- Open access
- Published: 09 July 2021

Using concept mapping to prioritize barriers to diabetes care and self-management for those who experience homelessness
- Eshleen K. Grewal 1 ,
- Rachel B. Campbell 1 ,
- Gillian L. Booth 2 , 3 , 4 , 5 ,
- Kerry A. McBrien 6 , 7 ,
- Stephen W. Hwang 2 , 3 , 4 , 5 ,
- Patricia O’Campo 2 , 4 , 5 &
- David J. T. Campbell ORCID: orcid.org/0000-0002-5570-3630 1 , 7 , 8
International Journal for Equity in Health volume 20 , Article number: 158 ( 2021 ) Cite this article
4429 Accesses
13 Citations
4 Altmetric
Metrics details
Diabetes is a chronic medical condition which demands that patients engage in self-management to achieve optimal glycemic control and avoid severe complications. Individuals who have diabetes and are experiencing homelessness are more likely to have chronic hyperglycemia and adverse outcomes. Our objective was to collaborate with individuals experiencing homelessness and care providers to understand the barriers they face in managing diabetes, as a first step in identifying solutions for enhancing diabetes management in this population.
We recruited individuals with lived experience of homelessness and diabetes (i.e. clients; n = 32) from Toronto and health and social care providers working in the areas of diabetes and/or homelessness (i.e. providers; n = 96) from across Canada. We used concept mapping, a participatory research method, to engage participants in brainstorming barriers to diabetes management, which were subsequently categorized into clusters, using the Concept Systems Global MAX software, and rated based on their perceived impact on diabetes management. The ratings were standardized for each participant group, and the average cluster ratings for the clients and providers were compared using t-tests.
The brainstorming identified 43 unique barriers to diabetes management. The clients’ map featured 9 clusters of barriers: Challenges to getting healthy food , Inadequate income , Navigating services, Not having a place of your own , Relationships with professionals , Diabetes education , Emotional wellbeing , Competing priorities , and Weather-related issues . The providers’ map had 7 clusters: Access to healthy food , Dietary choices in the context of homelessness , Limited finances, Lack of stable, private housing , Navigating the health and social sectors , Emotional distress and competing priorities , and Mental health and addictions . The highest-rated clusters were Challenges to getting healthy food (clients) and Mental health and addictions (providers). Challenges to getting healthy food was rated significantly higher by clients ( p = 0.01) and Competing priorities was rated significantly higher by providers ( p = 0.03).
Conclusions
Experiencing homelessness poses numerous barriers to managing diabetes, the greatest of which according to clients, is challenges to getting healthy food. This study showed that the way clients and providers perceive these barriers differs considerably, which highlights the importance of including clients’ insights when assessing needs and designing effective solutions.
Diabetes mellitus is a commonly occurring chronic medical condition that is associated with a high burden of mortality and morbidity. In 2018, 34.2 million Americans, or 10.5 % of the population, had diabetes and approximately 1.5 million Americans were newly diagnosed that year [ 1 ]. The risk of mortality for people with diabetes is two times greater than it is for people without diabetes, and having diabetes can reduce life expectancy by 5–15 years [ 2 ]. Chronically high blood glucose levels can result in an increased risk of diabetes-related complications over time, which include: nerve damage, kidney disease, blindness, and vascular disease [ 3 ]. To avoid adverse outcomes, people with diabetes must make decisions about their management frequently and on an ongoing basis. There is evidence to suggest that the combination of self-management education and self-management support can result in improvements in glycemic control through improved self-care behaviours, which in turn can reduce the risk of developing complications [ 4 ]. Participation in diabetes education, therefore, is critical for improving knowledge and self-efficacy, which enables patients to engage in healthy behaviours [ 4 ]. These healthy behaviours, including smoking cessation, dietary modification, and regular physical activity, in combination with pharmacotherapy, can reduce the risk for complications such as major adverse cardiac events [ 5 ]. Other behaviours such as self-monitoring of blood glucose levels can empower patients, improve treatment adherence, and assist diabetes care professionals in making decisions about treatment [ 6 ].
Among those with diabetes, people with lived experience of homelessness (PWLEH) are more likely than the general population to have elevated blood glucose levels [ 7 ]. Homelessness is defined by a lack of stable and safe housing, but it is often accompanied by inadequate income, mental and physical health problems, difficulty accessing health care and social supports, substance use disorders, previous involvement with the justice system, and adverse childhood experiences [ 8 , 9 ]. Although health issues may lead to homelessness, homelessness also greatly affects health, making it challenging for people who are experiencing homelessness to access care [ 8 , 10 ] and engage in self-management, especially when they have a chronic medical condition like diabetes, for which management is complex.
There are many barriers that can make it challenging to manage diabetes for PWLEH. Accessing health care services can involve long wait times and an appreciable amount of time may be spent travelling to and from appointments [ 11 ]. In addition to time, there is a financial burden associated with managing diabetes, as the costs of medications and blood glucose testing supplies may not be covered by public health insurance programs, even within Canada’s universal health system [ 7 , 11 , 12 ]. Barriers specific to homelessness that have been identified in the literature include concerns about food insecurity related to low-quality foods available in shelters, as well as challenges with safely storing medications and supplies, and strict shelter schedules with respect to eating meals and taking medications [ 7 , 13 ]. Travelling to appointments often involves the use of public transportation with associated costs. As many PWLEH do not have a fixed mailing address or reliable access to a phone, issues contacting patients are also common [ 8 , 14 ], making it difficult to schedule and notify patients of appointments [ 15 ]. Perceived feelings of being unwelcome in clinical settings can also prevent people who are experiencing homelessness from seeking health care services [ 16 ]. Other priorities, namely, obtaining the necessities of life (food, shelter, etc…), drug and alcohol use, and mental health or cognitive issues can also interfere with diabetes self-management [ 7 , 13 , 17 ].
While there are many barriers and challenges to diabetes management, the importance of these in relation to one another is not well known, nor is it well known if these priorities differ between providers and PWLEH. Other studies that have compared the perspectives of service users with those of service providers have found differences of opinions between the two groups [ 18 , 19 ]. One such study asking community members and service providers about which social and mental health services should be made available at a new medical clinic in the community found that community members and service providers had different views regarding which services were most needed [ 19 ]. Another study aimed to identify existing gaps in services for youth, where the opinions of the youth differed from those of the service providers regarding importance, but not in terms of ‘what to do first’ [ 18 ]. Traditionally, homeless-serving agencies have provided services based on their own beliefs about their clients’ needs instead of directly asking their clients what they need [ 20 ]. For instance, they may have focused on providing mental health and substance use services because the rates of mental illness and substance use are high among this population, or they may have prioritized housing because this population is characterized by a lack of a stable home, but those services may not address the most pressing issues for people who are experiencing homelessness [ 20 ] and may result in service gaps and barriers. The perspectives of service users, therefore, can be useful for service providers because those insights can help the providers understand how to tailor their services to better fill the gaps in service provision and remove barriers to accessing services, based on their clients’ priorities.
Given the complexity of diabetes management, myriad barriers that can affect adherence, and the potential for differences in perspectives between providers and PWLEH, we sought to collaborate with people who had lived experience of homelessness and diabetes, as well as health and social care providers who work with people experiencing homelessness and/or people with diabetes, to prioritize the challenges faced by this population in managing diabetes. The objective of this study was to determine the perceived relative impact of barriers to diabetes management and whether the perceptions about the impact of those barriers differed between providers and PWLEH.
Study design
We used a semi-quantitative, participatory methodology known as concept mapping. We used concept mapping because it can be used to create visual representations that depict the combined thoughts of a group, by integrating input from multiple people using quantitative data analysis techniques [ 21 ]. This methodology enabled us to gather insights from a group of PWLEH who have diabetes (herein referred to as the clients) and from various providers representing different areas of health and social care (herein referred to as the providers) and to quantitatively compare their collective feedback. Our study was approved by the research ethics boards of the University of Calgary and Unity Health Toronto/St. Michael’s Hospital.
Study participants & recruitment
The clients for this study were all recruited in Toronto, Ontario – Canada’s largest city and the city with the largest population of people experiencing homelessness [ 22 ]. The prevalence of diabetes among PWLEH in Toronto is thought to be similar to the prevalence among the general population [ 23 ] and barriers to managing diabetes previously identified by PWLEH in Toronto [ 7 ] are similar to the barriers identified by PWLEH in other cities [ 24 ].
Eight of the clients in this study were recruited as part of a larger community-based participatory research project designed to understand what it is like to live with diabetes while experiencing homelessness or housing instability and to propose and develop potential interventions for this population [ 25 ]. These eight participants met regularly in Toronto for study-related activities. In addition, we recruited several other participants to take part in this concept mapping exercise, to increase the sample size. To be eligible to participate, the clients had to: be older than 18 years, have a history of diabetes with a duration greater than two years, and have experienced homelessness within the previous two years. Homelessness in this study was defined similarly to the definition offered by the Canadian Observatory on Homelessness; we included participants whose living situations could be described as unsheltered, emergency sheltered, or provisionally sheltered [ 26 ]. Colleagues and advocates in the homeless-serving sector were consulted to determine the best places for recruiting the target population. Posters were put up in shelters, at homeless-serving agencies, and health clinics catering to the homeless population for recruitment. Established programs serving people who were experiencing homelessness or housing instability also helped with recruitment by advertising an information session to their program attendees. We explained the study to interested parties and obtained informed consent.
The service providers who took part in this study had previously been recruited as participants in another study of diabetes care for PWLEH [ 27 ]. They comprised professionals from four main categories of care: diabetes care professionals who worked primarily with inner-city or homeless populations, other health care professionals who worked primarily with inner-city or homeless populations, endocrinologists or diabetes care providers who did not specifically focus on inner-city or homeless populations, and other stakeholders, including frontline staff in shelters and social care providers. The providers were recruited from five major Canadian cities (Toronto, Ottawa, Edmonton, Calgary, and Vancouver), and they participated in this study remotely. Although the barriers to diabetes self-management may be similar across cities for PWLEH, the services available in each city differ [ 27 ]. Services in the health sector are largely impacted by funding and approval from provincial governments, which may have different priorities, and services in the homeless-serving sector are often provided by non-profit organizations, which rely to a great extent on donor funding for service provision. For these reasons, services that exist in one city may not exist in another, and we felt that it would be valuable to gain input from providers across different jurisdictions about their perspectives.
Data collection
The concept mapping process involves six steps and is depicted in Fig. 1 . The initial three steps relate to data collection: preparation, generation of statements, and structuring of statements [ 28 ].
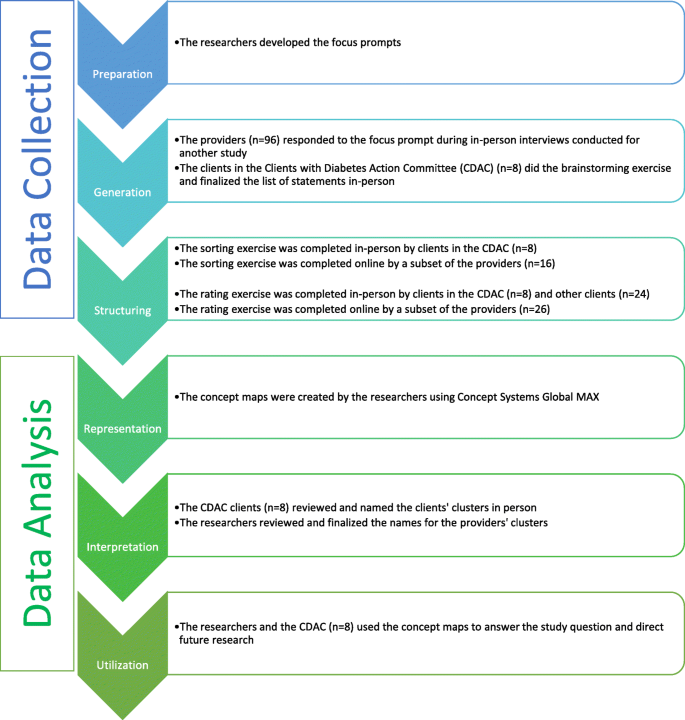
The concept mapping process
In the first step, preparation, the researchers must determine what the focus of the study will be. Usually, this involves two separate focus statements. The first statement is referred to as the focus prompt or the brainstorming focus, and it is developed to guide the brainstorming exercise in the second step. The second focus statement, called the rating focus, defines the factor(s) upon which the brainstormed statements will be rated in the rating exercise of the third step [ 28 , 29 ]. The focus prompt for the brainstorming exercise was, ‘What are some ways, good or bad, that diabetes might be affected by homelessness?’ . The rating prompt was: ‘What impact does [that factor] have on diabetes care and self-management (on a scale from no impact to high impact), specifically for people who are struggling with homelessness or housing instability?’ .
Generation involves a brainstorming exercise, in which the participants are provided with the focus prompt and asked to brainstorm statements in response [ 28 ]. The brainstorming exercise is done individually by each participant, and eventually, the ideas are combined and refined to form one set of statements [ 29 ]. Eight clients did the brainstorming exercise during an in-person group meeting. The providers had been individually interviewed by members of the research team, who then shared the providers’ ideas with the clients during their brainstorming session. The researchers recorded the ideas from the clients and the providers and refined the list of statements with the clients. The providers did not take part in the refinement of statements, as this aspect of the brainstorming exercise was done in person during a meeting with the clients.
Structuring involved two different exercises, sorting and rating. For the sorting exercise, each participant was asked to group individual statements into categories based on similarity, in a way that was meaningful to that individual [ 21 , 30 ]. The statements could not all be sorted into one pile, nor could each statement be in its own pile [ 29 ]. “Miscellaneous” piles with a group of statements that did not have a specific theme or link to each other were also discouraged. These instructions were explained to participants at the outset of the exercise and facilitators were present to help clarify instructions. The clients completed this exercise manually with statements printed on individual cue cards, while the providers completed this exercise using a tailor-made online platform. For the rating exercise, a Likert scale ranging from zero to four was used to rate each statement. A rating of zero meant the statement had no impact on diabetes control and self-management, and a rating of four meant it had an extreme impact on diabetes control and self-management. This exercise was done on paper forms by the clients and online by the providers.
Data analysis
The final three steps of the concept mapping process relate to data analysis: representation of statements, interpretation of maps, and utilization of maps [ 28 ].
In the representation step, sorting and rating data were analyzed using concept mapping software (Concept Systems Global Max, 2020, Ithaca NY) [ 30 , 31 ]. The representation step was done separately for the clients and the providers: the clients’ data were analyzed to create a clients’ cluster map and the providers’ data were analyzed to produce a providers’ cluster map. By having two cluster maps, rather than one, we were able to see how the number of clusters, the names of clusters, and the sorting of the statements, differed between the two participant groups.
The sorting data were analyzed using multidimensional scaling analysis, a technique that plots each statement as a point on a map. Statements that are closer together on the map were grouped together during the sorting exercise more often than statements that are farther apart. Multidimensional scaling was used to generate a matrix for each participant with one row and one column representing each of the statements [ 29 ]. In this study, the matrix had 43 rows and 43 columns. Each cell in the matrix corresponds to two statements, the row statement and the column statement. If those two statements were sorted into the same pile by the participant, the cell is given a value of one, and if they were not sorted into the same pile, the cell is assigned a value of zero [ 21 , 29 ]. This is done with each participant’s data so that there are as many separate matrices as there are participants in the study. All of the individual matrices are then summed to create a similarity matrix indicating how many participants sorted each pair of statements into the same pile [ 29 ]. This similarity data is used to create a two-dimensional point map, where the distance between two points on the map corresponds to their similarity [ 21 ].
These points were then grouped together to form clusters through hierarchical cluster analysis. Hierarchical cluster analysis uses the data from the point map to separate the points into non-overlapping clusters, developing a cluster map. The number of clusters in the final cluster map is determined by the participants and the researchers so that the map is presented in a way that is meaningful and useful to them [ 21 ]. This analysis begins by considering each statement to be in a cluster of its own, and it combines two clusters at a time, reducing the number of overall clusters until all the statements are in the same cluster. The statements are combined based on proximity, meaning that the two points that are closest together on the point map would be the first two points to form a cluster together [ 29 ]. The reliability, or goodness-of-fit of the map, is determined by calculating the final stress of the model [ 32 ]. Lower stress values suggest a better fit. Stress values in concept mapping data tend to be higher than in other multidimensional scaling analyses [ 33 ], therefore there is no accepted standard, however, it has been reported that an acceptable value for studies of this nature is less than 0.30 [ 34 ].
An average rating is then calculated for each cluster using the ratings for each of the individual statements in that cluster. Upon reviewing the average cluster ratings, it was clear that the clients and providers had rated the statements very differently, such that the clients had generally given lower ratings whereas the providers had given higher ratings, which resulted in lower average cluster ratings for the clients’ clusters and higher average cluster ratings for the providers’ clusters. To determine whether there was in fact a difference in the ratings between the two groups, the ratings were standardized and compared using unpaired two-sided t-tests, with an alpha of < 0.05. To standardize, the participants’ ratings for each statement were subtracted from the average rating of all the statements for their participant group (i.e., the clients’ average rating or the providers’ average rating). Both groups had different numbers of clusters with different numbers of statements in them, which would have been difficult to compare, so it was necessary to use the same cluster structure for both groups. We chose to compare based on the clients’ cluster structure because we wanted the analysis to be client-centred and because the clients had reviewed the clusters and the statements that were in each cluster, so the final structure reflected their feedback. We used unpaired t-tests to quantitatively compare the standardized cluster ratings to determine whether there was a statistically significant difference between the ratings of the clients and those of the providers for each cluster in the patient cluster map.
In the interpretation step, the maps and reports generated in the previous step are used to help frame the interpretation of the data. We assessed point maps, cluster maps, cluster reports with statements, and raw ratings reports. In this step, some of the clients were reconvened for an in-person meeting to discuss any changes that needed to be made to the maps and to provide input on the names of each of the clusters. The providers were not able to come together for a meeting, so their clusters were named by the researchers.
