An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List


Recent advances in understanding anorexia nervosa
Guido k.w. frank.
1 Department of Psychiatry, University of Colorado, Anschutz Medical Campus, Aurora, CO, 80045, USA
2 Neuroscience Program, University of Colorado, Anschutz Medical Campus, Aurora, CO, 80045, USA
Megan E. Shott
Marisa c. deguzman.
Anorexia nervosa is a complex psychiatric illness associated with food restriction and high mortality. Recent brain research in adolescents and adults with anorexia nervosa has used larger sample sizes compared with earlier studies and tasks that test specific brain circuits. Those studies have produced more robust results and advanced our knowledge of underlying biological mechanisms that may contribute to the development and maintenance of anorexia nervosa. It is now recognized that malnutrition and dehydration lead to dynamic changes in brain structure across the brain, which normalize with weight restoration. Some structural alterations could be trait factors but require replication. Functional brain imaging and behavioral studies have implicated learning-related brain circuits that may contribute to food restriction in anorexia nervosa. Most notably, those circuits involve striatal, insular, and frontal cortical regions that drive learning from reward and punishment, as well as habit learning. Disturbances in those circuits may lead to a vicious cycle that hampers recovery. Other studies have started to explore the neurobiology of interoception or social interaction and whether the connectivity between brain regions is altered in anorexia nervosa. All together, these studies build upon earlier research that indicated neurotransmitter abnormalities in anorexia nervosa and help us develop models of a distinct neurobiology that underlies anorexia nervosa.
Anorexia nervosa (AN) is characterized by a persistent restriction of energy intake and leads to a body weight that is significantly lower than what is expected for height and age 1 . There is either an intense fear of gaining weight or becoming fat or persistent behavior that interferes with weight gain (even though at significantly low weight). Individuals with AN experience a disturbance in the way one’s body weight or shape is experienced, undue influence of body shape and weight on self-evaluation, or persistent lack of recognition of the seriousness of the current low body weight. A restricting type has been distinguished from a binge eating/purging type; individuals in the latter group may intermittently have binge eating episodes or may use self-induced vomiting to avoid weight gain. AN shows a complex interplay between neurobiological, psychological, and environmental factors 2 and is a chronic disorder with frequent relapse, high treatment costs, and severe disease burden 3 , 4 . AN has a mortality rate 12 times higher than the death rate for all causes of death for females 15 to 24 years old 5 – 7 . Treatment success is modest, and no medication has been approved for AN treatment 8 .
Various psychological or psychodynamic theories have been developed in the past to explain the causes of AN but their underlying theories have been difficult to test 9 . On the contrary, neurobiological research using techniques such as human brain imaging leads to more directly testable hypotheses and holds promise to help us tease apart mechanisms that contribute to the onset of the illness, maintenance of AN behavior, and recovery from AN. This article will review recent advances in our understanding of the neurobiology of AN. Neurobiology is a branch of the life sciences, which deals with the anatomy, physiology, and pathology of the nervous system 10 . Neurobiology is closely associated with the field of neuroscience, a branch of biology, which tries to understand brain function, from gross anatomy to neural circuits and cells that comprise them 11 . The goal of neurobiological research in AN is to develop a medical model perspective to reduce stigma and help develop better treatments 12 . At the earlier stages of brain research in AN, study samples tended to be quite small, which made replication difficult 13 . Most frequently, altered serotonin function was associated with AN and anxiety in the disorder 14 . More recent brain research has built upon those studies and increased sample sizes in structural studies and introduced studying brain function in relation to specific tasks that are thought be related to food restriction, anxiety, and body image distortion. Most studies have been carried out in adults, although there is a growing body of literature that investigated youth with AN.
The most frequently applied brain imaging study design in the past studied brain volume in AN, and more recent research now allows cortical thickness of the brain to be investigated. For a long time, there was the notion that gray matter volume and cortical thickness are lower in patients with AN (when ill and after recovery) than in controls. This research was pioneered by Katzman et al . in adolescents with AN 15 , 16 . However, recent research by Bernardoni et al . 17 and King et al . 18 in adolescents and young adults indicated that such abnormalities are rather short-lived and that both lower volume and cortical thickness normalize with weight recovery. Animal studies suggest that those changes may be due to the effects of malnutrition and dehydration on astrocytes within the brain connective tissue 19 . Two studies from our group have found larger orbitofrontal cortex and insula volume in adults and adolescents with AN after 1 to 2 weeks of normalization of food intake or in individuals after recovery, and orbitofrontal cortex volume was related to taste pleasantness 20 , 21 . Those results were intriguing as they implicated taste perception in relation to brain volume but they need replication. New data from our group in healthy first-degree relatives of patients with AN also show larger orbitofrontal cortex volume, supporting a trait abnormality (unpublished data). Studies by Bernardoni et al . in young adults have found abnormalities in gray matter gyrification in AN, and nutritional rehabilitation seems to normalize altered cortical folding 22 . A valuable lesson from those studies is that food intake can have dramatic effects on brain structure. Whether lower or higher brain volume in AN has implications on illness behavior or is instead an effect of malnutrition without effects on behavior is still unclear and needs further research 23 , 24 .
Functional brain imaging provides the opportunity to tie behavior to brain activation and thus to distinct brain neurobiology, which could become a treatment target. Several aspects of behavior in AN stand out. One is the ability to restrict food intake to the point of emaciation while the typical mechanisms to maintain a healthy body weight are inefficient. Another is how the body can maintain this behavior even when AN patients in therapy are trying to break that behavior pattern.
Relevant to food avoidance behavior is the brain reward system, which processes the motivation to eat and hedonic experience after food intake, and also calculates and updates how valuable a specific food is to us 25 . This circuitry includes the insula, which contains the primary taste cortex, the ventral striatum that comprises dopamine terminals to drive food approach, and the orbitofrontal cortex that calculates a value, while the hypothalamus integrates body signals on hunger and satiety for higher-order decision making and food approach. Many studies have used visual food cues but it has been difficult to draw conclusions on the pathophysiology of AN from those studies 26 .
Several studies from our group using sugar taste stimuli have found that brain activation in adolescent and adult AN was elevated compared with controls in response to unexpected receipt or omission of sweet taste in the insula and striatum 27 , 28 . This so-called “prediction error” response has been associated with brain dopamine circuitry and serves as a learning signal to drive approach or avoidance of salient stimuli in the environment in the future. In addition, orbitofrontal cortex prediction error response correlated positively with anxiety measures in AN 28 , 29 . We found a similar pattern of elevated brain activation in AN to unexpected receipt or omission of monetary stimuli, suggesting a food-independent alteration of brain dopamine circuitry. Importantly, those studies have also shown that brain response was predictive of weight gain during treatment and that brain dopamine function could have an important role in weight recovery in AN. This was supported by a retrospective chart review in adolescents with AN that suggested that the dopamine D 2 receptor partial agonist aripiprazole was associated with higher weight gain in a structured treatment program in comparison with patients not on that medication 30 . Mechanistically, it was hypothesized that dopamine D 2 receptor stimulation might be desensitizing those receptors and normalize behavior response. This, however, is speculative and controlled studies are lacking.
Other lines of research on the pathophysiology of AN are directed toward feedback learning, and several studies have found that AN is associated with alterations, behaviorally or in brain response. A study by Foerde and Steinglass, who investigated learning using a picture association task in patients with AN before and after weight restoration, indicated deficits in feedback learning and generalization of learned information in comparison with controls 31 . Such alterations could translate directly into difficulties in behavior modification toward recovery. Studies from Ehrlich’s group found normal feedback learning in ill, but reduced performance on reversal learning in recovered AN, which made the impact of learning in ill AN less clear 32 , 33 . Furthermore, Bernardoni et al ., using a different study design, found that individuals with AN had an increased learning rate and elevated medial frontal cortex response following punishment 34 . That result supports previous findings of elevated sensitivity to punishment in AN as a possible biological trait 35 . Another very interesting study by Foerde et al . tested brain response to food choice presenting images of food and that research implicated the dorsal striatum in this process in AN 36 . The authors also found that the strength of connectivity between striatum and frontal cortex activation correlated inversely with actual caloric food intake in a test meal after the brain scan. The authors interpreted the findings to mean that this frontostriatal involvement in AN could contribute to habit formation of food restriction behavior. Behavioral research has provided evidence that habit formation or habit strength could be necessary for the perpetuation of AN behaviors and this concept is important to study further 37 – 39 .
The self-perception of being fat despite being underweight is another aspect of AN that the field continues to struggle with in finding its underlying pathophysiology. Some studies have found a specific brain response related to altered processing of visual information or tasks that tested interoception. For instance, Kerr et al . 40 found elevated insula activation during an abdomen perception task, and Xu et al . 41 found that a frontal and cingulate cortex response during a social evaluation task correlated with body shape concerns. A study by Hagman et al ., however, indicated a strong cognitive and emotional influence on body image distortion, and the intersection between altered perception and fear-driven self-perception needs further study 42 . Social interaction and its brain biology constitute another area that was hypothesized to be related to AN behaviors and some research is emerging on this topic. For instance, a study by McAdams et al . showed that the quality of the social relationship or social reciprocity tested in a trust game showed lower occipito-parietal brain response in patients with AN in comparison with a control group 43 . This research suggests altered reward experience from interpersonal contact in AN, which could impact emotional well-being and interfere with recovery. Oxytocin, a peptide hormone related to social behavior, could play a role but this requires more detailed research 44 .
Studies on brain connectivity can test either what brain regions work in concert during a specific task (functional connectivity) or what the hierarchical organization is between areas in the brain (that is, what region drives another) (effective connectivity). Several studies in the past have shown that resting-state functional connectivity is altered in patients with AN compared with control groups. Those studies repeatedly found altered connectivity that involved the insula, a region associated with taste perception, prediction error processing, and integration of body perception, as reviewed by Gaudio et al . 45 . More recent studies found higher or lower resting-state activation in AN across various networks and during rest or task conditions 39 , 46 – 49 . Longitudinal studies will need to test what might be the best resting-state network to focus on to predict, for instance, illness outcome or whether functional connectivity during specific tasks such as taste processing could be more informative. One study by Boehm et al . found normalization of functional connectivity in the default mode but continued abnormal frontoparietal network connectivity in recovered AN 50 . It remains to be seen whether functional connectivity will normalize with recovery or can identify long-lasting or maybe trait alterations.
Effective connectivity studies indicated that while viewing fearful faces, a group with AN had deficits of brain connectivity between prefrontal cortex and the amygdala, which correlated with measures for anxiety and eating behaviors in a study by Rangaprakash et al . 51 . Studies from our group that assessed effective connectivity during the tasting of sucrose solution found that, whereas in controls the hypothalamus drove ventral striatum response, in patients with AN, effective connectivity was directed from the ventral striatum to the hypothalamus 28 , 52 . Previously, a dopamine-dependent pathway from the ventral striatum to the hypothalamus that mediates fear was described and we hypothesized that this circuitry might be activated in AN to override appetitive hypothalamic signals 53 .
In summary, brain research has started to make inroads into the pathophysiology of AN. We have learned that malnutrition has significant effects on brain structure, changes that can recover with weight restoration, but whether those alterations have an impact on illness behavior remains unclear 23 . Research into the function of brain circuits has implicated reward pathways and malnutrition-driven alterations of dopamine responsiveness together with neuroendocrine changes, and high anxiety may interfere with normal mechanisms that drive eating behavior 54 . Habit learning and associated striatal-frontal brain connectivity could provide another mechanism of how brain function and interaction of cortical and sub-cortical regions may perpetuate illness behavior that is difficult to overcome. Those advances are promising to establish that AN is associated with a distinct brain pathophysiology. This will help researchers develop effective biological treatments that improve recovery and help prevent relapse. A significant challenge to overcome will be to integrate the differing brain research studies and develop a unified model 13 . Critical in this effort will be well-powered and comparable study designs across research groups, which take into account confounding factors such as comorbidity and medication use and which use rigorous standards for data analysis.
[version 1; peer review: 2 approved]
Funding Statement
This work was supported by National Institute of Mental Health grants MH096777 and MH103436 (both to GKWF) and by T32HD041697 (University of Colorado Neuroscience Program) and National Institutes of Health/National Center for Advancing Translational Sciences Colorado Clinical and Translational Science Awards grant TL1 TR001081 (both to MCD).
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Editorial Note on the Review Process
F1000 Faculty Reviews are commissioned from members of the prestigious F1000 Faculty and are edited as a service to readers. In order to make these reviews as comprehensive and accessible as possible, the referees provide input before publication and only the final, revised version is published. The referees who approved the final version are listed with their names and affiliations but without their reports on earlier versions (any comments will already have been addressed in the published version).
The referees who approved this article are:
- Carrie J McAdams , Department of Psychiatry, University of Texas at Southwestern Medical Center, Dallas, TX, USA No competing interests were disclosed.
- Janet Treasure , Section of Eating Disorders, Department of Psychological Medicine, Institute of Psychiatry, Psychology & Neuroscience, King's College London, London, UK No competing interests were disclosed.
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Eating Disorders: Current Knowledge and Treatment Update
- B. Timothy Walsh , M.D.
Search for more papers by this author
Although relatively uncommon, eating disorders remain an important concern for clinicians and researchers as well as the general public, as highlighted by the recent depiction of Princess Diana’s struggles with bulimia in “The Crown.” This brief review will examine recent findings regarding the diagnosis, epidemiology, neurobiology, and treatment of eating disorders.

Eight years ago, DSM-5 made major changes to the diagnostic criteria for eating disorders. A major problem in DSM-IV ’s criteria was that only two eating disorders, anorexia nervosa and bulimia nervosa, were officially recognized. Therefore, many patients presenting for treatment received the nonspecific diagnostic label of eating disorder not otherwise specified (EDNOS), which provided little information about the nature of the patient’s difficulties. This problem was addressed in several ways in DSM-5 (see DSM-5 Feeding and Eating Disorder list). The diagnostic criteria for anorexia nervosa and bulimia nervosa were slightly expanded to capture a few more patients in each category. But two other changes had a greater impact in reducing the use of nonspecific diagnoses.
The first of these was the addition of binge eating disorder (BED), which had previously been described in an appendix of DSM-IV . BED is the most common eating disorder in the United States, so its official recognition in DSM-5 led to a substantial reduction in the need for nonspecific diagnoses.
DSM-5 Feeding and Eating Disorder
Rumination Disorder
Avoidant/restrictive food intake disorder
Anorexia nervosa
Bulimia nervosa
Binge-eating disorder
Other specified feeding or eating disorder
Unspecified feeding or eating disorder
The second important change was the combination of the DSM-IV section titled “Feeding and Eating Disorders of Infancy or Early Childhood” with “Eating Disorders” to form an expanded section, “Feeding and Eating Disorders.” This change thereby included three diagnostic categories: pica, rumination disorder, and feeding disorder of infancy or early childhood. Pica and rumination disorder are infrequently diagnosed.
The other category, feeding disorder of infancy or early childhood, was rarely used and had been the subject of virtually no research since its inclusion in DSM-IV . The Eating Disorders Work Group responsible for reviewing the criteria for eating disorders for DSM-5 realized that there was a substantial number of individuals, many of them children, who severely restricted their food intake but did not have anorexia nervosa. For example, after a severe bout of vomiting after eating, some individuals attempt to prevent a recurrence by no longer eating at all, leading to potentially serious nutritional disturbances. No diagnostic category in DSM-IV existed for such individuals. Therefore, the DSM-IV category, feeding disorder of infancy or early childhood, was expanded and retitled “avoidant/restrictive food intake disorder” (ARFID). Combined, these changes led to a substantial reduction in the need for nonspecific diagnostic categories for eating disorders.
In the course of assessing the impact of the recommended changes in the diagnostic criteria for eating disorders, the Eating Disorders Work Group became aware of another group of individuals presenting for clinical care whose symptoms did not quite fit any of the existing or proposed categories. These were individuals, many of them previously overweight or obese, who had lost a substantial amount of weight and developed many of the signs and symptoms characteristic of anorexia nervosa. However, at the time of presentation, their weights remained within or above the normal range, therefore not satisfying the first diagnostic criterion for anorexia nervosa. The work group recommended that a brief description of such individuals be included in the DSM-5 diagnostic category that replaced DSM-IV ’s EDNOS: “other specified feeding and eating disorders” (OSFED); this description was labeled atypical anorexia nervosa. The degree to which the symptoms, complications, and course of individuals with atypical anorexia nervosa resemble and differ from those of individuals with typical anorexia nervosa remains an important focus of current research.
Epidemiology
Although eating disorders contribute significantly to the global burden of disease, they remain relatively uncommon. A study published in September 2018 by Tomoko Udo, Ph.D., and Carlos M. Grilo, Ph.D., in Biological Psychiatry examined data from a large, nationally representative sample of over 36,000 U.S. adults 18 years of age and older surveyed using a lay-administered diagnostic interview in 2012-2013. The 12-month prevalence estimates for anorexia nervosa, bulimia nervosa, and BED were 0.05%, 0.14%, and 0.44%, respectively. Although the relative frequencies of these disorders were similar to those described in prior studies, the absolute estimates were somewhat lower for unclear reasons. Consistent with clinical experience and prior reports, the eating disorders, especially anorexia nervosa and bulimia nervosa, were more prevalent among women (though men are also affected). Although eating disorders occurred across all ethnic and racial groups, there were fewer cases of anorexia nervosa among non-Hispanic and Hispanic Black respondents than among non-Hispanic White respondents. Consistent with long-standing clinical impression, individuals with lifetime anorexia nervosa reported higher incomes.
Finally, when BED was under consideration for official recognition in DSM-5 , some critics suggested that, since virtually everyone occasionally overeats, BED was an example of the misguided tendency of DSM to pathologize normal behavior. The low prevalence of BED reported in the study by Udo and Grilo documents that, when carefully assessed, BED affects only a minority of individuals and is therefore distinct from normality.
A subject of some debate and substantial uncertainty is whether the incidence of eating disorders (the number of new cases a year) is increasing. Some studies, such as that of Udo and Grilo, have found that the lifetime rates of eating disorders among older individuals are lower than those among younger individuals, suggesting that the frequency of eating disorders may be increasing. However, this might also reflect more recent awareness and knowledge of eating disorders. Other studies that conducted multiple examinations of the frequency of eating disorders in the same settings over time appear to suggest that, in the last several decades, the incidence of anorexia nervosa has remained roughly stable, whereas the incidence of bulimia nervosa has decreased. Presumably, this reflects changes in the sociocultural environment such as an increased acceptance of being overweight and reduced pressure to engage in inappropriate compensatory measures such as self-induced vomiting after binge eating.
The COVID-19 pandemic has impacted virtually every facet of life across the world and has produced severe financial, medical, and psychological stresses. Preliminary research suggests that such stresses have exacerbated the symptoms of individuals with preexisting eating disorders and have led to increased binge eating in the general population. Hopefully, these trends will improve with successful control of the pandemic.
Neurobiology
Much recent research on the mechanisms underlying the development and persistence of eating disorders has focused on the processing of rewarding and nonrewarding/punishing stimuli. Several studies have suggested that individuals with anorexia nervosa are less able to distinguish among stimuli with varying probabilities of obtaining a reward. Other studies suggest that, when viewing images of food during MRI scanning, individuals with anorexia nervosa tend to show less activation of brain reward areas than do controls. Such deficits may be related to disturbances in dopamine function in areas of the brain known to be involved in reward processing. Research based on emerging methods in computational psychiatry suggests that individuals with anorexia nervosa may be particularly sensitive to learning from punishment; for example, they may be very quick to learn what stimuli lead to a decrease in the amount of a reward. Conceivably, they may learn that eating high-fat foods prevents weight loss and produces undesirable weight gain, and they begin to avoid such foods. These studies, and a range of others, focus on probing basic brain mechanisms and how they may be disrupted in anorexia nervosa. A challenge for this “bottom-up” approach is to determine how exactly disturbances in such mechanisms are related to the eating disturbances characteristic of anorexia nervosa.
Other recent studies take a “top-down” approach, focusing on the neural circuitry underlying the persistent maladaptive choices made by individuals with anorexia nervosa when they decide what foods to eat. Such research successfully captures the well-established avoidance of high-fat foods by individuals with anorexia nervosa and has documented that such individuals utilize different neural circuits in making decisions about what to eat than do healthy individuals. These results are consistent with suggestions that the impressive persistence of anorexia nervosa in many individuals may be due to the establishment of automatic, stereotyped, and habitual behavior surrounding food choice. A challenge for such top-down research strategies is to determine how these maladaptive patterns develop so rapidly and become so ingrained.
Research on the neurobiology underlying bulimia nervosa is broadly similar. Although the results are complex, individuals with bulimia nervosa appear to find food stimuli more rewarding, and there are indications of disturbances in reward responsiveness to sweet tastes. Several studies have documented impairments in impulse control assessed using behavioral paradigms such as the Stroop Task. In this task, individuals are presented with a word naming a color (for example, “red”) but asked to name the color of the letters spelling the word (for example, the letters r, e, and d are green). Increased difficulties in performing such tasks have been described in individuals with bulimia nervosa and linked to reduced prefrontal cortical thickness.
It has long been known that eating disorders tend to run in families, and there has been strong evidence that this in part reflects the genes that individuals inherit from their parents. In recent decades, it has become clear that the risk of developing most complex human diseases, including obesity, hypertension, and eating disorders is related to many genes, each one of which contributes a small amount to the risk. Because the contribution of a single gene is so small, the DNA from a very large number of individuals with and without the disorder needs to be examined. For instance, genomewide association studies (GWAS) in schizophrenia have examined tens of thousands of individuals with schizophrenia and over 100,000 controls and identified well over 100 genetic loci that contribute to the risk of developing schizophrenia.
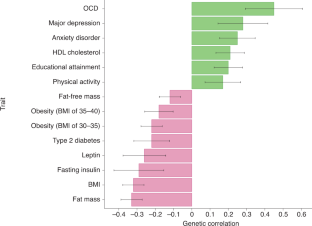
GWAS examining the genetic risk for eating disorders are under way but to date have focused primarily on anorexia nervosa. The Psychiatric Genetics Consortium has collected information from 10,000 to 20,000 individuals with anorexia nervosa and over 50,000 controls and has, so far, identified eight loci that contribute to the genetic risk for this disorder. In addition, this work has identified genetic correlations between anorexia nervosa and a range of other disorders known to be comorbid with anorexia nervosa such as anxiety disorders as well as a negative genetic correlation with obesity. These data suggest that the genetic risk for anorexia nervosa is based on a complex interplay between loci associated with a range of psychological and metabolic/anthropometric traits.
Although there have been no dramatic developments in our knowledge of how best to treat individuals with eating disorders, there have been some significant and useful advances in recent years.
For anorexia nervosa, arguably the most significant advance in treatment in the last quarter century has been family-based treatment for adolescents. In this approach, sometimes referred to as the “Maudsley method,” the family, guided by the therapist, becomes the primary agent of change and responsible for ensuring that eating behavior normalizes and weight increases. This approach differs markedly from prior treatment strategies that assumed parental involvement was not helpful or even detrimental. Family-based treatment is now widely viewed as a treatment of first choice for adolescents with anorexia nervosa and has also been adapted to treat bulimia nervosa.
Family-based treatment can be quite challenging for parents. The entire family is asked to attend treatment sessions, and one session early in treatment includes a family meal during which the parents are charged with the difficult task of persuading the adolescent to consume more food than he/she had intended. An alternative but related model, termed “parent-focused treatment,” has recently been explored in a few studies. In this approach, parents meet with a therapist without the affected adolescent or other members of the family and receive guidance regarding how to help the adolescent to alter his or her behavior following techniques virtually identical to those provided in traditional family-based treatment. Several small studies have examined this approach, and results suggest similar effectiveness. Although more research is needed, these findings suggest that parent-focused treatment may be an attractive alternative to family-based treatment for many parents and practitioners.
The COVID-19 pandemic has led to a dramatic acceleration in the provision of psychiatric care remotely, including family-based treatment. Work on providing family-based treatment via videoconference had begun prior to the arrival of COVID-19, as this specialized form of care is not widely available, and its provision via HIPAA-compliant video links would offer a substantial increase in accessibility. Several small studies suggested that remote provision of family-based treatment is feasible and likely to be efficacious. The restrictions imposed by COVID-19 on face-to-face contact have accelerated the remote delivery of family-based treatment; hopefully, new research will document its effectiveness. It should be noted, however, that, in most cases, local contact with a medical professional who can directly measure weight and oversee the patient’s physical state is required.
