Here’s how you know
- U.S. Department of Health and Human Services
- National Institutes of Health
NCCIH Clinical Digest
for health professionals

Massage Therapy for Health : What the Science Says
Clinical Guidelines, Scientific Literature, Info for Patients: Massage Therapy for Health

.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Low-Back Pain
Several reviews of research have found weak evidence that massage may be helpful for low-back pain. Clinical guidelines issued by the American College of Physicians in 2017 included massage as an option for treating acute/subacute low-back pain but did not include massage therapy among the options for treating chronic low-back pain.
What Does the Research Show?
- The Agency for Healthcare Research and Quality, in a 2016 evaluation of nondrug therapies for low-back pain, examined 20 studies that compared massage to usual care or other interventions and found that there was evidence that massage was helpful for chronic low-back pain but that the strength of evidence was low. The agency also looked at 6 studies that compared different types of massage but found that the evidence was insufficient to show whether any types were more effective than others.
- A 2015 Cochrane review found evidence that massage may provide short-term relief from low-back pain, but the evidence is not of high quality. The long-term effects of massage for low-back pain have not been established.
- Clinical practice guidelines issued by the American College of Physicians in 2017 included massage therapy as an option for treating acute/subacute low-back pain but did not include massage therapy among the options for treating chronic low-back pain.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Neck and Shoulder Pain
Massage therapy may provide short-term benefits for neck or shoulder pain.
- A 2016 review of four randomized controlled trials found that massage therapy may provide short-term benefits from neck pain. However, a 2012 Cochrane review of 15 trials on massage therapy for neck pain concluded that no recommendations for practice can be made at this time because the effectiveness of massage for neck pain remains uncertain.
- A 2013 review of 12 studies of massage for neck pain (757 total participants) found that massage therapy was more helpful for both neck and shoulder pain than inactive therapies but was not more effective than other active therapies. For shoulder pain, massage therapy had short-term benefits only.
- A 2014 randomized controlled trial involving 228 participants with chronic nonspecific neck pain found that 60-minute massages given multiple times per week was more effective than fewer or shorter sessions. The participants were randomized to 5 groups receiving various doses of massage (a 4-week course consisting of 30-minute visits 2 or 3 times weekly or 60-minute visits 1, 2, or 3 times weekly) or to a single control group (a 4-week period on a wait list).
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Osteoarthritis
Only a few studies have examined massage therapy for osteoarthritis, but results of some of these studies suggest that massage may have short-term benefits in relieving knee pain.
- A 2017 systematic review of seven randomized controlled trials involving 352 participants with arthritis found low- to moderate-quality evidence that massage therapy is superior to nonactive therapies in reducing pain and improving functional outcomes. A 2013 review of two randomized controlled trials found positive short-term (less than 6 months) effects in the form of reduced pain and improved self-reported physical functioning. Results of a 2006 randomized controlled trial of 68 adults with OA of the knee who received standard Swedish massage over 8 weeks demonstrated statistically significant improvements in pain and physical function.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Headache
Only a small number of studies have looked at massage for headache, and results have not been consistent.
- Limited evidence from two small studies suggests massage therapy is possibly helpful for migraines, but clear conclusions cannot be drawn. A 2011 systematic review of these two studies concluded that massage therapy might be equally effective as propranolol and topiramate in the prophylactic management of migraine.
- A 2016 randomized controlled trial with 64 participants evaluated 2 types of massage (lymphatic drainage and traditional massage), once a week for 8 weeks, in patients with migraine. The frequency of migraines decreased in both groups, compared with people on a waiting list.
- In a 2015 randomized controlled trial , 56 people with tension headaches were assigned to receive massage at myofascial trigger points or an inactive treatment (detuned ultrasound) twice a week for 6 weeks or to be on a waiting list. People who received either massage or the inactive treatment had a decrease in the frequency of headaches, but there was no difference between the two groups.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Cancer Symptoms and Treatment Side Effects
With appropriate precautions, massage therapy can be part of supportive care for cancer patients who would like to try it; however, the evidence that it can relieve pain and anxiety is not strong. 2014 clinical practice guidelines for the care of breast cancer patients include massage as one of several approaches that may be helpful for stress reduction, anxiety, depression, fatigue, and quality of life.
- Clinical practice guidelines issued in 2009 by the Society for Integrative Oncology recommends considering massage therapy delivered by an oncology-trained massage therapist as part of a multimodality treatment approach in patients experiencing anxiety or pain.
- In 2017 the Society for Integrative Oncology issued guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment, recommending the use of massage therapy to improve mood disturbance in breast cancer survivors after active treatment (grade B). This recommendation is based on results from six trials.
- In clinical practice guidelines issued by the American College of Chest Physicians in 2013, massage therapy is suggested as part of a multi-modality cancer supportive care program for lung cancer patients whose anxiety or pain is not adequately controlled by usual care.
- A 2016 Cochrane review of 19 small studies involving 1,274 participants found some studies suggesting that massage with or without aromatherapy may help relieve pain and anxiety in people with cancer; however, the quality of the evidence was very low and results were not consistent.
- Another 2016 systematic review and meta-analysis of 16 studies concluded that based on the available evidence, weak recommendations are suggested for massage therapy, compared to an active comparator, for the treatment of pain, fatigue, and anxiety.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Fibromyalgia
Results of research suggest that massage therapy may be helpful for some fibromyalgia symptoms.
- A 2014 systematic review and meta-analysis of 9 studies (404 total participants) concluded that massage therapy, if continued for at least 5 weeks, improved pain, anxiety, and depression in people with fibromyalgia but did not have an effect on sleep disturbance.
- A 2015 systematic review and meta-analysis of 10 studies (478 total participants) compared the effects of different kinds of massage therapy and found that most styles of massage had beneficial effects on the quality of life in fibromyalgia. Swedish massage may be an exception; 2 studies of this type of massage (56 total participants) did not show benefits.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} HIV/AIDS
There is some evidence that massage therapy may have benefits for anxiety, depression, and quality of life in people with HIV/AIDS, but the amount of research and number of people studied are small.
- A 2010 review of four studies involving a total of 178 participants concluded that massage therapy may help improve the quality of life for people with HIV or AIDS. A 2013 randomized controlled trial of 54 people suggested that massage may be helpful for depression in people with HIV; and a 2017 study of 29 people with HIV found that massage may be helpful for anxiety.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Infant Care
There is some evidence that premature infants who are massaged may have improved weight gain. No benefits of massage for healthy full-term infants have been clearly demonstrated.
- In a 2017 review of 34 randomized controlled trials of massage therapy for premature infants, 20 of the studies (1,250 total infants) evaluated the effect of massage on weight gain, with most showing an improvement. The mechanism by which massage therapy might increase weight gain is not well understood. Some studies suggested other possible benefits of massage but because the amount of evidence is small, no conclusions can be reached about effects other than weight gain.
- A 2013 Cochrane review of 34 studies of healthy full-term infants didn’t find clear evidence of beneficial effects of massage in these low-risk infants.
The risk of harmful effects from massage therapy appears to be low. However, there have been rare reports of serious side effects, such as blood clot, nerve injury, or bone fracture. Some of the reported cases have involved vigorous types of massage, such as deep tissue massage, or patients who might be at increased risk of injury.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} References
- Agency for Healthcare Research and Quality. Noninvasive Treatments for Low Back Pain. AHRQ Publication No. 16-EHC004-EF. February 2016.
- Bennett C, Underdown A, Barlow J. Massage for promoting mental and physical health in typically developing infants under the age of six months . Cochrane Database of Systematic Reviews . 2013;(4):CD005038. Accessed at https://www.cochranelibrary.com on January 21, 2017.
- Boyd C, Crawford C, Paat CF, et al. The impact of message therapy on function in pain populations: a systematic review and meta-analysis of randomized controlled trials: Part II, cancer pain populations . Pain Med . 2016;17(8):1553-1568.
- Chaibi A, Tuchin PJ, Russell MB. Manual therapies for migraine: a systematic review . J Headache Pain . 2011;12(2):127-133.
- Deng GE, Rausch SM, Jones LW, et al. Complementary therapies and integrative medicine in lung cancer: Diagnosis and management of lung cancer , 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest . 2013;143(5 Suppl):e420S-e436S.
- Furlan AD, Giraldo M, Baskwill A, et al. Massage for low-back pain . Cochrane Database of Systematic Reviews . 2015;(9):CD001929. Accessed at www.cochranelibrary.com on January 26, 2017.
- Greenlee H, Balneaves LG, Carlson LE, et al. Clinical practice guidelines on the use of integrative therapies as supportive care in patients treated for breast cancer . Journal of the National Cancer Institute Monographs . 2014;2014(50):346-358.
- Happe S, Peikert A, Siegert R, et al. The efficacy of lymphatic drainage and traditional massage in the prophylaxis of migraine: a randomized, controlled parallel group study. Neurological Sciences . 2016;37(10):1627-1632,
- Hillier SL, Louw Q, Morris L, et al. Massage therapy for people with HIV/AIDS . Cochrane Database of Systematic Reviews . 2010;(1):CD007502. Accessed at www.cochranelibrary.com on August 18, 2017.
- Kong LJ, Zhan HS, Cheng YW, et al. Massage therapy for neck and shoulder pain: a systematic review and meta-analysis . Evidence-Based Complementary and Alternative Medicine . 2013;2013;613279.
- Li Y-h, Wang F-y, Feng C-q et al. Massage therapy for fibromyalgia: a systematic review and meta-analysis of randomized controlled trials . PLoS One . 2014;9(2):e89304.
- Moraska AF, Stenerson L, Butryn N, et al. Myofascial trigger point-focused head and neck massage for recurrent tension-type headache: a randomized, placebo-controlled clinical trial . Clinical Journal of Pain . 2015;31(2):159-168.
- Nahin RL, Boineau R, Khalsa PS, Stussman BJ, Weber WJ. Evidence-based evaluation of complementary health approaches for pain management in the United States . Mayo Clinic Proceedings . September 2016;91(9):1292-1306.
- Nelson NL, Churilla JR. Massage therapy for pain and function in patients with arthritis: a systematic review of randomized controlled trials . Am J Phys Med Rehabil . 2017;96(9):665-672.
- Niemi A-K. Review of randomized controlled trials of massage in preterm infants . Children . 2017;4(4):pii:E21.
- Patel KC, Gross A, Graham N, Goldsmith CH, Ezzo J, Morien A, Peloso PMJ. Massage for mechanical neck disorders. Cochrane Database of Systematic Reviews. 2012;9:CD004871.
- Perlman AI, Ali A, Njike VY, et al. Massage therapy for osteoarthritis of the knee: a randomized dose-finding trial . PLoS One . 2012;7(2):e30248.
- Poland RE, Gertsik L, Favreau JT, et al. Open-label, randomized, parallel-group controlled clinical trial of massage for treatment of depression in HIV-infected subjects . Journal of Alternative and Complementary Medicine . 2013;19(4):334-340.
- Qaseem A, Wilt TJ, McLean RM et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians . Annals of Internal Medicine . 2017;166(7):514-530.
- Shengelia R, Parker SJ, Ballin M, et al. Complementary therapies for osteoarthritis: are they effective? Pain Manag Nurs . 2013;14(4):e274-e288.
- Sherman KJ, Cook AJ, Wellman RD, et al. Five-week outcomes from a dosing trial of therapeutic massage for chronic neck pain . Ann Fam Med . 2014;12(2):112-120.
- Shin ES, Seo KH, Lee SH, et al. Massage with or without aromatherapy for symptom relief in people with cancer . Cochrane Database of Systematic Reviews . 2016;(6):CD009873. Accessed at www.cochranelibrary.com on January 26, 2017.
- Yuan SLK, Matsutani LA, Marques AP. Effectiveness of different styles of massage therapy in fibromyalgia: a systematic review and meta-analysis . Manual Therapy . 2015;20(2):257-264.
NCCIH Clinical Digest is a service of the National Center for Complementary and Integrative Health, NIH, DHHS. NCCIH Clinical Digest, a monthly e-newsletter, offers evidence-based information on complementary health approaches, including scientific literature searches, summaries of NCCIH-funded research, fact sheets for patients, and more.
The National Center for Complementary and Integrative Health is dedicated to exploring complementary health products and practices in the context of rigorous science, training complementary health researchers, and disseminating authoritative information to the public and professionals. For additional information, call NCCIH’s Clearinghouse toll-free at 1-888-644-6226, or visit the NCCIH website at nccih.nih.gov . NCCIH is 1 of 27 institutes and centers at the National Institutes of Health, the Federal focal point for medical research in the United States.
Content is in the public domain and may be reprinted, except if marked as copyrighted (©). Please credit the National Center for Complementary and Integrative Health as the source. All copyrighted material is the property of its respective owners and may not be reprinted without their permission.
Subscriptions
NCCIH Clinical Digest is a monthly e-newsletter that offers evidence-based information on complementary and integrative health practices.
Clinical Digest Archive
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 08 April 2024
A systematic review and multivariate meta-analysis of the physical and mental health benefits of touch interventions
- Julian Packheiser ORCID: orcid.org/0000-0001-9805-6755 2 na1 nAff1 ,
- Helena Hartmann 2 , 3 , 4 na1 ,
- Kelly Fredriksen 2 ,
- Valeria Gazzola ORCID: orcid.org/0000-0003-0324-0619 2 ,
- Christian Keysers ORCID: orcid.org/0000-0002-2845-5467 2 &
- Frédéric Michon ORCID: orcid.org/0000-0003-1289-2133 2
Nature Human Behaviour ( 2024 ) Cite this article
Metrics details
- Human behaviour
- Paediatric research
- Randomized controlled trials
Receiving touch is of critical importance, as many studies have shown that touch promotes mental and physical well-being. We conducted a pre-registered (PROSPERO: CRD42022304281) systematic review and multilevel meta-analysis encompassing 137 studies in the meta-analysis and 75 additional studies in the systematic review ( n = 12,966 individuals, search via Google Scholar, PubMed and Web of Science until 1 October 2022) to identify critical factors moderating touch intervention efficacy. Included studies always featured a touch versus no touch control intervention with diverse health outcomes as dependent variables. Risk of bias was assessed via small study, randomization, sequencing, performance and attrition bias. Touch interventions were especially effective in regulating cortisol levels (Hedges’ g = 0.78, 95% confidence interval (CI) 0.24 to 1.31) and increasing weight (0.65, 95% CI 0.37 to 0.94) in newborns as well as in reducing pain (0.69, 95% CI 0.48 to 0.89), feelings of depression (0.59, 95% CI 0.40 to 0.78) and state (0.64, 95% CI 0.44 to 0.84) or trait anxiety (0.59, 95% CI 0.40 to 0.77) for adults. Comparing touch interventions involving objects or robots resulted in similar physical (0.56, 95% CI 0.24 to 0.88 versus 0.51, 95% CI 0.38 to 0.64) but lower mental health benefits (0.34, 95% CI 0.19 to 0.49 versus 0.58, 95% CI 0.43 to 0.73). Adult clinical cohorts profited more strongly in mental health domains compared with healthy individuals (0.63, 95% CI 0.46 to 0.80 versus 0.37, 95% CI 0.20 to 0.55). We found no difference in health benefits in adults when comparing touch applied by a familiar person or a health care professional (0.51, 95% CI 0.29 to 0.73 versus 0.50, 95% CI 0.38 to 0.61), but parental touch was more beneficial in newborns (0.69, 95% CI 0.50 to 0.88 versus 0.39, 95% CI 0.18 to 0.61). Small but significant small study bias and the impossibility to blind experimental conditions need to be considered. Leveraging factors that influence touch intervention efficacy will help maximize the benefits of future interventions and focus research in this field.
Similar content being viewed by others

Touching the social robot PARO reduces pain perception and salivary oxytocin levels
Nirit Geva, Florina Uzefovsky & Shelly Levy-Tzedek
The impact of mindfulness apps on psychological processes of change: a systematic review
Natalia Macrynikola, Zareen Mir, … John Torous
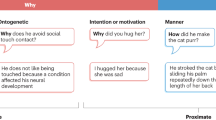
The why, who and how of social touch
Juulia T. Suvilehto, Asta Cekaite & India Morrison
The sense of touch has immense importance for many aspects of our life. It is the first of all the senses to develop in newborns 1 and the most direct experience of contact with our physical and social environment 2 . Complementing our own touch experience, we also regularly receive touch from others around us, for example, through consensual hugs, kisses or massages 3 .
The recent coronavirus pandemic has raised awareness regarding the need to better understand the effects that touch—and its reduction during social distancing—can have on our mental and physical well-being. The most common touch interventions, for example, massage for adults or kangaroo care for newborns, have been shown to have a wide range of both mental and physical health benefits, from facilitating growth and development to buffering against anxiety and stress, over the lifespan of humans and animals alike 4 . Despite the substantial weight this literature gives to support the benefits of touch, it is also characterized by a large variability in, for example, studied cohorts (adults, children, newborns and animals), type and duration of applied touch (for example, one-time hug versus repeated 60-min massages), measured health outcomes (ranging from physical health outcomes such as sleep and blood pressure to mental health outcomes such as depression or mood) and who actually applies the touch (for example, partner versus stranger).
A meaningful tool to make sense of this vast amount of research is through meta-analysis. While previous meta-analyses on this topic exist, they were limited in scope, focusing only on particular types of touch, cohorts or specific health outcomes (for example, refs. 5 , 6 ). Furthermore, despite best efforts, meaningful variables that moderate the efficacy of touch interventions could not yet be identified. However, understanding these variables is critical to tailor touch interventions and guide future research to navigate this diverse field with the ultimate aim of promoting well-being in the population.
In this Article, we describe a pre-registered, large-scale systematic review and multilevel, multivariate meta-analysis to address this need with quantitative evidence for (1) the effect of touch interventions on physical and mental health and (2) which moderators influence the efficacy of the intervention. In particular, we ask whether and how strongly health outcomes depend on the dynamics of the touching dyad (for example, humans or robots/objects, familiarity and touch directionality), demographics (for example, clinical status, age or sex), delivery means (for example, type of touch intervention or touched body part) and procedure (for example, duration or number of sessions). We did so separately for newborns and for children and adults, as the health outcomes in newborns differed substantially from those in the other age groups. Despite the focus of the analysis being on humans, it is widely known that many animal species benefit from touch interactions and that engaging in touch promotes their well-being as well 7 . Since animal models are essential for the investigation of the mechanisms underlying biological processes and for the development of therapeutic approaches, we accordingly included health benefits of touch interventions in non-human animals as part of our systematic review. However, this search yielded only a small number of studies, suggesting a lack of research in this domain, and as such, was insufficient to be included in the meta-analysis. We evaluate the identified animal studies and their findings in the discussion.
Touch interventions have a medium-sized effect
The pre-registration can be found at ref. 8 . The flowchart for data collection and extraction is depicted in Fig. 1 .
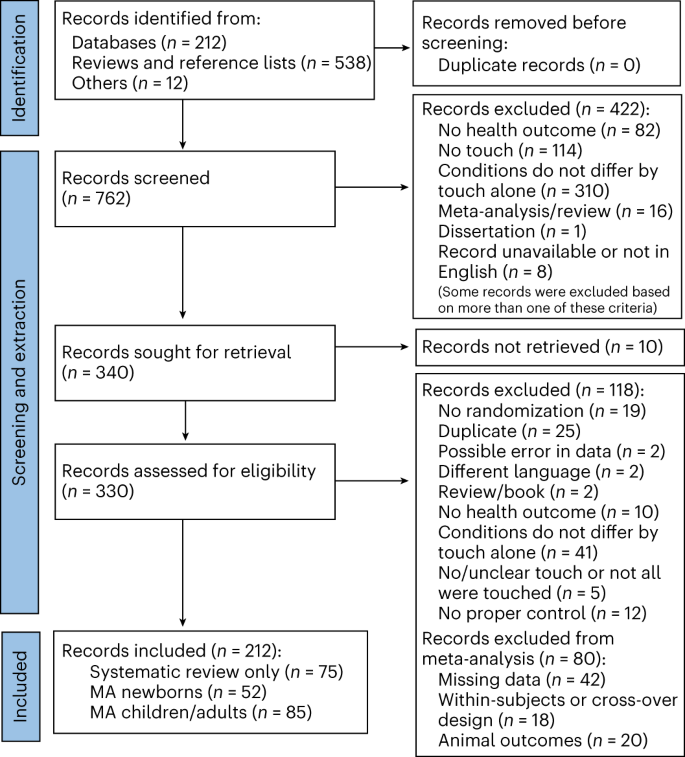
Animal outcomes refer to outcomes measured in non-human species that were solely considered as part of a systematic review. Included languages were French, Dutch, German and English, but our search did not identify any articles in French, Dutch or German. MA, meta-analysis.
For adults, a total of n = 2,841 and n = 2,556 individuals in the touch and control groups, respectively, across 85 studies and 103 cohorts were included. The effect of touch overall was medium-sized ( t (102) = 9.74, P < 0.001, Hedges’ g = 0.52, 95% confidence interval (CI) 0.42 to 0.63; Fig. 2a ). For newborns, we could include 63 cohorts across 52 studies comprising a total of n = 2,134 and n = 2,086 newborns in the touch and control groups, respectively, with an overall effect almost identical to the older age group ( t (62) = 7.53, P < 0.001, Hedges’ g = 0.56, 95% CI 0.41 to 0.71; Fig. 2b ), suggesting that, despite distinct health outcomes, touch interventions show comparable effects across newborns and adults. Using these overall effect estimates, we conducted a power sensitivity analysis of all the included primary studies to investigate whether such effects could be reliably detected 9 . Sufficient power to detect such effect sizes was rare in individual studies, as investigated by firepower plots 10 (Supplementary Figs. 1 and 2 ). No individual effect size from either meta-analysis was overly influential (Cook’s D < 0.06). The benefits were similar for mental and physical outcomes (mental versus physical; adults: t (101) = 0.79, P = 0.432, Hedges’ g difference of −0.05, 95% CI −0.16 to 0.07, Fig. 2c ; newborns: t (61) = 1.08, P = 0.284, Hedges’ g difference of −0.19, 95% CI −0.53 to 0.16, Fig. 2d ).
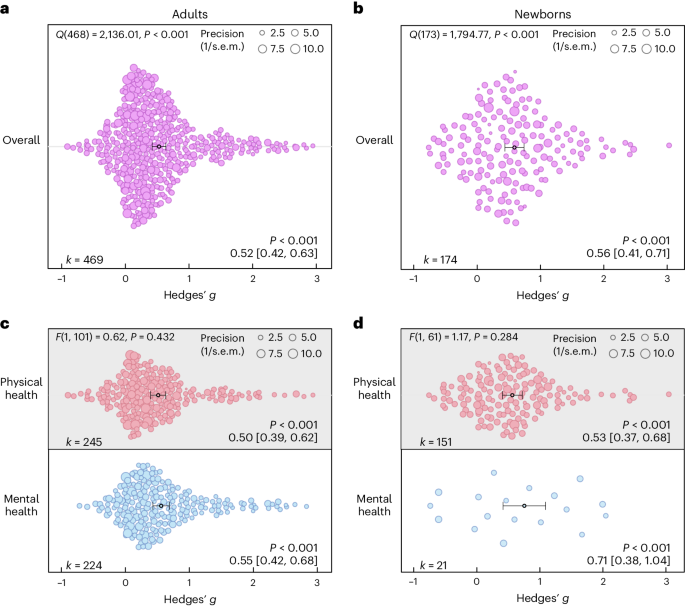
a , Orchard plot illustrating the overall benefits across all health outcomes for adults/children across 469 in part dependent effect sizes from 85 studies and 103 cohorts. b , The same as a but for newborns across 174 in part dependent effect sizes from 52 studies and 63 cohorts. c , The same as a but separating the results for physical versus mental health benefits across 469 in part dependent effect sizes from 85 studies and 103 cohorts. d , The same as b but separating the results for physical versus mental health benefits across 172 in part dependent effect sizes from 52 studies and 63 cohorts. Each dot reflects a measured effect, and the number of effects ( k ) included in the analysis is depicted in the bottom left. Mean effects and 95% CIs are presented in the bottom right and are indicated by the central black dot (mean effect) and its error bars (95% CI). The heterogeneity Q statistic is presented in the top left. Overall effects of moderator impact were assessed via an F test, and post hoc comparisons were done using t tests (two-sided test). Note that the P values above the mean effects indicate whether an effect differed significantly from a zero effect. P values were not corrected for multiple comparisons. The dot size reflects the precision of each individual effect (larger indicates higher precision). Small-study bias for the overall effect was significant ( F test, two-sided test) in the adult meta-analysis ( F (1, 101) = 21.24, P < 0.001; Supplementary Fig. 3 ) as well as in the newborn meta-analysis ( F (1, 61) = 5.25, P = 0.025; Supplementary Fig. 4 ).
Source data
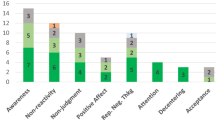
On the basis of the overall effect of both meta-analyses as well as their median sample sizes, the minimum number of studies necessary for subgroup analyses to achieve 80% power was k = 9 effects for adults and k = 8 effects for newborns (Supplementary Figs. 5 and 6 ). Assessing specific health outcomes with sufficient power in more detail in adults (Fig. 3a ) revealed smaller benefits to sleep and heart rate parameters, moderate benefits to positive and negative affect, diastolic blood and systolic blood pressure, mobility and reductions of the stress hormone cortisol and larger benefits to trait and state anxiety, depression, fatigue and pain. Post hoc tests revealed stronger benefits for pain, state anxiety, depression and trait anxiety compared with respiratory, sleep and heart rate parameters (see Fig. 3 for all post hoc comparisons). Reductions in pain and state anxiety were increased compared with reductions in negative affect ( t (83) = 2.54, P = 0.013, Hedges’ g difference of 0.31, 95% CI 0.07 to 0.55; t (83) = 2.31, P = 0.024, Hedges’ g difference of 0.27, 95% CI 0.03 to 0.51). Benefits to pain symptoms were higher compared with benefits to positive affect ( t (83) = 2.22, P = 0.030, Hedges’ g difference of 0.29, 95% CI 0.04 to 0.54). Finally, touch resulted in larger benefits to cortisol release compared with heart rate parameters ( t (83) = 2.30, P = 0.024, Hedges’ g difference of 0.26, 95% CI 0.04–0.48).
