Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.

Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What's a sunny-side up baby?

What happens to your baby right after birth

How your twins’ fetal positions affect labor and delivery

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

Where to go next

Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Why would posterior position matter in labor? The head is angled so that it measures larger. The top of the head molds less than the crown.
Baby’s spine is extended, not curled, so the crown of the head is not leading the way. Baby can’t help as much during the birth process to the same degree as the curled up baby.
Some posteriors are easy, while others are long and painful, and there are several ways to tell how your labor will be beforehand. After this, you may want to visit What to do when….in Labor .
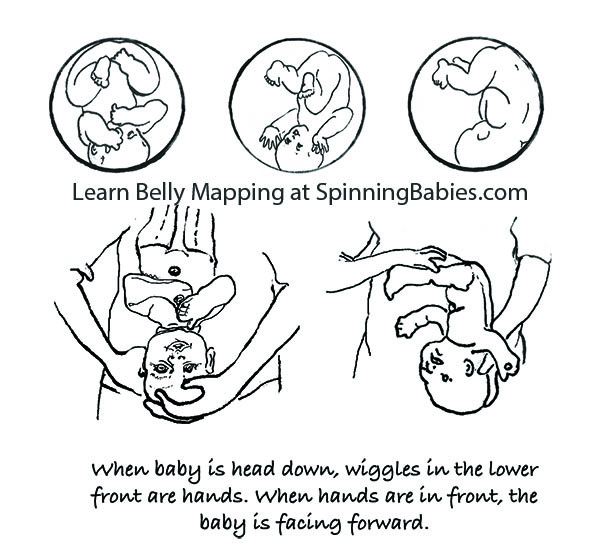
Belly Mapping ® Method tips: The Right side of the abdomen is almost always firmer, but the direct OP baby may not favor one side or the other. Baby’s limbs are felt in front, on both sides of the center line. A knee may slide past under the navel.

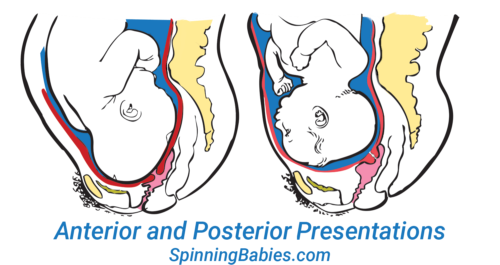
The OP position (occiput posterior fetal position) is when the back of the baby’s head is against the mother’s back. Here are drawings of an anterior and posterior presentation.
- When is Breech an Issue?
- Belly Mapping® Breech
- Flip a Breech
- When Baby Flips Head Down
- Breech & Bicornuate Uterus
- Breech for Providers
- What if My Breech Baby Doesn't Turn?
- Belly Mapping ®️ Method
- After Baby Turns
- Head Down is Not Enough
- Sideways/Transverse
- Asynclitism
- Oblique Lie
- Left Occiput Transverse
- Right Occiput Anterior
- Right Occiput Posterior
- Right Occiput Transverse
- Face Presentation
- Left Occiput Anterior
- OP Truths & Myths
- Anterior Placenta
- Body Balancing

Look at the above drawing. The posterior baby’s back is often extended straight or arched along the mother’s spine. Having the baby’s back extended often pushes the baby’s chin up.
Attention: Having the chin up is what makes the posterior baby’s head seem larger than the same baby when it’s in the anterior position.
Because the top of the head enters (or tries to enter) the pelvis first, baby seems much bigger by the mother’s measurements. A posterior head circumference measures larger than the anterior head circumference.
A large baby is not the same issue, however. The challenge with a posterior labor is that the top of the head, not the crown of the head leads the way.
A baby with their spine straight has less ability to wiggle and so the person giving birth has to do the work of two. This can be long and challenging or fast and furious. Also, there are a few posterior labors that are not perceived different than a labor with a baby curled on the left.
Why? Anatomy makes the difference. Learn to work with birth anatomy to reduce the challenge of posterior labor by preparing with our Three Balances SM and more.
What to do?
- Three Balances SM
- Dip the Hip
- Psoas Release
- Almost everything on this website except Breech Tilt
In Labor, do the above and add,
- Abdominal Lift and Tuck
- Other positions to Open the Brim
- Open the Outlet during pushing
There are four posterior positions
The direct OP is the classic posterior position with the baby facing straight forward. Right Occiput Transverse (ROT) is a common starting position in which the baby has a bit more likelihood of rotating to the posterior during labor than to the anterior. Right Occiput Posterior usually involves a straight back with a lifted chin (in the first-time mother). Left Occiput Posterior places the baby’s back opposite the maternal liver and may let the baby flex (curl) his or her back and therefore tuck the chin for a better birth. These are generalities, of course. See a bit more about posterior positions in Belly Mapping ® on this website. Want to map your baby’s position? Learn how with the Belly Mapping ® Workbook .
Pregnancy may or may not show symptoms. Just because a woman’s back doesn’t hurt in pregnancy doesn’t mean the baby is not posterior. Just because a woman is quite comfortable in pregnancy doesn’t mean the baby is not posterior. A woman can’t always feel the baby’s limbs moving in front to tell if the baby is facing the front.
The four posterior fetal positions
Four starting positions often lead to (or remain as) direct OP in active labor. Right Occiput Transverse (ROT), Right Occiput Posterior (ROP), and Left Occiput Posterior (LOP) join direct OP in adding labor time. The LOP baby has less distance to travel to get into an LOT position.
As labor begins, the high-riding, unengaged Right Occiput Transverse baby slowly rotates to ROA , working past the sacral promontory at the base of the spine before swinging around to LOT to engage in the pelvis. Most babies go on to OA at the pelvic floor or further down on the perineal floor.
If a baby engages as a ROT, they may go to OP or ROA by the time they descend to the midpelvis. The OP baby may stay OP. For some, once the head is lower than the bones and the head is visible at the perineum, the baby rotates and helpers may see the baby’s head turn then! These babies finish in the ROA or OA positions.
Feeling both hands in front, in two separate but low places on the abdomen, indicates a posterior fetal position. This baby is Left Occiput Posterior.
Studies estimate 15-30% of babies are OP in labor. Jean Sutton in Optimal Fetal Positioning states that 50% of babies trend toward posterior in early labor upon admission to the hospital. Strong latent labor swings about a third of these to LOT before dilation begins (in “pre-labor” or “false labor”).
Recent research shows about 50% of babies are in a posterior position when active labor begins, but of these, 3/4 of them rotate to anterior (or facing a hip in an occiput transverse, head down position.
Jean Sutton’s observations, reported in her 1996 book, indicates that some babies starting in a posterior position will rotate before arriving to the hospital. Ellice Lieberman observed most posteriors will rotate out of posterior into either anterior or to facing a hip throughout labor. Only 5-8% of all babies emerge directly OP (13% with an epidural in Lieberman’s study). At least 12% of all cesareans are for OP babies that are stuck due to the larger diameter of the OP head in comparison to the OA head. It’s more common for ROT, ROP, and OP babies to rotate during labor and to emerge facing back (OA). Some babies become stuck halfway through a long-arc rotation and some will need a cesarean anyway.
The three anterior starting positions for labor

Why not ROA? ROA babies may have their chins up and this deflexed position may lengthen the course of labor. Less than 4% of starting positions are ROA, according to a Birmingham study. This might not be ideal for first babies, but is not a posterior position either.
The spectrum of ease across posterior labors

Purchase Parent Class
Baby’s posterior position may matter in labor
With a posterior presentation, labor may or may not be significantly affected. There is a spectrum of possibilities with a posterior baby. Some women will not know they had a posterior baby because no one mentions it. Either the providers didn’t know, or didn’t notice. If labor moved along, they may not have looked at fetal position clues since there was no reason to figure out why labor wasn’t progressing. If a woman didn’t have back labor (more pain in her back than in her abdomen), the provider may not have been “clued into” baby’s position.
Some posterior babies are born in less than 8 hours and position did not slow down labor. Some posterior babies are born in less than 24 hours and position did not slow down labor enough to be out of the norm. Some posterior babies are born in less than 36-48 hours without the need for interventions.
Some posterior labors are manageable when women are mobile, supported, and eat and drink freely, as needed. Some posterior labor needs extra support that a well-trained and experienced doula may provide, but that typically a mate or loved one would not have the skills or stamina to keep up with. Some posterior labors progress only with the help of a highly-trained pregnancy bodyworker or deep spiritual, or otherwise a non-conventional model of care. Or, they seem only able to finish with medical intervention.
Some posterior labors are served by an epidural, meaning the pelvic floor relaxes enough for the baby to rotate and come out. Some epidurals, on the other hand, make it so that a woman can not finish the birth vaginally.
NOTE: Parents should know — some birth researchers, like Pediatrician John Kennell, are seriously asking whether a mother’s epidural turns off her body’s release of pain-relieving hormones which a baby relies on during childbirth. Some babies can’t turn and can’t be born vaginally and must be born by cesarean. This is a spectrum of possibilities. I’ve seen every one of the above possibilities several times and can add the wonderful experience of seeing a woman laughing pleasurably and squatting while her posterior baby slid out on to her bedroom floor.
Possible posterior effects, some women will have one or two and some will have many of these:

