Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 10, Issue 12
- Impact of the COVID-19 pandemic on mental health and well-being of communities: an exploratory qualitative study protocol
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-0180-0213 Anam Shahil Feroz 1 , 2 ,
- Naureen Akber Ali 3 ,
- Noshaba Akber Ali 1 ,
- Ridah Feroz 4 ,
- Salima Nazim Meghani 1 ,
- Sarah Saleem 1
- 1 Community Health Sciences , Aga Khan University , Karachi , Pakistan
- 2 Institute of Health Policy, Management and Evaluation , University of Toronto , Toronto , Ontario , Canada
- 3 School of Nursing and Midwifery , Aga Khan University , Karachi , Pakistan
- 4 Aga Khan University Institute for Educational Development , Karachi , Pakistan
- Correspondence to Ms Anam Shahil Feroz; anam.sahyl{at}gmail.com
Introduction The COVID-19 pandemic has certainly resulted in an increased level of anxiety and fear in communities in terms of disease management and infection spread. Due to fear and social stigma linked with COVID-19, many individuals in the community hide their disease and do not access healthcare facilities in a timely manner. In addition, with the widespread use of social media, rumours, myths and inaccurate information about the virus are spreading rapidly, leading to intensified irritability, fearfulness, insomnia, oppositional behaviours and somatic complaints. Considering the relevance of all these factors, we aim to explore the perceptions and attitudes of community members towards COVID-19 and its impact on their daily lives and mental well-being.
Methods and analysis This formative research will employ an exploratory qualitative research design using semistructured interviews and a purposive sampling approach. The data collection methods for this formative research will include indepth interviews with community members. The study will be conducted in the Karimabad Federal B Area and in the Garden (East and West) community settings in Karachi, Pakistan. The community members of these areas have been selected purposively for the interview. Study data will be analysed thematically using NVivo V.12 Plus software.
Ethics and dissemination Ethical approval for this study has been obtained from the Aga Khan University Ethical Review Committee (2020-4825-10599). The results of the study will be disseminated to the scientific community and to the research subjects participating in the study. The findings will help us explore the perceptions and attitudes of different community members towards the COVID-19 pandemic and its impact on their daily lives and mental well-being.
- mental health
- public health
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-041641
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
The mental health impact of the COVID-19 pandemic is likely to last much longer than the physical health impact, and this study is positioned well to explore the perceptions and attitudes of community members towards the pandemic and its impact on their daily lives and mental well-being.
This study will guide the development of context-specific innovative mental health programmes to support communities in the future.
One limitation is that to minimise the risk of infection all study respondents will be interviewed online over Zoom and hence the authors will not have the opportunity to build rapport with the respondents or obtain non-verbal cues during interviews.
The COVID-19 pandemic has affected almost 180 countries since it was first detected in Wuhan, China in December 2019. 1 2 The COVID-19 outbreak has been declared a public health emergency of international concern by the WHO. 3 The WHO estimates the global mortality to be about 3.4% 4 ; however, death rates vary between countries and across age groups. 5 In Pakistan, a total of 10 880 cases and 228 deaths due to COVID-19 infection have been reported to date. 6
The worldwide COVID-19 pandemic has not only incurred massive challenges to the global supply chains and healthcare systems but also has a detrimental effect on the overall health of individuals. 7 The pandemic has led to lockdowns and has created destructive impact on the societies at large. Most company employees, including daily wage workers, have been prohibited from going to their workplaces or have been asked to work from home, which has caused job-related insecurities and financial crises in the communities. 8 Educational institutions and training centres have also been closed, which resulted in children losing their routine of going to schools, studying and socialising with their peers. Delay in examinations is likewise a huge stressor for students. 8 Alongside this, parents have been struggling with creating a structured milieu for their children. 9 COVID-19 has hindered the normal routine life of every individual, be it children, teenagers, adults or the elderly. The crisis is engendering burden throughout populations and communities, particularly in developing countries such as Pakistan which face major challenges due to fragile healthcare systems and poor economic structures. 10
The COVID-19 pandemic has certainly resulted in an increased level of anxiety and fear in communities in terms of disease management and infection spread. 8 Further, the highly contagious nature of COVID-19 has also escalated confusion, fear and panic among community residents. Moreover, social distancing is often an unpleasant experience for community members and for patients as it adds to mental suffering, particularly in the local setting where get-togethers with friends and families are a major source of entertainment. 9 Recent studies also showed that individuals who are following social distancing rules experience loneliness, causing a substantial level of distress in the form of anxiety, stress, anger, misperception and post-traumatic stress symptoms. 8 11 Separation from family members, loss of autonomy, insecurity over disease status, inadequate supplies, inadequate information, financial loss, frustration, stigma and boredom are all major stressors that can create drastic impact on an individual’s life. 11 Due to fear and social stigma linked with COVID-19, many individuals in the community hide their disease and do not access healthcare facilities in a timely manner. 12 With the widespread use of social media, 13 rumours, myths and inaccurate information about COVID-19 are also spreading rapidly, not only among adults but are also carried on to children, leading to intensified irritability, fearfulness, insomnia, oppositional behaviours and somatic complaints. 9 The psychological symptoms associated with COVID-19 at the community level are also manifested as anxiety-driven panic buying, resulting in exhaustion of resources from the market. 14 Some level of panic also dwells in the community due to the unavailability of essential protective equipment, particularly masks and sanitisers. 15 Similarly, mental health issues, including depression, anxiety, panic attacks, psychotic symptoms and even suicide, were reported during the early severe acute respiratory syndrome outbreak. 16 17 COVID-19 is likely posing a similar risk throughout the world. 12
The fear of transmitting the disease or a family member falling ill is a probable mental function of human nature, but at some point the psychological fear of the disease generates more anxiety than the disease itself. Therefore, mental health problems are likely to increase among community residents during an epidemic situation. Considering the relevance of all these factors, we aim to explore the perceptions and attitudes towards COVID-19 among community residents and the impact of these perceptions and attitude on their daily lives and mental well-being.
Methods and analysis
Study design.
This study will employ an exploratory qualitative research design using semistructured interviews and a purposive sampling approach. The data collection methods for this formative research will include indepth interviews (IDIs) with community members. The IDIs aim to explore perceptions of community members towards COVID-19 and its impact on their mental well-being.
Study setting and study participants
The study will be conducted in two communities in Karachi City: Karimabad Federal B Area Block 3 Gulberg Town, and Garden East and Garden West. Karimabad is a neighbourhood in the Karachi Central District of Karachi, Pakistan, situated in the south of Gulberg Town bordering Liaquatabad, Gharibabad and Federal B Area. The population of this neighbourhood is predominantly Ismailis. People living here belong mostly to the middle class to the lower middle class. It is also known for its wholesale market of sports goods and stationery. Garden is an upmarket neighbourhood in the Karachi South District of Karachi, Pakistan, subdivided into two neighbourhoods: Garden East and Garden West. It is the residential area around the Karachi Zoological Gardens; hence, it is popularly known as the ‘Garden’ area. The population of Garden used to be primarily Ismailis and Goan Catholics but has seen an increasing number of Memons, Pashtuns and Baloch. These areas have been selected purposively because the few members of these communities are already known to one of the coinvestigators. The coinvestigator will serve as a gatekeeper for providing entrance to the community for the purpose of this study. Adult community members of different ages and both genders will be interviewed from both sites, as mentioned in table 1 . Interview participants will be selected following the eligibility criteria.
- View inline
Study participants for indepth interviews
IDIs with community members
We will conduct IDIs with community members to explore the perceptions and attitudes of community members towards COVID-19 and its effects on their daily lives and mental well-being. IDI participants will be identified via the community WhatsApp group, and will be invited for an interview via a WhatsApp message or email. Consent will be taken over email or WhatsApp before the interview begins, where they will agree that the interview can be audio-recorded and that written notes can be taken. The interviews will be conducted either in Urdu or in English language, and each interview will last around 40–50 min. Study participants will be assured that their information will remain confidential and that no identifying features will be mentioned on the transcript. The major themes will include a general discussion about participants’ knowledge and perceptions about the COVID-19 pandemic, perceptions on safety measures, and perceived challenges in the current situation and its impact on their mental well-being. We anticipate that 24–30 interviews will be conducted, but we will cease interviews once data saturation has been achieved. Data saturation is the point when no new themes emerge from the additional interviews. Data collection will occur concurrently with data analysis to determine data saturation point. The audio recordings will be transcribed by a transcriptionist within 24 hours of the interviews.
An interview guide for IDIs is shown in online supplemental annex 1 .
Supplemental material
Eligibility criteria.
The following are the criteria for inclusion and exclusion of study participants:
Inclusion criteria
Residents of Garden (East and West) and Karimabad Federal B Area of Karachi who have not contracted the disease.
Exclusion criteria
Those who refuse to participate in the study.
Those who have experienced COVID-19 and are undergoing treatment.
Those who are suspected for COVID-19 and have been isolated/quarantined.
Family members of COVID-19-positive cases.
Data collection procedure
A semistructured interview guide has been developed for community members. The initial questions on the guide will help to explore participants’ perceptions and attitudes towards COVID-19. Additional questions on the guide will assess the impact of these perceptions and attitude on the daily lives and mental health and well-being of community residents. All semistructured interviews will be conducted online via Zoom or WhatsApp. Interviews will be scheduled at the participant’s convenient day and time. Interviews are anticipated to begin on 1 December 2020.
Patient and public involvement
No patients were involved.
Data analysis
We will transcribe and translate collected data into English language by listening to the audio recordings in order to conduct a thematic analysis. NVivo V.12 Plus software will be used to import, organise and explore data for analysis. Two independent researchers will read the transcripts at various times to develop familiarity and clarification with the data. We will employ an iterative process which will help us to label data and generate new categories to identify emergent themes. The recorded text will be divided into shortened units and labelled as a ‘code’ without losing the main essence of the research study. Subsequently, codes will be analysed and merged into comparable categories. Lastly, the same categories will be grouped into subthemes and final themes. To ensure inter-rater reliability, two independent investigators will perform the coding, category creation and thematic analyses. Discrepancies between the two investigators will be resolved through consensus meetings to reduce researcher bias.
Ethics and dissemination
Study participants will be asked to provide informed, written consent prior to participation in the study. The informed consent form can be submitted by the participant via WhatsApp or email. Participants who are unable to write their names will be asked to provide a thumbprint to symbolise their consent to participate. Ethical approval for this study has been obtained from the Aga Khan University Ethical Review Committee (2020-4825-10599). The study results will be disseminated to the scientific community and to the research subjects participating in the study. The findings will help us explore the perceptions and attitudes of different community members towards the COVID-19 pandemic and its impact on their daily lives and mental well-being.
The findings of this study will help us to explore the perceptions and attitudes towards the COVID-19 pandemic and its impact on the daily lives and mental well-being of individuals in the community. Besides, an indepth understanding of the needs of the community will be identified, which will help us develop context-specific innovative mental health programmes to support communities in the future. The study will provide insights into how communities are managing their lives under such a difficult situation.
- World Health Organization
- Nielsen-Saines K , et al
- Worldometer
- Ebrahim SH ,
- Gozzer E , et al
- Snoswell CL ,
- Harding LE , et al
- Nargis Asad
- van Weel C ,
- Qidwai W , et al
- Brooks SK ,
- Webster RK ,
- Smith LE , et al
- Tripathy S ,
- Kar SK , et al
- Schwartz J ,
- Maunder R ,
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
ASF and NAA are joint first authors.
Contributors ASF and NAA conceived the study. ASF, NAA, RF, NA, SNM and SS contributed to the development of the study design and final protocols for sample selection and interviews. ASF and NAA contributed to writing the manuscript. All authors reviewed and approved the final version of the paper.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 11 February 2021
Methodological quality of COVID-19 clinical research
- Richard G. Jung ORCID: orcid.org/0000-0002-8570-6736 1 , 2 , 3 na1 ,
- Pietro Di Santo 1 , 2 , 4 , 5 na1 ,
- Cole Clifford 6 ,
- Graeme Prosperi-Porta 7 ,
- Stephanie Skanes 6 ,
- Annie Hung 8 ,
- Simon Parlow 4 ,
- Sarah Visintini ORCID: orcid.org/0000-0001-6966-1753 9 ,
- F. Daniel Ramirez ORCID: orcid.org/0000-0002-4350-1652 1 , 4 , 10 , 11 ,
- Trevor Simard 1 , 2 , 3 , 4 , 12 &
- Benjamin Hibbert ORCID: orcid.org/0000-0003-0906-1363 2 , 3 , 4
Nature Communications volume 12 , Article number: 943 ( 2021 ) Cite this article
13k Accesses
93 Citations
238 Altmetric
Metrics details
- Infectious diseases
- Public health
The COVID-19 pandemic began in early 2020 with major health consequences. While a need to disseminate information to the medical community and general public was paramount, concerns have been raised regarding the scientific rigor in published reports. We performed a systematic review to evaluate the methodological quality of currently available COVID-19 studies compared to historical controls. A total of 9895 titles and abstracts were screened and 686 COVID-19 articles were included in the final analysis. Comparative analysis of COVID-19 to historical articles reveals a shorter time to acceptance (13.0[IQR, 5.0–25.0] days vs. 110.0[IQR, 71.0–156.0] days in COVID-19 and control articles, respectively; p < 0.0001). Furthermore, methodological quality scores are lower in COVID-19 articles across all study designs. COVID-19 clinical studies have a shorter time to publication and have lower methodological quality scores than control studies in the same journal. These studies should be revisited with the emergence of stronger evidence.
Similar content being viewed by others
Clinical presentations, laboratory and radiological findings, and treatments for 11,028 COVID-19 patients: a systematic review and meta-analysis

Improving clinical paediatric research and learning from COVID-19: recommendations by the Conect4Children expert advice group
The effect of influenza vaccine in reducing the severity of clinical outcomes in patients with COVID-19: a systematic review and meta-analysis
Introduction.
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic spread globally in early 2020 with substantial health and economic consequences. This was associated with an exponential increase in scientific publications related to the coronavirus disease 2019 (COVID-19) in order to rapidly elucidate the natural history and identify diagnostic and therapeutic tools 1 .
While a need to rapidly disseminate information to the medical community, governmental agencies, and general public was paramount—major concerns have been raised regarding the scientific rigor in the literature 2 . Poorly conducted studies may originate from failure at any of the four consecutive research stages: (1) choice of research question relevant to patient care, (2) quality of research design 3 , (3) adequacy of publication, and (4) quality of research reports. Furthermore, evidence-based medicine relies on a hierarchy of evidence, ranging from the highest level of randomized controlled trials (RCT) to the lowest level of case series and case reports 4 .
Given the implications for clinical care, policy decision making, and concerns regarding methodological and peer-review standards for COVID-19 research 5 , we performed a formal evaluation of the methodological quality of published COVID-19 literature. Specifically, we undertook a systematic review to identify COVID-19 clinical literature and matched them to historical controls to formally evaluate the following: (1) the methodological quality of COVID-19 studies using established quality tools and checklists, (2) the methodological quality of COVID-19 studies, stratified by median time to acceptance, geographical regions, and journal impact factor and (3) a comparison of COVID-19 methodological quality to matched controls.
Herein, we show that COVID-19 articles are associated with lower methodological quality scores. Moreover, in a matched cohort analysis with control articles from the same journal, we reveal that COVID-19 articles are associated with lower quality scores and shorter time from submission to acceptance. Ultimately, COVID-19 clinical studies should be revisited with the emergence of stronger evidence.
Article selection
A total of 14787 COVID-19 papers were identified as of May 14, 2020 and 4892 duplicate articles were removed. In total, 9895 titles and abstracts were screened, and 9101 articles were excluded due to the study being pre-clinical in nature, case report, case series <5 patients, in a language other than English, reviews (including systematic reviews), study protocols or methods, and other coronavirus variants with an overall inter-rater study inclusion agreement of 96.7% ( κ = 0.81; 95% CI, 0.79–0.83). A total number of 794 full texts were reviewed for eligibility. Over 108 articles were excluded for ineligible study design or publication type (such as letter to the editors, editorials, case reports or case series <5 patients), wrong patient population, non-English language, duplicate articles, wrong outcomes and publication in a non-peer-reviewed journal. Ultimately, 686 articles were identified with an inter-rater agreement of 86.5% ( κ = 0.68; 95% CI, 0.67–0.70) (Fig. 1 ).
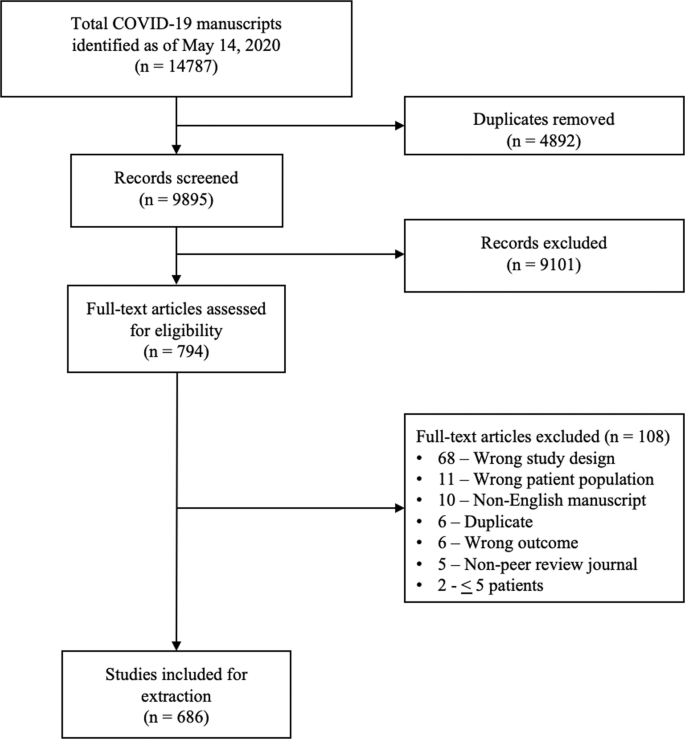
A total of 14787 articles were identified and 4892 duplicate articles were removed. Overall, 9895 articles were screened by title and abstract leaving 794 articles for full-text screening. Over 108 articles were excluded, leaving a total of 686 articles that underwent methodological quality assessment.
COVID-19 literature methodological quality
Most studies originated from Asia/Oceania with 469 (68.4%) studies followed by Europe with 139 (20.3%) studies, and the Americas with 78 (11.4%) studies. Of included studies, 380 (55.4%) were case series, 199 (29.0%) were cohort, 63 (9.2%) were diagnostic, 38 (5.5%) were case–control, and 6 (0.9%) were RCTs. Most studies (590, 86.0%) were retrospective in nature, 620 (90.4%) reported the sex of patients, and 7 (2.3%) studies excluding case series calculated their sample size a priori. The method of SARS-CoV-2 diagnosis was reported in 558 studies (81.3%) and ethics approval was obtained in 556 studies (81.0%). Finally, journal impact factor of COVID-19 manuscripts was 4.7 (IQR, 2.9–7.6) with a time to acceptance of 13.0 (IQR, 5.0–25.0) days (Table 1 ).
Overall, when COVID-19 articles were stratified by study design, a mean case series score (out of 5) (SD) of 3.3 (1.1), mean NOS cohort study score (out of 8) of 5.8 (1.5), mean NOS case–control study score (out of 8) of 5.5 (1.9), and low bias present in 4 (6.4%) diagnostic studies was observed (Table 2 and Fig. 2 ). Furthermore, in the 6 RCTs in the COVID-19 literature, there was a high risk of bias with little consideration for sequence generation, allocation concealment, blinding, incomplete outcome data, and selective outcome reporting (Table 2 ).
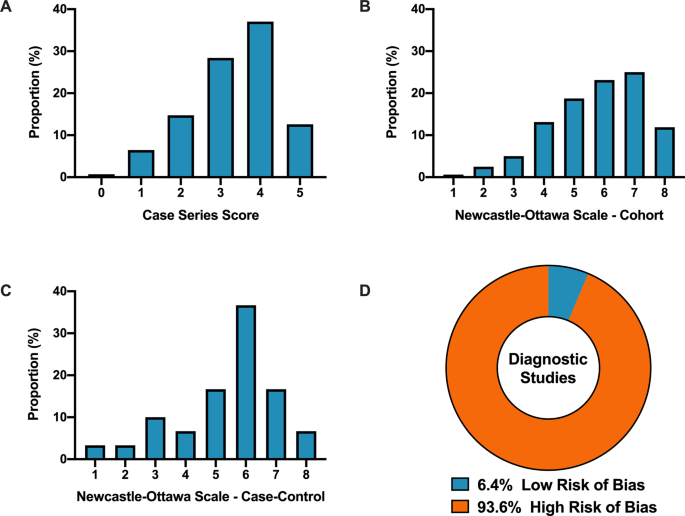
A Distribution of COVID-19 case series studies scored using the Murad tool ( n = 380). B Distribution of COVID-19 cohort studies scored using the Newcastle–Ottawa Scale ( n = 199). C Distribution of COVID-19 case–control studies scored using the Newcastle–Ottawa Scale ( n = 38). D Distribution of COVID-19 diagnostic studies scored using the QUADAS-2 tool ( n = 63). In panel D , blue represents low risk of bias and orange represents high risk of bias.
For secondary outcomes, rapid time from submission to acceptance (stratified by median time of acceptance of <13.0 days) was associated with lower methodological quality scores for case series and cohort study designs but not for case–control nor diagnostic studies (Fig. 3A–D ). Low journal impact factor (<10) was associated with lower methodological quality scores for case series, cohort, and case–control designs (Fig. 3E–H ). Finally, studies originating from different geographical regions had no differences in methodological quality scores with the exception of cohort studies (Fig. 3I–L ). When dichotomized by high vs. low methodological quality scores, a similar trend was observed with rapid time from submission to acceptance (34.4% vs. 46.3%, p = 0.01, Supplementary Fig. 1B ), low impact factor journals (<10) was associated with lower methodological quality score (38.8% vs. 68.0%, p < 0.0001, Supplementary Fig. 1C ). Finally, studies originating in either Americas or Asia/Oceania was associated with higher methodological quality scores than Europe (Supplementary Fig. 1D ).
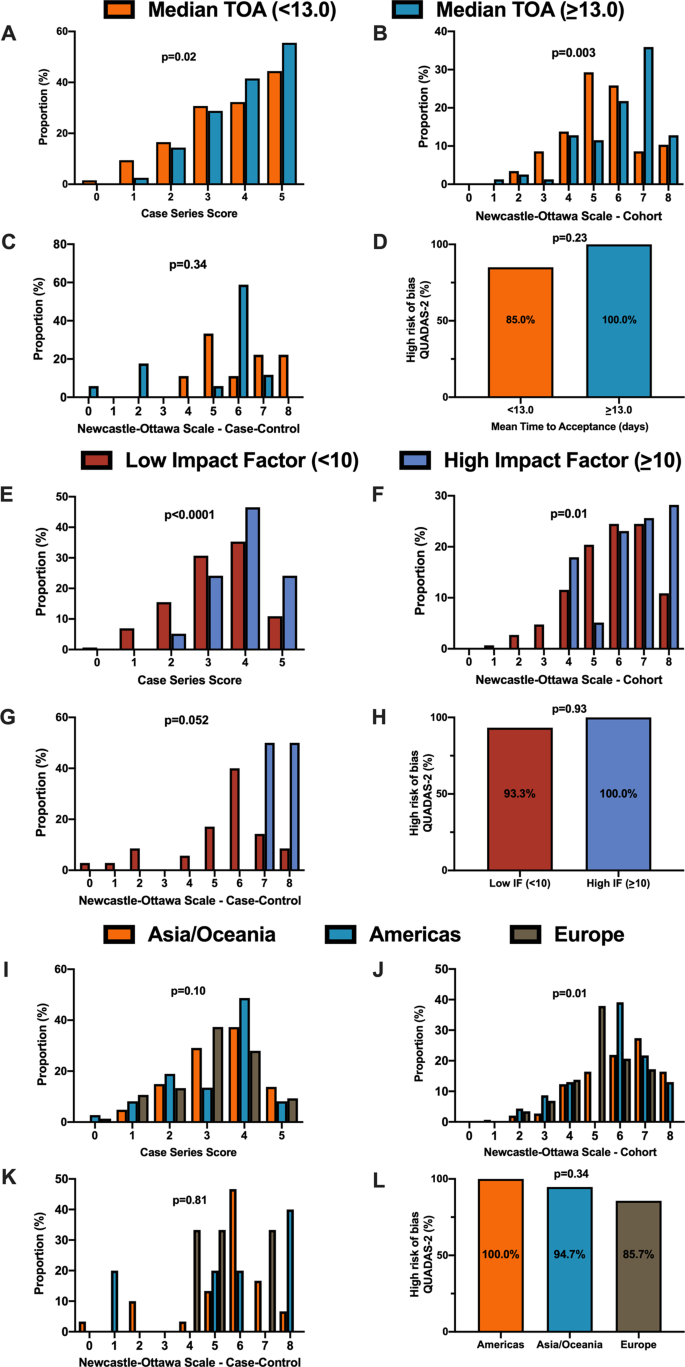
A When stratified by time of acceptance (13.0 days), increased time of acceptance was associated with higher case series score ( n = 186 for <13 days and n = 193 for >=13 days; p = 0.02). B Increased time of acceptance was associated with higher NOS cohort score ( n = 112 for <13 days and n = 144 for >=13 days; p = 0.003). C No difference in time of acceptance and case–control score was observed ( n = 18 for <13 days and n = 27 for >=13 days; p = 0.34). D No difference in time of acceptance and diagnostic risk of bias (QUADAS-2) was observed ( n = 43 for <13 days and n = 33 for >=13 days; p = 0.23). E When stratified by impact factor (IF ≥10), high IF was associated with higher case series score ( n = 466 for low IF and n = 60 for high IF; p < 0.0001). F High IF was associated with higher NOS cohort score ( n = 262 for low IF and n = 68 for high IF; p = 0.01). G No difference in IF and case–control score was observed ( n = 62 for low IF and n = 2 for high IF; p = 0.052). H No difference in IF and QUADAS-2 was observed ( n = 101 for low IF and n = 2 for high IF; p = 0.93). I When stratified by geographical region, no difference in geographical region and case series score was observed ( n = 276 Asia/Oceania, n = 135 Americas, and n = 143 Europe/Africa; p = 0.10). J Geographical region was associated with differences in cohort score ( n = 177 Asia/Oceania, n = 81 Americas, and n = 89 Europe/Africa; p = 0.01). K No difference in geographical region and case–control score was observed ( n = 37 Asia/Oceania, n = 13 Americas, and n = 14 Europe/Africa; p = 0.81). L No difference in geographical region and QUADAS-2 was observed ( n = 49 Asia/Oceania, n = 28 Americas, and n = 28 Europe/Africa; p = 0.34). In panels A – D , orange represents lower median time of acceptance and blue represents high median time of acceptance. In panels E – H , red is low impact factor and blue is high impact factor. In panels I – L , orange represents Asia/Oceania, blue represents Americas, and brown represents Europe. Differences in distributions were analysed by two-sided Kruskal–Wallis test. Differences in diagnostic risk of bias were quantified by Chi-squares test. p < 0.05 was considered statistically significant.
Methodological quality score differences in COVID-19 versus historical control
We matched 539 historical control articles to COVID-19 articles from the same journal with identical study designs in the previous year for a final analysis of 1078 articles (Table 1 ). Overall, 554 (51.4%) case series, 348 (32.3%) cohort, 64 (5.9%) case–control, 106 (9.8%) diagnostic and 6 (0.6%) RCTs were identified from the 1078 total articles. Differences exist between COVID-19 and historical control articles in geographical region of publication, retrospective study design, and sample size calculation (Table 1 ). Time of acceptance was 13.0 (IQR, 5.0–25.0) days in COVID-19 articles vs. 110.0 (IQR, 71.0–156.0) days in control articles (Table 1 and Fig. 4A , p < 0.0001). Case-series methodological quality score was lower in COVID-19 articles compared to the historical control (3.3 (1.1) vs. 4.3 (0.8); n = 554; p < 0.0001; Table 2 and Fig. 4B ). Furthermore, NOS score was lower in COVID-19 cohort studies (5.8 (1.6) vs. 7.1 (1.0); n = 348; p < 0.0001; Table 2 and Fig. 4C ) and case–control studies (5.4 (1.9) vs. 6.6 (1.0); n = 64; p = 0.003; Table 2 and Fig. 4D ). Finally, lower risk of bias in diagnostic studies was in 12 COVID-19 articles (23%; n = 53) compared to 24 control articles (45%; n = 53; p = 0.02; Table 2 and Fig. 4E ). A similar trend was observed between COVID-19 and historical control articles when dichotomized by good vs. low methodological quality scores (Supplementary Fig. 2 ).
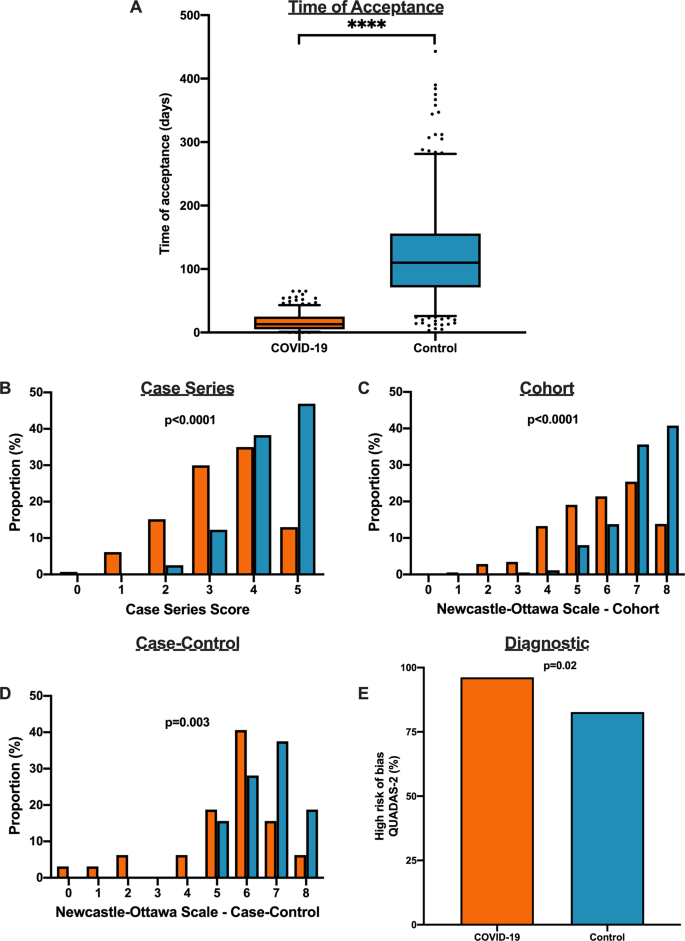
A Time to acceptance was reduced in COVID-19 articles compared to control articles (13.0 [IQR, 5.0–25.0] days vs. 110.0 [IQR, 71.0–156.0] days, n = 347 for COVID-19 and n = 414 for controls; p < 0.0001). B When compared to historical control articles, COVID-19 articles were associated with lower case series score ( n = 277 for COVID-19 and n = 277 for controls; p < 0.0001). C COVID-19 articles were associated with lower NOS cohort score compared to historical control articles ( n = 174 for COVID-19 and n = 174 for controls; p < 0.0001). D COVID-19 articles were associated with lower NOS case–control score compared to historical control articles ( n = 32 for COVID-19 and n = 32 for controls; p = 0.003). E COVID-19 articles were associated with higher diagnostic risk of bias (QUADAS-2) compared to historical control articles ( n = 53 for COVID-19 and n = 53 for controls; p = 0.02). For panel A , boxplot captures 5, 25, 50, 75 and 95% from the first to last whisker. Orange represents COVID-19 articles and blue represents control articles. Two-sided Mann–Whitney U-test was conducted to evaluate differences in time to acceptance between COVID-19 and control articles. Differences in study quality scores were evaluated by two-sided Kruskal–Wallis test. Differences in diagnostic risk of bias were quantified by Chi-squares test. p < 0.05 was considered statistically significant.
In this systematic evaluation of methodological quality, COVID-19 clinical research was primarily observational in nature with modest methodological quality scores. Not only were the study designs low in the hierarchy of scientific evidence, we found that COVID-19 articles were associated with a lower methodological quality scores when published with a shorter time of publication and in lower impact factor journals. Furthermore, in a matched cohort analysis with historical control articles identified from the same journal of the same study design, we demonstrated that COVID-19 articles were associated with lower quality scores and shorter time from submission to acceptance.
The present study demonstrates comparative differences in methodological quality scores between COVID-19 literature and historical control articles. Overall, the accelerated publication of COVID-19 research was associated with lower study quality scores compared to previously published historical control studies. Our research highlights major differences in study quality between COVID-19 and control articles, possibly driven in part by a combination of more thorough editorial and/or peer-review process as suggested by the time to publication, and robust study design with questions which are pertinent for clinicians and patient management 3 , 6 , 7 , 8 , 9 , 10 , 11 .
In the early stages of the COVID-19 pandemic, we speculate that an urgent need for scientific data to inform clinical, social and economic decisions led to shorter time to publication and explosion in publication of COVID-19 studies in both traditional peer-reviewed journals and preprint servers 1 , 12 . The accelerated scientific process in the COVID-19 pandemic allowed a rapid understanding of natural history of COVID-19 symptomology and prognosis, identification of tools including RT-PCR to diagnose SARS-CoV-2 13 , and identification of potential therapeutic options such as tocilizumab and convalescent plasma which laid the foundation for future RCTs 14 , 15 , 16 . A delay in publication of COVID-19 articles due to a slower peer-review process may potentially delay dissemination of pertinent information against the pandemic. Despite concerns of slow peer review, major landmark trials (i.e. RECOVERY and ACTT-1 trial) 17 , 18 published their findings in preprint servers and media releases to allow for rapid dissemination. Importantly, the data obtained in these initial studies should be revisited as stronger data emerges as lower quality studies may fundamentally risk patient safety, resource allocation and future scientific research 19 .
Unfortunately, poor evidence begets poor clinical decisions 20 . Furthermore, lower quality scientific evidence potentially undermines the public’s trust in science during this time and has been evident through misleading information and high-profile retractions 12 , 21 , 22 , 23 . For example, the benefits of hydroxychloroquine, which were touted early in the pandemic based on limited data, have subsequently failed to be replicated in multiple observational studies and RCTs 5 , 24 , 25 , 26 , 27 , 28 , 29 , 30 . One poorly designed study combined with rapid publication led to considerable investment of both the scientific and medical community—akin to quinine being sold to the public as a miracle drug during the 1918 Spanish Influenza 31 , 32 . Moreover, as of June 30, 2020, ClinicalTrials.gov listed an astonishing 230 COVID-19 trials with hydroxychloroquine/plaquenil, and a recent living systematic review of observational studies and RCTs of hydroxychloroquine or chloroquine for COVID-19 demonstrated no evidence of benefit nor harm with concerns of severe methodological flaws in the included studies 33 .
Our study has important limitations. We evaluated the methodological quality of existing studies using established checklists and tools. While it is tempting to associate methodological quality scores with reproducibility or causal inferences of the intervention, it is not possible to ascertain the impact on the study design and conduct of research nor results or conclusions in the identified reports 34 . Second, although the methodological quality scales and checklists used for the manuscript are commonly used for quality assessment in systematic reviews and meta-analyses 35 , 36 , 37 , 38 , they can only assess the methodology without consideration for causal language and are prone to limitations 39 , 40 . Other tools such as the ROBINS-I and GRADE exist to evaluate methodological quality of identified manuscripts, although no consensus currently exists for critical appraisal of non-randomized studies 41 , 42 , 43 . Furthermore, other considerations of quality such as sample size calculation, sex reporting or ethics approval are not considered in these quality scores. As such, the quality scores measured using these checklists only reflect the patient selection, comparability, diagnostic reference standard and methods to ascertain the outcome of the study. Third, the 1:1 ratio to identify our historical control articles may affect the precision estimates of our findings. Interestingly, a simulation of an increase from 1:1 to 1:4 control ratio tightened the precision estimates but did not significantly alter the point estimate 44 . Furthermore, the decision for 1:1 ratio in our study exists due to limitations of available historical control articles from the identical journal in the restricted time period combined with a large effect size and sample size in the analysis. Finally, our analysis includes early publications on COVID-19 and there is likely to be an improvement in quality of related studies and study design as the field matures and higher-quality studies. Accordingly, our findings are limited to the early body of research as it pertains to the pandemic and it is likely that over time research quality will improve over time.
In summary, the early body of peer-reviewed COVID-19 literature was composed primarily of observational studies that underwent shorter peer-review evaluation and were associated with lower methodological quality scores than comparable studies. COVID-19 clinical studies should be revisited with the emergence of stronger evidence.
A systematic literature search was conducted on May 14, 2020 (registered on June 3, 2020 at PROSPERO: CRD42020187318) and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses. Furthermore, the cohort study was reported according to the Strengthening The Reporting of Observational Studies in Epidemiology checklist. The data supporting the findings of this study is available as Supplementary Data 1 – 2 .
Data sources and searches
The search was created in MEDLINE by a medical librarian with expertise in systematic reviews (S.V.) using a combination of key terms and index headings related to COVID-19 and translated to the remaining bibliographic databases (Supplementary Tables 1 – 3 ). The searches were conducted in MEDLINE (Ovid MEDLINE(R) ALL 1946–), Embase (Ovid Embase Classic + Embase 1947–) and the Cochrane Central Register of Controlled Trials (from inception). Search results were limited to English-only publications, and a publication date limit of January 1, 2019 to present was applied. In addition, a Canadian Agency for Drugs and Technologies in Health search filter was applied in MEDLINE and Embase to remove animal studies, and commentary, newspaper article, editorial, letter and note publication types were also eliminated. Search results were exported to Covidence (Veritas Health Innovation, Melbourne, Australia) and duplicates were eliminated using the platform’s duplicate identification feature.
Study selection, data extraction and methodological quality assessment
We included all types of COVID-19 clinical studies, including case series, observational studies, diagnostic studies and RCTs. For diagnostic studies, the reference standard for COVID-19 diagnosis was defined as a nasopharyngeal swab followed by reverse transcriptase-polymerase chain reaction in order to detect SARS-CoV-2. We excluded studies that were exploratory or pre-clinical in nature (i.e. in vitro or animal studies), case reports or case series of <5 patients, studies published in a language other than English, reviews, methods or protocols, and other coronavirus variants such as the Middle East respiratory syndrome.
The review team consisted of trained research staff with expertise in systematic reviews and one trainee. Title and abstracts were evaluated by two independent reviewers using Covidence and all discrepancies were resolved by consensus. Articles that were selected for full review were independently evaluated by two reviewers for quality assessment using a standardized case report form following the completion of a training period where all reviewers were trained with the original manuscripts which derived the tools or checklists along with examples for what were deemed high scores 35 , 36 , 37 , 38 . Following this, reviewers completed thirty full-text extractions and the two reviewers had to reach consensus and the process was repeated for the remaining manuscripts independently. When two independent reviewers were not able reach consensus, a third reviewer (principal investigator) provided oversight in the process to resolve the conflicted scores.
First and corresponding author names, date of publication, title of manuscript and journal of publication were collected for all included full-text articles. Journal impact factor was obtained from the 2018 InCites Journal Citation Reports from Clarivate Analytics. Submission and acceptance dates were collected in manuscripts when available. Other information such as study type, prospective or retrospective study, sex reporting, sample size calculation, method of SARS-CoV-2 diagnosis and ethics approval was collected by the authors. Methodological quality assessment was conducted using the Newcastle–Ottawa Scale (NOS) for case–control and cohort studies 37 , QUADAS-2 tool for diagnostic studies 38 , Cochrane risk of bias for RCTs 35 and a score derived by Murad et al. for case series studies 36 .
Identification of historical control from identified COVID-19 articles
Following the completion of full-text extraction of COVID-19 articles, we obtained a historical control group by identifying reports matched in a 1:1 fashion. From the eligible COVID-19 article, historical controls were identified by searching the same journal in a systematic fashion by matching the same study design (“case series”, “cohort”, “case control” or “diagnostic”) starting in the journal edition 12 months prior to the COVID-19 article publication on the publisher website (i.e. COVID-19 article published on April 2020, going backwards to April 2019) and proceeding forward (or backward if a specific article type was not identified) in a temporal fashion until the first matched study was identified following abstract screening by two independent reviewers. If no comparison article was found by either reviewers, the corresponding COVID-19 article was excluded from the comparison analysis. Following the identification of the historical control, data extraction and quality assessment was conducted on the identified articles using the standardized case report forms by two independent reviewers and conflicts resolved by consensus. The full dataset has been made available as Supplementary Data 1 – 2 .
Data synthesis and statistical analysis
Continuous variables were reported as mean (SD) or median (IQR) as appropriate, and categorical variables were reported as proportions (%). Continuous variables were compared using Student t -test or Mann–Whitney U-test and categorical variables including quality scores were compared by χ 2 , Fisher’s exact test, or Kruskal–Wallis test.
The primary outcome of interest was to evaluate the methodological quality of COVID-19 clinical literature by study design using the Newcastle–Ottawa Scale (NOS) for case–control and cohort studies, QUADAS-2 tool for diagnostic studies 38 , Cochrane risk of bias for RCTs 35 , and a score derived by Murad et al. for case series studies 36 . Pre-specified secondary outcomes were comparison of methodological quality scores of COVID-19 articles by (i) median time to acceptance, (ii) impact factor, (iii) geographical region and (iv) historical comparator. Time of acceptance was defined as the time between submission to acceptance which captures peer review and editorial decisions. Geographical region was stratified into continents including Asia/Oceania, Europe/Africa and Americas (North and South America). Post hoc comparison analysis between COVID-19 and historical control article quality scores were evaluated using Kruskal–Wallis test. Furthermore, good quality of NOS was defined as 3+ on selection and 1+ on comparability, and 2+ on outcome/exposure domains and high-quality case series scores was defined as a score ≥3.5. Due to a small sample size of identified RCTs, they were not included in the comparison analysis.
The finalized dataset was collected on Microsoft Excel v16.44. All statistical analyses were performed using SAS v9.4 (SAS Institute, Inc., Cary, NC, USA). Statistical significance was defined as P < 0.05. All figures were generated using GraphPad Prism v8 (GraphPad Software, La Jolla, CA, USA).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The authors can confirm that all relevant data are included in the paper and in Supplementary Data 1 – 2 . The original search was conducted on MEDLINE, Embase and Cochrane Central Register of Controlled Trials.
Chen, Q., Allot, A. & Lu, Z. Keep up with the latest coronavirus research. Nature 579 , 193 (2020).
Article ADS CAS Google Scholar
Mahase, E. Covid-19: 146 researchers raise concerns over chloroquine study that halted WHO trial. BMJ https://doi.org/10.1136/bmj.m2197 (2020).
Chalmers, I. & Glasziou, P. Avoidable waste in the production and reporting of research evidence. Lancet 374 , 86–89 (2009).
Article Google Scholar
Burns, P. B., Rohrich, R. J. & Chung, K. C. The levels of evidence and their role in evidence-based medicine. Plast. Reconstr. Surg. 128 , 305–310 (2011).
Article CAS Google Scholar
Alexander, P. E. et al. COVID-19 coronavirus research has overall low methodological quality thus far: case in point for chloroquine/hydroxychloroquine. J. Clin. Epidemiol. 123 , 120–126 (2020).
Barakat, A. F., Shokr, M., Ibrahim, J., Mandrola, J. & Elgendy, I. Y. Timeline from receipt to online publication of COVID-19 original research articles. Preprint at medRxiv https://doi.org/10.1101/2020.06.22.20137653 (2020).
Chan, A.-W. et al. Increasing value and reducing waste: addressing inaccessible research. Lancet 383 , 257–266 (2014).
Ioannidis, J. P. A. et al. Increasing value and reducing waste in research design, conduct, and analysis. Lancet 383 , 166–175 (2014).
Chalmers, I. et al. How to increase value and reduce waste when research priorities are set. Lancet 383 , 156–165 (2014).
Salman, R. A.-S. et al. Increasing value and reducing waste in biomedical research regulation and management. Lancet 383 , 176–185 (2014).
Glasziou, P. et al. Reducing waste from incomplete or unusable reports of biomedical research. Lancet 383 , 267–276 (2014).
Bauchner, H. The rush to publication: an editorial and scientific mistake. JAMA 318 , 1109–1110 (2017).
He, X. et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 26 , 672–675 (2020).
Guaraldi, G. et al. Tocilizumab in patients with severe COVID-19: a retrospective cohort study. Lancet Rheumatol. 2 , e474–e484 (2020).
Duan, K. et al. Effectiveness of convalescent plasma therapy in severe COVID-19 patients. Proc. Natl Acad. Sci. USA 117 , 9490–9496 (2020).
Shen, C. et al. Treatment of 5 critically Ill patients with COVID-19 with convalescent plasma. JAMA 323 , 1582–1589 (2020).
Beigel, J. H. et al. Remdesivir for the treatment of covid-19—final report. N. Engl. J. Med. 383 , 1813–1826 (2020).
Group, R. C. et al. Dexamethasone in hospitalized patients with Covid-19—preliminary report. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa2021436 (2020).
Ramirez, F. D. et al. Methodological rigor in preclinical cardiovascular studies: targets to enhance reproducibility and promote research translation. Circ. Res 120 , 1916–1926 (2017).
Heneghan, C. et al. Evidence based medicine manifesto for better healthcare. BMJ 357 , j2973 (2017).
Mehra, M. R., Desai, S. S., Ruschitzka, F. & Patel, A. N. RETRACTED: hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. Lancet https://doi.org/10.1016/S0140-6736(20)31180-6 (2020).
Servick, K. & Enserink, M. The pandemic’s first major research scandal erupts. Science 368 , 1041–1042 (2020).
Mehra, M. R., Desai, S. S., Kuy, S., Henry, T. D. & Patel, A. N. Retraction: Cardiovascular disease, drug therapy, and mortality in Covid-19. N. Engl. J. Med. 382 , 2582–2582, https://doi.org/10.1056/NEJMoa2007621. (2020).
Article PubMed Google Scholar
Boulware, D. R. et al. A randomized trial of hydroxychloroquine as postexposure prophylaxis for Covid-19. N. Engl. J. Med. 383 , 517–525 (2020).
Gautret, P. et al. Clinical and microbiological effect of a combination of hydroxychloroquine and azithromycin in 80 COVID-19 patients with at least a six-day follow up: a pilot observational study. Travel Med. Infect. Dis. 34 , 101663–101663 (2020).
Geleris, J. et al. Observational study of hydroxychloroquine in hospitalized patients with Covid-19. N. Engl. J. Med. 382 , 2411–2418 (2020).
Borba, M. G. S. et al. Effect of high vs low doses of chloroquine diphosphate as adjunctive therapy for patients hospitalized with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection: a randomized clinical trial. JAMA Netw. Open 3 , e208857–e208857 (2020).
Mercuro, N. J. et al. Risk of QT interval prolongation associated with use of hydroxychloroquine with or without concomitant azithromycin among hospitalized patients testing positive for coronavirus disease 2019 (COVID-19). JAMA Cardiol. 5 , 1036–1041 (2020).
Molina, J. M. et al. No evidence of rapid antiviral clearance or clinical benefit with the combination of hydroxychloroquine and azithromycin in patients with severe COVID-19 infection. Médecine et. Maladies Infectieuses 50 , 384 (2020).
Group, R. C. et al. Effect of hydroxychloroquine in hospitalized patients with Covid-19. N. Engl. J. Med . 383, 2030–2040 (2020).