The treatment of adults with anorexia nervosa, who typically developed the disorder as teenagers and have been ill for five or more years, remains challenging. Structured behavioral interventions, such as those available in specialized inpatient, day program, or residential centers, typically lead to significant weight restoration and psychological and physiological improvement. However, the rate of relapse following acute care remains substantial. Furthermore, most adult patients with anorexia nervosa are very reluctant to accept treatment in such structured programs. A recent helpful development is evidence that olanzapine, at a dose of 5 mg/day to 10 mg/day, assists modestly with weight gain in adult outpatients with anorexia nervosa and is associated with few significant side effects. Unfortunately, it does not address core psychological symptoms and must be viewed as adjunctive to standard care.
There have been fewer recent developments in the treatment of patients with bulimia nervosa and of BED. For bulimia nervosa, cognitive-behavioral therapy remains the mainstay psychological treatment, and SSRIs continue to be the first-choice class of medication. For BED, multiple forms of psychological treatment are associated with substantial improvement in binge eating, and, in 2015, the FDA approved the use of the stimulant lisdexamfetamine (Vyvanse) for individuals with BED. Unlike most psychological treatments, lisdexamfetamine is associated with modest weight loss but has effects on pulse and blood pressure that may be of concern, especially for older individuals.
Also noteworthy are the development and application of new forms of psychological treatment for individuals with eating disorders. These include dialectical behavior therapy (DBT), acceptance and commitment therapy (ACT), and integrative cognitive-affective therapy (ICAT). Although only a few controlled studies have examined the effectiveness of these treatments, anecdotal information and the results of these studies suggest that such methods may be useful alternatives to more established interventions.
Conclusions
Eating disorders remain uncommon but clinically important problems characterized by persistent disturbances in eating or eating-related behavior. Cutting-edge research focuses on neurobiology and genetics, utilizing novel and rapidly evolving methodology. There have been modest advances in treatment approaches, including the COVID-19 pandemic’s acceleration of treatment delivery via video-link. Future studies will hopefully clarify the nature of ARFID and of atypical anorexia nervosa and lead to the development of more effective interventions, especially for individuals with long-standing eating disorders. ■
Additional Resources
Walsh BT. Diagnostic Categories for Eating Disorders: Current Status and What Lies Ahead. Psychiatr Clin North Am . 2019; 42(1):1-10.
Udo T, Grilo CM. Prevalence and Correlates of DSM-5 -Defined Eating Disorders in a Nationally Representative Sample of U.S. Adults. Biol Psychiatry . 2018; 84(5):345-354.
Van Hoeken D, Hoek HW. Review of the Burden of Eating Disorders: Mortality, Disability, Costs, Quality of Life, and Family Burden. Curr Opin Psychiatry . 2020; 33(6):521-527.
Bernardoni F, Geisler D, King JA, et al. Altered Medial Frontal Feedback Learning Signals in Anorexia Nervosa. Biol Psychiatry . 2018; 83(3):235-243.
Frank GKW, Shott ME, DeGuzman MC. The Neurobiology of Eating Disorders. Child Adolesc Psychiatr Clin N Am . 2019; 28(4):629-640.
Steinglass JE, Berner LA, Attia E. Cognitive Neuroscience of Eating Disorders. Psychiatr Clin North Am . 2019; 42(1):75-91.
Bulik CM, Blake L, Austin J. Genetics of Eating Disorders: What the Clinician Needs to Know. Psychiatr Clin North Am . 2019; 42(1):59-73.
Attia E, Steinglass JE, Walsh BT, et al. Olanzapine Versus Placebo in Adult Outpatients With Anorexia Nervosa: A Randomized Clinical Trial. Am J Psychiatry . 2019; 176(6):449-456.
Le Grange D, Hughes EK, Court A, et al. Randomized Clinical Trial of Parent-Focused Treatment and Family-Based Treatment for Adolescent Anorexia Nervosa. J Am Acad Child Adolesc Psychiatry . 2016; 55(8):683-92.
Pisetsky EM, Schaefer LM, Wonderlich SA, et al. Emerging Psychological Treatments in Eating Disorders. Psychiatr Clin North Am . 2019; 42:219-229.
B. Timothy Walsh, M.D., is a professor of psychiatry at the Columbia University Irving Medical Center and the founding director of the Columbia Center for Eating Disorders at the New York State Psychiatric Institute. He is the co-editor of the Handbook of Assessment and Treatment of Eating Disorders from APA Publishing.
Dr. Walsh reports receiving royalties or honoraria from UpToDate, McGraw-Hill, the Oxford University Press, the British Medical Journal, the Johns Hopkins Press, and Guidepoint Global

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 06 May 2022
Genetics and neurobiology of eating disorders
- Cynthia M. Bulik ORCID: orcid.org/0000-0001-7772-3264 1 , 2 , 3 ,
- Jonathan R. I. Coleman ORCID: orcid.org/0000-0002-6759-0944 4 , 5 ,
- J. Andrew Hardaway 6 ,
- Lauren Breithaupt 7 , 8 ,
- Hunna J. Watson 1 , 9 , 10 ,
- Camron D. Bryant ORCID: orcid.org/0000-0003-4505-5809 11 &
- Gerome Breen ORCID: orcid.org/0000-0003-2053-1792 4 , 5
Nature Neuroscience volume 25 , pages 543–554 ( 2022 ) Cite this article
9649 Accesses
27 Citations
56 Altmetric
Metrics details
- Feeding behaviour
- Psychiatric disorders
Eating disorders (anorexia nervosa, bulimia nervosa and binge-eating disorder) are a heterogeneous class of complex illnesses marked by weight and appetite dysregulation coupled with distinctive behavioral and psychological features. Our understanding of their genetics and neurobiology is evolving thanks to global cooperation on genome-wide association studies, neuroimaging, and animal models. Until now, however, these approaches have advanced the field in parallel, with inadequate cross-talk. This review covers overlapping advances in these key domains and encourages greater integration of hypotheses and findings to create a more unified science of eating disorders. We highlight ongoing and future work designed to identify implicated biological pathways that will inform staging models based on biology as well as targeted prevention and tailored intervention, and will galvanize interest in the development of pharmacologic agents that target the core biology of the illnesses, for which we currently have few effective pharmacotherapeutics.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
What next for eating disorder genetics? Replacing myths with facts to sharpen our understanding
Laura M. Huckins, Rebecca Signer, … Cynthia M. Bulik

Assessing a multivariate model of brain-mediated genetic influences on disordered eating in the ABCD cohort
Margaret L. Westwater, Travis T. Mallard, … Monique Ernst
Genome-wide association study identifies eight risk loci and implicates metabo-psychiatric origins for anorexia nervosa
Hunna J. Watson, Zeynep Yilmaz, … Cynthia M. Bulik
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (5th edn) (American Psychiatric Publishing, 2013).
Erskine, H. E., Whiteford, H. A. & Pike, K. M. The global burden of eating disorders. Curr. Opin. Psychiatry 29 , 346–353 (2016).
Article PubMed Google Scholar
Santomauro, D. F. et al. The hidden burden of eating disorders: an extension of estimates from the Global Burden of Disease Study 2019. Lancet Psychiatry 8 , 320–328 (2021).
Article PubMed PubMed Central Google Scholar
Schaumberg, K. et al. Patterns of diagnostic flux in eating disorders: a longitudinal population study in Sweden. Psychol. Med. 49 , 432–450 (2019).
Article Google Scholar
Southern, J. et al. Multi-scale computational modelling in biology and physiology. Prog. Biophys. Mol. Biol. 96 , 60–89 (2008).
Article CAS PubMed Google Scholar
Yilmaz, Z., Hardaway, J. & Bulik, C. Genetics and epigenetics of eating disorders. Adv. Genomics Genet. 5 , 131–150 (2015).
PubMed PubMed Central Google Scholar
Dellava, J. E., Thornton, L. M., Lichtenstein, P., Pedersen, N. L. & Bulik, C. M. Impact of broadening definitions of anorexia nervosa on sample characteristics. J. Psychiatr. Res. 45 , 691–698 (2011).
Watson, H. et al. Genome-wide association study identifies eight risk loci and implicates metabo-psychiatric origins for anorexia nervosa. Nat. Genet. 51 , 1207–1214 (2019).
Article CAS PubMed PubMed Central Google Scholar
Duncan, L. et al. Significant locus and metabolic genetic correlations revealed in genome-wide association study of anorexia nervosa. Am. J. Psychiatry 174 , 850–858 (2017).
Thornton, L. et al. The Anorexia Nervosa Genetics Initiative: overview and methods. Contemp. Clin. Trials 74 , 61–69 (2018).
Song, W., Wang, W., Yu, S. & Lin, G. N. Dissection of the genetic association between anorexia nervosa and obsessive–compulsive disorder at the network and cellular levels. Genes 12 , 491 (2021).
Munn-Chernoff, M. A. et al. Shared genetic risk between eating disorder- and substance-use-related phenotypes: evidence from genome-wide association studies. Addict. Biol. 26 , e12880 (2021).
Kaye, W. et al. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am. J. Psychiatry 161 , 2215–2221 (2004).
Cederlöf, M. et al. Etiological overlap between obsessive–compulsive disorder and anorexia nervosa: a longitudinal cohort, family and twin study. World Psychiatry 14 , 333–338 (2015).
Thornton, L. M., Welch, E., Munn-Chernoff, M. A., Lichtenstein, P. & Bulik, C. M. Anorexia nervosa, major depression, and suicide attempts: shared genetic factors. Suicide Life Threat. Behav. 46 , 525–534 (2016).
Dellava, J., Kendler, K. & Neale, M. Generalized anxiety disorder and anorexia nervosa: evidence of shared genetic variation. Depress. Anxiety 28 , 728–733 (2011).
Bulik-Sullivan, B. et al. An atlas of genetic correlations across human diseases and traits. Nat. Genet. 47 , 1236–1241 (2015).
Watson, H. J. et al. Common genetic variation and age at onset of anorexia nervosa. Biol. Psychiatry https://doi.org/10.1016/j.bpsgos.2021.09.001 (2021).
Solmi, F., Mascarell, M. C., Zammit, S., Kirkbride, J. B. & Lewis, G. Polygenic risk for schizophrenia, disordered eating behaviours and body mass index in adolescents. Br. J. Psychiatry 215 , 428–433 (2019).
Yilmaz, Z., Gottfredson, N., Zerwas, S., Bulik, C. & Micali, N. Developmental premorbid body mass index trajectories of adolescents with eating disorders in a longitudinal population cohort. J. Am. Acad. Child Adolesc. Psychiatry 58 , 191–199 (2019).
Abdulkadir, M. et al. Polygenic score for body mass index is associated with disordered eating in a general population cohort. J. Clin. Med. 9 , 1187 (2020).
Article PubMed Central Google Scholar
Hübel, C. et al. One size does not fit all. Genomics differentiates among anorexia nervosa, bulimia nervosa, and binge-eating disorder. Int. J. Eat. Disord. 54 , 785–793 (2021).
Murray, G. K. et al. Could polygenic risk scores be useful in psychiatry?: a review. JAMA Psychiatry 78 , 210–219 (2020).
Wray, N. et al. Research review: polygenic methods and their application to psychiatric traits. J. Child Psychol. Psychiatry 55 , 1068–1087 (2014).
Lee, P. H. et al. Genomic relationships, novel loci, and pleiotropic mechanisms across eight psychiatric disorders. Cell 179 , 1469–1482 (2019).
Article CAS Google Scholar
Lee, J. E., Namkoong, K. & Jung, Y.-C. Impaired prefrontal cognitive control over interference by food images in binge-eating disorder and bulimia nervosa. Neurosci. Lett. 651 , 95–101 (2017).
Yilmaz, Z. et al. Examination of the shared genetic basis of anorexia nervosa and obsessive–compulsive disorder. Mol. Psychiatry 25 , 2036–2046 (2020).
Reed, Z. E., Micali, N., Bulik, C. M., Davey Smith, G. & Wade, K. H. Assessing the causal role of adiposity on disordered eating in childhood, adolescence, and adulthood: a Mendelian randomization analysis. Am. J. Clin. Nutr. 106 , 764–772 (2017).
CAS PubMed PubMed Central Google Scholar
Tyrrell, J. et al. Genetic evidence for causal relationships between maternal obesity-related traits and birth weight. JAMA 315 , 1129–1140 (2016).
Adams, D. M., Reay, W. R., Geaghan, M. P. & Cairns, M. J. Investigating the effect of glycaemic traits on the risk of psychiatric illness using Mendelian randomisation. Neuropsychopharmacology 46 , 1093–1102 (2020).
Article PubMed PubMed Central CAS Google Scholar
Huckins, L. M. et al. Investigation of common, low-frequency and rare genome-wide variation in anorexia nervosa. Mol. Psychiatry 23 , 1169–1180 (2018).
PubMed Google Scholar
Scott-Van Zeeland, A. A. et al. Evidence for the role of EPHX2 gene variants in anorexia nervosa. Mol. Psychiatry 19 , 724–732 (2013).
Lutter, M. et al. Novel and ultra-rare damaging variants in neuropeptide signaling are associated with disordered eating behaviors. PLoS ONE 12 , e0181556 (2017).
Cui, H. et al. Eating disorder predisposition is associated with ESRRA and HDAC4 mutations. J. Clin. Invest. 123 , 4706–4713 (2013).
Lombardi, L. et al. Anorexia nervosa is associated with Neuronatin variants. Psychiatr. Genet. 29 , 103–110 (2019).
Wang, K. et al. A genome-wide association study on common SNPs and rare CNVs in anorexia nervosa. Mol. Psychiatry 16 , 949–959 (2011).
Yilmaz, Z. et al. Exploration of large, rare CNVs associated with psychiatric and neurodevelopmental disorders in individuals with anorexia nervosa. Psychiatr. Genet 27 , 152–158 (2017).
Boraska, V. et al. A genome-wide association study of anorexia nervosa. Mol. Psychiatry 19 , 1085–1094 (2014).
Chang, X. et al. Microduplications at the 15q11.2 BP1–BP2 locus are enriched in patients with anorexia nervosa. J. Psychiatr. Res. 113 , 34–38 (2019).
Bulik, C. M. et al. The Eating Disorders Genetics Initiative (EDGI): study protocol. BMC Psychiatry 21 , 234 (2021).
Co, M., Anderson, A. G. & Konopka, G. FOXP transcription factors in vertebrate brain development, function, and disorders. Wiley Interdiscip. Rev. Dev. Biol. 9 , e375 (2020).
Yengo, L. et al. Meta-analysis of genome-wide association studies for height and body mass index in ∼ 700,000 individuals of European ancestry. Hum. Mol. Genet. 27 , 3641–3649 (2018).
Zhang, M. et al. Axonogenesis is coordinated by neuron-specific alternative splicing programming and splicing regulator PTBP2. Neuron 101 , 690–706 (2019).
Arends, R. M. et al. Associations between the CADM2 gene, substance use, risky sexual behavior and self-control: a phenome-wide association study. Addict. Biol. 26 , e13015 (2021).
Rathjen, T. et al. Regulation of body weight and energy homeostasis by neuronal cell adhesion molecule 1. Nat. Neurosci. 20 , 1096–1103 (2017).
Gerson, S. L. MGMT: its role in cancer aetiology and cancer therapeutics. Nat. Rev. Cancer 4 , 296–307 (2004).
Reid, D. A. et al. Incorporation of a nucleoside analog maps genome repair sites in postmitotic human neurons. Science 372 , 91–94 (2021).
Wu, W. et al. Neuronal enhancers are hotspots for DNA single-strand break repair. Nature 593 , 440–444 (2021).
Finucane, H. et al. Partitioning heritability by functional annotation using genome-wide association summary statistics. Nat. Genet. 47 , 1228–1235 (2015).
Skene, N. G. et al. Genetic identification of brain cell types underlying schizophrenia. Nat. Genet. 50 , 825–833 (2018).
Chowdhury, T. G. et al. Voluntary wheel running exercise evoked by food-restriction stress exacerbates weight loss of adolescent female rats but also promotes resilience by enhancing GABAergic inhibition of pyramidal neurons in the dorsal hippocampus. Cereb. Cortex 29 , 4035–4049 (2019).
Klenowski, P. M. et al. Prolonged consumption of sucrose in a binge-like manner, alters the morphology of medium spiny neurons in the nucleus accumbens shell. Front. Behav. Neurosci. 10 , 54 (2016).
Wang, D. et al. Comprehensive functional genomic resource and integrative model for the human brain. Science 362 , eaat8464 (2018).
Rossi, M. A. & Stuber, G. D. Overlapping brain circuits for homeostatic and hedonic feeding. Cell Metab. 27 , 42–56 (2018).
Frank, G. K., Shott, M. E. & DeGuzman, M. C. Recent advances in understanding anorexia nervosa. F1000Res. 8 , 504 (2019).
Kaye, W. H., Wagner, A., Fudge, J. L. & Paulus, M. Neurocircuity of eating disorders. Curr. Top. Behav. Neurosci. 6 , 37–57 (2010).
Lammel, S., Lim, B. K. & Malenka, R. C. Reward and aversion in a heterogeneous midbrain dopamine system. Neuropharmacol 76 , 351–359 (2014).
Cowdrey, F. A., Park, R. J., Harmer, C. J. & McCabe, C. Increased neural processing of rewarding and aversive food stimuli in recovered anorexia nervosa. Biol. Psychiatry 70 , 736–743 (2011).
Kaye, W. H. et al. Neural insensitivity to the effects of hunger in women remitted from anorexia nervosa. Am. J. Psychiatry 177 , 601–610 (2020).
Bohon, C. & Stice, E. Reward abnormalities among women with full and subthreshold bulimia nervosa: a functional magnetic resonance imaging study. Int. J. Eat. Disord. 44 , 585–595 (2011).
Simon, J. J. et al. Neural signature of food reward processing in bulimic-type eating disorders. Soc. Cogn. Affect. Neurosci. 11 , 1393–1401 (2016).
Bailer, U. F. et al. Exaggerated 5-HT 1A but normal 5-HT 2 A receptor activity in individuals ill with anorexia nervosa. Biol. Psychiatry 61 , 1090–1099 (2007).
Broft, A. et al. Striatal dopamine type 2 receptor availability in anorexia nervosa. Psychiatry Res. 233 , 380–387 (2015).
Bailer, U. F. et al. Amphetamine induced dopamine release increases anxiety in individuals recovered from anorexia nervosa. Int. J. Eat. Disord. 45 , 263–271 (2012).
Broft, A. et al. Striatal dopamine in bulimia nervosa: a PET imaging study. Int. J. Eat. Disord. 45 , 648–656 (2012).
Mihov, Y. et al. Metabotropic glutamate receptor 5 in bulimia nervosa. Sci. Rep. 10 , 1–10 (2020).
Frank, G. K., Shott, M. E., Hagman, J. O. & Mittal, V. A. Alterations in brain structures related to taste reward circuitry in ill and recovered anorexia nervosa and in bulimia nervosa. Am. J. Psychiatry 170 , 1152–1160 (2013).
Craig, A. D. & Craig, A. How do you feel—now? The anterior insula and human awareness. Nat. Rev. Neurosci. 10 , 59–70 (2009).
Kerr, K. L. et al. Altered insula activity during visceral interoception in weight-restored patients with anorexia nervosa. Neuropsychopharmacology 41 , 521–528 (2016).
Zucker, N. L. et al. The clinical significance of posterior insular volume in adolescent anorexia nervosa. Psychosom. Med. 79 , 1025–1035 (2017).
Berner, L. A. et al. Altered anticipation and processing of aversive interoceptive experience among women remitted from bulimia nervosa. Neuropsychopharmacology 44 , 1265–1273 (2019).
Ting, J. T. & Feng, G. Neurobiology of obsessive–compulsive disorder: insights into neural circuitry dysfunction through mouse genetics. Curr. Opin. Neurobiol. 21 , 842–848 (2011).
Marsh, R. et al. An fMRI study of self-regulatory control and conflict resolution in adolescents with bulimia nervosa. Am. J. Psychiatry 168 , 1210–1220 (2011).
Skunde, M. et al. Neural signature of behavioural inhibition in women with bulimia nervosa. J. Psychiatry Neurosci. 41 , E69–E78 (2016).
Wierenga, C. et al. Altered BOLD response during inhibitory and error processing in adolescents with anorexia nervosa. PLoS ONE 9 , e92017 (2014).
Oberndorfer, T. A., Kaye, W. H., Simmons, A. N., Strigo, I. A. & Matthews, S. C. Demand‐specific alteration of medial prefrontal cortex response during an inhibition task in recovered anorexic women. Int. J. Eat. Disord. 44 , 1–8 (2011).
Finch, J. E., Palumbo, I. M., Tobin, K. E. & Latzman, R. D. Structural brain correlates of eating pathology symptom dimensions: a systematic review. Psychiatry Res. Neuroimaging 317 , 111379 (2021).
Geisler, D. et al. Altered white matter connectivity in young acutely underweight patients with anorexia nervosa. J. Am. Acad. Child Adolesc. Psychiatry 61 , 331–340 (2022).
Goodkind, M. et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry 72 , 305–315 (2015).
McTeague, L. M. et al. Identification of common neural circuit disruptions in emotional processing across psychiatric disorders. Am. J. Psychiatry 177 , 411–421 (2020).
Shanmugan, S. et al. Common and dissociable mechanisms of executive system dysfunction across psychiatric disorders in youth. Am. J. Psychiatry 173 , 517–526 (2016).
Wang, S. et al. Neurobiological commonalities and distinctions among 3 major psychiatric disorders: a graph theoretical analysis of the structural connectome. J. Psychiatry Neurosci. 45 , 15–22 (2020).
Xia, M. et al. Shared and distinct functional architectures of brain networks across psychiatric disorders. Schizophr Bull. 45 , 450–463 (2019).
Hudson, J. I., Hiripi, E., Pope, H. G. Jr. & Kessler, R. C. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol. Psychiatry 61 , 348–358 (2007).
Frank, G. K., Favaro, A., Marsh, R., Ehrlich, S. & Lawson, E. A. Toward valid and reliable brain imaging results in eating disorders. Int. J. Eat. Disord. 51 , 250–261 (2018).
Kaufmann, L.-K. et al. Fornix under water? Ventricular enlargement biases forniceal diffusion magnetic resonance imaging indices in anorexia nervosa. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2 , 430–437 (2017).
Gaudio, S., Carducci, F., Piervincenzi, C., Olivo, G. & Schiöth, H. B. Altered thalamo–cortical and occipital–parietal–temporal–frontal white matter connections in patients with anorexia and bulimia nervosa: a systematic review of diffusion tensor imaging studies. J. Psychiatry Neurosci. 44 , 324–339 (2019).
Thompson, P. M. et al. ENIGMA and global neuroscience: a decade of large-scale studies of the brain in health and disease across more than 40 countries. Transl. Psychiatry 10 , 100 (2020).
Gelegen, C. et al. Difference in susceptibility to activity-based anorexia in two inbred strains of mice. Eur. Neuropsychopharmacol. 17 , 199–205 (2007).
Gelegen, C. et al. Chromosomal mapping of excessive physical activity in mice in response to a restricted feeding schedule. Eur. Neuropsychopharmacol. 20 , 317–326 (2010).
Pjetri, E. et al. Identifying predictors of activity based anorexia susceptibility in diverse genetic rodent populations. PLoS ONE 7 , e50453 (2012).
Babbs, R. K. et al. Genetic differences in the behavioral organization of binge eating, conditioned food reward, and compulsive-like eating in C57BL/6J and DBA/2J strains. Physiol. Behav. 197 , 51–66 (2018).
Newmyer, B. A., Whindleton, C. M., Srinivasa, N., Jones, M. K. & Scott, M. M. Genetic variation affects binge feeding behavior in female inbred mouse strains. Sci. Rep. 9 , 1–10 (2019).
Kirkpatrick, S. L. et al. Cytoplasmic FMR1-interacting protein 2 is a major genetic factor underlying binge eating. Biol. Psychiatry 81 , 757–769 (2017).
Babbs, R. K. et al. Cyfip1 haploinsufficiency increases compulsive-like behavior and modulates palatable food intake in mice: dependence on Cyfip2 genetic background, parent of origin and sex. G3 9 , 3009–3022 (2019).
Farrell, M. et al. Treatment-resistant psychotic symptoms and the 15q11.2 BP1–BP2 (Burnside–Butler) deletion syndrome: case report and review of the literature. Transl. Psychiatry 10 , 1–8 (2020).
Yao, E. J. et al. Systems genetic analysis of binge-like eating in a C57BL/6J × DBA/2J-F2 cross. Genes Brain Behav. e12751 (2021).