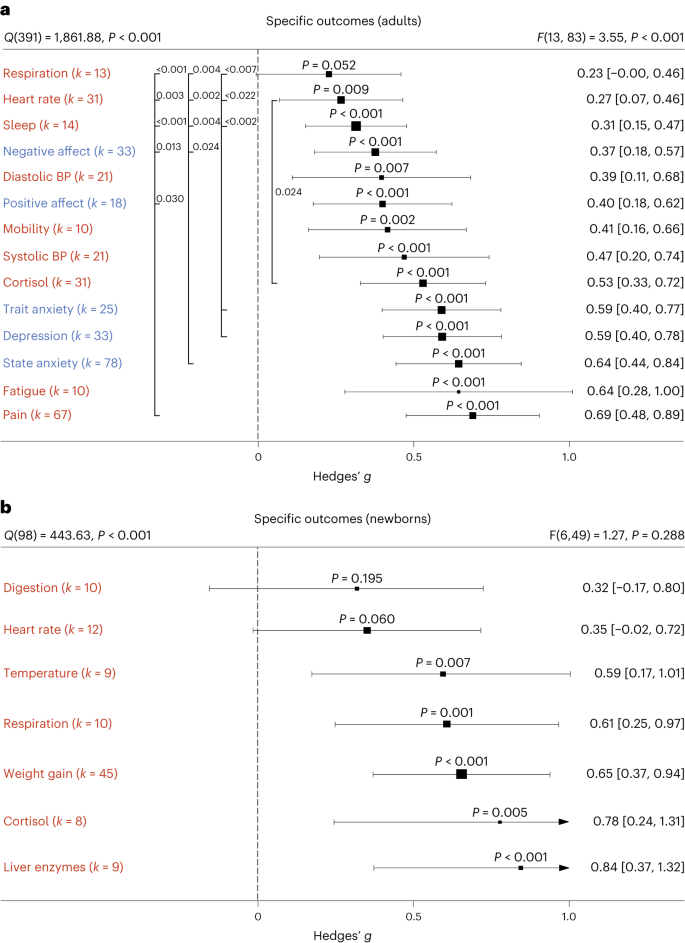
a , b , Health outcomes in adults analysed across 405 in part dependent effect sizes from 79 studies and 97 cohorts ( a ) and in newborns analysed across 105 in part dependent effect sizes from 46 studies and 56 cohorts ( b ). The type of health outcomes measured differed between adults and newborns and were thus analysed separately. Numbers on the right represent the mean effect with its 95% CI in square brackets and the significance level estimating the likelihood that the effect is equal to zero. Overall effects of moderator impact were assessed via an F test, and post hoc comparisons were done using t tests (two-sided test). The F value in the top right represents a test of the hypothesis that all effects within the subpanel are equal. The Q statistic represents the heterogeneity. P values of post hoc tests are depicted whenever significant. P values above the horizontal whiskers indicate whether an effect differed significantly from a zero effect. Vertical lines indicate significant post hoc tests between moderator levels. P values were not corrected for multiple comparisons. Physical outcomes are marked in red. Mental outcomes are marked in blue.
In newborns, only physical health effects offered sufficient data for further analysis. We found no benefits for digestion and heart rate parameters. All other health outcomes (cortisol, liver enzymes, respiration, temperature regulation and weight gain) showed medium to large effects (Fig. 3b ). We found no significant differences among any specific health outcomes.
Non-human touch and skin-to-skin contact
In some situations, a fellow human is not readily available to provide affective touch, raising the question of the efficacy of touch delivered by objects and robots 11 . Overall, we found humans engaging in touch with other humans or objects to have medium-sized health benefits in adults, without significant differences ( t (99) = 1.05, P = 0.295, Hedges’ g difference of 0.12, 95% CI −0.11 to 0.35; Fig. 4a ). However, differentiating physical versus mental health benefits revealed similar benefits for human and object touch on physical health outcomes, but larger benefits on mental outcomes when humans were touched by humans ( t (97) = 2.32, P = 0.022, Hedges’ g difference of 0.24, 95% CI 0.04 to 0.44; Fig. 4b ). It must be noted that touching with an object still showed a significant effect (see Supplementary Fig. 7 for the corresponding orchard plot).
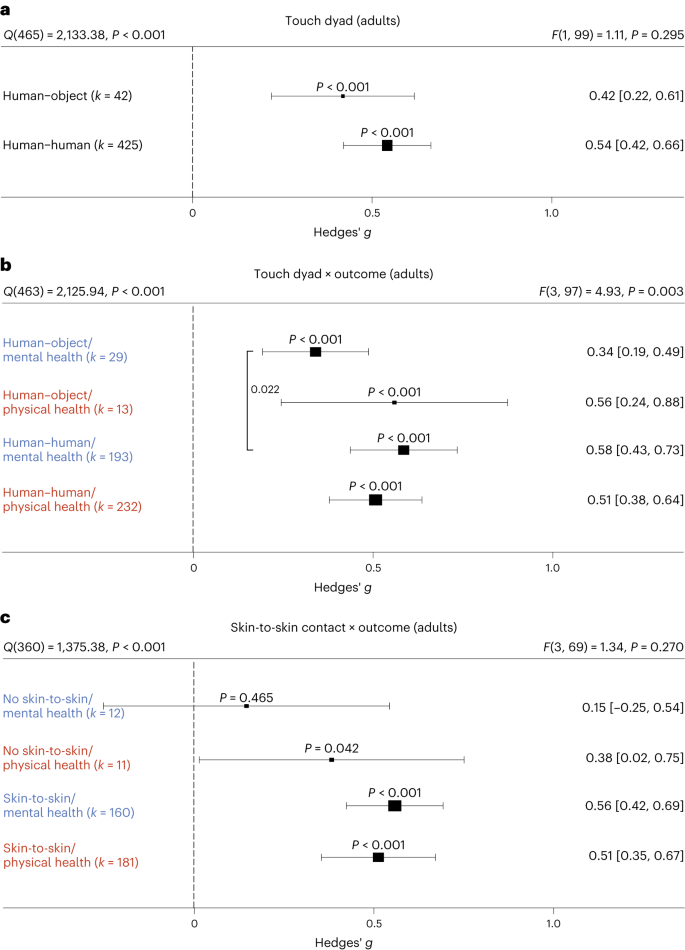
a , Forest plot comparing humans versus objects touching a human on health outcomes overall across 467 in part dependent effect sizes from 85 studies and 101 cohorts. b , The same as a but separately for mental versus physical health outcomes across 467 in part dependent effect sizes from 85 studies and 101 cohorts. c , Results with the removal of all object studies, leaving 406 in part dependent effect sizes from 71 studies and 88 cohorts to identify whether missing skin-to-skin contact is the relevant mediator of higher mental health effects in human–human interactions. Numbers on the right represent the mean effect with its 95% CI in square brackets and the significance level estimating the likelihood that the effect is equal to zero. Overall effects of moderator impact were assessed via an F test, and post hoc comparisons were done using t tests (two-sided test). The F value in the top right represents a test of the hypothesis that all effects within the subpanel are equal. The Q statistic represents the heterogeneity. P values of post hoc tests are depicted whenever significant. P values above the horizontal whiskers indicate whether an effect differed significantly from a zero effect. Vertical lines indicate significant post hoc tests between moderator levels. P values were not corrected for multiple comparisons. Physical outcomes are marked in red. Mental outcomes are marked in blue.
We considered the possibility that this effect was due to missing skin-to-skin contact in human–object interactions. Thus, we investigated human–human interactions with and without skin-to-skin contact (Fig. 4c ). In line with the hypothesis that skin-to-skin contact is highly relevant, we again found stronger mental health benefits in the presence of skin-to-skin contact that however did not achieve nominal significance ( t (69) = 1.95, P = 0.055, Hedges’ g difference of 0.41, 95% CI −0.00 to 0.82), possibly because skin-to-skin contact was rarely absent in human–human interactions, leading to a decrease in power of this analysis. Results for skin-to-skin contact as an overall moderator can be found in Supplementary Fig. 8 .
Influences of type of touch
The large majority of touch interventions comprised massage therapy in adults and kangaroo care in newborns (see Supplementary Table 1 for a complete list of interventions across studies). However, comparing the different types of touch explored across studies did not reveal significant differences in effect sizes based on touch type, be it on overall health benefits (adults: t (101) = 0.11, P = 0.916, Hedges’ g difference of 0.02, 95% CI −0.32 to 0.29; Fig. 5a ) or comparing different forms of touch separately for physical (massage therapy versus other forms: t (99) = 0.99, P = 0.325, Hedges’ g difference 0.16, 95% CI −0.15 to 0.47) or for mental health benefits (massage therapy versus other forms: t (99) = 0.75, P = 0.458, Hedges’ g difference of 0.13, 95% CI −0.22 to 0.48) in adults (Fig. 5c ; see Supplementary Fig. 9 for the corresponding orchard plot). A similar picture emerged for physical health effects in newborns (massage therapy versus kangaroo care: t (58) = 0.94, P = 0.353, Hedges’ g difference of 0.15, 95% CI −0.17 to 0.47; massage therapy versus other forms: t (58) = 0.56, P = 0.577, Hedges’ g difference of 0.13, 95% CI −0.34 to 0.60; kangaroo care versus other forms: t (58) = 0.07, P = 0.947, Hedges’ g difference of 0.02, 95% CI −0.46 to 0.50; Fig. 5d ; see also Supplementary Fig. 10 for the corresponding orchard plot). This suggests that touch types may be flexibly adapted to the setting of every touch intervention.
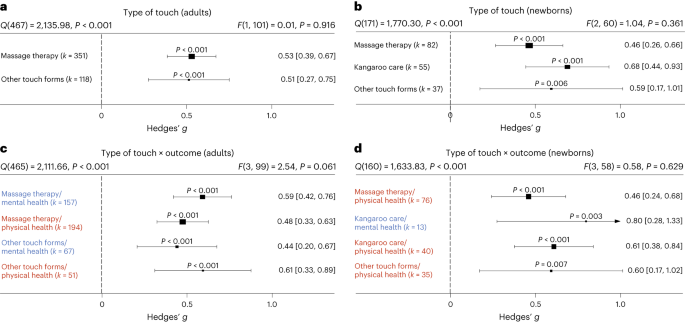
a , Forest plot of health benefits comparing massage therapy versus other forms of touch in adult cohorts across 469 in part dependent effect sizes from 85 studies and 103 cohorts. b , Forest plot of health benefits comparing massage therapy, kangaroo care and other forms of touch for newborns across 174 in part dependent effect sizes from 52 studies and 63 cohorts. c , The same as a but separating mental and physical health benefits across 469 in part dependent effect sizes from 85 studies and 103 cohorts. d , The same as b but separating mental and physical health outcomes where possible across 164 in part dependent effect sizes from 51 studies and 62 cohorts. Note that an insufficient number of studies assessed mental health benefits of massage therapy or other forms of touch to be included. Numbers on the right represent the mean effect with its 95% CI in square brackets and the significance level estimating the likelihood that the effect is equal to zero. Overall effects of moderator impact were assessed via an F test, and post hoc comparisons were done using t tests (two-sided test). The F value in the top right represents a test of the hypothesis that all effects within the subpanel are equal. The Q statistic represents heterogeneity. P values of post hoc tests are depicted whenever significant. P values above the horizontal whiskers indicate whether an effect differed significantly from a zero effect. Vertical lines indicate significant post hoc tests between moderator levels. P values were not corrected for multiple comparisons. Physical outcomes are marked in red. Mental outcomes are marked in blue.
The role of clinical status
Most research on touch interventions has focused on clinical samples, but are benefits restricted to clinical cohorts? We found health benefits to be significant in clinical and healthy populations (Fig. 6 ), whether all outcomes are considered (Fig. 6a,b ) or physical and mental health outcomes are separated (Fig. 6c,d , see Supplementary Figs. 11 and 12 for the corresponding orchard plots). In adults, however, we found higher mental health benefits for clinical populations compared with healthy ones (Fig. 6c ; t (99) = 2.11, P = 0.037, Hedges’ g difference of 0.25, 95% CI 0.01 to 0.49).
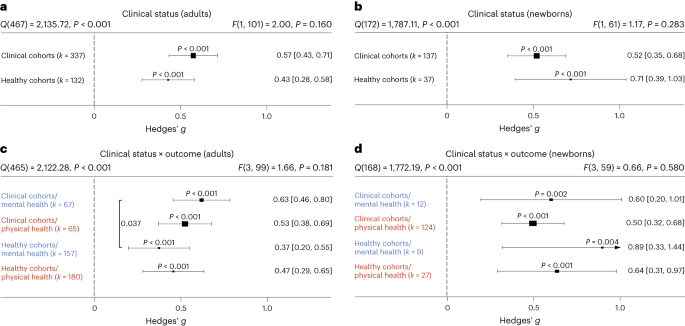
a , Health benefits for clinical cohorts of adults versus healthy cohorts of adults across 469 in part dependent effect sizes from 85 studies and 103 cohorts. b , The same as a but for newborn cohorts across 174 in part dependent effect sizes from 52 studies and 63 cohorts. c , The same as a but separating mental versus physical health benefits across 469 in part dependent effect sizes from 85 studies and 103 cohorts. d , The same as b but separating mental versus physical health benefits across 172 in part dependent effect sizes from 52 studies and 63 cohorts. Numbers on the right represent the mean effect with its 95% CI in square brackets and the significance level estimating the likelihood that the effect is equal to zero. Overall effects of moderator impact were assessed via an F test, and post hoc comparisons were done using t tests (two-sided test).The F value in the top right represents a test of the hypothesis that all effects within the subpanel are equal. The Q statistic represents the heterogeneity. P values of post hoc tests are depicted whenever significant. P values above the horizontal whiskers indicate whether an effect differed significantly from a zero effect. Vertical lines indicate significant post hoc tests between moderator levels. P values were not corrected for multiple comparisons. Physical outcomes are marked in red. Mental outcomes are marked in blue.
A more detailed analysis of specific clinical conditions in adults revealed positive mental and physical health benefits for almost all assessed clinical disorders. Differences between disorders were not found, with the exception of increased effectiveness of touch interventions in neurological disorders (Supplementary Fig. 13 ).
Familiarity in the touching dyad and intervention location
Touch interventions can be performed either by familiar touchers (partners, family members or friends) or by unfamiliar touchers (health care professionals). In adults, we did not find an impact of familiarity of the toucher ( t (99) = 0.12, P = 0.905, Hedges’ g difference of 0.02, 95% CI −0.27 to 0.24; Fig. 7a ; see Supplementary Fig. 14 for the corresponding orchard plot). Similarly, investigating the impact on mental and physical health benefits specifically, no significant differences could be detected, suggesting that familiarity is irrelevant in adults. In contrast, touch applied to newborns by their parents (almost all studies only included touch by the mother) was significantly more beneficial compared with unfamiliar touch ( t (60) = 2.09, P = 0.041, Hedges’ g difference of 0.30, 95% CI 0.01 to 0.59) (Fig. 7b ; see Supplementary Fig. 15 for the corresponding orchard plot). Investigating mental and physical health benefits specifically revealed no significant differences. Familiarity with the location in which the touch was applied (familiar being, for example, the participants’ home) did not influence the efficacy of touch interventions (Supplementary Fig. 16 ).
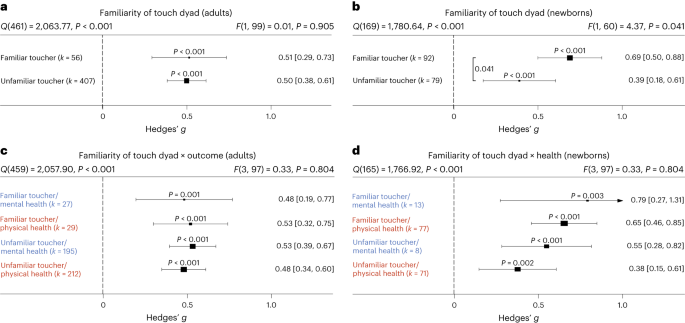
a , Health benefits for being touched by a familiar (for example, partner, family member or friend) versus unfamiliar toucher (health care professional) across 463 in part dependent effect sizes from 83 studies and 101 cohorts. b , The same as a but for newborn cohorts across 171 in part dependent effect sizes from 51 studies and 62 cohorts. c , The same as a but separating mental versus physical health benefits across 463 in part dependent effect sizes from 83 studies and 101 cohorts. d , The same as b but separating mental versus physical health benefits across 169 in part dependent effect sizes from 51 studies and 62 cohorts. Numbers on the right represent the mean effect with its 95% CI in square brackets and the significance level estimating the likelihood that the effect is equal to zero. Overall effects of moderator impact were assessed via an F test, and post hoc comparisons were done using t tests (two-sided test). The F value in the top right represents a test of the hypothesis that all effects within the subpanel are equal. The Q statistic represents the heterogeneity. P values of post hoc tests are depicted whenever significant. P values above the horizontal whiskers indicate whether an effect differed significantly from a zero effect. Vertical lines indicate significant post hoc tests between moderator levels. P values were not corrected for multiple comparisons. Physical outcomes are marked in red. Mental outcomes are marked in blue.
Frequency and duration of touch interventions
How often and for how long should touch be delivered? For adults, the median touch duration across studies was 20 min and the median number of touch interventions was four sessions with an average time interval of 2.3 days between each session. For newborns, the median touch duration across studies was 17.5 min and the median number of touch interventions was seven sessions with an average time interval of 1.3 days between each session.
Delivering more touch sessions increased benefits in adults, whether overall ( t (101) = 4.90, P < 0.001, Hedges’ g = 0.02, 95% CI 0.01 to 0.03), physical ( t (81) = 3.07, P = 0.003, Hedges’ g = 0.02, 95% CI 0.01–0.03) or mental benefits ( t (72) = 5.43, P < 0.001, Hedges’ g = 0.02, 95% CI 0.01–0.03) were measured (Fig. 8a ). A closer look at specific outcomes for which sufficient data were available revealed that positive associations between the number of sessions and outcomes were found for trait anxiety ( t (12) = 7.90, P < 0.001, Hedges’ g = 0.03, 95% CI 0.02–0.04), depression ( t (20) = 10.69, P < 0.001, Hedges’ g = 0.03, 95% CI 0.03–0.04) and pain ( t (37) = 3.65, P < 0.001, Hedges’ g = 0.03, 95% CI 0.02–0.05), indicating a need for repeated sessions to improve these adverse health outcomes. Neither increasing the number of sessions for newborns nor increasing the duration of touch per session in adults or newborns increased health benefits, be they physical or mental (Fig. 8b–d ). For continuous moderators in adults, we also looked at specific health outcomes as sufficient data were generally available for further analysis. Surprisingly, we found significant negative associations between touch duration and reductions of cortisol ( t (24) = 2.71, P = 0.012, Hedges’ g = −0.01, 95% CI −0.01 to −0.00) and heart rate parameters ( t (21) = 2.35, P = 0.029, Hedges’ g = −0.01, 95% CI −0.02 to −0.00).
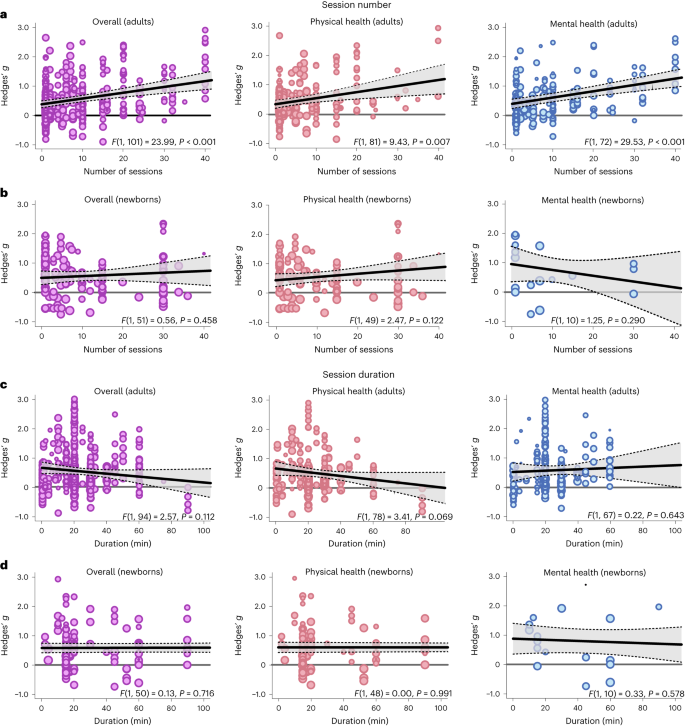
a , Meta-regression analysis examining the association between the number of sessions applied and the effect size in adults, either on overall health benefits (left, 469 in part dependent effect sizes from 85 studies and 103 cohorts) or for physical (middle, 245 in part dependent effect sizes from 69 studies and 83 cohorts) or mental benefits (right, 224 in part dependent effect sizes from 60 studies and 74 cohorts) separately. b , The same as a for newborns (overall: 150 in part dependent effect sizes from 46 studies and 53 cohorts; physical health: 127 in part dependent effect sizes from 44 studies and 51 cohorts; mental health: 21 in part dependent effect sizes from 11 studies and 12 cohorts). c , d the same as a ( c ) and b ( d ) but for the duration of the individual sessions. For adults, 449 in part dependent effect sizes across 80 studies and 96 cohorts were included in the overall analysis. The analysis of physical health benefits included 240 in part dependent effect sizes across 67 studies and 80 cohorts, and the analysis of mental health benefits included 209 in part dependent effect sizes from 56 studies and 69 cohorts. For newborns, 145 in part dependent effect sizes across 45 studies and 52 cohorts were included in the overall analysis. The analysis of physical health benefits included 122 in part dependent effect sizes across 43 studies and 50 cohorts, and the analysis of mental health benefits included 21 in part dependent effect sizes from 11 studies and 12 cohorts. Each dot represents an effect size. Its size indicates the precision of the study (larger indicates better). Overall effects of moderator impact were assessed via an F test (two-sided test). The P values in each panel represent the result of a regression analysis testing the hypothesis that the slope of the relationship is equal to zero. P values are not corrected for multiple testing. The shaded area around the regression line represents the 95% CI.
Demographic influences of sex and age
We used the ratio between women and men in the single-study samples as a proxy for sex-specific effects. Sex ratios were heavily skewed towards larger numbers of women in each cohort (median 83% women), and we could not find significant associations between sex ratio and overall ( t (62) = 0.08, P = 0.935, Hedges’ g = 0.00, 95% CI −0.00 to 0.01), mental ( t (43) = 0.55, P = 0.588, Hedges’ g = 0.00, 95% CI −0.00 to 0.01) or physical health benefits ( t (51) = 0.15, P = 0.882, Hedges’ g = −0.00, 95% CI −0.01 to 0.01). For specific outcomes that could be further analysed, we found a significant positive association of sex ratio with reductions in cortisol secretion ( t (18) = 2.31, P = 0.033, Hedges’ g = 0.01, 95% CI 0.00 to 0.01) suggesting stronger benefits in women. In contrast to adults, sex ratios were balanced in samples of newborns (median 53% girls). For newborns, there was no significant association with overall ( t (36) = 0.77, P = 0.447, Hedges’ g = −0.01, 95% CI −0.02 to 0.01) and physical health benefits of touch ( t (35) = 0.93, P = 0.359, Hedges’ g = −0.01, 95% CI −0.02 to 0.01). Mental health benefits did not provide sufficient data for further analysis.
The median age in the adult meta-analysis was 42.6 years (s.d. 21.16 years, range 4.5–88.4 years). There was no association between age and the overall ( t (73) = 0.35, P = 0.727, Hedges’ g = 0.00, 95% CI −0.01 to 0.01), mental ( t (53) = 0.94, P = 0.353, Hedges’ g = 0.01, 95% CI −0.01 to 0.02) and physical health benefits of touch ( t (60) = 0.16, P = 0.870, Hedges’ g = 0.00, 95% CI −0.01 to 0.01). Looking at specific health outcomes, we found significant positive associations between mean age and improved positive affect ( t (10) = 2.54, P = 0.030, Hedges’ g = 0.01, 95% CI 0.00 to 0.02) as well as systolic blood pressure ( t (11) = 2.39, P = 0.036, Hedges’ g = 0.02, 95% CI 0.00 to 0.04).
A list of touched body parts can be found in Supplementary Table 1 . For the touched body part, we found significantly higher health benefits for head touch compared with arm touch ( t (40) = 2.14, P = 0.039, Hedges’ g difference of 0.78, 95% CI 0.07 to 1.49) and torso touch ( t (40) = 2.23, P = 0.031; Hedges’ g difference of 0.84, 95% CI 0.10 to 1.58; Supplementary Fig. 17 ). Touching the arm resulted in lower mental health compared with physical health benefits ( t (37) = 2.29, P = 0.028, Hedges’ g difference of −0.35, 95% CI −0.65 to −0.05). Furthermore, we found a significantly increased physical health benefit when the head was touched as opposed to the torso ( t (37) = 2.10, P = 0.043, Hedges’ g difference of 0.96, 95% CI 0.06 to 1.86). Thus, head touch such as a face or scalp massage could be especially beneficial.
Directionality
In adults, we tested whether a uni- or bidirectional application of touch mattered. The large majority of touch was applied unidirectionally ( k = 442 of 469 effects). Unidirectional touch had higher health benefits ( t (101) = 2.17, P = 0.032, Hedges’ g difference of 0.30, 95% CI 0.03 to 0.58) than bidirectional touch. Specifically, mental health benefits were higher in unidirectional touch ( t (99) = 2.33, P = 0.022, Hedges’ g difference of 0.46, 95% CI 0.06 to 0.66).
Study location
For adults, we found significantly stronger health benefits of touch in South American compared with North American cohorts ( t (95) = 2.03, P = 0.046, Hedges’ g difference of 0.37, 95% CI 0.01 to 0.73) and European cohorts ( t (95) = 2.22, P = 0.029, Hedges’ g difference of 0.36, 95% CI 0.04 to 0.68). For newborns, we found weaker effects in North American cohorts compared to Asian ( t (55) = 2.28, P = 0.026, Hedges’ g difference of −0.37, 95% CI −0.69 to −0.05) and European cohorts ( t (55) = 2.36, P = 0.022, Hedges’ g difference of −0.40, 95% CI −0.74 to −0.06). Investigating the interaction with mental and physical health benefits did not reveal any effects of study location in both meta-analyses (Supplementary Fig. 18 ).
Systematic review of studies without effect sizes
All studies where effect size data could not be obtained or that did not meet the meta-analysis inclusion criteria can be found on the OSF project 12 in the file ‘Study_lists_final_revised.xlsx’ (sheet ‘Studies_without_effect_sizes’). Specific reasons for exclusion are furthermore documented in Supplementary Table 2 . For human health outcomes assessed across 56 studies and n = 2,438 individuals, interventions mostly comprised massage therapy ( k = 86 health outcomes) and kangaroo care ( k = 33 health outcomes). For datasets where no effect size could be computed, 90.0% of mental health and 84.3% of physical health parameters were positively impacted by touch. Positive impact of touch did not differ between types of touch interventions. These results match well with the observations of the meta-analysis of a highly positive benefit of touch overall, irrespective of whether a massage or any other intervention is applied.
We also assessed health outcomes in animals across 19 studies and n = 911 subjects. Most research was conducted in rodents. Animals that received touch were rats (ten studies, k = 16 health outcomes), mice (four studies, k = 7 health outcomes), macaques (two studies, k = 3 health outcomes), cats (one study, k = 3 health outcomes), lambs (one study, k = 2 health outcomes) and coral reef fish (one study, k = 1 health outcome). Touch interventions mostly comprised stroking ( k = 13 health outcomes) and tickling ( k = 10 health outcomes). For animal studies, 71.4% of effects showed benefits to mental health-like parameters and 81.8% showed positive physical health effects. We thus found strong evidence that touch interventions, which were mostly conducted by humans (16 studies with human touch versus 3 studies with object touch), had positive health effects in animal species as well.
