes, a discussion is needed to clearly outline the problem.
The next step is generating solutions without judgment. The "without judgment" part is crucial: Often when people are solving problems on their own, they will reject each potential solution as soon as they or someone else suggests it. This can lead to feeling helpless and also discarding solutions that would work.
The third step is evaluating the advantages and disadvantages of each solution. This is the step where judgment comes back.
Fourth, the client picks the most feasible solution that is most likely to work and they try it out.
The fifth step is evaluating whether the chosen solution worked, and if not, going back to step two or three to find another option. For step five, enough time has to pass for the solution to have made a difference.
This process is iterative, meaning the client and therapist always go back to the beginning to make sure the problem is resolved and if not, identify what needs to change.

Advantages of the problem-solving technique
The problem-solving technique might differ from ad hoc problem-solving in several ways. The most obvious is the suspension of judgment when coming up with solutions. We sometimes need to withhold judgment and see the solution (or problem) from a different perspective. Deliberately deciding not to judge solutions until later can help trigger that mindset change.
Another difference is the explicit evaluation of whether the solution worked. When people usually try to solve problems, they don’t go back and check whether the solution worked. It’s only if something goes very wrong that they try again. The problem-solving technique specifically includes evaluating the solution.
Lastly, the problem-solving technique starts with a specific definition of the problem instead of just jumping to solutions. To figure out where you are going, you have to know where you are.
One benefit of the cognitive behavioral therapy approach is the behavioral side. The behavioral part of therapy is a wide umbrella that includes problem-solving techniques among other techniques. Accessing multiple techniques means one is more likely to address the client’s main concern.

Salene M. W. Jones, Ph.D., is a clinical psychologist in Washington State.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
Problem solving therapy - use and effectiveness in general practice
Affiliation.
- 1 Department of Rural Health, Rural Health Academic Centre, the University of Melbourne, Ballarat, Victoria, Australia. [email protected]
- PMID: 22962642
Background: Problem solving therapy (PST) is one of the focused psychological strategies supported by Medicare for use by appropriately trained general practitioners.
Objective: This article reviews the evidence base for PST and its use in the general practice setting.
Discussion: Problem solving therapy involves patients learning or reactivating problem solving skills. These skills can then be applied to specific life problems associated with psychological and somatic symptoms. Problem solving therapy is suitable for use in general practice for patients experiencing common mental health conditions and has been shown to be as effective in the treatment of depression as antidepressants. Problem solving therapy involves a series of sequential stages. The clinician assists the patient to develop new empowering skills, and then supports them to work through the stages of therapy to determine and implement the solution selected by the patient. Many experienced GPs will identify their own existing problem solving skills. Learning about PST may involve refining and focusing these skills.
- General Practice / methods*
- National Health Programs
- Problem Solving*
- Psychotherapy / methods*
What is Problem-Solving Therapy? (The Pros and Cons)
When you’re navigating a difficult situation, it can feel like problems keep piling up. It’s easy to feel overwhelmed and discouraged when you can’t seem to find a solution to any of them.
Fortunately, problem-solving therapy can be a short-term, effective way to find the answers you need.
Here at KMA Therapy, we know that choosing a type of therapy should be the least of your problems. We’re passionate about educating our clients and community about the different types of therapy available, and how to know which ones could be a great choice for them.
After reading this article, you’ll know what problem-solving therapy is, what happens during problem-solving therapy, and its pros and cons.
What is Problem-Solving Therapy?
Problem-solving therapy is a short-form treatment that usually lasts between four and twelve sessions.
It is most frequently used to treat depression, with a primary focus on helping you build the tools needed to identify and solve problems.
The main goal of problem-solving therapy is to improve your overall quality of life by helping you reduce the impact of stressors and problems you’re facing.
Problem-solving therapy is used to treat:
- Suicidal ideation
- Self-harm behaviours
If you’re experiencing suicidal ideation or are having thoughts of harming yourself, you can connect with Talk Suicide Canada for immediate support.
What Happens During Problem-Solving Therapy?
During problem-solving therapy, your therapist will focus on two main components.
1. Positive problem-solving framework
Positive problem-solving involves creating a framework that allows you to view things in a positive way by allowing yourself to feel confident and capable when handling your problems.
This means figuring out how to accept that you’ll still face problems in your life, while feeling more sure about your ability to face, address, and overcome them.

2. Planful problem-solving
Planful problem-solving involves four steps that help you learn how to solve problems in a healthy way:
- Defining the problem that you need to solve in a way where potential solutions can be created
- Exploring alternative solutions to the problem you’re facing by listing as many creative solutions to your problem as you can
- Discussing decision-making strategies to help you know which solution to choose and how to adapt to overcome obstacles
- Implementing your solution for your problem and assessing whether it was the right choice
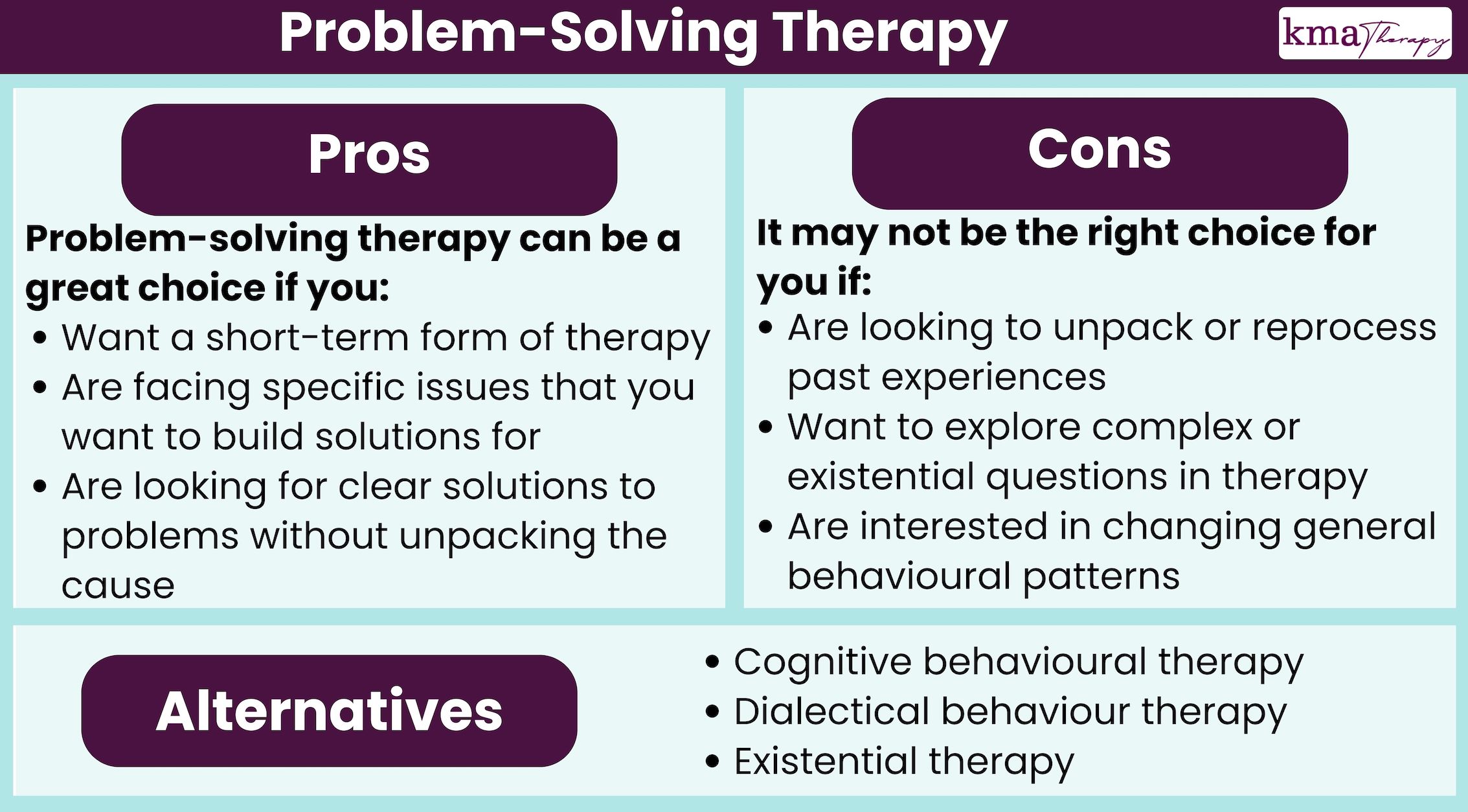
What are the Pros of Problem-Solving Therapy?
Problem-solving therapy is an effective and helpful form of therapy that can help you see meaningful changes in your life in a short amount of time.
Problem-solving therapy may be a great choice for you if:
- You want a short-term form of therapy
- You’re facing specific issues that you want to build solutions for
- You’re looking for clear solutions to problems without unpacking the cause
In general, problem-solving therapy is a great choice if there’s something specific in your life that’s causing additional problems.
For example, if you’re struggling with depression that makes you unable to keep in touch with loved ones or stay on top of your bills, problem-solving therapy can be a great choice to help you find solutions that work for these specific issues.
However, if you’re struggling to find the motivation to get out of bed in the morning because you want a deeper sense of purpose in your life, another form of therapy might be a better choice.
What are the Cons of Problem-Solving Therapy?
While problem-solving therapy can be quick, effective, and empowering, it’s not always the best choice if you’re interested in more in-depth conversations in therapy.
Problem-solving therapy may not be the right fit if you:
- Are looking to unpack or reprocess past experiences
- Want to explore complex or existential questions in therapy
- Are interested in changing general behavioural patterns (rather than specific problems)
Alternatives to Problem-Solving Therapy
After learning about the pros and cons of problem-solving therapy, you may be interested in some alternative forms of therapy to explore.
Alternatives to problem-solving therapy include:
- Existential therapy , which allows you to explore your sense of purpose and meaning in life
- Cognitive behavioural therapy , which focuses on helping you restructure your thought and behaviour patterns
- Dialectical behaviour therapy, which helps you build skills to change and solve problems, with an additional focus on mindfulness and relationships
Next Steps for Beginning Therapy
After reading this article, you know what problem-solving therapy is and how to know if it’s the right choice for you.
Here at KMA Therapy, our passionate team of therapists has been supporting our clients with tailored therapy plans for over 15 years.
You don’t have to know exactly what type of therapy you want to pursue when you meet a therapist for the first time, so don’t worry if you’re feeling overwhelmed.
It’s helpful to have a sense of what you like and dislike, and what types of therapy sound interesting to you - but your therapist will help you choose what will work best and create a treatment plan customized to you.
Register online for more information or download our free Therapy 101 Guide to learn more.
If you’d prefer to keep reading, explore these articles we’ve chosen for you:
- What is Psychodynamic Therapy? (The Pros and Cons)
- Therapy 101: The Ultimate Guide to Beginning Therapy
- What is a Therapy Introductory Session?
Register Online
What is systemic therapy (the pros and cons).
Our team of experts will support you throughout your mental health journey to help you become your most authentic self!
What’s the Difference Between Anxiety and Depression?
Are situationships good or bad 3 experts weigh in, or, are you all set and ready to book, ontario's premier counselling practice.

What is Solution-Focused Therapy: 3 Essential Techniques

You’re at an important business meeting, and you’re there to discuss some problems your company is having with its production.
At the meeting, you explain what’s causing the problems: The widget-producing machine your company uses is getting old and slowing down. The machine is made up of hundreds of small parts that work in concert, and it would be much more expensive to replace each of these old, worn-down parts than to buy a new widget-producing machine.
You are hoping to convey to the other meeting attendees the impact of the problem, and the importance of buying a new widget-producing machine. You give a comprehensive overview of the problem and how it is impacting production.
One meeting attendee asks, “So which part of the machine, exactly, is getting worn down?” Another says, “Please explain in detail how our widget-producing machine works.” Yet another asks, “How does the new machine improve upon each of the components of the machine?” A fourth attendee asks, “Why is it getting worn down? We should discuss how the machine was made in order to fully understand why it is wearing down now.”
You are probably starting to feel frustrated that your colleagues’ questions don’t address the real issue. You might be thinking, “What does it matter how the machine got worn down when buying a new one would fix the problem?” In this scenario, it is much more important to buy a new widget-producing machine than it is to understand why machinery wears down over time.
When we’re seeking solutions, it’s not always helpful to get bogged down in the details. We want results, not a narrative about how or why things became the way they are.
This is the idea behind solution-focused therapy . For many people, it is often more important to find solutions than it is to analyze the problem in great detail. This article will cover what solution-focused therapy is, how it’s applied, and what its limitations are.
Before you continue, we thought you might like to download our three Positive Psychology Exercises for free . These science-based exercises will explore fundamental aspects of positive psychology including strengths, values, and self-compassion, and will give you the tools to enhance the wellbeing of your clients, students, or employees.
This Article Contains:
What is solution-focused therapy, theory behind the solution-focused approach, solution-focused model, popular techniques and interventions, sfbt treatment plan: an example, technologies to execute an sfbt treatment plan (incl. quenza), limitations of sfbt counseling, what does sfbt have to do with positive psychology, a take-home message.
Solution-focused therapy, also called solution-focused brief therapy (SFBT), is a type of therapy that places far more importance on discussing solutions than problems (Berg, n.d.). Of course, you must discuss the problem to find a solution, but beyond understanding what the problem is and deciding how to address it, solution-focused therapy will not dwell on every detail of the problem you are experiencing.
Solution-focused brief therapy doesn’t require a deep dive into your childhood and the ways in which your past has influenced your present. Instead, it will root your sessions firmly in the present while working toward a future in which your current problems have less of an impact on your life (Iveson, 2002).
This solution-centric form of therapy grew out of the field of family therapy in the 1980s. Creators Steve de Shazer and Insoo Kim Berg noticed that most therapy sessions were spent discussing symptoms, issues, and problems.
De Shazer and Berg saw an opportunity for quicker relief from negative symptoms in a new form of therapy that emphasized quick, specific problem-solving rather than an ongoing discussion of the problem itself.
The word “brief” in solution-focused brief therapy is key. The goal of SFBT is to find and implement a solution to the problem or problems as soon as possible to minimize time spent in therapy and, more importantly, time spent struggling or suffering (Antin, 2018).
SFBT is committed to finding realistic, workable solutions for clients as quickly as possible, and the efficacy of this treatment has influenced its spread around the world and use in multiple contexts.
SFBT has been successfully applied in individual, couples, and family therapy. The problems it can address are wide-ranging, from the normal stressors of life to high-impact life events.

Download 3 Free Positive Psychology Exercises (PDF)
Enhance wellbeing with these free, science-based exercises that draw on the latest insights from positive psychology.
Download 3 Free Positive Psychology Tools Pack (PDF)
By filling out your name and email address below.
The solution-focused approach of SFBT is founded in de Shazer and Berg’s idea that the solutions to one’s problems are typically found in the “exceptions” to the problem, meaning the times when the problem is not actively affecting the individual (Iveson, 2002).
This approach is a logical one—to find a lasting solution to a problem, it is rational to look first at those times in which the problem lacks its usual potency.
For example, if a client is struggling with excruciating shyness, but typically has no trouble speaking to his or her coworkers, a solution-focused therapist would target the client’s interactions at work as an exception to the client’s usual shyness. Once the client and therapist have discovered an exception, they will work as a team to find out how the exception is different from the client’s usual experiences with the problem.
The therapist will help the client formulate a solution based on what sets the exception scenario apart, and aid the client in setting goals and implementing the solution.
You may have noticed that this type of therapy relies heavily on the therapist and client working together. Indeed, SFBT works on the assumption that every individual has at least some level of motivation to address their problem or problems and to find solutions that improve their quality of life .
This motivation on the part of the client is an essential piece of the model that drives SFBT (Miller & Rollnick, 2013).

Solution-focused theorists and therapists believe that generally, people develop default problem patterns based on their experiences, as well as default solution patterns.
These patterns dictate an individual’s usual way of experiencing a problem and his or her usual way of coping with problems (Focus on Solutions, 2013).
The solution-focused model holds that focusing only on problems is not an effective way of solving them. Instead, SFBT targets clients’ default solution patterns, evaluates them for efficacy, and modifies or replaces them with problem-solving approaches that work (Focus on Solutions, 2013).
In addition to this foundational belief, the SFBT model is based on the following assumptions:
- Change is constant and certain;
- Emphasis should be on what is changeable and possible;
- Clients must want to change;
- Clients are the experts in therapy and must develop their own goals;
- Clients already have the resources and strengths to solve their problems;
- Therapy is short-term;
- The focus must be on the future—a client’s history is not a key part of this type of therapy (Counselling Directory, 2017).
Based on these assumptions, the model instructs therapists to do the following in their sessions with clients:
- Ask questions rather than “selling” answers;
- Notice and reinforce evidence of the client’s positive qualities, strengths, resources, and general competence to solve their own problems;
- Work with what people can do rather than focusing on what they can’t do;
- Pinpoint the behaviors a client is already engaging in that are helpful and effective and find new ways to facilitate problem-solving through these behaviors;
- Focus on the details of the solution instead of the problem;
- Develop action plans that work for the client (Focus on Solutions, 2013).
SFBT therapists aim to bring out the skills, strengths, and abilities that clients already possess rather than attempting to build new competencies from scratch. This assumption of a client’s competence is one of the reasons this therapy can be administered in a short timeframe—it is much quicker to harness the resources clients already have than to create and nurture new resources.
Beyond these basic activities, there are many techniques and exercises used in SFBT to promote problem-solving and enhance clients’ ability to work through their own problems.