Nobis, S. et al. Alterations of proteome, mitochondrial dynamic and autophagy in the hypothalamus during activity-based anorexia. Sci. Rep. 8 , 1–15 (2018).
Nobis, S. et al. Colonic mucosal proteome signature reveals reduced energy metabolism and protein synthesis but activated autophagy during anorexia‐induced malnutrition in mice. Proteomics 18 , 1700395 (2018).
Breton, J. et al. Proteome modifications of gut microbiota in mice with activity-based anorexia and starvation: role in ATP production. Nutrition 67 , 110557 (2019).
Article PubMed CAS Google Scholar
Schroeder, M. et al. Placental miR-340 mediates vulnerability to activity based anorexia in mice. Nat. Commun. 9 , 1–15 (2018).
He, X., Stefan, M., Terranova, K., Steinglass, J. & Marsh, R. Altered white matter microstructure in adolescents and adults with bulimia nervosa. Neuropsychopharmacology 41 , 1841–1848 (2015).
Kaakoush, N. O. et al. Alternating or continuous exposure to cafeteria diet leads to similar shifts in gut microbiota compared to chow diet. Mol. Nutr. Food Res. 61 , 1500815 (2017).
Sweeney, P. & Yang, Y. Neural circuit mechanisms underlying emotional regulation of homeostatic feeding. Trends Endocrinol. Metab. 28 , 437–448 (2017).
Webber, E. S., Bonci, A. & Krashes, M. J. The elegance of energy balance: insight from circuit‐level manipulations. Synapse 69 , 461–474 (2015).
Andermann, M. L. & Lowell, B. B. Toward a wiring diagram understanding of appetite control. Neuron 95 , 757–778 (2017).
Welch, A. C. et al. Dopamine D2 receptor overexpression in the nucleus accumbens core induces robust weight loss during scheduled fasting selectively in female mice. Mol. Psychiatry 26 , 3765–3777 (2019).
Milton, L. K. et al. Suppression of corticostriatal circuit activity improves cognitive flexibility and prevents body weight loss in activity-based anorexia in rats. Biol. Psychiatry 90 , 819–828 (2021).
Zhang, J. & Dulawa, S. C. The utility of animal models for studying the metabo-psychiatric origins of anorexia nervosa. Front. Psychiatry 12 , 711181 (2021).
Foldi, C. J., Milton, L. K. & Oldfield, B. J. The role of mesolimbic reward neurocircuitry in prevention and rescue of the activity-based anorexia phenotype in rats. Neuropsychopharmacology 42 , 2292–2300 (2017).
Hebebrand, J., Muller, T., Holtkamp, K. & Herpertz-Dahlmann, B. The role of leptin in anorexia nervosa: clinical implications. Mol. Psychiatry 12 , 23–35 (2007).
Verhagen, L. A., Luijendijk, M. C. & Adan, R. A. Leptin reduces hyperactivity in an animal model for anorexia nervosa via the ventral tegmental area. Eur. Neuropsychopharmacol. 21 , 274–281 (2011).
Antel, J. et al. Rapid amelioration of anorexia nervosa in a male adolescent during metreleptin treatment including recovery from hypogonadotropic hypogonadism. Eur. Child Adolesc. Psychiatry https://doi.org/10.1007/s00787-021-01778-7 (2021).
Burghardt, P. R. et al. Leptin regulates dopamine responses to sustained stress in humans. J. Neurosci. 32 , 15369–15376 (2012).
Wu, Q., Han, Y. & Tong, Q. in Neural Regulation of Metabolism (eds. Wu, Q. & Zheng, R.) 211–233 (Springer, 2018).
Xu, P. et al. Activation of serotonin 2C receptors in dopamine neurons inhibits binge-like eating in mice. Biol. Psychiatry 81 , 737–747 (2017).
Marino, R. A. M. et al. Control of food approach and eating by a GABAergic projection from lateral hypothalamus to dorsal pons. Proc. Natl Acad. Sci. USA 117 , 8611–8615 (2020).
Wu, H. et al. Closing the loop on impulsivity via nucleus accumbens delta-band activity in mice and man. Proc. Natl Acad. Sci. USA 115 , 192–197 (2018).
Halpern, C. H. et al. Amelioration of binge eating by nucleus accumbens shell deep brain stimulation in mice involves D2 receptor modulation. J. Neurosci. 33 , 7122–7129 (2013).
London, T. D. et al. Coordinated ramping of dorsal striatal pathways preceding food approach and consumption. J. Neurosci. 38 , 3547–3558 (2018).
Livneh, Y. et al. Homeostatic circuits selectively gate food cue responses in insular cortex. Nature 546 , 611–616 (2017).
Kusumoto-Yoshida, I., Liu, H., Chen, B. T., Fontanini, A. & Bonci, A. Central role for the insular cortex in mediating conditioned responses to anticipatory cues. Proc. Natl Acad. Sci. USA 112 , 1190–1195 (2015).
Price, A. E., Stutz, S. J., Hommel, J. D., Anastasio, N. C. & Cunningham, K. A. Anterior insula activity regulates the associated behaviors of high fat food binge intake and cue reactivity in male rats. Appetite 133 , 231–239 (2019).
Wu, Y. et al. The anterior insular cortex unilaterally controls feeding in response to aversive visceral stimuli in mice. Nat. Commun. 11 , 640 (2020).
Spierling, S. et al. Insula to ventral striatal projections mediate compulsive eating produced by intermittent access to palatable food. Neuropsychopharmacology 45 , 579–588 (2020).
Anastasio, N. C. et al. Convergent neural connectivity in motor impulsivity and high-fat food binge-like eating in male Sprague-Dawley rats. Neuropsychopharmacology 44 , 1752–1761 (2019).
Newmyer, B. A. et al. VIPergic neurons of the infralimbic and prelimbic cortices control palatable food intake through separate cognitive pathways. JCI Insight 5 , e126283 (2019).
Mathis, A. et al. DeepLabCut: markerless pose estimation of user-defined body parts with deep learning. Nat. Neurosci. 21 , 1281–1289 (2018).
Maussion, G., Demirova, I., Gorwood, P. & Ramoz, N. Induced pluripotent stem cells: new tools for investigating molecular mechanisms in anorexia nervosa. Front. Nutr. 6 , 118 (2019).
Breen, G. et al. Translating genome-wide association findings into new therapeutics for psychiatry. Nat. Neurosci. 19 , 1392–1396 (2016).
Galmiche, M., Déchelotte, P., Lambert, G. & Tavolacci, M. P. Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. Am. J. Clin. Nutr. 109 , 1402–1413 (2019).
Papadopoulos, F., Ekbom, A., Brandt, L. & Ekselius, L. Excess mortality, causes of death and prognostic factors in anorexia nervosa. Br. J. Psychiatry 194 , 10–17 (2009).
Yao, S. et al. Familial liability for eating disorders and suicide attempts: evidence from a population registry in Sweden. JAMA Psychiatry 73 , 284–291 (2016).
Fichter, M. M., Quadflieg, N., Crosby, R. D. & Koch, S. Long-term outcome of anorexia nervosa: results from a large clinical longitudinal study. Int J. Eat. Disord. 50 , 1018–1030 (2017).
Berkman, N. et al. Management of eating disorders. Evid. Rep. Technol. Assess. 135 , 1–166 (2006).
Keski-Rahkonen, A. et al. Epidemiology and course of anorexia nervosa in the community. Am. J. Psychiatry 164 , 1259–1265 (2007).
Brownley, K. et al. Binge-eating disorder in adults: a systematic review and meta-analysis. Ann. Intern. Med. 165 , 409–420 (2016).
Fornaro, M. et al. Lisdexamfetamine in the treatment of moderate-to-severe binge eating disorder in adults: systematic review and exploratory meta-analysis of publicly available placebo-controlled, randomized clinical trials. Neuropsychiatr. Dis. Treat. 12 , 1827–1836 (2016).
Hall, J. F., Smith, K., Schnitzer, S. B. & Hanford, P. V. Elevation of activity level in the rat following transition from ad libitum to restricted feeding. J. Comp. Physiol. Psychol. 46 , 429–433 (1953).
Schalla, M. A. & Stengel, A. Activity based anorexia as an animal model for anorexia nervosa—a systematic review. Front Nutr. 6 , 69 (2019).
Novelle, M. G. & Diéguez, C. Food addiction and binge eating: lessons learned from animal models. Nutrients 10 , 71 (2018).
Article PubMed Central CAS Google Scholar
Corwin, R. L. & Babbs, R. K. Rodent models of binge eating: are they models of addiction? ILAR J. 53 , 23–34 (2012).
Moore, C. F., Sabino, V., Koob, G. F. & Cottone, P. Pathological overeating: emerging evidence for a compulsivity construct. Neuropsychopharmacology 42 , 1375–1389 (2017).
Rospond, B., Szpigiel, J., Sadakierska-Chudy, A. & Filip, M. Binge eating in preclinical models. Pharmacol. Rep. 67 , 504–512 (2015).
Cottone, P., Sabino, V., Steardo, L. & Zorrilla, E. P. Intermittent access to preferred food reduces the reinforcing efficacy of chow in rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 295 , R1066–R1076 (2008).
Hardaway, J. A. et al. Nociceptin receptor antagonist SB 612111 decreases high-fat diet binge eating. Behav. Brain Res. 307 , 25–34 (2016).
Download references
Acknowledgements
C.M.B. is supported by the National Institute of Mental Health (R01MH120170, R01MH124871, R01MH119084, R01MH118278 and R01MH124871), a Brain and Behavior Research Foundation Distinguished Investigator grant, the Swedish Research Council (Vetenskapsrådet, award no. 538-2013-8864), and the Lundbeck Foundation (grant no. R276-2018-4581). J.R.I.C. and G.B. acknowledge that the paper represents independent research part funded by the National Institute for Health Research (NIHR) Maudsley Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. J.A.H. is supported by K01DK115902. C.D.B. is supported by U01DA050243 and U01DA055299. L.B. is supported by T32MH112485, a Harvard Medical School Livingston Fellowship and the International OCD Foundation. G.B. is also supported by the UK Medical Research Council (MR/V012878/1, MR/V03605X/1 and MR/R024804/1) and Charlotte’s Helix.
Author information
Authors and affiliations.
Department of Psychiatry, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Cynthia M. Bulik & Hunna J. Watson
Department of Nutrition, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Cynthia M. Bulik
Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden
Social, Genetic and Developmental Psychiatry Centre, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK
Jonathan R. I. Coleman & Gerome Breen
National Institute of Health Research Maudsley Biomedical Research Centre, South London and Maudsley National Health Service Trust, London, UK
Department of Psychiatry and Behavioral Neurobiology, University of Alabama at Birmingham, Birmingham, AL, USA
J. Andrew Hardaway
Department of Psychiatry, Harvard Medical School, Boston, MA, USA
Lauren Breithaupt
Eating Disorders Clinical and Research Program, Massachusetts General Hospital, Boston, MA, USA
School of Psychology, Curtin University, Perth, Western Australia, Australia
Hunna J. Watson
Division of Paediatrics, School of Medicine, The University of Western Australia, Perth, Western Australia, Australia
Department of Pharmacology and Experimental Therapeutics and Psychiatry, Boston University School of Medicine, Boston, MA, USA
Camron D. Bryant
You can also search for this author in PubMed Google Scholar
Contributions
C.M.B., J.R.I.C., J.A.H., L.B., C.D.B., H.W. and G.B. all substantially contributed to the writing of the manuscript, approved the submitted version, are personally accountable for their own contribution, and ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Correspondence to Cynthia M. Bulik .
Ethics declarations
Competing interests.
C.M.B. reports the following competing interests: Shire (grant recipient, Scientific Advisory Board member); Idorsia (consultant); Pearson (author, royalty recipient); Equip Health (Clinical Advisory Board Member). G.B. reports the following competing interests: Otsuka Pharma (advisory board); Illumina (grant recipient, conference sponsorship). The other authors declare no competing interests.
Peer review
Peer review information.
Nature Neuroscience thanks Roger Adan, Sandra Sanchez-Roige, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Bulik, C.M., Coleman, J.R.I., Hardaway, J.A. et al. Genetics and neurobiology of eating disorders. Nat Neurosci 25 , 543–554 (2022). https://doi.org/10.1038/s41593-022-01071-z
Download citation
Received : 03 May 2020
Accepted : 01 April 2022
Published : 06 May 2022
Issue Date : May 2022
DOI : https://doi.org/10.1038/s41593-022-01071-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Unexpected identification of obesity-associated mutations in lep and mc4r genes in patients with anorexia nervosa.
- Luisa Sophie Rajcsanyi
- Yiran Zheng
- Anke Hinney
Scientific Reports (2024)
The multisensory mind: a systematic review of multisensory integration processing in Anorexia and Bulimia Nervosa
- Giulia Brizzi
- Maria Sansoni
- Giuseppe Riva
Journal of Eating Disorders (2023)
Psilocybin for the treatment of anorexia nervosa
- Tomislav Majić
- Stefan Ehrlich
Nature Medicine (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
Advertisement
Anorexia nervosa and familial risk factors: a systematic review of the literature
- Open access
- Published: 25 August 2022
- Volume 42 , pages 25476–25484, ( 2023 )
Cite this article
You have full access to this open access article
- Antonio Del Casale ORCID: orcid.org/0000-0003-2427-6944 1 ,
- Barbara Adriani 2 ,
- Martina Nicole Modesti 2 ,
- Serena Virzì 2 ,
- Giovanna Parmigiani 1 ,
- Alessandro Emiliano Vento 1 &
- Anna Maria Speranza 1
5913 Accesses
1 Altmetric
Explore all metrics
Anorexia Nervosa (AN) is a psychological disorder involving body manipulation, self-inflicted hunger, and fear of gaining weight.We performed an overview of the existing literature in the field of AN, highlighting the main intrafamilial risk factors for anorexia. We searched the PubMed database by using keywords such as “anorexia” and “risk factors” and “family”. After appropriate selection, 16 scientific articles were identified. The main intrafamilial risk factors for AN identified include: increased family food intake, higher parental demands, emotional reactivity, sexual family taboos, low familial involvement, family discord, negative family history for Eating Disorders (ED), family history of psychiatric disorders, alcohol and drug abuse, having a sibling with AN, relational trauma. Some other risk factors identified relate to the mother: lack of maternal caresses, dysfunctional interaction during feeding (for IA), attachment insecurity, dependence. Further studies are needed, to identify better personalized intervention strategies for patients suffering from AN.
Highlights:
This systematic review aims at identifying the main intrafamilial risk factors for anorexia nervosa, including maternal ones.
Intrafamilial risk factors identified mostly regard family environment and relational issues, as well as family history of psychiatric diseases.
Family risk factors identified may interact with genetic, environmental, and personal risk factors.
These findings may help develop tailored diagnostic procedures and therapeutic interventions.
Similar content being viewed by others

Factors predicting long-term weight maintenance in anorexia nervosa: a systematic review
Lydia Maurel, Molly MacKean & J. Hubert Lacey

An update on the prevalence of eating disorders in the general population: a systematic review and meta-analysis
Jie Qian, Ying Wu, … Dehua Yu

The Relationship Between Body Image Concerns, Eating Disorders and Internet Use, Part I: A Review of Empirical Support
Rachel F. Rodgers & Tiffany Melioli
Avoid common mistakes on your manuscript.
Introduction
Eating behavior encompasses all responses associated with the act of eating and is influenced by social conditions, individual perception, previous experiences, and nutritional status. Additional influencing factors include mass media and idealization of thinness. Anorexia nervosa (AN) is a psychological disorder concerning body manipulation, including fear of becoming fat and self-inflicted hunger. This disorder is interpreted as a response to the social context and a woman’s rejection of fat to deny mature sexuality (Gonçalves et al., 2013 ; Korb, 1994 ) and it was once supposed to have “hysterical” causes (Valente, 2016 ). The current definition of AN provided by the DSM-5 describes it as “a restriction of energy intake relative to requirements such as to lead to a significantly low body weight […]; intense fear of gaining weight or becoming fat, or persistence in behaviors that interfere with weight gain […]; alteration in the way weight or body shape are experienced […]” (Cuzzolaro, 2014 ). The lifetime prevalence of AN is estimated being of 1.4% (0.1–3.6%) in women and 0.2% (0-0.3%) in men (Galmiche et al., 2019 ). The lifetime prevalence rates of anorexia nervosa might be up to 4% among females and 0.3% among males (Van Eeden et al., 2021 ). AN finds its roots in biological, psychological, social, and familial risk factors.
More precisely, heritable risk factors for AN can be found in 48–74% of cases (Baker et al., 2017 ): for example, it has a higher prevalence in female relatives of individuals with AN (Bulik et al., 2019 ). The presence of genetic correlations between AN and metabolic and anthropometric traits may explain why people with AN achieve very low BMIs and may even maintain and relapse to low body weight despite clinical improvement (Bulik et al., 2019 ). On the other hand, psychological risk factors include excessive concerns about weight and figure, low self-esteem, and depression; while social risk factors are related to peer diet, peer criticism, and poor social support (Haynos et al., 2016 ). As far as family is concerned, it has been observed that anorexic girls’ families are often characterized by poor communication with one another, overprotection, conflicts, and hostility (Emanuelli et al., 2003 ; Horesh et al., 2015 ; Sim et al., 2009 ).
Overall, the puzzle of AN risk factors is still obscure and needs deeper investigations as far as some predisposing aspects are concerned, such as intrafamilial risk factors, which have been extensively analyzed but not properly clarified for clinical applications. Because of the multifactorial etiology of AN, intrafamilial risk factors identification can help to establish preventive interventions in at-risk individuals, and to provide tailored treatments from the earliest stages of the disorder. Our main hypothesis is that intrafamilial as well as maternal risk factors play an essential role in the development of the disease.
Therefore, the main objective of this work is to provide a scientific review of the existing literature about familial relational risk factors involved in the development of AN, with the aim of improving: prevention, establishment of an early diagnosis, and development of a tailored treatment.
Methodology
On February the 16th, 2022, a first research was conducted on PubMed with the title/abstract filter, using the terms “anorexia AND risk factors AND family” in the search bar. For eligibility, we included only randomized controlled studies and case-control studies focused on the issue, as well as case-control studies with at least 50 participants. We excluded reviews, single case studies, case reports, other types of articles and other studies that did not focus on the main topic. The system provided 76 articles, of which 24 were ignored for low relevance. Hence, 52 were assessed for eligibility, from which 26 articles were excluded for not respecting the inclusion criteria, and 12 were excluded for not analyzing the research subject specifically. To the remaining 14 articles, 2 were added from citation search.
In the PRISMA diagram below (Fig. 1 ), the articles identified for the review (76) are reported schematically: screened (76), assessed for eligibility (52) and included (16).
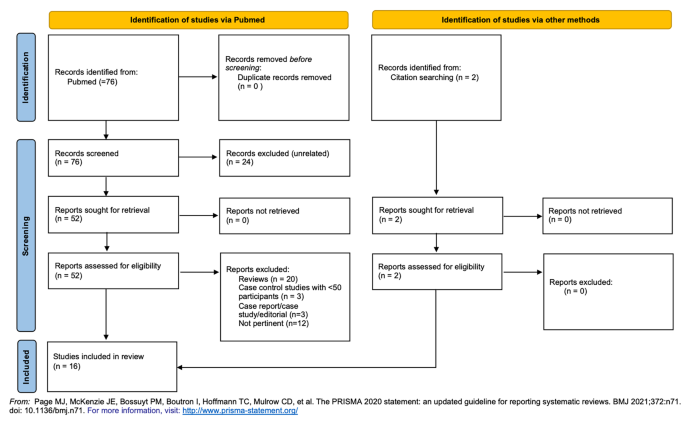
PRISMA diagram of the study
The main results of the studies analyzed are summarized in Table 1 .
Despite anorexia having been usually considered an expression of age-specific conflicts intensified by constrictive cultural ideas and certain kinds of familial constellations (Bemporad et al., 1988 ), having our review included studies from 1990 to 2021 and conducted across many countries (i.e. US, Japan, Poland, UK, etc.) we can hypothesize that such a condition just evolves with culture and time, still maintaining certain background issues that we are aiming to emphasize in order to recognize certain red flags.
Eating disorders mark deficits in the ability to be nourished and to symbolize embodied experience. Psychoanalytic theories suggest that mothers who are insufficiently developed leave the child either austerely avoiding intrusion or struggling to digest maternal provisions without becoming lost in them. (Charles, 2021 ). Infantile Anorexia (IA) has been defined as a child’s refusal of food for more than 1 month, between 6 months and 3 years of age; acute and/or chronic malnutrition; parental concern about the child’s eating; mother-child conflict, talk, and distraction during mealtime (Chatoor et al., 1998 ). Maternal risk factors for (IA) we have identified across the review can confirm this widely accepted theory, specifically lack of maternal caresses (Mangweth et al., 2005 ), dysfunctional interaction during feeding in IA (Ammaniti et al., 2010 ), and attachment insecurity (Chatoor et al., 2000 ). Regarding maternal history of psychiatric diseases, it has been noted that maternal depression has an influence on the development of conflicts during mother-child interaction in younger children, while maternal psychoticism predicts mother-child conflict during feeding in older children (Ammaniti et al., 2010 ). This means that depressed mothers engage in less positive interactions with their infants while breastfeeding, with difficulties in empathically recognizing their infant’s affective states at mealtimes (Ammaniti, Ambruzzi et al., 2004 ; Feldman et al., 2004 ).
In addition to the relational risk factors, maternal diet seems to play a role in the development of AN (Haynos et al., 2016 ). This mechanism seems to find its roots early during childhood, since the infant’s weight appears to be inversely related to the mother’s degree of concern about her body shape (Ammaniti, Lucarelli et al., 2004 ). The “modelling theory of AN” (Pike & Rodin, 1991 ) argues that adolescent girls begin the diet by mimicking their dieting mothers. It seems that family concerns about weight and appearance are directly linked to the development of low satisfaction with one’s body, and therefore directly or indirectly related to eating problems (Leung et al., 1996 ).
Maternal risk factors are synthesized in Table 2 .
Enlarging our highlight from the mother to the whole family nucleus, the onset and maintenance of AN seems to be closely related to familial risk factors, and knowing them is crucial to identify the best therapeutic approach in order to target the unhealthy family environment as well as the needs of the patient. In addition, being aware of the familiar background may help in strengthening the hypothesis of genetic correlates within Eating Disorders (ED). Intrafamilial risk factors for the development of ED seem to have a greater impact when they occur early in adolescence (Field et al., 2008 ), but most of them are chronic in time and one can suppose they can be found in a family at any time during the life of the patient.
The major intrafamilial risk factors identified in this review are summarized in the following Table 3 .
Increased food intake in the family (Hilbert et al., 2014 ) seems to play a role in the development of ED. This seems counterintuitive, but the discrepancy between one’s family food intake and peer and media influences on body ideals may contribute to triggering a subtle mechanism by which diet represents a way to affirm oneself in front of the family and reestablish social acceptance.
Perfectionism (Hilbert et al., 2014 ; Pike et al., 2008 , 2021 ) is widely recognized as a familiar risk factor across many studies, and it can be assimilated to higher parental demands (Pike et al., 2008 ). It surely contributes to creating a tense family environment in which the development of oneself is more difficult, therefore inhibiting progressive differentiation of self from other (Charles, 2021 ). Perfectionism itself will become a personal risk factor for the outcome and severity of disease (Longo, Aloi et al., 2021 ) in a way that could be mimicking the family environment.
In general, unhealthy family functioning is predictive of adolescence problems (Lyke & Matsen, 2013 ). General family malfunction is predictive for AD onset during adolescence, and the level of affective expression of the family seems to be relate to ED risk during adolescence (Felker & Stivers, 1994 ), but our review has highlighted that all those features of what could be described as a “toxic” family environment in the common sense play a role in the development of AN. Emotional reactivity (Lyke & Matsen, 2013 ), as well as family taboos regarding nudity and sexuality (Mangweth et al., 2005 ), low familial involvement (Haynos et al., 2016 ), negative affectivity (Pike et al., 2008 , 2021 ), and family discord (Pike et al., 2008 ) may lie in the background in the lives of a future AN patient, and should be recognized as environmental risk factors in order to develop a tailored psychotherapeutic intervention that may involve the family as well as the patient, since it seems clear that the quality of family functioning influences the development (McGrane & Carr, 2002 ) and maintenance of EDs (North et al., 1997 ; Strober et al., 1997 ; Wewetzer et al., 1996 ).