Shors, T. & McFadden, S. H. 1918 influenza: a Winnebago County, Wisconsin perspective. Clin. Med. Res. 7 , 147–156 (2009).
Stolberg, S. A Mad Scramble to Stock Millions of Malaria Pills, Likely for Nothing (The New York Times, 2020).
Hernandez, A. V., Roman, Y. M., Pasupuleti, V., Barboza, J. J. & White, C. M. Hydroxychloroquine or chloroquine for treatment or prophylaxis of COVID-19: a living systematic review. Ann. Int. Med. 173 , 287–296 (2020).
Glasziou, P. & Chalmers, I. Research waste is still a scandal—an essay by Paul Glasziou and Iain Chalmers. BMJ 363 , k4645 (2018).
Higgins, J. P. T. et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343 , d5928 (2011).
Murad, M. H., Sultan, S., Haffar, S. & Bazerbachi, F. Methodological quality and synthesis of case series and case reports. BMJ Evid. Based Med. 23 , 60–63 (2018).
Wells, G. S. B. et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analysis. http://wwwohrica/programs/clinical_epidemiology/oxfordasp (2004).
Whiting, P. F. et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 155 , 529–536 (2011).
Sanderson, S., Tatt, I. D. & Higgins, J. P. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int. J. Epidemiol. 36 , 666–676 (2007).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 25 , 603–605 (2010).
Guyatt, G. et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 64 , 383–394 (2011).
Quigley, J. M., Thompson, J. C., Halfpenny, N. J. & Scott, D. A. Critical appraisal of nonrandomized studies-A review of recommended and commonly used tools. J. Evaluation Clin. Pract. 25 , 44–52 (2019).
Sterne, J. A. et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355 , i4919 (2016).
Hamajima, N. et al. Case-control studies: matched controls or all available controls? J. Clin. Epidemiol. 47 , 971–975 (1994).
Download references
Acknowledgements
This study received no specific funding or grant from any agency in the public, commercial, or not-for-profit sectors. R.G.J. was supported by the Vanier CIHR Canada Graduate Scholarship. F.D.R. was supported by a CIHR Banting Postdoctoral Fellowship and a Royal College of Physicians and Surgeons of Canada Detweiler Travelling Fellowship. The funder/sponsor(s) had no role in design and conduct of the study, collection, analysis and interpretation of the data.
Author information
These authors contributed equally: Richard G. Jung, Pietro Di Santo.
Authors and Affiliations
CAPITAL Research Group, University of Ottawa Heart Institute, Ottawa, Ontario, Canada
Richard G. Jung, Pietro Di Santo, F. Daniel Ramirez & Trevor Simard
Vascular Biology and Experimental Medicine Laboratory, University of Ottawa Heart Institute, Ottawa, Ontario, Canada
Richard G. Jung, Pietro Di Santo, Trevor Simard & Benjamin Hibbert
Department of Cellular and Molecular Medicine, Faculty of Medicine, University of Ottawa, Ottawa, Ontario, Canada
Richard G. Jung, Trevor Simard & Benjamin Hibbert
Division of Cardiology, University of Ottawa Heart Institute, Ottawa, Ontario, Canada
Pietro Di Santo, Simon Parlow, F. Daniel Ramirez, Trevor Simard & Benjamin Hibbert
School of Epidemiology and Public Health, University of Ottawa, Ottawa, Ontario, Canada
Pietro Di Santo
Faculty of Medicine, University of Ottawa, Ontario, Canada
Cole Clifford & Stephanie Skanes
Department of Medicine, Cumming School of Medicine, Calgary, Alberta, Canada
Graeme Prosperi-Porta
Division of Internal Medicine, The Ottawa Hospital, Ottawa, Ontario, Canada
Berkman Library, University of Ottawa Heart Institute, Ottawa, Ontario, Canada
Sarah Visintini
Hôpital Cardiologique du Haut-Lévêque, CHU Bordeaux, Bordeaux-Pessac, France
F. Daniel Ramirez
L’Institut de Rythmologie et Modélisation Cardiaque (LIRYC), University of Bordeaux, Bordeaux, France
Department of Cardiovascular Medicine, Mayo Clinic, Rochester, MN, USA
Trevor Simard
You can also search for this author in PubMed Google Scholar
Contributions
R.G.J., P.D.S., S.V., F.D.R., T.S. and B.H. participated in the study conception and design. Data acquisition, analysis and interpretation were performed by R.G.J., P.D.S., C.C., G.P.P., S.P., S.S., A.H., F.D.R., T.S. and B.H. Statistical analysis was performed by R.G.J., P.D.S. and B.H. The manuscript was drafted by R.G.J., P.D.S., F.D.R., T.S. and B.H. All authors approved the final version of the manuscript and agree to be accountable to all aspects of the work.
Corresponding author
Correspondence to Benjamin Hibbert .
Ethics declarations
Competing interests.
B.H. reports funding as a clinical trial investigator from Abbott, Boston Scientific and Edwards Lifesciences outside of the submitted work. The remaining authors declare no competing interests.
Additional information
Peer review information Nature Communications Ian White and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, peer review file, description of additional supplementary files, supplementary data 1, supplementary data 2, reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Jung, R.G., Di Santo, P., Clifford, C. et al. Methodological quality of COVID-19 clinical research. Nat Commun 12 , 943 (2021). https://doi.org/10.1038/s41467-021-21220-5
Download citation
Received : 16 July 2020
Accepted : 13 January 2021
Published : 11 February 2021
DOI : https://doi.org/10.1038/s41467-021-21220-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Exploring covid-19 research credibility among spanish scientists.
- Eduardo Garcia-Garzon
- Ariadna Angulo-Brunet
- Guido Corradi
Current Psychology (2024)
Primary health care research in COVID-19: analysis of the protocols reviewed by the ethics committee of IDIAPJGol, Catalonia
- Anna Moleras-Serra
- Rosa Morros-Pedros
- Ainhoa Gómez-Lumbreras
BMC Primary Care (2023)
Identifying patterns of reported findings on long-term cardiac complications of COVID-19: a systematic review and meta-analysis
- Chenya Zhao
BMC Medicine (2023)
Implications for implementation and adoption of telehealth in developing countries: a systematic review of China’s practices and experiences
- Jiancheng Ye
- Molly Beestrum
npj Digital Medicine (2023)
Neuropsychological deficits in patients with persistent COVID-19 symptoms: a systematic review and meta-analysis
- Saioa Sobrino-Relaño
- Yolanda Balboa-Bandeira
- Natalia Ojeda
Scientific Reports (2023)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Public decisions about COVID-19 vaccines: A UK-based qualitative study
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations School of Psychology, Swansea University, Swansea, Wales, United Kingdom, Department of Medical Social Sciences, Feinberg School of Medicine, Northwestern University, Chicago, Illinois, United States of America
Roles Conceptualization, Funding acquisition, Investigation, Methodology, Writing – review & editing
Affiliations Manchester Centre for Health Psychology, University of Manchester, Manchester, United Kingdom, Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, Manchester, United Kingdom, NIHR Greater Manchester Patient Safety Translational Research Centre, University of Manchester, Manchester, United Kingdom
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Writing – review & editing
Affiliations School of Psychology, Swansea University, Swansea, Wales, United Kingdom, Manchester Centre for Health Psychology, University of Manchester, Manchester, United Kingdom
Roles Conceptualization, Supervision, Writing – review & editing
Affiliation University of Sussex, School of Psychology, Falmer, United Kingdom
Roles Conceptualization, Writing – review & editing
Affiliation Independent Researcher, Kassel, Germany
- Simon N. Williams,
- Christopher J. Armitage,
- Kimberly Dienes,
- John Drury,

- Published: March 6, 2023
- https://doi.org/10.1371/journal.pone.0277360
- Peer Review
- Reader Comments
To explore UK public decisions around whether or not to get COVID-19 vaccines, and the facilitators and barriers behind participants’ decisions.
This qualitative study consisted of six online focus groups conducted between 15 th March and 22 nd April 2021. Data were analysed using a framework approach.
Focus groups took place via online videoconferencing (Zoom).
Participants
Participants (n = 29) were a diverse group (by ethnicity, age and gender) UK residents aged 18 years and older.
We used the World Health Organization’s vaccine hesitancy continuum model to look for, and explore, three main types of decisions related to COVID-19 vaccines: vaccine acceptance, vaccine refusal and vaccine hesitancy (or vaccine delay). Two reasons for vaccine delay were identified: delay due to a perceived need for more information and delay until vaccine was “required” in the future. Nine themes were identified: three main facilitators (Vaccination as a social norm; Vaccination as a necessity; Trust in science) and six main barriers (Preference for “natural immunity”; Concerns over possible side effects; Perceived lack of information; Distrust in government;; Conspiracy theories; “Covid echo chambers”) to vaccine uptake.
In order to address vaccine uptake and vaccine hesitancy, it is useful to understand the reasons behind people’s decisions to accept or refuse an offer of a vaccine, and to listen to them and engage with, rather than dismiss, these reasons. Those working in public health or health communication around vaccines, including COVID-19 vaccines, in and beyond the UK, might benefit from incorporating the facilitators and barriers found in this study.
Citation: Williams SN, Armitage CJ, Dienes K, Drury J, Tampe T (2023) Public decisions about COVID-19 vaccines: A UK-based qualitative study. PLoS ONE 18(3): e0277360. https://doi.org/10.1371/journal.pone.0277360
Editor: Mohamed F. Jalloh, Centers for Disease Control and Prevention, UNITED STATES
Received: March 22, 2022; Accepted: October 26, 2022; Published: March 6, 2023
Copyright: © 2023 Williams et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Ethics was approved by Swansea University’s Department of Psychology Ethics Committee. As part of the ethics review process, participant confidentiality restrictions prohibit the authors from making the data set publicly available. During the consent process, participants were explicitly guaranteed that the data would only be seen my members of the study team. For any discussions about the data set please contact Swansea University’s Research Governance: [email protected] .
Funding: This research was supported by the Manchester Centre for Health Psychology based at the University of Manchester (£2000) and Swansea University’s ‘Greatest Need Fund’ (£3000). This research was supported by the Manchester Centre for Health Psychology based at the University of Manchester (£2000) and Swansea University’s ‘Greatest Need Fund’ (£3000). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: CJA is supported by NIHR Manchester Biomedical Research Centre and NIHR Greater Manchester Patient Safety Translational Research Centre. This does not alter our adherence to PLOS ONE policies on sharing data and materials. JD sits on SAGE SPI-B subgroup, and Independent Sage. TT currently works for the World Health Organization, but contributed to this paper as an independent researcher. This does not alter our adherence to PLOS ONE policies on sharing data and materials.” (as detailed online in our guide for authors http://journals.plos.org/plosone/s/competing-interests The authors have no other relationships or activities that could appear to have influenced the submitted work.
Introduction
Vaccine hesitancy is a complex and multifaceted problem, and one that is influenced by a range of contextual (e.g. historical, institutional, political) factors, as well as individual-level and vaccine specific factors (e.g. costs or design of a given vaccination program) [ 1 ]. Individual-level factors, include health-system and providers, knowledge and beliefs about health and prevention, personal perceptions about risk versus benefit and personal and family experiences with vaccination (including pain and side effects from past vaccines) [ 1 , 2 ]. Although they are shaped by contextual factors, this research is primarily interested in individual perceptions of UK residents around the decision to get vaccinated against COVID-19.
Vaccine hesitancy can be defined as “the delay in acceptance or refusal of vaccination despite availability of vaccination services” [ 2 ]. In this paper, we draw on The World Health Organization’s (WHO) SAGE Working Group on Vaccine Hesitancy’s ‘continuum of vaccine hesitancy’ model, which sees vaccine views to be set on a continuum between full acceptance of vaccines with no doubts, through to complete refusal with no doubts [ 1 , 2 ]. Vaccine hesitancy is seen as a heterogenous group in-between these diametric positions, including those who “delay” acceptance (i.e. do not get it when first offered or according to schedule).
Although the WHO continuum of vaccine hesitancy is a simple and useful heuristic to categorise individuals, especially in relation to individual-level perceptions or attitudes, it is important to acknowledge that these attitudes do not occur in a vacuum but are shaped and influenced by many social and contextual factors. Intentions and decisions around vaccine acceptance or refusal, and the reasons behind them, can also be understood in terms of the ‘5 C’s’ model of vaccine hesitancy. This model suggests that vaccine hesitancy is influenced by: Complacency —for example where the perceived risk of harm from the disease is low; convenience —for example where there are practical or logistical barriers to access vaccination; confidence —for example where there is a lack of trust in the safety or efficacy of the vaccine; communication –for example where misinformation can create distrust or confusion; and, context –for example certain social groups, including some ethnic minority communities might encounter additional barriers, including structural racism, which might affect vaccine uptake [ 1 , 3 ]. Another theoretical framework is the Behavioural and Social Drivers (BeSD) of vaccine uptake [ 4 ]. The BEsD framework suggests four main drivers of vaccination uptake: (1) people’s mental and emotional responses to vaccines ( thinking and feeling ); (2) social or group norms around vaccinations ( social processes ); (3) people’s willingness and intentions, or hesitancy, to get vaccinated ( motivation ); (4) contextual or structural barriers related to e.g costs or access ( practical issues ) [ 4 ]. It is important to note the inter-relatedness of the many drivers of vaccine acceptance or hesitancy. As such, a focus on individual level decisions or intentions around vaccines, as is the case in this study, needs to acknowledge the ways in which individual feelings, beliefs and motivations, are shaped by (and serve to shape) contextual and practical issues.
In terms of the reasons behind vaccine intentions and decisions, survey data on COVID-19 vaccine intentions and decisions suggests that most common reasons for vaccine hesitancy include: worries over side effects, worries over long term effects on health, as well as concerns over its efficacy [ 5 ]. Qualitative research on public views on COVID-19 vaccines is emerging. One study, from the UK, found that vaccine hesitancy was associated with three main factors: safety concerns, negative stories and personal knowledge, with those who were most confused, worried and mistrusting being the most hesitant [ 6 ]. Another study, from Canada, on overall attitudes to public health measures to reduce COVID-19 transmission found that many participants felt that vaccines were a means to “get back to normal life” while some were hesitant due to a lack of confidence in the potential efficacy of the vaccine and concerns over side-effects [ 7 ]. A study from Australia, with hesitant health or social care workers or clinically vulnerable adults, found that participants saw vaccination as beneficial for both individual and community protection, but also expressed safety concerns that made them feel like “guinea pigs” [ 8 ].
Ongoing research into vaccine hesitancy is needed to follow how attitudes and decisions around COVID-19 vaccines may be changing as the pandemic continues. Also, qualitative data can explore, in depth, the reasons behind why people are deciding to get vaccinated or not. In this paper, we explore participants’ decisions on COVID-19 vaccines in the UK during March and April 2021. For context, during this period the UK was experiencing a rapid roll out of COVID-19 vaccines (Astra Zeneca and Pfizer-BioNTech) via the National Health Service, with between January and 22nd April 2021, administered approximately 35 million total doses, with approximately 60% of the total population aged 16 and over having received at least one dose with doses being prioritised amongst older adults and those with certain underlying health conditions (clinically vulnerable and clinically extremely vulnerable adults) [ 9 ].
This paper explores participants’ intentions and decisions around whether or not to get vaccinated, and specifically the reasons behind them, thereby contributing to our understanding of the facilitators and barriers to vaccine uptake.
Materials and methods
Participants and data collection.
Data from this study came from the COVID Public Views (PVCOVID) study–a mixed-methods study using panel focus groups and surveys during the pandemic (commenced March 2020) [ 10 , 11 ]. Participants for the PVCOVID study were initially recruited to the study from March-July 2020, with a total of 53 participants initially enrolling into the study. Participants were all UK-based adults aged 18 years or older. Recruitment for the study took place primarily via non-probability, opportunity sampling. Recruitment included using social media advertising (Facebook ads and via posting ads on Twitter), other online advertising (e.g. online ‘free-ads’ such as Gumtree), as well as snowball sampling (e.g. asking participants who had taken part in a focus group to distribute the study ad to others they felt might be interested in participating). Recruitment sought as diverse a range of ages, genders, race/ethnicities, UK locations, and social backgrounds as possible (e.g. advertisements encouraged expressions of interest from individuals from Black and Asian Minority Ethnic (BAME) backgrounds; social media ads were designed to targeted users from across the UK and a wide age range). Although the study had a low number of individuals from older age groups (over 50 years of age) the over-representation of younger adults could be seen as beneficial because of their lower vaccination coverage [ 9 ].
Here we report on data from six online focus groups with 29 participants from within the overall PVCOVID study. Focus groups were not arranged according to any pre-existing views or decisions around vaccinations (i.e. we did not purposefully put those who were not intending on getting vaccinated in the same group for example). This was largely because of the longitudinal nature of the overall study, and our initial decision to try to keep the membership of each focus group the same over time in order to build rapport, familiarity and openness within the groups (we did not collect data on vaccine views during the initial recruitment and group allocation in March 2020). Each group contained a mixture of those who had already received at least one vaccine (n = 15) and those who had either already refused a vaccine or who were delaying their decision to get a vaccine (n = 14). One potential limitation of this focus group composition was that those who were refusing or delaying vaccination might have felt less comfortable expressing their opinion (since, generally getting vaccinated was seen by many as a social norm—see below). However, the focus group facilitator sought to ensure that all participants felt comfortable expressing their views, and that dialogue within the group was not hostile and as respectful and open as possible. Also, questions were phrased in non-leading, non-judgemental a way as possible.
In March 2021, participants were invited to take part in a rapid round of focus groups on the topic of vaccines. Participants took part in focus groups conducted between 15th March and 22nd April 2021. Further information about the participants discussed in the present paper are presented in Table 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0277360.t001
Online focus groups were necessary due to COVID-19 social distancing regulations, but have been seen to have benefits in general, as a means of eliciting public views from diverse and geographically dispersed participants [ 12 , 13 ]. Each focus group (of 4–6 participants) met virtually via the videoconferencing platform Zoom for approximately one hour. All focus groups discussed in the present paper were moderated by SW. Focus groups were recoded and transcribed. The topic guide for the focus groups (Appendix 1) was initially developed using existing literature on vaccination public attitudes and vaccine hesitancy discussed above, as well as rapidly emerging surveys on public attitudes to COVID-19 public attitudes.
Ethical approval was received by Swansea University’s School of Management Research Ethics Committee and Swansea University’s Department of Psychology Ethics Committee (Ref: 2020-4952-3957). All participants gave informed consent, both written and verbal. All data were kept securely and confidentially in line with ethical requirements, and where data is presented below, all quotes are anonymised to protect participants’ identities.
Data were analysed in accordance with a Framework Analysis (FA) approach [ 14 ]. FA is a flexible approach that is not aligned with a particular epistemological, philosophical or theoretical tradition. It can be either primarily inductive or deductive (or a combination thereof) and can be adapted with many qualitative approaches with the main aim being to generate themes [ 14 ]. Our use of FA combined elements of both induction and deduction in an abductive approach [ 15 , 16 ], whereby the researchers inductively coded for emergent facilitators and barriers to vaccine uptake as they emerged. The coding process was also broadly informed deductively by existing literature, including the WHO’s ‘continuum of vaccine hesitancy’ framework. Using the vaccine hesitancy continuum model [ 1 ], we analysed data to look for, and explore, three main types of vaccine decisions in the data: those who had accepted, or were planning on accepting, the vaccine; those who had refused, or were planning on refusing, the vaccine; and those who had not yet decided, or were delaying the decision of, whether or not to get the vaccine. As such, each participant was coded into one of these three main categories based on their decision or intention (e.g. statements that indicated they were not sure if they wanted a vaccine were coded into three main categories: accept, delay, refuse. Sub-coding sought to bring out the nuances within these simplified intention/decision types (e.g. “accept but unsure”). Inductive analysis was used to explore facilitators and barriers to vaccine acceptance (i.e. the reasons why people were getting or intending on accepting or refusing a vaccine or why they were unsure of or delaying their decision).
Two authors (SW and KD) primarily analysed the data, in consultation with the other three authors (CA, JD, TT). The first stage of FA is data familiarisation . SW and KD independently read three focus group transcripts initially, and independently assigned preliminary codes to specific lines or chunks of texts. The two authors met regularly (after each transcript) to identify commonalities and differences in their coding and discussed frequent or significant codes which were beginning to form emergent themes–i.e. patterns in the data, codes clustering around a common concept (e.g. ‘preference for natural immunity’) [ 16 , 17 ]. Following this, the third stage– data indexing– was performed, through which the two analysists systematically applied the thematic framework and the existing list of codes to the remaining transcripts. As FA is a flexible, iterative approach, new codes, and new themes (clusters of codes) were developed as they emerged. The fourth stage, data charting , enabled the analysts to refine, rearrange and focus (data reduction) on what they deemed the most prevalent and salient themes. The final stage– data mapping– enabled the analysts to review the main themes and organise them in relation to the study’s main objective–identifying facilitators and barriers to COVID-19 vaccine uptake using the accounts of the participants intentions and decisions around vaccines. The other three authors (CA, JD, TT) were not involved primarily in the data analysis but were consulted throughout the FA–and provided input into code definition and theme generation, they also provided comments which were used to resolve any disagreements between SW and KD’s coding.
Vaccine acceptance
One type of response, those who had already accepted or planned to accept (when they were offered one), a COVID-19 vaccine, held largely positive views around COVID-19 vaccines. In line with the vaccine hesitancy continuum [ 1 ], those accepting the vaccines fell into two subtypes: those who expressed little to no reservation about their decision to accept a vaccine (“full acceptance”) and those who had accepted, or were intending to accept, a vaccine, but who also expressed concerns or reservations about their decision (“accept but unsure”).
Those fully accepting tended to frame their decision as something that was quite “normal” to them (“I’ve had all my vaccines”—see vaccination as a social norm below):
“I had no problems getting the vaccines or any concerns about the efficacy of the vaccines … It was something I need to do to protect my family and loved ones … It was an easy decision to make, I’ve had all my vaccines all my life, because I see the value.” (Participant 44, Female 30s)
Those fully accepting also framed vaccination as a collective responsibility, and their decision as something that would “protect” others as well as themselves (especially vulnerable others) (“I don’t want to hurt anyone else” (Participant 19, Male, 20s)). This included some who saw themselves as not necessarily being at risk personally:
“I had my first one [vaccine dose] about a month ago … I was practically queuing up as soon as I heard … My biggest thing throughout the whole pandemic to protect others, not necessarily myself, because I’ve never seen myself as being particularly at risk but now, I am statistically less likely to catch and pass it on” (Participant 6, Male, 20s)
However, although some of those accepting were confident in their decision, others expressed concerns in spite of ultimately deciding to get vaccinated (akin to the Vaccine Hesitancy Continuum’s ‘accept but unsure’ vaccine attitude group) [ 1 , 2 ]:
“I was a bit suspicious. I suppose it’s only natural, everyone’s a little worried because you think it’s only been done in a year, but the science today compared to years ago is outstanding isn’t it, so they have more methods of testing to see if its effective, so I wasn’t really worried, and I’m glad I have got it” (Participant 42, Female 30s)
Those accepting a vaccine—including those in the “accept but unsure” category–expressed and emphasised a number of facilitators, including a trust in science and vaccination as a necessity (see below).
Vaccine refusal
A second type of response was from those who had already refused, or who were planning on refusing, a COVID-19 vaccine. Unlike those who were unsure of, or who were delaying, their decision of whether or not to get a vaccine (see below), those refusing explicitly stated that they were not going to have the vaccine (at least not for the “foreseeable future”):
“I’ve not had the vaccine and, to be honest with you, I don’t have any intention of getting the vaccine like in the foreseeable future, I just don’t see the point”. (Participant 3, Male, 20s)
Those refusing the vaccine tended to frame vaccination in terms of individual rather than collective responsibility; and as a personal choice (“It’s a choice I’ve made” (Participant 8, Female, 40s)). Those refusing were also less likely than others to frame their vaccination as something that would protect others and saw it as something that was primarily useful for those most vulnerable from serious COVID-19-related illness, for example older age groups (see preference for natural immunity below). Those refusing also emphasised the three main barriers, including a preference for natural immunity , concerns over side effects and distrust in government (see below).
Vaccine delay
A third type of response was from those who were still unsure of, or were delaying, the decision of whether or not to get the vaccine. These participants can be distinguished from those who had already made up their mind that they did not want to get vaccinated. These participants felt they needed more time to decide. Some of those delaying had already turned down or ignored their vaccination appointment invitations. However, they characterized their current position as subject to change–that is they did not want the vaccine yet but were aware that they might in future:
“I wouldn’t take it straight away… I’d rather just wait and make my own decision at my own pace really” (Participant 15, Male, 20s)
Some of those delaying tended to emphasise a need for more information about the efficacy and safety of the vaccine as a main reason for the delay in their decision (see perceived lack of information below) with some feeling they were being “pressured” (e.g. by the vaccination campaign and offer) into having to make a decision too quickly:
“I’m still holding out. I’ve been sent several letters and loads of text messages telling me that I needed to go for the vaccination, but I would rather wait at least four months to see exactly where it is all going… I don’t want to be sort of pressured into something that I might regret” (Participant 15, Male, 40s)
Like those refusing the vaccine, those delaying their decision were also concerned about the speed at which vaccines had been developed and were concerned over the possible longer-term side effects (see concerns over possible side effects below):
“I am a little bit nervous because I do feel like it’s all been rushed through incredibly quickly … have they done all the tests? I wanted to ensure that a lot more people had it before it was my turn, because I kind of figured that if there’s a problem, we’ll know” (Participant 50, Female, 50+)
Despite the feeling of “pressure”, some participants delaying tended to perceive themselves as having agency in their choice of whether to get vaccinated. However, others delaying tended to argue they felt as though they would be “forced to do it” (Participant 7, Female 20s):
“I don’t intend on taking it, unless it’s a must, unless, I heard you have [a vaccine] to go on holidays, but right now I am going to refuse it, until the very last moment. But I know at some point I will have to take it” (Participant 18, Female, 30s)
These participants tended to be quite hesitant about the idea of getting a COVID-19 vaccine but believed that they would “have” to get one in order to be able to engage in certain activities in future, particularly traveling internationally. Here, vaccination tended to be viewed as a personal choice rather than in terms of collective responsibility (“I have the say and right what I should accept into my body and nobody else should have a say” (Participant 22, Female, 20s)). They tended to perceive themselves as having little or no agency in regard to whether or not they would ultimately have a vaccine. The act of delaying may therefore be construed as a way to preserve agency while they could, or perhaps to recapture a sense of control over their lives that many felt they had lost during the pandemic [ 10 ].
Facilitators: Reasons for vaccine acceptance
Vaccination as a social norm..
Social norms are a means through which health behaviour and decisions can be influenced during the pandemic [ 18 ]. Those accepting a vaccine tended to discuss COVID-19 vaccination in relation to a personal willingness to be vaccinated in the past and in general (“I’ve had vaccines all my life for what is needed” (Participant 12, Male, 40s)), as well as in relation to a culture (the UK) within which vaccines were normative (including the fact that vaccinations were a “part of normal life” from a young age):
“For me, I’ve never been one to say no to a vaccine. Its part and parcel—as a child you are given various vaccines, and you don’t necessarily have a choice, but then when you have your boosters, you just go ahead and do it and to me that’s part of normal life” (Participant 10, Male, 40s)
For some, vaccination for COVID-19 was becoming more normative over the course of the pandemic. For some, hesitancy was decreasing, as more people started to get vaccinated, partly as a way to help get back to “normality” (see vaccination as a necessity ):
“Talking to people there’s a lot of people have taken it [the vaccine] and I’m surprised. They had said initially that they weren’t going to take it … [but] there’s just a lot of impatience and frustration at the minute you know people just want to get back to some sort of normality” (Participant 8, Female, 40s)
Others felt as though there was a pressure to get vaccinated, for example within some workplaces:
“Initially when it [vaccine] came out a lot of the [front line-workers] on my team were like ‘nope, not going to get it’ but that changed one-by-one, they started to go for it, and now I think there is only a handful who haven’t gone for it … its being monitored by senior management but they have got to ask have you had it or not, they are not asking why you haven’t had it, but I don’t know if that is something at some point, you know you have to justify your grounds as to why you haven’t” (Participant 5, Female, 30s)
For this participant, in their workplace, there was an implied expectation that they would, in the future, need to get the vaccine or justify why they hadn’t. This informal scrutiny of vaccine uptake may be functioning as an example of ‘norm-nudging’ [ 18 ]. In this participant’s workplace, although vaccination was not obligatory or coercive, and the reasons for ‘opting-out’ were not required, the implication was that opting-in was the default or normative position. The expectation that justification for opting out would be necessary in the future may have led to the change in decision (i.e. individuals opting to get vaccinated now, despite not initially wanting to, because they felt they would either be required to in the future or would have to justify their decision not to).
Vaccination as a necessity.
Vaccination as a social norm closely related to a second facilitator–vaccination a necessity. Participants discussed three main ways in which vaccination would be necessary or inevitable. These were framed either positively or negatively (related to whether participants were accepting of vaccines or not).
Firstly, those accepting a vaccine tended to refer to vaccination as being the way for them to “get back to normal” (Participant 20, Male, 20s) or “the only way forward, to get on with our lives” (Participant 12, Male, 40s). Secondly, a number of participants, including those accepting a vaccine and those delaying their decision, described an “acceptance” of the fact that they would need regular vaccinations or ‘boosters’ as a result of the continued emergence of new variants of the virus:
“My parents and I have already accepted that we will require boosters, they will be a fact of life, probably for the next four or five years, and it will be the same as our flu jab that we get every year” (Participant 2, Male, 40s)
In particular, concerns over new and emerging variants were cited as a reason as to why vaccination was not perceived to be a “one-off”, and so “regular” vaccination was seen to be necessary with “no other way out”.
“The virus is going to keep mutating, there is going to be different variants, I think that’s why the government is so hot on this vaccine because it is not going to stop. … It’s something that we’re going to have to live with this is not going to die out anytime soon… there is no other way out … we are going to have to go for our top-ups with the vaccine” (Participant 5, Female, 30s)
It is worth noting however, that refusers saw the possibility of regular vaccination as a deterrent to getting vaccinated currently:
“There’s a concern that, if one takes the vaccine have a variant of a new variant emerges. That could be resistant to the vaccine and then there’s a question of do you have to keep taking vaccines to protect yourself against each single various oh I don’t really have any intention of getting the vaccine” (Participant 3, Male, 20s)
Thirdly, immunity certificates or “vaccine passports” were also cited by some participants as a potential facilitator to vaccine uptake. One way in which they were framed was as a “necessary evil”—as something that were, begrudgingly, needed to help “save” the economy:
“I think it’s just it’s almost a necessary evil and it’s the way we’re going to go … I think it’s also going to save a lot of businesses and that will save you know; the economy and we all need the economy to be boisterous we all need a prominent economy”. (Participant 2, Male, 40s)
However, vaccine passports were a complex and controversial topic in the focus groups. Some delayers felt that vaccine passports were a reason why they would ultimately be “forced into” get a vaccine:
“I’m two minds really about whether to get the vaccine or not but I have a feeling people will be pressurised into having it through the vaccine passports or certificates, whether that could be for traveling or getting jobs, so I think people will be indirectly forced into getting it” (Participant 7, Male, 40s)
Trust in vaccine science.
Accepters expressed a higher trust in science, and to frame science as being relatively independent from government:
“I chose to be vaccinated because, not that I trust the government, but I trust the medicine and the science behind it. It’s not the government that produces the vaccine.” (Participant 11, Male, 50+)
Accepters were also more likely than others to associate the vaccination program with the health service (NHS):
“I know that the vaccine was developed really quickly … but I have faith in the health system and its testing” (Participant 10, Male, 40s)
Although some accepters expressed some concern at the speed at which the vaccines had been developed, they tended to contextualise this in terms of the fact that science was now more advanced than with many previous vaccines:
“I was a bit suspicious; I suppose it’s only natural, everyone’s a little worried because you think it’s only been don’t in a year, but the science today compared to years ago is outstanding isn’t it, so they have more methods of testing to see if its effective, so I wasn’t really worried, but I’m glad I have got it” (Participant 25, Female, 30s)
They also contextualised the speed of vaccine development in terms of what they perceived as rigorous testing, and the fact that there had been considerable scientific, medical and financial focus and investment in the vaccine development. This for them meant any potential risks from unforeseen issues due to safety or efficacy were likely to be minimal and outweighed by the benefits of the vaccination program:
“I believe it’s been so rigorously tested and it’s the only thing spoken about medically for the last 12 months and so the risk for me was just so minimal and benefits outweighed any risk for me” (Participant 6, Male, 20s)
Barriers: Reasons for vaccine delay or refusal
Preference for ‘natural immunity’..
Some participants argued that one of the reasons they were either hesitant about or did not want to get vaccinated was because they preferred to “fight” the virus “naturally”:
“For me personally I am not sure I would go for the vaccine… I just hope I have a strong immune system so I can fight the virus. We have this in-built immune system within our bodies…give them a chance to operate” (Participant 7, Male 40s)
In discussing their decision, refusers tended to frame COVID-19 as a disease which tended not to affect young and “healthy” people:
“I don’t have any intention of getting the vaccine in the foreseeable future, I just don’t see the point, because the virus is mainly fatal to those who are, like middle aged. (Participant 3, Male, 20s)
In doing so, they also emphasised their own healthiness as a reason as to why they didn’t need the vaccine, and drew comparisons to the fact they hadn’t needed vaccines in the past for other diseases:
“It just does not make sense to me to take a vaccine, it’s like a flu vaccine. I’ve never ever taken a flu vaccine, because I don’t get the flu.” (Participant 8, Female, 40s)
As noted above, refusers framed vaccination as an individual act rather than a collective act, and argued that the lack of personal benefit was outweighed by the perceived risks posed from potential side effects:
“I have no intentions of taking it, and I have focused a lot on my health over the years, I’m the healthiest I’ve ever been and I just don’t see I don’t the reason for me to take it … because from what I’ve read, there are risks with it so.” (Participant 8, Female, 40s)
Concerns over possible side effects.
One of the main reasons for vaccine hesitancy was a concern over side effects–something that accounted for why some people were delaying the decision to get vaccinated:
“I probably will have it [a vaccine], but I want to wait to see if people turn into zombies first. I’ll wait until a few hundred thousand have had it first” (Participant 28, Female, 20s).
Although the above quote was tongue-in-cheek, it was indicative of a wider concern over potentially unforeseen, longer-term, side effects. Delayers tended to frame these concerns in relation to what they knew about how vaccines were “normally” developed. They discussed how comparatively quickly COVID-19 vaccines had been developed and emphasized how not enough time had passed to be able to know long-term side effects:
“I do have like some concerns about how quickly they developed this vaccine, because most vaccines take like you know six five to six years to test and to make sure that you know they’ve seen all the side effects. But with this vaccine I still have that reservation that maybe it’s been too quick, and they’ve not really teased out all the long-term effects.” (Participant 3, Male, 20s)
Other delayers focused on short-term side effects or risks. In particular, recent reports of potential blood clots linked to vaccines were cited by a number of delayers. Interestingly, these participants were aware that any causal link between blood clots and vaccines had not been clearly demonstrated, or that any potential risk between vaccines and blood clots was considerably small. Nevertheless, they continued to cite blood clots as a cause for concern and framed their hesitancy in relation to it as an example of potential side effects (including unknown side effects that may emerge in the future):
“Right now, I am going to refuse it, until the very last moment. I feel like I’m a guinea pig. I don’t know if you heard the news that they have stopped one of the vaccines because there has [sic] been cases of blood clots of something. I know it’s a very, very, very, very tiny percentage but I feel like if I wait till the very last more [information] can come out”. (Participant 9, Female, 30s)
Some participants distinguished between vaccines, with those who did expressing personal concern, or observed concern in others, over the vaccine manufactured by the company AstraZeneca, which had been the focus of blood clot controversies in the media. For example, one participant, who was vaccine hesitant, stated that although they accepted the Pfizer vaccine (i.e. the vaccine manufactured by Pfizer-BioNTech), they would not have accepted the AstraZeneca vaccine:
“Now I’ve had it I feel okay about it, but I think that’s because with the Pfizer it doesn’t seem to be any negative reports, whereas with AstraZeneca there seems to be a lot of mixed communications, and I don’t think there is a lot of fault with the vaccine, it’s just I don’t think the company is very good at kind of being truthful and that makes people a bit doubtful … I don’t think I would have done it [had the AstraZeneca vaccine] (Participant 24, Female, 50+).
Another participant described how they had heard of others specifically opting out of vaccination, once they discovered they were to get the AstraZeneca vaccine:
“My aunt had hers and she said there was a huge queue in the surgery… but every single person that was offered the one that begins with an A [AstraZeneca] were actively declining it and walking out and she witnessed in ten minutes about 15 people turning up, being told what they were getting and walking out” (Participant 21, Female, 20s)
On the other hand, accepters, including those who had taken the vaccine with reservations (cf. The Vaccine Hesitancy Continuum’s [ 1 , 2 ] ‘accept but unsure’ group), were much less concerned over both short- and long-term side effects. They framed the issue in terms of a cost-benefit analysis, where for them, the perceived benefits (e.g. reducing the risk of “getting long Covid”) outweighed any potential risk of unknown, long-term side effects:
“I’m quite worried about, not any side effects now , but like maybe in ten years’ time … but then it seems like the risk from the vaccine is less than the risk of say getting long Covid … so the vaccine is the lesser of two evils” (Participant 24, Female, 50+)
They also made comparisons to what they saw as other equally rare side effects of common medications:
“I know there is this whole issue around blood clots, but people really need to get a grip, because you know, people die on a yearly basis from taking paracetamol, plenty of women die from blood clots as well …from taking the pill … that so the benefits outweigh the risks most definitely” (Participant 12, Male, 40s)
Perceived lack of information.
A perceived lack of information was a major factor for why some participants were either refusing or delaying vaccination:
“Whatever is going on with the vaccine, I don’t know, it really is a minefield of information” (Participant 8, Female, 40s)
Questions were scientific in nature and stemmed from the fact that COVID-19 was still such a new disease. For example, one participant (a refuser) questioned whether they would need to “keep taking” vaccines due to new variants (potentially “resistant” to the previous vaccines), something that deterred them from accepting their initial vaccine offer:
“There’s a concern that, if one takes the vaccine and a variant of a new variant emerges that could be resistant to the vaccine then there’s a question of do you have to keep taking vaccines to protect yourself against each single variant? I don’t really have any intention of getting the vaccine.” (Participant 3, Male, 20s)
Another participant (a delayer) questioned whether people still “need” a vaccine following infection with COVID-19:
“I am not against the vaccine, [but] for me there are so many unknowns, because It is so new there are so many questions that I want to ask, like if you have had Covid do you still need, in terms of the antibodies you have, or do you still need the protection from the vaccine? I’m very much in the middle, so once I get those answers, I will be leaning more towards getting it” (Participant 5, Female, 30s)
Distrust in government.
Refusers and some delayers tended to have less confidence in vaccine science and less trust in government (“I think a lot of my concerns are because of the government because I just don’t trust them at all” (Participant 29, Female, 50+)). They framed COVID-19 vaccine science as being closely linked to, or even compromised by, political or economic interests. Some justified their distrust in relation to historical controversies or examples of medical iatrogenesis:
“The government doesn’t have a very good track record with the sense that there was the Thalidomide tablets that were given to pregnant women back in the ‘60s, the blood transfusions that were imported from people volunteers in state penitentiaries in America that were contaminated, brought into the United Kingdom.… there’s been several vaccinations given to toddlers … that came from America—I think about 1000 children have died…. I’m not one to trust governments, they tend to rush into things.” (Participant 15, Male, 40s)
Although delayers generally recognised that the vaccines had been tested, they remained concerned or “sceptical” that testing had been done as extensively or for as long as was necessary. They tended to see vaccination as something that was still being tested (in the community):
“Even though there has been a lot of testing done, I still feel sceptical and quite scared to get it … technically it’s still in the testing phases even though it’s been approved, and so until I’m actually forced to do it, I don’t think I want to” (Participant 7, Female, 20s).
Although, as discussed above, some participants framed vaccine passports as a “necessary evil” to enable them to travel or to help the economy, others, including both refusers, framed them as “Orwellian” and argued that by using them, government were encroaching on their “freedom of choice” (Participant 13, Male, 40s) and “privacy”:
“[I’m] a hundred per cent against vaccine passports, I personally would rather just have the PCR [COVID-19 polymerase chain reaction] tests. … it is somewhat Orwellian … I ’m very, very concerned about things like surveillance and privacy” (Participant 3, Male, 20s)
Conspiracy theories and misinformation.
Those refusing a vaccine, and some of those delaying, linked their distrust in government to what they saw as conspiracies (things that “don’t seem to add up”), such as the perception that vaccines were driven by the “agenda” of the pharmaceutical companies involved in manufacturing them, in order to make profit.
“I mean distrust in government … the things that don’t seem to add up. I mean we have got the pharmaceutical companies, several of them creating a vaccine, some kind of race … and it’s just a win-win for them, if just everyone gets a vaccine and people can’t think for themselves … it a big agenda” (Participant 7, Male, 40s)
It is important to emphasise that, to the participants themselves, these were seen as plausible conspiracies.
Amongst the Black and Asian Minority Ethnic (BAME) participants in this study, most were critical of the circulation of conspiracy theories. However, many of them did also discuss how conspiracy theories and misinformation was quite prevalent in their communities (“It’s weird how it afflicts the Black community in terms of social media and WhatsApp conspiracy theories in circulation” (Participant 2, Male, 40s)). Some related the lower uptake in vaccination amongst BAME groups to the existence of ‘folk wisdom’ about what might help promote health or even protect against COVID-19:
“A few months back India was number two in the number of cases and deaths from Covid and one fine day it just vanished. So, everyone is trying to ask what is being done differently in India… and I guess that mindset is being transferred to racial communities here [in the UK]. So people are discussing our [Indian] food habits, and we do eat a lot of spicy food and spices so I’ve actually seen people talking about saying that ‘ok it’s our food which is different… There are people even saying ‘avoid the vaccines, stick to your spices, your curries and you’ll be fine’. So that is worrying but that is a topic which is being widely discussed in our Asian community” (Participant 4, Male, 30s)
However, a number of BAME participants linked the lower uptake in their communities to a distrust in government (see above) and thus a distrust in the vaccines. One example was the rumour that vaccines were being “tested” for side effects first amongst BAME patients:
“I think just from my experience, there’s a lot of conspiracies that I’ve heard about. Because I mean I identify myself as a Black British person and so within my community I’ve heard a lot of just not trusting the vaccine … somebody sent me a video about [UK Government Health Secretary] Matt Hancock …suggesting that the vaccine was tested first amongst the BAME group.” (Participant 5, Female)
These participants also discussed the issue of distrust as a wider issue, accounting for why there “is some cynicism in these communities” (Participant 2, Male, 40s). This lack of trust was seen to stem from a lack of information (cf. lack of information above), which in turn was seen to be the result of a lack of engagement with BAME communities, as well as a perceived lack of government accountability for the disparities that BAME communities have experienced during the pandemic:
“I just think within our community there needs to be a lot more education, especially if there are a lot of unknown questions that haven’t been answered … that needs to be advertised more as to where we can go to ask those questions to be more equipped with the knowledge around these vaccines, rather than listen to these conspiracies which a lot of them is [ sic ] fake news…. A lot of it [lack of trust] stems from the government; a lot of how it [pandemic] has been handled is embarrassing, a high number of deaths were from the Black and Asian community and so that mistrust in government along with them not really putting their hands up just makes us even more anxious” (Participant 5, Female)
Covid ‘echo chambers’.
One potential barrier to uptake is what might be seen as the emergence of ‘Covid echo-chambers’. Echo chambers can be defined as “polarized communities populated by like-minded” others and can be found particularly in online settings [ 19 ]:
“I also interact quite a lot on the internet and a lot of people that I speak to on the internet, they say the same thing that you know they just have this concern about the vaccine.” (Participant 3, Male, 20s)
The existence of polarized views, on an emotionally charged subject led some participants to argue that “everyone is extreme in their reactions” (Participant 26, Female, 20s):
“It really divides those who do have the vaccine and those who don’t, and I see quite a lot on social media people who post like very critical things of people who are on the opposite side” (Participant 15, Male, 20s)
As a result, some delayers felt ‘as though they didn’t ‘fit’ into either of the polarized attitude groups on vaccines, which may have been contributing to their uncertainty or hesitancy around whether or not to get vaccinated:
“Its either the people who [say] ‘don’t have the vaccine, it’s got 5G in it and the government are going to follow you and nobody should have it’ or you’ve got the people going ‘I’ve had the vaccine, and everyone should have the vaccine and you are stuffing it up for the rest of us” (Participant 26, Male, 30s)
Echo chambers are discrete and are characterised by a lack of communication across them. In our study we found evidence of a lack of communication between individuals with differing views on vaccines, for example between accepters and refusers. For example, one participant, an accepter, described how having conversations with a family member about vaccines was difficult given the latter’s opposing views on Covid:
“I’m happy to get the vaccine …but one family member isn’t keen on the vaccine, because they are just not convinced of the coronavirus in the first place…. I’ve not had a discussion with them about the vaccine because of his views on coronavirus in general” (Participant 6, Male, 20s)
Similarly, another participant, a refuser, described how she was reluctant to discuss the subject of vaccination with others, particularly those who she knew, or thought, may be in have strongly ‘pro-vaccination’ views:
“I don’t really bring it up now in conversation now with anyone … I don’t want to get into discussions. … I do find there is a lot more of two extreme sides (Participant 8, Female, 40s).
In keeping with the ‘continuum of vaccine hesitancy’ model [ 1 , 2 ], we found three main groups of participants, based on their decision or intention to receive a COVID-19 vaccine: Those who had accepted, or were planning on accepting, the vaccine; those who had refused, or were planning on refusing, the vaccine; and those who had not yet decided, or were delaying the decision of, whether or not to get the vaccine. In order to explain these different attitudes, we identified three facilitators (Vaccination as a social norm; Vaccination as a necessity; Trust in science) and six barriers (Preference for “natural immunity”; Concerns over possible side effects; Perceived lack of information; Distrust in government; Conspiracy theories; Covid echo chambers) to vaccine uptake. Although data on actual and eventual vaccine coverage changes rapidly [ 10 ], this study provides an in-depth account during the initial roll-out of the vaccines in the UK (during March-April 2021) into people’s decision-making process, including the reasons behind the decision to accept or refuse a vaccine and any hesitancy experienced.
The concept of ‘vaccine delay’ [ 1 , 2 ] can therefore be a useful concept (as a form of hesitancy, along with refusal) through which to understand why some are reluctant or unsure as to whether or when they will receive a COVID-19 vaccine, since many of those who were unsure, characterised their decision as one that was ongoing. We found two main reasons for the existence of vaccine delay. Firstly, some were delaying due to a perceived need for more information. Secondly, others were delaying until they were “required” to be vaccinated.