The key aim of the present study was twofold: (1) to provide an estimate of the effect size of touch interventions and (2) to disambiguate moderating factors to potentially tailor future interventions more precisely. Overall, touch interventions were beneficial for both physical and mental health, with a medium effect size. Our work illustrates that touch interventions are best suited for reducing pain, depression and anxiety in adults and children as well as for increasing weight gain in newborns. These findings are in line with previous meta-analyses on this topic, supporting their conclusions and their robustness to the addition of more datasets. One limitation of previous meta-analyses is that they focused on specific health outcomes or populations, despite primary studies often reporting effects on multiple health parameters simultaneously (for example, ref. 13 focusing on neck and shoulder pain and ref. 14 focusing on massage therapy in preterms). To our knowledge, only ref. 5 provides a multivariate picture for a large number of dependent variables. However, this study analysed their data in separate random effects models that did not account for multivariate reporting nor for the multilevel structure of the data, as such approaches have only become available recently. Thus, in addition to adding a substantial amount of new data, our statistical approach provides a more accurate depiction of effect size estimates. Additionally, our study investigated a variety of moderating effects that did not reach significance (for example, sex ratio, mean age or intervention duration) or were not considered (for example, the benefits of robot or object touch) in previous meta-analyses in relation to touch intervention efficacy 5 , probably because of the small number of studies with information on these moderators in the past. Owing to our large-scale approach, we reached high statistical power for many moderator analyses. Finally, previous meta-analyses on this topic exclusively focused on massage therapy in adults or kangaroo care in newborns 15 , leaving out a large number of interventions that are being carried out in research as well as in everyday life to improve well-being. Incorporating these studies into our study, we found that, in general, both massages and other types of touch, such as gentle touch, stroking or kangaroo care, showed similar health benefits.
While it seems to be less critical which touch intervention is applied, the frequency of interventions seems to matter. More sessions were positively associated with the improvement of trait outcomes such as depression and anxiety but also pain reductions in adults. In contrast to session number, increasing the duration of individual sessions did not improve health effects. In fact, we found some indications of negative relationships in adults for cortisol and blood pressure. This could be due to habituating effects of touch on the sympathetic nervous system and hypothalamic–pituitary–adrenal axis, ultimately resulting in diminished effects with longer exposure, or decreased pleasantness ratings of affective touch with increasing duration 16 . For newborns, we could not support previous notions that the duration of the touch intervention is linked to benefits in weight gain 17 . Thus, an ideal intervention protocol does not seem to have to be excessively long. It should be noted that very few interventions lasted less than 5 min, and it therefore remains unclear whether very short interventions have the same effect.
A critical issue highlighted in the pandemic was the lack of touch due to social restrictions 18 . To accommodate the need for touch in individuals with small social networks (for example, institutionalized or isolated individuals), touch interventions using objects/robots have been explored in the past (for a review, see ref. 11 ). We show here that touch interactions outside of the human–human domain are beneficial for mental and physical health outcomes. Importantly, object/robot touch was not as effective in improving mental health as human-applied touch. A sub-analysis of missing skin-to-skin contact among humans indicated that mental health effects of touch might be mediated by the presence of skin-to-skin contact. Thus, it seems profitable to include skin-to-skin contact in future touch interventions, in line with previous findings in newborns 19 . In robots, recent advancements in synthetic skin 20 should be investigated further in this regard. It should be noted that, although we did not observe significant differences in physical health benefits between human–human and human–object touch, the variability of effect sizes was higher in human–object touch. The conditions enabling object or robot interactions to improve well-being should therefore be explored in more detail in the future.
Touch was beneficial for both healthy and clinical cohorts. These data are critical as most previous meta-analytic research has focused on individuals diagnosed with clinical disorders (for example, ref. 6 ). For mental health outcomes, we found larger effects in clinical cohorts. A possible reason could relate to increased touch wanting 21 in patients. For example, loneliness often co-occurs with chronic illnesses 22 , which are linked to depressed mood and feelings of anxiety 23 . Touch can be used to counteract this negative development 24 , 25 . In adults and children, knowing the toucher did not influence health benefits. In contrast, familiarity affected overall health benefits in newborns, with parental touch being more beneficial than touch applied by medical staff. Previous studies have suggested that early skin-to-skin contact and exposure to maternal odour is critical for a newborn’s ability to adapt to a new environment 26 , supporting the notion that parental care is difficult to substitute in this time period.
With respect to age-related effects, our data further suggest that increasing age was associated with a higher benefit through touch for systolic blood pressure. These findings could potentially be attributed to higher basal blood pressure 27 with increasing age, allowing for a stronger modulation of this parameter. For sex differences, our study provides some evidence that there are differences between women and men with respect to health benefits of touch. Overall, research on sex differences in touch processing is relatively sparse (but see refs. 28 , 29 ). Our results suggest that buffering effects against physiological stress are stronger in women. This is in line with increased buffering effects of hugs in women compared with men 30 . The female-biased primary research in adults, however, begs for more research in men or non-binary individuals. Unfortunately, our study could not dive deeper into this topic as health benefits broken down by sex or gender were almost never provided. Recent research has demonstrated that sensory pleasantness is affected by sex and that this also interacts with the familiarity of the other person in the touching dyad 29 , 31 . In general, contextual factors such as sex and gender or the relationship of the touching dyad, differences in cultural background or internal states such as stress have been demonstrated to be highly influential in the perception of affective touch and are thus relevant to maximizing the pleasantness and ultimately the health benefits of touch interactions 32 , 33 , 34 . As a positive personal relationship within the touching dyad is paramount to induce positive health effects, future research applying robot touch to promote well-being should therefore not only explore synthetic skin options but also focus on improving robots as social agents that form a close relationship with the person receiving the touch 35 .
As part of the systematic review, we also assessed the effects of touch interventions in non-human animals. Mimicking the results of the meta-analysis in humans, beneficial effects of touch in animals were comparably strong for mental health-like and physical health outcomes. This may inform interventions to promote animal welfare in the context of animal experiments 36 , farming 37 and pets 38 . While most studies investigated effects in rodents, which are mostly used as laboratory animals, these results probably transfer to livestock and common pets as well. Indeed, touch was beneficial in lambs, fish and cats 39 , 40 , 41 . The positive impact of human touch in rodents also allows for future mechanistic studies in animal models to investigate how interventions such as tickling or stroking modulate hormonal and neuronal responses to touch in the brain. Furthermore, the commonly proposed oxytocin hypothesis can be causally investigated in these animal models through, for example, optogenetic or chemogenetic techniques 42 . We believe that such translational approaches will further help in optimizing future interventions in humans by uncovering the underlying mechanisms and brain circuits involved in touch.
Our results offer many promising avenues to improve future touch interventions, but they also need to be discussed in light of their limitations. While the majority of findings showed robust health benefits of touch interventions across moderators when compared with a null effect, post hoc tests of, for example, familiarity effects in newborns or mental health benefit differences between human and object touch only barely reached significance. Since we computed a large number of statistical tests in the present study, there is a risk that these results are false positives. We hope that researchers in this field are stimulated by these intriguing results and target these questions by primary research through controlled experimental designs within a well-powered study. Furthermore, the presence of small-study bias in both meta-analyses is indicative that the effect size estimates presented here might be overestimated as null results are often unpublished. We want to stress however that this bias is probably reduced by the multivariate reporting of primary studies. Most studies that reported on multiple health outcomes only showed significant findings for one or two among many. Thus, the multivariate nature of primary research in this field allowed us to include many non-significant findings in the present study. Another limitation pertains to the fact that we only included articles in languages mostly spoken in Western countries. As a large body of evidence comes from Asian countries, it could be that primary research was published in languages other than specified in the inclusion criteria. Thus, despite the large and inclusive nature of our study, some studies could have been missed regardless. Another factor that could not be accounted for in our meta-analysis was that an important prerequisite for touch to be beneficial is its perceived pleasantness. The level of pleasantness associated with being touched is modulated by several parameters 34 including cultural acceptability 43 , perceived humanness 44 or a need for touch 45 , which could explain the observed differences for certain moderators, such as human–human versus robot–human interaction. Moreover, the fact that secondary categorical moderators could not be investigated with respect to specific health outcomes, owing to the lack of data points, limits the specificity of our conclusions in this regard. It thus remains unclear whether, for example, a decreased mental health benefit in the absence of skin-to-skin contact is linked mostly to decreased anxiolytic effects, changes in positive/negative affect or something else. Since these health outcomes are however highly correlated 46 , it is likely that such effects are driven by multiple health outcomes. Similarly, it is important to note that our conclusions mainly refer to outcomes measured close to the touch intervention as we did not include long-term outcomes. Finally, it needs to be noted that blinding towards the experimental condition is essentially impossible in touch interventions. Although we compared the touch intervention with other interventions, such as relaxation therapy, as control whenever possible, contributions of placebo effects cannot be ruled out.
In conclusion, we show clear evidence that touch interventions are beneficial across a large number of both physical and mental health outcomes, for both healthy and clinical cohorts, and for all ages. These benefits, while influenced in their magnitude by study cohorts and intervention characteristics, were robustly present, promoting the conclusion that touch interventions can be systematically employed across the population to preserve and improve our health.
Open science practices
All data and code are accessible in the corresponding OSF project 12 . The systematic review was registered on PROSPERO (CRD42022304281) before the start of data collection. We deviated from the pre-registered plan as follows:
Deviation 1: During our initial screening for the systematic review, we were confronted with a large number of potential health outcomes to look at. This observation of multivariate outcomes led us to register an amendment during data collection (but before any effect size or moderator screening). In doing so, we aimed to additionally extract meta-analytic effects for a more quantitative assessment of our review question that can account for multivariate data reporting and dependencies of effects within the same study. Furthermore, as we noted a severe lack of studies with respect to health outcomes for animals during the inclusion assessment for the systematic review, we decided that the meta-analysis would only focus on outcomes that could be meaningfully analysed on the meta-analytic level and therefore only included health outcomes of human participants.
Deviation 2: In the pre-registration, we did not explicitly exclude non-randomized trials. Since an explicit use of non-randomization for group allocation significantly increases the risk of bias, we decided to exclude them a posteriori from data analysis.
Deviation 3: In the pre-registration, we outlined a tertiary moderator level, namely benefits of touch application versus touch reception. This level was ignored since no included study specifically investigated the benefits of touch application by itself.
Deviation 4: In the pre-registration, we suggested using the RoBMA function 47 to provide a Bayesian framework that allows for a more accurate assessment of publication bias beyond small-study bias. Unfortunately, neither multilevel nor multivariate data structures are supported by the RoBMA function, to our knowledge. For this reason, we did not further pursue this analysis, as the hierarchical nature of the data would not be accounted for.
Deviation 5: Beyond the pre-registered inclusion and exclusion criteria, we also excluded dissertations owing to their lack of peer review.
Deviation 6: In the pre-registration, we stated to investigate the impact of sex of the person applying the touch. This moderator was not further analysed, as this information was rarely given and the individuals applying the touch were almost exclusively women (7 males, 24 mixed and 85 females in studies on adults/children; 3 males, 17 mixed and 80 females in studied on newborns).
Deviation 7: The time span of the touch intervention as assessed by subtracting the final day of the intervention from the first day was not investigated further owing to its very high correlation with the number of sessions ( r (461) = 0.81 in the adult meta-analysis, r (145) = 0.84 in the newborn meta-analysis).
Inclusion and exclusion criteria
To be included in the systematic review, studies had to investigate the relationship between at least one health outcome (physical and/or mental) in humans or animals and a touch intervention, include explicit physical touch by another human, animal or object as part of an intervention and include an experimental and control condition/group that are differentiated by touch alone. Of note, as a result of this selection process, no animal-to-animal touch intervention study was included, as they never featured a proper no-touch control. Human touch was always explicit touch by a human (that is, no brushes or other tools), either with or without skin-to-skin contact. Regarding the included health outcomes, we aimed to be as broad as possible but excluded parameters such as neurophysiological responses or pleasantness ratings after touch application as they do not reflect health outcomes. All included studies in the meta-analysis and systematic review 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 , 141 , 142 , 143 , 144 , 145 , 146 , 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 , 162 , 163 , 164 , 165 , 166 , 167 , 168 , 169 , 170 , 171 , 172 , 173 , 174 , 175 , 176 , 177 , 178 , 179 , 180 , 181 , 182 , 183 , 184 , 185 , 186 , 187 , 188 , 189 , 190 , 191 , 192 , 193 , 194 , 195 , 196 , 197 , 198 , 199 , 200 , 201 , 202 , 203 , 204 , 205 , 206 , 207 , 208 , 209 , 210 , 211 , 212 , 213 , 214 , 215 , 216 , 217 , 218 , 219 , 220 , 221 , 222 , 223 , 224 , 225 , 226 , 227 , 228 , 229 , 230 , 231 , 232 , 233 , 234 , 235 , 236 , 237 , 238 , 239 , 240 , 241 , 242 , 243 , 244 , 245 , 246 , 247 , 248 , 249 , 250 , 251 , 252 , 253 , 254 , 255 , 256 , 257 , 258 , 259 , 260 , 261 , 262 , 263 are listed in Supplementary Table 2 . All excluded studies are listed in Supplementary Table 3 , together with a reason for exclusion. We then applied a two-step process: First, we identified all potential health outcomes and extracted qualitative information on those outcomes (for example, direction of effect). Second, we extracted quantitative information from all possible outcomes (for example, effect sizes). The meta-analysis additionally required a between-subjects design (to clearly distinguish touch from no-touch effects and owing to missing information about the correlation between repeated measurements 264 ). Studies that explicitly did not apply a randomized protocol were excluded before further analysis to reduce risk of bias. The full study lists for excluded and included studies can be found in the OSF project 12 in the file ‘Study_lists_final_revised.xlsx’. In terms of the time frame, we conducted an open-start search of studies until 2022 and identified studies conducted between 1965 and 2022.
Data collection
We used Google Scholar, PubMed and Web of Science for our literature search, with no limitations regarding the publication date and using pre-specified search queries (see Supplementary Information for the exact keywords used). All procedures were in accordance with the updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines 265 . Articles were assessed in French, Dutch, German or English. The above databases were searched from 2 December 2021 until 1 October 2022. Two independent coders evaluated each paper against the inclusion and exclusion criteria. Inconsistencies between coders were checked and resolved by J.P. and H.H. Studies excluded/included for the review and meta-analysis can be found on the OSF project.
Search queries
We used the following keywords to search the chosen databases. Agents (human versus animal versus object versus robot) and touch outcome (physical versus mental) were searched separately together with keywords searching for touch.
TOUCH: Touch OR Social OR Affective OR Contact OR Tactile interaction OR Hug OR Massage OR Embrace OR Kiss OR Cradling OR Stroking OR Haptic interaction OR tickling
AGENT: Object OR Robot OR human OR animal OR rodent OR primate
MENTAL OUTCOME: Health OR mood OR Depression OR Loneliness OR happiness OR life satisfaction OR Mental Disorder OR well-being OR welfare OR dementia OR psychological OR psychiatric OR anxiety OR Distress
PHYSICAL OUTCOME: Health OR Stress OR Pain OR cardiovascular health OR infection risk OR immune response OR blood pressure OR heart rate
Data extraction and preparation
Data extraction began on 10 October 2022 and was concluded on 25 February 2023. J.P. and H.H. oversaw the data collection process, and checked and resolved all inconsistencies between coders.
Health benefits of touch were always coded by positive summary effects, whereas adverse health effects of touch were represented by negative summary effects. If multiple time points were measured for the same outcome on the same day after a single touch intervention, we extracted the peak effect size (in either the positive or negative direction). If the touch intervention occurred multiple times and health outcomes were assessed for each time point, we extracted data points separately. However, we only extracted immediate effects, as long-term effects not controlled through the experimental conditions could be due to influences other than the initial touch intervention. Measurements assessing long-term effects without explicit touch sessions in the breaks were excluded for the same reason. Common control groups for touch interventions comprised active (for example, relaxation therapy) as well as passive control groups (for example, standard medical care). In the case of multiple control groups, we always contrasted the touch group to the group that most closely matched the touch condition (for example, relaxation therapy was preferred over standard medical care). We extracted information from all moderators listed in the pre-registration (Supplementary Table 4 ). A list of included and excluded health outcomes is presented in Supplementary Table 5 . Authors of studies with possible effects but missing information to calculate those effects were contacted via email and asked to provide the missing data (response rate 35.7%).
After finalizing the list of included studies for the systematic review, we added columns for moderators and the coding schema for our meta-analysis per our updated registration. Then, each study was assessed for its eligibility in the meta-analysis by two independent coders (J.P., H.H., K.F. or F.M.). To this end, all coders followed an a priori specified procedure: First, the PDF was skimmed for possible effects to extract, and the study was excluded if no PDF was available or the study was in a language different from the ones specified in ‘ Data collection ’. Effects from studies that met the inclusion criteria were extracted from all studies listing descriptive values or statistical parameters to calculate effect sizes. A website 266 was used to convert descriptive and statistical values available in the included studies (means and standard deviations/standard errors/confidence intervals, sample sizes, F values, t values, t test P values or frequencies) into Cohen’s d , which were then converted in Hedges’ g . If only P value thresholds were reported (for example, P < 0.01), we used this, most conservative, value as the P value to calculate the effect size (for example, P = 0.01). If only the total sample size was given but that number was even and the participants were randomly assigned to each group, we assumed equal sample sizes for each group. If delta change scores (for example, pre- to post-touch intervention) were reported, we used those over post-touch only scores. In case frequencies were 0 when frequency tables were used to determine effect sizes, we used a value of 0.5 as a substitute to calculate the effect (the default setting in the ‘metafor’ function 267 ). From these data, Hedges’ g and its variance could be derived. Effect sizes were always computed between the experimental and the control group.
Statistical analysis and risk of bias assessment
Owing to the lack of identified studies, health benefits to animals were not included as part of the statistical analysis. One meta-analysis was performed for adults, adolescents and children, as outcomes were highly comparable. We refer to this meta-analysis as the adult meta-analysis, as children/adolescent cohorts were only targeted in a minority of studies. A separate meta-analysis was performed for newborns, as their health outcomes differed substantially from any other age group.
Data were analysed using R (version 4.2.2) with the ‘rma.mv’ function from the ‘metafor’ package 267 in a multistep, multivariate and multilevel fashion.
We calculated an overall effect of touch interventions across all studies, cohorts and health outcomes. To account for the hierarchical structure of the data, we used a multilevel structure with random effects at the study, cohort and effects level. Furthermore, we calculated the variance–covariance matrix of all data points to account for the dependencies of measured effects within each individual cohort and study. The variance–covariance matrix was calculated by default with an assumed correlation of effect sizes within each cohort of ρ = 0.6. As ρ needed to be assumed, sensitivity analyses for all computed effect estimates were conducted using correlations between effects of 0, 0.2, 0.4 and 0.8. The results of these sensitivity analyses can be found in ref. 12 . No conclusion drawn in the present manuscript was altered by changing the level of ρ . The sensitivity analyses, however, showed that higher assumed correlations lead to more conservative effect size estimates (see Supplementary Figs. 19 and 20 for the adult and newborn meta-analyses, respectively), reducing the type I error risk in general 268 . In addition to these procedures, we used robust variance estimation with cluster-robust inference at the cohort level. This step is recommended to more accurately determine the confidence intervals in complex multivariate models 269 . The data distribution was assumed to be normal, but this was not formally tested.
To determine whether individual effects had a strong influence on our results, we calculated Cook’s distance D . Here, a threshold of D > 0.5 was used to qualify a study as influential 270 . Heterogeneity in the present study was assessed using Cochran’s Q , which determines whether the extracted effect sizes estimate a common population effect size. Although the Q statistic in the ‘rma.mv’ function accounts for the hierarchical nature of the data, we also quantified the heterogeneity estimator σ ² for each random-effects level to provide a comprehensive overview of heterogeneity indicators. These indicators for all models can be found on the OSF project 12 in the Table ‘Model estimates’. To assess small study bias, we visually inspected the funnel plot and used the standard error as a moderator in the overarching meta-analyses.
Before any sub-group analysis, the overall effect size was used as input for power calculations. While such post hoc power calculations might be limited, we believe that a minimum number of effects to be included in subgroup analyses was necessary to allow for meaningful conclusions. Such medium effect sizes would also probably be the minimum effect sizes of interest for researchers as well as clinical practitioners. Power calculation for random-effects models further requires a sample size for each individual effect as well as an approximation of the expected heterogeneity between studies. For the sample size input, we used the median sample size in each of our studies. For heterogeneity, we assumed a value between medium and high levels of heterogeneity ( I ² = 62.5% 271 ), as moderator analyses typically aim at reducing heterogeneity overall. Subgroups were only further investigated if the number of observed effects achieved ~80% power under these circumstances, to allow for a more robust interpretation of the observed effects (see Supplementary Figs. 5 and 6 for the adult and newborn meta-analysis, respectively). In a next step, we investigated all pre-registered moderators for which sufficient power was detected. We first looked at our primary moderators (mental versus physical health) and how the effect sizes systematically varied as a function of our secondary moderators (for example, human–human or human–object touch, duration, skin-to-skin presence, etc.). We always included random slopes to allow for our moderators to vary with the random effects at our clustering variable, which is recommended in multilevel models to reduce false positives 272 . All statistical tests were performed two-sided. Significance of moderators was determined using omnibus F tests. Effect size differences between moderator levels and their confidence intervals were assessed via t tests.
Post hoc t tests were performed comparing mental and physical health benefits within each interacting moderator (for example, mental versus physical health benefits in cancer patients) and mental or physical health benefits across levels of the interacting moderator (for example, mental health benefits in cancer versus pain patients). The post hoc tests were not pre-registered. Data were visualized using forest plots and orchard plots 273 for categorical moderators and scatter plots for continuous moderators.
For a broad overview of prior work and their biases, risk of bias was assessed for all studies included in both meta-analyses and the systematic review. We assessed the risk of bias for the following parameters:
Bias from randomization, including whether a randomization procedure was performed, whether it was a between- or within-participant design and whether there were any baseline differences for demographic or dependent variables.
Sequence bias resulting from a lack of counterbalancing in within-subject designs.
Performance bias resulting from the participants or experiments not being blinded to the experimental conditions.
Attrition bias resulting from different dropout rates between experimental groups.
Note that four studies in the adult meta-analysis did not explicitly mention randomization as part of their protocol. However, since these studies never showed any baseline differences in all relevant variables (see ‘Risk of Bias’ table on the OSF project ) , we assumed that randomization was performed but not mentioned. Sequence bias was of no concern for studies for the meta-analysis since cross-over designs were excluded. It was, however, assessed for studies within the scope of the systematic review. Importantly, performance bias was always high in the adult/children meta-analysis, as blinding of the participants and experimenters to the experimental conditions was not possible owing to the nature of the intervention (touch versus no touch). For studies with newborns and animals, we assessed the performance bias as medium since neither newborns or animals are likely to be aware of being part of an experiment or specific group. An overview of the results is presented in Supplementary Fig. 21 , and the precise assessment for each study can be found on the OSF project 12 in the ‘Risk of Bias’ table.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All data are available via Open Science Framework at https://doi.org/10.17605/OSF.IO/C8RVW (ref. 12 ). Source data are provided with this paper.
Code availability
All code is available via Open Science Framework at https://doi.org/10.17605/OSF.IO/C8RVW (ref. 12 ).
Fulkerson, M. The First Sense: a Philosophical Study of Human Touch (MIT Press, 2013).
Farroni, T., Della Longa, L. & Valori, I. The self-regulatory affective touch: a speculative framework for the development of executive functioning. Curr. Opin. Behav. Sci. 43 , 167–173 (2022).
Article Google Scholar
Ocklenburg, S. et al. Hugs and kisses—the role of motor preferences and emotional lateralization for hemispheric asymmetries in human social touch. Neurosci. Biobehav. Rev. 95 , 353–360 (2018).
Ardiel, E. L. & Rankin, C. H. The importance of touch in development. Paediatr. Child Health 15 , 153–156 (2010).
Article PubMed PubMed Central Google Scholar
Moyer, C. A., Rounds, J. & Hannum, J. W. A meta-analysis of massage therapy research. Psychol. Bull. 130 , 3–18 (2004).
Article PubMed Google Scholar
Lee, S. H., Kim, J. Y., Yeo, S., Kim, S. H. & Lim, S. Meta-analysis of massage therapy on cancer pain. Integr. Cancer Ther. 14 , 297–304 (2015).
LaFollette, M. R., O’Haire, M. E., Cloutier, S. & Gaskill, B. N. A happier rat pack: the impacts of tickling pet store rats on human–animal interactions and rat welfare. Appl. Anim. Behav. Sci. 203 , 92–102 (2018).
Packheiser, J., Michon, F. Eva, C., Fredriksen, K. & Hartmann H. The physical and mental health benefits of social touch: a comparative systematic review and meta-analysis. PROSPERO https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022304281 (2023).
Lakens, D. Sample size justification. Collabra. Psychol. 8 , 33267 (2022).
Quintana, D. S. A guide for calculating study-level statistical power for meta-analyses. Adv. Meth. Pract. Psychol. Sci. https://doi.org/10.1177/25152459221147260 (2023).
Eckstein, M., Mamaev, I., Ditzen, B. & Sailer, U. Calming effects of touch in human, animal, and robotic interaction—scientific state-of-the-art and technical advances. Front. Psychiatry 11 , 555058 (2020).
Packheiser, J. et al. The physical and mental health benefits of affective touch: a comparative systematic review and multivariate meta-analysis. Open Science Framework https://doi.org/10.17605/OSF.IO/C8RVW (2023).
Kong, L. J. et al. Massage therapy for neck and shoulder pain: a systematic review and meta-analysis. Evid. Based Complement. Altern. Med. 2013 , 613279 (2013).
Wang, L., He, J. L. & Zhang, X. H. The efficacy of massage on preterm infants: a meta-analysis. Am. J. Perinatol. 30 , 731–738 (2013).
Field, T. Massage therapy research review. Complement. Ther. Clin. Pract. 24 , 19–31 (2016).
Bendas, J., Ree, A., Pabel, L., Sailer, U. & Croy, I. Dynamics of affective habituation to touch differ on the group and individual level. Neuroscience 464 , 44–52 (2021).
Article CAS PubMed Google Scholar
Charpak, N., Montealegre‐Pomar, A. & Bohorquez, A. Systematic review and meta‐analysis suggest that the duration of Kangaroo mother care has a direct impact on neonatal growth. Acta Paediatr. 110 , 45–59 (2021).
Packheiser, J. et al. A comparison of hugging frequency and its association with momentary mood before and during COVID-19 using ecological momentary assessment. Health Commun. https://doi.org/10.1080/10410236.2023.2198058 (2023).
Whitelaw, A., Heisterkamp, G., Sleath, K., Acolet, D. & Richards, M. Skin to skin contact for very low birthweight infants and their mothers. Arch. Dis. Child. 63 , 1377–1381 (1988).
Article CAS PubMed PubMed Central Google Scholar
Yogeswaran, N. et al. New materials and advances in making electronic skin for interactive robots. Adv. Robot. 29 , 1359–1373 (2015).
