Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- How to Write a Literature Review | Guide, Examples, & Templates

How to Write a Literature Review | Guide, Examples, & Templates
Published on January 2, 2023 by Shona McCombes . Revised on September 11, 2023.
What is a literature review? A literature review is a survey of scholarly sources on a specific topic. It provides an overview of current knowledge, allowing you to identify relevant theories, methods, and gaps in the existing research that you can later apply to your paper, thesis, or dissertation topic .
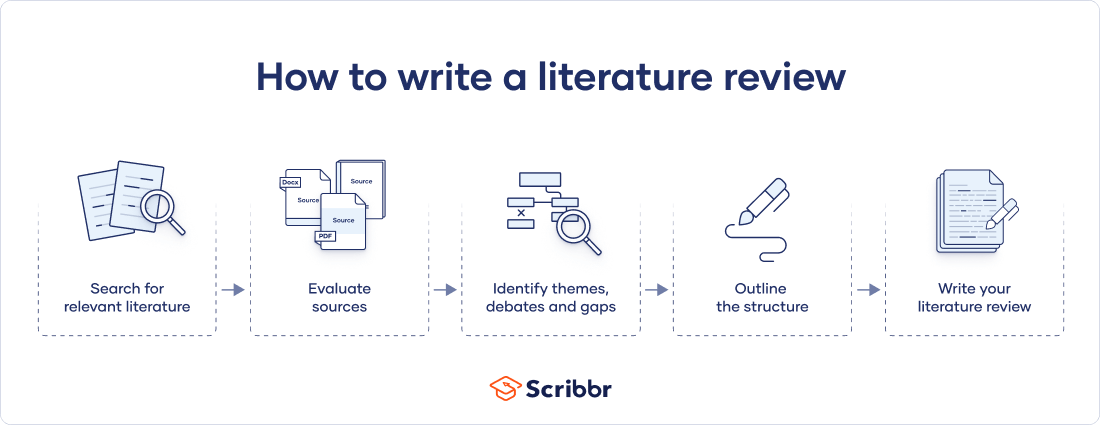
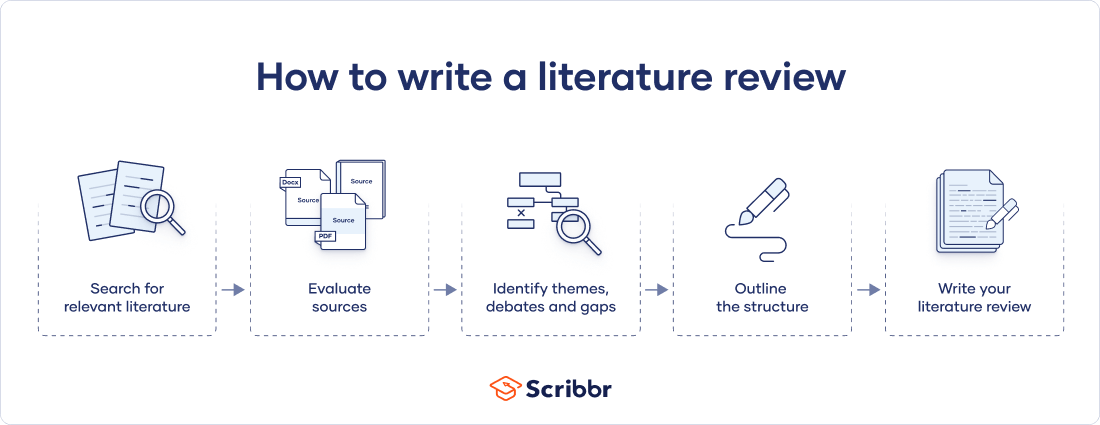
There are five key steps to writing a literature review:
- Search for relevant literature
- Evaluate sources
- Identify themes, debates, and gaps
- Outline the structure
- Write your literature review
A good literature review doesn’t just summarize sources—it analyzes, synthesizes , and critically evaluates to give a clear picture of the state of knowledge on the subject.
Instantly correct all language mistakes in your text
Upload your document to correct all your mistakes in minutes
Table of contents
What is the purpose of a literature review, examples of literature reviews, step 1 – search for relevant literature, step 2 – evaluate and select sources, step 3 – identify themes, debates, and gaps, step 4 – outline your literature review’s structure, step 5 – write your literature review, free lecture slides, other interesting articles, frequently asked questions, introduction.
- Quick Run-through
- Step 1 & 2
When you write a thesis , dissertation , or research paper , you will likely have to conduct a literature review to situate your research within existing knowledge. The literature review gives you a chance to:
- Demonstrate your familiarity with the topic and its scholarly context
- Develop a theoretical framework and methodology for your research
- Position your work in relation to other researchers and theorists
- Show how your research addresses a gap or contributes to a debate
- Evaluate the current state of research and demonstrate your knowledge of the scholarly debates around your topic.
Writing literature reviews is a particularly important skill if you want to apply for graduate school or pursue a career in research. We’ve written a step-by-step guide that you can follow below.
Here's why students love Scribbr's proofreading services
Discover proofreading & editing
Writing literature reviews can be quite challenging! A good starting point could be to look at some examples, depending on what kind of literature review you’d like to write.
- Example literature review #1: “Why Do People Migrate? A Review of the Theoretical Literature” ( Theoretical literature review about the development of economic migration theory from the 1950s to today.)
- Example literature review #2: “Literature review as a research methodology: An overview and guidelines” ( Methodological literature review about interdisciplinary knowledge acquisition and production.)
- Example literature review #3: “The Use of Technology in English Language Learning: A Literature Review” ( Thematic literature review about the effects of technology on language acquisition.)
- Example literature review #4: “Learners’ Listening Comprehension Difficulties in English Language Learning: A Literature Review” ( Chronological literature review about how the concept of listening skills has changed over time.)
You can also check out our templates with literature review examples and sample outlines at the links below.
Download Word doc Download Google doc
Before you begin searching for literature, you need a clearly defined topic .
If you are writing the literature review section of a dissertation or research paper, you will search for literature related to your research problem and questions .
Make a list of keywords
Start by creating a list of keywords related to your research question. Include each of the key concepts or variables you’re interested in, and list any synonyms and related terms. You can add to this list as you discover new keywords in the process of your literature search.
- Social media, Facebook, Instagram, Twitter, Snapchat, TikTok
- Body image, self-perception, self-esteem, mental health
- Generation Z, teenagers, adolescents, youth
Search for relevant sources
Use your keywords to begin searching for sources. Some useful databases to search for journals and articles include:
- Your university’s library catalogue
- Google Scholar
- Project Muse (humanities and social sciences)
- Medline (life sciences and biomedicine)
- EconLit (economics)
- Inspec (physics, engineering and computer science)
You can also use boolean operators to help narrow down your search.
Make sure to read the abstract to find out whether an article is relevant to your question. When you find a useful book or article, you can check the bibliography to find other relevant sources.
You likely won’t be able to read absolutely everything that has been written on your topic, so it will be necessary to evaluate which sources are most relevant to your research question.
For each publication, ask yourself:
- What question or problem is the author addressing?
- What are the key concepts and how are they defined?
- What are the key theories, models, and methods?
- Does the research use established frameworks or take an innovative approach?
- What are the results and conclusions of the study?
- How does the publication relate to other literature in the field? Does it confirm, add to, or challenge established knowledge?
- What are the strengths and weaknesses of the research?
Make sure the sources you use are credible , and make sure you read any landmark studies and major theories in your field of research.
You can use our template to summarize and evaluate sources you’re thinking about using. Click on either button below to download.
Take notes and cite your sources
As you read, you should also begin the writing process. Take notes that you can later incorporate into the text of your literature review.
It is important to keep track of your sources with citations to avoid plagiarism . It can be helpful to make an annotated bibliography , where you compile full citation information and write a paragraph of summary and analysis for each source. This helps you remember what you read and saves time later in the process.
The only proofreading tool specialized in correcting academic writing - try for free!
The academic proofreading tool has been trained on 1000s of academic texts and by native English editors. Making it the most accurate and reliable proofreading tool for students.
Try for free
To begin organizing your literature review’s argument and structure, be sure you understand the connections and relationships between the sources you’ve read. Based on your reading and notes, you can look for:
- Trends and patterns (in theory, method or results): do certain approaches become more or less popular over time?
- Themes: what questions or concepts recur across the literature?
- Debates, conflicts and contradictions: where do sources disagree?
- Pivotal publications: are there any influential theories or studies that changed the direction of the field?
- Gaps: what is missing from the literature? Are there weaknesses that need to be addressed?
This step will help you work out the structure of your literature review and (if applicable) show how your own research will contribute to existing knowledge.
- Most research has focused on young women.
- There is an increasing interest in the visual aspects of social media.
- But there is still a lack of robust research on highly visual platforms like Instagram and Snapchat—this is a gap that you could address in your own research.
There are various approaches to organizing the body of a literature review. Depending on the length of your literature review, you can combine several of these strategies (for example, your overall structure might be thematic, but each theme is discussed chronologically).
Chronological
The simplest approach is to trace the development of the topic over time. However, if you choose this strategy, be careful to avoid simply listing and summarizing sources in order.
Try to analyze patterns, turning points and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred.
If you have found some recurring central themes, you can organize your literature review into subsections that address different aspects of the topic.
For example, if you are reviewing literature about inequalities in migrant health outcomes, key themes might include healthcare policy, language barriers, cultural attitudes, legal status, and economic access.
Methodological
If you draw your sources from different disciplines or fields that use a variety of research methods , you might want to compare the results and conclusions that emerge from different approaches. For example:
- Look at what results have emerged in qualitative versus quantitative research
- Discuss how the topic has been approached by empirical versus theoretical scholarship
- Divide the literature into sociological, historical, and cultural sources
Theoretical
A literature review is often the foundation for a theoretical framework . You can use it to discuss various theories, models, and definitions of key concepts.
You might argue for the relevance of a specific theoretical approach, or combine various theoretical concepts to create a framework for your research.
Like any other academic text , your literature review should have an introduction , a main body, and a conclusion . What you include in each depends on the objective of your literature review.
The introduction should clearly establish the focus and purpose of the literature review.
Depending on the length of your literature review, you might want to divide the body into subsections. You can use a subheading for each theme, time period, or methodological approach.
As you write, you can follow these tips:
- Summarize and synthesize: give an overview of the main points of each source and combine them into a coherent whole
- Analyze and interpret: don’t just paraphrase other researchers — add your own interpretations where possible, discussing the significance of findings in relation to the literature as a whole
- Critically evaluate: mention the strengths and weaknesses of your sources
- Write in well-structured paragraphs: use transition words and topic sentences to draw connections, comparisons and contrasts
In the conclusion, you should summarize the key findings you have taken from the literature and emphasize their significance.
When you’ve finished writing and revising your literature review, don’t forget to proofread thoroughly before submitting. Not a language expert? Check out Scribbr’s professional proofreading services !
This article has been adapted into lecture slides that you can use to teach your students about writing a literature review.
Scribbr slides are free to use, customize, and distribute for educational purposes.
Open Google Slides Download PowerPoint
If you want to know more about the research process , methodology , research bias , or statistics , make sure to check out some of our other articles with explanations and examples.
- Sampling methods
- Simple random sampling
- Stratified sampling
- Cluster sampling
- Likert scales
- Reproducibility
Statistics
- Null hypothesis
- Statistical power
- Probability distribution
- Effect size
- Poisson distribution
Research bias
- Optimism bias
- Cognitive bias
- Implicit bias
- Hawthorne effect
- Anchoring bias
- Explicit bias
A literature review is a survey of scholarly sources (such as books, journal articles, and theses) related to a specific topic or research question .
It is often written as part of a thesis, dissertation , or research paper , in order to situate your work in relation to existing knowledge.
There are several reasons to conduct a literature review at the beginning of a research project:
- To familiarize yourself with the current state of knowledge on your topic
- To ensure that you’re not just repeating what others have already done
- To identify gaps in knowledge and unresolved problems that your research can address
- To develop your theoretical framework and methodology
- To provide an overview of the key findings and debates on the topic
Writing the literature review shows your reader how your work relates to existing research and what new insights it will contribute.
The literature review usually comes near the beginning of your thesis or dissertation . After the introduction , it grounds your research in a scholarly field and leads directly to your theoretical framework or methodology .
A literature review is a survey of credible sources on a topic, often used in dissertations , theses, and research papers . Literature reviews give an overview of knowledge on a subject, helping you identify relevant theories and methods, as well as gaps in existing research. Literature reviews are set up similarly to other academic texts , with an introduction , a main body, and a conclusion .
An annotated bibliography is a list of source references that has a short description (called an annotation ) for each of the sources. It is often assigned as part of the research process for a paper .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
McCombes, S. (2023, September 11). How to Write a Literature Review | Guide, Examples, & Templates. Scribbr. Retrieved April 9, 2024, from https://www.scribbr.com/dissertation/literature-review/
Is this article helpful?
Shona McCombes
Other students also liked, what is a theoretical framework | guide to organizing, what is a research methodology | steps & tips, how to write a research proposal | examples & templates, unlimited academic ai-proofreading.
✔ Document error-free in 5minutes ✔ Unlimited document corrections ✔ Specialized in correcting academic texts
Purdue Online Writing Lab Purdue OWL® College of Liberal Arts
Writing a Literature Review
Welcome to the Purdue OWL
This page is brought to you by the OWL at Purdue University. When printing this page, you must include the entire legal notice.
Copyright ©1995-2018 by The Writing Lab & The OWL at Purdue and Purdue University. All rights reserved. This material may not be published, reproduced, broadcast, rewritten, or redistributed without permission. Use of this site constitutes acceptance of our terms and conditions of fair use.
A literature review is a document or section of a document that collects key sources on a topic and discusses those sources in conversation with each other (also called synthesis ). The lit review is an important genre in many disciplines, not just literature (i.e., the study of works of literature such as novels and plays). When we say “literature review” or refer to “the literature,” we are talking about the research ( scholarship ) in a given field. You will often see the terms “the research,” “the scholarship,” and “the literature” used mostly interchangeably.
Where, when, and why would I write a lit review?
There are a number of different situations where you might write a literature review, each with slightly different expectations; different disciplines, too, have field-specific expectations for what a literature review is and does. For instance, in the humanities, authors might include more overt argumentation and interpretation of source material in their literature reviews, whereas in the sciences, authors are more likely to report study designs and results in their literature reviews; these differences reflect these disciplines’ purposes and conventions in scholarship. You should always look at examples from your own discipline and talk to professors or mentors in your field to be sure you understand your discipline’s conventions, for literature reviews as well as for any other genre.
A literature review can be a part of a research paper or scholarly article, usually falling after the introduction and before the research methods sections. In these cases, the lit review just needs to cover scholarship that is important to the issue you are writing about; sometimes it will also cover key sources that informed your research methodology.
Lit reviews can also be standalone pieces, either as assignments in a class or as publications. In a class, a lit review may be assigned to help students familiarize themselves with a topic and with scholarship in their field, get an idea of the other researchers working on the topic they’re interested in, find gaps in existing research in order to propose new projects, and/or develop a theoretical framework and methodology for later research. As a publication, a lit review usually is meant to help make other scholars’ lives easier by collecting and summarizing, synthesizing, and analyzing existing research on a topic. This can be especially helpful for students or scholars getting into a new research area, or for directing an entire community of scholars toward questions that have not yet been answered.
What are the parts of a lit review?
Most lit reviews use a basic introduction-body-conclusion structure; if your lit review is part of a larger paper, the introduction and conclusion pieces may be just a few sentences while you focus most of your attention on the body. If your lit review is a standalone piece, the introduction and conclusion take up more space and give you a place to discuss your goals, research methods, and conclusions separately from where you discuss the literature itself.
Introduction:
- An introductory paragraph that explains what your working topic and thesis is
- A forecast of key topics or texts that will appear in the review
- Potentially, a description of how you found sources and how you analyzed them for inclusion and discussion in the review (more often found in published, standalone literature reviews than in lit review sections in an article or research paper)
- Summarize and synthesize: Give an overview of the main points of each source and combine them into a coherent whole
- Analyze and interpret: Don’t just paraphrase other researchers – add your own interpretations where possible, discussing the significance of findings in relation to the literature as a whole
- Critically Evaluate: Mention the strengths and weaknesses of your sources
- Write in well-structured paragraphs: Use transition words and topic sentence to draw connections, comparisons, and contrasts.
Conclusion:
- Summarize the key findings you have taken from the literature and emphasize their significance
- Connect it back to your primary research question
How should I organize my lit review?
Lit reviews can take many different organizational patterns depending on what you are trying to accomplish with the review. Here are some examples:
- Chronological : The simplest approach is to trace the development of the topic over time, which helps familiarize the audience with the topic (for instance if you are introducing something that is not commonly known in your field). If you choose this strategy, be careful to avoid simply listing and summarizing sources in order. Try to analyze the patterns, turning points, and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred (as mentioned previously, this may not be appropriate in your discipline — check with a teacher or mentor if you’re unsure).
- Thematic : If you have found some recurring central themes that you will continue working with throughout your piece, you can organize your literature review into subsections that address different aspects of the topic. For example, if you are reviewing literature about women and religion, key themes can include the role of women in churches and the religious attitude towards women.
- Qualitative versus quantitative research
- Empirical versus theoretical scholarship
- Divide the research by sociological, historical, or cultural sources
- Theoretical : In many humanities articles, the literature review is the foundation for the theoretical framework. You can use it to discuss various theories, models, and definitions of key concepts. You can argue for the relevance of a specific theoretical approach or combine various theorical concepts to create a framework for your research.
What are some strategies or tips I can use while writing my lit review?
Any lit review is only as good as the research it discusses; make sure your sources are well-chosen and your research is thorough. Don’t be afraid to do more research if you discover a new thread as you’re writing. More info on the research process is available in our "Conducting Research" resources .
As you’re doing your research, create an annotated bibliography ( see our page on the this type of document ). Much of the information used in an annotated bibliography can be used also in a literature review, so you’ll be not only partially drafting your lit review as you research, but also developing your sense of the larger conversation going on among scholars, professionals, and any other stakeholders in your topic.
Usually you will need to synthesize research rather than just summarizing it. This means drawing connections between sources to create a picture of the scholarly conversation on a topic over time. Many student writers struggle to synthesize because they feel they don’t have anything to add to the scholars they are citing; here are some strategies to help you:
- It often helps to remember that the point of these kinds of syntheses is to show your readers how you understand your research, to help them read the rest of your paper.
- Writing teachers often say synthesis is like hosting a dinner party: imagine all your sources are together in a room, discussing your topic. What are they saying to each other?
- Look at the in-text citations in each paragraph. Are you citing just one source for each paragraph? This usually indicates summary only. When you have multiple sources cited in a paragraph, you are more likely to be synthesizing them (not always, but often
- Read more about synthesis here.
The most interesting literature reviews are often written as arguments (again, as mentioned at the beginning of the page, this is discipline-specific and doesn’t work for all situations). Often, the literature review is where you can establish your research as filling a particular gap or as relevant in a particular way. You have some chance to do this in your introduction in an article, but the literature review section gives a more extended opportunity to establish the conversation in the way you would like your readers to see it. You can choose the intellectual lineage you would like to be part of and whose definitions matter most to your thinking (mostly humanities-specific, but this goes for sciences as well). In addressing these points, you argue for your place in the conversation, which tends to make the lit review more compelling than a simple reporting of other sources.
Get science-backed answers as you write with Paperpal's Research feature
What is a Literature Review? How to Write It (with Examples)
A literature review is a critical analysis and synthesis of existing research on a particular topic. It provides an overview of the current state of knowledge, identifies gaps, and highlights key findings in the literature. 1 The purpose of a literature review is to situate your own research within the context of existing scholarship, demonstrating your understanding of the topic and showing how your work contributes to the ongoing conversation in the field. Learning how to write a literature review is a critical tool for successful research. Your ability to summarize and synthesize prior research pertaining to a certain topic demonstrates your grasp on the topic of study, and assists in the learning process.
Table of Contents
- What is the purpose of literature review?
- a. Habitat Loss and Species Extinction:
- b. Range Shifts and Phenological Changes:
- c. Ocean Acidification and Coral Reefs:
- d. Adaptive Strategies and Conservation Efforts:
- How to write a good literature review
- Choose a Topic and Define the Research Question:
- Decide on the Scope of Your Review:
- Select Databases for Searches:
- Conduct Searches and Keep Track:
- Review the Literature:
- Organize and Write Your Literature Review:
- Frequently asked questions
What is a literature review?
A well-conducted literature review demonstrates the researcher’s familiarity with the existing literature, establishes the context for their own research, and contributes to scholarly conversations on the topic. One of the purposes of a literature review is also to help researchers avoid duplicating previous work and ensure that their research is informed by and builds upon the existing body of knowledge.

What is the purpose of literature review?
A literature review serves several important purposes within academic and research contexts. Here are some key objectives and functions of a literature review: 2
- Contextualizing the Research Problem: The literature review provides a background and context for the research problem under investigation. It helps to situate the study within the existing body of knowledge.
- Identifying Gaps in Knowledge: By identifying gaps, contradictions, or areas requiring further research, the researcher can shape the research question and justify the significance of the study. This is crucial for ensuring that the new research contributes something novel to the field.
- Understanding Theoretical and Conceptual Frameworks: Literature reviews help researchers gain an understanding of the theoretical and conceptual frameworks used in previous studies. This aids in the development of a theoretical framework for the current research.
- Providing Methodological Insights: Another purpose of literature reviews is that it allows researchers to learn about the methodologies employed in previous studies. This can help in choosing appropriate research methods for the current study and avoiding pitfalls that others may have encountered.
- Establishing Credibility: A well-conducted literature review demonstrates the researcher’s familiarity with existing scholarship, establishing their credibility and expertise in the field. It also helps in building a solid foundation for the new research.
- Informing Hypotheses or Research Questions: The literature review guides the formulation of hypotheses or research questions by highlighting relevant findings and areas of uncertainty in existing literature.
Literature review example
Let’s delve deeper with a literature review example: Let’s say your literature review is about the impact of climate change on biodiversity. You might format your literature review into sections such as the effects of climate change on habitat loss and species extinction, phenological changes, and marine biodiversity. Each section would then summarize and analyze relevant studies in those areas, highlighting key findings and identifying gaps in the research. The review would conclude by emphasizing the need for further research on specific aspects of the relationship between climate change and biodiversity. The following literature review template provides a glimpse into the recommended literature review structure and content, demonstrating how research findings are organized around specific themes within a broader topic.
Literature Review on Climate Change Impacts on Biodiversity:
Climate change is a global phenomenon with far-reaching consequences, including significant impacts on biodiversity. This literature review synthesizes key findings from various studies:
a. Habitat Loss and Species Extinction:
Climate change-induced alterations in temperature and precipitation patterns contribute to habitat loss, affecting numerous species (Thomas et al., 2004). The review discusses how these changes increase the risk of extinction, particularly for species with specific habitat requirements.
b. Range Shifts and Phenological Changes:
Observations of range shifts and changes in the timing of biological events (phenology) are documented in response to changing climatic conditions (Parmesan & Yohe, 2003). These shifts affect ecosystems and may lead to mismatches between species and their resources.
c. Ocean Acidification and Coral Reefs:
The review explores the impact of climate change on marine biodiversity, emphasizing ocean acidification’s threat to coral reefs (Hoegh-Guldberg et al., 2007). Changes in pH levels negatively affect coral calcification, disrupting the delicate balance of marine ecosystems.
d. Adaptive Strategies and Conservation Efforts:
Recognizing the urgency of the situation, the literature review discusses various adaptive strategies adopted by species and conservation efforts aimed at mitigating the impacts of climate change on biodiversity (Hannah et al., 2007). It emphasizes the importance of interdisciplinary approaches for effective conservation planning.
How to write a good literature review
Writing a literature review involves summarizing and synthesizing existing research on a particular topic. A good literature review format should include the following elements.
Introduction: The introduction sets the stage for your literature review, providing context and introducing the main focus of your review.
- Opening Statement: Begin with a general statement about the broader topic and its significance in the field.
- Scope and Purpose: Clearly define the scope of your literature review. Explain the specific research question or objective you aim to address.
- Organizational Framework: Briefly outline the structure of your literature review, indicating how you will categorize and discuss the existing research.
- Significance of the Study: Highlight why your literature review is important and how it contributes to the understanding of the chosen topic.
- Thesis Statement: Conclude the introduction with a concise thesis statement that outlines the main argument or perspective you will develop in the body of the literature review.
Body: The body of the literature review is where you provide a comprehensive analysis of existing literature, grouping studies based on themes, methodologies, or other relevant criteria.
- Organize by Theme or Concept: Group studies that share common themes, concepts, or methodologies. Discuss each theme or concept in detail, summarizing key findings and identifying gaps or areas of disagreement.
- Critical Analysis: Evaluate the strengths and weaknesses of each study. Discuss the methodologies used, the quality of evidence, and the overall contribution of each work to the understanding of the topic.
- Synthesis of Findings: Synthesize the information from different studies to highlight trends, patterns, or areas of consensus in the literature.
- Identification of Gaps: Discuss any gaps or limitations in the existing research and explain how your review contributes to filling these gaps.
- Transition between Sections: Provide smooth transitions between different themes or concepts to maintain the flow of your literature review.
Conclusion: The conclusion of your literature review should summarize the main findings, highlight the contributions of the review, and suggest avenues for future research.
- Summary of Key Findings: Recap the main findings from the literature and restate how they contribute to your research question or objective.
- Contributions to the Field: Discuss the overall contribution of your literature review to the existing knowledge in the field.
- Implications and Applications: Explore the practical implications of the findings and suggest how they might impact future research or practice.
- Recommendations for Future Research: Identify areas that require further investigation and propose potential directions for future research in the field.
- Final Thoughts: Conclude with a final reflection on the importance of your literature review and its relevance to the broader academic community.

Conducting a literature review
Conducting a literature review is an essential step in research that involves reviewing and analyzing existing literature on a specific topic. It’s important to know how to do a literature review effectively, so here are the steps to follow: 1
Choose a Topic and Define the Research Question:
- Select a topic that is relevant to your field of study.
- Clearly define your research question or objective. Determine what specific aspect of the topic do you want to explore?
Decide on the Scope of Your Review:
- Determine the timeframe for your literature review. Are you focusing on recent developments, or do you want a historical overview?
- Consider the geographical scope. Is your review global, or are you focusing on a specific region?
- Define the inclusion and exclusion criteria. What types of sources will you include? Are there specific types of studies or publications you will exclude?
Select Databases for Searches:
- Identify relevant databases for your field. Examples include PubMed, IEEE Xplore, Scopus, Web of Science, and Google Scholar.
- Consider searching in library catalogs, institutional repositories, and specialized databases related to your topic.
Conduct Searches and Keep Track:
- Develop a systematic search strategy using keywords, Boolean operators (AND, OR, NOT), and other search techniques.
- Record and document your search strategy for transparency and replicability.
- Keep track of the articles, including publication details, abstracts, and links. Use citation management tools like EndNote, Zotero, or Mendeley to organize your references.
Review the Literature:
- Evaluate the relevance and quality of each source. Consider the methodology, sample size, and results of studies.
- Organize the literature by themes or key concepts. Identify patterns, trends, and gaps in the existing research.
- Summarize key findings and arguments from each source. Compare and contrast different perspectives.
- Identify areas where there is a consensus in the literature and where there are conflicting opinions.
- Provide critical analysis and synthesis of the literature. What are the strengths and weaknesses of existing research?
Organize and Write Your Literature Review:
- Literature review outline should be based on themes, chronological order, or methodological approaches.
- Write a clear and coherent narrative that synthesizes the information gathered.
- Use proper citations for each source and ensure consistency in your citation style (APA, MLA, Chicago, etc.).
- Conclude your literature review by summarizing key findings, identifying gaps, and suggesting areas for future research.
The literature review sample and detailed advice on writing and conducting a review will help you produce a well-structured report. But remember that a literature review is an ongoing process, and it may be necessary to revisit and update it as your research progresses.
Frequently asked questions
A literature review is a critical and comprehensive analysis of existing literature (published and unpublished works) on a specific topic or research question and provides a synthesis of the current state of knowledge in a particular field. A well-conducted literature review is crucial for researchers to build upon existing knowledge, avoid duplication of efforts, and contribute to the advancement of their field. It also helps researchers situate their work within a broader context and facilitates the development of a sound theoretical and conceptual framework for their studies.
Literature review is a crucial component of research writing, providing a solid background for a research paper’s investigation. The aim is to keep professionals up to date by providing an understanding of ongoing developments within a specific field, including research methods, and experimental techniques used in that field, and present that knowledge in the form of a written report. Also, the depth and breadth of the literature review emphasizes the credibility of the scholar in his or her field.
Before writing a literature review, it’s essential to undertake several preparatory steps to ensure that your review is well-researched, organized, and focused. This includes choosing a topic of general interest to you and doing exploratory research on that topic, writing an annotated bibliography, and noting major points, especially those that relate to the position you have taken on the topic.
Literature reviews and academic research papers are essential components of scholarly work but serve different purposes within the academic realm. 3 A literature review aims to provide a foundation for understanding the current state of research on a particular topic, identify gaps or controversies, and lay the groundwork for future research. Therefore, it draws heavily from existing academic sources, including books, journal articles, and other scholarly publications. In contrast, an academic research paper aims to present new knowledge, contribute to the academic discourse, and advance the understanding of a specific research question. Therefore, it involves a mix of existing literature (in the introduction and literature review sections) and original data or findings obtained through research methods.
Literature reviews are essential components of academic and research papers, and various strategies can be employed to conduct them effectively. If you want to know how to write a literature review for a research paper, here are four common approaches that are often used by researchers. Chronological Review: This strategy involves organizing the literature based on the chronological order of publication. It helps to trace the development of a topic over time, showing how ideas, theories, and research have evolved. Thematic Review: Thematic reviews focus on identifying and analyzing themes or topics that cut across different studies. Instead of organizing the literature chronologically, it is grouped by key themes or concepts, allowing for a comprehensive exploration of various aspects of the topic. Methodological Review: This strategy involves organizing the literature based on the research methods employed in different studies. It helps to highlight the strengths and weaknesses of various methodologies and allows the reader to evaluate the reliability and validity of the research findings. Theoretical Review: A theoretical review examines the literature based on the theoretical frameworks used in different studies. This approach helps to identify the key theories that have been applied to the topic and assess their contributions to the understanding of the subject. It’s important to note that these strategies are not mutually exclusive, and a literature review may combine elements of more than one approach. The choice of strategy depends on the research question, the nature of the literature available, and the goals of the review. Additionally, other strategies, such as integrative reviews or systematic reviews, may be employed depending on the specific requirements of the research.
The literature review format can vary depending on the specific publication guidelines. However, there are some common elements and structures that are often followed. Here is a general guideline for the format of a literature review: Introduction: Provide an overview of the topic. Define the scope and purpose of the literature review. State the research question or objective. Body: Organize the literature by themes, concepts, or chronology. Critically analyze and evaluate each source. Discuss the strengths and weaknesses of the studies. Highlight any methodological limitations or biases. Identify patterns, connections, or contradictions in the existing research. Conclusion: Summarize the key points discussed in the literature review. Highlight the research gap. Address the research question or objective stated in the introduction. Highlight the contributions of the review and suggest directions for future research.
Both annotated bibliographies and literature reviews involve the examination of scholarly sources. While annotated bibliographies focus on individual sources with brief annotations, literature reviews provide a more in-depth, integrated, and comprehensive analysis of existing literature on a specific topic. The key differences are as follows:
References
- Denney, A. S., & Tewksbury, R. (2013). How to write a literature review. Journal of criminal justice education , 24 (2), 218-234.
- Pan, M. L. (2016). Preparing literature reviews: Qualitative and quantitative approaches . Taylor & Francis.
- Cantero, C. (2019). How to write a literature review. San José State University Writing Center .
Paperpal is an AI writing assistant that help academics write better, faster with real-time suggestions for in-depth language and grammar correction. Trained on millions of research manuscripts enhanced by professional academic editors, Paperpal delivers human precision at machine speed.
Try it for free or upgrade to Paperpal Prime , which unlocks unlimited access to premium features like academic translation, paraphrasing, contextual synonyms, consistency checks and more. It’s like always having a professional academic editor by your side! Go beyond limitations and experience the future of academic writing. Get Paperpal Prime now at just US$19 a month!
Related Reads:
- Empirical Research: A Comprehensive Guide for Academics
- How to Write a Scientific Paper in 10 Steps
- Life Sciences Papers: 9 Tips for Authors Writing in Biological Sciences
- What is an Argumentative Essay? How to Write It (With Examples)
6 Tips for Post-Doc Researchers to Take Their Career to the Next Level
Self-plagiarism in research: what it is and how to avoid it, you may also like, ai + human expertise – a paradigm shift..., how to use paperpal to generate emails &..., ai in education: it’s time to change the..., is it ethical to use ai-generated abstracts without..., do plagiarism checkers detect ai content, word choice problems: how to use the right..., how to avoid plagiarism when using generative ai..., what are journal guidelines on using generative ai..., types of plagiarism and 6 tips to avoid..., how to write an essay introduction (with examples)....
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Dissertation
- What is a Literature Review? | Guide, Template, & Examples
What is a Literature Review? | Guide, Template, & Examples
Published on 22 February 2022 by Shona McCombes . Revised on 7 June 2022.
What is a literature review? A literature review is a survey of scholarly sources on a specific topic. It provides an overview of current knowledge, allowing you to identify relevant theories, methods, and gaps in the existing research.
There are five key steps to writing a literature review:
- Search for relevant literature
- Evaluate sources
- Identify themes, debates and gaps
- Outline the structure
- Write your literature review
A good literature review doesn’t just summarise sources – it analyses, synthesises, and critically evaluates to give a clear picture of the state of knowledge on the subject.
Instantly correct all language mistakes in your text
Be assured that you'll submit flawless writing. Upload your document to correct all your mistakes.
Table of contents
Why write a literature review, examples of literature reviews, step 1: search for relevant literature, step 2: evaluate and select sources, step 3: identify themes, debates and gaps, step 4: outline your literature review’s structure, step 5: write your literature review, frequently asked questions about literature reviews, introduction.
- Quick Run-through
- Step 1 & 2
When you write a dissertation or thesis, you will have to conduct a literature review to situate your research within existing knowledge. The literature review gives you a chance to:
- Demonstrate your familiarity with the topic and scholarly context
- Develop a theoretical framework and methodology for your research
- Position yourself in relation to other researchers and theorists
- Show how your dissertation addresses a gap or contributes to a debate
You might also have to write a literature review as a stand-alone assignment. In this case, the purpose is to evaluate the current state of research and demonstrate your knowledge of scholarly debates around a topic.
The content will look slightly different in each case, but the process of conducting a literature review follows the same steps. We’ve written a step-by-step guide that you can follow below.
The only proofreading tool specialized in correcting academic writing
The academic proofreading tool has been trained on 1000s of academic texts and by native English editors. Making it the most accurate and reliable proofreading tool for students.
Correct my document today
Writing literature reviews can be quite challenging! A good starting point could be to look at some examples, depending on what kind of literature review you’d like to write.
- Example literature review #1: “Why Do People Migrate? A Review of the Theoretical Literature” ( Theoretical literature review about the development of economic migration theory from the 1950s to today.)
- Example literature review #2: “Literature review as a research methodology: An overview and guidelines” ( Methodological literature review about interdisciplinary knowledge acquisition and production.)
- Example literature review #3: “The Use of Technology in English Language Learning: A Literature Review” ( Thematic literature review about the effects of technology on language acquisition.)
- Example literature review #4: “Learners’ Listening Comprehension Difficulties in English Language Learning: A Literature Review” ( Chronological literature review about how the concept of listening skills has changed over time.)
You can also check out our templates with literature review examples and sample outlines at the links below.
Download Word doc Download Google doc
Before you begin searching for literature, you need a clearly defined topic .
If you are writing the literature review section of a dissertation or research paper, you will search for literature related to your research objectives and questions .
If you are writing a literature review as a stand-alone assignment, you will have to choose a focus and develop a central question to direct your search. Unlike a dissertation research question, this question has to be answerable without collecting original data. You should be able to answer it based only on a review of existing publications.
Make a list of keywords
Start by creating a list of keywords related to your research topic. Include each of the key concepts or variables you’re interested in, and list any synonyms and related terms. You can add to this list if you discover new keywords in the process of your literature search.
- Social media, Facebook, Instagram, Twitter, Snapchat, TikTok
- Body image, self-perception, self-esteem, mental health
- Generation Z, teenagers, adolescents, youth
Search for relevant sources
Use your keywords to begin searching for sources. Some databases to search for journals and articles include:
- Your university’s library catalogue
- Google Scholar
- Project Muse (humanities and social sciences)
- Medline (life sciences and biomedicine)
- EconLit (economics)
- Inspec (physics, engineering and computer science)
You can use boolean operators to help narrow down your search:
Read the abstract to find out whether an article is relevant to your question. When you find a useful book or article, you can check the bibliography to find other relevant sources.
To identify the most important publications on your topic, take note of recurring citations. If the same authors, books or articles keep appearing in your reading, make sure to seek them out.
You probably won’t be able to read absolutely everything that has been written on the topic – you’ll have to evaluate which sources are most relevant to your questions.
For each publication, ask yourself:
- What question or problem is the author addressing?
- What are the key concepts and how are they defined?
- What are the key theories, models and methods? Does the research use established frameworks or take an innovative approach?
- What are the results and conclusions of the study?
- How does the publication relate to other literature in the field? Does it confirm, add to, or challenge established knowledge?
- How does the publication contribute to your understanding of the topic? What are its key insights and arguments?
- What are the strengths and weaknesses of the research?
Make sure the sources you use are credible, and make sure you read any landmark studies and major theories in your field of research.
You can find out how many times an article has been cited on Google Scholar – a high citation count means the article has been influential in the field, and should certainly be included in your literature review.
The scope of your review will depend on your topic and discipline: in the sciences you usually only review recent literature, but in the humanities you might take a long historical perspective (for example, to trace how a concept has changed in meaning over time).
Remember that you can use our template to summarise and evaluate sources you’re thinking about using!
Take notes and cite your sources
As you read, you should also begin the writing process. Take notes that you can later incorporate into the text of your literature review.
It’s important to keep track of your sources with references to avoid plagiarism . It can be helpful to make an annotated bibliography, where you compile full reference information and write a paragraph of summary and analysis for each source. This helps you remember what you read and saves time later in the process.
You can use our free APA Reference Generator for quick, correct, consistent citations.
To begin organising your literature review’s argument and structure, you need to understand the connections and relationships between the sources you’ve read. Based on your reading and notes, you can look for:
- Trends and patterns (in theory, method or results): do certain approaches become more or less popular over time?
- Themes: what questions or concepts recur across the literature?
- Debates, conflicts and contradictions: where do sources disagree?
- Pivotal publications: are there any influential theories or studies that changed the direction of the field?
- Gaps: what is missing from the literature? Are there weaknesses that need to be addressed?
This step will help you work out the structure of your literature review and (if applicable) show how your own research will contribute to existing knowledge.
- Most research has focused on young women.
- There is an increasing interest in the visual aspects of social media.
- But there is still a lack of robust research on highly-visual platforms like Instagram and Snapchat – this is a gap that you could address in your own research.
There are various approaches to organising the body of a literature review. You should have a rough idea of your strategy before you start writing.
Depending on the length of your literature review, you can combine several of these strategies (for example, your overall structure might be thematic, but each theme is discussed chronologically).
Chronological
The simplest approach is to trace the development of the topic over time. However, if you choose this strategy, be careful to avoid simply listing and summarising sources in order.
Try to analyse patterns, turning points and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred.
If you have found some recurring central themes, you can organise your literature review into subsections that address different aspects of the topic.
For example, if you are reviewing literature about inequalities in migrant health outcomes, key themes might include healthcare policy, language barriers, cultural attitudes, legal status, and economic access.
Methodological
If you draw your sources from different disciplines or fields that use a variety of research methods , you might want to compare the results and conclusions that emerge from different approaches. For example:
- Look at what results have emerged in qualitative versus quantitative research
- Discuss how the topic has been approached by empirical versus theoretical scholarship
- Divide the literature into sociological, historical, and cultural sources
Theoretical
A literature review is often the foundation for a theoretical framework . You can use it to discuss various theories, models, and definitions of key concepts.
You might argue for the relevance of a specific theoretical approach, or combine various theoretical concepts to create a framework for your research.
Like any other academic text, your literature review should have an introduction , a main body, and a conclusion . What you include in each depends on the objective of your literature review.
The introduction should clearly establish the focus and purpose of the literature review.
If you are writing the literature review as part of your dissertation or thesis, reiterate your central problem or research question and give a brief summary of the scholarly context. You can emphasise the timeliness of the topic (“many recent studies have focused on the problem of x”) or highlight a gap in the literature (“while there has been much research on x, few researchers have taken y into consideration”).
Depending on the length of your literature review, you might want to divide the body into subsections. You can use a subheading for each theme, time period, or methodological approach.
As you write, make sure to follow these tips:
- Summarise and synthesise: give an overview of the main points of each source and combine them into a coherent whole.
- Analyse and interpret: don’t just paraphrase other researchers – add your own interpretations, discussing the significance of findings in relation to the literature as a whole.
- Critically evaluate: mention the strengths and weaknesses of your sources.
- Write in well-structured paragraphs: use transitions and topic sentences to draw connections, comparisons and contrasts.
In the conclusion, you should summarise the key findings you have taken from the literature and emphasise their significance.
If the literature review is part of your dissertation or thesis, reiterate how your research addresses gaps and contributes new knowledge, or discuss how you have drawn on existing theories and methods to build a framework for your research. This can lead directly into your methodology section.
A literature review is a survey of scholarly sources (such as books, journal articles, and theses) related to a specific topic or research question .
It is often written as part of a dissertation , thesis, research paper , or proposal .
There are several reasons to conduct a literature review at the beginning of a research project:
- To familiarise yourself with the current state of knowledge on your topic
- To ensure that you’re not just repeating what others have already done
- To identify gaps in knowledge and unresolved problems that your research can address
- To develop your theoretical framework and methodology
- To provide an overview of the key findings and debates on the topic
Writing the literature review shows your reader how your work relates to existing research and what new insights it will contribute.
The literature review usually comes near the beginning of your dissertation . After the introduction , it grounds your research in a scholarly field and leads directly to your theoretical framework or methodology .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
McCombes, S. (2022, June 07). What is a Literature Review? | Guide, Template, & Examples. Scribbr. Retrieved 9 April 2024, from https://www.scribbr.co.uk/thesis-dissertation/literature-review/
Is this article helpful?
Shona McCombes
Other students also liked, how to write a dissertation proposal | a step-by-step guide, what is a theoretical framework | a step-by-step guide, what is a research methodology | steps & tips.
- Resources Home 🏠
- Try SciSpace Copilot
- Search research papers
- Add Copilot Extension
- Try AI Detector
- Try Paraphraser
- Try Citation Generator
- April Papers
- June Papers
- July Papers

How To Write A Literature Review - A Complete Guide

Table of Contents
A literature review is much more than just another section in your research paper. It forms the very foundation of your research. It is a formal piece of writing where you analyze the existing theoretical framework, principles, and assumptions and use that as a base to shape your approach to the research question.
Curating and drafting a solid literature review section not only lends more credibility to your research paper but also makes your research tighter and better focused. But, writing literature reviews is a difficult task. It requires extensive reading, plus you have to consider market trends and technological and political changes, which tend to change in the blink of an eye.
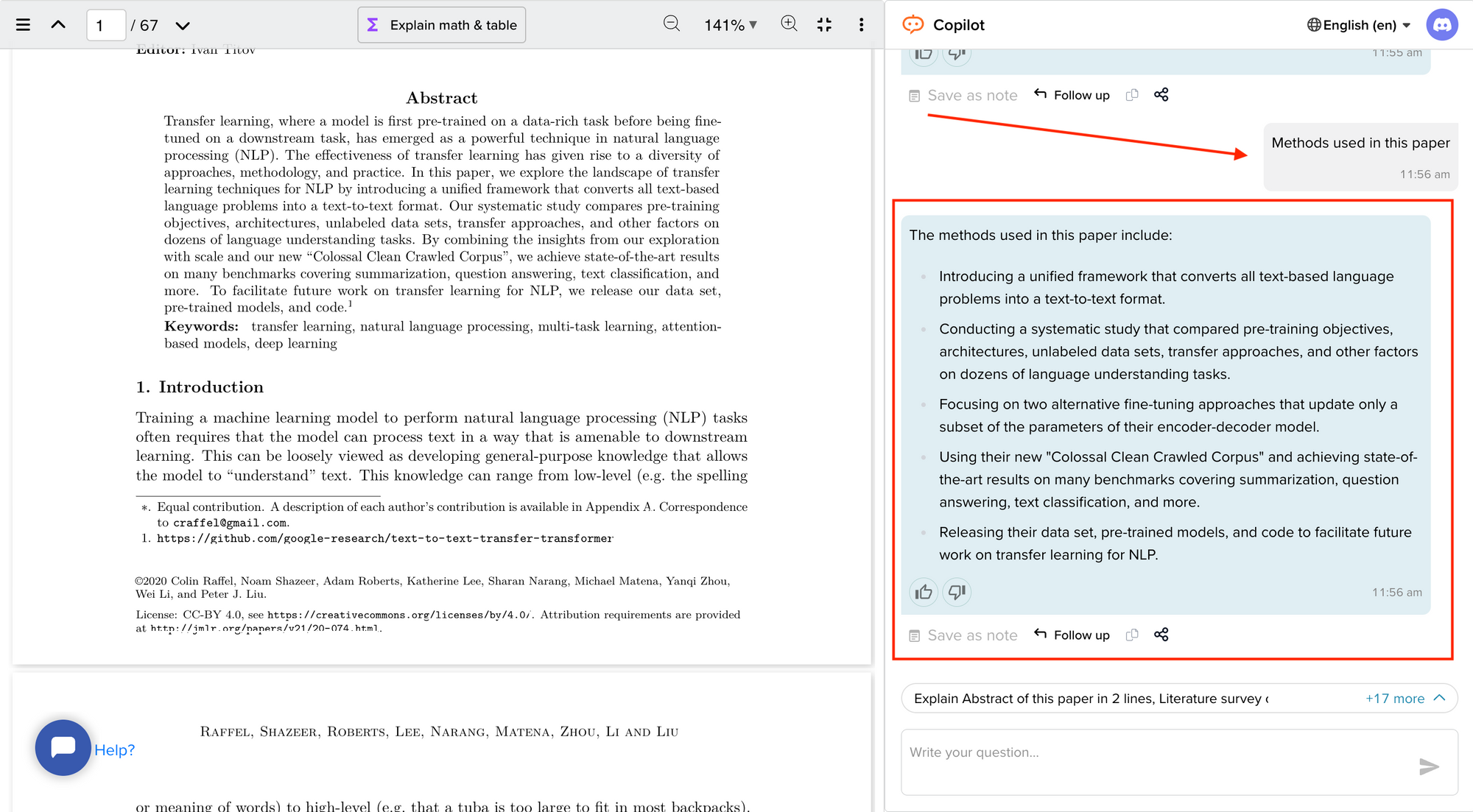
Now streamline your literature review process with the help of SciSpace Copilot. With this AI research assistant, you can efficiently synthesize and analyze a vast amount of information, identify key themes and trends, and uncover gaps in the existing research. Get real-time explanations, summaries, and answers to your questions for the paper you're reviewing, making navigating and understanding the complex literature landscape easier.
In this comprehensive guide, we will explore everything from the definition of a literature review, its appropriate length, various types of literature reviews, and how to write one.
What is a literature review?
A literature review is a collation of survey, research, critical evaluation, and assessment of the existing literature in a preferred domain.
Eminent researcher and academic Arlene Fink, in her book Conducting Research Literature Reviews , defines it as the following:
“A literature review surveys books, scholarly articles, and any other sources relevant to a particular issue, area of research, or theory, and by so doing, provides a description, summary, and critical evaluation of these works in relation to the research problem being investigated.
Literature reviews are designed to provide an overview of sources you have explored while researching a particular topic, and to demonstrate to your readers how your research fits within a larger field of study.”
Simply put, a literature review can be defined as a critical discussion of relevant pre-existing research around your research question and carving out a definitive place for your study in the existing body of knowledge. Literature reviews can be presented in multiple ways: a section of an article, the whole research paper itself, or a chapter of your thesis.
A literature review does function as a summary of sources, but it also allows you to analyze further, interpret, and examine the stated theories, methods, viewpoints, and, of course, the gaps in the existing content.
As an author, you can discuss and interpret the research question and its various aspects and debate your adopted methods to support the claim.
What is the purpose of a literature review?
A literature review is meant to help your readers understand the relevance of your research question and where it fits within the existing body of knowledge. As a researcher, you should use it to set the context, build your argument, and establish the need for your study.
What is the importance of a literature review?
The literature review is a critical part of research papers because it helps you:
- Gain an in-depth understanding of your research question and the surrounding area
- Convey that you have a thorough understanding of your research area and are up-to-date with the latest changes and advancements
- Establish how your research is connected or builds on the existing body of knowledge and how it could contribute to further research
- Elaborate on the validity and suitability of your theoretical framework and research methodology
- Identify and highlight gaps and shortcomings in the existing body of knowledge and how things need to change
- Convey to readers how your study is different or how it contributes to the research area
How long should a literature review be?
Ideally, the literature review should take up 15%-40% of the total length of your manuscript. So, if you have a 10,000-word research paper, the minimum word count could be 1500.
Your literature review format depends heavily on the kind of manuscript you are writing — an entire chapter in case of doctoral theses, a part of the introductory section in a research article, to a full-fledged review article that examines the previously published research on a topic.
Another determining factor is the type of research you are doing. The literature review section tends to be longer for secondary research projects than primary research projects.
What are the different types of literature reviews?
All literature reviews are not the same. There are a variety of possible approaches that you can take. It all depends on the type of research you are pursuing.
Here are the different types of literature reviews:
Argumentative review
It is called an argumentative review when you carefully present literature that only supports or counters a specific argument or premise to establish a viewpoint.
Integrative review
It is a type of literature review focused on building a comprehensive understanding of a topic by combining available theoretical frameworks and empirical evidence.
Methodological review
This approach delves into the ''how'' and the ''what" of the research question — you cannot look at the outcome in isolation; you should also review the methodology used.
Systematic review
This form consists of an overview of existing evidence pertinent to a clearly formulated research question, which uses pre-specified and standardized methods to identify and critically appraise relevant research and collect, report, and analyze data from the studies included in the review.
Meta-analysis review
Meta-analysis uses statistical methods to summarize the results of independent studies. By combining information from all relevant studies, meta-analysis can provide more precise estimates of the effects than those derived from the individual studies included within a review.
Historical review
Historical literature reviews focus on examining research throughout a period, often starting with the first time an issue, concept, theory, or phenomenon emerged in the literature, then tracing its evolution within the scholarship of a discipline. The purpose is to place research in a historical context to show familiarity with state-of-the-art developments and identify future research's likely directions.
Theoretical Review
This form aims to examine the corpus of theory accumulated regarding an issue, concept, theory, and phenomenon. The theoretical literature review helps to establish what theories exist, the relationships between them, the degree the existing approaches have been investigated, and to develop new hypotheses to be tested.
Scoping Review
The Scoping Review is often used at the beginning of an article, dissertation, or research proposal. It is conducted before the research to highlight gaps in the existing body of knowledge and explains why the project should be greenlit.
State-of-the-Art Review
The State-of-the-Art review is conducted periodically, focusing on the most recent research. It describes what is currently known, understood, or agreed upon regarding the research topic and highlights where there are still disagreements.
Can you use the first person in a literature review?
When writing literature reviews, you should avoid the usage of first-person pronouns. It means that instead of "I argue that" or "we argue that," the appropriate expression would be "this research paper argues that."
Do you need an abstract for a literature review?
Ideally, yes. It is always good to have a condensed summary that is self-contained and independent of the rest of your review. As for how to draft one, you can follow the same fundamental idea when preparing an abstract for a literature review. It should also include:
- The research topic and your motivation behind selecting it
- A one-sentence thesis statement
- An explanation of the kinds of literature featured in the review
- Summary of what you've learned
- Conclusions you drew from the literature you reviewed
- Potential implications and future scope for research
Here's an example of the abstract of a literature review
Is a literature review written in the past tense?
Yes, the literature review should ideally be written in the past tense. You should not use the present or future tense when writing one. The exceptions are when you have statements describing events that happened earlier than the literature you are reviewing or events that are currently occurring; then, you can use the past perfect or present perfect tenses.
How many sources for a literature review?
There are multiple approaches to deciding how many sources to include in a literature review section. The first approach would be to look level you are at as a researcher. For instance, a doctoral thesis might need 60+ sources. In contrast, you might only need to refer to 5-15 sources at the undergraduate level.
The second approach is based on the kind of literature review you are doing — whether it is merely a chapter of your paper or if it is a self-contained paper in itself. When it is just a chapter, sources should equal the total number of pages in your article's body. In the second scenario, you need at least three times as many sources as there are pages in your work.
Quick tips on how to write a literature review
To know how to write a literature review, you must clearly understand its impact and role in establishing your work as substantive research material.
You need to follow the below-mentioned steps, to write a literature review:
- Outline the purpose behind the literature review
- Search relevant literature
- Examine and assess the relevant resources
- Discover connections by drawing deep insights from the resources
- Structure planning to write a good literature review
1. Outline and identify the purpose of a literature review
As a first step on how to write a literature review, you must know what the research question or topic is and what shape you want your literature review to take. Ensure you understand the research topic inside out, or else seek clarifications. You must be able to the answer below questions before you start:
- How many sources do I need to include?
- What kind of sources should I analyze?
- How much should I critically evaluate each source?
- Should I summarize, synthesize or offer a critique of the sources?
- Do I need to include any background information or definitions?
Additionally, you should know that the narrower your research topic is, the swifter it will be for you to restrict the number of sources to be analyzed.
2. Search relevant literature
Dig deeper into search engines to discover what has already been published around your chosen topic. Make sure you thoroughly go through appropriate reference sources like books, reports, journal articles, government docs, and web-based resources.
You must prepare a list of keywords and their different variations. You can start your search from any library’s catalog, provided you are an active member of that institution. The exact keywords can be extended to widen your research over other databases and academic search engines like:
- Google Scholar
- Microsoft Academic
- Science.gov
Besides, it is not advisable to go through every resource word by word. Alternatively, what you can do is you can start by reading the abstract and then decide whether that source is relevant to your research or not.
Additionally, you must spend surplus time assessing the quality and relevance of resources. It would help if you tried preparing a list of citations to ensure that there lies no repetition of authors, publications, or articles in the literature review.
3. Examine and assess the sources
It is nearly impossible for you to go through every detail in the research article. So rather than trying to fetch every detail, you have to analyze and decide which research sources resemble closest and appear relevant to your chosen domain.
While analyzing the sources, you should look to find out answers to questions like:
- What question or problem has the author been describing and debating?
- What is the definition of critical aspects?
- How well the theories, approach, and methodology have been explained?
- Whether the research theory used some conventional or new innovative approach?
- How relevant are the key findings of the work?
- In what ways does it relate to other sources on the same topic?
- What challenges does this research paper pose to the existing theory
- What are the possible contributions or benefits it adds to the subject domain?
Be always mindful that you refer only to credible and authentic resources. It would be best if you always take references from different publications to validate your theory.
Always keep track of important information or data you can present in your literature review right from the beginning. It will help steer your path from any threats of plagiarism and also make it easier to curate an annotated bibliography or reference section.
4. Discover connections
At this stage, you must start deciding on the argument and structure of your literature review. To accomplish this, you must discover and identify the relations and connections between various resources while drafting your abstract.
A few aspects that you should be aware of while writing a literature review include:
- Rise to prominence: Theories and methods that have gained reputation and supporters over time.
- Constant scrutiny: Concepts or theories that repeatedly went under examination.
- Contradictions and conflicts: Theories, both the supporting and the contradictory ones, for the research topic.
- Knowledge gaps: What exactly does it fail to address, and how to bridge them with further research?
- Influential resources: Significant research projects available that have been upheld as milestones or perhaps, something that can modify the current trends
Once you join the dots between various past research works, it will be easier for you to draw a conclusion and identify your contribution to the existing knowledge base.
5. Structure planning to write a good literature review
There exist different ways towards planning and executing the structure of a literature review. The format of a literature review varies and depends upon the length of the research.
Like any other research paper, the literature review format must contain three sections: introduction, body, and conclusion. The goals and objectives of the research question determine what goes inside these three sections.
Nevertheless, a good literature review can be structured according to the chronological, thematic, methodological, or theoretical framework approach.
Literature review samples
1. Standalone
2. As a section of a research paper
How SciSpace Discover makes literature review a breeze?
SciSpace Discover is a one-stop solution to do an effective literature search and get barrier-free access to scientific knowledge. It is an excellent repository where you can find millions of only peer-reviewed articles and full-text PDF files. Here’s more on how you can use it:
Find the right information
Find what you want quickly and easily with comprehensive search filters that let you narrow down papers according to PDF availability, year of publishing, document type, and affiliated institution. Moreover, you can sort the results based on the publishing date, citation count, and relevance.
Assess credibility of papers quickly
When doing the literature review, it is critical to establish the quality of your sources. They form the foundation of your research. SciSpace Discover helps you assess the quality of a source by providing an overview of its references, citations, and performance metrics.
Get the complete picture in no time
SciSpace Discover’s personalized suggestion engine helps you stay on course and get the complete picture of the topic from one place. Every time you visit an article page, it provides you links to related papers. Besides that, it helps you understand what’s trending, who are the top authors, and who are the leading publishers on a topic.
Make referring sources super easy
To ensure you don't lose track of your sources, you must start noting down your references when doing the literature review. SciSpace Discover makes this step effortless. Click the 'cite' button on an article page, and you will receive preloaded citation text in multiple styles — all you've to do is copy-paste it into your manuscript.
Final tips on how to write a literature review
A massive chunk of time and effort is required to write a good literature review. But, if you go about it systematically, you'll be able to save a ton of time and build a solid foundation for your research.
We hope this guide has helped you answer several key questions you have about writing literature reviews.
Would you like to explore SciSpace Discover and kick off your literature search right away? You can get started here .
Frequently Asked Questions (FAQs)
1. how to start a literature review.
• What questions do you want to answer?
• What sources do you need to answer these questions?
• What information do these sources contain?
• How can you use this information to answer your questions?
2. What to include in a literature review?
• A brief background of the problem or issue
• What has previously been done to address the problem or issue
• A description of what you will do in your project
• How this study will contribute to research on the subject
3. Why literature review is important?
The literature review is an important part of any research project because it allows the writer to look at previous studies on a topic and determine existing gaps in the literature, as well as what has already been done. It will also help them to choose the most appropriate method for their own study.
4. How to cite a literature review in APA format?
To cite a literature review in APA style, you need to provide the author's name, the title of the article, and the year of publication. For example: Patel, A. B., & Stokes, G. S. (2012). The relationship between personality and intelligence: A meta-analysis of longitudinal research. Personality and Individual Differences, 53(1), 16-21
5. What are the components of a literature review?
• A brief introduction to the topic, including its background and context. The introduction should also include a rationale for why the study is being conducted and what it will accomplish.
• A description of the methodologies used in the study. This can include information about data collection methods, sample size, and statistical analyses.
• A presentation of the findings in an organized format that helps readers follow along with the author's conclusions.
6. What are common errors in writing literature review?
• Not spending enough time to critically evaluate the relevance of resources, observations and conclusions.
• Totally relying on secondary data while ignoring primary data.
• Letting your personal bias seep into your interpretation of existing literature.
• No detailed explanation of the procedure to discover and identify an appropriate literature review.
7. What are the 5 C's of writing literature review?
• Cite - the sources you utilized and referenced in your research.
• Compare - existing arguments, hypotheses, methodologies, and conclusions found in the knowledge base.
• Contrast - the arguments, topics, methodologies, approaches, and disputes that may be found in the literature.
• Critique - the literature and describe the ideas and opinions you find more convincing and why.
• Connect - the various studies you reviewed in your research.
8. How many sources should a literature review have?
When it is just a chapter, sources should equal the total number of pages in your article's body. if it is a self-contained paper in itself, you need at least three times as many sources as there are pages in your work.
9. Can literature review have diagrams?
• To represent an abstract idea or concept
• To explain the steps of a process or procedure
• To help readers understand the relationships between different concepts
10. How old should sources be in a literature review?
Sources for a literature review should be as current as possible or not older than ten years. The only exception to this rule is if you are reviewing a historical topic and need to use older sources.
11. What are the types of literature review?
• Argumentative review
• Integrative review
• Methodological review
• Systematic review
• Meta-analysis review
• Historical review
• Theoretical review
• Scoping review
• State-of-the-Art review
12. Is a literature review mandatory?
Yes. Literature review is a mandatory part of any research project. It is a critical step in the process that allows you to establish the scope of your research, and provide a background for the rest of your work.
But before you go,
- Six Online Tools for Easy Literature Review
- Evaluating literature review: systematic vs. scoping reviews
- Systematic Approaches to a Successful Literature Review
- Writing Integrative Literature Reviews: Guidelines and Examples
You might also like

Consensus GPT vs. SciSpace GPT: Choose the Best GPT for Research

Literature Review and Theoretical Framework: Understanding the Differences

Types of Essays in Academic Writing - Quick Guide (2024)
Literature Reviews
What this handout is about.
This handout will explain what literature reviews are and offer insights into the form and construction of literature reviews in the humanities, social sciences, and sciences.
Introduction
OK. You’ve got to write a literature review. You dust off a novel and a book of poetry, settle down in your chair, and get ready to issue a “thumbs up” or “thumbs down” as you leaf through the pages. “Literature review” done. Right?
Wrong! The “literature” of a literature review refers to any collection of materials on a topic, not necessarily the great literary texts of the world. “Literature” could be anything from a set of government pamphlets on British colonial methods in Africa to scholarly articles on the treatment of a torn ACL. And a review does not necessarily mean that your reader wants you to give your personal opinion on whether or not you liked these sources.
What is a literature review, then?
A literature review discusses published information in a particular subject area, and sometimes information in a particular subject area within a certain time period.
A literature review can be just a simple summary of the sources, but it usually has an organizational pattern and combines both summary and synthesis. A summary is a recap of the important information of the source, but a synthesis is a re-organization, or a reshuffling, of that information. It might give a new interpretation of old material or combine new with old interpretations. Or it might trace the intellectual progression of the field, including major debates. And depending on the situation, the literature review may evaluate the sources and advise the reader on the most pertinent or relevant.
But how is a literature review different from an academic research paper?
The main focus of an academic research paper is to develop a new argument, and a research paper is likely to contain a literature review as one of its parts. In a research paper, you use the literature as a foundation and as support for a new insight that you contribute. The focus of a literature review, however, is to summarize and synthesize the arguments and ideas of others without adding new contributions.
Why do we write literature reviews?
Literature reviews provide you with a handy guide to a particular topic. If you have limited time to conduct research, literature reviews can give you an overview or act as a stepping stone. For professionals, they are useful reports that keep them up to date with what is current in the field. For scholars, the depth and breadth of the literature review emphasizes the credibility of the writer in his or her field. Literature reviews also provide a solid background for a research paper’s investigation. Comprehensive knowledge of the literature of the field is essential to most research papers.
Who writes these things, anyway?
Literature reviews are written occasionally in the humanities, but mostly in the sciences and social sciences; in experiment and lab reports, they constitute a section of the paper. Sometimes a literature review is written as a paper in itself.
Let’s get to it! What should I do before writing the literature review?
If your assignment is not very specific, seek clarification from your instructor:
- Roughly how many sources should you include?
- What types of sources (books, journal articles, websites)?
- Should you summarize, synthesize, or critique your sources by discussing a common theme or issue?
- Should you evaluate your sources?
- Should you provide subheadings and other background information, such as definitions and/or a history?
Find models
Look for other literature reviews in your area of interest or in the discipline and read them to get a sense of the types of themes you might want to look for in your own research or ways to organize your final review. You can simply put the word “review” in your search engine along with your other topic terms to find articles of this type on the Internet or in an electronic database. The bibliography or reference section of sources you’ve already read are also excellent entry points into your own research.
Narrow your topic
There are hundreds or even thousands of articles and books on most areas of study. The narrower your topic, the easier it will be to limit the number of sources you need to read in order to get a good survey of the material. Your instructor will probably not expect you to read everything that’s out there on the topic, but you’ll make your job easier if you first limit your scope.
Keep in mind that UNC Libraries have research guides and to databases relevant to many fields of study. You can reach out to the subject librarian for a consultation: https://library.unc.edu/support/consultations/ .
And don’t forget to tap into your professor’s (or other professors’) knowledge in the field. Ask your professor questions such as: “If you had to read only one book from the 90’s on topic X, what would it be?” Questions such as this help you to find and determine quickly the most seminal pieces in the field.
Consider whether your sources are current
Some disciplines require that you use information that is as current as possible. In the sciences, for instance, treatments for medical problems are constantly changing according to the latest studies. Information even two years old could be obsolete. However, if you are writing a review in the humanities, history, or social sciences, a survey of the history of the literature may be what is needed, because what is important is how perspectives have changed through the years or within a certain time period. Try sorting through some other current bibliographies or literature reviews in the field to get a sense of what your discipline expects. You can also use this method to consider what is currently of interest to scholars in this field and what is not.
Strategies for writing the literature review
Find a focus.
A literature review, like a term paper, is usually organized around ideas, not the sources themselves as an annotated bibliography would be organized. This means that you will not just simply list your sources and go into detail about each one of them, one at a time. No. As you read widely but selectively in your topic area, consider instead what themes or issues connect your sources together. Do they present one or different solutions? Is there an aspect of the field that is missing? How well do they present the material and do they portray it according to an appropriate theory? Do they reveal a trend in the field? A raging debate? Pick one of these themes to focus the organization of your review.
Convey it to your reader
A literature review may not have a traditional thesis statement (one that makes an argument), but you do need to tell readers what to expect. Try writing a simple statement that lets the reader know what is your main organizing principle. Here are a couple of examples:
The current trend in treatment for congestive heart failure combines surgery and medicine. More and more cultural studies scholars are accepting popular media as a subject worthy of academic consideration.
Consider organization
You’ve got a focus, and you’ve stated it clearly and directly. Now what is the most effective way of presenting the information? What are the most important topics, subtopics, etc., that your review needs to include? And in what order should you present them? Develop an organization for your review at both a global and local level:
First, cover the basic categories
Just like most academic papers, literature reviews also must contain at least three basic elements: an introduction or background information section; the body of the review containing the discussion of sources; and, finally, a conclusion and/or recommendations section to end the paper. The following provides a brief description of the content of each:
- Introduction: Gives a quick idea of the topic of the literature review, such as the central theme or organizational pattern.
- Body: Contains your discussion of sources and is organized either chronologically, thematically, or methodologically (see below for more information on each).
- Conclusions/Recommendations: Discuss what you have drawn from reviewing literature so far. Where might the discussion proceed?
Organizing the body
Once you have the basic categories in place, then you must consider how you will present the sources themselves within the body of your paper. Create an organizational method to focus this section even further.
To help you come up with an overall organizational framework for your review, consider the following scenario:
You’ve decided to focus your literature review on materials dealing with sperm whales. This is because you’ve just finished reading Moby Dick, and you wonder if that whale’s portrayal is really real. You start with some articles about the physiology of sperm whales in biology journals written in the 1980’s. But these articles refer to some British biological studies performed on whales in the early 18th century. So you check those out. Then you look up a book written in 1968 with information on how sperm whales have been portrayed in other forms of art, such as in Alaskan poetry, in French painting, or on whale bone, as the whale hunters in the late 19th century used to do. This makes you wonder about American whaling methods during the time portrayed in Moby Dick, so you find some academic articles published in the last five years on how accurately Herman Melville portrayed the whaling scene in his novel.
Now consider some typical ways of organizing the sources into a review:
- Chronological: If your review follows the chronological method, you could write about the materials above according to when they were published. For instance, first you would talk about the British biological studies of the 18th century, then about Moby Dick, published in 1851, then the book on sperm whales in other art (1968), and finally the biology articles (1980s) and the recent articles on American whaling of the 19th century. But there is relatively no continuity among subjects here. And notice that even though the sources on sperm whales in other art and on American whaling are written recently, they are about other subjects/objects that were created much earlier. Thus, the review loses its chronological focus.
- By publication: Order your sources by publication chronology, then, only if the order demonstrates a more important trend. For instance, you could order a review of literature on biological studies of sperm whales if the progression revealed a change in dissection practices of the researchers who wrote and/or conducted the studies.
- By trend: A better way to organize the above sources chronologically is to examine the sources under another trend, such as the history of whaling. Then your review would have subsections according to eras within this period. For instance, the review might examine whaling from pre-1600-1699, 1700-1799, and 1800-1899. Under this method, you would combine the recent studies on American whaling in the 19th century with Moby Dick itself in the 1800-1899 category, even though the authors wrote a century apart.
- Thematic: Thematic reviews of literature are organized around a topic or issue, rather than the progression of time. However, progression of time may still be an important factor in a thematic review. For instance, the sperm whale review could focus on the development of the harpoon for whale hunting. While the study focuses on one topic, harpoon technology, it will still be organized chronologically. The only difference here between a “chronological” and a “thematic” approach is what is emphasized the most: the development of the harpoon or the harpoon technology.But more authentic thematic reviews tend to break away from chronological order. For instance, a thematic review of material on sperm whales might examine how they are portrayed as “evil” in cultural documents. The subsections might include how they are personified, how their proportions are exaggerated, and their behaviors misunderstood. A review organized in this manner would shift between time periods within each section according to the point made.
- Methodological: A methodological approach differs from the two above in that the focusing factor usually does not have to do with the content of the material. Instead, it focuses on the “methods” of the researcher or writer. For the sperm whale project, one methodological approach would be to look at cultural differences between the portrayal of whales in American, British, and French art work. Or the review might focus on the economic impact of whaling on a community. A methodological scope will influence either the types of documents in the review or the way in which these documents are discussed. Once you’ve decided on the organizational method for the body of the review, the sections you need to include in the paper should be easy to figure out. They should arise out of your organizational strategy. In other words, a chronological review would have subsections for each vital time period. A thematic review would have subtopics based upon factors that relate to the theme or issue.
Sometimes, though, you might need to add additional sections that are necessary for your study, but do not fit in the organizational strategy of the body. What other sections you include in the body is up to you. Put in only what is necessary. Here are a few other sections you might want to consider:
- Current Situation: Information necessary to understand the topic or focus of the literature review.
- History: The chronological progression of the field, the literature, or an idea that is necessary to understand the literature review, if the body of the literature review is not already a chronology.
- Methods and/or Standards: The criteria you used to select the sources in your literature review or the way in which you present your information. For instance, you might explain that your review includes only peer-reviewed articles and journals.
Questions for Further Research: What questions about the field has the review sparked? How will you further your research as a result of the review?
Begin composing
Once you’ve settled on a general pattern of organization, you’re ready to write each section. There are a few guidelines you should follow during the writing stage as well. Here is a sample paragraph from a literature review about sexism and language to illuminate the following discussion:
However, other studies have shown that even gender-neutral antecedents are more likely to produce masculine images than feminine ones (Gastil, 1990). Hamilton (1988) asked students to complete sentences that required them to fill in pronouns that agreed with gender-neutral antecedents such as “writer,” “pedestrian,” and “persons.” The students were asked to describe any image they had when writing the sentence. Hamilton found that people imagined 3.3 men to each woman in the masculine “generic” condition and 1.5 men per woman in the unbiased condition. Thus, while ambient sexism accounted for some of the masculine bias, sexist language amplified the effect. (Source: Erika Falk and Jordan Mills, “Why Sexist Language Affects Persuasion: The Role of Homophily, Intended Audience, and Offense,” Women and Language19:2).
Use evidence
In the example above, the writers refer to several other sources when making their point. A literature review in this sense is just like any other academic research paper. Your interpretation of the available sources must be backed up with evidence to show that what you are saying is valid.
Be selective
Select only the most important points in each source to highlight in the review. The type of information you choose to mention should relate directly to the review’s focus, whether it is thematic, methodological, or chronological.
Use quotes sparingly
Falk and Mills do not use any direct quotes. That is because the survey nature of the literature review does not allow for in-depth discussion or detailed quotes from the text. Some short quotes here and there are okay, though, if you want to emphasize a point, or if what the author said just cannot be rewritten in your own words. Notice that Falk and Mills do quote certain terms that were coined by the author, not common knowledge, or taken directly from the study. But if you find yourself wanting to put in more quotes, check with your instructor.
Summarize and synthesize
Remember to summarize and synthesize your sources within each paragraph as well as throughout the review. The authors here recapitulate important features of Hamilton’s study, but then synthesize it by rephrasing the study’s significance and relating it to their own work.
Keep your own voice
While the literature review presents others’ ideas, your voice (the writer’s) should remain front and center. Notice that Falk and Mills weave references to other sources into their own text, but they still maintain their own voice by starting and ending the paragraph with their own ideas and their own words. The sources support what Falk and Mills are saying.
Use caution when paraphrasing
When paraphrasing a source that is not your own, be sure to represent the author’s information or opinions accurately and in your own words. In the preceding example, Falk and Mills either directly refer in the text to the author of their source, such as Hamilton, or they provide ample notation in the text when the ideas they are mentioning are not their own, for example, Gastil’s. For more information, please see our handout on plagiarism .
Revise, revise, revise
Draft in hand? Now you’re ready to revise. Spending a lot of time revising is a wise idea, because your main objective is to present the material, not the argument. So check over your review again to make sure it follows the assignment and/or your outline. Then, just as you would for most other academic forms of writing, rewrite or rework the language of your review so that you’ve presented your information in the most concise manner possible. Be sure to use terminology familiar to your audience; get rid of unnecessary jargon or slang. Finally, double check that you’ve documented your sources and formatted the review appropriately for your discipline. For tips on the revising and editing process, see our handout on revising drafts .
Works consulted
We consulted these works while writing this handout. This is not a comprehensive list of resources on the handout’s topic, and we encourage you to do your own research to find additional publications. Please do not use this list as a model for the format of your own reference list, as it may not match the citation style you are using. For guidance on formatting citations, please see the UNC Libraries citation tutorial . We revise these tips periodically and welcome feedback.
Anson, Chris M., and Robert A. Schwegler. 2010. The Longman Handbook for Writers and Readers , 6th ed. New York: Longman.
Jones, Robert, Patrick Bizzaro, and Cynthia Selfe. 1997. The Harcourt Brace Guide to Writing in the Disciplines . New York: Harcourt Brace.
Lamb, Sandra E. 1998. How to Write It: A Complete Guide to Everything You’ll Ever Write . Berkeley: Ten Speed Press.
Rosen, Leonard J., and Laurence Behrens. 2003. The Allyn & Bacon Handbook , 5th ed. New York: Longman.
Troyka, Lynn Quittman, and Doug Hesse. 2016. Simon and Schuster Handbook for Writers , 11th ed. London: Pearson.
You may reproduce it for non-commercial use if you use the entire handout and attribute the source: The Writing Center, University of North Carolina at Chapel Hill
Make a Gift
- UConn Library
- Literature Review: The What, Why and How-to Guide
- Introduction
Literature Review: The What, Why and How-to Guide — Introduction
- Getting Started
- How to Pick a Topic
- Strategies to Find Sources
- Evaluating Sources & Lit. Reviews
- Tips for Writing Literature Reviews
- Writing Literature Review: Useful Sites
- Citation Resources
- Other Academic Writings
What are Literature Reviews?
So, what is a literature review? "A literature review is an account of what has been published on a topic by accredited scholars and researchers. In writing the literature review, your purpose is to convey to your reader what knowledge and ideas have been established on a topic, and what their strengths and weaknesses are. As a piece of writing, the literature review must be defined by a guiding concept (e.g., your research objective, the problem or issue you are discussing, or your argumentative thesis). It is not just a descriptive list of the material available, or a set of summaries." Taylor, D. The literature review: A few tips on conducting it . University of Toronto Health Sciences Writing Centre.
Goals of Literature Reviews
What are the goals of creating a Literature Review? A literature could be written to accomplish different aims:
- To develop a theory or evaluate an existing theory
- To summarize the historical or existing state of a research topic
- Identify a problem in a field of research
Baumeister, R. F., & Leary, M. R. (1997). Writing narrative literature reviews . Review of General Psychology , 1 (3), 311-320.
What kinds of sources require a Literature Review?
- A research paper assigned in a course
- A thesis or dissertation
- A grant proposal
- An article intended for publication in a journal
All these instances require you to collect what has been written about your research topic so that you can demonstrate how your own research sheds new light on the topic.
Types of Literature Reviews
What kinds of literature reviews are written?
Narrative review: The purpose of this type of review is to describe the current state of the research on a specific topic/research and to offer a critical analysis of the literature reviewed. Studies are grouped by research/theoretical categories, and themes and trends, strengths and weakness, and gaps are identified. The review ends with a conclusion section which summarizes the findings regarding the state of the research of the specific study, the gaps identify and if applicable, explains how the author's research will address gaps identify in the review and expand the knowledge on the topic reviewed.
- Example : Predictors and Outcomes of U.S. Quality Maternity Leave: A Review and Conceptual Framework: 10.1177/08948453211037398
Systematic review : "The authors of a systematic review use a specific procedure to search the research literature, select the studies to include in their review, and critically evaluate the studies they find." (p. 139). Nelson, L. K. (2013). Research in Communication Sciences and Disorders . Plural Publishing.
- Example : The effect of leave policies on increasing fertility: a systematic review: 10.1057/s41599-022-01270-w
Meta-analysis : "Meta-analysis is a method of reviewing research findings in a quantitative fashion by transforming the data from individual studies into what is called an effect size and then pooling and analyzing this information. The basic goal in meta-analysis is to explain why different outcomes have occurred in different studies." (p. 197). Roberts, M. C., & Ilardi, S. S. (2003). Handbook of Research Methods in Clinical Psychology . Blackwell Publishing.
- Example : Employment Instability and Fertility in Europe: A Meta-Analysis: 10.1215/00703370-9164737
Meta-synthesis : "Qualitative meta-synthesis is a type of qualitative study that uses as data the findings from other qualitative studies linked by the same or related topic." (p.312). Zimmer, L. (2006). Qualitative meta-synthesis: A question of dialoguing with texts . Journal of Advanced Nursing , 53 (3), 311-318.
- Example : Women’s perspectives on career successes and barriers: A qualitative meta-synthesis: 10.1177/05390184221113735
Literature Reviews in the Health Sciences
- UConn Health subject guide on systematic reviews Explanation of the different review types used in health sciences literature as well as tools to help you find the right review type
- << Previous: Getting Started
- Next: How to Pick a Topic >>
- Last Updated: Sep 21, 2022 2:16 PM
- URL: https://guides.lib.uconn.edu/literaturereview
- University of Texas Libraries
Literature Reviews
- What is a literature review?
- Steps in the Literature Review Process
- Define your research question
- Determine inclusion and exclusion criteria
- Choose databases and search
- Review Results
- Synthesize Results
- Analyze Results
- Librarian Support
What is a Literature Review?
A literature or narrative review is a comprehensive review and analysis of the published literature on a specific topic or research question. The literature that is reviewed contains: books, articles, academic articles, conference proceedings, association papers, and dissertations. It contains the most pertinent studies and points to important past and current research and practices. It provides background and context, and shows how your research will contribute to the field.
A literature review should:
- Provide a comprehensive and updated review of the literature;
- Explain why this review has taken place;
- Articulate a position or hypothesis;
- Acknowledge and account for conflicting and corroborating points of view
From S age Research Methods
Purpose of a Literature Review
A literature review can be written as an introduction to a study to:
- Demonstrate how a study fills a gap in research
- Compare a study with other research that's been done
Or it can be a separate work (a research article on its own) which:
- Organizes or describes a topic
- Describes variables within a particular issue/problem
Limitations of a Literature Review
Some of the limitations of a literature review are:
- It's a snapshot in time. Unlike other reviews, this one has beginning, a middle and an end. There may be future developments that could make your work less relevant.
- It may be too focused. Some niche studies may miss the bigger picture.
- It can be difficult to be comprehensive. There is no way to make sure all the literature on a topic was considered.
- It is easy to be biased if you stick to top tier journals. There may be other places where people are publishing exemplary research. Look to open access publications and conferences to reflect a more inclusive collection. Also, make sure to include opposing views (and not just supporting evidence).
Source: Grant, Maria J., and Andrew Booth. “A Typology of Reviews: An Analysis of 14 Review Types and Associated Methodologies.” Health Information & Libraries Journal, vol. 26, no. 2, June 2009, pp. 91–108. Wiley Online Library, doi:10.1111/j.1471-1842.2009.00848.x.
Meryl Brodsky : Communication and Information Studies
Hannah Chapman Tripp : Biology, Neuroscience
Carolyn Cunningham : Human Development & Family Sciences, Psychology, Sociology
Larayne Dallas : Engineering
Janelle Hedstrom : Special Education, Curriculum & Instruction, Ed Leadership & Policy
Susan Macicak : Linguistics
Imelda Vetter : Dell Medical School
For help in other subject areas, please see the guide to library specialists by subject .
Periodically, UT Libraries runs a workshop covering the basics and library support for literature reviews. While we try to offer these once per academic year, we find providing the recording to be helpful to community members who have missed the session. Following is the most recent recording of the workshop, Conducting a Literature Review. To view the recording, a UT login is required.
- October 26, 2022 recording
- Last Updated: Oct 26, 2022 2:49 PM
- URL: https://guides.lib.utexas.edu/literaturereviews

