- News & Events
- Faculty & Staff

A world-class city filled with art and culture and an incredible campus that offers cutting edge resources–that’s what students receive at Penn Nursing. And that’s just the start. Penn Nursing and the wider university offer something for everyone, as well as a lifelong community.

Penn Nursing is globally known for educating dynamic nurses—because our School values evidence-based science and health equity. That’s where our expertise lies, whether in research, practice, community health, or beyond. Everything we do upholds a through-line of innovation, encouraging our exceptional students, alumni, and faculty share their knowledge and skills to reshape health care.

Penn Nursing students are bold and unafraid, ready to embrace any challenge that comes their way. Whether you are exploring a career in nursing or interested in advancing your nursing career, a Penn Nursing education will help you meet your goals and become an innovative leader, prepared to change the face of health and wellness.

Penn Nursing is the #1-ranked nursing school in the world. Its highly-ranked programs help develop highly-skilled leaders in health care who are prepared to work alongside communities to tackle issues of health equity and social justice to improve health and wellness for everyone.

Penn Nursing’s rigorous academic curricula are taught by world renowned experts, ensuring that students at every level receive an exceptional Ivy League education . From augmented reality classrooms and clinical simulations to coursework that includes experiential global travel to clinical placements in top notch facilities, a Penn Nursing education prepares our graduates to lead.


American Nursing: An Introduction to the Past

Professional nursing holds a unique place in the American health care system. As members of the largest health care profession, the nation’s 3.1 million nurses work in diverse settings and fields and are frontline providers of health care services. While most nurses work in acute-care settings such as hospitals, nurses’ expertise and skills extend well beyond hospital walls. Working independently and with other health care professionals, nurses promote the health of individuals, families, and communities. Millions of Americans turn to nurses for delivery of primary health care services, health care education. and health advice and counseling. Nurses are critical links in maintaining a cutting-edge health care system.Nursing continues to be an indispensable service to the American public.

Florence Nightingale

Nursing and Hospital Care in the United States

The Beginnings of Nurse Education

The outbreak of the Civil War created an immediate need for capable nurses to care for the enormous number of sick and wounded. About 20,000 women and men served as nurses in both the North and the South. The commendable service rendered by Civil War nurses provided a rationale for future experiments in setting up training programs for nursing. One such program was initiated in Pennsylvania where the Women’s Hospital of Philadelphia offered a six months nurse training course, which graduated its first class in 1869. Similar courses, such as that offered by the New England Hospital for Women and Children were begun in other locales.
Professional Nurse Education Begins

The success of these first three so-called “Nightingale schools” led to a proliferation of similar nursing schools, or as they were most commonly called, nurse training programs. By 1900, somewhere between 400 to 800 schools of nursing were in operation in the country. These programs followed a fairly typical pattern. The school was either affiliated with or owned by a hospital that provided the students with the clinical experience considered necessary for the education of a nurse. Students received two to three years of training. While in the program students carried out the majority of patient care activities offered in the hospital, receiving only a modicum of classroom education in the form of lectures on patient care and related subjects. At the end of the educational program, students received a diploma and were eligible to seek work as a trained nurse .

The Profession of Nursing Organizes

These changes improved and reformed many aspects of the nurse training system, but problems remained. Reflecting the social and legal status of African Americans at the time, American professional nursing maintained strict racial segregation until the mid-twentieth century. African American individuals wanting to become nurses had to train in a separate educational system and faced a divided employment field in which white and black nurses did not participate equally. Nursing also remained a predominantly female profession. While a few schools admitted men, most schools refused them admission.
Challenges for Nursing
Employment conditions for nurses also presented challenges. In the early part of the twentieth century, hospitals employed only a few graduate nurses, mainly in supervisory positions. They relied instead on student nurses for the majority of the bedside care provided to patients. Most nurses, once they graduated from their educational program, entered the field of private duty nursing. Private duty nurses were employed by individual patients primarily in their homes. As institutions became the more normative site for delivery of sick care, private duty nurses moved with their patients into the hospital, delivering care to hospitalized individuals who could afford to pay for their own nurse. But for nurses, private duty often did not provide regular and dependable employment; nurses were hired on an ad hoc basis by patients and were oftentimes without a regular source of income. The cost of private duty was also quite high, limiting the number of patients employing private duty nurses. It was not until the mid-twentieth century that hospitals hired nurses as regular staff on a permanent basis, providing full professional nursing services to all hospitalized patients.
Nursing Diversifies
Despite the many difficulties within the profession, nursing continued to grow as an occupational field and became recognized as an essential health care service by the early twentieth century. Nurses fanned out into diverse fields delivering services to many people outside of hospitals. For example, Lillian Wald founded the Henry Street Settlement House in 1893, which provided nursing and other social services to impoverished populations on the Lower East Side of New York City. Replication of Wald’s work in other parts of the country led to the growth of the field of public health nursing, opening up new employment opportunities for nurses and expanding the type of services provided by nurses.

The special skills possessed by nurses were easily transferred to different fields of health care. For example, nurses were educated to administer anesthesia during surgery, leading to the specialty field of nurse anesthetists. By the early twentieth century it was quite common to find nurse anesthetists delivering anesthesia in many of the nation’s hospitals. By the 1920s, in some parts of the country, nurse-midwives delivered babies, in many cases to the most impoverished populations.

Mid-twentieth Century Nursing

The community college movement achieved only partial success. Community college programs did graduate many new nurses and often at a lower cost than traditional diploma programs. But, as the needs of late-twentieth-century patients became increasingly more complex, research studies indicated that being treated by nurses prepared at the baccalaureate level improved patient outcomes.
The Modern Practice of Nursing

Nursing education also thrived in the latter half of the twentieth century. Significant federal financial support for educating nurses, which became available beginning in the 1960s, permitted the revamping and modernizing of many nursing educational programs. Significantly, increased funding for nursing research permitted nursing to develop a sounder scientific basis for its practice. Nurse researchers today carry out cutting-edge studies that shed light on the ways and means of solving many health care problems and improving nursing services.

Historically, the nursing profession has consistently demonstrated its ability to adapt to changing and varied health care needs. It remains an exceedingly popular and highly respected profession that attracts large numbers of new recruits to its ranks. There is little doubt that nursing will continue to maintain its status as an extremely important profession, serving the health needs of the nation.
Jean C. Whelan (1949-2017) was Adjunct Assistant Professor of Nursing, University of Pennsylvania School of Nursing.
Related Links
Barbara Bates Center for the Study of the History of Nursing
See Yourself Here


Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
2 Health History
Learning objectives.
- Describe the purpose of a health history
- Enumerate the components of a health history.
- Discuss how culture, age and ethnicity influence obtaining a health history.
- Demonstrates therapeutic communication when obtaining a health history.
- Obtain a comprehensive health history
- Document the results of the health history
Overview of this chapter
This chapter presents the importance of a health history as a component of health assessment and the value of a health history obtained from the perspective of a nurse. This chapter will provide information on components of a health history, considerations in obtaining a health history and documentation.
Health History
The purpose of obtaining a health history is to gather subjective data from the patient and/or the patient’s family so that the health care team and the patient can collaboratively create a plan that will promote health, address acute health problems, and minimize chronic health conditions. The health history is typically done on admission to hospital, but a health history may be taken whenever additional subjective information from the patient may be helpful to inform care (Wilson & Giddens, 2013).
Subjective Data
Data gathered may be subjective or objective in nature. Subjective data is information reported by the patient and may include signs and symptoms described by the patient but not noticeable to others. Subjective data also includes demographic information, patient and family information about past and current medical conditions, and patient information about surgical procedures and social history. Objective data is information that the health care professional gathers during a physical examination and consists of information that can be seen, felt, smelled, or heard by the health care professional. Taken together, the data collected provides a health history that gives the health care professional an opportunity to assess health promotion practices and offer patient education (Stephen et al., 2012). The health history is the subjective data collection portion of the health assessment.
Components of a Health History
The health history obtained by nurses is framed from holistic perspectives of all factors that contributes to the patient’s current health status. The most common way of obtaining information is through an interview, primarily of the patient. When the patient is unable to provide information for various reasons, the nurse may obtain it from secondary sources.
Knowledge Check:
The checklist below provides steps of obtaining a nursing history based that reflects its components such as biographical data, reason for seeking care, history of present illness, past health history, family history, functional assessment, developmental functions and cultural assessment. Each healthcare facility will have electronic and/or paper forms based on these components.
Interview Guide
Introductory Information: Demographic and Biographic Data
Name/contact information and emergency information
- What is your full name?
- What name do you prefer to be called by?
- What is your address?
- What is your phone number?
- Who can we contact in an emergency? What is their relationship to you? What number can we reach them at?
Birthdate and age
- What is your birthdate?
- What is your age?
- Tell me what gender you identify with.
- What pronouns do you use? (If the person asks you to use a pronoun that you are not familiar with, it is okay for you to respectfully respond, “I am not familiar with that pronoun. Can you tell me more about it?”)
- Do you have any allergies?
- If so, what are you allergic to?
- How do you react to the allergy?
- What do you do to prevent or treat the allergy?
Note: You may need to prompt for information on medications, foods, etc.
Languages spoken and preferred language
- What languages do you speak?
- What language do you prefer to communicate in (verbally and written)?
Note: You may need to inquire and document if the client requires an interpreter.
Relationship status
- Tell me about your relationship status?
Occupation/school status
- What is your occupation? Where do you work?
- Do you go to school?
Resuscitation status
- We ask all clients about their resuscitation status, which refers to medical interventions that are used or not used in the case of an emergency (such as if your heart or breathing stops). You may need more time to think about this, and you may want to speak with someone you trust like a family member or friend. You should also know that you can change your mind. At this point, if any of this happens, would you like us to intervene?
Main Health Needs (Reasons for Seeking Care)
Presenting to a clinic or a hospital emergency or urgent care (first point of contact)
- Tell me about what brought you here today.
- Tell me more.
- How is that affecting you?
Already admitted, and you are starting your shift
- Tell me about your main health concerns today.
The PQRSTU Mnemonic
Provocative
- What makes your pain worse?
- What makes your pain feel better?
- What does the pain feel like?
- How bad is your pain?
- Where do you feel the pain?
- Point to where you feel the pain.
- Does the pain move around?
- Do you feel the pain elsewhere?
- How would you rate your pain on a scale of 0 to 10, with 0 being no pain and 10 being the worst pain you’ve ever experienced?
- When did the pain start?
- What were you doing when the pain started?
- Where were you when the pain started?
- Is the pain constant or does it come and go?
- If the pain is intermittent, when did it last occur?
- How long does the pain last?
- Have you taken anything to help relieve the pain?
- Have you tried any treatments at home for the pain?
Understanding
- What do you think is causing the pain?
Current and Past Health
Current health
- Are there any other issues affecting your current health?
Childhood illnesses
- Tell me about any significant childhood illnesses that you had.
- When did it occur?
- How did it affect you?
- How did it affect your day-to-day life?
- Were you hospitalized? Where? How was it treated?
- Who was the treating practitioner?
- Did you experience any complications?
- Did it result in a disability?
Chronic illnesses
- Tell me about any chronic illnesses you currently have or have had (e.g., cancer, cardiac, hypertension, diabetes, respiratory, arthritis).
- How has the illness affected you?
- How do you cope with the illness?
- When were you diagnosed?
- How was the illness being treated?
- Have you been hospitalized? Where?
- Have you experienced any complications?
- Has the illness resulted in a disability?
- How does the illness affect your day-to-day life?
Acute illnesses, accidents, or injuries
- Tell me about any acute illnesses that you have had.
- Tell me about any accidents or injuries you currently have or have had.
- Were you hospitalized? Where?
- How was it treated?
- Has it resulted in a disability?
Obstetrical health
- Have you ever been pregnant?
- Do you have plans to get pregnant in the future?
- Tell me about your pregnancies.
- Have you ever had difficulty conceiving?
- How was your labour and delivery?
- Tell me about your postpartum experience.
- Were there any issues or complications?
Mental Health and Mental Illnesses
Mental health is an important part of our lives and so I ask all clients about their mental health and any concerns or illnesses they may have.
Mental health
- Tell me about your mental health.
- Tell me about the stress in your life.
- How does stress affect you?
- How do you cope with this stress? (this may include positive or negative coping strategies.)
- Have you experienced a loss in your life or a death that is meaningful to you?
- Have you had a recent breakup or divorce?
- Have you recently lost your job or been off work?
- Have you recently had any legal issues?
- Have you purchased any weapons?
Mental illness
- How does that illness affect you?
- How does that illness affect your day-to-day life?
- What resources do you draw upon to cope with your illness?
- Tell me about your treatment (e.g., medications, counselling).
- Do you have any concerns that have not been addressed related to your illness?
Functional Health
- Tell me about your diet.
- What foods do you eat?
- What fluids do you drink? (Probe about caffeinated beverages, pop, and energy drinks.)
- What have you consumed in the last 24 hours? Is this typical of your usual eating pattern?
- Do you purchase and prepare your own meals?
- Tell me about your appetite. Have you had any changes in your appetite?
- Do you have any goals related to your nutrition?
- Do you have the financial capacity to purchase the foods you want to eat?
- Do you have the knowledge and time to prepare the meals you want to eat?
Elimination
- How often do you urinate each day?
- What colour is it (amber, clear, dark)?
- Have you noticed a strong odour?
- How often do you have a bowel movement?
- What colour is it (brown, black, grey)?
- Is it hard or soft?
- Do you have any problems with constipation or diarrhea? If so, how do you treat it?
- Do you take laxatives or stool softeners?
Sleep and rest
- Tell me about your sleep routine.
- How much do you sleep?
- Do you wake up at all?
- Do you feel rested when you wake? What do you do before you go to bed (e.g., use the phone, watch TV, read)?
- Do you take any sleep aids?
- Do you have any rests during the day?
Mobility, activity, exercise
- Tell me about your ability to move around.
- Do you have any problems sitting up, standing up or walking?
- Do you use any mobility aids (e.g., cane, walker, wheelchair)?
- Tell me about the activity and/or exercise that you engage in. What type? How frequent? For how long?
Violence and trauma
- Many clients experience violence or trauma in their lives. Can you tell me about any violence or trauma in your life?
- How has it affected you?
- Tell me about the ways you have coped with it.
- Have you ever talked with anyone about it before?
- Would you like to talk with someone?
Relationships and resources
- Tell me about the most influential relationships in your life.
- Tell me about the relationships you have with your family.
- Tell me about the relationships you have with your friends.
- Tell me about the relationships you have with any other people.
- How do these relationships influence your day-to-day life? Your health and illness?
- Who are the people that you talk to when you require support or are struggling in your life?
Intimate and sexual relationships
- I always ask clients about their intimate and sexual relationships. To start, tell me about what you think is important for me to know about your intimate and sexual relationships.
- Tell me about the ways that you ensure your safety when engaging in intimate and sexual practices.
- Do you have any concerns about your safety?
Substance use and abuse
- To better understand a client’s overall health, I ask everyone about substance use such as tobacco, herbal shisha, alcohol, cannabis, and illegal drugs.
- Do you or have you ever used any tobacco products (e.g., cigarettes, pipes, vaporizers, hookah)? If so, how much?
- When did you first start? If you used to use, when did you quit?
- Do you drink alcohol or have you ever? If so, how often do you drink?
- How many drinks do you have when you drink?
- When did you first start drinking? If you used to drink, when did you quit?
- Do you use or have you used any cannabis products? If so, how do you use them? How often do you use them?
- When did you first start using them?
- Do you purchase them from a regulated or unregulated place?
- If you used to use cannabis, when did you quit?
- Do you use any illegal drugs? If so, what type? How often do you use them?
- Tell me about the ways that you ensure your safety when using any of these substances.
- Have you ever felt you had a problem with any of these substances?
- Do you want to quit any of these substances?
- Have you ever tried to quit?
Environmental health and home/occupational/school health
- Tell me about any factors in your environment that may affect your health. Do you have any concerns about how your environment is affecting your health?
- Tell me about your home. Do you have any concerns about safety in your home or neighbourhood?
- Tell me about your workplace and/or school environment.
- What activities are you involved in or what does your day look like?
Self-concept and self-esteem
- Tell me what makes you who you are.
- Are you satisfied about where you are in your life?
- Can you share with me your life goals?
- Please explain.
- Tell me about how you take care of yourself and manage your home.
- Do you have sufficient finances to pay your bills and purchase food, medications, and other needed items?
- Do you have any current or future concerns about being able to function independently?
Preventive Treatments and Examinations
Medications
- Do you have the most current list of your medications?
- Do you have your medications with you? (If not, you should ask them to list each medication they are prescribed and if they know, the dose and frequency.)
- Can you tell me why you take this medication?
- How long have you been taking this medication?
- Do you take the medications as prescribed? (If they answer “no” or “sometimes,” ask them to tell you the reasons for not taking the medications as prescribed.)
Examination and diagnostic dates
- When was the last time you saw [name the primary care provider, nurse or specialist]?
- Can you share with me why you saw them?
- When was the last time you had your [name screening] tested?
- Do you know what the results were?
Vaccinations
- Can you tell me about your immunization status?
- Can you tell me what immunizations you have had, the dates you received them, and any significant reactions?
- Do you have your immunization record?
- When was your last flu vaccine?
If the client’s immunizations are not up-to-date or you noted vaccination hesitancy, you may ask:
- Can you tell me the reasons that your immunizations are not up-to-date?
- Can you tell me why you are hesitant to receive immunizations. (You may need to explore this further.)
Family Health
- Do they have any chronic or acute diseases (e.g., cardiac, cancer, mental health issues)?
- If so, do you know the cause of death?
- And at what age did they die?
- Has anyone been sick recently?
- If so, do you know the cause?
- What symptoms have they had?
- Have you been around anyone else who was sick recently (e.g., at work, at school, in a location that involved a close encounter such as a plane or an office)?
Cultural Health
- I am interested in your cultural background as it relates to your health. Can you share with me what is important about your cultural background that will help me care for you?
- How does that affect your health and illnesses?
- Is there anything else you want to share about how these factors act as resources in your life?
Learning Resource: Open the link below for more detailed information.
The Complete Subjective Health Assessment
Cultural factors in obtaining a health history
When interviewing a patient the nurse must be aware of cultural barriers and preferences in order to collect significant and complete subjective data.. For example due to age, culture, or ethnicity, some patients may believe that pain is to be expected and endured. The patient may not identify their pain as worthy of report unless the nurse is sensitive to this potential barrier of care. Due to age, culture or ethnicity, some patients may feel uncomfortable discussing sexual health. For example, where HIV is epidemic, it is the nurse’s responsibility (along with all other healthcare personal) to uncover risk factors that can address safety and early treatment for STIs (sexually transmitted diseases). Culture can have many meanings. Some of the many aspects that nurses need to be aware of that will impact information obtained in a health history include gender identity, religion, geographical region, and many diverse factors. The nurse must be open to learning about various cultures and ethnicity and be comfortable in initiating a cultural assessment, and use this knowledge to enhance communication to obtain the most accurate health history.
Health history and therapeutic communication