Working with a therapist is generally recommended when you are facing overwhelming or particularly difficult problems, but not all problems require a licensed professional to solve.
For each technique listed below, it will be noted if it can be used as a standalone technique.
Asking good questions is vital in any form of therapy, but SFBT formalized this practice into a technique that specifies a certain set of questions intended to provoke thinking and discussion about goal-setting and problem-solving.
One such question is the “coping question.” This question is intended to help clients recognize their own resiliency and identify some of the ways in which they already cope with their problems effectively.
There are many ways to phrase this sort of question, but generally, a coping question is worded something like, “How do you manage, in the face of such difficulty, to fulfill your daily obligations?” (Antin, 2018).
Another type of question common in SFBT is the “miracle question.” The miracle question encourages clients to imagine a future in which their problems are no longer affecting their lives. Imagining this desired future will help clients see a path forward, both allowing them to believe in the possibility of this future and helping them to identify concrete steps they can take to make it happen.
This question is generally asked in the following manner: “Imagine that a miracle has occurred. This problem you are struggling with is suddenly absent from your life. What does your life look like without this problem?” (Antin, 2018).
If the miracle question is unlikely to work, or if the client is having trouble imagining this miracle future, the SFBT therapist can use “best hopes” questions instead. The client’s answers to these questions will help establish what the client is hoping to achieve and help him or her set realistic and achievable goals.
The “best hopes” questions can include the following:
- What are your best hopes for today’s session?
- What needs to happen in this session to enable you to leave thinking it was worthwhile?
- How will you know things are “good enough” for our sessions to end?
- What needs to happen in these sessions so that your relatives/friends/coworkers can say, “I’m really glad you went to see [the therapist]”? (Vinnicombe, n.d.).
To identify the exceptions to the problems plaguing clients, therapists will ask “exception questions.” These are questions that ask about clients’ experiences both with and without their problems. This helps to distinguish between circumstances in which the problems are most active and the circumstances in which the problems either hold no power or have diminished power over clients’ moods or thoughts.
Exception questions can include:
- Tell me about the times when you felt the happiest;
- What was it about that day that made it a better day?
- Can you think of times when the problem was not present in your life? (Counselling Directory, 2017).
Another question frequently used by SFBT practitioners is the “scaling question.”
It asks clients to rate their experiences (such as how their problems are currently affecting them, how confident they are in their treatment, and how they think the treatment is progressing) on a scale from 0 (lowest) to 10 (highest). This helps the therapist to gauge progress and learn more about clients’ motivation and confidence in finding a solution.
For example, an SFBT therapist may ask, “On a scale from 0 to 10, how would you rate your progress in finding and implementing a solution to your problem?” (Antin, 2018).
Do One Thing Different
This exercise can be completed individually, but the handout may need to be modified for adult or adolescent users.
This exercise is intended to help the client or individual to learn how to break his or her problem patterns and build strategies to simply make things go better.
The handout breaks the exercise into the following steps (Coffen, n.d.):
- Think about the things you do in a problem situation. Change any part you can. Choose to change one thing, such as the timing, your body patterns (what you do with your body), what you say, the location, or the order in which you do things;
- Think of a time that things did not go well for you. When does that happen? What part of that problem situation will you do differently now?
- Think of something done by somebody else does that makes the problem better. Try doing what they do the next time the problem comes up. Or, think of something that you have done in the past that made things go better. Try doing that the next time the problem comes up;
- Think of something that somebody else does that works to make things go better. What is the person’s name and what do they do that you will try?
- Think of something that you have done in the past that helped make things go better. What did you do that you will do next time?
- Feelings tell you that you need to do something. Your brain tells you what to do. Understand what your feelings are but do not let them determine your actions. Let your brain determine the actions;
- Feelings are great advisors but poor masters (advisors give information and help you know what you could do; masters don’t give you choices);
- Think of a feeling that used to get you into trouble. What feeling do you want to stop getting you into trouble?
- Think of what information that feeling is telling you. What does the feeling suggest you should do that would help things go better?
- Change what you focus on. What you pay attention to will become bigger in your life and you will notice it more and more. To solve a problem, try changing your focus or your perspective.
- Think of something that you are focusing on too much. What gets you into trouble when you focus on it?
- Think of something that you will focus on instead. What will you focus on that will not get you into trouble?
- Imagine a time in the future when you aren’t having the problem you are having right now. Work backward to figure out what you could do now to make that future come true;
- Think of what will be different for you in the future when things are going better;
- Think of one thing that you would be doing differently before things could go better in the future. What one thing will you do differently?
- Sometimes people with problems talk about how other people cause those problems and why it’s impossible to do better. Change your story. Talk about times when the problem was not happening and what you were doing at that time. Control what you can control. You can’t control other people, but you can change your actions, and that might change what other people do;
- Think of a time when you were not having the problem that is bothering you. Talk about that time.
- If you believe in a god or a higher power, focus on God to get things to go better. When you are focused on God or you are asking God to help you, things might go better for you.
- Do you believe in a god or a higher power? Talk about how you will seek help from your god to make things go better.
- Use action talk to get things to go better. Action talk sticks to the facts, addresses only the things you can see, and doesn’t address what you believe another person was thinking or feeling—we have no way of knowing that for sure. When you make a complaint, talk about the action that you do not like. When you make a request, talk about what action you want the person to do. When you praise someone, talk about what action you liked;
- Make a complaint about someone cheating at a game using action talk;
- Make a request for someone to play fairly using action talk;
- Thank someone for doing what you asked using action talk.
Following these eight steps and answering the questions thoughtfully will help people recognize their strengths and resources, identify ways in which they can overcome problems, plan and set goals to address problems, and practice useful skills.
While this handout can be extremely effective for SFBT, it can also be used in other therapies or circumstances.
To see this handout and download it for you or your clients, click here .
Presupposing Change

The “presupposing change” technique has great potential in SFBT, in part because when people are experiencing problems, they have a tendency to focus on the problems and ignore the positive changes in their life.
It can be difficult to recognize the good things happening in your life when you are struggling with a painful or particularly troublesome problem.
This technique is intended to help clients be attentive to the positive things in their lives, no matter how small or seemingly insignificant. Any positive change or tiny step of progress should be noted, so clients can both celebrate their wins and draw from past wins to facilitate future wins.
Presupposing change is a strikingly simple technique to use: Ask questions that assume positive changes. This can include questions like, “What’s different or better since I saw you last time?”
If clients are struggling to come up with evidence of positive change or are convinced that there has been no positive change, the therapist can ask questions that encourage clients to think about their abilities to effectively cope with problems, like, How come things aren’t worse for you? What stopped total disaster from occurring? How did you avoid falling apart? (Australian Institute of Professional Counsellors, 2009).
The most powerful word in the Solution Focused Brief Therapy vocabulary – The Solution Focused Universe
A typical treatment plan in SFBT will include several factors relevant to the treatment, including:
- The reason for referral, or the problem the client is experiencing that brought him or her to treatment;
- A diagnosis (if any);
- List of medications taken (if any);
- Current symptoms;
- Support for the client (family, friends, other mental health professionals, etc.);
- Modality or treatment type;
- Frequency of treatment;
- Goals and objectives;
- Measurement criteria for progress on goals;
- Client strengths ;
- Barriers to progress.
All of these are common and important components of a successful treatment plan. Some of these components (e.g., diagnosis and medications) may be unaddressed or acknowledged only as a formality in SFBT due to its usual focus on less severe mental health issues. Others are vital to treatment progress and potential success in SFBT, including goals, objectives, measurement criteria, and client strengths.
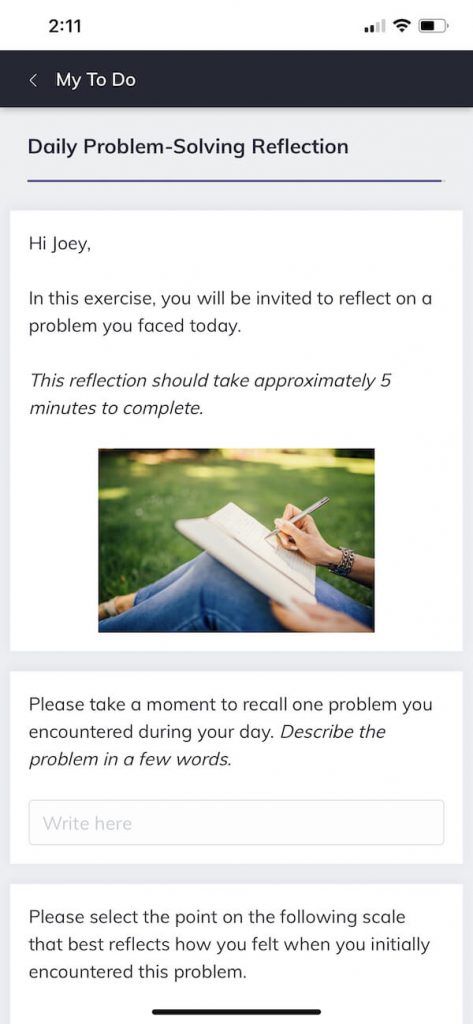
To this end, therapists are increasingly leveraging the benefits of technology to help develop, execute, and evaluate the outcomes of treatment plans efficiently.
Among these technologies are many digital platforms that therapists can use to carry out some steps in clients’ treatment plans outside of face-to-face sessions.
For example, by adopting a versatile blended care platform such as Quenza , an SFBT practitioner may carry out some of the initial steps in the assessment/diagnosis phase of a treatment plan, such as by inviting the client to complete a digital diagnostic questionnaire.
Likewise, the therapist may use the platform to send digital activities to the client’s smartphone, such as an end-of-day reflection inviting the client to recount their application of the ‘Do One Thing Different’ technique to overcome a problem.
These are just a few ideas for how you might use a customizable blended care tool such as Quenza to help carry out several of the steps in an SFBT treatment plan.

Some of the potential disadvantages for therapists include (George, 2010):
- The potential for clients to focus on problems that the therapist believes are secondary problems. For example, the client may focus on a current relationship problem rather than the underlying self-esteem problem that is causing the relationship woes. SFBT dictates that the client is the expert, and the therapist must take what the client says at face value;
- The client may decide that the treatment is successful or complete before the therapist is ready to make the same decision. This focus on taking what the client says at face value may mean the therapist must end treatment before they are convinced that the client is truly ready;
- The hard work of the therapist may be ignored. When conducted successfully, it may seem that clients solved their problems by themselves, and didn’t need the help of a therapist at all. An SFBT therapist may rarely get credit for the work they do but must take all the blame when sessions end unsuccessfully.
Some of the potential limitations for clients include (Antin, 2018):
- The focus on quick solutions may miss some important underlying issues;
- The quick, goal-oriented nature of SFBT may not allow for an emotional, empathetic connection between therapist and client.
- If the client wants to discuss factors outside of their immediate ability to effect change, SFBT may be frustrating in its assumption that clients are always able to fix or address their problems.
Generally, SFBT can be an excellent treatment for many of the common stressors people experience in their lives, but it may be inappropriate if clients want to concentrate more on their symptoms and how they got to where they are today. As noted earlier, it is also generally not appropriate for clients with major mental health disorders.
17 Top-Rated Positive Psychology Exercises for Practitioners
Expand your arsenal and impact with these 17 Positive Psychology Exercises [PDF] , scientifically designed to promote human flourishing, meaning, and wellbeing.
Created by Experts. 100% Science-based.
First, both SFBT and positive psychology share a focus on the positive—on what people already have going for them and on what actions they can take. While problems are discussed and considered in SFBT, most of the time and energy is spent on discussing, thinking about, and researching what is already good, effective, and successful.
Second, both SFBT and positive psychology consider the individual to be his or her own best advocate, the source of information on his or her problems and potential solutions, and the architect of his or her own treatment and life success. The individual is considered competent, able, and “enough” in both SFBT and positive psychology.
This assumption of the inherent competence of individuals has run both subfields into murky waters and provoked criticism, particularly when systemic and societal factors are considered. While no respectable psychologist would disagree that an individual is generally in control of his or her own actions and, therefore, future, there is considerable debate about what level of influence other factors have on an individual’s life.
While many of these criticisms are valid and bring up important points for discussion, we won’t dive too deep into them in this piece. Suffice it to say that both SFBT and positive psychology have important places in the field of psychology and, like any subfield, may not apply to everyone and to all circumstances.
However, when they do apply, they are both capable of producing positive, lasting, and life-changing results.
Solution-focused therapy puts problem-solving at the forefront of the conversation and can be particularly useful for clients who aren’t suffering from major mental health issues and need help solving a particular problem (or problems). Rather than spending years in therapy, SFBT allows such clients to find solutions and get results quickly.
Have you ever tried Solution-Focused Brief Therapy, as a therapist or as a client? What did you think of the focus on solutions? Do you think SFBT misses anything important by taking the spotlight off the client’s problem(s)? Let us know in the comments section.
We hope you enjoyed reading this article. Don’t forget to download our three Positive Psychology Exercises for free .
Antin, L. (2018). Solution-focused brief therapy (SFBT). Good Therapy. Retrieved from https://www.goodtherapy.org/learn-about-therapy/types/solution-focused-therapy
- Australian Institute of Professional Counsellors. (2009, March 30). Solution-focused techniques. Counseling Connection. Retrieved from http://www.counsellingconnection.com/index.php/2009/03/30/solution-focused-techniques/
- Berg, I. K. (n.d.). About solution-focused brief therapy. SFBTA . Retrieved from http://www.sfbta.org/about_sfbt.html
- Coffen, R. (n.d.). Do one thing different [Handout]. Retrieved from https://www.andrews.edu/~coffen/Do%20one%20thing%20different.pdf
- Focus on Solutions. (2013, October 28). The brief solution-focused model. Focus on solutions: Leaders in solution-focused training. Retrieved from http://www.focusonsolutions.co.uk/solutionfocused/
- George, E. (2010). Disadvantages of solution focus? BRIEF. Retrieved from https://www.brief.org.uk/resources/faq/disadvantages-of-solution-focus
- Iveson, C. (2002). Solution-focused brief therapy. Advances in Psychiatric Treatment, 8 (2), 149-156.
- Miller, W. R., & Rollnick, S. (2013). Motivational interviewing: Helping people change (3rd ed.). New York, NY: Guilford Press.
- Vinnicombe, G. (n.d.). Greg’s SFBT handout. Useful Conversations. Retrieved from http://www.usefulconversations.com/downloads
Share this article:
Article feedback
What our readers think.
Thank you. I’m about to start an MMFT internship, and SFBT is the model I prefer. You put everything in perspective.
Great insights. I have a client who has become a bit disengaged with our work together. This gives me a really helpful new approach for our upcoming sessions. He’s very focused on the problem and wanting a “quick fix.” This might at least get us on that path. Thank you!
Hi Courtney, great paper! I will like to know more about the limitations to SFT and noticed that you provided an intext citation to Antin 2016. Would you be able to provide the full reference? Thank you!
Thank you for bringing this to our attention. The reference has now been updated in the reference list — this should be Antin (2018):
– Nicole | Community Manager
The only thing tat was revealed to me while reading this article is the client being able to recognize the downfall of what got them into their problem in the first place. I felt that maybe a person should understand the problem to the extent that they may understand how to recognize what led to the problem in the first place. Understanding the process of how something broke down would give one knowledge and wisdom that may be able to be applied in future instances when something may go wrong again. Even if the thing is new (machine or person) having the wisdom and understanding of the cause that led to the effect may help prevent and or overcome an arising problem in the future. Not being able to recognize the process that brought down the machine and or human may be like adhering to ignorance, although they say ignorance is bliss in case of an emergency it would be better to be informed rather then blindly ignorant, as the knowledge of how the problem surfaced in the first place may alleviate unwarranted suffering sooner rather than later. But then again looking at it this way I may work myself out of a job if my clients never came back to see me. However is it about me or them or the greater societal structural good that we can induce through our education, skills, training, experience, and good will good faith effort to instill social justice coupled with lasting change for the betterment of human society and the world as a whole.
Very very helpful, thank you for writing. Just one point “While no respectable psychologist would disagree that an individual is generally in control of his or her own actions and, therefore, future, there is considerable debate about what level of influence other factors have on an individual’s life.” I think any psychologist that has worked in neurological dysfunction would probably acknowledge consciousness and ‘voluntary control’ are not that straight-forward. Generally though, I suppose there’s that whole debate of if we are ever in control of our actions or even our thoughts. It may well boil down to what we mean by ‘we’, as in what are we? A bundle of fibres acting on memories and impulses? A unique body of energy guided by intangible forces? Maybe I am not a respectable psychologist 🙂
This article provided me with insight on how to proceed with a role-play session in my CBT graduate course. Thank you!
Hi Derrick, That’s fantastic that you were able to find some guidance in this post. Best of luck with your grad students! – Nicole | Community Manager
Thank You…Great input and clarity . I now have light…
I was looking everywhere for a simple explanation for my essay and this is it!! thank you so much for this is was very useful and I learned a lot.
Very well done. Thank you for the multitude of insights.
Thank you for such a good passage discussed. I really have a great time understanding it.
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

Holistic Therapy: Healing Mind, Body, and Spirit
The term “holistic” in health care can be dated back to Hippocrates over 2,500 years ago (Relman, 1979). Hippocrates highlighted the importance of viewing individuals [...]

Trauma-Informed Therapy Explained (& 9 Techniques)
Trauma varies significantly in its effect on individuals. While some people may quickly recover from an adverse event, others might find their coping abilities profoundly [...]

Recreational Therapy Explained: 6 Degrees & Programs
Let’s face it, on a scale of hot or not, attending therapy doesn’t make any client jump with excitement. But what if that can be [...]
Read other articles by their category
- Body & Brain (49)
- Coaching & Application (57)
- Compassion (26)
- Counseling (51)
- Emotional Intelligence (24)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (20)
- Mindfulness (45)
- Motivation & Goals (45)
- Optimism & Mindset (34)
- Positive CBT (28)
- Positive Communication (20)
- Positive Education (47)
- Positive Emotions (32)
- Positive Leadership (17)
- Positive Parenting (3)
- Positive Psychology (33)
- Positive Workplace (37)
- Productivity (16)
- Relationships (46)
- Resilience & Coping (36)
- Self Awareness (21)
- Self Esteem (37)
- Strengths & Virtues (31)
- Stress & Burnout Prevention (34)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)
Download 3 Free Positive CBT Tools Pack (PDF)
3 Positive CBT Exercises (PDF)
Today's Therapist
What Is Problem Solving Therapy and Who Can It Help
February 1, 2017 By TodaysTherapist
Stressful events are part of everyday life. For some, coping with the negative effects of these events can be difficult, whether stressors are considered large (such as the death of a loved one) or small (like making a mistake at work). Stressors can create or exacerbate psychological and physical health problems. Problem solving therapy can help individuals develop effective coping methods for dealing with stressors in their lives by providing structured goals and coaching adaptation skills for decision-making situations. While this article provides some facts on problem solving therapy, it is strongly advised that individuals considering problem solving therapy receive care from licensed professionals.

What Is Problem Solving Therapy?
Problem Solving Therapy (PST), or structured problem solving, is psychological treatment used to help clients manage stressful life events. Therapists employ behavioral and cognitive intervention techniques to assist clients in establishing and actualizing goals and creating effective problem-solving, stress management techniques. Clients are encouraged and guided in how to be more proactive in their daily lives and make decisions that help them achieve goals. Core components of PST are addressing problem orientation, explicitly defining problems the client faces, coming up with and evaluating solutions, and breaking problems down into achievable, reasonable, and ultimately less stressful steps.
Solving Problems Outcomes
PST involves finding ways for individuals to change the stressful nature of situations and how they respond to stressors. Generally, problem-solving outcomes are based upon problem-solving style and problem orientation . Problem orientation is the feelings and thoughts a person has about their problems and perceived ability to resolve them. A positive problem orientation generally leads the person to enhance problem-solving efforts while a negative problem orientation tends to lead to the person being inhibited in solving their problems. Problem-solving style is behavioral and cognitive activities targeted at coping with stressors. Those with ineffective styles tend to report having more stressors and negative life events.
Problem solving therapy is essentially a series of training sessions in learning how to utilize adaptive problem solving skills that help clients better deal with and/or resolve problems that arise in their daily lives. Clients learn how to make more effective decisions for themselves, come up with their own creative ways to solve problems, and identify barriers or obstacles that surface when trying to reach their goals and how best to negate these hurdles. The overall intended outcome is that a client will feel more confident in their decision-making and problem-solving techniques and will be able to carry on their solutions as independently as possible.
Medical Conditions and Problem Solving Therapy
PST can be used by General Practitioners (GPs) to help treat difficult medical conditions, such as chronic pain management. As with a therapist, GPs have clients identify problems they want solved, set up goals, have clients come up with solutions for how they would like to solve the problem, weigh pros and cons of each solution in order to select the best one, and implement the solution. Together, a GP and client can review how well the selected solution is working and make any necessary changes. Again, this article is to provide helpful information in learning about PST; it is, therefore, highly recommended that one seeks help from a licensed, well-reputed professional who can help implement and analyze PST goals.
Developing and Achieving Problem Solving Therapy Goals
Therapists and GPs tend to use PST with clients who seem to be having difficulties coping with stressful life situations that can become confusing and overwhelming. The goals of PST revolve around meeting four key therapy objectives:
- Improving the client’s positive orientation;
- Reducing the client’s negative orientation;
- Enhancing the client’s ability to identify what is causing a problem, coming up with a few potential solutions, conducting cost-benefit analysis to determine the best solution, implementing the solution, then analyzing the outcome;
- Reducing impulsive and ultimately ineffective methods for attempting to solve problems.
Since every client is a different person and has diverse needs, therapists and doctors try to allow as much creative and analytic processing by the client as possible, although PST relies on the four basic components mentioned in the list above.
Therapists and clients alike should be aware of several obstacles that can occur during the PST process, including the client experiencing cognitive overload, difficulties with emotional regulation, usage of ineffective or maladaptive problem solving styles, feelings of hopelessness leading to decreased motivation to follow through on goals, and difficulties removing oneself from negative moods or thought patterns.
Who Can Benefit from Problem Solving Therapy?
Problem solving therapy can be beneficial for many different people. Since there is flexibility in regard to treatment goals and methods for achieving them, PST can be used in a group setting or one-on-one with an individual client. Since negative stressors are scientifically linked to mental and physical health problems, problem solving therapy can be beneficial to almost anyone, so long as they are open to the idea of pursuing treatment and engaging in the process.
PST has been found to be an effective therapeutic method for clients who are dealing with a vast array of mental, physical and emotional conditions. These conditions include some personality disorders, major depressive disorder, suicidal ideation, generalized anxiety disorder, relationship issues, emotional duress, and medically-based issues that result in emotional and physical pain (such as fibromyalgia, Hashimoto’s and hypothyroidism, diabetes, and cancer).
Problem solving therapy is a widely-acknowledged tool used by therapists and general medical practitioners alike to help clients find proactive and reasonable ways to deal with the stressful events that occur in their lives. Overall, PST can help people find meaningful, creative, and adjustable ways of reaching their problem-resolution goals and ultimately lead to a better quality of living for those dealing with major physical and mental health concerns. Anyone considering PST should contact a trained medical or counseling professional to inquire about how this type of therapy could potentially suit their needs.
Image from depositphotos.com.