- USC Libraries
- Research Guides
Organizing Your Social Sciences Research Paper
- 5. The Literature Review
- Purpose of Guide
- Design Flaws to Avoid
- Independent and Dependent Variables
- Glossary of Research Terms
- Reading Research Effectively
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Applying Critical Thinking
- Choosing a Title
- Making an Outline
- Paragraph Development
- Research Process Video Series
- Executive Summary
- The C.A.R.S. Model
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tiertiary Sources
- Scholarly vs. Popular Publications
- Qualitative Methods
- Quantitative Methods
- Insiderness
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Writing Concisely
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Generative AI and Writing
- USC Libraries Tutorials and Other Guides
- Bibliography
A literature review surveys prior research published in books, scholarly articles, and any other sources relevant to a particular issue, area of research, or theory, and by so doing, provides a description, summary, and critical evaluation of these works in relation to the research problem being investigated. Literature reviews are designed to provide an overview of sources you have used in researching a particular topic and to demonstrate to your readers how your research fits within existing scholarship about the topic.
Fink, Arlene. Conducting Research Literature Reviews: From the Internet to Paper . Fourth edition. Thousand Oaks, CA: SAGE, 2014.
Importance of a Good Literature Review
A literature review may consist of simply a summary of key sources, but in the social sciences, a literature review usually has an organizational pattern and combines both summary and synthesis, often within specific conceptual categories . A summary is a recap of the important information of the source, but a synthesis is a re-organization, or a reshuffling, of that information in a way that informs how you are planning to investigate a research problem. The analytical features of a literature review might:
- Give a new interpretation of old material or combine new with old interpretations,
- Trace the intellectual progression of the field, including major debates,
- Depending on the situation, evaluate the sources and advise the reader on the most pertinent or relevant research, or
- Usually in the conclusion of a literature review, identify where gaps exist in how a problem has been researched to date.
Given this, the purpose of a literature review is to:
- Place each work in the context of its contribution to understanding the research problem being studied.
- Describe the relationship of each work to the others under consideration.
- Identify new ways to interpret prior research.
- Reveal any gaps that exist in the literature.
- Resolve conflicts amongst seemingly contradictory previous studies.
- Identify areas of prior scholarship to prevent duplication of effort.
- Point the way in fulfilling a need for additional research.
- Locate your own research within the context of existing literature [very important].
Fink, Arlene. Conducting Research Literature Reviews: From the Internet to Paper. 2nd ed. Thousand Oaks, CA: Sage, 2005; Hart, Chris. Doing a Literature Review: Releasing the Social Science Research Imagination . Thousand Oaks, CA: Sage Publications, 1998; Jesson, Jill. Doing Your Literature Review: Traditional and Systematic Techniques . Los Angeles, CA: SAGE, 2011; Knopf, Jeffrey W. "Doing a Literature Review." PS: Political Science and Politics 39 (January 2006): 127-132; Ridley, Diana. The Literature Review: A Step-by-Step Guide for Students . 2nd ed. Los Angeles, CA: SAGE, 2012.
Types of Literature Reviews
It is important to think of knowledge in a given field as consisting of three layers. First, there are the primary studies that researchers conduct and publish. Second are the reviews of those studies that summarize and offer new interpretations built from and often extending beyond the primary studies. Third, there are the perceptions, conclusions, opinion, and interpretations that are shared informally among scholars that become part of the body of epistemological traditions within the field.
In composing a literature review, it is important to note that it is often this third layer of knowledge that is cited as "true" even though it often has only a loose relationship to the primary studies and secondary literature reviews. Given this, while literature reviews are designed to provide an overview and synthesis of pertinent sources you have explored, there are a number of approaches you could adopt depending upon the type of analysis underpinning your study.
Argumentative Review This form examines literature selectively in order to support or refute an argument, deeply embedded assumption, or philosophical problem already established in the literature. The purpose is to develop a body of literature that establishes a contrarian viewpoint. Given the value-laden nature of some social science research [e.g., educational reform; immigration control], argumentative approaches to analyzing the literature can be a legitimate and important form of discourse. However, note that they can also introduce problems of bias when they are used to make summary claims of the sort found in systematic reviews [see below].
Integrative Review Considered a form of research that reviews, critiques, and synthesizes representative literature on a topic in an integrated way such that new frameworks and perspectives on the topic are generated. The body of literature includes all studies that address related or identical hypotheses or research problems. A well-done integrative review meets the same standards as primary research in regard to clarity, rigor, and replication. This is the most common form of review in the social sciences.
Historical Review Few things rest in isolation from historical precedent. Historical literature reviews focus on examining research throughout a period of time, often starting with the first time an issue, concept, theory, phenomena emerged in the literature, then tracing its evolution within the scholarship of a discipline. The purpose is to place research in a historical context to show familiarity with state-of-the-art developments and to identify the likely directions for future research.
Methodological Review A review does not always focus on what someone said [findings], but how they came about saying what they say [method of analysis]. Reviewing methods of analysis provides a framework of understanding at different levels [i.e. those of theory, substantive fields, research approaches, and data collection and analysis techniques], how researchers draw upon a wide variety of knowledge ranging from the conceptual level to practical documents for use in fieldwork in the areas of ontological and epistemological consideration, quantitative and qualitative integration, sampling, interviewing, data collection, and data analysis. This approach helps highlight ethical issues which you should be aware of and consider as you go through your own study.
Systematic Review This form consists of an overview of existing evidence pertinent to a clearly formulated research question, which uses pre-specified and standardized methods to identify and critically appraise relevant research, and to collect, report, and analyze data from the studies that are included in the review. The goal is to deliberately document, critically evaluate, and summarize scientifically all of the research about a clearly defined research problem . Typically it focuses on a very specific empirical question, often posed in a cause-and-effect form, such as "To what extent does A contribute to B?" This type of literature review is primarily applied to examining prior research studies in clinical medicine and allied health fields, but it is increasingly being used in the social sciences.
Theoretical Review The purpose of this form is to examine the corpus of theory that has accumulated in regard to an issue, concept, theory, phenomena. The theoretical literature review helps to establish what theories already exist, the relationships between them, to what degree the existing theories have been investigated, and to develop new hypotheses to be tested. Often this form is used to help establish a lack of appropriate theories or reveal that current theories are inadequate for explaining new or emerging research problems. The unit of analysis can focus on a theoretical concept or a whole theory or framework.
NOTE : Most often the literature review will incorporate some combination of types. For example, a review that examines literature supporting or refuting an argument, assumption, or philosophical problem related to the research problem will also need to include writing supported by sources that establish the history of these arguments in the literature.
Baumeister, Roy F. and Mark R. Leary. "Writing Narrative Literature Reviews." Review of General Psychology 1 (September 1997): 311-320; Mark R. Fink, Arlene. Conducting Research Literature Reviews: From the Internet to Paper . 2nd ed. Thousand Oaks, CA: Sage, 2005; Hart, Chris. Doing a Literature Review: Releasing the Social Science Research Imagination . Thousand Oaks, CA: Sage Publications, 1998; Kennedy, Mary M. "Defining a Literature." Educational Researcher 36 (April 2007): 139-147; Petticrew, Mark and Helen Roberts. Systematic Reviews in the Social Sciences: A Practical Guide . Malden, MA: Blackwell Publishers, 2006; Torracro, Richard. "Writing Integrative Literature Reviews: Guidelines and Examples." Human Resource Development Review 4 (September 2005): 356-367; Rocco, Tonette S. and Maria S. Plakhotnik. "Literature Reviews, Conceptual Frameworks, and Theoretical Frameworks: Terms, Functions, and Distinctions." Human Ressource Development Review 8 (March 2008): 120-130; Sutton, Anthea. Systematic Approaches to a Successful Literature Review . Los Angeles, CA: Sage Publications, 2016.
Structure and Writing Style
I. Thinking About Your Literature Review
The structure of a literature review should include the following in support of understanding the research problem :
- An overview of the subject, issue, or theory under consideration, along with the objectives of the literature review,
- Division of works under review into themes or categories [e.g. works that support a particular position, those against, and those offering alternative approaches entirely],
- An explanation of how each work is similar to and how it varies from the others,
- Conclusions as to which pieces are best considered in their argument, are most convincing of their opinions, and make the greatest contribution to the understanding and development of their area of research.
The critical evaluation of each work should consider :
- Provenance -- what are the author's credentials? Are the author's arguments supported by evidence [e.g. primary historical material, case studies, narratives, statistics, recent scientific findings]?
- Methodology -- were the techniques used to identify, gather, and analyze the data appropriate to addressing the research problem? Was the sample size appropriate? Were the results effectively interpreted and reported?
- Objectivity -- is the author's perspective even-handed or prejudicial? Is contrary data considered or is certain pertinent information ignored to prove the author's point?
- Persuasiveness -- which of the author's theses are most convincing or least convincing?
- Validity -- are the author's arguments and conclusions convincing? Does the work ultimately contribute in any significant way to an understanding of the subject?
II. Development of the Literature Review
Four Basic Stages of Writing 1. Problem formulation -- which topic or field is being examined and what are its component issues? 2. Literature search -- finding materials relevant to the subject being explored. 3. Data evaluation -- determining which literature makes a significant contribution to the understanding of the topic. 4. Analysis and interpretation -- discussing the findings and conclusions of pertinent literature.
Consider the following issues before writing the literature review: Clarify If your assignment is not specific about what form your literature review should take, seek clarification from your professor by asking these questions: 1. Roughly how many sources would be appropriate to include? 2. What types of sources should I review (books, journal articles, websites; scholarly versus popular sources)? 3. Should I summarize, synthesize, or critique sources by discussing a common theme or issue? 4. Should I evaluate the sources in any way beyond evaluating how they relate to understanding the research problem? 5. Should I provide subheadings and other background information, such as definitions and/or a history? Find Models Use the exercise of reviewing the literature to examine how authors in your discipline or area of interest have composed their literature review sections. Read them to get a sense of the types of themes you might want to look for in your own research or to identify ways to organize your final review. The bibliography or reference section of sources you've already read, such as required readings in the course syllabus, are also excellent entry points into your own research. Narrow the Topic The narrower your topic, the easier it will be to limit the number of sources you need to read in order to obtain a good survey of relevant resources. Your professor will probably not expect you to read everything that's available about the topic, but you'll make the act of reviewing easier if you first limit scope of the research problem. A good strategy is to begin by searching the USC Libraries Catalog for recent books about the topic and review the table of contents for chapters that focuses on specific issues. You can also review the indexes of books to find references to specific issues that can serve as the focus of your research. For example, a book surveying the history of the Israeli-Palestinian conflict may include a chapter on the role Egypt has played in mediating the conflict, or look in the index for the pages where Egypt is mentioned in the text. Consider Whether Your Sources are Current Some disciplines require that you use information that is as current as possible. This is particularly true in disciplines in medicine and the sciences where research conducted becomes obsolete very quickly as new discoveries are made. However, when writing a review in the social sciences, a survey of the history of the literature may be required. In other words, a complete understanding the research problem requires you to deliberately examine how knowledge and perspectives have changed over time. Sort through other current bibliographies or literature reviews in the field to get a sense of what your discipline expects. You can also use this method to explore what is considered by scholars to be a "hot topic" and what is not.
III. Ways to Organize Your Literature Review
Chronology of Events If your review follows the chronological method, you could write about the materials according to when they were published. This approach should only be followed if a clear path of research building on previous research can be identified and that these trends follow a clear chronological order of development. For example, a literature review that focuses on continuing research about the emergence of German economic power after the fall of the Soviet Union. By Publication Order your sources by publication chronology, then, only if the order demonstrates a more important trend. For instance, you could order a review of literature on environmental studies of brown fields if the progression revealed, for example, a change in the soil collection practices of the researchers who wrote and/or conducted the studies. Thematic [“conceptual categories”] A thematic literature review is the most common approach to summarizing prior research in the social and behavioral sciences. Thematic reviews are organized around a topic or issue, rather than the progression of time, although the progression of time may still be incorporated into a thematic review. For example, a review of the Internet’s impact on American presidential politics could focus on the development of online political satire. While the study focuses on one topic, the Internet’s impact on American presidential politics, it would still be organized chronologically reflecting technological developments in media. The difference in this example between a "chronological" and a "thematic" approach is what is emphasized the most: themes related to the role of the Internet in presidential politics. Note that more authentic thematic reviews tend to break away from chronological order. A review organized in this manner would shift between time periods within each section according to the point being made. Methodological A methodological approach focuses on the methods utilized by the researcher. For the Internet in American presidential politics project, one methodological approach would be to look at cultural differences between the portrayal of American presidents on American, British, and French websites. Or the review might focus on the fundraising impact of the Internet on a particular political party. A methodological scope will influence either the types of documents in the review or the way in which these documents are discussed.
Other Sections of Your Literature Review Once you've decided on the organizational method for your literature review, the sections you need to include in the paper should be easy to figure out because they arise from your organizational strategy. In other words, a chronological review would have subsections for each vital time period; a thematic review would have subtopics based upon factors that relate to the theme or issue. However, sometimes you may need to add additional sections that are necessary for your study, but do not fit in the organizational strategy of the body. What other sections you include in the body is up to you. However, only include what is necessary for the reader to locate your study within the larger scholarship about the research problem.
Here are examples of other sections, usually in the form of a single paragraph, you may need to include depending on the type of review you write:
- Current Situation : Information necessary to understand the current topic or focus of the literature review.
- Sources Used : Describes the methods and resources [e.g., databases] you used to identify the literature you reviewed.
- History : The chronological progression of the field, the research literature, or an idea that is necessary to understand the literature review, if the body of the literature review is not already a chronology.
- Selection Methods : Criteria you used to select (and perhaps exclude) sources in your literature review. For instance, you might explain that your review includes only peer-reviewed [i.e., scholarly] sources.
- Standards : Description of the way in which you present your information.
- Questions for Further Research : What questions about the field has the review sparked? How will you further your research as a result of the review?
IV. Writing Your Literature Review
Once you've settled on how to organize your literature review, you're ready to write each section. When writing your review, keep in mind these issues.
Use Evidence A literature review section is, in this sense, just like any other academic research paper. Your interpretation of the available sources must be backed up with evidence [citations] that demonstrates that what you are saying is valid. Be Selective Select only the most important points in each source to highlight in the review. The type of information you choose to mention should relate directly to the research problem, whether it is thematic, methodological, or chronological. Related items that provide additional information, but that are not key to understanding the research problem, can be included in a list of further readings . Use Quotes Sparingly Some short quotes are appropriate if you want to emphasize a point, or if what an author stated cannot be easily paraphrased. Sometimes you may need to quote certain terminology that was coined by the author, is not common knowledge, or taken directly from the study. Do not use extensive quotes as a substitute for using your own words in reviewing the literature. Summarize and Synthesize Remember to summarize and synthesize your sources within each thematic paragraph as well as throughout the review. Recapitulate important features of a research study, but then synthesize it by rephrasing the study's significance and relating it to your own work and the work of others. Keep Your Own Voice While the literature review presents others' ideas, your voice [the writer's] should remain front and center. For example, weave references to other sources into what you are writing but maintain your own voice by starting and ending the paragraph with your own ideas and wording. Use Caution When Paraphrasing When paraphrasing a source that is not your own, be sure to represent the author's information or opinions accurately and in your own words. Even when paraphrasing an author’s work, you still must provide a citation to that work.
V. Common Mistakes to Avoid
These are the most common mistakes made in reviewing social science research literature.
- Sources in your literature review do not clearly relate to the research problem;
- You do not take sufficient time to define and identify the most relevant sources to use in the literature review related to the research problem;
- Relies exclusively on secondary analytical sources rather than including relevant primary research studies or data;
- Uncritically accepts another researcher's findings and interpretations as valid, rather than examining critically all aspects of the research design and analysis;
- Does not describe the search procedures that were used in identifying the literature to review;
- Reports isolated statistical results rather than synthesizing them in chi-squared or meta-analytic methods; and,
- Only includes research that validates assumptions and does not consider contrary findings and alternative interpretations found in the literature.
Cook, Kathleen E. and Elise Murowchick. “Do Literature Review Skills Transfer from One Course to Another?” Psychology Learning and Teaching 13 (March 2014): 3-11; Fink, Arlene. Conducting Research Literature Reviews: From the Internet to Paper . 2nd ed. Thousand Oaks, CA: Sage, 2005; Hart, Chris. Doing a Literature Review: Releasing the Social Science Research Imagination . Thousand Oaks, CA: Sage Publications, 1998; Jesson, Jill. Doing Your Literature Review: Traditional and Systematic Techniques . London: SAGE, 2011; Literature Review Handout. Online Writing Center. Liberty University; Literature Reviews. The Writing Center. University of North Carolina; Onwuegbuzie, Anthony J. and Rebecca Frels. Seven Steps to a Comprehensive Literature Review: A Multimodal and Cultural Approach . Los Angeles, CA: SAGE, 2016; Ridley, Diana. The Literature Review: A Step-by-Step Guide for Students . 2nd ed. Los Angeles, CA: SAGE, 2012; Randolph, Justus J. “A Guide to Writing the Dissertation Literature Review." Practical Assessment, Research, and Evaluation. vol. 14, June 2009; Sutton, Anthea. Systematic Approaches to a Successful Literature Review . Los Angeles, CA: Sage Publications, 2016; Taylor, Dena. The Literature Review: A Few Tips On Conducting It. University College Writing Centre. University of Toronto; Writing a Literature Review. Academic Skills Centre. University of Canberra.
Writing Tip
Break Out of Your Disciplinary Box!
Thinking interdisciplinarily about a research problem can be a rewarding exercise in applying new ideas, theories, or concepts to an old problem. For example, what might cultural anthropologists say about the continuing conflict in the Middle East? In what ways might geographers view the need for better distribution of social service agencies in large cities than how social workers might study the issue? You don’t want to substitute a thorough review of core research literature in your discipline for studies conducted in other fields of study. However, particularly in the social sciences, thinking about research problems from multiple vectors is a key strategy for finding new solutions to a problem or gaining a new perspective. Consult with a librarian about identifying research databases in other disciplines; almost every field of study has at least one comprehensive database devoted to indexing its research literature.
Frodeman, Robert. The Oxford Handbook of Interdisciplinarity . New York: Oxford University Press, 2010.
Another Writing Tip
Don't Just Review for Content!
While conducting a review of the literature, maximize the time you devote to writing this part of your paper by thinking broadly about what you should be looking for and evaluating. Review not just what scholars are saying, but how are they saying it. Some questions to ask:
- How are they organizing their ideas?
- What methods have they used to study the problem?
- What theories have been used to explain, predict, or understand their research problem?
- What sources have they cited to support their conclusions?
- How have they used non-textual elements [e.g., charts, graphs, figures, etc.] to illustrate key points?
When you begin to write your literature review section, you'll be glad you dug deeper into how the research was designed and constructed because it establishes a means for developing more substantial analysis and interpretation of the research problem.
Hart, Chris. Doing a Literature Review: Releasing the Social Science Research Imagination . Thousand Oaks, CA: Sage Publications, 1 998.
Yet Another Writing Tip
When Do I Know I Can Stop Looking and Move On?
Here are several strategies you can utilize to assess whether you've thoroughly reviewed the literature:
- Look for repeating patterns in the research findings . If the same thing is being said, just by different people, then this likely demonstrates that the research problem has hit a conceptual dead end. At this point consider: Does your study extend current research? Does it forge a new path? Or, does is merely add more of the same thing being said?
- Look at sources the authors cite to in their work . If you begin to see the same researchers cited again and again, then this is often an indication that no new ideas have been generated to address the research problem.
- Search Google Scholar to identify who has subsequently cited leading scholars already identified in your literature review [see next sub-tab]. This is called citation tracking and there are a number of sources that can help you identify who has cited whom, particularly scholars from outside of your discipline. Here again, if the same authors are being cited again and again, this may indicate no new literature has been written on the topic.
Onwuegbuzie, Anthony J. and Rebecca Frels. Seven Steps to a Comprehensive Literature Review: A Multimodal and Cultural Approach . Los Angeles, CA: Sage, 2016; Sutton, Anthea. Systematic Approaches to a Successful Literature Review . Los Angeles, CA: Sage Publications, 2016.
- << Previous: Theoretical Framework
- Next: Citation Tracking >>
- Last Updated: Apr 9, 2024 1:19 PM
- URL: https://libguides.usc.edu/writingguide
Harvey Cushing/John Hay Whitney Medical Library
- Collections
- Research Help
YSN Doctoral Programs: Steps in Conducting a Literature Review
- Biomedical Databases
- Global (Public Health) Databases
- Soc. Sci., History, and Law Databases
- Grey Literature
- Trials Registers
- Data and Statistics
- Public Policy
- Google Tips
- Recommended Books
- Steps in Conducting a Literature Review
What is a literature review?
A literature review is an integrated analysis -- not just a summary-- of scholarly writings and other relevant evidence related directly to your research question. That is, it represents a synthesis of the evidence that provides background information on your topic and shows a association between the evidence and your research question.
A literature review may be a stand alone work or the introduction to a larger research paper, depending on the assignment. Rely heavily on the guidelines your instructor has given you.
Why is it important?
A literature review is important because it:
- Explains the background of research on a topic.
- Demonstrates why a topic is significant to a subject area.
- Discovers relationships between research studies/ideas.
- Identifies major themes, concepts, and researchers on a topic.
- Identifies critical gaps and points of disagreement.
- Discusses further research questions that logically come out of the previous studies.
APA7 Style resources
APA Style Blog - for those harder to find answers
1. Choose a topic. Define your research question.
Your literature review should be guided by your central research question. The literature represents background and research developments related to a specific research question, interpreted and analyzed by you in a synthesized way.
- Make sure your research question is not too broad or too narrow. Is it manageable?
- Begin writing down terms that are related to your question. These will be useful for searches later.
- If you have the opportunity, discuss your topic with your professor and your class mates.
2. Decide on the scope of your review
How many studies do you need to look at? How comprehensive should it be? How many years should it cover?
- This may depend on your assignment. How many sources does the assignment require?
3. Select the databases you will use to conduct your searches.
Make a list of the databases you will search.
Where to find databases:
- use the tabs on this guide
- Find other databases in the Nursing Information Resources web page
- More on the Medical Library web page
- ... and more on the Yale University Library web page
4. Conduct your searches to find the evidence. Keep track of your searches.
- Use the key words in your question, as well as synonyms for those words, as terms in your search. Use the database tutorials for help.
- Save the searches in the databases. This saves time when you want to redo, or modify, the searches. It is also helpful to use as a guide is the searches are not finding any useful results.
- Review the abstracts of research studies carefully. This will save you time.
- Use the bibliographies and references of research studies you find to locate others.
- Check with your professor, or a subject expert in the field, if you are missing any key works in the field.
- Ask your librarian for help at any time.
- Use a citation manager, such as EndNote as the repository for your citations. See the EndNote tutorials for help.
Review the literature
Some questions to help you analyze the research:
- What was the research question of the study you are reviewing? What were the authors trying to discover?
- Was the research funded by a source that could influence the findings?
- What were the research methodologies? Analyze its literature review, the samples and variables used, the results, and the conclusions.
- Does the research seem to be complete? Could it have been conducted more soundly? What further questions does it raise?
- If there are conflicting studies, why do you think that is?
- How are the authors viewed in the field? Has this study been cited? If so, how has it been analyzed?
Tips:
- Review the abstracts carefully.
- Keep careful notes so that you may track your thought processes during the research process.
- Create a matrix of the studies for easy analysis, and synthesis, across all of the studies.
- << Previous: Recommended Books
- Last Updated: Jan 4, 2024 10:52 AM
- URL: https://guides.library.yale.edu/YSNDoctoral
How to Write a Literature Review

As every student knows, writing informative essay and research papers is an integral part of the educational program. You create a thesis, support it using valid sources, and formulate systematic ideas surrounding it. However, not all students know that they will also have to face another type of paper known as a Literature Review in college. Let's take a closer look at this with our custom essay writer .
Literature Review Definition
As this is a less common academic writing type, students often ask: "What is a literature review?" According to the definition, a literature review is a body of work that explores various publications within a specific subject area and sometimes within a set timeframe.
This type of writing requires you to read and analyze various sources that relate to the main subject and present each unique comprehension of the publications. Lastly, a literature review should combine a summary with a synthesis of the documents used. A summary is a brief overview of the important information in the publication; a synthesis is a re-organization of the information that gives the writing a new and unique meaning.
Typically, a literature review is a part of a larger paper, such as a thesis or dissertation. However, you may also be given it as a stand-alone assignment.
The Purpose
The main purpose of a literature review is to summarize and synthesize the ideas created by previous authors without implementing personal opinions or other additional information.
However, a literature review objective is not just to list summaries of sources; rather, it is to notice a central trend or principle in all of the publications. Just like a research paper has a thesis that guides it on rails, a literature review has the main organizing principle (MOP). The goal of this type of academic writing is to identify the MOP and show how it exists in all of your supporting documents.
Why is a literature review important? The value of such work is explained by the following goals it pursues:
- Highlights the significance of the main topic within a specific subject area.
- Demonstrates and explains the background of research for a particular subject matter.
- Helps to find out the key themes, principles, concepts, and researchers that exist within a topic.
- Helps to reveal relationships between existing ideas/studies on a topic.
- Reveals the main points of controversy and gaps within a topic.
- Suggests questions to drive primary research based on previous studies.
Here are some example topics for writing literature reviews:
- Exploring racism in "To Kill a Mockingbird," "The Adventures of Huckleberry Finn," and "Uncle Tom's Cabin."
- Isolationism in "The Catcher in the Rye," "Frankenstein," and "1984"
- Understanding Moral Dilemmas in "Crime and Punishment," "The Scarlet Letter," and "The Lifeboat"
- Corruption of Power in "Macbeth," "All the King's Men," and "Animal Farm"
- Emotional and Physical survival in "Lord of the Flies," "Hatchet," and "Congo."
How Long Is a Literature Review?
When facing the need to write a literature review, students tend to wonder, "how long should a literature review be?" In some cases, the length of your paper's body may be determined by your instructor. Be sure to read the guidelines carefully to learn what is expected from you.
Keeping your literature review around 15-30% of your entire paper is recommended if you haven't been provided with specific guidelines. To give you a rough idea, that is about 2-3 pages for a 15-page paper. In case you are writing a literature review as a stand-alone assignment, its length should be specified in the instructions provided.
Literature Review Format: APA, MLA, and Chicago
The essay format you use should adhere to the citation style preferred by your instructor. Seek clarification from your instructor for several other components as well to establish a desired literature review format:
- How many sources should you review, and what kind of sources should they be (published materials, journal articles, or websites)?
- What format should you use to cite the sources?
- How long should the review be?
- Should your review consist of a summary, synthesis, or a personal critique?
- Should your review include subheadings or background information for your sources?
If you want to format your paper in APA style, then follow these rules:
- Use 1-inch page margins.
- Unless provided with other instructions, use double-spacing throughout the whole text.
- Make sure you choose a readable font. The preferred font for APA papers is Times New Roman set to 12-point size.
- Include a header at the top of every page (in capital letters). The page header must be a shortened version of your essay title and limited to 50 characters, including spacing and punctuation.
- Put page numbers in the upper right corner of every page.
- When shaping your literature review outline in APA, don't forget to include a title page. This page should include the paper's name, the author's name, and the institutional affiliation. Your title must be typed with upper and lowercase letters and centered in the upper part of the page; use no more than 12 words, and avoid using abbreviations and useless words.
For MLA style text, apply the following guidelines:
- Double your spacing across the entire paper.
- Set ½-inch indents for each new paragraph.
- The preferred font for MLA papers is Times New Roman set to 12-point size.
- Include a header at the top of your paper's first page or on the title page (note that MLA style does not require you to have a title page, but you are allowed to decide to include one). A header in this format should include your full name; the name of your instructor; the name of the class, course, or section number; and the due date of the assignment.
- Include a running head in the top right corner of each page in your paper. Place it one inch from the page's right margin and half an inch from the top margin. Only include your last name and the page number separated by a space in the running head. Do not put the abbreviation p. before page numbers.
Finally, if you are required to write a literature review in Chicago style, here are the key rules to follow:
- Set page margins to no less than 1 inch.
- Use double spacing across the entire text, except when it comes to table titles, figure captions, notes, blockquotes, and entries within the bibliography or References.
- Do not put spaces between paragraphs.
- Make sure you choose a clear and easily-readable font. The preferred fonts for Chicago papers are Times New Roman and Courier, set to no less than 10-point size, but preferably to 12-point size.
- A cover (title) page should include your full name, class information, and the date. Center the cover page and place it one-third below the top of the page.
- Place page numbers in the upper right corner of each page, including the cover page.
Read also about harvard format - popular style used in papers.
Structure of a Literature Review
How to structure a literature review: Like many other types of academic writing, a literature review follows a typical intro-body-conclusion style with 5 paragraphs overall. Now, let’s look at each component of the basic literature review structure in detail:

- Introduction
You should direct your reader(s) towards the MOP (main organizing principle). This means that your information must start from a broad perspective and gradually narrow down until it reaches your focal point.
Start by presenting your general concept (Corruption, for example). After the initial presentation, narrow your introduction's focus towards the MOP by mentioning the criteria you used to select the literature sources you have chosen (Macbeth, All the King's Men, and Animal Farm). Finally, the introduction will end with the presentation of your MOP that should directly link it to all three literature sources.
Body Paragraphs
Generally, each body paragraph will focus on a specific source of literature laid out in the essay's introduction. As each source has its own frame of reference for the MOP, it is crucial to structure the review in the most logically consistent way possible. This means the writing should be structured chronologically, thematically or methodologically.
Chronologically
Breaking down your sources based on their publication date is a solid way to keep a correct historical timeline. If applied properly, it can present the development of a certain concept over time and provide examples in the form of literature. However, sometimes there are better alternatives we can use to structure the body.
Thematically
Instead of taking the "timeline approach," another option can be looking at the link between your MOP and your sources. Sometimes, the main idea will just glare from a piece of literature. Other times, the author may have to seek examples to prove their point. An experienced writer will usually present their sources by order of strength. For example, in "To Kill A Mockingbird," the entire novel was centralized around racism; in "The Adventures of Huckleberry Finn," racism was one of many themes.
Methodologically
As made obvious by the terminology, this type of structuring focuses on the methods used to present the central concept. For example, in "1984", George Orwell uses the law-and-order approach and shows the dangers of a dystopia for a social species.
In "Frankenstein," Mary Shelley exposes the character's physical traits as repulsive and horrifying, forcing him to suffer in an isolated environment. By showcasing the various methods used to portray the MOP, the writer can compare them based on things like severity, ethicality, and overall impact.
After presenting your key findings in the body paragraphs, there are 3 final objectives to complete in the essay's conclusion. First, the author should summarize the findings they have made or found, in other words, and briefly answer the question: "What have you learned?"
After discussing that information, the next step is to present the significance of the information about our current world today. In other words, how can the reader take the information and apply it to today's society? From that point, we finish off with a breadcrumb trail.
As the author, you want to leave the readers' trail of thought within the actual essay topic. This provides them with a means of further investigation—meaning that the reader may consider where the discussion will go next.
Writing an Outline for a Literature Review
Students often underestimate the importance of planning the structure of their papers in advance. However, this is not a wise approach. Having a rough APA literature review outline (or other style outlines) will not only help you follow the right format and structure but will also make the writing process simpler and help ensure that you include all of the important information without missing anything.
How to write a literature review outline: As you already know from the Structure section of this guide, every part of your literature review performs its own important role. Therefore, you should create your outline while keeping the general introduction-body-conclusion structure in mind and ensuring that each section meets its own objectives. However, it is important to remember that a literature review outline is slightly different from outlines of other types of essays because it does not provide new information. Instead, it focuses on existing studies relevant to the main topic.
Here is a literature review outline example on the subject of the Ebola virus to help you get it right:
- Introduce the general topic. Provide background information on the Ebola virus: genome, pathogenesis, transmission, epidemiology, treatment, etc.
- Shape the main research question: What is the potential role of arthropods (mechanical or biological vectors) in the distribution of the Ebola virus?
- Methodology: For example, the information was searched through X databases to find relevant research articles about the Ebola virus and arthropods' role in its spreading. The data was extracted using a standardized form.
- Expected outcomes
- Overall trends in the literature on this topic: While the natural reservoir of the virus is still not known with certainty, many researchers believe that arthropods (and fruit bats, in particular) pay a significant role in the distribution of the virus.
- Subject 1: A brief overview of the particular piece of literature in general terms; an analysis of the key aspects of the study; a review of the research questions, methods, procedures, and outcomes; and an overview of the strong and weak points, gaps, and contradictions.
- Subject 2: A brief overview of the particular piece of literature in general terms; an analysis of the key aspects of the study; a review of the research questions, methods, procedures, and outcomes; and an overview of the strong and weak points, gaps, and contradictions.
- Subject 3: A brief overview of the particular piece of literature in general terms; an analysis of the key aspects of the study; a review of the research questions, methods, procedures, and outcomes; and an overview of the strong and weak points, gaps, and contradictions.
- Indicate the relationships between the pieces of literature discussed. Emphasize key themes, common patterns, and trends. Talk about the pros and cons of the different approaches taken by the authors/researchers.
- State which studies seem to be the most influential.
- Emphasize the major contradictions and points of disagreement. Define the gaps still to be covered (if any).
- If applicable: define how your own study will contribute to further disclosure of the topic.
Hopefully, this sample outline will help you to structure your own paper. However, if you feel like you need some more advice on how to organize your review, don’t hesitate to search for more literature review outline examples in APA or other styles on the Web, or simply ask our writers to get a dissertation help .
Need Help With LITERATURE REVIEW?
Count on our literature review writing service to get it done! We will make your literature essay, we only need your paper requirements to save your precious time and nerves from writing it on your own!
How to Write a Good Literature Review
Whether you are writing a literature review within the framework of a large research project (e.g. thesis, dissertation, or other) or as a stand-alone assignment, the approach you should take to writing generally remains the same.

Whether you are writing a literature review within the framework of a large research project (e.g., thesis, dissertation, or other) or as a stand-alone assignment, the approach you should take to writing generally remains the same.
Now, as you know about the general rules and have a basic literature review outline template, let's define the steps to take to handle this task right with our service:
Step 1: Identifying the Topic
This is probably the only matter you may approach differently depending on whether your literature review comes within a research paper or a separate assignment altogether. If you are creating a literature review as a part of another work, you need to search for literature related to your main research questions and problems. Respectively, if you are writing it as a stand-alone task, you will have to pick a relevant topic and central question upon which you will collect the literature. Earlier in this guide, we suggested some engaging topics to guide your search.
Step 2: Conducting Research
When you have a clearly defined topic, it is time to start collecting literature for your review. We recommend starting by compiling a list of relevant keywords related to your central question—to make the entire research process much simpler and help you find relevant publications faster.
When you have a list of keywords, use them to search for valid and relevant sources. At this point, be sure to use only trusted sources, such as ones from university libraries, online scientific databases, etc.
Once you have found some sources, be sure to define whether or not they are actually relevant to your topic and research question. To save time, you can read abstracts to get general ideas of what the papers are about instead of the whole thing.
Pro Tip: When you finally find a few valid publications, take a look at their bibliographies to discover other relevant sources as well.
Step 3: Assess and Prioritize Sources
Throughout your research, you will likely find plenty of relevant literature to include in your literature review. At this point, students often make the mistake of trying to fit all the collected sources into their reviews. Instead, we suggest looking at what you've collected once more, evaluating the available sources, and selecting the most relevant ones. You most likely won't be able to read everything you find on a given topic and then be able to synthesize all of the sources into a single literature review. That's why prioritizing them is important.
To evaluate which sources are worth including in your review, keep in mind the following criteria:
- Credibility;
- Innovation;
- Key insights;
Furthermore, as you read the sources, don’t forget to take notes on everything you can incorporate into the review later. And be sure to get your citations in place early on. If you cite the selected sources at the initial stage, you will find it easier to create your annotated bibliography later on.
Step 4: Identify Relationships, Key Ideas, and Gaps
Before you can move on to outlining and writing your literature review, the final step is determining the relationships between the studies that already exist. Identifying the relationships will help you organize the existing knowledge, build a solid literature outline, and (if necessary) indicate your own research contribution to a specific field.
Some of the key points to keep an eye out for are:
- Main themes;
- Contradictions and debates;
- Influential studies or theories;
- Trends and patterns;
Here are a few examples: Common trends may include a focus on specific groups of people across different studies. Most researchers may have increased interest in certain aspects of the topic regarding key themes. Contradictions may include some disagreement concerning the theories and outcomes of a study. And finally, gaps most often refer to a lack of research on certain aspects of a topic.
Step 5: Make an Outline
Although students tend to neglect this stage, outlining is one of the most important steps in writing every academic paper. This is the easiest way to organize the body of your text and ensure that you haven't missed anything important. Besides, having a rough idea of what you will write about in the paper will help you get it right faster and more easily. Earlier in this guide, we already discussed the basic structure of a literature review and gave you an example of a good outline. At this workflow stage, you can use all of the knowledge you've gained from us to build your own outline.
Step 6: Move on to Writing
Having found and created all of your sources, notes, citations, and a detailed outline, you can finally get to the writing part of the process. At this stage, all you need to do is follow the plan you've created and keep in mind the overall structure and format defined in your professor's instructions.
Step 7: Adding the Final Touches
Most students make a common mistake and skip the final stage of the process, which includes proofreading and editing. We recommend taking enough time for these steps to ensure that your work will be worth the highest score. Do not underestimate the importance of proofreading and editing, and allocate enough time for these steps.
Pro Tip: Before moving on to proofreading and editing, be sure to set your literature review aside for a day or two. This will give you a chance to take your mind off it and then get back to proofreading with a fresh perspective. This tip will ensure that you won't miss out on any gaps or errors that might be present in your text.
These steps will help you create a top-notch literature review with ease! Want to get more advice on how to handle this body of work? Here are the top 3 tips you need to keep in mind when writing a literature review:
1. Good Sources
When working on a literature review, the most important thing any writer should remember is to find the best possible sources for their MOP. This means that you should select and filter through about 5-10 different options while doing initial research.
The stronger a piece of literature showcases the central point, the better the quality of the entire review.
2. Synthesize The Literature
Make sure to structure the review in the most effective way possible, whether it be chronologically, thematically, or methodologically. Understand what exactly you would like to say, and structure the source comparison accordingly.
3. Avoid Generalizations
Remember that each piece of literature will approach the MOP from a different angle. As the author, make sure to present the contrasts in approaches clearly and don't include general statements that offer no value.
Literature Review Examples
You can find two well-written literature reviews by the EssayPro writing team below. They will help you understand what the final product of a literature review should ideally look like.
The first literature review compares monolingual and bilingual language acquisition skills and uses various sources to prove its point:
The second literature review compares the impact of fear and pain on a protagonist’s overall development in various settings:
Both reviews will help you sharpen your skills and provide good guidelines for writing high-quality papers.
Get Help from an Essay Writer
Still aren’t sure whether you can handle literature review writing on your own? No worries because you can pay for essay writing and our service has got you covered! Boost your grades is to place an order in a few quick clicks and we will satisfy your write my paper request.
Related Articles
.webp)
- UWF Libraries
Literature Review: Conducting & Writing
- Sample Literature Reviews
- Steps for Conducting a Lit Review
- Finding "The Literature"
- Organizing/Writing
- APA Style This link opens in a new window
- Chicago: Notes Bibliography This link opens in a new window
- MLA Style This link opens in a new window
Sample Lit Reviews from Communication Arts
Have an exemplary literature review.
- Literature Review Sample 1
- Literature Review Sample 2
- Literature Review Sample 3
Have you written a stellar literature review you care to share for teaching purposes?
Are you an instructor who has received an exemplary literature review and have permission from the student to post?
Please contact Britt McGowan at [email protected] for inclusion in this guide. All disciplines welcome and encouraged.
- << Previous: MLA Style
- Next: Get Help! >>
- Last Updated: Mar 22, 2024 9:37 AM
- URL: https://libguides.uwf.edu/litreview
How to write a literature review introduction (+ examples)
The introduction to a literature review serves as your reader’s guide through your academic work and thought process. Explore the significance of literature review introductions in review papers, academic papers, essays, theses, and dissertations. We delve into the purpose and necessity of these introductions, explore the essential components of literature review introductions, and provide step-by-step guidance on how to craft your own, along with examples.
Why you need an introduction for a literature review
When you need an introduction for a literature review, what to include in a literature review introduction, examples of literature review introductions, steps to write your own literature review introduction.
A literature review is a comprehensive examination of the international academic literature concerning a particular topic. It involves summarizing published works, theories, and concepts while also highlighting gaps and offering critical reflections.
In academic writing , the introduction for a literature review is an indispensable component. Effective academic writing requires proper paragraph structuring to guide your reader through your argumentation. This includes providing an introduction to your literature review.
It is imperative to remember that you should never start sharing your findings abruptly. Even if there isn’t a dedicated introduction section .
Instead, you should always offer some form of introduction to orient the reader and clarify what they can expect.
There are three main scenarios in which you need an introduction for a literature review:
- Academic literature review papers: When your literature review constitutes the entirety of an academic review paper, a more substantial introduction is necessary. This introduction should resemble the standard introduction found in regular academic papers.
- Literature review section in an academic paper or essay: While this section tends to be brief, it’s important to precede the detailed literature review with a few introductory sentences. This helps orient the reader before delving into the literature itself.
- Literature review chapter or section in your thesis/dissertation: Every thesis and dissertation includes a literature review component, which also requires a concise introduction to set the stage for the subsequent review.
You may also like: How to write a fantastic thesis introduction (+15 examples)
It is crucial to customize the content and depth of your literature review introduction according to the specific format of your academic work.
In practical terms, this implies, for instance, that the introduction in an academic literature review paper, especially one derived from a systematic literature review , is quite comprehensive. Particularly compared to the rather brief one or two introductory sentences that are often found at the beginning of a literature review section in a standard academic paper. The introduction to the literature review chapter in a thesis or dissertation again adheres to different standards.
Here’s a structured breakdown based on length and the necessary information:
Academic literature review paper
The introduction of an academic literature review paper, which does not rely on empirical data, often necessitates a more extensive introduction than the brief literature review introductions typically found in empirical papers. It should encompass:
- The research problem: Clearly articulate the problem or question that your literature review aims to address.
- The research gap: Highlight the existing gaps, limitations, or unresolved aspects within the current body of literature related to the research problem.
- The research relevance: Explain why the chosen research problem and its subsequent investigation through a literature review are significant and relevant in your academic field.
- The literature review method: If applicable, describe the methodology employed in your literature review, especially if it is a systematic review or follows a specific research framework.
- The main findings or insights of the literature review: Summarize the key discoveries, insights, or trends that have emerged from your comprehensive review of the literature.
- The main argument of the literature review: Conclude the introduction by outlining the primary argument or statement that your literature review will substantiate, linking it to the research problem and relevance you’ve established.
- Preview of the literature review’s structure: Offer a glimpse into the organization of the literature review paper, acting as a guide for the reader. This overview outlines the subsequent sections of the paper and provides an understanding of what to anticipate.
By addressing these elements, your introduction will provide a clear and structured overview of what readers can expect in your literature review paper.
Regular literature review section in an academic article or essay
Most academic articles or essays incorporate regular literature review sections, often placed after the introduction. These sections serve to establish a scholarly basis for the research or discussion within the paper.
In a standard 8000-word journal article, the literature review section typically spans between 750 and 1250 words. The first few sentences or the first paragraph within this section often serve as an introduction. It should encompass:
- An introduction to the topic: When delving into the academic literature on a specific topic, it’s important to provide a smooth transition that aids the reader in comprehending why certain aspects will be discussed within your literature review.
- The core argument: While literature review sections primarily synthesize the work of other scholars, they should consistently connect to your central argument. This central argument serves as the crux of your message or the key takeaway you want your readers to retain. By positioning it at the outset of the literature review section and systematically substantiating it with evidence, you not only enhance reader comprehension but also elevate overall readability. This primary argument can typically be distilled into 1-2 succinct sentences.
In some cases, you might include:
- Methodology: Details about the methodology used, but only if your literature review employed a specialized method. If your approach involved a broader overview without a systematic methodology, you can omit this section, thereby conserving word count.
By addressing these elements, your introduction will effectively integrate your literature review into the broader context of your academic paper or essay. This will, in turn, assist your reader in seamlessly following your overarching line of argumentation.
Introduction to a literature review chapter in thesis or dissertation
The literature review typically constitutes a distinct chapter within a thesis or dissertation. Often, it is Chapter 2 of a thesis or dissertation.
Some students choose to incorporate a brief introductory section at the beginning of each chapter, including the literature review chapter. Alternatively, others opt to seamlessly integrate the introduction into the initial sentences of the literature review itself. Both approaches are acceptable, provided that you incorporate the following elements:
- Purpose of the literature review and its relevance to the thesis/dissertation research: Explain the broader objectives of the literature review within the context of your research and how it contributes to your thesis or dissertation. Essentially, you’re telling the reader why this literature review is important and how it fits into the larger scope of your academic work.
- Primary argument: Succinctly communicate what you aim to prove, explain, or explore through the review of existing literature. This statement helps guide the reader’s understanding of the review’s purpose and what to expect from it.
- Preview of the literature review’s content: Provide a brief overview of the topics or themes that your literature review will cover. It’s like a roadmap for the reader, outlining the main areas of focus within the review. This preview can help the reader anticipate the structure and organization of your literature review.
- Methodology: If your literature review involved a specific research method, such as a systematic review or meta-analysis, you should briefly describe that methodology. However, this is not always necessary, especially if your literature review is more of a narrative synthesis without a distinct research method.
By addressing these elements, your introduction will empower your literature review to play a pivotal role in your thesis or dissertation research. It will accomplish this by integrating your research into the broader academic literature and providing a solid theoretical foundation for your work.
Comprehending the art of crafting your own literature review introduction becomes significantly more accessible when you have concrete examples to examine. Here, you will find several examples that meet, or in most cases, adhere to the criteria described earlier.
Example 1: An effective introduction for an academic literature review paper
To begin, let’s delve into the introduction of an academic literature review paper. We will examine the paper “How does culture influence innovation? A systematic literature review”, which was published in 2018 in the journal Management Decision.
The entire introduction spans 611 words and is divided into five paragraphs. In this introduction, the authors accomplish the following:
- In the first paragraph, the authors introduce the broader topic of the literature review, which focuses on innovation and its significance in the context of economic competition. They underscore the importance of this topic, highlighting its relevance for both researchers and policymakers.
- In the second paragraph, the authors narrow down their focus to emphasize the specific role of culture in relation to innovation.
- In the third paragraph, the authors identify research gaps, noting that existing studies are often fragmented and disconnected. They then emphasize the value of conducting a systematic literature review to enhance our understanding of the topic.
- In the fourth paragraph, the authors introduce their specific objectives and explain how their insights can benefit other researchers and business practitioners.
- In the fifth and final paragraph, the authors provide an overview of the paper’s organization and structure.
In summary, this introduction stands as a solid example. While the authors deviate from previewing their key findings (which is a common practice at least in the social sciences), they do effectively cover all the other previously mentioned points.
Example 2: An effective introduction to a literature review section in an academic paper
The second example represents a typical academic paper, encompassing not only a literature review section but also empirical data, a case study, and other elements. We will closely examine the introduction to the literature review section in the paper “The environmentalism of the subalterns: a case study of environmental activism in Eastern Kurdistan/Rojhelat”, which was published in 2021 in the journal Local Environment.
The paper begins with a general introduction and then proceeds to the literature review, designated by the authors as their conceptual framework. Of particular interest is the first paragraph of this conceptual framework, comprising 142 words across five sentences:
“ A peripheral and marginalised nationality within a multinational though-Persian dominated Iranian society, the Kurdish people of Iranian Kurdistan (a region referred by the Kurds as Rojhelat/Eastern Kurdi-stan) have since the early twentieth century been subject to multifaceted and systematic discriminatory and exclusionary state policy in Iran. This condition has left a population of 12–15 million Kurds in Iran suffering from structural inequalities, disenfranchisement and deprivation. Mismanagement of Kurdistan’s natural resources and the degradation of its natural environmental are among examples of this disenfranchisement. As asserted by Julian Agyeman (2005), structural inequalities that sustain the domination of political and economic elites often simultaneously result in environmental degradation, injustice and discrimination against subaltern communities. This study argues that the environmental struggle in Eastern Kurdistan can be asserted as a (sub)element of the Kurdish liberation movement in Iran. Conceptually this research is inspired by and has been conducted through the lens of ‘subalternity’ ” ( Hassaniyan, 2021, p. 931 ).
In this first paragraph, the author is doing the following:
- The author contextualises the research
- The author links the research focus to the international literature on structural inequalities
- The author clearly presents the argument of the research
- The author clarifies how the research is inspired by and uses the concept of ‘subalternity’.
Thus, the author successfully introduces the literature review, from which point onward it dives into the main concept (‘subalternity’) of the research, and reviews the literature on socio-economic justice and environmental degradation.
While introductions to a literature review section aren’t always required to offer the same level of study context detail as demonstrated here, this introduction serves as a commendable model for orienting the reader within the literature review. It effectively underscores the literature review’s significance within the context of the study being conducted.
Examples 3-5: Effective introductions to literature review chapters
The introduction to a literature review chapter can vary in length, depending largely on the overall length of the literature review chapter itself. For example, a master’s thesis typically features a more concise literature review, thus necessitating a shorter introduction. In contrast, a Ph.D. thesis, with its more extensive literature review, often includes a more detailed introduction.
Numerous universities offer online repositories where you can access theses and dissertations from previous years, serving as valuable sources of reference. Many of these repositories, however, may require you to log in through your university account. Nevertheless, a few open-access repositories are accessible to anyone, such as the one by the University of Manchester . It’s important to note though that copyright restrictions apply to these resources, just as they would with published papers.
Master’s thesis literature review introduction
The first example is “Benchmarking Asymmetrical Heating Models of Spider Pulsar Companions” by P. Sun, a master’s thesis completed at the University of Manchester on January 9, 2024. The author, P. Sun, introduces the literature review chapter very briefly but effectively:
PhD thesis literature review chapter introduction
The second example is Deep Learning on Semi-Structured Data and its Applications to Video-Game AI, Woof, W. (Author). 31 Dec 2020, a PhD thesis completed at the University of Manchester . In Chapter 2, the author offers a comprehensive introduction to the topic in four paragraphs, with the final paragraph serving as an overview of the chapter’s structure:
PhD thesis literature review introduction
The last example is the doctoral thesis Metacognitive strategies and beliefs: Child correlates and early experiences Chan, K. Y. M. (Author). 31 Dec 2020 . The author clearly conducted a systematic literature review, commencing the review section with a discussion of the methodology and approach employed in locating and analyzing the selected records.
Having absorbed all of this information, let’s recap the essential steps and offer a succinct guide on how to proceed with creating your literature review introduction:
- Contextualize your review : Begin by clearly identifying the academic context in which your literature review resides and determining the necessary information to include.
- Outline your structure : Develop a structured outline for your literature review, highlighting the essential information you plan to incorporate in your introduction.
- Literature review process : Conduct a rigorous literature review, reviewing and analyzing relevant sources.
- Summarize and abstract : After completing the review, synthesize the findings and abstract key insights, trends, and knowledge gaps from the literature.
- Craft the introduction : Write your literature review introduction with meticulous attention to the seamless integration of your review into the larger context of your work. Ensure that your introduction effectively elucidates your rationale for the chosen review topics and the underlying reasons guiding your selection.
Get new content delivered directly to your inbox!
Subscribe and receive Master Academia's quarterly newsletter.
The best answers to "What are your plans for the future?"
10 tips for engaging your audience in academic writing, related articles.

How to peer review an academic paper
PhD thesis types: Monograph and collection of articles

How to disagree with reviewers (with examples!)

How to introduce yourself in a conference presentation (in six simple steps)
- Library Guides
- Literature Reviews
- Getting Started
Literature Reviews: Getting Started
What is a literature review.
A literature review is an overview of the available research for a specific scientific topic. Literature reviews summarize existing research to answer a review question, provide context for new research, or identify important gaps in the existing body of literature.
An incredible amount of academic literature is published each year, by estimates over two million articles .
Sorting through and reviewing that literature can be complicated, so this Research Guide provides a structured approach to make the process more manageable.
THIS GUIDE IS AN OVERVIEW OF THE LITERATURE REVIEW PROCESS:
- Getting Started (asking a research question | defining scope)
- Choosing a Type of Review
- Searching the Literature
- Organizing the Literature
- Writing the Literature Review (analyzing | synthesizing)
A literature search is a systematic search of the scholarly sources in a particular discipline. A literature review is the analysis, critical evaluation and synthesis of the results of that search. During this process you will move from a review of the literature to a review for your research. Your synthesis of the literature is your unique contribution to research.
WHO IS THIS RESEARCH GUIDE FOR?
— those new to reviewing the literature
— those that need a refresher or a deeper understanding of writing literature reviews
You may need to do a literature review as a part of a course assignment, a capstone project, a master's thesis, a dissertation, or as part of a journal article. No matter the context, a literature review is an essential part of the research process.
Literature Review Process

Purpose of a Literature Review
What is the purpose of a literature review.
A literature review is typically performed for a specific reason. Even when assigned as an assignment, the goal of the literature review will be one or more of the following:
- To communicate a project's novelty by identifying a research gap
- An overview of research issues , methodologies or results relevant to field
- To explore the volume and types of available studies
- To establish familiarity with current research before carrying out a new project
- To resolve conflicts amongst contradictory previous studies
Reviewing the literature helps you understand a research topic and develop your own perspective.
A LITERATURE REVIEW IS NOT :
- An annotated bibliography – which is a list of annotated citations to books, articles and documents that includes a brief description and evaluation for each entry
- A literary review – which is a critical discussion of the merits and weaknesses of a literary work
- A book review – which is a critical discussion of the merits and weaknesses of a particular book
Attribution
Thanks to Librarian Jamie Niehof at the University of Michigan for providing permission to reuse and remix this Literature Reviews guide.
The Library's Subject Specialists are happy to help with your literature reviews! Find your Subject Specialist here .

If you have questions about this guide, contact Librarians Matt Upson ([email protected]), Dr. Frances Alvarado-Albertorio ([email protected]), or Clarke Iakovakis ([email protected])
- Last Updated: Apr 9, 2024 3:50 PM
- URL: https://info.library.okstate.edu/literaturereviews
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Lau F, Kuziemsky C, editors. Handbook of eHealth Evaluation: An Evidence-based Approach [Internet]. Victoria (BC): University of Victoria; 2017 Feb 27.