The forehead that overlaps the pubic bone after labor starts must turn and drop into the pelvis to allow the birth to happen naturally. A cesarean finish of the labor is possible. Look at Abdominal Lift and Tuck in Techniques to guide you to solutions for easier engagement and progress.
- Longer pregnancy (some research shows this and some doesn’t)
- The amniotic sac breaking (water breaks, membranes open, rupture of membranes) before labor (1 in 5 OP labors)
- Not starting in time before induction is scheduled
- Labor is longer and stronger and less rhythmic than expected
- Start and stop labor pattern
- The baby may not engage, even during the pushing stage
- Longer early labor
- Longer active labor
- Back labor (in some cases)
- Pitocin may be used when labor stalls (but a snoring good rest followed by oatmeal may restore a contraction pattern, too)
- Longer pushing stage
- Maybe a woman has all three phases of labor lengthened by the OP labor or one or two of the three phases listed
- Sometimes the baby’s head gets stuck turned halfway to anterior – in the transverse diameter. This may be called a transverse arrest (not a transverse lie ).
- More likely to tear
- More likely to need a vacuum (ventouse) or forceps
- More likely to need a cesarean
These effects are in comparison to a baby in the left occiput anterior or left occiput transverse fetal position at the start of labor.
Who might have a hard time with a posterior baby?
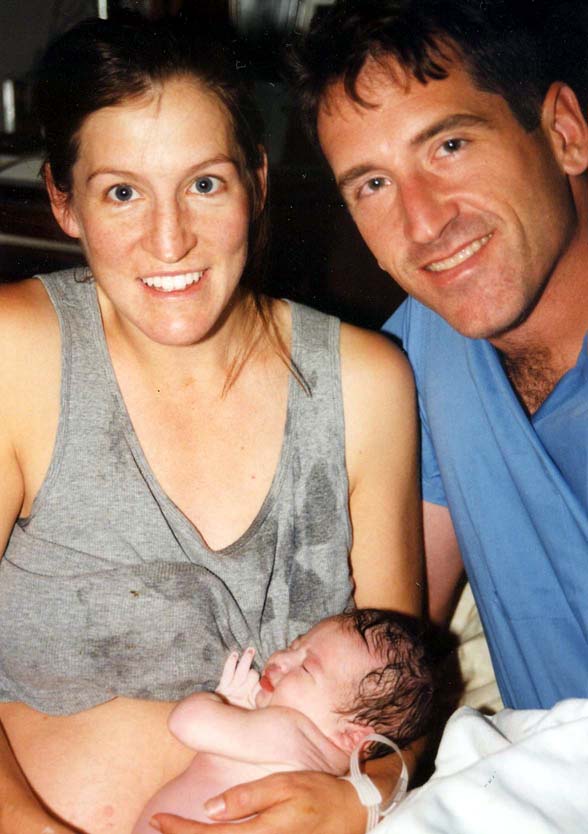
This family just had a fast posterior birth of their second child! Ease in labor includes other factors beyond baby position.
- A first-time mom
- A first-time mom whose baby hasn’t dropped into the pelvis by 38 weeks gestation (two weeks before the due date)
- A woman with an android pelvis (“runs like a boy,” often long and lanky, low pubis with narrow pubic arch and/or sitz bones close together, closer than or equal to the width of a fist)
- A woman whose baby, in the third trimester, doesn’t seem to change position at all, over the weeks. He or she kicks in the womb and stretches, but whose trunk is stationary for weeks. This mother’s broad ligament may be so tight that she may be uncomfortable when baby moves.
- A woman who has an epidural early in labor (data supports this), before the baby has a chance to rotate and come down.
- A woman who labors lying in bed
- Low-thyroid, low-energy woman who has gone overdue (this is my observation)
- A woman who lacks support by a calm and assured woman who is calming and reassuring to the birthing mother (a doula)
- A woman put on the clock
- A woman who refuses all help when the labor exceeds her ability to physically sustain her self (spilling ketones, dehydration, unable to eat or rest in a labor over X amount of hours which might be 24 for some or 48 for others)
- A woman whose birth team can’t match an appropriate technique to the needs of the baby for flexion, rotation, and/or descent from the level of the pelvis where the baby is currently at when stuck
Who is likely to have an easy time with a posterior baby?
- A second-time mom who’s given birth readily before (and pushing went well)
- A posterior baby with a tucked chin on his or her mama’s left side with a round pelvic brim
- An average-sized or smaller baby
- Someone whose posterior baby changes from right to left after doing inversions and other balancing work , though the baby is still posterior
- A woman with a baby in the Left Occiput Posterior, especially if the baby’s chin is tucked or flexed
- A woman who gets bodywork, myofascial release, etc.
- A woman whose posterior baby engages, and does not have an android (triangular) pelvis or a small outlet
- And of all of these, what is necessary is a pelvis big enough to accommodate the baby’s extra head size
- A woman who uses active birthing techniques — vertical positions, moves spontaneously and instinctively or with specific techniques from Spinning Babies ® , and other good advice
- A woman in a balanced nervous state, not so alert and “pumped up,” on guard, etc.
Any woman may also have an easier time than public opinion might indicate, too, just because she isn’t on this list. Equally, just because she is on the “hard” list doesn’t mean she will have a hard time for sure. These are general observations. They are neither condemnations nor promises. Overall, some posterior babies will need help getting born, while some posterior babies are born easily (easy being a relative term).
Let’s not be ideological about posterior labors.
While most posterior babies do eventually rotate, that can still mean there is quite a long wait – and a lot of physical labor during that wait. Sometimes it means the doula, midwife, nurse, or doctor is asking the mother to do a variety of position changes, techniques, and even medical interventions to help finish the labor. Patience works for many, but for some a cesarean is really the only way to be born. Read What To Do When…in Labor .
What causes a baby to be posterior?
There is a rising incidence of posterior babies at the time of birth. We know now that epidural anesthesia increases the rate of posterior position at the time of birth from about 4% (for women who don’t choose an epidural in a university birth setting) up to about 13% (Lieberman, 2005). Low thyroid function is associated with fetal malposition such as posterior or breech. (See Research & References .)
Most babies who are posterior early in labor will rotate to anterior once labor gets going. Some babies rotate late in labor, even just before emerging. Studies such as Lieberman’s show that at any given phase of labor, another 20% of posterior babies will rotate so that only a small number are still posterior as the head emerges.
My observations are that the majority of babies are posterior before labor. The high numbers of posterior babies at the end of pregnancy and in the early phase of labor is a change from what was seen in studies over ten years old. Perhaps this is from our cultural habits of sitting at desks, sitting in bucket seats (cars), and leaning back on the couch (slouching). Soft tissues such as the psoas muscle pair or the broad ligament also seem to be tight more often from these postures, from athletics (quick stops, jolts, and falls), from accidents, and from emotional or sexual assault.
Being a nurse or bodyworker who turns to care for people in a bed or on a table will also twist the lower uterine segment (along with some of the previously mentioned causes). This makes the baby have to compensate in a womb that is no longer symmetrical. Less often, the growing baby settles face-forward over a smaller pelvis, or a triangular-shaped pelvis (android). At the end of pregnancy, the baby’s forehead has settled onto a narrower than usual pubic bone, and if tight round ligaments hold the forehead there, the baby may have a tough time rotating. These are the moms and babies that I’m most concerned with in my work at Spinning Babies®. A baby that was breech beyond week 30 – 34 of pregnancy will flip head down in the posterior position. A woman with a history of breech or posterior babies is more likely to have a breech or posterior baby in the next pregnancy. However, she may not have an as long labor.
The best way to tell if your baby is OP or not, usually, is if you feel little wiggles in the abdomen right above your pubic bone. These are the fingers. They’d feel like little fingers wiggling, not like a big thunk or grinding from the head, though you might feel that, too. The little fingers will be playing by the mouth. This is the easiest indication of OP. The wiggles will be centered in the middle of your lower abdomen, close to the pubic bone. If you feel wiggles far to the right, near your hip, and kicks above on the right, but not near the center and none on the left, then those signal an OA or LOT baby (who will rotate to the OA easily in an active birth). After this, you might go to What to do when…in Labor.
Check out our current references in the Research & References section.

Pin It on Pinterest
- Trying to Conceive
- Signs & Symptoms
- Pregnancy Tests
- Fertility Testing
- Fertility Treatment
- Weeks & Trimesters
- Staying Healthy
- Preparing for Baby
- Complications & Concerns
- Pregnancy Loss
- Breastfeeding
- School-Aged Kids
- Raising Kids
- Personal Stories
- Everyday Wellness
- Safety & First Aid
- Immunizations
- Food & Nutrition
- Active Play
- Pregnancy Products
- Nursery & Sleep Products
- Nursing & Feeding Products
- Clothing & Accessories
- Toys & Gifts
- Ovulation Calculator
- Pregnancy Due Date Calculator
- How to Talk About Postpartum Depression
- Editorial Process
- Meet Our Review Board
Fetal Positions for Labor and Birth
Knowing your baby's position can you help ease pain and speed up labor
In the last weeks of pregnancy , determining your baby's position can help you manage pain and discomfort. Knowing your baby's position during early labor can help you adjust your own position during labor and possibly even speed up the process.
Right or Left Occiput Anterior
Illustration by JR Bee, Verywell
Looking at where the baby's head is in the birth canal helps determine the fetal position.The front of a baby's head is referred to as the anterior portion and the back is the posterior portion. There are two different positions called occiput anterior (OA) positions that may occur.
The left occiput anterior (LOA) position is the most common in labor. In this position, the baby's head is slightly off-center in the pelvis with the back of the head toward the mother's left thigh.
The right occiput anterior (ROA) presentation is also common in labor. In this position, the back of the baby is slightly off-center in the pelvis with the back of the head toward the mother's right thigh.
In general, OA positions do not lead to problems or additional pain during labor or birth.
Right or Left Occiput Transverse
Illustration by JR Bee, Verywell
When facing out toward the mother's right thigh, the baby is said to be left occiput transverse (LOT). This position is halfway between a posterior and anterior position. If the baby was previously in a posterior position (in either direction), the LOT position indicates positive movement toward an anterior position.
When the baby is facing outward toward the mother's left thigh, the baby is said to be right occiput transverse (ROT). Like the previous presentation, ROT is halfway between a posterior and anterior position. If the baby was previously in a posterior position, ROT is a sign the baby is making a positive move toward an anterior position.
When a baby is in the left occiput transverse position (LOT) or right occiput transverse (ROT) position during labor, it may lead to more pain and a slower progression.
Tips to Reduce Discomfort
There are several labor positions a mother can try to alleviate pain and encourage the baby to continue rotating toward an anterior position, including:
- Pelvic tilts
- Standing and swaying
A doula , labor nurse, midwife , or doctor may have other suggestions for positions.
Right or Left Occiput Posterior
When facing forward, the baby is in the occiput posterior position. If the baby is facing forward and slightly to the left (looking toward the mother's right thigh) it is in the left occiput posterior (LOP) position. This presentation can lead to more back pain (sometimes referred to as " back labor ") and slow progression of labor.
In the right occiput posterior position (ROP), the baby is facing forward and slightly to the right (looking toward the mother's left thigh). This presentation may slow labor and cause more pain.
To help prevent or decrease pain during labor and encourage the baby to move into a better position for delivery, mothers can try a variety of positions, including:
- Hands and knees
- Pelvic rocking
Mothers may try other comfort measures, including:
- Bathtub or shower (water)
- Counter pressure
- Movement (swaying, dancing, sitting on a birth ball )
- Rice socks (heat packs)
How a Doctor Determines Baby's Position
Leopold's maneuvers are a series of hands-on examinations your doctor or midwife will use to help determine your baby's position. During the third trimester , the assessment will be done at most of your prenatal visits. Knowing the baby's position before labor begins can help you prepare for labor and delivery.
Once labor begins, a nurse, doctor, or midwife will be able to get a more accurate sense of your baby's position by performing a vaginal exam. When your cervix is dilated enough, the practitioner will insert their fingers into the vagina and feel for the suture lines of the baby's skull as it moves down in the birth canal. It's important to ensure the baby is head down and moving in the right direction.
Labor and delivery may be more complicated if the baby is not in a head-down position, such as in the case of a breech presentation.
How You Can Determine Baby's Position
While exams by health practitioners are an important part of your care, from the prenatal period through labor and delivery, often the best person to assess a baby's position in the pelvis is you. Mothers should pay close attention to how the baby moves and where different movements are felt.
A technique called belly mapping can help mothers ask questions of themselves to assess their baby's movement and get a sense of the position they are in as labor approaches.
For example, the position of your baby's legs can be determined by asking questions about the location and strength of the kicking you feel. The spots where you feel the strongest kicks are most likely where your baby's feet are.
Other landmarks you can feel for include a large, flat plane, which is most likely your baby's back. Sometimes you can feel the baby arching his or her back.
At the top or bottom of the flat plane, you may feel either a hard, round shape (most likely your baby's head) or a soft curve (most likely to be your baby's bottom).
Guittier M, Othenin-Girard V, de Gasquet B, Irion O, Boulvain M. Maternal positioning to correct occiput posterior fetal position during the first stage of labour: a randomised controlled trial . BJOG: An International Journal of Obstetrics & Gynaecology . 2016;123(13):2199-2207. doi:10.1111/1471-0528.13855
Gizzo S, Di Gangi S, Noventa M, Bacile V, Zambon A, Nardelli G. Women’s Choice of Positions during Labour: Return to the Past or a Modern Way to Give Birth? A Cohort Study in Italy . Biomed Res Int . 2014;2014:1-7. doi:10.1155/2014/638093
Ahmad A, Webb S, Early B, Sitch A, Khan K, MacArthur C. Association between fetal position at onset of labor and mode of delivery: a prospective cohort study . Ultrasound in Obstetrics & Gynecology . 2014;43(2):176-182. doi:10.1002/uog.13189
Nishikawa M, Sakakibara H. Effect of nursing intervention program using abdominal palpation of Leopold’s maneuvers on maternal-fetal attachment . Reprod Health . 2013;10(1). doi:10.1186/1742-4755-10-12
Choi S, Park Y, Lee D, Ko H, Park I, Shin J. Sonographic assessment of fetal occiput position during labor for the prediction of labor dystocia and perinatal outcomes . The Journal of Maternal-Fetal & Neonatal Medicine . 2016;29(24):3988-3992. doi:10.3109/14767058.2016.1152250
Bamberg C, Deprest J, Sindhwani N et al. Evaluating fetal head dimension changes during labor using open magnetic resonance imaging . J Perinat Med . 2017;45(3). doi:10.1515/jpm-2016-0005
Gabbe S, Niebyl J, Simpson J et al. Obstetrics . Philadelphia, Pa.: Elsevier; 2012.
By Robin Elise Weiss, PhD, MPH Robin Elise Weiss, PhD, MPH is a professor, author, childbirth and postpartum educator, certified doula, and lactation counselor.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Your baby in the birth canal
During labor and delivery, your baby must pass through your pelvic bones to reach the vaginal opening. The goal is to find the easiest way out. Certain body positions give the baby a smaller shape, which makes it easier for your baby to get through this tight passage.
The best position for the baby to pass through the pelvis is with the head down and the body facing toward the mother's back. This position is called occiput anterior.
Information
Certain terms are used to describe your baby's position and movement through the birth canal.
FETAL STATION
Fetal station refers to where the presenting part is in your pelvis.
- The presenting part. The presenting part is the part of the baby that leads the way through the birth canal. Most often, it is the baby's head, but it can be a shoulder, the buttocks, or the feet.
- Ischial spines. These are bone points on the mother's pelvis. Normally the ischial spines are the narrowest part of the pelvis.
- 0 station. This is when the baby's head is even with the ischial spines. The baby is said to be "engaged" when the largest part of the head has entered the pelvis.
- If the presenting part lies above the ischial spines, the station is reported as a negative number from -1 to -5.
In first-time moms, the baby's head may engage by 36 weeks into the pregnancy. However, engagement may happen later in the pregnancy, or even during labor.
This refers to how the baby's spine lines up with the mother's spine. Your baby's spine is between their head and tailbone.
Your baby will most often settle into a position in the pelvis before labor begins.
- If your baby's spine runs in the same direction (parallel) as your spine, the baby is said to be in a longitudinal lie. Nearly all babies are in a longitudinal lie.
- If the baby is sideways (at a 90-degree angle to your spine), the baby is said to be in a transverse lie.
FETAL ATTITUDE
The fetal attitude describes the position of the parts of your baby's body.
The normal fetal attitude is commonly called the fetal position.
- The head is tucked down to the chest.
- The arms and legs are drawn in towards the center of the chest.
Abnormal fetal attitudes include a head that is tilted back, so the brow or the face presents first. Other body parts may be positioned behind the back. When this happens, the presenting part will be larger as it passes through the pelvis. This makes delivery more difficult.
DELIVERY PRESENTATION
Delivery presentation describes the way the baby is positioned to come down the birth canal for delivery.
The best position for your baby inside your uterus at the time of delivery is head down. This is called cephalic presentation.
- This position makes it easier and safer for your baby to pass through the birth canal. Cephalic presentation occurs in about 97% of deliveries.
- There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude).
If your baby is in any position other than head down, your doctor may recommend a cesarean delivery.
Breech presentation is when the baby's bottom is down. Breech presentation occurs about 3% of the time. There are a few types of breech:
- A complete breech is when the buttocks present first and both the hips and knees are flexed.
- A frank breech is when the hips are flexed so the legs are straight and completely drawn up toward the chest.
- Other breech positions occur when either the feet or knees present first.
The shoulder, arm, or trunk may present first if the fetus is in a transverse lie. This type of presentation occurs less than 1% of the time. Transverse lie is more common when you deliver before your due date, or have twins or triplets.
CARDINAL MOVEMENTS OF LABOR
As your baby passes through the birth canal, the baby's head will change positions. These changes are needed for your baby to fit and move through your pelvis. These movements of your baby's head are called cardinal movements of labor.
- This is when the widest part of your baby's head has entered the pelvis.
- Engagement tells your health care provider that your pelvis is large enough to allow the baby's head to move down (descend).
- This is when your baby's head moves down (descends) further through your pelvis.
- Most often, descent occurs during labor, either as the cervix dilates or after you begin pushing.
- During descent, the baby's head is flexed down so that the chin touches the chest.
- With the chin tucked, it is easier for the baby's head to pass through the pelvis.
Internal Rotation
- As your baby's head descends further, the head will most often rotate so the back of the head is just below your pubic bone. This helps the head fit the shape of your pelvis.
- Usually, the baby will be face down toward your spine.
- Sometimes, the baby will rotate so it faces up toward the pubic bone.
- As your baby's head rotates, extends, or flexes during labor, the body will stay in position with one shoulder down toward your spine and one shoulder up toward your belly.
- As your baby reaches the opening of the vagina, usually the back of the head is in contact with your pubic bone.
- At this point, the birth canal curves upward, and the baby's head must extend back. It rotates under and around the pubic bone.
External Rotation
- As the baby's head is delivered, it will rotate a quarter turn to be in line with the body.
- After the head is delivered, the top shoulder is delivered under the pubic bone.
- After the shoulder, the rest of the body is usually delivered without a problem.
Alternative Names
Shoulder presentation; Malpresentations; Breech birth; Cephalic presentation; Fetal lie; Fetal attitude; Fetal descent; Fetal station; Cardinal movements; Labor-birth canal; Delivery-birth canal

