An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.14(12); 2022 Dec


A Comprehensive Review on Postpartum Depression
Om suryawanshi, iv.
1 Obstetrics and Gynecology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, IND
Sandhya Pajai
One of the most common psychological effects following childbirth is postpartum depression. Postpartum depression (PPD) has a significant negative impact on the child's emotional, mental as well as intellectual development if left untreated, which can later have long-term complications. Later in life, it also results in the mother developing obsessive-compulsive disorder and anxiety. Many psychological risk factors are linked with PPD. The pathophysiology of the development of PPD is explained by different models like biological, psychological, integrated, and evolutionary models, which relate the result of the condition with particular conditions and factors. This article also explains the role of methyldopa as a medication used during pregnancy and the postpartum phase with the development of PPD. There are different mechanisms by which methyldopa causes depression. The large-scale screening of the condition can be done by Edinburgh Postnatal Depression Scale (EPDS). The diagnosis can be made by clinical assessment, simple self-report instruments, and questionnaires provided to mothers. Currently, there has not been any specific treatment for PPD, but selective serotonin reuptake inhibitors (SSRIs) like sertraline are effective in acute management. Venlafaxine and desvenlafaxine are serotonin-norepinephrine reuptake inhibitors used for the relief of symptoms. The SSRI and tricyclic antidepressants (TCA) used in combination have a prophylactic role in PPD. Nowadays, women prefer psychological therapies, complementary health practices, and neuromodulatory interventions like electroconvulsive therapy more than previous pharmacological treatments of depression. Allopregnanolone drug made into sterile solution brexanolone leads to a rapid decline of PPD symptoms. PPD is a common and severe disorder that affects many mothers following childbirth but is ignored and not given much importance. Later it affects the child's psychological and intellectual abilities and mother-child bonding. We can easily prevent it by early diagnosis and timely care and management of the mother. Understanding the underlying pathophysiology would also go a long way in preventing and managing the disorder.
Introduction and background
Postpartum depression (PPD) is a significant mental health constraint in females, which has an effect on nearly 13-19% of the females who newly attained motherhood [ 1 ]. PPD is identified by a continuous feeling of a low state of mind in new mothers, followed by sad feelings, less worthy, and despondence. It differs from baby blues, a short-lived period of emotional disruption that includes weeping, irritability, sleep troubles, and anxiety. It is identified and felt by every four in five women in very few days after child delivery and mostly remits by 10 days [ 1 , 2 ]. Currently, the Diagnostic and Statistical Manual for Mental Disorders-Fifth Edition (DSM-5) has classified depression associated with the onset of childbirth as starting in pregnancy or by the first month of postpartum [ 3 ]. According to the International Classification of Disease (ICD), postpartum depression is labeled as one beginning by the first six weeks of the postpartum phase [ 4 ]. Many research studies have further revised the guidelines for the first six months following childbirth, while few use the time frame for up to the first year following the period of delivery for the beginning of PPD [ 5 ].
In most aspects, PPD has many likely features with depression which occur at other times in a mother's life; in some prospects, it has few differences as many significant changes occur during pregnancy and the postpartum phase [ 1 , 6 ]. In approximation, nearly 80% of postpartum women face the prodrome of emotional disturbances in the first few days following childbirth [ 7 ]. More of, a large proportion of postpartum women following pregnancy experience symptoms attributed to depression-like disturbed appetite, lack of sleep, and low energy levels for working [ 8 ]. The above factors make it hard to separately identify the commonly occurring symptoms following childbirth and new infant care from those of a depressive condition. Sometimes the phase of postpartum depression in nearly 30% of women can continue for two years postpartum [ 9 ], while 50% of women have major depression throughout in which the course of depression may vary and have stable moderate depression, major stable depression, or repetitive intervals of significant depression [ 10 ]. A comparison of symptoms between postpartum blues, postpartum depression, and postpartum psychosis is shown in Table Table1 1 .
The table is adapted from Fishbein (2017) (Open source) [ 11 ].
Psychological risk factors of PPD
The risk factors can be grouped based on the strength of association with PPD. Depression and anxiety in pregnancy, postpartum blues, history of depression, neuroticism, excessive stress indulging life events, poor marital relations, lack of social support, and low self-esteem are strongly associated with postpartum depression [ 12 ]. On the other side, low socioeconomic status, single marital status, unwanted pregnancy, obstetrical stressors, and grieving infant temperament are reported to have a relatively weaker association [ 13 , 14 ]. The attitude of a mother [ 15 ] and her experience of different related complications like preterm delivery, prenatal hospitalization, emergency cesarean section, preeclampsia, and deceased infant health [ 16 ] are shown to have increased risk of developing PPD [ 17 - 19 ]. The above risk factors are more strongly associated with social and psychological aspects than biological aspects. A bar chart showing percentage of factors attributed to PPD is shown in Figure Figure1 1 .

The image is adapted from Shriraam et al. (2019) (Open source) [ 20 ].
Pathophysiology of PPD
The exact mechanism for the development of postpartum depression is still unknown. There are many different models and theories explaining the condition's cause over time. Biological model explains the development of the condition due to the drastic and sudden decrease in many pregnancy hormones like progesterone, estradiol, and cortisol. In the withdrawal model, stress and reproductive hormones increase in pregnancy and fall drastically during childbirth and in the postpartum phase, which leads to dysregulation of the system and causes PPD [ 21 - 23 ]. However, they fail to explain the mechanism of hormone withdrawal with depression and the depressive symptoms which begin during pregnancy. The depression model states the association of PPD with the stress hormones dysregulation, mainly cortisol [ 24 ]. There is a suggestion from a few recent reviews for the role of dysregulation of the hypothalamic-pituitary axis in the causation of PPD [ 25 , 26 ]. Declined dopaminergic regulation may also have a role in PPD [ 27 ]. Many neuroendocrine changes in pregnancy can also affect PPD development, including inhibited Gamma-aminobutyric acid (GABA) signaling and low levels of allopregnanolone [ 28 - 30 ].
Psychological models focus mainly on the effect of pregnancy, childbirth, and new parenthood as the major stress factors which cause PPD symptoms in women. There has been much support in the psychological literature [ 31 ]. Integrated models bridge the above and state the role of both biological factors, such as stress causing PPD symptoms in women having genetic and hormonal susceptibility [ 23 ]. Evolutionary models have an evolutionary perspective in which the PPD is believed to be due to human civilization because of psychological adaptation in the course of human evolution. A "mismatch hypothesis" of PPD was recently proposed by Hahn-Holbrook and Haselton that suggests that PPD might be a "disease of civilization" due to significant cultural shifts over the past century that have resulted in substantial deviations from typical human evolutionary lifestyles and the current high incidence rate [ 32 ].
Role of methyldopa in the induction of postpartum depression
Methyldopa, an agonist of presynaptic alpha-2 adrenergic receptors, prevents neurons from releasing norepinephrine and, consequently, inhibits the sympathetic nervous system. This medication is actively transported to the brain as an amino acid, where it is metabolized into the active form, -methyl norepinephrine. In the biosynthesis pathway of dopamine, norepinephrine, and epinephrine, methyldopa replaces dihydroxyphenylalanine (DOPA), forming inactive structures of neurotransmitters. Methyldopa blocks the baroreceptor signaling pathway by activating presynaptic 2-adrenergic receptors and altering a single nucleus through inactive neurotransmitters [ 33 ].
Methyldopa significantly raises the level of vascular endothelial growth factor (VEGF), which is both an angiogenic factor and a neurotrophic agent. Although neuronal function alteration is probably more complex, VEGF dysfunctions neurogenesis and the functioning of sustained neurons by decreasing serotonin concentration and catecholamine levels due to this property. These changes characterize the neurotrophic depression model.
Methyldopa reduces cerebral blood flow by impairing baroreceptor signaling pathways and decreasing sympathetic system stimulation. Impaired neuronal function, cognitive decline, and depression are all consequences of decreased cerebral blood flow, particularly in the orbitofrontal cortex. These modifications characterize the vascular model of depression.
Methyldopa raises nitric oxide (NO) levels by reducing nitric-compound excretion in the kidneys and increasing endothelial nitric oxide synthase (eNOS) expression. In high concentrations, NO is neurotoxic, causing mild inflammation and decreased levels of cofactors (tryptophan, tetrahydrobiopterin, and others).and decreased levels of catecholamines and serotonin; consequently, elevated NO levels can cause depression. Methyldopa lowers dopamine concentration by interfering with its production. The excretion of prolactin is controlled by dopamine. Low dopamine levels cause hyperprolactinemia, which impairs sexual behavior and contributes to depression. Disruption of the reward system is an integral part of the development of depression. Methyldopa lowers dopamine levels, a neurotransmitter essential to the reward system. Depression is brought on by methyl-dopa through this mechanism.
In light of the preceding, taking methyldopa can cause depression. Because methyl-dopa is the first-line treatment for preeclampsia and hypertension in pregnancy and because mood swings and sluggishness are common after labor, this side effect of methyldopa is more likely to occur in pregnant women. To fully understand the problem and provide appropriate mental health care for patients, extensive prospective studies evaluating depression that occurs during the treatment of methyldopa and identifying potential prevention and treatment are required in light of the solid theoretical foundation.
Methyldopa may be considered a depression risk factor, inducer in postpartum depression, with the cause of maternal blues in light of the preceding data. This process's pathomechanism is intricate and classified into following five categories: (1) neurotrophic alteration, (2) reduction of cerebral blood flow, (3) neurotoxicity induced by NO, (4) high levels of prolactin, and (5) reward system impairment (Figure (Figure2 2 ).

The image is adapted from Wicinski et al. (2020) (CC BY 4.0) [ 33 ].
Diagnosis of PPD
The criteria for when PPD first appears is still debatable [ 34 ]. The United States Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (DSM-5) includes episodes that begin during pregnancy and last for six months after birth [ 35 ]. Postpartum depression (PPD) has been estimated to occur up to one year after childbirth in clinical practice and published research. For example, DSM-IV’s Structured Clinical Interview can be used to diagnose PPD Simple self-report instruments like questionnaires have been used for many clinical assessments. The Edinburgh Postnatal Depression Scale (EPDS) is reliable, validated, frequently more practical, and economical in large-scale screenings for PPD risk and is the most well-known and widely used [ 36 ]. To lessen the burden placed on common symptoms experienced by most new mothers, EPDS emphasizes psychic depression symptoms. Two-item Patient Health Questionnaire (PHQ-2) and nine-item Patient Health Questionnaire (PHQ-9) questionnaire-based screening tools are familiar. The first two items of the PHQ-9 can be found in PHQ-2. A typical score of 10 or higher on the EPDS or PHQ-9 [ 37 - 40 ] is used as the threshold for being positive for PPD Many brief E.P.D.S. subscales, including three-item, seven-item, and -item subscales, have also been developed [ 41 ]. The Hamilton Rating Scale for Depression (HAM-D), which isn’t explicitly made for PPD, is one of the other screening tools [ 42 ]. HAM-D's reliability varies significantly between 0.46 and 0.98 in various evaluations [ 43 ]. The Bipolar Spectrum Diagnostic Scale (BSDS) for bipolar disorders (BD) and other scales for diagnosis of related mood disorders may also be functional in the perinatal period [ 44 ].
Present-day treatment options of PPD and its constraints
There are many therapeutic interventions in the treatment of PPD, most adapted from the treatment of the major depressive disorder (MDD), as to date, there aren't any pharmacological therapies explicitly approved for PPD
Acute Treatment
Selective serotonin reuptake inhibitors (SSRI): The primitive line treatment for moderate to severe PPD by use of an SSRI. Among all clinical trial drugs, Sertraline is the most effective drug among SSRIs for treating PPD [ 45 ]. De Crescenzo and colleagues conducted a systematic review in which they found psychotherapy, SSRIs, and Nortriptyline are adequate for the acute treatment of PPD [ 46 ]. However, insufficiently proven studies clearly distinguish one remedy from another.
Serotonin norepinephrine reuptake inhibitors (SNRIs) and antidepressants: There hasn't been much-randomized control trials (RCT) trial data for SNRIs and antidepressants. Open-label trials recommend venlafaxine [ 47 ] and desvenlafaxine [ 48 ] to relieve symptoms.
Tricyclic antidepressants (TCA) and monoamine oxidase inhibitors (MAOI): Till today, nortriptyline is one TCA used for PPD [ 49 ]. There are not much RCT-level data for MAOI.
Prophylactic Treatment
Selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCA's): The risk of recurrence for women who have previously experienced PPD is approximately 25% [ 50 ]. To conclude the efficacy of antidepressants in preventing PPD, a newly published Cochrane review found that additional studies involving more participants are required [ 51 ].
Psychotherapies, Complementary Health Practices, and Neuromodulatory Interventions
When considering antidepressant treatment, women having PPD experience mild to high rates of decisional conflict, particularly during pregnancy [ 52 ], and many prefer psychotherapies to pharmacotherapies [ 53 ]. Nearly 26-75% of pregnant women worldwide use complementary health practices due to their significant health-related advantages [ 54 ]. In the United States, 54% of women who suffer from depression say they have used complementary health practices in the past year [ 55 ]. In more severe and remitting cases of postpartum depression (PPD) and postpartum psychosis, an important neuromodulatory option is electroconvulsive therapy (ECT). Compared to treatment for non-postpartum depression or psychosis, ECT is said to have a higher response rate [ 56 ]. There are no RCT-level data for using ECT to treat PPD, despite the publication of guidelines for its use during Pregnancy [ 57 ]. For the treatment of PPD, additional neuromodulatory methods, such as transcranial direct current stimulation (TCCS) and repetitive transcranial magnetic stimulation (TMS), are in their initial trial stages [ 58 - 62 ]. Other non-invasive neuromodulation interventions and the effectiveness of ECT versus pharmacotherapy in severe PPD should be subject to additional RCT.
Implications for novel pharmacological treatment
A clinical study has used intravenous preparations for endogenous allopregnanolone CNS drugs due to its less oral bioavailability and excessive in vivo clearance. Allopregnanolone given intravenously has been shown to cause sedation and decreased saccadic eye velocity, with women experiencing these effects more than men [ 63 ]. Some women who receive intravenous allopregnanolone may experience only episodic and not semantic or working memory impairment [ 64 ]. Acute intravenous administration of allopregnanolone does not affect the startle response or prepulse inhibition of the startle reaction, indicating that it does not have anxiolytic effects on healthy women [ 65 ]. Allopregnanolone may regulate the hypothalamic-pituitary-gonadal axis through GABA-A receptor modulation, as evidenced by the fact that intravenous administration in healthy women during the follicular phase of a menstrual cycle is linked with decreased plasma concentration of luteinizing hormone and follicle-stimulating hormone but not plasma levels of estradiol or progesterone [ 66 ]. Investigation of synthetic Non-allogenic steroids (NAS) and their analogs as primary treatments for PPD is supported by the evidence mentioned above that NAS and GABA play a role in the pathophysiology of PPD Brexanolone (USAN) was developed by Sage Therapeutics, formerly known as SAGE-547 Injection), a proprietary, soluble synthetic allopregnanolone intravenous preparation. Brexanolone, which is a sterile solution of 5 mg/mL allopregnanolone in 250 mg/mL sulfobutylether-cyclodextrin buffered with citrate and diluted until it is isotonic with sterile water [ 67 ]. Brexanolone causes potent, dose-dependent activation of GABA-mediated currents in whole-cell patch electrophysiology studies. Studies on drug interactions have shown that co-administration of brexanolone can alter the metabolic rate of CYP2C9 substrates. Brexanolone in PPD was the subject of the latest series of open-label and few RCTs, which are placebo-controlled that demonstrated a rapid decline in PPD symptoms.
Consequences of PPD
There are few denotations related to women who experience postpartum depression being more likely to have comorbid obsessive-compulsive disorder and anxiety than women who experience depression at other times in their lives [ 68 ]. Postpartum depression is linked to various outcomes in other areas and an increased risk of comorbid disorders [ 69 ]. There have been reports of adverse long-term effects on infants' social, emotional, intellectual, and physical development [ 70 ]. Postpartum depression-afflicted mothers' children may also be more likely to have intellectual disabilities and psychosocial, emotional, or behavioral problems [ 71 ]. Deficient parenting and parental safety practices are also linked to postpartum depression and difficulties in bonding and mother-child interactions. Research must identify the significant risk factors and protective factors for postpartum depression because of the potentially devastating effects on the mother, the child, and their family postpartum depression.
Conclusions
PPD is a disorder that can be crippling and common. There are several effective pharmacological therapies, psychological therapies, psychosocial, and neuromodulation intercession, but the majority are understudied, particularly in RCT. Sadly, there is a significant underutilization of available treatments in the community. Even though PPD is now more readily discussed, a considerable stigma exists against few women seeking treatment. In low socioeconomic countries, mental health might not be prioritized; women may have restrictions in reaching out to providers specially trained in perinatal mental health even when they seek treatment. Because of the complexity of treatment modalities of peripartum psychiatric illness demands integrative work among multiple health service providers, including obstetrics, psychiatry, pediatrics, and nursing/midwifery. Reproductive psychiatric tutorials should be spread widely within the discipline of psychiatry in residency and fellowship programs.
It is necessary to develop novel therapeutics that specifically target the disorder's underlying pathophysiology and expand access to the treatments that are already in place and improve the quality of those treatments. The underlying neurobiology of PPD is still poorly understood, despite increased research into its causes. There is mounting evidence that psychiatric disorders are neural network disorders characterized by complex, multimodal patterns of neurobiological abnormalities. As a result, there is a pressing need for additional research into the underlying mechanisms of these disorders. We can detect, diagnose, and treat PPD more effectively during pregnancy and postpartum if we learn more about the neurobiology of PPD.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
- Open access
- Published: 14 May 2024
Exploring predictors and prevalence of postpartum depression among mothers: Multinational study
- Samar A. Amer ORCID: orcid.org/0000-0002-9475-6372 1 ,
- Nahla A. Zaitoun ORCID: orcid.org/0000-0002-5274-6061 2 ,
- Heba A. Abdelsalam 3 ,
- Abdallah Abbas ORCID: orcid.org/0000-0001-5101-5972 4 ,
- Mohamed Sh Ramadan 5 ,
- Hassan M. Ayal 6 ,
- Samaher Edhah Ahmed Ba-Gais 7 ,
- Nawal Mahboob Basha 8 ,
- Abdulrahman Allahham 9 ,
- Emmanuael Boateng Agyenim 10 &
- Walid Amin Al-Shroby 11
BMC Public Health volume 24 , Article number: 1308 ( 2024 ) Cite this article
345 Accesses
Metrics details
Postpartum depression (PPD) affects around 10% of women, or 1 in 7 women, after giving birth. Undiagnosed PPD was observed among 50% of mothers. PPD has an unfavorable relationship with women’s functioning, marital and personal relationships, the quality of the mother-infant connection, and the social, behavioral, and cognitive development of children. We aim to determine the frequency of PPD and explore associated determinants or predictors (demographic, obstetric, infant-related, and psychosocial factors) and coping strategies from June to August 2023 in six countries.
An analytical cross-sectional study included a total of 674 mothers who visited primary health care centers (PHCs) in Egypt, Yemen, Iraq, India, Ghana, and Syria. They were asked to complete self-administered assessments using the Edinburgh Postnatal Depression Scale (EPDS). The data underwent logistic regression analysis using SPSS-IBM 27 to list potential factors that could predict PPD.
