
- Why We Are Unique
- Annual Reports
- BCA Policies
- What We Fund

How To Apply
- Site Visits
- Ways To Give
- Host An Event
- Shop for BCA
- Go For Pink
- Newsletters
- Patient Resources
- Supplies & Wigs
Exceptional Project Grants
Breast Cancer Alliance invites clinical doctors and research scientists at any stage of their careers, including post docs, whose current proposal is focused on breast cancer, to apply for an Exceptional Project Grant. This award recognizes creative, unique and innovative research and is open to applicants at institutions in the contiguous United States. No for-profit institutions may apply. This is a one year grant for a total of $100,000.
The term of the Exceptional Project Grant is one year, beginning on March 1, 2025. Prior to submission of a formal grant proposal, BCA requires a Letter of Intent (LOI) and a separate CV that must be completed using the form linked here and must be submitted by midnight on March 31, 2024. The LOI must contain the applicant’s name, job title and institution, contact information, project title and hypothesis, outline the research aim(s) and methods, and include a brief discussion of the project’s potential impact. The CV should be in the current NIH biosketch format. The grant provides salary support and project costs for a total of $100,000 (distributed over the one-year period as noted above.) Indirect costs, which are included in the $100,000 award, must be limited to 8% of total direct costs.
Applicants will be informed by mid-May 2024 whether they have been invited to proceed with a formal application. Researchers should coordinate with their institutions, as BCA will accept a maximum of ONLY TWO LOIs PER INSTITUTION (YIG or XP.) References for the LOI are not required.
Full applications for the Exceptional Project Grant are due on or before midnight EDT on July 19, 2024 and are by invitation only. An Independent External Review Committee reviews and evaluates the applications. Based on their results and subsequent review by the Grants Committee, recommendations will be made to the BCA Board for final approval. Applicants will be notified by mid-February 2025 of the decision regarding their proposals. Winners must submit a midterm replrt by August 31, 2026 and a final report within 60 days of February 28, 2026. Failure to submit the midterm report will result in forfeiture of any remaining grant funds. A virtual site visit with BCA staff and supporters is also required.
For questions about the application process email: [email protected] or see the FAQ's below
**You may only submit an LOI for each proposal for either an Exceptional Project Grant or a Young Investigator Grant. It is your choice as to which application best suits your experience.
Young Investigator Grants
To encourage a commitment to breast cancer research, Breast Cancer Alliance invites clinical doctors and research scientists who are in the early stages of their careers, including post docs, whose current proposal is focused on breast cancer, to apply for funding for the Young Investigator Grant. This grant is open to applicants at institutions in the contiguous United States. No for-profit institutions may apply.This is a two-year grant for a total of $125,000, with half the grant award being paid out each year.
Applicants for the 2025 award must (i) not have held a tenure track faculty or tenure track research position for more than four years following completion of their training, as of March 1, 2025; (ii) not have been or are not a principal investigator on an NIH R01 or equivalent national/international non-mentored award as of March 1, 2025; and (iii) dedicate at least 50% of their work effort to research. This grant is intended to help advance the careers of young researchers who do not yet have their own major grant support but who design and conduct their own independent research projects .
The term of the Young Investigator Grant is two years, beginning on March 1, 2025. The grant provides salary support and project costs for a total of $125,000 (distributed over the two-year period as noted above.) Indirect costs, which are included in the $125,000 award, must be limited to 8% of total direct costs.
Prior to submission of a formal grant proposal, BCA requires a Letter of Intent (LOI) and a separate CV that must be completed using the form linked here and must be submitted by midnight on March 31, 2024. The LOI must contain the applicant’s name, job title and institution at the top of the page, and the applicant’s contact information. The document should state the project title and hypothesis, outline the research aim(s) and methods, and include a brief discussion of the project’s potential impact. The CV should be in the current NIH biosketch format.
Full applications for the Young Investigator Grant are due on or before midnight EDT on July 19, 2024 and are by invitation only. An Independent External Review Committee reviews and evaluates the applications. Based on their results and subsequent review by the Grants Committee, recommendations will be made to the BCA Board for final approval. Applicants will be notified by mid-February 2025 of the decision regarding their proposals. Winners must submit a midterm replrt by February 28, 2026 and a final report within 60 days of February 28, 2027. Failure to submit the midterm report will result in forfeiture of any remaining grant funds. A virtual site visit with BCA staff and supporters is also required.
**You may only submit an LOI for each proposal for either an Exceptional Project Grant or a Young Investigator Grant. It is your choice as to which application best suits your experience.
FAQs about Research Applications
Exceptional Project Applicants:
Question: Are Exceptional Projects open to clinical doctors and research scientists at any stage of their careers, including postdoctoral fellows?
Answer: Yes
Question: Is it permitted to have more than one PI on an Exceptional Project?
Question: If we submit with multi-PI’s, would we need a letter of support from both department heads?
Answer: If more than one individual will be formally listed as a PI on the project, and they are from different institutions, then a someone authorized to speak on behalf of the institution in terms of committing to support, and who has direct knowledge of the status and qualifications of the PI, should each sign off on behalf of his/her respective institution.
Question: Are there any specific eligibility requirements regarding the subject matter of the project and additional funding sources? For example, if I am working on a project that is partially funded by another source, would it be possible to apply for the BCA Exceptional Project Grant to cover a component of the project (for example, sequencing studies) that is not currently included in the budget of any other awarded grant?
Answer: There is no limitation on the subject matter of the project as long as it is reasonably related to the treatment, prevention or cure of breast cancer. However, the proposed project should be an exceptional project that can stand alone. Existing funding for a related aspect of the proposed project is not in itself disqualifying, but we would not, for example, consider the payment for sequencing studies in an otherwise funded project to be eligible for an exceptional project grant.
Question: Can affiliated institutions with separate DUNS numbers submit more than 2 applications?
Answer: If multiple affiliated institutions within a university or health care system each have separate DUNS numbers, each can submit up to 2 applications total, XP or YIG.
Young Investigator Grants:
Question: Are postdoctoral fellows eligible to apply for this award?
Answer: Yes, as long as they meet all the stated eligibility criteria for a Young Investigator. They must also provide a letter of support from their institution confirming that they will have institutional resources available to them throughout the two-year term of the grant.
Question: Is an LOI required for this type of grant?
Question: If an applicant for the Young Investigator Grant is currently funded by the R00 phase of an NIH K99/R00 Pathway to Independence Award, are they eligible to apply?
General and Application-related questions:
Question: What is the preferred format for submission of a full application?
Answer: The application should be submitted through the link on this page with all required components included in the document. Some individuals providing reference letters on behalf of an applicant prefer to send those separately; if this is the case, please let the Research Grants team know that a letter of reference will be arriving separately from the application.
Question: Is there a preferred format for the biohazards, human investigation and laboratory animal statements required for the application?
Answer: There content of each required statement should follow the NIH requirements for the corresponding statements.
Question: Do you require a hard copy of the application to accompany the emailed copy?
Answer: No, but the electronic submission must be submitted by the deadline date or it will not be considered for funding.
Question: Do you need to be a US citizen to apply for a BCA grant?
Answer: You do not have to be a US citizen to apply, but you must be affiliated with a US institution at which the grant project will be carried out.
Question: Does being a reviewer on BCA’s External Review Committee make you ineligible to submit an application for an Exceptional Project grant?
Answer: Being a current reviewer is not disqualifying for submission of an LOI or application, but an individual who is submitting an LOI, or is invited to submit a full application based on an LOI, would not be eligible to serve as a reviewer during the time his/her LOI or application are pending review.
Screening and Support Services Grants
Breast Cancer Alliance offers grants to providers that conduct screening and diagnostic breast cancer services for the underserved: screening and diagnostic mammograms, biopsies, ultrasounds and MRIs. The programs must be located in Connecticut and/or in Westchester County, New York. The term of the Screening and Support Services Grant is one calendar year beginning April 1. Breast Cancer Alliance does not fund patient counseling, patient navigation, office supplies, medical supplies, financial aid (i.e. gas bills, transportation, rent, overhead, grocery gift certificates, fringe benefits, etc.) printing costs, travel costs, marketing costs, recruitment costs or training programs.
- Regular applications are due by on or before midnight on December 11, 2024 .
- Applications received after the deadline will not be considered.
- Funding is determined on an annual basis, per each grant cycle. Prior gift allocations do not guarantee future grants.
- Grant recipients must submit the required midterm report by October 1, 2024 and a final report by April 30, 2025 .
- Any publicity associated with the program must acknowledge Breast Cancer Alliance as a supporter as much as is reasonably possible.
The Grants Committee of Breast Cancer Alliance reviews and evaluates each grant proposal. The results of the Grants Committee’s evaluations and subsequent recommendations are presented to the BCA Board for approval. Applicants are notified by March 2025 of the decision regarding their proposals.
The 2023 final report template is available here.
The 2024 midterm report template is available here and due no later than October 1, 2024.
The 2024 final report template is available here and due no later than April 30, 2025.
The 2025 application is available here . If you would like a pdf for drafting purposes, please email [email protected]
For questions about any education and outreach grants please email: [email protected]
Breast Surgery Fellowships
The term of the Breast Surgical Fellowship is one year with a grant award of $75,000, from August 1 through July 31. Institutions making application for the 2024 award must have an established breast fellowship program, be SSO accredited for a minimum of 2 years, and be located in Connecticut, New Jersey or New York.
Any publicity associated with this program and any papers published in association with the work done during or as a result of this fellowship must recognize the Breast Cancer Alliance. Institutions should only put forth applicants who are US citizens, are a MD, and have successfully completed a general surgery residency at a US medical center. No more than one CV may be submitted for consideration per institution, and no more than one fellowship will be awarded to any individual SSO accredited institution. For questions about fellowship funding please email: [email protected] . Applications are due on or before midnight on December 1, 2024 and should include two references to accompany the candidates CV . Applications after the deadline will not be considered. Applicants will be notified by March 2025 of the decision regarding their proposals.
The 2025 application is not yet available.

Sample Cancer Epidemiology Grant Applications
On this page..., orientation to sample applications, sample applications, links to other sample applications.

The National Cancer Institute (NCI) frequently receives questions from investigators for examples of successfully funded grant applications. Several investigators and their organizations agreed to let the Epidemiology and Genomics Research Program (EGRP) post excerpts of their grant applications online. The applications in the table below are excellent examples of grantsmanship.
EGRP is grateful to the investigators for enabling our Program to deliver this valuable resource. Certain details are redacted, such as social security numbers, budgets, home addresses, and phone numbers. Additionally, to minimize the file size, EGRP excluded sections of the original application that provide routine details, such as lists of performance sites and key personnel, biographical sketches, and bibliographies. As a result, the grant applications accessible through the links below do not include all sections that appear in the SF424 (R&R) used to apply for grants.
The text of the grant applications is copyrighted. Investigators and others may use the text from these same applications only for nonprofit educational purposes provided the content remains unchanged and the Principal Investigator(s), their organization(s), and NCI are credited.
Note: The table below highlights examples of grant applications that were submitted before January 25, 2023, the effective day of the NIH Data Management and Sharing (DMS) policy. EGRP anticipates updating the examples of grant applications that comply with the new DMS policy in the latter part of 2024. In the meantime, please refer to EGRP’s webpage on Data and Resource Management and Sharing Plans for more information on preparing DMS plans.
- Behavioral Research Program, Division of Cancer Control and Population Sciences, NCI
- Healthcare Delivery Research Program, Division of Cancer Control and Population Sciences, NCI
- Implementation Science Team, Division of Cancer Control and Population Sciences, NCI
- National Institute of Allergy and Infectious Diseases
Advances in Breast Cancer Research
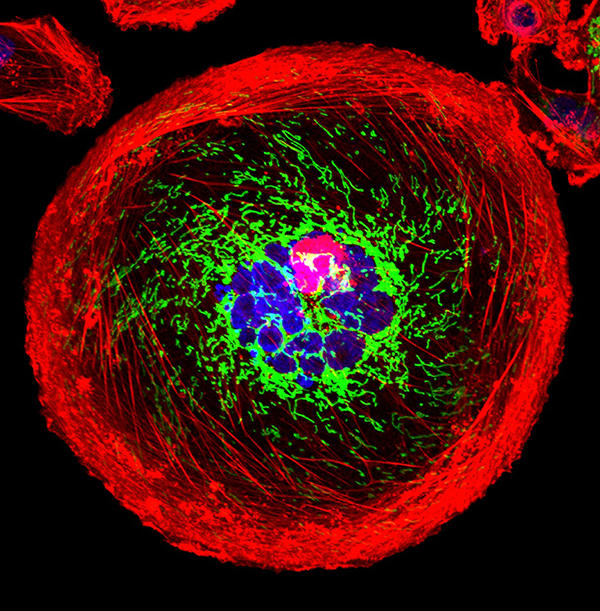
A polyploid giant cancer cell (PGCC) from triple-negative breast cancer.
NCI-funded researchers are working to advance our understanding of how to prevent, detect, and treat breast cancer. They are also looking at how to address disparities and improve quality of life for survivors of the disease.
This page highlights some of what's new in the latest research for breast cancer, including new clinical advances that may soon translate into improved care, NCI-supported programs that are fueling progress, and research findings from recent studies.
Early Detection of Breast Cancer
Breast cancer is one of a few cancers for which an effective screening test, mammography , is available. MRI ( magnetic resonance imaging ) and ultrasound are also used to detect breast cancer, but not as routine screening tools for people with average risk.
Ongoing studies are looking at ways to enhance current breast cancer screening options. Technological advances in imaging are creating new opportunities for improvements in both screening and early detection.
One technology advance is 3-D mammography , also called breast tomosynthesis . This procedure takes images from different angles around the breast and builds them into a 3-D-like image. Although this technology is increasingly available in the clinic, it isn’t known whether it is better than standard 2-D mammography , for detecting cancer at a less advanced stage.
NCI is funding a large-scale randomized breast screening trial, the Tomosynthesis Mammographic Imaging Screening Trial (TMIST) , to compare the number of advanced cancers detected in women screened for 5 years with 3-D mammography with the number detected in women screened with 2-D mammography.
Two concerns in breast cancer screening, as in all cancer screening, are:
- the potential for diagnosing tumors that would not have become life-threatening ( overdiagnosis )
- the possibility of receiving false-positive test results, and the anxiety that comes with follow-up tests or procedures
As cancer treatment is becoming more individualized, researchers are looking at ways to personalize breast cancer screening. They are studying screening methods that are appropriate for each woman’s level of risk and limit the possibility of overdiagnosis.
For example, the Women Informed to Screen Depending on Measures of Risk (WISDOM) study aims to determine if risk-based screening—that is, screening at intervals that are based on each woman’s risk as determined by her genetic makeup, family history , and other risk factors—is as safe, effective, and accepted as standard annual screening mammography.
WISDOM is also making a focused effort to enroll Black women in the trial. Past studies tended to contain a majority of White women and therefore, there is less data on how screening can benefit Black women. Researchers are taking a number of steps to include as many Black women as possible in the study while also increasing the diversity of all women enrolled.
Breast Cancer Treatment
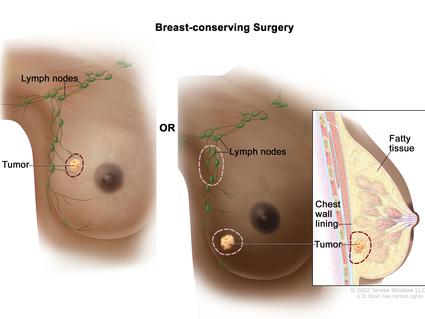
The mainstays of breast cancer treatment are surgery , radiation , chemotherapy , hormone therapy , and targeted therapy . But scientists continue to study novel treatments and drugs, along with new combinations of existing treatments.
It is now known that breast cancer can be divided into subtypes based on whether they:
- are hormone receptor (HR) positive which means they express estrogen and/or progesterone receptors ( ER , PR )
Shortening Radiation Therapy for Some with Early Breast Cancer
A condensed course was as effective and safe as the standard course for women with higher-risk early-stage breast cancer who had a lumpectomy.
As we learn more about the subtypes of breast cancer and their behavior, we can use this information to guide treatment decisions. For example:
- The NCI-sponsored TAILORx clinical trial. The study, which included patients with ER-positive, lymph node-negative breast cancer, found that a test that looks at the expression of certain genes can predict which women can safely avoid chemotherapy.
- The RxPONDER trial found that the same gene expression test can also be used to determine treatment options in women with more advanced breast cancer. The study found that some postmenopausal women with HR positive, HER-2 negative breast cancer that has spread to several lymph nodes and has a low risk of recurrence do not benefit from chemotherapy when added to their hormone therapy.
- The OFSET trial is comparing the addition of chemotherapy to usual treatment ( ovarian function suppression plus hormone therapy) to usual treatment alone in treating premenopausal estrogen receptor (ER)-positive/HER2-negative breast cancer patients who are at high risk of their cancer returning. This will help determine whether or not adding chemotherapy helps prevent the cancer from returning.
Genomic analyses, such as those carried out through The Cancer Genome Atlas (TCGA) , have provided more insights into the molecular diversity of breast cancer and eventually could help identify even more breast cancer subtypes. That knowledge, in turn, may lead to the development of therapies that target the genetic alterations that drive those cancer subtypes.
HR-Positive Breast Cancer Treatment
Hormone therapies have been a mainstay of treatment for HR-positive cancer. However, there is a new focus on adding targeted therapies to hormone therapy for advanced or metastatic HR-positive cancers. These treatments could prolong the time until chemotherapy is needed and ideally, extend survival. Approved drugs include:

Drug Combo Effective for Metastatic Breast Cancer in Younger Women
Ribociclib plus hormone therapy were superior to standard chemotherapy combos in a recent trial.
- Palbociclib (Ibrance) , ribociclib (Kisqali) , and everolimus (Afinitor) have all been approved by the FDA for use with hormone therapy for treatment of advanced or metastatic breast cancer. Ribociclib has been shown to increase the survival of patients with metastatic breast cancer . It has also shown to slow the growth of metastatic cancer in younger women when combined with hormone therapy.
- Elacestrant (Orserdu) is approved for HR-positive and HER2-negative breast cancer that has a mutation in the ESR1 gene, and has spread. It is used in postmenopausal women and in men whose cancer has gotten worse after at least one type of hormone therapy.
- Abemaciclib (Verzenio) can be used with or after hormone therapy to treat advanced or metastatic HR-positive, HER2-negative breast cancer. In October 2021, the Food and Drug Administration ( FDA ) approved abemaciclib in combination with hormone therapy to treat some people who have had surgery for early-stage HR-positive, HER2-negative breast cancer.
- Alpelisib (Piqray) is approved to be used in combination with hormone therapy to treat advanced or metastatic HR-positive, HER2-negative breast cancers that have a mutation in the PIK3CA gene .
- Sacituzumab govitecan-hziy (Trodelvy) is used for HR-positive and HER2-negative breast cancer that has spread or can't be removed with surgery. It is used in those who have received hormone therapy and at least two previous treatments. It has shown to extend the amount of time that the disease doesn't get worse ( progression-free survival ) and also shown to improve overall survival .
HER2-Positive Breast Cancer Treatment
The FDA has approved a number of targeted therapies to treat HER2-positive breast cancer , including:
- Trastuzumab (Herceptin) has been approved to be used to prevent a relapse in patients with early-stage HER2-positive breast cancer.
- Pertuzumab (Perjeta) is used to treat metastatic HER2-positive breast cancer, and also both before surgery ( neoadjuvant ) and after surgery ( adjuvant therapy ).
- Trastuzumab and pertuzumab together can be used in combination with chemotherapy to prevent relapse in people with early-stage HER2-positive breast cancer. Both are also used together in metastatic disease, where they delay progression and improve overall survival.
- Trastuzumab deruxtecan (Enhertu) is approved for patients with advanced or metastatic HER2-positive breast cancer who have previously received a HER2-targeted treatment. A 2021 clinical trial showed that the drug lengthened the time that people with metastatic HER2-positive breast cancer lived without their cancer progressing. The trial also showed that it was better at shrinking tumors than another targeted drug, trastuzumab emtansine (Kadcyla).
- Tucatinib (Tukysa) is approved to be used in combination with trastuzumab and capecitabine (Xeloda) for HER2-positive breast cancer that cannot be removed with surgery or is metastatic. Tucatinib is able to cross the blood–brain barrier, which makes it especially useful for HER2-positive metastatic breast cancer, which tends to spread to the brain.
- Lapatinib (Tykerb) has been approved for treatment of some patients with HER2-positive advanced or metastatic breast cancer, together with capecitabine or letrozole.
- Neratinib Maleate (Nerlynx) can be used in patients with early-stage HER2-positive breast cancer and can also be used together with capecitabine (Xeloda) in some patients with advanced or metastatic disease.
- Ado-trastuzumab emtansine (Kadcyla) is approved to treat patients with metastatic HER2-positive breast cancer who have previously received trastuzumab and a taxane . It's also used in some patients with early-stage HER2-positive breast cancer who have completed therapy before surgery ( neoadjuvant ) and have residual disease at the time of surgery.
HER2-Low Breast Cancer
A newly defined subtype, HER2-low, accounts for more than half of all metastatic breast cancers. HER2-low tumors are defined as those whose cells contain lower levels of the HER2 protein on their surface. Such tumors have traditionally been classified as HER2-negative because they did not respond to drugs that target HER2.
However, in a clinical trial, trastuzumab deruxtecan (Enhertu) improved the survival of patients with HER2-low breast cancer compared with chemotherapy , and the drug is approved for use in such patients.
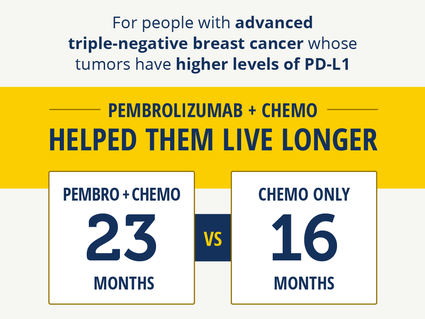
Immunotherapy Improves Survival in Triple-Negative Breast Cancer
For patients whose tumors had high PD-L1 levels, pembrolizumab with chemo helped them live longer.
Triple-Negative Breast Cancer Treatment
Triple-negative breast cancers (TNBC) are the hardest to treat because they lack both hormone receptors and HER2 overexpression , so they do not respond to therapies directed at these targets. Therefore, chemotherapy is the mainstay for treatment of TNBC. However, new treatments are starting to become available. These include:
- Sacituzumab govitecan-hziy (Trodelvy) is approved to treat patients with TNBC that has spread to other parts of the body . Patients must have received at least two prior therapies before receiving the drug.
- Pembrolizumab (Keytruda) is an immunotherapy drug that is approved to be used in combination with chemotherapy for patients with locally advanced or metastatic TNBC that has the PD-L1 protein. It may also be used before surgery (called neoadjuvant ) for patients with early-stage TNBC, regardless of their PD-L1 status.
- PARP inhibitors, which include olaparib (Lynparza) and talazoparib (Talzenna) , are approved to treat metastatic HER2-negative or triple-negative breast cancers in patients who have inherited a harmful BRCA gene mutation. Olaparib is also approved for use in certain patients with early-stage HER2-negative or triple-negative breast cancer.
- Drugs that block the androgen receptors or prevent androgen production are being tested in a subset of TNBC that express the androgen receptor.
For a complete list of drugs for breast cancer, see Drugs Approved for Breast Cancer .
NCI-Supported Breast Cancer Research Programs
Many NCI-funded researchers working at the NIH campus, as well as across the United States and world, are seeking ways to address breast cancer more effectively. Some research is basic, exploring questions as diverse as the biological underpinnings of cancer and the social factors that affect cancer risk. And some are more clinical, seeking to translate this basic information into improving patient outcomes. The programs listed below are a small sampling of NCI’s research efforts in breast cancer.
TMIST is a randomized breast screening trial that compares two Food and Drug Administration (FDA)-approved types of digital mammography, standard digital mammography (2-D) with a newer technology called tomosynthesis mammography (3-D).
The Breast Specialized Programs of Research Excellence (Breast SPOREs) are designed to quickly move basic scientific findings into clinical settings. The Breast SPOREs support the development of new therapies and technologies, and studies to better understand tumor resistance, diagnosis, prognosis, screening, prevention, and treatment of breast cancer.
The NCI Cancer Intervention and Surveillance Modeling Network (CISNET) focuses on using modeling to improve our understanding of how prevention, early detection, screening, and treatment affect breast cancer outcomes.
The Confluence Project , from NCI's Division of Cancer Epidemiology and Genetics (DCEG) , is developing a research resource that includes data from thousands of breast cancer patients and controls of different races and ethnicities. This resource will be used to identify genes that are associated with breast cancer risk, prognosis, subtypes, response to treatment, and second breast cancers. (DCEG conducts other breast cancer research as well.)
The Black Women’s Health Study (BWHS) Breast Cancer Risk Calculator allows health professionals to estimate a woman’s risk of developing invasive breast cancer over the next 5 years. With the NCI-funded effort, researchers developed a tool to estimate the risk of breast cancer in US Black women. The team that developed the tool hopes it will help guide more personalized decisions on when Black women—especially younger women—should begin breast cancer screening.
The goal of the Breast Cancer Surveillance Consortium (BCSC) , an NCI-funded program launched in 1994, is to enhance the understanding of breast cancer screening practices in the United States and their impact on the breast cancer's stage at diagnosis, survival rates, and mortality.
There are ongoing programs at NCI that support prevention and early detection research in different cancers, including breast cancer. Examples include:
- The Cancer Biomarkers Research Group , which promotes research in cancer biomarkers and manages the Early Detection Research Network (EDRN) . EDRN is a network of NCI-funded institutions that are collaborating to discover and validate early detection biomarkers. Within the EDRN, the Breast and Gynecologic Cancers Collaborative Group conducts research on breast and ovarian cancers.
- NCI's Division of Cancer Prevention houses the Breast and Gynecologic Cancer Research Group which conducts and fosters the development of research on the prevention and early detection of breast and gynecologic cancers.
Breast Cancer Survivorship Research
NCI’s Office of Cancer Survivorship, part of the Division of Cancer Control and Population Sciences (DCCPS), supports research projects throughout the country that study many issues related to breast cancer survivorship. Examples of studies funded include the impact of cancer and its treatment on physical functioning, emotional well-being, cognitive impairment , sleep disturbances, and cardiovascular health. Other studies focus on financial impacts, the effects on caregivers, models of care for survivors, and issues such as racial disparities and communication.
Breast Cancer Clinical Trials
NCI funds and oversees both early- and late-phase clinical trials to develop new treatments and improve patient care. Trials are available for breast cancer prevention , screening , and treatment .
Breast Cancer Research Results
The following are some of our latest news articles on breast cancer research and study updates:
- Can Some People with Breast Cancer Safely Skip Lymph Node Radiation?
- Study Adds to Debate about Mammography in Older Women
- Pausing Long-Term Breast Cancer Therapy to Become Pregnant Appears to Be Safe
- A Safer, Better Treatment Option for Some Younger Women with Breast Cancer
- Shorter Course of Radiation Is Effective, Safe for Some with Early-Stage Breast Cancer
- Pembrolizumab Improves Survival in Advanced Triple-Negative Breast Cancer
View the full list of Breast Cancer Research Results and Study Updates .
Sample Healthcare Delivery Research Grant Applications
The National Cancer Institute (NCI) frequently receives requests for examples of funded grant applications. Several investigators and their organizations agreed to let the Healthcare Delivery Research Program (HDRP) post excerpts of their healthcare delivery research grant applications online.
We are grateful to the investigators and their institutions for allowing us to provide this important resource to the community. We include a copy of the SF 424 R&R Face Page, Project Summary/Abstract (Description), Project Narrative, Specific Aims, and Research Strategy; we do not include other SF 424 (R&R) forms or requisite information found in the full grant application (e.g., performance sites, key personnel, biographical sketches). To maintain confidentiality, we have redacted some information from these documents (e.g., budgets, social security numbers, home addresses, introduction to revised application).
Sample Applications
R01: personalized screening for lung cancer: the importance of co-existing chronic conditions to clinical practice and policy, principal investigator.

Grant Mechanism & Award Number
R01CA249506-01
R01: Predicting and Addressing Colonoscopy Non-adherence in Community Settings

R01CA218923-01A1
R01: Using MOST to EMPOWER: Optimizing an Emotional Regulation Intervention to Enhance Well-being Among Young Adult Cancer Survivors
Principal investigators.

R01CA242849-01
R01: Improving Informal Caregivers' and Cancer Survivors' Psychological Distress, Symptom Management and Health Care Use

R01CA224282-01A1
R03: Statewide Assessment of HPV Vaccination Among Childhood Cancer Survivors

1R03CA216174-01A1
R03: Multi-center Evaluation of Digital Breast Tomosynthesis with Synthesized Two-dimensional Mammography for Breast Cancer Screening

R03CA223725-01
R21: Improving Transition Readiness in Adolescent and Young Adult (AYA) Survivors of Childhood Cancer

R21CA222936-01A1
R50: Natural History of Lung Cancer Diagnosed Within and Across Diverse Health Systems Implementing Lung Cancer Screening

R50CA251966-01
Additional Details
Copyright information.
The text of the grant applications is copyrighted. Investigators and others may use the text from these applications only for nonprofit educational purposes provided that the content remains unchanged and that the Principal Investigator(s), their organization(s), and NCI are credited.
Accessibility
Individuals using assistive technology (e.g., screen reader, Braille reader, etc.) who experience difficulty accessing any information should send an email to the HDRP team ( [email protected] ).
Other Sample Grants
See examples of successfully funded grant applications.
Currently Open Notice of Funding Opportunities Relevant to HDRP
See the currently open notice of funding opportunities (NOFOs) sponsored or co-sponsored by HDRP; other NOFOs relevant to HDRP; and NIH and NCI Parent and Omnibus NOFOs for investigator-initiated research.

Sample Behavioral Research Grant Applications
- Behavioral Research Program
- Funding Opportunities
- Sample Grant Applications
Fifteen investigators and their organizations agreed to let the Behavioral Research Program (BRP) post excerpts of their grant applications to demonstrate what a successful grant application looks like.
Sample Applications
R01: reducing chemotherapy toxicity in older adults, principal investigator.

Grant Mechanism & Award Number
R01CA177592-01
R01: Sleep Disturbance, Inflammation, and Cellular Aging in Breast Cancer Survivors

R01CA207130-01
R01: Disseminating Evidence-Based Interventions to Control Cancer

R01CA160327-01A1
R01: Increasing Implementation of Evidence-Based Interventions at Low-Wage Worksites

R01CA160217-01A1
R01: Establishing The Program Sustainability Action Planning Training Model

1R01CA203844-01A1
R01: Implementing Tobacco Use Treatment Guidelines in Community Health Centers in Vietnam

R01CA175329-01A1
R01: Using Technology to Scale-Up an Occupational Sun Protection Policy Program

1R01CA210259-01A1
R21: Effective Training Models for Implementing Health-Promoting Practices Afterschool

1R21CA201567-01A1
Preventing Falls and Frailty in Prostate Cancer Survivors: GET FIT Prostate

1R01CA222605-01A1
Sexual Health Empowerment for Cervical Health Literacy and Cancer Prevention

1R01CA181047-01A1
Vegetable Garden Feasibility Trial to Promote Function in Older Cancer Survivors

1R21CA182508-01
A Primary Care Multilevel mHealth Colorectal Cancer Screening (mCRC) Intervention

1R01CA178941-01
Participant Beliefs and Bias in a Randomized Controlled Trial

1R03CA178272-01
Constituent Yields and Biomarkers of Exposure for Tobacco Product Regulation

Irina Stepanov, Ph.D. University of Minnesota
1R01CA179246-01
Multisensory Processing Across Lifespan and Links to Cognition

