
- Sales CRM Software
- Application Portals
- Call Center CRM
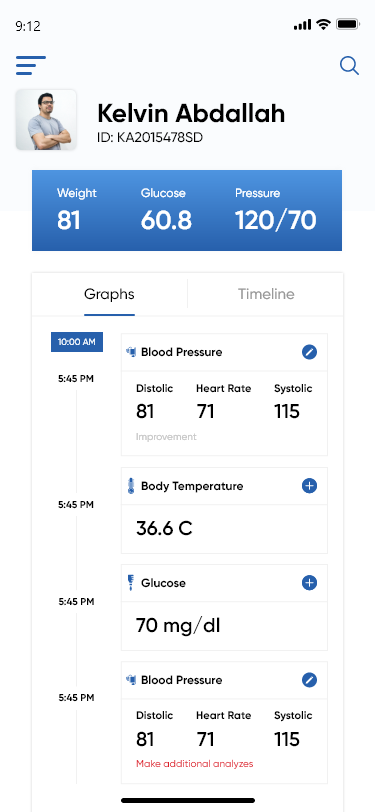
- Mobile CRM App
- Omnichannel Communication CONVERSE
- Reporting Dashboard SIERA
- Lead Management System
- Opportunity Management
- Sales Process Automation
- Sales Tracking
- Door-to-Door Sales
- Remote Team Management
- Field Sales CRM
- Merchant Onboarding App
- App UI/UX Customizer CASA
- Outside Sales CRM
- Field Force Automation
- Collections Management
- Field Force Tracking
- Event Campaign Management
- Bancassurance Management
- Marketing Automation
- Chatbot - Website
- Chatbot - WhatsApp
- Landing Pages
- Email Campaigns
- Lead Capture Automation
- Lead Engagement
- BTL Marketing Automation
- Advanced Marketing Analytics
- Hospitals and Clinics
- Hospice and Palliative Care
- Fertility Clinics
- Dental Care
- Diagnostics Labs
- ACQUISITION
- Patient Intake Automation
- Patient Appointment Scheduling
- Healthcare Call Center Solution
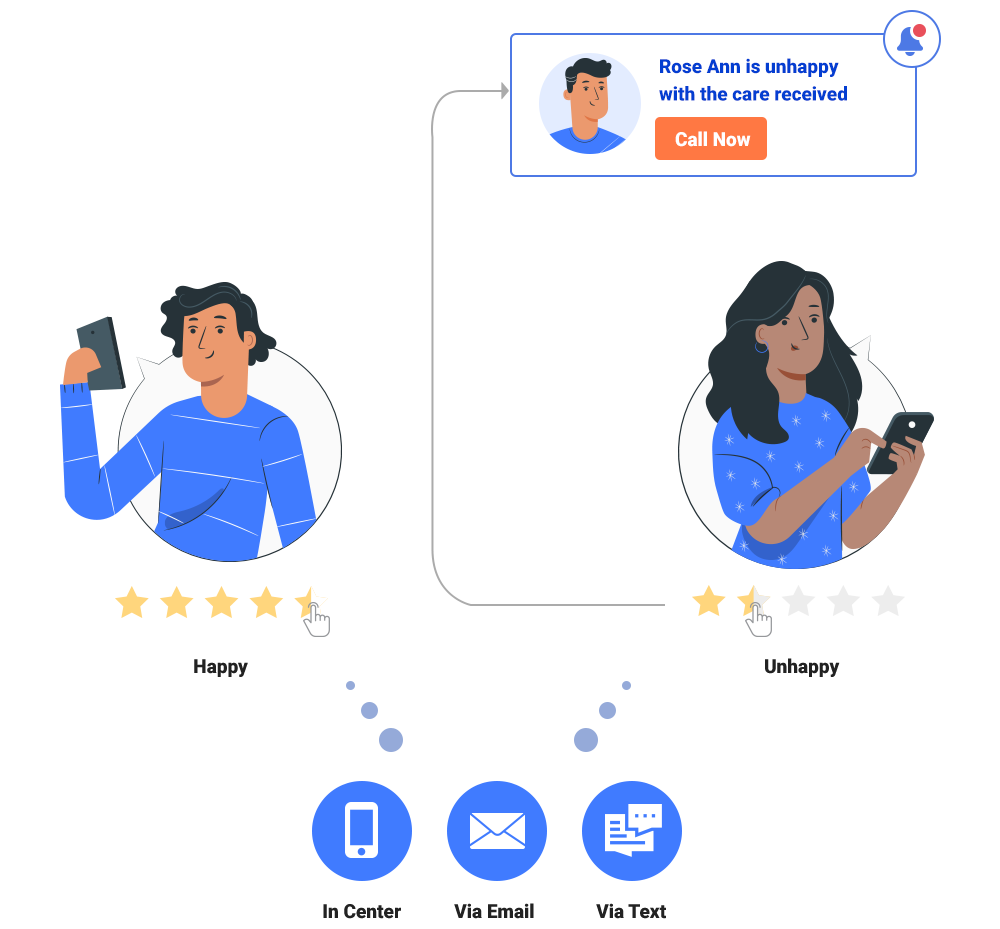
- Patient Experience Management
- Self-serve Patient Portals
- EHR Integration
- Physician Empanelment
- Security and Compliance
- Patient Engagement
- Higher Education
- Pre-schools and K12
- Training Institutions
- Student Recruitment Software
- Admission Portal
- Teacher Onboarding
- Publisher Portal
- Admission Software
- Credit Unions
- Securities and Trading
- Lending CRM
- Loan Origination System
- WhatsApp Lending Bot
- Debt Recovery Automation
- Bancassurance Solution
- PAPERLESS ONBOARDING
- e-KYC Solution
- Video KYC Solution
- Merchant Onboarding
- Merchant Lifecycle Management
- Travel and Hospitality
- Agriculture
- Home Improvement
- View by Industries
- 11 Modules of Hospital Management System and their Benefits

Ever wondered what it is like to manage an entire hospital?
It definitely sounds difficult.
Well, if you’ve landed on this article, you know that efficiently running an entire hospital isn’t a walk in the park. Although it is essential, it gets overwhelming at times.
Time is of the utmost importance when it comes to healthcare. Imagine the severity if there is even a minor delay or fault while sharing the results and diagnosis. To simplify operations and efficiently manage patient records, leading hospitals use a hospital management system. Employing hospital management software helps you reap the maximum benefits from your work.
Before discussing in detail how you can leverage an HMS to the fullest, let us understand what an HMS is and why it is needed.

What is a Hospital Management System?
A study showed that healthcare providers spend 35% of their time on documenting patient data. While paperwork is unavoidable in a hospital, you can automate the process and reduce the burden on the staff and doctors. Not just this, hundreds of other processes run parallel in a hospital. An HMS is a one-stop solution to manage all hospital processes and data transfer. You can use it to digitize and simplify activities like:
- Patient record management
- Tracking and managing appointments
- Maintaining staff records
- Billing and insurance claims
Overall, an HMS helps you improve patient experience and the quality of service provided in the hospital. At the same time it is also used to minimize operating expenses and improve the revenue cycle.
In a nutshell, Hospital Management System (HMS) creates a frictionless approach to managing the entire hospital and solving operational complexities.
However, HMS can be a complex system. For ease of understanding and implementation, it is divided into different modules. These modules are built depending on the needs of a department or a particular process. Let’s look at the 11 HMS modules that are essential for any hospital to improve end-to-end productivity.
11 Essential Hospital Management System Modules
Below we have discussed the 11 hospital management system modules in the same order that a hospital would need them, according to a patient’s journey.

1. Appointment Management
Managing appointments manually is not only tedious but also increases the chances of human errors. Even patients are inclined to choose a hospital with an option to book appointments online. In a recent study, 68% of patient s said they would prefer to schedule, modify, or cancel appointments online.
This hospital management system module enables you to add a scheduling option to your hospital’s website so that patients can easily schedule an appointment.
Once your patient has booked an appointment, the HMS software for hospitals will match the patient’s illness to the doctor’s area of expertise. It will then assign them to the next available specialist or the one they prefer. It also updates the available slots in real-time to avoid any confusion at the hospital. The next step in appointment booking is to collect medical documents. An HMS with a patient portal is used to collect documents and share the patient history with the doctors well in advance. If the patient requires assistance at his/her house, the system will check the doctors’ availability for the remote visit and allocate accordingly. In this way, you can create a smooth and error-free process by digitizing the appointment booking process.

2. Patient Management
After the patient onboarding is completed, the patient is moved to an IPD or OPD. The patient management module of HMS caters to the needs of the inpatient and outpatient departments. It captures and stores the medical history, treatment required, details of their previous visits, upcoming appointments, reports, insurance details, and more.
Patient management software also generates unique admissions numbers for each patient to easily manage admissions, discharges, and transfers. It also builds a comprehensive discharge summary to ensure smooth discharge. At the same time, it records and generates related documents, e.g., consent forms for electronic signature.
When you start collecting and storing details on hospital software systems, by default you also eliminate the need to get these details on every visit. HMS enables doctors and staff to focus more on treatment than administrative work.
Now, if you wish to automate other activities like patient communication, consider integrating your HMS with marketing automation software such as LeadSquared . It will enable you to automate communication with patients and doctors. You can send appointments and lab test reminders, or follow-ups, and build meaningful long-lasting relationships.