Barth WH. Malpresentations and malposition. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies . 8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
Kilpatrick SJ, Garrison E, Fairbrother E. Normal labor and delivery. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies . 8th ed. Philadelphia, PA: Elsevier; 2021:chap 11.
Review Date 11/10/2022
Updated by: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Childbirth Problems
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Delivery, face and brow presentation.
Julija Makajeva ; Mohsina Ashraf .
Affiliations
Last Update: January 9, 2023 .
- Continuing Education Activity
Face and brow presentation is a malpresentation during labor when the presenting part is either the face or, in the case of brow presentation, it is the area between the orbital ridge and the anterior fontanelle. This activity reviews the evaluation and management of these two presentations and explains the role of the interprofessional team in managing delivery safely for both the mother and the baby.
- Describe the mechanism of labor in the face and brow presentation.
- Summarize potential maternal and fetal complications during the face and brow presentations.
- Review different management approaches for the face and brow presentation.
- Outline some interprofessional strategies that will improve patient outcomes in delivery cases with face and brow presentation issues.
- Introduction
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin. The most common presentation in term labor is the vertex, where the fetal neck is flexed to the chin, minimizing the head circumference.
Face presentation – an abnormal form of cephalic presentation where the presenting part is mentum. This typically occurs because of hyperextension of the neck and the occiput touching the fetal back. Incidence of face presentation is rare, accounting for approximately 1 in 600 of all presentations. [1] [2] [3]
In brow presentation, the neck is not extended as much as in face presentation, and the leading part is the area between the anterior fontanelle and the orbital ridges. Brow presentation is considered the rarest of all malpresentation with a prevalence of 1 in 500 to 1 in 4000 deliveries. [3]
Both face and brow presentations occur due to extension of the fetal neck instead of flexion; therefore, conditions that would lead to hyperextension or prevent flexion of the fetal neck can all contribute to face or brow presentation. These risk factors may be related to either the mother or the fetus. Maternal risk factors are preterm delivery, contracted maternal pelvis, platypelloid pelvis, multiparity, previous cesarean section, black race. Fetal risk factors include anencephaly, multiple loops of cord around the neck, masses of the neck, macrosomia, polyhydramnios. [2] [4] [5]
These malpresentations are usually diagnosed during the second stage of labor when performing a digital examination. It is possible to palpate orbital ridges, nose, malar eminences, mentum, mouth, gums, and chin in face presentation. Based on the position of the chin, face presentation can be further divided into mentum anterior, posterior, or transverse. In brow presentation, anterior fontanelle and face can be palpated except for the mouth and the chin. Brow presentation can then be further described based on the position of the anterior fontanelle as frontal anterior, posterior, or transverse.
Diagnosing the exact presentation can be challenging, and face presentation may be misdiagnosed as frank breech. To avoid any confusion, a bedside ultrasound scan can be performed. [6] The ultrasound imaging can show a reduced angle between the occiput and the spine or, the chin is separated from the chest. However, ultrasound does not provide much predicting value in the outcome of the labor. [7]
- Anatomy and Physiology
Before discussing the mechanism of labor in the face or brow presentation, it is crucial to highlight some anatomical landmarks and their measurements.
Planes and Diameters of the Pelvis
The three most important planes in the female pelvis are the pelvic inlet, mid pelvis, and pelvic outlet.
Four diameters can describe the pelvic inlet: anteroposterior, transverse, and two obliques. Furthermore, based on the different landmarks on the pelvic inlet, there are three different anteroposterior diameters, named conjugates: true conjugate, obstetrical conjugate, and diagonal conjugate. Only the latter can be measured directly during the obstetric examination. The shortest of these three diameters is obstetrical conjugate, which measures approximately 10.5 cm and is a distance between the sacral promontory and 1 cm below the upper border of the symphysis pubis. This measurement is clinically significant as the fetal head must pass through this diameter during the engagement phase. The transverse diameter measures about 13.5cm and is the widest distance between the innominate line on both sides.
The shortest distance in the mid pelvis is the interspinous diameter and usually is only about 10 cm.
Fetal Skull Diameters
There are six distinguished longitudinal fetal skull diameters:
- Suboccipito-bregmatic: from the center of anterior fontanelle (bregma) to the occipital protuberance, measuring 9.5 cm. This is the presenting diameter in vertex presentation.
- Suboccipito-frontal: from the anterior part of bregma to the occipital protuberance, measuring 10 cm
- Occipito-frontal: from the root of the nose to the most prominent part of the occiput, measuring 11.5cm
- Submento-bregmatic: from the center of the bregma to the angle of the mandible, measuring 9.5 cm. This is the presenting diameter in face presentation where the neck is hyperextended.
- Submento-vertical: from the midpoint between fontanelles and the angle of the mandible, measuring 11.5cm
- Occipito-mental: from the midpoint between fontanelles and the tip of the chin, measuring 13.5 cm. It is the presenting diameter in brow presentation.
Cardinal Movements of Normal Labor
- Neck flexion
- Internal rotation
- Extension (delivers head)
- External rotation (Restitution)
- Expulsion (delivery of anterior and posterior shoulders)
Some of the key movements are not possible in the face or brow presentations.
Based on the information provided above, it is obvious that labor will be arrested in brow presentation unless it spontaneously changes to face or vertex, as the occipito-mental diameter of the fetal head is significantly wider than the smallest diameter of the female pelvis. Face presentation can, however, be delivered vaginally, and further mechanisms of face delivery will be explained in later sections.
- Indications
As mentioned previously, spontaneous vaginal delivery can be successful in face presentation. However, the main indication for vaginal delivery in such circumstances would be a maternal choice. It is crucial to have a thorough conversation with a mother, explaining the risks and benefits of vaginal delivery with face presentation and a cesarean section. Informed consent and creating a rapport with the mother is an essential aspect of safe and successful labor.
- Contraindications
Vaginal delivery of face presentation is contraindicated if the mentum is lying posteriorly or is in a transverse position. In such a scenario, the fetal brow is pressing against the maternal symphysis pubis, and the short fetal neck, which is already maximally extended, cannot span the surface of the maternal sacrum. In this position, the diameter of the head is larger than the maternal pelvis, and it cannot descend through the birth canal. Therefore the cesarean section is recommended as the safest mode of delivery for mentum posterior face presentations.
Attempts to manually convert face presentation to vertex, manual or forceps rotation of the persistent posterior chin to anterior are contraindicated as they can be dangerous.
Persistent brow presentation itself is a contraindication for vaginal delivery unless the fetus is significantly small or the maternal pelvis is large.
Continuous electronic fetal heart rate monitoring is recommended for face and brow presentations, as heart rate abnormalities are common in these scenarios. One study found that only 14% of the cases with face presentation had no abnormal traces on the cardiotocograph. [8] It is advised to use external transducer devices to prevent damage to the eyes. When internal monitoring is inevitable, it is suggested to place monitoring devices on bony parts carefully.
People who are usually involved in the delivery of face/ brow presentation are:
- Experienced midwife, preferably looking after laboring woman 1:1
- Senior obstetrician
- Neonatal team - in case of need for resuscitation
- Anesthetic team - to provide necessary pain control (e.g., epidural)
- Theatre team - in case of failure to progress and an emergency cesarean section will be required.
- Preparation
No specific preparation is required for face or brow presentation. However, it is essential to discuss the labor options with the mother and birthing partner and inform members of the neonatal, anesthetic, and theatre co-ordinating teams.
- Technique or Treatment
Mechanism of Labor in Face Presentation
During contractions, the pressure exerted by the fundus of the uterus on the fetus and pressure of amniotic fluid initiate descent. During this descent, the fetal neck extends instead of flexing. The internal rotation determines the outcome of delivery, if the fetal chin rotates posteriorly, vaginal delivery would not be possible, and cesarean section is permitted. The approach towards mentum-posterior delivery should be individualized, as the cases are rare. Expectant management is acceptable in multiparous women with small fetuses, as a spontaneous mentum-anterior rotation can occur. However, there should be a low threshold for cesarean section in primigravida women or women with large fetuses.
When the fetal chin is rotated towards maternal symphysis pubis as described as mentum-anterior; in these cases further descend through the vaginal canal continues with approximately 73% cases deliver spontaneously. [9] Fetal mentum presses on the maternal symphysis pubis, and the head is delivered by flexion. The occiput is pointing towards the maternal back, and external rotation happens. Shoulders are delivered in the same manner as in vertex delivery.
Mechanism of Labor in Brow Presentation
As this presentation is considered unstable, it is usually converted into a face or an occiput presentation. Due to the cephalic diameter being wider than the maternal pelvis, the fetal head cannot engage; thus, brow delivery cannot take place. Unless the fetus is small or the pelvis is very wide, the prognosis for vaginal delivery is poor. With persistent brow presentation, a cesarean section is required for safe delivery.
- Complications
As the cesarean section is becoming a more accessible mode of delivery in malpresentations, the incidence of maternal and fetal morbidity and mortality during face presentation has dropped significantly. [10]
However, there are still some complications associated with the nature of labor in face presentation. Due to the fetal head position, it is more challenging for the head to engage in the birth canal and descend, resulting in prolonged labor.
Prolonged labor itself can provoke foetal distress and arrhythmias. If the labor arrests or signs of fetal distress appear on CTG, the recommended next step in management is an emergency cesarean section, which in itself carries a myriad of operative and post-operative complications.
Finally, due to the nature of the fetal position and prolonged duration of labor in face presentation, neonates develop significant edema of the skull and face. Swelling of the fetal airway may also be present, resulting in respiratory distress after birth and possible intubation.
- Clinical Significance
During vertex presentation, the fetal head flexes, bringing the chin to the chest, forming the smallest possible fetal head diameter, measuring approximately 9.5cm. With face and brow presentation, the neck hyperextends, resulting in greater cephalic diameters. As a result, the fetal head will engage later, and labor will progress more slowly. Failure to progress in labor is also more common in both presentations compared to vertex presentation.
Furthermore, when the fetal chin is in a posterior position, this prevents further flexion of the fetal neck, as browns are pressing on the symphysis pubis. As a result, descend through the birth canal is impossible. Such presentation is considered undeliverable vaginally and requires an emergency cesarean section.
Manual attempts to change face presentation to vertex, manual or forceps rotation to mentum anterior are considered dangerous and are discouraged.
- Enhancing Healthcare Team Outcomes
A multidisciplinary team of healthcare experts supports the woman and her child during labor and the perinatal period. For a face or brow presentation to be appropriately diagnosed, an experienced midwife and obstetrician must be involved in the vaginal examination and labor monitoring. As fetal anomalies, such as anencephaly or goiter, can contribute to face presentation, sonographers experienced in antenatal scanning should also be involved in the care. It is advised to inform the anesthetic and neonatal teams in advance of the possible need for emergency cesarean section and resuscitation of the neonate. [11] [12]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Julija Makajeva declares no relevant financial relationships with ineligible companies.
Disclosure: Mohsina Ashraf declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Makajeva J, Ashraf M. Delivery, Face and Brow Presentation. [Updated 2023 Jan 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PubMed Links to PubMed
Similar articles in PubMed
- Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. [Am J Obstet Gynecol MFM. 2020] Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. Bellussi F, Livi A, Cataneo I, Salsi G, Lenzi J, Pilu G. Am J Obstet Gynecol MFM. 2020 Nov; 2(4):100217. Epub 2020 Aug 18.
- Review Sonographic evaluation of the fetal head position and attitude during labor. [Am J Obstet Gynecol. 2022] Review Sonographic evaluation of the fetal head position and attitude during labor. Ghi T, Dall'Asta A. Am J Obstet Gynecol. 2022 Jul 6; . Epub 2022 Jul 6.
- Stages of Labor. [StatPearls. 2024] Stages of Labor. Hutchison J, Mahdy H, Hutchison J. StatPearls. 2024 Jan
- Leopold Maneuvers. [StatPearls. 2024] Leopold Maneuvers. Superville SS, Siccardi MA. StatPearls. 2024 Jan
- Review Labor with abnormal presentation and position. [Obstet Gynecol Clin North Am. ...] Review Labor with abnormal presentation and position. Stitely ML, Gherman RB. Obstet Gynecol Clin North Am. 2005 Jun; 32(2):165-79.
Recent Activity
- Delivery, Face and Brow Presentation - StatPearls Delivery, Face and Brow Presentation - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches
suicide prevention
8 templates
46 templates
tropical rainforest
29 templates