Durkin, J., Jackson, D. & Usher, K. Touch in times of COVID‐19: touch hunger hurts. J. Clin. Nurs. https://doi.org/10.1111/jocn.15488 (2021).
Rokach, A., Lechcier-Kimel, R. & Safarov, A. Loneliness of people with physical disabilities. Soc. Behav. Personal. Int. J. 34 , 681–700 (2006).
Palgi, Y. et al. The loneliness pandemic: loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 275 , 109–111 (2020).
Heatley-Tejada, A., Dunbar, R. I. M. & Montero, M. Physical contact and loneliness: being touched reduces perceptions of loneliness. Adapt. Hum. Behav. Physiol. 6 , 292–306 (2020).
Article CAS Google Scholar
Packheiser, J. et al. The association of embracing with daily mood and general life satisfaction: an ecological momentary assessment study. J. Nonverbal Behav. 46 , 519–536 (2022).
Porter, R. The biological significance of skin-to-skin contact and maternal odours. Acta Paediatr. 93 , 1560–1562 (2007).
Hawkley, L. C., Masi, C. M., Berry, J. D. & Cacioppo, J. T. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol. Aging 21 , 152–164 (2006).
Russo, V., Ottaviani, C. & Spitoni, G. F. Affective touch: a meta-analysis on sex differences. Neurosci. Biobehav. Rev. 108 , 445–452 (2020).
Schirmer, A. et al. Understanding sex differences in affective touch: sensory pleasantness, social comfort, and precursive experiences. Physiol. Behav. 250 , 113797 (2022).
Berretz, G. et al. Romantic partner embraces reduce cortisol release after acute stress induction in women but not in men. PLoS ONE 17 , e0266887 (2022).
Gazzola, V. et al. Primary somatosensory cortex discriminates affective significance in social touch. Proc. Natl Acad. Sci. USA 109 , E1657–E1666 (2012).
Sorokowska, A. et al. Affective interpersonal touch in close relationships: a cross-cultural perspective. Personal. Soc. Psychol. Bull. 47 , 1705–1721 (2021).
Ravaja, N., Harjunen, V., Ahmed, I., Jacucci, G. & Spapé, M. M. Feeling touched: emotional modulation of somatosensory potentials to interpersonal touch. Sci. Rep. 7 , 40504 (2017).
Saarinen, A., Harjunen, V., Jasinskaja-Lahti, I., Jääskeläinen, I. P. & Ravaja, N. Social touch experience in different contexts: a review. Neurosci. Biobehav. Rev. 131 , 360–372 (2021).
Huisman, G. Social touch technology: a survey of haptic technology for social touch. IEEE Trans. Haptics 10 , 391–408 (2017).
Lewejohann, L., Schwabe, K., Häger, C. & Jirkof, P. Impulse for animal welfare outside the experiment. Lab. Anim. https://doi.org/10.17169/REFUBIUM-26765 (2020).
Sørensen, J. T., Sandøe, P. & Halberg, N. Animal welfare as one among several values to be considered at farm level: the idea of an ethical account for livestock farming. Acta Agric. Scand. A 51 , 11–16 (2001).
Google Scholar
Verga, M. & Michelazzi, M. Companion animal welfare and possible implications on the human–pet relationship. Ital. J. Anim. Sci. 8 , 231–240 (2009).
Coulon, M. et al. Do lambs perceive regular human stroking as pleasant? Behavior and heart rate variability analyses. PLoS ONE 10 , e0118617 (2015).
Soares, M. C., Oliveira, R. F., Ros, A. F. H., Grutter, A. S. & Bshary, R. Tactile stimulation lowers stress in fish. Nat. Commun. 2 , 534 (2011).
Gourkow, N., Hamon, S. C. & Phillips, C. J. C. Effect of gentle stroking and vocalization on behaviour, mucosal immunity and upper respiratory disease in anxious shelter cats. Prev. Vet. Med. 117 , 266–275 (2014).
Oliveira, V. E. et al. Oxytocin and vasopressin within the ventral and dorsal lateral septum modulate aggression in female rats. Nat. Commun. 12 , 2900 (2021).
Burleson, M. H., Roberts, N. A., Coon, D. W. & Soto, J. A. Perceived cultural acceptability and comfort with affectionate touch: differences between Mexican Americans and European Americans. J. Soc. Personal. Relatsh. 36 , 1000–1022 (2019).
Wijaya, M. et al. The human ‘feel’ of touch contributes to its perceived pleasantness. J. Exp. Psychol. Hum. Percept. Perform. 46 , 155–171 (2020).
Golaya, S. Touch-hunger: an unexplored consequence of the COVID-19 pandemic. Indian J. Psychol. Med. 43 , 362–363 (2021).
Ng, T. W. H., Sorensen, K. L., Zhang, Y. & Yim, F. H. K. Anger, anxiety, depression, and negative affect: convergent or divergent? J. Vocat. Behav. 110 , 186–202 (2019).
Maier, M., Bartoš, F. & Wagenmakers, E.-J. Robust Bayesian meta-analysis: addressing publication bias with model-averaging. Psychol. Methods 28 , 107–122 (2022).
Ahles, T. A. et al. Massage therapy for patients undergoing autologous bone marrow transplantation. J. Pain. Symptom Manag. 18 , 157–163 (1999).
Albert, N. M. et al. A randomized trial of massage therapy after heart surgery. Heart Lung 38 , 480–490 (2009).
Ang, J. Y. et al. A randomized placebo-controlled trial of massage therapy on the immune system of preterm infants. Pediatrics 130 , e1549–e1558 (2012).
Arditi, H., Feldman, R. & Eidelman, A. I. Effects of human contact and vagal regulation on pain reactivity and visual attention in newborns. Dev. Psychobiol. 48 , 561–573 (2006).
Arora, J., Kumar, A. & Ramji, S. Effect of oil massage on growth and neurobehavior in very low birth weight preterm neonates. Indian Pediatr. 42 , 1092–1100 (2005).
PubMed Google Scholar
Asadollahi, M., Jabraeili, M., Mahallei, M., Asgari Jafarabadi, M. & Ebrahimi, S. Effects of gentle human touch and field massage on urine cortisol level in premature infants: a randomized, controlled clinical trial. J. Caring Sci. 5 , 187–194 (2016).
Basiri-Moghadam, M., Basiri-Moghadam, K., Kianmehr, M. & Jani, S. The effect of massage on neonatal jaundice in stable preterm newborn infants: a randomized controlled trial. J. Pak. Med. Assoc. 65 , 602–606 (2015).
Bauer, B. A. et al. Effect of massage therapy on pain, anxiety, and tension after cardiac surgery: a randomized study. Complement. Ther. Clin. Pract. 16 , 70–75 (2010).
Beijers, R., Cillessen, L. & Zijlmans, M. A. C. An experimental study on mother-infant skin-to-skin contact in full-terms. Infant Behav. Dev. 43 , 58–65 (2016).
Bennett, S. et al. Acute effects of traditional Thai massage on cortisol levels, arterial blood pressure and stress perception in academic stress condition: a single blind randomised controlled trial. J. Bodyw. Mov. Therapies 20 , 286–292 (2016).
Bergman, N., Linley, L. & Fawcus, S. Randomized controlled trial of skin-to-skin contact from birth versus conventional incubator for physiological stabilization in 1200- to 2199-gram newborns. Acta Paediatr. 93 , 779–785 (2004).
Bigelow, A., Power, M., MacLellan‐Peters, J., Alex, M. & McDonald, C. Effect of mother/infant skin‐to‐skin contact on postpartum depressive symptoms and maternal physiological stress. J. Obstet. Gynecol. Neonatal Nurs. 41 , 369–382 (2012).
Billhult, A., Bergbom, I. & Stener-Victorin, E. Massage relieves nausea in women with breast cancer who are undergoing chemotherapy. J. Altern. Complement. Med. 13 , 53–57 (2007).
Billhult, A., Lindholm, C., Gunnarsson, R. & Stener-Victorin, E. The effect of massage on cellular immunity, endocrine and psychological factors in women with breast cancer—a randomized controlled clinical trial. Auton. Neurosci. 140 , 88–95 (2008).
Braun, L. A. et al. Massage therapy for cardiac surgery patients—a randomized trial. J. Thorac. Cardiovasc. Surg. 144 , 1453–1459 (2012).
Cabibihan, J.-J. & Chauhan, S. S. Physiological responses to affective tele-touch during induced emotional stimuli. IEEE Trans. Affect. Comput. 8 , 108–118 (2017).
Campeau, M.-P. et al. Impact of massage therapy on anxiety levels in patients undergoing radiation therapy: randomized controlled trial. J. Soc. Integr. Oncol. 5 , 133–138 (2007).
Can, Ş. & Kaya, H. The effects of yakson or gentle human touch training given to mothers with preterm babies on attachment levels and the responses of the baby: a randomized controlled trial. Health Care Women Int. 43 , 479–498 (2021).
Carfoot, S., Williamson, P. & Dickson, R. A randomised controlled trial in the north of England examining the effects of skin-to-skin care on breast feeding. Midwifery 21 , 71–79 (2005).
Castral, T. C., Warnock, F., Leite, A. M., Haas, V. J. & Scochi, C. G. S. The effects of skin-to-skin contact during acute pain in preterm newborns. Eur. J. Pain. 12 , 464–471 (2008).
Cattaneo, A. et al. Kangaroo mother care for low birthweight infants: a randomized controlled trial in different settings. Acta Paediatr. 87 , 976–985 (1998).
Charpak, N., Ruiz-Peláez, J. G. & Charpak, Y. Rey-Martinez kangaroo mother program: an alternative way of caring for low birth weight infants? One year mortality in a two cohort study. Pediatrics 94 , 804–810 (1994).
Chermont, A. G., Falcão, L. F. M., de Souza Silva, E. H. L., de Cássia Xavier Balda, R. & Guinsburg, R. Skin-to-skin contact and/or oral 25% dextrose for procedural pain relief for term newborn infants. Pediatrics 124 , e1101–e1107 (2009).
Chi Luong, K., Long Nguyen, T., Huynh Thi, D. H., Carrara, H. P. O. & Bergman, N. J. Newly born low birthweight infants stabilise better in skin-to-skin contact than when separated from their mothers: a randomised controlled trial. Acta Paediatr. 105 , 381–390 (2016).
Cho, E.-S. et al. The effects of kangaroo care in the neonatal intensive care unit on the physiological functions of preterm infants, maternal–infant attachment, and maternal stress. J. Pediatr. Nurs. 31 , 430–438 (2016).
Choi, H. et al. The effects of massage therapy on physical growth and gastrointestinal function in premature infants: a pilot study. J. Child Health Care 20 , 394–404 (2016).
Choudhary, M. et al. To study the effect of Kangaroo mother care on pain response in preterm neonates and to determine the behavioral and physiological responses to painful stimuli in preterm neonates: a study from western Rajasthan. J. Matern. Fetal Neonatal Med. 29 , 826–831 (2016).
Christensson, K. et al. Temperature, metabolic adaptation and crying in healthy full-term newborns cared for skin-to-skin or in a cot. Acta Paediatr. 81 , 488–493 (1992).
Cloutier, S. & Newberry, R. C. Use of a conditioning technique to reduce stress associated with repeated intra-peritoneal injections in laboratory rats. Appl. Anim. Behav. Sci. 112 , 158–173 (2008).
Cloutier, S., Wahl, K., Baker, C. & Newberry, R. C. The social buffering effect of playful handling on responses to repeated intraperitoneal injections in laboratory rats. J. Am. Assoc. Lab. Anim. Sci. 53 , 168–173 (2014).
CAS PubMed PubMed Central Google Scholar
Cloutier, S., Wahl, K. L., Panksepp, J. & Newberry, R. C. Playful handling of laboratory rats is more beneficial when applied before than after routine injections. Appl. Anim. Behav. Sci. 164 , 81–90 (2015).
Cong, X. et al. Effects of skin-to-skin contact on autonomic pain responses in preterm infants. J. Pain. 13 , 636–645 (2012).
Cong, X., Ludington-Hoe, S. M., McCain, G. & Fu, P. Kangaroo care modifies preterm infant heart rate variability in response to heel stick pain: pilot study. Early Hum. Dev. 85 , 561–567 (2009).
Cong, X., Ludington-Hoe, S. M. & Walsh, S. Randomized crossover trial of kangaroo care to reduce biobehavioral pain responses in preterm infants: a pilot study. Biol. Res. Nurs. 13 , 204–216 (2011).
Costa, R. et al. Tactile stimulation of adult rats modulates hormonal responses, depression-like behaviors, and memory impairment induced by chronic mild stress: role of angiotensin II. Behav. Brain Res. 379 , 112250 (2020).
Cutshall, S. M. et al. Effect of massage therapy on pain, anxiety, and tension in cardiac surgical patients: a pilot study. Complement. Ther. Clin. Pract. 16 , 92–95 (2010).
Dalili, H., Sheikhi, S., Shariat, M. & Haghnazarian, E. Effects of baby massage on neonatal jaundice in healthy Iranian infants: a pilot study. Infant Behav. Dev. 42 , 22–26 (2016).
Diego, M. A., Field, T. & Hernandez-Reif, M. Vagal activity, gastric motility, and weight gain in massaged preterm neonates. J. Pediatr. 147 , 50–55 (2005).
Diego, M. A., Field, T. & Hernandez-Reif, M. Temperature increases in preterm infants during massage therapy. Infant Behav. Dev. 31 , 149–152 (2008).
Diego, M. A. et al. Preterm infant massage elicits consistent increases in vagal activity and gastric motility that are associated with greater weight gain. Acta Paediatr. 96 , 1588–1591 (2007).
Diego, M. A. et al. Spinal cord patients benefit from massage therapy. Int. J. Neurosci. 112 , 133–142 (2002).
Diego, M. A. et al. Aggressive adolescents benefit from massage therapy. Adolescence 37 , 597–607 (2002).
Diego, M. A. et al. HIV adolescents show improved immune function following massage therapy. Int. J. Neurosci. 106 , 35–45 (2001).
Dieter, J. N. I., Field, T., Hernandez-Reif, M., Emory, E. K. & Redzepi, M. Stable preterm infants gain more weight and sleep less after five days of massage therapy. J. Pediatr. Psychol. 28 , 403–411 (2003).
Ditzen, B. et al. Effects of different kinds of couple interaction on cortisol and heart rate responses to stress in women. Psychoneuroendocrinology 32 , 565–574 (2007).
Dreisoerner, A. et al. Self-soothing touch and being hugged reduce cortisol responses to stress: a randomized controlled trial on stress, physical touch, and social identity. Compr. Psychoneuroendocrinol. 8 , 100091 (2021).
Eaton, M., Mitchell-Bonair, I. L. & Friedmann, E. The effect of touch on nutritional intake of chronic organic brain syndrome patients. J. Gerontol. 41 , 611–616 (1986).
Edens, J. L., Larkin, K. T. & Abel, J. L. The effect of social support and physical touch on cardiovascular reactions to mental stress. J. Psychosom. Res. 36 , 371–382 (1992).
El-Farrash, R. A. et al. Longer duration of kangaroo care improves neurobehavioral performance and feeding in preterm infants: a randomized controlled trial. Pediatr. Res. 87 , 683–688 (2020).
Erlandsson, K., Dsilna, A., Fagerberg, I. & Christensson, K. Skin-to-skin care with the father after cesarean birth and its effect on newborn crying and prefeeding behavior. Birth 34 , 105–114 (2007).
Escalona, A., Field, T., Singer-Strunck, R., Cullen, C. & Hartshorn, K. Brief report: improvements in the behavior of children with autism following massage therapy. J. Autism Dev. Disord. 31 , 513–516 (2001).
Fattah, M. A. & Hamdy, B. Pulmonary functions of children with asthma improve following massage therapy. J. Altern. Complement. Med. 17 , 1065–1068 (2011).
Feldman, R. & Eidelman, A. I. Skin-to-skin contact (kangaroo care) accelerates autonomic and neurobehavioural maturation in preterm infants. Dev. Med. Child Neurol. 45 , 274–281 (2003).
Feldman, R., Eidelman, A. I., Sirota, L. & Weller, A. Comparison of skin-to-skin (kangaroo) and traditional care: parenting outcomes and preterm infant development. Pediatrics 110 , 16–26 (2002).
Feldman, R., Singer, M. & Zagoory, O. Touch attenuates infants’ physiological reactivity to stress. Dev. Sci. 13 , 271–278 (2010).
Feldman, R., Weller, A., Sirota, L. & Eidelman, A. I. Testing a family intervention hypothesis: the contribution of mother–infant skin-to-skin contact (kangaroo care) to family interaction, proximity, and touch. J. Fam. Psychol. 17 , 94–107 (2003).
Ferber, S. G. et al. Massage therapy by mothers and trained professionals enhances weight gain in preterm infants. Early Hum. Dev. 67 , 37–45 (2002).
Ferber, S. G. & Makhoul, I. R. The effect of skin-to-skin contact (kangaroo care) shortly after birth on the neurobehavioral responses of the term newborn: a randomized, controlled trial. Pediatrics 113 , 858–865 (2004).
Ferreira, A. M. & Bergamasco, N. H. P. Behavioral analysis of preterm neonates included in a tactile and kinesthetic stimulation program during hospitalization. Rev. Bras. Fisioter. 14 , 141–148 (2010).
Fidanza, F., Polimeni, E., Pierangeli, V. & Martini, M. A better touch: C-tactile fibers related activity is associated to pain reduction during temporal summation of second pain. J. Pain. 22 , 567–576 (2021).
Field, T. et al. Leukemia immune changes following massage therapy. J. Bodyw. Mov. Ther. 5 , 271–274 (2001).
Field, T. et al. Benefits of combining massage therapy with group interpersonal psychotherapy in prenatally depressed women. J. Bodyw. Mov. Ther. 13 , 297–303 (2009).
Field, T., Delage, J. & Hernandez-Reif, M. Movement and massage therapy reduce fibromyalgia pain. J. Bodyw. Mov. Ther. 7 , 49–52 (2003).
Field, T. et al. Fibromyalgia pain and substance P decrease and sleep improves after massage therapy. J. Clin. Rheumatol. 8 , 72–76 (2002).
Field, T., Diego, M., Gonzalez, G. & Funk, C. G. Neck arthritis pain is reduced and range of motion is increased by massage therapy. Complement. Ther. Clin. Pract. 20 , 219–223 (2014).
Field, T., Diego, M., Hernandez-Reif, M., Deeds, O. & Figueiredo, B. Pregnancy massage reduces prematurity, low birthweight and postpartum depression. Infant Behav. Dev. 32 , 454–460 (2009).
Field, T. et al. Insulin and insulin-like growth factor-1 increased in preterm neonates following massage therapy. J. Dev. Behav. Pediatr. 29 , 463–466 (2008).
Field, T. et al. Yoga and massage therapy reduce prenatal depression and prematurity. J. Bodyw. Mov. Ther. 16 , 204–209 (2012).
Field, T., Diego, M., Hernandez-Reif, M., Schanberg, S. & Kuhn, C. Massage therapy effects on depressed pregnant women. J. Psychosom. Obstet. Gynecol. 25 , 115–122 (2004).
Field, T., Diego, M., Hernandez-Reif, M. & Shea, J. Hand arthritis pain is reduced by massage therapy. J. Bodyw. Mov. Ther. 11 , 21–24 (2007).
Field, T., Gonzalez, G., Diego, M. & Mindell, J. Mothers massaging their newborns with lotion versus no lotion enhances mothers’ and newborns’ sleep. Infant Behav. Dev. 45 , 31–37 (2016).
Field, T. et al. Children with asthma have improved pulmonary functions after massage therapy. J. Pediatr. 132 , 854–858 (1998).
Field, T., Hernandez-Reif, M., Diego, M. & Fraser, M. Lower back pain and sleep disturbance are reduced following massage therapy. J. Bodyw. Mov. Ther. 11 , 141–145 (2007).
Field, T. et al. Effects of sexual abuse are lessened by massage therapy. J. Bodyw. Mov. Ther. 1 , 65–69 (1997).
Field, T. et al. Pregnant women benefit from massage therapy. J. Psychosom. Obstet. Gynecol. 20 , 31–38 (1999).
Field, T. et al. Juvenilerheumatoid arthritis: benefits from massage therapy. J. Pediatr. Psychol. 22 , 607–617 (1997).
Field, T., Hernandez-Reif, M., Taylor, S., Quintino, O. & Burman, I. Labor pain is reduced by massage therapy. J. Psychosom. Obstet. Gynecol. 18 , 286–291 (1997).
Field, T. et al. Massage therapy reduces anxiety and enhances EEG pattern of alertness and math computations. Int. J. Neurosci. 86 , 197–205 (1996).
Field, T. et al. Brief report: autistic children’s attentiveness and responsivity improve after touch therapy. J. Autism Dev. Disord. 27 , 333–338 (1997).
Field, T. M. et al. Tactile/kinesthetic stimulation effects on preterm neonates. Pediatrics 77 , 654–658 (1986).
Field, T. et al. Massage reduces anxiety in child and adolescent psychiatric patients. J. Am. Acad. Child Adolesc. Psychiatry 31 , 125–131 (1992).
Field, T. et al. Burn injuries benefit from massage therapy. J. Burn Care Res. 19 , 241–244 (1998).
Filho, F. L. et al. Effect of maternal skin-to-skin contact on decolonization of methicillin-oxacillin-resistant Staphylococcus in neonatal intensive care units: a randomized controlled trial. BMC Pregnancy Childbirth https://doi.org/10.1186/s12884-015-0496-1 (2015).
Forward, J. B., Greuter, N. E., Crisall, S. J. & Lester, H. F. Effect of structured touch and guided imagery for pain and anxiety in elective joint replacement patients—a randomized controlled trial: M-TIJRP. Perm. J. 19 , 18–28 (2015).
Fraser, J. & Ross Kerr, J. Psychophysiological effects of back massage on elderly institutionalized patients. J. Adv. Nurs. 18 , 238–245 (1993).
Frey Law, L. A. et al. Massage reduces pain perception and hyperalgesia in experimental muscle pain: a randomized, controlled trial. J. Pain. 9 , 714–721 (2008).
Gao, H. et al. Effect of repeated kangaroo mother care on repeated procedural pain in preterm infants: a randomized controlled trial. Int. J. Nurs. Stud. 52 , 1157–1165 (2015).
Garner, B. et al. Pilot study evaluating the effect of massage therapy on stress, anxiety and aggression in a young adult psychiatric inpatient unit. Aust. N. Z. J. Psychiatry 42 , 414–422 (2008).
Gathwala, G., Singh, B. & Singh, J. Effect of kangaroo mother care on physical growth, breastfeeding and its acceptability. Trop. Dr. 40 , 199–202 (2010).
Geva, N., Uzefovsky, F. & Levy-Tzedek, S. Touching the social robot PARO reduces pain perception and salivary oxytocin levels. Sci. Rep. 10 , 9814 (2020).
Gitau, R. et al. Acute effects of maternal skin-to-skin contact and massage on saliva cortisol in preterm babies. J. Reprod. Infant Psychol. 20 , 83–88 (2002).
Givi, M. Durability of effect of massage therapy on blood pressure. Int. J. Prev. Med. 4 , 511–516 (2013).
PubMed PubMed Central Google Scholar
Glover, V., Onozawa, K. & Hodgkinson, A. Benefits of infant massage for mothers with postnatal depression. Semin. Neonatol. 7 , 495–500 (2002).
Gonzalez, A. et al. Weight gain in preterm infants following parent-administered vimala massage: a randomized controlled trial. Am. J. Perinatol. 26 , 247–252 (2009).
Gray, L., Watt, L. & Blass, E. M. Skin-to-skin contact is analgesic in healthy newborns. Pediatrics 105 , e14 (2000).
Grewen, K. M., Anderson, B. J., Girdler, S. S. & Light, K. C. Warm partner contact is related to lower cardiovascular reactivity. Behav. Med. 29 , 123–130 (2003).
Groër, M. W., Hill, J., Wilkinson, J. E. & Stuart, A. Effects of separation and separation with supplemental stroking in BALB/c infant mice. Biol. Res. Nurs. 3 , 119–131 (2002).
Gürol, A. P., Polat, S. & Nuran Akçay, M. Itching, pain, and anxiety levels are reduced with massage therapy in burned adolescents. J. Burn Care Res. 31 , 429–432 (2010).
Haley, S. et al. Tactile/kinesthetic stimulation (TKS) increases tibial speed of sound and urinary osteocalcin (U-MidOC and unOC) in premature infants (29–32 weeks PMA). Bone 51 , 661–666 (2012).
Harris, M., Richards, K. C. & Grando, V. T. The effects of slow-stroke back massage on minutes of nighttime sleep in persons with dementia and sleep disturbances in the nursing home: a pilot study. J. Holist. Nurs. 30 , 255–263 (2012).
Hart, S. et al. Anorexia nervosa symptoms are reduced by massage therapy. Eat. Disord. 9 , 289–299 (2001).
Hattan, J., King, L. & Griffiths, P. The impact of foot massage and guided relaxation following cardiac surgery: a randomized controlled trial. Issues Innov. Nurs. Pract. 37 , 199–207 (2002).
Haynes, A. C. et al. A calming hug: design and validation of a tactile aid to ease anxiety. PLoS ONE 17 , e0259838 (2022).
Henricson, M., Ersson, A., Määttä, S., Segesten, K. & Berglund, A.-L. The outcome of tactile touch on stress parameters in intensive care: a randomized controlled trial. Complement. Ther. Clin. Pract. 14 , 244–254 (2008).
Hernandez-Reif, M., Diego, M. & Field, T. Preterm infants show reduced stress behaviors and activity after 5 days of massage therapy. Infant Behav. Dev. 30 , 557–561 (2007).
Hernandez-Reif, M., Dieter, J. N. I., Field, T., Swerdlow, B. & Diego, M. Migraine headaches are reduced by massage therapy. Int. J. Neurosci. 96 , 1–11 (1998).
Hernandez-Reif, M. et al. Natural killer cells and lymphocytes increase in women with breast cancer following massage therapy. Int. J. Neurosci. 115 , 495–510 (2005).
Hernandez-Reif, M. et al. Children with cystic fibrosis benefit from massage therapy. J. Pediatr. Psychol. 24 , 175–181 (1999).
Hernandez-Reif, M., Field, T., Krasnegor, J. & Theakston, H. Lower back pain is reduced and range of motion increased after massage therapy. Int. J. Neurosci. 106 , 131–145 (2001).
Hernandez-Reif, M. et al. High blood pressure and associated symptoms were reduced by massage therapy. J. Bodyw. Mov. Ther. 4 , 31–38 (2000).
Hernandez-Reif, M. et al. Parkinson’s disease symptoms are differentially affected by massage therapy vs. progressive muscle relaxation: a pilot study. J. Bodyw. Mov. Ther. 6 , 177–182 (2002).
Hernandez-Reif, M., Field, T. & Theakston, H. Multiple sclerosis patients benefit from massage therapy. J. Bodyw. Mov. Ther. 2 , 168–174 (1998).
Hernandez-Reif, M. et al. Breast cancer patients have improved immune and neuroendocrine functions following massage therapy. J. Psychosom. Res. 57 , 45–52 (2004).