3. Facility Management
To provide a smooth experience for your patients, it is essential for your staff to have easy access to necessary hospital records. The facility management module of a healthcare management system helps you to maintain records of bed availability, occupancy status of rooms with specialized care, and more.
Healthcare management systems collect all such information and make it readily available to your receptionist.
If you have multiple facilities, then an HMS connects them to provide an overall picture. For example, doctors can access patient data from any hospital using an online hospital management system. Patients can visit any hospital according to their convenience, as all the records are available online.
4. Staff Management
The staff management module provides a concrete solution for the HR department. It contains records of your staff, job description, service domain, and other vital details.
It helps you to know your staff without going through a heavy bundle of files. Additionally, it enables you to plan the hiring process based on the requirements of the hospital.
5. Supply Management
A hospital cannot afford to be short of medical supplies. Not having the medicine at the right time or a minor delay in refill can lead to severe results. The supply management component of the HMS tracks the availability of medical stocks. It helps you calibrate the minimum quantity of supplies required without any hassle. It records the purchase date, quantity consumed, and supplier details. This way, you can calculate or predict the next purchase and reorder before the stock falls short. It also provides the details of the medicine available so that doctors can prescribe the ones in stock.
6. Financial Management
The financial management component of an HMS deals with the financial affairs of your hospital. It calculates, stores, and presents the billing information to the patients.
Additionally, it also records the expenses incurred by the hospital, revenue data, and other financial details of the hospital.
This consolidation saves you the trouble of analyzing a colossal pile of record books.
7. Insurance Management
An HMS’ insurance management component records and stores patients’ insurance details. On requirement, it presents the policy number, insurance company, and other associated information.
The hospital management software makes it easy to fetch these details, making insurance validation easier.
8. Laboratory Management
The laboratory management feature of hospital management software shows the details of various lab tests patients take. It furnishes reports when needed and maintains all records collectively. The doctors can easily access it. It also notifies the doctor and the patients when the results are ready.
9. Report Management
Report Management module, records and stores all the reports generated by the hospital.
In the case of financial reports, it analyzes performance metrics to check the business profitability. It also provides a comparison between performance reports for different years. An authorized person can access these hospital management system reports whenever required.
Furthermore, you can use healthcare dashboards to present these reports in an easy-to-read format.
10. Vaccination Management
A vaccination model of hospital management software keeps track of all the completed or upcoming vaccinations. It updates you about upcoming vaccinations and books a slot with the doctor. It also sends timely reminders to parents to ensure they don’t miss the slot.
11. Support Management
Patient satisfaction is of utmost importance for any hospital. This segment records data like inquiries, complaints, requests, and feedback from patients. It also ensures that you handle these requests and problems appropriately and at the soonest. You can automate the feedback collection process to reduce the staff’s workload, and everyone could fill out the feedback form.
If you are still thinking of whether or not to implement an HSM. To answer this let’s discuss the benefits you will observe after implementing an HMS.
Benefits of a Hospital Management System
1. enhanced communication between the patient and the hospital.
59% of millennials are willing to switch doctors for better online access. An HMS will improve communication between patients and hospitals by allowing patients to access their medical records, book appointments, receive reminders, and communicate online with their doctors and nurses. You will have improved patient engagement, a reduction in waiting times, and increased patient satisfaction.
2. Secured hospital data
Hospital management software must help you keep hospital data safe and secure. You can limit the access to authorized personnel only. Make sure to look for HIPAA Compliant software for PHI security.
3. Improved access to patient data
You can have easy entry to all patient-related data on a system using an HMS. You can also access data such as patient history, doctors engaged, test results, billing information, and many more with just a few clicks.
4. Reduced turnaround time
Streamline your hospital workflows by automating routine tasks like appointment or inventory management. This reduces the time and effort required to perform these tasks and the turnaround time. It also allows hospital staff to focus on more critical patient care areas.
5. Cost-effectiveness
Implementing hospital management software can lead to significant cost savings for hospitals. It helps by reducing administrative overheads, improving resource allocation, and minimizing the wastage of medical supplies. An HMS can also optimize revenue streams by ensuring timely billing and reducing claim denials.
6. Intelligent analytics with automatically generated reports
An HMS can provide valuable insights regarding operations by generating real-time reports on various metrics, such as patient flow, occupancy rates, and revenue generation. This enables you to make data-driven decisions, improve processes, and optimize resources.
7. Centralized administrative control
An HMS helps build a centralized platform for managing operations, allowing hospitals to streamline their administrative processes. It ensures consistency across departments. This can improve efficiency, reduce errors, and better overall patient care.
8. Reduced medical errors
An HMS can help reduce medical errors by providing doctors and nurses with up-to-date patient information. It minimizes the risk of misdiagnosis, incorrect treatment, or adverse drug interactions.
9. Reduced readmissions and rehospitalization rates
An HMS can also reduce readmissions and rehospitalization rates by ensuring timely follow-ups. This improves patient outcomes and reduces the risk of complications.
To get to know how effective a Hospital Management System can be for hospitals, let us have a look at the example of how Manipal Hospital benefited from it.
How LeadSquared Helped Manipal Hospitals to Improve Reporting and Lead Management
Manipal Hospitals is one of India’s largest healthcare providers, with over 27 multispecialty hospitals. They have multiple teams working together to enable a smooth patient experience.
With a high patient volume and each team working on a different platform, keeping track of each patient’s journey and managing appointments became increasingly hard for Manipal Hospitals. They needed to centralize leads across India while securely managing patient information. LeadSquared provided an all-in-one solution integrated with their existing HIS.
Key Results:
- Zero Lead Leakage
- 360° View Across Teams
- Better Patient Management
LeadSquared’s APIs and connectors help us collect detailed patient data and integrate it with our core HIS system. The dashboards and reports enable us to work with this data and derive great insights from it. Both these features help streamline processes, save time, and in turn boost team productivity. Kiran Ramakrishna, Assistant Manager, Manipal Hospitals
[Also read: Manipal Hospital Improves Reporting and Lead Management to know the complete story.]
Conclusion
Hospital Management System (HMS) is essential to the delivery of modern healthcare. It can boost patient outcomes, lower medical errors, and improve the overall quality of care. It enables hospitals with a centralized platform to manage their operations, automate mundane processes, and enhance communication.
Moreover, Healthcare CRM , when integrated with the Hospital Management System, helps you combine professional medical care with quality patient service.
To experience the benefits of an integrated HMS and Healthcare CRM system, get in touch with our team today!
Also read:
- What is Healthcare CRM?
- EHR integration with healthcare CRM software
- Patient satisfaction survey questions
- Healthcare CRM – A 61-question checklist to help you make the right decision
There are generally two types of HMS, cloud-based and on-premises. A cloud-based or web-based hospital management software is hosted on the provider’s server. In contrast, on-premises hospital management software is hosted on the hospital’s private server and data centers. A cloud-based hospital management system is more popular as it is cost-effective, and the provider can handle it remotely.
While implementing an HMS, you may face the following challenges: 1. Cybersecurity 2. Lack of technical team support 3. Complex interface 4. Higher initial implementation cost To overcome these challenges, you need the right provider. They will ensure data security and support the implementation and staff training.
An off-the-shelf CRM is popular as it is cost-effective and quick to implement. It is a great option for small to medium sized organizations looking for basic and essential features. Whereas a custom-built HMS provides more control over the usage and features.

Awantika is a healthcare marketer with LeadSquared. She has been a part of the content and product marketing game for almost 3 years. You can connect with her on LinkedIn or write to her at [email protected].
Table of Contents
- Share on Facebook
- Share on Twitter
- Share on WhatsApp
- Share on LinkedIn
Want to see LeadSquared in action?
- Customer Portal
- Performance Management
- Dev Platform LAPPS
- Help Portal
- Pricing SALES
- Pricing MARKETING
- Education CRM
- Healthcare CRM
- Insurance CRM
- Banking CRM
- Real Estate
- Marketplace CRM
- Manufacturing CRM
- What is CRM
- What is lead management
- What is vendor management
- What is sales management
- Case Studies
- Guides & Blogs
- Compare CRM
- CRM Glossary
- Sales Glossary
- Media & News
GET IN TOUCH
(+1) 732-385-3546 (US)
080-46971075 (India Sales)
080-46801265 (India Support)
62-87750-350-446 (ID)
- Legal & Compliance

An industry leading benefits package is just the beginning. A collaborative culture helps us thrive.