As far as the presence of other disorders in family members is concerned, our review established that a familiar history of almost any psychiatric disorder (Longo, Marzola et al., 2021 ; Pike et al., 2021 ), including depression (Lyon et al., 1997 ), affective disorders (Steinhausen et al., 2015 ), alcohol and drug abuse (Lyon et al., 1997 ) plays a role in the development of AN. Nevertheless, having a sibling with AN increases the risk of developing AN (Machado et al., 2014 ; Steinhausen et al., 2015 ). We can hypothesize that the role of genetics in this mechanism is crucial yet still obscure, and nevertheless, talking about the presence of these diseases in members of the family nucleus, having to cope and live with the difficulties of others’ conditions is what can predispose to AN. In addition, the opposite may happen as well: there is an increased risk for relatives of patients with AN and BN to develop subclinical forms of ED, major depressive disorder, obsessive-compulsive disorder, and anxiety disorders (Lilenfeld et al., 1998 ). What is curious to note is that, on the one hand, having a sibling with AN predisposes to the development of AN (Felker & Stivers, 1994 ; Machado et al., 2014 ; Steinhausen et al., 2015 ), probably because of shared intrafamilial risk factors, therefore underlining the importance of the aim of this review; but, on the other hand, negative family history for ED predicts poor outcome (Ackard et al., 2014 ), probably because of the familiar unpreparedness to cope with such a difficult condition and the discrepancy created between the healthy members and the patient, which remains alone and uncapable of sharing certain issues with the others, so close yet so far from them.
Another risk factor identified is having suffered a relational trauma (Longo, Marzola et al., 2021 ). In general, individuals who have suffered from traumatic events (physical violence, being threatened with a weapon, sexual violence, being a victim of robbery) more frequently develop maladaptive eating behaviors (Field et al., 2008 ). Some evidence also suggests an increase of severe life events in the year preceding the onset of AN (Råstam & Gillberg, 1991 ). Children of mothers who have experienced the loss of a vital member of their family (i.e. older child or partner) in the six months prior to pregnancy have a higher risk of ED than children and infants who have not been exposed to this risk factor (Su et al., 2015 ). Further confirming the possible role of relational trauma as a red flag not only in the development of AN, but also in determining the severity of the disease, patients with AN and comorbid Post Traumatic Stress Disorder (PTSD) show more severe concerns about body shape and weight (Field et al., 2008 ). Having suffered physical and sexual abuse during childhood appears to be related to the onset of psychiatric pathologies in general, and not specifically to the onset of EDs in the young adult (Bruch, 1977 ; McGrane & Carr, 2002 ; Smith et al., 1995 ): therefore, this risk factor needs further investigation to confirm its specific role in the development of AN.
Strength and limits
The strength of this work lies in the comparison between different studies regarding AN showing high level of evidence and providing a complete picture of the constellation of intrafamilial risk factors of anorexia nervosa. There main limit of this study is that few articles from those included are from the very last years, while many other studies were conducted and published earlier (1990–2014), underlining the need of further investigations.
Conclusions
The main intrafamilial risk factors for AN identified from this study are: increased food intake in the family, perfectionism, higher parental demands, emotional reactivity, family taboos regarding nudity and sexuality, low familial involvement, negative affectivity, family discord, dependence, negative family history for ED (as a predictor of poor outcome), family history of depression, positive family history for psychiatric disorders, affective disorders in family members, alcohol and drug abuse, having a sibling with AN, relational trauma. Some other risk factors identified may relate to the role of the mother during childhood especially, and are as follows: lack of maternal caresses, dysfunctional interaction during feeding (for IA), attachment insecurity, dependence, maternal diet.
Complex interactions occur between intrafamilial risk factors and other personal aspects and symptoms, including perfectionism, individual body image issues, social concerns, excessive preoccupation with weight control, stress and adjustment problems, lack of close friends, social prejudice.
In conclusion, further studies are needed to understand more clearly how intrafamilial risk factors for AN interact with other environmental, personal and genetic ones, in order to connect the dots that can lead to an improvement of diagnostic and therapeutic procedures, and to the development of tailored intervention strategies that may target multiple issues in the life of the patient, including intrafamilial mechanisms that may be identified precociously and addressed through familial therapy, for the sake of the whole family nucleus.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Ackard, D. M., Richter, S., Egan, A., & Cronemeyer, C. (2014). Poor outcome and death among youth, young adults, and midlife adults with eating disorders: An investigation of risk factors by age at assessment. International Journal of Eating Disorders , 47 (7), 825–835. https://doi.org/10.1002/eat.22346
Article PubMed Google Scholar
Ammaniti, M., Ambruzzi, A. M., Lucarelli, L., Cimino, S., & D’Olimpio, F. (2004). Malnutrition and dysfunctional mother-child feeding interactions: clinical assessment and research implications. Journal of the American College of Nutrition , 23 (3), 259–271. https://doi.org/10.1080/07315724.2004.10719369
Ammaniti, M., Lucarelli, L., Cimino, S., & D’Olimpio, F. (2004). Transmission intergénérationnelle: troubles alimentaires de l’enfance et psychopathologie maternelle. Devenir , 16 (3), 173. https://doi.org/10.3917/dev.043.0173
Article Google Scholar
Ammaniti, M., Lucarelli, L., Cimino, S., D’Olimpio, F., & Chatoor, I. (2010). Maternal psychopathology and child risk factors in infantile anorexia. International Journal of Eating Disorders , 43 (3), 233–240. https://doi.org/10.1002/eat.20688
Baker, J. H., Schaumberg, K., & Munn-Chernoff, M. A. (2017). Genetics of Anorexia Nervosa. Current Psychiatry Reports , 19 (11), 84. https://doi.org/10.1007/s11920-017-0842-2
Article PubMed PubMed Central Google Scholar
Bemporad, J. R., Ratey, J. J., O’Driscoll, G., & Daehler, M. L. (1988). Hysteria, Anorexia and the Culture of Self-Denial. Psychiatry (New York) , 51 (1), 96–103. https://doi.org/10.1521/00332747.1988.11024383
Bruch, H. (1977). Patologia del comportamento alimentare . Italian Tr). Feltrinelli.
Bulik, C. M., Flatt, R., Abbaspour, A., & Carroll, I. (2019). Reconceptualizing anorexia nervosa. Psychiatry and Clinical Neurosciences , 73 (9), 518–525. https://doi.org/10.1111/pcn.12857
Charles, M. (2021). Meaning, metaphor, and metabolization: the case of eating disorders. American Journal of Psychoanalysis , 81 (4), 444–466. https://doi.org/10.1057/s11231-021-09324-9
Chatoor, I., Hirsch, R., Ganiban, J., Persinger, M., & Hamburger, E. (1998). Diagnosing infantile anorexia: the observation of mother-infant interactions. Journal of the American Academy of Child and Adolescent Psychiatry , 37 (9), 959–967. https://doi.org/10.1097/00004583-199809000-00016
Chatoor, I., Ganiban, J., Hirsch, R., Borman-Spurrell, E., & Mrazek, D. A. (2000). Maternal characteristics and toddler temperament in infantile anorexia. Journal of the American Academy of Child and Adolescent Psychiatry , 39 (6), 743–751. https://doi.org/10.1097/00004583-200006000-00013
Cuzzolaro, M. (2014). Anoressie e bulimie . Il Mulino.
Emanuelli, F., Ostuzzi, R., Cuzzolaro, M., Watkins, B., Lask, B., & Waller, G. (2003). Family functioning in anorexia nervosa: British and Italian mothers’ perceptions. Eating Behaviors , 4 (1), 27–39. https://doi.org/10.1016/s1471-0153(02)00097-1
Feldman, R., Keren, M., Gross-Rozval, O., & Tyano, S. (2004). Mother-Child touch patterns in infant feeding disorders: relation to maternal, child, and environmental factors. Journal of the American Academy of Child and Adolescent Psychiatry , 43 (9), 1089–1097. https://doi.org/10.1097/01.chi.0000132810.98922.83
Felker, K. R., & Stivers, C. (1994). The relationship of gender and family environment to eating disorder risk in adolescents. Adolescence , 29 (116), 821–834. http://www.ncbi.nlm.nih.gov/pubmed/7892793
PubMed Google Scholar
Field, A. E., Javaras, K. M., Aneja, P., Kitos, N., Camargo, C. A., Taylor, C. B., & Laird, N. M. (2008). Family, peer, and media predictors of becoming eating disordered. Archives of Pediatrics & Adolescent Medicine , 162 (6), 574–579. https://doi.org/10.1001/archpedi.162.6.574
Galmiche, M., Déchelotte, P., Lambert, G., & Tavolacci, M. P. (2019). Prevalence of eating disorders over the 2000–2018 period: A systematic literature review. American Journal of Clinical Nutrition , 109 (5), 1402–1413. https://doi.org/10.1093/ajcn/nqy342
Gonçalves, J. A., Moreira, E. A. M., de Trindade, E. B. S. M., & Fiates, G. M. R. (2013). Eating disorders in childhood and adolescence.Revista Paulista de Pediatria: Orgao Oficial Da Sociedade de Pediatria de Sao Paulo, 31 (1),96–103. https://doi.org/10.1590/s0103-05822013000100016
Haynos, A. F., Watts, A. W., Loth, K. A., Pearson, C. M., & Neumark-Stzainer, D. (2016). Factors Predicting an Escalation of Restrictive Eating During Adolescence. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine , 59 (4), 391–396. https://doi.org/10.1016/j.jadohealth.2016.03.011
Hilbert, A., Pike, K. M., Goldschmidt, A. B., Wilfley, D. E., Fairburn, C. G., Dohm, F. A., Walsh, B. T., & Weissman, S., R (2014). Risk factors across the eating disorders. Psychiatry Research , 220 (1–2), 500–506. https://doi.org/10.1016/j.psychres.2014.05.054
Horesh, N., Sommerfeld, E., Wolf, M., Zubery, E., & Zalsman, G. (2015). Father-daughter relationship and the severity of eating disorders. European Psychiatry: The Journal of the Association of European Psychiatrists , 30 (1), 114–120. https://doi.org/10.1016/j.eurpsy.2014.04.004
Korb, M. (1994). Anorexia as Symbolic Expression of a Woman’s Rejection of Her Mother’s Life. Western Journal of Nursing Research , 16 (1), 69–80. https://doi.org/10.1177/019394599401600106
Leung, F., Schwartzman, A., & Steiger, H. (1996). Testing a dual-process family model in understanding the development of eating pathology: a structural equation modeling analysis. The International Journal of Eating Disorders , 20 (4), 367–375. https://doi.org/10.1002/(SICI)1098-108X(199612)20:4%3C367::AID-EAT4%3E3.0.CO;2-L
Lilenfeld, L. R., Kaye, W. H., Greeno, C. G., Merikangas, K. R., Plotnicov, K., Pollice, C., Rao, R., Strober, M., Bulik, C. M., & Nagy, L. (1998). A controlled family study of anorexia nervosa and bulimia nervosa: Psychiatric disorders in first-degree relatives and effects of proband comorbidity. Archives of General Psychiatry , 55 (7), 603–610. https://doi.org/10.1001/archpsyc.55.7.603
Longo, P., Aloi, M., Delsedime, N., Rania, M., Garcia, S., Abbate-Daga, C., G., & Marzola, E. (2021). Different clusters of perfectionism in inpatients with anorexia nervosa and healthy controls. Eating Disorders . https://doi.org/10.1080/10640266.2021.1938937
Longo, P., Marzola, E., De Bacco, C., Demarchi, M., & Abbate-Daga, G. (2021). Young patients with anorexia nervosa: The contribution of post-traumatic stress disorder and traumatic events. Medicina (Lithuania) , 57 (1), 1–10. https://doi.org/10.3390/medicina57010002
Lyke, J., & Matsen, J. (2013). Family functioning and risk factors for disordered eating. Eating Behaviors , 14 (4), 497–499. https://doi.org/10.1016/j.eatbeh.2013.08.009
Lyon, M., Chatoor, I., Atkins, D., Silber, T., Mosimann, J., & Gray, J. (1997). Testing the hypothesis of the multidimensional model of anorexia nervosa in adolescents. Adolescence , 32 (125), 101–111.
Machado, B. C., Gonçalves, S. F., Martins, C., Hoek, H. W., & Machado, P. P. (2014). Risk factors and antecedent life events in the development of anorexia nervosa: A Portuguese case-control study. European Eating Disorders Review , 22 (4), 243–251. https://doi.org/10.1002/erv.2286
Mangweth, B., Hausmann, A., Danzl, C., Walch, T., Rupp, C. I., Biebl, W., Hudson, J. I., & Pope, H. G. (2005). Childhood body-focused behaviors and social behaviors as risk factors of eating disorders. Psychotherapy and Psychosomatics , 74 (4), 247–253. https://doi.org/10.1159/000085149
McGrane, D., & Carr, A. (2002). Young Women at Risk for Eating Disorders: Perceived Family Dysfunction and Parental Psychological Problems. Contemporary Family Therapy , 24 , 385–395.
North, C., Gowers, S., & Byram, V. (1997). Family functioning and life events in the outcome of adolescent anorexia nervosa. The British Journal of Psychiatry: The Journal of Mental Science , 171 , 545–549. https://doi.org/10.1192/bjp.171.6.545
Pike, K. M., Hilbert, A., Wilfley, D. E., Fairburn, C. G., Dohm, F. A., Walsh, B. T., & Striegel-Moore, R. (2008). Toward an understanding of risk factors for anorexia nervosa: A case-control study. Psychological Medicine , 38 (10), 1443–1453. https://doi.org/10.1017/S0033291707002310
Pike, K. M., & Rodin, J. (1991). Mothers, daughters, and disordered eating. Journal of Abnormal Psychology , 100 (2), 198–204. https://doi.org/10.1037//0021-843x.100.2.198
Pike, K. M., So, M., Hilbert, A., Maekawa, H., Shimanouchi, T., Wilfley, D., Dohm, F. A., Fairburn, C. G., & Weissman, R. S. (2021). Risk factors for anorexia nervosa and bulimia nervosa in Japan and compared to a U.S. sample. International Journal of Eating Disorders , 54 (2), 155–167. https://doi.org/10.1002/eat.23442
Råstam, M., & Gillberg, C. (1991). The family background in anorexia nervosa: a population-based study. Journal of the American Academy of Child and Adolescent Psychiatry , 30 (2), 283–289. https://doi.org/10.1097/00004583-199103000-00018
Sim, L. A., Homme, J. H., Lteif, A. N., Voort, V., Schak, J. L., K. M., & Ellingson, J. (2009). Family functioning and maternal distress in adolescent girls with anorexia nervosa. The International Journal of Eating Disorders , 42 (6), 531–539. https://doi.org/10.1002/eat.20654
Smith, L. M., Mullis, R. L., & Hill, E. W. (1995). Identity Strivings within the Mother-Daughter Relationship. Psychological Reports , 76 (2), 495–503. https://doi.org/10.2466/pr0.1995.76.2.495
Steinhausen, H. C., Jakobsen, H., Helenius, D., Munk-Jørgensen, P., & Strober, M. (2015). A nation-wide study of the family aggregation and risk factors in anorexia nervosa over three generations. International Journal of Eating Disorders , 48 (1), 1–8. https://doi.org/10.1002/eat.22293
Strober, M., Freeman, R., & Morrell, W. (1997). The long-term course of severe anorexia nervosa in adolescents: survival analysis of recovery, relapse, and outcome predictors over 10–15 years in a prospective study. The International Journal of Eating Disorders , 22 (4), 339–360. https://doi.org/10.1002/(sici)1098-108x(199712)22:4%339::aid-eat1%3.0.co;2-n
Su, X., Xu, B., Liang, H., Olsen, J., Yuan, W., Cnattingius, S., László, K. D., & Li, J. (2015). Prenatal maternal bereavement and risk of eating disorders in infants and toddlers: a population-based cohort study. Bmc Psychiatry , 15 , 229. https://doi.org/10.1186/s12888-015-0612-9
Valente, S. (2016). The hysterical anorexia epidemic in the French nineteenth century. Dialogues in Philosophy Mental and Neuro Sciences , 9 (1), 22–23.
Google Scholar
Van Eeden, A. E., Van Hoeken, D., & Hoek, H. W. (2021). Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Current Opinion in Psychiatry , 34 (6), 515–524. https://doi.org/10.1097/YCO.0000000000000739
Wewetzer, C., Deimel, W., Herpertz-Dahlmann, B., Mattejat, F., & Remschmidt, H. (1996). Follow-up investigation of family relations in patients with anorexia nervosa. European Child & Adolescent Psychiatry , 5 (1), 18–24. https://doi.org/10.1007/BF00708210
Download references
Acknowledgement
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement.
Author information
Authors and affiliations.
Faculty of Medicine and Psychology, Department of Dynamic and Clinical Psychology, and Health Studies, Unit of Psychiatry ‘Sant’Andrea’ University Hospital, Sapienza University of Rome, Via di Grottarossa, 1035-1039, 00189, Rome, Italy
Antonio Del Casale, Giovanna Parmigiani, Alessandro Emiliano Vento & Anna Maria Speranza
Faculty of Medicine and Psychology, Sapienza University of Rome, Rome, Italy
Barbara Adriani, Martina Nicole Modesti & Serena Virzì
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: ADC, SV; Data curation ADC, GP; Investigation: SV, BA, MNM, AV, GP; Methodology: ADC; MNM; Supervision: ADC, AMS; Roles/Writing - original draft: ADC, SV, BA, MNM; Writing - review & editing: ADC, MNM.
Corresponding author
Correspondence to Antonio Del Casale .
Ethics declarations
Conflict of interest statement.
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Informed consent
Not applicable.
Conflict of interest
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Del Casale, A., Adriani, B., Modesti, M.N. et al. Anorexia nervosa and familial risk factors: a systematic review of the literature. Curr Psychol 42 , 25476–25484 (2023). https://doi.org/10.1007/s12144-022-03563-4
Download citation
Received : 09 May 2022
Revised : 09 May 2022
Accepted : 24 July 2022
Published : 25 August 2022
Issue Date : October 2023
DOI : https://doi.org/10.1007/s12144-022-03563-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Anorexia nervosa
- Risk factors
- Eating disorders
- Environment
Level of evidence:
- Find a journal
- Publish with us
- Track your research
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed

Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Anorexia Nervosa
- Evelyn Attia M.D.
- B. Timothy Walsh M.D.
Search for more papers by this author
At the suggestion of her pediatrician, “Rachel,” a 19-year-old college freshman at a competitive liberal arts college, was brought by her parents for psychiatric evaluation during spring break. According to her parents, Rachel had lost 16 lb since her precollege physical the previous August, falling to a weight of 104 lb at a height of 5 feet, 5 inches. Rachel’s chief complaint was that “everyone thinks I have an eating disorder.” She explained that she had been a successful student and field hockey player in high school. Having decided not to play field hockey in college, she began running several mornings each week during the summer and “cut out junk food” to protect herself from gaining “that freshman 10.” Rachel lost a few pounds that summer and received compliments from friends and family for looking so “fit.” She reported feeling more confident and ready for college than she had expected as the summer drew to a close. Once she began school, Rachel increased her running to daily, often skipped breakfast in order to get to class on time, and selected from the salad bar for her lunch and dinner. She worked hard in school, made the dean’s list the first semester, and announced to her family that she had decided to pursue a premed program. When Rachel returned home for Christmas vacation, her family noticed that she looked thin and tired. Despite encouragement to catch up on rest, she awoke early each morning to maintain her running schedule. She displayed a newfound interest in cooking and spent much of the day planning, shopping, and preparing dinner for her family. Rachel returned to school in January and thought she might be developing depression. Courses seemed less interesting, and she wondered whether the college she attended was right for her after all. She was sleeping less well and felt cold much of the day. Rachel’s parents asked her to step on the bathroom scale the night she returned home for spring break. Rachel was surprised to learn that her weight had fallen to 104 lb, and she agreed to a visit to her pediatrician, who found no evidence of a general medical illness and recommended a psychiatric consultation. Does Rachel have anorexia nervosa? If so, how should she be treated?
Anorexia nervosa is a serious mental illness characterized by the maintenance of an inappropriately low body weight, a relentless pursuit of thinness, and distorted cognitions about body shape and weight. Anorexia nervosa commonly begins during middle to late adolescence, although onsets in both prepubertal children and older adults have been described. Anorexia nervosa has a mortality rate as high as that seen in any psychiatric illness (1) and is associated with physiological alterations in virtually every organ system, although routine laboratory test results are often normal and physical examination may reveal only marked thinness.
Current Definition
DSM-IV (2) lists four criteria for the diagnosis of anorexia nervosa:
1. Refusal to maintain body weight at or above a minimally normal weight for age and height
2. Intense fear of gaining weight or becoming fat, even though underweight
3. Disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or denial of the seriousness of the current low body weight
4. In postmenarchal females, amenorrhea (i.e., the absence of at least three consecutive menstrual cycles)
DSM-IV describes two subtypes of anorexia nervosa—the restricting subtype, consisting of those individuals whose eating behavior is characterized by restriction of type and quantity of food without binge eating or purging behaviors, and the binge-purge subtype, consisting of those who also exhibit binge eating and/or purging behaviors, such as vomiting or misuse of laxatives.
Diagnostic Challenges
The DSM-IV criteria are most easily applied when patients are both sufficiently ill to fulfill all four diagnostic criteria and able to describe their ideation and behavior accurately. However, because ambivalence and denial frequently lead those with anorexia nervosa to minimize their symptoms, the clinician must make inferences about mental state and behavior.
An additional problem in diagnosis is that many individuals meet some but not all of the formal diagnostic criteria. For example, some women who meet all other criteria for anorexia nervosa continue to report some spontaneous menstrual activity. In a community-based sample of 84 female patients with full- or partial-syndrome anorexia nervosa, those with amenorrhea were not statistically different from those without across a number of clinical variables (3) , which raises questions about the utility of this diagnostic criterion (4 , 5) .
Differential Diagnosis
Proper diagnosis of any condition that includes low weight and restrictive eating must include consideration of other psychiatric and medical conditions that include these problems. Psychotic disorders, including schizophrenia and schizoaffective and delusional disorders, as well as anxiety disorders, such as obsessive-compulsive disorder, can include symptoms of food avoidance and distorted beliefs about one’s body. Medical conditions, including endocrine disturbances (such as thyroid disease and diabetes mellitus), gastrointestinal disturbances (such as inflammatory bowel and celiac disease), infections (such as hepatitis), and neoplastic processes may present with weight loss and should be considered when evaluating a patient for a possible eating disorder.
Anorexia nervosa has been recognized for centuries. Sir William Gull coined the term anorexia nervosa in 1873, but Richard Morton likely offered the first medical description of the condition in 1689 (6 , 7) . Despite its long-standing recognition, remarkably little is known about the etiology of, and effective treatment for, anorexia nervosa. A 2002 review in the American Journal of Psychiatry concluded that little progress was made during the second half of the 20th century in understanding the etiology, prognosis, or treatment of the disorder (8) .
Epidemiology
Prevalence rates for anorexia nervosa are generally described as ranging from 0.5% to 1.0% among females (9 , 10) , with males being affected about one-tenth as frequently (10 , 11) . A recent study describing a large population-based cohort of Swedish twins born between 1935 and 1958 found the overall prevalence of anorexia nervosa among the 31,406 study participants to be 1.20% and 0.29% for females and males, respectively; the prevalence of anorexia nervosa in both sexes was greater among those born after 1945 (12) .
Risk Factors
The identification of risk factors for anorexia nervosa is challenging because the low incidence of the disorder makes the conduct of prospective studies of sufficient size very difficult. A variety of possible risk factors have been identified, including early feeding difficulties, symptoms of anxiety, perfectionistic traits, and parenting style, but none can be considered to have been conclusively demonstrated (13 , 14) . Similarly, cultural factors undoubtedly play some role in the development of anorexia nervosa, although the disorder’s long history and its presence in regions around the globe (15 – 18) suggest that factors other than culture provide central contributions to the development of the disorder. In fact, one review that considers historical reports of eating disorders, data regarding changing incidence rates of eating disorders over time, and the prevalence of eating disorders in non-Western cultures concludes that anorexia nervosa is not a culture-bound syndrome (19) . Genetic factors are increasingly accepted as important contributors to the risk of anorexia nervosa. Twin studies of eating disorders have consistently found that a significant fraction of the variability in the occurrence of anorexia nervosa can be attributed to genetic factors, with heritability estimates ranging from 33% to 84% (20) .