Encyclopedia of Geropsychology pp 1874–1883 Cite as
Problem-Solving Therapy
- Sherry A. Beaudreau 2 , 3 , 4 ,
- Christine E. Gould 2 , 5 ,
- Erin Sakai 6 &
- J. W. Terri Huh 6 , 7
- Reference work entry
- First Online: 01 January 2017
101 Accesses
Behavioral intervention; Skills-based therapy; Treatment
Problem-solving therapy (PST), developed by Nezu and colleagues, is a non-pharmacological, empirically supported cognitive-behavioral treatment (D’Zurilla and Nezu 2006 ; Nezu et al. 1989 ). The problem-solving framework draws from a stress-diathesis model, namely, that life stress interacts with an individual’s predisposition toward developing a psychiatric disorder. The driving model behind PST posits that individuals who experience difficulty solving life’s problems or coping with stressors of everyday living struggle with psychiatric symptoms more often than individuals considered as good problem solvers. This psychological treatment teaches a step-by-step approach to the process of identifying and implementing adaptive solutions for daily problems. By teaching individuals to solve their problems more effectively and efficiently, this model assumes that their stress and related psychiatric symptoms will...
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Alexopoulos, G. S., Kiosses, D. N., Heo, M., Murphy, C. F., Shanmugham, B., & Gunning-Dixon, F. (2005). Executive dysfunction and the course of geriatric depression. Biological Psychiatry, 58 (3), 204–210.
Article PubMed Google Scholar
Areán, P. A., & Huh, J. W. T. (2006). Problem-solving therapy with older adults. In S. H. Qualls & B. G. Knight (Eds.), Psychotherapy for depression in older adults (1st ed., pp. 133–149). Hoboken: Wiley.
Google Scholar
Areán, P., Hegel, M., Vannoy, S., Fan, M. Y., & Unuzter, J. (2008). Effectiveness of problem-solving therapy for older, primary care patients with depression: Results from the IMPACT project. Gerontologist, 48 (3), 311–323.
Ciechanowski, P., Wagner, E., Schmaling, K., Schwartz, S., Williams, B., Diehr, P., Kulzer, J., Gray, S., Collier, C., & LoGerfo, J. (2004). Community-integrated home-based depression treatment in older adults: A randomized controlled trial. JAMA, 291 (13), 1569–1577.
Article CAS PubMed Google Scholar
Crabb, R. M., & Areán, P. A. (2015). Problem-solving treatment for late-life depression. In P. A. Areán (Ed.), Treatment of late-life depression, anxiety, and substance abuse (pp. 83–102). Washington, DC: American Psychological Association.
Chapter Google Scholar
D’Zurilla, T. J., & Nezu, A. M. (2006). Problem-solving therapy: A positive approach to clinical intervention (3rd ed.). New York: Springer.
D’Zurilla, T. J., Nezu, A. M., & Maydeu-Olivarez, A. (2002). Social problem-solving inventory – Revised (SPSI-R) . North Tonawanda: Multi-Health Systems.
Kiosses, D. N., & Alexopoulos, G. (2014). Problem-solving therapy in the elderly. Current Treatment Options in Psychiatry, 1 (1), 15–26.
Article PubMed PubMed Central Google Scholar
Knight, B. (2009). Adapting psychotherapy for working with older adults [DVD]. American Psychological Association. ISBN 9781433803666.
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping . New York: Springer.
Lynch, T. R., & Smoski, M. J. (2009). Individual and group psychotherapy. In M. D. Steffens, D. Blazer, D. C. Steffens, & M. E. Thakur (Eds.), The American Psychiatric Publishing text book of geriatric psychiatry (4th ed., pp. 521–538). Arlington: American Psychiatric Publishing.
Mikami, K., Jorge, R. E., Moser, D. J., Arndt, S., Jang, M., Solodkin, A., Small, S. L., Fonzetti, P., Hegel, M. T., & Robinson, R. G. (2014). Prevention of post-stroke generalized anxiety disorder, using escitalopram or problem-solving therapy. Journal of Neuropsychiatry and Clinical Neurosciences, 26 (4), 323–328.
Nezu, A. M., Nezu, C. M., & Perri, M. G. (1989). Problem-solving therapy for depression: Therapy, research, and clinical guidelines . New York: Wiley.
Nezu, A. M., Nezu, C. M., Friedman, S. H., Faddis, S., & Houts, P. S. (1998). Helping cancer patients cope: A problem-solving approach . Washington, DC: American Psychological Association.
Book Google Scholar
Nezu, A. M., Nezu, C. M., & D’Zurilla, T. J. (2007). Solving life’s problems: A 5 step guide to enhanced well-being . New York: Springer.
Shah, A., Scogin, F., & Floyd, M. (2012). Evidence-based psychological treatments for geriatric depression. In F. Scogin & A. Shah (Eds.), Making evidence-based psychological treatments work with older adults (1st ed., pp. 87–130). Washington, DC: American Psychological Association.
Sharpe, L., Gittins, C. B., Correia, H. M., Meade, T., Nicholas, M. K., Raue, P. J., McDonald, S., & Areán, P. A. (2012). Problem-solving versus cognitive restructuring of medically ill seniors with depression (PROMISE-D trial): Study protocol and design. BMC Psychiatry, 12 (1), 207–216.
Simon, S. S., Cordás, T. A., & Bottino, C. M. (2015). Cognitive behavioral therapies in older adults with depression and cognitive deficits: A systematic review. International Journal of Geriatric Psychiatry, 30 (3), 223–233.
Zarit, S. (1996). Interventions with family caregivers. In S. H. Zarit & B. G. Knight (Eds.), Effective clinical interventions in a life-stage context: A guide to psychotherapy and aging (1st ed., pp. 139–159). Washington, DC: American Psychological Association.
Download references
Author information
Authors and affiliations.
Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine, Stanford, CA, USA
Sherry A. Beaudreau & Christine E. Gould
Sierra Pacific Mental Illness Research Education and Clinical Center, VA Palo Alto Health Care System, Palo Alto, CA, USA
Sherry A. Beaudreau
School of Psychology, The University of Queensland, Brisbane, QLD, Australia
Geriatric Research, Education, and Clinical Center (GRECC), VA Palo Alto Health Care System, Palo Alto, CA, USA
Christine E. Gould
VA Palo Alto Health Care System, Palo Alto, CA, USA
Erin Sakai & J. W. Terri Huh
Stanford University School of Medicine, Stanford, CA, USA
J. W. Terri Huh
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sherry A. Beaudreau .
Editor information
Editors and affiliations.
The University of Queensland, Brisbane, QLD, Australia
Nancy A. Pachana
Rights and permissions
Reprints and permissions
Copyright information
© 2017 Springer Science+Business Media Singapore (outside the USA)
About this entry
Cite this entry.
Beaudreau, S.A., Gould, C.E., Sakai, E., Huh, J.W.T. (2017). Problem-Solving Therapy. In: Pachana, N.A. (eds) Encyclopedia of Geropsychology. Springer, Singapore. https://doi.org/10.1007/978-981-287-082-7_90
Download citation
DOI : https://doi.org/10.1007/978-981-287-082-7_90
Published : 31 January 2017
Publisher Name : Springer, Singapore
Print ISBN : 978-981-287-081-0
Online ISBN : 978-981-287-082-7
eBook Packages : Biomedical and Life Sciences Reference Module Biomedical and Life Sciences
Share this entry
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Free Therapy Techniques
- Anxiety Treatment
- Business and Marketing
- CBT Techniques
- Client Motivation
- Dealing With Difficult Clients
- Hypnotherapy Techniques
- Insomnia and Sleep
- Personal Skills
- Practitioner in Focus
- Psychology Research
- Psychotherapy Techniques
- PTSD, Trauma and Phobias
- Relationships
- Self Esteem
- Sensible Psychology Dictionary
- Smoking Cessation and Addiction
- The Dark Side of Your Emotional Needs
- Uncommon Philosophy
How to Use Problem-Solving Therapy with Your Clients
8 questions you can ask to help clients solve problems faster.
“Any idiot can face a crisis – it’s day to day living that wears you out.”
– Anton Chekhov
“Persistence and resilience only come from having been given the chance to work through difficult problems.”
– Gever Tulley
A common fantasy is of a golden and entirely problem-free future. Sound familiar? The assumption of such a fantasy is, of course, that a life free of problems is (a) possible and (b) by definition, one of happiness.
But could you really live without problems?
We are problem-solving creatures. 1 I suspect we can only be truly happy if we have problems, because rising to challenge gives life meaning. 2 But, paradoxically, we often feel un happy until we have solved our problems. Ah, the paradox of being human! But if we dig into this, the paradox dissolves.
This is because some problems are more problematic, depressing, and overwhelming than others. Some problems are intriguing and fun, while some are depressing and limiting, or at least seem like that. Problems are the fertilizer that helps us grow and develop. But, of course, it’s the kind of problems we have, and how we respond to them, that determines how meaningful life is for us.
Research has found that the kind of happiness associated with taking and getting is less physically beneficial for people than the kind we experience when we seek to help other people and make the world better in some way. The kind of happiness, or perhaps I should say enjoyment, associated with drug taking and drinking, for example, had similar effects on the body to the stress response from terrible adversity. 3
Which leads us to a cliché, but one worth considering.
The more you give, the more you get
When we help others, even when we help ‘us’ rather than simply ‘I’, we are seeking to solve problems that are connected to a sense of a wider, more meaningful life. This kind of satisfaction tends to be more nourishing. Simply looking for repeated thrills or highs can, pretty quickly, start to feel as meaningful as continually trying to fill a bucket with no bottom to it. A ‘bucket list’ is all very well… if the bucket being filled leads to fulfillment .
So, we can, I think, learn a lot about a person from their stated problems. Compare “My life isn’t providing me with meaning!” with “How can I make a difference?”
It’s a terrible cliché to say: “The more you give the more you get” but I would add to this truism “… especially when you forget about getting.”
But if finding solutions to problems and rising to the challenge of making things better can give us that all-important sense of meaning, what is the problem with problems?
Problematic problems
Problems become problematic when our clients lose hope that they can solve them, and especially when they can’t stop thinking about them.
Learned helplessness causes our clients to wrongly feel they’re less empowered than they actually are. They may have come to feel that life simply happens to them, and it had better treat them kindly because they don’t have any influence over life.
The other problem with problems is when people can think of nothing else. If we mull over our problems in the absence of hope, then we become dangerously vulnerable to depression. 4,5 If we feel we can’t solve problems, then we may substitute imagination and circular thinking for action.
If a person doesn’t have volition over where they place their attention, they will find that their focus becomes locked on what makes them feel bad. They will feel unable to withdraw their attention from that particular focus. We see this locking of attention, and difficulty withdrawing it, in addiction, obsession, and, of course, depression.
Sometimes, this kind of locked attention on problems can prove to be worse than the problems themselves.
The problem behind the problem
Because professionals like to slice reality thinly, problem-solving therapy has come to be seen as a type of therapy.
But all therapy is problem-solving therapy. Either we seek to help our clients ‘solve the problem’ by feeling and thinking differently about it, or we help them find ways to solve an actual practical problem (or both!).
Seek to establish how many of your clients’ problems are themselves maladaptive attempts to solve problems.
A client may have come to you for help because they are a control freak . But what problems is their control freakery maladaptively trying to solve? Anxiety ? Fear ? Jealousy ?
The first part of a therapy session, along with building rapport , is information gathering . So what questions can we ask our clients about their problems as a first step to helping them solve them?
Problem-solving therapy questions
Clients come to us when they have some kind of problem. Sometimes they have multiple problems. First off, we need to ask them if they feel the problem is soluble in practical terms or if they need to find ways to feel and think differently about the situation.
In addition, we can ask:
- Have they been using problem-solving strategies, consciously or otherwise, that cause them further problems? Examples might be trying to inflexibly exert control in ways that cause problems or excessive drinking as a way to self-medicate for anxiety.
- Have they been worrying about problems that could arise in the future? If so, it’s clear they’ve been misusing their imagination. We can help them imagine differently or even suspend imagination and therefore better tolerate uncertainty .
- To what extent does their life feel meaningful to them? We can ascertain through listening to our clients to what extent they have been meeting their primal emotional needs in balance.
- What was happening in their lives generally when the problem first developed?
- How do they generally go about solving problems? What is their problem-solving style? Displacement (alcohol or drugs)? Ignoring (head in the sand)? Anger ? Passivity ? Could they learn to think and solve problems differently?
- What ways they have already tried to deal with their problem? What has worked? What hasn’t worked? If I find my client has tried something before with success, I may want to do more of that with them. Reinventing the wheel is a waste of time.
- Do they normally solve problems well but have come to a situation that cannot simply be solved through common and generally effective problem-solving strategies? If so, they may simply need support and emotional help to lower anxiety around problematic situations. Sometimes the way to ‘solve a problem’ that can’t immediately be solved in a practical way is to deal with it better and respond differently on an emotional level .
- What resources do they have in terms of their environment, relationships, and personal resources? We can help them build up a sense of these resources and utilize them more fully.
Clients often have problems dealing with the uncertainties of life. We can remind them that the opposite of certainty needn’t necessarily be uncertainty, but rather can be an openness to discovery.
But we can also form problem-solving strategies with our clients.
Clients often come to us because they don’t know which way to go in life . They may not even know what they want. Maybe they have simply been living life in terms of what they don’t want.
We can help them clarify the problem, but also start to look beyond it.
You could be in a beautiful landscape with wonderful paths to follow, but if you walk around continually holding a large rock right in front of your eyes, that is all you will see. Talk of which path would be good for you to follow might feel meaningless, because all you see is the close-up rock.
We can help our clients put down their ‘rocks’ to see what path they might like to travel beyond the problem.
So how can we do this? Well, we can:
- calm them so that multiple perspectives are more easily perceived,
- use solution-focused language and questions ,
- get a sense of what they do want , not just what they don’t want,
- develop with them the steps to take along their desired path, and
- have them hypnotically rehearse their desired outcome.
A good practitioner will also be able to help their clients devise practical solutions sometimes. If we get a sense of the steps a client might need to take in order to solve some real-world problem, then we may be able to offer ideas or help them form a plan to get the help they need from other professionals. For example, I have put clients in touch with physiotherapists and even legal experts.
Clients may be our problems, but I prefer to think of them as challenges. Actually, better than that – we can see them as our guides to what is truly possible for people.
Watch problem-solving strategies inside Uncommon Practitioners TV
Our online resource for live therapy videos is a great place to watch problem-solving in action. If you’re not a member already and would like to join hundreds of therapy practitioners, you can sign up here to be notified when booking is open.
FREE Reframing Book! Just subscribe to my therapy techniques newsletter below.
Download my book on reframing, "New Ways of Seeing", when you subscribe for free email updates
Click to subscribe free now
About Mark Tyrrell
Psychology is my passion. I've been a psychotherapist trainer since 1998, specializing in brief, solution focused approaches. I now teach practitioners all over the world via our online courses .
You can get my book FREE when you subscribe to my therapy techniques newsletter. Click here to subscribe free now.
You can also get my articles on YouTube , find me on Instagram , Amazon , Twitter , and Facebook .
(1) http://www.i-c-r.org.uk/publications/monographarchive/Monograph33.pdf
(2) https://journals.sagepub.com/doi/abs/10.1177/0956797614531799
(3) https://www.pnas.org/content/early/2013/07/25/1305419110.short
(4) https://www.apa.org/monitor/nov05/cycle
(5) https://ijmhs.biomedcentral.com/articles/10.1186/1752-4458-8-53
Related articles:
Read more Psychotherapy Techniques therapy techniques »
Search for more therapy techniques:
- Odnoklassniki
- Facebook Messenger
- LiveJournal
Issues by year
Advertising
Volume 41, Issue 9, September 2012
Problem solving therapy Use and effectiveness in general practice
Problem solving therapy has been described as pragmatic, effective and easy to learn. It is an approach that makes sense to patients and professionals, does not require years of training and is effective in primary care settings. 1 It has been described as well suited to general practice and may be undertaken during 15–30 minute consultations. 2
Problem solving therapy takes its theoretical base from social problem solving theory which identifies three distinct sequential phases for addressing problems: 3
- discovery (finding a solution)
- performance (implementing the solution)
- verification (assessing the outcome).
Initially, the techniques of social problem solving emerged in response to empirical observations including that people experiencing depression exhibit a reduced capacity to resolve personal and social problems. 4,5 Problem solving therapy specifically for use in primary care was then developed. 6
Problem solving therapy has been shown to be effective for many common mental health conditions seen by GPs, including depression 7–9 and anxiety. 10,11 Most research has focused on depression. In randomised controlled trials, when delivered by appropriately trained GPs to patients experiencing major depression, PST has been shown to be more effective than placebo and equally as effective as antidepressant medication (both tricyclics and selective serotonin reuptake inhibitors [SSRIs]). 7,8 A recent meta-analysis of 22 studies reported that for depression, PST was as effective as medication and other psychosocial therapies, and more effective than no treatment. 9 For patients experiencing anxiety, benefit from PST is less well established. It has been suggested it is most effective with selected patients experiencing more severe symptoms who have not benefited from usual GP care. 10 Problem solving therapy may also assist a group of patients often seen by GPs: those who feel overwhelmed by multiple problems but who have not yet developed a specific diagnosis.
Although PST has been shown to be beneficial for many patients experiencing depression, debate continues about the mechanism(s) through which the observed positive impact of PST on patient affect is achieved. Two mechanisms have been proposed: the patient improves because they achieve problem resolution, or they improve because of a sense of empowerment gained from PST skill development. 12 Perhaps both factors play a part in achieving the benefits of PST as a therapeutic intervention. The observed benefit of PST for patients experiencing anxiety may be due to problem resolution and consequent reduction in distress from anticipatory concern about the identified but unsolved problem.
It is important to note that, while in the clinical setting we may find ourselves attempting to solve problems for patients and to advise them on what we think they should do, 13 this is not PST. Essential to PST, as an evidence based therapeutic approach, is that the clinician helps the patient to become empowered to learn to solve problems for themselves. The GP's role is to work through the stages of PST in a structured, sequential way to determine and to implement the solution selected by the patient. These stages have been described previously. 14 Key features of PST are summarised in Table 1 .
Using PST in general practice
Using PST, like any other treatment approach, depends on identifying patients for whom it may be useful. Patients experiencing a symptom relating to life difficulties, including relationship, financial or employment problems, which are seen by the patient in a realistic way, may be suitable for PST. Frequently, such patients feel overwhelmed and at times confused by these difficulties. Encouraging the patient to clearly define the problem(s) and deal with one problem at a time can be helpful. To this end, a number of worksheets have been developed. A simple, single page worksheet is shown in Figure 1 . A typical case study in which PST may be useful is presented in Table 2 . By contrast, patients whose thinking is typically characterised by unhelpful negative thought patterns about themself or their world may more readily benefit from cognitive strategies that challenge unhelpful negative thought patterns (such as cognitive behaviour therapy [CBT]). 15 Some problems not associated with an identifiable implementable solution, including existential questions related to life meaning and purpose, may not be suitable for PST. Identification of supportive and coping strategies along with, if appropriate, work around reframing the question may be more suitable for such patients.
Problem solving therapy may be used with patients experiencing depression who are also on antidepressant medication. It may be initiated with medication or added to existing pharmacotherapy. Intuitively, we might expect enhanced outcomes from combined PST and pharmacotherapy. However, research suggests this does not occur, with PST alone, medication alone and a combination of PST and medication each resulting in a similar patient outcomes.8 In addition to GPs, PST may be provided by a range of health professionals, most commonly psychologists. General practitioners may find they have a role in reinforcing PST skills with patients who developed their skills with a psychologist, especially if all Better Access Initiative sessions with the psychologist have been utilised.
The intuitive nature of PST means its use in practice is often straightforward. However, this is not always the case. Common difficulties using PST with patients and potential solutions to these difficulties have previously been discussed by the author 14 and are summarised in Table 3 . Problem solving therapy may also have a role in supporting marginalised patients such as those experiencing major social disadvantage due to the postulated mechanism of action of empowerment of patients to address symptoms relating to life problems. 12 of action includes empowerment of patients to address symptom causing life problems. Social and cultural context should be considered when using PST with patients, including conceptualisation of a problem, its significance to the patient and potential solutions.
General practitioners may be concerned that consultations that include PST will take too much time. 13 However, Australian research suggests this fear may not be justified with many GPs being able to provide PST to a simulated patient with a typical presentation of depression in 20 minutes. 15 Therefore, the concern over consultation duration may be more linked to established patterns of practice than the use of PST. Problem solving therapy may add an increased degree of structure to complex consultations that may limit, rather than extend, consultation duration.
Figure 1. Problem solving therapy patient worksheet
PST skill development for GPs
Many experienced GPs have intuitively developed valuable problem solving skills. Learning about PST for such GPs often involves refining and focusing those skills rather than learning a new skill from scratch. 13 A number of practical journal articles 16 and textbooks 10 that focus on developing PST skills in primary care are available. In addition, PST has been included in some interactive mental health continuing medical education for GPs. 17 This form of learning has the advantage of developing skills alongside other GPs.
Problem solving therapy is one of the Medicare supported FPS available to GPs. It is an approach that has developed from a firm theoretical basis and includes principles that will be familiar to many GPs. It can be used within the constraints of routine general practice and has been shown, when provided by appropriately skilled GPs, to be as effective as antidepressant medication for major depression. It offers an additional therapeutic option to patients experiencing a number of the common mental health conditions seen in general practice, including depression 7–9 and anxiety. 10,11
Conflict of interest: none declared.
- Gask L. Problem-solving treatment for anxiety and depression: a practical guide. Br J Psychiatry 2006;189:287–8. Search PubMed
- Hickie I. An approach to managing depression in general practice. Med J Aust 2000;173:106–10. Search PubMed
- D'Zurilla T, Goldfried M. Problem solving and behaviour modification. J Abnorm Psychol 1971;78:107–26. Search PubMed
- Gotlib I, Asarnow R. Interpersonal and impersonal problem solving skills in mildly and clinically depressed university students. J Consult Clin Psychol 1979;47:86–95. Search PubMed
- D'Zurilla T, Nezu A. Social problem solving in adults. In: Kendall P, editor. Advances in cognitive-behavioural research and therapy. New York: Academic Press, 1982. p. 201–74. Search PubMed
- Hegel M, Barrett J, Oxman T. Training therapists in problem-solving treatment of depressive disorders in primary care: lessons learned from the: "Treatment Effectiveness Project". Fam Syst Health 2000;18:423–35. Search PubMed
- Mynors-Wallis LM, Gath DH, Lloyd-Thomas AR, Tomlinson D. Randomised control trial comparing problem solving treatment with Amitryptyline and placebo for major depression in primary care. BMJ 1995;310:441–5. Search PubMed
- Mynors-Wallis LM, Gath DH, Day A, Baker F. Randomised controlled trial of problem solving treatment, antidepressant medication, and combined treatment for major depression in primary care. BMJ 2000;320:26–30. Search PubMed
- Bell A, D'Zurilla. Problem-solving therapy for depression: a meta-analysis. Clin Psychol Rev 2009;29:348–53. Search PubMed
- Mynors-Wallis L Problem solving treatment for anxiety and depression. Oxford: OUP, 2005. Search PubMed
- Seekles W, van Straten A, Beekman A, van Marwijk H, Cuijpers P. Effectiveness of guided self-help for depression and anxiety disorders in primary care: a pragmatic randomized controlled trial. Psychiatry Res 2011;187:113–20. Search PubMed
- Mynors- Wallis L. Does problem-solving treatment work through resolving problems? Psychol Med 2002;32:1315–9. Search PubMed
- Pierce D, Gunn J. GPs' use of problem solving therapy for depression: a qualitative study of barriers to and enablers of evidence based care. BMC Fam Pract 2007;8:24. Search PubMed
- Pierce D, Gunn J. Using problem solving therapy in general practice. Aust Fam Physician 2007;36:230–3. Search PubMed
- Pierce D, Gunn J. Depression in general practice, consultation duration and problem solving therapy. Aust Fam Physician 2011;40:334–6. Search PubMed
- Blashki G, Morgan H, Hickie I, Sumich H, Davenport T. Structured problem solving in general practice. Aust Fam Physician 2003;32:836–42. Search PubMed
- SPHERE a national mental health project. Available at www.spheregp.com.au [Accessed 17 April 2012]. Search PubMed
Also in this issue: Psychological strategies
Professional
Printed from Australian Family Physician - https://www.racgp.org.au/afp/2012/september/problem-solving-therapy © The Australian College of General Practitioners www.racgp.org.au
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Turk Psikiyatri Derg
- v.34(2); 2023
- PMC10552172

