An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Acta Biomed
- v.93(3); 2022


Factors associated with eating disorders in adolescents: a systematic review
Candy laurine suarez-albor.
1 Faculty of Nursing, Universidad Popular del Cesar, Valledupar, Colombia
Maura Galletta
2 Department of Medical Sciences and Public Health, University of Cagliari, Monserrato, Italy
Edna Margarita Gómez-Bustamante
3 Faculty of Nursing, University of Cartagena, Cartagena de Indias, Colombia
Background and aim:
The World Health Organization has placed eating disorders among the priority mental illnesses for children and adolescents given the risk they imply for their health. Recognizing the risk factors associated with this problem can serve as the basis for the design of timely and effective interventions. The objective of the study was to identify the factors associated with eating behavior in adolescents through a systematic review.
Systematic review. Search of the literature in the bibliographic sources CINAHL, CUIDEN, Pubmed, Dialnet, SCIELO and Science Direct. The search was conducted in October and November 2020. The search terms were Eating Disorders, Food Intake, and Adolescents. The evaluation of the methodological quality was carried out using a specific guide for observational epidemiological studies. A narrative synthesis of the findings was made. Additionally, the vote counting and sign test technique was applied.
25 studies were selected. The associated factors were body dissatisfaction, female gender, depression, low self-esteem, higher BMI that increases the risk of eating disorders.
Conclusions:
a high impact of psychological factors was observed. These should be considered in the design of effective interventions to prevent this disease, although the search needs to be broadened to identify larger and more complex studies that allow for a more comprehensive review. ( www.actabiomedica.it )
Introduction
Eating disorders (EDs) are complex and multifactorial pathologies that affect physical and mental health and are life threatening. They are characterized by an excessive preoccupation with the weight and shape of the body or a frank deviation of the body image, accompanied by voluntary restriction of the intake or the presence of episodes of binge eating that cause great suffering, impairment of health and quality of life ( 1 ). The prevalence of eating disorders is variable; in the last two decades several studies have been carried out, especially by the National Institute of Mental Health of the United States, which has compiled cases even from European countries. The countries with the highest cases are Switzerland 12%, Chile 8.3% and Spain 6.2% ( 2 ); Colombia is followed by 4.5% ( 3 ), the United Kingdom 3.7% ( 2 ) and Portugal 3.06% ( 2 ). Countries such as the United States, Italy, Costa Rica, Mexico, Honduras, Venezuela, have numbers between 0.5% -1.5% ( 4 , 5 ). Most of these disorders are more common in women and begin in adolescence, a stage of change where body image is consolidated. This in turn generates numerous crises of identity, physical appearance, friendly or sexual requirements and a struggle for autonomy, traits of perfectionism and self-demand that can lead to low self-esteem, dependence on the environment, difficulty in expressing emotions or expressing aggressiveness ( 6 , 7 ).
The World Health Organization (WHO) has placed eating disorders among the priority mental illnesses for children and adolescents given the risk they imply for their health and the great psychiatric comorbidity ( 8 ). Among the most frequent, depressive disorders 23.3%, anxiety disorders 10%, adaptive disorders 3.3% and negative perception of family relationships 43.3%, which aggravate the problem and cause important complications in the state of health ( 7 , 9 ). For this reason, EDs have become more relevant for the interest in the clinic, research and epidemiology ( 9 ). Various factors intervene in the occurrence of eating disorders and show a higher attributable risk such as biological, psychological, family and sociocultural ( 2 - 7 ). Thus, scientific evidence is abundant when addressing various aspects of eating disorders, however the state of the art revealed that in the last five years no literature review have been published on the subject, which is relevant to design or guide effective interventions that allow professionals to prevent these events. In this sense, the aim of this work was to carry out an exhaustive review of the published evidence about the factors associated with eating behaviour in adolescents.
A systematic review was carried out according to the guidelines of the PRISMA ( 10 ) statement, in the bibliographic sources LILACS, CUIDEN, Pubmed, Dialnet, SCIELO and Science Direct and MEDES. The search was carried out in October and November 2020. The search terms to be used were consulted in the DECS and MESH libraries, to guarantee their standardization, in English and Spanish, they were conjugated in search equations with the Boolean operators AND and OR thus: AND factors (Eating Disorders OR Food Intake OR Eating Behavior) AND adolescent.
Inclusion and exclusion criteria
Articles were selected from cohort, cross-sectional, and case control studies about factors associated with EDs in adolescents. The inclusion criteria were (a) free access articles in full text, (b) primary studies published between 2009 and 2020 to ensure that as many necessary and relevant studies as possible have been included in the review, (c) studies with a sample of adolescents aged from 10 to 19 years, according to the classification provided by the WHO ( 9 ). Dissertation, meta-analysis, review, experimental, intervention, or treatment studies were excluded, as well as studies with a mixed sample (children, adolescents, adults), and investigations without statistical information of association.
Article selection and evaluation of methodological quality
The selection of the articles was carried out in 4 phases. First, title and abstract were read to determine the suitability of the study and elimination of duplicates. Second, full text was read and the inclusion and exclusion criteria were applied. Third, a reverse and forward search was performed on the included studies to locate as many documents as possible. Fourth, the risk of bias was assessed through critical reading based on the Critical Reading Guide for Observational Studies in Epidemiology ( 11 , 12 ). A guide to assess cross-sectional studies was used ( 11 ). This instrument included 31 items that allow for minimizing biases and the confounding effect of internal validity. It was evaluated qualitatively using MB: very good, B: good, A: regular, and NI: does not report. A second guide was used to assess cohort studies and case-control studies ( 12 ). The instrument included 21 items and evaluated qualitatively the followings aspects: selection of subjects, validation of question, evaluation of the final outcomes, confounding factors, statistical analysis, general evaluation of the study, and description of the study, using A: adequately, B: partially, C: improperly, and D: I don’t know. This process was carried out by the first author and was audited by the other authors.
Data extraction
The data were consolidated through a structured booklet in Excel based on two types of information: (i) information about articles’ characteristics such as study sample, main author, year of publication, language, country, design; (ii) information about eating disorder risk factors such as biological, psychological, sociocultural, and family factors.
Data analysis
The information was treated qualitatively and analysed in a narrative way. The results were organized in tables and figures according to the PRISMA statement. Additionally, the found results exceeded the number of 20 articles, so the vote counting technique was applied. Such a technique consisted in granting a positive vote for studies with a statistically significant relationship between a risk factor and EDs, and a negative vote when there was no significant association. Subsequently, the sign test ( 13 , 14 ) was applied to determine if the difference in the number of positive studies was significantly greater than the opposite result. A significance value was established to be less than 0.05. It is important to notice that these techniques are limited but they can help to guide the results of the review in the absence of meta-analysis ( 14 ).

General diagram of the study
Methodological quality assessment
About the cross-sectional studies, 54.5% (n = 12) obtained high methodological quality, 27.2% (n = 7) medium quality, and 4.6% (n = 1) low methodological quality. This study was excluded by the revision. With regard to the cohort studies, it was assumed that studies with adequate rating in 23-26 items were considered to be of high methodological level; medium level was attributed to studies with adequate rating in 19-22 items, and low methodological level was attributed to studies with adequate rating in 18 items or less. In this sense, 100% (n = 3) of the cohort studies obtained a medium methodological quality ( Tab. 1 and Tab. 2 ).
Critical reading and assessment of methodological quality for cross-sectional studies.
Note . Internal validity. It defines whether the study design allows minimizing biases and the confounding effect ( 12 ).
The Items used were:
2. The inclusion and exclusion criteria of participants are indicated, as well as the sources and selection methods.
3. The selection criteria are adequate to answer the question or the objective of the study.
4. The study population, defined by the selection criteria, contains an adequate spectrum of the population of interest.
5. An estimate was made of the size, the level of confidence or the statistical power of the sample to estimate the measures of frequency or association that the study intended to obtain.
6. The number of potentially eligible people is reported, those initially selected, those who accept and those who finally participate or respond; fifteen. Statistical analysis was determined from the beginning of the study.
16. The statistical tests used are specified and appropriate
17. Participant losses, lost data or others were correctly treated
18. The main possible confounding elements were taken into account in the design and in the analysis.
Assessment: MB=very good; B=good; R=regular; NA=not applicable; NI=no information.
Critical reading and assessment of methodological quality for cohort studies.
Note . Cohort studies allow a direct determination of relative risk and allow calculation of the interval between exposure or risk factor and overall study disease ( 12 ). It was scored according to the validity of the question, selection of subjects, evaluation, confounding factors, statistical analysis, general assessment and description of the study. Rating: according to the author, the items were rated as follows: A: adequately; B: partially; C: improperly; D: I don’t know. For the purposes of this review, it was assumed that studies with adequate rating in 23-26 items were considered to be of high methodological level; medium level was attributed to studies with adequate rating in 19-22 items, and low methodological level was attributed to studies with adequate rating in 18 items or less.
Characteristics of the studies
Among the selected studies, 86.4% (n = 19) were cross-sectional design (15─33), 13.6% (n = 3) were cohort studies (34─36). Fifty-percent (n = 11) of the studies were conducted in Latin America (18, 20─22, 24─27, 31─33), 31.8% (n = 7) in Europe (15, 19, 23, 29, 30, 33, 34), 9% (n = 2) in Asia ( 16 , 34 ) 4.6% (n = 1) in Africa ( 17 ), and 4,6% (n = 1) in North America ( 28 ) ( Tab. 3 ).
Synthesis of the studies included in the review.
Factors associated with eating disorders
Different instruments were used to measure the factors associated with eating disorders. In 14.2% (n = 7) of the analysed studies, authors used the Eating Attitude Test (EAT-26) ( 17 , 18 , 20 , 21 , 25 , 30 , 31 ), 11% (n = 5) the Body Shape Questionnaire (BSQ) ( 21 , 25 , 27 , 29 , 31 ), and 9.5% (n = 4) the Sociocultural Attitudes Questionnaire towards appearance-3 (SATAQ-3) ( 20 , 28 , 32 , 36 ). About 93% (n = 14) of the studies analysed risk factors and about 7% (n = 1) analysed correct self-image and hours of practiced sport as protective factors (B = 0.11; p = 0.047) ( 30 ). Regarding the risk factors, psychological risks were the most frequently analysed by the studies (71%). They included dissatisfaction with body image, low self-esteem, high depression, high perfectionism, stress, impulsivity, personal and interpersonal insecurity, emotional dysregulation, and ineffectiveness. About 14% of the studies analysed sociocultural factors such as alcohol use-related problematics, internalization of the thinness ideal, influence of media, ridicule related to weight, and being an immigrant adolescent. Also, 7.1% of the studies analysed family factors such as authoritarian family style, family functioning, poor communication, and family care. Lastly, 7.1% of the studies analysed biological factors such as being female. The complete description of the factors is summarized in Tab. 3 .
Analysis of vote counting and sign test
It was found that there was a greater number of studies that reported statistically significant relationships between factors such as body dissatisfaction, female gender, depression, low self-esteem, and higher body mass index (BMI) with eating disorders ( Tab. 4 ). In this sense, adolescents with those risk factors are more likely developing eating disorders.
Analysis by vote counting and sign test.
In the present review, the results show that the main factors associated with eating disorders were psychological-type with a prevalence of the factor inherent the dissatisfaction with body image ( 16 ─ 18 , 21 , 25 , 27 , 29 , 31 , 32 , 35 ). Literature refers that dissatisfaction with body image increases significantly in adolescence due to environmental pressures like media (e.g., television, social networks, virtual and written press) ( 20 , 28 ). They represent channels of transmission of the current body aesthetic model and have a positive or negative impact on an adolescent’s body image. This is more common in women, as it was the biological factor reported in this review. However, the findings are consistent with other studies where dissatisfaction with body image occurs more frequently in females and is positively associated with BMI as a predictor of eating disorders. ( 37 , 38 ). Similarly, BMI appears directly related to dissatisfaction with one’s own body, namely the higher the BMI, the higher the body dissatisfaction ( 25 , 31 ─ 33 , 36 ). This association is more recurrent in female gender ( 17 , 22 , 26 , 28 , 30 ) as girls generally show greater instability of self-image, lower self-esteem and general dissatisfaction with their body, if compared to boys. In most studies, the sample studied was female ( 29 , 33 , 34 , 36 ). Other psychological factors were emerged from the review. They were: appearance orientation ( 28 ), high level of perfectionism ( 23 , 29 ), low self-esteem ( 18 , 29 , 33 , 34 , 36 ), impulsivity ( 22 ), stress, suicidal idea and depression ( 22 , 26 , 27 , 29 , 34 ), eat in the absence of hunger ( 28 ), concern about being overweight, submission ( 24 ), personal and interpersonal insecurity ( 29 , 36 ), and emotional dysregulation ( 33 ). A teenager with low self-esteem shows a negative attitude and evaluation towards himself. In fact, low self-esteem has been repeatedly considered as a relevant factor of vulnerability for the development of EDs. This evidence is supported by a previous review ( 39 ). It is also important to identify depressive and anxiety manifestations that have an impact on food restriction and concerns about figure and weight. The number of studies that supported the relationship between psychological factors and eating disorders was statistically significant according to the sign test.
Socio-cultural factors were analysed in 14.2% of the selected studies ( 15 , 16 , 20 , 24 , 26 , 32 , 36 ). The most frequently revealed were the internalization of the thin ideal followed by the influence of media, weight-related bullying , and immigrant adolescents. These sociocultural factors and the desire to conform to body aesthetic models promoted by media and advertising have a greater likelihood to developing perceptions of body dissatisfaction. Moreno ( 40 ) showed a very high relationship between the influence of the media and the presence of eating disorders in the adolescent population. This is a cultural problem that comes from long ago where the idea that a perfect body is thin and that this it is accepted by society. The media are very important agents in the transmission of messages about the desire for thinness that is constantly present in eating disorders; the media channel social pressure to be thin is obviously stronger on females than males ( 40 ).
A few studies analysed the relationship between family factors and eating disorders ( 19 , 21 , 34 ). However, family functioning, poor communication, family care, and authoritarian styles are factors described in the literature as predisposing to eating disorders by impacting the way adolescents worry about the amount of calories in food and obsessed with food and weight gain. In this sense, parents can play a protective role, but they can also represent a risk factor for their children’s eating behaviour, as adolescents regulate their behaviour according to their parental model from early childhood ( 40 , 41 ).
In this review, we found only one research that addressed protective factors related to physical exercise and correct ideas about body image. This could be due to the fact that research in the last two decades has focused on mitigating or controlling risk factors as the sole basis for interventions to prevent eating disorders in adolescents. However, protective factors make adolescents less vulnerable to the development of eating disorders and facilitate the achievement of physical and mental health, the quality of life of adolescents, the development of healthy habits and social welfare. Protective factors are susceptible to being modified and intensified and do not necessarily occur spontaneously or at random. In this sense, interventions focused on strengthening those factors could be effective to prevent eating disorders behaviours. This requires the development of research that identifies and analyses the protective factors that can be strengthened in adolescents ( 42 ─ 44 ).
Most of the studies included in this systematic review are cross-sectional and in a lower percentage are cohort studies. Spain is the country that has done the most research on the factors associated with eating disorders in adolescents, thus showing a particular interest in this topic. However, this review has shown that there is a plurality of studies in the scientific community from different sociocultural contexts. This can explain why there is variability of risk factors for eating behaviour, although body dissatisfaction is the most common factor emerged from the revision.
The limitations of the review reflect the heterogeneity of the study that does not allow to carry out a meta-analysis and statistic associations between factors. Although the vote count and the sign test allow giving an additional value to the narrative synthesis of the results, they are limited procedures to establish reliable statistical associations with data. In this sense, reviews around the subject with quantitative analysis procedures would be necessary.
Conclusions
Psychological factors were found to be the main risk factors directly related to eating disorders in adolescents. The most common were: dissatisfaction with body image, depression, low self-esteem and higher BMI. Being a woman was also identified as the most reported biological factor associated with eating disorders. These risk factors become relevant when guiding the creation of mental health promotion programs for adolescents and the prevention and early detection of the eating disorders in adolescents.
Conflict of Interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
- National Institute of Mental Health. Eating disorders: A problem that goes beyond food. 2018 [ Google Scholar ]
- Sánchez A. Prevalence of eating disorders in six European countries. Metas Enferm. 2017 Jun; 20 (5):66–73. Spanish. https://doi.org/10.35667/MetasEnf.2019.20.1003081094. [ Google Scholar ]
- Fajardo E, Méndez C, Jauregui A. Prevalence of risk of eating disorders in a population of secondary school students, Bogotá Colombia. Revista Med. 2017; 25 (1):46–57. Spanish. https://doi.org/10.18359/rmed.2917. [ Google Scholar ]
- Smink F, Daphne V, Hans H. Epidemiology of Eating Disorders; Incidence, prevalence and Mortality Rates. Curr Psychiatry Rep. 2012; 14 :406–14. doi: 10.1007 / s11920-012-0282-y. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Benjet C, Borges G, Medina M, et al. In: The Mental Health Survey in Adolescents in Mexico. Epidemiology of mental disorders in Latin America and the Caribbean. Rodríguez J, Kohn R, Aguilar S, editors. Washington: Pan American Health Organization; 2009. pp. 107–14. [ Google Scholar ]
- Ortiz Cuquejo LM, Aguiar C, Samudio Domínguez GC, et al. Eating disorders in adolescents: a growing pathology? Pediatr (Asunción) 2017 Apr; 44 (1):37–42. Spanish. https://doi.org/10.18004/ped.2017.abril.37-42. [ Google Scholar ]
- Gaete P V, López C C. Eating disorders in adolescents. A comprehensive approach. Rev Chil Pediatr. 2020 Oct; 91 (5):784–93. Spanish. doi: 10.32641/rchped.vi91i5.1534. PMID: 33399645. [ PubMed ] [ Google Scholar ]
- World Health Organization. Mental health in adolescents. 2020 [ Google Scholar ]
- World Health Organization. World Report on Adolescent Development. 2019 [ Google Scholar ]
- Urrutia G, Bonfill X. PRISMA statement: a proposal to improve the publication for systematic reviews and meta-analyzes: Rev. Medicina Clínica. 2010; 1 :507–511. [ PubMed ] [ Google Scholar ]
- Ciapponi A. Guide to critical reading of observational studies in epidemiology (first part)] Evid Actual Práct Ambul. 2010 Oct-Dec; 13 (1):135–40. Spanish. [ Google Scholar ]
- Ciapponi A. Critical reading guide of observational studies in epidemiology (second part) Evid Actual Práct Ambul. 2011 Mar; 14 :7–14. Spanish. [ Google Scholar ]
- Pino R, Frías A, Palomino P. The quantitative systematic review in nursing. RIDEC. 2014 Jan; 7 :24–40. Spanish. [ Google Scholar ]
- Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration. 2011 [ Google Scholar ]
- Esteban L, Veiga O, Gómez S, et al. Length of residence and risk of eating disorders in immigrant adolescents living in madrid. The AFINOS study. Nutr Hosp. 2014; 29 (5):1047–53. doi: 10.3305/nh.2014.29.5.7387. PMID: 24951984. [ PubMed ] [ Google Scholar ]
- Shahyad S, Pakdaman S, Shokri O, et al. The Role of Individual and Social Variables in Predicting Body Dissatisfaction and Eating Disorder Symptoms among Iranian Adolescent Girls: An Expanding of the Tripartite Influence Mode. Eur J Transl Myol. 2018; 28 (1):72–7. doi: 10.4081/ejtm.2018.7277. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yirga B, Assefa Y, Derso T, et al. Disordered eating attitude and associated factors among high school adolescents aged 12-19 years in Addis Ababa, Ethiopia: a cross-sectional study. BMC Res Notes. 2016; 9 (1):503. doi: 10.1186/s13104-016-2318-6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Altamirano Martínez MB, Vizmanos Lamotte B, Unikel Santoncini C. Continuum of risky eating behaviors in Mexican adolescents. Rev Panam Salud Publica. 2011 Nov; 30 (5):401–7. Spanish. doi: 10.1590/s1020-49892011001100001. [ PubMed ] [ Google Scholar ]
- Fuentes MC, García O. Influence of family socialization on satisfaction with body image in Spanish adolescents. Trastornos de la Conducta Alimentaria. 2015; 22 :2403–25. Spanish. [ Google Scholar ]
- Lazo Y, Quenaya A, Tristán P. Mass media influence and risk of developing eating disorders in female students from Lima, Peru. Arch Argent Pediatr. 2015; 113 (6):519–525. Spanish. [ PubMed ] [ Google Scholar ]
- Londoño-Pérez C, Moreno Ruge AM. Family and personal predictors of eating disorders in young people. Anal Psicol. 2017; 33 (2):235–42. Spanish. https://doi.org/10.6018/analesps.33.2.236781. [ Google Scholar ]
- Nuño-Gutiérrez BL, Celis-de la Rosa A, Unikel-Santoncini C. Prevalence and associated factors related to disordered eating in student adolescents of Guadalajara across sex. Rev Invest Clin. 2009; 61 (4):286–93. Spanish. [ PubMed ] [ Google Scholar ]
- Pamies L, Quiles Y. Perfectionism and risk factors for the development of eating disorders in Spanish adolescents of both genders. Anal Psicol. 2014; 30 (2):620–26. Spanish. https://dx.doi.org/10.6018/analesps.30.2.158441. [ Google Scholar ]
- Silva C, Millán B, González K. Gender role and eating attitudes in adolescents from two different socio-cultural contexts: Traditional vs. non-traditional. Rev Mex de Trastor Aliment. 2017; 8 (1):40–8. Spanish. https://doi.org/10.1016/j.rmta.2016.12.002. [ Google Scholar ]
- Fortes Lde S, Cipriani FM, Ferreira ME. Risk behaviors for eating disorder: factors associated in adolescent students. Trends Psychiatry Psychother. 2013; 35 (4):279–86. doi: 10.1590/2237-6089-2012-0055. [ PubMed ] [ Google Scholar ]
- Cogollo Z, Gómez E. Risk of eating behavior disorders in adolescents from Cartagena, Colombia. Invest Educ Enferm. 2013; 31 (3):450–6. Spanish. [ Google Scholar ]
- Caldera I, Martin P, Caldera J, et al. Predictors of risk eating behaviors in high school students. Rev Mex Trastor Aliment. 2019; 10 (1):22–31. http://dx.doi.org/10.22201/fesi.20071523e.2019.1.519. [ Google Scholar ]
- Reina SA, Shomaker LB, Mooreville M, et al. Sociocultural pressures and adolescent eating in the absence of hunger. Body Image. 2013; 10 (2):182–90. doi: 10.1016/j.bodyim.2012.12.004. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Laporta I, Delgado M, Reboyar S, et al. Perfectionism in adolescents with eating disorders. Eur J Health Research. 2020; 6 :97–107. Spanish. doi: 10.30552/ejhr.v6i1.205. [ Google Scholar ]
- Rod E, Pons R, Lajara F, et al. Influence of the habits of the adolescent population on self-image and the risk of eating disorder. Rev Pediatr Aten Primaria. 2011; 13 (51):387–96. [ Google Scholar ]
- De Sousa L, De Sousa S, Caputo E. Influence of psychological, anthropometric and sociodemographic factors on the symptoms of eating disorders in young athletes. Paidéia (Ribeirão Preto) 2014; 24 :21–7. Spanish. doi: 10.1590/1982-43272457201404. [ Google Scholar ]
- Castaño J, Giraldo D, Guevara J, et al. Prevalence of risk of eating disorders in a female population of high school students, Manizales, Colombia, 2011. Rev. Colomb. Obstet. Ginecol. 2012; 63 (1):46–56. Spanish. doi: https://doi.org/10.18597/rcog.202. [ Google Scholar ]
- Rutsztein G, Scappatura L, Murawski B. Perfectionism and low self-esteem across the continuum of eating disorders in adolescent girls from Buenos Aires. Rev Mex Trastor Aliment. 2014; 5 (1):39–49. Spanish. https://doi.org/10.1016/S2007-1523(14)70375-1. [ Google Scholar ]
- Haynos AF, Watts AW, Loth KA, et al. Factors Predicting an Escalation of Restrictive Eating During Adolescence. J Adolesc Health. 2016; 59 (4):391–6. doi: 10.1016/j.jadohealth.2016.03.011. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Maezono J, Hamada S, Sillanmäki L, et al. Cross-cultural, population-based study on adolescent body image and eating distress in Japan and Finland. Scand J Psychol. 2019; 60 (1):67–76. doi: 10.1111/sjop.12485. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Batista M, Žigić Antić L, Žaja O, et al. Predictors of eating disorder risk in anorexia nervosa adolescents. Acta Clin Croat. 2018; 57 (3):399–410. doi: 10.20471/acc.2018.57.03.01. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jiménez Flores P, Jiménez Cruz A, Bacardi Gascón M. Body-image dissatisfaction in children and adolescents: a systematic review. Nutr Hosp. 2017; 34 (2):479–89. Spanish. doi: 10.20960/nh.455. PMID: 28421808. [ PubMed ] [ Google Scholar ]
- Mancilla A, Vásquez R, Mantilla J, et al. Body dissatisfaction in children and preadolescents: A systematic review. Rev Mex Trastor Aliment. 2012; 3 (1):62–79. Spanish. [ Google Scholar ]
- Berkman ND, Lohr KN, Bulik CM. Outcomes of eating disorders: a systematic review of the literature. Int J Eat Disord. 2007; 40 (4):293–309. doi: 10.1002/eat.20369. [ PubMed ] [ Google Scholar ]
- Moreno J, Torres C. Revisión sistemática de los determinantes socioculturales asociados a los trastornos de la conducta alimentaria en adolescentes latinoamericanos entre 2004 y 2014. Bogotá: UCA publication; University Applied and Environmental Sciences. 2015 [ Google Scholar ]
- Ruíz A, Vázquez R, Mancilla J, et al. Family factors associated with Eating Disorders: a review. Rev Mex Trastor Aliment. 2013; 4 (1):45–57. Spanish. [ Google Scholar ]
- Góngora VC. Satisfaction with life, well-being, and meaning in life as protective factors of eating disorder symptoms and body dissatisfaction in adolescents. Eat Disord. 2014; 22 (5):435–49. doi: 10.1080/10640266.2014.931765. [ PubMed ] [ Google Scholar ]
- Levine MP, Smolak L. The role of protective factors in the prevention of negative body image and disordered eating. Eat Disord. 2016; 24 (1):39–46. doi: 10.1080/10640266.2015.1113826. [ PubMed ] [ Google Scholar ]
- Haines J, Kleinman KP, Rifas-Shiman SL, et al. Examination of shared risk and protective factors for overweight and disordered eating among adolescents. Arch Pediatr Adolesc Med. 2010; 164 (4):336–43. doi: 10.1001/archpediatrics.2010.19. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Eating Disorders in Adolescents Essay
Eating disorder as a severe health condition that can be manifested in many different ways may tackle a person of any age, gender, and socio-cultural background. However, adolescents, especially when it comes to female teenagers, are considered to be the most vulnerable in terms of developing this condition (Izydorczyk & Sitnik-Warchulska, 2018). According to the American Academy of Child & Adolescent Psychiatry (AACAP, 2018), 10 in 100 young women struggle with an eating disorder. Thus, the purpose of the present paper is to dwell on the specifics of external factors causing the disorder as well as the ways to deal with this issue.