Course of Illness
The course of anorexia nervosa is highly variable, with individual outcomes ranging from full recovery to a chronic and severe psychosocial disability accompanied by physical complications and death. Intervention early in the course of illness and full weight restoration appear to be associated with the best outcomes. Adolescent patients have a better prognosis than do adults. One-year relapse rates after initial weight restoration approach 50% (21) . Intermediate and long-term follow-up studies examining clinical samples find that while a significant fraction of patients achieve full psychological and physical recovery, at least 20% continue to meet full criteria for anorexia nervosa on follow-up assessment, with many others reporting significant residual eating disorder symptoms, even if they do not meet full criteria for anorexia nervosa (22) .
Physiological Disturbances
A multitude of biological disturbances may occur in underweight patients, but most appear to be normal physiological responses to starvation. Clinically significant abnormalities may develop in the cardiovascular, gastrointestinal, reproductive, and fluid and electrolyte systems (23) . These abnormalities usually do not require specific treatment beyond refeeding, and they return to normal on weight restoration. A worrisome possible exception is reduced bone density; since peak bone density is normally achieved during young adulthood, a prolonged episode of anorexia nervosa during this development stage may have a long-term impact on the risk of osteoporosis.
Neurobiological Hypotheses
The striking physical and behavioral characteristics of anorexia nervosa have prompted the development of a variety of neurobiological hypotheses over the years. Recently, results of several investigations have suggested that abnormalities in CNS serotonin function may play a role in the development and persistence of the disorder (24 , 25) . Notably, studies of long-term weight-recovered patients have described indications of increased serotonin activity, such as elevated levels of the serotonin metabolite 5-hydroxyindoleacetic acid in the CSF (26) and reduced binding potential of 5-HT 2A receptors, suggestive of higher levels of circulating CNS serotonin, in several brain regions (27) .
Kaye and colleagues (28) hypothesize that individuals with anorexia nervosa may have a trait disturbance characterized by high levels of CNS serotoninergic activity leading to symptoms of anxiety that are relieved by dieting, which leads to a reduction in serotonin production. However, this provocative hypothesis is based on assessments conducted after the onset of illness, which therefore cannot distinguish a predisposing trait from a long-lasting consequence of anorexia nervosa.
Another recent line of inquiry into the biological underpinnings of anorexia nervosa focuses on the perfectionistic and rigid behavioral style, including repetitive and stereotyped behaviors, characteristic of the syndrome. Investigators have hypothesized that these behaviors may result from a propensity to extreme fear conditioning and resistance to fear extinction (29) , suggesting that abnormalities may be present in limbic structures known to be involved in the acquisition of conditioned fear behavior. Other investigators have proposed that difficulties of individuals with anorexia nervosa in changing maladaptive behavior may relate to problems with set shifting, a function mediated by corticostriatothalamocortical neural circuits (30 , 31) .
Engaging a patient with anorexia nervosa to participate fully in the psychiatric evaluation may present a greater challenge than would be the case for patients with other disorders, including other eating disorders such as bulimia nervosa or binge eating disorder. Patients with anorexia nervosa often present for evaluation not because of their own interest in symptom relief but because of the concerns of family, friends, or health care providers. It may be necessary to obtain additional information from family members or others who know the patient well.
In addition, during the evaluation, it may be helpful to identify symptoms of the illness that are most likely to be ego-dystonic for the particular patient. Patients commonly minimize their concerns about low weight, but they may be more concerned, and therefore more likely to participate in the evaluation, if they recognize poor concentration, increased irritability, low bone density, hair loss, or feeling cold as developments associated with their restrictive eating pattern.
Medical issues should be reviewed, including weight and menstrual history. A complete review of systems is indicated, as anorexia nervosa can manifest a multitude of disturbances, including cardiovascular symptoms (e.g., bradycardia and other arrhythmias, including QTc prolongation, and hypotension), gastrointestinal symptoms (e.g., slow motility, esophageal inflammation associated with purging), endocrinologic symptoms (low estrogen in females, low testosterone in males, osteopenia, and osteoporosis), and dermatologic changes, such as the development of a layer of fine hair (lanugo) on the face and extremities.
The evaluation should include specific questions about eating behaviors, including the number and content of all meals and snacks on a recent day. The clinician should inquire about 1) restricting behaviors, including limiting permissible foods, as well as decreasing caloric amounts; 2) binge eating; 3) purging behaviors, including vomiting and misuse of laxatives and diuretics; and 4) exercise and hyperactive behaviors, including preferential walking and standing.
Given patients’ reluctance to endorse all of the diagnostic symptoms of anorexia nervosa on first meeting, the clinician may do well to identify the problem as “low weight” and explain that the treatment needs to include weight restoration, whether or not the patient meets full criteria for anorexia nervosa. Patients and their families are generally very interested in data from the World War II Minnesota study of semistarvation that documented the association between starvation and the development of psychological symptoms frequently identified with anorexia nervosa, such as depression, anxiety, obsessionality about food, and rigidity about eating behaviors (32) . The clinician may have better results engaging the patient with the identification of symptoms that are commonly associated with the state of starvation and that the patient has likely found troubling (such as thinking constantly about food) and therefore worth resolving.
Treatment Guidelines
All current treatment guidelines for anorexia nervosa emphasize weight restoration. There is no clearly defined algorithm for how to accomplish this goal, although common practice includes the selection of the least restrictive treatment setting that is likely to be effective. The APA practice guideline on treatment of eating disorders suggests that highly structured treatments are often needed to achieve weight gain for patients at weights <85% ideal body weight (33) . Hospital-based treatments may be used when weight is significantly low (e.g., <75% of ideal body weight) or when there has been rapid weight loss or medical signs of malnutrition, including significant bradycardia, hypotension, hypothermia, and so on.
Generally, outpatient treatments rely on a team of professionals. Medical monitoring, including weight and laboratory assessment, may be provided by an internist or pediatrician; psychological support is offered by a psychiatrist or other therapist; and nutritional counseling from a dietitian or nutritionist is often included. The team is generally led by the medical or psychiatric clinician—typically the one with the greatest expertise in the management of eating disorders.
Effective treatments generally assess outcome by weight and behavioral change. Nonspecific support needs to be paired with expectation of progress in measurable medical, behavioral, and psychological symptoms. Weight restoration is generally associated with improvement in a variety of psychological areas, including mood and anxiety symptoms (34 , 35) . In contrast, psychological improvement without accompanying changes in weight and eating behavior is of limited value. Patients and families should be informed about the physiology of weight gain, including the substantial number of calories required daily.
A family-based outpatient treatment for anorexia nervosa, also called the “Maudsley method,” may be helpful for younger patients (36) . This approach empowers the parents of a patient with anorexia nervosa to refeed their child, renegotiate the relationship between child and parents to involve issues other than food, and help their child resume normal adolescent development without an eating disorder. Several preliminary studies have shown promising results for family therapy with adolescent patients (37 , 38) .
For patients with anorexia nervosa who do not respond to outpatient treatments or those who do not have specialized outpatient treatments available in their vicinity, more structured treatments such as inpatient or partial hospital (day treatment) programs may be necessary. Structured treatments generally include observation during and after meals together with a consistently applied behavioral program that reinforces weight gain and normal eating behaviors. In recent years, the length of hospital stay for anorexia nervosa has decreased substantially because of economic limitations imposed by third-party payers; nonetheless, hospital programs can achieve a rate of weight gain of 2–4 pounds per week during active treatment (39) .
Controlled Treatment Trials
While structured settings have been used successfully for weight restoration treatments, there is little empirical support for a specific level of care or a particular psychosocial treatment for anorexia nervosa. As mentioned, a family-based approach appears promising for children and adolescents with anorexia nervosa; family therapy has been reported to be superior to individual therapy in two randomized controlled trials for adolescents with anorexia nervosa (40 , 41) . For adults with anorexia nervosa, a small study by Pike and colleagues (42) found cognitive behavior therapy superior to nutritional counseling in preventing relapse after hospital-based weight restoration. A recent study by McIntosh et al. (43) provocatively suggested that a patient-centered nonspecific supportive therapy may have been more helpful than cognitive behavior therapy or interpersonal therapy, as measured by a global rating of anorexia nervosa symptoms, in a sample of 56 underweight women with anorexia nervosa receiving treatment over a minimum of 20 weeks; unfortunately, the amount of weight gain was modest and not significantly different among the three study treatments.
Randomized controlled trials of medications for patients with anorexia nervosa have consistently reported disappointing results. Several psychopharmacologic agents have been studied, without identification of clear benefit, although studies have been limited by small sample sizes and the fact that most of the trials have been conducted in hospital settings where other treatment interventions are offered in addition to study medication (44) . While it has been suggested that psychotropic medications are rendered ineffective in underweight patients by the biological impact of starvation, a recent study comparing fluoxetine and placebo in weight-restored patients notably found no significant benefit to medication during the year following nutritional rehabilitation (45) .
Summary and Recommendations
Although recognized for centuries, anorexia nervosa remains enigmatic, often difficult to treat, and potentially lethal. The current approach to treatment includes careful medical assessment, ongoing medical and weight monitoring, and behaviorally oriented treatment aimed at normalizing weight and eating behaviors. Family-based treatment appears promising for younger patients.
With Rachel, the patient in the vignette, her typical presentation, her low weight (corresponding to a body mass index of 17.3), and her reluctance to restore her weight to its previously healthy level led the evaluating psychiatrist to conclude that Rachel indeed had anorexia nervosa. The psychiatrist recommended that Rachel attempt outpatient treatment but explained to her and her family that many patients require more structured settings for successful weight restoration. The psychiatrist recommended that Rachel see an eating disorder specialist knowledgeable about the characteristics of anorexia nervosa and experienced in dealing with the challenges of its treatment. The outpatient treatment plan included weekly psychotherapy sessions, along with regular visits with her pediatrician and a nutritionist. Although Rachel had complained of “depression,” the psychiatrist elected not to prescribe antidepressant medication, as there is no evidence of its utility in anorexia nervosa, and weight gain in this disorder is known to lead to improvement in mood. In the meetings with Rachel, the psychiatrist used cognitive behavior therapy techniques to help her in reevaluating her assumptions that low weight was somehow essential to her sense of self-worth. Treatment outcome was assessed by changes in weight and eating behavior. Rachel’s family participated by helping to supervise meals at the start of treatment and offering her more autonomy around eating as she made progress. Rachel was asked to gain weight at a rate of >1 lb per week and knew that failure to meet this goal would lead to transfer of treatment to a more structured setting. Rachel reached and maintained her premorbid weight and was able to return to school 6 months after initial presentation.
Received July 19, 2007; accepted Aug. 6, 2007 (doi: 10.1176/appi.ajp.2007.07071151). From the Department of Psychiatry, College of Physicians and Surgeons, Columbia University, New York; and the Eating Disorders Research Unit, New York State Psychiatric Institute, New York. Address correspondence and reprint requests to Dr. Attia, New York State Psychiatric Institute, 1051 Riverside Dr., Unit 98, New York, NY 10032; [email protected] (e-mail).
CME Disclosure: Dr. Attia has received research support from Pfizer and Eli Lilly. Dr. Walsh has received research support from Abbott Pharmaceuticals.
APA policy requires disclosure by CME authors of unapproved or investigational use of products discussed in CME programs. Off-label use of medications by individual physicians is permitted and common. Decisions about off-label use can be guided by scientific literature and clinical experience.
1. Sullivan PF: Mortality in anorexia nervosa. Am J Psychiatry 1995; 152:1073–1074 Google Scholar
2. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994 Google Scholar
3. Garfinkel PE, Lin E, Goering P, Spegg C, Goldbloom D, Kennedy S, Kaplan AS, Woodside DB: Should amenorrhea be necessary for the diagnosis of anorexia nervosa? evidence from a Canadian community sample. Br J Psychiatry 1996; 168:500–506 Google Scholar
4. Cachelin F, Maher B: Is amenorrhea a critical criterion for anorexia nervosa? J Psychosom Res 1998;44:435–440 Google Scholar
5. Watson T, Andersen A: A critical examination of the amenorrhea and weight criteria for diagnosing anorexia nervosa. Acta Psychiatr Scand 2003;108:175–182 Google Scholar
6. Pearce JM: Richard Morton: origins of anorexia nervosa. Eur Neurol 2004; 52:191–192 Google Scholar
7. Silverman JA: Sir William Gull (1819–1890): limner of anorexia nervosa and myxoedema: an historical essay and encomium. Eat Weight Disord 1997; 2:111–116 Google Scholar
8. Steinhausen H-C: The outcome of anorexia nervosa in the 20th century. Am J Psychiatry 2002; 159:1284–1293 Google Scholar
9. Hoek HW, van Hoeken D: Review of the prevalence and incidence of eating disorders. Int J Eat Disord 2003; 34:383–396 Google Scholar
10. Hudson JI, Hiripi E, Pope HG Jr, Kessler RC: The prevalence and correlates of eating disorders in the National Comorbidity Survey replication. Biol Psychiatry 2007; 61:348–358 Google Scholar
11. Lucas AR, Beard CM, O’Fallon WM, Kurland LT: 50-year trends in the incidence of anorexia nervosa in Rochester, Minn: a population-based study. Am J Psychiatry 1991; 148:917–922 Google Scholar
12. Bulik CM, Sullivan PF, Tozzi F, Furberg H, Lichtenstein P, Pedersen NL: Prevalence, heritability, and prospective risk factors for anorexia nervosa. Arch Gen Psychiatry 2006; 63:305–312 Google Scholar
13. Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras WC: Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy: Psychol Bull 2004; 130:19–65 Google Scholar
14. Striegel-Moore RH, Bulik CM: Risk factors for eating disorders. Am Psychologist 2007; 62:181–198 Google Scholar
15. Lee HY, Lee EL, Pathy P, Chan YH: Anorexia nervosa in Singapore: an eight-year retrospective study. Singapore Med J 2005; 46:275–281 Google Scholar
16. Njenga FG, Kangethe RN: Anorexia nervosa in Kenya. East Afr Med J 2004; 81:188–193 Google Scholar
17. Bennett D, Sharpe M, Freeman C, Carson A: Anorexia nervosa among female secondary school students in Ghana. Br J Psychiatry 2004; 185:312–317 Google Scholar
18. Hoek HW, van Harten PN, Hermans KME, Katzman MA, Matroos GE, Susser ES: The incidence of anorexia nervosa on Curaçao. Am J Psychiatry 2005; 162:748–752 Google Scholar
19. Keel PK, Klump KL: Are eating disorders culture-bound syndromes? implications for conceptualizing their etiology. Psychol Bull 2003; 129:747–769 Google Scholar
20. Bulik CM: Exploring the gene-environment nexus in eating disorders. J Psychiatry Neurosci 2005; 30:335–339 Google Scholar
21. Pike KM: Long-term course of anorexia nervosa: response, relapse, remission, and recovery. Clin Psychol Rev 1998; 18:447–475 Google Scholar
22. Fisher M: The course and outcome of eating disorders in adults and in adolescents: a review. Adolesc Med 2003; 14:149–158 Google Scholar
23. Walsh BT: Eating disorders, in Harrison’s Principles of Internal Medicine, 17th ed. Edited by Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL. New York, McGraw-Hill (in press) Google Scholar
24. Kaye WH, Frank GK, Bailer UF, Henry SE: Neurobiology of anorexia nervosa: clinical implications of alterations of the function of serotonin and other neuronal systems. Int J Eat Disord 2005; 37(suppl):S15–S19 Google Scholar
25. Attia E, Wolk S, Cooper T, Glasofer D, Walsh BT: Plasma tryptophan during weight restoration in patients with anorexia nervosa. Biol Psychiatry 2005; 57:674–678 Google Scholar
26. Kaye WH, Gwirtsman HE, George DT, Ebert MH: Altered serotonin activity in anorexia nervosa after long-term weight restoration: does elevated cerebrospinal fluid 5-hydroxyindoleacetic acid level correlate with rigid and obsessive behavior? Arch Gen Psychiatry 1991; 48:556–562 Google Scholar
27. Frank GK, Kaye WH, Meltzer CC, Price JC, Greer P, McConaha C, Skovira K: Reduced 5-HT 2A receptor binding after recovery from anorexia nervosa. Biol Psychiatry 2002; 52:896–906 Google Scholar
28. Kaye WH, Barbarich NC, Putnam K, Gendall KA, Fernstrom J, Fernstrom M, McConaha CW, Kishore A: Anxiolytic effects of acute tryptophan depletion in anorexia nervosa. Int J Eat Disord 2003; 33:257–267 Google Scholar
29. Strober M: Pathologic fear conditioning and anorexia nervosa: on the search for novel paradigms. Int J Eat Disord 2004; 35:504–508 Google Scholar
30. Holliday J, Tchanturia K, Landau S, Collier D, Treasure J: Is impaired set-shifting an endophenotype of anorexia nervosa? Am J Psychiatry 2005; 162:2269–2275 Google Scholar
31. Steinglass J, Walsh BT, Stern Y: Set shifting deficit in anorexia nervosa. J Int Neuropsychol Soc 2006; 12:431–435 Google Scholar
32. Schiele BC, Brozek J: “Experimental neurosis” resulting from semistarvation in man. Psychosom Med 1948; 10:31–50 Google Scholar
33. American Psychiatric Association: Practice Guideline for the Treatment of Patients With Eating Disorders, 3rd ed. Am J Psychiatry 2006; 163(Jul suppl) Google Scholar
34. Meehan KG, Loeb KL, Roberto CA, Attia E: Mood change during weight restoration in patients with anorexia nervosa. Int J Eat Disord 2006; 39:587–589 Google Scholar
35. Attia E, Haiman C, Walsh BT, Flater SR: Does fluoxetine augment the inpatient treatment of anorexia nervosa? Am J Psychiatry 1998; 155:548–551 Google Scholar
36. Lock J, le Grange D, Agras WS, Dare C: Treatment Manual for Anorexia Nervosa: A Family Based Approach. New York, Guilford, 2001 Google Scholar
37. Lock J, le Grange D, Forsberg S, Hewell K: Is family therapy useful for treating children with anorexia nervosa? results of a case series. J Am Acad Child Adolesc Psychiatry 2006; 45:1323–1328 Google Scholar
38. Lock J, Agras WS, Bryson S, Kraemer HC: A comparison of short- and long-term family therapy for adolescent anorexia nervosa. J Am Acad Child Adolesc Psychiatry 2005; 44:632–639 Google Scholar
39. Guarda AS, Heinberg LJ: Inpatient and partial hospital approaches to the treatment of eating disorders, in Handbook of Eating Disorders and Obesity. Edited by Thompson JK. Hoboken, NJ, John Wiley & Sons, 2004, pp 297–322 Google Scholar
40. Russell GF, Szmukler GI, Dare C, Eisler I: An evaluation of family therapy in anorexia nervosa and bulimia nervosa. Arch Gen Psychiatry 1987; 44:1047–1056 Google Scholar
41. Robin AL, Siegel PT, Moye AW, Gilroy M, Dennis AB, Sikand A: A controlled comparison of family versus individual therapy for adolescents with anorexia nervosa. J Am Acad Child Adolesc Psychiatry 1999; 38:1482–1489 Google Scholar
42. Pike KM, Walsh BT, Vitousek K, Wilson GT, Bauer J: Cognitive behavior therapy in the posthospitalization treatment of anorexia nervosa. Am J Psychiatry 2003; 160:2046–2049 Google Scholar
43. McIntosh VVW, Jordan J, Carter FA, Luty SE, McKenzie JM, Bulik CM, Frampton CMA, Joyce PR: Three psychotherapies for anorexia nervosa: a randomized, controlled trial. Am J Psychiatry 2005; 162:741–747 Google Scholar
44. Attia E, Schroeder L: Pharmacologic treatment of anorexia nervosa: where do we go from here? Int J Eat Disord 2005; 37(suppl):S60–S63 Google Scholar
45. Walsh BT, Kaplan AS, Attia E, Olmsted M, Parides M, Carter JC, Pike KM, Devlin MJ, Woodside B, Roberto CA, Rockert W: Fluoxetine after weight restoration in anorexia nervosa: a randomized controlled trial. JAMA 2006; 295:2605–2612 Google Scholar
- Musicothérapie réceptive et anorexie mentale. Évaluation du dispositif DéPi-AM de détente psychomusicale dans l’accompagnement d’adolescentes hospitalisées : étude pilote auprès de 8 patientes Neuropsychiatrie de l'Enfance et de l'Adolescence, Vol. 72, No. 2
- Anorexie mentale et musicothérapie Soins, Vol. 68, No. 881
- L’anorexie mentale, une pathologie familière et complexe Soins, Vol. 68, No. 881
- Cognitive flexibility and the risk of anorexia nervosa: An investigation using self-report and neurocognitive assessments Journal of Psychiatric Research, Vol. 151
- Eating Disorders 18 June 2021
- Severe and Enduring Anorexia Nervosa: Enduring Wrong Assumptions? 15 February 2021 | Frontiers in Psychiatry, Vol. 11
- Characterization of Anorexia Nervosa on Social Media: Textual, Visual, Relational, Behavioral, and Demographical Analysis 20 July 2021 | Journal of Medical Internet Research, Vol. 23, No. 7
- Cognitive flexibility in acute anorexia nervosa and after recovery: A systematic review Clinical Psychology Review, Vol. 81
- Exploring the Eating Disorder Examination Questionnaire, Clinical Impairment Assessment, and Autism Quotient to Identify Eating Disorder Vulnerability: A Cluster Analysis 2 September 2020 | Machine Learning and Knowledge Extraction, Vol. 2, No. 3
- A systematic review of blood-based serotonergic biomarkers in Bulimia Nervosa Psychiatry Research, Vol. 279
- Eating Disorders 12 March 2019
- Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity, Vol. 21, No. 2
- Anorexia Nervosa, Bulimia Nervosa, and Other Eating Disorders
- Impulse control in the dorsolateral prefrontal cortex counteracts post-diet weight regain in obesity NeuroImage, Vol. 109
- Anorexia Nervosa 23 January 2015
- Boletín Médico del Hospital Infantil de México, Vol. 72, No. 4
- The association between the development of weighing technology, possession and use of weighing scales, and self-reported severity of disordered eating 9 January 2014 | Irish Journal of Medical Science (1971 -), Vol. 183, No. 3
- Eating Disorders among Adolescents with a History of Obesity Pakistan Journal of Nutrition, Vol. 13, No. 8
- Risk Factors and Antecedent Life Events in the Development of Anorexia Nervosa: A Portuguese Case-Control Study 27 February 2014 | European Eating Disorders Review, Vol. 22, No. 4
- Anorexia nervosa in adolescents: challenges remain The Lancet, Vol. 383, No. 9924
- Family and Family Therapy, Vol. 22, No. 2
- Recognising anorexia nervosa: approaches to treatment British Journal of Mental Health Nursing, Vol. 2, No. 1
- Journal of Clinical Densitometry, Vol. 16, No. 4
- Open Journal of Preventive Medicine, Vol. 03, No. 02
- Food Restriction and Reward in Rats 24 August 2012
- Back to life: How to use positive psychology to beat anorexia? 25 January 2012 | International Journal of Research Studies in Psychology, Vol. 1, No. 2
- Osteopathic Family Physician, Vol. 4, No. 6
- Anorexie mentale par procuration : une présentation inhabituelle La Presse Médicale, Vol. 40, No. 5
- Recognising anorexia nervosa British Journal of Wellbeing, Vol. 1, No. 9
- Identification and Management of Eating Disorders in Children and Adolescents 1 December 2010 | Pediatrics, Vol. 126, No. 6
- Medical futility and psychiatry: Palliative care and hospice care as a last resort in the treatment of refractory anorexia nervosa 14 May 2009 | International Journal of Eating Disorders, Vol. 43, No. 4
- Neural processing of negative word stimuli concerning body image in patients with eating disorders: An fMRI study NeuroImage, Vol. 50, No. 3
- Anorexie mentale à l'adolescence EMC - Pédiatrie - Maladies infectieuses, Vol. 5, No. 1
- Journal de Pédiatrie et de Puériculture, Vol. 23, No. 1
- Scandinavian Journal of Caring Sciences, Vol. 24, No. 3
- Pro‐anorexia websites: What a clinician should know 29 November 2008 | International Journal of Eating Disorders, Vol. 42, No. 4
- Expert Opinion on Investigational Drugs, Vol. 18, No. 5

- International edition
- Australia edition
- Europe edition

Teasing children about weight increases risk of self-stigma as adults, study finds
Research reveals ‘long-lasting effects’ caused by pressure from parents, families, bullies and the media
Parents who tease their children about their weight are putting them at greater risk of feeling bad about their bodies decades later, regardless of whether they grow up to have obesity or not, a groundbreaking study has found.
Thirteen-year-olds who felt pressure from family members to shed pounds and endured weight-based teasing showed higher levels of internalised weight stigma when they turned 31, according to research by the University of Bristol published on Tuesday in the Lancet Regional Health Europe journal.