Our findings can be understood in relation to broader conceptual models of vaccine hesitancy, including the ‘Five C’s’ model [ 3 ] and the WHO SAGE Working Group on Vaccine Hesitancy Determinants Matrix [ 2 ], specifically to the case of COVID-19. Our findings suggest that, as per the ‘Five C’s’ model, particularly Confidence, and Complacency were major factors explaining vaccine hesitancy (concerns over convenience were not apparent in our study, perhaps due to the fact that at the time of data collection, the UK was seeing a rapid and lauded vaccine roll-out via its National Health Service (NHS) (the UK had between January and 22nd April 2021, administered approximately 35 million total doses, with approximately 60% of the total population aged 16 and over having received at least one dose [ 10 ]). For example, ‘confidence’ in the efficacy and safety of the vaccines was a major facilitator or barrier depending on a person’s perspective, especially in relation to the extent to which they trusted science or government (and the extent to which they saw the latter as influencing the former) [ 20 ]). Also, ‘complacency’ accounted for why some delayers and refusers were reluctant to be vaccinated. This complacency took the form of a perception of low personal risk and a valuing of “natural immunity” and might be better thought of as a form of ‘lay knowledge’ or ‘medical folk wisdom’ [ 21 , 22 ]. As such, rather than constructing it as ‘complacency’ per se, it might be more useful to understand how perceptions of low personal risk can be offset by constructing vaccination as a ‘collective responsibility–one that even those at relatively low personal risk from serious COVID-19 illness should do to protect others.
The Vaccine Hesitancy Determinants Matric holds that contextual, individual and group, and vaccine-specific issues all impact the extent to which people are accepting of or hesitant towards vaccination [ 1 ]. For instance, vaccination as a social norm was found to be an important individual and group influence. We found that a major barrier in the context of COVID-19 is the existence of conspiracy theories and Covid echo chambers. Thus, reducing the circulation and belief in conspiracy theories will likely help control the spread of COVID-19 [ 23 ], including in this case through potentially increasing vaccine uptake, perhaps particularly amongst BAME communities. Research suggests that people may be drawn to conspiracy theories when they promise to satisfy epistemic (e.g. desire for certainty), existential (e.g. a desire for control) and social (e.g. a desire to ‘fit in’ within a group) motives [ 24 ]. BAME communities may be particularly at risk from a lack of knowledge and safety, because of their historical marginalization in society and because of the fact that morbidity and mortality from COVID-19 has been higher. Research suggests that experiences of ostracism, including due to an individual’s race or ethnicity, may lead to greater belief in conspiracy theories, perhaps as a defence mechanism [ 24 , 25 ]. Further research on the role of ‘Covid echo chambers’ is needed. Our findings suggest that some people are reluctant to engage with others who hold, or may hold, differing opinions–particularly since COVID-19 policy is such a divisive and emotionally-charged issue. This lack of communication across echo chambers can have an ‘opinion reinforcing’ effect [ 25 ]. In the context of COVID-19 vaccination, strongly ‘pro-vaccination’ advertising or opinions may even be having a counterproductive effect for some, encouraging people to ‘double-down’ on their opposition or adding to their hesitancy. As such, working with individuals and communities, engaging with rather than criticising or dismissing their concerns (both legitimate and illegitimate) via mutually respectful dialogue is essential [ 26 ].
Vaccine delay may be usefully understood in relation to broader conceptual models on ‘patient delay’ [ 27 ]. In the context of COVID-19 vaccines, ‘appraisal delay’ (or decisional delay) [ 28 ] can be thought of as the question of ‘should I get vaccinated’? In order to reduce decisional delay, it is particularly important for policy and health organisations to address informational barriers, including some people’s perceived lack of information, the existence of conspiracy theories, and the existence of ‘Covid echo chambers’. For participants in this study, the lack of information was seen to be partly due to the fact that COVID-19 is a novel disease (i.e. scientists don’t yet have enough information) and due to the fact that insufficient or unclear information was being communicated to them (by e.g. medical or political agencies or individuals). Also, some felt that the information around vaccines and their efficacy or safety was at times too complex to understand, especially in light of new developments. This is perhaps another example of a phenomenon identified throughout the pandemic, referred to as ‘alert fatigue’. This is where frequently changing information (e.g. policies, guidelines, advisories) becomes increasingly difficult to interpret, comprehend and retain for members of the public [ 29 ]. Also, utilization delay (as a form of behavioural delay) can be understood as the time between when a person decides they will need medical intervention (i.e. a vaccine) and the deciding act on that decision (i.e. to get vaccinated). Delayers in this sense had already decided they were going to “need” to be vaccinated. Utilization delay entails the individual asking themselves, is the medical care (i.e. vaccination) worth the costs? In this case, many delayers had decided that the benefits of vaccination–as a ‘passport’ to international travel—were worth the perceived costs (e.g. the perceived infringement of their right to refuse a vaccine or concerns over potential future side effects). The decision to get vaccinated was perceived as not an entirely voluntary one, but one into which they were being ‘nudged’ or even indirectly forced—via the assumption that vaccine passports would be required in the future, especially for international travel.
Limitations
There are a number of limitations to note. Firstly, as with all qualitative studies, the generalizability of the findings is limited. As such, the study cannot be used to make generalisations about how prevalent vaccine acceptance or hesitancy is. Additionally, there was a particularly small number of those in our sample who had refused or were planning to refuse a vaccine and so further research specifically on a larger group of those who have refused the vaccine is needed.
Another limitation of the study is that although attempts were made to recruit and include as diverse a sample as possible, there is a relative underrepresentation of older adults (aged 50+ in the sample). However, for the purposes of the research question around vaccine uptake having a younger sample may be of benefit. Further strengths and limitations of the overall methodology and recruitment in the wider study are discussed in prior publications [ 10 , 11 ]. A further limitation is that the COVID-19 pandemic has (and at time of writing continues to) evolve rapidly, and so subsequent developments (e.g. new variants), may have affected peoples around vaccine uptake. Further research will explore evolving perceptions and any subsequent decisions. However, a particular strength of this study is its ability to provide in-depth and nuanced context as to the reasons behind vaccine acceptance, delay or refusal in the context of COVID-19 among residents in the UK.
This study has provided an in-depth examination of the reasons behind participants’ decisions around getting their initial COVID-19 vaccines. In order to address vaccine uptake and vaccine hesitancy, it is useful to understand the reasons behind people’s decisions to accept or refuse an offer of a vaccine. This qualitative study has suggested that, in the UK, three facilitators—Vaccination as a social norm; Vaccination as a necessity; Trust in science—and six barriers—Preference for “natural immunity”; Concerns over possible side effects; Distrust in government; Perceived lack of information; Conspiracy theories; Covid echo chambers–can help understand why people decide to get a COVID-19 vaccine or not. Future qualitative research looking at different countries is necessary to explore similarities and differences with this study’s findings, given the highly contextual nature of vaccine confidence and vaccine hesitancy.
The finding that convenience was not reported as an issue related to vaccine hesitancy in this study is also important to note. While there appears to have been good access to the vaccines among the general population during the study period, it is important for the key messaging to the community to be well thought out and in line with public belief systems, concerns, and potential misinformation. Findings from this study can help direct such messaging for clinicians/medical providers, community leaders, and public health practitioners. The COVID-19 pandemic, and its policy response, has, and will continue, to rapidly evolve. Further research, particularly longitudinal and comparative research, is needed to explore the evolution of attitudes to vaccines as the pandemic continues.
- View Article
- PubMed/NCBI
- Google Scholar
- 9. UK Government. Vaccinations in the United Coronavirus data: Vaccinations in the United Kingdom. Available at: https://coronavirus.data.gov.uk/details/vaccinations
- français
- español
- português
Related Links
Rapid qualitative research to increase covid-19 vaccination uptake: a research and intervention tool.

View Statistics
Description, document number, collections.
- Technical documents
Show Statistical Information
- 5. Regional Office for Europe
ORIGINAL RESEARCH article
Understanding health education needs of pregnant women in china during public health emergencies: a qualitative study amidst the covid-19 pandemic.

- 1 Department of Nursing, Quanzhou Medical College, Quanzhou, Fujian, China
- 2 Nursing Department, Quanzhou Women and Children's Hospital, Quanzhou, Fujian, China
- 3 Department of Imaging, Anxi County Hospital, Quanzhou, Fujian, China
- 4 Department of Child Health Care, Fujian Maternity and Child Health Hospital College of Clinical Medicine for Obstetrics and Gynecology and Pediatrics, Fujian Medical University, Fuzhou, Fujian, China
Background: Public health emergencies impose unique challenges on pregnant women, affecting their physiological, psychological, and social wellbeing. This study, focusing on the context of the corona virus disease in 2019 (COVID-19) pandemic in China, aims to comprehensively explore the experiences of pregnant women amidst diverse public health crises. Herein, we investigate the health education needs of pregnant Chinese women in regard to public health emergencies to provide a scientific foundation for the development of targeted health education strategies.
Objective: The study described in this article aims to explore the health education needs of pregnant Chinese women in the context of public health emergencies specifying the types of emergencies of pandemics and to provide a scientific basis for targeted health education interventions.
Methods: Thirteen pregnant women were purposively selected, and the rationale for this sample size lies in the qualitative nature of the study, seeking in-depth insights rather than generalizability. Data collection involved semi-structured interviews, and the Colaizzi, which is a structured qualitative technique used to extract, interpret, and organize significant statements from participant descriptions into themes, providing a comprehensive understanding of their lived experiences.
Results: The analysis yielded six prominent themes encompassing the following areas: I. Personal protection and vaccine safety; II. Knowledge of maternal health; III. Knowledge of fetal health; IV. Knowledge of childbirth; V. Knowledge of postpartum recovery; and VI. Knowledge sources of health education for pregnant women and their expectations of healthcare providers. Theme I was analyzed with two sub-themes (needs for personal protection knowledge, vaccine safety knowledge needs); Theme II was analyzed with three sub-themes (nutrition and diet, exercise and rest, sexual life); Theme III was analyzed with three sub-themes (medications and hazardous substances, pregnancy check-ups, and fetal movement monitoring); Theme IV was analyzed with three sub-themes (family accompaniment, analgesia in childbirth, and choice of mode of delivery); Theme V was analyzed with one sub-theme (knowledge of postnatal recovery); Theme VI was analyzed with one sub-theme (expectations of Healthcare providers). Sub-themes within each main theme were identified, offering a nuanced understanding of the multifaceted challenges faced by pregnant women during public health emergencies. The interrelation between sub-themes and main themes contributes to a holistic portrayal of their experiences.
Conclusion: The study emphasizes the need for healthcare professionals to tailor health education for pregnant women during emergencies, highlighting the role of the Internet in improving information dissemination. It recommends actionable strategies for effective health communication, ensuring these women receive comprehensive support through digital platforms for better health outcomes during public health crises.
1 Introduction
Pregnancy ushers in a period of diverse physiological, psychological, and social changes, necessitating specialized attention to address the unique needs of expectant women ( 1 ). The coronavirus disease outbreak in 2019 (COVID-19) has disproportionately affected pregnant individuals worldwide, with altered immune responses and compromised lung function placing them at heightened risk of infection ( 2 ). This increased susceptibility raises concerns about the potential for adverse pregnancy outcomes ( 3 ). In response to the COVID-19 pandemic, home isolation emerged as an important preventive measure against the spread of the virus, presenting pregnant women with the dual challenge of managing the inherent health challenges of pregnancy alongside the additional stresses and complexities introduced by the pandemic ( 4 ).
In this evolving landscape, the content and methods of delivering health education to pregnant women have significantly changed. Despite these developments, research on healthcare for pregnant women during epidemics, particularly within the Chinese context, remains scarce. Existing literature has largely focused on the psychological impacts of such crises on pregnant women ( 5 – 9 ).
In addition to focusing on the psychological wellbeing of pregnant women, it is also important to consider the broader spectrum of challenges they face, including physical health concerns and the need for social support during epidemics. Studies have demonstrated that epidemics like COVID-19 pose significant risks to the physical health of pregnant women, increasing the likelihood of complications such as preterm birth, preeclampsia, and gestational diabetes ( 10 , 11 ). Moreover, the impact of social distancing and healthcare system strain on the availability and quality of prenatal care further complicates these physical health challenges. In addition, social support plays a vital role in mitigating the psychological impact of epidemics on pregnant women ( 12 ). The reduction in face-to-face interactions and the increased reliance on virtual platforms for support have transformed the nature of social networks, with varying implications for maternal wellbeing. By integrating this broader spectrum of research, the complex interplay between psychological, physical and social factors affecting pregnant women during epidemics can be more clearly determined. This comprehensive approach not only enriches our understanding of their health education needs but also highlights the necessity for multifaceted health education strategies that address these interconnected aspects.
This study aims to fill this research gap by utilizing qualitative interviews to investigate the health education needs of pregnant Chinese women during public health emergencies, with a specific focus on the COVID-19 outbreak that began in China in 2021. The focus on China in this study is particularly relevant due to the country's unique challenges during the COVID-19 pandemic. China was the epicenter of the COVID-19 outbreak, facing unprecedented public health challenges that required rapid and large-scale interventions ( 13 ). This situation significantly impacted pregnant women, who faced heightened risks due to altered immune responses and compromised lung function, increasing their vulnerability to infection. Furthermore, the implementation of stringent lockdown measures and hospital visitation restrictions introduced additional complexities for accessing prenatal care and support systems ( 14 , 15 ). These factors underscore the importance of exploring the health education needs of pregnant Chinese women during such emergencies. By concentrating on the Chinese context, this study aims to uncover insights that can inform targeted health education strategies, acknowledging the nuanced ways in which cultural, social, and healthcare system factors intersect to influence health education needs and outcomes during public health crises.
Thus, we designed this present study to explore the specific health education requirements and information-seeking behaviors of pregnant Chinese women during the COVID-19 outbreak. The ultimate goal is to provide insights for healthcare institutions and professionals to develop effective health education strategies. These strategies are intended to safeguard the health and wellbeing of expectant mothers and their unborn children, offering a foundational framework to guide future research and practice in health education during similar health crises.
2 Research methodology
2.1 study participants.
A purposive sampling method was utilized to select 13 pregnant women for pre-interview participation who attended pregnancy healthcare examinations at an obstetrics outpatient clinic in a maternity and child healthcare hospital in Quanzhou City, Fujian Province, from December 2021 to June 2022. The selection process adhered to specific inclusion criteria: (1) Pregnant women aged 35 years or younger, with a gestational age of 12 weeks or more; (2) No presence of comorbidities or complications at the time of study; (3) A minimum education level of junior high school, ensuring adequate literacy for understanding and responding to the study's requirements; and (4) Willingness to provide informed consent. The study exclusion criteria were: (1) Severe audiovisual or cognitive impairments that could affect the participant's ability to understand questions or provide coherent responses; (2) A history of mental illness; and (3) Unwillingness to cooperate after the study's objectives and procedures had been explained by the investigator.
The study sample size was determined by the principle of information saturation, where the recruitment continued until no new themes were identified in the data. Following these criteria, 13 pregnant women were selected for the study, each assigned a unique identifier ranging from A to M.
2.2 Research instruments
2.2.1 basic information questionnaire.
This questionnaire was designed to collect baseline data from the pregnant women participating in the study, such as their gestational age, personal age, level of education, pregnancy type, and whether the pregnancy was intentional.
2.2.2 Interview outline
The interview outline was initially drafted by referring to the relevant literature ( 16 – 20 ) and by consultations with experts in nursing, obstetrics, and individuals outside the participant pool for pre-testing. After undergoing two rounds of revisions by nursing and obstetric experts and three pre-test sessions with non-participants, the final interview guide was established. The outline covered the following key questions:
(1) During the COVID-19 epidemic, what are your specific needs for health education, information, or healthcare services related to pregnancy?
(2) What are the primary methods or channels through which you seek out health education or information on pregnancy?
(3) How do you prefer to receive pregnancy-related health education and information from healthcare providers?
2.3 Research methods
2.3.1 data collection.
The study was approved by the Ethics Committee of Quanzhou Medical College (Approval No. 2021007). Using the phenomenological method, this qualitative research conducted in-depth, face-to-face interviews with each participant, lasting between 20 and 40 min. To ensure the accuracy and completeness of the data, follow-up telephone calls were made after each interview for content confirmation, allowing participants to add further insights or clarify previous statements.
Prior to conducting the interviews, necessary preparations were made, including the setup of tape recorders and notebooks to accurately capture the dialogue. Participants were informed about the study's objectives, its importance, the confidentiality of their responses, and their rights as participants, establishing a foundation of trust. Interviews were held in a private obstetrics room to guarantee confidentiality and create a comfortable setting for the participants.
To uphold the integrity of our study and minimize potential biases in data collection, rigorous steps were taken to train the interviewers and ensure their neutrality throughout the interviewing process. The following measures were implemented: (1) Interviewer training: prior to engaging with participants, interviewers underwent comprehensive training sessions conducted by experienced researchers in qualitative data collection. These sessions focused on the ethical considerations of interviewing pregnant women during public health emergencies, emphasizing the importance of neutrality, empathy, and open-mindedness. (2) Practice interviews: to refine their interviewing skills and familiarize themselves with potential challenges, interviewers conducted practice interviews with individuals who did not participate in the main study. Feedback from these practice sessions was critically reviewed, and additional training was provided where necessary to enhance the interviewers' proficiency. (3) Use of structured interview guides: interviewers utilized structured interview guides that were carefully designed and reviewed by the research team. These guides aimed to maintain consistency across interviews while allowing for flexibility to explore emergent themes. The questions were framed to minimize any inadvertent biases and to encourage participants to express their experiences openly. (4) Ongoing supervision and debriefing: throughout the data collection period, regular supervision meetings and debriefing sessions were conducted with the interviewers. This provided a platform to discuss any challenges faced during interviews and to address any potential biases that might have emerged. Consistent communication ensured that the research team remained vigilant in maintaining data collection standards.
Utilizing a semi-structured interview format based on a pre-developed outline allowed for the flexibility to adjust questions and their sequence as needed, tailoring the approach to each participant's responses. The researchers actively engaged with participants, guiding the conversation, posing questions, and seeking clarification when necessary, all the while maintaining a focus on the study's central theme.
A key aspect of the methodology was the emphasis on creating an environment conducive to open and honest communication. Participants were encouraged to share their thoughts and feelings freely. In addition to verbal responses, researchers also observed and noted non-verbal cues such as facial expressions, tone, pauses in speech, and body language. These observations were recorded and included in the data analysis to provide a comprehensive understanding of the participants' experiences.
2.3.2 Data organization
After each interview, we stored the original audio data and the general information questionnaire of the research subjects together in a designated folder. Within 2 days of concluding each interview, the audio data was transcribed into textual form and coded according to the alphabetical numbers assigned to each participant (A to M). The time and location of the interview were noted at the beginning of the text. After transcription, the texts underwent a meticulous review process to ensure their accuracy compared to the original recordings. Once validated, these accurate transcripts were saved in the unique digital folder for each participant, facilitating organized data retrieval for analysis.
To enhance the overall credibility of our study, we take the following approach:
Validation of findings: (1) Member checking: to enhance the credibility of our findings, we employed member checking as a form of validation. A subset of participants was provided with a summary of the identified themes and findings. Their feedback and reflections on whether these accurately represented their experiences were actively sought. This iterative process allowed us to refine and validate the interpretation of our data. (2) Peer debriefing: regular debriefing sessions were conducted within the research team. The interdisciplinary nature of our team facilitated a comprehensive discussion of the emerging themes, interpretations, and any potential biases. Peer debriefing served as a form of internal validation, ensuring that diverse perspectives were considered during the analysis. (3) Audit trail: an extensive audit trail was maintained throughout the research process. Detailed records of the data collection, coding, and analytical decisions were documented. This audit trail serves as a transparent account of our research journey, enabling others to follow our analytical processes and decisions.
Triangulation of findings: (1) Data source triangulation: we collected data through multiple sources, including individual interviews and, where applicable, relevant documents. Triangulating data from various sources enriched the depth and comprehensiveness of our findings, providing a more holistic understanding of pregnant women's experiences during public health emergencies. (2) Methodological triangulation: in addition to Colaizzi's phenomenological method, which served as our primary analytical approach, we applied methodological triangulation by exploring quantitative data related to demographic variables. This combination of qualitative and quantitative methods added layers to our understanding and strengthened the robustness of our findings.
3.1 Basic information
The baseline information of the study participants is shown in Table 1 .
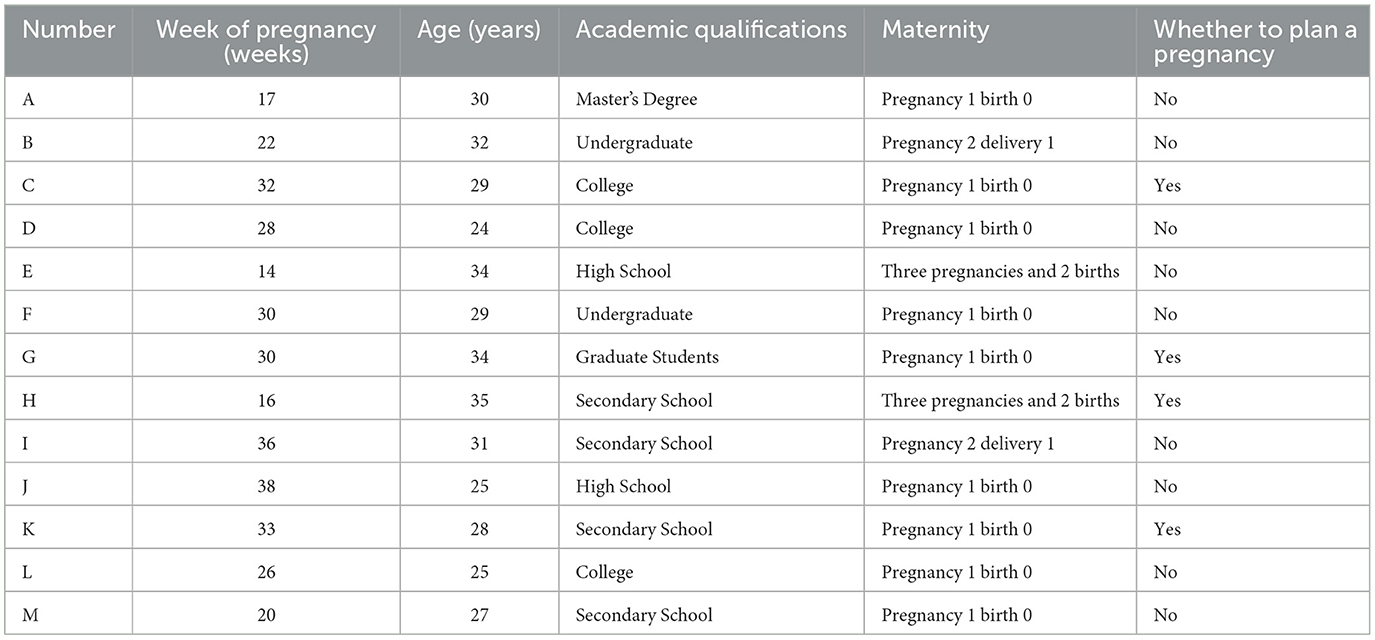
Table 1 . Basic information of pregnant women ( n = 13).
3.2 Findings
3.2.1 theme 1: personal protection and vaccine safety, 3.2.1.1 needs for personal protection knowledge.
Twelve of the study participants reported concerns about their knowledge regarding personal protective measures in the context of the epidemic. These individuals participated in regular maternity examinations and adopted a range of protective strategies to mitigate the risk of viral infection. Nonetheless, there was prevalent anxiety concerning the potential implications of maternal infection on both fetal and maternal health. While some adhered rigorously to prescribed protective guidelines, they further expressed a desire for healthcare facilities to strengthen their infection control protocols. Conversely, a subset of participants decided against attending hospital-based maternity check-ups, citing these concerns.
Participant A detailed the protective measures she adopted, saying, “For my pregnancy test last week, I wore two masks and goggles. Upon returning home, I immediately used alcohol for disinfection, changed, and thoroughly cleaned everything before going back to the hospital. My aim is to ensure complete protection and prevent any accidental virus transmission,” she added, visibly concerned (frowns).
Participant B expressed apprehension about hospital environments: “I avoid hospital visits unless absolutely necessary for my baby's health. Hospitals are crowded, and surfaces like door handles and elevator buttons might not be sanitized properly. I wish there were more rigorous disinfection practices in place.”
Participant C shared her unease about hospital visits, stating, “Even though I try to keep a distance, people often crowd together in lines. The hospital's lax approach to managing crowds increases my anxiety about obtaining a safe pregnancy test,” she remarked, frowning (frowns).
Participant D considered alternative preventive measures: “I've looked into mask effectiveness online and thought about herbal remedies for COVID-19 prevention. A neighbor knowledgeable in traditional medicine suggested a formula I'm thinking of trying.”
Participant E, recognizing the pandemic's severity, said, “With the current state of the COVID-19 epidemic, it's crucial for me to learn about protective measures during pregnancy and how to manage risks.”
Participant G, voicing her fears, mentioned, “The possibility of COVID-19 affecting my baby and me is a significant concern. I'm avoiding crowded places and taking all necessary precautions. I'm also looking for information on preventing infection during pregnancy.”
Participant H stressed the importance of medical advice: “I'm looking for guidance from healthcare professionals on how to protect myself and my fetus during the pandemic.”
During her second pregnancy, Participant H felt more anxious: “This pandemic has made me more worried than during my first pregnancy. I'm concerned about the virus's potential impact on my fetus during childbirth.”
Participant I was confused by conflicting information: “Although I've seen reports on TV and online about COVID-19′s effects on pregnant women and fetuses, I'm still unsure about the best actions to take.”
Approaching her due date, Participant J shared her concerns about hospital visits: “With my due date near, the thought of hospital visits is worrisome. Constantly wearing a mask is challenging, and my anxiety grows daily,” she said, frowning.
Participant K discussed the difficulties in accessing prenatal care: “Every maternity check-up requires health and travel code verification, which is tedious. Despite having appointments, long waits are common. The strict infection control and limited check-up slots often conflict with my schedule, leaving me worried about completing necessary checks for my fetus's health,” she explained, frowning.
Participant L contemplated the repercussions of contracting the virus: “If I were to catch the virus, I'm concerned about its impact on my unborn child, especially if it complicates hospital visits for labor or delivery.”
Expressing fears of reinfection, Participant M said, “Having had COVID-19 before, I'm worried about how it might affect my unborn child and the unsettling thought of getting the virus again,” her concern evident in her expression.
Collectively, while all participants expressed concerns about their knowledge of personal protective measures, their levels of anxiety and the extent of protective strategies they adopted varied significantly. For example, Participant A took extensive protective measures, including wearing multiple masks and goggles, which indicates a high level of anxiety and a strong desire for comprehensive protection. In contrast, other participants, like Participant D, explored alternative preventive measures, such as herbal remedies, suggesting a divergence in trust or confidence in conventional medical advice vs. traditional or alternative health practices.
3.2.1.2 Vaccine safety knowledge needs
Six participants highlighted their need for information on the safety of the COVID-19 vaccine during pregnancy. Concerns were focused on the potential adverse effects on the fetus, particularly when the vaccine was administered during unplanned pregnancies or within the first trimester. Questions also emerged regarding the effectiveness of partial vaccination with only three doses instead of the full series (COVID-19 vaccine full vaccination, meaning that the vaccine should be given in three consecutive doses, with the second dose to be completed as far as possible within 8 weeks of the first dose, and the third dose to be completed as far as possible within 6 months of the first dose).
Participant A shared her concerns about early vaccination: “I was vaccinated with the COVID-19 vaccine early in my pregnancy, which was unexpected. I'm worried about the possible negative effects on my baby's health.”
Participant E, who became pregnant soon after receiving the vaccine, expressed her fears: “I got pregnant 2 weeks after my third dose of the vaccine, without any plans for pregnancy at that time. Had I known, I might have reconsidered getting the vaccine, especially since there were advisories against pregnant women receiving it. The situation is quite worrying now.”
Participant H was confused by the varying advice: “The guidance regarding vaccination for pregnant women appears inconsistent. It's sometimes advised against, yet also presented as a protective measure against the virus. I'm unsure about the safety of receiving the vaccine during pregnancy.”
Participant K, nearing her due date, sought clarity: “With my baby's development well underway, is it safe for me to receive the vaccine now, or should I wait until after the delivery and breastfeeding period?”
Participant L had doubts about vaccine coverage: “After receiving one dose of the COVID-19 vaccine, I'm left wondering whether it fully protects against COVID-19-related pneumonia.”
Participant M, contemplating the need for a complete vaccination series, asked: “I had two doses before getting pregnant and didn't complete the third dose before conceiving. Is my vaccination still effective? And is completing the third dose crucial for ongoing protection?”
Here, we observed a clear division in attitudes toward hospital visits for maternity check-ups. Some participants, such as Participant B, avoided hospital visits due to concerns about insufficient sanitation and the risk of exposure in crowded settings. Others, however, despite sharing these concerns, continued to attend check-ups, emphasizing the importance of regular medical supervision for the baby's health. This divergence highlights a conflict between the perceived risk of exposure and the perceived necessity of prenatal care. Conflicting information and decision-making: participant I's confusion about the best actions to take due to conflicting information underscores a significant divergence in how participants processed and acted upon COVID-19-related health information. This variation suggests a need for clear, consistent, and trustworthy health communication tailored to pregnant women's concerns.
In addition, the participants' concerns also reflect divergent views on the efficacy and safety of the COVID-19 vaccine during pregnancy. For instance, Participant E's regret about receiving the vaccine close to conception due to advisories against pregnant women getting vaccinated highlights the confusion and mixed messages surrounding vaccination. Meanwhile, Participant L's uncertainty about the protection offered by a single vaccine dose points to a gap in understanding about vaccine efficacy and the importance of a complete series.
3.2.2 Theme II: maternal health
3.2.2.1 nutrition and diet.
Thirteen study participants, especially those in their first pregnancy, with unplanned pregnancies, experiencing severe early pregnancy symptoms, or concerned about excessive weight gain, expressed significant concerns about maintaining a healthy diet. They were in search of advice on appropriate dietary choices and what foods to avoid.
Participant A highlighted the challenge of balancing nutrition with early pregnancy symptoms: “Understanding the critical role of nutrition during pregnancy, I find it difficult to identify foods that are both nutritious and suitable for managing early pregnancy symptoms.”
Participant B, facing an unplanned pregnancy, sought guidance on nutrition: “Being unprepared due to my unplanned pregnancy, I am keen to learn what is best for the health of both myself and my baby, including how to maintain a healthy weight and ensure the baby's nutritional needs are met.”
Participant C, experiencing her first pregnancy, expressed concerns about weight management: “My family encourages me to eat more because it's my first pregnancy. However, I am worried about gaining too much weight and want to know how to balance getting enough nutrients without excessive weight gain.”
Participant D recognized the importance of dietary knowledge: “I know diet is important during pregnancy, but need information on specific foods that should be included or avoided.”
Participant E dealt with the impact of nausea on diet: “Dealing with constant nausea makes eating well difficult. I'm drawn to acidic foods like hawthorn (Hawthorn is a kind of sour fruit, and many pregnant women want to have sour food when they are pregnant and vomiting. Although food with sour flavor can relieve nausea and vomiting that occur in pregnant women, not all sour food is suitable for pregnant women to consume, and hawthorn is an exception. Hawthorn is an exception. Hawthorn has the effect of breaking blood and dispersing silt, which can stimulate uterine contraction and may induce miscarriage. Hawthorn contains a lot of fruit acids, which have the effect of astringency and stimulating the gastric mucosa. After pregnancy, pregnant women's spleen and stomach function is poor, eating more hawthorn is easy to reduce the digestive ability and cause indigestion) but am confused by mixed messages regarding their safety.”
Participant E also questioned the timing of folic acid intake: “I conceived unexpectedly and began folic acid late. Could this lead to developmental issues, as suggested online?”
Participant F emphasized the need for detailed guidance: “As this is my first pregnancy, I'm looking for detailed advice from healthcare providers on diet, exercise, and what symptoms to expect for a healthy pregnancy journey.”
Participant G discussed the need for a balanced diet: “It's vital for pregnant women to carefully manage their diet to ensure they're getting enough nutrients while avoiding too much caffeine, sugar, and other harmful substances. Following medical advice and regular check-ups are key.”
Participant H shared concerns about late folic acid supplementation: “This pregnancy was unexpected, and I started taking folic acid later than recommended. I'm worried about how this delay might affect my baby's development.”
Participant I focused on the importance of holistic health care: “Maintaining overall health through a balanced diet, sufficient rest, and regular exercise is essential for pregnant women.”
Participant J inquired about dietary management in late pregnancy: “As I approach the end of my pregnancy, I wonder if strict dietary control is still necessary.”
Participant K addressed the issue of weight management: “Finding a balance between the weight gain recommendations from doctors and family advice is difficult. I need guidance on how to provide the best nutrition for my baby without excessive weight gain.”
Participant L aimed for a balanced approach to health: “My main goal is to keep myself healthy while minimizing any negative impact on the fetus. I'm interested in learning about recommended dietary and exercise practices.”
Participant M desired comprehensive information: “I want to learn more about all aspects related to pregnancy, including diet, exercise, and mental health.”
The participants displayed varied strategies in managing nutritional intake, balancing between craving management and symptom alleviation. While some sought specific dietary advice to mitigate early pregnancy symptoms, others focused on weight management, indicating a spectrum of priorities and concerns related to diet. In addition, there was a clear divergence in approaches to weight management, with some participants concerned about excessive weight gain and seeking guidance to avoid it, while others felt pressure to eat more to support the baby's growth, reflecting varied familial and cultural influences on dietary practices during pregnancy.
3.2.2.2 Exercise and rest
During our interviews, nine participants shared insights into their experiences with exercise during pregnancy. It was observed that the comfort level and ability to engage in physical activity varied significantly across different pregnancy stages. Women in their mid-pregnancy often found it easier to participate in exercise, whereas early pregnancy symptoms and the fear of inducing premature labor were common deterrents. As pregnancy progressed, the intensity and variety of exercises diminished, with walking emerging as the most favored form of physical activity.
Participant B discussed her exercise routine: “I've been engaging in prenatal yoga and fitness routines tailored for pregnant women. I feel more comfortable being active in my mid-pregnancy despite early pregnancy discomforts. Before I exercise, I always check online to ensure the activities are safe.”
Participant C, in her thirties and nearing the third trimester, expressed interest in expanding her exercise options beyond walking, seeking safe activities suitable for this later stage of pregnancy.
Participant E encountered challenges with staying active due to early pregnancy symptoms like nausea and vomiting, which sometimes made even walking difficult.
Participant F, experiencing pregnancy for the first time, mentioned her simple exercise routine: “I take walks after dinner but am uncertain about other exercises that would be safe for me.”
Participant G, an older first-time pregnant woman, highlighted the importance of caution and the value of walking as a shared activity with her husband, emphasizing the need for precise guidance on safe exercises from professionals.
Participant H preferred walking as her main form of exercise, consistent with her activities in previous pregnancies, though she noted that hot weather often deterred her from going outside.
Participant I adjusted her activities to accommodate her growing belly, opting for evening walks as a cautious exercise option.
Participant L engaged with online exercise programs, focusing on stretching and gentle movements, and intentionally avoided intense activities such as hiking and sports.
Participant M found a suitable exercise in yoga, attending classes led by an instructor to ensure fitness while being mindful of her body's post-pregnancy changes.
These accounts reflect the diverse approaches to exercise among pregnant women, underscoring the importance of safety, comfort, and personal preferences in maintaining physical activity during pregnancy. Overall, the comfort and ability to engage in exercise varied, with some participants integrating specific prenatal routines comfortably into their daily lives, while others found even mild exercise challenging due to symptoms or concerns about safety, indicating a need for personalized exercise guidance. Moreover, the degree of engagement in physical activities showed divergence, with some participants actively seeking out safe exercises and others defaulting to walking as a safe option, highlighting differences in personal initiative, perceived safety, and available resources for exercise during pregnancy.
3.2.2.3 Sexual life
For this topic, discussions around sexual life during pregnancy revealed a notable reticence among participants, a reflection of broader cultural attitudes. Only a few women felt comfortable sharing their experiences, underscoring the sensitivity and privacy typically associated with this topic in Chinese culture. The primary concern for those who did speak on the matter was the safety of the fetus, influencing their decisions to engage in or abstain from sexual activity, especially during the early and late stages of pregnancy.
Participant B, drawing on her personal experience from a second pregnancy, noted that the middle trimester is often seen as a safer period for sexual activity. She emphasized the importance of proceeding with caution, acknowledging sexual intimacy as a part of life but one that requires careful consideration during pregnancy.
Participant L spoke openly about her experiences with intimacy, sharing that she and her husband had engaged in sexual activity with her husband on top, a position they found to be safe during what is considered a relatively safe month of pregnancy. Her openness highlighted a level of comfort and excitement in exploring intimacy within the perceived safety parameters of pregnancy.
Participant M, at 20 weeks pregnant, expressed a keen interest in exploring sexual intimacy discreetly with her husband. She valued conversations with individuals who had more experience in this area, indicating a desire for guidance and reassurance.
These accounts illustrate the varied approaches to navigating sexual intimacy during pregnancy among the participants. While some felt comfortable discussing and exploring this aspect of their lives, others preferred silence or abstention, guided by concerns for fetal health and influenced by cultural norms. These underscore the importance of providing personalized, flexible, and culturally sensitive health education and support to address the varied concerns and priorities of pregnant women effectively.
3.2.3 Theme III: fetal health
3.2.3.1 medications and hazardous substances.
Within the scope of concerns related to fetal health, some of our participants voiced apprehensions regarding the use of medications during pregnancy. The focus of their worry included antibiotics, exposure to chemicals, as well as the impact of smoking and alcohol consumption, all feared for their potential adverse effects on fetal development.
Participant D reflected on her actions before knowing she was pregnant, stating, “I was not aware of my pregnancy during the 1st to 2nd months, and during that time, I dyed my hair and frequently ate fast food. Now, I'm burdened with anxiety about how these actions may have affected my fetus.”
Participant H discussed the challenges posed by social obligations, “Due to my husband's work-related events, we often find ourselves in environments where smoking and drinking are prevalent. Discovering our unplanned pregnancy and with an NT scan [Nuchal Translucency scan] on the horizon, my concerns for the fetus's wellbeing have significantly heightened.”
Participant I recounted her dilemma with medication, “While we were planning for a pregnancy, I inadvertently took cold medicine shortly before learning I was pregnant. The uncertainty of how this might affect my baby's development is a constant worry, with the fear of potential abnormalities being particularly distressing.”
Here, we observed variance in participants' perceptions of risk regarding medication use and exposure to hazardous substances, with some expressing significant anxiety about accidental exposures early in pregnancy, while others were more concerned about social environments' impact on fetal health.
3.2.3.2 Pregnancy check-ups
The topic of pregnancy check-ups emerged as a point of concern for several participants, who were eager for clarity on the procedures involved, the implications for fetal health, and the necessary precautions to be observed before and after these check-ups.
Participant A was curious about the protocols for assessing the risk of Down's syndrome, asking, “Why are there different recommendations from doctors for Down's syndrome testing—between screening and non-invasive DNA tests? How do these methods operate, and is there any risk to the baby associated with them?”
Participant H brought up questions about a specific diagnostic procedure, “I'm trying to understand amniocentesis better. It was never suggested in my earlier pregnancies. What exactly does it involve, is it considered safe for someone of my age, and what are the risks to the baby?”
Participant L expressed concerns related to the scheduling of ultrasound appointments amid the ongoing pandemic, “The epidemic has led to the rescheduling of maternity exams, including my 21-week check-up. This has left me wondering about the best timing for undergoing a 3D or 4D ultrasound.”
Participant M sought detailed information on fetal development assessments, “I'm curious about macrosomia and what it entails. Which specific aspects of fetal development are examined for potential abnormalities? Is it necessary to fast before undergoing such an exam, given that my baby tends to be more active when I feel full? Could this activity level influence the results of the ultrasound?”
Overall, the participants differed in their information needs regarding pregnancy check-ups, with some seeking detailed explanations of specific procedures and their implications, while others were more concerned about the logistical aspects of scheduling and attending check-ups during the pandemic.
3.2.3.3 Fetal movement monitoring
Fetal movement is a significant indicator of a baby's wellbeing inside the womb, and it's understandable why it would be a source of concern for expecting mothers. The participants' experiences and questions highlight the need for clear, accessible information on what to expect and how to effectively monitor fetal movements.
Participant C's challenge with the impracticality of hourly movement counts due to a busy schedule is a common concern. Practical advice for busy mothers-to-be could involve setting aside specific times when they are more likely to notice movements, such as after meals or during periods of rest.
Participant F's experience of reduced fetal movement after overeating and the subsequent relief of finding everything was fine with her baby underlines the importance of awareness and prompt action when changes are noticed. It also points to the need for guidance on how normal physiological activities, like eating, can influence fetal movement.
Participant G's proactive approach, opting for an extra ultrasound after noticing changes in movement due to skipped meals, reflects the anxiety that can come with the responsibility of monitoring fetal health. This situation underscores the need for clear guidelines on when to seek medical advice and how maternal activities and behaviors can affect fetal movements.
Participant M's concern about not feeling fetal movements by 20 weeks and the resulting frequent hospital visits for reassurance speak to the anxiety first-time mothers, in particular, might experience. This highlights the necessity for education on the expected timeline for feeling fetal movements and when the lack of movement warrants medical attention.
Finally, Participant J's worry about decreased fetal movement as labor approaches and the reassurance received from a doctor touches on the need for continuous communication and reassurance from healthcare providers. It emphasizes the importance of understanding the normal changes in fetal movement patterns toward the end of pregnancy and when to seek help.
Overall, there was a range of practices and levels of concern regarding fetal movement monitoring. Some participants were proactive and sought additional check-ups upon noticing changes, while others experienced anxiety due to not feeling movements at expected times, highlighting varied responses to monitoring fetal health signs. These experiences point to a broader need for accessible, clear information and guidance for expectant mothers on monitoring fetal movements, understanding what is normal, and recognizing signs that may warrant further medical evaluation.
3.2.4 Theme IV: knowledge of childbirth
This theme encompasses the participants' perspectives and concerns regarding childbirth, highlighting their preferences for family accompaniment, considerations about labor analgesia, and choices regarding the mode of delivery. Each subtheme reflects a blend of personal desires, medical considerations, and emotional responses to the prospect of childbirth.
3.2.4.1 Family accompaniment
The desire for family support during childbirth was important for several participants, reflecting the emotional and psychological comfort it provides.
Participant C expressed a wish for her husband's presence to share in the birth experience.
Participant I hoped for her mother's support, emphasizing the value of maternal presence during such a significant life event.
Participant J, while valuing family support, acknowledged the critical role of medical staff in ensuring safety and wellbeing during childbirth.
Participant K offered a different perspective, preferring privacy over the presence of her husband during potentially messy childbirth moments.
Collectively, we observed that participants had divergent views on family support during childbirth, with some desiring the presence of their partner or mother for emotional support, while others preferred privacy, highlighting the personal nature of childbirth preferences.
3.2.4.2 Analgesia in childbirth
The discussion around labor analgesia revealed a range of emotions, from fear and confusion to the desire for a pain-free experience.
Participant G discussed the dilemma between fearing labor pain and worrying about the potential impact of analgesia on the baby.
Participant I, with a previous positive experience with painless labor, was open to using analgesia again, depending on the situation.
Participant J sought clarity on the availability and safety of painless labor options across hospitals, reflecting common concerns among expectant mothers.
Participant K, influenced by her friends' experiences, prioritized pain reduction in her childbirth plan.
From these, it can be observed that attitudes toward labor analgesia varied significantly, from fear of its effects on the baby to a strong preference for pain reduction. This diversity underscores the complexity of decisions around pain management in childbirth.
3.2.4.3 Choice of mode of delivery
The choice between vaginal birth and cesarean section was a topic of contemplation and concern for participants.
Participant G expressed a preference for vaginal birth but was wary of the potential for complications leading to emergency cesarean sections. She said “With the increasing prevalence of cesarean sections, I worry about unsuccessful attempts leading to further distress.”
Participant I felt encouraged by a smooth first delivery, hopeful for a similar experience the second time around, mentioning “A smooth first delivery suggests a smoother second one.”
Participant J, close to her due date, considered a cesarean section, influenced by fear of labor pain and the perceived control it offers over the birthing process. She revealed, “In my advanced stage, I'm unsure. I might defer to my doctor's recommendation, though I lean toward a cesarean due to fear of pain.”
Participant K aspired to a vaginal birth but was apprehensive about the associated pain. She mentioned “I aspire to a vaginal birth but dread the pain,” illustrating the complex considerations women navigate when deciding on their preferred mode of delivery.
Overall, the preferences for vaginal birth vs. cesarean section were mixed, influenced by previous experiences, fears of labor pain, and perceptions of control over the birthing process. This variation illustrates the personal and complex nature of deciding on a mode of delivery.
3.2.5 Theme V: knowledge of postnatal recovery
This part captures the concerns and anticipations of seven mothers regarding their recovery after childbirth. The focus on body image, abdominal skin recovery, and pelvic floor muscle strength reflects a blend of personal health priorities and societal influences. Traditional practices and cultural beliefs, such as the “sitting in the moonlight” period, play a significant role in shaping their recovery expectations and timelines.
Participant A worries about the impact of age on her postnatal recovery, highlighting a common concern that recovery might be more difficult for older mothers. This reflects a broader societal perception about the challenges of post-pregnancy body changes and weight loss in older women.
Participant D's experience brings attention to the physical and emotional impact of visible post-pregnancy changes, such as a prominent stomach and stretch marks, which can lead to uncomfortable social interactions and concerns about physical appearance.
Participant E, planning for weight loss after her third child, indicates a proactive approach to postnatal recovery, recognizing the importance of dedicating time and effort to regain pre-pregnancy body weight and shape.
Participant H's mention of temporary urinary incontinence after her second childbirth emphasizes the practical health concerns associated with pelvic floor recovery. Her commitment to rehabilitation post-birth underscores the importance of addressing these issues to improve quality of life and physical wellbeing.
Participant J's plan to rest for a month before focusing on weight loss suggests a balanced approach to recovery, acknowledging the need for physical rest and a gradual return to pre-pregnancy fitness and body shape.
Participant L's comment on the perceived benefits of early childbirth on recovery speed reflects cultural and societal beliefs about age and postnatal recovery. This belief may influence younger mothers' expectations and concerns about their post-pregnancy bodies.
Participant M's curiosity about specific postpartum changes, such as buttock enlargement and urinary leakage, highlights the desire for more comprehensive information on the physical recovery process. This interest in understanding the nuances of postnatal changes suggests a proactive approach to managing and mitigating these issues.
Collectively, these reflections underscore the complexity of postnatal recovery, encompassing physical, emotional, and societal dimensions. The mothers' concerns and plans reveal a deep-seated need for support, information, and practical strategies to navigate the postpartum period effectively.
3.2.6 Theme VI: sources of knowledge on health education for pregnant women and their expectations of healthcare providers
Participants in the study reported using a variety of sources for health education during pregnancy, including the Internet (via platforms like Baidu and mother-and-baby applications), WeChat groups, the experiences of friends, and the advice of healthcare professionals. They often combined these methods to gather necessary information, with thirteen participants particularly favoring online resources.
Participant A described her method: “During my first pregnancy, I used Baidu for dietary questions, adhered to the advice found in books, and consistently discussed any concerns with medical staff during check-ups.”
Participant B preferred direct consultation with healthcare experts: “My main sources are doctors and nurses. The epidemic makes hospital visits difficult, so I also participate in WeChat groups for updates, even though these discussions sometimes miss professional insights.”
Participant C highlighted the utility of digital applications: “I use a pregnancy app for intermittent insights and confirm its advice with doctors. Remote consultations would be a beneficial option under the current health advisories.”
Participant D suggested the importance of professional guidance in online forums: “I participate in WeChat groups for expectant mothers, recommending these forums host discussions led by healthcare experts.”