Effects of Problem Solving Therapy in Substance Use Disorder in Adolescents
Ömer kardaş.
1 Assis. Prof., Kocaeli University School of Medicine, Child and Adolescent Psychiatry Department, Kocaeli, Turkey
Burcu Kardaş
2 Assis. Prof., Kocaeli University School of Medicine, Child and Adolescent Psychiatry Department, Kocaeli, Turkey
Hozan Saatçioğlu
3 MD., Health Sciences University Şanlıurfa Training and Research Hospital, Child and Adolescent Psychiatry, Şanlıurfa, Turkey
Zeki Yüncü
4 Prof., Ege University School of Medicine, Child and Adolescent Psychiatry Department, İzmir, Turkey
In this study, it was aimed to examine the effects of problem solving therapy, which is a cognitive behavioral method, on adolescents diagnosed with alcohol and substance use disorder.
A semi-structured interview and intelligence test were administered to adolescents with diagnosis of substance use disorder to identify comorbidities. 46 adolescents who met the inclusion criteria were divided into two groups. Problem solving therapy was applied to the first group for 5 weeks, once a week, while the other group continued their routine controls in the center. Beck Depression Inventory, Screen for Child Anxiety Disorders, Revised Social Problem Solving Inventory, Addiction Profile Index and Treatment Motivation Questionnaire were administered to the groups at the beginning of the study and at the end of the 5th week and the results were analyzed.
Sociodemographic and substance use characteristics, comorbid psychopathologies and scale mean scores of the groups in the first evaluation were found to be similar to each other. Although the depression and anxiety scores decreased significantly in both groups, no significant difference was found between the groups. Problem-solving skills and treatment motivation increased in the therapy group and decreased in the control group. The difference between groups was found to be significant (p=0.045, 0.037 for problem solving and treatment motivation respectively). While the severity of addiction decreased in therapy group, it increased in control group, but the difference was not significant.
Conclusion:
This study is important in that it shows that psychosocial interventions strengthen the treatment of substance use disorder in adolescents. In our country, no other study was evaluating the effects of the intervention methods in addicted adolescents was found. Future studies with larger sample sizes and where the long-term results of substance use disorder are evaluated are needed.
INTRODUCTION
Problem Solving Therapy (PST) is a therapy method that uses Cognitive Behavioral Therapy (CBT) techniques to solve psychological problems caused by daily life’s challenges. The objective of PST is to teach individuals how to tackle encountered problems and also to teach about problem solving paths and strategies. The goal of PST is to cure the psychological distress caused by such problems and also prevent distress before it happens. In other words, PST is used both in therapy and in prevention; it is also utilized in gaining resilience or enhancing inherent capacity (Eskin 2011).
PST can be used in mental healthcare to treat different psychopathologies. A recently published meta-analysis encompassing 30 studies (with a total of 3530 patients) has concluded that PST is effective in the treatment of depression, with its impact dimension being found low yet comparable to other psychosocial treatment options (Cujipers et al. 2011). A meta-analysis that assesses PST use in primary healthcare found that PST is effective in anxiety disorders and depression (Zhang et al. 2018). A randomized controlled study comparing the use of PST with motivational interview (MI) in the treatment of substance use disorders has shown that, against MI only, the use of PST+MI together significantly decreased screening test scores (Sorsdahl et al. 2015). In another study investigating the use of PST in adolescents and young adults, results showed that there was a significant decrease in depression and suicide risk scores of the PST group compared to the wait list group (Eskin et al. 2007).
The treatment of addiction in adolescence is a long-term process as in all age groups. Adolescent addiction treatment should include multidimensional biopsychosocial interventions. Psychosocial interventions should be among the top priority approaches in adolescent addiction treatment. Such approaches include 12-step therapy, therapeutic communities, family-based therapies, behavioral approaches, individual and/or group Cognitive Behavioral Therapy (CBT) approaches. The purpose of CBT is to identify circumstances that trigger substance use in adolescents, develop coping mechanisms appropriate to these situations, and enhance communication and problem solving skills.
A study conducted with adolescents and young adults with substance use problems has shown that such individuals took up maladaptive problem solving methods to a greater extent. A 2009 study investigated the relationship between problem solving, personality characteristics and substance use among 307 high-school students. The study in question has revealed that hopelessness had a significant negative impact on rational problem solving skills (Winters et al. 2011). For such reasons, it is considered that applying problem solving therapy to adolescents who struggle with substance use disorders would increase their problem solving skills, decrease the intensity of comorbid conditions and contribute positively to addiction treatment.
There is a lack of studies which discuss non-pharmacologic treatment options and specialized intervention methods in adolescent addiction. Therefore, the purpose of the present study is to investigate the effects of “problem solving therapy” as an intervention method on adolescents who suffer from substance use disorders.
Study Design and Sample
This study was designed to be prospective and experimental. The blinding procedure was not applied during the assignment of cases included in the study to groups. At the beginning, it was planned to include 30 persons per group, totaling up to 60 people. Because of time limitations and the need to see the effectiveness of this application, cases included in the study were primarily assigned to the PST group. The control group was formed after the PST group. We were able to reach 16 cases for the control group. Following this, a power analysis was conducted as the study ran. Sample size of the study was calculated by using the G*Power software package (Faul et al. 2009). Duplicate measurement results showed that in order to achieve an 80% statistical power with an alpha error rate of 0.05 and Cohen’s effect size of 0.30, the required sample size was at least 12 participants per group. Due to time limitations and the fact that the required number of cases as calculated under the power analysis was reached, no further cases were added to the control group.
The study sample consists of 46 adolescents between the ages of 14-18 who are first application or follow-up patients diagnosed with alcohol/substance use disorder (ASUD) at Child and Adolescent Alcohol-Substance Addiction Research and Application Center. All subjects participated in the study on a voluntary basis. At the beginning 40 cases were included in PST group; however, 10 of them were subsequently excluded from the study. Of these 10 cases, 4 were excluded due to absenteeism, 2 due to displaying mental retardation (IQ<70) as a result of the intelligence tests performed, 1 due to attending the sessions under the influence and the remaining 3 cases due to missing data in the scales. The control group consisted of 20 cases, with 4 of them being excluded from the study later on. The reasons for exclusion for these 4 cases are as follows: according to the structured interview conducted, 1 of them had a psychotic disorder; 2 were excluded because of missing data in the second scale, and 1 case was excluded due to missing data in all scales. The study was completed with 46 participants with 30 cases in the PST group and 16 cases in the control group. Before participating in the study, a written statement of informed consent was taken from patients and their first degree relatives or their legal guardians (as per the Helsinki Declaration). An approval was received from Ege Faculty of Medicine Ethics Committee with the decision dated 29.06.2015 and numbered 15-5.1/5.
Inclusion and Exclusion Criteria
Volunteer cases between 14-18 years of age diagnosed with alcohol/substance use disorder (ASUD) according to the DSM-5 criteria (Diagnostic and Statistical Manual of Mental Disorders) (American Psychiatric Association 2013) were included in the study. Cases who had a mental retardation diagnosis or psychopathologies which prevent them from attending the sessions were excluded from the study. Cases who did not obey group rules, who were coming to sessions under the influence, absent for more than two sessions and wished to be excluded from study were also excluded from study.
Data Collection Tools
Socio-demographic information form.
This form was prepared by researchers to collect information on age, gender, educational status, family type, socioeconomic status, place of residence, status of parents, personal background, and family history.