Internalised weight stigma causes people to think they are less attractive, less competent, or less valuable as a person because of their weight, even if they do not have obesity or are underweight. It is linked to eating disorders and an increased drive for thinness.
The research found “strong and long-lasting effects on adult psychological health” caused by pressure from parents and families as well as bullies and the media.
The findings came from more than 4,000 children from in and around Bristol who were first studied in the 1990s and are now 33. It is the first study to explore the effects of such pressure across decades of people’s lives, the authors claim.
Obesity UK told a 2022 parliamentary inquiry into the impact of body image on physical and mental health that weight stigma was associated with depression and anxiety and compromised psychosocial wellbeing, could lead to avoidance or delay in adopting healthier habits and was associated with an increased risk of mortality independent of a person’s weight.
“Given substantial evidence that internalised weight stigma has serious implications for mental and other aspects of health, these findings will be crucial for targeting prevention programmes and supporting people most at risk,” the study authors concluded.
At age 13 the children were asked about how often their mother or father had made a comment about their weight and how much they were eating that made them feel bad, to what extent family members and people at school teased them about their weight or body shape, and how much pressure they felt to lose weight from family, friends and people they dated.
Eighteen years later, the same 4,060 people, now adults, were asked to rate their agreement with questions such as “I hate myself because of my weight” and “I am less attractive than most other people because of my weight”.
The researchers found that negative weight-related comments from parents, and feeling under pressure to lose weight from family and the media had the strongest associations with adults suffering with weight stigma and the connections were “robust”.
“The kids who get these comments from family members almost 20 years later have a more negative evaluation of themselves,” said Dr Amanda Hughes, a co-author of the report and a fellow at Bristol medical school’s department of population health science. “This is predicting a difference in people’s self-esteem and psychological health.”
She urged parents to “be really careful” when they talk to children about weight.
“This isn’t to say you shouldn’t be promoting healthy eating or saying exercise is a good thing, but it is about why you are making that case,” she said. “It’s about encouraging healthy eating practices for their own sake or because it makes you feel good. Don’t make it about ‘you need to be thin to be good’.”
Separately, people who were bullied as children also showed greater weight stigma, but the effect diminished depending on how long ago the bullying happened.
As the people in the study were children well before social media, the findings on the effects of media are likely to be out of date. Further research is needed to track the impact of the children’s exposure to social media later in life.
Hughes said it may not all be negative as social media could also be how people connected to body positive content.
- Children's health
- Parents and parenting
- Young people
Most viewed
2nd April 2024 Newsletter

This week we’re releasing another two resources from our new Schema series: Defectiveness and Coping Styles And Responses (Schema Therapy) . Our research roundup examines the impact of early life experiences on eating disorders, and explores how negative expectations can increase social anxiety.
Psychology Tools Schema Series
Launched earlier this year, our schema series breaks down the foundational ideas of schema therapy in an approachable and straightforward way. It also addresses the most common early maladaptive schemas (EMS) with a range of problem-specific handouts.
With illustrations, client-friendly explanations and schema-specific examples, the handouts offer accessible guidance for those working with schema therapy in-session. They’re a great learning tool for anyone wanting to become more familiar with this approach.
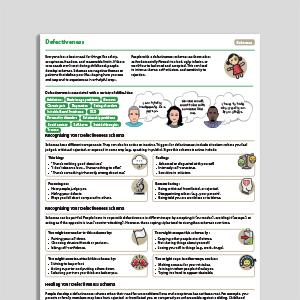
Defectiveness
Individuals with defectiveness experience a pervasive sense of inadequacy and inferiority. They see themselves as fundamentally flawed and defective, leading to deep-seated shame and unworthiness. Research suggests that it is one of the most pronounced early maladaptive schemas across psychological disorders, and is readily transmitted between parents and their children.
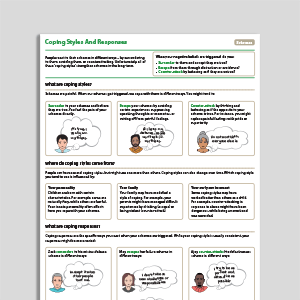
Coping Styles And Responses (Schema Therapy)
Coping styles refer to the characteristic ways individuals manage their EMS. They develop in childhood and operate outside of awareness, helping individuals adapt to their EMS, the intense affect accompanying them, and the environments in which they were formed. Much like EMS, factors that may influence the emergence of coping styles include temperament, modeling, conditioning, and culture.
Research Summaries
What role do early life experiences play in eating disorders?
What role do early life experiences play in the development of eating disorders? To address this question, a recent study explored the relationship between perceived parenting, temperament, early maladaptive schemas, and eating disorder symptoms. The findings revealed a direct linear impact pathway: maladaptive parenting predicted temperament, which in turn predicted maladaptive schemas, which ultimately influenced eating disorder symptoms. These results not only support the schema therapy model, but also offer valuable insights for broad, tailored treatment approaches for eating disorders.
"When treating patients with eating disorders, psychologists and other health professionals should consider individual differences in perceived parenting style, temperament, and early maladaptive schema levels and how these may impact the way an eating disorder manifests… More specifically, understanding the interplay of factors that contribute to the development of an eating disorder can potentially counteract the sense of personal shame and inadequacy that is often associated with a diagnosis."
Joshua, P. R., Lewis, V., Simpson, S., Kelty, S. F., & Boer, D. P. (2024). What role do early life experiences play in eating disorders? The impact of parenting style, temperament and early maladaptive schemas. Clinical Psychology & Psychotherapy , 31(1), e2904.
The legacy of social anxiety-linked negative expectancy
For therapists working with clients experiencing social anxiety, understanding the link between negative expectations, anxiety during interactions, and post-event negative thinking is crucial. This study indicates that increased negative expectations before social events amplifies state anxiety during interactions, which predicts post-event negative thinking. By recognizing the mediating role of pre-event negative expectancies, therapists can tailor interventions to address this aspect of social anxiety and the impact it has on post-event processing. However, it also highlights the need for further research exploring factors that contribute to post-event negativity.
Basanovic, J., Kowal, L., Millward, S., & MacLeod, C. (2024). The legacy of social anxiety-linked negative expectancy: A pathway from pre-event negative expectancies to post-event negative thinking. Journal of Behavior Therapy and Experimental Psychiatry , 83, 101937.
Get sent more useful pieces like this!
Sign up to our monthly newsletter full of helpful ideas, tools, and tips for mental health professionals like you. You'll find out about our latest resources, and you can also read our reviews of the latest research.
It's completely free and you can unsubscribe at any time.
- For clinicians
- For students
- Resources at your fingertips
- Designed for effectiveness
- Resources by problem
- Translation Project
- Help center
- Try us for free
- Terms & conditions
- Privacy Policy
- Cookies Policy
- Open access
- Published: 09 June 2023
A systematic review of people’s lived experiences of inpatient treatment for anorexia nervosa: living in a “bubble”
- Rebekah Rankin 1 ,
- Janet Conti 1 , 2 ,
- Lucie Ramjan 1 , 3 &
- Phillipa Hay 1 , 4
Journal of Eating Disorders volume 11 , Article number: 95 ( 2023 ) Cite this article
3230 Accesses
6 Citations
14 Altmetric
Metrics details
Treatment for anorexia nervosa (AN) is typically delivered on a continuum of care, starting with outpatient treatment, and moving onto intensive outpatient, day or residential treatment and/or inpatient hospitalisation. However, minimal attention has been afforded to the lived experiences of persons undergoing inpatient treatment for AN. In particular, qualitative literature pertaining to the lived experiences of specialist inpatient or residential treatment of AN remains fragmented and incomplete. The aim of this review was to synthesise current literature exploring patients’ lived experiences of residential and inpatient treatment for AN within eating disorder-specific treatment services.
Five databases were searched and a qualitative thematic systematic review and meta-synthesis of 11 studies were conducted.
Eleven studies of 159 participants were included. Four meta-themes were constructed from the data: (1) a medical discourse—“I don’t think it’s individualised here”; (2) restrictive practice—living in a “bubble”; (3) myself, others and “a similar demon”; and (4) I am “not just another anorexic”. The data also revealed two cross-cutting themes: (1) more than a single experience; and (2) meaning making and identity.
Conclusions
These findings highlight the complex and multifaceted nature of the inpatient treatment experience as well as the inherent conflicts in balancing the necessity of medical and psychological intervention with person-centred treatment approaches in the treatment of AN.
Plain English Summary
Treatment for anorexia nervosa (AN) is typically delivered on a continuum of care, starting with outpatient treatment, and moving onto intensive outpatient, day or residential treatment and/or inpatient hospitalisation. However, not much is known about the lived experiences of people going through inpatient treatment for AN. An improved understanding of individuals’ treatment experiences is essential in informing the development of new models of care with the potential to improve outcomes. In this systematic review, we examined the lived experiences of individuals going through inpatient treatment for AN available in the current literature. Searching in scientific databases resulted in 10,666 articles, 11 of which met the rigorous inclusion criteria. Four meta-themes and two cross-cutting themes were observed in patient experiences across the studies reviewed. These themes provide insight into the complex and multifaceted nature of the inpatient treatment experience as well as the inherent conflicts in balancing the necessity of medical and psychological intervention with person-centred treatment approaches in the treatment of AN.
Anorexia nervosa (AN) is a serious, complex and potentially life-threatening psychiatric illness, characterised by low body weight, body-image distortion and an intense fear of gaining weight [ 1 , 2 ]. This illness is indiscriminate—affecting individuals of all ages, genders, ethnicities, socioeconomic backgrounds and body weights—and ranges in both complexity and severity [ 3 ]. Based on epidemiological research, the mean-weighted lifetime prevalence rate of AN is 1.4% (range 0.1–3.6%) in women and 0.2% (range 0–0.3%) in men [ 4 ]. People with AN also experience lower levels of employment participation, high healthcare costs and early mortality [ 5 , 6 , 7 ].
Treatment for AN is typically delivered on a continuum of care, starting with outpatient treatment, and moving onto intensive outpatient, day or residential treatment, and/or inpatient hospitalisation [ 8 ]. An individual’s treatment journey through the various levels of care is unique, constantly changing and dependent on numerous factors such as treatment availability, patient motivation, and treatment history, symptom severity, medical stability, residential location and financial constraints [ 11 ]. Higher levels of care (e.g., day, residential treatment, and inpatient treatments) are reserved for those who are medically compromised and/or unable to be effectively treated in outpatient or community treatment settings [ 8 , 9 ]. Historically, hospital treatment programs for AN have focused on refeeding and medical stabilisation, applying a didactic ‘one-size-fits-all’ model of care, with community treatment teams only being developed within psychiatric or psychosomatic settings in the latter part of the twentieth century [ 10 ]. Despite ongoing advancements in the understanding of AN, research indicates that optimal care management has yet to be realised [ 8 , 11 , 12 , 13 ]. Long-term (10–20 years) follow-up studies [ 13 , 14 , 15 ] of those who have received inpatient treatment for eating disorders found that between 60 and 64% of individuals previously diagnosed with AN still met diagnostic criteria for an eating disorder at follow-up. While many people with severe and enduring AN are labelled as ‘treatment resistant’ [ 16 , 17 ], it is also possible that this group of individuals have simply been unable to access treatment that is suited to their unique needs and preferences that may support recovery [ 18 ]. These perceived deficiencies in care have driven alternate and more collaborative models of care with a much greater representation of people with lived experience on the treating team, such as the Carolyn Costin Monte Nido residential programs, which include the use of lived-experience peer mentors and clinical staff who have a lived experience of an eating disorder as a core component of their programs [ 19 , 20 ].
Most research regarding inpatient and residential treatment for AN has been quantitative and focused on treatment outcomes, measured mainly by ED symptoms or specific treatment factors such as the delivery of a particular intervention in an inpatient setting [ 20 , 21 , 22 ]. As such, minimal attention has been afforded to the lived experiences of persons undergoing inpatient treatment for AN. This is an important gap as improved understanding is essential to inform the development of new models of care with the potential to improve outcomes. While a small number of systematic reviews and meta-syntheses of the qualitative literature pertaining to the lived experience of eating disorder treatment and recovery exist [ 23 , 24 , 25 ], these reviews examine individuals’ treatment experiences across multiple treatment settings or focus on patients’ experiences of involuntary treatment [ 26 ]. Qualitative literature pertaining to the lived experiences of specialist inpatient or residential treatment of AN remains fragmented and incomplete.
To our knowledge there are no other published systematic reviews of qualitative literature regarding the lived experience of participants in eating disorder-specific treatment facilities that were inpatient specialist and/or residential. Thus, this paper aims to conduct a meta-synthesis of current literature pertaining to patients’ lived experiences of residential and inpatient treatment for AN within eating disorder-specific treatment services. This will provide a greater understanding of the contemporary literature and inform future research and interventions.
Study design
This meta-synthesis relies on the model of meta-ethnography and follows the procedures of the thematic synthesis described by Thomas and Harden [ 27 ]. In compliance with the Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) guidelines [ 28 ], this synthesis consisted of six stages: (1) defining the research question, the subjects and the types of studies to be included; (2) identifying and selecting the studies; (3) assessing the quality of the selected studies; (4) analysing the studies, identifying their themes and translating these themes across the studies; (5) generating meta-themes and structuring the synthesis; and (6) writing the synthesis findings. The thematic analysis contained two phases: one descriptive, which defined and compared the themes, and the other interpretive, which developed original ideas drawn from the review.
Search strategy
This systematic review search was conducted in accordance with the updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [ 29 ]. The protocol was approved by PROSPERO (ID number: CRD42023349066). A systematic electronic search of PubMed, PsychINFO, SCOPUS, Web of Science and ProQuest Psychology databases was conducted by the first author (RR) on April 27, 2023, following consultation with a health librarian. The following search terms and Boolean operators were employed where the terms appeared in either the title or abstract of the article: “eating disorder*” OR “ano-rex*” OR “anore*” AND “intervention*” OR “treat*” OR “residential*” OR “partial hospitalization” OR “inpatient*” AND “qualitative*” OR “perspective*” OR “experience*”. Given the shifts in inpatient treatment approaches in the twentieth century [ 12 ], the authors elected to focus on contemporary lived experiences of inpatient or other residential care. To capture patients’ lived experiences of eating disorder-specific treatment services, the search was limited to human subjects and articles published in peer-reviewed journals in the English language between January 2010 and April 2023.
Study selection
All search outputs were cross-referenced, and duplicate records removed using Covidence [ 30 ]. Screening of titles and abstracts was shared between authors to identify articles likely to be eligible. Full texts of identified studies were reviewed by two authors (RR, JC) to determine if studies met the following inclusion criteria: (a) qualitative research design or presented qualitative findings as a part of a mixed-methods design; (b) focused exclusively on the experience of inpatient and/or residential treatment for AN in an eating disorder-specific treatment setting; (c) all participants formally met Diagnostic and Statistical Manual of Mental Disorders (5th Edition) (DSM-5) [ 1 ] or World Health Organisation International Statistical Classification of Diseases and Related Health Problems (ICD-10) [ 2 ] diagnostic criterion for AN at the time of seeking treatment; and (d) published in a peer-reviewed journal.
Studies were excluded for the following reasons: (a) participants received inpatient treatment for a diagnosis other than an AN diagnosis; (b) treatment was provided in an outpatient or non-specified treatment setting; (c) the study focused on a specific treatment or intervention (e.g., family-based treatment) rather than the inpatient or residential experience; (d) the qualitative data presented were minimal (e.g., there were no extracts); (e) mixed or non-eating disorder-specific treatment setting; (f) published in a language other than English; and (g) was not published in a peer-reviewed journal. Any discrepancies in study selection were noted and resolved through discussion with a third author (LR). The final inclusion of the articles was based on consensus amongst three authors (RR, JC, LR).
Quality assessment
Articles were assessed by three authors (RR 100%; JC 50%; LR 50%) following guidance provided by the Critical Appraisal Skill Programme (CASP) [ 31 ] tool for qualitative research studies. The purpose of the tool is not to provide an absolute score of quality, but rather to facilitate consideration of clarity of aims, appropriateness of methods, design and recruitment methods, suitability of data collection, researcher reflexivity, ethics, analytic rigour and clarity of findings. Given the lack of consensus regarding the role and function of study quality in systematic reviews [ 32 , 33 ], for the purpose of the current review no papers were excluded based on their quality assessment scores. However, in keeping with the meta-ethnographic approach, studies of poorer quality contributed less to the synthesis. An outline of the quality assessment for each study can be found in Additional file 1 : Table A.
Data extraction and synthesis
Our analysis followed the procedure described by Sattar et al. [ 32 ] and Thomas and Harden [ 27 ], adapting them to the principles of the meta-ethnographic approach [ 32 , 34 ]. It began with an attentive reading and then repeated readings of the titles, abstracts and texts of each article. One author (RR) extracted the formal characteristics of the studies, and extracted and analysed the first-order results (that is, the qualitative extracts using pseudonyms chosen by original papers) and the second-order results (authors’ interpretations and discussions of the results) of each study using a custom template in Covidence [ 30 ]. No additional data were requested from the original investigators.
NVivo 12 [ 35 ] qualitative analysis software was used to manage all data and facilitate the generation of themes. Extracted data and analyses were coded and a set of themes and subthemes inductively developed (RR) according to Tomas and Harden’s [ 27 ] three-phase approach to thematic synthesis. Coding notes were collaboratively (JC; LR; PH; RR) reviewed for overlapping and repetitive codes by the research team prior to being collapsed into subthemes. Similar subthemes were clustered together to delineate major patterns in the data, creating overarching themes. Differences of opinion were resolved through discussion. Final themes were selected by all authors (JC; LR; PH; RR) and extracts embedded within the analytic narrative to create a coherent and meaningful representation of participants’ lived experience of inpatient or residential treatments for AN [ 36 ]. Researcher position statements are provided (see Additional file 2 ).
Presentation of studies
As outlined in Fig. 1 , the initial search identified a total of 10,666 articles—6806 following the removal of duplicates. Following title and abstract screening, 144 articles were selected for full text review. Of these, 11 met full inclusion criteria. The authors note that all studies were conducted in inpatient public and private settings. No publications qualitatively exploring the lived experience of individuals undergoing treatment for AN in residential settings were identified.
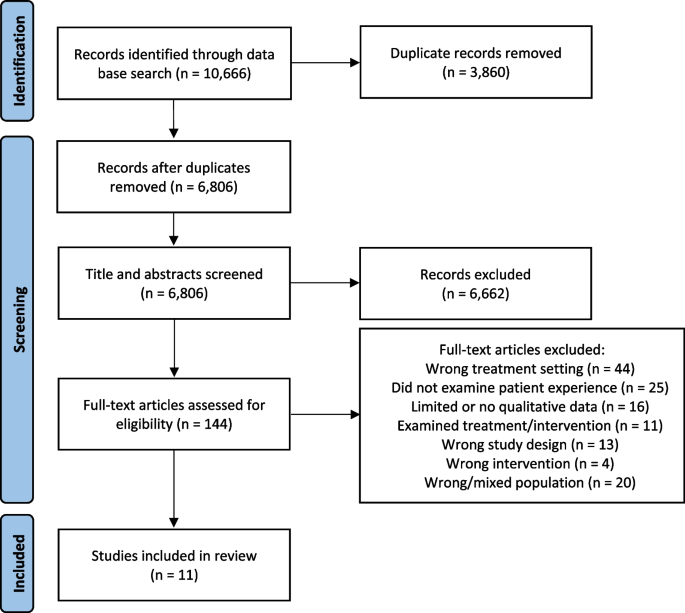
Flow of selecting and excluding studies according to the PRISMA guidelines for systematic reviews
From the 11 papers that met the search criteria, there were 159 participants (156 female; 3 male) ranging in age from 12 to 45 years. All studies included adolescent (age ≤ 18) participants, with four studies focusing solely on adolescent inpatient treatment experiences. Illness duration varied and was only reported in four studies. The included studies were conducted in five different countries: United Kingdom (n = 5); Australia (n = 2); New Zealand (n = 1); Israel (n = 1); Norway (n = 1); and Denmark (n = 1). Data were predominantly collected through semi-structured or in-depth interviews. Qualitative methods used among the studies included thematic analysis, grounded theory, interpretative phenomenological analysis, narrative analysis, discourse analysis and autoethnography. Table 1 provides a descriptive summary of the studies included in this review.
Quality assessment and risk of bias
The evaluation of the studies found variable quality across the articles (see Additional file 1 : Table A). The authors note that research design and rationale was unclear in five studies, and the consideration of the relationship between authors and participants was insufficient in three studies. Additionally, there was a paucity of information regarding in-patient treatment protocol, patient admission and eating disorder duration. Furthermore, there was variability in quality of rigour in data analyses, with approximately half of the studies producing more descriptive or superficial analysis while others were more in-depth.
Potential biases across studies included: inconsistency in the time-point of data collection (during, immediately post treatment or retrospectively); lack of consideration for key factors, such as illness severity/duration, length of admission and a number of therapies; lack of inclusion of interview questions to assess for potential biases in the collection of data and the interviews’ direction; and an over-reliance on single coders/data analysts and under-reliance on participant member checking. Within the studies, samples were not representative, with minimal male participants and a lack of cultural diversity (including Indigenous peoples).
Thematic findings
Four meta-themes were constructed from the data: (1) a medical discourse—“I don’t think it’s individualised here”; (2) restrictive practice—living in a “bubble”; (3) myself, others and “a similar demon”; and (4) I am not “just another anorexic”. Two themes cut across the data: (1) more than a single experience; and (2) meaning making and identity. As depicted in Fig. 2 , the four meta-themes connect through two cross-cutting themes. For example, participants’ positioning on the dominant medical discourse had implications on their meaning making throughout the treatment experience. As noted above, only previously published data are presented in these findings. Additional extracts from participants and from the authors of primary studies for each theme can be found in Additional file 3 : Table B).
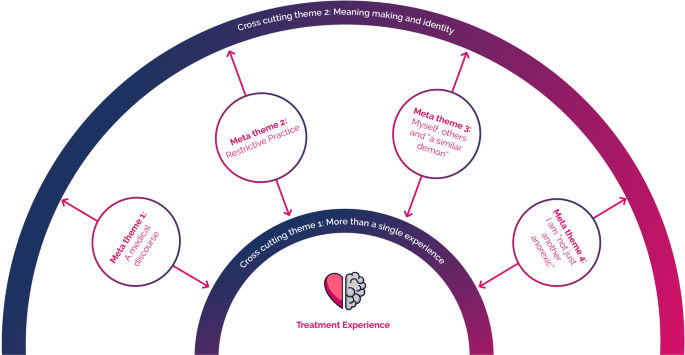
Relationships between meta-themes and cross-cutting themes observed in patient lived experiences of inpatient treatment for anorexia nervosa
Meta-theme 1: a medical discourse—“I don’t think it’s individualised here”
On admission to an inpatient facility for the treatment of AN, a patient’s family/carers and members of their treating teams will have legitimate concerns about an individual’s weight loss and the associated health complications [ 3 , 48 ]. As such, there is a strong focus on addressing physiological symptoms of an eating disorder (e.g., medical stabilisation, nutritional rehabilitation and weight restoration) through standardised phase-based treatment protocols [ 49 ]. Within this context, participant accounts of their inpatient treatment experiences highlighted challenges presented by the dominant medical discourse and the systemic focus on addressing physiological symptoms of an eating disorder [ 46 , 47 , 50 ].
Participants across seven studies [ 38 , 39 , 41 , 42 , 44 , 46 , 47 ] expressed disappointment and, at times, exasperation with what they felt was an almost exclusive focus on physiological rehabilitation at the perceived expense of their psychological wellbeing, individual identity, personal values and treatment goals. Colton and Pistrang [ 38 ] noted in their analysis that participants felt the main aim of the inpatient treatment unit was to “fatten them up” and restore weight, rather than support psychological recovery and wellbeing. This interpretation was supported by participants in Kezelman and colleagues’ study: “… essentially this place isn’t about getting better… psychologically, just… physically…” [ 42 ], P8]
Malson and colleagues suggested that the medical discourse, while necessary in the inpatient treatment setting, created an environment where “the eating disordered patient” may be constructed as being “entirely pathological” [ 37 ], p483]:
And they don’t listen to you at all. And whenever you try and like rationalize anything with them they just, you get told to sort of shut up because it’s the illness talking and you can’t possibly know any better than them because otherwise you wouldn’t be in here in the first place. [ 37 ] (Jessica M)
Similarly, in narrating her experience of multiple inpatient admissions, O’Connell wrote:
In treatment, anorexia was reductively constructed as a pathologised, medicalised condition, and while in some ways affirming, this also sometimes led me to feel misunderstood, invalidated and stereotyped. Anorexia became the overriding source of my identification, leading to my behaviour being automatically interpreted as symptomatic of illness, resulting in me feeling powerless. In addition, being unable to make my own decisions felt child-like and I found this humiliating. [ 47 ], p247–245]
Within the dominant medical discourse, the staff are in the position of being the expert authority (e.g., “you can’t possibly know any better… because otherwise you wouldn’t be in here in the first place.” [ 37 ] (Jessica M)). Thus, the patient was constituted as “powerless” [ 47 ] within their own treatment journey, as there was little or no place for them to be an “expert” in understanding their own symptoms through the lens of their lived experiences.
