Wait, but Wi-Fi?

Transmit Power Control Considerations
Proper configuration of Transmit Power Control (TPC) settings can help to ensure that your Access Point (AP) does not speak too loudly. If your AP is transmitting at 18dBm and an associated client station (STA) is at the cell edge and only capable of transmitting at 15dBm, your client will be able to hear the AP transmission, but the AP won’t be able to hear the client which leads to retransmissions and thus reduced performance.
Wireless network design is ultimately dependent upon the clients it is to support, so we will want to have an idea of what our intended clients are capable of. As an example, one of my customer’s clients is an HP EliteBook 8470p laptop workstation which has a Broadcom BCM943228HM4L Wi-Fi adapter. According to the product specification web page for this particular model, I was able to find that it is capable of transmitting at around 15dBm. If this is my customer’s least capable device, I would not want my AP to transmit louder than 15dBm either.
My customer is using a Cisco 3504 Wireless Controller running AireOS version 8.8. I am able to globally configure the Maximum Power Level Assignment to 15dBm.

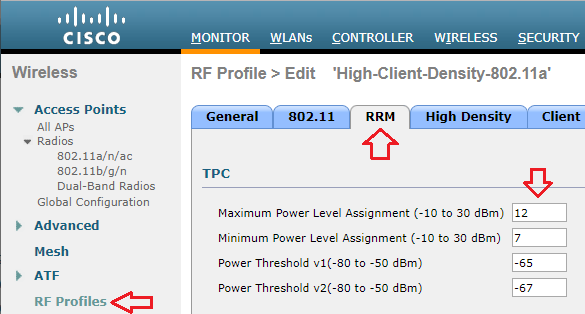
If the same controller were managing multiple locations with different requirements, I can also set a Maximum Power Level Assignment for different RF Profiles.
Though the maximum power level is configured in dBm, Cisco uses a series of numbers to represent levels of power. Phil Morgan of NC-Expert wrote an article titled WLC and AP Power settings in which he discusses Cisco power levels in further detail. In his article, he discusses how we can determine what the power levels represent as they vary by AP model, band (2.4 vs 5GHz), and even channel groupings (i.e. U-NII 1, 2, 2e, 3).
I also stumbled upon an excellent post by Maxim Risman in the Cisco Community titled Cisco Access point 2802i Tx Power Chart where he demonstrates the use of another very helpful command which summarizes the power levels of all APs: show advanced 802.11a txpower
Note that the range for the power levels actually does not change, but rather TPC is limiting the highest level that can be used.
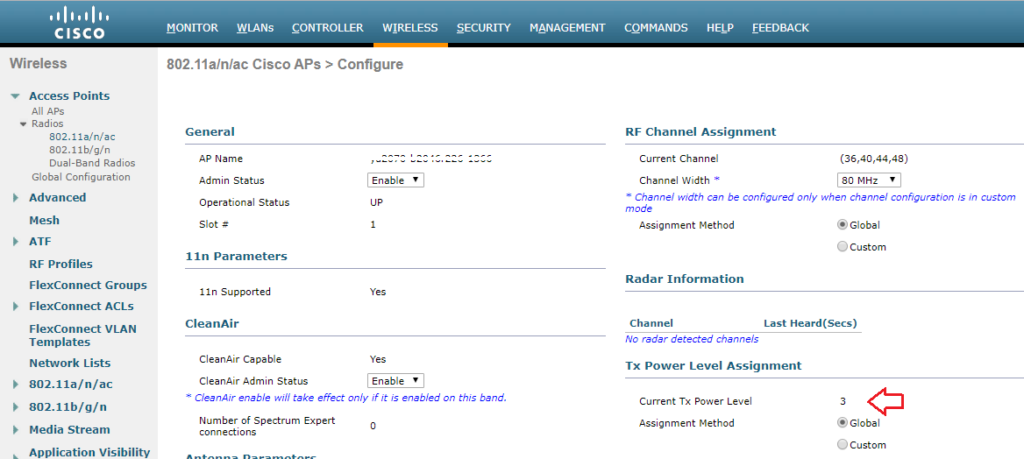
The current power level setting can also be found in the web GUI by navigating to Wireless > Access Points > Radios. There, you can see the power level for all of your APs in a column, or you can dive in to the configuration of a radio.
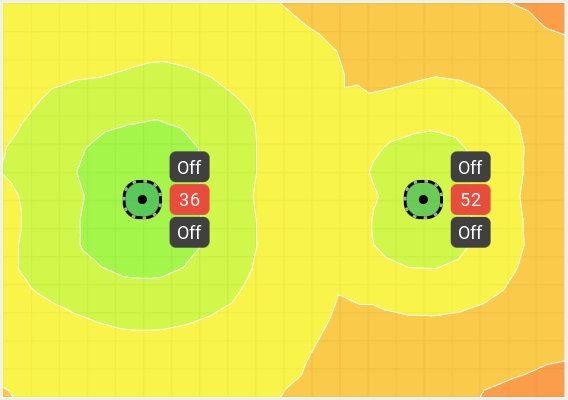
When performing predictive site surveys with Ekahau Pro site survey software, we have the ability to adjust the transmit power with which to generate our expected heat maps.
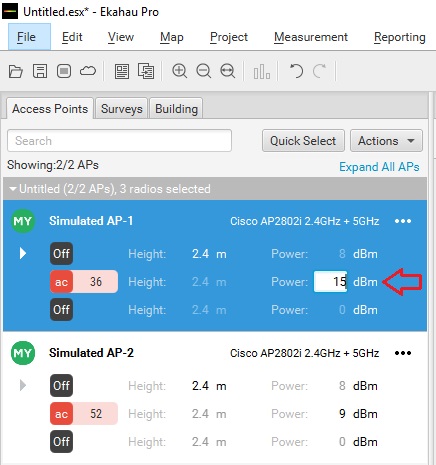
We can get an idea of how this difference may affect our design in the real world.
If you are interested in getting deeper into Cisco’s TPC implementation, you may want to check out a whitepaper they have published titled Transmit Power Control (TPC) Algorithm .
Published by Stephen
View all posts by Stephen

- Networking 101
Cisco Wireless Transmit Power Control

Power substation outside a VERY large data center in Atlanta,GA.
I’m going to start out by telling you something you probably already know. Every vendor has their own way of doing things. Sometimes it makes perfect sense, and other times you end up scratching your head wondering why that particular vendor implemented this feature or product. Since I have been spending a lot more time on wireless these days, I came across an issue that forced me to reconsider how transmit power control(TPC) actually works in a Cisco wireless deployment. I thought I would impart some of this information to you, dear reader, in the hopes that it may help you. If you spend a lot of time inside Cisco wireless LAN controllers, this may not be anything new to you.
The Need For TPC
If you have been around wireless long enough, you have probably dealt with wireless installs where all of the access points(AP) were functioning autonomously. While this isn’t a big deal in smaller environments, consider how much design work goes into a network with autonomous access points that number into the hundreds. It isn’t as simple as just deciding on channels and spinning all the access points up. You also have to consider the power levels of the respective access points. Failure to do so can result in the image below where the AP is clearly heard by the client device, but the AP cannot hear the client since it is transmitting at a higher power level than the client can match.
Now consider the use of a wireless LAN controller to manage all of those APs. In addition to things like dynamic channel assignment, you can also have it adjust the transmit power levels of the APs. This can come in handy when you have an AP fail and need the other APs to increase their transmit power to fill the gap that exists since that failed AP is no longer servicing clients. I should point out that proper design of a wireless network with respect to the client transmit power capabilities should NEVER be overlooked. You ALWAYS want to be aware of what power levels your clients can transmit at. It helps to reduce the problem in the image above.
There’s also the problem that can arise when too many APs can hear each other. It isn’t just about the clients. Wireless systems which adhere to the IEEE 802.11 standard are a half duplex medium. Only one device can talk at a time on a given channel. Either a client or the AP will talk, but not both at once. If an AP can hear another AP on the same channel at a usable signal, the airtime must be shared between those APs. Depending on the number of SSID’s in use, this can dramatically reduce the amount of airtime available for an AP to service a client. You can see some actual numbers with regard to SSIDs and APs in this blog post by Andrew von Nagy .
As you can see from two quick examples, there is a need to control the power level in which an AP will transmit. On controller based wireless networks(and even on the newer controller-less solutions), this is done automatically. I wouldn’t advise you turn that off unless you really know what you are doing and you have the time to plan it all out beforehand.
The Cisco Approach
On wireless LAN controllers, TPC is a function of Radio Resource Management(RRM). The specifics can be found here . I’ll spare you the read and give you the high points.
- The TPC algorithm is only concerned with reducing power levels. Increases in power levels are covered by Coverage Hole Detection and Correction algorithm.
- TPC runs in 10 minute intervals.
- A minimum of 4 APs are required for TPC to work.
It is the last point that I want to focus on, because the first two are pretty self explanatory. The reasoning behind the 4 AP minimum for TPC is as follows:
“For TPC to work ( or to even have a need for TPC ) 4 APS must be in proximity of each other. Why? Because on 2.4 GHz you only have three channels that do not overlap… Once you have a fourth AP you need to potentially adjust power down to avoid co channel interference. With 3 APS full power will not cause this issue.”
Those are not my words. They came from someone within Cisco that is focused on wireless. Since that person didn’t know I would publish that, I will not name said person. The explanation though, makes sense.
***Update – It appears that the Cisco documentation regarding TPC is a bit murky. Jeff Rensink pointed out in the comments below that TPC will also increase power levels. Although CHD will increase based on client information, I didn’t use any clients in my testing, as Jeff rightly assumed. The power increases I saw once I started removing AP’s from the WLC could not have been attributed to CHD adjustments. Read his comment below as he makes some very valid points. The NDP reference and accompanying link in his comment is fairly interesting.
Let’s see it in action to validate what Cisco’s documentation says.
TPC Testing
I happen to have a Cisco WLC 2504 handy with 4 APs. I set it up in my home office and only maintained about 10 feet separation from the APs. Ideally, I would test it with the APs a lot farther apart, but I did put some barriers around the APs to give some extra attenuation to the signal. I also only did testing on the 5GHz band. I disabled all of the 2.4GHz radios because I don’t need to give any of my neighbors a reason to hate me. Blasting 5GHz is less disruptive to their home wireless networks than 2.4GHz is due to the signals traveling farther / less attenuation of 2.4GHz vs 5GHz signals /antenna aperture. 🙂
Here you can see the available settings for TPC in the WLC GUI. This particular controller is running 7.6 code, so your version may vary.
- You can either set TPC to run automatically, on demand, or at a fixed power rate on all APs. TPC is band specific, so if you want different settings for 2.4GHz and 5GHz respectively, you can have that.
- Maximum and minimum settings for transmit power are available. The defaults are 30dBm for maximum power and -10dBm for minimum power.
- The power threshold is the minimum level at which you need to hear the third AP for the TPC algorithm to run. The default is -70dBm. You can set it higher or lower depending on your needs. High density environments might require a level stronger than -70dBm, with -50dBm being the strongest level supported. If you don’t necessarily need to run things like voice, you might be able to get away with a weaker threshold, but you cannot go beyond -80dBm.
A Quick Sidebar on Maximum Transmit Power in 5GHz
I set up the WLC with 3 APs active on 5GHz only. You can see that the power levels on the 3 APs are set to 1 in the image further down, which is maximum power according to Cisco. While it seems odd that max power would be a 1 and not some higher number, consider the fact that there are multiple maximum transmit power levels depending on which UNII band you are using in 5GHz. As a general reference, 20dBm would be 100mW and 14dBm would be 25mW. You could get 200mW(23dBm) of power using a UNII-3 channel vs UNII-1, which is maxed out 32mW(15dBm). That is a HUGE difference.
- 1 – 15dBm
- 2 – 12dBm
- 3 – 9dBm
- 4 – 6dBm
- 5 – 3dBm
- 1 – 17dBm
- 2 – 14dBm
- 3 – 11dBm
- 4 – 8dBm
- 5 – 5dBm
- 6 – 2dBm
- 1 – 23dBm
- 2 – 20dBm
- 3 – 17dBm
- 4 – 14dBm
- 5 – 11dBm
- 6 – 8dBm
- 7 – 5dBm
To see the supported power levels in terms of dBm on 5GHz, you can run the following command on the CLI of the WLC: show ap config 802.11a <ap name> The output will look something like this after you go through a handful of screens showing other stuff:
***Update – Brian Long wrote a blog post on this very thing! You can read it here .
Back To The Testing…
You can see in the image below that with 3 APs active, they are all running at power level 1, which is the default when the radios come online.
So let’s see what happens when I add the fourth AP. If our understanding of TPC is correct, we should see the power levels come down since the APs are so close to each other and will have a signal strength of well above -70dBm between each other.
Note – Power level decreases happen in single increments only, every time the TPC algorithm runs(every 10 minutes). To put it another way, it downgrades by 3dB max each cycle. Sam Clements pointed out to me via Twitter that when power levels increase, it can happen much more rapidly since the Coverage Hole Detection(CHD) and Correction algorithm is responsible for power increases.
If you want to see this work on the CLI in real time, you can issue the following command: debug airewave-director power enable
After I had waited for over half an hour, I decided to power off one more AP. When I brought it back online, I saw all 3 of the APs slowly go back to a power level of 1. Here’s the first change I saw in the 3 remaining APs:
It’s All In The Details
For wireless surveys, my company uses the Ekahau Site Survey product. It is a really neat survey tool and we use it for on site assessments as well as predictive surveys. When you define the requirements of the project, you can choose from a bunch of different vendor specific scenarios, or general wireless scenarios. I can apply those requirements to a predictive survey, or an on site survey where I am trying to determine if the existing coverage/capacity is good enough for the business needs.
Here’s a screen shot of the default requirements for the “Cisco Voice” scenario found in version 7.6.4 of Ekahau’s Site Survey program:
Closing Thoughts
Understanding how the TPC function works is pretty important when designing Cisco wireless networks. Failure to consider what all is involved in regards to transmit power on your APs could(not WILL, but COULD) lead to problems in the wireless network’s operation. However, if you want to manually set transmit power, that’s an option as well. Opinions differ on running RRM. I’m not sure there is a right or wrong answer. It depends. 🙂 I will say that I almost never see Cisco wireless implementations where RRM is not being used.
I don’t want to end this post without mentioning that some networks may be perfectly fine running APs at max power, especially on the 5GHz side. Your coverage may be enough to where there is minimal channel overlap(easily achievable in 5GHz with 20MHz channels and the use of all 3 UNII bands), and each AP can hear one or two neighboring APs at a decent level due to good cell overlap. You just might not have enough APs to trigger the TPC algorithm to run. That doesn’t mean “you are doing it wrong”. If it works for the business and all your users are fine, who am I to tell you that you need to “fix” it.
Hopefully this was beneficial to you if you needed a clearer understanding of how Cisco’s TPC function works. If you already have a good understanding of TPC and managed to read this far, feel free to shame humiliate correct me in the comments.
11 Responses to Cisco Wireless Transmit Power Control
Nice write up of the TPC process with actual testing. I would just make one correction.
The normal TPC algorithm should also raise power levels in addition to lowering them. This is evidenced in your testing as the powers raise up on the TCP interval when you took APs away. This is needed so that if an AP fails in real life, the surrounding APs can dynamically increase their power levels. The document that you linked actually says this. Although it also says that TCP is only used to decrease power (as you noted in your article). So it’s contradicting itself.
With coverage hole detection, the APs increase power in response to clients being connected at a low signal level. I haven’t seen any mention of CHD working to raise power in the absence of clients. So I don’t believe it has the capability to do so. Thus, if it were true that CHD was the only means to raise AP power, AP power would never raise without associated clients. I’ guessing in your tests, you didn’t have clients associated.
I don’t write this to pick on your article (it was very good). I just wanted to point out a common misconception that is unfortunately created by Cisco’s own documentation on the subject.
The other thing that bugs me about the RRM doc that you referenced is the inference that neighboring APs will be heard at lower RSSI levels as their power decreases. This is where they are talking about the TPC algorithm and how they use the power threshold value to determine if they should raise/lower power or not based on the 3rd loudest neighbor. The problem with that is that Neighbor Discovery Protocol (NDP) messages are always sent at the highest power/lowest data rate. So current AP power does not affect how loud a neighbor is heard, because TPC uses those NDP frames in its calculations. But part of the NDP information is the power level used to send the frame. So the TPC calculation can still do the math to figure out what power level is appropriate based on the threshold value.
For as important of a technology to understand as RRM is, Cisco definitely doesn’t make it easy to figure out. The article below helps fill in some information in regards to RRM. One of the nuggets is actually the reason why your power levels weren’t rising back up as quickly as you expected.
http://www.cisco.com/c/en/us/td/docs/wireless/controller/technotes/7-4/RRM_DG_74.html
Your comment is exactly the kind of additional information I was looking for in terms of corrections to my understanding of TPC, so I am grateful that you took the time to write it. There was a paragraph that I cut out of the blog post last night before publishing that I wish I would have left in after reading your comment. In that paragraph, I mentioned that when I powered off an AP, I still saw the TPC algorithm running via the “Last Power Level Assignment” field under the TPC page for 802.11a/n/ac. When I was proofreading, I pulled that paragraph because I thought it contradicted the RRM documentation stating that the TPC algorithm only cares about power decreases. It seemed like it would cause more confusion if I left it in.
After reading your comment, it makes a lot more sense now. I also appreciate the tidbit around NDP and how those messages actually work independent of the assigned power level to the AP.
Thanks again for the additional information. If I have some time, I will probably amend the post and reference your comment.
Great read Matthew. This is a keeper. 🙂
1. Regarding the comment from Cisco:
“For TPC to work (or to even have a need for TPC) 4 APs must be in proximity of each other. Why? Because on 2.4 GHz you only have three channels that do not overlap… Once you have a fourth AP you need to potentially adjust power down to avoid co-channel interference. With 3 APs full power will not cause this issue.”
DA > This is hideous…as you seemed to eluded to. The two major issues with this statement is that 1) it takes into consideration that you’re doing your testing inside a Faraday cage, and 2) there’s no such thing as adjacent channel interference. 🙁 I just had to get this off my chest. 🙂
While I can think of an advantage or two of using arbitrary numbers (e.g. 1-8) to represent power levels, the fact that they are so disparate across bands makes it non-intuitive for the Cisco novice. 1 should equal 1, 2 = 2, 3 = 3, etc…but no…of course not. 🙁 Confusion within the GUI is bad enough….but it’s much worse than that. Trying to assure maximum capacity, by uniformly mixing UNII-1 and UNII-3 channels (especially when DFS isn’t supported by many of your client devices), wouldn’t you end up with large cells and mid-sized cells unless TPC kicks in?
3. Question
It just seems silly to disable TPC unless there’s a 4th Cisco AP present in the network. Jeff mentioned that NDP is used in TPC calculations. Is that to say that neighboring APs can be used as TPC’s required-and-mysterious “4th AP”?
Again, great article. Very helpful.
Regarding your point number 1, I think they assume that anyone operating a wireless network will ONLY use 1, 6, and 11 inside the US. Of course, you and I both know that there are MANY networks run by people who just don’t seem to care about that.
As for point 2, it is fairly confusing when considering power levels at 5GHz. I would rather just have the scale start at 1 using the lowest level(-1dBm or 2dBm), and then go all the way up to whatever number on that scale represents 23dBm. You would still need to know what UNII band your 5GHz radio was on to know if you were at max power, but if I knew that power level 4 was always represented by 14dBm, I would know the radio was at 25mW. On the other hand, I can always look at power levels inside a Cisco WLC and know right away who is at max power, even though I still need to know what UNII band the radio is on.
To your point 3, my understanding of TPC is that it won’t even kick in until a 4th AP is heard. Although the AP’s are sending NDP messages to each other no matter what(I am going to verify this right now.), those messages are also used for other things like CleanAir and Rogue Detection according to the document that Jeff mentioned in his comment.
I just verified that NDP messages are still being sent every 60 seconds with just a single AP active on the WLC.
Awesome post and will be a great reference to customers we work with in Hospitals!
The fact that a ‘1’ is not a ‘1’ is definitely a challenge and can have a big effect on designs. Here is a reference ( http://blong1wifiblog.blogspot.com/2015/01/cisco-wireless-access-point-5ghz.html ) to output powers and the corresponding Cisco Power level for the 1131, 1242, 1142, 2602 and 3702 Cisco Access Points.
It was a hospital implementation that inspired this post. 🙂
Thanks for the link to the writeup you did. I will mention it when I update this post based on the comments received so far. TPC is definitely something that appears rather simple if you look at the settings within the WLC, but there is so much more to it. Even when I thought I understood it after testing, it turns out I really didn’t! Not sure I still do.
Great post, Matthew! On ESS and predictives for Cisco Voice, does it make sense to you to change the ESS defaults from 2 APs heard to min of 3 (plus dBm to -70, as you also suggest)? I am on conversation for tshoot of a poorly designed voice WLAN right now and if I have to go back out to do a predictive, I am just wondering if changing the defaults makes the best sense for a proper design. Thoughts?
Keep in mind that ESS is built with clients in mind. It isn’t necessarily concerned with AP to AP communication with respect to power levels. It does a great job of showing channel overlap, number of AP’s heard, etc. Without an understanding of how TPC works, you can layout AP’s to provide adequate coverage and capacity, but completely neglect how the AP’s will behave towards each other. By changing the defaults from 2 AP’s to 3 with a minimum signal level of -70dBm, you can ensure(as much as a predictive survey can) that your AP’s will see enough of each other to have the TPC algorithm run and let power levels adjust to something other than the maximum.
The “Network Issues” display in ESS will show areas in yellow that don’t meet this 3AP@-70dBm, or whatever value you set. You don’t need to try and get rid of all the yellow across the entire floor or area. You just need to get rid of it around the AP’s themselves. You will also have to ensure that the standard client coverage requirements(-67dBm for Cisco voice) are met, but with the amount of AP’s you will need to get TPC working, that shouldn’t be a problem. The alternative is to have all your AP’s running at max power since TPC didn’t have the right amount of AP’s at the right signal level to adjust power levels. While AP’s running at max power isn’t necessarily a bad thing, it will cause problems if you have an AP fail and none of the neighboring AP’s can increase power to offset the signal coverage gap from the failed AP. Additionally, with varying power levels across the UNII bands on 5GHz, max power could be anywhere from 25mW to 200mW. That could cause some big issues with voice deployments as you’ll run into the issue where the phone can hear the AP, but the AP can’t hear the phone.
My thoughts
I haven’t deployed a Cisco WLAN system (yet), but other vendors have the same or similar algorithm for that. But I haven’t used it once in my designs. Now I’m always open to rethink my designs, but relying on TPC (or similar) to cover holes if an AP fails or to reduce CCI just doesn’t seem quite right to me.
To cover holes upon an AP failure can be somewhat designed for with some proper cell overlap, however I would do that only in the 5GHz.
And CCI is not a factor of APs only, client devices are STAs too and they will equally effect other APs on the same channel. Plus lowering pwr for them completely obliterates your RSSI/SNR design. And lowering pwr also changes your MCS rates.
And just to compare, if a critical life-saving hospital component is low on battery and someone needs it immediately, those doctors won’t say: “Now, just try and hold on for a second while we charge this baby up. It really shouldn’t take long.” No, they’ll get a new one ASAP having it ready on standby. So the same must apply to APs if it’s a mission critical component.
So using something like TPC just doesn’t seem prudent to me. I’d rather use a fixed power value and design around that, but then again, I’m always open for new ideas.
I would be curious how you design around failure of an AP. Do your designs have enough cell overlap to where a failed AP would be covered by other AP’s nearby? Additionally, how do you deal with persistent interference and orchestrate cascading channel changes to compensate for that? This wouldn’t necessarily be an issue on 5GHz if you are using multiple UNII bands and 20MHz channels, but it would definitely be an issue on the 2.4GHz side.
I suppose it all depends on how responsive a company can be to failures in the network. TPC, or any other vendor implementation for that matter, can dynamically change based on the RF conditions. If everything is manually set, it requires manual intervention. I am not saying that there isn’t a use case for manually setting transmit power and channel assignments. I just think the majority of people supporting wireless networks out there would prefer to automate as much of the process as possible. Thanks for your viewpoint!
Comments are closed.
- December 2018
- January 2017
- October 2015
- February 2015
- January 2015
- October 2014
- September 2014
- August 2014
- February 2014
- November 2013
- October 2013
- January 2013
- December 2012
- September 2012
- August 2012
- February 2012
- January 2012
- December 2011
- November 2011
- September 2011
- August 2011
- February 2011
- January 2011
- December 2010
- November 2010
- October 2010
- September 2010
- August 2010
Recent Comments
- Matthew Norwood on Aerohive’s Private Pre-Shared Key Technology
- Lee Badman on Aerohive’s Private Pre-Shared Key Technology
- Matthew Norwood on Does Aerohive Scale?
- Chris Carlton on Does Aerohive Scale?
- Marc on From Multi-Vendor To Single-Vendor

