Government of Nepal
Ministry of health and population.
- Department of Health Services
- Organization Structure & DoHS Staff Profile
- NTD & Vector Born Disease Control Section
- Zoontic & Other Infectious Disease Control Section
- Disease Surveillance and Research Section
- Epidemiology & Epidemic Management Section
- NCD and Mental Health Section
- Leprosy Control and Disability Management Section
- Child Health and Immunization Section
- Maternal and Newborn Health Section
- Family Planning and Reproductive Health Section
- Nutrition Section
- Hospital Services Monitoring and Strengthening Section
- Basic & Emergency Management Section
- IENT and Oral Health Section
- Nursing Capacity Building Section
- Geriatric and Gender-violence Management Section
- Social Health Security Section
- Integrated Health Information Management Section
- Infrastructure Development Section
- Environment Health and Health Care Waste Management Section
- Logistic Management Section

HIV/AIDS and STI
- National Health Training Center
- National Public Health Laboratory
- National Health Education Information and Communication Center
- National Tuberculosis Control Center
- Integrated Health Information Management System
- Health Sector Information System
- Geographic Information System(GIS)
- Administration section
- Financial Administration Section
- Forms/Formats
- General Notice
- Public Health Facilities
- Non-Public/NGO Health Facilities
- Nursing Homes
- Medical Colleges
- Departments
- INGO/ NGO/ Donor Agencies
- Act/Regulations
- Plan/Policies
- धरौटी फिर्ता लिन आउने सम्वन्धी सुचना
- Annual Health Report 2079-80
- स्तरवृद्धि सम्बन्धि सूचना (स्तरवृद्धि पत्रहरु )
- स्तरवृद्धि सम्बन्धि सूचना
- HMIS बुलेटिन प्रकाशन सम्बन्धमा
- स्तरवृद्धि सम्बन्धि सूचना (स्तरवृद्धिपत्र नर्सिङ तर्फको)
- स्तरवृद्धि सम्बन्धि सूचना (स्तरवृद्धिपत्र पा.मे. तर्फको)
- स्तरवृद्धि सम्बन्धि सूचना (नर्सिङ- छैठौ र सातौ)
- स्तरवृद्धि सम्बन्धि सूचना (नर्सिङ)
Nepal’s response against HIV/AIDS begun with the launching of first National AIDS Prevention and Control Program in 1988. National HIV/AIDS Policy with 12 key policy statements and supportive structures like National AIDS Coordination Committee (NACC) and District AIDS coordination Committee to guide and coordinate the response at central and district level was endorsed in 1995.As directed by the National HIV/AIDS Policy, a multi-sector National AIDS Coordinating Committee (NACC) chaired by the Minister of Health and Population, members representation from different ministries, civil society, and private sector was established to coordinate, support and monitor the activities implemented through NCASC. Similarly, DACC was established to coordinate and monitor the activities at district level.
In 2002 a National AIDS Council (NAC) was established, chaired by the Prime Minister, to raise the profile of HIV/AIDS. The NAC was intended to set overall policy, lead high level advocacy, and provide overall guidance and direction to the national response to AIDS in Nepal. The latest national policy on HIV and AIDS (2010) have envisioned a more concrete policy framework for making AIDS free society with the overall policy aim of reducing impact of HIV among people by reducing new HIV infections.
Recently Nepal has expressed its high level political commitment to Political Declaration on HIV/AIDS: Intensifying our Efforts to Eliminate HIV/AIDS June 2011. The 2011 declaration builds on two previous political declarations: the 2001 Declaration of Commitment on HIV/AIDS and the 2006 Political Declaration on HIV/AIDS. At UNGASS, in 2001, Member States unanimously adopted the Declaration of Commitment on HIV/AIDS. This declaration reflected global consensus on a comprehensive framework to achieve Millennium Development Goal Six-: halting and beginning to reverse the HIV epidemic by 2015. Thus, to ensure the effective response to the HIV epidemic in Nepal and so to fulfil the accountability of the response, Nepal has already implemented three rounds national HIV/AIDS strategic plan. The recent National HIV/AIDS Strategy 2011-2016 has laid a concrete road map in planning, programming and reviewing of the national response to the epidemic.
Vision Nepal will become a place where new HIV infection are rare and when they do occur, every person will have access to high quality, life extending care without any form of discrimination.
To achieve universal access to HIV prevention, treatment, care and support.
- Reduce new HIV infections by 50 percent by 2016, compared to 2010;
- Reduce HIV-related deaths by 25 percent by 2016 (compared with a 2010 baseline) through universal access on treatment and care services; and
- Reduce new HIV infections in children by 90 percent by 2016 (compared with a 2010 baseline)
- Publications

New Life Center - HIV/AIDS
The new life center was created in 2006 and focused on pediatric hiv/aids until 2023. mother-to-child hiv transmission rates have plummeted in nepal, meaning the number of children requiring specialized care has also declined. this has enabled nyf to open this beautiful facility to a wider population of children, expanding the nlc’s mission effective in 2023 (read more on our new life center – medical recovery home page)., the services described below are still available for families in need of them. medical support is offered at the new life center. hiv/aids awareness & advocacy programming has now been absorbed into the work done through the nutritional rehabilitation home..
The New Life Center (NLC) is a residential health center which between 2006 and 2023 provided specialized, supportive care to Nepali children (age 0 to 14) living with HIV/AIDS.
These young patients and their caregivers stay here for months at a time, free of charge, receiving specialized medical and nutritional support, psychological counseling, tutoring services, cultural celebrations, and more – until they are healthy enough to return home. Caregivers of these children receive vital information on hygienic practices, nutrition, and the effective management of HIV/AIDS, plus counseling services in partnership with Ankur Counseling Center .
After discharge, families unable to access the free antiretroviral medicine provided by the Nepali government benefit from delivery services by NLC staff.

New Life Center nurses (in white) and two patient families pose in front of our beautiful facility at discharge. The New Life Center is located in Lalitpur, just outside of Kathmandu. Stigma against HIV is so great in Nepal that we can't show our patients' faces - but these moms are tremendously relieved to know the New Life Center is here to support them in managing their children's HIV.
How We Work
Because children’s immune systems are not fully developed, children living with HIV get much sicker than adults–and they do so more often as well. These children are exposed to all the same illnesses as other children, but even when their HIV is well-managed, their weakened immune systems struggle to fight effectively against common ailments like the flu, the common cold, urinary tract infections, and more. Tuberculosis and pneumonia are special dangers for Nepali children living with HIV.
The New Life Center provides these children with the support they need to survive and thrive with HIV.
Capable of treating up to 18 child-mother pairs on-site at a time, the NLC was built to provide holistic residential care to between 50 and 60 children living with HIV each year (often alongside their mothers, who are often also living with HIV).
Our NLC team helps children recover from illnesses, keep current on their medication, and perfect their HIV management practices at home. When an NLC child turns 15 (old enough for adult services), NYF matches them with their local HIV resources for adults, ensuring a smooth transition with no gaps in care.
Staff members include cooks, nurses, a nutritionist, a driver, and more, with hospital-based pediatricians visiting at least once a month.