Handbook of eHealth Evaluation: An Evidence-based Approach [Internet].
Chapter 9 methods for literature reviews.
Guy Paré and Spyros Kitsiou .
9.1. Introduction
Literature reviews play a critical role in scholarship because science remains, first and foremost, a cumulative endeavour ( vom Brocke et al., 2009 ). As in any academic discipline, rigorous knowledge syntheses are becoming indispensable in keeping up with an exponentially growing eHealth literature, assisting practitioners, academics, and graduate students in finding, evaluating, and synthesizing the contents of many empirical and conceptual papers. Among other methods, literature reviews are essential for: (a) identifying what has been written on a subject or topic; (b) determining the extent to which a specific research area reveals any interpretable trends or patterns; (c) aggregating empirical findings related to a narrow research question to support evidence-based practice; (d) generating new frameworks and theories; and (e) identifying topics or questions requiring more investigation ( Paré, Trudel, Jaana, & Kitsiou, 2015 ).
Literature reviews can take two major forms. The most prevalent one is the “literature review” or “background” section within a journal paper or a chapter in a graduate thesis. This section synthesizes the extant literature and usually identifies the gaps in knowledge that the empirical study addresses ( Sylvester, Tate, & Johnstone, 2013 ). It may also provide a theoretical foundation for the proposed study, substantiate the presence of the research problem, justify the research as one that contributes something new to the cumulated knowledge, or validate the methods and approaches for the proposed study ( Hart, 1998 ; Levy & Ellis, 2006 ).
The second form of literature review, which is the focus of this chapter, constitutes an original and valuable work of research in and of itself ( Paré et al., 2015 ). Rather than providing a base for a researcher’s own work, it creates a solid starting point for all members of the community interested in a particular area or topic ( Mulrow, 1987 ). The so-called “review article” is a journal-length paper which has an overarching purpose to synthesize the literature in a field, without collecting or analyzing any primary data ( Green, Johnson, & Adams, 2006 ).
When appropriately conducted, review articles represent powerful information sources for practitioners looking for state-of-the art evidence to guide their decision-making and work practices ( Paré et al., 2015 ). Further, high-quality reviews become frequently cited pieces of work which researchers seek out as a first clear outline of the literature when undertaking empirical studies ( Cooper, 1988 ; Rowe, 2014 ). Scholars who track and gauge the impact of articles have found that review papers are cited and downloaded more often than any other type of published article ( Cronin, Ryan, & Coughlan, 2008 ; Montori, Wilczynski, Morgan, Haynes, & Hedges, 2003 ; Patsopoulos, Analatos, & Ioannidis, 2005 ). The reason for their popularity may be the fact that reading the review enables one to have an overview, if not a detailed knowledge of the area in question, as well as references to the most useful primary sources ( Cronin et al., 2008 ). Although they are not easy to conduct, the commitment to complete a review article provides a tremendous service to one’s academic community ( Paré et al., 2015 ; Petticrew & Roberts, 2006 ). Most, if not all, peer-reviewed journals in the fields of medical informatics publish review articles of some type.
The main objectives of this chapter are fourfold: (a) to provide an overview of the major steps and activities involved in conducting a stand-alone literature review; (b) to describe and contrast the different types of review articles that can contribute to the eHealth knowledge base; (c) to illustrate each review type with one or two examples from the eHealth literature; and (d) to provide a series of recommendations for prospective authors of review articles in this domain.
9.2. Overview of the Literature Review Process and Steps
As explained in Templier and Paré (2015) , there are six generic steps involved in conducting a review article:
- formulating the research question(s) and objective(s),
- searching the extant literature,
- screening for inclusion,
- assessing the quality of primary studies,
- extracting data, and
- analyzing data.
Although these steps are presented here in sequential order, one must keep in mind that the review process can be iterative and that many activities can be initiated during the planning stage and later refined during subsequent phases ( Finfgeld-Connett & Johnson, 2013 ; Kitchenham & Charters, 2007 ).
Formulating the research question(s) and objective(s): As a first step, members of the review team must appropriately justify the need for the review itself ( Petticrew & Roberts, 2006 ), identify the review’s main objective(s) ( Okoli & Schabram, 2010 ), and define the concepts or variables at the heart of their synthesis ( Cooper & Hedges, 2009 ; Webster & Watson, 2002 ). Importantly, they also need to articulate the research question(s) they propose to investigate ( Kitchenham & Charters, 2007 ). In this regard, we concur with Jesson, Matheson, and Lacey (2011) that clearly articulated research questions are key ingredients that guide the entire review methodology; they underscore the type of information that is needed, inform the search for and selection of relevant literature, and guide or orient the subsequent analysis. Searching the extant literature: The next step consists of searching the literature and making decisions about the suitability of material to be considered in the review ( Cooper, 1988 ). There exist three main coverage strategies. First, exhaustive coverage means an effort is made to be as comprehensive as possible in order to ensure that all relevant studies, published and unpublished, are included in the review and, thus, conclusions are based on this all-inclusive knowledge base. The second type of coverage consists of presenting materials that are representative of most other works in a given field or area. Often authors who adopt this strategy will search for relevant articles in a small number of top-tier journals in a field ( Paré et al., 2015 ). In the third strategy, the review team concentrates on prior works that have been central or pivotal to a particular topic. This may include empirical studies or conceptual papers that initiated a line of investigation, changed how problems or questions were framed, introduced new methods or concepts, or engendered important debate ( Cooper, 1988 ). Screening for inclusion: The following step consists of evaluating the applicability of the material identified in the preceding step ( Levy & Ellis, 2006 ; vom Brocke et al., 2009 ). Once a group of potential studies has been identified, members of the review team must screen them to determine their relevance ( Petticrew & Roberts, 2006 ). A set of predetermined rules provides a basis for including or excluding certain studies. This exercise requires a significant investment on the part of researchers, who must ensure enhanced objectivity and avoid biases or mistakes. As discussed later in this chapter, for certain types of reviews there must be at least two independent reviewers involved in the screening process and a procedure to resolve disagreements must also be in place ( Liberati et al., 2009 ; Shea et al., 2009 ). Assessing the quality of primary studies: In addition to screening material for inclusion, members of the review team may need to assess the scientific quality of the selected studies, that is, appraise the rigour of the research design and methods. Such formal assessment, which is usually conducted independently by at least two coders, helps members of the review team refine which studies to include in the final sample, determine whether or not the differences in quality may affect their conclusions, or guide how they analyze the data and interpret the findings ( Petticrew & Roberts, 2006 ). Ascribing quality scores to each primary study or considering through domain-based evaluations which study components have or have not been designed and executed appropriately makes it possible to reflect on the extent to which the selected study addresses possible biases and maximizes validity ( Shea et al., 2009 ). Extracting data: The following step involves gathering or extracting applicable information from each primary study included in the sample and deciding what is relevant to the problem of interest ( Cooper & Hedges, 2009 ). Indeed, the type of data that should be recorded mainly depends on the initial research questions ( Okoli & Schabram, 2010 ). However, important information may also be gathered about how, when, where and by whom the primary study was conducted, the research design and methods, or qualitative/quantitative results ( Cooper & Hedges, 2009 ). Analyzing and synthesizing data : As a final step, members of the review team must collate, summarize, aggregate, organize, and compare the evidence extracted from the included studies. The extracted data must be presented in a meaningful way that suggests a new contribution to the extant literature ( Jesson et al., 2011 ). Webster and Watson (2002) warn researchers that literature reviews should be much more than lists of papers and should provide a coherent lens to make sense of extant knowledge on a given topic. There exist several methods and techniques for synthesizing quantitative (e.g., frequency analysis, meta-analysis) and qualitative (e.g., grounded theory, narrative analysis, meta-ethnography) evidence ( Dixon-Woods, Agarwal, Jones, Young, & Sutton, 2005 ; Thomas & Harden, 2008 ).
9.3. Types of Review Articles and Brief Illustrations
EHealth researchers have at their disposal a number of approaches and methods for making sense out of existing literature, all with the purpose of casting current research findings into historical contexts or explaining contradictions that might exist among a set of primary research studies conducted on a particular topic. Our classification scheme is largely inspired from Paré and colleagues’ (2015) typology. Below we present and illustrate those review types that we feel are central to the growth and development of the eHealth domain.
9.3.1. Narrative Reviews
The narrative review is the “traditional” way of reviewing the extant literature and is skewed towards a qualitative interpretation of prior knowledge ( Sylvester et al., 2013 ). Put simply, a narrative review attempts to summarize or synthesize what has been written on a particular topic but does not seek generalization or cumulative knowledge from what is reviewed ( Davies, 2000 ; Green et al., 2006 ). Instead, the review team often undertakes the task of accumulating and synthesizing the literature to demonstrate the value of a particular point of view ( Baumeister & Leary, 1997 ). As such, reviewers may selectively ignore or limit the attention paid to certain studies in order to make a point. In this rather unsystematic approach, the selection of information from primary articles is subjective, lacks explicit criteria for inclusion and can lead to biased interpretations or inferences ( Green et al., 2006 ). There are several narrative reviews in the particular eHealth domain, as in all fields, which follow such an unstructured approach ( Silva et al., 2015 ; Paul et al., 2015 ).
Despite these criticisms, this type of review can be very useful in gathering together a volume of literature in a specific subject area and synthesizing it. As mentioned above, its primary purpose is to provide the reader with a comprehensive background for understanding current knowledge and highlighting the significance of new research ( Cronin et al., 2008 ). Faculty like to use narrative reviews in the classroom because they are often more up to date than textbooks, provide a single source for students to reference, and expose students to peer-reviewed literature ( Green et al., 2006 ). For researchers, narrative reviews can inspire research ideas by identifying gaps or inconsistencies in a body of knowledge, thus helping researchers to determine research questions or formulate hypotheses. Importantly, narrative reviews can also be used as educational articles to bring practitioners up to date with certain topics of issues ( Green et al., 2006 ).
Recently, there have been several efforts to introduce more rigour in narrative reviews that will elucidate common pitfalls and bring changes into their publication standards. Information systems researchers, among others, have contributed to advancing knowledge on how to structure a “traditional” review. For instance, Levy and Ellis (2006) proposed a generic framework for conducting such reviews. Their model follows the systematic data processing approach comprised of three steps, namely: (a) literature search and screening; (b) data extraction and analysis; and (c) writing the literature review. They provide detailed and very helpful instructions on how to conduct each step of the review process. As another methodological contribution, vom Brocke et al. (2009) offered a series of guidelines for conducting literature reviews, with a particular focus on how to search and extract the relevant body of knowledge. Last, Bandara, Miskon, and Fielt (2011) proposed a structured, predefined and tool-supported method to identify primary studies within a feasible scope, extract relevant content from identified articles, synthesize and analyze the findings, and effectively write and present the results of the literature review. We highly recommend that prospective authors of narrative reviews consult these useful sources before embarking on their work.
Darlow and Wen (2015) provide a good example of a highly structured narrative review in the eHealth field. These authors synthesized published articles that describe the development process of mobile health ( m-health ) interventions for patients’ cancer care self-management. As in most narrative reviews, the scope of the research questions being investigated is broad: (a) how development of these systems are carried out; (b) which methods are used to investigate these systems; and (c) what conclusions can be drawn as a result of the development of these systems. To provide clear answers to these questions, a literature search was conducted on six electronic databases and Google Scholar . The search was performed using several terms and free text words, combining them in an appropriate manner. Four inclusion and three exclusion criteria were utilized during the screening process. Both authors independently reviewed each of the identified articles to determine eligibility and extract study information. A flow diagram shows the number of studies identified, screened, and included or excluded at each stage of study selection. In terms of contributions, this review provides a series of practical recommendations for m-health intervention development.
9.3.2. Descriptive or Mapping Reviews
The primary goal of a descriptive review is to determine the extent to which a body of knowledge in a particular research topic reveals any interpretable pattern or trend with respect to pre-existing propositions, theories, methodologies or findings ( King & He, 2005 ; Paré et al., 2015 ). In contrast with narrative reviews, descriptive reviews follow a systematic and transparent procedure, including searching, screening and classifying studies ( Petersen, Vakkalanka, & Kuzniarz, 2015 ). Indeed, structured search methods are used to form a representative sample of a larger group of published works ( Paré et al., 2015 ). Further, authors of descriptive reviews extract from each study certain characteristics of interest, such as publication year, research methods, data collection techniques, and direction or strength of research outcomes (e.g., positive, negative, or non-significant) in the form of frequency analysis to produce quantitative results ( Sylvester et al., 2013 ). In essence, each study included in a descriptive review is treated as the unit of analysis and the published literature as a whole provides a database from which the authors attempt to identify any interpretable trends or draw overall conclusions about the merits of existing conceptualizations, propositions, methods or findings ( Paré et al., 2015 ). In doing so, a descriptive review may claim that its findings represent the state of the art in a particular domain ( King & He, 2005 ).
In the fields of health sciences and medical informatics, reviews that focus on examining the range, nature and evolution of a topic area are described by Anderson, Allen, Peckham, and Goodwin (2008) as mapping reviews . Like descriptive reviews, the research questions are generic and usually relate to publication patterns and trends. There is no preconceived plan to systematically review all of the literature although this can be done. Instead, researchers often present studies that are representative of most works published in a particular area and they consider a specific time frame to be mapped.
An example of this approach in the eHealth domain is offered by DeShazo, Lavallie, and Wolf (2009). The purpose of this descriptive or mapping review was to characterize publication trends in the medical informatics literature over a 20-year period (1987 to 2006). To achieve this ambitious objective, the authors performed a bibliometric analysis of medical informatics citations indexed in medline using publication trends, journal frequencies, impact factors, Medical Subject Headings (MeSH) term frequencies, and characteristics of citations. Findings revealed that there were over 77,000 medical informatics articles published during the covered period in numerous journals and that the average annual growth rate was 12%. The MeSH term analysis also suggested a strong interdisciplinary trend. Finally, average impact scores increased over time with two notable growth periods. Overall, patterns in research outputs that seem to characterize the historic trends and current components of the field of medical informatics suggest it may be a maturing discipline (DeShazo et al., 2009).
9.3.3. Scoping Reviews
Scoping reviews attempt to provide an initial indication of the potential size and nature of the extant literature on an emergent topic (Arksey & O’Malley, 2005; Daudt, van Mossel, & Scott, 2013 ; Levac, Colquhoun, & O’Brien, 2010). A scoping review may be conducted to examine the extent, range and nature of research activities in a particular area, determine the value of undertaking a full systematic review (discussed next), or identify research gaps in the extant literature ( Paré et al., 2015 ). In line with their main objective, scoping reviews usually conclude with the presentation of a detailed research agenda for future works along with potential implications for both practice and research.
Unlike narrative and descriptive reviews, the whole point of scoping the field is to be as comprehensive as possible, including grey literature (Arksey & O’Malley, 2005). Inclusion and exclusion criteria must be established to help researchers eliminate studies that are not aligned with the research questions. It is also recommended that at least two independent coders review abstracts yielded from the search strategy and then the full articles for study selection ( Daudt et al., 2013 ). The synthesized evidence from content or thematic analysis is relatively easy to present in tabular form (Arksey & O’Malley, 2005; Thomas & Harden, 2008 ).
One of the most highly cited scoping reviews in the eHealth domain was published by Archer, Fevrier-Thomas, Lokker, McKibbon, and Straus (2011) . These authors reviewed the existing literature on personal health record ( phr ) systems including design, functionality, implementation, applications, outcomes, and benefits. Seven databases were searched from 1985 to March 2010. Several search terms relating to phr s were used during this process. Two authors independently screened titles and abstracts to determine inclusion status. A second screen of full-text articles, again by two independent members of the research team, ensured that the studies described phr s. All in all, 130 articles met the criteria and their data were extracted manually into a database. The authors concluded that although there is a large amount of survey, observational, cohort/panel, and anecdotal evidence of phr benefits and satisfaction for patients, more research is needed to evaluate the results of phr implementations. Their in-depth analysis of the literature signalled that there is little solid evidence from randomized controlled trials or other studies through the use of phr s. Hence, they suggested that more research is needed that addresses the current lack of understanding of optimal functionality and usability of these systems, and how they can play a beneficial role in supporting patient self-management ( Archer et al., 2011 ).
9.3.4. Forms of Aggregative Reviews
Healthcare providers, practitioners, and policy-makers are nowadays overwhelmed with large volumes of information, including research-based evidence from numerous clinical trials and evaluation studies, assessing the effectiveness of health information technologies and interventions ( Ammenwerth & de Keizer, 2004 ; Deshazo et al., 2009 ). It is unrealistic to expect that all these disparate actors will have the time, skills, and necessary resources to identify the available evidence in the area of their expertise and consider it when making decisions. Systematic reviews that involve the rigorous application of scientific strategies aimed at limiting subjectivity and bias (i.e., systematic and random errors) can respond to this challenge.
Systematic reviews attempt to aggregate, appraise, and synthesize in a single source all empirical evidence that meet a set of previously specified eligibility criteria in order to answer a clearly formulated and often narrow research question on a particular topic of interest to support evidence-based practice ( Liberati et al., 2009 ). They adhere closely to explicit scientific principles ( Liberati et al., 2009 ) and rigorous methodological guidelines (Higgins & Green, 2008) aimed at reducing random and systematic errors that can lead to deviations from the truth in results or inferences. The use of explicit methods allows systematic reviews to aggregate a large body of research evidence, assess whether effects or relationships are in the same direction and of the same general magnitude, explain possible inconsistencies between study results, and determine the strength of the overall evidence for every outcome of interest based on the quality of included studies and the general consistency among them ( Cook, Mulrow, & Haynes, 1997 ). The main procedures of a systematic review involve:
- Formulating a review question and developing a search strategy based on explicit inclusion criteria for the identification of eligible studies (usually described in the context of a detailed review protocol).
- Searching for eligible studies using multiple databases and information sources, including grey literature sources, without any language restrictions.
- Selecting studies, extracting data, and assessing risk of bias in a duplicate manner using two independent reviewers to avoid random or systematic errors in the process.
- Analyzing data using quantitative or qualitative methods.
- Presenting results in summary of findings tables.
- Interpreting results and drawing conclusions.
Many systematic reviews, but not all, use statistical methods to combine the results of independent studies into a single quantitative estimate or summary effect size. Known as meta-analyses , these reviews use specific data extraction and statistical techniques (e.g., network, frequentist, or Bayesian meta-analyses) to calculate from each study by outcome of interest an effect size along with a confidence interval that reflects the degree of uncertainty behind the point estimate of effect ( Borenstein, Hedges, Higgins, & Rothstein, 2009 ; Deeks, Higgins, & Altman, 2008 ). Subsequently, they use fixed or random-effects analysis models to combine the results of the included studies, assess statistical heterogeneity, and calculate a weighted average of the effect estimates from the different studies, taking into account their sample sizes. The summary effect size is a value that reflects the average magnitude of the intervention effect for a particular outcome of interest or, more generally, the strength of a relationship between two variables across all studies included in the systematic review. By statistically combining data from multiple studies, meta-analyses can create more precise and reliable estimates of intervention effects than those derived from individual studies alone, when these are examined independently as discrete sources of information.
The review by Gurol-Urganci, de Jongh, Vodopivec-Jamsek, Atun, and Car (2013) on the effects of mobile phone messaging reminders for attendance at healthcare appointments is an illustrative example of a high-quality systematic review with meta-analysis. Missed appointments are a major cause of inefficiency in healthcare delivery with substantial monetary costs to health systems. These authors sought to assess whether mobile phone-based appointment reminders delivered through Short Message Service ( sms ) or Multimedia Messaging Service ( mms ) are effective in improving rates of patient attendance and reducing overall costs. To this end, they conducted a comprehensive search on multiple databases using highly sensitive search strategies without language or publication-type restrictions to identify all rct s that are eligible for inclusion. In order to minimize the risk of omitting eligible studies not captured by the original search, they supplemented all electronic searches with manual screening of trial registers and references contained in the included studies. Study selection, data extraction, and risk of bias assessments were performed independently by two coders using standardized methods to ensure consistency and to eliminate potential errors. Findings from eight rct s involving 6,615 participants were pooled into meta-analyses to calculate the magnitude of effects that mobile text message reminders have on the rate of attendance at healthcare appointments compared to no reminders and phone call reminders.
Meta-analyses are regarded as powerful tools for deriving meaningful conclusions. However, there are situations in which it is neither reasonable nor appropriate to pool studies together using meta-analytic methods simply because there is extensive clinical heterogeneity between the included studies or variation in measurement tools, comparisons, or outcomes of interest. In these cases, systematic reviews can use qualitative synthesis methods such as vote counting, content analysis, classification schemes and tabulations, as an alternative approach to narratively synthesize the results of the independent studies included in the review. This form of review is known as qualitative systematic review.
A rigorous example of one such review in the eHealth domain is presented by Mickan, Atherton, Roberts, Heneghan, and Tilson (2014) on the use of handheld computers by healthcare professionals and their impact on access to information and clinical decision-making. In line with the methodological guidelines for systematic reviews, these authors: (a) developed and registered with prospero ( www.crd.york.ac.uk/ prospero / ) an a priori review protocol; (b) conducted comprehensive searches for eligible studies using multiple databases and other supplementary strategies (e.g., forward searches); and (c) subsequently carried out study selection, data extraction, and risk of bias assessments in a duplicate manner to eliminate potential errors in the review process. Heterogeneity between the included studies in terms of reported outcomes and measures precluded the use of meta-analytic methods. To this end, the authors resorted to using narrative analysis and synthesis to describe the effectiveness of handheld computers on accessing information for clinical knowledge, adherence to safety and clinical quality guidelines, and diagnostic decision-making.
In recent years, the number of systematic reviews in the field of health informatics has increased considerably. Systematic reviews with discordant findings can cause great confusion and make it difficult for decision-makers to interpret the review-level evidence ( Moher, 2013 ). Therefore, there is a growing need for appraisal and synthesis of prior systematic reviews to ensure that decision-making is constantly informed by the best available accumulated evidence. Umbrella reviews , also known as overviews of systematic reviews, are tertiary types of evidence synthesis that aim to accomplish this; that is, they aim to compare and contrast findings from multiple systematic reviews and meta-analyses ( Becker & Oxman, 2008 ). Umbrella reviews generally adhere to the same principles and rigorous methodological guidelines used in systematic reviews. However, the unit of analysis in umbrella reviews is the systematic review rather than the primary study ( Becker & Oxman, 2008 ). Unlike systematic reviews that have a narrow focus of inquiry, umbrella reviews focus on broader research topics for which there are several potential interventions ( Smith, Devane, Begley, & Clarke, 2011 ). A recent umbrella review on the effects of home telemonitoring interventions for patients with heart failure critically appraised, compared, and synthesized evidence from 15 systematic reviews to investigate which types of home telemonitoring technologies and forms of interventions are more effective in reducing mortality and hospital admissions ( Kitsiou, Paré, & Jaana, 2015 ).
9.3.5. Realist Reviews
Realist reviews are theory-driven interpretative reviews developed to inform, enhance, or supplement conventional systematic reviews by making sense of heterogeneous evidence about complex interventions applied in diverse contexts in a way that informs policy decision-making ( Greenhalgh, Wong, Westhorp, & Pawson, 2011 ). They originated from criticisms of positivist systematic reviews which centre on their “simplistic” underlying assumptions ( Oates, 2011 ). As explained above, systematic reviews seek to identify causation. Such logic is appropriate for fields like medicine and education where findings of randomized controlled trials can be aggregated to see whether a new treatment or intervention does improve outcomes. However, many argue that it is not possible to establish such direct causal links between interventions and outcomes in fields such as social policy, management, and information systems where for any intervention there is unlikely to be a regular or consistent outcome ( Oates, 2011 ; Pawson, 2006 ; Rousseau, Manning, & Denyer, 2008 ).
To circumvent these limitations, Pawson, Greenhalgh, Harvey, and Walshe (2005) have proposed a new approach for synthesizing knowledge that seeks to unpack the mechanism of how “complex interventions” work in particular contexts. The basic research question — what works? — which is usually associated with systematic reviews changes to: what is it about this intervention that works, for whom, in what circumstances, in what respects and why? Realist reviews have no particular preference for either quantitative or qualitative evidence. As a theory-building approach, a realist review usually starts by articulating likely underlying mechanisms and then scrutinizes available evidence to find out whether and where these mechanisms are applicable ( Shepperd et al., 2009 ). Primary studies found in the extant literature are viewed as case studies which can test and modify the initial theories ( Rousseau et al., 2008 ).
The main objective pursued in the realist review conducted by Otte-Trojel, de Bont, Rundall, and van de Klundert (2014) was to examine how patient portals contribute to health service delivery and patient outcomes. The specific goals were to investigate how outcomes are produced and, most importantly, how variations in outcomes can be explained. The research team started with an exploratory review of background documents and research studies to identify ways in which patient portals may contribute to health service delivery and patient outcomes. The authors identified six main ways which represent “educated guesses” to be tested against the data in the evaluation studies. These studies were identified through a formal and systematic search in four databases between 2003 and 2013. Two members of the research team selected the articles using a pre-established list of inclusion and exclusion criteria and following a two-step procedure. The authors then extracted data from the selected articles and created several tables, one for each outcome category. They organized information to bring forward those mechanisms where patient portals contribute to outcomes and the variation in outcomes across different contexts.
9.3.6. Critical Reviews
Lastly, critical reviews aim to provide a critical evaluation and interpretive analysis of existing literature on a particular topic of interest to reveal strengths, weaknesses, contradictions, controversies, inconsistencies, and/or other important issues with respect to theories, hypotheses, research methods or results ( Baumeister & Leary, 1997 ; Kirkevold, 1997 ). Unlike other review types, critical reviews attempt to take a reflective account of the research that has been done in a particular area of interest, and assess its credibility by using appraisal instruments or critical interpretive methods. In this way, critical reviews attempt to constructively inform other scholars about the weaknesses of prior research and strengthen knowledge development by giving focus and direction to studies for further improvement ( Kirkevold, 1997 ).
Kitsiou, Paré, and Jaana (2013) provide an example of a critical review that assessed the methodological quality of prior systematic reviews of home telemonitoring studies for chronic patients. The authors conducted a comprehensive search on multiple databases to identify eligible reviews and subsequently used a validated instrument to conduct an in-depth quality appraisal. Results indicate that the majority of systematic reviews in this particular area suffer from important methodological flaws and biases that impair their internal validity and limit their usefulness for clinical and decision-making purposes. To this end, they provide a number of recommendations to strengthen knowledge development towards improving the design and execution of future reviews on home telemonitoring.
9.4. Summary
Table 9.1 outlines the main types of literature reviews that were described in the previous sub-sections and summarizes the main characteristics that distinguish one review type from another. It also includes key references to methodological guidelines and useful sources that can be used by eHealth scholars and researchers for planning and developing reviews.
Typology of Literature Reviews (adapted from Paré et al., 2015).
As shown in Table 9.1 , each review type addresses different kinds of research questions or objectives, which subsequently define and dictate the methods and approaches that need to be used to achieve the overarching goal(s) of the review. For example, in the case of narrative reviews, there is greater flexibility in searching and synthesizing articles ( Green et al., 2006 ). Researchers are often relatively free to use a diversity of approaches to search, identify, and select relevant scientific articles, describe their operational characteristics, present how the individual studies fit together, and formulate conclusions. On the other hand, systematic reviews are characterized by their high level of systematicity, rigour, and use of explicit methods, based on an “a priori” review plan that aims to minimize bias in the analysis and synthesis process (Higgins & Green, 2008). Some reviews are exploratory in nature (e.g., scoping/mapping reviews), whereas others may be conducted to discover patterns (e.g., descriptive reviews) or involve a synthesis approach that may include the critical analysis of prior research ( Paré et al., 2015 ). Hence, in order to select the most appropriate type of review, it is critical to know before embarking on a review project, why the research synthesis is conducted and what type of methods are best aligned with the pursued goals.
9.5. Concluding Remarks
In light of the increased use of evidence-based practice and research generating stronger evidence ( Grady et al., 2011 ; Lyden et al., 2013 ), review articles have become essential tools for summarizing, synthesizing, integrating or critically appraising prior knowledge in the eHealth field. As mentioned earlier, when rigorously conducted review articles represent powerful information sources for eHealth scholars and practitioners looking for state-of-the-art evidence. The typology of literature reviews we used herein will allow eHealth researchers, graduate students and practitioners to gain a better understanding of the similarities and differences between review types.
We must stress that this classification scheme does not privilege any specific type of review as being of higher quality than another ( Paré et al., 2015 ). As explained above, each type of review has its own strengths and limitations. Having said that, we realize that the methodological rigour of any review — be it qualitative, quantitative or mixed — is a critical aspect that should be considered seriously by prospective authors. In the present context, the notion of rigour refers to the reliability and validity of the review process described in section 9.2. For one thing, reliability is related to the reproducibility of the review process and steps, which is facilitated by a comprehensive documentation of the literature search process, extraction, coding and analysis performed in the review. Whether the search is comprehensive or not, whether it involves a methodical approach for data extraction and synthesis or not, it is important that the review documents in an explicit and transparent manner the steps and approach that were used in the process of its development. Next, validity characterizes the degree to which the review process was conducted appropriately. It goes beyond documentation and reflects decisions related to the selection of the sources, the search terms used, the period of time covered, the articles selected in the search, and the application of backward and forward searches ( vom Brocke et al., 2009 ). In short, the rigour of any review article is reflected by the explicitness of its methods (i.e., transparency) and the soundness of the approach used. We refer those interested in the concepts of rigour and quality to the work of Templier and Paré (2015) which offers a detailed set of methodological guidelines for conducting and evaluating various types of review articles.
To conclude, our main objective in this chapter was to demystify the various types of literature reviews that are central to the continuous development of the eHealth field. It is our hope that our descriptive account will serve as a valuable source for those conducting, evaluating or using reviews in this important and growing domain.
- Ammenwerth E., de Keizer N. An inventory of evaluation studies of information technology in health care. Trends in evaluation research, 1982-2002. International Journal of Medical Informatics. 2004; 44 (1):44–56. [ PubMed : 15778794 ]
- Anderson S., Allen P., Peckham S., Goodwin N. Asking the right questions: scoping studies in the commissioning of research on the organisation and delivery of health services. Health Research Policy and Systems. 2008; 6 (7):1–12. [ PMC free article : PMC2500008 ] [ PubMed : 18613961 ] [ CrossRef ]
- Archer N., Fevrier-Thomas U., Lokker C., McKibbon K. A., Straus S.E. Personal health records: a scoping review. Journal of American Medical Informatics Association. 2011; 18 (4):515–522. [ PMC free article : PMC3128401 ] [ PubMed : 21672914 ]
- Arksey H., O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005; 8 (1):19–32.
- A systematic, tool-supported method for conducting literature reviews in information systems. Paper presented at the Proceedings of the 19th European Conference on Information Systems ( ecis 2011); June 9 to 11; Helsinki, Finland. 2011.
- Baumeister R. F., Leary M.R. Writing narrative literature reviews. Review of General Psychology. 1997; 1 (3):311–320.
- Becker L. A., Oxman A.D. In: Cochrane handbook for systematic reviews of interventions. Higgins J. P. T., Green S., editors. Hoboken, nj : John Wiley & Sons, Ltd; 2008. Overviews of reviews; pp. 607–631.
- Borenstein M., Hedges L., Higgins J., Rothstein H. Introduction to meta-analysis. Hoboken, nj : John Wiley & Sons Inc; 2009.
- Cook D. J., Mulrow C. D., Haynes B. Systematic reviews: Synthesis of best evidence for clinical decisions. Annals of Internal Medicine. 1997; 126 (5):376–380. [ PubMed : 9054282 ]
- Cooper H., Hedges L.V. In: The handbook of research synthesis and meta-analysis. 2nd ed. Cooper H., Hedges L. V., Valentine J. C., editors. New York: Russell Sage Foundation; 2009. Research synthesis as a scientific process; pp. 3–17.
- Cooper H. M. Organizing knowledge syntheses: A taxonomy of literature reviews. Knowledge in Society. 1988; 1 (1):104–126.
- Cronin P., Ryan F., Coughlan M. Undertaking a literature review: a step-by-step approach. British Journal of Nursing. 2008; 17 (1):38–43. [ PubMed : 18399395 ]
- Darlow S., Wen K.Y. Development testing of mobile health interventions for cancer patient self-management: A review. Health Informatics Journal. 2015 (online before print). [ PubMed : 25916831 ] [ CrossRef ]
- Daudt H. M., van Mossel C., Scott S.J. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. bmc Medical Research Methodology. 2013; 13 :48. [ PMC free article : PMC3614526 ] [ PubMed : 23522333 ] [ CrossRef ]
- Davies P. The relevance of systematic reviews to educational policy and practice. Oxford Review of Education. 2000; 26 (3-4):365–378.
- Deeks J. J., Higgins J. P. T., Altman D.G. In: Cochrane handbook for systematic reviews of interventions. Higgins J. P. T., Green S., editors. Hoboken, nj : John Wiley & Sons, Ltd; 2008. Analysing data and undertaking meta-analyses; pp. 243–296.
- Deshazo J. P., Lavallie D. L., Wolf F.M. Publication trends in the medical informatics literature: 20 years of “Medical Informatics” in mesh . bmc Medical Informatics and Decision Making. 2009; 9 :7. [ PMC free article : PMC2652453 ] [ PubMed : 19159472 ] [ CrossRef ]
- Dixon-Woods M., Agarwal S., Jones D., Young B., Sutton A. Synthesising qualitative and quantitative evidence: a review of possible methods. Journal of Health Services Research and Policy. 2005; 10 (1):45–53. [ PubMed : 15667704 ]
- Finfgeld-Connett D., Johnson E.D. Literature search strategies for conducting knowledge-building and theory-generating qualitative systematic reviews. Journal of Advanced Nursing. 2013; 69 (1):194–204. [ PMC free article : PMC3424349 ] [ PubMed : 22591030 ]
- Grady B., Myers K. M., Nelson E. L., Belz N., Bennett L., Carnahan L. … Guidelines Working Group. Evidence-based practice for telemental health. Telemedicine Journal and E Health. 2011; 17 (2):131–148. [ PubMed : 21385026 ]
- Green B. N., Johnson C. D., Adams A. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. Journal of Chiropractic Medicine. 2006; 5 (3):101–117. [ PMC free article : PMC2647067 ] [ PubMed : 19674681 ]
- Greenhalgh T., Wong G., Westhorp G., Pawson R. Protocol–realist and meta-narrative evidence synthesis: evolving standards ( rameses ). bmc Medical Research Methodology. 2011; 11 :115. [ PMC free article : PMC3173389 ] [ PubMed : 21843376 ]
- Gurol-Urganci I., de Jongh T., Vodopivec-Jamsek V., Atun R., Car J. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database System Review. 2013; 12 cd 007458. [ PMC free article : PMC6485985 ] [ PubMed : 24310741 ] [ CrossRef ]
- Hart C. Doing a literature review: Releasing the social science research imagination. London: SAGE Publications; 1998.
- Higgins J. P. T., Green S., editors. Cochrane handbook for systematic reviews of interventions: Cochrane book series. Hoboken, nj : Wiley-Blackwell; 2008.
- Jesson J., Matheson L., Lacey F.M. Doing your literature review: traditional and systematic techniques. Los Angeles & London: SAGE Publications; 2011.
- King W. R., He J. Understanding the role and methods of meta-analysis in IS research. Communications of the Association for Information Systems. 2005; 16 :1.
- Kirkevold M. Integrative nursing research — an important strategy to further the development of nursing science and nursing practice. Journal of Advanced Nursing. 1997; 25 (5):977–984. [ PubMed : 9147203 ]
- Kitchenham B., Charters S. ebse Technical Report Version 2.3. Keele & Durham. uk : Keele University & University of Durham; 2007. Guidelines for performing systematic literature reviews in software engineering.
- Kitsiou S., Paré G., Jaana M. Systematic reviews and meta-analyses of home telemonitoring interventions for patients with chronic diseases: a critical assessment of their methodological quality. Journal of Medical Internet Research. 2013; 15 (7):e150. [ PMC free article : PMC3785977 ] [ PubMed : 23880072 ]
- Kitsiou S., Paré G., Jaana M. Effects of home telemonitoring interventions on patients with chronic heart failure: an overview of systematic reviews. Journal of Medical Internet Research. 2015; 17 (3):e63. [ PMC free article : PMC4376138 ] [ PubMed : 25768664 ]
- Levac D., Colquhoun H., O’Brien K. K. Scoping studies: advancing the methodology. Implementation Science. 2010; 5 (1):69. [ PMC free article : PMC2954944 ] [ PubMed : 20854677 ]
- Levy Y., Ellis T.J. A systems approach to conduct an effective literature review in support of information systems research. Informing Science. 2006; 9 :181–211.
- Liberati A., Altman D. G., Tetzlaff J., Mulrow C., Gøtzsche P. C., Ioannidis J. P. A. et al. Moher D. The prisma statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Annals of Internal Medicine. 2009; 151 (4):W-65. [ PubMed : 19622512 ]
- Lyden J. R., Zickmund S. L., Bhargava T. D., Bryce C. L., Conroy M. B., Fischer G. S. et al. McTigue K. M. Implementing health information technology in a patient-centered manner: Patient experiences with an online evidence-based lifestyle intervention. Journal for Healthcare Quality. 2013; 35 (5):47–57. [ PubMed : 24004039 ]
- Mickan S., Atherton H., Roberts N. W., Heneghan C., Tilson J.K. Use of handheld computers in clinical practice: a systematic review. bmc Medical Informatics and Decision Making. 2014; 14 :56. [ PMC free article : PMC4099138 ] [ PubMed : 24998515 ]
- Moher D. The problem of duplicate systematic reviews. British Medical Journal. 2013; 347 (5040) [ PubMed : 23945367 ] [ CrossRef ]
- Montori V. M., Wilczynski N. L., Morgan D., Haynes R. B., Hedges T. Systematic reviews: a cross-sectional study of location and citation counts. bmc Medicine. 2003; 1 :2. [ PMC free article : PMC281591 ] [ PubMed : 14633274 ]
- Mulrow C. D. The medical review article: state of the science. Annals of Internal Medicine. 1987; 106 (3):485–488. [ PubMed : 3813259 ] [ CrossRef ]
- Evidence-based information systems: A decade later. Proceedings of the European Conference on Information Systems ; 2011. Retrieved from http://aisel .aisnet.org/cgi/viewcontent .cgi?article =1221&context =ecis2011 .
- Okoli C., Schabram K. A guide to conducting a systematic literature review of information systems research. ssrn Electronic Journal. 2010
- Otte-Trojel T., de Bont A., Rundall T. G., van de Klundert J. How outcomes are achieved through patient portals: a realist review. Journal of American Medical Informatics Association. 2014; 21 (4):751–757. [ PMC free article : PMC4078283 ] [ PubMed : 24503882 ]
- Paré G., Trudel M.-C., Jaana M., Kitsiou S. Synthesizing information systems knowledge: A typology of literature reviews. Information & Management. 2015; 52 (2):183–199.
- Patsopoulos N. A., Analatos A. A., Ioannidis J.P. A. Relative citation impact of various study designs in the health sciences. Journal of the American Medical Association. 2005; 293 (19):2362–2366. [ PubMed : 15900006 ]
- Paul M. M., Greene C. M., Newton-Dame R., Thorpe L. E., Perlman S. E., McVeigh K. H., Gourevitch M.N. The state of population health surveillance using electronic health records: A narrative review. Population Health Management. 2015; 18 (3):209–216. [ PubMed : 25608033 ]
- Pawson R. Evidence-based policy: a realist perspective. London: SAGE Publications; 2006.
- Pawson R., Greenhalgh T., Harvey G., Walshe K. Realist review—a new method of systematic review designed for complex policy interventions. Journal of Health Services Research & Policy. 2005; 10 (Suppl 1):21–34. [ PubMed : 16053581 ]
- Petersen K., Vakkalanka S., Kuzniarz L. Guidelines for conducting systematic mapping studies in software engineering: An update. Information and Software Technology. 2015; 64 :1–18.
- Petticrew M., Roberts H. Systematic reviews in the social sciences: A practical guide. Malden, ma : Blackwell Publishing Co; 2006.
- Rousseau D. M., Manning J., Denyer D. Evidence in management and organizational science: Assembling the field’s full weight of scientific knowledge through syntheses. The Academy of Management Annals. 2008; 2 (1):475–515.
- Rowe F. What literature review is not: diversity, boundaries and recommendations. European Journal of Information Systems. 2014; 23 (3):241–255.
- Shea B. J., Hamel C., Wells G. A., Bouter L. M., Kristjansson E., Grimshaw J. et al. Boers M. amstar is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. Journal of Clinical Epidemiology. 2009; 62 (10):1013–1020. [ PubMed : 19230606 ]
- Shepperd S., Lewin S., Straus S., Clarke M., Eccles M. P., Fitzpatrick R. et al. Sheikh A. Can we systematically review studies that evaluate complex interventions? PLoS Medicine. 2009; 6 (8):e1000086. [ PMC free article : PMC2717209 ] [ PubMed : 19668360 ]
- Silva B. M., Rodrigues J. J., de la Torre Díez I., López-Coronado M., Saleem K. Mobile-health: A review of current state in 2015. Journal of Biomedical Informatics. 2015; 56 :265–272. [ PubMed : 26071682 ]
- Smith V., Devane D., Begley C., Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. bmc Medical Research Methodology. 2011; 11 (1):15. [ PMC free article : PMC3039637 ] [ PubMed : 21291558 ]
- Sylvester A., Tate M., Johnstone D. Beyond synthesis: re-presenting heterogeneous research literature. Behaviour & Information Technology. 2013; 32 (12):1199–1215.
- Templier M., Paré G. A framework for guiding and evaluating literature reviews. Communications of the Association for Information Systems. 2015; 37 (6):112–137.
- Thomas J., Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. bmc Medical Research Methodology. 2008; 8 (1):45. [ PMC free article : PMC2478656 ] [ PubMed : 18616818 ]
- Reconstructing the giant: on the importance of rigour in documenting the literature search process. Paper presented at the Proceedings of the 17th European Conference on Information Systems ( ecis 2009); Verona, Italy. 2009.
- Webster J., Watson R.T. Analyzing the past to prepare for the future: Writing a literature review. Management Information Systems Quarterly. 2002; 26 (2):11.
- Whitlock E. P., Lin J. S., Chou R., Shekelle P., Robinson K.A. Using existing systematic reviews in complex systematic reviews. Annals of Internal Medicine. 2008; 148 (10):776–782. [ PubMed : 18490690 ]
This publication is licensed under a Creative Commons License, Attribution-Noncommercial 4.0 International License (CC BY-NC 4.0): see https://creativecommons.org/licenses/by-nc/4.0/
- Cite this Page Paré G, Kitsiou S. Chapter 9 Methods for Literature Reviews. In: Lau F, Kuziemsky C, editors. Handbook of eHealth Evaluation: An Evidence-based Approach [Internet]. Victoria (BC): University of Victoria; 2017 Feb 27.
- PDF version of this title (4.5M)
- Disable Glossary Links
In this Page
- Introduction
- Overview of the Literature Review Process and Steps
- Types of Review Articles and Brief Illustrations
- Concluding Remarks
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Chapter 9 Methods for Literature Reviews - Handbook of eHealth Evaluation: An Ev... Chapter 9 Methods for Literature Reviews - Handbook of eHealth Evaluation: An Evidence-based Approach
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 24, Issue 2
- Five tips for developing useful literature summary tables for writing review articles
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-0157-5319 Ahtisham Younas 1 , 2 ,
- http://orcid.org/0000-0002-7839-8130 Parveen Ali 3 , 4
- 1 Memorial University of Newfoundland , St John's , Newfoundland , Canada
- 2 Swat College of Nursing , Pakistan
- 3 School of Nursing and Midwifery , University of Sheffield , Sheffield , South Yorkshire , UK
- 4 Sheffield University Interpersonal Violence Research Group , Sheffield University , Sheffield , UK
- Correspondence to Ahtisham Younas, Memorial University of Newfoundland, St John's, NL A1C 5C4, Canada; ay6133{at}mun.ca
https://doi.org/10.1136/ebnurs-2021-103417
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Literature reviews offer a critical synthesis of empirical and theoretical literature to assess the strength of evidence, develop guidelines for practice and policymaking, and identify areas for future research. 1 It is often essential and usually the first task in any research endeavour, particularly in masters or doctoral level education. For effective data extraction and rigorous synthesis in reviews, the use of literature summary tables is of utmost importance. A literature summary table provides a synopsis of an included article. It succinctly presents its purpose, methods, findings and other relevant information pertinent to the review. The aim of developing these literature summary tables is to provide the reader with the information at one glance. Since there are multiple types of reviews (eg, systematic, integrative, scoping, critical and mixed methods) with distinct purposes and techniques, 2 there could be various approaches for developing literature summary tables making it a complex task specialty for the novice researchers or reviewers. Here, we offer five tips for authors of the review articles, relevant to all types of reviews, for creating useful and relevant literature summary tables. We also provide examples from our published reviews to illustrate how useful literature summary tables can be developed and what sort of information should be provided.
Tip 1: provide detailed information about frameworks and methods
- Download figure
- Open in new tab
- Download powerpoint
Tabular literature summaries from a scoping review. Source: Rasheed et al . 3
The provision of information about conceptual and theoretical frameworks and methods is useful for several reasons. First, in quantitative (reviews synthesising the results of quantitative studies) and mixed reviews (reviews synthesising the results of both qualitative and quantitative studies to address a mixed review question), it allows the readers to assess the congruence of the core findings and methods with the adapted framework and tested assumptions. In qualitative reviews (reviews synthesising results of qualitative studies), this information is beneficial for readers to recognise the underlying philosophical and paradigmatic stance of the authors of the included articles. For example, imagine the authors of an article, included in a review, used phenomenological inquiry for their research. In that case, the review authors and the readers of the review need to know what kind of (transcendental or hermeneutic) philosophical stance guided the inquiry. Review authors should, therefore, include the philosophical stance in their literature summary for the particular article. Second, information about frameworks and methods enables review authors and readers to judge the quality of the research, which allows for discerning the strengths and limitations of the article. For example, if authors of an included article intended to develop a new scale and test its psychometric properties. To achieve this aim, they used a convenience sample of 150 participants and performed exploratory (EFA) and confirmatory factor analysis (CFA) on the same sample. Such an approach would indicate a flawed methodology because EFA and CFA should not be conducted on the same sample. The review authors must include this information in their summary table. Omitting this information from a summary could lead to the inclusion of a flawed article in the review, thereby jeopardising the review’s rigour.
Tip 2: include strengths and limitations for each article
Critical appraisal of individual articles included in a review is crucial for increasing the rigour of the review. Despite using various templates for critical appraisal, authors often do not provide detailed information about each reviewed article’s strengths and limitations. Merely noting the quality score based on standardised critical appraisal templates is not adequate because the readers should be able to identify the reasons for assigning a weak or moderate rating. Many recent critical appraisal checklists (eg, Mixed Methods Appraisal Tool) discourage review authors from assigning a quality score and recommend noting the main strengths and limitations of included studies. It is also vital that methodological and conceptual limitations and strengths of the articles included in the review are provided because not all review articles include empirical research papers. Rather some review synthesises the theoretical aspects of articles. Providing information about conceptual limitations is also important for readers to judge the quality of foundations of the research. For example, if you included a mixed-methods study in the review, reporting the methodological and conceptual limitations about ‘integration’ is critical for evaluating the study’s strength. Suppose the authors only collected qualitative and quantitative data and did not state the intent and timing of integration. In that case, the strength of the study is weak. Integration only occurred at the levels of data collection. However, integration may not have occurred at the analysis, interpretation and reporting levels.
Tip 3: write conceptual contribution of each reviewed article
While reading and evaluating review papers, we have observed that many review authors only provide core results of the article included in a review and do not explain the conceptual contribution offered by the included article. We refer to conceptual contribution as a description of how the article’s key results contribute towards the development of potential codes, themes or subthemes, or emerging patterns that are reported as the review findings. For example, the authors of a review article noted that one of the research articles included in their review demonstrated the usefulness of case studies and reflective logs as strategies for fostering compassion in nursing students. The conceptual contribution of this research article could be that experiential learning is one way to teach compassion to nursing students, as supported by case studies and reflective logs. This conceptual contribution of the article should be mentioned in the literature summary table. Delineating each reviewed article’s conceptual contribution is particularly beneficial in qualitative reviews, mixed-methods reviews, and critical reviews that often focus on developing models and describing or explaining various phenomena. Figure 2 offers an example of a literature summary table. 4
Tabular literature summaries from a critical review. Source: Younas and Maddigan. 4
Tip 4: compose potential themes from each article during summary writing
While developing literature summary tables, many authors use themes or subthemes reported in the given articles as the key results of their own review. Such an approach prevents the review authors from understanding the article’s conceptual contribution, developing rigorous synthesis and drawing reasonable interpretations of results from an individual article. Ultimately, it affects the generation of novel review findings. For example, one of the articles about women’s healthcare-seeking behaviours in developing countries reported a theme ‘social-cultural determinants of health as precursors of delays’. Instead of using this theme as one of the review findings, the reviewers should read and interpret beyond the given description in an article, compare and contrast themes, findings from one article with findings and themes from another article to find similarities and differences and to understand and explain bigger picture for their readers. Therefore, while developing literature summary tables, think twice before using the predeveloped themes. Including your themes in the summary tables (see figure 1 ) demonstrates to the readers that a robust method of data extraction and synthesis has been followed.
Tip 5: create your personalised template for literature summaries
Often templates are available for data extraction and development of literature summary tables. The available templates may be in the form of a table, chart or a structured framework that extracts some essential information about every article. The commonly used information may include authors, purpose, methods, key results and quality scores. While extracting all relevant information is important, such templates should be tailored to meet the needs of the individuals’ review. For example, for a review about the effectiveness of healthcare interventions, a literature summary table must include information about the intervention, its type, content timing, duration, setting, effectiveness, negative consequences, and receivers and implementers’ experiences of its usage. Similarly, literature summary tables for articles included in a meta-synthesis must include information about the participants’ characteristics, research context and conceptual contribution of each reviewed article so as to help the reader make an informed decision about the usefulness or lack of usefulness of the individual article in the review and the whole review.
In conclusion, narrative or systematic reviews are almost always conducted as a part of any educational project (thesis or dissertation) or academic or clinical research. Literature reviews are the foundation of research on a given topic. Robust and high-quality reviews play an instrumental role in guiding research, practice and policymaking. However, the quality of reviews is also contingent on rigorous data extraction and synthesis, which require developing literature summaries. We have outlined five tips that could enhance the quality of the data extraction and synthesis process by developing useful literature summaries.
- Aromataris E ,
- Rasheed SP ,
Twitter @Ahtisham04, @parveenazamali
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:

Citation Styles
- Chicago Style
- Annotated Bibliographies

What is a Lit Review?
How to write a lit review.
- Video Introduction to Lit Reviews
Main Objectives
Examples of lit reviews, additional resources.
- Zotero (Citation Management)
What is a literature review?
- Either a complete piece of writing unto itself or a section of a larger piece of writing like a book or article
- A thorough and critical look at the information and perspectives that other experts and scholars have written about a specific topic
- A way to give historical perspective on an issue and show how other researchers have addressed a problem
- An analysis of sources based on your own perspective on the topic
- Based on the most pertinent and significant research conducted in the field, both new and old

- A descriptive list or collection of summaries of other research without synthesis or analysis
- An annotated bibliography
- A literary review (a brief, critical discussion about the merits and weaknesses of a literary work such as a play, novel or a book of poems)
- Exhaustive; the objective is not to list as many relevant books, articles, reports as possible
- To convey to your reader what knowledge and ideas have been established on a topic
- To explain what the strengths and weaknesses of that knowledge and those ideas might be
- To learn how others have defined and measured key concepts
- To keep the writer/reader up to date with current developments and historical trends in a particular field or discipline
- To establish context for the argument explored in the rest of a paper
- To provide evidence that may be used to support your own findings
- To demonstrate your understanding and your ability to critically evaluate research in the field
- To suggest previously unused or underused methodologies, designs, and quantitative and qualitative strategies
- To identify gaps in previous studies and flawed methodologies and/or theoretical approaches in order to avoid replication of mistakes
- To help the researcher avoid repetition of earlier research
- To suggest unexplored populations
- To determine whether past studies agree or disagree and identify strengths and weaknesses on both sides of a controversy in the literature

- Choose a topic that is interesting to you; this makes the research and writing process more enjoyable and rewarding.
- For a literature review, you'll also want to make sure that the topic you choose is one that other researchers have explored before so that you'll be able to find plenty of relevant sources to review.

- Your research doesn't need to be exhaustive. Pay careful attention to bibliographies. Focus on the most frequently cited literature about your topic and literature from the best known scholars in your field. Ask yourself: "Does this source make a significant contribution to the understanding of my topic?"
- Reading other literature reviews from your field may help you get ideas for themes to look for in your research. You can usually find some of these through the library databases by adding literature review as a keyword in your search.
- Start with the most recent publications and work backwards. This way, you ensure you have the most current information, and it becomes easier to identify the most seminal earlier sources by reviewing the material that current researchers are citing.
The organization of your lit review should be determined based on what you'd like to highlight from your research. Here are a few suggestions:
- Chronology : Discuss literature in chronological order of its writing/publication to demonstrate a change in trends over time or to detail a history of controversy in the field or of developments in the understanding of your topic.
- Theme: Group your sources by subject or theme to show the variety of angles from which your topic has been studied. This works well if, for example, your goal is to identify an angle or subtopic that has so far been overlooked by researchers.
- Methodology: Grouping your sources by methodology (for example, dividing the literature into qualitative vs. quantitative studies or grouping sources according to the populations studied) is useful for illustrating an overlooked population, an unused or underused methodology, or a flawed experimental technique.