To begin with, it is necessary to define which diseases are meant under the notion of an eating disorder. Generally, eating disorders encompass such conditions as anorexia nervosa, bulimia, binge eating, and avoidant/restrictive food intake disorder (ARFID) (AACAP, 2018). Although these conditions have different manifestations in the context of eating patterns, all of them affect teenager’s nutrition patterns and average weight. According to the researchers, there exist common external stressors that lead to an eating disorder, such as:
- Socio-cultural appearance standards. For the most part, modern culture and mass media promote certain body images as a generally accepted ideal, which causes many teenage girls to doubt their appearance and follow the mass trends.
- Biological factors. Some teenagers might have a genetic predisposition for certain disorders if anyone in the family struggled with the disease at some point in the past.
- Emotional factors. Children, who are at risk of being affected by such mental disorders as anxiety and depression, are likely to disrupt their nutrition patterns.
- Peer pressure. Similar to socio-cultural standards, peer pressure dictates certain criteria for the teenagers’ body image, eventually impacting their perception of food and nutrition (Izydorczyk & Sitnik-Warchulska, 2018).
With such a variety of potential stressors, it is imperative for both medical professionals and caregivers to pay close attention to the teenager’s eating habits. Thus, in order to assess the issue, any medical screening should include weight and height measurements. In such a way, medical professionals are able to define any discrepancies in the measurements over time and bring this issue up with a patient. When working with adolescents, it is of paramount importance to establish a trusting relationship with a patient, as teenagers are extremely vulnerable at this age. After identifying any issue related to weight and body image, nurses and physicians need to ask the patient whether they have any problems with eating. In case they are not willing to talk on the matter, it is necessary to emphasize that their response will not be shared with caregivers unless they want it. It is also necessary to ask questions regarding the child’s relationship with peers carefully, as they may easily become an emotional trigger.
In order to avoid such complications as eating disorders, it is vital for caregivers to talk with their children on the topic of the aforementioned stressors. Firstly, they need to promote healthy eating patterns by explaining why it is important for one’s body instead of giving orders to the child. For additional support, they may ask a medical professional to justify this information. Secondly, the caregivers need to dedicate time to explain the inappropriateness of body standards promoted by the mass media and promote diversity and positive body image within the family. Lastly, caregivers are to secure a safe environment for the teenager’s fragile self-esteem and self-actualization in order for them to feel more confident among peers (Boberová & Husárová, 2021). These steps, although frequently undermined, contribute beneficially in terms of dealing with eating disorders external stressors among adolescents.
American Academy of Child & Adolescent Psychiatry [AACAP]. (2018). Eating disorders in teens. Web.
Boberová, Z., & Husárová, D. (2021). What role does body image in relationship between level of health literacy and symptoms of eating disorders in adolescents?. International Journal of Environmental Research and Public Health , 18 (7), 3482.
Izydorczyk, B., & Sitnik-Warchulska, K. (2018). Socio-cultural appearance standards and risk factors for eating disorders in adolescents and women of various ages. Frontiers in psychology , 9 , 429.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, June 23). Eating Disorders in Adolescents. https://ivypanda.com/essays/eating-disorders-in-adolescents/
"Eating Disorders in Adolescents." IvyPanda , 23 June 2022, ivypanda.com/essays/eating-disorders-in-adolescents/.
IvyPanda . (2022) 'Eating Disorders in Adolescents'. 23 June.
IvyPanda . 2022. "Eating Disorders in Adolescents." June 23, 2022. https://ivypanda.com/essays/eating-disorders-in-adolescents/.
1. IvyPanda . "Eating Disorders in Adolescents." June 23, 2022. https://ivypanda.com/essays/eating-disorders-in-adolescents/.
Bibliography
IvyPanda . "Eating Disorders in Adolescents." June 23, 2022. https://ivypanda.com/essays/eating-disorders-in-adolescents/.
- External Stressors in Adolescents
- Eating Disorders in Adolescent Girls
- Influence of Modelling in Teenager’s Eating Disorders
- Socio-Cultural Approach of Humanity Examination
- Eating and Mood Disorders Among Adolescents
- Stressors in Nursing Workplace
- Environmental Stressors
- Organizational Stressors, Their Results and Types
- Eating Disorders in Male Adolescents as Health Topic
- The Socialization of the Caregivers
- Discussion Board Post: Distinction between the Public and Private
- Cyberbullying: Definition, Forms, Groups of Risk
- Human Trafficking and Healthcare Organizations
- The Politics of Abortion in Modern Day Jamaica
- Challenges of Prisoner Re-Entry Into Society
- Share full article
Advertisement
Supported by
Adolescence
Eating Disorders in Teens Have ‘Exploded’ in the Pandemic
Here’s what parents need to know.

By Lisa Damour
As a psychologist who cares for adolescents I am well aware of the prevalence of eating disorders among teenagers . Even still, I am stunned by how much worse the situation has become in the pandemic.
According to the psychologist Erin Accurso, the clinical director of the eating disorders program at the University of California, San Francisco, “our inpatient unit has exploded in the past year,” taking in more than twice as many adolescent patients as it did before the pandemic. Dr. Accurso explained that outpatient services are similarly overwhelmed: “Providers aren’t taking new clients, or have wait-lists up to six months.”
The demand for eating disorder treatment “is way outstretching the capacity to address it,” said the epidemiologist S. Bryn Austin, a professor at the T.H. Chan School of Public Health and research scientist in the Division of Adolescent and Young Adult Medicine at Boston Children’s Hospital. “I’m hearing this from colleagues all across the country.” Even hotlines are swamped. The National Eating Disorders Association helpline has had a 40 percent jump in overall call volume since March 2020. Among callers who shared their age over the last year, 35 percent were 13 to 17 years old, up from 30 percent in the year before the pandemic.
What has changed in the pandemic?
There are several possible explanations for this tsunami of eating concerns in teenagers. When adolescents lost the familiar rhythm of the school day and were distanced from the support of their friends, “many of the things that structured a teenager’s life evaporated in one fell swoop,” said Dr. Walter Kaye, a psychiatrist and the founder and executive director of the eating disorders program at the University of California, San Diego. “People who end up with eating disorders tend to be anxious and stress sensitive — they don’t do well with uncertainty.”
Further, eating disorders have long been linked with high achievement . Driven adolescents who might have normally poured their energy into their academic, athletic or extracurricular pursuits suddenly had too much time on their hands. “Some kids turned their attention toward physical health or appearance as a way to cope with anxiety or feel productive,” Dr. Accurso said. “Their goals around ‘healthy’ eating or getting ‘in shape’ got out of hand” and quickly caused significant weight loss.
For some, an increase in emotional eating in the pandemic has been part of the problem. Attending school from a home where food is constantly available may lead some young people to eat more than usual as a way to manage pandemic-related boredom or stress . “Being at school presents a barrier to using food as a coping mechanism; at home, we don’t have that barrier,” noted Kelly Bhatnagar, psychologist and co-founder of the Center for Emotional Wellness in Beachwood, Ohio, a practice specializing in the treatment of eating disorders.
In many households the pandemic has heightened food insecurity and its attendant anxieties, which can increase the risk of eating disorders. Research shows that, compared to teenagers whose families have enough food, those in homes where food is scarce are more likely to fast, to skip meals, and to abuse laxatives and diuretics with the aim of controlling their weight.
The Instagram influence
What teens see on their screens is also a factor. During the pandemic, teenagers have spent more time than usual on social media . While that can be a source of much needed connection and comfort , scrutinizing images of peers and influencers on highly visual social media has been implicated in body dissatisfaction and disordered eating . Dr. Austin noted that teenagers can be prone to comparing their own bodies to the images they see online. “That comparison creates a downward spiral in terms of body image and self-esteem. It makes them more likely to adopt unhealthy weight control behaviors.”
When adolescents take an interest in managing their weight, they often go looking for guidance online. Indeed, a new Common Sense Media survey found that among teenagers who sought health information online between September and November of 2020, searches on fitness and exercise information came second only to searches for content related to Covid-19 — and ahead of searches on anxiety, stress and depression.
What young people find when they go looking for fitness information can be highly problematic. They are likely to come across harmful “thinspiration” and “fitspiration” posts celebrating slim or sculpted bodies, or even sites that encourage eating disordered behavior . Worse, algorithms record online search information and are “deliberately designed to feed harmful weight loss content to users who are already struggling with body image,” such as advertisements for dangerous diet supplements, Dr. Austin said.
When to worry
With so many forces contributing to teenagers’ body dissatisfaction and eating disordered behavior, how do parents know when to worry?
Parents should be alarmed, Dr. Kaye said, “if your child suddenly loses 10 to 20 pounds, becomes secretive about eating, or if you are seeing food disappear,” as becoming furtive about what, how and when one eats is a common occurrence in anorexia, bulimia and other eating disorders.
Experts agree that adults should be on the lookout for behaviors that veer from previous norms, such as suddenly skipping family meals or refusing to eat food from entire categories, such as carbohydrates or processed foods. Worth concern, too, is the teenager who develops fixations such as carefully counting calories, exercising obsessively or hoarding food, which may be a sign of a binge eating disorder. Parents should also pay close attention, said Dr. Accurso, if adolescents express a lot of guilt or anxiety around food or eating, or feel unhappy or uncomfortable with their bodies.
According to Dr. Bhatnagar, the view of eating disorders as a “white girls’ illness” can keep teens who are not white girls from seeking help or being properly screened for eating disorders by health professionals, even though eating disorders regularly occur across both sexes and all ethnic groups .
“Boys are having the same troubles,” said Dr. Bhatnagar, “but heterosexual boys may talk about body image a little differently. They tend to talk in terms of getting fit, getting lean or being muscular.”
Dr. Austin also noted that it is common to see elevated rates of eating disorders in lesbian, gay and bisexual youth of all genders as well as transgender and gender diverse young people.
“Eating disorders,” Dr. Accurso said, “don’t discriminate.”
How to help
Research shows that early identification and intervention play a key role in the successful treatment of eating disorders. Accordingly, parents who have questions about their teen’s relationship with eating, weight or exercise should not hesitate to seek an evaluation from their pediatrician or family health provider. Trustworthy eating disorder information, screening tools and support can also be found online. And when necessary, online resources can provide guidance and support to those on treatment waiting lists. “It may not be ideal for many,” Dr. Kaye said, “but it’s the reality of the situation we’re in.”
Parents can also take steps to reduce the likelihood that an eating disorder will take hold in the first place. Experts encourage adults to model a balanced approach to eating and to create enjoyable opportunities for being physically active while steering clear of negative comments about their teenager’s body or their own. Parents should also openly address the dangers of a ubiquitous diet culture that emphasizes appearance over well-being, creates stigma and shame around weight and links body size to character and worth. As Dr. Accurso noted, “We are not defined by a number on a scale.”
Where to find help
The National Eating Disorders Association , or NEDA, is a good starting place. It supports individuals and families affected by eating disorders.
F.E.A.S.T. is an international nonprofit organization run by caregivers of those suffering from eating disorders, meant to help others.
Maudsley Parents was created by parents who helped their children recover with family-based treatment , to offer hope and help to other families confronting eating disorders.
The Academy for Eating Disorders offers many resources, as do the Eating Disorders Center for Treatment and Research at University of California, San Diego, and the Eating Disorders Program at Boston Children’s Hospital.
Lisa Damour is a psychologist and the author of the New York Times best sellers “Untangled” and “Under Pressure.” Dr. Damour also co-hosts the podcast “Ask Lisa: The Psychology of Parenting.” More about Lisa Damour
How to Communicate Better With the Teens in Your Life
Simple strategies can go a long way toward building a stronger, more open relationship..
Active listening is an essential skill when seeking to engage any family member in conversation — teens included. Here is how to get better at it .
There are many reasons why a teen might not be opening up to you. These are the most common explanations for their silence .
Is your kid dismissing your solutions to their problems as irritating or irrelevant? It is usually because they’re not looking for you solve their problems.
Developing a healthy relationship with social media can be tricky. Here is how to talk to teens about it .
If your teen is surly or standoffish, these strategies can help you reconnect .
Are you worried that your kid might be struggling with his or her mental health? Understand the warning signs and make sure to approach the issue with the utmost sensitivity.
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
INTRODUCTION
Definitions, epidemiology, screening for eating disorders, assessment of children and adolescents with suspected eating disorders, laboratory evaluation, medical complications in patients with eating disorders, psychological and neurologic effects, dermatologic effects, dental and/or oral effects, cardiovascular effects, gastrointestinal tract effects, renal and electrolyte effects, endocrine effects, treatment principles across the eating disorder spectrum, the pediatrician’s role in care, financial considerations, pediatrician’s role in prevention and advocacy, guidance for pediatricians, lead authors, committee on adolescence, 2018–2019, identification and management of eating disorders in children and adolescents.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Laurie L. Hornberger , Margo A. Lane , THE COMMITTEE ON ADOLESCENCE , Laurie L. Hornberger , Margo Lane , Cora C. Breuner , Elizabeth M. Alderman , Laura K. Grubb , Makia Powers , Krishna Kumari Upadhya , Stephenie B. Wallace , Laurie L. Hornberger , Margo Lane , MD FRCPC , Meredith Loveless , Seema Menon , Lauren Zapata , Liwei Hua , Karen Smith , James Baumberger; Identification and Management of Eating Disorders in Children and Adolescents. Pediatrics January 2021; 147 (1): e2020040279. 10.1542/peds.2020-040279
Download citation file:
- Ris (Zotero)
- Reference Manager
Eating disorders are serious, potentially life-threatening illnesses afflicting individuals through the life span, with a particular impact on both the physical and psychological development of children and adolescents. Because care for children and adolescents with eating disorders can be complex and resources for the treatment of eating disorders are often limited, pediatricians may be called on to not only provide medical supervision for their patients with diagnosed eating disorders but also coordinate care and advocate for appropriate services. This clinical report includes a review of common eating disorders diagnosed in children and adolescents, outlines the medical evaluation of patients suspected of having an eating disorder, presents an overview of treatment strategies, and highlights opportunities for advocacy.
Although the earliest medical account of an adolescent patient with an eating disorder was more than 300 years ago, 1 a thorough understanding of the pathophysiology and psychobiology of eating disorders remains elusive today. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition ( DSM-5 ) includes the latest effort to describe and categorize eating disorders, 2 placing greater emphasis on behavioral rather than physical and cognitive criteria, thereby clarifying these conditions in those children who do not express body or weight distortion. DSM-5 diagnostic criteria for several of the eating disorders commonly seen in children and adolescents are presented in Table 1 .
Diagnostic Features of Eating Disorders Commonly Seen in Children and Adolescents
Adapted from the DSM-5 , American Psychiatric Association, 2013. 2
Notable changes in DSM-5 since the previous edition include the elimination of amenorrhea and specific weight percentiles in the diagnosis of anorexia nervosa (AN) and a reduction in the frequency of binge eating and compensatory behaviors required for the diagnosis of bulimia nervosa (BN). The diagnosis “eating disorder not otherwise specified” has been eliminated, and several diagnoses have been added, including binge-eating disorder (BED) and avoidant/restrictive food intake disorder (ARFID). 3 – 5 The diagnosis of ARFID encompasses feeding behaviors previously categorized in the fourth edition ( DSM-IV ) as “feeding disorder of infancy and early childhood” and expands these into adolescence and adulthood. Individuals with ARFID intentionally limit intake for reasons other than for concern for body weight, such as the sensory properties of food, a lack of interest in eating, or a fear of adverse consequences with eating (eg, choking or vomiting). As a result, they may experience weight loss or failure to achieve expected weight gain, malnutrition, dependence on nutritional supplementation, and/or interference with psychosocial functioning. 6 – 9 The category “other specified feeding and/or eating disorder” is now applied to patients whose symptoms do not meet the full criteria for an eating disorder despite causing significant distress or impairment. Among these disorders is atypical AN in which diminished self-worth, nutritional restriction, and weight loss mirrors that seen with AN, although body weight at presentation is in the normal or above-normal range. Efforts are ongoing to further categorize abnormal eating behaviors and refine diagnoses. 10
Prevalence data for eating disorders vary according to study populations and the criteria used to define an eating disorder. 11 A systematic review of prevalence studies published between 1994 and 2013 found widely varied estimates in the lifetime prevalence of eating disorders, with a range from 1.0% to 22.7% for female individuals and 0.3% to 0.6% for male indnividuals. 12 A 2011 cross-sectional survey of more than 10 000 nationally representative US adolescents 13 to 18 years of age estimated prevalence rates of AN, BN, and BED at 0.3%, 0.9%, and 1.6%, respectively. Behaviors suggestive of AN and BED but not meeting diagnostic thresholds were identified in another 0.8% and 2.5%, respectively. The mean age of onset for each of these disorders was 12.5 years. 13 Several studies have suggested higher BED prevalence rates of 2% to 4%, with a more equal distribution between girls and boys, making it perhaps the most common eating disorder among adolescents. 14 In contrast, the diagnoses seen in treatment may belie the relative prevalence of these disorders. In a review of 6 US adolescent eating disorder treatment programs, the distribution of diagnoses was 32% AN, 30% atypical AN, 9% BN, 19% ARFID, 6% purging disorder, and 4% others. 15 This may reflect the underrecognition and/or undertreatment of disorders such as BED.