I don’t think it’s individualised in here…. They have their formula and they just put everyone on it… [but] everyone’s problems here are completely different…. [ 42 ], p10]
Participants’ experience of being “othered” [ 47 ] within the dominant medical discourse was most apparent in the frequent expressions of frustration regarding the perceived lack of individualisation in treatment, particularly during the initial phases of treatment [ 37 , 39 , 41 , 43 , 44 , 46 , 47 ]. Where participants felt “othered” during their treatment, they reported questioning treatment efficacy and goodness of fit—“is the right sort of treatment for me…” [ 37 ] (Clare)—and reported engaging in acts of resistance in an attempt to preserve their identity in the face of a dominant medical discourse:
… even if they get a guardianship order, what are they going to do? Stand around and psychoanalyse you against your will…. It’s only physical things that they can only do to me really. [ 39 ] (Jessica B)
Meta-theme 2: restrictive practice—living in a “bubble”
Participants across all the studies described the inpatient treatment setting as being one of highly regimented schedules and practices that spatially, relationally and temporally separated them from external experiences. As highlighted by Eli [ 41 ] and others [ 42 , 44 , 45 , 46 , 47 ], the majority of participants regarded the restrictive treatment environment with a sense of ambivalence. While many participants expressed a strong dislike of the restrictive treatment environment [ 37 , 39 , 41 , 43 , 44 , 46 ]—“It’s a place for hell… you’re stuck here and you can’t get out and you can’t do anything” [ 38 ] P17]—they also perceived the same environment as being instrumental in creating a “safe space” or “safety bubble” [ 43 ], P4] that separated them from the “real world” [ 47 ] or “outside world” [ 41 ]: “It kind of became your safe haven.”.[ 44 ], P6]
Many participants reflected that the restrictive treatment environment allowed them to engage in treatment by removing opportunities to engage in unhelpful behaviours associated with the eating disorder [ 38 , 41 , 43 , 44 , 46 , 47 ]. For example:
It [the ward] was a little lab like that, that you could be inside…. A lab in the sense that it was very sterile, it was – very very exact and measured conditions, and – you knew that you, it’s not like the real world, so it eased [our burden]. [ 41 ] (Grace) You don’t have to control it [the eating disorder] anymore and you can give over that control… it feels as if you are in that stage where you can’t make any decisions… so it is nice to have other people take over. [ 43 ] (Participant 17)
As exemplified in the extracts above, the treatment environment—with its clear daily routines, activities and dietary programs—provided participants with a clear anchor and structure within which to relinquish control of the eating disorder [ 41 , 42 , 43 , 44 ]. The physical separation from their external world also provided some participants with a space for self-discovery and growth [ 41 , 43 , 47 ] Meital explained:
The first hospitalization (laughs) – its funny to say but I enjoyed it. Like, suddenly I had friends, and it was really pleasant, and it was also, somehow, [a way of] getting out of home, something that I wanted. I wanted my privacy and my independence, and I had it there. [ 41 ]
While many participants expressed their dislike of the inpatient treatment environment, several studies [ 38 , 41 , 42 , 44 , 46 , 47 ] highlighted participants’ apparent reluctance or apprehension to leave treatment and the perceived safety of the structured/boundaried treatment environment. For example, one participant in Smith and colleagues’ study stated, “You become dependent on it… you feel it is your safe place almost. I am almost afraid to be here now because I have become quite attached.” [ 43 ] (Participant 6) Tali, meanwhile, stated, “I didn’t want to leave, I didn’t want to leave, no one wanted to leave… as difficult as it was, there were many difficult things, but—but it was sort of a greenhouse” [ 41 ].
The transition away from high-intensity, wrap-around supports back into the community was experienced as a source of fear for many participants—“I didn’t want to leave” [ 41 ] (Tali)—with participants citing a perceived lack of support in the community [ 43 , 47 ]. Other participants questioned their ability to take a stand against their eating disorder alone outside of the ward: “I worry about going home full time… I hear this voice saying… it will be you and me again.”.[ 43 ] (Participant 3)
Meta-theme 3: myself, others and “a similar demon”
A unique aspect of inpatient treatment for AN is living in an environment with others experiencing the same condition. For many participants, admission to an inpatient facility is the first time they had met or interacted with other individuals with an eating disorder [ 38 , 41 , 44 ]. Participants across six studies described fellow patients as having a major impact—for better and for worse—on their inpatient experience [ 37 , 38 , 41 , 42 , 43 , 44 ]. For many participants, the inpatient community functioned as a formative experience that was central to the narrative of their inpatient treatment experience. As Alon explained:
… getting there, and sitting in groups, and hearing people talking about things that you’re also going through – there’s something very powerful in this, in this sense of ‘I’m not alone’… [we] feel like, we’re all dealing here with a similar demon, and there’s some sense of shared destiny. [ 41 ]
Participants in six studies [ 37 , 38 , 41 , 43 , 44 , 47 ] spoke of the importance of identification with other patients in reducing isolation, as well as normalising and validating their affective experience:
… you can talk to them [patients] so much easier than what you can when you’re out of here. Do you know what I mean, you can talk about anorexia just as you can talk about Coronation Street [a television show] … whereas at home, that issue would be totally avoided and I would not even talk about it. [ 38 ], P10]
Participants also spoke of learning effective coping skills from their peers, as well as finding hope for recovery: “It is really good in terms of being able to hear how other people have gotten over the drive to exercise and how they have managed to eat certain foods.”.[ 43 ] (Participant 3)
Despite the positive aspects of being part of an inpatient community, participants in seven studies [ 38 , 41 , 42 , 43 , 44 , 46 , 47 ] spoke of making physical and behavioural comparisons with others: “I saw other people that were thinner than me and it made me feel like I had failed at my eating disorder.” [ 44 ], P2] Participants described experiencing feelings of “envy” towards their “emaciated peers” [ 43 ], p23] and competing to be “the best anorexic” [ 38 ], P8]. Over half of participants in Eli’s [ 41 ] study reported feeling “triggered” by the close proximity of other patients and being able to “observe” other patients’ appearance, progress and “everyday practices”, with one participant explaining, “Since we’re all eating in the same room, you’re experiencing everyone else’s troubles.”.[ 44 ], P6]
The presence of other patients at different recovery stages also appeared to, at times, exacerbate the distress associated with between-patient comparison. As the following participants explained:
When you reach a condition that’s relatively healthy and fine and you’re halfway there… suddenly a girl who weighs 20 kilos shows up… I don’t want to see it…. It’s not that it’s the sick side [of me], it’s like – it’s the side I never had. So why do I need to get acquainted with it? [ 41 ] (Natalie) It really screws me up seeing extremely thin people [. . .] they are pleased they are not as fat as I am. [ 47 ] (Diary, 18th January 2007)
Furthermore, several participants described a contagion effect among the inpatient community. Participants reflected that living with other patients made them more aware of and susceptible to adopting the unhelpful behaviours of others. For example, one young person stated: “I didn’t really know … about self-harm, um, about pacing to stop your weight going up, you know, walking around, exercise. I soon cottoned on.” [ 38 ], p311] Another said, “Seeing what they [other patients] did kind of gives you ideas about being sneaky.”.[ 44 ], P1]
Meta-theme 4: I am “not just another anorexic”
Participants repeatedly emphasised the importance of healthcare professionals and treating teams seeing them as individuals. Colton and Pistrang [ 38 ] noted that a “key dimension” (p310) used by participants in describing their experiences of inpatient treatment was whether they felt staff viewed them as being an individual or “just another anorexic” (p310) coming through the program. For example:
I miss just being me, not a patient in need of help and support. [ 45 ], p5] It’s sort of like speaking to him [a doctor] is like bashing your head up against a wall… Because everything you say is part of the disease. No matter what it is… And you’re like: I’m a person. There’s a personality in here you know?… You know I’m not just anorexic. [ 37 ] (T6A—interviewer responses removed)
Across several studies, participants perceived staff as being too busy and not having enough time to listen to them or care about what they did, provided they complied with treatment [ 38 , 39 , 41 , 42 , 43 , 47 ] Participants frequently expressed their frustration at the perceived lack of individualisation in their treatment planning and often reported feeling “pigeonholed” [ 37 ] (Polly) by clinical staff (e.g., “I also frequently felt ‘unheard’ and my reasoning invalidated due to my inability to escape an anorexic framing” [ 47 ], p274]), particularly during assessment and the initial phases of treatment [ 39 , 41 , 42 , 43 ].
Participants’ feelings of being misunderstood by clinical staff appeared to foster a climate of resistance within the inpatient treatment setting [ 39 , 41 , 44 ]: “it makes you not want to cooperate because they don’t really want to understand.” [ 42 ] Conversely, “good staff” [ 43 , 44 , 45 ] were described as able to “… see the person behind the anorexia.” [ 38 ], P5] As Grace reflected:
They knew about me much more than I knew about myself… things that even I wasn’t aware of, but that they could see from the outside.... It always gave me a good feeling – that I don’t have to talk and they still know. [ 41 ]
Where participants felt seen and acknowledged as an individual—not merely the bearer of an eating disorder diagnosis—they reported increased engagement in recovery-orientated/help-seeking behaviours. For example:
When they’re more encouraging and supportive it makes me want to try harder and when they’re more forceful it makes me always want to pull against and try harder at doing the wrong things. [ 38 ] (Participant 9) … you build up trust… you know you can say things to them and they understand a bit more because they know more about your past. [ 43 ] (Participant 2)
Boughtwood and Halse suggested that “recognizing the differences between individual patients and respecting the meanings they attach to their illness is central to the therapeutic alliance in the treatment of anorexia.” [ 39 ], p92] Furthermore, the ability of staff to “hold hope” [ 23 ] for a patient’s recovery appeared to strengthen participant motivation and connection to a sense of self or identity beyond their eating disorder [ 38 , 39 , 41 , 44 ]. As a participant in Kezelman and colleagues’ study recalled, “Wow, these people… [have] faith in me, I need to have faith in myself.”.[ 42 ], P8]
Cross-cutting theme 1: more than single experience
Inpatient treatment for AN typically entails several weeks or months of living away from home. In reflecting on treatment experiences, participants across all studies outlined a multidimensional experience characterised by a series of non-liner—often recursive—phases or transitions. Kezelman and colleagues [ 42 ] observed three broad phases in their analysis of the adolescent inpatient treatment experience: (1) reconciling with the AN diagnosis and understanding the necessity of medical intervention; (2) adjustment to treatment and the treatment environment; and (3) reflection and integration. They noted that participant accounts of treatment experience demonstrated a “complex and often ambivalent psychological process” whereby individuals’ understandings and “acceptance of their physical and medical needs were often in conflict” (p228) with their “affective experiences” and beliefs regarding recovery.
The concept of transitions during treatment were exemplified throughout O’Connell’s [ 47 ] autoethnographic account of her inpatient treatment experience across multiple admissions, and further highlighted by Smith and colleagues in their theme “Experience of transition” [ 43 ], p21]. They noted participants’ initial struggle to adjust to the treatment environment—“at the start, I didn’t want to be here” (p21)—before coming to see “treatment as a safe environment” (p21) they felt reliant on prior to discharge. Patients’ experience of transitioning between phases during treatment for AN were directly and indirectly observed across all studies in this synthesis. As demonstrated in meta-themes 1 to 4, participants’ experiences appeared to be influenced by how they navigated and made meaning of these transitions during treatment.
Cross-cutting theme 2: meaning making and identity
Participant accounts of inpatient treatment experience across all studies were characterised by conflicts and dilemmas, or the experiences of ambivalence and liminality throughout treatment. Although participants varied in their views regarding the helpfulness of inpatient treatment, most individuals reported a sense of duality—both positive and negative feelings—regarding multiple aspects of the inpatient treatment experience (meta-theme 1 to 4). At times, participants appeared overwhelmed by internal conflicts regarding their diagnosis and the necessity of inpatient treatment (meta-theme 1 and 2), their experience of staff (meta-theme 1 to 3) and other patients (meta-theme 4), and the restrictive treatment environment (meta-theme 2 to 4).
Participants’ ability to make meaning of their experiences and resolve ambivalence at various phases throughout the inpatient treatment journey appeared to shape their global perception(s) of the inpatient treatment. For example, as outlined in meta-theme 2, Meita [ 41 ] described her first inpatient experience as being a positive experience that provided her with independence. However, she described her second inpatient experience extremely differently:
The second hospitalization, in comparison, was very traumatic. I felt really bad there. I couldn’t find myself…. Being in a closed ward with very tough discipline, very clear rules, where they decide for you when you’ll eat, when you’ll have time for breaks, like – it didn’t suit me anymore. I needed my freedom, to decide on my own structure.(p7)
In analysing this shift, Eli [ 41 ] noted that while the “ward itself had remained the same”, Meital’s desire for “freedom”, likely her definition of what independence looked like, and priority to “find myself” (p7) had shifted between admissions, thus leading her to experience and engage with the same treatment facility and protocol in two very different ways.
Participant meaning making also appeared to be influenced by individual readiness for change. A central conflict described by many participants was whether or not they were willing to “let go” of the eating disorder and participate collaboratively in treatment. For example, O’Connell reflected that in “wanting something different, I tentatively opened up in my mind to the idea of letting go of anorexia.” [ 47 ], p275]. While participants consistently identified that their own willingness for recovery was central to treatment success—“I have to wait ‘till I am ready” [ 38 ], P6]—Broughtwood and Halse [ 39 ] observed that some patients managed this conflict by temporarily performing the role of the “perfect (obedient) patient” (p89), as yielding to the clinical team at times served their longer-term personal agenda.
There is an ‘us versus them’ mentality though, like [the doctors] want me to put on [a certain amount of weight] by Wednesday and um I can’t believe it, and you know. Yeah it’s hard to explain but, there is a real ‘I’ll do it [gain weight] just to make them happy so that I can get home’. Ah, rather than ‘they think that it’s best that I put on this amount of weight, and they know what they’re doing because they’re medical professionals, so I guess it is best for me.(Renee)
Renee’s engagement with the medical discourse was more complex than simply “obeying or rejecting” (p880) her clinical team or treatment; rather, her position in this discourse was one of ambivalence regarding whether the treatment goals proposed by her treating team were of benefit to her. Renee’s positioning in relation to the dominant medical discourse appeared to impact her motivation and the way in which she interpreted clinical staff actions and the restrictive treatment environment.
Participants’ values, treatment goals and connection to an identity outside of their eating disorder identity also appeared to have an impact on how participants made meaning of their eating disorder diagnosis and treatment experiences. Throughout treatment narratives [ 37 , 40 , 41 , 43 , 44 , 45 , 46 , 47 ], AN was experienced by participants as being both a “friend” and identity investment — “a shield to hide behind, and something which gave confidence and security”—as well as being an “enemy” or a “suffocating, frightening and depriving” [ 38 ], p310] identity thief (see Additional file 3 : Table B for exemplar quotes). Thus, treatment engagement and recovery for participants was not simply a process of choosing to disengage from a set of unhelpful behaviours associated with their eating disorder, but rather the acknowledgment of AN and the consideration one’s own identity, values and purpose outside of the eating disorder [ 38 , 41 , 43 , 44 , 46 , 47 ]. As one participant explained:
I find it difficult to distinguish… what is me and what is the eating disorder… a lot of what my treatment has been is actually finding my own identity. [ 43 ] (Participant 3)
This meta-analysis sought to synthesise contemporary literature pertaining to individuals’ lived experiences of residential and inpatient treatment for AN within eating disorder-specific treatment services. Eleven qualitative studies were selected with a total of 159 participants with lived experience of inpatient treatment for AN. Four meta-themes emerged from the data: (1) a medical discourse—“I don’t think it’s individualised here”; (2) living in a “bubble”; (3) myself, others and “a similar demon”; and (4) I am more than “just another anorexic”. The data also revealed two cross-cutting themes: (1) more than a single experience; and (2) meaning-making. These themes highlight the complex and multifaceted nature of inpatient treatment experiences.
Findings from this synthesis suggest that, while many individuals retrospectively acknowledge the necessity of medical intervention as part of their treatment journey, the restrictive treatment environment and biomedical focus of inpatient treatment facilities often disqualifies the patient’s voice, individual identity, lived experience, personal values and understandings of their symptoms. These findings are consistent with the broader body of literature pertaining to inpatient experiences of hospitalisation for psychiatric care, which highlight patients’ sense of feeling restricted or trapped in a different world during admission [ 26 , 51 , 52 , 53 ]. Within the dominant medical discourse, clinical staff are frequently positioned as being expert authorities and may be perceived as “prison wardens”, thus leaving little or no space for patients to be an “expert” in understanding their own symptoms through the lens of their lived experiences [ 25 , 53 , 54 , 55 ].
Inpatient admissions for psychiatric care represent a significant disruption to an individual’s life narrative, sense of self and identity [ 25 , 52 ]. As such, inpatient treatment may be one of the “most challenging experiences” [ 51 ], p329] over the course of an individual’s illness and recovery journey. Participant accounts of inpatient treatment of AN in this synthesis were characterised by the experiences of ambivalence and liminality. While many individuals expressed a desire for recovery and a life beyond AN, the concept of recovery was closely associated with complex identity negotiations and hindered by a fear of the unknown in recovery [ 23 , 56 , 57 , 58 , 59 ]. These findings speak to the ego-syntonic nature of AN (e.g., the way in which AN behaviours may align with an individual’s ideal self, values and identity) [ 57 , 60 ] and highlight the paradoxical way in which those with AN may simultaneously wish for recovery while actively resisting treatment [ 61 ].
As inpatient treatment for AN typically occurs at critical points in an individual’s treatment journey, participant treatment experiences may reflect their broader experience of liminality in their relationship with themselves and AN. The concept of recovery was associated with complex identity negotiations across participant narratives in this study. Thus, treatment engagement was not simply a process of an individual choosing to disengage from a set of unhelpful behaviours associated with an eating disorder, but rather the acknowledgment of AN and the consideration of one’s own identity, values and purpose outside of the eating disorder. This is consistent with research indicating that recovery from AN is more about the reclamation of self and identity outside of AN than it is the illness process [ 25 , 58 , 62 , 63 ]. The way in which patients made meaning of their experiences and resolved ambivalence throughout their inpatient treatment journey shaped their global perception(s) of the inpatient treatment. As such, factors independent of treatment (e.g., life events, personal values, identity, self-reflection, life goals, personal understandings of AN) are likely to influence individual motivation for change [ 56 , 59 , 64 ].
Participant narratives across all studies highlighted the inherent conflicts between service providers administration of standardised phase-based treatment protocols, the broader therapeutic milieu and patients’ desire for person-centred care. For example, many participants felt the inpatient treatment programs focused too heavily on the physiological symptoms of AN and provided a lack of assistance in addressing the underlying psychological difficulties and the distress associated with weight gain. This finding is consistent with current literature [ 25 ] and adds weight to outcome studies suggesting the presence of a gap between physiological (e.g., weight) and psychological (e.g., eating disorder cognitions, level of distress relating to weight and shape) improvements following inpatient treatment for AN [ 65 , 66 ]. Evidence suggests without improvements in both physiological and psychological aspects of the AN, there exists a risk of a pseudo-recovery—that is, a physical recovery in the absence of psychological recovery—which may place an individual at higher risk of relapse following discharge [ 67 , 68 ]. Thus, while nutrition rehabilitation is essential in ameliorating both psychological and psychosocial symptoms of AN [ 49 , 68 , 69 ], individual aspects such as motivation for change are also important to consider in predicting treatment adherence and patient outcomes [ 22 , 70 ].
Clinical staff were found to play a critical role in the formation of patient treatment experiences and in the creation of the ward milieu. As with previous literature [ 25 , 53 , 61 , 71 ], where patients feel seen as an individual—“more than just anorexic”—they were more likely to engage in recovery-orientated behaviours [ 65 , 70 ]. Furthermore, the ability of staff to “hold hope” [ 23 ] for a patient’s recovery appeared to strengthen participant motivation and connection to a sense of self or identity beyond their eating disorder. Similarly, the inpatient community was seen as a formative experience—for better or for worse—for many participants and was central to their narrative of their inpatient treatment experience. While patient peers served to normalise and validate the inpatient treatment experiences, several participants described a contagion effect among the inpatient community.
Clinical implications
The tensions between administering replicable standardised phase-based treatment protocols and patients’ desire for person-centred care are many (e.g., the conflict between the necessity of medical interventions and treatment non-negotiables vs the development of positive therapeutic relationships and maintenance of a positive patient milieu) and may pose the greatest challenge for healthcare professionals in treating AN in the inpatient setting [ 25 , 53 , 68 , 72 ]. Participant narratives of inpatient treatment indicate that addressing these conflicts is of the utmost importance. Explicitly acknowledging conflicts—where clinically relevant—may allow healthcare providers to provide patients with appropriate and timely information regarding treatment decisions. For example, the provision of a clear and individualised treatment rationale—that includes the persons’ own goals along with treatment non-negotiables [ 73 ]—maximises client autonomy in the face of a dominant medical discourse [ 26 , 70 , 71 , 74 , 75 ].
Eliciting patients’ own treatment goals and understandings of the function(s) of their illness early in treatment may create opportunities for the exploration of non-treatment related factors associated with the tipping point of change (e.g., values, relationships and individual identity separate from AN) later in treatment. It may also facilitate the development co-ownership in patient treatment journeys, particularly where patients are unable to provide consent due to involuntary admission [ 26 , 46 , 76 ]. Furthermore, adopting a person-centred treatment approaches, which keep the individual with their unique experiences at the core of treatment planning and assessment, may enhance the effectiveness of tailored inpatient treatments for sub-populations of those presenting with AN (e.g., ethnic minorities, individuals with a trauma history or a co-occurring diagnosis such as autism) [ 74 , 77 , 78 , 79 ]. Treatment context may also have influenced participant experiences; for example, inpatient treatments may be more prohibitive and focus more on eating behaviour change/symptom management to mitigate medical risk.
Clinical practice guidelines for the treatment of eating disorders [ 49 ], suggest that treatment for those with AN be provided within a treatment framework that “supports the values of recovery-oriented care”. (p6) This approach recognises that no two individuals are the same and recognises the inherent strengths and capacity each individual holds within themselves. As such, recovery-orientated approaches to mental health treatment aim to promote self-direction, self-determination, self-management and autonomy, in the context of individualised, holistic and evidenced based person-centred treatment.
Adopting person-centred and recovery-orientated treatment approaches that prioritise patient safety and autonomy needs to be balanced with safety and broader/stakeholder considerations (e.g., the ability to operationalise quality interventions in a replicable way). Findings in this review support the view that inpatient treatment may be more efficacious when focused on both the physiological and psychological symptoms of AN. Building patients’ ability to cope with and tolerate distress associated with weight gain during inpatient treatment may assist in closing the gap [ 65 , 66 ] between physiological and psychological improvements following inpatient treatment, thus reducing participant risk of relapse following discharge [ 67 , 68 ].
Strengths and limitations
The findings from this study need to be interpreted in the context of several limitations. First, given the exclusion criterion, the authors may have excluded pertinent research published in grey literature or languages other than English. Second, the authors only included previously published data in this meta-synthesis. As such, a significant proportion of original transcript data were not synthesised in this study. Third, the themes generated in this paper are influenced and shaped by the authors’ focus on participant lived experiences.
A strength of this study was its exploration of a combined 159 participants’ lived experience of inpatient treatment for AN from 11 separate studies. Overall, the included studies were of good quality. However, the authors note that descriptions of participant demographics (e.g., age, ethnicity, socio-economic status, severity of illness and treatment history) were limited. Similarly, the descriptions of treatment programs and settings—including the structure, delivery and content of treatment modalities—were limited. The authors also noted an underrepresentation of male participants and the absence of qualitative literature regarding patient lived experiences of residential care. The lack of consistent descriptive data limited the authors’ ability to assess patient and treatment variables that contribute to patient lived experiences and limits the generalisability of the findings. Furthermore, variability in sampling and recruitment strategies used in the included studies may have led to the possibility of selection bias and skewed views of treatment. Further research is also needed to determine if there are differences in patient experiences across the lifespan and, if so, how interventions may be best tailored to meet the needs of patients in different life phases (e.g., young persons and adults).