spring season
34 templates
american football
16 templates

32 templates
Baby Presentation templates
When a baby arrives in a family, the reasons for joy are endless. these little creatures change our lives forever with their laughter and even their crying. to accompany you and your family in everything related to newborns, we want to do it with these google slides and powerpoint templates about babies..

Premium template
Unlock this template and gain unlimited access
My Baby's Yearbook
Welcome to your baby’s yearbook! Capture all the precious moments of your baby's first year with this beautiful and unique template. You can now easily create a stunning yearbook full of photographs and other memorabilia, perfect for a keepsake. Write down all the details and information in the helpful resources....

Complications During Fetal Growth Clinical Case
Download the "Complications During Fetal Growth Clinical Case" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare...

Fetal Monitoring Case Report
Download the "Fetal Monitoring Case Report" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare professionals to...

Cute Mother and Baby Minitheme
This template is dedicated to the loving relationship mothers have with their babies, that’s why it’s so heartwarming, calming and beautiful. With this template you can speak about your baby in a creative way: what are their favorite clothes? And what’s their favorite game? There’s no one that knows your...


Stages of a Baby
A new member of the family has arrived! Now, this newborn baby must go through all the stages a baby goes through. Their first steps, their first words... How sweet! With this medical template, you will be able to talk about all these stages, from the first months of life...

Watercolor Baby Toys Minitheme
This presentation template is perfect for any audience, featuring an explosion of creativity and cuteness! It includes a variety of playful watercolor baby toys that will engage your viewers and draw their attention. There are vibrant colors and layouts to create the perfect atmosphere - plus custom designs and fonts...
Sexual and Reproductive Health Center
Download the "Sexual and Reproductive Health Center" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare professionals...

Baby Race Competition Planning for MK
Are you running constantly after your baby because he or she can't keep still? Maybe your baby is a natural-born athlete! There are some competitions that involve, just as it sounds, babies racing against each other! You've probably seen it on TV: parents encouraging and telling their children to come...

Cute Watercolor Baby Shower Minitheme
Invite your family and loved ones to a baby shower they will never forget and use this cute template to speak about your little baby, how it has grown, what were their first words, what’s their favourite toy and food… The design is super cute and includes illustrations in watercolor!...

Baby Shower and Gender Reveal Party
What's better than celebrating a new bundle of joy? Celebrating the gender of a new bundle of joy! A baby shower and gender reveal party are the perfect way to bring family and friends together to share in the excitement of the upcoming arrival. A cute template like this one...

Virtual Baby Shower Invitations
Welcoming a baby is always a beautiful event, and if the situation doesn’t allow your family and friends to get together, a good solution is to have an online baby shower! Invite everyone to enjoy some online time with your baby and have an amazing evening with these cute printable...

Postpartum Ischemic Stroke Case Report
Download the "Postpartum Ischemic Stroke Case Report" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare professionals...

US' National Neonatal Nurses Day
We want to show nurses the love and appreciation they deserve. Especially neonatal ones! With this template for the National Neonatal Nurses Day in the US you can celebrate September 15th with a presentation full of data, statistics, information and respect. When a postcard is not enough, an editable template...

Kindergarten Day
Download the "Kindergarten Day" presentation for PowerPoint or Google Slides and create big learning experiences for the littlest students! Dynamic and adorable, this template provides the visual stimuli that Pre-K students thrive on and makes your lessons more playful and exciting — after all, Pre-K education is all about playing...

Crisis Pregnancy Center (CPC)
Download the "Crisis Pregnancy Center (CPC)" presentation for PowerPoint or Google Slides. Hospitals, private clinics, specific wards, you know where to go when in need of medical attention. Perhaps there’s a clinic specialized in treating certain issues, or a hospital in your area that is well-known for its state-of-the-art technology....

Patient with Gestational Diabetes Case Report
Download the "Patient with Gestational Diabetes Case Report" presentation for PowerPoint or Google Slides. A clinical case is more than just a set of symptoms and a diagnosis. It is a unique story of a patient, their experiences, and their journey towards healing. Each case is an opportunity for healthcare...

Neonatal Jaundice Disease
We know that being a mom or a dad is hard and scary, but when it comes to Jaundice, we recommend you not to panic. If your newborn’s eyes turn a bit yellow, it could be Jaundice, a condition that is common in babies and that is usually non-threatening. It...