The overall frequency of PPD in the total sample was 92(13.6%). It ranged from 2.3% in Syria to 26% in Ghana. Only 42 (6.2%) were diagnosed. Multiple logistic regression analysis revealed there were significant predictors of PPD. These factors included having unhealthy baby adjusted odds ratio (aOR) of 11.685, 95% CI: 1.405–97.139, p = 0.023), having a precious baby (aOR 7.717, 95% CI: 1.822–32.689, p = 0.006), who don’t receive support (aOR 9.784, 95% CI: 5.373–17.816, p = 0.001), and those who are suffering from PPD. However, being married and comfortable discussing mental health with family relatives are significant protective factors (aOR = 0.141 (95% CI: 0.04–0.494; p = 0.002) and (aOR = 0.369, 95% CI: 0.146–0.933, p = 0.035), respectively.
The frequency of PPD among the mothers varied significantly across different countries. PPD has many protective and potential factors. We recommend further research and screenings of PPD for all mothers to promote the well-being of the mothers and create a favorable environment for the newborn and all family members.
Peer Review reports
Introduction
Postpartum depression (PPD) is among the most prevalent mental health issues [ 1 ]. The onset of depressive episodes after childbirth occurs at a pivotal point in a woman’s life and can last for an extended period of 3 to 6 months; however, this varies based on several factors [ 2 ]. PPD can develop at any time within the first year after childbirth and last for years [ 2 ]. It refers to depressive symptoms that a mother experiences during the postpartum period, which are vastly different from “baby blues,” which many mothers experience within three to five days after the birth of their child [ 3 ].
Depressive episodes are twice as likely to occur during pregnancy compared to other times in a woman’s life, and they frequently go undetected and untreated [ 4 ]. According to estimates, almost 50% of mothers with PPD go undiagnosed [ 4 ]. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria for PPD include mood instability, loss of interest, feelings of guilt, sleep disturbances, sleep disorders, and changes in appetite [ 5 ], as well as decreased libido, crying spells, anxiety, irritability, feelings of isolation, mental liability, thoughts of hurting oneself and/or the infant, and even suicidal ideation [ 6 ].
Approximately 1 in 10 women will experience PPD after giving birth, with some studies reporting 1 in 7 women [ 7 ]. Globally, the prevalence of PPD is estimated to be 17.22% (95% CI: 16.00–18.05) [ 4 ], with a prevalence of up to 15% in the previous year in eighty different countries or regions [ 1 ]. This estimate is lower than the 19% prevalence rate of PPD found in studies from low- and middle-income countries and higher than the 13% prevalence rate (95% CI: 12.3–13.4%) stated in a different meta-analysis of data from high-income countries [ 8 ].
The occurrence of postpartum depression is influenced by various factors, including social aspects like marital status, education level, lack of social support, violence, and financial difficulties, as well as other factors such as maternal age (particularly among younger women), obstetric stressors, parity, and unplanned pregnancy [ 4 ]. When a mother experiences depression, she may face challenges in forming a satisfying bond with her child, which can negatively affect both her partner and the emotional and cognitive development of infants and adolescents [ 4 ]. As a result, adverse effects may be observed in children during their toddlerhood, preschool years, and beyond [ 9 ].
Around one in seven women can develop PPD [ 7 ]. While women experiencing baby blues tend to recover quickly, PPD tends to last longer and severely affects women’s ability to return to normal function. PPD affects the mother and her relationship with the infant [ 7 ]. The prevalence of postpartum depression varies depending on the assessment method, timing of assessment, and cultural disparities among countries [ 7 ]. To address these aspects, we conducted a cross-sectional study focusing on mothers who gave birth within the previous 18 months. Objectives: to determine the frequency of PPD and explore associated determinants or predictors, including demographic, obstetric, infant-related, and psychosocial factors, and coping strategies from June to August 2023 in six countries.
Study design and participants
This is an analytical cross-sectional design and involved 674 mothers during the childbearing period (CBP) from six countries, based on the authors working settings, namely Egypt, Syria, Yemen, Ghana, India, and Iraq. It was conducted from June to August 2023. It involved all mothers who gave birth within the previous 18 months, citizens of one of the targeted countries, and those older than 18 years and less than 40 years. Women who visited for a routine postpartum follow-up visit and immunization of their newborns were surveyed.
Multiple pregnancies, illiteracy, or anyone deemed unfit to participate in accordance with healthcare authorities, mothers who couldn’t access or use the Internet, mothers who couldn’t read or speak Arabic or English and couldn’t deal with the online platform or smart devices, mothers whose babies were diagnosed with serious health problems, were stillborn, or experienced intrauterine fetal death, and participants with complicated medical, mental, or psychological disorders that interfered with completing the questionnaire were all exclusion criteria. There were no incentives offered to encourage participation.
Sample size and techniques
The sample size was estimated according to the following equation: n = Z 2 P (1-P)/d 2 . This calculation was based on the results of a systematic review and meta-analysis in 2020 of 17% as the worldwide prevalence of PPD and 12% as the worldwide incidence of PPD, as well as a 5% precision percentage, 80% power of the study, a 95% confidence level, and an 80% response rate [ 11 ]. The total calculated sample size is 675. The sample was diverse in terms of nationality, with the majority being Egyptian (16.3%), followed by Yemeni (24.3%) and Indian (19.1%), based on many factors discussed in the limitation section.
The sampling process for recruiting mothers utilized a multistage approach. Two governorates were randomly selected from each country. Moreover, we selected one rural and one urban area from each governorate. Through random selection, participants were chosen for the study. Popular and officially recognized online platforms, including websites and social media platforms such as Facebook, Twitter, WhatsApp groups, and registered emails across various health centers, were utilized for reaching out to participants. Furthermore, a community-based sample was obtained from different public locations, including well-baby clinics, PHCs, and family planning units.
Mothers completed the questionnaire using either tablets or cellphones provided by the data collectors or by scanning the QR code. All questions were mandatory to prevent incomplete forms. Once they provided their informed consent, they received the questionnaire, which they completed and submitted. To enhance the response rate, reminder messages and follow-up communications were employed until the desired sample size was achieved or until the end of August. To avoid seasonal affective disorders, the meteorological autumn season began on the 1st day of September, which may be associated with Autum depressive symptoms that may confound or affect our results.
Data collection tool
Questionnaire development and structure.
The questionnaire was developed and adapted based on data obtained from previous studies [ 7 , 8 , 9 , 10 , 11 , 12 ]. Initially, it was created in English and subsequently translated into Arabic. To ensure accuracy, a bilingual panel consisting of two healthcare experts and an externally qualified medical translator translated the English version into Arabic. Additionally, two English-speaking translators performed a back translation, and the original panel was consulted if any concerns arose.
Questionnaire validation
To collect the data, an online, self-administered questionnaire was utilized, designed in Arabic with a well-structured format. We conducted an assessment of the questionnaire’s reliability and validity to ensure a consistent interpretation of the questions. The questionnaire underwent validation by psychiatrists, obstetricians, and gynecologists. Furthermore, in a pilot study involving 20 women of CBA, the questionnaire’s clarity and comprehensibility were evaluated. It is important to note that the findings from the pilot study were not included in our main study.
The participants were asked to rate the questionnaire’s organization, clarity, and length, as well as provide a general opinion. Following that, certain questions were revised in light of their input. To check for reliability and reproducibility, the questionnaire was tested again on the same people one week later. The final data analysis will not include the data collected during the pilot test. We calculated a Cronbach’s alpha of 0.76 for the questionnaire.
The structure of the questionnaire
After giving their permission to take part in the study. The questionnaire consisted of the following sections:
Study information and electronic solicitation of informed consent.
Demographic and health-related factors: age, gender, place of residence, educational level, occupation, marital status, weight, height, and the fees of access to healthcare services.
Obstetric history: number of pregnancies, gravida, history of abortions, number of live children, history of dead children, inter-pregnancy space (y), current pregnancy status, type of the last delivery, weight gain during pregnancy (kg), baby age (months), premature labor, healthy baby, baby admitted to the NICU, Feeding difficulties, pregnancy problems, postnatal problems, and natal problems The nature of baby feeding.
Assessment of postpartum depression (PPD) levels using the Edinburgh 10-question scale: This scale is a simple and effective screening tool for identifying individuals at risk of perinatal depression. The EPDS (Edinburgh Postnatal Depression Scale) is a valuable instrument that helps identify the likelihood of a mother experiencing depressive symptoms of varying severity. A score exceeding 13 indicates an increased probability of a depressive illness. However, clinical discretion should not be disregarded when interpreting the EPDS score. This scale captures the mother’s feelings over the past week, and in cases of uncertainty, it may be beneficial to repeat the assessment after two weeks. It is important to note that this scale is not capable of identifying mothers with anxiety disorders, phobias, or personality disorders.
For Questions 1, 2, and 4 (without asterisks): Scores range from 0 to 3, with the top box assigned a score of 0 and the bottom box assigned a score of 3. For Questions 3 and 5–10 (with asterisks): Scores are reversed, with the top box assigned a score of 3 and the bottom box assigned a score of 0. The maximum score achievable is 30, and a probability of depression is considered when the score is 10 or higher. It is important to always consider item 10, which pertains to suicidal ideation [ 12 ].
Psychological and social characteristics: received support or treatment for PPD, awareness of symptoms and risk factors, experienced cultural stigma or judgment about PPD in the community, suffer from any disease or mental or psychiatric disorder, have you ever been diagnosed with PPD, problems with the husband, and financial problems.
Coping strategies and causes for not receiving the treatment and reactions to PPD, in descending order: social norms, cultural or traditional beliefs, personal barriers, 48.5% geographical or regional disparities in mental health resources, language or communication barriers, and financial constraints.
Statistical analysis
The collected data was computerized and statistically analyzed using the SPSS program (Statistical Package for Social Science), version 27. The data was tested for normal distribution using the Shapiro-Walk test. Qualitative data was represented as frequencies and relative percentages. Quantitative data was expressed as mean ± SD (standard deviation) if it was normally distributed; otherwise, median and interquartile range (IQR) were used. The Mann-Whitney test (MW) was used to calculate the difference between quantitative variables in two groups for non-parametric variables. Correlation analysis (using Spearman’s method) was used to assess the relationship between two nonparametric quantitative variables. All results were considered statistically significant when the significant probability was < 0.05. The chi-square test (χ 2 ) and Fisher exact were used to calculate the difference between qualitative variables.
The frequency of PPD among mothers (Fig. 1 )
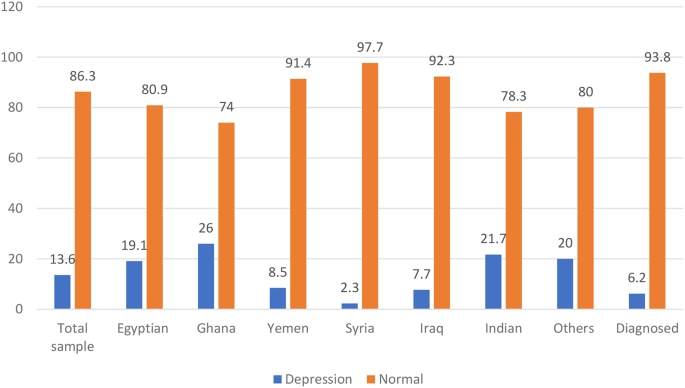
The frequency of PPD among the studied mothers
The frequency of PPD in the total sample using the Edinburgh 10-question scale was 13.5% (Table S1) and 92 (13.6%). Which significantly ( p = 0.001) varied across different countries, being highest among Ghana mothers 13 (26.0%) out of 50 and Indians 28 (21.7%) out of 129. Egyptian 21 (19.1) out of 110, Yemen 14 (8.5%) out of 164, Iraq 13 (7.7%) out of 168, and Syria 1 (2.3%) out of 43 in descending order. Nationality is also significantly associated with PPD ( p = 0.001).
Demographic, and health-related characteristics and their association with PPD (Table 1 )
The study included 674 participants. The median age was 27 years, with 407 (60.3%) of participants falling in the >25 to 40-year-old age group. The majority of participants were married, 650 (96.4%), had sufficient monthly income, 449 (66.6%), 498 (73.9%), had at least a preparatory or high school level of education, and were urban. Regarding health-related factors, 270 (40.01%) smoked, 645 (95.7%) smoked, 365 (54.2%) got the COVID-19 vaccine, and 297 (44.1%) got COVID-19. Moreover, 557 (82.6%) had no comorbidities, 623 (92.4%) had no psychiatric illness or family history, and they charged for health care services for themselves 494 (73.3%).
PPD is significant ( p < 0.05). Higher among single or widowed women 9 (56.3%) and mothers who had both medical, mental, or psychological problems 2 (66.7%), with ex-cigarette smoking 5 (35.7%) ( p = 0.033), alcohol consumption ( p = 0.022) and mothers were charged for the health care services for themselves 59 (11.9%).
Obstetric, current pregnancy, and infant-related characteristics and their association with PPD (Table 2 )
The majority of the studied mothers were on no hormonal treatment or contraceptive pills 411 (60.9%), the current pregnancy was unplanned and wanted 311 (46.1%), they gained 10 ≥ kg 463 (68.6%), 412 (61.1%) delivered vaginal, a healthy baby 613 (90.9%), and, on breastfeeding, only 325 (48.2%).
There was a significant ( P < 0.05) association observed between PPD, which was significantly higher among mothers on contraceptive methods, and those who had 1–2 live births (76.1%) and mothers who had interpregnancy space for less than 2 years. 86 (93.5%), and those who had a history of dead children. Moreover, among those who had postnatal problems (27.2%).
The psychosocial characteristics and their association with PPD (Table 3 )
Regarding the psychological and social characteristics of the mothers, the majority of mothers were unaware of the symptoms of PPD (75%), and only 236 (35.3%) experienced cultural stigma or judgment about PPD in the community. About 41 (6.1%) were diagnosed with PPD during the previous pregnancy, and only 42 (6.2%) were diagnosed and on medications.
A p -value of less than 0.001 demonstrates a highly statistically significant association with the presence of PPD. Mothers with PPD were significantly more likely to have a history of or be currently diagnosed with PPD, as well as financial and marital problems. Experienced cultural stigma or judgment about PPD and received more support.
Coping strategies and causes for not receiving the treatment and reaction to PPD (Table 3 ; Fig. 2 )
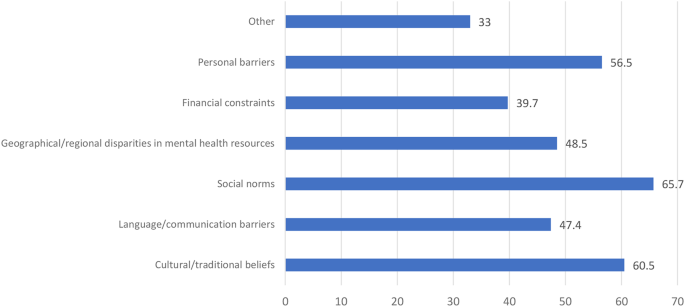
Causes for not receiving the treatment and reaction to PPD
Around half of the mothers didn’t feel comfortable discussing mental health: 292 (43.3%) with a physician, 307 (45.5%) with a husband, 326 (48.4%) with family, and 472 (70.0%) with the community. Moreover, mothers with PPD felt significantly more comfortable discussing mental health in descending order: 46 (50.0%) with a physician, 41 (44.6%) with a husband, and 39 (42.3%) with a family (Table 3 ).
There were different causes for not receiving the treatment and reactions to PPD, in descending order: 65.7% social norms, 60.5% cultural or traditional beliefs, 56.5% personal barriers, 48.5% geographical or regional disparities in mental health resources, 47.4% language or communication barriers, and 39.7% financial constraints.
Prediction of PPD (significant demographics, obstetric, current pregnancy, and infant-related, and psychosocial), and coping strategies derived from multiple logistic regression analysis (Table 4 ).
Significant demographic predictors of ppd.
Marital Status (Married or Single): The adjusted odds ratio (aOR) among PPD mothers who were married in comparison to their single counterparts was 0.141 (95% CI: 0.04–0.494; p -value = 0.002).
Nationality: For PPD Mothers of Yemeni nationality compared to those with Egyptian nationality, the aOR was 0.318 (95% CI: 0.123–0.821, p = 0.018). Similarly, for Syrian nationality in comparison to Egyptian nationality, the aOR was 0.111 (95% CI: 0.0139–0.887, p = 0.038), and for Iraqi nationality compared to Egyptian nationality, the aOR was 0.241 (95% CI: 0.0920–0.633, p = 0.004).
Significant obstetric, current pregnancy, and infant-related characteristics predictors of PPD
Current Pregnancy Status (Precious Baby—Planned): The aOR for the occurrence of PPD among women with a “precious baby” relative to those with a “planned” pregnancy was 7.717 (95% CI: 1.822–32.689, p = 0.006).
Healthy Baby (No-Yes): The aOR for the occurrence of PPD among women with unhealthy babies in comparison to those with healthy ones is 11.685 (95% CI: 1.405–97.139, p = 0.023).
Postnatal Problems (No–Yes): The aOR among PPD mothers reporting postnatal problems relative to those not reporting such problems was 0.234 (95% CI: 0.0785–0.696, p = 0.009).
Significant psychological and social predictors of PPD
Receiving support or treatment for PPD (No-Yes): The aOR among PPD mothers who were not receiving support or treatment relative to those receiving support or treatment was 9.784 (95% CI: 5.373–17.816, p = 0.001).
Awareness of symptoms and risk factors (No-Yes): The aOR among PPD mothers who lack awareness of symptoms and risk factors relative to those with awareness was 2.902 (95% CI: 1.633–5.154, p = 0.001).
Experienced cultural stigma or judgement about PPD in the community (No-Yes): The aOR among PPD mothers who had experienced cultural stigma or judgment in the community relative to those who have not was 4.406 (95% CI: 2.394–8.110, p < 0.001).
Suffering from any disease or mental or psychiatric disorder: For “Now I am suffering—not at all,” the aOR among PPD mothers was 12.871 (95% CI: 3.063–54.073, p = 0.001). Similarly, for “Had a past history but was treated—not at all,” the adjusted odds ratio was 16.6 (95% CI: 2.528–108.965, p = 0.003), and for “Had a family history—not at all,” the adjusted odds ratio was 3.551 (95% CI: 1.012–12.453, p = 0.048).
Significant coping predictors of PPD comfort: discussing mental health with family (maybe yes)
The aOR among PPD mothers who were maybe more comfortable discussing mental health with family relatives was 0.369 (95% CI: 0.146–0.933, p = 0.035).
PDD is a debilitating mental disorder that has many potential and protective risk factors that should be considered to promote the mental and psychological well-being of the mothers and to create a favorable environment for the newborn and all family members. This multinational cross-sectional survey was conducted in six different countries to determine the frequency of PDD using EPDS and to explore its predictors. It was found that PPD was a prevalent problem that varied across different nations.
The frequency of PPD across the studied countries
Using the widely used EPDS to determine the current PPD, we found that the overall frequency of PPD in the total sample was 92 (13.6%). Which significantly ( p = 0.001) varied across different countries, being highest among Ghana mothers 13 (26.0%) out of 50 and Indians 28 (21.7%) out of 129. Egyptian 21 (19.1) out of 110, Yemen 14 (8.5%) out of 164, Iraq 13 (7.7%) out of 169, and Syria 1 (2.3%) out of 43 in descending order. This prevalence was similar to that reported by Hairol et al. (2021) in Malaysia (14.3%) [ 13 ], Yusuff et al. (2010) in Malaysia (14.3%) [ 14 ], and Nakku et al. (2006) in New Delhi (12.75%) [ 15 ].
While the frequency of PPD varied greatly based on the timing, setting, and existence of many psychosocial and post-partum periods, for example, it was higher than that reported in Italy (2012), which was 4.7% [ 16 ], in Turkey (2017) was 9.1%/110 [ 17 ], 9.2% in Sudan [ 18 ], Eritrea (2020) was 7.4% [ 19 ], in the capital Kuala Lumpur (2001) was (3.9%) [ 20 ], in Malaysia (2002) was (9.8%) [ 21 ], and in European countries. (2021) was 13–19% [ 22 ].