Although previously mischaracterized as diseases of non-Hispanic white, affluent adolescent girls, eating disorder behaviors are increasingly recognized across all racial and ethnic groups 16 – 20 and in lower socioeconomic classes, 21 preadolescent children, 22 males, and children and adolescents perceived as having an average or increased body size.
Preteens with eating disorders are more likely than older adolescents to have premorbid psychopathology (depression, obsessive-compulsive disorder, or other anxiety disorders) and less likely to have binge and purge behaviors. There is a more equal distribution of illness by sex among younger patients and, frequently, more rapid weight loss, leading to earlier presentation to health care providers. 23
Although diagnosis in males may increase with the more inclusive DSM-5 criteria, 24 , 25 it is often delayed because of the misperception of health care providers that eating disorders are female disorders. 26 In addition, disordered eating attitudes may differ in male individuals, 27 focusing on leanness, weight control, and muscularity. Purging, use of muscle-building supplements, substance abuse, and comorbid depression are common in males. 28 – 30
Eating disorders can occur in individuals with various body habitus, and their presence in those of larger body habitus is increasingly apparent. 31 – 34 Weight stigma (the undervaluation or negative stereotyping of individuals because they have overweight or obesity) seems to play a role. Adolescents with larger body habitus are exposed to weight stigma through the media, their families, peers, and teachers, and health care professionals, resulting in depression, anxiety, poor body image, social isolation, unhealthy eating behaviors, and worsening obesity. 35 When presenting with significant weight loss but a BMI still classified in the “healthy,” overweight, or obese ranges, patients with eating disorders such as atypical AN may be overlooked by health care providers 36 , 37 but may experience the same severe medical complications as those who are severely underweight. 38 – 40
Increased rates of disordered eating may be found in sexual minority youth. 41 – 43 Analysis of Youth Risk Behavior Survey data reveals lesbian, gay, and bisexual high school students have significantly higher rates of unhealthy and disordered weight-control behaviors than their heterosexual peers. 44 , 45 Transgender youth may be at particular risk. 46 , 47 In a survey of nearly 300 000 college students, transgender students had the highest rates of self-reported eating disorder diagnoses and compensatory behaviors (ie, use of diet pills or laxatives or vomiting) compared with all cisgender groups. Nearly 16% of transgender respondents reported having been diagnosed with an eating disorder, as compared with 1.85% of cisgender heterosexual women. 48
Adolescents with chronic health conditions requiring dietary control (eg, diabetes, cystic fibrosis, inflammatory bowel disease, and celiac disease) may also be at increased risk of disordered eating. 49 – 51 Among teenagers with type 1 diabetes mellitus, at least one-third may engage in binge eating, self-induced vomiting, insulin omission for weight loss, and excessive exercise, 52 , 53 resulting in poorer glycemic control. 54
Many adolescents engage in dietary practices that may overlap with or disguise eating disorders. The lay term "orthorexia" describes the behavior of individuals who become increasingly restrictive in their food consumption, not based on concerns for quantity of food but the quality of food (eg, specific nutritional content or organically produced). The desire to improve one’s health through optimal nutrition and food quality is the initial focus of the patient, and weight loss and/or malnutrition may ensue as various foods are eliminated from the diet. Individuals with orthorexia may spend excessive amounts of time in meal planning and experience extreme guilt or frustration when their food-related practices are interrupted. 55 , 56 Psychologically, this behavior appears to be related to AN and obsessive-compulsive disorder 57 and is considered by some to be a subset within the restrictive eating disorders. Vegetarianism is a lifestyle choice adopted by many adolescents and young adults that may sometimes signal underlying eating pathology. 58 , 59 In a comparison of adolescent and young adult females with and without a history of eating disorders, those with eating disorders were more likely to report ever having been vegetarian. Many of these young women acknowledged that their decision to become vegetarian was primarily motivated by their desire for weight loss, and most reported that they had done so at least a year after first developing eating disorder symptoms. 60
In an attempt to improve performance or achieve a desired physique, adolescent athletes may engage in unhealthy weight-control behaviors. 61 The term “female athlete triad” has historically referred to (1) low energy availability that may or may not be related to disordered eating; (2) menstrual dysfunction; and (3) low bone mineral density (BMD) in physically active females. 62 – 65 Inadequate caloric intake in comparison to energy expenditure is the catalyst for endocrine changes and leads to decreased bone density and menstrual irregularities. Body weight may be stable. This energy imbalance may result from a lack of knowledge regarding nutritional needs in the athlete or from intentional intake restriction associated with disordered eating.
Hormonal disruption and low BMD can occur in undernourished male athletes as well. 66 Increased recognition of the role of energy deficiency in disrupting overall physiologic function in both male and female individuals led a 2014 International Olympic Committee consensus group to recommend replacing the term female athlete triad to the more inclusive term, “relative energy deficiency in sport.” 67 , 68 Athletes participating in sports involving endurance, weight requirements, or idealized body shapes may be at particular risk of relative energy deficiency in sport. Signs and symptoms of relative energy deficiency, such as amenorrhea, bradycardia, or stress fractures, may alert pediatricians to this condition.
Pediatricians are in a unique position to detect eating disorders early and interrupt their progression. Annual health supervision visits and preparticipation sports examinations offer opportunities to screen for eating disorders. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents , fourth edition, offers sample screening questions about eating patterns and body image. 69 Reported dieting, body image dissatisfaction, experiences of weight-based stigma, or changes in eating or exercise patterns invite further exploration. Positive responses on a standard review of symptoms may need further probing. For example, oligomenorrhea or amenorrhea (either primary or secondary) may indicate energy deficiency. 70 Serial weight and height measurements plotted on growth charts are invaluable. Weight loss or the failure to make expected weight gain may be more obvious when documented on a graph. Similarly, weight fluctuations or rapid weight gain may cue a health care provider to question binge eating or BN symptoms. Recognizing that many patients who present to eating disorder treatment programs have or previously had elevated weight according to criteria from the Centers for Disease Control and Prevention, 71 it is worthwhile to carefully inquire about eating and exercise patterns when weight loss is noted in any child or adolescent. Screening for unhealthy and extreme weight-control measures before praising desirable weight loss can avoid inadvertently reinforcing these practices.
A comprehensive assessment of a child or adolescent suspected of having an eating disorder includes a thorough medical, nutritional, and psychiatric history, followed by a detailed physical examination. A useful web resource for assessment is published in multiple languages by the Academy for Eating Disorders. 72 Relevant interview questions are listed in Table 2 . A collateral history from a parent may reveal abnormal eating-related behaviors that were denied or minimized by the child or adolescent.
Example Questions to Ask Adolescents With a Possible Eating Disorder
Adapted from Rome and Strandjord. 89 LMP, last menstrual period.
A full psychosocial assessment, including a home, education, activities, drugs/diet, sexuality, suicidality/depression (HEADSS) assessment is vital. This evaluation includes screening for physical or sexual abuse by using the principles of trauma-informed care and responding according to American Academy of Pediatrics guidance on suspected physical or sexual abuse or sexual assault 73 – 75 as well as state laws. Vital to the HEADSS assessment is an evaluation for symptoms of other potential psychiatric diagnoses, including suicidal thinking, which may have been unrecognized previously.
A comprehensive physical examination, including close attention to growth parameters and vital signs, allows the pediatrician to assess for signs of medical compromise and for signs and symptoms of eating disorder behaviors; findings may be subtle and, thus, overlooked without careful notice. For accuracy, weights are best obtained after the patient has voided and in an examination gown without shoes. Weight, height, and BMI can be evaluated by using appropriate growth charts. Low body temperature, resting blood pressure (BP), or resting heart rate (HR) for age may suggest energy restriction. Because a HR of 50 beats per minute or less is unusual even in college-aged athletes, 76 the finding of a low HR may be a sign of restrictive eating. Orthostatic vital signs (HR and BP, obtained after 5 minutes of supine rest and repeated after 3 minutes of standing) 77 , 78 revealing a systolic BP drop greater than 20 mm Hg, a diastolic BP drop greater than 10 mm Hg, or tachycardia may suggest volume depletion from restricted fluid intake or purging or a compromised cardiovascular system.
Pertinent physical findings in children and adolescents with eating disorders are summarized in Table 3 . A differential diagnosis for the signs and symptoms of an eating disorder is found in Table 4 , and selected medical complications of eating disorders are provided in Table 5 .
Notable Physical Examination Features in Children and Adolescents With Eating Disorders
Adapted from Rosen; American Academy of Pediatrics. 208
Selected Differential Diagnosis for Eating Disorders According to Presentation
Adapted from Rome and Strandjord 89 and Rosen; American Academy of Pediatrics. 208
Selected Medical Complications Resulting From Eating Disorders
Initial laboratory evaluation is performed to screen for medical complications of eating disorders or to rule out alternate diagnoses ( Tables 4 and 5 ). Typical initial laboratory testing includes a complete blood cell count; serum electrolytes, calcium, magnesium, phosphorus, and glucose; liver transaminases; urinalysis; and thyroid-stimulating hormone concentration. 72 Screening for specific vitamin and mineral deficiencies (eg, vitamin B 12 , vitamin D, iron, and zinc) may be indicated on the basis of the nutritional history of the patient. Laboratory investigations are often normal in patients with eating disorders; normal results do not exclude the presence of serious illness with an eating disorder or the need for hospitalization for medical stabilization. An electrocardiogram is important for those with significant weight loss, abnormal cardiovascular signs (such as orthostasis or bradycardia), or an electrolyte abnormality. A urine pregnancy test and serum gonadotropin and prolactin levels may be indicated for girls with amenorrhea; a serum estradiol concentration may serve as a baseline for reassessment during recovery. 79 Similarly, serum gonadotropin and testosterone levels can be useful to assess and monitor for central hypogonadism in boys with restrictive eating. Bone densitometry, by using dual radiograph absorptiometry analyzed with age-appropriate software, may be considered for those with amenorrhea for more than 6 to 12 months. 80 , 81 If there is uncertainty about the diagnosis, other studies including inflammatory markers, serological testing for celiac disease, serum cortisol concentrations, testing stool for parasites, or radiographic imaging of the brain or gastrointestinal tract may be considered. In the occasional patient, both an eating disorder and an organic illness, such as celiac disease, may be discovered. 82
Eating disorders can affect every organ system 83 , 84 with potentially serious medical complications that develop as a consequence of malnutrition, weight changes, or purging. Details of complications are described in reviews 85 – 89 and are summarized in Table 5 . Most medical complications resolve with weight normalization and/or resolution of purging. Complications of BED can include those of obesity; these are summarized in other reports and not reiterated here. 84 , 90
Psychological symptoms can be primary to the eating disorder, a feature of a comorbid psychiatric disorder, or secondary to starvation. Initial symptoms of depression and anxiety may abate with refeeding. 91 Rumination about body weight and size is a core feature of AN, whereas rumination about food decreases as starvation reverses. 92 Difficulty in emotion regulation occurs across the spectrum of eating disorders but is more severe in those who binge eat or purge. 93 Cognitive function studies in a large population-based sample of adolescents revealed eating disorder participants had deficits in executive functioning, including global processing and cognitive flexibility but performed better than control participants on measures of visual attention and vigilance. 94
Structural brain imaging studies to date have yielded inconsistent results, likely explained, at least in part, by methodologic differences and the need to control for many variables, including nutritional state, hydration, medication use, and comorbid illness. 95 A longitudinal study revealed that global cortical thinning in acutely ill adolescents and young adults with AN normalized with weight restoration over a period of approximately 3 months. 96
Common skin changes in underweight patients include lanugo, hair thinning, dry scaly skin, and yellow discoloration related to carotenemia. Brittle nails and angular cheilitis may also be observed. Acrocyanosis can be observed in underweight patients and may be a protective mechanism against heat loss. Abrasions and calluses over the knuckles can occur from cutting the skin on incisors while self-inducing emesis. 97
Patients with eating disorders experience higher rates of dental erosion and caries. This occurs more frequently in those who self-induce emesis but can also be observed in those who do not. 98 Normal dental findings do not preclude the possibility that purging is occurring. 99 Hypertrophy of the parotid and other salivary glands, accompanied by elevations in serum amylase concentrations with normal lipase concentrations, may be a clue to vomiting. 99 Xerostomia, from either salivary gland dysfunction or psychiatric medication side effect, can reduce the oral pH, which can lead to increased growth of cariogenic oral bacteria. 98 , 100
Reports of cardiac complications in eating disorders are focused predominantly on restrictive eating disorders. Common cardiovascular signs include low HR, orthostasis, and poor peripheral perfusion. Orthostatic intolerance symptoms (eg, lightheadedness) and vital sign findings may resemble those of postural orthostatic tachycardia syndrome 101 , 102 and may contribute to a delay in referral to appropriate care if eating disorder behaviors are not disclosed or appreciated.
Cardiac structural changes include decreased left ventricular (LV) mass, LV end diastolic and LV end systolic volumes, functional mitral valve prolapse, pericardial effusion, and myocardial fibrosis (noted in adults). 103 – 105 Electrocardiographic abnormalities, including sinus bradycardia, and lower amplitude LV forces are more common in AN than in nonrestrictive eating disorders. 106 One study reported a nearly 10% prevalence of prolonged (>440 milliseconds) QTc interval in hospitalized adolescents and young adults with a restrictive eating disorder. 107 Repolarization abnormalities, a potential precipitant to lethal arrhythmia, 108 may prompt clinicians to also consider other factors, such as medication use or electrolyte abnormalities, that may affect cardiac conduction. 107 , 109
Gastrointestinal complaints are common and sometimes precede the diagnosis of the eating disorder. Delayed gastric emptying and slow intestinal transit time often contribute to reported sensations of nausea, bloating, and postprandial fullness 110 and may be a presenting feature of restrictive eating. Constipation is a frequent experience for patients and multifactorial in etiology. 111 Esophageal mucosal damage from self-induced vomiting, including scratches, and bleeding secondary to Mallory-Weiss tears can occur. 99 Superior mesenteric artery syndrome may develop in the setting of severe weight loss. 111 Hepatic transaminase concentrations and coagulation times can be elevated as a consequence of malnutrition and, typically, normalize with appropriate nutrition. 110
Fluid and electrolyte abnormalities may occur as a result of purging or cachexia. 99 , 112 Dehydration can be present in any patient with an eating disorder. Disordered osmotic regulation can present in many patterns (central and renal diabetes insipidus, syndrome of inappropriate antidiuretic hormone). 112 Patients who vomit may have a hypokalemic, hypochloremic metabolic alkalosis resulting from loss of gastric hydrochloric acid, chronic dehydration, and the subsequent increase in aldosterone that promotes sodium reabsorption in exchange for potassium and acid at the distal tubule level. 113 Patients who abuse laxatives may experience a variety of electrolyte and acid-base derangements. 113 Dilutional hyponatremia can be observed in patients who intentionally water load to induce satiety or to misrepresent their weight at clinic visits. Abrupt cessation of laxative use may be associated with peripheral edema and, therefore, motivate further laxative 114 or diuretic misuse.
Restrictive eating disorders commonly cause endocrine dysfunction. 80 , 115 Euthyroid sick syndrome (low triiodothyronine, elevated reverse triiodothyronine, or normal or low thyroxine and thyroid-stimulating hormone) is the most common thyroid abnormality. 116 Functioning as an adaptive mechanism to starvation, supplemental thyroid hormone is not indicated when this pattern is noted. 116 Hypercortisolemia may be seen in AN. 81 , 116 Hypothalamic-pituitary-gonadal axis suppression may be attributable to weight loss, physical overactivity, or stress. Female individuals with AN may have amenorrhea, and male individuals can have small testicular volumes 117 and low testosterone concentrations. 118
Growth retardation, short stature, and pubertal delay may all be observed in prepubertal and peripubertal children and adolescents with eating disorders. 115 AN is associated with low levels of insulin-like growth factor-1 and growth hormone resistance. 119 Catch-up growth has been inconsistently reported in the literature; younger patients may have greater and more permanent effects on growth. 120 , 121 Adolescent boys may be at an even greater risk for height deficits than girls; because boys typically enter puberty later than girls and experience their peak growth at a later sexual maturity stage, they are less likely to have completed their growth if an eating disorder develops in the middle teenage years. 119
Low BMD is a frequent complication of eating disorders in both male and female patients 117 and is a risk in both AN and BN. 122 Low BMD is worrisome not only because of the increased risk of fractures in the short-term 123 but, also, because of the potential to irreversibly compromise skeletal health in adulthood. 124
The ultimate goals of care in eating disorders are that children and adolescents are nourished back to their full healthy weight and growth trajectory, that their eating patterns and behaviors are normalized, and that they establish a healthy relationship with food and their body weight, shape, and size as well as a healthy sense of self. Independent of a specific DSM diagnosis, treatment is focused on nutritional repletion and psychological therapy. Psychotropic medication can be a useful adjunct in select circumstances.
After diagnosing an eating disorder, the pediatrician arranges appropriate care. Patients who are medically unstable may require urgent referral to a hospital ( Table 6 ). Patients with mild nutritional, medical, and psychological dysfunction may be managed in the pediatrician’s office in collaboration with outpatient nutrition and mental health professionals with specific expertise in eating disorders. Because an early response to treatment may be associated with better outcomes, 125 , 126 timely referral to a specialized multidisciplinary team is preferred, when available. If resources do not exist locally, pediatricians may need to partner with health experts who are farther away for care. For patients who do not improve promptly with outpatient care, more intensive programming (eg, day-treatment programs or residential settings) may be indicated.
Indications Supporting Hospitalization in an Adolescent With an Eating Disorder
Reprinted with permission from the Society for Adolescent Health and Medicine. 85 ECG, electrocardiogram.
Often, an early task of the pediatrician is to identify a treatment goal weight. This goal weight may be determined in collaboration with a registered dietitian. Pediatricians who are planning to refer the patient to a specialized treatment team may opt to defer the task to the team. Acknowledging that body weights naturally fluctuate, the treatment goal weight is often expressed as a goal range. Individualized treatment goal weights are formulated on the basis of age, height, premorbid growth trajectory, pubertal stage, and menstrual history. 87 , 127 In a study of adolescent girls with AN, of those who resumed menses during treatment, this occurred, on average, at 95% of the treatment goal weight. 128 Health care providers may be pressured by patients, their patients’ parents, or other health care providers to target a treatment goal weight that is lower than the previous growth trajectory or other clinical indicators would suggest is appropriate. If a treatment goal weight is inappropriately low, there is an inherent risk of offering only partial weight restoration and insufficient treatment. 129 The treatment goal weight is reassessed at regular intervals (eg, every 3–6 months) to account for changes in physical growth and development (in particular, age, height, and sexual maturity). 87 , 127
An important role for the pediatrician is to offer guidance regarding eating and to manage the physical aspects of the illnesses. For all classifications of eating disorders, reestablishing regular eating patterns is a fundamental early step. Meals and snacks are reintroduced or improved in a stepwise manner, with 3 meals and frequent snacks per day. Giving the message that “food is the medicine that is required for recovery” and promoting adherence to taking that medicine at scheduled intervals often helps patients and families get on track. 130 A multivitamin with minerals can help ensure that deficits in micronutrients are addressed. To optimize bone health, calcium and vitamin D supplements can be dosed to target recommended daily amounts (elemental calcium: 1000 mg for patients 4–8 years of age, or 1300 mg for patients 9–18 years of age; vitamin D: 600 IU for patients 4–18 years of age). 87 , 131 Patients can be reassured that the bloating discomfort caused by slow gastric emptying improves with regular eating. When constipation is troubling, nutritional strategies, including weight restoration, are the treatments of choice. 111 When these interventions are inadequate to alleviate constipation, osmotic (eg, polyethylene glycol 3350) or bulk-forming laxatives are preferred over stimulant laxatives. The use of nonstimulant laxatives decreases the risks of electrolyte derangement and avoids the potential hazard of “cathartic colon syndrome” that may be associated with abuse of stimulant cathartics (senna, cascara, bisacodyl, phenolphthalein, anthraquinones). 99 , 114
To optimize dental outcomes, patients can be encouraged to disclose their illness to their dentist. Current dental hygiene recommendations for patients who vomit include the use of topical fluoride, applied in the dental office or home, or use of a prescription fluoride (5000 ppm) toothpaste. Because brushing teeth immediately after vomiting may accelerate enamel erosion, patients can be advised to instead rinse with water, followed by using a sodium fluoride rinse whenever possible. 132
Collaborative Outpatient Care
Most patients with AN are treated in outpatient settings. 85 , 133 Pediatricians play an important role in the medical management and coordination of the treatment of these patients. The pediatrician plays a primary role in assessing for and managing acute and long-term medical complications, monitoring treatment progress, and coordinating care with nutritional and mental health colleagues. 85 , 130 , 134 Although some primary care pediatricians feel comfortable coordinating care, others choose to refer patients to providers with expertise in pediatric eating disorders. Ideally, all members of the treatment team are sensitive to the unique developmental needs of children and adolescents. 133
Educating young people and their parents about the physiologic and psychological effects of food restriction is an early component of care. Parents are empowered to feed their children regularly (typically 3 meals and 2–3 snacks per day) and adjust portion size and energy richness based on weight progress. Many parents are amazed to discover the amount of energy (3500 kcal or more) that may be required to restore weight for their children. Detailed tracking of caloric intake is not necessary. Serving foods with high caloric density and ensuring that beverages are energy rich (eg, choosing fruit juice or milk instead of water) are effective strategies to maximize energy intake without requiring large increases in volume. Parents can relieve adolescents of having to decide on appropriate serving sizes by plating meals for them. Accommodating special diets, such as vegetarian or vegan, can make meeting nutritional goals especially challenging. Reintroducing foods that have been avoided or that induce fear of weight gain are essential steps on the path to recovery.