- Be selective. Highlight only the most important and relevant points from a source in your review.
- Use quotes sparingly. Short quotes can help to emphasize a point, but thorough analysis of language from each source is generally unnecessary in a literature review.
- Synthesize your sources. Your goal is not to make a list of summaries of each source but to show how the sources relate to one another and to your own work.
- Make sure that your own voice and perspective remains front and center. Don't rely too heavily on summary or paraphrasing. For each source, draw a conclusion about how it relates to your own work or to the other literature on your topic.
- Be objective. When you identify a disagreement in the literature, be sure to represent both sides. Don't exclude a source simply on the basis that it does not support your own research hypothesis.
- At the end of your lit review, make suggestions for future research. What subjects, populations, methodologies, or theoretical lenses warrant further exploration? What common flaws or biases did you identify that could be corrected in future studies?
- Double check that you've correctly cited each of the sources you've used in the citation style requested by your professor (APA, MLA, etc.) and that your lit review is formatted according to the guidelines for that style.
Your literature review should:
- Be focused on and organized around your topic.
- Synthesize your research into a summary of what is and is not known about your topic.
- Identify any gaps or areas of controversy in the literature related to your topic.
- Suggest questions that require further research.
- Have your voice and perspective at the forefront rather than merely summarizing others' work.
- Cyberbullying: How Physical Intimidation Influences the Way People are Bullied
- Use of Propofol and Emergence Agitation in Children
- Eternity and Immortality in Spinoza's 'Ethics'
- Literature Review Tutorials and Samples - Wilson Library at University of La Verne
- Literature Reviews: Introduction - University Library at Georgia State
- Literature Reviews - The Writing Center at UNC Chapel Hill
- Writing a Literature Review - Boston College Libraries
- Write a Literature Review - University Library at UC Santa Cruz
- << Previous: Annotated Bibliographies
- Next: Zotero (Citation Management) >>
- Last Updated: Jan 17, 2024 2:47 PM
- URL: https://researchguides.elac.edu/Citation
Warwick Business School
How to write a literature review.
Not sure what a literature review is or how to structure it? In this session, we will examine the function of a literature review and the importance of showing where your own piece of research fits into the overall context of research in your particular research field. We will focus on the importance of ensuring your literature review is both evaluative and critical. You will be given some samples of writing and be required to identify the typical conventions for paragraph structure, tense usage, and signposting language.
Please complete the form below to request a place on the session running
8 th june 11am-1pm (uk time).
This form is closed and is no longer accepting any submissions. Thank you for your time.
- Open access
- Published: 06 December 2022
What improves access to primary healthcare services in rural communities? A systematic review
- Zemichael Gizaw 1 ,
- Tigist Astale 2 &
- Getnet Mitike Kassie 2
BMC Primary Care volume 23 , Article number: 313 ( 2022 ) Cite this article
13k Accesses
9 Citations
1 Altmetric
Metrics details
To compile key strategies from the international experiences to improve access to primary healthcare (PHC) services in rural communities. Different innovative approaches have been practiced in different parts of the world to improve access to essential healthcare services in rural communities. Systematically collecting and combining best experiences all over the world is important to suggest effective strategies to improve access to healthcare in developing countries. Accordingly, this systematic review of literature was undertaken to identify key approaches from international experiences to enhance access to PHC services in rural communities.
All published and unpublished qualitative and/or mixed method studies conducted to improvement access to PHC services were searched from MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar. Articles published other than English language, citations with no abstracts and/or full texts, and duplicate studies were excluded. We included all articles available in different electronic databases regardless of their publication years. We assessed the methodological quality of the included studies using mixed methods appraisal tool (MMAT) version 2018 to minimize the risk of bias. Data were extracted using JBI mixed methods data extraction form. Data were qualitatively analyzed using emergent thematic analysis approach to identify key concepts and coded them into related non-mutually exclusive themes.
Our analysis of 110 full-text articles resulted in ten key strategies to improve access to PHC services. Community health programs or community-directed interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telemedicine, working with traditional healers, working with non-profit private sectors and non-governmental organizations including faith-based organizations are the key strategies identified from international experiences.
This review identified key strategies from international experiences to improve access to PHC services in rural communities. These strategies can play roles in achieving universal health coverage and reducing disparities in health outcomes among rural communities and enabling them to get healthcare when and where they want.
Peer Review reports
Introduction
Universal health coverage (UHC) is used to provide expanding services to eliminate access barriers. Universal health coverage is defined by the world health organization (WHO) as access to key promotional, preventive, curative and rehabilitative health services for all at an affordable rate and ensuring equity in access. The term universal has been described as the State's legal obligation to provide healthcare to all its citizens, with particular attention to ensuring that all poor and excluded groups are included [ 1 , 2 , 3 ].
Strengthening primary healthcare (PHC) is the most comprehensive, reliable and productive approach to improving people's physical and mental wellbeing and social well-being, and that PHC is a pillar of a sustainable health system for UHC and health-related sustainable development goals [ 4 , 5 ]. Despite tremendous progress over the last decades, there are still unaddressed health needs of people in all parts of the world [ 6 , 7 ]. Many people, particularly the poor and people living in rural areas and those who are in vulnerable circumstances, face challenges to remain healthy [ 8 ].
Geographical and financial inaccessibility, inadequate funding, inconsistent medication supply and equipment and personnel shortages have left the reach, availability and effect of PHC services in many countries disappointingly limited [ 9 , 10 ]. A recent Astana Declaration recognized those aspects of PHC need to be changed to adapt adequately to current and emerging threats to the healthcare system. This declaration discussed that implementation of a need-based, comprehensive, cost-effective, accessible, efficient and sustainable healthcare system is needed for disadvantaged and rural populations in more local and convenient settings to provide care when and where they want it [ 8 ].
Different innovative approaches have been practiced in different parts of the world to improve access to essential healthcare services in rural communities. Systematically collecting and combining best experiences all over the world is important to suggest effective strategies to improve access to healthcare in developing countries. Accordingly, this systematic review of literature was undertaken to identify key approaches from international experiences to enhance access to PHC services in rural communities. The findings of this systematic literature review can be used by healthcare professionals, researchers and policy makers to improve healthcare service delivery in rural communities.
Methodology
Research question.
What improves access to PHC services in rural communities? We used the PICO (population, issue/intervention, comparison/contrast, and outcome) construct to develop the search question [ 11 ]. The population is rural communities or remote communities in developing countries who have limited access to healthcare services. Moreover, we extended the population to developed countries to capture experiences of both developing and developed countries. The issue/intervention is implementation of different community-based health interventions to access to essential healthcare services. In this systematic review, we focused on PHC health services, mainly essential or basic healthcare services, community or public health services, and health promotion or health education. Primary healthcare is “a health care system that addressed social, economic, and political causes of poor health promotes health though health services at the primary care level enhances health of the community” [ 12 ]. Comparison/contrast is not appropriate for this review. The outcome is improved access to essential healthcare services.
Outcome measures
The outcome of this review is access to PHC services, such as preventive, promotive, curative, rehabilitative, and palliative health services which are affordable, convenient or acceptable, and available to all who need care.
Criteria for considering studies for this review
All published and unpublished qualitative and/or mixed method studies conducted to improve access to PHC services were included. Government and international or national organizations reports were also included. Different organizations whose primary mission is health or promotion of community health were selected. We included articles based on these eligibility criteria: context or scope of studies (access to PHC services), article type (primary studies), and publication language (English). Articles published other than English language, citations with no abstracts and/or full texts, reviews, and duplicate studies were excluded. We included all articles available in different electronic databases regardless of their publication years. We didn’t use time of publication for screening.
Information sources and search strategy
We searched relevant articles from MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar to access all forms of evidence. An initial search of MEDLINE was undertaken followed by analysis of the text words contained in the title and abstract, and of the index terms used to describe articles. We used the aforementioned performance indicators of PHC delivery and the PICO as we described above to choose keywords. A second search using all identified keywords and index terms was undertaken across all included databases. Thirdly, references of all identified articles were searched to get additional studies. The full electronic search strategy for MEDLINE, a major database we used for this review is included as a supplementary file (Additional file 1 : Appendix 1).
Study selection and assessment of methodological quality
Search results from different electronic databases were exported to Endnote reference manager version 7 to remove duplication. Two independent reviewers (ZG and BA) screened out records. An initial screening of titles and abstracts was done based on the PICO criteria and language of publication. Secondary screening of full-text papers was done for studies we included at the initial screening phase. We further investigated and assessed records included in the full-text articles against the inclusion and exclusion criteria. We sat together and discussed the eligibility assessment. The interrater agreement was 90%. We resolved disagreements by consensus for points we had different rating. We used the PRISMA flow diagram to summarize the study selection processes.
Methodological quality of the included studies was assessed using mixed methods appraisal tool (MMAT) version 2018 [ 13 ]. As it is clearly indicated in the user guide of the MMAT tool, it is discouraged to calculate an overall score from the ratings of each criterion. Instead, it is advised to provide a more detailed presentation of the ratings of each criterion to better inform quality of the included studies. The rating of each criterion was, therefore, done as per the detail explanations included in the guideline. Almost all the included full text articles fulfilled the criteria and all the included full text articles were found to be better quality.
Data extraction
We independently extracted data from papers included in the review using JBI mixed methods data extraction form. This form is only used for reviews that follow a convergent integrated approach, i.e. integration of qualitative data and qualitative data [ 14 ]. The data extraction form was piloted on randomly selected papers and modified accordingly. One reviewer extracted the data from the included studies and the second reviewer checked the extracted data. Disagreements were resolved by discussion between the two reviewers. Information was extracted from each included study on: list of authors, year of publication, study area, population of interest, study type, methods, focus of the studies, main findings, authors’ conclusion, and limitations of the study.
Synthesis of findings
The included full-text articles were qualitatively analyzed using emergent thematic analysis approach to identify key concepts and coded them into related non-mutually exclusive themes. Themes are strategies mentioned or discussed in the included records to improve access to PHC services. Themes were identified manually by reading the included records again and again. We then synthesized each theme by comparing the discussion and conclusion of the included articles.
Systematic review registration number
The protocol of this review is registered in PROSPERO (the registration number is: CRD42019132592) to avoid unplanned duplication and to enable comparison of reported review methods with what was planned in the protocol. It is available at https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019132592 .
Schematic of the systematic review and reporting of the search
We used PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2009 checklist [ 15 ] for reporting of this systematic review.
Study selection
The search strategy identified 1148 titles and abstracts [914 from PubMed (Table 1 ) and 234 from other sources] as of 10 March 2022. We obtained 900 after we removed duplicated articles. Following assessment by title and abstract, 485 records were excluded because these records did not meet the criteria as mentioned in the method section. Additional 256 records were discarded because the records did not discuss the outcome of interest well and some records were systematic reviews. The full text of the remaining 159 records was examined in more detail. It appeared that 49 studies did not meet the inclusion criteria as described in the method section. One hundred ten records met the inclusion criteria and were included in the systematic review or synthesis (Fig. 1 ).
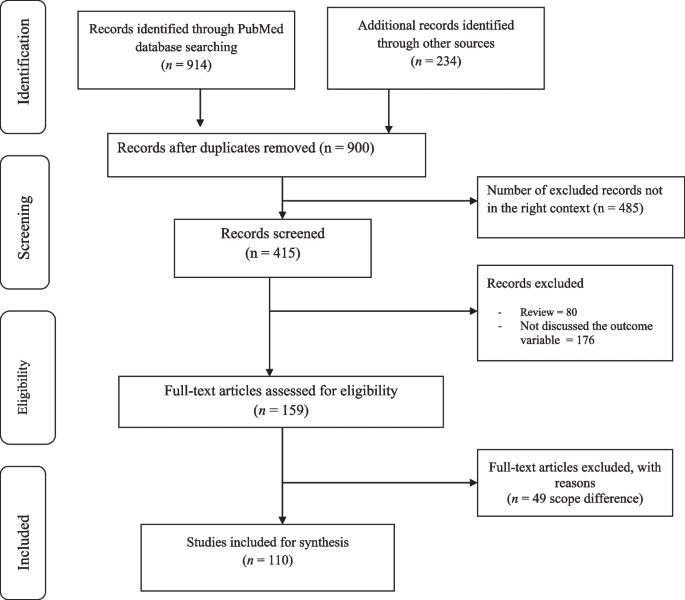
Study selection flow diagram
Of 900 articles resulting from the search term, 110 (12.2%) met the inclusion criteria. The included full-text articles were published between 1993 and 2021. Ninety-two (83.6%) of the included full-text articles were research articles, 5(4.5%) were technical reports, 3 (2.7%) were perspective, 4 (3.6%) was discussion paper, 3(2.7%) were dissertation or thesis, 2 (1.8%) were commentary, and 1 (0.9) was a book. Thirty-six (33%) and 29 (26%) of the included full-text articles were conducted in Africa and North America, respectively (Fig. 2 ).
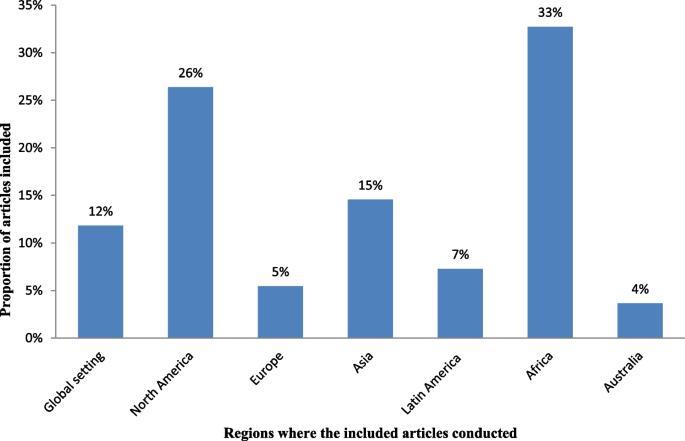
Regions where the included full-test articles conducted
Key strategies identified
The analysis of 110 full-text articles resulted in 10 themes. The themes are key strategies to improve access to PHC services in rural communities. The key strategies identified are community health programs or community-directed healthcare interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telemedicine, promoting the role of traditional medicine, working with non-profit private sectors and non-governmental organizations (NGOs) including faith-based organizations (Table 2 ).
Description of strategies
a. Community health programs or community-directed healthcare interventions
Twenty-four (21.8%) of the full-text articles included in this review discussed that community health programs (CHPs) or community-directed healthcare interventions are best strategies to provide basic health and medical care close to the community to increase access and coverage of essential health services. Community health programs are locally based health promotion, disease prevention, and treatment programs available typically to communities in need and community-directed intervention strategy is an approach in which communities themselves direct the planning and implementation of intervention delivery. Rural communities, especially, in developing countries have no access to healthcare facilities in the near distance and have less chance to receive healthcare from doctors, health officers, nurses or midwives. In response to this critical problems, many countries have been investing heavily in community based primary health care to bring services to rural and remote areas where most of the population lives. Community health programs include construction of health posts or community health centers close to the community and deployment of community health workers (CHWs), such as health extension workers, to reach-out every village, who play a prominent role as the gatekeepers of healthcare in rural communities. Community-directed healthcare intervention is an approach in which communities themselves direct the planning and implementation of healthcare interventions. Community participation remains crucial in the identification of health problems, planning or designing of health interventions and implementation of the interventions, which enhances need-based and demand-driven provision of health services while promoting sustainability and ownership (Additional file 2 : Appendix 2, Table A1).
b. School-based primary healthcare
In this review, 9 of 110 (8.2%) of the included full-text articles pointed out that school-based healthcare services can be effective to improve access to PHC services. School-based health services are health programs that offer health care to children and youth either in a school or on school grounds and usually staffed according to school community needs and resources. School-based health services provide a variety of healthcare services to underserved children, youth and vulnerable populations in a convenient and accessible environment. Access to comprehensive health services via schools leads to improved access to healthcare (Additional file 3 : Appendix 3, Table A2).
c. Student-led healthcare services
In this review, 5 of 110 (4.5%) of the full-text articles discussed that the use of medical and health science students as healthcare service providers can minimize problems related with shortage of health professionals in rural healthcare system and can play appreciable roles to minimize healthcare service access problems in rural communities. Student-led healthcare services are developed through consultation between universities and local health providers and are purposefully designed clinical placements with a focus on clinical educational activities for pre-registration students. Student-led clinics link students, healthcare professionals, community-based organizations, universities, and communities. In this approach, students can gain practical experience in an interdisciplinary setting and through exposure to a community with unique and severe needs (Additional file 4 : Appendix 4, Table A3).
d. Outreach services or mobile clinics
In this systematic literature review, 18 of 110 (16.4%) of the included studies discussed that outreach services or mobile clinics in primary care and rural hospital settings can improve access to PHC services in rural communities. Mobile outreach service is defined as healthcare services provided by a mobile team of trained providers, from a higher-level health facility to a lower-level health facilities or locally available community facilities that are not used for clinical services, such as schools, health posts, or other community structures. Outreach services improve access to specialists and hospital-based services, strengthen connections between specialists and PHC providers, and give the benefits of consultations in primary care settings. Specialist outreach services have the potential to overcome access barriers faced by disadvantaged rural and remote communities. Furthermore, a community-based mobile clinics can be effective in uncovering illness and in directing patients to a healthcare home (Additional file 5 : Appendix 5, Table A4).
e. Family health program
Four (3.6%) of the included full-text articles discussed that family health program (FHP) is highly cost-effective tool for improving access to healthcare services for deprived areas (such as rural communities). Family health program means the program is a program designed to provide primary care as well as the prevention and early treatment of communicable and non-communicable diseases in defined populations by deploying interdisciplinary healthcare teams include physicians, nurses, nurse assistants, and full-time community health agents. It has evolved into a robust approach to providing primary care for defined populations by deploying interdisciplinary healthcare teams. The nucleus of each team includes a physician, a nurse, a nurse assistant, and full-time community health agents. This approach is effective on improving access to healthcare and eliminating health disparities (Additional file 6 : Appendix 6, Table A5).
f. Empanelment
This systematic review of literature identified that empanelment (also known as rostering) is a best strategy to proactively provide coordinated primary healthcare towards achieving universal health coverage. Empanelment is a continuous, iterative set of processes that identify and assign populations to facilities, care teams, or primary care providers who have a responsibility to know their assigned population. It enables health systems to improve health outcomes and to reduce costs. Empanelment establishes a point of care for individuals and simultaneously holds primary healthcare providers and care teams accountable for actively managing care for a specific group of individuals (Additional file 7 : Appendix 7, Table A6).
g. Community health funding schemes
In this systematic review of literature, 11 (10%) of the included articles discussed that community health funding schemes such as community-based health insurance (CBHI) increases access to healthcare services in low-income rural communities. Community-based health insurance schemes are usually voluntary and characterized by community members pooling funds to offset the cost of healthcare. Moreover, this approach is effective to mobilize domestic resources for health at low income levels. For low-income countries, community health financing has modest ability to increase the total amount of funds for healthcare. Properly structured community health financing system can significantly improve efficiency, reduce the cost of healthcare, improve quality and health outcomes, and pool risks. Community-financing schemes could improve preventive services and reduce the incidence of diseases. It could also improve people’s access to healthcare and the quality of services, thus improving their health status. Community health financing could also improve risk pooling and reduce health-induced impoverishment. Community health insurance has potential positive impacts on health and social security (Additional file 8 : Appendix 8, Table A7).
h. Telemedicine
In this review, 13 of 110 (11.8%) articles discussed that telemedicine is one of the solutions for rural subspecialty healthcare delivery. Telemedicine can be defined as the use of technology (computers, video, phone, messaging) by a medical professional to diagnose and treat patients in a remote location. The provision of subspecialty services using telemedicine to a remote and medically underserved population provides improved access to subspecialty care. Telemedicine brings sustainable healthcare to rural populations. Use of information and communication technologies in support of health and health-related fields, including healthcare services, health surveillance, health education, and health research has the potential to greatly improve health service efficiency, expand or scale up treatment delivery to thousands of patients in the rural populations (Additional file 9 : Appendix 9, Table A8).
i. Promoting the role of traditional medicine
Seven (6.4%) of the included articles showed that incorporating traditional healers into public health system addresses healthcare needs of people with limited access to allopathic medicine. Traditional medicine is the sum total of the knowledge, skill, and practices based on the theories, beliefs, and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health as well as in the prevention, diagnosis, improvement or treatment of physical and mental illness. Knowledge about traditional medicine has a catalyzing effect in meeting health sector development objectives. Integrating traditional medicine into national health systems in combination with national policy and regulation for products, practices and providers can enhance access to PHC services in remote populations (Additional file 10 : Appendix 10, Table A9).
j. Working with non-profit private sectors and non-governmental organizations
In this systematic review, 15 of 110 (13.6%) of the included articles revealed that working with non-profit private sectors and NGOs strengthens the healthcare system. Involving the non-profit private sectors, faith-based organizations (FBOs), and NGOs for health system strengthening eventually contributes to create a healthcare system reflecting an increased efficiency, more equity and good governance in health. International and local NGOs have endeavored to fill the gaps in access to healthcare services, research and advocacy. Non-profit private sectors and NGOs have a key role in improving health in low- and middle-income countries. With networks that reach even the most remote communities, many FBOs are well positioned to promote demand and access for healthcare services. Partnership among FBOs is critical in increasing access to healthcare services, and ensuring sustainability by influencing behaviors at the community, family and individual level. Faith-based organizations play an integral role in the healthcare system by increasing health seeking behaviors and delivering supportive services that address common access and cultural barriers (Additional file 11 : Appendix 11, Table A10).
This systematic literature review found that community health programs or community-directed healthcare interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telehealth, integrative medicine, and working with non-profit private sectors and NGOs are key strategies to improve access to PHC services in rural communities. The identified strategies address the four major pillars of primary healthcare (i.e., community participation, inter-sectoral coordination, appropriate technology, and support mechanism made available) [ 126 ]. Moreover, the identified strategies are effective to improve access to healthcare services to rural communities. Moreover, the identified strategies are effective to solve shortage of manpower and to build knowledge and skill of the local health workforces in rural healthcare system. The ability of a healthcare system to meet health needs of the population depends largely on the knowledge, skills, motivation and deployment of the people responsible for organizing and delivering health services. The results of this review can strengthen the health information system, which are core elements of the healthcare system that ensure community engagement through dissemination and use of timely and reliable health information to rural populations. This review also suggests strategies to narrow down the health disparities among rural populations, which is wide in most Least and Middle Income Countries (LMICs). Healthcare services are usually disproportionately concentrated in major urban areas. As a result, rural communities face growing health disparities, largely attributed to weak policies, inefficiencies, poor leadership, and governance in healthcare system.
This review identified that community health programs or community-directed healthcare interventions address health disparities by ensuring equitable access to health resources in communities where health equity is limited by socioeconomic and geographical factors. Community health programs include identifying and prioritizing public health problems in a specific geographic area; designing and implementing public health interventions (such as establishing community health centers, mobile clinics, and outreach programs); providing services (such as health education, screenings, social support, and counseling), and deploying community health workers to promote healthy behaviors; advocating for improved care for populations at risk; and working with stakeholders to address community healthcare needs [ 16 , 17 , 18 , 127 , 128 , 129 , 130 ]. The community-oriented PHC model which is socially responsive medicine makes a healthcare system more rational, accountable, appropriate, and socially relevant to the public. Consequently, this model serves as a paradigm for reforming healthcare systems. Community-directed interventions can be considered as a realistic means to increase accessibility of interventions at community-level in rural areas [ 32 , 33 , 34 , 35 , 36 , 37 , 38 ]. This approach is best in situations where there are cultural barriers to implement interventions because this strategy is effective to develop ownership in the community. In-service and on-the-job training for community health workers, close supervision and government support, and program evaluation is very important to strengthen the community health program [ 131 , 132 , 133 ].
This review identified that school-based PHC services are effective strategies to improve access to PHC services. School-based health services provide a variety of healthcare services to children, youth and vulnerable populations in a convenient and accessible environment which indirectly improve leadership and governance. Science teachers and home room teachers play important roles to implement this strategy. It impacts on delivering preventive care such as immunizations, managing chronic illnesses and providing reproductive health services for adolescents. Comprehensive health services via schools improve access to healthcare information [ 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ]. Access to school around the world increased drastically in the last century [ 134 ]. This high schooling rate is a good opportunity to provide healthcare services to school learners in accessible places and to disseminate health messages to families. Prior researches suggest that school-based healthcare services increase access to healthcare by increasing utilization of primary care, prevention services, and health maintenance visits [ 135 , 136 ]. Including science teachers, home room teachers, school principals, students, communities, community health workers, and other interested parties in the school-based healthcare system as main actors or promoters must be considered to sustain the impact. Health and education sectors should work in collaboration with the above-mentioned actors to plan, implement and monitor the progress. School-based healthcare services are preferable in situations when there is high schooling rate and limited access to healthcare institutions. This strategy is also an alternative way in areas where the health seeking behavior of the community is low.
The use of medical and health science students in rural healthcare system was identified as a key strategy to minimize health inequalities in rural communities due to shortages in health workforce and distribution of healthcare resources [ 49 , 50 , 51 , 52 , 53 ]. Student-led health intervention is an alternative approach to provide essential healthcare services to the community where there is shortage of healthcare workers [ 137 , 138 ]. Students will have opportunities to learn professional skills and competencies while they are providing healthcare services to the community. Moreover, benefits for student learning include increased communication, collaboration, and leadership skills [ 53 , 139 ]. Student-led health intervention also enables increased access to services, more time for assessments and treatments, increased depth of health teaching, holistic and integrated healthcare, and free health supports [ 140 , 141 , 142 , 143 ]. However, the use of medical and health science students in the rural healthcare system may have ethical and competency issues. Supporting strategies such as close supervision, preparing clear protocols, and including senior experts in the team should be considered.
This systematic review of literature found that outreach services or mobile clinics can improve access to PHC service delivery in rural populations [ 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 ]. In developing countries, the highest proportion of people lives in rural areas where doctor services are not available. Rural communities travel to major cities to get specialist services. This reflects a desire for closer integration between primary and secondary care. Specialist outreach services or mobile clinics have become one of the effective solution to solve health disparities, to improve access to healthcare services, and to build capacity of local healthcare workforces. This strategy is preferable in situations when there are high loads in tertiary or referral level hospitals and when there is high patient leakage in the referral system [ 63 , 64 , 65 , 66 , 67 , 68 , 69 ]. However, the implementation may not be easy. It needs well established healthcare system and budget. Moreover, the efficiency of care may be lower compared with hospital-based cares and the effect on patients’ health outcomes might be small [ 56 , 57 , 61 ] . Irregular specialist visits in rural areas may not have real impacts unless the services are sustainable with a strong commitment at national and local levels. Outreach activities should be included in health policies with strong leadership, healthcare financing, and private initiatives must be encouraged to maintain the activities over time.
This review revealed that FHP is highly effective tool for improving health for rural communities. The FHP has provided a new, more robust model of primary healthcare services designed to provide accessible, first contact, comprehensive, and whole person care that is coordinated with other healthcare services. It has positive results to improved availability, access to, and use of health services, and improved health indicators, such as reduced infant mortality, improved detection of cases of neglected diseases, and reduced health disparities [ 73 , 144 , 145 , 146 ]. The FHP deploys interdisciplinary healthcare teams. The team includes a physician, a nurse, a nurse assistant, and full-time community health agents. Family health teams are organized geographically. The teams are responsible for delivering public health interventions [ 72 , 74 ]. Family health program is an alternative strategy in rural healthcare system in situations when there are inequities in access to care; when there is high hospitalization rate; when there is low health seeking behavior in the community; and when there is poor case detecting and reporting system. Despite these remarkable achievements, the FHP has some challenges include difficulties in the recruitment and retention of doctors trained appropriately to deliver primary healthcare, large variations in quality of local care, patchy integration of primary care services with existing secondary and tertiary care, and slow adoption of FHP in large population [ 147 ].
In this review, empanelment has been identified as a best strategy to deliver coordinated primary healthcare towards achieving universal health coverage [ 76 , 77 , 78 , 79 ]. The goal of empanelment is provide people-centered healthcare services based on their needs to ensure that every established patient receives optimal care, whether he/she regularly visits healthcare centers. Major activities in this approach include assignment of all patients to a healthcare provider panel; update panel assignments on a regular basis; and use panel data to educate, and track patients [ 79 ]. Empanelment enables healthcare systems to improve patient experiences, reduce costs, and improve health outcomes. Empanelment is an effective strategy to deliver four key functions: first-contact accessibility, continuity, comprehensiveness, and coordination [ 148 ]. Effective empanelment requires responsibility for the health of a target population, including providing healthcare services based on their health status, which is an important step in moving towards people-centered integrated healthcare [ 79 ].
This review identified that community health funding schemes such as community-based health insurance (CBHI) increases access to healthcare in low-income rural communities. Moreover, this approach is effective to mobilize domestic resources for health at low income levels [ 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 ]. Community-based health insurance is an emerging strategy to provide financial protection against the cost of illness. It is an effective strategy to improve access to quality health services for low-income rural households [ 149 ]. Existence of social capital in the community is a determinant factor for the effectiveness of CBHI as social capital has a positive effect on the community's demand for insurance [ 150 , 151 ]. Moreover, solidarity and trust between the members are the key principles for the good functioning of a CBHI. Solidarity and trust stir-up members who are susceptible to risk to put together their resources for common use [ 149 , 152 , 153 ]. Affordability of premiums or contributions, technical arrangements made by the scheme management, timing of collecting the contributions, trust in the integrity and competence of the managers of the CBHI, The quality of care offered through the CBHI, accessible across different population groups are some of the determinant factors to be considered to increase people’s decision to join the CBHI schemes [ 154 , 155 ].
In this review, telemedicine has been identified as one of the many possible solutions for rural subspecialty healthcare delivery. Telemedicine is a vital technological tool to increase healthcare access, improve care delivery systems, engage in culturally competent outreach, health workforce development, and health information system [ 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 ]. Telemedicine can be a great alternative to the traditional healthcare system in situations like diagnoses of common medical problems; inquiries about various medical issues for home treatments; post-treatment check-ins or follow-up for chronic care; holidays, weekends, late night or any other situation when regular medical care is not possible; patient inability to leave the house; patients who lack regular access to relevant medical expertise in their geographic area ; and etc. However, technological issues are challenges when dealing with telemedicine, especially in developing countries. General problems of Internet connectivity and access to infrastructure can minimize benefits of this strategy. Costs associated with technology can also be a barrier. Furthermore, health technology requires human capacity to use it. Therefore, strengthening the information communication technologies (ICT) and human capacity building on ICT are important to address the health needs of the rural communities.
This systematic review of literature identified that promoting the role of TM solves problems of access to allopathic medicine. Integration of TM in health system will result in increased coverage and access to healthcare services. The role of complementary and alternative medicine for health is undisputed particularly in light of its role in health promotion and well-being. It also supports local health workforces [ 104 , 105 , 106 , 107 , 108 , 109 ]. Incorporating traditional healers into the public health system addresses healthcare needs [ 156 , 157 ]. However, integrating TM to the public healthcare system is challenging. It is a general belief that TM defies scientific procedures in terms of objectivity, measurement, codification and classification [ 157 ]. If integrated, who provides training to medical doctors on the ontology, epistemology and the efficacies of TM in modern medicine [ 157 ]. Due to these, some scholars suggest that both TM and modern medicine be allowed to operate and develop independent of one another [ 158 , 159 ]. Another fundamental challenge to TM is the widespread reported cases of fake healers and healings [ 157 ]. Generally, this strategy is more of feasible in areas where formal trainings on integrative medicine are available. Even though the integration is challenging, the health sector can use traditional healers as health educators or health promoters by providing training and continuous support. It can be also possible to use traditional healers as facilitators in the community-directed approaches. In general TM can be used in the primary healthcare system where no access to allopathic medicine and when conventional medicine is ineffective in treatment of disease [ 160 ].
Working with non-profit private sectors and NGOs has been identified as effective strategies to strengthen the healthcare system in developing countries [ 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 ]. Since governments in developing countries are challenged to meet the health needs of their populations because of financial constraints, limited human resources, and weak health infrastructure; the private sector (especially the non-profit private sectors) and non-governmental organizations can help expand access to healthcare services through its resources, expertise, and infrastructure. However, the presence of an NGO in the operation, may contribute to unrealistic expectations of health services, affecting perceptions of the latter negatively [ 113 ]. Moreover, reports have it that besides other issues in many instances NGOs allocated funds only to disease specific projects (vertical programming) rather than to broad based investments (horizontal programming) [ 161 ]. There are also concerns that donor expenditures in developing countries are not only unsustainable but may be considered as inadequate considering the enormous healthcare burden [ 161 , 162 , 163 , 164 ]. To avoid unrealistic expectations and dissatisfaction, and to increase and sustain the population’s trust in the organization, NGOs should operate in a manner that is as integrated as possible within the existing structure and should work close to the population it serves, with services anchored in the community. Moreover, faith-based organizations contribute in health such as disease prevention, health education or promotion, and community health development beyond psychological and spiritual care [ 119 , 120 , 121 , 122 , 123 , 124 ]. Religious organizations can reach all segments of rural populations. Therefore, integrating PHC services, especially health education and promotion, diseases prevention and community health development with religious organizations intensifies delivery of healthcare services. Working with FBOs is a best way in situations where cultural and faith-based barriers are common and in areas, where access problems are often related to lack of providers. However, religious organizations need intensive training on health promotion and health system to enable them to respond to local contexts within the framework of national policies. Moreover, there should be strong partnership with government agenesis to sustain the effort [ 165 , 166 , 167 , 168 ].
Contribution of this review
Various studies reported one or more strategies to improve access to primary healthcare services. However, the strategies reported by individual studies are not compiled together and there is lack of pooled evidence on effective strategies to improve access to healthcare system. This systematic literature review was, therefore, conducted to compile effective strategies to improve access to healthcare services in rural communities. The review suggests key strategies to improve access to PHC services in rural communities. These suggested strategies are implementable in countries that suffer from shortage of health workers and healthcare financing because all the strategies used locally available opportunities. The local healthcare system needs, therefore, scan the available opportunities in the locality for implementing the suggested strategies and needs to integrate the strategies in the healthcare system to sustain the impacts. Healthcare providers, researchers and policy makers could use the results of this systematic literature review to increase access to healthcare services in hard-to-reach areas. As the strategies are compiled from experiences of different countries (developed and least developed countries), there might be contextual differences like socio-economic, cultural, institutional, and geographical challenges to adopt the identified strategies. Moreover, some of the experiences only come from one or two countries. Therefore, strategy developers and implementers need to consider these contextual challenges or variation during adopting and implementing different strategies.
Strengths and limitations of the study
As a strength, this systematic review explores international (both developed and developing countries) best experiences on primary healthcare service delivery and identified ten key approaches to improve access to PHC services in rural communities. We also searched relevant published or unpublished articles, dissertations or theses, discussion papers, and perspectives from a wide range of sources, such as MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar.
As a limitation, we entirely relied on electronic databases to search relevant articles. We didn’t include locally available printed out records. We also applied limits for language. We excluded articles published other than English language. We believed we could get more relevant articles if we had access to records available in prints and if we include articles published other than English language. Furthermore, since the strategies are compiled from experiences of different countries (developed and least developed countries), there might be contextual differences like socio-economic, cultural, institutional and geographical challenges to adopt the identified strategies. There was also limited evidence for some articles, especially reports to rate their methodological quality. Readers should also note that our review might missed some important work in improving access to PHC services and the identified strategies are not the only strategies to improve access to PHC services. There might be other effective strategies which are not included in this review. In addition generalizability might be affected since some of the experiences only come from one or two countries. Moreover, this review focuses on access not quality of care delivered.
This review identified key strategies from international experiences to improve access to PHC services in rural communities. These strategies are effective to improve access to healthcare services in rural or remote communities. They can also play roles in achieving UHC and reducing disparities in health outcomes and increase access to rural communities to get healthcare when and where they want. Therefore, incorporating these key strategies suggested by this review in to the healthcare system is useful to enhance PHC services and to minimize impacts of health disparity in rural communities. However, the identified strategies may not be easy to implement. Increasing number and capacity of human resource for health; strengthening the healthcare financing system; improving medicine and supplies; working in different partners and communities; establishing monitoring and evaluation system; strong and committed leadership; and encouraging private initiatives must be considered to implement and maintain these strategies over time. Moreover, policy makers, program planners and implementers who want to utilize findings of this review should be aware that these are not the only effective strategies to improve access to primary healthcare services.
Availability of data and materials
All the extracted data are included in the manuscript.
Abbreviations
Community-based health insurance
Faith-based organizations
Family health program
Information communication technologies
Mixed methods appraisal tool
Non-governmental organizations
- Primary healthcare
Primary Health Care Performance Initiative
Population, phenomena of interest and context)
Traditional medicine
Universal health coverage
Hampton MB, Kettle AJ, Winterbourn CC. Inside the neutrophil phagosome: oxidants, myeloperoxidase, and bacterial killing. Blood. 1998;92(9):3007–17.
Article CAS Google Scholar
Kirby M. The right to health fifty years on: Still skeptical? Health Hum Rights. 1999;4(1):6–25.
O’Connell T, Rasanathan K, Chopra M. What does universal health coverage mean? The Lancet. 2014;383(9913):277–9.
White F. Primary health care and public health: foundations of universal health systems. Med Princ Pract. 2015;24(2):103–16.
Article Google Scholar
Sanders D, Nandi S, Labonté R, Vance C, Van Damme W. From primary health care to universal health coverage—one step forward and two steps back. The Lancet. 2019;394(10199):619–21.
Brezzi M, Luongo P. Regional Disparities In Access To Health Care. 2016.
Google Scholar
Hartley D. Rural health disparities, population health, and rural culture. Am J Public Health. 2004;94(10):1675–8.
Walraven G. The 2018 Astana declaration on primary health care, is it useful? J Glob Health. 2019;9(1).
Gillam S. Is the declaration of Alma Ata still relevant to primary health care? BMJ (Clinical research ed). 2008;336(7643):536–8.
Tollman S, Doherty J, Mulligan JA. General Primary Care. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, Jha P, Mills A, Musgrove P, editors. Disease Control Priorities in Developing Countries. Washington: World Bank The International Bank for Reconstruction and Development/The World Bank Group; 2006. Available at https://www.ncbi.nlm.nih.gov/books/NBK11789/pdf/Bookshelf_NBK11789.pdf .
Stern C, Jordan Z, McArthur A. Developing the review question and inclusion criteria. AJN The Am J Nurs. 2014;114(4):53–6.
World Health Organization. losing the gap in a generation. Commission on Social Determinants of Health FINAL REPORT. 2008. Available at https://www.who.int/social_determinants/final_report/csdh_finalreport_2008.pdf . Accessed on 22 March 2022.
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, GagnonM-P GF, Nicolau B, O’Cathain A. Mixed methods appraisal tool (MMAT), version 2018. Canada: IC Canadian Intellectual Property Office, Industry; 2018. Available at https://mixedmethodsappraisaltoolpublicpbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf .
JBI Manual for Evidence Synthesis. Appendix 8.1 JBI Mixed Methods Data Extraction Form following a Convergent Integrated Approach. Available at https://jbi-global-wiki.refined.site/space/MANUAL/3318284375/Appendix+8.1+JBI+Mixed+Methods+Data+Extraction+Form+following+a+Convergent+Integrated+Approach . Accessed on 12 August 2021.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Assefa Y, Gelaw YA, Hill PS, Taye BW, Van Damme W. Community health extension program of Ethiopia, 2003–2018: successes and challenges toward universal coverage for primary healthcare services. Glob Health. 2019;15(1):1–11.
Admassie A, Abebaw D, Woldemichael AD. Impact evaluation of the Ethiopian health services extension programme. J Dev Eff. 2009;1(4):430–49.
Yitayal M, Berhane Y, Worku A, Kebede Y. The community-based Health extension Program significantly improved contraceptive utilization in West gojjam Zone, ethiopia. J Multidiscip Healthc. 2014;7:201.
Croke K, Mengistu AT, O’Connell SD, Tafere K. The impact of a health facility construction campaign on health service utilisation and outcomes: analysis of spatially linked survey and facility location data in Ethiopia. BMJ Glob Health. 2020;5(8):e002430.
Arwal S. Health Posts in Afghanistan. J Gen Practice. 2015;3(213):2.
Negussie A, Girma G. Is the role of Health Extension Workers in the delivery of maternal and child health care services a significant attribute? The case of Dale district, southern Ethiopia. BMC Health Serv Res. 2017;17(1):1–8.
Than KK, Mohamed Y, Oliver V, Myint T, La T, Beeson JG, Luchters S. Prevention of postpartum haemorrhage by community-based auxiliary midwives in hard-to-reach areas of Myanmar: a qualitative inquiry into acceptability and feasibility of task shifting. BMC Pregnancy Childbirth. 2017;17(1):1–10.
Medhanyie A, Spigt M, Kifle Y, Schaay N, Sanders D, Blanco R, GeertJan D, Berhane Y. The role of health extension workers in improving utilization of maternal health services in rural areas in Ethiopia: a cross sectional study. BMC Health Serv Res. 2012;12(1):1–9.
Sakeah E, McCloskey L, Bernstein J, Yeboah-Antwi K, Mills S, Doctor HV. Can community health officer-midwives effectively integrate skilled birth attendance in the community-based health planning and services program in rural Ghana? Reprod Health. 2014;11(1):1–13.
Sarmento DR. Traditional birth attendance (TBA) in a health system: what are the roles, benefits and challenges: a case study of incorporated TBA in Timor-Leste. Asia Pac Fam Med. 2014;13(1):1–9.
Rahmawati R, Bajorek B. Peer Reviewed: A Community Health Worker-Based Program for Elderly People with Hypertension in Indonesia: A Qualitative Study, 2013. Prev Chronic Dis. 2015;12:E175.
Feltner FJ, Ely GE, Whitler ET, Gross D, Dignan M. Effectiveness of community health workers in providing outreach and education for colorectal cancer screening in Appalachian Kentucky. Soc Work Health Care. 2012;51(5):430–40.
Hughes MM, Yang E, Ramanathan D, Benjamins MR. Community-based diabetes community health worker intervention in an underserved Chicago population. J Community Health. 2016;41(6):1249–56.
Panday S, Bissell P, Van Teijlingen E, Simkhada P. The contribution of female community health volunteers (FCHVs) to maternity care in Nepal: a qualitative study. BMC Health Serv Res. 2017;17(1):1–11.
Datiko DG, Lindtjørn B. Health extension workers improve tuberculosis case detection and treatment success in southern Ethiopia: a community randomized trial. PLoS ONE. 2009;4(5):e5443.
le Roux KW, Almirol E, Rezvan PH, Le Roux IM, Mbewu N, Dippenaar E, Stansert-Katzen L, Baker V, Tomlinson M, Rotheram-Borus M. Community health workers impact on maternal and child health outcomes in rural South Africa–a non-randomized two-group comparison study. BMC Public Health. 2020;20(1):1–14.
Witmer A, Seifer SD, Finocchio L, Leslie J, O’Neil EH. Community health workers: integral members of the health care work force. Am J Public Health. 1995;85(8 Pt 1):1055–8.
Wright RA. Community-oriented primary care. The cornerstone of health care reform. Jama. 1993;269(19):2544–7.
Makaula P, Bloch P, Banda HT, Mbera GB, Mangani C, de Sousa A, Nkhono E, Jemu S, Muula AS. Primary Health Care in rural Malawi - a qualitative assessment exploring the relevance of the community-directed interventions approach. BMC Health Serv Res. 2012;12:328.
Katabarwa MN, Habomugisha P, Richards FO Jr, Hopkins D. Community-directed interventions strategy enhances efficient and effective integration of health care delivery and development activities in rural disadvantaged communities of Uganda. Trop Med Int Health : TM & IH. 2005;10(4):312–21.
Madon S, Malecela MN, Mashoto K, Donohue R, Mubyazi G, Michael E. The role of community participation for sustainable integrated neglected tropical diseases and water, sanitation and hygiene intervention programs: A pilot project in Tanzania. Soc Sci Med. 1982;2018(202):28–37.
Okeibunor JC, Orji BC, Brieger W, Ishola G, Otolorin E, Rawlins B, Ndekhedehe EU, Onyeneho N, Fink G. Preventing malaria in pregnancy through community-directed interventions: evidence from Akwa Ibom State, Nigeria. Malaria J. 2011;10:227.
Brieger WR, Sommerfeld JU, Amazigo UV. The Potential for Community-Directed Interventions: Reaching Underserved Populations in Africa. Int Q Community Health Educ. 2015;35(4):295–316.
Braimah JA, Sano Y, Atuoye KN, Luginaah I. Access to primary health care among women: the role of Ghana’s community-based health planning and services policy. Prim Health Care Res Dev. 2019;20:e82.
Kaplan DW, Brindis CD, Phibbs SL, Melinkovich P, Naylor K, Ahlstrand K. A comparison study of an elementary school–based health center: effects on health care access and use. Arch Pediatr Adolesc Med. 1999;153(3):235–43.
Allison MA, Crane LA, Beaty BL, Davidson AJ, Melinkovich P, Kempe A. School-based health centers: improving access and quality of care for low-income adolescents. Pediatrics. 2007;120(4):e887–94.
Keeton V, Soleimanpour S, Brindis CD. School-based health centers in an era of health care reform: Building on history. Curr Probl Pediatr Adolesc Health Care. 2012;42(6):132–56.
Brindis CD, Klein J, Schlitt J, Santelli J, Juszczak L, Nystrom RJ. School-based health centers: Accessibility and accountability. J Adolesc Health. 2003;32(6):98–107.
Hutchinson P, Carton TW, Broussard M, Brown L, Chrestman S. Improving adolescent health through school-based health centers in post-Katrina New Orleans. Child Youth Serv Rev. 2012;34(2):360–8.
Paschall MJ, Bersamin M. School-based health centers, depression, and suicide risk among adolescents. Am J Prev Med. 2018;54(1):44–50.
Minguez M, Santelli JS, Gibson E, Orr M, Samant S. Reproductive health impact of a school health center. J Adolesc Health. 2015;56(3):338–44.
Gibson EJ, Santelli JS, Minguez M, Lord A, Schuyler AC. Measuring school health center impact on access to and quality of primary care. J Adolesc Health. 2013;53(6):699–705.
Bozigar M. A Cross-Sectional Survey to Evaluate Potential for Partnering With School Nurses to Promote Human Papillomavirus Vaccination. Prev Chronic Dis. 2020;17:E111.
Suen J, Attrill S, Thomas JM, Smale M, Delaney CL, Miller MD. Effect of student-led health interventions on patient outcomes for those with cardiovascular disease or cardiovascular disease risk factors: a systematic review. BMC Cardiovasc Disord. 2020;20(1):1–10.
Atuyambe LM, Baingana RK, Kibira SP, Katahoire A, Okello E, Mafigiri DK, Ayebare F, Oboke H, Acio C, Muggaga K. Undergraduate students’ contributions to health service delivery through communitybased education. BMC Med Educ. 2016;16:123.
Stuhlmiller CM, Tolchard B. Developing a student-led health and wellbeing clinic in an underserved community: collaborative learning, health outcomes and cost savings. BMC Nurs. 2015;14(1):1–8.
Campbell DJ, Gibson K, O’Neill BG, Thurston WE. The role of a student-run clinic in providing primary care for Calgary’s homeless populations: a qualitative study. BMC Health Serv Res. 2013;13(1):1–6.
Simpson SA, Long JA. Medical student-run health clinics: important contributors to patient care and medical education. J Gen Intern Med. 2007;22(3):352–6.
Gruen RL, O’Rourke IC, Bailie RS, d’Abbs PH, O’Brien MM, Verma N. Improving access to specialist care for remote Aboriginal communities: evaluation of a specialist outreach service. Med J Aust. 2001;174(10):507–11.
Gruen RL, Weeramanthri T, Bailie R. Outreach and improved access to specialist services for indigenous people in remote Australia: the requirements for sustainability. J Epidemiol Community Health. 2002;56(7):517–21.
Gruen RL, Bailie RS, Wang Z, Heard S, O’Rourke IC. Specialist outreach to isolated and disadvantaged communities: a population-based study. The Lancet. 2006;368(9530):130–8.
Bond M, Bowling A, Abery A, McClay M, Dickinson E. Evaluation of outreach clinics held by specialists in general practice in England. J Epidemiol Community Health. 2000;54(2):149–56.
Irani M, Dixon M, Dean JD. Care closer to home: past mistakes, future opportunities. J R Soc Med. 2007;100(2):75–7.
Bailey JJ, Black ME, Wilkin D. Specialist outreach clinics in general practice. BMJ (Clinical research ed). 1994;308(6936):1083–6.
De Roodenbeke E, Lucas S, Rouzaut A, Bana F. Outreach services as a strategy to increase access to health workers in remote and rural areas. Geneva: WHO; 2011.
Bowling A, Stramer K, Dickinson E, Windsor J, Bond M. Evaluation of specialists’ outreach clinics in general practice in England: process and acceptability to patients, specialists, and general practitioners. J Epidemiol Community Health. 1997;51(1):52–61.
Spencer N. Consultant paediatric outreach clinics–a practical step in integration. Arch Dis Child. 1993;68(4):496–500.
Aljasir B, Alghamdi MS. Patient satisfaction with mobile clinic services in a remote rural area of Saudi Arabia. East Mediterr Health J. 2010;16(10):1085–90.
Lee EJ, O’Neal S. A mobile clinic experience: nurse practitioners providing care to a rural population. J Pediatr Health Care. 1994;8(1):12–7.
Cone PH, Haley JM. Mobile clinics in Haiti, part 1: Preparing for service-learning. Nurse Educ Pract. 2016;21:1–8.
Diaz-Perez Mde J, Farley T, Cabanis CM. A program to improve access to health care among Mexican immigrants in rural Colorado. J Rural Health. 2004;20(3):258–64.
Hill C, Zurakowski D, Bennet J, Walker-White R, Osman JL, Quarles A, Oriol N. Knowledgeable Neighbors: a mobile clinic model for disease prevention and screening in underserved communities. Am J Public Health. 2012;102(3):406–10.
Edgerley LP, El-Sayed YY, Druzin ML, Kiernan M, Daniels KI. Use of a community mobile health van to increase early access to prenatal care. Matern Child Health J. 2007;11(3):235–9.
Peters G, Doctor H, Afenyadu G, Findley S, Ager A. Mobile clinic services to serve rural populations in Katsina State, Nigeria: perceptions of services and patterns of utilization. Health Policy Plan. 2014;29(5):642–9.
Neke NM, Gadau G, Wasem J. Policy makers’ perspective on the provision of maternal health services via mobile health clinics in Tanzania—Findings from key informant interviews. PLoS ONE. 2018;13(9):e0203588.
Padmadas SS, Johnson FA, Leone T, Dahal GP. Do mobile family planning clinics facilitate vasectomy use in Nepal? Contraception. 2014;89(6):557–63.
Macinko J, Harris MJ. Brazil’s family health strategy—delivering community-based primary care in a universal health system. N Engl J Med. 2015;372(23):2177–81.
Macinko J, Lima Costa MF. Access to, use of and satisfaction with health services among adults enrolled in Brazil’s Family Health Strategy: evidence from the 2008 National Household Survey. Tropical Med Int Health. 2012;17(1):36–42.
Dourado I, Oliveira VB, Aquino R, Bonolo P, Lima-Costa MF, Medina MG, Mota E, Turci MA, Macinko J. Trends in primary health care-sensitive conditions in Brazil: the role of the Family Health Program (Project ICSAP-Brazil). Medical care. 2011;49:577–84.
Aquino R, De Oliveira NF, Barreto ML. Impact of the family health program on infant mortality in Brazilian municipalities. Am J Public Health. 2009;99(1):87–93.
Chong P-N, Tang WE. Transforming primary care—the way forward with the TEAMS2 approach. Fam Pract. 2019;36(3):369–70.
Primary Health Care Performance Initiatives (phcpi). Improvement strategies model: Population health management: Empanelment. Available at https://improvingphc.org/sites/default/files/Empanelment%20-%20v1.2%20-%20last%20updated%2012.13.2019.pdf . Accessed on 18 March 2022.
McGough P, Chaudhari V, El-Attar S, Yung P. A health system’s journey toward better population health through empanelment and panel management. Healthcare. 2018;6(66):1–9.
Bearden T, Ratcliffe HL, Sugarman JR, Bitton A, Anaman LA, Buckle G, Cham M, Quan DCW, Ismail F, Jargalsaikhan B. Empanelment: A foundational component of primary health care. Gates Open Res. 2019;3:1654.
Hsiao WC. Unmet health needs of two billion: is community financing a solution? 2001.
Wang W, Temsah G, Mallick L. The impact of health insurance on maternal health care utilization: evidence from Ghana, Indonesia and Rwanda. Health Policy Plan. 2017;32(3):366–75.
Atnafu DD, Tilahun H, Alemu YM. Community-based health insurance and healthcare service utilisation, North-West, Ethiopia: a comparative, cross-sectional study. BMJ Open. 2018;8(8):e019613.
USAID. Ethiopia’s Community-based Health Insurance: A Step on the Road to Universal Health Coverage. Available at https://www.hfgproject.org/ethiopias-community-based-health-insurance-step-road-universal-health-coverage/ . Accessed on 18 March 2022.
Blanchet NJ, Fink G, Osei-Akoto I. The effect of Ghana’s National Health Insurance Scheme on health care utilisation. Ghana Med J. 2012;46(2):76–84.
CAS Google Scholar
Nshakira-Rukundo E, Mussa EC, Nshakira N, Gerber N, von Braun J. Impact of community-based health insurance on utilisation of preventive health services in rural Uganda: a propensity score matching approach. Int J Health Econ Manag. 2021;21(2):203–27.
Mwaura JW, Pongpanich S. Access to health care: the role of a community based health insurance in Kenya. Pan Afr Med J. 2012;12(1):35.
Jutting JP. The Impact Of Health Insurance On The Access To Health Care And Financial Protection In Rural Developing Countries: The Example of Senegal. HNP discussion paper series;. World Bank, Washington, DC. © World Bank. 2011. https://openknowledge.worldbank.org/handle/10986/13774 . License: CC BY 3.0 IGO.
Balamiento NC. The impact of social health insurance on healthcare utilization outcomes: evidence from the indigent program of the Philippine National Health Insurance. International Institute of Social Studies. 2018. Available at https://thesis.eur.nl/pub/46445/Balamiento,%20Neeanne_MA_2017_18%20_ECD.pdf . Accessed 30 Nov 2022.
Farrell CM, Gottlieb A. The effect of health insurance on health care utilization in the justice-involved population: United States, 2014–2016. Am J Public Health. 2020;110(S1):S78–84.
Thuong NTT. Impact of health insurance on healthcare utilisation patterns in Vietnam: a survey-based analysis with propensity score matching method. BMJ Open. 2020;10(10):e040062.
Custodio R, Gard AM, Graham G. Health information technology: addressing health disparity by improving quality, increasing access, and developing workforce. J Health Care Poor Underserved. 2009;20(2):301–7.
Meier CA, Fitzgerald MC, Smith JM. eHealth: extending, enhancing, and evolving health care. Annu Rev Biomed Eng. 2013;15:359–82.
Anstey Watkins JOT, Goudge J, Gomez-Olive FX, Griffiths F. Mobile phone use among patients and health workers to enhance primary healthcare: A qualitative study in rural South Africa. Soc Sci Med. 1982;2018(198):139–47.
Kuntalp M, Akar O. A simple and low-cost Internet-based teleconsultation system that could effectively solve the health care access problems in underserved areas of developing countries. Comput Methods Programs Biomed. 2004;75(2):117–26.
Price M, Yuen EK, Goetter EM, Herbert JD, Forman EM, Acierno R, Ruggiero KJ. mHealth: a mechanism to deliver more accessible, more effective mental health care. Clin Psychol Psychother. 2014;21(5):427–36.
Bashshur RL, Shannon GW, Krupinski EA, Grigsby J, Kvedar JC, Weinstein RS, Sanders JH, Rheuban KS, Nesbitt TS, Alverson DC, et al. National telemedicine initiatives: essential to healthcare reform. Telemed J E Health. 2009;15(6):600–10.
Norton SA, Burdick AE, Phillips CM, Berman B. Teledermatology and underserved populations. Arch Dermatol. 1997;133(2):197–200.
Raza T, Joshi M, Schapira RM, Agha Z. Pulmonary telemedicine–a model to access the subspecialist services in underserved rural areas. Int J Med Informatics. 2009;78(1):53–9.
Shouneez YH. Smartphone hearing screening in mHealth assisted community-based primary care. UPSpace Institutional Repository, Department of Liberary Service. Dissertation (MCommPath)--University of Pretoria. 2016. Available at http://hdl.handle.net/2263/53477 . Accessed 17 Mar 2022.
Marcin JP, Ellis J, Mawis R, Nagrampa E, Nesbitt TS, Dimand RJ. Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community. Pediatrics. 2004;113(1 Pt 1):1–6.
Olu O, Muneene D, Bataringaya JE, Nahimana M-R, Ba H, Turgeon Y, Karamagi HC, Dovlo D. How can digital health technologies contribute to sustainable attainment of universal health coverage in Africa? A perspective. Front Public Health. 2019;7:341.
Ryan MH, Yoder J, Flores SK, Soh J, Vanderbilt AA. Using health information technology to reach patients in underserved communities: A pilot study to help close the gap with health disparities. Global J Health Sci. 2016;8(6):86.
Buckwalter KC, Davis LL, Wakefield BJ, Kienzle MG, Murray MA. Telehealth for elders and their caregivers in rural communities. Fam Community Health. 2002;25(3):31–40.
WHO Regional Committee for Africa. Promoting the role of traditional medicine in health systems: a strategy for the African Region. World Health Organization. Regional Office for Africa. Available at http://www.who.int/iris/handle/10665/95467. .
Mishra SR, Neupane D, Kallestrup P. Integrating complementary and alternative medicine into conventional health care system in developing countries: an example of Amchi. J Evid-Based Complementary Altern Med. 2015;20(1):76–9.
Mbwambo ZH, Mahunnah RL, Kayombo EJ. Traditional health practitioner and the scientist: bridging the gap in contemporary health research in Tanzania. Tanzan Health Res Bull. 2007;9(2):115–20.
Poudyal AK, Jimba M, Murakami I, Silwal RC, Wakai S, Kuratsuji T. A traditional healers’ training model in rural Nepal: strengthening their roles in community health. Trop Med Int Health : TM & IH. 2003;8(10):956–60.
Payyappallimana U. Role of Traditional Medicine in Primary Health Care: An Overview of Perspectives and Challenges. Yokohama J Social Sciences. 2009;14(6):723–43.
Kange’ethe SM. Traditional healers as caregivers to HIV/AIDS clients and other terminally challenged persons in Kanye community home-based care programme (CHBC), Botswana. SAHARA J. 2009;6(2):83–91.
Habtom GK. Integrating traditional medical practice with primary healthcare system in Eritrea. J Complement Integr Med. 2015;12(1):71–87.
Ejaz I, Shaikh BT, Rizvi N. NGOs and government partnership for health systems strengthening: a qualitative study presenting viewpoints of government, NGOs and donors in Pakistan. BMC Health Serv Res. 2011;11(1):1–7.
Wu FS. International non-governmental actors in HIV/AIDS prevention in China. Cell Res. 2005;15(11):919–22.
Biermann O, Eckhardt M, Carlfjord S, Falk M, Forsberg BC. Collaboration between non-governmental organizations and public services in health–a qualitative case study from rural Ecuador. Glob Health Action. 2016;9(1):32237.
Mercer A, Khan MH, Daulatuzzaman M, Reid J. Effectiveness of an NGO primary health care programme in rural Bangladesh: evidence from the management information system. Health Policy Plan. 2004;19(4):187–98.
Baqui AH, Rosecrans AM, Williams EK, Agrawal PK, Ahmed S, Darmstadt GL, Kumar V, Kiran U, Panwar D, Ahuja RC. NGO facilitation of a government community-based maternal and neonatal health programme in rural India: improvements in equity. Health Policy Plan. 2008;23(4):234–43.
Ricca J, Kureshy N, LeBan K, Prosnitz D, Ryan L. Community-based intervention packages facilitated by NGOs demonstrate plausible evidence for child mortality impact. Health Policy Plan. 2014;29(2):204–16.
Ahmed N, DeRoeck D, Sadr-Azodi N. Private sector engagement and contributions to immunisation service delivery and coverage in Sudan. BMJ Glob Health. 2019;4(2):e001414.
Edimond BJ. The Contribution of Non-Governmental Organizations in Delivery of Basic Health Services in Partnership with Local Government. Doctoral Dissertation, Uganda Martyrs University. 2014.
Chand S, Patterson J: Faith-Based Models for Improving Maternal and Newborn Health. IMA World Health and ActionAid International USA, 2007 Available at https://imaworldhealthorg/wp-content/uploads/2014/06/faith_based_models_for_improving_maternal_and_newborn_health.pdf
Magezi V. Churchdriven primary health care: Models for an integrated church and community primary health care in Africa (a case study of the Salvation Army in East Africa). HTS Teologiese Studies/ Theological Studies. 2018;74(2):4365.
Villatoro AP, Dixon E, Mays VM. Faith-based organizations and the Affordable Care Act: Reducing Latino mental health care disparities. Psychol Serv. 2016;13(1):92–104.
Levin J. Faith-based initiatives in health promotion: history, challenges, and current partnerships. American journal of health promotion : AJHP. 2014;28(3):139–41.
Green A, Shaw J, Dimmock F, Conn C. A shared mission? Changing relationships between government and church health services in Africa. Int J Health Plann Manage. 2002;17(4):333–53.
Bandy G, Crouch A. Building from common foundations : the World Health Organization and faith-based organizations in primary healthcare. World Health Organization; 2008. Available at https://apps.who.int/iris/handle/10665/43884 . Accessed 16 Mar 2022.
Zahnd WE, Jenkins WD, Shackelford J, Lobb R, Sanders J, Bailey A. Rural cancer screening and faith community nursing in the era of the Affordable Care Act. J Health Care Poor Underserved. 2018;29(1):71–80.
Wagle K. Primary Health Care (PHC): History, Principles, Pillars, Elements & Challenges. Global Health, 2020. Available at https://www.publichealthnotes.com/primary-health-care-phc-history-principles-pillars-elements-challenges/ . Accessed 4 June 2022.
Bhatt J, Bathija P. Ensuring access to quality health care in vulnerable communities. Acad Med. 2018;93(9):1271.
Arvey SR, Fernandez ME. Identifying the core elements of effective community health worker programs: a research agenda. Am J Public Health. 2012;102(9):1633–7.
Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D, Wang J. Community health needs assessment: potential for population health improvement. Popul Health Manag. 2016;19(3):178–86.
Chudgar RB, Shirey LA, Sznycer-Taub M, Read R, Pearson RL, Erwin PC. Local health department and academic institution linkages for community health assessment and improvement processes: a national overview and local case study. J Public Health Manag Pract. 2014;20(3):349–55.
Desta FA, Shifa GT, Dagoye DW, Carr C, Van Roosmalen J, Stekelenburg J, Nedi AB, Kols A, Kim YM. Identifying gaps in the practices of rural health extension workers in Ethiopia: a task analysis study. BMC Health Serv Res. 2017;17(1):1–9.
Lehmann U, Sanders D. Community health workers: what do we know about them. The state of the evidence on programmes, activities, costs and impact on health outcomes of using community health workers Geneva: World Health Organization; 2007. Available at https://www.hrhresourcecenter.org/node/1587.html . Accessed 17 Mar 2022.
Chen N, Raghavan M, Albert J, McDaniel A, Otiso L, Kintu R, West M, Jacobstein D. The community health systems reform cycle: strengthening the integration of community health worker programs through an institutional reform perspective. Global Health: Sci Practice. 2021;9(Supplement 1):S32–46.
Roser M, Ortiz-Ospina E: Global rise of education. Our World in Data 2017. Available at https://ourworldindata.org/global-rise-of-education . Accessed on 29 May 2019.
Santelli J, Morreale M, Wigton A, Grason H. School health centers and primary care for adolescents: a review of the literature. J Adolesc Health. 1996;18(5):357–66.
Wade TJ, Mansour ME, Guo JJ, Huentelman T, Line K, Keller KN. Access and utilization patterns of school-based health centers at urban and rural elementary and middle schools. Public Health Reports. 2008;123(6):739–50.
Johnson I, Hunter L, Chestnutt IG. Undergraduate students’ experiences of outreach placements in dental secondary care settings. Eur J Dent Educ. 2012;16(4):213–7.
Ndira S, Ssebadduka D, Niyonzima N, Sewankambo N, Royall J. Tackling malaria, village by village: a report on a concerted information intervention by medical students and the community in Mifumi Eastern Uganda. Afr Health Sci. 2014;14(4):882–8.
Frakes K-a, Brownie S, Davies L, Thomas JB, Miller M-E, Tyack Z. Capricornia Allied Health Partnership (CAHP): a case study of an innovative model of care addressing chronic disease through a regional student-assisted clinic. Aust Health Rev. 2014;38(5):483–6.
Frakes KA, Brownie S, Davies L, Thomas J, Miller ME, Tyack Z. The sociodemographic and health-related characteristics of a regional population with chronic disease at an interprofessional student-assisted clinic in Q ueensland C apricornia A llied H ealth P artnership. Aust J Rural Health. 2013;21(2):97–104.
Frakes K-A, Tyzack Z, Miller M, Davies L, Swanston A, Brownie S. The Capricornia Project: Developing and implementing an interprofessional student-assisted allied health clinic. 2011.
Frakes K-A, Brownie S, Davies L, Thomas J, Miller M-E, Tyack Z. Experiences from an interprofessional student-assisted chronic disease clinic. J Interprof Care. 2014;28(6):573–5.
Schutte T, Tichelaar J, Dekker RS, van Agtmael MA, de Vries TP, Richir MC. Learning in student-run clinics: A systematic review. Med Educ. 2015;49(3):249–63.
Paim J, Travassos C, Almeida C, Bahia L, Macinko J. The Brazilian health system: history, advances, and challenges. The Lancet. 2011;377(9779):1778–97.
Rocha R, Soares RR. Evaluating the impact of community-based health interventions: evidence from Brazil’s Family Health Program. Health Econ. 2010;19(S1):126–58.
Rasella D, Harhay MO, Pamponet ML, Aquino R, Barreto ML. Impact of primary health care on mortality from heart and cerebrovascular diseases in Brazil: a nationwide analysis of longitudinal data. BMJ (Clinical research ed). 2014;349:g4014.
Harris M. Brazil’s Family Health Programme: A cost effective success that higher income countries could learn from. BMJ: Br Med J. 2010;341(7784):1171–2.
Starfield B. Is primary care essential? The lancet. 1994;344(8930):1129–33.
Donfouet HPP, Mahieu P-A. Community-based health insurance and social capital: a review. Heal Econ Rev. 2012;2(1):1–5.
Zhang L, Wang H, Wang L, Hsiao W. Social capital and farmer’s willingness-to-join a newly established community-based health insurance in rural China. Health Policy. 2006;76(2):233–42.
Donfouet HPP. Essombè J-RE, Mahieu P-A, Malin E: Social capital and willingness-to-pay for community-based health insurance in rural Cameroon. Global J Health Sci. 2011;3(1):142.
Grunau J. Exploring people’s motivation to join or not to join the community-based health insurance’Sina Passenang’in Sotouboua, Togo. 2013.
Gitahi JW. Innovative Healthcare Financing and Equity through Community Based Health Insurance Schemes (CBHHIS) In Kenya. United States International University-Africa Digital Repository. Available at http://erepo.usiu.ac.ke/11732/3654 . Accessed 18 May 2022.
Carrin G, Waelkens MP, Criel B. Community-based health insurance in developing countries: a study of its contribution to the performance of health financing systems. Tropical Med Int Health. 2005;10(8):799–811.
Umeh CA, Feeley FG. Inequitable access to health care by the poor in community-based health insurance programs: a review of studies from low-and middle-income countries. Global Health: Science And Practice. 2017;5(2):299–314.
Odebiyi AI. Western trained nurses’ assessment of the different categories of traditional healers in southwestern Nigeria. Int J Nurs Stud. 1990;27(4):333–42.
Abdullahi AA. Trends and challenges of traditional medicine in Africa. Afr J Tradit Complement Altern Med : AJTCAM. 2011;8(5 Suppl):115–23.
Taye OR. Yoruba Traditional Medicine and the Challenge of Integration. The J Pan Afr Studies. 2009;3(3):73–90.
Konadu K. Medicine and Anthropology in Twentieth Century Africa: Akan Medicine and Encounters with (Medical) Anthropology. African Studies Quarterly. 2008;10(2 & 3).
Benzie IF, Wachtel-Galor S: Herbal medicine: biomolecular and clinical aspects. 2nd Ed. 2011. Available at https://www.crcpress.com/Herbal-Medicine-Biomolecular-and-Clinical-Aspects-Second-Edition/Benzie-Wachtel-Galor/p/book/9781439807132 . Accessed 21 May 2022.
Ejughemre U. Donor support and the impacts on health system strengthening in sub-saharan africa: assessing the evidence through a review of the literature. Am J Public Health Res. 2013;1(7):146–51.
Seppey M, Ridde V, Touré L, Coulibaly A. Donor-funded project’s sustainability assessment: a qualitative case study of a results-based financing pilot in Koulikoro region. Mali Globalization and health. 2017;13(1):1–15.
Shaw RP, Wang H, Kress D, Hovig D. Donor and domestic financing of primary health care in low income countries. Health Systems & Reform. 2015;1(1):72–88.
Gotsadze G, Chikovani I, Sulaberidze L, Gotsadze T, Goguadze K, Tavanxhi N. The challenges of transition from donor-funded programs: results from a theory-driven multi-country comparative case study of programs in Eastern Europe and Central Asia supported by the Global Fund. Global Health: Science and Practice. 2019;7(2):258–72.
Ascroft J, Sweeney R, Samei M, Semos I, Morgan C. Strengthening church and government partnerships for primary health care delivery in Papua New Guinea: Lessons from the international experience. Health policy and health finance knowledge hub Working paper series. 2011(16).
Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213–34.
Olivier J, Wodon Q. The role of faith-inspired health care providers in Sub-Saharan Africa and public private partnerships: Strengthening the Evidence for faith-inspired health engagement in Africa, Volume 1. Health, Nutrition and Population (HNP) Discussion Paper Series 76223v1. Available at https://documents1.worldbank.org/curated/en/851911468203673017 . Accessed 20 May 2022.
Schumann C, Stroppa A, Moreira-Almeida A. The contribution of faith-based health organisations to public health. Int Psychiatry. 2011;8(3):62–4.
Download references
Acknowledgements
The author would like to thank IPHC- E for funding this review.
This review was funded by International Institute for Primary Health Care- Ethiopia (IPHC- E).
Author information
Authors and affiliations.
Department of Environmental and Occupational Health and Safety, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Zemichael Gizaw
International Institute for Primary Health Care- Ethiopia, Ethiopian Public Health Institute, Addis Ababa, Ethiopia
Tigist Astale & Getnet Mitike Kassie
You can also search for this author in PubMed Google Scholar
Contributions
ZG prepared the manuscript. TA and GMK critically reviewed the protocol and manuscript. All the authors read and approved the final manuscript.
Corresponding author
Correspondence to Zemichael Gizaw .
Ethics declarations
Ethics approval and consent to participate.
Systematic review does not required ethics approval.
Consent for publication
This manuscript does not contain any individual person’s data.
Competing interests
The authors declared that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: .
Searchstrategy. MEDLINE (PubMed).
Additional file 2: Appendix 2: Table A1.
Description of full-text articles which discussed community health programs or community-directed interventions as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 3:
Appendix 3: Table A2. Description of full-text articles which discussed school-based healthcareservices as a strategy to improve PHCservice delivery in rural communities.
Additional file 4:
Appendix 4: Table A3. Description of full-text articles which discussed student-led healthcareservices as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 5: Appendix 5: Table A4
. Descriptionof full-text articles which discussed outreach services or mobile clinics as astrategy to improve PHC service delivery in ruralcommunities.
Additional file 6:
Appendix 6: Table A5. Description of full-text articles which discussed family health program as astrategy to improve PHC service delivery in rural,communities.
Additional file 7:
Appendix 7: Table A6. Description of full-text articles whichdiscussed empanelment as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 8:
Appendix 9: Table A8. Description of full-text articles which discussed telemedicine or mobile healthas a strategy to improve PHC service delivery in ruralcommunities.
Additional file 9:
Appendix 8: Table A7. Description of full-text articles which discussed community health funding schemes as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 10:
Appendix 10: Table A9. Description of full-text articles which discussed promoting the role of workingwith traditional healers as a strategy toimprove PHC service delivery in rural communities.
Additional file 11:
Appendix 11: Table A10. Description of full-text articles which discussed working with non-profitprivate sectors and non-governmental organizations as a strategy to improve PHC service delivery in rural communities.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gizaw, Z., Astale, T. & Kassie, G.M. What improves access to primary healthcare services in rural communities? A systematic review. BMC Prim. Care 23 , 313 (2022). https://doi.org/10.1186/s12875-022-01919-0
Download citation
Received : 09 August 2022
Accepted : 18 November 2022
Published : 06 December 2022
DOI : https://doi.org/10.1186/s12875-022-01919-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Access to PHC services
- Rural communities
- Key strategies to improve access to PHC services
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
- Open access
- Published: 05 September 2022
Psychiatric and medical comorbidities of eating disorders: findings from a rapid review of the literature
- Ashlea Hambleton 1 ,
- Genevieve Pepin 2 ,
- Anvi Le 3 ,
- Danielle Maloney 1 , 4 ,
- National Eating Disorder Research Consortium ,
- Stephen Touyz 1 , 4 &
- Sarah Maguire 1 , 4
Journal of Eating Disorders volume 10 , Article number: 132 ( 2022 ) Cite this article
17k Accesses
40 Citations
65 Altmetric
Metrics details
Eating disorders (EDs) are potentially severe, complex, and life-threatening illnesses. The mortality rate of EDs is significantly elevated compared to other psychiatric conditions, primarily due to medical complications and suicide. The current rapid review aimed to summarise the literature and identify gaps in knowledge relating to any psychiatric and medical comorbidities of eating disorders.
This paper forms part of a rapid review) series scoping the evidence base for the field of EDs, conducted to inform the Australian National Eating Disorders Research and Translation Strategy 2021–2031, funded and released by the Australian Government. ScienceDirect, PubMed and Ovid/Medline were searched for English-language studies focused on the psychiatric and medical comorbidities of EDs, published between 2009 and 2021. High-level evidence such as meta-analyses, large population studies and Randomised Control Trials were prioritised.
A total of 202 studies were included in this review, with 58% pertaining to psychiatric comorbidities and 42% to medical comorbidities. For EDs in general, the most prevalent psychiatric comorbidities were anxiety (up to 62%), mood (up to 54%) and substance use and post-traumatic stress disorders (similar comorbidity rates up to 27%). The review also noted associations between specific EDs and non-suicidal self-injury, personality disorders, and neurodevelopmental disorders. EDs were complicated by medical comorbidities across the neuroendocrine, skeletal, nutritional, gastrointestinal, dental, and reproductive systems. Medical comorbidities can precede, occur alongside or emerge as a complication of the ED.
Conclusions
This review provides a thorough overview of the comorbid psychiatric and medical conditions co-occurring with EDs. High psychiatric and medical comorbidity rates were observed in people with EDs, with comorbidities contributing to increased ED symptom severity, maintenance of some ED behaviours, and poorer functioning as well as treatment outcomes. Early identification and management of psychiatric and medical comorbidities in people with an ED may improve response to treatment and overall outcomes.
Plain English Summary
The mortality rate of eating disorders is significantly elevated compared to other psychiatric conditions, primarily due to medical complications and suicide. Further, individuals with eating disorders often meet the diagnostic criteria of at least one comorbid psychiatric or medical disorder, that is, the individual simultaneously experiences both an ED and at least one other condition. This has significant consequences for researchers and health care providers – medical and psychiatric comorbidities impact ED symptoms and treatment effectiveness. The current review is part of a larger Rapid Review series conducted to inform the development of Australia’s National Eating Disorders Research and Translation Strategy 2021–2031. A Rapid Review is designed to comprehensively summarise a body of literature in a short timeframe, often to guide policymaking and address urgent health concerns. The Rapid Review synthesises the current evidence base and identifies gaps in eating disorder research and care. This paper gives a critical overview of the scientific literature relating to the psychiatric and medical comorbidities of eating disorders. It covers recent literature regarding psychiatric comorbidities including anxiety disorders, mood disorders, substance use disorders, trauma and personality disorders and neurodevelopmental disorders. Further, the review discusses the impact and associations between EDs and medical comorbidities, some of which precede the eating disorder, occur alongside, or as a consequence of the eating disorder.
Introduction
Eating Disorders (EDs) are often severe, complex, life-threatening illnesses with significant physiological and psychiatric impacts. EDs impact individuals across the entire lifespan, affecting all age groups (although most often they emerge in childhood and adolescence), genders, socioeconomic groups and cultures [ 1 ]. EDs have some of the highest mortality rates of all psychiatric illnesses and carry a significant personal, interpersonal, social and economic burdens [ 2 , 3 ].
Adding to the innate complexity of EDs, it is not uncommon for people living with an ED to experience associated problems such as psychological, social, and functional limitations [ 2 ] in addition to psychiatric and medical comorbidities [ 4 , 5 , 6 ]. Comorbidity is defined as conditions or illnesses that occur concurrently to the ED. Evidence suggests that between 55 and 95% of people diagnosed with an ED will also experience a comorbid psychiatric disorder in their lifetime [ 4 , 6 ]. Identifying psychiatric comorbidities is essential because of their potential impact on the severity of ED symptomatology, the individual’s distress and treatment effectiveness [ 7 , 8 ].
The mortality rate of EDs is significantly higher than the general population, with the highest occurring in Anorexia Nervosa (AN) due to impacts on the cardiovascular system [ 9 ] and suicide. [ 10 ] Mortality rates are also heightened in Bulimia Nervosa (BN) and Other Specified Feeding and Eating Disorder (OSFED) [ 11 ]. Suicide rates are elevated across the ED spectrum, and higher rates are observed in patients with a comorbid psychiatric disorder [ 10 , 12 ]. Of concern, the proportion of people with an ED not accessing treatment is estimated to be as high as 75% [ 13 ], potentially a consequence of comorbidities which impact on motivation, the ability to schedule appointments or require clinical prioritisation (i.e., self-harm or suicidal behaviours) [ 14 ]. Further, for many of those diagnosed with an ED who access treatment, recovery is a lengthy process. A longitudinal study found approximately two-thirds of participants with AN or BN had recovered by 22 years follow-up [ 15 ]. Although recovery occurred earlier for those with BN, illness duration was lengthy for both groups with quality of life and physical health impacts [ 15 ]. Further, less is known regarding the illness trajectory for those who do not receive treatment.
Medical comorbidities associated with EDs can range from mild to severe and life-threatening, with complications observed across all body systems, including the cardiac, metabolic and gastrointestinal, and reproductive systems [ 5 ]. These comorbidities and complications can place people at increased risk of medical instability and death [ 5 ]. Therefore, understanding how co-occurring medical comorbidities and complications impact EDs is critical to treatment and recovery.
In addition to ED-associated medical comorbidities, EDs often present alongside other psychiatric conditions. Psychiatric comorbidities in people with EDs are associated with higher health system costs, emergency department presentations and admissions [ 16 ]. Comorbidities may precede the onset of the ED, be co-occurring, or result from symptoms and behaviours associated with the ED [ 17 , 18 ]. Individuals with an ED, their carers and care providers often face a complex and important dilemma; the individual with an ED requires treatment for their ED but also for their psychiatric comorbidities, and it can be difficult for treatment providers to determine which is the clinical priority [ 19 ]. This is further complicated by the fact that EDs and comorbidities may have a reciprocal relationship, whereby the presence of one impact the pathology, treatment and outcomes of the other.
The current Rapid Review (RR) forms part of a series of reviews commissioned by the Australian Federal Government to inform the Australian National Eating Disorders Research and Translation Strategy 2021–2031 [ 20 ]. In response to the impact of psychiatric and medical comorbidities on outcomes, this rapid review summarises the recent literature on the nature and implications of psychiatric and medical comorbidities associated with EDs.
The Australian Government Commonwealth Department of Health funded the InsideOut Institute for Eating Disorders (IOI) to develop the Australian Eating Disorders Research and Translation Strategy 2021–2031 [ 20 ] under the Psych Services for Hard to Reach Groups initiative (ID 4-8MSSLE). The strategy was developed in partnership with state and national stakeholders including clinicians, service providers, researchers, and experts by lived experience (both consumers and families/carers). Developed through a two-year national consultation and collaboration process, the strategy provides the roadmap to establishing EDs as a national research priority and is the first disorder-specific strategy to be developed in consultation with the National Mental Health Commission. To inform the strategy, IOI commissioned Healthcare Management Advisors (HMA) to conduct a series of RRs to assess all available peer-reviewed literature on all DSM-5 listed EDs.
A RR Protocol [ 21 ] was utilised to allow swift synthesis of the evidence in order to guide public policy and decision-making [ 22 ]. This approach has been adopted by several leading health organisations including the World Health Organisation [ 17 ] and the Canadian Agency for Drugs and Technologies in Health Rapid Response Service [ 18 ], to build a strong evidence base in a timely and accelerated manner, without compromising quality. A RR is not designed to be as comprehensive as a systematic review—it is purposive rather than exhaustive and provides actionable evidence to guide health policy [ 23 ].
The RR is a narrative synthesis adhering to the PRISMA guidelines [ 24 ]. It is divided by topic area and presented as a series of papers. Three research databases were searched: ScienceDirect, PubMed and Ovid/Medline. To establish a broad understanding of the progress made in the field of EDs, and to capture the largest evidence base from the past 12 years (originally 2009–2019, but expanded to include the preceding two years), the eligibility criteria for included studies were kept broad. Therefore, included studies were published between 2009 and 2021, written in English, and conducted within Western healthcare systems or health systems comparable to Australia in terms of structure and resourcing. The initial search and review process was conducted by three reviewers between 5 December 2019 and 16 January 2020. The re-run for the years 2020–2021 was conducted by two reviewers at the end of May 2021.
The RR had a translational research focus with the objective of identifying evidence relevant to developing optimal care pathways. Searches therefore used a Population, Intervention, Comparison, Outcome (PICO) approach to identify literature relating to population impact, prevention and early intervention, treatment, and long-term outcomes. Purposive sampling focused on high-level evidence studies encompassing meta-analyses; systematic reviews; moderately sized randomised controlled studies (RCTs) (n > 50); moderately sized controlled-cohort studies (n > 50); and population studies (n > 500). However, the diagnoses ARFID and UFED necessitated less stringent eligibility criteria due to a paucity of published articles. As these diagnoses are newly captured in the DSM-5 (released in 2013, within the allocated search timeframe), the evidence base is still emerging, and few studies have been conducted. Thus, smaller studies (n = ≤ 20) and narrative reviews were also considered and included. Grey literature, such as clinical or practice guidelines, protocol papers (without results) and Masters’ theses or dissertations, were excluded. Other sources (which may not be replicable when applying the current methodology) included the personal libraries of authors, yielding two additional studies (see Additional file 1 ). This extra step was conducted in line with the PRISMA-S: an extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews [ 25 ].
Full methodological details including eligibility criteria, search strategy and terms and data analysis are published in a separate protocol paper, which included a total of 1320 studies [ 26 ] (see Additional file 1 : Fig. S1 for PRISMA flow diagram). Data from included studies relating to psychiatric and medical comorbidities of EDs were synthesised and are presented in the current review. No further analyses were conducted.
The search included articles published in the period January 2009 to May 2021. The RR identified 202 studies for inclusion. Of these, 58% related to psychiatric comorbidities (n = 117) and 42% to medical comorbidities (n = 85). A full list of the studies included in this review and information about population, aims and results can be found in Additional file 2 : Tables S3, S4. Results are subdivided into two categories: (1) psychiatric comorbidities and (2) medical complications. Tables 1 and 2 provide high-level summaries of the results.
Psychiatric comorbidities
The study of psychiatric comorbidities can assist with developing models of ED aetiology, conceptualising psychopathology and has relevance for treatment development and outcomes. Given that common psychological factors are observed across psychiatric disorders [ 87 ], it is not surprising that there are high prevalence rates of co-occurring psychiatric conditions with EDs. Comorbidity rates of EDs and other psychiatric conditions are elevated further in ethnic/racial minority groups [ 88 ]. When looking at the evidence from studies conducted with children and young people, one study of children with ARFID found that 53% of the population had a lifetime comorbid psychiatric disorder [ 89 ]. It emerged from the RR that research regarding psychiatric comorbidities generally focussed on the prevalence rates of comorbidities among certain ED subgroups, with some also exploring implications for treatment and ED psychopathology.
Anxiety disorders
Research indicates that EDs and anxiety disorders frequently co-occur [ 8 , 27 ]. The high prevalence rates of anxiety disorders in the general population are also observed in people with EDs; with a large population study finding anxiety disorders were the most frequently comorbid conditions reported [ 8 ]. In a study of women presenting for ED treatment, 65% also met the criteria for at least one comorbid anxiety disorder [ 28 ]. Of note, 69% of those endorsing the comorbidity also reported that the anxiety disorder preceded the onset of the ED [ 28 ]. Another study explored anxiety across individuals with an ED categorised by three weight ranges (individuals whose weight is in the ‘healthy weight’ range, individuals in the ‘overweight’ range and individuals in the ‘obese’ range). While anxiety was elevated across all groups, the authors did note that individuals in the overweight group reported significantly higher rates of anxiety than individuals within the healthy weight group [ 90 ]. One study that explored temperamental factors provided some insight into factors that may mediate this association; anxiety sensitivity (a predictor of anxiety disorders) was associated with greater ED severity among individuals in a residential ED treatment facility [ 29 ]. Further, this association was mediated by a tendency to engage in experiential avoidance—the authors noting that individuals with greater ED symptoms were more likely to avoid distressing experiences [ 29 ].
Generalised anxiety disorder (GAD)
Studies have noted the potential genetic links between EDs and GAD, noting that the presence of one significantly increases the likelihood of the other [ 8 , 30 ]. Further, there appears to be a relationship between the severity of ED behaviours and the co-occurrence of GAD, with comorbidity more likely when fasting and excessive exercise are present, as well as a lower BMI [ 30 ]. The authors noted the particularly pernicious comorbidity of EDs (specifically AN) and GAD may be amplified by the jointly anxiolytic and weight loss effects of food restriction and excessive exercise [ 30 ].
Social anxiety
A meta-analysis of 12 studies found higher rates of social anxiety across all ED diagnoses, with patients with BN demonstrating the highest rate of comorbidity at 84.5%, followed by both BED and AN-BP both at 75% [ 31 ]. High levels of social anxiety were also associated with more severe ED psychopathology [ 31 ] and higher body weight [ 91 ]. This particular comorbidity may also impact on access to treatment for the ED; a large follow-up study of adolescents found that self-reported social phobia predicted not seeking treatment for BN symptoms [ 32 ]. Interestingly, two studies noted that anxiety symptoms improved following psychological treatments that targeted ED symptoms, possibly due to a shared symptom profile [ 29 , 31 ].
Obsessive–compulsive disorder
Similarities between the symptoms of Obsessive–Compulsive Disorder (OCD) and EDs, such as cognitive rigidity, obsessiveness, detail focus, perfectionism and compulsive routines have long been reported in the literature [ 34 ]. Given the symptom overlap, a meta-analysis sought to clarify the lifetime and current (that is, a current diagnosis at the time of data collection) comorbidity rates of OCD and EDs, noting the lifetime comorbidity rate was 18% and current comorbidity rate was 15% [ 33 ]. However, the authors noted that this prevalence may double over longer periods of observation, with some follow-up data demonstrating comorbidity rates of 33% [ 33 ]. Prevalence rates of OCD seemed to be highest among people with AN (lifetime = 19% and current = 14%) compared to other ED subtypes. In addition to the symptom crossover, this RR found evidence of a complex relationship between OCD and EDs, including a potential association between OCD and greater ED severity [ 34 ].
Network analysis found that doubts about simple everyday things and repeating things over and over bridged between ED and OCD symptoms. Further, a pathway was observed between restricting and checking compulsions and food rigidity as well as binge eating and hoarding. However, as the data was cross-sectional, directional inferences could not be made [ 36 ]. An earlier study explored how changes in OCD symptoms impact ED symptoms among an inpatient sample [ 35 ]. As was hypothesised, decreases in OCD symptoms accounted for significant variance in decreases in ED symptoms, and this effect was strongest among ED patients with comorbid OCD. The study also found that irrespective of whether patients had comorbid OCD or not, when ED symptoms improved, so did symptoms of OCD [ 35 ]. The authors concluded that perhaps there is a reciprocal relationship between OCD and ED symptoms, whereby symptoms of both conditions interact in a synergistic, bidirectional manner, meaning that improvement in one domain can lead to improvement in another [ 35 ]. These findings were somewhat supported in a study by Simpson and colleagues (2013), which found exposure and response prevention (a specialised OCD treatment) resulted in a significant reduction in OCD severity, as was expected, and an improvement in ED symptoms. In their study, individuals with BN showed more improvement than those with AN–nevertheless, BMI still increased among those underweight [ 92 ].