New Life Center nurses (in white coats) administer medicine to several children receiving care for HIV - as well as their mothers, also living with HIV. Stigma around HIV is so strong in Nepal that NYF must obscure the faces of these individuals, but here at the New Life Center, everyone is treated like family.
Beginning in 2022, in response to lessons learned during the COVID-19 pandemic, we expanded our outreach capabilities to provide home-based care options for rural families who are unable to spend months out of the year in Kathmandu Valley. Mothers in need of income generation help became eligible for some of our programs aimed at small business start-ups. (See Vocational Education & Career Counseling .)
HIV/AIDS Awareness & Advocacy
In coordination with our hospital friends and grassroots partners, NYF expanded our HIV/AIDS Awareness efforts in 2022 and 2023. This included a telephone helpline for those hoping to keep their status private, as well as the production and distribution of Nepali-language educational resources for caregivers. Our hope is that by expanding our reach in this way, we can save and enrich many more lives – and help Nepal continue its progress in addressing this global challenge.
We’re proud to have a developed a clear, illustrated Nepali-language HIV/AIDS information and home health guide to help families understand and manage this challenging diagnosis. Copies of this booklet have been distributed to individual families and to local health posts and the offices of other Nepali NGOs working to address HIV in their communities. (You can download the booklet below or view it as Flipbook on our website).
Our team released two radio public service announcements, each recorded in Nepali and the Bhojpuri language. For one year, these brief clips played several times a day (including prime time) through the Ujjyalo Network—a nationwide network of FM radio stations throughout Nepal, with millions of listeners a day. FM radio is the most popular information source in Nepal, reaching rural and urban listeners alike.
The sound files below include translations into English of the important information shared over Nepal’s radio waves to challenge social stigmas, prevent further spread, and empower individuals living with HIV to access important health resources.
HIV/AIDS Awareness Campaign Booklet
Radio Announcement #1
Radio Announcement #2
Pediatric hiv in nepal.
People living with HIV/AIDS in Nepal face social isolation, medical neglect, and physical and emotional abandonment. Though the Nepali government offers HIV medication and other treatment programs free of charge, these services are difficult to access for patients in remote villages. Some hospitals still refuse care to affected people.
Many children are only diagnosed after their fathers, and sometimes both parents, have died of the disease. Tragically, low diagnosis rates have resulted in some mothers unknowingly passing the virus to multiple children. These children are at extremely high risk. HIV/AIDS is one of the most stigmatized illnesses in Nepal. Schools shut their doors. Non-infected children won’t play with them, and they’re banned from village activities. As kids living with HIV/AIDS become desperately sick with opportunistic diseases and feel brutally ostracized, their quality of life plummets.

A group of children enjoy a sunny afternoon on a balcony area at the New Life Center. Times like this - coloring and enjoying the simple medicine of sunshine and good company - help these kids feel less alone, and more like children.
Problems related specifically to HIV/AIDS in Nepal – in particular where children are concerned – include:
- Scarce specialized programs for people living with HIV/AIDS
- Limited access to available programs and resources, particularly for families in geographically remote villages
- Cultural stigma and superstition around HIV/AIDS status
- Low and late diagnosis rates, especially for rural communities
- Parental death leaving behind orphan children unable to access care
- Large families prioritizing uninfected children
- Necessarily-long hospital stays for children receiving care
- Endemic malnutrition throughout the country
NYF works closely with many other local organizations serving communities living with HIV to respond to these problems as effectively as possible.

The New Life Center is located in Kathmandu Valley, next to NYF's flagship Nutritional Rehabilitation Home. Here, our incredible team (pictured above) ensures families living with HIV are safe, nurtured, and supported in their journeys of becoming.
Fortunately, facilities and programs like those offered through the New Life Center and our community partners empower children and families to harness their potential and live full, rich, joyful lives. Building on a strong foundation of nutritional care, attention to a medical routine, and psychological counseling, the New Life Center helps children and families regain control of their health and chase their dreams.
Related Articles

An Expanded Mission for the New Life Center
An expanded mission for the New Life Center (NLC) began effective July 2023, thanks to tremendous progress made in Nepal’s […]

AIDS Awareness Month & NYF’s New Life Center
AIDS Awareness Month AIDS Awareness Month occurs each October. This is an opportunity to share science-based, factual, and clear information […]