Needless to say, therapeutic communication techniques are essential in obtaining a health history. However, due to many reasons, healthcare professionals, including nurses, oftentimes fail to establish a therapeutic relationship or to deliver therapeutic communication. The following are examples :
- Have you ever been to see a healthcare provider and when they walk in the room they are not looking at you but are looking at the chart, or tapping on a computer.
- Have you ever felt rushed by their questions, like they are in a hurry and need to move on to the next patient?
- Have you ever had the healthcare provider give you a diagnosis, provide you with a treatment and you left with a prescription but you didn’t grasp the entire explanation?
The nurse should apply communication and interpersonal skills to create, maintain, and terminate a nurse-client relationship. [] Nurses and other healthcare professionals need to use therapeutic communication techniques at all times.
Open the link below for more detailed information
Therapeutic Communication
Documentation of Health History:
The patient’s health history is initially obtained during admission or initial visit, and constantly updated with subsequent interactions or visits. Documentation of information obtained during the nurse-patient interview, and/or secondary sources will need to be documented on a format that the healthcare facility uses. Nowadays, most healthcare facilities use electronic health records (EHR). EHRs are accessed by various members of the healthcare team in real-time, and this indicates that information obtained can be recorded during the interview process as well. The nurse needs to develop the competency to maintain therapeutic communication techniques while attending to the electronic health record keeping. Healthcare facilities use different documentation systems. Nurses will need to learn facility specific documentation system, whether electronic or paper, but the contents of a patient history will largely be similar.
Learning Exercises
LaPierre, D. (2010). Clinical assessment. Sharing in health.ca:open access training in healthcare.Retrieved at http://www.sharinginhealth.ca/clinical_assessment/clinical_assessment.html
Nursing Documentation https://hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/provider-portal/QMP/NurseDocumentationPPT.pdf
Sharma, N and Gupta, V ( 2021). Therapeutic Communication. https://www.statpearls.com/articlelibrary/viewarticle/127665/?utm_source=pubmed&utm_campaign=reviews&utm_content=127665#
Taylor, C., Lillis, C., Lynn, P., & LeMone, P. (2015). Fundamentals of nursing: The art and science of person-centered nursing care(8th ed.). Philadelphia: Wolters Kluwer Health.
Wilson, S., Giddens, J., (2013). Health assessment for nursing
https://pressbooks.library.ryerson.ca/documentation/
Health Assessment Guide for Nurses Copyright © by Ching-Chuen Feng; Michelle Agostini; and Raquel Bertiz is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
- Pre-Nursing
- Nursing School
- After Graduation
Health History Data Collection in Nursing Assessments: A Guide

As aspiring nurses, understanding the significance of health history data collection in nursing assessments is paramount. It forms the foundation for delivering exceptional client care and developing personalized treatment plans.
Effectively conducting health history assessments is integral to a nurse’s role in delivering client-centered care. By meticulously collecting and documenting essential health information, nurses can assist health care teams in making well-informed decisions and implementing personalized treatment plans.
Health history data collection is a dynamic process that requires active listening, empathy, and strong communication skills. As nursing students, practice active listening during client interviews and take notes meticulously. Be mindful of verbal and non-verbal cues that provide additional insights into the client’s health concerns.
Moreover, always approach health history assessments without judgment. Clients may feel vulnerable sharing sensitive information, and creating a safe and non-threatening environment to facilitate open and honest conversations is essential.
How to Assess Health History
Nurses play a pivotal role in gathering vital information about clients’ health and medical backgrounds when conducting health history assessments.
During the interview, encourage clients to express their thoughts and concerns freely. Avoid interrupting them. And if necessary, use open-ended questions to elicit more detailed responses. Remember, client-centered care is all about empowering individuals to actively participate in their health management.
This process involves thorough client interviews, careful documentation, and attention to detail.
Let’s explore the essential steps for assessing health history:
- Establish Rapport: Building a strong rapport is crucial before diving into a client’s health history. Establishing a trusting and compassionate relationship with the client will encourage open communication and lead to more accurate information.
- Collect Demographic Information: Begin the assessment by gathering basic demographic details, such as the client’s name, age, gender, and contact information. This information is essential for creating accurate and organized client records.
- Comprehensive Medical History: Ask about any previous medical conditions, surgeries, or hospitalizations the client has experienced. Pay close attention to chronic illnesses, allergies, and family medical history, as they can significantly impact current and future treatments.
- Medication and Allergies: Document the client’s current medications, including prescription drugs, over-the-counter medicines, and herbal supplements. Be sure to inquire about any allergies to medications or specific substances to prevent adverse reactions.
- Lifestyle Factors: Understanding a client’s lifestyle choices, such as diet, exercise routine, smoking habits, and alcohol consumption, can help identify potential risk factors and develop tailored health promotion strategies.
- Psychosocial History: Inquire about the client’s social support system, occupation, living environment, and any significant life events. These factors can influence the client’s well-being and healthcare decisions.
Example of Nursing Health History Assessment
To better grasp the concept of health history documentation, let’s walk through an example of a nursing assessment for a fictional client named Mr. Smith, a 55-year-old man seeking treatment for persistent lower back pain.
Client: Mr. Smith
Gender: Male
Contact: 555-123-4567
Medical History:
- Hypertension (diagnosed at age 45)
- Hyperlipidemia (diagnosed at age 48)
- Appendectomy at age 32
- Allergic to Penicillin
Medications:
- Lisinopril 10mg once daily for hypertension
- Simvastatin 20mg once daily for hyperlipidemia
- Sedentary lifestyle, no regular exercise routine
- Occasional alcohol consumption (social gatherings)
Psychosocial:
- Married, living with wife and two adult children
- Retired accountant
- Significant life event: Recent loss of his mother, whom he was very close to
Enhance Your Nursing Assessments
As you embark on your nursing journey, remember that health history data collection is the foundation of providing quality client care. Practice your interviewing and documentation skills regularly to become a skilled and compassionate nurse.
Utilizing digital nursing study tools can enhance your learning experience and prepare you to significantly impact the healthcare field.
SimpleNursing offers personalized study plans, question banks, lecture series, videos with rationales, and much more to boost your nursing knowledge.
Start with a free trial today .
Want to ace Nursing School Exams & the NCLEX?
Make topics click with easy-to-understand videos & more. We've helped over 1,000,000 students & we can help you too.
Share this post
Nursing students trust simplenursing.

SimpleNursing Student Testimonial
Most recent posts.

How to Accurately Measure on a Syringe
What’s one of the most important aspects of using a syringe correctly? The ability to…

What do You Bring to the NCLEX on Exam Day?
It's the day of the exam... the day you've been anticipating for quite some time.…

Biceps Brachii
If you've ever flexed your arm to see if all the hard work you put…

Last-Minute NCLEX Tips & Day-Before Strategies
After graduating from nursing school, the culmination of your education and training is put to…
Find what you are interested in
- History Classics
- Your Profile
- Find History on Facebook (Opens in a new window)
- Find History on Twitter (Opens in a new window)
- Find History on YouTube (Opens in a new window)
- Find History on Instagram (Opens in a new window)
- Find History on TikTok (Opens in a new window)
- This Day In History
- History Podcasts
- History Vault
Florence Nightingale
By: History.com Editors
Updated: April 24, 2023 | Original: November 9, 2009