Mood disorders
Depression and major depressive disorder (mdd).
This RR also found high levels of comorbidity between major depression and EDs. A longitudinal study of disordered eating behaviours among adolescents found that disordered eating behaviours and depressive symptoms developed concurrently [ 37 ]. Among the sample, over half the adolescent sample had a depressive disorder. Prevalence rates were similar for AN (51.5%) and BN (54%) [ 37 ]. The study also explored the neurological predictors of comorbid depression in individuals with EDs, noting that lower grey matter volumes in the medial orbitofrontal, dorsomedial, and dorsolateral prefrontal cortices predicted the concurrent development of purging and depressive symptoms [ 37 ]. The results suggested that alterations in frontal brain circuits were part of a neural aetiology common to EDs and depression [ 37 ].
This RR found much support for a strong relationship between depression and ED symptomatology. In a study of patients with AN, comorbid MDD was associated with a greater AN symptom severity [ 93 ], and this relationship between the symptoms of MDD and AN was bidirectional in a study of adolescents undergoing treatment for AN, whereby dietary restraint predicted increased guilt and hostility (symptoms of low mood) and fear predicted further food restriction [ 94 ]. Further studies noted the association between BN, BED and NES, with a higher prevalence of depression and more significant depression symptoms [ 95 , 96 , 97 ]. However, other studies have failed to find support for this association–for example, a Swedish twin study found no association between NES and other mental health disorders [ 98 ].
The impact of the relationship between depression and EDs on treatment outcomes was variable across the studies identified by the RR. One study noted the impact of depression on attrition; patients with BN and comorbid depression attending a university clinic had the highest rates of treatment drop-out [ 99 ]. However, in a sample of patients with AN, the comorbidity of depression (or lack of) did not impact treatment outcome and the severity of depression was not associated with changes in ED symptoms [ 100 ]. This finding was supported in another study of inpatients with AN; pre-treatment depression level did not predict treatment outcome or BMI [ 101 ].
Bipolar disorders
Notable comorbidity rates between bipolar disorders (BD) and EDs were reported in the literature reviewed, however evidence about the frequency of this association was mixed. Studies noted comorbidity rates of BD and EDs ranging between 1.9% to as high as 35.8% [ 38 , 39 , 40 ]. In order to better understand the nature of comorbidity, a recent systematic review and meta-analysis found BD (including bipolar 1 disorder and bipolar 2 disorder) and ED comorbidity varied across different ED diagnostic groups (BED—12.5%, BN—7.4%, AN—3.8%) [ 102 ]. However, the authors noted the scant longitudinal studies available, particularly in paediatric samples. An analysis of comorbidity within a sample of patients with BD identified that 27% of participants also met criteria for an ED; 15% had BN, 12% had BED, and 0.2% had AN [ 103 ]. Two other studies noted considerable comorbidity rates of BD; 18.6% for binge eating [ 104 ] and 8.8% for NES [ 105 ]. Some studies suggested the co-occurrence of BD and EDs were seen most in people with AN-BP, BN and BED—all of which share a binge and/or purge symptom profile [ 38 , 106 ]. Specifically, BED and BN were the most common co-occurring EDs with BD [ 40 ], however, these EDs are also the most prevalent in the population. Therefore, it is unclear if this finding is reflective of the increased prevalence of BN and BED, or if it reflects a shared underlying psychopathology between BD and these EDs [ 40 ].
Comorbid ED-BD patients appear to experience increased ED symptom severity, poorer daily and neuropsychological functioning than patients with only a ED or BD diagnosis [ 107 ]. In an effort to understand which shared features in ED-BD relate to quality of life, one study assessed an adult sample with BD [ 108 ]. Binge eating, restriction, overevaluation of weight and shape, purging and driven exercise were associated with poorer clinical outcomes, quality of life and mood regulation [ 108 ]. Additionally, a study of patients undergoing treatment for BD noted patients with a comorbid ED had significantly poorer clinical outcomes and higher scores of depression [ 109 ]. Further, quality of life was significantly lower among patients with comorbid ED-BD [ 109 ]. The comorbidity of ED and BD has implications for intervention and clinical management, as at least one study observed higher rates of alcohol abuse and suicidality among patients with comorbid ED and BD compared to those with BD only [ 40 ].
Personality disorders
This RR identified limited research regarding the comorbidity between personality disorders (PD) and EDs. A meta-analysis sought to summarise the proportion of comorbid PDs among patients with AN and BN [ 41 ]. There was a heightened association between any type of ED and PDs, and this was significantly different to the general population. For specific PDs, the proportions of paranoid, borderline, avoidant, dependant and obsessive–compulsive PD were significantly higher in EDs than in the general population. For both AN and BN, Cluster C PDs (avoidant, dependant and obsessive–compulsive) were most frequent. The authors noted that the specific comorbidity between specific EDs and PDs appears to be associated with common traits—constriction/perfectionism and rigidity is present in both AN and obsessive–compulsive PD (which had a heightened association), as was the case with impulsivity, a characteristic of both BN and borderline PD [ 41 ]. This symptom association was also observed in a study of adolescents admitted to an ED inpatient unit whereby a significant interaction between binge-purge EDs (AN-BP and BN), childhood emotional abuse (a risk factor for PD) and borderline personality style was found [ 110 ].
This comorbidity may be associated with greater patient distress and have implications for patient outcomes [ 41 , 42 ]. Data from a nine-year observational study of individuals with BN reported that comorbidity with a PD was strongly associated with elevated mortality risk [ 111 ]. In terms of treatment outcomes, an RCT compared the one- and three-year treatment outcomes of four subgroups of women with BN, defined by PD complexity; no comorbid PD (health control), personality difficulties, simple PD and complex PD [ 112 ]. At pre-treatment, the complex PD group had greater ED psychopathology than the other three groups. Despite this initial difference, there were no differences in outcomes between groups at one-year and three-year follow up [ 112 ]. The authors suggested this result could be due to the targeting of the shared symptoms of BN and PD by the intervention delivered in this study, and that as ED symptoms improve, so do PD symptoms [ 112 ]. Suggesting that beyond symptom overlap, perhaps some symptoms attributed to the PD are better explained by the ED. This was consistent with Brietzke and colleagues’ (2011) recommendation that for individuals with ED and a comorbid PD, treatment approaches should target both conditions where possible [ 113 ].
Substance use disorders
Comorbid substance use disorders (SUDs) are also often noted in the literature as an issue that complicates treatment and outcomes of EDs [ 114 ]. A meta-analysis reported the lifetime prevalence of EDs and comorbid SUD was 27.9%, [ 43 ] with a lifetime prevalence of comorbid illicit drug use of 17.2% for AN and 18.6% for BN [ 115 ]. Alcohol, caffeine and tobacco were the most frequently reported comorbidities [ 43 ]. Further analysis of SUDs by substance type in a population-based twin sample indicated that the lifetime prevalence of an alcohol use disorder among individuals with AN was 22.4% [ 115 ]. For BN, the prevalence rate was slightly higher at 24.0% [ 115 ].
The comorbidity of SUD is considered far more common among individuals with binge/purge type EDs, evidenced by a meta-analysis finding higher rates of comorbid SUD among patients with AN-BP and BN than AN-R [ 44 ]. This trend was also observed in population data [ 116 ]. Further, a multi-site study found that patients with BN had higher rates of comorbid SUD than patients with AN, BED and Eating Disorder Not Otherwise Specific (EDNOS) (utilised DSM-IV criteria) [ 117 ]. Behaviourally, there was an association between higher frequencies of binge/purge behaviours with high rates of substance use [ 117 ]. The higher risk of substance abuse among patients with binge/purge symptomology was also associated with younger age of binge eating onset [ 118 ]. A study explored whether BN and ED subtypes with binge/purge symptoms predicted adverse outcomes and found that adolescent girls with purging disorder were significantly more likely to use drugs or frequently binge drink [ 119 ]. This association was again observed in a network analysis of college students, whereby there was an association between binge drinking and increased ED cognitions [ 120 ].
Psychosis and schizophrenia
The RR identified a small body of literature with mixed results regarding the comorbidity of ED and psychosis-spectrum symptoms. A study of patients with schizophrenia found that 12% of participants met full diagnostic criteria for NES, with a further 10% meeting partial criteria [ 45 ]. Miotto and colleagues’ (2010) study noted higher rates of paranoid ideation and psychotic symptoms in ED patients than those observed in healthy controls [ 121 ]. However, the authors concluded that these symptoms were better explained by the participant's ED diagnosis than a psychotic disorder [ 121 ]. At a large population level, an English national survey noted associations between psychotic-like experiences and uncontrolled eating, food dominance and potential EDs [ 122 ]. In particular, these associations were stronger in males [ 122 ]. However, the true comorbidity between psychotic disorders and ED remains unclear and further research is needed.
Body dysmorphic disorder
While body image disturbances common to AN, BN and BED are primarily related to weight and shape concerns, individuals with body dysmorphic disorder (BDD) have additional concerns regarding other aspects of their appearance, such as facial features and skin blemishes [ 46 , 123 ]. AN and BDD share similar psychopathology and both have a peak onset period in adolescence, although BDD development typically precedes AN [ 46 ]. The prevalence rates of BDD among individuals with AN are variable. In one clinical sample of female AN patients, 26% met BDD diagnostic criteria [ 124 ]. However, much higher rates were observed in another clinical sample of adults with AN, where 62% of patients reported clinically significant 'dysmorphic concern' [ 125 ].
As the RR has found with other mental health comorbidities, BDD contributes to greater symptom severity in individuals with AN, making the disorder more difficult to treat. However, some research suggested that improved long-term outcomes from treatments for AN are associated with the integration of strategies that address dysmorphic concerns [ 124 , 126 ]. However, there remains little research on the similarities, differences and co-occurrence of BDD and AN, and with even less research on the cooccurrence of BDD and other EDs.
Neurodevelopmental disorders
Attention deficit hyperactivity disorder
Several studies noted the comorbidity between Attention Deficit Hyperactivity Disorder (ADHD) and EDs. A systematic review found moderate evidence for a positive association between ADHD and disordered eating, particularly between overeating and ADHD [ 47 ]. The impulsivity symptoms of ADHD were particularly associated with BN for all genders, and weaker evidence was found for the association between hyperactivity and restrictive EDs (AN and ARFID) for males, but not females [ 47 ]. Another meta-analysis reported a two-fold increased risk of ADHD in individuals with an ED [ 48 ] and studies have noted particularly strong associations between ADHD and BN [ 49 , 50 ]. In a cohort of adults with a diagnosis of an ED, 31.3% had a 'possible' ADHD [ 127 ]. Another study considered sex differences; women with ADHD had a significantly higher lifetime prevalence of both AN and BN than women without ADHD [ 128 ]. Further, the comorbidity rates for BED were considerably higher among individuals with ADHD for both genders [ 128 ].
Further evidence for a significant association between ADHD and EDs was reported in a population study of children [ 51 ]. Results revealed that children with ADHD were more like to experience an ED or binge, purge, or restrictive behaviours above clinical threshold [ 51 ]. Another study of children with ADHD considered gender differences; boys with ADHD had a greater risk of binge eating than girls [ 129 ]. However, the study found no significant difference in AN's prevalence between ADHD and non-ADHD groups. Further, among patients attending an ED specialist clinic, those with comorbid ADHD symptoms had poorer outcomes at one-year follow-up [ 130 ].
Autism spectrum disorder
There is evidence of heightened prevalence rates of autism spectrum disorder (ASD) among individuals with EDs. A systematic review found an average prevalence of ASD with EDs of 22.9% compared with 2% observed in the general population [ 52 ]. With regards to AN, several studies have found symptoms of ASD to be frequently exhibited by patients with AN [ 53 , 54 ]. An assessment of common phenomena between ARFID and ASD in children found a shared symptom profile of eating difficulties, behavioural problems and sensory hypersensitivity beyond what is observed in typically developing children (the control group) [ 55 ]. While research in this area is developing, the findings indicated these comorbidities would likely have implications for the treatment and management of both conditions [ 55 ].
Post traumatic stress disorder
Many individuals with EDs report historical traumatic experiences, and for a proportion of the population, symptoms of post traumatic stress disorder (PTSD). A broad range of prevalence rates between PTSD and EDs have been reported; between 16.1–22.7% for AN, 32.4–66.2% for BN and 24.02–31.6% for BED [ 56 ]. A review noted self-criticism, low self-worth, guilt, shame, depression, anxiety, emotion dysregulation, anger and impulsivity were linked to the association between EDs and trauma [ 57 ]. It was suggested that for individuals with trauma/PTSD, EDs might have a functional role to manage PTSD symptoms and reduce negative affect [ 57 ]. Further, some ED behaviours such as restriction, binge eating, and purging may be used to avoid hyperarousal, in turn maintaining the association between EDs and PTSD [ 57 ].
Few studies have explored the impact of comorbid PTSD on ED treatment outcomes. A study of inpatients admitted to a residential ED treatment service investigated whether PTSD diagnosis at admission was associated with symptom changes [ 56 ]. Cognitive and behavioural symptoms related to the ED had decreased at discharge, however, they increased again at six-month follow up. In contrast, while PTSD diagnosis was associated with higher baseline ED symptoms, it was not related to symptom change throughout treatment or treatment dropout [ 56 ]. Given previous research identified that PTSD and EDs tend to relate to more complex courses of illness, greater rates of drop out and poorer outcomes, a study by Brewerton and colleagues [ 131 ], explored the presence of EDs in patients with PTSD admitted to a residential setting. Results showed that patients with PTSD had significantly higher scores of ED psychopathology, as well as depression, anxiety and quality of life. [ 131 ]. Further, those with PTSD had a greater tendency for binge-type EDs.
Suicidality
Suicide is one of the leading causes of death for individuals with EDs [ 58 ]. In a longitudinal study of adolescents, almost one quarter had attempted suicide, and 65% reported suicidal ideation within the past 6 months [ 37 ]. EDs are a significant risk factor for suicide, with some evidence suggesting a genetic association between suicide risk and EDs [ 59 , 60 ]. This association was supported in the analysis of Swedish population registry data, which found that individuals with a sibling with an ED had an increased risk of suicide attempts with an odds ratio of 1.4 (relative cohort n = 1,680,658) [ 61 ]. For suicide attempts, this study found an even higher odds ratio of 5.28 (relative cohort n = 2,268,786) for individuals with an ED and 5.39 (relative cohort n = 1,919,114) for death by suicide [ 61 ]. A comparison of individuals with AN and BN indicated that risk for suicide attempts was higher for those with BN compared to AN [ 61 ]. However, the opposite was true for death by suicide; which was higher in AN compared to BN [ 61 ]. This result is consistent with the findings of a meta-analysis—the incidence of suicide was higher among patients with AN compared to those with BN or BED [ 62 ].
The higher incidence of suicide in adults with AN [ 132 ] is potentially explained by the findings from Guillaume and colleagues (2011), which suggested that comparative to BN, AN patients are more likely to have more serious suicide attempts resulting in a higher risk of death [ 133 ]. However, death by suicide remains a significant risk for both diagnoses. As an example, Udo and colleagues (2019) study reported that suicide attempts were more common in those with an AN-BP subtype (44.1%) than AN-R (15.7%), or BN (31.4%) [ 134 ]. Further, in a large cohort of transgender college students with EDs, rates of past-year suicidal ideation (a significant risk factor for suicide attempts) was 75.2%, and suicide attempts were 74.8%, significantly higher than cisgender students with EDs and transgender students without EDs [ 135 ]. The RR found that the risk of suicidal ideation and behaviour was associated with ED diagnosis and the presence of other comorbidities. Among a community-based sample of female college students diagnosed with an ED, 25.6% reported suicidal ideation, and this was positively correlated with depression, anxiety and purging [ 136 ]. In support of this evidence, Sagiv and Gvion (2020) proposed a dual pathway model of risk of suicide attempt in individuals with ED, which implicates trait impulsivity and comorbid depression [ 137 ]. In two large transdiagnostic ED patient samples, suicidal ideation was associated with different aspects of self-image between ED diagnoses. For example, suicidal ideation was associated with higher levels of self-blame among individuals with BED, while among patients with AN and OSFED, increased suicidal ideation was associated with a lack of self-love [ 138 , 139 ].
Anorexia nervosa
Amongst adults with AN, higher rates of suicide have been reported amongst those with a binge-purge subtype (25%) than restrictive subtype (8.65%) [ 58 , 140 ]. Further, comorbid depression and prolonged starvation were strongly associated with elevated suicide attempts for both subtypes [ 58 , 140 ]. In another study, the risk of attempted suicide was associated with depression, but it was moderated by hospital treatment [ 93 ]. Further, suicidal ideation was related to depression. A significant 'acquired' suicide risk in individuals with AN has been identified by Selby et al. (2010) through an increased tolerance for pain and discomfort resultant from repeated exposure to painful restricting and purging behaviours [ 141 ].
Bulimia nervosa
Further research among individuals diagnosed with BN found an increased level of suicide risk [ 142 ]. Results from an extensive study of women with BN indicated that the lifetime prevalence of suicide attempts in this cohort was 26.9% [ 143 ]. In one study of individuals diagnosed with severe BN, 60% of deaths were attributed to suicide [ 144 ]. The mean age at the time of death was 29.6 years, and predictive factors included previous suicide attempts and low BMI. Further, in a sample of children and adolescents aged 7 to 18 years, higher rates of suicidal ideation were associated with BN, self-induced vomiting and a history of trauma [ 12 ].
A large population-based study of adolescents and adults explored the frequency and correlates of suicidal ideation and attempts in those who met the criteria for BN [ 145 ]. Suicidal ideation was highest in adolescents with BN (53%), followed by BED (34.4%), other non-ED psychopathology (21.3%) or no psychopathology (3.8%). A similar trend was observed for suicide plans and attempts [ 145 ]. However, for adults, suicidality was more prevalent in the BN group compared to no psychopathology, but not statistically different to the AN, BED or other psychopathology groups [ 145 ].
Consistent with Crow and colleagues’ (2014) results, in a sample of women with BN, depression had the strongest association with lifetime suicide attempts [ 146 ]. There were also associations between identity problems, cognitive dysregulation, anxiousness, insecure attachment and lifetime suicide attempts among the sample. Depression was the most pertinent association, suggesting that potential comorbid depression should be a focus of assessment and treatment among individuals with BN due to the elevated suicide risk for this group [ 146 ]. Insecure attachment is associated with childhood trauma, and a systematic review found that suicide attempts in women with BN were significantly associated with childhood abuse and familial history of EDs [ 58 ].
Binge eating disorder
The RR found mixed evidence for the association between suicidal behaviour and BED. A meta-analysis found no suicides for patients with BED [ 62 ]. However, evidence from two separate large national surveys found that a significant proportion of individuals who had a suicide attempt also had a diagnosis of BED [ 134 , 147 ].
Non-suicidal self injury
Non-suicidal self-injury (NSSI), broadly defined, is the intentional harm inflicted to one’s body without intent to die [ 148 ]. Recognising NSSI is often a precursor for suicidal ideation and behaviour [ 149 ], together with the already heightened mortality rate for EDs, several studies have examined the association between EDs and NSSI. Up to one-third of patients with EDs report NSSI at some stage in their lifetime, with over one quarter having engaged in NSSI within the previous year [ 63 ]. Similarly, a cohort study [ 148 ] found elevated rates of historical NSSI amongst patients with DSM-IV EDs; specifically EDNOS (49%), BN (41%) and AN (26%). In a Spanish sample of ED patients, the most prevalent form of NSSI was banging (64.6%) and cutting (56.9%) [ 63 ].
Further research has explored the individual factors associated with heightened rates of NSSI. Higher levels of impulsivity among patients with EDs have been associated with concomitant NSSI [ 64 ]. This was demonstrated in a longitudinal study of female students, whereby NSSI preceded purging, marking it a potential risk factor for ED onset [ 65 ]. In a study of a large clinical sample of patients with EDs and co-occurring NSSI, significantly higher levels of emotional reactivity were observed [ 150 ]. The highest levels of emotional reactivity were reported by individuals with a diagnosis of BN, who were also more likely to engage in NSSI than those with AN [ 150 ]. In Olatunji and colleagues’ (2015) cohort study, NSSI was used to regulate difficult emotions, much like other ED behaviours. NSSI functioning as a means to manage negative affect associated with EDs was further supported by Muehlenkamp and colleagues’ [ 66 ] study exploring the risk factors in inpatients admitted for an ED. The authors found significant differences in the prevalence of NSSI across ED diagnoses, although patients with binge/purge subtype EDs were more likely to engage in poly-NSSI (multiple types of NSSI). Consistent with these findings, a study of patients admitted to an ED inpatient unit found that 45% of patients displayed at least one type of NSSI [ 151 ]. The function of NSSI among ED patients was explored in two studies, one noting that avoiding or suppressing negative feelings was the most frequently reported reason for NSSI [ 151 ]. The other analysed a series of interviews and self-report questionnaires and found patients with ED and comorbid Borderline Personality Disorder (BPD) engaged in NSSI as a means of emotion regulation [ 152 ].
Medical comorbidities
The impact of EDs on physical health and the consequential medical comorbidities has been a focus of research. Many studies reported medical comorbidities resulting from prolonged malnutrition, as well as excessive exercise, binging and purging behaviours.
Cardiovascular complications
As discussed above, although suicide is a significant contributor to the mortality rate of EDs, physical and medical complications remain the primary cause of death, particularly in AN, with a high proportion of deaths thought to result from cardiovascular complications [ 153 ]. AN has attracted the most research focus given its increased risk of cardiac failure due to severe malnutrition, dehydration and electrolyte imbalances [ 67 ].
Cardiovascular complications in AN can be divided by conduction, structural and ischemic diseases. A review found that up to 87% of patients experience cardiovascular compromise shortly following onset of AN [ 153 ]. Within conduction disease, bradycardia and QT prolongation occur at a high frequency, largely due to low body weight and resultant decreased venous return to the heart. Whereas, atrioventricular block and ventricular arrhythmia are more rare [ 153 ]. Various structural cardiomyopathies are observed in AN, such as low left ventricular mass index (occurs frequently), mitral prolapse and percardial effusion (occurs moderately). Ischemic diseases such as dyslipidemia or acute myocardial infarction are more rare.
Another review identified cardiopulmonary abnormalities that are frequently observed in AN; mitral valve prolapse occurred in 25% of patients, sinus bradycardia was the most common arrhythmia, and pericardial effusion prevalence rates ranged from 15 to 30%. [ 68 ] Sudden cardiac death is thought to occur due to increased QT interval dispersion and heart rate variability. [ 68 ] A review of an inpatient database in a large retrospective cohort study found that coronary artery disease (CAD) was lower in AN patients than the general population (4.4% and 18.4%, respectively). Consistent with trends in the general population, the risk of cardiac arrest, arrhythmias and heart failure was higher in males with AN than females with AN [ 69 ].
Given that individuals with AN have compromised biology, may avoid medical care, and have higher rates of substance use, research has examined cancer incidence and prognosis among individuals with AN. A retrospective study noted higher mortality from melanoma, cancers of genital organs and cancers of unspecified sites among individuals with AN, however, there was no statistically significant difference compared to the general population [ 70 ]. No further studies of cancer in EDs were identified.
Gastrointestinal disorders
The gastrointestinal (GI) system plays a pivotal role in the development, maintenance, and treatment outcomes for EDs, with changes and implications present throughout the GI tract. More than 90% of AN patients report fullness, early satiety, abdominal distention, pain and nausea [ 68 ]. Although it is well understood that GI system complaints are complicated and exacerbated by malnutrition, purging and binge eating [ 154 , 155 ], the actual cause of the increased prevalence of GI disorders and their contribution to ED maintenance remain poorly understood.
To this end, a review aimed to determine the GI symptoms reported in two restrictive disorders (AN and ARFID), as well as the physiologic changes as a result of malnutrition and function of low body weight and the contribution of GI diseases to the disordered eating observed in AN and ARFID [ 156 ]. The review found mixed evidence regarding whether GI issues were increased in patients with AN and ARFID. This was partly due to the relatively limited amount of research in this area and mixed results across the literature. The review noted that patients with AN and ARFID reported a higher frequency of symptoms of gastroparesis. Further, there was evidence for a bidirectional relationship between AN and functional gastrointestinal disorders (FGIDs) contributing to ongoing disordered eating. The review found that GI symptoms observed in EDs develop due to (1) poorly treated medical conditions with GI-predominant symptoms, (2) the physiological and anatomical changes that develop due to malnutrition or (3) FGIDs.
There was a high rate of comorbidity (93%) between ED and FGIDs, including oesophageal, bowel and anorectal disorders, in a patient sample with AN, BN and EDNOS [ 157 ]. A retrospective study investigating increased rates of oesophageal cancer in individuals with a history of EDs could not conclude that risk was associated with purging over other confounding factors such as alcohol abuse and smoking [ 158 ].
Given that gut peptides like ghrelin, cholecystokinin (CCK), peptide tyrosine (PYY) and glucagon-like peptide 1 (GLP-1) are known to influence food intake, attention has focussed on the dysregulation of gut peptide signalling in EDs [ 159 ]. A review aimed to discuss how these peptides or the signals triggered by their release are dysregulated in EDs and whether they are normalised following weight restoration or weight loss (in the case of people with higher body weight) [ 159 ]. The results were inconsistent, with significant variability in peptide dysregulation observed across EDs [ 159 ]. A systematic review and meta-analysis explored whether ghrelin is increased in restrictive AN. The review found that all forms of ghrelin were raised in AN’s acute state during fasting [ 160 ]. In addition, the data did not support differences in ghrelin levels between AN subtypes [ 160 ]. Another study examined levels of orexigenic ghrelin and anorexigenic peptide YY (PYY) in young females with ARFID, AN and healthy controls (HC) [ 161 ]. Results demonstrated that fasting and postprandial ghrelin were lower in ARFID than AN, but there was no difference between ARFID and AN for fasting and postprandial PYY [ 161 ].
Oesophageal and gastrointestinal dysfunction have been observed in patients with AN and complicate nutritional and refeeding interventions [ 155 ]. Findings from a systematic review indicated that structural changes that occurred in the GI tract of patients with AN impacted their ability to swallow and absorb nutrients [ 162 ]. Interestingly, no differences in the severity of gastrointestinal symptoms were observed between AN-R and AN-BP subtypes [ 155 ].
A systematic review of thirteen studies aimed to identify the most effective treatment approaches for GI disorders and AN [ 163 ]. An improvement in at least one or more GI symptoms was reported in 11 of the 13 studies, with all studies including nutritional rehabilitation, and half also included concurrent psychological treatment [ 163 ]. Emerging evidence on ED comorbidity with chronic GI disorders suggested that EDs are often misdiagnosed in children and adolescents due to the crossover of symptoms. Therefore, clinicians treating children and adolescents for GI dysfunction should be aware of potential EDs and conduct appropriate screening [ 164 ]. There has been an emerging focus on the role of the gut microbiome in the regulation of core ED symptoms and psychophysiology. Increased attention is being paid to how the macronutrient composition of nutritional rehabilitation should be considered to maximise treatment outcomes. A review found that high fibre consumption in addition to prebiotic and probiotic supplementation helped balance the gut microbiome and maintained the results of refeeding [ 165 ].
Bone health
The RR found evidence for bone loss/poor bone mineral density (BMD) and EDs, particularly in AN. The high rates of bone resorption observed in patients with AN is a consequence of chronic malnutrition leading to osteoporosis (weak and brittle bones), increased fracture risk and scoliosis [ 166 ]. The negative impacts of bone loss are more pronounced in individuals with early-onset AN when the skeleton is still developing [ 67 ] and among those who have very low BMI [ 71 ], with comorbidity rates as high as 46.9% [ 71 ]. However, lowered BMD was also observed among patients with BN [ 72 ].
A review [ 167 ] explored the prevalence and differences in pathophysiology of osteoporosis and fractures in patients with AN-R and AN-BP. AN-R patients had a higher prevalence of osteoporosis, and AN-BP patients had a higher prevalence of osteopenia (loss of BMD) [ 167 ]. Further, the authors noted the significant increase in fracture risk that starts at disease onset and lasts throughout AN, with some evidence that risk remains increased beyond remission and recovery [ 167 ]. Findings from a longitudinal study of female patients with a history of adolescent AN found long-term bone thinning at five and ten-year follow-up despite these patients achieving weight restoration [ 168 ].
Given this, treatment to increase BMD in individuals with AN has been the objective of many pharmacotherapy trials, mainly investigating the efficacy of hormone replacement [ 169 , 170 ]. Treatments include oestrogen and oral contraceptives [ 169 , 170 , 171 , 172 ]; bisphosphonates [ 169 , 173 ]; other hormonal treatment [ 174 , 175 , 176 , 177 ] and vitamin D [ 178 ]. However, the outcomes of these studies were mixed.
Refeeding syndrome
Nutritional rehabilitation of severely malnourished individuals is central to routine care and medical stabilisation of patients with EDs [ 179 ]. Within inpatient treatment settings, reversing severe malnutrition is achieved using oral, or nasogastric tube feeding. However, following a period of starvation, initiating/commencing feeding has been associated with ‘refeeding syndrome’ (RFS), a potentially fatal electrolyte imbalance caused by the body's response to introducing nutritional restoration [ 180 , 181 ]. The studies identified in the RR focused predominantly on restrictive EDs/on this population group—results regarding RFS risk were mixed [ 73 ].
A retrospective cohort study of inpatients diagnosed with AN with a very low BMI implemented a nasogastric feeding routine with vitamin, potassium and phosphate supplementation [ 182 ]. All patients achieved a significant increase in body weight. None developed RFS [ 182 ], suggesting that even with extreme undernutrition, cautious feeding within a specialised unit can be done safely without RFS. For adults with AN, aminotransferases are often high upon admission, however are normalised following four weeks of enteral feeding [ 183 , 184 ]. Further, the RR identified several studies demonstrating the provision of a higher caloric diet at intake to adolescents with AN led to faster recoveries and fewer days in the hospital with no observed increased risk for RFS [ 75 , 76 , 77 ]. These findings were also noted in a study of adults with AN [ 179 ].
However, the prevalence of RFS among inpatients is highly variable, with one systematic review noting rates ranging from 0 to 62% [ 74 ]. This variability was largely a reflection of the different definitions of RFS used across the literature [ 74 ]. A retrospective review of medical records of patients with AN admitted to Intensive Care Units (ICUs) aimed to evaluate complications, particularly RFS, that occurred during the ICU stay and the impact of these complications on treatment outcomes [ 185 ]. Of the 68 patients (62 female), seven developed RFS (10.3%) [ 185 ].
Although easily detectable and treatable, hypophosphatemia (a low serum phosphate concentration) may lead to RFS which is the term used to describe severe fluid and electrolyte shifts that can occur when nutrition support is introduced after a period of starvation. Untreated hypophosphatemia may lead to characteristic signs of the RFS such as respiratory failure, heart failure, and seizures [ 76 , 179 , 186 , 187 , 188 ]. A retrospective case–control study of inpatients with severe AN identified [ 189 ]. A retrospective study of AN and atypical AN patients undergoing refeeding found that the risk of hypophosphatemia was associated with a higher level of total weight loss and recent weight loss rather than the patient’s weight at admission [ 190 ]. The safe and effective use of prophylactic phosphate supplementation during refeeding was supported by the results from Agostino and colleagues’ chart review study [ 191 ], where 90% of inpatients received supplementation during admission.
Higher calorie refeeding approaches are considered safe in most cases, however the steps necessitated to monitor health status are costly to health services [ 192 ]. The most cost-effective approach would likely involve prophylactic electrolyte supplementation in addition to high calorie refeeding, which would decrease the need for daily laboratory monitoring as well as shortening hospital stays [ 75 , 191 , 192 ]. A systematic review noted that much of the research regarding refeeding, particularly in children and young people, has been limited by small sample sizes, single-site studies and heterogeneous designs [ 181 ]. Further, the differing definitions of RFS, recovery, remission and outcomes leading to variable results. While RFS appears safe for many people requiring feeding, the risk and benefits of it are unclear [ 193 ] due to the limited research on this topic. Following current clinical practice guidelines on the safe introduction of nutrition is recommended.
Metabolic syndrome
Metabolic syndrome refers to a group of factors that increase risks for heart disease, diabetes, stroke and other related conditions [ 194 ]. Metabolic syndrome is conceptualised as five key criteria; (1) elevated waist circumference, (2) elevated triglyceride levels, (3) reduced HDL-C, (4) elevated blood pressure and (5) elevated fasting glucose. The binge eating behaviours exhibited in BN, BED and NES have been linked to the higher rates of metabolic syndrome observed in these ED patients [ 78 , 195 ].
An analysis of population data of medical comorbidities with BED noted the strongest associations were with diabetes and circulatory systems, likely indexing components of metabolic syndrome [ 196 ]. While type 1 diabetes is considered a risk factor for ED development, both BN and BED have increased risk for type 2 diabetes [ 78 ]. A 16-year observation study found that the risk of type 2 diabetes was significantly increased in male patients with BED compared to the community controls [ 78 ]. By the end of the observation period, 33% of patients with BED had developed type 2 diabetes compared to 1.7% of the control group. The prevalence of type 2 diabetes among patients with BN was also slightly elevated at 4.4% [ 78 ]. Importantly, the authors were not able to control for BMI in this study. In another study, BED was the most prevalent ED in a cohort of type 2 diabetes patients [ 197 ]. Conversely, the prevalence of AN among patients with type 2 diabetes is significantly lower, with a review of national data reporting comorbidity rates to be 0.06% [ 198 ].
Metabolic dysfunction was observed in a relatively large sample of individuals with NES, including metabolic syndrome and type 2 diabetes, with women reporting slightly higher rates (13%) than men (11%) [ 199 ]. In another group of adults with type 2 diabetes, 7% met the diagnostic criteria for NES [ 200 ]. These findings suggested a need for increased monitoring and treatment of type 2 diabetes in individuals with EDs, particularly BED and NES. Another study found BED had a significant impact on metabolic abnormalities, including elevated cholesterol and poor glycaemic control [ 201 ].
The RR identified one intervention study, which examined an intervention to address medical comorbidities associated with BN and BED [ 195 ]. The study compared cognitive behaviour therapy (CBT) to an exercise and nutrition intervention to increase physical fitness, decrease body fat percentage and reduce the risk for metabolic syndrome. While the exercise intervention improved participants' physical fitness and body composition, neither group reduced cardiovascular risk at one-year follow-up [ 195 ].
Oral health
Purging behaviour, particularly self-induced vomiting, has been associated with several oral health and gastrointestinal dysfunctions in patients with EDs. A case–control study of ED patients with binge/purge symptomology found that despite ED patients reporting an increased concern for dental issues and engaging in more frequent brushing, their oral health was poorer than controls. [ 79 ] Further, a systematic review and meta-analysis aimed to explore whether EDs increase the risk of tooth erosion [ 80 ]. The analysis found that patients with EDs had more risk of dental erosion, especially among those who self-induced vomiting [ 80 ]. These findings were also found in a large cohort study, where the increased risk for BN was associated with higher rates of dental erosion but not dental cavities [ 81 ].
However, a systematic review of 10 studies suggested that poor oral health may be common among ED patients irrespective of whether self-induced vomiting forms part of their psychopathology [ 202 ]. One study reported that AN-R patients had poorer oral health outcomes and tooth decay than BN patients [ 203 ]. Two studies identified associations between NES and poor oral health, including higher rates of missing teeth, periodontal disease [ 204 , 205 ]. Another study of a group of patients with AN, BN and EDNOS, demonstrated the impact of ED behaviours on dental soft tissue, whereby 94% of patients had oral mucosal lesions, and 3% were found to have dental erosion [ 206 ].
Vitamin deficiencies
The prolonged periods of starvation, food restriction (of caloric intake and/or food groups), purging and excessive exercise observed across the ED spectrum have detrimental impacts on micronutrient balances [ 207 ]. The impact of prolonged vitamin deficiencies in early-onset EDs can also impair brain development, substantially reducing neurocognitive function in some younger patients even after weight restoration [ 82 ]. Common micronutrient deficiencies include calcium, fat soluble vitamins, essential fatty acids selenium, zinc and B vitamins [ 183 ]. One included study looked at prevalence rates of cerebral atrophy and neurological conditions, specifically Wernicke's encephalopathy in EDs and found that these neurological conditions were very rare in people with EDs [ 208 ].
Cognitive functioning
The literature included in RR regarding the cognitive changes in ED patients with AN following weight gain was sparse. It appears that some cognitive functions affected by EDs recover following nutritional restoration, whereas others persist. Cognitive functions, such as flexibility, central coherence, decision making, attention, processing speed and memory, are hypothesised to be impacted by, and influence the maintenance of EDs. A systematic review explored whether cognitive functions improved in AN following weight gain [ 83 ]. Weight gain appeared to be associated with improved processing speed in children and adolescents. However, no improvement was observed in cognitive flexibility following weight gain. Further, the results for adults were inconclusive [ 83 ].
Reproductive health
Infertility and higher rates of poor reproductive health are strongly associated with EDs, including miscarriages, induced abortions, obstetric complications, and poorer birth outcomes [ 84 , 85 ]. Although amenorrhea is a known consequence of AN, oligomenorrhea (irregular periods) was common among individuals with BN and BED [ 86 ]. A twin study found women diagnosed with BN and BED were also more likely to have poly cystic ovarian syndrome (PCOS), leading to menstrual irregularities [ 209 ]. The prevalence of lifetime amenorrhea in this sample was 10.4%, and lifetime oligomenorrhea was 33.7%. An epidemiological study explored the association of premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD) in women with BN and BED and found prevalence rates as high as 42.4% for PMS and 4.2% for PMDD [ 210 ].
Given the increased rates of menstrual irregularities and issues, questions have been raised regarding whether this complication is reversed or improves with recovery. A review of five studies monitoring reproductive functions during recovery over a 6- to 18-year follow up period [ 211 ] noted no significant difference between the pooled odds of childbirth rates between the AN and general population—demonstrating that if patients undergo treatment for AN, achieve weight restoration, and continue to maintain wellness, reproductive functions can renormalise [ 211 ].
An observational study of women with AN, BN or EDNOS found higher rates of low birth rate, pre-term deliveries, caesarean deliveries, and intrauterine growth restrictions [ 84 ]. Increased caesarean delivery was also observed in a large cohort of women diagnosed with BED [ 212 ]. However, these women had higher birth weight babies [ 212 ]. Further, women with comorbid ED and epilepsy were found to have an increased risk of pregnancy-related comorbidities, including preeclampsia (gestational hypertension and signs of damage to the liver and kidneys ) , gestational diabetes and perinatal depression [ 213 ].
The results from this review identified that the symptomology and outcomes of EDs are impacted by both psychiatric and medical factors. Further, EDs have a mortality rate substantially higher than the general population, with a significant proportion of those who die from an ED dying by suicide or as a result of severe medical complications.
This RR noted high rates of psychiatric and medical comorbidities in people with EDs, with comorbidities contributing to increased ED symptom severity, maintenance of some ED behaviours, compromised functioning, and adverse treatment outcomes. Evidence suggested that early identification and management of psychiatric and medical comorbidities in people with an ED may improve response to treatment and outcomes [ 29 , 35 , 83 ].
EDs and other psychiatric conditions often shared symptoms and high levels of psychopathology crossover were noted. The most prevalent psychiatric comorbidities were anxiety disorders, mood disorders and substance use disorders [ 8 , 100 , 119 ]. perhaps unsurprising given the prevalence of these illnesses in the general population. Of concern is the elevated suicide rate noted across the ED spectrum, the highest observed in AN [ 58 , 140 , 149 ]. For people with AN, suicide attempts were mostly associated with comorbid mood and anxiety disorders [ 136 ]. The review noted elevated rates of NSSI were particularly associated with binge/purge subtype EDs [ 150 ], impulsivity and emotional dysregulation (again, an example of psychopathological overlap).
With regards to PDs, studies were limited to EDs with binge-purge symptomology. Of those included, the presence of a comorbid personality disorder and ED was associated with childhood trauma [ 110 ] and elevated mortality risk [ 111 ]. There appeared to be a link between the clinical characteristics of the ED (e.g., impulsivity, rigidity) and the comorbid PD (cluster B PDs were more associated with BN/BED and cluster C PDs were more associated with AN). There was mixed (albeit limited) evidence regarding the comorbidity between EDs and psychosis and schizophrenia, with some studies noting an association between EDs and psychotic experiences [ 45 ]. Specifically, there was an association between psychotic experiences and uncontrolled eating and food dominance, which were stronger in males [ 122 ]. In addition, the review noted the association between EDs and neurodevelopmental disorders-specifically ADHD—was associated with features of BN and ASD was more prevalent among individuals with AN [ 53 , 54 ] and ARFID [ 55 ].
EDs are complicated by medical comorbidities across the neuroendocrine, skeletal, nutritional, gastrointestinal, dental, and reproductive systems that can occur alongside, or result from the ED. The RR noted mixed evidence regarding the effectiveness and safety of enteral feeding [ 180 , 181 ], with some studies noting that RFS could be safely managed with supplementation [ 191 ]. Research also described the impacts of restrictive EDs on BMD and binge eating behaviour on metabolic disorders [ 78 , 195 ]. Purging behaviours, particularly self-induced vomiting [ 79 ], were found to increase the risk of tooth erosion [ 81 ] and damage to soft tissue within the gastrointestinal tract [ 206 ]. Further, EDs were associated with a range of reproductive health issues in women, including infertility and birth complications [ 84 ].
Whilst the RR achieved its aim of synthesising a broad scope of literature, the absence of particular ED diagnoses and other key research gaps are worth noting. A large portion of the studies identified focused on AN, for both psychiatric and medical comorbidities. This reflects the stark lack of research exploring the comorbidities for ARFID, NES, and OSFED compared to that seen with AN, BN and BED. There were no studies identified exploring the psychiatric and medical comorbidities of Pica. These gaps could in part be due to the timeline utilised in the RR search strategy, which included the transition from DSM-IV to DSM-5. The update in the DSM had significant implications for psychiatric diagnosis, with the addition of new disorders (such as Autism Spectrum Disorder and various Depressive Disorders), reorganisation (for example, moving OCD and PTSD out of anxiety disorders and into newly defined chapters) and changes in diagnostic criteria (including for AN and BN, and establishing BED as a discrete disorder). Although current understanding suggests EDs are more prevalent in females, research is increasingly demonstrating that males are not immune to ED symptoms, and the RR highlighted the disproportionate lack of male subjects included in recent ED research, particularly in the domain of psychiatric and medical comorbidities.
As the RR was broad in scope and policy-driven in intent, limitations as a result of this methodology ought to be considered. The RR only considered ‘Western’ studies, leading to the potential of important pieces of work not being included in the synthesis. In the interest of achieving a rapid synthesis, grey literature, qualitative and theoretical works, case studies or implementation research were not included, risking a loss of nuance in developing fields, such as the association and prevalence of complex/developmental trauma with EDs (most research on this comorbidity focuses on PTSD, not complex or developmental trauma) or body image dissatisfaction among different gender groups. No studies regarding the association between dissociative disorders and EDs were included in the review. However, dissociation can co-occur with EDs, particularly AN-BP and among those with a trauma history [ 214 ]. Future studies would benefit from exploring this association further, particularly as trauma becomes more recognised as a risk factor for ED development.
The review was not designed to be an exhaustive summary of all medical comorbidities. Thus, some areas of medical comorbidity may not be included, or there may be variability in the level of detail included (such as, limited studies regarding the association between cancer and EDs). Studies that explored the association between other autoimmune disorders (such as Type 1 Diabetes, Crohn’s disease, Addison’s disease, ulcerative colitis, and coeliac disease) and EDs [ 215 , 216 ] were not included. Future reviews and research should examine the associations between autoimmune disorders and the subsequent increased risk of EDs, and likewise, the association between EDs and the subsequent risk of autoimmune disorders.
An important challenge for future research is to explore the impact of comorbidity on ED identification, development and treatment processes and outcomes. Insights could be gained from exploring shared psychiatric symptomology (i.e., ARFID and ASD, BN/BED and personality disorders, and food addiction). Particularly in disorders where the psychiatric comorbidity appears to precede the ED diagnosis (as may be the case in anxiety disorders [ 28 ]) and the unique physiological complications of these EDs (e.g., the impact of ARFID on childhood development and growth). Further, treatment outcomes would benefit from future research exploring the nature of the proposed reciprocal nature between EDs and comorbidities, particularly in those instances where there is significant shared psychopathology, or the presence of ED symptoms appears to exacerbate the symptoms of the other condition—and vice versa.
The majority of research regarding the newly introduced EDs has focused on understanding their aetiology, psychopathology, and what treatments demonstrate efficacy. Further, some areas included in the review had limited included studies, for example cancer and EDs. Thus, in addition to the already discussed need for further review regarding the association between EDs and autoimmune disorders, future research should explore the nature and prevalence of comorbidity between cancers and EDs. There was variability regarding the balance of child/adolescent and adult studies across the various comorbidities. Some comorbidities are heavily researched in child and adolescent populations (such as refeeding syndrome) and others there is stark child and adolescent inclusion, with included studies only looking at adult samples. Future studies should also address specific comorbidities as they apply to groups underrepresented in current research. This includes but is not limited to gender, sexual and racial minorities, whereby prevalence rates of psychiatric comorbidities are elevated. [ 88 ] In addition, future research would benefit from considering the nature of psychiatric and medical comorbidity for subthreshold and subclinical EDs, particularly as it pertains to an opportunity to identify EDs early within certain comorbidities where ED risk is heightened.
This review has identified the psychiatric and medical comorbidities of EDs, for which there is a substantial level of literature, as well as other areas requiring further investigation. EDs are associated with a myriad of psychiatric and medical comorbidities which have significant impacts on the symptomology and outcomes of an already difficult to treat, and burdensome illness.
Availability of data and materials
Not applicable—all citations provided.
Abbreviations
Anorexia nervosa—restricting type
Anorexia nervosa—binge-purge type
Avoidant restrictive food intake disorder
Body mass index
Borderline personality disorder
Diagnostic and statistical manual of mental disorders, 5th edition
Eating disorder
Generalised anxiety disorder
International classification of diseases, 11th edition
Major depressive disorder
Night eating syndrome
Other specified feeding or eating disorder
Post-traumatic stress disorder
Rapid review
Brandsma L. Eating disorders across the lifespan. J Women Aging. 2007;19(1–2):155–72.
Article PubMed Google Scholar
van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr Opin Psychiatry. 2020;33(6):521–7.
Article PubMed PubMed Central Google Scholar
Weigel A, Löwe B, Kohlmann S. Severity of somatic symptoms in outpatients with anorexia and bulimia nervosa. Eur Eat Disord Rev. 2019;27(2):195–204.
Hudson JI, Hiripi E, Pope HG Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61(3):348–58.
Jahraus J. Medical complications of eating disorders. Psychiatr Ann. 2018;48(10):463–7.
Article Google Scholar
Udo T, Grilo CM. Psychiatric and medical correlates of DSM-5 eating disorders in a nationally representative sample of adults in the United States. Int J Eat Disord. 2019;52(1):42–50.
Grenon R, Tasca GA, Cwinn E, Coyle D, Sumner A, Gick M, et al. Depressive symptoms are associated with medication use and lower health-related quality of life in overweight women with binge eating disorder. Womens Health Issues. 2010;20(6):435–40.
Ulfvebrand S, Birgegård A, Norring C, Högdahl L, von Hausswolff-Juhlin Y. Psychiatric comorbidity in women and men with eating disorders results from a large clinical database. Psychiatry Res. 2015;230(2):294–9.
Sachs KV, Harnke B, Mehler PS, Krantz MJ. Cardiovascular complications of anorexia nervosa: a systematic review. Int J Eat Disord. 2016;49(3):238–48.
Smith AR, Zuromski KL, Dodd DR. Eating disorders and suicidality: what we know, what we don’t know, and suggestions for future research. Curr Opin Psychol. 2018;22:63–7.
Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68(7):724–31.
Mayes SD, Fernandez-Mendoza J, Baweja R, Calhoun S, Mahr F, Aggarwal R, et al. Correlates of suicide ideation and attempts in children and adolescents with eating disorders. Eat Disord. 2014;22(4):352–66.
Hart LM, Granillo MT, Jorm AF, Paxton SJ. Unmet need for treatment in the eating disorders: a systematic review of eating disorder specific treatment seeking among community cases. Clin Psychol Rev. 2011;31(5):727–35.
Kaplan AS, Garfinkel PE. Difficulties in treating patients with eating disorders: A review of patient and clinician variables. Can J Psychiatry. 1999;44(7):665–70.
Eddy KT, Tabri N, Thomas JJ, Murray HB, Keshaviah A, Hastings E, et al. Recovery from anorexia nervosa and bulimia nervosa at 22-year follow-up. J Clin Psychiatry. 2017;78(2):184–9.
John A, Marchant A, Demmler J, Tan J, DelPozo-Banos M. Clinical management and mortality risk in those with eating disorders and self-harm: e-cohort study using the SAIL databank. BJPsych Open. 2021;7(2):1–8.
Monteleone P, Brambilla F. Multiple comorbidities in people with eating disorders. In: Comorbidity of mental and physical disorders. vol. 179. Karger Publishers; 2015. p. 66-80.
Van Alsten SC, Duncan AE. Lifetime patterns of comorbidity in eating disorders: an approach using sequence analysis. Eur Eat Disord Rev. 2020;28(6):709–23.
National Institute of Health and Care Excellence. Managing comorbid health problems in people with eating disorders. United Kingdom: National Institute of Health and Care Excellence. 2019.
Institute InsideOut. Australian Eating Disorders Research and Translation Strategy 2021–2031. Sydney: The University of Sydney; 2021.
Google Scholar
Virginia Commonwealth University. Rapid review protocol. 2018.
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20.
Hamel C, Michaud A, Thuku M, Skidmore B, Stevens A, Nussbaumer-Streit B, et al. Defining rapid reviews: a systematic scoping review and thematic analysis of definitions and defining characteristics of rapid reviews. J Clin Epidemiol. 2020;129:74–85.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 2009;6(7):1–6.
Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, et al. PRISMA-S: an extension to the PRISMA statement for reporting literature searches in systematic reviews. Syst Rev. 2021;10(1):39.
Aouad P, Bryant E, Maloney D, Marks P, Le A, Russell H, et al. Informing the development of Australia’s national eating disorders research and translation strategy: a rapid review methodology. J Eat Disord. 2022;10(1):31.
Godart N, Radon L, Curt F, Duclos J, Perdereau F, Lang F, et al. Mood disorders in eating disorder patients: prevalence and chronology of ONSET. J Affect Disord. 2015;185:115–22.
Swinbourne J, Hunt C, Abbott M, Russell J, St Clare T, Touyz S. The comorbidity between eating disorders and anxiety disorders: Prevalence in an eating disorder sample and anxiety disorder sample. Aust N Z J Psychiatry. 2012;46(2):118–31.
Espel-Huynh HM, Muratore AF, Virzi N, Brooks G, Zandberg LJ. Mediating role of experiential avoidance in the relationship between anxiety sensitivity and eating disorder psychopathology: a clinical replication. Eat Behav. 2019;34:101308.
Thornton LM, Dellava JE, Root TL, Lichtenstein P, Bulik CM. Anorexia nervosa and generalized anxiety disorder: further explorations of the relation between anxiety and body mass index. J Anxiety Disord. 2011;25(5):727–30.
Kerr-Gaffney J, Harrison A, Tchanturia K. Social anxiety in the eating disorders: a systematic review and meta-analysis. Psychol Med. 2018;48(15):2477–91.
Ranta K, Väänänen J, Fröjd S, Isomaa R, Kaltiala-Heino R, Marttunen M. Social phobia, depression and eating disorders during middle adolescence: longitudinal associations and treatment seeking. Nord J Psychiatry. 2017;71(8):605–13.
Mandelli L, Draghetti S, Albert U, De Ronchi D, Atti A-R. Rates of comorbid obsessive-compulsive disorder in eating disorders: a meta-analysis of the literature. J Affect Disord. 2020;277:927–39.
Finzi-Dottan R, Zubery E. The role of depression and anxiety in impulsive and obsessive-compulsive behaviors among anorexic and bulimic patients. Eat Disord. 2009;17(2):162–82.
Olatunji BO, Tart CD, Shewmaker S, Wall D, Smits JA. Mediation of symptom changes during inpatient treatment for eating disorders: the role of obsessive–compulsive features. J Psychiatr Res. 2010;44(14):910–6.
Vanzhula IA, Kinkel-Ram SS, Levinson CA. Perfectionism and difficulty controlling thoughts bridge eating disorder and obsessive-compulsive disorder symptoms: a network analysis. J Affect Disord. 2021;283:302–9.
Zhang Z, Robinson L, Jia T, Quinlan EB, Tay N, Chu C, et al. Development of disordered eating behaviors and comorbid depressive symptoms in adolescence: neural and psychopathological predictors. Biol Psychiatry. 2020;90(12):853–62.
Thiebaut S, Godart N, Radon L, Courtet P, Guillaume S. Crossed prevalence results between subtypes of eating disorder and bipolar disorder: a systematic review of the literature. L’encephale. 2019;45(1):60–73.
Crow S, Blom TJ, Sim L, Cuellar-Barboza AB, Biernacka JM, Frye MA, et al. Factor analysis of the eating disorder diagnostic scale in individuals with bipolar disorder. Eat Behav. 2019;33:30–3.
McDonald CE, Rossell SL, Phillipou A. The comorbidity of eating disorders in bipolar disorder and associated clinical correlates characterised by emotion dysregulation and impulsivity: a systematic review. J Affect Disord. 2019;259:228–43.
Martinussen M, Friborg O, Schmierer P, Kaiser S, Øvergård KT, Neunhoeffer A-L, et al. The comorbidity of personality disorders in eating disorders: a meta-analysis. Eat Weight Disord Stud Anorex Bulim Obes. 2017;22(2):201–9.
Vrabel KR, Rø Ø, Martinsen EW, Hoffart A, Rosenvinge JH. Five-year prospective study of personality disorders in adults with longstanding eating disorders. Int J Eat Disord. 2010;43(1):22–8.
PubMed Google Scholar
Bahji A, Mazhar MN, Hudson CC, Nadkarni P, MacNeil BA, Hawken E. Prevalence of substance use disorder comorbidity among individuals with eating disorders: A systematic review and meta-analysis. Psychiatry Res. 2019;273:58–66.
Calero-Elvira A, Krug I, Davis K, Lopez C, Fernández-Aranda F, Treasure J. Meta-analysis on drugs in people with eating disorders. Eur Eat Disord Rev Prof J Eat Disord Assoc. 2009;17(4):243–59.
Palmese LB, Ratliff JC, Reutenauer EL, Tonizzo KM, Grilo CM, Tek C. Prevalence of night eating in obese individuals with schizophrenia and schizoaffective disorder. Compr Psychiatry. 2013;54(3):276–81.
Hartmann AS, Greenberg JL, Wilhelm S. The relationship between anorexia nervosa and body dysmorphic disorder. Clin Psychol Rev. 2013;33(5):675–85.
Kaisari P, Dourish CT, Higgs S. Attention deficit hyperactivity disorder (ADHD) and disordered eating behaviour: a systematic review and a framework for future research. Clin Psychol Rev. 2017;53:109–21.
Nazar BP, Bernardes C, Peachey G, Sergeant J, Mattos P, Treasure J. The risk of eating disorders comorbid with attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Int J Eat Disord. 2016;49(12):1045–57.
Seitz J, Kahraman-Lanzerath B, Legenbauer T, Sarrar L, Herpertz S, Salbach-Andrae H, et al. The role of impulsivity, inattention and comorbid ADHD in patients with bulimia nervosa. PLoS ONE. 2013;8(5):e63891.
Ziobrowski H, Brewerton TD, Duncan AE. Associations between ADHD and eating disorders in relation to comorbid psychiatric disorders in a nationally representative sample. Psychiatry Res. 2018;260:53–9.
Bleck JR, DeBate RD, Olivardia R. The comorbidity of ADHD and eating disorders in a nationally representative sample. J Behav Health Serv Res. 2015;42(4):437–51.
Huke V, Turk J, Saeidi S, Kent A, Morgan JF. Autism spectrum disorders in eating disorder populations: a systematic review. Eur Eat Disord Rev. 2013;21(5):345–51.
Westwood H, Mandy W, Tchanturia K. Clinical evaluation of autistic symptoms in women with anorexia nervosa. Mol Autism. 2017;8(1):1–9.
Dell’Osso L, Carpita B, Gesi C, Cremone I, Corsi M, Massimetti E, et al. Subthreshold autism spectrum disorder in patients with eating disorders. Compr Psychiatry. 2018;81:66–72.
Dovey TM, Kumari V, Blissett J. Eating behaviour, behavioural problems and sensory profiles of children with avoidant/restrictive food intake disorder (ARFID), autistic spectrum disorders or picky eating: same or different? Eur Psychiatry. 2019;61:56–62.
Mitchell KS, Singh S, Hardin S, Thompson-Brenner H. The impact of comorbid posttraumatic stress disorder on eating disorder treatment outcomes: investigating the unified treatment model. Int J Eat Disord. 2021;54(7):1260–9.
Mitchell KS, Scioli ER, Galovski T, Belfer PL, Cooper Z. Posttraumatic stress disorder and eating disorders: maintaining mechanisms and treatment targets. Eat Disord. 2021;29(3):292–306.
Goldstein A, Gvion Y. Socio-demographic and psychological risk factors for suicidal behavior among individuals with anorexia and bulimia nervosa: a systematic review. J Affect Disord. 2019;245:1149–67.
Pisetsky EM, Peterson CB, Mitchell JE, Wonderlich SA, Crosby RD, Le Grange D, et al. A comparison of the frequency of familial suicide attempts across eating disorder diagnoses. Int J Eat Disord. 2017;50(6):707–10.
Thornton LM, Welch E, Munn-Chernoff MA, Lichtenstein P, Bulik CM. Anorexia nervosa, major depression, and suicide attempts: shared genetic factors. Suicide Life Threat Behav. 2016;46(5):525–34.
Yao S, Kuja-Halkola R, Thornton LM, Runfola CD, D’Onofrio BM, Almqvist C, et al. Familial liability for eating disorders and suicide attempts: evidence from a population registry in Sweden. JAMA Psychiatry. 2016;73(3):284–91.
Preti A, Rocchi MBL, Sisti D, Camboni M, Miotto P. A comprehensive meta-analysis of the risk of suicide in eating disorders. Acta Psychiatr Scand. 2011;124(1):6–17.
Pérez S, Marco JH, Cañabate M. Non-suicidal self-injury in patients with eating disorders: prevalence, forms, functions, and body image correlates. Compr Psychiatry. 2018;84:32–8.
Claes L, Islam MA, Fagundo AB, Jimenez-Murcia S, Granero R, Agüera Z, et al. The relationship between non-suicidal self-injury and the UPPS-P impulsivity facets in eating disorders and healthy controls. PLoS ONE. 2015;10(5):e0126083.
Riley EN, Davis HA, Combs JL, Jordan CE, Smith GT. Nonsuicidal self-injury as a risk factor for purging onset: Negatively reinforced behaviours that reduce emotional distress. Eur Eat Disord Rev. 2016;24(1):78–82.
Muehlenkamp JJ, Claes L, Smits D, Peat CM, Vandereycken W. Non-suicidal self-injury in eating disordered patients: a test of a conceptual model. Psychiatry Res. 2011;188(1):102–8.
Gosseaume C, Dicembre M, Bemer P, Melchior J-C, Hanachi M. Somatic complications and nutritional management of anorexia nervosa. Clin Nutr Exp. 2019;28:2–10.
Cass K, McGuire C, Bjork I, Sobotka N, Walsh K, Mehler PS. Medical complications of anorexia nervosa. Psychosomatics. 2020;61(6):625–31.
Kalla A, Krishnamoorthy P, Gopalakrishnan A, Garg J, Patel N, Figueredo V. Gender and age differences in cardiovascular complications in anorexia nervosa patients. Int J Cardiol. 2017;227:55–7.
Karamanis G, Skalkidou A, Tsakonas G, Brandt L, Ekbom A, Ekselius L, et al. Cancer incidence and mortality patterns in women with anorexia nervosa. Int J Cancer. 2014;134(7):1751–7.
Hofman M, Landewé-Cleuren S, Wojciechowski F, Kruseman AN. Prevalence and clinical determinants of low bone mineral density in anorexia nervosa. Eur J Intern Med. 2009;20(1):80–4.
Robinson L, Aldridge V, Clark E, Misra M, Micali N. A systematic review and meta-analysis of the association between eating disorders and bone density. Osteoporos Int. 2016;27(6):1953–66.
Rizzo SM, Douglas JW, Lawrence JC. Enteral nutrition via nasogastric tube for refeeding patients with anorexia nervosa: a systematic review. Nutr Clin Pract. 2019;34(3):359–70.
Cioffi I, Ponzo V, Pellegrini M, Evangelista A, Bioletto F, Ciccone G, et al. The incidence of the refeeding syndrome. A systematic review and meta-analyses of literature. Clin Nutr. 2021;40(6):3688–701.
Golden NH, Keane-Miller C, Sainani KL, Kapphahn CJ. Higher caloric intake in hospitalized adolescents with anorexia nervosa is associated with reduced length of stay and no increased rate of refeeding syndrome. J Adolesc Health. 2013;53(5):573–8.
Garber AK, Mauldin K, Michihata N, Buckelew SM, Shafer M-A, Moscicki A-B. Higher calorie diets increase rate of weight gain and shorten hospital stay in hospitalized adolescents with anorexia nervosa. J Adolesc Health. 2013;53(5):579–84.
O’Connor G, Nicholls D, Hudson L, Singhal A. Refeeding low weight hospitalized adolescents with anorexia nervosa: a multicenter randomized controlled trial. Nutr Clin Pract. 2016;31(5):681–9.
Raevuori A, Suokas J, Haukka J, Gissler M, Linna M, Grainger M, et al. Highly increased risk of type 2 diabetes in patients with binge eating disorder and bulimia nervosa. Int J Eat Disord. 2015;48(6):555–62.
Conviser JH, Fisher SD, Mitchell KB. Oral care behavior after purging in a sample of women with bulimia nervosa. J Am Dent Assoc. 2014;145(4):352–4.
Hermont AP, Oliveira PA, Martins CC, Paiva SM, Pordeus IA, Auad SM. Tooth erosion and eating disorders: a systematic review and meta-analysis. PLoS ONE. 2014;9(11):e111123.
Hermont AP, Pordeus IA, Paiva SM, Abreu MHNG, Auad SM. Eating disorder risk behavior and dental implications among adolescents. Int J Eat Disord. 2013;46(7):677–83.
Peebles R, Sieke EH. Medical complications of eating disorders in youth. Child Adolesc Psychiatr Clin. 2019;28(4):593–615.
Hemmingsen SD, Wesselhoeft R, Lichtenstein MB, Sjögren JM, Støving RK. Cognitive improvement following weight gain in patients with anorexia nervosa: a systematic review. Eur Eat Disord Rev. 2021;29(3):402–26.
Pasternak Y, Weintraub AY, Shoham-Vardi I, Sergienko R, Guez J, Wiznitzer A, et al. Obstetric and perinatal outcomes in women with eating disorders. J Womens Health. 2012;21(1):61–5.
Linna MS, Raevuori A, Haukka J, Suvisaari JM, Suokas JT, Gissler M. Reproductive health outcomes in eating disorders. Int J Eat Disord. 2013;46(8):826–33.
Martini MG, Solmi F, Krug I, Karwautz A, Wagner G, Fernandez-Aranda F, et al. Associations between eating disorder diagnoses, behaviors, and menstrual dysfunction in a clinical sample. Arch Womens Ment Health. 2016;19(3):553–7.
Clarke E, Kiropoulos LA. Mediating the relationship between neuroticism and depressive, anxiety and eating disorder symptoms: The role of intolerance of uncertainty and cognitive flexibility. J Affect Disord Rep. 2021;4:100101.
Grilo CM, White MA, Barnes RD, Masheb RM. Psychiatric disorder co-morbidity and correlates in an ethnically diverse sample of obese patients with binge eating disorder in primary care settings. Compr Psychiatry. 2013;54(3):209–16.
Kambanis PE, Kuhnle MC, Wons OB, Jo JH, Keshishian AC, Hauser K, et al. Prevalence and correlates of psychiatric comorbidities in children and adolescents with full and subthreshold avoidant/restrictive food intake disorder. Int J Eat Disord. 2020;53(2):256–65.
Balantekin KN, Grammer AC, Fitzsimmons-Craft EE, Eichen DE, Graham AK, Monterubio GE, et al. Overweight and obesity are associated with increased eating disorder correlates and general psychopathology in university women with eating disorders. Eat Behav. 2021;41:101482.
Spettigue W, Obeid N, Santos A, Norris M, Hamati R, Hadjiyannakis S, et al. Binge eating and social anxiety in treatment-seeking adolescents with eating disorders or severe obesity. Eat Weight Disord Stud Anorex Bulim Obes. 2020;25(3):787–93.
Simpson HB, Wetterneck CT, Cahill SP, Steinglass JE, Franklin ME, Leonard RC, et al. Treatment of obsessive-compulsive disorder complicated by comorbid eating disorders. Cogn Behav Ther. 2013;42(1):64–76.
Fennig S, Hadas A. Suicidal behavior and depression in adolescents with eating disorders. Nord J Psychiatry. 2010;64(1):32–9.
Pila E, Murray SB, Le Grange D, Sawyer SM, Hughes EK. Reciprocal relations between dietary restraint and negative affect in adolescents receiving treatment for anorexia nervosa. J Abnorm Psychol. 2019;128(2):129–39.
Touchette E, Henegar A, Godart NT, Pryor L, Falissard B, Tremblay RE, et al. Subclinical eating disorders and their comorbidity with mood and anxiety disorders in adolescent girls. Psychiatry Res. 2011;185(1–2):185–92.
Carriere C, Michel G, Féart C, Pellay H, Onorato O, Barat P, et al. Relationships between emotional disorders, personality dimensions, and binge eating disorder in French obese adolescents. Arch Pediatr. 2019;26(3):138–44.
Kucukgoncu S, Tek C, Bestepe E, Musket C, Guloksuz S. Clinical features of night eating syndrome among depressed patients. Eur Eat Disord Rev. 2014;22(2):102–8.
Lundgren JD, Allison KC, Stunkard AJ, Bulik CM, Thornton LM, Lindroos AK, et al. Lifetime medical and psychiatric comorbidity of night eating behavior in the Swedish Twin Study of Adults: Genes and Environment (STAGE). Psychiatry Res. 2012;199(2):145–9.
Schnicker K, Hiller W, Legenbauer T. Drop-out and treatment outcome of outpatient cognitive–behavioral therapy for anorexia nervosa and bulimia nervosa. Compr Psychiatry. 2013;54(7):812–23.
Calugi S, El Ghoch M, Conti M, Dalle GR. Depression and treatment outcome in anorexia nervosa. Psychiatry Res. 2014;218(1–2):195–200.
Voderholzer U, Witte S, Schlegl S, Koch S, Cuntz U, Schwartz C. Association between depressive symptoms, weight and treatment outcome in a very large anorexia nervosa sample. Eat Weight Disord Stud Anorex Bulim Obes. 2016;21(1):127–31.
Fornaro M, Daray FM, Hunter F, Anastasia A, Stubbs B, De Berardis D, et al. The prevalence, odds and predictors of lifespan comorbid eating disorder among people with a primary diagnosis of bipolar disorders, and vice-versa: systematic review and meta-analysis. J Affect Disord. 2021;280:409–31.
McElroy SL, Crow S, Blom TJ, Biernacka JM, Winham SJ, Geske J, et al. Prevalence and correlates of DSM-5 eating disorders in patients with bipolar disorder. J Affect Disord. 2016;191:216–21.
Boulanger H, Tebeka S, Girod C, Lloret-Linares C, Meheust J, Scott J, et al. Binge eating behaviours in bipolar disorders. J Affect Disord. 2018;225:482–8.
Melo MCA, de Oliveira RM, de Araújo CFC, de Mesquita LMF, de Bruin PFC, de Bruin VMS. Night eating in bipolar disorder. Sleep Med. 2018;48:49–52.
McElroy SL, Frye MA, Hellemann G, Altshuler L, Leverich GS, Suppes T, et al. Prevalence and correlates of eating disorders in 875 patients with bipolar disorder. J Affect Disord. 2011;128(3):191–8.
Thiebaut S, Jaussent I, Maïmoun L, Beziat S, Seneque M, Hamroun D, et al. Impact of bipolar disorder on eating disorders severity in real-life settings. J Affect Disord. 2019;246:867–72.
McAulay C, Mond J, Outhred T, Malhi GS, Touyz S. Eating disorder features in bipolar disorder: clinical implications. J Mental Health. 2021:1–11.
Seixas C, Miranda-Scippa Â, Nery-Fernandes F, Andrade-Nascimento M, Quarantini LC, Kapczinski F, et al. Prevalence and clinical impact of eating disorders in bipolar patients. Braz J Psychiatry. 2012;34(1):66–70.
Spiegel J, Arnold S, Salbach H, Gotti E, Pfeiffer E, Lehmkuhl U, et al. Emotional abuse interacts with borderline personality in adolescent inpatients with binge-purging eating disorders. Eat Weight Disord Stud Anorex Bulim Obes. 2021;27:131–8.
Himmerich H, Hotopf M, Shetty H, Schmidt U, Treasure J, Hayes RD, et al. Psychiatric comorbidity as a risk factor for the mortality of people with bulimia nervosa. Soc Psychiatry Psychiatr Epidemiol. 2019;54(7):813–21.
Rowe SL, Jordan J, McIntosh VV, Carter FA, Frampton C, Bulik CM, et al. Complex personality disorder in bulimia nervosa. Compr Psychiatry. 2010;51(6):592–8.
Brietzke E, Moreira CL, Toniolo RA, Lafer B. Clinical correlates of eating disorder comorbidity in women with bipolar disorder type I. J Affect Disord. 2011;130(1–2):162–5.
Harrop EN, Marlatt GA. The comorbidity of substance use disorders and eating disorders in women: prevalence, etiology, and treatment. Addict Behav. 2010;35(5):392–8.
Baker JH, Mitchell KS, Neale MC, Kendler KS. Eating disorder symptomatology and substance use disorders: prevalence and shared risk in a population based twin sample. Int J Eat Disord. 2010;43(7):648–58.
Root TL, Pisetsky EM, Thornton L, Lichtenstein P, Pedersen NL, Bulik CM. Patterns of co-morbidity of eating disorders and substance use in Swedish females. Psychol Med. 2010;40(1):105–15.
Fouladi F, Mitchell JE, Crosby RD, Engel SG, Crow S, Hill L, et al. Prevalence of alcohol and other substance use in patients with eating disorders. Eur Eat Disord Rev. 2015;23(6):531–6.
Brewerton TD, Rance SJ, Dansky BS, O’Neil PM, Kilpatrick DG. A comparison of women with child-adolescent versus adult onset binge eating: Results from the national women’s study. Int J Eat Disord. 2014;47(7):836–43.
Field AE, Sonneville KR, Micali N, Crosby RD, Swanson SA, Laird NM, et al. Prospective association of common eating disorders and adverse outcomes. Pediatrics. 2012;130(2):e289–95.
Cusack CE, Christian C, Drake JE, Levinson CA. A network analysis of eating disorder symptoms and co-occurring alcohol misuse among heterosexual and sexual minority college women. Addict Behav. 2021;118:106867.
Miotto P, Pollini B, Restaneo A, Favaretto G, Sisti D, Rocchi MB, et al. Symptoms of psychosis in anorexia and bulimia nervosa. Psychiatry Res. 2010;175(3):237–43.
Koyanagi A, Stickley A, Haro JM. Psychotic-like experiences and disordered eating in the English general population. Psychiatry Res. 2016;241:26–34.
Phillipou A, Castle DJ, Rossell SL. Direct comparisons of anorexia nervosa and body dysmorphic disorder: a systematic review. Psychiatry Res. 2019;274:129–37.
Cerea S, Bottesi G, Grisham JR, Ghisi M. Non-weight-related body image concerns and body dysmorphic disorder prevalence in patients with anorexia nervosa. Psychiatry Res. 2018;267:120–5.
Beilharz F, Phillipou A, Castle D, Jenkins Z, Cistullo L, Rossell S. Dysmorphic concern in anorexia nervosa: implications for recovery. Psychiatry Res. 2019;273:657–61.
Beilharz F, Castle D, Grace S, Rossell S. A systematic review of visual processing and associated treatments in body dysmorphic disorder. Acta Psychiatr Scand. 2017;136(1):16–36.
Svedlund NE, Norring C, Ginsberg Y, von Hausswolff-Juhlin Y. Symptoms of attention deficit hyperactivity disorder (ADHD) among adult eating disorder patients. BMC Psychiatry. 2017;17(1):1–9.
Brewerton TD, Duncan AE. Associations between attention deficit hyperactivity disorder and eating disorders by gender: results from the national comorbidity survey replication. Eur Eat Disord Rev. 2016;24(6):536–40.
Bisset M, Rinehart N, Sciberras E. DSM-5 eating disorder symptoms in adolescents with and without attention-deficit/hyperactivity disorder: a population-based study. Int J Eat Disord. 2019;52(7):855–62.
Svedlund NE, Norring C, Ginsberg Y, von Hausswolff-Juhlin Y. Are treatment results for eating disorders affected by ADHD symptoms? A one-year follow-up of adult females. Eur Eat Disord Rev. 2018;26(4):337–45.
Brewerton TD, Perlman MM, Gavidia I, Suro G, Genet J, Bunnell DW. The association of traumatic events and posttraumatic stress disorder with greater eating disorder and comorbid symptom severity in residential eating disorder treatment centers. Int J Eat Disord. 2020;53(12):2061–6.
Bühren K, Schwarte R, Fluck F, Timmesfeld N, Krei M, Egberts K, et al. Comorbid psychiatric disorders in female adolescents with first-onset anorexia nervosa. Eur Eat Disord Rev. 2014;22(1):39–44.
Guillaume S, Jaussent I, Olie E, Genty C, Bringer J, Courtet P, et al. Characteristics of suicide attempts in anorexia and bulimia nervosa: a case–control study. PLoS ONE. 2011;6(8):e23578.
Udo T, Bitley S, Grilo CM. Suicide attempts in US adults with lifetime DSM-5 eating disorders. BMC Med. 2019;17(1):1–13.
Duffy ME, Henkel KE, Joiner TE. Prevalence of self-injurious thoughts and behaviors in transgender individuals with eating disorders: a national study. J Adolesc Health. 2019;64(4):461–6.
Goel NJ, Sadeh-Sharvit S, Flatt RE, Trockel M, Balantekin KN, Fitzsimmons-Craft EE, et al. Correlates of suicidal ideation in college women with eating disorders. Int J Eat Disord. 2018;51(6):579–84.
Sagiv E, Gvion Y. A multi factorial model of self-harm behaviors in Anorexia-nervosa and Bulimia-nervosa. Compr Psychiatry. 2020;96:152142.
Andersén M, Birgegård A. D iagnosis-specific self-image predicts longitudinal suicidal ideation in adult eating disorders. Int J Eat Disord. 2017;50(8):970–8.
Runfola CD, Thornton LM, Pisetsky EM, Bulik CM, Birgegård A. Self-image and suicide in a Swedish national eating disorders clinical register. Compr Psychiatry. 2014;55(3):439–49.
Forcano L, Álvarez E, Santamaría JJ, Jimenez-Murcia S, Granero R, Penelo E, et al. Suicide attempts in anorexia nervosa subtypes. Compr Psychiatry. 2011;52(4):352–8.
Selby EA, Smith AR, Bulik CM, Olmsted MP, Thornton L, McFarlane TL, et al. Habitual starvation and provocative behaviors: two potential routes to extreme suicidal behavior in anorexia nervosa. Behav Res Ther. 2010;48(7):634–45.
Bodell LP, Joiner TE, Keel PK. Comorbidity-independent risk for suicidality increases with bulimia nervosa but not with anorexia nervosa. J Psychiatr Res. 2013;47(5):617–21.
Forcano L, Fernández-Aranda F, Alvarez-Moya E, Bulik C, Granero R, Gratacos M, et al. Suicide attempts in bulimia nervosa: personality and psychopathological correlates. Eur Psychiatry. 2009;24(2):91–7.
Huas C, Godart N, Caille A, Pham-Scottez A, Foulon C, Divac SM, et al. Mortality and its predictors in severe bulimia nervosa patients. Eur Eat Disord Rev. 2013;21(1):15–9.
Crow SJ, Swanson SA, le Grange D, Feig EH, Merikangas KR. Suicidal behavior in adolescents and adults with bulimia nervosa. Compr Psychiatry. 2014;55(7):1534–9.
Pisetsky EM, Wonderlich SA, Crosby RD, Peterson CB, Mitchell JE, Engel SG, et al. Depression and personality traits associated with emotion dysregulation: correlates of suicide attempts in women with bulimia nervosa. Eur Eat Disord Rev. 2015;23(6):537–44.
Brown KL, LaRose JG, Mezuk B. The relationship between body mass index, binge eating disorder and suicidality. BMC Psychiatry. 2018;18(1):1–9.
Olatunji BO, Cox R, Ebesutani C, Wall D. Self-harm history predicts resistance to inpatient treatment of body shape aversion in women with eating disorders: The role of negative affect. J Psychiatr Res. 2015;65:37–46.
Pérez S, Ros MC, Folgado JEL, Marco JH. Non-suicidal self-injury differentiates suicide ideators and attempters and predicts future suicide attempts in patients with eating disorders. Suicide Life Threat Behav. 2019;49(5):1220–31.
Smith KE, Hayes NA, Styer DM, Washburn JJ. Emotional reactivity in a clinical sample of patients with eating disorders and nonsuicidal self-injury. Psychiatry Res. 2017;257:519–25.
Claes L, Klonsky ED, Muehlenkamp J, Kuppens P, Vandereycken W. The affect-regulation function of nonsuicidal self-injury in eating-disordered patients: which affect states are regulated? Compr Psychiatry. 2010;51(4):386–92.
Navarro-Haro MV, Wessman I, Botella C, García-Palacios A. The role of emotion regulation strategies and dissociation in non-suicidal self-injury for women with borderline personality disorder and comorbid eating disorder. Compr Psychiatry. 2015;63:123–30.
Giovinazzo S, Sukkar S, Rosa G, Zappi A, Bezante G, Balbi M, et al. Anorexia nervosa and heart disease: a systematic review. Eat Weight Disord Stud Anorex Bulim Obes. 2019;24(2):199–207.
Bouquegneau A, Dubois BE, Krzesinski J-M, Delanaye P. Anorexia nervosa and the kidney. Am J Kidney Dis. 2012;60(2):299–307.
Benini L, Todesco T, Frulloni L, Dalle Grave R, Campagnola P, Agugiaro F, et al. Esophageal motility and symptoms in restricting and binge-eating/purging anorexia. Dig Liver Dis. 2010;42(11):767–72.
Gibson D, Watters A, Mehler PS. The intersect of gastrointestinal symptoms and malnutrition associated with anorexia nervosa and avoidant/restrictive food intake disorder: Functional or pathophysiologic? A systematic review. Int J Eat Disord. 2021.
Abraham S, Kellow J. Exploring eating disorder quality of life and functional gastrointestinal disorders among eating disorder patients. J Psychosom Res. 2011;70(4):372–7.
Brewster DH, Nowell SL, Clark DN. Risk of oesophageal cancer among patients previously hospitalised with eating disorder. Cancer Epidemiol. 2015;39(3):313–20.
Smith KR, Moran TH. Gastrointestinal peptides in eating-related disorders. Physiol Behav. 2021;238:113456.
Seidel M, Markmann Jensen S, Healy D, Dureja A, Watson HJ, Holst B, et al. A systematic review and meta-analysis finds increased blood levels of all forms of ghrelin in both restricting and binge-eating/purging subtypes of anorexia nervosa. Nutrients. 2021;13(2):709.
Becker KR, Mancuso C, Dreier MJ, Asanza E, Breithaupt L, Slattery M, et al. Ghrelin and PYY in low-weight females with avoidant/restrictive food intake disorder compared to anorexia nervosa and healthy controls. Psychoneuroendocrinology. 2021;129:105243.
Schalla MA, Stengel A. Gastrointestinal alterations in anorexia nervosa—A systematic review. Eur Eat Disord Rev. 2019;27(5):447–61.
West M, McMaster CM, Staudacher HM, Hart S, Jacka FN, Stewart T, et al. Gastrointestinal symptoms following treatment for anorexia nervosa: A systematic literature review. Int J Eat Disord. 2021;54(6):936–51.
Avila JT, Park K, Golden NH. Eating disorders in adolescents with chronic gastrointestinal and endocrine diseases. Lancet Child Adolesc Health. 2019;3(3):181–9.
Ruusunen A, Rocks T, Jacka F, Loughman A. The gut microbiome in anorexia nervosa: relevance for nutritional rehabilitation. Psychopharmacology. 2019;236(5):1545–58.
Zaina F, Pesenti F, Persani L, Capodaglio P, Negrini S, Polli N. Prevalence of idiopathic scoliosis in anorexia nervosa patients: results from a cross-sectional study. Eur Spine J. 2018;27(2):293–7.
Hung C, Muñoz M, Shibli-Rahhal A. Anorexia nervosa and osteoporosis. Calcif Tissue Int. 2021;110(5):562–75.
Mumford J, Kohn M, Briody J, Miskovic-Wheatley J, Madden S, Clarke S, et al. Long-term outcomes of adolescent anorexia nervosa on bone. J Adolesc Health. 2019;64(3):305–10.
Robinson L, Aldridge V, Clark EM, Misra M, Micali N. Pharmacological treatment options for low bone mineral density and secondary osteoporosis in anorexia nervosa: a systematic review of the literature. J Psychosom Res. 2017;98:87–97.
Sim LA, McGovern L, Elamin MB, Swiglo BA, Erwin PJ, Montori VM. Effect on bone health of estrogen preparations in premenopausal women with anorexia nervosa: A systematic review and meta-analyses. Int J Eat Disord. 2010;43(3):218–25.
Lebow J, Sim L. The influence of estrogen therapies on bone mineral density in premenopausal women with anorexia nervosa and amenorrhea. Vitam Horm. 2013;92:243–57.
Maïmoun L, Renard E, Lefebvre P, Bertet H, Philibert P, Sénèque M, et al. Oral contraceptives partially protect from bone loss in young women with anorexia nervosa. Fertil Steril. 2019;111(5):1020–9.
Miller KK, Meenaghan E, Lawson EA, Misra M, Gleysteen S, Schoenfeld D, et al. Effects of risedronate and low-dose transdermal testosterone on bone mineral density in women with anorexia nervosa: a randomized, placebo-controlled study. J Clin Endocrinol Metab. 2011;96(7):2081–8.
Bloch M, Ish-Shalom S, Greenman Y, Klein E, Latzer Y. Dehydroepiandrosterone treatment effects on weight, bone density, bone metabolism and mood in women suffering from anorexia nervosa—a pilot study. Psychiatry Res. 2012;200(2–3):544–9.
Vajapeyam S, Ecklund K, Mulkern RV, Feldman HA, O’Donnell JM, DiVasta AD, et al. Magnetic resonance imaging and spectroscopy evidence of efficacy for adrenal and gonadal hormone replacement therapy in anorexia nervosa. Bone. 2018;110:335–42.
DiVasta AD, Feldman HA, Beck TJ, LeBoff MS, Gordon CM. Does hormone replacement normalize bone geometry in adolescents with anorexia nervosa? J Bone Miner Res. 2014;29(1):151–7.
Fazeli PK, Wang IS, Miller KK, Herzog DB, Misra M, Lee H, et al. Teriparatide increases bone formation and bone mineral density in adult women with anorexia nervosa. J Clin Endocrinol Metab. 2014;99(4):1322–9.
Giollo A, Idolazzi L, Caimmi C, Fassio A, Bertoldo F, Dalle Grave R, et al. V itamin D levels strongly influence bone mineral density and bone turnover markers during weight gain in female patients with anorexia nervosa. Int J Eat Disord. 2017;50(9):1041–9.
Davies JE, Cockfield A, Brown A, Corr J, Smith D, Munro C. The medical risks of severe anorexia nervosa during initial re-feeding and medical stabilisation. Clin Nutr ESPEN. 2017;17:92–9.
Hale MD, Logomarsino JV. The use of enteral nutrition in the treatment of eating disorders: a systematic review. Eat Weight Disord Stud Anorex Bulim Obes. 2019;24(2):179–98.
Rocks T, Pelly F, Wilkinson P. Nutrition therapy during initiation of refeeding in underweight children and adolescent inpatients with anorexia nervosa: a systematic review of the evidence. J Acad Nutr Diet. 2014;114(6):897–907.
Gentile MG, Pastorelli P, Ciceri R, Manna GM, Collimedaglia S. Specialized refeeding treatment for anorexia nervosa patients suffering from extreme undernutrition. Clin Nutr. 2010;29(5):627–32.
Hanachi M, Melchior JC, Crenn P. Hypertransaminasemia in severely malnourished adult anorexia nervosa patients: risk factors and evolution under enteral nutrition. Clin Nutr. 2013;32(3):391–5.
Rosen E, Sabel AL, Brinton JT, Catanach B, Gaudiani JL, Mehler PS. Liver dysfunction in patients with severe anorexia nervosa. Int J Eat Disord. 2016;49(2):151–8.
Vignaud M, Constantin J-M, Ruivard M, Villemeyre-Plane M, Futier E, Bazin J-E, et al. Refeeding syndrome influences outcome of anorexia nervosa patients in intensive care unit: an observational study. Crit Care. 2010;14(5):R172.
Whitelaw M, Gilbertson H, Lam P-Y, Sawyer SM. Does aggressive refeeding in hospitalized adolescents with anorexia nervosa result in increased hypophosphatemia? J Adolesc Health. 2010;46(6):577–82.
Leclerc A, Turrini T, Sherwood K, Katzman DK. Evaluation of a nutrition rehabilitation protocol in hospitalized adolescents with restrictive eating disorders. J Adolesc Health. 2013;53(5):585–9.
Leitner M, Burstein B, Agostino H. Prophylactic phosphate supplementation for the inpatient treatment of restrictive eating disorders. J Adolesc Health. 2016;58(6):616–20.
Brown C, Sabel A, Gaudiani J, Mehler PS. Predictors of hypophosphatemia during refeeding of patients with severe anorexia nervosa. Int J Eat Disord. 2015;48(7):898–904.
Whitelaw M, Lee KJ, Gilbertson H, Sawyer SM. Predictors of complications in anorexia nervosa and atypical anorexia nervosa: degree of underweight or extent and recency of weight loss? J Adolesc Health. 2018;63(6):717–23.
Agostino H, Erdstein J, Di Meglio G. Shifting paradigms: continuous nasogastric feeding with high caloric intakes in anorexia nervosa. J Adolesc Health. 2013;53(5):590–4.
Ridout KK, Kole J, Fitzgerald KL, Ridout SJ, Donaldson AA, Alverson B. Daily laboratory monitoring is of poor health care value in adolescents acutely hospitalized for eating disorders. J Adolesc Health. 2016;59(1):104–9.
Nehring I, Kewitz K, Von Kries R, Thyen U. Long-term effects of enteral feeding on growth and mental health in adolescents with anorexia nervosa—results of a retrospective German cohort study. Eur J Clin Nutr. 2014;68(2):171–7.
National Heat LaBI. Metabolic syndrome: US Department of Health and Human Services. 2020.
Mathisen TF, Sundgot-Borgen J, Rosenvinge JH, Bratland-Sanda S. Managing risk of non-communicable diseases in women with bulimia nervosa or binge eating disorders: A randomized trial with 12 months follow-up. Nutrients. 2018;10(12):1887.
Article PubMed Central Google Scholar
Thornton LM, Watson HJ, Jangmo A, Welch E, Wiklund C, von Hausswolff-Juhlin Y, et al. Binge-eating disorder in the Swedish national registers: Somatic comorbidity. Int J Eat Disord. 2017;50(1):58–65.
Nicolau J, Simó R, Sanchís P, Ayala L, Fortuny R, Zubillaga I, et al. Eating disorders are frequent among type 2 diabetic patients and are associated with worse metabolic and psychological outcomes: results from a cross-sectional study in primary and secondary care settings. Acta Diabetol. 2015;52(6):1037–44.
Jaworski M, Panczyk M, Śliwczyński AM, Brzozowska M, Janaszek K, Małkowski P, et al. A ten-year longitudinal study of prevalence of eating disorders in the general polish type 2 diabetes population. Med Sci Monit Int Med J Exp Clin Res. 2018;24:9204.
Gallant A, Drapeau V, Allison KC, Tremblay A, Lambert M, O’Loughlin J, et al. Night eating behavior and metabolic heath in mothers and fathers enrolled in the QUALITY cohort study. Eat Behav. 2014;15(2):186–91.
Hood MM, Reutrakul S, Crowley SJ. Night eating in patients with type 2 diabetes. Associations with glycemic control, eating patterns, sleep, and mood. Appetite. 2014;79:91–6.
Udo T, McKee SA, White MA, Masheb RM, Barnes RD, Grilo CM. Menopause and metabolic syndrome in obese individuals with binge eating disorder. Eat Behav. 2014;15(2):182–5.
Kisely S, Baghaie H, Lalloo R, Johnson NW. Association between poor oral health and eating disorders: systematic review and meta-analysis. Br J Psychiatry. 2015;207(4):299–305.
Pallier A, Karimova A, Boillot A, Colon P, Ringuenet D, Bouchard P, et al. Dental and periodontal health in adults with eating disorders: a case-control study. J Dent. 2019;84:55–9.
Lundgren JD, Smith BM, Spresser C, Harkins P, Zolton L, Williams K. The relationship of night eating to oral health and obesity in community dental clinic patients. Age (Years). 2010;57(15):12.
Lundgren JD, Williams KB, Heitmann BL. Nocturnal eating predicts tooth loss among adults: results from the Danish MONICA study. Eat Behav. 2010;11(3):170–4.
Panico R, Piemonte E, Lazos J, Gilligan G, Zampini A, Lanfranchi H. Oral mucosal lesions in anorexia nervosa, bulimia nervosa and EDNOS. J Psychiatr Res. 2018;96:178–82.
Setnick J. Micronutrient deficiencies and supplementation in anorexia and bulimia nervosa: a review of literature. Nutr Clin Pract. 2010;25(2):137–42.
Oudman E, Wijnia JW, Oey MJ, van Dam MJ, Postma A. Preventing Wernicke’s encephalopathy in anorexia nervosa: A systematic review. Psychiatry Clin Neurosci. 2018;72(10):774–9.
Ålgars M, Huang L, Von Holle AF, Peat CM, Thornton LM, Lichtenstein P, et al. Binge eating and menstrual dysfunction. J Psychosom Res. 2014;76(1):19–22.
Nobles CJ, Thomas JJ, Valentine SE, Gerber MW, Vaewsorn AS, Marques L. Association of premenstrual syndrome and premenstrual dysphoric disorder with bulimia nervosa and binge-eating disorder in a nationally representative epidemiological sample. Int J Eat Disord. 2016;49(7):641–50.
Chaer R, Nakouzi N, Itani L, Tannir H, Kreidieh D, El Masri D, et al. Fertility and Reproduction after recovery from anorexia nervosa: a systematic review and meta-analysis of long-term follow-up studies. Diseases. 2020;8(4):46.
Bulik CM, Von Holle A, Siega-Riz AM, Torgersen L, Lie KK, Hamer RM, et al. Birth outcomes in women with eating disorders in the Norwegian Mother and Child cohort study (MoBa). Int J Eat Disord. 2009;42(1):9–18.
Kolstad E, Gilhus NE, Veiby G, Reiter SF, Lossius MI, Bjørk M. Epilepsy and eating disorders during pregnancy: prevalence, complications and birth outcome. Seizure. 2015;28:81–4.
Longo P, Panero M, Amodeo L, Demarchi M, Abbate-Daga G, Marzola E. Psychoform and somatoform dissociation in anorexia nervosa: a systematic review. Clin Psychol Psychother. 2021;28(2):295–312.
Zerwas S, Larsen JT, Petersen L, Thornton LM, Quaranta M, Koch SV, et al. Eating disorders, autoimmune, and autoinflammatory disease. Pediatrics. 2017;140(6):e20162089.
Wotton CJ, James A, Goldacre MJ. Coexistence of eating disorders and autoimmune diseases: record linkage cohort study, UK. Int J Eat Disord. 2016;49(7):663–72.
Download references
Acknowledgements
The authors would like to thank and acknowledge the hard work of Healthcare Management Advisors (HMA) who were commissioned to undertake the Rapid Review. Additionally, the authors would like to thank all members of the consortium and consultation committees for their advice, input, and considerations during the development process. Further, a special thank you to the carers, consumers and lived experience consultants that provided input to the development of the Rapid Review and wider national Eating Disorders Research & Translation Strategy. Finally, thank you to the Australian Government—Department of Health for their support of the current project.
National Eating Disorder Research Consortium: Phillip Aouad, Sarah Barakat, Robert Boakes, Leah Brennan, Emma Bryant, Susan Byrne, Belinda Caldwell, Shannon Calvert, Bronny Carroll, David Castle, Ian Caterson, Belinda Chelius, Lyn Chiem, Simon Clarke, Janet Conti, Lexi Crouch, Genevieve Dammery, Natasha Dzajkovski, Jasmine Fardouly, Carmen Felicia, John Feneley, Amber-Marie Firriolo, Nasim Foroughi, Mathew Fuller-Tyszkiewicz, Anthea Fursland, Veronica Gonzalez-Arce, Bethanie Gouldthorp, Kelly Griffin, Scott Griffiths, Ashlea Hambleton, Amy Hannigan, Mel Hart, Susan Hart, Phillipa Hay, Ian Hickie, Francis Kay-Lambkin, Ross King, Michael Kohn, Eyza Koreshe, Isabel Krug, Anvi Le, Jake Linardon, Randall Long, Amanda Long, Sloane Madden, Sarah Maguire, Danielle Maloney, Peta Marks, Sian McLean, Thy Meddick, Jane Miskovic-Wheatley, Deborah Mitchison, Richard O’Kearney, Shu Hwa Ong, Roger Paterson, Susan Paxton, Melissa Pehlivan, Genevieve Pepin, Andrea Phillipou, Judith Piccone, Rebecca Pinkus, Bronwyn Raykos, Paul Rhodes, Elizabeth Rieger, Sarah Rodan, Karen Rockett, Janice Russell, Haley Russell, Fiona Salter, Susan Sawyer, Beth Shelton, Urvashnee Singh, Sophie Smith, Evelyn Smith, Karen Spielman, Sarah Squire, Juliette Thomson, Marika Tiggemann, Stephen Touyz, Ranjani Utpala, Lenny Vartanian, Andrew Wallis, Warren Ward, Sarah Wells, Eleanor Wertheim, Simon Wilksch & Michelle Williams
The RR was in-part funded by the Australian Government Department of Health in partnership with other national and jurisdictional stakeholders. As the organisation responsible for overseeing the National Eating Disorder Research & Translation Strategy, InsideOut Institute commissioned Healthcare Management Advisors to undertake the RR as part of a larger, ongoing, project. Role of Funder: The funder was not directly involved in informing the development of the current review.
Author information
Authors and affiliations.
InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, Charles Perkins Centre (D17), University of Sydney, Camperdown, NSW, 2006, Australia
Ashlea Hambleton, Danielle Maloney, Stephen Touyz & Sarah Maguire
School of Health and Social Development, Faculty of Health, Deakin University, Geelong, VIC, 3220, Australia
Genevieve Pepin
Healthcare Management Advisors, Melbourne, VIC, Australia
Sydney Local Health District, Camperdown, NSW, Australia
Danielle Maloney, Stephen Touyz & Sarah Maguire
You can also search for this author in PubMed Google Scholar
National Eating Disorder Research Consortium
- Phillip Aouad
- , Sarah Barakat
- , Robert Boakes
- , Leah Brennan
- , Emma Bryant
- , Susan Byrne
- , Belinda Caldwell
- , Shannon Calvert
- , Bronny Carroll
- , David Castle
- , Ian Caterson
- , Belinda Chelius
- , Lyn Chiem
- , Simon Clarke
- , Janet Conti
- , Lexi Crouch
- , Genevieve Dammery
- , Natasha Dzajkovski
- , Jasmine Fardouly
- , Carmen Felicia
- , John Feneley
- , Amber-Marie Firriolo
- , Nasim Foroughi
- , Mathew Fuller-Tyszkiewicz
- , Anthea Fursland
- , Veronica Gonzalez-Arce
- , Bethanie Gouldthorp
- , Kelly Griffin
- , Scott Griffiths
- , Ashlea Hambleton
- , Amy Hannigan
- , Susan Hart
- , Phillipa Hay
- , Ian Hickie
- , Francis Kay-Lambkin
- , Ross King
- , Michael Kohn
- , Eyza Koreshe
- , Isabel Krug
- , Jake Linardon
- , Randall Long
- , Amanda Long
- , Sloane Madden
- , Sarah Maguire
- , Danielle Maloney
- , Peta Marks
- , Sian McLean
- , Thy Meddick
- , Jane Miskovic-Wheatley
- , Deborah Mitchison
- , Richard O’Kearney
- , Shu Hwa Ong
- , Roger Paterson
- , Susan Paxton
- , Melissa Pehlivan
- , Genevieve Pepin
- , Andrea Phillipou
- , Judith Piccone
- , Rebecca Pinkus
- , Bronwyn Raykos
- , Paul Rhodes
- , Elizabeth Rieger
- , Sarah Rodan
- , Karen Rockett
- , Janice Russell
- , Haley Russell
- , Fiona Salter
- , Susan Sawyer
- , Beth Shelton
- , Urvashnee Singh
- , Sophie Smith
- , Evelyn Smith
- , Karen Spielman
- , Sarah Squire
- , Juliette Thomson
- , Marika Tiggemann
- , Stephen Touyz
- , Ranjani Utpala
- , Lenny Vartanian
- , Andrew Wallis
- , Warren Ward
- , Sarah Wells
- , Eleanor Wertheim
- , Simon Wilksch
- & Michelle Williams
Contributions
DM, PM, ST and SM oversaw the Rapid Review process; AL carried out and wrote the initial review; AH and GP wrote the first manuscript; all authors edited and approved the final manuscript.
Corresponding author
Correspondence to Ashlea Hambleton .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
ST receives royalties from Hogrefe and Huber, McGraw Hill and Taylor and Francis for published books/book chapters. He has received honoraria from the Takeda Group of Companies for consultative work, public speaking engagements and commissioned reports. He has chaired their Clinical Advisory Committee for Binge Eating Disorder. He is the Editor in Chief of the Journal of Eating Disorders. ST is a committee member of the National Eating Disorders Collaboration as well as the Technical Advisory Group for Eating Disorders. AL undertook work on this RR while employed by HMA. A/Prof Sarah Maguire is a guest editor of the special issue “Improving the future by understanding the present: evidence reviews for the field of eating disorders.”
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
PRISMA diagram.
Additional file 2.
Studies included in the Rapid Review.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hambleton, A., Pepin, G., Le, A. et al. Psychiatric and medical comorbidities of eating disorders: findings from a rapid review of the literature. J Eat Disord 10 , 132 (2022). https://doi.org/10.1186/s40337-022-00654-2
Download citation
Received : 08 July 2022
Accepted : 15 August 2022
Published : 05 September 2022
DOI : https://doi.org/10.1186/s40337-022-00654-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychiatric
- Comorbidities
- Eating disorders
Journal of Eating Disorders
ISSN: 2050-2974
- General enquiries: [email protected]
What Is A Literature Review?
A plain-language explainer (with examples).
By: Derek Jansen (MBA) & Kerryn Warren (PhD) | June 2020 (Updated May 2023)
If you’re faced with writing a dissertation or thesis, chances are you’ve encountered the term “literature review” . If you’re on this page, you’re probably not 100% what the literature review is all about. The good news is that you’ve come to the right place.
Literature Review 101
- What (exactly) is a literature review
- What’s the purpose of the literature review chapter
- How to find high-quality resources
- How to structure your literature review chapter
- Example of an actual literature review
What is a literature review?
The word “literature review” can refer to two related things that are part of the broader literature review process. The first is the task of reviewing the literature – i.e. sourcing and reading through the existing research relating to your research topic. The second is the actual chapter that you write up in your dissertation, thesis or research project. Let’s look at each of them:
Reviewing the literature
The first step of any literature review is to hunt down and read through the existing research that’s relevant to your research topic. To do this, you’ll use a combination of tools (we’ll discuss some of these later) to find journal articles, books, ebooks, research reports, dissertations, theses and any other credible sources of information that relate to your topic. You’ll then summarise and catalogue these for easy reference when you write up your literature review chapter.
The literature review chapter
The second step of the literature review is to write the actual literature review chapter (this is usually the second chapter in a typical dissertation or thesis structure ). At the simplest level, the literature review chapter is an overview of the key literature that’s relevant to your research topic. This chapter should provide a smooth-flowing discussion of what research has already been done, what is known, what is unknown and what is contested in relation to your research topic. So, you can think of it as an integrated review of the state of knowledge around your research topic.