Premature Birth
Download the "Premature Birth" presentation for PowerPoint or Google Slides. Healthcare goes beyond curing patients and combating illnesses. Raising awareness about diseases, informing people about prevention methods, discussing some good practices, or even talking about a balanced diet—there are many topics related to medicine that you could be sharing with...
- Page 1 of 8
New! Make quick presentations with AI
Slidesgo AI presentation maker puts the power of design and creativity in your hands, so you can effortlessly craft stunning slideshows in minutes.
Register for free and start editing online
Trending Topics:
- Say Kaddish Daily
- Passover 2024

Jewish Newborn Ceremonies 101
An overview of ceremonies to welcome baby boys and girls.
By My Jewish Learning
History and Development
The practice of circumcising baby boys ( brit milah , or “the covenant of circumcision”) has its roots in Abraham’s circumcising the male members of his household, as recorded in the biblical Book of Genesis . It is a deep and persistent symbol of covenant and continuity for the Jewish people.
A parallel ceremony for girls (often called a simchat bat , “celebration of a daughter,” or brit banot, “daughters’ covenant”) is a contemporary development with historical and cultural predecessors, inspired by Jewish feminism , and practiced in most liberal and some traditional communities. Families and communities have also acknowledged and celebrated the arrival of babies in many other ways throughout Jewish history, and in different Jewish traditions throughout the world, with a variety of home and synagogue rituals of celebration and naming.
Liturgy, Ritual, and Custom
For boys, the ceremony for brit milah (also known as a “bris”) traditionally takes place on the eighth day of life, and includes words of blessing, the circumcision itself, and the giving of a name. Traditionally the responsibility of the baby’s father, the act of circumcision is usually performed (according to prescribed custom) by a mohel , an individual trained in the practice and its rituals. For many girls, the much newer simchat bat or brit banot (frequently referred to in English as a “baby naming”) can take place on a variety of days. It often follows a similar structure as the brit milah, with one of several covenantal or welcoming acts (e.g., candlelighting, footwashing, or being wrapped in a tallit [prayer shawl]) as the ritual centerpiece. Some families follow the simpler and longer-standing custom of having their new daughter receive her Hebrew or Yiddish name during a synagogue Torah-reading service, rather than holding a freestanding simchat bat.
Just as the longstanding tradition of brit milah for boys inspired the creation of parallel ceremonies for girls, the creative approach to tradition that has marked simchat bat ceremonies has in many cases shaped the way that brit milah is celebrated, for example, with fuller involvement of the mother, and an emphasis on themes equally applicable to girls and boys.
In Practice
A ceremony and celebration for a Jewish baby is often planned in a hurry after the baby is born. Fortunately, there are many resources available to parents and families to help with the planning a brit milah or a simchat bat . Those attending such an event have a special role to play as family and community members. Enjoying the festive meal (or seudah) is considered a sacred obligation. Families may mark the occasion with a tzedakah (charity) donation or other social action project, or continue the ancient custom of planting a tree in honor of each child.
Pidyon HaBen
Jewish tradition mandates a ceremony in which first-born Jewish males (those who are the first to “open the womb” of their mother) are “ redeemed ” from the service of the ancient priests. It is usually a small, private ceremony in which someone who is believed to be a descendant from the priestly class (a cohen) symbolically releases the child back to his parents. It is mainly practiced today by traditionally observant Jews.
The encounter between tradition and modernity, and between different Jewish customs, raises interesting questions about ceremonies of welcoming, naming, and covenant. What are the connections and differences between ceremonies for girls and those for boys? Is there a move toward standardization or diversity in ceremonies for girls? And what happens when Jewish tradition collides with contemporary debates about the morality and effects of circumcision ? Finally with a large percentage of Jews marrying non-Jews, some couples debate what faith tradition to raise their child, and if both, then how are newborn ceremonies reflecting those decisions?
For more Jewish parenting help, visit our partner site Kveller.
Pronounced: breet mee-LAH, Origin: Hebrew, literally “covenant of circumcision,” the Jewish circumcision ceremony for an 8-day-old boy, marking the covenant between God and the Jews. Also known as a bris.
simchat bat
Pronounced: SEEM-khat BAHT, Origin: Hebrew, ceremony welcoming a Jewish baby girl, also known as a brit bat.
Pronounced: tzuh-DAH-kuh, Origin: Hebrew, from the Hebrew root for justice, charitable giving.
Join Our Newsletter
Empower your Jewish discovery, daily
Discover More

Weddings & Marriage
36 Questions for Jewish Lovers
Rabbi and marriage counselor Ari Sytner offers 36 questions for Jewish couples to achieve greater intimacy and harmony.

The Kabbalistic Secret of Kissing
What the Zohar teaches about love-making and the coming of the messiah.

How to Pray Through Infertility
Jewish tradition is no stranger to infertility, but it is only recently that liturgical responses to this struggle have emerged.
Need to talk? Call 1800 882 436. It's a free call with a maternal child health nurse. *call charges may apply from your mobile
Is it an emergency? Dial 000 If you need urgent medical help, call triple zero immediately.
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
Malpresentation
8-minute read
If you feel your waters break and you have been told that your baby is not in a head-first position, seek medical help immediately .
- Malpresentation is when your baby is not facing head-first down the birth canal as birth approaches.
- The most common type of malpresentation is breech — when your baby’s bottom or feet are facing downwards.
- A procedure called external cephalic version can sometimes turn a breech baby into a head-first position at 36 weeks.
- Most babies with malpresentation are born by caesarean, but you may be able to have a vaginal birth if your baby is breech.
- There is a serious risk of cord prolapse if your waters break and your baby is not head-first.
What are presentation and malpresentation?
‘Presentation’ describes how your baby is facing down the birth canal. The ‘presenting part’ is the part of your baby’s body that is against the cervix .
The ideal presentation is head-first, with the crown (top) of the baby’s head against the cervix, with the chin tucked into the baby’s chest. This is called ‘vertex presentation’.
If your baby is in any other position, it’s called ‘malpresentation’. Malpresentation can mean your baby’s face, brow, buttocks, foot, back, shoulder, arms or legs or the umbilical cord are against the cervix.
It’s safest for your baby’s head to come out first. If any other body part goes down the birth canal first, the risks to you and your baby may be higher. Malpresentation increases the chance that you will have a more complex vaginal birth or a caesarean.
If my baby is not head-first, what position could they be in?
Malpresentation is caused by your baby’s position (‘lie’). There are different types of malpresentation.
Breech presentation
This is when your baby is lying with their bottom or feet facing down. Sometimes one foot may enter the birth canal first (called a ‘footling presentation’).
Breech presentation is the most common type of malpresentation.
Face presentation
This is when your baby is head-first but stretching their neck, with their face against the cervix.
Transverse lie
This is when your baby is lying sideways. Their back, shoulders, arms or legs may be the first to enter the birth canal.
Oblique lie
This is when your baby is lying diagonally. No particular part of their body is against the cervix.
Unstable lie
This is when your baby continually changes their position after 36 weeks of pregnancy.
Cord presentation
This is when the umbilical cord is against the cervix, between your baby and the birth canal. It can happen in any situation where your baby’s presenting part is not sitting snugly in your pelvis. It can become an emergency if it leads to cord prolapse (when the cord is born before your baby, potentially reducing placental blood flow to your baby).
What is malposition?
If your baby is lying head-first, the best position for labour is when their face is towards your back.
If your baby is facing the front of your body (posterior position) or facing your side (transverse position) this is called malposition. Transverse position is not the same as transverse lie. A transverse position means your labour may take a bit longer and you might feel more pain in your back. Often your baby will move into a better position before or during labour.
Why might my baby be in the wrong position?
Malpresentation may be caused by:
- a low-lying placenta
- too much or too little amniotic fluid
- many previous pregnancies, making the muscles of the uterus less stable
- carrying twins or more
Often no cause is found.
Is it likely that my baby will be in the wrong position?
Many babies are in a breech position during pregnancy. They usually turn head-first as pregnancy progresses, and more than 9 in 10 babies in Australia have a vertex presentation (ideal presentation, head-first) at birth.
You are more likely to have a malpresentation if:
- this is your first baby
- you are over 40 years old
- you've had a previous breech baby
- you go into labour prematurely
How is malpresentation diagnosed?
Malpresentation is normally diagnosed when your doctor or midwife examines you, from 36 weeks of pregnancy. If it’s not clear, it can be confirmed with an ultrasound.
Can my baby’s position be changed?
If you are 36 weeks pregnant , it may be possible to gently turn your baby into a head-first position. This is done by an obstetrician using a technique called external cephalic version (ECV).
Some people try different postures or acupuncture to correct malpresentation, but there isn’t reliable evidence that either of these work.
Will I need a caesarean if my baby has a malpresentation?
Most babies with a malpresentation close to birth are born by caesarean . You may be able to have a vaginal birth with a breech baby, but you will need to go to a hospital that can offer you and your baby specialised care.
If your baby is breech, an elective (planned) caesarean is safer for your baby than a vaginal birth in the short term. However, in the longer term their health will be similar, on average, regardless of how they were born.
A vaginal birth is safer for you than an elective caesarean. However, about 4 in 10 people planning a vaginal breech birth end up needing an emergency caesarean . If this happens to you, the risk of complications will be higher.
Your doctor can talk to you about your options. Whether it’s safe for you to try a vaginal birth will depend on many factors. These include how big your baby is, the position of your baby, the structure of your pelvis and whether you’ve had a caesarean in the past.
What are the risks if I have my baby when it’s not head-first?
If your waters break when your baby is not head-first, there is a risk of cord prolapse. This is an emergency.
Vaginal breech birth
Risks to your baby can include:
- Erb’s palsy
- fractures, dislocations or other injuries
- bleeding in your baby’s brain
- low Apgar scores
- their head getting stuck – this is an emergency
Risks to you include:
- blood loss or blood clots
- infection in the wound
- problems with the anaesthetic
- damage to other organs nearby, such as your bladder
- a higher chance of problems in future pregnancies
- a longer recovery time than after a vaginal birth
Risks to your baby include:
- trouble with breathing — this is temporary
- getting a small cut during the surgery
Will I have a malpresentation in my future pregnancies?
If you had a malpresentation in one pregnancy, you have a higher chance of it happening again, but it won’t necessarily happen in future pregnancies. If you’re worried, it may help to talk to your doctor or midwife so they can explain what happened.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call . Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: July 2022
Related pages
Labour complications.
- Interventions during labour
- Giving birth - stages of labour
Breech pregnancy
Search our site for.
- Caesarean Section
- Foetal Version
Need more information?
Top results
When a baby is positioned bottom-down late in pregnancy, this is called the breech position. Find out about 3 main types and safe birthing options.
Read more on Pregnancy, Birth & Baby website

Breech Presentation at the End of your Pregnancy
Breech presentation occurs when your baby is lying bottom first or feet first in the uterus (womb) rather than the usual head first position. In early pregnancy, a breech position is very common.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website

External Cephalic Version for Breech Presentation - Pregnancy and the first five years
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website