Lower frequencies were than those reported; PPD is a predominant problem in Asia, e.g., in Pakistan, the three-month period after childbirth, ranging from 28.8% in 2003 to 36% in 2006 to 94% in 2007, while after 12 months after childbirth, it was 62% in 2021 [ 23 – 24 ]. While in 2022 Afghanistan 45% after their first labour [ 25 ] in Canada (2015) was 40% [ 26 ], in India, the systematic review in 2022 was 22% of Primipara [ 27 ], in Malaysia (2006) was 22.8% [ 28 ], in India (2019) was 21.5% [ 29 ], in the Tigray zone in Ethiopia (2017) was 19% [ 30 ], varied in Iran between 20.3% and 35% [ 31 – 32 ], and in China was 499 (27.37%) out of 1823 [ 33 ]. A possible explanation might be the differences in the study setting and the type of design utilized. Other differences should be considered, like different populations with different socioeconomic characteristics and the variation in the timing of post-partum follow-up. It is vital to consider the role of culture, the impact of patients’ beliefs, and the cultural support for receiving help for PPD.
Demographic and health-related associations, or predictors of PPD (Tables 1 and 4 )
Regarding age, our study found no significant difference between PPD and non-PPD mothers with regard to age. In agreement with our study [ 12 , 34 , 35 ], other studies [ 36 , 37 , 38 ] found an inverse association between women’s age and PPD, with an increased risk of PPD (increases EPDS scores) at a younger age significantly, as teenage mothers, being primiparous, encounter difficulty during the postpartum period due to their inability to cope with financial and emotional difficulties, as well as the challenge of motherhood. Cultural factors and social perspectives of young mothers in different countries could be a reason for this difference. [ 38 – 39 ] and Abdollahi et al. [ 36 ] reported that older mothers were a protective factor for PPD (OR = 0.88, 95% CI: 0.84–0.92].
Regarding marital status, after controlling for other variables, married mothers exhibited a significantly diminished likelihood of experiencing PPD in comparison to single women (0.141; 95% CI: 0.04–0.494; p = 0.002). Also, Gebregziabher et al. [ 19 ] reported that there were statistically significant differences in proportions between mothers’ PPD and marital status.
Regarding the mother’s education, in agreement with our study, Ahmed et al. [ 34 ] showed that there was no statistically significant difference between PPD and a mother’s education. While Agarwala et al. [ 29 ] showed that a higher level of mother’s education. increases the risk of PPD, Gebregziabher et al. [ 19 ] showed that the housewives were 0.24 times less likely to develop PPD as compared to the employed mothers (aOR = 0.24, 95% CI: 0.06–0.97; p = 0.046); those mothers who perceived their socioeconomic status (SES) as low were 13 times more likely to develop PPD as compared to the mothers who had good SES (aOR = 13.33, 95% CI: 2.66–66.78; p = 0.002).
Regarding the SES or monthly income, while other studies [ 18 , 40 ] found that there was a statistically significant association between PPD mothers and different domains of SES, 34% of depressed women were found to live under low SES conditions in comparison to only 15.4% who were found to live in high SES and experienced PPD. In disagreement with our study, Hairol et al. [ 12 ] demonstrated that the incidence of PPD was significantly p = 0.01 higher for participants from the low-income group (27.27%) who were 2.58 times more likely to have PDD symptoms (OR: 2.58, 95% CI: 1.23–5.19; p = 0.01 compared to those from the middle- and high-income groups (8.33%), and low household income (OR = 3.57 [95% CI: 1.49–8.5] increased the odds of PPD [ 41 ].
Adeyemo et al. (2020),and Al Nasr et al. (2020) revealed that there was no significant difference between the occurrence of PPD and socio-demographic characteristics. This difference may be due to a different sample size and ethnicity [ 42 , 43 ]. In agreement with our findings, Abdollahi et al. [ 36 ] demonstrated that after multiple logistic regression analyses, there were increased odds of PPD with a lower state of general health (OR = 1.08 [95% CI: 1.06–1.11]), gestational diabetes (OR = 2.93 [95% CI = 1.46–5.88]), and low household income (OR = 3.57 [95% CI: 1.49–8.5]). The odds of PPD decreased.
Regarding access to health care, in agreement with studies conducted at Gondar University Hospital, Ethiopia [ 18 ], North Carolina, Colorado [ 21 ], Khartoum, Sudan [ 44 ], Asaye et al. [ 45 ], the current study found that participants who did not have free access to the healthcare system were riskier for the development of PPD. the study results may be affected by the care given during the antenatal care (ANC) visits. This can be explained by the fact that PPD was four times higher than that of mothers who did not have ANC, where counseling and anticipatory guidance care are given that build maternal self-esteem and resiliency, along with knowledge about normal and problematic complications to discuss at care visits and their right to mental and physical wellness, including access to care. The increased access to care (including postpartum visits) will increase the diagnosis of PPD and provide guidance, reassurance, and appropriate referrals. Healthcare professionals have the ability to both educate and empower mothers as they care for their babies, their families, and themselves [ 46 ].
Regarding nationality, for PPD mothers of Yemeni nationality compared to those of Egyptian nationality, the aOR is 0.318 (95% CI: 0.123–0.821, p = 0.018). Similarly, for Syrian nationality in comparison to Egyptian nationality, the aOR is 0.111 (95% CI: 0.0139–0.887, p = 0.038), and for Iraqi nationality compared to Egyptian nationality, the aOR is 0.241 (95% CI: 0.0920–0.633, p = 0.004). These findings indicated that, while accounting for other covariates, individuals from the aforementioned nationalities were less predisposed to experiencing PPD than their Egyptian counterparts. These findings can be explained by the fact that, in Egypt, the younger age of marriage, especially in rural areas, poor mental health services, being illiterate, dropping out of school early, unemployment, and the stigma of psychiatric illnesses are cultural factors that hinder the diagnosis and treatment of PPD [ 40 ].
Obstetric, current pregnancy, and infant-related characteristics and their association or predictors of PPD (Tables 2 and 4 )
In the present study, the number of dead children was significantly associated with PPD. This report was supported by studies conducted with Gujarati postpartum women [ 41 ] and rural southern Ethiopia [ 43 ]. This might be because mothers who have dead children pose different psychosocial problems and might regret it for fear of complications developing during their pregnancy. Agarwala et al. [ 29 ] found that a history of previous abortions and having more than two children increased the risk of developing PPD due to a greater psychological burden. The inconsistencies in the findings of these studies indicate that the occurrence of postpartum depression is not solely determined by the number of childbirths.
In obstetric and current pregnancy , there was no significant difference regarding the baby’s age, number of miscarriages, type of last delivery, premature labour, healthy baby, baby admitted to the neonatal intensive care unit (NICU), or feeding difficulties. In agreement with Al Nasr et al. [ 42 ], inconsistent with Asaye et al. [ 45 ], they showed that concerning multivariable logistic regression analysis, abortion history, birth weight, and gestational age were significant associated factors of postpartum depression at a value of p < 0.05.
However, a close association was noted between the mode of delivery and the presence of PPD in mothers, with p = 0.107. There is a high tendency towards depression seen in mothers who have delivered more than three times (44%). In disagreement with what was reported by Adeyemo et al. [ 41 ], having more than five children ( p = 0.027), cesarean section delivery ( p = 0.002), and mothers’ poor state of health since delivery ( p < 0.001) are associated with an increase in the risk of PPD [ 47 ]. An increased risk of cesarean section as a mode of delivery was observed (OR = 1.958, p = 0.049) in a study by Al Nasr et al. [ 42 ].
We reported breastfeeding mothers had a lower, non-significant frequency of PPD compared to non-breast-feeding mothers (36.6% vs. 45%). In agreement with Ahmed et al. [ 34 ], they showed that with respect to breastfeeding and possible PPD, about 67.3% of women who depend on breastfeeding reported no PPD, while 32.7% only had PP. Inconsistency with Adeyemo et al. [ 41 ], who reported that unexclusive breastfeeding ( p = 0.003) was associated with PPD, while Shao et al. [ 40 ] reported that mothers who were exclusively formula feeding had a higher prevalence of PPD.
Regarding postnatal problems, our results revealed that postnatal problems display a significant association with PPD. In line with our results, Agarwala et al. [ 29 ] and Gebregziabher et al. [ 19 ] showed that mothers who experienced complications during childbirth, those who became ill after delivery, and those whose babies were unhealthy had a statistically significant higher proportion of PPD.
Hormone-related contraception methods were found to have a statistically significant association with PPD, consistent with the literature [ 46 ]; this can be explained by the hormones and neurotransmitters as biological factors that play significant roles in the onset of PPD. Estrogen hormones act as regulators of transcription from brain neurotransmitters and modulate the action of serotonin receptors. This hormone stimulates neurogenesis, the process of generating new neurons in the brain, and promotes the synthesis of neurotransmitters. In the hypothalamus, estrogen modulates neurotransmitters and governs sleep and temperature regulation. Variations in the levels of this hormone or its absence are linked to depression [ 19 ].
Participants whose last pregnancy was unplanned were 3.39 times more likely to have postpartum depression (aOR = 3.39, 95% CI: 1.24–9.28; p = 0.017). Mothers who experienced illness after delivery were more likely to develop PPD as compared to their counterparts (aOR = 7.42, 95% CI: 1.44–34.2; p = 0.016) [ 40 ]. In agreement with Asaye et al. [ 45 ] and Abdollahi et al. [ 36 ], unplanned pregnancy has been associated with the development of PPD (aOR = 2.02, 95% CI: 1.24, 3.31) and OR = 2.5 [95% CI: 1.69–3.7] than those of those who had planned, respectively.
The psychosocial characteristics and their association with PPD
Mothers with a family history of mental illness were significantly associated with PPD. This finding was in accordance with studies conducted in Istanbul, Turkey [ 47 ], and Bahrain [ 48 ]. Other studies also showed that women with PPD were most likely to have psychological symptoms during pregnancy [ 43 , 44 , 45 , 46 , 47 , 48 , 49 ]. A meta-analysis of 24,000 mothers concluded that having depression and anxiety during pregnancy and a previous history of psychiatric illness or a history of depression are strong risk factors for developing PPD [ 50 , 51 , 52 ]. Asaye et al. [ 45 ], mothers whose relatives had mental illness history were (aOR = 1.20, 95% CI: 1.09, 3.05 0) be depressed than those whose relatives did not have mental illness history.
This can be attributed to the links between genetic predisposition and mood disorders, considering both nature and nurture are important to address PDD. PPD may be seen as a “normal” condition for those who are acquainted with relatives with mood disorders, especially during the CBP. A family history of mental illness can be easily elicited in the ANC first visit history and requires special attention during the postnatal period. There are various risk factors for PPD, including stressful life events, low social support, the infant’s gender preference, and low income [ 53 ].
Concerning familial support and possible PPD, a statistically significant association was found between them. We reported that mothers who did not have social support (a partner or the father of the baby) had higher odds (aOR = 5.8, 95% CI: 1.33–25.29; p = 0.019) of experiencing PPD. Furthermore, Al Nasr et al. [ 42 ] revealed a significant association between the PPD and an unsupportive spouse ( P value = 0.023). while it was noted that 66.5% of women who received good familial support after giving birth had no depression, compared to 33.5% who only suffered from possible PPD [ 40 ]]. Also, Adeyemo et al. [ 41 ] showed that some psychosocial factors were significantly associated with having PPD: having an unsupportive partner ( p < 0.001), experiencing intimate partner violence ( p < 0.001), and not getting help in taking care of their baby ( p < 0.001). Al Nasr et al. (2020) revealed that the predictor of PPD was an unsupportive spouse (OR = 4.53, P = 0.049) [ 48 ].
Regarding the perceived stigma, in agreement with our study, Bina (2020) found that shame, stigma, the fear of being labeled mentally ill, and language and communication barriers were significant factors in women’s decisions to seek treatment or accept help [ 53 ]. Other mothers were hesitant about mental health services [ 54 ]. It is noteworthy that some PPD mothers refused to seek treatment due to perceived insufficient time and the inconvenience of attending appointments [ 55 ].
PPD was significantly higher among mothers with financial problems or problems with their husbands. This came in agreement with Ahmed et al. [ 34 ], who showed that, regarding stressful conditions and PPD, there was a statistically significant association with a higher percentage of PPD among mothers who had a history of stressful conditions (59.3%), compared to those with no history of stressful conditions (40.7%). Furthermore, Al Nasr et al. (2020) revealed that stressful life events contributed significantly ( P value = 0.003) to the development of PPD in the sample population. Al Nasr et al. stressful life events (OR = 2.677, p = 0.005) [ 42 ].
Coping strategies: causes of fearing and not seeking
Feeling at ease discussing mental health topics with one’s husband, family, community, and physician and experiencing cultural stigma or judgment regarding PPD within the community was significantly associated with the presence of PPD. In the current study, there were different reasons for not receiving the treatment, including cultural or traditional beliefs, language or communication barriers, social norms, and geographical or regional disparities in mental health resources. Haque and Malebranche [ 56 ] portrayed culture and the various conceptualizations of the maternal role as barriers to women seeking help and treatment.
In the present study, marital status, nationality, current pregnancy status, healthy baby, postnatal problems, receiving support or treatment for PPD, having awareness of symptoms and risk factors of PPD, suffering from any disease or mental or psychiatric disorder, comfort discussing mental health with family, and experiencing cultural stigma or judgment about PPD in the community were the significant predictors of PPD. In agreement with Ahmed et al. [ 34 ], the final logistic regression model contained seven predictors for PPD symptoms: SES, history of depression, history of PPD, history of stressful conditions, familial support, unwanted pregnancy, and male preference.
PPD has been recognized as a public health problem and may cause negative consequences for infants. It is estimated that 20 to 40% of women living in low-income countries experience depression during pregnancy or the postpartum period. The prevalence of PPD shows a wide variation, affecting 8–50% of postnatal mothers across countries [ 19 ].
Strengths and limitations
Strengths of our study include its multinational scope, which involved participants from six different countries, enhancing the generalizability of the findings. The study also boasted a large sample size of 674 participants, increasing the statistical power and reliability of the results. Standardized measures, such as the Edinburgh Postnatal Depression Scale (EPDS), were used for assessing postpartum depression, ensuring consistency and comparability across diverse settings. Additionally, the study explored a comprehensive range of predictors and associated factors of postpartum depression, including demographic, obstetric, health-related, and psychosocial characteristics. Rigorous analysis techniques, including multiple logistic regression analyses, were employed to identify significant predictors of postpartum depression, controlling for potential confounders and providing robust statistical evidence.
However, the study has several limitations that should be considered. Firstly, its cross-sectional design limits causal inference, as it does not allow for the determination of temporal relationships between variables. Secondly, the reliance on self-reported data, including information on postpartum depression symptoms and associated factors, may be subject to recall bias and social desirability bias. Thirdly, the use of convenience sampling methods may introduce selection bias and limit the generalizability of the findings to a broader population. Lastly, cultural differences in the perception and reporting of postpartum depression symptoms among participants from different countries could influence the results.
Moreover, the variation in sample size and response rates among countries can be attributed to two main variables. (1) The methodology showed that the sample size was determined by considering several parameters, such as allocating proportionately to the mothers who gave birth and fulfilling the selection criteria during the data collection period served by each health center. (2) The political turmoil in Syria affects how often and how well people can use the Internet, especially because the data was gathered using an online survey link, leading to a relatively low number of responses from those areas. (3) Language barrier in Ghana: as we used the Arabic and English-validated versions of the EPDS, Ghana is a multilingual country with approximately eighty languages spoken. Although English is considered an official language, the primarily spoken languages in the southern region are Akan, specifically the Akuapem Twi, Asante Twi, and Fante dialects. In the northern region, primarily spoken are the Mole-Dagbani ethnic languages, Dagaare and Dagbanli. Moreover, there are around seventy ethnic groups, each with its own unique language [ 57 ]. (4) At the end of the data collection period, to avoid seasonal affective disorders, the meteorological autumn season began on the 1st day of September, which may be associated with autumm depressive symptoms that may confound or affect our results. Furthermore, the sampling methods were not universal across all Arabic countries, potentially constraining the generalizability of our findings.
Recommendations
The antenatal programme should incorporate health education programmes about the symptoms of PPD. Health education programs about the symptoms of PPD should be included in the antenatal program.
Mass media awareness campaigns have a vital role in raising public awareness about PPD-related issues. Mass media.
The ANC first visit history should elicit a family history of mental illness, enabling early detection of risky mothers. Family history of mental illness can be easily elicited in the ANC first visit history.
For effective management of PPD, effective support (from husband, friends, and family) is an essential component. For effective management of PPD effectiveness of support.
The maternal (antenatal, natal, and postnatal) services should be provided for free and of high quality The maternal (antenatal, natal, postnatal) services should be provided free and of high quality.
It should be stressed that although numerous studies have been carried out on PPD, further investigation needs to be conducted on the global prevalence and incidence of depressive symptoms in pregnant women and related risk factors, especially in other populations.
Around 14% of the studied mothers had PPD, and the frequency varies across different countries and half of them do not know. Our study identified significant associations and predictors of postpartum depression (PPD) among mothers. Marital status was significantly associated with PPD, with married mothers having lower odds of experiencing PPD compared to single mothers. Nationality also emerged as a significant predictor, with Yemeni, Syrian, and Iraqi mothers showing lower odds of PPD compared to Egyptian mothers. Significant obstetric, current pregnancy, and infant-related predictors included the pregnancy status, the health status of the baby, and the presence of postnatal problems. Among psychological and social predictors, receiving support or treatment for PPD, awareness of symptoms and risk factors, experiencing cultural stigma or judgment about PPD, and suffering from any disease or mental disorder were significantly associated with PPD. Additionally, mothers who were maybe more comfortable discussing mental health with family relatives had lower odds of experiencing PPD.
These findings underscore the importance of considering various demographic, obstetric, psychosocial, and coping factors in the identification and management of PPD among mothers. Targeted interventions addressing these predictors could potentially mitigate the risk of PPD and improve maternal mental health outcomes.
Data availability
Yes, I have research data to declare.The data is available when requested from the corresponding author [email protected].
Abbreviations
Adjusted Odds Ratio
- Postpartum depression
Primary Health Care centers
Socioeconomic Status
program (Statistical Package for Social Science
The Edinburgh Postnatal Depression Scale
The Neonatal Intensive Care Unit
Sultan P, Ando K, Elkhateb R, George RB, Lim G, Carvalho B et al. (2022). Assessment of Patient-Reported Outcome Measures for Maternal Postpartum Depression Using the Consensus-Based Standards for the Selection of Health Measurement Instruments Guideline: A Systematic Review. JAMA Network Open; 1;5(6).
Crotty F, Sheehan J. Prevalence and detection of postnatal depression in an Irish community sample. Ir J Psychol Med. 2004;21:117–21.
Article PubMed Google Scholar
Goodman SH, Brand SR. Parental psychopathology and its relation to child psychopathology. In: Hersen M, Gross AM, editors. Handbook of clinical psychology vol 2: children and adolescents. Hoboken, NJ: Wiley; 2008. pp. 937–65.
Google Scholar
Wang Z, Liu J, Shuai H, Cai Z, Fu X, Liu Y, Xiao et al. (2021). Mapping global prevalence of depression among postpartum women. Transl Psychiatry. 2021;11(1):543. https://doi.org/10.1038/s41398-021-01663-6 . Erratum in: Transl Psychiatry; 20;11(1):640. PMID: 34671011IF: 6.8 Q1 B1; PMCID: PMC8528847IF: 6.8 Q1 B1.Lase accessed Jan 2024.