Family-Based Treatment and Parent-Focused Therapy
Over the past 2 decades, a specialized eating disorder–focused, family-based intervention, commonly referred to as family-based treatment (FBT), has emerged as the leading first-line treatment approach for pediatric eating disorders. 135 Effectiveness is well established for AN. 133 , 136 Rather than dwelling on possible causes of the eating disorder, FBT is focused on recovery from the disease. FBT consists of 3 phases and contends that parents are not to blame for their child’s illness, eating disorders are not caused by dysfunctional families, and parents play an essential role in recovery. 136 During appointments, the entire family unit meets with the therapist. In phase 1, weight restoration is the primary goal. Parents, supported by the therapist, take responsibility to ensure that their child eats sufficiently and limit pathologic weight-control behaviors. Parents are encouraged to take responsibility for meal planning and preparation. Pediatricians can be helpful by reminding parents of the importance of fighting the disease effectively in the early stages, with the goals of reaching a truly healthy weight, resuming pubertal development, reversing medical complications, and restoring normal cognitions. Early weight gain (4–5 pounds by session 4, typically correlating with 4 weeks of treatment) is predictive of better outcomes in adolescents. 126 , 137 , 138 By phase 2, substantial weight recovery has occurred, and the adolescent gradually resumes responsibility for his or her own eating. By phase 3, weight has been restored, and the therapy shifts to address general issues of adolescent psychosocial development. 136 This therapy is detailed in manuals for providers 137 and families. 139 FBT with experienced providers is not available in all communities. Nevertheless, community providers may integrate the essential principles of FBT in their work with patients and families. 130
Parent-focused therapy is an adaptation of FBT wherein the therapist supports the parents to renourish the patient and limit weight-control behaviors but, after the initial appointment, meets only with the parents. 140 The patient has brief visits with a nurse or physician for the assessment of weight and acute mental health issues but is not directly involved with a therapist.
The role pediatricians serve in the care of an adolescent in FBT differs from the customary role of a physician with patients. 134 In the FBT setting, the pediatrician does not weigh the patient because that task is performed by the therapist. The pediatrician directs the care only when there are immediate medical safety concerns. If the pediatrician identifies an urgent medical issue that requires intervention or hospitalization, he or she is obligated to provide recommendations to the patient, the parents, and the primary therapist. For the medically stable patient, the pediatrician acts as a consultant to the parents and primary therapist. When a parent asks a question related to treatment, instead of directly advising the parents what to do, the pediatrician, ideally, redirects that treatment decision back to the parent: “You know your child the best. What do you think will best help in your child’s recovery?” In this way, the physician empowers parents to make their own decisions, enhancing their confidence to care for their ill child.
Day-Treatment Programs
Day-treatment programs (day hospitalization and partial hospitalization) provide an intermediate level of care for patients with eating disorders who are medically stable and do not require 24-hour supervision but need more than outpatient care. 133 , 141 These programs may prevent the need for higher levels of care or may be a “step-down” from inpatient or residential to outpatient care. Day treatment typically involves 8 to 10 hours per day of care (including meals, therapy, groups, and other activities) by a multidisciplinary staff 5 days per week. Reported evaluations of child and adolescent day-treatment programs are few and observational in design. 142 – 145 Despite the absence of systematic data supporting their usefulness, these programs are generally believed to have an important role in the continuum of care.
Residential Treatment
Residential treatment may be necessary for a minority of medically stable patients with eating disorders. Indications for residential treatment include a poor motivation for recovery, need for structure and supervision to prevent unhealthy behaviors (eg, food restriction, compulsive exercise), lack of a supportive family environment, absence of outpatient treatment in the patient’s locale, 146 or outpatient interventions having been unsuccessful. 133 Residential treatment typically includes 24 hour per day supervision, medical oversight, group-based psychoeducational therapy, nutritional counseling, individual therapy, and family therapy. The length of stay can be weeks to months, depending on the severity of illness and financial resources. Outcome studies reported by residential programs, generally, reveal improved symptomatology at discharge, 147 but the results at long-term follow-up are mixed. 148 , 149 However, few outcome studies are focused on adolescents, compare the efficacy of residential to outpatient treatment, or make comparisons across programs or treatment modalities.
Although some adolescents require this higher level of care, health care providers and families are encouraged to exercise caution when selecting a residential treatment program. The number of residential programs has more than tripled in the last decade, with many operated by for-profit companies. Marketing practices by some are questionable. 150 Outcome studies demonstrating program efficacy may be misleading because of a lack of rigorous design or peer review. 151 Until recently, there was no certification process to ensure program quality and safety. In 2016, The Joint Commission implemented new accreditation standards for behavioral health care organizations that provide outpatient or residential eating disorder treatment. 152 It remains to be seen how many programs will pursue this accreditation.
The National Eating Disorders Association Web site offers useful suggestions for evaluating treatment programs ( www.nationaleatingdisorders.org ).
Hospital-Based Stabilization
Suggested indications for the hospitalization of children and adolescents with eating disorders published by the Society for Adolescent Health and Medicine are listed in Table 6 .
The most common goal for hospital-based stabilization is nutritional restoration. Variation occurs with regard to how quickly hospitalized patients with AN are refed. 153 , 154 It is important to balance 2 competing goals: achieve weight gain swiftly and avoid refeeding syndrome. 155 Refeeding syndrome refers to the metabolic and clinical changes that occasionally occur when a malnourished patient is aggressively nutritionally rehabilitated; the hallmarks are hypophosphatemia and multiorgan dysfunction. 155 – 157 A systematic review of hospitalized adolescents with AN reported an average incidence of refeeding hypophosphatemia (without necessarily organ dysfunction) of 14%. 158 Over the past decade, a long followed maxim, “start low and go slow,” has been challenged. 87 , 155 Several centers have described starting calories at 1400 kcal or more per day, 154 including recent reports demonstrating safe treatment of mildly and moderately malnourished adolescents by using initial caloric prescriptions of 2200 to 2600 kcal per day, while achieving a weight gain of approximately 3 to 4.5 pounds per week. 159 , 160 Because the risk of refeeding hypophosphatemia may correlate with the degree of starvation, pediatricians may opt to take a more cautious approach in severely malnourished (<70% median BMI) children until further studies are reported. 87 , 154
Nasogastric tube (NGT) feeding may be necessary for some hospitalized adolescents, but opinions vary regarding when they should be initiated. 161 Most North American programs reserve NGT feeds for when patients are not able to complete meals; however, internationally, some centers report the routine use of NGT feeding, either exclusively at first or in combination with meals. 162 , 163 Potential benefits of NGT feeding include faster weight gain and medical stabilization, with a possibility for a reduced hospital length of stay. 162 , 163 Although viewed by some health care providers as invasive or punitive, others view NGT feeding as empathic, by reducing both physical and psychological pain in the early treatment stages. 161 There is insufficient evidence to recommend one approach over another. 154 Independent of whether NGT feeds are used routinely, physicians involved in the treatment of hospitalized medically unstable patients may be called on to provide nutrition via an NGT when nutritional needs are not being met. The use of total parenteral nutrition carries higher risks of medical complications, is costly, and is not recommended unless other forms of refeeding are not possible. 154
High-quality studies in which researchers examine the impact of inpatient care are limited, and the best end point for hospital treatment of children and adolescents is unclear. A US multicenter research collaborative showed that, in a national cohort of low-weight 9- to 21-year-olds with restrictive eating disorders, those who were hospitalized had a greater odds of being at 90% of the median BMI at 1-year follow-up. 164 However, a randomized controlled trial (RCT) of treatment of adolescent AN in the United Kingdom revealed no benefits of inpatient over outpatient care 165 ; this study was limited by poor adherence to the allocated treatment. An RCT in Germany in 2014 revealed that inpatient adolescents discharged earlier to outpatient treatment fared as well as those discharged later. 141 Similarly, an RCT conducted in Australia in 2015 revealed that adolescents who were discharged to FBT as soon as they were medically stable fared at least as well as adolescents who remained inpatients until achieving 90% of their treatment goal weight. 166 The recently reported average length of stay in the United States for patients admitted for medical stabilization by using higher caloric prescriptions was 3 to 12 days. 159 , 167 , 168
Pharmacotherapy for AN
A variety of medications have been studied for the treatment of AN, primarily in adults, but none have been approved for this indication by the US Food and Drug Administration (FDA). 169 Despite their demonstrated ineffectiveness, 170 more than one-half of adolescents with restrictive eating disorders are prescribed psychotropic medications, most likely in attempts to treat comorbid conditions, such as depression and anxiety. 171 Selective serotonin-reuptake inhibitors (SSRIs) have been tried but are not effective in acutely ill, malnourished patients and have not been shown to prevent disease relapse in those who are weight restored. 172 – 174 A number of atypical antipsychotic medications have also been studied, including quetiapine, risperidone, and olanzapine. Results have generally revealed little benefit in weight gain or improvement in eating-disorder thinking. 169 , 175 – 178 Initial studies of augmentation of SSRIs with atypical antipsychotics in adult patients have been promising. 179
The current recommendations to optimize bone health are full weight restoration with physiologic resumption of menses and supplementation with calcium and vitamin D. 79 , 81 , 87 , 115 Bisphosphonate treatment is not recommended. 79 , 87 , 115 Estrogen supplementation in the form of combined estrogen-progesterone oral contraceptive pills is not effective in enhancing BMD in adolescents with AN. 81 Small trials with transdermal estrogen 180 or with low-dose combined oral contraceptive pills plus dehydroepiandrosterone 181 have shown a positive effect on BMD compared with controls, but further studies are needed before these are considered standard care. Although cyclic vaginal bleeding may be induced with the use of exogenous hormones, this may reinforce a patient’s denial of the medical consequences of her disease and masks the spontaneous return of menses.
Most patients with BN and BED are managed in outpatient settings with the collaboration of a medical and mental health care providers as well as a dietitian, as needed.
Psychological treatment studies are more limited in BN compared with AN and are especially lacking in BED. 133 Cognitive behavioral therapy (CBT) has a modest evidence-base for BN and BED. 133 , 182 CBT explicitly recognizes the interrelationships among an individual’s thoughts, feelings, and actions, and its principles can be used by all disciplines. Reestablishing regular eating patterns is a central goal, and educating patients about the perpetuating nature of the restriction-binge-purge cycle is an early focus. Patients with BN and BED can minimize the urge to binge that is typically experienced late in the day, if they eat regularly throughout the day. Decreasing the binge amount and frequency may decrease guilt and shame and the ensuing negative self-assessment. During CBT, patients are taught to question their distorted thoughts and remodel their eating behaviors. 182
Although there is a manual to guide FBT for patients with BN, 183 it is based on more limited evidence than FBT for AN. 182 An RCT comparing FBT with CBT revealed patients in the FBT group were more likely to abstain from binge eating and purging at the end of the 18-week treatment (39% vs 20%) with no statistical difference (49% vs 32%) at 1-year follow-up. 184 There are no published studies in which researchers examine FBT for BED.
Pharmacotherapy for BN
As with other pharmacotherapy research, studies of treatment of BN have primarily been in adult subjects. Several pharmacologic agents, including SSRIs, have been demonstrated to be effective for the treatment of adult BN, although only fluoxetine has FDA approval. Although not approved for pediatric BN, fluoxetine is FDA approved for child and adolescent depression and obsessive-compulsive disorder, so it is a reasonable option if pharmacologic treatment of BN is considered. 169 The antiepileptic topiramate has been shown to significantly decrease binge eating in adults who do not respond to or are not able to tolerate SSRIs. However, cases of topiramate triggering eating disorder symptoms in adolescents have been reported. 185 Other drugs, including naltrexone and ondansetron, are being used with some success in adult BN, although data are lacking to recommend their use more broadly. 169
Pharmacotherapy for BED
Research on the treatment of binge eating lags behind that for other eating disorders and has been focused on adult subjects. SSRIs have rarely differed from placebo in their effect on BED and show no better outcome than behavioral therapy alone. Although the use of topiramate has been shown to reduce binge eating and help with weight loss, the rates of adverse effects are relatively high. 186 Lisdexamfetamine, a central nervous system stimulant approved for treatment of attention-deficit/hyperactivity disorder, was approved by the FDA in 2015 for the treatment of moderate to severe BED in adults. Although it has been demonstrated to reduce the frequency of binge-eating episodes, lisdexamfetamine is not indicated for weight loss. As with the use of other central nervous system stimulants, there is a potential for abuse and dependence as well as serious cardiovascular reactions. 187
ARFID is a relatively new diagnosis, and, consequently, there is limited literature describing treatment. 188 , 189 Because patients with ARFID vary in terms of underlying psychological motivations for restrictive eating, individualized behavioral treatment strategies are needed. 182 , 190 Despite varying characteristics of the disorder, the dual goals of refeeding and normalization of eating align with the goals of treating other eating disorders. A study of pediatric and young adult patients admitted with ARFID at a single academic medical center reported that ARFID patients were more likely to require enteral nutrition and stayed in the hospital longer than patients with AN. 9
No medication is specifically indicated for use in ARFID; pharmacotherapy is directed at treating underlying comorbid illness (eg, anxiety) as necessary.
The treatment of eating disorders is multidisciplinary, often long-term, and may require expensive, high-level care, such as inpatient stabilization or residential or partial hospitalization programs. The costs associated with treatment can create substantial financial burdens for families. 191 Having medical insurance, public or private, is no guarantee that these costs will be covered. 192 Insurance carriers are able to define their own criteria for eating disorder treatment, leading to wide variations in coverage from state to state. Some states do not identify eating disorders as life-threatening conditions, thereby limiting treatment coverage. State-sponsored public insurance plans may not cover out-of-state treatment programs, even when no comparable treatment programs exist within that state. Outpatient mental health providers who are willing to accept the lower payments from public insurance may have no expertise in treating eating disorders. Those who do and will see publicly insured patients or those in managed care plans typically limit the number of these patients in their panels. Private insurance may increase access to treatment but dictate lower levels and shorter periods of care than is indicated by a patient’s clinical status and health care provider recommendation. Families of patients with eating disorders typically will need assistance navigating the financial aspects of treatment. The National Eating Disorders Association offers general information online for families regarding financial coverage for treatment ( www.nationaleatingdisorders.org ).
The prognoses reported for adolescents with eating disorders vary widely, depending on research methodology, definitions of recovery, and duration of follow-up. Generally, adolescents have greater success in recovery from eating disorders than their adult counterparts, 193 with overall recovery rates of approximately 70%. 194
In a review of 11 adolescent eating disorder treatment programs, 54% of patients treated for restrictive disorders had restored to at least 90% of their median body weight (MBW) for age and height at 1-year follow-up. This is essential for catch-up growth and resumption of menses in girls. Two significant predictors of weight recovery were a higher percentage of MBW at initial presentation and shorter duration of symptoms, highlighting the importance of early identification of these disorders. Outcomes did not vary meaningfully across programs, suggesting that all treatment models were helpful. 195
In a more-recent study, researchers examined the weight restoration of patients from 14 adolescent treatment programs with a diagnosis of a restrictive eating disorder by DSM-5 criteria. At 1-year follow-up, those with ARFID were the least likely (43%) to have regained ≥90% MBW and were also more likely to be younger, have had a longer duration of symptoms, and have left treatment prematurely. Eighty-two percent of those with atypical AN and 64% of those with AN had regained ≥90% MBW. Having received a higher level of care (eg, partial hospitalization and/or residential care) did not increase the likelihood of weight recovery. Again, there were no significant differences in outcomes between programs, despite various treatment modalities. 196
Information on the long-term prognosis of adolescents with AN is limited. In a study of adolescents who completed a 12-month outpatient AN treatment study (either FBT or adolescent-focused therapy), approximately one-third of patients were in full remission 1 year after completion, with better rates in the FBT group (49%) than in the adolescent-focused therapy group (23%). 197 Follow-up in a convenience sample of the original study 2 to 4 years after treatment revealed less than 10% of patients relapsed, with no difference between the 2 groups. 198 An RCT comparing parent-focused therapy with FBT demonstrated equivalent outcomes between the groups at 12-month follow-up (37% vs 29%). 140
Information about recovery from BN, BED, and purging disorder in adolescents is less available but suggests higher rates of relapse and the development of comorbidities. Outcome studies on BN in adults reveal variable recovery rates, ranging from approximately 50% to 70% at 4- to 6-year follow-up, with relapse rates of 30% and about 25% having chronic disease. 194 A longitudinal study of adolescent girls with BED and purging disorders into early adulthood revealed that one-quarter of these girls started to use drugs other than marijuana, more than one-third began to binge drink frequently, and 27% demonstrated high levels of depressive symptoms. 199 Not surprisingly, misuse of drugs and alcohol among patients with eating disorders is associated with a poorer outcome or death. 193
Mortality rates among individuals with eating disorders are substantially elevated in comparison with those of the general population, with death typically occurring in adulthood. Premature death is 4 to 5 times higher for patients with AN and 2 to 3 times as high for those with BN. 200 – 203 Suicide rates are increased among patients with eating disorders 204 and, in one study, accounted for 30% deaths. 203 In a national survey of adolescents, 35% of those meeting criteria for BN, 15% of those meeting criteria for BED, and 8% of those meeting criteria for AN reported having made a suicide attempt. 205 The risk of suicide among patients with eating disorders appears to be declining and has been attributed to an increased recognition of eating disorders and effective treatment. 206
Efforts to prevent eating disorders may occur in clinical practice and community settings. By using sensitive, nonstigmatizing language and demonstrating supportive attitudes toward children and adolescents of all body shapes and sizes, pediatricians create a welcoming clinical setting for discussions about weight and weight-related behaviors. The American Academy of Pediatrics clinical report “Preventing Obesity and Eating Disorders in Adolescents” highlights steps that pediatricians can take to prevent both conditions. 207 These steps include focusing on healthy habits with patients and families rather than weight and dieting, encouraging more frequent family meals, discouraging “weight talk” and “weight teasing” in the home, closely monitoring weight loss in patients advised to lose weight, and promoting a healthy body image in all children and adolescents. 207 Pediatricians may also advise teachers, coaches, and athletic trainers about healthy approaches to nutrition and exercise, raise awareness of the detrimental effects of weight stigmatization, and alert them to the warning signs of eating disorders.
Pediatricians can join others in advocating for improved access to quality eating disorder treatment services. The limited availability of developmentally appropriate mental health services, lack of mental health parity, and service “carve-outs” all have been barriers to patients and families who seek necessary treatment and seem to be disproportionately problematic for patients with eating disorders. Despite evidence of its effectiveness, FBT is not available in many communities. Through advocacy, pediatricians can help support health care reform efforts that will enable children and adolescents with eating disorders to access necessary care.
Pediatricians should be knowledgeable about the variety of risk factors and early signs and symptoms of eating disorders in both male and female children and adolescents. Pediatricians should screen patients for disordered eating and unhealthy weight-control behaviors at annual health supervision visits. Pediatricians should evaluate weight, height, and BMI by using age- and sex-appropriate charts, assess menstrual status in girls, and recognize the changes in vital signs that may signal the presence of an eating disorder.
When an eating disorder is suspected, pediatricians, in conjunction with appropriate consultants, should initiate a comprehensive evaluation of the patient that includes both medical and psychological assessments as well as suicide risk appraisal. Once diagnosed, patients should be monitored for medical and nutritional complications by their pediatrician or referred to other qualified practitioners for medical oversight.
To facilitate multidisciplinary care, pediatricians should refer their patients with eating disorders to treatment resources in their region when available. Ideally, these treatment program providers should have expertise in the unique developmental needs of this age group.
Pediatricians are encouraged to advocate for legislation and policy changes that ensure appropriate services for patients with eating disorders, including medical care, nutritional intervention, mental health treatment, and care coordination, in settings that are appropriate for the developmental level of the patient and severity of the illness.
Clinical reports from the American Academy of Pediatrics benefit from expertise and resources of liaisons and internal (AAP) and external reviewers. However, clinical reports from the American Academy of Pediatrics may not reflect the views of the liaisons or the organizations or government agencies that they represent.
The guidance in this report does not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate.
All clinical reports from the American Academy of Pediatrics automatically expire 5 years after publication unless reaffirmed, revised, or retired at or before that time.
Drs Hornberger and Lane were equally responsible for conceptualizing, writing, and revising the manuscript and considering input from all reviewers and the board of directors; and all authors approve the final manuscript as submitted.
This document is copyrighted and is property of the American Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American Academy of Pediatrics. Any conflicts have been resolved through a process approved by the Board of Directors. The American Academy of Pediatrics has neither solicited nor accepted any commercial involvement in the development of the content of this publication.