Updates from NYF President Som Paneru
Dear NYF Community, I hope you are all continuing to stay safe and healthy. Earlier this month, the Nepal government […]
HIV/AIDS prevention in the Nepalese context
Affiliation.
- 1 University of Southern California, CA, USA.
- PMID: 18349353
- DOI: 10.1177/0163278708315924
With their numbers now approaching almost 30 million, Nepalese feature importantly in the South Asian demography. Yet, it has been only 60 years since Nepal gained international recognition as a nation-state. Nepal at present is one of the world's poorest countries and is in dire need of development, especially in the area of health. Given the current civil instability coupled with rapid modernization, the health and well-being of the Nepalese people have been increasingly affected by newer threats, such as HIV/AIDS. The present study discusses the uniqueness of the Nepalese context in relation to HIV/AIDS prevention. The authors suggest that HIV/AIDS prevention programs in Nepal should now focus more on adolescents from rural regions. The authors also suggest the ways one may approach the task of developing a prevention program targeting rural youths.
- Adolescent Behavior
- Communication Barriers
- Cultural Characteristics
- HIV Infections / ethnology*
- HIV Infections / prevention & control*
- Health Promotion / organization & administration*
- Nepal / epidemiology
- Residence Characteristics
- Sexual Behavior / ethnology
- Socioeconomic Factors
- Understanding The HIV Epidemic
At a glance: HIV in Nepal
A regional leader on sexual and gender minority rights
Key statistics: 2021
- 30,000 people with HIV
- 0.1% adult HIV prevalence
- <1,000 new HIV infections
- <1,000 AIDS-related deaths
- 22,000 people on antiretroviral treatment
Progress towards targets
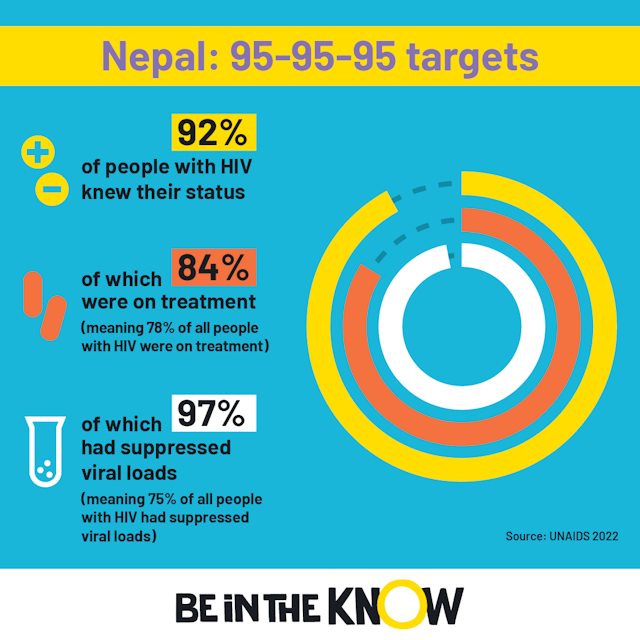
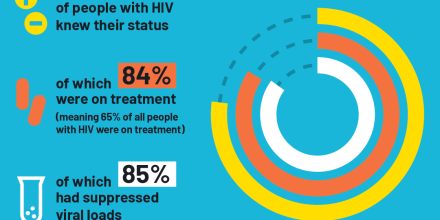
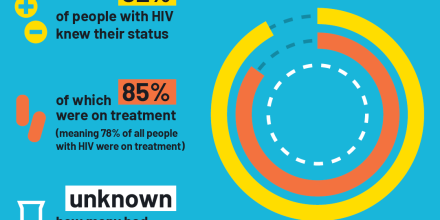
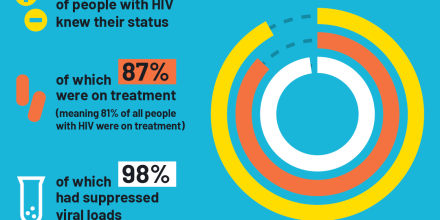
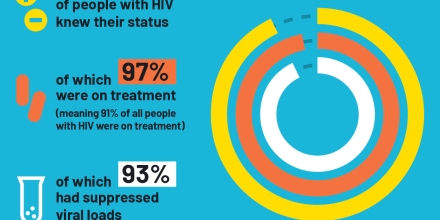
The current targets for HIV testing and treatment are called the 95-95-95 targets and must be reached by 2025 in order to end AIDS by 2030.
In 2021 in Nepal:
Did you know?
Community and home-based care programmes run by and for people with HIV are playing a key role in addressing access to treatment, and have been very effective at keeping people in care.
Preventing HIV in Nepal focuses on:
- prevention of mother-to-child transmission (PMTCT)
- harm reduction (needle and syringe programmes and opioid agonist therapy)
- comprehensive sexuality education in secondary schools
- condom distribution
- PrEP (small-scale pilot)
- behaviour change communication.
Nepal has scaled up PMTCT services in recent years. In 2021, around 70% of pregnant women were offered an HIV test, and only 83% of pregnant women diagnosed with HIV were on treatment.
Testing for HIV is:
- available in HIV testing clinics, HIV care clinics, mobile facilities, antenatal care and labour rooms, opioid agonist therapy sites, tuberculosis clinics and private clinics
- encouraged for the partners and children of people newly diagnosed with HIV (called index testing)
- can be carried out by trained peer providers in community settings
- linked to HIV prevention services (for people who test negative)
- linked to HIV treatment services, with immediate treatment is available.
Nepal focuses its testing programme on communities most affected by HIV. As part of this, mobile testing units staffed by healthcare workers and peers go to nightclubs and bars, neighbourhoods where people sell sex, remote birthing sites, injecting dens, and areas where high numbers of male labour migrants and their partners live and work.
Treatment for HIV is:
- available immediately after diagnosis
- provided as part of a ‘one-stop shop’ approach, alongside services for sexually transmitted infections and tuberculosis
- monitored by viral load testing, although this is not available everywhere
- available in most health facilities
- includes home-based or community-based adherence support for individuals, or as part of an adherence support group.
AIDS-related deaths are declining fast in Nepal, falling by 65% since 2010.
Local context
Nepal’s HV epidemic used to be driven by injecting drug use , but now the main way HIV spreads is through sex. But people who inject drugs are still one of the population groups most affected by HIV in Nepal. The other groups most at risk are migrant workers, transgender people , sex workers , prisoners , young people , men who have sex with men and military personnel. Half of all HIV infections occur among sex workers (4.8%), their clients (36.7%) and migrant workers (7.2%).
Men are disproportionately affected: 60% of people with HIV in Nepal are male. This is due to high HIV prevalence rates among the male clients of sex workers, people who inject drugs and migrant labourers. Men are also more likely to die from an AIDS-related illness than women.
HIV prevalence varies across the country. The Kathmandu Valley, the highway districts and the far-western development region are home to the greatest number of people with HIV. These areas are highly populated and home to large migrant populations. Community-based organisations and networks led by people with HIV can be found across the country and are involved in supporting HIV treatment and care, as well as overall wellbeing, for almost 17,000 people.
Late diagnosis is a problem in Nepal – around one third of people are diagnosed with HIV after it has already progressed to AIDS.
HIV-related stigma is also an issue. The most recent data (2016) suggests around one-third of Nepalese people hold discriminatory attitudes towards people with HIV. In recent years, Nepal has made reducing stigma and discrimination against people with HIV a priority of its HIV response.
Nepal was the first Asian country to identify the existence of ‘gender and sexual minorities’ in its constitution. Same-sex acts are legal. Abortion is legal, but it must be carried out in the first 12 weeks of pregnancy.
Nepal has a national strategy to address gender-based violence and violence against women, including women with HIV. The country also provides HIV and sexuality education in secondary schools. And it has recently changed laws and policies so that adolescents can access HIV testing and other HIV services more easily. All of these factors have aided the response to the HIV epidemic in the country.
Nepal’s National HIV Strategic Plan 2016-2021 aimed to reach UNAIDS’ targets through a rights-based and decentralised HIV programme. Every year, around three-quarters of funding for its HIV response goes towards reaching key populations with HIV prevention; targeted HIV testing to find people with HIV who are not diagnosed, and ensuring people are linked to testing and treatment.
Nepal’s HIV programme remains heavily dependent on international assistance – donors provide seven times more investment in the country’s HIV response than the Nepalese Government.
Get the latest news
Keep up-to-date with new developments, research breakthroughs and evidence for what works in sexual health and the HIV response, with our news service.
Explore more

At a glance: HIV in Bangladesh
At a glance: HIV in India
At a glance: HIV in Kenya
At a glance: HIV in Lesotho
At a glance: HIV in Malawi
Still can't find what you're looking for, share this page.
- Last updated: 31 March 2023
- Last full review: 01 March 2022
- Next full review: 01 March 2025
HIV/AIDS in Nepal
Context, Current Situation, Response
Cite this chapter
- Ganesh Gurung 4 &
- B. K. Suvedi 5
151 Accesses
Nepal is one of the least developed countries in Asia, having a population of 23.1 million with an annual growth rate of 2.2% (CBS, 2001). Even though Nepal allocates five to six percent of its total national budget to the health sector every year, indicators demonstrate the relatively poor health of the Nepali population. The infant mortality rate is as high as 64.2 deaths/1000 live births, and the maternal mortality rate is 415/100,000. In addition, the fertility rate is 4.1%, with the contraceptiveusing rate being 39.3%; the average life expectancy is 61.9 years (NPC/CBS, 2001).
This is a preview of subscription content, log in via an institution to check access.

Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Unable to display preview. Download preview PDF.
AIDS Program Effort Index (API). (2003). USAID, UN-AIDS, WHO, and the Policy Project. ( December 2003 ).
Google Scholar
Central Bureau of Statistics (CBS). (2001). Population Census of 2001. In Collaboration with United Nations Population Fund (UNFPA). Kathmandu.
Dixit, H. (1999). The Quest for Health . Educational Enterprise Ltd, Kathmandu.
Ministry of Health (MoH). (2002a). Annual Report of Department of Health Services, Nepal. Kathmandu.
Ministry of Health (MoH). (2002b). Nepal Demographic and Health Survey 2001. Department of Health Services, Family Health Division. (unpublished)
Ministry of Health, Nepal (MoH) and National Centre for HIV/AIDS and STDs (NCASC). (2002). National HIV/AIDS Strategy (2002–2006). Kathmandu.
Ministry of Health, Nepal (MoH) and National Centre for HIV/AIDS and STDs (NCASC). (2003). National Operational Plan for HIV/AIDS Control (20032004). Kathmandu.
National Planning Commission (NPC)/ Central Bereau of Statististic (CBS). (2001). Stastistical Year Book of Nepal. Kathmandu.
Poudel, K.C., Okulura, J., Wasai, M., Sherchand, J.B., Zimba, M., Murakami, M. (2001). HIV/STI Survey in Nepal, Preliminary Findings. Kathmandu. (unpublished paper).
Suvedi, B.K. (1990). On the Road to Primary Health Care: Health Aspects of Baitadi. Kathmandu. (unpublished paper).
Suvedi, B.K. (1994). HIV/AIDS Manual. STD/AIDS Counseling and Training Services. Kathmandu.
Suvedi, B.K. (1997). Mapping the Trend of HIV/AIDS in Nepal. J Nepal Med Assoc . Kathmandu.
Suvedi, B.K., Gurubacharya, V.L. (1992). Sexual behavior patterns in Nepal. J. Inst. Med . 14(4): 298305.
Suvedi, B.K., Gurubacharya, V.L. and Thapa, K. (1994). Seasonal Migration in Western Nepal and its Relation to HIV Transmission. J Nepal Med Assoc . Kathmandu.
New ERA and STD/AIDS Counselling and Framing Series (SACTS). (2002). HIV/STD Prevalence and Risk Factors Among Migrants and Non Migrant Males of Achham District of Far Western Nepal. Family Health International Nepal. Kathmandu.
UNAIDS and National Centre for AIDS and STD Control (NCASC). (2003). The HIV/AIDS/STD Situation and National Response in Nepal: A Profile. Kathmandu.
Download references
Author information
Authors and affiliations.
Nepal Institute of Development Studies, Kathmandu, Nepal
Ganesh Gurung
Ministry of Health, Kathmandu, Nepal
B. K. Suvedi
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Harvard AIDS Institute, Harvard School of Public Health, Boston, Massachusetts, USA
Yichen Lu PhD ( Principal Research Scientist, Special Professor ) & Ellen Stiefvater MPP ( Principal Research Scientist, Special Professor ) &
Nankai University, Tianjin, China
Yichen Lu PhD ( Principal Research Scientist, Special Professor ) ( Principal Research Scientist, Special Professor )
Harvard AIDS Institute, Department of Immunology and Infectious Diseases, Harvard School of Public Health, Boston, Massachusetts, USA
Max Essex DVM, PhD ( Chairman, Mary Woodard Lasker Professor of Health Sciences ) ( Chairman, Mary Woodard Lasker Professor of Health Sciences )
Rights and permissions
Reprints and permissions
Copyright information
© 2004 Springer Science+Business Media New York
About this chapter
Gurung, G., Suvedi, B.K. (2004). HIV/AIDS in Nepal. In: Lu, Y., Essex, M., Stiefvater, E. (eds) AIDS in Asia. Springer, Boston, MA. https://doi.org/10.1007/978-0-306-48536-7_10
Download citation
DOI : https://doi.org/10.1007/978-0-306-48536-7_10
Publisher Name : Springer, Boston, MA
Print ISBN : 978-1-4419-3452-9
Online ISBN : 978-0-306-48536-7
eBook Packages : Springer Book Archive
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Perceived social support, hope, and quality of life of persons living with HIV/AIDS: a case study from Nepal