Hertenstein, M. J. & Campos, J. J. Emotion regulation via maternal touch. Infancy 2 , 549–566 (2001).
Hinchcliffe, J. K., Mendl, M. & Robinson, E. S. J. Rat 50 kHz calls reflect graded tickling-induced positive emotion. Curr. Biol. 30 , R1034–R1035 (2020).
Hodgson, N. A. & Andersen, S. The clinical efficacy of reflexology in nursing home residents with dementia. J. Altern. Complement. Med. 14 , 269–275 (2008).
Hoffmann, L. & Krämer, N. C. The persuasive power of robot touch. Behavioral and evaluative consequences of non-functional touch from a robot. PLoS ONE 16 , e0249554 (2021).
Holst, S., Lund, I., Petersson, M. & Uvnäs-Moberg, K. Massage-like stroking influences plasma levels of gastrointestinal hormones, including insulin, and increases weight gain in male rats. Auton. Neurosci. 120 , 73–79 (2005).
Hori, M. et al. Tickling during adolescence alters fear-related and cognitive behaviors in rats after prolonged isolation. Physiol. Behav. 131 , 62–67 (2014).
Hori, M. et al. Effects of repeated tickling on conditioned fear and hormonal responses in socially isolated rats. Neurosci. Lett. 536 , 85–89 (2013).
Hucklenbruch-Rother, E. et al. Delivery room skin-to-skin contact in preterm infants affects long-term expression of stress response genes. Psychoneuroendocrinology 122 , 104883 (2020).
Im, H. & Kim, E. Effect of yakson and gentle human touch versus usual care on urine stress hormones and behaviors in preterm infants: a quasi-experimental study. Int. J. Nurs. Stud. 46 , 450–458 (2009).
Jain, S., Kumar, P. & McMillan, D. D. Prior leg massage decreases pain responses to heel stick in preterm babies. J. Paediatr. Child Health 42 , 505–508 (2006).
Jane, S.-W. et al. Effects of massage on pain, mood status, relaxation, and sleep in Taiwanese patients with metastatic bone pain: a randomized clinical trial. Pain 152 , 2432–2442 (2011).
Johnston, C. C. et al. Kangaroo mother care diminishes pain from heel lance in very preterm neonates: a crossover trial. BMC Pediatr. 8 , 13 (2008).
Johnston, C. C. et al. Kangaroo care is effective in diminishing pain response in preterm neonates. Arch. Pediatr. Adolesc. Med. 157 , 1084–1088 (2003).
Jung, M. J., Shin, B.-C., Kim, Y.-S., Shin, Y.-I. & Lee, M. S. Is there any difference in the effects of QI therapy (external QIGONG) with and without touching? a pilot study. Int. J. Neurosci. 116 , 1055–1064 (2006).
Kapoor, Y. & Orr, R. Effect of therapeutic massage on pain in patients with dementia. Dementia 16 , 119–125 (2017).
Karagozoglu, S. & Kahve, E. Effects of back massage on chemotherapy-related fatigue and anxiety: supportive care and therapeutic touch in cancer nursing. Appl. Nurs. Res. 26 , 210–217 (2013).
Karbasi, S. A., Golestan, M., Fallah, R., Golshan, M. & Dehghan, Z. Effect of body massage on increase of low birth weight neonates growth parameters: a randomized clinical trial. Iran. J. Reprod. Med. 11 , 583–588 (2013).
Kashaninia, Z., Sajedi, F., Rahgozar, M. & Noghabi, F. A. The effect of kangaroo care on behavioral responses to pain of an intramuscular injection in neonates . J. Pediatr. Nurs. 3 , 275–280 (2008).
Kelling, C., Pitaro, D. & Rantala, J. Good vibes: The impact of haptic patterns on stress levels. In Proc. 20th International Academic Mindtrek Conference 130–136 (Association for Computing Machinery, 2016).
Khilnani, S., Field, T., Hernandez-Reif, M. & Schanberg, S. Massage therapy improves mood and behavior of students with attention-deficit/hyperactivity disorder. Adolescence 38 , 623–638 (2003).
Kianmehr, M. et al. The effect of massage on serum bilirubin levels in term neonates with hyperbilirubinemia undergoing phototherapy. Nautilus 128 , 36–41 (2014).
Kim, I.-H., Kim, T.-Y. & Ko, Y.-W. The effect of a scalp massage on stress hormone, blood pressure, and heart rate of healthy female. J. Phys. Ther. Sci. 28 , 2703–2707 (2016).
Kim, M. A., Kim, S.-J. & Cho, H. Effects of tactile stimulation by fathers on physiological responses and paternal attachment in infants in the NICU: a pilot study. J. Child Health Care 21 , 36–45 (2017).
Kim, M. S., Sook Cho, K., Woo, H.-M. & Kim, J. H. Effects of hand massage on anxiety in cataract surgery using local anesthesia. J. Cataract Refr. Surg. 27 , 884–890 (2001).
Koole, S. L., Tjew A Sin, M. & Schneider, I. K. Embodied terror management: interpersonal touch alleviates existential concerns among individuals with low self-esteem. Psychol. Sci. 25 , 30–37 (2014).
Krohn, M. et al. Depression, mood, stress, and Th1/Th2 immune balance in primary breast cancer patients undergoing classical massage therapy. Support. Care Cancer 19 , 1303–1311 (2011).
Kuhn, C. et al. Tactile-kinesthetic stimulation effects sympathetic and adrenocortical function in preterm infants. J. Pediatr. 119 , 434–440 (1991).
Kumar, J. et al. Effect of oil massage on growth in preterm neonates less than 1800 g: a randomized control trial. Indian J. Pediatr. 80 , 465–469 (2013).
Lee, H.-K. The effects of infant massage on weight, height, and mother–infant interaction. J. Korean Acad. Nurs. 36 , 1331–1339 (2006).
Leivadi, S. et al. Massage therapy and relaxation effects on university dance students. J. Dance Med. Sci. 3 , 108–112 (1999).
Lindgren, L. et al. Touch massage: a pilot study of a complex intervention. Nurs. Crit. Care 18 , 269–277 (2013).
Lindgren, L. et al. Physiological responses to touch massage in healthy volunteers. Auton. Neurosci. Basic Clin. 158 , 105–110 (2010).
Listing, M. et al. Massage therapy reduces physical discomfort and improves mood disturbances in women with breast cancer. Psycho-Oncol. 18 , 1290–1299 (2009).
Ludington-Hoe, S. M., Cranston Anderson, G., Swinth, J. Y., Thompson, C. & Hadeed, A. J. Randomized controlled trial of kangaroo care: cardiorespiratory and thermal effects on healthy preterm infants. Neonatal Netw. 23 , 39–48 (2004).
Lund, I. et al. Corticotropin releasing factor in urine—a possible biochemical marker of fibromyalgia. Neurosci. Lett. 403 , 166–171 (2006).
Ma, Y.-K. et al. Lack of social touch alters anxiety-like and social behaviors in male mice. Stress 25 , 134–144 (2022).
Massaro, A. N., Hammad, T. A., Jazzo, B. & Aly, H. Massage with kinesthetic stimulation improves weight gain in preterm infants. J. Perinatol. 29 , 352–357 (2009).
Mathai, S., Fernandez, A., Mondkar, J. & Kanbur, W. Effects of tactile-kinesthetic stimulation in preterms–a controlled trial. Indian Pediatr. 38 , 1091–1098 (2001).
CAS PubMed Google Scholar
Matsunaga, M. et al. Profiling of serum proteins influenced by warm partner contact in healthy couples. Neuroenocrinol. Lett. 30 , 227–236 (2009).
CAS Google Scholar
Mendes, E. W. & Procianoy, R. S. Massage therapy reduces hospital stay and occurrence of late-onset sepsis in very preterm neonates. J. Perinatol. 28 , 815–820 (2008).
Mirnia, K., Arshadi Bostanabad, M., Asadollahi, M. & Hamid Razzaghi, M. Paternal skin-to-skin care and its effect on cortisol levels of the infants. Iran. J. Pediatrics 27 , e8151 (2017).
Mitchell, A. J., Yates, C., Williams, K. & Hall, R. W. Effects of daily kangaroo care on cardiorespiratory parameters in preterm infants. J. Neonatal-Perinat. Med. 6 , 243–249 (2013).
Mitchinson, A. R. et al. Acute postoperative pain management using massage as an adjuvant therapy: a randomized trial. Arch. Surg. 142 , 1158–1167 (2007).
Modrcin-Talbott, M. A., Harrison, L. L., Groer, M. W. & Younger, M. S. The biobehavioral effects of gentle human touch on preterm infants. Nurs. Sci. Q. 16 , 60–67 (2003).
Mok, E. & Pang Woo, C. The effects of slow-stroke back massage on anxiety and shoulder pain in elderly stroke patients. Complement. Ther. Nurs. Midwifery 10 , 209–216 (2004).
Mokaberian, M., Noripour, S., Sheikh, M. & Mills, P. J. Examining the effectiveness of body massage on physical status of premature neonates and their mothers’ psychological status. Early Child Dev. Care 192 , 2311–2325 (2021).
Mori, H. et al. Effect of massage on blood flow and muscle fatigue following isometric lumbar exercise. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 10 , CR173–CR178 (2004).
Moyer-Mileur, L. J., Haley, S., Slater, H., Beachy, J. & Smith, S. L. Massage improves growth quality by decreasing body fat deposition in male preterm infants. J. Pediatr. 162 , 490–495 (2013).
Moyle, W. et al. Foot massage and physiological stress in people with dementia: a randomized controlled trial. J. Altern. Complement. Med. 20 , 305–311 (2014).
Muntsant, A., Shrivastava, K., Recasens, M. & Giménez-Llort, L. Severe perinatal hypoxic-ischemic brain injury induces long-term sensorimotor deficits, anxiety-like behaviors and cognitive impairment in a sex-, age- and task-selective manner in C57BL/6 mice but can be modulated by neonatal handling. Front. Behav. Neurosci. 13 , 7 (2019).
Negahban, H., Rezaie, S. & Goharpey, S. Massage therapy and exercise therapy in patients with multiple sclerosis: a randomized controlled pilot study. Clin. Rehabil. 27 , 1126–1136 (2013).
Nelson, D., Heitman, R. & Jennings, C. Effects of tactile stimulation on premature infant weight gain. J. Obstet. Gynecol. Neonatal Nurs. 15 , 262–267 (1986).
Griffin, J. W. Calculating statistical power for meta-analysis using metapower. Quant. Meth. Psychol . 17 , 24–39 (2021).
Nunes, G. S. et al. Massage therapy decreases pain and perceived fatigue after long-distance Ironman triathlon: a randomised trial. J. Physiother. 62 , 83–87 (2016).
Ohgi, S. et al. Comparison of kangaroo care and standard care: behavioral organization, development, and temperament in healthy, low-birth-weight infants through 1 year. J. Perinatol. 22 , 374–379 (2002).
O′Higgins, M., St. James Roberts, I. & Glover, V. Postnatal depression and mother and infant outcomes after infant massage. J. Affect. Disord. 109 , 189–192 (2008).
Okan, F., Ozdil, A., Bulbul, A., Yapici, Z. & Nuhoglu, A. Analgesic effects of skin-to-skin contact and breastfeeding in procedural pain in healthy term neonates. Ann. Trop. Paediatr. 30 , 119–128 (2010).
Oliveira, D. S., Hachul, H., Goto, V., Tufik, S. & Bittencourt, L. R. A. Effect of therapeutic massage on insomnia and climacteric symptoms in postmenopausal women. Climacteric 15 , 21–29 (2012).
Olsson, E., Ahlsén, G. & Eriksson, M. Skin-to-skin contact reduces near-infrared spectroscopy pain responses in premature infants during blood sampling. Acta Paediatr. 105 , 376–380 (2016).
Pauk, J., Kuhn, C. M., Field, T. M. & Schanberg, S. M. Positive effects of tactile versus kinesthetic or vestibular stimulation on neuroendocrine and ODC activity in maternally-deprived rat pups. Life Sci. 39 , 2081–2087 (1986).
Pinazo, D., Arahuete, L. & Correas, N. Hugging as a buffer against distal fear of death. Calid. Vida Salud 13 , 11–20 (2020).
Pope, M. H. et al. A prospective randomized three-week trial of spinal manipulation, transcutaneous muscle stimulation, massage and corset in the treatment of subacute low back pain. Spine 19 , 2571–2577 (1994).
Preyde, M. Effectiveness of massage therapy for subacute low-back pain: a randomized controlled trial. Can. Med. Assoc. J. 162 , 1815–1820 (2000).
Ramanathan, K., Paul, V. K., Deorari, A. K., Taneja, U. & George, G. Kangaroo mother care in very low birth weight infants. Indian J. Pediatr. 68 , 1019–1023 (2001).
Reddan, M. C., Young, H., Falkner, J., López-Solà, M. & Wager, T. D. Touch and social support influence interpersonal synchrony and pain. Soc. Cogn. Affect. Neurosci. 15 , 1064–1075 (2020).
Rodríguez-Mansilla, J. et al. The effects of ear acupressure, massage therapy and no therapy on symptoms of dementia: a randomized controlled trial. Clin. Rehabil. 29 , 683–693 (2015).
Rose, S. A., Schmidt, K., Riese, M. L. & Bridger, W. H. Effects of prematurity and early intervention on responsivity to tactual stimuli: a comparison of preterm and full-term infants. Child Dev. 51 , 416–425 (1980).
Scafidi, F. A. et al. Massage stimulates growth in preterm infants: a replication. Infant Behav. Dev. 13 , 167–188 (1990).
Scafidi, F. A. et al. Effects of tactile/kinesthetic stimulation on the clinical course and sleep/wake behavior of preterm neonates. Infant Behav. Dev. 9 , 91–105 (1986).
Scafidi, F. & Field, T. Massage therapy improves behavior in neonates born to HIV-positive mothers. J. Pediatr. Psychol. 21 , 889–897 (1996).
Scarr-Salapatek, S. & Williams, M. L. A stimulation program for low birth weight infants. Am. J. Public Health 62 , 662–667 (1972).
Serrano, B., Baños, R. M. & Botella, C. Virtual reality and stimulation of touch and smell for inducing relaxation: a randomized controlled trial. Comput. Hum. Behav. 55 , 1–8 (2016).
Seyyedrasooli, A., Valizadeh, L., Hosseini, M. B., Asgari Jafarabadi, M. & Mohammadzad, M. Effect of vimala massage on physiological jaundice in infants: a randomized controlled trial. J. Caring Sci. 3 , 165–173 (2014).
Sharpe, P. A., Williams, H. G., Granner, M. L. & Hussey, J. R. A randomised study of the effects of massage therapy compared to guided relaxation on well-being and stress perception among older adults. Complement. Therap. Med. 15 , 157–163 (2007).
Sherman, K. J., Cherkin, D. C., Hawkes, R. J., Miglioretti, D. L. & Deyo, R. A. Randomized trial of therapeutic massage for chronic neck pain. Clin. J. Pain. 25 , 233–238 (2009).
Shiloh, S., Sorek, G. & Terkel, J. Reduction of state-anxiety by petting animals in a controlled laboratory experiment. Anxiety, Stress Coping 16 , 387–395 (2003).
Shor-Posner, G. et al. Impact of a massage therapy clinical trial on immune status in young Dominican children infected with HIV-1. J. Altern. Complement. Med. 12 , 511–516 (2006).
Simpson, E. A. et al. Social touch alters newborn monkey behavior. Infant Behav. Dev. 57 , 101368 (2019).
Smith, S. L., Haley, S., Slater, H. & Moyer-Mileur, L. J. Heart rate variability during caregiving and sleep after massage therapy in preterm infants. Early Hum. Dev. 89 , 525–529 (2013).
Smith, S. L. et al. The effect of massage on heart rate variability in preterm infants. J. Perinatol. 33 , 59–64 (2013).
Solkoff, N. & Matuszak, D. Tactile stimulation and behavioral development among low-birthweight infants. Child Psychiatry Hum. Dev. 6 , 3337 (1975).
Srivastava, S., Gupta, A., Bhatnagar, A. & Dutta, S. Effect of very early skin to skin contact on success at breastfeeding and preventing early hypothermia in neonates. Indian J. Public Health 58 , 22–26 (2014).
Stringer, J., Swindell, R. & Dennis, M. Massage in patients undergoing intensive chemotherapy reduces serum cortisol and prolactin: massage in oncology patients reduces serum cortisol. Psycho-Oncol. 17 , 1024–1031 (2008).
Suman Rao, P. N., Udani, R. & Nanavati, R. Kangaroo mother care for low birth weight infants: a randomized controlled trial. Indian Pediatr. 45 , 17–23 (2008).
Sumioka, H. et al. A huggable device can reduce the stress of calling an unfamiliar person on the phone for individuals with ASD. PLoS ONE 16 , e0254675 (2021).
Sumioka, H., Nakae, A., Kanai, R. & Ishiguro, H. Huggable communication medium decreases cortisol levels. Sci. Rep. 3 , 3034 (2013).
Suzuki, M. et al. Physical and psychological effects of 6-week tactile massage on elderly patients with severe dementia. Am. J. Alzheimer’s Dis. Other Dement. 25 , 680–686 (2010).
Thomson, L. J. M., Ander, E. E., Menon, U., Lanceley, A. & Chatterjee, H. J. Quantitative evidence for wellbeing benefits from a heritage-in-health intervention with hospital patients. Int. J. Art. Ther. 17 , 63–79 (2012).
Triplett, J. L. & Arneson, S. W. The use of verbal and tactile comfort to alleviate distress in young hospitalized children. Res. Nurs. Health 2 , 17–23 (1979).
Walach, H., Güthlin, C. & König, M. Efficacy of massage therapy in chronic pain: a pragmatic randomized trial. J. Altern. Complement. Med. 9 , 837–846 (2003).
Walker, S. C. et al. C‐low threshold mechanoafferent targeted dynamic touch modulates stress resilience in rats exposed to chronic mild stress. Eur. J. Neurosci. 55 , 2925–2938 (2022).
Weinrich, S. P. & Weinrich, M. C. The effect of massage on pain in cancer patients. Appl. Nurs. Res. 3 , 140–145 (1990).
Wheeden, A. et al. Massage effects on cocaine-exposed preterm neonates. Dev. Behav. Pediatr. 14 , 318–322 (1993).
White, J. L. & Labarba, R. C. The effects of tactile and kinesthetic stimulation on neonatal development in the premature infant. Dev. Psychobiol. 9 , 569–577 (1976).
Wilkie, D. J. et al. Effects of massage on pain intensity, analgesics and quality of life in patients with cancer pain: a pilot study of a randomized clinical trial conducted within hospice care delivery. Hosp. J. 15 , 31–53 (2000).
Willemse, C. J. A. M., Toet, A. & van Erp, J. B. F. Affective and behavioral responses to robot-initiated social touch: toward understanding the opportunities and limitations of physical contact in human–robot interaction. Front. ICT 4 , 12 (2017).
Willemse, C. J. A. M. & van Erp, J. B. F. Social touch in human–robot interaction: robot-initiated touches can induce positive responses without extensive prior bonding. Int. J. Soc. Robot. 11 , 285–304 (2019).
Woods, D. L., Beck, C. & Sinha, K. The effect of therapeutic touch on behavioral symptoms and cortisol in persons with dementia. Res. Complement. Med. 16 , 181–189 (2009).
Yamaguchi, M., Sekine, T. & Shetty, V. A salivary cytokine panel discriminates moods states following a touch massage intervention. Int. J. Affect. Eng. 19 , 189–198 (2020).
Yamazaki, R. et al. Intimacy in phone conversations: anxiety reduction for Danish seniors with hugvie. Front. Psychol. 7 , 537 (2016).
Yang, M.-H. et al. Comparison of the efficacy of aroma-acupressure and aromatherapy for the treatment of dementia-associated agitation. BMC Complement. Altern. Med. 15 , 93 (2015).
Yates, C. C. et al. The effects of massage therapy to induce sleep in infants born preterm. Pediatr. Phys. Ther. 26 , 405–410 (2014).
Yu, H. et al. Social touch-like tactile stimulation activates a tachykinin 1-oxytocin pathway to promote social interactions. Neuron 110 , 1051–1067 (2022).
Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t -tests and ANOVAs. Front. Psychol. 4 , 863 (2013).
Page, M. J., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst. Rev. https://doi.org/10.1186/s13643-021-01626-4 (2021).
Wilson, D. B. Practical meta-analysis effect size calculator (Version 2023.11.27). https://campbellcollaboration.org/research-resources/effect-size-calculator.html (2023).
Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw https://doi.org/10.18637/jss.v036.i03 (2010).
Scammacca, N., Roberts, G. & Stuebing, K. K. Meta-analysis with complex research designs: dealing with dependence from multiple measures and multiple group comparisons. Rev. Educ. Res. 84 , 328–364 (2014).
Pustejovsky, J. E. & Tipton, E. Meta-analysis with robust variance estimation: expanding the range of working models. Prev. Sci. Off. J. Soc. Prev. Res. 23 , 425–438 (2022).
Cook, R. D. in International Encyclopedia of Statistical Science (ed. M. Lovric) S. 301–302 (Springer, 2011).
Higgins, J. P. T., Thompson, S. & Deeks, J. Measuring inconsistency in meta-analyses. BMJ https://doi.org/10.1136/bmj.327.7414.557 (2003).
Oberauer, K. The importance of random slopes in mixed models for Bayesian hypothesis testing. Psychol. Sci. 33 , 648–665 (2022).
Nakagawa, S. et al. The orchard plot: cultivating a forest plot for use in ecology, evolution, and beyond. Res. Synth. Methods 12 , 4–12 (2021).
Download references
Acknowledgements
We thank A. Frick and E. Chris for supporting the initial literature search and coding. We also thank A. Dreisoerner, T. Field, S. Koole, C. Kuhn, M. Henricson, L. Frey Law, J. Fraser, M. Cumella Reddan, and J. Stringer, who kindly responded to our data requests and provided additional information or data with respect to single studies. J.P. was supported by the German National Academy of Sciences Leopoldina (LPDS 2021-05). H.H. was supported by the Marietta-Blau scholarship of the Austrian Agency for Education and Internationalisation (OeAD) and the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation, project ID 422744262 – TRR 289). C.K. received funding from OCENW.XL21.XL21.069 and V.G. from the European Research Council (ERC) under European Union’s Horizon 2020 research and innovation programme, grant ‘HelpUS’ (758703) and from the Dutch Research Council (NWO) grant OCENW.XL21.XL21.069. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Open access funding provided by Ruhr-Universität Bochum.
Author information
Julian Packheiser
Present address: Social Neuroscience, Faculty of Medicine, Ruhr University Bochum, Bochum, Germany
These authors contributed equally: Julian Packheiser, Helena Hartmann.
Authors and Affiliations
Social Brain Lab, Netherlands Institute for Neuroscience, Royal Netherlands Academy of Art and Sciences, Amsterdam, the Netherlands
Julian Packheiser, Helena Hartmann, Kelly Fredriksen, Valeria Gazzola, Christian Keysers & Frédéric Michon
Center for Translational and Behavioral Neuroscience, University Hospital Essen, Essen, Germany
Helena Hartmann
Clinical Neurosciences, Department for Neurology, University Hospital Essen, Essen, Germany
You can also search for this author in PubMed Google Scholar
Contributions
J.P. contributed to conceptualization, methodology, formal analysis, investigation, data curation, writing the original draft, review and editing, visualization, supervision and project administration. HH contributed to conceptualization, methodology, formal analysis, investigation, data curation, writing the original draft, review and editing, visualization, supervision and project administration. K.F. contributed to investigation, data curation, and review and editing. C.K. and V.G. contributed to conceptualization, and review and editing. F.M. contributed to conceptualization, methodology, formal analysis, investigation, writing the original draft, and review and editing.
Corresponding author
Correspondence to Julian Packheiser .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Human Behaviour thanks Ville Harjunen, Rebecca Boehme and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information.
Supplementary Figs. 1–21 and Tables 1–4.
Reporting Summary
Peer review file, supplementary table 1.
List of studies included in and excluded from the meta-analyses/review.
Supplementary Table 2
PRISMA checklist, manuscript.
Supplementary Table 3
PRISMA checklist, abstract.
Source Data Fig. 2
Effect size/error (columns ‘Hedges_g’ and ‘variance’) information for each study/cohort/effect included in the analysis. Source Data Fig. 3 Effect size/error (columns ‘Hedges_g’ and ‘variance’) together with moderator data (column ‘Outcome’) for each study/cohort/effect included in the analysis. Source Data Fig. 4 Effect size/error (columns ‘Hedges_g’ and ‘variance’) together with moderator data (columns ‘dyad_type’ and ‘skin_to_skin’) for each study/cohort/effect included in the analysis. Source Data Fig. 5 Effect size/error (columns ‘Hedges_g’ and ‘variance’) together with moderator data (column ‘touch_type’) for each study/cohort/effect included in the analysis. Source Data Fig. 6 Effect size/error (columns ‘Hedges_g’ and ‘variance’) together with moderator data (column ‘clin_sample’) for each study/cohort/effect included in the analysis. Source Data Fig. 7 Effect size/error (columns ‘Hedges_g’ and ‘variance’) together with moderator data (column ‘familiarity’) for each study/cohort/effect included in the analysis. Source Data Fig. 7 Effect size/error (columns ‘Hedges_g’ and ‘variance’) together with moderator data (columns ‘touch_duration’ and ‘sessions’) for each study/cohort/effect included in the analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Packheiser, J., Hartmann, H., Fredriksen, K. et al. A systematic review and multivariate meta-analysis of the physical and mental health benefits of touch interventions. Nat Hum Behav (2024). https://doi.org/10.1038/s41562-024-01841-8
Download citation
Received : 16 August 2023
Accepted : 29 January 2024
Published : 08 April 2024
DOI : https://doi.org/10.1038/s41562-024-01841-8

Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Massage therapy for the treatment of attention deficit/hyperactivity disorder (ADHD) in children and adolescents: A systematic review and meta-analysis
Affiliations.
- 1 School of Nursing, The Hong Kong Polytechnic University, Hong Kong SAR, China.
- 2 Pediatric Tuina Health Care Clinic, Shandong University of Traditional Chinese Medicine Affiliated Hospital, China.
- 3 Department of Psychology, The Chinese University of Hong Kong, China.
- 4 School of Chinese Medicine, Hong Kong Baptist University, China.
- 5 School of Nursing, The Hong Kong Polytechnic University, Hong Kong SAR, China. Electronic address: [email protected].
- PMID: 30670272
- DOI: 10.1016/j.ctim.2018.12.011
Objective: To summarize the current evidence on the effects and safety of massage therapy for the treatment of ADHD in children and adolescents.
Method: A systematic review of 8 randomized controlled trials (RCTs) and 3 case series studies was conducted with a meta-analysis of 4 of the RCTs.
Results: Pooled analysis showed that massage produced more improvement in ADHD symptoms in terms of effective rate compared to Ritalin (risk ratio: 1.39, 95%CI: 1.16 - 1.66; P = 0.0004). Individual RCTs suggested that massage was differed significantly from waitlist control in improving the conditions of anxious-passive (mean difference: -11.7; 95%CI [-17.84, -5.56]; P = 0.0002), and asocial behavior (mean difference = - 8.60; 95%CI [-15.87, -1.33]; P = 0.02).