1R21CA183492-01
BRP is grateful to the investigators who enabled our program to deliver this valuable resource. Please note that certain details are redacted, such as social security numbers, budgets, and home addresses. Additionally, to minimize the file size, BRP excluded sections of the original application that provide routine details, such as lists of performance sites and key personnel, biographical sketches, and bibliographies. As a result, SF424 (R&R) sections do not appear in these samples.
The text of the grant applications is copyrighted. Investigators and others may use the text from these applications only for nonprofit educational purposes provided that the content remains unchanged and that the Principal Investigator(s), their organization(s), and NCI are credited.
Accessibility. If you are using assistive technology, such as a screen reader or Braille reader, and have trouble accessing information from the sample applications, please send an email to [email protected] .
Other Cancer Grant Applications
See examples of successfully funded grant applications from other NCI programs.
- Epidemiology Research Grant Applications
- Healthcare Delivery Research Grant Applications
Current BRP Funding Opportunities
BRP provides funding support for a comprehensive program of research, ranging from basic behavioral research to the development, testing, and dissemination of interventions in areas including, but not limited to, tobacco use, screening, dietary behavior, sun protection, emotion regulation, and physical activity.
- Find Funding Opportunities
- BRP-Funded Grants
- How to Apply
- Featured Grantees
- Affective Science, Decision-Making, and Emotion
- Aging and Cancer
- Alcohol and Cancer
- Nutrition and Dietary Behaviors
- Obesity and Energy Balance
- Perception, Attention, and Cognition
- Physical Activity
- Social Media
- Sun Protection Behaviors
- Tobacco Control
- Research Resources and Tools
- Adherence to Oral Anticancer Agents
- Biobehavioral Pathways Network
- Cognitive Changes
- Communication and Decision-Making
- Multimorbidity and Cancer Control
- Medical Imaging Workshop
- Sleep and Circadian Function
- Alcohol & Cancer
- Behavioral Genetics
- Dyadic Processes
- Environment & Policy Context
- Nutrition & Dietary Behaviors
- Trans-NCI Obesity & Cancer Working Group
- Sleep & Circadian Function
- Translational Research
- FLASHE Insights: Parent–Adolescent Dyads
- FLASHE Publications
- FLASHE Study Webinars
- Food Attitudes & Behaviors
- NCI-CRUK Sandpit Workshops
- TREC Centers
- ENICTO Consortium
- Digital Health
- Addressing Communication Inequalities to Advance Health Equity
- Health and Science Misinformation
- CEBP Focus Issue
- Special Section
- Smart and Connected Health
- Social Media and Health
- Assessing Cancer Patient Tobacco Use
- Cancer Center Cessation Initiative
- Collaborative Research on Addiction at NIH
- Co-Use of Tobacco with Alcohol and Cannabis
- Electronic Nicotine Delivery Systems (ENDS) Use
- Smokeless Tobacco and Public Health
- SCALE Collaboration
- Secondhand Smoke Exposure
- Smoking Cessation
- Tobacco and HIV
- Monograph 1
- Monograph 2
- Monograph 3
- Monograph 4
- Monograph 5
- Monograph 6
- Monograph 7
- Monograph 8
- Monograph 9
- Monograph 10
- Monograph 11
- Monograph 12
- Monograph 13
- Monograph 14
- Monograph 15
- Monograph 16
- Monograph 17
- Monograph 18
- Monograph 19
- Monograph 20
- Monograph 21
- Monograph 22
- Monograph 23
- Tobacco Regulatory Science
- Survey Topics
- 2022-2023 TUS-CPS Data
- 2018–2019 Technical Notes
- Table 1: Smoking Status
- Table 2: Home & Work Environment
- Table 3: E-Cigarette Use
- 2014–2015 Technical Notes
- Table 2: Home and Work Environment
- Table 3: Quit Attempts & Cessation
- Tables 4a/4b/4c: Use of Other Tobacco Products
- Table 5: Various Unique Items
- Table 6: Attitudes Toward Smoking in Public
- 2010–2011 Technical Notes
- Tables 4/4b: Use of Other Tobacco Products
- Table 7: Cessation Treatments & Methods
- 2006–2007 Technical Notes
- Table 4: Use of Other Tobacco Products
- 2003 Technical Notes
- 2001–2002 Technical Notes
- Table 3: Attitudes Toward Smoking in Public
- Table 4: Quit Attempts and Cessation
- 2000 TUS-CPS Data
- 1998–1999 Technical Notes
- Table 4. Quit Attempts and Cessation
- 1995-1996 TUS-CPS Data
- 1992-1993 TUS-CPS Data
- 2007 State Data Tables
- Health Professional Advice to Quit Smoking
- Attitudes Toward Smoking in Restaurants, Hospitals, & Indoor Work Areas
- Attitudes Toward Smoking in Indoor Sporting Events & Shopping Malls
- Attitudes Toward Smoking in Bars & Cocktail Lounges
- Quit Attempts & Cessation
- 2009 Workshop
- 2013 Webinar
- Publications
- Career and Training
- BRP Scientific News
- Research article
- Open access
- Published: 01 October 2013
Critical research gaps and translational priorities for the successful prevention and treatment of breast cancer
- Suzanne A Eccles 17 ,
- Eric O Aboagye 1 ,
- Simak Ali 1 ,
- Annie S Anderson 2 ,
- Jo Armes 7 ,
- Fedor Berditchevski 4 ,
- Jeremy P Blaydes 3 ,
- Keith Brennan 5 ,
- Nicola J Brown 6 ,
- Helen E Bryant 6 ,
- Nigel J Bundred 5 ,
- Joy M Burchell 7 ,
- Anna M Campbell 2 ,
- Jason S Carroll 9 ,
- Robert B Clarke 5 ,
- Charlotte E Coles 34 ,
- Gary JR Cook 7 ,
- Angela Cox 6 ,
- Nicola J Curtin 10 ,
- Lodewijk V Dekker 11 ,
- Isabel dos Santos Silva 12 ,
- Stephen W Duffy 13 ,
- Douglas F Easton 9 ,
- Diana M Eccles 3 ,
- Dylan R Edwards 15 ,
- Joanne Edwards 14 ,
- D Gareth Evans 5 ,
- Deborah F Fenlon 3 ,
- James M Flanagan 1 ,
- Claire Foster 3 ,
- William M Gallagher 16 ,
- Montserrat Garcia-Closas 17 ,
- Julia M W Gee 18 ,
- Andy J Gescher 28 ,
- Vicky Goh 7 ,
- Ashley M Groves 8 ,
- Amanda J Harvey 33 ,
- Michelle Harvie 5 ,
- Bryan T Hennessy 20 ,
- Stephen Hiscox 18 ,
- Ingunn Holen 6 ,
- Sacha J Howell 5 ,
- Anthony Howell 5 ,
- Gill Hubbard 21 ,
- Nick Hulbert-Williams 22 ,
- Myra S Hunter 7 ,
- Bharat Jasani 18 ,
- Louise J Jones 13 ,
- Timothy J Key 23 ,
- Cliona C Kirwan 5 ,
- Anthony Kong 23 ,
- Ian H Kunkler 24 ,
- Simon P Langdon 24 ,
- Martin O Leach 17 ,
- David J Mann 1 ,
- John F Marshall 13 ,
- Lesley Ann Martin 17 ,
- Stewart G Martin 11 ,
- Jennifer E Macdougall 25 ,
- David W Miles 7 ,
- William R Miller 24 ,
- Joanna R Morris 4 ,
- Sue M Moss 13 ,
- Paul Mullan 26 ,
- Rachel Natrajan 17 ,
- James PB O’Connor 5 ,
- Rosemary O’Connor 27 ,
- Carlo Palmieri 31 ,
- Paul D P Pharoah 9 ,
- Emad A Rakha 11 ,
- Elizabeth Reed 29 ,
- Simon P Robinson 17 ,
- Erik Sahai 32 ,
- John M Saxton 15 ,
- Peter Schmid 30 ,
- Matthew J Smalley 18 ,
- Valerie Speirs 19 ,
- Robert Stein 8 ,
- John Stingl 9 ,
- Charles H Streuli 5 ,
- Andrew N J Tutt 7 ,
- Galina Velikova 19 ,
- Rosemary A Walker 28 ,
- Christine J Watson 9 ,
- Kaye J Williams 5 ,
- Leonie S Young 20 &
- Alastair M Thompson 2
Breast Cancer Research volume 15 , Article number: R92 ( 2013 ) Cite this article
131k Accesses
278 Citations
69 Altmetric
Metrics details
Introduction
Breast cancer remains a significant scientific, clinical and societal challenge. This gap analysis has reviewed and critically assessed enduring issues and new challenges emerging from recent research, and proposes strategies for translating solutions into practice.
More than 100 internationally recognised specialist breast cancer scientists, clinicians and healthcare professionals collaborated to address nine thematic areas: genetics, epigenetics and epidemiology; molecular pathology and cell biology; hormonal influences and endocrine therapy; imaging, detection and screening; current/novel therapies and biomarkers; drug resistance; metastasis, angiogenesis, circulating tumour cells, cancer ‘stem’ cells; risk and prevention; living with and managing breast cancer and its treatment. The groups developed summary papers through an iterative process which, following further appraisal from experts and patients, were melded into this summary account.
The 10 major gaps identified were: (1) understanding the functions and contextual interactions of genetic and epigenetic changes in normal breast development and during malignant transformation; (2) how to implement sustainable lifestyle changes (diet, exercise and weight) and chemopreventive strategies; (3) the need for tailored screening approaches including clinically actionable tests; (4) enhancing knowledge of molecular drivers behind breast cancer subtypes, progression and metastasis; (5) understanding the molecular mechanisms of tumour heterogeneity, dormancy, de novo or acquired resistance and how to target key nodes in these dynamic processes; (6) developing validated markers for chemosensitivity and radiosensitivity; (7) understanding the optimal duration, sequencing and rational combinations of treatment for improved personalised therapy; (8) validating multimodality imaging biomarkers for minimally invasive diagnosis and monitoring of responses in primary and metastatic disease; (9) developing interventions and support to improve the survivorship experience; (10) a continuing need for clinical material for translational research derived from normal breast, blood, primary, relapsed, metastatic and drug-resistant cancers with expert bioinformatics support to maximise its utility. The proposed infrastructural enablers include enhanced resources to support clinically relevant in vitro and in vivo tumour models; improved access to appropriate, fully annotated clinical samples; extended biomarker discovery, validation and standardisation; and facilitated cross-discipline working.
Conclusions
With resources to conduct further high-quality targeted research focusing on the gaps identified, increased knowledge translating into improved clinical care should be achievable within five years.
Globally, breast cancer is the most frequently diagnosed cancer in women, with an estimated 1.38 million new cases per year. Fifty thousand cases in women and 400 in men are recorded each year in the UK alone. There are 458,000 deaths per year from breast cancer worldwide making it the most common cause of female cancer death in both the developed and developing world [ 1 ].
In the UK, the age-standardised incidence of breast cancer in women has increased by 6% over the last decade, between 1999 to 2001 and 2008 to 2010 [ 2 ]. It is estimated that around 550,000-570,000 people are living with or after a diagnosis of breast cancer in the UK [ 3 ] and, based on current projections, this figure is expected to triple by 2040 due to an ageing population and continued improvements in survival [ 4 ]. Recent research indicates that the annual cost of breast cancer to the UK economy is £1.5bn, with just over a third of that cost (£0.6bn) from healthcare alone [ 5 ]. Yet the annual spend on breast cancer research by partners of the National Cancer Research Institute has reduced in recent years despite the level of cancer research spend being generally maintained [ 6 ].
In 2006, the charity Breast Cancer Campaign facilitated a meeting of leading breast cancer experts in the United Kingdom to explore which gaps in research, if filled, would make the most impact on patient benefit. The subsequent paper [ 7 ] has helped shape the direction of breast cancer research since that time. One overarching need identified was the ‘lack of access to appropriate and annotated clinical material’, which directly led to the formation of the UK’s first multi-centre, breast-specific tissue bank [ 8 ].
This new gap analysis represents an expanded, evidence-based follow-on developed collaboratively by clinicians, scientists and healthcare professionals. The aim is to ensure that the roadmap for breast cancer research remains a relevant, consensual and authoritative resource to signpost future needs. It builds upon the previous gap analysis by briefly reviewing the current status of key areas, critically assessing remaining issues and new challenges emerging from recent research findings and proposes strategies to aid their translation into practice. Whilst a survey of progress during the last five years is not the intention of this article, the preparatory detailed discussions and data analysis could provide the basis for such a retrospective review.
During 2012, Breast Cancer Campaign facilitated a series of workshops, each covering a specialty area of breast cancer (Figure 1 ). These working groups covered genetics, epigenetics and epidemiology; molecular pathology and cell biology; hormonal influences and endocrine therapy; imaging, detection and screening; current and novel therapies and associated biomarkers; drug resistance; invasion, metastasis, angiogenesis, circulating tumour cells, cancer ‘stem’ cells; breast cancer risk and prevention; living with and managing breast cancer and its treatment. Working group leaders and their multidisciplinary teams (comprising a representative cross-section of breast cancer clinicians, scientists, and healthcare professionals) participated in iterative cycles of presentation and discussion, offering a subjective consideration of the recent relevant peer-reviewed literature. Summary reports were prepared by each group, collated, condensed and edited into a draft, which was critically appraised by an external Executive Advisory Board of international experts. This position paper highlights the key gaps in breast cancer research that were identified, together with detailed recommendations for action.
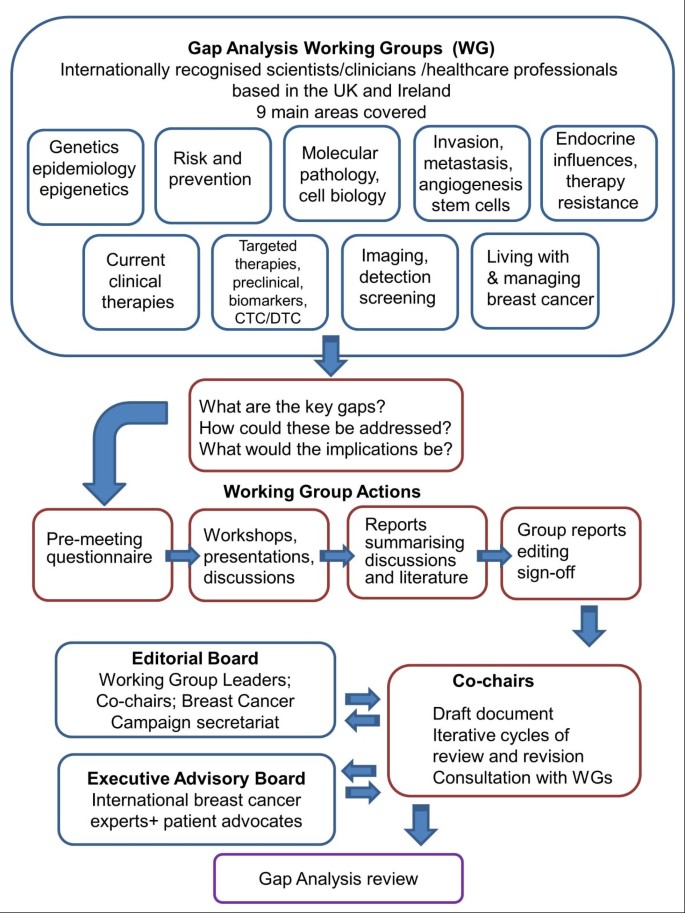
Gap analysis methodology. The flow chart illustrates the concept, processes and procedures devised to generate the gap analysis review.
Genetics, epigenetics and epidemiology
Current status, genetic predisposition.
Our knowledge of the heritability of breast cancer has increased significantly since 2007. Known breast cancer genes (BRCA1, BRCA2, CHEK2, ATM, PALB2, BRIP1, TP53, PTEN, CDH1 and STK11) make up 25 to 30% of the heritability [ 9 ]. Genome-wide association studies (GWAS) and the recent international collaborative analyses have confirmed 77 common polymorphisms individually associated with breast cancer risk, which add a further 14% [ 9 – 11 ]. Evidence from an Illumina collaborative oncological gene-environment study (iCOGS) experiment suggests that further single nucleotide polymorphisms (SNPs) may contribute at least 14% to the heritability, leaving only approximately 50% as ‘missing heritability’ (Figure 2 ).
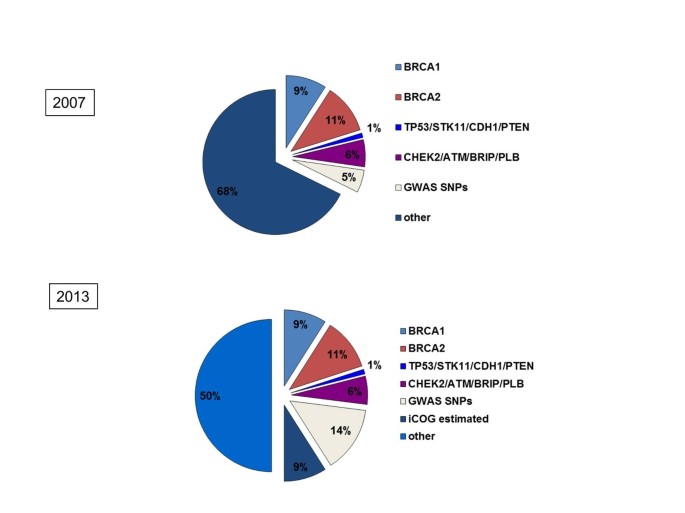
Familial cancer genetics. The proportion of the familial component of breast cancers that can be ascribed to specific genetic defects. The difference between June 2007 and 2013 shows the impact of genome-wide association studies (GWAS) that have now identified 77 common low-risk SNPs. Courtesy of Professor Douglas Easton (University of Cambridge). Reprinted by permission from Macmillan Publishers Ltd: Nature Genetics (45,345-348), copyright 2013.
If we assume the risk estimates for polygenic markers are log additive, the cumulative risk associated with these SNPs has a median of 9% to age 80 (95% confidence intervals 5 to 15%). In the familial setting, we have learnt that common genetic SNPs can modify the risk associated with BRCA2, which may be relevant when considering risk-reducing surgery [ 12 , 13 ].
BRCA1 and BRCA2
There is improved understanding of the function of BRCA1 and BRCA2 in relation to DNA repair and therapeutic responses. For example, BRCA2 functions in RAD51 loading and BRCA1 in countering 53BP1-mediated blocking of homologous recombinational (HR)-DNA repair; hence poly (ADP-ribose) polymerase (PARP) inhibitors have been developed and trialled against BRCA-driven cancers [ 14 ]. Several additional genes associated with breast cancer risk are part of the BRCA network and there is a clear relationship with the Fanconi pathway [ 9 ]. Genes in this network point to reduced HR-DNA repair as the mechanism underlying cancer susceptibility, although the precise functions of associated signalling proteins (for example PTEN, CHK2, ATM and N-terminal BRCA1) that relate to cancer development are unknown. Gene interactions of some higher risk alleles are recognised to be sub-multiplicative, whereas low risk alleles are log-additive [ 15 ]. Some susceptibility SNPs may function at the level of chromatin remodelling/enhancer activity related to nearby gene expression.
Epigenetics
Epigenetic alterations are frequent and cancer-specific methylation in circulating tumour (ct)DNA in serum can be used as an early detection biomarker, or as a prognostic indicator [ 16 , 17 ]. The recent ENCODE study provided a wide-ranging analysis of epigenetic marks on a small fraction of the genome [ 18 ]. The first candidate gene epigenetic risk factor that could usefully be included in breast cancer risk models (once fully validated) has been identified [ 19 ]. Epigenetic factors also provide molecular measures of long-term exposure to potentially oncogenic agents. Epigenetic alterations are reversible; preclinical and recent clinical testing of epigenetic-targeted therapies such as etinostat (a DNA methylation inhibitor) and vorinostat (a histone deacetylase inhibitor) indicate that such drugs may prove effective in combination with other therapies [ 20 , 21 ].
Psychosocial considerations
Predictive genetic testing for breast cancer predisposition genes can increase distress in the short term (which reduces over time) for those identified as gene carriers, whilst non-carriers report lower levels of concern following genetic testing [ 22 ]. A number of interventions have now been developed and tested to support the genetic testing process and have been shown to reduce distress, improve the accuracy of the perceived risk of breast cancer, and increase knowledge about breast cancer and genetics [ 23 ]. Examples introduced since the last gap analysis include education using tailored information technology to prepare women for genetic counselling [ 24 ]; interventions to support women’s decisions about whether or not to have genetic testing [ 25 ] and support for gene carriers thus identified [ 12 ].
What are the key gaps in our knowledge and how might they be filled?
Moderate risk alleles.
Remaining ‘moderate risk’ alleles will be found within the short term by exome sequencing and extended GWAS studies will identify additional lower risk alleles. If up to 28% of the risk from known SNPs could be explained, while the median of the risk distribution changes little, confidence limits would change dramatically, such that the women in the top 5% at risk would have >15% lifetime risk, compared with <3% lifetime risk at the lower end. A prospective analysis will be required to show that genetic risk assessment can predict risk when combined with mammographic screening. We need to determine if or how common SNPs modify the contributions of BRCA1-associated and moderate risk genes (such as CHEK2, ATM) and whether this is influenced by oestrogen levels or risk management using, for example, lifestyle or chemopreventive approaches.
Functional implications of unclassified variants in BRCA1/BRCA2, fine-mapping of risk-associated variants (from GWAS) and understanding the functional impact of the more common SNPs such as TOX3 and the role of FOXA1 remain to be determined. Similarly, deconvoluting the functional interactions between susceptibility genes and known breast cancer-associated proteins require systems biology approaches. Can we achieve a clear clinical use of the knowledge gained by GWAS, SNP and BRCA studies by validation of risk models incorporating SNPs and moderate risk alleles (in particular in the familial setting) to improve risk management? A randomised trial for population screening with mammography stratified on individual genetic risk estimates (combined with other key risk factors) is warranted.
BRCA1 and 2
A scheme to define categories of risk for variants in BRCA (and other) cancer genes is needed to provide specific clinical recommendations. BRCA variants of uncertain significance occur in approximately 5% of all genetic tests for BRCA1/BRCA2 mutations [ 26 ]. A range of in silico and functional assays is available to provide evidence for or against a genetic variant being pathogenic. A calculation combining all lines of evidence can estimate the posterior probability that a particular gene variant is predisposing to disease. The expression of breast cancer genes in normal breast tissue and pathways that may underlie cancer risk (such as DNA damage response) could be used to identify tractable markers and to direct treatment choice. Additional BRCA-deficient human tumour cell lines and animal models of breast cancer are required.
There is a gap in our understanding of cause or consequence between epigenetic traits and gene transcription. Translational studies are needed to investigate epigenetic patterns in clinical material and from clinical trials to identify and validate prognostic markers. The extent to which epigenetic markers can be incorporated into risk models alongside genetic and lifestyle factors is not yet known. Understanding how cancer risk factors impact on the epigenome and whether this provides a mechanism for increased risk associated with those exposures is poorly understood.
Further research is needed to support informed decision making about risk management options and to assess the psychosocial implications of changing behaviour and anxiety about cancer [ 27 ]. Interventions to support discussions with those newly diagnosed with breast cancer are being developed to improve understanding of risk to individuals and their families [ 28 ]. Interventions are also required to support conversations within the family about genetic risk and its implications, given that the onus is often on the patient [ 29 ]. Research involving women at increased genetic risk for breast cancer should assess the psychosocial impact on partners and the implications for their relationships [ 30 ]. Evidence from this research needs to inform services and direct resources to support those at increased risk of breast cancer.
Risk and prevention
Risk estimation.
We know little about the exact cause(s) of the majority of breast cancers. The major challenge for prevention is to identify women at risk as precisely as possible and then to apply measures such as chemoprevention and lifestyle changes. Current models can predict probable numbers of breast cancer cases in specific risk factor strata, but have modest discriminatory accuracy at the individual level [ 31 ]. The publication of more than 70 common genetic susceptibility factors via large-scale collaborative efforts [ 10 , 32 ] and the realisation that mammographic density is a major risk factor is important, but the major gap in our knowledge is how to incorporate these factors into our current risk prediction models [ 33 ].
Automated methods for estimation of mammographic density require further evaluation for its potential use as a biomarker for risk stratification in screening and changes in density as a biomarker of responsiveness to preventive approaches. Studies of chest irradiation for lymphomas and carcinogens in rodent models suggest the importance of exposure to radiation during puberty [ 34 , 35 ].
There is a need to assess the value of several new approaches to discovering biomarkers including adductomics, transcriptomics, metabolomics [ 36 ] and epigenomics and to determine how well-established measurements (for example oestrogen levels) can be incorporated into risk models [ 37 ].
Chemoprevention
An overview of all trials of selective oestrogen receptor modulators (SERMs) as chemopreventive agents indicates that risk is reduced by 38% for up to 10 years from the start of five years’ treatment [ 38 ]. An issue is predicting those women who will benefit from SERM treatment. Lasofoxifene appears to be the most active SERM and its further development is desirable [ 39 ]. In postmenopausal women, the MA P3 trial indicated that exemestane reduced risk by 65% after 35 months median follow-up [ 40 ] requiring confirmation with additional aromatase inhibitor (AI) prevention studies. The value of low-dose tamoxifen and fenretinide also needs to be established [ 41 ]. Since SERMs and AIs reduce only oestrogen receptor positive (ER+ve) disease, there is a need for agents to prevent ER negative (ER-ve) disease, to distinguish between ER- and progesterone receptor (PR)-related disease [ 42 ] and to develop better animal models [ 43 ]. There is a need to confirm that oestrogen-only hormone replacement therapy (HRT) reduces risk whereas combined HRT increases risk in the Women’s Health Initiative (WHI) trials and to establish the mechanism of this dichotomy [ 44 , 45 ].
Lifestyle changes
Most studies related to breast cancer risk and lifestyles are observational. Favourable changes in lifestyle including reduction of calorie excess, increasing exercise, reducing alcohol intake and less environmental exposures to disturbance of circadian rhythm could reduce breast cancer by one third [ 46 – 49 ]. Communicating the potential benefits of lifestyle change, identifying teachable moments and using health services to endorse lifestyle change for prevention will require additional studies to determine why health beliefs translate poorly into action [ 50 ].
Marked adult weight gain in premenopausal women is associated with a doubling of risk of postmenopausal breast cancer compared with no or little weight gain [ 51 ]. Conversely, weight loss of 3kg or more is associated with a 25 to 40% reduction of cancer in older women compared with those who continue to gain weight. [ 52 – 54 ]. It is not clear whether to focus on all overweight women, those with gynoid or abdominal obesity or those with metabolic syndrome. Weight gain after surgery for breast cancer increases risk of relapse [ 55 ]; there is a need for further randomised trials to determine whether reducing weight in the overweight, or preventing weight gain after surgery prevents relapse. Weight management strategies seeking efficacy in the long term may be particularly difficult to sustain.
The effect of individual components of diet is controversial. The risk of ER-ve tumours may be reduced by high vegetable intake [ 56 ] while lowering fat intake may reduce both breast cancer risk and relapse after surgery. However, two of the three randomised trials of lower fat intake are confounded by concomitant weight loss [ 57 , 58 ] and the one study without weight loss showed no effect of reduction of fat intake on breast cancer relapse after surgery [ 59 ].
There is evidence for breast cancer prevention with habitual exercise [ 60 ]. Observational evidence shows that a physically active lifestyle after cancer treatment prevents relapse and reduces the risk of all-cause mortality [ 61 ]. The optimal exercise regime and timing are uncertain and randomised trials are required to assess the preventive benefits. There is a need to understand the mechanism of the apparent beneficial effects of caloric restriction and exercise.
Effective and sustainable lifestyle changes (diet, exercise and weight) need to be agreed and effective routes to initiation and maintenance identified. Further work needs to be undertaken in chemoprevention strategies and adherence to effective agents.
Prospective cohort studies are needed to develop and validate risk models, which may need to incorporate polygenic risks, mammographic density and measures of body composition. Risks may be refined by the discovery and validation of novel biomarkers such as epigenetic markers [ 19 ] and prospective validation of known markers such as serum oestrogen [ 62 , 63 ]. Effectiveness and cost-effectiveness, analyses to evaluate possible personalised screening and prevention programmes [ 64 ] and pilot studies to evaluate delivery options followed by large randomised trials are required. Polygenic and other biomarkers should be used to distinguish between the development of ER +ve, ER+ve/PR +ve and ER–ve cancers.
Many breast cancers arise in women without apparent risk factors; current studies suggest that polygenic risk factors and mammographic density add only a little to the Gail model [ 65 ]. Precision is required using polygenic approaches to decide whether or not to give preventive tamoxifen. Currently, about 10% of breast cancers arise in women with a 10-year risk above 5%. Taking this at-risk group and increasing the frequency of screening would be of some benefit, but more effective risk-adapted screening will depend upon a better definition of risk.
Further improvement and cost-effectiveness of the NHS breast cancer screening programme could include tomography, ultrasound and automated methods for the measurement of volumetric mammographic density (using software programs such as Quantra or Volpara) and automatically using these for risk stratification to adapt screening interval to risk. Experimentally, there are now opportunities for determining whether high breast density alters the response of breast epithelial cells to DNA damage or oncogene activation. This may provide prognostic value if we can define novel biomarkers to distinguish which women with high mammographic density will develop cancer [ 66 , 67 ].
Uptake of tamoxifen and raloxifene is variable and optimal methods need to be developed to explain risk, the benefit/risk ratio of treatment and to identify women who will benefit. The benefit from tamoxifen may be determined by changes in mammographic density [ 68 ] but needs confirmation. Identification of women who could develop ER-ve tumours should become possible (for example by polygenic scores). Work is required to corroborate the efficacy of lasofoxifene; the use of AIs in the preventive setting should be clarified by the International Breast Cancer Intervention Study II (IBIS II) trial, while the use of low-dose tamoxifen and retinoids also await trial results. Further studies are required to develop new preventive agents; those which might be pursued further include rexinoids, omega 3 fatty acids, sulphorophane, antiprogestins and insulin-like growth factor 1 (IGF1) inhibitors [ 409 ].
The widespread introduction of preventive agents depends upon efficient methods for identifying risk and effective counselling. Neither has been widely taken up, particularly in postmenopausal women, but the recently published NICE guidelines may signal a change for the use of tamoxifen in chemoprevention. Identification within screening programmes may be a valid approach [ 64 ]. However, since trials of chemoprevention require long duration and are costly, the development of biomarkers as indicators of effectiveness and their acceptance by regulatory agencies is attractive.
Lifestyle change for breast cancer prevention
A precise definition of interventions for diet and exercise and the relative importance for reduction of ER+ve or ER-ve breast cancer is unclear. The effect of caloric restriction by age and the duration of interventions remain unknown as do the underlying mechanisms of action. Identifying successful methods to translate prevention evidence into public health policy including effective behaviour change programmes and convincing clinicians to change practice in favour of prevention are required. Most evidence for lifestyle change is observational and confirmatory data from prospective randomised controlled trials (RCTs) with long-term follow-up and clinical endpoints may be needed. A breast cancer prevention trial using exercise would require a sample size of 25,000 to 35,000 and an eight to ten-year follow-up to observe a 20 to 25% decrease in risk for a moderate-to-vigorous physical activity programme. Such a large-scale study is not currently possible so the focus has been on a RCT of exercise in breast cancer patients to determine how exercise influences survival. The AMBER cohort study in 1,500 breast cancer patients measures physical activity, fitness and other indicators to determine exactly how physical activity influences survival [ 69 ].
Nevertheless, the beneficial effects demonstrated in randomised trials to prevent diabetes and cardiovascular disease need to be balanced against the enormous size and cost that would be required for such trials in breast cancer. For secondary prevention of disease recurrence after surgery, trials are due to report on caloric restriction and exercise in 2014 and 2018 [ 70 , 71 ].
There are teachable moments within the breast screening programmes for links to prevention through changes in lifestyle [ 50 , 64 ]. Reduction in alcohol consumption using community/class/cultural approaches, analogous to those for smoking, needs to be explored using social marketing approaches within a research context. It is likely that energy restriction and exercise will not be a complete answer to prevention and efforts should be made to design lifestyle prevention trials with and without energy restriction mimetic agents such as mTOR inhibitors, resveratrol, and metformin. mTOR inhibitors such as everolimus (RAD001) are effective in advanced breast cancer [ 72 ] although toxicities will prevent its use as a preventive agent; rapamycin in animal models reduces tumour incidence and increases longevity [ 73 ]. There is a need to translate these important findings into the clinic, perhaps by low dose or intermittent regimens to avoid toxicity [ 74 ]. Metformin is in clinical trial as an adjuvant for breast cancer treatment and demonstration of effectiveness in this situation could lead to assessment for prevention including in prediabetic populations [ 75 ].
Molecular pathology
Breast cancer classification and issues of heterogeneity.
During the last five years several high-profile studies have significantly advanced the molecular subclassification of breast cancer (reviewed in [ 76 ] and [ 77 ]). Intratumoral heterogeneity in both pre-malignant and invasive breast cancer is well documented. It is likely that both genetic and epigenetic instability, combined with microenvironmental and therapy-induced selective pressures lead to clonal evolution, which continues during metastatic progression. However, whether heterogeneity arises from cancer stem cell plasticity and a hierarchy of aberrant differentiation or stochastic events is a moot point (Figure 3 ). Genomic studies have been used to develop both prognostic biomarkers and to identify biomarkers to predict response to therapy. Nevertheless, ‘driver’ genetic changes in breast cancer will need to be filtered from the background, clinically inconsequential changes [ 78 ].
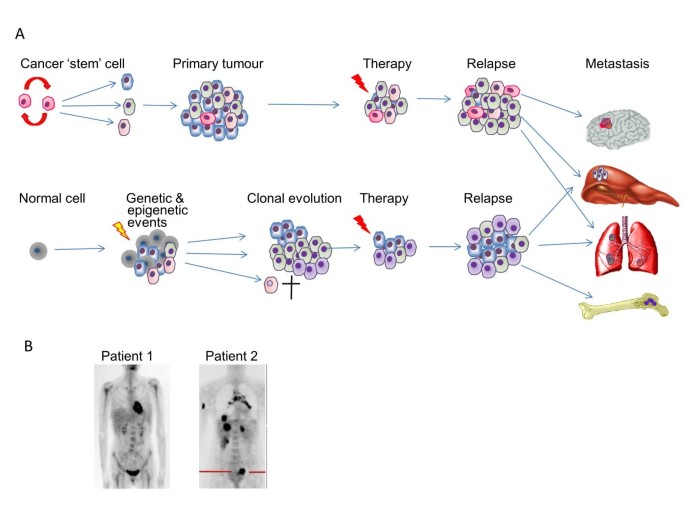
Tumour heterogeneity. (A) Recent molecular and genetic profiling has demonstrated significant intratumoural heterogeneity that can arise through genomic instability (leading to mutations), epigenetic events and/or microenvironmental influences. The stem cell hypothesis proposes that tumour-initiating cells are pluripotent and can thus give rise to progeny of multiple phenotypes; alternatively heterogeneity could be due to stochastic events. Temporal heterogeneity can be exacerbated by therapy (theoretically due to clonal evolution as some clones are eliminated whilst others expand). The significant molecular/genetic differences between cells in different areas within individual cancers, between primary and metastatic tumours (and potentially between cancer cells that successfully colonise different organs) have implications for the reliability of primary tumour biopsies for diagnosis, seeking biomarkers for treatment planning and responses to therapy. In addition, there is substantial inter-tumour heterogeneity. (B) shows images of two patients who presented with breast cancers of identical histological type and biochemical parameters. Four years later, one patient is clear of disease, while the other has evidence of multiple distant metastases, illustrative of between-patient heterogeneity in terms of response to therapy (clinical images kindly provided by Professor William Gallagher, with thanks to Dr Rut Klinger and Dr Donal Brennan (UCD Conway Institute).
Exploring the diversity and inter-tumour heterogeneity of breast cancer has led to the development of a novel classification that integrates genomic and transcriptomic information to classify 10 subtypes with distinct clinical outcomes [ 79 ]. Triple-negative breast cancer (TNBC) in particular is now recognised to demonstrate heterogeneity at the molecular, pathological and clinical levels. [ 80 ]. Such analyses, together with advanced next-generation sequencing have significant implications for improved understanding of basic tumour biology and will potentially enable the identification of new molecular targets for personalised treatment plans [ 81 , 82 ] Additionally, identification of non-coding RNAs is showing potential in diagnosis, prognosis and therapy [ 83 ].
Microenvironmental influences and tumour - host interactions
Breast development is critically reliant upon cell polarity [ 84 ], choreographed cell death pathways and interactions between epithelial cells and stroma; all processes which when deregulated are implicated in oncogenesis and tumour progression [ 85 – 87 ]. The tumour microenvironment, comprising a community of both malignant and non-malignant cells, significantly influences breast cancer cell behaviour [ 88 , 89 ]. Recently, progress has been made in understanding the bidirectional interplay between tumours and surrounding stromal cells/extracellular matrix (ECM), which can potentiate resistance to targeted therapies including endocrine therapy [ 90 , 91 ]. Consequently, components of the tumour microenvironment may represent targets for therapeutic intervention alongside the tumour to improve response to treatment [ 92 ].
Hypoxia reflects dynamic microenvironmental conditions in solid tumours, limits responses to radiotherapy [ 93 ] and some chemotherapeutic and anti-endocrine agents [ 94 , 95 ], drives genomic instability and is generally associated with progression to invasive/metastatic disease [ 96 , 97 ]. Tumour-stromal interactions change under hypoxic conditions to promote tumour progression via the activity of enzymes such as LOX [ 98 ], angiogenic factors and infiltrating macrophages [ 99 , 100 ]. A stem-like breast cancer cell subpopulation with an epithelial-mesenchymal transition (EMT) phenotype is expanded during repetitive hypoxia/reoxygenation cycles [ 101 ]. Hypoxia also contributes to cancer stem cell plasticity and niche formation [ 102 ] potentially explaining the relationship between hypoxia and chemotherapy resistance [ 103 ]. Finally, at the physiological level, host metabolic, inflammatory and immunological factors can impact on cancer development and progression, and these processes are further modified by the physical environments in which we live (Figure 4 ).

Microenvironmental influences on breast cancer. Breast cancer biology, progression and response to therapy is influenced at many levels from epigenetic effects on gene expression (for example methylation) through soluble and cell-mediated stromal interactions, intratumoural inflammatory and angiogenic components, hypoxia, host endocrinological and immunological status through to exposure to multiple agents in the environment in which we live.