PST: Problem Solving Therapy, IQ: Intelligence Quotient
Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL)
K-SADS-PL is a semi-structured interview form that aims to identify present and lifetime psychopathologies in children and adolescents. The form consists of three sections. Reliability and validity of the scale for the Turkish sample was ensured (Kaufman et al. 1997, Gökler et al. 2004).
Beck Depression Inventory (BDI)
Beck depression inventory (BDI) is a self-report scale developed by Beck in 1961 for the purpose of evaluating emotional, cognitive, somatic and motivational components of depression. Even though its primary aim is to assess depressive symptoms it also enables the evaluation of cognitive contents. Scale scores range between 0-63. Any score equal to or above 10 is considered as a signifier for depression. Validity and reliability of BDI for the Turkish society was provided (Beck 1969, Hisli 1989).
Treatment Motivation Questionnaire (TMQ)
It is a self-report 5 point Likert scale with 26 items, developed to measure reasons of participating and continuing alcohol/substance use treatment. Scale was developed by Ryan et al. in 1995 and in 2006 reliability and validity study was conducted by Evren et al. (Ryan et al. 1995, Evren 2006).
Social Problem-Solving Inventory-Revised (SPSI-R)
The scale developed by Maydeu-Olivares and D’Zurilla between 1995-96 was revised later on in 2002. The inventory consists of 2 main domains that identify problem orientation and problem solving methods with subdomains for each domain. These are:
“Positive Problem Orientation, Negative Problem Orientation, Reasoning, Handicapping, Failure Avoidance, Problem Solving”. Social Problem-Solving Inventory-Revised (SPSI-R) was translated into Turkish and its reliability and validity was ensured by Eskin and Aycan (D’Zurilla et al. 2002, Eskin 2009).
Addiction Profile Index (API) Adolescent form
API was developed by Ögel et al. They also provided the reliability and validity of this scale. The scale consists of 25 items and 5 subdomains (diagnosis, characteristics of substance use, the effect of the substance on person’s life, craving and motivation). It is a self-report, 5-point Likert scale (Ögel et al. 2012).
Screen for Child Anxiety Related Emotional Disorders (SCARED)
Screen for Child Anxiety Related Emotional Disorders (SCARED) scale was developed by Birmaher et al. (1999) for screening childhood anxiety disorders. Its reliability and validity was ensured by Çakmakçı (2004). Child and parent forms of the scale are available. The SCARED scale consists of 41 items, with a total score of 25 and above being considered as a warning sign for anxiety disorder (Birmaher et al. 1999, Çakmakçı 2004).
Wechsler Intelligence Scale for Children-Revised (WISC-R)
Wechsler Intelligence Scale for Children was developed by Wechsler in 1949 to measure the intelligence of children between the ages of 5-15. In 1974, it was revised and the applicable age group was updated to between 6-16 years old. Adaptation of WISC-R for the Turkish culture was performed by Savaşır and Şahin (Wechsler 1974, Savaşır 1995).
Wechsler Adult Intelligence Scale (WAIS)
WAIS is a scale that evaluates intelligence on a multidimensional level and is applied individually. In 1945 when Wechsler developed WAIS, it could be administered to individuals at the age of 16 and above, with 11 sub-tests evaluating verbal and performance skills. Reliability and validity of the Turkish version of the scale was provided by Epir and İskit. Even though the reliability and validity of the scale was ensured, Turkish norms are not yet available (Wechsler 1974, Epir 1972).
This study started after introducing the aim of the research, answering the questions of volunteers and signing of the informed consent forms. All cases included in the study were administered with the K-SADS-PL, which is a test assessing sociodemographic characteristics and comorbid psychiatric disorders, during a clinical interview in the first application. After that, in order to determine intelligence level of cases, WISC-R was administered to cases under 16 years old and WAIS was administered to cases who were aged 16 years and above. The PST group consisted of 30 cases, and the study was completed by dividing them to sub groups with each group including a minimum of 5 and maximum 10 cases.
Two specialists ran the PST sessions together the first is a lecturer and Mental Health Specialist as well as a cognitive behavioral therapist; the second one is a Research Assistant in Child and Adolescent Psychiatry. Before starting the procedure, a meeting was held with Prof. Dr. Mehmet Eskin who pioneered the use of PST in Türkiye and conducted studies in this area. The researchers received training on problem solving therapy. The training materials were obtained and studies in the field of PST were examined. The contents of structured sessions were prepared together.
All cases included in the study group were administered with problem solving therapy. PST involves 8 stages. In this study, for the regular attendance of adolescents, therapy sessions were planned to be completed in 5 weeks and each session lasted 45 minutes. During this time, outpatient follow-up controls of cases continued without interruption. In sessions participants played warm-up games; then the agenda was set with theoretical explanations always being supported with practice, and at the end homework was given. During the sessions, the story of an addicted adolescent was told; examples from this story were given to facilitate the active participation of the cases in detecting problems and finding solution options. Cases included in the control group continued their regular follow-ups in the center. Social Problem-Solving Inventory-Revised (SPSI-R), Beck depression inventory (BDI), Screen for Child Anxiety Related Emotional Disorders (SCARED), Addiction profile index (API) (adolescent form) and Treatment motivation questionnaire (TMQ) were administered to all cases at the beginning of study and on the 5 th week of the study.
Stages of Problem Solving Therapy
Evaluation and debriefing interview: This constitutes the first interview with participants. The aim of this stage is to create a collaborative trust environment by evaluating the individual’s existing complaints and their problem solving skill levels and informing them about the content of therapy.
Problem orientation training: The purpose of this second session is to assist individuals in recognizing their existing problems and exhibiting positive attitude while tackling these problems. In this stage, our aim was to develop a mindset of positive problem orientation in our cases. This mindset involves believing that problems can be solved, seeing problems as a part of life, and not evading the issues.
Describing problems: In this stage, reasons or problems that contribute to existing distress or complaints of individuals are identified and formulated. The aim is to evaluate and describe problems that can cause distress by answering the questions of where, when, how often and with whom these problems occur.
Setting goals: After overcoming existing problems, the individual tries to evaluate his/her current situation and set goals with a realistic attitude. This session is centered around the question of whether the goals set by the individual have to do with changing the problem or decreasing the emotional impact thereof.
Coming up with possible solution options: The aim of this stage is to create as many solutions as possible to the existing problem. All possible solutions are noted down without discussing whether it is suitable or effective.
Choosing a suitable solution option: All solution options are evaluated according to their problem solving and goal achieving power and acceptability and applicability with the highest rated option being selected at the end.
Implementing the solution: This is the stage where the individual is prepared for the implementation. For this, all advantages and disadvantages of such implementation are discussed with the person in advance.
Evaluation of the Procedure: At this stage, results of the implementation are evaluated by asking whether the problem is solved or not, and whether the goal is achieved or not. In the case of an unsuccessful implementation, all stages are reviewed. If there is an error in the implementation of a particular stage, the procedure is backtracked and started again from there.
In our study, the 8-stage PST sessions were administered as follows:
- Week: Evaluation, debriefing, and problem orientation training (1. and 2. stages)
- Week: Describing problems (3. stage)
- Week: Setting goals and coming up with possible solution options (4. and 5. stages)
- Week: Choosing the suitable solution option and implementing the chosen solution (6. and 7. stages)
- Week: Evaluating the whole procedure (8. stage)
Statistical Method
The data was evaluated with the SPSS (The Statistical Package for Social Sciences) 22.0 software package. Normality assumption was evaluated by using the Shapiro-Wilk and Kolmogorov-Smirnov tests for normality. Chi-Square test, independent samples T-test and McNemar test were used for the comparison of the groups. In repeated application of scales for evaluating the potential differences between groups, “repeated measures analysis of variance” was used, with p<0.05 being accepted as statistically significant. In order to show the significance level of findings, the p value was input directly.
The PST group consisted of 16 (53.3%) girls and 14 (46.7%) boys. The control group consisted of 5 (31.2%) girls and 11 (68.8%) boys. The mean age of participants was 16.3 (PST: 16.2, control: 16.5). Groups were similar to each other in terms of the mean age of participants and gender distribution (p=0.124, 0.152). Nearly half of participants were not attending school (52.2%). Looking at the rates of psychiatric comorbidities, attention deficit and hyperactivity was found to be (ADHD) 82.6% (n=38), conduct disorder (CD) 30.4% (n=14), oppositional defiant disorder (ODD) 63% (n=29), major depressive disorder (MDD) 41% (n=19), and anxiety disorder (AD) 28.4% (n=13). It was found that sociodemographic and clinical characteristics of groups were similar to each other. The relevant data are shown in detail under Table 1 .
Comparison of Sociodemographic and Clinical Characteristics of PST and Control Groups
PST: Problem Solving Therapy, SD: Standard Deviation, SES: Socioeconomic Status, ADHD: Attention Deficit Hyperactivity Disorder, CD: Conduct Disorder, ODD: Oppositional Defiant Disorder, MDD: Major Depressive Disorder, AD: Anxiety Disorder. a: Chi Square Test, b: Independent Sample T-Test, p<0.05
Tobacco and substance use rates of groups are as follows: tobacco 91.3%, alcohol 93.5%, cannabis 93.5%, ecstasy 69.6%, synthetic cannabinoids 69.6%, inhalants 45.7%, heroin 8.7%. Starting ages are; for tobacco use 12.3, for alcohol 13.4, for cannabis 13.8, for ecstasy 14.5, for synthetic cannabinoids 15.1, for inhalants 14.6, and for benzodiazepines 14.8 years old. Tobacco, alcohol, ecstasy, synthetic cannabinoids, inhalants, benzodiazepines, and heroin rate of use (p=0.759, 1.000, 0.274, 0.316, 0.512, 0.095, 1.000, 0.602), starting ages (p=0.532, 0.818, 0.527, 0.609, 0.667, 0.440, 0.724) and amounts of tobacco use (p=0.286) of groups were found to be similar.
The groups’ initial BDI, SCARED, TMQ, API, SPSI-R average scores were found to be similar (p=0.702, 0.523, 0.318, 0.344, 0.091). After 5 weeks a significant decrease was observed in BDI and SCARED scores of both groups (p=0.001); but in terms of such decrease there was no significant difference between the groups (p=0.645, 0.654). It was seen that TMQ and SPSI-R scores increased in the PST group and decreased in the control group; however, the rate of change was not significant (p=0.998, 0.961). In the course of time, SPSI-R and TMQ scores increased in the PST group and decreased in the control group. As a consequence, a significant difference was found between groups (p=0.045, 0.037). Changes in scale scores are presented in detail in Table 2 .
Comparison of Baseline Values and Changes in Scale Scores
PST: Problem Solving Therapy, BDI: Beck Depression Inventory, SCARED: Screen for Child Anxiety Related Emotional Disorders, TMQ: Treatment Motivation Questionnaire, API: Addiction Profile Index, SPSI-R: Social Problem Solving Inventory-Revised
When the groups were evaluated in terms of BDI cutoff scores, it was seen that in the first measurement, 80% of the PST group was in the “depressed” category (n=24). In the second measurement this rate decreased with only 30% of group falling in the “depressed” category (n=6). This change was statistically significant (p=0.001). In the control group, it was observed that in the first measurement 81.2% of the group was in the “depressed” category (n=13) and in the second measurement that the same rate decreased down to 56.2% (n=9). This change was found not to be statistically significant (p=0.125). Table 3 presents the changes in BDI cutoff scores.
Comparison of the Change of BDI According to the Cut-off Score
PST: Problem Solving Therapy, BDI: Beck Depression Inventory
This study intends to examine the effects of PST, a cognitive behavioral therapy method, on adolescents who have substance use disorder. At the end of study, BDI and SCARED scores decreased significantly in both groups but a statistically significant difference was not found between the two groups. While mean SPSI-R and mean TMQ scores increased in the PST group, these scores decreased in the control group and a significant difference was found between the groups. As mean API scores decreased in the PST group, the same increased in the control group. However, there was no significant difference between the groups. When the groups were compared according to their BDI score categories, in the PST group the number of cases in the “depressed” category significantly decreased; yet there was no significant decrease in the control group.
Cognitive Behavioral Therapy (CBT) methods are used effectively in depression treatment by themselves or in combination with pharmacotherapy. In the treatment of children and adolescents who are diagnosed with mild to moderate major depressive disorder (MDD), CBT is recommended as the first option (Melvin et al. 2006). In studies falling within the scope of Treatment of Adolescent with Depression (TADS) wherein 4 different treatment methods (medication, medication+CBT, CBT, and placebo) are compared, it was reported that medication+CBT treated depression faster than fluoxetine treatment or CBT treatment alone (AACAP 2007, TADS Team 2009). Similarly, in the study titled “Treatment of SSRI-Resistant Depression in Adolescents (TORDIA)” it was found that on the 12th week, medication+CBT was more effective than only medication (AACAP 2007). The present study confirms the findings in the literature in that PST administered in addition to routine treatment gives way to a more positive change according to evaluations made over the BDI cutoff scores.
In a study including 6050 adults who use alcohol, it was reported that the group that was diagnosed with alcohol addiction diagnosis according to DSM-IV had 4 times higher MDD comorbidity when compared to the group that was not diagnosed with alcohol addiction (Hasin & Grant 2002). ASUD may give way to other disorders or, more frequently, it follows other disorders. It is known that adolescents diagnosed with ASUD have a psychological disorder which possibly had its outset in childhood, that affects etiology and treatment (Kaplan & Sadock 2012). Considering the fact that MDD is a disorder that disrupts the psychosocial adaptation of an individual, similarly to our study, it could be said that treating this disorder will positively contribute to ASUD treatment.
Looking at the efficacy of PST in the treatment of MDD in adolescents, a study conducted in Türkiye included 27 adolescents and young adults in the problem solving group and 19 adolescents and young adults in the wait list, all between the ages of 15-18. Said cases were administered with 6 sessions of PST. BDI scores showed that in the PST group 77.8% of participants were considered to be treated; however, in the control group only 15.8% of participants were treated. In addition to this, researchers conducted a follow-up interview one year after the study, with results showing that treatment gains were maintained (Eskin et al. 2008). In another study, 22 cases were included in the problem solving group and 23 in the waitlist group, with the ages of the participants ranging between 12-21 years old. This study revealed that depression scores of the PST group decreased significantly (Hoek et al. 2012). Our study was found to confirm these two studies evaluating depression scores. On the other hand, our study differs from other studies in that it only involves adolescents.
In a meta-analysis examining the effects of CBT on adolescents who are diagnosed with anxiety disorder (AD) a comparison of 3 treatment types as CBT+medication, CBT treatment alone and medication alone was performed. In turn, response to treatment rates were reported to be 68%, 46% and 46% respectively. 36 weeks later, response treatment rates were reported to be 73%, 52% and 52% in the same order (Kendall & Peterman 2015). In a controlled study where a CBT method titled “Coping Cat Program” was applied to 488 children and adolescents between 7-17 years old, it was found that all CBT, medication and CBT+medication methods were effective, as well as CBT+medication being found superior to other methods (Kendall et al. 2016). In another meta-analysis encompassing 44 different studies comparing different CBT methods in treatment of anxiety disorders as counselling, CBT and PST, all methods were found effective but differences between the methods were not statistically significant (Cape et al. 2010).
Our study found that the decrease in mean SCARED scores was statistically significant in the PST group, which corresponds to other studies in the literature that state combined treatment approaches are effective in the treatment of anxiety disorders. However, no studies were found in the literature wherein the implementation of problem solving therapy in the treatment of anxiety disorder in children and adolescents was practiced.
Patients who present with ASUD-comorbid anxiety disorder display the following characteristics: higher levels of incapacity, heavier drinking/smoking, worse social adaptation, higher hospitalization numbers and more severe psychiatric distress (Grant et al. 2005, Burns et al. 2005). A longitudinal follow-up study on generalized anxiety disorder patients reported that ASUD comorbidity decreases the possibility of treatment for generalized anxiety disorder and also increases its recurrence probability (Bruce et al. 2005). It is observed that there is a frequent comorbidity between ASUD and anxiety disorder (as well as other mental disorders) and that this comorbidity affects response to treatment rates. It could be deduced that the treatment of anxiety disorder is an effective option in treating ASUD.
Motivation is an internal state affected by external factors and is therefore changeable. Motivation is necessary in the treatment of addiction. In a study assessing 170 adolescents between 13-18 years old who are diagnosed with ASUD, the cases received CBT for 10 weeks and it was reported that their treatment motivation increased. The same study emphasizes that with the increase of treatment motivation, the amount of substance use decreased (Kaminer et al. 2016). A longitudinal follow-up study conducted in 2011 evaluated addiction severity and treatment motivation of 167 adults diagnosed with ASUD through psychometric scales. As a result it was stated that high treatment motivation was a predictor of low addiction severity (Korcha et al. 2011). During a study wherein 142 patients who were receiving smoking cessation treatment were evaluated, all cases were examined 3 times; before treatment, after CBT+medication treatment and 6 months after treatment, and it was emphasized that the success of treatment was significantly related to low levels of anxiety and depression and to high levels of treatment motivation (Pawlina et al. 2015). In our study, it was found that receiving PST in addition to regular treatment increased treatment motivation and this result is compatible with literature.
Cognitive behavioral group therapy (CBGT) seem to be more practical in terms of its low cost and power of reaching more people. In a review study assessing CBGT involving the adult age group, it was found that CBGT is generally more efficient than standard treatments. In the same study, CBGT was compared with pharmacotherapy and it was found that the efficiency of CBGT alone is similar to medication treatments (Yıldırım & Sütçü 2016). In a study published in 2014, 279 cannabis addicts between 16-63 years old were examined, with 149 of them receiving combined treatment (CBT, motivational therapy and problem solving training together) and the remaining 130 being kept the in waitlist group. At the end of treatment, it was reported that cannabis use decreased in a statistically significant manner in the therapy group compared to the waitlist group. Also, the amount of cannabis use and problems associated with cannabis use decreased significantly in the therapy group (Hoch et al. 2014). Another study was conducted with 240 young adults who had cannabis dependence according to DSM-IV with all participants being randomly assigned to 4 groups. Each group received different modes of treatment as follows: the 1 st group had a standard psychiatric interview, the 2 nd group motivational interview and CBT, the 3 rd group contingency management and avoidance reinforcement approach, and the 4 th group motivational therapy, CBT and additionally, contingency management. At the end of treatment these four groups were compared and it was seen that the decrease in substance use frequency and intensity was lowest in the standard therapy group and such frequency and intensity was significantly decreased in the contingency management group. 1 year later cases were evaluated again and it was determined that individuals in the combined therapy group used significantly less amounts substance and that the severity of their addiction decreased (Kadden et al. 2007). In 2009, a controlled study was conducted with adolescents who were between 14-18 years of age and had cannabis addiction; one group received motivational therapy+CBT+contingency management and psychoeducation was delivered to their families, and the other group was included in the waitlist. 69 adolescents were included in this study and 3 months, 6 months and 9 months after treatment, the cases were evaluated in terms of their restarting cannabis use. In all measurements, restarting rates were significantly less in the group receiving therapy when compared to the control group (Stranger et al. 2009).
In the literature, we found a study wherein PST was administered in substance use disorder treatment in the adolescent age group. In this study, 29 cases received family supported behavioral therapy, and 27 cases were included in the individual PST group. Results of satisfaction scale for young people, satisfaction scale for family and urine tests showed that there was a statistically significant decrease in substance use for both groups; besides this, it was emphasized that none of the methods applied was superior to the others (Azrin et al. 2000).
In the literature there were 7 studies practicing CBGT including problem solving therapy in the treatment of alcohol use disorder in adults. In a study involving 78 convicted adult males diagnosed with alcohol addiction according to DSM-IV, it was found that CBGT including problem solving training is superior to 12-step programs (Easton et al. 2007). In another study comparing naltrexone, CBGT and placebo, it was emphasized that CBGT including naltrexone+problem solving training reduced cravings for alcohol more (O’Malley et al. 2007). In a study comparing CBGT including problem solving training to motivational group intervention (MGI), it was reported that CBGT including problem solving training is superior to motivational group intervention (Rosenblum et al. 2005). In a study conducted in our country which examined 90 alcohol dependent patients, CBGT including problem solving training was administered alongside standard therapy procedures; yet a control group was not established for the study. In the follow-up it was found that 72.3% of cases were in remission (Türkcan et al. 2001). Our study shows that adding PST to regular interviews decreases addiction severity and also that CBT approaches decrease addiction severity; thus, the findings of our study are in accord with the literature. However, the difference between groups was not statistically significant. This could be explained with the inadequate size of the sample, methodological differences and the application of a different intervention method.
The literature includes a study wherein SPSI-R is administered to adolescents diagnosed with ASUD. In said study it was reported that with PST, the subscale mean scores for PPO (positive problem orientation) and RPS (rational problem solving) increased whereas NPO (negative problem orientation), ICPSS (impulsive-careless problem solving style), APSS (avoidant problem solving style) subscale mean scores decreased (Azrin et al. 2001). In our study, mean SPSI-R scores increased in the PST group and decreased in the control group. It was seen that such changes were statistically significant (p=0.037). When evaluated in terms of subscale scores, there was no statistically significant difference between the groups.
CONCLUSION AND LIMITATIONS
In ASUD treatment for adolescents, in addition to pharmacotherapy, psychosocial interventions are needed. Nowadays CBT techniques are practiced in centers that administer such treatment, but this procedure is not prevalent and has not become the standard. As a cognitive behavioral intervention method, PST could be considered as an effective option. Our study is the first one in Türkiye examining an intervention method applied to adolescents with addiction. The limitations of our study were as follows: low number of cases, case numbers in the groups not being equalized, gender distribution not being homogenous, blind procedure not being used while forming and evaluating the groups, interventions administered to groups not starting at the same time, case numbers included in groups not being equal, and power analysis not being performed at the beginning of the study. Different studies which do away with these limitations and evaluate the long term results are needed.
Acknowledgement:
We would like to thank Prof. Dr. Mehmet Eskin, Ebru Gürçay and Cansu Bingül for their contributions to the study .

17 Fun Problem Solving Activities for Kids
There might be affiliate links on this page, which means we get a small commission of anything you buy. As an Amazon Associate we earn from qualifying purchases. Please do your own research before making any online purchase.
As a child, I would spend hours putting together puzzles… whether it was 3-D puzzles or figuring out a crossword. I also loved it when teachers would give the class an open-ended question and we had to work in groups to figure out the answer in our own way.
Even something as simple as playing checkers with my brothers gave me the chance to use strategy as a way to win the game. I honestly believe that it’s so important for kids to solve problems at a young age, as it helps them think critically and outside the box.
Table of Contents
So, Why Is It Important To Teach Kids Problem Solving?
I think these kinds of activities are so important for kids to do because it helps them learn how to think analytically and solve problems on their own. It's a great way to get kids to use their imaginations and be creative.
Rote memorization simply does not have the same effect. This type of learning is great for learning facts like historical dates, but it’s not going to help kids figure out how events in history happened and the results.
We take these problem-solving skills into college, the workforce, and travel . My ability to problem solve since childhood has certainly got me through many sticky situations while in a new city or country.
Additionally, problem-solving helps children learn how to find creative solutions to challenges they may face both in and out of the classroom . These activities can also be fun and used in cohesion with school or playtime.
17 Fun Problem-Solving Activities for Kids
1. marble mazes.
This activity was selected because it requires them to think spatially. Spatial learning will benefit kids when they start driving, riding a bike, playing sports,etc.
To do this activity in its simplest form, you will need a piece of paper, a pencil, and some marbles. First, draw a maze on a piece of paper using a pencil.
Make sure to create a start and finish point. Then, place the marbles at the start of the maze. The goal is to get the marbles from the start to the finish by tilting the paper and using gravity to guide the marbles through the maze.
Another example of a marble maze can involve using toilet paper rolls taped together to create a three-dimensional maze. The larger the maze, the harder you can make it.

Check Price on Amazon!
If you are not into the DIY method, you can always buy a toy maze on Amazon. A good 48 piece puzzle is the Melissa & Doug Underwater Ocean Floor puzzle.
2. The Tower Challenge
Building a tower gives kids the chance to think about gravity, structure, and balance.
To do this activity, you will need some building materials like legos, blocks, or even toilet paper rolls. The challenge is to see how high they can stack the materials without the tower toppling over.
This can be done individually or in teams. An activity like this is good for younger kids and is the building block to learning about harder topics like engineering.
3. The Egg Drop Challenge
The egg drop challenge helps kids learn how to engineer a solution that prevents something from breaking. It requires them to think critically about which materials will best protect something fragile like an egg when dropped from a height.
To do this activity, you will need some eggs and various materials such as straws, cotton balls, bubble wrap, etc. The goal is to construct a device that will protect an egg from breaking upon impact.
This can be done individually or in teams . Teams can even have a competition for the best egg drop device.
As children begin handling, shopping for, and cooking their own food, activities like this will help them understand how to handle breakable items like bottles, eggs, delicate fruit,.etc. Ideally, this is best for age groups 8 and up.
4. The Penny Drop Challenge
This activity was selected because it requires kids to think about physics and how different materials affect sound.
To do this activity, you will need a penny ( or another coin), a cup, and various materials such as paper towels, cotton balls, etc.
The goal is to drop the penny into the cup without making any noise. Begin by placing different materials into the cup and then drop the penny into it. The children should also drop the penny from different heights into the same material to see if/how the impact from a higher drop affects sound.
Group kids into teams or let them try it on their own.
Kids should make note of what type of sounds are made when the penny hits different materials. This is a great activity for kids who are interested in science and physics.
5. The Balloon Race Challenge
This activity was selected because it helps kids learn about aerodynamics and Bernoulli’s principle . It also requires them to think creatively about how to design a balloon-powered vehicle.
To do this activity, you will need balloons, straws, masking tape, and markers. The goal is to design a balloon-powered vehicle that can travel a distance of at least 10 feet. Kids can begin this activity by sketching out their designs on paper.
After they have a basic design, they can begin building their vehicle from various materials. Then kids can explain why they think the balloon traveled or did not travel as far as it did.
6. The Marshmallow Challenge
Marshmallows are not only delicious, but they are also soft and malleable. So kids can have fun using it for some construction projects.
This activity was selected because it requires kids to think creatively about how to build a structure using limited materials. It also helps them learn about engineering and work as a team.
To do this activity, you will need marshmallows and spaghetti noodles. The goal is to build the tallest free-standing structure possible using only marshmallows and spaghetti noodles. If you don't have spaghetti noodles, use something similar like pretzel sticks.
You may even want to establish certain rules like each team can only use a certain number of marshmallows or noodles. A time limit can also make it more fun and challenging.
For more fun activities, check out our post on problem solving exercises for team building .
7. The Balloon Pop Challenge
If you remember your childhood, you probably remember popping balloons for fun at times. But this activity is different because it requires kids to use strategy and critical thinking.
This activity was selected because it helps kids learn about patterns and problem-solving. It is also a lot of fun for kids who like popping balloons. The goal is to create a device that will allow them to pop a balloon without using their hands.
To do this activity, you will need balloons and various materials such as straws, string, paper clips, etc.
8. Picture Pieces Puzzle Game
As mentioned earlier, puzzles are a great pastime – especially in childhood. Kids must think critically about how to put the pieces together to create a certain picture. It also helps them learn about shapes, colors, and other concepts.