What’s the purpose of a literature review?
The literature review chapter has a few important functions within your dissertation, thesis or research project. Let’s take a look at these:
Purpose #1 – Demonstrate your topic knowledge
The first function of the literature review chapter is, quite simply, to show the reader (or marker) that you know what you’re talking about . In other words, a good literature review chapter demonstrates that you’ve read the relevant existing research and understand what’s going on – who’s said what, what’s agreed upon, disagreed upon and so on. This needs to be more than just a summary of who said what – it needs to integrate the existing research to show how it all fits together and what’s missing (which leads us to purpose #2, next).
Purpose #2 – Reveal the research gap that you’ll fill
The second function of the literature review chapter is to show what’s currently missing from the existing research, to lay the foundation for your own research topic. In other words, your literature review chapter needs to show that there are currently “missing pieces” in terms of the bigger puzzle, and that your study will fill one of those research gaps . By doing this, you are showing that your research topic is original and will help contribute to the body of knowledge. In other words, the literature review helps justify your research topic.
Purpose #3 – Lay the foundation for your conceptual framework
The third function of the literature review is to form the basis for a conceptual framework . Not every research topic will necessarily have a conceptual framework, but if your topic does require one, it needs to be rooted in your literature review.
For example, let’s say your research aims to identify the drivers of a certain outcome – the factors which contribute to burnout in office workers. In this case, you’d likely develop a conceptual framework which details the potential factors (e.g. long hours, excessive stress, etc), as well as the outcome (burnout). Those factors would need to emerge from the literature review chapter – they can’t just come from your gut!
So, in this case, the literature review chapter would uncover each of the potential factors (based on previous studies about burnout), which would then be modelled into a framework.
Purpose #4 – To inform your methodology
The fourth function of the literature review is to inform the choice of methodology for your own research. As we’ve discussed on the Grad Coach blog , your choice of methodology will be heavily influenced by your research aims, objectives and questions . Given that you’ll be reviewing studies covering a topic close to yours, it makes sense that you could learn a lot from their (well-considered) methodologies.
So, when you’re reviewing the literature, you’ll need to pay close attention to the research design , methodology and methods used in similar studies, and use these to inform your methodology. Quite often, you’ll be able to “borrow” from previous studies . This is especially true for quantitative studies , as you can use previously tried and tested measures and scales.