Presentation and position of baby through pregnancy and at birth
Presentation and position refer to where your baby’s head and body is in relation to your birth canal. Learn why it’s important for labour and birth.
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Call us and speak to a Maternal Child Health Nurse for personal advice and guidance.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
2:21-24 The presentation of baby Jesus
Luke 2:21-24 “On the eighth day, when it was time to circumcise him, he was named Jesus, the name the angel had given him before he had been conceived. When the time of their purification according to the Law of Moses had been completed, Joseph and Mary took him to Jerusalem to present him to the Lord (as it is written in the Law of the Lord, ‘Every firstborn male is to be consecrated to the Lord’), and to offer a sacrifice in keeping with what is said in the Law of the Lord: ‘a pair of doves or two young pigeons’.”
When she was a little girl her mother brought her to church, but there was always a barrier she put up between herself and the congregation. At the earliest opportunity, when she was in her mid-teens, she stopped attending church. She got a job and lived like a modern girl, not keen on the institution of marriage or having a family. That was as old-fashioned as worshipping the living God, but then she fell in love with a kind man and she moved in with him. However, after a time that relationship of ‘living together’ didn’t satisfy them. They got married, and then when her sister had children and she saw babies close up her early opinions about not wanting to be a mother also changed, in fact her views about many things began to change as she matured. She watched her mother who had gone through a number of great crises and yet kept trusting in God. She couldn’t have got by, her mother told her, without knowing that Lord was in control and was helping her day by day. The daughter saw that, how her mother was given strength outside herself by the Lord, and she found herself praying, praying for motherhood in particular. Then she started to go to church each Sunday with her husband, and then they did become parents. A month or so ago she made a profession of faith that she had become a Christian and she got confirmed. I had sowed and watered for many years and in his time God gave the increase.
There is a longing in every heart to know God, and when this is joined with a longing for other great realities, like a life-long marriage to someone who loves you, and for children then your yearning after God grows. God has said that it is not good for man to be alone. When God gives you children you have enormous new responsibilities. How are you going to raise them? Are you going to put a barrier between them and their knowing the living God by your apathy and ignorance? Are you going to say to them, “God is unimportant and unknowable”? Or will you help them to know and serve God in a way you yourself have not been knowing him?
In our text we are told of the response of Joseph and Mary to the arrival of their new born baby boy, and that is what we are going to study today. What attitudes should be displayed by a young husband and wife to honour the Lord in dealing with their children? I am going to look at their attitude through the prism of four or five words and events mentioned in verses 21 through 24.
1. CIRCUMCISION: JOSEPH AND MARY HAD JESUS CIRCUMCISED.
We are told, “On the eighth day . . . it was time to circumcise him” (v.21). In other words the eighth day in Jesus’ life – as it was for every Jewish boy – was the prescribed day for circumcision. God required it; he had said in Leviticus chapter twelve and verse three, “On the eighth day the boy is to be circumcised.” So if Joseph and Mary were going to be God-fearing parents then they had to start right by doing everything that God said, trusting and obeying Jehovah. That was the beginning of wisdom and the beginning of blessed parenthood. So they had their darling baby boy circumcised, and Joseph himself would have had to do it; it was not for some centuries that rabbis took on the responsibility of circumcising baby boys. Eight days earlier young Joseph had had to assist Mary in giving birth to Jesus in the stable cave. There was no one else there but Joseph to help his wife in childbirth. Now he had to circumcise the baby; he had to do it. Think of it! You are holding in your arms your tiny adorable newborn son. Maybe you are twenty-one years of age, and now you are going to get the razor out and circumcise your son! Joseph had been told just how important this baby was – Christ the Lord, the Son of the Highest! Would you sleep the night before you were to do this? You’d pray together, your wife and yourself, and you’d ask God to help you, to stop your hand from trembling. You wouldn’t be aware of one interesting fact, that God has so designed the human body that around the eighth day of life the blood clotting factor is the highest, but you did know that circumcision was done to every single Jewish baby boy, with no fatalities, as it had been done to you, and God required it.
Why had it to be done? Jesus had to be circumcised for a number of reasons. It was a welcoming ceremony for every Jew; it said that this baby boy was welcome in the covenant community of Israel. A person circumcised was uniquely aware that he was of the seed of Abraham, and that Jesus was also the lawful, circumcised son of circumcised David. There were privileges that came from this; for example, Jesus couldn’t have been accepted as a teacher in Israel unless he’d been circumcised. There’d have been no possibility of him standing in the Temple courts and crying to the crowds of people hanging onto his words, “If anyone is thirsty, let him come to me and drink. Whoever believes in me, as the Scripture has said, streams of living water will flow from within him.” (Jn.7:37&38). An uncircumcised Jesus could have had no admission to any lawful Jewish assembly. He couldn’t have preached in a synagogue. He’d have been regarded by the Jews as an uncircumcised Gentile, an apostate from the faith of the patriarchs. By circumcision he had a right to the national privileges of Israel.
Again, submission to circumcision was saying that this child was born under the law of God, and as Jesus had begun so he would go on. Jesus’ whole life was going to be one of fulfilling all righteousness in keeping God’s commandments. Please grasp this, because it will be life for you; it’s going to be that righteousness of Christ, worked out in his daily obedience, which is going to save everyone who believes. The great champion of historic Christianity in the last century was Dr. J. Gresham Machen of Philadelphia and in the 1930s he was asked a couple of times to preach on the radio a series of broadcasts. In fact there were two series of messages, one called The Christian Faith in the Modern World and the other The Christian View of Man. Dr. Machen’s academic specialty was as Professor of New Testament, and he needed help in a better understanding of the theology of the Bible to broadcast it all over Philadelphia. He got this wisdom through a young Scotsman called John Murray. Dr. Machen was especially enlightened by Mr. Murray to understand how we are saved not only by Christ dying for us on the cross but by living for us, actively obeying God on our behalf. Of course our sin is imputed to Christ on Calvary, but also the daily righteousness of the God-man is imputed to us who believe in him; we are made the righteousness of God in Christ. Gresham Machen saw that truth as he had never seen it before and experienced the wonderful comfort it brings.
In late December 1936 Dr. Machen said good-bye to John Murray as he went out by train for a week to the freezing heartland of America, the state was north Dakota and it was mid-winter. Dr Machen went there at the request of a preacher who was trying to bring his muddled little congregation to understand and accept the teaching of the Bible and resist modernism. Dr. Machen was not a fit man going there but he couldn’t turn down this request for help and disappoint an old student. So he went, and as soon as he arrived there he fell ill with pneumonia and pleurisy. The day before he died, still only in his fifties, he sent a telegram to John Murray which told Mr. Murray what his hope was founded on as death was coming near. The telegram read, “I am so thankful for the active obedience of Christ. No hope without it.” Our hope is that Jesus Christ fulfilled all the righteousness God demands from us. We are saved by his righteousness not our own.
Why am I telling you this moving story? Because we are seeing the very first evidence of Christ’s obedience to the law, and his fulfilling the righteousness which we fail to fulfil. We see it here in Jesus’ submission to the rite of circumcision. God said in his word, “On the eighth day the boy is to be circumcised,” and we must notice that God’s law was kept by Joseph, Mary but especially Jesus who fulfilled the ceremonial law in our place. So in accepting this pain Jesus declared that henceforth his life was going to be one of fulfilling all our righteousness by keeping the law on behalf of every one of his people.
But there was even more significance to circumcising a baby boy besides it being a sign of his Jewishness, and that he was living under the law of Jehovah. Circumcision was a sign of regeneration; God was saying by this sign to the people of God during their state of childhood under the old covenant dispensation, “As a people your greatest need is a circumcised heart. Sin has put its roots down and down into your innermost beings and it’s stopping you loving the Lord with every bit of your hearts. Circumcision is a sign that that sinful attitude has to be cut out of your lives in a great definitive act of renewal.” We’d say that this sign of circumcision in the Old Testament period pointed to the fulfillment and reality of a new heart during the New Covenant. So the question we have to ask is obvious, why should Jesus – of all people – have to be submitted to this? He had no need of his heart being circumcised because he never had any sin – even as a baby. He wasn’t born in sin or shapen in iniquity. Mary did not conceive him in sin. He was from his begetting God’s holy child Jesus. So what spiritual need was there of his being circumcised? Doesn’t it deny his perfection?
No, it shows us Jesus’ mission in life from a week old. It shows us why he came from heaven to the womb of Mary. Circumcision declared Jesus’ solidarity with us. Christ has taken a sinner’s religion along with all the other baby boys who were submitted to circumcision that month all over Israel. Thirty years later our Lord will stand in a line of sinners waiting to be baptized by John in the river Jordan. Two people in front of him there stands a man who used to hit his wife. The man directly in front of him was a thief. The man behind him is a drunkard, and the man behind him is a liar, and the man behind him a blasphemer, and these sinners have all come to repentance for their sin, and now they are confessing their sins and they’ve known God’s forgiveness. They are waiting to be baptized by John in the river Jordan. And there in the midst of this long line of confessing sinners is the holy and sinless Son of God, Jesus the Messiah, the one who again is showing us that he has taken a sinners’ religion and is standing in solidarity with them.
There was a missionary working in the Hawaiian Islands named Joseph Damian. He preached to a colony of lepers, lovingly and faithfully serving and pastoring them for years. Then one day he spilt some hot water on his foot but he couldn’t feel anything. He touched his foot but his foot couldn’t feel his probing finger. Joe realized that he also had contracted leprosy. He went to church that morning and began his sermon not with the words “My fellow believers . . .” but, “My fellow lepers . . .” Now he could identify completely, utterly and totally with his congregation. I am saying that at the moment of our Lord’s circumcision we first meet Jehovah Jesus, the God of the Bible, identifying with us as one who has been made in the likeness of sinful flesh, humbling himself to death, even the death of the cross. God was willing to come so low to raise us, not a God pulling puppet strings, not a God simply spectating our agony but one who submitted to bloody circumcision, who sweated drops of blood and threw himself onto the ground and prayed in agony. That is the God who comes close to us and understands us.
So here is the week old baby Jesus bleeding after his circumcision, and crying with pain. When a hymnist wrote a Christmas carol with the line “but little Lord Jesus no crying he makes,” he surely was referring to the absence of petulant, selfish, ego-endorsing crying. When babies cry they can be communicating that they are in pain, or that they are hungry, or wet, or cold, and that isn’t sinful, it’s human. So Jesus at eight days was already into the pain and bloodiness of fallen human existence. The blood of Mary’s boy-child is being shed. His life begins with bloodshed. It ends with bloodshed. Down and down and down our Lord was willing to descend for our salvation. So the first thing we are told was Jesus’ circumcision.
2. IDENTIFICATION: JOSEPH AND MARY GAVE HIM HIS NAME JESUS.
We are told, “he was named Jesus, the name the angel had given him before he had been conceived” (v.21). My daughter and her husband have chosen the name for their unborn son and they’ve prayed for him by name every day for weeks ever since a scan revealed that the baby was a boy. His date of birth is not for another five or six weeks. When we ask them, “So what’s his name?” They say, “We’re not telling you that yet. We want to have something with which to surprise you in November.” Now you will remember that Jesus’ parents did not choose his name, that both to Mary (as recorded in Luke chapter one and verse thirty-one), and to Joseph on a separate occasion (as recorded in Matthew chapter one and verse twenty-one) they were told separately by messengers from God that the name of the child was to be ‘Jesus.’ It was God’s chosen name for his own Son. In a sense the name of every one of us was chosen by God, wasn’t it? He is the ultimate first cause for everything, and so, though some of you may not be very fond of your names, God did have some part to play in permitting your parents to make that choice, and it is good to think of your name, its choice and its meaning as one given you by God. Let me give you two illustrations of people considering their names. At a time when John Bunyan began to feel the power of the written word and his books were spreading all over the country he was rearranging the letters of his name. He came up with “NU HONY IN A B”. That was the effect of God’s grace in his life. The new sweetness of the divine mercy had totally transformed Mr. B.