Florence Nightingale (1820-1910), known as “The Lady With the Lamp,” was a British nurse, social reformer and statistician best known as the founder of modern nursing. Her experiences as a nurse during the Crimean War were foundational in her views about sanitation. She established St. Thomas’s Hospital and the Nightingale Training School for Nurses in 1860. Her efforts to reform healthcare greatly influenced the quality of care in the 19 and 20 centuries.
Florence Nightingale: Early Life
Florence Nightingale was born on May 12, 1820, in Florence, Italy to Frances Nightingale and William Shore Nightingale. She was the younger of two children. Nightingale’s affluent British family belonged to elite social circles. Her mother, Frances, hailed from a family of merchants and took pride in socializing with people of prominent social standing. Despite her mother’s interest in social climbing, Florence herself was reportedly awkward in social situations. She preferred to avoid being the center of attention whenever possible. Strong-willed, Florence often butted heads with her mother, whom she viewed as overly controlling. Still, like many daughters, she was eager to please her mother. “I think I am got something more good-natured and complying,” Florence wrote in her own defense, concerning the mother-daughter relationship.
Florence’s father was William Shore Nightingale, a wealthy landowner who had inherited two estates—one at Lea Hurst, Derbyshire, and the other in Hampshire, Embley Park—when Florence was five years old. Florence was raised on the family estate at Lea Hurst, where her father provided her with a classical education, including studies in German, French and Italian.
From a very young age, Florence Nightingale was active in philanthropy, ministering to the ill and poor people in the village neighboring her family’s estate. By the time she was 16 years old, it was clear to her that nursing was her calling. She believed it to be her divine purpose.
When Nightingale approached her parents and told them about her ambitions to become a nurse, they were not pleased. In fact, her parents forbade her to pursue nursing. During the Victorian Era , a young lady of Nightingale’s social stature was expected to marry a man of means—not take up a job that was viewed as lowly menial labor by the upper social classes.
When Nightingale was 17 years old, she refused a marriage proposal from a “suitable” gentleman, Richard Monckton Milnes. Nightingale explained her reason for turning him down, saying that while he stimulated her intellectually and romantically, her “moral…active nature…requires satisfaction, and that would not find it in this life.” Determined to pursue her true calling despite her parents’ objections, in 1844, Nightingale enrolled as a nursing student at the Lutheran Hospital of Pastor Fliedner in Kaiserwerth, Germany.
Florence Nightingale and Nursing
In the early 1850s, Nightingale returned to London, where she took a nursing job in a Middlesex hospital for ailing governesses. Her performance there so impressed her employer that Nightingale was promoted to the superintendent within just a year of being hired. The position proved challenging as Nightingale grappled with a cholera outbreak and unsanitary conditions conducive to the rapid spread of the disease. Nightingale made it her mission to improve hygiene practices, significantly lowering the death rate at the hospital in the process. The hard work took a toll on her health. She had just barely recovered when the biggest challenge of her nursing career presented itself.
Florence Nightingale and the Crimean War
In October of 1853, the Crimean War broke out. The British Empire was at war against the Russian Empire for control of the Ottoman Empire . Thousands of British soldiers were sent to the Black Sea, where supplies quickly dwindled. By 1854, no fewer than 18,000 soldiers had been admitted into military hospitals.
At the time, there were no female nurses stationed at hospitals in Crimea. The poor reputation of past female nurses had led the war office to avoid hiring more. But, after the Battle of Alma, England was in an uproar about the neglect of their ill and injured soldiers, who not only lacked sufficient medical attention due to hospitals being horribly understaffed but also languished in appallingly unsanitary and inhumane conditions.
In late 1854, Nightingale received a letter from Secretary of War Sidney Herbert, asking her to organize a corps of nurses to tend to the sick and fallen soldiers in the Crimea. Nightingale rose to her calling. She quickly assembled a team of 34 nurses from a variety of religious orders and sailed with them to the Crimea just a few days later.
Although they had been warned of the horrid conditions there, nothing could have prepared Nightingale and her nurses for what they saw when they arrived at Scutari, the British base hospital in Constantinople . The hospital sat on top of a large cesspool, which contaminated the water and the hospital building itself. Patients lay on in their own excrement on stretchers strewn throughout the hallways. Rodents and bugs scurried past them. The most basic supplies, such as bandages and soap, grew increasingly scarce as the number of ill and wounded steadily increased. Even water needed to be rationed. More soldiers were dying from infectious diseases like typhoid and cholera than from injuries incurred in battle.
The no-nonsense Nightingale quickly set to work. She procured hundreds of scrub brushes and asked the least infirm patients to scrub the inside of the hospital from floor to ceiling. Nightingale herself spent every waking minute caring for the soldiers. In the evenings she moved through the dark hallways carrying a lamp while making her rounds, ministering to patient after patient. The soldiers, who were both moved and comforted by her endless supply of compassion, took to calling her “the Lady with the Lamp.” Others simply called her “the Angel of Crimea.” Her work reduced the hospital’s death rate by two-thirds.
In addition to vastly improving the sanitary conditions of the hospital , Nightingale created a number of patient services that contributed to improving the quality of their hospital stay. She instituted the creation of an “invalid’s kitchen” where appealing food for patients with special dietary requirements was cooked. She established a laundry so that patients would have clean linens. She also instituted a classroom and a library for patients’ intellectual stimulation and entertainment. Based on her observations in Crimea, Nightingale wrote Notes on Matters Affecting the Health, Efficiency and Hospital Administration of the British Army , an 830-page report analyzing her experience and proposing reforms for other military hospitals operating under poor conditions. The book would spark a total restructuring of the War Office’s administrative department, including the establishment of a Royal Commission for the Health of the Army in 1857.
Nightingale remained at Scutari for a year and a half. She left in the summer of 1856, once the Crimean conflict was resolved, and returned to her childhood home at Lea Hurst. To her surprise, she was met with a hero’s welcome, which the humble nurse did her best to avoid. The Queen rewarded Nightingale’s work by presenting her with an engraved brooch that came to be known as the “Nightingale Jewel” and by granting her a prize of $250,000 from the British government.
Florence Nightingale, Statistician
With the support of Queen Victoria , Nightingale helped create a Royal Commission into the health of the army. It employed leading statisticians of the day, William Farr and John Sutherland, to analyze army mortality data, and what they found was horrifying: 16,000 of the 18,000 deaths were from preventable diseases—not battle. But it was Nightingale’s ability to translate this data into a new visual format that really caused a sensation. Her polar area diagram, now known as a “Nightingale Rose Diagram,” showed how the Sanitary Commission’s work decreased the death rate and made the complicated data accessible to all, inspiring new standards for sanitation in the army and beyond. She became the first female member of the Royal Statistical Society and was named an honorary member of the American Statistical Association.
Florence Nightingale’s Impact on Nursing
Nightingale decided to use the money to further her cause. In 1860, she funded the establishment of St. Thomas’ Hospital, and within it, the Nightingale Training School for Nurses. Nightingale became a figure of public admiration. Poems, songs and plays were written and dedicated in the heroine’s honor. Young women aspired to be like her. Eager to follow her example, even women from the wealthy upper classes started enrolling at the training school. Thanks to Nightingale, nursing was no longer frowned upon by the upper classes; it had, in fact, come to be viewed as an honorable vocation.
While at Scutari, Nightingale had contracted “Crimean fever” and would never fully recover. By the time she was 38 years old, she was homebound and bedridden and would be so for the remainder of her life. Fiercely determined and dedicated as ever to improving health care and alleviating patients’ suffering, Nightingale continued her work from her bed.
Residing in Mayfair, she remained an authority and advocate of health care reform, interviewing politicians and welcoming distinguished visitors from her bed. In 1859, she published Notes on Hospitals , which focused on how to properly run civilian hospitals.
Throughout the U.S. Civil War , she was frequently consulted about how to best manage field hospitals. Nightingale also served as an authority on public sanitation issues in India for both the military and civilians, although she had never been to India herself.
In 1908, at the age of 88, she was conferred the merit of honor by King Edward. In May of 1910, she received a congratulatory message from King George on her 90th birthday.
Florence Nightingale: Death and Legacy
In August 1910, Florence Nightingale fell ill but seemed to recover and was reportedly in good spirits. A week later, on the evening of Friday, August 12, 1910, she developed an array of troubling symptoms. She died unexpectedly at 2 p.m. the following day, Saturday, August 13, 1910, at her home in London.
Characteristically, she had expressed the desire that her funeral be a quiet and modest affair, despite the public’s desire to honor Nightingale—who tirelessly devoted her life to preventing disease and ensuring safe and compassionate treatment for the poor and the suffering. Respecting her last wishes, her relatives turned down a national funeral. The “Lady with the Lamp” was laid to rest in Hampshire, England.
The Florence Nightingale Museum, which sits at the site of the original Nightingale Training School for Nurses, houses more than 2,000 artifacts commemorating the life and career of the “Angel of the Crimea.” To this day, Florence Nightingale is broadly acknowledged and revered as the pioneer of modern nursing.
Florence Nightingale: Saving Lives With Statistics. BBC. Florence Nightingale. The National Archives, UK.

Sign up for Inside History
Get HISTORY’s most fascinating stories delivered to your inbox three times a week.
By submitting your information, you agree to receive emails from HISTORY and A+E Networks. You can opt out at any time. You must be 16 years or older and a resident of the United States.
More details : Privacy Notice | Terms of Use | Contact Us

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.


2.2: Health History Basic Concepts
- Last updated
- Save as PDF
- Page ID 44505

- Ernstmeyer & Christman (Eds.)
- Chippewa Valley Technical College via OpenRN
During a health history, the nurse collects subjective data from the patient, their caregivers, and/or family members using focused and open-ended questions. Before discussing the components of a health history, let’s review some important concepts related to assessment and communicating effectively with patients.
Subjective Versus Objective Data
Obtaining a patient’s health history is a component of the Assessment phase of the nursing process. Information obtained while performing a health history is called subjective data. Subjective data is information obtained from the patient and/or family members and can provide important cues about functioning and unmet needs requiring assistance. Subjective data is considered a symptom because it is something the patient reports. When documenting subjective data in a progress note, it should be included in quotation marks and start with verbiage such as, “The patient reports…” or “The patient’s wife states…” An example of subjective data is when the patient reports, “I feel dizzy.”
A patient is considered the primary source of subjective data. Secondary sources of data include information from the patient’s chart, family members, or other health care team members. Patients are often accompanied by their care partners. Care partners are family and friends who are involved in helping to care for the patient. For example, parents are care partners for children; spouses are often care partners for each other, and adult children are often care partners for their aging parents. When obtaining a health history, care partners may contribute important information related to the health and needs of the patient. If data is gathered from someone other than the patient, the nurse should document where the information is obtained.
Objective data is information observed through your senses of hearing, sight, smell, and touch while assessing the patient. Objective data is obtained during the physical examination component of the assessment process. Examples of objective data are vital signs, physical examination findings, and laboratory results. An example of objective data is recording a blood pressure reading of 140/86. Subjective data and objective data are often recorded together during an assessment. For example, the symptom the patient reports, “I feel itchy all over,” is documented in association with the sign of an observed raised red rash located on the upper back and chest.
Addressing Barriers and Adapting Communication
It is vital to establish rapport with a patient before asking questions about sensitive topics to obtain accurate data regarding the mental, emotional, and spiritual aspects of a patient’s condition. When interviewing a patient, also consider the patient’s developmental status and level of understanding. Ask one question at a time and allow adequate time for the patient to respond. If the patient does not provide an answer even with additional time, try rephrasing the question in a different way for improved understanding.
If any barriers to communication exist, adapt your communication to that patient’s specific needs. For more information about potential communication barriers and strategies for adapting communication, visit the “ Communication ” chapter in Open RN Nursing Fundamentals .
Cultural Safety
It is important to conduct a health history in a culturally safe manner. Cultural safety refers to the creation of safe spaces for patients to interact with health professionals without judgment or discrimination. Focus on factors related to a person’s cultural background that may influence their health status. It is helpful to use an open-ended question to allow the patient to share what they believe to be important. For example, ask “I am interested in your cultural background as it relates to your health. Can you share with me what is important to know about your cultural background as part of your health care?”
If a patient’s primary language is not English, it is important to obtain a medical translator, as needed, prior to initiating the health history. The patient’s family member or care partner should not interpret for the patient. The patient may not want their care partner to be aware of their health problems or their care partner may not be familiar with correct medical terminology that can result in miscommunication.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Skills [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021.