2010, Quality of Life Research
Purpose This study investigates the relationship among perceived satisfaction from social support, hope, and QOL of PLWHA. Method A cross-sectional in design was applied, among a sample of 160 HIV-infected persons receiving treatment, care, and support from eight community-based NGOs. QOL was assessed using the WHO (QOL)-26 tool, and social support was assessed by use of a modified Sarason’s Social Support Questionnaire. A Hope Assessment Scale was also developed. Results The non-family support network was greater than family support network. Overall satisfaction from social support and hope was significantly correlated with QOL; the greatest effect of social support was on environmental functioning, and the lowest was on social relationships, emotional support was less a predictor of social relationship than other types of supports. Conclusion The effect of perceived satisfaction from social support was through the mediation variable hope. As it has widely been recognized that community-based support is vital for issues of quality of life, strategies to improve social support and hope intervention programs are strongly encouraged. The results of the study have implications for providing care, treatment, and psycho-social support to maintain or enhance quality of life of PLWHA.
Related Papers
Nimona Shaka
People living with HIV/AIDS (PLWHA) report feelings of self-doubt, self-consciousness, and negative interpersonal interactions, and feelings of hopelessness and despair related to their illness. Understanding about the social support available and received by PLWHA is important as it impacts their psychological well being. In-depth interviews were carried out with PLWHA receiving treatment and support from a Charity organisation at Fitchewereda. Fitcheis in Oromia region, Ethiopia. Participant recruitment was terminated when saturation of themes was obtained in qualitative interviews, totaling 12 participants. Acceptance of HIV status was difficult. A majority chose to seclude themselves and not face discrimination and a similar number were thinking others are discriminating them because of their HIV status. So self-stigma was also affecting psychological wellbeing more than experience of stigma. Being a member of the charity organisation and getting support from that organisation a...
AIDS and Behavior
Susan McHale
Social support (SS) plays a key role for HIV/ AIDS prevention and disease management. Numerous gen-eral and disease-specific SS instruments have been developed and perception of support has been increasingly considered, though no scales have been specifically developed to measure perceived social support (PSS) in HIV/AIDS. To help fill this gap a 12-item scale was developed. The study comprised 406 (HIV(?) and HIV(-)) participants from Chile and the UK. A principal component factor analysis yielded three factors explaining 77.0 % of the total variance: Belonging, Esteem and Self-development with Cronbach a of 0.759, 0.882 and 0.927 respectively and 0.893 on the full scale. The PSS-HIV is brief, easy-to-apply, available in English and Spanish and evaluates the perception of supportive social interactions. Further research is needed to corroborate its capacity to detect
Sexuality and Disability
Sevban Arslan
Behailu Tariku
Background Globally, millions of people are affected by human immunodeficiency virus (HIV). Acquired immunodeficiency was linked with psychosocial problems, whereby stigma and discrimination are the most common. Therefore, this study was aimed at assessing the level of the social support problem in people living with human immunodeficiency virus (PLHIV) and factors associated with it at selected hospitals of North Shewa Zone, Amhara Region, Ethiopia. Method An institution-based cross-sectional study design was employed. A total of 422 PLHIV were involved in the study. A multidimensional perceived social support scale (MPSSS) for the measurement of social support problems was implemented. Systematic random sampling was used to recruit the study population after selecting study areas by lottery methods. Multivariate logistic regression analyses were performed via SPSS software. The statistical association was declared at a p value of less than 0.05 in the final model. Result The preva...
DOAJ (DOAJ: Directory of Open Access Journals)
Dipendra Khatiwada
Journal of AIDS & Clinical Research
Mohammad Amin Wani
International Journal of STD and AIDS
Karen Angulo
Aids Care-psychological and Socio-medical Aspects of Aids/hiv
Keiko Nanishi
RELATED PAPERS
Kieler Notizen zur Pflanzenkunde
Jürgen Hebbel
Academic Pediatrics
Thaiane Defalco
SSRN Electronic Journal
anita bocker
PAINEL 20: "Reparações históricas e a desmontagem do passado colonial", Vítor de Sousa/Sheila Khan
Vitor de Sousa
Journal of the American Chemical Society
Ralph Connor
International Journal of Science and Engineering Invention
aekram faisal
Studies in Business and Economics
Abdulrasaki Saka
Tourism Economics
Michał Rudnicki
Jenna Valdez
Maria Antònia Font Fernández
Nuclear Fusion
Young-soon Bae
Journal of the science of food and agriculture
Tim Goulette
Applied Ecology and Environmental Research
Oğuzhan Yanar
International Journal of Biosciences (IJB)
SHAH FAISAL
Emblemas - Revista do Departamento de História e Ciências Sociais - UFG/CAC
Sandra Dantas
European Journal of Medicinal Chemistry
Bharat Dond
New Journal of Chemistry
Eugeniya V Nikitina
Filologia modernă: realizări şi perspective în context european
Ion Barbuta
Publizistik
Esteban Lopez-Escobar
Revista Conexões de Saberes
DALILA XAVIER DE FRANCA
International Journal of Pharmaceutics
Rosa Piedade
The Journal of rheumatology
Ganesh Raghu
Journal of Clinical Psychopharmacology
Carole Martin
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Nepal J Epidemiol
- v.5(3); 2015 Sep
Economic Burden of HIV/AIDS Upon Households in Nepal: A Critical Review
Ak narayan poudel.
1 Post-doctoral Internship Fellow, Centre for Public Health, Liverpool John Moores University, United Kingdom
David Newlands
2 Senior Lecturer, Institute for International Health & Development, Queen Margret University, United Kingdom.
Padam Simkhada
3 Professor, Centre for Public Health, Liverpool John Moores University, United Kingdom
Thousands of people are infected with HIV/AIDS in Nepal and most of them are adults of working age. Therefore, HIV/AIDS is a big burden in Nepal. This review was conducted to find the existing knowledge gap about the economic burden of HIV/AIDS at the household level in Nepal, the extent of economic burden exerted by the disease, and to provide policy recommendations. It is concluded that there was a considerable knowledge gap about the issue, and the economic burden exerted by HIV/AIDS was big enough to push the affected households into poverty. It is suggested that more studies need to be conducted to fill the knowledge gap. Similarly, Government of Nepal and other organisations working in the field of HIV/AIDS need to provide economic supports (e.g.- support for travel costs) to the HIV positive people and need to increase the awareness level among general population for reducing stigma and discrimination, and reducing economic burden on them.
Introduction
Economic burden of hiv/aids.
Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome (HIV/AIDS) has health, economic and social consequences. HIV/AIDS causes health consequences resulting to the morbidity and mortality of infected people [ 1 , 2 ]. People with advanced HIV status are vulnerable to infections and malignancies, due to their poor immune system, called ‘opportunistic infections’. Many of the opportunistic infections occur during the advanced condition of HIV and can be fatal [ 3 ]. Increased adult morbidity and mortality due to HIV/AIDS are likely to have important consequences for households, communities and health systems [ 4 ]. The death of a HIV positive individual results in a permanent loss of income from less labour on the farm, lower remittances from jobs, costs associated with the funeral and mourning, and a possible removal of children from school in order to save on educational expenses and to increase household labour and income, resulting in a severe loss of future earning potential for the family [ 5 ]. Therefore, the health consequences of HIV/AIDS have an economic impact on the household.
The HIV/AIDS-affected households need to pay a substantial amount of money for the care and treatment of their ill family members [ 6 ]. The disease affects the earning capacity of the person and other members of the households too. The HIV positive person may be very weak and may be absent from work or may lose their job due to the illness [ 7 ]. The working time of household members may be shifted from productive activities to the care of the sick family members, and thus household income declines further [ 8 ]. Thus, the economic consequences can be divided into- direct costs, productivity costs and other hidden costs (e.g. – loss of income).
HIV/AIDS exerts social impacts and consequences too. HIV/AIDS is perhaps the most stigmatized disease in the world [ 9 ]. The disease is more prevalent in female sex workers, the clients of sex workers, injecting drug users and men who have sex with men (MSM) and it is often seen as a disease directly linked with personal behaviour. Therefore, people infected with HIV/AIDS face stigma and discrimination [ 10 ]. Stigma and discrimination in HIV/AIDS may result in either not seeking treatment [ 11 ] or seeking treatment far from the home where the patient is not known by the health care professionals and others [ 12 ]. This behaviour also has economic consequences because not seeking treatment means premature mortality and seeking treatment far from home means increased costs for the HIV-affected household. People living with HIV/AIDS (PLHA) might lose jobs due to stigma and discrimination from employers if known to them [ 13 , 14 ]. Rejection, isolation, less support from family, relatives, neighbours, friends, and community are also another consequence of the stigma and discrimination related to HIV/AIDS [ 13 , 15 ]. Therefore, these social consequences also have an economic impact on the household.