You can take a medium to large picture and cut it into pieces. If you have younger kids, you may want to make the pieces larger. However, if you have kids closer to the 8-11 age range, you should be able to provide a challenge and make the pieces smaller.
9. Copy the Block Model
For this challenge, you can build a model out of blocks for the kids to copy. Put kids into groups and make sure each group has the same number of blocks you used for your model.
Make your model block as simple or complex as needed for your child's age group.
Set a time limit and make sure each group starts at the same time.
10. Team Scavenger Hunt
A scavenger hunt is great for kids because they have to search for items and use investigative skills. It is also a lot of fun and can be done both indoors and outdoors .
To do this activity, you will need to create a list of items for the kids to find. The items can be anything from common household items to things you would find outside.
These types of activities can also revolve around a theme like a holiday, movie, or book. For example, if the kids are fans of “Harry Potter” you can make a list of items to find that are related to the movie.
11. Obstacle Course
This activity requires kids to think creatively about how to get from one point to another while maneuvering around obstacles. If you have outdoor space, this can be done with common objects such as hula hoops, cones, etc.
If you don't have access to an outdoor space, you can use common household items to create an indoor obstacle course. For example, you can use chairs, blankets, pillows, etc.
Begin by setting up the course and then timing each child as they complete it. You can also have them race against each other to make it more fun.
Obstacle courses are also great because kids get to be physically active while they are thinking critically.
12. Reading Storybooks
There are many great benefits for kids that read storybooks. One of the excellent benefits is the ability to problem-solve. When they read the stories in the books, they see scenarios that cause them to be attached to the various characters they read about.
So, when they encounter a real-life problem, it is often productive to ask a child how their favorite character would solve that problem. Your kids can also be encouraged to come up with various options and possible outcomes for some of the situations they may encounter.
This not only helps kids solve various problems but become more independent as well.
13. Ask Them Open-Ended Questions
A good way to improve a child's ability to think critically and creatively and improve their ability to solve problems is by asking open-ended questions. It also helps them to develop healthy personalities .
There are no right or wrong answers to these questions. In addition, the solution requires more than a simple “yes” or “no” answer. Furthermore, it allows kids to put some extra thought into their responses.
Here are some examples of open-ended questions you may want to ask.
- What did this experience teach you?
- Was this easy? What was easy about it?
- What this difficult? What is complicated about it?
- What may happen next in this situation?
- How did you come to this solution?
- What, if anything, would you do differently next time?
- What can we do to make things more fun next time?
14. Build Various Structures with Toys
Whether wooden blocks, LEGO blocks, or engineering blocks… giving your kid blocks to build whatever their minds can dream up is fun. In addition, it requires them to think about how they will make a structure, put the pieces together, and creatively ensure the building's function and design.

You may also want to challenge them to build something more complicated and watch them use their brain power to make it happen.
15. Acting Out Skits
Impromptu activities like acting out skits help kids identify problems, develop solutions, and execute them. This process works with multiple kids being divided into teams.
First, you will want to write down different situations, such as resolving a disagreement between siblings or dealing with bullying on the playground on a piece of paper. Second, you will fold the paper and place it in a hat or bowl.
Third, each team will pick a scenario out of the hat. Finally, you can give the kids a few minutes to discuss their solution and act out.
16. Solving Moral Dilemmas
In this simple game, you will help your kids solve simple dilemmas they may find themselves in. You could write down a situation your child may find themselves in and help them learn the moral way to solve the problem.
For instance, “The cashier gave them an additional $5 change back on my purchase. What should they do?” Another scenario could be, “I saw my friend cheating on a test. Should I tell on them or let it go?” A third one could be, “I caught my friends stealing some gum from the store. What should I do?”
After writing down the dilemmas and placing them in a bowl, get each child to select one and read it aloud. Finally, you will help them devise morally correct solutions to the moral dilemma.
17. Animal Pairing Game
This is a fun and creative game to help your kids with focus, critical thinking, and team building skills . In addition, this activity requires an even number of players to participate (4, 6, 8, etc.)
Before starting the game, you will want to write the names of different animals twice, each on a separate slip of paper. Then pass out the slips of paper to each individual or team member, instructing them not to share with anyone the name of the animal they received.
Then the children will perform activities the animals might do without talking or making sounds. Some of these activities might include:
- The way the animal cleans or grooms itself
- The way the animal sleeps
- The way the animal fights
- The way the animal eats or drinks
- The way the animal walks or runs
The goal is for each child to successfully pair up with the other child who has selected the same animal.
How Problem Solving in Childhood Helps in Adulthood
Children are not born with problem-solving skills. It is something that needs to be learned and developed over time .
From babies who learn how to communicate their needs to toddlers who figure out how to get what they want, to children who are starting to understand the consequences of their actions – problem-solving is a process that begins in childhood and continues into adulthood.
Some of the benefits of teaching problem-solving skills to children include:
- Improved critical thinking skills
- Better decision-making skills
- Enhanced creativity
- Improved communication and collaboration skills
- Increased confidence
There are many ways to teach problem-solving skills to children. The activities mentioned above are just a few examples. It is important to find activities that are appropriate for the age and abilities of the child.
With practice, children will develop these skills and be better prepared to face challenges in both childhood and adulthood.
Final Thoughts About Fun Problem Solving Activities For Kids
These are just a few ideas to get you started on teaching your child crucial problem solving skills. Perhaps they’ve inspired to come with some of your own, or seek out others? The important thing is to make sure the activity is age-appropriate and challenging enough to engage the kids.
Problem-solving skills are important for kids to learn because they can be applied to various situations in life. These skills also promote critical thinking, which is an important life skill.
There are many other problem-solving activities for kids out there. In time, you’ll find the ones that work best for your child. And be sure not to forget about your own needs and self-improvement, both of which will make you a better parent and mentor. Here are some useful activities for adults to get your started.
Finally, if you want to level up your parenting skills, then check out this resource that will show you how to get your kids to listen WITHOUT yelling, nagging, or losing control .
- Share full article
Advertisement
Supported by
the new old age
Why Are Older Americans Drinking So Much?
The pandemic played a role in increased consumption, but alcohol use among people 65 and older was climbing even before 2020.