What are the key gaps in our knowledge and how might these be filled?
Normal breast development and the origins of cancer.
It is not known how many breast epithelial cell subpopulations function as stem cells (capable of self-renewal) or progenitor cells (which proliferate expansively) [ 104 – 106 ]. Clearer understanding of cell lineages, changes in transcription factor expression during breast development and definition of the nature of stem and progenitor cells is fundamental to delineating relationships between normal and malignant cells.
Current cancer stem cell (CSC) assays have limitations: dormant cells cannot be detected and cell subpopulations that give rise to clones in vivo may not be active in ‘mammosphere’ cultures. There is no clear consensus on markers that define functional breast CSC in mouse and human. Indeed, they may not represent a fixed subpopulation, but instead exist in specific niches in flexible equilibrium with non-CSCs, with the balance depending on interactions between them as well as external selective pressures [ 107 – 109 ]. Understanding this plasticity [ 110 ] and its therapeutic implications are key areas for future investigation.
Breast cancer subtypes: genomics and bioinformatics
Several large-scale, cross-sectional, integrated molecular studies have established comprehensive molecular portraits of invasive primary breast cancers [ 111 – 114 ]. The International Cancer Genome Consortium (ICGC), The Cancer Genome Atlas (TCGA) and individual studies have released sequence data; however, gaining access to and interrogating this information requires expert bioinformatic collaborations. Relating these advances in genomic knowledge to improving clinical care has yet to be achieved. Knowledge of genetic, epigenetic and host factors underpinning distinct subtypes of breast cancer (plus their associated aberrant signalling pathways) and predictive biomarkers will be essential in targeting new therapeutic agents to the right patients.
For ductal carcinoma in situ (DCIS), an increased understanding is required of molecular markers of prognosis, thus providing key information to avoid overtreatment. We need to know which DCIS lesions will recur if adequate surgery is performed with wide, clear margins. Biological markers of DCIS should aim at defining which lesions are likely to progress, in order to avoid radiotherapy or even surgery if the risk of invasive cancer is sufficiently remote [ 115 ]. Markers for response to radiotherapy or endocrine therapy and the need for these therapies (particularly in low-risk patients) remain unclear.
Tumour microenvironment and stromal influences
Paget’s venerable ‘seed and soil’ analogy - recognising that tumour-initiating cells require a permissive host environment to thrive - is beginning to be deciphered at the molecular level. [ 42 ]. The composition and biophysical characteristics of the breast matrisome [ 116 ] and how it controls different stages of gland development and in early breast cancer requires definition. It is important to identify the transcription factors that define luminal and myoepithelial cells and to understand whether additional microenvironmental factors such as the ECM and fibroblast growth factor (FGF), Notch or Wnt signalling can switch their fate. Specialised niches defined by specific cell-cell/cell-matrix interactions in the microenvironment together with soluble, ECM-bound and microvesicle-associated host factors regulate CSC activation [ 117 ]. Further research on such CSC niches, their role in dormancy and the complex relationships between CSCs and metastasis is essential [ 118 – 120 ].
Stromal changes predict early progression of disease [ 121 ] and in-depth knowledge of how these conditions can be manipulated for therapeutic benefit is required [ 122 ]. Advances in the field of mechanotransduction are shedding light on the mechanisms by which altered matrix density or ‘stiffness’ can influence cell behaviour, and enzymes such as lysyl oxidases (LOX) are potential targets for therapy [ 123 ].
There is a need for better biomarkers of hypoxia including gene expression profiles [ 124 ] serum proteins, circulating tumour cells (CTCs) or functional imaging that could be used non-invasively in patients to enable more rigorous testing of its prognostic/predictive value. Although hypoxia-targeted therapies have proven disappointing to date, new approaches are emerging. In common with other targeted therapies for systemic disease, methods for measuring efficacy will need to be redesigned [ 124 – 126 ].
Tumours have an increased dependence on aerobic glycolysis. We need to understand how hypoxia affects the tumour metabolome and thus may determine therapeutic responses [ 96 ]. The dependence of metabolically adapted breast cancer cells on altered biochemical pathways presents new therapeutic targets linked to aerobic glycolysis, acidosis and the hypoxic response [ 127 , 128 ]. Since these pathways also interact with classical survival and proliferation signalling pathways via PKB/mTOR, there are opportunities to develop new combinatorial therapeutic strategies.
Breast cancer development and progression
Mammary stem cells.
There is increased understanding of stem cell hierarchies and their potential roles in breast development [ 129 – 131 ], but debate continues on the relationship between normal stem and progenitor cells, their dysregulation in cancer and the nature of putative CSCs [ 132 – 135 ]. Most data suggest that breast CSCs are a defined population with basal-like or mesenchymal-like features [ 136 – 138 ]. There is emerging data from cell line models that the CSC state is dynamic and can be induced by the tumour microenvironment [ 110 ], and this requires further investigation in human cancers. It is not known whether there are differences in CSC phenotype between breast cancer subtypes such as luminal vs. TNBC [ 139 , 140 ]. An emerging consensus is that CSCs initiate metastases and tumour regrowth after therapy, but do not necessarily generate the majority cell population in primary tumours.
Circulating tumour cells
Blood-borne tumour cells are routinely identified in breast cancer patients but their scoring can depend upon the method used [ 141 ]. Their relationship to disseminated tumour cells (DTCs) in tissues is unclear, although a recent publication showed that the presence of CD44+CD24 -/lo cells (putative CSCs) in the bone marrow is an independent adverse prognostic indicator in patients with early stage breast cancer [ 142 ]. A population of CTCs from patients with primary luminal cancer (expressing EPCAM, CD44, CD47 and MET) generated multi-site metastases when injected into mice. Hence it is likely that a subset of CTCs have metastatic potential [ 143 ], which may equate to CSCs. CTCs may occur in heterogeneous emboli of multiple cell types; perhaps those containing stem-like cells and/or ‘feeder’ cells are more likely to survive and grow at distant sites.
This key hallmark of breast cancer occurs when cancer cells access lymphatic and vascular systems, enabling dissemination via lymph nodes and then via the venous and arterial vascular system to distant organs. Once the disease has spread, it becomes life-threatening and patients require systemic treatment. Metastatic relapse typically occurs many months to decades after surgery, thus we need a greater understanding of the processes that occur following tumour cell dissemination, including the phenomenon of dormancy. Recent mathematical modelling using relapse data has provided interesting insights and proposals for hypothesis testing [ 144 ]. CTCs and DTCs that generate metastases are, by definition, tumour-initiating cells; hence their study needs to relate to CSC research [ 145 , 146 ]. Since the last gap analysis, there has been a paradigm shift in this area with the discovery of ‘pre-metastatic niches’ (analogous to stem cell niches) in organs destined to develop metastases [ 147 , 148 ].
In addition, seminal research using animal models has identified tumour and host genes associated with metastatic capacity (quite distinct from tumorigenic potential), and also organotropism [ 149 – 151 ]. The relevance of these experimental observations to human breast cancer and the translation of these findings into clinical studies require confirmation but may provide additional predictive value [ 152 ].
Reversible EMT, regulated by many factors including transforming growth factor beta (TGFβ) signalling, Slug and Snail transcription factors and hypoxia may be linked to invasion, dissemination and drug resistance [ 153 – 156 ]. The role of EMT in human cancer metastasis is still controversial and the underlying molecular mechanisms are not fully understood [ 157 ]. However, mesenchymal/stromal gene signatures have been identified which relate to TNBC subtypes, bone metastasis and resistance to neoadjuvant therapies [ 158 ].
Circulating tumour cells and nucleic acids
It is unclear whether CTCs originate from primary tumours, micro-metastases or multiple primary and secondary sites. Indeed, CTCs from distant metastases can potentially reseed the primary tumour [ 159 , 160 ]. More research is needed to define the origins of these cells. Importantly, analysis of CTCs needs to be carried out as far as possible in the clinical context, where their biology can be correlated with patient outcomes. CTCs and ctDNA are particularly useful where accessible breast cancer material is not available, or to obtain serial samples during therapy, providing a window on response and relapse.
To enable further progress, systems and protocols for isolating and characterising CTCs need to be rigorously defined and standardised, with an analysis of whether all systems identify/isolate the same cells (or indeed all CTCs, since EMT may preclude identification using epithelial markers [ 141 , 161 – 163 ]). We need to know the proportion of live, quiescent and apoptotic CTCs, their characteristics and malignant potential and to understand their relationship to the primary tumour and whether different subsets of CTCs have different predictive value.
The use of ctDNA is increasing as a potentially useful further source of information on breast cancer biology and response to therapy [ 164 – 166 ]. miRNAs identified in the systemic circulation (free or exosome-associated) [ 167 ] may also serve as diagnostic or prognostic biomarkers and/or as therapeutic targets. Indeed, it has been suggested that exosomes themselves, with their emerging roles in bidirectional signalling, immune suppression, subversion of targeted therapy and potentiation of metastasis [ 168 ] could be removed (for example by plasmapheresis) for therapeutic benefit [ 169 ].
Metastatic disease
Metastasis is the major cause of treatment failure, but it is far from clear why some patients with apparently similar disease succumb and not others [ 170 ]. We need to identify key signalling pathways linked to organotropism [ 171 ] and to develop new therapies for micro-and macro-metastatic disease [ 172 ]. Given the multiple breast cancer subtypes (and associated oncogenic drivers), it will be important to try to align genotypes/epigenotypes to metastatic patterns, in order to predict likely sites of relapse. Treatment decisions are generally based on the profile of the primary cancer, but information about the evolution of the disease from CTC, DTC or (where possible) metastases at different sites is essential, since both gains and losses of potential therapeutic targets have been observed in these distinct tumour cell populations.
We need to understand how the host microenvironment at secondary sites influences tumour cell survival and to define similarities and differences between ‘permissive’ microenvironments in organs favoured by breast cancer cells such brain, bone or liver. We have learned a good deal since the last gap analysis about the ‘vicious cycle’ of bone metastasis, whereby tumour cell interactions within this unique microenvironment mutually promote metastatic outgrowth and bone remodelling via hormonal, immunological and inflammatory mediators. These findings need to be translated into new therapies targeting both tumour and host components [ 173 ] with the paradigm extended to other specialised sites such as brain [ 174 ].
Current therapies
Clinical therapies.
Current clinical therapies for breast cancer are offered on an individual patient basis via a multidisciplinary team and comprise surgery, radiotherapy and drug therapies targeting oncogenic processes. Selection of therapy is based on Level 1 evidence from large RCTs or meta-analyses of such RCTs [ 175 – 177 ]. Increasingly, correlative translational studies are integrated prospectively into clinical trials, aiming to define the optimal target population and provide insight into mechanisms of resistance. The individualisation of treatment, optimal duration of treatments, prediction of metastasis or drug resistance remain challenging and reflect incomplete understanding of the underlying biology of breast cancer. However, up-to-date guidelines are useful to determine the best therapy for individual patients [ 178 ].
Immunohistochemical (IHC) analyses for selecting therapeutic options generally lack reproducibility and standardization resulting in poor concordance between laboratories. The Quality Assurance programme for ER, PR and human epidermal growth factor receptor 2 (HER2) in the UK has to some extent addressed this, but for other biomarkers, including Ki67, there clearly remain problems. We need to develop standardised protocols for better quantification of biomarkers [ 179 ], especially optimised methods of sample collection/storage to ensure that unstable or transient biomarkers (such as phosphoproteins or histone marks) are retained. This is especially important for predictive markers such as HER2, together with those which report on the efficacy of HER2-directed therapies and other emerging targets.
Health inequalities remain in relation to treatment. Older people diagnosed with cancer are more likely to experience undertreatment, potentially having poorer clinical outcomes than younger women for example [ 180 , 181 ]. Indeed, there is a lack of data to inform decision making about treatment for the elderly patient with breast cancer in part attributable to their under-representation in trials, but clinical teams may make inadvertent ageist decisions [ 182 , 183 ]. In addition, breast cancer and its treatment can have a considerable impact on women and their families [ 184 ]. Psychological distress is common, although not inevitable, and is associated with poorer quality of life [ 185 , 186 ]. Regular distress screening is recommended as a core component of good quality cancer care [ 187 , 188 ] in order to provide appropriate support.
Surgery remains the primary treatment for most women, with breast conservation (plus whole breast radiotherapy) providing similar outcomes to mastectomy. Following mastectomy, breast reconstruction should be considered, although uptake is incomplete. Axillary surgery has moved from clearance via node sampling techniques to sentinel node biopsy as the preferred means for assessment of axillary metastasis in early breast cancer. Neoadjuvant therapy, initially implemented to down-stage inoperable cancers, is increasingly used to assess drug efficacy in individuals and to reduce the extent of surgery required in good responders [ 189 ].
Radiotherapy
Radiotherapy is both clinically effective and cost-effective in the adjuvant and palliative settings. The Oxford overview of adjuvant radiotherapy trials [ 177 ] showed a halving of risk of first recurrence in all risk groups and favourable effects of local control on long-term survival. There is long-term confirmation of the value of boost irradiation to the site of excision after breast-conserving surgery in all subgroups, including women >60 years [ 190 ]. The long-term safety and efficacy of hypo-fractionated radiotherapy after breast-conserving surgery and mastectomy for operable breast cancer has recently been confirmed: (10-year results of Canadian [ 191 ] and Standardisation of Breast Radiotherapy (START) trials also suggesting generalisability to all subgroups of patients [ 192 , 193 ].
Trials of partial breast irradiation evaluating intraoperative radiotherapy in comparison to external beam radiotherapy [ 194 , 195 ] or brachytherapy [ 196 ] have short follow-up, but guidelines on partial breast irradiation [ 197 , 198 ] have encouraged off-study use of partial breast irradiation in advance of clinical trial results. Omission of postoperative radiotherapy after breast-conserving surgery in older, lower-risk women suggests the differential in local recurrence rates may be acceptable with a cumulative in breast recurrence of 2.5% in breast conservation surgery alone vs. 0.7% for surgery and postoperative radiotherapy (median follow-up 53 months age 55 to 75 years [ 199 ]) and at 10 years local recurrence, nine for conservation alone vs. 2% for surgery and radiotherapy in the =/>70 years, ER+ve group [ 200 ].
Decision making
Clinical decision-making tools to support individualised treatment can influence patients’ treatment choices and experiences [ 201 ] and communication training for oncology professionals is now widely available throughout the UK to improve the delivery of information and support to patients [ 202 ]. A recent national survey of over 40,000 patients with a broad range of cancers identified the fact that younger patients and ethnic minorities in particular reported substantially less positive experiences of involvement in decision making [ 203 ].
Overtreatment
A significant number of patients are overtreated to achieve the improved survival overall in early breast cancer, since we cannot define individual risks of disease recurrence or sensitivity to treatment. For survivors, the long-term side effects of treatment may be significant; individualised treatment so that patients only receive the treatment they require to achieve cure remains elusive. This is relevant to surgery, radiotherapy, chemotherapy and endocrine therapy.
With the widespread adoption of sentinel node biopsy (SNB)-limiting surgery to the axilla has substantially reduced arm morbidity [ 204 ]. A detailed understanding of underlying tumour biology is required to support decisions around surgical management, (for example axillary node clearance or not after positive sentinel nodes). No further axillary surgery even for one to two positive nodes [ 205 ] and the equivalence of axillary clearance to axillary radiotherapy for local disease recurrence (despite the differing morbidities) in the presence of a low disease burden [ 206 ] demonstrate further progress in this surgical setting. However, the optimal design of radiation treatment fields for SNB-positive patients is not known.
For postoperative radiotherapy after breast-conserving therapy, we do not have reliable ways of identifying low risk, particularly in elderly patients for whom radiotherapy might be omitted. While even low-risk patients have an approximately 50% reduction in first recurrence [ 177 ], the absolute gain for low-risk breast cancer patients (older age, small, ER+ve cancers) after breast-conserving surgery is very modest. We need reliable molecular markers of identifying such low-risk groups or individuals.
Further work is required to clarify whether the response to neoadjuvant chemotherapy can be used to guide the selection of patients for regional nodal irradiation [ 207 ] or whether patients who are clinically node positive before neoadjuvant chemotherapy and are converted to node negative after neoadjuvant chemotherapy on SNB require axillary nodal irradiation.
Individualisation of treatment
Understanding the optimal treatment strategies for an individual patient remains elusive. A number of genomic (for example Mammaprint, Oncotype Dx, PAM50) and immunohistochemical (for example IHC 4) tests have been developed to predict prognosis and latterly, response to chemotherapy; however, prospective trial evidence is still awaited [ 208 ]. Recently, serum metabolite profiling using a combination of nuclear magnetic resonance (NMR) spectroscopy and liquid chromatography-mass spectrometry (LC-MS) correctly identified 80% of breast cancer patients whose tumours failed to respond adequately to chemotherapy, showing promise for more personalized treatment protocols [ 209 ].
Increased understanding of the dynamic changes that occur over time is critical and will require repeated assessment of tumour profiles. Genomic tests predict response to endocrine or chemotherapy and those at highest risk of relapse [ 210 – 212 ], but prospective trials are required to determine whether axillary clearance or chemotherapy can be avoided in node-positive patients. Similarly, biological markers of radiosensitivity (tumour and normal tissue) require better characterisation and implementation into clinical strategies to allow personalisation of treatment and avoidance of late radiation-induced toxicity [ 213 ].
CNS metastatic disease
As a result of improved outcome for patients with metastatic breast cancer (MBC), central nervous system (CNS) metastatic disease is an increasing therapeutic challenge [ 214 ]. Optimal treatment strategies have yet to be defined including sequencing or combination of stereotactic and whole brain radiotherapy, systemic treatments, intrathecal treatment approaches for leptomeningeal disease and prophylactic interventions.
Bone metastatic disease
Bisphosphonates reduce the risk of developing breast cancer in osteoporotic and osteopenic women by approximately 30% and the risk of recurrence in early breast cancer when used at the time of diagnosis [ 215 , 216 ].The interaction between the internal endocrine environment and the effect of bisphosphonates is complex and poorly understood. While negative results overall were reported in the large UK AZURE trial [ 217 ] women more than five years postmenopausal benefitted, consistent with data from the NSABP-34 trial [ 218 ]. In premenopausal women, bisphosphonates can abrogate the bone loss associated with use of an AI. In addition, recurrence and death rates were reduced when used in combination with either tamoxifen or an AI after treatment with the LHRH agonist goserelin (ABCSG12: [ 219 ]. Taken together, these studies suggest that a bisphosphonate may have its greatest effect in a low-oestrogen environment.
The impact of bone-targeted therapy on extra-skeletal metastases and locoregional relapse also highlights the need to better understand experimental observations concerning reseeding of tumours from dormant cells within the bone microenvironment [ 220 ]. Additionally, the role of RANK-RANKL signalling in mammary stem cell biology allows for the possibility that targeting this pathway with agents such as denosumab may offer a prevention strategy for bone metastasis [ 221 , 222 ].
Oligometastatic disease
The role of localised treatment of oligometastatic disease for example in the form of selective stereotactic body radiotherapy, radiofrequency ablation or surgery is currently unclear. The impact of irradiating the primary tumour, biological communications between treated primary site and distant metastases and whether radiation therapy can convert the primary tumour into an in situ vaccine [ 223 ] are relatively unexplored. Prospective randomised trials are required, which should ideally incorporate comprehensive molecular studies to define subtypes most likely to respond; a related question is how to treat primary breast cancer in patients presenting with metastatic disease.
The molecular basis of chemo-radiosensitivity, biomarkers (including specific gene signatures, proteomic markers) of tumour and/or normal tissue sensitivity is required to allow selection of patients who may benefit from adjuvant radiotherapy and avoid toxicity to those who will not. Explanations for the mechanism(s) of favourable impacts of locoregional control from radiotherapy (RT) on survival are needed [ 224 ] and may include in vivo real time biosensors of tumour biology to capture transient changes in the tumour microenvironment that drive metastasis.
Hypofractionated adjuvant radiotherapy
Even shorter-dose fractionation schedules (that is one week of whole breast radiotherapy) might achieve equivalent locoregional control with comparable toxicity [ 225 , 226 ]. Partial breast irradiation appears promising, but the long-term safety and efficacy is still uncertain [ 197 , 198 ]. In addition, it appears likely that there is a subgroup of low-risk, older patients from whom postoperative radiotherapy can be safely omitted [ 227 , 228 ]. The role of postmastectomy radiotherapy in intermediate risk breast cancer [ 229 ], axillary irradiation in sentinel node positive macro- or micro-metastases [ 230 ] or boost dose in DCIS following breast-conserving surgery [ 231 ] are all currently unclear. Further definition of the role of stereotactic body radiotherapy, accounting for tumour motion [ 232 ], in combination with neoadjuvant systemic therapy, to liver or bone metastases for oligometastatic disease are required. Similarly, the optimal dose fractionation for locally advanced disease needs to be established [ 233 ].
Molecularly targeted therapies
Anti-endocrine agents.
Multiple lines of clinical and translational evidence have increased our knowledge of the risk of recurrence, particularly for ER+ve disease [ 212 , 234 – 236 ]. The optimal duration of treatment remains incompletely defined but several RCTs have provided important new data: eight to ten years of adjuvant treatment for ER+ve breast cancers is more effective than five years of letrozole or tamoxifen [ 237 – 239 ].
Endocrine therapy resistance
Comprehensive guidelines to define endocrine resistance have now been agreed [ 240 ]. Clinical studies of various agents alone and in combination with signalling inhibitors have been completed since the last gap analysis. [ 241 – 243 ]. The biology of ERs, including the importance of phosphorylation [ 244 ], ER co-regulators [ 245 ], cross-talk with kinases [ 246 ] and altered ER-binding events [ 247 ] nevertheless requires further elucidation. MicroRNAs regulate ER activity and endocrine responses, [ 248 ], while epigenetic events promote ER loss or tumour suppressor silencing [ 249 ]. Cancer stem cells may also be implicated in endocrine resistance [ 250 ].
The multiple cell-signalling changes driving resistance and associated disease progression, nevertheless reveal potential cancer cell vulnerabilities [ 251 ] for example mTOR [ 72 ], EGFR/HER2 [ 252 ] and Src kinase [ 253 ]. New methodologies such as large-scale siRNA screens have also provided novel therapeutic targets such as CDK10 and fibroblast growth factor receptor 1(FGFR1) [ 254 , 255 ].
Oncogenic signalling inhibitors
Several molecularly targeted therapies have been licensed since the last gap analysis including lapatinib and pertuzumab in HER2+ cancers [ 31 ] and the mTOR inhibitor everolimus in ER+ve disease [ 72 , 256 ], which can overcome endocrine resistance [ 257 ]. Agents targeting signal transduction pathways (notably HER2) have had a significant impact in the treatment of certain breast cancer subtypes [ 258 ]. However, there is still limited understanding of the oncogenic pathways that control the progression of premalignant breast diseases or rare, but often aggressive, breast cancers (for example metaplastic breast cancer) [ 259 ]. Molecules may have distinct functions in different cellular contexts, therefore rigorous target validation is critical [ 260 , 261 ]; if a signalling protein has a scaffold function, disruption of protein-protein interactions may be required for efficacy. This requires a detailed biophysical analysis of protein structures and their key interactions.
For HER-2 positive disease, dual HER-receptor blockade is more effective than monotherapy and may help prevent or overcome resistance [ 262 , 263 ]. Two years of adjuvant trastuzumab offers no benefit over one year [ 264 ] but the utility of shorter trastuzumab therapy is, as yet, unconfirmed [ 265 ]. In metastatic breast cancer, serum metabolomic analyses may help to select patients with HER2+ cancers with greater sensitivity to paclitaxel plus lapatinib [ 266 ]. Multiple clinical trials are evaluating PI3K pathway inhibitors; other new agents under development include HSP90 inhibitors (for example NVP-AUY922 and ganetespib); panHER, irreversible inhibitors including neratinib and afatinib; monoclonal antibodies directed against human epidermal growth factor receptor 3 (HER3) and Src inhibitors such as saracatinib.
Resistance to signalling inhibitors
Resistance to targeted signal transduction agents is common, arising via multiple mechanisms including utilisation of compensatory feedback loops or alternative signalling pathways. Systems biology applications have begun to describe these dynamic changes [ 267 , 268 ], and are critical to identify key target points for effective therapeutic intervention.
Robust guidelines (akin to REMARK) are not yet employed in studies assessing the efficacy of novel therapeutics. Such rigour is essential to ensure that both appropriate models and quantitative outputs are fully utilised. The best drug combinatorial approaches could then be developed based on mechanistic insight into opportunities afforded by synthetic lethality [ 269 , 270 ]. More sophisticated experimental models of DNA-damage response (DDR) defects and those that accurately reflect mechanisms of therapy resistance will enable the design of targeted therapies to overcome these clinically relevant issues.
Drug responses
We lack a comprehensive understanding of the exact mechanisms (both on- and off-target) by which drugs exert anti-cancer effects in vivo ; this is exacerbated by our incomplete appreciation of networks, cross-talk and redundancy in cell signalling. Given that multiple inhibitors of specific pathways are now available (for example PI3K/PKB/mTOR), harmonised approaches to prioritisation of specific inhibitors/inhibitor classes and of research objectives in clinical trials are required.
Clinical determinants of intrinsic and acquired resistance
There is incomplete understanding of the role of diverse gene expression, epigenetic, protein and non-coding RNA changes in the heterogeneous manifestations of clinical resistance, [ 271 ]. There is a lack of equivalence between clinical, pathological, proliferative and molecular resistance that needs to be addressed and single genes or a canonical pathway are unlikely to be responsible. Furthermore, multiple mechanisms have also been implicated in acquired resistance, but their relationship to intrinsic resistance remains to be defined. Figure 5 illustrates the heterogeneity in patterns of gene expression in clinical endocrine resistance, suggesting that at least three major molecular mechanisms could be involved [ 272 ].
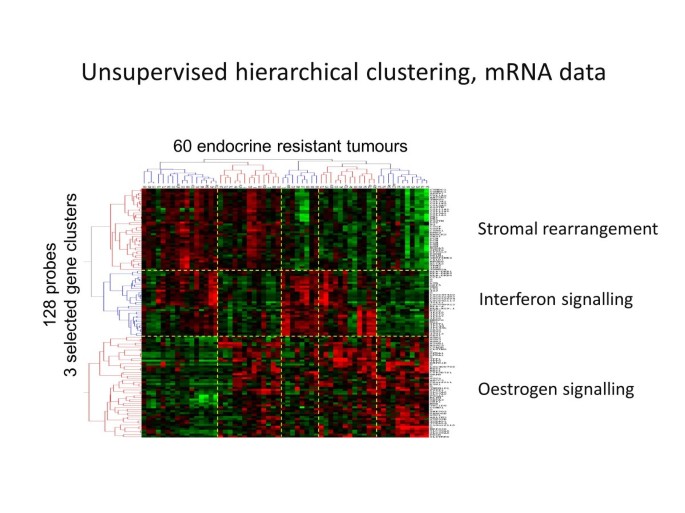
Molecular heterogeneity of endocrine resistance. Unsupervised hierarchical clustering of mRNA from 60 endocrine-resistant breast cancers shows heterogeneity in gene expression suggesting a multiplicity of underlying mechanisms including changes in oestrogen and interferon signalling and stromal genes. Courtesy of Professor William Miller and Dr Alexey Larionov, based on a poster presentation at the thirty-second annual CTRC-AACR San Antonio Breast Cancer Symposium, Dec 10–13, 2009 [ 272 ].
There is a need to understand the clinical impact of additional hormone receptors besides ERα, especially the progesterone receptor (PR): whilst PR is prognostic, the TEAM study has not demonstrated a predictive value [ 273 ]. Similar considerations apply to ERβ [ 274 , 275 ] and the androgen receptor (AR) [ 276 ], since trials of anti-androgens are currently underway in metastatic breast cancer [ 277 ].
It is not clear whether there are differences in ER+ve premenopausal vs. postmenopausal endocrine resistance [ 278 ]. As with other targeted therapies, the microenvironment, therapy-induced signalling reprogramming and stem cells are likely to play key roles. Proteomic profiling and protein functionality are particularly poorly characterised in the clinical resistance setting and such measurements remain challenging but essential.
It is important to define the contribution of CSCs to relapse on endocrine therapy, determine their sensitivity to existing agents or identify the unique signalling pathways that sustain their clonogenic potential. Diagnostic or prognostic tests based on ‘whole’ tumour samples may fail to address these potentially significant minority subpopulations of cells.
The few prospective studies to date have demonstrated that changes in management for one in six patients could be advised based on changes in breast cancer biomarkers on relapse, particularly ER, PR and HER2 [ 279 – 281 ]. Consequently, important clinical questions such as whether changes in the frequency of drug administration or alternating drug therapy could avoid or contribute to this process need to be addressed. Considering host factors such as adherence to medication [ 282 ], drug metabolism [ 283 ] and immune mechanisms [ 284 ], alongside molecular characteristics of tumours and the host microenvironment is essential.
Combinations and sequencing of targeted agents with conventional agents
Despite high-level evidence for isolated treatment situations (for example adjuvant treatment with AIs) [ 210 , 285 , 286 ], these have not been integrated into sequential treatment strategies, for example for adjuvant or first- or second-line palliative treatment. As treatment standards change (with AIs as standard adjuvant therapy), the sequence of tamoxifen as adjuvant therapy with AIs for first-line metastatic ER+ve disease may require adaptation. Such trials apply standard treatments that manufacturers may have little interest in supporting; new ways of supporting these trials will need to be explored.
Models are needed for the longitudinal study of hypoxic ‘microniches’ to inform timing of delivery of sequential targeted therapies or chemotherapy with radiation; to test real-time robotically controlled RT delivery to motion-affected hypoxic regions of primary breast tumours; and RT in combination with novel agents targeting pH regulatory mechanisms. Similarly, novel early-phase clinical trials of preoperative RT + targeted therapy or neoadjuvant hormonal therapy with baseline on-treatment biopsies for markers and gene signatures of radiosensitivity (the window of opportunity design) could complement the development of trials of stereotactic body RT to primary + neoadjuvant systemic therapy for limited-volume metastases in liver and bone.
Practical considerations include the risk/benefit of combining signalling inhibitors with anti-hormones, sequencing of tamoxifen and AIs [ 287 ] and targeting additional steroidogenic enzymes [ 288 ]. Recent randomised clinical studies have demonstrated substantial benefits for combinations of targeted agents such as endocrine therapy and mTOR inhibitors in ER+ve MBC [ 72 ] or horizontal dual HER-receptor blockade [ 289 – 292 ]. This results in several new challenges. Many patients benefit from single agent endocrine therapy or HER2-blockade and could avoid, at least initially, the toxicity of combination therapy if these cancers could be identified. There is a clear need to identify patients who respond adequately to targeted therapy (for example anti-HER-2 agents +/− endocrine agents) and do not need chemotherapy. Rational combinations need to be explored in the appropriate setting, taking into consideration compensatory induction of alternative signal transduction pathways bypassing targeted treatments. Treatment benefits in MBC or the neoadjuvant setting need converting into a potential survival benefit in early breast cancer.
New therapeutic approaches
Although phenotypically similar to BRCA1 mutant breast cancers, TNBC are heterogeneous and lack of expression of ER, PR and HER2 is not a good predictor of homologous recombination repair (HRR) status [ 293 ] Prognostic and predictive biomarkers of response for TNBC are obvious gaps which need to be addressed [ 294 ], complemented by an expanded and representative panel of fully characterised tumour cell lines and models [ 295 ]. More emphasis should be directed at developing markers of drug resistance and markers of resistance to current basal-like breast cancer/TNBC therapies [ 296 ]. Better biomarker-led characterisation could assist in patient stratification and hopefully improved treatment responses. Similarly, additional targets are required for other molecular subtypes that fail to respond to existing therapies.
Lymphangiogenesis and angiogenesis
Current understanding the role of lymphangiogenesis in metastasis (and thus its potential as a therapeutic target akin to neoangiogenesis) is limited [ 297 ]. In contrast, given the morbidity associated with lymphoedema following extensive lymph node dissection, identifying a means of inducing local regeneration of lymphatic vessels postoperatively could be envisaged. The contribution of the lymphatic system to immune responses to tumours is also underexplored [ 298 ]. Better in vitro and in vivo models are required to understand the cellular and molecular complexities of pathological angiogenesis and lymphangiogenesis, tumour cell intravasation, extravasation, organ colonisation and strategies for effective therapeutic interventions [ 299 ].
Anti-angiogenic therapies have been extensively trialled but have not yet lived up to their promise, with bevacizumab no longer approved for breast cancer by the FDA [ 300 – 302 ]. Tumour vasculature is heterogeneous [ 303 ] and multiple, temporally dynamic mechanisms contribute to the lack of durable responses [ 304 ]. The main focus has been vascular endothelial growth factor (VEGF)-driven angiogenesis but there is considerable redundancy in angiogenic signalling pathways [ 305 ]. Also, there are no validated biomarkers of response to anti-angiogenic therapies and it is likely that the vasculature of anatomically dispersed metastases will demonstrate further functional heterogeneity.
Exploiting the immune system
Although generally considered to be immunosuppressive, some chemotherapeutic agents (and indeed monoclonal antibodies) may involve an immune element; thus the combination of immunotherapy and chemotherapy becomes a real possibility [ 306 , 307 ]. In node-positive, ER-/HER2- disease, lymphocytic infiltration was associated with good prognosis in the BIG 02–98 adjuvant phase III trial [ 284 ]. There needs to be a systematic quantification of immune infiltration of breast cancer subtypes and how this relates to tumour progression, response to therapy or changes during treatment.
Cancer immunotherapy is gaining ground, whether antibody-based or cell-based, with an increasing emphasis on targeting the tumour microenvironment (for example macrophages or cancer-associated fibroblast (CAFs)) with DNA vaccines [ 308 ]. In addition, several immunogenic antigens (such as cancer testis antigens) have been detected in poor-prognosis breast cancers, which may serve as targets for therapy or chemoprevention [ 309 , 310 ]. New strategies for enhancing natural immunity or eliminating suppressor functions are required. There is a need for better animal models for evaluating immunotherapeutic strategies and in deciphering possible contributions to lack of responsiveness.
Living with and managing breast cancer and its treatment
Survivorship.
Cancer and its treatment have a considerable and long-term impact on everyday life [ 311 – 313 ]. Consequences may be physical (for example pain, fatigue, lymphoedema, hot flushes, night sweats and sexual problems), or psychological (cognitive function, anxiety, depression, fear of recurrence) and directly affect relationships, social activities and work. The relationship between the cancer patient and his/her partner will have a bearing on the level of distress: if communication is good, psychological distress will be lower [ 314 ]. Women may feel abandoned once treatment is completed with low confidence as a result [ 312 , 315 ]. The current system does not meet their needs [ 184 ] and the National Cancer Survivorship Initiative has been established to investigate new models of aftercare.
A recent framework publication highlights the importance of providing support to enable people to self-manage their aftercare [ 315 ]. Patients benefit from improved sense of control and ability to effect change together with an increased likelihood of seeking health information [ 316 , 317 ].
Living with advanced breast cancer
Quality of life in women with metastatic breast cancer is poor [ 318 ] with many experiencing uncontrolled symptoms [ 319 ]. Pain is a significant problem throughout the illness, not just with the end of life [ 318 ]. Depression, anxiety and traumatic stress also require intervention [ 320 , 321 ]. Those with metastatic breast cancer receiving social support report more satisfaction and a sense of fulfilment. Fewer avoidance-coping strategies are associated with better social functioning and a larger social network. Social stress has been found to increase pain and mood disturbance and has been associated with isolation. In addition, self-image and a decrease in sexual functioning challenge self-esteem and relationships at a time when support is most needed [ 322 ].
The impact of medical management on quality of life and decision making regarding palliative chemotherapy [ 323 , 324 ] and a lack of rehabilitation services [ 325 , 326 ] has been recognised. The convergence of palliative treatments and the end of life may impact on symptom control and care provision as well as place of death [ 327 , 328 ].
Supportive interventions
The main physical symptoms associated with breast cancer treatment are fatigue, pain, hot flushes, night sweats, cognitive and sexual problems and lymphoedema. Some interventions have demonstrated benefit with specific side effects [ 329 – 331 ]. Meta-analysis demonstrates that psychological interventions can reduce distress and anxiety [ 332 ], provide some physiological benefit, but with weak evidence regarding survival benefit [ 333 ]. Overall the evidence focuses on short-term benefit while the longer-term implications are unknown.
Group interventions are less effective in reducing anxiety and depression than individualised interventions such as cognitive behaviour therapy (CBT); [ 334 ], but do result in social and emotional improvements [ 335 ] and greater patient satisfaction [ 336 ]. Psycho-educational interventions show improvements in physical and psychosocial wellbeing [ 337 ] and reduced anxiety [ 338 ].
CBT reduces fatigue [ 339 ], insomnia [ 340 ] improves physical activity and quality of life [ 341 ]. CBT appears to be effective at all stages of breast cancer: group CBT can significantly reduce the impact of menopausal symptoms in breast cancer patients [ 342 , 343 ] with effects maintained over six months. Care packages to help improve coping skills, including group counselling sessions and/or telephone-based prompts has shown supportive care in the extended and permanent phases of survival to be effective [ 344 ]. Mindfulness-based stress reduction and cognitive therapy can improve mood, endocrine-related quality of life, and wellbeing at least in the short term [ 345 ].
Much evidence demonstrates the benefits of physical activity for breast cancer patients [ 346 ]. RCTs show that physical activity interventions during treatment show small to moderate beneficial effects on cardiovascular fitness, muscular strength and can reduce deconditioning. Post treatment, physical activity interventions result in a reduction in body fat and increase in fat-free mass, a moderate to large effect on cardiovascular and muscular strength, small to moderate effect on quality of life, fatigue, anxiety and depression and some evidence of reduced lymphoedema and osteoporosis [ 347 , 348 ].
The translation of physical activity research into clinical practice is a challenge. Currently, exercise-based cancer rehabilitation is not routinely incorporated into breast cancer care. However, from the National Cancer Survivorship Initiative, Macmillan Cancer Support is evaluating around 12 physical activity programmes and evaluating physical, psychological and cost benefits. One exercise intervention during therapy reassessed participants after five years and showed that those from the exercise group were still incorporating approximately 2.5 hours more physical activity a week and were more positive than control patients [ 349 ]. Furthermore, other charities are starting up similar programmes, such as Breast Cancer Care’s ‘Best Foot Forward’. There are very few intervention studies involving women with advanced metastatic cancer; these predominantly focus on supportive-expressive therapy and have been found to reduce distress [ 350 ] but the benefits are not maintained in the long term [ 334 ].
Inadequate translation of research findings into practice
While the problems are well recognised, there is inadequate clinical translation: for example, recognising the benefits of physical activity requires incorporating and testing intervention(s) in clinical practice. There is also a lack of representation and sensitivity to the needs of diverse groups. Similarly, the impact of breast cancer goes beyond the patient; more attention should be paid to their families, partners and children.
CBT is becoming integrated into clinical practice with training for clinical nurse specialists but there is still a need to consider how CBT and other interventions can be better integrated to widen access. Novel interventions must be developed and validated using methods based upon sound theoretical principles, with demonstrable effectiveness (both clinical and financial) that can be deployed as widely as possible to maximise benefit. A clear understanding of the components of interventions that promote uptake, adherence and long-term benefit is required. Funding for research into living with and managing the consequences of breast cancer and its treatment is very limited, adversely impacting the building of research capacity and expertise.
Establishing a multidisciplinary research consortium to develop a theoretical framework to inform research addressing the needs of those living with and managing the broad ranging consequences of breast cancer and its treatment would inform choice of outcome measures, innovative approaches to intervention design and testing. Alternative trial designs to RCTs need to be considered that incorporate patient preferences. It would also be of great benefit to the field to draw up guidance on implementing successful evidence into clinical practice.
Longitudinal studies are required to assess the recovery of health and wellbeing and the long-term adjustment of women and men who have a diagnosis of breast cancer. This will allow investigation of how unmet psychosocial needs and psychological morbidity during diagnosis and treatment relate to quality of life, sexuality, physical wellbeing and the effects of other illnesses later in life. The long-term impacts of breast cancer and therapy on everyday life need further investigation [ 351 ]. There are implications for cardiac functioning, osteoporosis, neuropathy, cognitive dysfunction, lymphoedema and shoulder mobility on the ability to maintain independence [ 352 ].
There is insufficient epidemiological data on the problems of women who have recurrence and metastatic disease. Research into integrated oncology and palliative care models are needed to determine which approaches improve quality of life, psychological wellbeing, palliation of symptoms, treatment decisions and end of life care. The needs of the families of women with advanced metastatic cancer and how to support them and their carers most effectively are unclear. Decision making at the end of life and the development of tools to assist women and healthcare professionals to choose appropriate treatment and place of death is needed.
Specialist breast care nurses have also been found to enhance the supportive care of women with metastatic breast cancer. [ 353 ]. However, there is a need to identify the active components of interventions and an individual’s preference for different types of interventions to determine what works best for him or her.
Development of mindfulness and third-wave approaches (for example Acceptance and Commitment Therapy) may be effective. More RCTs of theory-based interventions for treatment-related symptoms and innovative trial designs are needed (with longer follow-up, analysis of moderators and mediators and identified components) to support women to manage their everyday lives. Interventions to address specific psychological needs such as low self-confidence and fear of recurrence also need to be tested. Interventions are required to support women to increase their physical activity, reduce the risk of recurrence and examine the impact on late effects. The frequency, intensity, type and timing of physical activity for maximum benefit needs to be established. Effective means are required to support women to manage impaired sexuality/sexual function, altered body image, lymphoedema, weight gain [ 354 ], fear of recurrence, hormone therapy-related symptoms [ 341 , 343 , 355 , 356 ], cognitive problems [ 357 ][ 358 ] and post-surgical problems [ 359 , 360 ]. Alternative delivery of intervention needs to be explored, such as self-management, telephone or online support and non-specialist delivery: for example comparison of home-based versus hospital-based interventions on physical activity levels, patient satisfaction and motivation.
Strategic approaches to enable progress
Experimental models of breast cancer, improved tissue culture models.
There is now a greater appreciation of the importance of employing appropriate human cancer cells. [ 361 ]. Commonly used breast cancer cell lines are derived from metastases or pleural effusions and fail to adequately represent the diversity and complexity of breast cancer [ 362 ]. It has proven difficult to establish human tumour cell cultures representative of the major subtypes and to maintain their genomic and phenotypic integrity. In addition, inter-patient variability and inadvertent selection of the most malignant subtypes, skews availability of representative material.
Better representation of breast cancer subtypes is required. Material from normal mammary tissue, premalignant breast conditions, different ER+ve (and rare) subtypes of breast cancers and ideally metastases from all major sites are needed to cover the full spectrum of breast cancer development and progression. Primary or minimally passaged cell cultures will avoid issues of misidentification, contamination or long-term culture artefacts. Ideally, a central repository of well-annotated human primary breast cancer cells, associated host cells and cell lines should be available to researchers linked to a searchable, open-access database. Maintaining breast tumour tissue in culture with its essential characteristics intact will enable prognostic screening and testing of potential therapeutic agents.
Reliable cell-type-specific markers are required and it is also important to be able to recognise cancer stem cell subpopulations (or transient phenotypes). Identification of promoters for distinct cell subpopulations will enhance the number and scope of available in vitro models. [ 363 ] and enable conditional genetic modifications for mechanistic and target validation studies [ 364 ]. Ideally, co-cultures (of both normal and precancerous breast cells) with host cell populations such as fibroblasts, myoepithelial cells, macrophages, adipocytes or vascular endothelial cells are needed for studies of cellular interactions within the appropriate ECM microenvironment.
Three-dimensional culture models can recapitulate the tissue architecture of the breast and its characteristic invasion patterns [ 89 , 365 ] especially if host stromal components are incorporated [ 366 ]. Three-dimensional heterotypic model systems are also enabling dissection of the effect of cell-cell interactions and stromal elements in drug resistance. Three-dimensional cultures require additional refinement, higher throughput, quantitative assays [ 367 ] and a move towards more physiologically relevant conditions, for example by the use of bioreactors, enabling long-term cultures under flow conditions; especially appropriate for invasion assays [ 368 , 369 ].
Animal tumour models
In the last five years there has been an expansion in the use of orthotopic (anatomically correct) breast cancer xenografts [ 370 ] and significant advances in developing patient-derived xenografts (PDX) [ 371 ]. These models better reflect the human cancers from which they were derived and ER+ve tumours respond appropriately to oestrogen ablation [ 372 ]. Increased use of genetically engineered mouse (GEM) models driven by relevant abnormalities such as BRCA mutations, HER2 overexpression and so on have enabled the study of naturally occurring tumours in immunocompetent hosts and evaluation of new targeted therapies such as PARP inhibitors and the emergence of resistance [ 373 ]. Pros and cons of different models are shown in Figure 6 .
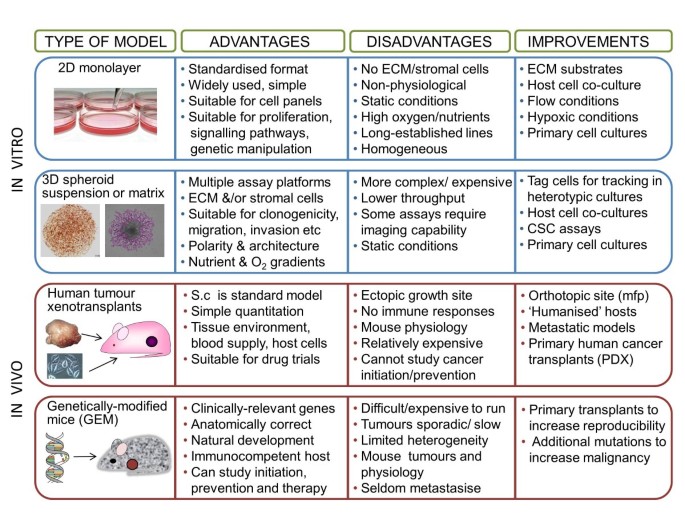
Comparative properties of experimental tumour models. In vitro assays of tumour growth and response to therapy can be conducted in two dimensions or three dimensions - the latter more closely approximating the biology of solid tumours than a simple monolayer. Cultures can be enhanced by the addition of matrix proteins and/or host cells and can be adapted to measure not only tumour cell proliferation, but also additional cancer hallmarks such as invasion. Standard in vivo assays depend upon the transplantation of established human tumour cell lines into athymic (immune-incompetent) hosts. These models are relatively simple and easy to use, but are increasingly complemented by genetically engineered mice harbouring targeted genetic mutations which render them susceptible to developing mammary cancers. The figure summarises key advantages and disadvantages of each model and means by which their clinical relevance and utility might be enhanced. Based on a figure provided courtesy of Claire Nash in Dr Valerie Speirs’ group (University of Leeds).
Expansion of PDX models will be required to cover all the main breast cancer phenotypes [ 374 ] and to address the contribution of ethnic diversity [ 375 ]. Advanced GEM models with multiple genetic abnormalities, able to generate both hormone sensitive and insensitive tumours and in which metastasis occurs at clinically relevant sites will also be a desirable refinement [ 376 , 377 ]. However, all such animal models will require validation of any findings in the clinical setting [ 296 , 378 , 379 ]. Models are also required to investigate mechanisms of the induction of (and escape from) long-term tumour dormancy [ 380 ], a unique feature of breast cancer.
Invasive behaviour does not occur uniformly or synchronously within a tumour [ 381 ] and this heterogeneity is not easily reproduced in vitro . Improved tumour models and methods are required to understand the localised and possibly transient factors involved in temporal and spatial heterogeneity that promote invasion and metastasis.
Models for testing novel targeted agents against disseminated disease
Novel agents designed for systemic administration are rarely tested against established invasive/metastatic disease in preclinical animal models [ 382 , 383 ]. There is an urgent need to develop better models for the discovery and development of therapies targeting metastases that are effective against all sites of disease [ 384 ].
In around 20% of women, complete resection of primary tumours does not prevent distant metastases because dissemination has already occurred. In these cases, agents targeting cell motility or invasion may have limited value. It is therefore critical that preclinical models used for testing such therapies incorporate established micrometastases [ 385 ]. Similarly, there is a preponderance of lung metastasis models in routine use. Other important sites of breast cancer metastasis (for example bone, brain and, liver) are relatively poorly represented, and this needs remedying in preclinical drug evaluation [ 386 – 388 ]. Human tissue (such as bone) transplanted into mice can provide a more relevant microenvironment [ 389 ].
Preclinical or clinical trials focused on tumour shrinkage are not appropriate for testing the efficacy of anti-invasive or anti-metastatic agents that may reduce metastasis without significantly impacting primary tumour growth [ 390 ]. Such approaches would likely fail current response evaluation criteria in solid tumors (RECIST) criteria and show little activity in the neoadjuvant setting or in late stage patients with advanced metastatic disease. The potential to utilise veterinary models for testing novel therapies or RT-systemic therapy combinations and cross-disciplinary collaboration with other scientific disciplines to develop real-time in vivo biosensors of tumour biology offer novel opportunities for significant progress.
Modelling drug resistance
While challenging, establishing cell lines, tissue slice models and PDX from relapsed and resistant cancers should be the ultimate goal in order to provide a window on the mechanisms that occur in patients where therapies fail. This would also allow ex vivo targeting studies, employing signalling analyses and imaging systems to track resistance mechanisms and progression.
Preclinical endocrine resistant models have largely been derived from ER+ve MCF7 cells in vitro , either by transfection of potential signalling molecules such as HER2 or from continuous exposure to anti-endocrine agents. Extensive panels of relapsed human tumour cell lines are required to reflect the heterogeneity of clinical resistant disease. This will allow assessment of the impact of genetic background, duration, sequence and type of endocrine agent (including AI) and rational evaluation of agents to reverse resistance [ 391 ]. It is critical to validate mechanisms identified in vitro with clinical resistance.
Longitudinal clinical samples and associated biological studies
Biobanking has substantially improved and is seen as a significant outcome of the last gap analysis [ 7 ] but the systematic analysis of clinical material collected from serial tumour biopsies/ fine-needle aspiration (FNA) (or ideally less invasive means such as ‘liquid biopsy’) before, during and following resistance development is lacking. Procurement of matched materials remains challenging but is critical to establishing clinically relevant signalling mechanisms that culminate in acquired resistance, allowing tracking of the dynamics and prevalence of molecular events during response through to any subsequent relapse. Care must be taken to provide adequate sampling of inherently heterogeneous tumours in their primary, recurrent and disseminated settings, which may also provide material for study of site-specific metastasis. [ 392 ] and samples must be full annotated, ideally with ‘omics’ profiling and immunohistochemistry. The biopsy of metastatic lesions is challenging and will require systematic introduction of a ‘warm autopsy’ programme [ 393 ]. A more realistic alternative is to further exploit the preoperative neoadjuvant setting, despite the potential issues of heterogeneity and sampling [ 394 ]. Collection of such samples is a particularly valuable resource to address mechanisms of intrinsic resistance and to track early therapy-associated signalling changes (Figure 7 ).
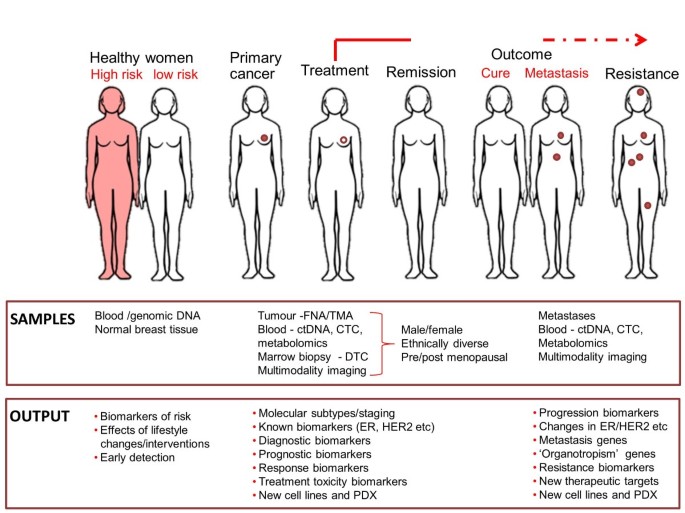
Longitudinal sampling and enhanced biobanks. The longitudinal collection of blood and samples from normal breasts, primary cancers and relapsed/metastatic/treatment-resistant disease is essential in order to address the origins, heterogeneity and evolution of breast cancers. Samples are required from as broad a patient population as possible to understand ethnic, age-related and gender differences in incidence, molecular subtypes, prognosis and response to treatment. Sequential samples (ideally patient-matched) from primary tumours and metastases will enable detailed studies of tumour evolution/progression and provide material for generating new cell lines and patient-derived xenografts for translational research. Multimodality imaging and metabolomic analyses will add further dimensions of valuable information. Based on a figure provided courtesy of Professor William Gallagher, with thanks to Dr Rut Klinger (UCD Conway Institute).
Increased use of clinical relapse material will determine the relevance of preclinical findings and identify potential candidates for detailed mechanistic evaluation in appropriate tumour model systems. Ultimately the goal is to determine if patients can be better stratified to allow rational, personalised choices for further therapy. This aspiration requires better integration between clinicians and scientists, trial providers and pharmaceutical companies and would benefit from data sharing. Tissue-based analyses from clinical trials need to be expanded to incorporate all of the next generation sequencing studies for research. These initiatives need to be co-ordinated with cancer registry/ British Association of Surgical Oncology (BASO) breast cancer data.
Blood samples for early diagnosis, monitoring treatment response, early indicators of disease relapse (and revealing increased heterogeneity) are imperative as our ability to generate new biomarkers through emerging technologies increases. These include detection of CTCs, miRNAs, ctDNA, exosomes, and so on. Serum HER2 measurement may be another promising biomarker with prognostic and predictive value [ 395 – 398 ].
Biomarkers of response or relapse
With the exception of ER and HER2, the availability of biomarkers to accurately identify which patients will receive benefit from targeted treatment, and indicators of patients at high risk of progression or relapse remains limited. Further advances in molecularly targeted and anti-endocrine therapy require clinically applicable predictive biomarkers to enable appropriate patient recruitment and to track responses to treatment [ 399 , 400 ]. These analyses should be applied both to primary tumours and recurrent/metastatic lesions to accommodate the profound heterogeneity within individual cancers, which increases further during disease progression. Understanding which molecular markers are ‘drivers’ of breast cancer and their functional roles at different stages of disease will be key to designing more effective targeted agents.
Validation of predictive markers for drug response could be better facilitated by the routine inclusion of such approaches into clinical trials rather than retrospective analyses of archived material. Any new biomarkers should have well-defined cut-off points, be thoroughly validated and robust. We require biomarkers to identify patients who will not respond to trastuzumab (primary resistance) in addition to the development of secondary acquired resistance. Discriminatory biomarkers are required for combination therapies such as lapatinib and trastuzumab in HER2-positive breast cancers. We lack preclinical data that can predict which combination of anti-HER2 therapies is optimal. There is also a need for biomarkers that can identify patients who may be more suitably treated with a tyrosine kinase inhibitor (TKI) rather than trastuzumab or combination anti-HER2 therapy. New irreversible TKIs currently in clinical trials, (for example afatinib and neratinib) have shown increased potency in preclinical studies - could these now become the mainstay for HER2-positive tumours?
Knowledge of the therapeutic benefits of mTOR inhibitors and of newer PI3K pathway inhibitors in breast cancer subtypes is rudimentary and we have no biomarkers that can be used to optimise their therapeutic index. In addition, knowledge of how important genomic (for example PIK3CA mutations) and proteomic (for example PTEN loss) biomarkers impact the efficacy of specific PI3K pathway inhibitors in the clinical setting is limited. Further preclinical research on the functional proteomic effects of genomic abnormalities in the PI3K pathway in breast cancer is essential.
ER+ve tumour heterogeneity remains a challenge: luminal A vs. luminal B subgroups impact on prognosis; however, the mechanisms of endocrine failure remain largely unknown. In ER+ve disease there is a lack of accepted biomarkers/signatures to distinguish endocrine-sensitive patients from those with intrinsic insensitivity or who will develop early or late resistance.
There is a need to develop non-invasive means of detecting risk of subsequent relapse. In addition to serial tumour samples, serum samples are warranted as these may ultimately provide less invasive indicators of acquisition of resistance. It remains unclear if single or multiple biomarkers or transcriptional profiles are optimal, or even if basic endocrinological markers may prove valuable in the context of predicting resistance.
While imaging (at least with some modalities) is routinely applied to the early detection and follow-up of breast cancers, there is a need to increase the use of functional screening techniques to better understand tumour heterogeneity, identify features associated with response or resistance to treatment and more rapidly translate promising new preclinical methodologies to clinical evaluation. It is important to evaluate emerging imaging biomarkers of primary and metastatic breast cancer and there is a requirement for new, more specific and clinically translatable radiotracers for positron emission tomography/single-photon emission computed tomography (PET/SPECT) [ 401 , 402 ]. We also need to identify and assess the utility of imaging biomarkers associated with other hallmarks of cancer beyond proliferation for example invasion, altered metabolism, hypoxia. Attention needs to be given as to how to validate novel imaging biomarkers in adequately powered multi-centre clinical trials. The funding available from most grant-awarding bodies is insufficient to cover this, suggesting the need to consider larger collaborative trials funded by more than one agency.
Imaging may also be able to report on intratumoural heterogeneity and identify the most significant region (for example more aggressive/invasive areas via diffusion-weighted magnetic resonance imaging (MRI)), to more accurately direct biopsies or radiotherapy. EMT could be addressed by the increased use of cluster, histogram and/or texture analyses, but it will be necessary to define the correct metrics to assess and quantify such phenotypes [ 403 ]. It would be desirable to extend these techniques to define different tumour subtypes such as DCIS, luminal or TNBC non-invasively (which may identify mixed lesions missed by homogenised or limited sample analyses) and assess heterogeneity between metastases. Ideally, imaging studies (both preclinical and clinical) should be co-registered with linked genomic and proteomic information in order to fully interpret the biological relevance of the images obtained [ 404 – 406 ]. However, tissue collection is often not co-ordinated with imaging studies and the added benefit not always appreciated.
A key achievable goal is to non-invasively evaluate predictive biomarkers of therapeutic responses. Increased adoption of more clinically relevant orthotopic xenograft and transgenic murine models of primary and metastatic breast cancer will demand robust preclinical imaging approaches. The use of such models in imaging-embedded trials of novel agents will improve the accuracy of preclinical data, accelerating the development of promising drugs, or enabling early closure of suboptimal programmes. Such refined preclinical trial designs will also prove highly informative in establishing combination and/or sequential treatment regimes.
Clinical trial design and patient involvement
Clinical trial design should be adapted to use preoperative and neoadjuvant models to allow novel therapies to be tested in patients [ 394 , 407 ], identify de novo resistant cancers and investigate how such resistance can be counteracted. These approaches are particularly relevant for therapeutic strategies that target cancer stem cells, residual (dormant) cancer cells or influence the tumour microenvironment. Future trial design will also have to incorporate dynamic strategies, such as using the response to short-term treatment to guide the use of additional preoperative treatment. Given the increasing focus on small target populations (for example molecular subtypes of breast cancer), clinical trial strategies for effective patient stratification or selection based on molecular characteristics are required to allow routine integration into large-scale clinical trials. In addition, the relatively long period between surgery and relapse in breast cancer patients impacts negatively on the economic feasibility of such clinical trials. New thinking will be required to modify clinical trial design, and to consider biomarkers that relate to invasive and metastatic phenotypes, for example as in trials with denosumab where the development of skeletal-related events (SRE) was an accepted and measurable endpoint [ 221 ].
Patient reported outcomes
There is a need to incorporate standardised patient-reported outcome measures (PROMs) both within clinical trials and in everyday clinical practice. Currently, many trial reports are reliant on the common terminology criteria for adverse events (CTCAE) gradings about side effects, which show alarming discrepancies with data actually collected from patients [ 408 ].
Further research is needed to support the use of decision aids around surgery and treatment and to define any benefits. There is also a need for prospective research to identify consequences of treatment and the impact of co-morbidities on the lives of women with breast cancer so that future patients can consider these as part of their decision making. The experiences of minority ethnic groups, younger (<45 years) and older (>70 years) women in relation to their treatment choices and management need further research. Addressing non-adherence to endocrine therapy and understanding the biological mechanisms of significant side effects such as menopausal symptoms are poorly understood. The value of incorporating lifestyle recommendations as part of routine care and its impact on recovery and quality of life should be further explored.
Multidisciplinary collaborations and resources
Increased resources are required to support core (for example biochemical/IHC) as well as new ‘omics technologies; to develop improved in vitro / in vivo / ex vivo model development, serial clinical sample collection, advanced bioinformatic/systems biology analysis, clinical biomarker validation and ‘bench to bedside’ drug development. Stronger multidisciplinary collaborations between laboratory scientists, clinicians, bioinformaticians and engineers (and in turn with funding bodies and industry) must be encouraged. Much better integration of computer science, database engineering, data analytics and visualisation, hardware and software engineering within biological research will be essential to effectively read and translate increasingly complex data. Convincing drug companies of the benefits of a co-ordinated approach (tissue collection before, during and after treatments) in clinical trials of new drugs is problematic, and access of material for research purposes is limited. Companies must be convinced of the benefits of accurate biomarkers to allow for the better stratification of patients. Even though this will limit their target population, this should be offset by higher response rates and faster regulatory approval.
Continued support is required for basic biological research and understanding of cell signalling processes with emphasis on interactions, cross-talk and microenvironmental regulation. It is important that approaches in this area are linked to systematic investigations and precise analyses of cell responses to a wide range (and combination) of inhibitors, tested in clinically relevant breast cancer model systems. A key element is open discussion and learning from negative results to avoid unnecessary duplication of research. Sharing of information, best practice, optimised model systems, technologies and resources is essential, perhaps through developing web-based analysis portals. Such approaches are needed to integrate and interpret diverse sources of data to understand the plasticity of signalling emerging during treatment though to resistance (Figure 8 ).
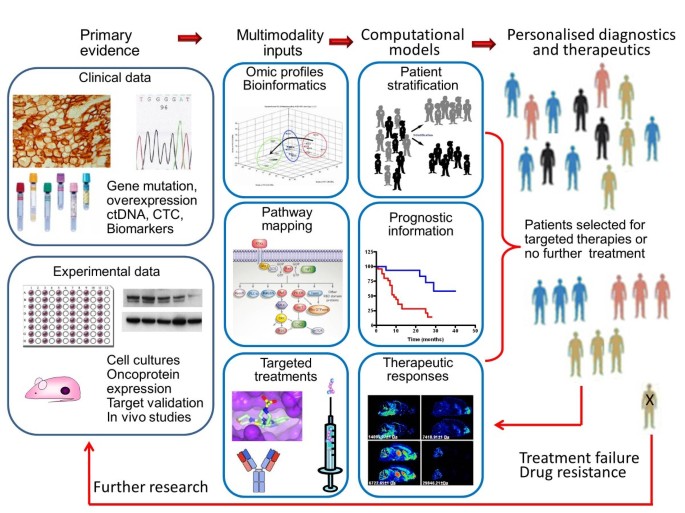
Integrated vision of multidisciplinary research. Enhanced integration and utilisation of the vast amount of clinical and experimental observations relating to breast cancer is urgently required. Clinical observations generate hypotheses relating to the origins of cancer, its underlying molecular pathology and potential vulnerabilities that could be exploited for therapeutic benefit. Such insights provide opportunities for testing and validation in in vitro, in vivo and in silico models. Drug discovery aims to provide inhibitors of major oncogenic ‘drivers’ for use singly or in combination with conventional therapies; such personalised medicine requires the co-development of predictive and pharmacodynamic biomarkers of response. Results from preclinical therapy studies and clinical trials should be fed back into searchable databases to reveal reasons for treatment failure and allow new strategies to be tested and deployed. Based on a figure provided courtesy of Professor William Gallagher, with thanks to Professor Walter Kolch (UCD Conway Institute).
A co-operative network of advanced radiotherapy facilities, analogous to the Experimental Cancer Medicine Centres is needed to ensure adequate patient numbers for clinical trials. Engaging patients and healthcare teams is critical to enable complex biological studies (especially longitudinal biomarker studies). Lack of academic clinicians (particularly in radiation oncology), radiobiology and physics staff nationally and rising service pressures on NHS staff are all detrimental to delivery of clinical translational research.
While substantial advances have been made in breast cancer research and treatment in the last five years, there remain significant gaps in translating this newly acquired knowledge into clinical improvements.
Understanding the specific functions and contextual interactions of genetic and epigenetic advances and applying this knowledge to clinical practice, including tailored screening, will require deeper understanding of molecular mechanisms and prospective clinical validation. Even with clinically actionable tests, decision making, support for patients and their families and overcoming the barriers to lifestyle change (diet, exercise and weight) alongside chemopreventive strategies are required to optimise health outcomes.
Genomic profiling of sequential clinical samples (primary, relapsed and secondary cancers, CTC, ctDNA, before, during and following therapy) is required to identify specific biomarkers of inter-/intra-tumour spatial and temporal heterogeneity, metastatic potential, sensitivity to radiotherapy and different forms of chemotherapy, de novo or acquired resistance. This will significantly improve patient stratification for existing therapies and identify key nodes in these dynamic processes as potential new therapeutic targets. Validated markers of these processes (including minimally invasive multimodality imaging and metabolomics methodologies) will benefit from synergies between laboratory and clinical interactions. Improved understanding of the interactions, duration, sequencing and optimal combinations of therapy should allow better stratification of patients and reduce overtreatment (or undertreatment) enhancing prevention or survival while reducing morbidity.
Further genetic, epigenetic and molecular profiling of breast cancers and their associated stroma would be significantly enhanced by expanded panels of cell lines representing all major breast cancer subtypes and three-dimensional tumour-host heterotypic co-culture systems. This would enable increased understanding of the molecular drivers behind specific cancer subtypes and their role (together with microenvironmental modifiers) in treatment resistance and metastasis. Deciphering tumour-stromal interactions incorporating metabolic and immunological host mechanisms and intracellular/extracellular signalling pathways would have therapeutic implications for prevention and therapy. Advanced high-content analytical methods will enable consideration of additional key cancer ‘hallmarks’ beyond proliferation (for example cell motility and invasion) and enable screening for inhibitors under more physiologically relevant conditions. Better preclinical animal models (for example genetically engineered mice expressing relevant human oncogenes, which develop widespread metastases; patient-derived xenografts) are required. Such models would enable testing of hypotheses derived from clinical observations and rigorous target validation and evaluation of novel therapies in the metastatic setting (and where desirable in immunocompetent hosts).
Underpinning these advances, optimised multimodality imaging for diagnosis and therapeutic monitoring should enable better evaluation of primary and metastatic disease. Clinically annotated tissues for translational research must be linked to bioinformatics as key contributors to interdisciplinary research, essential for rapid future advances. Increasing numbers of women and men are surviving breast cancer. Alongside advances in understanding the disease and using that knowledge for prevention, earlier detection and successful treatment of breast cancer, interventions to improve the survivorship experience require innovative approaches to address the consequences of diagnosis and treatment.
Top 10 gaps:
Understanding the specific functions and contextual interactions of genetic and epigenetic changes in the normal breast and the development of cancer
Effective and sustainable lifestyle changes (diet, exercise and weight) alongside chemopreventive strategies
Tailored screening approaches including clinically actionable tests
Molecular drivers behind breast cancer subtypes, treatment resistance and metastasis
Mechanisms of tumour heterogeneity, tumour dormancy, de novo or acquired resistance; how to target the key nodes in these dynamic processes
Validated markers of chemosensitivity and radiosensitivity
Interactions, duration, sequencing and optimal combinations of therapy for improved individualisation of treatment
Optimised multimodality imaging for diagnosis and therapeutic monitoring should enable better evaluation of primary and metastatic disease
Interventions and support to improve the survivorship experience including physical symptoms such as hot flushes and lymphoedema
Clinically annotated tissues for translational research including tumour, non-tumour and blood based materials from primary cancers, relapsed and metastatic disease
Proposed strategic solutions:
For significant progress to be made in treating and supporting those impacted by breast cancer (and ultimately preventing and overcoming this disease) basic and translational research scientists in academia and industry, funding bodies, government and patients need to work together to achieve the following key strategic solutions
To reverse the decline in resources targeted towards breast cancer research, funding must be increased and strategically directed to enhance our current knowledge, develop the talent pool, and apply evidence-based findings to improve clinical care
A fully cohesive and collaborative infrastructure must be developed to support breast cancer research; this requires improved access to appropriate, well-annotated clinical material including longitudinal sample collection with expert bioinformatics support and data sharing.
Building on sound investment and infrastructure, all stakeholders (researchers, funders, government, industry and patients) must work together on the clinical development and translation of research knowledge to patient benefit. For example, enhanced, clinically relevant, in vitro and in vivo models are required for evaluation of new therapies together with validated biomarkers, which should then be embedded in clinical practice.
Research funders, government and industry should provide innovative programmes to encourage collaborative cross-disciplinary working practices, including the training of more physician-scientists and integration of physical sciences, technology and engineering.
Improving clinical trial methodologies, including patient involvement, recognising that a changing global environment is required to ensure that all clinical developments can be tested and ultimately implemented for patient benefit.
Abbreviations
Aromatase inhibitor
Androgen receptor
Ataxia telangiectasia mutated
British Association of Surgical Oncology
Cancer-associated fibroblast
Cognitive behavioural therapy
Cyclin-dependent kinase 10
CHK2 checkpoint homolog
Checkpoint kinase 2
Central nervous system
Cancer stem cell
Circulating tumour cell (in blood)
Common terminology criteria for adverse events
Circulating tumour DNA
Ductal carcinoma in situ
DNA damage response
Deoxyribonucleic acid
Disseminated tumour cell (usually in marrow nodes or tissue)
Extracellular matrix
Epithelial-mesenchymal transition
Oestrogen receptor
Fibroblast growth factor
Fibroblast growth factor receptor 1
Fine-needle aspiration
Forkhead box protein A1
Genetically engineered mouse
Genome-wide association studies
Human epidermal growth factor receptor 2
Human epidermal growth factor receptor 3
Homologous recombination repair
Hormone replacement therapy
Heat shock protein 90
Ipsilateral breast tumour recurrence
International Cancer Genome Consortium
Illumina collaborative oncological gene-environment study
Insulin-like growth factor 1
Immunohistochemical
Induced pluripotent stem cells
Chromatography-mass spectrometry
Metastatic breast cancer
Magnetic resonance imaging
Nuclear magnetic resonance
Representing the whole HER family
Poly (ADP-ribose) polymerase
Patient-derived xenografts
Positron emission tomography/single-photon emission computed tomography
Phosphatidylinositide-3 kinase
Gene encoding PI3 kinase alpha
Protein kinase B
Progesterone receptor
Patient-reported outcome measures
Randomised controlled trial
Response evaluation criteria in solid tumors
Ribonucleic acid
Selective oestrogen receptor modulators
Short inhibitory RNAs
Sentinel node biopsy
Single nucleotide polymorphism
Skeletal-related events
Standardisation of Breast Radiotherapy (START) trial A
Standardisation of Breast Radiotherapy (START) trial B
The Cancer Genome Atlas
Transforming growth factor beta
Tyrosine kinase inhibitor
Tissue microarray
Triple-negative breast cancer
Vascular endothelial growth factor
Women’s Health Initiative.
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM: Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010, 127: 2893-2917.
Article CAS PubMed Google Scholar
Breast cancer incidence statistics. http://www.cancerresearchuk.org/cancer-info/cancerstats/types/breast/incidence/#trends ,
Maddams JBD, Gavin A, Steward J, Elliott J, Utley M, Møller H: Cancer prevalence in the United Kingdom: estimates for 2008. Br J Cancer. 2009, 101: 541-547.
Article CAS PubMed PubMed Central Google Scholar
Maddams J, Utley M, Moller H: Projections of cancer prevalence in the United Kingdom, 2010–2040. Br J Cancer. 2012, 107: 1195-1202.
Leal J: The economic burden of cancer across the European Union. Proceedings of the National Cancer Research Institute Conference: 4–7. 2012, Liverpool, November
Google Scholar
Data package. http://www.ncri.org.uk/includes/Publications/general/Data_package_12.xls ,
Thompson A, Brennan K, Cox A, Gee J, Harcourt D, Harris A, Harvie M, Holen I, Howell A, Nicholson R, Steel M, Streuli C: Evaluation of the current knowledge limitations in breast cancer research: a gap analysis. Breast Cancer Res : BCR. 2008, 10: R26-
Article PubMed PubMed Central Google Scholar
Tissue Bank. http://breastcancertissuebank.org/about-tissue-bank.php ,
Melchor L, Benitez J: The complex genetic landscape of familial breast cancer. Hum Genet. 2013
Michailidou K, Hall P, Gonzalez-Neira A, Ghoussaini M, Dennis J, Milne RL, Schmidt MK, Chang-Claude J, Bojesen SE, Bolla MK, Wang Q, Dicks E, Lee A, Turnbull C, Rahman N, Fletcher O, Peto J, Gibson L, Dos Santos Silva I, Nevanlinna H, Muranen TA, Aittomäki K, Blomqvist C, Czene K, Irwanto A, Liu J, Waisfisz Q, Meijers-Heijboer H, Adank M, Breast and Ovarian Cancer Susceptibility Collaboration, et al: Large-scale genotyping identifies 41 new loci associated with breast cancer risk. Nat Genet. 2013, 45: 353-361. 361e351-352
Sakoda LC, Jorgenson E, Witte JS: Turning of COGS moves forward findings for hormonally mediated cancers. Nat Genet. 2013, 45: 345-348.
Antoniou AC, Beesley J, McGuffog L, Sinilnikova OM, Healey S, Neuhausen SL, Ding YC, Rebbeck TR, Weitzel JN, Lynch HT, Isaacs C, Ganz PA, Tomlinson G, Olopade OI, Couch FJ, Wang X, Lindor NM, Pankratz VS, Radice P, Manoukian S, Peissel B, Zaffaroni D, Barile M, Viel A, Allavena A, Dall'Olio V, Peterlongo P, Szabo CI, Zikan M, Claes K, et al: Common breast cancer susceptibility alleles and the risk of breast cancer for BRCA1 and BRCA2 mutation carriers: implications for risk prediction. Cancer Res. 2010, 70: 9742-9754.
Ingham S, Warwick J, Byers H, Lalloo F, Newman W, Evans D: Is multiple SNP testing in BRCA2 and BRCA1 female carriers ready for use in clinical practice? Results from a large Genetic Centre in the UK. Clin Genet. 2013, 84: 37-42.
Audeh MW, Carmichael J, Penson RT, Friedlander M, Powell B, Bell-McGuinn KM, Scott C, Weitzel JN, Oaknin A, Loman N, Lu K, Schmutzler RK, Matulonis U, Wickens M, Tutt A: Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and recurrent ovarian cancer: a proof-of-concept trial. Lancet. 2010, 376: 245-251.
Turnbull C, Seal S, Renwick A, Warren-Perry M, Hughes D, Elliott A, Pernet D, Peock S, Adlard JW, Barwell J, Berg J, Brady AF, Brewer C, Brice G, Chapman C, Cook J, Davidson R, Donaldson A, Douglas F, Greenhalgh L, Henderson A, Izatt L, Kumar A, Lalloo F, Miedzybrodzka Z, Morrison PJ, Paterson J, Porteous M, Rogers MT, Shanley S, et al: Gene-gene interactions in breast cancer susceptibility. Hum Mol Genet. 2012, 21: 958-962.
Muller HM, Widschwendter A, Fiegl H, Ivarsson L, Goebel G, Perkmann E, Marth C, Widschwendter M: DNA methylation in serum of breast cancer patients: an independent prognostic marker. Cancer Res. 2003, 63: 7641-7645.
PubMed Google Scholar
Yazici H, Terry MB, Cho YH, Senie RT, Liao Y, Andrulis I, Santella RM: Aberrant methylation of RASSF1A in plasma DNA before breast cancer diagnosis in the Breast Cancer Family Registry. Cancer Epidemiol Biomarkers Prev. 2009, 18: 2723-2725.
Bernstein BE, Birney E, Dunham I, Green ED, Gunter C, Snyder M, ENCODE Project Consortium: An integrated encyclopedia of DNA elements in the human genome. Nature. 2012, 489: 57-74.
Article CAS Google Scholar
Brennan K, Garcia-Closas M, Orr N, Fletcher O, Jones M, Ashworth A, Swerdlow A, Thorne H, Investigators KC, Riboli E, Vineis P, Dorronsoro M, Clavel-Chapelon F, Panico S, Onland-Moret NC, Trichopoulos D, Kaaks R, Khaw KT, Brown R, Flanagan JM: Intragenic ATM methylation in peripheral blood DNA as a biomarker of breast cancer risk. Cancer Res. 2012, 72: 2304-2313.
Azad N, Zahnow CA, Rudin CM, Baylin SB: The future of epigenetic therapy in solid tumours–lessons from the past. Nat Rev Clin Oncol. 2013, 10: 256-266.
Tsai HC, Li H, Van Neste L, Cai Y, Robert C, Rassool FV, Shin JJ, Harbom KM, Beaty R, Pappou E, Harris J, Yen RW, Ahuja N, Brock MV, Stearns V, Feller-Kopman D, Yarmus LB, Lin YC, Welm AL, Issa JP, Minn I, Matsui W, Jang YY, Sharkis SJ, Baylin SB, Zahnow CA: Transient low doses of DNA-demethylating agents exert durable antitumor effects on hematological and epithelial tumor cells. Cancer Cell. 2012, 21: 430-446.
Foster C, Watson M, Eeles R, Eccles D, Ashley S, Davidson R, Mackay J, Morrison PJ, Hopwood P, Evans DG, Psychosocial Study Collaborators: Predictive genetic testing for BRCA1/2 in a UK clinical cohort: three-year follow-up. Br J Cancer. 2007, 96: 718-724.
Hilgart JS, Coles B, Iredale R: Cancer genetic risk assessment for individuals at risk of familial breast cancer. Cochrane Database Syst Rev. 2012, 2: CD003721
Albada A, Werrett J, Van Dulmen S, Bensing JM, Chapman C, Ausems MG, Metcalfe A: Breast cancer genetic counselling referrals: how comparable are the findings between the UK and the Netherlands?. J Comm Gen. 2011, 2: 233-247.
Article Google Scholar
Wakefield CE, Meiser B, Homewood J, Peate M, Taylor A, Lobb E, Kirk J, Young MA, Williams R, Dudding T, Tucker K, AGenDA Collaborative Group: A randomized controlled trial of a decision aid for women considering genetic testing for breast and ovarian cancer risk. Breast Cancer Res Treat. 2008, 107: 289-301.
Article PubMed Google Scholar
Lindor NM, Goldgar DE, Tavtigian SV, Plon SE, Couch FJ: BRCA1/2 Sequence variants of uncertain significance: a primer for providers to assist in discussions and in medical management. Oncol. 2013, 18: 518-524.
Hallowell N, Baylock B, Heiniger L, Butow PN, Patel D, Meiser B, Saunders C, Price MA, kConFab Psychosocial Group on behalf of the kConFab I: Looking different, feeling different: women’s reactions to risk-reducing breast and ovarian surgery. Fam Cancer. 2012, 11: 215-224.
Watts KJ, Meiser B, Mitchell G, Kirk J, Saunders C, Peate M, Duffy J, Kelly PJ, Gleeson M, Barlow-Stewart K, Rahman B, Friedlander M, Tucker K, TFGT Collaborative Group: How should we discuss genetic testing with women newly diagnosed with breast cancer? Design and implementation of a randomized controlled trial of two models of delivering education about treatment-focused genetic testing to younger women newly diagnosed with breast cancer. BMC Cancer. 2012, 12: 320-
Chivers Seymour K, Addington-Hall J, Lucassen AM, Foster CL: What facilitates or impedes family communication following genetic testing for cancer risk? A systematic review and meta-synthesis of primary qualitative research. J Genet Couns. 2010, 19: 330-342.
Mireskandari S, Sherman KA, Meiser B, Taylor AJ, Gleeson M, Andrews L, Tucker KM: Psychological adjustment among partners of women at high risk of developing breast/ovarian cancer. Genet Med. 2007, 9: 311-320.
Amir E, Freedman OC, Seruga B, Evans DG: Assessing women at high risk of breast cancer: a review of risk assessment models. J Natl Cancer Inst. 2010, 102: 680-691.
Dite GS, Mahmoodi M, Bickerstaffe A, Hammet F, Macinnis RJ, Tsimiklis H, Dowty JG, Apicella C, Phillips KA, Giles GG, Southey MC, Hopper JL: Using SNP genotypes to improve the discrimination of a simple breast cancer risk prediction model. Breast Cancer Res Treat. 2013, 139: 887-896.
Eriksson L, Hall P, Czene K, Dos Santos SI, McCormack V, Bergh J, Bjohle J, Ploner A: Mammographic density and molecular subtypes of breast cancer. Br J Cancer. 2012, 107: 18-23.
Swerdlow AJ, Cooke R, Bates A, Cunningham D, Falk SJ, Gilson D, Hancock BW, Harris SJ, Horwich A, Hoskin PJ, Linch DC, Lister TA, Lucraft HH, Radford JA, Stevens AM, Syndikus I, Williams MV: Breast cancer risk after supradiaphragmatic radiotherapy for Hodgkin’s lymphoma in England and Wales: a National Cohort Study. J Clin Oncol. 2012, 30: 2745-2752.
Aupperlee MD, Leipprandt JR, Bennett JM, Schwartz RC, Haslam SZ: Amphiregulin mediates progesterone-induced mammary ductal development during puberty. Breast Cancer Res BCR. 2013, 15: R44-
Denkert C, Bucher E, Hilvo M, Salek R, Oresic M, Griffin J, Brockmoller S, Klauschen F, Loibl S, Barupal DK, Budczies J, Iljin K, Nekljudova V, Fiehn O: Metabolomics of human breast cancer: new approaches for tumor typing and biomarker discovery. Genome Med. 2012, 4: 37-
CAS PubMed PubMed Central Google Scholar
Santen RJ, Boyd NF, Chlebowski RT, Cummings S, Cuzick J, Dowsett M, Easton D, Forbes JF, Key T, Hankinson SE, Howell A, Ingle J, Breast Cancer Prevention Collaborative Group: Critical assessment of new risk factors for breast cancer: considerations for development of an improved risk prediction model. Endocr Relat Cancer. 2007, 14: 169-187.
Cuzick J, Sestak I, Bonanni B, Costantino JP, Cummings S, DeCensi A, Dowsett M, Forbes JF, Ford L, LaCroix AZ, Mershon J, Mitlak BH, Powles T, Veronesi U, Vogel V, Wickerham DL, SERM Chemoprevention of Breast Cancer Overview Group: Selective oestrogen receptor modulators in prevention of breast cancer: an updated meta-analysis of individual participant data. Lancet. 2013, 381: 1827-1834.
LaCroix AZ, Powles T, Osborne CK, Wolter K, Thompson JR, Thompson DD, Allred DC, Armstrong R, Cummings SR, Eastell R, Ensrud KE, Goss P, Lee A, Neven P, Reid DM, Curto M, Vukicevic S, PEARL Investigators: Breast cancer incidence in the randomized PEARL trial of lasofoxifene in postmenopausal osteoporotic women. J Natl Cancer Inst. 2010, 102: 1706-1715.
Goss PE, Ingle JN, Ales-Martinez JE, Cheung AM, Chlebowski RT, Wactawski-Wende J, McTiernan A, Robbins J, Johnson KC, Martin LW, Winquist E, Sarto GE, Garber JE, Fabian CJ, Pujol P, Maunsell E, Farmer P, Gelmon KA, Tu D, Richardson H, NCIC CTG MAP.3 Study Investigators: Exemestane for breast-cancer prevention in postmenopausal women. N Engl J Med. 2011, 364: 2381-2391.
Decensi A, Gandini S, Serrano D, Cazzaniga M, Pizzamiglio M, Maffini F, Pelosi G, Daldoss C, Omodei U, Johansson H, Macis D, Lazzeroni M, Penotti M, Sironi L, Moroni S, Bianco V, Rondanina G, Gjerde J, Guerrieri-Gonzaga A, Bonanni B: Randomized dose-ranging trial of tamoxifen at low doses in hormone replacement therapy users. J Clin Oncol. 2007, 25: 4201-4209.