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders. 5th edition. Arlington, VA: American Psychiatric Association; Lase accessed October 2023.
Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26:289–95.
Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, Brody S, Miller WC. Perinatal depression: prevalence, screening accuracy, and screening outcomes: Summary. AHRQ evidence report summaries; 2005. pp. 71–9.
O’hara MW, Swain AM. (1996). Rates and risk of postpartum depression: a meta-analysis. Int Rev Psychiatry. 1996; 8:37–54.
Goodman SH, Brand SR. (2008). Parental psychopathology and its relation to child psychopathology. In: Hersen M, Gross AM, editors. Handbook of clinical psychology Vol 2: Children and adolescents. Hoboken, NJ: John Wiley & Sons; 2008. pp. 937–65.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150:782–6.
Article CAS PubMed Google Scholar
Martín-Gómez C, Moreno-Peral P, Bellón J, SC Cerón S, Campos-Paino H, Gómez-Gómez I, Rigabert A, Benítez I, Motrico E. Effectiveness of psychological, psychoeducational and psychosocial interventions to prevent postpartum depression in adolescent and adult mothers: study protocol for a systematic review and meta-analysis of randomised controlled trials. BMJ open. 2020;10(5):e034424. [accessed Mar 16 2024].
Article PubMed PubMed Central Google Scholar
Sehairi Z. (2020). Validation Of The Arabic Version Of The Edinburgh Postnatal Depression Scale And Prevalence Of Postnatal Depression On An Algerian Sample. https://api.semanticscholar.org/CorpusID:216391386 . Accessed August 2023.
Hairol MI, Ahmad SA, Sharanjeet-Kaur S et al. (2021). Incidence and predictors of postpartum depression among postpartum mothers in Kuala Lumpur, Malaysia: a cross-sectional study. PLoS ONE, 16(11), e0259782.
Yusuff AS, Tang L, Binns CW, Lee AH. Prevalence and risk factors for postnatal depression in Sabah, Malaysia: a cohort study. Women Birth. 2015;1(1):25–9. pmid:25466643
Article Google Scholar
Nakku JE, Nakasi G, Mirembe F. Postpartum major depression at six weeks in primary health care: prevalence and associated factors. Afr Health Sci. 2006;6(4):207–14. https://doi.org/10.5555/afhs.2006.6.4.207 . PMID: 17604509IF: 1.0 Q4 B4; PMCID: PMC1832062
Clavenna A, Seletti E, Cartabia M, Didoni A, Fortinguerra F, Sciascia T, et al. Postnatal depression screening in a paediatric primary care setting in Italy. BMC Psychiatry. 2017;17(1):42. pmid:28122520
Serhan N, Ege E, Ayrancı U, Kosgeroglu N. (2013). Prevalence of postpartum depression in mothers and fathers and its correlates. Journal of clinical nursing; 1;22(1–2):279–84. pmid:23216556
Deribachew H, Berhe D, Zaid T, et al. Assessment of prevalence and associated factors of postpartum depression among postpartum mothers in eastern zone of Tigray. Eur J Pharm Med Res. 2016;3(10):54–60.
Gebregziabher NK, Netsereab TB, Fessaha YG, et al. Prevalence and associated factors of postpartum depression among postpartum mothers in central region, Eritrea: a health facility based survey. BMC Public Health. 2020;20:1–10.
Grace J, Lee K, Ballard C, et al. The relationship between post-natal depression, somatization and behaviour in Malaysian women. Transcult Psychiatry. 2001;38(1):27–34.
Mahmud WMRW, Shariff S, Yaacob MJ. Postpartum depression: a survey of the incidence and associated risk factors among malay women in Beris Kubor Besar, Bachok, Kelantan. The Malaysian journal of medical sciences. Volume 9. MJMS; 2002. p. 41. 1.
Anna S. Postpartum depression and birthexperience in Russia. Psychol Russia: State Theart. 2021;14(1):28–38.
Yadav T, Shams R, Khan AF, Azam H, Anwar M et al. (2020).,. Postpartum Depression: Prevalence and Associated Risk Factors Among Women in Sindh, Pakistan. Cureus.22;12(12):e12216. https://doi.org/10.7759/cureus.12216 . PMID: 33489623IF: 1.2 NA NA; PMCID: PMC7815271IF: 1.2 NA NA.
Abdullah M, Ijaz S, Asad S. (2024). Postpartum depression-an exploratory mixed method study for developing an indigenous tool. BMC Pregnancy Childbirth 24, 49 (2024). https://doi.org/10.1186/s12884-023-06192-2 .
Upadhyay RP, Chowdhury R, Salehi A, Sarkar K, Singh SK, Sinha B et al. (2022). Postpartum depression in India: a systematic review and meta-analysis. Bull World Health Organ [Internet]. 2017 October 10 [cited 2022 October 6];95(10):706. https://doi.org/10.2471/BLT.17.192237/ .
Khalifa DS, Glavin K, Bjertness E et al. (2016). Determinants of postnatal depression in Sudanese women at 3 months postpartum: a cross-sectional study. BMJ open, 6(3), e00944327).
Khadija Sharifzade BK, Padhi S, Manna etal. (2022). Prevalence and associated factors of postpartum depression among Afghan women: a phase-wise cross-sectional study in Rezaie maternal hospital in Herat province.; Razi International Medical Journa2| 2|59| https://doi.org/10.56101/rimj.v2i2.59 .
Azidah A, Shaiful B, Rusli N, et al. Postnatal depression and socio-cultural practices among postnatal mothers in Kota Bahru, Kelantan, Malaysia. Med J Malay. 2006;61(1):76–83.
CAS Google Scholar
Agarwala A, Rao PA, Narayanan P. Prevalence and predictors of postpartum depression among mothers in the rural areas of Udupi Taluk, Karnataka, India: a cross-sectional study. Clin Epidemiol Global Health. 2019;7(3):342–5.
Arikan I, Korkut Y, Demir BK et al. (2017). The prevalence of postpartum depression and associated factors: a hospital-based descriptive study.
Azimi-Lolaty HMD, Hosaini SH, Khalilian A, et al. Prevalence and predictors of postpartum depression among pregnant women referred to mother-child health care clinics (MCH). Res J Biol Sci. 2007;2:285–90.
Najafi KFA, Nazifi F, Sabrkonandeh S. Prevalence of postpartum depression in Alzahra Hospital in Rasht in 2004. Guilan Univ Med Sci J. 2006;15:97–105. (In Persian.).
Deng AW, Xiong RB, Jiang TT, Luo YP, Chen WZ. (2014). Prevalence and risk factors of postpartum depression in a population-based sample of women in Tangxia Community, Guangzhou. Asian Pacific journal of tropical medicine; 1;7(3):244–9. pmid:24507649
Ahmed GK, Elbeh K, Shams RM, et al. Prevalence and predictors of postpartum depression in Upper Egypt: a multicenter primary health care study. J Affect Disord. 2021;290:211–8.
Cantilino A, Zambaldi CF, Albuquerque T, et al. Postpartum depression in Recife–Brazil: prevalence and association with bio-socio-demographic factors. J Bras Psiquiatr. 2010;59:1–9.
Abdollahi F, Zarghami M, Azhar MZ, et al. Predictors and incidence of post-partum depression: a longitudinal cohort study. J Obstet Gynecol Res. 2014;40(12):2191–200.
McCoy SJB, Beal JM, et al. Risk factors for postpartum depression: a retrospective investigation at 4-weeks postnatal and a review of the literature. JAOA. 2006;106:193–8.
PubMed Google Scholar
Sierra J. (2008). Risk Factors Related to Postpartum Depression in Low-Income Latina Mothers. Ann Arbor: ProQuest Information and Learning Company, 2008.
Çankaya S. The effect of psychosocial risk factors on postpartum depression in antenatal period: a prospective study. Arch Psychiatr Nurs. 2020;34(3):176–83.
Shao HH, Lee SC, Huang JP, et al. Prevalence of postpartum depression and associated predictors among Taiwanese women in a mother-child friendly hospital. Asia Pac J Public Health. 2021;33(4):411–7.
Adeyemo EO, Oluwole EO, Kanma-Okafor OJ, et al. Prevalence and predictors of postpartum depression among postnatal women in Lagos. Nigeria Afr Health Sci. 2020;20(4):1943–54.
Al Nasr RS, Altharwi K, Derbah MS et al. (2020). Prevalence and predictors of postpartum depression in Riyadh, Saudi Arabia: a cross sectional study. PLoS ONE, 15(2), e0228666.
Desai ND, Mehta RY, Ganjiwale J. Study of prevalence and risk factors of postpartum depression. Natl J Med Res. 2012;2(02):194–8.
Azale T, Fekadu A, Medhin G, et al. Coping strategies of women with postpartum depression symptoms in rural Ethiopia: a cross-sectional community study. BMC Psychiatry. 2018;18(1):1–13.
Asaye MM, Muche HA, Zelalem ED. (2020). Prevalence and predictors of postpartum depression: Northwest Ethiopia. Psychiatry journal, 2020.
Ayele TA, Azale T, Alemu K et al. (2016). Prevalence and associated factors of antenatal depression among women attending antenatal care service at Gondar University Hospital, Northwest Ethiopia. PLoS ONE, 11(5), e0155125.
Saraswat N, Wal P, Pal RS et al. (2021). A detailed Biological Approach on Hormonal Imbalance Causing Depression in critical periods (Postpartum, Postmenopausal and Perimenopausal Depression) in adult women. Open Biology J, 9.
Guida J, Sundaram S, Leiferman J. Antenatal physical activity: investigating the effects on postpartum depression. Health. 2012;4:1276–86.
Robertson E, Grace S, Wallington T, et al. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26:289–95.
Watanabe M, Wada K, Sakata Y, et al. Maternity blues as predictor of postpartum depression: a prospective cohort study among Japanese women. J Psychosom Obstet Gynecol. 2008;29:211–7.
Kirpinar I˙, Gözüm S, Pasinliog˘ lu T. Prospective study of post-partum depression in eastern Turkey prevalence, socio- demographic and obstetric correlates, prenatal anxiety and early awareness. J Clin Nurs. 2009;19:422–31.
Zhao XH, Zhang ZH. Risk factors for postpartum depression: an evidence-based systematic review of systematic reviews and meta-analyses. Asian J Psychiatry. 2020;53:102353.
Bina R. Predictors of postpartum depression service use: a theory-informed, integrative systematic review. Women Birth. 2020;33(1):e24–32.
Jannati N, Farokhzadian J, Ahmadian L. The experience of healthcare professionals providing mental health services to mothers with postpartum depression: a qualitative study. Sultan Qaboos Univ Med J. 2021;21(4):554.
Dennis CL, Chung-Lee L. Postpartum depression help‐seeking barriers and maternal treatment preferences: a qualitative systematic review. Birth. 2006;33(4):323–31.
Haque S, Malebranche M. (2020). Impact of culture on refugee women’s conceptualization and experience of postpartum depression in high-income countries of resettlement: a scoping review. PLoS ONE, 15(9), e0238109.
https:// www.statista.com/statistics/1285335/population-in-ghana-by-languages-spoken/ .
Download references
Acknowledgements
We would like to express our deep thanks to Rovan Hossam Abdulnabi Ali for her role in completing this study and her unlimited support. Special thanks to Dr. Mohamed Liaquat Raza for his role in reviewing the questionnaire. Moreover, we would like to thank all the mothers who participated in this study.
No funding for this project.
Author information
Authors and affiliations.
Department of Public Health and Community Medicine, Faculty of Medicine, Zagazig University, Zagazig, Egypt
Samar A. Amer
Department of Family Medicine, Faculty of Medicine, Zagazig University, Zagazig, Egypt
Nahla A. Zaitoun
Department of Psychiatry, Faculty of Medicine, Zagazig University, Zagazig, Egypt
Heba A. Abdelsalam
Faculty of Medicine, Al-Azhar University, Damietta, Egypt
Abdallah Abbas
Department of Obstetrics and Gynecology, Faculty of Medicine, Zagazig University, Zagazig, Egypt
Mohamed Sh Ramadan
Hammurabi Medical College, University of Babylon, Al-Diwaniyah, Iraq
Hassan M. Ayal
Hardamout University College of Medicine, Almukalla, Yemen
Samaher Edhah Ahmed Ba-Gais
Department of General Medicine, Shadan Institute of Medical Science, Hyderabad, India
Nawal Mahboob Basha
College of Medicine, Sulaiman Alrajhi University, Albukayriah, Al-Qassim, Saudi Arabia
Abdulrahman Allahham
Department of Virology, Noguchi Memorial Institute for Medical Research, University of Ghana Legon, Accra, Ghana
Emmanuael Boateng Agyenim
Department of Public Health and Community Medicine, Faculty of Medicine, Beni-Suef University, Beni-Suef, Egypt
Walid Amin Al-Shroby
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: Samar A. Amer (SA); Methodology: SA, Nahal A. Zaitoun (NZ); Validation: Mohamed Ramadan Ali Shaaban (MR), Hassan Majid Abdulameer Aya (HM), Samaher Edhah Ahmed Ba-Gais (SG), Nawal Mahboob Basha (NB), Abdulrahman Allahham (AbAl), Emmanuael Boateng Agyenim (EB); Formal analysis: Abdallah Abbas (AA); Data curation: MR, HM, SG, NB, AbAl, NZ, and EB; Writing original draft preparation: SA, Heba Ahmed Abdelsalam (HAA), and NZ; Writing review and editing: MR, AA, Walid Amin Elshrowby (WE); Visualization: SA, AA; Supervision: SA; Project administration: AA. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Samar A. Amer .
Ethics declarations
Ethical approval and consent to participate.
All participants were provided with electronic informed consent after receiving clear explanations regarding the study’s objectives, data confidentiality, voluntary participation, and the right to withdraw. The questionnaire did not contain any sensitive questions, and data collection was performed anonymously. We affirm that all relevant ethical guidelines have been adhered to, and any necessary approvals from the ethics committee have been obtained. Approval was received from the ethical committee of the family medicine department, the faculty of medicine at Zagazig University, and from the patients included in the study. IRP#ZU-IRP#11079-8/10-2023.
Practicing ethical decision-making is crucial for providing clinical treatment. Such decisions are frequently made challenging due to a lack of knowledge and the mother’s ability to handle the associated complexities and uncertainties that affect the patient’s current level of functioning and ability to take care of her child. At the end of the survey, we raised concerns regarding the red flags, such as suicidal thoughts, and called for a revisit for the psychiatrist’s evaluation of the discussion of the risks, benefits, and alternatives to using medication.
Consent for publication
All authors have read and agreed to the published version of the manuscript.
Previous publication
We declare that this research paper has not been published elsewhere in any other academic journal or platform.
Generative AI in scientific writing
We declare that we have not used AI in writing any part of this manuscript.

Conflict of interest
No conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Amer, S.A., Zaitoun, N.A., Abdelsalam, H.A. et al. Exploring predictors and prevalence of postpartum depression among mothers: Multinational study. BMC Public Health 24 , 1308 (2024). https://doi.org/10.1186/s12889-024-18502-0
Download citation
Received : 06 February 2024
Accepted : 02 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12889-024-18502-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- The Edinburgh postnatal depression scale (EPDS)
- Determinants
- Psychosocial
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
ORIGINAL RESEARCH article
A comprehensive analysis of post-partum depression risk factors: the role of socio-demographic, individual, relational, and delivery characteristics.

- 1 Department of Surgical, Medical and Molecular Pathology and Critical Care Medicine, University of Pisa, Pisa, Italy
- 2 Department of Educations, Languages, Intercultures, Literatures and Psychology, University of Florence, Florence, Italy
- 3 Division of Obstetrics and Gynaecology, Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy
Postpartum depression is a common and complex phenomenon that can cause relevant negative outcomes for children, women and families. Existing literature highlights a wide range of risk factors. The main focus of this paper is to jointly investigate different types of risk factors (socio-demographic, psychopathological, relational, and related to labor and birth experience) in post-partum depression onset in women during first-child pregnancy, identifying which of these are the most important predictors. A cohort longitudinal study was conducted on 161 Italian nulliparous low-risk women ( M age = 31.63; SD = 4.88) without elective cesarean. Data was collected at three different times: Socio-demographic, prenatal anxiety and depression, and quality of close relationship network (with mother, father and partner, and the prenatal attachment to child) were assessed at T1 (week 31–32 of gestation); clinical data on labor and childbirth (mode and typology of delivery, duration of labor, duration of eventual administration of epidural analgesia, and child's APGAR index at birth) were registered at T2 (the day of childbirth); and the degree of post-natal depression symptomatology was measured at T3 (1 month after birth). Postpartum depression is associated with several risk factors (woman's age, woman's prenatal psychopathological characteristics, the level of prenatal attachment to child, the quality of romantic relationship, and some clinical delivery difficulties). Overall, the level of prenatal attachment to child was the most important predictor of post-partum depression. These findings emphasize the very important role of prenatal attachment for the onset of postpartum depression and the need to promote adequate and targeted prevention interventions. Limitations, strengths, and theoretical and clinical implications are discussed.
Introduction
For a woman, the gestation of her first child has been identified as a central life event ( 1 ). From a psychological perspective, in fact, the pregnancy of the first baby involves the transition to motherhood, a major developmental period with important implications for mothers, for the infant-mother relationship, and the infant's development ( 2 ). During the first pregnancy, a woman's maternal identity develops through the reorganization of mental self-representation and the elaboration of other significant relationships ( 3 , 4 ). The woman's mental self-representation enriches with the maternal component, thus leading her to review the relationship with her own mother; the mental couple image gradually modifies with integration of the family image, and the marital relationship is reorganized with the parental component. With the birth of the first child, the quality of the couple relationship may undergo temporary changes that are influenced by the ability of the parents to adapt to new needs ( 5 ).
The transition to parenthood (transition to parenthood—TTP) has often been associated with marital crisis, and the premise in literature was that parenthood creates serious individual and relationship distress ( 6 , 7 ). Parenting can be an improvement factor for some couple relationships; however, it can also be disruptive and increase problems ( 8 ). While some couples may develop new skills in resolving difficulties, others find themselves running aground trying to develop these skills ( 6 ).
All the above physical, psychological, and relational changes that occur during the perinatal period may increase the risk for maternal emotional vulnerability, such as depressed emotions. The DSM-5 proposes the term “peripartum onset” as a major depressive episode during pregnancy or in the weeks or months following delivery ( 9 ). This condition is characterized by sad mood, anxiety, irritability, lack of positive emotions, loss of pleasure, interests and energy, decreased appetite, inability to cope, fear of hurting self and baby, and suicidal thoughts ( 10 , 11 ). Both anxiety and depression can occur in the perinatal period (up to 1 year after delivery) ( 9 ) and these conditions present high rates of co-morbidity ( 12 ). The first weeks immediately after childbirth are the most critical ( 13 ), and although the increased vulnerability continues for the following 6 months ( 14 – 16 ), post-partum depression (PPD) generally occurs within the first month after delivery ( 9 ).
This vulnerability is higher for primiparous mothers, who present an increased risk for depression in the postpartum period ( 12 , 17 , 18 ), especially in the first 90 days after delivery ( 19 ). Although contrasting results emerged about the prevalence of postpartum depression in relation to parity ( 20 , 21 ), studies conducted in the European context showed that the prevalence for PPD in primiparas was 11.8 vs. 8.6% in multiparas ( 21 ).
In fact, maternal inexperience leads new mothers to have greater difficulty in early interactions with their children, and research has reported that the effect of maternal depression is greater in nulliparas compared to multiparas ( 22 ).
Although from a psychiatric perspective postpartum depression is no longer classified as a distinct entity, from a psychological perspective, depression occurring during the postpartum period has particular relevance in a woman's life.