Our Results
We work to improve the health care continuum, based on our extensive research and experience.
Read Case Studies
% INCREASE IN PATIENT VOLUME
Clinical Locations
If you have a location in mind, use our Locations search to find clinical careers.
Search Locations by State
- For Patients
NEWS & RESOURCES
At USACS, we are always gathering – and sharing – information. It’s through the process of documenting best practices, reviewing metrics and adopting innovative solutions that we find success with our nationwide partners.
General News
Mar 7, 2024

USACS Announces Annual Clinical Excellence Award Winners
CANTON, Ohio, March 7, 2024 – US Acute Care Solutions (USACS), the nation’s largest physician-owned provider of hospital-based emergency and inpatient medicine, is pleased to announce eight clinicians who have been named recipients of the National Clinical Governance Board’s (NCGB) Clinical Excellence Award. These recipients were honored during USACS’ annual Assembly meeting held in Denver, CO, last month. The Clinical Excellence Award was created to recognize outstanding clinical care by individual physicians and advanced practice providers (APPs) who do not serve in leadership or management roles and represent each USACS service line. Nominations are submitted year-round by clinical colleagues and are reviewed at the beginning of each calendar year. Recipients are selected and notified before the annual spring Assembly meeting. Congratulations to the following recipients of the 2024 Clinical Excellence Award: Matthew Baltz, MD, Bon Secours Memorial Regional Medical Center— Mechanicsville, VA Calen Hart, MD, AdventHealth Tampa—Tampa, FL Waleed Hussein, MD, Hazel Hawkins Memorial Hospital—Hollister, CA Omar Naji, MD, StoneSprings Hospital Center—Dulles, VA Ryan Nguyen, PA-C, Dell Children's Medical Center of Central Texas—Austin, TX James (Ian) Richardson, DO, Bon Secours Memorial Regional Medical Center—Mechanicsville, VA Nathan Scherer, DO, AdventHealth ER and Urgent Care at Meridian—Parker, CO Melissa Volpe, PA-C, Sentara Martha Jefferson Hospital—Charlottesville, VA National Director of Clinical Education and Vice Chair of the NCGB, Roya Caloia, DO, MPH, FACEP, shared, “These are the people you work alongside who make you want to be a better physician or APP. Their efforts and commitment to high-quality patient care remind you of why you chose to go into medicine in the first place. Congratulations to each recipient, I am honored to call each of you colleagues!” About USACS Founded by emergency medicine and inpatient physicians across the country, USACS is solely owned by its physicians and hospital system partners. The group is a national leader in integrated acute care, including emergency medicine, hospitalist, and critical care services. USACS provides high-quality care to approximately ten million patients annually across more than 400 programs and is aligned with many of the leading health systems in the country. Visit usacs.com for more. ### Media Contact Marty Richmond Corporate Communications Department US Acute Care Solutions 330.493.4443 x1406 [email protected]
OWNERSHIP MATTERS
When physicians own the business, they’re empowered to make the best decisions.

HOSPITAL MANAGEMENT CASE STUDIES
As a physician-owned organization, we value results. Enhancing the quality and efficiency of hospital management, while improving patient outcomes, is our goal. We continually measure real-life results to demonstrate success. Looking for information related to a specific measurement goal? Filter our case studies by selected outcomes below.
% PATIENT SATISFACTION SCORE
From Failure to Success
TH PERCENTILE OR HIGHER FOR PATIENT SATISFACTION
Observation Care That Works
MILLION DOLLARS SAVED IN PROGRAM'S FIRST YEAR
Reducing the Flow of Blood ... and Money
% LWBS RATE AND REDUCTION IN DOOR-TO-PROVIDER TIME
The Meritus Medical Center Turnaround
MINUTE REDUCTION IN TOTAL LENGTH OF STAY
The Most Efficient Gatekeeper
TIPS TO ENSURE HIGHER STANDARD OF CARE IS MET
Building Better Clinicians
% LWBS RATES, DOWN FROM 5%
Reducing ER Overcrowding Without Adding Beds
HOUR SPRINT STARTS RELATIONSHIPS ON THE RIGHT FOOT
Achieving Minimal Blowback and Maximum Buy-in
% DECREASE IN WAIT TIME TO SEE A DOCTOR
Increased ED Efficiency for a Newly Built Hospital
NEW PARTNERSHIPS NEW OPPORTUNITIES
If you’d like to explore all USACS can offer your facility and join our nationwide network of partners, contact us today.
Contact Us +
Tell us about yourself
Know more about our vision & mission at Zenkins.
Learn more about our process and how we work?
Contact today! Ready to help you with all tech challenges.
Stay updated with latest technologies and tools.
SAAS Product Development
Empowering Your Vision with Expert SAAS Product Development Services
IT Staff Augmentation
Boosting Your IT Capabilities with Staff Augmentation Solutions
Product Engineering
Crafting Innovation Through Product Engineering Services
Platform and Infrastructure
Elevating Your Digital Foundation: Our Platform and Infrastructure Expertise
Digital Transformation
Unlocking Your Digital Potential: Transformation Services for the Modern Age
Data Engineering
Unlocking the Power of Data: Our Expert Data Engineering Services
IT Consulting
Navigating IT Excellence: Our Comprehensive Consulting Services
- Maintenance And Support
Safeguarding Your Success: Exceptional Maintenance and Support Services
Core Expertise
- .NET Development
- ASP.NET MVC Web Dev.
- ASP.NET Core Web Dev.
- ASP.NET Web Form Dev.
- .NET Windows App Dev.
- .NET WPF Application Dev.
- .NET Core API Development
- .NET WCF Services
- .NET CMS Development
- C# Development
- .NET Core Development
- Full-Stack Web App Dev.
- Agile, Scrum & DevOps
- Integration Services
- Mobile App Development
- AI ML Development
- Legacy .NET App Modernization
- E-Commerce Solutions
- Enterprise Application Dev.
- Database Design And Mgmt
- Cloud Integration
- Azure / AWS / GCP
- Migration Services
- Third-Party Integrations
- UI/ UX Design
- Quality Assurance & Testing
- Security And Compliance
- Consulting And Strategy
- Content Management
- Performance Optimization
- IoT Hardware & Software
- .NET Developers
- C# Developers
- VB.NET Developers
- .NET Core Developers
- Windows Desktop Application Developers
- Azure Developers
- SQL Server Developers
- ASP.NET MVC Developers
- Blazor Developers
- Angular Developers
- Full-Stack .NET Developers
- HTML / CSS Developers
- JavaScript Developers
- Xamarin Developers
- Kentico CMS Developers
- Sitecore Developers
- Umbraco Developers
- Orchard CMS Developers
- DNN (DotNetNuke) Developers
- Sitefinity Developers
- NopCommerce Developers
- mojoPortal Developers
- DevOps Engineers
- UI/UX Designers
- Quality Assurance (QA) Testers
- Security Experts
Build Your Team
We help companies transform, scale, and gain a competitive edge with robust, customized, and innovative digital solutions.
- Technologies
- Entity Framework
- Razor Pages
- Razor Views
- Microservices
- IdentityServer
- Visual Studio
- Visual Studio Code
- Azure DevOps
- SQL Server Management Studio (SSMS)
- AWS (Amazon Web Services)
- GCP (Google Cloud Platform)
- Azure Functions
- Distributed Platforms
Our expertise spans all major technologies and platforms, and advances to innovative technology trends.
Can't find what you need?
- Case Studies
Hospital Management Software: A Case Study
- Post author: Maryliya M J
- Post published: January 12, 2024
- Reading time: 11 mins read

Hospital Management Software (HMS): A Case Study
Table of contents.
Hospital Management Software (HMS) has revolutionized the way healthcare organizations operate, streamlining administrative tasks, improving patient care, and enhancing overall efficiency.
Introduction to Hospital Management Software (HMS)
What is hospital management software.
Hospital management software, also known as HMS, is a digital solution that helps healthcare institutions streamline their administrative and operational processes. It provides a centralized system for managing various aspects of a hospital, including patient registration, appointment scheduling, billing, pharmacy management, and electronic health records.
Importance of HMS in the Healthcare Industry
In an industry where time is of the essence and accuracy is crucial, hospital management software plays a vital role. It eliminates the need for manual paperwork and reduces the chances of errors, improving overall efficiency. HMS provides real-time insights into patient data, allows seamless communication between departments, and enables hospitals to deliver better patient care. With the ever-increasing complexity of healthcare, HMS has become an indispensable tool for modern hospitals.
Key Features and Benefits of HMS
Streamlining patient registration and admission.
Gone are the days of long queues and paperwork during patient registration. HMS simplifies the process by digitizing patient information, streamlining the admission process, and reducing wait times. It ensures accurate data entry, minimizes errors, and improves the overall patient experience.
Efficient Appointment Scheduling and Management
Efficient appointment scheduling is essential for both patients and healthcare providers. HMS allows patients to book appointments online, check availability, and receive reminders. It also helps hospitals optimize their scheduling, reduce no-shows, and effectively manage their resources.
Simplifying Billing and Revenue Management
Billing and revenue management can be complex and time-consuming. HMS automates the billing process, generates accurate invoices, and integrates with insurance providers. It ensures transparency, reduces billing errors, and helps hospitals manage their finances effectively.
Enhancing Inventory and Pharmacy Management
Keeping track of inventory and managing pharmacy operations can be a daunting task. HMS enables hospitals to track stock levels, automate reordering, and ensure seamless supply chain management. It improves medication safety, reduces wastage, and enhances overall efficiency.