Unlimited Access
Exam 350-401 topic 1 question 407 discussion.
If the maximum power level assignment for global TPC 802.11a/n/ac is configured to 10 dBm. which power level effectively doubles the transmit power?
siteoforigin
Rafaelinho88, get it certification.
Unlock free, top-quality video courses on ExamTopics with a simple registration. Elevate your learning journey with our expertly curated content. Register now to access a diverse range of educational resources designed for your success. Start learning today with ExamTopics!
Log in to ExamTopics
Report comment.
- Skip to content
- Skip to search
- Skip to footer
Enhanced Classic LAN, Release Release 12.2.1
New and changed information, general parameters, spanning tree, manageability, configuration backup, flow monitor.
The following table provides an overview of the significant changes up to this current release. The table does not provide an exhaustive list of all changes or of the new features up to this release.
Creating an Enhanced Classic LAN Fabric
This document describes how to create a new Enhanced Classic LAN fabric using the Enhanced Classic LAN fabric template.
Note that this document gives information specifically for the fields that you will see in the Enhanced Classic LAN fabric template. See the Managing Legacy/Classic Networks in Cisco Nexus Dashboard Controller document for detailed procedures around managing legacy/classic networks in NDFC using the Enhanced Classic LAN fabric template.
Navigate to the LAN Fabrics page:
Manage > Fabrics
Click Actions > Create Fabric .
The Create Fabric window appears.
Enter a unique name for the fabric in the Fabric Name field, then click Choose Fabric .
A list of all available fabric templates are listed.
From the available list of fabric templates, choose the Enhanced Classic LAN template, then click Select .
Enter the necessary field values to create a fabric.
The tabs and their fields in the screen are explained in the following sections. The fabric level parameters are included in these tabs.
When you have completed the necessary configurations, click Save .
Click on the fabric to display a summary in the slide-in pane.
Click on the Launch icon to display the Fabric Overview.
The General Parameters tab is displayed by default. The fields in this tab are described in the following table.
What’s next: Complete the configurations in another tab if necessary, or click Save when you have completed the necessary configurations for this fabric.
The fields in the Spanning Tree tab are described in the following table. All of the fields are automatically populated based on Cisco-recommended best practice configurations, but you can update the fields if needed.
The fields in the VPC tab are described in the following table. All of the fields are automatically populated based on Cisco-recommended best practice configurations, but you can update the fields if needed.
The fields in the Protocols tab are described in the following table. Most of the fields are automatically populated based on Cisco-recommended best practice configurations, but you can update the fields if needed.
The fields in the Advanced tab are described in the following table. All of the fields are automatically populated based on Cisco-recommended best practice configurations, but you can update the fields if needed.
The fields in the Resources tab are described in the following table. Most of the fields are automatically populated based on Cisco-recommended best practice configurations, but you can update the fields if needed.
The fields in the Manageability tab are described in the following table. Most of the fields are automatically populated based on Cisco-recommended best practice configurations, but you can update the fields if needed.
The fields in the Bootstrap tab are described in the following table. Most of the fields are automatically populated based on Cisco-recommended best practice configurations, but you can update the fields if needed.
The fields in the Configuration Backup tab are described in the following table. Most of the fields are automatically populated based on Cisco-recommended best practice configurations, but you can update the fields if needed.
The fields in the Flow Monitor tab are described in the following table. Most of the fields are automatically populated based on Cisco-recommended best practice configurations, but you can update the fields if needed.
In the Netflow Exporter area, click Actions > Add to add one or more Netflow exporters. This exporter is the receiver of the netflow data. The fields on this screen are:
Exporter Name - Specifies the name of the exporter.
IP - Specifies the IP address of the exporter.
VRF - Specifies the VRF over which the exporter is routed.
Source Interface - Enter the source interface name.
UDP Port - Specifies the UDP port over which the netflow data is exported.
Click Save to configure the exporter. Click Cancel to discard. You can also choose an existing exporter and select Actions > Edit or Actions > Delete to perform relevant actions.
In the Netflow Record area, click Actions > Add to add one or more Netflow records. The fields on this screen are:
Record Name - Specifies the name of the record.
Record Template - Specifies the template for the record. Enter one of the record templates names. The following two record templates are available for use. You can create custom netflow record templates. Custom record templates saved in the template library are available for use here.
netflow_ipv4_record - to use the IPv4 record template.
netflow_l2_record - to use the Layer 2 record template.
Is Layer2 Record - Check this check box if the record is for Layer2 netflow.
Click Save to configure the report. Click Cancel to discard. You can also choose an existing record and select Actions > Edit or Actions > Delete to perform relevant actions.
In the Netflow Monitor area, click Actions > Add to add one or more Netflow monitors. The fields on this screen are:
Monitor Name - Specifies the name of the monitor.
Record Name - Specifies the name of the record for the monitor.
Exporter1 Name - Specifies the name of the exporter for the netflow monitor.
Exporter2 Name - (optional) Specifies the name of the secondary exporter for the netflow monitor.
The record name and exporters referred to in each netflow monitor must be defined in " Netflow Record " and " Netflow Exporter ".
In the Netflow Sampler area, click Actions > Add to add one or more Netflow samplers. These are optional fields and are applicable only when there are N7K aggregation switches in the fabric. The fields on this screen are:
Sampler Name - Specifies the name of the sampler.
Number of Samples
Number of Packets in Each Sampling
Click Save to configure the monitor. Click Cancel to discard. You can also choose an existing monitor and select Actions > Edit or Actions > Delete to perform relevant actions.
THE SPECIFICATIONS AND INFORMATION REGARDING THE PRODUCTS IN THIS MANUAL ARE SUBJECT TO CHANGE WITHOUT NOTICE. ALL STATEMENTS, INFORMATION, AND RECOMMENDATIONS IN THIS MANUAL ARE BELIEVED TO BE ACCURATE BUT ARE PRESENTED WITHOUT WARRANTY OF ANY KIND, EXPRESS OR IMPLIED. USERS MUST TAKE FULL RESPONSIBILITY FOR THEIR APPLICATION OF ANY PRODUCTS.
THE SOFTWARE LICENSE AND LIMITED WARRANTY FOR THE ACCOMPANYING PRODUCT ARE SET FORTH IN THE INFORMATION PACKET THAT SHIPPED WITH THE PRODUCT AND ARE INCORPORATED HEREIN BY THIS REFERENCE. IF YOU ARE UNABLE TO LOCATE THE SOFTWARE LICENSE OR LIMITED WARRANTY, CONTACT YOUR CISCO REPRESENTATIVE FOR A COPY.
The Cisco implementation of TCP header compression is an adaptation of a program developed by the University of California, Berkeley (UCB) as part of UCB’s public domain version of the UNIX operating system. All rights reserved. Copyright © 1981, Regents of the University of California.
NOTWITHSTANDING ANY OTHER WARRANTY HEREIN, ALL DOCUMENT FILES AND SOFTWARE OF THESE SUPPLIERS ARE PROVIDED “AS IS" WITH ALL FAULTS. CISCO AND THE ABOVE-NAMED SUPPLIERS DISCLAIM ALL WARRANTIES, EXPRESSED OR IMPLIED, INCLUDING, WITHOUT LIMITATION, THOSE OF MERCHANTABILITY, FITNESS FOR A PARTICULAR PURPOSE AND NONINFRINGEMENT OR ARISING FROM A COURSE OF DEALING, USAGE, OR TRADE PRACTICE.
IN NO EVENT SHALL CISCO OR ITS SUPPLIERS BE LIABLE FOR ANY INDIRECT, SPECIAL, CONSEQUENTIAL, OR INCIDENTAL DAMAGES, INCLUDING, WITHOUT LIMITATION, LOST PROFITS OR LOSS OR DAMAGE TO DATA ARISING OUT OF THE USE OR INABILITY TO USE THIS MANUAL, EVEN IF CISCO OR ITS SUPPLIERS HAVE BEEN ADVISED OF THE POSSIBILITY OF SUCH DAMAGES.
Any Internet Protocol (IP) addresses and phone numbers used in this document are not intended to be actual addresses and phone numbers. Any examples, command display output, network topology diagrams, and other figures included in the document are shown for illustrative purposes only. Any use of actual IP addresses or phone numbers in illustrative content is unintentional and coincidental.
The documentation set for this product strives to use bias-free language. For the purposes of this documentation set, bias-free is defined as language that does not imply discrimination based on age, disability, gender, racial identity, ethnic identity, sexual orientation, socioeconomic status, and intersectionality. Exceptions may be present in the documentation due to language that is hardcoded in the user interfaces of the product software, language used based on RFP documentation, or language that is used by a referenced third-party product.
Cisco and the Cisco logo are trademarks or registered trademarks of Cisco and/or its affiliates in the U.S. and other countries. To view a list of Cisco trademarks, go to this URL: http://www.cisco.com/go/trademarks . Third-party trademarks mentioned are the property of their respective owners. The use of the word partner does not imply a partnership relationship between Cisco and any other company. (1110R)
© 2017-2024 Cisco Systems, Inc. All rights reserved.
Bias-Free Language
The documentation set for this product strives to use bias-free language. For the purposes of this documentation set, bias-free is defined as language that does not imply discrimination based on age, disability, gender, racial identity, ethnic identity, sexual orientation, socioeconomic status, and intersectionality. Exceptions may be present in the documentation due to language that is hardcoded in the user interfaces of the product software, language used based on RFP documentation, or language that is used by a referenced third-party product. Learn more about how Cisco is using Inclusive Language.
- Open a Support Case
- (Requires a Cisco Service Contract )
eating disorder in adolescence essay
Eating disorders in adolescents essay.
Eating disorder as a severe health condition that can be manifested in many different ways may tackle a person of any age, gender, and socio-cultural background. However, adolescents, especially when it comes to female teenagers, are considered to be the most vulnerable in terms of developing this condition (Izydorczyk & Sitnik-Warchulska, 2018). According to the American Academy of Child & Adolescent Psychiatry (AACAP, 2018), 10 in 100 young women struggle with an eating disorder. Thus, the purpose of the present paper is to dwell on the specifics of external factors causing the disorder as well as the ways to deal with this issue.
To begin with, it is necessary to define which diseases are meant under the notion of an eating disorder. Generally, eating disorders encompass such conditions as anorexia nervosa, bulimia, binge eating, and avoidant/restrictive food intake disorder (ARFID) (AACAP, 2018). Although these conditions have different manifestations in the context of eating patterns, all of them affect teenager’s nutrition patterns and average weight. According to the researchers, there exist common external stressors that lead to an eating disorder, such as:
- Socio-cultural appearance standards. For the most part, modern culture and mass media promote certain body images as a generally accepted ideal, which causes many teenage girls to doubt their appearance and follow the mass trends.
- Biological factors. Some teenagers might have a genetic predisposition for certain disorders if anyone in the family struggled with the disease at some point in the past.
- Emotional factors. Children, who are at risk of being affected by such mental disorders as anxiety and depression, are likely to disrupt their nutrition patterns.
- Peer pressure. Similar to socio-cultural standards, peer pressure dictates certain criteria for the teenagers’ body image, eventually impacting their perception of food and nutrition (Izydorczyk & Sitnik-Warchulska, 2018).
With such a variety of potential stressors, it is imperative for both medical professionals and caregivers to pay close attention to the teenager’s eating habits. Thus, in order to assess the issue, any medical screening should include weight and height measurements. In such a way, medical professionals are able to define any discrepancies in the measurements over time and bring this issue up with a patient. When working with adolescents, it is of paramount importance to establish a trusting relationship with a patient, as teenagers are extremely vulnerable at this age. After identifying any issue related to weight and body image, nurses and physicians need to ask the patient whether they have any problems with eating. In case they are not willing to talk on the matter, it is necessary to emphasize that their response will not be shared with caregivers unless they want it. It is also necessary to ask questions regarding the child’s relationship with peers carefully, as they may easily become an emotional trigger.
In order to avoid such complications as eating disorders, it is vital for caregivers to talk with their children on the topic of the aforementioned stressors. Firstly, they need to promote healthy eating patterns by explaining why it is important for one’s body instead of giving orders to the child. For additional support, they may ask a medical professional to justify this information. Secondly, the caregivers need to dedicate time to explain the inappropriateness of body standards promoted by the mass media and promote diversity and positive body image within the family. Lastly, caregivers are to secure a safe environment for the teenager’s fragile self-esteem and self-actualization in order for them to feel more confident among peers (Boberová & Husárová, 2021). These steps, although frequently undermined, contribute beneficially in terms of dealing with eating disorders external stressors among adolescents.
American Academy of Child & Adolescent Psychiatry [AACAP]. (2018). Eating disorders in teens. Web.
Boberová, Z., & Husárová, D. (2021). What role does body image in relationship between level of health literacy and symptoms of eating disorders in adolescents?. International Journal of Environmental Research and Public Health , 18 (7), 3482.
Izydorczyk, B., & Sitnik-Warchulska, K. (2018). Socio-cultural appearance standards and risk factors for eating disorders in adolescents and women of various ages. Frontiers in psychology , 9 , 429.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, June 23). Eating Disorders in Adolescents. https://ivypanda.com/essays/eating-disorders-in-adolescents/
"Eating Disorders in Adolescents." IvyPanda , 23 June 2022, ivypanda.com/essays/eating-disorders-in-adolescents/.
IvyPanda . (2022) 'Eating Disorders in Adolescents'. 23 June.
IvyPanda . 2022. "Eating Disorders in Adolescents." June 23, 2022. https://ivypanda.com/essays/eating-disorders-in-adolescents/.
1. IvyPanda . "Eating Disorders in Adolescents." June 23, 2022. https://ivypanda.com/essays/eating-disorders-in-adolescents/.
Bibliography
IvyPanda . "Eating Disorders in Adolescents." June 23, 2022. https://ivypanda.com/essays/eating-disorders-in-adolescents/.
- External Stressors in Adolescents
- Eating Disorders in Adolescent Girls
- Influence of Modelling in Teenager’s Eating Disorders
- Socio-Cultural Approach of Humanity Examination
- Eating and Mood Disorders Among Adolescents
- Stressors in Nursing Workplace
- Environmental Stressors
- The Socialization of the Caregivers
- Organizational Stressors, Their Results and Types
- Eating Disorders in Male Adolescents as Health Topic
- Discussion Board Post: Distinction between the Public and Private
- Cyberbullying: Definition, Forms, Groups of Risk
- Human Trafficking and Healthcare Organizations
- The Politics of Abortion in Modern Day Jamaica
- Challenges of Prisoner Re-Entry Into Society
Home — Essay Samples — Nursing & Health — Eating Disorders — Eating Disorders in Adolescents
Eating Disorders in Adolescents
- Categories: Eating Disorders
About this sample