Participant E utilized a mix of past experiences and digital tools: “With two pregnancies behind me, I rely on my own experiences and conversations with friends who are pregnant, along with updates from a pregnancy app named ‘Beauty Grapefruit.”'
Participant F mentioned the logistical challenges of attending hospital classes: “Hospital maternity classes are useful but scheduling conflicts arise. Having the option to replay these classes would aid in learning.”
Participant G described a proactive strategy: “I independently researched and read literature on pregnancy, supplementing this with insights from friends and family.”
Participant H used a blend of historical knowledge and current discussions: “I base my understanding on previous pregnancies and enhance it with current group discussions.”
Participant I engaged with local support networks: “I join a local WeChat group of pregnant women for active discussions on health topics. My attendance at in-person classes is sporadic due to the epidemic.”
Participant J sought information online: “I use the internet to investigate practices related to pregnancy.”
Participant K called for clear communication from healthcare providers: “It's crucial that healthcare providers offer detailed, patient-focused explanations. Online platforms could help address our questions more efficiently, considering their tight schedules.”
Participant L adopted a multifaceted approach: “Being my first pregnancy, I extensively read and seek out online consultations.”
Participant M interacted within digital communities cautiously: “I participate in WeChat discussions, but direct responses from doctors are rare due to their obligations. I limit my interactions to reduce any risk of complications.”
Overall, this theme illustrates the diverse and adaptive strategies pregnant women employ to educate themselves about health during pregnancy and their expectation for accessible and clear communication from healthcare providers.
4 Discussion
4.1 personal protection and vaccine safety.
This study highlights the measures Chinese pregnant women undertake to protect themselves and their unborn children amidst public health crises, such as the COVID-19 pandemic. Participants exhibited a readiness to self-isolate and curtail routine pregnancy check-ups, motivated by the objective to avert potential infections. Nonetheless, it is crucial to acknowledge that excessive anxiety during epidemics can lead to negative outcomes, as highlighted in prior research ( 21 ). The Chinese government has recommended a prudent approach, advising pregnant women to minimize non-essential medical visits while emphasizing the importance of attending essential prenatal examinations ( 22 ). Furthermore, healthcare facilities have adopted stringent infection control protocols, including facility disinfection, the provision of one-on-one consultations, and the enforcement of social distancing during wait times ( 23 ) Media and internet resources have been instrumental in communicating protective strategies, thus reducing the anxiety of pregnant women before consultations and enhancing their safety during medical visits ( 17 ).
Moreover, participants expressed significant concerns regarding the safety and efficacy of the COVID-19 vaccine. Given their dual role as healthcare recipients and guardians of their own and their fetuses' wellbeing, they sought affirmation on the vaccine's appropriateness. Although public health guidelines such as social distancing and mask usage are critical, the introduction of the COVID-19 vaccine presented an additional layer of preventive measures ( 24 , 25 ). Initially, the National Health and Wellness Commission advised against administering the COVID-19 vaccine to women of childbearing potential and those breastfeeding. However, subsequent studies have validated the vaccine's safety and efficacy for pregnant individuals ( 26 – 29 ). Research indicates that COVID-19 vaccination does not increase the likelihood of teratogenic effects, congenital anomalies, spontaneous abortions, or low birth weights in comparison to those who are unvaccinated ( p < 0.05).
4.2 Knowledge needs of pregnant women and fetal health
This study highlights the critical need to address the knowledge gaps among pregnant women regarding dietary practices essential for fetal development. Participants expressed a strong desire for information on nutritious dietary choices, underscoring the need for comprehensive and actionable counseling from healthcare providers. Such counseling should provide clear guidelines on prenatal nutrition, focusing on the consumption of nutrient-dense foods, the avoidance of potentially harmful substances, and methods to alleviate common pregnancy-related discomforts.
Collaboration between healthcare providers and dietitians is essential in delivering accurate information and personalized dietary advice that meets individual preferences and needs. Given the unique challenges and uncertainties presented by public health crises, healthcare professionals have a significant duty to educate and support pregnant women in making informed dietary decisions that promote maternal and fetal health. Proper nutrition during pregnancy is vital for the health of both the mother and the fetus ( 30 ). By offering evidence-based guidance, healthcare providers can enable pregnant women to make wise dietary choices, thus improving health outcomes.
During public health emergencies, the mental health of pregnant women has become a critical concern ( 31 ). Insights from interviews conducted in this study indicate that participants experienced increased stress, anxiety, and emotional instability, particularly highlighted during the COVID-19 pandemic. It is essential to develop targeted mental health resources and support mechanisms to assist pregnant women in effectively managing these challenges. Initiatives should include stress management techniques, counseling services, and awareness campaigns about available support networks. The integration of mental health support into routine prenatal care is crucial for addressing the psychological wellbeing of pregnant women during public health crises ( 31 ). This approach should include systematic screening for mental health issues, offering counseling services, and ensuring timely referrals to specialized resources. Evidence-based interventions, such as the Centering Pregnancy (CP) model of care, positive cognitive exercises, and peer support, have shown effectiveness in enhancing emotional wellbeing during pregnancy ( 32 – 36 ). CP originated in the United States ( 36 ) and consists of three main components, as follows: (1) Creation of a discussion group: 8–12 pregnant women of similar gestational weeks are divided into a group, and each group is led by a doctor and a midwife, respectively (the families of the pregnant women may also participate). (2) Pregnancy self-management: doctors or midwives conduct one-on-one antenatal check-ups for pregnant women. Pregnant women are instructed and encouraged to complete simple examinations such as weight, blood pressure, abdominal circumference, and fetal heartbeat monitoring on their own and record them. After the check-up, the pregnant woman can consult the midwife about her problems. If it is a common problem during pregnancy, the midwife encourages her to solve it together as a group. Between examinations, pregnant women can communicate and discuss freely. (3) Group discussion: starting from 12 to 16 weeks, group discussion is organized on a regular basis, 0.5–2 h each time for a total of 10 sessions. Pregnant women are encouraged to speak and discuss, share their feelings and experiences, guide the content of the discussion, and answer the questions raised by the pregnant women. Currently, CP is widely used in Western countries, including North America, Australia, the United Kingdom, and Africa ( 37 – 39 ), and it is agreed that CP is the best model of maternal health care, which promotes active participation of pregnant women, improves their mental health, and enhances satisfaction with care, prenatal knowledge, and ownership of self-care; and reduces the risk of preterm labor and cesarean section ( 40 – 43 ), while in China, the use of CP is still in its infancy. In China, the use of CP is still in its infancy, and some studies have found that CP can reduce pregnant women's fear of labor, enhance their breastfeeding self-efficacy ( 44 , 45 ), promote comprehensive support from midwives, family members, and peers at the same time, and improve coping with perinatal problems ( 46 ). Mindfulness is the ability to describe an individual's awareness of being in the present moment. The level of mindfulness can be a useful predictor of depression to some extent, with higher levels of mindfulness being associated with lower levels of depression ( 33 ). When the level of positive thinking of pregnant women is low, they are unable to focus on the present moment and frequently focus on negative life events during pregnancy or after delivery, which may cause them to have negative emotions such as irritability and depression. Research has shown that a certain period of positive thinking training can improve the participants' positive thinking level and negative emotions ( 33 ). Currently, the most important positive thinking interventions include positive thinking stress reduction therapy and positive thinking cognitive behavioral therapy ( 33 ), which can reduce the generation of negative emotions, improve the quality of life, and promote the emotional stability of the mind during pregnancy and postpartum care.
4.3 Improving health education and guidance during pregnancy
Public health emergencies can restrict pregnant women's access to routine antenatal screening services due to hospital limitations and concerns for the safety of both the women and their fetuses. These restrictions may affect the detection of pregnancy complications and their overall management. To maintain continuous care, healthcare systems must adopt innovative methods for providing remote prenatal monitoring, health education, and guidance, such as through telemedicine and virtual counseling. Since the beginning of the COVID-19 pandemic in 2019, there has been a notable increase in pregnant women seeking personal protection against the novel coronavirus infection during pregnancy and childbirth ( 9 ). Furthermore, about 71.0% of Chinese pregnant women have turned to health apps, official microblogs, and WeChat public channels for information, highlighting the Internet's critical role during public health crises as an essential resource for pregnant women to obtain pregnancy-related information ( 47 , 48 ).
The study revealed that participants predominantly utilized internet searches, pregnancy health applications, WeChat groups, and public forums for acquiring health-related information during public health emergencies. Nonetheless, skepticism concerning the expertise of information sources, including biomedical professionals, led to pregnant women harboring reservations about the reliability of health knowledge obtained online. They exhibited a greater trust in health education and information disseminated by certified biomedical practitioners. It is observed that medical professionals participating in group chats, such as on WeChat, may find it challenging to meet the personalized health education needs of each pregnant woman effectively. While telemedicine serves as a feasible option for certain prenatal care aspects, it faces limitations, such as the incapacity to perform specific physical examinations or tests remotely ( 49 ). As healthcare systems endeavor to provide continuous care amidst public health crises, it is imperative for providers, community-based organizations, and policymakers to develop and advocate for virtual support groups, online forums, and educational resources specifically designed for the needs of pregnant women. These initiatives can cultivate a sense of community, offer emotional support, and ensure access to trustworthy information, thereby mitigating isolation and improving overall wellbeing. Therefore, establishing robust communication channels between healthcare providers and pregnant women is essential for conveying accurate information, addressing concerns, and enabling shared decision-making.
4.4 Limitations
This study acknowledges the potential influence of social desirability bias on our findings, given the sensitive nature of the topics discussed. While measures were taken to ensure a comfortable and confidential environment for participants, the possibility that respondents might tailor their answers to what they perceive as more socially acceptable cannot be entirely ruled out. This bias could affect the authenticity and depth of the data collected, as participants might underreport or alter their experiences and needs. Additionally, its qualitative approach, while insightful, limits the ability to quantify the prevalence of specific needs or opinions, as it lacks quantitative data. This restricts the generalizability of findings and the measurement of opinion distribution among the broader population. Future research could benefit from employing mixed methods or anonymous data collection techniques to mitigate this limitation and capture a more authentic range of responses.
5 Conclusion
This study sheds light on the critical health education needs of pregnant women during public health emergencies during the COVID-19 pandemic. The empirical evidence provided serves as a valuable foundation, offering guidance for health education practitioners to develop targeted and impactful educational content. Nevertheless, this study is constrained by its limited sample size, the geographical limitation of the sample, and the potential for sample selection bias. To strengthen these findings, future research could include a broader and more diverse participant base and employ a variety of data collection techniques. In summary, this research emphasizes the vital role of health education for pregnant women during the COVID-19 pandemic, providing meaningful insights for healthcare providers and setting a direction for future investigations in this field. The insights from this pandemic highlight the importance of encouraging pregnant women to attend maternity examinations in a timely manner and to utilize biomedical resources wisely, ensuring the health and safety of both mothers and infants during public health challenges. By adopting comprehensive safety measures and isolation protocols, access to medical care for pregnant women can be improved, and leveraging internet resources can effectively promote the dissemination of healthcare knowledge related to pregnancy.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Research Ethics Review Committee of Ethics Committee of Quanzhou Medical College (the code of ethics: No. 2021007). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XS: Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. YZ: Data curation, Funding acquisition, Methodology, Project administration, Resources, Supervision, Visualization, Writing – review & editing, Conceptualization. MC: Data curation, Formal analysis, Funding acquisition, Investigation, Project administration, Resources, Validation, Visualization, Writing – review & editing. XX: Data curation, Formal analysis, Investigation, Software, Writing – review & editing, Resources. GL: Conceptualization, Data curation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by the Fundamental Project: Guided Science and Technology Plan Project of Quanzhou City (2021N137S).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Chauhan A, Potdar J. Maternal mental health during pregnancy: a critical review. Cureus. (2022) 14:e30656. doi: 10.7759/cureus.30656
PubMed Abstract | Crossref Full Text | Google Scholar
2. Tai D, Shah A, Doubeni CA, Sia IG, Wieland ML. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. (2021) 72:703–6. doi: 10.1093/cid/ciaa815
3. Wang Y, Wu Q, Zhou Y, Ma Y, Sun X. Development of cesarean section nursing process for pregnant women with coronavirus disease. Chin J Nurs. (2020) 55:511–4. doi: 10.3761/j.issn.0254-1769.2020.04.006
Crossref Full Text | Google Scholar
4. Chiesa V, Antony G, Wismar M, Rechel B. COVID-19 pandemic: health impact of staying at home, social distancing and “lockdown” measures-a systematic review of systematic reviews. J Public Health. (2021) 43:e462–81. doi: 10.1093/pubmed/fdab102
5. Chen Y, Deng Y, Huang X, Luo T. A survey on the current psychological and sleep status of pregnant women during the new coronary pneumonia epidemic and analysis of the influencing factors. Acad J Guangzhou Med Coll. (2022) 50:150–5. doi: 10.3969/j.issn.2095-9664.2022.03.30
6. Zhang S, Zeng L, Huang T, Lu Y, Zhou Y, Mai B, et al. A survey analysis of the prenatal psychological status of pregnant women during the prevention and control of novel coronavirus pneumonia epidemic. J Med Theor Pract. (2022) 35:507–9. doi: 10.19381/j.issn.1001-7585.2022.03.065
7. Liu X, Liu Y, Gu X. Analysis of the depression status of pregnant women during the new coronary pneumonia epidemic. Today Nurse. (2021) 28:29–31. doi: 10.19791/j.cnki.1006-6411.2021.07.012
8. Shen W, Zhang H, Lai S, Aimei F. Anxiety and depression state and the influencing factors in pregnant women in 2019-nCoV epidemic. Jilin Med J. (2021) 42:62–5. doi: 10.3969/j.issn.1004-0412.2021.01.019
9. Chen Y, Sun X, Li M, Xu Y. Investigation on the psychological status and coping style of pregnant women during the outbreak of COVID-19. Chin Nurs Manag. (2020) 20:1827–30. doi: 10.21203/rs.3.rs-34763/v2
10. van Baar J, Kostova EB, Allotey J, Thangaratinam S, Zamora JR, Bonet M, et al. COVID-19 in pregnant women: a systematic review and meta-analysis on the risk and prevalence of pregnancy loss. Hum Reprod Update. (2023) 2023:39. doi: 10.1093/humrep/deac105.039
11. Mahajan NN, Kesarwani S, Kumbhar P, Kuppusamy P, Pophalkar M, Thamke P, et al. Increased risk of early-onset preeclampsia in pregnant women with COVID-19. Hypert Pregn. (2023) 42:2187630. doi: 10.1080/10641955.2023.2187630
12. Li F, Luo S, Mu W, Li Y, Ye L, Zheng X, et al. Effects of sources of social support and resilience on the mental health of different age groups during the COVID-19 pandemic. BMC Psychiatry. (2021) 21:16. doi: 10.1186/s12888-020-03012-1
13. Liu W, Yue XG, Tchounwou PB. Response to the COVID-19 epidemic: the Chinese experience and implications for other countries. Int J Environ Res Public Health . (2020) 17:72304. doi: 10.3390/ijerph17072304
14. Avercenc L, Ngueyon SW, Bertholdt C, Baumont S, Freitas AC, Morel O, et al. Improving prenatal care during lockdown: comparing telehealth and in-person care for low-risk pregnant women in the protect pilot study. J Gynecol Obstet Hum Reprod. (2022) 51:102445. doi: 10.1016/j.jogoh.2022.102445
15. Justman N, Shahak G, Gutzeit O, Ben ZD, Ginsberg Y, Solt I, et al. Lockdown with a price: the impact of the COVID-19 pandemic on prenatal care and perinatal outcomes in a tertiary care center. Isr Med Assoc J. (2020) 22:533–7.
PubMed Abstract | Google Scholar
16. Shi K, Zhang G, Bi X, Yin Y, Gu X. A qualitative study on the health needs of primiparous mothers during pregnancy. Today Nurse. (2021) 28:73–8. doi: 10.19793/j.cnki.1006-6411.2021.36.025
17. Li Y, Shao Q, Fu W, Bai R, Xu X. Qualitative interviews on the prenatal screening behavior of pre women during the novel coronavirus epidemic. Henan Med Res. (2021) 30:6191–3. doi: 10.3969/j.issn.1004-437X.2021.33.014
18. Wu X, Ding Y, Zhu C, Xie F. Experiences of primiparas participating in the antenatal clinic service: a qualitative research. J Nurs Sci. (2012) 27:4–6. doi: 10.3870/hlxzz.2012.12.004
19. Mu T, Li Y, Wu D, Yin M, Cheng J, Gao Y, et al. Health education needs of women in different stages of pregnancy: a qualitative research. Nurs J Chin People's Liberat Army. (2018) 35:15–8. doi: 10.3969/j.issn.1008-9993.2018.14.004
20. Zhong S. A qualitative study of psychological experiences and pregnancy health care needs of elderly second-trimester pregnant. Chin Gen Practice Nursing. (2021) 19:3275–8. doi: 10.12104/ji.ssn.1674-4748.2021.23.030
21. Yang X, Zhang Y, Zhang W, Shi Q, Zhao X, Cao D, et al. Response and process recommendations for obstetrics departments in sentinel hospitals under novel coronavirus infection outbreaks. Modern advances in obstetrics and gynecology. Progr Obstetr Gynecol. (2020) 29:243–5. doi: 10.13283/j.cnki.xdfckjz.2020.04.002
22. The State Council. Joint prevention and control mechanism of the State Council in response to the pneumonia epidemic with novel coronavirus infection. Notice on strengthening maternal disease treatment and safe delivery assistance during the prevention and control of novel coronavirus pneumonia epidemic . (2020). Available online at: http://www.gov.cn/xinwen/2020-02/10/content_5476731.html
Google Scholar
23. Ying LX, Zhang Y, Tu HX, Leck A. Cleaning and disinfection in health care settings during the COVID-19 outbreak. Commun Eye Health. (2020) 33:36–7.
24. Chen E. Prevention and control strategy of COVID-19 in the vaccine era. J Prev Med. (2021) 33:221–5. doi: 10.19485/j.cnki.issn2096-5087.2021.03.002
25. China NHC. Technological guideline for COVID-19 vaccination. Infect Dis Inform. (2021) 34:97–8. doi: 10.3969/j.issn.1007-8134.2021.02.001
26. Dagan N, Barda N, Biron-Shental T, Makov-Assif M, Key C, Kohane IS, et al. Effectiveness of the BNT162B2 mRNA COVID-19 vaccine in pregnancy. Nat Med. (2021) 27:1693–5. doi: 10.1038/s41591-021-01490-8
27. Kharbanda EO, Haapala J, DeSilva M, Vazquez-Benitez G, Vesco KK, Naleway AL, et al. Spontaneous abortion following COVID-19 vaccination during pregnancy. J Am Med Assoc. (2021) 326:1629–31. doi: 10.1001/jama.2021.15494
28. Li Y, Tang H, Zhang J, Ting Z, Lin S. Safety evaluation of novel coronavirus vaccine during pregnancy. Progr Obstetr Gynecol. (2023) 32:161–5. doi: 10.13283/j.cnki.xdfckjz.2023.03.001
29. Hua Q, Xu X, Lü H, Zhang H. Research progress on the safety and efficacy of COVID-19 vaccine among special populations. J Prev Med. (2022) 34:479–82. doi: 10.19485/j.cnki.issn2096-5087.2022.05.011
30. Qin Y, Xie L. Nutrition and supplements during pregnancy: a vital component in building the health and well-being of both the mother and the developing baby. Nutrients . (2023) 15:153395. doi: 10.3390/nu15153395
31. Lopez-Morales H, Del VM, Canet-Juric L, Andres ML, Galli JI, Poo F, et al. Mental health of pregnant women during the COVID-19 pandemic: a longitudinal study. Psychiatry Res. (2021) 295:113567. doi: 10.1016/j.psychres.2020.113567
32. Yang H, Yan X, Chen Y, Ma X, Du Y. Effect of mindfulness training on young and middle-aged central post-stroke pain. Nurs Rehabil J. (2023) 22:14–8. doi: 10.3969/j.issn.1671-9875.2023.01.003
33. Zhang X, Wang Y, Li Y, Wang H, Wang Y. Effect of mindfulness and emotion regulation on maternal depression. Chin J Health Educ. (2022) 38:1072–6. doi: 10.16168/j.cnki.issn.1002-9982.2022.12.003
34. Yu W, Chi J, Gao X, Tang J, ZhangG X, Yang L. Advances of peer support in young cancer patients. Occup Health. (2023) 39:850–4. Available online at: https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjMxMjI2Eg56eXlqazIwMjMwNjAyORoIbnRidzc1dTg%3D
35. Liu J, Jiang Q, Liu J, Liu A, Wang C. Study on the application of peer support group education in patients with inflammatory bowel disease. Nurs Rehabil J . (2023) 22:39–42. doi: 10.3969/j.issn.1671-9875.2023.02.008
36. Rising SS. Centering pregnancy. An interdisciplinary model of empowerment. J Nurse Midwifery. (1998) 43:46–54. doi: 10.1016/S0091-2182(97)00117-1
37. McNeil DA, Vekved M, Dolan SM, Siever J, Horn S, Tough SC, et al. qualitative study of the experience of centeringpregnancy group prenatal care for physicians. BMC Pregn Childb. (2013) 13(Suppl.1):S6. doi: 10.1186/1471-2393-13-S1-S6
38. Allen J, Kildea S, Stapleton H. How does group antenatal care function within a caseload midwifery model? A critical ethnographic analysis. Midwifery. (2015) 31:489–97. doi: 10.1016/j.midw.2015.01.009
39. Patil CL, Abrams ET, Klima C, Kaponda CP, Leshabari SC, Vonderheid SC, et al. Centering pregnancy-Africa: a pilot of group antenatal care to address millennium development goals. Midwifery. (2013) 29:1190–8. doi: 10.1016/j.midw.2013.05.008
40. Eluwa GI, Adebajo SB, Torpey K, Shittu O, Abdu-Aguye S, Pearlman D, et al. The effects of centering pregnancy on maternal and fetal outcomes in northern Nigeria: a prospective cohort analysis. BMC Pregn Childb. (2018) 18:158. doi: 10.1186/s12884-018-1805-2
41. Teate A, Leap N, Rising SS, Homer CS. Women's experiences of group antenatal care in Australia—the centering pregnancy pilot study. Midwifery. (2011) 27:138–45. doi: 10.1016/j.midw.2009.03.001
42. Cunningham SD, Grilo S, Lewis JB, Novick G, Rising SS, Tobin JN, et al. Group prenatal care attendance: determinants and relationship with care satisfaction. Matern Child Health J. (2017) 21:770–6. doi: 10.1007/s10995-016-2161-3
43. Ickovics JR, Earnshaw V, Lewis JB, Kershaw TS, Magriples U, Stasko E, et al. Cluster randomized controlled trial of group prenatal care: perinatal outcomes among adolescents in new york city health centers. Am J Public Health. (2016) 106:359–65. doi: 10.2105/AJPH.2015.302960
44. Yuan C, Liu Y, Liu G, Ye D. The effect of health education based on centering pregnancy model on fear of childbirth. J Nurs Sci. (2017) 32:27–9. doi: 10.3870/j.issn.1001-4152.2017.18.027
45. Zheng Y, Ding Y, Wu Y. Effect of self-efficacy-based focus group care model on improving of breastfeeding rate. J Nurs. (2018) 25:75–8. doi: 10.16460/j.issn1008-9969.2018.05.075
46. Chen D, Li Y, Zhou L, Tan H. Primiparas, experiences of participating in a midwife-led centering pregnancy program: a qualitative research. J Nurs Sci. (2018) 33:32–4.
47. Javanmardi M, Noroozi M, Mostafavi F, Ashrafi-Rizi H. Internet usage among pregnant women for seeking health information: a review article. Iran J Nurs Midwifery Res. (2018) 23:79–86. doi: 10.4103/ijnmr.IJNMR_82_17
48. Sayakhot P, Carolan-Olah M. Internet use by pregnant women seeking pregnancy-related information: a systematic review. BMC Pregn Childb. (2016) 16:65. doi: 10.1186/s12884-016-0856-5
49. Herman H, Faridova A, Tefr O, Farid S, Ayayee N, Trojanova K, et al. Telemedicine in prenatal care. Cent Eur J Public Health. (2022) 30:131–5. doi: 10.21101/cejph.a7458
Keywords: pregnant women, health education, public health emergencies, qualitative research, COVID-19
Citation: Su X, Zhang Y, Chen M, Xu X and Liu G (2024) Understanding health education needs of pregnant women in China during public health emergencies: a qualitative study amidst the COVID-19 pandemic. Front. Public Health 12:1271327. doi: 10.3389/fpubh.2024.1271327
Received: 12 September 2023; Accepted: 22 April 2024; Published: 02 May 2024.
Reviewed by:
Copyright © 2024 Su, Zhang, Chen, Xu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuezhen Zhang, 499368300@qq.com
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Research article
- Open access
- Published: 07 April 2021
Learning about COVID-19: a qualitative interview study of Australians’ use of information sources
- Deborah Lupton 1 &
- Sophie Lewis 2
BMC Public Health volume 21 , Article number: 662 ( 2021 ) Cite this article
13k Accesses
25 Citations
106 Altmetric
Metrics details
A multitude of information sources are available to publics when novel infectious diseases first emerge. In this paper, we adopt a qualitative approach to investigate how Australians learnt about the novel coronavirus and COVID-19 and what sources of information they had found most useful and valuable during the early months of the pandemic.
In-depth semi-structured telephone interviews were conducted with a diverse group of 40 Australian adults in mid-2020 about their experiences of the COVID-19 crisis. Participants were recruited through Facebook advertising. Detailed case studies were created for each participant, providing the basis of a thematic analysis which focused on the participants’ responses to the questions about COVID-19-related information sources.
Diverse sources of COVID-19-related information, including traditional media, online media and in-person interactions, were actively accessed, appraised and engaged with by participants. There was a high level of interest in COVID-19 information as people grappled with uncertainty, anxiety and feeling overwhelmed. Certain key events or experiences made people become aware that the outbreak was threatening Australia and potentially themselves. Most people demonstrated keen awareness that misinformation was rife in news outlets and social media sites and that they were taking steps to determine the accuracy of information. High trust was placed in health experts, scientists and government sources to provide reliable information. Also important to participants were informal discussions with friends and family members who were experts or working in relevant fields, as well as engaging in-person in interactions and hearing from friends and family who lived overseas about what COVID-19 conditions were like there.
A constantly changing news environment raises challenges for effective communication of risk and containment advice. People can become confused, distressed and overwhelmed by the plethora of information sources and fast-changing news environment. On the other hand, seeking out information can provide reassurance and comfort in response to anxiety and uncertainty. Clarity and consistency in risk messaging is important, as is responding quickly to changes in information and misinformation. Further research should seek to identify any changes in use of and trust in information sources as time goes by.
Peer Review reports
News and social media can play an important role in providing information to publics in cases of new or emerging diseases. It is vital to reach people quickly and share details in a situation in which medical and public health authorities are grappling with how the disease spreads and can best be controlled [ 1 , 2 , 3 , 4 , 5 ]. Major infectious disease outbreaks are highly newsworthy, typically attracting dramatic statements concerning risk [ 6 , 7 , 8 ]. News media coverage is often a starting point at which people start to reflect on the seriousness of pandemic risk and its implications for their own lives [ 2 , 9 ]. However, news reports can also become hyperbolic or convey misinformation, leading to scepticism and lack of trust in official sources, unfounded complacency or alternatively, generating heightened feelings of fear, uncertainty, depression and anxiety [ 2 , 10 , 11 ].
The COVID-19 outbreak began to receive public attention in early January 2020, following reports by Wuhan health officials of a cluster of viral pneumonia cases of unknown cause affecting people in that large Chinese city in Hubei province [ 12 ]. The news and public health communication environment responding to the COVID-19 crisis has been fraught, frequently characterised by conflicting or rapidly changing information as health authorities and governments struggled to make sense of this new outbreak and identify the best way to control its spread [ 13 , 14 , 15 ]. COVID-19 news reporters and creators and sharers of social media content have been subjected to continual criticism for disseminating misleading or false information. The term ‘infodemic’ has been used in some popular media outlets and academic analyses to describe the wealth of ‘fake news’ and conspiracy theories circulating, particularly in online news sites and social media platforms [ 16 , 17 , 18 , 19 , 20 ].
Analyses of how news reporting and social media content have framed COVID-19 issues across different countries have identified marked variances. Ageism in social media content has been identified, with older people positioned as both more vulnerable and more expendable than other age groups [ 21 ]. Racism has also featured in some countries’ news reporting, particularly against Chinese people, who have been frequently positioned as to blame for the emergence of the novel coronavirus in Wuhan [ 22 ]. Politicisation and polarisation of opinion has characterised COVID-19 news in US television networks and newspapers [ 23 ], whereas strong support for government measures was evident in South Korean newspaper reporting [ 24 ]. A focus on prevention and control measures, medical treatment and research, and global or local socioeconomic influences was identified in an analysis of Chinese news articles [ 25 ].
Information provided in news coverage of COVID-19 in Australia has included reporting of the first cases and deaths and the subsequent rapid spread of the novel coronavirus around the world, accounts of statements, decisions and press conferences held by political leaders and health authorities, strategies to avoid infection, medical controversies and debates and progress towards treatments for COVID-19 and vaccines [ 5 , 26 , 27 ]. In Australia, very early news reporting (January 2020) focused on the ‘mystery Chinese virus’ and made continual comparisons to SARS [ 26 ]. A study of two major Australian newspapers’ COVID-19 coverage found that they were quite slow to begin covering the emerging outbreak, suggesting an initial lack of awareness that it might pose a threat to Australians. Subsequent news reporting largely focused on the social and economic impacts of the crisis. There was little blame or judgement directed at any social or national groups, although panic buyers did receive some criticism [ 27 ].
Quantitative surveys to determine how publics were responding to coverage of the COVID-19 crisis in news and social media have identified an association between COVID-19-related news and social media consumption and heightened anxiety and distress in Russia [ 28 ], China [ 29 , 30 ] and USA [ 31 ]. Malaysian research found that respondents mainly used television and internet news portals to access COVID-19 information. Those who preferred government sources of information were more confident about the control of COVID-19 and believed their government was handling the crisis well [ 32 ]. Research in the UK found that people’s news consumption surged in the early months of the crisis but gradually returned to pre-crisis levels, with evidence of a growing avoidance of news. A decline in respondents’ trust in key sources of COVID-19-related news and information was also noted: particularly in relation to social media sites and government sources [ 33 ].
A comparative international online survey included nationally representative samples from Australia, New Zealand, UK, USA, Italy and South Korea [ 34 ]. For respondents in most of these countries, government and friends and family were the most trusted sources of COVID-19 information, ranked above the news media and social media. Together with New Zealanders (89%), Australians evidenced the highest levels of trust in their government (78%) to give clear and accurate advice on COVID-19. While 58% of Australians said they trusted the news media in general for COVID-19 advice, only 30% trusted information found or shared on social media more specifically.
Another online survey conducted early in the Australian nation-wide lockdown (April 2020) [ 35 ] found that Australians were consuming news media more than usual due to their interest in and concern about the pandemic. More than two-thirds said that they had been accessing news more than once a day since the outbreak. Half of the respondents were using television reporting as their main COVD news source, while 22% were accessing online news coverage and 18% news on social media. The respondents reported high levels of satisfaction with news coverage of COVID-19 (73%), but it was contributing to people’s feelings of anxiety, particularly for women and younger people. Most respondents said that they trusted health experts and scientists (85%) and to a lesser degree, government (66%) to provide information about COVID-19. Just over half said that they trusted news organisations but less than a quarter of respondents reported that they had encountered high levels of misinformation in the news or social media about COVID-19. Australians agreed that the federal government had done a good job of informing them about the pandemic (75%) and how they should respond (81%).
The surveys reviewed above are valuable in identifying trends across large populations in attitudes and practices related to COVID-19 information sources. To complement and extend such findings, qualitative social research methods provide a way of investigating people’s engagements with personal sources of information about emerging health risks such as family members and healthcare providers as well as with government sources and news and social media reporting in greater depth. This approach provides for explorations of lived experiences in sociocultural contexts [ 1 , 2 , 11 , 36 ]. Thus far, few qualitative analyses of Australians’ responses to news and social media coverage of COVID-19 have been published. Among other issues, the ‘Australians’ Experiences of COVID-19′ study investigated people’s use and appraisal of information about COVID-19. We wanted to surface the full range of information sources upon which participants relied and those they most trusted: including but beyond media or government sources.
The study took place during the first 6 months of the COVID-19 crisis in Australia, following the identification of the first Australian COVID-19 cases on 25 January 2020 and the implementation of a nation-wide lockdown from mid-March 2020 [ 37 ]. Forty indepth, semi-structured interviews with adults living in Australia were conducted by the second author between late May and late July 2020. In addition to the closing of international borders and some national state borders, the national lockdown included directives for people to work at home where possible, limits on household visitors, bans on public gatherings, the closing of non-essential services and schools, and physical distancing rules. The spread of COVID-19 began to be slowed by April 2020. Restrictions were progressively eased from mid-May 2020 onwards but fluctuated in response to the incidence of COVID-19 community case numbers. Restrictions were re-introduced in the state of Victoria from July until November 2020, following a significant second wave of infection in that state [ 37 ].
Due to physical distancing restrictions, the interviews for this study were conducted by telephone. This method also ensured that people living across the nation, including in regional and remote areas, had the opportunity to participate in the study. Interested potential participants responded to an advertisement about the study on Facebook. Participants were offered a gift card to compensate them for their time. Sub-quotas were set and achieved in recruitment to ensure a heterogeneous interviewee group with a spread of participants across gender, age group, and place of residence (metropolitan, regional and rural/remote areas). Facebook was chosen to advertise for recruitment because of its popularity among Australian adults. At the time this study was carried out, figures on Australian Facebook use show that 60% of all Australians (of any age) were regular Facebook users, with 50% of the Australian population logging on at least once a day [ 38 ]. Using this method of recruitment therefore proved to be fast and effective, and we easily met our sub-quotas. Table 1 shows the sociodemographic characteristics of the participants.
The study adopted a qualitative approach that was focused on a wide-ranging interview about the participants’ experiences of the novel coronavirus/COVID-19 during the 6 month period following identification of the first Australian cases. All interviews were audio-recorded and professionally transcribed in full. A narrative case study approach was adopted in compiling and analysing the interview materials. This approach sees the indepth interview as a form of shared storytelling, in which participants recount narratives in response to interview questions and researchers formulate their accounts into narratives [ 39 , 40 ]. The second author wrote fieldnotes for each participant soon after she conducted each interview. These fieldnotes were presented in narrative form, drawing on the author’s impressions and recollections of how the participants responded to the questions. Once each interview was transcribed by a professional service and returned to the authors, both authors then used the transcripts to augment these notes, inserting illustrative direct quotations from them to configure a detailed narrative case study for each interviewee. These case studies, together with the full transcripts, comprise our research materials for analysis.
Some of our findings are reported thematically across the case studies, while in other analyses we present case studies to provide a detailed biographical narrative. For the purposes of the present paper, the set of detailed case studies formed the basis of a topical thematic analysis which focused on the participants’ responses to the questions about sources of information about COVID-19. These themes were derived as an iterative analytical process involving both authors working with the research materials of case studies we had developed together with the interview transcripts. This approach to social inquiry is directed at identifying ‘making the mundane, taken-for-granted, everyday world visible’ through interpretative and narrative practices ( [ 41 ] , p. 723). As Denzin ( [ 41 ] , p. 722) puts it, human experience (and by extension, social inquiry) ‘is a process. It is messy, open-ended, inconclusive, tangled up’. Hence our focus on interpretation and narrative as modes of analysis: the interviewees interpreted our questions in formulating their responses, and we in turn interpreted their responses in configuring the case studies, identifying themes across the cases and presenting our findings.
The first question in the interview prompted participants to think back to how and when they had first heard about COVID-19 and to provide narratives of how they felt about it at that time. This question was followed up by asking participants ‘Since that first time of hearing about the coronavirus/COVID-19, what has been the most helpful or useful sources of information for you to learn about the virus?’ and ‘What has made these sources so helpful or useful for you?’. It is on their responses to these three opening questions that we focus in this article.
Initial reactions to COVID-19-related information
Given that initial news reports in Australian outlets focused on China and SARS [ 26 ], it is not surprising that most participants had first heard about the new infectious disease outbreak through news media sources reporting on the ‘mystery SARS-like’ cluster of cases in China. The location of the outbreak in first news reports and the comparison with SARS in this early news coverage led people to think that it was a faraway problem that would not directly affect them. Several people drew on their memories of previous outbreaks of novel infectious diseases such as SARS, MERS and Ebola in their responses. For example, Michael (aged 56) initially heard about the virus in Wuhan through television news reporting. He recalls hearing about coronavirus as it was being compared with SARS. He remembered that the SARS epidemic had not affected Australia, so did not think COVID-19 would either.
SARS seemed to affect other countries around the world but not Australia. So, I didn’t think that it would be as severe as what it ended up, so widespread across the world. So no, I didn’t really worry at the time.
Greg (aged 69) was even less concerned about the threat of COVID-19 at first, as his initial exposure to news about the coronavirus was via jokes that circulated on Facebook. He remembered that Facebook friends at first tended to make light of the threat of the outbreak: ‘I wasn’t too sure what to make of it, and enjoyed a couple of jokes when people said “I’m having a corona attack!” and put a photo of a [Corona brand] beer up on Facebook’. It was when Greg heard projections of the number of people that might be hospitalised with the virus in Australia on television news reporting in early March that he began to realise that it was a serious problem. The initial joking on Facebook was countered by the dramatic television news reports of the growing threat posed by COVID-19 to Australians.
I had listened to all the news broadcasts: listened with some trepidation to the forecasts of 'the hospitals are going to need thousands of beds', and concerned about that … By early March, I started to pay attention.
The initial sheer volume of news reporting and other public messaging about the spread of the coronavirus and measures needed to contain it could be overwhelming for some people. Because of the novel nature of the COVID-19 pandemic and the fast-changing news about it and its potential impacts on Australia, it was common for the participants to observe that they found themselves not being able to look away from news reporting about the crisis once the serious nature and rapid spread of the pandemic worldwide began to be reported in Australian news outlets. Participants commented on the importance of judicious consumption of news and information about the virus to avoid becoming overly obsessed and anxious after realising the risks to Australians of COVID-19. Several participants commented that they began to feel that there was saturation of ‘bad news’ and fear-inducing announcements from government officials in press conferences and health communication campaigns.
Some participants noted the tendency for sensationalism in news reporting and social media activity and the deleterious effects on their feelings of wellbeing. They often talked about ‘switching off’ from or limiting their exposure to news about the virus as time went on as a way of managing their distress and supporting their mental wellbeing. As Joe (aged 41) commented:
when I have looked at the international news and looking at what’s happening in America and that sort of stuff, it gets me really worked up and I get very upset about it. I find that quite challenging, and at the same time, I find it very difficult not to look. So, I found it really hard, particularly in the early days, in terms of just not constantly having the news on and constantly hearing about what was going on. It’s only probably been in the last two weeks that I’ve managed to sort of cut that down to maybe two or three times a week, whereas it was two or three times a day. It was just, I had to know what was going on all the time.
Several others reported difficulty in keeping up with all the new information being issued from these sources: some of which could be contradictory. For example, Emma (aged 29) described the government-provided information in press conferences or public health campaigns concerning restrictions as often ‘confusing’. She noted that some of the restrictions imposed by the government were ‘arbitrary’ or hard to make sense of. Emma gave the example of the number of people allowed at a wedding or a funeral, a rule which she remembered was constantly changed during the early months of the pandemic: ‘It’s, like, bizarre and kind of hard to understand’.
Blame, misinformation and conspiracy theories
Many participants were highly aware of the potential for news reporting or social media content to be misleading or inaccurate: problems which themselves have received attention from the news media itself as well as public health authorities in Australia [ 5 , 15 ]. Some people expressed feelings such as frustration, distress or anger around the kinds of information (conspiracies, misinformation, concerns about bias or fake news) circulating social media platforms. One example is Sarah (aged 54), whose husband is an essential worker in health services. She was concerned that the misinformation about COVID-19 in the news media and social media could reinforce or sanction careless or negligent behaviours that would place her husband and other frontline healthcare workers at increased risk of infection. She knew from her husband’s first-hand experience that the threat of COVID-19 was not exaggerated.
My husband was dealing with those patients who are highly contagious, and he was told not to wear full protection and that was frightening. So when people were saying ‘It’s a hoax, don’t worry about it,’ I’m like, ‘Well, you’re putting my husband’s life in danger’. So it was really distressing.
Other participants demonstrated a high level of scepticism towards the accuracy of information they encountered in the news media. They said that they were careful to try to evaluate the level of risk as it was reported in news outlets, given the news media’s tendency towards hyperbole to attract viewers. As James (aged 26) commented:
[The media] are going to catastrophise everything and anything, all the information. So, whatever I’m reading, I’ve got to make sure that I don’t just believe it straight away and look into it a bit more and ask some more questions, rather than just saying, yep, okay, I believe that.
For Greg (aged 69), the main source of information to learn about the novel coronavirus and COVID-19 has been television news reporting. He talked about the importance of ‘reading between the lines’ and being mindful of the polarisation and ‘bias of the media’ in reporting about the coronavirus. Greg was also concerned about some of the conspiracy theories that were circulating initially, and that the outbreak was not being taken seriously by a section of the community. He was even more vigilant in appraising the validity of news and commentary on Facebook: his second main source of information.
I must admit I’ve become quite careful about reading conspiracy-type theories on Facebook. Yeah, it’s a platform for everyone to have their say, but I’ve discovered that in my own opinion, some theories are quite farfetched. People can be sincerely wrong.
Joe (aged 41) said he is surprised by how many people he knows have ‘bought into’ the conspiracy theories, including his own elderly mother. He perceives these theories as expressed by people who need someone to blame. Joe said that he does his best to counter these claims where he has seen them expressed: which includes in face-to-face interactions or telephone conversations with close family members as well as in social media outlets such as Facebook.
There has been some discussion that I’ve had with family that has been just ridiculous. My mother, who’s a bit older and just, I don’t know, a bit susceptible to bad information, says all sorts of conspiracy-type things to me, which I’ve just told her is ridiculous. At one point, I think she was saying that China’s done this deliberately, and this was to break the world economy. I mean, the worst one I’ve seen and heard of, which was from an associate on Facebook, was the 5G theory, which – I just think – I don’t know … it seems to – a lot of people were buying into that, which surprised me. I think they were desperate to have a cause of something they could point at.
Most trustworthy information sources
Given their caution about news reporting and social media content, many participants talked about being judicious around what sources of information they used to learn about the COVID-19 crisis. They placed an emphasis on trusted, unbiased, reliable sources of information that they assumed were founded on expert medical and scientific advice and research, or on personal experience of the pandemic.
Natalia (aged 67) was born overseas and keeps in close contact with friends and family there: including viewing content about COVID-19 they have shared on Facebook. She said that she is careful to check that any news items she sees her friends or family members sharing comes from ‘a well-known news source’ such as the ABC (Australian Broadcasting Corporation) or the Washington Post (USA) news outlet or quoting a scientific study: ‘I try to do that, because well, I know how fake news creates fear or hopes for nothing’. Ruth (aged 70) also referred to the ABC as well as the BBC (British Broadcasting Corporation) as trustworthy, noting that she uses her smartphone to access their news reporting.
I just keep reading on my phone and some articles I discount because I think they’re crap, and other articles I think, well, yeah, this seems to make sense … I take the ABC and the BBC as being okay.
For most participants, government sources such as the federal government health minister and state premiers and health authorities such as Chief Medical Officers were also viewed as credible. Greg (aged 69) said that he finds information from these sources to be the most helpful, mainly because he believes that ultimately, they have the country’s and its citizens’ best interests at heart. He positioned himself and other Australians as responsible for following government advice for the collective good of the community and as a way of demonstrating good citizenship.
Well that was pretty much the bottom line for me. That, okay, if the government says you’ve got to socially isolate, well that’s what I’ll do. I’ll take precautions, I’ll wear a mask, I’ll wear gloves when I go shopping. I did all of that in the early stages.
Max (aged 52) spoke about the value he placed on the federal government response communicated in regular news conferences that were closely covered by the news media. He liked keeping up to date with reporting of these news conferences because he thought that they provided the most current and local information about the pandemic and the current restrictions in a situation in which these details could change from day to day. Max found it reassuring and informative that these news conferences and announcements were predictable and appreciated being able to readily access these details using digital news outlets.
Even though those news conferences became a bit tedious and repetitive, it was good to know that they were regular conferences … and that you knew that a couple of times a day we were being updated as to what’s going on.
High value and trust were also placed on the information provided by people known personally to the participants who were considered to have expert knowledge or personal experience of the pandemic. Such sources included friends or family members who work in healthcare, government or science domains. They were viewed as unbiased and therefore more credible than some of the news media reporting. For example, Ruth (age 70) said that she trusts both her doctor and her brother, who is a scientist, to give her authoritative and fact-based advice about COVID-19.
I actually discussed it with my doctor, probably three or four weeks ago, because I see him frequently … He said in our particular district there hasn’t been any coronavirus cases for three or four weeks and he thought it was quite safe. So, I talked to him about it … I talk to my brother about it – he’s a scientist. I think it’s factual information and people with scientific backgrounds that provide the information.
Sarah (aged 54) noted that with her husband working in a hospital, their family had received a proliferation of COVID-19-related information from his workplace even before the national lockdown took place. She knew from her husband’s work experiences that hospitals were engaged in rushed preparations for a predicted surge of patients needing care for COVID-19: ‘Yeah that was the word of mouth we were getting. So that was, yeah, it was good in some respects and terrifying in others’.
Participants who had family members or friends living overseas also often nominated these people as important sources of details about what life was like in countries such as the USA, UK, Spain and Italy where the COVID-19 crisis was much further advanced than in Australia. Riley (aged 29), who was born in the USA and still has family and friends living there, observed that: ‘certainly once it hit New York, then I was getting inundated with messages from my parents, because it was affecting them very directly obviously’.
A small number of participants mentioned faith-based communities or teachings as contributing to their sense-making around COVID-19. For Greg (aged 69), it was his fundamentalist Christian teachings that contributed to his growing awareness that the COVID-19 outbreak in China could be serious globally, resulting in the ‘end times’ he believes is forecast in the Bible. For Riley (aged 29), the personal risk of infection was really brought home by new measures introduced into the synagogue that Riley regularly attends.
I was involved in a lot of stuff in the synagogue and about early to mid-March, early March, they were starting to say we can’t shake hands anymore and we can’t come close to each other anymore. When they started talking about that in the synagogue, I was starting to really pay attention, I was like ‘They’re telling me this for a reason!’. I started to take it a bit more seriously, so I’m glad that the people in my religious community were taking it seriously before I started to.
Bringing sources together
As is evident from the participants’ accounts outlined above, many used a range of information sources about COVID-19. The relative influence of these sources in some cases changed as the pandemic gathered momentum or as key details about COVID-19 changed over the first 6 months when medical and public health experts were still learning about the ways the novel coronavirus spread, the effects of COVID-19 and how best to contain the pandemic and governments and health officials were struggling to find the most effective and least harmful policy settings.