In the final step, utilization, the concept maps are reviewed to determine how they can be utilized to answer the study question [ 30 ]. In this study, the findings from the clients’ concept mapping research informed the subsequent research program in providing the topics of interest for the participatory photovoice project that ensued [ 35 ].
There were 32 clients and 96 providers who took part in this study: Although there were 128 participants altogether, only a subset of those participants took part in each stage of the concept mapping process (Fig. 1 ). For instance, only eight of the 32 clients took part in the brainstorming and sorting exercises, but all 32 took part in the rating exercise. For the providers, all 96 took part in the brainstorming exercise, but only 16 and 26 of these individuals took part in the sorting and rating exercises, respectively. The final sample size is consistent with what has typically been reported in other concept mapping projects [ 34 ].
Characteristics of the clients
The demographic characteristics of the clients are presented in Table 1 . All of the clients were over the age of 25 and just over half identified as men. None of the clients were sleeping rough at the time of this study, while a quarter of the clients were in private housing with the remainder in shelter or tenuous, transitional, or community housing. Collectively, they had experienced homelessness or housing instability for a median length of two years and had been living with diabetes for a median length of seven years. A majority of the clients had experienced some diabetes-related complications and had physical or mental health comorbidities as well. The most commonly reported method of managing diabetes was the use of oral medications, which were utilized by three-quarters of the clients, although approximately one-third of the clients used injectable agents (including insulin). The clients also saw a variety of care providers for the treatment of their diabetes; about three-quarters saw a family physician, one-fifth saw a pharmacist, and one-third saw a medical specialist, a diabetes nurse, and a diabetes dietitian, respectively.
Characteristics of the providers
Only eight of the providers completed the demographic survey. Most (6/8) were women, half were between the ages of 55 and 64, and 5/8 had 20 or more years of experience working with patients that have diabetes and/or complex social needs, while the rest had 15–19 years of experience. The providers also had a variety of different qualifications and titles including, registered dietitian, registered nurse, certified diabetes educator, family physician, program administrator/manager, and executive director. They also worked in a variety of settings such as community/private family medicine practices, specialty practices, community health centres, community pharmacies, academic/public family medicine practices, and homeless shelters.
Concept mapping
During the brainstorming exercise, the participants generated a list of statements representing barriers to self-management, starting with a large list, which was then refined by removing duplicates and combining similar statements. The resulting, final version of the list contained 43 statements (Table 2 ).
Using the data from the sorting exercises, the statements were plotted in relation to one another and presented as point maps through multidimensional scaling, and the points were then grouped to form cluster maps (Fig. 2 a and b) through hierarchical cluster analysis. The clients’ cluster map is based on sorting data from eight participants, and it consists of nine clusters, with a final stress value of 0.2987. Those clusters were named: (1) Challenges to getting healthy food , (2) Inadequate income , (3) Navigating services , (4) Not having a place of your own , (5) Relationships with professionals , (6) Diabetes education , (7) Emotional well-being , (8) Competing priorities , and (9) Weather-related issues . The providers’ cluster map had seven clusters, made using sorting data from 16 participants, and had a final stress value of 0.2521. The clusters were named: (1) Access to healthy food , (2) Dietary choices in the context of homelessness , (3) Limited finances , (4) Lack of stable, private housing , (5) Navigating the health and social sectors , (6) Emotional distress and competing priorities , and (7) Mental health and addictions . Appendix A (see Additional File 1 ) contains tables that list which statements were in each cluster for both the clients and the providers.

Cluster maps for the clients and the providers. a . Clients’ cluster map. b . Providers’ cluster map
The rating exercise was completed by 32 clients and 26 providers. The ratings for the individual statements were used to calculate an average cluster rating. The clients’ clusters, arranged from the cluster with the highest average rating to the cluster with the lowest average rating, with the average rating in parentheses (out of a total of four), are: (1) Challenges to getting healthy food (2.08), (2) Weather-related issues (1.83), (3) Emotional well-being (1.65), (4) Inadequate income (1.65), (5) Competing priorities (1.60), (6) Relationships with professionals (1.43), (7) Diabetes education (1.35), (8) Not having a place of your own (1.23), and (9) Navigating services (1.18). Providers’ clusters, by contrast, were: (1) Mental health and addictions (3.54), (2) Emotional distress and competing priorities (3.42), (3) Dietary choices in the context of homelessness (3.12), (4) Navigating the health and social sectors (3.00), (5) Limited finances (2.97), (6) Lack of stable, private housing (2.88), and (7) Access to healthy food (2.79).
Using the grouping of clusters defined by clients, we calculated standardized cluster averages for the two groups (Fig. 3 ). There were two clusters for which the standardized averages differed in a statistically significant manner, Challenges to getting healthy food (standardized difference = 0.6396; p = 0.013) and Competing priorities (standardized difference=-0.5250; p = 0.026). The clients had a higher rating for Challenges to getting healthy food than the providers and the providers had a higher rating for Competing priorities . While trends were suggesting potential differences in the other clusters, these were the only two that reached statistical significance, due to the relatively small sample size for this quantitative analysis.
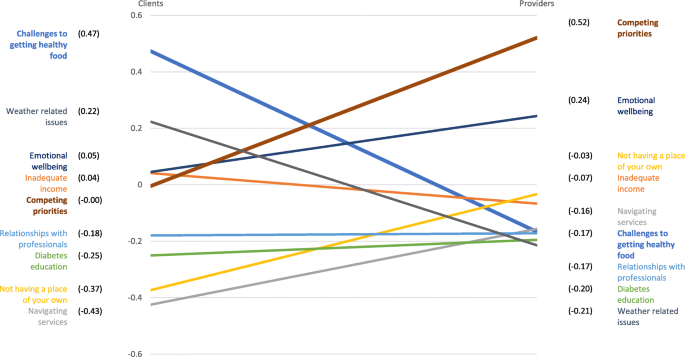
Graphical representation of the average standardized cluster ratings
The clients and providers identified a plethora of barriers to diabetes management, ultimately resulting in a refined list of 43 unique barriers. The clients’ and providers’ sorting data resulted in concept maps with distinct cluster names and configurations representing differing perceptions of barriers to managing diabetes while experiencing homelessness. Both the clients’ and the providers’ clusters represented themes related to access to healthy food; financial limitations; housing; health and social care; and psychosocial wellbeing. The clients chose to have a cluster titled Relationships with professionals , whereas the providers’ map included those barriers in the Navigating the health and social sectors and Lack of stable, private housing clusters. While the clients’ map has two clusters representing similar themes: Navigating services and Not having a place of your own , the clients saw the barriers related to relationships as being distinct from those related to navigation issues or housing issues and chose to have a separate cluster for them. These findings confirm the notion that the perspectives of clients/patients/service users and service providers regarding barriers to diabetes management may be different, and that the reasoning behind patients’ differing perspectives may not be evident to the providers. Traditionally, the identification of barriers and the creation of solutions has not meaningfully considered input from the individuals who have the most at stake, the patients/clients. Our findings highlight the importance of considering the patient perspective when designing solutions for enhancing diabetes management to address the barriers which have the greatest impact, according to patients.
Comparisons of the cluster ratings indicated that there were significant differences between the clients and the providers in the perceived impact of the barriers faced in diabetes management. The cluster related to challenges to accessing healthy food was the most influential from the client perspective, and it was rated significantly higher by the clients than the providers. The cluster representing priorities that compete with diabetes management was thought to be the most impactful by providers, and the rating for this cluster was significantly higher for the providers compared to the clients.
There are many reasons why accessing healthy food can be challenging for PWLEH. Many may rely on shelters or community kitchens for food so they must eat whatever is available, even if they have been advised to avoid such food by their healthcare providers [ 36 ]. The meals in shelters often have high amounts of sugar, starch and fat, and there are few fruits and vegetables available, which results in diets that are likely to be inappropriate for people with diabetes [ 7 ]. These shelters and community kitchens, however, also have limited resources and must often rely on food that is donated to them [ 24 ]. Sometimes, PWLEH may be unable to get three meals in a day so they are often eating when they can and hoarding extra food, so they have something to eat later. Alternatively, if they had access to affordable, nutritious food, they would not be worried about where their next meal is going to come from [ 37 ] and they would have greater diabetes self-management self-efficacy [ 38 ]. The lack of access to food is especially concerning for people who are using insulin, as they may use less than the prescribed amount of insulin for fear of developing hypoglycemia if they are not able to predict mealtimes reliably [ 15 ]. It is likely that because PWLEH need to negotiate their dietary intake daily, this rose to the top of the priority list for them. Providers may benefit from knowing that for PWLEH this is the most troubling aspect of diabetes self-management.
With regards to competing priorities, studies have noted that PWLEH tend to have many demands and prioritize things such as food, shelter, and employment above diabetes care and self-management practices [ 13 ]. When they continually face difficulties in meeting these basic needs, people may forego preventative care or sacrifice self-care [ 39 ]. This may partially explain why the providers believed that competing priorities have a great effect on diabetes management. As for why this cluster of factors was rated lower by clients, we hypothesize that this discrepancy may relate to lower health-related self-awareness in this population [ 40 ], or because clients did not fully grasp how their other issues may affect their diabetes, likely due to the fact that their social networks are often comprised of others who face similar issues. This is consistent with literature documenting that non-clinically trained people are typically less aware of the impact of the social determinants of health [ 41 ]. By contrast, healthcare providers are more likely to be informed about the social determinants of health and how diabetes care is affected significantly by the complete picture of patients’ lives [ 42 ]. It is also possible that barriers related to competing priorities were deemed less impactful by the clients because their greatest competing priority is accessing food, which had a separate cluster of its own, and had the highest average rating for the clients. The clients may also have felt that accessing healthy food is more important than other aspects of self-management if the diabetes education they received emphasized the importance of diet above all else.
The second highest-rated cluster for the clients was focused on issues related to the weather. Cold-related injuries are very common amongst PWLEH in Canada and they often result in emergency department visits [ 43 ]. One of the many complications of diabetes is reduced circulation, especially in the feet, so in cold weather foot care becomes even more important, as the winter weather can increase the risk for infections, frostbite and amputations [ 44 , 45 ].
The providers’ third highest-rated cluster focused on a lack of stable, secure housing and while the clients had a similar cluster, for them, it received the second-lowest rating. Understandably, providers would consider this an important barrier, given that there is much in the literature describing the need to treat homelessness as a health issue [ 46 ] and suggesting that it is important for providers to help address housing concerns [ 15 ]. It is surprising, however, that this cluster was given such a low rating relative to the other clusters by the clients because participants in other qualitative studies have described housing as a foundational need that affects diabetes self-management in numerous ways [ 36 , 47 ]. In one study, participants reported that being unstably housed is emotionally and physically draining, which makes it difficult to prioritize diabetes, and when the need for shelter is not met, there is no foundation from which they can pursue their health goals [ 47 ]. This view is in accordance with Maslow’s hierarchy of needs, which places basic needs such as food and shelter ahead of health [ 8 , 15 , 48 ]. Not having housing also means not having a secure place to store diabetes testing supplies such as glucometers or medications and insulin, and there is a fear that they may be stolen in a communal living arrangement such as an emergency shelter [ 36 ]. Furthermore, stable housing can provide a sense of consistency and control that can help with the routinization of diabetes care and allow some control over diet, while high housing costs can compete with the cost of diabetes care [ 47 ].
One of the strengths of this study is its participatory nature. We gathered input from PWLEH as well as a variety of providers who work in health and social settings, which ensured that we had diverse perspectives represented. The clients were able to review the concept maps and name the clusters, which meant that the final maps reflected their perspectives rather than the opinions of the researchers. This is important because the participants may see the value of having certain themes or representing the barriers a different way than the researchers. Concept mapping incorporates both qualitative and quantitative analyses in one process, which enables complex ideas to be explored in a short period of time, and the output of the quantitative analyses supplements and enhances the qualitative interpretations. Furthermore, the creation of visual representations through this combination of analyses provides structure and credibility to the results [ 30 ]. Additionally, it includes both individual and group activities, and the process in which these activities occur avoids some of the issues that are commonly experienced when using qualitative methodologies such as, the monopolization of group discussion time by one or two individuals, the likelihood of conformity bias, or the need for individuals to publicly discuss their personal opinions or experiences [ 30 ]. Another strength is that the participants were involved in the analysis of the data and they were able to interpret the concept maps that were created using their data. This methodology ensures that the thoughts of the participants are accurately reflected [ 28 , 30 ]. The visual concept maps allowed us to display the associations between multiple themes and the rating data enabled comparison of the relative importance of each theme [ 28 , 30 ].
There are also limitations to this study, one of which is that only eight clients completed the sorting exercise. This was due to the time commitment required of participants and the complexity of the task. Ideally, participants must take part in the brainstorming, sorting, and rating exercises, and then review the results and provide feedback, but it may be difficult to keep participants engaged throughout the whole process. However, despite this small sample, the resultant map still had an acceptable final stress value. Another limitation of this study is the lack of available demographic data about the providers, as only a small proportion of the providers completed the demographic survey. While it is unfortunate that we are unable to fully describe the group of providers who participated in this study, we do know that the roles they had and the settings they worked in varied considerably. Additionally, the providers did not have the opportunity to reflect on the concept map that was produced with their data. The research team decided to finalize the cluster map on their own because the providers were from five different cities, and it was not possible to plan a meeting for all of the providers.
The participants in our study identified many of the same barriers that are described in other studies. However, this study is unique in that it allowed participants to rank these barriers from most to least impactful on diabetes management – and compared these rankings between PWLEH and providers. The results show that clients and providers differ in their understanding of barriers and the impact they have on diabetes management. Given that the clients in this study have indicated that difficulties with accessing healthy food are the greatest barriers to managing diabetes, future research and interventions aimed at improving diabetes management among PWLEH who have diabetes could focus on determining how to improve access to diabetes-appropriate food for this population.
Availability of data and materials
The data pertaining to this study may be available upon request from the corresponding author.
Abbreviations
people with lived experience of homelessness
Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta: US Department of Health and Human Services; 2020.
Public Health Agency of Canada. Diabetes in Canada: Facts and figures from a public health perspective. Ottawa: Government of Canada; 2011.
Diabetes Canada. Diabetes 360: A framework for a diabetes strategy for Canada. 2018.
Sherifali D, Berard LD, Gucciardi E, MacDonald B, MacNeill G. Self-Management Education and Support. Can J Diabetes. 2018;42(Suppl 1):36-s41.
Google Scholar
Stone JA, Houlden RL, Lin P, Udell JA, Verma S. Cardiovascular Protection in People With Diabetes. Can J Diabetes. 2018;42(Suppl 1):162-s9.
Berard LD, Siemens R, Woo V. Monitoring Glycemic Control. Can J Diabetes. 2018;42(Suppl 1):47-s53.
Hwang SW, Bugeja AL. Barriers to appropriate diabetes management among homeless people in Toronto. CMAJ. 2000;163(2):161–5.
CAS PubMed PubMed Central Google Scholar
Davies A, Wood LJ. Homeless health care: meeting the challenges of providing primary care. Med J Aust. 2018;209(5):230–4.
Article Google Scholar
Gaetz S, Backgrounder: “What is homelessness?” 2009 [Available from: https://homelesshub.ca/resource/what-homelessness .
Campbell DJT, O’Neill BG, Gibson K, Thurston WE. Primary healthcare needs and barriers to care among Calgary’s homeless populations. BMC Fam Practice. 2015;16(1):139.
Canada. Standing Committee on Health. A diabetes strategy for Canada. 2019.
Campbell DJT, Manns BJ, Hemmelgarn BR, Sanmartin C, Edwards A, King-Shier K. Understanding Financial Barriers to Care in Patients With Diabetes: an Exploratory Qualitative Study. Diabetes Educ. 2017;43(1):78–86.
Elder NC, Tubb MR. Diabetes in homeless persons: barriers and enablers to health as perceived by patients, medical, and social service providers. Soc Work Public Health. 2014;29(3):220–31.
Mancini NL, Campbell RB, Yaphe HM, Tibebu T, Grewal EK, Saunders-Smith T, et al. Identifying challenges and solutions to providing diabetes care for the homeless. Diabetes Can. 2020.
Nickasch B, Marnocha SK. Healthcare experiences of the homeless. J Am Acad Nurse Pract. 2009;21(1):39–46.
Wen CK, Hudak PL, Hwang SW. Homeless people’s perceptions of welcomeness and unwelcomeness in healthcare encounters. J Gen Intern Med. 2007;22(7):1011–7.
Campbell RB, Saunders-Smith T, Tibebu T, Grewal EK, Yaphe HM, Mancini NL, et al. Patient-level barriers to diabetes management among those with housing instability. Can J Diabetes. 2020;44(7):S22.
Minh A, Patel S, Bruce-Barrett C, O’Campo P. Letting Youths Choose for Themselves: Concept Mapping as a Participatory Approach for Program and Service Planning. Fam Community Health. 2015;38(1):33–43.
Velonis AJ, Molnar A, Lee-Foon N, Rahim A, Boushel M, O’Campo P. “One program that could improve health in this neighbourhood is ____?“ using concept mapping to engage communities as part of a health and human services needs assessment. BMC Health Serv Res. 2018;18(1):150-.
Acosta O, Toro PA. Let’s ask the homeless people themselves: a needs assessment based on a probability sample of adults. Am J Community Psychol. 2000;28(3):343–66.
Article CAS Google Scholar
Trochim W, Kane M. Concept mapping: an introduction to structured conceptualization in health care. Int J Qual Health Care. 2005;17(3):187–91.
Gaetz S, Donaldson J, Richter T, Gulliver T. The State of Homelessness in Canada 2013. Toronto: Canadian Homelessness Research Network Press; 2013.
Lee TC, Hanlon JG, Ben-David J, Booth GL, Cantor WJ, Connelly PW, et al. Risk factors for cardiovascular disease in homeless adults. Circulation. 2005;111(20):2629–35.