Households use a range of strategies to cope with the burden of illness (for both treatment costs and productivity losses) [ 16 ]. The immediate coping method of illness for those households who have cash or savings is to use the available cash and mobilise savings [ 17 , 18 ]. Another frequently used strategy for those households who do not have cash or savings at all or have an insufficient amount is borrowing from family and friends or taking loan from money lenders, or sale of assets [ 18 ]. The effect of loans on households can be severe. Some studies show that households remain in debt for a considerable time after the illness, which created the debt [ 19 ]. If assets like land and livestock are sold by a poor household, they put the household into a vicious circle of poverty [ 16 ]. Other strategies for dealing with the direct costs of illness include diversifying income by engaging in activities other than their normal work or selling their labour [ 18 ]. In relation to coping with the productivity costs of illness, tasks are re-allocated among household members (intra-household labour substitution), in some cases external labour may be hired to take on the responsibilities of the ill household members, and children may be taken out of school [ 20 ]. Intra-household labour substitution may have adverse consequences particularly when children are removed from school to take on the work activities of a sick parent [ 21 ].
In summary, HIV/AIDS is a disease, which has health, economic and social consequences. Thus, it not only affects the victim, but also affects the households. Morbidity and mortality, income losses (due to direct costs for treatment and reduced productivity), and stigma and discrimination are the health, economic and social consequences of HIV/AIDS respectively. The end impact of all these consequences is ‘economic’. This means that all these consequences affect the income, expenditure and savings of HIV/AIDS affected households. These consequences finally push the HIV/AIDS affected households into poverty, which can be classified as a catastrophic, impoverishing and poverty trap impacts.
Findings of the previous studies are evident that HIV-affected households generate relatively lower household income than HIV-unaffected households [ 22 , 23 ]. HIV-infected people are compelled to stop their employment or business due to their illness [ 7 ]. The burden of treatment is significantly greater in HIV-affected households than HIV-unaffected households. This burden increases as the PLHA decline in health and that produces an even greater impact on the household [ 6 , 23 ] . The households have to spend a higher proportion of their monthly income on the care and support of PLHA [ 24 ]. The long-term treatment for HIV/AIDS can have lifelong financial implications on HIV-affected households [ 25 ].
Health insurance is either unavailable for HIV-infected people in developing countries [ 24 ] or people are not aware of health insurance [ 26 ]. Therefore, out-of-pocket payment for health care is widely used by HIV-affected households in developing countries. In case of Nepal, 81.4 % of total health care costs in 2012 were contributed out-of-pocket from households and the rest of the costs (18.6%) were contributed by the government, private companies and donors [ 27 ]. This also includes the health care of HIV/AIDS in Nepal. Moreover, there is no social security (e.g. - allowances) in Nepal to the PLHA.
HIV/AIDS in Nepal
The first case of HIV/AIDS was reported in 1988 in Nepal. After that the nature of the HIV epidemic has gradually moved from being a ‘low prevalence’ to ‘concentrated epidemic’ [ 28 ]. In 2014, an estimated 39,249 people were living with HIV/AIDS and an estimated 2,576 people died due to the disease. An estimated number of 1,493 people were newly infected by HIV/AIDS and HIV prevalence rate among adult population was 0.02% [ 29 ]. However, the total reported HIV cases were 25,838 as of December 2014. According to the reported cases, 88 % of people living with HIV/AIDS were between the working age of 15-49 years and the majority of them were male (63%) [ 30 ]. The above evidences suggest that HIV/AIDS is a big burden in Nepal because it is concentrated on thousands of working age adults.
Despite considerable efforts from donors, government, non-governmental organisations (NGOs), and international non-governmental organisations (INGOs); people living with HIV/AIDS have to pay a significant amount of money for their treatment and care. PLHA need to pay travel costs, most diagnostic test costs, medicine costs (except ART), lodging and food cost. The government provides only Cluster of Differentiation 4 (CD4) test services and ART medicines free of cost. Wasti et al. reported that PLHA in Nepal faces financial constraints for HIV/AIDS treatment. Their report states that PLHA are facing difficulty to manage out-of-pocket expenses like diagnostic test costs, additional costs incurred through travel, nutritional and other user charges [ 11 ]. Moreover, CD4 count and Facs calibre sites were limited only in 28 treatment centres in Nepal, which compelled PLHA to travel further for CD4 count tests from time to time. Wasti et al. highlighted distance as a major problem because treatment centres were concentrated in urban areas or town centres. PLHA in the rural hill areas are dying without getting treatment because of the lack of travel costs. If the PLHA has to go to Kathmandu for CD4 tests, the travel costs are six times higher than the average daily income of many Nepalese people [ 11 ].
HIV/AIDS is one of the biggest burdens of diseases in Nepal as thousands of adults are affected by it. The disease has multiple consequences (e.g. - health, economic and social). Therefore, it is an important public health issue. However, it was assumed that there were only limited numbers of relevant studies conducted and no one knows how many published or unpublished papers are in Nepal on this issue till date. Moreover, there was no review paper published on this topic which could be useful to the policy makers at the government level and other stakeholders working in the field. Likewise, there was no idea among public health researchers about the existing knowledge gap on economic burden of HIV/AIDS in Nepal.
This review is conducted to find the existing knowledge gap about the economic burden of HIV/AIDS, extent of economic burden exerted by the disease at the household level, and to provide policy recommendation to the Nepalese Government for the welfare of HIV positive people. Therefore, it is believed that the results of the review will be helpful to the public health researchers, policy makers and other stakeholders working in the field of HIV/AIDS in Nepal.
Methodology
This paper is prepared by reviewing published and unpublished literature concerning the economic burden of HIV/AIDS in Nepal. Based on the consequences of HIV/AIDS, the economic burden was sub-divided into five components namely- direct costs, productivity costs, economic consequences of stigma and discrimination related to HIV/AIDS, coping strategies, and catastrophic and impoverishing impacts.
Five different search strategies were used to find the studies related to the economic burden of HIV/AIDS. The first search strategy used in the study was the direct costs for HIV/AIDS in Nepal. The second was studies related to productivity costs and the third one dealt with the economic consequences of stigma and discrimination. The fourth was the coping strategies and the fifth related to the catastrophic and impoverishing impacts due to out-of-pocket payment.
The literature was searched in the Medline (Ovid) search engine by using different search words from the records ranging from 1990 to Week 2 September 2015. But, the search results were limited by full-text and English. However, Google (scholar) search and manual search were also carried out to find the additional studies for review.
The major search words used to search the literature were- “HIV" or "HIV/AIDS" or "human immunodeficiency virus”; “cost$" or "economic burden" or "socioeconomic impact" or "economic impact$"; “expenditure" or "health expenditure" or "economic consequence$"; "financial impact$" or "financial burden" or “productivity loss$" or "productivity cost$" or "morbidity"; "work productivity" or "labour productivity" or "days lost"; “absenteeism" or "presenteeism" or "disability”; “coping strateg$" or "strateg$ to cope" or "coping measure$"; “catastrophic" or "catastrophe" or "impoverishment" or "impoverishing"; “stigma" or "discrimination"; and “Nepal”.
While combining all the relevant search words from the aforementioned search strategies, a total of 42 studies were retrieved from Medline (Ovid); a total of five studies were found from Google scholar, and one study was found from manual search. After checking the relevancy, a total of seven studies were selected for the review.
The inclusion criteria for the literature were – the research which is conducted on HIV/AIDS in Nepal and related to direct costs, productivity costs, economic consequences of stigma and discrimination, coping strategies (financial), catastrophic and impoverishing impacts, the article which full text is available, published after 1990 to Week 2 September 2015, and in English.
The exclusion criteria for the literature were the research articles whose full text were not available, not related to Nepal, not related to the household level of economic burden (or related to the burden at national level), not related to economic consequences of stigma and discrimination, published before 1990, and in other languages than English.
After searching the studies, we synthesised the important information from each study about the research methods, sample size, study location, and main findings. We contrasted and compared these findings based on the similarities, differences and represented critically in this paper.
A total of seven studies were selected based on the criteria set above for the review. Among them, three studies were related to direct costs of HIV/AIDS treatment [ 31-33 ], one of them also touched a little about the productivity costs of HIV/AIDS [ 33 ]. Other four studies were related to the economic consequences of stigma and discrimination associated with HIV/AIDS [ 13-15 , 34 ]. However, there was no study which investigated the coping strategies, catastrophic and impoverishing impacts of HIV/AIDS in Nepal. Details about the results and findings of the review are presented below.