FUNDING: No external funding.
anorexia nervosa
avoidant/restrictive food intake disorder
binge-eating disorder
bone mineral density
bulimia nervosa
blood pressure
cognitive behavioral therapy
Diagnostic and Statistical Manual of Mental Disorders Fifth Edition
family-based treatment
Food and Drug Administration
home, activities, drugs/diet, sexuality, suicidality/depression
left ventricular
median body weight
nasogastric tube
randomized controlled trial
selective serotonin-reuptake inhibitor
Laurie L. Hornberger, MD, MPH
Margo A. Lane, MD, FRCPC
Cora C. Breuner, MD, MPH, Chairperson
Elizabeth M. Alderman, MD, FSAHM
Laura K. Grubb, MD, MPH
Makia Powers, MD, MPH
Krishna Kumari Upadhya, MD
Stephenie B. Wallace, MD
Laurie L. Hornberger, MD, MPH – Section on Adolescent Health
Margo A. Lane, MD FRCPC – Canadian Pediatric Society
Meredith Loveless, MD – American College of Obstetricians and Gynecologists
Seema Menon, MD – North American Society of Pediatric and Adolescent Gynecology
Lauren Zapata, PhD, MSPH – Centers for Disease Control and Prevention
Liwei Hua, MD, PhD – American Academy of Child and Adolescent Psychiatry
Karen Smith
James Baumberger, MPP
Competing Interests
Advertising Disclaimer »
Citing articles via
Email alerts.

Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Connection denied by Geolocation Setting.
Reason: Blocked country: Russia
The connection was denied because this country is blocked in the Geolocation settings.
Please contact your administrator for assistance.
- Open access
- Published: 29 April 2024
Self-reported health related quality of life in children and adolescents with an eating disorder
- A. Wever ORCID: orcid.org/0000-0002-8877-5876 1 ,
- E. van Gerner 2 ,
- J.C.M Jansen 3 &
- B. Levelink 1
BMC Psychology volume 12 , Article number: 242 ( 2024 ) Cite this article
Metrics details
Eating disorders in children and adolescents can have serious medical and psychological consequences. The objective of this retrospective quantitative study is to gain insight in self-reported Health Related Quality of Life (HRQoL) of children and adolescents with a DSM-5 diagnosis of an eating disorder.
Collect and analyse data of patients aged 8–18 years, receiving treatment for an eating disorder. At the start and end of treatment patients completed the KIDSCREEN-52, a questionnaire measuring HRQoL.
Data of 140 patients were analysed. Children diagnosed with Anorexia Nervosa, Bulimia Nervosa, and Other Specified Feeding or Eating Disorder all had lower HRQoL on multiple dimensions at the start of treatment, there is no statistically significant difference between these groups. In contrast, patients with Avoidant Restrictive Food Intake Disorder only had lower HRQoL for the dimension Physical Well-Being. HRQoL showed a significant improvement in many dimensions between start and end of treatment, but did not normalize compared to normative reference values of Dutch children.
The current study showed that self-reported HRQoL is low in children with eating disorders, both at the beginning but also at the end of treatment. This confirms the importance of continuing to invest in the various HRQoL domains.
Peer Review reports
Eating disorders in children and adolescents can have serious medical and psychological consequences and rank 12th on the list of physical and mental conditions amongst woman aged 15–19 years in high-income countries when looking at the global burden of disease [ 1 , 2 ]. The estimated lifetime prevalence of Anorexia Nervosa (AN) in woman is 1–4% and 1–2% for Bulimia Nervosa (BN), and the epidemiology is changing, with increasing rates of eating disorders in younger children, boys and minority groups [ 2 , 3 ].
The past two decades research on health-related quality of life (HRQoL) in patients with an eating disorder has increased [ 4 , 5 , 6 , 7 , 8 ]. HRQoL is a subjective evaluation of the overall health of an individual, as well as the health of underlying subdimensions of physical, psychological and social functioning [ 9 ]. Most studies have been conducted in adults and a recent review and meta-analysis both show that eating disorders are associated with significant impaired HRQoL compared with the healthy population [ 10 , 11 ]. To our knowledge only one other study evaluated the impact of eating disorders on HRQoL in children and adolescents. Jenkins et al. looked at the impact of eating disorders in a group of adolescents seeking treatment for AN, BN or eating disorder not otherwise specified (EDNOS) [ 6 ]. This study reported a poorer HRQoL measured with the SF-36 Health Survey in adolescents with an eating disorder compared with adolescent norms for the Swedish population [ 6 ]. Two studies included both children and adolescents. Weigel et al. examined the association between disorder specific factors, comorbidity and HRQoL in anorexia nervosa in adolescents and adults. HRQoL was measured using the visual analogue scale (EQ-VAS) a generic scale that does not look to different HRQoL domains [ 12 ]. Ackard et al. assessed quality of life in patients diagnosed with an eating disorder, mean age at initial assessment was 20.6 years (SD 5 8.3 years), with a range of 12–53 years. Children were not assessed separatly. Other studies in children and adolescents focused on disordered eating behaviours, but not diagnosed eating disorders [ 4 ]. A review of population-based studies showed that disordered eating attitudes and behaviours were associated with lower HRQoL in children and adolescents [ 9 ]. Herpertz-Dahlmann and colleagues found a poorer HRQoL in adolescents with self-reported disordered eating, and an association between eating disorder symptoms and psychopathology [ 13 ].
Because treating an eating disorder encompasses more than weight gain alone it is important to know the possible impact of an eating disorder on HRQoL [ 14 ]. As there are still few studies on self-reported HRQoL in children and adolescents with a diagnosed eating disorder, the primary aim of this study is to gain more insight in the different domains of self-reported HRQoL in a clinical sample of children and adolescents with a DSM-5 diagnosis of an eating disorder at the beginning of treatment. In addition, changes of HRQoL between start and end of treatment were evaluated to determine whether treatment influences HRQoL and if so which domains.
Participant
Data of patients who were diagnosed conform the Diagnostic and Statistical Manual of Mental Disorders (DSM) -IV-TR/DSM-5 criteria for an eating disorder, and receiving treatment between November 2006 and April 2019 at The Mutsaersstichting were used [ 15 , 16 ]. The Mutsaersstichting is a mental healthcare institute specialised in eating disorders in the Netherlands where children between 0 and 18 years receive both in- and outpatient treatment. At first presentation, every patient received an extensive consultation with a child and youth psychologist, a child and youth psychiatrist and a paediatrician. Based on this information DSM-IV-TR and DSM-5 classification were made. Patients diagnosed before 2014 were rediagnosed using the DSM-5 classification, especially using the new criteria for Avoidant Restrictive Food Intake Disorder (ARFID). Subsequently, a personalized treatment plan was presented to the family. Treatment always consisted of a combination of family-based treatment, individual treatment, group treatment and physical follow-up. Data from patients who met the DSM-5 diagnosis for AN, BN, ARFID, Binge Eating Disorder (BED), or OSFED were considered eligible for analyses. Because the study specifically focused on self-reported HRQoL, only data of children between the ages of 8 and 18 were included, since for younger children the parents completed the HRQoL questionnaire. Children and adolescents who only had HRQoL reports completed by the parents were excluded. Ethical approval was obtained from the medical ethics committee of the Maastricht University Medical Centre.
As part of the Routine Outcome Monitoring the KIDSCREEN-52 questionnaire was sent to every patient who sought treatment for an eating disorder at the Mutsaersstichting. Baseline characteristics and clinical data were collected at the start and end of treatment. At first consultation, patient characteristics including age, sex, underlying diseases, eating attitudes and behaviours, compensatory behaviour and sociodemographic data were obtained. Heart rate and blood pressure were measured with an oscillometric blood pressure machine and evaluated according to the Clinical Practice Guidline of the American Acadamy of Pediatrics [ 17 ]. In addition, a full physical examination was performed. Body Mass Index (BMI) was calculated from measured weight and height [ 18 ]. Growth charts designed by the Dutch organization for applied scientific research (TNO) were used to determine height for age (standard deviation, SD) and weight for height (SD) [ 19 , 20 ]. At the end-evaluation data was collected concerning most recent height, weight, BMI and eating attitudes and behaviours.
The KIDSCREEN-52 is a validated self-report questionnaire for measuring HRQoL in European children between 8 and 18 years old [ 21 , 22 , 23 , 24 , 25 ]. It consists of 52 questions, divided into 10 dimensions: Physical Well-being, Psychological Well-being, Moods and Emotions, Self-Perception, Autonomy, Parent Relations and Home Life, Social Support and Peers, School Environment, Social Acceptance (Bullying), and Financial Resources. The KIDSCREEN-52 uses 5-point Likert scale responses, within each different dimension the results are converted into a Rasch scale. Cronbach–alpha’s vary between 0.77 and 0.89 [ 25 ]. The results are transformed to a t-score, giving the children in the total reference population a mean t-score of 50 with a SD of 10. Specific reference populations are made by country, gender and age groups. The results of this study are compared with the validated normative reference values of Dutch children in the age between 8 and 18 years old [ 25 ]. Ulrike Ravens-Sieberer defined a mean t-score 0.5 SD below the mean t-score of the specific referential population of a country as a low HRQoL and a t-score 0.5 SD above the mean t-score of the referential population as high HRQoL [ 25 ].
Data analysis
All statistical analyses were performed using IBM SPSS Statistics version 25 [ 26 ]. The Mann-Withney U, χ 2 , and fisher exact test were used to determine whether there were statistical differences between all the children and adolescents included in this study and the children who completed the questionnaire at intake and end-evaluation. Paired t test was used to test for statistically significant differences in HRQoL between start- and end of treatment. To test the differences in t-score on the KIDSCREEN-52 stratified for DSM-classification, a one-way ANOVA and Welch test was done, with the Tukey’s Test as a post-hoc analysis. Statistically significance was considered when the result had a p value of < 0.05. Univariate regression analysis was done in the group diagnosed with AN to test whether there is an association between HRQoL and BMI, BMI SD, age, excessive exercise and binge eating. Since purging only occurred in four patients this could not be included in the analysis. Other DSM-5 diagnoses where not included due to small subgroup sample size.
Baseline characteristics
Data of 276 patients were analysed of which 140 were found eligible for this study (Fig. 1 ). Baseline characteristics are presented in Table 1 . The total population consisted primarily of female children and adolescents ( n = 119; 85%) with a mean age of 15.0 years ranging from 8 to 18 years. Almost half of the population was classified as AN ( n = 68; 48.6%). The mean weight for children with AN ( n = 67) was 44.1 kg (minimal weight 25 kg– maximal weight 59 kg) with a mean weight SD of -1.6 and mean BMI of 15.9 kg/m 2 (minimal BMI 11.9 kg/m 2 – maximal BMI 19.9 kg/m 2 ). Children with ARFID had a mean weight of 31.9 kg (minimal weight 18 kg– maximal weight 105 kg), mean weight SD– 0.6, mean BMI 15.9 kg/m 2 (minimal BMI 12.1 kg/m 2 – maximal BMI 36.3 kg/m 2 ). Only two patients were diagnosed with BED, this was too small a sample size to be included in results stratified for the DSM-5 criteria. No significant differences were found in the baseline characteristics between children who completed the KIDSCREEN-52 only at the beginning of treatment, and those who completed the questionnaire both at the start and end-evaluation ( n = 47), except for psychiatric co-morbidities ( X 2 (1) = 4.97; p = 0.026). Even though the effect size for this finding, Cramer’s V = 0.188, was weak, due to the known association between psychiatric co-morbidities and eating disorder symptoms, a comparison between HRQoL at the beginning and end of treatment was only made within the group of 47 patients that completed both questionnaires [ 13 , 27 , 28 ].
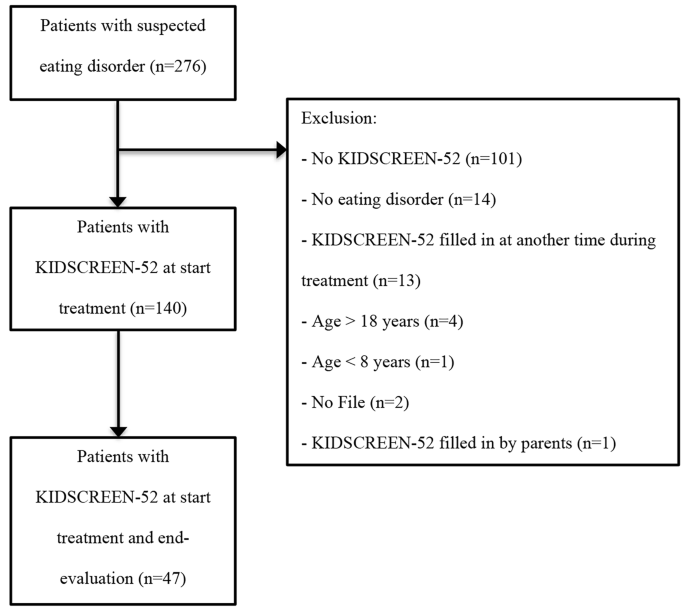
HRQoL at the start of treatment
Table 2 shows mean t-scores scored by children and adolescents on the KIDSCREEN-52 at the start of treatment, stratified for the DSM-5 criteria. Children with the diagnosis AN, BN and OSFED all had a lower HRQoL (≤ 0.5 SD of mean score) than the reference population for the dimensions Physical Well-being, Psychological Well-being, Moods and Emotions, Self-Perception, Autonomy, Financial Resources, Peers and Social Support, School Environment and Bullying. There were no statistically significant differences in t-scores between AN, BN and OSFED. This was confirmed with a Turkey’s post hoc test. Compared with the reference population the HRQoL in patients with ARFID was only lower for the dimension Physical Well-Being. For the dimensions Physical Well-being, Psychological Well-being, Moods and Emotions, Self-Perception, Autonomy, Parent Relations and Home Life and School Environment the t-scores of children with ARFID were significantly higher than those of the children who met criteria of all other eating disorders. Social Support and Peers was significantly higher in patients with ARFID compared to AN, but not with BN and OSFED. Univariate regression analysis in the group diagnosed with AN showed a significant association between a higher t-score on the domain Physical Well-being and higher BMI, BMI SD. Other variables were not associated with a higher or lower t-score.
HRQoL change between start and end of treatment
In Table 3 mean t-scores of the KIDSCREEN-52 at the start of treatment are compared with t-scores at the end evaluation. HRQoL showed a significant improvement in mean t-scores before and after treatment for Physical Well-being (t (46) = -4.4, p < 0.001), Psychological Well-being (t (45) = − 3.0, P = 0.004), Moods and emotions (t (45) = -3.3, p = 0.002) Self Perception (t (45) = -3.7, p = 0.001) and School environment (t (44) = -2.8, p = 0.008). However, after treatment the HRQoL for these dimensions did not normalize compared to normative reference values of Dutch children. The subgroup sample sizes were too small for findings relating to change in QoL before and after treatment to be stratified by diagnosis.
This study shows that the self-reported HRQoL in children and adolescents receiving outpatient treatment in the Netherlands for an eating disorder is significantly lower on multiple dimensions at the beginning and end of treatment compared with the reference population. Most studies that have been conducted in children and adolescents are population-based studies that focus on disordered eating behaviours, yet they also show a significantly decreased mental HRQoL [ 9 , 13 , 29 , 30 , 31 , 32 , 33 , 34 ]. The study of Jenskins, showed similar results in a group of sixty-seven adolescents seeking treatment for an eating disorder [ 6 ].
The domain physical well-being is significantly lower for all types of eating disorders. This finding replicates that of Winkler et al. in which compared to the controls, adult women with AN had significantly impaired HRQoL as measured by the Eating Disorders Quality of Life (EDQOL) scale including lower physical functioning [ 35 ]. Yet several other studies showed only a significantly lower mental component summary and normal levels in the psychical component summary scored with Short Form-36 Health Survey (SF-36) [ 4 , 6 , 14 , 36 ]. This difference could partially be explained by the use of different questionnaires, where some questionnaires could reflect the physical pathology of eating disorders rather than real physical health. The KIDSCREEN-52 for example specifically asked for fatigue, where other questionnaires ask for the ability to walk the stairs. When diagnosed with AN extensive exercise might be associated with the disease itself. Disease severity and duration of the eating disorder might also influence results. Children and adolescents in our study received one or more previous treatments in 55% of the patients and in 34% had a disease duration of more than one year. To gain more insight a univariate regression analysis was done in the group diagnosed with AN, which showed a significant association between a higher BMI and higher t-score on the domain Physical Well-being, suggesting that the results as shown within this study might be a reflection of real physical health rather than psychopathology.
When comparing AN, BN and OSFED this study does not find statistically significant differences similar as the meta-analysis on quality of life by Winkler et al. suggesting a similarity between these eating disorders with regard to HRQoL [ 35 ]. Notable exception to this are the children and adolescents with ARFID, who only score lower on the item Physical Well-being, unlike the children and adolescents classified with all other eating disorders who have lower scores on almost all HRQoL dimensions. This suggests that HRQoL affects children with ARFID differently. Hay et al. compared adults and adolescents from the age of 15 years with ARFID in the Australian population to other eating disorders and found, unlike the current study, a normal physical HRQoL and a significantly lower mental HRQoL [ 37 ]. A Dutch study by Krom et al., in which children were treated for ARFID in a Diagnostic Centre for Feeding Problems showed that the HRQoL, reported by their parents using TNO-AZL Preschool Children Quality of Life (TAPQOL) was significantly lower on the subscales appetite, lungs, stomach, motor functioning, and positive mood and liveliness, suggesting that both physical and mental HRQoL was affected [ 38 ]. The difference in mental HRQoL between the current study and the study by Krom et al. might be explained by an overestimation by parents of the child’s psychosocial functioning due to parent’s own concerns, and besides that it might be caused by age differences. Another explanation could be that ARFID differs from longer recognised disorders such as anorexia nervosa and bulimia nervosa in that they do not have a core psychopathology of body image disturbance or weight/shape overvaluation. Given that in adolescent and young adult women at least, it is clear that overvaluation of weight/shape is very strongly associated with impairment in quality of life including but not limited to the mental health domain, it is not too surprising that children and adolescents with a diagnosis of ARFID report relatively little impairment in mental HRQoL [ 39 , 40 ]. The lower physical HRQoL that is seen in the current study might be explained by nutritional deficits often seen in children with ARFID [ 41 ].
The HRQoL shows significant improvement after treatment in all dimensions except for Autonomy and Social Support and Peers. However, HRQoL does not normalize compared to the reference population, and stays significantly impaired. This finding is consistent with considerations of other studies, namely that symptom remission alone is not sufficient for improvement in quality of life [ 42 ]. Studies looking at the long-term effects of eating disorders show that the long-term HRQoL after treatment continues to improve but is still not normalized after 8- or 30-years [ 14 , 42 , 43 , 44 ]. Thus follow-up, with paying attention to HRQoL, should continue longer than the initial treatment. Similar to our results, greatest improvement in HRQoL was noted in the physical functioning domain [ 43 , 44 ]. With childhood and adolescence being a critical period of development, the current study underlines the importance of treatment in which the success of the treatment is not based on BMI or amount of food intake alone, but focuses on other quality of life factors, such as psychological well-being, autonomy and social support.
There are limitations to this study. Due to the small subgroup sample size findings in the change in HRQoL before and after treatment could not be stratified by diagnosis. This study enrolled participants during a 14-year period, this longer period could have confounded the results due to changes in the care and treatments. Also, the retrospective nature of this study and the use of a generic HRQoL scale needs to be taken into consideration. Using generic HRQoL scales could give an over or underestimation of the HRQoL, since it does not focus specific on eating disorders, and questions for example about physical wellbeing could be an expression of the eating disorder rather than healthy behaviour. Our patients received both in- and outpatient treatment, which implies a certain disease severity and might not be generalizable to patients in other settings. HRQoL at the start of treatment could be lower or higher depending on the setting. Even though the children who completed the KIDSCREEN-52 only at the beginning of treatment and those who completed the questionnaire both at the start and end-evaluation are comparable, a large number of patients did not fill in the KIDSCREEN-52 at end-evaluation which might influence the outcome of quality of life after treatment, especially if the patients that did recover are the ones that did not fill in the questionnaire.
However, despite the limitations this descriptive study gives insight in the self-reported HRQoL of children and adolescents in the Netherlands treated for an eating disorder. It shows a significant reduction in both mental and physical HRQoL compared to the reference population with the exception of ARFID in which only physical HRQoL is impaired. This study also shows that even after treatment, children do not achieve normal HRQoL, which poses a potential risk to their development. Long-term follow-up of these children seems important, and more research is needed focusing on the effect of using quality of life parameters as most important measurements for recovery.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
Anorexia Nervosa
Avoidant Restrictive Food Intake Disorder
Binge Eating Disorder
Body Mass Index
Bulimia Nervosa
Diagnostic and Statistical Manual of Mental Disorders
Eating Disorders Quality of Life
Eating disorder not otherwise specified
Health-related quality of life
Standard deviation
36-Short Form-36 Health Survey
TNO-AZL Preschool Children Quality of Life
Erskine HE, Whiteford HA, Pike KM. The global burden of eating disorders. Curr Opin Psychiatry. 2016;29(6):346–53.
Article PubMed Google Scholar
Campbell K, Peebles R. Eating disorders in children and adolescents: state of the art review. Pediatrics. 2014;134(3):582–92.
Keski-Rahkonen A, Mustelin L. Epidemiology of eating disorders in Europe: prevalence, incidence, comorbidity, course, consequences, and risk factors. Curr Opin Psychiatry. 2016;29(6):340–5.
Ackard DM, Richter S, Egan A, Engel S, Cronemeyer CL. The meaning of (quality of) life in patients with eating disorders: a comparison of generic and disease-specific measures across diagnosis and outcome. Int J Eat Disord. 2014;47(3):259–67.
Engel SG, Adair CE, Las Hayas C, Abraham S. Health-related quality of life and eating disorders: a review and update. Int J Eat Disord. 2009;42(2):179–87.
Jenkins PE, Hoste RR, Doyle AC, Eddy K, Crosby RD, Hill L, et al. Health-related quality of life among adolescents with eating disorders. J Psychosom Res. 2014;76(1):1–5.