Davachi S, Ferrari I. Homelessness and Diabetes: Reducing Disparities in Diabetes Care Through Innovations and Partnerships. Can J Diabetes. 2012;36(2):75–82.
Campbell DJT, Campbell RB, DiGiandomenico A, Larsen M, Davidson MA, McBrien KA, Booth GL, Hwang SW. Using community-based participatory research approaches to meaningfully engage those with lived experience of diabetes and homelessness. BMJ Open Diabetes Research & Care. 2021;9:e002154. https://doi.org/10.1136/bmjdrc-2021-002154 .
Gaetz S, Barr C, Friesen A, Harris B, Hill C, et al. Kovacs-Burns. Canadian Definition of Homelessness. Toronto: Canadian Observatory on Homelessness; 2012.
Campbell DJT, Campbell RB, Booth GL, Hwang SW, McBrien KA. Innovations in Providing Diabetes Care for Individuals Experiencing Homelessness: An Environmental Scan. Can J Diabetes. 2020;44(7):643–50.
Trochim WM. An introduction to concept mapping for planning and evaluation. Eval Prog Plan. 1989;12(1):1–16.
Kane M, Trochim W. M. K. Concept Mapping for Planning and Evaluation. Thousand Oaks: SAGE; 2007. Available from: https://methods.sagepub.com/book/concept-mapping-for-planning-and-evaluation .
Burke JG, O’Campo P, Peak GL, Gielen AC, McDonnell KA, Trochim WM. An introduction to concept mapping as a participatory public health research method. Qual Health Res. 2005;15(10):1392–410.
Concept Systems Inc. The Concept System® Global MAX™. Ithaca: Concept Systems Inc; 2020. p. Web-based Platform.
Kruskal JB. Multidimensional scaling by optimizing goodness of fit to a nonmetric hypothesis. Psychometrika. 1964;29(1):1–27.
Trochim WMK. The reliability of concept mapping. Annual Conference of the American Evaluation Association; Dallas. 1993.
Rosas SR, Kane M. Quality and rigor of the concept mapping methodology: a pooled study analysis. Eval Prog Plan. 2012;35(2):236–45.
Campbell R, Larsen M, DiGiandomenico A, Davidson M, Booth G, Hwang S, et al. Illustrating challenges of managing diabetes while homeless using photovoice methodology. Can Med Assoc J. 2021;193.
Rojas-Guyler L, Inniss-Richter ZM, Lee R, Bernard AL, King K, editors. Factors Predictive of Knowledge and Self-Management Behaviors among Male Military Veterans with Diabetes Residing in a Homeless Shelter for People Recovering from Addiction. 2014.
Lee BA, Greif MJ. Homelessness and hunger. J Health Soc Behav. 2008;49(1):3–19.
Vijayaraghavan M, Jacobs EA, Seligman H, Fernandez A. The association between housing instability, food insecurity, and diabetes self-efficacy in low-income adults. J Health Care Poor Underserved. 2011;22(4):1279–91.
Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87(2):217–20.
Rew L. A Theory of Taking Care of Oneself Grounded in Experiences of Homeless Youth. Nurs Res. 2003;52(4):234–41.
Robert SA, Booske BC, Rigby E, Rohan AM. Public views on determinants of health, interventions to improve health, and priorities for government. WMJ. 2008;107(3):124–30.
PubMed Google Scholar
Willems S, Van Roy K, De Maeseneer J. Appendix A Educating health professionals to address the social determinants of health. A Framework for Educating Health Professionals to Address the Social Determinants. of Health. Washington, DC: National Academies Press (US); 2016.
Zhang P, Bassil K, Gower S, Katj M, Kiss A, Gogosis E, et al. Cold-related injuries in a cohort of homeless adults. J Soc Distress Homeless. 2019;28:85–9.
Hillson R. Diabetes and temperature. Pract Diabetes. 2016;33(2):45–6.
Spero D. Diabetes Self-Management 2019. Available from: https://www.diabetesselfmanagement.com/blog/eight-ways-manage-diabetes-cold-weather/ .
Stafford A, Wood L. Tackling Health Disparities for People Who Are Homeless? Start with Social Determinants. Int J Environ Res Public Health. 2017;14(12):1535.
Keene DE, Guo M, Murillo S. “That wasn’t really a place to worry about diabetes”: Housing access and diabetes self-management among low-income adults. Soc Sci Med. 2018;197:71–7.
Maslow AH. Motivation and Personality, 3rd Ed. New York: Harper and Row; 1987.
Download references
Acknowledgements
Not applicable.
This study received funding from Alberta Innovates, the O’Brien Institute for Public Health and the Cal Wenzel Cardiometabolic Fund.
Author information
Authors and affiliations.
Department of Medicine, Cumming School of Medicine, University of Calgary, Calgary, Canada
Eshleen K. Grewal, Rachel B. Campbell & David J. T. Campbell
Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
Gillian L. Booth, Stephen W. Hwang & Patricia O’Campo
Department of Medicine, Faculty of Medicine, University of Toronto, Toronto, Canada
Gillian L. Booth & Stephen W. Hwang
MAP Centre for Urban Health Solutions, St. Michael’s Hospital, Unity Health Toronto, Toronto, Canada
Institute for Clinical Evaluative Sciences, Toronto, Canada
Department of Family Medicine, Cumming School of Medicine, University of Calgary, Calgary, Canada
Kerry A. McBrien
Department of Community Health Sciences, Cumming School of Medicine, University of Calgary, Calgary, Canada
Kerry A. McBrien & David J. T. Campbell
Department of Cardiac Sciences, Cumming School of Medicine, University of Calgary, Calgary, Canada
David J. T. Campbell
You can also search for this author in PubMed Google Scholar
Contributions
The study was conceived by DJTC and RBC with meaningful contributions from GLB, KAM, SWH, and PO. Data collection and analysis were conducted by EKG, RBC and DJTC. The initial draft of the manuscript was written by EKG and DJTC and was revised with feedback from RBC, GLB, KAM, SWH, and PO. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to David J. T. Campbell .
Ethics declarations
Ethics approval and consent to participate.
This study received ethics approval from the institutional review boards at the University of Calgary (REB 18-1663) and St. Michael’s Hospital/Unity Health Toronto (REB 18–288). All participants provided informed consent.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Statements organized by cluster. Tables displaying the clients’ clusters with statements and the providers’ clusters with statements.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Grewal, E.K., Campbell, R.B., Booth, G.L. et al. Using concept mapping to prioritize barriers to diabetes care and self-management for those who experience homelessness. Int J Equity Health 20 , 158 (2021). https://doi.org/10.1186/s12939-021-01494-3
Download citation
Received : 22 February 2021
Accepted : 08 June 2021
Published : 09 July 2021
DOI : https://doi.org/10.1186/s12939-021-01494-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Diabetes mellitus
- Homeless persons
- Patient engagement research
- Patient priorities
- Community-based participatory research
International Journal for Equity in Health
ISSN: 1475-9276
- General enquiries: [email protected]
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- For Health Professionals
- Diabetes Discoveries & Practice Blog
Every Person with Diabetes Needs Ongoing Self-Management Education and Support
- Patient Self-Management
- Medication and Monitoring
- Patient Communication

You prescribe medications for type 2 diabetes, but what about diabetes education and support? It can be just as essential.
Research shows that diabetes self-management education and support (DSMES) can improve A1C levels and have a positive effect on other clinical, psychosocial, and behavioral aspects of diabetes. Margaret (Maggie) Powers, PhD, RD, CDE, a clinician and research scientist at the International Diabetes Center in Park Nicollet in Minneapolis, explains how.
Q: Why should health care providers promote diabetes self-management education and support (DSMES) for their patients with type 2 diabetes?
A: It’s important because over 90 percent of diabetes care is self-care; provided by the person with diabetes. Diabetes self-management education and support enables people to be the best self-managers possible.
Q: When should that educational support be provided?
A: Our goal in writing the DSMES joint position statement was to provide clear guidance on the four critical times when a person with type 2 diabetes might need more attention to diabetes self-management. The objective was to encourage health care professionals to assess, provide, and adjust DSMES. This can help to avoid crisis management and support people with diabetes to be comfortable and confident in their decision making.
The position statement includes an algorithm of care that addresses four critical time points; these time points also are relevant for the other aspects of diabetes care.
- Fourth time point: When transitions in care occur, such as when someone is transitioning from the hospital to home or from home to assisted living. These transitions can affect an individual’s activity or ability to function, and we want to be on top of that, while also attending to other adjustments that might influence daily choices.
In clinical care at these different times, there is often a focus on, “Do we need to adjust the medication?” Yet, there’s also this whole aspect of actually taking the medication, the daily self-management, and nutrition. We want the health care system to be aware of these four critical time points and refer people appropriately to recognized and certified diabetes self-management education programs, registered dietitians, and mental health professionals, or to provide that care in the clinical setting.
Q: How can clinicians be encouraged to provide diabetes education, or make referrals for that education, at these time points for their patients?
A: We recommend embedding a diabetes self-management education and support checklist into clinical health records so that referrals for diabetes education are systematized. When you have someone who’s newly diagnosed with diabetes, or who’s experiencing another health problem, even if it’s a broken elbow—as their health care provider you may not be thinking, “I need to figure out how they’re going to stay active” or “How are they going to check their blood glucose?” or “Can they do that with one hand?” If the referral process is embedded in the clinical health record for the four critical time points, it can improve clinical outcomes, quality of care, and patient satisfaction.
Q: Can you provide more in-depth information on what is involved in DSMES?
A: If you’re the primary care provider, you can answer questions and provide emotional support regarding the diagnosis. But you might not have the time to ask and problem-solve important questions for the patient such as, “What times do you eat? When do you eat? How are you going to prepare foods now? When are you going to take the medication? How are you going to remember to take the medication?”
As diabetes educators, when we meet with someone at diagnosis, our role is to assess the factors that influence the individual’s decision making—like lifestyle, cultural influences, health beliefs, current knowledge, physical limitations, family support, financial status, medical history, even literacy and numeracy—we use a lot of numbers in diabetes. And we cover a lot of ground. We work with the person on medication adherence, monitoring of blood glucose, the food plan, physical activity, prevention of heart disease, and dealing with other acute and chronic complications. Diabetes education is also about risk reduction, such as smoking cessation, daily foot checks at home, and developing personal strategies to address psychosocial issues and concerns.
Q: What’s the evidence that diabetes education improves outcomes?
A: When I was president of the ADA, I did a talk on this topic, which is reprinted in the article, “If DSME Were a Pill, Would You Prescribe It?” Typically, when somebody is diagnosed with diabetes, they’re prescribed metformin. But why is diabetes education or nutrition therapy not automatically prescribed? The ADA goes through a process of evaluating medications and they look at efficacy—does it reduce A1C? What’s the risk of hypoglycemia with the medication? Is it weight neutral? What are the side effects? What are the costs? What I did in my talk was look at the efficacy of diabetes education using the same parameters. It reduces A1C; we have that data from diabetes education programs. We know that when people are initially diagnosed with diabetes, we can actually reduce or delay the initiation of medication with nutrition therapy.
Also, research shows that diabetes education improves the quality of life, self-efficacy, empowerment, healthy coping strategies, self-care behaviors, and adherence to the food plan. It also leads to healthier food choices, more activity, and use of glucose monitoring, and it lowers blood pressure and lipids. This is all referenced and cited in the article.
Q: Is diabetes education covered by Medicare and private insurance?
A: Medicare definitely believes in the value of education and reimburses for diabetes education and medical nutrition therapy. Private insurance also reimburses, especially for nutrition therapy. However, we've found that very few people are using the reimbursement benefits .
Q: What's preventing everyone with diabetes from receiving diabetes education?
A: I don’t think that there’s been a clear expectation by health care providers that they should write a referral or by people with diabetes that they should expect to receive referrals to a dietitian and a diabetes educator. But the ADA’s Standards of Medical Care in Diabetes—2019 recommend that everybody should receive nutrition therapy from a qualified person and they should receive diabetes education. People living with diabetes need to have clear expectations for this, and the health system—including primary care providers—needs to make the referrals. Clinical systems management can help by providing automatic referrals at the four critical time points.
There are still barriers that we're working through with Medicare. For example, you can't receive nutrition therapy and diabetes education at the same time. Another barrier is that Medicare requires diabetes education to be offered within the health system. We cannot offer our program at the local church, community center, or library—Medicare will not reimburse for those programs, even though we would like to make our programs more accessible in the community.
Another barrier is that the referral to diabetes education must come from the primary care provider. It can’t be the cardiologist, for example, and the patient cannot self-refer.
Q: The 2018 update of the ADA/EASD consensus report reinforces the importance of DSMES. What do you think will be the impact of this report?
A: I am thrilled that this consensus report supports the concept of four critical time points for diabetes education as well as individualized programs of medical nutrition therapy. The original version primarily focused on medication selection, but with each revision there’s been a much clearer indication of the value of diabetes education and medical nutrition therapy. I think this report can have a major impact on diabetes education by reducing the barriers to access and supporting the self-management needs of people with diabetes.
How do you ensure that your patients with diabetes receive education and support at critical times? Share below in the comments.
Editor’s Note: Learn more by viewing Discovering the Full Super Powers of DSMES (PDF, 1.96 MB) , a National Diabetes Education Program (NDEP) webinar and related continuing education credit available through CDC Training and Continuing Education Online .
Subscribe to get blog updates.
Share this page
We welcome comments; all comments must follow our comment policy .
Blog posts written by individuals from outside the government may be owned by the writer and graphics may be owned by their creator. In such cases, it is necessary to contact the writer, artist, or publisher to obtain permission for reuse.
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 4: Ambulatory Care—Type 2 Diabetes Management
Bradley Phillips; Michelle Farland
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book

Jump to a Section
Chapter aims, introduction.
- OUR PRACTICE—AN OUTPATIENT INTERDISCIPLINARY ENDOCRINOLOGY PRACTICE
- UTILIZING CRITICAL THINKING SKILLS IN OUR PRACTICE
- APPLICATION OF THE PPCP IN OUR PRACTICE
- THE COLLECTION OF PATIENT INFORMATION IN OUR PRACTICE
- CLINICAL REASONING, CRITICAL THINKING, AND THE PPCP FOR THE CARE OF CARLOS P.
- Full Chapter
- Supplementary Content
The aims of this chapter are to:
Discuss the roles of a systematic patient care process and clinical reasoning in assessing and resolving medication-related problems as part of a collaborative effort to provide patient-centered care in type 2 diabetes mellitus (T2DM) management.
Incorporate the elements of the Pharmacists’ Patient Care Process (PPCP) in a simulated patient case while outlining critical thought processes and clinical reasoning as it relates to the care of a person with T2DM.
• Type 2 diabetes • critical thinking • clinical reasoning • medication optimization • chronic disease state management • Pharmacists’ Patient Care Process • patient-centered care
Providing care for patients with diabetes mellitus (DM) requires a multifactorial approach and is ideally conducted in an interdisciplinary practice. The World Health Organization describes diabetes as “a chronic disease that occurs either when the pancreas does not produce enough insulin or when the body cannot effectively use the insulin it produces.” 1 The primary concern of the resultant hyperglycemia is the negative impact on nerves and blood vessels. These negative impacts result in chronic complications of diabetes, including microvascular complications (eg, retinopathy, nephropathy, neuropathy) and macrovascular complications (eg, transient ischemic attack, cerebral vascular accident, myocardial infarction).
According to the American Diabetes Association (ADA), Standards of Medical Care in Diabetes 2023, the diagnosis of DM is made following a fasting plasma glucose (≥126 mg/dL), 2-hour oral glucose tolerance test (≥200 mg/dL following 75 g anhydrous glucose), random plasma glucose (≥200 mg/dL with classic symptoms of hyperglycemia such as polyuria, polydipsia, polyphagia), or A1C (≥6.5%). 2 Confirmation of the diagnostic test is needed in the absence of unequivocal hyperglycemia.
Over 37 million Americans have a diagnosis of diabetes, with about 90% having type 2 diabetes mellitus (T2DM). The cost of diabetes care in the United States has risen significantly in recent years, with a 26% increase between 2012 and 2017. In 2017, the estimated cost of diabetes was $327 billion (US dollars), with direct medical costs contributing $237 billion and reduced productivity contributing $90 billion. 3
Diabetes management requires active participation from the patient in many aspects of their lives, and accordingly, it requires healthcare providers to actively engage in the biopsychosocial model when applying a multifactorial approach to providing care to each patient. Therefore, the ADA recommends “people with diabetes can benefit from a coordinated multidisciplinary team that may include and is not limited to diabetes care and education specialists, primary care and subspecialty clinicians, nurses, registered dietitian nutritionists, exercise specialists, pharmacists, dentists, podiatrists, and mental health professionals.” 4
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait

- Previous Article
- Next Article
What Is Professional Competency?
Elements of a glycemic management education program, institutional culture, diabetes education in the hospital: establishing professional competency.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Carol S. Manchester; Diabetes Education in the Hospital: Establishing Professional Competency. Diabetes Spectr 1 October 2008; 21 (4): 268–271. https://doi.org/10.2337/diaspect.21.4.268
Download citation file:
- Ris (Zotero)
- Reference Manager
Establishing and maintaining professional competency is essential for the successful delivery of diabetes care and education. An interdisciplinary approach to education is effective for facilitating the delivery of knowledge and supporting glycemic control efforts in the hospital. Educational programs should be designed to promote and develop critical thinking skills and clinical judgment using a variety of media and resources targeted to adult learners. A competent professional staff will provide care that is evidence-based, safe, effective, and appropriate for the population served. These efforts have the potential to improve quality outcome measures and enhance patient satisfaction.