Words: 568 |
Published: Feb 12, 2024
Words: 568 | Page: 1 | 3 min read
Table of contents
Introduction, types of eating or feeding disorders in adolescents, causes and risk factors of eating disorders in adolescents, treating eating disorders.
Fairburn, C.G. (2008). Cognitive Behavior Therapy and Eating Disorders . New York: Guilford Press.
Grilo, C.M., & Mitchell, J.E. (2012). Treatment of Eating Disorders . New York: Guilford Press.
- Herrin, M., & Larkin, M. (2013). Nutrition Counseling in the Treatment of Eating Disorders . California: Routledge.
Hornbacher, M. (2009). Wasted: A Memoir of Anorexia and Bulimia . New York: John Wiley & Sons.
Lock, J., & Grange, D.L. (2005). Help Your Teenager Beat an Eating Disorder . New York: Guilford Press.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Heisenberg
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
5 pages / 2332 words
5 pages / 2196 words
2 pages / 799 words
4 pages / 1677 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Eating Disorders
Jane Martin's play "Beauty" is a thought-provoking exploration of society's obsession with physical appearance and the detrimental impact of consumerism on individual self-esteem. In this essay, we will delve into the portrayal [...]
Psychological disorders are more commonly diagnosed in today’s society. Years ago, a psychological disorder was easily overlooked. In today’s society, it is easier to tell if someone has a psychological disorder because of all [...]
According to “Number of Adults with Eating Disorders in The U.S in 2008-2012, by Age Group (in 1,000) on Statista, there were eleven thousand people between the age of eighteen to twenty-five years old who were diagnosed with [...]
First of foremost, the subject at hand is still in constant debates; whether food addiction truly exist or not, for as we all know food is vital to our survival as a living organism. Also, we all have this tendency to get [...]
Eating disorders have become a prevalent issue in today's society, affecting individuals of all ages and backgrounds. From anorexia nervosa to bulimia to binge eating disorder, these conditions not only impact physical health [...]
The global rise in obesity has reached alarming levels, presenting a significant public health challenge. This essay delves into the multifaceted nature of obesity and examines a range of solutions to address this complex issue. [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Introduction
- Conclusions
- Article Information
SCOFF indicates Sick, Control, One, Fat, Food.
a Data from KiGGS baseline, 2003-2006. 34
b Data from KiGGS wave 2, 2014-2017. 34
eTable 1. Electronic search strategy
eTable 2. Excluded studies and reasons for exclusion
eTable 3. Results of the quality assessment checklist for prevalence studies
eFigure. Doi plot and Luis Furuya-Kanamori index determining the publication bias of the studies analyzed for proportion of disordered eating
Data sharing statement
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
López-Gil JF , García-Hermoso A , Smith L, et al. Global Proportion of Disordered Eating in Children and Adolescents : A Systematic Review and Meta-analysis . JAMA Pediatr. 2023;177(4):363–372. doi:10.1001/jamapediatrics.2022.5848
Manage citations:
© 2024
- Permissions
Global Proportion of Disordered Eating in Children and Adolescents : A Systematic Review and Meta-analysis
- 1 Health and Social Research Center, Universidad de Castilla-La Mancha, Cuenca, Spain
- 2 Department of Environmental Health, T.H. Chan School of Public Health, Harvard University, Boston, Massachusetts
- 3 Navarrabiomed, Hospital Universitario de Navarra (HUN), Universidad Pública de Navarra (UPNA), IdiSNA, Pamplona, Navarra, Spain
- 4 Centre for Health, Performance and Wellbeing, Anglia Ruskin University, Cambridge, United Kingdom
- 5 Division of Psychology and Mental Health, University of Manchester, Manchester Academic Health Science Centre, Manchester, United Kingdom
- 6 Greater Manchester Mental Health NHS Foundation Trust, Manchester Academic Health Science Centre, Manchester, United Kingdom
- 7 Centre for Public Health, Queen’s University, Belfast, United Kingdom
- 8 Postgraduate Program in Public Health, Universidade Estadual de Londrina, Londrina, Brazil
- 9 Escuela de Fisioterapia, Universidad de las Américas, Quito, Ecuador
- 10 Faculty of Nursing, Universidad de Castilla-La Mancha, Albacete, Spain
- 11 Faculty of Health Sciences, San Antonio Catholic University of Murcia, Murcia, Spain
Question What is the global proportion of disordered eating in children and adolescents?
Findings In this systematic review and meta-analysis of 32 studies including 63 181 participants from 16 countries, 22% reported that children and adolescents showed disordered eating. The proportion was further elevated among girls, older adolescents, and those with higher body mass index.
Meaning Identifying the magnitude of disordered eating and its distribution in at-risk populations is crucial for planning and executing actions aimed at preventing, detecting, and dealing with them.
Importance The 5-item Sick, Control, One, Fat, Food (SCOFF) questionnaire is the most widely used screening measure for eating disorders. However, no previous systematic review and meta-analysis determined the proportion of disordered eating among children and adolescents.
Objective To establish the proportion among children and adolescents of disordered eating as assessed with the SCOFF tool.
Data Sources Four databases were systematically searched (PubMed, Scopus, Web of Science, and the Cochrane Library) with date limits from January 1999 to November 2022.
Study Selection Studies were required to meet the following criteria: (1) participants: studies of community samples of children and adolescents aged 6 to 18 years and (2) outcome: disordered eating assessed by the SCOFF questionnaire. The exclusion criteria included (1) studies conducted with young people who had a diagnosis of physical or mental disorders; (2) studies that were published before 1999 because the SCOFF questionnaire was designed in that year; (3) studies in which data were collected during COVID-19 because they could introduce selection bias; (4) studies based on data from the same surveys/studies to avoid duplication; and (5) systematic reviews and/or meta-analyses and qualitative and case studies.
Data Extraction and Synthesis A systematic review and meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline.
Main Outcomes and Measures Proportion of disordered eating among children and adolescents assessed with the SCOFF tool.
Results Thirty-two studies, including 63 181 participants, from 16 countries were included in this systematic review and meta-analysis. The overall proportion of children and adolescents with disordered eating was 22.36% (95% CI, 18.84%-26.09%; P < .001; n = 63 181) ( I 2 = 98.58%). Girls were significantly more likely to report disordered eating (30.03%; 95% CI, 25.61%-34.65%; n = 27 548) than boys (16.98%; 95% CI, 13.46%-20.81%; n = 26 170) ( P < .001). Disordered eating became more elevated with increasing age ( B , 0.03; 95% CI, 0-0.06; P = .049) and body mass index ( B , 0.03; 95% CI, 0.01-0.05; P < .001).
Conclusions and Relevance In this systematic review and meta-analysis, the available evidence from 32 studies comprising large samples from 16 countries showed that 22% of children and adolescents showed disordered eating according to the SCOFF tool. Proportion of disordered eating was further elevated among girls, as well as with increasing age and body mass index. These high figures are concerning from a public health perspective and highlight the need to implement strategies for preventing eating disorders.
Eating disorders are psychiatric disorders characterized by abnormal eating or weight control behaviors, which can lead to serious health problems. 1 These disorders include anorexia nervosa, bulimia nervosa, binge eating disorder, and eating disorder–not otherwise specified. 2 , 3 They are defined according to individual signs and symptoms and with degrees of severity detailed in the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) ( DSM-5 ), 2 as well as in the World Health Organization International Classification of Diseases, 11th Revision (ICD-11) . 3 Similarly, they are recognized within the mental disorders included in the Global Burden of Diseases, Injuries, and Risk Factors Study 2019 4 and are currently a public health concern in most mid- and high-income countries because their prevalence in young people has markedly increased over the past 50 years. 1 Furthermore, eating disorders are among the most life-threatening of all mental health conditions 5 and accounted for 17 361.5 years of life lost (between 1990 and 2019) and caused 318.3 deaths worldwide in 2019. 4
The etiology of eating disorders is very complex and, similar to other psychiatric disorders such as depression and anxiety, arises from the intersection of many risk factors. 6 Although the prevalence varies according to study populations and definitions used, 7 it is recognized that eating disorders are common in adolescents and even more common in young adults. 8 Based on the DSM-5 , the prevalence of eating disorders in children and adolescents (aged 11-19 years) has been stated to be between 1.2% (boys) and 5.7% (girls), with increasing incidence over recent decades. 7 Considering that mid to late adolescence is a peak period of eating disorders and their symptoms, knowing and understanding the proportion of disordered eating among youths is a crucial issue. 9
Because some children and adolescents with eating disorders may hide the core symptoms of the illness and delay seeking specialized care due to feelings of shame or stigmatization, 10 it is reasonable to consider that eating disorders are underdiagnosed and undertreated. 11 In addition to diagnosed eating disorders, parents, guardians, and health care professionals should be aware of symptoms of disordered eating, which include behaviors such as weight loss dieting, binge eating, self-induced vomiting, excessive exercise, and the use of laxatives or diuretics (although not to the level to warrant a clinical diagnosis of an eating disorder). 12 Although these symptoms predict outcomes related to eating disorders and obesity in adolescents 5 years later, 13 it is important to distinguish disordered eating from eating disorders. 14 The term disordered eating is often used to describe and identify some of the different eating behaviors that do not necessarily meet the diagnostic criteria for an eating disorder and therefore cannot be classified as eating disorders per se. 15 Notwithstanding, although its impact on health is often minimized, disordered eating should be closely evaluated because it can evolve into eating disorders. 12
The Sick, Control, One, Fat, Food (SCOFF) questionnaire, developed in 1999 by Morgan et al, 16 is the most widely used screening measure for eating disorders. 17 It consists of 5 questions with dichotomic answers options (ie, yes or no) 16 : (1) Do you make yourself sick because you feel uncomfortably full? (2) Do you worry you have lost control over how much you eat? (3) Have you recently lost more than 1 stone in a 3-month period? (4) Do you believe yourself to be fat when others say you are too thin? (5) Would you say that food dominates your life? A positive screen is provided when a participant answers yes to 2 or more questions, 16 which denotes a suspicion of an existing eating disorder (ie, disordered eating). 17 Previous systematic reviews have examined the SCOFF questionnaire as a screening tool in primary care setting. 17 , 18 For instance, a recent systematic review with meta-analysis including 25 validation studies found that the validity of the cutoff point of 2 or more on the SCOFF questionnaire was high across samples with a pooled sensitivity of 86.0% and specificity of 83.0%. Another recent systematic review for populations and settings relevant to primary care in the US found that a cutoff point of 2 or more on the SCOFF questionnaire had a pooled sensitivity of 84% and pooled specificity of 80% among adults. 18 Among young people, previous studies have found that the cutoff point of 2 or more on the SCOFF questionnaire provided a sensitivity ranging from 64.1% to 81.9% and a specificity ranging from 77.7% to 87.2%. 19 - 22
Despite the above, thus far, no previous systematic review and meta-analysis determined the proportion of disordered eating among children and adolescents. From an epidemiological perspective, identifying the magnitude of disordered eating and its distribution in at-risk populations is crucial for planning and executing actions aimed at preventing, detecting, and dealing with them. 23 Therefore, the aim of the present study was to establish the proportion among children and adolescents of disordered eating as assessed with the SCOFF tool, one of the most widely used methods to study disordered eating in this population. 8
This systematic review and meta-analysis was registered in the International Prospective Register of Systematic Reviews (PROSPERO) ( CRD42022350837 ) and conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses ( PRISMA ) reporting guideline. 24
Studies were required to meet the following criteria: (1) participants: studies of community samples of children and adolescents aged 6 to 18 years and (2) outcome: disordered eating assessed by the SCOFF questionnaire. Searching was not restricted to articles published in peer-reviewed journals of any particular language. For studies that included children/adolescents and adults, the articles were reviewed and, if reported, the child/adolescent samples were included.
The exclusion criteria included (1) studies conducted with young people who had a diagnosis of physical or mental disorders; (2) studies that were published before 1999 because the SCOFF questionnaire was designed in that year 16 ; (3) studies in which data were collected during COVID-19 because they could introduce selection bias; (4) studies based on data from the same surveys/studies to avoid duplication; and (5) systematic reviews and/or meta-analyses and qualitative and case studies.
Two researchers (J.F.L.-G. and D.V.-M.) systematically searched PubMed, Scopus, Web of Science, and the Cochrane Library with date limits from January 1999 to November 2022. Based on the participants, outcome, and study criteria, studies were identified using all possible combinations of the following groups of search terms: (1) child* OR adolescent* OR youth* OR teen* OR young* and (2) Sick, Control, One, Fat, Food OR SCOFF. The complete search strategy for each database is shown in eTable 1 in Supplement 1 . In addition, the list of references of the studies included in this review and in a previous systematic review 17 was thoroughly reviewed to ensure that no eligible studies were missed.
After identifying eligible studies, Mendeley (version for Windows 10; Elsevier) was used to remove duplicate studies. Two members of the research team (J.F.L.-G. and D.V.-M.) conducted the selection process independently and screened every title and abstract to identify potentially relevant articles to be reviewed in the full-text phase. A third researcher (A.G.-H.) participated to resolve any discrepancies.
The proportion of participants with disordered eating (ie, cutoff point ≥2 on the SCOFF questionnaire) was extracted by 1 researcher (D.V.-M.). Another researcher (J.F.L.-G.) checked the data for accuracy. In case of a discrepancy between these 2 researchers, a third researcher (A.G.-H.) reviewed the information.
Information on the authors, affiliations, date, and source of each study included in this review was hidden to avoid bias in the assessment of the methodological quality of the articles. Two researchers (D.V.-M. and J.F.L.-G.) independently assessed the risk of study bias of the included studies. This assessment was performed using a specific tool by Hoy et al 25 for prevalence studies. The tool consists of 10 items that address both the external and internal validity of prevalence studies. Each item can be classified as yes (low risk) or no (high risk), which equals 0 and 1 point, respectively. The overall risk of study bias is deemed to be at low risk of bias, moderate risk of bias, or high risk of bias if the points scored are 0 to 3, 4 to 6, or 7 to 9, respectively.
Proportion of disordered eating was computed based on the raw numerators (ie, participants who scored ≥2 on SCOFF questionnaire) and denominators (ie, total sample) found among the studies.
Using RStudio software version 2022.07.2 + 576 (R Group for Statistical Computing) with the meta package, 26 a meta-analysis of single proportions (ie, metaprop ) was pooled by applying a random-effects model that displayed the results as forest plots using the inverse variance method. The exact or Clopper-Pearson method was used to establish 95% CIs for proportion from the selected individual studies, 27 and a Freeman-Tukey double arcsine transformation was used to normalize the results before calculating the pooled proportion. 28 A continuity correction of 0.5 was used both to calculate individual study results with confidence limits and to conduct meta-analysis.
Heterogeneity between the included studies was determined by the I 2 statistic and its P value. Small study effects and publication bias were examined using the Doi plot and the Luis Furuya-Kanamori index. 29 No asymmetry, minor asymmetry, or major asymmetry were considered with values of less than −2, between −2 and −1, and more than −1, respectively. 29
Subgroup analyses were conducted by gender. Furthermore, random-effects meta-regression analyses using the method of moments were estimated to independently assess whether disordered eating differed by mean age or body mass index (BMI) (both as continuous variables).
A total of 628 records were identified through database searches ( Figure 1 ). After screening for duplicates, gray literature, and other reasons, 302 records remained. Finally, 97 records were obtained for full-text review. Of those studies, 67 were excluded for several reasons (eTable 2 in Supplement 1 ). Two studies were included via other methods (ie, citation searching). Finally, 32 studies, including 63 181 participants, were included in this systematic review, and all studies were included in the meta-analysis.
The main characteristics of the 32 included studies are summarized in the Table . Twenty-six of the studies were cross-sectional, 19 , 20 , 30 , 31 , 34 , 36 , 37 , 39 , 41 - 46 , 48 - 59 4 were longitudinal, 32 , 33 , 35 , 40 1 was a quasi-experimental study, 47 and 1 was a randomized clinical trial. 38 A total of 63 181 participants (51.8% girls) aged 7 to 18 years were included in this systematic review and meta-analysis.
According to gender, 22 studies reported the overall proportion of children and adolescents with disordered eating in both girls and boys, and 2 studies included only 1 gender (ie, only girls 44 , 55 ). The remaining 8 studies did not report proportion segmented by gender. In terms of geographical regions, 16 different countries were identified, including 21 studies in Europe, 19 , 20 , 30 , 34 - 36 , 40 - 43 , 45 , 46 , 48 - 53 , 56 , 57 , 59 5 in Asia, 33 , 37 , 47 , 55 , 58 4 in North America, 31 , 32 , 44 , 54 1 in South America, 38 and 1 in Africa. 39 All the studies were conducted with participants from only 1 country.
All studies were deemed to be at low risk of bias, presenting scores ranging between 0 and 2 points (with the exception of the study by Hicks et al, 44 which presented 3 points). The main sources of bias were associated with the representativeness of the analyzed sample. 19 , 20 , 30 , 31 , 35 - 39 , 41 , 44 , 46 , 47 , 50 , 52 , 54 , 55 A summary of the risk of bias scoring is shown in eTable 3 in Supplement 1 .
Figure 2 shows that the overall proportion of children and adolescents with disordered eating was 22.36% (95% CI, 18.84%-26.09%; P < .001; n = 63 181) ( I 2 = 98.58%). The Luis Furuya-Kanamori index for the Doi plot showed no asymmetry, indicating no risk of publication bias (Luis Furuya-Kanamori index = −0.58) (eFigure in Supplement 1 ).
Figure 3 depicts the subgroup analysis according to gender. Girls were significantly more likely to report disordered eating (30.03%; 95% CI, 25.61%-34.65%; n = 27 548) than boys (16.98%; 95% CI, 13.46%-20.81%; n = 26 170) ( P < .001).
The random-effects meta-regression models between proportion of disordered eating and mean age or BMI are shown in Figure 4 . Disordered eating became more elevated with increasing age ( B , 0.03; 95% CI, 0-0.06; P = .049) ( Figure 4 A) and BMI ( B , 0.03; 95% CI, 0.01-0.05; P < .001) ( Figure 4 B).
To our knowledge, this is the first meta-analysis that has comprehensively examined the overall proportion of children and adolescents with disordered eating in terms of gender, mean age, and BMI. The main findings of this study are as follows: (1) a total of 14 856 of 63 181 children and adolescents (22.36%) from 16 countries showed disordered eating; (2) the proportion of children and adolescents with disordered eating was significantly higher in girls than in boys; and (3) the proportion of disordered eating among children and adolescents was positively associated with mean age and BMI. These findings can inform intervention priorities for disordered eating as a global health initiative to prevent possible health problems among young people, 60 particularly in girls and young people with higher BMI.
Our findings indicate that more than 1 in 5 children and adolescents presented with disordered eating. It is noteworthy that disordered eating and eating disorders are not similar because not all children and adolescents who reported disordered eating behaviors will necessarily be diagnosed with an eating disorder. 15 However, disordered eating in childhood/adolescence may predict outcomes associated with eating disorders in early adulthood. 13 For this reason, this high proportion found is worrisome and call for urgent action to try to address this situation. In 2019, 14 million people experienced eating disorders including almost 3 million children and adolescents. 61 The behaviors related to eating disorders may lead to greater risk or damage to health, significant distress, or significant impairment of functioning. 60 Indeed, eating disorders are among the most life-threatening psychiatric problems, and people with these conditions die 10 to 20 years younger than the general population. 5
Our findings also indicated that the proportion of children and adolescents with disordered eating was higher in girls than in boys. Although sex differences in disordered eating seem to be relatively minor in adolescence, 62 it is well known that these disorders are more prevalent among girls. 63 Conventionally, studies have focused principally on the female sex, but currently this is not considered as a female-specific matter. The reasons for sex disagreement in the prevalence are not well known. 62 It has been pointed out that disordered eating is frequently unobserved among boys. 64 Boys are presumed to underreport the problem because of the societal perception that these disorders mostly affect girls 65 and because disordered eating has usually been thought by the general population to be exclusive to girls and women. 64 Additionally, it has been noted that the current diagnostic criteria of eating disorder 2 fail to detect disordered eating behaviors more commonly observed in boys than in girls, such as intensely engaging in muscle mass and weight gain with the goal of improving body image satisfaction. 64
On the other hand, the proportion of young people with disordered eating increased with increasing age. This finding is in line with the scientific literature. 66 - 68 The age at onset of eating disorders has classically been described in adolescence. 68 Adolescence represents a critical period for the onset of eating disorders. 66 Similarly, Swanson et al 67 found that the median age at onset of some eating disorders (eg, anorexia nervosa, bulimia nervosa, binge eating disorder) ranged from 12.3 to 12.6 years in a US nationally representative sample including 10 123 adolescents. As the analyzed sample in the present systematic review and meta-analysis ranged from age 7 to 18 years and only 3 studies included only children (ie, aged 7-10 years), it seems to corroborate these ages at onset.
Importantly, we found that the proportion of children and adolescents with disordered eating became more evaluated with increasing BMI. In this sense, the proportion of disordered eating is higher in young people with excess weight than in their counterparts with normal weight. 37 , 69 , 70 Young people who have excess weight may follow disordered eating behaviors while attempting to lose body weight. 71 Therefore, it has been described that young people with excess weight is the population that appears to experience symptoms of disordered eating most frequently (eg, unsupervised weight loss dieting may lead to eating disorder risk 72 ). Although most adolescents who develop an eating disorder do not report prior excess weight problems, some adolescents could misinterpret what eating healthy consists of and engage in unhealthy behaviors (eg, skipping meals to generate a caloric deficit), which could then lead to development of an eating disorder. 73
The WHO’s Comprehensive Mental Health Action Plan 2013-2030 recognizes the essential role of mental health in achieving health for all people, establishing some objectives/priorities. 60 For instance, among others, this plan tries to strengthen information systems, evidence, and research for mental health. In this sense, our systematic review and meta-analysis contributes to this aim by providing epidemiological evidence on the current situation of disordered eating that, if undetected and untreated, can lead to eating disorders with their harmful consequences for the individual, the family, and society. Similarly, the high proportion of disordered eating found in this systematic review and meta-analysis reinforce the importance of screening eating disorders in primary care setting. This is in line with the recommendations by the American Academy of Pediatrics 74 and the American Academy of Child and Adolescent Psychiatry, 75 which advise screening young people through longitudinal height and weight monitoring and looking for symptoms of disordered eating. In this sense, the SCOFF questionnaire is simple, memorable, and easy for applying and scoring, 16 which may be considered the first approach to identify the need for a more detailed and specialized evaluation. 20 However, positive results should be followed by further questioning, prior to an automatic referral to mental health professionals. 76
The present study has certain limitations that must be acknowledged. First, only studies that analyzed disordered eating using the SCOFF questionnaire were included. This decision is justified by the intention of homogenizing the proportion of global proportion of children and adolescents with disordered eating. In this sense, the SCOFF questionnaire is the most widely used screening tool for eating disorders, has been adapted and validated for its use in several languages, seems to be highly effective as a screening tool, and has been extensively used to raise the suspicion level of an eating disorder. Second, because of the cross-sectional nature of most of the included studies, a causal relationship cannot be established. Third, due to the inclusion of binge eating disorder and other specified eating disorders in the DSM-5 , there is not enough evidence to support the use of SCOFF in primary care and community-based settings for screening all the range of eating disorders. However, a meta-analysis by Kutz et al 17 concluded that the SCOFF is a useful and simple screening tool for the most prevalent eating disorders (ie, bulimia nervosa, anorexia nervosa). Fourth, we included studies based on self-report questionnaires to assess disordered eating, and consequently, both social desirability and recall bias could influence the findings.
The available evidence from 32 studies comprising large samples from 16 countries showed that approximately 22% of children and adolescents showed disordered eating according to the SCOFF tool. The proportion of disordered eating was further elevated among girls as well as with increasing age and BMI. This high proportion is worrisome from a public health perspective and highlights the need to implement strategies for preventing eating disorders. 60
Accepted for Publication: November 30, 2022.
Published Online: February 20, 2023. doi:10.1001/jamapediatrics.2022.5848
Corresponding Authors: José Francisco López-Gil, PhD, Health and Social Research Center, Universidad de Castilla-La Mancha, Cuenca 16071, Spain ( [email protected] ); Héctor Gutiérrez-Espinoza, PhD, Escuela de Fisioterapia, Universidad de las Américas, Quito 170504, Ecuador ( [email protected] ).
Author Contributions: Dr López-Gil had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: López-Gil, García-Hermoso, Mesas, Tárraga-López, Victoria-Montesinos.
Acquisition, analysis, or interpretation of data: López-Gil, Smith, Firth, Trott, Mesas, Jiménez-López, Gutiérrez-Espinoza, Tárraga-López.
Drafting of the manuscript: López-Gil, García-Hermoso, Smith, Firth.
Critical revision of the manuscript for important intellectual content: López-Gil, Victoria-Montesinos, Smith, Firth, Trott, Mesas, Jiménez-López, Gutiérrez-Espinoza, Tárraga-López.
Statistical analysis: López-Gil, Tárraga-López.
Administrative, technical, or material support: López-Gil, García-Hermoso, Victoria-Montesinos.
Supervision: Smith, Firth, Trott, Tárraga-López.
Conflict of Interest Disclosures: Dr López-Gil is a Margarita Salas Fellow (Universidad de Castilla-La Mancha; 2021-MS-20563). Dr García-Hermoso is a Miguel Servet Fellow (Instituto de Salud Carlos III; CP18/0150). No other disclosures were reported.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
INTRODUCTION
Definitions, epidemiology, screening for eating disorders, assessment of children and adolescents with suspected eating disorders, laboratory evaluation, medical complications in patients with eating disorders, psychological and neurologic effects, dermatologic effects, dental and/or oral effects, cardiovascular effects, gastrointestinal tract effects, renal and electrolyte effects, endocrine effects, treatment principles across the eating disorder spectrum, the pediatrician’s role in care, financial considerations, pediatrician’s role in prevention and advocacy, guidance for pediatricians, lead authors, committee on adolescence, 2018–2019, identification and management of eating disorders in children and adolescents.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Laurie L. Hornberger , Margo A. Lane , THE COMMITTEE ON ADOLESCENCE , Laurie L. Hornberger , Margo Lane , Cora C. Breuner , Elizabeth M. Alderman , Laura K. Grubb , Makia Powers , Krishna Kumari Upadhya , Stephenie B. Wallace , Laurie L. Hornberger , Margo Lane , MD FRCPC , Meredith Loveless , Seema Menon , Lauren Zapata , Liwei Hua , Karen Smith , James Baumberger; Identification and Management of Eating Disorders in Children and Adolescents. Pediatrics January 2021; 147 (1): e2020040279. 10.1542/peds.2020-040279
Download citation file:
- Ris (Zotero)
- Reference Manager
Eating disorders are serious, potentially life-threatening illnesses afflicting individuals through the life span, with a particular impact on both the physical and psychological development of children and adolescents. Because care for children and adolescents with eating disorders can be complex and resources for the treatment of eating disorders are often limited, pediatricians may be called on to not only provide medical supervision for their patients with diagnosed eating disorders but also coordinate care and advocate for appropriate services. This clinical report includes a review of common eating disorders diagnosed in children and adolescents, outlines the medical evaluation of patients suspected of having an eating disorder, presents an overview of treatment strategies, and highlights opportunities for advocacy.
Although the earliest medical account of an adolescent patient with an eating disorder was more than 300 years ago, 1 a thorough understanding of the pathophysiology and psychobiology of eating disorders remains elusive today. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition ( DSM-5 ) includes the latest effort to describe and categorize eating disorders, 2 placing greater emphasis on behavioral rather than physical and cognitive criteria, thereby clarifying these conditions in those children who do not express body or weight distortion. DSM-5 diagnostic criteria for several of the eating disorders commonly seen in children and adolescents are presented in Table 1 .
Diagnostic Features of Eating Disorders Commonly Seen in Children and Adolescents
Adapted from the DSM-5 , American Psychiatric Association, 2013. 2
Notable changes in DSM-5 since the previous edition include the elimination of amenorrhea and specific weight percentiles in the diagnosis of anorexia nervosa (AN) and a reduction in the frequency of binge eating and compensatory behaviors required for the diagnosis of bulimia nervosa (BN). The diagnosis “eating disorder not otherwise specified” has been eliminated, and several diagnoses have been added, including binge-eating disorder (BED) and avoidant/restrictive food intake disorder (ARFID). 3 – 5 The diagnosis of ARFID encompasses feeding behaviors previously categorized in the fourth edition ( DSM-IV ) as “feeding disorder of infancy and early childhood” and expands these into adolescence and adulthood. Individuals with ARFID intentionally limit intake for reasons other than for concern for body weight, such as the sensory properties of food, a lack of interest in eating, or a fear of adverse consequences with eating (eg, choking or vomiting). As a result, they may experience weight loss or failure to achieve expected weight gain, malnutrition, dependence on nutritional supplementation, and/or interference with psychosocial functioning. 6 – 9 The category “other specified feeding and/or eating disorder” is now applied to patients whose symptoms do not meet the full criteria for an eating disorder despite causing significant distress or impairment. Among these disorders is atypical AN in which diminished self-worth, nutritional restriction, and weight loss mirrors that seen with AN, although body weight at presentation is in the normal or above-normal range. Efforts are ongoing to further categorize abnormal eating behaviors and refine diagnoses. 10
Prevalence data for eating disorders vary according to study populations and the criteria used to define an eating disorder. 11 A systematic review of prevalence studies published between 1994 and 2013 found widely varied estimates in the lifetime prevalence of eating disorders, with a range from 1.0% to 22.7% for female individuals and 0.3% to 0.6% for male indnividuals. 12 A 2011 cross-sectional survey of more than 10 000 nationally representative US adolescents 13 to 18 years of age estimated prevalence rates of AN, BN, and BED at 0.3%, 0.9%, and 1.6%, respectively. Behaviors suggestive of AN and BED but not meeting diagnostic thresholds were identified in another 0.8% and 2.5%, respectively. The mean age of onset for each of these disorders was 12.5 years. 13 Several studies have suggested higher BED prevalence rates of 2% to 4%, with a more equal distribution between girls and boys, making it perhaps the most common eating disorder among adolescents. 14 In contrast, the diagnoses seen in treatment may belie the relative prevalence of these disorders. In a review of 6 US adolescent eating disorder treatment programs, the distribution of diagnoses was 32% AN, 30% atypical AN, 9% BN, 19% ARFID, 6% purging disorder, and 4% others. 15 This may reflect the underrecognition and/or undertreatment of disorders such as BED.
Although previously mischaracterized as diseases of non-Hispanic white, affluent adolescent girls, eating disorder behaviors are increasingly recognized across all racial and ethnic groups 16 – 20 and in lower socioeconomic classes, 21 preadolescent children, 22 males, and children and adolescents perceived as having an average or increased body size.
Preteens with eating disorders are more likely than older adolescents to have premorbid psychopathology (depression, obsessive-compulsive disorder, or other anxiety disorders) and less likely to have binge and purge behaviors. There is a more equal distribution of illness by sex among younger patients and, frequently, more rapid weight loss, leading to earlier presentation to health care providers. 23
Although diagnosis in males may increase with the more inclusive DSM-5 criteria, 24 , 25 it is often delayed because of the misperception of health care providers that eating disorders are female disorders. 26 In addition, disordered eating attitudes may differ in male individuals, 27 focusing on leanness, weight control, and muscularity. Purging, use of muscle-building supplements, substance abuse, and comorbid depression are common in males. 28 – 30
Eating disorders can occur in individuals with various body habitus, and their presence in those of larger body habitus is increasingly apparent. 31 – 34 Weight stigma (the undervaluation or negative stereotyping of individuals because they have overweight or obesity) seems to play a role. Adolescents with larger body habitus are exposed to weight stigma through the media, their families, peers, and teachers, and health care professionals, resulting in depression, anxiety, poor body image, social isolation, unhealthy eating behaviors, and worsening obesity. 35 When presenting with significant weight loss but a BMI still classified in the “healthy,” overweight, or obese ranges, patients with eating disorders such as atypical AN may be overlooked by health care providers 36 , 37 but may experience the same severe medical complications as those who are severely underweight. 38 – 40
Increased rates of disordered eating may be found in sexual minority youth. 41 – 43 Analysis of Youth Risk Behavior Survey data reveals lesbian, gay, and bisexual high school students have significantly higher rates of unhealthy and disordered weight-control behaviors than their heterosexual peers. 44 , 45 Transgender youth may be at particular risk. 46 , 47 In a survey of nearly 300 000 college students, transgender students had the highest rates of self-reported eating disorder diagnoses and compensatory behaviors (ie, use of diet pills or laxatives or vomiting) compared with all cisgender groups. Nearly 16% of transgender respondents reported having been diagnosed with an eating disorder, as compared with 1.85% of cisgender heterosexual women. 48
Adolescents with chronic health conditions requiring dietary control (eg, diabetes, cystic fibrosis, inflammatory bowel disease, and celiac disease) may also be at increased risk of disordered eating. 49 – 51 Among teenagers with type 1 diabetes mellitus, at least one-third may engage in binge eating, self-induced vomiting, insulin omission for weight loss, and excessive exercise, 52 , 53 resulting in poorer glycemic control. 54
Many adolescents engage in dietary practices that may overlap with or disguise eating disorders. The lay term "orthorexia" describes the behavior of individuals who become increasingly restrictive in their food consumption, not based on concerns for quantity of food but the quality of food (eg, specific nutritional content or organically produced). The desire to improve one’s health through optimal nutrition and food quality is the initial focus of the patient, and weight loss and/or malnutrition may ensue as various foods are eliminated from the diet. Individuals with orthorexia may spend excessive amounts of time in meal planning and experience extreme guilt or frustration when their food-related practices are interrupted. 55 , 56 Psychologically, this behavior appears to be related to AN and obsessive-compulsive disorder 57 and is considered by some to be a subset within the restrictive eating disorders. Vegetarianism is a lifestyle choice adopted by many adolescents and young adults that may sometimes signal underlying eating pathology. 58 , 59 In a comparison of adolescent and young adult females with and without a history of eating disorders, those with eating disorders were more likely to report ever having been vegetarian. Many of these young women acknowledged that their decision to become vegetarian was primarily motivated by their desire for weight loss, and most reported that they had done so at least a year after first developing eating disorder symptoms. 60
In an attempt to improve performance or achieve a desired physique, adolescent athletes may engage in unhealthy weight-control behaviors. 61 The term “female athlete triad” has historically referred to (1) low energy availability that may or may not be related to disordered eating; (2) menstrual dysfunction; and (3) low bone mineral density (BMD) in physically active females. 62 – 65 Inadequate caloric intake in comparison to energy expenditure is the catalyst for endocrine changes and leads to decreased bone density and menstrual irregularities. Body weight may be stable. This energy imbalance may result from a lack of knowledge regarding nutritional needs in the athlete or from intentional intake restriction associated with disordered eating.
Hormonal disruption and low BMD can occur in undernourished male athletes as well. 66 Increased recognition of the role of energy deficiency in disrupting overall physiologic function in both male and female individuals led a 2014 International Olympic Committee consensus group to recommend replacing the term female athlete triad to the more inclusive term, “relative energy deficiency in sport.” 67 , 68 Athletes participating in sports involving endurance, weight requirements, or idealized body shapes may be at particular risk of relative energy deficiency in sport. Signs and symptoms of relative energy deficiency, such as amenorrhea, bradycardia, or stress fractures, may alert pediatricians to this condition.
Pediatricians are in a unique position to detect eating disorders early and interrupt their progression. Annual health supervision visits and preparticipation sports examinations offer opportunities to screen for eating disorders. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents , fourth edition, offers sample screening questions about eating patterns and body image. 69 Reported dieting, body image dissatisfaction, experiences of weight-based stigma, or changes in eating or exercise patterns invite further exploration. Positive responses on a standard review of symptoms may need further probing. For example, oligomenorrhea or amenorrhea (either primary or secondary) may indicate energy deficiency. 70 Serial weight and height measurements plotted on growth charts are invaluable. Weight loss or the failure to make expected weight gain may be more obvious when documented on a graph. Similarly, weight fluctuations or rapid weight gain may cue a health care provider to question binge eating or BN symptoms. Recognizing that many patients who present to eating disorder treatment programs have or previously had elevated weight according to criteria from the Centers for Disease Control and Prevention, 71 it is worthwhile to carefully inquire about eating and exercise patterns when weight loss is noted in any child or adolescent. Screening for unhealthy and extreme weight-control measures before praising desirable weight loss can avoid inadvertently reinforcing these practices.
A comprehensive assessment of a child or adolescent suspected of having an eating disorder includes a thorough medical, nutritional, and psychiatric history, followed by a detailed physical examination. A useful web resource for assessment is published in multiple languages by the Academy for Eating Disorders. 72 Relevant interview questions are listed in Table 2 . A collateral history from a parent may reveal abnormal eating-related behaviors that were denied or minimized by the child or adolescent.
Example Questions to Ask Adolescents With a Possible Eating Disorder
Adapted from Rome and Strandjord. 89 LMP, last menstrual period.
A full psychosocial assessment, including a home, education, activities, drugs/diet, sexuality, suicidality/depression (HEADSS) assessment is vital. This evaluation includes screening for physical or sexual abuse by using the principles of trauma-informed care and responding according to American Academy of Pediatrics guidance on suspected physical or sexual abuse or sexual assault 73 – 75 as well as state laws. Vital to the HEADSS assessment is an evaluation for symptoms of other potential psychiatric diagnoses, including suicidal thinking, which may have been unrecognized previously.