Again the father of Mary Steele (a relation of the hymn-writer Anne Steele) gave his six year-old daughter a book and wrote inside the cover this acrostic;
My God, my refuge and delight,
Attend my humble cry;
Remember I’m a sinner great,
Yet Thou canst me supply.
So shall I love and live Thy praise,
Till I resign my breath;
Eternally adore Thy name,
Ev’n now and after death.
Lord, lead me by Thy Spirit still,
Ev’n guide me to Thy holy hill.
So God chose the name ‘Jesus.’ He could have given his Son the name ‘Moreh’ meaning ‘teacher’ because Jesus was the most inspiring teacher that this world has ever heard. Or God could have given him the name ‘Mehlech’ meaning ‘king’ because Jesus had power over creation, over men, over demons, over disease and over death itself. Supreme authority was his, but neither was he named ‘Mehlech.’ God passed by titles like that and he selected a name which speaks of deliverance, grace and help for lost men and women. He was named ‘Jesus,’ and that name means ‘Saviour’, or ‘He saves’, or ‘Jehovah the Saviour,’ or ‘the Lord saves.’ This is how he principally wants to be known, as the Redeemer of men and women.
There is no Saviour like him on earth or in heaven; there is no Saviour who has achieved what he has achieved; there is no Saviour who has earned the exaltation he has earned; there is no Saviour doing what he is doing today. He is the unique Saviour because he has done the impossible. By his life and death he has saved us (past tense) from the condemnation of sin by taking that condemnation in our place. He is saving us (present tense) from the power of sin by actually indwelling us and giving us strength to resist sin changing us year by year. He will save us (future tense) from the very presence of sin because when we see him then we shall be like him, totally freed from sin. He has taken the supreme responsibility for the salvation of all his people – and they are more in number than the stars of heaven – from the beginning to the end he saves. His name will always be ‘Jesus’ and so Charles Wesley says,
“Happy, if with my latest breath
I might but gasp His name:
Preach Him to all. And cry in death
Behold, behold the Lamb!”
Jesus is the one and only Saviour. There is none other name under heaven given amongst men whereby we must be saved. The folly of our human nature is that it wants to put something else alongside Christ in our salvation; “Jesus does a part, but I do my part too.” Our very nature itches to make some contribution to our salvation, towards what I call “Jesus plus.” But your name is not ‘Jesus’; that is his name uniquely. He alone is the Saviour. My salvation before God is not in the least dependent upon myself or anyone at all except Jesus only. All by himself he became the Lamb of God and he suffered and bled alone. When you stand before God in that tremendous day Jesus, as the only Mediator, will present your soul unblemished and complete to his Father. He will do it and he will do it without any assistance from man. Christ only for your salvation. Rest your confidence where it must rest. When you sin then grieve for it please, but don’t think that your grief must be added to Jesus’ salvation. When you witness for him speak wisely please, but don’t think that your boldness must be added to Jesus’ salvation. Remember that just as your righteousness can never make Christ’s righteousness any better, so your sin can never make Christ’s righteousness any worse. If you are clothed in Christ’s righteousness, even though you see yourself black with sin, you may stand now, and stand at the Judgment Day, and say I have a Saviour who lived and died for me, and that fact will see you through. Please be always abounding in the work of the Lord Jesus, and be happy to be a mere disciple of Christ, but don’t do those things to be safe. Your good works add nothing whatsoever to the work of Christ’s salvation. It is Christ who died. It is Christ who rose and now lives in heaven and in you. It is Christ who is at the right hand of God, and it is Christ who makes intercession for us and so saves us to the uttermost when we come to God by him. The parents identified their baby as ‘Jesus,’ the Saviour. Is he your Saviour? Let’s not be content to be church attenders, or admirers of Jesus, but let’s make sure that he knows us and we know him who is the Deliverer from the guilt and power of sin and Redeemer from Satan’s bondage. Let’s make sure we can say, “The Saviour from God is my eternal friend.” The third word, what is that?
3. PURIFICATION: JOSEPH AND MARY PURIFIED THEMSELVES.
We are told, “the time of their purification according to the Law of Moses had been completed” (v.22). What’s all this about? Again it was an Old Testament ceremonial requirement found in the book of Leviticus chapter twelve; “The LORD said to Moses, ‘Say to the Israelites: A woman who becomes pregnant and gives birth to a son will be ceremonially unclean for seven days, just as she is unclean during her monthly period. On the eighth day the boy is to be circumcised. Then the woman must wait thirty-three days to be purified from her bleeding. She must not touch anything sacred or go to the sanctuary until the days of her purification are over’” (Lev. 12:1-4). Now you may complain about this being in the Bible, that it is boring, that it is anti-women or demeaning to women, and that it is irrelevant to us today, but let me say a word in its defence and about its relevance to all of us.
By this law, and many like it, the children of Israel were being taught some simple lessons about living pure lives (remember that during this Old Testament time they were, as it were, in the childhood of their faith). “The God you serve is a pure God and he wants you to live a pure life.” That was the basic lesson. Those of you who’ve read the Old Testament through from Genesis chapter one onwards have often met these teachings about cleanness and uncleanness in the first five books of Moses. For example, there were rules about what happened if you had skin disease, or bodily discharges, or if you touched unclean things, or ate unclean foods. Then you had to purify yourself ceremonially, wash yourself and make a sacrifice because of this contact. So Mary had had a baby and Joseph had assisted her in the birth, and that might be the reason Luke writes about the time of their purification, not just Mary’s. Or Luke might be referring to Joseph’s involvement in the purification ceremony that he was the one who got the pigeons and sacrificed them for Mary. Paul explains in Colossians 2:16 and 17 that those laws are the shadow of Christ who is the substance. Every time a baby was born, or a certain time each month for women, or with other bodily discharges then Old Testament Christians had to relate them in their minds to the fascinating issue of living a pure life. If you took them in that way they became a divine teaching device. So you hear the prophet Isaiah talking to the people about their sin and saying, “But we are all as an unclean thing” (Isa. 64:6), and the people listened and they had a picture of living a clean and pure life which pleased God in all of life and everything, in what they ate, and wore, and how they washed themselves. Isaiah was exhorting them to always think of the purity of God and the pure Spirit.
So the people were taught during the Old Testament dispensation that after the birth of a baby, for forty days the mother was in this category of ‘unclean.’ Now there were some compassionate reasons for this law; it protected the woman for six entire weeks immediately after the pains and occasional tearing of childbirth from a demanding husband. He shouldn’t bother her. Let her heal! Then there is the reason of hygiene; let these weeks after the birth of the baby be a time when the mother enjoys washing and luxuriating regularly in her bath. People of two or three thousand years ago in the Middle East knew little about how essential cleanliness was when there were open wounds, but God here provides this good rule. Let the new mother spend some time washing and lying in warm water after the baby was born. God insists on this no matter if her boorish husband complains. That is the sort of God who reigns in heaven and in his church on earth, how kind and understanding he is to the needy and weak, the woman with child or to one just getting over having a child.
What is the big message of purification? Please associate our loving Lord in heaven with the fulness of life and wholeness and purity, not with death and defilement and disorder. God commands that all of life be lived under his direction, the food we eat, our monthly cycles, the birth of our children – it is all to be connected with honouring God. He was warning them at that time, “Don’t you or your husband run to the temple immediately with the newborn baby because that is what the priests of the fertility gods demand, claiming that it’s their idols who’ve caused this. Don’t give them publicity by parading a newly born baby in the temple of Baal. No! Let the weeks go by; there is no connection between worship and sex – in spite of what’s said by the Baals, the fertility cults in the nations all around Israel with their lurid priestesses. You children of Abraham are not to be like the Gentiles all around you; you are not to pick up their attitudes to women and child-bearing and their obscene temples.”
But the most important message conveyed by these laws about ritual purity is that God is pure, and man, conversely, is contaminated and unfit, in and of himself, to approach a holy God and only by the sacrifice can cleansing come to you. That is the main thrust of this teaching. Mary and Joseph needed to be purified, but they didn’t realize that the actual way of their purification lay in the baby they had circumcised, and named. So it was strange that one the one hand because of Jesus’ birth they needed to be purified, but on the other hand purification came to them only because Jesus had been born. We need purity for everything we do, and we find the mainspring of pure living in a living relationship with the Lord Jesus. What is the fourth word?
4. PRESENTATION: JOSEPH AND MARY PRESENTED JESUS AT THE TEMPLE.
We are told that after the days of purification had ended, and Jesus was six weeks old, that then, “Joseph and Mary took him to Jerusalem to present him to the Lord” (v.22). “Son we are taking you to your Father’s house,” Joseph might have said as he smiled down at his baby boy. They took him there that first definitive time, and they could have said to Jehovah, “Here he is, your blessed Son. Help us to care for him and put no stumbling block in the way of raising him to love and serve you.” Then to the feasts in Jerusalem a few times each year they took Jesus, and then their other children, so that Jesus became very familiar with the Temple, his true Father’s home, and knew it was his home too. You remember Hannah, the mother of Samuel presenting him at the Temple, how she had prayed long for a son, and then God heard her prayer, and soon she brought him, young as he was, to the house of the Lord and she said to Eli the priest, “‘As surely as you live, my lord, I am the woman who stood here beside you praying to the LORD. I prayed for this child, and the LORD has granted me what I asked of him. So now I give him to the LORD. For his whole life he shall be given over to the LORD.’ And he worshipped the LORD there” (I Sam. 1:26-28). Hannah had said to the Lord, “If you should give a child to me, then I will give that child to you for all the days of his life.” That is the movement and model for every Christian parent. Children are an inheritance from the Lord, and we give them back to God to serve him all their days.
5. CONSECRATION: JOSEPH AND MARY COMMITTED JESUS AS HOLY TO THE LORD.
We are told, “(as it is written in the Law of the Lord, ‘Every firstborn male is to be consecrated to the Lord’), and to offer a sacrifice in keeping with what is said in the Law of the Lord: ‘a pair of doves or two young pigeons’” (vv. 23&24).So here we are told the last step that these two young Old Testament parents took in presenting their first born child to God. On the fortieth day of the life of Jesus he was consecrated in the Temple to the Lord. You may not remember this, that every single firstborn son in Israel was considered to belong to the Lord, to spend his life working for the Lord in the Temple. But exemption was obtained for those firstborn by paying at the Temple five shekels’ redemption fee (except in the case of the tribe of Levi whose firstborn did give lifelong service in the Temple). That redemption price for Jesus was paid by Joseph and Mary. He was consecrated to the Lord but not to work only as a priest in the temple but to work as a prophet preaching the word all over the land, and to work as a king showing his power over creation, demons, sin and death, and especially as a priest and sacrifice laying himself on the altar of Golgotha. Here is the incarnate eternal Son of God, Jesus, and yet he was born under the law in order to redeem us from the curse of the law. That means he was born under sentence of death and he bore that sentence absolutely and voluntarily and he also satisfied the law’s demand for perfect obedience. The Son of Man came to give his life a ransom for many.
Then Joseph and Mary finally purchased the purification sacrifice for cleansing from their own impurity, and the sacrifice was the very cheapest, the kind of sacrifice poor folks bought, a couple of pigeons. What an elaborate business! Five great acts that every godly family under the Old Covenant should have gone through to present Jesus Christ to a life, not of being served, but to serve. But having children and raising a family is enormously influential. Raise up a child in the way that he should go and when he is old he will not depart from it.
30th September 2007 GEOFF THOMAS
Share This Sermon
- Skip to main content
- Keyboard shortcuts for audio player