Between 1980 and 2003, hospital discharges coded with a diagnosis of diabetes increased from 2.2 to 5.1 million, representing a 132% increase in 23 years. 1 The economic burden of diabetes care was estimated at $174 billion in 2007, of which $116 billion was spent on medical expenditures, including $58 million on hospital inpatient care. 2 These figures continue to increase at a time when the management of acute care diabetes and hyperglycemia has undergone intensification and rapid change. 3 – 5 Thus, health care systems are gaining an awareness of the importance of glycemic control, the impact that provision of diabetes care has on resources,and the need to redesign systems and processes that will optimize diabetes care delivery.
How, then, can national standards for diabetes care and education be met;staff knowledge be maintained at cost-neutral levels; lengths of stay,readmission rates, and hospital-acquired complications be reduced; and cost savings be achieved? 6 – 15 The establishment of an interdisciplinary team of clinical experts and“champions” can help achieve all of these goals and facilitate the delivery of diabetes self-management education in the acute care setting.
In a 2004 article, Abbate 16 stated that, “Improving diabetes care requires competent providers to be actively involved in quality improvement in order to build a system capable of translating their knowledge into optimal outcomes for patients.” To state that one is competent is to say that one has sufficient knowledge and ability and is capable of the task or position. A definition of competency that can be applied to all disciplines is, “a level of performance demonstrating the effective application of knowledge, skill, and judgment.” 17 In its scope of practice document, the International Council of Nurses states that, “The registered nurse attains knowledge and competency that reflects current nursing practice.” 18 And the American Nurses Association adds that, “Although registered nurses have the most contact with the acutely ill patient and are often the main providers of survival skills education, all health care providers need sufficient diabetes knowledge to provide safe, competent care to persons with or at risk for diabetes.” 19
Ensuring the professional competency of an entire clinical staff is essential to the successful delivery of evidence-based, safe, effective,respectful, and appropriate care.
Studies have reported the lack of diabetes knowledge prevalent in a variety of provider disciplines. 20 – 23 This lack of knowledge includes unawareness of current practice standards,insufficient understanding of pharmacological agents including insulin and oral diabetes agents, inaccurate carbohydrate counting, and an inability to critically assess patient characteristics crucial to individualized diabetes management. Add to this the need to carefully evaluate concomitant therapies,treat comorbidities, and provide diabetes self-management knowledge and skills to patients, and it becomes clear that providers are lacking crucial skills and knowledge essential to managing these complex tasks.
Key elements of a successful inpatient glycemic management education program include core competencies, knowledge assessment, development of a strategic education plan, and continuing education. These must be established by an interdisciplinary team composed of individuals knowledgeable about diabetes and willing to serve as champions of efforts to improve glycemic control. The complementary knowledge and skill sets of the various disciplines represented in a diabetes care team allow the team to develop an educational program that will disseminate the wide range of requisite knowledge and training necessary to ensure professional competency throughout the health care system.
Core competencies must be established for physicians, nurses, dietitians,and pharmacists as the primary providers of patients care and education. A competency is “verification that required skills, processes, or concepts are done/understood correctly as determined by an expert.” 24 Competencies are used to validate and verify the scientific knowledge base and skills of staff members. Core competencies related to hospital glycemic management and diabetes care include the proper use of insulin and other diabetes medications, nutrition therapy, point-of-care testing, hypoglycemia treatment, and concomitant therapies.
Methods that can be used to successfully evaluate competencies include case scenarios that require critical thinking and problem-solving skills with a focus on assessment, prioritization, and accurate clinical decision making, as well as simulation exercises that entail observation of skills (process audits) and can incorporate written exercises. Internet-based competency tests can also be created, allowing individuals to take a competency test at any time. Table 1 identifies key elements to be included in a core competencies test for insulin; Table 2 provides an example of an insulin competency checklist and questions designed to promote critical thinking and clinical judgment skills. It is important to consider the Joint Commission's requirements for age-related competencies and incorporate these into core competency tests developed for specific populations and staff members. 25
Core Competency Content for Insulin

Example of a Competency Question for Insulin

Before developing a strategic plan for diabetes staff education, a thorough assessment of each professional discipline's current knowledge and skills must be conducted. Valid tools are available or can be developed to test the basic knowledge necessary for safe care delivery and effective problem solving,prioritization, and assessment. It is extremely helpful to have an awareness of the educational preparation and training of the staff; recognizing the composition of the staff will help the team tailor educational offerings for specific groups or individuals using appropriate teaching methodologies. 26
A review and inventory of available tools, reference materials, and Internet-based resources must be completed. Determining the actual availability of these resources to staff is important. If the resources exist but staff members are unable to access them easily and in a timely manner, the benefit is lost. Additionally, an education budget must be discussed with administration so that it is clear how many non-patient–care hours can be used for learning.
Providing education to all staff members who deal with diabetic patients anywhere along the health care continuum presents significant challenges. Factors that can affect the success of educational initiatives include the varying work schedules of staff, paid versus unpaid time for training,inclusion of “nice to know” versus “need to know”information, and the linking of performance to clinical excellence and peer review. 27 Another major challenge is “information acquisition fatigue,” the constant introduction of new information, new equipment and technology, and new processes and changes that can lead to an inability to process, integrate, and internalize newly acquired knowledge. An educational plan should be multifaceted, realistic, and flexible and should have established measurable learning outcomes for staff.
Some components of a successful plan for acute care include employee orientation, tests of medication knowledge, preceptor clinical guidelines and curriculum, annual competency testing for each discipline (e.g., physicians,nurses, dietitians, and pharmacists), professional development and continuing education, and resource support. Facilities that are associated with an academic health center must also plan to review curriculum and provide orientation to faculty and students. Strong collaborative partnerships with schools can be established to provide graduate student preceptorships in diabetes care and education.
New employee orientation is an excellent opportunity to establish the standard of practice and impart necessary knowledge and understanding of glycemic management. This can include a review of the classifications of diabetes, the rationale for tight glycemic control, acute care glycemic targets, and the treatment modalities used in the hospital (e.g., basal-bolus insulin therapy). This is also a good time to stress the importance of educating patients to perform diabetes self-care sooner rather than later.
Incorporating relevant diabetes scenarios on a new employee test allows for assessment of their level of knowledge before they finish formal orientation. Preceptors of the new employees, who have had their knowledge validated before they model diabetes care for new staff, can then be aware of the new employees' strengths and identify appropriate learning opportunities.
Administration can be supportive by allowing time for new employees to be trained to competency rather than to a specific duration of time. 28 This is especially important when training new graduates. A study conducted by Forneris and Peden-McAlpine 29 with novice nurses identified the emergence of the intentional critical thinker at 4–6 months, with intentional coaching and narrative reflective journaling as part of the process. This confirms that critical-thinking skills are developed and nurtured by the professionals and experiences encountered over time.
Professional development or continuing education can be targeted at a basic or an advanced level. Special population needs and research can be incorporated into these offerings. Methods to facilitate learning include the development and use of case studies and case scenarios, Grand Rounds presentations, Internet-based learning modules, journal clubs, resource toolkits, and medication charts. Clinical rounding, clinical coaching,observation and shadowing, and cross-discipline training should be considered an integral part of the staff development plan. 27 , 30 – 34 A creative and innovative approach to education has resulted in sustained knowledge and professional growth. 35
In addition to the interdisciplinary team and education plan, the culture of the institution will have a significant impact on staff behaviors and clinical outcomes. Studies in the intensive care units of the Johns Hopkins Quality and Safety Research Group have shown that a “culture of safety,particularly a teamwork climate, is a predictor for many clinically important outcomes.” 36 Professionals must believe they are functioning in a safe environment where mutual trust and respect exist, collaboration is fostered, and a common goal for care delivery is shared. 37
Educational materials and curriculum content should be developed using the national standards 30 , 38 of the professional organizations such as the American Diabetes Association,the American College of Endocrinology, the American Association of Clinical Endocrinologists, the American Association of Diabetes Educators, and the Joint Commission. Reviewing teaching and learning principles, curriculum development materials and guidelines, and tools created for testing will help facilitate new knowledge and promote the design of a hospital-based professional education program.
Organizations specific to staff development, education, and health education have abundant resources available. As technology continues to advance, information system technicians can assist in the development and implementation of Internet-based programs that appeal to younger professionals and fulfill a need for education in real-time, which is at the time the information is actually needed by the staff member. Workshops and written materials on coaching, mentoring, and modeling can provide the foundation for a well-rounded, diverse educational program to meet the diverse needs of adult learners.
Ensuring professional competency is an important strategy for improving diabetes care and education in acute care settings. As the prevalence of diabetes continues to rise and health care costs soar, professionals are called on to provide quality clinical care and education to achieve optimal clinical and behavioral outcomes. Staff members are being asked to do this concurrently with a multitude of other tasks, while facing competing demands,budget restrictions, and time constraints. Investing in the development of a strategic diabetes education plan by a dedicated interdisciplinary team not only will improve outcomes, but also will improve staff satisfaction with their work, enhance retention of dedicated staff members, increase employee engagement, and promote patient satisfaction.
The time is now for diabetes care providers to work in concert with administrators of institutions and health care systems to redesign inpatient health care delivery for diabetic patients. This can start with a redesign of professional education as we have known it in the past, moving away from didactic presentations toward thought-provoking case simulations, from classroom learning to hands-on clinical rounding, from self-learning packets to Internet-based learning modules and from standard testing to simulation experiences. 27 , 39 With this, the realization of the importance of glycemic management will become the norm, and the integration of clinical protocols, policies, and patient education for diabetes care and glycemic management will be the standard of practice.
Carol S. Manchester, MSN, APRN, BC-ADM, CDE, is a diabetes clinical nurse specialist at the University of Minnesota Medical Center and the University of Minnesota Children's Hospital in Fairview and an adjunct faculty member at the University of Minnesota School of Nursing in Minneapolis.
Email alerts
- Inpatient Management of Hyperglycemia and Diabetes
- Online ISSN 1944-7353
- Print ISSN 1040-9165
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account

- Center on Health Equity and Access
- Health Care Cost
- Health Care Delivery
- Value-Based Care
The Role of Clinical Care Pathways in Diabetes Management: A Guide to Designing a Clinical Care Pathway at Your Institution
This publication was developed in conjunction with Eli Lilly and Company. Its content does not constitute an endorsement of the company or its products by the contributors.
A clinical care pathway , also known as a care pathway or integrated care pathway, is designed to guide clinicians regarding the optimal approach to treatment selection for a patient with a specific condition or disease, with the primary goals of improving quality of care, reducing variations in clinical practice, and promoting efficient use of health care resources. 1 Based on evidence-based clinical practice guidelines, clinical care pathways include recommendations for screening, diagnosis, monitoring, treatment goals, and interventions over the course of a disease or continuum of care, and thus have the potential to influence quality of care and patient outcomes. 1 Clinical care pathways for chronic conditions such as type 2 diabetes are designed to provide different levels of support across multidisciplinary teams throughout the disease continuum, from precursor risk to advanced disease. 2
Benefits of Clinical Care Pathways
Reflecting the best clinical evidence available, clinical care pathways can provide health systems with a roadmap for providing the most appropriate treatment based on the latest clinical evidence and current guidelines, delivered in a timely manner and without unnecessary variation. 2 Outcome metrics that show optimization of delivery of care may include: clinical outcomes, patient knowledge and self-management, implementation of evidence-based practices, and level of multidisciplinary teamwork. 2
Standardized clinical care pathways that reduce variation in treatment and improve adherence to evidence-based guidelines among providers in a health care system may in turn reduce cumulative incidence of diabetes-related complications and all-cause mortality, reduce cardiovascular risk, 3 and result in health care savings. 4
According to 2017-2018 CDC data on adults diagnosed with diabetes in the United States, target goals for A 1C (< 8%), blood pressure (< 140/90 mm Hg), and cholesterol levels (non–high-density lipoprotein < 130 mg/dL) were met by 75%, 70%, and 56% of patients, respectively. 5 However, just 26% met all 3 care goals and were nonsmokers, highlighting the potential to increase the proportion of patients who achieve multiple target goals for diabetes management.
Although numerous interventions to improve adherence have been implemented, a highly fragmented care delivery system that lacks clinical information capabilities, duplicates services, and is poorly designed to coordinate delivery of chronic care remains a major barrier. 6 The implementation in health care systems of standardized clinical care pathways based on guideline-recommended targets and goals of diabetes care may help bridge this gap to delivering optimal care for patients. Well-developed multidisciplinary clinical care pathways provide structure when choosing an individual’s care plan, while keeping important considerations at the forefront.
Developing Clinical Care Pathways in Diabetes
The primary goal for management and treatment of diabetes is to prevent or delay complications and maximize quality of life. 6 Evidence-based guidelines from leading organizations such as the American Diabetes Association (ADA), the American Association of Clinical Endocrinology (AACE), and the American College of Endocrinology (ACE) provide a framework for developing clinical care pathways for populations with diabetes. In 2015, AACE and ACE published joint guidelines for developing a comprehensive care plan for diabetes. 7 In 2020, as a supplement to the 2015 guidelines, AACE and ACE jointly published an algorithm for the comprehensive management of patients with type 2 diabetes. 8 This algorithm provides clinicians with a practical guide to comprehensive management of the entire patient and uses evidence-based approaches to treatment that take into account individual risks and complications.
The latest ADA guidelines (2021) suggest a patient-centered approach to the management of diabetes, using a chronic care model that involves close working relationships between patients and clinicians. The chronic nature of diabetes and its multiple associated comorbidities warrant a multidisciplinary approach to management, which may include physicians, nurse practitioners, physician assistants, nurses, dietitians, exercise specialists, pharmacists, dentists, podiatrists, and mental health professionals. 6
Although health systems create clinical care pathways for diabetes management based on information from the ADA and AACE/ACE guidelines and cost-benefit analyses of treatment, variability in following best practices may depend on several influences. These include health system formularies, differences in stated goals, composition of multidisciplinary teams, patient characteristics, number of patients, and treatment settings. This variability can occur even among clinical care pathways considered to reflect “good practice.” 9 Therefore, considering variances in clinical care pathways and working toward a standardized approach to care may be beneficial. 9 The availability of treatment options may be limited by an approved formulary, value-based agreements with the manufacturer, or the limitation of treatment options to those available on the electronic health record, introducing variability into management pathways among health systems. Moreover, affordability of diabetes medications can be a substantial barrier to achieving glycemic goals. Therefore, considering variances in pathways and working toward a standardized approach to care may be beneficial.
Implementing Clinical Care Pathways in Diabetes
Clinical care pathways include evidence- and expert-driven recommendations and are evidence-driven, multidisciplinary and collaborative, electronically-integrated, outcome-oriented, and reflective (see Table ). 9 As an agreed-upon plan for clinical management of a group of patients with a particular medical problem, a clinical care pathway provides a multidisciplinary template of the plan of care for leading each patient through the health care system to a desired outcome. In diabetes, this includes monitoring of complications, escalation of glycemic-control treatment, dietary management, and achievement of identified treatment goals. 2 Although treatment guidelines, which are embedded into the clinical care pathway itself, are usually developed in a top-down fashion, clinical care pathways are more often developed from the bottom up so they closely fit the configuration of the particular health care organization. Adaptations for particular institutional cultures can be accommodated by including local teams in the creation and implementation of the clinical care pathway. 10
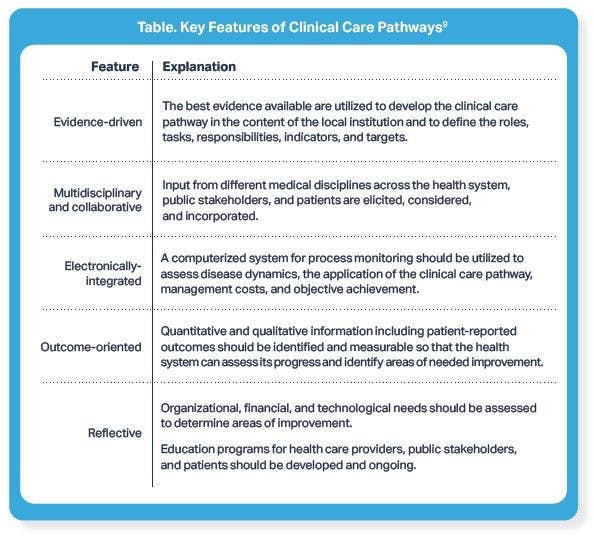
Click to view larger image.
The Importance of Multidisciplinary Involvement
Multidisciplinary involvement is essential to the development and launch of a successful clinical care pathway, since implementation depends on both clinical service providers and managers. Engagement of staff in all areas is necessary at each stage, from adoption to implementation to maintenance. 10 A review of 32 studies of integrated care interventions for type 2 diabetes, published in 2016, found that most facilitators to the implementation process were found at the social context level, including staff involvement in decision-making and planning, the ability to recruit committed staff and ensure buy-in, good leadership, and intra- and inter-practice cooperation and sharing of resources. 11
These findings align with those of the ADA, which lists delivery system design in which medical visits are coordinated with a team-based approach, decision support based on evidence-based guidelines, clinical information systems that can provide both patient-specific and population-based information, and a quality-oriented culture among the core elements of its Chronic Care Model. Expanding the role of teams in implementing more intensive disease-management strategies, implementing electronic health records, and tracking medication history at a systems level are key to improving the quality of diabetes care overall. 6
Addressing Barriers to Successful Implementation of Clinical Care Pathways
Barriers impeding adoption of clinical care pathways may occur at the level of staff (clinician or management) or health care organization (management, resources, or institutional structure). They may also be influenced by external factors, such as social policies or patient characteristics. 10 Analyses of situations in which guideline implementation failed to achieve the desired outcomes concluded that factors such as patient education and communication, doubts among physicians about the validity of the recommendations, overly complex algorithms for diagnosis and treatment determination, excessive workload for physicians, and demands for unnecessary tests by patients need to be considered when developing clinical care pathways. 12 Furthermore, diabetes has multiple potential comorbidities and related complications; effective management of patients requires a collaborative care approach with providers from multiple specialties, including diabetes care and education specialists, physicians, nurse practitioners, physician assistants, nurses, dieticians, exercise specialists, pharmacists, dentists, podiatrists, and mental health professionals. 6 Therefore, a clinical care pathway for diabetes needs to address these complexities of care and encourage all stakeholders to buy into it.
