John Money Gender Experiment: Reimer Twins
Julia Simkus
Editor at Simply Psychology
BA (Hons) Psychology, Princeton University
Julia Simkus is a graduate of Princeton University with a Bachelor of Arts in Psychology. She is currently studying for a Master's Degree in Counseling for Mental Health and Wellness in September 2023. Julia's research has been published in peer reviewed journals.
Learn about our Editorial Process
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
The John Money Experiment involved David Reimer, a twin boy raised as a girl following a botched circumcision. Money asserted gender was primarily learned, not innate.
However, David struggled with his female identity and transitioned back to male in adolescence. The case challenged Money’s theory, highlighting the influence of biological sex on gender identity.
- David Reimer: David was born in 1965; he had a MZ twin brother. When he was 8 months old his penis was accidentally cut off during surgery.
- His parents contacted John Money, a psychologist who was developing a theory of gender neutrality. His theory claimed that a child would take the gender identity he/she was raised with rather than the gender identity corresponding to the biological sex.
- David’s parents brought him up as a girl and Money wrote extensively about this case claiming it supported his theory. However, Brenda as he was named was suffering from severe psychological and emotional difficulties and in her teens, when she found out what had happened, she reverted back to being a boy.
- This case study supports the influence of testosterone on gender development as it shows that David’s brain development was influenced by the presence of this hormone and its effects on gender identity was stronger that the influence of social factors.

What Did John Money Do To The Twins
David Reimer was an identical twin boy born in Canada in 1965. When he was 8 months old, his penis was irreparably damaged during a botched circumcision.
John Money, a psychologist from Johns Hopkins University, had a prominent reputation in the field of sexual development and gender identity.
David’s parents took David to see Dr. Money at Johns Hopkins Hospital in Baltimore where he advised that David be “sex reassigned” as a girl through surgical, hormonal, and psychological treatments.
John Money believed that gender identity is primarily learned through one’s upbringing (nurture) as opposed to one’s inborn traits (nature). He proposed that gender identity could be changed through behavioural interventions, and he advocated that gender reassignment was the solution for treating any child with intersex traits or atypical sex anatomies.
Dr. John Money argued that it’s possible to habilitate a baby with a defective penis more effectively as a girl than a boy.
At the age of 22 months, David underwent extensive surgery in which his testes and penis were surgically removed and rudimentary female genitals were constructed.
David’s parents raised him as a female and gave him the name Brenda (this name was chosen to be similar to his birth name, Bruce). David was given estrogen during adolescence to promote the development of breasts.
He was forced to wear dresses and was directed to engage in typical female norms, such as playing with dolls and mingling with other girls.
Throughout his childhood, David was never informed that he was biologically male and that he was an experimental subject in a controversial investigation to bolster Money’s belief in the theory of gender neutrality – that nurture, not nature, determines gender identity and sexual orientation.
David’s twin brother, Brian, served as the ideal control because the brothers had the same genetic makeup, but one was raised as a girl and the other as a boy. Money continued to see David and Brian for consultations and check ups annually.
During these check-ups, Money would force the twins to rehearse sexual acts and inspect one another’s genitals. On some occasions, Money would even photograph the twins doing these exercises. Money claimed that childhood sexual rehearsal play was important for healthy childhood sexual exploration.
David also recalls receiving anger and verbal abuse from Money if they resisted participation.
Money (1972) reported on Reimer’s progress as the “John/Joan case” to keep the identity of David anonymous. Money described David’s transition as successful.
He claimed that David behaved like a little girl and did not demonstrate any of the boyish mannerisms of his twin brother Brian. Money would publish this data to reinforce his theories on gender fluidity and to justify that gender identity is primarily learned.
In reality, though, David was never happy as a girl. He rejected his female identity and experienced severe gender dysphoria . He would complain to his parents and teachers that he felt like a boy and would refuse to wear dresses or play with dolls.
He was severely bullied in school and experienced suicidal depression throughout adolescence. Upon learning about the truth about his birth and sex of rearing from his father at the age of 15, David assumed a male gender identity, calling himself David.
David Reimer underwent treatments to reverse the assignment such as testosterone injections and surgeries to remove his breasts and reconstruct a penis.
David married a woman named Jane at 22 years and adopted three children.
Dr. Milton Diamond, a psychologist and sexologist at the University of Hawaii and a longtime academic rival of Money, met with David to discuss his story in the mid-1990s.
Diamond (1997) brought David’s experiences to international attention by reporting the true outcome of David’s case to prevent physicians from making similar decisions when treating other infants. Diamond helped debunk Money’s theory that gender identity could be completely learned through intervention.
David continued to suffer from psychological trauma throughout adulthood due to Money’s experiments and his harrowing childhood experiences. David endured unemployment, the death of his twin brother Brian, and marital difficulties.
At the age of thirty-eight, David committed suicide.
David’s case became the subject of multiple books, magazine articles, and documentaries. He brought to attention to the complications of gender identity and called into question the ethicality of sex reassignment of infants and children.
Originally, Money’s view of gender malleability dominated the field as his initial report on David was that the reassignment had been a success. However, this view was disproved once the truth about David came to light.
His case led to a decline in the number of sex reassignment surgeries for unambiguous XY male infants with a micropenis and other congenital malformations and brought into question the malleability of gender and sex.
At present, however, the clinical literature is still deeply divided on the best way to manage cases of intersex infants.
Colapinto, J. (2000). As nature made him: The boy who was raised as a girl. New York, NY: Harper Collins.
Colapinto, J. (2018). As nature made him: The boy who was raised as a girl. Langara College.
Diamond, M., & Sigmundson, H. K. (1997). Sex reassignment at birth: Long-term review and clinical implications . Archives of pediatrics & adolescent medicine, 151(3), 298-304.
Money, J., & Ehrhardt, A. A. (1972). Man & Woman, Boy & Girl : The Differentiation and Dimorphism of Gender Identity from Conception to Maturity. Baltimore, Maryland: Johns Hopkins University Press.
Money, J., & Tucker, P. (1975). Sexual signatures: On being a man or a woman.
Money, J. (1994). The concept of gender identity disorder in childhood and adolescence after 39 years . Journal of sex & marital therapy, 20(3), 163-177.
David Reimer and John Money Gender Reassignment Controversy: The John/Joan Case
In the mid-1960s, psychologist John Money encouraged the gender reassignment of David Reimer, who was born a biological male but suffered irreparable damage to his penis as an infant. Born in 1965 as Bruce Reimer, his penis was irreparably damaged during infancy due to a failed circumcision. After encouragement from Money, Reimer’s parents decided to raise Reimer as a girl. Reimer underwent surgery as an infant to construct rudimentary female genitals, and was given female hormones during puberty. During childhood, Reimer was never told he was biologically male and regularly visited Money, who tracked the progress of his gender reassignment. Reimer unknowingly acted as an experimental subject in Money’s controversial investigation, which he called the John/Joan case. The case provided results that were used to justify thousands of sex reassignment surgeries for cases of children with reproductive abnormalities. Despite his upbringing, Reimer rejected the female identity as a young teenager and began living as a male. He suffered severe depression throughout his life, which culminated in his suicide at thirty-eight years old. Reimer, and his public statements about the trauma of his transition, brought attention to gender identity and called into question the sex reassignment of infants and children.
Bruce Peter Reimer was born on 22 August 1965 in Winnipeg, Ontario, to Janet and Ron Reimer. At six months of age, both Reimer and his identical twin, Brian, were diagnosed with phimosis, a condition in which the foreskin of the penis cannot retract, inhibiting regular urination. On 27 April 1966, Reimer underwent circumcision, a common procedure in which a physician surgically removes the foreskin of the penis. Usually, physicians performing circumcisions use a scalpel or other sharp instrument to remove foreskin. However, Reimer’s physician used the unconventional technique of cauterization, or burning to cause tissue death. Reimer’s circumcision failed. Reimer’s brother did not undergo circumcision and his phimosis healed naturally. While the true extent of Reimer’s penile damage was unclear, the overwhelming majority of biographers and journalists maintained that it was either totally severed or otherwise damaged beyond the possibility of function.
In 1967, Reimer’s parents sought the help of John Money, a psychologist and sexologist who worked at the Johns Hopkins Hospital in Baltimore, Maryland. In the mid twentieth century, Money helped establish the views on the psychology of gender identities and roles. In his academic work, Money argued in favor of the increasingly mainstream idea that gender was a societal construct, malleable from an early age. He stated that being raised as a female was in Reimer’s interest, and recommended sexual reassignment surgery. At the time, infants born with abnormal or intersex genitalia commonly received such interventions.
Following their consultation with Money, Reimer’s parents decided to raise Reimer as a girl. Physicians at the Johns Hopkins Hospital removed Reimer’s testes and damaged penis, and constructed a vestigial vulvae and a vaginal canal in their place. The physicians also opened a small hole in Reimer’s lower abdomen for urination. Following his gender reassignment surgery, Reimer was given the first name Brenda, and his parents raised him as a girl. He received estrogen during adolescence to promote the development of breasts. Throughout his childhood, Reimer was not informed about his male biology.
Throughout his childhood, Reimer received annual checkups from Money. His twin brother was also part of Money’s research on sexual development and gender in children. As identical twins growing up in the same family, the Reimer brothers were what Money considered ideal case subjects for a psychology study on gender. Reimer was the first documented case of sex reassignment of a child born developmentally normal, while Reimer’s brother was a control subject who shared Reimer’s genetic makeup, intrauterine space, and household.
During the twin’s psychiatric visits with Money, and as part of his research, Reimer and his twin brother were directed to inspect one another’s genitals and engage in behavior resembling sexual intercourse. Reimer claimed that much of Money’s treatment involved the forced reenactment of sexual positions and motions with his brother. In some exercises, the brothers rehearsed missionary positions with thrusting motions, which Money justified as the rehearsal of healthy childhood sexual exploration. In his Rolling Stone interview, Reimer recalled that at least once, Money photographed those exercises. Money also made the brothers inspect one another’s pubic areas. Reimer stated that Money observed those exercises both alone and with as many as six colleagues. Reimer recounted anger and verbal abuse from Money if he or his brother resisted orders, in contrast to the calm and scientific demeanor Money presented to their parents. Reimer and his brother underwent Money’s treatments at preschool and grade school age. Money described Reimer’s transition as successful, and claimed that Reimer’s girlish behavior stood in stark contrast to his brother’s boyishness. Money reported on Reimer’s case as the John/Joan case, leaving out Reimer’s real name. For over a decade, Reimer and his brother unknowingly provided data that, according to biographers and the Intersex Society of North America, was used to reinforce Money’s theories on gender fluidity and provided justification for thousands of sex reassignment surgeries for children with abnormal genitals.
Contrary to Money’s notes, Reimer reports that as a child he experienced severe gender dysphoria, a condition in which someone experiences distress as a result of their assigned gender. Reimer reported that he did not identify as a girl and resented Money’s visits for treatment. At the age of thirteen, Reimer threatened to commit suicide if his parents took him to Money on the next annual visit. Bullied by peers in school for his masculine traits, Reimer claimed that despite receiving female hormones, wearing dresses, and having his interests directed toward typically female norms, he always felt that he was a boy. In 1980, at the age of fifteen, Reimer’s father told him the truth about his birth and the subsequent procedures. Following that revelation, Reimer assumed a male identity, taking the first name David. By age twenty-one, Reimer had received testosterone therapy and surgeries to remove his breasts and reconstruct a penis. He married Jane Fontaine, a single mother of three, on 22 September 1990.
In adulthood, Reimer reported that he suffered psychological trauma due to Money’s experiments, which Money had used to justify sexual reassignment surgery for children with intersex or damaged genitals since the 1970s. In the mid-1990s, Reimer met Milton Diamond, a psychologist at the University of Hawaii, in Honolulu, Hawaii, and academic rival of Money. Reimer participated in a follow-up study conducted by Diamond, in which Diamond cataloged the failures of Reimer’s transition.
In 1997, Reimer began speaking publicly about his experiences, beginning with his participation in Diamond’s study. Reimer’s first interview appeared in the December 1997 issue of Rolling Stone magazine. In interviews, and a later book about his experience, Reimer described his interactions with Money as torturous and abusive. Accordingly, Reimer claimed he developed a lifelong distrust of hospitals and medical professionals.
With those reports, Reimer caused a multifaceted controversy over Money’s methods, honesty in data reporting, and the general ethics of sex reassignment surgeries on infants and children. Reimer’s description of his childhood conflicted with the scientific consensus about sex reassignment at the time. According to NOVA, Money led scientists to believe that the John/Joan case demonstrated an unreservedly successful sex transition. Reimer’s parents later blamed Money’s methods and alleged surreptitiousness for the psychological illnesses of their sons, although the notes of a former graduate student in Money’s lab indicated that Reimer’s parents dishonestly represented the transition’s success to Money and his coworkers. Reimer was further alleged by supporters of Money to have incorrectly recalled the details of his treatment. On Reimer’s case, Money publicly dismissed his criticism as antifeminist and anti-trans bias, but, according to his colleagues, was personally ashamed of the failure.
In his early twenties, Reimer attempted to commit suicide twice. According to Reimer, his adult family life was strained by marital problems and employment difficulty. Reimer’s brother, who suffered from depression and schizophrenia, died from an antidepressant drug overdose in July of 2002. On 2 May 2004, Reimer’s wife told him that she wanted a divorce. Two days later, at the age of thirty-eight, Reimer committed suicide by firearm.
Reimer, Money, and the case became subjects of numerous books and documentaries following the exposé. Reimer also became somewhat iconic in popular culture, being directly referenced or alluded to in the television shows Chicago Hope , Law & Order , and Mental . The BBC series Horizon covered his story in two episodes, “The Boy Who Was Turned into a Girl” (2000) and “Dr. Money and the Boy with No Penis” (2004). Canadian rock group The Weakerthans wrote “Hymn of the Medical Oddity” about Reimer, and the New York-based Ensemble Studio Theatre production Boy was based on Reimer’s life.
- Carey, Benedict. “John William Money, 84, Sexual Identity Researcher, Dies.” New York Times , 11 July 2016.
- Colapinto, John. "The True Story of John/Joan." Rolling Stone 11 (1997): 54–73.
- Colapinto, John. As Nature Made Him: The Boy who was Raised as a Girl . New York: HarperCollins Publishers, 2000.
- Colapinto, John. "Gender Gap—What were the Real Reasons behind David Reimer’s Suicide." Slate (2004).
- Dr. Money and the Boy with No Penis , documentary, written by Sanjida O’Connell (BBC, 2004), Film.
- The Boy Who Was Turned Into a Girl , documentary, directed by Andrew Cohen (BBC, 2000.), Film.
- “Who was David Reimer (also, sadly, known as John/Joan)?” Intersex Society of North America . http://www.isna.org/faq/reimer (Accessed October 31, 2017).
How to cite
Articles rights and graphics.
Copyright Arizona Board of Regents Licensed as Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported (CC BY-NC-SA 3.0)
Last modified
Share this page.
- Share full article
Advertisement
Supported by
David Reimer, 38, Subject of the John/Joan Case
By The Associated Press
- May 12, 2004
Correction Appended
David Reimer, a man who was born a boy but raised as a girl in a famous medical experiment, only to reassert his male identity in the last 20 years of his life, died on May 4. He was 38. His family says he committed suicide.
Mr. Reimer shared his story about his life in the pages of a book and on Oprah Winfrey's television show.
His mother, Janet Reimer, said she believed that her son would still be alive had it not been for the devastating experiment, which led to much emotional hardship.
''He managed to have so much courage,'' she said Sunday. ''I think he felt he had no options. It just kept building up and building up.''
After a botched circumcision operation when he was a toddler, David Reimer became the subject of a study that became known as the John/Joan case in the 60's and 70's. His mother said she was still angry with the Baltimore doctor who persuaded her and her husband, Ron, to give female hormones to their son and raise him as a daughter.
As he grew up as Brenda in Winnipeg, he faced cruelty from the other children. ''They wouldn't let him use the boys' washroom or the girls','' Ms. Reimer recalled. ''He had to go in the back alley.''
His sexual reassignment was then widely reported as a success and proof that children are not by nature feminine or masculine but through nurture are socialized to become girls or boys. David's identical twin brother, Brian, offered researchers a matched control subject.
But when, as a teenager, he discovered the truth about his past , he resumed his male identity, eventually marrying and becoming a stepfather to three children.
In 2000, John Colapinto wrote ''As Nature Made Him: The Boy Who Was Raised as a Girl,'' providing David an opportunity to tell his story. He wanted to save other children from a similar fate, his mother said.
While he had spoken anonymously in the past, he entered the public eye after the book was published, beginning with an appearance on ''Oprah'' in February 2000.
His mother said he had recently become depressed after losing his job and separating from his wife. He was also still grieving over the death of his twin brother two years earlier, she said.
Correction: May 18, 2004, Tuesday Because of an editing error, an erroneous credit appeared on Wednesday on the obituary of David Reimer, who was reared as a girl after botched surgery in a famous medical experiment but reclaimed his male identity. It was by The Canadian Press, not The Associated Press.

A Boy Raised as a Girl Killed Himself 19 Years Ago Today
Upbringing has limited power to impose gender identity..
Posted May 5, 2023 | Reviewed by Tyler Woods
- An experiment was performed on an unknowing child by raising him as a girl, following his botched circumcision, with disastrous results.
- Western society is often cruel to children with atypical genitals, but genital surgery on infants—without their consent—is not justified.
- Societal acceptance of the real nuances of sex and gender would be a better approach to infants who have ambiguous or atypical genitals.
Today, May 5 th , is the 19 th anniversary of David Reimer’s suicide .
Raising a child with atypical genitals
David, born Bruce, lost his penis to a botched circumcision as an infant in 1966. After this event, his parents, Janet and Ron, though they lived in Canada, were referred to the leading “sexologist” at the time, John Money. Money was a psychologist who ran a clinic at Johns Hopkins University, where surgeons performed pediatric genital constructions. Genitals, then and now, are what we rely on to define an infant’s sex . It’s easier to "make a hole" than to "build a pole,” as one surgeon put it, so Money advised that Bruce be castrated and have his genitals modified to look as typically female as possible, then be raised as a girl, while keeping the real story secret.
Money hypothesized that a consistent and unambiguous upbringing as either a boy or a girl is sufficient to impart a clear gender identity to the child. He felt that such an upbringing is necessary for a child’s well-being, given how poorly other children and Western society generally treat children of ambiguous sex, including intersex children. The Reimers took Money’s advice, renamed their child Brenda, dressed Brenda in typical girl’s clothing, encouraged Brenda to participate in traditionally feminine activities, and so on, while visiting Money’s clinic annually for psychological check-ups and progress reports.
The perfect case study
Meanwhile, Money regularly published research reports about Brenda and spoke about the case (without identifying information) at seminars and conferences. Money saw this case as an ideal test of his hypothesis about the potency of consistent and unambiguous gender-specific upbringing, for two reasons.
First, unlike the intersex infants that Money’s clinic typically treated, there was no ambiguity or mismatch in this child’s genetic or hormonal makeup. Bruce/Brenda had typical male chromosomes— XY —and had experienced typical male prenatal hormones from the fetal testes— testosterone and other androgens—“male sex hormones.” So if Brenda became a happy and typical girl, this would mean that upbringing was key to gender identity , trumping chromosomes and prenatal hormones, even for infants who were unambiguously of the opposite sex biologically.
Second, Bruce/Brenda had an identical twin, Brian, who avoided a similar fate just by chance, having been the second in line for circumcision. The existence of a perfectly matched control child made the case study even more compelling.
Tragic consequences
Money always portrayed this case as an unadulterated success, but it was not. Despite the best efforts of Janet and Ron to bring up Brenda as a typical girl, Brenda never felt comfortable in this gender role and suffered greatly in childhood trying to act like a typical girl, especially in school. The situation got worse and worse until Ron finally told 14-year-old Brenda what had really happened. Brenda immediately asserted a masculine identity and became David.
David felt much more comfortable as a boy and later a man. He married a woman and became stepfather to her children. But he was always haunted by his horrific childhood. This reached a crescendo on May 5 th , 2004, soon after his wife said she was leaving him and two years after his twin, Brian, died of a drug overdose. David shot and killed himself that day .
Although Money never admitted failure in this case, the truth was eventually revealed in research articles by other scientists and physicians, notably Milton Diamond , and in an exposé by journalist John Colapinto in Rolling Stone magazine and later in a book, As Nature Made Him: The Boy Who was Raised as a Girl.
One obvious lesson from David Reimer’s story is that gender identity cannot be imposed by upbringing alone. Genes and prenatal hormones do matter.
Another lesson—perhaps less obvious—is that nuances of sex and gender exist, and if we ignore them, this can endanger those who do not fit neatly into a male or female box.
In some ways, John Money knew this very well. Money was well aware that biological sex characteristics, including chromosomes, gonads, hormones, hormone receptors, and genitals, can be a mixture of typically male and typically female, or be intermediate between them, as his practice focused on such intersex children . Money also opened the first gender identity clinic in the U.S. in 1965, where he and colleagues helped transgender (then called transexual) adults with hormones and surgery to adjust their biological traits to match their gender identity. And although treating intersex infants with surgery and hormones should have been regarded quite differently than treating adults—because infants can’t consent to such treatments—Money was aware that intersex children could grow up to be well-adjusted adults even without surgery, because that had been the subject of his own Ph.D. dissertation. But Money was also aware that Western society is cruel to children with ambiguous genitals. Ultimately, he apparently felt that avoiding society’s cruelties outweighed the possible negative consequences of infant genital surgeries.

Thus, although it would be easy to view Money simply as the villain of this story, we might take a more nuanced view of him as well and recognize that he had some good intentions to help people with ambiguous sex and/or gender characteristics, though the consequences of his actions were nonetheless tragic for David Reimer, as well as for many intersex children.
Colapinto, J. (2000). As Nature Made Him: The Boy Who was Raised as a Girl. New York, NY: Harper Perennial.
Fausto-Sterling, A. (2000). Sexing the Body: Gender Politics and the Construction of Sexuality. New York, NY: Basic Books.
Karkazis, K. (2008) Fixing Sex: Intersex, Medical Authority, and Lived Experience. Durham, NC: Duke University Press.