Rosner B, Glynn RJ, Tamimi RM, Chen WY, Colditz GA, Willett WC, Hankinson SE: Breast cancer risk prediction with heterogeneous risk profiles according to breast cancer tumor markers. Am J Epidemiol. 2013, 178: 296-308.
Uray IP, Brown PH: Chemoprevention of hormone receptor-negative breast cancer: new approaches needed. Recent Results Cancer Res. 2011, 188: 147-162.
Chlebowski RT, Anderson GL, Gass M, Lane DS, Aragaki AK, Kuller LH, Manson JE, Stefanick ML, Ockene J, Sarto GE, Johnson KC, Wactawski-Wende J, Ravdin PM, Schenken R, Hendrix SL, Rajkovic A, Rohan TE, Yasmeen S, Prentice RL, WHI Investigators: Estrogen plus progestin and breast cancer incidence and mortality in postmenopausal women. JAMA. 2010, 304: 1684-1692.
Anderson GL, Chlebowski RT, Aragaki AK, Kuller LH, Manson JE, Gass M, Bluhm E, Connelly S, Hubbell FA, Lane D, Martin L, Ockene J, Rohan T, Schenken R, Wactawski-Wende J: Conjugated equine oestrogen and breast cancer incidence and mortality in postmenopausal women with hysterectomy: extended follow-up of the Women’s Health Initiative randomised placebo-controlled trial. Lancet Oncol. 2012, 13: 476-486.
Wiseman M: The second World Cancer Research Fund/American Institute for Cancer Research expert report. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Proc Nutr Soc. 2008, 67: 253-256.
Parkin DM, Boyd L, Walker LC: 16. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Br J Cancer. 2011, 105: S77-S81.
Li CI, Chlebowski RT, Freiberg M, Johnson KC, Kuller L, Lane D, Lessin L, O’Sullivan MJ, Wactawski-Wende J, Yasmeen S, Prentice R: Alcohol consumption and risk of postmenopausal breast cancer by subtype: the women’s health initiative observational study. J Natl Cancer Inst. 2010, 102: 1422-1431.
Hansen J, Stevens RG: Case–control study of shift-work and breast cancer risk in Danish nurses: impact of shift systems. Eur J Cancer. 2012, 48: 1722-1729.
Anderson AS, Mackison D, Boath C, Steele R: Promoting changes in diet and physical activity in breast and colorectal cancer screening settings: an unexplored opportunity for endorsing healthy behaviors. Cancer Prev Res. 2013, 6: 165-172.
Huang Z, Hankinson SE, Colditz GA, Stampfer MJ, Hunter DJ, Manson JE, Hennekens CH, Rosner B, Speizer FE, Willett WC: Dual effects of weight and weight gain on breast cancer risk. JAMA. 1997, 278: 1407-1411.
Harvie M, Howell A, Vierkant RA, Kumar N, Cerhan JR, Kelemen LE, Folsom AR, Sellers TA: Association of gain and loss of weight before and after menopause with risk of postmenopausal breast cancer in the Iowa women’s health study. Cancer Epidemiol Biomarkers Prev. 2005, 14: 656-661.
Eliassen AH, Colditz GA, Rosner B, Willett WC, Hankinson SE: Adult weight change and risk of postmenopausal breast cancer. JAMA. 2006, 296: 193-201.
Teras LR, Goodman M, Patel AV, Diver WR, Flanders WD, Feigelson HS: Weight loss and postmenopausal breast cancer in a prospective cohort of overweight and obese US women. CCC. 2011, 22: 573-579.
Niraula S, Ocana A, Ennis M, Goodwin PJ: Body size and breast cancer prognosis in relation to hormone receptor and menopausal status: a meta-analysis. Breast Cancer Res Treat. 2012, 134: 769-781.
Jung S, Spiegelman D, Baglietto L, Bernstein L, Boggs DA, van den Brandt PA, Buring JE, Cerhan JR, Gaudet MM, Giles GG, Goodman G, Hakansson N, Hankinson SE, Helzlsouer K, Horn-Ross PL, Inoue M, Krogh V, Lof M, McCullough ML, Miller AB, Neuhouser ML, Palmer JR, Park Y, Robien K, Rohan TE, Scarmo S, Schairer C, Schouten LJ, Shikany JM, Sieri S, et al: Fruit and vegetable intake and risk of breast cancer by hormone receptor status. J Natl Cancer Inst. 2013, 105: 219-236.
Prentice RL, Caan B, Chlebowski RT, Patterson R, Kuller LH, Ockene JK, Margolis KL, Limacher MC, Manson JE, Parker LM, Paskett E, Phillips L, Robbins J, Rossouw JE, Sarto GE, Shikany JM, Stefanick ML, Thomson CA, Van Horn L, Vitolins MZ, Wactawski-Wende J, Wallace RB, Wassertheil-Smoller S, Whitlock E, Yano K, Adams-Campbell L, Anderson GL, Assaf AR, Beresford SA, et al: Low-fat dietary pattern and risk of invasive breast cancer: the Women’s Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006, 295: 629-642.
Chlebowski RT, Rose D, Buzzard IM, Blackburn GL, Insull W, Grosvenor M, Elashoff R, Wynder EL: Adjuvant dietary fat intake reduction in postmenopausal breast cancer patient management. The Women’s Intervention Nutrition Study (WINS). Breast Cancer Res Treat. 1992, 20: 73-84.
Pierce JP, Natarajan L, Caan BJ, Parker BA, Greenberg ER, Flatt SW, Rock CL, Kealey S, Al-Delaimy WK, Bardwell WA, Carlson RW, Emond JA, Faerber S, Gold EB, Hajek RA, Hollenbach K, Jones LA, Karanja N, Madlensky L, Marshall J, Newman VA, Ritenbaugh C, Thomson CA, Wasserman L, Stefanick ML: Influence of a diet very high in vegetables, fruit, and fiber and low in fat on prognosis following treatment for breast cancer: the Women’s Healthy Eating and Living (WHEL) randomized trial. JAMA. 2007, 298: 289-298.
Friedenreich CM: Physical activity and breast cancer: review of the epidemiologic evidence and biologic mechanisms. Recent Results Cancer Res. 2011, 188: 125-139.
Fontein DB, de Glas NA, Duijm M, Bastiaannet E, Portielje JE, Van de Velde CJ, Liefers GJ: Age and the effect of physical activity on breast cancer survival: A systematic review. Cancer Treat Rev. 2013, 39: 958-965.
Key TJ: Endogenous oestrogens and breast cancer risk in premenopausal and postmenopausal women. Steroids. 2011, 76: 812-815.
Farhat GN, Cummings SR, Chlebowski RT, Parimi N, Cauley JA, Rohan TE, Huang AJ, Vitolins M, Hubbell FA, Manson JE, Cochrane BB, Lane DS, Lee JS: Sex hormone levels and risks of estrogen receptor-negative and estrogen receptor-positive breast cancers. J Natl Cancer Inst. 2011, 103: 562-570.
Evans DG, Warwick J, Astley SM, Stavrinos P, Sahin S, Ingham S, McBurney H, Eckersley B, Harvie M, Wilson M, Beetles U, Warren R, Hufton A, Sergeant JC, Newman WG, Buchan I, Cuzick J, Howell A: Assessing individual breast cancer risk within the U.K. National Health Service Breast Screening Program: a new paradigm for cancer prevention. Cancer Prev Res. 2012, 5: 943-951.
Darabi H, Czene K, Zhao W, Liu J, Hall P, Humphreys K: Breast cancer risk prediction and individualised screening based on common genetic variation and breast density measurement. BCR. 2012, 14: R25-
Brower V: Homing in on mechanisms linking breast density to breast cancer risk. J Natl Cancer Inst. 2010, 102: 843-845.
Martin LJ, Boyd NF: Mammographic density. Potential mechanisms of breast cancer risk associated with mammographic density: hypotheses based on epidemiological evidence. BCR. 2008, 10: 201-
Article PubMed PubMed Central CAS Google Scholar
Cuzick J, Warwick J, Pinney E, Duffy SW, Cawthorn S, Howell A, Forbes JF, Warren RM: Tamoxifen-induced reduction in mammographic density and breast cancer risk reduction: a nested case–control study. J Natl Cancer Inst. 2011, 103: 744-752.
Courneya KS, Karvinen KH, McNeely ML, Campbell KL, Brar S, Woolcott CG, McTiernan A, Ballard-Barbash R, Friedenreich CM: Predictors of adherence to supervised and unsupervised exercise in the Alberta Physical Activity and Breast Cancer Prevention Trial. J Phys Act Health. 2012, 9: 857-866.
Rack B, Andergassen U, Neugebauer J, Salmen J, Hepp P, Sommer H, Lichtenegger W, Friese K, Beckmann MW, Hauner D, Hauner H, Janni W: The German SUCCESS C Study - the first European lifestyle study on breast cancer. Breast Care (Basel). 2010, 5: 395-400.
Villarini A, Pasanisi P, Traina A, Mano MP, Bonanni B, Panico S, Scipioni C, Galasso R, Paduos A, Simeoni M, Bellotti E, Barbero M, Macellari G, Venturelli E, Raimondi M, Bruno E, Gargano G, Fornaciari G, Morelli D, Seregni E, Krogh V, Berrino F: Lifestyle and breast cancer recurrences: the DIANA-5 trial. Tumori. 2012, 98: 1-18.
CAS PubMed Google Scholar
Baselga J, Campone M, Piccart M, Burris HA, Rugo HS, Sahmoud T, Noguchi S, Gnant M, Pritchard KI, Lebrun F, Beck JT, Ito Y, Yardley D, Deleu I, Perez A, Bachelot T, Vittori L, Xu Z, Mukhopadhyay P, Lebwohl D, Hortobagyi GN: Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med. 2012, 366: 520-529.
Anisimov VN, Zabezhinski MA, Popovich IG, Piskunova TS, Semenchenko AV, Tyndyk ML, Yurova MN, Rosenfeld SV, Blagosklonny MV: Rapamycin increases lifespan and inhibits spontaneous tumorigenesis in inbred female mice. Cell Cycle. 2011, 10: 4230-4236.
Longo VD, Fontana L: Intermittent supplementation with rapamycin as a dietary restriction mimetic. Aging. 2011, 3: 1039-1040.
Goodwin PJ, Thompson AM, Stambolic V: Diabetes, metformin, and breast cancer: lilac time?. J Clin Oncol. 2012, 30: 2812-2814.
Reis-Filho JS, Pusztai L: Gene expression profiling in breast cancer: classification, prognostication, and prediction. Lancet. 2011, 378: 1812-1823.
Baird RD, Caldas C: Genetic heterogeneity in breast cancer: the road to personalized medicine?. BMC Med. 2013, 11: 151-
Lawrence MS, Stojanov P, Polak P, Kryukov GV, Cibulskis K, Sivachenko A, Carter SL, Stewart C, Mermel CH, Roberts SA, Kiezun A, Hammerman PS, McKenna A, Drier Y, Zou L, Ramos AH, Pugh TJ, Stransky N, Helman E, Kim J, Sougnez C, Ambrogio L, Nickerson E, Shefler E, Cortés ML, Auclair D, Saksena G, Voet D, Noble M, DiCara D, et al: Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature. 2013, 499: 214-218.
Dawson SJ, Rueda OM, Aparicio S, Caldas C: A new genome-driven integrated classification of breast cancer and its implications. EMBO J. 2013, 32: 617-628.
Metzger-Filho O, Tutt A, de Azambuja E, Saini KS, Viale G, Loi S, Bradbury I, Bliss JM, Azim HA, Ellis P, Di Leo A, Baselga J, Sotiriou C, Piccart-Gebhart M: Dissecting the heterogeneity of triple-negative breast cancer. J Clin Oncol. 2012, 30: 1879-1887.
Russnes HG, Navin N, Hicks J, Borresen-Dale AL: Insight into the heterogeneity of breast cancer through next-generation sequencing. J Clin Invest. 2011, 121: 3810-3818.
Samuel N, Hudson TJ: Translating genomics to the clinic: implications of cancer heterogeneity. Clin Chem. 2013, 59: 127-137.
Jansson MD, Lund AH: MicroRNA and cancer. Mol Oncol. 2012, 6: 590-610.
Akhtar N, Streuli CH: An integrin-ILK-microtubule network orients cell polarity and lumen formation in glandular epithelium. Nat Cell Biol. 2013, 15: 17-27.
Bazzoun D, Lelievre S, Talhouk R: Polarity proteins as regulators of cell junction complexes: Implications for breast cancer. Pharmacol Ther. 2013, 138: 418-427.
Lelievre SA: Tissue polarity-dependent control of mammary epithelial homeostasis and cancer development: an epigenetic perspective. J Mammary Gland Biol Neoplasia. 2010, 15: 49-63.
Xue B, Krishnamurthy K, Allred DC, Muthuswamy SK: Loss of Par3 promotes breast cancer metastasis by compromising cell-cell cohesion. Nat Cell Biol. 2013, 15: 189-200.
Martin FT, Dwyer RM, Kelly J, Khan S, Murphy JM, Curran C, Miller N, Hennessy E, Dockery P, Barry FP, O'Brien T, Kerin MJ: Potential role of mesenchymal stem cells (MSCs) in the breast tumour microenvironment: stimulation of epithelial to mesenchymal transition (EMT). Breast Cancer Res Treat. 2010, 124: 317-326.
Weigelt B, Lo AT, Park CC, Gray JW, Bissell MJ: HER2 signaling pathway activation and response of breast cancer cells to HER2-targeting agents is dependent strongly on the 3D microenvironment. Breast Cancer Res Treat. 2010, 122: 35-43.
Pontiggia O, Sampayo R, Raffo D, Motter A, Xu R, Bissell MJ, Joffe EB, Simian M: The tumor microenvironment modulates tamoxifen resistance in breast cancer: a role for soluble stromal factors and fibronectin through beta1 integrin. Breast Cancer Res Treat. 2012, 133: 459-471.
Martinez-Outschoorn UE, Goldberg A, Lin Z, Ko YH, Flomenberg N, Wang C, Pavlides S, Pestell RG, Howell A, Sotgia F, Lisanti MP: Anti-estrogen resistance in breast cancer is induced by the tumor microenvironment and can be overcome by inhibiting mitochondrial function in epithelial cancer cells. Cancer Biol Ther. 2011, 12: 924-938.
Hanahan D, Coussens LM: Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell. 2012, 21: 309-322.
He WS, Dai XF, Jin M, Liu CW, Rent JH: Hypoxia-induced autophagy confers resistance of breast cancer cells to ionizing radiation. Oncol Res. 2012, 20: 251-258.
Article PubMed CAS Google Scholar
Tan EY, Yan M, Campo L, Han C, Takano E, Turley H, Candiloro I, Pezzella F, Gatter KC, Millar EK, O'Toole SA, McNeil CM, Crea P, Segara D, Sutherland RL, Harris AL, Fox SB: The key hypoxia regulated gene CAIX is upregulated in basal-like breast tumours and is associated with resistance to chemotherapy. Br J Cancer. 2009, 100: 405-411.
Milas L, Hittelman WN: Cancer stem cells and tumor response to therapy: current problems and future prospects. Semin Radiat Oncol. 2009, 19: 96-105.
Mimeault M, Batra SK: Hypoxia-inducing factors as master regulators of stemness properties and altered metabolism of cancer- and metastasis-initiating cells. J Cell Mol Med. 2013, 17: 30-54.
Rundqvist H, Johnson RS: Hypoxia and metastasis in breast cancer. Curr Top Microbiol Immunol. 2010, 345: 121-139.
Postovit LM, Abbott DE, Payne SL, Wheaton WW, Margaryan NV, Sullivan R, Jansen MK, Csiszar K, Hendrix MJ, Kirschmann DA: Hypoxia/reoxygenation: a dynamic regulator of lysyl oxidase-facilitated breast cancer migration. J Cell Biochem. 2008, 103: 1369-1378.
Obeid E, Nanda R, Fu YX, Olopade OI: The role of tumor-associated macrophages in breast cancer progression (Review). Int J Oncol. 2013, 43: 5-12.
Lewis CE, Hughes R: Inflammation and breast cancer. Microenvironmental factors regulating macrophage function in breast tumours: hypoxia and angiopoietin-2. BCR. 2007, 9: 209-
Louie E, Nik S, Chen JS, Schmidt M, Song B, Pacson C, Chen XF, Park S, Ju J, Chen EI: Identification of a stem-like cell population by exposing metastatic breast cancer cell lines to repetitive cycles of hypoxia and reoxygenation. BCR. 2010, 12: R94-
Dittmer J, Rody A: Cancer stem cells in breast cancer. Histol Histopathol. 2013, 28: 827-838.
Mao Q, Zhang Y, Fu X, Xue J, Guo W, Meng M, Zhou Z, Mo X, Lu Y: A tumor hypoxic niche protects human colon cancer stem cells from chemotherapy. J Cancer Res Clin Oncol. 2013, 139: 211-222.
Van Keymeulen A, Rocha AS, Ousset M, Beck B, Bouvencourt G, Rock J, Sharma N, Dekoninck S, Blanpain C: Distinct stem cells contribute to mammary gland development and maintenance. Nature. 2011, 479: 189-193.
van Amerongen R, Bowman AN, Nusse R: Developmental stage and time dictate the fate of Wnt/beta-catenin-responsive stem cells in the mammary gland. Cell Stem Cell. 2012, 11: 387-400.
de Visser KE, Ciampricotti M, Michalak EM, Tan DW, Speksnijder EN, Hau CS, Clevers H, Barker N, Jonkers J: Developmental stage-specific contribution of LGR5(+) cells to basal and luminal epithelial lineages in the postnatal mammary gland. J Pathol. 2012, 228: 300-309.
Smalley M, Piggott L, Clarkson R: Breast cancer stem cells: Obstacles to therapy. Cancer Lett. 2012, 338: 57-62.
Iliopoulos D, Hirsch HA, Wang G, Struhl K: Inducible formation of breast cancer stem cells and their dynamic equilibrium with non-stem cancer cells via IL6 secretion. Proc Natl Acad Sci U S A. 2011, 108: 1397-1402.
Sarrio D, Franklin CK, Mackay A, Reis-Filho JS, Isacke CM: Epithelial and mesenchymal subpopulations within normal basal breast cell lines exhibit distinct stem cell/progenitor properties. Stem Cells. 2012, 30: 292-303.
Chaffer CL, Marjanovic ND, Lee T, Bell G, Kleer CG, Reinhardt F, D’Alessio AC, Young RA, Weinberg RA: Poised chromatin at the ZEB1 promoter enables breast cancer cell plasticity and enhances tumorigenicity. Cell. 2013, 154: 61-74.
Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, Hastie T, Eisen MB, van de Rijn M, Jeffrey SS, Thorsen T, Quist H, Matese JC, Brown PO, Botstein D, Lønning PE, Børresen-Dale AL: Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci U S A. 2001, 98: 10869-10874.
Banerji S, Cibulskis K, Rangel-Escareno C, Brown KK, Carter SL, Frederick AM, Lawrence MS, Sivachenko AY, Sougnez C, Zou L, Cortes ML, Fernandez-Lopez JC, Peng S, Ardlie KG, Auclair D, Bautista-Piña V, Duke F, Francis J, Jung J, Maffuz-Aziz A, Onofrio RC, Parkin M, Pho NH, Quintanar-Jurado V, Ramos AH, Rebollar-Vega R, Rodriguez-Cuevas S, Romero-Cordoba SL, Schumacher SE, Stransky N: Sequence analysis of mutations and translocations across breast cancer subtypes. Nature. 2012, 486: 405-409.
Shah SP, Roth A, Goya R, Oloumi A, Ha G, Zhao Y, Turashvili G, Ding J, Tse K, Haffari G, Bashashati A, Prentice LM, Khattra J, Burleigh A, Yap D, Bernard V, McPherson A, Shumansky K, Crisan A, Giuliany R, Heravi-Moussavi A, Rosner J, Lai D, Birol I, Varhol R, Tam A, Dhalla N, Zeng T, Ma K, Chan SK, et al: The clonal and mutational evolution spectrum of primary triple-negative breast cancers. Nature. 2012, 486: 395-399.
Cancer Genome Atlas N: Comprehensive molecular portraits of human breast tumours. Nature. 2012, 490: 61-70.
Solin LJ, Gray R, Baehner FL, Butler SM, Hughes LL, Yoshizawa C, Cherbavaz DB, Shak S, Page DL, Sledge GW, Davidson NE, Ingle JN, Perez EA, Wood WC, Sparano JA, Badve S: A multigene expression assay to predict local recurrence risk for ductal carcinoma in situ of the breast. J Natl Cancer Inst. 2013, 105: 701-710.
Naba A, Clauser KR, Hoersch S, Liu H, Carr SA, Hynes RO: The matrisome: in silico definition and in vivo characterization by proteomics of normal and tumor extracellular matrices. MCP. 2012, 11: M111.014647-
Glukhova MA, Streuli CH: How integrins control breast biology. Curr Opin Cell Biol. 2013, 25: 633-641.
Ito Y, Iwase T, Hatake K: Eradication of breast cancer cells in patients with distant metastasis: the finishing touches?. Breast Cancer. 2012, 19: 206-211.
Sampieri K, Fodde R: Cancer stem cells and metastasis. Semin Cancer Biol. 2012, 22: 187-193.
Takebe N, Warren RQ, Ivy SP: Breast cancer growth and metastasis: interplay between cancer stem cells, embryonic signaling pathways and epithelial-to-mesenchymal transition. BCR. 2011, 13: 211-
Finak G, Bertos N, Pepin F, Sadekova S, Souleimanova M, Zhao H, Chen H, Omeroglu G, Meterissian S, Omeroglu A, Hallett M, Park M: Stromal gene expression predicts clinical outcome in breast cancer. Nat Med. 2008, 14: 518-527.
Kalluri R, Zeisberg M: Fibroblasts in cancer. Nat Rev Cancer. 2006, 6: 392-401.
Barker HE, Cox TR, Erler JT: The rationale for targeting the LOX family in cancer. Nat Rev Cancer. 2012, 12: 540-552.
Favaro E, Lord S, Harris AL, Buffa FM: Gene expression and hypoxia in breast cancer. Genome Med. 2011, 3: 55-
Milani M, Harris AL: Targeting tumour hypoxia in breast cancer. Eur J Cancer. 2008, 44: 2766-2773.
Lundgren K, Holm C, Landberg G: Hypoxia and breast cancer: prognostic and therapeutic implications. CMLS. 2007, 64: 3233-3247.
Ward C, Langdon SP, Mullen P, Harris AL, Harrison DJ, Supuran CT, Kunkler IH: New strategies for targeting the hypoxic tumour microenvironment in breast cancer. Cancer Treat Rev. 2013, 39: 171-179.
Bailey KM, Wojtkowiak JW, Hashim AI, Gillies RJ: Targeting the metabolic microenvironment of tumors. Adv Pharmacol. 2012, 65: 63-107.
Dos Santos CO, Rebbeck C, Rozhkova E, Valentine A, Samuels A, Kadiri LR, Osten P, Harris EY, Uren PJ, Smith AD, Hannon GJ: Molecular hierarchy of mammary differentiation yields refined markers of mammary stem cells. Proc Natl Acad Sci U S A. 2013, 110: 7123-7130.
Makarem M, Spike BT, Dravis C, Kannan N, Wahl GM, Eaves CJ: Stem cells and the developing mammary gland. J Mammary Gland Biol Neoplasia. 2013, 18: 209-219.
Visvader JE: Keeping abreast of the mammary epithelial hierarchy and breast tumorigenesis. Genes Dev. 2009, 23: 2563-2577.
Ablett MP, Singh JK, Clarke RB: Stem cells in breast tumours: are they ready for the clinic?. Eur J Cancer. 2012, 48: 2104-2116.
Badve S, Nakshatri H: Breast-cancer stem cells-beyond semantics. Lancet Oncol. 2012, 13: e43-e48.
Kaimala S, Bisana S, Kumar S: Mammary gland stem cells: more puzzles than explanations. J Biosci. 2012, 37: 349-358.
La Porta CA: Thoughts about cancer stem cells in solid tumors. World J Stem Cells. 2012, 4: 17-20.
Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan A, Zhou AY, Brooks M, Reinhard F, Zhang CC, Shipitsin M, Campbell LL, Polyak K, Brisken C, Yang J, Weinberg RA: The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008, 133: 704-715.
Polyak K, Weinberg RA: Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer. 2009, 9: 265-273.
Scheel C, Weinberg RA: Phenotypic plasticity and epithelial-mesenchymal transitions in cancer and normal stem cells?. Int J Cancer. 2011, 129: 2310-2314.
Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF: Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci U S A. 2003, 100: 3983-3988.
Harrison H, Farnie G, Howell SJ, Rock RE, Stylianou S, Brennan KR, Bundred NJ, Clarke RB: Regulation of breast cancer stem cell activity by signaling through the Notch4 receptor. Cancer Res. 2010, 70: 709-718.
Muller V, Riethdorf S, Rack B, Janni W, Fasching P, Solomayer E, Aktas B, Kasimir-Bauer S, Pantel K, Fehm T, DETECT study group: Prognostic impact of circulating tumor cells assessed with the Cell Search AssayTM and AdnaTest BreastTM in metastatic breast cancer patients: the DETECT study. BCR. 2012, 14: R118-
Giordano A, Gao H, Cohen EN, Anfossi S, Khoury J, Hess K, Krishnamurthy S, Tin S, Cristofanilli M, Hortobagyi GN, Woodward WA, Lucci A, Reuben JM: Clinical of cancer stem cells in bone marrow of early breast cancer patients. Ann Oncol. 2013, [Epud ahead of print]
Baccelli I, Schneeweiss A, Riethdorf S, Stenzinger A, Schillert A, Vogel V, Klein C, Saini M, Bauerle T, Wallwiener M, Holland-Letz T, Höfner T, Sprick M, Scharpff M, Marmé F, Sinn HP, Pantel K, Weichert W, Trumpp A: Identification of a population of blood circulating tumor cells from breast cancer patients that initiates metastasis in a xenograft assay. Nat Biotechnol. 2013, 31: 539-544.
Willis L, Graham TA, Alarcon T, Alison MR, Tomlinson IP, Page KM: What can be learnt about disease progression in breast cancer dormancy from relapse data?. PloS one. 2013, 8: e62320-
Balic M, Lin H, Williams A, Datar RH, Cote RJ: Progress in circulating tumor cell capture and analysis: implications for cancer management. Expert Rev Mol Diagn. 2012, 12: 303-312.
Barriere G, Riouallon A, Renaudie J, Tartary M, Rigaud M: Mesenchymal and stemness circulating tumor cells in early breast cancer diagnosis. BMC Cancer. 2012, 12: 114-
Sceneay J, Smyth MJ, Moller A: The pre-metastatic niche: finding common ground. Cancer Metastasis Rev. 2013, [Epud ahead of print]
Peinado H, Lavotshkin S, Lyden D: The secreted factors responsible for pre-metastatic niche formation: old sayings and new thoughts. Semin Cancer Biol. 2011, 21: 139-146.
Nguyen DX, Bos PD, Massague J: Metastasis: from dissemination to organ-specific colonization. Nat Rev Cancer. 2009, 9: 274-284.
Hu G, Kang Y, Wang XF: From breast to the brain: unraveling the puzzle of metastasis organotropism. J Mole Cell Biol. 2009, 1: 3-5.
Hsieh SM, Look MP, Sieuwerts AM, Foekens JA, Hunter KW: Distinct inherited metastasis susceptibility exists for different breast cancer subtypes: a prognosis study. BCR. 2009, 11: R75-
Scheel C, Weinberg RA: Cancer stem cells and epithelial-mesenchymal transition: concepts and molecular links. Semin Cancer Biol. 2012, 22: 396-403.
Dave B, Mittal V, Tan NM, Chang JC: Epithelial-mesenchymal transition, cancer stem cells and treatment resistance. BCR. 2012, 14: 202-
Drasin DJ, Robin TP, Ford HL: Breast cancer epithelial-to-mesenchymal transition: examining the functional consequences of plasticity. BCR. 2011, 13: 226-
Giordano A, Gao H, Anfossi S, Cohen E, Mego M, Lee BN, Tin S, De Laurentiis M, Parker CA, Alvarez RH, Valero V, Ueno NT, De Placido S, Mani SA, Esteva FJ, Cristofanilli M, Reuben JM: Epithelial-mesenchymal transition and stem cell markers in patients with HER2-positive metastatic breast cancer. Mol Cancer Ther. 2012, 11: 2526-2534.
Kasimir-Bauer S, Hoffmann O, Wallwiener D, Kimmig R, Fehm T: Expression of stem cell and epithelial-mesenchymal transition markers in primary breast cancer patients with circulating tumor cells. BCR. 2012, 14: R15-
Chui MH: Insights into cancer metastasis from a clinicopathologic perspective: Epithelial-Mesenchymal Transition is not a necessary step. Int J Cancer. 2013, 132: 1487-1495.
Marchini C, Montani M, Konstantinidou G, Orru R, Mannucci S, Ramadori G, Gabrielli F, Baruzzi A, Berton G, Merigo F, Fin S, Iezzi M, Bisaro B, Sbarbati A, Zerani M, Galiè M, Amici A: Mesenchymal/stromal gene expression signature relates to basal-like breast cancers, identifies bone metastasis and predicts resistance to therapies. PloS one. 2010, 5: e14131-
Kim MY, Oskarsson T, Acharyya S, Nguyen DX, Zhang XH, Norton L, Massague J: Tumor self-seeding by circulating cancer cells. Cell. 2009, 139: 1315-1326.
Comen E, Norton L: Self-seeding in cancer. Recent Res Cancer Res. 2012, 195: 13-23.
Gorges TM, Tinhofer I, Drosch M, Rose L, Zollner TM, Krahn T, von Ahsen O: Circulating tumour cells escape from EpCAM-based detection due to epithelial-to-mesenchymal transition. BMC Cancer. 2012, 12: 178-
Kallergi G, Papadaki MA, Politaki E, Mavroudis D, Georgoulias V, Agelaki S: Epithelial to mesenchymal transition markers expressed in circulating tumour cells of early and metastatic breast cancer patients. BCR. 2011, 13: R59-
Yu M, Bardia A, Wittner BS, Stott SL, Smas ME, Ting DT, Isakoff SJ, Ciciliano JC, Wells MN, Shah AM, Concannon KF, Donaldson MC, Sequist LV, Brachtel E, Sgroi D, Baselga J, Ramaswamy S, Toner M, Haber DA, Maheswaran S: Circulating breast tumor cells exhibit dynamic changes in epithelial and mesenchymal composition. Science. 2013, 339: 580-584.
De Mattos-Arruda L, Cortes J, Santarpia L, Vivancos A, Tabernero J, Reis-Filho JS, Seoane J: Circulating tumour cells and cell-free DNA as tools for managing breast cancer. Nat Rev Clin Oncol. 2013, 10: 377-389.
Murtaza M, Dawson SJ, Tsui DW, Gale D, Forshew T, Piskorz AM, Parkinson C, Chin SF, Kingsbury Z, Wong AS, Marass F, Humphray S, Hadfield J, Bentley D, Chin TM, Brenton JD, Caldas C, Rosenfeld N: Non-invasive analysis of acquired resistance to cancer therapy by sequencing of plasma DNA. Nature. 2013, 497: 108-112.
Zhang F, Chen JY: Breast cancer subtyping from plasma proteins. BMC Med Genomics. 2013, 6: S6-
Corcoran C, Friel AM, Duffy MJ, Crown J, O’Driscoll L: Intracellular and extracellular microRNAs in breast cancer. Clin Chem. 2011, 57: 18-32.
Hendrix A, Hume AN: Exosome signaling in mammary gland development and cancer. Int J Dev Biol. 2011, 55: 879-887.
Marleau AM, Chen CS, Joyce JA, Tullis RH: Exosome removal as a therapeutic adjuvant in cancer. J Transl Med. 2012, 10: 134-
Eccles SA, Paon L: Breast cancer metastasis: when, where, how?. Lancet. 2005, 365: 1006-1007.
Eccles: Growth regulatory pathways contributing to organ selectivity of metastasis. Cancer Metastasis: Biologic Basis and Therapeutics. 2011, Cambridge: Cambridge University Press, 204-214.
Chapter Google Scholar
Mina LA, Sledge GW: Rethinking the metastatic cascade as a therapeutic target. Nat Rev Clin Oncol. 2011, 8: 325-332.
Wilson C, Holen I, Coleman RE: Seed, soil and secreted hormones: potential interactions of breast cancer cells with their endocrine/paracrine microenvironment and implications for treatment with bisphosphonates. Cancer Treat Rev. 2012, 38: 877-889.
Fidler IJ: The role of the organ microenvironment in brain metastasis. Semin Cancer Biol. 2011, 21: 107-112.
Peto R, Davies C, Godwin J, Gray R, Pan HC, Clarke M, Cutter D, Darby S, McGale P, Taylor C, Wang YC, Bergh J, Di Leo A, Albain K, Swain S, Piccart M, Pritchard K, Early Breast Cancer Trialists’ Collaborative G: Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet. 2012, 379: 432-444.
Darby S, McGale P, Correa C, Taylor C, Arriagada R, Clarke M, Cutter D, Davies C, Ewertz M, Godwin J, Gray R, Pierce L, Whelan T, Wang Y, Peto R, Early Breast Cancer Trialists’ Collaborative G: Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011, 378: 1707-1716.
Davies C, Godwin J, Gray R, Clarke M, Cutter D, Darby S, McGale P, Pan HC, Taylor C, Wang YC, Dowsett M, Ingle J, Peto R, Early Breast Cancer Trialists’ Collaborative G: Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet. 2011, 378: 771-784.
Senkus EKS, Penault-Llorca F, Poortmans P, Thompson A, Zackrisson S, Cardoso F: ESMO Guidelines Working Group. Ann Oncol. 2013, doi: 10.1093/annonc/mdt284
Khoury T: Delay to formalin fixation alters morphology and immunohistochemistry for breast carcinoma. Appl Immunohistochem Mol Morphol. 2012, 20: 531-542.
Dale DC: Poor prognosis in elderly patients with cancer: the role of bias and undertreatment. J Support Oncol. 2003, 1: 11-17.
Seah MD, Chan PM: Rethinking undertreatment in elderly breast cancer patients. Asian J Surg. 2009, 32: 71-75.
Harder H, Ballinger R, Langridge C, Ring A, Fallowfield LJ: Adjuvant chemotherapy in elderly women with breast cancer: patients’ perspectives on information giving and decision making. Psychooncology. 2013, doi: 10.1002/pon.3338
Ring A, Harder H, Langridge C, Ballinger RS, Fallowfield LJ: Adjuvant chemotherapy in elderly women with breast cancer (AChEW): an observational study identifying MDT perceptions and barriers to decision making. Ann Oncol. 2013, 24: 1211-1219.
Armes J, Crowe M, Colbourne L, Morgan H, Murrells T, Oakley C, Palmer N, Ream E, Young A, Richardson A: Patients’ supportive care needs beyond the end of cancer treatment: a prospective, longitudinal survey. J Clin Oncol. 2009, 27: 6172-6179.
Maguire P: Psychological aspects. ABC of Breast Diseases. 2002, London: BMJ Books, 150-153. 2nd Edition. Edited by Dixon M.
Hulbert-Williams N, Neal R, Morrison V, Hood K, Wilkinson C: Anxiety, depression and quality of life after cancer diagnosis: what psychosocial variables best predict how patients adjust?. Psychooncology. 2011, doi: 10.1002/pon.1980
Jacobsen PB: Screening for psychological distress in cancer patients: challenges and opportunities. J Clin Oncol. 2007, 25: 4526-4527.
The International. Psycho-Oncology Society. http://www.ipos-society.org/about/news/standards_news.aspx ,
Thompson AM, Moulder-Thompson SL: Neoadjuvant treatment of breast cancer. Ann Oncol. 2012, 23: x231-x236.
Bartelink H, Horiot JC, Poortmans PM, Struikmans H, Van den Bogaert W, Fourquet A, Jager JJ, Hoogenraad WJ, Oei SB, Warlam-Rodenhuis CC, Pierart M, Collette L: Impact of a higher radiation dose on local control and survival in breast-conserving therapy of early breast cancer: 10-year results of the randomized boost versus no boost EORTC 22881–10882 trial. J Clin Oncol. 2007, 25: 3259-3265.
Whelan TJ, Pignol JP, Levine MN, Julian JA, MacKenzie R, Parpia S, Shelley W, Grimard L, Bowen J, Lukka H, Perera F, Fyles A, Schneider K, Gulavita S, Freeman C: Long-term results of hypofractionated radiation therapy for breast cancer. N Engl J Med. 2010, 362: 513-520.
Group ST, Bentzen SM, Agrawal RK, Aird EG, Barrett JM, Barrett-Lee PJ, Bliss JM, Brown J, Dewar JA, Dobbs HJ, Haviland JS, Hoskin PJ, Hopwood P, Lawton PA, Magee BJ, Mills J, Morgan DA, Owen JR, Simmons S, Sumo G, Sydenham MA, Venables K, Yarnold JR: The UK Standardisation of Breast Radiotherapy (START) Trial A of radiotherapy hypofractionation for treatment of early breast cancer: a randomised trial. Lancet Oncol. 2008, 9: 331-341.
Group ST, Bentzen SM, Agrawal RK, Aird EG, Barrett JM, Barrett-Lee PJ, Bentzen SM, Bliss JM, Brown J, Dewar JA, Dobbs HJ, Haviland JS, Hoskin PJ, Hopwood P, Lawton PA, Magee BJ, Mills J, Morgan DA, Owen JR, Simmons S, Sumo G, Sydenham MA, Venables K, Yarnold JR: The UK Standardisation of Breast Radiotherapy (START) Trial B of radiotherapy hypofractionation for treatment of early breast cancer: a randomised trial. Lancet. 2008, 371: 1098-1107.
Vaidya JS, Joseph DJ, Tobias JS, Bulsara M, Wenz F, Saunders C, Alvarado M, Flyger HL, Massarut S, Eiermann W, Keshtgar M, Dewar J, Kraus-Tiefenbacher U, Sütterlin M, Esserman L, Holtveg HM, Roncadin M, Pigorsch S, Metaxas M, Falzon M, Matthews A, Corica T, Williams NR, Baum M: Targeted intraoperative radiotherapy versus whole breast radiotherapy for breast cancer (TARGIT-A trial): an international, prospective, randomised, non-inferiority phase 3 trial. Lancet. 2010, 376: 91-102.
Rampinelli C, Bellomi M, Ivaldi GB, Intra M, Raimondi S, Meroni S, Orecchia R, Veronesi U: Assessment of pulmonary fibrosis after radiotherapy (RT) in breast conserving surgery: comparison between conventional external beam RT (EBRT) and intraoperative RT with electrons (ELIOT). Technol Cancer Res Treat. 2011, 10: 323-329.
Hannoun-Levi JM, Resch A, Gal J, Kauer-Dorner D, Strnad V, Niehoff P, Loessl K, Kovacs G, Van Limbergen E, Polgar C, On behalf of the GEC-ESTRO Breast Cancer Working Group: Accelerated partial breast irradiation with interstitial brachytherapy as second conservative treatment for ipsilateral breast tumour recurrence: Multicentric study of the GEC-ESTRO Breast Cancer Working Group. Radiother Oncol. 2013, doi: 1016/j.radonc.2013.03.026
Smith BD, Arthur DW, Buchholz TA, Haffty BG, Hahn CA, Hardenbergh PH, Julian TB, Marks LB, Todor DA, Vicini FA, Whelan TJ, White J, Wo JY, Harris JR: Accelerated partial breast irradiation consensus statement from the American Society for Radiation Oncology (ASTRO). Int J Radiat Oncol Biol Phys. 2009, 74: 987-1001.
Polgar C, Van Limbergen E, Potter R, Kovacs G, Polo A, Lyczek J, Hildebrandt G, Niehoff P, Guinot JL, Guedea F, Johansson B, Ott OJ, Major T, Strnad V, GEC-ESTRO Breast Cancer Working Group: Patient selection for accelerated partial-breast irradiation (APBI) after breast-conserving surgery: recommendations of the Groupe Europeen de Curietherapie-European Society for Therapeutic Radiology and Oncology (GEC-ESTRO) breast cancer working group based on clinical evidence (2009). Radiother Oncol. 2010, 94: 264-273.
Tinterri C, Gatzemeier W, Zanini V, Regolo L, Pedrazzoli C, Rondini E, Amanti C, Gentile G, Taffurelli M, Fenaroli P, Tondini C, Saccetto G, Sismondi P, Murgo R, Orlandi M, Cianchetti E, Andreoli C: Conservative surgery with and without radiotherapy in elderly patients with early-stage breast cancer: a prospective randomised multicentre trial. Breast. 2009, 18: 373-377.
Hughes KS, Schnaper LA, Cirrincione C, Berry DA, McCormick B, Muss HB, Shank B, Hudis C, Winer EP, Smith BL: ASCO Annual Meeting 2010. 2010, Lumpectomy plus tamoxifen with or without irradiation in women age 70 or older with early breast cancer, Journal of Clinical Oncology,
Lipkus IM, Peters E, Kimmick G, Liotcheva V, Marcom P: Breast cancer patients’ treatment expectations after exposure to the decision aid program adjuvant online: the influence of numeracy. Med Decis Making. 2010, 30: 464-473.
Fallowfield L, Jenkins V, Farewell V, Saul J, Duffy A, Eves R: Efficacy of a Cancer Research UK communication skills training model for oncologists: a randomised controlled trial. Lancet. 2002, 359: 650-656.
El Turabi A, Abel GA, Roland M, Lyratzopoulos G: Variation in reported experience of involvement in cancer treatment decision making: evidence from the National Cancer Patient Experience Survey. Br J Cancer. 2013, 109: 780-787.
Fleissig A, Fallowfield LJ, Langridge CI, Johnson L, Newcombe RG, Dixon JM, Kissin M, Mansel RE: Post-operative arm morbidity and quality of life. Results of the ALMANAC randomised trial comparing sentinel node biopsy with standard axillary treatment in the management of patients with early breast cancer. Breast Cancer Res Treat. 2006, 95: 279-293.
Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, Leitch AM, Saha S, McCall LM, Morrow M: Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011, 305: 569-575.
Rutgers EJ, Donker M, Straver ME, Meijnen P, Van De Velde CJ, Mansel RE, Westenberg H, Orzales L, Bouma WH, van der Mijle H, Nieuwenhuijzen P, Sanne C, Veltkamp LS, Messina CGM, Duez NJ, Hurkmans C, Bogaerts J, van Tienhoven G: ASCO Annual Meeting. 2013, Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer patients: final analysis of the EORTC AMAROS trial (10981/22023), Journal of Clinical Oncology,
Smith BD: Using chemotherapy response to personalize choices regarding locoregional therapy: a new era in breast cancer treatment?. J Clin Oncol. 2012, 30: 3913-3915.
Azim HA, Michiels S, Zagouri F, Delaloge S, Filipits M, Namer M, Neven P, Symmans WF, Thompson A, Andre F, Loi S, Swanton C: Utility of prognostic genomic tests in breast cancer practice: The IMPAKT 2012 Working Group Consensus Statement. Ann Oncol. 2013, 24: 647-654.
Wei S, Liu L, Zhang J, Bowers J, Gowda GA, Seeger H, Fehm T, Neubauer HJ, Vogel U, Clare SE, Raferty D: Metabolomics approach for predicting response to neoadjuvant chemotherapy for breast cancer. Mol Oncol. 2013, 7: 297-307.
Dowsett M, Cuzick J, Wale C, Forbes J, Mallon EA, Salter J, Quinn E, Dunbier A, Baum M, Buzdar A, Howell A, Bugarini R, Baehner FL, Shak S: Prediction of risk of distant recurrence using the 21-gene recurrence score in node-negative and node-positive postmenopausal patients with breast cancer treated with anastrozole or tamoxifen: a TransATAC study. J Clin Oncol. 2010, 28: 1829-1834.
Albain KS, Barlow WE, Shak S, Hortobagyi GN, Livingston RB, Yeh IT, Ravdin P, Bugarini R, Baehner FL, Davidson NE, Sledge GW, Winer EP, Hudis C, Ingle JN, Perez EA, Pritchard KI, Shepherd L, Gralow JR, Yoshizawa C, Allred DC, Osborne CK, Hayes DF, Breast Cancer Intergroup of North America: Prognostic and predictive value of the 21-gene recurrence score assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on chemotherapy: a retrospective analysis of a randomised trial. Lancet Oncol. 2010, 11: 55-65.
Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M, Baehner FL, Walker MG, Watson D, Park T, Hiller W, Fisher ER, Wickerham DL, Bryant J, Wolmark N: A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004, 351: 2817-2826.
Coates PJ, Appleyard MV, Murray K, Ackland C, Gardner J, Brown DC, Adamson DJ, Jordan LB, Purdie CA, Munro AJ, Wright EG, Dewar JA, Thompson AM: Differential contextual responses of normal human breast epithelium to ionizing radiation in a mouse xenograft model. Can Res. 2010, 70: 9808-9815.
Arslan UY, Oksuzoglu B, Aksoy S, Harputluoglu H, Turker I, Ozisik Y, Dizdar O, Altundag K, Alkis N, Zengin N: Breast cancer subtypes and outcomes of central nervous system metastases. Breast. 2011, 20: 562-567.
Rennert G, Pinchev M, Rennert HS: Use of bisphosphonates and risk of postmenopausal breast cancer. J Clin Oncol. 2010, 28: 3577-3581.
Chlebowski RT, Col N: Bisphosphonates and breast cancer prevention. Anticancer Agents Med Chem. 2012, 12: 144-150.
Coleman RE: Adjuvant bone-targeted therapy to prevent metastasis: lessons from the AZURE study. Curr Opin Support Palliat Care. 2012, 6: 322-329.
Paterson AH, Anderson SJ, Lembersky BC, Fehrenbacher L, Falkson CI, King KM, Weir LM, Brufsky AM, Dakhil S, Lad T, Baez-Diaz L, Gralow JR, Robidoux A, Perez EA, Zheng P, Geyer CE, Swain S, Costantino JP, Mamounas EP, Wolmark N: Oral clodronate for adjuvant treatment of operable breast cancer (National Surgical Adjuvant Breast and Bowel Project protocol B-34): a multicentre, placebo-controlled, randomised trial. Lancet Oncol. 2012, 13: 734-742.
Gnant M, Dubsky P, Hadji P: Bisphosphonates: prevention of bone metastases in breast cancer. Recent Results Cancer Res. 2012, 192: 65-91.
Comen E, Norton L, Massague J: Clinical implications of cancer self-seeding. Nat Rev Clin Oncol. 2011, 8: 369-377.
Azim H, Azim HA: Targeting RANKL in breast cancer: bone metastasis and beyond. Expert Rev Anticancer Ther. 2013, 13: 195-201.
Drooger JC, van der Padt A, Sleijfer S, Jager A: Denosumab in breast cancer treatment. Eur J Pharmacol. 2013, doi: 10.1016/j.ejphar.2013.03.034
Formenti SC, Demaria S: Radiation therapy to convert the tumor into an in situ vaccine. Int J Radiat Oncol Biol Phys. 2012, 84: 879-880.
Liauw SL, Connell PP, Weichselbaum RR: New paradigms and future challenges in radiation oncology: an update of biological targets and technology. Sci Transl Med. 2013, 5: 173sr172-
Coles CE, Brunt AM, Wheatley D, Mukesh MB, Yarnold JR: Breast radiotherapy: less is more?. Clin Oncol (R Coll Radiol). 2013, 25: 127-134.
Yarnold J, Bentzen SM, Coles C, Haviland J: Hypofractionated whole-breast radiotherapy for women with early breast cancer: myths and realities. Int J Radiat Oncol Biol Phys. 2011, 79: 1-9.
Mannino M, Yarnold JR: Local relapse rates are falling after breast conserving surgery and systemic therapy for early breast cancer: can radiotherapy ever be safely withheld?. Radiother Oncol. 2009, 90: 14-22.
Blamey RW, Bates T, Chetty U, Duffy SW, Ellis IO, George D, Mallon E, Mitchell MJ, Monypenny I, Morgan DA, Macmillan RD, Patnick J, Pinder SE: Radiotherapy or tamoxifen after conserving surgery for breast cancers of excellent prognosis: British Association of Surgical Oncology (BASO) II trial. Eur J Cancer. 2013, 49: 2294-2302.
Kunkler I: Adjuvant chest wall radiotherapy for breast cancer: black, white and shades of grey. Eur J Surg Oncol. 2010, 36: 331-334.
Critchley AC, Thompson AM, Chan HY, Reed MW: Current controversies in breast cancer surgery. Clin Oncol (R Coll Radiol). 2013, 25: 101-108.
Riou O, Lemanski C, Guillaumon V, Lauche O, Fenoglietto P, Dubois JB, Azria D: Role of the radiotherapy boost on local control in ductal carcinoma in situ. Int J Surg Oncol. 2012, 2012: 748196-
PubMed PubMed Central Google Scholar
Kirkbride P, Hoskin PJ: Implementation of stereotactic ablative radiotherapy (stereotactic body radiotherapy). Clin Oncol (R Coll Radiol). 2012, 24: 627-628.
Somaiah N, Yarnold J, Lagerqvist A, Rothkamm K, Helleday T: Homologous recombination mediates cellular resistance and fraction size sensitivity to radiation therapy. Radiother Oncol. 2013, 1008: 155-1561.
Dowsett M, Nielsen TO, A’Hern R, Bartlett J, Coombes RC, Cuzick J, Ellis M, Henry NL, Hugh JC, Lively T, McShane L, Paik S, Penault-Llorca E, Prudkin L, Regan M, Salter J, Sotiriou C, Smith IE, Viale G, Zujewski JA, Hayes DF, International Ki-67 in Breast Cancer Working Group: Assessment of Ki67 in breast cancer: recommendations from the International Ki67 in Breast Cancer working group. J Natl Cancer Inst. 2011, 103: 1656-1664.
Paik S, Tang G, Shak S, Kim C, Baker J, Kim W, Cronin M, Baehner FL, Watson D, Bryant J, Costantino JP, Geyer CE JR, Wickerham DL, Wolmark N: Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006, 24: 3726-3734.
van de Vijver MJ, He YD, van’t Veer LJ, Dai H, Hart AA, Voskuil DW, Schreiber GJ, Peterse JL, Roberts C, Marton MJ, Parrish M, Atsma D, Witteveen A, Glas A, Delahaye L, van der Velds T, Bartelink H, Rodenhuis S, Rutgers ET, Friend SH, Bernards R: A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med. 2002, 347: 1999-2009.
Goss PE, Ingle JN, Martino S, Robert NJ, Muss HB, Piccart MJ, Castiglione M, Tu D, Shepherd LE, Pritchard KI, Livingston RB, Davidson NE, Norton L, Peres ES, Abrams JS, Cameron DA, Palmer MJ, Pater JL, et al: Randomized trial of letrozole following tamoxifen as extended adjuvant therapy in receptor-positive breast cancer: updated findings from NCIC CTG MA.17. J Natl Cancer Inst. 2005, 97: 1262-1271.
Davies C, Pan H, Godwin J, Gray R, Arriagada R, Raina V, Abraham M, Medeiros Alencar VH, Badran A, Bonfill X, Bradbury J, Clarke M, Collins R, Davis SR, Delmestri A, Fores JF, Haddad P, Hou MF, Inbar M, Khaled H, Kielanowska J, Kwan WH, Mathew BS, Mittra I, Muller B, Nicolucci A, Peralta O, Pernas F, Petruzelka L, Pienkowski T, et al: Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013, 381: 805-816.
Jakesz R, Jonat W, Gnant M, Mittlboeck M, Greil R, Tausch C, Hilfrich J, Kwasny W, Menzel C, Samonigg H, Seifert M, Gademann G, Kaufmann M, Woldgang J, ABCSG and the GABG: Switching of postmenopausal women with endocrine-responsive early breast cancer to anastrozole after 2 years’ adjuvant tamoxifen: combined results of ABCSG trial 8 and ARNO 95 trial. Lancet. 2005, 366: 455-462.
Goldhirsch A, Ingle JN, Gelber RD, Coates AS, Thurlimann B, Senn HJ: Panel m: Thresholds for therapies: highlights of the St Gallen International Expert Consensus on the primary therapy of early breast cancer 2009. Ann Oncol. 2009, 20: 1319-1329.
Osborne CK, Neven P, Dirix LY, Mackey JR, Robert J, Underhill C, Schiff R, Gutierrez C, Migliaccio I, Anagnostou VK, Rimm DL, Magill P, Sellers M: Gefitinib or placebo in combination with tamoxifen in patients with hormone receptor-positive metastatic breast cancer: a randomized phase II study. Clin Cancer Res. 2011, 17: 1147-1159.
Carlson RW, O’Neill A, Vidaurre T, Gomez HL, Badve SS, Sledge GW: A randomized trial of combination anastrozole plus gefitinib and of combination fulvestrant plus gefitinib in the treatment of postmenopausal women with hormone receptor positive metastatic breast cancer. Breast Cancer Res Treat. 2012, 133: 1049-1056.
Baselga J, Bradbury I, Eidtmann H, Di Cosimo S, de Azambuja E, Aura C, Gomez H, Dinh P, Fauria K, Van Dooren V, Aktan G, Goldkirsch A, Chang TW, Horvath Z, Coccia-Portugal M, Dormont J, Tseng LM, Kunz G, Sohn JH, Semiglazov V, Lerzo G, Palacova M, Probachai V, Pusztai L, Untch M, Gelber RD, Piccart-Gebhart M, NeoALTTO Study Team: Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2012, 379: 633-640.
Hamilton-Burke W, Coleman L, Cummings M, Green CA, Holliday DL, Horgan K, Maraqa L, Peter MB, Pollock S, Shaaban AM, Smith L, Speirs V: Phosphorylation of estrogen receptor beta at serine 105 is associated with good prognosis in breast cancer. Am J Pathol. 2010, 177: 1079-1086.
O’Hara J, Vareslija D, McBryan J, Bane F, Tibbitts P, Byrne C, Conroy RM, Hao Y, Gaora PO, Hill AD, McIlroy M, Young LS: AIB1:ERalpha transcriptional activity is selectively enhanced in aromatase inhibitor-resistant breast cancer cells. Clin Cancer Res. 2012, 18: 3305-3315.
Santen RJ, Fan P, Zhang Z, Bao Y, Song RX, Yue W: Estrogen signals via an extra-nuclear pathway involving IGF-1R and EGFR in tamoxifen-sensitive and -resistant breast cancer cells. Steroids. 2009, 74: 586-594.
Ross-Innes CS, Stark R, Teschendorff AE, Holmes KA, Ali HR, Dunning MJ, Brown GD, Gojis O, Ellis IO, Green AR, Ali S, Chin SF, Palmieri C, Caldas C, Carroll JS: Differential oestrogen receptor binding is associated with clinical outcome in breast cancer. Nature. 2012, 481: 389-393.
Di Leva G, Gasparini P, Piovan C, Ngankeu A, Garofalo M, Taccioli C, Iorio MV, Li M, Volinia S, Alder H, Nakamura T, Nuovo G, Liu Y, Nephew KP, Croce CM: MicroRNA cluster 221–222 and estrogen receptor alpha interactions in breast cancer. J Natl Cancer Inst. 2010, 102: 706-721.
Dunn BK, Jegalian K, Greenwald P: Biomarkers for early detection and as surrogate endpoints in cancer prevention trials: issues and opportunities. Recent Results Cancer Res. 2011, 188: 21-47.
Pece S, Tosoni D, Confalonieri S, Mazzarol G, Vecchi M, Ronzoni S, Bernard L, Viale G, Pelicci PG, Di Fiore PP: Biological and molecular heterogeneity of breast cancers correlates with their cancer stem cell content. Cell. 2010, 140: 62-73.
Giamas G, Filipovic A, Jacob J, Messier W, Zhang H, Yang D, Zhang W, Shifa BA, Photiou A, Tralau-Stewart C, Castellano L, Green AR, Coombes RC, Ellis IO, Ali S, Lenz HJ, Stebbing J: Kinome screening for regulators of the estrogen receptor identifies LMTK3 as a new therapeutic target in breast cancer. Nat Med. 2011, 17: 715-719.
Johnston S, Pippen J, Pivot X, Lichinitser M, Sadeghi S, Dieras V, Gomez HL, Romieu G, Manikhas A, Kennedy MJ, Press MF, Maltzman J, Florance A, O’Rourke L, Oliva C, Stein S, Pegram M: Lapatinib combined with letrozole versus letrozole and placebo as first-line therapy for postmenopausal hormone receptor-positive metastatic breast cancer. J Clin Oncol. 2009, 27: 5538-5546.
Elsberger B, Paravasthu DM, Tovey SM, Edwards J: Shorter disease-specific survival of ER-positive breast cancer patients with high cytoplasmic Src kinase expression after tamoxifen treatment. J Cancer Res Clin Oncol. 2012, 138: 327-332.
Iorns E, Turner NC, Elliott R, Syed N, Garrone O, Gasco M, Tutt AN, Crook T, Lord CJ, Ashworth A: Identification of CDK10 as an important determinant of resistance to endocrine therapy for breast cancer. Cancer Cell. 2008, 13: 91-104.
Turner N, Pearson A, Sharpe R, Lambros M, Geyer F, Lopez-Garcia MA, Natrajan R, Marchio C, Iorns E, Mackay A, Gillett C, Grigoriadis A, Tutt A, Reis-Filho JS: FGFR1 amplification drives endocrine therapy resistance and is a therapeutic target in breast cancer. Cancer Res. 2010, 70: 2085-2094.
Higgins MJ, Baselga J: Targeted therapies for breast cancer. J Clin Invest. 2011, 121: 3797-3803.
Gnant M: Overcoming endocrine resistance in breast cancer: importance of mTOR inhibition. Expert Rev Anticancer Ther. 2012, 12: 1579-1589.
Zardavas D, Baselga J, Piccart M: Emerging targeted agents in metastatic breast cancer. Nat Rev Clin Oncol. 2013, 10: 191-210.
Moulder S, Moroney J, Helgason T, Wheler J, Booser D, Albarracin C, Morrow PK, Koenig K, Kurzrock R: Responses to liposomal Doxorubicin, bevacizumab, and temsirolimus in metaplastic carcinoma of the breast: biologic rationale and implications for stem-cell research in breast cancer. J Clin Oncol. 2011, 29: e572-e575.
Hoelder S, Clarke PA, Workman P: Discovery of small molecule cancer drugs: successes, challenges and opportunities. Mol Oncol. 2012, 6: 155-176.
Kauselmann G, Dopazo A, Link W: Identification of disease-relevant genes for molecularly-targeted drug discovery. Curr Cancer Drug Targets. 2012, 12: 1-13.
Swain SM, Kim SB, Cortes J, Ro J, Semiglazov V, Campone M, Ciruelos E, Ferrero JM, Schneeweiss A, Knott A, Clark E, Ross G, Benyunes MC, Baselga J: Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic breast cancer (CLEOPATRA study): overall survival results from a randomised, double-blind, placebo-controlled, phase 3 study. Lancet Oncol. 2013, 14: 461-471.
Criscitiello C, Azim HA, Agbor-Tarh D, de Azambuja E, Piccart M, Baselga J, Eidtmann H, Di Cosimo S, Bradbury I, Rubio IT: Factors associated with surgical management following neoadjuvant therapy in patients with primary HER2-positive breast cancer: results from the NeoALTTO phase III trial. Ann Oncol. 2013, 24: 1980-1985.
Goldhirsch A, Piccart-Gebhart MJ, Procter M, Azambuja E de, Weber HA, Untch M, Smith I, Gianni L, Jackisch C, Cameron D, Bell R, Dowsett M, Gelber RD, Leyland-Jones B, Baselga J: The HERA Study Team HERA TRIAL: 2 years versus 1 year of trastuzumab after adjuvant chemotherapy in women with HER2-positive early breast cancer at 8 years of median follow up. Cancer Research. 72 (24): December 15, 2012 Supplement 3;
Pivot X, Romieu G, Debled M, Pierga JY, Kerbrat P, Bachelot T, Lortholary A, Espie M, Fumoleau P, Serin D, Jacquin JP, Jouannaud C, Rios M, Abadie-Lacourtoisie S, Tubiana-Mathieu N, Cany L, Catala S, Khayat D, Pauporte I, Kramar A, PHARE trial investigators: 6 months versus 12 months of adjuvant trastuzumab for patients with HER2-positive early breast cancer (PHARE): a randomised phase 3 trial. Lancet Oncol. 2013, 14: 741-748.
Tenori L, Oakman C, Claudino WM, Bernini P, Cappadona S, Nepi S, Biganzoli L, Arbushites MC, Luchinat C, Bertini I, Di Leo A: Exploration of serum metabolomic profiles and outcomes in women with metastatic breast cancer: a pilot study. Mol Oncol. 2012, 6: 437-444.
Duncan JS, Whittle MC, Nakamura K, Abell AN, Midland AA, Zawistowski JS, Johnson NL, Granger DA, Jordan NV, Darr DB, Usary J, Kuan PF, Smalley DM, Major B, He X, Hoadley KA, Zhou B, Sharpless NE, Perou C, Kim WY, Gomez SM, Chen X, Jin J, Frye SV, Earp HS, Graves LM, Johnson GL: Dynamic reprogramming of the kinome in response to targeted MEK inhibition in triple-negative breast cancer. Cell. 2012, 149: 307-321.
Heiser LM, Sadanandam A, Kuo WL, Benz SC, Goldstein TC, Ng S, Gibb WJ, Wang NJ, Ziyad S, Tong F, Bayani N, Hu Z, Billig JI, Dueregger A, Lewis S, Jakkula L, Korkola JE, Durinck S, Pepin F, Guan Y, Purdom E, Neuvial P, Bengtsson H, Wood KW, Smith PG, Vassiley LT, Hennessy BT, Greshock J, Bachman KE, Hardwicke MA, et al: Subtype and pathway specific responses to anticancer compounds in breast cancer. Proc Natl Acad Sci U S A. 2012, 109: 2724-2729.
Kelly CM, Buzdar AU: Using multiple targeted therapies in oncology: considerations for use, and progress to date in breast cancer. Drugs. 2013, 73: 505-515.
Sultana R, Abdel-Fatah T, Abbotts R, Hawkes C, Albarakati N, Seedhouse C, Ball G, Chan S, Rakha EA, Ellis IO, Madhusudan S: Targeting XRCC1 deficiency in breast cancer for personalized therapy. Cancer Res. 2013, 73: 1621-1634.
Miller WR, Larionov A, Anderson TJ, Evans DB, Dixon JM: Sequential changes in gene expression profiles in breast cancers during treatment with the aromatase inhibitor, letrozole. Pharmacogenomics J. 2012, 12: 10-21.
Larionov AFD, Caldwell H, Sims A, Fawkes A, Murphy L, Renshaw L, Dixon J: Gene expression profiles of endocrine resistant breast tumours. Cancer Res. 2009, 69: 809-810.
Bartlett JM, Brookes CL, Robson T, van de Velde CJ, Billingham LJ, Campbell FM, Grant M, Hasenburg A, Hille ET, Kay C, Kieback DG, Putter H, Markopoulos C, Kranenbarg E, Mallon EA, Dirix L, Seynaeve C, Rea D: Estrogen receptor and progesterone receptor as predictive biomarkers of response to endocrine therapy: a prospectively powered pathology study in the Tamoxifen and Exemestane Adjuvant Multinational trial. J Clin Oncol. 2011, 29: 1531-1538.
Honma N, Horii R, Iwase T, Saji S, Younes M, Takubo K, Matsuura M, Ito Y, Akiyama F, Sakamoto G: Clinical importance of estrogen receptor-beta evaluation in breast cancer patients treated with adjuvant tamoxifen therapy. J Clin Oncol. 2008, 26: 3727-3734.
Yan Y, Li X, Blanchard A, Bramwell VH, Pritchard KI, Tu D, Shepherd L, Myal Y, Penner C, Watson PH, Leygue E, Murphy LC: Expression of both estrogen receptor-beta 1 (ER-beta1) and its co-regulator steroid receptor RNA activator protein (SRAP) are predictive for benefit from tamoxifen therapy in patients with estrogen receptor-alpha (ER-alpha)-negative early breast cancer (EBC). Ann Oncol. 2013, 24: 1986-1993.
De Amicis F, Thirugnansampanthan J, Cui Y, Selever J, Beyer A, Parra I, Weigel NL, Herynk MH, Tsimelzon A, Lewis MT, Chamness GC, Hilsenbeck SG, Ando S, Fuqua SA: Androgen receptor overexpression induces tamoxifen resistance in human breast cancer cells. Breast Cancer Res Treat. 2010, 121: 1-11.
Garay JP, Park BH: Androgen receptor as a targeted therapy for breast cancer. Am J Cancer Res. 2012, 2: 434-445.
Fan P, Yue W, Wang JP, Aiyar S, Li Y, Kim TH, Santen RJ: Mechanisms of resistance to structurally diverse antiestrogens differ under premenopausal and postmenopausal conditions: evidence from in vitro breast cancer cell models. Endocrinology. 2009, 150: 2036-2045.
Thompson AM, Jordan LB, Quinlan P, Anderson E, Skene A, Dewar JA, Purdie CA: Prospective comparison of switches in biomarker status between primary and recurrent breast cancer: the Breast Recurrence In Tissues Study (BRITS). Breast Cancer Res. 2010, 12: R92-
Amir E, Clemons M, Purdie CA, Miller N, Quinlan P, Geddie W, Coleman RE, Freedman OC, Jordan LB, Thompson AM: Tissue confirmation of disease recurrence in breast cancer patients: pooled analysis of multi-centre, multi-disciplinary prospective studies. Cancer Treat Rev. 2012, 38: 708-714.
Moussa O, Purdie C, Vinnicombe S, Thompson AM: Biomarker discordance: prospective and retrospective evidence that biopsy of recurrent disease is of clinical utility. Cancer Biomark. 2012, 12: 231-239.
Makubate B, Donnan PT, Dewar JA, Thompson AM, McCowan C: Cohort study of adherence to adjuvant endocrine therapy, breast cancer recurrence and mortality. Br J Cancer. 2013, 108: 1515-1524.
Thompson AM, Johnson A, Quinlan P, Hillman G, Fontecha M, Bray SE, Purdie CA, Jordan LB, Ferraldeschi R, Latif A, Hadfield KD, Clarke RB, Ashcroft L, Evans DG, Howell A, Nikoloff M, Lawrence J, Newman WG: Comprehensive CYP2D6 genotype and adherence affect outcome in breast cancer patients treated with tamoxifen monotherapy. Breast Cancer Res Treat. 2011, 125: 279-287.
Loi S, Sirtaine N, Piette F, Salgado R, Viale G, Van Eenoo F, Rouas G, Francis P, Crown JP, Hitre E, de Azambuja E, Quinaux E, Di Leo A, Michiels S, Piccart MJ, Sotiriou C: Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02–98. J Clin Oncol. 2013, 31: 860-867.
Group BIGC, Mouridsen H, Giobbie-Hurder A, Goldhirsch A, Thurlimann B, Paridaens R, Smith I, Mauriac L, Forbes J, Price KN, Regan MM, Gelber RD, Coates AS: Letrozole therapy alone or in sequence with tamoxifen in women with breast cancer. N Engl J Med. 2009, 361: 766-776.
Coombes RC, Kilburn LS, Snowdon CF, Paridaens R, Coleman RE, Jones SE, Jassem J, Van de Velde CJ, Delozier T, Alvarez I, Del Mastro L, Ortmann O, Diedrich K, Coates AS, Bajetta E, Homberg SB, Dodwell D, Mickiewicz E, Anderson J, Lonning PE, Cocconi G, Forbes J, Castiglione M, Stuart N, Stewart A, Fallowfield LJ, Bertelli G, Hall E, Bogle RG, Carpentieri M, et al: Survival and safety of exemestane versus tamoxifen after 2–3 years’ tamoxifen treatment (Intergroup Exemestane Study): a randomised controlled trial. Lancet. 2007, 369: 559-570.
Palmieri C, Shah D, Krell J, Gojis O, Hogben K, Riddle P, Ahmad R, Tat T, Fox K, Porter A, Mahmoud S, Kirschke S, Shousha S, Gudi M, Coombes RC, Leonard R, Cleator S: Management and outcome of HER2-positive early breast cancer treated with or without trastuzumab in the adjuvant trastuzumab era. Clin Breast Cancer. 2011, 11: 93-102.
Fontein DB, Seynaeve C, Hadji P, Hille ET, van de Water W, Putter H, Kranenbarg EM, Hasenburg A, Paridaens RJ, Vannetzel JM, Markopoulos C, Hoxumi Y, Bartlett JM, Jones SE, Rea DW, Nortier JW, van de Velde CJ: Specific adverse events predict survival benefit in patients treated with tamoxifen or aromatase inhibitors: an international tamoxifen exemestane adjuvant multinational trial analysis. J Clin Oncol. 2013, 31: 2257-2264.
Blackwell KL, Burstein HJ, Storniolo AM, Rugo HS, Sledge G, Aktan G, Ellis C, Florance A, Vukelja S, Bischoff J, Baselga J, O’Shaughnessy J: Overall survival benefit with lapatinib in combination with trastuzumab for patients with human epidermal growth factor receptor 2-positive metastatic breast cancer: final results from the EGF104900 Study. J Clin Oncol. 2012, 30: 2585-2592.
Gianni L, Pienkowski T, Im YH, Roman L, Tseng LM, Liu MC, Lluch A, Staroslawska E, de la Haba-Rodriguez J, Im SA, Pedrini JL, Poirier B, Pedrini JL, Poirier B, Morandi P, Semiglazov V, Srimuninnimi V, Bianchi G, Szado T, Ratnayake J, Ross G, Valagussa P: Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol. 2012, 13: 25-32.
Baselga J, Bradbury I, Eidtmann H, Di Cosimo S, de Azambuja E, Aura C, Gomez H, Dinh P, Fauria K, Van Dooren V, Aktan G, Goldhirsch A, Chang TW, Horvath Z, Coccia-Portugal M, Domant J, Tseng LM, Kunz G, Sohn JH, Semiglazov V, Lerzo G, Palacova M, Probachai V, Pusztai L, Untch M, Gelber RD, Piccart-Gebhart M, NeoALTTO Study Team: Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2012, 379: 633-640.
Baselga J, Cortes J, Kim SB, Im SA, Hegg R, Im YH, Roman L, Pedrini JL, Pienkowski T, Knott A, Clark E, Benyunes MC, Ross G, Swain SM, CLEOPATRA Study Group: Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med. 2012, 366: 109-119.
Gelmon KA, Tischkowitz M, Mackay H, Swenerton K, Robidoux A, Tonkin K, Hirte H, Huntsman D, Clemons M, Gilks B, Yerushalmi R, Macpherson E, Carmichael J, Oza A: Olaparib in patients with recurrent high-grade serous or poorly differentiated ovarian carcinoma or triple-negative breast cancer: a phase 2, multicentre, open-label, non-randomised study. Lancet Oncol. 2011, 12: 852-861.
Cleator S, Heller W, Coombes RC: Triple-negative breast cancer: therapeutic options. Lancet Oncol. 2007, 8: 235-244.
Molyneux G, Smalley MJ: The cell of origin of BRCA1 mutation-associated breast cancer: a cautionary tale of gene expression profiling. J Mammary Gland Biol Neoplasia. 2011, 16: 51-55.
Michalak EM, Jonkers J: Studying therapy response and resistance in mouse models for BRCA1-deficient breast cancer. J Mammary Gland Biol Neoplasia. 2011, 16: 41-50.
Ran S, Volk L, Hall K, Flister MJ: Lymphangiogenesis and lymphatic metastasis in breast cancer. Pathophysiology. 2010, 17: 229-251.
Ferris RL, Lotze MT, Leong SP, Hoon DS, Morton DL: Lymphatics, lymph nodes and the immune system: barriers and gateways for cancer spread. Clin Exp Metastasis. 2012, 29: 729-736.
Gomes FG, Nedel F, Alves AM, Nor JE, Tarquinio SB: Tumor angiogenesis and lymphangiogenesis: tumor/endothelial crosstalk and cellular/microenvironmental signaling mechanisms. Life Sci. 2013, 92: 101-107.
Lenzer J: FDA committee votes to withdraw bevacizumab for breast cancer. BMJ. 2011, 343: d4244-
D’Agostino RB: Changing end points in breast-cancer drug approval–the Avastin story. N Engl J Med. 2011, 365: e2-
Shojaei F: Anti-angiogenesis therapy in cancer: current challenges and future perspectives. Cancer Lett. 2012, 320: 130-137.
Nagy JA, Benjamin L, Zeng H, Dvorak AM, Dvorak HF: Vascular permeability, vascular hyperpermeability and angiogenesis. Angiogenesis. 2008, 11: 109-119.
Kerbel RS: Strategies for improving the clinical benefit of antiangiogenic drug based therapies for breast cancer. J Mammary Gland Biol Neoplasia. 2012, 17: 229-239.
Sitohy B, Nagy JA, Dvorak HF: Anti-VEGF/VEGFR therapy for cancer: reassessing the target. Cancer Res. 2012, 72: 1909-1914.
Chew V, Toh HC, Abastado JP: Immune microenvironment in tumor progression: characteristics and challenges for therapy. J Oncol. 2012, 2012: 608406-
Andre F, Dieci MV, Dubsky P, Sotiriou C, Curigliano G, Denkert C, Loi S: Molecular pathways: involvement of immune pathways in the therapeutic response and outcome in breast cancer. Clin Cancer Res. 2013, 19: 28-33.
Reisfeld RA: The tumor microenvironment: a target for combination therapy of breast cancer. Crit Rev Oncog. 2013, 18: 115-133.
Chen YT, Ross DS, Chiu R, Zhou XK, Chen YY, Lee P, Hoda SA, Simpson AJ, Old LJ, Caballero O, Neville A: Multiple cancer/testis antigens are preferentially expressed in hormone-receptor negative and high-grade breast cancers. PloS one. 2011, 6: e17876-
Adams S, Greeder L, Reich E, Shao Y, Fosina D, Hanson N, Tassello J, Singh B, Spagnoli GC, Demaria S, Jungbluth AA: Expression of cancer testis antigens in human BRCA-associated breast cancers: potential targets for immunoprevention?. Cancer Immunol Immunother. 2011, 60: 999-1007.
Corner J, Wright D, Hopkinson J, Gunaratnam Y, McDonald JW, Foster C: The research priorities of patients attending UK cancer treatment centres: findings from a modified nominal group study. Br J Cancer. 2007, 96: 875-881.
Hewitt M, Rowland JH, Yancik R: Cancer survivors in the United States: age, health, and disability. J Geront A, Biol Sci Med Sci. 2003, 58: 82-91.
Foster C, Wright D, Hill H, Hopkinson J, Roffe L: Psychosocial implications of living 5 years or more following a cancer diagnosis: a systematic review of the research evidence. Eur J Cancer Care (Engl). 2009, 18: 223-247.
Hubbard G, Menzies S, Flynn P, Adams S, Haseen F, Thomas I, Scanlon K, Reed L, Forbat L: Relational mechanisms and psychological outcomes in couples affected by breast cancer: a systematic review of the literature. BMJ, Supportive and Palliative Care. 2013, 3: 1-7.
Foster C, Fenlon D: Recovery and self-management support following primary cancer treatment. Br J Cancer. 2011, 105: S21-S28.
Cimprich B, Janz NK, Northouse L, Wren PA, Given B, Given CW: Taking CHARGE: A self-management program for women following breast cancer treatment. Psychooncology. 2005, 14: 704-717.
Bloom JR, Stewart SL, D’Onofrio CN, Luce J, Banks PJ: Addressing the needs of young breast cancer survivors at the 5 year milestone: can a short-term, low intensity intervention produce change?. J Cancer Surviv. 2008, 2: 190-204.
Reed E, Simmonds P, Haviland J, Corner J: Quality of life and experience of care in women with metastatic breast cancer: a cross-sectional survey. J Pain Symptom Manage. 2012, 43: 747-758.
Aranda S, Schofield P, Weih L, Yates P, Milne D, Faulkner R, Voudouris N: Mapping the quality of life and unmet needs of urban women with metastatic breast cancer. Eur J Cancer Care (Engl). 2005, 14: 211-222.
Hopwood P, Howell A, Maguire P: Psychiatric morbidity in patients with advanced cancer of the breast: prevalence measured by two self-rating questionnaires. Br J Cancer. 1991, 64: 349-352.
Pinder KL, Ramirez AJ, Black ME, Richards MA, Gregory WM, Rubens RD: Psychiatric disorder in patients with advanced breast cancer: prevalence and associated factors. Eur J Cancer. 1993, 29A: 524-527.
Kissane DW, Grabsch B, Love A, Clarke DM, Bloch S, Smith GC: Psychiatric disorder in women with early stage and advanced breast cancer: a comparative analysis. Aust N Z J Psychiatry. 2004, 38: 320-326.
Grunfeld EA, Maher EJ, Browne S, Ward P, Young T, Vivat B, Walker G, Wilson C, Potts HW, Westcombe AM, Richards MA, Ramirez AJ: Advanced breast cancer patients’ perceptions of decision making for palliative chemotherapy. J Clin Oncol. 2006, 24: 1090-1098.
Karamouzis MV, Ioannidis G, Rigatos G: Quality of life in metastatic breast cancer patients under chemotherapy or supportive care: a single-institution comparative study. Eur J Cancer Care. 2007, 16: 433-438.
Cheville AL, Troxel AB, Basford JR, Kornblith AB: Prevalence and treatment patterns of physical impairments in patients with metastatic breast cancer. J Clin Oncol. 2008, 26: 2621-2629.
Headley JA, Ownby KK, John LD: The effect of seated exercise on fatigue and quality of life in women with advanced breast cancer. Oncol Nurs forum. 2004, 31: 977-983.
Asola R, Huhtala H, Holli K: Intensity of diagnostic and treatment activities during the end of life of patients with advanced breast cancer. Breast Cancer Res Treat. 2006, 100: 77-82.
Gagnon B, Mayo NE, Hanley J, MacDonald N: Pattern of care at the end of life: does age make a difference in what happens to women with breast cancer?. J Clin Oncol. 2004, 22: 3458-3465.
Richardson A, Addington-Hall J, Amir Z, Foster C, Stark D, Armes J, Brearley SG, Hodges L, Hook J, Jarrett N, Stamataki Z, Scott I, Walker J, Ziegler L, Sharpe MS: Knowledge, ignorance and priorities for research in key areas of cancer survivorship: findings from a scoping review. Br J Cancer. 2011, 105: S82-S94.
Stanton AL, Luecken LJ, MacKinnon DP, Thompson EH: Mechanisms in psychosocial interventions for adults living with cancer: opportunity for integration of theory, research, and practice. J Consult Clin Psychol. 2013, 81: 318-335.
Fenlon DR, Corner JL, Haviland JS: A randomized controlled trial of relaxation training to reduce hot flashes in women with primary breast cancer. J Pain Symptom Manage. 2008, 35: 397-405.
Osborn RL, Demoncada AC, Feuerstein M: Psychosocial interventions for depression, anxiety, and quality of life in cancer survivors: meta-analyses. Int J Psychiatry Med. 2006, 36: 13-34.
Spiegel D, Bloom JR, Kraemer HC, Gottheil E: Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet. 1989, 2: 888-891.
Edwards AG, Hulbert-Williams N, Neal RD: Psychological interventions for women with metastatic breast cancer. Cochrane Database Syst Rev. 2008, 3: CD004253
Emilsson S, Svensk AC, Tavelin B, Lindh J: Support group participation during the post-operative radiotherapy period increases levels of coping resources among women with breast cancer. Eur J Cancer Care (Engl). 2012, 21: 591-598.
Hoey LM, Ieropoli SC, White VM, Jefford M: Systematic review of peer-support programs for people with cancer. Patient Educ Couns. 2008, 70: 315-337.
Ganz PA, Kwan L, Stanton AL, Bower JE, Belin TR: Physical and psychosocial recovery in the year after primary treatment of breast cancer. J Clin Oncol. 2011, 29: 1101-1109.
Capozzo MA, Martinis E, Pellis G, Giraldi T: An early structured psychoeducational intervention in patients with breast cancer: results from a feasibility study. Cancer Nurs. 2010, 33: 228-234.
Gielissen MF, Verhagen CA, Bleijenberg G: Cognitive behaviour therapy for fatigued cancer survivors: long-term follow-up. Br J Cancer. 2007, 97: 612-618.
Ritterband LM, Bailey ET, Thorndike FP, Lord HR, Farrell-Carnahan L, Baum LD: Initial evaluation of an Internet intervention to improve the sleep of cancer survivors with insomnia. Psychooncology. 2012, 21: 695-705.
Armes J, Chalder T, Addington-Hall J, Richardson A, Hotopf M: A randomized controlled trial to evaluate the effectiveness of a brief, behaviorally oriented intervention for cancer-related fatigue. Cancer. 2007, 110: 1385-1395.
Mann E, Smith M, Hellier J, Hunter MS: A randomised controlled trial of a cognitive behavioural intervention for women who have menopausal symptoms following breast cancer treatment (MENOS 1): trial protocol. BMC Cancer. 2011, 11: 44-
Duijts SF, van Beurden M, Oldenburg HS, Hunter MS, Kieffer JM, Stuiver MM, Gerritsma MA, Menke-Pluymers MB, Plaisier PW, Rijna H, Lopes Cardozo AM, Timmers G, van der Meij S, van der Veen H, Bijker N, de Widt-Levert LN, Geenen MM, Heuff G, van Dulken EJ, Aaronson NK BE: Efficacy of cognitive behavioral therapy and physical exercise in alleviating treatment-induced menopausal symptoms in patients with breast cancer: results of a randomized, controlled, multicenter trial. J Clin Oncol. 2012, 30: 4124-4133.
Thompson J, Cocker H, Coleman RE, Colwell B, Freeman JV, Holmes K, Reed MW, Anthony C, Greenfield D: Breast cancer aftercare; preparing patients for discharge from routine hospital follow-up (PREP). Proceedings of the British Psychosocial Oncology Society Conference: 3–4 December 2009. 2009, Cardiff, Wales: Psycho-Oncology, 19(Suppl. 3):S1–S20 (2010)
Shennan C, Payne S, Fenlon D: What is the evidence for the use of mindfulness-based interventions in cancer care? A review. Psychooncology. 2011, 20: 681-697.
Campbell KL, Neil SE, Winters-Stone KM: Review of exercise studies in breast cancer survivors: attention to principles of exercise training. Br J Sports Med. 2011, 46: 909-916.
Speck RM, Courneya KS, Masse LC, Duval S, Schmitz KH: An update of controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv. 2010, 4: 87-100.
Fong DY, Ho JW, Hui BP, Lee AM, Macfarlane DJ, Leung SS, Cerin E, Chan WY, Leung IP, Lam SH, Taylor AJ, Cheng KK: Physical activity for cancer survivors: meta-analysis of randomised controlled trials. BMJ. 2012, 344: e70-
Mutrie N, Campbell A, Barry S, Hefferon K, McConnachie A, Ritchie D, Tovey S: Five-year follow-up of participants in a randomised controlled trial showing benefits from exercise for breast cancer survivors during adjuvant treatment. Are there lasting effects?. J Cancer Surviv. 2012, 6: 420-430.
Classen C, Butler LD, Koopman C, Miller E, DiMiceli S, Giese-Davis J, Fobair P, Carlson RW, Kraemer HC, Spiegel D: Supportive-expressive group therapy and distress in patients with metastatic breast cancer: a randomized clinical intervention trial. Arch Gen Psychiatry. 2001, 58: 494-501.
Watson EK, Rose PW, Neal RD, Hulbert-Williams N, Donnelly P, Hubbard G, Elliott J, Campbell C, Weller D, Wilkinson C: Personalised cancer follow-up: risk stratification, needs assessment or both?. Br J Cancer. 2012, 106: 1-5.
Fenlon D, Frankland J, Foster CL, Brooks C, Coleman P, Payne S, Seymour J, Simmonds P, Stephens R, Walsh B, Addington-Hall JM: Living into old age with the consequences of breast cancer. Eur J Oncol Nurs. 2013, 17: 311-316.
Watts K, Meiser B, Conlon H, Rovelli S, Tiller K, Zorbas H, Lewis C, Neil G, Friedlander M: A specialist breast care nurse role for women with metastatic breast cancer: enhancing supportive care. Oncol Nurs Forum. 2011, 38: 627-631.
Absolom K, Eiser C, Michel G, Walters SJ, Hancock BW, Coleman RE, Snowden JA, Greenfield DM: Follow-up care for cancer survivors: views of the younger adult. Br J Cancer. 2009, 101: 561-567.
Fenlon DR, Corner JL, Haviland J: Menopausal hot flushes after breast cancer. Eur J Cancer Care (Engl). 2009, 18: 140-148.
Mann E, Smith MJ, Hellier J, Balabanovic JA, Hamed H, Grunfeld EA, Hunter MS: Cognitive behavioural treatment for women who have menopausal symptoms after breast cancer treatment (MENOS 1): a randomised controlled trial. Lancet Oncol. 2012, 13: 309-318.
Castellon SA, Ganz PA, Bower JE, Petersen L, Abraham L, Greendale GA: Neurocognitive performance in breast cancer survivors exposed to adjuvant chemotherapy and tamoxifen. J Clin Exp Neuropsychol. 2004, 26: 955-969.
Rausch R, Kraemer S, Pietras CJ, Le M, Vickrey BG, Passaro EA: Early and late cognitive changes following temporal lobe surgery for epilepsy. Neurology. 2003, 60: 951-959.
Oliveri JM, Day JM, Alfano CM, Herndon JE, Katz ML, Bittoni MA, Donohue K, Paskett ED: Arm/hand swelling and perceived functioning among breast cancer survivors 12 years post-diagnosis: CALGB 79804. J Cancer Surviv. 2008, 2: 233-242.
Fourie WJ, Robb KA: Physiotherapy management of axillary web syndrome following breast cancer treatment: discussing the use of soft tissue techniques. Physiotherapy. 2009, 95: 314-320.
Holliday DL, Speirs V: Choosing the right cell line for breast cancer research. Breast Cancer Res. 2011, 13: 215-
Lacroix M, Leclercq G: Relevance of breast cancer cell lines as models for breast tumours: an update. Breast Cancer Res Treat. 2004, 83: 249-289.
Liu X, Ory V, Chapman S, Yuan H, Albanese C, Kallakury B, Timofeeva OA, Nealon C, Dakic A, Simic V, Haddad BR, Rhim JS, Dritschilo A, Riegel A, McBride A, Schlegel R: ROCK inhibitor and feeder cells induce the conditional reprogramming of epithelial cells. Am J Pathol. 2012, 180: 599-607.
Yuan H, Myers S, Wang J, Zhou D, Woo JA, Kallakury B, Ju A, Bazylewicz M, Carter YM, Albanese C, Grant N, Shad A, Dritschilo A, Liu X, Schlegel R: Use of reprogrammed cells to identify therapy for respiratory papillomatosis. N Engl J Med. 2012, 367: 1220-1227.
Lee GY, Kenny PA, Lee EH, Bissell MJ: Three-dimensional culture models of normal and malignant breast epithelial cells. Nat Methods. 2007, 4: 359-365.
Calvo F, Sahai E: Cell communication networks in cancer invasion. Curr Opin Cell Biol. 2011, 23: 621-629.
Vinci M, Gowan S, Boxall F, Patterson L, Zimmermann M, Court W, Lomas C, Mendiola M, Hardisson D, Eccles SA: Advances in establishment and analysis of three-dimensional tumor spheroid-based functional assays for target validation and drug evaluation. BMC Biol. 2012, 10: 29-
Krishnan V, Shuman LA, Sosnoski DM, Dhurjati R, Vogler EA, Mastro AM: Dynamic interaction between breast cancer cells and osteoblastic tissue: comparison of two- and three-dimensional cultures. J Cell Physiol. 2011, 226: 2150-2158.
Quail DF, Maciel TJ, Rogers K, Postovit LM: A unique 3D in vitro cellular invasion assay. J Biomol Screen. 2012, 17: 1088-1095.
Ho KS, Poon PC, Owen SC, Shoichet MS: Blood vessel hyperpermeability and pathophysiology in human tumour xenograft models of breast cancer: a comparison of ectopic and orthotopic tumours. BMC Cancer. 2012, 12: 579-
DeRose YS, Gligorich KM, Wang G, Georgelas A, Bowman P, Courdy SJ, Welm AL, Welm BE, et al: Patient-derived models of human breast cancer: protocols for in vitro and in vivo applications in tumor biology and translational medicine. Current protocols in pharmacology. Edited by: Enna SJ, John Wiley & Sons . 2013, Chapter 14:Unit14 23
Kabos P, Finlay-Schultz J, Li C, Kline E, Finlayson C, Wisell J, Manuel CA, Edgerton SM, Harrell JC, Elias A, Sartorius CA: Patient-derived luminal breast cancer xenografts retain hormone receptor heterogeneity and help define unique estrogen-dependent gene signatures. Breast Cancer Res Treat. 2012, 135: 415-432.
Rottenberg S, Jaspers JE, Kersbergen A, van der Burg E, Nygren AO, Zander SA, Derksen PW, de Bruin M, Zevenhoven J, Lau A, Boulter R, Cranston A, O’Conner MJ, Martin NM, Borst P, Jonkers J: High sensitivity of BRCA1-deficient mammary tumors to the PARP inhibitor AZD2281 alone and in combination with platinum drugs. Proc Natl Acad Sci U S A. 2008, 105: 17079-17084.
Mollard S, Mousseau Y, Baaj Y, Richard L, Cook-Moreau J, Monteil J, Funalot B, Sturtz FG: How can grafted breast cancer models be optimized?. Cancer Biol Ther. 2011, 12: 855-864.
Zhang X, Claerhout S, Prat A, Dobrolecki LE, Petrovic I, Lai Q, Landis MD, Wiechmann L, Schiff R, Giuliano M, Wong H, Fuqua SW, Contreras A, Gutierrez C, Huang J, Mao S, Pavlick AC, Froehlich AM, Wu MF, Tsimelzon A, Hilsenbeck SG, Chen ES, Zuloaga P, Shaw CA, Rimawi MF, Perou CM, Mills GB, Chang JC, Lewis MT: A renewable tissue resource of phenotypically stable, biologically and ethnically diverse, patient-derived human breast cancer xenograft models. Cancer Res. 2013, 73: 4885-4897.
Borowsky AD: Choosing a mouse model: experimental biology in context–the utility and limitations of mouse models of breast cancer. Cold Spring Harb Perspect Biol. 2011, 3: a009670-
Andrechek ER, Nevins JR: Mouse models of cancers: opportunities to address heterogeneity of human cancer and evaluate therapeutic strategies. J Mol Med. 2010, 88: 1095-1100.
Caligiuri I, Rizzolio F, Boffo S, Giordano A, Toffoli G: Critical choices for modeling breast cancer in transgenic mouse models. J Cell Physiol. 2012, 227: 2988-2991.
Kirma NB, Tekmal RR: Transgenic mouse models of hormonal mammary carcinogenesis: advantages and limitations. J Steroid Biochem Mol Biol. 2012, 131: 76-82.
Uhr JW, Pantel K: Controversies in clinical cancer dormancy. Proc Natl Acad Sci U S A. 2011, 108: 12396-12400.
Giampieri S, Manning C, Hooper S, Jones L, Hill CS, Sahai E: Localized and reversible TGFbeta signalling switches breast cancer cells from cohesive to single cell motility. Nat Cell Biol. 2009, 11: 1287-1296.
Eccles SA, Welch DR: Metastasis: recent discoveries and novel treatment strategies. Lancet. 2007, 369: 1742-1757.
Francia G, Cruz-Munoz W, Man S, Xu P, Kerbel RS: Mouse models of advanced spontaneous metastasis for experimental therapeutics. Nat Rev Cancer. 2011, 11: 135-141.
Eckhardt BL, Francis PA, Parker BS, Anderson RL: Strategies for the discovery and development of therapies for metastatic breast cancer. Nature Rev Drug Dis. 2012, 11: 479-497.
Guerin E, Man S, Xu P, Kerbel RS: A model of postsurgical advanced metastatic breast cancer more accurately replicates the clinical efficacy of antiangiogenic drugs. Cancer Res. 2013, 73: 2743-2748.
Kievit FM, Stephen ZR, Veiseh O, Arami H, Wang T, Lai VP, Park JO, Ellenbogen RG, Disis ML, Zhang M: Targeting of primary breast cancers and metastases in a transgenic mouse model using rationally designed multifunctional SPIONs. ACS Nano. 2012, 6: 2591-2601.
Fang Y, Chen Y, Yu L, Zheng C, Qi Y, Li Z, Yang Z, Zhang Y, Shi T, Luo J, Liu M: Inhibition of breast cancer metastases by a novel inhibitor of TGFbeta receptor 1. J Natl Cancer Inst. 2013, 105: 47-58.
Palmieri D, Lockman PR, Thomas FC, Hua E, Herring J, Hargrave E, Johnson M, Flores N, Qian Y, Vega-Valle E, Tasker KS, Rudraraju V, Mittapalli RK, Gaasch JA, Bohn KA, Thorsheim HR, Liewehr DJ, Davis S, Reilly JF, Walker R, Bronder JL, Feigenbaum L, Steinberg S, Camphausen K, Meltzer PS, Richon VM, Smith QR, Steeq PS: Vorinostat inhibits brain metastatic colonization in a model of triple-negative breast cancer and induces DNA double-strand breaks. Clin Cancer Res. 2009, 15: 6148-6157.
Xia TS, Wang J, Yin H, Ding Q, Zhang YF, Yang HW, Liu XA, Dong M, Du Q, Ling LJ, Zha XM, Fu W, Wang S: Human tissue-specific microenvironment: an essential requirement for mouse models of breast cancer. Oncol Rep. 2010, 24: 203-211.
Steeg PS: Perspective: the right trials. Nature. 2012, 485: S58-S59.
Wong AL, Lee SC: Mechanisms of resistance to trastuzumab and novel therapeutic strategies in HER2-positive breast cancer. Int J Breast Cancer. 2012, 2012: 415170-
Polyak K: Heterogeneity in breast cancer. J Clin Invest. 2011, 121: 3786-3788.
Lindell KO, Erlen JA, Kaminski N: Lessons from our patients: development of a warm autopsy program. PLoS medicine. 2006, 3: e234-
Hadad S, Iwamoto T, Jordan L, Purdie C, Bray S, Baker L, Jellema G, Deharo S, Hardie DG, Pusztai L, Moulder-Thompson S, Dewar JA, Thompson AM: Evidence for biological effects of metformin in operable breast cancer: a pre-operative, window-of-opportunity, randomized trial. Breast Cancer Res Treat. 2011, 128: 783-794.
Leary AF, Hanna WM, van de Vijver MJ, Penault-Llorca F, Ruschoff J, Osamura RY, Bilous M, Dowsett M: Value and limitations of measuring HER-2 extracellular domain in the serum of breast cancer patients. J Clin Oncol. 2009, 27: 1694-1705.
Witzel I, Loibl S, von Minckwitz G, Mundhenke C, Huober J, Hanusch C, Henschen S, Hauschild M, Lantzsch T, Tesch H, Latos K, Just M, Hilfrich J, Barinoff J, Eulenburg CZ, Roller M, Untch M, Muller V: Monitoring serum HER2 levels during neoadjuvant trastuzumab treatment within the GeparQuattro trial. Breast Cancer Res Treat. 2010, 123: 437-445.
Thureau S, Clatot F, Laberge-Le-Couteulx S, Baron M, Basuyau JP, Blot E: Elevated HER2 extracellular domain level in primary breast cancer with HER2 overexpression predicts early failure of adjuvant trastuzumab. Anticancer Res. 2012, 32: 1429-1433.
Molina R, Escudero JM, Munoz M, Auge JM, Filella X: Circulating levels of HER-2/neu oncoprotein in breast cancer. Clin Chem Lab Med. 2012, 50: 5-21.
Dietel M, Johrens K, Laffert M, Hummel M, Blaker H, Muller BM, Lehmann A, Denkert C, Heppner FL, Koch A, Sers C, Anagnostopoulos I: Predictive molecular pathology and its role in targeted cancer therapy: a review focussing on clinical relevance. Cancer Gene Ther. 2013, 20: 211-221.
Modur V, Hailman E, Barrett JC: Evidence-based laboratory medicine in oncology drug development: from biomarkers to diagnostics. Clin Chem. 2013, 59: 102-109.
Knowles SM, Wu AM: Advances in immuno-positron emission tomography: antibodies for molecular imaging in oncology. J Clin Oncol. 2012, 30: 3884-3892.
Capala J, Bouchelouche K: Molecular imaging of HER2-positive breast cancer: a step toward an individualized ‘image and treat’ strategy. Curr Opin Oncol. 2010, 22: 559-566.
Asselin MC, O’Connor JP, Boellaard R, Thacker NA, Jackson A: Quantifying heterogeneity in human tumours using MRI and PET. Eur J Cancer. 2012, 48: 447-455.
Waterton JC, Pylkkanen L: Qualification of imaging biomarkers for oncology drug development. Eur J Cancer. 2012, 48: 409-415.
Segal E, Sirlin CB, Ooi C, Adler AS, Gollub J, Chen X, Chan BK, Matcuk GR, Barry CT, Chang HY, Kuo MD: Decoding global gene expression programs in liver cancer by noninvasive imaging. Nat Biotechnol. 2007, 25: 675-680.
Lambin P, Rios-Velazquez E, Leijenaar R, Carvalho S, van Stiphout RGPM, Granton P, Zegers CML, Gillies R, Boellard R, Dekker A, Aerts HJ: Radiomics: extracting more information from medical images using advanced feature analysis. Eur J Cancer. 2012, 48: 441-446.
Macaskill EJ, Bartlett JM, Sabine VS, Faratian D, Renshaw L, White S, Campbell FM, Young O, Williams L, Thomas JS, Barber MD, Dixon JM: The mammalian target of rapamycin inhibitor everolimus (RAD001) in early breast cancer: results of a pre-operative study. Breast Cancer Res Treat. 2011, 128: 725-734.
Basch E, Jia X, Heller G, Barz A, Sit L, Fruscione M, Appawu M, Iasonos A, Atkinson T, Goldfarb S, Culkin A, Kris MG, Schrag D: Adverse symptom event reporting by patients vs clinicians: relationships with clinical outcomes. J Natl Cancer Inst. 2009, 101: 1624-1632.
Dietary Fish and Omega 3 Fatty Acids for Breast Cancer Prevention. [ http://clinicaltrials.gov/show/NCT01282580 ]
Download references
Acknowledgements
We would like to acknowledge the helpful contributions to the final manuscript from the Executive Advisory Board: Kevin Brindle, Robert E Coleman, Charles Coombes, Jack Cuzick, Mitchell Dowsett, Lesley Fallowfield, Christine Friedenreich, William J Gullick, Barry Gusterson, Craig Jordan, Sunil Lakhani, Bettina Meiser, Emma Pennery, Rebecca Riggins and Stephen Johnston. We would also like to acknowledge the contributions of the patient advocate representatives Mairead McKenzie and Marion Lewis from Breast Cancer Care’s Service User Research Panel.
SAE acknowledges support from the NIHR RM/ICR Biomedical Research Centre, ICR and Cancer Research UK.
AMT acknowledges support from Breast Cancer Campaign, Breakthrough Breast Cancer and CR-UK.
Breast Cancer Campaign staff Lisa Wilde, Phyllis Quinn and Stuart Griffiths assisted in the design and implementation of the gap analysis initiative and acted as facilitators throughout the process. Geraldine Byrne was responsible for co-ordinating and delivering the logistics and acted as a facilitator at the nine gap analysis workshops that were held at the Breast Cancer Campaign offices.
We thank Dr Alexis Willet who provided editorial assistance on behalf of Punch Consulting.
Author information
Authors and affiliations.
Imperial College London, Exhibition Rd, London, SW7 2AZ, UK
Eric O Aboagye, Simak Ali, James M Flanagan & David J Mann
University of Dundee, Perth Road, Dundee, DD1 4HN, UK
Annie S Anderson, Anna M Campbell & Alastair M Thompson
University of Southampton, University Road, Southampton, SO17 1BJ, UK
Jeremy P Blaydes, Diana M Eccles, Deborah F Fenlon & Claire Foster
University of Birmingham, Edgbaston, Birmingham, B15 2TT, UK
Fedor Berditchevski & Joanna R Morris
University of Manchester, Oxford Road, Manchester, M13 9PL, UK
Keith Brennan, Nigel J Bundred, Robert B Clarke, D Gareth Evans, Michelle Harvie, Sacha J Howell, Anthony Howell, Cliona C Kirwan, James PB O’Connor, Charles H Streuli & Kaye J Williams
University of Sheffield, Western Bank, Sheffield, S10 2TN, UK
Nicola J Brown, Helen E Bryant, Angela Cox & Ingunn Holen
Kings College London, Strand, London, WC2R 2LS, UK
Jo Armes, Joy M Burchell, Gary JR Cook, Vicky Goh, Myra S Hunter, David W Miles & Andrew N J Tutt
University College London, Gower Street, London, WC1E 6BT, UK
Ashley M Groves & Robert Stein
Cancer Research UK, Cambridge Research Institute/University of Cambridge, Trinity Lane, Cambridge, CB2 1TN, UK
Jason S Carroll, Douglas F Easton, Paul D P Pharoah, John Stingl & Christine J Watson
Newcastle University, Claremont Road, Newcastle upon Tyne, NE1 7RU, UK
Nicola J Curtin
University of Nottingham, University Park, Nottingham, NG7 2RD, UK
Lodewijk V Dekker, Stewart G Martin & Emad A Rakha
London School of Hygiene and Tropical Medicine, Keppel Street, London, WC1E 2HT, UK
Isabel dos Santos Silva
Queen Mary University of London, Mile End Road, London, E1 4NS, UK
Stephen W Duffy, Louise J Jones, John F Marshall & Sue M Moss
University of Glasgow, University Avenue, Glasgow, G12 8QQ, UK
Joanne Edwards
University of East Anglia, Earlham Road, Norwich, NR4 7TJ, UK
Dylan R Edwards & John M Saxton
University College Dublin, Belfield, Dublin 4, Ireland
William M Gallagher
The Institute of Cancer Research, 15 Cotswold Road, London, SM2 5MG, UK
Suzanne A Eccles, Montserrat Garcia-Closas, Martin O Leach, Lesley Ann Martin, Rachel Natrajan & Simon P Robinson
University of Cardiff, Park Place, Cardiff, CF10 3AT, UK
Julia M W Gee, Stephen Hiscox, Bharat Jasani & Matthew J Smalley
University of Leeds, Woodhouse Lane, Leeds, LS2 9JT, UK
Valerie Speirs & Galina Velikova
Royal College of Surgeons Ireland, 123, St Stephen’s Green, Dublin 2, Ireland
Bryan T Hennessy & Leonie S Young
University of Stirling, Stirling, FK9 4LA, UK
Gill Hubbard
University of Chester, Parkgate Road, Chester, CH1 4BJ, UK
Nick Hulbert-Williams
University of Oxford, Wellington Square, Oxford, OX1 2JD, UK
Timothy J Key & Anthony Kong
University of Edinburgh, South Bridge, Edinburgh, EH8 9YL, UK
Ian H Kunkler, Simon P Langdon & William R Miller
National Cancer Research Institute, 407 St John Street, London, EC1V 4AD, UK
Jennifer E Macdougall
Queen’s University Belfast, University Road, Belfast, BT7 1NN, UK
Paul Mullan
University College Cork, College Road, Cork, Ireland
Rosemary O’Connor
University of Leicester, University Road, Leicester, LE1 4RH, UK
Andy J Gescher & Rosemary A Walker
Princess Alice Hospice, West End Lane, Esher, KT10 8NA, UK
Elizabeth Reed
Brighton and Sussex Medical School, University of Sussex, Brighton, East Sussex, BN1 9PX, UK
Peter Schmid
The University of Liverpool, Brownlow Hill, Liverpool, L69 7ZX, UK
Carlo Palmieri
London Research Institute, 44 Lincoln’s Inn Fields, London, WC2A 3LY, UK
Brunel University, Kingston Lane, Uxbridge, UB8 3PH, UK
Amanda J Harvey
Cambridge University Hospitals NHS Foundation Trust, Hills Road, Cambridge, CB2 0QQ, UK
Charlotte E Coles
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Suzanne A Eccles or Alastair M Thompson .
Additional information
Competing interests.
Dr Galina Velikova: Chair of a working group of the National Cancer Survivorship Initiative led by Macmillan Cancer Support.
Drs Helen Bryant and Dr Nicola Curtin: hold patents for PARP inhibitors.
Professor William Gallagher: co-Founder and part-time Chief Scientific Officer of OncoMark, a molecular diagnostics company.
Dr Martin Leach: director of Specialty Scanners plc, developing MRI-based diagnosis and treatment systems.
Dr Sacha Howell: Advisory Board honoraria from AstraZeneca, Roche, Novartis, Genomic Health and Celgene.
Dr Robert Stein: shareholder in GlaxoSmithKline and chief investigator of the OPTIMA study; travel funds received from Celgene, Roche, BristolMeyersSquibb, SanofiAventis and Novartis; Advisory Board fees from Novartis, Amgen, GSK, Roche and AstraZeneca.
Dr Nigel Bundred has received paid honoraria from Genomic Health.
The remaining authors declare that they have no competing interests.
Authors’ contributions
*denotes recipient of Breast Cancer Campaign funding in the last five years. ≠ denotes current Breast Cancer Campaign Scientific Advisory Board membership. # denotes current Breast Cancer Campaign Board of Trustees membership. Chairs: SAE # and AMT # conceived the overall strategy, designed the workshop formats and authored the manuscript on the basis of the final reports submitted by the nine working groups. Group Leaders: RBC, IDSS, DGE* ≠ , CF ≠ ,WMG ≠ , AH ≠ , IH* ≠ , LJJ*, SPL, SPR ≠ , PS* ≠ , and VS* led their respective groups with the help of the Deputy Group Leaders, co-ordinated responses from a pre-circulated questionnaire, and wrote and submitted final reports. Deputy Group Leaders: EOA, NJB a , JMF* ≠ , JMWG*, AJH*, MH, AK, JRM*, PM* ≠ , ES, MJS* ≠ , ER, and RN* supported the activities of the Group Leaders in contributing to collating workshop presentations and discussions and producing the final reports from each group. Working group members: SA*, ASA , JA*, FB*, JPB*, KB* ≠ , NJB b , HEB ≠ , JMB, AMC*, JSC*, CEC*, GJRC*, AC, NJC, LVD* ≠ , SWD, DFE, DME, DRE*, JE, DFF*, MGC, AJG, VG, AMG, BTH, SH, SJH ≠ , GH, NHW, MSH, BJ, TJK, CCK, IHK*, MOL, DJM, JFM* ≠ , LAM, SGM ≠ , JEM, DWM, WRM, JRM, SMM*, JPBOC, ROC*, CP, PDPP*, EAR ≠ , JMS*, RS ≠ , JS, CHS, ANJT, GV, RAW*, CJW, KJW ≠ and LSY all participated in/contributed to the gap analysis workshops, discussions and in generating the respective reports. NJB a Nigel J Bundred. NJB b Nicola J Brown. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, authors’ original file for figure 4, authors’ original file for figure 5, authors’ original file for figure 6, authors’ original file for figure 7, authors’ original file for figure 8, authors’ original file for figure 9, rights and permissions.
Reprints and permissions
About this article
Cite this article.
Eccles, S.A., Aboagye, E.O., Ali, S. et al. Critical research gaps and translational priorities for the successful prevention and treatment of breast cancer. Breast Cancer Res 15 , R92 (2013). https://doi.org/10.1186/bcr3493
Download citation
Received : 08 August 2013
Accepted : 12 September 2013
Published : 01 October 2013
DOI : https://doi.org/10.1186/bcr3493
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breast Cancer
- Circulating Tumor Cells (CTCs)
- Current Cancer Stem Cell (CSC)
- Mammographic Density
- Triple-negative Breast Cancer (TNBC)
Breast Cancer Research
ISSN: 1465-542X
- Submission enquiries: [email protected]
Together we are beating cancer
About cancer
Cancer types
- Breast cancer
- Bowel cancer
- Lung cancer
- Prostate cancer
Cancers in general
- Clinical trials
Causes of cancer
Coping with cancer
- Managing symptoms and side effects
- Mental health and cancer
- Money and travel
- Death and dying
- Cancer Chat forum
Health Professionals
- Cancer Statistics
- Cancer Screening
- Learning and Support
- NICE suspected cancer referral guidelines
Get involved
- Make a donation
By cancer type
- Leave a legacy gift
- Donate in Memory
Find an event
- Race for Life
- Charity runs
- Charity walks
- Search events
- Relay For Life
- Volunteer in our shops
- Help at an event
- Help us raise money
- Campaign for us
Do your own fundraising
- Fundraising ideas
- Get a fundraising pack
- Return fundraising money
- Fundraise by cancer type
- Set up a Cancer Research UK Giving Page
- Find a shop or superstore
- Become a partner
- Cancer Research UK for Children & Young People
- Our We Are campaign
Our research
- Brain tumours
- Skin cancer
- All cancer types
By cancer topic
- New treatments
- Cancer biology
- Cancer drugs
- All cancer subjects
- All locations
By Researcher
- Professor Duncan Baird
- Professor Fran Balkwill
- Professor Andrew Biankin
- See all researchers
- Our achievements timeline
- Our research strategy
- Involving animals in research
Funding for researchers
Research opportunities
- For discovery researchers
- For clinical researchers
- For population researchers
- In drug discovery & development
- In early detection & diagnosis
- For students & postdocs
Our funding schemes
- Career Development Fellowship
- Discovery Programme Awards
- Clinical Trial Award
- Biology to Prevention Award
- View all schemes and deadlines
Applying for funding
- Start your application online
How to make a successful application
- Funding committees
Successful applicant case studies
How we deliver research
- Our research infrastructure
- Events and conferences
- Our research partnerships
- Facts & figures about our funding
- Develop your research career
Recently funded awards
- Manage your research grant
- Notify us of new publications
Find a shop
- Volunteer in a shop
- Donate goods to a shop
- Our superstores
Shop online
- Wedding favours
- Cancer Care
- Flower Shop
Our eBay store
- Shoes and boots
- Bags and purses
- We beat cancer
- We fundraise
- We develop policy
- Our global role
Our organisation
- Our strategy
- Our Trustees
- CEO and Executive Board
- How we spend your money
- Early careers
Cancer news
- Cancer News
- For Researchers
- For Supporters
- Press office
- Publications
- Update your contact preferences
ABOUT CANCER
GET INVOLVED
NEWS & RESOURCES
FUNDING & RESEARCH
You are here