How do I find articles for my literature review?
Finding quality journal articles is essential to crafting a rock-solid literature review. As you probably already know, not all research is created equally, and so you need to make sure that your literature review is built on credible research .
We could write an entire post on how to find quality literature (actually, we have ), but a good starting point is Google Scholar . Google Scholar is essentially the academic equivalent of Google, using Google’s powerful search capabilities to find relevant journal articles and reports. It certainly doesn’t cover every possible resource, but it’s a very useful way to get started on your literature review journey, as it will very quickly give you a good indication of what the most popular pieces of research are in your field.
One downside of Google Scholar is that it’s merely a search engine – that is, it lists the articles, but oftentimes it doesn’t host the articles . So you’ll often hit a paywall when clicking through to journal websites.
Thankfully, your university should provide you with access to their library, so you can find the article titles using Google Scholar and then search for them by name in your university’s online library. Your university may also provide you with access to ResearchGate , which is another great source for existing research.
Remember, the correct search keywords will be super important to get the right information from the start. So, pay close attention to the keywords used in the journal articles you read and use those keywords to search for more articles. If you can’t find a spoon in the kitchen, you haven’t looked in the right drawer.
Need a helping hand?
How should I structure my literature review?
Unfortunately, there’s no generic universal answer for this one. The structure of your literature review will depend largely on your topic area and your research aims and objectives.
You could potentially structure your literature review chapter according to theme, group, variables , chronologically or per concepts in your field of research. We explain the main approaches to structuring your literature review here . You can also download a copy of our free literature review template to help you establish an initial structure.
In general, it’s also a good idea to start wide (i.e. the big-picture-level) and then narrow down, ending your literature review close to your research questions . However, there’s no universal one “right way” to structure your literature review. The most important thing is not to discuss your sources one after the other like a list – as we touched on earlier, your literature review needs to synthesise the research , not summarise it .
Ultimately, you need to craft your literature review so that it conveys the most important information effectively – it needs to tell a logical story in a digestible way. It’s no use starting off with highly technical terms and then only explaining what these terms mean later. Always assume your reader is not a subject matter expert and hold their hand through a journe y of the literature while keeping the functions of the literature review chapter (which we discussed earlier) front of mind.
Example of a literature review
In the video below, we walk you through a high-quality literature review from a dissertation that earned full distinction. This will give you a clearer view of what a strong literature review looks like in practice and hopefully provide some inspiration for your own.
Wrapping Up
In this post, we’ve (hopefully) answered the question, “ what is a literature review? “. We’ve also considered the purpose and functions of the literature review, as well as how to find literature and how to structure the literature review chapter. If you’re keen to learn more, check out the literature review section of the Grad Coach blog , as well as our detailed video post covering how to write a literature review .
Psst… there’s more!
This post is an extract from our bestselling Udemy Course, Literature Review Bootcamp . If you want to work smart, you don't want to miss this .
You Might Also Like:
16 Comments
Thanks for this review. It narrates what’s not been taught as tutors are always in a early to finish their classes.
Thanks for the kind words, Becky. Good luck with your literature review 🙂
This website is amazing, it really helps break everything down. Thank you, I would have been lost without it.
This is review is amazing. I benefited from it a lot and hope others visiting this website will benefit too.
Timothy T. Chol [email protected]
Thank you very much for the guiding in literature review I learn and benefited a lot this make my journey smooth I’ll recommend this site to my friends
This was so useful. Thank you so much.
Hi, Concept was explained nicely by both of you. Thanks a lot for sharing it. It will surely help research scholars to start their Research Journey.
The review is really helpful to me especially during this period of covid-19 pandemic when most universities in my country only offer online classes. Great stuff
Great Brief Explanation, thanks
So helpful to me as a student
GradCoach is a fantastic site with brilliant and modern minds behind it.. I spent weeks decoding the substantial academic Jargon and grounding my initial steps on the research process, which could be shortened to a couple of days through the Gradcoach. Thanks again!
This is an amazing talk. I paved way for myself as a researcher. Thank you GradCoach!
Well-presented overview of the literature!
This was brilliant. So clear. Thank you
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
- Open access
- Published: 10 April 2024
A systematic review of the association between history of sexually transmitted infections and subsequent condom use in adolescents
- Frédérique Tremblay 1 , 2 ,
- Yohann Courtemanche 1 ,
- Richard E. Bélanger 2 , 4 &
- Anne-Marie Turcotte-Tremblay 2 , 3
BMC Public Health volume 24 , Article number: 1000 ( 2024 ) Cite this article
Metrics details
Sexually transmitted infections (STIs) are common among adolescents. According to the Health Belief Model, cues to action influence preventive behaviors. Cues to action can include health experiences such as being diagnosed with an STI. The impact of a history of STIs on subsequent condom use among adolescents remains largely unexamined, despite high rates of recurrence and their health impacts. This project aimed to systematically review the literature on the association between curable STIs and subsequent condom use among adolescents. The systematic review, reported following PRISMA guidelines, was conducted using the Joanna Briggs Institute method. Eligible studies, in the form of cohort studies, case-control studies, or cross-sectional studies, targeted adolescents aged 10 to 24, with or without a history of curable STIs; the outcome was subsequent condom use. MEDLINE (Ovid), Embase (Elsevier), and Web of Science were searched from January 2012 to December 2022 with the assistance of an information specialist. Two reviewers independently selected articles and extracted data. Risk of bias analysis was performed using ROBINS-E. The review explores results, with tables, based on population characteristics, exposure, and outcome, and addresses the influence of gender, ethnicity, and age. Of 3088 articles identified, seven studies were retained. Almost all the studies focused on African-American, Nigerian, or Rwandan adolescents, and several included only girls. Among girls, a history of STI increased subsequent condom use in combination with other contraceptive methods ( n = 4). Among boys and older adolescents of both genders, a history of STI was associated with a decrease in condom use ( n = 3). No study distinguished between different STIs. While all the studies ( n = 7) presented a high risk of bias, six did not present a threat to conclusion validity. All the studies indicated that a history of STI could influence subsequent protective behaviors, possibly by acting as a cue to action, as posited by the Health Belief Model. This information enhances our understanding of factors leading to the adoption of preventive health measures among adolescents and could apply to other infectious experiences.
Registration The protocol is registered in PROSPERO (CRD42023397443).
Peer Review reports
Sexually active adolescents do not always use condoms during sex. Indeed, while more than 50% of 15–24-year-olds have experienced their first sexual intercourse by age 18 [ 1 ], 40–50% of youths nevertheless report not having used condoms during their most recent sexual intercourse [ 2 , 3 ], which increases their risks of acquiring STIs. Worldwide, there are approximately 333 million new cases of STIs annually, with the highest rates occurring among 15–24-year-olds [ 4 ]. STI incidence is rising, with the largest increase being in adolescents [ 5 , 6 ]. Adolescents represent at least one-third of cases of chlamydia, with the highest levels being seen in younger adolescent girls [ 4 ]. Adolescents and youths between the ages of 10 and 24 years [ 7 ] are particularly susceptible to STIs due to biological, behavioral, and social factors [ 8 , 9 ]. Adolescents from lower socioeconomic backgrounds [ 10 ], ethnic minorities [ 11 ], and sexual orientation minorities [ 12 ] face even higher odds of infection.
Condoms, used during sexual intercourse, are effective in reducing STIs by acting as a barrier to transmission [ 13 , 14 ]. Some STIs remain asymptomatic but transmissible [ 15 ]. Transmission can occur through vaginal, anal, or oral sex [ 15 ]. Chlamydia (including lymphogranuloma venereum, or LGV), gonorrhea, syphilis, and trichomoniasis are curable [ 16 ], and condoms remain the most effective method for reducing the risks of those STIs during sex [ 17 ].
Not using condoms during sex can lead to STIs, which, if left untreated, may result in severe physical consequences such as blindness, cancer, cardiovascular diseases, sterility, and even death [ 18 ]. While adolescents may not frequently experience these consequences, they may develop such problems later in adulthood [ 18 ]. Worldwide, 50% of the most common STIs are curable (chlamydia, gonorrhea, syphilis, and trichomoniasis), with the most common being chlamydia [ 19 ]. Gonorrhea is the second most reported bacterial STI [ 19 ] and, although rare, can cause infertility in both sexes if untreated [ 20 ]. Clinical conditions can include pelvic inflammatory disease, chronic pelvic pain, ectopic pregnancy in girls, and epididymitis in boys [ 20 ]. STIs also entail an important economic burden. For example, the 26 million new STIs in 2018 in the United States of America (USA) are estimated to have incurred $16 billion in direct medical costs for the American healthcare system [ 21 , 22 ], with 15–24-year-olds accounting for up to 26% of the total cost [ 22 ]. Therefore, understanding the factors that influence preventive health behaviors in this area has important implications for the healthcare system.
In public health, the Health Belief Model (HBM) is often used to explain health-related behaviors [ 23 , 24 ], such as condom use. In the HBM, the adoption of preventive health behaviors is influenced indirectly by cues to action, which can be events experienced by the individual [ 23 , 24 ]. According to that model, a history of STI could influence an individual’s subsequent protective behavior by acting as a cue to action such as using a condom during sexual intercourse. Studies in behavioral change psychology and in neurobiology suggest that memories of a past STI could activate or alter subsequent actions, such as the adoption of protective sexual behavior [ 25 , 26 ].
Understanding the impact of an STI on subsequent condom use in adolescents could be particularly important. In one study, a history of STI and related shame were positively associated with condom use in African-American female adolescents [ 27 ]. However, in another, condom use was negatively associated with history of STI in sexually active adolescents [ 28 ]. In a 2002 survey in the USA, adolescents with a history of STI reported less condom use at most recent intercourse [ 29 ]. Other studies on this association have reached conflicting conclusions, with a history of STI associated with either higher or lower subsequent use of condoms [ 30 , 31 , 32 , 33 , 34 , 35 , 36 ]. Adolescents who have had curable infections may use condoms differently from those with chronic infections, as the latters’ motivation may also be linked to the protection of uninfected partners [ 37 ]. Furthermore, even curable infections can recur, which can be avoided if adequate behavior changes are implemented [ 38 ]. Consequently, a synthesis and critical appraisal of the scientific literature on the relation between a history of curable STIs and subsequent condom use in adolescents would be useful to clarify the state of knowledge.
To the best of our knowledge, there is no systematic literature review that would provide a complete picture of the influence of curable STIs on condom use in adolescents. A better understanding of the impacts of those STIs on subsequent condom use would help guide clinical and public health approaches to effective interventions in this population particularly susceptible to STIs and reinfections [ 39 ]. Our review will focus on those infections as cues to action related to condom use in adolescents. It will provide information on factors influencing their sexual preventive behaviors that could be of interest to professionals seeking to help adolescents improve their responses to STIs that could have serious consequences for their future health. Hence, the research question is: what effect does a history of STI have on subsequent condom use in adolescents? In particular, the objective of this review is to synthesize and critically appraise the literature on the association between curable STIs and subsequent condom use among adolescents.
The protocol for this review is registered in PROSPERO (CRD42023397443) [ 40 ]. The Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines were followed [ 41 ]. The Joanna Briggs Institute (JBI) method for a systematic review of etiology was used [ 42 ].
Eligibility criteria
The eligibility criteria for the studies refer to the JBI method [ 42 ], which is the PECOSS approach (P = population, E = exposure C = comparison (non-exposure), O = outcome, S = study design, S = study setting).
Adolescents were the target study population. The age range used was that defined recently by Sawyer et al. in The Lancet , i.e., 10–24-year-olds [ 7 ]. In our protocol, we had predetermined that if the age range was not reported in the article, the population was considered to be within the age range if it concerned “high school students”, “adolescents”, or “young adults”. However, all included studies reported the ages of their participants. Papers reporting exclusively on younger children and/or adults were excluded. Studies had to report on sexual activity. Sexually active youth were defined as having had at least one type of sexual contact (e.g., vaginal, anal, oral) with another person of any gender [ 43 ] as self-reported [ 44 ]. Papers only about sex workers (e.g., exotic dancers, adult film performers) were excluded, on the basis that their activities involve significantly more risky sexual behaviors and higher risk of contracting STIs than those of adolescents in the general population [ 45 ].
Eligible STIs included curable infections (chlamydia or LGV, gonorrhea, syphilis, and trichomoniasis), which represent the most frequent infections in the adolescent population [ 16 , 46 ]. Articles focusing only on incurable STIs (HIV, genital herpes, or HPV) were excluded, as this review was aimed specifically at behaviors that could avoid STI recurrences [ 38 ], which could not be studied in chronically infected individuals. Studies that included multiple curable STIs or that did not distinguish between curable and incurable STIs (e.g., “do you have an STI?”) were eligible for this review. Both objective (i.e., laboratory results or diagnostic tests) and subjective (i.e., self-reported) measures for the STI were acceptable for inclusion. History of STI among some participants included in the study was required for eligibility.
Comparison (non-exposure)
Non-exposure was considered as adolescents’ not having experienced an STI during their lifetime.
Outcome of interest
The outcome of interest was condom use measured after an STI among those who had experienced STIs. Condom use was defined as using or not using a condom during vaginal, anal, or oral sex [ 47 ]. Condom use had to be stated as an outcome of interest in the studies. Papers about unprotected intercourse or composite measures including condoms were eligible. Eligible condom types included any type of equally effective condom (male/female condoms) [ 48 , 49 , 50 , 51 ]. Although any type of condom use reporting was allowed, condom use is most often self-reported [ 52 ]. Any type of measurement was included (yes/no, count, proportion, etc.), any recall period, any partner specificity, and any sexual act [ 17 ].
Study design
Observational studies were required [ 42 , 53 ]. Studies were included if they reported results specifically on the association of interest (STI history and subsequent condom use). Prospective and retrospective cohort studies, case-control studies, and cross-sectional studies were included in the review [ 53 ]. Cross-sectional studies were considered if it was clear that individuals who had experienced an STI reported on their infection history and subsequent condom use.
Study setting
To obtain a generational portrait of adolescents, studies published from January 2012 to December 2022 were included in the review. The decision was taken to cover the last decade, as major behavioral trends can differ between generations that are exposed to different historical events and context during particular life stages [ 54 , 55 ].
Information sources
MEDLINE (Ovid), Embase (Elsevier), and Web of Science were searched [ 56 , 57 ]. All the reference lists of the included studies from the databases were evaluated for inclusion. A list of all the included studies ( n = 7) was forwarded to the systematic review team. Only published studies were searched; given the etiological perspective of the systematic review, the grey literature was not considered.
Search strategy
The search strategy (see Additional file 1 ) was developed through an iterative process between FT (first author) and the information specialist and subsequently approved by the systematic review team. It was then performed in the selected databases. The concepts considered were: adolescent population, STIs (gonorrhea, syphilis, chlamydia or LGV, and trichomoniasis), condom use, and observational studies, as indicated in the study design section above. The search strategy for observational studies was inspired by the strategies used by Li et al. [ 58 ] and Avau et al. [ 59 ]. Cross-sectional studies in the form of surveys or questionnaires were included [ 58 , 59 ]. Given the evolution in terminology in recent years, the term sexually transmitted disease (STD) was included, along with STI, in the literature search. No restrictions were applied on language and year of publication.
Selection process
The selection process was completed in four steps using Covidence. The first consisted of a pilot selection from 10% of the total number of unique references, randomly chosen. Two reviewers independently selected studies based on the eligibility criteria. This pilot selection ensured a shared comprehension of the eligibility criteria among all members involved in the selection process, using the kappa statistic (> 0.7 considered satisfactory) [ 60 , 61 ]. When the conclusion was unsatisfactory, the criteria were adjusted. The second step was the selection by two reviewers once the pilot test was concluded. The two reviewers independently selected studies based on titles and abstracts. When there was consensus, the article was included or excluded [ 62 ] for full-text screening. The third step consisted of independent selection based on full-text screening by two reviewers, with disagreements resolved through discussion. If disagreements were due to a difference in interpretation, arbitration by a third reviewer was sought. No contact with the authors of the studies was needed. Agreement was again assessed using the kappa statistic [ 60 ]. In the fourth step, the included studies were discussed by the reviewers for final selection.
Data collection process and data items
To extract the variables of interest, an Excel [ 63 ] data extraction form was developed based on a coding guide that included definitions of those variables and the extraction modalities. The following variables were considered, in five categories: 1) study characteristics included name of first author, year of publication, country in which the study was conducted, study setting, and study design; 2) population characteristics included race/ethnicity, gender, sample size, mean, minimum and maximum age, sexual activity, and socioeconomic status; 3) STI history characteristics included type of STI, frequency of STI history, type of measure of STI history, and recall period; 4) condom use characteristics included frequency of outcome use (for each possible outcome: condom use alone, dual method, multiple methods, unprotected sex acts, protected sex acts, consistent condom use, and risky sexual behavior), condom type, temporal period for each possible outcome, types of response choices presented for condom measurement questions, consistency of condom use, type of sexual act in which the condom outcome was used, abstinence, type of partner, effect measure used (i.e., odds ratio, relative risk), group in which the effect was assessed, adjusted and crude effect measures, and standard error for further calculation of the 95% confidence interval (CI); and 5) characteristics of the method used included the regression model for each outcome and the handling of missing data. Pilot extraction was carried out independently on two studies by two reviewers prior to the main data extraction to ensure a shared comprehension and fine-tuning of the extraction guide as needed. The two reviewers then independently carried out the extraction. Disagreements were discussed and resolved with the help of a third reviewer as needed.
Study risk of bias assessment
Risk of bias in the studies was independently assessed by two reviewers after a pilot step was concluded. Since only cohort and cross-sectional studies were identified, risk of bias was assessed using the Risk Of Bias In Non-randomized Studies—of Exposure (ROBINS-E) tool [ 64 ]. This tool covers seven domains of risk of bias related to: 1) confounding; 2) measurement of exposure; 3) selection of participants into the study or into the analysis; 4) post-exposure interventions; 5) missing data; 6) measurement of the outcome; and 7) selection of the reported result [ 64 ]. Each of these domains and overall risk of bias were rated as low risk of bias , some concerns , high risk of bias , or very high risk of bias , according to the ROBINS-E algorithms [ 64 ]. The conclusion of those algorithms could be overridden if the authors of the review deemed that it did not yield an appropriate risk of bias judgment, as recommended by the ROBINS-E Development Group (2023) [ 64 ]. Disagreements were discussed and resolved by the two reviewers, with arbitration by a third reviewer as needed. Confounders were selected based on an a priori literature screening, which identified the following as determinants of exposure and outcome: social and sexual network [ 65 , 66 ]; risky sexual behavior tendencies [ 67 , 68 ]; education [ 18 , 69 , 70 ]; knowledge and awareness [ 71 , 72 , 73 ]; socioeconomic status [ 65 , 74 ]; healthcare resources [ 65 , 74 , 75 ]; age [ 8 , 9 , 65 ]; gender [ 76 , 77 ]; ethnicity [ 11 , 78 ]; and cultural and religious beliefs [ 65 , 79 ].
Data synthesis
The study selection process was reported with the number of identified studies, the number of studies retained based on title and abstract, and the number of studies selected by full-text screening based on the eligibility criteria. The extracted data were synthesized using tables and in narrative form regarding the studies, population, exposure, and outcomes characteristics. The associations between STI history and different types of condom use outcomes were individually explored to assess the impact of STI history on different behaviors in different contexts. Further narrative exploration of the associations was based on different outcomes, gender, race/ethnicity, and age. The effect of an STI infection on condom use by adolescents was reported with the effect measure used in the eligible studies and its 95%CI. Where missing, the 95%CI was calculated [ 80 ]. When a study did not present an adjusted effect measure, one was calculated, if possible, when data were available. Authors were contacted if information necessary for analysis was missing in the reviewed papers. Given the high heterogeneity of the studies, no meta-analysis was performed. A table was produced presenting the risk of bias of each study according to the ROBINS-E and the relevant domain. Risk of bias was considered in the interpretation of results. Certainty assessment, publication bias assessment, and subgroup analyses were not conducted.
Study selection process and study characteristics
From a total of 3088 articles retrieved, seven (Walsh et al. 2014; Kottke et al. 2015; Wallace et al. 2015; Clarke et al. 2016; Chambliss et al. 2021; Ebuenyi et al. 2021; and Kawuki et al. 2022) met the criteria (Fig. 1 ) [ 33 , 36 , 81 , 82 , 83 , 84 , 85 ]. Among these included studies, five were cross-sectional [ 33 , 36 , 82 , 83 , 84 ], one was a repeated cross-sectional study [ 81 ], and one was a prospective cohort study [ 85 ]. The included studies were published between 2014 [ 85 ] and 2022 [ 83 ], and were conducted in the USA ( n = 5) [ 33 , 36 , 81 , 84 , 85 ], in Nigeria ( n = 1) [ 82 ], and in Rwanda ( n = 1) [ 83 ] (Table 1 ). Three studies were conducted in clinical settings [ 33 , 36 , 84 ], two were community-based, either in an ongoing survey or a demographic survey [ 81 , 83 ], and two were conducted in schools [ 82 , 85 ] (Table 1 ).
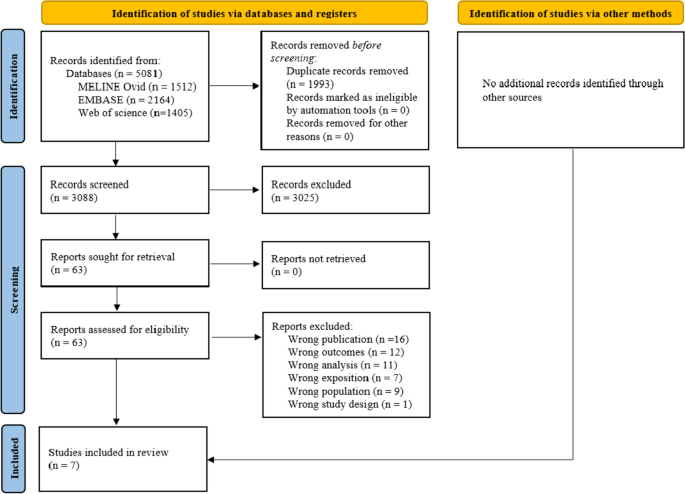
PRISMA 2020 flow diagram for systematic review [ 41 ]
Characteristics of the study population
The mean age of participants ranged from 16.0 [ 81 ] to 21.3 years [ 36 ] (Table 1 ), with an age range of 14 to 24 years (Table 1 ). One study [ 85 ] did not report the maximum age. All studies reported on origins [ 33 , 81 , 82 , 83 , 84 ] or race [ 36 , 85 ] (Table 2 ). Participants were African-American [ 33 , 81 , 84 ], a majority of Black non-Hispanic (61% of the sample) [ 36 ], only Nigerian [ 82 ], or only Rwandan [ 83 ], and in one study, 71% of participants were White [ 85 ] (Table 2 ). Five studies reported on some socioeconomic indicators [ 33 , 82 , 83 , 84 , 85 ], while two reported no information on socioeconomic indicators. The most frequent indicator used was education ( n = 3) of either a family member [ 84 ] or the participant [ 82 , 83 ]. Gender was reported by all studies, with four studies about girls only [ 33 , 83 , 84 , 85 ], one about boys only [ 81 ], and two about both [ 36 , 82 ] (Table 2 ). Six of the seven studies only included sexually active participants [ 33 , 36 , 81 , 83 , 84 , 85 ] and limited the analysis to them, while one study included sexually abstinent participants in the main analysis [ 82 ] (Table 2 ).
Characteristics of STI history
None of the studies differentiated among STI types or noted whether the STI was curable or not [ 33 , 36 , 81 , 82 , 83 , 84 , 85 ]. Questions were often general, with participants being asked: “Ever been told you had an STD” [ 36 , 81 ] or whether they had a “previous STD” [ 84 ]. Almost all the studies ( n = 6) reported on what proportion of the participants had a history of STI [ 33 , 36 , 82 , 83 , 84 , 85 ], ranging from 2.6% to 43.7% (Table 2 ). All studies asked about STI history through survey questions [ 33 , 36 , 81 , 82 , 83 , 84 , 85 ]. Regarding recall, four studies asked about lifetime exposure [ 33 , 82 , 84 , 85 ], two asked about history of STI within the past year [ 81 , 83 ] and one asked specifically about more than three months ago [ 36 ] (Table 1 ).
Characteristics of condom use
Three types of outcomes regarding condom use were identified: 1) use of condom alone (condom use [ 81 , 84 ], consistent condom use [ 36 ], and percentage of protected vaginal sex acts out of the total number of sex acts [proportional condom use] [ 36 ]); 2) use of condom simultaneously with a contraceptive method (dual method [ 84 , 85 ], or multiple methods of contraception including condoms [ 33 , 83 ]); and 3) unprotected sex (number of unprotected sex acts [ 36 ] or risky sexual behaviors [ 82 ]) (Table 1 ). In the three studies reporting on the use of condom alone, the proportion of participants using condoms ranged from 20.6% to 56.9% [ 81 , 84 ] (Table 3 ). Only one study reported the proportion of participants consistently using a condom (19.0%); this study also reported 54.7% of proportional condom use [ 36 ] (Table 3 ). Four studies also used dual method or multiple methods as outcomes [ 33 , 83 , 84 , 85 ]. Of the studies reporting on frequency of use, dual or multiple methods were used by 17.4% to 63.1% of participants [ 33 , 83 , 84 ] (Table 3 ). Two studies reported on unprotected sex acts, either reporting the number of unprotected vaginal sex acts in the past three months (mean (SD): 12.0 (18.7)) [ 36 ] or the proportion of participants using risky sexual behaviors, including condomless sex (46.8%) [ 82 ] (Table 3 ). In the remainder of this paper, “condom use” is an umbrella term for all condom use possible outcomes.
Characteristics of reporting
Five studies did not mention condom type [ 33 , 36 , 81 , 82 , 84 ], one specifically referred to male condoms [ 83 ], and one did not differentiate between types of condoms [ 85 ] (Table 3 ). Last sex [ 33 , 81 , 84 ] and sex in the past three months [ 36 , 82 , 85 ] were each used three times for the outcome timeline (Table 1 ), while one study did not mention any timeline [ 83 ]. Almost all studies ( n = 6) asked about the use of condoms using a dichotomous yes/no question [ 33 , 81 , 82 , 83 , 84 , 85 ], while one asked about number of times condoms were used during a given time period [ 36 ] (Table 3 ). Only two studies reported on consistency of condom use [ 36 , 85 ], and none clearly addressed the type of partner with regard to the sexual activity under study (Table 3 ). Three studies indicated the type of sex act, all vaginal [ 33 , 36 , 85 ] (Table 3 ).
Characteristics of statistical methods
Five studies used logistic regression [ 33 , 36 , 81 , 82 , 83 ], one used linear regression [ 36 ], one used generalized estimating equation to account for dependency in observations [ 84 ], and one used multilevel modeling [ 85 ] (Table 3 ). Five studies had no missing values [ 33 , 36 , 82 , 83 , 84 ], one excluded participants based on missing values [ 81 ], and one practiced multiple imputation [ 85 ] (Table 3 ).
Risk of bias
Figure 2 presents the risk of bias assessment of the included studies. All studies presented a high risk of bias [ 33 , 36 , 81 , 82 , 83 , 84 , 85 ]. Five presented some concerns or a high risk of bias due to confounding [ 33 , 36 , 81 , 82 , 85 ] from a lack of consideration of confounders, which could lead to underestimation of the effect measure. No study presented a risk of bias arising from the measurement of the exposure. One study presented some concerns regarding the selection of participants into the study, while the three studies conducted in a clinical setting (either adolescent clinics or STI clinics) presented a high risk of bias [ 33 , 36 , 84 ]. No bias was found regarding post-exposure intervention, and only one study presented concerns due to missing data [ 81 ]. All studies presented a high risk of bias arising from the measurement of condom use, given the possibility of differential information bias regarding outcomes as reported by people with an STI history and those without. Two studies presented a high risk of bias regarding the selection of reported results [ 33 , 85 ]. Despite the biases identified, most studies still produced interpretable conclusions with respect to predicted directions and the context leading to the conclusions, particularly regarding the 1 st and 6 th risk of bias domains. Considering this, studies that were classified as having a very high risk of bias using the ROBINS-E’s algorithm were classified as having a high risk of bias. Three studies probably had a larger effect measure than they should have had, while three noted a weaker effect than they should have had.
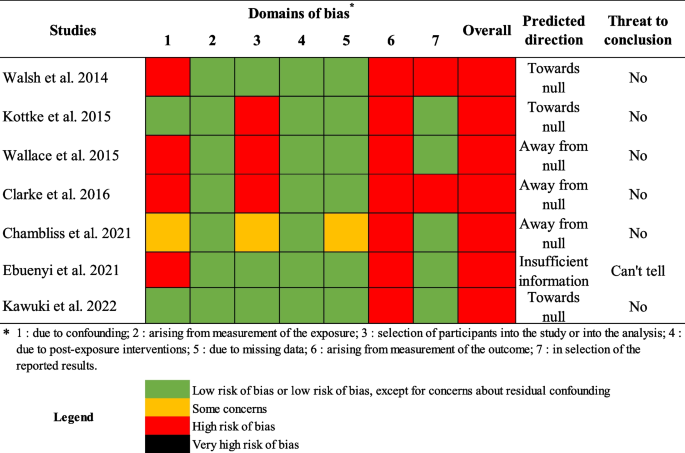
Risk of bias assessment with the Risk of Bias In Non-randomized Studies – of Exposure (ROBINS-E)
Association between history of STI and condom use outcomes
The exposure and outcome timelines and types of outcomes are presented in Table 1 , along with crude effects and adjusted effects with 95%CI of the association between an STI history and subsequent condom use, where reported by individual studies. Other details about exposure and outcomes can be found in Tables 2 and 3 respectively.
Results of synthesis
Sti history and condom use alone.
Three studies examined the association between STI history and condom use alone [ 36 , 81 , 84 ] (Table 1 ). When condom use alone was observed, only one study found that STI history in the past year was associated with a reduction in condom use at last sex (OR 0.37, 95%CI; 0.16–0.89) [ 81 ] (Table 1 ). This effect was only found in one wave of a repeated cross-sectional study. This study was rated with a high risk of bias without threat to conclusion validity (Fig. 2 ). Other studies examining the association between STI history and condom use alone did not find a similar association [ 36 , 84 ] and were also rated with a high risk of bias (Fig. 2 ).
STI history and dual method
Two studies examined the association between STI history and the dual method [ 84 , 85 ]. When condom use was coupled with another method to prevent pregnancy, one study found statistically significant higher odds of dual method use at last intercourse (adjusted odd ratios [AOR] 2.30, 95%CI; 1.26–4.18) with a lifetime history of STI [ 84 ]. The other found higher odds of dual method use in the past three months (AOR 2.88, 95%CI; 1.17–4.59) with a lifetime history of STI [ 85 ] (Table 1 ). While both studies had a high risk of bias, no threat to conclusion validity was found (Fig. 2 ).
STI history and multiple methods
Two studies examined the association between STI history and multiple methods [ 33 , 83 ]. When condom use was combined with other methods or considered in the pooled result of multiple methods examined, one study found higher odds of use at last sex in adolescents 14–16 years old who had a lifetime history of STI (AOR 4.80, 95%CI; 1.80–13.10) [ 33 ]. The other also found higher odds of use, but in sexually active adolescents 15–19 years old who had an STI within the past year (AOR 8.27, 95%CI; 2.54–26.10) [ 83 ] (Table 1 ). Kawuki et al. [ 83 ] also reported an AOR including non-sexually active participants (AOR 38.89, 95%CI; 10.28–147.10) (Table 1 ). Both studies had a high risk of bias without threat to conclusion validity (Fig. 2 ).
STI history and unprotected sexual acts
Two studies examined the association between STI history and unprotected sexual acts [ 36 , 82 ]. One study found that having had an STI more than three months ago was significantly associated with an increase in unprotected vaginal sex in the past three months in 18–24-year-old participants (β 5.32, 95%CI; 0.52–10.12) [ 36 ]. Another found that the odds of risky sexual behavior were higher in 15–19-year-old participants previously diagnosed with an STI (AOR 2.08, 95%CI; 1.12–3.96) [ 82 ] (Table 1 ). Only the study reporting on risky sexual behavior had a possible threat to conclusion validity [ 82 ] (Fig. 2 ).
STI history and condom use, according to gender
All studies that examined the effect of a history of STI on condom use only in girls ( n = 4) inspected either dual method or multiple methods as outcomes [ 33 , 83 , 84 , 85 ] (Tables 1 and 2 ). According to the results with these outcomes, all were statistically significant and associated with higher use, while none presented any threat to conclusion validity regarding risk of bias assessment [ 33 , 83 , 84 , 85 ] (Fig. 2 ). No association with STI history was found regarding condom use alone in girls [ 84 ]. The study that included only boys ( n = 1) found that adolescent boys with a history of STI had lower odds of using a condom at last sex than those without such history [ 81 ], with no threat to conclusion validity (Fig. 2 ). Two studies included both boys and girls. Both studies, when inspecting unprotected sex acts or risky sexual behaviors, found a positive association with STI history [ 36 , 82 ]. However, no association was found regarding condom use alone [ 36 ]. Possible threats to conclusion validity remained regarding Ebuenyi et al. [ 82 ] (Fig. 2 ).
STI history and condom use, according to ethnicity or race
Three studies were conducted with African-Americans; these examined condom use alone and dual method [ 84 ], multiple methods [ 33 ], and condom use alone [ 81 ] (Tables 1 and 2 ). All three studies found statistically significant effects toward a positive association between history of STI and dual method or multiple methods (Table 1 ). One study conducted with a majority of Black non-Hispanic Americans (61%) found an increase in unprotected vaginal sex acts in boys diagnosed with an STI more than three months ago [ 36 ], with no threat to conclusion validity (Fig. 2 ). The one study conducted with Nigerians presented a threat to conclusion validity regarding the positive association found between STI history and risky sexual behavior (Table 1 and Fig. 2 ) [ 82 ]. The study conducted with Rwandans found a positive association between STI history in the past year and the use of multiple methods (Table 1 ), with no threat to conclusion validity [ 83 ] (Fig. 2 ). Finally, only one study was conducted with a majority of White Americans, which found a positive association between lifetime history of STI and dual method use in the past three months (Table 1 ) [ 85 ], with no threat to conclusion validity arising from bias (Fig. 2 ).
STI history and condom use, according to age
Two studies examined the association between STI history and condom use in adolescent populations with mean age above 20 years [ 36 , 82 ]. One found a positive statistically significant association between STI history and unprotected vaginal sex acts [ 36 ], while the other found a statistically significant association with risky sexual behaviors [ 82 ] (Table 1 ). Both were assessed as having a high risk of bias, with only the one regarding risky sexual behaviors presenting a possible threat to conclusion validity (Fig. 2 ). The remaining studies ( n = 5) examined the association between STI history and condom use in younger participants (≤ 18.1 mean years of age) and examined either condom use alone or dual method/multiple methods (Table 1 ) [ 33 , 81 , 83 , 84 , 85 ]. Those studies found the previously stated results regarding dual method/multiple methods and condom use alone, with the respective risks of bias (Fig. 2 ).
Summary of evidence
Three types of outcomes regarding condom use were identified in only seven studies over the last decade. Most of those studies presented interpretable conclusions even in the presence of a risk of bias. Our review found that: 1) a history of STI was rarely associated with condom use alone, except when analyzed only in boys, who tended to use condoms less after having recovered from an infection; 2) younger girls with a history of STI increased their use of dual/multiple methods; 3) both boys and girls of older age reported increased unprotected sex acts after an STI; and 4) race/ethnicity cannot, at this point, be stated as influencing the association between STI history and subsequent condom use. Due to the small number of studies, the findings should be interpreted with care.
Explanatory hypotheses supported by literature
In one of the included studies, STI history in boys was associated with a reduction in subsequent use of condom alone. Some studies showed that the association between STI history and condom use was influenced by gender. The association between a history of STI and subsequent condom use alone may disappear when the two genders are combined in the analysis. Studies that did not differentiate by gender in their analysis possibly confounded the effect. The studies that included boys did not inspect the association with the dual method or multiple methods of protection including condoms. Those two outcomes referred mostly to pregnancy prevention methods only used by girls [ 87 ]. However, studies examining contraception in adolescence have historically analyzed it in girls, who still often assume responsibility for reproductive planning and childcare [ 88 , 89 ]. The lack of association or possible negative association with condom use alone could be due to adolescent boys’ taking more sexual risks than girls [ 90 ]. Boys-only analyses could show an increase in risk-taking behavior considering that tendency of higher risk-taking [ 90 , 91 ]. Moreover, one of the most common STIs, chlamydia, has few complications in boys, which could influence their subsequent behaviors after infection [ 92 ]. However, the one study that found an association between STI history and condom use alone only reported it in one of the waves of their repeated cross-sectional survey, which suggests that it could not be replicated in different years [ 81 ]. This could also mean, as the authors concluded, that STI history is not a consistent predictor of condom use alone [ 81 ].
Remarkably, STI history was associated with subsequent unprotected sexual acts and risky sexual behaviors in both boys and girls, even when a history of STI appeared to increase subsequent condom use in combination with other contraceptive methods in girls. Determinants of preventive health behaviors may help explain this. In fact, those two studies combining boys and girls each had a population with a mean age over 20 years, and older adolescents are known to be more prone to adopting negative attitudes toward condom use [ 36 ]. As condom use is significantly influenced by attitudes [ 93 ], this could potentially explain the direction of the association. Studies should be replicated in older adolescents with a rigorous methodology to eliminate the risk of threat to conclusion validity that is present in one of those studies.
Girls with a history of STI increased their dual/multiple methods use. Several factors contribute to the importance of condom use in adolescent girls [ 74 , 94 ]. Girls are disproportionately affected by STIs [ 95 ], and those who are infected may be warned about the serious potential impacts of STIs on their fertility [ 96 , 97 , 98 ]. The effects are particularly important on their reproductive health because of their anatomy, in that female fertility is vulnerable to STIs due in part to delicate vaginal mucosa [ 97 ] and possible damage and occlusion of the fallopian tubes from previous infection [ 98 ]. Moreover, these vulnerabilities can be exacerbated when girls are living in unfavorable sociocultural and economic conditions [ 97 ]. It is plausible that the clinical approach taken with girls infected by STIs may be different from that with boys. This could explain the divergence between genders with regard to the impact of STI history on subsequent condom use and extra protection regarding pregnancy.
With regard to race or ethnicity, no clear pattern appeared to influence the association between STI history and subsequent condom use. Three studies found a positive association with the dual method or multiple methods, while three others found associations with unprotected sexual acts. The only study in a White population found a positive association with dual method use. This could potentially mean that neither race nor ethnicity explain all the relationships between STI history and subsequent condom use, as gender appears to do in those seven studies. African-American girls are often disproportionately negatively affected by sexual and reproductive health conditions compared with girls from other races or ethnicities, in part because of socioeconomic factors [ 99 ]. The higher odds of infection in ethnic minorities [ 11 , 100 ] could partially explain their high representation in the studies included in the systematic review. Race and ethnicity remain important in health research, notably to highlight health disparities. However, given the lack of clear consensus definitions regarding race and ethnicity in some research areas, researchers should consider carefully the definitions they apply when creating classifications for their research objectives [ 101 ]. The contexts of health determinants likely play an important role when the association of interest is observed. The sociocultural context of the individuals included in the study should also be considered.
Limitations of the evidence
An important limitation is the small number of studies included in the review, which limited our data analysis and quantification of the effect of interest on the outcomes found. More studies could help to clarify the conclusions coming from the small number of studies, as well as to generalize findings to more populations. Most of the studies included focused on African-American adolescent girls in the USA or in African countries (Nigeria and Rwanda). The results should be interpreted with caution when applied to contexts other than those studied. These studies would need to be replicated in other contexts and with more diverse populations to enhance the external validity of the findings [ 102 ].
While STI history and subsequent condom use could be studied with longitudinal studies, cross-sectional surveys were almost always used (85.7%). Cross-sectional surveys are sources of reliable information representative of the populations under study [ 102 ]. However, longitudinal studies could be beneficial, in order to establish the important temporal sequence to causality, to exclude recall bias, and to observe changes over time [ 102 , 103 ].
None of the studies included in this review differentiated between curable and incurable STIs. Future research should distinguish between different types of STIs (e.g., curable vs incurable), as they may affect preventive behaviours differently. This would help clarify the association between STI history and subsequent condom use with regard to different types of exposure.
Almost all the studies used dichotomous questions regarding condom use. A 2014 systematic review of condom use measurement called for a standardization of measures [ 104 ], as the lack of standards for condom use measurement hinders the comparability of findings across studies. According to that systematic review of 215 studies, six dimensions could be considered when condom use is the outcome of interest: partner type, temporal period, measurement scale, consistency of use, controlling for abstinence, and type of sex [ 104 ]. In particular, some studies did not limit their analysis to sexually active participants, which could confound the association between STI history and condom use. This could explain, in part, why Kawuki et al. [ 83 ] found such a high odds ratio when including all samples, which would have included low numbers of participants with STI history. While exposure timeline was variable in the studies, the temporal periods for condom use were similar in most cases. However, most of the studies did not report on consistency of use, and consistency plays an important part in the reduction of transmission during condom use [ 105 ]. It was not possible to ascertain what type of partner the condom use involved: in fact, it is known that condom use varies by partner type, being lower with a primary partner and in long-term relationships [ 106 ]. Taking into account all these elements could significantly enhance the study of the association between STI history and subsequent condom use. On the other hand, almost all the studies ( n = 5) included socioeconomic indicators, which is sometimes an important gap in the scientific literature, even in the highest-ranked medical journal, as reported in a recent literature review [ 107 ].
The three studies conducted in a clinical setting presented a risk of selection bias. Both STI history and condom use can lead people to seek clinical consultation, which could result in a possible collider bias [ 102 , 108 ]. When selecting participants in a clinical context, attention should be given to ensuring that the association of interest is free of such bias. Another important selection bias can arise when excluding participants based on missing values, especially if those values are not missing at random [ 109 ], which was done in one study without consideration of the mechanism responsible for the missing data. Multiple imputation is a useful method for handling missing values [ 109 ]. Results should be presented even when not statistically significant, which sometimes leads to selecting a high risk of bias in the 7 th domain of ROBINS-E.
Many other psychosocial variables could explain behavior change, such as perceived susceptibility, perceived severity, health motivation, self-efficacy, or perceived benefits or barriers [ 110 ]. However, none of the articles included in the literature review elaborated on such psychosocial variables. Future research should explore how psychosocial variables and past experiences can influence preventive actions such as condom use.
Limitations of the review process
As mentioned earlier, articles from inception to 2012 in MEDLINE, Embase, and Web of Science were excluded, in order to focus on a ten-year generational context [ 54 , 55 , 111 ]. Hence, one limitation of this systematic review is that the conclusions cannot be generalized to earlier time periods. However, the results will be useful for decision-makers focused on the behaviors of contemporary youth.
Future research
Multiple studies in this review did not consider important confounding factors, such as social and sexual networks [ 65 , 66 ], other risky sexual behaviors [ 67 , 68 ], education [ 18 , 69 , 70 ], knowledge and awareness [ 71 , 72 , 73 ], socioeconomic status [ 65 , 74 ], healthcare resources [ 65 , 75 ], and cultural and religious beliefs [ 65 , 79 ]. However, those confounders are known to have a positive association with STI history and a negative association with condom use, which suggests a possible underestimation of the effect measure. Even in the presence of a high risk of bias, the conclusions about the association for many of the studies would still be the same. Furthermore, the high risk of bias concluded in all the studies also results from bias arising from the measurement of condom use. This stems from the fact that people who had STIs and those who did not could potentially have given differential information regarding condom use outcomes. However, information about condom use is a self-reported measure [ 104 ], and such a requirement could not be taken into account in ROBINS-E. All our studies were ultimately classified with a high risk of bias. It is important to note that greater attention should be given to threats to conclusion validity regarding the reasons behind the categorization in the 1 st and 6 th domains.
Implications of research findings
The differences in the association between STI history and condom use detected between girls and boys, and between the different age groups, call for a rethinking of clinical approaches and awareness-raising interventions after an STI diagnosis. Gender-specific approaches in clinical and research settings have been beneficial in fields related to psychiatry [ 112 ], cardiovascular diseases, and osteoporosis [ 113 ]. Such approaches are, in fact, a step closer to gender equity, as they take into account the specific needs of both men and women [ 114 ]. The same can be said for age-specific interventions targeting adolescents [ 115 ]. Tailoring counseling and education practices to specific groups could minimize the risks of transmission and reinfection.
Conclusions
Condom use in adolescents who have experienced STIs is important, as they must protect themselves from reinfections and further transmission. In line with the HBM, these results highlight factors that can influence the adoption of preventive health measures, such as condom use, among adolescents who experienced STIs. The results could help in tailoring gender-sensitive clinical approaches to STI diagnosis in adolescents. As STIs are transmitted via sexual interactions, both girls and boys should be involved in decisions on their subsequent condom use and reminded of the impact of STIs. Even in older adolescent populations, with their higher possibility of perpetuating risky sexual behaviors, STIs require serious consideration. Further studies should differentiate this issue by gender and adolescent age, examining the different potential impacts on behavior. More studies, with rigorous epidemiologic methods, should also investigate the association in young boys [ 88 , 89 ]. Such results could also apply to other infectious experiences, as a curable infection could potentially modulate subsequent behaviors in adolescence.
Availability of data and materials
All data and materials used in the present systematic review are available from the corresponding author.
Abbreviations
Confidence interval
- Health Belief Model
Human immunodeficiency virus
Human papillomavirus
Joanna Briggs Institute
Lymphogranuloma venereum
Population, Exposure, Comparison, Outcome, Study design, Study setting
Preferred Reporting Items for Systematic reviews and Meta-Analyses
Risk Of Bias In Non-randomized Studies – of Exposure
Sexually transmitted disease
Sexually transmitted infection
United States of America
Finer LB, Philbin JM. Sexual initiation, contraceptive use, and pregnancy among young adolescents. Pediatrics. 2013;131(5):886–91.
Article PubMed PubMed Central Google Scholar
Rotermann M, McKay A. Sexual behaviours, condom use and other contraceptive methods among 15- to 24-year-olds in Canada. Health Rep. 2020;31(9):3–11.
PubMed Google Scholar
Jing Z, Li J, Wang Y, Zhou C. Prevalence and trends of sexual behaviors among young adolescents aged 12 years to 15 years in low and middle-income countries: population-based study. JMIR Public Health Surveill. 2023;9: e45236.
Dehne K, Riedner G. Sexually transmitted infections among adolescents. The need for adequate health services. Geneva: World Health Organization. 2005 [Available from: https://www.who.int/publications/i/item/9241562889 .
Shannon CL, Klausner JD. The growing epidemic of sexually transmitted infections in adolescents: a neglected population. Curr Opin Pediatr. 2018;30(1):137–43.
Zhang J, Ma B, Han X, Ding S, Li Y. Global, regional, and national burdens of HIV and other sexually transmitted infections in adolescents and young adults aged 10–24 years from 1990 to 2019: a trend analysis based on the Global Burden of Disease Study 2019. Lancet Child Adolesc Health. 2022;6(11):763–76.
Article PubMed Google Scholar
Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health. 2018;2(3):223–8.
Hitchcock PJ. Adolescents and sexually transmitted diseases. AIDS patient care STDs. 1996;10(2):79–85.
Article CAS PubMed Google Scholar
Lindberg LD, Firestein L, Beavin C. Trends in U.S. adolescent sexual behavior and contraceptive use, 2006–2019. Contracept X. 2021;3:100064.
The Lancet Child Adolescent Health. Youth STIs: an epidemic fuelled by shame. Lancet Child Adolesc Health. 2022;6(6):353.
Ojukwu EN, Okoye HU, Saewyc E. Social correlates of HIV-risky behaviours among African Canadian adolescents living in British Columbia, Canada: a secondary data analysis. Int J Environ Res Public Health. 2023;20(11):6031.
Everett BG. Sexual orientation disparities in sexually transmitted infections: examining the intersection between sexual identity and sexual behavior. Arch Sex Behav. 2013;42(2):225–36.
Holmes KK, Levine R, Weaver M. Effectiveness of condoms in preventing sexually transmitted infections. Bull World Health Organ. 2004;82(6):454–61.
PubMed PubMed Central Google Scholar
Mahdy H, Shaeffer AD, McNabb DM. Condoms. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 [Available from: https://www.ncbi.nlm.nih.gov/books/NBK470385/ .
CDC. CDC Fact Sheet: Information for teens and young adults: staying healthy and preventing STDs. Centers for Disease Control and Prevention 2022 [Available from: https://www.cdc.gov/std/life-stages-populations/stdfact-teens.htm .
WHO. Sexually transmitted infections (STIs) [Internet]. Geneva: World Health Organization. 2023 [Available from: https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis ).
Noar SM, Cole C, Carlyle K. Condom use measurement in 56 studies of sexual risk behavior: review and recommendations. Arch Sex Behav. 2006;35(3):327–45.
Yarber WL, Parrillo AV. Adolescents and sexually transmitted diseases. J Sch Health. 1992;62(7):331–8.
Garcia MR, Leslie SW, Wray AA. Sexually transmitted infections. In: StatPearls [Internet]: Treasure Island (FL): StatPearls Publishing; 2023 [Available from: https://www.ncbi.nlm.nih.gov/books/NBK560808/ .
Choudhri Y, Miller J, Sandhu J, Leon A, Aho J. Gonorrhea in Canada, 2010–2015. Can Commun Dis Rep. 2018;44(2):37–42.
Article CAS PubMed PubMed Central Google Scholar
CDC. 1 in 5 people in the U.S. have a sexually transmitted infection. Centers for Disease Control and Prevention; 2021 [Available from: https://www.cdc.gov/nchhstp/newsroom/2021/2018-STI-incidence-prevalence-estimates.html .
Chesson HW, Spicknall IH, Bingham A, Brisson M, Eppink ST, Farnham PG, et al. The estimated direct lifetime medical costs of sexually transmitted infections acquired in the United States in 2018. Sex Transm Dis. 2021;48(4):215–21.
Becker MH. The Health belief model and personal health behavior. Thorofare (NJ): Slack; 1974.
Google Scholar
Becker MH, Drachman RH, Kirscht JP. A new approach to explaining sick-role behavior in low-income populations. Am J Public Health. 1974;64(3):205–16.
Duckworth AL, Gross JJ. Behavior change. Organ Behav Hum Decis Process. 2020;161(Suppl):39–49.
Shors TJ. Significant life events and the shape of memories to come: a hypothesis. Neurobiol Learn Mem. 2006;85(2):103–15.
Sales JM, DiClemente RJ, Rose ES, Wingood GM, Klein JD, Woods ER. Relationship of STD-related shame and stigma to female adolescents’ condom-protected intercourse. J Adolesc Health. 2007;40(6):573.e1–6.
Upchurch DM, Kusunoki Y. Associations between forced sex, sexual and protective practices, and sexually transmitted diseases among a national sample of adolescent girls. Womens Health Issues. 2004;14(3):75–84.
Diclemente RJ, Wingood GM, Sionean C, Crosby R, Harrington K, Davies S, et al. Association of adolescents’ history of sexually transmitted disease (STD) and their current high-risk behavior and STD status: a case for intensifying clinic-based prevention efforts. Sex Transm Dis. 2002;29(9):503–9.
Kowalczyk Mullins TL, Ding L, Huang B, Kahn JA. HPV vaccine risk perceptions and subsequent sexual behaviors and sexually transmitted infections among adolescent girls. J Adolesc Health. 2015;56(2):S14.
Article Google Scholar
Crosby RA, DiClemente RJ, Wingood GM, Sionéan C, Cobb BK, Harrington K. Correlates of unprotected vaginal sex among African American female adolescents: importance of relationship dynamics. Arch Pediatr Adolesc Med. 2000;154(9):893–9.
Davies SL, DiClemente RJ, Wingood GM, Person SD, Dix ES, Harrington K, et al. Predictors of inconsistent contraceptive use among adolescent girls: findings from a prospective study. J Adolesc Health. 2006;39(1):43–9.
Clarke KEN, Kraft JM, Wiener JB, Hatfield-Timajchy K, Kottke M, Sales JM, et al. Factors associated with contraceptive use differ between younger and older African-American female adolescents. J Pediatr Adolesc Gynecol. 2016;29(5):448–53.
Shew ML, Remafedi GJ, Bearinger LH, Faulkner PL, Taylor BA, Potthoff SJ, et al. The validity of self-reported condom use among adolescents. Sex Transm Dis. 1997;24(9):503–10.
Appelgren KE, Kraft JM, Hatfield-Timajchy K, Kottke M, Sales J, Goedken P, et al. Predictors of condom and contraceptive use differ between younger and older adolescents. J Adolesc Health. 2015;56(2):S36–7.
Wallace AR, Blood EA, Crosby RA, Shrier LA. Differences in correlates of condom use between young adults and adults attending sexually transmitted infection clinics. Int J STD AIDS. 2015;26(8):526–33.
Farrington EM, Bell DC, DiBacco AE. Reasons people give for using (or not using) condoms. AIDS Behav. 2016;20(12):2850–62.
Shain RN, Perdue ST, Piper JM, Holden AE, Champion JD, Newton ER, et al. Behaviors changed by intervention are associated with reduced STD recurrence: the importance of context in measurement. Sex Transm Dis. 2002;29(9):520–9.
Batteiger BE, Tu W, Ofner S, Van Der Pol B, Stothard DR, Orr DP, et al. Repeated Chlamydia trachomatis genital infections in adolescent women. J Infect Dis. 2010;201(1):42–51.
NIHR. PROSPERO : International prospective register of systematic reviews. York: National Institute for Health Research; 2022. [Available from: https://www.crd.york.ac.uk/prospero/ .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Chapter 7: Systematic reviews of etiology and risk: In: Aromataris E, Munn Z, editors. JBI manual for evidence synthesis. JBI 2020. [Available from: https://synthesismanual.jbi.global .
Gebgard PH. Human sexual activity. In: Encyclopedia Britannica; 2022. [Available from: https://www.britannica.com/topic/human-sexual-activity .
Fenton KA, Johnson AM, McManus S, Erens B. Measuring sexual behaviour: methodological challenges in survey research. Sex Transm Infect. 2001;77(2):84–92.
CDC. HIV risk among persons who exchange sex for money or nonmonetary items. Centers for Disease Control and Prevention; 2022. [Available from: https://www.cdc.gov/hiv/group/sexworkers.html .
Sieving RE, Gewirtz O’Brien JR, Saftner MA, Argo TA. Sexually transmitted diseases among US adolescents and young adults: patterns, clinical considerations, and prevention. Nurs Clin North Am. 2019;54(2):207–25.
Government of Canada. Safer condom use. Public Health Agency of Canada; 2022. [Available from: https://www.canada.ca/en/public-health/services/sexual-health/safer-condom-use.html .
de Wit JBF, Adam PCG, den Daas C, Jonas K. Sexually transmitted infection prevention behaviours: health impact, prevalence, correlates, and interventions. Psychol Health. 2022;38(6):675–700.
MacDonald NE, Wells GA, Fisher WA, Warren WK, King MA, Doherty JA, et al. High-risk STD/HIV behavior among college students. JAMA. 1990;263(23):3155–9.
Minnis AM, Padian NS. Effectiveness of female controlled barrier methods in preventing sexually transmitted infections and HIV: current evidence and future research directions. Sex Transm Infect. 2005;81(3):193–200.
Steen R, Wi TE, Kamali A, Ndowa F. Control of sexually transmitted infections and prevention of HIV transmission: mending a fractured paradigm. Bull World Health Organ. 2009;87(11):858–65.
Smelser NJ, Baltes PB, editors. International encyclopedia of the social & behavioral sciences. Amsterdam: Elsevier; 2001.
Aromataris E, Munn Z, editors. JBI manual for evidence synthesis. JBI; 2020. [Available from: https://doi.org/10.46658/JBIMES-20-01 .
Elder GH Jr. The life course as developmental theory. Child Dev. 1998;69(1):1–12.
Elder GH Jr, Johnson MK, Crosnoe R, Mortimer JT, Shanahan MJ. The emergence and development of life course theory. In: Mortimer JT, Shanahan MJ, editors. Handbook of the life course. Boston (MA): Springer; 2003. p. 3–19.
Chapter Google Scholar
Clarivate. Scientific & Academic Research, Discovery and Workflow Solutions : Web of Science Core Collection. Clarivate; 2022. [Available from: https://clarivate.com/products/scientific-and-academic-research/research-discovery-and-workflow-solutions/web-of-science/web-of-science-core-collection/ .
St Vincent's Hospital. Literature searching : database years of coverage. [Internet]. Library Service, St. Vincent's Hospital Melbourne, Australia; 2022. [Available from: https://library.svhm.org.au/literature_searching/coverageyears .
Li L, Smith HE, Atun R, Tudor Car L. Search strategies to identify observational studies in MEDLINE and Embase. Cochrane Database Syst Rev. 2019;3(3):MR000041.
Avau B, Van Remoortel H, De Buck E. Translation and validation of PubMed and Embase search filters for identification of systematic reviews, intervention studies, and observational studies in the field of first aid. J Med Libr Assoc. 2021;109(4):599–608.
Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33(2):363–74.
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276–82.
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane handbook for systematic reviews of interventions. Cochrane; 2023. [Available from: www.training.cochrane.org/handbook .
Microsoft Corporation. Microsoft Excel; 2018. [Available from: https://office.microsoft.com/excel .
ROBINS-E Development Group (Higgins J, Morgan R, Rooney A, Taylor K, Thayer K, Silva R, et al. Risk Of Bias In Non-randomized Studies - of Exposure (ROBINS-E). 2022. [Available from: https://www.riskofbias.info/welcome/robins-e-tool .
Aventin Á, Gordon S, Laurenzi C, Rabie S, Tomlinson M, Lohan M, et al. Adolescent condom use in Southern Africa: narrative systematic review and conceptual model of multilevel barriers and facilitators. BMC Public Health. 2021;21(1):1228.
Kenyon CR, Delva W. It’s the network, stupid: a population’s sexual network connectivity determines its STI prevalence. F1000Res. 2018;7:1880.
Menon J, Mwaba S, Thankian K, Lwatula C. Risky sexual behaviour among university students. Int STD Res Rev. 2016;4(1):1–7.
Omisore A, Oyerinde I, Abiodun O, Aderemi Z, Adewusi T, Ajayi I, et al. Factors associated with risky sexual behaviour among sexually experienced undergraduates in Osun state. Nigeria Afr Health Sci. 2022;22(1):41–50.
Huneeus A, Deardorff J, Lahiff M, Guendelman S. Type of primary education is associated with condom use at sexual debut among chilean adolescents. Sex Transm Dis. 2014;41(5):306–11.
David JS, Bénédique P, Kiragu A, Olorunsaiye CZ, Fanor J, Joseph G, et al. Prevalence and factors associated with condom use among sexually active young women in Haiti: evidence from the 2016/17 Haiti demographic and health survey. BMC Womens Health. 2023;23(1):146.
Dula J, Oljira L, Geda B, Kinati T. Knowledge of sexually transmitted disease and barriers to seeking sexual and reproductive health care among Chercher high school students. Adv Pharmacoepidemiol Drug Saf. 2017;6(1):216.
Farshbaf-Khalili A, Shahnazi M, Salehi-Pourmehr H, Faridvand F, Asgarloo Z. Behavioral prevention regarding sexually transmitted infections and its predictors in women. Iran Red Crescent Med J. 2014;16(8):e18346.
Nigussie T, Yosef T. Knowledge of sexually transmitted infections and its associated factors among polytechnic college students in Southwest Ethiopia. Pan Afr Med J. 2020;37:68.
Harling G, Subramanian S, Bärnighausen T, Kawachi I. Socioeconomic disparities in sexually transmitted infections among young adults in the United States: examining the interaction between income and race/ethnicity. Sex Transm Dis. 2013;40(7):575–81.
Haley DF, Edmonds A, Belenky N, Hickson DA, Ramirez C, Wingood GM, et al. Neighborhood health care access and sexually transmitted infections among women in the southern United States: a cross-sectional multilevel analysis. Sex Transm Dis. 2018;45(1):19–24.
Government of Canada. Report on sexually transmitted infection surveillance in Canada, 2019 Public Health Agency of Canada; 2022. [Available from: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/report-sexually-transmitted-infection-surveillance-canada-2019.html .
Siu WHS, Li PR, See LC. Rate of condom use among sexually active adolescents: a nationwide cross-sectional study in Taiwan from 2012 to 2016. BMJ Open. 2021;11(8):e047727.
Farmer MA, Meston CM. Predictors of condom use self-efficacy in an ethnically diverse university sample. Arch Sex Behav. 2006;35(3):313–26.
Shaw SA, El-Bassel N. The influence of religion on sexual HIV risk. AIDS Behav. 2014;18(8):1569–94.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. 2nd ed. Hoboken (NJ): John Wiley & Sons; 2021.
Book Google Scholar
Chambliss JT, Evans R, Bolland A, Wingate MS, Bolland JM. Exploring condom use behaviors among African American adolescent boys in the deep south. Am J Mens Health. 2021;15(2):15579883211009040.
Ebuenyi ID, Chikezie UE, Nwoke EA. Psychosocial correlates of risky sexual behaviour amongst students in Niger Delta University. Bayelsa Pan Afr Med J. 2021;38:7.
Kawuki J, Gatasi G, Sserwanja Q, Mukunya D, Musaba MW. Utilisation of modern contraceptives by sexually active adolescent girls in Rwanda: a nationwide cross-sectional study. BMC Womens Health. 2022;22(1):369.
Kottke M, Whiteman MK, Kraft JM, Goedken P, Wiener J, Kourtis AP, et al. Use of dual methods for protection from unintended pregnancy and sexually transmitted diseases in adolescent African American women. J Pediatr Adolesc Gynecol. 2015;28(6):543–8.
Walsh JL, Fielder RL, Carey KB, Carey MP. Dual method use among a sample of first-year college women. Perspect Sex Reprod Health. 2014;46(2):73–81.
National Institute of Statistics of Rwanda, Ministry of Health, ICF. Rwanda demographic and health survey 2019–20. Final report. Kigali (Rwanda) and Rockville (MD): NISR and ICF2021 [Available from: https://www.statistics.gov.rw/publication/1724 .
Bansode OM, Sarao MS, Cooper DB. Contraception. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. [Available from: https://www.ncbi.nlm.nih.gov/books/NBK536949/ .
Borges ALV, Duarte LS, Cabral CDS, Lay AAR, Viana OA, Fujimori E. Male condom and dual protection use by adolescent men in Brazil. Rev Saude Publica. 2021;55:109.
Saewyc EM. What about the boys? The importance of including boys and young men in sexual and reproductive health research. J Adolesc Health. 2012;51(1):1–2.
Puente D, Zabaleta E, Rodríguez-Blanco T, Cabanas M, Monteagudo M, Pueyo MJ, et al. Gender differences in sexual risk behaviour among adolescents in Catalonia. Spain Gac Sanit. 2011;25(1):13–9.
Harris CR, Jenkins M, Glaser D. Gender differences in risk assessment: why do women take fewer risks than men? Judgm and Decis Mak. 2006;1(1):48.
CDC. Chlamydia – CDC basic fact sheet. Centers for Disease Control and Prevention; 2022. [Available from: https://www.cdc.gov/std/chlamydia/stdfact-chlamydia.htm .
Espada JP, Morales A, Guillén-Riquelme A, Ballester R, Orgilés M. Predicting condom use in adolescents: a test of three socio-cognitive models using a structural equation modeling approach. BMC Public Health. 2016;16:35.
Geller RJ, Decker MR, Adedimeji AA, Weber KM, Kassaye S, Taylor TN, et al. A prospective study of exposure to gender-based violence and risk of sexually transmitted infection acquisition in the Women’s Interagency HIV Study, 1995–2018. J Womens Health (Larchmt). 2020;29(10):1256–67.
Kreisel KM, Spicknall IH, Gargano JW, Lewis FMT, Lewis RM, Markowitz LE, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2018. Sex Transmi Dis. 2021;48(4):208–14.
Smolarczyk K, Mlynarczyk-Bonikowska B, Rudnicka E, Szukiewicz D, Meczekalski B, Smolarczyk R, et al. The impact of selected bacterial sexually transmitted diseases on pregnancy and female fertility. Int J Mol Sci. 2021;22(4):2170.
Van Gerwen OT, Muzny CA, Marrazzo JM. Sexually transmitted infections and female reproductive health. Nat Microbiol. 2022;7(8):1116–26.
Svenstrup HF, Fedder J, Kristoffersen SE, Trolle B, Birkelund S, Christiansen G. Mycoplasma genitalium, Chlamydia trachomatis, and tubal factor infertility–a prospective study. Fertil Steril. 2008;90(3):513–20.
Prather C, Fuller TR, Marshall KJ, Jeffries WLt. The impact of racism on the sexual and reproductive health of African American women. J Womens Health (Larchmt). 2016;25(7):664–71.
Boutrin MC, Williams DR. What racism has to do with it: understanding and reducing sexually transmitted diseases in youth of color. Healthcare (Basel). 2021;9(6):673.
Lu C, Ahmed R, Lamri A, Anand SS. Use of race, ethnicity, and ancestry data in health research. PLOS Glob Public Health. 2022;2(9): e0001060.
Lash TL, VanderWeele TJ, Haneuse S, Rothman KJ. Modern epidemiology. 4th ed. Philadelphia (PA): Wolters Kluwer; 2021.
Caruana EJ, Roman M, Hernández-Sánchez J, Solli P. Longitudinal studies. J Thorac Dis. 2015;7(11):E537–40.
Fonner VA, Kennedy CE, O’Reilly KR, Sweat MD. Systematic assessment of condom use measurement in evaluation of HIV prevention interventions: need for standardization of measures. AIDS Behav. 2014;18(12):2374–86.
Weller SC, Davis-Beaty K. Condom effectiveness in reducing heterosexual HIV transmission. Cochrane Database Syst Rev. 2022;2022(1):CD003255.
Williams M, Ross MW, Bowen AM, Timpson S, McCoy HV, Perkins K, et al. An investigation of condom use by frequency of sex. Sex Transm Infect. 2001;77(6):433–5.
Buttery SC, Philip KEJ, Alghamdi SM, Williams PJ, Quint JK, Hopkinson NS. Reporting of data on participant ethnicity and socioeconomic status in high-impact medical journals: a targeted literature review. BMJ Open. 2022;12(8):e064276.
Holmberg MJ, Andersen LW. Collider bias. JAMA. 2022;327(13):1282–3.
Kang H. The prevention and handling of the missing data. Korean J Anesthesiol. 2013;64(5):402–6.
Conner M, et al. Models of health behaviors. In: Llewellyn CD, Ayers S, McManus C, Newman S, Petrie KJ, Revenson TA, et al., editors. Campbridge handbook of psychology, health and medicine. Campbridge University Press; 2019. p. 55–60.
Witwer E, Jones R, Lindberg L. Sexual behavior and contraceptive and condom use among U.S. high school students, 2013–2017. New York (NY): Guttmacher Institute; 2018.
Franceschini A, Fattore L. Gender-specific approach in psychiatric diseases: because sex matters. Eur J Pharmacol. 2021;896: 173895.
Baggio G, Corsini A, Floreani A, Giannini S, Zagonel V. Gender medicine: a task for the third millennium. Clin Chem Lab Med. 2013;51(4):713–27.
Pederson A, Greaves L, Poole N. Gender-transformative health promotion for women: a framework for action. Health Promot Int. 2015;30(1):140–50.
Das JK, Salam RA, Lassi ZS, Khan MN, Mahmood W, Patel V, et al. Interventions for adolescent mental health: an overview of systematic reviews. J Adolesc Health. 2016;59(4s):S49–60.
Download references
Acknowledgements
We thank Dr. Hervé Tchala Vignon Zomahoun, who commented on a preliminary version of the review, and the information specialist, Frédéric Bergeron, who helped developed the literature search review.
FT received scholarships from the “Fonds de Recherche du Québec – Santé” (FRQS) and the Canadian Institutes of Health Research (CIHR). All authors thank the Quebec Population Health Research Network (QPHRN) for its contribution to the financing of this publication in open access.
Author information
Authors and affiliations.
Department of Social and Preventive Medicine, Faculty of Medicine, Université Laval, 1050, avenue de la Médecine, Room 4633, Québec, (QC), G1V 0A6, Canada
Frédérique Tremblay & Yohann Courtemanche
Projet COMPASS Québec, VITAM – Centre de recherche en santé durable, CIUSSS-CN and Université Laval, GMF-U Maizerets, 2480, chemin de la Canardière, Québec, (QC), G1J 2G1, Canada
Frédérique Tremblay, Richard E. Bélanger & Anne-Marie Turcotte-Tremblay
Faculy of Nursing, Université Laval, 1050, avenue de la Médecine, Room 3645, Québec, (QC), G1V 0A6, Canada
Anne-Marie Turcotte-Tremblay
Department of Pediatrics, Faculty of Medicine, Université Laval, 1050, avenue de la Médecine, Room 4633, Québec, (QC), G1V 0A6, Canada
Richard E. Bélanger
You can also search for this author in PubMed Google Scholar
Contributions
FT drafted the manuscript. FT, AMTT, and RB contributed to the development of the selection criteria. FT developed the search strategy. FT and YC conducted the pilot selection of the studies, the further selection by title and abstracts, the selection by full text, the extraction, and the risk of bias evaluation. RB provided expertise on sexually transmitted infections in adolescence, as a pediatrician. AMTT provided expertise in the development and direction of the systematic review. All authors read, provided feedback, and approved the final manuscript.
Corresponding author
Correspondence to Frédérique Tremblay .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Search strategies for MEDLINE (Ovid), Embase (Elsevier), and Web of Science.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Tremblay, F., Courtemanche, Y., Bélanger, R.E. et al. A systematic review of the association between history of sexually transmitted infections and subsequent condom use in adolescents. BMC Public Health 24 , 1000 (2024). https://doi.org/10.1186/s12889-024-18322-2
Download citation
Received : 28 September 2023
Accepted : 10 March 2024
Published : 10 April 2024
DOI : https://doi.org/10.1186/s12889-024-18322-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescents
- Sexually transmitted infections
- Preventive behaviors
- Sexual behaviors
- Systematic review
- Epidemiology
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Methodology
- Open access
- Published: 06 April 2024
Consolidated guidance for behavioral intervention pilot and feasibility studies
- Christopher D. Pfledderer ORCID: orcid.org/0000-0001-7503-8554 1 , 2 ,
- Lauren von Klinggraeff 3 ,
- Sarah Burkart 3 ,
- Alexsandra da Silva Bandeira 3 ,
- David R. Lubans 4 ,
- Russell Jago 5 ,
- Anthony D. Okely 6 ,
- Esther M. F. van Sluijs 7 ,
- John P. A. Ioannidis 11 , 12 , 8 , 9 , 10 ,
- James F. Thrasher 3 ,
- Xiaoming Li 3 &
- Michael W. Beets 3
Pilot and Feasibility Studies volume 10 , Article number: 57 ( 2024 ) Cite this article
454 Accesses
21 Altmetric
Metrics details
In the behavioral sciences, conducting pilot and/or feasibility studies (PFS) is a key step that provides essential information used to inform the design, conduct, and implementation of a larger-scale trial. There are more than 160 published guidelines, reporting checklists, frameworks, and recommendations related to PFS. All of these publications offer some form of guidance on PFS, but many focus on one or a few topics. This makes it difficult for researchers wanting to gain a broader understanding of all the relevant and important aspects of PFS and requires them to seek out multiple sources of information, which increases the risk of missing key considerations to incorporate into their PFS. The purpose of this study was to develop a consolidated set of considerations for the design, conduct, implementation, and reporting of PFS for interventions conducted in the behavioral sciences.
To develop this consolidation, we undertook a review of the published guidance on PFS in combination with expert consensus (via a Delphi study) from the authors who wrote such guidance to inform the identified considerations. A total of 161 PFS-related guidelines, checklists, frameworks, and recommendations were identified via a review of recently published behavioral intervention PFS and backward/forward citation tracking of a well-known PFS literature (e.g., CONSORT Ext. for PFS). Authors of all 161 PFS publications were invited to complete a three-round Delphi survey, which was used to guide the creation of a consolidated list of considerations to guide the design, conduct, and reporting of PFS conducted by researchers in the behavioral sciences.
A total of 496 authors were invited to take part in the three-round Delphi survey (round 1, N = 46; round 2, N = 24; round 3, N = 22). A set of twenty considerations, broadly categorized into six themes (intervention design, study design, conduct of trial, implementation of intervention, statistical analysis, and reporting) were generated from a review of the 161 PFS-related publications as well as a synthesis of feedback from the three-round Delphi process. These 20 considerations are presented alongside a supporting narrative for each consideration as well as a crosswalk of all 161 publications aligned with each consideration for further reading.
We leveraged expert opinion from researchers who have published PFS-related guidelines, checklists, frameworks, and recommendations on a wide range of topics and distilled this knowledge into a valuable and universal resource for researchers conducting PFS. Researchers may use these considerations alongside the previously published literature to guide decisions about all aspects of PFS, with the hope of creating and disseminating interventions with broad public health impact.
Peer Review reports
Key messages regarding feasibility
• There are more than 160 published guidelines, reporting checklists, frameworks, and recommendations related to PFS. All these publications offer some form of guidance on PFS, but many focus on one or a few topics, making it difficult for researchers wanting to gain a broader understanding of all the relevant and important aspects of PFS and requires them to seek out multiple sources of information, which increases the risk of missing key considerations to incorporate into their PFS.
• We present a set of consolidated considerations for behavioral intervention pilot and/or feasibility studies based on a review of the literature and a Delphi study with the authors who wrote this literature.
• We believe this consolidated set of considerations can be a “go-to” resource for any behavioral interventionist wanting to design, conduct, and report on their pilot and/or feasibility study.
In the behavioral sciences, conducting pilot and/or feasibility studies (PFS) is a key step that occurs early in the translational science continuum. PFS provide essential information to inform the design, conduct, and implementation of larger-scale trials, although not all studies follow the traditional roadmap to scale-up [ 1 ]. PFS are designed to answer questions surrounding uncertainty (feasibility) and potential impact (preliminary efficacy) and to inform gaps in knowledge about the various aspects of the intervention or conduct of the study. In turn, this information is used to make decisions regarding scale-up and future plans for a larger-scale trial.
There are more than 160 published guidelines, checklists, frameworks, and recommendations related to the design, conduct, and reporting of PFS. These publications offer some form of guidance on PFS, but many focus on a specific aspect of design, conduct, and reporting considerations. This makes it difficult for researchers who want to gain a broader understanding of all the relevant and important aspects of PFS and forces them to seek out multiple sources of information, which increases the risk of missing key considerations to incorporate into their PFS. Because of this, we believe a consolidated list of considerations, drawing on the breadth and depth of knowledge that has already been published on the topic, would have high utility for researchers and assist them in understanding important considerations and nuances when conducting a PFS.
Throughout this paper, we refer to PFS as early-stage studies designed to inform larger-scale, well-powered trials. We recognize that there are numerous labels for such studies (e.g., “proof-of-concept”, “evidentiary”, “vanguard”). We also realize that the terms “pilot” and “feasibility” evoke different meanings [ 2 , 3 ] and are used interchangeably and, in some instances, simultaneously. We address this issue in this consolidation of considerations. We also recognize that not all PFS will include or need to consider all the identified considerations. In many instances, however, a single PFS is designed to cover all of the data needed to inform a larger-scale trial [ 4 ]. This includes everything from estimating recruitment/retention rates, participant satisfaction and engagement, fidelity, and a host of other feasibility indicators, as well as providing some preliminary indications of change in one or more outcomes of interest. Researchers often deliberately design a PFS to collect information across these multiple dimensions, though their decision making is often largely driven by such issues as available resources and abbreviated timelines.
The purpose of this study was to develop a consolidated set of considerations for the design, conduct, implementation, and reporting of PFS for interventions in the fields of behavioral sciences. The considerations presented herein were developed through any extensive review of the literature and a Delphi study of experts who wrote the existing literature on PFS. The consolidated set of considerations was developed for universal application across interventions in the behavioral sciences and across the study designs one may choose. We expect this consolidation will serve as a valuable resource for all behavioral science interventionists who design and conduct PFS, regardless of the intervention mechanism, target population, or study design.
To ensure rigor and methodological quality throughout the consolidation of previously published guidelines, checklists, frameworks, and recommendations, we relied on guidance from Moher et al., [ 5 , 6 ] which details the main steps in the development of evidence-based consensus in health fields. These steps included developing a strong rationale for the consolidation, necessary preparatory work conducted by the study team, consensus activities, and development of the final consolidation. These steps are detailed below. When relevant, we also drew on similar consensus studies conducted in the behavioral sciences [ 2 , 3 , 7 , 8 ].
Review of previously published guidelines, checklists, frameworks, and recommendations for PFS
A scoping bibliometric review of published PFS-related guidelines, checklists, frameworks, and recommendations was conducted prior to developing the Delphi survey, which has been reported elsewhere [ 9 ]. Briefly, we identified 4143 PFS from which we then identified 90 guidelines, checklists, frameworks, and recommendations cited in that literature. We then continued searching for relevant literature via backward citation tracking of known publications, including the CONSORT Extension for Pilot and Feasibility Studies [ 7 ], Medical Research Council guidance [ 10 ], and publications such as Bowen et al. [ 11 ] and Pearson et al. [ 12 ] A total of 161 publications were identified that encompassed nine thematic domains: adaptations , definitions of pilot and feasibility studies , design and interpretation , feasibility , implementation , intervention development , progression criteria , sample size , and scale-up . The 161 publications guided our inclusion of the sample of respondents for the Delphi survey, which is detailed in the next section. It is worth noting that after this review, we identified an additional relevant publication published after the completion of the study, which is included in our final sample (bringing the total number of studies to 162) but was not used to inform the Delphi study.
Participant selection and recruitment for the Delphi survey
Lead, second, corresponding, and senior authors of the 161 published guidelines, checklists, frameworks, and recommendations for PFS were invited via email to complete a three-round Delphi study. Contact information was retrieved from published article meta-data and when not found in the published articles, emails were retrieved from another publicly available source, such as faculty pages or university websites. This resulted in 496 potential participants, who were sent an individualized invitation email via Qualtrics for round 1 of the Delphi study. For round 2, only participants who completed round 1 were invited to take part in the survey. We then sent the round 3 survey back to the original pool of 496 potential participants, regardless of whether they completed round 1. This process is summarized in Fig. 1 and took place between May 2022 and January 2023. Ethical approval was granted by the University of South Carolina’s Institutional Review Board (IRB # Pro00120890) prior to the start of the study.
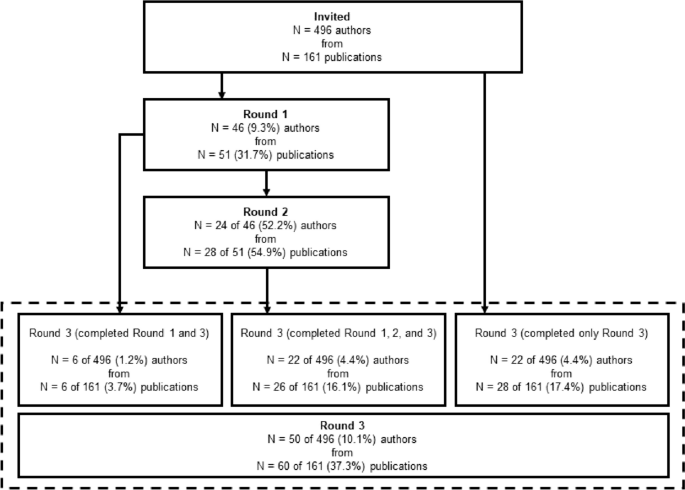
Participant flow through each round of the Delphi survey process
Delphi survey
Each round of the Delphi survey process was guided by established protocols [ 13 , 14 ] and is detailed below.
Round 1—Delphi survey
In round 1 of the Delphi process, participants were asked to provide the most important considerations regarding the design, conduct, analysis, or reporting of behavioral pilot and/or feasibility intervention studies in separate free-text fields via Qualtrics. Before beginning the survey, participants were provided with operational definitions of both “behavioral interventions” and “preliminary studies” for context. No other prompts were provided. In round 1 of the Delphi study, we referred to PFS as “preliminary” studies, but after receiving comments about the use of this term, this was changed to “pilot and/or feasibility” studies in round 2. Survey distribution for round 1 took place in May and June 2022.
Preparation for round 2
Participants’ responses from round 1 were exported from Qualtrics to a.csv file in Microsoft Excel, collated into individual Microsoft Word documents for each participant, converted to PDFs, and imported into NVivo for thematic coding. Prior to coding responses in NVivo, we simplified and revised our original nine thematic domains from the scoping bibliometric review into six overarching themes: intervention design , study design , conduct of trial , implementation of intervention , statistical analysis , and reporting . This revision was conducted after an initial review of responses from round 1 of the Delphi survey in an effort to simplify themes and to allow for maximum parsimony across expert perspectives. Specifically, we identified overlap in several of the original nine themes and made a decision to include them as subthemes in the revision to six overarching themes. The titles of the original nine thematic domains were largely retained and can be found embedded as subthemes in the six revised overarching themes. A two-step thematic coding process followed. First, individual participant responses were coded into a corresponding theme based on the content of their response. This was completed by two members of the research team (CDP and MWB). Disagreements were brought to the larger research team (LV, SB, and AB) during weekly meetings and were resolved at that time. Once participant responses were coded into one of the six overarching themes, our research team coded responses into one of 20 subthemes based on qualitative analysis of participants’ responses by theme. These 20 subthemes served as the coding framework for the second step of the thematic coding process, and responses were coded as such by two members of the research team (CDP and MWB).
Round 2—Delphi survey
In round 2 of the Delphi study, participants were re-oriented to the study with a brief narrative and were presented with the six overarching themes and 20 subthemes generated via qualitative analysis of the results from round 1. To give participants context, we provided select, representative quotes for each subtheme from round 1 of the survey. After being presented with the theme, subtheme, and select quotes, participants were asked to provide a recommendation for each subtheme for inclusion in a consolidated framework for behavioral intervention PFS. Participants were also given the chance to indicate if they felt a subtheme should not be included in a consolidated framework. The survey was organized such that each theme (along with the corresponding subthemes) was presented as a randomized block, meaning individual participants were presented with a unique order of themes and asked to provide their considerations. Block randomization of themes was performed to prevent the possibility of homogenous burnout across participants as they reached the last theme of the survey. The last question of the survey was a free-text field in which participants could indicate if there were any additional considerations that were not mentioned in the survey that should be added to a consolidated framework for pilot and/or feasibility behavioral intervention studies. Survey distribution for round 2 took place in September and October 2022.
Preparation for round 3
Participant responses from round 2 were exported from Qualtrics to a.csv file in Microsoft Excel and collated into individual Microsoft Word documents for each of the 20 subthemes. A collection of considerations for each subtheme was written based on participant responses from rounds 1 and 2 and from information provided throughout the previously identified 161 pilot and/or feasibility-related guidelines, checklists, frameworks, and recommendations. Weekly research group meetings were used to further refine the considerations.
Round 3—Delphi survey
In the final round of the Delphi study, participants were first asked to provide basic demographic information including age, sex, race/ethnicity, and the year in which they received their terminal degree. Demographic information was not collected from participants in round 1 or 2 of the Delphi survey to limit participant burden in the initial rounds of the survey. We then provided participants with an outline of the six themes and 20 subthemes that emerged from rounds 1 and 2 of the study, a description of the final recommendation for the study, and instructions for the final survey. For each of the 20 subthemes, participants were given an operational definition of the subtheme and a list of considerations, which were generated based on the comments from rounds 1 and 2. They were then asked to rate their level of agreement with the considerations (0–10 Likert scale from Strongly Disagree to Strongly Agree). An optional free-text field was provided for additional information about what we should add to/change about the considerations. Participants were presented with each subtheme in block-randomized order just as in round 2. Survey distribution for round 3 took place in December 2022 and January 2023.
Final consolidation of considerations
The final set of considerations was written in a similar manner to round 2. Responses were collated into separate working documents for each of the 20 subthemes, which also included the list of previously written considerations drafted for round 2. The previously written considerations were altered based on participant feedback from round 3 and from further supporting information from the 161 pilot and/or feasibility-related guidelines, checklists, frameworks, and recommendations. Primary changes to the considerations were made by two members of the research team (CDP and MWB) and further refined by members of our larger research team (LV, SB, and AB).
Analysis of quantitative data
There were two forms of quantitative data gathered from participants during round 3 of the Delphi survey process. The first was demographic information, which was summarized descriptively as means, standard deviations, and ranges where appropriate. The second were the participant’s Likert-scale ratings of each set of considerations for each of the 20 subthemes. These data were summarized visually with boxplots and descriptively with means, standard deviations, medians, ranges, and interquartile ranges. All quantitative analysis was performed in STATA v17.0 statistical software package (College Station, TX, USA).
Participant characteristics and survey completion
A total of 46 of the 496 (9.3%) invited authors representing 51 of the 161 (31.7%) identified publications completed round 1 of the Delphi study. In round 1, where respondents were asked to provide up to 20 considerations regarding the design, conduct, analysis, or reporting of behavioral pilot and/or feasibility intervention studies, participants gave a mean of 8 ± 4 (range = 1–20, median = 7, IQR = 5–10) considerations. Of the 46 participants who completed round 1, 24 (52.2%) completed round 2. A total of 50 (10.1%) of the original pool of 496 participants representing 60 (37.3%) publications completed round 3. For the 161 publications that were represented by authors in the Delphi study, the median year of publication was 2015 (range = 1998–2022, IQR = 2013–2018). Comparatively, across all possible 161 identified publications, the median year of publication was 2013 (range = 1989–2022, IQR = 2009–2017). A visual summary of participant flow through each of the three rounds of the Delphi survey process is provided in Fig. 1 . Demographic information for participants who completed round 3 is presented in Table 1 .
Likert ratings of the considerations
Likert scale ratings (0–10 scale) of each of the considerations for the 20 subthemes were provided by 50 out of 50 (100%) participants during round 3 of the Delphi survey. These are summarized in Table 2 . Average ratings for considerations across all 20 subthemes ranged from 7.6 to 8.8, with medians ranging from 8 to 10.
Consolidated considerations for PFS
For each subtheme, we provide an operational definition of the subtheme, a consolidated list of considerations based on the review of pilot and/or feasibility literature and the three-round Delphi study, and a narrative summary of the subtheme. We also provide a crosswalk of 161 guidelines, checklists, frameworks, and recommendations, mapped on to the subthemes identified and an additional publication that was published after the Delphi process, but was relevant to include in the list [ 15 ]. The crosswalk is found in Additional file 1 and can be used to identify supporting literature for each of the subthemes and considerations we have consolidated. Of the 161 publications, 15 are reporting guidelines/checklists, 44 are guidelines/recommendations, 18 are reviews that offer recommendations, 37 are frameworks/models, and 47 are commentaries/editorials that offer recommendations or guidance for preliminary studies. For the narrative summary, wherever possible, we have identified relevant examples across widely used study designs for PFS which range from “N of 1” studies, micro-randomized trials, single and multiple group designs, and those involving traditional randomization, to highlight the universality of the consolidated considerations.
Intervention design
Adaptations and tailoring.
Adaptations and tailoring refer to any deliberate changes to the design or delivery of an intervention, with the goal of improving fit or effectiveness in a given context [ 16 ].
Considerations
Where components of the intervention are adapted/tailored, details of who was involved (e.g., investigative team, key stakeholders, participants) in the decisions (see 1.3. Stakeholder Engagement and Co-Production ), when the adaptations/tailoring occurred, and how and why the modification(s) were made need to be clearly reported.
How the proposed adaptations/tailoring address the issues/challenges observed in the intervention need to be clearly reported along with justification for why these changes should result in an improved design.
Whether the adaptations/tailoring occurred a priori or during the conduct of the study should be clearly described.
The intervention component of PFS can be conducted in a rigorous fashion yet be flexible enough to allow for minor adaptations or tailoring (in composition, format, design, etc.) when justified and in response to emerging feasibility indicators.
If substantial adaptations are made to the intervention, such that the adaptations may influence feasibility indicators or behavioral outcomes, re-testing of the PFS prior to progression is justifiable (see 2.1. Iteration and Intervention Refinement ). Adaptations/tailoring occurring under these circumstances should refer to any a priori progression criteria specifications (see 2.2. Progression Criteria ).
Often, existing evidence-based interventions are modified (i.e., adapted/tailored) for delivery to a new sample or in a new setting that is different from where the intervention was originally implemented and evaluated. In these situations, a PFS may be conducted to establish whether the modifications are appropriate in the new sample/setting [ 17 , 18 ]. Adaptations are often made to increase relevance and participant engagement, with the assumption the adaptations would lead to better outcomes in the target populations and settings of eventual interest [ 19 , 20 ].
Adaptations can consist of changes to intervention materials to make them culturally relevant to the target population (race/ethnicity, country/setting, norms/values) [ 19 , 21 ]. Adaptations may also include changes to the intervention itself, such as how it is delivered (e.g., combining sessions, online vs. face-to-face), delivery location, who it is delivered by, or the length of the sessions/intervention [ 22 , 23 ]. Adaptations may occur at any point in the design, implementation, and evaluation/interpretation of a PFS. These include a priori adaptations of existing interventions, those that occur as a result of the evaluation of an intervention, or adaptations made on an ongoing basis throughout a PFS [ 19 , 21 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 ].
Where adaptations/tailoring occur, reasons for the adaptations and who participated in the decision-making process should be reported. Often, the adaptation process includes coproduction/codesign methods that can involve focus groups, feedback sessions, and key patient, participant, and public involvement [ 17 ] to justify and inform the relevancy of the adaptations [ 19 , 34 , 35 , 36 ] (see 1.3. Stakeholder Engagement and Co-Production). If coproduction/codesign methods are used, these should be clearly reported.
Site selection and context
Site selection refers to the location in which a PFS will be conducted. Context refers to the factors that form the setting of the intervention, including location, culture, environment, and situation [ 12 , 37 ].
Whenever feasible, researchers should choose sites for PFS that are representative of those anticipated in the future larger-scale trial.
Purposeful selection of sites can be used to ensure an intervention is tested in an appropriate range of contexts.
A rationale for the sites selected should be clearly stated along with how the sites and context reflect what is anticipated in the future larger-scale trial.
Key characteristics of the sites and context should be reported.
The context of intervention delivery and any information that suggests contextual elements may impact the feasibility or future efficacy of the intervention should be clearly reported.
Where context is known or hypothesized to influence the implementation and/or feasibility of an intervention, including more than one site may be necessary.
Setting and contextual characteristics are known factors that can influence intervention outcomes. For PFS testing interventions that rely on a setting as part of the delivery process or are embedded naturally within existing settings, site selection and context become key factors to understand at the early stages of the design and evaluation of an intervention. Setting and context may represent static (e.g., hospital serving low-resource area) or dynamic (e.g., weather, day-to-day variability) characteristics [ 38 ]. Reasons why sites are selected in a PFS can include a range of pragmatic considerations. These include the need for representation of a diverse range of characteristics (e.g., geography, populations served), facilities/infrastructure required for the project (e.g., cell phone connectivity, low-resource settings), and proximity to the investigative team [ 39 , 40 , 41 , 42 , 43 , 44 , 45 ]. These decisions may also be based on the ability to refer sufficient numbers of participants at a given site [ 43 , 46 , 47 ]. Descriptions of the context and setting and how these might influence intervention outcomes should be clearly reported [ 38 , 48 , 49 ].
In some PFS, understanding setting complexity and how an intervention fits within a broader system may be the primary research questions that need to be answered prior to conducting a larger-scale trial. Studies investigating setting or context are useful for the identification of whether an intervention is appropriate or feasible to deliver for a given setting [ 50 , 51 , 52 , 53 ]. This allows for understanding uncertainties about the setting and how differences across settings may influence implementation [ 54 , 55 , 56 , 57 ]. In some situations, where an existing intervention is adapted to be delivered in a different setting, understanding how the intervention interacts with the new context becomes a key feasibility outcome to evaluate.
Stakeholder engagement and co-production
Stakeholder engagement and co-production refers to the use of partnerships with individuals, communities, and service providers to aid in the development and implementation of an intervention [ 58 ].
PFS should be, whenever possible, co-designed/co-created or informed by key stakeholder (e.g., community and professional) perspectives throughout all stages of design and implementation.
Whenever possible, pro-equity approaches that ensure the unique considerations and perspectives around an intervention’s acceptability, safety, etc., and participation in and ownership of research from minority and vulnerable populations, should be used.
The processes by which the PFS was co-designed, including who was consulted, why, when they were consulted, and how their input was obtained, should be clearly described.
Stakeholder engagement and co-production methods are commonly used in PFS to ensure the relevance of a number of intervention-related facets. These include the relevance of intervention materials, how an intervention is delivered, whether the content is appropriate, and if any important components are missing [ 59 , 60 , 61 ]. Employing stakeholder engagement and co-production methods can be useful to ensure ownership of the developed intervention by recipients and end-users [ 62 ]. Where these methods are employed, it is important to report who is involved in co-production (participants, interventionists, members of the public, other key stakeholders) and a rationale for their involvement in the process [ 63 , 64 , 65 ]. The process of engaging stakeholders in co-production can take many forms, including “think aloud”—commonly used for useability testing, questionnaires, and/or interviews [ 66 , 67 , 68 , 69 , 70 ]. What participants did during the co-production process, such as reviewing qualitative interviews or initial testing of intervention materials, should be reported. Details of how participants were engaged in the co-production (e.g., time dedicated, number of rounds of review/workshops, the total number of individuals involved) should also be included [ 71 , 72 ]. In some instances, it may be appropriate to describe details of the training required to facilitate a co-production process [ 61 ].
Theory usage
Theory usage refers to the utilization of any conceptual or theoretical model to inform aspects of the PFS that are mechanisms of change [ 8 ].
Researchers, where relevant, should include details about one or more behavior change theories (e.g., intervention activities, mechanisms) which informed aspects of the PFS, including whether components of the intervention are theoretically or practically informed.
The theoretical foundation of an intervention should be clearly stated. The components of an intervention may directly map on to one or more theories of change. These could be specific theories, mechanisms, or conceptual frameworks informed by practice. Theories of change should refer to intervention resources, activities, mechanisms, and intermediate and final outcomes. This information can be presented in the form of a logic model of change or conceptual frameworks depicting the theory of change or program theory [ 50 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 ]. Details of the theory of change and how this informed intervention development can be presented alongside pilot and/or feasibility outcomes, but could also be published separately, such as in a protocol overview [ 81 , 82 ].
Well-defined problem and aims
Well-defined problems and aims refers to the focused research questions/objectives used to guide the design, conduct, and analyses of PFS [ 8 ].
PFS should be guided by clear and focused research questions related primarily to the feasibility of the intervention and prospects of subsequent scale-up to a larger-scale trial. These well-formulated research questions should be answered by an appropriate and transparent methodology that uses both quantitative and qualitative data.
Where appropriate, the PFS proposal and report should define a clinically important public health problem for which researchers are designing, refining, or adapting an intervention.
PFS are designed primarily to answer key aspects regarding the feasibility of an intervention. These include addressing uncertainties about the intervention and the implications of the findings for larger-scale trials [ 83 ]. Questions of uncertainty are the basis for well-defined problems and aims of PFS. These can include understanding researchers’ access to the population of interest (recruitment); acceptability of randomization (for certain study designs); developing, refining, and finalizing intervention protocols; acceptability of the intervention for the target population; intervention deliverers and other key personnel; and other feasibility-related outcomes including fidelity, cost, equity, and cultural appropriateness [ 70 , 84 , 85 , 86 , 87 ].
In certain situations, the aims of a PFS can be more exploratory in nature. But this does not preclude the study from having a set of well-defined problems and aims. Examples may include learning about the assets, values, and/or history of the community in which an intervention could potentially be delivered and learning about the processes in which co-design and collaboration with community members could naturally take place prior to delivering an intervention.
Study design
Iteration and intervention refinement.
Iteration and intervention refinement refers to the re-testing of an intervention in PFS to further refine intervention components before scaling to a larger trial [ 88 ].
If the conclusion of the PFS is to make significant adjustments to either the study design or the intervention, then it should be acknowledged that the results do not justify proceeding further and a second PFS is necessary to establish feasibility before testing the intervention in a larger-scale, well-powered trial. Any potential changes (adaptations/tailoring) should be clearly documented along with information about how and why the changes are to be made (see 1.1. Adaptations and Tailoring ).
The decision to conduct multiple iterations of a PFS can be pragmatic or theoretical and based on factors including the perceived confidence the redesign will sufficiently address the identified problems.
Conclusions from a PFS should include whether the intervention, in its current form, is ready for a future trial or if modifications are needed (and if so, details of them), and whether they are substantial enough to warrant another PFS.
Iterations refer to the re-testing of an intervention in another PFS [ 89 , 90 , 91 , 92 ]. This can be done based upon findings from a previous PFS trial where minor and/or major adjustments to the intervention, its delivery, or other aspects of the study were found. Initial evaluations of an intervention may even pre-plan for multiple iterations. The iterations create a sequence of trialing and modifying prior to any well-powered trials. At the conclusion of a PFS, investigators can make the decision, based upon progression criteria and other findings, whether additional testing of the intervention needs to ensue prior to scale-up. This decision should be left to the interventionists and co-developers and be based on the evidence collected from the PFS, available resources, and time. Decisions can be pragmatic but also important are theoretical considerations that can inform whether or why alterations to the intervention may or may not result in anticipated or unanticipated changes.
Progression criteria
Progression criteria are a set of a priori benchmarks or thresholds regarding key feasibility markers that inform decisions about whether to proceed, to proceed with changes, or not to proceed from the PFS to a future study, either a main trial or another PFS [ 15 ].
PFS should include a set of progression criteria which are used to inform decisions about whether to proceed, proceed with changes, or not to proceed to a larger-scale study.
Progression criteria should be determined a priori and be based on either evidence from previously published/conducted research or a sound rationale provided.
Decisions on whether to proceed should also be informed by contextual, temporal, and partnership factors that evolve over the course of the pilot and/or feasibility.
Progression criteria should be made for feasibility metrics such as recruitment rate, retention/drop-out rate, acceptability, implementation/fidelity, and other appropriate feasibility indicators where appropriate.
Progression decisions can also include evidence of potential impact (see 5.2. Preliminary Impact ).
Progression criteria decisions can be in the form of a “Go/No Go” system or a “Stop Light” (red/amber/green) system, indicating no progression, progression with changes, or progression with no changes.