Kessler, S. J. (1998) Lessons from the Intersexed. New Brunswick, NJ: Rutgers University Press.

Ari Berkowitz, Ph.D., is a Presidential Professor of Biology at the University of Oklahoma and author of Governing Behavior.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
David Reimer, 38; After Botched Surgery, He Was Raised as a Girl in Gender Experiment
- Show more sharing options
- Copy Link URL Copied!
David Reimer, the Canadian man raised as a girl for most of the first 14 years of his life in a highly touted medical experiment that seemed to resolve the debate over the cultural and biological determinants of gender, has died at 38. He committed suicide May 4 in his hometown of Winnipeg, Canada.
At 8 months of age, Reimer became the unwitting subject of “sex reassignment,” a treatment method embraced by his parents after his penis was all but obliterated during a botched circumcision. The American doctor whose advice they sought recommended that their son be castrated, given hormone treatments and raised as a girl. The physician, Dr. John Money, supervised the case for several years and eventually wrote a paper declaring the success of the gender conversion.
For the record:
12:00 a.m. May 15, 2004 For The Record Los Angeles Times Saturday May 15, 2004 Home Edition Main News Part A Page 2 National Desk 0 inches; 25 words Type of Material: Correction Reimer obituary -- The obituary of David Reimer in Thursday’s California section said the doctor who botched Reimer’s circumcision was female. The doctor was male.
Known as the “John/Joan” case, it was widely publicized and gave credence to arguments presented in the 1970s by feminists and others that humans are sexually neutral at birth and that sex roles are largely the product of social conditioning.
But, in fact, the gender conversion was far from successful. Money’s experiment was a disaster for Reimer that created psychological scars he ultimately could not overcome.
Reimer’s story was told in the 2000 book “As Nature Made Him,” by journalist John Colapinto. Reimer said he cooperated with Colapinto in the hope that other children could be spared the miseries he experienced.
Reimer was born on Aug. 22, 1965, 12 minutes before his identical twin brother. His working-class parents named him Bruce and his brother Brian. Both babies were healthy and developed normally until they were seven months old, when they were discovered to have a condition called phimosis, a defect in the foreskin of the penis that makes urination difficult.
The Reimers were told that the problem was easily remedied with circumcision. During the procedure at the hospital, a doctor who did not usually perform such operations was assigned to the Reimer babies. She chose to use an electric cautery machine with a sharp cutting needle to sever the foreskin.
But something went terribly awry. Exactly where the error lay -- in the machine, or in the user -- was never determined. What quickly became clear was that baby Bruce had been irreparably maimed.
(The doctors decided not to try the operation on his brother Brian, whose phimosis later disappeared without treatment.)
The Reimers were distraught. Told that phallic reconstruction was a crude option that would never result in a fully functioning organ, they were without hope until one Sunday evening after the twins’ first birthday when they happened to tune in to an interview with Money on a television talk show. He was describing his successes at Johns Hopkins University in changing the sex of babies born with incomplete or ambiguous genitalia.
He said that through surgeries and hormone treatments he could turn a child into whichever sex seemed most appropriate, and that such reassignments were resulting in happy, healthy children.
Money, a Harvard-educated native of New Zealand, had already established a reputation as one of the world’s leading sex researchers, known for his brilliance and his arrogance. He was credited with coining the term “gender identity” to describe a person’s innate sense of maleness or femaleness.
The Reimers went to see Money, who with unwavering confidence told them that raising Bruce as a girl was the best course, and that they should never say a word to the child about ever having been a boy.
About six weeks before his second birthday, Bruce became Brenda on an operating table at Johns Hopkins. After bringing the toddler home, the Reimers began dressing her like a girl and giving her dolls.
She was, on the surface, an appealing little girl, with round cheeks, curly locks and large, brown eyes. But Brenda rebelled at her imposed identity from the start. She tried to rip off the first dress that her mother sewed for her. When she saw her father shaving, she wanted a razor, too. She favored toy guns and trucks over sewing machines and Barbies. When she fought with her brother, it was clear that she was the stronger of the two. “I recognized Brenda as my sister,” Brian was quoted as saying in the Colapinto book. “But she never, ever acted the part.”
Money continued to perform annual checkups on Brenda, and despite the signs that Brenda was rejecting her feminized self, Money insisted that continuing on the path to womanhood was the proper course for her.
In 1972, when Brenda was 7, Money touted his success with her gender conversion in a speech to the American Assn. for the Advancement of Science in Washington, D.C., and in the book, “Man & Woman, Boy & Girl,” released the same day. The scientists in attendance recognized the significance of the case as readily as Money had years earlier. Because Brenda had an identical male twin, they offered the perfect test of the theory that gender is learned, not inborn.
Money already was the darling of radical feminists such as Kate Millett, who in her bestselling “Sexual Politics” two years earlier had cited Money’s writings from the 1950s as proof that “psychosexual personality is therefore postnatal and learned.”
Now his “success” was written up in Time magazine, which, in reporting on his speech, wrote that Money’s research provided “strong support for a major contention of women’s liberationists: that conventional patterns of masculine and feminine behavior can be altered.” In other words, nurture had trumped nature.
The Reimer case quickly was written into textbooks on pediatrics, psychiatry and sexuality as evidence that anatomy was not destiny, that sexual identity was far more malleable than anyone had thought possible. Money’s claims provided powerful support for those seeking medical or social remedies for gender-based ills.
What went unreported until decades later, however, was that Money’s experiment actually proved the opposite -- the immutability of one’s inborn sense of gender.
Money stopped commenting publicly on the case in 1980 and never acknowledged that the experiment was anything but a glowing success. Dr. Milton Diamond, a sexologist at the University of Hawaii at Manoa, had long been suspicious of Money’s claims. He was finally able to locate Reimer through a Canadian psychiatrist who had seen Reimer as a patient.
In an article published in the Archives of Pediatric and Adolescent Medicine in 1997, Diamond and the psychiatrist, Dr. H. Keith Sigmundson, showed how Brenda had steadily rejected her reassignment from male to female. In early adolescence, she refused to continue receiving the estrogen treatments that had helped her grow breasts. She stopped seeing Money. Finally, at 14, she refused to continue living as a girl.
When she confronted her father, he broke down in tears and told her what had happened shortly after her birth. Instead of being angry, Brenda was relieved. “For the first time everything made sense,” the article by Diamond and Sigmundson quoted her as saying, “and I understood who and what I was.”
She decided to reclaim the identity she was born with by taking male hormone shots and undergoing a double mastectomy and operations to build a penis with skin grafts. She changed her name to David, identifying with the Biblical David who fought Goliath. “It reminded me,” David told Colapinto, “of courage.”
David developed into a muscular, handsome young man. But the grueling surgeries spun him into periods of depression and twice caused him to attempt suicide. He spent months living alone in a cabin in the woods. At 22, he prayed to God for the first time in his life, begging for the chance to be a husband and father.
When he was 25, he married a woman and adopted her three children. Diamond reported that while the phallic reconstruction was only partially successful, David could have sexual intercourse and experience orgasm. He worked in a slaughterhouse and said he was happily adjusted to life as a man.
In interviews for Colapinto’s book, however, he acknowledged a deep well of wrenching anger that would never go away.
“You can never escape the past,” he told the Seattle Post-Intelligencer in 2000. “I had parts of my body cut away and thrown in a wastepaper basket. I’ve had my mind ripped away.”
His life began to unravel with the suicide of his brother two years ago. Brian Reimer had been treated for schizophrenia and took his life by overdosing on drugs. David visited his brother’s grave every day. He lost his job, separated from his wife and was deeply in debt after a failed investment.
He is survived by his wife, Jane; his parents, and his children.
Despite the hardships he experienced, he said he did not blame his parents for their decision to raise him as a girl. As he told Colapinto, “Mom and Dad wanted this to work so I’d be happy. That’s every parent’s dream for their child. But I couldn’t be happy for my parents. I had to be happy for me. You can’t be something that you’re not. You have to be you.”

Elaine Woo is a Los Angeles native who has written for her hometown paper since 1983. She covered public education and filled a variety of editing assignments before joining “the dead beat” – news obituaries – where she has produced artful pieces on celebrated local, national and international figures, including Norman Mailer, Julia Child and Rosa Parks. She left The Times in 2015.
More From the Los Angeles Times

Science & Medicine
Canny as a crocodile but dumber than a baboon — new research ponders T. rex’s brain power
April 29, 2024

Climate & Environment
You’re gonna need a bigger number: Scientists consider a Category 6 for mega-hurricane era
April 26, 2024

Opinion: America’s ‘big glass’ dominance hangs on the fate of two powerful new telescopes
April 25, 2024

Mosquito season is upon us. So why are Southern California officials releasing more of them?
- Skip to main content
- Keyboard shortcuts for audio player
All Things Considered
- Latest Show
- Consider This Podcast
- About The Program
- Contact The Program
- Corrections
Remembering David Reimer
Melissa Block
NPR's Melissa Block talks with John Colapinto, author of As Nature Made Him: The Boy Who Was Raised as a Girl , about David Reimer, who killed himself at the age of 38 years on May 4. Reimer had become a focus in the "nature vs. nurture" debate after he was raised as a girl, along with his identical twin brother. But, Reimer later in life decided to live as a boy. He decided to go public after the publishing of the book in an effort to reverse the findings of the study.
Critical Essays on John Money’s Diagnostic Concepts
Lisa Downing , Iain Morland , and Nikki Sullivan
224 pages | 2 halftones, 1 table | 6 x 9 | © 2014
Gay and Lesbian Studies
Gender and Sexuality
History: History of Ideas
History of Science
Psychology: Experimental, Comparative, and Physiological Psychology
- Table of contents
- Author Events
Related Titles
“In Fuckology , Downing and co-authors capture Money’s story ably.”
New Scientist
“Downing, Morland, and Sullivan provide a critical exposition of John Money’s extensive oeuvre, introducing original, and illuminative debates regarding the historical context and intellectual stimuli behind his work whilst conjointly—in their own words—‘fucking with’ Money’s frequently destructive dogma. . . . The authors competently elucidate the nuances of Money’s expansive and controversial career and make use of the ‘plasticity’ of his arguments to narrativise conflicts which were fundamental to his, and others’, conceptualizations of the moral, humanist, and medical implications of coining diagnostic concepts relating to sex, as well as the resulting implementation of behavioral, juridical, and surgical responses. This will be hugely beneficial to scholars of medicine and further afield, medical practitioners, and to academics and postgraduates with interests in gender, sex and sexuality.”
Journal of Gender Studies
“ Fuckology is a groundbreaking intervention. The authors not only historicize Money’s diagnostic categories but also rethink his impact on contemporary understandings of sex, gender, and sexuality writ large. Moreover, Downing, Morland, and Sullivan develop unique interdisciplinary insights that only a theoretical humanities-based collaborative inquiry into the biopolitics and bioethics of the human sciences can offer. . . . Fuckology provides vital critical tools for rethinking the legacies of sexology as they crystallize and come undone in the present.”
“John Money’s influential and controversial career has never received the careful, critical, and nuanced attention it deserves—until now. Coauthors Downing, Morland, and Sullivan bring three very different forms of expertise to bear on Money’s work and its legacy, in a study that should be of interest to scholars of medicine and sexuality alike.”
Susan Stryker | University of Arizona
“One of the most prominent and prolific sexologists of the second half of the twentieth century, John Money coined the term “gender” and pioneered the use of surgical procedures to treat intersex and transgender subjects. In this timely and important critical reassessment of Money’s work, Downing, Morland, and Sullivan lay bare the inconsistencies and assumptions embedded in his conceptualisation of sex. The title of the book derives from Money’s own term for his particular brand of sexology while also, as the authors astutely point out, providing the critical tools with which to fuck with sexology itself.”
Elizabeth Stephens | University of Queensland
“This book makes a unique and exciting contribution to the field, examining in detail Money’s work on the concepts of ‘hermaphroditism’, ‘transsexualism’, and ‘paraphilia.’ It is a well-founded critique that goes to the heart of sexological research methodology and its underpinning assumptions. This work is queer, critical, historically astute, and politically engaged—offering an analysis that many of us have been looking forward to, and that will certainly contribute to our work.”
Katrina Roen | University of Oslo
“What this collection of critical essays does best is paint a convincing portrait of the contradictions riddling Money’s arguments. . . I suspect that few of us would come out smelling entirely of intellectual roses if our lifework were put under the microscope as Money’s has been here, but Fuckology unravels something deeper and more worrisome than the average scholarly waffling. Money suffered the pathology of rigid certainty; his ego refused to bend to conflicting data. . . Fuckology is a revealing look at a deliberately complex mind.”
Journal of Sex & Marital Therapy
“In their piercing, sophisticated, and well-researched book Fuckology , coauthors Downing, Morland and Sullivan bring nuance to these interpretations of Money’s work in sexology. This long-overdue critical reanalysis of John Money and his contributions embraces, rather than discounts, the tensions, complexities, and contradictions throughout Money’s scholarly corpus. . . . An honest reading of Money, whose diffuse body of work is fraught with rifts and contradictions, demands a multi-faceted analysis. Downing, Morland and Sullivan’s success in producing such an analysis renders the book pertinent to categories of scholars as disparate and varied as Money’s own oeuvre: historians, scholars of gender and sexuality studies, sexologists, ethicists and others will all find relevant insights in this compelling new book.”
Sexualities
“We see here critical sexuality studies confronting the work of the most influential of modern sexologists, John Money. The point is not to dismiss sexology – that has been done too often and too quickly in queer studies – but to engage with it in a sustained, scholarly manner. Downing, Morland, and Sullivan do that admirably, identifying the casual contradictions and unpacking the constitutive tensions in Money’s thinking.”
Peter Cryle | University of Queensland
Table of Contents
The two-parent privilege.
Melissa S. Kearney
Touchy Subject
Lauren Bialystok
Sentimental Savants
Meghan K. Roberts
The Book of Minor Perverts
Benjamin Kahan
Be the first to know
Get the latest updates on new releases, special offers, and media highlights when you subscribe to our email lists!
Sign up here for updates about the Press
- Newsletters
- Account Activating this button will toggle the display of additional content Account Sign out
What were the real reasons behind David Reimer’s suicide?
Just shy of a month ago, I got a call from David Reimer’s father telling me that David had taken his own life. I was shocked, but I cannot say I was surprised. Anyone familiar with David’s life—as a baby, after a botched circumcision, he underwent an operation to change him from boy to girl—would have understood that the real mystery was how he managed to stay alive for 38 years, given the physical and mental torments he suffered in childhood and that haunted him the rest of his life. I’d argue that a less courageous person than David would have put an end to things long ago.
After David’s suicide, press reports cited an array of reasons for his despair: bad investments, marital problems, his brother’s death two years earlier. Surprisingly little emphasis was given to the extraordinary circumstances of his upbringing. This was unfortunate because to understand David’s suicide, you first need to know his anguished history, which I chronicled in my book As Nature Made Him:The Boy Who Was Raised As a Girl .
David Reimer was one of the most famous patients in the annals of medicine. Born in 1965 in Winnipeg, he was 8 months old when a doctor used an electrocautery needle, instead of a scalpel, to excise his foreskin during a routine circumcision, burning off his entire penis as a result. David’s parents (farm kids barely out of their teens) were referred to Johns Hopkins Hospital in Baltimore, home of the world’s leading expert in gender identity, psychologist Dr. John Money, who recommended a surgical sex change, from male to female. David’s parents eventually agreed to the radical procedure, believing Dr. Money’s claims that this was their sole hope for raising a child who could have heterosexual intercourse—albeit as a sterile woman with a synthetic vagina and a body feminized with estrogen supplements.
For Dr. Money, David was the ultimate experiment to prove that nurture, not nature, determines gender identity and sexual orientation—an experiment all the more irresistible because David was an identical twin. His brother, Brian, would provide the perfect matched control, a genetic clone raised as a boy.
David’s infant “sex reassignment” was the first ever conducted on a developmentally normal child. (Money had helped to pioneer the procedure in hermaphrodites.) And according to Money’s published reports through the 1970s, the experiment was a success. The twins were happy in their assigned roles: Brian a rough and tumble boy, his sister Brenda a happy little girl. Money was featured in Time magazine and included a chapter on the twins in his famous textbook Man & Woman, Boy & Girl .
The reality was far more complicated. At age 2, Brenda angrily tore off her dresses. She refused to play with dolls and would beat up her brother and seize his toy cars and guns. In school, she was relentlessly teased for her masculine gait, tastes, and behaviors. She complained to her parents and teachers that she felt like a boy; the adults—on Dr. Money’s strict orders of secrecy—insisted that she was only going through a phase. Meanwhile, Brenda’s guilt-ridden mother attempted suicide; her father lapsed into mute alcoholism; the neglected Brian eventually descended into drug use, pretty crime, and clinical depression.
When Brenda was 14, a local psychiatrist convinced her parents that their daughter must be told the truth. David later said about the revelation: “Suddenly it all made sense why I felt the way I did. I wasn’t some sort of weirdo. I wasn’t crazy.”
David soon embarked on the painful process of converting back to his biological sex. A double mastectomy removed the breasts that had grown as a result of estrogen therapy; multiple operations, involving grafts and plastic prosthesis, created an artificial penis and testicles. Regular testosterone injections masculinized his musculature. Yet David was depressed over what he believed was the impossibility of his ever marrying. He twice attempted suicide in his early 20s.
David did eventually marry a big-hearted woman named Jane, but his dark moods persisted. He was plagued by shaming memories of the frightening annual visits to Dr. Money, who used pictures of naked adults to “reinforce” Brenda’s gender identity and who pressed her to have further surgery on her “vagina.”
When David was almost 30, he met Dr. Milton Diamond, a psychologist at the University of Hawaii and a longtime rival of Dr. Money. A biologist by training, Diamond had always been curious about the fate of the famous twin, especially after Money mysteriously stopped publishing follow-ups in the late 1970s. Through Diamond, David learned that the supposed success of his sex reassignment had been used to legitimize the widespread use of infant sex change in cases of hermaphroditism and genital injury. Outraged, David agreed to participate in a follow-up by Dr. Diamond, whose myth-shattering paper (co-authored by Dr. Keith Sigmundson) was published in Archives of Pediatrics and Adolescent Medicine in March 1997 and was featured on front pages across the globe.
I met David soon after, when he agreed to be interviewed by me for a feature story in Rolling Stone. He subsequently agreed to collaborate with me on a book about his life, As Nature Made Him , published in February 2000. In the course of our interviews, David told me that he could never forget his nightmare childhood, and he sometimes hinted that he was living on borrowed time.
Most suicides, experts say, have multiple motives, which come together in a perfect storm of misery. So it was with David. After his twin Brian died of an overdose of antidepressants in the spring of 2002, David sank into a depression. Though the two had been estranged, David had, in recent months, taken to visiting Brian’s grave, leaving flowers and, at some point prior to his own suicide, a note.
David also had marital difficulties. He was not easy to live with, given his explosive anger, his cyclical depressions, his fears of abandonment—all of which Jane weathered for almost 14 years. But with David spiraling ever deeper into sloth and despair, she told him on the weekend of May 2 that they should separate for a time. David stormed out of the house. Two days later, Jane received a call from the police, saying that they had found David but that he did not want her to know his location. Two hours after that, Jane got another call. This time the police told her that David was dead.
Genetics almost certainly contributed to David’s suicide. His mother has been a clinical depressive all her life; his brother suffered from the same disease. How much of the Reimers’ misery was due to inherited depression, and how much to the nightmare circumstances into which they had been thrown? David’s mutilation and his parents’ guilt were tightly entwined, multiplying the mental anguish to which the family members were already prone.
In some press reports, financial problems were given as the sole motive in David’s suicide. While this is absurdly reductive, it is true that last fall David learned that he was the victim of an alleged con man who had hoodwinked him out of $65,000—a loss that ate at him and no doubt contributed to his despair.
In his final months, David was unemployed—for him, a disastrous circumstance. When I first met him, seven years ago, he was a janitor in a slaughter house—tough, physically demanding work that he loved. But when the plant closed a few years ago, David never found another full-time job. And thanks to me, he didn’t have to. I split all profits from the book with David, 50-50. This brought him a substantial amount of money, as did a subsequent movie deal with Peter Jackson, the director of the Lord of the Rings trilogy. With no compelling financial need to work, David was able to sit around his house and brood—a state of affairs for which I feel some guilt.
In the end, of course, it was what David was inclined to brood about that killed him. David’s blighted childhood was never far from his mind. Just before he died, he talked to his wife about his sexual “inadequacy,” his inability to be a true husband. Jane tried to reassure him. But David was already heading for the door.
On the morning of May 5, he retrieved a shotgun from his home while Jane was at work and took it into the garage. There, with the terrible, methodical fixedness of the suicide, he sawed off the barrel. Then he drove to the nearby parking lot of a grocery store, parked, raised the gun, and, I hope, ended his sufferings forever.
Title: David Reimer's Legacy: Limiting parental discretion
Authors: Hazel Glenn Beh and Milton Diamond Ph.D.
Published in: Cardozo Journal of Law & Gender . Vol. 12:(1):5-30, 2005
Hazel Glenn Beh, Ph.D., J.D., Wm. S. Richardson School of Law, University of Hawai‘i and Milton Diamond, Ph.D., John A. Burns School of Medicine, University of Hawai‘i. Support for Milton Diamond’s work comes from the Eugene Garfield Foundation, Philadelphia, Pennsylvania.
I. Introduction
- II. Intersexuality
A. David Reimer and the Failure of Surgical Sex Assignment
B. the traditional approach: fear and the allure of the quick fix, c. the current debate: moratorium or improved informed consent, a. surgery merely to normalize genitalia poses substantial risks of harm without evidence of benefits, b. consent to genital surgery exceeds the limits of parental authority to make medical decisions for their children.