We fund research that makes a clear link with our research priorities and look for the best researchers in their field.
Below is some simple advice from our research funding team that will help you make a great application. Each funding scheme has its own application guidelines so it's vital that you read these too before submitting an application. If you have any questions about these specific guidelines then you should get in touch with the person who manages that scheme. If you'd like to know more, you can also read advice from our current grantees .
What you will be judged on
- Relevance to our research priorities - read our Research Strategy and clearly state how your research relates to cancer research. Make sure you read the eligibility information for your chosen scheme.
- The originality of your ideas and proposal - make sure your research is answering an important and valid research question.
- Your knowledge of relevant literature and developments in your area.
- The quality of your experimental design – think about feasibility and identify what could go wrong. Show preliminary data if relevant.
- Value for money – your funding panel will want to know that the money we invest will be spent well. Make sure you leave enough time to budget accurately and that your costs are realistic. You should also justify all your costs.
- Your research team – make sure the people you choose have the right expertise. Check if there are other areas they can help with outside of the obvious scientific requirements of the project. For example, do they have a background in public policy that will help you share your findings?
- You – it’s important the funding panel trust their investment in you. Identify your unique strengths and draw on your previous successes.
Remember, it helps to know your audience. Find out who sits on the funding committee relevant to your scheme and what they’re interested in. They may even be a member of your current institution and you’ll be able to speak to them directly. Take a look at our funding committee pages.
Advice from our decision makers (funding committees)
1. show clearly how the application builds on existing knowledge.
Your research must be based on solid principles.
2. Spend time on the abstract
- Include all aspects of the study so the reviewers can immediately see everything you plan to do.
- Make sure it’s clear, concise, and thorough.
3. Make every step of the methods 100% clear
- Including the procedure, sample size, why you have chosen that sample and how you will collect and analyse the data.
- Make sure you clearly show how your objectives or research questions will be addressed.
4. Tell a coherent, easily understood story
- Why you are doing the study.
- What you plan to do.
- How you will go about this.
- When you plan to do it and timings.
- What the impact will be.
- Who your team are.
- How you will resource the work.
5. Remember that simple ideas appeal
If your plan includes too many studies with too many components the research questions can become lost.
6. Take time on the analysis section
Some grant applications fail through imprecise descriptions of analysis of the data. Make sure you demonstrate your understanding of data, whether it’s statistical or qualitative.
Filling in the online form
- Work with the grants/research office at your host institution – they can offer support and advice, particularly around costing your research proposal.
- Gather relevant additional information, such as ethical/regulatory approval, equipment quotes, letters of support, commercial interactions and other awards.
- Contact the grants helpline if you have questions about our online grants management system: [email protected] .
Contact the grants team
Find funding
Find a funding opportunity that suits your career and research area.
Search all funding
Find out how our current grantees successfully applied for funding.
Recently funded awards by Cancer Research UK
Find out more
Help elsewhere
NIHR Research Design Service
Health and Care Research Wales: Research Design and Conduct Service
MRC Guidance for complex interventions
Call for proposals
Applicants for funding from Against Breast Cancer (ABC) should familiarise themselves with the funding process before applying . Calls for Proposals will be issued by Against Breast Cancer (ABC) and researchers are invited to apply before the advertised deadline date using the template forms provided.
Against Breast Cancer Seed Grants are intended for innovative research projects that have the potential to impact the way metastatic breast cancer is diagnosed, treated or even prevented.
Seed grants are for up to £50,000 and designed for a maximum term of 1 year and can be used for the following purposes
- preliminary data to be gathered to support a larger grant application
- for a stand-alone project to achieve a stated goal
- to enhance an existing funded project if it can be shown that such funding would add significant value and advance the research
Researchers considering submitting an application are required to hold a doctoral degree and be working in a UK based institution.
All proposals should be in line with our Research Strategy and lead applicants will have a strong publishing record. Collaborative applications involving researchers or institutions from anywhere in the world are invited, as long as the lead applicant’s host institution is in the UK and the majority of the research takes place in the UK. If collaborators are included in the proposal, they will be required to provide a letter of support for the project as part of the application.
Apply for funding here and read the Terms and Conditions of funding (PDF, 240 KB)
If you have any questions, please contact Dr. Bryony Gray, Research Manager, on 01235 534211 or email [email protected]
Closing date: We have no current call for proposals .
Something isn't right with my breast...
Take part in a research study
Share this page
- Share full article