Are you struggling to keep up with your software development needs? Are you looking for a team of dedicated developers who can work on your project full-time and deliver high-quality results? So why wait? Contact us today to learn more about our services and to start the process of hiring your own dedicated development team. Let us help you take your project to the next level! Contact Now!
Improving electronic health records ( ehr ) and documentation.
Maintaining accurate electronic health records is essential for providing quality healthcare. HMS digitizes patient records, making them easily accessible, securely stored, and retrievable when needed. It improves data accuracy, enhances collaboration between healthcare professionals, and simplifies documentation processes.
About the Client
Our client, a large hospital, faced challenges in patient record management, appointment scheduling, and interdepartmental coordination. Recognizing the need for a comprehensive solution, they sought a Hospital Management Software (HMS) to enhance patient care and administrative efficiency.
Project Overview
The project aimed to develop a robust Hospital Management Software using .NET to address the client’s challenges. The primary objectives included electronic health records, appointment scheduling, inventory management of medical supplies, and seamless communication between various departments for a more integrated healthcare system.
The Challenges
- Patient Record Management: The existing systems struggled with efficient and secure management of electronic health records.
- Appointment Scheduling: Inefficient appointment scheduling processes led to long waiting times and patient dissatisfaction.
- Interdepartmental Coordination: Lack of seamless communication hindered collaboration between different departments.
The Solution
Our experienced team of developers and project managers collaborated to design and implement a comprehensive .NET-based Hospital Management Software (HMS). The solution incorporated features such as electronic health records, appointment scheduling, and inventory management, promoting seamless communication between departments.
Key Features of the HMS
- Electronic Health Records (EHR): The HMS enabled efficient and secure management of electronic health records, ensuring easy access for authorized personnel.
- Appointment Scheduling: Advanced scheduling algorithms optimized appointments, reducing waiting times and improving patient satisfaction.
- Inventory Management: The software facilitated real-time tracking and management of medical supplies, preventing shortages and optimizing inventory levels.
- Interdepartmental Communication: Robust communication tools were integrated to enhance collaboration and coordination between different hospital departments.
The Outcome
The Hospital Management Software was successfully deployed, resulting in significant improvements in patient care and administrative efficiency. Efficient EHR management, optimized appointment scheduling, and seamless communication between departments enhanced overall healthcare services.
Our team’s expertise in developing a tailored Hospital Management Software using .NET technologies addressed the client’s challenges effectively. The implementation of features like EHR, appointment scheduling, and interdepartmental communication contributed to a more integrated and efficient healthcare system.
In conclusion, Hospital Management Software (HMS) has proven to be a game-changer in healthcare management, revolutionizing the way hospitals operate and improving patient care. The successful case study of this hospital showcases the transformative power of HMS, highlighting its benefits, challenges, and lessons learned throughout the implementation process.
As we look ahead, the future of HMS holds promising advancements, including artificial intelligence, cloud-based solutions, and interoperability with other systems. With continued innovation and adoption of HMS, we can expect further improvements in hospital operations, patient experiences, and overall healthcare outcomes. Embracing the potential of Hospital Management Software is crucial for healthcare organizations seeking to thrive in a rapidly evolving industry.
Are you facing challenges in patient record management and hospital administration? Contact us today to explore how our expertise in HMS development can transform your healthcare operations and enhance patient care.
Get 50% off on your first project with us! Join our community of satisfied customers and experience the power of our software team today. Contact now and get 50% off your first software project/ product. Don’t miss out on this exclusive offer! Your Name * Your Email * Contact Number * Brief Your Requirement * 0 / 500 Claim Your Discount Please do not fill in this field.
You might also like.

Our approach for offering our SmartX bank the greatest banking software development services

Our way to offer HealthCare CRM to our clients

Hotel Management Software: A Case Study
Book a free consultation.
Tailored Solutions, Expert Advice, and Project Estimates Await.
Expect a Prompt Call from one of our Account Managers.
- Top .NET Talent
- Time Zone Aligned
- Experienced Team
At Zenkins, we understand the importance of having skilled and dedicated .NET professionals on your side. Our team consists of top .NET talent with a proven track record of delivering high-quality solutions. Whether you need custom .NET application development or require expertise in ASP.NET, C#, or .NET Core, our talented developers are ready to bring your vision to life.
We recognize that time zone differences can often be a challenge in global collaborations. Zenkins addresses this issue by ensuring that our development teams are time zone-aligned with your operations. This means you can expect real-time communication, rapid responses, and a seamless workflow, reducing project delays and ensuring effective collaboration, no matter where you are in the world.
Experience matters in the world of software development, and our team has it in abundance. Zenkins’ experienced team brings a wealth of knowledge and expertise to the table. From legacy .NET application modernization to building cutting-edge cloud-native solutions using the .NET framework, our team has successfully handled a wide array of projects. You can trust us to navigate your software development journey with precision and care.
+91 70690 18504
[email protected]
Zenkins is a leading .NET development company in India, with over 10 years of experience in developing high-quality, scalable, and secure .NET applications. The company has a team of experienced and certified .NET developers who are experts in all aspects of .NET development, including ASP.NET, WPF, Windows Forms, WCF, Xamarin, and more.
- Methodologies
- Our Services
- IT Staffing Services
- Software Outsourcing
- Careers @Zenkins
- Current Openings
- Technology Insights
- Careers Insights

326, Naroda Business Point, Vasant Vihar 2, Nava Naroda, Ahmedabad, Gujarat 382330
Opening soon in Pune Baner, Pune, Maharashtra 411045 - India
Opening soon in Bangalore Vasanth Nagar, Bengaluru, Karnataka, 560020 - India
Privacy Overview
Get 50% off your first project with us.
Join our community of satisfied customers and experience the power of our software team today. Contact now and get 50% off your first software project/ product. Don’t miss out on this exclusive offer!
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