- V. Supporting Parents in Raising Healthy Children
- VI. Conclusion
In this essay, the authors examine parental decision-making and challenge parental authority to consent to infant surgery to “normalize” ambiguous genitalia of intersexed infants. The authors contend that consent to sex assignment and genital normalizing surgery in particular exceeds parental authority because it unnecessarily forecloses the child’s right to an open future. Moreover, conflicted by their own anxieties, guilt, shame, or repugnance, parents may not be able to act solely in their child’s best interest. Making matters worse, the lack of adequate long-term follow-up studies as well as clinical experience suggests that parents often decide with incomplete information about surgical outcomes and the psychosocial adjustment of intersex individuals who have not had surgery. This article is not intended as criticism of parents for past decisions, but rather to encourage parents now making medical decisions not to yield to unwarranted fears about their child’s future. The increasing activism of the intersex community, the extraordinary resources available on the internet, and a growing body of evidence suggests that genitalia are of little consequence to gender identity, and this knowledge should empower parents to resist what has been characterized as a “monster approach” to treating ambiguous genitalia. The law has a role to play in diffusing the terror, and in supporting parents who are faced with the prospect of raising children with genitalia that fall outside of the “normal” standards, the narrow limits of which are imposed and perpetuated by intolerance.
Accounts from parents of children with ambiguous genitalia reported in recent news articles about intersex surgery illustrate the nature of their concerns regarding their children’s future:
My problem is the adolescent period … Growing up a teenage girl is hard enough. I never want her to feel different. I never want her to have extra issues to deal with. … When she’s a teenager, and she’s in a girl’s locker room, it’s not going to be a cute situation Society is a big issue here. I tell my husband, if we lived on a deserted island she’d never need this. 1 It’s hard for a parent not to think of the psychological damage. 2 You’re the parent, you make the decisions … We felt this needed to be done right now. 3 The doctor said that the surgery preserves the blood supply and the nerves, so she will be able to have an orgasm. Anita [the mother] wondered whether, even if [her daughter] Emma’s responsiveness is reduced, she would be able to tell the difference. Wouldn’t it be more difficult to have a sensitive but “weird” set of genitals, which might make it too embarrassing to wear a bathing suit, let alone be naked with another person? 4 In an ideal world, I would do what is medically necessary and leave her alone. And she would be absolutely accepted for who she is, the special person she will be. … But that’s not the way our world works. 5
These quotes illustrate how parental fear that their child will endure a blighted childhood and adolescence overwhelms parents and leads them to consent to surgery on their intersex infants despite increasing evidence that cosmetic surgery on intersex infants may be unwarranted and improvident. Pressured and isolated in a medical quandary, these parents are discouraged by the prospect that their children might be reviled and rejected during their formative childhood and teen years, and want to spare them such pain. They are convinced that a cosmetic “fix” is preferable to a later locker room revelation that their child has ambiguous genitals, even if a satisfactory psychological and physical outcome cannot be assured.
The following quote, taken from a respected medical text published in 1969, reveals how physicians viewed the fate of intersex infants:
One of the few fundamental aspects of life is that of sex. Its normal functioning is vital to the survival of our race, essential for our full assimilation as individuals into society, and pervades every aspect of our lives. To visualize individuals who properly belong neither to one sex nor to the other is to imagine freaks, misfits, curiosities, rejected by society and condemned to a solitary existence of neglect and frustration. Few of these unfortunate people meet with tolerance and understanding from their fellows and fewer still find even limited acceptance in a small section of society: all are constantly confronted with reminders of their unhappy situation. The tragedy of their lives is the greater since it may be remediable; with suitable management and treatment, especially if this is begun soon after birth, many of these people can be helped to live happy well adjusted lives, and some may even be fertile and be enabled to enjoy a normal family life. 6
Thus, physicians since the latter half of the twentieth century have persuaded parents to embrace a surgical solution to intersexuality by fueling parental fears that their infant would otherwise be doomed to a freakish future.
The story of David Reimer, now with its very sad postscript, 7 has been extensively discussed in medical literature and elsewhere 8 since his story was published as Sex Reassignment at Birth: Long Term Review and Clinical Implications in the Archives of Pediatric and Adolescent Medicine in 1997. 9 There, and subsequently, Diamond and others have challenged the premise that surgical sex assignment and other cosmetic genital surgery on intersexed infants and children is clinically appropriate 10
David’s death should serve as a reminder and a warning to those involved in the issue of surgical treatment of infants that the problem here is not merely an intellectual debate over the use of an experimental procedure; many people have been and continue to be affected by these decisions. 11 After David’s suicide, John Colapinto, the author who collaborated with David to write As Nature Made Him reflected on his death. 12 While acknowledging David had “multiple motives” for suicide, Colapinto wrote: “[I]n the end, of course, it was what David was inclined to brood about that killed him. David’s blighted childhood was never far from his mind.” 13
This article pays tribute to David Reimer by questioning parental authority to consent to surgical interventions. Both children and parents will be best served if treatment decisions preserve the child’s bodily integrity, autonomy, and open future. The authors acknowledge that raising a child with nonconforming genitalia may challenge parents, but these children are not freaks or monsters, and need not be perceived as such. 14 To be sure, society’s narrow construction of gender tormented David throughout his life. When he was an infant, without a penis, it led his loving but distressed parents to consent to radical surgery to turn him into a girl. When he was a girl, his classmates relentlessly ridiculed him because he acted like the boy he was, and school officials failed to protect him. As a young adult, when David reclaimed his male identity and briefly became a cause célèbre, he still could not move beyond what had been done to him and how he then saw himself. However, what truly tortured David throughout his life was not the loss of his penis but the imposition of surgical and social interventions that made him someone he was not and did not want to be. David reflected,
If I had grown up as a boy without a penis? Oh, I would still have had my problems, but they wouldn’t have been compounded. … I would have been way better off if they had just left me alone, because when I switched back over, then I had two problems on my hands, not just one, because of them trying to brainwash me into accepting myself as a girl. 15
How is it that the repugnance associated with ambiguous genitalia is so great that caring physicians advise, and good, loving parents consent to radical surgery on infants? Alice Dreger characterized the current response to such intersex conditions as the “monster” ethics approach: 16 “Unfortunately, the present treatment of intersexuality in the U.S. seems to be deeply informed by the monster approach; ethical guidelines that would be applied in nearly any other medical intervention are, in cases of intersexuality, ignored.” 17 Monster ethics allow parents and doctors to ignore sound medical practice in treating intersex infants.
Secrecy, shame, and stigma are common among intersex children and may well produce lasting impressions. 18 However, adults recall that the shame, stigma, and secrecy came from being treated as medical oddities. Parents who demedicalize the intersex child rather than adopting the “monster” approach can ameliorate such social scars. Interviewing intersex adults, Celia Kitzinger observed that “[t]he hushed conversations, the embarrassment of doctors, the explanations which don’t add up, lead women and girls with [Androgen Insensitivity Syndrome] to the belief that they have a defect so monstrous that nobody is willing to discuss it.” 19
In the 1990s, and particularly after David Reimer’s case was reintroduced into the medical literature in 1997, activists called for a moratorium on genital surgery which was intended to “normalize” the appearance of a child’s genitals. 20 Although some in the medical community accepted this premise until more could be known about the proper treatment of intersex infants, others argued that fuller disclosure of the medical uncertainty of the procedures would suffice and the traditional method of “normalization” should continue. While fuller informed consent is laudable, informed consent by parents alone cannot legitimize surgery to normalize infant genitalia when it is not medically necessary. Parents do not have the authority to consent to genital normalizing and sex assignment surgery on behalf of their infants. In the spirit of optimism, this article also addresses how the law can best support parents and give them the strength of parental character to love, cherish, and nurture the child that is. Ultimately, law informed by the truth will best serve the children.
II. INTERSEXUALITY
Atypical sexual differentiation occurs in more than one percent of live births. 21 The incongruities may be of a genetic, gonadal, hormonal and/or genital nature 22 and can occur at the time of gamete formation, fertilization or during fetal development. 23 Medical science, like western society, has long assumed that “there is a single universally correct development pathway” and that variations in sexual dimorphism are based on error. 24 Increasingly, biologists questioned “a priori belief in complete genital dimorphism” and expressed the view that intersex conditions may instead represent normal and to-be-expected biological variation in humans. 25
Infants with intersex conditions may be born with visible genital ambiguities or their circumstance may not become apparent until adolescence or later. 26 There are well over a dozen intersex conditions, each having unique and different characteristics. 27 In some conditions, such as Complete Androgen Insensitivity Syndrome (CAIS) or Klinefelter’s syndrome (KS), an infant’s genitals typically do not reveal a problem. 28 For instance, because of a genetic mutation to the androgen receptor gene, an XY (male) infant with CAIS will be born with female-appearing genitalia and will likely be reared as a girl unless some medical condition prompts early medical testing. At puberty, the condition may be diagnosed when the child fails to menstruate or has some other developmental anomaly. 29 In contrast, infants with Partial AIS (PAIS) often are noticed soon after birth when parents and physicians observe incomplete masculinization of the genitals. 30 Congenital adrenal hyperplasia (CAH), a disorder that results in the prenatal overproduction of androgens, shows up at birth in affected female infants. An XX (female) infant with CAH will have virilized genitalia, ranging from “minor clitoral enlargement or labial fusion to virilization so severe that the infant is mistaken for a male at birth.” 31
Most intersex babies probably do not have surgery in infancy. Some intersex conditions do not manifest in infancy and there is no genital ambiguity in others. Gauging the number of infants that undergo genital surgery is difficult. However, estimates of the number of candidates for genital surgery vary from 1.62% to “between one and two in a thousand” infants. 32
III. THE MONSTER IN THE LOCKER ROOM
In 1997, the case of John/Joan told the story of the person we now know as David Reimer. 33 The account described the failed sex reassignment of a child who had been originally presented to the medical world as a case success. 34 David Reimer and his twin brother were born as normal boys. However, David’s “penis was accidentally burned to ablation during phimosis repair by cautery” at eight months of age. 35 His distraught parents eventually consulted with John Money, a leading psychologist at The Johns Hopkins Hospital at the time. David’s parents were advised that while their son’s penis could not be repaired, he could be raised as a girl with surgically reassigned genitalia. The parents deliberated and ultimately decided to accept the offer to change David into a girl. 36 David’s testicles were removed and a rudimentary vaginal exterior was fashioned from his scrotal tissue. 37 In effect, David, a 46 XY male who was not born intersexed, was treated as if he were. His testicles were removed, female-appearing genitalia were constructed, and he was raised as a girl.
According to Colapinto’s account, the information the Reimers—neither of whom had finished high school—received about the surgery was woefully inadequate. 38 Indeed, they could not have been assured of any particular outcome since this treatment was entirely experimental. 39 David’s parents did not appreciate that the treatment had never been attempted on a child born with an established typical sex. Anxious for a good outcome, however, they were impressed with Money’s confidence and optimism that the operation would be successful. In fact, Janet Reimer said, “I looked up to [John Money] like a god … . I accepted whatever he said.” 40 They also recalled being rushed to decide because Money believed that there was a short window of opportunity; they were even accused of “procrastinating.” 41
It is now well known that David’s family struggled mightily to carry out the doomed treatment plan for over a decade. 42 Yet it all collapsed in adolescence when David could not deny his own innate gender. 43 At the age of fourteen he threatened suicide unless he could live as a male. 44 David was then finally told the truth about his birth, the loss of his penis, the surgery, and the highly secret treatment plan to raise him as a girl. David thereafter reclaimed his male identity and lived as a man. He underwent four surgeries to construct a penis. He eventually married and adopted his wife’s children. David later collaborated with John Colapinto on a book about his life, As Nature Made Him. The Boy Who Was Raised as a Girl. 45 On May 4, 2004, David ended his life at the age of 38. 46 David’s twin brother, Brian, had died of a drug overdose two years earlier. 47
When an intersex condition or genital ambiguity is apparent in infancy, parents and physicians must consider how to proceed. Sometimes, medical intervention is essential to preserve the child’s life, such as in the case of cloacal exstrophy 48 and more commonly in cases known as salt-losing CAH. 49 Such medically necessary management must be distinguished from sex reassignment or genital “normalization” surgery. 50 Cosmetic surgery to “normalize” the appearance of genitalia stands on a different footing than medically necessary treatment.
After birth, parents are anxious to know the sex of their child and to announce it to others. The inability to identify the sex of the child has been characterized as a social emergency. 51 This so-called emergency, including the theoretically associated parental crisis, has for many years justified early surgery on children with visibly ambiguous genitalia. It is these decisions to “normalize” the genitals rather than life-saving surgery or tentative gender assignment without surgery that has become most controversial.
Misinterpretation of earlier studies involving intersexed persons drove the idea that that surgical sex reassignment of David Reimer and of infants born with ambiguous genitalia could be successful. In a summary of findings of their work with hermaphrodites, the term for those intersexed in the 1950s, John Money and others advanced the theory that the gender in which the child was reared could determine the child’s own sexual identification. 52 Therefore, they suggested that surgical assignment to achieve a good aesthetic appearance was a primary consideration in the case of intersex infants:
In briefest summary, our findings point to the extreme desirability of deciding, with as little diagnostic delay as possible, on the sex of assignment and rearing when a hermaphroditic baby is born. Thereafter, uncompromising adherence to the decision is desirable. The chromosomal sex should not be the ultimate criterion, nor should the gonadal sex. By contrast, a great deal of emphasis should be placed on the morphology of the external genitals and the ease with which these organs can be surgically reconstructed to be consistent with the assigned sex. 53
One caveat was that reassignment must be done in the “early months of life,” in the “critical period” or else it would be “psychologically injurious.” 54 Money and his colleagues were strong proponents of surgical assignment and not just social assignment, stating that “[t]hough the sex of rearing could transcend external genital morphology in psychologic importance, absence or correction of ambiguous genital appearance was psychologically beneficial.” 55 Furthermore, Money wrote confidently about surgery on female genitalia: “Clitoral amputation in patients living as girls does not, so far as our evidence goes, destroy erotic sensitivity and responsiveness, provided the vagina is well developed. If clitoridectomy is performed in early infancy, the chances of undesirable psychologic sequelae are negligible.” 56
A psychologist by training, Money believed that parents, and ultimately the intersexed child, could not come to terms with the social and psychological ramifications of ambiguity. 57 “Before contemporary medical interventions, many children with a defect of the sex organs were condemned to grow up as they were born, stigmatized and traumatized.” 58 Money perceived parents as unable to cope, insistent on a definite sex assignment, and willing to surrender to medical authority.
[O]ne may infer that the linguistic need to have either a him or a her is so great that parents do not argue the issue, even on the basis of common- sense evidence that all is not well with their baby’s sex organs. Instead, when in doubt, they seek an authoritative decision. 59
Money often wrote about how to counsel parents to re-announce the sex of their child with the least social trauma; if properly done, re-announcement presented a short-lived and minor crisis that would resolve with “consistency of rearing” in the assigned gender. 60
Money attempted to fight against cruel stereotypes by calling intersex conditions “errors.” Apparently, he thought that simply by referring to intersex conditions as “sex errors,” he was triumphing over stigmatizing stereotypes:
Words can wound. Medicine can be very cruel in diagnostic terms as gruesome as bird-faced dwarfism and prune-belly syndrome. That is why serious thought went into the decision to continue using Sex Errors in the title of this second revised and enlarged edition. Medical terms such as hermaphroditism or intersex are too stigmatizing for people born with a syndrome that affects the sex organs. They find it stigmatizing to have to talk about themselves as having an abnormality, anomaly, defect, deviance, deficiency, or handicap. They would rather use the term sex error. It implicates their anatomy, not themselves. 61
Thus it was, with well-meant intent, that Money viewed intersex conditions as errors of the anatomy which could be corrected with surgery. The authors observe that it is less stigmatizing to characterize intersex conditions as to be expected and not uncommon developmental variations.
The sentiment that intersex conditions were monstrous defects is reflected in a medical text published in 1969 by Dewhurst and Gordon. 62 They wrote:
That a newborn child should have deformity of any magnitude is a distressing thing, but that so fundamental an issue as the very sex of the child should be in doubt is a tragic event which immediately conjures up visions of a hopeless psychologic misfit doomed to live always as a sexual freak in loneliness and frustration. 63
Fear of the monster still continues to dominate the decisional process. In Lessons From the Intersexed, Suzanne Kessler explored the distress of parents in the first few months after the birth of their intersex child and how the allure of a medical cure can indeed overwhelm parents. 64 The crisis begins at birth when everyone asks whether the child is a boy or a girl, and apparently, the choice is between only one of two answers: “it is a boy” or “it is a girl.” The urgency related to providing an answer for that question can only derive from parental and societal need as a newborn infant hardly finds it necessary to provide an answer to such a seemingly weighty question. Quoting an interview with an endocrinologist, Kessler wrote:
Very frequently a decision is made before all this information is available, simply because it takes so long to make the correct diagnosis. And you cannot let a child go indefinitely, not in this society you can’t. … There’s pressure on parents [for a decision], and the parents transmit that pressure onto physicians. 65
During the waiting period, parents are typically advised not to make a premature announcement about the sex of the infant and to altogether refrain from discussing the condition in order to avoid insistent questioning. 66 Kessler commented, “[Physicians] talk as though they have no choice but to respond to the parents’ pressure for a resolution of psychological discomfort and as though they have no choice but to use medical technology in the service of a two gender-culture.” 67 The advice to keep the condition secret 68 isolated parents within the medical arena, since physicians were the only ones with whom parents believed they were free to discuss the condition. It reinforced a sense of shame. “In short, parents are asked to sidestep the infant’s gender rather than admit that the gender is unknown [or in doubt], thereby collaborating in a web of white lies, ellipses, and mystifications.” 69
Reiner described the traditional medical approach that became entrenched for more than four decades as follows:
[I]nfluenced initially by Money’s work, varying clinical algorithms gradually evolved into a treatment paradigm: • Assign neonates who have anomalous genitalia to female sex-of- rearing if they are genetically female or if they are genetically male but do not have an adequate phallus • Perform Feminizing genitoplasty • Instruct parents to inform no one of this birth history 70
So it was that the physician’s construction of gender became the parents’ construction as well. The parents were educated that there were two sexes—male and female. 71 They were informed that their child, by an error of nature, was not apparently male or female. They were told to delay any announcement of a sex, to confide in only a few discreet friends and family. They were told to act quickly because the condition required urgent treatment and surgical assignment could treat the condition. They were led to believe that if the genitals were normalized and if they raised their child with a consistent gender identity, a crisis could be averted, even if the infant underwent surgical sex re-assignment. Thus, parents were induced to simplistically believe that although their child was born intersexed, he or she need not remain so. 72
The confidence in surgical intervention as a solution, and the absolute imperative to project such surety, is remarkable. Perhaps signaling their acknowledgment that such treatment may in fact be a house of cards, Dewhurst and Gordon admonished:
At the risk of repetition, we emphasize again that whatever is decided this decision must be underlined by appropriate surgical measures to make the genitalia conform to the chosen sex. Above all, unwanted gonadal tissue must be removed to prevent the appearance of heterosexual manifestations about the time of puberty, for these might destroy the confidence of the parents so carefully built up and would certainly have a distressing effect upon the child. 73
Secrecy, shame, overwhelming isolation, and medical dependency were certainly part of the Reimer family experience. When Janet and Ron Reimer, David’s parents, first discovered John Money, they had some doubts about surgery. Eventually, however, their concern that David could not be a normal boy prevailed. With Dr. Money’s advice in mind, Janet Reimer stated: “But I thought, with his injury, it would be easier for Bruce to be raised as a girl—to be raised gently. He wouldn’t have to prove anything like a man had to do.” 74 Ron Reimer recalled thinking: “You know how little boys are … ‘Who can pee the furthest?’ Whip out the wiener and whiz against the fence. Bruce wouldn’t be able to do that, and the other kids would wonder why.” 75 Colapinto wrote of his interviews with Ron:
“Ron could not even imagine the humiliations and frustrations that would entail. As a girl or a woman, though, Bruce wouldn’t face all that. … If what Dr. Money told them was true, she could live a normal life, she could get married, she could be happy.” 76
The Reimers were incredibly diligent in implementing the plan, as they were told to do. They went to extraordinary lengths to follow the treatment plan. 77 Although twin brothers Brian and David began to dread returning to Johns Hopkins for annual visits, the Reimers insisted. 78 Eventually, “they sweeten[ed] the pill … with a family vacation.” 79 David and Brian recollected emotionally painful, humiliating, and invasive psychiatric sessions at Johns Hopkins. 80 Significantly, invasive and personally embarrassing situations are a common recollection of intersex children. 81
Despite the general acceptance of early surgery as a treatment of intersex for more than four decades, many in the medical community began to question the premises of sex assignment following revelations about David Reimer in 1997. 82 For example, William Reiner, a pediatric urologist who formerly performed surgeries on intersex infants, observed that sex assignment surgeries were not altogether satisfactory. 83 In recent years, Reiner not only stopped performing surgeries and trained as a child psychiatrist, but also became a vocal opponent of surgical sex assignment in infants. 84 In reviewing the development of the surgical standard, Reiner noted that the “clinical vacuum” that existed at the time Money began his studies allowed his views on gender fluidity during childhood to flourish. 85 Reiner commented that although “[d]ata remained sparse … [t]he notion that gender-typical behaviors and gender identity could be products of surgical and social technique was appended to the clinical teaching repertoire as spoken truths of clinical practice.” 86 The “blank slate” concept of infant gender neces 87 “This intervention model—although it preceded research, so that the model was in search of data—became definitive treatment. It also transformed a broad psychologic conception into an inflexible clinical concept.” 88
Importantly, by observing patients over time, Reiner concluded that sex and social gender assignment could not necessarily prevail over prenatal influences. 89 When Diamond and Sigmundson reported on the failure of the David Reimer case, Reiner wrote an editorial supporting their findings and conclusions. 90 Initially, the medical community engaged in substantial reflection in both the literature and at professional meetings after the reports of failure in David’s case. As a result, there has been increasing acceptance of the view that surgeries performed on infants for the sake of appearance alone are unjustified. For example, in 2004, a fifteen-member multidisciplinary panel convened by the Hastings Center concluded: “None of the appearance-altering surgeries need be done urgently. Surgery to normalize appearance without the consent of the patient lacks ethical justification in most cases.” 91
However, many in the medical community did not and still do not embrace the moratorium position. 92 Those against a moratorium adhere to the view that not doing surgery also has its own inherent risks, principally related to social stigma and parental rejection of the infant. Pediatric urologist Kenneth Glassberg called for increased research but justified the continuation of surgery by pointing to intersex adults reportedly satisfied by infant surgery: “What about all of those patients who have done well after gender assignment? Should they have been condemned to growing up as what would inevitably be considered freaks by their classmates?” 93 Proponents of at least some continuation of surgical treatment advocate more attention to informed consent until efficacy of surgical treatment is established or refuted. Physician Erica Eugster, criticizing the Hastings Center panel’s position, summarized the view of surgery proponents:
If parents maintain a strong prejudice in favor of surgery despite a complete education about its potential risks, the effects of unilaterally denying the option for a decade or more could surely be disastrous. Therefore, until rigorous comparisons of psychosexual functions in patients receiving early genital surgery using modern techniques versus no early genital surgery have been conducted, only TWO conclusions may safely be made. First, the ultimate decision regarding early surgery rests with the parents and should be made in the context of their own cultural beliefs only after a detailed and comprehensive review of all options, opinions, and available outcome data. Affording parents this authority does not present an ethical dilemma, since in our society all major decisions regarding minor children are traditionally made by parents. Second, when early genital surgery is performed, it should be undertaken by surgeons in centers of excellence with particular expertise in the care of patients with intersex conditions. 94
In keeping with such reasoning, proponents of early surgery have attempted to legitimize questionable surgery by heightening the informed consent process provided to parents. This approach, characterized as the “middle ground” between a moratorium and the traditional approach, has been advanced by others as well. 95 Some legal commentators have also opposed a moratorium; Laura Hermer summed up the argument in favor of parental choice:
It must be recognized that, if we choose the latter course [a moratorium], we will have again used intersex individuals as guinea pigs of sorts, this time in a cultural experiment. However much any of us may wish to see Fausto-Sterling’s latter course prevail, the outcome is not certain. Thus, a physician cannot, in good conscience, assure the parents of an intersex infant that they ought not to choose cosmetic or sex assignment surgery for their child, on the ground that the unaltered child, along with his/her intersexual forebears and brethren, will (over time) alter our present sex and gender systems to make space for those who do not conform to the present norms. Given our present state of knowledge concerning the long-term outcomes of intersex individuals (both those who have and have not had surgery), and our current sex and gender systems and the fact that intersex individuals have no choice but to cope with them one way or another, there can presently be no reasonably certain “right” answer for physicians and parents of intersex children with respect to surgery. 96
IV. WHY INFORMED CONSENT CANNOT LEGITIMIZE MEDICALLY UNNECESSARY SURGERY
The fallacy of the argument in favor of heightened informed consent in lieu of a moratorium on surgery is that the argument presumes that parental informed consent can legitimize a surgical treatment that lacks a therapeutic rationale and poses a substantial risk of harm over the lifetime of the patient. 97 The so-called “middle ground” position assumes that in the absence of knowledge about the outcome, the medical profession is entitled to proceed with surgery provided that there is fully informed parental consent. Implicitly, the position presupposes that surgery can be justified based on the risk of social stigma in childhood, parental distress, and parental preferences.