Several people explained the complex processes by which they appraised and made sense of COVID-19 information through a range of sources. For example, Georgia (aged 24) commented that she likes the immediacy of sources of information like Twitter and television news reports but considers them not always trustworthy or reliable. Typically, she will supplement this information through her own online research using government websites and through word of mouth from friends who live overseas and have been more seriously affected or exposed to the COVID-19 crisis. Georgia explained that the government-sourced information is the most helpful for her because it is ‘verifiable’. She knows that the government draws on health expertise in formulating its COVID-19 advice and policy. In particular, she finds localised information most useful: for instance when and where it is safe to go outside in her local area, and what actions she should be taking to reduce her own risk of COVID-19 as well as risks to others. It is less important for her to learn about the ‘bigger picture’ of the pandemic. These practices also help Georgia deal with the plethora of information available about COVID-19: ‘Anything where the information is bite sized and verifiable, I appreciate, so I guess in that sense, Twitter is good as long as I then go fact check’.
Emma (aged 29) also receives a lot of news through Twitter, preferring to read a range of different sources on that platform so that she is then able to formulate her own views about the issue. She also recounted hearing in the news and social media about people’s real-life experiences of becoming ill with COVID-19 and how that was particularly powerful for her. Emma described herself as already living with anxiety pre-COVID-19. She noted that accessing more information and gaining knowledge about COVID-19 made her feel less worried: in part, because it gave her the knowledge to take precautions to avoid contracting the novel coronavirus. Emma was also keen to be aware of what the government was doing to handle the crisis, including how she as an individual could help the collective response.
Personally, I find it really helpful to have as much information as possible on things. I think that helps me relax a bit more. I know certain people, it’s the opposite, where the more you know about something, reading about something a lot, will make you more agitated. But it was the opposite for me – where I was like, I would like to know as much as possible about this so I can avoid it and knowing what the governments are doing and knowing what you can do personally to help and so on and so forth.
Another example of bringing different information sources together is provided by Darren (aged 64). He said that he has relied on government-related information in finding out and learning more about the coronavirus and COVID-19. He accesses this information via online government health websites. Darren commented that he finds this kind of information more truthful than the news media ‘spin’ that is imposed on government-based information.
I saw the media reports where health ministers and health advisors were giving information out, but to be quite honest I didn’t pay too much attention to it, because attached to all that was the media spin afterwards. So I left it alone to a great extent and just relied on the government website and blogs that were from medical personnel.
Darren noted that he is cautious about the circulation of ‘false information’ and ‘fake news’ on social media. However, he is willing to use social media to access websites and ‘serious’ bloggers which he accesses as more truthful and trustworthy: ‘They are either scientific or they are reliable blogs, if you know what I mean. They are ones that I have read for many, many years’.
The description of his evaluation of COVID-19 information sources provided by Mark (aged 48) highlights the importance of the advice offered both by international bodies that can provide general advice and local sources of information, as well as demonstrating that social media sites can be vital platforms for disseminating these details. Mark said that he has ‘never trusted the media for reporting anything’. He preferred the World Health Organization’s (WHO) regular media briefings hosted on social media outlets as his chief source of information about the novel coronavirus and COVID-19. Mark said that he used Australian government sources of information as a secondary source to the WHO, to provide more localised information and advice: for instance about guidelines and directives for daily living and how to prevent against contracting or spreading the coronavirus.
Similar to previous qualitative research on publics’ responses to information sources about new disease outbreaks [ 1 , 2 , 11 , 36 ], our findings show that participants were active users of information sources rather than passively accepting news accounts, government spokespeople or social media content as authoritative. The participants demonstrated awareness that misinformation was rife in news outlets – and especially social media sites – and that they were taking steps to determine the accuracy of information. Their accounts also highlight the interactions of different forms of information sources, and the sophistication with which participants engage with these different kinds of information. Diverse sources of COVID-19-related information, both international and local, were actively accessed, appraised and engaged with by participants.
As was found in survey findings in Australia [ 35 ] and other countries [ 32 ], traditional media (television and radio news reports) were important sources for participants, as were government sources such as press conferences, health campaigns and websites [ 34 , 35 ] and friends and family [ 34 ]. Despite contentions that Australian publics have lost confidence in the advice of public health authorities and governments due to conflicting and rapidly changing information provided [ 13 ], our participants demonstrated willingness to trust these sources for information and advice about how to respond to the crisis. Indeed, other research conducted around the same time as our study showed that Australians’ trust in government had increased dramatically since the outbreak of COVID-19: largely because they assess government interventions to manage COVID-19 as appropriate and effective [ 42 ]. Regular press conferences with government and health officials were important in gaining people’s trust and reassuring them that the federal and state governments were working hard to control the crisis. People wanted both very localised information that was directly relevant to them and general information from trusted global health organisations such as the WHO.
Healthcare professionals personally known to people, such as their regular general practitioner, were also trusted sources of information. Illustrative of the importance placed on experiential knowledge, the participants referred to the value of having informal discussions with friends and family members who were experts or working in relevant fields, such as healthcare or science, as well as engaging in-person in interactions with groups such as faith-based communities and simply hearing from friends and family who lived overseas about what COVID-19 conditions were like there.
Our findings support and extend other research that has highlighted the affective dimensions of engaging with information sources in relation to major health crisis such as outbreaks of new infectious diseases [ 2 , 9 , 10 , 11 ]. Similar to survey-based research in Australia [ 35 ] and internationally [ 28 , 29 , 30 , 31 , 33 ], our study’s participants reported a high interest in COVID-19 news reports in the initial stages of the pandemic. Some people described feelings of anxiety or distress in response to the plethora of information continually published in news reports and on social media. Others were angry and frustrated about the extent of misinformation that was circulating in the community and online and the potential for it to contribute to the spread of the coronavirus and pose a risk to others. However for many people, keeping up to date with changes in information and news in the rapidly changing environment of the COVID-19 crisis was a form of reassurance and helpful in ensuring they were conforming to best-practice risk avoidance and management.
The findings also show how certain key events or experiences made people become aware that the outbreak was threatening Australia and potentially themselves. For some people, this was hearing in the news media about the growing number of cases in their region, drastic government interventions imposed to contain the spread or the identification of infected people in their immediate locale. For others, it was face-to-face encounters or telephone conversations with trusted people or viewing content from friends and family members overseas on social media about how they were experiencing the pandemic in their countries that really brought home the dire threats posed by COVID-19 and what could happen to Australia if the outbreak were not contained.
A limitation of our study is that it did not involve a representative sample of Australian adults and therefore the findings are not generalisable to the population as a whole. However, a diverse group of participants was included, and the findings support and provide further detail about the trends identified in large-scale surveys of Australians’ news consumption and trust in information sources during the initial months of the COVID-19 crisis [ 34 , 35 ].
Conclusions
Our findings provide further contextual insights into the complexities and social contexts of these practices and sense-making responses, including how people bring together information from different sources in understanding the threat of COVID-19 and the interactions of digital with non-digital sources. A constantly changing news environment, as was the case during the first 6 months of the COVID-19 crisis, raises challenges for effective communication of risk and containment advice. People can become confused, distressed and overwhelmed by the plethora of information sources and fast-changing news environment. On the other hand, seeking out information can provide reassurance and comfort in response to anxiety and uncertainty. Clarity and consistency in risk messaging is important, as is responding quickly to changes in information and misinformation.
Our interview study took place at a certain point in the Australian experience of the COVID-19 crisis (towards the end of the national lockdown). Given the rapidly changing nature of the spread of COVID-19 in Australia since then, including a major outbreak in the state of Victoria and an extended second lockdown in that state, continuing and follow-up research is recommended to better understand how Australians have made sense of and protected themselves against the COVID-19 crisis and which sources have been most helpful for them in doing so.
Availability of data and materials
No data or materials are publicly available as the participants did not consent to open sharing of their interview transcripts or other personal information. Anonymised interview transcripts may be made available from the corresponding author on reasonable request.
Linde-Arias AR, Roura M, Siqueira E. Solidarity, vulnerability and mistrust: how context, information and government affect the lives of women in times of Zika. BMC Infect Dis. 2020;20(1). https://doi.org/10.1186/s12879-020-04987-8 .
Davis M, Lohm D. Pandemics, publics, and narrative. Oxford: Oxford University Press; 2020. https://doi.org/10.1093/oso/9780190683764.001.0001 .
Book Google Scholar
McCauley M, Minsky S, Viswanath K. The H1N1 pandemic: media frames, stigmatization and coping. BMC Public Health. 2013;13(1). https://doi.org/10.1186/1471-2458-13-1116 .
Lwin MO, Lu J, Sheldenkar A, Cayabyab YM, Yee AZH, Smith HE. Temporal and textual analysis of social media on collective discourses during the Zika virus pandemic. BMC Public Health. 2020;20(1). https://doi.org/10.1186/s12889-020-08923-y .
Hooker C, Leask J. Risk communication should be explicit about values. A perspective on early communication during COVID-19. J Bioethical Inquiry. 2020;17(4):581–9. https://doi.org/10.1007/s11673-020-10057-0 .
Article Google Scholar
Lupton D. Moral threats and dangerous desires: AIDS in the news media. Bristol: Taylor & Francis; 1994.
Google Scholar
Duncan B. How the media reported the first days of the pandemic (H1N1) 2009: results of EU-wide media analysis. Eurosurveillance. 2009, 2020;14(30) Available from: https://www.eurosurveillance.org/content/10.2807/ese.14.30.19286-en . Accessed 1 Mar 2021.
Klemm C, Das E, Hartmann T. Swine flu and hype: a systematic review of media dramatization of the H1N1 influenza pandemic. J Risk Res. 2016;19(1):1–20. https://doi.org/10.1080/13669877.2014.923029 .
Mesch GS, Schwirian KP, Kolobov T. Attention to the media and worry over becoming infected: the case of the swine flu (H1N1) epidemic of 2009. Sociol Health Illn. 2013;35(2):325–31. https://doi.org/10.1111/j.1467-9566.2012.01500.x .
Article PubMed Google Scholar
Garfin DR, Silver RC, Holman EA. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Health Psychol. 2020;39(5):355–7. https://doi.org/10.1037/hea0000875 .
Article PubMed PubMed Central Google Scholar
Davis M, Lohm D, Flowers P, Waller E, Stephenson N. “We became sceptics”: fear and media hype in general public narrative on the advent of pandemic influenza. Sociol Inq. 2014;84(4):499–518.
World Health Organization. Timeline: WHO's COVID-19 response2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline?gclid=CjwKCAiA17P9BRB2EiwAMvwNyGWSa7LCiCAgb9r1TIgGmjmcYnZzOj7_zVA80ZeeVZyUsfqM35BvrhoCofQQAvD_BwE#event-7 . Accessed 1 Mar 2021.
Maher R, Murphet B. Community engagement in Australia’s COVID-19 communications response: learning lessons from the humanitarian sector. Media Int Australia. 2020;177(1):113–8. https://doi.org/10.1177/1329878X20948289 .
Bernadas JMAC, Ilagan K. Journalism, public health, and COVID-19: some preliminary insights from the Philippines. Media Int Australia. 2020;177(1):132–8. https://doi.org/10.1177/1329878X20953854 .
Pickles K, Cvejic E, Nickel B, Copp T, Bonner C, Leask J, et al. COVID-19 misinformation trends in Australia: prospective longitudinal national survey. J Med Internet Res. 2021; 23(1). Available from: https://www.jmir.org/2021/1/e23805 . Accessed 1 Mar 2021.
Orso D, Federici N, Copetti R, Vetrugno L, Bove T. Infodemic and the spread of fake news in the COVID-19-era. Eur J Emerg Med. 2020;27(5):327–8. https://doi.org/10.1097/MEJ.0000000000000713 .
Rodrigues UM, Xu J. Regulation of COVID-19 fake news infodemic in China and India. Media Int Australia. 2020;177(1):125–31. https://doi.org/10.1177/1329878X20948202 .
Bruns A, Harrington S, Hurcombe E. ‘Corona? 5G? Or both?’: The dynamics of COVID-19/5G conspiracy theories on Facebook. Media Int Australia. 2020;177(1):12–29. https://doi.org/10.1177/1329878X20946113 .
Meese J, Frith J, Wilken R. COVID-19, 5G conspiracies and infrastructural futures. Media Int Australia. 2020;177(1):30–46. https://doi.org/10.1177/1329878X20952165 .
Irwin RE. Misinformation and de-contextualization: international media reporting on Sweden and COVID-19. Globalization and Health [Internet]. 2020; 16(1). doi: https://doi.org/10.1186/s12992-020-00588-x
Meisner BA. Are you OK, Boomer? Intensification of ageism and intergenerational tensions on social media amid COVID-19. Leisure Sciences. 2021;43(1-2):56–61.
Wen J, Aston J, Liu X, Ying T. Effects of misleading media coverage on public health crisis: a case of the 2019 novel coronavirus outbreak in China. Anatolia. 2020;31(2):331–6. https://doi.org/10.1080/13032917.2020.1730621 .
Hart PS, Chinn S, Soroka S. Politicization and polarization in COVID-19 news coverage. Sci Commun. 2020;42(5):679–97. https://doi.org/10.1177/1075547020950735 .
Article PubMed Central Google Scholar
Jo W, Chang D. Political consequences of COVID-19 and media framing in South Korea. Front Public Health. 2020; 8(425). Available from: https://www.frontiersin.org/article/10.3389/fpubh.2020.00425 . Accessed 1 Mar 2021.
Liu Q, Zheng Z, Zheng J, Chen Q, Liu G, Chen S, et al. Health communication through news media during the early stage of the COVID-19 outbreak in China: digital topic modeling approach. J Med Internet Res. 2020;22(4):e19118 Available from: http://www.jmir.org/2020/4/e19118/ .
Lupton D. A ‘mystery SARS-like illness’. How did Australian news outlets cover the COVID-19 outbreak when it first emerged in early 2020? Medium. 2021; Available from: https://deborahalupton.medium.com/its-been-a-year-since-the-first-australian-covid-19-cases-d7e4df44a550 . Accessed 1 Mar 2021.
Thomas T, Wilson A, Tonkin E, Miller ER, Ward PR. How the media places responsibility for the COVID-19 pandemic—an Australian media analysis. Front Public Health. 2020; 8(483). Available from: https://www.frontiersin.org/article/10.3389/fpubh.2020.00483 . Accessed 1 Mar 2021.
Nekliudov NA, Blyuss O, Cheung KY, Petrou L, Genuneit J, Sushentsev N, et al. Excessive media consumption about COVID-19 is associated with increased state anxiety: outcomes of a large online survey in Russia. J Med Internet Res. 2020; 22(9). Available from: https://www.jmir.org/2020/9/e20955 . Accessed 1 Mar 2021.
Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental health problems and social media exposure during COVID-19 outbreak. Plos One. 2020;15(4):e0231924. https://doi.org/10.1371/journal.pone.0231924 .
Article CAS PubMed PubMed Central Google Scholar
Liu M, Zhang H, Huang H. Media exposure to COVID-19 information, risk perception, social and geographical proximity, and self-rated anxiety in China. BMC Public Health. 2020;20(1). https://doi.org/10.1186/s12889-020-09761-8 .
Riehm KE, Holingue C, Kalb LG, Bennett D, Kapteyn A, Jiang Q, et al. Associations between media exposure and mental distress among U.S. adults at the beginning of the COVID-19 pandemic. Am J Prev Med. 2020;59(5):630–8. https://doi.org/10.1016/j.amepre.2020.06.008 .
Mohamad E, Tham JS, Ayub SH, Hamzah MR, Hashim H, Azlan AA. Relationship between COVID-19 information sources and attitudes in battling the pandemic among the Malaysian public: cross-sectional survey study. J Med Internet Res. 2020; 22(11). Available from: http://www.jmir.org/2020/11/e23922/ . Accessed 1 Mar 2021.
Nielsen RK, Fletcher R, Kalogeropoulos A, Simon F. Communications in the coronavirus crisis: lessons for the second wave. Reuters Institute. 2020. Available from: https://reutersinstitute.politics.ox.ac.uk/communications-coronavirus-crisis-lessons-second-wave . Accessed 1 Mar 2021.
Browne B. Global attitudes to COVID-19 pandemic and response. Online: The Australia Institute; 2020.
Park S, Fisher C, Lee JY, McGinness K. COVID-19: Australian news and misinformation. Canberra: News and Media Research Centre; 2020.
Davis MD, Stephenson N, Lohm D, Waller E, Flowers P. Beyond resistance: social factors in the general public response to pandemic influenza. BMC Public Health. 2015; 15(1). Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-015-1756-8 . Accessed 1 Mar 2021.
Lupton D. Timeline of COVID-19 in Australia. Medium. 2020. Available from: https://medium.com/@deborahalupton/timeline-of-covid-19-in-australia-1f7df6ca5f23 . Accessed 1 Mar 2021.
Social Media News. Social media statistics in Australia - June 20202020 6 August 2020. Available from: https://www.socialmedianews.com.au/social-media-statistics-australia-january-2020/ . Accessed 1 Mar 2021.
Rodríguez-Dorans E, Jacobs P. Making narrative portraits: a methodological approach to analysing qualitative data. Int J Soc Res Methodol. 2020;23(6):611–23.
McDougall A, Kinsella EA, Goldszmidt M, Harkness K, Strachan P, Lingard L. Beyond the realist turn: a socio-material analysis of heart failure self-care. Sociol Health Illn. 2018;40(1):218–33. https://doi.org/10.1111/1467-9566.12675 .
Denzin NK. The death of data in neoliberal times. Qual Inq. 2019;25(8):721–4. https://doi.org/10.1177/1077800419847501 .
Goldfinch S, Taplin R, Gauld R. Trust in government increased during the Covid-19 pandemic in Australia and New Zealand. Australian J Public Adm. 2021;80(1):3–11.
Download references
Acknowledgements
We thank the participants for giving their time to be interviewed for this study.
The study was funded by personal research support awarded to DL by UNSW Sydney as part of her SHARP Professorship.

Author information
Authors and affiliations.
Vitalities Lab, Centre for Social Research in Health and Social Policy Research Centre, UNSW Sydney, Sydney, Australia
Deborah Lupton
Centre for Social Research in Health, UNSW Sydney, Sydney, Australia
Sophie Lewis
You can also search for this author in PubMed Google Scholar
Contributions
DL conceived the project, conducted the literature review, contributed to the analysis, interpretation and discussion of the research materials and wrote the manuscript. SL conducted the interviews, wrote the case studies, contributed to the analysis, interpretation and discussion of the materials and reviewed and commented on the manuscript draft. Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Deborah Lupton .
Ethics declarations
Consent to publication.
Not applicable, as no identifying images of participants or identity revealing data are present in the study.
Ethics approval and consent to participate
The study was conducted according to the guidelines of the National Research and Medical Council of Australia. It was approved by the UNSW human research ethics committee (approval number HC200292). All participants provided informed consent prior to the interview. To maintain confidentiality, participants were assigned a pseudonym and all contextual identifiers were removed from the transcripts. To further preserve anonymity, the participants’ specific location of residence is not disclosed in the findings.
Competing interests
None to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lupton, D., Lewis, S. Learning about COVID-19: a qualitative interview study of Australians’ use of information sources. BMC Public Health 21 , 662 (2021). https://doi.org/10.1186/s12889-021-10743-7
Download citation
Received : 28 November 2020
Accepted : 19 March 2021
Published : 07 April 2021
DOI : https://doi.org/10.1186/s12889-021-10743-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Supplements
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 9, Issue 4
- The downstream effects of COVID-19 on adolescent girls in the Peruvian Amazon: qualitative findings on how the pandemic affected education and reproductive health
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-4892-909X Lisa L Woodson 1 ,
- Adriana Garcia Saldivar 2 ,
- http://orcid.org/0000-0001-8578-5510 Heidi E Brown 1 ,
- http://orcid.org/0000-0001-8526-458X Priscilla A Magrath 3 ,
- Nicolas Antunez de Mayolo 4 ,
- http://orcid.org/0000-0001-6877-8490 Sydney Pettygrove 1 ,
- http://orcid.org/0000-0001-7455-8531 Leslie V Farland 1 ,
- http://orcid.org/0000-0001-7818-3394 Purnima Madhivanan 3 ,
- http://orcid.org/0000-0002-3008-1695 Magaly M Blas 5
- 1 Department of Epidemiology and Biostatistics , The University of Arizona Mel and Enid Zuckerman College of Public Health , Tucson , Arizona , USA
- 2 Universidad Peruana Cayetano Heredia , Lima , Peru
- 3 Department of Health Promotion Sciences , The University of Arizona Mel and Enid Zuckerman College of Public Health , Tucson , Arizona , USA
- 4 School of Medicine , Universidad Peruana Cayetano Heredia , Lima , Peru
- 5 School of Public Health and Administration , Universidad Peruana Cayetano Heredia , Lima , Peru
- Correspondence to Lisa L Woodson; lisalabita{at}arizona.edu
Due to COVID-19, schools were closed to mitigate disease spread. Past studies have shown that disruptions in education have unintended consequences for adolescents, including increasing their risk of school dropout, exploitation, gender-based violence, pregnancy and early unions. In Peru, the government closed schools from March 2020 to March 2022, declaring a national emergency that affected an estimated 8 million children. These closures may have unintended consequences, including increased adolescent pregnancy, particularly in Peru’s rural, largely indigenous regions. Loreto, located in the Peruvian Amazon, has one of the highest adolescent pregnancy rates in the country and poor maternal and child health outcomes. The underlying causes may not be fully understood as data are limited, especially as we transition out of the pandemic. This qualitative study investigated the downstream effects of COVID-19 on adolescent education and reproductive health in Loreto’s districts of Nauta and Parinari. In-depth interviews (n=41) were conducted with adolescents and community leaders. These were held in June 2022, 3 months after the reinstitution of in-person classes throughout Peru. Focus group discussions (FGDs) were also completed with community health workers and educators from the same study area in October 2022 to supplement our findings (3 FGDs, n=15). We observed that the economic, educational and health effects of the COVID-19 pandemic contributed to reduced contraceptive use, and increased school abandonment, early unions and adolescent pregnancy. The interplay between adolescent pregnancy and both early unions and school abandonment was bidirectional, with each acting as both a cause and consequence of the other.
- Qualitative study
- Global Health
Data availability statement
Data not available due to ethical restrictions. Qualitative data collected for this study are not publicly available as they contain potentially identifying information of the research participants. Due to the participants residing in small and remote communities in Nauta and Parinari, the research team ensured that the data presented were de-identified in a manner that preserves their confidentiality, including the use of generic participant labels for quotes used in the report.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjgh-2023-012391
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Disruptions to education have been shown to have adverse effects on adolescent girls. Longitudinal studies in Malawi and Kenya showed that COVID-19 led to lower school re-enrolment rates, higher dropout among older adolescent girls and increased pregnancy risk for girls aged 15–19 years. A systematic review across low-income and middle-income countries found varying increases in adolescent pregnancy during the pandemic due to factors like school closures, peer pressure and economic challenges. However, data from Brazil showed a decrease in unplanned adolescent pregnancy, likely due to social distancing measures.
WHAT THIS STUDY ADDS
We provide a better understanding of the effects of the COVID-19 pandemic on the education and reproductive health of adolescent indigenous girls in the Amazon basin of Peru. This study also highlights three key factors affecting adolescent pregnancy during COVID-19: economics, education and healthcare access.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The pandemic may have long-lasting sexual and reproductive health consequences for adolescent girls whose education was severely disrupted. The knowledge gained from this research can be used to inform interventions and policies that may be implemented in this region to reduce the risk of adolescent pregnancy and school dropout, especially targeted towards indigenous youth.
Introduction
Adolescent pregnancy (AP) has adverse maternal and perinatal outcomes with increased risk of morbidity and mortality. 1 Globally, pregnancy and childbirth complications are the leading cause of death among girls 15–19 years of age. 2 3 To improve adolescent sexual and reproductive health (SRH) outcomes, increasing the educational attainment of girls is an effective strategy. 4 5 However, school closures to mitigate COVID-19 spread had unintentional consequences. It was estimated that 11–20 million children globally dropped out of school due to economic shocks of the pandemic, 6 7 a majority were secondary school-aged girls. 8 9 Dropout was more profound among girls in vulnerable and marginalised communities. 6 Girls who dropped out of school were at increased risk of exploitation, gender-based violence and child marriage. 10 Decreased female schooling is associated with low contraceptive use 11 and in turn, decreased contraceptive use has been shown to increase adolescent fertility. 12 13 Conversely, higher education levels deter AP, especially in low-income and middle-income countries. 14
A longitudinal study in Malawi of pre-COVID-19 and post-COVID-19 data found that extended school closures resulted in lower school re-enrolment rates and higher dropout rates, especially among older adolescent girls. 15 In Kenya, there were observed significant differences in secondary school-aged girls between the pre-COVID-19 and COVID-19 cohorts, with the latter group reporting a twofold to threefold higher risk of pregnancy and dropout. 16 A systematic review examining the effect of COVID-19 on adolescent health, education, and other social and economic factors in low-income and middle-income countries found that increased AP rates were influenced by school closures, peer pressure, lack of family planning and economic pressures. 17 Conversely, Latin America, particularly Brazil, experienced a decrease in unplanned adolescent pregnancies during the first year of the pandemic likely due to enforced social distancing measures. 18 These data, however, may not have fully captured the long-term risks of AP due to COVID-19 mitigation efforts, did not differentiate between high-risk groups and were not representative of all Latin American countries. 19
In Peru, there was a slight increase in AP in 2021, especially in the selva or jungle region, although it is unclear if this was a result of the pandemic as the study used live birth certificate data. 20 The study furthermore does not take into account Peru’s COVID-19 migration efforts put into effect on 12 March 2020. The government imposed some of the earliest and strictest lockdowns in the world and mandated school closures nationwide 21 affecting over 8 million children from pre-primary to secondary school. 22 23
Latin America and the Caribbean have the second-highest rate of AP in the world despite reductions made in the past two decades. 6 24 In Peru, the fertility rate among adolescents 15–19 years was 58.0 in 2020 and remains considerably high when compared with other middle-income countries. 24 Moreover, these rates are considerably higher among adolescent girls residing in rural areas, the selva (jungle) regions and within the lowest wealth quintiles of Peru. 25 Thus, it is not surprising that Loreto, located in the Amazonian basin of northeastern Peru with a predominately rural population and high rates of poverty, has one of the highest rates of AP in the country. 25 Loreto also has some of the country’s poorest maternal and child health outcomes. 26
Peru’s COVID-19 containment measures may have unintentionally affected adolescent girls in the Loreto region. However, available data are limited, making it challenging to fully understand the extent of these effects. The purpose of the study was to gain greater insight into the downstream effects of the COVID-19 pandemic on the educational and reproductive health outcomes of adolescents within the Amazon basin—specifically focusing on school dropout and AP.
Study sites
The study sites were located in Nauta and Parinari districts of Loreto, Peru along 210 km of the Marañón River, a major tributary of the upper Amazon River. We conducted research in 11 communities. The study sites ranged in size from 120 to over 400 people and were largely designated by the Peruvian government as indigenous population centres or communities. Most were only accessible by boat.
Less than 15 000 people reside in the rural communities of Nauta and Parinari of our study area, a majority identifying as either Catholic or Evangelical and indigenously as Kukama. 27–29 The predominant language spoken is Spanish. The main livelihood activities are fishing and farming; communities closer to the capital city of Iquitos also make and sell handicrafts.
Communities had limited access to health centres along the Marañón River depending on location and population density. In Peru, primary health centres are divided into four types from lowest (I-1) to highest (I-4) service provision. The urban centre of Nauta, which has the only paved road to Iquitos, services a larger population with I-4 and I-3 health centres. The population centre of Parinari has the other I-3 health centre. In our study area, there are 11 I-1, 1 I-2, 2 I-3 and 1 I-4 health centres (see figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
Map of communities in the districts of Nauta and Parinari, Loreto, Peru embedded with community health workers (CHWs) through Mamás del Río service area. Primary health centres are divided into four types from the lowest (I-1) and highest (I-4). I-1 refers to health posts which usually include one nurse’s aide, nurse or nurse midwife. I-2 refers to a health post with a medical doctor which includes one of the personnel/services from an I-1 establishment and a general physician or surgeon. I-3 refers to a health centre and includes personnel/services from I-1 and I-2, a dentist, laboratory technician, pharmacy technician and a statistical technician. I-4 refers to a health centre with an inpatient facility and includes personnel/services from I-1 to I-3, a specialist physician and professional pharmacist.
Not all communities have a secondary school. There are 38 secondary schools in our study area including 10 located within and directly around the port city of Nauta. Secondary school consists of 5 years from grades 7 to 11, with students typically aged 13–18 years. 30
Study design
We conducted both in-depth interviews (IDIs) and focus group discussions (FGDs). For the IDIs, we collected data from adolescents defined as either a pregnant girl, non-pregnant girl, or boy, and community leaders. Inclusion criteria for adolescent IDIs were Spanish-speaking youth between the ages of 15 and 17 years who attended school full-time before March 2020. Pregnant adolescents included those who were primigravida or primiparous (having become pregnant after August 2020 or 6 months after the start of the pandemic). Non-pregnant adolescent girls were nulliparous. Adolescent boys had no paternity exclusion criteria. We included male participants to enhance our comprehension of peer and relationship dynamics, aiming for a more comprehensive understanding of the experience of the pandemic for adolescents. Community leaders were identified as those who hold a place or occupation of distinction in our study sites, including certified medical professionals, and indigenous or youth leaders. Participants were required to be Spanish speaking and either worked or resided in Nauta or Parinari.
FGDs were conducted with educators and community health workers (CHWs) who volunteered to participate in the study. Educators eligible for inclusion had to be Spanish speaking and had current or prior experience working as an educator, staff, or administrator in a local secondary school in Nauta or Parinari. CHWs were required to be Spanish speaking, residents of Nauta or Parinari, had previous experience as a CHW before the pandemic and be current active members of Mamás del Río, a project through Universidad Peruana Cayetano Heredia. Mamás del Río is a community-based health intervention project focused on improving maternal and neonatal health outcomes in rural Amazonian communities of Peru. 31–36 We sampled CHWs and educators in key access points along the Marañón River. The FGDs were held in larger population centres because of the availability of secure and private spaces. Gender-specific FGDs were held with the CHWs. However, owing to the small number of educators, we did not separate these participants by gender for the FGDs.
We used purposive sampling using the snowball principle to identify interview participants for the study. We first identified pregnant adolescent girls in Nauta and Parinari with the help of local obstetricians and CHWs. In study sites with identified pregnant adolescents, we first introduced our research to the indigenous community leader or apu when available. Once permitted to conduct the study in the community, we would interview the apu. Next, we would interview the pregnant adolescent and ask her to refer an adolescent boy and a never-pregnant adolescent girl for an interview. In circumstances where they could not make a referral, we relied on the CHW or local obstetrician for the recruitment of participants in the same community who met our inclusion criteria.
Guides for the IDIs and FGDs were developed to gain a contextual understanding of factors that directly and indirectly influenced adolescent educational attainment and reproductive health during the pandemic. Additionally, our semistructured interview guides included sensitive SRH topics, which participants may under-report because of confidentiality concerns and reluctance to disclose potentially embarrassing personal information. 37 To address this, SRH questions were phrased to capture the experiences of adolescents in their community rather than of the individual. This technique was adapted from Westgard et al . 38
The numbers of IDIs and FGDs were determined by thematic saturation, 39 conducted in Spanish, and lasted approximately 45–90 min. Demographic data were collected from each participant at the start of the interview or FGD. IDIs and FGDs were recorded using a voice recording device. If the participant declined to be recorded, notes were handwritten.
Study participants
Table 1 shows that the mean age of adolescent participants was 15.9 years. Over half (55.2%) self-identified as indigenous. 44.8% did not specify an ethnic identity despite living in a recognised indigenous population centre or community. All adolescent participants were enrolled in secondary school before the pandemic, of which 58.6% were currently enrolled and 27.6% had since graduated. Four adolescents (13.8%) permanently dropped out of school between March 2020 and March 2022.
- View inline
Demographic characteristics of study participants in the study sites of Nauta and Parinari by type, n=56
IDIs with community leaders included seven apus, four medical professionals and one youth leader. Not all apus were available in the study sites for an interview; however, none had declined our request to conduct the study. Only one study site did not have an apu. All male community leaders in this sample were apus. Female community leaders consisted of obstetricians, a medical technician and a youth leader. The mean age of community leaders was 44.5 years with two-thirds (66.7%) having completed secondary school or higher. Most community leaders were indigenous (75.0%).
The mean age of the FGD participants was 45.7 years with 33.3% having completed primary school and 53.3% having completed secondary school or higher. All CHW participants identified as indigenous while educators identified as non-indigenous.
Data collection
Field observations were conducted in June and October 2022. Field notes were compiled and organised by date. This included notes on adolescent interactions and SRH education. Brochures and other health materials provided by the local health clinics of the ‘Decidamos Ya! Reducir el Embarazo Adolescente en Loreto’ campaign were also collected and reviewed. 40 41 We used these data to triangulate the findings from IDIs and FGDs on how and in what context SRH information was provided to adolescents.
IDIs were conducted in June 2022, 3 months after the reinstitution of in-person classes throughout Peru. Empirically, to reach thematic saturation, we had aimed to complete 12 IDIs among each homogeneous group 42 ; however, we had difficulty recruiting adolescents for the study due to the sensitive nature of discussing SRH, the unfamiliarity of participating in qualitative studies and time constraints. In total, we completed 41 IDIs consisting of 11 pregnant adolescents, 9 never-pregnant adolescent girls, 9 adolescent boys and 12 community leaders in Nauta and Parinari. FGDs with educators and CHWs were conducted in October 2022 to supplement interview findings.
Data analysis
Notes and recordings were transcribed and uploaded to ATLAS.ti Windows (V.22.0.6.0). 43 Using a thematic approach, we derived patterns from our qualitative data. Themes with subthemes were identified through an iterative process using notes gathered from field observations, field debriefings and IDIs across participant groups. Codes were developed both inductively and deductively. Broader code categories included: social norms, SRH access, SRH outcomes, contraceptive use, confidence/aspiration, COVID-19 effects, education, mobility, social interactions and technology use. For this paper, we only present data that were expressively linked to youth’s COVID-19 experience. A more in-depth examination of social norms is referenced in a compendium paper. 44 No new codes emerged from the FGDs. Once the codebook was finalised in Excel, codes were uploaded to ATLAS.ti and used by the research team to code each interview and FGD. Six IDIs were selected to test intercoder reliability with a Krippendorff alpha-binary of 0.80 or greater across code groups. Identified discrepancies were reviewed and discussed between coders, then recoded through a consensus process.
The design, data collection and analysis phases of the research were informed by the interdisciplinary expertise and experiential backgrounds of our research team in the fields of public health, medicine, sociology, epidemiology and anthropology. See the online supplemental appendix for reflexivity statement.
Supplemental material
Effects of covid-19-related restrictions.
Adolescents clearly remembered the day when they received news of the emergency declaration by the Peruvian government of a country-wide shut down due to the COVID-19 pandemic. The initial 15-day lockdown was extended for 2 years, and community members were severely restricted in their movement outside their homes.
At the time of the pandemic, it was different… For example, you couldn’t go out to play, you couldn’t go out to have fun in the street, everything was controlled, sometimes security took care of us, and you couldn’t go out anywhere. (adolescent boy, IDI)
With consecutive lockdown periods under the state of emergency, adolescents grew more hopeless. They also described this period as sad, fearful, lonely and boring.
That’s how we went and until I think the month of June when there was an indefinite lockdown. There we lost hope of everything. (non-pregnant adolescent, IDI) I gained a lot of weight because, what were we doing? In the house, we made our breakfast, our lunch, our dinner. We ate and laid down… everything was boring. We didn’t go out, we just looked out the window. We closed it because we were afraid of getting infected. (non-pregnant adolescent, IDI)
Drinking and smoking also increased during this time as a coping mechanism.
Well, here was a time that… they were a lot into alcohol. Yes, alcohol, and they [adolescent boys] smoked a lot… Yes, they were like that for a while. (non-pregnant adolescent, IDI)
The COVID-19 pandemic had negatively affected communities along the Amazon basin. Due to a growing fear of contagion, rural communities along the Marañón River closed their ports and followed strict social distancing precautions starting in early 2020 as the rapid spread of disease, and a large number of deaths were reported from Iquitos. In addition, adolescents feared leaving their homes. Despite these mitigation efforts, ‘in the end, we all ended up getting the disease’ (pregnant adolescent, IDI). Some shared personal experiences of deaths in their families; others recalled hearing about people dying of COVID-19 at the health posts. Yet, these restrictions may have been hard to enforce in rural areas, and over time, communities eased their COVID-19 restrictions as it became economically unviable to continue strict isolation measures.
Households reported a loss of income during the pandemic. Fishing, as the primary livelihood activity and part of the cultural identity of the Kukama people in this region, was affected by mobility restrictions along the Marañón River and port closures. The trade linkages were severely disrupted as fish and products could not be sold in the urban markets of Nauta and Iquitos, and family businesses were unable to get supplies.
It was pure state law. The other communities too, are a bit difficult to enter another community. In other words, they locked us up. (male community leader, IDI) There has been a port blockade here, right? No exit or entry, right? But that led to chaos. There was no rice, there was no chicken, there wasn’t much. (male community leader, IDI)
Households experienced financial hardships which were further exacerbated by increased food prices during COVID-19. Households faced food insecurity and resorted to negative coping strategies such as reduced food intake, selling non-essential household items, relocating, and/or subsistence fishing and farming.
Here are times, like they say, we don’t have the money. Sometimes, uhum (laughs) we eat little. Or sometimes my partner goes to look for work… on the farm; [what] he produces, he sells. Sometimes we have [money], we just buy it… sometimes you have little and you can’t buy so many things [like] what you want to eat sometimes… I know that a lot has gone up [in price]. What you could eat before… with little money and now it’s no longer possible. (pregnant adolescent, IDI)
Additionally, many fathers were forced to find work outside of the community leaving adolescents with less parental supervision. There was also a growing demand for adolescents to work in the chacras or farm/fields, family gardens or fish to supplement household food.
[We] sold everything. I didn’t know how; all the money had gone down the drain. We were left without money and so we went to the farm. (pregnant adolescent, IDI)
Other youth went ‘to look for work in the city’ (pregnant adolescent, IDI), which usually consisted of informal or labour-intensive employment such as construction. Adolescent girls hired as domestic workers reported unpaid and exploitative working conditions:
During the pandemic, I could not go out because, because I did not live with my mother. I lived with another lady, that is, she made us work a lot… What did I not do!? I didn’t rest. I [worked] mostly the fields, cultivated [all day] in the sun, sometimes washed clothes, and had no rest. (pregnant adolescent, IDI)
Young girls forced to work outside of their homes in larger urban areas due to economic insecurity during the pandemic were more vulnerable to early unions and AP; some girls had sexual relations with men in the home or extended family of their employer. However, from the accounts of the participants, it is unclear how these relationships were initiated.
Access to healthcare
Health centres, sporadically spread along the Marañón River, were not accessible as movement was severely restricted, and many facilities were closed during the pandemic. If open, they were understaffed and diverted their limited resources toward the COVID-19 response.
Additionally, health staff did not travel to the communities, and medicine was scarce, further disrupting regularly provided services, including contraceptive access, during this time.
Many continued to take care of themselves, and many did not because, as I say, they did not have as much access since the medicines did not arrive at the clinics. (female community leader, IDI) Yes, it has changed with the pandemic. The nurses are in charge of giving contraceptive methods but in the pandemic, they were not here [in the community], and there was no one to turn to. (adolescent boy, IDI)
Botiquines, or community medicine cabinets, were quickly depleted of their medical supplies and were not replenished, forcing participants to rely more heavily on CHWs and locally available medicinal plants or remedio vegetal for the treatment of COVID-19, other ailments and family planning. The use of medicinal plants was not uncommon to prevent unwanted pregnancies and may have had increased use during the pandemic as formal SRH services and modern contraceptives were severely limited.
I believe that there are, uh, enough plant medicines to take care of ourselves, as you say, ‘toronja’ [grapefruit] is one, for me, it is a very effective remedy. I took care of myself just like that… I cannot get pregnant. (female CHW, FGD)
Adolescent girls refrained from seeking reproductive healthcare beyond their community because of COVID-19-related restrictions. When intercommunity travel was permitted, girls were required to travel to the health post by boat chaperoned by a parent or older adult male relative. Unaccompanied travel was not permitted. This prompted concerns from girls about accessing confidential and private SRH services.
SRH information
Before the pandemic, adolescents accessed SRH education from visiting organisations or in school. Health clinics also provided SRH information to adolescents primarily during on-site appointments or health checks. When financed, the obstetrician from the health clinic visited neighbouring communities through campaigns to provide abstinence-based SRH education in schools (as noted in our field observations), at church or in other open community spaces. However, the subject matter varied depending on the instructor. Despite formal efforts to provide adolescents with SRH information, it was considered inefficient, inconsistent and at times, incorrect.
That is, they gave us talks but… we couldn’t prevent ourselves. In other words, even though they gave us instructions on how to take care of ourselves with the methods… most of my classmates have gone out… like this… that is, they are all moms. (pregnant adolescent, IDI) The teacher told them that they can also be infected [with HIV] when they use the same bathroom: ‘You have to wash the bathroom with bleach, do that… when you sneeze the virus spreads, just like COVID, you have to take care of yourself.’ (adolescent boy, IDI)
Regardless of how effective formal SRH education was perceived among adolescents, during the pandemic, it was largely absent or unavailable despite calls from Peru’s Ministry of Education to teach contraceptive methods to youth.
In the pandemic, in the first year they didn’t talk…, and now it [is said] that the Ministry of Education itself tells teachers to come and talk about contraceptive methods. (non-pregnant adolescent, IDI)
This can be attributed to lockdown measures that restricted adolescents from accessing education at the health posts. Also, virtual SRH education was considered less optimal and largely halted as schools and obstetricians lacked the resources to effectively teach the subject.
In the absence of formal SRH education during the pandemic, adolescents relied on informal networks for information and advice. For many, parents were identified as primary source of SRH information. However, the extent of information shared is unclear as one adolescent boy described it as ‘not enough’. The conversation between parents and daughters centred around ‘[taking] care not to get pregnant’, while conversations with sons had greater emphasis on ‘[taking] care of themselves’ (pregnant adolescent, IDI).
Thus, adolescents depended on friends for more explicit information on sexual intercourse and contraceptive methods, sharing what they learnt from personal experience, health posts, previous SRH workshops at school, parents, older siblings, partners or the internet. Due to increased access to technology during COVID-19, adolescents turned to this resource to obtain SRH information.
Prior to the pandemic, secondary schools located in the Marañón River employed teachers from urban areas who stayed for short periods with a schedule that allowed them to travel back and forth. The quality of teaching was considered low due to the poor recruitment of qualified teachers. Many also did not ethnically identify as indigenous. Not all communities had secondary schools and students had to travel by peke-peke or gasoline-powered wooden boats to attend in person. This presented challenges in terms of increased transportation costs and the dangers of traversing hazardous river conditions and inclement weather. In cases where students had to attend school in another community, they needed to rent accommodations in a dormitory, home or a designated hostel nearby, incurring additional educational costs.
During the pandemic, schools were closed, teachers did not travel and students were socially isolated in their homes. To meet the educational needs, teachers would make photocopies of the homework to be sent by boat to the communities each month. When available, the Peruvian government distributed tablets to promote virtual education. Households were required to pay for photocopy charges and to recharge mobile data plans for the tablets; however, many could not afford these additional costs as they were already experiencing economic hardships because of the pandemic. Furthermore, several communities in the Amazon basin do not have reliable access to electricity or internet via cellular towers. Government-issued tablets came with data plans from a single telecom company that were not uniformly available across communities. This rendered online education as an impractical option for many students. To help offset the educational costs during the pandemic, parents gathered small groups of students to share resources.
It was something…not as normal as it was before. You didn’t see your classmates anymore, it’s not like being at school with everyone together…it was something separate, we only met as a group [with] some of our classmates, that’s how it was. (adolescent boy, IDI)
Adolescents were less motivated to attend classes online. Some expressed frustration in adapting to this new format of learning and felt that it was less engaging, of lower quality, inconsistent and less productive. Virtual classes were offered less frequently and in shorter duration than in-person classes had been before the pandemic. Students, during this period, temporarily abandonado or abandoned virtual classes and stopped submitting homework; however, many did not consider this dropping out or leaving school permanently. In the end, students passed or graduated regardless of meeting academic proficiency or performance for their grade level by government order (Vice-Ministerial Resolution No. 193-2020-Minedu) 45 :
Yes, there were some changes as everything was virtual. All the students passed [their] grade, just like that, without knowing anything… that we have learned almost nothing. (adolescent boy, IDI)
Teachers recounted that when schools reopened for in-person classes in March 2022, many students could not be accounted for. It was assumed that these students dropped out.
I have students who have not been on my attendance list since March [2022] … and there are at least five in each classroom. We have not heard from them since March to this day [October 2022]. I don’t even know them either because they didn’t attend [school]. (male educator, FGD)
Adolescents were more likely to drop out in their final years of secondary school, usually reflecting changing life priorities related to work, relationships or having children.
I think now just to raise my child. Because I’m not thinking about going back to school… Everything is different – I mean that’s your reality, and besides that, the jobs that come don’t give you time for anything. (pregnant adolescent, IDI) Falling in love along the way, so after that, many do not finish secondary school. (male community leader, IDI)
During the pandemic, many adolescents were also pressured to discontinue their education due to the economic stress of the pandemic, choosing instead to support their families and, in some cases, work outside of their communities. Many did not re-enrol when schools reopened in their communities.
Interviewer: In the pandemic years, who has left school the most? Participant: The girls… Sometimes some young people, for work reasons, money…yes, mostly for that reason. (adolescent boy, IDI) [My friends/classmates] they didn’t want to go [to school] because maybe… well, it was boring, they worked, they saw the money and they didn’t want to study anymore. (pregnant adolescent, IDI)
Technology use
Communities along the Marañón River have limited access to the internet, and electricity was largely restricted to nightly use. However, our findings suggested that adolescents in this region used technology in a greater capacity than before the pandemic. Adolescents increasingly relied on technology to access virtual education through government-distributed tablets or personal cellphones, and as a means for social engagement when strict COVID-19 mitigation efforts limited individual movement and required youth to self-isolate. Adolescents also sought SRH information online because personal devices provided greater privacy. Yet, the use of technology for this purpose is not well supervised and community leaders were concerned about the growing technology use among adolescents and increased access to pornography.
They get into some programs, uh, let’s say that does a lot of harm to the child, to the adolescent… they use it [the internet] for bad things… and that is the issue for us; it is really worrying to see the child go crazy, right? (male community leader, IDI)
Early unions/AP
Many participants believed that the pandemic led to more unions and partnerships in their communities despite having limited social interactions during the pandemic.
No, the pandemic has made even more couples join together, and there have been even more couples here in the community because they did not go out, they did not go out to any town, and no town was allowed to enter… And that has meant that everyone… with that, the number of young people who have their partners within the community has increased. (male community leader, IDI)
Sexual and romantic relations were maintained in ‘secret’ (male community leader, IDI), using online platforms to connect and coordinate meetings in person despite strict lockdown restrictions.
Yes, sometimes when we go out there alone, we find ourselves, sometimes a chair, a bench, in a dark place as they say. (pregnant adolescent, IDI)
Many of the partnerships were observed between underage girls (<18 years) and older adult men 8–15 years their senior, with unions/cohabitation becoming obligatory upon pregnancy. The pandemic may have pushed more adolescent girls into relationships with older partners for economic stability and pressure to find a suitable partner. For example, the adult male partner of one pregnant adolescent was identified by his prominent position in the community and reported by the study participant and others as being ‘a good person’. The subsequent quote from a non-pregnant adolescent provided valuable insight into the dynamics of these relationships:
He is supporting me a lot, well, I tell you that from a very young age. Many girls always say: ‘I like older people’, right? (laughs) Because I think that an older person can help you, I say, or can guide you. (non-pregnant adolescent, IDI)
However, not all pregnancies result in a union. Some pregnant adolescents experienced abandonment during the pandemic.