- LISTEN & FOLLOW
- Apple Podcasts
- Google Podcasts
- Amazon Music
Your support helps make our show possible and unlocks access to our sponsor-free feed.
A nervous parent's guide to starting your baby on solid foods

Andee Tagle

To ensure your baby is ready to eat solid food, check for these developmental markers: good head control, the ability to sit upright with minimal support, loss of the tongue thrust reflex and an interest in food. Lindsey Balbierz for NPR hide caption
To ensure your baby is ready to eat solid food, check for these developmental markers: good head control, the ability to sit upright with minimal support, loss of the tongue thrust reflex and an interest in food.
When Marina Chaparro's baby was 6 months old, she felt that her daughter was ready to start eating solid foods. But when Chaparro offered some to her, "she would not open her mouth. Wouldn't even pick up the food!" she says.
Eventually, her baby started eating bananas three weeks later. But it made Chaparro, who is a pediatric dietician, realize, "Wow — feeding kids is hard. I had questions. I had doubts. I just imagined what other parents who didn't have the knowledge I had were going through."
Introducing your baby to solid foods can be an anxiety-inducing experience. Parents may be unsure about what to feed their baby, how to feed them or how to deal with allergies and choking hazards.

The emotional roller coaster of being a new mom
But with a little preparation and patience, you can feed your baby with confidence — and even make it "a fun, enjoyable experience," says Dr. Amna Husain, a pediatrician based in South Carolina who shares baby and child health resources on her Instagram account.
She and Chaparro, who runs Nutrichicos , a kids' nutrition organization targeted to the Latino community, answer common questions on the topic.
When should I introduce solids to my baby?
Infants should be introduced to solid foods at about 6 months of age , according to the American Academy of Pediatrics. But don't just go by the calendar. Instead, look out for these developmental markers.
- Head control: Your baby should be able to hold their head upright and steady throughout the duration of a meal, about 15 minutes.
- Sitting upright . Make sure your baby has enough trunk strength to sit up straight with minimal support to avoid choking. If you put them in a high chair and they immediately tilt over or slump down, it might not be time yet.
- Loss of tongue thrust reflexes. "They stick out their tongue if something is introduced into their mouth before they're ready," says Husain.
- Interest. "They might be curious about your food. They might open their mouth or follow it with their eyes" as you're eating, says Chaparro.

What you need to know about preparing financially for a baby
What should i feed my baby.
Babies who have shown signs of readiness should eat small amounts of soft, nutritious foods throughout the day, about a tablespoon at a time . Think mashed fruits and veggies; ground meat, fish or poultry; and grains like porridge or fortified infant cereal.
The key at this stage is to introduce a wide range of foods, says Husain. It doesn't matter if it's homemade, store-bought or takeout. Encourage your baby to eat the foods of your culture. Chaparro, who is Latina, fed her baby beans and tortillas, for example. And experiment with spices (though, when it comes to salt, be mindful — the evidence is mixed on its effect on babies).
There are benefits to variety. A baby's first year of life is a small window of opportunity in which they are extra receptive to all types of flavors and textures, according to recent research . And when they try new foods, it pays off down the line. It may increase their willingness to eat fruits and veggies later in life and decrease their risk of developing food allergies.
How should I feed my baby?
The baby is in the high chair. They've got their bib on. You're ready to feed them. But err — how? Here are a few approaches, each with their own pros and cons.

I flew to Japan with my baby. Here's the travel advice that helped me survive the trip

There are pros and cons to baby-led weaning and spoon feeding. Here, three foods are prepared in each style. On the left, avocado, banana and cooked butternut squash are sliced for a 6-month-old baby who is baby-led weaning. On the right, the same foods are prepared as soft purees for spoon feeding. Lindsey Balbierz for NPR hide caption
Baby-led weaning
In this process, babies feed themselves whole pieces of soft foods, says Husain — like slices of banana or avocado or wedges of baked sweet potato.
It can be a messy process and lead to a lot of waste, Husain says. Your little one may be interested in squishing and throwing the food rather than chewing and swallowing it. And you're likely to see a lot more gagging earlier on (more about that later) since you're starting with whole pieces of food rather than easier-to-manage purees.
But there are upsides. Advocates say BLW can foster independent eating and discourage pickiness , says Husain. And it "can help with appetite control, especially because a child is feeding themselves," not getting spoon after spoon from a parent.
Spoon feeding
With spoon feeding, parents take control of the process. You choose what your baby eats (often a spoonable food like a puree, cereal or porridge), hold the spoon and bring it to the baby's mouth.
The upside is that your baby may eat more and waste less, says Husain. The downside is that it may take your baby longer to eat independently. And some studies have shown that babies who were introduced to textures later on were more likely to develop preferences for softer foods and displayed more pickiness.
Combo-feeding
As the name implies, this is a combination of spoon feeding purees and baby-led weaning hand-held foods. Mixing the two may lead to confusion for the baby, says Husain. When should they eat with their hands? When should they eat with a spoon?
Whichever approach you use, remember that there's no right way to feed your baby. Be responsive to their needs, follow their hunger and fullness cues and let your baby lead the way, says Chaparro.
When should I introduce potential allergens to my baby? And how?
This might come as a surprise, but research shows strong evidence that introducing common allergens like eggs, peanuts, tree nuts and shellfish as soon as your baby starts solids can reduce the risk of allergies. In fact, one landmark 2015 study showed that introducing even at-risk babies to peanuts early on reduced the risk of allergy by 81%.
Introduce allergens one at a time in small amounts. Solid Starts , an online resource and app, suggests an eighth of a teaspoon. You may want to mix an allergen, say, peanut butter, into other foods like applesauce. Offer it early in the day so you'll have time to spot or treat any reactions, says Chaparro.
Watch out for allergic reactions
Hives, rash, and itching are some of the most common mild reactions . Monitor for any changes on the skin, as well as scratching, hoarse cries or other unusual behavior that might suggest discomfort.
Keep your pediatrician's phone number nearby and some allergy medication in case of more severe reactions like vomiting or diarrhea.
If there's no immediate reaction, wait a few days before introducing a new food. That way, you can be sure which new food was safe or caused a reaction, says Chaparro.
Then keep offering those common allergens. Just because your baby didn't have a reaction the first time doesn't mean it can't happen the next time, says Chaparro. And regular exposure is important for maintaining tolerance .
How do I prevent my baby from choking?
Choking can happen at any time and with anything, even liquids. To set up for success, make your baby's eating practices as safe as possible.

"If you can smush it in your hand, it should be OK for those little gums to play with," says pediatrician Dr. Amna Husain. Avoid firm, round and slippery foods, like grapes, nuts and popcorn, which can get stuck in a young child's airway. Lindsey Balbierz for NPR hide caption
Serve 'smushable' foods
"If you can smush it in your hand, it should be OK for those little gums to play with," says Husain. Think avocados, oatmeal, shredded chicken, scrambled eggs and rice.
Avoid firm, round and slippery foods, like grapes, nuts, popcorn and hard candies, says Husain. These foods can get stuck in a young child's airway, which is "about the size of a drinking straw in diameter."
Gagging vs. choking
What do you do if your baby starts sputtering? First, understand the difference between a gag and a choke.
Gags are often noisy and accompanied by a cough. "Gagging can be very frightening. But when the child is coughing or gagging, [it means] something tried to tickle their airway in such a way that their airway and their larynx spasmed and led to the gagging, but their airway is intact. They are moving air in and out because they are coughing," says Husain.
If your child is gagging, stay calm so your little one doesn't panic. Let them work through it on their own. "Watch them, comfort them, offer them small sips [of water], but don't offer another bite of food. Let them take a minute to get their bearings," says Husain.
"Choking, on the other hand, is silent," says Husain. "There is something obstructing or impacting your child's airway, so there is no noise coming out of your child." In some cases, you may hear a high-pitched noise called a stridor . It's usually caused by an obstruction in or narrowing of the airway. And you may possibly see a very panicked look on your child's face.
If a baby is choking, the evidence-backed and proven method is to do back blows followed by chest blows on your child — and then, if they're unresponsive, proceed to call 911 and do CPR .
Beware of anti-choking devices
You might have seen anti-choking devices on commercials or social media. Husain says not to rely on them. They may create a false sense of security for parents. Her No. 1 advice? Take infant CPR or brush up on that class you took already. If you have a pamphlet on it, keep that next to baby's eating area.
How do I make mealtime fun for my baby?
Create a peaceful environment, says Husain. "If your child refuses to eat, don't force them. You don't want this to be stressful for them."
And remember, introducing solids to your baby is a journey. Savor the experience, says Chaparro, and remember that "food is about family, memories and love."
The digital story was written by Malaka Gharib and edited by Andee Tagle and Meghan Keane. The visual editor is Beck Harlan. We'd love to hear from you. Leave us a voicemail at 202-216-9823, or email us at [email protected].
Listen to Life Kit on Apple Podcasts and Spotify , and sign up for our newsletter .
- Life Kit: Parenting

IMAGES
VIDEO
COMMENTS
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech ...
Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left. This is called left occiput anterior or right ...
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.. In brow presentation, the neck is moderately arched so that the brow presents first.. Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor.
Baby's head is near their mama's ribs, with their feet or knees below their buttocks. Head up, one leg up and one leg down (Incomplete or Footling Breech Presentation) In this position, one or both feet or knees are below baby's buttocks. One of baby's feet points towards the cervix and is in position be delivered first.
The vertex presentation describes the orientation a fetus should be in for a safe vaginal delivery. It becomes important as you near your due date because it tells your pregnancy care provider how they may need to deliver your baby. Vertex means "crown of the head.". This means that the crown of the fetus's head is presenting towards the ...
Usually when a baby is being born in a vertex presentation the back of the baby's head, which is called the occiput, is towards the front or anterior of your pelvis and their back is towards your belly. Their chin is also typically in a flexed position, tucked into their chest. Occiput anterior is the best and safest position for a baby to be ...
Presentation of twins in Der Rosengarten ("The Rose Garden"), a standard medical text for midwives published in 1513. In obstetrics, the presentation of a fetus about to be born specifies which anatomical part of the fetus is leading, that is, is closest to the pelvic inlet of the birth canal. According to the leading part, this is identified as a cephalic, breech, or shoulder presentation.
There are four posterior positions. The direct OP is the classic posterior position with the baby facing straight forward. Right Occiput Transverse (ROT) is a common starting position in which the baby has a bit more likelihood of rotating to the posterior during labor than to the anterior. Right Occiput Posterior usually involves a straight back with a lifted chin (in the first-time mother).
When the baby is facing outward toward the mother's left thigh, the baby is said to be right occiput transverse (ROT). Like the previous presentation, ROT is halfway between a posterior and anterior position. If the baby was previously in a posterior position, ROT is a sign the baby is making a positive move toward an anterior position.
Cephalic presentation occurs in about 97% of deliveries. There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude). If your baby is in any position other than head down, your doctor may recommend a cesarean delivery. Breech presentation is when the baby's bottom is down ...
Presentation refers to which part of your baby's body is facing towards your birth canal. Position refers to the direction your baby's head or back is facing. Your baby's presentation will be checked at around 36 weeks of pregnancy. Your baby's position is most important during labour and birth.
👉I know OB-Maternity can be overwhelming. Let me help YOU!👉Fetal Positioning, Presentation, and Station can be complex concepts that I tried to break down ...
Posterior: The head is down, and the back is in line with the pregnant person's. Transverse lie: The fetus is lying horizontally on its back. Breech: The fetus's feet point down. A fetus ...
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin.
This exhibit depicts delivery the fetus in utero with face presentation. The animation shows the baby in Right Mentum Transverse Position (RMT) and then slow...
Baby Presentation templates. When a baby arrives in a family, the reasons for joy are endless. These little creatures change our lives forever with their laughter and even their crying. To accompany you and your family in everything related to newborns, we want to do it with these Google Slides and PowerPoint templates about babies.
A baby is born or adopted into a Jewish family, and through that, into a covenantal community. From the ancient tradition of circumcision to contemporary, innovative ceremonies, a new Jewish boy or girl becomes a focal point for ritual and celebration. The choosing of a name becomes an opportunity to connect with people, stories, events, and associations that are significant to the parents.
If your baby is in any other position, it's called 'malpresentation'. Malpresentation can mean your baby's face, brow, buttocks, foot, back, shoulder, arms or legs or the umbilical cord are against the cervix. It's safest for your baby's head to come out first. If any other body part goes down the birth canal first, the risks to you ...
2:21-24 The presentation of baby Jesus. Luke 2:21-24 "On the eighth day, when it was time to circumcise him, he was named Jesus, the name the angel had given him before he had been conceived. When the time of their purification according to the Law of Moses had been completed, Joseph and Mary took him to Jerusalem to present him to the Lord ...
What should I feed my baby? Babies who have shown signs of readiness should eat small amounts of soft, nutritious foods throughout the day, about a tablespoon at a time.Think mashed fruits and ...