A comprehensive physical examination, including close attention to growth parameters and vital signs, allows the pediatrician to assess for signs of medical compromise and for signs and symptoms of eating disorder behaviors; findings may be subtle and, thus, overlooked without careful notice. For accuracy, weights are best obtained after the patient has voided and in an examination gown without shoes. Weight, height, and BMI can be evaluated by using appropriate growth charts. Low body temperature, resting blood pressure (BP), or resting heart rate (HR) for age may suggest energy restriction. Because a HR of 50 beats per minute or less is unusual even in college-aged athletes, 76 the finding of a low HR may be a sign of restrictive eating. Orthostatic vital signs (HR and BP, obtained after 5 minutes of supine rest and repeated after 3 minutes of standing) 77 , 78 revealing a systolic BP drop greater than 20 mm Hg, a diastolic BP drop greater than 10 mm Hg, or tachycardia may suggest volume depletion from restricted fluid intake or purging or a compromised cardiovascular system.
Pertinent physical findings in children and adolescents with eating disorders are summarized in Table 3 . A differential diagnosis for the signs and symptoms of an eating disorder is found in Table 4 , and selected medical complications of eating disorders are provided in Table 5 .
Notable Physical Examination Features in Children and Adolescents With Eating Disorders
Adapted from Rosen; American Academy of Pediatrics. 208
Selected Differential Diagnosis for Eating Disorders According to Presentation
Adapted from Rome and Strandjord 89 and Rosen; American Academy of Pediatrics. 208
Selected Medical Complications Resulting From Eating Disorders
Initial laboratory evaluation is performed to screen for medical complications of eating disorders or to rule out alternate diagnoses ( Tables 4 and 5 ). Typical initial laboratory testing includes a complete blood cell count; serum electrolytes, calcium, magnesium, phosphorus, and glucose; liver transaminases; urinalysis; and thyroid-stimulating hormone concentration. 72 Screening for specific vitamin and mineral deficiencies (eg, vitamin B 12 , vitamin D, iron, and zinc) may be indicated on the basis of the nutritional history of the patient. Laboratory investigations are often normal in patients with eating disorders; normal results do not exclude the presence of serious illness with an eating disorder or the need for hospitalization for medical stabilization. An electrocardiogram is important for those with significant weight loss, abnormal cardiovascular signs (such as orthostasis or bradycardia), or an electrolyte abnormality. A urine pregnancy test and serum gonadotropin and prolactin levels may be indicated for girls with amenorrhea; a serum estradiol concentration may serve as a baseline for reassessment during recovery. 79 Similarly, serum gonadotropin and testosterone levels can be useful to assess and monitor for central hypogonadism in boys with restrictive eating. Bone densitometry, by using dual radiograph absorptiometry analyzed with age-appropriate software, may be considered for those with amenorrhea for more than 6 to 12 months. 80 , 81 If there is uncertainty about the diagnosis, other studies including inflammatory markers, serological testing for celiac disease, serum cortisol concentrations, testing stool for parasites, or radiographic imaging of the brain or gastrointestinal tract may be considered. In the occasional patient, both an eating disorder and an organic illness, such as celiac disease, may be discovered. 82
Eating disorders can affect every organ system 83 , 84 with potentially serious medical complications that develop as a consequence of malnutrition, weight changes, or purging. Details of complications are described in reviews 85 – 89 and are summarized in Table 5 . Most medical complications resolve with weight normalization and/or resolution of purging. Complications of BED can include those of obesity; these are summarized in other reports and not reiterated here. 84 , 90
Psychological symptoms can be primary to the eating disorder, a feature of a comorbid psychiatric disorder, or secondary to starvation. Initial symptoms of depression and anxiety may abate with refeeding. 91 Rumination about body weight and size is a core feature of AN, whereas rumination about food decreases as starvation reverses. 92 Difficulty in emotion regulation occurs across the spectrum of eating disorders but is more severe in those who binge eat or purge. 93 Cognitive function studies in a large population-based sample of adolescents revealed eating disorder participants had deficits in executive functioning, including global processing and cognitive flexibility but performed better than control participants on measures of visual attention and vigilance. 94
Structural brain imaging studies to date have yielded inconsistent results, likely explained, at least in part, by methodologic differences and the need to control for many variables, including nutritional state, hydration, medication use, and comorbid illness. 95 A longitudinal study revealed that global cortical thinning in acutely ill adolescents and young adults with AN normalized with weight restoration over a period of approximately 3 months. 96
Common skin changes in underweight patients include lanugo, hair thinning, dry scaly skin, and yellow discoloration related to carotenemia. Brittle nails and angular cheilitis may also be observed. Acrocyanosis can be observed in underweight patients and may be a protective mechanism against heat loss. Abrasions and calluses over the knuckles can occur from cutting the skin on incisors while self-inducing emesis. 97
Patients with eating disorders experience higher rates of dental erosion and caries. This occurs more frequently in those who self-induce emesis but can also be observed in those who do not. 98 Normal dental findings do not preclude the possibility that purging is occurring. 99 Hypertrophy of the parotid and other salivary glands, accompanied by elevations in serum amylase concentrations with normal lipase concentrations, may be a clue to vomiting. 99 Xerostomia, from either salivary gland dysfunction or psychiatric medication side effect, can reduce the oral pH, which can lead to increased growth of cariogenic oral bacteria. 98 , 100
Reports of cardiac complications in eating disorders are focused predominantly on restrictive eating disorders. Common cardiovascular signs include low HR, orthostasis, and poor peripheral perfusion. Orthostatic intolerance symptoms (eg, lightheadedness) and vital sign findings may resemble those of postural orthostatic tachycardia syndrome 101 , 102 and may contribute to a delay in referral to appropriate care if eating disorder behaviors are not disclosed or appreciated.
Cardiac structural changes include decreased left ventricular (LV) mass, LV end diastolic and LV end systolic volumes, functional mitral valve prolapse, pericardial effusion, and myocardial fibrosis (noted in adults). 103 – 105 Electrocardiographic abnormalities, including sinus bradycardia, and lower amplitude LV forces are more common in AN than in nonrestrictive eating disorders. 106 One study reported a nearly 10% prevalence of prolonged (>440 milliseconds) QTc interval in hospitalized adolescents and young adults with a restrictive eating disorder. 107 Repolarization abnormalities, a potential precipitant to lethal arrhythmia, 108 may prompt clinicians to also consider other factors, such as medication use or electrolyte abnormalities, that may affect cardiac conduction. 107 , 109
Gastrointestinal complaints are common and sometimes precede the diagnosis of the eating disorder. Delayed gastric emptying and slow intestinal transit time often contribute to reported sensations of nausea, bloating, and postprandial fullness 110 and may be a presenting feature of restrictive eating. Constipation is a frequent experience for patients and multifactorial in etiology. 111 Esophageal mucosal damage from self-induced vomiting, including scratches, and bleeding secondary to Mallory-Weiss tears can occur. 99 Superior mesenteric artery syndrome may develop in the setting of severe weight loss. 111 Hepatic transaminase concentrations and coagulation times can be elevated as a consequence of malnutrition and, typically, normalize with appropriate nutrition. 110
Fluid and electrolyte abnormalities may occur as a result of purging or cachexia. 99 , 112 Dehydration can be present in any patient with an eating disorder. Disordered osmotic regulation can present in many patterns (central and renal diabetes insipidus, syndrome of inappropriate antidiuretic hormone). 112 Patients who vomit may have a hypokalemic, hypochloremic metabolic alkalosis resulting from loss of gastric hydrochloric acid, chronic dehydration, and the subsequent increase in aldosterone that promotes sodium reabsorption in exchange for potassium and acid at the distal tubule level. 113 Patients who abuse laxatives may experience a variety of electrolyte and acid-base derangements. 113 Dilutional hyponatremia can be observed in patients who intentionally water load to induce satiety or to misrepresent their weight at clinic visits. Abrupt cessation of laxative use may be associated with peripheral edema and, therefore, motivate further laxative 114 or diuretic misuse.
Restrictive eating disorders commonly cause endocrine dysfunction. 80 , 115 Euthyroid sick syndrome (low triiodothyronine, elevated reverse triiodothyronine, or normal or low thyroxine and thyroid-stimulating hormone) is the most common thyroid abnormality. 116 Functioning as an adaptive mechanism to starvation, supplemental thyroid hormone is not indicated when this pattern is noted. 116 Hypercortisolemia may be seen in AN. 81 , 116 Hypothalamic-pituitary-gonadal axis suppression may be attributable to weight loss, physical overactivity, or stress. Female individuals with AN may have amenorrhea, and male individuals can have small testicular volumes 117 and low testosterone concentrations. 118
Growth retardation, short stature, and pubertal delay may all be observed in prepubertal and peripubertal children and adolescents with eating disorders. 115 AN is associated with low levels of insulin-like growth factor-1 and growth hormone resistance. 119 Catch-up growth has been inconsistently reported in the literature; younger patients may have greater and more permanent effects on growth. 120 , 121 Adolescent boys may be at an even greater risk for height deficits than girls; because boys typically enter puberty later than girls and experience their peak growth at a later sexual maturity stage, they are less likely to have completed their growth if an eating disorder develops in the middle teenage years. 119
Low BMD is a frequent complication of eating disorders in both male and female patients 117 and is a risk in both AN and BN. 122 Low BMD is worrisome not only because of the increased risk of fractures in the short-term 123 but, also, because of the potential to irreversibly compromise skeletal health in adulthood. 124
The ultimate goals of care in eating disorders are that children and adolescents are nourished back to their full healthy weight and growth trajectory, that their eating patterns and behaviors are normalized, and that they establish a healthy relationship with food and their body weight, shape, and size as well as a healthy sense of self. Independent of a specific DSM diagnosis, treatment is focused on nutritional repletion and psychological therapy. Psychotropic medication can be a useful adjunct in select circumstances.
After diagnosing an eating disorder, the pediatrician arranges appropriate care. Patients who are medically unstable may require urgent referral to a hospital ( Table 6 ). Patients with mild nutritional, medical, and psychological dysfunction may be managed in the pediatrician’s office in collaboration with outpatient nutrition and mental health professionals with specific expertise in eating disorders. Because an early response to treatment may be associated with better outcomes, 125 , 126 timely referral to a specialized multidisciplinary team is preferred, when available. If resources do not exist locally, pediatricians may need to partner with health experts who are farther away for care. For patients who do not improve promptly with outpatient care, more intensive programming (eg, day-treatment programs or residential settings) may be indicated.
Indications Supporting Hospitalization in an Adolescent With an Eating Disorder
Reprinted with permission from the Society for Adolescent Health and Medicine. 85 ECG, electrocardiogram.
Often, an early task of the pediatrician is to identify a treatment goal weight. This goal weight may be determined in collaboration with a registered dietitian. Pediatricians who are planning to refer the patient to a specialized treatment team may opt to defer the task to the team. Acknowledging that body weights naturally fluctuate, the treatment goal weight is often expressed as a goal range. Individualized treatment goal weights are formulated on the basis of age, height, premorbid growth trajectory, pubertal stage, and menstrual history. 87 , 127 In a study of adolescent girls with AN, of those who resumed menses during treatment, this occurred, on average, at 95% of the treatment goal weight. 128 Health care providers may be pressured by patients, their patients’ parents, or other health care providers to target a treatment goal weight that is lower than the previous growth trajectory or other clinical indicators would suggest is appropriate. If a treatment goal weight is inappropriately low, there is an inherent risk of offering only partial weight restoration and insufficient treatment. 129 The treatment goal weight is reassessed at regular intervals (eg, every 3–6 months) to account for changes in physical growth and development (in particular, age, height, and sexual maturity). 87 , 127
An important role for the pediatrician is to offer guidance regarding eating and to manage the physical aspects of the illnesses. For all classifications of eating disorders, reestablishing regular eating patterns is a fundamental early step. Meals and snacks are reintroduced or improved in a stepwise manner, with 3 meals and frequent snacks per day. Giving the message that “food is the medicine that is required for recovery” and promoting adherence to taking that medicine at scheduled intervals often helps patients and families get on track. 130 A multivitamin with minerals can help ensure that deficits in micronutrients are addressed. To optimize bone health, calcium and vitamin D supplements can be dosed to target recommended daily amounts (elemental calcium: 1000 mg for patients 4–8 years of age, or 1300 mg for patients 9–18 years of age; vitamin D: 600 IU for patients 4–18 years of age). 87 , 131 Patients can be reassured that the bloating discomfort caused by slow gastric emptying improves with regular eating. When constipation is troubling, nutritional strategies, including weight restoration, are the treatments of choice. 111 When these interventions are inadequate to alleviate constipation, osmotic (eg, polyethylene glycol 3350) or bulk-forming laxatives are preferred over stimulant laxatives. The use of nonstimulant laxatives decreases the risks of electrolyte derangement and avoids the potential hazard of “cathartic colon syndrome” that may be associated with abuse of stimulant cathartics (senna, cascara, bisacodyl, phenolphthalein, anthraquinones). 99 , 114
To optimize dental outcomes, patients can be encouraged to disclose their illness to their dentist. Current dental hygiene recommendations for patients who vomit include the use of topical fluoride, applied in the dental office or home, or use of a prescription fluoride (5000 ppm) toothpaste. Because brushing teeth immediately after vomiting may accelerate enamel erosion, patients can be advised to instead rinse with water, followed by using a sodium fluoride rinse whenever possible. 132
Collaborative Outpatient Care
Most patients with AN are treated in outpatient settings. 85 , 133 Pediatricians play an important role in the medical management and coordination of the treatment of these patients. The pediatrician plays a primary role in assessing for and managing acute and long-term medical complications, monitoring treatment progress, and coordinating care with nutritional and mental health colleagues. 85 , 130 , 134 Although some primary care pediatricians feel comfortable coordinating care, others choose to refer patients to providers with expertise in pediatric eating disorders. Ideally, all members of the treatment team are sensitive to the unique developmental needs of children and adolescents. 133
Educating young people and their parents about the physiologic and psychological effects of food restriction is an early component of care. Parents are empowered to feed their children regularly (typically 3 meals and 2–3 snacks per day) and adjust portion size and energy richness based on weight progress. Many parents are amazed to discover the amount of energy (3500 kcal or more) that may be required to restore weight for their children. Detailed tracking of caloric intake is not necessary. Serving foods with high caloric density and ensuring that beverages are energy rich (eg, choosing fruit juice or milk instead of water) are effective strategies to maximize energy intake without requiring large increases in volume. Parents can relieve adolescents of having to decide on appropriate serving sizes by plating meals for them. Accommodating special diets, such as vegetarian or vegan, can make meeting nutritional goals especially challenging. Reintroducing foods that have been avoided or that induce fear of weight gain are essential steps on the path to recovery.
Family-Based Treatment and Parent-Focused Therapy
Over the past 2 decades, a specialized eating disorder–focused, family-based intervention, commonly referred to as family-based treatment (FBT), has emerged as the leading first-line treatment approach for pediatric eating disorders. 135 Effectiveness is well established for AN. 133 , 136 Rather than dwelling on possible causes of the eating disorder, FBT is focused on recovery from the disease. FBT consists of 3 phases and contends that parents are not to blame for their child’s illness, eating disorders are not caused by dysfunctional families, and parents play an essential role in recovery. 136 During appointments, the entire family unit meets with the therapist. In phase 1, weight restoration is the primary goal. Parents, supported by the therapist, take responsibility to ensure that their child eats sufficiently and limit pathologic weight-control behaviors. Parents are encouraged to take responsibility for meal planning and preparation. Pediatricians can be helpful by reminding parents of the importance of fighting the disease effectively in the early stages, with the goals of reaching a truly healthy weight, resuming pubertal development, reversing medical complications, and restoring normal cognitions. Early weight gain (4–5 pounds by session 4, typically correlating with 4 weeks of treatment) is predictive of better outcomes in adolescents. 126 , 137 , 138 By phase 2, substantial weight recovery has occurred, and the adolescent gradually resumes responsibility for his or her own eating. By phase 3, weight has been restored, and the therapy shifts to address general issues of adolescent psychosocial development. 136 This therapy is detailed in manuals for providers 137 and families. 139 FBT with experienced providers is not available in all communities. Nevertheless, community providers may integrate the essential principles of FBT in their work with patients and families. 130
Parent-focused therapy is an adaptation of FBT wherein the therapist supports the parents to renourish the patient and limit weight-control behaviors but, after the initial appointment, meets only with the parents. 140 The patient has brief visits with a nurse or physician for the assessment of weight and acute mental health issues but is not directly involved with a therapist.
The role pediatricians serve in the care of an adolescent in FBT differs from the customary role of a physician with patients. 134 In the FBT setting, the pediatrician does not weigh the patient because that task is performed by the therapist. The pediatrician directs the care only when there are immediate medical safety concerns. If the pediatrician identifies an urgent medical issue that requires intervention or hospitalization, he or she is obligated to provide recommendations to the patient, the parents, and the primary therapist. For the medically stable patient, the pediatrician acts as a consultant to the parents and primary therapist. When a parent asks a question related to treatment, instead of directly advising the parents what to do, the pediatrician, ideally, redirects that treatment decision back to the parent: “You know your child the best. What do you think will best help in your child’s recovery?” In this way, the physician empowers parents to make their own decisions, enhancing their confidence to care for their ill child.
Day-Treatment Programs
Day-treatment programs (day hospitalization and partial hospitalization) provide an intermediate level of care for patients with eating disorders who are medically stable and do not require 24-hour supervision but need more than outpatient care. 133 , 141 These programs may prevent the need for higher levels of care or may be a “step-down” from inpatient or residential to outpatient care. Day treatment typically involves 8 to 10 hours per day of care (including meals, therapy, groups, and other activities) by a multidisciplinary staff 5 days per week. Reported evaluations of child and adolescent day-treatment programs are few and observational in design. 142 – 145 Despite the absence of systematic data supporting their usefulness, these programs are generally believed to have an important role in the continuum of care.
Residential Treatment
Residential treatment may be necessary for a minority of medically stable patients with eating disorders. Indications for residential treatment include a poor motivation for recovery, need for structure and supervision to prevent unhealthy behaviors (eg, food restriction, compulsive exercise), lack of a supportive family environment, absence of outpatient treatment in the patient’s locale, 146 or outpatient interventions having been unsuccessful. 133 Residential treatment typically includes 24 hour per day supervision, medical oversight, group-based psychoeducational therapy, nutritional counseling, individual therapy, and family therapy. The length of stay can be weeks to months, depending on the severity of illness and financial resources. Outcome studies reported by residential programs, generally, reveal improved symptomatology at discharge, 147 but the results at long-term follow-up are mixed. 148 , 149 However, few outcome studies are focused on adolescents, compare the efficacy of residential to outpatient treatment, or make comparisons across programs or treatment modalities.
Although some adolescents require this higher level of care, health care providers and families are encouraged to exercise caution when selecting a residential treatment program. The number of residential programs has more than tripled in the last decade, with many operated by for-profit companies. Marketing practices by some are questionable. 150 Outcome studies demonstrating program efficacy may be misleading because of a lack of rigorous design or peer review. 151 Until recently, there was no certification process to ensure program quality and safety. In 2016, The Joint Commission implemented new accreditation standards for behavioral health care organizations that provide outpatient or residential eating disorder treatment. 152 It remains to be seen how many programs will pursue this accreditation.
The National Eating Disorders Association Web site offers useful suggestions for evaluating treatment programs ( www.nationaleatingdisorders.org ).
Hospital-Based Stabilization
Suggested indications for the hospitalization of children and adolescents with eating disorders published by the Society for Adolescent Health and Medicine are listed in Table 6 .
The most common goal for hospital-based stabilization is nutritional restoration. Variation occurs with regard to how quickly hospitalized patients with AN are refed. 153 , 154 It is important to balance 2 competing goals: achieve weight gain swiftly and avoid refeeding syndrome. 155 Refeeding syndrome refers to the metabolic and clinical changes that occasionally occur when a malnourished patient is aggressively nutritionally rehabilitated; the hallmarks are hypophosphatemia and multiorgan dysfunction. 155 – 157 A systematic review of hospitalized adolescents with AN reported an average incidence of refeeding hypophosphatemia (without necessarily organ dysfunction) of 14%. 158 Over the past decade, a long followed maxim, “start low and go slow,” has been challenged. 87 , 155 Several centers have described starting calories at 1400 kcal or more per day, 154 including recent reports demonstrating safe treatment of mildly and moderately malnourished adolescents by using initial caloric prescriptions of 2200 to 2600 kcal per day, while achieving a weight gain of approximately 3 to 4.5 pounds per week. 159 , 160 Because the risk of refeeding hypophosphatemia may correlate with the degree of starvation, pediatricians may opt to take a more cautious approach in severely malnourished (<70% median BMI) children until further studies are reported. 87 , 154
Nasogastric tube (NGT) feeding may be necessary for some hospitalized adolescents, but opinions vary regarding when they should be initiated. 161 Most North American programs reserve NGT feeds for when patients are not able to complete meals; however, internationally, some centers report the routine use of NGT feeding, either exclusively at first or in combination with meals. 162 , 163 Potential benefits of NGT feeding include faster weight gain and medical stabilization, with a possibility for a reduced hospital length of stay. 162 , 163 Although viewed by some health care providers as invasive or punitive, others view NGT feeding as empathic, by reducing both physical and psychological pain in the early treatment stages. 161 There is insufficient evidence to recommend one approach over another. 154 Independent of whether NGT feeds are used routinely, physicians involved in the treatment of hospitalized medically unstable patients may be called on to provide nutrition via an NGT when nutritional needs are not being met. The use of total parenteral nutrition carries higher risks of medical complications, is costly, and is not recommended unless other forms of refeeding are not possible. 154
High-quality studies in which researchers examine the impact of inpatient care are limited, and the best end point for hospital treatment of children and adolescents is unclear. A US multicenter research collaborative showed that, in a national cohort of low-weight 9- to 21-year-olds with restrictive eating disorders, those who were hospitalized had a greater odds of being at 90% of the median BMI at 1-year follow-up. 164 However, a randomized controlled trial (RCT) of treatment of adolescent AN in the United Kingdom revealed no benefits of inpatient over outpatient care 165 ; this study was limited by poor adherence to the allocated treatment. An RCT in Germany in 2014 revealed that inpatient adolescents discharged earlier to outpatient treatment fared as well as those discharged later. 141 Similarly, an RCT conducted in Australia in 2015 revealed that adolescents who were discharged to FBT as soon as they were medically stable fared at least as well as adolescents who remained inpatients until achieving 90% of their treatment goal weight. 166 The recently reported average length of stay in the United States for patients admitted for medical stabilization by using higher caloric prescriptions was 3 to 12 days. 159 , 167 , 168
Pharmacotherapy for AN
A variety of medications have been studied for the treatment of AN, primarily in adults, but none have been approved for this indication by the US Food and Drug Administration (FDA). 169 Despite their demonstrated ineffectiveness, 170 more than one-half of adolescents with restrictive eating disorders are prescribed psychotropic medications, most likely in attempts to treat comorbid conditions, such as depression and anxiety. 171 Selective serotonin-reuptake inhibitors (SSRIs) have been tried but are not effective in acutely ill, malnourished patients and have not been shown to prevent disease relapse in those who are weight restored. 172 – 174 A number of atypical antipsychotic medications have also been studied, including quetiapine, risperidone, and olanzapine. Results have generally revealed little benefit in weight gain or improvement in eating-disorder thinking. 169 , 175 – 178 Initial studies of augmentation of SSRIs with atypical antipsychotics in adult patients have been promising. 179
The current recommendations to optimize bone health are full weight restoration with physiologic resumption of menses and supplementation with calcium and vitamin D. 79 , 81 , 87 , 115 Bisphosphonate treatment is not recommended. 79 , 87 , 115 Estrogen supplementation in the form of combined estrogen-progesterone oral contraceptive pills is not effective in enhancing BMD in adolescents with AN. 81 Small trials with transdermal estrogen 180 or with low-dose combined oral contraceptive pills plus dehydroepiandrosterone 181 have shown a positive effect on BMD compared with controls, but further studies are needed before these are considered standard care. Although cyclic vaginal bleeding may be induced with the use of exogenous hormones, this may reinforce a patient’s denial of the medical consequences of her disease and masks the spontaneous return of menses.
Most patients with BN and BED are managed in outpatient settings with the collaboration of a medical and mental health care providers as well as a dietitian, as needed.
Psychological treatment studies are more limited in BN compared with AN and are especially lacking in BED. 133 Cognitive behavioral therapy (CBT) has a modest evidence-base for BN and BED. 133 , 182 CBT explicitly recognizes the interrelationships among an individual’s thoughts, feelings, and actions, and its principles can be used by all disciplines. Reestablishing regular eating patterns is a central goal, and educating patients about the perpetuating nature of the restriction-binge-purge cycle is an early focus. Patients with BN and BED can minimize the urge to binge that is typically experienced late in the day, if they eat regularly throughout the day. Decreasing the binge amount and frequency may decrease guilt and shame and the ensuing negative self-assessment. During CBT, patients are taught to question their distorted thoughts and remodel their eating behaviors. 182
Although there is a manual to guide FBT for patients with BN, 183 it is based on more limited evidence than FBT for AN. 182 An RCT comparing FBT with CBT revealed patients in the FBT group were more likely to abstain from binge eating and purging at the end of the 18-week treatment (39% vs 20%) with no statistical difference (49% vs 32%) at 1-year follow-up. 184 There are no published studies in which researchers examine FBT for BED.
Pharmacotherapy for BN
As with other pharmacotherapy research, studies of treatment of BN have primarily been in adult subjects. Several pharmacologic agents, including SSRIs, have been demonstrated to be effective for the treatment of adult BN, although only fluoxetine has FDA approval. Although not approved for pediatric BN, fluoxetine is FDA approved for child and adolescent depression and obsessive-compulsive disorder, so it is a reasonable option if pharmacologic treatment of BN is considered. 169 The antiepileptic topiramate has been shown to significantly decrease binge eating in adults who do not respond to or are not able to tolerate SSRIs. However, cases of topiramate triggering eating disorder symptoms in adolescents have been reported. 185 Other drugs, including naltrexone and ondansetron, are being used with some success in adult BN, although data are lacking to recommend their use more broadly. 169
Pharmacotherapy for BED
Research on the treatment of binge eating lags behind that for other eating disorders and has been focused on adult subjects. SSRIs have rarely differed from placebo in their effect on BED and show no better outcome than behavioral therapy alone. Although the use of topiramate has been shown to reduce binge eating and help with weight loss, the rates of adverse effects are relatively high. 186 Lisdexamfetamine, a central nervous system stimulant approved for treatment of attention-deficit/hyperactivity disorder, was approved by the FDA in 2015 for the treatment of moderate to severe BED in adults. Although it has been demonstrated to reduce the frequency of binge-eating episodes, lisdexamfetamine is not indicated for weight loss. As with the use of other central nervous system stimulants, there is a potential for abuse and dependence as well as serious cardiovascular reactions. 187
ARFID is a relatively new diagnosis, and, consequently, there is limited literature describing treatment. 188 , 189 Because patients with ARFID vary in terms of underlying psychological motivations for restrictive eating, individualized behavioral treatment strategies are needed. 182 , 190 Despite varying characteristics of the disorder, the dual goals of refeeding and normalization of eating align with the goals of treating other eating disorders. A study of pediatric and young adult patients admitted with ARFID at a single academic medical center reported that ARFID patients were more likely to require enteral nutrition and stayed in the hospital longer than patients with AN. 9
No medication is specifically indicated for use in ARFID; pharmacotherapy is directed at treating underlying comorbid illness (eg, anxiety) as necessary.
The treatment of eating disorders is multidisciplinary, often long-term, and may require expensive, high-level care, such as inpatient stabilization or residential or partial hospitalization programs. The costs associated with treatment can create substantial financial burdens for families. 191 Having medical insurance, public or private, is no guarantee that these costs will be covered. 192 Insurance carriers are able to define their own criteria for eating disorder treatment, leading to wide variations in coverage from state to state. Some states do not identify eating disorders as life-threatening conditions, thereby limiting treatment coverage. State-sponsored public insurance plans may not cover out-of-state treatment programs, even when no comparable treatment programs exist within that state. Outpatient mental health providers who are willing to accept the lower payments from public insurance may have no expertise in treating eating disorders. Those who do and will see publicly insured patients or those in managed care plans typically limit the number of these patients in their panels. Private insurance may increase access to treatment but dictate lower levels and shorter periods of care than is indicated by a patient’s clinical status and health care provider recommendation. Families of patients with eating disorders typically will need assistance navigating the financial aspects of treatment. The National Eating Disorders Association offers general information online for families regarding financial coverage for treatment ( www.nationaleatingdisorders.org ).
The prognoses reported for adolescents with eating disorders vary widely, depending on research methodology, definitions of recovery, and duration of follow-up. Generally, adolescents have greater success in recovery from eating disorders than their adult counterparts, 193 with overall recovery rates of approximately 70%. 194
In a review of 11 adolescent eating disorder treatment programs, 54% of patients treated for restrictive disorders had restored to at least 90% of their median body weight (MBW) for age and height at 1-year follow-up. This is essential for catch-up growth and resumption of menses in girls. Two significant predictors of weight recovery were a higher percentage of MBW at initial presentation and shorter duration of symptoms, highlighting the importance of early identification of these disorders. Outcomes did not vary meaningfully across programs, suggesting that all treatment models were helpful. 195
In a more-recent study, researchers examined the weight restoration of patients from 14 adolescent treatment programs with a diagnosis of a restrictive eating disorder by DSM-5 criteria. At 1-year follow-up, those with ARFID were the least likely (43%) to have regained ≥90% MBW and were also more likely to be younger, have had a longer duration of symptoms, and have left treatment prematurely. Eighty-two percent of those with atypical AN and 64% of those with AN had regained ≥90% MBW. Having received a higher level of care (eg, partial hospitalization and/or residential care) did not increase the likelihood of weight recovery. Again, there were no significant differences in outcomes between programs, despite various treatment modalities. 196
Information on the long-term prognosis of adolescents with AN is limited. In a study of adolescents who completed a 12-month outpatient AN treatment study (either FBT or adolescent-focused therapy), approximately one-third of patients were in full remission 1 year after completion, with better rates in the FBT group (49%) than in the adolescent-focused therapy group (23%). 197 Follow-up in a convenience sample of the original study 2 to 4 years after treatment revealed less than 10% of patients relapsed, with no difference between the 2 groups. 198 An RCT comparing parent-focused therapy with FBT demonstrated equivalent outcomes between the groups at 12-month follow-up (37% vs 29%). 140
Information about recovery from BN, BED, and purging disorder in adolescents is less available but suggests higher rates of relapse and the development of comorbidities. Outcome studies on BN in adults reveal variable recovery rates, ranging from approximately 50% to 70% at 4- to 6-year follow-up, with relapse rates of 30% and about 25% having chronic disease. 194 A longitudinal study of adolescent girls with BED and purging disorders into early adulthood revealed that one-quarter of these girls started to use drugs other than marijuana, more than one-third began to binge drink frequently, and 27% demonstrated high levels of depressive symptoms. 199 Not surprisingly, misuse of drugs and alcohol among patients with eating disorders is associated with a poorer outcome or death. 193
Mortality rates among individuals with eating disorders are substantially elevated in comparison with those of the general population, with death typically occurring in adulthood. Premature death is 4 to 5 times higher for patients with AN and 2 to 3 times as high for those with BN. 200 – 203 Suicide rates are increased among patients with eating disorders 204 and, in one study, accounted for 30% deaths. 203 In a national survey of adolescents, 35% of those meeting criteria for BN, 15% of those meeting criteria for BED, and 8% of those meeting criteria for AN reported having made a suicide attempt. 205 The risk of suicide among patients with eating disorders appears to be declining and has been attributed to an increased recognition of eating disorders and effective treatment. 206
Efforts to prevent eating disorders may occur in clinical practice and community settings. By using sensitive, nonstigmatizing language and demonstrating supportive attitudes toward children and adolescents of all body shapes and sizes, pediatricians create a welcoming clinical setting for discussions about weight and weight-related behaviors. The American Academy of Pediatrics clinical report “Preventing Obesity and Eating Disorders in Adolescents” highlights steps that pediatricians can take to prevent both conditions. 207 These steps include focusing on healthy habits with patients and families rather than weight and dieting, encouraging more frequent family meals, discouraging “weight talk” and “weight teasing” in the home, closely monitoring weight loss in patients advised to lose weight, and promoting a healthy body image in all children and adolescents. 207 Pediatricians may also advise teachers, coaches, and athletic trainers about healthy approaches to nutrition and exercise, raise awareness of the detrimental effects of weight stigmatization, and alert them to the warning signs of eating disorders.
Pediatricians can join others in advocating for improved access to quality eating disorder treatment services. The limited availability of developmentally appropriate mental health services, lack of mental health parity, and service “carve-outs” all have been barriers to patients and families who seek necessary treatment and seem to be disproportionately problematic for patients with eating disorders. Despite evidence of its effectiveness, FBT is not available in many communities. Through advocacy, pediatricians can help support health care reform efforts that will enable children and adolescents with eating disorders to access necessary care.
Pediatricians should be knowledgeable about the variety of risk factors and early signs and symptoms of eating disorders in both male and female children and adolescents. Pediatricians should screen patients for disordered eating and unhealthy weight-control behaviors at annual health supervision visits. Pediatricians should evaluate weight, height, and BMI by using age- and sex-appropriate charts, assess menstrual status in girls, and recognize the changes in vital signs that may signal the presence of an eating disorder.
When an eating disorder is suspected, pediatricians, in conjunction with appropriate consultants, should initiate a comprehensive evaluation of the patient that includes both medical and psychological assessments as well as suicide risk appraisal. Once diagnosed, patients should be monitored for medical and nutritional complications by their pediatrician or referred to other qualified practitioners for medical oversight.
To facilitate multidisciplinary care, pediatricians should refer their patients with eating disorders to treatment resources in their region when available. Ideally, these treatment program providers should have expertise in the unique developmental needs of this age group.
Pediatricians are encouraged to advocate for legislation and policy changes that ensure appropriate services for patients with eating disorders, including medical care, nutritional intervention, mental health treatment, and care coordination, in settings that are appropriate for the developmental level of the patient and severity of the illness.
Clinical reports from the American Academy of Pediatrics benefit from expertise and resources of liaisons and internal (AAP) and external reviewers. However, clinical reports from the American Academy of Pediatrics may not reflect the views of the liaisons or the organizations or government agencies that they represent.
The guidance in this report does not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate.
All clinical reports from the American Academy of Pediatrics automatically expire 5 years after publication unless reaffirmed, revised, or retired at or before that time.
Drs Hornberger and Lane were equally responsible for conceptualizing, writing, and revising the manuscript and considering input from all reviewers and the board of directors; and all authors approve the final manuscript as submitted.
This document is copyrighted and is property of the American Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American Academy of Pediatrics. Any conflicts have been resolved through a process approved by the Board of Directors. The American Academy of Pediatrics has neither solicited nor accepted any commercial involvement in the development of the content of this publication.
FUNDING: No external funding.
anorexia nervosa
avoidant/restrictive food intake disorder
binge-eating disorder
bone mineral density
bulimia nervosa
blood pressure
cognitive behavioral therapy
Diagnostic and Statistical Manual of Mental Disorders Fifth Edition
family-based treatment
Food and Drug Administration
home, activities, drugs/diet, sexuality, suicidality/depression
left ventricular
median body weight
nasogastric tube
randomized controlled trial
selective serotonin-reuptake inhibitor
Laurie L. Hornberger, MD, MPH
Margo A. Lane, MD, FRCPC
Cora C. Breuner, MD, MPH, Chairperson
Elizabeth M. Alderman, MD, FSAHM
Laura K. Grubb, MD, MPH
Makia Powers, MD, MPH
Krishna Kumari Upadhya, MD
Stephenie B. Wallace, MD
Laurie L. Hornberger, MD, MPH – Section on Adolescent Health
Margo A. Lane, MD FRCPC – Canadian Pediatric Society
Meredith Loveless, MD – American College of Obstetricians and Gynecologists
Seema Menon, MD – North American Society of Pediatric and Adolescent Gynecology
Lauren Zapata, PhD, MSPH – Centers for Disease Control and Prevention
Liwei Hua, MD, PhD – American Academy of Child and Adolescent Psychiatry
Karen Smith
James Baumberger, MPP
Competing Interests
Advertising Disclaimer »
Citing articles via
Email alerts.

Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Share full article
Advertisement
Supported by
Adolescence
Eating Disorders in Teens Have ‘Exploded’ in the Pandemic
Here’s what parents need to know.

By Lisa Damour
As a psychologist who cares for adolescents I am well aware of the prevalence of eating disorders among teenagers . Even still, I am stunned by how much worse the situation has become in the pandemic.
According to the psychologist Erin Accurso, the clinical director of the eating disorders program at the University of California, San Francisco, “our inpatient unit has exploded in the past year,” taking in more than twice as many adolescent patients as it did before the pandemic. Dr. Accurso explained that outpatient services are similarly overwhelmed: “Providers aren’t taking new clients, or have wait-lists up to six months.”
The demand for eating disorder treatment “is way outstretching the capacity to address it,” said the epidemiologist S. Bryn Austin, a professor at the T.H. Chan School of Public Health and research scientist in the Division of Adolescent and Young Adult Medicine at Boston Children’s Hospital. “I’m hearing this from colleagues all across the country.” Even hotlines are swamped. The National Eating Disorders Association helpline has had a 40 percent jump in overall call volume since March 2020. Among callers who shared their age over the last year, 35 percent were 13 to 17 years old, up from 30 percent in the year before the pandemic.
What has changed in the pandemic?
There are several possible explanations for this tsunami of eating concerns in teenagers. When adolescents lost the familiar rhythm of the school day and were distanced from the support of their friends, “many of the things that structured a teenager’s life evaporated in one fell swoop,” said Dr. Walter Kaye, a psychiatrist and the founder and executive director of the eating disorders program at the University of California, San Diego. “People who end up with eating disorders tend to be anxious and stress sensitive — they don’t do well with uncertainty.”
Further, eating disorders have long been linked with high achievement . Driven adolescents who might have normally poured their energy into their academic, athletic or extracurricular pursuits suddenly had too much time on their hands. “Some kids turned their attention toward physical health or appearance as a way to cope with anxiety or feel productive,” Dr. Accurso said. “Their goals around ‘healthy’ eating or getting ‘in shape’ got out of hand” and quickly caused significant weight loss.
For some, an increase in emotional eating in the pandemic has been part of the problem. Attending school from a home where food is constantly available may lead some young people to eat more than usual as a way to manage pandemic-related boredom or stress . “Being at school presents a barrier to using food as a coping mechanism; at home, we don’t have that barrier,” noted Kelly Bhatnagar, psychologist and co-founder of the Center for Emotional Wellness in Beachwood, Ohio, a practice specializing in the treatment of eating disorders.
In many households the pandemic has heightened food insecurity and its attendant anxieties, which can increase the risk of eating disorders. Research shows that, compared to teenagers whose families have enough food, those in homes where food is scarce are more likely to fast, to skip meals, and to abuse laxatives and diuretics with the aim of controlling their weight.
The Instagram influence
What teens see on their screens is also a factor. During the pandemic, teenagers have spent more time than usual on social media . While that can be a source of much needed connection and comfort , scrutinizing images of peers and influencers on highly visual social media has been implicated in body dissatisfaction and disordered eating . Dr. Austin noted that teenagers can be prone to comparing their own bodies to the images they see online. “That comparison creates a downward spiral in terms of body image and self-esteem. It makes them more likely to adopt unhealthy weight control behaviors.”
When adolescents take an interest in managing their weight, they often go looking for guidance online. Indeed, a new Common Sense Media survey found that among teenagers who sought health information online between September and November of 2020, searches on fitness and exercise information came second only to searches for content related to Covid-19 — and ahead of searches on anxiety, stress and depression.
What young people find when they go looking for fitness information can be highly problematic. They are likely to come across harmful “thinspiration” and “fitspiration” posts celebrating slim or sculpted bodies, or even sites that encourage eating disordered behavior . Worse, algorithms record online search information and are “deliberately designed to feed harmful weight loss content to users who are already struggling with body image,” such as advertisements for dangerous diet supplements, Dr. Austin said.
When to worry
With so many forces contributing to teenagers’ body dissatisfaction and eating disordered behavior, how do parents know when to worry?
Parents should be alarmed, Dr. Kaye said, “if your child suddenly loses 10 to 20 pounds, becomes secretive about eating, or if you are seeing food disappear,” as becoming furtive about what, how and when one eats is a common occurrence in anorexia, bulimia and other eating disorders.
Experts agree that adults should be on the lookout for behaviors that veer from previous norms, such as suddenly skipping family meals or refusing to eat food from entire categories, such as carbohydrates or processed foods. Worth concern, too, is the teenager who develops fixations such as carefully counting calories, exercising obsessively or hoarding food, which may be a sign of a binge eating disorder. Parents should also pay close attention, said Dr. Accurso, if adolescents express a lot of guilt or anxiety around food or eating, or feel unhappy or uncomfortable with their bodies.
According to Dr. Bhatnagar, the view of eating disorders as a “white girls’ illness” can keep teens who are not white girls from seeking help or being properly screened for eating disorders by health professionals, even though eating disorders regularly occur across both sexes and all ethnic groups .
“Boys are having the same troubles,” said Dr. Bhatnagar, “but heterosexual boys may talk about body image a little differently. They tend to talk in terms of getting fit, getting lean or being muscular.”
Dr. Austin also noted that it is common to see elevated rates of eating disorders in lesbian, gay and bisexual youth of all genders as well as transgender and gender diverse young people.
“Eating disorders,” Dr. Accurso said, “don’t discriminate.”
How to help
Research shows that early identification and intervention play a key role in the successful treatment of eating disorders. Accordingly, parents who have questions about their teen’s relationship with eating, weight or exercise should not hesitate to seek an evaluation from their pediatrician or family health provider. Trustworthy eating disorder information, screening tools and support can also be found online. And when necessary, online resources can provide guidance and support to those on treatment waiting lists. “It may not be ideal for many,” Dr. Kaye said, “but it’s the reality of the situation we’re in.”
Parents can also take steps to reduce the likelihood that an eating disorder will take hold in the first place. Experts encourage adults to model a balanced approach to eating and to create enjoyable opportunities for being physically active while steering clear of negative comments about their teenager’s body or their own. Parents should also openly address the dangers of a ubiquitous diet culture that emphasizes appearance over well-being, creates stigma and shame around weight and links body size to character and worth. As Dr. Accurso noted, “We are not defined by a number on a scale.”
Where to find help
The National Eating Disorders Association , or NEDA, is a good starting place. It supports individuals and families affected by eating disorders.
F.E.A.S.T. is an international nonprofit organization run by caregivers of those suffering from eating disorders, meant to help others.
Maudsley Parents was created by parents who helped their children recover with family-based treatment , to offer hope and help to other families confronting eating disorders.
The Academy for Eating Disorders offers many resources, as do the Eating Disorders Center for Treatment and Research at University of California, San Diego, and the Eating Disorders Program at Boston Children’s Hospital.
Lisa Damour is a psychologist and the author of the New York Times best sellers “Untangled” and “Under Pressure.” Dr. Damour also co-hosts the podcast “Ask Lisa: The Psychology of Parenting.” More about Lisa Damour
How to Communicate Better With the Teens in Your Life
Simple strategies can go a long way toward building a stronger, more open relationship..
Active listening is an essential skill when seeking to engage any family member in conversation — teens included. Here is how to get better at it .
There are many reasons why a teen might not be opening up to you. These are the most common explanations for their silence .
Is your kid dismissing your solutions to their problems as irritating or irrelevant? It is usually because they’re not looking for you solve their problems.
Developing a healthy relationship with social media can be tricky. Here is how to talk to teens about it .
If your teen is surly or standoffish, these strategies can help you reconnect .
Are you worried that your kid might be struggling with his or her mental health? Understand the warning signs and make sure to approach the issue with the utmost sensitivity.
Essay on Eating Disorders in Adolescents
Essay on eating disorders: introduction, types of eating or feeding disorders in adolescents, causes and risk factors of eating disorders in adolescents, treating eating disorders, conclusion of eating disorders essay.
There are various types of feeding or eating disorders that affect adolescents. The prevalence rate of eating or feeding disorders depends on the different types and various risk factors. Young people have issues with their body weight and image, thus often suffer from eating disorders because they have a preference for certain food types. Eating or feeding disorders have numerous associated problems that require early treatment as soon as they are diagnosed.
There are four types of eating disorders diagnosed among adolescents. Studies have established that various factors cause and predispose adolescents to the various types of eating disorders.
These causes belong to three categories, namely biological, environmental and psychological. Eating disorders are treated according to their type and symptoms. Effective treatment requires one to have a plan that will help to monitor the disappearance of various symptoms and their body weight.
A feeding or eating disorder is defined as a physical, medical or psychological condition in an individual that makes them unable to consume certain types of food (Hornbacher, 2009). They influence an individual’s emotions and behavior towards certain food groups.
There are various types of feeding or eating disorders that affect adolescents. Studies have established that the number of young adults suffering from eating disorders has been rising over the last couple of years. The prevalence rate of eating or feeding disorders depends on the different types and various risk factors. This group of people consists of people between the onset of puberty and maturity (Lock & Grange, 2005).
This illness is common among adolescents who diet and have low self esteem due to negative perceptions of their body images. According to experts, young people have issues with their body weight and image, thus often suffer from eating disorders because they have a preference for certain food types. Eating disorders have various causes, risk factors, symptoms, treatment options, and associated myths (Hornbacher, 2009).
According to experts, eating or feeding disorders have numerous associated problems that require early treatment as soon as they are diagnosed. Eating disorders that are left untreated have serious consequences.
According to nutritionists, people should have regular checkups for any disorders, especially when they start noticing body changes anytime they eat a certain type of food (Hornbacher, 2009). In addition, friends and family members should provide moral support to someone diagnosed with an eating disorder in order to aid their effective recovery.
According to experts, there are four types of eating disorders diagnosed among adolescents, namely anorexia, bulimia, binge and other specified feeding disorder (Lock & Grange, 2005). Anorexia refers to a prolonged disorder of eating due to loss of appetite.
This disorder affects adolescents who limit themselves to certain groups of foods for fear of being overweight (Hornbacher, 2009). This disorder is common among adolescents because at this stage people are very conscious about various developments in their body and the impacts they have on their image.
Some symptoms of this disorder include skipping of meals, prioritizing of exercise, making up excuses for not eating, watching ones diet, and avoiding eating food they prepare for others. Other notable red flags include obsession with nutrition shows, avoiding certain types of food, checking one’s weight regularly, and drinking a lot of water among others (Hornbacher, 2009).
The second disorder is bulimia. It refers to an eating disorder common among adolescent who engage in excessive eating, which is followed by acts of clearing their bodies from any form of stigma. This disorder is characterized by people eating a lot of food, which is followed by doing too much exercise to avoid gaining weight (Hornbacher, 2009).
Symptoms of this disorder include one using the bathroom during or after a meal, eating too much food, regular dieting, secretive disposal of used food wrappers, lack of control over the amount of food to eat and forceful vomiting (Hornbacher, 2009).
The third type of eating disorder is binge. It refers to an eating disorder that involves immoderate indulgence. Unlike in bulimia where victims engage in purging activities, binge eating disorder leads people to having feelings of culpability, despair and self-criticism (Lock & Grange, 2005).
According to experts, this disorder is common among adolescents suffering from depression and low self esteem. Symptoms of this disorder include eating even one is not hungry, eating alone, lack of emotional control over food, taking too much food in a single meal, as well as constant complaints from friends and family about ones eating habits. The final category is made up of other specified eating disorders.
This category involves a permutation of symptoms of all the other eating disorders (Lock & Grange, 2005). Adolescents suffering from this disorder often experience different phases in their eating habits where they are either obsessed about food or gaining weight.
Studies have established that various factors cause and predispose adolescents to the various types of eating disorders. These causes belong to three categories, namely biological, environmental and psychological. However, experts argue that factors under the three categories have not been clearly defined as the main causes of eating disorders (Hornbacher, 2009).
There are two biological factors that cause eating disorders in adolescents or predispose them to the illness. The first factor is the genetic history of a family. According to experts, a family that has a history of having any eating disorder puts people in subsequent generations at a higher risk of suffering the same (Grilo & Mitchell, 2012). In addition, the kind of upbringing a family adopts can also lead to someone suffering from any type of eating disorder.
The second factor is brain activity. According to experts, the brain produces certain chemical substances that regulate important processes such as digestion, feelings of hunger, and desire for food. Depending on one’s brain activity, an individual can suffer from any of the four categories of eating disorders (Grilo & Mitchell, 2012).
Psychological factors also cause eating disorders or predispose adolescents to the illness. According to experts, the psychological condition of an adolescent can influence their eating habits, which eventually lead to a disorder (Fairburn, 2008). Some of the psychological factors that cause eating disorders include depression, anxiety, low self-esteem, societal values, individual traits, lack of self control, traumatic experiences (Herrin & Larkin, 2013).
According to experts, the pessimistic sense of inadequacy and a despondent lack of activity caused by depression often make people to change their eating habits. Some people start eating too much food, while others tend to reduce the amount of food they take.
Depression also makes adolescents to skip a meal, as they lose their emotional control when around food. Anxiety is another psychological factor that can cause eating disorders in adolescents (Fairburn, 2008). Psychiatrists argue that adolescents often experience cycles of worry and nervousness, which influence their eating habits. Adolescents are also prone to suffering from low self-esteem issues.
This is mainly caused by peer pressure for one to achieve perfection (Grilo & Mitchell, 2012). Societal or family values also influence on the eating habits of adolescents. Societies that hold a lot of value on elements such as body size, physical appearance and certain food types influence on the development of eating disorders among adolescents.
Environmental factors also cause eating disorders in adolescents or predispose them to the illness. In this context, the environment refers to the totality of conditions surrounding adolescents (Grilo & Mitchell, 2012). The conditions surrounding adolescents, both at home and schools often affect the kind of foods they will eat.
Some of the environmental factors that cause eating disorders include societal values, cultural attitudes, troubled relationships, and nature of activities one engages in among others (Hornbacher, 2009). According to experts, the values that a society places on an individual being thin or fat create an environment that creates bias towards people with certain body types.
Cultural attitudes regarding the ideal physical image of a man or woman also cause eating disorders among adolescents. During adolescence, many people start developing a certain degree of consciousness towards their body image (Fairburn, 2008). Most adolescents aim at meeting or bettering the standards set by a society regarding how someone should look like. This affects their eating habits, which in turn results in the development of a disorder.
Troubled relationships can lead to someone suffering from effects such as depression, which often influence on an individual’s eating habits (Hornbacher, 2009). A highly stressful environment can make someone to either consume a lot of food or vice versa.
Experts also argue that the kind of activities that adolescents pick out in schools also influence their eating habits. Those who engage in sports, athletics, and dancing are often conscious about staying fit and may avoid eating certain foods (Grilo & Mitchell, 2012). Those who choose to engage in less active engagements have little worry over their eating habits.
According to experts, eating disorders are treated according to their type and symptoms. The best treatment option for eating disorders is therapy, whereby a patient gets to express themselves and learn a few things about nutrition (Herrin & Larkin, 2013). In some instances, patients can receive medication if symptoms of a disorder indicate the possibility of an underlying medical condition responsible for the illness.
Studies have established that if certain eating disorders are not treated in time, they can lead to life-threatening complications. Effective treatment requires one to have a plan that will help to monitor the disappearance of various symptoms and their body weight (Herrin & Larkin, 2013). An eating disorder patient should go for regular therapy sessions with a registered dietitian, as well as ensuring they have the support of their family and friends.
Eating disorders are among the common illnesses that affect adolescents across the world. Studies have established that eating disorders are caused by a combination of biological, psychological and environmental factors. Experts argue that it is important for an eating disorder to be treated as soon as it is diagnosed, because any delays can lead to life-threatening complications.
There are numerous treatment options for eating disorders that patients can take up depending on the symptoms they show. One of the most important elements for achieving effective treatment of eating disorders is ensuring the support of friends and family members. The prevalence rate of eating or feeding disorders depends on the different types and various risk factors.
Herrin, M., & Larkin, M. (2013). Nutrition Counseling in the Treatment of Eating Disorders. California: Routledge.
Cite this paper
StudyCorgi. (2020, January 9). Essay on Eating Disorders in Adolescents. https://studycorgi.com/feeding-and-eating-disorders-in-adolescents/
"Essay on Eating Disorders in Adolescents." StudyCorgi , 9 Jan. 2020, studycorgi.com/feeding-and-eating-disorders-in-adolescents/.
StudyCorgi . (2020) 'Essay on Eating Disorders in Adolescents'. 9 January.
1. StudyCorgi . "Essay on Eating Disorders in Adolescents." January 9, 2020. https://studycorgi.com/feeding-and-eating-disorders-in-adolescents/.
StudyCorgi . "Essay on Eating Disorders in Adolescents." January 9, 2020. https://studycorgi.com/feeding-and-eating-disorders-in-adolescents/.
StudyCorgi . 2020. "Essay on Eating Disorders in Adolescents." January 9, 2020. https://studycorgi.com/feeding-and-eating-disorders-in-adolescents/.
This paper, “Essay on Eating Disorders in Adolescents”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: February 23, 2023 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.