Should Alcoholic Beverages Have Cancer Warning Labels?
Ireland will require them starting in 2026, and there are nascent efforts elsewhere to add more explicit labeling about the health risks of drinking.
An example of a label that will be added in 2026 to all beer, wine and liquor sold in Ireland, emphasizing ties between alcohol use and liver disease or cancer. Credit... Alcohol Action Ireland
Supported by
By Ted Alcorn
- Published April 9, 2024 Updated April 11, 2024
Fifteen words are roiling the global alcohol industry.
Beginning in 2026, containers of beer, wine and liquor sold in Ireland will be required by law to bear a label in red capital letters with two warnings: “THERE IS A DIRECT LINK BETWEEN ALCOHOL AND FATAL CANCERS” and “DRINKING ALCOHOL CAUSES LIVER DISEASE.”
The requirement, signed into law last year, is backed by decades of scientific research and goes much further than any country has thus far communicated the health risks of alcohol consumption. It has sparked fierce opposition from alcohol businesses worldwide, but it is also inspiring a push in some other countries to pursue similar measures.
“It’s an important step,” said Dr. Timothy Naimi, the director of the Canadian Institute for Substance Use Research at the University of Victoria. “People who drink should have the right to know basic information about alcohol, just as they do for other food and beverage products.”
In Thailand, the government is in the final stages of drafting a regulation requiring alcohol products to carry graphic images accompanied by text warnings such as “alcoholic beverages can cause cancer,” according to The Bangkok Post .
A bill has been introduced in the Canadian Parliament that would require labels on all alcoholic beverages to communicate a “direct causal link between alcohol consumption and the development of fatal cancers.”
Last week, the Alaska State Legislature held a committee hearing on a bill that would require businesses selling alcohol to post signs carrying a cancer warning.
Norway, which already heavily regulates the sale of alcohol, is developing proposals for introducing cancer warning labels. The country’s state secretary, Ole Henrik Krat Bjorkholt, who followed Ireland’s effort with great interest, said in an interview, “I think it’s probable that we will implement something similar.”
Ireland has been a trailblazer in setting aggressive public health policies before. In 2004, it became the first country to ban smoking in indoor workplaces, including bars and restaurants, a policy since adopted in over 70 countries. The warning label requirement for alcohol could be the start of a similar change in how beverages are packaged, and a vehicle for raising awareness about the dangers of drinking, however small the amount.
A long fight
The evidence linking drinking and cancer is well established. In 1988, the World Health Organization’s International Agency for Research on Cancer concluded that alcohol is carcinogenic to humans. Research in the decades since has only strengthened the conclusion, including for breast, liver, colorectal and esophageal cancers. In November, the W.H.O. and the I.A.R.C. declared in a joint statement : “No safe amount of alcohol consumption for cancers can be established.”
Despite this, the connection between alcohol and cancer isn’t well known. In the United States, a recent nationwide survey found that about one in three Americans was aware that drinking increased the risk of cancer.
Globally, only a quarter of countries require any kind of health warning on alcohol, according to a recent study , and the mandated language is generally imprecise. The United States last altered its warning labels in 1989 , when it introduced language that discouraged drinking during pregnancy, or before driving or operating heavy machinery, and that vaguely acknowledged that alcohol “may cause health problems.”