Direct Costs
While looking at the literatures related to direct costs of HIV/AIDS, only three studies were found. Two studies were from published articles [ 31 , 32 ] and one from unpublished MSc thesis [ 33 ]. Puri et al. and Thapa did cross-sectional survey [ 32 , 33 ], but research method is not clear in the study by Pradhan et al. [ 31 ]. Puri et al. conducted studies on nine cities of Nepal about the costs of sexual and reproductive health in 2006 with 1,669 respondents [ 32 ]. Thapa conducted small survey with 50 respondents who came to take anti-retroviral medicine (ART) at Teaching Hospital, Kathmandu in 2007 [ 33 ]. Pradhan et al. calculated costs of care for children affected by HIV/AIDS, but their study is silent about sample size [ 31 ].
Puri et al. reported the out-of-pocket costs for HIV/AIDS treatment for a three month period was only NRs 541 (US$ 7.5) (NRs 180.3/month) [ 32 ]. Thapa found more than double the direct costs to visit treatment centre than reported by Puri et al. [ 32 , 33 ]. She found the direct costs of NRs 404 ($7.27) per visit to get ART medicine [ 33 ]. Considerably lower treatment costs in Puri et al.’s study than Thapa’s study may be due to two reasons- 38 % of respondents in Puri et al.’s study did self-treatment by visiting local pharmacy and they included many cities in their study (geographical variations) [ 32 , 33 ]. However, both of the studies did not include costs for the accompanying person while visiting the treatment centres, only concentrated in the cities and excluded the remote rural parts of the country where the HIV positive people need to pay up to six times of their daily wage for travel costs for their treatment [ 11 ]. Moreover, these studies did not include diagnostic costs while calculating direct costs of treatment [ 33 ]. Unlike the above two studies, a study by Pradhan et al. reported the actual care costs for HIV-affected child per month from societal perspectives- NRs 6,763 (US$ 93.9), NRs 9,269 (US$ 128.7) and NRs 42,602 (US$ 591.7) in community based care, home based care and comprehensive institutional care respectively [ 31 ]. It should be noted that the study by Pradhan et al. is completely different from Puri et al. and Thapa because it employs three different models and the costing was done from societal perspectives [ 31-33 ]. They did not separate costs of HIV/AIDS treatment in their study. Therefore, their findings are not directly comparable to the other two studies, although they are related.
The studies reviewed above shows that there are only a limited number of studies assessing direct costs of HIV/AIDS treatment in Nepal. These studies [ 32 , 33 ] did not include all the costs components for HIV/AIDS treatment and only concentrated in the urban areas. Therefore, if the costs calculations were done properly, the direct costs for HIV/AIDS treatment would have been considerably higher than reported in these studies, although the studies reported the costs which are big enough to push HIV-affected households into poverty.
Productivity Costs
There has been no study to measure the productivity costs of HIV positive people in Nepal. However, Thapa tried to calculate the value of time lost while visiting treatment centres to get ART medicine by HIV positive patients in Kathmandu valley (NRs 105.2 or US$ 1.5 per visit) [ 33 ]. The study did not investigate the actual productivity costs of HIV/AIDS in Nepal. Here, actual productivity costs mean costs incurred due to ill health, which include monetary value of absenteeism and presenteeism caused by HIV/AIDS. Therefore, actual productivity costs due to HIV/AIDS among HIV positive people is still unknown in Nepal.
Economic Consequences of Stigma and Discrimination
As there were no proper studies investigating the economic consequences of stigma and discrimination related to HIV/AIDS in Nepal, all the studies reporting some sorts of economic issues are reviewed in this paper.
There were four studies which touched the economic consequences of stigma and discrimination related to HIV/AIDS in Nepal. Three of the studies were focussed broadly on HIV/AIDS related stigma and discrimination in general [ 13-15 ] but one study was focussed solely on women’s issues related to HIV/AIDS [ 34 ]. FHI [ 34 ] and FHI [ 13 ] conducted interviews with 57 respondents in each study but Rai conducted mixed methods of interviews (with 7 respondents) and literature reviews [ 15 ]. However, Nepal and Ross used secondary data which contained information of 80 individuals and 12 focus groups discussions [ 14 ].
A study by FHI [ 13 ] reported that there was a separation of PLHA from communities and families, loss of employment and restrictions on movement and activities in communities [ 13 ]. Moreover, it was reported that HIV positive women were discriminated greatly compared to men and more often faced permanent loss of family support. FHI [ 34 ] also reported similar findings. According to FHI [ 34 ], HIV positive women were not accepted and supported by their family compared to their husbands who were also HIV positive. Many women faced serious loss of social and economic support from their family and society. They also found that deteriorating economic conditions with women and their children once their husband died [ 34 ]. Similar to these findings, Rai reported that women face a lack of acceptance and support from family members more than their HIV positive husbands. Some PLHA, generally women are forced to leave home after the detection of HIV status. Moreover, most PLHA face the problem of finding work and contributing economically to the household [ 15 ]. Nepal and Ross also reported that PLHA were excluded and rejected from home and society which greatly stressed their economic status [ 14 ]. Similar to findings reported by FHI [ 13 ], they also reported that more than 20 % of PLHA’s employment was affected negatively after the detection of the disease [ 14 ].
The review found that the study findings are very general and not quantified in numbers or figures (e.g. – percentage). Isolation, rejection, exclusion (from job, family or society), less supports were major forms of stigma and discrimination which had economic consequences on PLHA. Although all PLHA were discriminated, it was found that HIV positive women faced more discrimination and less support from their family and society, which makes them more vulnerable. There is also a need of further study which explores the consequences in detail.
Coping Strategies, Catastrophic and Impoverishing Impacts
The literature review concluded that there were no studies relating to the coping strategies (financial) used by HIV/AIDS affected households. Likewise, there were no studies reporting the catastrophic and impoverishing impacts due to HIV/AIDS in Nepal till the date. Therefore, there is a complete knowledge gap in these economic issues.
The review found that there was insufficient research concerning economic burden of HIV/AIDS in Nepal. Three of the studies assessed the direct costs of HIV/AIDS treatment. Nevertheless, these studies did not include all the components of the direct costs and did not cover rural and remote areas of Nepal. There was no study in Nepal which reported the actual productivity costs caused by HIV/AIDS. There were four studies which slightly touched the economic consequences of stigma and discrimination related to HIV/AIDS in Nepal. There were no studies which explored the coping strategies used by HIV/AIDS affected households. Likewise, there was no study which quantified the catastrophic and impoverishing impacts due to HIV/AIDS. Therefore, it is concluded that there was no research which assessed the economic burden of HIV/AIDS in Nepal covering all the cost components and geographical locations. Thus, there is a big knowledge gap about the burden in the Nepalese context and we strongly recommend conducting further studies which can explore all the issues relating to the economic burden of HIV/AIDS in depth covering all geographical locations.
While looking at the extent of economic burden of HIV/AIDS at the household level, it is concluded that the reviewed studies under reported the direct costs as they did not include all the components (e.g. - diagnostic costs, costs for accompanying person) while calculating. They did not calculate the productivity costs (value of absenteeism and presentism due to HIV/AIDS) too in their studies, which also share big proportion of economic burden. Therefore, it was concluded that the economic burden exerted by the disease would have been very high if they calculated the burden by including all the cost items. However, the review findings and available evidences suggest that the economic burden of HIV/AIDS is big enough to push the HIV-affected households into poverty in Nepal.
We cannot recommend many policies from this review as there were limited studies which could not provide sufficient knowledge about the economic burden. However, based on the available studies and evidences, the review concluded that the economic burden of the disease is high at the household level. Therefore, the Government of Nepal and other organisations working in the field of HIV/AIDS need to focus on reducing the economic burden by providing economic supports (e.g. – allowances for treatment costs, support for travel costs) to the PLHA and increasing awareness level of the general people about the HIV/AIDS through trainings and other programmes (like radio programme) for reducing stigma and discrimination, and thus reducing economic burden on them. Moreover, female PLHA need more attention and supports than their male counterparts as they were more discriminated from their family and society.
Limitation of the Paper
This review paper is mainly based on the published studies available online (Ovid-Medline and Google scholar) and very few unpublished studies (available from manual search). There might be other unpublished studies too which we could not manage to find manually and did not include in this study. This might limit the findings of our study.