Nursing Skills [Internet].
- About Open RN
Chapter 2 Health History
2.1. health history introduction, learning objectives.
- Establish a therapeutic nurse-patient relationship
- Use effective verbal and nonverbal communication techniques
- Collect health history data
- Modify assessment techniques to reflect variations across the life span and cultural variations
- Document actions and observations
- Recognize and report significant deviations from norms
“‘Sickness’ is what is happening to the patient. Listen to them.” [ 1 ]
The profession of nursing is defined by the American Nurses Association as “the protection, promotion, and optimization of health and abilities, prevention of illness and injury, facilitation of healing, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, groups, communities, and populations.” [ 2 ] Simply put, nurses treat human responses to health problems and/or life processes. Nurses look at each person holistically, including emotional, spiritual, psychosocial, and physical health needs. They also consider problems and issues that the person experiences as a part of a family and a community. To collect detailed information about a patient’s human response to illness and life processes, nurses perform a health history. A health history is part of the Assessment phase of the nursing process. It consists of using directed, focused interview questions and open-ended questions to obtain symptoms and perceptions from the patient about their illnesses, functioning, and life processes. While obtaining a health history, the nurse is also simultaneously performing a general survey. Visit the “ General Survey Assessment ” chapter more information.
2.2. HEALTH HISTORY BASIC CONCEPTS
During a health history, the nurse collects subjective data from the patient, their caregivers, and/or family members using focused and open-ended questions. Before discussing the components of a health history, let’s review some important concepts related to assessment and communicating effectively with patients.
Subjective Versus Objective Data
Obtaining a patient’s health history is a component of the Assessment phase of the nursing process. Information obtained while performing a health history is called subjective data. Subjective data is information obtained from the patient and/or family members and can provide important cues about functioning and unmet needs requiring assistance. Subjective data is considered a symptom because it is something the patient reports. When documenting subjective data in a progress note, it should be included in quotation marks and start with verbiage such as, “The patient reports…” or “The patient’s wife states…” An example of subjective data is when the patient reports, “I feel dizzy.”
A patient is considered the primary source of subjective data. Secondary sources of data include information from the patient’s chart, family members, or other health care team members. Patients are often accompanied by their care partners. Care partners are family and friends who are involved in helping to care for the patient. For example, parents are care partners for children; spouses are often care partners for each other, and adult children are often care partners for their aging parents. When obtaining a health history, care partners may contribute important information related to the health and needs of the patient. If data is gathered from someone other than the patient, the nurse should document where the information is obtained.
Objective data is information observed through your senses of hearing, sight, smell, and touch while assessing the patient. Objective data is obtained during the physical examination component of the assessment process. Examples of objective data are vital signs, physical examination findings, and laboratory results. An example of objective data is recording a blood pressure reading of 140/86. Subjective data and objective data are often recorded together during an assessment. For example, the symptom the patient reports, “I feel itchy all over,” is documented in association with the sign of an observed raised red rash located on the upper back and chest.
Addressing Barriers and Adapting Communication
It is vital to establish rapport with a patient before asking questions about sensitive topics to obtain accurate data regarding the mental, emotional, and spiritual aspects of a patient’s condition. When interviewing a patient, also consider the patient’s developmental status and level of understanding. Ask one question at a time and allow adequate time for the patient to respond. If the patient does not provide an answer even with additional time, try rephrasing the question in a different way for improved understanding.
If any barriers to communication exist, adapt your communication to that patient’s specific needs. For more information about potential communication barriers and strategies for adapting communication, visit the “ Communication ” chapter in Open RN Nursing Fundamentals .
Cultural Safety
It is important to conduct a health history in a culturally safe manner. Cultural safety refers to the creation of safe spaces for patients to interact with health professionals without judgment or discrimination. Focus on factors related to a person’s cultural background that may influence their health status. It is helpful to use an open-ended question to allow the patient to share what they believe to be important. For example, ask “I am interested in your cultural background as it relates to your health. Can you share with me what is important to know about your cultural background as part of your health care?”
If a patient’s primary language is not English, it is important to obtain a medical translator, as needed, prior to initiating the health history. The patient’s family member or care partner should not interpret for the patient. The patient may not want their care partner to be aware of their health problems or their care partner may not be familiar with correct medical terminology that can result in miscommunication.
2.3. COMPONENTS OF A HEALTH HISTORY
The purpose of obtaining a health history is to gather subjective data from the patient and/or their care partners to collaboratively create a nursing care plan that will promote health and maximize functioning. A comprehensive health history is completed by a registered nurse and may not be delegated. It is typically done on admission to a health care agency or during the initial visit to a health care provider, and information is reviewed for accuracy and currency at subsequent admissions or visits.
A comprehensive health history investigates several areas:
- Demographic and biological data
- Reason for seeking health care
- Current and past medical history
- Family health history
- Functional health and activities of daily living
- Review of body systems
Each of these areas is further described in the following sections.
The “History and Physical” documentation in a patient’s medical record is completed by a health care provider on admission to a health care agency. It is very similar to the health history obtained by a nurse and is helpful to read when caring for a patient for an overview of their treatment plan.
2.4. DEMOGRAPHIC AND BIOLOGICAL DATA
Demographic and biographic data includes basic characteristics about the patient, such as their name, contact information, birthdate, age, gender and preferred pronouns, allergies, languages spoken and preferred language, relationship status, occupation, and resuscitation status. [ 1 ] See Table 2.4a for sample focused questions used to gather demographic and biological data.
- Demographic and Biological Data
View in own window
See Table 2.4b for a sample demographic form used during a complete health history.
Sample Demographic Form [ 2 ]
2.5. REASON FOR SEEKING HEALTH CARE
It is helpful to begin the health history by obtaining the reason why the patient is seeking health care in their own words. During a visit to a clinic or emergency department or on admission to a health care agency, the patient’s reasons for seeking care are referred to as the chief complaint . After a patient has been admitted, the term main health needs is used to classify what the patient feels is most important at that time. Whichever term is used, it recognizes that patients are complex beings, with potentially multiple coexisting health needs, but there is often a pressing issue that requires most immediate care. This is not to suggest that other issues be ignored, but rather it allows health care team members to prioritize care and address more urgent needs first. [ 1 ] See Table 2.5a for suggested focused interview questions to use to investigate the reason a patient is seeking care based on the health care setting.
The nurse is always aware of critical assessment findings requiring immediate notification of a health care provider or the initiation of emergency care according to agency policy. For example, if a patient reports chest pain, difficulty breathing, sudden changes in vision or the ability to speak, sudden weakness or paralysis, uncontrolled bleeding, or thoughts of self-harm, the provider should immediately be notified with possible initiation of emergency care.
Focused Questions for Reasons for Seeking Health Care by Setting [ 2 ]
Chief Complaint
After identifying the reason why the patient is seeking health care, additional focused questions are used to obtain detailed information about this concern. The mnemonic PQRSTU is often used to ask the patient questions in an organized fashion. See Figure 2.1 [ 3 ] for an image of PQRSTU.
PQRSTU Mnemonic
The PQRSTU mnemonic is often used to assess pain, but it can also be used to assess many other symptoms. See Table 2.5b for suggested focus questions for pain and other symptoms using the PQRSTU mnemonic. [ 4 ]
Sample PQRSTU Focused Questions for Pain and Other Symptoms
While interviewing a patient about their chief complaint, use open-ended questions to allow the patient to elaborate on information that further improves your understanding of their health concerns. If their answers do not seem to align, continue to ask focused questions to clarify information. For example, if a patient states that “the pain is tolerable” but also rates the pain as a “7” on a 0-10 pain scale, these answers do not align, and the nurse should continue to use follow-up questions using the PQRSTU framework. For example, upon further questioning the patient explains they rate the pain as a “7” in their knee when participating in physical therapy exercises, but currently feels the pain is tolerable while resting in bed. This additional information will help the nurse customize interventions for effective treatment.
2.6. CURRENT AND PAST MEDICAL HISTORY
After exploring a patient’s chief complaint, their current and past medical histories are reviewed to obtain a full understanding of their “human response” to medical conditions and life processes. While obtaining this information, it is also helpful to determine their understanding of the condition and its associated treatment. If a patient has a prior medical diagnosis, but is unaware of what it means or does not understand the recommended treatment, they may not be following instructions intended. For example, a patient diagnosed with “high blood pressure” may erroneously think they only need to take their medications when they feel as if their blood pressure is high, instead of daily at the recommended doses.
Categories included in past medical history include current health, medications, childhood illnesses, chronic illnesses, acute illnesses, accidents, injuries, and obstetrical health for females. Medication reconciliation is a comparison of a list of current medications with a previous list and is completed at every hospitalization and clinic visit. Not all categories of current and past health histories apply to every patient, so only ask questions that are relevant to the patient you are interviewing. See Table 2.6 [ 1 ] for suggested focused interview questions related to current and past medical history.
Sample Focused Questions for Current and Past Health History
2.7. FAMILY HEALTH HISTORY
Many diseases have a genetic component. It is important to understand the risk and likelihood of a patient developing illnesses based on their family health. Ask about the health status, age, and, if applicable, cause of death of immediate blood relatives (parents, grandparents, and siblings). Questions to ask include the following:
- Tell me about the health of your blood relatives. Does anyone have diseases like cancer, heart problems, or respiratory problems?
- Have any of your blood relatives died? If so, do you know the cause of death? What age did they die?
2.8. FUNCTIONAL HEALTH AND ACTIVITIES OF DAILY LIVING
Functional health assessment collects data related to the patient’s functioning and their physical and mental capacity to participate in Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs). Activities of Daily Living (ADLs) are daily basic tasks that are fundamental to everyday functioning (e.g., hygiene, elimination, dressing, eating, ambulating/moving). See Figure 2.2 [ 1 ] for an illustration of ADLs.
Activities of Daily Living (ADLs)
Instrumental Activities of Daily Living (IADL) are more complex daily tasks that allow patients to function independently such as managing finances, paying bills, purchasing and preparing meals, managing one’s household, taking medications, and facilitating transportation. See Figure 2.3 [ 2 ] for an illustration of IADLs. Assessment of IADLs is particularly important to inquire about with young adults who have just moved into their first place, as well as with older patients with multiple medical conditions and/or disabilities.
Instrumental Activities of Daily Living (IADLs)
Information obtained when assessing functional health provides the nurse a holistic view of a patient’s human response to illness and life conditions. It is helpful to use an assessment framework, such as Gordon’s Functional Health Patterns, [ 3 ] to organize interview questions according to evidence-based patterns of human responses. Using this framework provides the patient and their family members an opportunity to identify health-related concerns to the nurse that may require further in-depth assessment. It also verifies patient understanding of conditions so that misperceptions can be clarified. This framework includes the following categories:
- Nutritional-Metabolic: Food and fluid consumption relative to metabolic need
- Elimination: Excretion including bowel and bladder
- Activity-Exercise: Activity and exercise
- Sleep-Rest: Sleep and rest
- Cognitive-Perceptual: Cognition and perception
- Role-Relationship: Roles and relationships
- Sexuality-Reproductive: Sexuality and reproduction
- Coping-Stress Tolerance: Coping and effectiveness of managing stress
- Value-Belief: Values, beliefs, and goals that guide choices and decisions
- Self-Perception and Self-Concept: Self-concept and mood state [ 4 ]