It took over a decade for Ireland’s labeling requirement to become a reality, according to Sheila Gilheany, chief executive of the advocacy organization Alcohol Action Ireland, who described it as “the most contested piece of legislation in Irish history.” She said that the effort began in 2012, when a steering group assigned to address the country’s high rate of alcohol-related deaths recommended a raft of measures, including warning labels.
Many of the recommendations were watered down by the time they became law in 2018, but the labeling requirement made it through unscathed. It took another four years for lawmakers to hammer out the specific wording and the design that would be required.
As those details were decided, alcohol companies stepped up their protests. In late 2022, a group of major alcohol-exporting European countries submitted formal objections to the European Commission, the European Union’s executive branch, arguing that Ireland’s labels impeded free trade and were not appropriate or proportionate to the objective of reducing alcohol’s harms.
When the commission raised no objection, Antonio Tajani, Italy’s foreign minister, called the Irish proposal “an attack on the Mediterranean diet.” The language in the labels “doesn’t take into account the difference between moderate consumption and alcohol abuse,” he said on Twitter .
Coordinated industry opposition
Alcohol businesses are fighting on multiple fronts to keep the Irish labeling requirement from taking effect. At committee meetings of the World Trade Organization in June and November, trade groups and eleven alcohol-exporting countries, including the United States, expressed concerns, questioned the scientific validity of the cancer warning and argued that Ireland’s labels would infringe on free trade.
In comments submitted to the World Trade Organization, the Distilled Spirits Council of the United States called the labels “inaccurate” and “misleading.” The group also suggested that “this important public health objective would be best managed” as part of a parallel effort to address cancer in the European Union, an area where the alcohol industry has proved to have greater influence.
The European Commission was supposed to propose language for alcohol health warnings as part of the its Beating Cancer Plan by the end of 2023 but failed to meet that deadline. In December, over the objections of the World Health Organization , the European Parliament approved a report that did not affirm the need for warning labels, instead calling for information on “moderate and responsible drinking.”
In the final report, its authors repeatedly watered down language about alcohol’s role in disease, narrowly warning only about “harmful” or “excess” consumption.
Size and design
Cormac Healy, the director of Drinks Ireland, a trade group, said that his organization wasn’t entirely utterly opposed to health warnings. But he said that the mandated size of the labels would be impractical for use on smaller products, picking a 50-milliliter bottle up from his desk to demonstrate. And the warning language itself was “disproportionate and inaccurate,” he said, and primarily geared toward scaring people.
“To inform, to educate — you can’t really do that on a label,” he added.
In the United States, alcohol warning labels are typically on the back of the bottle or can, where they blend in with other graphic features. Dr. Marissa Hall, an assistant professor in the department of health behavior at the University of North Carolina at Chapel Hill, said that the labels would be more effective at catching a purchaser’s eye if they were on the front, included an image or icon, and featured one of a rotating group of brief messages.
Dr. Hall recently received a grant from the National Institutes of Health to test the impact of stronger design features. When she tells friends about her research, many are surprised to learn the United States requires warning labels at all, she said, because the existing ones so easily go unnoticed.
“They have no idea,” she said.
In the last 15 years, a few countries have proposed stronger alcohol warning labels, but each has been met with fierce opposition, said Paula O’Brien, a professor of law at the University of Melbourne. In 2010, Thailand proposed requiring a rotating group of warnings accompanied by graphic color imagery; O’Brien called it “the high-water mark for alcohol labeling.” But at the World Trade Organization, other countries raised concerns that the labels would restrain free trade, and the measure stalled.
In 2016, South Korea overcame similar objections to mandate a group of warning labels, some of which link alcohol with cancer, that alcohol makers can choose from to put on their products.
Even research on the topic has been contentious. In 2017, Yukon, a sparsely populated territory in northwest Canada, forged a partnership with scientists to introduce and test the impact of brightly colored warning labels, one of which included the phrase “alcohol can cause cancer.” But after alcohol trade groups complained, the local government paused the study out of fear it would face a lawsuit that it could not afford to fight.
“I was a bit surprised about the strength of the reaction,” said Dr. Erin Hobin, a scientist at Public Health Ontario who led the project in Yukon.
When the researchers resumed the study several months later, on the condition that the cancer warning be omitted, they found that people buying alcoholic beverages featuring the labels were still more likely to notice the messages, and reported reducing their drinking. Sales of products carrying the labels also fell by around 7 percent during the intervention and several months that followed.
Most importantly, Dr. Hobin said, as drinkers grew more informed about the link between alcohol and cancer, they also became more likely to support policies for controlling alcohol availability, pricing and marketing, which have been shown to reduce drinking even more.
If the alcohol industry dissuaded the European Union from adopting warning labels, it would keep Ireland isolated and out of harmony with European law. That could ultimately form a basis for challenging the labeling requirement in Irish courts, said Dr. Ollie Bartlett, an assistant professor of law at Maynooth University in Ireland. But he said that such efforts were unlikely to prevail because Ireland’s alcohol warning labels are “proportionate to the objective of protecting public health.”
Observers say the European Union isn’t likely to take any further action until after parliamentary elections this summer. And there’s no indication that Ireland will retreat from its commitment to require the labels starting in May 2026.
Dr. Gauden Galea, a strategic adviser at the World Health Organization, said he was confident that broader labeling efforts would eventually succeed. At 63, he’s old enough to recall how cigarette companies once advertises on the front pages of newspapers, he added.
Eventually, he hopes, “People will not remember the time when you needed a warning on pesticides, but could sell an unlabeled carcinogen like alcohol with impunity.”
The Fight Against Cancer
Colon and rectal cancers are increasing among people younger than 50. Experts have a few ideas about why .
Should alcoholic beverages have cancer warning labels? Ireland will require them starting in 2026, and there are nascent efforts elsewhere .
Risk calculators can offer a more personalized picture of an individual patient’s breast cancer risk. But experts warn that the results need to be interpreted with the help of a doctor .
The human papillomavirus vaccine provides powerful protection against the leading cause of cervical cancer and against a strong risk factor for anal cancer. Here’s what to know about the shot .
A recent study adds to growing evidence that exercise is an important part of preventing prostate cancer , the second most common and second most fatal cancer in the United States for men.
No single food can prevent cancer on its own, but experts say that there are some that may help you build the best defense .
Advertisement