During the pandemic, participants believed that there was an increase in APs in their communities. A pregnant adolescent shared that before the pandemic, many young girls played outside in the afternoons but afterward, she noticed most now have children. Others believed that AP was most common among girls aged 14–15 years but also included those as young as 12 years:
Well, in the pandemic it did affect a lot because people, students ah, about 15, 12 years old, 13, 14, 17, not much 17; more were 15 to 14 years old; there were quite a lot that they were gestating. (non-pregnant adolescent, IDI)
Causal diagram
Based on our research, we developed a causal diagram illustrating how COVID-19 affected education, health access and economics/household financial stability, and in turn, AP and school dropout (see figure 2 ). COVID-19 also inadvertently affected early unions and contraceptive use. The relationship between AP, school dropout/abandonment and early unions is bidirectional, indicating that AP is both a consequence and a cause.
Causal diagram of the effects of the COVID-19 pandemic on education and sexual and reproductive health of adolescents in the Amazon basin, Peru. Arrows indicate directionality, dashed lines indicate bidirectionality; red lines represent a negative relationship; black lines represent a positive relationship; outcomes are in grey boxes; the primary outcome of interest (adolescent pregnancy) is in the red diamond.
We observed that girls dropped out of school during the pandemic because they became pregnant or were forced to work due to economic insecurity. They migrated for work, often under exploitative conditions. They were vulnerable to advances made by adult men in the households they were employed and may have been subject to coercive sexual relations. Many returned to their communities pregnant; however, this would need further exploration as it was unclear from participant accounts how these relationships were formed. Likewise, girls may have also sought these relationships for greater economic stability.
Our research aimed to understand how adolescent SRH and education were affected during the COVID-19 pandemic. We were able to access remote indigenous communities in the Amazon basin of Peru and learn from vulnerable youth in this region. We found from our thematic analysis that the economic, educational and health effects of COVID-19 contributed to school dropout/abandonment, decreased contraceptive use, early unions and AP. However, the relationship between AP was not unidirectional between school dropout and early unions. In a longitudinal study in Peru, cohabitation and early unions were found to be intrinsically related to and often a result of pregnancy. 46
Economically during the pandemic, Peru experienced the greatest drop in gross domestic product among all Latin American countries, an estimated contraction of 11%. This decline can be attributed to the government’s COVID-19 mitigation efforts, and its effect on education, health and mobility. 47 Additionally, the pandemic pushed more families into poverty as unemployment increased. The informal job sector was particularly affected. 47 The financial repercussions of COVID-19 may have elevated the risk of AP, given that both low socioeconomic status and lack of employment opportunities in low-income and middle-income countries are associated with an increased likelihood of AP. 48
Likewise, the COVID-19 policies lacked cultural appropriateness and consideration for Peru’s indigenous people. The emergency declaration of compulsory social isolation by the Peruvian government gave little advance notice and left many indigenous groups without supplies and food. 49 When products were available locally, many households were priced out due to the high demand for these products when available. 49 The economic pressure of the pandemic not only pushed girls to drop out of school to seek employment outside of their communities, increasing their risk of AP, but changed nuclear family structures. Fathers, in particular, were forced to find work outside of the community resulting in a single-parent household, which may help drive AP. 46 50
COVID-19 mitigation efforts had further detrimental SRH consequences for adolescents. The pandemic made it difficult for youth to access SRH services. 51 This was affected by factors such as fear of COVID-19 contagion, access restrictions and cost. 17 52 Concerns around accessing confidential and private healthcare may have also reduced the utilisation of SRH services and contraceptives among adolescents. 52 Indigenous girls in our study sites were required to travel to the health post accompanied by a parent or adult man, potentially creating impediments to accessing these services. Such factors increased their susceptibility to AP as they face greater geographical, economic and cultural/linguistic barriers to accessing appropriate education and healthcare compared with their non-indigenous counterparts. 53
Education serves as a buffer against AP. 14 Favara et al found that in Peru, attendance and better school performance were associated with increased age of sexual initiation and a lower risk of early childbearing. 46 Conversely, girls with lower education levels were less likely to use contraceptives and were at a higher risk of pregnancy. 13 School retention is a key AP prevention strategy for secondary school-aged girls. 54 However, COVID-19 school closures affected how youth were able to access education. 17 Disadvantaged children in Peru (those whose parents did not complete secondary school) lost an average of 34% instructional time during the pandemic. 55 Ultimately, this may lead to wider educational inequalities and greater dropout, especially among poorer households like those in our study sites. 56 57
SRH information was largely absent during the pandemic and is unlikely to be compensated for in the future. 52 Even so, formal health education may have limited effectiveness in reducing AP among this population even before COVID-19 due to inconsistent programming and incomplete information. It has also been shown that SRH interventions based solely on school curricula have limited evidence of changing the sexual practices and behaviours of adolescents. 58 Apart from formal SRH education, adolescents also relied on parents, peers and the internet to acquire more knowledge. The reliability and accuracy of this information remain unclear and need further investigation as cultural taboos may restrict what is shared. 59 Notably, previous research in Peru’s central jungle region, as demonstrated in a case–control study, highlighted the protective effect of adolescent SRH communication with parents against AP. 60 While our study sample was of a different indigenous background, this finding underscores the significance of parent–adolescent communication and parent-sourced SRH education in AP prevention.
Furthermore, early unions between pregnant adolescent girls and older adult men were observed in our study and reportedly increased during the pandemic. Adolescent girls may be motivated to seek out relationships with older men for financial security or out of fear of not finding a suitable partner. 61 Studies have shown that adolescent girls were at higher risk of engaging in exploitative work during COVID-19 and were subject to unwanted sexual advances, 51 a known determinant of unintended pregnancies. 54 It is important to also consider the unequal gender power relationships between adolescent girls and their adult partners in the Amazon basin. Girls lacked agency to make decisions around their reproductive health. 62 The COVID-19 pandemic likely intensified these concerns. However, our data were limited as older male partners were not included as participants in our current research, restricting us from gaining deeper insight into this phenomenon within the specific cultural context of our study site.
Other limitations of our study included possible recall and social desirability bias. Participants may have had difficulty recalling events over the last 2 years since the national school closures in March 2020. To reduce this bias, we conducted IDIs with adolescents and community leaders within 3 months of school reopening in Peru.
We also recognise that social desirability may have influenced responses among adolescent participants when discussing SRH and education. In the demographic survey, only four adolescent study participants (13.8%) had declared that they had permanently dropped out of school during the pandemic; however, in interviews, we found that a larger number may have temporarily ‘abandoned’ school during this same period. Using other terminologies or descriptions in the demographic survey and interviews may help elicit this information better.
Due to the nature of how participants for the FGDs and IDIs were recruited, they may not have been representative of the population. CHWs who volunteered to be in our study could easily travel to the location of the FGDs; however, this inadvertently may have biased our sample as more isolated communities along the Marañón River may not have been represented. Likewise, educators for our FGD were only recruited from one secondary school in our study site, and medically trained community leaders did not identify as indigenous although they lived in these communities. Adolescents who agreed to participate in interviews may also be inherently different from those who declined. For future research, we would include adult male partners of adolescent girls, a group not originally part of the study design. It was only through IDIs and FGDs that we identified this knowledge gap.
Other effects of COVID-19 on adolescent health were not explicitly explored in our research. These include mental health, gender-based violence and poverty. However, we found that participants often alluded to these topics when relating their experiences of the pandemic in terms of their relationships, AP and school. These factors would need further investigation as they are important to uncovering the gaps in current knowledge of the pandemic’s effect on our study population.
Conclusions
As we transition out of the COVID-19 pandemic, we recommend concentrated efforts to counteract the effect COVID-19 had on adolescent girls in the Amazon who are the most vulnerable in Peru. This includes specific strategies aimed at reducing their risk of AP. The insight gained from our research, especially around how youth access and use information, health resources and technology, can help inform and develop post-pandemic interventions that aim to reduce the incidence of AP in these communities. Overall, our research underscores the growing importance of investing in tailored, comprehensive and consistent SRH education in indigenous communities that involves a broader network of formal and informal educators. Furthermore, we propose leveraging the increased use of technology by integrating it into SRH education. This approach must be paired with more accessible, adolescent-friendly, confidential and private SRH services. It is crucial to ensure that SRH services and education are culturally appropriate and readily accessible for indigenous populations, particularly during future pandemics, to effectively address their unique needs and geographical isolation.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
Ethical approval for the research was obtained from Universidad Peruana Cayetano Heredia as the IRB of record (SIDISI Code: 2071919) approved on 13 May 2022, and with amendments on 6 June 2022 and 3 October 2022. The University of Arizona served as the external IRB (STUDY00001109). Before data collection, we obtained written informed participant consent. For participants under the age of 18 years, we obtained both assent from minors and parental consent. Informed consent was obtained prior to community leader interviews and FGDs. Adolescent participants received a compensation of S/10 PEN (equivalent to US$2.50) per interview, whereas community leaders, CHWs and educators were given S/15 PEN (equivalent to US$3.75). For CHWs who incurred travel costs to attend the FGDs, we provided reimbursement for the cost of gasoline used (~S/20 PEN per gallon).
Acknowledgments
We would like to thank the Agentes Comuntarios de Salud of Mamás del Río, the community leaders, local health staff, teachers and adolescents of the communities of Nauta and Parinari for their contribution to our research. We would also like to acknowledge the support and guidance of Mamás del Río, Universidad Peruana Cayetano Heredia, Gerencia Regional de Salud de Loreto and the University of Arizona. Special thanks also go to Elizabeth Jacobs and Cory Mabel for their contributions.
- Conde-Agudelo A ,
- Belizán JM ,
- World Health Organization
- Chandra-Mouli V , et al
- Estrada F ,
- Atienzo EE ,
- Cruz-Jiménez L , et al
- Azevedo JP ,
- Goldemberg D , et al
- Schmidt D ,
- United Nations Educational Scientific and Cultural Organization (UNESCO)
- Bandiera O ,
- Buehren N ,
- Goldstein M , et al
- United Nations Children’s Fund
- Ainsworth M ,
- Sánchez-Páez DA ,
- Starrs AM ,
- Barker G , et al
- Carbajal J ,
- Behrman J , et al
- Zulaika G ,
- Bulbarelli M ,
- Nyothach E , et al
- Ramaiya A ,
- Chandra-Mouli V ,
- Both R , et al
- Monteiro DLM ,
- Monteiro IP ,
- Machado MSC , et al
- Gutierrez M ,
- de Hoyos R , et al
- Román-Lazarte VE ,
- Fernández-Fernández MF ,
- Huanco-Apaza DD
- End Coronavirus.org
- Instituto Nacional de Estadística e Informática
- Ministerio de Cultura
- Social Innovation in Health Initiative
- Reinders S ,
- Neuman M , et al
- Lange IL , et al
- Castro-Arroyave D ,
- Del Mastro N I ,
- Tejada-Llacsa PJ ,
- Reinders S , et al
- Huicho L , et al
- Brener ND ,
- Billy JOG ,
- Westgard CM ,
- Bello G , et al
- PLAN International Peru
- ↵ ATLAS.Ti scientific software development GmbH . ATLAS.ti 22 Windows ,
- Woodson LL ,
- Garcia Saldivar A ,
- Brown HE , et al
- Ministerio de Educación del Perú
- favara marta ,
- Pradhan R ,
- Cherofsky J
- Lopez-Calva LF ,
- Meherali S ,
- Adewale B ,
- Ali S , et al
- Lindberg LD ,
- Equipo de Seguimiento Concertado a las Políticas de Salud Sub Grupo
- Neidhöfer G ,
- Chaabane S ,
- Doraiswamy S ,
- Chaabna K , et al
- Garzón-Orjuela N ,
- Samacá-Samacá D ,
- Moreno-Chaparro J , et al
- Quincho-Estares ÁJ ,
- Flores-Rondon AJ , et al
- Techasrivichien T ,
- Suguimoto SP , et al
- Del Mastro N. I
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
PM and MMB are joint senior authors.
Handling editor Manasee Mishra
PM and MMB contributed equally.
Presented at The research was previously presented as a poster presentation at the Ninth Annual Stanford Global Health Research Convening at Stanford University, California on 25 January 2023.
Contributors LW, PM and MMB led the conception and design of the study with input from PAM, LVF, SP and HEB. LW, PM, HEB and MMB helped to secure funding for the research. LW, PM and MMB coordinated efforts for ethics approval through the University of Arizona and Universidad Peruana Cayetano Heredia. Study site logistics were coordinated with MMB, NAdM and AGS. LW and AGS conducted data collection, codebook development and analysis. LW and AGS interpreted the data with guidance from MMB. LW drafted the manuscript. PAM, MMB, HEB, PM, AGS and NAdM provided revisions to the manuscript. All authors reviewed the final manuscript for publication. LW, as the guarantor, accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding This work was supported by the Fulbright-Fogarty and Global Health Equity Scholar’s Programme (grant #: D43TW010540). Additional funding was provided by the University of Arizona’s College of Public Health Dean’s Fund (grant #: N/A) and the Graduate and Professional Student Council Research and Project grant (grant #: N/A).
Map disclaimer The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests None declared.
Patient and public involvement Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review Not commissioned; internally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- Open access
- Published: 29 April 2024
Impact of COVID-19 pandemic among patients with lung and head and neck cancer assisted in a public cancer center in Brazil
- Gilson Gabriel Viana Veloso 1 ,
- Flávia Duarte Amaral 2 &
- Angélica Nogueira-Rodrigues 3
BMC Cancer volume 24 , Article number: 539 ( 2024 ) Cite this article
149 Accesses
Metrics details
There is no updated national data regarding the real impact of the COVID-19 pandemic on delaying diagnosis and treatment among patients with lung, and head, and neck cancers in Brazil. This study aimed to analyze the COVID-19 pandemic impact on cancer diagnosis and clinical outcomes among lung, head, and neck cancer patients assisted in a tertiary cancer center in Southeastern Brazil, as well as to analyze these patients’ pretreatment clinical features.
Retrospective cohort of patients with lung or head and neck cancer assisted in a tertiary cancer center in southeastern Brazil between January/2019 and December/2021. To assess statistical differences among groups [i.e., cohort 2019 versus (vs.) 2020 and 2019 vs. 2021] chi-square test was used with a 5% significance level and 90% power for sample size calculation. Differences among baseline clinical features and sociodemographic characteristics were evaluated either by T-test for two samples or Fisher’s or Pearson’s chi-square test (for quantitative or qualitative variables). All utilized tests had a 5% significance level.
Six hundred fifty-two patients were included, 332 with lung and 320 with head and neck cancer; it was observed a significant decrease in oncologic treatment recommendations and increase in palliative care recommendation for patients with lung cancer, despite similar stages at diagnosis. During the COVID-19 pandemic, more pain symptoms were reported at the first Oncology assessment for patients with head and neck cancer ( p < 0.05). Compared to 2019, head and neck cancer patients diagnosed in 2021 presented a worse initial performance status ( p = 0.008). There was a statistically significant increase in survival for patients diagnosed with head and neck cancer in 2021 when compared to 2019 ( p = 0.003).
Conclusions
This research highlights low survival rates for patients with lung and head and neck cancer in Brazil, even before the pandemic started, as consequence of advanced diseases at diagnosis at the public health system and clinical degrading features. Additionally, there was an increase incidence in both lung cancer and head and neck cancer despite no differences in clinical stage. This reflects how fragile is the public healthcare system even before facing an acute public health crisis such as the COVID-19 pandemic. Yet, the total impact on public health may follow for many years.
Peer Review reports
Cancer is now the first or second leading cause of death in over 60% of the countries, according to the World Health Organization (WHO) [ 1 ], and nearly 70% of cancer deaths occur in middle and low-income countries (LMICs) [ 2 ]. In 2020, 225,830 Brazilians died from the disease [ 3 ].
The Brazilian Ministry of Health estimates nearly 704,000 new cancer cases in the country for each year between 2023 and 2025 [ 3 ]. Regarding lung cancer, 32,560 new cases are expected per year, placing this tumor as the fourth most common cancer in the country [ 3 ]. Focusing on oral cavity and laryngeal cancers, nearly 15,100 and 7,790 new cases per year are expected, respectively [ 3 ].
Since the beginning of the coronavirus-19 pandemic (COVID-19), by the end of January 2023, over 6,7 million people have died from the disease worldwide, including nearly 700,000 Brazilians [ 4 ], and since its’ beginning, oncologists were concerned about its impact on patient care [ 5 ].
The overall distraction among health care systems due to COVID-19 may implicate deleterious effects on cancer patient assistance in the short and long-term follow-up [ 6 ] and quantifying the impact of delayed cancer diagnosis and treatment due to the pandemic in both the clinical stage and the prognosis is a complex task [ 7 ].
The main objective of this study was to analyze COVID-19 pandemic impact on cancer diagnosis among lung and head and neck cancer patients assisted in a tertiary cancer center in Southeastern Brazil as well as to analyze these patients’ pretreatment clinical features.
Materials and methods
Study protocol.
This was a retrospective cohort study at Santa Casa de Misericórdia de Belo Horizonte , a tertiary cancer center in Belo Horizonte, Southeastern Brazil. This study aimed to analyze whether the COVID-19 pandemic harmed patients with lung and head and neck cancers, yielding delayed diagnosis, more advanced clinical stage at diagnosis, and poorer outcomes in comparison with 2019, the year before the pandemic. For that aim, three cohorts were defined including patients diagnosed between 2019 and 2021, one cohort for each year. To proper collect and access data, two separate comparisons were defined: 2019 vs. 2020 and 2019 vs. 2021. In 2020 Brazil had major changes concerning lockdowns, restructure in the hospital to become a respiratory hospital for COVID-19 patients and major impact on increased deaths. In 2021, Brazil’s scenario started to change with vaccination coverage in January 2021, flexibilization of lockdown regimens and hospital’s regaining the opportunity to fully work as they usually did before the pandemic has started (i.e., 2019).
Population of analysis
Inclusion criteria included patients with a confirmed diagnosis of either head and neck cancer or lung cancer, above 18 years old, who had their first oncology assessment between January first, 2019, and December thirty first, 2021. Subjects could have had their first oncology assessment either by a hospital admission or on an ambulatory basis.
Exclusion criteria included: patients with inconclusive biopsies for malignant neoplasia, thyroid cancer, thymic tumors, and pleural mesothelioma. Those tumors were excluded from the final analysis due to different biological behavior in comparison to the other tumors here assessed.
Tumors were codified according to the International Classification of Diseases 10th edition (ICD-10) [ 8 ] as here described: C00, C01, C02, C03, C04, C05, C06, C07, C08, C09, C10, C11, C12, C13, C30, C31, C32, C33, C34, C43 and C80.
Data collection
Data collection was performed through a structured questionnaire developed by the authors aiming to assess all proposed objectives in this research. All charts were available for consultation at the hospital’s electronic system for assistant physicians.
For lifestyle habits associated with head and neck cancer, the following variables were included in the questionnaire: smoking and alcohol intake histories, divided into 2 categories: current or former and never; and, and body mass index (BMI – kg/m²), analyzed continuously and then categorized based on cutoffs for malnutrition (< 18,5 kg/m²), adequate (18,5–24,9 kg/m²), overweight (≥ 25,0 kg/m²), and obesity (≥ 30,0 kg/m²).
Sociodemographic variables included race and education level. Race was categorized into four categories: undeclared, Caucasian, black, and mixed race. Education level was categorized into 2 categories: ≤ 8 years of formal education and > 8 years of formal education. Financial status was initially included as a sociodemographic variable, however, due to a lack of data on charts (100% of misinformation) it was excluded.
To assess patients’ clinical features the following variables were included: clinical or pathologic stage, performance status at first oncologic assessment and after 6 months, treatment indication (including all modalities, i.e., surgery, chemotherapy, and/or radiotherapy), the indication of exclusive palliative care at first oncology assessment, pain symptoms reported, necessity of enteral nutrition, the indication of tracheostomy, and dental work-up before treatment started. The latter was used solely for patients with head and neck cancer. A dichotomized strategy was used (i.e., yes, or no) for the necessity of enteral nutrition, the indication of treatment, the indication of exclusive palliative care at first oncology assessment, pain symptoms, the indication of tracheostomy, and dental work-up before treatment.
Patients were staged accordingly to the TNM Classification of Malignant Tumors 8th edition by the American Joint Committee on Cancer [ 9 ]. Performance statuses were assessed based on the Eastern Cooperative Oncology Group (ECOG) scale, divided into six categories (range 0 to 5) [ 10 ]. Outcome analysis and objective response rate were based on the guideline for Response Evaluation Criteria for Solid Tumors (RECIST) 1.1 [ 11 ].
Two other variables included in this research were the time between primary biopsy and first oncology assessment and the time between the first appointment with an oncologist and the date of the first treatment. Means and standard deviation were calculated.
Overall survival analysis was calculated based on the date of diagnosis and date of death registered on the chart or loss of follow-up. Cutoff date for overall survival was January 15th, 2023. For the cause of death, patients were stratified into death due to baseline disease, due to COVID-19 infection or due to other cause (yes or no categories for all). Additionally, a dichotomous variable “death before treatment start” was included for those patients with treatment indication but who died before its’ beginning, also categorized into “yes” or “no”.
Statistical analysis
To assess statistical differences among groups [i.e., 2019 versus (vs.) 2020 and 2019 vs. 2021] a chi-square (χ²) test was used for two independent groups with a 5% significance level and 90% power for sample size calculation. To estimate measurement effectiveness a pilot study was performed by an independent statistician with 40 patients randomly selected from the patients described in Table 1 . Based on these data, the sample size was calculated on R statistic software version 3.5.1 with an effect of 0,2182. The minimum sample size for our planned analysis was then 298 patients (Fig. 1 ).
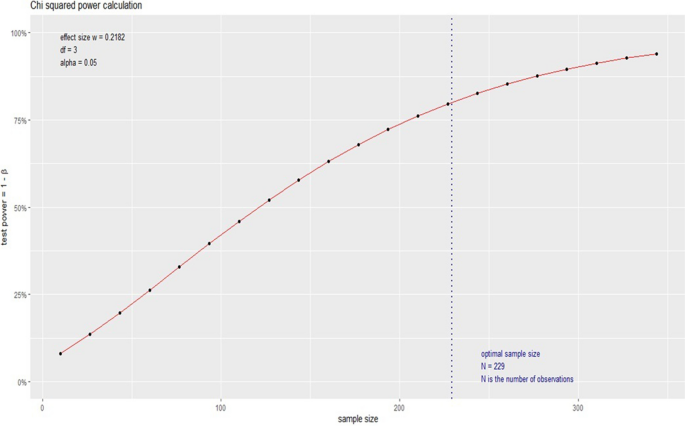
Sample size calculation
Differences among baseline clinical features and sociodemographic characteristics were evaluated either by T-test for two samples or Fisher’s or Pearson’s chi-square test (for quantitative or qualitative variables). T-test for 2 samples was used based on the central limit theorem, which states that in sample sizes above 5 or 10 per group, all means present with normal distribution, independently of data distribution [ 12 ]. All utilized tests had a 5% significance level (meaning a p -value ≤ 0,05).
All statistical analyses were performed on IBM SPSS Statistics (SPSS, version 23.0 for Windows; SPSS Inc, Chicago, Ill).
This study was submitted and approved by the Ethics Committee of Santa Casa de Misericórdia de Belo Horizonte (approval number 39,115,720,900,005,138). Since this is a retrospective cohort and there was a substantial number of reported deaths on the medical charts with no possibility for verbal or written consent, the need for informed consent was waived by Ethics Committee of Santa Casa de Misericórdia de Belo Horizonte .
Population characteristics
Six hundred fifty-two patients were included in the current analysis, 332 with lung cancer and 320 with head and neck cancer.
Focusing on the lung cancer patients, 87 patients were diagnosed in 2019, 124 in 2020 and 121 in 2021. In 2019 and 2020, the mean age at diagnosis was 66 years old, and 65 in 2021 (Table 1 ). In 2020, females were predominant; in 2019 and 2021 men were the majority. Baseline characteristics that showed a significant statistical difference among groups were smoking status (25% never smokers in 2020 compared to 10% in 2019, p -value 0.027) and race (25% of Caucasians in 2020 and 29% in 2021, compared to 17% in 2019, p -values 0.001 for both comparisons). Although non-significant, patients diagnosed during the pandemic presented with more pain symptoms (6% increase in 2020 and 12% increase in 2021, p -value 1.000 and 0.132, respectively) (Table 2 ). The time frame between first oncology assessment and initial treatment was shorter 20 days in 2020 compared to 2019 ( p -value 0.029). For the time gap analysis, we included patients with treatment recommendations (i.e., 68 patients in 2019, and = 74 patients in 2020). There was no difference when it comes to clinical stage and metastatic disease at diagnosis to all comparisons for patients with lung cancer (2019 vs. 2020 and 2019 vs. 2021).
Regarding the group with head and neck cancer, the mean age at diagnosis was 55.49 in 2019, 58.50 years in 2021, and 60.05 years in 2021 (Table 3 ); the latter with a statistically significant difference ( p -value 0.012). Males were predominant in all three years. The sole baseline characteristic that showed a significant statistical difference among groups was race (25% Caucasians in 2020 compared to 17% in 2019, and 28.9% of Caucasians in 2021 compared to 17% in 2019; p -value 0.000 for both comparisons). There was a 22% increase in primary tumor size (tumors classified as “T4”) among patients with head and neck cancer in 2020 in comparison to 2019 ( p -value 0.017). Presence of pain symptoms had nearly a 11% increase in 2020, and a 18% increase in 2021 when compared to 2019 ( p -value 0.002 and 0.029, respectively) (Table 4 ). In 2021, for the initial performance status, there was a 11% increase in category “2” ( p -value 0.008). Also, in 2021 the indication of tracheostomy had a 15% increase in comparison to 2019 ( p -value 0.043). For patients in the head and cancer group, there was no difference when it comes to clinical stage and metastatic disease at diagnosis to all comparisons (2019 vs. 2020 and 2019 vs. 2021). However, there was a tendency to the increased clinical stage in 2021 ( p -value 0.058 for the stratified clinical stage).
Outcomes and survival analysis
Regarding treatment recommendation for patients with lung cancer, including chemotherapy indication, it was observed a 12% decrease in treatment recommendations in 2020 compared to 2019 ( p -value 0.031), and 16% decrease in 2021 ( p -value 0.006), irrespectively of curative intention (i.e., first-line treatment also). Moreover, there was a 11% increase in the indication of exclusive palliate care at first oncology assessment in 2020 ( p -value 0.015) and 18% in 2021 ( p -value 0.001). All comparisons were with patients diagnosed in 2019, the year before the pandemic.
There were no statistically significant differences between patients’ outcomes for lung cancer when patients from 2019 to 2020 were compared (Table 5 ). For overall survival there was a non-significant reduction in 2020 survival [6 months (95% CI 3.18–8.81 months) in 2019 vs. 3 months in 2020 (95% CI 1.18–4.81)] (Table 5 ; Fig. 2 ). There was no statistically significant difference in objective rate response among patients with lung cancer in 2019 vs. 2021 group. Performance status after 6 months of first oncology assessment showed an increase in death rate after 6 months for 2021’s patients ( p = 0.001). Even though there was a statistically significant difference regarding survival rate ( p = 0.005), overall survival showed a non-significant 33% decrease in 2021 survival [6 months (95% CI 3.18–8.81 months) vs. 4 months (95% CI 2.41–5.59)] (Table 5 ; Fig. 2 ).
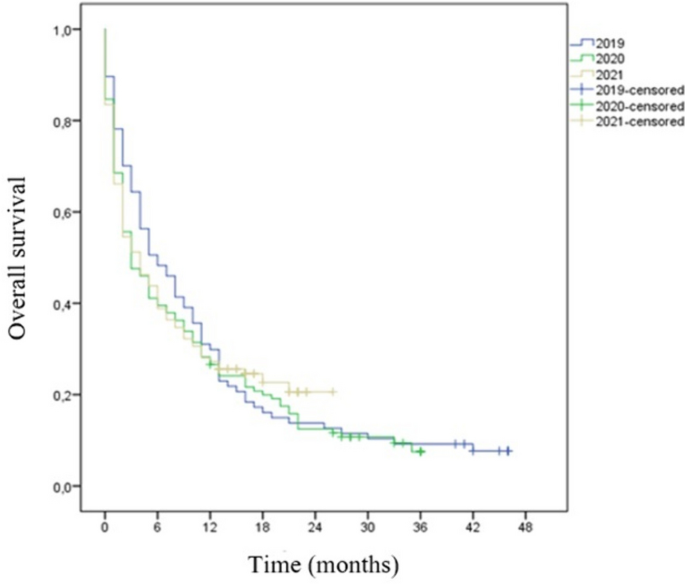
– Overall survival for patients with lung cancer, 2019–2021
There were no statistically significant differences between patients’ outcomes for head and neck cancer when patients from 2019 to 2020 were compared (Table 6 ). There was a statistically significant difference in survival rate in 2019 vs. 2021 group for patients with head and neck cancer, with a 20% decrease for patients from 2021 ( p -value 0.003). Additionally, performance status after 6 months of first oncology assessment showed an improvement after treatment with a 20% increase among patients categorized as “0” ( p = 0.013). Differently from the lung cancer cohort, it was not observed a significant decrease in treatment recommendation or an increase in palliative care recommendation during the pandemic in the head and neck cancer cohort. Kaplan Meier’s curve for overall survival for head and neck cancer to all three years is demonstrated in Fig. 3 .
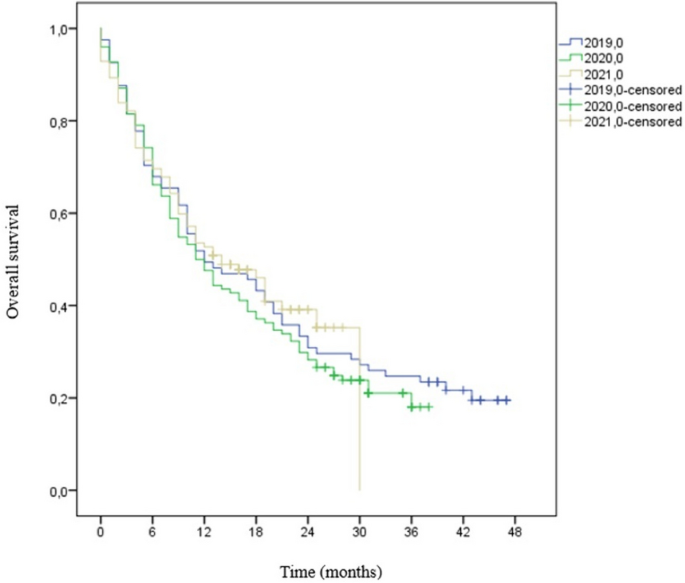
– Overall survival for patients with head and neck cancer, 2019–2021
The Santa Casa de Misericórdia de Belo Horizonte is a hospital with 1000 beds destined for public health care and is one of the biggest cancer centers in Minas Gerais state. The hospital is responsible for one-third of all oncology treatments on the providence. In 2019 24,666 oncology appointments, including patients for first assessment (hospital or ambulatory basis), patients in current anti-cancer treatment, patients in exclusive palliative care, and patients on follow-up after cancer remission. For 2020, the number of appointments were 24,547 and in 2021, 32,850. In addition, the Oncology service did not interrupt treatment assistance for cancer patients receiving chemotherapy and/or radiotherapy due to the pandemic. However, many surgeries were canceled due lack of beds in intensive care units (ICU) for post-operation observance since the ICU beds were relocated to patients with confirmed COVID-19 or acute respiratory distress. Also, during the COVID-19 pandemic, over 70% of these 1000 beds were turned into respiratory wings; such approach was also observed in other cancer centers in the country [ 13 ]. Worldwide the COVID-19 pandemic impacted cancer care; a global collaborative study across 54 countries [ 14 ] reported that in over 88% of the participating cancer centers there was challenges in providing adequate cancer care during the pandemic, including number of medical appointments, restricted access to medications, and missing on chemotherapy cycles. However, in this cancer center we were able to maintain the oncology wing in its’ full capacity and were able to increase the number of patients assisted.
Brazil is a middle-income country with over 207 million inhabitants (according to the 2022 census) [ 15 ]. Several low and middle-income countries are not prepared to provide adequate care to cancer patients, one of the reasons why high-income countries have higher survival rates [ 1 ]. The pillars of Brazil’s public health policies include equity, equality, and integrity to whoever seeks medical care in public health centers and Brazil’s Brazilian public health system provides free treatment to over 190 million people [ 16 ], including all cancer treatment modalities (i.e., surgery, chemotherapy, and radiotherapy) [ 17 ]. Since all these treatment options are fully funded by Brazilian’s government, patients’ assistance is completely free of charges, so, the resources offered to each patient is the same. Nonetheless, it is worth mentioning that the system may work with an important waiting list of medical appointments, diagnostic assessment, and treatment itself. Based on that, a Brazilian oncology patient loses nearly double of health years in comparison to some European countries and triple the time when compared to the United States of America [ 18 ]. Another fact that may impact overall cancer survival in Brazil is the difference between public health care and private care since there are several disparities among treatment options for locally advanced and advance diseases among these two groups. All these variables combined yield in low survival rate among cancer patients as it was demonstrated among the subjects included in this research.
Brazil has two specific laws regarding cancer treatment; the first one from 2012, known as the “60-day law” meaning that cancer patients have an upper limit of 60 days to initiate specific cancer treatment after diagnosis. The second one from 2019 is known as the “30-day law” meaning that highly suspicious patients have 30 days to fulfill all necessary diagnostic tests after symptoms have been reported to a medical physician [ 17 ]. Based on that, it was decided to assess among the subjects the time gap between the first oncology assessment and initial treatment; it was reported that in 2019 and 2021, the estimated time was close to 74 days, and for 2020, the estimated time was 53 days. National data indicates that most Brazilians receive a cancer diagnosis in the metastatic stage, reaching a peak of 200 days between the first reported symptom and biopsy release [ 17 ].
In this cohort, lung cancer patients diagnosed after the pandemic started shad a higher probability of not receiving chemotherapy and had a higher indication of exclusive palliative care, even though there was not a significant difference in clinical stage at diagnosis. To better define indication of best supportive care usually there’s a combination of ECOG scale plus functionality and nutritional status, and it was observed that patients were much more fragile than the pre-pandemic era and for our surprise, this scenario was irrespectively of clinical stage. Differences in treatment indication have not been observed in the head and neck cohort, but higher pain level at diagnosis was also observed.
In the lung cancer cohort 17.7% of patients had malnutrition, as for 35.6% in the head and neck cancer cohort. Brazilian nutritional status was updated in 2019, and results showed that 63% were above weight (overweight or obesity), 34.5% were eutrophic, and 2.5% were considered malnutrition [ 19 ]. In comparison to this study population, these updates showed that cancer patients may present with worst nutritional status than the general population, which is expected since involuntary weight loss is one of the first cancer symptoms. Moreover, patients with head and neck cancer may already experience reduced food intake before treatment starts [ 20 , 21 , 22 ], and patients with malnutrition have a higher risk of poor prognosis and worst treatment outcomes [ 23 ]. In this cohort, over 50% of patients with head and neck cancer patients needed enteral nutrition during treatment and that one-third suffered from malnutrition. Several aspects of the patient with head and cancer may alter due to malnutrition, such as impaired immune function, decrease in quality of life and interrupted treatments [ 20 ]. Pain tumor-related is an additional factor in weight loss [ 22 ], and we presented data with an increase in pain symptoms reported at diagnosis. The combination of our data based on nutritional status, and decreased functionality due to pain symptoms reinforce the findings of increased indication for exclusive palliative care it was found in this research.
Overall, pain symptoms were reported by 54.7% of the study population; 38% of patients in 2019 had pain symptoms reported. This number increased to 57% in 2020 and escalated to 31% in 2021. Here it must be highlighted that among patients with head and neck cancer, pain symptoms significantly increased after the COVID-19 pandemic started, whereas for lung cancer patients the reported increase was statistically non-significant. Since pain is one of the most challenging clinical features in cancer patients, it must be identified correctly and properly treated. Nearly 51% of all cancer patients report pain symptoms at some point during the disease (diagnosis, treatment, or exclusive palliative care) [ 24 ]. Patients with pain symptoms and delay medical care tend to seek self-medication, which may enhance treatment and clinical complications secondly to the mistreatment of their condition [ 25 ]. Lung cancer patients often report pain symptoms at diagnosis due to anatomic features of the tumor, such as bone and nerve invasion or metastatic disease, while patients with head and neck cancer may experience pain either due to the primary tumor or due to the treatment consequences, including surgery, radiation, or chemotherapy [ 24 ].
There was an increased number of lung cancer diagnoses on the hospital during the pandemic. For the lung cancer cohort, in 2020 there was an increase of 42.5% and in 2021 an increase of 39.1%. Concepcion et al. [ 26 ] reported an increase of 2.9% in 2020 and 3.34% in 2021 in total lung cancers diagnosed after the pandemic started but in much lower scale than it was found in this study. However, differently from what it was reported here, they showed a decrease in lung cancer death reports (-4.87% in 2020 and − 7.56% in 2021). Even though it was found an increased number of cancer diagnoses, Brazil had a decrease in such aspects during the pandemic, ranging from − 24.3% to -42.7% in some regions [ 27 ]; overall, up to 15,000 new cases were not diagnosed monthly due to COVID-19 [ 27 ]. Such data inference that oncology care varied in Brazilian territory during the pandemic – mainly due to lockdown recommendations and closed ambulatory services. Also, in contrast to these findings, a decreased incidence of lung cancer was observed by Kasymjanova et al. [ 28 ], with 34.7% less diagnosis but with more advanced stages during the COVID-19 pandemic. Regarding starting treatment with chemotherapy and/or radiotherapy, there was no significant delay.
Overall, there was no identification of statistical differences for the clinical stage at the lung cancer group, and it is worth mentioning that over 70% of subjects were metastatic at diagnosis [ 29 ]. The results presented by Lou et al. [ 30 ] also demonstrated no change in clinical stage at diagnosis for patients with lung cancer besides a shorter time-to-treatment in 2020 (38.92 days), like what it was found in this research. No change in clinical stage at diagnosis was also presented by Kizilirmak et al. [ 31 ]; stage IV disease was present in 59.31% of the pre-pandemic group and 65.35% of the pandemic group. Even though they did not find differences in lung cancer incidence between 2019 and 2020, Park et al. [ 32 ] identified a higher proportion of patients with locally advanced or metastatic disease after the COVID-19 pandemic started (2020 74.7% vs. 2109 62.7%).
Brazil does not provide thorax computerized tomography scans regularly due to high costs to the public health care system. There is no screening program for lung cancer in the country approved by Brazilian’s Ministry of Health, which might explain why Brazil has such high numbers of metastatic disease at diagnosis on a public health basis, which later will reflect in poorer outcomes since delayed diagnosis of lung cancer results in upper staging, decreased prognosis and lower survival rates [ 33 ]. Lung cancer has a 22.9% combined survival rate in five years [ 34 ], and clinical stage has an important role on these statistics, since clinical stage I ranges in survival rate from 92–68% in 5 years whereas patients with metastatic disease at diagnosis have a five-year survival rate of 10% [ 35 ].
Regarding the patients with head and neck cancer, there was an increase of 52.43% in 2020 and 37.8% in 2021. Nonetheless, Solis et al. [ 36 ] showed a 5–10% decrease in the number of new patients diagnosed with head and neck cancer after the COVID-19 pandemic, while several other international reports have documented a 22–43% decrease in the number of new diagnoses. Also, it was demonstrated patients with more advanced diseases when primary tumor size in 2020 was evaluated. In addition to the data here presented, the increased number of patients with tracheostomy indication may be related to such delayed diagnosis. Similarly, Tevetoğlu et al. [ 37 ], Flynn et al. [ 38 ], and Popovic et al. [ 39 ] also presented a cohort with patients presenting increased clinical stage at diagnosis among patients with head and neck cancer after the pandemic started. Although lymph node status is an important prognostic factor for these patients [ 40 ], this study did not find significant differences among all compared groups to this variable. The subgroup from 2021 did not showed differences among clinical stage, there was a tendency of more advanced diseased on the stratified staging. Similar results were presented by Clements et al. [ 41 ] who also did not find differences on symptoms and patients’ ECOG. The 5-year survival rates for head and neck cancer patients in general have a poor prognosis. The five-year survival rate varies between 30 and 70%, depending on the stage and location of the tumor [ 42 ]. In 2020 this cohort demonstrated a decreased survival in comparison to the pre-pandemic period. Similar results were cited by Peacok et al. [ 43 ]. As for 2021, there was a 20% increase in survival in comparison to 2019, but such significant difference may be due to a shorter follow-up in comparison to those patients from 2019, and perhaps such difference will balance after a 5-year follow-up.
In Brazil, public cancer centers receive a monthly amount of approximately $200,00 (R$ 1,100 Brazilian reais) from the government to treat patients with advanced lung cancer. For head and neck cancer the monthly amount of money range between $100,00 and $235,00 (R$ 571,00–1,300 Brazilian reais), irrespectively of clinical stage. The Brazilian healthcare system does not afford immunotherapy or direct target therapies for these tumors, except for gefitinib in patients with epidermal growth factor receptor (EGFR) mutations. In this context, that’s why Brazilian patients with lung, head and, neck cancer have access only to cytotoxic chemotherapy in contrast to all major recommendations for treatment worldwide [ 44 , 45 ]. While lung cancer survival improved tremendously over the past 15 years since precision medicine arose, the main goal for thoracic oncologists is to overcome the median overall survival of 8 months that chemotherapy usually achieves [ 46 ]. Over 85% of patients with lung cancer included in this study died. For patients with head and neck cancer, over 71% have passed. These data put in evidence the disparities when adequate treatment access is not available, setting back the recent advances in modern oncology.
The data collected had an expressive amount of missing data for baseline characteristics, especially for 2019’s patients, with special attention to sociodemographic features, which may have increased the statistical differences among groups in those aspects. That is one of the pitfalls that follow retrospective studies; such differences in exposure data among groups may alter the study estimates [ 47 ].
In conclusion, in a cohort of 652 lung and head and neck cancer patients treated in Brazil from 2019 to 2021, it was observed a significant decrease in oncologic treatment recommendations and increase in palliative care indication during the first two years of the pandemic in the lung cancer group, despite similar stages at diagnosis. Increased pain levels at diagnosis were observed in all patients during the pandemic compared to patients diagnosed at the year before it. This study also highlights low survival rates for patients with lung and head and neck cancer in Brazil, even before the pandemic, as a probable consequence of advanced diseases at diagnosis and limited access to best treatment options at the publica health system.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
Body mass index
Confidence interval
Coronavirus disease
Eastern Cooperative Oncology Group
Faculdades Ciências Médicas de Minas Gerais
Global Cancer Statistics
International Classification of Diseases
Intensive Care Unit
Low-and middle-income countries
Response evaluation criteria in solid tumors
Standard deviation
Standard error
Surveillance, epidemiology, and end results program
Classification of tumors
World Health Organization
World Health Organization. Cancer. Available at: https://www.who.int/health-topics/cancer#tab=tab_1 . Access 1 Feb 2023
World Health Organization. IAEA/WHO Joint Statement on Reducing Inequity in Access to Cancer Care through Rays of Hope Initiative. Available at: https://www.who.int/news/item/04-02-2022-iaea-who-joint-statement-on-reducing-inequity-in-access-to-cancer-care-through-rays-of-hope-initiative#:~:text=World%20Health%20Organization,expected%20to%20occur%20in%20LMICs . Access 1 Feb 2023.
Brasil. Instituto Nacional De Câncer (Brasil). Estimativa 2023: incidência de câncer no Brasil / Instituto Nacional De Câncer. – Rio de Janeiro: INCA; 2022. 160 p.: il. color.
World Health Organization. Coronavirus disease (COVID-19). Available at: https://covid19.who.int/ . Access 1 Feb 2023.
Shah MA, Mayer S, Emlen F, et al. Clinical screening for COVID-19 in asymptomatic patients with Cancer. JAMA Netw Open. 2020;3(9):e2023121. https://doi.org/10.1001/jamanetworkopen.2020.23121 .
Article PubMed PubMed Central Google Scholar
Cortiula F, Pettke A, Bartoletti M, Puglisi F, Helleday T. Managing COVID-19 in the oncology clinic and avoiding the distraction effect. Ann Oncol Off J Eur Soc Med Oncol. 2020;31(5):P553–555. https://doi.org/10.1016/j.annonc.2020.03.286 .
Article Google Scholar
Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullian R, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21(8):1023–34. https://doi.org/10.1016/S1470-2045(20)30388-0 .
Article CAS PubMed PubMed Central Google Scholar
World Health Organization. ICD-10: international statistical classification of diseases and related health problems: tenth revision, 2nd ed. World Health Organization; 2004.
Amin MB, Edge S, Greene F, Byrd DR, Brookland RK, Washington MK, et al. AJCC Cancer Staging Manual (8th edition). Springer International Publishing: American Joint Commission on Cancer; 2017
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP. Toxicity and response criteria of the Eastern cooperative oncology group. Am J Clin Oncol. 1982;5(6):649–55.
Article CAS PubMed Google Scholar
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47. https://doi.org/10.1016/j.ejca.2008.10.026 .
Norman G. Likert scales, levels of measurement and the ‘“laws”’of statistics. Adv Health Sci Educ Theory Pract. 2010;15(5):625–32. https://doi.org/10.1007/s10459-010-9222-y .
Article PubMed Google Scholar
Caminha I, Távora F, Sousa J, Martins Neto F, Cavalcanti LPG. Impacto Da Pandemia De COVID-19 no diagnóstico de câncer de pulmão no nordeste brasileiro. J Bras Pneumol. 2022;48(6):e20220248.
PubMed PubMed Central Google Scholar
Jazieh AR, Akbulut H, Curigliano G, Rogado A, Alsharm AA, Razis ED, et al. Impact of the COVID-19 pandemic on cancer care: a global collaborative study. JCO Glob Oncol. 2020;6:1428–38.
Brasil. Instituto Brasileiro de Geografia e Estatística. Censo Demográfico. https://www.ibge.gov.br/estatisticas/sociais/rendimento-despesa-e-consumo/22827-censo-demografico-2022.html . Access 1 Mar 2023.
Brasil. Ministério da Saúde. Secretaria de Estado de Saúde. Disponível em: < https://www.saude.mg.gov.br/sus . Access 1 Oct 2022.
Brasil. Sociedade Brasileira de Oncologia clínica. Disponível em: < https://sboc.org.br/noticias/item/1717-nova-lei-obriga-a-realizacao-de-exame-para-diagnostico-de-cancer-em-ate-30-dias. Access 1 Oct 2022.
Brasil. Sociedade Brasileira de Oncologia clínica. Disponível em: https://sboc.org.br/noticias/item/1733-brasil-apresenta-piores-indicadores-no-investimento-em-cancer-se-comparado-a-pares-da-america-latina-revela-pesquisa#:~:text=Diante%20disso%2C%20o%20levantamento%20%E2%80%9CC%C3%A2ncer,suplementar%20(planos%20de%20sa%C3%BAde) . Access 1 Oct 2022
Brasil. Ministério da Saúde. Situação alimentar e nutricional no Brasil: excesso de peso e obesidade da população adulta na Atenção Primária à Saúde. 2020.