In the following text, experts from Cleveland Clinic, Geisinger, and Primary PartnerCare , discuss how they implemented clinical care pathways for diabetes treatment at their institutions. Guidance on implementing clinical care pathways into the electronic health record system is provided by experts from the Cerner Corporation and Epic Systems Corporation .
Assess Your Populations
The experts agreed that the first step in establishing a clinical care pathway in diabetes is to focus on primary care physicians (PCPs). “Primary care manages 90% of the patients with type 2 diabetes,” said Kevin Pantalone, DO, ECNU, FACE, director of diabetes initiatives, and staff endocrinologist in the department of endocrinology at Cleveland Clinic. Clinical care pathways are designed to help guide treatment decisions, particularly at a time where multiple treatments are available to meet different needs. “We are seeing literally an explosion in [new] diabetes medications,” Harry Jacob, MD, chief medical officer at Primary PartnerCare explained. “It is becoming increasingly difficult for PCPs to know which treatments to prescribe.
Developing a clinical care pathway that meets the needs of a specific institution’s patient population is important and may require combining recommendations from multiple guidelines. The diabetes clinical care pathway at Cleveland Clinic combines the ADA, the American College of Cardiology (ACC), and the AACE/ACE guidelines to aid PCPs in sifting through the recommendations and making a decision that is right for their patients.
“Compared with when they were first introduced, now the guidelines are similar,” said Pantalone. “But then you add in the American College of Physician’s (ACP) guidelines, which suggest A 1C targets of 8%, 13 which was against what the ADA was saying, and I think you can appreciate if you are a [PCP] and you are hearing different things from different organizations, you say, ‘What’s the right thing to do?’ Overall, that was leading to a lot of the therapeutic inertia.”
Therapeutic inertia refers to the point at which providers fail to intensify therapy in a patient even though it is indicated by an elevated A 1C . 14
“[At Cleveland Clinic,] we found a very high rate of therapeutic inertia, where patients were being seen [by providers] and their A 1C was above target, yet when we looked [at data] 6 months after the visit, we did not see any evidence of an intervention,” Pantalone explained.
He went on to explain that there is a tendency for patients and providers to feel that they are providing better care than they are. Moreover, patients and providers will often talk themselves out of intensifying treatment. “For example, the patient may say, ‘Dr Smith, it was the holidays. I’m really going to try, give me a second chance. I don’t want any more meds,’” Pantalone explained. “However, when you look back, the patient’s A 1C has been above goal for 2 years.” He went on to say, “Generally speaking, when an A 1C is above target, without an intervention being performed, it will either remain elevated or slowly worsen; it’s not magically going to get better.”
Primary PartnerCare found similar results when looking at their data, according to Marion Davis, MBA , chief executive officer, “The physician leadership was clearly surprised that some patients with diabetes were only getting one A 1C [measurement] per year. What the physicians think they are doing is not always what they are [actually] doing. Having population-level data really helps change behavior and focus their attention.”
Assemble All Stakeholders
“Collaboration between specialty and primary care in developing and implementing these clinical care pathways is a must,” said Christopher Babiuch, MD, medical director of specialty integration at Cleveland Clinic. “Each group brings certain perspectives and needs to the table. Understanding these allows for a better end product. For example, hypertension control is key to improved cardiovascular outcomes. Multiple touch points to manage this improve the likelihood of good control. When a patient is identified as having uncontrolled hypertension in the endocrinology office, communication between teams ensures faster medication titration and follow-up than if we were not working as a team.”
Anita D. Misra-Hebert, MD, MPH, associate professor of medicine at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University and center director of the Healthcare Delivery and Implementation Science Center, also at Cleveland Clinic, echoed Babiuch’s comments. “Collaboration between primary care and endocrinology is critical to achieve optimal diabetes care outcomes,” she explained. “We are fortunate that, within our integrated health system [we have] a shared electronic medical record; communication can occur seamlessly.” Although the primary care and endocrinology departments have the same goals of optimizing diabetes care, she said, clinical workflows may differ significantly between the 2 specialties. “Through close collaboration, workflows can be optimized [to] both settings with coordinated and appropriate management.”
"We are seeing literally an explosion in [new] diabetes medications." Harry Jacob, MD
Ensuring pharmacists are also part of the care plan can aid in maintaining an optimal standard of care. According to Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES, a clinical pharmacy specialist and the continuous glucose monitoring program coordinator at Cleveland Clinic , “It is easy [for a provider] to become complacent when a patient has their A 1C close to goal. But what we know now is that when patients have heart failure, high cardiovascular risk, or already established cardiovascular or kidney disease, irrespective of their A 1C , we should be putting them on [different treatments].”
Create Committees
Engaging stakeholders involved in initiating the clinical care pathway in teams can ensure all stakeholders’ goals are met. One way to do this is to establish committees, said Juliann Molecavage, DHA, MHA, BSHCM, associate vice president, quality & primary care services at Geisinger. “Our diabetes transformation committee includes endocrinologists and a quality medical director, nurses, pharmacists, and dieticians, all working together utilizing their content expertise and to develop the pathway.” The committee meets monthly to review analytics and ensure the clinical care pathway is having a positive impact, she added.
"Frequently, the hardest part is putting your providers in the room and getting them to agree. [But] that’s what you must do; that governance is important." Jeffrey Wall, MD
Emily Barey, MSN, vice president at Epic, agreed that it is important to gather all stakeholders and work to achieve consensus. “Like any good process improvement work, it starts with an executive sponsor, a physician champion pulling in key stakeholders,” she said, adding that project management support is also important. After workflows have been analyzed and clinical best practices have been established, “operationalizing [the clinical care pathway] takes project management to coordinate all the stakeholders and the decisions, not just regarding the handoffs but also for coordinating the care. Oftentimes, that is a big paradigm shift for many organizations to make.
Determine Electronic Health Record Capabilities
Implementation of clinical care pathways into the electronic health record system is key to ensuring decisions can be made in real-time at the point of care. For this reason, the team at Geisinger ensures that information technology (IT) staff are involved in development meetings. “We include an IT member in the actual meetings to help us understand what [our electronic health record vendor] allowed for,” Molecavage explained. It is important to ensure that point-of-care tools, such as best practice alerts (BPAs) and health maintenance topics, definitions of patient population, and testing intervals are all aligned in the electronic health record, she said.
The electronic health record system is also important for ensuring the adaptability of the care plan across multiple encounters in the organization. “One of our most important learnings from our initial implementation of an electronic medical record tool to improve diabetes management was the need to adapt our educational tools to be available asynchronous to the actual office visit,” said Misra-Hebert. For example, she explained that because diabetes management decisions often are made in response to a subsequent A 1C result and reconsidered at the time when a refill on a current medication is being requested, or when a patient may be communicating blood sugar results through the electronic record, having an integrated clinical support tool available at those times, as well as during an office visit, may substantially affect provider uptake and improve diabetes management overall.
A number of electronic health record systems have been developed to be able to handle clinical care pathway integration. “Our care pathway framework allows us to build, or the client or third-party companies to build algorithms, questions, answers, prompts, recommendations, and treatments into the Cerner environment natively, to cover not just diabetes, but other chronic conditions,” said Jeffrey Wall, MD, senior director, clinical innovation, at Cerner Corporation, a health information technology company.
Development of the clinical care pathway in the electronic health record also necessitates a strong relationship with an electronic health record vendor, as well as physician leaders who will meet with the vendor. “Your ability to alter your electronic health record is somewhat limited to what [your] vendor can allow you to do,” Pantalone explained. “It may sound silly, but an extra click can be a huge barrier if you do not have the ability to make the adjustments. It is very important for organizations to have a good relationship with their electronic vendor and have a vendor that continuously tries to improve its products. With continued dialogue with [our vendor] and using our physician leaders who oversee leading our enterprise-wide electronic health record, we have been able to slowly but surely make the changes necessary to help improve care.”
“Frequently, the hardest part is putting your providers in the room and getting them to agree,” according to Wall. “[But] that’s what you must do; that governance is important.”
Health information technology organizations work to have meaningful conversations with their physician clients to understand the adjustments that are needed in the electronic health record to best meet the needs of the provider and patient populations. “We will ask the physician if the issue stems from a compliance problem or a care variance problem,” explained David Nill, MD, vice president and chief medical officer at Cerner Corporation. “From there, we can then drill down and say, ‘Okay, what do we need to standardize for the providers? Where are they tripping up?’ Notably, it is at that point where care pathways can help nudge providers in the right direction.”
Determine Funding Sources
Cost can also be a barrier to the implementation of clinical care pathways. Some organizations may have the opportunity to apply for grants or other philanthropic sources to fund their clinical care pathway. “Our intensification tool project was funded by a grant through a pharma company,” Pantalone said. “They were very concerned about the high rates of therapeutic inertia. In addition, [Cleveland Clinic] has a very strong philanthropy base. I can appreciate where smaller organizations may struggle to try to develop these types of system-wide intervention simply because of the resources being more limited.”
The implementation of clinical care pathways at an organization requires buy-in from several different stakeholders, which can be a challenge; however, bringing in the right individuals early in the process can help stave off a number of issues. “The sooner you get started on [development], the better,” Pantalone explained. “There is a lot of red tape, there are a lot of stakeholders, and it takes time to slowly move through the bureaucratic process. With billing, nursing, etc, there are a lot of resources that need to be allocated.”
Molecavage agreed that many organizations do not implement clinical care pathways because they have limited resources. “You must spend money to make money sometimes,” she said. “However, [that can be] difficult for organizations that are smaller or that do not have a structure in place. We’re lucky; Geisinger’s a large system, so we can tap into resources that not all areas have.” She suggests that smaller health care systems incorporate discussions on implementing clinical care pathways into existing physician meetings. “We would also start with the leaders. The leadership in community medicine would be sort of the stakeholders. We would present it to them and help them understand the importance of it and what the workflow is, so they’re the ones who are helping to support it with the frontline physicians, getting it to the department meetings.”
"One of our most important learnings from our initial implementation of an electronic medical record tool to improve diabetes management was the need to adapt our educational tools to be available asynchronous to the actual office visit." Anita D. Misra-Hebert, MD, MPH
Build the Clinical Care Pathway
One of the first steps in building a clinical care pathway is focusing on a few key goals. “Most of our customers who have started down the path of using a clinical [care] pathway have done so with quality, cost, and patient experience in mind,” said Barey. “Nonetheless, [it is advisable] to usually start with 1 or 2 [goals] to get a template approach to understanding how to solve the process problem, and then reaffirm that all departments are on the same page. Then determine how to use technology to make it highly reliable, measurable, and as efficient as possible.”
One of the main goals of the clinical care pathway program at Cleveland Clinic was to overcome therapeutic inertia by making sure that elevated A 1C levels were brought to the attention of each health care professional the patients encountered. “If we only make a change when a patient is in front of us [specialists] in the office, we are not going to make much progress because most patients may only see us 2 or 3 times a year at most,” said Pantelone. For that reason, alerts were implemented in the electronic health record system to ensure each person seeing the patient is aware of an elevated A 1C . “Whether it’s the PCP, me, or the pharmacist, if someone sees that the control is not good, even if [we] do not have time to deal with it that day during the visit for back pain, [we ensure] that we refer the patient or do something to ensure that they are intervened upon by another means within the next couple of weeks to months.” For example, if a patient has had an A 1C of 8% or higher for 6 months, a BPA will pop up in the electronic health record. The provider can then consult an endocrinologist, nutritionist, diabetes educator, or pharmacist, and place medication orders directly from the electronic health record.
The overall goal of the clinical care pathway is to make prescribing easier for PCPs, who can sometimes be overwhelmed by the number of medications available for diabetes. “Embedded in our electronic health record, we have 5 goals of care from which a provider can select which goals are most important for that particular patient,” Pantelone explained. When a provider chooses 1 of the goals of care—A 1C reduction, weight loss, hypoglycemia, costs (medication costs), and cardiovascular risk—the intensification tool lists the drug classes (in descending order, based on recommendation) that will help the patient attain that goal. If a provider chooses multiple goals (eg, weight loss and A 1C reduction), the tool lists medication choices that would help attain all of the goals selected.
"Most of our customers who have started down the path of using a clinical care pathway have done so with quality, cost, and patient experience in mind. Nonetheless, [it is advisable] to usually start with 1 or 2 [goals] to get a template approach to understanding how to solve the process problem, and then reaffirm that all departments are on the same page. Then determine how to use technology to make it highly reliable, measurable, and as efficient as possible." Emily Barey, RN, MSN
Geisinger has followed a similar approach, according to Molecavage. “We worked with both endocrinologists and our PCPs to come up with a pathway for first-line and second-line medication and treatment for our patients with diabetes, as well as the right time to refer [to an endocrinologist] and then transition the care back to primary care. They were able to do so in a way where the PCPs had a good feel for what that care plan is, and they could then go ahead with the treatment.” For example, BPAs were added to the electronic health record that would alert the user that a patient had not had their A 1C checked in the last 6 months, or that a prescribed medication was not on the active list. “If the patient was not on a [recommended] medication, the alert would prompt an order set, which would go through the first-line and second-line medications,” she explained.
The creation of patient registries is also a key goal for monitoring high-risk patients and ensuring an organization remains in contact with them. “[Through our] diabetes registry we were able to identify those patients with an A 1C above 9%, for example,” Pantalone said. “About 10% of patients had A 1C above 9%, which translated to about 7000 patients. [That is] a tremendous opportunity to engage with patients.”
Another goal making sure that Cleveland Clinic had ambulatory care pharmacists embedded at most of its family health centers. “[They] were well-versed in diabetes and hypertension management,” Pantalone explained. “Embedding them in the community family health centers was very important as this would be a means for PCPs to help refer their patients and to help assist with diabetes management as well as blood pressure control.”
Determine Referral Pathways
Part of the clinical care pathway at Cleveland Clinic is identifying patients who are newly diagnosed and referring them to a specialist, then being very aggressive in terms of a structured follow-up program for 6 to 9 months to get the patient’s A 1C under control before transitioning them back to primary care. Pantalone explained that the goal is to have specialists returning to acting as a consultant, which can only be achieved by referring the patients early on, intervening where necessary in treatment, and then transitioning back to primary care. “These pathways and processes must be developed through a strong collaboration with primary care to ensure their effectiveness and compliance by all parties involved,” he said. “This strong collaboration at Cleveland Clinic is referred to as the ‘Diabetes Neighborhood,’ and leaders from pharmacy, primary care, endocrinology, etc, meet weekly to review the progress and implementation of the various initiatives being developed. This helps to ensure the early referral of patients with uncontrolled type 2 diabetes to the specialists, followed by a smooth and clear transition back to their primary provider once the goals of care have been met.”
"We worked with both endocrinologists and our PCPs to come up with a pathway for first-line and second-line medication and treatment for our patients with diabetes, as well as the right time to refer [to an endocrinologist] and then transition the care back to primary care." Juliann Molecavage, DHA, MHA, BSHCM
“One of the biggest things we’ve noticed in developing a registry is we’ve been able to identify patients and a pathway for referral,” he said. “[For example,] a patient with an A 1C above 9% for 6 months would be referred to an endocrinologist. After that appointment, the patient will follow up with a pharmacist or nurse practitioner within a month, then follow up with a mid-level provider in 3 months, and then ultimately come back to see the physician at 6 months. The goal is to then have the patient’s A 1C be at target and to transition them back to primary care. We are trying to get patients referred early in the [course of the] disease where we feel we can have the biggest impact as a specialist team and then get them back to their PCP for ongoing management.”
Isaacs explained that the collaborative practice agreements among pharmacists in Ohio enables them to serve as mid-level providers who are able to adjust medications. Thus, pharmacists can interact with patients in between their usual care visits and provide medication intensification support, as needed, an important part of Cleveland Clinic’s diabetes clinical care pathway.
The value of having a pharmacist as part of the clinical care pathway is that pharmacists have specialized knowledge of medications, she explained, which can help providers save time in looking up information about drug interactions, adverse effects, and more. “Combined with the ability to be able to adjust the medications, [the availability of a pharmacist] helps to overcome therapeutic inertia and helps to get patients to their glucose targets more quickly,” she said.
“The most important message that a [patient] receives is a personalized one [from their provider] that tells them there is an opportunity for them and their care. We have seen incredible results [by] going direct to [the patient] on gaps in care, follow-up visits, and closure of those gaps." Ray Herschman, MS
Determine How Success Will Be Measured
The determinants of success should be decided before implementing the clinical care pathway and agreed upon by all stakeholders. Consistent metrics are important, advised Barey. “That process can be a challenge; oftentimes groups use different metrics as a baseline for what a successful diabetes care looks like,” she said. Different plans, payers, and contracts specify different numerators and denominators for success, and the more these can be standardized into a single metric, the easier it is to gain support among staff. “It is hard to receive 4 different report cards on diabetes care, or any chronic disease,” she explained. “In my experience, the groups that completed that normalization [upfront] have been more successful in bringing people along.”
“Everything we do, we try to incorporate analytics with it because you cannot improve what you cannot measure,” added Molecavage. It is important to identify groups of individuals who are doing well and those have opportunities for improvement. “We will work with them to understand: Is it that they are not following the process, or that they are not [completing] the workflows? Do their populations have the resources they need? Understanding that compounding factors come into play is important, and a lot of that goes back to the leaders being responsible and holding them accountable.”
The team at Geisinger has implemented analytics at the regional, site, and provider levels to find deviations from the clinical care pathway. It is then the responsibility of the respective medical director or clinical leader to follow up and determine why the deviation is occurring. National Committee for Quality Assurance benchmarks are employed to ensure the program is paying off. “For A 1C levels greater than 9%, our benchmark is 14%, meaning 86% of our patients should be at less than 9%. If it’s neuropathy screening, we should have 90% of our population living with diabetes [passing] that. Geisinger’s not coming up with what we think we should be doing; we are relying on the regulations and the national bodies to do that,” Molecavage added.