Cognitive Behavioral Therapy
How intensive cbt-e can help adolescents with anorexia, the duration of anorexia doesn't influence the benefit of enhanced cognitive-behavioral therapy (cbt-e)..
Posted March 18, 2024 | Reviewed by Abigail Fagan
- What Is Cognitive Behavioral Therapy?
- Find a therapist who practices CBT
- Treatment studies in adolescents with anorexia typically involve patients with less than 3 years of illness.
- Little data is available on treatment outcomes for those with an illness duration of more than 3 years.
- A study found that adolescents from both groups have similar benefits from CBT-E.
The role of illness duration as a predictor and moderator of treatment outcomes has been extensively studied in adult patients with eating disorders. Surprisingly, findings suggest this variable does not seem to influence clinical outcomes. In contrast, limited research has evaluated the impact of illness duration on treatment outcomes in adolescent patients. This lack of data may stem from more uniformity in illness duration among adolescents than adults. Alternatively, it could be attributed to a general preference for considering patients' age, which is more straightforward to assess and appears closely linked to the duration of illness.
Family-based treatment (FBT) has the highest level of evidence regarding efficacy in adolescents with eating disorders. The first randomized controlled trial of FBT, initially known as Maudsley family therapy or "the Maudsley approach," compared it with individual supportive therapy. The study found that FBT proved more effective for adolescent patients who had anorexia nervosa for less than three years. Subsequent investigations into FBT have predominantly concentrated on adolescents with an illness duration of less than three years. Nevertheless, research exploring predictors of FBT has produced conflicting results regarding the role of illness duration in adolescent patients with eating disorders, both in both randomized clinical trials and observational longitudinal studies.
Enhanced cognitive-behavioral therapy (CBT-E) is a specialized psychological transdiagnostic treatment for all forms of eating disorders, including anorexia nervosa, bulimia nervosa, binge eating disorder , and other similar states. CBT-E was developed as an outpatient treatment for adults but then adapted by my team for adolescents and intensive care settings.
The effectiveness of CBT-E for adolescents has been confirmed through longitudinal studies conducted in outpatient and intensive (day-hospital and residential) real-world settings. These results led the National Institute for Health and Care and Clinical Excellence to recommend CBT for adolescents with eating disorders when FBT is deemed unacceptable, contraindicated, or ineffective.
Intensive CBT-E
Intensive CBT-E never adopts coercive or prescriptive attitudes or procedures, and patients are never expected to do anything they do not agree to. The aim is to actively involve adolescent patients in decision-making throughout treatment, enhancing their sense of empowerment and control. Patients eligible for intensive CBT-E (i.e., those who do not respond to a well-delivered outpatient treatment) attend four preparatory sessions in which they are introduced to the nature and aims of the treatment. Since patients are expected to address weight restoration from the first day of residential treatment, it is vital that they have decided to commit to this goal before they are admitted.
The treatment is delivered in a specialized unit for eating disorders by a ''non-eclectic'' multidisciplinary team (physicians, psychologists, nurses, and dieticians) all trained in CBT-E. The treatment lasts 20 weeks (13 of residential treatment followed by seven weeks of day-hospital).
Intensive maintains all the main strategies and procedures of outpatient CBT-E, which are delivered in both individual sessions and in a group format, but with three main features that distinguish it from the outpatient-based version. First, the treatment is delivered by a non-eclectic multidisciplinary team comprising physicians, psychologists, dieticians, and nurses, all fully trained in CBT-E. Second, assistance with eating is provided in the first weeks of treatment to help patients overcome their difficulties in real time. Third, the adolescent patients continue their course of study during the treatment. Intensive CBT-E also includes additional elements designed to reduce the high rate of relapse that typically follows discharge from residential treatments. For instance, the unit is open, and patients are free to go outside. In this way, they continue to be exposed to the types of environmental stimuli that tend to provoke their eating disorder psychopathology, but with full access to staff support. Furthermore, during the weeks immediately preceding discharge, a concerted effort is made to identify likely environmental setback triggers, which are then addressed during the individual CBT-E sessions. Moreover, towards the end of treatment, parents are helped to create a positive, stress -free home environment in readiness for the patient’s return. Before discharge, patients collaborate on identifying setbacks, including joint sessions.