- Health Perception-Health Management: A patient’s perception of their health and well-being and how it is managed. This is an umbrella category of all the categories above and underlies performing a health history.
The functional health section can be started by saying, “I would like to ask you some questions about factors that affect your ability to function in your day-to-day life. Feel free to share any health concerns that come to mind during this discussion.” Focused interview questions for each category are included in Table 2.8 . Each category is further described below.
The nutritional category includes, but is not limited to, food and fluid intake, usual diet, financial ability to purchase food, time and knowledge to prepare meals, and appetite. This is also an opportune time to engage in health promotion discussions about healthy eating. Be aware of signs for malnutrition and obesity, especially if rapid and excessive weight loss or weight gain have occurred.
Life Span Considerations
When assessing nutritional status, the types of questions asked and the level of detail depend on the developmental age and health of the patient. Family members may also provide important information.
- Infants: Ask parents about using breast milk or formula, amount, frequency, supplements, problems, and introductions of new foods.
- Pregnant women: Include questions about the presence of nausea and vomiting and intake of folic acid, iron, omega-3 fatty acids, vitamin D, and calcium.
- Older adults or patients with disabling illnesses: Inquire about the ability to purchase and cook their food, decreased sense of taste, ability to chew or swallow foods, loss of appetite, and enough fiber and nutrients. [ 5 ]
For more information about nutrition, visit the “ Nutrition ” chapter in Open RN Nursing Fundamentals .
Elimination.
Elimination refers to the removal of waste products through the urine and stool. Health care professionals refer to urinating as voiding and stool elimination as having a bowel movement. Familiar terminology may need to be used with patients, such as “pee” and “poop.” Constipation commonly occurs in hospitalized patients, so it is important to assess the date of their last bowel movement and monitor the frequency, color, and consistency of their stool. Assess urine concentration, frequency, and odor, especially if concerned about urinary tract infection, incontinence, or incontinence. Findings that require further investigation include dysuria (pain or difficulty upon urination), blood in the stool, melena (black, tarry stool), constipation, diarrhea, or excessive laxative use. [ 6 ]
When assessing elimination, the types of questions asked and the level of detail depends on the developmental age and health of the patient.
Toddlers: Ask parents or guardians about toilet training. Toilet training takes several months, occurs in several stages, and varies from child to child. It is influenced by culture and depends on physical and emotional readiness, but most children are toilet trained between 18 months and three years.
Older Adults: Constipation and incontinence are common symptoms associated with aging. Additional focused questions may be required to further assess these issues. [ 7 ]
For more information about elimination, visit the “ Elimination ” chapter in Open RN Nursing Fundamentals .
Mobility, activity, and exercise.
Mobility refers to a patient’s ability to move around (e.g., sit up, sit down, stand up, walk). Activity and exercise refer to informal and/or formal activity (e.g., walking, swimming, yoga, strength training). In addition to assessing the amount of exercise, it is also important to assess activity because some people may not engage in exercise but have an active lifestyle (e.g., walk to school or work in a physically demanding job).
Findings that require further investigation include insufficient aerobic exercise and identified risks for falls. [ 8 ]
Mobility and activity depend on developmental age and a patient’s health and illness status. With infants, it is important to assess their ability to meet specific developmental milestones at each well-baby visit. Mobility can become problematic for patients who are ill or are aging and can result in self-care deficits. Thus, it is important to assess how a patient’s mobility is affecting their ability to perform ADLs and IADLs. [ 9 ]
For more information, visit the “ Mobility ” chapter in Open RN Nursing Fundamentals .
Sleep and rest.
The sleep and rest category refers to a patient’s pattern of rest and sleep and any associated routines or sleeping medications used. Although it varies for different people and their life circumstances, obtaining eight hours of sleep every night is a general guideline. Findings that require further investigation include disruptive sleep patterns and reliance on sleeping pills or other sedative medications. [ 10 ]
Older Adults: Disruption in sleep patterns can be especially troublesome for older adults. Assessing sleep patterns and routines will contribute to collaborative interventions for improved rest. [ 11 ]
For more information, visit the “ Sleep and Rest ” chapter in Open RN Nursing Fundamentals .
Cognitive and perceptual.
The cognitive and perceptual category focuses on a person’s ability to collect information from the environment and use it in reasoning and other thought processes. This category includes the following:
- Adequacy of vision, hearing, taste, touch, feeling, and smell
- Any assistive devices used
- Pain level and pain management
- Cognitive functional abilities, such as orientation, memory, reasoning, judgment, and decision-making [ 12 ]
If a patient is experiencing pain, it is important to perform an in-depth assessment using the PQRSTU method described in the “ Reason for Seeking Health Care ” section of this chapter. It is also helpful to use evidence-based assessment tools when assessing pain, especially for patients who are unable to verbally describe the severity of their pain. See Figure 2.4 [ 13 ] for an image of the Wong-Baker FACES tool that is commonly used in health care.
The Wong-Baker FACES Pain Rating Scale. Used with permission from http://www.WongBakerFACES.org.
Older Adults : Older adults are especially at risk for problems in the cognitive and perceptual category. Be alert for cues that suggest deficits are occurring that have not been previously diagnosed.
Roles – Relationships
Quality of life is greatly influenced by the roles and relationships established with family, friends, and the broader community. Roles often define our identity. For example, a patient may describe themselves as a “mother of an 8 year old.” This category focuses on roles and relationships that may be influenced by health-related factors or may offer support during illness. [ 14 ] Findings that require further investigation include indications that a patient does not have any meaningful relationships or has “negative” or abusive relationships in their lives.
Be sensitive to cues when assessing individuals with any of the following characteristics: isolation from family and friends during crisis, language barriers, loss of a significant person or pet, loss of job, significant home care needs, prolonged caregiving, history of abuse, history of substance abuse, or homelessness. [ 15 ]
Sexuality – Reproduction
Sexuality and sexual relations are an aspect of health that can be affected by illness, aging, and medication. This category includes a person’s gender identity and sexual orientation , as well as reproductive issues. It involves a combination of emotional connection, physical companionship (holding hands, hugging, kissing) and sexual activity that impact one’s feeling of health. [ 16 ]
The Joint Commission has defined terms to use when caring for diverse patients. Gender identity is a person’s basic sense of being male, female, or other gender. [ 17 ] Gender expression are characteristics in appearance, personality, and behavior that are culturally defined as masculine or feminine. [ 18 ] Sexual orientation is the preferred term used when referring to an individual’s physical and/or emotional attraction to the same and/or opposite gender. [ 19 ] LGBTQ is an acronym standing for the lesbian, gay, bisexual, transgender, and queer population. It is an umbrella term that generally refers to a group of people who are diverse in gender identity and sexual orientation. It is important to provide a safe environment to discuss health issues because the LGBTQ population experiences higher rates of smoking, alcohol use, substance abuse, HIV and other STD infections, anxiety, depression, suicidal ideation and attempts, and eating disorders as a result of stigma and marginalization. [ 20 ]
Although sexuality is frequently portrayed in the media, individuals often consider these topics as private subjects. Use sensitivity when discussing these topics with different age groups across cultural beliefs while maintaining professional boundaries.
For more information, read the Joint Commission’s PDF Field Guide called Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community.
Coping-stress tolerance.
Individuals experience stress that can lead to dysfunction if not managed in a healthy manner. Throughout life, healthy and unhealthy coping strategies are learned. Coping strategies are behaviors used to manage anxiety. Effective strategies control anxiety and lead to problem solving but ineffective strategies can lead to abuse of food, tobacco, alcohol, or drugs. [ 21 ] Nurses teach and reinforce effective coping strategies.
Substance Use and Abuse
Alcohol, tobacco products, marijuana, and drugs are often used as ineffective coping strategies. It is important to use a nonjudgmental approach when assessing a patient’s use of substances so they do not feel stigmatized. Substance abuse can affect people of all ages. Make a distinction between use and abuse as you assess frequency of use and patterns of behavior. Substance abuse often causes disruption in everyday function (e.g., loss of employment, deterioration of relationships, or precarious living circumstances) because of dependence on a substance. Action is needed if patients indicate that they have a problem with substance use or show signs of dependence, addiction, or binge drinking. [ 22 ]
Some individuals are at increased risk for problems with coping strategies and stress management. Be sensitive to cues when assessing individuals with characteristics such as uncertainty in medical diagnosis or prognosis, financial problems, marital problems, poor job fit, or few close friends and family members. [ 23 ]
Value-Belief
This category includes values and beliefs that guide decisions about health care and can also provide strength and comfort to individuals. It is common for a person’s spirituality and values to be influenced by religious faith. A value is an accepted principle or standard of an individual or group. A belief is something accepted as true with a sense of certainty. Spirituality is a way of living that comes from a set of values and beliefs that are important to a person. The Joint Commission asks health care professionals to respect patients’ cultural and personal values, beliefs, and preferences and accommodate patients’ rights to religious and other spiritual services. [ 24 ] When performing an assessment, use open-ended questions to allow the patient to share values and beliefs they believe are important. For example, ask, “I am interested in your spiritual and religious beliefs and how they relate to your health. Can you share with me any spiritual beliefs or religious practices that are important to you during your stay?”
For more information about assessing and providing for patients’ spiritual needs, visit the “ Spirituality ” chapter in Open RN Nursing Fundamentals .
Self-perception and self-concept.
The focus of this category is on the subjective thoughts, feelings, and attitudes of a patient about themself. Self-concept refers to all the knowledge a person has about themself that makes up who they are (i.e., their identity). Self-esteem refers to a person’s self-evaluation of these items as being worthy or unworthy. Body image is a mental picture of one’s body related to appearance and function. It is best to assess these items toward the end of the interview because you will have already collected data that contributes to an understanding of the patient’s self-concept. Factors that influence a patient’s self-concept vary from person to person and include elements of life they value, such as talents, education, accomplishments, family, friends, career, financial status, spirituality, and religion. [ 25 ] The self-perception and self-concept category also focuses on feelings and mood states such as happiness, anxiety, hope, power, anger, fear, depression, and control. [ 26 ]
Some individuals are at risk for problems with self-perception and self-concept. Be sensitive to cues when assessing individuals with characteristics such as uncertainty regarding a medical diagnosis or surgery, significant personal loss, history of abuse or neglect, loss of body part or function, or history of substance abuse. [ 27 ]
Violence and Trauma
There are many types of violence that a person may experience, including neglect or physical, emotional, mental, sexual, or financial abuse. You are legally mandated to report suspected cases of child abuse or neglect, as well as suspected cases of elder abuse. At any time, if you or the patient is in immediate danger, follow agency policy and procedure.
Trauma results from violence or other distressing events in a life. Collaborative intervention with the patient is required when violence and trauma are identified. People respond in different ways to trauma. It is important to use a trauma-informed approach when caring for patients who have experienced trauma. For example, a patient may respond to the traumatic situation in a way that seems unfitting (such as with laughter, ambivalence, or denial). This does not mean the patient is lying but can be a symptom of trauma. To reduce the effects of trauma, it is important to implement collaborative interventions to support patients who have experienced trauma. [ 28 ]
Loss of Body Part
A person can have negative feelings or perceptions about the characteristics, function, or limits of a body part as a result of a medical condition, surgery, trauma, or mental condition. Pay attention to cues, such as neglect of a body part or negative comments about a body part, and use open-ended questions to obtain additional information.
Mental Health
Mental health is frequently underscreened and unaddressed in health care. The mental health of all patients should be assessed, even if they appear well or state they have no mental health concerns so that any changes in condition are quickly noticed and treatment implemented. Mental health includes emotional and psychological symptoms that can affect a patient’s day-to-day ability to function. The World Health Organization (2014) defines mental health as “a state of well-being in which every individual realizes their own potential, can cope with normal stresses of life, can work productively and fruitfully, and is able to make a contribution to their community.” [ 29 ] Mental illness includes conditions diagnosed by a health care provider, such as depression, anxiety, addiction, schizophrenia, post-traumatic stress disorder, and others. Mental illness can disrupt everyday functioning and affect a person’s employment, education, and relationships.