Despite these limitations, this synthesis has a number of strengths, including being a response to the paucity of research in relation to the lived experience of inpatient treatment for AN. The authors also employed a rigorous methodological process in the selection, evaluation and interpretation of the studies in this synthesis. This included several authors working in parallel on steps in the interpretation and analysis of data drawn from a number of studies. By drawing on the voice of those with a lived experience of inpatient treatment for AN within eating disorder-specific treatment services, this study may generate a map for healthcare professionals as they navigate the inherent conflicts between administering standardised phase-based treatment protocols and patients’ desire for person-centred care.
Results of this synthesis suggest that the lived experience of inpatient treatment for AN within eating disorder-specific treatment services is complex and multifaceted. Inpatient treatment for AN typically occurs at critical points through a patient’s treatment journey and represent a significant disruption to an individual’s life narrative, sense of self and identity. As such, patient narratives are marked by conflicts and reflect participants’ sense of liminality in their relationship with themselves and AN. This supports research indicating that recovery from AN is more about the reclamation of self and identity outside of AN than it is the illness process [ 25 , 59 , 64 , 73 ].
While many individuals retrospectively acknowledge the necessity of medical intervention as part of their treatment journey, the restrictive treatment environment and biomedical focus of inpatient treatment facilities often disqualifies the patient’s voice, individual identity, lived experience, personal values and understandings of their symptoms. Furthermore, without improvements in both physiological and psychological aspects of the AN, there exists a risk of a pseudo-recovery, which may place an individual at higher risk of relapse following discharge. Adopting person-centred and recovery-oriented treatment approaches may serve to maximise client autonomy in the face of a dominant medical discourse and support patient reclamation of identity. However, further research is needed to identify how service providers may best navigate the inherent conflicts in balancing the necessity of medical and psychological intervention within phase-based treatment protocols with person-centred treatment approaches in the treatment of AN.
Availability of data and materials
The additional files document contains the following data and materials for the meta-synthesis: Assessment of quality of included papers (Additional file 1 : Table A), researcher position statements (Additional file 2 ) and Exemplar data extracts for Metathemes in the Metasynthesis (Additional file 3 : Table B). No additional data is available.
Abbreviations
- Anorexia nervosa
Diagnostic and Statistical Manual of Mental Disorders (5th Edition)
World Health Organisation International Statistical Classification of Diseases and Related Health Problems
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed Text-Revision. Washington: American Psychiatric Association; 2022.
Book Google Scholar
World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 11th Revision (ICD-11). Geneva: World Health Organization, 2019. https://icd.who.int/en . Accessed 04 Apr 2023.
Santomauro DF, Melen S, Mitchison D, Vos T, Whiteford H, Ferrari AJ. The hidden burden of eating disorders: an extension of estimates from the Global Burden of Disease Study 2019. Lancet Psychiatry. 2021;8(4):320–8.
Article PubMed PubMed Central Google Scholar
Galmiche M, Déchelotte P, Lambert G, Tavolacci MP. Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. Am J Clin Nutr. 2019;109(5):1402–13.
Article PubMed Google Scholar
Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13(2):153–60.
Fichter MM, Quadflieg N. Mortality in eating disorders-results of a large prospective clinical longitudinal study. Int J Eat Disord. 2016;49(4):391–401.
van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr Opin Psychiatry. 2020;33(6):521.
National Guideline Alliance (UK). Eating disorders: recognition and treatment. National Institute for Health and Care Excellence (NICE), 2017.
Hilbert A, Hoek HW, Schmidt R. Evidence-based clinical guidelines for eating disorders: international comparison. Translator. Curr Opin Psychiatry. 2017;30(6):423–37.
Treasure J, Oyeleye O, Bonin EM, Zipfel S, Fernandez-Aranda F. Optimising care pathways for adult anorexia nervosa. What is the evidence to guide the provision of high-quality, cost-effective services? Eur Eat Disord Rev. 2021;29(3):306–15.
Bohrer BK, Foye U, Jewell T. Recovery as a process: exploring definitions of recovery in the context of eating-disorder-related social media forums. Int J Eat Disord. 2020;53(8):1219–23.
de Vos JA, LaMarre A, Radstaak M, Bijkerk CA, Bohlmeijer ET, Westerhof GJ. Identifying fundamental criteria for eating disorder recovery: a systematic review and qualitative meta-analysis. J Eat Disord. 2017;5(1):1–4.
Google Scholar
Vinchenzo C, McCombie C, Lawrence V. The experience of patient dropout from eating disorders treatment: a systematic review and qualitative synthesis. BJPsych Open. 2021;7(S1):S299.
Article PubMed Central Google Scholar
Fichter MM, Quadflieg N, Crosby RD, Koch S. Long-term outcome of anorexia nervosa: results from a large clinical longitudinal study. Int J Eat Disord. 2017;50(9):1018–30.
Strobel C, Quadflieg N, Naab S, Voderholzer U, Fichter MM. Long-term outcomes in treated males with anorexia nervosa and bulimia nervosa—a prospective, gender-matched study. Int J Eat Disord. 2019;52(12):1353–64.
Halmi KA. Perplexities of treatment resistence in eating disorders. BMC Psychiatry. 2013;13(1):1–6.
Article Google Scholar
Kotilahti E, West M, Isomaa R, Karhunen L, Rocks T, Ruusunen A. Treatment interventions for severe and enduring eating disorders: systematic review. Int J Eat Disord. 2020;53(8):1280–302.
Hay PJ, Park RJ, Touyz SW. toward an improved understanding of severe and enduring anorexia nervosa. Front Psych. 2021;12:698194.
Brewerton TD, Costin C. Long-term outcome of residential treatment for anorexia nervosa and bulimia nervosa. Eat Disord. 2011;19(2):132–44.
Peckmezian T, Paxton SJ. A systematic review of outcomes following residential treatment for eating disorders. Eur Eat Disord Rev. 2020;28(3):246–59.
Kan C, Hawkings YR, Cribben H, Treasure J. Length of stay for anorexia nervosa: systematic review and meta-analysis. Eur Eat Disord Rev. 2021;29(3):371–92.
Murray SB, Quintana DS, Loeb KL, Griffiths S, Le Grange D. Treatment outcomes for anorexia nervosa: a systematic review and meta-analysis of randomized controlled trials. Psychol Med. 2019;49(4):535–44.
Conti JE, Joyce C, Hay P, Meade T. “Finding my own identity”: a qualitative metasynthesis of adult anorexia nervosa treatment experiences. BMC Psychol. 2020;8(1):1–4.
Richardson C, Paslakis G. Men’s experiences of eating disorder treatment: a qualitative systematic review of men-only studies. J Psychiatr Ment Health Nurs. 2021;28(2):237–50.
Stockford C, Stenfert Kroese B, Beesley A, Leung N. Women’s recovery from anorexia nervosa: a systematic review and meta-synthesis of qualitative research. Eat Disord. 2019;27(4):343–68.
Akther SF, Molyneaux E, Stuart R, Johnson S, Simpson A, Oram S. Patients’ experiences of assessment and detention under mental health legislation: systematic review and qualitative meta-synthesis. Br J Psychiatry Open. 2019;5(3):e37.
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):1.
Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12(1):1–8.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. www.covidence.org .
Critical Appraisal Skills Programme (CASP). CASP qualitative research checklist: 10 questions to help you make sense of qualitative research, 2022. https://casp-uk.b-cdn.net/wp-content/uploads/2018/03/CASP-Qualitative-Checklist-2018_fillable_form.pdf . Cited 1 Jan 2023.
Sattar R, Lawton R, Panagioti M, Johnson J. Meta-ethnography in healthcare research: a guide to using a meta-ethnographic approach for literature synthesis. BMC Health Serv Res. 2021;21:1–3.
Siddaway AP, Wood AM, Hedges LV. How to do a systematic review: a best practice guide for conducting and reporting narrative reviews, meta-analyses, and meta-syntheses. Annu Rev Psychol. 2019;70:747–70.
Atkins S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Health Serv Res. 2008;8(1):1.
NVivo. Qualitative data analysis software. 12th ed. QSR International Pty Ltd; 2022.
Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16(1):1609406917733847.
Malson H, Finn DM, Treasure J, Clarke S, Anderson G. Constructing ‘The Eating Disordered Patient’1: a discourse analysis of accounts of treatment experiences. J Community Appl Soc Psychol. 2004;14(6):473–89.
Colton A, Pistrang N. Adolescents’ experiences of inpatient treatment for anorexia nervosa. Eur Eat Disord Rev. 2004;12(5):307–16.
Boughtwood D, Halse C. Other than obedient: Girls’ constructions of doctors and treatment regimes for anorexia nervosa. J Community Appl Soc Psychol. 2010;20(2):83–94.
Long S, Wallis D, Leung N, Meyer C. “All eyes are on you”: anorexia nervosa patient perspectives of in-patient mealtimes. J Health Psychol. 2012;17(3):419–28.
Eli K. Between difference and belonging: Configuring self and others in inpatient treatment for eating disorders. PLoS ONE. 2014;9(9):e105452.
Kezelman S, Rhodes P, Hunt C, Anderson G, Clarke S, Crosby RD, Touyz S. Adolescent patients’ perspectives on rapid-refeeding: a prospective qualitative study of an inpatient population. Adv Eat Disord. 2016;4(3):277–92.
Smith V, Chouliara ZO, Morris PG, Collin P, Power K, Yellowlees A, Grierson D, Papageorgiou E, Cook M. The experience of specialist inpatient treatment for anorexia nervosa: a qualitative study from adult patients’ perspectives. J Health Psychol. 2016;21(1):16–27.
Thabrew H, Mairs R, Taylor-Davies G. Young people’s experiences of brief inpatient treatment for anorexia nervosa. J Pediatr Child Health Care. 2020;56(1):30–3.
Solhaug Storli C, Alsaker S. Treatment of eating disorders: voices from a ward. Int J Qual Stud Health Well-being. 2021;16(1):1983948.
Mac Donald B, Gustafsson SA, Bulik CM, Clausen L. Living and leaving a life of coercion: a qualitative interview study of patients with anorexia nervosa and multiple involuntary treatment events. J Eat Disord. 2023;11(1):1–9.
O’Connell L. Being and doing anorexia nervosa: an autoethnography of diagnostic identity and performance of illness. Health. 2023;27(2):263–78.
Heruc G, Hurst K, Casey A, Fleming K, Freeman J, Fursland A, Hart S, Jeffrey S, Knight R, Roberton M, Roberts M. ANZAED eating disorder treatment principles and general clinical practice and training standards. J Eat Disord. 2020;8(1):1–9.
Hay P, Chinn D, Forbes D, Madden S, Newton R, Sugenor L, Touyz S, Ward W. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders. Aust N Z J Psychiatry. 2014;48(11):977–1008.
Hepworth J. The social construction of anorexia nervosa. Thousand Oaks: Sage Publications; 2012.
Roe D, Ronen YI. Hospitalization as experienced by the psychiatric patient: a therapeutic jurisprudence perspective. Int J Law Psychiatry. 2003;26(3):317–32.
Staniszewska S, Mockford C, Chadburn G, Fenton SJ, Bhui K, Larkin M, Newton E, Crepaz-Keay D, Griffiths F, Weich S. Experiences of in-patient mental health services: systematic review. BJPsych. 2019;214(6):329–38.
PubMed Google Scholar
Ramjan LM, Gill BI. An inpatient program for adolescents with anorexia experienced as a metaphoric prison. Am J Nurs. 2012;112(8):24–33.
Malson H, Burns M. Re-theorising the slash of dis/order: an introduction to critical feminist approaches to eating dis/orders. In: Critical feminist approaches to eating dis/orders. Routledge, 2009. p. 23–8.
Sibeoni J, Orri M, Valentin M, Podlipski MA, Colin S, Pradere J, Revah-Levy A. Metasynthesis of the views about treatment of anorexia nervosa in adolescents: perspectives of adolescents, parents, and professionals. PLoS ONE. 2017;12(1):e0169493.
Fogarty S, Ramjan LM. The tipping point of change in anorexia nervosa (AN): qualitative findings from an online study. Women Health. 2018;58(9):1050–61.
Gregertsen EC, Mandy W, Serpell L. The egosyntonic nature of anorexia: an impediment to recovery in anorexia nervosa treatment. Front Psychol. 2017;8:2273.
Lewke-Bandara RS, Thapliyal P, Conti J, Hay P. “It also taught me a lot about myself”: a qualitative exploration of how men understand eating disorder recovery. J Eat Disord. 2020;8:1–9.
Rankin R, Conti J, Touyz S, Arcelus J, Meyer C, Hay P. Dancing with change: a qualitative exploration of in-session motivation to change in the treatment of anorexia nervosa. Aust Psychol. 2023;58:1–2.
Forrest LN, Jones PJ, Ortiz SN, Smith AR. Core psychopathology in anorexia nervosa and bulimia nervosa: a network analysis. Int J Eat Disord. 2018;51(7):668–79.
Eaton CM. Eating disorder recovery: a metaethnography. J Am Psychiatr Nurses Assoc. 2020;26(4):373–88.
Conti JE. Recovering identity from anorexia nervosa: Women’s constructions of their experiences of recovery from anorexia nervosa over 10 years. J Constr Psychol. 2018;31(1):72–94.
Rance N, Moller NP, Clarke V. ‘Eating disorders are not about food, they’re about life’: client perspectives on anorexia nervosa treatment. J Health Psychol. 2017;22(5):582–94.
Hay P. A systematic review of evidence for psychological treatments in eating disorders: 2005–2012. Int J Eat Disord. 2013;46(5):462–9.
Castro J, Gila A, Puig J, Rodriguez S, Toro J. Predictors of rehospitalization after total weight recovery in adolescents with anorexia nervosa. Int J Eat Disord. 2004;36(1):22–30.
Fennig S, Brunstein Klomek A, Shahar B, Sarel-Michnik Z, Hadas A. Inpatient treatment has no impact on the core thoughts and perceptions in adolescents with anorexia nervosa. Early Interv Psychiatry. 2017;11(3):200–7.
Bardone-Cone AM, Hunt RA, Watson HJ. An overview of conceptualizations of eating disorder recovery, recent findings, and future directions. Curr Psychiatry Rep. 2018;20:1–8.
Voderholzer U, Haas V, Correll CU, Körner T. Medical management of eating disorders: an update. Curr Opin Psychiatry. 2020;33(6):542–53.
Frank GK, DeGuzman MC, Shott ME. Motivation to eat and not to eat–The psycho-biological conflict in anorexia nervosa. Physiol Behav. 2019;206:185–90.
Vall E, Wade TD. Predictors of treatment outcome in individuals with eating disorders: a systematic review and meta-analysis. Int J Eat Disord. 2015;48(7):946–71.
Belsiyal CX, Rentala S, Das A. Use of therapeutic milieu interventions in a psychiatric setting: a systematic review. J Educ Health Promot. 2022;11(1):234.
Marzola E, Albini E, Delsedime N, Fassino S, Abbate-Daga G. Therapeutic alliance in inpatients with severe anorexia nervosa. Translator. Eur Eat Disord Rev. 2019;27(6):671–581.
Geller J, Srikameswaran S. Treatment non-negotiables: why we need them and how to make them work. Eur Eat Disord Rev. 2006;14(4):212–7.
Longo P, Bertorello A, Panero M, Abbate-Daga G, Marzola E. Traumatic events and post-traumatic symptoms in anorexia nervosa. Eur J Psychotraumatol. 2019;10(1):1682930.
Tiles-Shields C, Bamford BH, Touyz S, Le Grange D, Hay P, Lacey H. Predictors of therapeutic alliance in two treatments for adults with severe and enduring anorexia nervosa. J Eat Disord. 2016;4:1–7.
Atti AR, Mastellari T, Valente S, Speciani M, Panariello F, De Ronchi D. Compulsory treatments in eating disorders: a systematic review and meta-analysis. Eat Weight Disord. 2021;26:1037–48.
Babb C, Brede J, Jones CR, Elliott M, Zanker C, Tchanturia K, Serpell L, Mandy W, Fox JR. It’s not that they don’t want to access the support... it’s the impact of the autism’: the experience of eating disorder services from the perspective of autistic women, parents and healthcare professionals. Autism. 2021;25(5):1409–21.
Brede J, Babb C, Jones C, Elliott M, Zanker C, Tchanturia K, Serpell L, Fox J, Mandy W. “For me, the anorexia is just a symptom, and the cause is the autism”: investigating restrictive eating disorders in autistic women. J Autism Dev Disord. 2020;50:4280–96.
Kronenfeld LW, Reba-Harrelson L, Von Holle A, Reyes ML, Bulik CM. Ethnic and racial differences in body size perception and satisfaction. Body Image. 2010;7(2):131–6.
Download references
Acknowledgements
Not applicable.
This study was funded Rebekah Rankin is a doctoral student currently supported by the Western Sydney University Butterfly Foundation Postgraduate Research Scholarship which is jointly funded by Western Sydney University and the Butterfly Foundation. She is also recipient of the DHCRC top up scholarship. The funding bodies were not involved in the design of the study and collection, analysis and interpretation of data and in writing the manuscript.
Author information
Authors and affiliations.
Translational Health Research Institute, School of Medicine, Western Sydney University, Sydney, Australia
Rebekah Rankin, Janet Conti, Lucie Ramjan & Phillipa Hay
School of Psychology, Western Sydney University, Sydney, Australia
Janet Conti
School of Nursing and Midwifery, Western Sydney University, Sydney, Australia
Lucie Ramjan
Campbelltown Hospital, South West Sydney Local Health District (SWSLHD), Sydney, Australia
Phillipa Hay
You can also search for this author in PubMed Google Scholar
Contributions
The first author wrote the main manuscript text, prepared all initial tables and figures, and supporting documentation. All authors participated in the edited and review of the manuscript.
Corresponding author
Correspondence to Rebekah Rankin .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
Rebekah Rankin is a doctoral student currently supported by the Western Sydney University Butterfly Foundation Postgraduate Research Scholarship which is jointly funded by Western Sydney University and the Butterfly Foundation. She is also recipient of the DHCRC top up scholarship. Phillipa Hay receives/has received sessional fees and lecture fees from the Australian Medical Council, Therapeutic Guidelines publication, and HETI (New South Wales and the former NSW Institute of Psychiatry) and royalties/honoraria from Hogrefe and Huber, McGraw Hill Education, and Blackwell Scientific Publications, Biomed Central and PlosMedicine and she has received research grants from the NHMRC and ARC. She is Chair of the National Eating Disorders Collaboration Steering Committee in Australia (2019-) and was Member of the ICD-11 Working Group for Eating Disorders and was Chair Clinical Practice Guidelines Project Working Group (eating disorders) of RANZCP (2012–2015). She is the editor-in-chief of the Journal of Eating Disorders. She has prepared a report under contract for Takeda (formerly Shire) Pharmaceuticals in regard to Binge Eating Disorder (July 2017) and is a consultant to Takeda Pharmaceuticals. All views in this paper are her own. All other authors declare that they have no conflict of interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Table A: Quality assessment of papers included in review.
Additional file 2.
Researcher position statements.
Additional file 3.
Table B: Exemplar data extracts for metathemes in the metasynthesis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Rankin, R., Conti, J., Ramjan, L. et al. A systematic review of people’s lived experiences of inpatient treatment for anorexia nervosa: living in a “bubble”. J Eat Disord 11 , 95 (2023). https://doi.org/10.1186/s40337-023-00820-0
Download citation
Received : 15 March 2023
Accepted : 06 June 2023
Published : 09 June 2023
DOI : https://doi.org/10.1186/s40337-023-00820-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Eating disorder
- Inpatient treatment
- Systematic review
- Meta-synthesis
- Qualitative
- Intervention
- Lived experience
Journal of Eating Disorders
ISSN: 2050-2974
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Anorexia nervosa is a complex psychiatric illness associated with food restriction and high mortality. Recent brain research in adolescents and adults with anorexia nervosa has used larger sample sizes compared with earlier studies and tasks that test specific brain circuits. Those studies have produced more robust results and advanced our ...
Epidemiology. Although eating disorders contribute significantly to the global burden of disease, they remain relatively uncommon. A study published in September 2018 by Tomoko Udo, Ph.D., and Carlos M. Grilo, Ph.D., in Biological Psychiatry examined data from a large, nationally representative sample of over 36,000 U.S. adults 18 years of age and older surveyed using a lay-administered ...
Anorexia nervosa is associated with a high incidence of coexisting psychiatric conditions, marked treatment resistance, frequent medical complications, and a substantial risk of death. Several psyc...
Anorexia nervosa is a serious psychiatric illness with medical as well as behavioural health manifestations. It is associated with high rates of morbidity and a mortality rate as high as that of any other psychiatric illness.1 It is an old illness2 and a challenge to treat, especially in adults, who might have been ill for several years.3 Although outpatient treatments to target anorexia ...
On average, only 50% of people with an eating disorder make a full recovery, and anorexia nervosa has one of the highest mortality rates of all psychiatric disorders. Eating disorders cost between £3·9 and £4·6 billion per year to the National Health Service (NHS) and result in losses of between £6·8 and £8 billion to the economy.
Abstract. Eating disorders (anorexia nervosa, bulimia nervosa and binge-eating disorder) are a heterogeneous class of complex illnesses marked by weight and appetite dysregulation coupled with ...
54 studies, of which 36 were from high-income countries, were included in the analysis. The number of global eating disorder cases in 2019 that were unrepresented in GBD 2019 was 41·9 million (95% UI 27·9-59·0), and consisted of 17·3 million (11·3-24·9) people with binge-eating disorder and 24·6 million (14·7-39·7) people with OSFED (vs 13·6 million [10·2-17·5] people with ...
Eating disorders (ED), especially Anorexia Nervosa (AN), are internationally reported to have amongst the highest mortality and suicide rates in mental health. With limited evidence for current pharmacological and/or psychological treatments, there is a grave responsibility within health research to better understand outcomes for people with a lived experience of ED, factors and interventions ...
Aims and scope. Journal of Eating Disorders is the first open access, peer-reviewed journal publishing leading research in the science and clinical practice of eating disorders. It disseminates research that provides answers to the important issues and key challenges in the field of eating disorders and to facilitate translation of evidence ...
To synthesise the evidence on the relationships between internalised weight bias (IWB) and biopsychosocial health outcomes in individuals ≤ 25 years. Tiarna Foster, Melissa Eaton and Yasmine Probst. Journal of Eating Disorders 2024 12 :38. Review Published on: 15 March 2024. Full Text.
Anorexia Nervosa (AN) is a psychological disorder involving body manipulation, self-inflicted hunger, and fear of gaining weight.We performed an overview of the existing literature in the field of AN, highlighting the main intrafamilial risk factors for anorexia. We searched the PubMed database by using keywords such as "anorexia" and "risk factors" and "family". After appropriate ...
e among younger persons (aged <15 years) has increased. It is unclear whether this reflects earlier detection or earlier age of onset. Nevertheless, it has implications for future research into risk factors and for prevention programs. For bulimia nervosa, there has been a decline in overall incidence rate over time. The lifetime prevalence rates of anorexia nervosa might be up to 4% among ...
DSM-IV (2) lists four criteria for the diagnosis of anorexia nervosa: 1. Refusal to maintain body weight at or above a minimally normal weight for age and height. 2. Intense fear of gaining weight or becoming fat, even though underweight. 3. Disturbance in the way in which one's body weight or shape is experienced, undue influence of body ...
It is linked to eating disorders and an increased drive for thinness. The research found "strong and long-lasting effects on adult psychological health" caused by pressure from parents and ...
2nd April 2024 Newsletter. This week we're releasing another two resources from our new Schema series: Defectiveness and Coping Styles And Responses (Schema Therapy). Our research roundup examines the impact of early life experiences on eating disorders, and explores how negative expectations can increase social anxiety.
Treatment for anorexia nervosa (AN) is typically delivered on a continuum of care, starting with outpatient treatment, and moving onto intensive outpatient, day or residential treatment and/or inpatient hospitalisation. However, minimal attention has been afforded to the lived experiences of persons undergoing inpatient treatment for AN. In particular, qualitative literature pertaining to the ...
In the last two decades, the scientific literature on so-called body representations has been increasing, and the notion of body awareness (BA) is particularly interesting for neurorehabilitation. In this article, we present results derived from recent studies on this representation, considering the different definitions and explicative models proposed as well as the empirical settings used to ...