Notably, in defending the surgery option, proponents of surgery mischaracterize the position of moratorium proponents, suggesting that the Intersex Society of North America (ISNA) and others are actually calling on parents to raise their intersex children as a “third” sex. For example, Diamond’s position has been summarized as: “Diamond is of the opinion that sex assignment and genital surgery should be delayed until the child can decide for itself. This means that child should neither be raised as a boy nor a girl, but as an intersex person.” 98 Yet those opposed to surgery have never suggested that parents raise their child without assignment or subject them to a “cultural experiment” by raising them as genderless as Hermer, for example, characterized the non-surgical approach. 99
We are not suggesting that intersexed children should be raised without gender … The aim must be to raise infants in a way that will most probably turn out to be comfortable for the maturing child. But gender assignment has to be provisional, subject to revision by the intersexed child as he or she matures 100
Thus, opponents of surgery simply seek to stop infant surgery to allow for the possibility that the gender of rearing might be wrong. The so-called cultural experiment is hardly as radical as proponents of surgery suggest. 101 Although proponents postulate that gender of rearing and genital appearance must match for gender development, this proposition is doubtful and has not been established. 102 Proponents assert that the social stigma suffered by intersex individuals warrants medical intervention. Yet, experiences within the intersex adult community suggest another entirely possible reality—that as opposed to Dewhurst and Gordon’s prediction, being intersexed does not doom them as “freaks, misfits, curiosities, rejected by society and condemned to a solitary existence of neglect and frustration.” 103
In fact, such prediction of doom was not the case historically before surgery was possible, 104 nor is it the case today. 105 According to Colapinto, Money’s own doctoral dissertation studies in the 1950s supported the fact that intersex individuals can have satisfying and rewarding lives without surgical alteration. 106 Alice Dreger’s historical account of the lives of intersexed individuals prior to the “medicalization” of intersex also supports the view that these individuals can lead satisfied lives without surgery. 107 Reiner’s follow-up study of cloacal exstrophy patients who were not sex reassigned as female suggests that individuals can enjoy a positive psychosexual outcome. He noted that “[t]he few male children who have cloacal exstrophy and were raised as male do well psychosocially and psychosexually.” 108 Significantly, Reiner also noted that those male children who were initially assigned to female and later rejected the assignment transitioned successfully. 109 Studies of males with micropenis also indicate that such men can firmly establish a male role and successful sexual relationships. 110 Additionally, personal testimonies of intersexed individuals about their reaction to surgery sheds light on whether surgery should be postponed until consent may be obtained from the individual:
My condition (PAIS) [partial androgen insensitivity syndrome] means that I would have been born a “normal” boy if my body responded normally to the testosterone my testes were producing (i.e. my body only partially responds to testosterone). Even though doctors knew this, they still decided to continue with their plan to raise me as a girl. I agree they had to make a decision, and that raising me as a girl was appropriate, but what I don’t agree with was their decision to perform irreversible, non-therapeutic treatment on me without my consent. Part of their ‘treatment’ plan was to also withhold the truth about my condition from my family, and from me as I got older. They also somehow believed that being a (non-identical) twin sister would help me grow comfortable as a girl. They were very wrong. 111 Not that I would necessarily have kept my phalloclit … But I would have liked to have been able to choose for myself. I would have liked to have grown up in the body I was born with … But physically, someone else made the decision of what and who I would always “be” before I even knew who and what I “was”. … [The doctors] used surgical force to make my appearance coincide with the medical and social standards of a “normal” female body, thereby attempting to permanently jettison any trace of intersexuality. 112 As a woman, I am less than whole—I have a secret past, I lack important parts of my genitals and sexual response. When a lover puts her hand to my genitals for the first time, the lack is immediately obvious to her. Finally, I simply do not feel myself a woman (even less a man). But the hermaphrodite identity was too monstrous, too other, too freakish, for me to easily embrace. A medical anomaly, patched up as best the surgeons could manage. 113
A study involving twenty-one parents of intersex children—46 XX children with CAH and genital ambiguity—between the ages of eight months and thirteen years was recently reported. 114 Eighty-nine percent of the parents had consented to genital surgery. 115 The study reported one finding that 100 % of those parents who had consented to surgery “cited [among other reasons] the potential for a more natural genital appearance” when recalling “their reasoning and motivation for consenting” to genital surgery. 116 Furthermore, when asked if they would consent to genital surgery if a reduction in sexual sensation/responsiveness were certain , 95% of the parents indicated that the physical and psychological benefits of surgery in infancy permitted a more normal childhood by avoiding ostracism from others. Moreover, all the parents disagreed with postponing genital surgery until the children were old enough to consent. 117
One need only consider the contrast between the above findings with the personal testimonies of the now adult children to realize that parents should not be asked to give informed consent to surgery without external safeguards. How can parents presume to know whether sexual function or appearance in adulthood would serve the best interests of their child over the child’s lifetime? The fact is, whether genital function and pleasure should be paramount to appearance is a question so essential to one’s own bodily integrity, autonomy, and privacy that a parent cannot make the decision for a child absent a medical justification. When the decision can be postponed, it should be. The law, as it now exists, supports that position.
Traditionally, parental medical decisions on behalf of children are accorded deference in recognition “that natural bonds of affection lead parents to act in the best interests of their children.” 118 However, there are limits to such deference. The United States Supreme Court observed that “parents cannot always have absolute and unreviewable discretion to decide.” 119
Professor Jennifer Rosato has identified traditional instances where either categorical or situational conflicts call for placing limits on a parent’s authority to consent to medical decisions for the child. 120 Drawing lessons from bioethics, she has concluded: “1) Family members do not possess an inherent right to decide forthe patient; 2) deference to family members usually furthers beneficence; and 3) conflicts of interest provide a reasoned basis for interfering with family decision-makers.” 121 According to Rosato, categorical conflicts of interests between parents and children:
include those in which the decision-maker makes treatment decisions that fall outside the range of reasonableness; where extraordinary medical treatment is involved; or where the treatment decision involves a countervailing constitutional right of the patient that, when exercised, is likely to interfere with the family member’s decision. When a categorical conflict exists, a neutral third party, such as a judge, must determine whether the decision of the proxy accords with the beneficence principle. 122
The law has recognized such categorical conflicts when treatment implicates the child’s sexuality, reproduction, or privacy interests, or that involve consent to non-therapeutic treatment. 123
Genital normalizing surgery raises issues common to the types of categorical conflicts Rosato has identified. It is an unreasonable, 124 extraordinary 125 medical intervention 126 that impacts significant constitutional interests of the child. 127 Rosato has also described “situational conflicts” between parent and child that limit parental authority to consent to treatment; these conflicts may be “financial, emotional, or value-based.” 128 These conflicts arise where parents do not necessarily share an identity ‘of interests with the child and therefore may not act in accord with the child’s best interests. 129 To understand the full extent of the conflicts, one need only note that when an intersex child is born, a primary focus of physicians is the emotional needs of the parent. 130 Indeed, one premise that has continued to justify infant surgery has been the concern that the appearance and uncertainty of the infant’s sex was so distressing to parents that it jeopardized the parent-child relationship. 131 The fact that physicians have seemingly regarded the parent instead of the child as the patient, and focused so much attention on parental discomfort and embarrassment exacerbates the situational emotional conflict of interest. 132
As evidenced from the selection of quotes cited in the Introduction of this article, parents largely focus on short period of time—childhood and adolescence—when they discuss their reasons for agreeing to infant surgery. Notably, this is the period of a child’s life when parents will be most involved and affected by the appearance of the child’s genitals. Yet childhood, and to a lesser extent adolescence, represents a period of life when the genitals are less sexually significant than during adulthood. Thus it may be that parents place greater emphasis on appearance than sexual function because problems related to appearance are more immediate and of more consequence to them than that of the sexual, erotic and/or gender issues in adulthood, if surgery proves improvident.
V. SUPPORTING PARENTS IN RAISING HEALTHY CHILDREN
Recently, Alice Dreger challenged physicians to recognize that they can perpetuate or work to eliminate harmful social norms:
[W]hat I’m looking for in medicine today—at least around the treatment of children born with socially-challenging anatomies—is a radical change. … [W]hat I hope I’m starting to work towards—is a radical medicine that recognizes and confronts the oppressive nature of social anatomical norms and questions the use of medicine to uphold, and even advance, particularly oppressive norms. 133
Concerned about the vulnerability of infants with congenital or genetic conditions that fall outside societal views of the normal, Professor Wendy Anton Fitzgerald similarly challenged the law to “work toward a jurisprudence which will embrace all of human difference, genetic and congenital included.” 134 She further challenged lawyers to “work toward broadening our jurisprudence to include children, indeed all human difference, in our legal understanding of personhood, hoping thus to transform our culture to become more inclusive as well.” 135
No doubt parenting has a substantial and lasting impact on children. However, there is no need to assume that parental reaction always dictates the proper, or the best, treatment of infants. In fact, it would be a disservice to parents and to the trust placed upon the irrationality 136 of parental love, if one assumes parents cannot cope with babies who have nonconforming genitals. As their children’s guardians, parents are expected to rise to the challenges of countless uncertainties.
Consider these conclusions of a researcher comparing the experiences of children with micropenis raised by “different generations of parents”:
Half of the older group remembered unhappy experiences of teasing by their peers, while the younger group was more confidant, only one being considered rather shy. In the younger group all eight were able to change and shower without comment from their peers, while half of the post-pubertal group were too embarrassed to do so. These differences are attributed to better counseling of parents. Supportive parents who encourage ‘normality’ produce confident and well-adjusted children. 137
It is increasingly recognized that parental rights do not give parents blanket authority to make decisions on behalf of their children. 138 Rather, parents have the responsibility to make decisions based on the child’s best interests. Similarly, parents of children within a sexual minority must act in their child’s best interest. Parental interests, biases and preferences are necessarily and correctly subservient to the child’s needs and rights.
But what of stigma, teasing and bullying? It is true that such possibilities face the intersex child and adolescent. Parental and societal responsibility must mean that neither parents nor the courts tolerate the victimization of sexual minorities. In this regard, the authors note with approval the recent judicial decisions that require schools to protect sexual minority students and allow them to be who they are with the full protection of the law. 139 Parents must be assured that the courts will join them in their endeavor to protect their child. 140 While there can be no guarantee to parents that intersexed children will be free from stigma, will never be teased, and will never be bullied, it also cannot be denied that no child has ever come with such a guarantee.
VI. CONCLUSION
In this article, the authors have continued their criticism of traditional surgical interventions on children born with ambiguous genitalia. The developing “middle ground” approach is not appropriate because it attempts to legitimize surgical procedures that have not proven to be more beneficial than lesser interventions such as counseling, education, advocacy and protection against stigmatization. Furthermore, surgery has been shown to have catastrophic consequences for some. Surgery was premised on concerns about parental reaction, social stigma, and a theory that gender and genitalia must match to yield a solid gender identity. Before surgery was possible, it was known that intersexed individuals historically led private and satisfied lives. It is immoral to blame and punish the victim of bigotry rather than to use our efforts to resist the bigot. Moreover, it is questionable as to whether parents and infants share a community of interests sufficient to grant parental authority, and whether informed consent of parents can be valid.
We end with hope and expectation that parents will love and raise their children to be confident and satisfied, while preserving their child’s right to make decisions so central to their identity and sexuality for themselves.
1 Mirreya Navarro, When Gender Isn’t a Given, N.Y. TIMES, Sept. 19, 2004, § 9, at 1, 6 (interviewing anonymous parents who opted for clitoroplasty on a four year old with CAH).
2 Id. (interviewing Lisa Greene, mother of infant with CAH who opted for surgery to create a vaginal opening and rebuild urethra, but not clitoroplasty).
3 Id. (interviewing Jeff Spear, who consented to clitoroplasty and other surgeries on a six month old infant).
4 Emily Nussbaum, A Question of Gender, DISCOVER, Jan. 2002, at 92, 97 (explaining why the infant’s mother consented to surgery on Emma, diagnosed XY/XO mosaic).
6 CHRISOPHER J. DEWHURST & RONALD R. GORDON, TI-rE INTERSEXUAL DISORDERS vii (1969) (emphasis added).
7 David Reimer committed suicide in 2004. David was born a boy. During phimosis repair at the age of eight months, his penis was destroyed. His parents eventually located a psychologist at Johns Hopkins Hospital who proposed that the parents change David into a girl through surgery and raise him as a girl. David was renamed Brenda. and the reported success of his case became the basis of surgical standard of care for intersex infants for the next three decades. See generally Hazel Glenn Beh & Milton Diamond, An Emerging Ethical and Medical Dilemma: Should Physicians Perform Sex Assignment Surgery on Infants with Ambiguous Genitalia?, 7 MICH. J. GENDER & L. 1 (2000); Milton Diamond, Pediatric Management of Ambiguous and Traumatized Genitalia, 162 J. UROLOGY 1021 (1999).
8 See, e.g.. JOHN COLAPINTO, AS NATURE MADE HIM: THE BOY WHO WAS RAISED AS A GIRL (2000); NOVA: Sex: Unknown (PBS television broadcast Oct. 10, 2001).
9 Milton Diamond & Keith Sigmundson, Sex Reassignment at Birth: Long Term Review and Clinical Implications, 151 ARCHIVES PEDIATRIC & ADOLESCENT MED. 298-304 (1997). See also Kenneth Kipnis & Milton Diamond. Pediatric Ethics and the Surgical Assignment of Sex, 9 J. CLINICAL ETHICS 398 (1998).
10 The authors have argued elsewhere that doctors should stop performing sex assignment surgery on intersex infants until much more is known about the long-term consequences of surgery. They also argued that parents exceeded their authority by consenting to this needless, unproven, and life-altering surgery. Further, it constituted malpractice for physicians to persist in performing surgery without evidence that the treatment would yield satisfactory results. Physicians were obligated, when obtaining informed consent, to inform parents that the surgery proposed had not yet been validated. Moreover, the authors noted that there was a paucity of scientific studies to support a surgical standard of care. To date, the anecdotal reports and limited reported hindsight studies from intersex adults who have had surgery as children suggested that in many cases, surgery did not bring about the positive results predicted. See Beh & Diamond, supra note 7.
11 Ironically, David was not intersexed. yet his case became the standard for treating intersex conditions. It was reasoned that if a typical male could be successfully reared as a girl, then surely an intersexed male could also be. Likewise, when the failure of his treatment became known, it affected intersex treatment. See Milton Diamond, Sex, Gender, and identity over the Years: A Changing Perspective, in 13 CHILD & ADOLESCENT PSYCHIATRIC CLINICS: SEX & GENDER 591-607 (Milton Diamond & Alayne Yates, eds. 2004) [hereinafter SEX & GENDER].
12 See generally COLAPINTO, supra note 8.
13 John Colapinto, Gender Gap: What Were the Real Reasons Behind David Reimer’s Suicide?, SLATE, June 3, 2004, http://slate.msn.com/id/210168J (last visited Dec. 31, 2005).
14 We are in no waycriticizing David’s parents. They, as many other well-intentioned parents, did what they were led to believe as best for their son. David himself had forgiven his parents for being misinformed. In fact, their own anguish and guilt is testament to the harm of leaving such a monumental decision to parents. See COLAPINTO, supra note 8, at 256.
15 COLAPINTO, supra note 8, at 262.
16 Dreger borrowed the term from George Annas, who discussed the monster approach in connection with medical decisions concerning conjoined twins. Alice Domurat Dreger, “Ambiguous Sex”—or Ambivalent Medicine? Ethical issues in the Treatment of Intersexuality, 28 HASTINGS CENTER REP. 24, 33 (1998) (citing George Annas, Siamese Twins: Killing One to Save the Other, 17 HASTINGS CENTER REP. 27 (1987)), available at http://www.isna.org/articles/ambivalent_medicine .
17 Dreger, supra note 16, at 33.
18 Milton Diamond & Linda A. Watson, Androgen Insensitivity Syndrome and Klinefelter’s Syndrome: Sex and Gender Considerations, in SEX & GENDER, supra note 11, at 623. See also SHARON E. PREVES, INTERSEX AND IDENTITY: THE CONTESTED SELF (2003).
19 Celia Kitzinger, Women with Androgen Insensitivity Syndrome, in WOMEN’S HEALTH CONTEMPORARY INTERNATIONAL PERSPECTIVES 387 (Jane M. Ussher ed., 2000).
20 Diamond & Sigmundson, supra note 9; see also Kipnis & Diamond, supra note 9, at 398-410. This is also the position of different intersex groups, such as the Intersex Society of North America (ISNA), http://www.isna.org ; Bodies Like Ours, http://www.BodiesLikeOurs.org ; and A Kindred Spirit, http://www.kindredspiritlakeside.homestead.com .
21 Melanie Blackless et al., How Sexually Dimorphic Are We? Review and Synthesis, 12 AM. J. HUM. BIOLOGY 151 (2000). See also SUZANNE J. KESSLER, LESSONS FROM THE INTERSEXED 135 n.4 (1998) (discussing difficulty of establishing accurate rates).
22 PEGGY T. COHEN-KETTENIS & FRIEDMAN PFÄFFLIN, TRANSGENDERISM AND INTERSEXUALITY IN CHILDHOOD AND ADOLESCENTS 25 (2003):
Sexual differentiation disorders can be classified in various ways. Traditionally, genetic sex or gonadal histology is used as an organizing principle. Female and male pseudohermaphroditism, true hermaphroditism, and gonadal differentiation disorders are then the resulting categories. In true hermaphroditism both testicular and ovarian tissue are present. Female or male pseudohermaphroditism indicates that respectively only ovarian or testicular tissue is present. In incomplete or complete gonadal dysgenesis one or both gonads are streak gonads. Some of these conditions co-occur with sex chromosome anomalies, while others do not, but the two phenomena are frequently associated.
23 Id. at 49.
24 Blackless et al., supra note 21, at 151. See also JOHN MONEY, SEX ERRORS OF THE BODY (1968); JOHN MONEY, SEX ERRORS OF THE BODY AND RELATED SYNDROMES: A GUIDE TO COUNSELING CHILDREN, ADOLESCENTS, AND THEIR FAMILIES (2d ed. 1994).
25 Blackless et al., supra note 21, at 151 (summarizing literature). In fact, while medicine has adhered to a view of absolute sexual dimorphism in “sex chromosome composition, gonadal structure, hormone levels, and the structure of genital duct systems and external genitalia,” people culturally recognize that other traits of male and female are not so absolute. “Our culture acknowledges the wide variety of body shapes and sizes characteristic of males and females. Most sexual dimorphisms involve quantitative traits, such as height, build, and voice timbre, for which considerable overlap exists between males and females.” Id. at 15 I, 161. See also Milton Diamond et al., From Fertilization to Adult Sexual Behavior: Nonhormonal Influences on Sexual Behavior, 30 HORMONES & BEHAV. 333-53 (1996).
26 Blackless et al., supra note 21, at 161.
27 Beh & Diamond, supra note 7, at 2 n.2. See generally MELVIN M. GRUMBACH ET AL., DISORDERS OF SEX DIFFERENTIATION 842-1002 (2003).
28 Although there may be some physical clues, Klinefelter’s syndrome, a sex chromosome disorder, is often not diagnosed until breast development at puberty. Both CAIS and KS may only be diagnosed with a work-up for infertility after marriage. Diamond & Watson, supra note 18, at 631-32.