It is helpful to begin this component of a mental health assessment with a statement such as, “Mental health is an important part of our lives, so I ask all patients about their mental health and any concerns or questions they may have.” [ 30 ] Be attentive of critical findings that require intervention. For example, if a patient talks about feeling hopeless or depressed, it is important to screen for suicidal thinking. Begin with an open-ended question, such as, “Have you ever felt like hurting yourself?” If the patient responds with a “Yes,” then progress with specific questions that assess the immediacy and the intensity of the feelings. For example, you may say, “Tell me more about that feeling. Have you been thinking about hurting yourself today? Have you put together a plan to hurt yourself?” When assessing for suicidal thinking, be aware that a patient most at risk is someone who has a specific plan about self-harm and can specify how and when they will do it. They are particularly at risk if planning self-harm within the next 48 hours. The age of the patient is not a factor in this determination of risk. If you believe the patient is at high risk, do not leave the patient alone. Collaborate with them regarding an immediate plan for emergency care. [ 31 ]
Health Perception-Health Management
Health perception-health management is an umbrella term encompassing all of the categories described above, as well as environmental health.
Environmental Health
Environmental health refers to the safety of a patient’s physical environment, also called a social determinant of health. Examples of environmental health include, but are not limited to, exposure to violence in the home or community; air pollution; and availability of grocery stores, health care providers, and public transportation. Findings that require further investigation include a patient living in unsafe environments. [ 32 ]
See Table 2.8 for sample focused questions for all categories related to functional health. [ 33 ]
Focused Interview Questions for Functional Health Categories [ 34 ] . Begin this section by saying, “I would like to ask you some questions about factors that affect your ability to function in your day-to-day life. Feel free to share any health concerns that come to mind during this discussion.”
2.9. REVIEW OF BODY SYSTEMS
A body system review asks focused questions related to overall health status and body systems such as cardiac, respiratory, neurological, gastrointestinal, urinary, and musculoskeletal systems. See “ Chapter Resources A ” for a sample health history form that contains brief questions according to body systems. Nurses often incorporate review of system questions into the physical examination of each system. For example, while listening to bowel sounds in the abdomen, a nurse often inquires about the patient’s bowel pattern. Additional focused assessment questions related to each body system are found in each assessment chapter of this book.
2.10. SAMPLE DOCUMENTATION
Information obtained during a health history interview is typically documented on agency-specific forms. See “ Chapter Resources A ” for a sample health history form used for documentation purposes. Additional information collected that is not included on the form should be documented in an associated progress note.
2.11. CHECKLIST FOR OBTAINING A HEALTH HISTORY
Use the checklist below to review the steps for completion of “Obtaining a Health History.”
Disclaimer: Always review and follow agency policy regarding this specific skill.
Gather supplies: health history agency form.
Knock, enter the room, greet the patient, and provide for privacy.
Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient and ask if they have any questions.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs.
Address patient needs (pain, toileting, glasses/hearing aids) prior to starting. Note if the patient has signs of distress such as difficulty breathing or chest pain. If signs are present, defer the health history and obtain emergency assistance per agency policy.
Complete a health history interview, including the following components per your instructor’s instructions:
- Reason for Seeking Health Care
- Current and Past Medical History
- Family History
- Functional Health
- Review of Body Systems
Ensure five safety measures before leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
Document the health history findings and report any concerns according to agency policy.
2.12. LEARNING ACTIVITIES
Learning activities.
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
You are admitting a patient with a new diagnosis of type 2 diabetes. During the admission assessment, you note that the patient identifies as Muslim. How could you explore the patient’s cultural background to better understand how the patient’s culture might influence the patient’s health status and decisions?
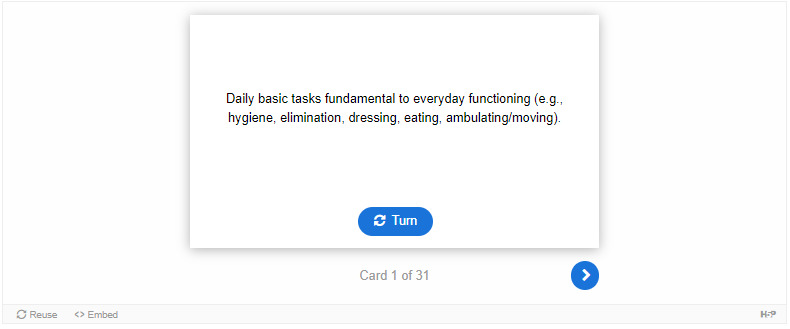
- II. GLOSSARY
Daily basic tasks fundamental to everyday functioning (e.g., hygiene, elimination, dressing, eating, ambulating/moving).
Something accepted as true with a sense of certainty. [ 1 ]
A mental picture of one’s body related to appearance and function. [ 2 ]
Family and friends who are involved in helping to care for the patient.
The reason a patient is seeking health care during a visit to a clinic or on admission to a health care facility.
The creation of safe spaces for patients to interact with health professionals without judgment or discrimination.
Discomfort or pain on urinating.
Refers to the removal of waste products through the urine and stool.
The patient’s physical and mental capacity to participate in activities of daily living (ADLs) and instrumental activities of daily living (IADLs).
Characteristics in appearance, personality, and behavior, culturally defined as masculine or feminine. [ 3 ]
One’s basic sense of being male, female, or other gender. [ 4 ]
The process of using directed interview questions to obtain symptoms and perceptions about a patient’s illness or life condition. The purpose of obtaining a health history is to gather subjective data from the patient and/or the patient’s family so that the health care team and the patient can collaboratively create a plan that will promote health, address acute health problems, and minimize chronic health conditions.
Complex daily tasks that allow patients to function independently such as managing finances, paying bills, purchasing and preparing meals, managing one’s household, taking medications, and facilitating transportation.
An acronym standing for lesbian, gay, bisexual, transgender, and queer is an umbrella term that generally refers to a group of people who are diverse with regard to their gender identity and sexual orientation. There are expanded versions of this acronym. [ 5 ]
Term used to classify what needs the patient feels are most important to address after admission to a health care agency.
A comparison of a list of current medications with a previous list and is completed at every hospitalization and clinic visit.
Dark, tarry-looking stool due to the presence of digested blood.
A state of well-being in which every individual realizes their own potential, can cope with normal stresses of life, can work productively and fruitfully, and is able to make a contribution to their community. [ 6 ]
A patient’s ability to move around (e.g., sit up, sit down, stand up, walk).
The protection, promotion, and optimization of health and abilities, prevention of illness and injury, facilitation of healing, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, groups, communities, and population. [ 7 ]
Information observed through your sense of hearing, sight, smell, and touch while assessing the patient.
Information obtained directly from the patient.
Information from the patient’s chart, family members, or other health care team members.
Knowledge a person has about themselves that makes up who they are (i.e., their identity).
A person’s self-evaluation of their self-concept as being worthy or unworthy.
The preferred term used when referring to an individual’s physical and/or emotional attraction to the same and/or opposite gender. [ 8 ]
Objective data found by the nurse or health care provider when assessing a patient.
A way of living that comes from a set of meanings, values, and beliefs that are important to a person. [ 9 ]
Information obtained from the patient and/or family members that offers important cues from their perspectives.
Subjective data that the patient reports, such as “I feel dizzy.”
An accepted principle or standard of an individual or group. [ 10 ]
Medical terminology used for urinating.
- CHAPTER RESOURCES A: SAMPLE HEALTH HISTORY FORM
Please view a Sample Health History Form
Licensed under a Creative Commons Attribution 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/ .
- Cite this Page Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Skills [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021. Chapter 2 Health History.
- PDF version of this title (449M)
In this Page
- HEALTH HISTORY INTRODUCTION
- HEALTH HISTORY BASIC CONCEPTS
- COMPONENTS OF A HEALTH HISTORY
- DEMOGRAPHIC AND BIOLOGICAL DATA
- REASON FOR SEEKING HEALTH CARE
- CURRENT AND PAST MEDICAL HISTORY
- FAMILY HEALTH HISTORY
- FUNCTIONAL HEALTH AND ACTIVITIES OF DAILY LIVING
- REVIEW OF BODY SYSTEMS
- SAMPLE DOCUMENTATION
- CHECKLIST FOR OBTAINING A HEALTH HISTORY
- LEARNING ACTIVITIES
Other titles in this collection
- Open RN OER Textbooks
Related Items in Bookshelf
- All Textbooks
Bulk Download
- Bulk download content from FTP
Recent Activity
- Chapter 2 Health History - Nursing Skills Chapter 2 Health History - Nursing Skills
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Chapter Resources A: Sample Health History Form
View a Sample Health History Form.
Nursing Skills - 2e Copyright © 2023 by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
Domain 1: Knowledge for Nursing Practice
Descriptor: Integration, translation, and application of established and evolving disciplinary nursing knowledge and ways of knowing, as well as knowledge from other disciplines, including a foundation in liberal arts and natural and social sciences. This distinguishes the practice of professional nursing and forms the basis for clinical judgment and innovation in nursing practice.
Contextual Statement: Knowledge for Nursing Practice provides the context for understanding nursing as a scientific discipline. The lens of nursing, informed by nursing history, knowledge, and science, reflects nursing’s desire to incorporate multiple perspectives into nursing practice, leading to nursing’s unique way of knowing and caring.
Preparation in both liberal arts and sciences and professional nursing coursework provides graduates with the essential abilities to function as independent, intellectually curious, socially responsible, competent practitioners (Tobbell, 2018). A liberal education creates the foundation for the development of intellectual and practical abilities within the context of nursing. Further, liberal education is the key to understanding self and others; contributes to safe, quality care; and informs the development of clinical judgment.
Search for Resources
Entry-Level Domain 1 Competencies
1.1 Demonstrate an understanding of the discipline of nursing’s distinct perspective and where shared perspectives exist with other disciplines
1.1a Identify concepts, derived from theories from nursing and other disciplines, which distinguish the practice of nursing.
1.1b Apply knowledge of nursing science that develops a foundation for nursing practice.
1.1c Understand the historical foundation of nursing as the relationship developed between the individual and nurse.
1.1d Articulate nursing’s distinct perspective to practice.
1.2 Apply theory and research-based knowledge from nursing, the arts, humanities, and other sciences.
1.2a Apply or employ knowledge from nursing science as well as the natural, physical, and social sciences to build an understanding of the human experience and nursing practice.
1.2b Demonstrate intellectual curiosity
1.2c Demonstrate social responsibility as a global citizen who fosters the attainment of health equity for all.
1.2d Examine influence of personal values in decision making for nursing practice.
1.2e Demonstrate ethical decision making.
1.3 Demonstrate clinical judgment founded on a broad knowledge base.
1.3a Demonstrate clinical reasoning.
1.3b Integrate nursing knowledge (theories, multiple ways of knowing, evidence) and knowledge from other disciplines and inquiry to inform clinical judgment.
1.3c Incorporate knowledge from nursing and other disciplines to support clinical judgment.
Advanced-Level Domain 1 Competencies
1.1e Translate evidence from nursing science as well as other sciences into practice.
1.1f Demonstrate the application of nursing science to practice.
1.1g Integrate an understanding of nursing history in advancing nursing’s influence in health care.
1.2f Synthesize knowledge from nursing and other disciplines to inform education, practice, and research.
1.2g Apply a systematic and defendable approach to nursing practice decisions.
1.2h Employ ethical decision making to assess, intervene, and evaluate nursing care.
1.2i Demonstrate socially responsible leadership.
1.2j Translate theories from nursing and other disciplines to practice.
1.3d Integrate foundational and advanced specialty knowledge into clinical reasoning.
1.3e Synthesize current and emerging evidence to influence practice.
1.3f Analyze decision models from nursing and other knowledge domains to improve clinical judgment.
Taking a comprehensive health history: learning through practice and reflection
Affiliation.
- 1 Registered Advanced Nurse Practitioner (Cardiology) and Registered Nurse Prescriber (Cardiology), Tallaght Hospital (a Trinity College Dublin Teaching Hospital), Dublin, Republic of Ireland.
- PMID: 29034702
- DOI: 10.12968/bjon.2017.26.18.1033
Taking a comprehensive health history is a core competency of the advanced nursing role. The purpose of the health history is to source important and intimate knowledge about the patient and allow the nurse and patient to establish a therapeutic relationship. Reflective practice, a core value of nursing in Ireland, means learning from experience. This article demonstrates how a recorded comprehensive health history simulation, coupled with reflection, provided insight into an advanced nurse practitioner's history-taking skills, thereby enhancing clinical practice.
Keywords: Advanced nursing; Assessment; Clinical history taking; Core values; Reflection.
- Advanced Practice Nursing
- Documentation
- Medical History Taking / methods*
- Nurse-Patient Relations
- Nursing Assessment / methods*