Develop Educational Materials Needed for Rollout
Education initiatives that meet the needs of the institution must be developed and put in place in time for rollout. “I think it is very important that when you develop care pathways, you pay attention to how you implement [them] so that you can learn the best approach. Oftentimes, the biggest driver of whether something is used or not is how it is implemented rather than how great it is or how it is designed,” Pantalone said.
“We will implement trainings and department meetings and identify key stakeholders and super users,” Molecavage explained. “A lot of times we designate champions in each location who are passionate about the pathway, and who can answer questions as they come up throughout the day or throughout what we’re doing.” Training related to aspects of the program that impact workflows is especially important. “Everyone enjoys efficient workflows and doing what they are used to doing,” she said. “If you make a change, it always adds more time.” Health care providers may not have been trained in using analytics tools and applications with dashboards, so Geisinger ensured training was provided.
All trainings at Geisinger are followed up by a 1-page document providers can refer to going forward. “We supplement all our training with a step-by-step document that is disseminated down to all the people it relates to, so they have a resource to look back on,” Molecavage said. Trainees are also assigned a contact person on the appropriate committee. “When they see an issue, they know they have someone to talk to about it,” she said, and the contact people gain valuable information for improving the program. “We are constantly fed that [information] back and forth to one another.”
Test the Clinical Care Pathway in the Electronic Health Record
Convenience is key to ensuring providers utilize any type of clinical care pathway in the electronic health record. “You need to have something that is very simple, easy, and convenient for the clinician to act on,” Pantalone explained. “A BPA sounds nice, but PCPs get inundated with 10 different BPAs, [leading to] BPA fatigue.” To circumvent this issue, the teams at Geisinger and Cleveland Clinic implemented functionalities that save providers time. For example, A 1C BPAs link with a Smartset with orders for diabetes-related supplies and type 2 diabetes medications prepopulated in both 30- and 90-day supplies. In addition, if a patient has not had a foot exam or an eye exam, for example, the provider can choose an option to populate an order to fulfill that gap in care directly from the patients’ health maintenance summary section. “That closes the loop directly by eliminating the 3 steps in between (putting in an order, associating it with a diagnosis, and filing it),” he said. “This can have a tremendous impact on increasing the number of patients becoming compliant. The take-home learning point is that simple is better because it is more efficient.”
Barey agreed that convenience is important and smart utilization of alerts or pop-ups can affect usability and avert BPA fatigue. “The Epic care pathway is a step-by-step workflow process that was seen as much more helpful than pop-ups. And a reference tool is embedded in the workflow; the provider does not have to go anyplace else [within the electronic health record]. Furthermore, the visual workflow component ensures that [providers] do not get distracted by it,” she explained. Decision-support alerts are used as a safety net; the provider sees a pop-up only if the right decision was not made or an opportunity was missed. “In terms of key performance indicators or data-driven improvement, we can track how often decision support is utilized, and with who and where, and then what [the provider] did with the decision support,” she added. “You would want to absolutely bake the review of decision support utilization and usability in as best practice for implementing [the clinical care pathway] in an electronic health record.”
Electronic health records are also available to patients, and so consideration of their needs and actions in the clinical care pathway is also important to consider. “When we identify these gaps in care, we also develop technology that [utilizes] the same analytic and performance measures that are being presented to the provider,” explained Ray Herschman, MS, vice president and general manager of Value Based Care and Risk Solutions at Cerner Corporation. “The most important message that a [patient] receives is a personalized one [from their provider] that tells them there is an opportunity for them and their care. We have seen incredible results [by] going directly to [the patient] about gaps in care, follow-up visits, and closure of those gaps.”
Pilot the Program Among Select Providers
Geisinger took 6 months to plan its clinical care pathway implementation, and then piloted the program at a few of its sites. “We always do a pilot because everything in theory seems like it’s going to work until you get to implementing it and you find areas for improvement or areas that just are not working,” shared Molecavage. “During that pilot phase, we are focused on [learning] what works, what does not work, and what needs to change. Once we feel comfortable with that, we put the educational pieces in place.” The educational pieces, in turn, offer feedback for fine-tuning the program before launch.“Often it will be a physician champion in each location who is passionate about what we are doing who can answer questions as they come up throughout the day,” she explained. “Then we are constantly feeding that back to the larger group to make sure we’re improving what we can and what we need to.”
Pilot testing to ensure the clinical care pathway is working as designed in the electronic health record prior to launch is also very important. According to Eric Boose, MD, associate chief medical information officer at Cleveland Clinic, the multidisciplinary steering committee worked together from the beginning to test and refine the tool at Cleveland Clinic. “It was interesting because it was done at rapid iterations,” he explained. “[We had] almost weekly meetings and the IT teams would build [the tool] and come back. From there, we kept refining it and refining it, and at the end we came to this consensus. With the functionality changing, we’ve been optimizing it more and more.”
"Initial education is important when rolling out any new process, but reinforcing it is probably more important. Regular touch points with the providers to assess usage and obtain feedback for improvement is key." Christopher Babiuch, MD
Rollout the Clinical Care Pathway
Once the clinical care pathway is functioning appropriately in the electronic health record and education materials and trainings are in place, the clinical care pathway is ready for rollout; however, encouraging providers to use it can be challenging due to time constraints. “This is a very useful tool,” Pantalone said, “But, what we found was it is challenging to get providers to deviate from their normal workflow, because many providers are very busy, and they tend to keep doing whatever they’re doing just to get through their busy schedule. We are currently working on ways where we can help increase the utilization of this tool by simplifying it and optimizing its incorporation into provider workflows.” For example, he said, use of the tool to intensify therapy in patients with uncontrolled type 2 diabetes may need to be positioned asynchronous to the office visits (ie, in telephone and refill encounters that do not have the same time constraints as office-based encounters) in order to facilitate more consistent utilization.
Providers also may be hesitant to utilize the tool because they do not see the value it will add to their practice. Understanding the providers who will be using it, as well as their needs and concerns, can be key to ensuring its uptake. “Adoption is always a concern with any [clinical] care pathway,” Wall explained. “There are doctors who have been in practice for 30 years, and may say, ‘I know how to take care of patients living with diabetes. I do not need your pathway.’ However, you may look at the patient record and notice they are using a medication that is [no longer recommended in first line for that patient].” Providers need to be shown that the clinical care pathway will simplify their work by prepopulating notes, teeing up orders, and so on, he said. “[The clinical care pathway] can be an easier way or a quicker way to see the patient, which allows the provider to get a lunch break or see more patients.”
Perform Continued Assessment and Updates
Meeting regularly after a clinical care pathway has been implemented is important. “Before COVID-19, we had a lot of meetings,” explained Jacob of Primary PartnerCare. “We [held] community physician groups run by regional medical directors, and broke those into smaller panels of 10 to 15 physicians [who met] either monthly or bi-monthly to review all the projects, the data, the issues, etc.”
“Initial education is important when rolling out any new process, but reinforcing it is probably more important,” agreed Babiuch of Cleveland Clinic. “Regular touch points with the providers to assess usage and obtain feedback for improvement is key.” Assessing impact and providing that information to the providers is also important for reinforcing the value of the clinical care pathway,” he added. “We are all used to seeing reports showing how many of our patients with diabetes are uncontrolled. Although that is good to know, having a ready-made tool to help improve that care is powerful.”
Quality reporting also can ensure accountability and uptake of the clinical care pathway. “Under the Medicare Shared Savings Program, we must report quality, and diabetes care is a major quality parameter focus that we complete through our physician portal,” said Jacob. “By using the quality reporting tools relating to diabetes and sharing that data with the doctors and their peers in the ACO [accountable care organization], we can drive high quality care.”
Transparency in provider data across the institution increases provider accountability and can aid in ensuring adherence to the clinical care pathway. “One thing that has really helped move the needle [at Cleveland Clinic] is the transparency,” Pantalone explained. “When we get reports and see the providers in the department, and [for example] if I see that my name is near the bottom of the list for percentage of patients with A 1C less than 7%... I don’t want to be down there! That type of accountability is very important. We have seen that that really helps to move the needle. No one wants to be at the bottom of the list.”
Data should be analyzed further to determine why providers may not be hitting goals, as differences in practice sites and patient populations can have an impact, Pantalone cautioned. “You must take [the data] with a grain of salt,” he said. “[For example,] a provider in our department who always has the best A 1C data was the one who cared for all the pregnant patients [which is a different patient population compared with] other providers who may be in the inner city and seeing patients with a low socioeconomic status. It is important to do those sorts of exercises from a department level so that organizations can identify the ‘positive deviants’ that are doing a good job and find out what it is they are doing so that you can determine if that is something you can implement across your department.”
Tackling Updates
Because new evidence is published frequently, care should be taken to ensure the clinical care pathway can be updated easily. “Updating [clinical care pathways] is a challenge because new evidence becomes available quickly,” Isaacs of Cleveland Clinic explained. “For example, when a new drug gets a new labeled indication, then you must reevaluate it. Overall, ensuring [the clinical care pathway] is as current as possible is important. Collecting feedback on an ongoing basis can help.”
Good governance is key to keeping the electronic health record tool in line with current guidelines, said Boose. “There’s always supposed to be an expert group for each functionality,” he added. “They’re the ones who are supposed to watch it over time.” An expert group for each functionality conducts a regular review to make sure the tools are consistent with current guidelines.
Formularies are updated on a monthly schedule. “Regarding ADA standards and others, even though the big update is annually, there are more updates [online],” said Isaacs. “I think that ideally [clinical care pathway tools] should be reviewed quarterly or every 6 months to stay relevant.”
Conclusions
However daunting, the developing and launching of a clinical care pathway is not impossible. “The key is that you must break it down into very small parts and do 1 thing at a time,” Pantalone said.
“Even if you just tackle 1 condition out of the gate and develop confidence, that is the best way to go,” said Nill. “Start with your easiest condition first to get your physicians on board and saying, ‘Okay. This is making my life easier.’”
“From conceptualization, meeting, and receiving the sign-off from physician leadership and Accountable Care Organization Board, to launching the first step took less than a month,” shared Davis. “The harder part was educating the physicians that [this clinical care pathway] mattered and what was included in the data analysis. Because doctors are scientists, they wanted to understand the full data from what we were including. After that, it was easy to get the doctors on board. Doctors want to provide good care, and population data and analyses are powerful tools in helping them achieve this goal.”
“Multidisciplinary collaboration is key,” Babiuch said. “Having all the stakeholders pushing toward the same goal is where this will be successful.”
“Start small,” Molecavage agreed. “Start with 1 [objective], which could be as easy as identifying the population and the measure you want to start with—A 1C or retinopathy or nephropathy. Find key stakeholders who are passionate, and don’t overcomplicate it.”
Key Learnings
- Use the latest guidelines to create a clinical care pathway that focuses on PCPs; they manage 90% of patients with type 2 diabetes and may be overwhelmed by the number of new diabetes medications available.
- Start small with 1 or 2 goals and develop a template approach to expanding capabilities.
- Aim to seamlessly integrate the clinical care pathway into the existing electronic health record to enable all medical professionals who see the patient to make real-time decisions by employing minimal, action-oriented best practice alerts.
- Test and reassess; use data-driven metrics and make them fully transparent. Maintain expert committees to keep electronic tools updated per association guidelines.
Lilly would like to thank the experts at Cleveland Clinic, Geisinger Health System, Primary PartnerCare, Epic, and Cerner Corporation, whose guidance heavily contributed to the development of this publication.

Download PDF
- Chawla A, Westrich K, Matter S, Kaltenboeck A, Dubois R. Care pathways in US healthcare settings: current successes and limitations, and future challenges. Am J Manag Care. 2016;22(1):53-62.
- Grant P, Chika-Ezerioha I. Evaluating diabetes integrated care pathways. Practical Diabetes. 2014; 31(8):319-322. doi:10.1002/pdi.1894
- Wan EYF, Fung CSC, Jiao FF, et al. Five-year effectiveness of the multidisciplinary risk assessment and management programme-diabetes mellitus (RAMP-DM) on diabetes-related complications and health service uses-a population-based and propensity-matched cohort study. Diabetes Care. 2018;41(1):49-59. doi:10.2337/dc17-0426
- Jiao FF, Fung CSC, Wan EYF, et al. Five-Year Cost-effectiveness of the Multidisciplinary Risk Assessment and Management Programme-Diabetes Mellitus (RAMP-DM). Diabetes Care. 2018;41(2):250-257. doi:10.2337/dc17-1149
- Only 1 in 4 adults with diagnosed diabetes achieve combined diabetes care goals. CDC. Accessed February 1, 2021. https://www.cdc.gov/diabetes/research/reports/diabetes-abcs.html
- American Diabetes Association. Standards of Medical Care in Diabetes—2021. Diabetes Care. 2021;44(suppl 1):S1-S232. doi:10.2337/dc21-Sint
- Handelsman Y, Bloomgarden ZT, Grunberger G, et al. American Association of Clinical Endocrinologists and American College of Endocrinology - clinical practice guidelines for developing a diabetes mellitus comprehensive care plan - 2015. Endocr Pract. 2015;21(suppl 1):1-87. doi:10.4158/EP15672.GL
- Garber AJ, Handelsman Y, Grunberger G, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm - 2020 executive summary. Endocr Pract. 2020;26(1):107-139. doi:10.4158/CS-2019-0472
- Vrijhoef HJ, de Belvis AG, de la Calle M, et al. IT-supported integrated care pathways for diabetes: a compilation and review of good practices. Int J Care Coord. 2017;20(1-2):26-40. doi:10.1177/2053434517714427
- Evans-Lacko S, Jarrett M, McCrone P, Thornicroft G. Facilitators and barriers to implementing clinical care pathways. BMC Health Serv Res. 2010;10:182. doi:10.1186/1472-6963-10-182
- Busetto L, Luijkx KG, Elissen AMJ, Vrijhoef HJM. Context, mechanisms and outcomes of integrated care for diabetes mellitus type 2: a systematic review. BMC Health Serv Res. 2016;16:18. doi:10.1186/s12913-015-1231-3
- Grol R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care. 2001;39(8 suppl 2):46-54. doi:10.1097/00005650-200108002-00003
- Qaseem A, Wilt TJ, Kansagara D, et al. Hemoglobin A 1C Targets for glycemic control with pharmacologic therapy for nonpregnant adults with type 2 diabetes mellitus: a guidance statement update from the American College of Physicians. Ann Intern Med. 2018;168(8):569-576. doi:10.7326/M17-0939
- Khunti K, Davies MJ. Clinical inertia-Time to reappraise the terminology?. Prim Care Diabetes. 2017;11(2):105-106. doi:10.1016/j.pcd.2017.01.007
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Equity Health

Using concept mapping to prioritize barriers to diabetes care and self-management for those who experience homelessness
Eshleen k. grewal.
1 Department of Medicine, Cumming School of Medicine, University of Calgary, Calgary, Canada
Rachel B. Campbell
Gillian l. booth.
2 Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
3 Department of Medicine, Faculty of Medicine, University of Toronto, Toronto, Canada
4 MAP Centre for Urban Health Solutions, St. Michael’s Hospital, Unity Health Toronto, Toronto, Canada
5 Institute for Clinical Evaluative Sciences, Toronto, Canada
Kerry A. McBrien
6 Department of Family Medicine, Cumming School of Medicine, University of Calgary, Calgary, Canada
7 Department of Community Health Sciences, Cumming School of Medicine, University of Calgary, Calgary, Canada
Stephen W. Hwang
Patricia o’campo, david j. t. campbell.
8 Department of Cardiac Sciences, Cumming School of Medicine, University of Calgary, Calgary, Canada
Associated Data
The data pertaining to this study may be available upon request from the corresponding author.
Diabetes is a chronic medical condition which demands that patients engage in self-management to achieve optimal glycemic control and avoid severe complications. Individuals who have diabetes and are experiencing homelessness are more likely to have chronic hyperglycemia and adverse outcomes. Our objective was to collaborate with individuals experiencing homelessness and care providers to understand the barriers they face in managing diabetes, as a first step in identifying solutions for enhancing diabetes management in this population.
We recruited individuals with lived experience of homelessness and diabetes (i.e. clients; n = 32) from Toronto and health and social care providers working in the areas of diabetes and/or homelessness (i.e. providers; n = 96) from across Canada. We used concept mapping, a participatory research method, to engage participants in brainstorming barriers to diabetes management, which were subsequently categorized into clusters, using the Concept Systems Global MAX software, and rated based on their perceived impact on diabetes management. The ratings were standardized for each participant group, and the average cluster ratings for the clients and providers were compared using t-tests.
The brainstorming identified 43 unique barriers to diabetes management. The clients’ map featured 9 clusters of barriers: Challenges to getting healthy food , Inadequate income , Navigating services, Not having a place of your own , Relationships with professionals , Diabetes education , Emotional wellbeing , Competing priorities , and Weather-related issues . The providers’ map had 7 clusters: Access to healthy food , Dietary choices in the context of homelessness , Limited finances, Lack of stable, private housing , Navigating the health and social sectors , Emotional distress and competing priorities , and Mental health and addictions . The highest-rated clusters were Challenges to getting healthy food (clients) and Mental health and addictions (providers). Challenges to getting healthy food was rated significantly higher by clients ( p = 0.01) and Competing priorities was rated significantly higher by providers ( p = 0.03).
Conclusions
Experiencing homelessness poses numerous barriers to managing diabetes, the greatest of which according to clients, is challenges to getting healthy food. This study showed that the way clients and providers perceive these barriers differs considerably, which highlights the importance of including clients’ insights when assessing needs and designing effective solutions.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12939-021-01494-3.