29 Id. at 624.
30 Id. at 624-2 5.
31 Melissa Hines, Psychosexual Development in Individuals Who Have Female Pseudohermaphroditism, in SEX & GENDER, supra note 11. A male (XY) may also have CAH, but that child will not have genital ambiguities and may be diagnosed later.
32 Blackless et al., supra note 21, at 161.
33 John/Joan was the pseudonym Diamond and Sigmundson assigned to David Reimer. David was given the name Bruce Reimer by his parents in infancy. Following surgery at twenty-two months of age, his parents named him Brenda. When he re-established his male identity, he took the name David. See COLAPINTO, supra note 8, at 9,53, 182.
34 See Diamond & Sigmundson, supra note 9; see also Milton Diamond, Pediatric Management of Ambiguous and Traumatized Genitalia, 162 J. UROLOGY 1021-28 (2000); Milton Diamond, The Joan/Joan Case: Another Perspective, THE POSITION (2000), available at http://www.hawaii.edu/PCSS/biblio/2000to2004/2000-another-perspective.html . See also Diamond & Watson, supra note 18, at 629 (citing another case of sex reassignment originally published as a success that was later found not to be so).
35 COLAPINTO, supra note 8, at 11.
36 Id. at 51-54.
37 Id. at 53-54.
38 Id. at 50.
39 Dr. Money predicated his treatment on his reasoning from intersexed cases he had studied and his having worked with transsexuals. See The Joan/Joan Case: Another Perspective, supra note 34.
40 COLAPINTO, supra note 8, at 50.
41 Id. at 51.
42 See, e.g., id. at 58-59.
43 Id. at 178-80.
44 See Diamond & Sigmundson, supra note 9.
45 COLAPINTO, supra note 8.
46 See supra text accompanying note 14. For a media account of Brian’s death, see CBC News Online, May 10, 2004, available at http://www.cbc.ca/news/background/reimer/ .
47 BBC Science & Nature: TV & Radio Follow-up, Dr. Money and the Boy with No Penis, available at http://www.bbc.co.uk/sn/tvradio/programmes/horizon/dr_money_trans.shtml (last visited February 19, 2006).
48 An infant with cloacal exstrophy has not only “anomalous genitalia,” but also “a devastating pelvic field defect” that compromises survival. According to Dr. William Reiner, forty years ago, “survival was apparently nil; with vast improvements in neonatal medical and surgical care in the last 30 years approximately 90% or more babies who are born with this defect survive into adulthood. Surgical reconstruction of pelvic organs is medically necessary; however, sex re-assignment is not.” William Reiner, Psychosexual Development in Genetic Males Assigned Female: The Cloacal Exstrophy Experience, in SEX & GENDER, supra note 11, at 657,659-60, 662.
49 Melissa Hines, Congenital Adrenal Hyperplasia, in SEX & GENDER, supra note II, at 643.
50 See Reiner, supra note 48, at 659.
51 AMERICAN ACADEMY OF PEDIATRICS, Evaluation of the Newborn with Developmental Anomalies of the External Genitalia, 106 PEDIATRICS 138, 138 (2000) (“The birth of a child with ambiguous genitalia constitutes a social emergency.”); KESSLER, supra note 21, at 15.
52 John Money et al., Imprinting and the Establishment of Gender Role, 77 ARCHIVES NEUROLOGY & PSYCHIATRY 333 (1957).
53 Id. at 334.
54 Id. at 336. Timing became ever more determinative to Money’s evolving sex assignment theory but what remained a constant in his writing was that the time to indisputably make a boy or a girl was not fixed until sometime after birth.
Taking into account many components and factoring in a time variable makes possible the formulation of the proposition nature/critical period/nurture in place of the outworn proposition, nature/nurture. The critical period signifies that the interaction of nature and nurture together advances development, but only if that interaction takes place at the critical period, neither too soon or too late, but precisely on time. Then, once the critical period passes, there is no backtracking. The outcome is fixed and immutable.
SEX ERRORS OF THE BODY AND RELATED SYNDROMES, supra note 24, at 6. The critical period was supposed to extend until about two years after birth. John Money, Joan G. Hampson & John L. Hampson, Hermaphroditism: Recommendations Concerning Assignment of Sex, Change of Sex, and Psychologic Management, 97 BULL. JOHNS HOPKINS HOSP. 284-300 (1955).
55 Money et al., supra note 52, at 336.
56 Id. Evidence suggests otherwise. See Catherine Minto et al., The Effect of Clitoral Surgery on Sexual Outcome in Individuals Who Have Intersex Conditions with Ambiguous Genitalia: A Cross- sectional Study, 361 LANCET 1252-57 (2003) (reporting findings that erotic sensitivity is reduced by such surgery).
57 In the preface to Money’s text, Gooren wrote about this fear : “We have a need to feel normal. We all need to feel that others are normal. Nowhere is this need so strong, or so laden with emotion, as in the area of sex. Is it an “it”? No parent asks this question, but all fear the answer.” Louis Gooren, Preface to the Second Edition, SEX ERRORS OF THE BODY AND RELATED SYNDROMES, supra note 24, at ix.
Without doubt, Money’s recommendation to perform early surgery and unequivocal social assignment was widely influential. See, e.g., DEWHURST & GORDON, supra note 6, at 39, 53, 148 (citing and propounding the recommendations of Money and the Hampsons).
58 SEX ERRORS OF THE BODY AND RELATED SYNDROMES, supra note 24, at 6.
59 John Money et al., Micropenis, Family Mental Health, and Neonatal Management: A Report on 14 Patients Reared as Girls, I. J. PREVENTIVEPSYCHOL. 17 (1981).
60 Id. at 25-26. See also SEX ERRORS OF THE BODY AND RELATED SYNDROMES, supra note 24, at 65-66; John Money, Birth Defect of the Sex Organs: Telling the Parents and the Patient, 10 BRIT. J. SEXUAL MED. 14(1983).
61 SEX ERRORS OF THE BODY AND RELATED SYNDROMES, supra note 24, at xiv.
62 DEWHURST & GORDON, supra note 6, at 1.
63 Id. at 1. In their preface, Dewhurst and Gordon wrote:
One of the few fundamental aspects of life is that of sex. Its normal functioning is vital to the survival of our race, essential for our full assimilation as individuals into society, and pervades every aspect of our lives. To visualize individuals who properly belong neither to one sex nor to the other is to imagine freaks, misfits, curiosities, rejected by society and condemned to a solitary existence of neglect and frustration. Few of these unfortunate people meet with tolerance and understanding from their fellows and fewer still find even limited acceptance in a small section of society: all are constantly confronted with reminders of their unhappy situation. The tragedy of their lives is the greater since it may be remediable; with suitable management and treatment, especially if this is begun soon after birth, many of these people can be helped to live happy well adjusted lives, and some may even be fertile and be enabled to enjoy a normal family life.
Id. at vii.
64 KESSLER, supra note 21.
65 Id. at 20.
66 Id at 21-22.
67 Id. at 32.
68 SEX ERRORS OF THE BODY AND RELATED SYNDROMES, supra note 24, at 22 (advising parents to tell few people outside the family).
69 KESSLER, supra note 21. at 22: see also Id. at 99.
70 Reiner, supra note 48, at 658.
71 See generally Beh & Diamond, supra note 7, at 42-59 (critiquing the informed consent process).
73 DEWHURST & GORDON, supra note 6. Notice that Dewhurst and Gordon were concerned that if all of the gonadal tissue was not removed, heterosexual manifestations resulting from remaining gonadal tissue might emerge that for the reassigned adolescent would appear as a same-sex attraction. Christina Matta, tracing the historical development of the surgery postulates that concern about homosexuality among hermaphrodites contributed to an upswing in infant surgeries. Christina Matta, Ambiguous Bodies and Deviant Sexualities: Hermaphrodites, Homosexuality, and Surgery in the U.S. 1850-1904, 48 PERSPECTIVES BIOLOGY & MED. 74-83 (2005) (claiming it was concern with homosexuality among hermaphrodites that led to the upswing in infant surgeries). Note also that there was the underlying assumption that the tendency to be heterosexual would be conflicted by a reassignment of sex and the reassigned individual “should” now exhibit behaviors that would be called homosexual.
74 COLAPINTO, supra note 8, at 52.
77 Id. at 98-99, 114-15.
78 Brian and David resisted because the sessions were humiliating and degrading. Money discussed sexual matters well beyond what the children’s sexual maturity warranted. In some sessions, they were coerced to engage in “coital mimicry” and “sexual rehearsal play” in which they acted out sex play with one another. The treatment theory was based on the assumption that by doing so David would learn assume a female role. To their mortification, photos were also taken. COLAPINTO, supra note 8, at 86-90.
79 COLAPINTO, supra note 8, at 91; Diamond & Sigmundson, supra note 9.
80 Id. at 86-88, 91-94, 129-30, 136-41.
81 Sherry A. Groveman, The Hanukkah Bush: Ethical Implications in the Clinical Management of Intersex, 9 J. CLINICAL ETHICS 356(1998). Perhaps most disturbing are the descriptions in published interviews with children. JOHN MONEY, BIOGRAPHIES OF GENDER AND HERMAPHRODITISM IN PAIRED COMPARISONS (1991). The interviews with children are surprisingly graphic and one might question whether they were age-appropriate. For example, Case #2: Sex Reassigned as Boy, there is a lengthy description of numerous medical interventions and psychiatric interviews. At one point, the child remains in the hospital for eleven months, during the course of several failed surgeries. Id. at 276-7 The child was pressed at length about whether to become a boy through surgery or to remain a girl. Id. at 289-92. Ultimately, he returned “reluctantly” at twenty-four years of age, but as Money described, “he had long ago had his fill of doctors and their hospital, and wanted to be left alone.” Id. at 293. Frequently, Money employed so-called “parables,” a technique he believed could advance therapeutic goals. He would obliquely impart information and guide children to imagine the future as it could be with intervention. Id. at 441-43.
82 Diamond, supra note 11, at 59 1-607.
83 See Melissa Hendricks, Into the Hands of Babes, JOHNS HOPKINS MAGAZINE, Sept. 2000 available at http://www.jhu.edu/~jhumag/0900web/babes.html .
Reiner had wholeheartedly subscribed to this model throughout the 1970s and ’80s, first as a urology resident at Hopkins and then as a [sic] urologist in private practice in central California. But over the course of his career, he had become troubled by a dearth of information on the psychological and sexual outcome of children with urogenital conditions.
84 Id. Reiner himself was confronted by a case of mistaken sex reassignment. See William Reiner, Case Study: Sex Reassignment in a Teenage Girl, 35 J. AM. ACADEMY CHILD & ADOLESCENT PSYCHOL. 799-803 (1996).
85 See Reiner, supra note 48, at 661.
89 Id. at 659. Reiner’s work with cloacal exstrophy patients is illuminating. Cloacal exstrophy is a rare condition; it occurs in approximately one in 400,000 births. Reiner estimates about ten such children are born a year in the United States. These children are either genetically and hormonally male or female, but they are born with severe and often life-threatening pelvic field defects, including among others, defects to the bowel, bladder and lower vertebrae. They also have “severe inadequacy or absence of genitalia.”
In his follow-up study, twenty-four of the genetic males with cloacal exstrophy were assigned female, underwent feminizing genitoplasty and castration, and raised female. Reiner noted, “Of the 24 subjects who were sex-assigned female, 13 have declared themselves male[.]” Id. at 664. He further noted that they “all reported an aversion to strictly feminine attire ... after the age of approximately 3 years.” Id. “Of the subjects who continue to be reared as girls, parents have been conscious of their child’s male-typical behaviors and attitudes.” Id. at 665 . In sum, he concluded, “neonatal castration plus feminizing genitoplasty—coupled with social and legal assignment to female—does not seem to override the neurobiologic underpinnings of male sexual identity and male gender role preferences. Therefore, female sex assignment in genetically—and hormonally—male neonates risks personal internal confusion and social external conflict and contradiction.” Id at 671.
Other look-back studies on adults with other conditions show mixed satisfaction about their pediatric care. For instance, in one study, it was found that for a majority of seventy-two intersex adults with varying intersex conditions, “long term outcome appears to be more favorable than some current rhetoric suggests.” However, the study also observed “a small minority of adult intersex patients are dissatisfied with their gender,” and that a “more substantial [minority] are dissatisfied with genital status and sexual functioning, and they support policy changes.” H.F.L. Meyer-Bahlburg et al., Attitudes of Adult 46 XY Intersex Persons to Clinical Management Policies, 171 J. UROLOGY 1615, 1618 (2004). That same study is notable in another respect. Of forty-five individuals that had genital surgery, in hindsight, a total of 46% believed surgery should be postponed—22% supported postponing until adulthood and 24% until adolescence. On the other hand, 47% believe the surgery should be done in infancy. Id. at 1617. Furthermore, fewer than half, only 45% of those surveyed reported being “mainly satisfied” with sexual functioning. Id.
90 William Reiner, To Be Male or Female—That Is the Question, 151 ARCHIVES PEDIATRIC & ADOLESCENT MED. 224-25 (1997).
91 Joel Frader et al., Health Care Professionals and Intersex Conditions , 158 ARCHIVES PEDIATRIC & ADOLESCENT MED. 426, 427 (2004).
92 See, e.g., Peter Lee & Philip A. Gruppuso, Should Cosmetic Surgery Be Performed on the Genitals of Children Born with Ambiguous Genitals, PHYSICIAN’S WKLY, Aug. 16, 1999, available at http://www.physiciansweekly.com/archive/99/08_16_99/pc.html .
93 Kenneth I. Glassberg, Gender Assignment and the Pediatric Urologist, 161 J. UROLOGY I 3C 1309 (1999).
94 Erica A. Eugster, Invited Critique , 158 ARCHIVES PEDIATRIC & ADOLESCENT MED. 426, 4 (2004).
95 See, e.g., Robert M. Blizzard, Intersex Issues: A Series of Continuing Conundrums, 110 PEDIATRICS 616, 620 (2003); S.F. Ahmed et al., Intersex and Gender Assignment: The Third Way?, 89 ARCHIVES DISEASE CHILDHOOD 847, 849 (2003).
96 Laura Hermer, Paradigms Revised: Intersex Children, Bioethics & the Law, 11 ANN. HEALTH L. 195, 228 (2002). See also Julie Greenberg, Legal Aspects of Gender Assignment, 13 THE ENDOCRINOLOGIST 277, 279, 285 (2003) (calling for a “middle ground approach” of “qualified persistent informed consent” and commenting that “[u]ntil long-term studies prove that the dominant treatment protocol provides a better psychological outcome than the alternative treatment proposed, physicians need to ensure that any consent provided by parents is based on full information”).
97 Dissatisfaction with the assigned sex occurs with significant frequency, depending on the intersex condition. See Diamond, supra note 11, at 602-03. See also websites of ISNA, Bodies Like Ours and A Kindred Spirit, supra note 20.
98 Froukje M.E. Slijper et al., Long-Term Psychological Evaluation of Intersex Children , 27 ARCHIVES SEXUAL BEHAV. 125, 142 (1998). See also Ahmed et al., supra note 95, at 849.
99 Hermer, supra note 96, at 228.
100 Kipnis & Diamond, supra note 9, at 406. See also Milton Diamond, Pediatric Management of Ambiguous and Traumatized Genitalia, 162 J. UROLOGY 1021, 1025 (1999). ISNA advises that children be raised with a gender assignment, just not a surgical assignment. See http://www.isna.org/articles/tips_for_parents . Dreger also has not advocated raising children without a gender. See Alice Domurat Dreger, A History of Intersexuality: From the Age of Gonads to the Age of Consent, 9 J. CLINICAL ETHICS 345, 353 (1998) (“All children—no matter how intersexed—can and should be assigned a male or female gender.”).
101 In light of the fact that genitals are covered by clothing and intersex children will be raised as boys or girls, it is hard to see why leaving a healthy body part alone is particularly radical. This is especially so, given the ability of children to be as modest and private as they deem fit. The locker room fear of exposure is also largely overrated. In recent years, group showers in public schools have become the exception, rather than the rule. See Randy Dotinga, Where Have All the Showers Gone?, CHRISTIAN SCI. MONITOR, Feb. 3, 2004, available at http://www.csmonitor.com/2004/0203/p12s01-legn.htm ; see also Valerie Bonney, Squeaky Clean, AM. SCH. & U. MAG, July 1, 2004, available at http://asumag.com/mag/university_squeaky_clean/ .
102 There is a paucity of evidence that surgery provides any benefit to gender development and in fact, there is accumulating evidence about its irrelevance to gender development:
There are scarce data on how children with complex genital anomalies perceive their genitals and how this relates to their gender development. Long term outcome studies of such boys indicate that male gender development does develop in the absence of gender specific genitalia. A systematic examination of the relation between genital appearance and gender identity in a group of girls with congenital adrenal hyperplasia, showed a link between atypical gender identity and prenatal androgen exposure, but not with the degree of virilisation. Taken together, this research suggests that genital appearance may not be as crucial a determinant in gender identity as once thought, although further research is necessary to clarify this observation.
Id.; see also Milton Diamond, Biased-Interaction Theory of Psychosexual Development: How Does One Know If He Is Male or Female, in SEX ROLES (forthcoming 2006).
Ahmed et al., supra note 95, at 848. See also Jorge J. Daaboul, Does the Study of History Affect Clinical Practice? Intersex as a Case Study: The Physician's View, ISNA, http://www.isna.org/articles/daaboul_history :
The thrust of medicine in the last century has been to “cure” intersexed individuals by using surgical, hormonal and psychological therapies to make them unequivocally male or female. However, the functional and psychological results of this approach have been poor. Many intersexed individuals have suffered severe psychological and physical damage from medicine’s attempts to make them male or female. Nonetheless, physicians continue to consider intersex a disease to be fixed because they have no concept that intersexed individuals can lead normal lives as intersexed individuals. History, however, provides strong empirical evidence that, in the past, intersexed individuals have lived normal, happy lives without medical treatment. The empirical evidence derived from the study of history complements and gives practical weight to the ethical proposition that individuals with intersex have a right to autonomously decide their futures and be free from medical intervention.
103 DEWHURST & GORDON, supra note 6, at vii. For life stories, see, e.g., websites of ISNA and Bodies Like Ours, supra note 20.
104 Daaboul, supra note 102. See also Matta, supra note 73, at 77 (tracing the history of surgery for intersex conditions and observing that “[p]hysicians who proposed surgery also found that their patients had different ideas about their bodies. Physicians could no more force patients to undergo surgery than they could force them to wear trousers instead of dresses, and as a result, patients often shrugged off their uncommon bodies as harmless and went about business as usual.”).
105 See Justine Marut Schoeber, A Surgeon’s Response to the Intersex Controversy , 9 J. CLINICAL ETHICS 393, 394 (1998) (noting that although surgery proponents postulated that genitals that conform to gender of rearing are necessary to the development of a solid gender identity, “[w]hether genital appearance significantly impacts a firm gender conviction remains undetermined”); see also A Conversation with Milton Diamond, in DEAN KOTULA, THE PHALLUS PALACE: FEMALE TO MALE TRANSSEXUALS 35-56 (William E. Parker ed., 2002) (stating that it is also significant to consider that all transsexuals are brought up with typical genitalia and rearing yet conclude from internal cues that they must switch from their gender of rearing), available at http://www.kindredspiritlakeside.homestead.com/P_Dr_Diamond.html .
106 COLAPINTO, supra note 8, at 232-35. See also Justine M. Reilly & C.R.J. Woodhouse, Small Penis and the Male Sexual Role, 142 J. UROLOGY 569 (1989); C.R.J. Woodhouse, Ambiguous Genitalia and Intersexuality—Micropenis, in PEDIATRIC UROLOGY 689, 692 (Barry O’Donnell & Stephen A. Koff eds., 3d ed. 1997).
107 See ALICE DOMURAT DREGER, HERMAPHRODITES AND THE MEDICAL INVENTION OF SEX (1998).
108 Reiner, supra note 48, at 670.
109 Id. at 664-65.
110 C.R.J. Woodhouse, supra note 106, at 690.
111 Personal letter from Tony Briffa in an online communication that was removed from the website, http://www.vicnet.net.au/~/tonybriffa.htm , as part of a court case, in which Mr. Briffa was attempting to sue his physicians for their treatment (on file with the authors).
112 Morgan Holmes, Medical Politics and Cultural Imperatives: Intersexuality Beyond Pathology and Erasure (1994) (unpublished M.A. thesis, York University, England).
113 Cheryl Chase, Affronting Reason, in LOOKING QUEER: BODY IMAGE AND GAY IDENTITY IN LESBIAN, BISEXUAL, GAY, AND TRANSGENDER COMMUNITIES 205-219 (Dawn Atkins ed., 1998).
114 The 46 XX “children had congenital adrenal hyperplasia (CAH), were virilized at birth and were being raised as girls.” Jennifer E. Dayner et al., Medical Treatment of Intersex: Parental Perspectives, 172 J. UROLOGY 1762, 1762-63 (2004).
115 Id. at 1763.
118 Parham v. JR., 442 U.S. 582, 602 (1979).
119 Id. at 604. See also Planned Parenthood of Central Mo. v. Danforth, 428 U.S. 52, 74 (1976) (“Constitutional rights do not mature and come into being magically only when one attains the state-defined age of majority. Minors, as well as adults, are protected by the Constitution and possess constitutional rights.”).
120 See Jennifer Rosato, Using Bioethics Discourse to Determine When Parents Should Make Health Care Decisions for Their Children: Is Deference Justified, 73 TEMP. L. REV. 1 (2000).