Sandmæl JA, Sand K, Bye A, Solheim TS, Oldervoll L, Helvik A-S. Nutritional experiences in head and neck cancer patients. Eur J Cancer Care. 2019;28:e13168. https://doi.org/10.1111/ecc.13168 .
Oliveira KG, von Zeidler SV, Podestá JR, et al. Influence of pain severity on the quality of life in patients with head and neck cancer before antineoplastic therapy. BMC Cancer. 2014;14: 39. https://doi.org/10.1186/1471-2407-14-39 .
Bossi P, Giusti R, Tarsitano A, Airoldi M, De Sanctis V, Caspiani O, et al. The point of pain in head and neck cancer. Crit Rev Oncol/Hematol. 2019;138:51–9. https://doi.org/10.1016/j.critrevonc.2019.04.001 .
Park S, Park S, Lee SH, Suh B, Keam B, Kim TM, et al. Nutritional status in the era of target therapy: poor nutrition is a prognostic factor in non-small cell lung cancer with activating epidermal growth factor receptor mutations. Korean J Intern Med. 2016;31(6):1140–9. https://doi.org/10.3904/kjim.2015.062 .
Hochberg U, Elgueta MF, Perez J. Interventional analgesic management of lung cancer pain. Front Oncol. 2017;7: 17. https://doi.org/10.3389/fonc.2017.00017 .
Mahl C, Melo LRS, Almeida MHA, Carvalho CS, Santos LLS, Nunes OS, et al. Delay in head and neck cancer care during the COVID-19 pandemic and its impact on health outcomes. Braz Oral Res. 2020;34:e126. https://doi.org/10.1590/1807-3107bor-2020.vol34.0126 .
Concepcion J, Yeager M, Alfaro S, Newsom K, Ibrahim J, Bilski T, et al. Trends of cancer screenings, diagnoses, and mortalities during the COVID-19 pandemic: implications and future recommendations. Am Surg. 2022. https://doi.org/10.1177/00031348221091948 .
Marques NP, Silveira DMM, Marques NCT, Martelli DRB, Oliveira EA, Martelli-Júnior H. Cancer diagnosis in Brazil in the COVID-19 era. Seminars in Oncology. 2021;48(2):156–9. https://doi.org/10.1053/j.seminoncol.2020.12.002 . ISSN 0093-7754.
Kasymjanova G, Anwar A, Cohen V, Sultanem K, Pepe C, Sakr L, et al. The impact of COVID-19 on the diagnosis and treatment of lung cancer at a canadian academic center: a retrospective chart review. Curr Oncol. 2021;28:4247–55. https://doi.org/10.3390/curroncol28060360 .
Bersani F, Morena D, Picca F, et al. Future perspectives from lung cancer pre-clinical models: new treatments are coming? Transl lung cancer Res. 2020;9(6):2629–44. https://doi.org/10.21037/tlcr-20-189 .
Lou J, Kooragayala K, Williams JP, Sandilos Georgianna, Butchy MV, Yoon-Flannery KDO et al. The Early Impact of the COVID-19 Pandemic on Lung, Colorectal, and Breast Cancer Screening and Treatment at a Tertiary Cancer Center. American Journal of Clinical Oncology 45(9):p 381–390, September 2022. | https://doi.org/10.1097/COC.0000000000000936 .
Kızılırmak D, Yılmaz Z, Havlucu Y, Çelik P. Impact of the COVID-19 pandemic on diagnosis of lung cancer. SN Compr Clin Med. 2023;5:23. https://doi.org/10.1007/s42399-022-01366-z .
Park JY, Lee YJ, Kim T, Lee CY, Kim HI, Kim JH, et al. Collateral effects of the coronavirus disease 2019 pandemic on lung cancer diagnosis in Korea. BMC Cancer. 2020;20:1040. https://doi.org/10.1186/s12885-020-07544-3 .
Keogh JAJ, Chhor AD, Begum H, Akhtar-Danesh N, Finley C. Impact of the COVID-19 pandemic on non–small-cell lung cancer pathologic stage and presentation. Can J Surg. 2022;65(4):E496. https://doi.org/10.1503/cjs.016721 .
National Cancer Institute. Cancer Stat Facts: Lung and Bronchus. https://seer.cancer.gov/statfacts/html/lungb.html . Access 1 Mar 2023.
Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WE, Nicholson AG, Groome P, Mitchell A, Bolejack V, International Association for the Study of Lung Cancer Staging and Prognostic Factors Committee, Advisory Boards, and Participating Institutions, International Association for the Study of Lung Cancer Staging and Prognostic Factors Committee Advisory Boards and Participating Institutions. The IASLC Lung Cancer Staging Project: proposals for revision of the TNM Stage groupings in the Forthcoming (Eighth) Edition of the TNM classification for Lung Cancer. J Thorac Oncol. 2016;11(1):39–51. https://doi.org/10.1016/j.jtho.2015.09.009 .
Solis RN, Mehrzad M, Faiq S, Frusciante RP, Sekhon HK, Abouyared M, et al. The impact of COVID-19 on head and neck cancer treatment: before and during the pandemic. OTO Open. 2021;5(4). https://doi.org/10.1177/2473974X211068075 .
Tevetoğlu F, Kara S, Aliyeva C, Yildirim R, Yener HM. Delayed presentation of head and neck cancer patients during COVID-19 pandemic. Eur Arch Otorhinolaryngol. 2021;278:5081–5. https://doi.org/10.1007/s00405-021-06728-2 .
Flynn W, Maqsood R, Maseland T, Montgomery J, Douglas C. Advancing head and neck cancer following the coronavirus disease 2019 pandemic. J Laryngol Otol. 2022:1–7. https://doi.org/10.1017/S0022215122000950 .
Popovic M, Fiano V, Moirano G, Chiusa L, Conway DI, Garzino Demo P, Gilardetti M, Iorio GC, Moccia C, Ostellino O, Pecorari G, Ramieri G, Ricardi U, Riva G, Virani S, Richiardi L. The impact of the COVID-19 pandemic on Head and Neck Cancer diagnosis in the Piedmont Region, Italy: interrupted time-series analysis. Front Public Health. 2022;10: 809283. https://doi.org/10.3389/fpubh.2022.809283 .
Burusapat C, Jarungroongruangchai W, Charoenpitakchai M. Prognostic factors of cervical node status in head and neck squamous cell carcinoma. World J Surg Oncol. 2015;13:51. https://doi.org/10.1186/s12957-015-0460-6 .
Clements K, Cowell A, White G, Flynn W, Conway DI, Douglas CM, Paterson C. The COVID-19 pandemic has not changed stage at presentation nor treatment patterns of head and neck cancer: a retrospective cohort study. Clin Otolaryngol. 2023;48(4):587–94. https://doi.org/10.1111/coa.14048 .
Hoesseini A, Offerman MPJ, van de Wall-Neecke BJ, Sewnaik A, Wieringa MH, Baatenburg de Jong RJ. Physicians’ clinical prediction of survival in head and neck cancer patients in the palliative phase. BMC Palliat Care. 2020;19(1):176. https://doi.org/10.1186/s12904-020-00682-2 .
Peacock HM, De Gendt C, Silversmit G, Nuyts S, Casselman J, Machiels JP, Giusti F, van Gool B, Vander Poorten V, Van Eycken L. Stage shift and relative survival for head and neck cancer during the 2020 COVID-19 pandemic: a population-based study of temporal trends. Front Oncol. 2023;13: 1253968. https://doi.org/10.3389/fonc.2023.1253968 .
National Comprehensive Cancer Network. Non-small cell lung cancer (version 2.2023). 2023. Retrieved from https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf .
National Comprehensive Cancer Network. (2022). Head and Neck Cancers (version 1.2023) . Retrieved from https://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf .
Schiller JH, Harrington D, Belani CP, et al. Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med. 2002;346(2):92–8. https://doi.org/10.1056/NEJMoa011954 .
Karahalios A, Baglietto L, Carlin JB, English DR, Simpson JA. A review of the reporting and handling of missing data in cohort studies with repeated assessment of exposure measures. BMC Med Res Methodol. 2012;12: 96. https://doi.org/10.1186/1471-2288-12-96 .
Download references
Acknowledgements
Not applicable.
No specific funding for this project.
Author information
Authors and affiliations.
MD, Post-Graduate Program in Health Sciences, Faculdade Ciências Médicas de, Minas Gerais – FCM-MG, Oncologist, Oncoclínicas&Co/MedSir, Belo Horizonte, MG, Brazil
Gilson Gabriel Viana Veloso
Oncoclínicas&Co/MedSir, Belo Horizonte, MG, Brazil
Flávia Duarte Amaral
Post-Graduate Program in Health Sciences, Faculdade Ciências Médicas de Minas Gerais – FCM-MG, Federal University of Minas Gerais – UFMG, Brazilian Group of Gynecologic Oncology (EVA), Oncoclínicas&Co/MedSir, DOM Oncologia, Belo Horizonte, MG, Brazil
Angélica Nogueira-Rodrigues
You can also search for this author in PubMed Google Scholar
Contributions
GGVV was responsible for data collection, interpretation and writing. FDA and ANR participated in writing the final report. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Angélica Nogueira-Rodrigues .
Ethics declarations
Ethics approval and consent to participate.
This study was submitted and approved by the Ethics Committee of Santa Casa de Misericórdia de Belo Horizonte (approval number 39115720900005138). All experiments were performed in accordance with relevant guidelines and regulations (such as the Declaration of Helsinki). The need for informed consent was waived by Ethics Committee of Santa Casa de Misericórdia de Belo Horizonte.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Viana Veloso, G.G., Amaral, F.D. & Nogueira-Rodrigues, A. Impact of COVID-19 pandemic among patients with lung and head and neck cancer assisted in a public cancer center in Brazil. BMC Cancer 24 , 539 (2024). https://doi.org/10.1186/s12885-024-12255-0
Download citation
Received : 03 April 2023
Accepted : 11 April 2024
Published : 29 April 2024
DOI : https://doi.org/10.1186/s12885-024-12255-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical oncology
- Head and Neck tumors
- Lung tumors
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Qualitative study of the psychological experience of COVID-19 patients during hospitalization
Affiliations.
- 1 Humanities Teaching and Research Office, School of Nursing, Henan University of Science and Technology, The First Affiliated Hospital of Henan University of Science and Technology, Luoyang, China.
- 2 Department of Infection, The First Affiliated Hospital, and College of Clinical Medicine of Henan University of Science and Technology, Luoyang, China.
- 3 Department of Infection, The First Affiliated Hospital, and College of Clinical Medicine of Henan University of Science and Technology, Luoyang, China. Electronic address: [email protected].
- 4 Department of Infection, The First Affiliated Hospital, and College of Clinical Medicine of Henan University of Science and Technology, Luoyang, China. Electronic address: [email protected].
- PMID: 32949869
- PMCID: PMC7444461
- DOI: 10.1016/j.jad.2020.08.040
Background: Coronavirus disease 2019 (COVID-19) continues to spread across the globe, but patient experiences are rarely documented.
Objective: To explore the psychology of COVID-19 patients during hospitalization.
Methods: A phenomenological and robust sampling approach was employed. Sixteen patients admitted to the First Affiliated Hospital of Henan University of Science and Technology with COVID-19 from 20th January to 1st March 2020 were selected. Data were collected through semi-structured interviews, phone calls, or face-to-face interviews using quarantine measures. Data were analyzed using the Colaizzi method.
Results: The psychological experience of COVID-19 patients during hospitalization could be summarized into five themes. Firstly, attitudes toward the disease included fear, denial, and stigma during the early stages, which gradually developed into acceptance in the later stages. Secondly, the major source of stress included the viral nature of the disease, quarantine measures, and concerns regarding the health of family members. Thirdly, reactions of body and mind included disease stage-dependent emotional responses, excessive attention to symptoms, rumination, and changes in diet, sleep, and behavior. Fourthly, supportive factors included psychological adjustments, medical care, and family and social support. Finally, the disease resulted in psychological growth and patients viewed problems with gratitude through the cherishing of life, family, bravery, and tenacity.
Conclusion: COVID-19 patients gradually changed their attitude toward the disease and displayed emotional responses dependent on the stage of the disease. Negative emotions dominated during the early stages but gradually gave way to mixed positive and negative emotions. Active guidance of psychological growth may therefore promote physical and mental recovery in COVID-19 patients.
Keywords: Coronavirus disease 2019; Emergencies; Pandemic; Patients; Psychological experience; Qualitative study.
Copyright © 2020. Published by Elsevier B.V.
Publication types
- Evaluation Study
- Research Support, Non-U.S. Gov't
- Adaptation, Psychological
- Attitude to Health*
- COVID-19 / psychology*
- COVID-19 / therapy
- Hospitalization*
- Inpatients / psychology*
- Middle Aged
- Qualitative Research
- Young Adult
This paper is in the following e-collection/theme issue:
Published on 30.4.2024 in Vol 8 (2024)
Expanding Youth-Friendly HIV Self-Testing Services During the COVID-19 Pandemic: Qualitative Analysis of a Crowdsourcing Open Call in Nigeria
Authors of this article:

Original Paper
- Onyekachukwu Anikamadu 1 , MPH ;
- Oliver Ezechi 2 , MD, PhD ;
- Alexis Engelhart 3 , MPH ;
- Ucheoma Nwaozuru 4 , PhD ;
- Chisom Obiezu-Umeh 5 , MPH ;
- Ponmile Ogunjemite 2, 6 , BSc ;
- Babatunde Ismail Bale 2, 7 , OD ;
- Daniel Nwachukwu 2 , BSc ;
- Titilola Gbaja-biamila 2, 5 , MBBS ;
- David Oladele 2, 5 , MBBS ;
- Adesola Z Musa 2 , PhD ;
- Stacey Mason 5 , MPH ;
- Temitope Ojo 3 , MPH, PhD ;
- Joseph Tucker 8, 9 , AM, MD, PhD ;
- Juliet Iwelunmor 3 , PhD
1 Brown School of Social Work, Washington University in St. Louis, St Louis, MO, United States
2 Clinical Sciences Department, Nigerian Institute of Medical Research, Lagos, Nigeria
3 Division of Infectious Disease, Washington University School of Medicine in St. Louis, St Louis, MO, United States
4 Department of Implementation Science, Wake Forest School of Medicine, Winston-Salem, NC, United States
5 Department of Behavioral Science and Health Education, College for Public Health and Social Justice, Saint Louis University, St Louis, MO, United States
6 Department of Human Anatomy, Federal University of Technology, Akure, Nigeria
7 Department of Optometry, University of Benin, Benin City, Nigeria
8 Division of Infectious Diseases, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
9 Faculty of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London, United Kingdom
Corresponding Author:
Onyekachukwu Anikamadu, MPH
Brown School of Social Work
Washington University in St Louis
1 Brookings Drive
St Louis, MO, 63130
United States
Phone: 1 314 935 6600
Email: [email protected]
Background: HIV self-testing (HIVST) among young people is an effective approach to enhance the uptake of HIV testing recommended by the World Health Organization. However, the COVID-19 pandemic disrupted conventional facility-based HIV testing services, necessitating the exploration of innovative strategies for the effective delivery of HIVST.
Objective: This study analyzed the outcomes of a digital World AIDS Day crowdsourcing open call, designed to elicit youth responses on innovative approaches to promote HIVST among young people (14-24 years) in Nigeria during COVID-19 restrictions.
Methods: From November 2 to 22, 2020, a World AIDS Day 2020 crowdsourcing open call was held digitally due to COVID-19 restrictions. The crowdsourcing open call followed World Health Organization standardized steps, providing a structured framework for participant engagement. Young people in Nigeria, aged 10-24 years, participated by submitting ideas digitally through Google Forms or email in response to this crowdsourcing open call prompt: “How will you promote HIV self-testing among young people during COVID-19 pandemic?” Data and responses from each submission were analyzed, and proposed ideas were closely examined to identify common themes. Four independent reviewers (AE, SM, AZM, and TG) judged each submission based on the desirability, feasibility, and impact on a 9-point scale (3-9, with 3 being the lowest and 9 being the highest).
Results: The crowdsourcing open call received 125 eligible entries, 44 from women and 65 from men. The median age of participants was 20 (IQR 24-20) years, with the majority having completed their highest level of education at the senior secondary school level. The majority of participants lived in the South-West region (n=61) and Lagos state (n=36). Of the 125 eligible entries, the top 20 submissions received an average total score of 7.5 (SD 2.73) or above. The panel of judges ultimately selected 3 finalists to receive a monetary award. Three prominent themes were identified from the 125 crowdsourcing open call submissions as specific ways that HIVST can adapt during the COVID-19 pandemic: (1) digital approaches (such as gamification, photoverification system, and digital media) to generate demand for HIVST and avoid risks associated with attending clinics, (2) awareness and sensitization through existing infrastructures (such as churches, schools, and health facilities), and (3) partnerships with influencers, role models, and leaders (such as religious and youth leaders and social influencers in businesses, churches, organizations, and schools) to build trust in HIVST services.
Conclusions: The crowdsourcing open call effectively engaged a diverse number of young people who proposed a variety of ways to improve the uptake of HIVST during the COVID-19 pandemic. Findings contribute to the need for innovative HIVST strategies that close critical knowledge and practice gaps on ways to reach young people with HIVST during and beyond the pandemic.
Trial Registration: ClinicalTrials.gov NCT04710784; https://clinicaltrials.gov/study/NCT04710784
Introduction
Nigeria stands as the fourth-highest contributor to the global burden of HIV and has the largest HIV burden in sub-Saharan Africa [ 1 , 2 ]. An estimated 1.9 million Nigerians were living with HIV in 2018, setting the national HIV prevalence among those aged 15 to 49 years at 1.5% [ 3 ]. Since then, as of 2020, rates have remained constant, with only 67% of those affected aware of their status and only 53% receiving treatment [ 3 ]. Even with strengthened interventions over the past few decades, Nigeria still has a high burden of HIV, and a high number of young people (14-24 years) acquire the virus [ 3 ].
HIV self-testing (HIVST) is an important step that can enhance the uptake of essential HIV prevention services and is recommended by the World Health Organization [ 4 ]. HIVST is an antibody test that allows individuals to conveniently test themselves at home or in a private setting, yielding results within 20 minutes [ 5 ]. Recognized as a safe and effective method for increasing testing rates, especially among young people, HIVST has long been considered an alternative to clinical testing [ 4 ]. With the ability to collect their own samples and conduct the test at their own convenience, individuals gain autonomy in the testing process [ 4 ]. Although HIVST had been gaining traction prior to the COVID-19 pandemic, COVID-19 regulations hampered HIV testing, hastening the creation and scale-up of HIVST services [ 6 ].
The COVID-19 pandemic significantly impacted and disturbed the global health care system to varying degrees, with HIV prevention and treatment programs among those that were not spared [ 7 ]. A shift in the health system’s focus impacted all health programs not only in Nigeria but around the world. Many resources were redirected due to the COVID-19 pandemic, causing disruptions in existing clinical and community-based services surrounding prevention, treatment, and curative services, including those of HIV [ 8 , 9 ]. HIVST can play a critical role in decentralizing services, guaranteeing the use of HIV testing services during periods of uncertainties. It allows both beneficiaries and health care providers to adhere to physical distancing guidelines and limits the danger of exposure to transmission. While certain populations of Nigerian young people are at high risk of being infected with HIV, there is minimal evidence on measures to improve HIVST uptake among young people in Nigeria during the COVID-19 pandemic. An understanding of the strategies would be valuable to Nigerian young people and policy makers as well as global researchers implementing interventions in Nigeria or those who desire to adapt interventions to different contexts, particularly during disruptions such as those caused by the pandemic. To address this gap, we launched a digital crowdsourcing open call to elicit ideas for promoting HIVST during the pandemic. Crowdsourcing is an open innovation approach, often used as a tool to gather ideas, innovations, or information for specific purposes [ 10 ]. It is an effective strategy for communicating and designing interventions related to HIV and sexual health [ 11 , 12 ]. The goal of this qualitative study was to uncover recurring themes in a digital World AIDS Day (WAD) crowdsourcing open call for youth responses on how to increase HIVST among Nigerian young people during the COVID-19 pandemic.
Our crowdsourcing open call consisted of a 5-step process including digital crowdsourcing open call, web-based submissions, judging, analysis of themes, and common themes identified ( Figure 1 ) throughout the design and implementation, data collection, and data analysis phases.

Digital Crowdsourcing Open Call Design and Implementation
For this study, we used crowdsourcing, which involves a group of individuals working together to solve a problem and then publicly share the solutions [ 13 , 14 ]. The 4 Youth By Youth (4YBY) team announced a crowdsourcing open call to promote HIVST among young people in Nigeria from November 2 to 22, 2020. 4YBY is a team of young people, health professionals, activists, and entrepreneurs from diverse backgrounds, who are united by the shared passion to advance Nigerian youth participation in creating innovative, sustainable HIV prevention services. The “World’s AIDS Day HIV Self-Testing Contest” was held on December 1, 2020, to commemorate the annual WAD celebration. Due to the COVID-19 pandemic, we only used web-based engagement to recruit Nigerian young people between the ages of 14 and 24 years to take part in the crowdsourcing open call. To guarantee that a varied range of Nigerian young people from various backgrounds were involved, purposive sampling procedures were used [ 15 ]. The 4YBY team sent the crowdsourcing open call information to youth listservs and advertised on all social media platforms, including Instagram, Facebook, WhatsApp, and a website. The goal of the digital crowdsourcing open call was to provide open and safe areas for Nigerian young people to express their thoughts and ideas about how to promote HIVST during the pandemic. Individual demographic and contact information such as name, number, age, gender identity, education, and location were collected for each entrant.
Web-Based Collection of Submission Data
Participants responded to the prompt “How might you promote HIV self-testing among young people during COVID-19 measures?” using either Google Forms or email. Each submission had a word limit of 150 words to succinctly capture their unique ideas for HIV promotion throughout the pandemic. Consent to participate and demographic information were also obtained from each participant. The requested demographic information included contact information, age, gender, relationship status, current location, highest level of completed education, and occupation. Individuals had the option of not reporting sociodemographic characteristics.
Two research members (CO-U and UN) checked for the eligibility of each submission. Four independent reviewers (AE, SM, AZM, and TG) rated participant entries based on defined judging criteria, which included desirability, feasibility, and impact ( Textbox 1 ). Each submission received either a 1 (low), 2 (moderate), or 3 (high) for each of the 3 defined judging criteria, with the highest overall combined score being 9. This process was adapted from the human-centered, design thinking framework [ 15 , 16 ]. The first, second, and third place contestants each earned a monetary prize for their outstanding submission: 50,000 Naira (approximately US $139) for third place, 150,000 Naira (approximately US $417) for second place, and 250,000 Naira (approximately US $694) for third place.
Desirability (1-3): Concept is appealing to young people and is affordable, accessible, and confidential.
Feasibility (1-3): Concept is practical in terms of implementation and resource availability.
Impact (1-3): Concept has the ability to influence young people to self-test for HIV and can reach young people in Nigeria.
Data Analysis
Following the crowdsourcing open call’s conclusion, staff deidentified each entry and used summary statistics to compile the participants’ demographic data. A thematic analysis was conducted using open coding that assigns themes to capture specific ideas and axial coding, which explores linkages between concepts and categories and determines common themes [ 17 , 18 ]. The coding exercises were completed in a Google Spreadsheet by trained staff who were not part of the study team, and then a thematic codebook was constructed and used to assess qualitative data. Each of the 2 staff members (OA and AE) coded the crowdsourcing open call entries separately before meeting to resolve any discrepancies in coding judgments. The codebook was then created by consensus between the 2 researchers (CO-U and UN) [ 18 ]. Throughout the coding process, recurring themes were identified, and codes were created to meet the HIVST promotion themes. The staff members reread each submission a final time after developing the initial codebook to fine-tune the final codebook. Snapshots of entries that fit in each code were included in the final codebook. This was then forwarded to a third party for final examination and approval.
Ethical Considerations
Regulatory approval to conduct the research was received from the Nigerian Institute of Medical Research Institutional Review Board (Project #: IRB 18/028). Informed consent was obtained from all participants involved in the study. Following the conclusion of the crowdsourcing open call, each entry was deidentified to ensure anonymity. These measures were implemented to uphold ethical standards, ensuring participant protection and transparency throughout the research process. Additionally, monetary compensation was awarded to first-, second-, and third-place submissions.
Characteristics of Entrant Submissions
The 2020 digital WAD crowdsourcing open call received a total of 153 entries from Nigerians aged 14 to 24 years, of which 83.7% (n=128) were through Google Forms, and 16.3% (n=25) were by email. Of the 153 entries, there were 125 unique submissions identified after duplicates (n=24), and those submissions that could not be scored based on our inclusion criteria (n=4) were removed. Characteristics and demographics were collected for the 125 eligible, unique submissions.
The majority of the entrants were male (n=65, 52%). There were 44 (35.2%) female individuals, 1 (0.8%) individual preferred not to say their gender, and 15 (12%) gender responses were left missing. The average age of the entrants was 19.96 (SD 2.73) years, and the median age was also 20 (IQR 24-20) years. The breakdown of the number of individuals per age group is as follows: 48 (38.4%) individuals aged 14-19 years and 64 (51.2%) individuals aged 20-24 years. The highest level of education obtained by participants was mostly senior secondary school (n=61, 48.8%), followed by some tertiary school (n=22, 17.6%), bachelor’s degree (n=17, 13.6%), junior secondary school (n=4, 3.2%), primary school (n=2, 1.6%), and master’s degree (n=2, 1.6%). In total, 15 (12%) individuals did not report their highest level of education. The majority of entrants lived in Lagos state (n=36, 28.8%) and in the South-West region (n=61, 48.8%). Table 1 includes the characteristics of the eligible submissions.
Of the 125 eligible submissions, the mean score of the submissions was 5.42 (1.65). In total, 20 participants were selected as finalists with their submissions scoring as 7.5 or above. Three submissions were selected as the top submissions and were given a prize ( Multimedia Appendix 1 ).
The average word count of Google Forms submissions was 425.27 (SD 392.91) words. Two videos were submitted with lengths of 4.3 and 6.4 minutes. A total of 5 submissions included images, 1 submission consisted of a video and images, 1 entrant submitted a PowerPoint (Microsoft Corp) presentation file, and 4 submissions included a combination of images and text. All other entries were text submissions.
Analysis of Themes
After analyzing all 125 eligible submissions, 3 key themes were identified from the crowdsourcing open call submissions as specific ways that HIVST can adapt to the COVID-19 pandemic (theme 1) and the possibilities as well as facilitators of HIVST during the COVID-19 pandemic (themes 2 and 3). Common strategies to promote HIVST during and after COVID-19 were through (1) digital approaches (such as gamification, photoverification system, and digital media) to generate demand for HIVST and avoid risks associated with attending clinics, (2) awareness and sensitization through existing infrastructures (such as churches, schools, and health facilities), and (3) partnerships with influencers, role models, and leaders (such as religious and youth leaders and social influencers in businesses, churches, organizations, and schools) to build trust in HIVST services ( Multimedia Appendix 2 ).
Theme 1: Digital Approaches to Generate Demand for HIVST and Avoid Risks Associated With Attending Clinics
This was a recurring theme that appeared to be desirable, feasible, and impactful to young people in Nigeria. Because COVID-19 can be spread through airborne transmission and social distancing regulations were put into place, young people saw digital media as a safe method to transmit awareness and information regarding HIV and HIVST. Young people established ideas to educate and promote HIVST through digital media engagement avenues such as Facebook, Twitter, Instagram, WhatsApp, gamification, and mobile apps. For example, entrants proposed creating mobile apps that provide knowledge on HIVST and COVID-19 testing as well as linkage to testing facilities ( Figure 2 ). The top finalist suggested an interactive health gaming app called “Bambam” that allows users to access and monitor their health and HIV status coupled with competitive incentives to keep users engaged and encourage peer synergy. Because many young people in Nigeria have access to the internet and digital devices, participants mentioned the importance of using digital approaches as a medium for HIV and HIVST awareness campaigns to limit social gatherings and limit the influx of people to high-traffic areas such as hospitals. Submission examples are presented in Multimedia Appendix 2 .

Theme 2: Awareness and Sensitization Through Existing Infrastructures
This was a common theme that arose even during the COVID-19 pandemic. Many submissions suggested that existing facilities and infrastructures can still be used as resources for HIV information and as testing sites. They emphasized the importance of wearing face masks, applying hand sanitizer, and social distancing while at these places. A few participants mentioned the idea of creating awareness through religious gatherings, as churches and religious bodies were still allowed to be open during the pandemic. Other participants made it clear that holding discussions and seminars in physical locations gives rise to more social and personal connections. However, participants mentioned it is important to avoid large gatherings. Submission examples are presented in Multimedia Appendix 2 .
Theme 3: Partnerships With Influencers, Role Models, and Leaders to Build Trust in HIVST Testing Services
This was portrayed as a strategy that would impact young people in Nigeria and influence them to self-test for HIV. Participants mentioned collaborating with people such as social media influencers, religious and community leaders, and physicians to educate and sensitize young people in Nigeria on HIV and link them to self-testing kits and testing services. Participants suggested using celebrities as ambassadors to promote and encourage HIVST among young people ( Figure 3 ). Entrants also proposed the idea of leaders reaching out, through trained personnel and volunteers, to individuals in rural and more local areas, as these individuals may not have access to internet services. Submission examples are presented in Multimedia Appendix 2 .
Additionally, a few participants also mentioned similarities between the fight against COVID-19 with that of HIV. Participants recognized the comparability between COVID-19 and HIV and how HIV facility-based testing is stalled due to COVID-19 regulations such as facilities shutting down or social distancing guidelines being initiated. Participants highlighted the accessibility of HIVST, in which self-testing for HIV can be administered in an individual’s own home and privacy.

Follow-Up Activities
Following the conclusion of the digital crowdsourcing event, the top-scored ideas generated informed the refinement of a youth-friendly HIVST intervention delivery, particularly focusing on enhancing linkage to care. This refined intervention is to be evaluated in a randomized controlled trial (ClinicalTrials.gov NCT04710784).
Principal Findings
This digital WAD crowdsourcing open call administered during the COVID-19 pandemic generated ideas on how HIVST uptake can be increased among Nigerians in the course of the COVID-19 pandemic. The study illustrated efforts to reach young people creatively to facilitate HIVST while being compliant with the COVID-19 pandemic. Our findings also highlight accessible, affordable, and feasible ways to create awareness of HIVST throughout the COVID-19 pandemic and after the pandemic.
Our data suggest that HIVST can be effectively used to meet the demands of young people’s HIV testing during the pandemic. The COVID-19 pandemic created countless barriers that required the public to rethink a way around the norm and develop new strategies to overcome the obstacles, specifically reconsidering how to promote and fulfill HIVST services [ 19 ]. For example, across Nigeria, there were many disruptions to health care services [ 20 ], including those of HIV and sexually transmitted infections [ 9 , 21 ]. Yet, there was a need for innovative public health and social measures to reduce the disruptions caused by the pandemic [ 22 ]. Our crowdsourcing open call illustrated how a digital program can be used as a strategy to promote HIVST services that are compliant with the COVID-19 guidelines carried out in Nigeria [ 23 ]. Digital activities such as our crowdsourcing open call allowed for COVID-19 mitigation measures to continue to occur successfully while being compliant with government guidance [ 24 , 25 ].
Participants generated ideas on how HIVST distribution can be modified to adhere to the ongoing restrictions caused by the pandemic through channels that are digital as well as existing infrastructures and partnerships with key players. The ideas proposed can help form future campaigns, specifically during a time of limited physical interaction, and can pave the way toward more innovative and cost-saving techniques.
This study was held completely digitally due to the COVID-19 pandemic. It was a safe way to connect with individuals across Nigeria and administer new ideas that followed COVID-19 regulations. Although a large number of individuals participated in our crowdsourcing open call, it was significantly less than our crowdsourcing open calls in previous years 2018 and 2019 [ 15 ]. This could be related to competing COVID-19 demands. Though we gave the options of both web-based or offline submissions, all submissions were received via email or Google Forms. We recognize that technological advancements are continually occurring globally, and many young people have access to a mobile device, laptop, or computer [ 26 ]. In Nigeria, 63.8% of the population had internet access in 2020 [ 27 ]. However, internet connections are not always reliable and lead to issues during web-based learning or streaming [ 26 ]. Because our digital crowdsourcing open call was held via Zoom (Zoom Video Communications), this may have averted individuals from the crowdsourcing open call, knowing that they may have a possibility of internet connection issues.
However, as in previous years, the crowdsourcing open call engaged a wide range of young people and allowed them to voice their ideas on how to promote HIVST through various innovative strategies [ 15 ]. Crowdsourcing is not only a strategic way to receive solutions [ 9 , 10 ] but also very unique in the way that it includes individuals with different perspectives and creates meaningful participation among young people [ 13 , 14 , 28 ]. Our crowdsourcing open call accentuated this with youth participation and the development of ideas to prospectively scale up HIVST among young people and in communities throughout Nigeria. Harnessing young people’s concepts through crowdsourcing open calls captivates young people’s perspectives and potentially enhances mobilization efforts. Young people generated adapted, effective, and original strategies relating to the design, distribution, and education of HIVST kits during the COVID-19 era. We showed how young people can engage, produce innovative approaches, and create in-person or web-based connections.
Limitations
This study has several limitations. First, most ineligible entries were those submitted via Google Forms, with 24 as duplicates and 2 as submissions that could not be scored. Second, many submissions included text that did not specifically answer the crowdsourcing open-call question, such as those that defined HIV and those that described the burden of HIV in Nigeria. These limitations highlight a need for better communication and marketing of the crowdsourcing event so individuals fully understand the objective of the crowdsourcing open call and prompt being asked. Third, this study inevitably had selection bias, in which some individuals may have been more likely selected than others, and the group of participants may not have been equally representative of all ages of young people in Nigeria (14 to 24 years). In addition, the crowdsourcing open call was completely web-based, and submissions were submitted through Google Forms and email, which may have excluded individuals who wanted to participate but had limited or no access to the internet. Fourth, analytical bias may have been introduced during the evaluation or scoring process. Finally, demographic information was more frequently missing in email submissions (ie, age and gender), whereas participants who submitted via Google Forms filled in the age and gender question.
Findings from this study will help inform and improve strategies of HIVST to increase HIVST uptake in Nigeria during the COVID-19 pandemic and for years to come in the postpandemic era. This study implies that crowdsourcing and involvement of young people are valuable in identifying current and unconventional HIVST uptake strategies, particularly during an ongoing pandemic, and should also be considered in other aspects of research.
Conclusions
Though the study has many limitations, the crowdsourcing open call engaged a large, diverse number of young people through digital connections. The entrants suggested a diverse range of innovative techniques to increase the uptake of HIVST for vulnerable young people in Nigeria. Their tailored strategies to promote HIVST during the COVID-19 pandemic indicate that HIVST is a feasible method of testing despite barriers relating to physical interactions and in-person testing facilities. Findings from our crowdsourcing open call will inform future research on promoting HIVST and can contribute to the sustainability of HIVST even in times of unprecedented crises.
Acknowledgments
The authors extend their thanks to the I-TEST team at Saint Louis University, the University of North Carolina at Chapel Hill, and Nigerian Institute of Medical Research; 4 Youth By Youth; Youth Ambassadors; and other groups that helped to organize the challenge. The authors would also like to thank the program officers and members of the Prevention and Treatment Through a Comprehensive Care Continuum for HIV-Affected Adolescents in Resource Constrained Settings Consortium.
Data Availability
The data generated and analyzed in this study are not publicly available due to privacy and confidentiality considerations but are available from the corresponding author on reasonable request.
Authors' Contributions
OE, JT, and JI led the study’s conceptualization, methodology, project administration, and supervision, as well as reviewed and edited the paper. OA and AE conducted data curation, formal analysis, and visualization, as well as drafted the original paper. UN, CO-U, TG, DO, and AZM served as investigators and administrators, contributing to the paper review and editing. PO, BIB, DN, SM, and TO also reviewed and edited the paper. All authors have read and approved the paper.
Conflicts of Interest
None declared.
Top 3 submissions identified.
Emerging themes and examples of submissions.
- Country progress report—Nigeria. UNAIDS. URL: https://www.unaids.org/sites/default/files/country/documents/NGA_2020_countryreport.pdf [accessed 2024-03-06]
- Nigeria prevalence rate. National Agency for the Control of AIDS (NACA). 2019. URL: https://naca.gov.ng/nigeria-prevalence-rate/ [accessed 2024-03-06]
- Nigeria overview. UNAIDS. 2018. URL: https://www.unaids.org/en/regionscountries/countries/nigeria [accessed 2024-03-06]
- Guidelines on HIV self-testing and partner notification: supplement to consolidated guidelines on HIV testing services. World Health Organization. 2016. URL: https://apps.who.int/iris/bitstream/handle/10665/251655/9789241549868-eng.pdf [accessed 2024-03-06]
- HIV self-testing. Centers for Disease Control and Prevention. 2022. URL: https://www.cdc.gov/hiv/basics/hiv-testing/hiv-self-tests.html#:~:text=An%20HIV%20self%2Dtest%20(or,test%20results%20within%2020%20minutes [accessed 2024-03-06]
- Mhango M, Chitungo I, Dzinamarira T. COVID-19 lockdowns: impact on facility-based HIV testing and the case for the scaling up of home-based testing services in Sub-Saharan Africa. AIDS Behav. 2020;24(11):3014-3016. [ FREE Full text ] [ CrossRef ] [ Medline ]
- SeyedAlinaghi S, Mirzapour P, Pashaei Z, Afzalian A, Tantuoyir MM, Salmani R, et al. The impacts of COVID-19 pandemic on service delivery and treatment outcomes in people living with HIV: a systematic review. AIDS Res Ther. 2023;20(1):4. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chavez J, Worth K. Learning from the past to guide the future: HIV and COVID-19. Clin Nurse Spec. 2021;35(2):54-55. [ CrossRef ] [ Medline ]
- COVID-19 and HIV: 1 Moment 2 Epidemics 3 Opportunities how to seize the moment to learn, leverage and build a new way forward for everyone's health and rights. UNAIDS Joint United Nations Programme on HIV/AIDS. 2020. URL: https://www.unaids.org/sites/default/files/media_asset/20200909_Lessons-HIV-COVID19.pdf [accessed 2024-03-06]
- Aitamurto T, Leiponen A, Tee R. The promise of idea crowdsourcing—benefits, contexts, limitations. Nokia Ideasproject White Paper. 2011. URL: https://www.researchgate.net/publication/257926136_The_Promise_of_Idea_Crowdsourcing-Benefits_Contexts_Limitations [accessed 2024-03-06]
- Wang C, Han L, Stein G, Day S, Bien-Gund C, Mathews A, et al. Crowdsourcing in health and medical research: a systematic review. Infect Dis Poverty. 2020;9(1):8. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tang W, Ritchwood TD, Wu D, Ong JJ, Wei C, Iwelunmor J, et al. Crowdsourcing to improve HIV and sexual health outcomes: a scoping review. Curr HIV/AIDS Rep. 2019;16(4):270-278. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tahlil KM, Obiezu-Umeh C, Gbajabiamila T, Nwaozuru U, Oladele D, Musa AZ, et al. A designathon to co-create community-driven HIV self-testing services for Nigerian youth: findings from a participatory event. BMC Infect Dis. 2021;21(1):505. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Han L, Chen A, Ong JJ, Iwelunmor J, Tucker JD. Crowdsourcing in health and health research: a practical guide. World Health Organization. 2018. URL: https://www.who.int/tdr/publications/year/2018/crowdsourcing-practical-guide/en/ [accessed 2024-04-05]
- Iwelunmor J, Ezechi O, Obiezu-Umeh C, Gbaja-Biamila T, Nwaozuru U, Oladele D, et al. The 4 Youth by Youth HIV self-testing crowdsourcing contest: a qualitative evaluation. PLoS One. 2020;15(5):e0233698. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Carlgren L, Rauth I, Elmquist M. Framing design thinking: the concept in idea and enactment. Creat Innov Manage. 2016;25(1):38-57. [ CrossRef ]
- Presmeg N, Kaiser G, editors. Compendium for Early Career Researchers in Mathematics Education. Cham. Springer International Publishing; 2019.
- Mathews A, Conserve D, Mason H, Alston LM, Rennie S, Tucker J. 'Informed and empowered': a mixed-methods study of crowdsourcing contests to promote uptake of HIV self-testing kits among African Americans. J Virus Erad. 2020;6(2):74-80. [ FREE Full text ] [ CrossRef ]
- Ponticiello M, Mwanga-Amumpaire J, Tushemereirwe P, Nuwagaba G, King R, Sundararajan R. "Everything is a mess": how COVID-19 is impacting engagement with HIV testing services in rural Southwestern Uganda. AIDS Behav. 2020;24(11):3006-3009. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Responding to COVID-19 in Africa: using data to find a balance. Partnership for Evidence-Based Response to COVID-19. 2020. URL: https://reliefweb.int/sites/reliefweb.int/files/resources/PERC_RespondingtoCovidData.pdf [accessed 2024-03-06]
- Disruption in HIV, hepatitis and STI services due to COVID-19. World Health Organization. 2020. URL: https://www.who.int/docs/default-source/hiv-hq/disruption-hiv-hepatitis-sti-services-due-to-covid19.pdf?sfvrsn=5f78b742_6 [accessed 2024-03-06]
- Overview of public health and social measures in the context of COVID-19. World Health Organization. 2020. URL: https://www.who.int/publications/i/item/overview-of-public-health-and-social-measures-in-the-context-of-covid-19 [accessed 2024-03-06]
- Nigeria. Department of Foreign Affairs. URL: https://www.dfa.ie/travel/travel-advice/a-z-list-of-countries/nigeria/ [accessed 2021-10-26]
- Mukerjee S, Chow CM, Li M. Mitigation strategies and compliance in the COVID-19 fight; how much compliance is enough? PLoS One. 2021;16(8):e0239352. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Padidar S, Liao S, Magagula S, Mahlaba TAM, Nhlabatsi NM, Lukas S. Assessment of early COVID-19 compliance to and challenges with public health and social prevention measures in the Kingdom of Eswatini, using an online survey. PLoS One. 2021;16(6):e0253954. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Abdulmajeed K, Joyner DA, McManus C. Challenges of online learning in Nigeria. 2020. Presented at: L@S '20: Proceedings of the Seventh ACM Conference on Learning @ Scale; August 12-14, 2020;417-420; Virtual Event, USA. URL: https://dl.acm.org/doi/proceedings/10.1145/3386527 [ CrossRef ]
- Telecoms data: active voice and internet per state, porting and tariff information (Q4 2017). National Bureau of Statistics. 2018. URL: https://tinyurl.com/ye36acpx [accessed 2024-03-06]
- Hildebrand M, Ahumada C, Watson S. CrowdOutAIDS: crowdsourcing youth perspectives for action. Reprod Health Matters. 2013;21(41):57-68. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by A Mavragani; submitted 03.03.23; peer-reviewed by T Lillie; comments to author 03.10.23; revised version received 22.01.24; accepted 23.01.24; published 30.04.24.
©Onyekachukwu Anikamadu, Oliver Ezechi, Alexis Engelhart, Ucheoma Nwaozuru, Chisom Obiezu-Umeh, Ponmile Ogunjemite, Babatunde Ismail Bale, Daniel Nwachukwu, Titilola Gbaja-biamila, David Oladele, Adesola Z Musa, Stacey Mason, Temitope Ojo, Joseph Tucker, Juliet Iwelunmor. Originally published in JMIR Formative Research (https://formative.jmir.org), 30.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR Formative Research, is properly cited. The complete bibliographic information, a link to the original publication on https://formative.jmir.org, as well as this copyright and license information must be included.
- Open access
- Published: 01 May 2024
Health system lessons from the global fund-supported procurement and supply chain investments in Zimbabwe: a mixed methods study
- Abaleng Lesego 1 ,
- Lawrence P. O. Were 1 , 2 ,
- Tsion Tsegaye 1 ,
- Rafiu Idris 3 ,
- Linden Morrison 3 ,
- Tatjana Peterson 3 ,
- Sheza Elhussein 3 ,
- Esther Antonio 4 ,
- Godfrey Magwindiri 4 ,
- Ivan Dumba 5 ,
- Cleyland Mtambirwa 5 ,
- Newman Madzikwa 5 ,
- Raiva Simbi 5 ,
- Misheck Ndlovu 6 &
- Tom Achoki 1
BMC Health Services Research volume 24 , Article number: 557 ( 2024 ) Cite this article
30 Accesses
Metrics details
The Global Fund partnered with the Zimbabwean government to provide end-to-end support to strengthen the procurement and supply chain within the health system. This was accomplished through a series of strategic investments that included infrastructure and fleet improvement, training of personnel, modern equipment acquisition and warehouse optimisation. This assessment sought to determine the effects of the project on the health system.
This study employed a mixed methods design combining quantitative and qualitative research methods. The quantitative part entailed a descriptive analysis of procurement and supply chain data from the Zimbabwe healthcare system covering 2018 – 2021. The qualitative part comprised key informant interviews using a structured interview guide. Informants included health system stakeholders privy to the Global Fund-supported initiatives in Zimbabwe. The data collected through the interviews were transcribed in full and subjected to thematic content analysis.
Approximately 90% of public health facilities were covered by the procurement and distribution system. Timeliness of order fulfillment (within 90 days) at the facility level improved from an average of 42% to over 90% within the 4-year implementation period. Stockout rates for HIV drugs and test kits declined by 14% and 49% respectively. Population coverage for HIV treatment for both adults and children remained consistently high despite the increasing prevalence of people living with HIV. The value of expired commodities was reduced by 93% over the 4-year period.
Majority of the system stakeholders interviewed agreed that support from Global Fund was instrumental in improving the country's procurement and supply chain capacity. Key areas include improved infrastructure and equipment, data and information systems, health workforce and financing. Many of the participants also cited the Global Fund-supported warehouse optimization as critical to improving inventory management practices.
It is imperative for governments and donors keen to strengthen health systems to pay close attention to the procurement and distribution of medicines and health commodities. There is need to collaborate through joint planning and implementation to optimize the available resources. Organizational autonomy and sharing of best practices in management while strengthening accountability systems are fundamentally important in the efforts to build institutional capacity.
Peer Review reports
The Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund), together with its Zimbabwean national and international stakeholders have continued to invest in health system strengthening to improve public health in the country. These investments have been guided by systemwide strategic assessments to understand the fundamental challenges facing the Zimbabwean health system [ 1 , 2 , 3 , 4 ].
Given the strategic importance of access to essential medicines, vaccines, and other health technologies as a strategic pillar of any health system [ 4 , 5 ], the Global Fund supported the Ministry of Health and Child Care (MOHCC) through the United Nations Development Program (UNDP) to undertake a comprehensive assessment of the national procurement and supply chain management (PSCM) system in 2013 [ 6 ]. This assessment aimed to develop a strategic vision and costed action plan for improvement. This covered both upstream and downstream aspects of PSCM. The strategic purpose was to help the MOHCC launch a coordinated approach to invest in PSCM improvements and enhance coordination and cooperation in managing all health commodities across the health system [ 3 , 6 , 7 ].
Subsequently, the Global Fund supported several initiatives aimed at the realization of the improvements proposed by the comprehensive assessment undertaken by UNDP [ 6 ]. These initiatives primarily encompassed end-to-end supply chain assistance in critical areas, including demand quantification and forecasting, warehousing capacity development, fleet improvement, distribution systems, and waste management systems. Other support aspects focused on warehouse optimization, data and information management systems, and personnel training [ 7 , 8 ]. In general, warehouse optimization is the process of improving the efficiency and effectiveness of warehouse operations. It involved refining workflows, leveraging technology, enhancing spatial utilization, and ensuring precise inventory management [ 6 , 7 ].