In fact, it enhances the risk of a multitude of negative consequences for children, women, and families, including poor infant physical health and more frequent sickness, and physiological, psychological, emotional, and psychomotor delays during infancy and early childhood ( 23 ).
Moreover, PPD can negatively affect the ability and the availability of women to adequately take care of their children. Henderson et al. ( 24 ) have shown the important negative outcomes that PPD can have on mother-infant interactions, the child's growth, and the tendency to quit breastfeeding earlier. Moreover, children of mothers with PPD tend to establish insecure attachment bonds and develop social difficulties with peers ( 25 , 26 ).
Because of these relevant consequences, it is important to identify the risk factors that can be involved in the development of PPD in first-time mothers.
Several factors, both internal and external, have been found to be related to PPD, and it is plausible that a complex interplay of these can be the cause of greater vulnerability ( 27 ), especially in women during their first pregnancy, compared to those who already have a child. Alongside psychological risk factors, such as a lifetime history of depression, and a presence of antenatal depression and prenatal anxiety ( 28 , 29 ), many authors have shown that relational variables constitute significant risk factors for post-partum depression development. Problems in maternal and romantic relationships, such as marital instability, and low level of maternal ( 30 , 31 ) and marital support ( 32 ) have been found to be linked with PPD. Priel and Besser ( 33 ) have also found that antenatal attachment was closely linked to PPD. A higher level of antenatal attachment to child predicted a lower level of depressive symptomatology after birth. The presence of stressful life events, or the lack of social support from peer and health professionals, can foster the subsequent development of PPD ( 34 – 36 ).
There are other clinical aspects linked to pregnancy and delivery that are associated to the PPD condition. A complicated labor and birth characterized by longer length of labor and greater pain, or medical intervention during delivery, can result in negative consequences, varying from maternal distress to PPD ( 31 , 37 ). Given that the nulliparous tend to be less self-confident in the maternal role, and that being less self-confident has been associated with postpartum depression ( 38 ), labor and delivery complications can be particularly difficult for first-time mothers.
Finally, some socio-demographic characteristics, such as a young age, or low level of education, or low income, may be considered linked to a higher probability of developing PPD ( 39 , 40 ).
Despite the relevance of these risk factors, most studies have focused on psychopathology and social network aspects linked to maternal and romance relationships, and less attention has been directed to the exploration of these factors jointly.
The aims of this study were: (1) to confirm previous results exploring the role that several sets of variables, such as socio-demographic, individual, relational, and related to delivery characteristics, separately considered, play as risk factors for the onset of postpartum depression; and (2) to verify which, among the above risk factors, have a more significant influence when they are considered together.
In accordance with literature, it was hypothesized that: (1) young age, low level of education, low employment status, and not planned pregnancy, could positively predict levels of PPD; (2) prenatal anxiety and depression positively predict PPD; (3) an affectionate prenatal attachment, and a good quality romantic and parental relationship negatively predict PPD; (4) a more complicated labor (in terms of duration and duration of epidural and oxytocin administration), the modality of delivery (cesarean section vs. vaginal birth) and a worse index of newborn well-being (in terms of lower Apgar score) positively predict PPD. No hypotheses were developed about the strongest predictor for PPD.
Materials and Methods
Procedure and participants.
The study was conducted in accordance with the guidelines for the ethical treatment of human participants of the Italian Psychological Association. The Ethical Committee of Azienda USL 4 Prato, Italy, had previously approved the study (no 780/2013). Data were collected during 2014 in the maternity ward of a public hospital of the metropolitan area of Prato (Italy), a unit with about 1,130 deliveries per year (69% Italian women), from January to December 2014, during delivery preparation courses organized for pregnant women (>30 weeks of gestation).
A cohort longitudinal study was carried out. Data were collected at three different time points: (1) 31–32 week of gestation; (2) the day of delivery; and (3) 1 month after childbirth.
Inclusion criteria were: Italian women, age >18 years, physically and psychologically healthy nulliparous women with singleton low-risk pregnancies, gestational age >31 weeks. Exclusion criteria were: twin pregnancy, maternal pathologies during pregnancy, fetal pathologies, the presence of depressive pathologies documented in clinical records, and planned elective cesarean. Planned elective cesarean was an exclusion criterium because we were interested in examining the roles of labor and delivery as predictors of PPD. Therefore, we excluded from the study women who underwent planned elective cesarean, but not those who experienced emergency cesarean after labor.
The participants ( n = 191) were informed about the aims of the study and signed a written informed consent form. They could withdraw from participation at any time. Ninety-four percent of the women who were contacted consented to participate in the survey ( n = 179) and, of them, 90% completed the entire follow-up (Time 1, 2, and 3). At T1 we recruited 179 women, but by T3 we lost 18 women who did not return the completed questionnaire. The final sample consisted of 161 nulliparous pregnant women aged 18–42 years ( M = 31.63, SD = 4.88). Our sample is representative regarding both size and age of the general population of women giving birth in Prato that meet our inclusion criteria.
At time 1, all participants received a battery of questionnaires for the collection of socio-demographic, clinical, psychological and relational data. In particular:
Socio-Demographic and Clinical Measures
Participants provided their age, educational level, work status, marital status, information about the number of years of their couple relationship, and information about planned or not pregnancy.
Psychological Measures
Participants were asked to complete psychological questionnaires to assess psychopathological characteristics. To assess the women's anxiety level, the State Anxiety Inventory (STAI_Y2) ( 41 , 42 ) was used. This questionnaire is the most widely used measure of anxiety during pregnancy, especially in association with postnatal depression ( 43 ). The STAI_Y2 is a 20-item self-report questionnaire asking to report how often the anxiety state was experienced. Responses were rated on a 4-point Likert scale, from 1 (never) to 4 (very often) The total score is obtained by summing all items, after some items are overturned, and can range from 20 to 80. A high score indicates a high level of anxiety. For the current study, Cronbach's alpha was 0.90.
To detect the level of women's depression, the Beck Depression Inventory (BDI) ( 44 , 45 ) was used. The BDI is a 21-item self-report inventory used for measuring the severity of symptoms. Each item had a set of four responses ranging in intensity from 0 to 3. The total score is obtained by summing all items and can range from 0 to 63. High scores indicate high depressive symptomatology. In the present sample, Cronbach's value was 0.84.
Relational Measures
All women were asked to complete four questionnaires assessing the quality of their close relationship network, with their mother, father and partner, and the level of their prenatal attachment to child. In particular, the quality of women's relationships with mothers and fathers was assessed using the Parental Bonding Instrument (PBI) ( 46 , 47 ). The PBI consists of two parallel versions of 21 items, ranging from 0 (Very likely) to 3 (Very unlikely), which assessed three dimensions: Care, Encouragement toward autonomy, and Overprotection. In the present sample, Cronbach's values for the paternal version were 0.98, 0.98, and 0.96 for Care, Encouragement toward autonomy, and Overprotection, respectively. For the maternal version, Cronbach's values for Care, Encouragement toward autonomy, and Overprotection were 0.98, 0.96, and 0.87, respectively. In this study, we used a global dimension of the relationship quality, summing the above three dimensions, according to the procedure described in the results section. The total score for PBI is obtained by summing all items and can range from 0 to 63. High scores on this dimension indicate that the women perceive a good quality of their maternal and paternal relationships.
The quality of the women's romantic relationships was assessed using the Romance Qualities Scale (RQS) ( 48 ). The RQS is a 22-item self-report instrument, ranging from 1 (Absolutely false) to 5 (Absolutely true), which assesses five main qualitative dimensions of the relationship with partner (companionship, conflict, help, security and closeness) and a global score of the romantic relationship quality. The total score is obtained by summing all items and can range from 22 to 110. High scores on this dimension indicate that women perceive a good quality of their romantic relationships. In the present sample, Cronbach's value was 0.84.
The Prenatal Attachment Inventory (PAI) ( 49 , 50 ) was used to measure the mother's attachment bond to her child during pregnancy. The PAI is a self-report questionnaire with 21 items from 1 (Almost never) to 4 (Almost always). The total score is obtained by summing all items and can range from 21 to 84. High scores indicate a good quality of prenatal attachment bond. For the present sample, the Cronbach's alpha was 0.93.
At time 2, clinical information regarding labor, delivery and birth outcomes was extracted from hospital records after childbirth. In particular:
Labor measures including three indices: (a) modality of labor (induced vs. spontaneous); (b) duration of labor in hours; (c) administration of epidural analgesia in hours (no analgesia administration = 0).
Mode of delivery, recorded according to category: vaginal (natural and operative vaginal delivery) vs. emergency cesarean delivery.
Birth outcomes, assessed via APGAR scores at 1 min. APGAR score index at birth was determined by evaluating the newborn baby on: color, heart rate, reflexes, muscle tone, respiration). Scores ≤3 are generally regarded as critically low, 4–6 fairly low, and 7–10 generally normal.
At time 3, women were requested to fill out a psychological questionnaire to assess the degree of postnatal depression symptomatology. Diagnosing depression in post-partum may be particularly challenging due to the overlap of diagnostic depressive symptoms with those of a normal post-partum period for women (e.g., fatigue, decreased libido, and sleep or appetite change). Nevertheless, as documented by several authors, the Edinburgh Postnatal Depression Scale (EPDS) ( 51 , 52 ), originally devised for the identification of postpartum depression disorders, allows us to measure affective aspects rather than physical symptoms of depression that may be affected by the perinatal period ( 52 ). The EPDS is a self-report questionnaire consisting of 10 items ranging from 0 to 3, according to increasing severity of the symptom. The total score is obtained by summing all items and can range from 0 to 30 with higher scores on this scale indicating higher levels of postnatal depression symptomatology. For the current sample, Cronbach's alpha was 0.88.
Data Analysis
Data were analyzed using SPSS version 24 (2017). Frequency, means, standard deviation, and bivariate correlation were calculated for all variables. To determine the relationship between predictor variables and postpartum depression, linear regression analyses were separately undertaken for each set of risk factor variables considered.
Regarding parental relationships, we were interested in creating an aggregate score of the quality of maternal and paternal relationship. To verify the possibility to use a single score for the quality of maternal and paternal relationships to include in the regression analysis, two factorial analyses with the three dimensions of the PBI were conducted, separately for the mother and father versions.
Subsequently, to explore the stronger risk factors, a linear regression (stepwise method) was conducted with post-partum depression as the dependent variable, and the significant risk factors were entered as predictors. An alpha level of 0.05 was used for all statistical tests.
All the women had a middle or high socioeconomic level; 87% had a high school diploma or bachelor's degree (13% of women had a secondary school diploma, 54% had a high school diploma, and 33% a bachelor's degree or more) and 81.4% of the women had a job. Regarding marital status, 100% of participants lived with their partners, and 59.1% were married. The length of romantic relationships ranged from 1 to 17 years ( M = 6.25, SD = 3.81). Pregnancy was planned in 82.6%.
The regression analysis with socio-demographic characteristics as independent variables and the score of PPD as a dependent variable showed that the model composed by age, length of the romantic relationship, level of education (dummy variable: 1 = high school or university degree; 0 = middle school or elementary school degree), employment status (dummy variable: 1 = employed; 0 = unemployed), and planned pregnancy (dummy variable = 1 = non-planned; 0 = planned) explained only 6% of the variance ( Table 1 ). Specifically, data showed that the severity of PPD was positively affected by the age of women. On the contrary, the length of the relationship with partner, level of education, employment status, and planned pregnancy did not significantly affect the level of PPD.
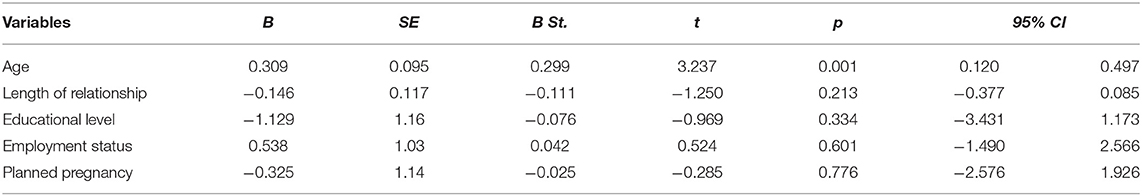
Table 1 . Summary of the linear regression analysis with socio-demographical characteristics as independent variables for PPD score.
Psychopathological Characteristics and PPD Condition
Table 2 shows the means, standard deviations, and pair-wise correlation coefficients for the two dimensions of psychopathological antenatal characteristics (anxiety and depression) and the PPD condition. A high level of PPD was associated with a high level of prenatal anxiety and depression. Moreover, prenatal anxiety and depression were significantly and positively correlated.
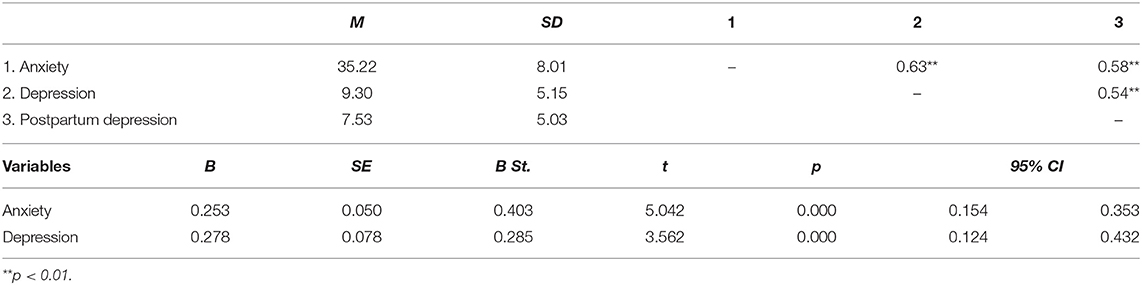
Table 2 . Descriptive statistics, correlations and summary of the linear regression analysis with psychopathological characteristics as independent variables for PPD score.
The linear regression performed with prenatal anxiety and depression on PPD score explained 38% of the variance (see Table 2 ). Both these variables positively affect the level of PPD.
Close Relationships Network and PPD Condition
To obtain a global score of the women's relationship quality with their mothers and fathers, two factor analyses were conducted with the three dimensions of the PBI, for mother and father, separately. Because correlation analyses between the three dimensions of the PBI in relation to the maternal and paternal versions showed that the Overprotection dimension is negatively correlated with Care (maternal: r = −0.77; paternal: r = −0.58) and Encouragement toward autonomy (maternal: r = −0.89; paternal: r = −0.93) dimensions, the Overprotection score was reversed before carrying out the factorial analyses to obtain saturations of the same mark on the hypothetical common factor (the single score of the PBI measure).
The results of the factor analyses showed that the dimensions of the PBI (Care, Encouragement toward autonomy and Low Overprotection) loaded into a single factor for both the maternal and paternal versions. Specifically, regarding the maternal version, the three dimensions accounted for 86.15% of total variance. Regarding the paternal version, the three dimensions accounted for 83.99% of total variance.
In conclusion, both for the mother and father versions, high scores on this dimension express warm, positive and supportive parental behaviors, reflecting a good quality of parental relationships.
In Table 3 , the descriptive statistics of the close relationship variables and their pair-wise correlation coefficients with PPD are shown. The level of PPD was negatively and significantly correlated with the women's relationship quality with their mothers, fathers and romantic partners, and their prenatal attachment to child. Moreover, the prenatal attachment was positively correlated with the quality of the three close relationships (mother, father and partner). Finally, the quality of maternal relationship was significantly and positively correlated with the quality of paternal relationship. Given the high correlation between maternal and paternal relationships ( r = 0.87), in order to avoid multicollinearity problems, a single score of these aspects was calculated. In other words, we composed a score of parental relationship by calculating the mean of the two scores.
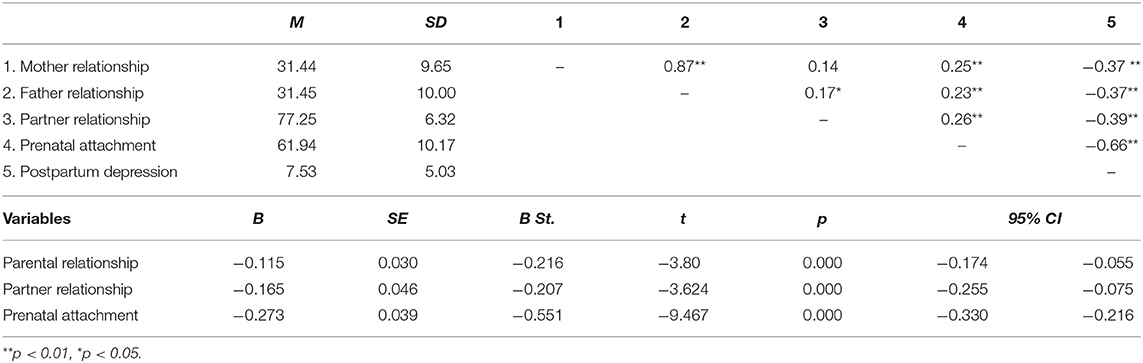
Table 3 . Descriptive statistics, correlations and summary of the linear regression analysis with the quality of parental, romantic and prenatal relationships as independent variables for PPD score.
The linear regression showed that the model composed by parental relationship, romantic relationship and prenatal attachment explained 52% of the variance (see Table 3 ). The quality of parental and romantic relationship and prenatal attachment to child seems to positively affect the level of PPD.
Labor, Delivery, and Birth Outcome Characteristics and PPD Condition
87.6% of the women had spontaneous labor, and in the remaining 12.4% labor was induced. 89.4% of women had vaginal deliveries, and 10.6% had emergency cesarean deliveries. Significant differences emerged with respect to PPD regarding the mode of labor [spontaneous vs. induced: t (159) = −5.311; p = 0.000] and mode [vaginal vs. cesarean: t (159) = 7.429; p = 0.000] of delivery. Specifically, women who had an induced labor showed a higher level of PPD than women who had a spontaneous one. In the same way, women who had a cesarean delivery reported a higher level of PPD than women with vaginal delivery.
Table 4 presents the descriptive statistics and correlation coefficients of all continuous delivery variables.
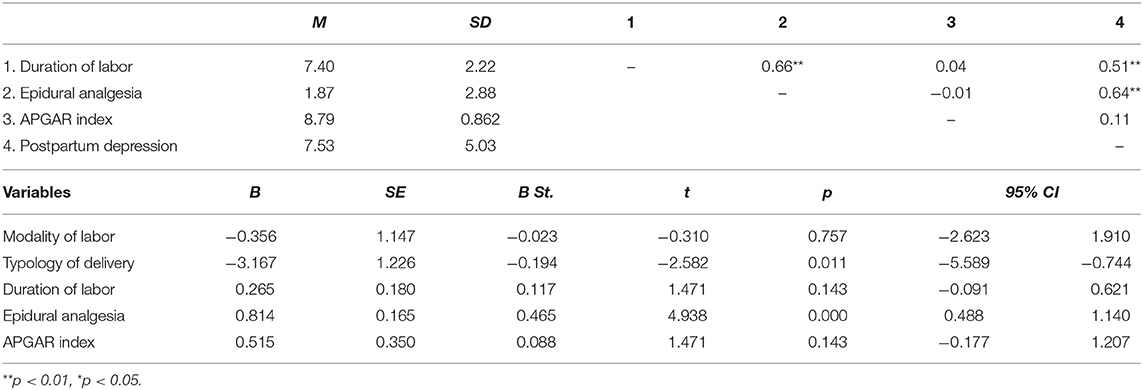
Table 4 . Descriptive statistics, correlations and summary of the linear regression analysis with the delivery characteristics as independent variables for PPD score.
The level of PPD is positively and significantly correlated with the length of labor and the duration of the administration of epidural analgesia. On the contrary, the correlation between PPD and the child's APGAR index is not significant. Finally, the duration of labor is positively and significantly correlated with the duration of the administration of epidural analgesia.