CASE STUDY OF HOSPITAL MANAGEMENT SYSTEM (HMS

Related Papers
International Journal of Clinical Monitoring and Computing
International Journal for Research in Applied Science & Engineering Technology (IJRASET)
IJRASET Publication
Hospital Management System includes registration of patients, storing the details into the system and appointing doctors online. Our software has the facility to give a unique id for every patient and stores the details of every patient and list of all the doctors which work in the hospital. It includes a search availability of a doctor and the details of a patient using the id. Our system gives each doctor a unique code due to which patients can book their appointments online. The Hospital Management System can be entered using a username and a password. It is accessible by an administrator, doctor and the patient as well. Each doctor has their unique username and password which can be logged in by their correspond email-id , like the doctor patient also have their unique username and pass. But the admin has access to both the doctors and patients details and everything which would help the admin to keep an eye over its hospital management. The interface is simple and userfriendly. The data are well protected for personal use and makes the data processing very fast.
Ijaems Journal
— Health institution requires quality data and information management to function effectively and efficiently. It is an understatement to say that many organizations, institutions or government agencies have become critically dependent on the use of database system for their successes especially in the hospital. This work aims at developing an improved hospital information management system using a function-based approach. An efficient HIMS that can be used to manage patient information and its administration is presented in this work. This is with the goal of eradicating the problem of improper data keeping, inaccurate reports, wastage of time in storing, processing and retrieving information faced by the existing hospital information system in order to improve the overall efficiency of the health institution. The system was developed with Hypertext Markup Language (HTML), Cascading Style Sheets (CSS), Hypertext Preprocessor (PHP), and My Structured Query Language (MySQL). The new system was tested using data collected from Renewal Clinic, Ibadan, Nigeria was used as case study were the data for the research was collected and the system was tested. The system provides a vital platform of information storage and retrieval in hospitals.
The paper developed an automated system that is used to manage patient information and its administration. This was with a view to eliminate the problem of inappropriate data Keeping, inaccurate reports, time wastage in storing, processing and retrieving information encountered by the traditional hospital system in order to improve the overall efficiency of the organization. The tools used to implement the system are Hypertext Markup Language (HTML), Cascading Style Sheets (CSS), Hypertext Preprocessor (PHP), and My Structured Query Language(MySQ).The Proposed system was tested using the information collected from Murab Hospital, Ilorin, kwara State , Nigeria and compared with the existing traditional hospital system. The design provides excellent patient services and improved information infrastructure.
Mohammed Aman
OBJECTIVE : Hospitals currently use a manual system for the management and maintenance of critical information. The current system requires numerous paper forms, with data stores spread throughout the hospital management infrastructure. Often information (on forms) is incomplete, or does not follow management standards. Forms are often lost in transit between departments requiring a comprehensive auditing process to ensure that no vital information is lost. Multiple copies of the same information exist in the hospital and may lead to inconsistencies in data in various data stores. A significant part of the operation of any hospital involves the acquisition, management and timely retrieval of great volumes of information. This information typically involves; patient personal information and medical history, staff information, room and ward scheduling, staff scheduling, operating theater scheduling and various facilities waiting lists. All of this information must be managed in an efficient and cost wise fashion so that an institution's resources may be effectively utilized HMS will automate the management of the hospital making it more efficient and error free. It aims at standardizing data, consolidating data ensuring data integrity and reducing inconsistencies. PROJECT OVERVIEW : The Hospital Management System (HMS) is designed for Any Hospital to replace their existing manual, paper based system. The new system is to control the following information; patient information, room availability, staff and operating room schedules, and patient invoices. These services are to be provided in an efficient, cost effective manner, with the goal of reducing the time and resources currently required for such tasks. A significant part of the operation of any hospital involves the acquisition, management and timely retrieval of great volumes of information. This information typically involves; patient personal information and medical history, staff information, room and ward scheduling, staff scheduling, operating theater scheduling and various facilities waiting lists. All of this
International Journal of Computer Theory and Engineering
Ezenwa Nwawudu
emeka ajoku
ABSTRACT This study investigated online hospital management system as a tool to revolutionize medical profession. With many writers decrying how patients queue up for hours in order to receive medical treatment, and some end-up being attended to as „spillover‟, the analyst investigated the manual system in detail with a view to finding out the need to automate the system. Subsequently, a computer-aided program was designed to bring about improvement in the care of individual patients, taking the advantage of computer speed, storage and retrieved facilities. The software designed will take care of patient‟s registration, billing, treatment and payments. The programming language employed in this work was Microsoft C#.
RELATED PAPERS
GERMAN ANDRÉS GIL LOVERA
IOSR Journals
Siti Chairani
British journal of cancer
J. Ciccolini
Nuclear Engineering and Design
Thomas GELAIN
Eduardo Campazzo
Lecture Notes in Computer Science
Mike Brayshaw
2019 27th Iranian Conference on Electrical Engineering (ICEE)
Ali Poureslami
Luca Iandoli
Ryan Hayhurst
Henk Bloemhoff
خالد ي ح ي محمد
Biochimica et Biophysica Acta (BBA) - Biomembranes
Martial Ruat
The Handbook of Environmental Chemistry
Journal of digital imaging
Andreas Brühschwein
arXiv: Number Theory
Mariusz Skałba
Central European Journal of Public Health
Revista Española de Enfermedades Digestivas
José Antonio Rodríguez Montes
Applied Sciences
Rafael Jiménez Castañeda
Acta Neurochirurgica
Gilles Perrin
HERNAN ALEJANDRO OLANO GARCIA
Yaron Dagan
Aziz A Elfazziki
Corinna Nicosia
Wahana Fisika
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Support is what makes healthcare faster.
We have everything you need.
Communication is the key to patient care.
Your own ideas integrated into EMR.
Innovation at your finger tips.
We have everything you need for a startup.
Data at your fingertips.
Bring ideas to real life.
All in one integrated solution.
Making healthcare easy and affordable.
Your own telehealth solution.
- CASE STUDIES
Learn what we’re all about.
See through our heads and heart.
How we rise and shine?
How we stand out?
We’re looking for you.
See research’s and latest trends.
- FUND MY START-UP
Leveraging data for efficient resource management
A single hospital produces terabytes of data every day. Here’s how we used machine learning algorithms to sort through all this data to find patterns and room for improvement.
Explore Our Methodology
We have deployed mobile and web products that grow at scale, from mobile applications to enterprise-grade platforms across a wide variety of industries.
“The beauty of SyS Creations team is their healthcare knowledge. They built everything simple yet future-ready. We shifted to new tech with almost zero effort. Having a healthcare-focused IT company as a tech partner makes a whole lot of difference!”
Introduction
The client was a prominent multispecialty hospital with separate departments for everything from pediatrics to plastic surgery. Their problem was that individual departments had their workflows and systems, which created separate data silos. And they wanted to bring together all this data under a single platform for better management.
United Kingdom
Challenges & goals.
Once we spoke to the different department heads, doctors, other healthcare professionals, and the hospital, we knew what we had to do.
- Departments had different workflows to serve their patients better.
- Every department had its systems for organizing and storing data
- Interdepartmental data transfer was completely manual
- To create a unified data collection platform
- Maintain the diverse workflows of different departments
- Analyze the data and make the organization more efficient.
Our Engagement
We designed a platform that brought together the data from all the departments. Cutting edge AI we developed gave accurate and actionable insights to prevent wastage of resources within the organization.
We created a solution that produces our client an estimated saving of 1 million USD annually.
Technologies We Utilized
By using the latest technology, we ensure our solutions are future-proof.
To design and develop an intuitive and easy-to-navigate interface.
To We used our proprietary HIPAA compliant EMR technology to store patient details securely.
We used AWS AI systems to implement machine learning and artificial intelligence into the system.
To store the system data in a safe, secure, and scalable manner.
For building an effective software backend.
Android/iOS
For building the mobile apps.
Project Media
Our work produced measurable results for our clients.
Better inventory management
Wastage of material resources was reduced by 56%.
Smoother operations
The average patient wait time was reduced by 67%.
Reduced expenditure
The system created close to 1million USD in annual savings for the organization.
Reduced workload for the hospital staff
98% of the hospital staff reported a massive decrease in their daily workload.
Let's Build Great Things Together!
Free technical consultation, connect with the tech team, onboarding the team, let's build great things together, we support game-changing early-stage healthcare technology leaders who are building the future..
Experiences of implementing hospital management information system (HMIS) at a tertiary care hospital, India
Vilakshan - XIMB Journal of Management
ISSN : 0973-1954
Article publication date: 19 November 2021
Issue publication date: 2 February 2023
Mumbai needs to be transformed into a world-class city as stated in the 2005–2025 development plan of Municipal Corporation. For this initiative, hospital management information system (HMIS) has to be implemented across 400+ health facilities in the city.
Design/methodology/approach
A case study methodology was adopted to study HMIS implementation. Wave 1 of Phase 1 implementation of HMIS is carried out as a pilot project at Film City’s Hospital, Mumbai, which “go-live” on 21st June 2018. The work for hardware and software implementation was awarded to HardSystems and Solutions Limited and SoftSolutions India Private Limited, respectively, through e-tender.
Provision of inadequate quantity of hardware, slowness of network or system, non-satisfactory training after observation confirmation and sign-off process, lack of data entry operators, mismatch in numbering systems in blood bank and many other challenges concerned with the specific departments had become a major impediment in the efforts to maximize number of patients registered into HMIS.
Practical implications
Even after providing many clinical and managerial benefits, being the first cloud-based centrally located HMIS in any of the hospitals in the city, it imposes a major challenge for the management in terms of resistance of employees toward technology and need for the adoption of theoretical models for implementing change for the overall organizational development.