121 Id . at35.
122 Id. at 43 (internal citations omitted).
123 Categorical conflicts include procedures such as: female genital mutilation, see Criminalization of Female Genital Mutilation Act, Pub. L. No. 104-208, § 645, 110 Stat. 3009, 3009-708 (1996) (codified as amended at 18 U.S.C. § 116); reproductive decisions of mature minors, see, e.g., Bellotti v. Baird, 443 U.S. 622, 633 (1979); sterilization, see, e.g., Matter of A.W., 637 P.2d 366 (Cob. 1981) (en banc); denial of lifesaving treatment based on religious beliefs, see, e.g., In re McCauley, 565 N.E.2d 411, 413 (Mass. 1991); Novak v. Cobb-County Kennestone Hosp. Auth., 849 F. Supp. 1559 (ND. Ga. 1994); non-therapeutic research posing greater than minimal risk, see, e.g., Grimes v. Kennedy Krieger Institute, Inc., 782 A.2d 807, 853 (Md. App. 2001); organ donation from a minor to another, see, e.g., Hart v. Brown, 289 A.2d 386 (Conn. Super. 1972) (“natural parents of a minor should have the right to give their consent to an isograft kidney transplantation procedure when their motivation and reasoning are favorably reviewed by a community representation which includes a court of equity”). Some courts have refused to allow donation by a person deemed incompetent. See, e.g., In re Richardson, 284 So.2d 185 (La. App. 1973) (holding that neither parents nor the courts could authorize kidney transplant of mentally retarded minor to his sister); In re Guardianship of Pescinski, 226 N.W.2d 180 (Wis. 1975).
124 Strictly speaking, the surgery might not meet Rosato’s concept of unreasonableness because while the surgery is controversial, it remains for the time being an accepted medical practice among a minority of physicians. “A recent survey of pediatric urologists found two-thirds would call genetically male babies boys even if they have no penis—while five years ago almost all would have recommended raising them as girls.” Surgery May Be Hasty for Unclear Gender Intersex, SCI. LETTER, Mar. 15, 2005, at 989, available at 2005 WLNR 3750081.
125 Australia, as a matter of national common law, has developed a categorical standard for extraordinary medical treatment for children: “Court authorisation to medical treatment is required where there is a significant risk of making the wrong decision, either as to a child’s present or future capacity to consent or about what are the best interests of a child who cannot consent, and where the consequences of a wrong decision are particularly grave.” Sec’y Dep’t of Health and Cmty. Servs. v. JWB & SMB (1992) 175 C.L.R. 218. Notably, this standard has also been applied to intersex surgery. See Re A (1993) 16 Fam. L. R. 715 (giving permission to a minor—fourteen-year-old genetic female with Congenital Adrenal Hyperplasia identifying as a male—who was unable give informed consent for gender reassignment surgery). See also Margaret O’Rourke, Dilemmas When Gender Is Uncertain, AUSTRALIAN, Mar. 19, 2005, at C31, available at 2005 WLNR 4210025.
126 In Rosato’s construction of categorical conflicts, genital normalizing and sex assignment surgeries are also extraordinary medical treatment, which is defined as a “‘momentous’ decision[] … that would ... cause a permanent or unavoidable loss or impairment of important physical or psychological functions.” Rosato, supra note 120, at 45 (discussing and quoting ALLEN E. BUCHANAN & DAN W. BROCK, DECIDING FOR OTHERS: THE ETHICS OF SURROGATE DECISION MAKING 142-43 (1990)).
127 Rosato, supra note 120, at 45. Genital normalizing and sex assignment surgery involves countervailing constitutional rights of privacy related to self-identity, sexuality, and in some instances, procreation. Although children may lack the ability to exercise these nascent rights, the right to make these choices should be preserved until they are able to do so. As the United States Supreme Court has stated, “Parents may be free to become martyrs themselves. But it does not follow they are free, in identical circumstances, to make martyrs of their children before they have reached the age of full and legal discretion when they can make that choice for themselves.” Prince v. Mass., 321 U.S. 158, 170 (1944) (emphasis added).
128 Rosato, supra note 120, at 51.
129 See, e.g., Matter of A. W. ,637 P.2d 366:
Consent by parents to the sterilization of their mentally retarded offspring has a history of abuse which indicates that parents, at least in this limited context, cannot be presumed to have an identity of interest with their children. ... The inconvenience of caring for the incompetent child coupled with fears of sexual promiscuity or exploitation may lead parents to seek a solution which infringes their offspring’s fundamental procreative rights.
130 See COHEN-KETTENIS & PFÄFFLIN, supra note 22, at 85 (“When the children themselves are too young to understand their situation, the first psychological care concerns the parents.”); KESSLER, supra note 21,at 12-32.
131 See AMERICAN ACADEMY OF PEDIATRICS, supra note 51,at 138; KESSLER, supra note 21, at 12-32 (discussing parental distress as a motivation for treatment); see also DEWHURST & GORDON, supra note 6, at 4 (“At this early age the emotional reactions of the parents only and not of the child need be considered.”).
132 KESSLER, supra note 21,at 16.
133 Alice Dreger, Intersex Treatment as Standard Medical Practice, or How Wrong I Was, Oct. 1, 2004, ISNA, http://www.isna.org/articles/howwrongiwas .
134 Wendy Anton Fitzgerald, Engineering Perfect Offspring: Devaluing Children and Childhood, 24 HASTINGS CONST. L.Q. 833, 857-58 (1997).
136 Professor Barbara Woodhouse commented about a news article regarding a father saving his child from a burning building and she parenthetically quoted the local fire marshall who said, “That guy went through hell to get that baby out!”:
Perhaps my method seeks to remind the reader of something that is easy to forget in the quest for rigorous models: parents are not rational actors in the commonly accepted meaning of the term. Yet their seemingly irrational acts make perfect sense in the context of the human experience of parenthood.
Barbara Bennett Woodhouse, Of Babies, Bonding and Burning Buildings: Discerning Parenthood in Irrational Action, 81 VA. L. REV. 2493, 2496-97 (1995).
137 Woodhouse, supra note 106, at 690.
138 For a contemporary view of child-centered framework to understanding the source of parental authority and responsibility, see generally Barbara B. Woodhouse, Hatching the Egg: A Child-Centered Perspective on Parents’ Rights, 14 CARDOZO L. REV. 1747 (1993); Barbara Woodhouse, “Out of Children’s Needs, Children’s Rights”: The Child’s Voice in Defining Family, 8 B.Y.U. J. PUB. L. 321 (1994); Barbara Bennett Woodhouse, Speaking Truth to Power: Challenging “The Power of Parents to Control the Education of Their Own”, 11 CORNELL J.L. & PUB. POL’Y 481 (2002).
139 In this regard, Matter of Shane T, 453 N.Y.S.2d 590 (Fam. Ct. 1982), is noteworthy. There, a father repeatedly called his son “fag,” “faggot” and “queer.” The father claimed this was “a form of legitimate parental discipline to cure the child of certain unspecified ‘girlie’ behavior.” The father stated “that it would be embarrassing for him if [his son] were queer.” Id. at 593. The court found the conduct constituted child abuse, as did the child’s mother’s failure to stop the conduct and to protect the child.
While a parent’s right to raise his or her child remains fundamental ... it is equally fundamental that children have constitutional rights which must be respected by all, including their parents. ... [T]he bill of rights is not for adults alone. Time and again, courts have reiterated the validity of state interference in the parental-child relationship when necessary to protect the child’s health and welfare. Id. at 593-94.
140 For example, two recent decisions in New York and Massachusetts have required schools to accommodate transgendered students in their real life transition. See Jean Doe v. Bell, 754 N.Y.S.2d 846 (Sup. Ct. 2003) (holding that an all-male city-sponsored foster facility did not make a reasonable accommodation under New York law when the facility refused to allow male-to-female seventeen year old youth to dress as a girl as recommended by minor’s psychiatrist); Doe v. Yuntis, 2001 WL 664947 (Mass. Super. 2001) (under Massachusetts law, public junior high school officials may be subject to liability for refusing to allow male-to-female, fifteen year old to dress as a girl as recommended in her psychiatric treatment plan). There have been other positive developments for young victims of harassment. See, e.g., Nabozny v. Podlesny, 92 F.3d 446 (7th Cir. 1996). The United States Supreme Court recently held that school officials who act with “deliberate indifference” to known acts of student- on-student sexual harassment may be subject to liability. Harassment must extend beyond “mere teasing” and must be “so severe, pervasive, and objectively offensive that it effectively bars the victim’s access to an educational opportunity or benefit.” Davis v. Monroe County Bd. of Educ., 526U.S. 629, 633 (1999).
Back to top
Open Education Sociology Dictionary
nature versus nurture
Table of Contents
Definition of Nature Versus Nurture
( noun ) A debate between the influence of genetics ( nature ) and social environments ( nurture ) on the development of individual or group and which one is more dominant.
Nature Versus Nurture Pronunciation
Pronunciation Usage Guide
Syllabification : na·ture ver·sus nur·ture
Audio Pronunciation
Phonetic Spelling
- American English – /nAY-chuhr vUHR-suhz nUHR-chuhr/
- British English – /nAY-chuh vUHR-suhs nUHR-chuh/
International Phonetic Alphabet
- American English – /ˈneɪʧər ˈvɜrsəs ˈnɜrʧər/
- British English – /ˈneɪʧə ˈvɜːsəs ˈnɜːʧə/
Usage Notes
- An oft debated topic in the social sciences is whether nature or nurture exerts more control on an individual or society .
- The story of David Reimer, also known as the David/Brenda case study or the John/Joan case study , is an important one for theories of nature vs. nurture. David was born male and as an infant his penis was destroyed in a botched circumcision. Medical and Psychological intervention ensued which saw David renamed Brenda and raised as a girl. He failed to identify as a girl and transitioned back to male status as a teenager. He lived and functioned as a male before committing suicide in 2004, aged 38. This case study portrays different views on what constitutes gender, identity and sexuality and the problems each school of thought faces in their arguments and the consequences of belief and action following those arguments.
- In some cultures, intersexed infants are seen as normal, sometimes special, beings, and these views run counter to those found in industrialized or Western societies, which see such bodies as abnormal and in need of correction.
- nature-nurture
- nature v nurture
- nature vs nurture
- Also called: nature-nurture debate

Related Quotations
- “Biological models for understanding human behavior rely on the idea that innate biological differences between males and females ‘program’ distinct social behaviors for men and women. This is called biological determinism . Socially based frameworks, such as those coming from the fields of cultural anthropology or sociology , look at variations in behaviors and gender attributes . These approaches highlight the socialization process that teaches boys and girls to live up to the expectations for their respective genders . Either approach on its own—biology or socialization , nature or nurture—is inadequate for explaining complex human beings and why we do what we do” (Tarrant 2009:67).
- “ Feminism explicitly examines women’s roles and experiences in society , working to fully uncover women’s contributions to social life and the nature of the structures and processes that maintain gender inequality” (Hughes and Kroehler 2008:17).
- “The source of much of the heat in the incest debate is the friction incident on rubbing two very different views of human nature against the same problem. The conventionalist view is that human beings are born with a few ‘basic drives,’ all of which are asocial if not antisocial and some of which are so dangerous they must be constrained. The rest of what humans are, and the larger part by far, is learned and thus varies from society to society —a view that is commonly taken to mean that utopia or something like it is possible. Constitutionalists, in contrast, are committed to the view that while human beings are far from complete at birth, they typically develop along lines laid out by an innate plan. The variation touted by conventionalists is largely ephemeral if not the result of distortion occasioned by abnormal circumstances. Most constitutionalists argue that if we were really as pliable as conventionalists claim, we would all be slaves molded to serve one master or another. Where conventionalists, optimistic on principle, pit their hope for the future on a pliable human nature , constitutionalists, typically pessimistic, allay their fears for the future by holding fast to the view that human nature is stubborn” (Wolf 2014:4).
Related Video
Additional Information
- Sex and Gender Resources – Books, Journals, and Helpful Links
- Word origin of “nature” and “versus” and “nurture” – Online Etymology Dictionary: etymonline.com
Related Terms
- discrimination
- role taking
- socialization
Hughes, Michael, and Carolyn J. Kroehler. 2008. Sociology: The Core . 8th ed. Boston: McGraw-Hill.
Tarrant, Shira. 2009. Men and Feminism . Berkeley, CA: Seal Press.
Wolf, Arthur P. 2014. Incest Avoidance and the Incest Taboos: Two Aspects of Human Nature . Stanford, CA: Stanford Briefs.
Works Consulted
Ferris, Kerry, and Jill Stein. 2010. The Real World: An Introduction to Sociology . 2nd ed. New York: Norton.
Merriam-Webster. (N.d.) Merriam-Webster Dictionary . ( http://www.merriam-webster.com/ ).
Oxford University Press. (N.d.) Oxford Dictionaries . ( https://www.oxforddictionaries.com/ ).
Ravelli, Bruce, and Michelle Webber. 2016. Exploring Sociology: A Canadian Perspective . 3rd ed. Toronto: Pearson.
Thompson, William E., and Joseph V. Hickey. 2012. Society in Focus: An Introduction to Sociology . 7th ed. Boston: Allyn & Bacon.
Tischler, Henry L. 2011. Introduction to Sociology . 10th ed. Belmont, CA: Wadsworth.
Wikipedia contributors. (N.d.) Wikipedia, The Free Encyclopedia . Wikimedia Foundation. ( https://en.wikipedia.org/ ).
Cite the Definition of Nature Versus Nurture
ASA – American Sociological Association (5th edition)
Bell, Kenton, ed. 2013. “nature versus nurture.” In Open Education Sociology Dictionary . Retrieved April 30, 2024 ( https://sociologydictionary.org/nature-versus-nurture/ ).
APA – American Psychological Association (6th edition)
nature versus nurture. (2013). In K. Bell (Ed.), Open education sociology dictionary . Retrieved from https://sociologydictionary.org/nature-versus-nurture/
Chicago/Turabian: Author-Date – Chicago Manual of Style (16th edition)
Bell, Kenton, ed. 2013. “nature versus nurture.” In Open Education Sociology Dictionary . Accessed April 30, 2024. https://sociologydictionary.org/nature-versus-nurture/ .
MLA – Modern Language Association (7th edition)
“nature versus nurture.” Open Education Sociology Dictionary . Ed. Kenton Bell. 2013. Web. 30 Apr. 2024. < https://sociologydictionary.org/nature-versus-nurture/ >.
- International edition
- Australia edition
- Europe edition

Radio review: Case Study
T here was a big "eek" moment at the start of Case Study (Radio 4). We heard from the mother of the programme's subject – David Reimer, born a boy but raised as a girl – about the medical catastrophe that led to a disastrous experiment of gender reassignment.
She remembered the call from the hospital where her twin baby sons were due to be circumcised. The first procedure had been a disaster. "The penis had been burned off," she said. Eek. Her speech was slow, slurred almost, and sounded haunted by what she had endured, allowed, in the years that followed. And little wonder: one twin, who continued as a boy, died of a drugs overdose, and Reimer (pictured) killed himself in 2004.
The programme told Reimer's devastating story well, and presenter Claudia Hammond extended it to consider the ramifications for medical research since. Part of Reimer's horror, she explained, was that his case was reported in the literature as a complete success, though it was nothing of the sort. "I tried to put makeup on," we heard Reimer say in an archive clip, "but I looked like Bozo the Clown. It's in you, it's in your genetics – nobody has to tell you what you are." His voice too sounded scarred, as he grappled for composure but remained audibly all at sea.
- Radio review
Comments (…)
Most viewed.
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- Auto Racing
- 2024 Paris Olympic Games
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Retired pro wrestler, failed congressional candidate indicted in Vegas murder case
FILE - Daniel Rodimer leaves court after his initial appearance on murder charges at the Regional Justice Center in Las Vegas, Wednesday, April 10, 2024. Rodimer, a retired professional wrestler and former congressional candidate in Nevada and Texas, has been indicted on a murder charge in the death of an Idaho man who suffered a head injury during a Halloween Party at a Las Vegas Strip hotel. (Bizuayehu Tesfaye/Las Vegas Review-Journal via AP, File)
- Copy Link copied
LAS VEGAS (AP) — A retired professional wrestler and former congressional candidate in Nevada and Texas has been indicted on a murder charge in the death of an Idaho man who suffered a head injury during a Halloween Party at a Las Vegas Strip hotel.
Daniel Rodimer, 45, who now lives in Texas, is expected to appear before a Nevada judge May 8 following his indictment Friday in the death of Christopher Tapp.
His defense attorneys, David Chesnoff and Richard Schonfeld, said Friday that Rodimer “maintains his complete innocence and looks forward to his day in court.”
Tapp, 47, of Idaho Falls, was injured Oct. 29 at the Resorts World hotel and taken to a hospital, where he died several days later, police said. He had served more than 20 years in prison in Idaho in a 1996 killing before receiving an $11.7 million settlement from Idaho Falls in 2022 in a wrongful conviction lawsuit.
Investigators initially believed Tapp had been fatally injured in a fall, but they later learned that he had been in an argument with Rodimer.
Rodimer, a Republican who lost bids for Congress in Nevada in 2020 and in Texas in 2021 , surrendered to Las Vegas police for his arrest March 6 and remains free on a $200,000 bail.
- Open access
- Published: 25 April 2024
The maternal factors associated with infant low birth weight: an umbrella review
- Hoda Arabzadeh 1 ,
- Amin Doosti-Irani 1 , 2 ,
- Sima Kamkari 3 ,
- Maryam Farhadian 4 ,
- Elahe Elyasi 1 &
- Younes Mohammadi 1 , 5
BMC Pregnancy and Childbirth volume 24 , Article number: 316 ( 2024 ) Cite this article
128 Accesses
Metrics details
In this umbrella review, we systematically evaluated the evidence from meta-analyses and systematic reviews of maternal factors associated with low birth weight.
PubMed, Scopus, and Web of Science were searched to identify all relevant published studies up to August 2023. We included all meta-analysis studies (based on cohort, case-control, cross-sectional studies) that examined the association between maternal factors (15 risk factors) and risk of LBW, regardless of publication date. A random-effects meta-analysis was conducted to estimate the summary effect size along with the 95% confidence interval (CI), 95% prediction interval, and heterogeneity (I 2 ) in all meta-analyses. Hedges’ g was used as the effect size metric. The effects of small studies and excess significance biases were assessed using funnel plots and the Egger’s test, respectively. The methodological quality of the included studies was assessed using the AMSTAR 2 tool.
We included 13 systematic Review with 15 meta-analysis studies in our study based on the inclusion criteria. The following 13 maternal factors were identified as risk factors for low birth weight: crack/cocaine (odds ratio [OR] 2.82, 95% confidence interval [CI] 2.26–3.52), infertility (OR 1.34, 95% CI 1.2–1.48), smoking (OR 2.00, 95% CI 1.76–2.28), periodontal disease (OR 2.41, 95% CI 1.67–3.47), depression (OR 1.84, 95% CI 1.34–2.53), anemia (OR 1.32, 95% CI 1.13–1.55), caffeine/coffee (OR 1.34, 95% CI 1.14–1.57), heavy physical workload (OR 1.87, 95% CI 1.00-3.47), lifting ≥ 11 kg (OR 1.59, 95% CI 1.02–2.48), underweight (OR 1.79, 95% CI 1.20–2.67), alcohol (OR 1.23, 95% CI 1.04–1.46), hypertension (OR 3.90, 95% CI 2.73–5.58), and hypothyroidism (OR 1.40, 95% CI 1.01–1.94). A significant negative association was also reported between antenatal care and low birth weight.
Conclusions
This umbrella review identified drug use (such as crack/cocaine), infertility, smoking, periodontal disease, depression, caffeine and anemia as risk factors for low birth weight in pregnant women. These findings suggest that pregnant women can reduce the risk of low birth weight by maintaining good oral health, eating a healthy diet, managing stress and mental health, and avoiding smoking and drug use.
Peer Review reports
Introduction
Low birth weight (LBW), defined by the World Health Organization as a weight under 2500 g at birth, stands as a formidable global public health challenge [ 1 , 2 , 3 ]. Far beyond a numerical classification, LBW represents a pivotal health metric and a key indicator of intrauterine growth retardation (IUGR). It intricately weaves together the dynamics of fetal development, gestational duration, and birth outcomes, underscoring its significance [ 4 ]. LBW contributes to a spectrum of adverse outcomes throughout the life course. Infants with LBW are more susceptible to stunted growth, infectious diseases, neurodevelopmental impairments, compromised cognitive function, and academic performance challenges in childhood and adulthood [ 5 , 6 ]. In addition to the immediate health consequences, low birth weight can also have long-term effects on a child’s cognitive and physical development. Children born with low birth weight may experience delays in speech, language, and motor skills development, and may be at increased risk of attention deficit hyperactivity disorder (ADHD) and other behavioral problems [ 7 , 8 ]. LBW is responsible for 60–80% of deaths in the first month of life, LBW significantly heightens the risk of diverse adverse outcomes [ 1 , 9 , 10 , 11 , 12 , 13 , 14 , 15 ]. Moreover, the socioeconomic costs entwined with LBW reverberate across the lifespan, affecting both individuals and society at large [ 16 , 17 ]. Recognizing the magnitude of health and economic burdens linked with LBW, the World Health Organization has prioritized the reduction of LBW prevalence as a critical public health goal and therefore, sets an ambitious target, aiming for a 30% reduction in prevalence of LBW worldwide between 2012 and 2025 [ 1 , 18 ]. To attain this ambitious goal, a profound understanding of modifiable determinants of intrauterine growth restriction is essential. This entails a comprehensive exploration of biological, socioeconomic, environmental, and behavioral factors that collectively influence fetal development and contribute to LBW risk [ 19 , 20 ]. Notably, maternal health conditions and exposures during pregnancy emerge as especially crucial factors amenable to intervention [ 19 , 21 , 22 , 23 ]. Despite the extensive literature on maternal factors associated with LBW, existing studies yield mixed or inconclusive findings. The absence of a systematic compilation of collective meta-analytic evidence linking various maternal determinants to LBW risk underscores the need for an umbrella review. This unique endeavor is poised to clarify maternal factors with the strongest and most consistent associations with LBW. Its significance lies in elucidating maternal exposures that significantly contribute to LBW risk, thereby informing targeted clinical and public health strategies to address this critical global health issue. Therefore, the primary objective of this umbrella review is to comprehensively synthesize available meta-analytic evidence, with a particular emphasis on evaluating the association between various maternal risk factors and low birth weight (LBW). This meticulous approach ensures a profound exploration of LBW within the intricate context of poor growth and shorter gestation, contributing to a nuanced understanding of this complex public health challenge.
This umbrella review was conducted and reported by following the PRISMA guideline [ 24 ].