Results of the linear regression showed that the model composed by the variables regarding labor, delivery and birth characteristics explained 44% of the variance (see Table 4 ). Specifically, cesarean delivery (dummy variable: 0 = cesarean delivery; 1 = vaginal delivery), and the duration of the administration of epidural analgesia seem to positively affect the severity of PPD. On the contrary, the results showed the no-significant influences of the modality of labor (dummy variable: 1 = induced labor; 0 = spontaneous labor) and the duration of labor, or the child's APGAR index, in affecting the severity of PPD.
The Stronger Predictors of PPD Condition
Finally, a multiple regression was conducted to explore which of the significant risk factors found in the previously reported analyses make meaningful contributions to the overall prediction of the severity of PPD, which are: age, anxiety, depression, parental relationship, romantic relationship, prenatal attachment, typology of delivery, and epidural analgesia. All these predictors were entered at the first step, using a stepwise method.
Results showed that the model is composed of only four variables, which explain 61% of the PPD total score variance. Specifically, prenatal attachment to child entered into the equation in Step 1, which accounted for the greatest portion of the variance in PPD scores. The duration of the administration of epidural analgesia entered in Step 2, which contributed an additional 10% of variance. The anxiety score entered in Step 3, which contributed an additional 6%. Finally, the quality of romantic relationships entered in Step 4, which contributed an additional 3%. In Table 5 , all statistical results are reported.
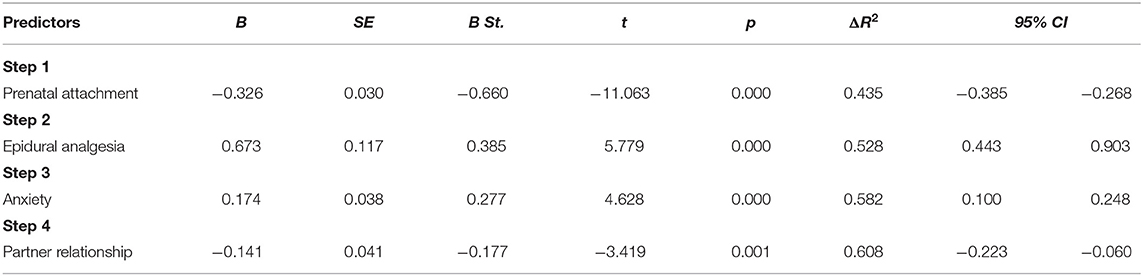
Table 5 . Summary of the linear regression analysis using stepwise method with all risk significant factors as independent variables for PPD score.
Pregnancy and the postpartum period is a delicate moment in a woman's life, characterized by biological, psychological and social change, during which women are at increased risk of emotional vulnerability and depressive symptomatology ( 1 ). This is especially true for nulliparous women, who, in addition to the normal psychic, psychological and relational changes typical of the pregnancy period, are dealing with more specific challenges, such as the transition to motherhood, or the reorganization of mental self-representation. At the first pregnancy, all these changes and reorganizations can represent challenges which are particularly relevant for women, and the presence of problems that prevent them from reaching a good transition to motherhood puts them at greater risk of developing a subsequent depressive symptomology. According to literature, primiparous mothers present an enhanced risk for depression in the postpartum period ( 17 , 18 ) and more severe effects of depression in early interactions with their infants ( 22 ), due to their inexperience compared to multiparous mothers.
In literature, several factors have been found related to PPD, and we believe that the complex interplay of these can be the cause of greater vulnerability in nulliparous women ( 27 – 29 ). For this reason, the main purpose of this study was to explore the role that several sets of variables, such as socio-demographic, individual, relational, and related to delivery characteristics, separately considered, play as risk factors for the onset of postpartum depression in nulliparas. However, to date, no studies have jointly analyzed all these different risk factors. Consequently, the main and second purpose was to verify which have a more significant influence when they are considered together, in order to identify the more important risk factors.
Overall, our results show that, in reference to socio-demographic characteristics, only the age of women was a significant predictor of PPD scores. Older women seem have a higher probability of developing a depressive symptomatology 1 month after childbirth. On the contrary, in line with Roomruangwong's results ( 29 ), we found no significant influences of the level of education, employment status, the length of the romantic relationship, or planned pregnancy.
In reference to psychopathological characteristics, our results showed a strong association between prenatal psychopathology and the possibility to develop PPD. According to previous studies ( 28 , 29 , 53 ), nulliparous with a high level of anxiety and depression during pregnancy tend to develop PPD symptomatology more than women with a low level of these characteristics before delivery. Not surprisingly, due to the high association between antenatal and post-partum depression, the last edition of the DSM ( 9 ) proposed the term “peripartum onset” to indicate the depressive episode occurring during the pregnancy and the first 4 weeks after delivery.
Regarding the relational variables, our results indicated that only the prenatal attachment to child and the quality of romantic relationship affect the level of PPD ( 30 , 32 ). In particular, prenatal attachment, defined as the emotional bond experienced by the parent toward the infant ( 54 ), seems to play a very important role in PPD, given that it involves the maternal disposition toward fetus and a protection attitude toward baby ( 55 , 56 ). New research has suggested that this type of attachment is an indicator of the caregiving system ( 56 , 57 ).
Interestingly, it is not the length of the relationship but its quality that better influences the security and well-being of nulliparous women. In has been widely recognized that the quality of the romantic relationship is a strong protective factor in the life-span ( 58 , 59 ), and this could play an important role, especially in certain periods of life, such as the puerperium ( 60 ). During the transition to parenthood, the couple relationship may be negatively affected during pregnancy, given that birth of the first child leads to partnership re-organization of responsibilities and reciprocal routines, thus decreasing relationship quality ( 61 ). Therefore, a high quality of couple relationship constitutes a protective factor, and a low quality of romantic relationship constitutes a significant risk factor for the development of psychological diseases, such as a higher probability to develop depressive symptoms ( 62 ) and other forms of psychopathology ( 63 ).
The quality of relationship with parents also affects the level of PPD. In reference to a woman's relationship with her parents, this result is convergent with previous studies that have found that the bond quality to mother significantly influences a woman's well-being during pregnancy and after delivery, considerably reducing the risk to develop a PPD condition ( 64 ). Tani et al. ( 65 , 66 ) have shown that the security of attachment to mother affects the quality of prenatal attachment and the consequent ability of the new mother to be sensitive to her newborn's needs, promoting spontaneous caregiving and attachment behavior. Maternal perceived support could also be considered a relevant protector factor: women who reported a high level of maternal social support showed a lower level of PPD symptomatology after labor ( 31 ). However, although in line with previous studies, this study expands on existing literature, showing the protective role of both maternal and paternal relationships on nulliparous women postnatal depression. It is reasonable to suppose that quality of relationship with parents is relevant during the first pregnancy, given that it can help women in the transition to motherhood and the assumption of the maternal role.
Finally, regarding labor factors, our data showed that a longer duration of the administration of epidural analgesia could be considered significant predictors of PPD in nulliparous. As suggested by previous studies, these factors can negatively influence the quality of the birth experience, fostering the possibility of developing a depressive mood, while an easier childbirth experience can act as a protective factor during the vulnerable period after delivery ( 31 , 67 – 69 ). Regarding delivery factors, our findings suggest that emergency cesarean delivery affects post-partum depression in the nulliparous. This seems to confirm that women who express a strong desire to have a natural childbirth during pregnancy, but who must undergo cesarean section, are more prone to risk of postpartum depression ( 70 ).
Finally, our results highlighted no significant influences of the other variables considered, such as the length and the modality of labor and the APGAR index. In our sample, newborns showed good general condition. In fact, only three children (1.9%) obtained a score lower than 7, and no scores lower than six.
The second aim of this study was to explore which, among the above considered risk factors, were the stronger ones. Our analysis showed that, despite the marginal role of variables linked to clinical delivery difficulties, prenatal women's psychopathological characteristics and poor quality of couple relationship, prenatal attachment to child was the most important predictor of PPD, which, by itself, explains almost all the variance of the tested model.
Prenatal attachment expresses the first internalized representation that a pregnant woman develops of her unborn child and the emotional tie with him/her. Therefore, it is reasonable to hypothesize that a nulliparous with a good representation of her future child could experience her pregnancy with positive feelings, and that this, in turn, could improve the transition to her parenting role and well-being.
Extensive literature has shown that women who felt more affection toward their unborn children have more compliance with health practices during pregnancy ( 71 , 72 ), present less clinical complications during delivery, and show less difficulty, more confidence and better adjustment in assuming the new parenting role ( 73 ). Moreover, it has been found that prenatal attachment to the fetus plays a positive and significant role in promoting more adequate mother-child interactions ( 61 ) and spontaneous caregiving and attachment behavior after childbirth ( 65 ). Therefore, it is not surprising that the mother's prenatal attachment to child could represent a key element to improving the health of the mother and child, the outcome being a significant protective factor to prevent PPD onset.
Despite the doubtless interest of these results, there are some limitations to this study. The first is the inclusion criteria. Only nulliparous women with no risk pregnancy, no twins, or previous miscarriage or abortion, were included in this study. Therefore, future research should extend study to samples of women who have twin pregnancies, or with high-risk pregnancies. A second limitation is that our study only investigated the role of relational variables connected to the women's close relationship network, not considering the role that relationships with gynecologists, midwives, and medical and nursing staff play in influencing the mothers' delivery experience during pregnancy and childbirth, and postpartum depression outcomes. An important direction for future research would be to extend this study to other aspects of the women's social network. Providing these additional data could allow us to develop specific and targeted preventive interventions for PPD, and a better understanding of which variables could be important in women with a more complicated history of pregnancy. A third limitation to this study is that PPD was assessed at 1 month post birth. Although it has been recognized that the vulnerability for depression continues for 6 months after delivery ( 14 – 16 ), according to DSM-5, depression with postpartum onset is an episode of major depression that occurs in the 4 weeks following delivery. In any case, further research should extend the follow-up to a longer period of time, for example, 4–6 months of the child's life. It is necessary to underline that the number of comparisons between the methods of birth is very different. In future research, it would be appropriate to have a more homogeneous sample, to compare PPD both after cesarean and after spontaneous or induced vaginal birth.
Finally, further studies with larger samples are desirable to replicate our findings.
Overall, the results of the present study have great relevance for clinical practice. Perinatal depression is an important public health issue with aftermath for mothers, children, and families. This is especially true for women during the first pregnancy, because of their greater emotional vulnerability. Timely screening and appropriate treatment are needed to prevent unnecessary suffering. Until now, screening and preventive health programs have given attention to medical and clinical risk factors. However, our results stress the importance of new focus on more comprehensive care and wellness, suggesting the promotion of mothers' and children's health in perinatal phases by expanding initiatives in clinical practice to additional behavioral and psychosocial screenings. Besides the importance of an early detection of depressive and anxious symptoms in nulliparous women, the present results highlight the relevant role played by relational factors, such as the quality of prenatal attachment to child, the relationship with partner, and the relationship with parents. All these relationships need to be taken into consideration to guarantee a more positive outcome toward the transition to motherhood. Moreover, it may be important to provide more information to women about the various possibilities of labor and delivery: what they are, what consequences they have, not only on the health of the mother and child, but also on the mother-child relationship, in order to allow women to have a more comprehensive understanding of these important aspects.
In conclusion, we believe that these results could have relevant clinical and social implications. Understanding the most important relevant risk factors for PPD is essential for identifying nulliparous pregnant women at risk and promptly intervening with specific preventive health care programs.
Data Availability Statement
The dataset analyzed during the current study is available from the corresponding author on reasonable request.
Ethics Statement
The study was conducted in accordance with the guidelines for the ethical treatment of human participants of the Italian Psychological Association. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the Ethical Committee of Azienda USL 4 Prato, Italy (no 780/2013).
Author Contributions
MS participated in the development of protocol and analytical framework for the study. Moreover, she contributed to the drafting of the introduction and discussion sections of the manuscript. LP had primary responsibility for protocol development, patient screening, and participant's enrolment. Moreover, she performed the data analysis and contributed to draft the Methods and Materials section. FP revised the manuscript critically for important intellectual content.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Darvill R, Skirton H, Farrand P. Psychological factors that impact on women's experiences of first-time motherhood: a qualitative study of the transition. Midwifery. (2010) 26:3. doi: 10.1016/j.midw.2008.07.006
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Deave T, Johnson D, Ingram J. Transition to parenthood: the needs of parents in pregnancy and early parenthood. BMC Pregnancy Childbirth. (2008) 8:30. doi: 10.1186/1471-2393-8-30
3. Stern DN. The Motherhood Constellation: A Unified View of Parent-infant Psychotherapy . New York, NY: Basic Books (1995).
Google Scholar
4. Slade A, Cohen LJ, Sadler LS, Miller M. The psychology and psychopathology of pregnancy: reorganization and transformation. In: Zeanah CH, editor. Handbook of Infant Mental Health . New York, NY: The Gilford Press (2009). p. 22–39.
5. Cast AD. Well-being and the transition to parenthood: An identity theory approach. Sociol Perspect. (2004) 47:1. doi: 10.1525/sop.2004.47.1.55
CrossRef Full Text | Google Scholar
6. Cox M, Paley B, Burchinal M, Payne C. Marital perceptions and interactions across the transition to parenthood. JMF. (1999) 61:611–25. doi: 10.2307/353564
7. Condon J, Boyce P, Corkindale C. The first time fathers study: a prospective study of the mental health and wellbeing of men during the transition to parenthood. Aust N Z J Psychiatry. (2004) 38:56–64. doi: 10.1111/j.1440-1614.2004.01298.x
8. Banse R. Adult attachment and marital satisfaction: evidence for dyadic configuration effects. JSPR. (2004) 21:273–82. doi: 10.1177/0265407504041388
9. APA (2013). American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed . Arlington, VA: American Psychiatry Publishing. doi: 10.1176/appi.books.9780890425596
PubMed Abstract | CrossRef Full Text
10. Beck C. (1993). Teetering on the edge: a substantive theory of postpartum depression. Nurs Res. 42:42–8. doi: 10.1097/00006199-199301000-00008
11. McCarthy A. Postnatal depression: diagnosis and treatment. Ir Med. (1998) 91:44.
PubMed Abstract | Google Scholar
12. Dennis CL, Falah-Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry. (2017) 210:315–23. doi: 10.1192/bjp.bp.116.187179
13. Cox JL, Murray D, Chapman GA. Controlled study of onset, duration and prevalence of postnatal depression. Br J Psychiatry. (1993) 163:27–31. doi: 10.1192/bjp.163.1.27
14. Evans J, Heron J, Francomb H, Oke S, Golding J. Cohort study of depressed mood during pregnancy and after childbirth. BMJ. (2001) 323:257–60. doi: 10.1136/bmj.323.7307.257
15. Huang YC, Mathers N. Postnatal depression—Biological or cultural? A comparative study of postnatal women in the UK and Taiwan. J Adv Nurs. (2011) 33:279–87. doi: 10.1046/j.1365-2648.2001.01664.x
16. Vismara L, Rollè L, Agostini F, Sechi C, Fenaroli V, Molgora S, et al. Perinatal parenting stress, anxiety, and depression outcomes in first-time mothers and fathers: a 3- to 6-months postpartum follow-up study. Front Psychol. (2016) 7:938. doi: 10.3389/fpsyg.2016.00938
17. Satoh A, Kitamiya C, Kudoh H, Watanabe M, Menzawa K, Sasaki H. Factors associated with late post-partum depression in Japan. Jpn J Nurs Sci. (2009) 6:1. doi: 10.1111/j.1742-7924.2009.00121.x
18. Zubaran C, Foresti K. Investigating quality of life and depressive symptoms in the postpartum period. Women Birth. (2011) 24:1. doi: 10.1016/j.wombi.2010.05.002
19. Munk-Olsen T, Laursen TM, Pedersen CB, Mors O, Mortensen PB. New parents and mental disorders: a population-based register study. JAMA. (2006) 296:2582–9. doi: 10.1001/jama.296.21.2582
20. Mancini F, Carlson C, Albers L. Use of the postpartum depression screening scale in a collaborative obstetric practice. JMWH. (2007) 52:429–34. doi: 10.1016/j.jmwh.2007.03.007
21. Glavin K, Smith L, Sørum R. Prevalence of postpartum depression in two municipalities in Norway. Scand J Caring Sci. (2009) 23:705–10. doi: 10.1111/j.1471-6712.2008.00667.x
22. Righetti-Veltema M, Conne-Perréard E, Bousquet A, Manzano J. Postpartum depression and mother-infant relationship at 3 months old. J Affect Disord. (2002) 70:291–306. doi: 10.1016/S0165-0327(01)00367-6
23. Van den Bergh BRH, Mulder EJH, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: links and possible mechanisms. A review. Neurosci Biobehav Rev. (2005) 29:237–58. doi: 10.1016/j.neubiorev.2004.10.007
24. Henderson JJ, Evans SF, Straton JA, Priest SR, Hagan R. Impact of postnatal depression on breastfeeding duration. Birth. (2003) 30:175–80. doi: 10.1046/j.1523-536X.2003.00242.x
25. Bagner DM, Pettit JW, Lewinsohn PM, Seeley JR. Effect of maternal depression on child behavior: a sensitive period? J Am Acad Child Adolesc Psychiatry. (2010) 49:7. doi: 10.1016/j.jaac.2010.03.012
26. Glasheen C, Richardson GA, Fabio A. (2010). A systematic review of the effects of postnatal maternal anxiety on children. Arch Womens Ment Health. (2010) 13:1. doi: 10.1007/s00737-009-0109-y
27. Ross LE, Sellers EM, Gilbert Evan SE, Romach MK. Mood changes during pregnancy and the postpartum period: development of a biopsychosocial model. Acta Psychiatr Scand. (2004) 109:457–66. doi: 10.1111/j.1600-0047.2004.00296.x
28. Coelho HF, Murray L, Royal-Lawson M, Cooper PJ. Antenatal anxiety disorder as a predictor of postnatal depression: a longitudinal study. J Affect Disord. (2011) 129:1–3. doi: 10.1016/j.jad.2010.08.002
29. Roomruangwong C, Withayavanitchai S, Maes M. (2016). Antenatal and postnatal risk factors of postpartum depression symptoms in Thai women: a case-control study. Sex Reprod Healthc. (2016) 10:25–31. doi: 10.1016/j.srhc.2016.03.001
30. Brugha TS, Wheatley S, Taub NA, Culverwell A, Friedman T, Kirwan PH, et al. Pragmatic randomized trial of antenatal intervention to prevent post-natal depression by reducing psychosocial risk factors. Psychol Med. (2000) 30:1273–81. doi: 10.1017/S0033291799002937
31. Tani F, Castagna V. Maternal social support, quality of birth experience, and post-partum depression in primiparous women. J Matern Fetal Neonatal Med. (2016) 30:6. doi: 10.1080/14767058.2016.1182980
32. Sapkota S, Kobayashi T, Takase M. Husbands' experiences of supporting their wives during childbirth in Nepal. Midwifery. (2012) 28:1. doi: 10.1016/j.midw.2010.10.010
33. Priel B, Besser A. Vulnerability to postpartum depressive symptomatology: dependency, self-criticism and the moderating role of antenatal attachment. J Soc Clin Psychol. (1999) 18:2. doi: 10.1521/jscp.1999.18.2.240
34. Brealey SD, Hewitt C, Green JM, Morrell J, Gilbody S. Screening for postnatal depression: is it acceptable to women and healthcare professionals? A systematic review and meta-synthesis. J Reprod Infant Psychol. (2010) 28:4. doi: 10.1080/02646838.2010.513045
35. Mustaffa MS, Marappan D, Abu MS, Khan A, Ahmad R. Social support during prenatal and postnatal stage: influence on maternal depression and mental well-being. Procedia Soc Behav Sci. (2014) 143:417–22. doi: 10.1016/j.sbspro.2014.07.506
36. Scope A, Booth A, Morrell CJ, Sutcliffe P, Cantrell A. Perceptions and experiences of interventions to prevent postnatal depression. A systematic review and qualitative evidence synthesis. J Affect Disord. (2017) 210:1. doi: 10.1016/j.jad.2016.12.017
37. McCoy SJB, Beal JM, Shipman SBM, Payton ME, Watson GH. (2006). Risk factors for postpartum depression: a retrospective investigation at 4-weeks postnatal and a review of the literature. J Am Osteopath Assoc. (2006) 106:193–8.