Conclusion: Evidence suggests that massage therapy is beneficial for treating ADHD in children and adolescents.
Keywords: ADHD; Massage; Meta-analysis; Systematic review.
Copyright © 2018 Elsevier Ltd. All rights reserved.
Publication types
- Meta-Analysis
- Systematic Review
- Adolescent Behavior
- Attention Deficit Disorder with Hyperactivity / complications
- Attention Deficit Disorder with Hyperactivity / therapy*
- Child Behavior
- Child, Preschool
- Methylphenidate
- Waiting Lists
Research Literacy: Massage & Sleep
Does massage therapy improve sleep in infants and their mothers?
By Martha Brown Menard, Ph.D., LMT, February 1, 2020

The Study Question
Sleep issues are common among infants and toddlers, and are estimated to occur in 20 to 30 percent of children under 3 years of age. When children experience poor sleep, mothers are also affected. While implementing a bedtime routine is often recommended, there is little research on its efficacy separate from other treatments, or on which components of a bedtime routine help to improve infant sleep. Previous research has shown that massage can have a positive effect on sleep for preterm infants, infants and young children. This study examined the impact of a massage-based bedtime routine on infant sleep, maternal sleep and maternal mood.
The Study Methods
Participants were recruited through an independent clinical research organization and offered a financial incentive for completing the study. Inclusion criteria were that children had an identified sleep problem as noted by the mother, with all mothers endorsing that their child had a sleep problem that ranged from “small” to “severe.” Families were excluded if the child was reported to wake more than three times a night, stayed awake more than 60 minutes per night and had a total daily sleep duration of less than nine hours. Additional exclusion criteria were non-English speaking, current acute or chronic illness, and if the child was routinely bathed or had lotion applied in the hour before bedtime four or more times per week.
There were 123 families recruited and randomly assigned to continue their child’s usual bedtime practices during the study period (the control condition) or to implement a new nightly two-step bedtime routine: following a one-week baseline period during which mothers followed their child’s usual bedtime practices, for the next two weeks mothers included a massage (using a provided massage product in a blinded container and instructional materials including possible massage techniques), and quiet activities such as cuddling and singing a lullaby.
Instructions were given for massaging the baby’s chest, arms and hands, stomach, back, and legs and feet. Mothers continued to put their child to bed as they normally did, whether they put their child to bed awake or stayed with their child until asleep, and had lights out within 30 minutes of completing the massage, so that the only change was the new bedtime routine.
The massage intervention included 64 families, and 59 families participated in the control condition. Mothers were aged 18–45 years, with a mean age of 30.6 years; infants were aged 3–18 months with a mean age of 8.96 months, and 46 percent were male.
Outcomes measures included the Brief Infant Sleep Questionnaire (BISQ), completed on a weekly basis, and the Pittsburgh Sleep Quality Index (PSQ J), Epworth Sleepiness Scale, Edinburgh Postnatal Depression Scale, Brief Mood Introspection Scale, Parenting Stress Index and State-Trait Anxiety Inventory, completed at baseline and at the end of the study. All questionnaires were completed online.
Independent samples t-tests and chi-square tests were conducted to determine any pre-existing demographic or sleep differences between the control group and the intervention group; none were found. No differences were found across demographic variables, or baseline maternal or child sleep variables between the two groups.
The Results
Analyses showed a significant reduction in the number of nighttime wakings for children and mothers in the intervention group, but not for those in the control group. Overall, mothers perceived improvements in their child’s sleep for all variables measured for the intervention group, with no changes reported in the control group. Mothers reported improvements in bedtime difficulty, how well their child slept, child morning mood and their confidence in managing child sleep issues.
Mothers in the intervention group reported improved sleep quality as measured by the PSQI. There was also a decreased perception by mothers of sleep as a problem. The percent of mothers who reported their child had a sleep problem decreased from 78.1 percent at baseline to 60.9 percent after the first week of intervention, and to 46.9 percent at the end of the two-week intervention period. No significant differences were found for those in the control group. Mothers in the intervention group were also more likely to report feeling “somewhat” or “very confident” in managing their child’s sleep compared to the control group, and were highly likely to continue to use the prescribed routine.
There were no changes for the majority of mood and behavior scales for the mothers. No differences were found for depressive symptomatology (EPDS), daytime sleepiness (ESS), parenting stress (PSI) or state anxiety (STAI).
Limitations of the Study
This study has several limitations. The massage instructions are not described. Many of the outcomes are selfreported, and there were no objective measures of infant and toddler sleep, such as actigraphy.
Results may have been due to participant expectations that sleep would improve, although not all self-reported outcomes showed improvement. While participants reported being satisfied with the bedtime intervention and likely to continue it, there was no longer term follow-up of reported massage effects or whether participants actually did continue the intervention.
Implications for Evidence-Informed Practice
In this study, massage therapy as part of a consistent bedtime routine appears to offer benefits to both infants and mothers related to improved sleep quality. Practitioners who have clients with young children and who report sleep difficulties may want to offer to teach the parents how to give a simple massage to their child as part of a bedtime routine.
Related Resources
Continuing education massage therapy research ce.
Research literacy helps you market your massage practice to clients and health care professionals.
Massage Therapy Journal Is Massage Nature's Sleep Aid?
For millions of restless Americans, massage therapy could be the secret to a better night's sleep.
Advertisement
Evaluation of Serum Reaction to Low-Intensity Laser Exposure by Its Solid Phase Structure
- Published: 25 October 2016
- Volume 161 , pages 841–844, ( 2016 )
Cite this article
- V. V. Shabalin 1 &
- S. N. Shatokhina 2
35 Accesses
2 Citations
Explore all metrics
The effects of various modes of low-intensity laser exposure on the sera of healthy subjects and patients are studied. It is shown by the cuneiform dehydration method that the serum structure is liable to change in response to certain modes of low-intensity laser exposure. The structure of patients’ sera is more sensitive to low-intensity laser exposure.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Delayed effects of neutron radiation on human serum.
Anna Michnik, Kinga Polaczek-Grelik, … Zofia Drzazga
Infrared Spectroscopy of Blood Serum from Patients with Oncohematological Diseases
E. A. Telnaya, L. V. Plotnikova, … A. M. Polyanichko

The influence of sugar molecule type on the stability of lyophilized human serum albumin (HSA) nanocolloid kit
Ratna Dini Haryuni, Wening Lestari, … Triningsih
Devyatkov ND, Golant MB, Betskii OV. Millimeter Waves and Their Role in Life Processes. Moscow, 1991. Russian.
Zaguskin SL. A hypothesis of possible physical nature of signals of intracellular and intercellular synchronization of protein synthesis rhythms. Biol. Bull. 2004;31(4):319-323.
Article CAS Google Scholar
Illarionov VE. Bases of Laser Therapy. Moscow, 1992. Russian.
Kudryashov YuB, Perov YuF, Rubin AB. Radiation Biophysics: RF and Microwave Electromagnetic Radiation. Moscow, 2008. Russian.
Sakhenko KI, Seteikin AYu. Research on the effects of laser radiation on ionic composition of biological fluid. in: Physics: Basic and Applied Research, and Education. Blagoveshchensk, 2012. pp. 150-154. Russian.
Seteikin AYu, Mitrofanova VI, Malinovskaya OV. Spectroscopic analysis of changes in the physical properties of blood serum samples exposed to low-intensity laser irradiation .Vestn. Amur. Gos. Univer. Ser. Estesv. Ekonom. Nauki. 2007; (37):31-33. Russian.
Shabalin VN, Shatokhina SN. Autogenous rhythms and self-organization of biological fluids. Bull. Exp. Biol. Med. 1996;122(4):967-973.
Article Google Scholar
Download references
Author information
Authors and affiliations.
St. Petersburg Institute of the Ear, Nose, and Throat, Ministry of Health of the Russian Federation, St. Petersburg, Russia
V. V. Shabalin
M. F. Vladimirsky Moscow Regional Research Clinical Institute, Moscow, Russia
S. N. Shatokhina
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to S. N. Shatokhina .
Additional information
Translated from Byulleten’ Eksperimental’noi Biologii i Meditsiny , Vol. 161, No. 6, pp. 803-806, June, 2016
Rights and permissions
Reprints and permissions
About this article
Shabalin, V.V., Shatokhina, S.N. Evaluation of Serum Reaction to Low-Intensity Laser Exposure by Its Solid Phase Structure. Bull Exp Biol Med 161 , 841–844 (2016). https://doi.org/10.1007/s10517-016-3525-9
Download citation
Received : 12 March 2015
Published : 25 October 2016
Issue Date : October 2016
DOI : https://doi.org/10.1007/s10517-016-3525-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- low-intensity laser exposure
- cuneiform dehydration
- Find a journal
- Publish with us
- Track your research
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- Winter 2024 | VOL. 22, NO. 1 Reproductive Psychiatry: Postpartum Depression is Only the Tip of the Iceberg CURRENT ISSUE pp.1-142
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Massage Therapy for Psychiatric Disorders
- Mark Hyman Rapaport , M.D. ,
- Pamela J. Schettler , Ph.D. ,
- Erika R. Larson , M.S., L.M.T. ,
- Dedric Carroll , L.M.T. ,
- Margaret Sharenko , L.M.T., C.P.T. ,
- James Nettles , Ph.D., L.M.T. ,
- Becky Kinkead , Ph.D.
Search for more papers by this author
This article reviews the current state of knowledge of the role of massage therapy in the treatment of common psychiatric disorders and symptoms. It briefly discusses the prevalence of psychiatric disorders and the popularity of complementary and integrative treatments in the general population. The authors touch on the growing literature describing the biology and neurobiology of massage therapy. The impact of massage as both a therapy for major psychiatric disorders and a treatment for psychiatric symptoms is reviewed, and how massage therapists conceptualize and treat their patients with psychiatric complaints is discussed. If psychiatrists are going to partner with massage therapists, they need to understand how massage therapists’ perspectives differ from those of traditional practitioners of allopathic medicine. A model of how psychiatrists and other mental health professionals can work with massage therapists to care for patients is proposed, followed by a summary of the article’s key points.
Of the top 25 disorders associated with years lost because of disability, seven are major psychiatric disorders ( 1 ). Major depression is the second leading cause of years living with disability in the world, anxiety disorders are the ninth leading cause, and schizophrenia is the 11th leading cause. Thus, major psychiatric syndromes are clearly associated with a major cost to society. Major psychiatric syndromes are also remarkably prevalent. One in four individuals will have a major psychiatric syndrome at some point in their lifetime ( 2 ). This means that everyone knows someone with a major psychiatric disorder, and every family is touched by the presence of these diseases. Despite significant advances toward both understanding the neuroscience of and developing new psychotherapies and pharmacotherapies to treat these disorders, a great unmet treatment need still exists. Using major depressive disorder as an example, we know from the National Institute of Mental Health–funded Sequenced Treatment Alternatives to Relieve Depression study that only one-third of individuals go into remission with initial treatment for depression ( 3 ). Furthermore, although close to two-thirds may enter remission with multiple successive treatments, the majority of these individuals will relapse within one year of reaching remission status ( 3 ). Thus, there is clearly a need for additional options to treat people with depression. It is reasonable to extrapolate from depression to other psychiatric disorders for which there are even fewer available treatment options. We contend that approaches to identifying potential treatment interventions for patients need to be broadened.
Systematic investigation into the popularity of complementary and alternative medicine (CAM) for treatment in the United States began in 1990 with the survey spearheaded by Eisenberg and colleagues ( 4 ). In this initial report in the New England Journal of Medicine, they documented that 33.8% of the adults surveyed had used some type of alternative or complementary medical service in the past 12 months. These findings were a revelation to most individuals in traditional Western or allopathic medical communities. Eisenberg and colleagues followed this report with a paper that compared and contrasted their 1990 data with those from a survey conducted in 1997 ( 5 ). This later publication documented an increase in the use of alternative therapies from 33.8% to 42.0%, with herbal medicine, massage, megavitamins, self-help groups, folk remedies, homeopathy, and energy healing increasing the most. They reported that some of the most frequent reasons for using complementary and alternative therapies included back pain, anxiety, depression, and headaches. In the 1997 paper, they estimated that the cost for services provided was $21.2 billion, with at least $12.2 billion being paid out of pocket. These initial findings by Eisenberg and colleagues were updated in the 2002 and 2007 Centers for Disease Control and Prevention–sponsored CAM surveys. In both of these surveys ( 6 , 7 ), approximately 40% of adults reported having used some type of complementary and alternative therapy in the past 12 months. Also, both of these surveys indicated that approximately 5% of the U.S. adult population had used massage therapy. Purohit and colleagues ( 8 ) performed a reanalysis of the 2007 National Health Interview data of 23,393 adults that focused on the presence of neuropsychiatric symptoms and their impact on CAM usage. The prevalence of the use of CAM therapies was 43.78% for individuals with self-reported symptoms of depression, insomnia, headaches, memory deficits, attention deficits, and sleep problems versus 29.7% for individuals who did not report any of these symptoms. Of those individuals with at least one neuropsychiatric symptom who used CAM therapies, 20% used CAM therapy because they felt that standard treatments were either too expensive or ineffective, and 25% used CAM therapies because they were recommended by their traditional medical provider.
In conclusion, there is an interface between psychiatric disorders and complementary and alternative therapies such as massage. Accordingly, validated alternative therapies are now being integrated within the medical mainstream under the rubric “complementary and integrative medicine” (CIM). Consistent with this, and reflecting an emphasis on well-being and treatment of disease, the National Institutes of Health have renamed the center addressing CAM therapies the National Center for Complementary and Integrative Health. Psychiatric disorders are common and disabling, and current treatment methods, although helpful for many, are not the treatment of choice for many patients and are insufficient to alleviate disability and suffering for many others. This suggests that allopathic practitioners should think about two questions: What is the body of evidence supporting CIM interventions, and what is the best way for a psychiatrist or other mental health service provider and a CIM practitioner to interact with each other in the care of a patient? We address these two important issues.
Biology of Massage
Rigorous study of the biology of therapeutic massage is still in a relatively nascent phase. Although studies have attempted to understand the impact of various forms of massage on the body since the early 1990s, the research has been fraught with problems, in particular a lack of consistent funding for investigation of the biological effects of massage. Another challenge faced by the field is that there are many different types of massage and great variation in research study designs. As a result, current knowledge of the biology of massage rests mainly on a number of small studies investigating very different interventions that have been done for different lengths of time and at different frequencies. Despite these limitations, certain biological patterns seem to have emerged from recent studies.
Human Studies of the Neurobiology of Massage
A few EEG and imaging studies have investigated the impact of massage on brain circuitry or brain regions. One of the first studies was performed by the Touch Institute. In this study, 26 adults were given chair massage for 15 minutes twice weekly for five weeks, and 24 adults were asked to sit quietly in the massage chair twice weekly for five weeks ( 9 ). Field and colleagues found that twice-weekly massage was associated with an increase in frontal delta power in the EEG and a decrease in frontal alpha and beta power. This pattern is consistent with increased relaxation yet enhanced alertness, which was supported by the massage group’s having increased speed and accuracy on mathematical computations and decreased levels of anxiety. Salivary cortisol levels were also lower in the massage condition but not in the control condition. In a study of an aromatherapy massage intervention versus no treatment, Wu and colleagues ( 10 ) were able to replicate an increase in alpha wave activity in their aromatherapy massage sample, but they found a reduction in delta wave activity. However, they reported decreases in state anxiety and depression and an increase in psychological well-being as well as a reduction in salivary cortisol levels and an increase in plasma brain-derived neurotrophic factor in the aromatherapy group.
Neuroimaging studies investigating the impact of massage on the brain have been limited. In a small positron emission tomography study in 2006, Ouchi and colleagues ( 11 ) reported that being placed in the scanner in a prone position versus a supine position caused increased activation in the precuneus. This activation was further enhanced by both four minutes and 20 minutes of palm pressure massage applied to participants’ backs. The 20 minutes of massage also caused a greater increase in parasympathetic tone as well as activation of the parieto-occipital region. Ouchi and colleagues also reported activation in the cerebellum associated with massage. The authors concluded that this pattern of activation of the precuneus with back massage might reflect augmentation of arousal in consciousness functions associated with positive affect and that their findings of increased activity in the forebrain-amygdala system might be responsible for an increase in parasympathetic tone in the brain. The latter would also be consistent with a cerebellar increase in blood flow, which again would help regulate parasympathetic tone. These findings were partially replicated and extended by Sliz and colleagues ( 12 ), who looked at the neurocorrelates of a single session of massage versus those of a resting control condition, reflexology and massage with an object. They found that Swedish massage of the right foot while the participant performed a cognitive task in the scanner was associated with increased activation of the subgenual anterior and retrosplenial-posterior cingulate cortices. This increased activation of the retrosplenial-posterior cingulate cortex was sustained even without activation by the task.
If one integrates these findings investigating the impact of massage with those of a series of elegant studies that have been performed to attempt to understand the basic neurobiology of touch, one can come up with unifying theory of the impact of massage on the brain. An MRI study by Golaszewski and colleagues ( 13 ) demonstrated that vibrating tactile stimulation of the plantar surface of the foot increased activity in the inferior and posterior cingulate gyri along with the somatosensory cortex, insula, thalamus, caudate, and cerebellum. These brain regions integrate tactile and sensory information from mechanoreceptors, the myelinated A-beta and A-alpha afferents, and the unmyelinated sensory nerve fibers called c-tactile afferents that are thought to be associated with positive affect. The c-tactile afferents are stimulated by gentle stroking of hairy skin surfaces. They project to the limbic cortex, including the orbital frontal cortex and posterior insulate bilaterally.
In summary, although the data on the impact of massage on EEG and neuroimaging changes in the brain are limited, when these data are combined with the emerging data on somatic sensory pleasure circuitry, it is reasonable to postulate that massage’s beneficial effects on affiliation and feelings of well-being may be due to stimulation of specific brain circuits involved in pleasure and reward ( 14 ).
Impact of Massage on the Hypothalamic-Pituitary-Adrenal Axis and Neurohormones
A myriad of small studies of massage have measured either salivary or plasma cortisol levels. Many of these studies investigated only single time-point measures of cortisol before and after a series of massage interventions. The consensus of existing meta-analyses as well as of this review is that massage tends to decrease measures of plasma and salivary cortisol versus either a wait-list or a no-treatment condition ( 15 ). However, in general these studies have not looked at the sustained impact of massage after cessation of treatment. Rapaport and colleagues ( 16 ) have compared and contrasted the impact of a single 45-minute session of manualized Swedish massage with that of a manualized light-touch control condition in adults with no psychiatric disorder. They sampled cortisol, oxytocin, vasopressin, and adrenocorticotropic hormone after a 30-minute accommodation period at two points before initiation of massage or touch and then at several time points during the hour after the intervention. These authors found that a single session of either massage or touch was associated with a small effect-size decrease in cortisol levels in healthy young participants as well as a large effect-size increase in oxytocin in both groups. However, compared with changes found in cortisol and oxytocin, the massage group showed a profound significant decrease in vasopressin compared with the touch control group.
In a subsequent study, Rapaport and colleagues investigated the impact of weekly massage versus weekly touch for five weeks, as well as the impact of twice-weekly massage or twice-weekly touch for five weeks ( 17 ). Weekly massage versus weekly touch was associated with a pattern of results similar to that observed with a single session of massage. However, twice-weekly massage caused a significantly greater cumulative increase in oxytocin and decrease in vasopressin than twice-weekly touch. Although these data are of interest and consistent with previous studies reporting a decrease in cortisol levels and an increase in sense of affiliation associated with massage, these small studies require replication with larger cohorts of participants.
In summary, data suggest that massage may be associated with a decrease in hypothalamic-pituitary-adrenal activation and possibly with an increase in oxytocin levels. However, larger rigorous studies are needed.
Impact of Massage on the Immune System
A great deal of the pioneering work investigating the relationship between massage and the immune system occurred at the University of Miami. This group investigated the impact of massage on immune function in a variety of different patient populations including depressed individuals, HIV-positive young women, and HIV-positive adolescents ( 18 – 20 ). In general, this group reported an increase in natural killer (NK) cells and an increase in NK cell activity associated with massage compared with control conditions such as muscle relaxation. Rapaport and colleagues reported that a single session of Swedish massage versus a touch control condition caused a leukocytosis with a moderate effect-size increase in CD56+ NK cells and an increase in activated T cells ( 16 ). They have also reported that massage was associated with a significant decrease in Type 2 T helper (TH2) mitogen-stimulated cytokines compared with both baseline levels and the touch control condition ( 16 ). Massage was also associated with a decrease in mitogen-stimulated proinflammatory cytokine production when contrasted with the touch control condition. In 2012, Rapaport and colleagues reported that these effects were sustained for at least one week and that they were specific to individuals who received one massage per week in contrast to the groups receiving two massages per week ( 17 ). These findings are consistent with a report by Donoyama and Ohkoshi ( 21 ), who reported that two healthy female participants had an increase in gene expressions associated with immune response in the immune system compared with a 40-minute resting control condition. These findings are also consistent with work that has been done to investigate the local impact of massage on muscles that have been injured during exercise ( 22 ). Consistent with reports of both a single session of massage and repeated massage on TH2 cytokine production is a paper by Loft and colleagues that reports that massage decreased antibody responses after hepatitis B vaccination ( 23 ). In summary, although these findings require replication, they suggest that massage may affect the immune system in a way that enhances immune surveillance and NK cell activity while decreasing inflammation and TH2-type responses.
Summary of the Biology of Massage
In summary, although much more extensive investigation of the neurobiology of massage is needed, the data suggest that there is a parsimonious way of conceptualizing the mechanisms underlying its beneficial effects. The brain circuitry stimulated by c fibers is associated with feelings of positive affect and well-being. Massage also stimulates brain circuits involved in the control of sympathetic and parasympathetic activity, with an enhancement of parasympathetic tone. These effects could in turn lead to a decrease in stress response as well as modulation of certain aspects of immune function, such as a decrease in inflammatory response. Thus, it is possible to synthesize the existing data regarding the biology of massage into a cogent working hypothesis about its benefits for certain psychiatric disorders.
Massage, Depression, and Depressive Symptoms
As previously discussed, the use of CAM to treat depressive symptoms and major depression is common ( 5 , 24 ). A reanalysis of a national survey by Kronenberg and colleagues ( 25 , 26 ) that focused on 220 women with depression who were part of a national telephone survey of 3,060 women indicated that 54% of the depressed women reported using CAM in the past year and that half of those respondents indicated that they used some form of manual therapy. Despite the clear data suggesting that many patients with major depression or depressive symptoms are interested in CIM therapies and, in particular, manual therapies, the data have significant limitations. A meta-analysis by Coelho and colleagues ( 27 ) reviewed 595 articles and excluded all but four from their meta-analysis of massage therapy for treatment of major depression or depressive symptoms. A more recent meta-analysis of massage therapy for depressed people by Hou and colleagues ( 28 ) used less stringent criteria and identified 17 studies with 786 participants from among 246 references. This meta-analysis included many studies whose participants were recruited because of a primary disorder other than depression, including insomnia, breast cancer, fibromyalgia, HIV infection, and low back pain. They concluded that these clinical trials were of moderate quality and that the pooled standardized mean differences from fixed and random effects models were .76 and .73, respectively. However, they cautioned that these 17 studies had considerable heterogeneity and that standardized protocols for massage therapy are needed, using validated depression scales with larger and more homogeneous participant populations.
In a comprehensive review of the use of CAM for perinatal depression, Deligiannidis and Freeman ( 29 ) suggested that a growing body of literature supports the use of antenatal massage therapy either in combination with psychotherapy or as a monotherapy to treat pregnant women with mild depressive symptomatology. Poland and colleagues ( 30 ) published results of a randomized, parallel-group, open-label controlled trial of massage versus light touch and wait-list control for the treatment of major depressive disorder in individuals infected with HIV. They reported that twice-weekly massage therapy was effective in decreasing depressive symptoms as measured by both the Hamilton Depression Rating Scale and the Beck Depression Inventory, beginning at week 4 and continuing throughout the eight-week trial period.
When the data presented here are synthesized with those of previous meta-analyses investigating the biology and efficacy of massage therapy across multiple disorders, they suggest that massage may be beneficial, at least as an adjuvant treatment, for depressed patients interested in a manual alternative therapy ( 15 , 31 , 32 ).
Massage and Anxiety Symptoms and Disorders
Not surprisingly, similar to the findings about the use of complementary and alternative therapies for the treatment of depressive symptoms, massage and other complementary and alternative therapies are frequently used to treat symptoms of anxiety by the general population as well as by individuals with a host of different medical conditions ( 4 – 7 ). In fact, 43% of people who were treated in the National Institutes of Health–funded Coordinated Anxiety and Learning Management study reported using some type of complementary and alternative treatment for their anxiety disorder ( 33 ). These individuals met the DSM-IV criteria for generalized anxiety disorder, panic disorder, social anxiety disorder, or posttraumatic stress disorder. However, despite the high rate of use of complementary and alternative treatments for anxiety disorders as well as for symptoms of anxiety, very little systematic research has investigated massage therapy as a treatment for the anxiety disorders. Four published studies have investigated the use of massage for patients with generalized anxiety disorder. Billhult and Määttä ( 34 ) reported that eight women with generalized anxiety disorder who were treated twice weekly with one-hour massages had decreased feelings of anxiety and increased feelings of self-confidence associated with this open-label pilot treatment.
In contrast, Sherman and colleagues ( 35 ) compared and contrasted therapeutic massage with thermal therapy and relaxing room therapy for 10 sessions over a 12-week period. They reported that all three treatments were equally as effective in decreasing symptoms of anxiety. The patients in this study were allowed to be medicated and the treatment protocols were flexible in terms of the 10 intervention sessions. McPherson and McGraw ( 36 ) reported results of a multimodule intervention with 25 individuals with generalized anxiety disorder and comorbid disorders. In this multimodule therapy that included partner-assisted massage, they found significant reductions on the GAD-7, decreased anxiolytic medication use, and decreased pain scale ratings. In a randomized, single blind comparison of massage and light touch for patients with generalized anxiety disorder, Rapaport and colleagues found that the group randomized to twice-weekly Swedish massage therapy had significant improvements in both clinician and self-report ratings of anxiety ( 37 ). They further observed significant improvement in both clinician and self-report ratings of depression. There currently are no published studies evaluating massage as a treatment for posttraumatic stress disorder, social anxiety disorder, or panic disorder.
In conclusion, a growing body of evidence has suggested that massage may be a beneficial intervention either as an adjuvant or as a monotherapy for decreasing anxiety symptoms. The data demonstrating the efficacy of massage in specific psychiatric disorders are quite limited, and more rigorous studies are needed.