What is the outcome of intensive CBT-E in adolescents?
So far, no study has compared the outcomes of CBT-E in adolescent patients with illness durations of less than three years versus those with durations of three years or more.
Our recent study published in the International Journal of Eating Disorders has addressed this research gap, assessing the effectiveness of intensive CBT-E in adolescents with anorexia nervosa and duration of illness exceeding three years, as compared to those with a shorter duration of illness.
One hundred and fifty-nine consecutive patients who have failed outpatient treatment were enrolled (n=122 with a duration of illness <3 years and n=37 ≥ 3 years). The key findings can be summarized as follows.
- Regarding the acceptability of intensive CBT-E, more than 80% of eligible patients agreed to commence treatment, and 81% completed it.
- A substantial proportion of adolescents (23.3%) with anorexia nervosa, contrary to those usually included in the FBT studies, had a duration of illness ≥3 years.
- The duration of illness was not associated with differences in the severity of psychopathological features.
- No discernible differences were found between adolescents with a duration of illness <3 or ≥3 years across various outcome measures (dropout rates, improvements in body weight, and psychopathology). Furthermore, more than 70% of adolescents achieved good body mass index (BMI = kg/m2) outcomes, and approximately 60% maintained a full response at 20-week follow-up in both illness duration groups.
Clinical implications
The findings support the use of intensive CBT-E in adolescents with anorexia nervosa who have failed previous outpatient treatments, irrespective of whether the duration of illness is equal to or longer than three years. With over 80% of patients completing treatment and demonstrating substantial improvement, the study reveals sustained positive changes until the 20-week follow-up, with approximately 60% achieving a full response.

In conclusion, this new study suggests that the outcome of intensive CBT-E is not influenced by the duration of illness in adolescents with anorexia nervosa, and there is a concrete possibility of recovery in those with a duration of ≥ 3 years who have failed previous outpatient treatment.
Calugi, S., Dalle Grave, A., Chimini, M., Lorusso, A., & Dalle Grave, R. (2024). Illness duration and treatment outcome of intensive cognitive‐behavioral therapy in adolescents with anorexia nervosa. International Journal of Eating Disorders . doi: https://doi.org/10.1002/eat.24196

Riccardo Dalle Grave, M.D., is head of the Department of Eating and Weight Disorders at the Villa Garda Hospital in Italy. He is the author of Cognitive Behavior Therapy for Adolescents with Eating Disorders.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Types of Eating Disorders
Do i have an eating disorder.
- Treatment and Resources
- Risks in Teens
- Finding Help
- Next in Eating Disorders Guide What Are the Signs of Disordered Eating?
Eating disorders are serious medical conditions that affect both physical and mental health. These disorders are not a choice and can be life-threatening. Fortunately, it is possible to recover from an eating disorder.
Common types of eating disorders include anorexia nervosa, bulimia nervosa , and binge eating disorder . Other types include avoidant/restrictive food intake disorder (ARFID) and other specified feeding and eating disorders (OSFED). Eating disorders can affect people of all ages, races, ethnicities, body weights, and genders.
Verywell / Danie Drankwalter
You may be wondering if you have an eating disorder or disordered eating. An eating disorder is a clinical diagnosis. Disordered eating refers to abnormal eating patterns that do not fit the criteria for an eating disorder. See your healthcare provider if you believe that you could be experiencing an eating disorder.
This article will provide an overview of eating disorders, including the signs and symptoms, how to recognize one in someone else, and the treatment options.
Defining an Eating Disorder
An eating disorder is a serious mental health disorder. It affects your thoughts about your body, food, and eating behaviors. An eating disorder often causes disturbing thoughts and emotions. People experiencing an eating disorder often feel obsessed with thoughts of food and body weight.
An eating disorder can significantly impact your physical and mental health. It may even be life-threatening when left untreated. Eating disorders are most commonly diagnosed in young people assigned female at birth but can affect anyone.
There are different types of eating disorders. They each require their own interventions and treatment plans. The signs and symptoms of eating disorders vary by type.
Anorexia Nervosa
Anorexia nervosa is an eating disorder characterized by restricting the amount of food or calories consumed. People with anorexia nervosa may feel preoccupied with thoughts of restricting certain types of food. They also usually have a disordered view of their body and feel overweight when they are dangerously underweight.
Possible symptoms of anorexia nervosa include:
- Preoccupation with food, calories, and body weight
- Frequent thoughts about dieting
- Restricting the amount of food you consume
- Resisting a healthy weight for your height and age
- Fear of gaining weight
- Frequent exercising that feels rigid
- Dry, brittle hair and nails
- Constipation
- Fine hair all over the body
Possible signs of anorexia nervosa in someone else include:
- Dramatic weight loss
- Always dressing in layers (for warmth or to hide weight loss)
- Rigid exercise routine
- Making excuses to skip meals
Complications
Over time, anorexia nervosa can lead to serious health complications, including:
- Low red blood cell count (anemia)
- Muscle wasting and weakness
- Weak bones (osteoporosis)
- Low blood pressure
- Slowed breathing rate and heart rate
- Infertility
Bulimia Nervosa
Bulimia nervosa is an eating disorder that usually involves consuming large amounts of food, followed by purging the food through vomiting or the use of laxatives .
Possible symptoms of bulimia nervosa include:
- Binging large amounts of food
- Feeling the need to purge after a large meal or snack
- Forcing yourself to vomit after eating
- Frequently taking laxatives or diuretics after eating
- Acid reflux
- Severe dehydration
- Chronic sore throat
- Swollen salivary glands
- Drinking excessive amounts of water or non-calorie beverages to try to feel full
- Dental problems such as cavities , the discoloration of teeth, and sensitivity
Possible signs of bulimia nervosa in someone else include:
- Food seems to disappear quickly
- Evidence of lots of food having been eaten, such as empty wrappers and food containers
- They often seem to go to the bathroom soon after eating
- Evidence of vomiting (smell or sight of it in the bathroom)
- Using mouthwash, mints, or gum constantly throughout the day
- Calluses on the backs of hands from self-induced vomiting
Binge Eating Disorder
Binge eating disorder is the most common eating disorder in the United States. It is characterized by binging large amounts of food and feeling guilty or ashamed afterward. Unlike bulimia, people with binge eating disorder do not purge after eating.
Possible symptoms of binge eating disorder include:
- Feeling out of control while eating (unable to stop)
- Feelings of disgust, shame, guilt, and depression after eating
- Stealing or hoarding food to eat in secret
- Creating schedules or rituals around binge eating
Possible signs of binge eating disorder in someone else include:
- Food disappearing quickly
- Hidden empty wrappers and food containers
- Weight gain or obesity
Avoidant Restrictive Food Intake Disorder
Avoidant restrictive food intake disorder (ARFID) is an eating disorder that involves not consuming enough calories to grow and develop properly.
Many children go through phases of “picky” eating. People with ARFID are unable to consume enough calories for proper growth. They may restrict several categories of food. Unlike people with anorexia, people with ARFID do not fear weight gain.
Possible symptoms of avoidant restrictive food intake disorder include:
- Minimal range of preferred foods
- Fears of choking or vomiting when eating
- Craving non-food items like dirt, hair, or paint chips (known as pica)
Possible signs of avoidant restrictive food intake disorder in someone else include:
- Refusal to eat several types of food
Other Specified Feeding and Eating Disorders
Other specified feeding and eating disorders (OSFED) are a group of eating disorders that do not meet the criteria for any of the previously mentioned eating disorders. People with these types of disorders experience disordered eating patterns.
Possible symptoms of OSFED include:
- Frequent episodes of binging food
- Feeling as though your self-esteem is tied to your body image
- Feeling consumed with dieting
- Intense need to exercise after eating
Possible signs of OSFED in someone else include:
- Frequent talk of dieting or “burning off” calories
- Disappearance of large amounts of food in a short period
- Hidden empty wrappers and food containers
You may be wondering if you have an eating disorder. The best way to figure this out is to see a healthcare provider. The healthcare provider will conduct a physical exam and medical history. Plan to answer questions about your eating habits, exercise routines, and overall health.
Your provider may recommend medical tests, including :
- Blood tests : To test for anemia and electrolyte imbalances (an imbalance of important charged minerals in the blood)
- Urine tests : To assess hydration status
- Kidney function tests : To detect kidney damage
- Electrocardiogram (EKG or ECG) : To check heart health
If you feel that your eating habits, exercise routines, or purging episodes are beyond your control, it’s important to see your healthcare provider right away.
Causes and Risk Factors
The exact cause of an eating disorder is unknown. Researchers believe that most eating disorders are caused by a combination of genetic, biological, psychological, and social factors.
Eating disorders can affect people of all ages, genders, weights, races, and ethnicities. Young people assigned female at birth are most likely to be diagnosed.
Risk factors for an eating disorder include:
- Poor body image
- Beginning to diet at a young age
- Family history of eating disorders
- Participation in certain sports that focus on weight or body size (such as wrestling, ballet, gymnastics, and ice skating)
- History of anxiety or depression
Eating Disorder Treatment and Resources
Eating disorders are serious medical conditions that require treatment. When left untreated, eating disorders like anorexia nervosa can cause life-threatening health complications. Fortunately, they are treatable. See your healthcare provider and a mental health professional for treatment.
The primary goals of eating disorder treatment are to:
- Restore adequate nutrition
- Achieve and maintain a healthy weight
- Reduce excessive exercise
- Stop binge-purge behaviors
- Treat any underlying mental health disorders
Treatment options for most eating disorders may include:
- Therapy : Individual, group, or family psychotherapy
- Medications : Antidepressants, antipsychotics, mood stabilizers
- Nutritional counseling : Meal planning and eating goals with a registered dietitian
- Medical care : Treatment of any health complications such as dehydration or heart damage
Risks of Eating Disorders in Teens
It is estimated that up to 1 in 10 adolescents assigned female at birth will experience an eating disorder. It is also possible for adolescents assigned male at birth to experience an eating disorder.
A 2019 study found that exposure to media can increase the risk of eating disorders in adolescents because it promotes dissatisfaction with body image. Teens exposed to media such as television, magazines, and social media may feel increased pressure to achieve a certain beauty standard. This may happen around the same time as puberty, a process that usually causes weight gain and bodily changes.
Research shows that family-based therapy is an effective treatment for teens with eating disorders. This type of therapy empowers parents to take over the responsibility of feeding their children to ensure they receive enough nutrients.
Not Just Teens
While teens may be at a higher risk of developing eating disorders, people of all ages can be affected.
Where to Go If You Think You Have an Eating Disorder
If you think you may have an eating disorder, seek help right away. Reach out to your healthcare provider to determine your diagnosis and treatment plan. Eating disorders can lead to serious medical complications and a higher risk of suicide. It is critical to seek help as soon as possible.
Resources that may help you include:
- Eating Disorders Helpline
- Eating Disorder Peer Support Groups
- Eating Disorder Recovery Mentor
- National Eating Disorder Association
- National Association of Anorexia Nervosa and Associated Disorders
- National Institute of Mental Health
- Substance Abuse and Mental Health Services Administration
If you are having any thoughts of self-harm or suicide, seek immediate care at an emergency department or by calling the 988 Suicide & Crisis Lifeline or 911.
An eating disorder is a serious medical condition that affects physical and mental health. It is not a choice and can be life-threatening if left untreated. Common types of eating disorders include anorexia nervosa and bulimia nervosa. Binge eating disorder is the most common type of eating disorder in the United States. Other types of eating disorders include avoidant restrictive food intake disorder and other specified feeding and eating disorders.
Eating disorders are most common in young people assigned female at birth but can affect people of all ages, genders, races, ethnicities, and body weights. Eating disorders can cause serious medical complications and need to be treated as soon as possible. See your healthcare provider if you are concerned that you may be experiencing disordered eating or an eating disorder.
A Note on Gender and Sex Terminology
Verywell Health acknowledges that sex and gender are related concepts, but they are not the same. To accurately reflect our sources, this article uses terms like “female,” “male,” “woman,” and “man” as the sources use them.
National Institute of Mental Health. Eating disorders: about more than food .
Academy of Nutrition and Dietetics. Disordered eating .
Feng B, Harms J, Chen E, Gao P, Xu P, He Y. Current discoveries and future implications of eating disorders . Int J Environ Res Public Health . 2023;20(14):6325. doi:10.3390/ijerph20146325
Anxiety and Depression Association of America. Types of eating disorders .
Anxiety and Depression Association of America. Eating disorders .
MedlinePlus. Eating disorders .
Nemours Teens Health. Eating disorders (for teens) .
National Institute of Mental Health. Eating disorders .
American Academy of Child and Adolescent Psychiatry. Eating disorders in teens .
Uchôa FNM, Uchôa NM, Daniele TMDC, et al. Influence of the mass media and body dissatisfaction on the risk in adolescents of developing eating disorders . Int J Environ Res Public Health . 2019;16(9):1508. doi:10.3390/ijerph16091508
By Carrie Madormo, RN, MPH Carrie Madormo, RN, MPH, is a health writer with over a decade of experience working as a registered nurse. She has practiced in a variety of settings including pediatrics, oncology, chronic pain, and public health.
- Conditionally
- Newsletter Signup
Dead Weight: Essays on Hunger and Harm Is Our March SELF Well-Read Book Club Pick
By Hannah Dylan Pasternak
.png)
All products are independently selected by our editors. If you buy something, we may earn an affiliate commission.
.png)
Each month, the SELF Well-Read Book Club highlights a timely, delightful, and crucial book on a subject that helps readers live better lives. So far, we’ve covered everything from the politics of running to the state of modern motherhood .
It’s more likely than not that you know someone—if not yourself—who has lived with an eating disorder ; almost one out of every 10 people in the United States will have one in their lifetime. According to the National Eating Disorders Association, 22% of children and adolescents around the world show symptoms of disordered eating, and eating disorders have the second-highest mortality rate of any mental illness. These statistics are jarring, though to many of us, not so shocking. But there are other facts, stories, and histories that are given far less space in the discourse—and that’s exactly what author Emmeline Clein works to untangle in Dead Weight: Essays on Hunger and Harm , SELF’s March Well-Read Book Club pick.
In each essay, Clein takes a close, empathetic look at the cultural frameworks that destroyed nearly any possibility of a positive body image for people alive in the early 2000s. If you were a young person with a TV or internet connection at that time, you’re probably very familiar: the “pro-ana” Tumblrs, the trajectories of It girls like Lindsay Lohan and Nicole Richie, and dangerous monoliths like Weight Watchers and MyFitnessPal. Clein tackles these topics in a sensitive and conscientious way, which is both extremely rare and extremely important, as a lot of eating disorder coverage can operate as a manual rather than a warning. By the end of the book, you’ll be left with a better understanding of how society at large failed you—and not the other way around.
Other notable parts of the book include a close look at binge eating disorder (and, more broadly, the types of EDs that are considered more socially acceptable); questions around sex, consumption, and the things women are “allowed” to devour; the genuinely shocking difficulty of getting effective treatment; and the ways disordered eating disproportionally affects underserved communities, like queer, fat, or Black people, along with those who have lived in poverty or with food insecurity.
So, on the heels of National Eating Disorders Awareness Week, we’re eager to come together and read something that will hopefully act like a little bit of salve to a wound that runs deep for so many of us. For a few suggested reading pairings from SELF, see the list below. Grab your copy of the book here , and stay tuned for a Q&A with Clein coming soon.
‘Dead Weight: Essays on Hunger and Harm’ by Emmeline Clein
Suggested reading:
- How to Get Help If You Think Your Eating Might Be Disordered
- A Chatbot Replaced Workers at an Eating Disorder Helpline. It Went Horribly Wrong.
- The New Obesity Guidelines for Kids Are Appalling
- ‘Heroin Chic’ Wasn’t OK in the ‘90s and It’s Not OK Now
- Growing Up With ‘Almond Mom’
- How to Maintain a Healthy Body Image in College
- I Wish ‘Don’t Weigh Me’ Cards Existed When I Was Young. Here’s What I Did Instead
- 7 Ways to Heal Your Relationship With Your ‘Trigger Foods’

SELF does not provide medical advice, diagnosis, or treatment. Any information published on this website or by this brand is not intended as a substitute for medical advice, and you should not take any action before consulting with a healthcare professional.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Pediatr
Adolescents With Eating Disorders in Pediatric Practice – The European Academy of Paediatrics Recommendations
Agnieszka rynkiewicz.
1 Department of Psychiatry, College of Medical Sciences, Institute of Medical Sciences, University of Rzeszow, Rzeszow, Poland
2 Center for Diagnosis, Therapy and Education SPECTRUM ASC-MED, Gdańsk, Poland
Łukasz Dembiński
3 The European Academy of Paediatrics (EAP), Brussels, Belgium
4 Department of Pediatric Gastroenterology and Nutrition, Medical University of Warsaw, Warsaw, Poland
Berthold Koletzko
5 Department of Paediatrics, Dr. von Hauner Children’s Hospital, University of Munich Medical Centre, Ludwig-Maximilians-Universität Munich, Munich, Germany
Pierre-André Michaud
6 Faculté de Biologie et de Médecine, Université de Lausanne, Lausanne, Switzerland
Adamos Hadjipanayis
7 School of Medicine, European University Cyprus, Nicosia, Cyprus
8 Department of Paediatrics, Larnaca General Hospital, Larnaca, Cyprus
Zachi Grossman
9 Adelson School of Medicine, Ariel University, Ariel, Israel
10 Maccabi Health Services, Tel Aviv, Israel
Kathryn Korslund
11 THIRA Health, Bellevue, WA, United States
Bryan H. King
12 Department of Psychiatry and Behavioral Sciences, Weill Institute for Neurosciences, University of California, San Francisco, San Francisco, CA, United States
Janet Treasure
13 Eating Disorder Unit, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, United Kingdom
Jarosław Peregud-Pogorzelski
14 Department of Pediatrics, Pediatric Oncology and Immunology, Pomeranian Medical University, Szczecin, Poland
15 Polish Society of Paediatrics, Warsaw, Poland
Stefano del Torso
16 ChildCare WorldWide-CCWWItalia OdV, Padova, Italy
Arunas Valiulis
17 Clinic of Children’s Diseases, Institute of Clinical Medicine, Vilnius University Medical Faculty, Vilnius, Lithuania
18 Department of Public Health, Institute of Health Sciences, Vilnius University Medical Faculty, Vilnius, Lithuania
Artur Mazur
19 Department of Paediatrics, College of Medical Sciences, Institute of Medical Sciences, University of Rzeszow, Rzeszow, Poland
Associated Data
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
In the face of the growing number of adolescents suffering from eating disorders (EDs) and access to psychiatric care limited by the epidemiological and demographic situation, the primary care pediatrician’s role in diagnosing and treating EDs is growing. The European Academy of Paediatrics (EAP) decided to summarize knowledge about EDs and formulate recommendations to support European pediatricians and improve care for adolescents with EDs.
Pediatricians commonly encounter patients with suspected or confirmed eating disorders (EDs), who carry a considerable risk of morbidity and even mortality. Early detection, appropriate diagnostic workup, and effective treatment require transdisciplinary collaboration. They are all essential for improving the patients’ prognosis. Here we aim to review current knowledge relevant for practicing pediatricians and provide recommendations of the European Academy of Paediatrics (EAP) on the role of pediatricians in caring for adolescents with ED and for actions of authorities and pediatric societies aiming to improve healthcare for these patients.
Classification
The Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) and the 11th revision of the International Classification of Diseases (ICD-11) define ED as persistent abnormal eating behaviors that significantly impair physical health or psychosocial functioning ( 1 , 2 ). The diagnostic criteria and characteristics of the most common ED in the adolescent population – anorexia nervosa (AN), bulimia nervosa (BN), binge-eating disorder (BED), avoidant/restrictive food intake disorder (ARFID) – are presented in Table 1 ( 2 ).
Diagnostic criteria for selected eating disorders ( 1 , 3 ).
Other less common EDs include:
- • Atypical AN – AN with normal body weight;
- • Rumination-regurgitation disorder – repeated regurgitation of food not associated with other medical conditions;
- • Pica – persistent eating of non-nutritive/non-food substances;
- • Purging disorder – recurrent purging behavior to influence weight or shape (e.g., vomiting, misuse of laxatives or diuretics, or other medications) in the absence of BED.
In practice, one type of ED may shift to another over time, and in some patients, it is difficult to diagnose a particular type of ED precisely.
Epidemiology
As the onset of the disease is usually in the teenage years, pediatricians are the most likely to suspect a diagnosis of ED ( 4 , 5 ). Data on the prevalence of ED are quite varied and depend on the population and diagnostic criteria used. Large-scale population surveys also have an underestimation bias due to patients’ tendency to minimize symptoms or deny the disease ( 6 ). However, the overall prevalence of ED is estimated from 2% to even 6%, with a nearly five times greater frequency of BED than other types of ED ( 7 – 10 ). The COVID-19 pandemic also contributed to a significant increase in stress, disturbances in school and family relations, and often limited access to psychological counseling, which increased the frequency of ED and deterioration of the prognosis ( 11 ).
Statistically, ED are more common in females, although in BED, the proportion of male patients is higher approximately a third ( 12 ).
Episodes of behavior typical of ED but not meeting all criteria may occur in up to one in five adolescents ( 13 ). However, some behaviors may mask or mimic ED at this age, which is mainly related to the adolescent gaining influence on their own nutrition and focusing attention on external appearance ( 14 ). Autism spectrum disorder shares some common features with ED, especially the restrictive ones, which should be considered in the differential diagnosis ( 15 , 16 ). ED can also coexist with other mental or organic disorders, such as depression, celiac disease, or diabetes ( 17 ).
A specific cause of ED has not been established, but potential etiology includes genetic predisposition, cognitive and emotional vulnerability, social and environmental factors, such as pressure of the dominant cultural patterns and weight stigma ( 18 ). Moreover, in the group of children with ED, there are increased risks of emotional or behavioral disorders, attention-deficit/hyperactivity disorder and autism spectrum disorders ( 19 , 20 ).
It should also be noted that an increased risk of ED occurs in children struggling with the lack of social acceptance (e.g., overweight, ethnic, racial, or sexual minorities) ( 21 , 22 ).
Impact on Health
Eating disorder should be seen not only as a mental illness but as a threat to health and even to life. Chronic malnutrition, nutritional deficiencies, frequent vomiting, and misuse of drugs can lead to irreversible effects that impair adolescents’ health and development. Chronic undernutrition can lead to long-term effects, such as diminished bone density or even cognitive impairment ( 23 ). Moreover, the consequences of ED can cause secondary peer acceptance problems, bullying, symptoms of post-traumatic stress disorder, and an increased risk of self-injury ( 24 – 26 ). ED has the second-highest mortality rate of all mental health disorders due to the increased frequency of suicide attempts but also due to the health consequences of cachexia (e.g., electrolyte problems, dehydration, heart failure) ( 27 , 28 ).
The main health problems that adolescents with ED may report to a pediatrician are summarized in Table 2 .
Major health complaints, symptoms, and signs in adolescents with eating disorders.
Screening and Early Diagnosis
Due to the fatal consequences of untreated ED, early diagnosis and therapeutic intervention improve outcomes. Awareness of the various ED symptoms and screening in risk groups is an essential role of the primary care pediatrician and nurse. Vaccination visits and annual health check-ups provide a unique opportunity to spot the first signs of ED. Therefore, assessing the nutritional status with reference to growth charts at each visit is essential ( 29 ).
Apart from the findings in the physical examination described in Table 2 , blood pressure and heart rate should be assessed. Lowering these values in relation to age references may be a symptom of cachexia and (e.g., in the case of significant bradycardia) indicate the need for hospitalization.
In the ED risk assessment, several available tools can be used. To date, many different physician-filled or self-assessed screening questionnaires, which can help to detect abnormal behaviors and lead to earlier diagnosis, have been developed, e.g.:
- • SCOFF questionnaire – containing five short questions about eating and its impact on life ( 30 );
- • Eating disorder Screen for Primary care (ESP) – containing questions about eating patterns and previous ED episodes ( 31 );
- • Eating Disorders Assessment for DSM-5 (EDA-5) – containing questions based on the DSM-5 diagnosis criteria ( 32 );
- • Child Eating Disorder Examination (ChEDE) – containing 28 questions to assess diagnostic criteria for BED and BN ( 33 );
- • Bright Futures Questionnaires – a relatively extensive questionnaire from the American Academy of Pediatrics containing questions about eating patterns and body image ( 34 ).
However, the results of questionnaires, especially those self-reported, should be interpreted with caution and in the context of the entire clinical picture. Due to the lack of an unequivocal advantage of one questionnaire, pediatricians should use the one with the interpretation of which they have the most experience and is available in the national language.
The primary care pediatrician can also directly ask questions about, e.g., inducing vomiting, using laxatives, or self-image, but it is essential to maintain an atmosphere of respect and trust. A comprehensive psychosocial assessment is also necessary, emphasizing the possibility of coexistence of addictions, bullying, and physical or sexual abuse ( 35 , 36 ).
Laboratory tests should be considered in patients with suspected ED to exclude anemia, disturbances of electrolyte equilibrium, thyroid dysfunction, and celiac disease – Table 3 . However, the diagnosis of ED is purely clinical, and diagnostic procedures mentioned above mainly aim to identify metabolic and physiological disturbances that are consequences of ED. Among patients with severe cachexia, cardiological evaluation (electrocardiogram and echocardiogram) is vital to exclude cardiac arrhythmias and pericardial effusion ( 37 ). Some patients may require additional radiological, gastroenterological, endocrinological, or neurological workup to rule out causes of symptoms other than ED.
Recommended diagnostics in patients with suspected ED in primary pediatric care.
Most adolescents with ED can be treated in an outpatient setting provided that a patient and family are motivated to cooperate, and there are no severe malnutrition, somatic complications, or other psychiatric problems requiring hospitalization ( 38 ). In such cases, cooperation between a psychiatrist and a psychologist with a primary care pediatrician is essential to optimize treatment strategies and ensure patient safety. In addition, since treatment of EDs requires an interdisciplinary approach, dietitians, family therapists, social workers, and teachers, whenever possible, should be involved in treating patients with ED.
Family based treatment is the recommended front-line treatment for ED in childhood and adolescents. However, Cognitive Behavior Therapy or its modification – Dialectical Behavior Therapy – can be a useful supplement ( 39 ). However, in addition, regular monitoring of the patient’s nutritional status by the primary care pediatrician is vital especially in cases of AN.
Hospitalization should be considered in adolescents who develop life-threatening complications of ED or have failed to restore weight with outpatient treatment. Effective hospital treatment needs a professional, multidisciplinary team with expertise and experience dealing with ED patients and a structured treatment plan that is regularly re-evaluated and revised when necessary. In addition, patients with coexisting mental and organic diseases, pericardial effusion, electrolyte disorders, and a high risk of developing the refeeding syndrome require special supervision ( 40 , 41 ).
Pharmacotherapy (e.g., antidepressants or neuroleptics) is also used in the treatment of ED, but it should be carried out with the leading role of a psychiatrist.
Pediatricians should consider that, as with many chronic diseases, ED affects the patient’s entire family. For example, many parents can be depressed, grieve, or express guilt because of their child’s illness ( 42 ). Also, siblings may develop their own psychological and psychiatric problems ( 43 ).
Early diagnosis and adequate treatment can produce a partial remission in over 60% of patients ( 44 , 45 ).
The Role of Pediatricians
Primary care pediatricians play a crucial role in screening and early diagnosis of ED because they have the unique opportunity to monitor adolescents’ health regularly, and they have the chance, to some extent, assess adolescents’ family and social situations. Therefore, a mandatory part of the examination should be the assessment of nutritional status, as it may be the first sign of ED.
The role of pediatricians is also to educate and inform the community about ED and advocate for these patients. Moreover, in the face of the shortage of child psychiatrists in many European countries, the pediatrician often will have to act as the treatment coordinator ( 46 ).
Recommendations
For international and national state, health, and education authorities
- • Adolescents with ED require multidisciplinary care. Therefore, this issue should be present in undergraduate and postgraduate medical education.
- • National health authorities should provide adolescents with ED with multidisciplinary care and support for their families.
For European and national pediatric societies
- • Pediatric societies should support their members through ongoing training in ED.
- • Pediatric societies should advocate in increasing the availability of psychiatric and psychological care for adolescents with ED.
For pediatricians
- • An integral part of each patient visit should be the assessment of their nutritional status.
- • Measurement of blood pressure and heart rate should be a part of every physical examination of adolescents with ED.
- • When assessing the risk of ED, pediatricians should use the questionnaires with which they have the most experience and are available in the local language.
- • The role of a pediatrician is to cooperate with a psychiatrist and psychologist in the therapeutic process, with particular emphasis on regular assessment of the nutritional status and early identification of health risk signs.
- • Adolescents with life-threatening complications of ED and those who have failed in weight normalization efforts should be referred to the hospital.
Data Availability Statement
Author contributions.
AR, ŁD, BK, AH, and AM: study design. AR and ŁD: data collection. AR, ŁD, BK, and P-AM: data analysis and interpretation. AR, ŁD, BK, P-AM, AH, ZG, KK, BHK, JT, JP-P, ST, AV, and AM: manuscript preparation and critical revision. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.