Krom H, van der Sluijs Veer L, van Zundert S, Otten MA, Benninga M, Haverman L, Kindermann A. Health related quality of life of infants and children with avoidant restrictive food intake disorder. Int J Eat Disord. 2019;52(4):410–8.
Article PubMed PubMed Central Google Scholar
Chou B, Bohn JA, Mairs R. Acute abdominal pain caused by hematometra in an adolescent female: a case report. J Med Case Rep. 2016;10(1):369.
Wu XY, Yin WQ, Sun HW, Yang SX, Li XY, Liu HQ. The association between disordered eating and health-related quality of life among children and adolescents: a systematic review of population-based studies. PLoS ONE. 2019;14(10):e0222777.
Ágh T, Kovács G, Supina D, Pawaskar M, Herman BK, Vokó Z, Sheehan DV. A systematic review of the health-related quality of life and economic burdens of anorexia nervosa, bulimia nervosa, and binge eating disorder. Eat Weight Disord. 2016;21(3):353–64.
Winkler LA, Christiansen E, Lichtenstein MB, Hansen NB, Bilenberg N, Støving RK. Quality of life in eating disorders: a meta-analysis. Psychiatry Res. 2014;219(1):1–9.
Weigel A, Konig HH, Gumz A, Lowe B, Brettschneider C. Correlates of health related quality of life in anorexia nervosa. Int J Eat Disord. 2016;49(6):630–4.
Herpertz-Dahlmann B, Wille N, Holling H, Vloet TD, Ravens-Sieberer U, group Bs. Disordered eating behaviour and attitudes, associated psychopathology and health-related quality of life: results of the BELLA study. Eur Child Adolesc Psychiatry. 2008;17(Suppl 1):82–91.
de la Rie SM, Noordenbos G, van Furth EF. Quality of life and eating disorders. Qual Life Res. 2005;14(6):1511–22.
[APA] APA. Diagnostic and statistical manual of mental disorders: DSM-IV. (1994). Washington, DC:1994.
Association AP. Diagnostic and Statistical Manual of Mental Disorders. Diagnostic and Statistical Manual of Mental Disorders. Fifth ed2013.
Abaied JL, Wagner C, Breslend NL, Flynn M. Respiratory sinus arrhythmia as a predictor of eating disorder symptoms in college students: moderation by responses to stress and parent psychological control. Eat Behav. 2016;21:109–15.
Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;7(4):284–94.
Schonbeck Y, Talma H, van Dommelen P, Bakker B, Buitendijk SE, HiraSing RA, van Buuren S. The world’s tallest nation has stopped growing taller: the height of Dutch children from 1955 to 2009. Pediatr Res. 2013;73(3):371–7.
Schonbeck Y, van Dommelen P, HiraSing RA, van Buuren S. Trend in height of Turkish and Moroccan children living in the Netherlands. PLoS ONE. 2015;10(5):e0124686.
Ravens-Sieberer U, Erhart M, Rajmil L, Herdman M, Auquier P, Bruil J, et al. Reliability, construct and criterion validity of the KIDSCREEN-10 score: a short measure for children and adolescents’ well-being and health-related quality of life. Qual Life Res. 2010;19(10):1487–500.
Ravens-Sieberer U, Gosch A, Rajmil L, Erhart M, Bruil J, Duer W, et al. KIDSCREEN-52 quality-of-life measure for children and adolescents. Expert Rev Pharmacoecon Outcomes Res. 2005;5(3):353–64.
Ravens-Sieberer U, Gosch A, Rajmil L, Erhart M, Bruil J, Power M, et al. The KIDSCREEN-52 quality of life measure for children and adolescents: psychometric results from a cross-cultural survey in 13 European countries. Value Health. 2008;11(4):645–58.
Ravens-Sieberer U, Herdman M, Devine J, Otto C, Bullinger M, Rose M, Klasen F. The European KIDSCREEN approach to measure quality of life and well-being in children: development, current application, and future advances. Qual Life Res. 2014;23(3):791–803.
Ravens-Sieberer U. The Kidscreen questionnaires: quality of life questionnaires for children and adolescents; handbook. Pabst Science Publ.; 2006.
IBM Corp. Released 2017. IBM SPSS statistics for Windows VA, NY: IBM Corp.
Padierna A, Quintana JM, Arostegui I, Gonzalez N, Horcajo MJ. The health-related quality of life in eating disorders. Qual Life Res. 2000;9(6):667–74.
Jenkins PE, Hoste RR, Meyer C, Blissett JM. Eating disorders and quality of life: a review of the literature. Clin Psychol Rev. 2011;31(1):113–21.
Ackard DM, Fulkerson JA, Neumark-Sztainer D. Psychological and behavioral risk profiles as they relate to eating disorder diagnoses and symptomatology among a school-based sample of youth. Int J Eat Disord. 2011;44(5):440–6.
Zeiler M, Waldherr K, Philipp J, Nitsch M, Dur W, Karwautz A, Wagner G. Prevalence of eating Disorder Risk and associations with Health-related quality of life: results from a large school-based Population Screening. Eur Eat Disord Rev. 2016;24(1):9–18.
Stice E, Marti CN, Shaw H, Jaconis M. An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. J Abnorm Psychol. 2009;118(3):587–97.
Gelin Z, Fuso S, Hendrick S, Cook-Darzens S, Simon Y. The effects of a multiple family therapy on adolescents with eating disorders: an outcome study. Fam Process. 2015;54(1):160–72.
Kenny B, Bowe SJ, Taylor CB, Moodie M, Brown V, Hoban E, Williams J. Longitudinal relationships between sub-clinical depression, sub-clinical eating disorders and health-related quality of life in early adolescence. Int J Eat Disord. 2023;56(6):1114–24.
Mitchell TB, Steele RG. Bidirectional associations between Disordered Eating and Health-Related Quality of Life in Elementary School-Age Youth. J Pediatr Psychol. 2017;42(3):315–24.
PubMed Google Scholar
Winkler LA, Gudex C, Lichtenstein MB, Roder ME, Adair CE, Sjogren JM, Stoving RK. Explanatory factors for Disease-Specific Health-Related Quality of Life in Women with Anorexia Nervosa. J Clin Med. 2021;10(8).
Mitchison D, Hay P, Mond J, Slewa-Younan S. Self-reported history of anorexia nervosa and current quality of life: findings from a community-based study. Qual Life Res. 2013;22(2):273–81.
Hay P, Mitchison D, Collado AEL, Gonzalez-Chica DA, Stocks N, Touyz S. Burden and health-related quality of life of eating disorders, including Avoidant/Restrictive Food Intake Disorder (ARFID), in the Australian population. J Eat Disord. 2017;5:21.
Krom H, van Oers HA, van der Sluijs Veer L, van Zundert SMC, Otten MGM, Haverman L, et al. Health-Related Quality of Life and Distress of parents of children with avoidant restrictive food intake disorder. J Pediatr Gastroenterol Nutr. 2021;73(1):115–24.
Mond JM, Hay PJ, Rodgers B, Owen C. Mental health impairment associated with eating-disorder features in a community sample of women. J Ment Health. 2011;20(5):456–66.
Wagner AF, Stefano EC, Cicero DC, Latner JD, Mond JM. Eating disorder features and quality of life: does gender matter? Qual Life Res. 2016;25(10):2603–10.
Bryant-Waugh R. Avoidant/Restrictive food intake disorder. Child Adolesc Psychiatr Clin N Am. 2019;28(4):557–65.
Pohjolainen V, Koponen S, Rasanen P, Roine RP, Sintonen H, Karlsson H. Long-term health-related quality of life in eating disorders. Qual Life Res. 2016;25(9):2341–6.
Dobrescu SR, Dinkler L, Gillberg C, Rastam M, Gillberg C, Wentz E. Anorexia nervosa: 30-year outcome. Br J Psychiatry. 2020;216(2):97–104.
Padierna A, Quintana JM, Arostegui I, Gonzalez N, Horcajo MJ. Changes in health related quality of life among patients treated for eating disorders. Qual Life Res. 2002;11(6):545–52.
Download references
Acknowledgements
Not applicable.
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and affiliations.
Department of Paediatrics, Maastricht University Medical Centre (MUMC+), P. Debyelaan 25, 6229 HX, Maastricht, The Netherlands
A. Wever & B. Levelink
Department of Primary care, Radboud University Medical Centre, Geert Grooteplein Zuid 10, 6525 GA, Nijmegen, The Netherlands
E. van Gerner
Department of Child and Youth Psychiatry, Postweg 88, 5915 HB, De Mutsaersstichting, Venlo, The Netherlands
J.C.M Jansen
You can also search for this author in PubMed Google Scholar
Contributions
CRediT author statement: A Wever: Writing - Original Draft, E. van Gerner: Formal analysis and Investigation, J.C.M. Jansen: Conceptualization and Writing - Review & Editing, B Levelink: Conceptualization and Writing - Review & Editing.
Corresponding author
Correspondence to A. Wever .

Ethics declarations
Ethics approval and consent to participate.
The medical ethics committee of the Maastricht University Medical Centre was consulted for ethical approval (METC 2019 − 1027). The medical ethics committee stated that the Medical Research Involving Human Subjects Act (WMO) does not apply to this study. The need for informed consent was waived by medical ethics committee of the Maastricht University Medical Centre, because Medical Research Involving Human Subjects Act (WMO) does not apply to this study. This research was performed following the Dutch legislation that applies to retrospective research, Agreement on Medical Treatment Act (Wet op de geneeskundige behandelingsovereenkomst, WGBO, in Dutch), from the Dutch Civil Code.
Consent for publication
Competing interests.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wever, A., van Gerner, E., Jansen, J. et al. Self-reported health related quality of life in children and adolescents with an eating disorder. BMC Psychol 12 , 242 (2024). https://doi.org/10.1186/s40359-024-01684-y
Download citation
Received : 27 November 2023
Accepted : 25 March 2024
Published : 29 April 2024
DOI : https://doi.org/10.1186/s40359-024-01684-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health Related Quality of Life
- Adolescents
- Eating disorder
- Anorexia nervosa
- Avoidant/Restrictive food intake disorder
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
Logo Left Content

Logo Right Content
Stanford University School of Medicine blog

More kids are being hospitalized for eating disorders — researchers learned why
Over the last decade, physicians have taken a broader view of adolescent eating disorders, thanks to a growing recognition of the variety of disordered eating patterns that can harm patients' health, especially their heart function.
As a result, hospitalization rates for adolescent eating disorders have climbed six- to seven-fold since 2010, according to a new Stanford Medicine-led study published recently in Hospital Pediatrics .
Much of the increase comes from patients who might not have been diagnosed with disordered eating in the past, including young people treated for atypical anorexia. These individuals are not underweight when diagnosed, but have undergone dangerously rapid weight loss.
More teens are also being diagnosed with a condition called avoidant/restrictive food intake disorder. In ARFID, which was formally recognized in 2013, patients struggle to eat enough for reasons that aren't related to body image.
Like other eating disorders with a longer medical history -- including typical anorexia nervosa and bulimia nervosa -- atypical anorexia and ARFID can cause dangerously low blood pressure and very slow, unstable heart rate, sometimes leading to heart failure.
Eating disorders have the highest mortality rate of any psychiatric disorder. We have an opportunity here to save lives. Megen Vo
"Eating disorders have the highest mortality rate of any psychiatric disorder," said the study's senior author, Megen Vo , MD, medical director of the Eating Disorders Outpatient Clinic at Stanford Medicine. "We have an opportunity here to save lives."
Because speedy intervention is the best predictor of successful eating disorder treatment, parents also need to recognize that eating disorders may look different from what they expect, Vo said. The study helps confirm what she sees in her treatment of patients through the Comprehensive Eating Disorders Program at Stanford Medicine Children's Health: Young people benefit when parents quickly realize that their children are in crisis and when their pediatricians are ready to take immediate action.
"We live in a time where there is a crisis of body shaming, body image dissatisfaction and diet culture," Vo said. "Eating disorders are not within a person's control; they're not something someone chooses or knows how to stop. That's why outside expert help is imperative."
A wider variety of patients
Both cultural pressures and stress play a role in the development of eating disorders, Vo said, adding that in the first year of the COVID-19 pandemic, as the stress of prolonged stay-at-home orders took hold, experts noticed a jump in the number of young people who needed hospital care.

To get a sense of how these changes related to trends over a longer period, Vo and her colleagues examined hospital admission data from 2010 to 2022 at 12 children's hospitals and medical systems across the country, including Stanford Medicine Children's Health .
Their analysis showed a fairly steady increase in eating disorder hospital admissions for adolescents aged 12 to 21 from 2010 to 2020, a large spike in 2021, and a slight decline in 2022. At the 12 hospitals, a total of 294 adolescents were hospitalized for eating disorders in 2010; hospitalizations peaked at 2,135 in 2021.
These figures represent only a small part of the problem of eating disorders, Vo noted, adding that prior studies estimate 10% of the population meets diagnostic criteria for an eating disorder at some point in their lives. Most patients receive treatment outside the hospital.
About the same number of patients were hospitalized with severe malnutrition during the years examined in the study, but over time, more patients had either no malnutrition, or it was mild to moderate. Admissions for bulimia did not change. Among those with anorexia -- which is characterized by very low food intake, inaccurate body image and a fear of weight gain -- a growing proportion had atypical anorexia, which was first recognized as a distinct diagnosis in 2013. Doctors are becoming more aware of the risks for patients who start out heavier and lose a lot of weight quickly through unsafe dieting, Vo said.
"They may not look like the traditional person you think of who has an eating disorder," Vo said. "People who start higher on the growth curve can lose more weight, faster, and go undetected even though they may have the same, if not more severe, cardiac abnormalities" as underweight patients.
They may not look like the traditional person you think of who has an eating disorder. Megen Vo
Since the diagnosis was formally introduced, also in 2013, doctors have also hospitalized more teens for ARFID.
"The overarching theme is, they are not driven by a desire to change their body weight, shape or size; it's truly that they can't get enough calories in for whatever reason," Vo said.
Kids with ARFID may have extreme sensory sensitivities to many foods, might not respond to their body's hunger cues or may have had a bad experience with food such as an episode of choking that left them afraid to eat. These challenges may be manageable during earlier stages of childhood, but become problematic when their puberty growth spurt arrives and they suddenly need more nutrients. "You see their needs go way up but the foods they find acceptable don't change," Vo said.
What parents should know
Parents of teenagers need to be aware that traditional characteristics of an eating disorder, such as being underweight, are not the only warning signs. Skipping meals, secretive eating behavior, new aversions to foods the teen has typically eaten and becoming absorbed in fad diets can all be red flags.
What patients say about their bodies may vary depending on the person -- instead of focusing on thinness, as girls often do, a boy might say he hopes to be lean and muscular. Transgender teens may express weight and shape concerns that are linked to their gender identity which, if paired with eating changes, may raise concern for an eating disorder.
Because eating disorders can vary, parents should trust their gut if they are worried about a child's or teen's eating. The best predictor of successful treatment is intervening early, so parents should not hesitate to reach out to their pediatrician for help.
"Parents know their kids better than anyone else in the world," Vo said. "If they think something's up, something's usually up."
Supporting healthy growth
For all kids and teens, a healthy family culture focuses on everyone's inherent value rather than their body size or physical appearance. Parents can talk about all foods having a place in a balanced diet: "There's room in a day for ice cream, there's room in a day for kale," Vo said. "No foods are off limits. It's balance that is important."
Avoiding dietary comparisons between siblings is also vital, as children and teens naturally need different amounts of food at different stages of growth.
Both teens and their parents should know that continued growth is normal throughout adolescence, Vo added. Their weight is supposed to increase because of bone mineral density accrual, organ growth and muscle growth.
"Even though teens may not be growing a lot in height past their growth spurt, they are still supposed to be growing into their early 20s," she said. "If their weight is stagnating or they are worried about weight loss, we suggest coming in to their physician."
Researchers contributed to the study from Nemours Children's Hospital of Delaware in Wilmington, Delaware and Thomas Jefferson University in Philadelphia, Pennsylvania. The study did not have external funding.
Photo: Tero Vesalainen
Related posts
Binge eating linked to habit circuitry in the brain
How hypnosis can alter the brain’s perception of pain
Popular posts.

Is an increase in penile length cause for concern?

Could anesthesia-induced dreams wipe away trauma?
- Open access
- Published: 22 April 2024
Meal support intervention for eating disorders: a mixed-methods systematic review
- Aleshia Ellis 1 ,
- Kerri Gillespie 1 ,
- Laura McCosker 1 ,
- Carly Hudson 2 ,
- Gideon Diamond 1 ,
- Tawanda Machingura 2 ,
- Grace Branjerdporn 1 , 2 &
- Sabine Woerwag-Mehta 1 , 2
Journal of Eating Disorders volume 12 , Article number: 47 ( 2024 ) Cite this article
349 Accesses
2 Altmetric
Metrics details
Mealtimes are a period of heightened distress for individuals with eating disorders. Patients frequently display maladaptive coping strategies, such as hiding food and using distraction techniques to avoid eating. The aim of this systematic review is to evaluate the evidence for meal support interventions as a first-line intervention for eating disorders.
Six databases were systematically searched in January 2024. Papers including patients with an eating disorder, and meal support or meal supervision, were examined. Quality appraisal was conducted.
Ten studies met inclusion criteria. Meal support was conducted individually and in group settings. Two studies examined the practical or interpersonal processes of meal support. Carers and trained clinicians implemented meal support. Individuals across the lifespan were examined. Settings included inpatient units, community clinics, and the home. Studies were heterogeneously evaluated with retrospective chart audits, pre- and post- cohort studies, semi-structured interviews, video analysis, and surveys.
Meal support intervention is potentially suitable and beneficial for patients of various age groups and eating disorder diagnoses. Due to the lack of consistent approaches, it is apparent there is no standardised framework and manualised approach. This highlights the need for the development of a co-designed approach, adequate training, and rigorous evaluation.
Plain English summary
Previous research indicates that meal support may be potentially beneficial as an independent intervention in the treatment of eating disorders, but inconsistent approaches and a lack of standardization make evaluations challenging. The current study aims to provide an overview of current meal support interventions, how they are implemented, and their impacts on health outcomes and hospital admissions in people experiencing an eating disorder. Gaps in current knowledge and research highlight the need for further investigation, and the development of a co-designed approach, adequate training, and rigorous evaluation.
Eating and drinking are fundamental and life sustaining activities. Eating is a learnt behaviour, contrary to thoughts it is innate [ 1 ]. Findings from a large number of studies indicates that eating meals together as a family is associated with favourable dietary patterns and improved physical and psychosocial outcomes in children, including fewer rates of obesity, decreased risk for eating disorders, and improved academic achievement [ 2 ]. An inverse correlation between family meal frequency and weight-control behaviour, binge eating, and chronic dieting, for females has been reported [ 3 , 4 , 5 ].
For individuals with eating disorders, meal times are a period of heightened distress [ 6 ]. Negative emotions, such as fear, anxiety, disgust, irritability, anger and depression increase during mealtimes [ 7 , 8 , 9 , 10 ]. To cope with these feelings patients frequently display maladaptive coping strategies, such as avoiding eating certain foods, avoiding eating with others, hiding food, covertly exercising, and using distraction techniques to avoid eating [ 7 , 11 , 12 ].
Whilst a strong predictor of clinical outcome is eating behaviour, directly or indirectly related to weight restoration [ 13 , 14 ], support during meal times is a critical and effective component of nutritional rehabilitation [ 15 ]. There is no consistent approach consensus or guideline on how to best support an individual with disordered eating behaviours during meal times [ 10 , 16 , 17 ].
The most researched and utilised form of meal support is the family meal, a component of Maudsley Family Based Therapy (MFBT), Family Therapy (FBT) and Multifamily Therapy (MFT), the current gold standards of treatment for children with anorexia nervosa and bulimia nerviosa. The family meal is typically conducted during the first phase of treatment. The focus, approach and number of family meals conducted is highly variable with some models emphasising normalising eating, whilst others focus on the improvement of family relations and interactions [ 18 , 19 ].
Clinicians and personal supports (including families and caregivers) of those with eating disorders report mealtimes as being distressing, putting caregivers and clinicians at risk of emotional burn out [ 20 , 21 , 22 , 23 ]. The family meal has been described as particularly challenging and experienced by some as a cause for therapeutic breakdown and subsequent disengagement of families from therapy. Hence, adherence to this element of treatment is poor, with approximately 40.0% of clinicians reportedly not pursuing a family meal during MFBT/FBT [ 15 , 24 , 25 ]. An investigation of therapist perspectives on MFBT and FBT found highly inconsistent implementation of the family meal as a standard part of treatment, with only 25.0% conducting a meal on a regular basis [ 26 ]. Limited training in these specific therapeutic components, reluctance to view them as part of their therapeutic role, and a sense of intimidation and anxiety were reported reasons for the lack of adherence to the treatment protocol. Over a third (36.5%) of clinicians who reported using FBT rarely include the family meal in their practice [ 25 ]. In a study that investigated carers’ views on single and dual-family treatment for AN, some caregivers viewed the family meal as beneficial, but many perceived it as anxiety provoking or ‘‘false” [ 24 ]. A recent systematic review concluded that the usefulness of family meals in family therapy for eating disorders is not clear [ 27 ]. On the other hand, emerging evidence for alternative approaches to family meals, such as direct advice or DVDs, have shown to be acceptable and effective in inducing weight gain and reducing caregiver distress [ 28 , 29 , 30 ].