Originality/value
To the best of the authors’ knowledge, no other teaching case study is conducted to study the HMIS implementation in large-scale public health-care services. This is a dummy case study for teaching exercises. The identity of the stakeholders, organizations and events has been masked to maintain confidentiality.
- Change management
- Organizational development
- Health-care services management
- Hospital management information systems
- Pilot project
Arora, L. and Ikbal, F. (2023), "Experiences of implementing hospital management information system (HMIS) at a tertiary care hospital, India", Vilakshan - XIMB Journal of Management , Vol. 20 No. 1, pp. 59-81. https://doi.org/10.1108/XJM-09-2020-0111
Emerald Publishing Limited
Copyright © 2021, Lakshya Arora and Feroz Ikbal.
Published in Vilakshan – XIMB Journal of Management . Published by Emerald Publishing Limited. This article is published under the Creative Commons Attribution (CC BY 4.0) licence. Anyone may reproduce, distribute, translate and create derivative works of this article (for both commercial and non-commercial purposes), subject to full attribution to the original publication and authors. The full terms of this licence maybe seen at http://creativecommons.org/licences/by/4.0/legalcode
It was a dewy evening of Mumbai in July 2018 and a biscuit falls into the hot coffee which Medical Superintendent of Film City’s Hospital, Mumbai was dunking into his huge vintage cup.
Deputy Medical Superintendent and hospital management information system (HMIS) Nodal Officer at Film City’s Hospital bought a letter sent by one of the Heads of a Clinical Department to his office. It was mentioned in the letter that in most domains of the HMIS, the providers have not completed the modules and required integration which they have requested them to make as per the departments’ clinical and documentation requirements. The letter added that the training team was helping them only with cursory skills which they could learn by themselves once the modules would be effectively designed and given. Hence, the representatives of SoftSolutions India Private Limited were suggested to be called in a meeting along with Heads of all the Departments and other users of the system in the presence of Medical Superintendent and Director to avoid financial losses to the health-care system.
The Deputy Medical Superintendent and the HMIS Nodal Officer discussed with the Medical Superintendent that it was only one among many letters received by HOD of many departments of the hospital where HMIS was implemented as a pilot project by the Director in the past few months.
Informatics involves information acquisition, organization, validation, storage, retrieval, integration, analysis, communication and presentation, using IT as a key resource ( Lifshitz et al. , 2007 ; Sinard, 2006 ). HMIS is defined as the “computer system designed to ease the management of all the hospital’s medical and administrative information and to improve the quality of healthcare” ( Degoulet and Fieschi, 1997 ). An EHR system comprises “the longitudinal collection of electronic health information for and about persons, where health information is defined as information pertaining to the health of an individual or health care provided to an individual. Critical building blocks of an EHR system are the electronic health records (EHR) maintained by provider…and by individuals” ( National Institutes of Health, 2003 ).
At present, most of the Indian hospitals are adopting HMIS as a way of automation and digitalization of their health-care records.
Film City’s Hospital, Mumbai
Bombay, the very first possession of Britishers in India, came to King Charles II of England in 1661, when he married the Portuguese queen, as part of the royal dowry. Through Corporation Resolution No. 512 which was dated August 12, 1996 under Maharashtra Act, XXV, 1996, the name “Bombay” has been changed as “Mumbai.”
Greater Mumbai is presently a metropolitan aggregation of around 18 million residents (world’s six largest and largest in India). The port city accounts for most of foreign trade in India as well as government revenues, being one of the major hubs for education, research, development and technology in India ( MCGM, 2019 ).
The Film City’s Hospital situated in the heart of Mumbai is a 1,000-bedded tertiary care facility with around 30 clinical departments where every year more than 55,400 patients are admitted and more than 280,000 patients (new and old) are treated in out-patient department. More than 21,000 operations (major and minor) are performed and 4,200 deliveries are done every year.
In addition to the routine medical services, it also offers various super-specialty services in nephrology, neurosurgery, endocrinology, gastroenterology, cardiology and cardiac vascular and thoracic surgery. This hospital has well-equipped intensive care units for medical, surgical, cardiac and neonate patients. The hospital has its own blood bank and component therapy unit, which provides services round the clock. A whole body CT scanner, cardiac catheterization system and spect camera, etc. are also installed at the hospital. It also has independent hyperbaric oxygen therapy chambers.
The hospital levies fees from the patients at subsidies rate and efforts are made to provide the best and excellent patient care ( MCGM Health Department, 2019 ).
Why hospital management information system…?
India’s 12th 5-year plan highlights the need to improve HMIS throughout the nation and a possible investment in health IT in the public health system (Twelfth Five year Plan Draft 2012, 2017). Multiple findings have reported the advantages of HMIS implementation ( Hillestad R et al. , 2005 ; Wang et al. , 2003 ; Frisse and Holmes, 2007 ; Shekelle et al. , 2006 ).
HMIS is considered to be the most promising instrument to improve the overall efficiency, safety and efficacy of the health service (Basit et al. , 2006). Wide and effective use of HMIS improves the quality of health care ( Frere, 1987 ); minimize adverse events; reduce the cost of medical care ( Lun, 1995 ); increase administrative productivity improvements ( Kuruvilla et al. , 2004 ); reduce documentation as well as enhance access to affordable treatment (Basit et al. , 2006; Yasnoff et al. , 2000 ).
Municipal Corporation aspires Mumbai to be transformed into a millennium and world-class city as stated in the development plan 2005–2025. For this to happen, Mumbai requires to be distinguished about the quality of life aspect by improving the quality of citizen welfare services. As part of this initiative, the HMIS has to be implemented across 400+ health facilities across the city.
There is the availability of digital access original data through HMIS which can be used as a strong tool in the decision support system for the Film City’s Hospital management. The HMIS data can be used for analysis as well as for forecasting purposes. The electronic medical records (EMRs) as well as picture archiving and communication system (PACS) generated can be of great use for the clinical purposes for better diagnosis and treatment. The HMIS data can also be used for drug calculations and better scientific inventory management practices at the hospital.
Hospital management information system implementation at Film City’s Hospital
Literature have shown that implementation and improvement in HMIS to guide policy and management decisions has found essential space in countries such as Peru, Tanzania, Solomon Islands, Caribbean, Lesotho, Honduras, India (Uttar Pradesh) and Kryragya Republic (World Bank Reports , 1993 , 1999, 2000, 2001; Commission on Health Research for Development, 1990 ).
The work of software implementation and post-implementation of HMIS in the film city covering 4 major hospitals, 1 dental hospital, 18 peripheral hospitals, 5 specialty hospitals, 28 maternity homes, 161 dispensaries and 183 health posts was awarded to SoftSolutions India Private Limited.
As per the directives, Wave 1 of Phase 1 implementation of HMIS is carried out at Film City’s Hospital as a pilot project. Wave 2 of Phase 1 was planned to be implemented at other three major hospitals in the city and thereafter at balance health-care locations ( Mukul, 2018 ).
It was decided to form a committee to commence the viability and feasibility of Wi-Fi services project at Film City’s Hospital and the standing committee sanction was received for awarding the work for hardware and network implementation at the Phase I Hospitals and the LOI of worth Rs. 50+ crores for the prestigious project is issued to HardSystems and Solutions Limited. Further, a pilot implementation is planned to be carried out at few departments in Film City’s Hospital which “go-live” on 21st June 2018 ( MCGM IT Department, 2019 ).
Bid document for hospital management information system
The HMIS software pilot project at Film City’s Hospital was awarded to SoftSolutions Private Limited through evaluation of technical and commercial bids by e-tender process, initiated in July 2016. SoftSolutions, also as part of their scope, conducted a site survey for hardware infrastructure for all health-care institutions in the city. The exact quantity and minimum specifications for various hardware and infrastructure have been provided by SoftSolutions post site survey.
The purpose of this bid document is to select an agency for not only the supply but also the hardware and network components’ installation, testing, commissioning and maintenance for the health institutions.
A Bid Evaluation Committee (BEC) was appointed to examine and assess the submitted technical as well as commercial bids. The BEC reviewed the bids to decide if they’re really complete, able to respond and if the bid format complies with the bid specifications. In a bid that does not represent a material variance, it was waived for any informality or nonconformity and the bidder with the lowest cost submitted (L1 rate) in the commercial bid opening was awarded the contract.
Submission of inception report.
Supply, installation and commission of various hardware and network components along with required accessories at health institution.
Undertake required passive structured cabling (including patch chord, faceplate with input/output connector, laying of LAN and fiber cable (if required) with proper labeling, testing certificate and others).
The device should be tested before mass-installation (operating system compatibility, software, drivers, etc.).
The supplier should take care of all installation and support issues that are faced by the end-user, for all hardware and software supplied as part of the purchase order. This would include installation and support for security functions, user configuration, LAN configuration, etc.
Addition of a desktop PC to the security device is to be done by the implementation agency.
In-warranty annual technical support for hardware and network components services for a period of five years.
The following are additional points for the scope of the implementation agency:
The Wi-Fi/network device shall be connected to the local area network.
The supplier shall disable unnecessary services, protocols and ports.
When installing software, ensure that only required software is installed and the latest versions of all software including all recommended security patches are updated.
Disable or remove redundant software/services (including program, machine utilities and network services).
Pre-requisites for hospital management information system pilot project
The Assistant Medical Officer (AMO) of the hospital was appointed as the HMIS implementation nodal person from Film City’s Hospital for coordinating with the internet service provider and hardware supplier appointed by HardSystems and Solutions Limited, implementation of software by SoftSolutions and coordinating with various departments for providing solutions to any challenges faced.
Site readiness – the representative of SoftSolutions visited each department of the hospital for finalizing the network points, in consultation with the Head of Departments (HODs).