38. Porter CL, Hsu HC. First-time mothers' perceptions of efficacy during the transition to motherhood: links to infant temperament. J Fam Psychol. (2003) 17:1. doi: 10.1037//0893-3200.17.1.54
39. Davis L, Edwards H, Mohay H, Wollin J. The impact of very premature birth on the psychological health of mothers. Early Hum Dev. (2003) 73:61–70. doi: 10.1016/S0378-3782(03)00073-2
40. Rubertsson C, Waldenstrom U., Wickberg B. (2003). Depressive mood in early pregnancy: prevalence and women at risk in a national Swedish sample. J Reprod Infant Psychol. 21:2. doi: 10.1080/0264683031000124073
41. Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. (1983). State-Trait Anxiety Inventory for Adults: Manual, Instrument and Scoring Guide . Mind Garden: Consulting Psychologists Press (1983). doi: 10.1037/t06496-000
CrossRef Full Text
42. Predabissi L, Santinello M. Edizione Italiana STAI . Firenze: Giunti OS (1989).
43. Chinchilla-Ochoa D, Barriguete-Chávez Peón P, Farfán-Labonne BE, Garza-Morales S, Leff-Gelman P, Flores-Ramos M. Depressive symptoms in pregnant women with high trait and state anxiety during pregnancy and postpartum. Int J Womens Health. (2019) 11:257–65. doi: 10.2147/IJWH.S194021
44. Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression . New York, NY: Guilford Press (1979).
45. Ghisi M, Flebus GB, Montano A, Sanavio E, Sica C. Beck Depression Inventory, 2nd ed . Firenze: Organizzazioni Speciali (2006).
46. Parker G, Tupling H, Brown LB. A parental bonding instrument. Br J Med Psychol. (1979) 52:1. doi: 10.1111/j.2044-8341.1979.tb02487.x
47. Bonaiuto M, Perucchini P, Pierro A. L'adolescente e i membri significativi della sua rete sociale [Adolescent and significant members of his social network]. Età Evol. (1997) 57:40–56.
48. Ponti L, Guarnieri S, Smorti A, Tani F. A measure for the study of friendship and romantic relationship quality from adolescence to early-adulthood. TOPSY J. (2010) 12:3. doi: 10.2174/1874350101003010076
49. Müller ME. Development of the prenatal attachment inventory. West J Nurs Res. (1993) 15:2. doi: 10.1177/019394599301500205
50. Della Vedova AM, Dabrassi F, Imbasciati A. (2008). Assessing prenatal attachment in an Italian women sample. J Reprod Infant Psychol. (2008) 26:86–98. doi: 10.1080/02646830701805349
51. Benvenuti P, Ferrara M, Niccolai C, Valoriani V, Cox JL. The Edimburgh Postnatal Depression Scale: validation for an Italian sample. J Affect Disord. (1999) 53:2. doi: 10.1037/t11281-000
52. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. (1987) 150:782–6. doi: 10.1192/bjp.150.6.782
53. Norhayati MN, Hazlina NH, Asrenee AR, Emilin WM. Magnitude and risk factors for postpartum symptoms: a literature review. J Affect Disord. (2015) 175:1. doi: 10.1016/j.jad.2014.12.041
54. Condon JT, Corkindale CJ. The assessment of parent-to-infant attachment: development of a self-report questionnaire instrument. J Reprod Infant Psychol. (1998) 16:1. doi: 10.1080/02646839808404558
55. Condon JT. The assessment of antenatal emotional attachment: development of a questionnaire instrument. Br J Med Psychol. (1993) 66:2. doi: 10.1111/j.2044-8341.1993.tb01739.x
56. Walsh J, Hepper EG, Marshall BJ. Investigating attachment, caregiving, and mental health: a model of maternal-fetal relationships. BMC Pregnancy Childbirth. (2014) 14:383. doi: 10.1186/s12884-014-0383-1
57. Brandon AR, Pitts S, Denton WH, Stringer CA, Evans HM. A history of the theory of prenatal attachment. J Prenat Perinat Psychol Health. (2009) 23:201–22.
58. Diener M, Diener McGravan MB. What makes people happy? A developmental approach to the literature on family relationships and well-being. In: Eid M, Larsen RJ, editor. The Science of Subjective Well-being . New York, NY: Guilford (2008). p. 347–75.
59. Guarnieri S, Smorti M, Tani F. Attachment relationships and life satisfaction during emerging adulthood. Soc Indic Res. (2015) 121:3. doi: 10.1007/s11205-014-0655-1
60. Yusuff ASM, Tang L, Binns CW, Lee AH. Prevalence and risk factors for postnatal depression in Sabah, Malaysia: a cohort study. Women Birth. (2015) 28:1. doi: 10.1016/j.wombi.2014.11.002
61. Mazzeschi C, Pazzagli C, Radi G, Raspa V, Buratta L. Antecedents of maternal parenting stress: the role of attachment style, prenatal attachment, and dyadic adjustment in first-time mothers. Front Psychol. (2015) 6:1443. doi: 10.3389/fpsyg.2015.01443
62. Beach SH, Katz J, Kim S, Brody GH. Prospective effects of marital satisfaction on depressive symptoms in established marriages: a dyadic model. J Soc Pers Relat. (2003) 20:6. doi: 10.1177/0265407503020003005
63. South SC, Krueger RF. Understanding general and specific connections between psychopathology and marital distress: a model based approach. J Abnorm Psychol. (2011) 120:4. doi: 10.1037/a0025417
64. McMahon CA, Barnett B, Kowalenko NM, Tennant CC. Maternal attachment state of mind moderates the impact of postnatal depression on infant attachment. J Child Psychol Psychiatry (2006) 47:660–9. doi: 10.1111/j.1469-7610.2005.01547.x
65. Tani F, Castagna V, Ponti L. Women who had positive relationships with their own mothers reported good attachments to their first child before and after birth. Acta Paediatr. (2017) 107:4. doi: 10.1111/apa.14162
66. Tani F, Castagna V, Ponti L. Mothers' social perceived support, anxiety and prenatal attachment to child: which direct and indirect influences on delivery clinical indices? Int J Health Sci Res. (2017) 7:346–52.
67. Blom EA, Jansen PW, Verhulst FC, Hofman A, Raat H, Jaddoe VWV, et al. Perinatal complications increase the risk of postpartum depression. The Generation R Study. BJOG. (2010) 117:11. doi: 10.1111/j.1471-0528.2010.02660.x
68. Smorti M, Ponti L, Tani F. Maternal depressive symptomatology during pregnancy is relevant risk factor affecting newborn's health: a longitudinal study. J Reprod Infant Psychol. (2019) 39:492–7. doi: 10.1080/02646838.2019.1581919
69. Smorti M, Ponti L, Tani F. The effect of maternal depression and anxiety on labour and the well-bing of the newborn. J Obstet Gynaecol. (2019) 39:492–7. doi: 10.1080/01443615.2018.1536697
70. Houston KA, Kaimal AJ, Nakagawa S, Gregorich SE, Yee LM, Kuppermann M. Mode of delivery and postpartum depression: the role of patient preferences. Am J Obstet Gynecol. (2015) 212:2. doi: 10.1016/j.ajog.2014.09.002
71. Alhusen JL, Gross D, Hayat MJ, Rose L, Sharps P. The role of mental health on maternal-fetal attachment in low-income women. J Obstet Gynecol Neonatal Nurs. (2012) 41:6. doi: 10.1111/j.1552-6909.2012.01385.x
72. Sadat Maddahi M, Dolatian M, Khoramabadi M, Talebi A. Correlation of maternal-fetal attachment and health practiced during pregnancy with neonatal outcomes. Elecron Psys. (2016) 8:7. doi: 10.19082/2639
73. Shah PE, Fonagy P, Strathearn L. Is attachment transmitted across generations? The plot thickens. Clin Child Psychol Psychiatry. (2010) 15:3. doi: 10.1177/1359104510365449
Keywords: postnatal depression, childbirth, maternal mental health, risk factor, nulliparous women
Citation: Smorti M, Ponti L and Pancetti F (2019) A Comprehensive Analysis of Post-partum Depression Risk Factors: The Role of Socio-Demographic, Individual, Relational, and Delivery Characteristics. Front. Public Health 7:295. doi: 10.3389/fpubh.2019.00295
Received: 03 April 2019; Accepted: 01 October 2019; Published: 24 October 2019.
Reviewed by:
Copyright © 2019 Smorti, Ponti and Pancetti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Martina Smorti, martina.smorti@unipi.it ; Lucia Ponti, pontilucia@gmail.com
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Undergraduate
- High School
- Architecture
- American History
- Asian History
- Antique Literature
- American Literature
- Asian Literature
- Classic English Literature
- World Literature
- Creative Writing
- Linguistics
- Criminal Justice
- Legal Issues
- Anthropology
- Archaeology
- Political Science
- World Affairs
- African-American Studies
- East European Studies
- Latin-American Studies
- Native-American Studies
- West European Studies
- Family and Consumer Science
- Social Issues
- Women and Gender Studies
- Social Work
- Natural Sciences
- Pharmacology
- Earth science
- Agriculture
- Agricultural Studies
- Computer Science
- IT Management
- Mathematics
- Investments
- Engineering and Technology
- Engineering
- Aeronautics
- Medicine and Health
- Alternative Medicine
- Communications and Media
- Advertising
- Communication Strategies
- Public Relations
- Educational Theories
- Teacher's Career
- Chicago/Turabian
- Company Analysis
- Education Theories
- Shakespeare
- Canadian Studies
- Food Safety
- Relation of Global Warming and Extreme Weather Condition
- Movie Review
- Admission Essay
- Annotated Bibliography
- Application Essay
- Article Critique
- Article Review
- Article Writing
- Book Review
- Business Plan
- Business Proposal
- Capstone Project
- Cover Letter
- Creative Essay
- Dissertation
- Dissertation - Abstract
- Dissertation - Conclusion
- Dissertation - Discussion
- Dissertation - Hypothesis
- Dissertation - Introduction
- Dissertation - Literature
- Dissertation - Methodology
- Dissertation - Results
- GCSE Coursework
- Grant Proposal
- Marketing Plan
- Multiple Choice Quiz
- Personal Statement
Power Point Presentation
- Power Point Presentation With Speaker Notes
- Questionnaire
- Reaction Paper
Research Paper
- Research Proposal
- SWOT analysis
- Thesis Paper
- Online Quiz
- Literature Review
- Movie Analysis
- Statistics problem
- Math Problem
- All papers examples
- How It Works
- Money Back Policy
- Terms of Use
- Privacy Policy
- We Are Hiring
Postpartum Depression, Research Paper Example
Pages: 9
Words: 2422
Hire a Writer for Custom Research Paper
Use 10% Off Discount: "custom10" in 1 Click 👇
You are free to use it as an inspiration or a source for your own work.
Introduction
Postpartum depression is a complex condition that is characterized by emotional and psychological responses to the birth of a child. This set of circumstances poses a high risk to some mothers in the form of depression and other concerns that impact mental health and wellbeing. The issues related to postpartum depression are often poorly understood because they contribute to a difficult state for new mothers to manage if they are unsure of how to manage motherhood and the experiences that are inevitable with this process. Therefore, a comprehensive theoretical approach must be considered that has a significant impact on outcomes for new mothers.
Postpartum depression creates a set of complex circumstances that have a lasting impact on many new mothers, thereby necessitating an evaluation that includes the concepts associated with self-care and the ability to overcome the symptoms of postpartum depression and to be effective in advancing patient care outcomes for this group. When postpartum depression is evident, there may be periods whereby self-care is difficult to achieve under normal circumstances. This contributes to a negative set of complications for some women with this condition and requires a level of attention and focus in order to ensure that self-care needs are met in the desired manner. However, this practice is difficult on many levels because it limits the ability of Orem’s theory to be applicable when patients are unable to administer self-care when postpartum depression is evident. Therefore, an evaluation of Orem’s Self-Care theory is essential to the discovery of new concepts to alleviate this state of depression and to improve the bonding experience between mother and child (Larsen, 2011). These issues must be addressed in the context of their impact on women who have recently given birth and how Orem’s theory may be applied to these circumstances in order to determine how depression impacts patient care outcomes for new mothers (Larsen, 2011). The following discussion will address Orem’s Theory of Self-Care in greater detail and will provide a basis for examining the needs of new mothers who face postpartum depression after birth.
Description of the Theory: Purpose
Orem’s Self-Care Theory supports individuals who seek to perform self-care activities as part of the daily routine to provide a positive impact for patients (Larsen, 20110. Most importantly, this theory supports patients who seek therapeutic interventions to perform self-care in the home environment over time (Larsen, 2011). This practice supports the participation of patients with postpartum depression and other issues to be effective in supporting a change effort for patients (Larsen, 2011). Most importantly, it is necessary to evaluate the circumstances under which Orem’s theory of self-care may apply during the postpartum period because many women struggle with their emotions, thereby making self-care and acceptance more difficult for patients (Larsen, 2011).
Concepts and Definitions
According to Orem’s Theory of Self-Care, self-care is a regulatory function, whereby individuals are given and assume the functions and responsibility of care for themselves, and when individuals are not willing or able to perform these functions, there are self-care deficits. Patients engage in self-care maintenance—tasks to prevent symptoms, such as adhering to sodium restrictions—and self-care management—activities to respond to symptoms—to prevent these deficits, i.e., improve or maintain their functioning” (Yehle, 2014, p. 5). Therefore, this concept must be well represented through the activities that are conducted to administer self-care for patients who struggle with postpartum depression.
Relationships and Structure
In a study by Nazik & Eryilmaz (2013), it was determined that “the care given to women in the postpartum period using Orem’s self-care model prevented postpartum complications and increased the self-care agency of postpartum women” (P. 360). This practice requires further consideration because it has a significant impact on how mothers respond to postpartum depression and whether or not they are able to administer quality self-care during this period, given the emotional and psychological difficulties that they might face during this stage (Nazik & Eryilmaz, 2013). This practice requires an individual to examine her inner strength and to obtain support from her peers and from clinicians in order to perform self-care at the desired level (Chen, 2014). These practices support and encourage the development of new directions in advancing Orem’s theory of self-care so that it is fully applicable to female patients experiencing postpartum depression. Patients with this condition require a level of support and encouragement so that they recognize their ability to overcome personal challenges and other considerations that impact their wellbeing and self-care capabilities (Chen, 2014).
Assumptions
With the utilization of Orem’s theory of self-care for patients with postpartum depression, it is believed that each mevaluated individually in order to determine her mental and psychological state after birth so that all possible ideas and concepts are explored to address the condition and to improve outcomes. This theory makes a number of assumptions, including the belief that all mothers with postpartum depression are seeking help and are able to administer self-care activities in the home environment. It is also believed that the ability of patients to overcome their own challenges related to self-care is instrumental in supporting an agenda that will positively impact this group and enable them to once again recognize the importance of carinthat bvg for themselves and in performing self-care activities at the expected level (Yehle, 2014). Self-care in patients with postpartum depression must be well understood and capture the ability to reflect upon new directions and a focus on new strategies to support motivation and strength in caring for oneself effectively in a complex environment where emotions and other considerations get in the way (Chen, 2014). It is expected women who experience postpartum depression will be challenged by their own limitations and eventually recognize that these limitations are real and wreak havoc on their ability to perform self-care and to communicate ideas effectively so that patients receive the assistance that is needed to achieve the intended results (Chen, 2014).
Self-care activities require a level of knowledge and acceptance of individual characteristics and strengths that will facilitate motivation in mothers experiencing postpartum depression. However, this process also demonstrates that women with this condition may face risks that are beyond their control and for which they have no immediate short-term solution because they do not recognize the nature of their own inner strength. It is important for women with postpartum depression to recognize the overarching nature of the condition and to be effective in recognizing that it is temporary and will not debilitate a person over the long term.
Many women with postpartum depression appear to be hopeless and helpless because the condition debilitates their natural logical sensibilities and their ability to make practical decisions that will have a positive impact on their health ; therefore, the condition must be examined under a different lens and must capture the overarching perspective that will have a lasting impact on outcomes and on relationships in supporting a new direction in facilitating change and progress within one’s own life and to overcome the emotions and feelings related to postpartum depression within this population.
Reflection on the Theory: Clarity
This theory requires nurses to examine how patients with postpartum depression might benefit their morale and overall wellbeing; therefore, this practice requires patients to on administering their self-care activities effectively. This practice will demonstrate the significance of these activities and will support and encourage nurse who face their own risks, such as postpartum depression, to improve their own health through these efforts. Women with postpartum depression become inundated with feelings and emotions for which they have no real understanding and acceptance; therefore, they may have a tendency to become lost in the moment and cannot recover from these conditions without extreme difficulty. In these instances, women must be provide with support and guidance to recognize that their needs are of critical importance and that they must tend to those needs as best as possible.
Self-care offers an opportunity to examine a woman’s core strengths and to be effective in meeting her own personal needs as best as possible. However, when struggles occur in this area, it becomes necessary to evaluate other possibilities and to be understanding of the different elements which capture core needs and expectations. Although women may feel as if they face postpartum depression alone, they nonetheless have many opportunities to experience support from friends and family members in order to enable them to recognize their self-worth and contributions. It is hopeful that these experiences will provide a basis for examining other areas that will have a lasting impact on conditions and that will provide a means of performing self-care activities effectively to gain a greater sense of self-worth, self-confidence, and inner strength.
Generalizability
Orem’s Theory of Self-Care is a dominant perspective regarding the nature of the human condition and the ability to recognize what each individual requires to achieve survival within a given environment. For women who have recently given birth for the first time or on multiple occasions, hormonal changes reflect a set of important challenges that require further evaluation, given the limitations that may persist with the emotional vulnerability of this stage. The practical nature of this practice supports the ability to adapt effectively to a variety of situations that require self-care so that patients with postpartum depression are able to overcome any limitations that stand in the way of these activities. This process also requires nurses to be effective promoters of the self-care concept so that patients receive optimal focus and attention to address their concerns. The administration of self-care must be generalizable to the extent that it supports the application of key principles to a variety of settings.
Accessibility
When women experience what is considered to be true clinical postpartum depression, they may have a tendency to ignore themselves and to refrain from administering self-care within their own environments. This is a difficult set of circumstances to witness from an outsider’s perspective, but it also demonstrates a need to understand why this motivation disappears to begin with and how to overcome these emotions and experience a return to normalcy. The accessibility of this theory is necessary to ensure that patients receive the necessary attention to be able to administer self-care at the desired level. Women with postpartum depression must gain support from others so that they are able to recognize the importance of self-care as part of a larger framework in overcoming this condition. Therefore, the accessibility of self-care is critical to the wellbeing of patients with postpartum depression, particularly if they believe that they do not have a chance for a viable recovery from this condition.
It is necessary for women who are experiencing postpartum depression to recognize that they are not alone and that even if their ability to perform self-care is currently limited, this is not a permanent condition. It is expected that this will change over time and that women will begin to again experience feelings of self-worth and acceptance of their new status as mothers. This also reflects their understanding that they are not only responsible for themselves, but also for another person, and this supports a greater understanding of their inner strengths and abilities as human beings to be successful as mothers. Although postpartum depression is a highly individualistic condition, it nonetheless reflects a situation whereby making sense of the circumstances is a challenging consideration and requires a high level of support and encouragement from those surrounding the person.