Identifying potential risk factors
In order to pinpoint the potential risk factors associated with Low Birth Weight (LBW), a systematic search was conducted across various online sources to identify all conceivable maternal risk factors linked to LBW. Subsequently, in collaboration with a gynecologist and obstetrician, key risk factors were selected for further investigation in the subsequent phase, which involved locating pertinent meta-analyses.
Search strategy and eligibility criteria
We conducted a systematic search of PubMed, Scopus, and Web of Science, for meta-analyses published on the association between maternal factors and low birth weight (LBW). The search was conducted on August 2023, without limitations in time, language, and place. We used the following relevant MeSH terms and keywords: Maternal exposure, Smoking, Anemia, Periodontal diseases, Depression, Anxiety, Hypertension, High blood pressure, Body mass index, Quetelet index, Women working, Antenatal care, Alcoholism, Drug use disorders, Caffeine, Thyroid diseases, Infertility female, Infant, Low birth weight, Meta-analysis, Systematic review, Synthesis. The detailed search strategy is included in the supplementary material (Table 1 ).
Two authors (HA and EE) independently screened the titles and abstracts of all identified studies and then reviewed the full texts of eligible studies. Disagreements were resolved through discussion with YM. We included all published meta-analyses of cohort, case-control, and cross-sectional studies that examined the association between maternal factors (15 risk factors) and risk of LBW, regardless of publication date. For each factor, we selected the meta-analysis with the highest quality score based on the AMSTAR 2 tool. If two or more meta-analyses had the same quality score, we prioritized the meta-analysis with the latest publication date and the largest sample size.
Data extraction
Two authors (HA and EE) independently extracted data from the selected studies using a pre-specified form in Microsoft Excel. The extracted data included the following: Factors associated with LBW, First author of the paper, Publication year, Number of participants, Number of studies in the meta-analysis, Study design of included studies, Results of heterogeneity tests, Random effect P-values and the measure of association (e.g., risk ratio, odds ratio) with 95% CI.
Quality assessment
We assessed the quality of the selected studies using the AMSTAR 2 tool [ 25 ]. Any disagreements between the two reviewers were resolved through discussion with a third author (YM). The AMSTAR 2 is a validated and critical appraisal tool for evaluating systematic reviews of randomized trials. It contains 16 items, seven of which are critical items and nine are non-critical items. The rating method was as follows:
Studies with no non-critical items or one non-critical item were defined as high quality.
Studies with more than one non-critical item were defined as medium quality.
Studies with one critical item and with or without non-critical items were defined as low quality.
Studies with more than one critical item with or without non-critical items were defined as critically low quality.
Statistical analysis
We performed all statistical analyses using the meta-umbrella R package. The meta-umbrella R package is a tool that allows users to perform umbrella reviews with the stratification of evidence. All studies reported odds ratios and relative risks with 95% confidence intervals (CIs) for risk factors of LBW. We used a random-effects model to calculate the pooled odds ratios and relative risks, and we calculated P-values for each risk factor. A significance level of P < 0.05 was considered statistical significancy. We assessed heterogeneity among the primary studies using Cochran’s Q test and I2 statistic [ 26 ]. The I2 statistic is a measure of the percentage of variation across studies that is due to heterogeneity rather than chance. An I2 statistic of > 50% was considered to indicate high heterogeneity. We also estimated the 95% prediction interval (95% PI) for each risk factor. The 95% PI is a range of values that is likely to contain the value of a single new observation given the specified settings of the predictors [ 27 ]. We used Egger’s regression asymmetry test to assess publication bias [ 28 ]. Egger’s test is a statistical test that can be used to detect publication bias in meta-analyses. A P-value < 0.05 on Egger’s test was considered to indicate evidence of publication bias. We used Ioannidis test for excess of significance bias to assess the overall bias of the meta-analyses [ 29 ]. Ioannidis’ test is a statistical test that can be used to detect bias in meta-analyses, such as selective reporting bias or publication bias. A P-value < 0.05 on Ioannidis test was considered to indicate evidence of overall bias. We also reported the Hedges’ g value for each risk factor. Hedges’ g is a measure of effect size which tells you how much one group differs from another—usually a difference between an experimental group and a control group [ 30 ]. Cohen suggested using the following rule of thumb for interpreting results: Small effect (cannot be discerned by the naked eye) = 0.2, Medium Effect = 0.5, Large Effect (can be seen by the naked eye) = 0.8 [ 31 ].
Strength of existing evidence
We used the Ioannidis criteria classification to assess the strength of the evidence of factors for Low Birth Weight. This classification proposes to stratify evidence into five ordinal classes: convincing (class I), highly suggestive (class II), suggestive (class III), weak (class IV), and not significant (ns) (Table 1 )
Study selection
The initial database search yielded 1,292 records. After removing 601 duplicates, 691 articles underwent title and abstract screening. A further 49 full-text articles were assessed for eligibility, of which 13 meta-analyses were included in the qualitative synthesis (Fig. 1 ). The list of excluded studies is provided in Supplementary Table 2 .
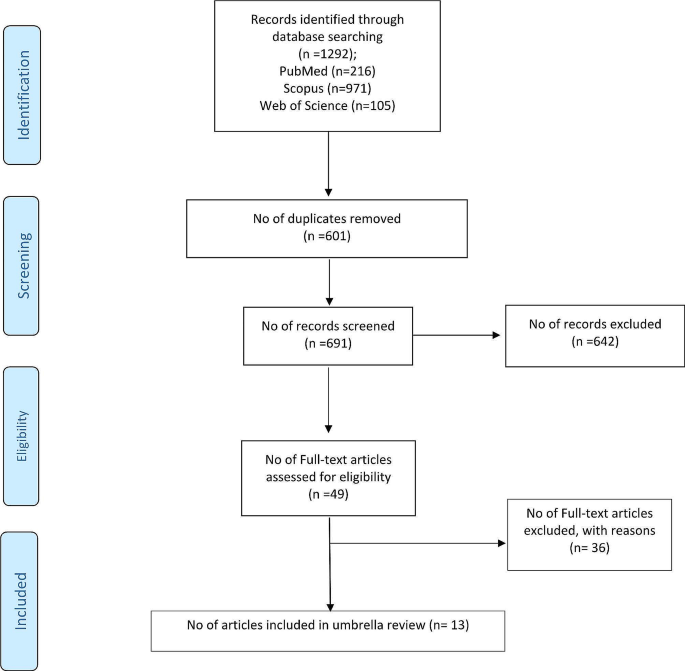
Flowchart of study selection process of the included meta-analyses in umbrella review
Study characteristics
The 13 included meta-analyses comprised a total of 15 separate meta-analyses examining different maternal risk factors for low birth weight (LBW). Collectively, these 15 meta-analyses included 119,358 LBW cases and 5,084,217 participants across 198 individual studies [ 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 ]. The sample size exceeded 1,000 in all meta-analyses except one ( n < 500). Publication years they were ranged from 2013 to 2023. The selected meta-analyses included observational study designs including case-control, cohort, and cross-sectional. The meta-analyses examined the following 15 maternal factors about LBW risk: cocaine/crack use, caffeine intake, hypertension, smoking, periodontal disease, depression, anemia, heavy physical workload, heavy lifting, underweight, overweight/obesity, alcohol use, antenatal care, infertility, and hypothyroidism. Detailed characteristics of each meta-analysis are presented in Table 2 .
Methodological quality
The methodological quality of all included meta-analyses was rated as “critically low” based on the AMSTAR-2 tool. Individual quality assessment scores are provided in Supplementary file, Table 3 .
Summary effect sizes
Of the 15 maternal factors examined, 13 demonstrated statistically significant associations with LBW risk at p ≤ 0.05 and were considered as risk factors: periodontal disease, depression, smoking, hypertension, cocaine/crack use, anemia, heavy physical workload, heavy lifting, underweight, alcohol use, hypothyroidism, caffeine intake, and infertility. One factor, antenatal care, showed a significant protective effect against LBW ( p < 0.001). Overweight/obesity was not significantly associated with LBW ( p = 0.054).
Based on the evaluation of effect size and evidence strength, cocaine/crack use (OR 2.82, 95% CI: 2.26–3.52) and infertility (OR 1.33, 95% CI: 1.2–1.48) were classified as convincing risk factors (Class I). Antenatal care (OR 0.47, 95% CI: 0.36–0.61) and smoking (OR 2.00, 95% CI: 1.75–2.28) showed highly suggestive evidence (Class II). Periodontal disease, depression, anemia, and caffeine intake were considered suggestive evidence (Class III). The remaining risk factors demonstrated weak evidence (Class IV). Summary effect sizes and evidence grades are presented in Table 3 ; Fig. 2 .
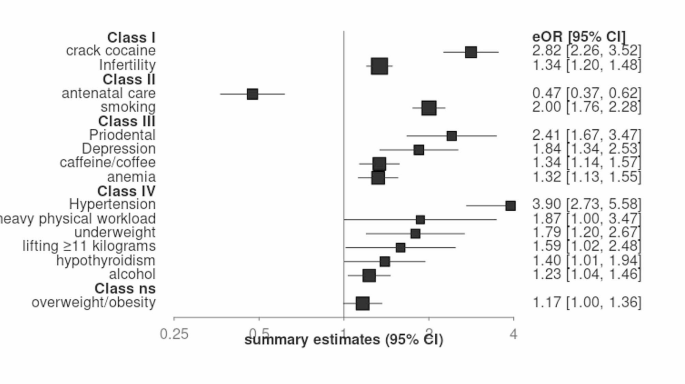
Summary estimates with 95% confidence intervals from 15 associations for LBW
Heterogeneity and bias
Across the 15 associations, 12 (80%) exhibited high heterogeneity (I2 > 50%) and three (20%) had low heterogeneity (I2 < 50%). The 95% prediction interval included the null value for 11 associations (73%) and excluded the null for four associations (27%). Small study bias was indicated in three meta-analyses based on significant Egger’s tests ( p < 0.05) for periodontal disease, depression, and anemia. No evidence of excess significance bias was found for 10 factors according to Ioannidis testing; the remaining five showed potential excess significance bias. According to Hedges’ g values, effect sizes were small for seven factors, medium for six factors, and large for two factors. Detailed results for heterogeneity and bias assessments are presented in Table 3 .
This umbrella review aimed to examine the connection between maternal factors and the risk of low birth weight (LBW). We analyzed 15 maternal factors based on 13 systematic review and meta-analysis studies involving 119,358 LBW cases. Our findings revealed that periodontal disease, anemia, depression, hypertension, hypothyroidism, infertility, underweight, heavy physical workload, lifting ≥ 11 kg, smoking and alcohol, caffeine, and crack/cocaine use during pregnancy were identified as risk factors for LBW. Additionally, antenatal care was found to be a protective factor against LBW.
Our study found highly suggestive evidence that antenatal care can decrease the risk of low birth weight. Specifically, our results showed that mothers who received prenatal care at least once during pregnancy had a lower risk of LBW in their infants [ 44 ]. Furthermore, we did not identify significant publication bias or excess significant bias (publication bias) in our study. Our findings are consistent with other studies [ 45 , 46 , 47 ], which support the notion that promoting prenatal care for pregnant women can serve as a valuable and essential strategy to enhance newborn health outcomes and mitigate the risk of LBW.
Our study provides convincing evidence that infertility is a risk factor for low birth weight (LBW). In our study, infertility was defined as pregnancy occurring after 12 months of trying [ 48 , 49 ]. Our results are consistent with a published meta-analysis, which found that twins conceived through in vitro fertilization (IVF) have a higher risk of LBW [ 50 ]. Given that various underlying pathologies can lead to infertility, some of these mechanisms may also contribute to adverse pregnancy outcomes [ 51 , 52 ].
Our study found suggestive evidence that smoking, caffeine intake, and narcotics such as crack/cocaine use during pregnancy are risk factors for low birth weight (LBW). Additionally, we found weak evidence that alcohol can increase the risk of LBW. Previous studies have attributed the negative effects of smoking on LBW to nicotine, which affects the cardiovascular system of the mother, leading to tachycardia and peripheral vasoconstriction [ 53 , 54 , 55 ]. This results in hypoxia and low levels of nutrients delivered to the placenta, ultimately causing fetal growth restriction [ 56 , 57 ]. Alcohol and crack/cocaine use can also interfere with the transfer of important nutrients for growth by the placenta and affect the fetus’s ability to receive sufficient oxygen and nourishment, leading to LBW [ 56 , 58 , 59 ].
However, in the included meta-analysis that examined the effect of alcohol on LBW, high heterogeneity and publication bias were reported, and it was classified as weak evidence. This heterogeneity may be due to differences in methodology, sample size, and specificities. Therefore, we must be careful when interpreting the association between alcohol and LBW. Caffeine metabolism is slower in pregnant women, and caffeine can easily be transmitted across the placenta due to its presence in amniotic fluid, umbilical cord, urine, and plasma. The fetus cannot produce enough enzymes for caffeine metabolism due to liver immaturity, leading to an increased risk of LBW [ 60 ]. Previous dose-response meta-analyses have shown that there is a graded relationship between caffeine consumption and LBW, with every 100 mg of maternal caffeine consumption per day (about one cup of coffee) increasing the risk of LBW [ 61 , 62 ]. However, evidence from previous dose-response meta-analyses has also shown that there is no identifiable threshold for caffeine intake to be a risk factor for adverse pregnancy outcomes such as LBW [ 63 ].
Our umbrella review found that diseases such as hypertension, periodontitis, depression, anemia, and hypothyroidism are associated with an increased risk of low birth weight (LBW). The study by Rahman et al. demonstrated that pregnancy-induced hypertension is an independent risk factor for LBW, In the results of a WHO secondary analysis survey conducted in low- and middle-income countries, pregnancy with hypertension was associated with a double risk of LBW [ 64 , 65 ]. Our meta-analysis showed that almost one-third of pregnancies with hypertension result in the birth of LBW infants, although the results may have been influenced by several confounders and high heterogeneity (I2 = 75%), However, another meta-analysis study conducted on cohort studies yielded results that are consistent with our findings [ 66 ].
Depression during pregnancy has been associated with poorer maternal health behaviors, such as unhealthy diet, physical weakness, poverty, unhealthy lifestyle, and smoking, which could increase the risk of LBW [ 21 , 67 ]. A meta-analysis published in 2017 indicated a decrease in maternal hemoglobin level during the first pregnancy is significantly related to the risk of LBW, although there was no significant relationship with the second and third trimesters [ 68 ]. Periodontitis can directly cause infection of the placenta and fetus through periodontal bacteria, and several published studies have confirmed that periodontal disease is significantly associated with adverse pregnancy outcomes [ 69 , 70 , 71 ]. However, a case-control study showed that periodontal disease is not significantly associated with LBW, even after controlling for potential confounders [ 72 ], which may be due to recall bias or selection bias.
Thyroid disorders such as hypothyroidism in pregnant women can be a risk factor for LBW because thyroid hormone regulates fetal growth and development throughout pregnancy. The fetus needs placental hormone transfer from the mother to access thyroid hormone, especially during the first 18 to 20 weeks of gestation [ 73 ]. It is important to note that I2 > 65 was reported in these four meta-analyses, and publication bias and publication bias were significant in periodontal diseases, depression, and anemia. However, these factors were classified as suggestive evidence (class III), while hypertension was placed in the category of weak evidence despite having an OR of 3.8. These points should be considered when interpreting these associations.
Over the past few decades, there has been an increase in the proportion of working women. However, past studies have shown that physical work can be a factor for adverse pregnancy outcomes, including low birth weight and preterm delivery. Heavy physical activity can lead to the contraction of the uterus and increase the risk of premature labor by increasing the level of noradrenaline [ 43 , 74 , 75 ].
The meta-analysis we reviewed showed a positive and significant correlation between heavy physical workload, lifting ≥ 11 kg, and low birth weight. However, this meta-analysis had high heterogeneity (> 80) and was classified as weak evidence (class IV). Significant excess bias was also reported for lifting ≥ 11 kg. Other meta-analysis studies have shown that long working hours compared to standard hours and standing at work for > 4 h per day during pregnancy are associated with an increased risk of miscarriage, low birth weight, and preterm delivery [ 76 , 77 ].
Several previously published studies have demonstrated that maternal body mass index (BMI) during pre-pregnancy or early pregnancy can affect the health of both mothers and infants [ 78 , 79 , 80 , 81 ]. In our investigation, we found that maternal underweight was positively and significantly related to low birth weight, while the relationship between obesity/overweight and low birth weight was not significant. Another meta-analysis, which was based on cohort studies and adjusted for confounders, supports our claim that maternal underweight is a risk factor for low birth weight in infants [ 82 ].
Implication
Given the significance of understanding the determinants influencing low birth weight to mitigate and diminish this unfavorable pregnancy outcome, our findings hold the potential to assist policymakers and healthcare practitioners in sustaining and enhancing the well-being of both mothers and infants. Various recommendations for prospective research endeavors can be proposed, including the imperative to undertake meta-analyses on unexplored factors impacting low birth weight, such as infectious diseases, which were not investigated in our study.
Strengths and limitations
An umbrella review serves as a comprehensive document that provides a useful overview of reviews on a specific topic, including all relevant reviews [ 83 , 84 , 85 ], Our study represents the first umbrella review conducted on risk factors for low birth weight (LBW). Additionally, significant publication bias, as determined by Egger’s test, was observed in only three meta-analyses (Periodontal Disease, Depression, Anemia), while most of the others did not report significant publication bias.
However, it is important to acknowledge the limitations of our study when interpreting the findings. Firstly, the search was limited to three databases (PubMed, Scopus, and Web of Sciences), potentially introducing selection bias despite their extensive coverage. Secondly, we focused solely on the association between certain maternal factors and the risk of LBW, neglecting other potential factors that may contribute to LBW risk. Thirdly, some of the included meta-analyses exhibited high heterogeneity, and the underlying factors contributing to this heterogeneity (such as age, gender, nationality, and study region) were not further explored, which may have influenced our results. Lastly, the validity of umbrella reviews relies on the quality of the included meta-analyses, and since all the meta-analyses in our study were of low quality, we express concern regarding the robustness of our findings.
It is important to acknowledge that certain risk factors, such as periodontal disease, may have been subject to varying degrees of scrutiny in the literature, with some more rigorous studies suggesting limited impact on outcomes. While our review accurately reflects the existing evidence, it is essential to note the nuanced nature of certain risk factors and their potential influence on outcomes. Additionally, concerns have been raised about the analyses of cocaine effects, with criticisms centered on the adequacy of controlling associated risk factors. Recognizing these nuances is crucial in interpreting our findings, and future research endeavors may benefit from addressing these concerns and incorporating diverse study designs for a more comprehensive understanding of the complex interplay between risk factors and outcomes.
This umbrella review aimed to systematically and comprehensively collect available data from published meta-analyses that investigated the association between maternal factors and the risk of low birth weight. The goal was to provide clinical decision-makers and researchers with a robust evaluation of these associations, with the ultimate aim of preserving and improving the health of mothers and babies and preventing low birth weight.
Our findings suggest that periodontal disease, anemia, depression, infertility, smoking, and substance use (such as crack/cocaine) during pregnancy are associated with an increased risk of low birth weight, supported by suggestive evidence.
Data availability
No datasets were generated or analysed during the current study.
Fite MB, Tura AK, Yadeta TA, Oljira L, Roba KT. Prevalence, predictors of low birth weight and its association with maternal iron status using serum ferritin concentration in rural Eastern Ethiopia: a prospective cohort study. BMC Nutr. 2022;8(1):1–10.
Article Google Scholar
Gupta MK, Kakkar M, Sethi C, Malhotra A. Pattern of morbidity and mortality in LBW neonates: a study from Jaipur. J Evol Med Dent Sci. 2014;3(6):1339–45.
Lin S, Li J, Wu J, Yang F, Pei L, Shang X. Interactive effects of maternal exposure to chemical fertilizer and socio-economic status on the risk of low birth weight. BMC Public Health. 2022;22(1):1206.
Article PubMed PubMed Central Google Scholar
Ramankutty P, TIKREETI RAS, RASAAM KW, AL-THAMERY DM, YACOUB AA, MAHMOOD DA. A study on birth weight of Iraqi children. J Trop Pediatr. 1983;29(1):5–10.
Article CAS PubMed Google Scholar
Williams RL, Creasy RK, Cunningham GC, Hawes WE, Norris FD, Tashiro M. Fetal growth and perinatal viability in California. Obstet Gynecol. 1982;59(5):624–32.
CAS PubMed Google Scholar
Yilgwan C, Abok I, Yinnang W, Vajime B. Prevalence and risk factors of low birth weight in Jos. Jos J Med. 2009;4(1):13–5.
Google Scholar
Gebregzabiherher Y, Haftu A, Weldemariam S, Gebrehiwet H. The prevalence and risk factors for low birth weight among term newborns in Adwa General Hospital, Northern Ethiopia. Obstetrics and Gynecology International. 2017;2017.
Oluwafemi RO, Adesina FP, Hassan AO. Outcomes and Disease Spectrum of LBW neonates in a secondary health facility. J Healthc Eng. 2022;2022:9974636.
Endalamaw A, Engeda EH, Ekubagewargies DT, Belay GM, Tefera MA. Low birth weight and its associated factors in Ethiopia: a systematic review and meta-analysis. Ital J Pediatr. 2018;44(1):1–12.
Sema A, Tesfaye F, Belay Y, Amsalu B, Bekele D, Desalew A. Associated factors with low birth weight in Dire Dawa City, Eastern Ethiopia: a cross-sectional study. BioMed research international. 2019;2019.
Upadhyay RP, Taneja S, Ranjitkar S, Mazumder S, Bhandari N, Dua T, et al. Factors determining cognitive, motor and language scores in low birth weight infants from North India. PLoS ONE. 2021;16(5):e0251387.
Article CAS PubMed PubMed Central Google Scholar
Louis B, Steven B, Margret N, Ronald N, Emmanuel L, Tadeo N, et al. Prevalence and factors associated with low birth weight among teenage mothers in new Mulago hospital: a cross sectional study. J Health Sci (El Monte). 2016;4:192.
PubMed Google Scholar
Khan MMA, Mustagir MG, Islam MR, Kaikobad MS, Khan HT. Exploring the association between adverse maternal circumstances and low birth weight in neonates: a nationwide population-based study in Bangladesh. BMJ open. 2020;10(10):e036162.