For the implementation of HMIS, one server room and one room for hardware and software support staff for the hospital and UPS room per building were identified and subsequently handed over to HardSystems and Solutions Limited, as per the specification ( The Hindu, 2018 ).
The support staff room was used by HardSystems and Solutions Limited for storing the equipment during the installation.
The civil work, if any, required for the network installation, server room and UPS room readiness was carried out by the Hospital Assistant Engineer (AE), Civil Department.
The furniture, if any, required for the HMIS hardware was identified and procurement was carried out by the Hospital M&E department.
The electrical work for HMIS implementation was carried out through the Chief Engineer (M&E) department. The concerned M&E engineer from the hospital coordinated with the representative of SoftSolutions and HardSystems and Solutions Limited.
Hardware and software implementation
As the number of patients was increasing in the waiting areas of the clinical departments, Deputy Medical Superintendent took a round with HMIS nodal officer to locate any patient-free area or store rooms in IPD building.
After the functional requirement study and the hardware survey did from June to September, 2016, the Digital Laboratory and Security room on ground floor of IPD building of the Film City’s Hospital was allotted for hardware storage. A 24 × 7 helpdesk was also created to give instant solutions to the arising issues in the software or hardware.
As per directives, 200 customized portable computer trolleys (to be used for computer-on-wheels) were provided as per the requirements and storage area in the departments.
Under Software Research Survey (SRS) up to September 2016, software customization for medical specialties was done after studying the workflow of major hospitals of Mumbai, for surgical specialties, radiology and central sterile services. Sub-committees were formed in each of these hospitals to monitor the process of customization of software, and sessions to sensitize nursing staff, technicians, pharmacists, registration attendants, etc. were conducted across all the hospitals. Weekly or sometimes fortnightly review meetings were held at the Film City’s Hospital. Also, various teams visited multiple public, private and trust hospitals across the city to study already existing HMIS implemented in these hospitals ( MCGM IT Department, 2019 ).
User acceptance tests and finalization of hospital management information system modules
Documented literature suggests that the degree of end-user satisfaction is a pivotal factor of an information system’s success ( Bailey and Pearson, 1983 ). Many other studies have stressed the significance of levels of end-user satisfaction ( Doll and Torkzadeh, 1988 ; DeLone and McLean, 1992 ).
During the user acceptance test-1 (UAT-1), there were 517 observations noted in module testing which was carried out up to March 21, 2017, by the doctors and other representatives.
Thereafter, in April 2017, a UAT observation confirmation process (also known as system requirement specification reconfirmation) was carried out by SoftSolutions with representatives from various health-care facilities who were assigned for each module so as to prepare SRS 1.1 with more precise information and requirement to aid the development of HMIS.
With reference to the OPD module, about 318 proformas from 29 departments were handed over to SoftSolutions on 9th June 2017 for developing the EMR for the OPD module. Considering each proforma was unique and also an easy-to-use system is to be developed, SoftSolutions has developed a solution and the same was shown to a team of doctors of each department concerned with the OPD module to check the functionality and provide their inputs for the same, so that the precise requirement can be incorporated in the SRS 1.1.
Further, SoftSolutions have documented the information provided during and after the UAT 1 and UAT/SRS reconfirmation in the latest SRS version 1.1 and the same was ascertained by the team of representatives who had provided the information during the UAT/SRS reconfirmation and corrected the same if necessary and provided the sign-off for the respective module SRS 1.1. On completion of the activity, UAT-2 (inter-module) and thereafter UAT-3 (integrated) were planned to be conducted.
On the basis of all the three UAT and UAT observation confirmation processes conducted for different modules, there were a number of change requests made by concerned HODs/departments which after approval from nodal officers were incorporated through some policy decisions for requirements which were taken by the administration.
It was finalized by the management that the short message service (SMS) would be used for registration and inpatient referral only. It is not necessary to send SMS for every activity. For easy workflow of IT services, digital signatures were assigned for important decisions, for legal, medico-legal cases, birth and death certificates.
Recruitment of data entry operators and training of hospital staffs
Deployment of data entry operators (DEOs) for assisting the hospital staff related to the implementation of HMIS was done through prescribed norms of recruitment for different departments for three working shifts.
The training was well planned by a team of SoftSolutions and all the requirements including space and other resources were allocated. Training was done in two parts, which involved orientation lectures and hands-on session conducted in the first and second weeks of February 2018, respectively.
It was decided to use India’s first indigenous Web-based PACS Medsynapse for training doctors and staff of radiology department. It is developed on advanced technologies and provided a full range of features and tools for image processing, distribution and archival. It is very user-friendly, scalable and affordable PACS with more than 20,000 installations in 40 countries.
A training completion certificate on specific HMIS module was awarded to each employee after successful completion of training.
For the purpose of logging into HMIS computers and application, employee’s ID-based default login and password systems were generated, which were later allowed to reset by the users. Thus, all the resident doctors and other staff got access to the HMIS system.
An HMIS refreshment training with proper consultation with Team SoftSolutions was provided once again in October 2018 after proper implementation of all the 32 modules in the system.
Dry run and go-live
A dry run was conducted in the selected clinical and supportive services departments of Film City’s Hospital in Phase 1 from April to June 2018. After the required improvements needed the pilot project “go-live” for Phase 1 of Wave 1 from 21st June 2018 ( MCGM RTI, 2019 ).
Overcoming hospital management information system challenges
Provision of an inadequate quantity of hardware either because of lack of storage space or because of unavailability of furniture and computer trolleys had become a major impediment in the efforts to maximize the number of patients registered into HMIS at Film City’s Hospital, e.g. super-specialties such as nephrology and gastroenterology have an average outpatient load of around 100–150 patients per OPD. But only three computers have been provided for doctors and one for the nursing staff in the OPD of super-specialties.
Because of the slowness of the network or the system, particularly after 11:00 a.m., patients are inconvenienced as they have to wait for long periods till the EMRs are filled and prescriptions and laboratory/radiology requisitions are generated. At times, patients are reluctant to wait for the procedure to be completed. Consequently, only a few requisitions of laboratory and radiology investigations had been processed through the system. It was decided to put more LAN cables but when the issues persist, new Wi-Fi dongles were thought to be procured for every department in the future ( DNA, 2019 ).
Also, a major challenge is that integration of HMIS with various government and insurance schemes is to be undertaken and also a separate budget is to be allocated for HMIS consumables.
HMIS Nodal Officer conducted an immediate evaluation and the following challenges were reported to be faced by some important clinical and supportive services departments.
Department of gastroenterology
One of the issues of the gastroenterology was that all the hospitals in the film city were using different systems for capturing endoscopy reports. Also other investigations such as manometry, PH, fibroscan and breath hydrogen were intended to be managed well so that different reports and PDF can be uploaded in HMIS. The report’s structure given in HMIS was discussed with concerned IT team to check for the network link to the system.
Department of psychiatry
As soon as the recreational activities started for the admitted patients, the HOD of Psychiatry Department entered the IPD area. HMIS Nodal Officer was waiting for him to ask for required modifications.
He said, “Wires need to be covered to protect against damage by the psychiatric patients. Sub-departments like Psychology, Social worker and EEG are also to be included in the system.” HMIS Nodal Officer carefully noted the desired changes. When inquired about the psychiatric OPD, implementation of electronic queue management system monitor was suggested.
Pediatrics department
On meeting with the Professor of Pediatrics while he was checking the nutritional chart for a three-year-old child, the Nodal Officer asks her to raise the concerns regarding HMIS implementation. She swiftly enumerated that the weight, age and height data have to be integrated for making relevant WHO charts and growth curves for classifying patients with severe acute malnutrition or moderate acute malnutrition. She added, immunization record is also to be included in IPD paper. If a vaccine is missing as per national immunization program, a warning has to come on the system. Automatic calculation of surface area is required for prescribing certain drugs. Integration with certain government schemes is also required.
Opening her smart tablet, the HMIS Nodal Officer checked the relevant schemes available in the Film City’s Hospital and asked, “Should Janani Suraksha Scheme also be integrated?” for which she got the affirmative response.
Professor of Pediatrics explained to the Nodal Officer that daily reporting/monthly data have to be available disaggregated in terms of age, gender, notifiable diseases and monsoon-related illness. In addition, the multiple diagnoses have to get sited separately because they are not mutually exclusive. Also, referral list has to be made comprehensive to include physiotherapy, occupational therapy, dietetics and speech therapy in addition to clinical/lab departments.
Radiology department
With the use of Digital Imaging and Communications in Medicine standard and Health Level 7 communication protocol, vendors communicate with the radiology imaging management system termed PACS. Undoubtedly, a major concern in radiology department is to combine the images of each analysis with other important patient records and enhance interoperability with radiology information system and HMIS ( Cummings, 1995 ; Offenmuller, 1997 ).
According to recommendations of PACS Support Engineer given to HMIS Nodal Officer of Film City’s Hospital, “open office” does not support PACS reporting. In addition, the automatic transfer of stored images from USG machine to HMIS was not taking place. Therefore, the HOD of Radiology requested that the licensed access to 3D-MPR viewing be provided to all the radiology employees, including CT/MRI technicians. Furthermore, with the view of additional CT and MRI machines being instilled with additional workload in the near future, approximately 70 licensed accesses needed to be made available to increase the ease, efficiency and speed of reporting. The licensed MS office is also preferred to maintain the integrity and uniformity of the departmental work.
Also, while reporting the patient on PACS, considerable time was consumed in logging in as well as in opening a particular patient. It was difficult to interpret whether the slowness could be attributed to the slow speed of the network or slowness of the operating software.