More specifically, the Global Fund provided funds for the construction of warehouses for the National Pharmaceutical Company of Zimbabwe (NATPHARM) to facilitate the smooth handling of health commodities. Additionally, this support extended to water supplies (in terms of sinking boreholes) for various warehouses, water tanks, and booster pumps for the other branches. Global Fund also supported NATPHARM in constructing two incinerators in the two main cities, Harare, and Bulawayo to handle pharmaceutical waste effectively [ 9 , 10 ].
Through Global Fund support, NATPHARM also received modern warehouse equipment such as forklifts, pallet jacks and rolling ladders, and data and information management system support for better visibility and effective handling of health commodities. The support further extended to optimising the Harare branch warehouse with modern receiving and transit capabilities to serve other feeder locations and the procurement of modern delivery trucks to facilitate the distribution of commodities. Global Fund support also extended to personnel training and retention for the effective functioning of NATPHARM and the broader procurement and supply system [ 3 , 6 , 9 ].
Focusing on quality assurance and safety of medicines and other health commodities, Global Fund supported the Medicines Control Authority of Zimbabwe (MCAZ) to develop capacity in quality testing of all commodities procured through grants. MCAZ was also supported with the installation of solar panels that allowed for an uninterrupted power supply to facilitate smooth operations at the organization. The Global Fund support was also critical in the upgrading of the biology and chemistry laboratories to attain WHO prequalification standards [ 8 , 9 , 11 ]. Similarly, there was direct support from the Global Fund to facilitate pharmacovigilance activities, such as adverse drug reactions reporting using electronic systems. All these measures were meant to ensure that the medicines and health commodities consumed in the Zimbabwean health system were safe and quality-assured [ 4 , 5 , 9 , 11 ].
The overarching project by the Global Fund to support the Zimbabwean government was designed and implemented in response to the nationally identified gaps and opportunities that were established through various research and consultative efforts [ 3 , 4 , 6 , 8 ]. The project was kickstarted in the first quarter of 2019 and continued through 2021, with various project components being implemented in a phased approach to achieve the national targets [ 3 , 4 , 7 , 10 , 11 ]. To ensure effective coordination, accountability, and avoidance of duplicative efforts, the project was designed and implemented in close coordination with other partners represented in the National Health Development Partners Coordination Forum (HDPCF), Health Sector Technical Working Group (HSTWG), and the Global Fund Country Coordination Mechanism (CCM), among others [ 3 , 4 , 6 , 8 , 10 ]. There was regular reporting to the respective coordination mechanisms to track progress as well as troubleshoot any implementation issues as they arose [ 6 , 9 ].
Overall, the gaps identified through the various assessments commissioned by the Global Fund included a lack of effective coordination, poor inventory and order management, human resource constraints, and warehousing and storage inefficiencies [ 12 , 13 ]. Therefore, the focus of the Global Fund support was to retool the Zimbabwean PSCM system to be efficient, cost-effective and responsive to the population's health needs, particularly in the face of global epidemics and pandemics such as HIV/AIDS and COVID-19 [ 14 , 15 , 16 , 17 , 18 ].
In an attempt to resolve these issues, healthcare systems around the world are working on streamlining their supply chains through various health system strengthening measures [ 19 , 20 , 21 , 22 ]. Therefore, the objective of this analysis was to assess the overall effects of the Global Fund-supported investments in the Zimbabwean PSCM system and document the lessons learned to inform future programming efforts to strengthen healthcare systems.
The assessment covered a period of 2018 -2021 and employed both qualitative and quantitative research methods. Figure 1 . illustrates the convergent mixed methods study design that was applied. In this study design, both the qualitative and quantitative data collection and analyses are implemented simultaneously, and the insights merged to provide a fuller picture [ 23 ].
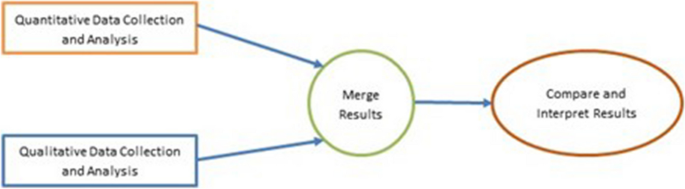
Convergent mixed methods design
The quantitative part of the study entailed collecting and analysing administrative data covering priority indicators that are routinely reported on the Zimbabwe PSCM. Meanwhile, the qualitative part comprised of key informant interviews (KII) focusing on stakeholders within the healthcare system to give perspective to the observed data trends. Insight from the two parts of the analysis were merged and subjected to comparative assessment and interpretation to ensure that a consistent picture emerged [ 23 , 24 ]. More details on the methods are provided in later sections.
Analytical framework
The overall analytical approach espoused in this assessment was anchored on the logical relationships of the building blocks of the health system as described by the World Health Organization (WHO) health system framework [ 5 ]. Figure 2 shows the analytical framework, which illustrates the results chain cascading from the Global Fund-supported initiatives to the expected improvements in intermediate and long-term outcomes related to PSCM, including the availability of medicines, reduced wastage, and overall improvements in population-level coverage [ 4 , 5 ].
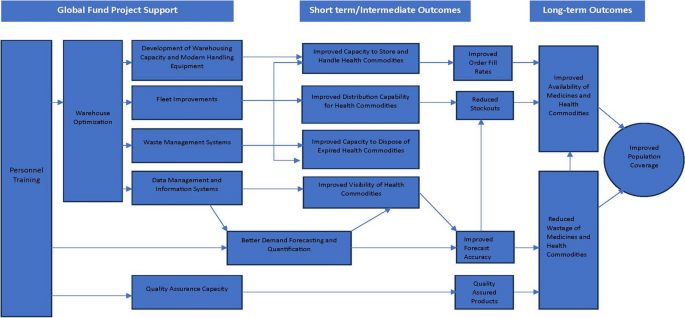
Analytic framework
Overall, the framework graphically displays the results Global Fund intended to achieve through its support to the Zimbabwean PSCM. The "theory of change" that underlies the Global Fund’s strategy is revealed through the arrows in the diagram that identify “causal” linkages through which various intermediate results interact to make progress toward the overall goal of improving health system performance [ 3 , 5 ].
Quantitative research
The quantitative research entailed a detailed descriptive analysis of the operational data that was routinely reported across the Zimbabwe PSCM system. Table 1 . shows some of the key performance indicators (KPI) that were considered in our analysis.
Data collection, management and analysis
The data used in this analysis were obtained from the routinely reported operational data that included the NATPHARM-operated warehouses and healthcare facilities in the country. The data were extracted from the various data management systems operated by the different institutions, cleaned, and collated into a comprehensive dataset in the form of a spreadsheet covering the period of the assessment. The database was examined for completeness and accuracy by cross-referencing the corresponding progress reports for specific periods. Trends of priority indicators were compared over time, as they related to Global Fund support to the PSCM space.
Qualitative research
The qualitative assessment entailed KIIs with health system stakeholders who were knowledgeable and intimately involved in the Global Fund-supported initiatives and its intended beneficiaries. This included provincial and district management teams, hospital and clinic personnel, and other stakeholders in the Zimbabwe health system. Informed consent was obtained from each study participant involved in the study. The data collection protocol ensured that all study participants fully understood the objectives of the study and consented verbally to provide the required information.
As previously stated, the literature review helped map and identify critical organisations involved in the PSCM space, and more specifically, those involved in the procurement and health system strengthening activities supported by the Global Fund. A full list of those organisations is provided on Table 2 .
Sampling techniques
Convenience purposive sampling was used to select key informants and in-depth interviews [ 23 ]. Our sample was supplemented using snowball sampling methods (also called chain sampling). The initial respondents referred other potential respondents until no new information was forthcoming or achieved saturation. Efforts were made to be all-inclusive, involving various stakeholder groups and organisations intimately linked to the operations of the Zimbabwe PSCM landscape.
This comprised of KIIs using a structured interview guide that covered various thematic areas relevant to the assessment to obtain a comprehensive perspective of the impact of the Global Fund-supported initiatives in the country. In its development, testing and validation, the key informant guide was pretested and adapted to ensure suitability for the task. In view of the restrictions imposed to prevent the spread of COVID-19 infections at the time of the study, some KIIs were conducted online using multimedia channels such as Zoom, Skype, and telephonically.
Three research assistants supported the two project leaders in conducting the KIIs. After each interview, all notes taken by the research assistant were checked by the two project leaders to ensure completeness and readability to minimise recording errors. In addition, a tape recorder was used for interviews to assist with reference post data collection. All the recordings were stored in a pin-protected cloud storage which was only accessible by the two project evaluation leaders. Qualitative data obtained from the KIIs were transcribed in full and then manually analysed applying thematic content analysis. Where there was a divergence of opinion, an agreement was established through discussion with three members of the project evaluation team. In thematic analysis, data from interview transcripts were grouped into similar concepts. This approach was appropriate for semi-structured expert interviews as it is used to code text with a predefined coding system that can then be refined and completed with new themes emerging [ 23 , 24 ]. Our initial coding system was defined during the desk review stage and continuously updated in the successive phases of data collection employing a deductive approach of qualitative research. The emerging themes were not preconceived (desk review) but emerged from the data during the coding process, while the global themes were the highest-order themes that emerged from the data and were broad enough to capture the essence of the entire dataset [ 23 ]. The codes are presented in a tabular format in the results section below.
This section presents both the quantitative and qualitative research results from the study. The quantitative results comprise of trends of the priority operational PSCM indicators for the relevant period. The qualitative results present the perspectives of the key health stakeholders involved in the Zimbabwe healthcare system.
Quantitative results
Table 3 shows that the total warehouse capacity across the Zimbabwean health system increased by 37.8% between 2018 and 2021.
Of the 1500 public health facilities in Zimbabwe coverage by the PSCM system was consistently high between the years 2018 and 2021, averaging 94%, and increasing by 13.6% over the same period. However, order fulfillment rate within 90 days, for 1410 reporting health facilities was consistently below 50% from 2018 to 2020, despite the reported high coverage for the health facilities by the PSCM in the country. Notably, this indicator showed remarkable improvement to 91% in 2021, from an average of 42% from the previous three years. More specifically, the order fill rate for Tenofovir 300mg/ lamivudine 300mg/efavirenz 600mg (TLE 600mg) improved despite the significant drop observed in 2020. However, when comparing 2018 and 2021, the order fill rate for this specific HIV drug increased by around 36.5%, while the stockout rates for the same drug at the central stores declined by about 14.5% over the same period.
Table 3 further shows a 44% drop of order fill rates for the Determine HIV Test Kit between 2018 and 2020 for the 1410 reporting health facilities, only to recover in the year 2021, where order fill rates improved to 83%. At the same time, the stockout rates for the Determine HIV Test Kit at the central stores declined by 49% between 2018 and 2021.
Figure 3 shows the estimated average population coverage for HIV treatment for adults and children, from 2018 to 2020, at 92% and 71%, respectively. The figure shows that there was limited variation in the population level coverage over the years, despite the estimated increase in the number of people living with HIV over the same period. The national target for this indicator is 95%.
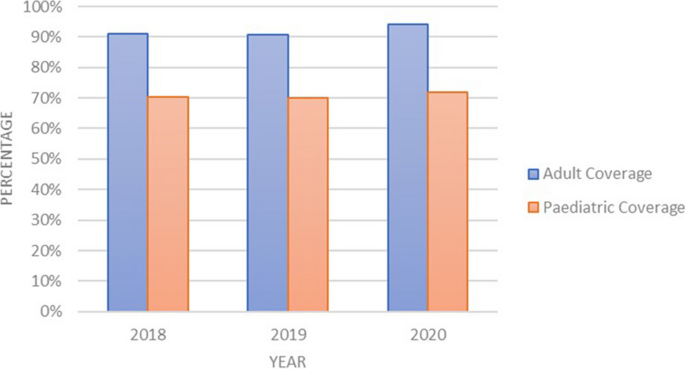
Adult and paediatric HIV treatment population coverage
Figure 4 shows the proportion of the value of the expired stock in the 7 warehouses, over three years, between 2019 and 2021, which demonstrates a declining trend over time. The highest expiry was in quarter 4 2019 at 1.9%, compared with the lowest in quarter 3 2021 at 0.1%. This represents a 93% reduction in value of expired stock.
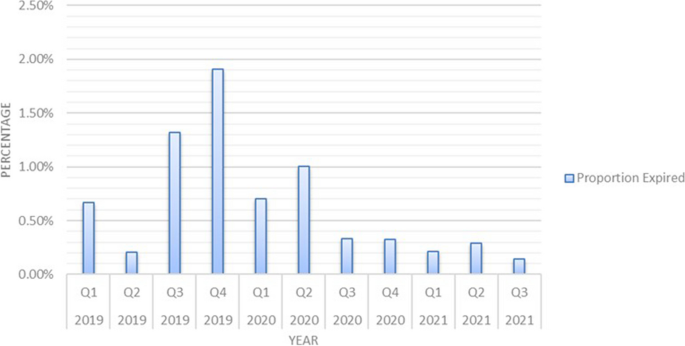
Percentage value of expired stock
Figure 5 shows the combined stock-taking variance valued in United States Dollar terms across 7 warehouses over a three-year period. The stock variance shows a declining trend over the three-year period to negligible values at the end of 2021.
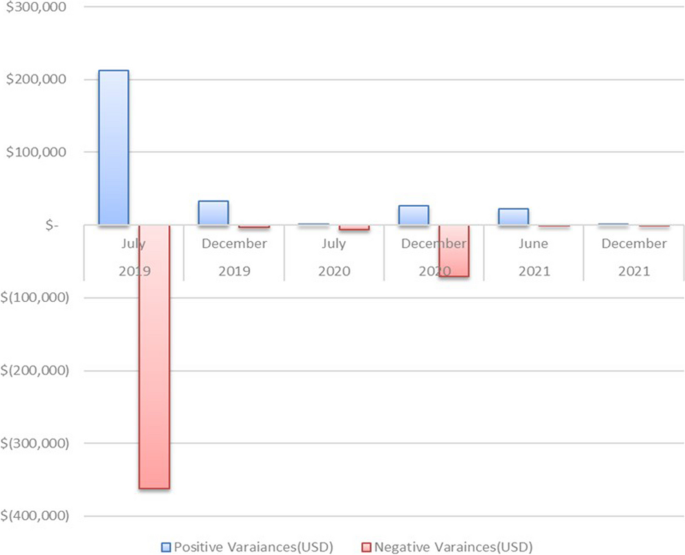
Stock-taking variance
Figure 6 shows the temporal trend of the number of days that it took NATPHARM to resolve the stock variances across the different warehouses in the country. Overall, there is a decline from the average of 8 days from the December 2018 stocktake (with Harare warehouse as an outliner at 25 days), to an average of 1 day in the December 2021 stocktake, where all warehouses converge.
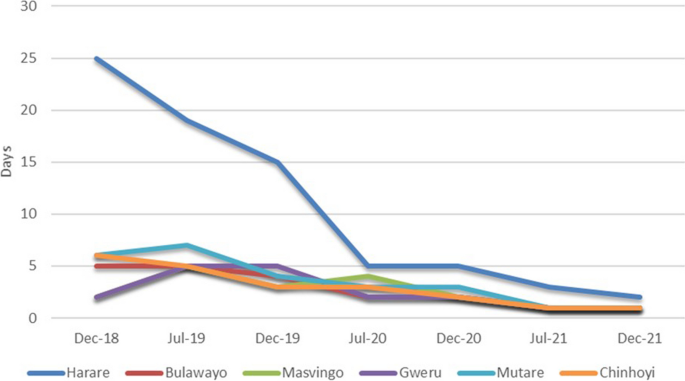
Duration to resolve stock variance
Table 4 shows the funding levels in USD$ to support the diagnostic capacity for Covid-19, comprising of the polymerase chain reaction test (PCR) and rapid diagnostic tests (RDT). The table further shows the PSCM related costs, the total test done, and positive cases identified over the two-year period. The total funding between 2020 and 2021 increased by 290%, with testing levels increasing by 490% over the same period. The average Covid-19 positivity rate in 2020 was 6.4% while the positivity rate for 2021, was 3.1%, indicating a greater than 50% drop.
Qualitative results
Most of the participants interviewed acknowledged that the Global Fund support to NATPHARM and the broader Zimbabwean health system had been central in improving the overall performance of the health system through improved availability of essential medicines and other health commodities. This was largely achieved by ramping up the various components of the PSCM value chain and related operations, leading to efficiency, effectiveness and reliability.
Table 5 shows the codes, emerging and global themes from the thematic content analysis. The emerging themes revolved around the lack of infrastructure and equipment curtailing warehouse operations before the Global Fund support. Data gaps and poor product visibility were also emerging themes, as were the effects of the old fleet on the overall supply and distribution system. Similarly, issues of infrastructure, capacity, and personnel training gaps emerged as crucial themes hindering quality assurance within the PSCM. Global themes also largely focused on infrastructural inadequacy leading to underperformance. Improvements leading to better handling of commodities; data and information systems, enhancing visibility and supporting accuracy in forecasts; improvements in the distribution systems enabled by newer fleets also featured as global themes. Similarly, better trained and motivated personnel, able to perform critical functions; capacity to ensure the quality and safety of medicines and other health commodities; and the need for effective multistakeholder partnerships to improve effectiveness and sustainability of health systems, were key themes.
NATPHARM operations
According to the NATPHARM management, warehouse improvement and optimisation exercise resulted in better visibility and improved efficiency in the operations related to the commodity handling across the entire value chain. More specifically, the processes related to stock taking improved markedly over time according to the reports presented by various organizations that had been commissioned to undertake the stock audits.
“ …. warehouse optimisation supported implementing an inventory management system which conformed with bin location and variant codes, according to different donors. The result was improved, faster and more accurate stock takes, a sharp reduction of variances and more streamlined order processing ” Participant, NATPHARM.
Further, it was reported by various participants that order processing and deliveries had improved to be timely and on schedule as a result of the improved visibility and efficiency harnessed across the PSCM. Similarly, there was consensus that receiving processes and documentation had significantly improved through the support offered by Global Fund particularly towards warehouse optimization. The improvements in the data management systems and related trainings were also cited as contributory to the overall trend that was observed.
“ Reporting quality has greatly improved and is now timely, accurate and complete. This helps in accurate forecasting of demand, which in turn avoids unnecessary wastage and expiries” Participant MOHCC.
There was consensus from the majority of participants interviewed that the fleet improvements had improved the availability of essential commodities vital for the effective management of high burden diseases; HIV/AIDS, Malaria and Tuberculosis in Zimbabwe. According to participants from a local health facility, this was evidenced by low stockout rates for the key commodities needed to manage these three conditions effectively. The new fleet was reported to facilitate deliveries from various warehouses to the recipient health facilities on a regular basis. This level of distributional access coupled with better demand forecasting as a result of improved data use, was noted as critical in the improved availability of medicines and health commodities at the health facility levels.
Further, respondents in the leadership of NATPHARM revealed that the Global Fund support had benefited the overall financial position of the organisation by tapping into efficiencies harnessed through the various measures that have been implemented. Some of the support measures that resulted in efficiency improvements include, the warehouse optimization, pharmaceutical waste management and fleet improvements, which ultimately reduced operational costs.
For example, it was noted that running a newer fleet of vehicles led to lower maintenance and fuelling costs than previously was the case, when deliveries were done using older vehicles. Similarly, it was noted that pharmaceutical waste resulting from expired medicines and other health commodities was expensive to store and dispose, particularly when engaging third party organizations. However, this additional cost was reportedly in the decline, as a result of the investment in the incinerators for waste management.
“ The provision of incinerators for waste management has resulted in huge savings in terms of the cost of waste destruction. It has also resulted in significant compliance with environmental health regulations.”, Participant, NATPHARM.
MCAZ operations
Majority of the participants agreed that the Global Fund support to MCAZ strengthened its overall capacity to handle the requisite safety and quality assurance needs to effectively support the procurement functions for medicines and other health commodities within the country and regionally. The installation of solar panels to provide uninterrupted electricity power supply for the operations of the organization was cited as a huge advantage allowing for improved performance, in a country where power supply is unreliable. Similarly, other participants cited, the support for MCAZ laboratories to obtain the WHO prequalification status, as a major step towards effectiveness and sustainability for the organization; citing the fact that MCAZ is offering quality assurance services regionally at a fee.
“ We [MCAZ] now have the capacity to conduct the safety and quality assurance tests needed to support the procurement of commodities in the country and the region. We [MCAZ] even recently won the tender to support the regional procurement activities ”, Participant, MCAZ.
Based on the results framework provided in Fig. 3 , there is clear evidence that the Global Fund-supported initiatives resulted in positive improvements in the overall performance of the Zimbabwean PSCM system. However, it is important to recognise some of the assessment’s limitations in interpreting these findings. First, the results reported are for a limited observation period and a limited set of indicators, which are largely confined to the national level analysis, missing out on granular subnational and commodity-specific analysis that could be more informative. Secondly, this study was not conceptualised before the onset of the intervention reported here (i.e., Global Fund-supported initiatives), and therefore, no specific steps were taken to develop an appropriate prospective research design and data collection strategy to support a more rigorous assessment. Therefore, the study relied on secondary PSCM data that were sparse and covered a limited period. Third, the study could be subject to confounding relationships with other concurrent interventions being implemented by other health system stakeholders that have direct or indirect effects on the PSCM system, complicating impact attribution to specific interventions. Forth, the analysis focused only on a narrow subset of medicines and commodities related to HIV/AIDS and COVID-19. However, despite these limitations, every effort has been made to use the most up-to-date and complete information available, including validation using official reports and collaborative reported data with key informant interviews.
The estimated population coverage for HIV treatment for both adults and children remained consistently high despite the increasing prevalence in the country. It was estimated that adults living with HIV increased by 10% from a baseline of 2018, to reach 1.3M in 2020, while children living with HIV increased by 24%, from a baseline of 2018, to reach 75 000 in 2020 [ 3 , 4 , 9 ]. As a key last mile population outcome, it can be rightly assumed that high HIV treatment coverage in the Zimbabwean system emanated from strengthened inventory management functionality and improved delivery of orders supported by a modern fleet of vehicles, which allowed for meeting the supply target of four quarterly rounds [ 3 , 8 ]. Population coverage is an important performance measure for a health system. It unites two important concepts; need and utilisation of an intervention to improve health [ 25 ]. In our case, the intervention is HIV treatment and the population in need is those living with HIV needing treatment; and the proportion with access and able to use the treatment they need, represents population coverage. This is a fundamentally important consideration as various health systems, including low- and middle-income countries, are making universal health coverage (UHC) efforts. There is no question, that improved access to essential medicines and other health technologies is a fundamental cornerstone towards UHC [ 1 , 5 , 26 ].
Other intermediate indicators that are critical for progress towards improved availability of medicines and other health commodities and hence UHC, also showed significant improvements that could be attributed to Global Fund-supported initiatives. For example, reduced wastage and decreasing value of expired health commodities reported, point towards improving efficiency across the value chain. As noted earlier, efficiency is one of the fundamental expectations of an effective health system outlined in the WHO health system framework [ 3 , 5 ]. The diminishing value of expiries could be ascribed to various factors, including the improved workflow processes and data accuracy at NATPHARM. This improvement which is associated with better visibility of commodities across the value chain could be attributed to investments made by Global Fund such as the enterprise resource planning platform, coupled with concomitant training and supervision.
Through Global Fund’s assistance to NATPHARM, automation of tasks such as stock management, ordering, and other operational activities was central and contributory to driving the observed improvements in the handling of commodities; reduction of wastage and expiries and improving availability. Similarly, better inventory management and warehouse optimization activities such as decongestion resulted in quicker, timely, more accurate, and well-documented stock takes, improving overall commodity management.
Variances between stock on hand and physical counts were used to determine whether facilities are conducting period checks on their stocks and therefore calculating monthly consumption of commodities accurately. As such the variance across commodities should be zero. Low variance indicates that the stocks at hand are generally similar and do not vary widely from the physical stock counts, while high variance indicates that the respective values have greater variability and are more widely dispersed from one another. There is clear evidence pointing towards the reduction in stock variances when comparing stock on hand and physical counts across the different warehouses in the country over time. This trend can be attributed to better visibility of commodities at the warehouses and training of personnel which was supported by the Global Fund [ 2 , 9 ]. Similarly, the number of days it took the NATPHARM personnel to resolve stock variances showed a dramatic reduction, from an average of 8 days to 1 day in a span of 3 years. This observed trend could also further support the claim that overall, the Global Fund supported initiatives produced the desired results.
With the advent of Covid-19, the effects of the Global Fund support on the PSCM became evident considering the robust response the country was able to mount particularly in terms of diagnostics [ 9 ]. The country was able to rapidly roll out COVID-19 testing, reaching many people between 2020 and 2021. Similarly, the Covid-19 positivity rates declined from 6.4% to about 3.1% over the same period. High positivity rates may indicate that the health system is only testing the sickest patients who seek medical attention and is not casting a wide enough net to know how much of the virus is spreading within its communities. A low rate of positivity on the other hand, can be seen as a sign that a health system has sufficient testing capacity for the size of the Covid-19 outbreak and is testing enough of its population to make informed decisions about reopening the economy. The WHO guidance is that countries which have conducted extensive testing for COVID-19, should remain at 5% or lower positivity rate for at least 14 days.
Safe pharmaceutical waste management and disposal is a primary consideration of any effective health system in completing the PSCM loop [ 27 ]. The Global Fund supported the investment in MOHCC operated incinerators. These investments could largely be associated with reduction in the cost of storage, handling and disposal of the expired stock, particularly when considering that certain space was rented from third parties which often charged a premium. Safe pharmaceutical waste disposal also became more priority with the increased supplies that resulted from the efforts to tackle the Covid-19 pandemic.
Despite signs of progress, there was temporary faltering of indicators- namely, order fill and stockout rates; associated with key commodities for effective management of HIV in the year 2020, warranting an explanation. The drop in Tenofovir/Lamivudine/Efavirenz (TLE 600mg) in 2020 could be linked to several factors. In the year 2019, the Zimbabwe MOHCC adopted new treatment regimens containing Dolutegravir. This means, newly HIV positive clients were started on Dolutegravir regimen as standard of care rather than the previous first line treatment which then surged Tenofovir/Lamivudine/Dolutegravir 50mg order fill rate, while having the opposite effect on the old regimen. Lastly, the effects of COVID-19 pandemic cannot be underestimated as the global supply chain systems were logged with delays which caused disruptions and inefficiencies in health systems in many countries [ 28 ]. In the same period, Determine HIV Test Kit rebounded from stocking out in central stores because of strengthened warehouse optimization activities, including better inventory management, purposeful stock taking, and approval processes contributed to the lowering of stockout rates.
The Global Fund-supported initiatives were also instrumental in building capacity by training key personnel for the effective implementation of activities related to the procurement and supply chain management function [ 8 , 29 , 30 ]. Better quantification and forecasting capabilities (due to data availability through e-LMIS and personnel training), improved warehousing capacity to hold a wide portfolio of products, and direct delivery to facilities through a modern fleet could have contributed to the high population coverage reported [ 26 , 30 , 31 ]. According to the WHO health system framework, effective leadership is required to coordinate all the functions of the health system in order to achieve the desired outcomes [ 5 ]. Therefore, it is sensible to conclude that, the reported health system improvements could not have happened without effective leadership and well-trained staff tasked with coordination and management across the PSCM value chain. It can be further inferred that the training and capacity development measures offered to the NATPHARM personnel were consequential in supporting the broader health system to meet its overall objectives, including improving PSCM performance [ 2 , 7 , 29 ].
Similarly, adequate infrastructure, equipment, data, and information management systems are crucial ingredients for a well-functioning health system, according to the WHO health system framework [ 4 , 5 , 9 ]. The Global Fund-supported initiatives were central in supporting these aspects of the health system through improved warehousing capacity, of modern equipment, installation of solar panels, fleet improvement and deployment of an electronic-logistic management information system (e-LMIS). The cumulative benefits of these investments include optimised procurement and distribution of commodities leading to a reduction in stockout rates and timely order refills to meet the population health needs [ 9 ].
Based on these findings, it would be reasonable to conclude that the Global Fund-supported initiatives in Zimbabwe contributed positively to strengthening the health system, particularly through the improved performance of the various indicators linked to the PSCM system at national and regional warehouses, as well as health facilities. Considering the prevailing health needs in the country, the implementation of this project and the manner of investments provide a basis and playbook for further support to make progress. This is particularly true considering the various competing priorities in the Zimbabwean healthcare system amidst resource constraints [ 3 , 6 , 8 ]. This was largely underpinned on the overarching focus on UHC and the critical role that an effective PSCM plays towards that very objective [ 3 , 12 , 13 , 14 ].
The Global Fund-supported project in Zimbabwe worked through the existing national coordination mechanisms where various key stakeholders, including MOHCC and NATPHARM, were involved in all key strategic planning and implementation decisions, ensuring country leadership and ownership. It was clear from the outset that this approach required sound partnership, transparency, and accountability among all the involved stakeholders, to deliberate and find common ground, guided by the overarching objective to make progress towards UHC.
The question of securing the gains and ensuring sustainability is fundamental for donor supported health programs in low- and middle- income countries. To make progress, it is imperative for health system stakeholders, including governments and donor organizations that are keen to sustainably strengthen health systems to pay close attention to critical areas like the procurement and distribution of health commodities. It is critical to collaborate with key stakeholders through joint planning and implementation to optimize the available resources. Organizational autonomy coupled with strong data driven accountability systems and the sharing of best management practices are fundamentally important in this discourse.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request and once written permission is obtained from NATPHARM.
Abbreviations
Country Coordination Mechanism
Health Development Partners Coordination Forum
Health Sector Technical Working Group
Key Informant Interview
Medicines Control Authority of Zimbabwe
Ministry of Health and Child Care
National Pharmaceutical Company of Zimbabwe
Polymerase Chain Reaction
Procurement and Supply Chain Management
Rapid Diagnostic Tests
Tenofovir Lamivudine Efavirenz
Universal Health Coverage
United Nations Development Program
World Health Organization
UNDP. Healthy systems for healthy people: UNDP and Global Fund support to strengthen financial and risk management for the delivery of health services in Zimbabwe. New York: United Nations Development Programme; 2020.
UNDP. Healthy systems for healthy people: UNDP and Global Fund support to strengthen the national health management information system. New York: United Nations Development Programme; 2020.
MOHCC. Investment case for the national health strategy 2021-2025. Harare: Accelerating investments towards Universal Health Coverage; 2020.
Google Scholar
MOHCC. National health strategy 2021–2025. Harare: Ministry of Health and Child Care; 2020.
WHO. Everybody business: strengthening health systems to improve health outcomes: WHO’s framework. Geneva: WHO; 2007.
Group EH. Comprehensive assessment of the supply chain for health commodities in the public sector in Zimbabwe. Harare: United Nations Development Programme; 2013.
MOHCC. Analysis and findings from the Zimbabwe supply chain human resource assessment. Harare: Ministry of Health and Child Care; 2012.
UNDP. Healthy systems for healthy people: the impact of UNDP-managed Global Fund investments in procurement and supply chain systems in Zimbabwe. Harare: United Nations Development Programme ; 2020.
Global Fund. Audit report: Global Fund Grants in Zimbabwe. Geneva: The Global Fund; 2020
MOHCC. Zimbabwe electronic logistics management information system baseline assessment report December 2018 to January 2019. Harare: Ministry of Health and Child Care ; 2019.
MOHCC. Zimbabwe comprehensive laboratory assessment. Harare: Ministry of Health and Child Care; 2016.
Privett N, Gonsalvez D. The top ten global health supply chain issues: perspectives from the field. ORHC. 2014;3(4):226–30. https://doi.org/10.1016/j.orhc.2014.09.002 .
Article Google Scholar
Yadav P. Health product supply chains in developing countries: diagnosis of the root causes of underperformance and an agenda for reform. Health Syst Reform. 2015;1(2):142–54. https://doi.org/10.4161/23288604.2014.968005 .
Article PubMed Google Scholar
Seidman G, Atun R. Do changes to supply chains and procurement processes yield cost savings and improve availability of pharmaceuticals, vaccines or health products? A systematic review of evidence from low-income and middle-income countries. BMJ Global Health. 2017;2:e000243.
Article PubMed PubMed Central Google Scholar
Windisch R, Waiswa P, Neuhann F, Scheibe F, Savigny DD. Scaling up antiretroviral therapy in Uganda: using supply chain management to appraise health systems strengthening. Global Health. 2011;7:25. https://doi.org/10.1186/1744-8603-7-25 .
Cyn-Young P, Kijin K, Susann R, Steven B, Woo KJ, Tayag MC, et al. This brief examines the global shortage of the personal protective equipment (PPE) needed to tackle COVID-19 and suggests policy implications. Manila: Asian Development Bank; 2020.
Dai T, Zaman MH, Padula WV, Davidson PM. Supply chain failures amid Covid-19 signal a new pillar for global health preparedness. J Clin Nurs. 2021;30(1–2):e1–3. https://doi.org/10.1111/jocn.15400 .
Ghaffar A, Rashidian A, Khan W, Tariq M. Verbalising importance of supply chain management in access to health services. J Pharm Policy Pract. 2021;14(Suppl 1):91. https://doi.org/10.1186/s40545-021-00352-5 . ( 1–3 ).
Jahre M, Dumoulin L, Greenhalgh LB, Hudspeth C, Limlim P, Spindler A. Improving health in developing countries: reducing complexity of drug supply chains. JHLSCM. 2012;2(1):54–84. https://doi.org/10.1108/20426741211226000 .
Vledder M, Friedman J, Sjoblom M, Brown T, Yadav P. Improving supply chain for essential drugs in low-income countries: results from a large scale randomized experiment in Zambia. Health Syst Reform. 2019;5(2):158–77. https://doi.org/10.1080/23288604.2019.1596050 .
Agrawal P, Barton I, Bianco RD, Hovig D, Sarley D, Yadav P. Moving medicine, moving minds: helping developing countries overcome barriers to outsourcing health commodity distribution to boost supply chain performance and strengthen health systems. Glob Health Sci Pract. 2016;4(3):359–65. https://doi.org/10.9745/GHSP-D-16-00130 .
Arora M, Gigras Y. Importance of supply chain management in healthcare of third world countries. IJSOM. 2018;5(1):101–6. https://doi.org/10.22034/2018.1.7 .
Creswell J, Creswell JD. Research design: qualitative, quantitative, and mixed methods approaches. London: Sage; 2018.
Achoki T, Lesego A. The imperative for systems thinking to promote access to medicines, efficient delivery, and cost-effectiveness when implementing health financing reforms: a qualitative study. Int J Equity Health. 2017;16:53. https://doi.org/10.1186/s12939-017-0550-x . (1-13).
Colson KE, Dwyer-Lindgren L, Achoki T, Fullman N, Schneider M, Mulenga P, et al. Benchmarking health system performance across districts in Zambia: a systematic analysis of levels and trends in key maternal and child health interventions from 1990 to 2010. BMC Med. 2015;13:69. https://doi.org/10.1186/s12916-015-0308-5 . 1-14.
Githendu P, Morrison L, Silaa R, Pothapregada S, Asiimwe S, Idris R, et al. Transformation of the Tanzania medical stores department through global fund support: an impact assessment study. BMJ Open. 2020;10(e040276):1–12. https://doi.org/10.1136/bmjopen-2020-040276 .
MOHCC. Infection Control and Waste Management Plan (ICWMP). Harare: Ministry of Health and Child Care; 2022.
Moosavi J, Fathollahi-Fard AM, Dulebenets MA. Supply chain disruption during the COVID-19 pandemic: recognizing potential disruption management strategies. Int J Disaster Risk Reduct. 2022;75:102983. https://doi.org/10.1016/j.ijdrr.2022.102983 .
Albano GL, Ballarin A, Sparro M. Framework agreements and repeated purchases: the basic economics and a case study on the acquisition of it services. In: International Public Procurement Conference. Milan: The International Public Procurement Conference; 2010.
OECD. Manual for framework agreements. Paris: Organization for Economic Co-operation and Development; 2014.
Arney L, Yadav P, Miller R, Wilkerson T. Strategic contracting practices to improve procurement of health commodities. Glob Health Sci Pract. 2014;2(3):295–306. https://doi.org/10.9745/GHSP-D-14-00068 .
Download references
Acknowledgements
The authors would like to thank the participants from the different organizations in Zimbabwe that provided feedback during the study. They are also grateful to the management of the various organizations that allowed their staff to participate and provided premises and other resources that were used during the interviews. Gratitude to Sarah Gurrib who proofread the manuscript and offered useful comments.
The study was funded by the Global Fund to Fight AIDs, Tuberculosis and Malaria. The funder had no role in the study design, data collection, data analysis, data interpretation, or writing of the article. All authors had full access to study data and had final responsibility for the decision to submit for publication.
Author information
Authors and affiliations.
Africa Institute for Health Policy, P.O. Box 57266-00200, Nairobi, Kenya
Abaleng Lesego, Lawrence P. O. Were, Tsion Tsegaye & Tom Achoki
Department of Health Sciences & Department of Global Health, Boston University, Boston, U.S.A.
Lawrence P. O. Were
Global Fund to Fight AIDs, Tuberculosis and Malaria, Geneva, Switzerland
Rafiu Idris, Linden Morrison, Tatjana Peterson & Sheza Elhussein
PricewaterhouseCoopers, Harare, Zimbabwe
Esther Antonio & Godfrey Magwindiri
National Pharmaceutical Company of Zimbabwe, Harare, Zimbabwe
Ivan Dumba, Cleyland Mtambirwa, Newman Madzikwa & Raiva Simbi
Medicines Control Authority of Zimbabwe, Harare, Zimbabwe
Misheck Ndlovu
You can also search for this author in PubMed Google Scholar
Contributions
Tom Achoki (TA), Rafiu Idris (RI), Lawrence Were (LW) and Abaleng Lesego (AL) conceptualized and designed the study. AL, TA, and Godfrey Magwindiri (GM) collected and analyzed data. TA and AL drafted the manuscript. Tsion Tsegaye (TT), Linden Morrison (LM), Tatjana Peterson (TP), Sheza Elhussein (SE), Esther Antonio(EA), Ivan Dumba (ID), Cleyland Mtambirwa (CM), Newman Madzikwa(NM), Raiva Simbi (RS), Misheck Ndlovu (MN) and LW did the critical revisions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Tom Achoki .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval including the consent procedure for participants was obtained from the Ethics Committee of the MOHCC Department of Research and NATPHARM, Harare Zimbabwe. The conduct and methods of this study adhered to the tenets outlined in the Declaration of Helsinki. Informed consent was obtained from each study participant involved in the study. The data collection protocol ensured that all study participants fully understood the objectives of the study and consented in writing to provide the required information. Before the interview commenced, the participants also consented verbally and confirmed that they had understood the objectives of the study and that they could opt out of the interview at any time without prejudice. No sensitive or personally identifying information was collected regarding the study participants.
Consent for publication
Not applicable.
Competing Interests
RI, LM, TP and SE declare that they are fulltime employees at the Global Fund to Fight AIDs, Tuberculosis and Malaria. EA and GM declare that they are fulltime employees at PricewaterhouseCoopers. ID, CM, NM and RS are fulltime employees at National Pharmaceutical Company of Zimbabwe. The rest of the authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lesego, A., Were, L.P.O., Tsegaye, T. et al. Health system lessons from the global fund-supported procurement and supply chain investments in Zimbabwe: a mixed methods study. BMC Health Serv Res 24 , 557 (2024). https://doi.org/10.1186/s12913-024-11028-6
Download citation
Received : 06 March 2023
Accepted : 22 April 2024
Published : 01 May 2024
DOI : https://doi.org/10.1186/s12913-024-11028-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health systems
- Procurement and supply chain management
- Global fund
- Donor funded programs
- Development assistance for health
- Health systems strengthening
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

IMAGES
COMMENTS
Methods and analysis This formative research will employ an exploratory qualitative research design using semistructured interviews and a purposive sampling approach. The data collection methods for this formative research will include indepth interviews with community members. ... Introduction The COVID-19 pandemic has certainly resulted in an ...
The COVID-19 model digraph can be expressed as a graph G = ( N, L), where G is the model graph, N = ( S, I, U, W, R) is the set of nodes (states), L = { v 1, v 2, v 3, v 4, v 5, v 6, v 7 } is the set of links (reactions). The model interaction individuals for the COVID-19 epidemic outbreak with reaction rates.
A study of 1,210 respondents from 194 cities in China found that during the beginning of the COVID-19 outbreak, more than 50% had moderate to severe psychological impact, with ~30% reporting moderate to severe anxiety ( Wang et al., 2020a ). Mental patients displayed more serious symptoms relating to physical health and suicidal ideation ( Hao ...
Qualitative research carried out during the COVID-19 pandemic can ask and answer questions which complement epidemiological data by providing insight into people's lived experiences of disease, care, and epidemic response efforts ( Teti et al., 2020 ). The exacerbation of social, health, and economic inequalities; the implementation of health ...
The conducted qualitative research was aimed at capturing the biggest challenges related to the beginning of the COVID-19 pandemic. The interviews were carried out in March-June (five stages of the research) and in October (the 6th stage of the research). A total of 115 in-depth individual interviews were conducted online with 20 respondents, in 6 stages. The results of the analysis showed ...
Abstract. With COVID-19 affecting all types of research, the authors of this article contribute to the discussions on how COVID-19 affects the world of qualitative nursing research in irrefutable ways. Underrepresented and vulnerable populations are faced with higher rates and severity of COVID-19, heightening the need to better address their ...
The COVID-19 pandemic has forced both quantitative and qualitative health researchers to adapt and strategize data collection strategies without causing any harm to the participants or researchers. This has resulted in utilizing various types of strategies such as online surveys and synchronous virtual platforms such as Zoom and Webex.
We performed a systematic review to evaluate the methodological quality of currently available COVID-19 studies compared to historical controls. A total of 9895 titles and abstracts were screened ...
As the COVID-19 pandemic has shown, setting up studies in time to gather relevant, real-world data enables researchers to capture current views and experiences, focus on practicalities on the ground, and deliver actionable results. ... and consequently contribute to the development of the rapid qualitative research.
Background The impact of the Covid-19 pandemic on young people's (YP) mental health has been mixed. Systematic reviews to date have focused predominantly on quantitative studies and lacked involvement from YP with lived experience of mental health difficulties. Therefore, our primary aim was to conduct a qualitative systematic review to examine the perceived impact of the Covid-19 pandemic ...
In South Africa, public perceptions of the COVID-19 pandemic and risk mitigation measures remain mixed. To better understand health behaviours in the context of COVID-19, a qualitative study was conducted, which aimed to investigate perceptions relating to the COVID-19 pandemic among the South African adult population. Twelve online focus groups were conducted across the following age groups ...
We documented low COVID-19 vaccination intentions (e.g., the need to wait and see) and specific concerns around the COVID-19 vaccines (e.g., about rapid development and side effects), which are consistent with similar qualitative research in racially/ethnically diverse populations (including Black Americans) and quantitative evidence that ...
Objective To explore UK public decisions around whether or not to get COVID-19 vaccines, and the facilitators and barriers behind participants' decisions. Design This qualitative study consisted of six online focus groups conducted between 15th March and 22nd April 2021. Data were analysed using a framework approach. Setting Focus groups took place via online videoconferencing (Zoom ...
This qualitative tool provides step by step guidance on how to design and conduct rapid qualitative research with different target groups to understand their barriers and drivers to COVID-19 vaccination. These insights can then be used to inform the development of interventions tailored to the target groups for successful COVID-19 vaccination ...
Research surrounding the psychological impacts of the COVID-19 pandemic suggests that many people experience feelings of grief due to loss of loved ones, loss of a sense of normalcy, or both . However, this study found that even though individuals were limited in their capacity to change their current situation, many remained optimistic with ...
Qualitative research is a process of understanding and discovery based on distinct methodological traditions of inquiry that explore social or human experiences. ... However, the COVID-19 pandemic has forced qualitative health researchers to rapidly adapt their tried and true in-person methods and to explore, innovate, and quickly overcome ...
This qualitative study was conducted to collect the opinions of experts on the identification of the Information challenges of COVID-19 during March-June 2020. The research population included all health professionals and experts. The sampling method was initially purposive and continued to saturate the data as snowball technique.
Two main challenges associated with the development of qualitative research in the COVID-19 context, namely "time constraints" and "physical distancing" are addressed and reflections on how to undertake qualitative healthcare research given the evolving restrictions are provided. The global response to mitigate the spread of the COVID-19 pandemic brought about massive health, social ...
In this paper I examine how the pandemic and quarantine of 2020 affected qualitative research. Employing personal narrative as a method, I show what disadvantages researchers may have met with whilst conducting their studies. The unprecedented circumstances of the restrictions and uncertainty caused by the Covid-19 crisis have had a dramatic impact on the public mental health of individuals ...
Keywords: pregnant women, health education, public health emergencies, qualitative research, COVID-19. Citation: Su X, Zhang Y, Chen M, Xu X and Liu G (2024) Understanding health education needs of pregnant women in China during public health emergencies: a qualitative study amidst the COVID-19 pandemic. Front.
A multitude of information sources are available to publics when novel infectious diseases first emerge. In this paper, we adopt a qualitative approach to investigate how Australians learnt about the novel coronavirus and COVID-19 and what sources of information they had found most useful and valuable during the early months of the pandemic. In-depth semi-structured telephone interviews were ...
These techniques, in contrast to rapid qualitative research approaches, can be also used as part of longer-term studies (Vindrola-Padros and Johnson, 2020). As qualitative researchers wanted to produce meaningful yet rapid research findings during the COVID-19 pandemic, the use of rapid qualitative research methods has seen an increase.
Due to COVID-19, schools were closed to mitigate disease spread. Past studies have shown that disruptions in education have unintended consequences for adolescents, including increasing their risk of school dropout, exploitation, gender-based violence, pregnancy and early unions. In Peru, the government closed schools from March 2020 to March 2022, declaring a national emergency that affected ...
Study protocol. This was a retrospective cohort study at Santa Casa de Misericórdia de Belo Horizonte, a tertiary cancer center in Belo Horizonte, Southeastern Brazil.This study aimed to analyze whether the COVID-19 pandemic harmed patients with lung and head and neck cancers, yielding delayed diagnosis, more advanced clinical stage at diagnosis, and poorer outcomes in comparison with 2019 ...
Background: Coronavirus disease 2019 (COVID-19) continues to spread across the globe, but patient experiences are rarely documented. Objective: To explore the psychology of COVID-19 patients during hospitalization. Methods: A phenomenological and robust sampling approach was employed. Sixteen patients admitted to the First Affiliated Hospital of Henan University of Science and Technology with ...
Abstract. In late 2020 and the first semester of 2021, in Santiago de Chile, five women researchers who work with qualitative methodologies, based on their reflections on how the context of the COVID-19 pandemic has impacted on their doctoral research or their role as thesis advisors, conducted a reflective exploration of the conditions and ...
However, the COVID-19 pandemic disrupted conventional facility-based HIV testing services, necessitating the exploration of innovative strategies for the effective delivery of HIVST. ... (795) Focus Groups and Qualitative Research for Human Factors Research (722) Theme Issue: Novel Coronavirus (COVID-19) Outbreak Rapid Reports (1449) Infectious ...
This study employed a mixed methods design combining quantitative and qualitative research methods. The quantitative part entailed a descriptive analysis of procurement and supply chain data from the Zimbabwe healthcare system covering 2018 - 2021. ... The average Covid-19 positivity rate in 2020 was 6.4% while the positivity rate for 2021 ...