Deviations from the application of progression criteria may be justified if researchers are confident that a proposed solution will address the problem at a larger scale and can provide strong theoretical and/or empirical evidence to support their assertion (see 1.1. Adaptations/Tailoring ).
Across all feasibility metrics, some form of progression criteria thresholds and classification systems should be pre-defined [ 74 , 80 , 93 , 94 , 95 , 96 , 97 , 98 ]. The thresholds are commonly study- and intervention-specific, and these thresholds can be designated by investigators and any co-designers. Common classification schemes include red/amber/green and go/no-go. Often, these criteria are pre-registered and/or appear in protocol documents. Progression criteria can be used to gauge whether certain aspects of the intervention and its delivery along with other aspects of the study need to be modified. This information can be used to inform decisions about whether a subsequent test of the intervention should be conducted in another PFS (see 2.1. Iteration and Intervention Refinement ).
Randomization and control groups
Randomization refers to the process of using random chance to allocate units (individuals or settings/clusters) to one or more intervention conditions. Randomization can be used to separate units into distinct groups or randomization within a unit for when and what intervention(s) they may receive (order and timing). A control/comparator condition serves as the counterfactual. A control/comparator group is a group of participants (and/or settings/clusters) allocated to receive differing amounts, orders, or types of intervention(s) being tested [ 99 , 100 , 101 ]. A baseline period can serve as a control/comparator condition for studies employing single-arm or individual-level interventions (e.g., N-of-1) [ 102 ].
Not every PFS needs to include two or more groups or employ random allocation.
The presence of a control/comparator group or randomization can be included if it reflects the aims and objectives of the study.
Control groups can take numerous forms and should be reflective of the objectives of the study, the context within which the intervention is tested, and acceptability by the target population.
When randomization is employed, methods of randomization should be clearly described to ensure reproducibility.
If a control/comparator group is present, feasibility indicators collected on the intervention group should also be collected on the control group where appropriate (e.g., feasibility of data collection, acceptability of randomization, retention).
PFS can employ a range of designs. These include N-of-1 [ 103 ], micro-randomized trials [ 104 ], single-group [ 105 ], quasi-experimental [ 106 ], and multi-group/multi-setting designs [ 107 ]. Despite these design options, not every PFS needs to employ randomization or include more than one group. The use of randomization and multi-group design features should be based on the objectives of the PFS. Randomization in PFS can take the form of allocating groups to different interventions or varying levels of the same intervention (doses). Randomization can also take the form of within-person or group allocation of the timing and/or varying interventions participants may receive. Where multiple groups are included, “what” they receive (i.e., allocated to) should be based on the nature of the intervention and be consistent with conventions within the field of study. This can range from a purely no-treatment comparator to standard practice to alternate active interventions. Where some form of a comparator group is used, researchers should evaluate feasibility metrics to understand such things as the ability to retain those not receiving the intervention and acceptability of randomization. Incorporating either randomization or multiple groups can increase the scientific rigor of the PFS but is not necessary to evaluate most feasibility metrics of an intervention.
Scale-up refers to the process of delivering and evaluating an intervention in progressively larger studies, beginning with testing an intervention within one or more PFS and moving towards larger studies of the same, or similar, interventions. It is a “deliberate effort to increase the impact of successfully tested health intervention so as to benefit more people and foster policy and program development on a lasting basis” [ 108 , 109 ].
PFS should be designed with the intent for future testing of an intervention in large-scale trials and beyond.
Researchers should consider plans for later-phase research on the intervention and explain how information gathered from the PFS will be used to answer key questions surrounding the uncertainty of the intervention or the design or conduct of a progressively larger future study.
Issues regarding the adoption, implementation, and maintenance of the intervention over progressively larger studies can be considered at both the design and conduct phases of the PFS.
Efforts should be made to ensure key features of the PFS be similar to those in the future large-scale trial. These include the amount of support to implement the intervention, characteristics of who delivers the intervention, the target population, the duration under which the intervention is tested, and the measures employed.
Where differences are anticipated between pilot and/or feasibility testing and the larger-scale trial, a description of these differences should be provided along with a clear justification of how the changes may or may not impact the intervention.
PFS should be designed and conducted with the idea the information collected will be used to inform the testing of an intervention in progressively larger sample sizes and/or settings [ 85 , 110 , 111 , 112 , 113 , 114 , 115 , 116 ]. This implies researchers who conduct PFS intend to continue to refine and optimize an intervention for maximal impact along a translational science continuum [ 117 , 118 , 119 ]. With this in mind, understanding early on how an intervention could be delivered to progressively larger numbers of individuals and/or settings should be incorporated into the early stages of the design and conduct of PFS. Considerations for scaling can include characteristics of those who deliver an intervention, the resources required to train and deliver an intervention, and to whom an intervention is delivered. How these aspects can change as one progresses from commonly smaller-sized PFS to evaluating an intervention for broader population-level impact should inform what transpires in a PFS. Researchers should, therefore, consider whether what they can accomplish on a smaller scale can similarly be accomplished on a larger scale [ 120 , 121 ].
Conduct of trial
Measurement and data collection
Measurement and data collection refer to any tools, devices, instruments, personnel, and time required to assess feasibility or outcomes related to an intervention.
PFS can assess the feasibility and appropriateness of measurement and data collection procedures including the following:
How or if the data can be collected
The acceptability of the measurements and data collection procedures (e.g., burden)
If the measures are valid for the population/outcomes in question
Where applicable, measurements and data collection procedures should closely resemble those anticipated for the well-powered trial.
The reporting of measurement and data collection procedures should be sufficiently detailed to permit standardized data collection, including information about why the measurements were selected and how they were administered, scored, and interpreted.
Information about the feasibility and appropriateness of measurement and data collection procedures can consist of both quantitative and qualitative data sources.
The process of collecting outcome data in a PFS serves to demonstrate the feasibility of data collection methods—whether explicitly stated or not [ 122 ]. However, some PFS may be designed to answer whether outcome measures proposed for the larger-scale trial can be collected. This can include the ability to collect data using more invasive/burdensome methods (e.g., urine/hair samples, blood draws) [ 123 , 124 ]. Additional metrics associated with the feasibility of measurement and data collection may include determining rates of missing data, participant response rates, and any time/resource costs associated with data collection [ 125 , 126 , 127 ]. This information can be used to reduce participant burden and costs associated with data collection as well as refine protocols in the larger-scale trial [ 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 ].
Recruitment
Recruitment refers to the procedures used to identify and select potential participants (individuals and/or settings/clusters) and enroll them into a PFS. The recruitment rate is the proportion of eligible participants or settings/clusters who are enrolled at the baseline of an intervention trial compared to the invited/eligible target population [ 137 ].
Recruitment procedures should be clearly described, with any strategies designed to maximize recruitment fully detailed.
Information should include details of procedures used to recruit at the individual and setting/cluster levels, where appropriate.
Recruitment information should include the following, where appropriate:
Proportion of eligible units (e.g., individuals, settings) recruited
The start and end dates of the recruitment periods
Number of participants recruited per setting/cluster, overall, and number of settings/clusters
Number of potential participants screened, eligible, consented, and enrolled in the study
Reasons for non-recruitment/non-consent
Acceptability of recruitment strategies
Details should be provided about the recruitment strategies used, measures of their success, what worked, and what may need to be altered for future studies.
Participant recruitment is a key marker of intervention feasibility. Identifying optimal recruitment strategies in a PFS plays a critical role in determining whether the specified sample size can be achieved in the well-powered trial. Recruitment strategies may include opt-out methods (passive consent), telephone reminders, open designs (participants know what arm of the trial they are in), referrals, modalities of communication with potential participants (e.g., phone calls, emailing, text, mailings), convenient study location, and partnering with community members/settings [ 138 , 139 , 140 , 141 ]. The specific recruitment strategies used can influence the demographic makeup of participants. Different recruitment strategies can also yield varying amounts of eligible participants. In addition, each recruitment strategy has an associated cost. It may also be important to identify reasons why participants refused to participate in the study and record these reasons quantitatively and/or qualitatively. This information should be collected at the individual and/or setting level where appropriate. These can be important to establish during a PFS to optimize recruitment procedures in the larger-scale trial, especially in situations where there are uncertainties around recruiting the target population. At times, it may even be appropriate to formally test recruitment strategies, particularly when there is uncertainty about the best approach. For example, by embedding a “Study Within A Trial” (SWAT), researchers may gain answers to uncertainties around methodological decisions regarding a number of feasibility outcomes, including recruitment [ 142 , 143 ].
Retention (attrition/drop-out) is the proportion of enrolled participants who are present throughout the full length of the intervention [ 137 ].
Researchers conducting PFS should ensure retention rates are measured.
Where possible, assessments can be made to identify differences in retention across groups or intervention conditions.
Reasons why individuals leave a study can be collected and analyzed to investigate whether particular factors are associated with retention.
Procedures should clearly describe strategies used to assist with retaining participants during the delivery of the intervention and any post-intervention follow-up time periods, where appropriate.
Retention-related information can include both quantitative and qualitative data sources.
Retention is a commonly assessed marker of intervention feasibility. Retaining participants throughout an intervention is important to ensure participants receive the full dose of intervention components as designed and whether selective attrition is present. Retention-related information also helps to understand issues regarding missing data and low statistical power in future studies. Ultimately, retention is a marker of intervention viability. In other words, if participants do not want to receive an intervention it is unlikely to be impactful.
For a given intervention, a clear definition of retention should be reported. This can include participants staying for the duration of study-related procedures/measures (e.g., data collection), completing intervention components, and/or attendance at intervention sessions [ 22 , 92 , 128 , 144 ]. Depending on the nature of the intervention and the outcomes targeted, PFS may be designed specifically to address issues regarding retention in samples that have been historically challenging to engage/retain in interventions [ 145 , 146 ].
Retention strategies, such as flexible scheduling, reminders, compensation, consistency in study staff (continuity of relationships), gathering multiple contacts, thank you and birthday cards, and follow-up phone calls within a given period, can reduce the rate of participant drop-out [ 139 , 147 , 148 , 149 ]. Where dropouts occur, reasons for withdrawal from the study can be collected [ 128 , 150 ]. Factors influencing retention, both positively and negatively, including participant motivation/aspirations, expectations, the perceived need for an intervention, and accessibility of intervention (location delivered), can be collected from both participants and intervention deliverers [ 151 , 152 , 153 , 154 , 155 ].
Implementation of intervention
Acceptability.
Acceptability is a perception/notion that an intervention or various aspects of an intervention are favorable, agreeable, palatable, enjoyable, satisfactory, valued, appropriate from the perspectives of participants or communities receiving the intervention, and/or have a wider fit within a system. It relates to how users “feel” about an intervention [ 156 ].
Researchers should clearly define what is meant by “acceptability” for a given study, at what levels (e.g., individual, deliverer, setting) it will be assessed, and by what methods (e.g., surveys, interviews). This should be based on the nature of the intervention and its constituent components, target population, setting level characteristics, and key stakeholders.
Measures of acceptability can be pre-defined and included in both the PFS and large-scale trial stages.
Acceptability should be captured, at minimum, from the end user (intervention participants). Acceptability can also be captured from those involved with delivering the intervention, along with anyone else involved in the implementation process.
Acceptability, as defined for a given study, can be assessed for participants in control conditions where appropriate (e.g., acceptability of randomization to active comparator, acceptability of data collection procedures).
Researchers can use both quantitative (e.g., surveys) and qualitative (e.g., interviews) methods to assess acceptability.
In most behavioral interventions, it is important to understand whether those receiving an intervention, those delivering an intervention, and any other key individual(s) find the intervention, either in its entirely or in relevant parts, to be “acceptable” to inform whether the intervention would be used or tolerated. Acceptability encompasses a range of aspects related to impressions of an intervention. These can be gathered anytime along the intervention development continuum. At the earliest stages of conceptualization, prior to packaging and preliminary testing of an intervention, assessments of acceptability (preferences) can include participants’ views of whether the proposed intervention could be appropriate for addressing a given outcome, whether they (the participants) would be willing to adhere to an intervention, the suitability of intervention materials, or whether they perceive the intervention to be useful. During intervention delivery, ongoing assessment of likeability, satisfaction, metrics of engagement with an intervention, and utility can be collected periodically [ 45 , 157 , 158 , 159 ]. Once an intervention is completed, post-assessment markers of acceptability can include perceptions of the length or overall burden of the intervention, what strategies/components of an intervention were liked best, referral of the intervention to others, or whether the intervention met their (the recipients, deliverers, others) preferences/expectations. Where an intervention is delivered by individuals outside the intervention-development team, assessing their perspectives on the acceptability of an intervention may be necessary.
Assessments of acceptability can include both qualitative and quantitative measures. User-centered design [ 160 ] and “think aloud” protocols [ 161 ] can be used in the early stages of intervention conceptualization/formulization. Exit interviews, upon intervention completion, from recipients, deliverers, and other key individuals involved in the intervention, are often employed to evaluate markers of acceptability. Quantitative measures typically include items developed specifically for a given study. Alternatively, existing scales assessing acceptability can be used or modified accordingly for a given application [ 162 , 163 , 164 ]. Acceptability can also cover other aspects of the evaluation process of an intervention. This includes such areas as whether completing the proposed measures is feasible, acceptability of being randomized, or whether recipients were satisfied with the location where an intervention was delivered.
Fidelity is the degree to which an intervention is delivered as intended and the quality of that delivery [ 165 , 166 ].
Researchers should clearly define what is meant by “fidelity” for a given study, at what levels (e.g., individual, deliverer, setting) it will be assessed, and by what methods (e.g., surveys, interviews).
Measures of fidelity should be pre-defined with all intervention components listed.
Fidelity can consist of information about how an intervention will be delivered, for whom, what the intervention consists of, and when and where (context) the intervention will be delivered.
If strategies are used to encourage fidelity (e.g., a manualized intervention, feedback to those delivering the intervention), these should be reported.
Factors influencing fidelity can be assessed and, where appropriate, linked to feasibility outcomes.
Fidelity is often a primary marker of implementation. Assessment of an intervention’s fidelity provides key information regarding whether an intervention, either the testing of individual components or in their entirety, can be delivered as intended. In PFS where initial evaluations of an intervention are conducted, fidelity plays an important role in identifying whether the intervention can be delivered as intended. Evaluation of fidelity implies a working understanding of the intervention and some pre-planned, a priori expected delivery [ 167 , 168 ]. Measuring fidelity can be useful where adaptations (or changes) to the materials may take place (either planned or unplanned). Systematically documenting deviations from the original intervention can yield important insights into whether adaptations were beneficial or detrimental to the outcomes [ 169 ].
Fidelity can include many aspects of an intervention. These include adherence to intervention materials (what was done), quality of delivery (how it was done), and the dose of what was received [ 166 , 170 ]. Assessing fidelity can take many forms. This includes the creation of study-specific fidelity checklists which capture the presence of key components that should be delivered during an intervention (e.g., key material to be delivered in session one or a multi-session intervention) and how they were delivered [ 134 , 171 ]. Response ranges vary from present/absent, yes/no, to Likert-scaled items. Fidelity checklists can be completed either in real-time or reviewed later through the use of recorded video or audio of completed sessions [ 172 , 173 , 174 ]. Checklists can be completed by either someone external to the delivery agent via structured observations/recordings or completed by the delivery agent (e.g., self-report, logbooks) immediately following the delivery [ 175 , 176 , 177 ].
Qualitative interviews of delivery agents can also be conducted to gauge views regarding aspects of an intervention such as the training received to deliver, confidence in delivering, and any perceived barriers to delivering an intervention as planned [ 172 ]. Factors affecting fidelity can be collected to understand what, if anything, may influence departures from delivering an intervention as designed [ 22 , 132 , 173 , 178 ]. Common ways to encourage fidelity are through the use of a manualized package of procedures, training materials, and ongoing review of sessions accompanied by feedback.
Cost and resources
Costs and resources refer to the investments and assets required to develop, implement, and sustain an intervention [ 12 , 179 ].
PFS can include assessments of the costs and required resources of conducting an intervention.
In PFS costs and resources mIn PFS costs and resources may include the following:ay include the following:
Monetary costs associated with training, supervision, and recruitment of both stakeholders and participants, incentivization, facilities, materials, and intervention component development and delivery.
Opportunity costs/time demands associated with completing the intervention by participants and delivering the intervention by providers.
Researchers can collect information to determine the feasibility of measuring the costs associated with the intervention, with this information used to inform a more well-defined cost analysis/economic evaluation in a larger-scale trial.
Researchers should keep in mind that some costs associated with the intervention will be fixed (one-time costs) and some will be recurring during the successful scale-up and sustainment of the intervention.
For some PFS, collecting the costs associated with delivering an intervention may be necessary to inform a larger-scale trial. In PFS, this is often referred to as conducting an economic evaluation, costing, or cost analysis [ 125 , 180 , 181 , 182 , 183 ]. Studies may collect cost data to “rehearse” cost-effectiveness evaluations (economic evaluations) or evaluate the feasibility of collecting cost-related data [ 169 , 184 ]. Where cost data are collected, micro-costing approaches that inventory all associated costs with an intervention are often conducted and used to generate a total cost per unit estimate, often expressed as a cost per participant. Costs can be fixed, variable, or projected future estimates, and they may vary according to the desired fidelity and rigor of the implementation of the interventions. Common resources inventoried for cost include the costs of consumables, staff time, services received, transportation, room hires, and refreshments. Costs can be separated into the costs associated with the initial design/development, set up of the intervention, training of staff to deliver, and the costs associated with intervention delivery. The inclusion of cost data is not study-design specific and spans a wide range of designs from N of 1 to cluster randomized studies [ 185 , 186 , 187 ].
Statistical analysis
Sample size.
Sample size refers to the number of participants (or groups/clusters) in a given study [ 188 ].
The sample size of a PFS should be based on the feasibility objectives of the study.
Sample sizes do not have to be based upon a formal sample size calculation (i.e., power).
Sample sizes should be pre-specified and justified.
Sample size estimates should consider the representativeness of the target population or subgroup, setting, and other relevant contextual aspects that may influence how and why an intervention works.
Sample characteristics should be clearly described and may refer to individuals and/or clusters (e.g., churches, workplaces, neighborhoods, schools).
Where relevant, studies should clearly report factors impacting the sample size (e.g., availability of funds, time constraints).
Investigators are encouraged to report the a priori power achieved by the sample size selected for a PFS.
It is widely recognized that most PFS are underpowered to detect clinically significant/public health important effects in outcomes. Selecting the appropriate sample size for a PFS, however, can vary across studies based on the objectives. In some instances, formal power calculations can be conducted/presented, but one should avoid the temptation of presenting a PFS as being well-powered by assuming implausibly large effects and/or event rates and using non-relevant outcomes. Sample size justification can be made based on other factors including, but not limited to, the availability of resources, the number of potential participants within a given setting, representativeness of the sample to the target population, complexities regarding the intervention, or the experiences of the investigators working with the population/setting [ 189 , 190 , 191 , 192 , 193 ]. Regardless of the approach taken, researchers need to ensure they have sufficient numbers (i.e., sample size) to make informed decisions based on the feasibility metrics and objectives of a PFS and acknowledge any limitations that the usually small sample size confers.
Preliminary impact
Preliminary impact is the ability of an intervention, during a PFS to produce a desired or intended result [ 194 ].
PFS need not be powered to detect statistically significant differences in outcomes, but one or more outcomes, as appropriate to the research, can be assessed.
When outcomes are collected, changes in outcome data (e.g., estimated effect sizes) can be used to aid in decisions regarding the conduct of a subsequent larger-scale trial (e.g., sample size needed).
In many cases, it may be necessary to demonstrate an intervention “moves” outcomes in the appropriate direction and is not causing harm. In this scenario, it is recommended statistical testing can be performed but to avoid the interpretation of p values as conclusive evidence of an intervention’s impact in a larger-scale trial.
Interpretations of performed statistical tests should not include a justification for (or against) proceeding to a subsequent large-scale intervention or for making claims about the likely success of the study. Interpretations should help guide, but not dominate, the decision to proceed to a large-scale intervention.
Investigators should avoid misusing language such as “statistically significant” to describe their interpretation of outcomes from a PFS.
Where pilot and/or feasibility estimates of impact on primary, secondary, or tertiary outcomes are reported these should be pre-specified, with point estimates and a measure of variability reported for all time points.
For studies presenting both feasibility and outcome data, outcome data should be relegated to a secondary or exploratory focus.
In some circumstances, it may be appropriate to evaluate, in a preliminary/exploratory fashion, the potential impact of an intervention on proximal or distill outcomes in a PFS. Where outcomes are assessed and reported, researchers need to understand the evidence is neither definitive nor necessarily very indicative of an intervention’s impact within a larger-scale trial. Nevertheless, the evaluation of outcomes within a PFS can provide useful, additional information to help inform decisions about whether the intervention is ready to be tested at a larger scale. When reporting outcomes, researchers should avoid using misleading language centered on the presence or lack of “statistical significance”. All reported outcome assessments should be secondary to feasibility metrics, which are the primary focus of most PFS. Further, it is suggested that journals should not require by default outcome assessments and/or formal hypothesis testing for manuscripts that report on PFS nor base publishing decisions on the outcomes of potential efficacy analyses if reported.
Pre-registration and protocol publishing
Pre-registration and protocol publishing refers to an a priori process of documenting planned intervention design and analyses [ 195 ].
Pre-registration and a protocol made publicly available (via peer-reviewed journal, pre-print server, or other forms of public dissemination) contributes to transparency and ensures that changes between what is planned, what is conducted, and what is ultimately reported are communicated and justified.
We acknowledge there is a certain degree of flexibility when it comes to PFS between what is proposed and what actually transpires in the execution of the study. Pre-registration of PFS needs to balance the developmental/exploratory nature of these types of studies with the need to document and adhere to general protocols that are the foundation of rigorous and transparent science. The goal of pre-registration is not to create an inflexible scope of work that cannot adapt to uncertainties encountered in the study, but to communicate changes to a protocol and to justify why those changes were made.
Pre-registration of study objectives can be appropriate and at times required based upon funding stipulations. While some PFS are not pre-registered, many can be found on existing trial registries. These include Clinical Trials [ 196 ] and other emerging pre-print servers and open-science repositories, such as Open Science Framework [ 197 , 198 ]. Protocol publishing is also becoming increasingly common for PFS. Pre-registration and protocol publishing may help to provide details about a PFS as well as ensure deviations, although necessary at times, are clearly documented.
Study labeling
Study labeling refers to naming/presenting a PFS with appropriate naming conventions for the study being conducted [ 2 , 3 ].
At a minimum, researchers should make sure studies are clearly labeled to indicate their preliminary nature and reflect the aims and objectives of the study in both the title and abstract with either “pilot”, “feasibility”, “proof-of-concept”, “formative”, or other relevant label(s).
PFS should be clearly labeled to identify and separate them within the intervention development and evaluation literature. One of the benefits of clearly labeling PFS is the ease of identification of these types of studies to understand the evolution of behavioral interventions. Because PFS are often smaller in scale, clear identification also helps to distinguish these types of studies from studies that are small in scale and lack an emphasis on intervention development, refinement, and scaling.
A number of different taxonomies have been proposed to label these types of studies. However, we recognize researchers can and do use terms referring to preliminary studies interchangeably or utilize a combination of them to describe a single study [ 79 , 136 , 167 , 199 , 200 , 201 , 202 , 203 , 204 , 205 , 206 , 207 , 208 , 209 , 210 ]. In the absence of a universal consensus of terms, it is recommended investigators clearly label their PFS with one or more widely used terms that identify the preliminary nature of the study. These terms could include “pilot”, “feasibility”, “proof-of-concept”, “preliminary”, “evidentiary”, “vanguard”, and/or “exploratory”. Thus, investigators should identify the most appropriate term(s) that describe the objective of their study. This should consider the stage and number of tests/evaluations of an intervention.
Framework and guideline usage
The utilization of published frameworks/guidelines to guide the development, implementation, and reporting of PFS.
Where possible, researchers should choose an appropriate framework to structure PFS and use it to guide the design, conduct, analysis, and reporting of said study.
Findings from PFS should be disseminated in a way that adheres to reporting guidelines to facilitate transparency and allow for replication.
There are many existing guidelines, checklists, frameworks, and recommendations that can be useful for the design, conduct, implementation, analysis, and reporting of PFS [ 9 , 211 ]. The use of these publications is associated with higher study quality and reporting [ 9 ]. Guidelines include those developed specifically for PFS and also include those designed outside of the preliminary study context but are highly relevant to many aspects of PFS. Investigators should be familiar with existing guidance and utilize it appropriately, based on the specific objectives of their PFS.
PFS play a pivotal role in the development, refinement, implementation, and sustainability of successful behavioral interventions. This is evidenced by their emphasis on funding agencies [ 4 , 212 , 213 , 214 , 215 , 216 ] and depiction within translational science frameworks [ 117 , 118 , 217 , 218 ]. We identified 161 publications offering some form of guidelines, checklists, frameworks, or recommendations for PFS. Through a Delphi study utilizing expert perspectives, we developed a comprehensive set of considerations which span the continuum of development, conduct, implementation, evaluation, and reporting of behavioral intervention PFS. We believe this will serve as a valuable resource for researchers in the behavioral sciences.
Continued challenges with PFS
While this consolidation of considerations for PFS was developed for broad applicability, there were strong opposing views among the Delphi study participants on some of the considerations that represent continued challenges with PFS. The most striking opposing opinions were observed within the “statistical analysis” theme and were present in both the “sample size” and “preliminary impact” considerations. For example, several respondents in the Delphi study believed sample size estimates for a larger-scale trial can be informed by the estimated intervention effect sizes generated from a PFS, and formal hypothesis testing can be performed and associated p values interpreted in a preliminary study. Other respondents expressed strong opinions that the sample of a PFS need not be representative of the target population. Conversely, the vast majority of respondents agreed that sample size justifications should be based on the feasibility objectives of a given PFS and argued against hypothesis testing (i.e., formal statistical testing and interpretation of p values) during the early phases of intervention development. There have been arguments made for reporting confidence intervals instead of p values for any non-feasibility-related outcomes assessed during PFS [ 219 , 220 , 221 , 222 ]. However, respondents of our Delphi study were quick to point out there is little practical difference between the use of p values or confidence intervals, especially if the PFS is underpowered from the start.
Opposing views were identified throughout the Delphi process for other considerations as well, including “study labeling” and “pre-registration and protocol publishing”. For study labeling, some respondents appreciated the distinction between “pilot”, “feasibility”, and other “preliminary study” terminology, while others worried that these distinctions were not well known and may cause undue confusion. Many participants of the Delphi study indicated they would rather there be no distinction, voicing concerns that adopting rigid taxonomies would create research silos and hinder cross-purpose innovation. Ultimately, we chose not to take a definitive stance on this issue, but rather make researchers aware they should be labeling PFS in some way to aid in the identification of these types of studies. On the topic of pre-registration and protocol publishing, some Delphi respondents argued that pre-registration and protocol publishing for PFS was asking too much and that this type of work should be reserved only for larger-scale trials. Others fully supported the idea of pre-registration and protocol publishing for PFS, arguing it aids in transparency and reproducibility. Again, these are decisions ultimately left up to the researchers conducting PFS, but it is likely that registration will be increasingly requested and enforced (e.g., by funders). The lack of registration of all PFS means that one cannot understand the totality of the efforts that are made in that space for developing and assessing the feasibility of an intervention.
It is important to understand that what may be viewed as common and accepted practice may not be widely held everywhere and the reasons for this vary according to country, funder, and disciplinary norms. It may be that differing opinions stem from differences between what commonly accepted/promoted translational science frameworks espouse and the realities of conducting PFS, which are often conducted with limited resources and abbreviated timelines. In addition, there may be different levels of expectations about what is proposed in these frameworks and the expectations of funding agencies and grant reviewers [ 223 ]. Such disagreements can prove problematic for behavioral scientists when seeking funding or wanting to publish findings from their PFS. Reconciliation on these topics is unlikely, and perhaps unnecessary, yet it is important to acknowledge what can and cannot be accomplished by a PFS. We believe appropriately tending to these issues throughout all phases of design, conduct, interpretation, and reporting should help preemptively dissuade critiques that could stymie the progress of intervention development and implementation.
Progress for PFS
While disagreements were noted for a few considerations, most respondents agreed on the content of most topics. For example, participants of the Delphi study agreed that feasibility outcomes, including recruitment, retention, acceptability, and fidelity should take priority over preliminary impact and should be used and presented as the primary outcomes of PFS. This also aligns with developing well-designed problems and aims of PFS, most of which should answer questions regarding uncertainties (feasibility) of an intervention. Respondents also agreed progression criteria are useful when developing and deploying PFS, although some recommended caution on the use of progression criteria that are too rigid when making decisions about scaling up PFS to the next stage. Finally, and perhaps most salient, participants agreed on the importance of PFS as a critical step in successful large-scale intervention development and implementation. However, one cannot exclude the presence of selection bias in favor of the importance of PFS among authors who have authored guidelines on them and even more so among authors who responded to our surveys.
Use of the considerations
We believe the considerations in this paper span the continuum of PFS, from development to reporting, and will be useful for researchers planning to conduct their very first PFS to well-seasoned interventionists. We envision these consolidated considerations being used in practice and as an educational tool for trainees. On a broader scale, we are hopeful this consolidation may improve PFS in the future, reducing research waste and leading to the development of high-quality, scalable behavioral interventions with maximal reach and public health impact. In addition to the considerations themselves, we provide a crosswalk of all published guidelines, checklists, frameworks, and recommendations related to PFS in Additional file 2 in an effort to amplify the voices of experts in this field. Researchers reading this study and those who want to know more about a particular consideration are encouraged to utilize the crosswalk located in Additional file 1 to identify further reading, which may provide more specific guidance on a particular topic. While not the focus of this consolidation, we also believe many of the considerations are cross-cutting with large-scale implementation and dissemination research. Researchers doing this type of work may look to certain considerations to guide aspects of their larger-scale study as well.
Strengths and limitations
These consolidated considerations have several strengths. First, they were created based on information gathered from 161 published guidelines, checklists, frameworks, and recommendations on the topic of PFS. We relied on authors from these very same 161 publications to voice their opinions about the most important PFS-related topics via a three-round Delphi study. The total sample of participants across three rounds of the Delphi process represented over 35% of the 161 publications. Participants had, on average, 23 years of experience since their terminal degree, representing a collective 1150 years of experience across respondents. Moreover, we supplement this consolidation with a review of those 161 guidelines, checklists, frameworks, and recommendations, creating one of the largest collective sources of information on PFS published to date. This study is not without limitations. While we had a moderate representation of Delphi participants across publications, we were only able to recruit 10% (50 out of 496 identified authors) of our target population for the Delphi process. Further, while there was an equal distribution of males and females, the sample was largely White. Other than age and years of terminal degree, we did not collect other demographic information on the Delphi participants, although the median year of publication for the publications represented in our sample was slightly more recent (2015) than the total sample of possible publications (2013) from which authors were sampled. For the considerations themselves, there is still no true consensus on many of the topics presented. Differences of opinion were observed throughout the Delphi process and can be found across the published literature. Despite this, we believe the consolidated considerations could be a valuable resource for behavioral interventionists conducting PFS on a broad range of public health topics.
This is one of the first studies to attempt to garner consensus on a broad range of considerations regarding PFS for the behavioral sciences. We leveraged expert opinion from researchers who have published PFS-related guidelines, checklists, frameworks, and recommendations on a wide range of topics and distilled this knowledge into a valuable and universal resource for researchers conducting PFS. We identified 20 considerations for PFS, which fall into six categories, including intervention design , study design , conduct of trial , implementation of intervention , statistical analysis , and reporting . We also provide a list of the available publications on each of the specific considerations for further reading and use and have aligned these publications with the considerations set forth in this paper. Researchers may use these considerations alongside the previously published literature to guide decision making about all aspects of PFS, with the hope of creating and disseminating interventions with broad public health impact.
Availability of data and materials
The datasets used and analyzed during the current study are freely available at https://osf.io/kyft7/ .
Indig D, Lee K, Grunseit A, Milat A, Bauman A. Pathways for scaling up public health interventions. BMC Public Health. 2018;18(1):68. https://doi.org/10.1186/s12889-017-4572-5 .
Article Google Scholar
Eldridge SM, Lancaster GA, Campbell MJ, et al. Defining feasibility and pilot studies in preparation for randomised controlled trials: development of a conceptual framework. Plos One. 2016;11(3):e0150205. https://doi.org/10.1371/journal.pone.0150205 . Lazzeri C, ed.
Article CAS PubMed PubMed Central Google Scholar
Bond C, Lancaster GA, Campbell M, et al. Pilot and feasibility studies: extending the conceptual framework. Pilot Feasibil Stud. 2023;9(1):24. https://doi.org/10.1186/s40814-023-01233-1 .
National Institutes of Health. NIH Planning Grant Program (R34) .; 2019. https://grants.nih.gov/grants/funding/r34.htm . Accessed 13 July, 2023
Moher D, Altman DG, Schulz KF, Simera I. How to develop a reporting guideline. In: Moher D, Altman DG, Schulz KF, Simera I, Wager E, eds. Guidelines for Reporting Health Research: A User’s Manual. John Wiley & Sons, Ltd; 2014:14–21. https://doi.org/10.1002/9781118715598.ch2
Moher D, Schulz KF, Simera I, Altman DG. Guidance for developers of health research reporting guidelines. Plos Med. 2010;7(2):e1000217. https://doi.org/10.1371/journal.pmed.1000217 .
Article PubMed PubMed Central Google Scholar
Eldridge SM, Chan CL, Campbell MJ, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ. Published online October 24 2016;i5239. https://doi.org/10.1136/bmj.i5239
O’Cathain A, Croot L, Duncan E, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019;9(8):e029954. https://doi.org/10.1136/bmjopen-2019-029954 .
Pfledderer CD, Von Klinggraeff L, Burkart S, et al. Use of guidelines, checklists, frameworks, and recommendations in behavioral intervention preliminary studies and associations with reporting comprehensiveness: a scoping bibliometric review. Pilot Feasibil Stud. 2023;9:161. https://doi.org/10.1186/s40814-023-01389-w .
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. Published online September 29, 2008:a1655. https://doi.org/10.1136/bmj.a1655
Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med. 2009;36(5):452–7. https://doi.org/10.1016/j.amepre.2009.02.002 .
Pearson N, Naylor PJ, Ashe MC, Fernandez M, Yoong SL, Wolfenden L. Guidance for conducting feasibility and pilot studies for implementation trials. Pilot Feasibil Stud. 2020;6(1):167. https://doi.org/10.1186/s40814-020-00634-w .
Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique: Delphi survey technique. J Adv Nurs. 2000;32(4):1008–15. https://doi.org/10.1046/j.1365-2648.2000.t01-1-01567.x .
Article CAS PubMed Google Scholar
Keeney S, Hasson F, McKenna HP. The Delphi Technique in Nursing and Health Research. Oxford: Wiley-Blackwell; 2011.
Mellor K, Albury C, Dutton SJ, Eldridge S, Hopewell S. Recommendations for progression criteria during external randomised pilot trial design, conduct, analysis and reporting. Pilot Feasibil Stud. 2023;9(1):59. https://doi.org/10.1186/s40814-023-01291-5 . s40814-023-01291-01295.
Stirman SW, Miller CJ, Toder K, Calloway A. Development of a framework and coding system for modifications and adaptations of evidence-based interventions. Implement Sci. 2013;8(1):65. https://doi.org/10.1186/1748-5908-8-65 .
Swindle T, Martinez A, Børsheim E, Andres A. Adaptation of an exercise intervention for pregnant women to community-based delivery: a study protocol. BMJ Open. 2020;10(9):e038582. https://doi.org/10.1136/bmjopen-2020-038582 .
Sizemore KM, Gray S, Wolfer C, et al. A proof of concept pilot examining feasibility and acceptability of the positively healthy just-in-time adaptive, ecological momentary, intervention among a sample of sexual minority men living with HIV. J Happiness Stud. 2022;23(8):4091–118. https://doi.org/10.1007/s10902-022-00587-2 .
Duarte N, Hughes SL, Paúl C. Cultural adaptation and specifics of the fit & strong! program in Portugal. Transl Behav Med. 2019;9(1):67–75. https://doi.org/10.1093/tbm/iby003 .
Article PubMed Google Scholar
Eylem O, Van Straten A, De Wit L, Rathod S, Bhui K, Kerkhof AJFM. Reducing suicidal ideation among Turkish migrants in the Netherlands and in the UK: the feasibility of a randomised controlled trial of a guided online intervention. Pilot Feasibil Stud. 2021;7(1):30. https://doi.org/10.1186/s40814-021-00772-9 .
Mathews E, Thomas E, Absetz P, et al. Cultural adaptation of a peer-led lifestyle intervention program for diabetes prevention in India: the Kerala diabetes prevention program (K-DPP). BMC Public Health. 2017;17(1):974. https://doi.org/10.1186/s12889-017-4986-0 .
Zullig LL, McCant F, Silberberg M, Johnson F, Granger BB, Bosworth HB. Changing CHANGE: adaptations of an evidence-based telehealth cardiovascular disease risk reduction intervention. Transl Behav Med. 2018;8(2):225–32. https://doi.org/10.1093/tbm/ibx030 .
Hill JL, Zoellner JM, You W, et al. Participatory development and pilot testing of iChoose: an adaptation of an evidence-based paediatric weight management program for community implementation. BMC Public Health. 2019;19(1):122. https://doi.org/10.1186/s12889-019-6450-9 .
Sánchez-Franco S, Arias LF, Jaramillo J, et al. Cultural adaptation of two school-based smoking prevention programs in Bogotá Colombia. Transl Behav Med. 2021;11(8):1567–78. https://doi.org/10.1093/tbm/ibab019 .
Lloyd J, Bjornstad G, Borek A, et al. Healthy parent carers programme: mixed methods process evaluation and refinement of a health promotion intervention. BMJ Open. 2021;11(8):e045570. https://doi.org/10.1136/bmjopen-2020-045570 .
Meiksin R, Allen E, Crichton J, et al. Protocol for pilot cluster RCT of project respect: a school-based intervention to prevent dating and relationship violence and address health inequalities among young people. Pilot Feasibil Stud. 2019;5(1):13. https://doi.org/10.1186/s40814-019-0391-z .
Sebire SJ, Banfield K, Jago R, et al. A process evaluation of the PLAN-A intervention (Peer-Led physical Activity iNtervention for Adolescent girls). BMC Public Health. 2019;19(1):1203. https://doi.org/10.1186/s12889-019-7545-z .
Mueller S, Soriano D, Boscor A, et al. MANTRA: development and localization of a mobile educational health game targeting low literacy players in low and middle income countries. BMC Public Health. 2020;20(1):1171. https://doi.org/10.1186/s12889-020-09246-8 .
Gaume J, Grazioli VS, Paroz S, Fortini C, Bertholet N, Daeppen JB. Developing a brief motivational intervention for young adults admitted with alcohol intoxication in the emergency department – results from an iterative qualitative design. Plos One. 2021;16(2):e0246652. https://doi.org/10.1371/journal.pone.0246652 . Alam A (Neeloy, ed).
Siu AL, Zimbroff RM, Federman AD, et al. The effect of adapting Hospital at Home to facilitate implementation and sustainment on program drift or voltage drop. BMC Health Serv Res. 2019;19(1):264. https://doi.org/10.1186/s12913-019-4063-8 .
Martin S, Rassi C, Antonio V, et al. Evaluating the feasibility and acceptability of a community dialogue intervention in the prevention and control of schistosomiasis in Nampula province, Mozambique. Plos One. 2021;16(8):e0255647. https://doi.org/10.1371/journal.pone.0255647 . Diemert DJ, ed.
Ellis-Hill C, Thomas S, Gracey F, et al. HeART of Stroke: randomised controlled, parallel-arm, feasibility study of a community-based arts and health intervention plus usual care compared with usual care to increase psychological well-being in people following a stroke. BMJ Open. 2019;9(3):e021098. https://doi.org/10.1136/bmjopen-2017-021098 .
Walton A, Nahum-Shani I, Crosby L, Klasnja P, Murphy S. Optimizing digital integrated care via micro-randomized trials. Clin Pharmacol Ther. 2018;104(1):53–8. https://doi.org/10.1002/cpt.1079 .
Odukoya OO, Manortey S, Takemoto M, Alder S, Okuyemi KS. Body, Soul and Spirit, an adaptation of two evidence-based interventions to promote physical activity and healthy eating among adults in churches in Lagos Nigeria: a three-arm cluster randomized controlled pilot trial. Pilot Feasibil Stud. 2020;6(1):59. https://doi.org/10.1186/s40814-020-00600-6 .
Malden S, Hughes AR, Gibson AM, et al. Adapting the ToyBox obesity prevention intervention for use in Scottish preschools: protocol for a feasibility cluster randomised controlled trial. BMJ Open. 2018;8(10):e023707. https://doi.org/10.1136/bmjopen-2018-023707 .
Istanboulian L, Rose L, Yunusova Y, Dale CM. Protocol for a mixed method acceptability evaluation of a codesigned bundled COmmunication intervention for use in the adult ICU during the COVID-19 PandEmic: the COPE study. BMJ Open. 2021;11(9):e050347. https://doi.org/10.1136/bmjopen-2021-050347 .
McKay H, Nettlefold L, Bauman A, et al. Implementation of a co-designed physical activity program for older adults: positive impact when delivered at scale. BMC Public Health. 2018;18(1):1289. https://doi.org/10.1186/s12889-018-6210-2 .
Klasnja P, Smith S, Seewald NJ, et al. Efficacy of contextually tailored suggestions for physical activity: a micro-randomized optimization trial of HeartSteps. Ann Behav Med. 2019;53(6):573–82. https://doi.org/10.1093/abm/kay067 .
Murray E, Daff K, Lavida A, Henley W, Irwin J, Valabhji J. Evaluation of the digital diabetes prevention programme pilot: uncontrolled mixed-methods study protocol. BMJ Open. 2019;9(5):e025903. https://doi.org/10.1136/bmjopen-2018-025903 .
Rodrigues AmorimAdegboye A, Cocate PG, Benaim C, et al. Recruitment of low-income pregnant women into a dietary and dental care intervention: lessons from a feasibility trial. Trials. 2020;21(1):244. https://doi.org/10.1186/s13063-020-4142-5 .
Northridge ME, Metcalf SS, Yi S, Zhang Q, Gu X, Trinh-Shevrin C. A protocol for a feasibility and acceptability study of a participatory, multi-level, dynamic intervention in urban outreach centers to improve the oral health of low-income Chinese Americans. Front Public Health. 2018;6:29. https://doi.org/10.3389/fpubh.2018.00029 .
Nicolson GH, Hayes C, Darker C. A theory-based multicomponent intervention to reduce occupational sedentary behaviour in professional male workers: protocol for a cluster randomised crossover pilot feasibility study. Pilot Feasibil Stud. 2020;6(1):175. https://doi.org/10.1186/s40814-020-00716-9 .
Thomas DSK, Bull S, Nyanza EC, Hampanda K, Liedtke M, Ngallaba SE. An mHealth pilot designed to increase the reach of prevention of mother-to-child transmission of HIV (PMTCT) across the treatment cascade in a resource-constrained setting in Tanzania. Plos One. 2019;14(2):e0212305. https://doi.org/10.1371/journal.pone.0212305 . Biemba G, ed.
Lemanska A, Poole K, Griffin BA, et al. Community pharmacy lifestyle intervention to increase physical activity and improve cardiovascular health of men with prostate cancer: a phase II feasibility study. BMJ Open. 2019;9(6):e025114. https://doi.org/10.1136/bmjopen-2018-025114 .
Logie CH, Daniel C, Newman PA, Loutfy MR. An HIV/STI prevention intervention for internally displaced women in Leogane, Haiti: study protocol for an N-of-1 pilot study. BMJ Open. 2012;2(4):e001634. https://doi.org/10.1136/bmjopen-2012-001634 .
Coulman E, Hastings R, Gore N, et al. The Early Positive Approaches to Support (E-PAtS) study: study protocol for a feasibility cluster randomised controlled trial of a group programme (E-PAtS) for family caregivers of young children with intellectual disability. Pilot Feasibil Stud. 2020;6(1):147. https://doi.org/10.1186/s40814-020-00689-9 .
Njuguna IN, Beima-Sofie K, Mburu CW, et al. Adolescent transition to adult care for HIV-infected adolescents in Kenya (ATTACH): study protocol for a hybrid effectiveness-implementation cluster randomised trial. BMJ Open. 2020;10(12):e039972. https://doi.org/10.1136/bmjopen-2020-039972 .
Bradford N, Condon P, Pitt E, Tyack Z, Alexander K. Optimising symptom management in children with cancer using a novel mobile phone application: protocol for a controlled hybrid effectiveness implementation trial (RESPONSE). BMC Health Serv Res. 2021;21(1):942. https://doi.org/10.1186/s12913-021-06943-x .
Maughan-Brown B, Smith P, Kuo C, et al. A conditional economic incentive fails to improve linkage to care and antiretroviral therapy initiation among HIV-positive adults in Cape Town South Africa. AIDS Patient Care STDs. 2018;32(2):70–8. https://doi.org/10.1089/apc.2017.0238 .
Kramer F, Labudek S, Jansen CP, et al. Development of a conceptual framework for a group-based format of the Lifestyle-integrated Functional Exercise (gLiFE) programme and its initial feasibility testing. Pilot Feasibil Stud. 2020;6(1):6. https://doi.org/10.1186/s40814-019-0539-x .
Doody P, Lord JM, Whittaker AC. Assessing the feasibility and impact of an adapted resistance training intervention, aimed at improving the multi-dimensional health and functional capacity of frail older adults in residential care settings: protocol for a feasibility study. Pilot Feasibil Stud. 2019;5(1):86. https://doi.org/10.1186/s40814-019-0470-1 .
Morris AS, Murphy RC, Shepherd SO, Healy GN, Edwardson CL, Graves LEF. A multi-component intervention to sit less and move more in a contact centre setting: a feasibility study. BMC Public Health. 2019;19(1):292. https://doi.org/10.1186/s12889-019-6615-6 .
Millar A, Tip L, Lennon R, et al. The introduction of mindfulness groups to a psychiatric rehabilitation in-patient setting: a feasibility study. BMC Psychiatry. 2020;20(1):322. https://doi.org/10.1186/s12888-020-02725-7 .
Rasheed MA, Bharuchi V, Mughis W, Hussain A. Development and feasibility testing of a play-based psychosocial intervention for reduced patient stress in a pediatric care setting: experiences from Pakistan. Pilot Feasibil Stud. 2021;7(1):63. https://doi.org/10.1186/s40814-021-00781-8 .
Azar KMJ, Nasrallah C, Szwerinski NK, et al. Implementation of a group-based diabetes prevention program within a healthcare delivery system. BMC Health Serv Res. 2019;19(1):694. https://doi.org/10.1186/s12913-019-4569-0 .
Tsakos G, Brocklehurst PR, Watson S, et al. Improving the oral health of older people in care homes (TOPIC): a protocol for a feasibility study. Pilot Feasibil Stud. 2021;7(1):138. https://doi.org/10.1186/s40814-021-00872-6 .
Clemson L, Laver K, Jeon YH, et al. Implementation of an evidence-based intervention to improve the wellbeing of people with dementia and their carers: study protocol for ‘Care of People with dementia in their Environments (COPE)’ in the Australian context. BMC Geriatr. 2018;18(1):108. https://doi.org/10.1186/s12877-018-0790-7 .
Hawkins J, Madden K, Fletcher A, et al. Development of a framework for the co-production and prototyping of public health interventions. BMC Public Health. 2017;17(1):689. https://doi.org/10.1186/s12889-017-4695-8 .
Gillespie J, Hughes A, Gibson AM, Haines J, Taveras E, Reilly JJ. Protocol for Healthy Habits Happy Homes (4H) Scotland: feasibility of a participatory approach to adaptation and implementation of a study aimed at early prevention of obesity. BMJ Open. 2019;9(6):e028038. https://doi.org/10.1136/bmjopen-2018-028038 .
Griva K, Chia JMX, Goh ZZS, et al. Effectiveness of a brief positive skills intervention to improve psychological adjustment in patients with end-stage kidney disease newly initiated on haemodialysis: protocol for a randomised controlled trial (HED-Start). BMJ Open. 2021;11(9):e053588. https://doi.org/10.1136/bmjopen-2021-053588 .
Chudleigh J, Holder P, Moody L, et al. Process evaluation of co-designed interventions to improve communication of positive newborn bloodspot screening results. BMJ Open. 2021;11(8):e050773. https://doi.org/10.1136/bmjopen-2021-050773 .
Maindal HT, Timm A, Dahl-Petersen IK, et al. Systematically developing a family-based health promotion intervention for women with prior gestational diabetes based on evidence, theory and co-production: the Face-it study. BMC Public Health. 2021;21(1):1616. https://doi.org/10.1186/s12889-021-11655-2 .
Bray EA, George A, Everett B, Salamonson Y, Ramjan L. Protocol for developing a healthcare transition intervention for young people with spinal cord injuries using a participatory action research approach. BMJ Open. 2021;11(7):e053212. https://doi.org/10.1136/bmjopen-2021-053212 .
Goffe L, Hillier-Brown F, Hildred N, et al. Feasibility of working with a wholesale supplier to co-design and test acceptability of an intervention to promote smaller portions: an uncontrolled before-and-after study in British Fish & Chip shops. BMJ Open. 2019;9(2):e023441. https://doi.org/10.1136/bmjopen-2018-023441 .
Livings R, Naylor JM, Gibson K, et al. Implementation of a community-based, physiotherapy-led, multidisciplinary model of care for the management of knee osteoarthritis: protocol for a feasibility study. BMJ Open. 2020;10(7):e039152. https://doi.org/10.1136/bmjopen-2020-039152 .
Guagliano JM, Brown HE, Coombes E, et al. The development and feasibility of a randomised family-based physical activity promotion intervention: the Families Reporting Every Step to Health (FRESH) study. Pilot Feasibil Stud. 2019;5(1):21. https://doi.org/10.1186/s40814-019-0408-7 .
Kassavou A, Houghton V, Edwards S, Brimicombe J, Sutton S. Development and piloting of a highly tailored digital intervention to support adherence to antihypertensive medications as an adjunct to primary care consultations. BMJ Open. 2019;9(1):e024121. https://doi.org/10.1136/bmjopen-2018-024121 .
Payne Riches S, Piernas C, Aveyard P, Sheppard JP, Rayner M, Jebb SA. The Salt Swap intervention to reduce salt intake in people with high blood pressure: protocol for a feasibility randomised controlled trial. Trials. 2019;20(1):584. https://doi.org/10.1186/s13063-019-3691-y .
Degroote L, Van Dyck D, De Bourdeaudhuij I, De Paepe A, Crombez G. Acceptability and feasibility of the mHealth intervention ‘MyDayPlan’ to increase physical activity in a general adult population. BMC Public Health. 2020;20(1):1032. https://doi.org/10.1186/s12889-020-09148-9 .
Bodschwinna D, Lorenz I, Bauereiss N, Gündel H, Baumeister H, Hoenig K. PartnerCARE—a psycho-oncological online intervention for partners of patients with cancer: study protocol for a randomised controlled feasibility trial. BMJ Open. 2020;10(10):e035599. https://doi.org/10.1136/bmjopen-2019-035599 .
Lowthian JA, Green M, Meyer C, et al. Being Your Best: protocol for a feasibility study of a codesigned approach to reduce symptoms of frailty in people aged 65 years or more after transition from hospital. BMJ Open. 2021;11(3):e043223. https://doi.org/10.1136/bmjopen-2020-043223 .
Goff LM, Moore AP, Rivas C, Harding S. Healthy Eating and Active Lifestyles for Diabetes (HEAL-D): study protocol for the design and feasibility trial, with process evaluation, of a culturally tailored diabetes self-management programme for African-Caribbean communities. BMJ Open. 2019;9(2):e023733. https://doi.org/10.1136/bmjopen-2018-023733 .
Vandervelde S, Scheepmans K, Milisen K, et al. Reducing the use of physical restraints in home care: development and feasibility testing of a multicomponent program to support the implementation of a guideline. BMC Geriatr. 2021;21(1):77. https://doi.org/10.1186/s12877-020-01946-5 .
Simpson S, Wyke S, Mercer SW. Adaptation of a mindfulness-based intervention for incarcerated young men: a feasibility study. Mindfulness. 2019;10(8):1568–78. https://doi.org/10.1007/s12671-018-1076-z .
Jumbe S, James WY, Madurasinghe V, et al. Evaluating NHS Stop Smoking Service engagement in community pharmacies using simulated smokers: fidelity assessment of a theory-based intervention. BMJ Open. 2019;9(5):e026841. https://doi.org/10.1136/bmjopen-2018-026841 .
Langford R, Jago R, White J, et al. A physical activity, nutrition and oral health intervention in nursery settings: process evaluation of the NAP SACC UK feasibility cluster RCT. BMC Public Health. 2019;19(1):865. https://doi.org/10.1186/s12889-019-7102-9 .
Appel JM, Fullerton K, Hennessy E, et al. Design and methods of shape up under 5: integration of systems science and community-engaged research to prevent early childhood obesity. Plos One. 2019;14(8):e0220169. https://doi.org/10.1371/journal.pone.0220169 . Nkomazana O, ed.
Myers B, Carney T, Browne FA, Wechsberg WM. A trauma-informed substance use and sexual risk reduction intervention for young South African women: a mixed-methods feasibility study. BMJ Open. 2019;9(2):e024776. https://doi.org/10.1136/bmjopen-2018-024776 .
Brewer LC, Hayes SN, Caron AR, et al. Promoting cardiovascular health and wellness among African-Americans: community participatory approach to design an innovative mobile-health intervention. Plos One. 2019;14(8):e0218724. https://doi.org/10.1371/journal.pone.0218724 . Newton RL, ed.
Mitchell KR, Purcell C, Simpson SA, et al. Feasibility study of peer-led and school-based social network Intervention (STASH) to promote adolescent sexual health. Pilot Feasibil Stud. 2021;7(1):125. https://doi.org/10.1186/s40814-021-00835-x .
on behalf of the REACH-HF investigators, Greaves CJ, Wingham J, et al. Optimising self-care support for people with heart failure and their caregivers: development of the Rehabilitation Enablement in Chronic Heart Failure (REACH-HF) intervention using intervention mapping. Pilot Feasibil Stud. 2016;2(1):37. https://doi.org/10.1186/s40814-016-0075-x .
Lang CC, Smith K, Wingham J, et al. A randomised controlled trial of a facilitated home-based rehabilitation intervention in patients with heart failure with preserved ejection fraction and their caregivers: the REACH-HFpEF Pilot Study. BMJ Open. 2018;8(4):e019649. https://doi.org/10.1136/bmjopen-2017-019649 .
Abuhaloob L, Helles N, Mossey P, Freeman R. An ADePT evaluation for incorporating the TIPPS periodontal health intervention into primary care antenatal programmes to enhance infant birth weight in Palestine: a feasibility study. Pilot Feasibil Stud. 2021;7(1):91. https://doi.org/10.1186/s40814-021-00827-x .
Davis M, Wolk CB, Jager-Hyman S, et al. Implementing nudges for suicide prevention in real-world environments: project INSPIRE study protocol. Pilot Feasibil Stud. 2020;6(1):143. https://doi.org/10.1186/s40814-020-00686-y .
Barnett M, Miranda J, Kia-Keating M, Saldana L, Landsverk J, Lau AS. Developing and evaluating a lay health worker delivered implementation intervention to decrease engagement disparities in behavioural parent training: a mixed methods study protocol. BMJ Open. 2019;9(7):e028988. https://doi.org/10.1136/bmjopen-2019-028988 .
Lucas-Thompson R, Seiter N, Broderick PC, et al. Moving 2 Mindful (M2M) study protocol: testing a mindfulness group plus ecological momentary intervention to decrease stress and anxiety in adolescents from high-conflict homes with a mixed-method longitudinal design. BMJ Open. 2019;9(11):e030948. https://doi.org/10.1136/bmjopen-2019-030948 .
Clouse K, Phillips TK, Camlin C, et al. CareConekta: study protocol for a randomized controlled trial of a mobile health intervention to improve engagement in postpartum HIV care in South Africa. Trials. 2020;21(1):258. https://doi.org/10.1186/s13063-020-4190-x .
McCrabb S, Mooney K, Elton B, Grady A, Yoong SL, Wolfenden L. How to optimise public health interventions: a scoping review of guidance from optimisation process frameworks. BMC Public Health. 2020;20(1):1849. https://doi.org/10.1186/s12889-020-09950-5 .
Neuhaus M, Healy GN, Fjeldsoe BS, et al. Iterative development of Stand Up Australia: a multi-component intervention to reduce workplace sitting. Int J Behav Nutr Phys Act. 2014;11(1):21. https://doi.org/10.1186/1479-5868-11-21 .
Fanning J, Brooks AK, Ip E, et al. A mobile health behavior intervention to reduce pain and improve health in older adults with obesity and chronic pain: the MORPH pilot trial. Front Digit Health. 2020;2:598456. https://doi.org/10.3389/fdgth.2020.598456 .
Larsen B, Greenstadt ED, Olesen BL, Marcus BH, Godino J, Zive MM. An mHealth physical activity intervention for latina adolescents: iterative design of the Chicas Fuertes study. JMIR Form Res. 2021;5(6):e26195. https://doi.org/10.2196/26195 .
Pagoto S, Tulu B, Agu E, Waring ME, Oleski JL, Jake-Schoffman DE. Using the Habit App for weight loss problem solving: development and feasibility study. JMIR MHealth UHealth. 2018;6(6):e145. https://doi.org/10.2196/mhealth.9801 .
Forsyth R, Purcell C, Barry S, et al. Peer-led intervention to prevent and reduce STI transmission and improve sexual health in secondary schools (STASH): protocol for a feasibility study. Pilot Feasibil Stud. 2018;4(1):180. https://doi.org/10.1186/s40814-018-0354-9 .
Nixon AC, Bampouras TM, Gooch HJ, et al. The EX-FRAIL CKD trial: a study protocol for a pilot randomised controlled trial of a home-based EXercise programme for pre-frail and FRAIL, older adults with chronic kidney disease. BMJ Open. 2020;10(6):e035344. https://doi.org/10.1136/bmjopen-2019-035344 .
Woodford J, Wikman A, Cernvall M, et al. Study protocol for a feasibility study of an internet-administered, guided, CBT-based, self-help intervention (ENGAGE) for parents of children previously treated for cancer. BMJ Open. 2018;8(6):e023708. https://doi.org/10.1136/bmjopen-2018-023708 .
Huang H, Yang P, Xue J, et al. Evaluating the individualized treatment of traditional Chinese medicine: a pilot study of N-of-1 trials. Evid Based Complement Alternat Med. 2014;2014:1–10. https://doi.org/10.1155/2014/148730 .
Hernandez LM, Wetter DW, Kumar S, Sutton SK, Vinci C. Smoking cessation using wearable sensors: protocol for a microrandomized trial. JMIR Res Protoc. 2021;10(2):e22877. https://doi.org/10.2196/22877 .
Militello L, Sobolev M, Okeke F, Adler DA, Nahum-Shani I. Digital prompts to increase engagement with the Headspace App and for stress regulation among parents: feasibility study. JMIR Form Res. 2022;6(3):e30606. https://doi.org/10.2196/30606 .
Kang M, Ragan BG, Park JH. Issues in outcomes research: an overview of randomization techniques for clinical trials. J Athl Train. 2008;43(2):215–21. https://doi.org/10.4085/1062-6050-43.2.215 .
Nair B. Clinical trial designs. Indian Dermatol Online J. 2019;10(2):193–201. https://doi.org/10.4103/idoj.IDOJ_475_18 .
Kendall JM. Designing a research project: randomised controlled trials and their principles. Emerg Med J. 2003;20(2):164–8. https://doi.org/10.1136/emj.20.2.164 .
D’Agostino RB, Kwan H. Measuring effectiveness What to expect without a randomized control group. Med Care. 1995;33(4 Suppl):AS95-105.
PubMed Google Scholar
Kravitz RL, Aguilera A, Chen EJ, et al. Feasibility, acceptability, and influence of mHealth-supported N-of-1 trials for enhanced cognitive and emotional well-being in US volunteers. Front Public Health. 2020;8:260. https://doi.org/10.3389/fpubh.2020.00260 .
Golbus JR, Dempsey W, Jackson EA, Nallamothu BK, Klasnja P. Microrandomized trial design for evaluating just-in-time adaptive interventions through mobile health technologies for cardiovascular disease. Circ Cardiovasc Qual Outcomes. 2021;14(2):e006760. https://doi.org/10.1161/CIRCOUTCOMES.120.006760 .
Pratt D, Mitchell H, Fitzpatrick L, Lea J. A single-group pilot feasibility and acceptability study of the broad minded affective coping technique for suicidal adults in crisis. J Behav Cogn Ther. 2022;32(4):290–6. https://doi.org/10.1016/j.jbct.2022.07.002 .
Dierick F, Bouché AF, Guérin S, et al. Quasi-experimental pilot study to improve mobility and balance in recurrently falling nursing home residents by voluntary non-targeted side-stepping exercise intervention. BMC Geriatr. 2022;22(1):1006. https://doi.org/10.1186/s12877-022-03696-y .
Agarwal G, Gaber J, Richardson J, et al. Pilot randomized controlled trial of a complex intervention for diabetes self-management supported by volunteers, technology, and interprofessional primary health care teams. Pilot Feasibil Stud. 2019;5(1):118. https://doi.org/10.1186/s40814-019-0504-8 .
Milat AJ, King L, Bauman AE, Redman S. The concept of scalability: increasing the scale and potential adoption of health promotion interventions into policy and practice. Health Promot Int. 2013;28(3):285–98. https://doi.org/10.1093/heapro/dar097 .
Smith JM, De Graft-Johnson J, Zyaee P, Ricca J, Fullerton J. Scaling up high-impact interventions: how is it done? Int J Gynecol Obstet. 2015;130:S4–10. https://doi.org/10.1016/j.ijgo.2015.03.010 .
Wulandari LPL, Kaldor J, Guy R. Uptake and acceptability of assisted and unassisted HIV self-testing among men who purchase sex in brothels in Indonesia: a pilot intervention study. BMC Public Health. 2020;20(1):730. https://doi.org/10.1186/s12889-020-08812-4 .
Thomas ED, Zohura F, Hasan MT, et al. Formative research to scale up a handwashing with soap and water treatment intervention for household members of diarrhea patients in health facilities in Dhaka, Bangladesh (CHoBI7 program). BMC Public Health. 2020;20(1):831. https://doi.org/10.1186/s12889-020-08727-0 .
Gagnon MP, Ndiaye MA, Larouche A, et al. Optimising patient active role with a user-centred eHealth platform (CONCERTO+) in chronic diseases management: a study protocol for a pilot cluster randomised controlled trial. BMJ Open. 2019;9(4):e028554. https://doi.org/10.1136/bmjopen-2018-028554 .
Bowden JL, Egerton T, Hinman RS, et al. Protocol for the process and feasibility evaluations of a new model of primary care service delivery for managing pain and function in patients with knee osteoarthritis (PARTNER) using a mixed methods approach. BMJ Open. 2020;10(2):e034526. https://doi.org/10.1136/bmjopen-2019-034526 .
Whittaker SL, Taylor NF, Hill KD, Ekegren CL, Brusco NK. Self-managed occupational therapy and physiotherapy for adults receiving inpatient rehabilitation (‘My Therapy’): protocol for a mixed-methods process evaluation. BMC Health Serv Res. 2021;21(1):810. https://doi.org/10.1186/s12913-021-06463-8 .
Bloom I, Welch L, Vassilev I, et al. Findings from an exploration of a social network intervention to promote diet quality and health behaviours in older adults with COPD: a feasibility study. Pilot Feasibil Stud. 2020;6(1):15. https://doi.org/10.1186/s40814-020-0553-z .
Jackson C, Huque R, Ahmed F, et al. Children Learning About Second-hand Smoke (CLASS II): a mixed methods process evaluation of a school-based intervention. Pilot Feasibil Stud. 2021;7(1):112. https://doi.org/10.1186/s40814-021-00853-9 .
Czajkowski SM, Powell LH, Adler N, et al. From ideas to efficacy: The ORBIT model for developing behavioral treatments for chronic diseases. Health Psychol. 2015;34(10):971–82. https://doi.org/10.1037/hea0000161 .
Onken LS, Carroll KM, Shoham V, Cuthbert BN, Riddle M. Reenvisioning clinical science: unifying the discipline to improve the public health. Clin Psychol Sci. 2014;2(1):22–34. https://doi.org/10.1177/2167702613497932 .
Onken L. Implementation science at the national institute on aging: the principles of it. Public Policy Aging Rep. 2022;32(1):39–41. https://doi.org/10.1093/ppar/prab034 . Kaskie B, ed.
Beets MW, Von Klinggraeff L, Weaver RG, Armstrong B, Burkart S. Small studies, big decisions: the role of pilot/feasibility studies in incremental science and premature scale-up of behavioral interventions. Pilot Feasibil Stud. 2021;7(1):173. https://doi.org/10.1186/s40814-021-00909-w .
Von Klinggraeff L, Dugger R, Okely AD, et al. Early-stage studies to larger-scale trials: investigators’ perspectives on scaling-up childhood obesity interventions. Pilot Feasibil Stud. 2022;8(1):31. https://doi.org/10.1186/s40814-022-00991-8 .
Pressman A, Law H, Stahl R, et al. Conducting a pilot randomized controlled trial of community-based mindfulness-based stress reduction versus usual care for moderate-to-severe migraine: protocol for the Mindfulness and Migraine Study (M&M). Trials. 2019;20(1):257. https://doi.org/10.1186/s13063-019-3355-y .
on behalf of the PD_Manager consortium, Antonini A, Gentile G, et al. Acceptability to patients, carers and clinicians of an mHealth platform for the management of Parkinson’s disease (PD_Manager): study protocol for a pilot randomised controlled trial. Trials. 2018;19(1):492. https://doi.org/10.1186/s13063-018-2767-4 .
Cardwell K, Smith SM, Clyne B, et al. Evaluation of the General Practice Pharmacist (GPP) intervention to optimise prescribing in Irish primary care: a non-randomised pilot study. BMJ Open. 2020;10(6):e035087. https://doi.org/10.1136/bmjopen-2019-035087 .
Adams N, Skelton DA, Howel D, et al. Feasibility of trial procedures for a randomised controlled trial of a community based group exercise intervention for falls prevention for visually impaired older people: the VIOLET study. BMC Geriatr. 2018;18(1):307. https://doi.org/10.1186/s12877-018-0998-6 .
Sahota P, Christian M, Day R, Cocks K. The feasibility and acceptability of a primary school-based programme targeting diet and physical activity: the PhunkyFoods Programme. Pilot Feasibil Stud. 2019;5(1):152. https://doi.org/10.1186/s40814-019-0542-2 .
Huberty J, Matthews J, Leiferman J, Cacciatore J, Gold KJ. A study protocol of a three-group randomized feasibility trial of an online yoga intervention for mothers after stillbirth (The Mindful Health Study). Pilot Feasibil Stud. 2018;4(1):12. https://doi.org/10.1186/s40814-017-0162-7 .
Yang MJ, Sutton SK, Hernandez LM, et al. A Just-In-Time Adaptive intervention (JITAI) for smoking cessation: feasibility and acceptability findings. Addict Behav. 2023;136:107467. https://doi.org/10.1016/j.addbeh.2022.107467 .
Karkar R, Schroeder J, Epstein DA, et al. TummyTrials: a feasibility study of using self-experimentation to detect individualized food triggers. In: Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems. ACM; 2017:6850–6863. https://doi.org/10.1145/3025453.3025480
Munson SA, Schroeder J, Karkar R, Kientz JA, Chung CF, Fogarty J. The importance of starting with goals in N-of-1 studies. Front Digit Health. 2020;2:3. https://doi.org/10.3389/fdgth.2020.00003 .
McGrattan AM, McEvoy CT, Vijayakumar A, et al. A mixed methods pilot randomised controlled trial to develop and evaluate the feasibility of a Mediterranean diet and lifestyle education intervention ‘THINK-MED’ among people with cognitive impairment. Pilot Feasibil Stud. 2021;7(1):3. https://doi.org/10.1186/s40814-020-00738-3 .
Davies M, Kristunas CA, Huddlestone L, et al. Increasing uptake of structured self-management education programmes for type 2 diabetes in a primary care setting: a feasibility study. Pilot Feasibil Stud. 2020;6(1):71. https://doi.org/10.1186/s40814-020-00606-0 .
Jobst S, Leppla L, Köberich S. A self-management support intervention for patients with atrial fibrillation: a randomized controlled pilot trial. Pilot Feasibil Stud. 2020;6(1):87. https://doi.org/10.1186/s40814-020-00624-y .
Tarrant M, Carter M, Dean SG, et al. Singing for people with aphasia (SPA): results of a pilot feasibility randomised controlled trial of a group singing intervention investigating acceptability and feasibility. BMJ Open. 2021;11(1):e040544. https://doi.org/10.1136/bmjopen-2020-040544 .
Mama SK, Bhuiyan N, Bopp MJ, McNeill LH, Lengerich EJ, Smyth JM. A faith-based mind–body intervention to improve psychosocial well-being among rural adults. Transl Behav Med. 2020;10(3):546–54. https://doi.org/10.1093/tbm/ibz136 .
Stephenson A, Garcia-Constantino M, Murphy MH, McDonough SM, Nugent CD, Mair JL. The “Worktivity” mHealth intervention to reduce sedentary behaviour in the workplace: a feasibility cluster randomised controlled pilot study. BMC Public Health. 2021;21(1):1416. https://doi.org/10.1186/s12889-021-11473-6 .
Hallingberg B, Turley R, Segrott J, et al. Exploratory studies to decide whether and how to proceed with full-scale evaluations of public health interventions: a systematic review of guidance. Pilot Feasibil Stud. 2018;4(1):104. https://doi.org/10.1186/s40814-018-0290-8 .
Chatters R, Newbould L, Sprange K, et al. Recruitment of older adults to three preventative lifestyle improvement studies. Trials. 2018;19(1):121. https://doi.org/10.1186/s13063-018-2482-1 .
DeFrank G, Singh S, Mateo KF, et al. Key recruitment and retention strategies for a pilot web-based intervention to decrease obesity risk among minority youth. Pilot Feasibil Stud. 2019;5(1):109. https://doi.org/10.1186/s40814-019-0492-8 .
Greidanus MA, De Rijk AE, De Boer AGEM, et al. A randomised feasibility trial of an employer-based intervention for enhancing successful return to work of cancer survivors (MiLES intervention). BMC Public Health. 2021;21(1):1433. https://doi.org/10.1186/s12889-021-11357-9 .
Kroska EB, Hoel S, Victory A, et al. Optimizing an acceptance and commitment therapy microintervention via a mobile app with two cohorts: protocol for micro-randomized trials. JMIR Res Protoc. 2020;9(9):e17086. https://doi.org/10.2196/17086 .
Treweek S, Bevan S, Bower P, et al. Trial forge guidance 1: what is a Study Within A Trial (SWAT)? Trials. 2018;19(1):139. https://doi.org/10.1186/s13063-018-2535-5 .
Treweek S, Bevan S, Bower P, et al. Trial forge guidance 2: how to decide if a further Study Within A Trial (SWAT) is needed. Trials. 2020;21(1):33. https://doi.org/10.1186/s13063-019-3980-5 .
Vetrovsky T, Cupka J, Dudek M, et al. A pedometer-based walking intervention with and without email counseling in general practice: a pilot randomized controlled trial. BMC Public Health. 2018;18(1):635. https://doi.org/10.1186/s12889-018-5520-8 .
Smith JD, Berkel C, Rudo-Stern J, et al. The family check-up 4 Health (FCU4Health): applying implementation science frameworks to the process of adapting an evidence-based parenting program for prevention of pediatric obesity and excess weight gain in primary care. Front Public Health. 2018;6:293. https://doi.org/10.3389/fpubh.2018.00293 .
Dillingham R, Ingersoll K, Flickinger TE, et al. PositiveLinks: a mobile health intervention for retention in HIV care and clinical outcomes with 12-month follow-up. AIDS Patient Care STDs. 2018;32(6):241–50. https://doi.org/10.1089/apc.2017.0303 .
Orkin A, Campbell D, Handford C, et al. Protocol for a mixed-methods feasibility study for the surviving opioid overdose with naloxone education and resuscitation (SOONER) randomised control trial. BMJ Open. 2019;9(11):e029436. https://doi.org/10.1136/bmjopen-2019-029436 .
Krutsinger DC, Yadav KN, Cooney E, Brooks S, Halpern SD, Courtright KR. A pilot randomized trial of five financial incentive strategies to increase study enrollment and retention rates. Contemp Clin Trials Commun. 2019;15:100390. https://doi.org/10.1016/j.conctc.2019.100390 .
Phillips S, Kanter J, Mueller M, et al. Feasibility of an mHealth self-management intervention for children and adolescents with sickle cell disease and their families. Transl Behav Med. 2021;11(3):724–32. https://doi.org/10.1093/tbm/ibaa132 .
Nikles J, Mitchell GK, Schluter P, et al. Aggregating single patient (n-of-1) trials in populations where recruitment and retention was difficult: the case of palliative care. J Clin Epidemiol. 2011;64(5):471–80. https://doi.org/10.1016/j.jclinepi.2010.05.009 .
Taylor G, Aveyard P, Bartlem K, et al. IntEgrating Smoking Cessation treatment As part of usual Psychological care for dEpression and anxiety (ESCAPE): protocol for a randomised and controlled, multicentre, acceptability, feasibility and implementation trial. Pilot Feasibil Stud. 2019;5(1):16. https://doi.org/10.1186/s40814-018-0385-2 .
Clouse K, Mongwenyana C, Musina M, et al. Acceptability and feasibility of a financial incentive intervention to improve retention in HIV care among pregnant women in Johannesburg South Africa. AIDS Care. 2018;30(4):453–60. https://doi.org/10.1080/09540121.2017.1394436 .
Ortiz JA, Smith BW, Shelley BM, Erickson KS. Adapting mindfulness to engage latinos and improve mental health in primary care: a pilot study. Mindfulness. 2019;10(12):2522–31. https://doi.org/10.1007/s12671-019-01229-0 .
Fuchs JD, Stojanovski K, Vittinghoff E, et al. A mobile health strategy to support adherence to antiretroviral preexposure prophylaxis. AIDS Patient Care STDs. 2018;32(3):104–11. https://doi.org/10.1089/apc.2017.0255 .
Myers ND, Lee S, Bateman AG, et al. Accelerometer-based assessment of physical activity within the fun for wellness online behavioral intervention: protocol for a feasibility study. Pilot Feasibil Stud. 2019;5(1):73. https://doi.org/10.1186/s40814-019-0455-0 .
Gooding K, Phiri M, Peterson I, Parker M, Desmond N. Six dimensions of research trial acceptability: how much, what, when, in what circumstances, to whom and why? Soc Sci Med. 2018;213:190–8. https://doi.org/10.1016/j.socscimed.2018.07.040 .
Hoel S, Victory A, Sagorac Gruichich T, et al. A mixed-methods analysis of mobile ACT responses from two cohorts. Front Digit Health. 2022;4:869143. https://doi.org/10.3389/fdgth.2022.869143 .
Coughlin LN, Nahum-Shani I, Bonar EE, et al. Toward a just-in-time adaptive intervention to reduce emerging adult alcohol use: testing approaches for identifying when to intervene. Subst Use Misuse. 2021;56(14):2115–25. https://doi.org/10.1080/10826084.2021.1972314 .
Mande A, Moore SL, Banaei-Kashani F, Echalier B, Bull S, Rosenberg MA. Assessment of a mobile health iPhone app for semiautomated self-management of chronic recurrent medical conditions using an N-of-1 trial framework: feasibility pilot study. JMIR Form Res. 2022;6(4):e34827. https://doi.org/10.2196/34827 .
Dopp AR, Parisi KE, Munson SA, Lyon AR. A glossary of user-centered design strategies for implementation experts. Transl Behav Med. 2019;9(6):1057–64. https://doi.org/10.1093/tbm/iby119 .
Rose H, McKinley J, eds. The Routledge Handbook of Research Methods in Applied Linguistics. London: Routledge; 2020.
Lewis JR. The system usability scale: past, present, and future. Int J Human-Computer Interact. 2018;34(7):577–90. https://doi.org/10.1080/10447318.2018.1455307 .
Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2(3):197–207. https://doi.org/10.1016/0149-7189(79)90094-6 .
Sidani S, Epstein DR, Bootzin RR, Moritz P, Miranda J. Assessment of preferences for treatment: validation of a measure: PREFERENCE MEASURE. Res Nurs Health. 2009;32(4):419–31. https://doi.org/10.1002/nur.20329 .
An M, Dusing SC, Harbourne RT, Sheridan SM, START-Play Consortium. What really works in intervention? Using fidelity measures to support optimal outcomes. Phys Ther. 2020;100(5):757–65. https://doi.org/10.1093/ptj/pzaa006 .
Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol. 2008;41(3–4):327–50. https://doi.org/10.1007/s10464-008-9165-0 .
Rivard M, Mello C, Mestari Z, et al. Using prevent teach reinforce for young children to manage challenging behaviors in public specialized early intervention services for autism. J Autism Dev Disord. 2021;51(11):3970–88. https://doi.org/10.1007/s10803-020-04856-y .
Stagg HR, Abubakar I, Campbell CN, et al. IMPACT study on intervening with a manualised package to achieve treatment adherence in people with tuberculosis: protocol paper for a mixed-methods study, including a pilot randomised controlled trial. BMJ Open. 2019;9(12):e032760. https://doi.org/10.1136/bmjopen-2019-032760 .
Kilbride C, Scott DJM, Butcher T, et al. Rehabilitation via HOMe Based gaming exercise for the Upper-limb post Stroke (RHOMBUS): protocol of an intervention feasibility trial. BMJ Open. 2018;8(11):e026620. https://doi.org/10.1136/bmjopen-2018-026620 .
Dumas JE, Lynch AM, Laughlin JE, Phillips Smith E, Prinz RJ. Promoting intervention fidelity. Am J Prev Med. 2001;20(1):38–47. https://doi.org/10.1016/S0749-3797(00)00272-5 .
Walton H, Spector A, Roberts A, et al. Developing strategies to improve fidelity of delivery of, and engagement with, a complex intervention to improve independence in dementia: a mixed methods study. BMC Med Res Methodol. 2020;20(1):153. https://doi.org/10.1186/s12874-020-01006-x .
Nomikos PA, Hall M, Fuller A, et al. Fidelity assessment of nurse-led non-pharmacological package of care for knee pain in the package development phase of a feasibility randomised controlled trial based in secondary care: a mixed methods study. BMJ Open. 2021;11(7):e045242. https://doi.org/10.1136/bmjopen-2020-045242 .
Hall M, Fuller A, Nomikos PA, et al. East Midlands knee pain multiple randomised controlled trial cohort study: cohort establishment and feasibility study protocol. BMJ Open. 2020;10(9):e037760. https://doi.org/10.1136/bmjopen-2020-037760 .
Horne JC, Hooban KE, Lincoln NB, Logan PA. Regaining Confidence after Stroke (RCAS): a feasibility randomised controlled trial (RCT). Pilot Feasibil Stud. 2019;5(1):96. https://doi.org/10.1186/s40814-019-0480-z .
Porter KJ, Brock DJ, Estabrooks PA, et al. SIPsmartER delivered through rural, local health districts: adoption and implementation outcomes. BMC Public Health. 2019;19(1):1273. https://doi.org/10.1186/s12889-019-7567-6 .
Watson A, Timperio A, Brown H, Hesketh KD. Process evaluation of a classroom active break (ACTI-BREAK) program for improving academic-related and physical activity outcomes for students in years 3 and 4. BMC Public Health. 2019;19(1):633. https://doi.org/10.1186/s12889-019-6982-z .
Hind D, Drabble SJ, Arden MA, et al. Feasibility study for supporting medication adherence for adults with cystic fibrosis: mixed-methods process evaluation. BMJ Open. 2020;10(10):e039089. https://doi.org/10.1136/bmjopen-2020-039089 .
Tibbitts B, Porter A, Sebire SJ, et al. Action 3:30R: process evaluation of a cluster randomised feasibility study of a revised teaching assistant-led extracurricular physical activity intervention for 8 to 10 year olds. BMC Public Health. 2019;19(1):1111. https://doi.org/10.1186/s12889-019-7347-3 .
Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health Ment Health Serv Res. 2011;38(2):65–76. https://doi.org/10.1007/s10488-010-0319-7 .
Wijana MB, Feldman I, Ssegonja R, Enebrink P, Ghaderi A. A pilot study of the impact of an integrated individual- and family therapy model for self-harming adolescents on overall healthcare consumption. BMC Psychiatry. 2021;21(1):374. https://doi.org/10.1186/s12888-021-03375-z .
Roberts JL, Williams J, Griffith GM, et al. Soles of the feet meditation intervention for people with intellectual disability and problems with anger and aggression—a feasibility study. Mindfulness. 2020;11(10):2371–85. https://doi.org/10.1007/s12671-020-01454-y .
Fallin-Bennett A, Lofwall M, Waters T, et al. Behavioral and Enhanced Perinatal Intervention (B-EPIC): a randomized trial targeting tobacco use among opioid dependent pregnant women. Contemp Clin Trials Commun. 2020;20:100657. https://doi.org/10.1016/j.conctc.2020.100657 .
Krebs P, Sherman SE, Wilson H, et al. Text2Connect: a health system approach to engage tobacco users in quitline cessation services via text messaging. Transl Behav Med. 2020;10(1):292–301. https://doi.org/10.1093/tbm/ibz033 .
Bailey DP, Edwardson CL, Pappas Y, et al. A randomised-controlled feasibility study of the REgulate your SItting Time (RESIT) intervention for reducing sitting time in individuals with type 2 diabetes: study protocol. Pilot Feasibil Stud. 2021;7(1):76. https://doi.org/10.1186/s40814-021-00816-0 .
Karnon J, Qizilbash N. Economic evaluation alongsiden-of-1 trials: getting closer to the margin. Health Econ. 2001;10(1):79–82. https://doi.org/10.1002/1099-1050(200101)10:1%3c79::AID-HEC567%3e3.0.CO;2-Z .
Dichter MN, Berg A, Hylla J, et al. Evaluation of a multi-component, non-pharmacological intervention to prevent and reduce sleep disturbances in people with dementia living in nursing homes (MoNoPol-sleep): study protocol for a cluster-randomized exploratory trial. BMC Geriatr. 2021;21(1):40. https://doi.org/10.1186/s12877-020-01997-8 .
Williams J, Fairbairn E, McGrath R, et al. A feasibility hybrid II randomised controlled trial of volunteer ‘Health Champions’ supporting people with serious mental illness manage their physical health: study protocol. Pilot Feasibil Stud. 2021;7(1):116. https://doi.org/10.1186/s40814-021-00854-8 .
Teare MD, Dimairo M, Shephard N, Hayman A, Whitehead A, Walters SJ. Sample size requirements to estimate key design parameters from external pilot randomised controlled trials: a simulation study. Trials. 2014;15(1):264. https://doi.org/10.1186/1745-6215-15-264 .
Azariah S, Saxton P, Franklin R, Forster R, Werder S, Jenkins R. NZPrEP Demonstration Project: protocol for an open-label, single-arm trial of HIV pre-exposure prophylaxis (PrEP) to determine feasibility, acceptability, adverse and behavioural effects of PrEP provision to gay and bisexual men in publicly funded sexual health clinics in Auckland, New Zealand. BMJ Open. 2019;9(6):e026363. https://doi.org/10.1136/bmjopen-2018-026363 .
Dawkins L, Bauld L, Ford A, et al. A cluster feasibility trial to explore the uptake and use of e-cigarettes versus usual care offered to smokers attending homeless centres in Great Britain. Plos One. 2020;15(10):e0240968. https://doi.org/10.1371/journal.pone.0240968 . Leroyer C, ed.
Farragher JF, Thomas C, Ravani P, Manns B, Elliott MJ, Hemmelgarn BR. Protocol for a pilot randomised controlled trial of an educational programme for adults on chronic haemodialysis with fatigue (Fatigue-HD). BMJ Open. 2019;9(7):e030333. https://doi.org/10.1136/bmjopen-2019-030333 .
Shani P, Raeesi K, Walter E, et al. Qigong mind-body program for caregivers of cancer patients: design of a pilot three-arm randomized clinical trial. Pilot Feasibil Stud. 2021;7(1):73. https://doi.org/10.1186/s40814-021-00793-4 .
Croke A, Moriarty F, Boland F, et al. Integrating clinical pharmacists within general practice: protocol for a pilot cluster randomised controlled trial. BMJ Open. 2021;11(3):e041541. https://doi.org/10.1136/bmjopen-2020-041541 .
Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45(5):626–9. https://doi.org/10.1016/j.jpsychires.2010.10.008 .
American Psychological Association. Preregistration .; 2021. https://www.apa.org/pubs/journals/resources/preregistration . Accessed 12 July, 2023
National Library of Medicine. Clinical trials. Published online 2023. https://clinicaltrials.gov/ . Accessed 12 July, 2023
Center for Open Science. Open Science Framework. Published online 2023. https://osf.io/ . Accessed 12 July, 2023
Foster ED, Deardorff A. Open Science Framework (OSF). J Med Libr Assoc. 2017;105(2):203. https://doi.org/10.5195/jmla.2017.88 .
Article PubMed Central Google Scholar
Murphy ME, McSharry J, Byrne M, et al. Supporting care for suboptimally controlled type 2 diabetes mellitus in general practice with a clinical decision support system: a mixed methods pilot cluster randomised trial. BMJ Open. 2020;10(2):e032594. https://doi.org/10.1136/bmjopen-2019-032594 .
Torres S, Sales CMD, Guerra MP, Simões MP, Pinto M, Vieira FM. Emotion-focused cognitive behavioral therapy in comorbid obesity with binge eating disorder: a pilot study of feasibility and long-term outcomes. Front Psychol. 2020;11:343. https://doi.org/10.3389/fpsyg.2020.00343 .
Ritchwood TD, Massa C, Kamanga G, Pettifor A, Hoffman I, Corneli A. Understanding of perceived infectiousness and its influence on sexual behavior among individuals with acute HIV infection in Lilongwe, Malawi (HPTN 062). AIDS Educ Prev. 2020;32(3):260–70. https://doi.org/10.1521/aeap.2020.32.3.260 .
Eaton AD, Chan Carusone S, Craig SL, et al. The ART of conversation: feasibility and acceptability of a pilot peer intervention to help transition complex HIV-positive people from hospital to community. BMJ Open. 2019;9(3):e026674. https://doi.org/10.1136/bmjopen-2018-026674 .
Holliday R, Preshaw PM, Ryan V, et al. A feasibility study with embedded pilot randomised controlled trial and process evaluation of electronic cigarettes for smoking cessation in patients with periodontitis. Pilot Feasibil Stud. 2019;5(1):74. https://doi.org/10.1186/s40814-019-0451-4 .
Wilchesky M, Mueller G, Morin M, et al. The OptimaMed intervention to reduce inappropriate medications in nursing home residents with severe dementia: results from a quasi-experimental feasibility pilot study. BMC Geriatr. 2018;18(1):204. https://doi.org/10.1186/s12877-018-0895-z .
Garcia DO, Valdez LA, Bell ML, et al. A gender- and culturally-sensitive weight loss intervention for Hispanic males: the ANIMO randomized controlled trial pilot study protocol and recruitment methods. Contemp Clin Trials Commun. 2018;9:151–63. https://doi.org/10.1016/j.conctc.2018.01.010 .
Johannessen T, Ree E, Strømme T, Aase I, Bal R, Wiig S. Designing and pilot testing of a leadership intervention to improve quality and safety in nursing homes and home care (the SAFE-LEAD intervention). BMJ Open. 2019;9(6):e027790. https://doi.org/10.1136/bmjopen-2018-027790 .
Deady M, Johnston D, Milne D, et al. Preliminary effectiveness of a smartphone app to reduce depressive symptoms in the workplace: feasibility and acceptability study. JMIR MHealth UHealth. 2018;6(12):e11661. https://doi.org/10.2196/11661 .
Juszczyk D, Gillison F. Juicy June: a mass-participation snack-swap challenge—results from a mixed methods feasibility study. Pilot Feasibil Stud. 2018;4(1):119. https://doi.org/10.1186/s40814-018-0310-8 .
Beasley JM, Kirshner L, Wylie-Rosett J, Sevick MA, DeLuca L, Chodosh J. BRInging the Diabetes prevention program to GEriatric populations (BRIDGE): a feasibility study. Pilot Feasibil Stud. 2019;5(1):129. https://doi.org/10.1186/s40814-019-0513-7 .
Prochilo GA, Costa RJS, Hassed C, Chambers R, Molenberghs P. A 16-week aerobic exercise and mindfulness-based intervention on chronic psychosocial stress: a pilot and feasibility study. Pilot Feasibil Stud. 2021;7(1):64. https://doi.org/10.1186/s40814-020-00751-6 .
Enhancing the QUAlity and Transparency Of health Research (EQUATOR) Network. https://www.equator-network.org/ . Accessed 22 Aug, 2023
National Institute of Diabetes and Digestive and Kidney Diseases. U34: Implementation Planning Cooperative Agreement .; 2023. https://www.niddk.nih.gov/research-funding/process/apply/funding-mechanisms/u34-multi-center-clinical-studies . Accessed 13 July, 2023
NIH Central Resource for Grants and Funding Information. Grants & Funding: P20 .; 2023. https://grants.nih.gov/grants/funding/ac_search_results.htm?text_curr=p20 . Accessed 13 July, 2023
UK Research and Innovation. Funding for Biomedical Research and Innovation .; 2022. https://www.ukri.org/what-we-do/developing-people-and-skills/mrc/funding-for-biomedical-research-and-innovation/pilot-projects-and-small-grants/ . Accessed 13 July, 2023
Canadian Institutes of Health Research. Health Research Training Platform Pilot .; 2022. https://cihr-irsc.gc.ca/e/52278.html . Accessed 13, 2023
National Health and Medical Research Council. Research Translation .; 2023. Accessed July 13, 2023. https://www.nhmrc.gov.au/research-policy/research-translation-and-impact
National Institute of Environmental Health Sciences. Translational Research Framework .; 2019. https://www.niehs.nih.gov/research/programs/translational/framework-details/index.cfm . Accessed 13 July, 2023
Wichman C, Smith LM, Yu F. A framework for clinical and translational research in the era of rigor and reproducibility. J Clin Transl Sci. 2021;5(1):e31. https://doi.org/10.1017/cts.2020.523 .
Lee EC, Whitehead AL, Jacques RM, Julious SA. The statistical interpretation of pilot trials: should significance thresholds be reconsidered? BMC Med Res Methodol. 2014;14(1):41. https://doi.org/10.1186/1471-2288-14-41 .
Sim J. Should treatment effects be estimated in pilot and feasibility studies? Pilot Feasibil Stud. 2019;5(1):107. https://doi.org/10.1186/s40814-019-0493-7 .
Teresi JA, Yu X, Stewart AL, Hays RD. Guidelines for designing and evaluating feasibility pilot studies. Med Care. 2022;60(1):95–103. https://doi.org/10.1097/MLR.0000000000001664 .
Moore CG, Carter RE, Nietert PJ, Stewart PW. Recommendations for planning pilot studies in clinical and translational research. Clin Transl Sci. 2011;4(5):332–7. https://doi.org/10.1111/j.1752-8062.2011.00347.x .
Beets MW, Pfledderer C, Von Klinggraeff L, Burkart S, Armstrong B. Fund behavioral science like the frameworks we endorse: the case for increased funding of preliminary studies by the National Institutes of Health. Pilot Feasibil Stud. 2022;8(1):218. https://doi.org/10.1186/s40814-022-01179-w .
Download references
Acknowledgements
The authors would like to thank all experts who provided valuable input through the Delphi process of this study.
Research reported in this abstract was supported by The National Heart, Lung, and Blood Institute of the National Institutes of Health under award number R01HL149141 (Beets), F31HL158016 (von Klinggraeff), and F32HL154530 (Burkart) as well as by the Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under award number P20GM130420 for the Research Center for Child Well-Being. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and affiliations.
Department of Health Promotion and Behavioral Sciences, The University of Texas Health Science Center at Houston, School of Public Health in Austin, Austin, TX, 78701, USA
Christopher D. Pfledderer
Michael and Susan Dell Center for Healthy Living, The University of Texas Health Science Center at Houston, School of Public Health in Austin, Austin, TX, 78701, USA
Arnold School of Public Health, University of South Carolina, Columbia, SC, 29205, USA
Lauren von Klinggraeff, Sarah Burkart, Alexsandra da Silva Bandeira, James F. Thrasher, Xiaoming Li & Michael W. Beets
College of Human and Social Futures, The University of Newcastle Australia, Callaghan, NSW, 2308, Australia
David R. Lubans
Bristol Medical School, Population Health Sciences, University of Bristol, Bristol, BS8 1QU, UK
Russell Jago
Faculty of Arts, Social Sciences and Humanities, School of Health and Society, University of Wollongong, Wollongong, NSW, 2522, Australia
Anthony D. Okely
MRC Epidemiology Unit, University of Cambridge, Cambridge, CB2 0QQ, UK
Esther M. F. van Sluijs
Department of Medicine, Stanford University, Stanford, CA, USA
John P. A. Ioannidis
Department of Epidemiology and Population Health, Stanford University, Stanford, CA, USA
Department of Biomedical Data Science, Stanford University, Stanford, CA, USA
Department of Statistics, Stanford University, Stanford, CA, USA
Meta-Research Innovation Center at Stanford (METRICS), Stanford University, Stanford, CA, USA
You can also search for this author in PubMed Google Scholar
Contributions
CDP - Conceptualization; methodology; software; formal analysis; investigation; data curation; writing—original draft; writing—review and editing; visualization; and supervision. LV—Methodology; investigation; data curation; writing—original draft; writing—review and editing; and formal analysis. SB—Methodology; investigation; data curation; writing—original draft; writing—review and editing; and formal analysis. AB—Methodology; writing—original draft; writing—review and editing; and formal analysis. DL—Writing—original draft and writing—review and editing. RJ—Writing—original draft and writing—review and editing. AO—Writing—original draft and writing—review and editing. ES—Writing—original draft and writing—review and editing. JPA—Writing—original draft; writing—review and editing; and formal analysis. JT—Writing—original draft and writing—review and editing. XL—Writing—original draft and writing—review and editing. MWB—Conceptualization; methodology; software; formal analysis; investigation; data curation; writing—original draft; writing—review and editing; visualization; supervision; and funding acquisition. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Christopher D. Pfledderer .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was granted by the University of South Carolina’s Institutional Review Board (IRB # Pro00120890) prior to the start of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Literature crosswalk.
Additional file 2.
Summary table of considerations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pfledderer, C.D., von Klinggraeff, L., Burkart, S. et al. Consolidated guidance for behavioral intervention pilot and feasibility studies. Pilot Feasibility Stud 10 , 57 (2024). https://doi.org/10.1186/s40814-024-01485-5
Download citation
Received : 20 September 2023
Accepted : 26 March 2024
Published : 06 April 2024
DOI : https://doi.org/10.1186/s40814-024-01485-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Pilot and Feasibility Studies
ISSN: 2055-5784
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Examples of literature reviews. Step 1 - Search for relevant literature. Step 2 - Evaluate and select sources. Step 3 - Identify themes, debates, and gaps. Step 4 - Outline your literature review's structure. Step 5 - Write your literature review.
A literature review is a document or section of a document that collects key sources on a topic and discusses those sources in conversation with each other (also called synthesis ). The lit review is an important genre in many disciplines, not just literature (i.e., the study of works of literature such as novels and plays).
Okay - with the why out the way, let's move on to the how. As mentioned above, writing your literature review is a process, which I'll break down into three steps: Finding the most suitable literature. Understanding, distilling and organising the literature. Planning and writing up your literature review chapter.
The literature review template includes the following sections: Before you start - essential groundwork to ensure you're ready. The introduction section. The core/body section. The conclusion /summary. Extra free resources. Each section is explained in plain, straightforward language, followed by an overview of the key elements that you ...
Option 1: Chronological (according to date) Organising the literature chronologically is one of the simplest ways to structure your literature review. You start with what was published first and work your way through the literature until you reach the work published most recently. Pretty straightforward.
A literature review is a critical analysis and synthesis of existing research on a particular topic. It provides an overview of the current state of knowledge, identifies gaps, and highlights key findings in the literature. 1 The purpose of a literature review is to situate your own research within the context of existing scholarship ...
A literature review is a survey of scholarly sources on a specific topic. It provides an overview of current knowledge, allowing you to identify relevant theories, methods, and gaps in the existing research. There are five key steps to writing a literature review: Search for relevant literature. Evaluate sources. Identify themes, debates and gaps.
A literature review is much more than just another section in your research paper. It forms the very foundation of your research. It is a formal piece of writing where you analyze the existing theoretical framework, principles, and assumptions and use that as a base to shape your approach to the research question.
A literature review discusses published information in a particular subject area, and sometimes information in a particular subject area within a certain time period. A literature review can be just a simple summary of the sources, but it usually has an organizational pattern and combines both summary and synthesis.
Example: Predictors and Outcomes of U.S. Quality Maternity Leave: A Review and Conceptual Framework: 10.1177/08948453211037398 ; Systematic review: "The authors of a systematic review use a specific procedure to search the research literature, select the studies to include in their review, and critically evaluate the studies they find." (p. 139).
Literature reviews are in great demand in most scientific fields. Their need stems from the ever-increasing output of scientific publications .For example, compared to 1991, in 2008 three, eight, and forty times more papers were indexed in Web of Science on malaria, obesity, and biodiversity, respectively .Given such mountains of papers, scientists cannot be expected to examine in detail every ...
A literature or narrative review is a comprehensive review and analysis of the published literature on a specific topic or research question. The literature that is reviewed contains: books, articles, academic articles, conference proceedings, association papers, and dissertations. It contains the most pertinent studies and points to important ...
A literature review may consist of simply a summary of key sources, but in the social sciences, a literature review usually has an organizational pattern and combines both summary and synthesis, often within specific conceptual categories.A summary is a recap of the important information of the source, but a synthesis is a re-organization, or a reshuffling, of that information in a way that ...
A literature review is an integrated analysis-- not just a summary-- of scholarly writings and other relevant evidence related directly to your research question.That is, it represents a synthesis of the evidence that provides background information on your topic and shows a association between the evidence and your research question.
A literary review template is a type of written work that discusses published information about a specific subject matter. The length of the review doesn't matter. It can be as simple as a summary of sources or can be as long as several pages. An outline for literature review can also evaluate these sources and advise to the readers regarding ...
Here is a literature review outline example on the subject of the Ebola virus to help you get it right: Introduction; Introduce the general topic. Provide background information on the Ebola virus: genome, pathogenesis, transmission, epidemiology, treatment, etc. ... The data was extracted using a standardized form. Expected outcomes; Overall ...
Steps for Conducting a Lit Review; Finding "The Literature" Organizing/Writing; APA Style This link opens in a new window; Chicago: Notes Bibliography This link opens in a new window; MLA Style This link opens in a new window; Sample Literature Reviews. Sample Lit Reviews from Communication Arts; Have an exemplary literature review? Get Help!
These sections serve to establish a scholarly basis for the research or discussion within the paper. In a standard 8000-word journal article, the literature review section typically spans between 750 and 1250 words. The first few sentences or the first paragraph within this section often serve as an introduction.
A literature review is an overview of the available research for a specific scientific topic. Literature reviews summarize existing research to answer a review question, provide context for new research, or identify important gaps in the existing body of literature.. An incredible amount of academic literature is published each year, by estimates over two million articles.
If you're working on a dissertation or thesis and are looking for an example of a strong literature review chapter, you've come to the right place.. In this video, we walk you through an A-grade literature review from a dissertation that earned full distinction.We start off by discussing the five core sections of a literature review chapter by unpacking our free literature review template.
Literature reviews can take two major forms. The most prevalent one is the "literature review" or "background" section within a journal paper or a chapter in a graduate thesis. This section synthesizes the extant literature and usually identifies the gaps in knowledge that the empirical study addresses (Sylvester, Tate, & Johnstone, 2013).
Literature reviews offer a critical synthesis of empirical and theoretical literature to assess the strength of evidence, develop guidelines for practice and policymaking, and identify areas for future research.1 It is often essential and usually the first task in any research endeavour, particularly in masters or doctoral level education. For effective data extraction and rigorous synthesis ...
Step 4: Write. Be selective. Highlight only the most important and relevant points from a source in your review. Use quotes sparingly. Short quotes can help to emphasize a point, but thorough analysis of language from each source is generally unnecessary in a literature review. Synthesize your sources.
We will focus on the importance of ensuring your literature review is both evaluative and critical. You will be given some samples of writing and be required to identify the typical conventions for paragraph structure, tense usage, and signposting language. Please complete the form below to request a place on the session running
Accordingly, this systematic review of literature was undertaken to identify key approaches from international experiences to enhance access to PHC services in rural communities. All published and unpublished qualitative and/or mixed method studies conducted to improvement access to PHC services were searched from MEDLINE, Scopus, Web of ...
The current rapid review aimed to summarise the literature and identify gaps in knowledge relating to any psychiatric and medical comorbidities of eating disorders. This paper forms part of a rapid review) series scoping the evidence base for the field of EDs, conducted to inform the Australian National Eating Disorders Research and Translation ...
The word "literature review" can refer to two related things that are part of the broader literature review process. The first is the task of reviewing the literature - i.e. sourcing and reading through the existing research relating to your research topic. The second is the actual chapter that you write up in your dissertation, thesis or ...
The systematic review, reported following PRISMA guidelines, was conducted using the Joanna Briggs Institute method. Eligible studies, in the form of cohort studies, case-control studies, or cross-sectional studies, targeted adolescents aged 10 to 24, with or without a history of curable STIs; the outcome was subsequent condom use.
In the behavioral sciences, conducting pilot and/or feasibility studies (PFS) is a key step that provides essential information used to inform the design, conduct, and implementation of a larger-scale trial. There are more than 160 published guidelines, reporting checklists, frameworks, and recommendations related to PFS. All of these publications offer some form of guidance on PFS, but many ...
Creative territories are geographic spaces of collaboration between different social actors, driving innovations and requiring regulatory mechanisms for sustainability and growth. This paper aims to synthesize available evidence on creative territories through a systematic literature review to analyze the significant actors in creative territories, the type of partnerships between them, the ...