Common Eating Disorders Explained. Symptoms & Treatments
E ating disorders affect almost 5% of the population worldwide. These disorders usually develop during adolescence but can develop in adulthood as well.
Some disorders, such as anorexia nervosa, are more common in women. However, these disorders can affect anyone irrespective of gender, age, or other characteristics.
Eating disorders are severe conditions that can cause numerous complex medical issues and result in severe emotional distress.
People with severe eating disorders may require help from more than one medical professional to recover. To root out the issue in its entirety, not only is medical assistance required, but mental health counseling is also paramount since eating disorders are mainly psychological issues.
Some serious eating disorders may require daily supervision. Nurses can play a significant role in this regard. From the point a patient walks through the hospital doors until they leave, nurses are the primary point of contact for most patients.
From this critical position, nurses can help patients identify their eating disorders earlier.
These disorders almost always stay under the radar until they’ve progressed in severity. Developing the eye to recognize the signs of an eating disorder in a patient requires exceptional knowledge and skill.
To develop and gain that knowledge, nurses can pursue an MSN or DNP degree.
Defining Eating Disorders
Eating disorders can be defined as certain behavioral conditions characterized by severe and persistent disturbances in an individual’s eating behaviors.
Eating disorders are considered among the deadliest of mental illnesses . They can impair a person’s social, psychological, and physiological functioning.
So, let’s take a closer look at some of the common eating disorders:
Anorexia nervosa is one of the most commonly known eating disorders. This disorder is prevalent among women more than men and often starts during adolescence or early adulthood.
People suffering from anorexia view themselves as overweight despite often being severely underweight. They restrict their food intake and try to eat as little as possible.
Some common symptoms of anorexia nervosa are:
- Considerably underweight as compared to other people of their age
- Engaging in restricted eating behaviors
- Intense fear of gaining weight
- Engaging in behaviors that will prevent them from gaining weight
- They have a distorted body image and may face self-esteem issues due to it
- They deny accepting that they are underweight
- May also develop depression and anxiety
- They may use laxatives, diet pills and often fall ill
There can be many long-term side effects of anorexia nervosa if it goes undiagnosed and untreated for a long time. For instance, such people may face fertility issues, weak or brittle nails, and hair.
Moreover, the lack of important nutrients can also lead to organ failure.
Bulimia is characterized by binge eating episodes where they eat till it is painful. This is followed by purging. This includes behaviors like forced vomiting, excessive exercise, using laxatives, and so on.
Common symptoms include:
- Recurring episodes of binge eating and inability to control them
- Frequently engaging in purging behaviors to avoid weight gain
- Self-esteem and body image issues
Bulimia nervosa can negatively impact one’s physical health if not treated. People with this disorder may experience a sore throat, digestive problems, dehydration, and hormonal imbalances. Moreover, they also have higher chances of experiencing a stroke.
This is one of the most common eating disorders in the United States. It often gets confused with bulimia nervosa. However, it does not include purging behaviors.
People with BED eat large amounts of food and cannot control themselves.
This disorder is characterized by the following:
- Eating large amounts of food in a short time, even if they do not feel hungry
- Unable to control or stop eating
- Feelings of guilt and shame regarding this behavior
- Absence of purging behaviors
Pica is a disorder in which a person craves non-food items like sand, soap, paper, chalk, ice, and more. It is commonly found in children, pregnant women, or people with mental disabilities.
Such people are at a higher risk of poisoning, gut injuries, and various deficiencies.
Rumination Disorder
This disorder can affect anyone, irrespective of their age. In this disorder, a person tends to regurgitate food, swallow it, chew it again then swallow or spit it out.
It can also result in severe malnutrition and extreme weight loss if it is not properly treated.
Avoidant/Restrictive Food Intake Disorder (ARFID)
ARFID starts during infancy or early childhood but can also persist into adulthood. Furthermore, it is commonly found in both men and women.
In this disorder, the person has disturbed eating patterns due to a lack of interest in eating or dislike towards certain tastes and smells.
- Avoiding or restricting food intake
- Eating habits interfere with normal social functioning
- Malnutrition and weight loss
- May also be dependent on supplements of tube feeding
How Can An Eating Disorder Be Treated?
Even though eating disorders are severe and can cause numerous problems, they are treatable. People suffering from disorders can recover and lead healthy lives with the help of early detection and the proper treatment.
Some treatment methods for eating disorders are:
Psychotherapy
This is effective for all eating disorders. It helps identify underlying issues, which helps understand the causes of the disorder. Moreover, it helps establish healthy eating patterns and coping mechanisms.
It is also used to deal with the psychological side effects of eating disorders, such as depression, anxiety, and low self-esteem. Commonly used therapeutic interventions include CBT, behavioral therapy, and family therapy.
Medication can be used for treating the side effects of eating disorders. For instance, anti-depressants can be prescribed to fight off depression and increase serotonin levels.
Nutritional Counseling
Nutritional counseling helps the patient in learning about healthy eating habits.
It helps you recognize signs of hunger and satiation. Furthermore, following a healthy diet plan helps you maintain body weight and overcome any deficiencies caused by the disorder.
Hospitalization
This option is often required for severe cases requiring intensive treatment and care. However, it is not very common.
In Conclusion
Eating disorders are mental health conditions that involve disturbed eating behaviors.
Moreover, these disorders can hurt a person’s mental and physical health. Therefore, they require effective and immediate treatment as they can worsen if left untreated.
Next Up From ChaChingQueen
- Nursing And Nutrition: How To Combine Your Love Of Both
- Is Your 3 Year Old Exhibiting Sign Of Autism?
- Overcoming Low Self-Esteem
- Dietician Shares 12 Foods You Can Eat A Lot Of Without Getting Fat

We will write a custom essay on your topic. To begin with, it is necessary to define which diseases are meant under the notion of an eating disorder. Generally, eating disorders encompass such conditions as anorexia nervosa, bulimia, binge eating, and avoidant/restrictive food intake disorder (ARFID) (AACAP, 2018).
In the present review, the results show that the main factors associated with eating disorders were psychological-type with a prevalence of the factor inherent the dissatisfaction with body image ( 16 ─ 18, 21, 25, 27, 29, 31, 32, 35 ). Literature refers that dissatisfaction with body image increases significantly in adolescence due to ...
1. Introduction: Eating Disorders in Adolescence. Eating disorders in adolescence are among the most important public health problems in the world [1,2,3,4,5], and they affect a predominantly female population of adolescent girls and young women, from 13 to 25/30 years of age, with a male/female ratio of about 1 out of 10 [6,7,8].Regarding the adolescent population, epidemiological studies ...
Types of eating or feeding disorders in adolescents. There are four main types of eating disorders diagnosed among adolescents: anorexia, bulimia, binge eating disorder, and other specified eating disorders (Lock & Grange, 2005). Anorexia is characterized by a loss of appetite and a restriction of certain food groups in order to avoid weight gain.
Eating disorders in childhood and adolescence present a serious threat to health and well-being, including medical consequences ranging from growth delay to life-threatening effects of starvation and refeeding (Reference Nicholls, Hudson and Mahomed Nicholls 2011a).Anorexia nervosa is frequently cited as the third most common chronic illness of adolescence (Reference Lucas, Beard and O'Fallon ...
The etiology of eating disorders is very complex and, similar to other psychiatric disorders such as depression and anxiety, arises from the intersection of many risk factors. 6 Although the prevalence varies according to study populations and definitions used, 7 it is recognized that eating disorders are common in adolescents and even more ...
Eating disorders are severe conditions that often affect young people during a developmentally important stage in life. 1, 2 Although both men and women of all ages can be affected, those who are diagnosed with an eating disorder are mainly female adolescents and young women. 1, 3 First symptoms often occur in early adolescence or the late ...
Binge-eating disorder (BED) is the most common ED in children and adolescents and is more prevalent in females than males. EDs may present differently in children and adolescents than in adults, and parents or caregivers may be the first to notice changes in eating patterns or body weight.
The Facts. 28.8 million Americans will have an eating disorder in their lifetime. Eating disorders have the HIGHEST risk of death of any mental illness. Eating disorders affect all genders, all races and every ethnic group. Genetics, environmental factors and personality traits all contribute to the risk of developing an eating disorder.
Anorexia symptoms include: intense fear of increasing weight. highly restricted eating. denial or distorted view of their body. refusal to gain weight or maintain a moderate weight. self-esteem ...
Although the earliest medical account of an adolescent patient with an eating disorder was more than 300 years ago, 1 a thorough understanding of the pathophysiology and psychobiology of eating disorders remains elusive today. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) includes the latest effort to describe and categorize eating disorders, 2 placing ...
Many kinds of eating disorders may affect children and teens: Anorexia nervosa is an eating disorder characterized by an extreme fear of gaining weight. People with anorexia nervosa often see themselves as overweight when they are at a healthy weight, and even when they are greatly underweight. There are two forms of anorexia nervosa: The ...
It supports individuals and families affected by eating disorders. F.E.A.S.T. is an international nonprofit organization run by caregivers of those suffering from eating disorders, meant to help ...
Eating disorders are complex illnesses that are affecting adolescents with increasing frequency [1]. They rank as the third most common chronic illness in adolescent females, with an incidence of up to 5% [1-3]. Three major subgroups are recognized: a restrictive form in which food intake is severely limited (anorexia nervosa); a bulimic form in which binge-eating episodes are followed by ...
With regard to CBT studies, DeBar et al79 have used an adolescent adaptation of CBT in a sample of female adolescents with BED (52%), recurrent binge eating episodes (32%), or bulimia spectrum disorders (16%). Subjects in CBT group were compared with a usual-delayed treatment (TAU-DT) control group (N=13), in which adolescents received CBT 6 ...
A feeding or eating disorder is defined as a physical, medical or psychological condition in an individual that makes them unable to consume certain types of food (Hornbacher, 2009). They influence an individual's emotions and behavior towards certain food groups. There are various types of feeding or eating disorders that affect adolescents.
The most commonly used model of treatment for adolescents with AN is family-based treatment (FBT), while CBT is preferred therapy for BN (Lock & Fitzpatrick, 2009).Treatment approaches for adolescents living with EDNOS depend upon how closely the symptoms align with either BN or AN (Yager et al., 2012).Multifamily therapy (MFT) is posited a promising group model for young people, given its ...
It was shown previously that eating disorders (EDs) most often develop in adolescence and just after age 20 [21]. The results of this research in males and females aged 18-26 showed that a risk of ...
This paper will cover several statistics along with the three primary eating disorders faced in adolescence. The three eating disorders covered are anorexia nervosa, bulimia nervosa, and binge-eating disorder. Anorexia nervosa is an eating disorder that is noted by irrational and persistent fears of gaining weight.
Introduction. Eating disorder (ED) describe sicknesses that are represented by constant disturbance of eating patterns and extreme unhappiness or worry about body weight/shape which leads to poor physical and/or mental health. Over the past few decades there has been an increase in the prevalence of eating disorder especially among adolescents.
Eating disorders are complex illnesses that affect adolescents with increasing frequency. They rank as the third most common chronic illness in adolescent females (), with an incidence of up to 5% (2,3), a rate that has increased dramatically over the past three decades.Two major subgroups of the disorders are recognized: a restrictive form, in which food intake is severely limited (anorexia ...
Family-based treatment (FBT) has the highest level of evidence regarding efficacy in adolescents with eating disorders. The first randomized controlled trial of FBT, initially known as Maudsley ...
An eating disorder is a serious medical condition that affects physical and mental health. It is not a choice and can be life-threatening if left untreated. Common types of eating disorders include anorexia nervosa and bulimia nervosa. Binge eating disorder is the most common type of eating disorder in the United States.
According to the National Eating Disorders Association, 22% of children and adolescents around the world show symptoms of disordered eating, and eating disorders have the second-highest mortality ...
Classification. The Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) and the 11th revision of the International Classification of Diseases (ICD-11) define ED as persistent abnormal eating behaviors that significantly impair physical health or psychosocial functioning (1, 2).The diagnostic criteria and characteristics of the most common ED in the adolescent ...
Eating disorders affect almost 5% of the population worldwide. These disorders usually develop during adolescence but can develop in adulthood as well. Some disorders, such as anorexia nervosa ...

IMAGES
VIDEO
COMMENTS
TPC Min and Max settings are entered in dBm NOT Power level index. For this you will want to know the allowed powers for the AP model you are configuring. Power level index is a scale 1-8 from (1)Max to (8) Minimum power for the AP.
The maximum and minimum TPC power settings apply to all the access points through RF profiles in a RF network. To set the Maximum Power Level Assignment and Minimum Power Level Assignment, enter the maximum and minimum transmit power used by RRM in the fields in the Tx Power Control window. The range for these parameters is -10 to 30 dBm.
To set the Maximum Power Level Assignment and Minimum Power Level Assignment, ... If Dynamic Channel Assignment (DCA)/Transmit Power Control (TPC) is turned off on the RF group member, and auto is set on RF group leader, the channel or TX power on a member gets changed as per the algorithm that is run on the RF group leader. ... Check the Avoid ...
TPC adjusts the Tx power up or down to meet the required coverage level indicated by the TPC Threshold. In order to configure RRM to do the TPC calculations, you need to set the txPower assignment to global with the command config { 802.11a | 802.11b } txPower global auto .
TPC page also shows few non-configurable parameter settings. 1 Power Neighbor Count : The minimum number of neighbors an AP must have for TPC algorithm to run. 2.Power Assignment Leader: The IP Address of RF group leader, who is responsible for power level assignment. 3.Last Power Level Assignmnet: The last time RRM evaluated current TPC ...
The TPC parameters can be configured under the RRM tab of our RF profile. We can then amend the following configuration parameters: Maximum Power Level Assignment. Minimum Power Level Assignment. Power Threshold v1. Power Threshold v2. One of the functions that makes up the RRM operations is Transmit Power Control (TPC).
Though the maximum power level is configured in dBm, Cisco uses a series of numbers to represent levels of power. Phil Morgan of NC-Expert wrote an article titled WLC and AP Power settings in which he discusses Cisco power levels in further detail. In his article, he discusses how we can determine what the power levels represent as they vary by AP model, band (2.4 vs 5GHz), and even channel ...
Maximum and minimum settings for transmit power are available. The defaults are 30dBm for maximum power and -10dBm for minimum power. The power threshold is the minimum level at which you need to hear the third AP for the TPC algorithm to run. The default is -70dBm. You can set it higher or lower depending on your needs.
(Cisco Controller) > config 802.11b channel global auto. Auto Transmit Power Control. Description—Auto TPC should be enabled to allow RRM to select best transmit power for each radio. Clicking Fix it Now enables Auto TPC. The Cisco WLC dynamically controls the access point transmit power based on real-time wireless LAN conditions.
If the maximum power level assignment for global Transmit Power Control (TPC) for 802.11a/n/ac is configured to 10 dBm, then doubling the transmit power would require an increase of 3 dBm. A 3 dBm increase represents a doubling of the power level, so a power level of 13 dBm would effectively double the transmit power.
Note On a Cisco Nexus 5000 Series switch that runs Cisco NX-OS Release 4.2(2), you can configure the 8-Gbps administrative speed only on an M1060 switch module. You can configure the speed to 1 Gbps, 2 Gbps, or 4 Gbps on all switch modules on a Cisco Nexus 5000 Series switch that runs Cisco NX-OS Release 4.2(2) or earlier releases.
Power Supply Mode: Choose the appropriate power supply mode. ... one per syslog server. The minimum value is 0 and the maximum value is 7. To specify a higher severity, enter a higher number. ... (EVPN is disabled), at the fabric level, you can select the first hop redundancy protocol (FHRP) for host traffic to be either HSRP or VRRP. HSRP is ...
Navigate to LAN > Fabrics. From the Actions drop-down list, click Create Fabric. Enter a unique name for the fabric in the Fabric Name field, then click Choose Fabric. A list of all available fabric templates are listed. From the available list of fabric templates, choose the BGP Fabric template, then click Select.
Navigate to the LAN Fabrics page:. Manage > Fabrics. Click Actions > Create Fabric.. The Create Fabric window appears.. Enter a unique name for the fabric in the Fabric Name field, then click Choose Fabric.. A list of all available fabric templates are listed. From the available list of fabric templates, choose the Enhanced Classic LAN template, then click Select.
12 Maximum power level assignment Vs TX power levels Go to solution Majid Jalinousi Beginner Options 02-29-2016 09:35 PM - edited 07-05-2021 04:41 AM Hi, I want to know if I change maximum power level assignment, how it's gonna affect the TX power levels?... Tags RRM, TPC Controllers use the TPC (Tx Power Control) algorithm to determine whether the power of an AP needs to be adjusted down.