Diabetes mellitus is a commonly occurring chronic medical condition that is associated with a high burden of mortality and morbidity. In 2018, 34.2 million Americans, or 10.5 % of the population, had diabetes and approximately 1.5 million Americans were newly diagnosed that year [ 1 ]. The risk of mortality for people with diabetes is two times greater than it is for people without diabetes, and having diabetes can reduce life expectancy by 5–15 years [ 2 ]. Chronically high blood glucose levels can result in an increased risk of diabetes-related complications over time, which include: nerve damage, kidney disease, blindness, and vascular disease [ 3 ]. To avoid adverse outcomes, people with diabetes must make decisions about their management frequently and on an ongoing basis. There is evidence to suggest that the combination of self-management education and self-management support can result in improvements in glycemic control through improved self-care behaviours, which in turn can reduce the risk of developing complications [ 4 ]. Participation in diabetes education, therefore, is critical for improving knowledge and self-efficacy, which enables patients to engage in healthy behaviours [ 4 ]. These healthy behaviours, including smoking cessation, dietary modification, and regular physical activity, in combination with pharmacotherapy, can reduce the risk for complications such as major adverse cardiac events [ 5 ]. Other behaviours such as self-monitoring of blood glucose levels can empower patients, improve treatment adherence, and assist diabetes care professionals in making decisions about treatment [ 6 ].
Among those with diabetes, people with lived experience of homelessness (PWLEH) are more likely than the general population to have elevated blood glucose levels [ 7 ]. Homelessness is defined by a lack of stable and safe housing, but it is often accompanied by inadequate income, mental and physical health problems, difficulty accessing health care and social supports, substance use disorders, previous involvement with the justice system, and adverse childhood experiences [ 8 , 9 ]. Although health issues may lead to homelessness, homelessness also greatly affects health, making it challenging for people who are experiencing homelessness to access care [ 8 , 10 ] and engage in self-management, especially when they have a chronic medical condition like diabetes, for which management is complex.
There are many barriers that can make it challenging to manage diabetes for PWLEH. Accessing health care services can involve long wait times and an appreciable amount of time may be spent travelling to and from appointments [ 11 ]. In addition to time, there is a financial burden associated with managing diabetes, as the costs of medications and blood glucose testing supplies may not be covered by public health insurance programs, even within Canada’s universal health system [ 7 , 11 , 12 ]. Barriers specific to homelessness that have been identified in the literature include concerns about food insecurity related to low-quality foods available in shelters, as well as challenges with safely storing medications and supplies, and strict shelter schedules with respect to eating meals and taking medications [ 7 , 13 ]. Travelling to appointments often involves the use of public transportation with associated costs. As many PWLEH do not have a fixed mailing address or reliable access to a phone, issues contacting patients are also common [ 8 , 14 ], making it difficult to schedule and notify patients of appointments [ 15 ]. Perceived feelings of being unwelcome in clinical settings can also prevent people who are experiencing homelessness from seeking health care services [ 16 ]. Other priorities, namely, obtaining the necessities of life (food, shelter, etc…), drug and alcohol use, and mental health or cognitive issues can also interfere with diabetes self-management [ 7 , 13 , 17 ].
While there are many barriers and challenges to diabetes management, the importance of these in relation to one another is not well known, nor is it well known if these priorities differ between providers and PWLEH. Other studies that have compared the perspectives of service users with those of service providers have found differences of opinions between the two groups [ 18 , 19 ]. One such study asking community members and service providers about which social and mental health services should be made available at a new medical clinic in the community found that community members and service providers had different views regarding which services were most needed [ 19 ]. Another study aimed to identify existing gaps in services for youth, where the opinions of the youth differed from those of the service providers regarding importance, but not in terms of ‘what to do first’ [ 18 ]. Traditionally, homeless-serving agencies have provided services based on their own beliefs about their clients’ needs instead of directly asking their clients what they need [ 20 ]. For instance, they may have focused on providing mental health and substance use services because the rates of mental illness and substance use are high among this population, or they may have prioritized housing because this population is characterized by a lack of a stable home, but those services may not address the most pressing issues for people who are experiencing homelessness [ 20 ] and may result in service gaps and barriers. The perspectives of service users, therefore, can be useful for service providers because those insights can help the providers understand how to tailor their services to better fill the gaps in service provision and remove barriers to accessing services, based on their clients’ priorities.
Given the complexity of diabetes management, myriad barriers that can affect adherence, and the potential for differences in perspectives between providers and PWLEH, we sought to collaborate with people who had lived experience of homelessness and diabetes, as well as health and social care providers who work with people experiencing homelessness and/or people with diabetes, to prioritize the challenges faced by this population in managing diabetes. The objective of this study was to determine the perceived relative impact of barriers to diabetes management and whether the perceptions about the impact of those barriers differed between providers and PWLEH.
Study design
We used a semi-quantitative, participatory methodology known as concept mapping. We used concept mapping because it can be used to create visual representations that depict the combined thoughts of a group, by integrating input from multiple people using quantitative data analysis techniques [ 21 ]. This methodology enabled us to gather insights from a group of PWLEH who have diabetes (herein referred to as the clients) and from various providers representing different areas of health and social care (herein referred to as the providers) and to quantitatively compare their collective feedback. Our study was approved by the research ethics boards of the University of Calgary and Unity Health Toronto/St. Michael’s Hospital.
Study participants & recruitment
The clients for this study were all recruited in Toronto, Ontario – Canada’s largest city and the city with the largest population of people experiencing homelessness [ 22 ]. The prevalence of diabetes among PWLEH in Toronto is thought to be similar to the prevalence among the general population [ 23 ] and barriers to managing diabetes previously identified by PWLEH in Toronto [ 7 ] are similar to the barriers identified by PWLEH in other cities [ 24 ].
Eight of the clients in this study were recruited as part of a larger community-based participatory research project designed to understand what it is like to live with diabetes while experiencing homelessness or housing instability and to propose and develop potential interventions for this population [ 25 ]. These eight participants met regularly in Toronto for study-related activities. In addition, we recruited several other participants to take part in this concept mapping exercise, to increase the sample size. To be eligible to participate, the clients had to: be older than 18 years, have a history of diabetes with a duration greater than two years, and have experienced homelessness within the previous two years. Homelessness in this study was defined similarly to the definition offered by the Canadian Observatory on Homelessness; we included participants whose living situations could be described as unsheltered, emergency sheltered, or provisionally sheltered [ 26 ]. Colleagues and advocates in the homeless-serving sector were consulted to determine the best places for recruiting the target population. Posters were put up in shelters, at homeless-serving agencies, and health clinics catering to the homeless population for recruitment. Established programs serving people who were experiencing homelessness or housing instability also helped with recruitment by advertising an information session to their program attendees. We explained the study to interested parties and obtained informed consent.
The service providers who took part in this study had previously been recruited as participants in another study of diabetes care for PWLEH [ 27 ]. They comprised professionals from four main categories of care: diabetes care professionals who worked primarily with inner-city or homeless populations, other health care professionals who worked primarily with inner-city or homeless populations, endocrinologists or diabetes care providers who did not specifically focus on inner-city or homeless populations, and other stakeholders, including frontline staff in shelters and social care providers. The providers were recruited from five major Canadian cities (Toronto, Ottawa, Edmonton, Calgary, and Vancouver), and they participated in this study remotely. Although the barriers to diabetes self-management may be similar across cities for PWLEH, the services available in each city differ [ 27 ]. Services in the health sector are largely impacted by funding and approval from provincial governments, which may have different priorities, and services in the homeless-serving sector are often provided by non-profit organizations, which rely to a great extent on donor funding for service provision. For these reasons, services that exist in one city may not exist in another, and we felt that it would be valuable to gain input from providers across different jurisdictions about their perspectives.
Data collection
The concept mapping process involves six steps and is depicted in Fig. 1 . The initial three steps relate to data collection: preparation, generation of statements, and structuring of statements [ 28 ].

The concept mapping process
In the first step, preparation, the researchers must determine what the focus of the study will be. Usually, this involves two separate focus statements. The first statement is referred to as the focus prompt or the brainstorming focus, and it is developed to guide the brainstorming exercise in the second step. The second focus statement, called the rating focus, defines the factor(s) upon which the brainstormed statements will be rated in the rating exercise of the third step [ 28 , 29 ]. The focus prompt for the brainstorming exercise was, ‘What are some ways, good or bad, that diabetes might be affected by homelessness?’ . The rating prompt was: ‘What impact does [that factor] have on diabetes care and self-management (on a scale from no impact to high impact), specifically for people who are struggling with homelessness or housing instability?’ .
Generation involves a brainstorming exercise, in which the participants are provided with the focus prompt and asked to brainstorm statements in response [ 28 ]. The brainstorming exercise is done individually by each participant, and eventually, the ideas are combined and refined to form one set of statements [ 29 ]. Eight clients did the brainstorming exercise during an in-person group meeting. The providers had been individually interviewed by members of the research team, who then shared the providers’ ideas with the clients during their brainstorming session. The researchers recorded the ideas from the clients and the providers and refined the list of statements with the clients. The providers did not take part in the refinement of statements, as this aspect of the brainstorming exercise was done in person during a meeting with the clients.
Structuring involved two different exercises, sorting and rating. For the sorting exercise, each participant was asked to group individual statements into categories based on similarity, in a way that was meaningful to that individual [ 21 , 30 ]. The statements could not all be sorted into one pile, nor could each statement be in its own pile [ 29 ]. “Miscellaneous” piles with a group of statements that did not have a specific theme or link to each other were also discouraged. These instructions were explained to participants at the outset of the exercise and facilitators were present to help clarify instructions. The clients completed this exercise manually with statements printed on individual cue cards, while the providers completed this exercise using a tailor-made online platform. For the rating exercise, a Likert scale ranging from zero to four was used to rate each statement. A rating of zero meant the statement had no impact on diabetes control and self-management, and a rating of four meant it had an extreme impact on diabetes control and self-management. This exercise was done on paper forms by the clients and online by the providers.
Data analysis
The final three steps of the concept mapping process relate to data analysis: representation of statements, interpretation of maps, and utilization of maps [ 28 ].
In the representation step, sorting and rating data were analyzed using concept mapping software (Concept Systems Global Max, 2020, Ithaca NY) [ 30 , 31 ]. The representation step was done separately for the clients and the providers: the clients’ data were analyzed to create a clients’ cluster map and the providers’ data were analyzed to produce a providers’ cluster map. By having two cluster maps, rather than one, we were able to see how the number of clusters, the names of clusters, and the sorting of the statements, differed between the two participant groups.
The sorting data were analyzed using multidimensional scaling analysis, a technique that plots each statement as a point on a map. Statements that are closer together on the map were grouped together during the sorting exercise more often than statements that are farther apart. Multidimensional scaling was used to generate a matrix for each participant with one row and one column representing each of the statements [ 29 ]. In this study, the matrix had 43 rows and 43 columns. Each cell in the matrix corresponds to two statements, the row statement and the column statement. If those two statements were sorted into the same pile by the participant, the cell is given a value of one, and if they were not sorted into the same pile, the cell is assigned a value of zero [ 21 , 29 ]. This is done with each participant’s data so that there are as many separate matrices as there are participants in the study. All of the individual matrices are then summed to create a similarity matrix indicating how many participants sorted each pair of statements into the same pile [ 29 ]. This similarity data is used to create a two-dimensional point map, where the distance between two points on the map corresponds to their similarity [ 21 ].
These points were then grouped together to form clusters through hierarchical cluster analysis. Hierarchical cluster analysis uses the data from the point map to separate the points into non-overlapping clusters, developing a cluster map. The number of clusters in the final cluster map is determined by the participants and the researchers so that the map is presented in a way that is meaningful and useful to them [ 21 ]. This analysis begins by considering each statement to be in a cluster of its own, and it combines two clusters at a time, reducing the number of overall clusters until all the statements are in the same cluster. The statements are combined based on proximity, meaning that the two points that are closest together on the point map would be the first two points to form a cluster together [ 29 ]. The reliability, or goodness-of-fit of the map, is determined by calculating the final stress of the model [ 32 ]. Lower stress values suggest a better fit. Stress values in concept mapping data tend to be higher than in other multidimensional scaling analyses [ 33 ], therefore there is no accepted standard, however, it has been reported that an acceptable value for studies of this nature is less than 0.30 [ 34 ].
An average rating is then calculated for each cluster using the ratings for each of the individual statements in that cluster. Upon reviewing the average cluster ratings, it was clear that the clients and providers had rated the statements very differently, such that the clients had generally given lower ratings whereas the providers had given higher ratings, which resulted in lower average cluster ratings for the clients’ clusters and higher average cluster ratings for the providers’ clusters. To determine whether there was in fact a difference in the ratings between the two groups, the ratings were standardized and compared using unpaired two-sided t-tests, with an alpha of < 0.05. To standardize, the participants’ ratings for each statement were subtracted from the average rating of all the statements for their participant group (i.e., the clients’ average rating or the providers’ average rating). Both groups had different numbers of clusters with different numbers of statements in them, which would have been difficult to compare, so it was necessary to use the same cluster structure for both groups. We chose to compare based on the clients’ cluster structure because we wanted the analysis to be client-centred and because the clients had reviewed the clusters and the statements that were in each cluster, so the final structure reflected their feedback. We used unpaired t-tests to quantitatively compare the standardized cluster ratings to determine whether there was a statistically significant difference between the ratings of the clients and those of the providers for each cluster in the patient cluster map.
In the interpretation step, the maps and reports generated in the previous step are used to help frame the interpretation of the data. We assessed point maps, cluster maps, cluster reports with statements, and raw ratings reports. In this step, some of the clients were reconvened for an in-person meeting to discuss any changes that needed to be made to the maps and to provide input on the names of each of the clusters. The providers were not able to come together for a meeting, so their clusters were named by the researchers.
In the final step, utilization, the concept maps are reviewed to determine how they can be utilized to answer the study question [ 30 ]. In this study, the findings from the clients’ concept mapping research informed the subsequent research program in providing the topics of interest for the participatory photovoice project that ensued [ 35 ].
There were 32 clients and 96 providers who took part in this study: Although there were 128 participants altogether, only a subset of those participants took part in each stage of the concept mapping process (Fig. 1 ). For instance, only eight of the 32 clients took part in the brainstorming and sorting exercises, but all 32 took part in the rating exercise. For the providers, all 96 took part in the brainstorming exercise, but only 16 and 26 of these individuals took part in the sorting and rating exercises, respectively. The final sample size is consistent with what has typically been reported in other concept mapping projects [ 34 ].
Characteristics of the clients
The demographic characteristics of the clients are presented in Table 1 . All of the clients were over the age of 25 and just over half identified as men. None of the clients were sleeping rough at the time of this study, while a quarter of the clients were in private housing with the remainder in shelter or tenuous, transitional, or community housing. Collectively, they had experienced homelessness or housing instability for a median length of two years and had been living with diabetes for a median length of seven years. A majority of the clients had experienced some diabetes-related complications and had physical or mental health comorbidities as well. The most commonly reported method of managing diabetes was the use of oral medications, which were utilized by three-quarters of the clients, although approximately one-third of the clients used injectable agents (including insulin). The clients also saw a variety of care providers for the treatment of their diabetes; about three-quarters saw a family physician, one-fifth saw a pharmacist, and one-third saw a medical specialist, a diabetes nurse, and a diabetes dietitian, respectively.
Demographic characteristics of the clients ( n = 32)
a one participant chose 2 housing options, therefore n sums to 33
Characteristics of the providers
Only eight of the providers completed the demographic survey. Most (6/8) were women, half were between the ages of 55 and 64, and 5/8 had 20 or more years of experience working with patients that have diabetes and/or complex social needs, while the rest had 15–19 years of experience. The providers also had a variety of different qualifications and titles including, registered dietitian, registered nurse, certified diabetes educator, family physician, program administrator/manager, and executive director. They also worked in a variety of settings such as community/private family medicine practices, specialty practices, community health centres, community pharmacies, academic/public family medicine practices, and homeless shelters.
Concept mapping
During the brainstorming exercise, the participants generated a list of statements representing barriers to self-management, starting with a large list, which was then refined by removing duplicates and combining similar statements. The resulting, final version of the list contained 43 statements (Table 2 ).
List of unranked and unsorted statements from the brainstorming exercise
Using the data from the sorting exercises, the statements were plotted in relation to one another and presented as point maps through multidimensional scaling, and the points were then grouped to form cluster maps (Fig. 2 a and b) through hierarchical cluster analysis. The clients’ cluster map is based on sorting data from eight participants, and it consists of nine clusters, with a final stress value of 0.2987. Those clusters were named: (1) Challenges to getting healthy food , (2) Inadequate income , (3) Navigating services , (4) Not having a place of your own , (5) Relationships with professionals , (6) Diabetes education , (7) Emotional well-being , (8) Competing priorities , and (9) Weather-related issues . The providers’ cluster map had seven clusters, made using sorting data from 16 participants, and had a final stress value of 0.2521. The clusters were named: (1) Access to healthy food , (2) Dietary choices in the context of homelessness , (3) Limited finances , (4) Lack of stable, private housing , (5) Navigating the health and social sectors , (6) Emotional distress and competing priorities , and (7) Mental health and addictions . Appendix A (see Additional File 1 ) contains tables that list which statements were in each cluster for both the clients and the providers.

Cluster maps for the clients and the providers. a . Clients’ cluster map. b . Providers’ cluster map
The rating exercise was completed by 32 clients and 26 providers. The ratings for the individual statements were used to calculate an average cluster rating. The clients’ clusters, arranged from the cluster with the highest average rating to the cluster with the lowest average rating, with the average rating in parentheses (out of a total of four), are: (1) Challenges to getting healthy food (2.08), (2) Weather-related issues (1.83), (3) Emotional well-being (1.65), (4) Inadequate income (1.65), (5) Competing priorities (1.60), (6) Relationships with professionals (1.43), (7) Diabetes education (1.35), (8) Not having a place of your own (1.23), and (9) Navigating services (1.18). Providers’ clusters, by contrast, were: (1) Mental health and addictions (3.54), (2) Emotional distress and competing priorities (3.42), (3) Dietary choices in the context of homelessness (3.12), (4) Navigating the health and social sectors (3.00), (5) Limited finances (2.97), (6) Lack of stable, private housing (2.88), and (7) Access to healthy food (2.79).