Inmproving the support provided at mealtimes is a core component of ED treatments, that aim to not only normalise weight, but also nromalise meal eating behaviours, and progress patients toward independence [ 15 , 31 ]. Previous research into the efficacy of meal support has predominantly investigated techniques that are part of a larger, family-based treatment model. A dearth of research relates to the potential benefit of meal support as a first-line intervention. Treatment Modalities to improve support during meal times are rooted in family therapy and have been used predominantly in child and adolescent populations. Little is currently understood about the impacts of meal support in adults compared to younger populations. We have therefore included all age groups in this review in an attempt to further understand the impacts of meal support in different age groups, and determine any differential effects. The differential impacts of meal support for different diagnoses (specifically AN compared to ARFID in younger cohorts) is also poorly understood and requires further investigation. The aim of this systematic review is to investigate whether meal support is being used as a first-line intervention, how these interventions are being implemented and for whom, and the characteristics of these interventions and where they take place. A secondary aim of the review is to evaluate the evidence for meal support interventions as a first-line treatment for eating disorders by identifying the outcomes of these interventions in terms of patient health and satisfaction of patients, parents and staff. While “meal support” and “meal supervision” was used interchangeably across studies, the term “meal support” will be used for the purpose of this review.
This systematic review was conducted according to the 2020 PRISMA reporting guidelines for Systematic Reviews and Meta-Analyses [ 32 ]. The review protocol was registered on the PROSPERO database (registration no. CRD42022311374). A narrative synthesis was conducted where papers were too heterogeneous or contained too little data to conduct meta-analysis.
Research questions
The systematic review will provide an exploratory investigation of the evidence for meal support interventions as a first-line treatment, by answering the following research questions:
What are the characteristics of existing, first-line, meal support interventions described in the literature?
What are the outcomes of first-line meal support interventions, in terms of patient health (weight gain, food consumption, length of stay)?
What are the qualitative outcomes of first-line meal support interventions, in terms of patient, parent, or staff satisfaction and opinions.
Search strategy
Search terms were chosen after investigation of the literature, and consultation with eating disorder researchers and clinicians. Preliminary searches were conducted to identify the optimal search strategy and to eliminate overly broad terms and abbreviations that retrieved excessive numbers of unrelated articles (such as AN, ED, and BED). The search strategy, outlined in Table 1 , contained keywords and MeSH terms relevant to meal support and meal supervision for people with a diagnosis of an eating disorder. Six online databases were systematically searched in December 2021: CINAHL, EMBASE, PsycInfo, PubMed, Scopus, and Web of Science. A manual, hand search of reference lists of included papers, and of related systematic reviews, was also conducted.
Selection criteria
Papers were included based on the following criteria:
Patients had a diagnosis of an eating disorder [anorexia nervosa, bulimia nervosa, binge eating disorder, avoidant and restrictive food intake disorder (ARFID)].
Meal support or meal supervision was used.
Papers with no empirical data, or which were not available in English were excluded. There were no restrictions on the type of study setting in which the meal support intervention occurred (e.g., inpatient, ambulatory clinics, home, public and private); type of methodology employed (e.g., qualitative, quantitative or mixed methods); or age of the participant.
Screening process
Duplicate papers were removed from the original yield of the databases. Titles and abstracts were reviewed by two independent raters based on the inclusion criteria. The full-texts of remaining articles were also independently reviewed by two raters. In cases of disagreement, the suitability of the article was discussed and consensus reached, or another researcher mediated the discussion to make a final determination about the article’s inclusion.
Quality assessment
The McMaster Quantitative and Qualitative Assessment Tools, and the Mixed-Methods Appraisal Tool (MMAT) [ 33 ] were used to appraise the quality of included articles. The MMAT is a 19-item checklist designed to concomitantly appraise the methodological quality of quantitative, qualitative and mixed methods studies. Studies were independently assessed by two raters and the findings were compared. In cases where there was discrepancy, results were discussed until a consensus was reached.
Study selection
14,096 studies were identified through database searching. Once duplicates were removed, the title and abstracts of 5,173 studies were screened, excluding 5,129 studies. Forty-four full-texts were then reviewed for eligibility, resulting in 34 articles being excluded. Reasons for exclusion were that studies were not focused on meal support as a first-line intervention ( n = 20), were a conference abstract, poster, dissertation or other non-eligible paper type ( n = 11), included the wrong patient population ( n = 2), or not available in English ( n = 1). A PRISMA flowchart of the study screening and selection process is presented in Fig. 1 .
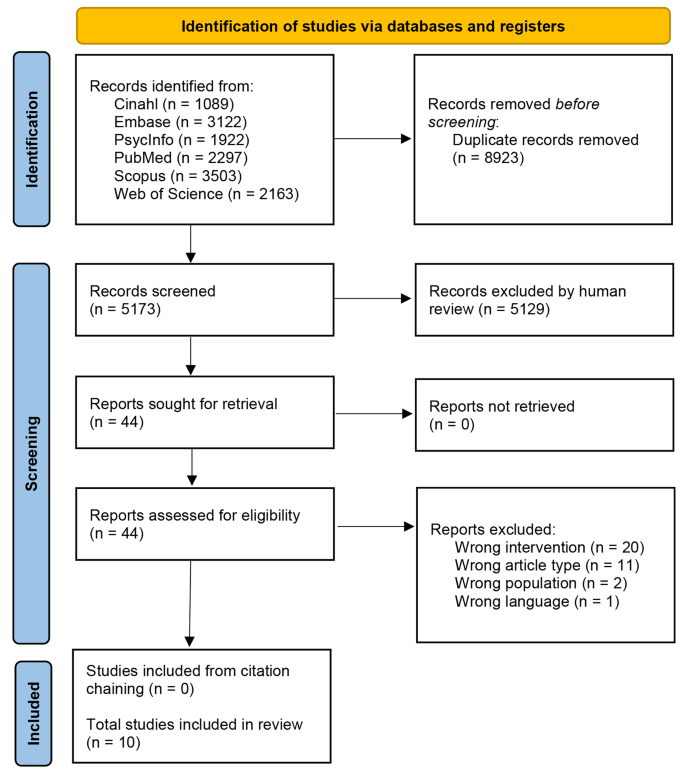
PRISMA flow diagram
Methodological quality of studies
Quality assessment results are displayed in Supplementary Tables 1 , 2 , and 3 . Purpose, background literature, study design and type, results’ statistical significance, analyses clinical importance and conclusions were described well for quantitative studies ( n = 4) [ 15 , 34 , 35 , 36 ]. Two studies did not include one or more of the following details: sample size justification, validity of outcome measures, description of the intervention, contamination and cointervention avoided, and drop-out reporting [ 35 , 36 ]. Qualitative studies ( n = 4) [ 37 , 38 , 39 , 40 ] mostly met the quality appraisal criteria except for two studies [ 39 , 40 ] which did not report, or provided inadequate detail, for one or more of the following aspects: theoretical perspective, obtaining informed consent, identifying assumptions and biases of the researcher and reporting on the decision trail. Kells (2013) reported better outcomes in patients who received meal support compared to patients who did not receive meal support; however, it is unclear whether patient characteristics, severity of illness, length of diagnosis, and physical compromise were comparable to the intervention group. Mixed-methods studies ( n = 2) [ 10 , 41 ] tended to meet the quality appraisal criteria except for not integrating quantitative and qualitative results, and addressing inconsistencies in the results between these two components.
Study characteristics
Quantitative ( n = 4) [ 15 , 34 , 35 , 36 ], qualitative ( n = 4) [ 37 , 38 , 39 , 40 ], and mixed-methods design ( n = 2) [ 10 , 41 ] were identified. Specific methodologies included retrospective chart audits [ 15 , 35 , 36 ], a pre- and post- cohort study [ 34 ], semi-structured interviews [ 10 , 39 , 40 ], video analyses [ 37 , 38 ], and surveys [ 10 , 41 ].
Most studies ( n = 7) were conducted within an inpatient specialist eating disorders unit [ 10 , 15 , 35 , 36 , 37 , 38 , 40 ]. A private eating disorders clinic [ 34 ], child and adolescent public tertiary mental health community service [ 41 ], and home were also identified [ 34 , 39 ]. The sample size ranged between 9 and 56 participants.
Study participants
Study participants included patients diagnosed with an eating disorder (anorexia nervosa, bulimia nervosa, ARFID, binge eating disorder) ( n = 5) [ 15 , 34 , 35 , 36 , 40 ] and in two, linked studies, a mixed group of patients with an eating disorder and some patients with a diagnosis of disordered eating not meeting diagnostic threshold [ 35 , 36 ] receiving meal support; clinicians providing meal support ( n = 4) [ 10 , 37 , 39 , 39 ]; and parents and carers of patients with eating disorders ( n = 1) [ 41 ].
Patient characteristics
As seen in Table 2 , most studies ( n = 7) examined patients with a primary diagnosis of anorexia nervosa [ 15 , 35 , 36 , 37 , 38 , 40 , 41 ]. Patients with an eating disorder not otherwise specified (EDNOS) were investigated in two studies [ 36 , 41 ]. Diagnoses of bulimia nervosa [ 41 ] and ARFID [ 34 ] were included in one study each. One study also included in their cohort some patients who did not meet the diagnostic threshold fo an eating disorder diagnosis [ 36 ]. Average Body Mass Index (BMI) ranged between 14 and 16.1 in the three studies that reported BMI [ 35 , 36 , 38 ].
Most ( n = 6) studies included adolescents between 12 and 18 years old [ 15 , 35 , 36 , 41 ], staff and patients at facilities that catered for adolescents aged 12 to 18 [ 37 ], or staff that treated adolescents 16 and over [ 38 ]. Two studies included patients under 12 years [ 34 , 35 ]. Three studies included patients over the age of 18 [ 35 , 36 , 40 ]. One study included staff members for facilities treating patients of all ages [ 10 ]. Three studies involved exclusively [ 40 ] or predominantly [ 15 , 35 ] female patients, and one study focused on mostly male patients [ 34 ]. Studies that did not specify gender focused on study characteristics and / or included staff members as participants.5)
Clinician characteristics
Three studies, reported on clinicians of varying professional backgrounds delivering meal support: including nursing staff; clinical support staff; consultant psychiatrists; social workers, and; child welfare officers [ 37 , 38 , 39 ].
Intervention characteristics
As seen in Table 3 , staff to patient ratios varied across inpatient units starting from 1:1 [ 10 , 34 , 39 ] and ranging up to 1:10 [ 10 ]. Most ( n = 9) studies provided meal support by a trained clinician [ 10 , 15 , 34 , 35 , 36 , 37 , 38 , 39 , 40 ].
Two studies examined the practical [ 38 ] or interpersonal [ 37 ] processes of meal support delivered within inpatient units. Practical processes consisted of three phases: preparatory (meals are served, and patients are asked to be seated at the table with their food), eating (patients and inpatient staff sit at the table and eat their meals, with support from the staff), and post-meal (patients finish eating and leave the dining room with the staff) [ 38 ]. Interpersonal aspects of meal support included: monitoring food intake, providing mealtime instruction, motivating and encouraging patients to complete the meal, expressing support and understanding, and providing psychoeducation [ 37 ].
The length of time of mealtimes varied from 30 min [ 34 , 37 , 38 ], to 60 min [ 10 ]. Supervised rest period immediately after the meal ranged from 15 to 60 min [ 10 , 15 , 38 , 39 ]. While it is common practice in eatig disorder treatments (e.g., CBT) to use graduated exposure to ‘fear-foods’ in ARFID and AN, none of the articles described implementing a graduated approach to meal supervision.
Aesthetics of the dining room (e.g., size, shape, and setting of the dining table), timing of the meals to avoid delays, and consistency in approach were important aspects identified to alleviate distress in patients [ 10 , 40 ]. Familiarity with the clinicians and having a standardised training approach were facilitators of meal support effectiveness [ 39 ]. Furthermore, clinicians providing empathic emotional support during mealtimes, such as encouraging patients to continue eating and reducing feelings of anxiety [ 10 , 15 ], whilst also being assertive and firm around food consumption [ 10 , 15 , 37 ] was reported being effective. Distraction techniques utilised and identified as helpful included discussing unrelated topics, employing breathing techniques, playing games, and watching television or listening to radio [ 10 , 15 ]. Staff, however, were uncertain around appropriate topics to discuss [ 10 ] and voiced that distraction could prolong eating time [ 40 ]. Peer support was found to be beneficial to instil hope that recovery was possible [ 37 ]. Interviews relating to patient experience of mealtimes revealed three themes: mealtime delivery (logistical factors influencing meals), individual outcomes (cognitions, emotions, behaviours, and physical sensations during meals), mealtime characteristics disengagement, perceived battlegrounds, and a desire for involvement in more decision making at mealtimes [ 40 ].
The importance of training parents and carers in providing meal support post-discharge was acknowledged in three studies [ 34 , 39 , 41 ]. Rigorous training of parents and carers of patients with ARFID in the provision of meal support at home was shown to be a successful alternative to long-term eating disorder outpatient treatment. Parental satisfaction and treatment acceptability were reported high and treatment gains were maintained during follow-up at a mean of 2.3 years [ 34 ].. Distribution of a manual and DVD for psychoeducation and meal support training was described as effective and valuable to parents and carers [ 41 ].
Quantitative outcomes
Three studies found positive outcomes with increased weight gain and fewer episodes of bradycardia [ 35 ], shorter hospital stays [ 36 ], reduced incidence of nasogastric feeding [ 15 ], and reduced incidence of inappropriate mealtime behaviours [ 34 ]. However, Kells and colleagues [ 35 ] found that meal supervision was associated with longer hospital stays. Two studies also found no differences between supervised (meal support) and non-supervised meals in terms of weight gain [ 15 , 36 ], electrolytes or vital signs [ 36 ], length of hospital stay [ 15 ], or rate of readmission [ 15 ]. All of these studies were conducted in child, adolescent, and young adult cohorts.
Experiences with meal support
Patients suggested simulating post-discharge meals, and reported that staff who eat alongside them and provide both empathic support and understanding of negative cognitions was important [ 10 ]. Parents and caregivers were satisfied with resources as it empowered them and increased their understanding; however, the stage of readiness of the patient needed to be considered [ 41 ]. Two studies explored clinicians’ experiences and feedback with regards to delivering meal support and supervision, suggesting that training in a uniform approach and debriefing sessions supported patient outcomes [ 37 , 39 ].
This literature review identified ten studies, that examine the role of meal support as a standalone intervention for eating disorders, using quantitative, qualitative and mixed methods approaches. Most studies met quality appraisal criteria with average ratings. Due to small numbers and heterogeneity in design and methodology comparisons between studies was not possible.
Retrospective chart audits, pre and post comparisons, interviews, surveys and video analyses were used to explore the significance of meal support from a patient, clinician and parent / carer perspective. Whilst most studies were conducted in inpatient settings, meal support was also examined in a mental health community service and the home environment. This suggests that a meal support intervention can potentially be used across inpatient and outpatient settings as well as the home environment. Patients predominately had a diagnosis of anorexia nervosa, and were adolescents, however meal support was also utilised forbulimia nervosa and ARFID in children and adults. Meal support intervention is potentially suitable and beneficial for patients of all age groups and can be applied for a range of eating disorder diagnoses. Two studies that included patients who did not meet the diagnostic threshold for a diagnosis, found a beneficial impact of meal support on patient outcomes [ 35 , 36 ], indicating the possible use of meal support as a preventive measure. Meal support was provided by clinicians from multi-professional backgrounds and in one study parents / carers were upskilled to deliver the intervention. Hence meal support could be conceptualised as a generic intervention, i.e., an intervention that could potentially be delivered by anyone, involved in the care of the patient, with adequate training.
In inpatient units, staffing levels available for the delivery of a meal support intervention varied significantly between studies. Practical and interpersonal aspects of the meal support intervention were explored and evaluated. Interpersonal aspects of meal support included: monitoring food intake, providing mealtime instruction, motivating and encouraging patients to complete the meal, expressing support and understanding, and providing psychoeducation [ 37 ].The included studies mainly focused on meal support within an inpatient setting. Supervised meals are assumed to be standard practice within specialised disorder inpatient units, and are considered best practice in facilitating refeeding in patients with eating disorders [ 42 ], however implementation across various settings has not been adequately researched. Our findings identified mixed results in terms of weight gain, length of stay, and future admissions, indicating that further research into this area is necessary. A complete lack of quantitative findings in adult groups means that findings of children and adolescents is potnentially being extrapolated to adult populations that may not be generalisable. Further studies into the benefits of meal support in adult populations is particularly warranted.
There was a lack of literature on provision of meal support in community settings or by parents and carers in the home environment; only three studies were conducted at home [ 34 , 39 , 41 ], with only two of these having meal support provided by the patients’ parents or carers [ 34 , 41 ]. It has been identified as essential that meals should reflect ‘normal’ situations, to facilitate a positive transition back to regular eating habits [ 39 , 40 ] Therefore, further research is needed to understand how meal support can be used in this way and how the intervention can be adapted and used in the transition from inpatient settings to both community and home environments. In the two studies where parents and carers provided meal support at home [ 34 , 41 ], it was emphasised that provision of training and support resources were required for them to be able to adequately deliver meal support. Parents appreciated an intensive, tailored training approach that provided them with the skills needed to support their child [ 43 ]. Similarly, a meal support manual and DVD resource were rated favourably by parents, who reported they provide empowerment and the ability to implement empathic emotional and practical meal support at home [ 41 ]. However, further exploration of access to continued support in their use and implementation, as well as avenues for troubleshooting, would help provide a more robust framework to which the intervention is based and practiced. The review also revealed that each setting delivered meal support differently, however all studies reported that the intervention generally consisted of supervised eating followed by a rest period, with staff providing emotional and practical support throughout.
The evidence examined in this review shows that there is currently no agreed standardised, manualised, consistent approach to meal support available. This has been highlighted as problematic and being distressing for patients, carers and clinicians. Uncertainty and variation in the intervention provided across different environments has the potential to affect treatment outcomes and lead to inconsistencies in approach. It also increases missed opportunities to provide valuable interventions to people across various settings and in some ways could lead to negatives experiences and a change in the trajectory of the participants recovery journey. Developing a manualised meal support approach, co-designed with patients, caregivers, and healthcare clinicians is vital in integrating the experiences of those involved in the intervention.
Furthermore, significant variation in the outcomes measured in each of these studies was observed; including recovery outcomes (e.g., weight gain, length of stay, food consumption), experience outcomes, and satisfaction outcomes. In some studies, these outcomes were measured using non-validated, unstandardised measures. Inconsistency for key recovery outcomes were reported; for instance Kells et al. [ 35 ] reported a mean weight increase following meal support, whilst Couturier et al. [ 15 ] observed no change. Hence the clinical impact of meal support as an intervention is not yet clearly established.
Limitations
This review synthesised the existing literature on meal support as an intervention for those with eating disorders and several limitations could be identified. The included studies were heterogenous in methodology and scope, which prevented the use of a meta-analysis to compare results across studies. Given that the literature on meal support is currently limited, none of the included studies were randomised controlled trials, which are the gold standard in assessing effectiveness of an intervention.
In a limited number of studies, the parent or carer of the patient, delivered the meal support intervention. Given that meal support is aligned with the person’s progress, and not the setting it is delivered in, further research involving caregivers would be beneficial in supporting recovery post-hospital discharge.
Although patients with a variety of eating disorder diagnoses were included in the studies, there is a need for further examination of how meal support intervention could be used and adapted for each diagnosis. In several of the studies, key demographic and clinical information, such as patients’ age and BMI was not reported. Reporting these variables is essential in understanding the patient population for which meal support might be suitable. However, these data were predominantly missing from papers focussed on describing the characteristics of the service, and not on patient outcomes. We therefore did not reach out to individual authors to request missing information. We acknowledge that failing to do so was another limitation of the study.
Clinical implications
Due to the lack of evidence, meal support is rarely referenced in guidelines. More rigorously designed studies are required to ascertain its potential in the field eating disorder treatment. Meal support intervention as a standalone treatment is unique as it is based on a pragmatic, as opposed to a systemic, approach. It focuses solely on practical skills required during mealtime and can potentially be used across all ages. Delivery of the meal support intervention is anticipated to be fluid, and adapted in keeping with the patient’s recovery journey. For instance, the intervention might be directive in the initial phase of recovery, with the person providing meal support taking on a deliberate authoritative approach. However, as recovery progresses the style of support is anticipated to transition to a more collaborative approach in line with the patients increasing ability to make healthy choices over food intake. This is in keeping with existing models, in which advice on meal management is embedded in either systemic or cognitive behavioural concepts. In a family environment, the nature of meal time interactions are reported as imperative to recovery outcomes and family mealtime interactions commonly consist of both direct and indirect eating prompts and the provision of information, incentivising eating [ 44 ]. Training parents and carers in meal support can foster these interactions and provide the practical skills required to enable continued care at home outside of the inpatient setting.
Whilst this intervention might potentially be beneficial in treating eating disorders, it is essential to improve the understanding of individual differences, interpersonal components, environmental factors and how practical support is best delivered. Effectiveness may vary dependent upon where in the recovery process the patient is, as well as the level of family/caregiver support that the patient has, and social influences that are at play [ 41 , 45 ]. Therefore, whilst the proposed manualised approach to meal support should outline a consistent assessment of needs and method for delivering the intervention, meal support approaches also need to be flexible and tailored to the needs of the patient and their available family and personal supports.
It is of note, that meal support is an important aspect of clinical care not only for patients with eating disorders. Meal support models outside the field of eating disorders might provide valuable insights on transferable skills, and concepts to meal support intervention. For instance, research into provision of meal support for patients with dementia identified core attitudes to its delivery that are potentially applicable and valuable for patients with eating disorders: i.e., the support person being able to establish a core connection, tailoring the intervention to the needs of the patient, whilst being receptive to the idea that needs may change [ 46 ] and recognising that good mealtime care helps patients to be empowered, and enables carers to respond in a way that encourages (but does not coerce) the patient to eat more [ 47 ]. However, due to the food-related distress observed in the disordered eating population, mealtime interventions are often seen as coercive, and it is uncertain how non-coercive, encouraging meal support could be implemented or whether it would be useful. This may be a differentiating factor between age cohorts that has not yet been investigated. Another example is the Altered Eating Framework, developed collaboratively with cancer survivors, to support disordered eating in cancer patients. It conceptualises seven core domains for assessment and meal support provision: physical anatomical, physical functional, sensory, behavioural, cognitive, cultural/social and emotional. This framework is an example for engaging in patient co-design to develop a comprehensive approach to meet clinical needs of a specific patient group while the outcome demonstrates potential for broader application. In addition, valuable insights for the development of a standalone meal support intervention could potentially be drawn from learnings and experiences gathered delivering the family meal as part of family therapy.