Evidence Supporting the Use of Massage for Other Psychiatric Symptom Clusters
A growing number of studies have suggested that a variety of massage interventions may facilitate greater sleep quality and sleep length for patients with primary and postpartum insomnia, insomnia and fatigue secondary to renal failure and hemodialysis, post–coronary bypass graft surgery sleep disturbance, and insomnia secondary to perimenopausal and postmenopausal symptoms ( 38 – 42 ). Massage therapy has also been linked to both improvement in sleep and improvement in behavior for patients with dementia ( 43 , 44 ). Other studies have also suggested that massage interventions may decrease anxiety and enhance mood in nursing home residents with cognitive impairment ( 45 , 46 ). The data on the use of massage therapy to decrease symptoms of autism are relatively limited ( 47 ), but one recently published trial of Qigong massage delivered by the parents of preschool children with autism reported improvement on measures of autism as well as in sensory and self-regulation responses ( 48 ). Although a comprehensive review of the complex literature investigating the relationship of decreasing pain and massage is beyond the scope of this review, data suggesting that massage may be useful in decreasing a variety of forms of musculoskeletal pain are increasing ( 49 – 51 ).
In summary, the extant, albeit limited, data on the relationships between the treatment of sleep, agitation, climacteric symptoms associated with menopause, and pain have suggested that massage may be helpful for at least some patients. Clearly, more rigorous study is needed before definitive conclusions can be reached about the value of massage therapy, especially in light of the marked variety of massage interventions and the cultural and societal factors influencing their use.
How Massage Therapists Conceptualize and Treat Clients With Psychiatric Complaints
Therapeutic massage is an intentionally holistic treatment approach that can complement the traditional practice of medicine. Massage therapy is not a substitute for traditional medical care, and the massage therapist cannot diagnose. The community practice of therapeutic massage has three basic themes: It is client centered, its practice has a formal structure, and factors influence practice ( 52 ). Establishing trust is the basis for a therapeutic relationship forged between practitioner and client. The emphasis on shared decision making in CIM empowers clients to take an active role in their health ( 53 ). A typical outline of activities involved in the practice of massage therapy includes ongoing assessment and evaluation, development of a treatment plan, treatment, health messages, documentation, and closure ( 52 ). Assessment starts when a client enters the treatment space; basic massage therapy education includes postural analysis and instruction in observing other cues such as breathing patterns. Massage therapists are trained to conceptualize health as a natural relaxed and aware state and any disease as an imbalance in that state. Accordingly, therapeutic massage assessment and treatment focuses on promoting interoceptive awareness (of both individuals in the therapeutic dyad), allowing the individual to feel more relaxed and comfortable in his or her body. The massage therapist may use special orthopedic assessment tests before continuing with a tactile assessment (often using broad holistic strokes to palpate the underlying tissues). An individualized treatment plan—including type of massage, session frequency, and session length—is developed on the basis of a combination of the client’s health history and current health status, balancing client goals with reality, referencing the best available evidence (research and resources such as pharmacology textbooks) and the massage therapist’s clinical expertise ( 52 , 54 ). Assessment of the client through conversation and nonverbal clues is continuous both during the session and after the session is completed.
The literature has no consensus regarding the optimal type of massage therapy, frequency of treatment, or length of the sessions. All modalities of massage therapy are performed with intention and presence, providing an opportunity for the client to interact with another human being (the massage therapist) in a safe environment. Initial contact with the patient during treatment allows the massage therapist to gauge surface tension or ease before systematically progressing deeper or working a larger area. Most massage therapists are trained in a variety of modalities, allowing them to choose the tools best suited to the client’s current needs. In a treatment session, the client is in control of his or her experience ( 54 ).
Few studies have reported attempts to identify clinically relevant massage therapy frequency and dose ( 17 , 55 , 56 ). In practice, considerations of budget, schedule, accessibility, and acuity of symptoms are considered in determining the individualized treatment plan. Massage therapists on our team who have a community practice generally recommend that sessions occur every 10–14 days. In follow-up interviews for a recent study on massage for cancer-related fatigue, several participants indicated that the positive effects of the sessions lasted for days beyond completion of treatment. This is consistent with Rapaport and colleagues’ findings that the biological effects of massage were sustained for at least a week after the last session ( 17 ), as well as with those of the study by Perlman and colleagues ( 55 ), who reported that the positive effects of a massage intervention were sustained throughout the follow-up period for their study of osteoarthritis of the knee.
Along with the aforementioned factors, session length depends on techniques used and could vary in length from 15 to 90 minutes. Relaxing and revitalizing techniques are used at the end of a treatment session and establish closure. Finally, an exit interview is conducted, which may include home care suggestions relevant to the massage experience. All sessions should be formally documented, typically using SOAP (subjective, objective, assessment, and plan) note format.
Two factors influence the practice of massage therapy in the community: scope of practice and professional standards and ethics ( 52 ). Massage therapy is often thought of as a treatment for soft tissue dysfunction (i.e., muscle aches, tightness, and pain). However, an individual massage therapist’s scope of practice depends on his or her training, education, and location of practice. Basic educational requirements for massage therapy vary from state to state, as do regulatory laws (which can also vary by municipality). A massage therapist may choose to specialize in a certain type of treatment or work with a particular population. The practice of therapeutic massage is not static but continues to evolve as parameters change ( 57 ). Participation in continuing education classes, professional meetings, and experience continually shapes and refines a massage therapist’s practice and potentially expands the scope of practice.
Professional massage therapy organizations maintain and refine a repository of professional standards and ethics statements to guide the practice of massage therapy ( https://www.amtamassage.org/articles/3/MTJ/detail/2493 ). In the case of a client currently in the care of a psychiatrist, collaboration between the psychiatrist and the massage therapist may be beneficial in establishing boundaries to preserve safety of the client and the massage therapist.
How Psychiatrists and Massage Therapists Can Work Together
Many individuals with psychiatric disorders are already using CIM. A mail survey of adults with serious mental illness found that 31% of respondents reported using massage therapy ( 58 ). A starting point may be to begin by asking which of your existing clients uses massage therapy, which massage therapist they frequent, and what the massage therapist’s intake process entails. This query may lead the psychiatrist to seek out massage therapy to better understand available treatment options, but it may also prove helpful in identifying characteristics of individuals who may benefit most from referrals to therapeutic massage.
Communication is key to facilitating collaboration and ensuring that the patient is given consistent messages. Collaboration between psychiatrists and massage therapists can yield an integrated approach that capitalizes on the benefits of both forms of treatment while incorporating patient preferences and priorities. In addition, collaboration can expand treatment options, potentially allowing patients to have a more active role in their health care. Therapeutic massage invites a patient to actively engage in optimizing his or her mind-body awareness. The massage therapist serves as a witness to changes the patient undergoes through treatment, both conventional and complementary or integrative. Massage therapy is best viewed as an adjunct therapy rather than as an alternative to conventional treatment.
Identification of a well-suited massage therapist to add to your professional network can be accomplished through word of mouth or professional associations. For a successful partnership, the massage therapist will have a treatment philosophy that aligns with the physician’s treatment philosophy and a basic understanding of psychiatric disorders. Professional massage therapy organizations offer massage therapist locator services, and these services only list members in good standing ( https://www.amtamassage.org/findamassage/index.html )
In closing, patients accept and commonly use complementary and integrative therapies. They frequently seek out massage therapy to treat symptoms of depression and anxiety. Although data have suggested that massage may help decrease problems with depressed mood or acute anxiety, less information is available regarding the use of massage as a therapy for depression or anxiety disorders. Current data do suggest that massage may have some benefit as at least an adjuvant to conventional therapies. Although the data are limited, some findings have suggested that massage may acutely decrease hypothalamic-pituitary-adrenal activity, have a positive effect on immune function, enhance parasympathetic tone, and modulate brain circuitry. The approach and philosophy of well-trained massage therapists is complementary to conventional psychiatric training and can thus be an important additional resource in treating patients. A respectful and collaborative approach to care may truly help patients.
Dr. Schettler reports being a statistical analysis consultant to LivaNova. Dr. Nettles reports participation in the Novartis Employees Retirement Fund, being a consultant to Wolf Greenfield—Boston Drug Discovery IP, and serving as an expert witness. Dr. Rapaport, Ms. Larson, Mr. Carroll, Ms. Sharenko, and Dr. Kinkead report no financial relationships with commercial interests.
1 Global Burden of Disease Study 2013 Collaborators : Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013 . Lancet 386:743–800, 2015 Crossref , Google Scholar
2 Kessler RC, Chiu WT, Demler O, et al. : Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication . Arch Gen Psychiatry 62:617–627, 2005 Crossref , Google Scholar
3 Rush AJ, Trivedi MH, Wisniewski SR, et al. : Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report . Am J Psychiatry 163:1905–1917, 2006 Crossref , Google Scholar
4 Eisenberg DM, Kessler RC, Foster C, et al. : Unconventional medicine in the United States. Prevalence, costs, and patterns of use . N Engl J Med 328:246–252, 1993 Crossref , Google Scholar
5 Eisenberg DM, Davis RB, Ettner SL, et al. : Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey . JAMA 280:1569–1575, 1998 Crossref , Google Scholar
6 Barnes PM, Bloom B, Nahin RL : Complementary and alternative medicine use among adults and children: United States, 2007 . Natl Health Stat Rep 12:1–23, 2008 Google Scholar
7 Barnes PM, Powell-Griner E, McFann KK, et al. Complementary and alternative medicine use among adults: United States . Adv Data 343:1–19, 2004 Google Scholar
8 Purohit MP, Wells RE, Zafonte RD, et al. : Neuropsychiatric symptoms and the use of complementary and alternative medicine . PM R 5:24–31, 2013 Crossref , Google Scholar
9 Field T, Ironson G, Scafidi F, et al. : Massage therapy reduces anxiety and enhances EEG pattern of alertness and math computations . Int J Neurosci 86:197–205, 1996 Crossref , Google Scholar
10 Wu JJ, Cui Y, Yang YS, et al. : Modulatory effects of aromatherapy massage intervention on electroencephalogram, psychological assessments, salivary cortisol and plasma brain-derived neurotrophic factor . Complement Ther Med 22:456–462, 2014 Crossref , Google Scholar
11 Ouchi Y, Kanno T, Okada H, et al. : Changes in cerebral blood flow under the prone condition with and without massage . Neurosci Lett 407:131–135, 2006 Crossref , Google Scholar
12 Sliz D, Smith A, Wiebking C, et al. : Neural correlates of a single-session massage treatment . Brain Imaging Behav 6:77–87, 2012 Crossref , Google Scholar
13 Golaszewski SM, Siedentopf CM, Koppelstaetter F, et al. : Human brain structures related to plantar vibrotactile stimulation: a functional magnetic resonance imaging study . Neuroimage ; 29:923–929, 2006 Crossref , Google Scholar
14 Lloyd DM, McGlone FP, Yosipovitch G : Somatosensory pleasure circuit: from skin to brain and back . Exp Dermatol 24:321–324, 2015 Crossref , Google Scholar
15 Labyak SE, Metzger BL : The effects of effleurage backrub on the physiological components of relaxation: a meta-analysis . Nurs Res 46:59–62, 1997 Crossref , Google Scholar
16 Rapaport MH, Schettler P, Breese C : A preliminary study of the effects of a single session of Swedish massage on hypothalamic-pituitary-adrenal and immune function in normal individuals . J Altern Complement Med 16:1079–1088, 2010 Crossref , Google Scholar
17 Rapaport MH, Schettler P, Bresee C : A preliminary study of the effects of repeated massage on hypothalamic-pituitary-adrenal and immune function in healthy individuals: a study of mechanisms of action and dosage . J Altern Complement Med 18:789–797, 2012 Crossref , Google Scholar
18 Ironson G, Field T, Scafidi F, et al. : Massage therapy is associated with enhancement of the immune system’s cytotoxic capacity . Int J Neurosci 84:205–217, 1996 Crossref , Google Scholar
19 Diego MA, Field T, Hernandez-Reif M, et al. : HIV adolescents show improved immune function following massage therapy . Int J Neurosci 106:35–45, 2001 Crossref , Google Scholar
20 Shor-Posner G, Miguez MJ, Hernandez-Reif M, et al. : Massage treatment in HIV-1 infected Dominican children: a preliminary report on the efficacy of massage therapy to preserve the immune system in children without antiretroviral medication . J Altern Complement Med 10:1093–1095, 2004 Crossref , Google Scholar
21 Donoyama N, Ohkoshi N : Effects of traditional Japanese massage therapy on gene expression: preliminary study . J Altern Complement Med 17:553–555, 2011 Crossref , Google Scholar
22 Crane JD, Ogborn DI, Cupido C, et al. : Massage therapy attenuates inflammatory signaling after exercise-induced muscle damage . Sci Transl Med 4:119ra13, 2012 Crossref , Google Scholar
23 Loft P, Petrie KJ, Booth RJ, et al. : Effects of massage on antibody responses after hepatitis B vaccination . Psychosom Med 74:982–987, 2012 Crossref , Google Scholar
24 Kessler RC, Soukup J, Davis RB, et al. : The use of complementary and alternative therapies to treat anxiety and depression in the United States . Am J Psychiatry 158:289–294, 2001 Crossref , Google Scholar
25 Wu P, Fuller C, Liu X, et al. : Use of complementary and alternative medicine among women with depression: results of a national survey . Psychiatr Serv 58:349–356, 2007 Crossref , Google Scholar
26 Kronenberg F, Cushman LF, Wade CM, et al. : Race/ethnicity and women’s use of complementary and alternative medicine in the United States: results of a national survey . Am J Public Health 96:1236–1242, 2006 Crossref , Google Scholar
27 Coelho HF, Boddy K, Ernst E : Massage therapy for the treatment of depression: a systematic review . Int J Clin Pract 62:325–333, 2008 Crossref , Google Scholar
28 Hou WH, Chiang PT, Hsu TY, et al. : Treatment effects of massage therapy in depressed people: a meta-analysis . J Clin Psychiatry 71:894–901, 2010 Crossref , Google Scholar
29 Deligiannidis KM, Freeman MP : Complementary and alternative medicine therapies for perinatal depression . Best Pract Res Clin Obstet Gynaecol 28:85–95, 2014 Crossref , Google Scholar
30 Poland RE, Gertsik L, Favreau JT, et al. : Open-label, randomized, parallel-group controlled clinical trial of massage for treatment of depression in HIV-infected subjects . J Altern Complement Med 19:334–340, 2013 Crossref , Google Scholar
31 Moyer CA, Rounds J, Hannum JW : A meta-analysis of massage therapy research . Psychol Bull 130:3–18, 2004 Crossref , Google Scholar
32 Ottenbacher KJ, Muller L, Brandt D, et al. : The effectiveness of tactile stimulation as a form of early intervention: a quantitative evaluation . J Dev Behav Pediatr 8:68–76, 1987 Crossref , Google Scholar
33 Bystritsky A, Hovav S, Sherbourne C, et al. : Use of complementary and alternative medicine in a large sample of anxiety patients . Psychosomatics 53:266–272, 2012 Crossref , Google Scholar
34 Billhult A, Määttä S : Light pressure massage for patients with severe anxiety . Complement Ther Clin Pract 15:96–101, 2009 Crossref , Google Scholar
35 Sherman KJ, Ludman EJ, Cook AJ, et al. : Effectiveness of therapeutic massage for generalized anxiety disorder: a randomized controlled trial . Depress Anxiety 27:441–450, 2010 Crossref , Google Scholar
36 McPherson F, McGraw L : Treating generalized anxiety disorder using complementary and alternative medicine . Altern Ther Health Med 19:45–50, 2013 Google Scholar
37 Rapaport MH, Schettler P, Larson ER, et al. : Acute Swedish massage monotherapy successfully remediates symptoms of generalized anxiety disorder: a proof-of-concept, randomized controlled study . J Clin Psychiatry 77:e883–e891, 2016 Crossref , Google Scholar
38 Ko YL, Lee HJ : Randomised controlled trial of the effectiveness of using back massage to improve sleep quality among Taiwanese insomnia postpartumwomen . Midwifery 30:60–64, 2014 Crossref , Google Scholar
39 Unal KS, Balci Akpinar R : The effect of foot reflexology and back massage on hemodialysis patients’ fatigue and sleep quality . Complement Ther Clin Pract 24:139–144, 2016 Crossref , Google Scholar
40 Nerbass FB, Feltrim MI, Souza SA, et al. : Effects of massage therapy on sleep quality after coronary artery bypass graft surgery . Clinics (Sao Paulo) 65:1105–1110, 2010 Crossref , Google Scholar
41 Oliveira D, Hachul H, Tufik S, et al. : Effect of massage in postmenopausal women with insomnia: a pilot study . Clinics (Sao Paulo) 66:343–346, 2011 Crossref , Google Scholar
42 Oliveira DS, Hachul H, Goto V, et al. : Effect of therapeutic massage on insomnia and climacteric symptoms in postmenopausal women . Climacteric 15:21–29, 2012 Crossref , Google Scholar
43 Rodriguez-Mansilla J, Gonzalez-Lopez-Arza MV, Varela-Donoso E, et al. : Ear therapy and massage therapy in the elderly with dementia: a pilot study. J Tradit Chinese Med 33:461–467, 2013 Crossref , Google Scholar
44 Harris M, Richards KC, Grando VT : The effects of slow-stroke back massage on minutes of nighttime sleep in persons with dementia and sleep disturbances in the nursing home: a pilot study . J Holist Nurs 30:255–263, 2012 Crossref , Google Scholar
45 Moyle W, Cooke ML, Beattie E, et al. : Foot massage versus quiet presence on agitation and mood in people with dementia: a randomised controlled trial . Int J Nurs Stud 51:856–864, 2014 Crossref , Google Scholar
46 Holliday-Welsh DM, Gessert CE, Renier CM : Massage in the management of agitation in nursing home residents with cognitive impairment . Geriatr Nurs 30:108–117, 2009 Crossref , Google Scholar
47 Lee MS, Kim JI, Ernst E : Massage therapy for children with autism spectrum disorders: a systematic review . J Clin Psychiatry 72:406–411, 2011 Crossref , Google Scholar
48 Silva LM, Schalock M, Gabrielsen K . Early intervention for autism with a parent-delivered Qigong massage program: a randomized controlled trial . Am J Occup Ther 65:550-559, 2011 Crossref , Google Scholar
49 Netchanok S, Wendy M, Marie C, et al. : The effectiveness of Swedish massage and traditional Thai massage in treating chronic low back pain: a review of the literature . Complement Ther Clin Pract 18:227–234, 2012 Crossref , Google Scholar
50 Furlan AD, Pennick V, Bombardier C, et al. : 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group . Spine 34:1929–1941, 2009 Crossref , Google Scholar
51 Bervoets DC, Luijsterburg PA, Alessie JJ, et al. : Massage therapy has short-term benefits for people with common musculoskeletal disorders compared to no treatment: a systematic review . J Physiother 61:106–116, 2015 Crossref , Google Scholar
52 Kennedy AB, Cambron JA, Sharpe PA, et al. : Process for massage therapy practice and essential assessment . J Bodyw Mov Ther 20:484–496, 2016 Crossref , Google Scholar
53 Berger S, Braehler E, Ernst J : The health professional-patient-relationship in conventional versus complementary and alternative medicine: a qualitative study comparing the perceived use of medical shared decision-making between two different approaches of medicine . Patient Educ Couns 88:129–137, 2012 Crossref , Google Scholar
54 Fortune LD, Hymel GM : Creating integrative work: a qualitative study of how massage therapists work with existing clients . J Bodyw Mov Ther 19:25–34, 2015 Crossref , Google Scholar
55 Perlman AI, Ali A, Njike VY, et al. : Massage therapy for osteoarthritis of the knee: a randomized dose-finding trial . PLoS One 7:e30248, 2012 Crossref , Google Scholar
56 Sherman KJ, Cook AJ, Wellman RD, et al. : Five-week outcomes from a dosing trial of therapeutic massage for chronic neck pain . Ann Fam Med 12:112–120, 2014 Crossref , Google Scholar
57 Porcino AJ, Boon HS, Page SA, et al. : Exploring the nature of therapeutic massage bodywork practice . Int J Ther Massage Bodywork 6:15–24, 2013 Google Scholar
58 Russinova Z, Wewiorski NJ, Cash D : Use of alternative health care practices by persons with serious mental illness: perceived benefits . Am J Public Health 92:1600–1603, 2002 Crossref , Google Scholar
- The skin‐brain connection and pleasant touch as supportive care for psychocutaneous disorders 1 December 2023 | Skin Health and Disease, Vol. 4, No. 1
- Effect of massage on blood pressure in patients with hypertension: A meta-analysis Journal of Bodywork and Movement Therapies, Vol. 37
- Patient Attitudes and Perceived Barriers Toward Mental Health Treatment Options in a Rural Student-Run Clinic Cureus, Vol. 4
- Utilization of massage chairs for promoting overall health and wellness: A rapid scoping review EXPLORE, Vol. 31
- Effects of aromatherapy on depression: A meta-analysis of randomized controlled trials General Hospital Psychiatry, Vol. 84
- Effects of Massages and Other Touch Interventions on Various Diseases 28 October 2023
- AIM in Alternative Medicine 1 January 2022
- Berührung ein Lebensmittel: Einfluss auf die körperliche und geistige Gesundheit 12 May 2022
- The Effect of Foot Reflexology on Amnesia in Patients Undergoing Electroconvulsive Therapy: A Randomized Clinical Trial 28 February 2021 | Journal of Caring Sciences, Vol. 10, No. 1
- Touch Research–Quo Vadis? A Plea for High-Quality Clinical Trials 28 December 2020 | Brain Sciences, Vol. 11, No. 1
- AIM in Alternative Medicine 11 August 2021
- A reformulated contextual model of psychotherapy for treating anxiety and depression Clinical Psychology Review, Vol. 80
- Model structure for protocol adherence utilizing a manualized therapeutic massage intervention 12 October 2018 | Journal of Complementary and Integrative Medicine, Vol. 16, No. 2
- Medical Hypotheses, Vol. 128
- Psychoneuroendocrinology, Vol. 101
- complementary and integrative medicine
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Focus (Am Psychiatr Publ)
- v.16(1); Winter 2018

Massage Therapy for Psychiatric Disorders
This article reviews the role of massage therapy in the treatment of common psychiatric disorders and briefly discusses the prevalence and popularity of complementary and integrative treatments in the general population and touches on the literature on the biology and neurobiology of massage therapy.
This article reviews the current state of knowledge of the role of massage therapy in the treatment of common psychiatric disorders and symptoms. It briefly discusses the prevalence of psychiatric disorders and the popularity of complementary and integrative treatments in the general population. The authors touch on the growing literature describing the biology and neurobiology of massage therapy. The impact of massage as both a therapy for major psychiatric disorders and a treatment for psychiatric symptoms is reviewed, and how massage therapists conceptualize and treat their patients with psychiatric complaints is discussed. If psychiatrists are going to partner with massage therapists, they need to understand how massage therapists’ perspectives differ from those of traditional practitioners of allopathic medicine. A model of how psychiatrists and other mental health professionals can work with massage therapists to care for patients is proposed, followed by a summary of the article’s key points.
Of the top 25 disorders associated with years lost because of disability, seven are major psychiatric disorders ( 1 ). Major depression is the second leading cause of years living with disability in the world, anxiety disorders are the ninth leading cause, and schizophrenia is the 11th leading cause. Thus, major psychiatric syndromes are clearly associated with a major cost to society. Major psychiatric syndromes are also remarkably prevalent. One in four individuals will have a major psychiatric syndrome at some point in their lifetime ( 2 ). This means that everyone knows someone with a major psychiatric disorder, and every family is touched by the presence of these diseases. Despite significant advances toward both understanding the neuroscience of and developing new psychotherapies and pharmacotherapies to treat these disorders, a great unmet treatment need still exists. Using major depressive disorder as an example, we know from the National Institute of Mental Health–funded Sequenced Treatment Alternatives to Relieve Depression study that only one-third of individuals go into remission with initial treatment for depression ( 3 ). Furthermore, although close to two-thirds may enter remission with multiple successive treatments, the majority of these individuals will relapse within one year of reaching remission status ( 3 ). Thus, there is clearly a need for additional options to treat people with depression. It is reasonable to extrapolate from depression to other psychiatric disorders for which there are even fewer available treatment options. We contend that approaches to identifying potential treatment interventions for patients need to be broadened.
Systematic investigation into the popularity of complementary and alternative medicine (CAM) for treatment in the United States began in 1990 with the survey spearheaded by Eisenberg and colleagues ( 4 ). In this initial report in the New England Journal of Medicine, they documented that 33.8% of the adults surveyed had used some type of alternative or complementary medical service in the past 12 months. These findings were a revelation to most individuals in traditional Western or allopathic medical communities. Eisenberg and colleagues followed this report with a paper that compared and contrasted their 1990 data with those from a survey conducted in 1997 ( 5 ). This later publication documented an increase in the use of alternative therapies from 33.8% to 42.0%, with herbal medicine, massage, megavitamins, self-help groups, folk remedies, homeopathy, and energy healing increasing the most. They reported that some of the most frequent reasons for using complementary and alternative therapies included back pain, anxiety, depression, and headaches. In the 1997 paper, they estimated that the cost for services provided was $21.2 billion, with at least $12.2 billion being paid out of pocket. These initial findings by Eisenberg and colleagues were updated in the 2002 and 2007 Centers for Disease Control and Prevention–sponsored CAM surveys. In both of these surveys ( 6 , 7 ), approximately 40% of adults reported having used some type of complementary and alternative therapy in the past 12 months. Also, both of these surveys indicated that approximately 5% of the U.S. adult population had used massage therapy. Purohit and colleagues ( 8 ) performed a reanalysis of the 2007 National Health Interview data of 23,393 adults that focused on the presence of neuropsychiatric symptoms and their impact on CAM usage. The prevalence of the use of CAM therapies was 43.78% for individuals with self-reported symptoms of depression, insomnia, headaches, memory deficits, attention deficits, and sleep problems versus 29.7% for individuals who did not report any of these symptoms. Of those individuals with at least one neuropsychiatric symptom who used CAM therapies, 20% used CAM therapy because they felt that standard treatments were either too expensive or ineffective, and 25% used CAM therapies because they were recommended by their traditional medical provider.
In conclusion, there is an interface between psychiatric disorders and complementary and alternative therapies such as massage. Accordingly, validated alternative therapies are now being integrated within the medical mainstream under the rubric “complementary and integrative medicine” (CIM). Consistent with this, and reflecting an emphasis on well-being and treatment of disease, the National Institutes of Health have renamed the center addressing CAM therapies the National Center for Complementary and Integrative Health. Psychiatric disorders are common and disabling, and current treatment methods, although helpful for many, are not the treatment of choice for many patients and are insufficient to alleviate disability and suffering for many others. This suggests that allopathic practitioners should think about two questions: What is the body of evidence supporting CIM interventions, and what is the best way for a psychiatrist or other mental health service provider and a CIM practitioner to interact with each other in the care of a patient? We address these two important issues.
Biology of Massage
Rigorous study of the biology of therapeutic massage is still in a relatively nascent phase. Although studies have attempted to understand the impact of various forms of massage on the body since the early 1990s, the research has been fraught with problems, in particular a lack of consistent funding for investigation of the biological effects of massage. Another challenge faced by the field is that there are many different types of massage and great variation in research study designs. As a result, current knowledge of the biology of massage rests mainly on a number of small studies investigating very different interventions that have been done for different lengths of time and at different frequencies. Despite these limitations, certain biological patterns seem to have emerged from recent studies.