COMMENTS
The development and evolution of the nursing profession is intricately connected to historical influences throughout the ages, beginning in. antiquity. The study of the history of nursing helps us to better understand the societal forces and issues that continue to confront the profession. Understanding the history of nursing also allows nurses ...
Nursing and Hospital Care in the United States. The Philadelphia Almshouse, 1835 Throughout history most sick care took place in the home and was the responsibility of family, friends, and neighbors with knowledge of healing practices. In the United States, family-centered sickness care remained traditional until the nineteenth century.
Q-Chat. Created by. raaaahatm. Teacher. Study with Quizlet and memorize flashcards containing terms like Which war helped to expand the role of the nurse practitioner to include advanced emergency procedures??, What nurse was an expert on cholera, who paid her own way to help wounded soldiers on the battlefield?, Which nurse was appointed as ...
The health history is the subjective data collection portion of the health assessment. Components of a Health History. The health history obtained by nurses is framed from holistic perspectives of all factors that contributes to the patient's current health status. The most common way of obtaining information is through an interview ...
Nurses in Wars Fought by the United States. During and following the American Revolution, men served as corpsmen, providing nursing care for soldiers. Following the Civil War and before the Spanish American War in 1898, nurses in the United States Army were also men. These men were known as hospital corpsmen.
NURSING HISTORY. Nursing History Assignment. One of the greatest advancements in the history of nursing was the opening of Nightingale influenced nursing schools. The schools opened in 1873. Florence Nightingale became a nurse and provided nursing care for soldiers in Turkey (PowerPoint slide 10). She also published "Notes on Nursing" and ...
As the nursing history framework illustrates, nursing history could be included in every nursing course regardless of the course's focus. Table 1 illustrates one nursing history topic idea for both entry-level and advanced-level education with its related framework purpose(s) and its alignment to a competency and sub-competency(ies) for each of the 10 Domains for Nursing within the 2021 AACN ...
The Bellevue Hospital School of Nursing is America's first nursing school that applied Florence Nightingale's principles. Her principles included strict rules of hygiene and cleanliness as well as a staff of trained nurses supervised by a more experienced nurse who oversees the overall nursing services at the hospital.
nursing, profession that assumes responsibility for the continuous care of the sick, the injured, the disabled, and the dying. Nursing is also responsible for encouraging the health of individuals, families, and communities in medical and community settings. Nurses are actively involved in health care research, management, policy deliberations ...
The History of Nursing in the United States the·sis: a statement or theory that is put forward as a premise to be ... this assignment; the student's thesis can be up to 300 words. Their challenge in creating a thesis statement for this assignment is to choose one word from the list of "foundational
Health history data collection is a dynamic process that requires active listening, empathy, and strong communication skills. As nursing students, practice active listening during client interviews and take notes meticulously. Be mindful of verbal and non-verbal cues that provide additional insights into the client's health concerns.
Nursing History. Nursing history was defined as a disciplinary sub-topic in academe, similar to 'medical history' or 'labour history' and therefore a curriculum topic as distinct from history of nursing which is considered a broad term referring to the past of nursing, including histories of nursing (Fealy, 2008). ... Written assignment ...
Ancient history. The early history of nurses suffers from a lack of source material, but nursing in general has long been an extension of the wet-nurse function of women.. Buddhist Indian ruler (268 BC to 232 BC) Ashoka erected a series of pillars, which included an edict ordering hospitals to be built along the routes of travelers, and that they be "well provided with instruments and medicine ...
nurse's uniform, cap. Who is Mary Adelaide Nutting? 1907. first nursing professor in the world and first nurse to occupy a chair on university faculty. Who is Lillian Wald? observed horrendous conditions on Lower East Side (NY) provided care with Mary Brewster. What nurse corps formed in WW2? Cadet Nurse Corps.
Florence Nightingale (1820-1910), known as "The Lady With the Lamp," was a British nurse, social reformer and statistician best known as the founder of modern nursing. Her experiences as a ...
Obtaining a patient's health history is a component of the Assessment phase of the nursing process. Information obtained while performing a health history is called subjective data. Subjective data is information obtained from the patient and/or family members and can provide important cues about functioning and unmet needs requiring ...
Chapter 2 Health History - Nursing Skills - NCBI Bookshelf is a comprehensive guide for nurses to conduct effective health assessments and interventions for their patients. It covers topics such as communication skills, cultural competence, physical examination, and documentation. Learn from the experts and improve your nursing practice with this valuable resource.
Chapter 2 Health History. 2.1 Health History Introduction. 2.2 Health History Basic Concepts. 2.3 Components of a Health History. 2.4 Demographic and Biological Data. ... 21.8 Applying the Nursing Process to Catheterization. 21.9 Sample Documentation. 21.10 Checklist for Foley Catheter Insertion (Male) 21.11 Checklist for Foley Catheter ...
1.2a Apply or employ knowledge from nursing science as well as the natural, physical, and social sciences to build an understanding of the human experience and nursing practice. 1.2b Demonstrate intellectual curiosity. 1.2c Demonstrate social responsibility as a global citizen who fosters the attainment of health equity for all.
Abstract. Taking a comprehensive health history is a core competency of the advanced nursing role. The purpose of the health history is to source important and intimate knowledge about the patient and allow the nurse and patient to establish a therapeutic relationship. Reflective practice, a core value of nursing in Ireland, means learning from ...
Medication History. Current medications: none. Vitamins: no, feels she should. Herbal remedies/health supplements: none. Past medication: Albuterol, d/c'd 2 years ago. Dose: 1 to 2 puffs as needed. Reason for taking: asthma. Reason for d/c: no need for it; Past medication: Benzaclyn d/c'd six months ago.
It has clues to the information you need. It provides the framework for the assignment-making process, including staff constraints, additional duties that must be covered, and patient factors most impor-tant on your unit. Use the electronic health record (EHR) to generate various useful pieces of patient in-formation.
The earliest known nursing assignment samples date back to the 19th century when nursing was still a relatively new profession. These assignments were often simple tasks, such as keeping records ...