A woman who gives birth to a child often experiences a myriad of feelings and emotions that are often overwhelming and that create difficult challenges in balancing the needs of the child and in providing care for oneself. When this balance is distorted, it often becomes difficult for a woman to recognize her own inner strength when her emotions get in the way. Therefore, self-care may fall by the wayside and may be ignored. When this situation occurs, it is necessary to develop a strategy that will have a lasting impact on a person so that she is able to gain the support that she needs to be successful not only as a mother, but as a human being who is capable of self-care and treatment at the desired level.
These issues also require a high level understanding and acceptance of the issues that impact women who have recently had children and who are struggling to overcome the changes that have occurred with this process. It is believed that when self-care is ignored or neglected for a period of time, a woman is unable to exercise sound and reasonable judgment in many ways, thereby creating disconnect between her own needs and the needs of her child. Women who experience these changes must be provided with support and guidance in an effort to overcome adversity and to be effective as human beings. Therefore, self-care must remain a key priority for women in this state, even if they do not recognize this to be the case.
The evolution of postpartum depression is a challenging condition because it often leads a woman to evaluate her own self-worth and to understand why she is not currently motivated to perform self-care activities at the necessary level. These issues require a greater understanding of the nature of the condition and its impact on female health during this stage. Furthermore, it requires women to be patient and to begin to recognize their own self-worth, even during periods of darkness when it appears that all hope is lost and patients are unable to effectively cope with the condition and its impact on daily activities, wellbeing, and general quality of life for this patient population.
These experiences support the understanding and purpose of Orem’s Theory of Self-Care in order to enable women to take back their lives and to overcome postpartum depression with the guidance and encouragement of a strong support system to ensure that they will experience success and achievement in this area. It is expected that self-care activities will resume at the necessary in women experiencing postpartum depression, and that these experiences may serve as a learning curve in order to determine how to overcome adversity, to recognize inner strength, and to be proactive in meeting personal needs through self-care activities at the desired level.
Chen, A. M., Yehle, K. S., Albert, N. M., Ferraro, K. F., Mason, H. L., Murawski, M. M., & Plake, K. S. (2014). Relationships between health literacy and heart failure knowledge, self-efficacy, and self-care adherence. Research in Social and Administrative Pharmacy , 10 (2), 378-386.
Larsen, A. (2011). A supportive education program for perinatal depression utilizing Orem’s Theory of Self-Care. 139st APHA Annual Meeting and Exposition.
Nazik, E., & Eryilmaz, G. (2013). The Prevention And Reduction Of Postpartum Complications Orem’s Model. Nursing science quarterly , 26 (4), 360-364.
Stuck with your Research Paper?
Get in touch with one of our experts for instant help!
Antibodies and the Immune System, Power Point Presentation Example
Elements of Empiric Versus Aesthetic Critical Appraisal of Nursing Theory, Essay Example
Time is precious
don’t waste it!
Plagiarism-free guarantee
Privacy guarantee
Secure checkout
Money back guarantee

Related Research Paper Samples & Examples
The risk of teenagers smoking, research paper example.
Pages: 11
Words: 3102
Impacts on Patients and Healthcare Workers in Canada, Research Paper Example
Pages: 7
Words: 1839
Death by Neurological Criteria, Research Paper Example
Words: 2028
Ethical Considerations in End-Of-Life Care, Research Paper Example
Pages: 5
Words: 1391
Ethical Dilemmas in Brain Death, Research Paper Example
Words: 2005
Politics of Difference and the Case of School Uniforms, Research Paper Example
Pages: 2
Words: 631
Postpartum Depression: Treatment and Therapy Essay
Introduction, postpartum depression.
Although for many people the birth of a child is an exciting part of life, for some it may cause adverse health outcomes. One of them is postpartum depression that can be characterized by mood swings, sleep deprivation, and anxiety. This paper discusses a patient that presented in the clinic with these symptoms. It outlines the possible treatment and therapy methods, as well as the implications of the condition.
A 28-year-old patient presented in the office three weeks after giving birth to her first son with the symptoms of postpartum depression. The woman was a single mother; she did not have a strong support system as her former partner refused to help her and her family lived in a different state. She noted that she was sleep-deprived, she felt apathetic, sad, experienced anxiety, and had a decreased appetite.
The patient reported that she was diagnosed with depression seven years ago but underwent treatment and had not had the symptoms for a long time. The woman noted that her mother also had signs of a mental disorder but never sought professional help. The patient cried while talking to me; her emotional state was poor. In addition, the woman admitted that she had thought of harming her newborn son because she felt that she was tired of taking care of him.
The typical signs of postpartum depression include the presence of sleep disorder, fatigue, crying, anxiety, changes in appetite, and feelings of inadequacy (Tharpe, Farley, & Jordan, 2017). The patient has these symptoms, which allowed for establishing the diagnosis. Drug therapy included the prescription of tricyclic antidepressants, as they do not pose risks to infants during breastfeeding (Anxiety and Depression Association of America, 2018). Additional therapies included adequate nutrition with the exclusion of caffeine and herbal remedies, such as 2 cups of lemon balm tea daily (Tharpe et al., 2017).
Moreover, I advised the woman to participate in support groups’ meetings and have a scheduled time for personal care, hobbies, and favorite activities, as well as sleep. In addition, I asked the patient to try to have some time away from her child as it could improve her mental state as well. As for follow-up care measures, I suggested that the woman could document her thoughts and feelings and update me on the changes in her condition by visiting my office in two weeks. Moreover, I invited the patient to participate in an educational session on the aspects of postpartum depression.
The primary implication of the woman’s condition is that it is vital to educate individuals on its symptoms and assure them that this experience is common. Moreover, it is necessary to continue establishing support groups and psychotherapy sessions aimed to eliminate this issue. Postpartum depression may affect not only this woman but her entire family unit as the individuals close to the patient can also start experiencing emotional distress and other related symptoms. In the case of my patient, the condition may affect her relationships with her child, potentially causing a poor emotional bond and behavioral problems in the infant.
Postpartum depression is a severe condition that may affect a patient’s life significantly. It can cause individuals to feel anxious, experience mood swings and changes in appetite, and have thoughts of harming their newborn children. The management strategy for this illness can include drug therapy along with alternative remedies. It is vital to establish support groups and educational training for people having postpartum depression to decrease its incidence.
Anxiety and Depression Association of America. (2018). Postpartum depression . Web.
Tharpe, N. L., Farley, C., & Jordan, R. G. (2017). Clinical practice guidelines for midwifery & women’s health (5th ed.). Burlington, MA: Jones & Bartlett Publishers.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, July 9). Postpartum Depression: Treatment and Therapy. https://ivypanda.com/essays/postpartum-depression-discussion/
"Postpartum Depression: Treatment and Therapy." IvyPanda , 9 July 2021, ivypanda.com/essays/postpartum-depression-discussion/.
IvyPanda . (2021) 'Postpartum Depression: Treatment and Therapy'. 9 July.
IvyPanda . 2021. "Postpartum Depression: Treatment and Therapy." July 9, 2021. https://ivypanda.com/essays/postpartum-depression-discussion/.
1. IvyPanda . "Postpartum Depression: Treatment and Therapy." July 9, 2021. https://ivypanda.com/essays/postpartum-depression-discussion/.
Bibliography
IvyPanda . "Postpartum Depression: Treatment and Therapy." July 9, 2021. https://ivypanda.com/essays/postpartum-depression-discussion/.
- Postpartum Depression and Acute Depressive Symptoms
- Technology to Fight Postpartum Depression in African American Women
- Supporting the Health Needs of Patients With Parkinson’s, Preeclampsia, and Postpartum Depression
- Anxiety Disorder: Psychological Studies Comparison
- Mental Illness With Mass Shootings
- A Review of Postpartum Depression and Continued Post Birth Support
- Role of Behavioral Science in Treatment of Dyslexia and Dyscalculia
- The Psychological and Social Problems in Students
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Breastfeeding Special Circumstances
- Contraindications to Breastfeeding
- Breastfeeding: Diet, Vitamins, and Minerals
- Environmental and Chemical Exposures
- Travel and Breastfeeding
- Illnesses or Conditions and Breastfeeding
- Relactation
Postpartum Depression
At a glance.
Mothers with postpartum depression (following childbirth) can usually continue to breastfeed. Health care providers should work with mothers experiencing postpartum depression to ensure they receive appropriate treatment, support, and safe medications while breastfeeding.

There is not enough evidence to know if breastfeeding is associated with a higher or lower risk of postpartum depression (following childbirth). According to a 2018 systematic review by the Agency for Healthcare Research and Quality (AHRQ) , understanding the relationship is challenging "because women with depression may have difficulty initiating and sustaining breastfeeding, and women who experience breastfeeding difficulties may develop depression" (p. 107).
Antidepressants while breastfeeding
It may be safe to take antidepressant medications while breastfeeding. Although many medications pass into breast milk, most have little or no effect on milk supply or infant well-being.
When discussing depression medications , the health care provider needs to ask a mother if she is breastfeeding. Together, they can decide which medications are right for her and safe to use while breastfeeding.
LactMed® is a database of information on medications to which breastfeeding mothers may be exposed.
Breastfeeding with postpartum depression
Mothers with postpartum depression can usually continue to breastfeed. While some mothers experience positive feelings from breastfeeding, others may not. Health care providers can:
- Address mothers' depression promptly and help them reach their breastfeeding goals.
- Talk to mothers about treatment options, including medications and non-pharmacological options, such as individual or group therapy.
- Help mothers access professional breastfeeding support as needed.
Learn more:
Postpartum Depression —Office on Women's Health
Incorporating Recognition and Management of Perinatal Depression Into Pediatric Practice —American Academy of Pediatrics
ABM Clinical Protocol #18: Use of Antidepressants in Breastfeeding Mothers —Academy of Breastfeeding Medicine
Breastfeeding special circumstances
Health care providers and public health practitioners will find information about breastfeeding in special circumstances.
For Everyone
Health care providers.
- Share full article
Advertisement
Supported by
Ad for Lactation Cookies Returns to Times Square
After Clear Channel, which manages many of the advertisements in the area, said a provocative billboard for a Molly Baz recipe was “flagged for review,” two companies stepped in to offer new space.

By Alisha Haridasani Gupta
Molly Baz, the cookbook author, and her pregnant belly, rhinestone bikini and breasts will be back up in Times Square, uncensored.
A week after The New York Times reported that her billboard for lactation cookies had been “flagged for review” and swapped out for a more conservative image by the company that powered the billboard, Clear Channel, the ad has found a new home. The probiotics supplement and microbiome research brand Seed has donated their billboard to Swehl, the breastfeeding start-up that created the cookie campaign with Ms. Baz. Clear Channel still has not responded to requests for comment.
The original imagery, with the words “Just Add Milk,” will now run for the next three weeks alongside a Seed billboard with a clear message: “Dear Molly, Thankfully we’re not (lactose) intolerant.”
The partnership was the direct result of the anger and backlash on social media over what many called unjust censorship, said Ara Katz, a co-chief executive and a co-founder of Seed. The ad that featured Ms. Baz included no nudity — her breasts were covered by her cookies — yet was flagged despite the fact that Times Square billboards regularly run sensual lingerie ads.
Ms. Katz read the original Times story last week and was determined to help. She reached out to the company that powers her company’s billboards, Lightyear Media, which did not just agree to bring Ms. Baz back. “The women who work there gave us additional ad inventory for free,” Ms. Katz said. That would allow the ad to run more frequently.
“It feels so much bigger than this campaign and this ad,” said Elizabeth Myer, who founded Swehl with Betsy Riley. “It is actually this moment of time we’re in — women are really tired of the double standard around our bodies.”
After the original ad was removed from circulation, several brands reached out to Swehl to find ways to help get it back up. One advertising company put the ad up on a truck on Tuesday and drove it around Times Square for eight hours.
But given that Ms. Katz founded Seed because of her own personal struggles with breastfeeding, the company felt like the most organic partner for Swehl, Ms. Myer said, even though the founders had not known each other before this week.
“We’ve all become really fast friends,” Ms. Katz said.
Advertising has long had an ambivalent relationship with women’s health content. It was not until 2017 that an ad for period products was allowed to run using red liquid , as opposed to what had been deemed the more palatable blue. In 2020, an ad by the mother and baby care brand Frida that realistically depicted the pain of postpartum recovery was barred from airing during the Oscars . And online content related to women’s health or breastfeeding is often censored on social media , as was the case for the baby care company Tommee Tippee , which ran a campaign titled “Boob Life” for its breast pumps, depicting a montage of realistic breastfeeding vignettes and breasts.
The rejection of an ad, however, can prove to be great publicity, thanks to the reach of social media.
The controversy around Ms. Baz’s ad drove more than 200,000 new users to Swehl’s website, representing a 500 percent increase in traffic, and Ms. Myer said the company’s sales on Amazon had doubled, though Swehl did not share exact sales figures.
“It’s been a really, really wild roller coaster of a week,” she said.
Alisha Haridasani Gupta is a Times reporter covering women’s health and health inequities. More about Alisha Haridasani Gupta
Pregnancy, Childbirth and Postpartum Experiences
Aspirin’s Benefits: Not enough pregnant women at risk of developing pre-eclampsia, life-threatening high blood pressure, know that low-dose aspirin can help lower that risk. Leading experts are hoping to change that.
‘A Chance to Live’: Cases of trisomy 18 may rise as many states restrict abortion. Some women have chosen to have these babies , love them tenderly and care for them devotedly.
Teen Pregnancies: A large study in Canada found that women who were pregnant as teenagers were more likely to die before turning 31 .
Weight-Loss Drugs: Doctors say they are seeing more women try weight-loss medications in the hopes of having a healthy pregnancy. But little is known about the impact of those drugs on a fetus.
Premature Births: After years of steady decline, premature births rose sharply in the United States between 2014 and 2022. Experts said the shift might be partly the result of a growing prevalence of health complications among mothers .
Depression and Suicide: Women who experience depression during pregnancy or in the year after giving birth have a greater risk of suicide and attempted suicide .

IMAGES
VIDEO
COMMENTS
Postpartum depression (PPD) has a significant negative impact on the child's emotional, mental as well as intellectual development if left untreated, which can later have long-term complications. Later in life, it also results in the mother developing obsessive-compulsive disorder and anxiety. Many psychological risk factors are linked with PPD.
Background Since the last decade, postpartum depression (PPD) has been recognized as a significant public health problem, and several factors have been linked to PPD. Mothers at risk are rarely undetected and underdiagnosed. Our study aims to determine the factors leading to symptoms of depression using Structural Equation Modeling (SEM) analysis. In this research, we introduced a new ...
Background Postpartum depression (PPD) affects around 10% of women, or 1 in 7 women, after giving birth. Undiagnosed PPD was observed among 50% of mothers. PPD has an unfavorable relationship with women's functioning, marital and personal relationships, the quality of the mother-infant connection, and the social, behavioral, and cognitive development of children. We aim to determine the ...
Postpartum depression and pain negatively affect maternal well-being, and postpartum depression has been associated with adverse outcomes in children. However, there is a dearth of information about the effects of postpartum depression and pain on infant care and development. ... Depression Research & Treatment, 2019. 2016; (Article 4518979 ...
Postpartum depression (PPD) is a significant health issue for many new mothers in the weeks and months following a child's birth. Quantitative data suggest that a mother's PPD negatively impacts healthcare decision-making for the child via routine well-baby visits and pediatric care.
Although it has been recognized that the vulnerability for depression continues for 6 months after delivery (14-16), according to DSM-5, depression with postpartum onset is an episode of major depression that occurs in the 4 weeks following delivery. In any case, further research should extend the follow-up to a longer period of time, for ...
P ostpartum depression (PPD) is a mood disorder that a ects 10 to 15% of new. mothers. In the United States the prevalence of PPD ranges from 7 to 20%, but. most studies suggest rates between 10 ...
Background/Objectives: Postpartum depression is usually defined as a major depressive episode that occurs shortly after childbirth. This condition is most commonly found in females; however, paternal postpartum depression has begun to attract more research attention. This study aims to identify different instruments for measuring this mental health problem and to detect risk factors as well as ...
Postpartum depression is widely recognized as a significant health threat to the mother and the rest of the family, and thus to society, but the biggest threat is to the lifetime health prospects of the newborn infant. Given the health significance of postpartum depression, recent research about the risk factors for this condition, and ...
Postpartum emotional issues, including postpartum blues, postpartum psychosis, and postpartum depression (PPD), affect many mothers worldwide. The prevalence of postpartum blues ranges from 300 to 750 per 1,000 mothers, while postpartum psychosis has a prevalence of 0.89-2.6 cases per 1,000 births.
Introduction. Postpartum depression is a complex condition that is characterized by emotional and psychological responses to the birth of a child. This set of circumstances poses a high risk to some mothers in the form of depression and other concerns that impact mental health and wellbeing. The issues related to postpartum depression are often ...
The article "Understanding the needs of women with postnatal depression" is a 2010 publication in the journal of Nursing Standard volume 24, issue 46, from page 47 to 56 authored by Karen Robertson. The author of this article focuses on the topic of postpartum depression with special attention to diagnosing the disorder, and some of the ...
Stigma and Postpartum Depression CDC research shows that nationally, about 1 in 8 women experience symptoms of postpartum depression. While 80 percent of new moms may experience baby blues during the first two weeks following the birth of their child, postpartum depression impacts 15-20 percent of moms. Left untreated,
Activity During Pregnancy and Postpartum Depression. Studies have shown that women's mood and cardiorespiratory fitness improve when they engage in moderate-intensity physical activity in the weeks and months after giving birth to a child. Complementary Therapy for Postpartum Depression in Primary Care. Thus, the woman faced frustration and ...
Depression in the postpartum period has been linked to poor parental bonding, child abuse, and neglect. Furthermore, poor bonding has been found consistently with more cesarean births than vaginal. For years, researchers have been searching for a correlation between obstetric method of delivery and incidence of PPD.
What causes postpartum depression? More research is needed to determine the link between the rapid drop in hormones after delivery and depression. The levels of estrogen and progesterone increase tenfold during pregnancy but drop sharply after delivery. By three days postpartum, levels of these hormones drop back to pre-pregnancy levels.
Postpartum depression is a severe condition that may affect a patient's life significantly. It can cause individuals to feel anxious, experience mood swings and changes in appetite, and have thoughts of harming their newborn children. The management strategy for this illness can include drug therapy along with alternative remedies.
A total of 122 studies (out of 3712 references retrieved from bibliographic databases) were included in this systematic review. The results of the studies were synthetized into three categories: (a) the maternal consequences of postpartum depression, including physical health, psychological health, relationship, and risky behaviors; (b) the infant consequences of postpartum depression ...
Postpartum Depression has many underlying causes and cannot be narrowed down to one single factor. However, mental and physical changes after birth can definitely make an impact on the manifestation of PPD. Every woman experiences changes in their body after giving birth. However, the body changes come with hormone changes, and the hormones ...
According to a 2018 systematic review by the Agency for Healthcare Research and Quality (AHRQ), understanding the relationship is challenging "because women with depression may have difficulty initiating and sustaining breastfeeding, and women who experience breastfeeding difficulties may develop depression" (p. 107).
According to research from the International Journal of Public Health Science, postpartum rage is defined as an emotional state that can occur in young mothers after giving birth. It involves ...
The probiotics supplement and microbiome research brand Seed has donated their billboard to Swehl, the breastfeeding start-up that created the cookie campaign with Ms. Baz. Clear Channel still has ...