Human Studies of the Neurobiology of Massage
A few EEG and imaging studies have investigated the impact of massage on brain circuitry or brain regions. One of the first studies was performed by the Touch Institute. In this study, 26 adults were given chair massage for 15 minutes twice weekly for five weeks, and 24 adults were asked to sit quietly in the massage chair twice weekly for five weeks ( 9 ). Field and colleagues found that twice-weekly massage was associated with an increase in frontal delta power in the EEG and a decrease in frontal alpha and beta power. This pattern is consistent with increased relaxation yet enhanced alertness, which was supported by the massage group’s having increased speed and accuracy on mathematical computations and decreased levels of anxiety. Salivary cortisol levels were also lower in the massage condition but not in the control condition. In a study of an aromatherapy massage intervention versus no treatment, Wu and colleagues ( 10 ) were able to replicate an increase in alpha wave activity in their aromatherapy massage sample, but they found a reduction in delta wave activity. However, they reported decreases in state anxiety and depression and an increase in psychological well-being as well as a reduction in salivary cortisol levels and an increase in plasma brain-derived neurotrophic factor in the aromatherapy group.
Neuroimaging studies investigating the impact of massage on the brain have been limited. In a small positron emission tomography study in 2006, Ouchi and colleagues ( 11 ) reported that being placed in the scanner in a prone position versus a supine position caused increased activation in the precuneus. This activation was further enhanced by both four minutes and 20 minutes of palm pressure massage applied to participants’ backs. The 20 minutes of massage also caused a greater increase in parasympathetic tone as well as activation of the parieto-occipital region. Ouchi and colleagues also reported activation in the cerebellum associated with massage. The authors concluded that this pattern of activation of the precuneus with back massage might reflect augmentation of arousal in consciousness functions associated with positive affect and that their findings of increased activity in the forebrain-amygdala system might be responsible for an increase in parasympathetic tone in the brain. The latter would also be consistent with a cerebellar increase in blood flow, which again would help regulate parasympathetic tone. These findings were partially replicated and extended by Sliz and colleagues ( 12 ), who looked at the neurocorrelates of a single session of massage versus those of a resting control condition, reflexology and massage with an object. They found that Swedish massage of the right foot while the participant performed a cognitive task in the scanner was associated with increased activation of the subgenual anterior and retrosplenial-posterior cingulate cortices. This increased activation of the retrosplenial-posterior cingulate cortex was sustained even without activation by the task.
If one integrates these findings investigating the impact of massage with those of a series of elegant studies that have been performed to attempt to understand the basic neurobiology of touch, one can come up with unifying theory of the impact of massage on the brain. An MRI study by Golaszewski and colleagues ( 13 ) demonstrated that vibrating tactile stimulation of the plantar surface of the foot increased activity in the inferior and posterior cingulate gyri along with the somatosensory cortex, insula, thalamus, caudate, and cerebellum. These brain regions integrate tactile and sensory information from mechanoreceptors, the myelinated A-beta and A-alpha afferents, and the unmyelinated sensory nerve fibers called c-tactile afferents that are thought to be associated with positive affect. The c-tactile afferents are stimulated by gentle stroking of hairy skin surfaces. They project to the limbic cortex, including the orbital frontal cortex and posterior insulate bilaterally.
In summary, although the data on the impact of massage on EEG and neuroimaging changes in the brain are limited, when these data are combined with the emerging data on somatic sensory pleasure circuitry, it is reasonable to postulate that massage’s beneficial effects on affiliation and feelings of well-being may be due to stimulation of specific brain circuits involved in pleasure and reward ( 14 ).
Impact of Massage on the Hypothalamic-Pituitary-Adrenal Axis and Neurohormones
A myriad of small studies of massage have measured either salivary or plasma cortisol levels. Many of these studies investigated only single time-point measures of cortisol before and after a series of massage interventions. The consensus of existing meta-analyses as well as of this review is that massage tends to decrease measures of plasma and salivary cortisol versus either a wait-list or a no-treatment condition ( 15 ). However, in general these studies have not looked at the sustained impact of massage after cessation of treatment. Rapaport and colleagues ( 16 ) have compared and contrasted the impact of a single 45-minute session of manualized Swedish massage with that of a manualized light-touch control condition in adults with no psychiatric disorder. They sampled cortisol, oxytocin, vasopressin, and adrenocorticotropic hormone after a 30-minute accommodation period at two points before initiation of massage or touch and then at several time points during the hour after the intervention. These authors found that a single session of either massage or touch was associated with a small effect-size decrease in cortisol levels in healthy young participants as well as a large effect-size increase in oxytocin in both groups. However, compared with changes found in cortisol and oxytocin, the massage group showed a profound significant decrease in vasopressin compared with the touch control group.
In a subsequent study, Rapaport and colleagues investigated the impact of weekly massage versus weekly touch for five weeks, as well as the impact of twice-weekly massage or twice-weekly touch for five weeks ( 17 ). Weekly massage versus weekly touch was associated with a pattern of results similar to that observed with a single session of massage. However, twice-weekly massage caused a significantly greater cumulative increase in oxytocin and decrease in vasopressin than twice-weekly touch. Although these data are of interest and consistent with previous studies reporting a decrease in cortisol levels and an increase in sense of affiliation associated with massage, these small studies require replication with larger cohorts of participants.
In summary, data suggest that massage may be associated with a decrease in hypothalamic-pituitary-adrenal activation and possibly with an increase in oxytocin levels. However, larger rigorous studies are needed.
Impact of Massage on the Immune System
A great deal of the pioneering work investigating the relationship between massage and the immune system occurred at the University of Miami. This group investigated the impact of massage on immune function in a variety of different patient populations including depressed individuals, HIV-positive young women, and HIV-positive adolescents ( 18 – 20 ). In general, this group reported an increase in natural killer (NK) cells and an increase in NK cell activity associated with massage compared with control conditions such as muscle relaxation. Rapaport and colleagues reported that a single session of Swedish massage versus a touch control condition caused a leukocytosis with a moderate effect-size increase in CD56+ NK cells and an increase in activated T cells ( 16 ). They have also reported that massage was associated with a significant decrease in Type 2 T helper (TH2) mitogen-stimulated cytokines compared with both baseline levels and the touch control condition ( 16 ). Massage was also associated with a decrease in mitogen-stimulated proinflammatory cytokine production when contrasted with the touch control condition. In 2012, Rapaport and colleagues reported that these effects were sustained for at least one week and that they were specific to individuals who received one massage per week in contrast to the groups receiving two massages per week ( 17 ). These findings are consistent with a report by Donoyama and Ohkoshi ( 21 ), who reported that two healthy female participants had an increase in gene expressions associated with immune response in the immune system compared with a 40-minute resting control condition. These findings are also consistent with work that has been done to investigate the local impact of massage on muscles that have been injured during exercise ( 22 ). Consistent with reports of both a single session of massage and repeated massage on TH2 cytokine production is a paper by Loft and colleagues that reports that massage decreased antibody responses after hepatitis B vaccination ( 23 ). In summary, although these findings require replication, they suggest that massage may affect the immune system in a way that enhances immune surveillance and NK cell activity while decreasing inflammation and TH2-type responses.
Summary of the Biology of Massage
In summary, although much more extensive investigation of the neurobiology of massage is needed, the data suggest that there is a parsimonious way of conceptualizing the mechanisms underlying its beneficial effects. The brain circuitry stimulated by c fibers is associated with feelings of positive affect and well-being. Massage also stimulates brain circuits involved in the control of sympathetic and parasympathetic activity, with an enhancement of parasympathetic tone. These effects could in turn lead to a decrease in stress response as well as modulation of certain aspects of immune function, such as a decrease in inflammatory response. Thus, it is possible to synthesize the existing data regarding the biology of massage into a cogent working hypothesis about its benefits for certain psychiatric disorders.
Massage, Depression, and Depressive Symptoms
As previously discussed, the use of CAM to treat depressive symptoms and major depression is common ( 5 , 24 ). A reanalysis of a national survey by Kronenberg and colleagues ( 25 , 26 ) that focused on 220 women with depression who were part of a national telephone survey of 3,060 women indicated that 54% of the depressed women reported using CAM in the past year and that half of those respondents indicated that they used some form of manual therapy. Despite the clear data suggesting that many patients with major depression or depressive symptoms are interested in CIM therapies and, in particular, manual therapies, the data have significant limitations. A meta-analysis by Coelho and colleagues ( 27 ) reviewed 595 articles and excluded all but four from their meta-analysis of massage therapy for treatment of major depression or depressive symptoms. A more recent meta-analysis of massage therapy for depressed people by Hou and colleagues ( 28 ) used less stringent criteria and identified 17 studies with 786 participants from among 246 references. This meta-analysis included many studies whose participants were recruited because of a primary disorder other than depression, including insomnia, breast cancer, fibromyalgia, HIV infection, and low back pain. They concluded that these clinical trials were of moderate quality and that the pooled standardized mean differences from fixed and random effects models were .76 and .73, respectively. However, they cautioned that these 17 studies had considerable heterogeneity and that standardized protocols for massage therapy are needed, using validated depression scales with larger and more homogeneous participant populations.
In a comprehensive review of the use of CAM for perinatal depression, Deligiannidis and Freeman ( 29 ) suggested that a growing body of literature supports the use of antenatal massage therapy either in combination with psychotherapy or as a monotherapy to treat pregnant women with mild depressive symptomatology. Poland and colleagues ( 30 ) published results of a randomized, parallel-group, open-label controlled trial of massage versus light touch and wait-list control for the treatment of major depressive disorder in individuals infected with HIV. They reported that twice-weekly massage therapy was effective in decreasing depressive symptoms as measured by both the Hamilton Depression Rating Scale and the Beck Depression Inventory, beginning at week 4 and continuing throughout the eight-week trial period.
When the data presented here are synthesized with those of previous meta-analyses investigating the biology and efficacy of massage therapy across multiple disorders, they suggest that massage may be beneficial, at least as an adjuvant treatment, for depressed patients interested in a manual alternative therapy ( 15 , 31 , 32 ).
Massage and Anxiety Symptoms and Disorders
Not surprisingly, similar to the findings about the use of complementary and alternative therapies for the treatment of depressive symptoms, massage and other complementary and alternative therapies are frequently used to treat symptoms of anxiety by the general population as well as by individuals with a host of different medical conditions ( 4 – 7 ). In fact, 43% of people who were treated in the National Institutes of Health–funded Coordinated Anxiety and Learning Management study reported using some type of complementary and alternative treatment for their anxiety disorder ( 33 ). These individuals met the DSM-IV criteria for generalized anxiety disorder, panic disorder, social anxiety disorder, or posttraumatic stress disorder. However, despite the high rate of use of complementary and alternative treatments for anxiety disorders as well as for symptoms of anxiety, very little systematic research has investigated massage therapy as a treatment for the anxiety disorders. Four published studies have investigated the use of massage for patients with generalized anxiety disorder. Billhult and Määttä ( 34 ) reported that eight women with generalized anxiety disorder who were treated twice weekly with one-hour massages had decreased feelings of anxiety and increased feelings of self-confidence associated with this open-label pilot treatment.
In contrast, Sherman and colleagues ( 35 ) compared and contrasted therapeutic massage with thermal therapy and relaxing room therapy for 10 sessions over a 12-week period. They reported that all three treatments were equally as effective in decreasing symptoms of anxiety. The patients in this study were allowed to be medicated and the treatment protocols were flexible in terms of the 10 intervention sessions. McPherson and McGraw ( 36 ) reported results of a multimodule intervention with 25 individuals with generalized anxiety disorder and comorbid disorders. In this multimodule therapy that included partner-assisted massage, they found significant reductions on the GAD-7, decreased anxiolytic medication use, and decreased pain scale ratings. In a randomized, single blind comparison of massage and light touch for patients with generalized anxiety disorder, Rapaport and colleagues found that the group randomized to twice-weekly Swedish massage therapy had significant improvements in both clinician and self-report ratings of anxiety ( 37 ). They further observed significant improvement in both clinician and self-report ratings of depression. There currently are no published studies evaluating massage as a treatment for posttraumatic stress disorder, social anxiety disorder, or panic disorder.
In conclusion, a growing body of evidence has suggested that massage may be a beneficial intervention either as an adjuvant or as a monotherapy for decreasing anxiety symptoms. The data demonstrating the efficacy of massage in specific psychiatric disorders are quite limited, and more rigorous studies are needed.
Evidence Supporting the Use of Massage for Other Psychiatric Symptom Clusters
A growing number of studies have suggested that a variety of massage interventions may facilitate greater sleep quality and sleep length for patients with primary and postpartum insomnia, insomnia and fatigue secondary to renal failure and hemodialysis, post–coronary bypass graft surgery sleep disturbance, and insomnia secondary to perimenopausal and postmenopausal symptoms ( 38 – 42 ). Massage therapy has also been linked to both improvement in sleep and improvement in behavior for patients with dementia ( 43 , 44 ). Other studies have also suggested that massage interventions may decrease anxiety and enhance mood in nursing home residents with cognitive impairment ( 45 , 46 ). The data on the use of massage therapy to decrease symptoms of autism are relatively limited ( 47 ), but one recently published trial of Qigong massage delivered by the parents of preschool children with autism reported improvement on measures of autism as well as in sensory and self-regulation responses ( 48 ). Although a comprehensive review of the complex literature investigating the relationship of decreasing pain and massage is beyond the scope of this review, data suggesting that massage may be useful in decreasing a variety of forms of musculoskeletal pain are increasing ( 49 – 51 ).
In summary, the extant, albeit limited, data on the relationships between the treatment of sleep, agitation, climacteric symptoms associated with menopause, and pain have suggested that massage may be helpful for at least some patients. Clearly, more rigorous study is needed before definitive conclusions can be reached about the value of massage therapy, especially in light of the marked variety of massage interventions and the cultural and societal factors influencing their use.
How Massage Therapists Conceptualize and Treat Clients With Psychiatric Complaints
Therapeutic massage is an intentionally holistic treatment approach that can complement the traditional practice of medicine. Massage therapy is not a substitute for traditional medical care, and the massage therapist cannot diagnose. The community practice of therapeutic massage has three basic themes: It is client centered, its practice has a formal structure, and factors influence practice ( 52 ). Establishing trust is the basis for a therapeutic relationship forged between practitioner and client. The emphasis on shared decision making in CIM empowers clients to take an active role in their health ( 53 ). A typical outline of activities involved in the practice of massage therapy includes ongoing assessment and evaluation, development of a treatment plan, treatment, health messages, documentation, and closure ( 52 ). Assessment starts when a client enters the treatment space; basic massage therapy education includes postural analysis and instruction in observing other cues such as breathing patterns. Massage therapists are trained to conceptualize health as a natural relaxed and aware state and any disease as an imbalance in that state. Accordingly, therapeutic massage assessment and treatment focuses on promoting interoceptive awareness (of both individuals in the therapeutic dyad), allowing the individual to feel more relaxed and comfortable in his or her body. The massage therapist may use special orthopedic assessment tests before continuing with a tactile assessment (often using broad holistic strokes to palpate the underlying tissues). An individualized treatment plan—including type of massage, session frequency, and session length—is developed on the basis of a combination of the client’s health history and current health status, balancing client goals with reality, referencing the best available evidence (research and resources such as pharmacology textbooks) and the massage therapist’s clinical expertise ( 52 , 54 ). Assessment of the client through conversation and nonverbal clues is continuous both during the session and after the session is completed.
The literature has no consensus regarding the optimal type of massage therapy, frequency of treatment, or length of the sessions. All modalities of massage therapy are performed with intention and presence, providing an opportunity for the client to interact with another human being (the massage therapist) in a safe environment. Initial contact with the patient during treatment allows the massage therapist to gauge surface tension or ease before systematically progressing deeper or working a larger area. Most massage therapists are trained in a variety of modalities, allowing them to choose the tools best suited to the client’s current needs. In a treatment session, the client is in control of his or her experience ( 54 ).
Few studies have reported attempts to identify clinically relevant massage therapy frequency and dose ( 17 , 55 , 56 ). In practice, considerations of budget, schedule, accessibility, and acuity of symptoms are considered in determining the individualized treatment plan. Massage therapists on our team who have a community practice generally recommend that sessions occur every 10–14 days. In follow-up interviews for a recent study on massage for cancer-related fatigue, several participants indicated that the positive effects of the sessions lasted for days beyond completion of treatment. This is consistent with Rapaport and colleagues’ findings that the biological effects of massage were sustained for at least a week after the last session ( 17 ), as well as with those of the study by Perlman and colleagues ( 55 ), who reported that the positive effects of a massage intervention were sustained throughout the follow-up period for their study of osteoarthritis of the knee.
Along with the aforementioned factors, session length depends on techniques used and could vary in length from 15 to 90 minutes. Relaxing and revitalizing techniques are used at the end of a treatment session and establish closure. Finally, an exit interview is conducted, which may include home care suggestions relevant to the massage experience. All sessions should be formally documented, typically using SOAP (subjective, objective, assessment, and plan) note format.
Two factors influence the practice of massage therapy in the community: scope of practice and professional standards and ethics ( 52 ). Massage therapy is often thought of as a treatment for soft tissue dysfunction (i.e., muscle aches, tightness, and pain). However, an individual massage therapist’s scope of practice depends on his or her training, education, and location of practice. Basic educational requirements for massage therapy vary from state to state, as do regulatory laws (which can also vary by municipality). A massage therapist may choose to specialize in a certain type of treatment or work with a particular population. The practice of therapeutic massage is not static but continues to evolve as parameters change ( 57 ). Participation in continuing education classes, professional meetings, and experience continually shapes and refines a massage therapist’s practice and potentially expands the scope of practice.
Professional massage therapy organizations maintain and refine a repository of professional standards and ethics statements to guide the practice of massage therapy ( https://www.amtamassage.org/articles/3/MTJ/detail/2493 ). In the case of a client currently in the care of a psychiatrist, collaboration between the psychiatrist and the massage therapist may be beneficial in establishing boundaries to preserve safety of the client and the massage therapist.
How Psychiatrists and Massage Therapists Can Work Together
Many individuals with psychiatric disorders are already using CIM. A mail survey of adults with serious mental illness found that 31% of respondents reported using massage therapy ( 58 ). A starting point may be to begin by asking which of your existing clients uses massage therapy, which massage therapist they frequent, and what the massage therapist’s intake process entails. This query may lead the psychiatrist to seek out massage therapy to better understand available treatment options, but it may also prove helpful in identifying characteristics of individuals who may benefit most from referrals to therapeutic massage.
Communication is key to facilitating collaboration and ensuring that the patient is given consistent messages. Collaboration between psychiatrists and massage therapists can yield an integrated approach that capitalizes on the benefits of both forms of treatment while incorporating patient preferences and priorities. In addition, collaboration can expand treatment options, potentially allowing patients to have a more active role in their health care. Therapeutic massage invites a patient to actively engage in optimizing his or her mind-body awareness. The massage therapist serves as a witness to changes the patient undergoes through treatment, both conventional and complementary or integrative. Massage therapy is best viewed as an adjunct therapy rather than as an alternative to conventional treatment.
Identification of a well-suited massage therapist to add to your professional network can be accomplished through word of mouth or professional associations. For a successful partnership, the massage therapist will have a treatment philosophy that aligns with the physician’s treatment philosophy and a basic understanding of psychiatric disorders. Professional massage therapy organizations offer massage therapist locator services, and these services only list members in good standing ( https://www.amtamassage.org/findamassage/index.html )
In closing, patients accept and commonly use complementary and integrative therapies. They frequently seek out massage therapy to treat symptoms of depression and anxiety. Although data have suggested that massage may help decrease problems with depressed mood or acute anxiety, less information is available regarding the use of massage as a therapy for depression or anxiety disorders. Current data do suggest that massage may have some benefit as at least an adjuvant to conventional therapies. Although the data are limited, some findings have suggested that massage may acutely decrease hypothalamic-pituitary-adrenal activity, have a positive effect on immune function, enhance parasympathetic tone, and modulate brain circuitry. The approach and philosophy of well-trained massage therapists is complementary to conventional psychiatric training and can thus be an important additional resource in treating patients. A respectful and collaborative approach to care may truly help patients.
Dr. Schettler reports being a statistical analysis consultant to LivaNova. Dr. Nettles reports participation in the Novartis Employees Retirement Fund, being a consultant to Wolf Greenfield—Boston Drug Discovery IP, and serving as an expert witness. Dr. Rapaport, Ms. Larson, Mr. Carroll, Ms. Sharenko, and Dr. Kinkead report no financial relationships with commercial interests.

IMAGES
VIDEO
COMMENTS
Massage therapy is one of the most effective and widely used alternative therapies. Although most massage therapy sessions are for pain, recent research suggests that it is effective for other conditions including growth of premature infants, ADHD, depression, and immune conditions, most especially cancer (see Field, Diego, &; Hernandez-Reif, 2007 for a review). 1 In this paper recent data are ...
This analysis was designed to contribute to the field in the following ways: (a) begin to more clearly define concepts of massage therapy and function as it relates to pain and other clinical outcomes in order to guide future research; (b) determine the efficacy of massage therapy for treating individuals who would typically visit their general ...
Since a rather extensive massage therapy research review by Field was published in 2014, a significant literature has amassed on massage therapy effects on a variety of conditions that are reviewed here [].Empirical studies, systematic reviews and meta-analyses on massage therapy effects were found on a Pubmed search for the years 2013-2016.
Research article. The effect of therapeutic massage on patients with obesity: A systematic review and meta-analysis. Author links open overlay panel Zhengri Cong a 1, ... Compared with conventional therapy, massage therapy were more effective, mainly in terms of (1) weight [mean difference (MD) = -3.71, 95%CI = −6.51,-0.88]; (2) body mass ...
We have conducted several studies showing that massage therapy by a therapist and by significant others reduces prenatal depression and in turn increases gestational age and birthweight (see Field 2014 for a review) [1]. In a recent study, massage therapy was compared to yoga, with yoga being considered a form of self-massage [3].
Massage Therapy Journal. AMTA's award-winning publication focuses on massage therapy techniques and research, practical self-care tips, and business practices. Each issue of Massage Therapy Journal features research-based articles on the practice of massage to provide you the most up-to-date information to help serve your clients.
Massage therapy may provide short-term benefits for neck or shoulder pain. What Does the Research Show? A 2016 review of four randomized controlled trials found that massage therapy may provide short-term benefits from neck pain. However, a 2012 Cochrane review of 15 trials on massage therapy for neck pain concluded that no recommendations for practice can be made at this time because the ...
named COVID-19 (coronavirus disease 2019) by the World Health Organization (WHO). Tuina (massage) therapy is 1 of the widely employed complementary and alternative medicine interventions in the world. As a useful therapy implemented on human's skin, muscles and joints, tuina (massage) has unique advantages in the field of medicine. This systematic review and meta-analysis will summarize the ...
A meta-analysis of massage therapy research. Psychol Bull 2004; 130: 3-18. Article Google Scholar Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Rompay MV et al. Trends in alternative ...
The large majority of touch interventions comprised massage therapy in adults and kangaroo care ... Rounds, J. & Hannum, J. W. A meta-analysis of massage therapy research. Psychol. Bull. 130, 3 ...
The first massage therapy research agenda was developed by the MTF in 1991 and outlined five key goals: 1) Build a research infrastructure within the massage therapy profession; 2) Fund research into the safety and efficacy of massage therapy; 3) Fund studies on physiological and other mechanisms by which massage therapy achieves its effects; 4 ...
Objective: To summarize the current evidence on the effects and safety of massage therapy for the treatment of ADHD in children and adolescents. Method: A systematic review of 8 randomized controlled trials (RCTs) and 3 case series studies was conducted with a meta-analysis of 4 of the RCTs. Results: Pooled analysis showed that massage produced more improvement in ADHD symptoms in terms of ...
Since a rather extensive massage therapy research review by Field was published in 2014, a significant literature has amassed on massage therapy effects on a variety of conditions that are reviewed here [1].Empirical studies, systematic reviews and meta-analyses on massage therapy effects were found on a Pubmed search for the years 2013-2016.
Massage was more effective than simple-touch for immediate pain relief and mood shifts. Similar data have been reported for breast cancer patients [38]. A review of 19 empirical studies and 8 review articles confirmed these data [39]. According to these authors, 73% of cancer patients use massage therapy in the U.S.
The Value of Massage Research. Research is essential to verify the many benefits of massage therapy. A growing body of research supports massage therapy for health and wellness. Use research to explain the health benefits of massage to your clients and reference our research on the profession's growth in business planning.
Consumer Views & Use of Massage Therapy; The Value of Massage Research; Publications & Research Overview; Massage Therapy Journal . Our award-winning magazine features compelling articles on massage techniques, the science of how massage can help for client conditions, business guidance, self-care tips and more. Explore Massage Therapy Journal
3.1. The Effect of Massage Therapy on Motor Abilities. The effects of massage therapy on motor abilities are presented in Table 1, in which 73 studies were included. Force, strength, speed, endurance, and flexibility are the main motor abilities that were examined in the reported research.
K. A. Kokushkin's 38 research works with 17 citations and 1,190 reads, including: Clinical and economic assessment of feasibility of using quadritherapy in patients with reduced ejection fraction ...
Massage therapy has been notably effective in preventing prematurity, enhancing growth of infants, increasing attentiveness, decreasing depression and aggression, alleviating motor problems, reducing pain, and enhancing immune function. This review covers massage therapy research from the last decade, as an update to the American Psychologist ...
The effects of various modes of low-intensity laser exposure on the sera of healthy subjects and patients are studied. It is shown by the cuneiform dehydration method that the serum structure is liable to change in response to certain modes of low-intensity laser exposure. The structure of patients' sera is more sensitive to low-intensity laser exposure.
In 2015, research estimates that massage therapy was a $12.1 billion industry. All but six states require massage therapists to be licensed, and licensure requires the applicant to receive training at an accredited school, and to pass a comprehensive exam. Those states that require licensure also typically require continuing education in ...
Alla Kholmogorova currently works at the Moscow State University of Psychology and Education (dean of the faculty of Counseling and Clinical Psychology). Alla does research in Health Psychology ...
Massage was used by 5.2% of those with anxiety, making it the fourth most commonly used CAM therapy for this problem, after relaxation, imagery, and spiritual healing . "Anxiety or depression" was the patient's primary complaint in 5% - 9% of consecutive visits to massage therapists in two states [ 6 ].
Biology of Massage. Rigorous study of the biology of therapeutic massage is still in a relatively nascent phase. Although studies have attempted to understand the impact of various forms of massage on the body since the early 1990s, the research has been fraught with problems, in particular a lack of consistent funding for investigation of the biological effects of massage.
THERAPY INTERVENTIONS A 2-Day Master Class September 22 and 23, 2018 Presented by: Joan Farrell, PhD. & Ida Shaw, MA. Potential audience: people who had basic schema-therapy training and already actively practicing individual therapy sessions. Day 1 will focus on the conceptualization of impasses with client and therapist during therapy
This article reviews the role of massage therapy in the treatment of common psychiatric disorders and briefly discusses the prevalence and popularity of complementary and integrative treatments in the general population and touches on the literature on the biology and neurobiology of massage therapy. Keywords: anxiety, depression, complementary ...