HIV/AIDS and its possible consequences (Source: Literature reviews)

Flow diagram of the literature selection process for the review study
Pricing depends on the type of task you wish to be completed, the number of pages, and the due date. The longer the due date you put in, the bigger discount you get!
Article Sample
- bee movie script
- hills like white elephants
- rosewood movie
- albert bandura
- young goodman brown
John N. Williams
Testimonials
PenMyPaper: a student-friendly essay writing website
We, at PenMyPaper, are resolute in delivering you professional assistance to write any kind of academic work. Be it marketing, business, or healthcare sector, we can prepare every kind of draft efficiently, meeting all the points of the question brief. Also, we believe in 'research before drafting'. Any work without ample research and evidence will be a flawed one and thus we aim to make your drafts flawless with exclusive data and statistics. With us, you can simply relax while we do the hard work for you.
Diane M. Omalley

Laura V. Svendsen

COMMENTS
प्रत्येक वर्ष 1 दिसम्बरलाई 'विश्व स्वास्थ्य सङ्गठन'ले 'विश्व एड्स दिवस ...
Background. Nepal's response against HIV/AIDS begun with the launching of first National AIDS Prevention and Control Program in 1988. National HIV/AIDS Policy with 12 key policy statements and supportive structures like National AIDS Coordination Committee (NACC) and District AIDS coordination Committee to guide and coordinate the response at central and district level was endorsed in 1995 ...
The Human Immunodeficiency Virus (HIV) infects cells of the immune system, destroying or impairing their function. This leads to progressive deterioration of the immune system, leading to "Acquired Immune Deficiency Syndrome (AIDS)". The immune deficient system can no longer fulfill its role of fighting infection and person starts getting various "opportunistic infections".
The NAC was intended to set overall policy, lead high level advocacy, and provide overall guidance and direction to the national response to AIDS in Nepal. The latest national policy on HIV and AIDS (2010) have envisioned a more concrete policy framework for making AIDS free society with the overall policy aim of reducing impact of HIV among ...
With the objective of providing updated, evidence-based clinical recommendations outlining a public health approach to providing ARV drugs for HIV treatment and prevention in the context of the continuum of HIV care, Ministry of Health and Population, National Center for AIDS & STD Control revised the National ART Guidelines developed in 2012, based on the recommendations adopted to Nepal ...
HIV/AIDS Awareness & Advocacy. In coordination with our hospital friends and grassroots partners, NYF expanded our HIV/AIDS Awareness efforts in 2022 and 2023. This included a telephone helpline for those hoping to keep their status private, as well as the production and distribution of Nepali-language educational resources for caregivers.
This volume examines the meaning and cultural contexts of HIV/AIDS in Nepal, where AIDS is relatively new and rapidly growing. Until now little has been known about how Nepalis understand the illness locally known as "AIDS rog.". This book presents the first long-term field study of the cultural dimensions of HIV/AIDS in South Asia.
6.3.1 Linkages between MNH and clinical HIV services 93 6.3.2 Linkages with other health programmes for special needs 93 6.3.2 Linkages to community-based AIDS service organisations 93 6.4. Maternal prophylaxis and treatment for opportunistic infections 94 6.5. Prevention of unintended pregnancies in HIV-infected women 96 6.5.1.
The present study discusses the uniqueness of the Nepalese context in relation to HIV/AIDS prevention. The authors suggest that HIV/AIDS prevention programs in Nepal should now focus more on adolescents from rural regions. The authors also suggest the ways one may approach the task of developing a prevention program targeting rural youths.
This guideline is intended for all stakeholders engaged in HIV and sexually transmitted infections (STIs) response. It will serve as guidance to fast-track the HIV response in the country, province, and at the local level. vi National Consolidated Guidelines on Strategic Information of HIV Response in Nepal.
The present study discusses the uniqueness of the Nepalese context in relation to HIV/AIDS prevention. The authors suggest that HIV/AIDS prevention programs in Nepal should now focus more on adolescents from rural regions. The authors also suggest the ways one may approach the task of developing a prevention program targeting rural youths.
Nepal's HV epidemic used to be driven by injecting drug use, but now the main way HIV spreads is through sex.But people who inject drugs are still one of the population groups most affected by HIV in Nepal. The other groups most at risk are migrant workers, transgender people, sex workers, prisoners, young people, men who have sex with men and military personnel.
The first HIV / AIDS cases in Nepal were reported in 1988. The HIV epidemic is largely attributed to sexual transmissions and account for more than 85% of the total new HIV infections. Coinciding with the outbreak of civil unrest, there was a drastic increase in the new cases in 1996. The infection rate of HIV/AIDS in Nepal among the adult ...
HIV prevalence among the age group of 15-24 years was 0.02 percent in 2019Thenew infection was peaked in 1999 with almost 4,250 new cases in a calendar year which has declined to 790 in 2019. The 2019 national HIV infection estimation shows that AIDS-related deaths are in declining trend (895 deaths in 2018 compared to 739 deaths in 2019).
NHSP NHSP (2021-2026) (2021-2026) AT AT A A GLANCE GLANCE. With With the the National National HIV HIV Strategic Strategic Track Track approach approach towards towards ending ending threat threat by by 2030, 2030, through through achieving achieving. Plan, Plan, Nepal Nepal has has embarked embarked on on a Fast- a Fast-.
Abstract. Nepal is one of the least developed countries in Asia, having a population of 23.1 million with an annual growth rate of 2.2% (CBS, 2001). Even though Nepal allocates five to six percent of its total national budget to the health sector every year, indicators demonstrate the relatively poor health of the Nepali population.
The number of officially reported cases of HIV infection and of AIDS in Nepal remains low, but Nepal's open border with India and the high level of physical mobility within Nepal and abroad, associated with widespread labor migration and encouraged by the recent development of road transport, means that there is a real danger of a rapid spread of HIV within Nepal.
Abstract. Stigma related to HIV and AIDS in Nepal is an issue that requires better understanding. Some prevention efforts, because of lack of cultural understanding, have paradoxically amplified ...
The modified version of HIV-specific social support questionnaire was translated from English into Nepali language and translated back from Nepali into English by independent translators. Each of the domains in the Nepali version of the scale showed good internal reliability, yielding Cronbach's alpha of .89 emotional, .86 informational, .82 ...
In 2014, an estimated 39,249 people were living with HIV/AIDS and an estimated 2,576 people died due to the disease. An estimated number of 1,493 people were newly infected by HIV/AIDS and HIV prevalence rate among adult population was 0.02% [ 29 ]. However, the total reported HIV cases were 25,838 as of December 2014.
Order. To get the online essay writing service, you have to first provide us with the details regarding your research paper. So visit the order form and tell us a paper type, academic level, subject, topic, number and names of sources, as well as the deadline. Also, don't forget to select additional services designed to improve your online ...
100% Success rate. NursingManagementBusiness and EconomicsEconomics+69. John N. Williams. #16 in Global Rating. Essay On Hiv Aids In Nepali Language. 4.9/5. Services. 2640Orders prepared. 63Customer reviews.
Hiv Aids Essay In Nepali Language - Show More. Translate » 4.9/5. Essay writing help has this amazing ability to save a student's evening. For example, instead of sitting at home or in a college library the whole evening through, you can buy an essay instead, which takes less than one minute, and save an evening or more. ...