Suggestions for future research
Most studies were conducted in AN, with only one study in ARFID that did find beneficial results. The differences between these diagnostic groups in terms of their benefit from meal support interventions should be further investigated. Cost effectiveness analyses are also missing from the literature, which may elucidate further evidence to support or rebuke the use of meal support strategies in inpatient settings. We also recommend the development and evaluation of a multidisciplinary and lived experience co-designed framework for a standardised, yet adaptable, manualised approach for meal support interventions.
This systematic review has synthesised the current literature on meal support intervention for eating disorders. Studies have highlighted the benefits of meal support in facilitating recovery, however a number of gaps and opportunities for improvement are noted. The studies examined highlight the need for a framework and manualised approach to meal support intervention.
Data availability
Not applicable.
Abbreviations
Maudsley Family Based Therapy
Family Based Therapy
Multifamily Therapy
Avoidant/restrictive food intake disorder
Mixed-Methods Appraisal Tool
Body Mass Index
Eating Disorder Not Otherwise Specified
Satter E. Secrets of feeding a healthy family: how to eat, how to raise good eaters. How to Cook: Kelcy; 2011.
Google Scholar
Glanz K, Metcalfe JJ, Folta SC, Brown A, Fiese B. Diet and Health benefits Associated with In-Home eating and sharing meals at home: a systematic review. Int J Environ Res Public Health. 2021;18(4).
Harrison ME, Norris ML, Obeid N, Fu M, Weinstangel H, Sampson M. Systematic review of the effects of family meal frequency on psychosocial outcomes in youth. Can Fam Physician. 2015;61(2):e96–106.
PubMed PubMed Central Google Scholar
Neumark-Sztainer D, Eisenberg ME, Fulkerson JA, Story M, Larson NI. Family meals and disordered eating in adolescents: longitudinal findings from project EAT. Arch Pediatr Adolesc Med. 2008;162(1):17–22.
Article PubMed Google Scholar
Loth K, Wall M, Choi CW, Bucchianeri M, Quick V, Larson N, et al. Family meals and disordered eating in adolescents: are the benefits the same for everyone? Int J Eat Disord. 2015;48(1):100–10.
Russell GF. Anorexia nervosa: its identity as an illness and its treatment. Mod Trends Psychol Med. 1970;2(1):56–62.
Harvey T, Troop NA, Treasure JL, Murphy T. Fear, disgust, and abnormal eating attitudes: a preliminary study. Int J Eat Disord. 2002;32(2):213–8.
Lawson EA, Holsen LM, Santin M, DeSanti R, Meenaghan E, Eddy KT, et al. Postprandial oxytocin secretion is associated with severity of anxiety and depressive symptoms in anorexia nervosa. J Clin Psychiatry. 2013;74(5):e451–7.
Article PubMed PubMed Central Google Scholar
Tobey JA. The Biology of Human Starvation. Am J Public Health. 1951;41(2):236–7.
Article Google Scholar
Long S, Wallis DJ, Leung N, Arcelus J, Meyer C. Mealtimes on eating disorder wards: a two-study investigation. Int J Eat Disord. 2012b;45(2):241–6.
Vanzhula IA, Sala M, Christian C, Hunt RA, Keshishian AC, Wong VZ, et al. Avoidance coping during mealtimes predicts higher eating disorder symptoms. Int J Eat Disord. 2020;53(4):625–30.
Lobera IJ, Estébanez S, Fernández MS, Bautista EA, Garrido O. Coping strategies in eating disorders. Eur Eat Disorders Review: Prof J Eat Disorders Association. 2009;17(3):220–6.
Gowers SG, Edwards VJ, Fleminger S, Massoubre C, Wallin U, Canalda G et al. Treatment aims and philosophy in the treatment of adolescent anorexia nervosa in Europe. 2002;10(4):271–80.
Guarda AS. Treatment of anorexia nervosa: insights and obstacles. Physiol Behav. 2008;94(1):113–20.
Couturier J, Mahmood A. Meal support therapy reduces the use of nasogastric feeding for adolescents hospitalized with anorexia nervosa. Eat Disord. 2009;17(4):327–32.
Psychiatrists RCo. Standards for adult inpatient eating disorder services. In: Improvement RCoPCfQ, editor. London2017.
Hay P, Chinn D, Forbes D, Madden S, Newton R, Sugenor L et al. Clinical practice guidelines for the treatment of eating disorders. In: Psychiatrists RAaNZCo, editor. 2022.
Agras WS, Lock J, Brandt H, Bryson SW, Dodge E, Halmi KA, et al. Comparison of 2 family therapies for adolescent anorexia nervosa: a randomized parallel trial. JAMA Psychiatry. 2014;71(11):1279–86.
Gelin Z, Cook-Darzens S, Simon Y, Hendrick S. Two models of multiple family therapy in the treatment of adolescent anorexia nervosa: a systematic review. Eat Weight Disorders: EWD. 2016;21(1):19–30.
Treasure J. How do families cope when a relative has an eating disorder? The Clinician’s Guide to Collaborative Caring in Eating Disorders. Routledge; 2009. pp. 61–75.
Warren CS, Schafer KJ, Crowley ME, Olivardia R. A qualitative analysis of job burnout in eating disorder treatment providers. Eat Disord. 2012;20(3):175–95.
Thompson-Brenner H, Satir DA, Franko DL, Herzog DB. Clinician reactions to patients with eating disorders: a review of the literature. Psychiatric Serv (Washington DC). 2012;63(1):73–8.
Leichner P, Hall D, Calderon R. Meal support training for friends and families of patients with eating disorders. Eat Disord. 2005;13(4):407–11.
Whitney J, Currin L, Murray J, Treasure J. Family work in anorexia nervosa: a qualitative study of carers’ experiences of two methods of family intervention. Eur Eat Disorders Review: J Eat Disorders Association. 2012;20(2):132–41.
Kosmerly S, Waller G, Lafrance Robinson A. Clinician adherence to guidelines in the delivery of family-based therapy for eating disorders. Int J Eat Disord. 2015;48(2):223–9.
Couturier J, Kimber M, Jack S, Niccols A, Van Blyderveen S, McVey G. Understanding the uptake of family-based treatment for adolescents with anorexia nervosa: therapist perspectives. Int J Eat Disord. 2013;46(2):177–88.
Cook-Darzens S. The role of family meals in the treatment of eating disorders: a scoping review of the literature and implications. Eat Weight Disord. 2016;21(3):383–93.
Hughes EK, Le Grange D, Court A, Yeo MS, Campbell S, Allan E, et al. Parent-focused treatment for adolescent anorexia nervosa: a study protocol of a randomised controlled trial. BMC Psychiatry. 2014;14:105.
Månsson J, Parling T, Swenne I. Favorable effects of clearly defined interventions by parents at the start of treatment of adolescents with restrictive eating disorders. Int J Eat Disord. 2016;49(1):92–7.
Sepulveda AR, Lopez C, Todd G, Whitaker W, Treasure J. An examination of the impact of the Maudsley eating disorder collaborative care skills workshops on the well being of carers: a pilot study. Soc Psychiatry Psychiatr Epidemiol. 2008;43(7):584–91.
Gardner L, Trueman H. Improving mealtimes for patients and staff within an eating disorder unit: understanding of the problem and first intervention during the pandemic-an initial report. BMJ Open Qual. 2021;10(2).
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health. 2014;35:29–45.
Taylor T, Blampied N, Roglić N. Controlled case series demonstrates how parents can be trained to treat paediatric feeding disorders at home. Acta Paediatr. 2021;110(1):149–57.
Kells M, Davidson K, Hitchko L, O’Neil K, Schubert-Bob P, McCabe M. Examining supervised meals in patients with restrictive eating disorders. Appl Nurs Res. 2013;26(2):76–9.
Kells M, Schubert-Bob P, Nagle K, Hitchko L, O’Neil K, Forbes P, et al. Meal supervision during medical hospitalization for eating disorders. Clin Nurs Res. 2017;26(4):525–37.
Beukers L, Berends T, de Man-van Ginkel JM, van Elburg AA, van Meijel B. Restoring normal eating behaviour in adolescents with anorexia nervosa: a video analysis of nursing interventions. Int J Ment Health Nurs. 2015;24(6):519–26.
Hage TW, Rø Ø, Moen A. Time’s up– staff’s management of mealtimes on inpatient eating disorder units. J Eat Disorders. 2015;3(1):13.
Watt J, Dickens GL. Community-based mealtime management for adolescents with anorexia nervosa: a qualitative study of clinicians’ perspectives and experiences. J Child Adolesc Psychiatr Nurs. 2018;31(1):30–8.
Long S, Wallis D, Leung N, Meyer C. All eyes are on you: anorexia nervosa patient perspectives of in-patient mealtimes. J Health Psychol. 2012a;17(3):419–28.
Cairns JC, Styles LD, Leichner P. Evaluation of meal support training for parents and caregivers using a video and a manual. J Can Acad Child Adolesc Psychiatry. 2007;16(4):164–6.
Hay P, Chinn D, Forbes D, Madden S, Newton R, Sugenor L, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders. Australian New Z J Psychiatry. 2014;48(11):977–1008.
Leadley S, Taylor T. The distance between empirically-supported treatment and actual practice for paediatric feeding problems: an international clinical perspective. 2021:0–00.
White HJ, Haycraft E, Madden S, Rhodes P, Miskovic-Wheatley J, Wallis A, et al. How do parents of adolescent patients with anorexia nervosa interact with their child at mealtimes? A study of parental strategies used in the family meal session of family‐based treatment. Int J Eat Disord. 2015;48(1):72–80.
Macdonald P, Rhind C, Hibbs R, Goddard E, Raenker S, Todd G, et al. Carers’ assessment, skills and information sharing (CASIS) trial: a qualitative study of the experiential perspective of caregivers and patients. Eur Eat Disorders Rev. 2014;22(6):430–8.
Driessen A, Ibáñez Martín R. Attending to difference: enacting individuals in food provision for residents with dementia. 2020;42(2):247–61.
Liu W, Tripp-Reimer T, Williams K, Shaw C. Facilitators and barriers to optimizing eating performance among cognitively impaired older adults: a qualitative study of nursing assistants’ perspectives. Dement (London England). 2020;19(6):2090–113.
Download references
Acknowledgements
We would like to acknowledge Bond University for a grant to fund Carly Hudson as a research assistant.
Author information
Authors and affiliations.
Gold Coast Hospital and Health Services, 1 Hospital Boulevard, Southport, QLD, 4215, Australia
Aleshia Ellis, Kerri Gillespie, Laura McCosker, Gideon Diamond, Grace Branjerdporn & Sabine Woerwag-Mehta
Bond University, 14 University Drive, Robina, QLD, 4226, Australia
Carly Hudson, Tawanda Machingura, Grace Branjerdporn & Sabine Woerwag-Mehta
You can also search for this author in PubMed Google Scholar
Contributions
The study was conceptualised by SW and TM. Study methodology was designed by TM, GB, and SW. Literature searches and screening was conducted by CH, GD, KG, and LM. Formal analysis was performed by GB, CH, and KG. Supervision and resources were provided by GB, SW, and TM. The findings were validated by AE and SW. The original draft manuscript was completed by CH, GB, SW, and AE. Review and editing of the final manuscript was conducted by TM, GD, SW, GB, KG, and LM. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Grace Branjerdporn or Sabine Woerwag-Mehta .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ellis, A., Gillespie, K., McCosker, L. et al. Meal support intervention for eating disorders: a mixed-methods systematic review. J Eat Disord 12 , 47 (2024). https://doi.org/10.1186/s40337-024-01002-2
Download citation
Received : 08 February 2023
Accepted : 03 April 2024
Published : 22 April 2024
DOI : https://doi.org/10.1186/s40337-024-01002-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Meal support
- Intervention
- Systematic review
- Eating disorders
- Multidisciplinary
Journal of Eating Disorders
ISSN: 2050-2974
- General enquiries: [email protected]

Why Aren't Our Girls and Women Eating?
There are some unique reasons why females diet..
Posted April 27, 2024 | Reviewed by Pam Dailey
- Anorexic women often experience shame and seek to numb this feeling.
- They attempt to numb the shame with perfectionism.
- The vicious cycle of shame and perfectionism should be addressed in therapy.
What is going on with our girls, teens, and women? Why are eating and weight such hot topics? Why do so many females feel that dieting and losing weight are such major accomplishments? I am referring to females of all ages who engage in the relentless pursuit of thinness and take pride in dietary restraint. Being a healthy weight is certainly important, but focusing on dieting and restraining food intake does in many cases lead to eating disorders like anorexia nervosa which are extremely resistant to treatment. In addition, they are associated with depression , isolation, and health problems.
The thinking among professionals who are treating females with eating disorders seems to be concentrated on the treatment of depression and anxiety while also working on cognitive restructuring, particularly around such negative thoughts as, "I will be seen as a glutton if I gain a pound." Therapists also tend to work in conjunction with nutritionists who aim to normalize healthy eating habits to restore body weight. Additionally, the therapy often includes a physician who monitors physical health.
More recent research particularly that of Howard et al. (2023) has had a very interesting and unique focus. I found this research particularly refreshing because it adds an additional lens from which to view anorexia nervosa and dietary restraint in general. I think this perspective has been largely overlooked in the treatment of females with eating and body image issues. Howard et al. (2023) interviewed 11 females over the age of 18 who were receiving outpatient treatment for anorexia nervosa in a community eating-disorders service. They were assessed with the Eating Disorder Examination Questionnaire, a demographics questionnaire, and a face-to-face interview.
The focus of the study was on the relationship between anorexia and the self-conscious emotions of shame and perfectionism . The findings indicated that anorexia was clearly driven in part by the vicious cycle of shame and perfectionism. The relationship was as follows: Anorexics tend to deal with their feelings of shame by striving for perfectionism. It is not entirely clear why these women were so full of shame, although those who had a history of trauma reported experiencing shame prior to perfectionism. The women who did not report a history of trauma were either unsure of which feeling came first or sometimes reported that perfectionism preceded shame. Regardless of the directionality of these two self-conscious emotions, they coexisted to form a vicious cycle for these women. Many reported trying to minimize feelings of shame by setting high standards for themselves. In this group, perfectionism was centered around the body and dietary restraint. They were striving for the perfect body by controlling their eating. And recovery was particularly difficult for several reasons, including the need to be perfect at recovery.
While the findings may have implications for the successful treatment of anorexics, there are several limitations of this study. The sample size was small. We also do not know if the same degree of shame and perfectionism would be found in younger and older females who are not in treatment or who are at different stages of their eating disorder. The most important question is whether or not the shame-perfectionism cycle precedes the development of body image and eating issues or if this cycle is preceded by the development of full-blown anorexia nervosa. We could learn the answers to these questions by replicating this study with both a large control group and a large number of females of all ages pretreatment, during treatment, and during recovery. In the meantime, issues of shame and perfectionism should be addressed with females who present with body image issues and eating/dieting issues.
Howard,T.L.M.,Williams.M.O.Woodward.,D.&Fox, J.R.E. (2023)The relationship between shame, perfectionism, and Anorexia Nervosa:A grounded theory study. Psychology and Psychotherapy:Theory, Research, and Practice, 96,40-55.

Barbara Greenberg, Ph.D., is a clinical psychologist who specializes in the treatment of adolescents and their well-intentioned but exhausted parents.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

IMAGES
VIDEO
COMMENTS
In the present review, the results show that the main factors associated with eating disorders were psychological-type with a prevalence of the factor inherent the dissatisfaction with body image ( 16 ─ 18, 21, 25, 27, 29, 31, 32, 35 ). Literature refers that dissatisfaction with body image increases significantly in adolescence due to ...
We will write a custom essay on your topic. To begin with, it is necessary to define which diseases are meant under the notion of an eating disorder. Generally, eating disorders encompass such conditions as anorexia nervosa, bulimia, binge eating, and avoidant/restrictive food intake disorder (ARFID) (AACAP, 2018).
Binge-eating disorder (BED) is the most common ED in children and adolescents and is more prevalent in females than males. EDs may present differently in children and adolescents than in adults, and parents or caregivers may be the first to notice changes in eating patterns or body weight.
Types of eating or feeding disorders in adolescents. There are four main types of eating disorders diagnosed among adolescents: anorexia, bulimia, binge eating disorder, and other specified eating disorders (Lock & Grange, 2005). Anorexia is characterized by a loss of appetite and a restriction of certain food groups in order to avoid weight gain.
Eating disorders in childhood and adolescence present a serious threat to health and well-being, including medical consequences ranging from growth delay to life-threatening effects of starvation and refeeding (Reference Nicholls, Hudson and Mahomed Nicholls 2011a).Anorexia nervosa is frequently cited as the third most common chronic illness of adolescence (Reference Lucas, Beard and O'Fallon ...
Eating disorders are complex illnesses that are affecting adolescents with increasing frequency [1]. They rank as the third most common chronic illness in adolescent females, with an incidence of up to 5% [1-3]. Three major subgroups are recognized: a restrictive form in which food intake is severely limited (anorexia nervosa); a bulimic form in which binge-eating episodes are followed by ...
It supports individuals and families affected by eating disorders. F.E.A.S.T. is an international nonprofit organization run by caregivers of those suffering from eating disorders, meant to help ...
Bulimia nervosa. Bulimia nervosa, or bulimia, is characterized by compulsive eating followed by compensatory behaviors. Examples include vomiting, excessive exercise, and laxative use. Symptoms ...
Although the earliest medical account of an adolescent patient with an eating disorder was more than 300 years ago, 1 a thorough understanding of the pathophysiology and psychobiology of eating disorders remains elusive today. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) includes the latest effort to describe and categorize eating disorders, 2 placing ...
Introduction. Eating disorders have their peak onset in adolescence and a severe impact on physical and mental health (Qian et al., Citation 2022).At the core of eating disorders is concern over eating, shape, weight and their control (Fairburn et al., Citation 2003b).Disordered eating behaviours may consist of overeating or insufficient food intake and be associated with compensatory ...
rank as the third most common chronic condition among adolescent females [2] Anorexia. nervosa, characterized by severe food restriction, and bulimia nervosa, characterized b y binge. eating ...
Disordered eating related to stress, poor nutritional habits, and food fads are relatively common problems for youth. In addition, two psychiatric eating disorders, anorexia nervosa and bulimia, are on the increase among teenage girls and young women and often run in families. These two eating disorders also occur in boys, but less often.
Eating disorders are not uncommon among teens. Take "Kerri" (not her real name) for example. Upset with a sudden weight gain, the 15-year-old forced herself to throw up after eating her school ...
Eating disorders are disabling, deadly, and costly mental disorders that considerably impair physical health and disrupt psychosocial functioning. Disturbed attitudes towards weight, body shape, and eating play a key role in the origin and maintenance of eating disorders. Eating disorders have been increasing over the past 50 years and changes in the food environment have been implicated.
Eating disorders are complex diseases that affect mostly. adolescents and are considered to be the third m ost common. chronic disease in ad olescent women (Gold en et al., 2 003). Currently, they ...
Eating disorders in children and adolescents can have serious medical and psychological consequences and rank 12th on the list of physical and mental conditions amongst woman aged 15-19 years in high-income countries when looking at the global burden of disease [1, 2].The estimated lifetime prevalence of Anorexia Nervosa (AN) in woman is 1-4% and 1-2% for Bulimia Nervosa (BN), and the ...
Their analysis showed a fairly steady increase in eating disorder hospital admissions for adolescents aged 12 to 21 from 2010 to 2020, a large spike in 2021, and a slight decline in 2022. At the 12 hospitals, a total of 294 adolescents were hospitalized for eating disorders in 2010; hospitalizations peaked at 2,135 in 2021.
Group modalities are commonly used in the treatment of adolescent eating disorders both nationally and internationally, for example, Southern Health Butterfly Day Program (Victoria, Australia) and the Renfrew Centre ... (Wanlass et al., 2005) with no published papers presenting a compilation of evidenced-based group therapy for the adolescent ...
Introduction. Eating disorder (ED) describe sicknesses that are represented by constant disturbance of eating patterns and extreme unhappiness or worry about body weight/shape which leads to poor physical and/or mental health. Over the past few decades there has been an increase in the prevalence of eating disorder especially among adolescents.
Results: Thirty-six percent of adolescents with BP I experienced lifetime eating disorder symptoms; among comorbid adolescents, 74% reported eating disorder cognitions and 40% reported symptoms related to bingeing, 25% purging, and 17% restricting. BP I adolescents with (vs. without) eating disorder symptoms had higher Children's Depression Rating Scale-Revised scores (40.5 vs. 34.5; p < 0.001 ...
Objective Mealtimes are a period of heightened distress for individuals with eating disorders. Patients frequently display maladaptive coping strategies, such as hiding food and using distraction techniques to avoid eating. The aim of this systematic review is to evaluate the evidence for meal support interventions as a first-line intervention for eating disorders. Method Six databases were ...
Howard et al. (2023) interviewed 11 females over the age of 18 who were receiving outpatient treatment for anorexia nervosa in a community eating-disorders service.
Introduction: As part of an exploratory and hypothesis-generating study, we developed the Sports Preference Questionnaire (SPOQ) to survey the athletic behavior of mentally ill children and adolescents, subjectively assessed physical fitness and perceived psychological effects of physical activity. Methods: In a department of child and adolescent psychiatry, we classified 313 patients (6-18 ...