IMAGES
VIDEO
COMMENTS
prevalent cases of cancer and about 35,000 new cases are added to this every year. Based on the. (18.5%) it ranks second to cervical cancer. The burden of breast cancer is increasing in both. rate ...
More than half a million of the world's women died from breast cancer in 2012, making it one of the leading (BC) causes of cancer-related deaths in women across the world (Ferlay et al., 2015). The phosphatidylinositol 3-kinase (PI3K)/Akt pathway represents a complex signalling network that integrates numerous upstream stimuli to
insight into prevention, detection, diagnosis or treatment of breast cancer. • How the outcomes from the proposed research plan will advance our knowledge of breast cancer in an important way and/or contribute to the way that we conduct breast cancer research. 3. Project Description (Narrative):
We are committed to supporting young investigators in breast cancer research and encourage applications from talented new postdoctoral researchers. 2. Eligibility ... research proposal for a different award (for example, a rejected fellowship resubmitted as a project grant), you must include a covering letter acknowledging the rejected grant ...
This is a one year grant for a total of $100,000. The term of the Exceptional Project Grant is one year, beginning on March 1, 2025. Prior to submission of a formal grant proposal, BCA requires a Letter of Intent (LOI) and a separate CV that must be completed using the form linked here and must be submitted by midnight on March 31, 2024.
Title of Project. Grant Mechanism & Award Number. Elizabeth Kantor, PhD, MPH, Memorial Sloan Kettering Cancer Center. Obesity, Chemotherapy Dosing, and Breast Cancer Outcomes. View Abstract. R37 CA222793-04. View Grant Application. [PDF - 1.48 MB] Anna Prizment, PhD, University of Minnesota.
Research Proposal PDF Available. ... Breast cancer is the most common diagnosed malignancy in women worldwide (22%) and in India (18.5%) it ranks second to cervical cancer. ... for example, to.
Sample Research Proposal for the Department of Psychology Chair's Minority/Underrepresented Research Grant The Roles of Body Image and Self-Esteem in Breast Cancer Treatment Decisions Project Overview Breast cancer is the second most commonly diagnosed cancer among women, and has the second ...
1) utilize existing and develop new national and state-level partnerships to carry out dissemination research, 2) recruit practitioners into our studies with high response rates, 3) train practitioners on use of EBPPs, and 4) conduct large-scale dissemina- tion research. C.3. Expertise of research team members .
Eye-Opening Breast Cancer Statistics on Racial Disparities. 0.5%. average increase in breast cancer incidence rates each year since the. mid-2000s. 200%. increased likelihood Black women have of developing triple-negative breast cancer. 41%. increase in the breast cancer death rate for Black women compared with White women.
We also only include a copy of the SF 424 R&R Face Page, Project Summary/Abstract (Description), Project Narrative, Specific Aims, and Research Strategy. We do not include other SF 424 (R&R) forms or basic information found in full grant applications, such as performance sites, key personnel, or biographical sketches.
Breast Cancer Now is the UK's largest dedicated breast cancer research funder. To date, we have invested over £250 million in ground-breaking research. We also provide life-changing care and support services for people affected by breast cancer, and we campaign to make sure that everyone affected by breast cancer
The Breast Cancer Now Catalyst Programme promotes innovation and excellence in breast cancer research, through collaboration in the UK and across Europe. Right now, we're funding over 80 cutting-edge projects worth just over £29 million to discover how we can prevent breast cancer, save lives, and help people to live well with and beyond the ...
RESEARCH PROPOSAL Hypothesis: Cancer associated fibroblasts cause drug resistance in mutant KRAS-driven colon and lung cancers by altering signal transduction in cancer cells. Establishing an assay to determine drug resistance associated with co-culture of cancer cells with cancer- associated fibroblasts ...
NCI is funding a large-scale randomized breast screening trial, the Tomosynthesis Mammographic Imaging Screening Trial (TMIST), to compare the number of advanced cancers detected in women screened for 5 years with 3-D mammography with the number detected in women screened with 2-D mammography. Two concerns in breast cancer screening, as in all ...
Who Can Apply: Awarded to institutions as block grants to provide seed money for newly independent investigators to initiate cancer research projects. The principal investigator of the grant should be a senior faculty member. Funding: 1 to 3 years with an average of $120K a year, renewable. Deadline: April 1*.
R03 Small Research Grant. Small Research Grants (R03s) provide research support specifically limited in time and amount for studies in categorical program areas. Small research grants provide flexibility for initiating studies that are generally for preliminary short-term projects. These grants are non-renewable.
Funding. The National Cancer Institute (NCI) frequently receives requests for examples of funded grant applications. Several investigators and their organizations agreed to let the Healthcare Delivery Research Program (HDRP) post excerpts of their healthcare delivery research grant applications online. We are grateful to the investigators and ...
BRP provides funding support for a comprehensive program of research, ranging from basic behavioral research to the development, testing, and dissemination of interventions in areas including, but not limited to, tobacco use, screening, dietary behavior, sun protection, emotion regulation, and physical activity.
Breast cancer remains a significant scientific, clinical and societal challenge. This gap analysis has reviewed and critically assessed enduring issues and new challenges emerging from recent research, and proposes strategies for translating solutions into practice. More than 100 internationally recognised specialist breast cancer scientists, clinicians and healthcare professionals ...
Including the procedure, sample size, why you have chosen that sample and how you will collect and analyse the data. Make sure you clearly show how your objectives or research questions will be addressed. 4. Tell a coherent, easily understood story. Why you are doing the study. What you plan to do. How you will go about this.
Calls for Proposals will be issued by Against Breast Cancer (ABC) and researchers are invited to apply before the advertised deadline date using the template forms provided. Against Breast Cancer Seed Grants are intended for innovative research projects that have the potential to impact the way metastatic breast cancer is diagnosed, treated or ...
•This is the proposal for our new insight and involvement community •Breast Cancer Voices and Insight & Experience Panel will be replaced by a single, but multi-layered, community •The community exists: •to serve the organisation in helping to shape its work through the views and perspectives of those affected by breast cancer
Norway, which already heavily regulates the sale of alcohol, is developing proposals for introducing cancer warning labels. The country's state secretary, Ole Henrik Krat Bjorkholt, who followed ...