Viengsakhone L, Yoshida Y, Harun-Or-Rashid M, Sakamoto J. Factors affecting low birth weight at four central hospitals in vientiane, Lao PDR. Nagoya J Med Sci. 2010;72(1–2):51–8.
Pereira PPS, Da Mata FA, Figueiredo ACG, de Andrade KRC, Pereira MG. Maternal active smoking during pregnancy and low birth weight in the Americas: a systematic review and meta-analysis. Nicotine Tob Res. 2017;19(5):497–505.
Article PubMed Google Scholar
Xiong X, Buekens P, Vastardis S, Stella MY. Periodontal disease and pregnancy outcomes: state-of-the-science. Obstet Gynecol Surv. 2007;62(9):605–15.
Marvin-Dowle K, Soltani H. A comparison of neonatal outcomes between adolescent and adult mothers in developed countries: a systematic review and meta-analysis. Eur J Obstet Gynecol Reproductive Biology: X. 2020;6:100109.
Patra J, Bakker R, Irving H, Jaddoe VW, Malini S, Rehm J. Dose–response relationship between alcohol consumption before and during pregnancy and the risks of low birthweight, preterm birth and small for gestational age (SGA)—a systematic review and meta-analyses. BJOG: Int J Obstet Gynecol. 2011;118(12):1411–21.
Article CAS Google Scholar
Hulse G, English D, Milne E, Holman C, Bower C. Maternal cocaine use and low birth weight newborns: a meta-analysis. Addiction. 1997;92(11):1561–70.
Haider BA, Olofin I, Wang M, Spiegelman D, Ezzati M, Fawzi WW. Anaemia, prenatal iron use, and risk of adverse pregnancy outcomes: systematic review and meta-analysis. BMJ (Clinical Res ed). 2013;346.
Accortt EE, Cheadle AC, Dunkel Schetter C. Prenatal depression and adverse birth outcomes: an updated systematic review. Matern Child Health J. 2015;19:1306–37.
Bian Y, Zhang Z, Liu Q, Wu D, Wang S. Maternal risk factors for low birth weight for term births in a developed region in China: a hospital-based study of 55,633 pregnancies. J Biomedical Res. 2013;27(1):14.
Murphy CC, Schei B, Myhr TL, Du Mont J. Abuse: a risk factor for low birth weight? A systematic review and meta-analysis. CMAJ. 2001;164(11):1567–72.
CAS PubMed PubMed Central Google Scholar
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ (Clinical research ed). 2015;349.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358.
Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10(1):101–29.
Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ (Clinical Res ed). 2011;342.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical Res ed). 1997;315(7109):629–34.
Ioannidis JP, Trikalinos TA. An exploratory test for an excess of significant findings. Clin Trails. 2007;4(3):245–53.
Hedges LV, Olkin I. Statistical methods for meta-analysis. Academic; 2014.
Cohen J. The t Test for Means. I Statistical Power Analysis for the Behavioral Sciences (2. utg., s. 19–74). New York: Routledge; 1977.
Zhang Y, Feng W, Li J, Cui L, Chen ZJ. Periodontal Disease and adverse neonatal outcomes: a systematic review and Meta-analysis. Front Pead. 2022;10.
Rahman MM, Abe SK, Rahman MS, Kanda M, Narita S, Bilano V, et al. Maternal anemia and risk of adverse birth and health outcomes in low- and middle-income countries: systematic review and meta-analysis. Am J Clin Nutr. 2016;103(2):495–504.
Pereira PPS, Da Mata FAF, Figueiredo ACG, de Andrade KRC, Pereira MG. Maternal active smoking during pregnancy and low birth weight in the americas: a systematic review and meta-analysis. Nicotine Tob Res. 2017;19(5):497–505.
Pereira P, Mata F, Figueiredo A, Silva RB, Pereira MG. Maternal exposure to Alcohol and low birthweight: a systematic review and Meta-analysis. Revista Brasileira De Ginecol E Obstetricia: Revista da Federacao Brasileira das Sociedades de Ginecol E Obstet. 2019;41(5):333–47.
Messerlian C, Maclagan L, Basso O. Infertility and the risk of adverse pregnancy outcomes: a systematic review and meta-analysis. Hum Reprod (Oxford England). 2013;28(1):125–37.
Liu L, Ma Y, Wang N, Lin W, Liu Y, Wen D. Maternal body mass index and risk of neonatal adverse outcomes in China: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2019;19(1):105.
Jin F, Qiao C. Association of maternal caffeine intake during pregnancy with low birth weight, childhood overweight, and obesity: a meta-analysis of cohort studies. International journal of obesity (2005). 2021;45(2):279 – 87.
Hou J, Yu P, Zhu H, Pan H, Li N, Yang H, et al. The impact of maternal hypothyroidism during pregnancy on neonatal outcomes: a systematic review and meta-analysis. Gynecol Endocrinology: Official J Int Soc Gynecol Endocrinol. 2016;32(1):9–13.
Ghimire U, Papabathini SS, Kawuki J, Obore N, Musa TH. Depression during pregnancy and the risk of low birth weight, preterm birth and intrauterine growth restriction- an updated meta-analysis. Early Hum Dev. 2021;152:105243.
Getaneh T, Negesse A, Dessie G, Desta M. The impact of pregnancy induced hypertension on low birth weight in Ethiopia: systematic review and meta-analysis. Ital J Pediatr. 2020;46(1):174.
Dos Santos JF, de Melo Bastos Cavalcante C, Barbosa FT, Gitaí DLG, Duzzioni M, Tilelli CQ, et al. Maternal, fetal and neonatal consequences associated with the use of crack cocaine during the gestational period: a systematic review and meta-analysis. Arch Gynecol Obstet. 2018;298(3):487–503.
Cai C, Vandermeer B, Khurana R, Nerenberg K, Featherstone R, Sebastianski M, et al. The impact of occupational activities during pregnancy on pregnancy outcomes: a systematic review and meta-analysis. Am J Obstet Gynecol. 2020;222(3):224–38.
Engdaw GT, Tesfaye AH, Feleke M, Negash A, Yeshiwas A, Addis W, et al. Effect of antenatal care on low birth weight: a systematic review and meta-analysis in Africa, 2022. Front Public Health. 2023;11:1158809.
Fonseca J, Silva A, Rocha P, Batista R, Thomaz E, Lamy-Filho F et al. Racial inequality in perinatal outcomes in two Brazilian birth cohorts. Braz J Med Biol Res. 2021;54.
Cunningham SD, Lewis JB, Shebl FM, Boyd LM, Robinson MA, Grilo SA, et al. Group prenatal care reduces risk of preterm birth and low birth weight: a matched cohort study. J Women’s Health. 2019;28(1):17–22.
Ghimire PR, Agho KE, Akombi BJ, Wali N, Dibley M, Raynes-Greenow C, et al. Perinatal mortality in South Asia: systematic review of observational studies. Int J Environ Res Public Health. 2018;15(7):1428.
Basso O, Baird DD. Infertility and preterm delivery, birthweight, and caesarean section: a study within the Danish National Birth Cohort. Hum Reprod. 2003;18(11):2478–84.
Thomson F, Shanbhag S, Templeton A, Bhattacharya S. Obstetric outcome in women with subfertility. BJOG: Int J Obstet Gynecol. 2005;112(5):632–7.
McDonald SD, Han Z, Mulla S, Ohlsson A, Beyene J, Murphy KE, et al. Preterm birth and low birth weight among in vitro fertilization twins: a systematic review and meta-analyses. Eur J Obstet Gynecol Reproductive Biology. 2010;148(2):105–13.
Saunders D, Mathews M, Lancaster P. The Australian Register: current research and future role a: a preliminary Report. Ann N Y Acad Sci. 1988;541(1):7–21.
Tan S-L, Doyle P, Campbell S, Beral V, Rizk B, Brinsden P, et al. Obstetric outcome of in vitro fertilization pregnancies compared with normally conceived pregnancies. Am J Obstet Gynecol. 1992;167(3):778–84.
Jauniaux E, Burton GJ. Morphological and biological effects of maternal exposure to tobacco smoke on the fetoplacental unit. Early Hum Dev. 2007;83(11):699–706.
Ko T-J, Tsai L-Y, Chu L-C, Yeh S-J, Leung C, Chen C-Y, et al. Parental smoking during pregnancy and its association with low birth weight, small for gestational age, and preterm birth offspring: a birth cohort study. Pediatr Neonatology. 2014;55(1):20–7.
Chiolero A, Bovet P, Paccaud F. Association between maternal smoking and low birth weight in Switzerland: the EDEN study. Swiss Med Wkly. 2005;135(35–36):525–30.
Wang N, Tikellis G, Sun C, Pezic A, Wang L, Wells JC, et al. The effect of maternal prenatal smoking and alcohol consumption on the placenta-to-birth weight ratio. Placenta. 2014;35(7):437–41.
Lambers DS, Clark KE, editors. The maternal and fetal physiologic effects of nicotine. Seminars in perinatology. Elsevier; 1996.
Borges G, Lopez-Cervantes M, Medina-Mora ME, Tapia-Conyer R, Garrido F. Alcohol consumption, low birth weight, and preterm delivery in the National Addiction Survey (Mexico). Int J Addictions. 1993;28(4):355–68.
Sprauve ME, Lindsay MK, Herbert S, Graves W. Adverse perinatal outcome in parturients who use crack cocaine. Obstet Gynecol. 1997;89(5):674–8.
Chen L-W, Wu Y, Neelakantan N, Chong MF-F, Pan A, van Dam RM. Maternal caffeine intake during pregnancy is associated with risk of low birth weight: a systematic review and dose-response meta-analysis. BMC Med. 2014;12(1):1–12.
Chen LW, Wu Y, Neelakantan N, Chong MF, Pan A, van Dam RM. Maternal caffeine intake during pregnancy is associated with risk of low birth weight: a systematic review and dose-response meta-analysis. BMC Med. 2014;12:174.
Rhee J, Kim R, Kim Y, Tam M, Lai Y, Keum N, et al. Maternal caffeine consumption during pregnancy and risk of low Birth Weight: a dose-response Meta-analysis of Observational studies. PLoS ONE. 2015;10(7):e0132334.
Greenwood DC, Thatcher NJ, Ye J, Garrard L, Keogh G, King LG, et al. Caffeine intake during pregnancy and adverse birth outcomes: a systematic review and dose-response meta-analysis. Eur J Epidemiol. 2014;29(10):725–34.
Rahman LA, Hairi NN, Salleh N. Association between pregnancy induced hypertension and low birth weight; a population based case-control study. Asia Pac J Public Health. 2008;20(2):152–8.
Bilano VL, Ota E, Ganchimeg T, Mori R, Souza JP. Risk factors of pre-eclampsia/eclampsia and its adverse outcomes in low-and middle-income countries: a WHO secondary analysis. PLoS ONE. 2014;9(3):e91198.
Li F, Wang T, Chen L, Zhang S, Chen L, Qin J. Adverse pregnancy outcomes among mothers with hypertensive disorders in pregnancy: a meta-analysis of cohort studies. Pregnancy Hypertens. 2021;24:107–17.
Rahman A, Bunn J, Lovel H, Creed F. Association between antenatal depression and low birthweight in a developing country. Acta Psychiatrica Scandinavica. 2007;115(6):481–6.
Rahmati S, Delpishe A, Azami M, Ahmadi MRH, Sayehmiri K. Maternal Anemia during pregnancy and infant low birth weight: a systematic review and Meta-analysis. Int J Reproductive Biomed. 2017;15(3):125.
Cetin I, Pileri P, Villa A, Calabrese S, Ottolenghi L, Abati S. Pathogenic mechanisms linking periodontal diseases with adverse pregnancy outcomes. Reproductive Sci. 2012;19(6):633–41.
Komine-Aizawa S, Aizawa S, Hayakawa S. Periodontal diseases and adverse pregnancy outcomes. J Obstet Gynecol Res. 2019;45(1):5–12.
Saddki N, Bachok Na, Hussain NHN, Zainudin SLA, Sosroseno W. The association between maternal periodontitis and low birth weight infants among malay women. Commun Dent Oral Epidemiol. 2008;36(4):296–304.
Souza LM, Cruz SSd, Gomes-Filho IS, Barreto ML, Passos-Soares JS, Trindade SC, et al. Effect of maternal periodontitis and low birth weight—A case control study. Acta Odontol Scand. 2016;74(1):73–80.
Derakhshan A, Peeters RP, Taylor PN, Bliddal S, Carty DM, Meems M, et al. Association of maternal thyroid function with birthweight: a systematic review and individual-participant data meta-analysis. Lancet Diabetes Endocrinol. 2020;8(6):501–10.
Knudsen IR, Bonde JP, Petersen SB. Physically strenuous work during pregnancy and risk of preterm birth. Arch Environ Occup Health. 2018;73(4):236–42.
Kramer MS, McDonald SW. Aerobic exercise for women during pregnancy. Cochrane database of systematic reviews. 2006(3).
Palmer KT, Bonzini M, Harris EC, Linaker C, Bonde JP. Work activities and risk of prematurity, low birth weight and pre-eclampsia: an updated review with meta-analysis. Occup Environ Med. 2013;70(4):213–22.
Cai C, Vandermeer B, Khurana R, Nerenberg K, Featherstone R, Sebastianski M, et al. The impact of occupational shift work and working hours during pregnancy on health outcomes: a systematic review and meta-analysis. Am J Obstet Gynecol. 2019;221(6):563–76.
Liu X, Du J, Wang G, Chen Z, Wang W, Xi Q. Effect of pre-pregnancy body mass index on adverse pregnancy outcome in north of China. Arch Gynecol Obstet. 2011;283:65–70.
Chen Z, Du J, Shao L, Zheng L, Wu M, Ai M, et al. Prepregnancy body mass index, gestational weight gain, and pregnancy outcomes in China. Int J Gynecol Obstet. 2010;109(1):41–4.
Kumar A, Chaudhary K, Prasad S. Maternal indicators and obstetric outcome in the north Indian population: a hospital-based study. J Postgrad Med. 2010;56(3):192.
Rahman MM, Abe SK, Kanda M, Narita S, Rahman MS, Bilano V, et al. Maternal body mass index and risk of birth and maternal health outcomes in low- and middle-income countries: a systematic review and meta-analysis. Obes Rev. 2015;16(9):758–70.
Han Z, Mulla S, Beyene J, Liao G, McDonald SD. Maternal underweight and the risk of preterm birth and low birth weight: a systematic review and meta-analyses. Int J Epidemiol. 2011;40(1):65–101.
Becher L, Thomson D, Caldwell D, editors. Addressing multiple treatments I: Cochrane Overviews. Basic Workshops; 2009.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J. 2009;26(2):91–108.
Booth A. EVIDENT Guidance for reviewing the evidence: a compendium of methodological literature and websites. Volume 13. Sheffield: University of Sheffield; 2016.
Download references
Acknowledgements
Not applicable.
The study has been supported by the Hamadan University of Medical Sciences with grant number 1401120210487.
Author information
Authors and affiliations.
Department of Epidemiology, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran
Hoda Arabzadeh, Amin Doosti-Irani, Elahe Elyasi & Younes Mohammadi
Research Center for Health Sciences, Hamadan University of Medical Sciences, Hamadan, Iran
Amin Doosti-Irani
Department of Obstetrics and Gynecology, Fatemiyeh Hospital Research Center, Hamadan, Iran
Sima Kamkari
Department of Biostatistics, School of Public Health, Hamadan University of Medical Science, Hamadan, Iran
Maryam Farhadian
Modeling of Noncommunicable Diseases Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
Younes Mohammadi
You can also search for this author in PubMed Google Scholar
Contributions
H.A participated in data collection, analysis, drafting and final approval of manuscript. A.D.I participated in study design, critically revising manuscript and final approval of the manuscript.S.K participated in conception of the study, critically revising manuscript and final approval of the manuscript.M.F participated in analysis of the study, critically revising manuscript and final approval of the manuscript.E.E participated in data collection, drafting and final approval of manuscript.Y. M Participated in conception, study design, analysis, drafting and final approval of manuscript. All authors have agreed to be responsible for all aspects of the work.
Corresponding author
Correspondence to Younes Mohammadi .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
The ethics committees of Hamadan University of Medical Sciences have approved this study with the reference number IR.UMSHA.REC.1401.1026.
Consent for publication
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Arabzadeh, H., Doosti-Irani, A., Kamkari, S. et al. The maternal factors associated with infant low birth weight: an umbrella review. BMC Pregnancy Childbirth 24 , 316 (2024). https://doi.org/10.1186/s12884-024-06487-y
Download citation
Received : 15 November 2023
Accepted : 05 April 2024
Published : 25 April 2024
DOI : https://doi.org/10.1186/s12884-024-06487-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Low birth weight
- Periodontal disease
- Maternal factors
- Umbrella review
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]

COMMENTS
The John Money Experiment involved David Reimer, a twin boy raised as a girl following a botched circumcision. Money asserted gender was primarily learned, not innate. However, David struggled with his female identity and transitioned back to male in adolescence. The case challenged Money's theory, highlighting the influence of biological sex on gender identity.
Updated March 12, 2024. David Reimer was born a boy in Winnipeg, Canada in 1965 — but following a botched circumcision at the age of eight months, his parents raised him as a girl. Facebook Although David Reimer's story was initially seen as a success by his family and Dr. John Money, his story would eventually prove to have a tragic end.
In the mid-1960s, psychologist John Money encouraged the gender reassignment of David Reimer, who was born a biological male but suffered irreparable damage to his penis as an infant. Born in 1965 as Bruce Reimer, his penis was irreparably damaged during infancy due to a failed circumcision. After encouragement from Money, Reimer's parents decided to raise Reimer as a girl.
After a botched circumcision operation when he was a toddler, David Reimer became the subject of a study that became known as the John/Joan case in the 60's and 70's.
David Reimer (born Bruce Peter Reimer; 22 August 1965 - 4 May 2004) was a Canadian man raised as a girl following medical advice and intervention after his penis was severely injured during a botched circumcision in infancy.. The psychologist John Money oversaw the case and reported the reassignment as successful and as evidence that gender identity is primarily learned.
Today, May 5 th, is the 19 th anniversary of David Reimer's suicide. Raising a child with atypical genitals David, born Bruce, lost his penis to a botched circumcision as an infant in 1966.
REIMER's case became a landmark because of its value to the study of nature vs. nurture. He's the subject of the new book, "As Nature Made Him: The Boy Who was Raised as a Girl" (HarperCollins) by ...
David Reimer, the Canadian man raised as a girl for most of the first 14 years of his life in a highly touted medical experiment that seemed to resolve the debate over the cultural and biological ...
Summary. In 1966, at the age of eight months, Bruce Reimer and his twin brother, Brian, were admitted to the hospital for circumcisions that were meant to cure difficulties both were having in urinating. Yet Brian never underwent the procedure because Bruce's circumcision went disastrously awry. The general practitioner used an electrocautery ...
Claudia Hammond revisits the classic case studies that have advanced psychological research. Janet and Ron Reimer's twin sons, Bruce and Brian, were born in Winnipeg in Canada in August 1965. All ...
But, Reimer later in life decided to live as a boy. He decided to go public after the publishing of the book in an effort to reverse the findings of the study. NPR's Melissa Block talks with John ...
In his most publicized case study, Money oversaw the reassignment of David Reimer as female following a circumcision accident in infancy. Heralded by many as proof that gender is pliable, the case was later discredited when Reimer revealed that he had lived as a male since his early teens. In ...
Bruce Reimer started to become Brenda on July 3, 1967. Physicians at Johns Hopkins surgically castrated him, and the remaining skin was used to forge a "cosmetic vaginal cleft". Money sent the ...
In some press reports, financial problems were given as the sole motive in David's suicide. While this is absurdly reductive, it is true that last fall David learned that he was the victim of an ...
There was a case just like this in the 1960s, a case which ended in tragedy. Twins Bruce and Brian Reimer were born in Canada as two perfectly normal boys. But after seven months, both were having ...
The Tragic Story Of David Reimer, The Boy Forced To Live As A Girl. Famed sex psychologist John Money convinced David Reimer's parents to raise him as a girl after his penis was irreparably damaged in a botched circumcision when he was an infant. The case of David Reimer is a complicated one. Throughout his short life, he was known by three ...
A. David Reimer and the Failure of Surgical Sex Assignment. In 1997, the case of John/Joan told the story of the person we now know as David Reimer. 33 The account described the failed sex reassignment of a child who had been originally presented to the medical world as a case success. 34 David
The story of David Reimer, also known as the David/Brenda case study or the John/Joan case study, is an important one for theories of nature vs. nurture. David was born male and as an infant his penis was destroyed in a botched circumcision. Medical and Psychological intervention ensued which saw David renamed Brenda and raised as a girl.
Thu 19 Aug 2010 02.59 EDT. T here was a big "eek" moment at the start of Case Study (Radio 4). We heard from the mother of the programme's subject - David Reimer, born a boy but raised as a girl ...
Jesse Walker | 5.24.2004 12:00 AM. On May 4, 2004, David Reimer committed suicide in Winnipeg. Thirty-eight years old, he had been a slaughterhouse worker and an odd-job man. He had also been both ...
On 4 May, Reimer took his own life. While his recent ills surely contributed to the despair, his mother knows there was more to it than that. His death was the final coda to a life that became a ...
David Reimer, the 38-year-old man who was raised as a girl ("Brenda") following a botched circumcision in infancy, committed suicide on May 4, 2004. As the left rushes to validate sodomy by judicial fiat and "homosexual marriage," perhaps now is an appropriate time to revisit his case. It reveals.
Retired pro wrestler, failed congressional candidate indicted in Vegas murder case. FILE - Daniel Rodimer leaves court after his initial appearance on murder charges at the Regional Justice Center in Las Vegas, Wednesday, April 10, 2024. Rodimer, a retired professional wrestler and former congressional candidate in Nevada and Texas, has been ...
In this umbrella review, we systematically evaluated the evidence from meta-analyses and systematic reviews of maternal factors associated with low birth weight. PubMed, Scopus, and Web of Science were searched to identify all relevant published studies up to August 2023. We included all meta-analysis studies (based on cohort, case-control, cross-sectional studies) that examined the ...