By Paula Span
The phone awakened Doug Nordman at 3 a.m. A surgeon was calling from a hospital in Grand Junction, Colo., where Mr. Nordman’s father had arrived at the emergency room, incoherent and in pain, and then lost consciousness.
At first, the staff had thought he was suffering a heart attack, but a CT scan found that part of his small intestine had been perforated. A surgical team repaired the hole, saving his life, but the surgeon had some questions.
“Was your father an alcoholic?” he asked. The doctors had found Dean Nordman malnourished, his peritoneal cavity “awash with alcohol.”
The younger Mr. Nordman, a military personal finance author living in Oahu, Hawaii, explained that his 77-year-old dad had long been a classic social drinker: a Scotch and water with his wife before dinner, which got topped off during dinner, then another after dinner, and perhaps a nightcap.
Having three to four drinks daily exceeds current dietary guidelines , which define moderate consumption as two drinks a day for men and one for women, or less. But “that was the normal drinking culture of the time,” said Doug Nordman, now 63.
At the time of his 2011 hospitalization, though, Dean Nordman, a retired electrical engineer, was widowed, living alone and developing symptoms of dementia. He got lost while driving, struggled with household chores and complained of a “slipping memory.”
He had waved off his two sons’ offers of help, saying he was fine. During that hospitalization, however, Doug Nordman found hardly any food in his father’s apartment. Worse, reviewing his father’s credit card statements, “I saw recurring charges from the Liquor Barn and realized he was drinking a pint of Scotch a day,” he said.
Public health officials are increasingly alarmed by older Americans’ drinking. The annual number of alcohol-related deaths from 2020 through 2021 exceeded 178,000, according to recently released data from the Centers for Disease Control and Prevention : more deaths than from all drug overdoses combined.
An analysis by the National Institute on Alcohol Abuse and Alcoholism shows that people over 65 accounted for 38 percent of that total. From 1999 to 2020, the 237 percent increase in alcohol-related deaths among those over age 55 was higher than for any age group except 25- to 34-year-olds.
Americans largely fail to recognize the hazards of alcohol, said George Koob, the director of the institute. “Alcohol is a social lubricant when used within the guidelines, but I don’t think they realize that as the dose increases it becomes a toxin,” he said. “And the older population is even less likely to recognize that.”
The growing number of older people accounts for much of the increase in deaths, Dr. Koob said. An aging population foreshadows a continuing surge that has health care providers and elder advocates worried, even if older people’s drinking behavior doesn’t change.
But it has been changing . The proportions of people over 65 who report using alcohol in the past year (about 56 percent) and the past month (about 43 percent) are lower than for all other groups of adults. But older drinkers are markedly more likely to do it frequently, on 20 or more days a month, than younger ones.
Moreover, a 2018 meta-analysis found that binge drinking (defined as four or more drinks on a single occasion for women, five or more for men) had climbed nearly 40 percent among older Americans over the past 10 to 15 years.
What’s going on here?
The pandemic has clearly played a role. The C.D.C. reported that deaths attributable directly to alcohol use, emergency room visits associated with alcohol, and alcohol sales per capita all rose from 2019 to 2020, as Covid arrived and restrictions took hold.
“A lot of stressors impacted us: the isolation, the worries about getting sick,” Dr. Koob said. “They point to people drinking more to cope with that stress.”
Researchers also cite a cohort effect. Compared to those before and after them, “the boomers are a substance-using generation,” said Keith Humphreys, a psychologist and addiction researcher at Stanford. And they’re not abandoning their youthful behavior, he said.
Studies show a narrowing gender divide, too. “Women have been the drivers of change in this age group,” Dr. Humphreys said.
From 1997 to 2014, drinking rose an average of 0.7 percent a year for men over 60, while their binge drinking remained stable. Among older women, drinking climbed by 1.6 percent annually, with binge drinking up 3.7 percent.
“Contrary to stereotypes, upper-middle-class, educated people have higher rates of drinking,” Dr. Humphreys explained. In recent decades, as women grew more educated, they entered workplaces where drinking was normative; they also had more disposable income. “The women retiring now are more likely to drink than their mothers and grandmothers,” he said.
Yet alcohol use packs a greater wallop for older people, especially for women, who become intoxicated more quickly than men because they’re smaller and have fewer of the gut enzymes that metabolize alcohol.
Seniors may argue that they are merely drinking the way they always have, but “equivalent amounts of alcohol have much more disastrous consequences for older adults,” whose bodies cannot process it as quickly, said Dr. David Oslin, a psychiatrist at the University of Pennsylvania and the Veterans Affairs Medical Center in Philadelphia.
“It causes slower thinking, slower reaction time and less cognitive capacity when you’re older,” he said, ticking off the risks.
Long associated with liver diseases, alcohol also “exacerbates cardiovascular disease, renal disease and, if you’ve been drinking for many years, there’s an increase in certain kinds of cancers,” he said. Drinking contributes to falls, a major cause of injury as people age, and disrupts sleep.
Older adults also take a lot of prescription drugs, and alcohol interacts with a long list of them. These interactions can be particularly common with pain medications and sleep aids like benzodiazepines, sometimes causing over-sedation. In other cases, alcohol can reduce a drug’s effectiveness.
Dr. Oslin cautions that, while many prescription bottles carry labels that warn against using those drugs with alcohol, patients may shrug that off, explaining that they take their pills in the morning and don’t drink until evening.
“Those medications are in your system all day long, so when you drink, there’s still that interaction,” he tells them.
One proposal for combating alcohol misuse among older people is to raise the federal tax on alcohol, for the first time in decades. “Alcohol consumption is price-sensitive, and it’s pretty cheap right now relative to income,” Dr. Humphreys said.
Resisting industry lobbying and making alcohol more expensive, the way higher taxes have made cigarettes more expensive, could reduce use.
So could eliminating barriers to treatment. Treatments for excessive alcohol use, including psychotherapy and medications, are no less effective for older patients , Dr. Oslin said. In fact, “age is actually the best predictor of a positive response,” he said, adding that “treatment doesn’t necessarily mean you have to become abstinent. We work with people to moderate their drinking.”
But the 2008 federal law requiring health insurers to provide parity — meaning the same coverage for mental health, including substance use disorders, as for other medical conditions — doesn’t apply to Medicare. Several policy and advocacy groups are working to eliminate such disparities.
Dean Nordman never sought treatment for his drinking, but after his emergency surgery, his sons moved him into a nursing home, where antidepressants and a lack of access to alcohol improved his mood and his sociability. He died in the facility’s memory care unit in 2017.
Doug, whom his father had introduced to beer at 13, had been a heavy drinker himself, he said, “to the point of blackout” as a college student, and a social drinker thereafter.
But as he watched his father decline, “I realized this was ridiculous,” he recalled. Alcohol can exacerbate the progression of cognitive decline, and he had a family history.
He has remained sober since that pre-dawn phone call 13 years ago.
- Open access
- Published: 08 April 2024
Occupational therapy students' perceptions of their experience in a role-emerging Level II fieldwork within higher education student services
- Marie-Christine Potvin 1 ,
- Alexis N. Morales 1 ,
- Erin K. West 1 ,
- Mika Kalimi 1 &
- Jeanne M. Coviello 2
BMC Medical Education volume 24 , Article number: 384 ( 2024 ) Cite this article
153 Accesses
Metrics details
Role-emerging settings – those where occupational therapy (OT) services have not traditionally been provided – are common sites for practice placements of entry-level occupational therapy students. A growing body of literature has attempted to determine the value and drawbacks of such practice placements on the professional preparedness of OT students with mixed findings. Benefits have been identified, including increased cultural understanding, advocacy, creativity, initiative, and problem-solving skills. However, OT students have been reported to perceive such placement as limiting their professional growth and preparedness to practice compared to traditional placements.
A phenomenological study was conducted seeking the perceptions of OT students ( n = 14) about their clinical placement at a role-emerging site. Recorded semi-structured interviews were conducted by trained interviewers within two weeks of the end of clinical placement. The recordings were transcribed verbatim and then coded using an iterative multi-coder inductive approach. Inter-coder agreement, reflectivity, and audit trail were maintained.
Three themes emerged from the analysis: (1) integrating independence and support, (2) becoming occupational therapists, and (3) filling a gap. These themes reflect students’ positive perceptions of their role-emerging clinical placement. They felt that this placement allowed them to develop self-confidence and professional identity as occupational therapists and learn new skills while simultaneously filling a gap in services for clients. Most importantly, they felt that this placement prepared them for their future OT practice.
This finding and their resounding support of the experience suggest that OT students can perceive role-emerging placement as a solid foundation for clinical practice. Factors, included in this placement, that may have contributed to their experience include the level of support provided, time available for learning including space to make mistakes, and freedom from productivity and payor requirements.
Peer Review reports
Practice placements are mandatory for occupational therapy education programs to be recognized as meeting the minimum standard by the World Federation of Occupational Therapy [ 1 ]. In the United States (US), practice placements for master and doctoral degree occupational therapy students are known as fieldwork and are divided into Level I and Level II, with the latter being a more substantial experience (i.e., typically full-time for 12 weeks; Accreditation Council for Occupational Therapy Education [ 2 ]. Level II fieldwork provides students with opportunities for practical application of newly acquired occupational therapy knowledge and skills under the guidance of a licensed occupational therapist within traditional or non-traditional settings [ 2 ]. Occupational therapy practice settings categorized as “traditional” are those where the role of occupational therapy is already clearly established. In the US, these include hospitals, outpatient clinics, schools, and skilled nursing facilities. Any occupational therapy practice outside of these areas is labeled “non-traditional” or “role-emerging” to indicate settings where occupational therapy services are being developed [ 1 , 3 , 4 ].
In recent years, in the United States, there has been a rise in occupational therapists branching out of traditional occupational therapy practice and establishing occupational therapy services in role-emerging settings such as county jails, drug and alcohol rehabilitation centers, and universities [ 4 , 5 , 6 , 7 , 8 , 9 ]. This shift from traditional to role-emerging practice has been attributed to both economic and philosophical principles that allow clinicians to provide holistic care to address clients’ health, wellness, and quality of life while not being dependent on third-party reimbursement [ 10 ]. As a result, there is an increased demand for occupational therapists who are skilled to work in these settings [ 6 , 7 , 8 , 9 ]. In parallel, there is thus a growing need to train future occupational therapists to be competent in role-emerging practice, which can be accomplished, in part, by providing fieldwork experiences in such settings [ 6 , 7 , 11 , 12 , 13 , 14 ]. In fact, some have stated that providing training to occupational therapy students in role-emerging practice settings is imperative to the profession [ 6 , 13 , 15 ]. This mirrors what has been documented recently in the US with an increase in the use of role-emerging settings for fieldwork in response to the increase in the need for sites as more occupational therapy programs have been accredited [ 8 , 16 ].
Both traditional and role-emerging fieldwork align with US accreditation standards and provide FW students with exposure to persons and/or groups across the lifespan with varying conditions in settings that reflect current professional practice [ 2 , 3 ]. Based on review of a wide range of studies, some benefits and challenges of role-emerging fieldwork have been identified. In these settings, students build confidence in the use of occupational therapy skills, increase their cultural understanding, and develop advocacy skills [ 6 , 9 , 17 ]. Furthermore, self-directed learning, which is a hallmark of such placements, results in students experiencing an increase in creativity, initiative, and problem-solving skills [ 8 ]. Critical, role-emerging placements were found to promote the development of occupational therapy students’ professional identity [ 8 , 16 ]. On the other hand, occupational therapy students commonly perceive role-emerging fieldwork placements as lacking the same opportunities for professional growth as traditional placements [ 6 , 8 , 9 ], and in some studies, students reported feeling that role-emerging fieldwork placement failed to prepare them adequately to be competent entry-level practitioners [ 8 , 9 ]. Studies found that students identified challenges with defining professional roles, anticipated difficulties relating to shared versus individualized supervision and caseloads, experienced strained peer dynamics, limitations within the physical environment, lack of support throughout their placement, taxing physical demands of placement, need for clearly defined expectations and effectiveness of communication between all constituents, and difficulty managing the high level of responsibility [ 16 , 18 , 19 ]. There are thus both benefits and challenges of role-emerging fieldwork placements identified in the literature, however further research on occupational therapy student perceptions of specific types of role-emerging placements is needed to minimize perceived challenges and create beneficial learning environments that facilitate the development of self-confidence and perceived readiness for practice [ 7 , 8 , 9 , 16 ].
A few higher education institutions in the US have started to use occupational therapy expertise to support the academic success of students with disabilities on their campuses [ 20 , 21 , 22 , 23 ]. The GOALS 2 Program intends to enhance the academic attainment of college students with disabilities and therefore, is a novel and under-researched, role-emerging Level II fieldwork placement (Boney et al., 2019, Harrington et al., 2021). The development of this role-emerging fieldwork program was informed by evidentiary literature relating to best practice to maximize the learning experience of the occupational therapy students. For example, a collaborative fieldwork model was used, as past research found that students benefit of peer support and positive peer pressure and value being in pairs or groups to share the lived experience when placed in a role-emerging setting for fieldwork [ 16 , 18 ]. We intended to explore whether the integration of these practices alleviated occupational therapy students' concerns with being placed in role-emerging settings for fieldwork.
A study was conducted to explore the GOALS 2 Program Level II occupational therapy fieldwork students’ perceptions of the value of this role-emerging placement on their preparation for clinical practice and their vision of their future practice.
An inductive phenomenological qualitative study was conducted to investigate occupational therapy Level II fieldwork student impressions of placement in this role-emerging setting. Phenomenological studies are used to explore the perspective about events or experiences from an individual or a group’s perspective [ 24 ], which matches the intent of this study. An inductive method was used, as the analysis was conducted without the use of a preexisting coding frame, frame of reference, or the researchers' preconceptions [ 25 ].
Participants
The cohort of occupational therapy students ( n = 14), who completed their Level II fieldwork with the GOALS 2 Program, were invited to participate in the study. We projected that 9–12 interviews would allow a point of saturation to be reached. All 14 students who were eligible for the study (hereafter referred to as “participants”) agreed to participate; their choice to participate had no impact on their ability to complete their Level II fieldwork with the program. Participants could withdraw from the study at any time for any reason without consequences. Ethical approval was secured from the university institutional review board prior to the beginning of the study, and all participants signed written consent forms after participating in the informed consent process.
Fieldwork setting
The GOALS 2 Program offers free services to university students with disabilities whose needs fall within the occupational therapy scope of practice and were not fully met by pre-existing campus services at a mid-Atlantic private not-for-profit university. The primary approach used within the program is coaching, but services also include assistive technology needs identification and training, adaptation of learning tasks and environments, and advocacy to and education of the clients’ educational units and other students’ services. In addition, the fieldwork students performed administrative tasks related to the range of services provided since they were the primary staff of the program. Finally, the fieldwork students engaged in program development (e.g., attracting clients, bringing awareness of the program within the university, as well as developing and refining intake, documentation, and discharge planning processes), as this was a new program at the inception of the study. All fieldwork students completed at least one project that ranged in type and style (e.g., disability awareness month campaign on campus, spearheading a disability advocacy group on campus, presentation about person-first language and disability-supportive interactions for safety and security personnel). The program’s location on campus was a small conference room on the main campus, although services were provided in different locations based on need. Services were mostly offered Monday through Friday during regular business hours, with flexibility to meet clients’ needs.
Two Level II fieldwork students supported the program each semester with supervision from two occupational therapists onsite for a total minimum of eight hours per week (range: 8–16 h). In addition, at least one occupational therapist was always available via email, text, or phone for time-sensitive needs. Finally, the Level II occupational therapy fieldwork students had access to the support of the director of the students’ accessibility office and the dean of students if needed. One of the supervising occupational therapists had four years of clinical experience primarily in community mental health and the second 20 years of experience primarily in pediatrics at the beginning of the study. Both had limited experience as fieldwork educators.
The occupational therapy fieldwork students with the GoALS 2 Program who became participants in this study completed the didactic portion of their occupational therapy education in one of three programs (i.e., two master-level and one doctorate-level) within one university. This was the same university where the clients of the GOALS 2 Program were students. The participants had completed their Level I fieldwork experiences at a variety of sites, and all had a role-emerging Level I fieldwork experience. The participants were either completing their first or second Level II fieldwork experience with the GOALS 2 Program. Data for this study were collected within 2 weeks of the end of their Level II fieldwork with the Program. As commonly used in role-emerging fieldwork, the GOALS 2 Program uses a collaborative fieldwork model, where a group of students actively learn and work together on all aspects throughout their experience [ 3 , 16 ].
Research team
The research team was composed of five authors, and their work was supported by several graduate assistants. All members of the research team self-identified as female and white; one self-identified their ethnicity as Hispanic/Latina. All research team members were occupational therapists (1st and 5th authors) or occupational therapy students (authors 2–4) at the time of the study. The first and fifth authors had experience in qualitative and quantitative research methodologies. The 1st author was an occupational therapy faculty member at the university and the administrator and one of the fieldwork supervisors of the GOALS 2 Program. To minimize the potential effect of the 1st author’s multiple roles with the participants, safeguards were put in place: (1) the informed consent process was completed by the graduate assistants; (2) the data analysis was completed by the 2nd and 3rd authors with the 1st author’s role confined to discrepancy resolution. Authors 2–3 completed their doctoral experiential and capstone project within the GOALS 2 Program during the academic years that followed the end of the data collection for this study. The fifth author has extensive experience in fieldwork coordination and role-emerging fieldwork but was not involved with the GOALS 2 Program beyond this study. The graduate assistants were not involved with the GOALS 2 Program beyond the study.
Data collection
The data for the study were collected through semi-structured interviews conducted in person or via Zoom by one of the trained graduate assistants using an interview guide (see Fig. 1 ). The interviews ranged in length from 30 to 45 min. To increase the study results’ trustworthiness and minimize potential bias, an audit trail, decision-making processes, and reflexive journals, to document self-evaluation of insights, personal reflection, and provide context for researchers’ reactions, were maintained throughout the data collection and data analysis process [ 26 ]. All data, audio recordings, and text files were saved on password-protected servers and accessed through password-protected computers by study personnel only.
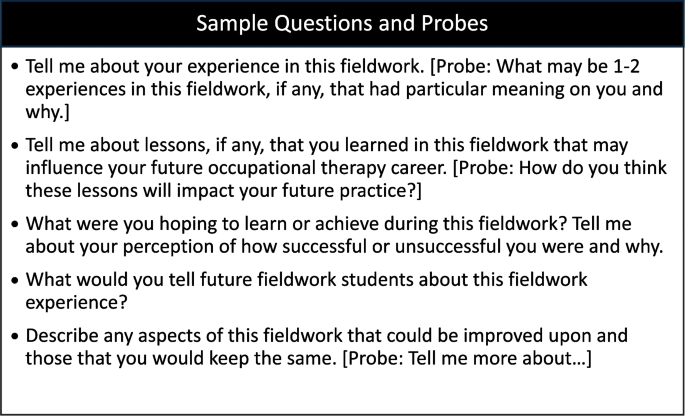
Semi-structured interview guide used in the study
Data analysis and preparation
All interviews were audio-recorded, transcribed verbatim using a transcription protocol, checked for reliability, and de-identified to prepare the data for analysis by trained graduate research assistants who did not conduct the interviews. The data were then analyzed in a multi-step iterative process that included developing the codebook, coding, and deductive interpretation.
Codebook development
The inductive approach, described by [ 27 ], was utilized to develop the codebook using an iterative multi-coder process involving (1) reading the interview transcripts to identify potential codes and code definitions to capture the interviewees’ messages; (2) adjusting codes, definitions, and hierarchies as more transcripts were read; and (3) calibrating the hierarchically organized codes until no new insights or understandings emerged and saturation was achieved. This process was completed by two researchers (the second and third authors) via discussion of rationale until codes were reliably coded using the definitions. They discussed their approach, codes, and interpretation with the lead researcher (the first author) throughout the process.
Data coding
Once the codebook was finalized, all transcripts were uploaded into NVivo (Version 12). The second and third authors coded all 14 transcripts independently and then compared their coding to establish intercoder reliability across all transcripts, achieving ~ 95% intercoder agreement. Any differences in coding were resolved through discussion with the lead author.
Data interpretation
Once all interviews were coded, the second and third authors independently identified themes using a non-linear, phenomenological, narrative inquiry process in which the data were organized by codes to illuminate themes and then conducted peer debriefing [ 26 ]. They reviewed the audit trails and reflexive journals to ensure that their interpretation had not missed key elements. Expert debriefing with the lead researcher (first author) occurred to confirm the rigor and interpretation of the analysis. Interpretation of data was confirmed via member checking with four past fieldwork students involved with the GOALS 2 Program.
The participants’ socio-demographic information, collected verbally and by email, is summarized (see Table 1 ). These variables were selected to describe the participants to ascertain the transferability of results for this qualitative study. Thirteen of the participants identified as women and as white, which is reflective of the degree of diversity within the US occupational therapy workforce [ 27 ]. The mean age of the participants was 30.6 years old (SD = 7.6). Of the 14 participants, 50% reported that occupational therapy was not their first career. This was expected as one of the occupational therapy programs from which the Level II students were drawn was hybrid and intended for non-traditional students.
The qualitative analysis identified three major themes: Integrating Independence and Support is Key , Becoming an Occupational Therapist , and Filling a Gap, and seven subcomponents (see Fig. 2 ). In the theme Integrating Independence and Support is Key students spoke of the importance of both being autonomous in their evaluation and treatment of clients while simultaneously having a support system through their peer partner and fieldwork educators. Becoming an Occupational Therapist captured participants’ perceptions of the spectrum of skills that they developed during this placement, which they believed were both uniquely gained in a role-emerging setting and fundamental to occupational therapy practice. Last, the theme Filling a Gap emerged from fieldwork students’ perception of the impact that they made on this university campus by providing necessary services to address any barrier faced by their clients, including but not limited to, academic achievements such as social participation and community mobility. These themes and their subcomponents are further described and illustrated through exemplary quotes in the following paragraphs.
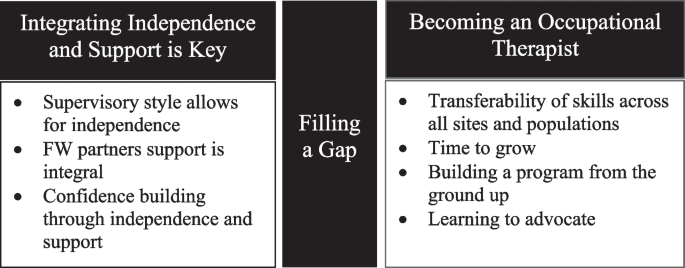
Themes and subcomponents that emerged from the study
Integrating independence and support is key
Most participants (13/14) spoke of the need to be self-directed in this fieldwork setting because of the distant supervision model. Participants also spoke of the collaborative learning model used, and its importance in gaining independence while feeling supported. Participants reflected on the importance of the support they received from their fieldwork educators, as well as from their peer partner, which allowed them to build their independence. Participants explained how independence and support came together allowing them to gain greater confidence in themselves, contributing to the development of their professional identity as occupational therapists. The participants emphasized the effectiveness of this dual approach, and within this broad theme, three subcomponents emerged: supervisory style allows for independence, fieldwork partner support is integral, and confidence building through independence and support.
Supervisory style allows for independence
All but one of the participants credited support from their fieldwork educators, which came in the form of trust, availability, and weekly supervisory meetings, for fieldwork placement success. Participants felt that the fieldwork educators trusted them to get the work done. One participant noted, “there was a lot of independence and… trust in us as students to move forward and to handle things. That was great” (P7, L436-437). Even with distant supervision, participants never felt alone. A participant noted, “Both [fieldwork educators] provided excellent preceptorship. The amount of time that they spent with us was adequate. They were supportive. They gave you responsibility. I wouldn’t change that. It felt like the right balance of independent responsibility and leadership” (P12, L182-189). Participants also felt that their fieldwork educators were available to them outside the designated eight hours of supervisory time. One participant stated, “I always felt [that] if I had a question, I could go to her” (P1, L477-481). The structure of weekly meetings to debrief and discuss caseloads with the fieldwork educators allowed students not to feel isolated. In addition, it provided an opportunity to cultivate professional skills. “We had weekly clinical meetings that were really effective. [We] touched base and saw where we were. It really helped develop our professional reasoning” (P1, L449-451).
Fieldwork partner support is integral
Of the participants, 12/14 identified the collaborative learning model as another major contributor to their success. They found that having a fieldwork partner at the site was an asset. In the participants’ words, “the multiple fieldwork students’ dynamic is really important” (P4, L221). Participant Four stated, “having less hands-on supervisor time, it's important to have someone you can bounce ideas off of…and just work closely with so you’re not alone” (L221-223). Partners were able to complement each other's strengths and function as a team. A participant stated, "a total benefit for us was that me and my partner had two different skill sets. So, we were able to complement each other very well” (P12, L220-222). When reflecting on their future practice, participants expressed that working so closely with a peer mirrored the team approach in many other settings, and it served them well to develop those skills in this fieldwork experience. Participant Fourteen stated, “the idea of having to work in a team and make those decisions as a partnership was really valuable… because [in future practice] we never are going to be making our decisions alone, even though we might be treating alone” (L507-509).
Confidence building through independence and support
Participants appreciated that the supervision and collaborative learning model of this placement which they felt promoted their autonomy and increased self-confidence. A participant noted, “[I found] my independence and my confidence on my own, without someone holding my hand” (P2, L435-436). Clients in the GOALS 2 Program are typically in stable health with no immediate safety risks or medical complications, which creates a lower-pressure environment. Therefore, participants were apt to independently make mistakes and learn from them, a process that helped them gain self-confidence. Participant Four notes, “I think starting out with a slightly more low-pressure setting was really helpful in building my self-confidence” (L179-181).
Becoming an occupational therapist
All participants spoke about the skills gained through their time in this fieldwork and how it contributed to their development as occupational therapists and would be valuable in their future practice. They valued the opportunities to develop skills outside of those typically learned during fieldwork. For example, during this fieldwork placement, participants learned professional coaching techniques which they employed with clients. Further, their projects and the administration of the GOALS 2 Program led them to discover a new passion for advocacy and develop an understanding of program development. Four subcomponents emerged as participants shared the role of this fieldwork placement in their development as occupational therapists: transferability of skills across all sites and populations, time to grow, building a program from the ground up, and learning to advocate.
Transferability of skills across all occupational therapy sites and populations
All of the participants spoke positively about their perception of the transferability of the skills learned in this setting to their next Level II fieldwork and their future careers. Specifically, they mentioned interviewing skills and professionalism as transferable aspects. Referring to the coaching skills learned, one participant stated, “any [occupational therapy] student can benefit from what you learn [with GOALS 2 ]… the interactions, interviewing, talking to clients, … they’re all valuable skills… it’s everything you do as an occupational therapist” (P3, L185-192). Participants also mentioned time management as another transferable skill that they developed. Participant Four noted, “not only the communication and professionalism to bring into my future placements but my future career… but also those little things like creating my own schedule and managing my time… as a professional versus a student” (L64-66). When speaking about the development of occupational therapy-specific skills, participants identified building therapeutic relationships as a transferable skill acquired (P12, L117-119) through this specific experience.