Using the grouping of clusters defined by clients, we calculated standardized cluster averages for the two groups (Fig. 3 ). There were two clusters for which the standardized averages differed in a statistically significant manner, Challenges to getting healthy food (standardized difference = 0.6396; p = 0.013) and Competing priorities (standardized difference=-0.5250; p = 0.026). The clients had a higher rating for Challenges to getting healthy food than the providers and the providers had a higher rating for Competing priorities . While trends were suggesting potential differences in the other clusters, these were the only two that reached statistical significance, due to the relatively small sample size for this quantitative analysis.

Graphical representation of the average standardized cluster ratings
The clients and providers identified a plethora of barriers to diabetes management, ultimately resulting in a refined list of 43 unique barriers. The clients’ and providers’ sorting data resulted in concept maps with distinct cluster names and configurations representing differing perceptions of barriers to managing diabetes while experiencing homelessness. Both the clients’ and the providers’ clusters represented themes related to access to healthy food; financial limitations; housing; health and social care; and psychosocial wellbeing. The clients chose to have a cluster titled Relationships with professionals , whereas the providers’ map included those barriers in the Navigating the health and social sectors and Lack of stable, private housing clusters. While the clients’ map has two clusters representing similar themes: Navigating services and Not having a place of your own , the clients saw the barriers related to relationships as being distinct from those related to navigation issues or housing issues and chose to have a separate cluster for them. These findings confirm the notion that the perspectives of clients/patients/service users and service providers regarding barriers to diabetes management may be different, and that the reasoning behind patients’ differing perspectives may not be evident to the providers. Traditionally, the identification of barriers and the creation of solutions has not meaningfully considered input from the individuals who have the most at stake, the patients/clients. Our findings highlight the importance of considering the patient perspective when designing solutions for enhancing diabetes management to address the barriers which have the greatest impact, according to patients.
Comparisons of the cluster ratings indicated that there were significant differences between the clients and the providers in the perceived impact of the barriers faced in diabetes management. The cluster related to challenges to accessing healthy food was the most influential from the client perspective, and it was rated significantly higher by the clients than the providers. The cluster representing priorities that compete with diabetes management was thought to be the most impactful by providers, and the rating for this cluster was significantly higher for the providers compared to the clients.
There are many reasons why accessing healthy food can be challenging for PWLEH. Many may rely on shelters or community kitchens for food so they must eat whatever is available, even if they have been advised to avoid such food by their healthcare providers [ 36 ]. The meals in shelters often have high amounts of sugar, starch and fat, and there are few fruits and vegetables available, which results in diets that are likely to be inappropriate for people with diabetes [ 7 ]. These shelters and community kitchens, however, also have limited resources and must often rely on food that is donated to them [ 24 ]. Sometimes, PWLEH may be unable to get three meals in a day so they are often eating when they can and hoarding extra food, so they have something to eat later. Alternatively, if they had access to affordable, nutritious food, they would not be worried about where their next meal is going to come from [ 37 ] and they would have greater diabetes self-management self-efficacy [ 38 ]. The lack of access to food is especially concerning for people who are using insulin, as they may use less than the prescribed amount of insulin for fear of developing hypoglycemia if they are not able to predict mealtimes reliably [ 15 ]. It is likely that because PWLEH need to negotiate their dietary intake daily, this rose to the top of the priority list for them. Providers may benefit from knowing that for PWLEH this is the most troubling aspect of diabetes self-management.
With regards to competing priorities, studies have noted that PWLEH tend to have many demands and prioritize things such as food, shelter, and employment above diabetes care and self-management practices [ 13 ]. When they continually face difficulties in meeting these basic needs, people may forego preventative care or sacrifice self-care [ 39 ]. This may partially explain why the providers believed that competing priorities have a great effect on diabetes management. As for why this cluster of factors was rated lower by clients, we hypothesize that this discrepancy may relate to lower health-related self-awareness in this population [ 40 ], or because clients did not fully grasp how their other issues may affect their diabetes, likely due to the fact that their social networks are often comprised of others who face similar issues. This is consistent with literature documenting that non-clinically trained people are typically less aware of the impact of the social determinants of health [ 41 ]. By contrast, healthcare providers are more likely to be informed about the social determinants of health and how diabetes care is affected significantly by the complete picture of patients’ lives [ 42 ]. It is also possible that barriers related to competing priorities were deemed less impactful by the clients because their greatest competing priority is accessing food, which had a separate cluster of its own, and had the highest average rating for the clients. The clients may also have felt that accessing healthy food is more important than other aspects of self-management if the diabetes education they received emphasized the importance of diet above all else.
The second highest-rated cluster for the clients was focused on issues related to the weather. Cold-related injuries are very common amongst PWLEH in Canada and they often result in emergency department visits [ 43 ]. One of the many complications of diabetes is reduced circulation, especially in the feet, so in cold weather foot care becomes even more important, as the winter weather can increase the risk for infections, frostbite and amputations [ 44 , 45 ].
The providers’ third highest-rated cluster focused on a lack of stable, secure housing and while the clients had a similar cluster, for them, it received the second-lowest rating. Understandably, providers would consider this an important barrier, given that there is much in the literature describing the need to treat homelessness as a health issue [ 46 ] and suggesting that it is important for providers to help address housing concerns [ 15 ]. It is surprising, however, that this cluster was given such a low rating relative to the other clusters by the clients because participants in other qualitative studies have described housing as a foundational need that affects diabetes self-management in numerous ways [ 36 , 47 ]. In one study, participants reported that being unstably housed is emotionally and physically draining, which makes it difficult to prioritize diabetes, and when the need for shelter is not met, there is no foundation from which they can pursue their health goals [ 47 ]. This view is in accordance with Maslow’s hierarchy of needs, which places basic needs such as food and shelter ahead of health [ 8 , 15 , 48 ]. Not having housing also means not having a secure place to store diabetes testing supplies such as glucometers or medications and insulin, and there is a fear that they may be stolen in a communal living arrangement such as an emergency shelter [ 36 ]. Furthermore, stable housing can provide a sense of consistency and control that can help with the routinization of diabetes care and allow some control over diet, while high housing costs can compete with the cost of diabetes care [ 47 ].
One of the strengths of this study is its participatory nature. We gathered input from PWLEH as well as a variety of providers who work in health and social settings, which ensured that we had diverse perspectives represented. The clients were able to review the concept maps and name the clusters, which meant that the final maps reflected their perspectives rather than the opinions of the researchers. This is important because the participants may see the value of having certain themes or representing the barriers a different way than the researchers. Concept mapping incorporates both qualitative and quantitative analyses in one process, which enables complex ideas to be explored in a short period of time, and the output of the quantitative analyses supplements and enhances the qualitative interpretations. Furthermore, the creation of visual representations through this combination of analyses provides structure and credibility to the results [ 30 ]. Additionally, it includes both individual and group activities, and the process in which these activities occur avoids some of the issues that are commonly experienced when using qualitative methodologies such as, the monopolization of group discussion time by one or two individuals, the likelihood of conformity bias, or the need for individuals to publicly discuss their personal opinions or experiences [ 30 ]. Another strength is that the participants were involved in the analysis of the data and they were able to interpret the concept maps that were created using their data. This methodology ensures that the thoughts of the participants are accurately reflected [ 28 , 30 ]. The visual concept maps allowed us to display the associations between multiple themes and the rating data enabled comparison of the relative importance of each theme [ 28 , 30 ].
There are also limitations to this study, one of which is that only eight clients completed the sorting exercise. This was due to the time commitment required of participants and the complexity of the task. Ideally, participants must take part in the brainstorming, sorting, and rating exercises, and then review the results and provide feedback, but it may be difficult to keep participants engaged throughout the whole process. However, despite this small sample, the resultant map still had an acceptable final stress value. Another limitation of this study is the lack of available demographic data about the providers, as only a small proportion of the providers completed the demographic survey. While it is unfortunate that we are unable to fully describe the group of providers who participated in this study, we do know that the roles they had and the settings they worked in varied considerably. Additionally, the providers did not have the opportunity to reflect on the concept map that was produced with their data. The research team decided to finalize the cluster map on their own because the providers were from five different cities, and it was not possible to plan a meeting for all of the providers.
The participants in our study identified many of the same barriers that are described in other studies. However, this study is unique in that it allowed participants to rank these barriers from most to least impactful on diabetes management – and compared these rankings between PWLEH and providers. The results show that clients and providers differ in their understanding of barriers and the impact they have on diabetes management. Given that the clients in this study have indicated that difficulties with accessing healthy food are the greatest barriers to managing diabetes, future research and interventions aimed at improving diabetes management among PWLEH who have diabetes could focus on determining how to improve access to diabetes-appropriate food for this population.
Acknowledgements
Not applicable.
Abbreviation
Authors’ contributions.
The study was conceived by DJTC and RBC with meaningful contributions from GLB, KAM, SWH, and PO. Data collection and analysis were conducted by EKG, RBC and DJTC. The initial draft of the manuscript was written by EKG and DJTC and was revised with feedback from RBC, GLB, KAM, SWH, and PO. The author(s) read and approved the final manuscript.
This study received funding from Alberta Innovates, the O’Brien Institute for Public Health and the Cal Wenzel Cardiometabolic Fund.
Availability of data and materials
Declarations.
This study received ethics approval from the institutional review boards at the University of Calgary (REB 18-1663) and St. Michael’s Hospital/Unity Health Toronto (REB 18–288). All participants provided informed consent.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Eshleen K. Grewal, Email: ac.yraglacu@lawergke .
Rachel B. Campbell, Email: [email protected] .
Gillian L. Booth, Email: [email protected] .
Kerry A. McBrien, Email: ac.yraglacu@eirbcmak .
Stephen W. Hwang, Email: [email protected] .
Patricia O’Campo, Email: [email protected] .
David J. T. Campbell, Email: ac.yraglacu@lebpmacd .
MindMap Gallery Diabetes Mellitus
Diabetes Mellitus
Diabetes mellitus (DM), commonly known as diabetes, is a group of metabolic disorders characterized by a high blood sugar level over a prolonged period of time.
- Recommended to you
Mind-Map-Diabetes-Mellitus
- Autosomal Dominate
- Insulin Resistance
- MODY: mature onset diabetes of youth
- Cause:Mutations of Glucokinase genesand 5 other genes that regulate insulin inthe pancreas
- Gene mutations
- KCNJ11; Potassium channel glucosesecretion pathology
- TCF 12; endcodes for secretion of insulin
- PPAR-y; adpocyte differentiation &amp; glucosemetabolization
- Carbohydrate limitation
- Exercise: increases insulin sensitivity
Diagnostic Test
- Blood Glucose Monitoring
- Genetic marker testing
Pathophysiology
- Blindness
- Heart Disease
- Kidney Failure
- Elevated Blood Glucose
Chromosome 11
- Mutations on CTLA 4 ; cytotoxiclymphosyte
- PTPN22; lymphoid tyrosine phosphate
- negatively regulates T-cell activation, alsolinked to Lupus, Arthritis, Thyroid disease
Type 1 insulin dep
- Pathophyology
- T-cells infiltrate pancreas kill insulinproducing B cells
- Autoantibiodies are formed againstpancreatic cells
- Genetic Risk factors
- HLA 2 Allels gene mutation; HLA DR3,4,inappropriate autoimmune activation
- Aspartic acid on position 57 mutates andchanges shape of the molecule
- Causitive Factors
- Genetic factors not exclusively responsiblefor disorder, viral infections activateautoimmune response
A Critical-Thinking Acronym for Diabetes Care
- PMID: 26863708
- Abbreviations as Topic*
- Clinical Competence / standards*
- Diabetes Mellitus / drug therapy*
- Diabetes Mellitus / nursing*
- Nursing Care / standards*
- Nursing Staff, Hospital / education*
- Practice Guidelines as Topic*
- United States

IMAGES
VIDEO
COMMENTS
Diabetes Mellitus Type I Hyperlipidemia Chronic Kidney Disease Vascular Dementia Behavioral Disturbance Alcohol/stimulant dependent, currently in remission HIV ... Name: Alyssa Mon tgomery Critical Thinking Map Date 1/25/ 2022. Medical Diagnosis: Diabetes M ellitus T ype I . Hyperlipidemia . Chroni c Kidney Disease . V ascular Dementia .
Here at the American Diabetes Association® (ADA), we hope that you are doing well and staying safe during these uncertain times.This fall we are excited to announce a few publication updates as well as new education resources for your participants. What's New Healthy Interactions Virtual Diabetes Conversation Map® Program Is Now Available!
Diabetes mellitus is a commonly occurring chronic medical condition that is associated with a high burden of mortality and morbidity. In 2018, 34.2 million Americans, or 10.5 % of the population, had diabetes and approximately 1.5 million Americans were newly diagnosed that year [].The risk of mortality for people with diabetes is two times greater than it is for people without diabetes, and ...
It can be just as essential. Research shows that diabetes self-management education and support (DSMES) can improve A1C levels and have a positive effect on other clinical, psychosocial, and behavioral aspects of diabetes. Margaret (Maggie) Powers, PhD, RD, CDE, a clinician and research scientist at the International Diabetes Center in Park ...
This presentation is geared toward nursing students and nurses and is a narrated power point on the concept map or mind map of the medical diagnosis of diabe...
The UMass Memorial Diabetes Center of Excellence (DCOE) offers an extensive self-management education program recognized by the American Diabetes Association. It's designed to provide information, motivation and support. Diabetes educators at UMass Memorial utilize Conversation Maps® during to help people with lifestyle changes such as healthy eating, medication management, physical ...
the US Diabetes Conversation Map tools. Map tool topics include "On the Road to Better Managing your Diabetes"; "Diabetes and Healthy Eating"; "Monitoring Your Blood Glucose"; "Continuing Your Journey with Diabetes"; and "Caring for Gestational Diabetes". The maps are interactive and provide a "game-like" approach. Group
According to the American Diabetes Association (ADA), Standards of Medical Care in Diabetes 2023, the diagnosis of DM is made following a fasting plasma glucose (≥126 mg/dL), 2-hour oral glucose tolerance test (≥200 mg/dL following 75 g anhydrous glucose), random plasma glucose (≥200 mg/dL with classic symptoms of hyperglycemia such as polyuria, polydipsia, polyphagia), or A1C (≥6.5% ...
The major findings of the study include; concept maps are important for developing clear understanding of concepts in Biology, concept maps refrains rote learning thus promotes critical thinking ...
The IDEA Study enrolled 623 participants with a history of suboptimally controlled type 2 diabetes through HP and LCF from June 2008 to May 2009, with the purpose of evaluating the effectiveness of an interactive, group-based diabetes educational experience using the Conversation Map tools. Individuals interested in the study were eligible to participate if they had an A1C value within the ...
Introduction. The patients' involvement in their own care is a cornerstone of diabetes care and the health care providers' role is to stimulate and support patients' self-management and problem-solving skills. 1, 2 Self-management behaviors are needed for the successful implementation of every intervention that improves metabolic control in patients with diabetes or delays the onset of ...
Keywords: pharmacy education, teaching and learning, critical thinking, diabetes management. 1. Introduction. More than 34 million people in the United States have diabetes, and diabetes is the seventh leading cause of death . ... MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
) Ongoing support is critical to sustain progress made by participants during the DSME program.) Behavioral goal setting is an effective strategy to sup-port self-management behaviors. The U.S. Diabetes Conversation Map tools are available in English and Spanish. The Spanish language version is cultural relevant to Spanish speaking audiences. Merck
Between 1980 and 2003, hospital discharges coded with a diagnosis of diabetes increased from 2.2 to 5.1 million, representing a 132% increase in 23 years. 1 The economic burden of diabetes care was estimated at $174 billion in 2007, of which $116 billion was spent on medical expenditures, including $58 million on hospital inpatient care. 2 These figures continue to increase at a time when the ...
Abstract. Attitudes, knowledge, and skills of critical thinking are developed in a role-playing simulation. Using diabetes mellitus, students solve lifelike problems within the role-playing experience, develop sensitivity and awareness of another's life experience with illness, and generate empathy toward persons with diabetes.
Critical thinking Diabetes mellitus. 1960s. Click the card to flip 👆. major public health emphasis focused on smoking cessation and prevention. as smoking declined in the U.S. over the next 30 years we saw a rapid decline in smoking related deaths from cancer, stroke and cardiovascular disease. Click the card to flip 👆.
In 2015, AACE and ACE published joint guidelines for developing a comprehensive care plan for diabetes. 7 In 2020, as a supplement to the 2015 guidelines, AACE and ACE jointly published an ...
The brainstorming identified 43 unique barriers to diabetes management. The clients' map featured 9 clusters of barriers: Challenges to getting healthy food, Inadequate income, ... Participation in diabetes education, therefore, is critical for improving knowledge and self-efficacy, which enables patients to engage in healthy behaviours .
A mind map about diabetes mellitus. You can edit this mind map or create your own using our free cloud based mind map maker. MindMap Gallery Diabetes Mellitus. 715 2 2 Release time:2020-10-08 Diabetes Mellitus. Diabetes mellitus (DM), commonly known as diabetes, is a group of metabolic disorders characterized by a high blood sugar level over ...
A Critical-Thinking Acronym for Diabetes Care. A Critical-Thinking Acronym for Diabetes Care Medsurg Nurs. 2015 Nov-Dec;24(6):432-3. Authors Vicki Chase, Mavis Strakal, Timothy K Jackson. PMID: 26863708 No abstract available. MeSH terms Abbreviations as Topic* Clinical Competence / standards* ...
Critical Thinking Map - Diabetes.pdf - Doc Preview. Pages 2. Total views 18. Great Basin College. NURS. NURS 158. ally191221. 2/28/2021. View full document. Students also studied. Module 2 - Critical Thinking.pdf. Colorado State University, Global Campus. ACT 360. Critical Thinking Map - TB.pdf. Great Basin College.