Time to grow
In the host fieldwork placement, occupational therapy students were not held to productivity standards dictated by employers’ or payors’ reimbursement policies. Rather, expectations of workload were incumbent on client needs and fieldwork student readiness. The participants appreciated the amount of time they were afforded to build meaningful therapeutic relationships with their clients. Participant Twelve stated, “the value of the GOALS 2 Program is that you’re really able to develop therapeutic relationships with people. Other placements don’t just allow you the time to do that” (L157-160). Additional time with clients was attributed to not being bound to productivity markers. One participant stated, “I could develop the skills of doing what was important for the person that I [was] working with versus what an administrator or an insurance company is telling me is important” (P7, L274-282). They added “we were not subject to productivity demand” (P7, L274-282).
Building a program from the ground up
All participants said that they appreciated being able to hone their program development skills within this fieldwork, an aspect that they were not expecting. Participant Twelve commented, “we performed administrative duties such as scheduling, email correspondence, collaborating and talking with different departments about the program” (L12-14). Regarding the work required to create new systems for the program, one participant remarked, “[we] were working on program development for the program itself, so we actually created a whole discharge process” (P7, L90-91). Participants were tasked not only with running the program but also with continuing to enlarge the program. One participant stated, “one thing that I am proud of is trying to get more clients and expand the program” (P10, L13-14).
Learning to advocate
All participants repeatedly described having the opportunity to develop skills in advocacy and a “passion to advocate” (P8, L172). Advocacy came in three main forms for participants: collaborating with clients to advocate for themselves, advocating on behalf of their clients, and advocating for the unique value of occupational therapy. In the participants’ view, these advocacy efforts were met with success as well as challenges. Eight of the fourteen participants reflected on how commonly clients wanted support related to self-advocacy. A participant remarked, “I’d say that happened for the majority of our clients” (P8, L176-178). Thus, participants learned how to advocate on behalf of their clients, a skill they mentioned as useful to their future career, as illustrated in this excerpt, “[working with a client to obtain reasonable accommodations] taught me a lot about how we, as occupational therapists, will always need to advocate for our clients” (P5 L129-130). Participants also advocated for the distinct value of occupational therapy while simultaneously building skills in communicating with other members of an interprofessional team. A participant stated, “I grew by collaborating with other offices and having to explain and advocate about the importance of the GOALS 2 Program [and] occupational therapy” (P10, L181-183). Although advocating was mostly a positive experience, participants had to overcome challenges when university professors demonstrated reluctance to adapt. As one participant commented, “one thing that [was] negative or discouraging is that we have a client that needs accommodations. In her program, there was a lot of push back [against these]. That was pretty eye opening” (P6, L82-91).
Filling a gap
The last theme, Filling a Gap, does not have subcomponents. Throughout the interviews, participants reflected on the work being done through the GOALS 2 Program and its potential wider impact on colleges and universities and the scope of occupational therapy practice. While recognizing that accommodations are being offered to college students, participants noted gaps in what is provided that can be filled with services offered by the GOALS 2 Program. Participant Fourteen reflected, “they had needs that just weren’t being met by all of the supports that were already on campus” (L49-51). The support and services provided by the GOALS 2 Program give clients more opportunities for success in an environment where they may have otherwise fallen off the radar. A participant remarked, “we’re really filling a gap. There are students whose services dropped off when they graduated high school. When they move to college, they kind of get lost through the cracks” (P1, L135-138).
Filling a gap through occupational therapy service was perceived by participants to be needed not only in terms of supplementing support offered by colleges and universities but also in terms of the major life transition that occurs at that age. Participants recognized the services occupational therapists could provide to support that transition. Participant Eight noted, “it’s such a huge life transition and such an unmet need for all students transitioning to college” (L158-159). This transition could be addressed by occupational therapists and occupational therapy assistants prior to attending university. One participant realized the potential usefulness of this service for high school students, stating, “especially as occupational therapists… how can [we] be a part of that transition? Whether it's socially, academically… the big picture academics, and being successful in that setting, how can we be a part of that?” (P4, L207-209).
Studies have found that occupational therapy fieldwork students learn similar skills in role-emerging and traditional fieldwork settings [ 6 , 9 ]. However, students have the impression that role-emerging fieldwork placements are not adequate preparation for clinical practice [ 8 , 9 , 18 , 19 ]. Further research on students’ experiences in various role-emerging settings is critical to creating beneficial learning environments that translate to student readiness and self-confidence as occupational therapists [ 7 , 8 , 9 ]. Our qualitative study explored occupational therapy students’ perceptions of their fieldwork site, identifying three main themes described in the following paragraphs.
Integrating Independence and Support is a key theme that reflects the duality between the independence afforded and the need for support within role-emerging fieldwork. The independence afforded by the distance supervision fieldwork placement was perceived as beneficial. This theme also reinforces previous studies that found that students reported increased self-confidence following role-emerging fieldwork placements [ 5 , 6 , 9 , 16 , 17 ]. Our participants attributed their confidence building to the support they received from their fieldwork educators through weekly feedback meetings and having a peer partner with whom to debrief. This allowed them to feel supported despite the distant supervision model. This seems unique, as previous studies primarily identified role-emerging fieldwork students feeling a lack of supervisor support which affected their overall feelings of success [ 8 , 16 , 18 , 19 , 28 ]. The elements of the supervision that were deemed beneficial by the participants included feeling trusted with the responsibilities given, their supervisor’s availability to answer questions outside of the eight hours a week of preceptorship, the effectiveness of the weekly supervision meeting, and the supportive nature of the fieldwork educators. These elements are found in other role-emerging fieldwork literature especially when a collaborative model is used [ 19 , 29 , 30 ], thus these findings are unlikely to fully explain the positive perspective of these students regarding their experience in their host role-emerging fieldwork site.
Our study’s findings affirm recent studies that found that having a peer partner, or collaborative learning, was perceived as essential in role-emerging fieldwork where a fieldwork educator is not available full-time [ 17 , 18 , 19 , 28 , 31 , 32 ]. The collaborative learning model has been cited as a successful tool to increase students’ problem-solving and communication skills and develop their ability to be a leader and work in a team [ 4 , 33 ]. Participants in this study noted these benefits and recognized the transferability of these skills to their future career. Studies have frequently identified the importance of a peer partner in role-emerging fieldwork settings [ 4 , 9 , 16 , 19 , 29 , 30 , 32 , 33 ], but only a few studies have noted the increase in students’ overall confidence as a result of collaborating with a peer partner [ 17 , 28 ]. In addition, participants reported that the low-pressure nature of this placement was a further catalyst for building self-confidence and autonomy. Research to date has echoed this point, showing that students in role-emerging placements found that without having an established role of occupational therapy at their site, their professional reasoning skills could grow without constraints [ 8 , 9 , 16 ].
The Becoming an Occupational Therapist theme emerged as participants spoke of the skills they learned in this setting and the value of these skills for their future occupational therapy practice. This is important since the literature to date has shown mixed student perceptions on the transferability of skills learned in role-emerging fieldwork to more traditional occupational therapy settings [ 8 , 9 ]. The occupational therapy fieldwork students in this study did not express this ambivalence, clearly expressing that the skills they learned (e.g., communication, interviewing, professionalism, and time management) could be applied in their future practice. Among other skills, they most frequently noted that developing strong therapeutic relationships with clients was a major takeaway from this placement, a finding that aligns with past research findings [ 9 , 16 , 32 , 33 ]. Given that in this role-emerging setting, participants learned to coach, a skillset that, in part, builds one therapeutic use of self, it is surmised that those were some of the skills participants found transferable [ 34 ]. Future studies should explore whether this transferability of the coaching skills was actuated.
According to the participants, a major factor that promoted the building of strong therapeutic relationships was being afforded the time to grow and the freedom from the productivity and payor requirements associated with traditional occupational therapy settings. At this fieldwork site, billing was not a factor, and prior research suggests that students appreciate the general freedom to treat using their autonomy and clinical and professional reasoning without the need to meet billing standards or emulate their fieldwork educator [ 5 , 32 ]. The participants in this study also reported that they developed time management skills in this setting. Time management is a skill that students have identified as facile and challenging in role-emerging placements [ 9 , 32 ]. Additionally, participants noted that they gained valuable skills in program development and management of occupational therapy services that will be essential to their future practice. Previous studies have cited program development as a key aspect of role-emerging settings [ 4 , 6 , 7 ]. However, Lau and Ravenek [ 16 ], found that students reported having difficulties establishing the occupational therapy role and finding their place within an organization during role-emerging fieldwork placement.
Within this theme, the need and opportunity to learn to advocate emerged from the data, with participants commenting on the need to advocate on behalf of their clients but also to help other services on campus understand the distinct value of occupational therapy. This development of advocacy skills may be a benefit of this setting and of role-emerging fieldwork settings at large, given that this finding is consistent in the literature [ 17 ]. In this fieldwork placement, advocacy came in many forms, but projects were frequently mentioned by participants as opportunities to advocate. The literature has yet to link projects with the opportunity to advocate, such as what was described by participants in this study. Advocacy is closely related to the Filling a Gap theme, which highlights the opportunity for occupational therapy to address an untapped need unfilled by other services. During their time in the GOALS 2 Program, the participants were able to understand the impact of occupational therapy on client progress and success, the wide scope of occupational therapy service provision needed, and the way occupational therapy fits into a university setting.
Limitations
The sample size ( n = 14) was appropriate for a qualitative study, and data saturation was reached. Transferability of the study results should be done cautiously for a few reasons. First, all participants had completed a Level I role-emerging placement and may have thus been better prepared for this fieldwork experience. They also all completed their Level II fieldwork within the same role-emerging site and with the same fieldwork educators, limiting our ability to differentiate between the impact of the educational practices used within this novel fieldwork placement vs the experience and skills of the fieldwork educators themselves. It should be noted that both fieldwork educators had limited experience in that role at the beginning of the study. Finally, half of the participants in this study were second career students. It is possible that their previous professional experience influenced their perception of this fieldwork placement. Efforts were also made to minimize the risk of researcher bias (i.e., reflexive journaling, an audit trail, multiple coders, independent thematic analysis, member checking, and peer debriefing with the lead researcher); however, the results may still be inadvertently biased.
Future directions
A valid and reliable questionnaire of fieldwork students’ perceptions of role-emerging settings could provide additional perspectives from a larger number of students. Additionally, a study comparing the knowledge and skills of practicing clinicians who completed a fieldwork placement in a role-emerging setting in comparison to those who did not would benefit the field.
Conclusions
Role-emerging practice settings bring the profession back to its roots of occupation as a means of intervention. They meet crucial societal needs and are here to stay, and as a result, occupational therapy students need to develop the unique skills such settings require. The results of this study indicate that occupational therapy students can overwhelmingly perceive role-emerging fieldwork settings as valuable. They saw opportunities to learn skills and know when to seek support, to collaborate intraprofessionally and interprofessionally, to develop programs, and to advocate for the profession, all of which can be used in traditional practice. Some of the features of this placement that are thought to have contributed to the students’ positive experience include the level of support provided, time available for learning including space to make mistakes, and freedom from productivity and payor requirements. Building on the current literature, the findings of this study can be used within future role-emerging placements to enhance students' experience.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
World Federation of Occupational Therapists. Minimum standards for education of occupational therapist revised 2016. World Federation of Occupational Therapists; 2016 [cited 2021 May 30]. Available from: https://www.wfot.org/assets/resources/COPYRIGHTED-World-Federation-of-Occupational-Therapists-Minimum-Standards-for-the-Education-of-Occupational-Therapists-2016a.pdf . Accessed Dec 2022.
2018 accreditation council for occupational therapy education (ACOTE®) standards and interpretive guide (Effective July 31, 2020). Occup Ther Educ. 2018 Nov 19;72(2):7212410005p1–83. doi: https://doi.org/10.5014/ajot.2018.72s217 .
American Occupational Therapy Association. COE guidelines for an occupational therapy fieldwork experience-Level II [Internet]. American Occupational Therapy Association; 2012 [cited 2021 Jun 01]. Available from: https://www.aota.org/-/media/corporate/files/educationcareers/educators/fieldwork/levelii/coe-guidelines-for-an-occupational-therapy-fieldwork-experience-level-ii-final.pdf
Hunter H, Volkert A. Issues and challenges of role-emerging placements. World Federation of Occupational Therapists Bulletin. 2016;73(1):57–65. https://doi.org/10.1080/14473828.2016.1162485 . Cited 2021 Jun 01.
Clarke C, Martin M, Sadlo G, de-Visser R. The development of an authentic professional identity on role-emerging placements. British J Occup Ther. 2014;77(5):222–9. https://doi.org/10.4276/030802214x13990455043368 . Cited 2021 June 01.
Gat S, Ratzon NZ. Comparison of occupational therapy students’ perceived skills after traditional and nontraditional fieldwork. Occup Ther. 2014;68(2):47–57. https://doi.org/10.5014/ajot.2014.007732 . Cited 2021 June 01.
Provident IM, Joyce-Gaguzis K. Creating an occupational therapy level II fieldwork experience in a county jail setting. Occup Ther. 2005;59(1):101–6. https://doi.org/10.5014/ajot.59.1.101 . Cited 2021 June 06.
Overton A, Clark M, Thomas Y. A review of non-traditional occupational therapy practice placement education: a focus on role-emerging and project placements. Occup Ther. 2009;72(7):294–301. https://doi.org/10.1177/030802260907200704 . Cited 2021 May 25.
Smith YJ, Cornella E, Williams N. Working with populations from a refugee background: an opportunity to enhance the occupational therapy educational experience. Popul Occup Ther Educ. 2013;61(1):20–7. https://doi.org/10.1111/1440-1630.12037 . Cited 20 May 2021.
Meyers SK. Community practice in occupational therapy: A guide to serving the community. 1st ed. Sudbury: Jones & Bartlett Publishers; 2009.
Cooper R, Raine R. Role-emerging placements are an essential risk for the development of the occupational therapy profession: the debate. Occup Ther Prof. 2009;72(9):301–9. https://doi.org/10.1177/030802260907200910 . Cited 2021 Jun 16.
Friedland J, Polatajko H, Gage M. Expanding the boundaries of occupational therapy practice through student fieldwork experiences: description of a provincially-funded community development project. Occup Ther. 2001;68(5):301–9. https://doi.org/10.1177/000841740106800506 . Cited 2021 Jun 11.
Hoppes S, Hellman CM. Understanding occupational therapy students’ attitudes, intentions, and behaviors regarding community service. Occup Ther Behav. 2007;61(5):527–34. https://doi.org/10.5014/ajot.61.5.527 . Cited 2021 Jun 07.
Roberts ME, Hooper BR, Wood WH, King RM. An international systematic mapping review of fieldwork education in occupational therapy. Educ Occup Ther. 82(2):106–18. https://doi.org/10.1177/0008417414552187 . Cited 2021 May 16.
Wilburn VG, DeCleene-Huber KE, Gahimer J, Beitman C, Moore ES. Perceptions of academic fieldwork coordinators regarding the value of fieldwork in emerging areas of practice. 2016;4(4):10–7 https://scholarworks.iupui.edu/handle/1805/17622 .
Lau M, Ravenek M. The student perspective on role-emerging fieldwork placements in occupational therapy: a review of the literature. Occup Ther. 2019;7(3):1–21. https://doi.org/10.15453/2168-6408.1544 . Cited 2021 Jun 22.
Nielsen S, Jedlicka JS, Hanson D, Fox L, Graves C. Student perceptions of non-traditional level I fieldwork. J Occup Ther Educ. 2017;1(2). https://doi.org/10.26681/jote.2017.010206 . Cited 2021 May 28.
Kinsella AT, Piersol CV. Development and evaluation of a collaborative model level II fieldwork program. J Postsecondary Educ Disability. 2018;6(3):14.
Tokolahi E, Robinson R. A scoping review of role-emerging, school-based fieldwork placements in occupational therapy education. New Zealand Journal of Occupational Therapy. 2021;68(2):26–33.
Boney JD, Potvin M, Chabot M. The GOALS 2 program: expanded supports for students with disabilities in postsecondary education (practice brief). 2019;32(3):321–329.
Harrington EE, Santos GO, Potvin M. Postsecondary education students with disabilities’ perceptions of occupational therapy-led coaching. Occup Ther. 2021;9(2):1–13. https://doi.org/10.15453/2168-6408.1790 . Cited 2021 May 19.
Schindler V. Outcomes of an occupational therapy–supported education program for college students with autism spectrum disorder, learning disability, and mental health diagnoses. Occup Ther Educ. 2017;41(4). https://doi.org/10.5014/ajot.2017.71s1-po7127 . Cited 2021 Jun 19.
Schindler V. An occupational therapy-based supported education program for university students with various DSM-5 diagnoses: program description and academic outcomes. Open J Occup Ther. 2019;7(2). https://doi.org/10.15453/2168-6408.1549 . Cited [2021 May 24.
Leedy PD, Ormrod JE. Practical research: planning and design. 11th ed. Boston: Pearson; 2016.
Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis. International Journal of Qualitative Methods. 2017;16(1). https://doi.org/10.1177/1609406917733847 . Cited 2021 Jun 17.
DePoy E, Gitlin LN. Introduction to research: understanding and applying multiple strategies. 5th ed. Missouri: Elsevier; 2015.
Bernard HR, Wutich A, Ryan GW. Chapter 6: codebooks and coding. In: Bernard HR, Wutich A, Ryan GW, editors. Analyzing qualitative data: Systematic approaches. 2nd ed. Los Angeles: Sage; 2016. p. 125–59.
Golos A, Tekuzener E. Student and supervisor perspectives on the effectiveness of community-based placements for occupational therapy students. Occup Ther. 2021;21(1):1–12. https://doi.org/10.1186/s12909-021-02492-3 . Cited 2021 May 19.
Schaaf RC, Carroll AP, Toth-Cohen S, Burke JP, Johnson C, Herge E. Promoting environments that measure outcomes: partnerships for change. J Occup Ther Educ. 2017;1(2). https://doi.org/10.26681/jote.2017.010204s .
Golos A, Tekuzener E. Student and supervisor perspectives on the effectiveness of community-based placements for occupational therapy students. BMC Med Educ. 2021;21:1–11.
Coviello JM, Potvin M, Lockhart-Keene L. Occupational therapy assistant students’ perspectives about the development of clinical reasoning. Occup Ther Dev. 2019;7(2):1–16. https://doi.org/10.15453/2168-6408.1533 . Cited 2021 Jun 14.
Potvin M, Coviello JM, Rothacker E, Taylor C, Pettigrew T, Thomas MB, Lockhart-Keene L. Clinical and professional reasoning development in level II fieldwork: occupational therapy assistant students’ perception. Dev Occup Ther. 2021;5(3):1–27. https://doi.org/10.26681/jote.2021.050311 . Cited 2021 Jun 01.
Mattila AM, Dolhi C. Transformative experience of master of occupational therapy students in a non-traditional fieldwork setting. Occup Ther. 2016;32(1):16–31. https://doi.org/10.1080/0164212x.2015.1088424 . Cited 2021 Jun 23.
Potvin M-C, West E, Morales A, Coronado N, Sailor K. I could really use this": Occupational therapy students’ perceptions of coaching. Occupational therapy international. https://doi.org/10.1155/2022/2266326 .
Download references
Acknowledgements
We want to acknowledge the support of graduate assistants and students Michael Barret, Caitlin Beach, Janette Boney, Kathleen Carr, Briona Stauffer, and Lisa Zolotnitsky without whom this study would not have been possible. We thank Jennifer Wilson for her editorial support.
The Department of Occupational Therapy and the Dean of Students Office at Thomas Jefferson University funded this role-emerging fieldwork placement.
Author information
Authors and affiliations.
Department of Occupational Therapy, Thomas Jefferson University, 901 Walnut Street, 6th Floor, Philadelphia, PA, 19107, USA
Marie-Christine Potvin, Alexis N. Morales, Erin K. West & Mika Kalimi
College of Public Health, Temple University, Mitten Hall, Room 201E, 1913 North Broad Street, Philadelphia, PA, 19122, USA
Jeanne M. Coviello
You can also search for this author in PubMed Google Scholar
Contributions
MCP was the primary investigator, conceptualized the study, and supervised all parts of the study from recruitment through preparing the manuscript; ANM and EKW analyzed the data and drafted the manuscript; MK participated in the data preparation and contributed to the writing of the manuscript; and JMC participated in the writing of the discussion of the manuscript and conceptually edited the introduction.
Corresponding author
Correspondence to Marie-Christine Potvin .
Ethics declarations
Ethics approval and consent to participate.
The Thomas Jefferson University’s Institutional Review Board approved this study. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’ s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Potvin, MC., Morales, A.N., West, E.K. et al. Occupational therapy students' perceptions of their experience in a role-emerging Level II fieldwork within higher education student services. BMC Med Educ 24 , 384 (2024). https://doi.org/10.1186/s12909-024-05303-7
Download citation
Received : 12 October 2023
Accepted : 12 March 2024
Published : 08 April 2024
DOI : https://doi.org/10.1186/s12909-024-05303-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical rotation
- Experimental Learning
- Occupational Therapy
- Role-Emerging
- Non-Traditional
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Problem-solving therapy is a brief intervention that provides people with the tools they need to identify and solve problems that arise from big and small life stressors. It aims to improve your overall quality of life and reduce the negative impact of psychological and physical illness. Problem-solving therapy can be used to treat depression ...
Problem-solving therapy (PST) is an intervention with cognitive and behavioral influences used to assist individuals in managing life problems. Therapists help clients learn effective skills to address their issues directly and make positive changes. PST is used in various settings to address mental health concerns such as depression, anxiety, and more.
Problem-solving therapy (PST) takes a results-oriented approach to managing issues. PST is rooted in cognitive behavioral therapy (CBT) and can also be referred to as problem-solving brief therapy (PSBT). It's growing in popularity thanks to evidence showing it can effectively treat a variety of health and mental health problems, such as ...
Problem-Solving Therapy aims to reduce the incidence and impact of mental health disorders and improve wellbeing by helping clients face life's difficulties (Dobson, 2011). This article introduces Problem-Solving Therapy and offers techniques, activities, and worksheets that mental health professionals can use with clients.
Key points. Problem-solving is one technique used on the behavioral side of cognitive-behavioral therapy. The problem-solving technique is an iterative, five-step process that requires one to ...
Problem solving therapy is suitable for use in general practice for patients experiencing common mental health conditions and has been shown to be as effective in the treatment of depression as antidepressants. Problem solving therapy involves a series of sequential stages. The clinician assists the patient to develop new empowering skills, and ...
Problem-solving therapy is a cognitive-behavioral intervention geared to improve an individual's ability to cope with stressful life experiences. The underlying assumption of this approach is that symptoms of psychopathology can often be understood as the negative consequences of ineffective or maladaptive coping.
Problem-solving therapy is a short-form treatment that usually lasts between four and twelve sessions. It is most frequently used to treat depression, with a primary focus on helping you build the tools needed to identify and solve problems.
Therapists use cognitive behavioral therapy to help people with mental and physical health challenges like: ... The skills CBT often emphasizes, like problem-solving, personal interaction, and ...
Solution-focused therapy puts problem-solving at the forefront of the conversation and can be particularly useful for clients who aren't suffering from major mental health issues and need help solving a particular problem (or problems). Rather than spending years in therapy, SFBT allows such clients to find solutions and get results quickly. ...
This review assessed the efficacy of problem-solving therapy (PST) in helping individuals to overcome any type of health problem. The authors concluded that there is strong evidence for the effectiveness of PST. The conclusion was derived from a meta-analysis of clinically and statistically variable data and there were a number of methodological concerns, therefore it may not be reliable.
Problem solving therapy is a widely-acknowledged tool used by therapists and general medical practitioners alike to help clients find proactive and reasonable ways to deal with the stressful events that occur in their lives. Overall, PST can help people find meaningful, creative, and adjustable ways of reaching their problem-resolution goals ...
Problem-solving therapy (PST), developed by Nezu and colleagues, is a non-pharmacological, empirically supported cognitive-behavioral treatment (D'Zurilla and Nezu 2006; Nezu et al. 1989 ). The problem-solving framework draws from a stress-diathesis model, namely, that life stress interacts with an individual's predisposition toward ...
Problem-Solving Therapy (PST) is an evidenced-based intervention to facilitate behavioral changes through a variety of skill training. PST identifies strategies to support people to cope with difficulties in life and take the initiative to solve everyday problems. Using cognitive behavioral theories, effective and successful problem solving
Problem-Solving Therapy for Primary Care was developed as an efficient modality to treat patients in busy primary care settings over the course of 4-8 sessions. It has been found that as few as three sessions of PST-PC could be beneficial ( Mynors-Wallis et al., 2000 ; Hegel et al., 2004 ; Arean et al., 2008 ).
46Problem-Solving Therapy. Step 4. Follow the breathing directions for about 5 minutes. Inhale slowlyand deeplythrough your nose into your abdomen, fi lling all the spaces in your belly with air (if you have diffi culty breathing through your nose, go ahead and breathe through your mouth).
By speaking openly and honestly with your mental health provider about mixed feelings you may have about a change you are considering, you can work together to explore and use your motivation for change. Problem-Solving Therapy (PST) PST is a therapy for Veterans who are experiencing depression or suicidal thoughts. PST can help you recover ...
But all therapy is problem-solving therapy. Either we seek to help our clients 'solve the problem' by feeling and thinking differently about it, or we help them find ways to solve an actual practical problem (or both!). Seek to establish how many of your clients' problems are themselves maladaptive attempts to solve problems.
Problem-solving therapy refers to a psychological treatment that helps to teach you to effectively manage the negative effects of stressful events that can occur in life. Such stressors can be rather large, such as getting a divorce, experiencing the death of a loved one, losing a job, or having a chronic medical illness like cancer or heart ...
Problem solving therapy is suitable for use in general practice for patients experiencing common mental health conditions and has been shown to be as effective in the treatment of depression as antidepressants. Problem solving therapy involves a series of sequential stages. The clinician assists the patient to develop new empowering skills, and ...
Problem-solving skills and treatment motivation increased in the therapy group and decreased in the control group. The difference between groups was found to be significant (p=0.045, 0.037 for problem solving and treatment motivation respectively). While the severity of addiction decreased in therapy group, it increased in control group, but ...
Additionally, problem-solving helps children learn how to find creative solutions to challenges they may face both in and out of the classroom. These activities can also be fun and used in cohesion with school or playtime. 17 Fun Problem-Solving Activities for Kids 1. Marble Mazes. This activity was selected because it requires them to think ...
In the latest edition of the Army War College journal Parameters, Andrew Carr argues that the rising level of complexity in the world necessitates a change in how we define strategy away from a math problem of ends + ways + means and instead look to strategy as problem-solving.1 Carr's idea is that as the amount of complexity in a situation increases, the strategy should be less focused on ...
The pandemic played a role in increased consumption, but alcohol use among people 65 and older was climbing even before 2020. By Paula Span The phone awakened Doug Nordman at 3 a.m. A surgeon was ...
In these settings, students build confidence in the use of occupational therapy skills, increase their cultural understanding, and develop advocacy skills [6, 9, 17]. Furthermore, self-directed learning, which is a hallmark of such placements, results in students experiencing an increase in creativity, initiative, and problem-solving skills .
864 likes, 2 comments - occupational_therapy_verticlesOctober 7, 2023 on : "This activity works on child's ️ Attention Concentration Visual memory Working memory Problem solving Timing and sequencing Start with two sequence and gradually build more steps and sequence. ⚠️For added challenge use timer or metronome!
In solving descriptive geometry (DG) problems, board (i.e., hand drawing) methods are frequently used, despite this discipline is still very important to enhance spatial vision. These methods are very different from CAD tools which are used in the field of design. CAD facilitates the realization of geometric constructions and transformations (i.e., rotation, translation, copying, scaling ...