In addition to this, there was the need for early integration of revenue counter and the central laboratory with the HMIS system for the better functioning.
Laboratory and diagnostics services
Diagnostics is a data-intensive specialty, and laboratory data is often used in addition to patient services to record continuous improvement, performance management, outcome analyses and research studies ( Cowan, 2005 ; Young, 2000 ). At the center of most laboratory activities is the laboratory information system. Workflow management, specimen monitoring, data entry and reporting, regulatory enforcement assistance, code acquisition, interfacing with several other applications, archiving, inventory management and provision of billing information are its features (Eleveitch and Spackman, 2001; Pearson et al. , 2006 ).
For appointment generation counter: token generation facility for the same-day blood collection of patients has to be incorporated in the system. For the token generation, a fast printer device was required as a large number of patients need to be handed over in a short period of time.
For labeling counter
Quality of bar code labels need to be improved. Printouts sometimes are not readable and may face problem in scanning. The problem was discussed with the Project Director, HMIS.
Consumables such as printer roll, appropriate sized labels are not easily available in the hospital.
For collection table: It was discussed with the IT in charge, SoftSolutions, that wall-mounted all-in-one PC units with bar code scanner facility or tablets with in-built scanner need to be installed in OPD for scanning the collected blood samples.
Blood sample processing: Appropriate diagnostic equipment such as blood cell counter and automated biochemistry analyzer have to be procured, which can be integrated with HMIS.
Blood bank services
The blood bank system consists of an autonomous blood center responsible for human blood procurement, storage and distribution ( Li et al. , 2007 ). Because blood bank services are vital segment of the Film City’s Hospital and there were major concerns raised by the employees in the department, Medical Superintendent called for an urgent board meeting ( Tables 1 ).
A unique number was given to each blood bag in the blood bank. This number is followed through the life of that blood bag, i.e. the same number applies at blood group, serological tests, stock taking, cross-matching and issue of blood bag to patients. As on 30th July 2018, the blood bank numbers were at “Indoor 905,” “Outdoor 9888” and “Brought from i.e. BF 1186.”
The HMIS data entries in Blood Bank were attempted since 26th July 2018; however, the HMIS software is unable to match the actual bag numbers because it begins by default 001, 002, 003, etc. Because of this error, the outdoor bag number 8434 may be entered in HMIS as bag number 0004, indoor bag number 894 entered in HMIS as bag number 0005 and so on.
This numbering system, if continued, could have created utter chaos at all levels. Online bloodstock will show wrong bag numbers available to technicians for a cross-match. Issued bags will not correspond to the actual blood bag issued, thus resulting in confusion at a blood bank and clinician level.
In addition, serious mistakes in identifying and discarding of seropositive bags (HIV, Hepatitis B, etc.) can occur because of an incorrect numbering system.
Given the sensitive nature of blood bank work, the slightest error in numbering can cause disastrous results for the patient’s life. Any kind of dual numbering system, as suggested by the HMIS technical team, will further compound the problem, double the workload and invite severe adverse remarks from the FDA.
Because Film City’s Hospital is stationed for the pilot study, any errors can get carried forward and adversely affect the working of other hospitals and other blood banks too. In view of this serious medico-legal and ethical implications, it is essential that HMIS number entries have to categorically match with available numbering for blood bags.
Pharmacy prescriptions and dispensary services
In outpatient health care, the drug management process is a multifaceted relationship between patients, prescribers and pharmacists, which is also enabled by HMIS ( Tamblyn, 2004 ). Electronic medication management has the ability to allow a secure process, but errors may also be created ( Bates et al. , 2001 ).
At Film City’s Hospital, after consultation with head pharmacist, HMIS Nodal Officer noted that a standard prescription format should include name of the drug, preparation, strength, dose, route of administration, frequency and number of days. The route of drug administration should be comprehensive and must also include intradermal, intra-thecal and intra-ocular routes.
It was recommended that the prescriptions need to be in terms of both generic and brand names. Allergies must be a mandatory field, which needs to be pop out during prescriptions. Starting and end dates should be integrated especially for drugs with progressive decreasing doses. At once, no medicines should be prescribed for more than one month.
It was suggested to improvise the SAP system, based on the positive features of government’s “e-Aushadi program” which includes:
Need for surplus and shortage alerts.
Rigorous quality control of medicines should be mandatory and built-in using impaneled NABL-accredited laboratory.
Achieving the milestones
The HMIS is being implemented to improve the quality and responsiveness of health-care services in health-care network in the film city ( Tables 2 and 3 ).
Features of hospital management information system implementation at Film City’s Hospital
The unique features of the HMIS system at Film City’s Hospital are that this system is first of its kind in any of the city’s hospitals that uses a cloud-based centrally located system in which as much as 32 clinical and supportive services HMIS modules are covered. It is made possible to achieve inter-departmental and intra-departmental connectivity in Film City’s Hospital through this system. In addition, this cloud-based system also allows central access to data through any city’s health-care systems, thus enhancing inter-hospitals connectivity ( MCGM RTI, 2019 ).
Hospital management information system implementation – the road ahead
There is a lack of DEOs in some departments. To enhance the time and cost-effectiveness and to achieve digitization through increasing reach to more number of patients, it was decided to implement “Speech to Text” software in the OPDs based on the principle of “machine learning.” The SoftSolutions team has already started taking voice samples of the doctors in the OPDs, and to test the effectiveness of the software, the trial run has been started in the Psychiatry and General Medicine OPD of Film City’s Hospital.
Also, at the registration department, issue of digitalized health card to every patient with Unique Hospital Identification Number and bar coding on it has been started. In the future, the bar scanners will be incorporated to save time at various points in the hospital.
Most of the users are still very resistant in the use of technology in the hospital as they are adapted to traditional manual data entry and calculation methods. The percentage of EMR completion still has to be improved.
Deputy Medical Superintendent along with the HMIS Nodal Officer discussed with the Medical Superintendent, Film City’s Hospital that there is a need for adoption of “John Kotter’s Eight-Step Plan” for implementing change for user acceptability for the overall organizational development and to reinforce the future dream which she had seen of digitalized health-care systems in digitalized India.
Several studies on implementation of HMIS in developed countries ( Ash et al. , 2003 ; Ball, 2003 ; Berg, 2001 ; Benson, 2002 ; Little Johns et al. , 2003 , Joel Rodrigues, 2009 ; Lippeveld et al. , 1992 ; Dudeck et al. , 1997 ) had reported various challenges, including those in managing infrastructure, integration, inter-departmental issues, technical requirements, data and software issues, end-user contribution, standardization of terminologies, training needs and ignorance of hospital administration. In developing nations, numerous health-care professionals associate information systems with filling of infinite registers, collecting information and submitting reports without sufficient input, making HMIS “data-driven” instead of “action-driven” ( Sandiford et al. , 1992 ; Smith et al. , 1988 ). Similarly, in this case study, although being an Indian hospital, managing infrastructure in terms of space for computers, trolleys and other accessories became a major challenge. Allocating areas for installing LAN and rooms for information technologist in a crowded hospital was not that easy task. In this case study, the hospital also faced inter-departmental and inter-hospitals issues with respect to integration and standardization of clinical domains and report structures, respectively. Even after adopting the HMIS principles in several trainings, many employees, especially elder age, felt the need for technical assistance. In addition, the poor doctor–patient ratio and the downtime of the server made the work more complicated as in some of the departments, employees started doing dual entries (both in register and computer) to prevent loss of any data.
Several issues have been identified in the review of reports and studies in low-income countries ( Gladwin, 1999 ), such as general organizational and management difficulties ( Campbell et al. , 1996 ; Braa et al. , 1997 ; Azubuike and Ehiri, 1999 ); data acquisition and processing concerns ( Robey and Lee, 1990 ; Jayasuiriya, 1999 ; Lippeveld et al. , 2000 ); inadequate use of information (WHO, 1994b, 1999; Braa et al. , 1997 ); over-reliance on epidemiological data or specific surveys ( Husein et al. , 1993 ; Sapirie and Orzeszyna, 1995 ); and paucity of an integrated information strategy for the organization ( Van Der Lei et al. , 1993 ). In a similar way, in this case study also, many departments in the hospitals faced challenges around complexity, inconsistency and poor integrity of the system. Although the management tried to ensure the effectiveness, incidents such as mismatch in blood bag numbering in HMIS posed a major ethical issue. There were multiple concerns around data acquisition at revenue and cost centers of the hospital. Although management took corrective and preventive actions, it was reflective of a strategy which would have been well integrated prior with clinical understanding and principles of change management.
Several studies have been conducted on interface design methodologies ( Shearer et al. , 1997 ; Arreola et al. , 1997 ), and among the unidirectional, bidirectional and integrated workstations ( Levine, 1990 ), the interface with more consistent information base is most preferred ( Veader, 1997 ). Studies have reported that an integrated radiology network enhances the efficacy of physicians, minimizes costs, decreases the amount of repetitive or unnecessary tests and increases the quality of care ( Gibby and Mciff, 1997 ). In addition, owing to the extensive adoption of electronic radiology reporting systems, filmless radiology systems and speech recognition, there have also been considerable radiology workflow efficiency improvements ( Mariani et al. , 2006 ; Gay et al. , 2002 ; White, 2005 ; Ralston et al. , 2004 ). Similarly, in this case study, it was observed that with administrative efforts and understanding employee training needs, the number of repetitive tests was reduced. There was a direct benefit in lowering turnaround time and publishing more reports. The better integration and consistency of the PACS will help in increasing the profit per unit volume for the radiology department.
HMIS is important in its ability to resolve issues such as increasing laboratory volume with outreach programs; intensified EMRs integration; and the subsequent need to combine fragmented information systems, laboratory resource shortages, patient safety, cost control, central control of subspecialties, rising demand for laboratory diagnostics and customized intervention ( Becich et al. , 2004 ; Sinard and Morrow, 2001 ). In this case study also, HMIS-integrated EMR played a significant role in decreasing the average waiting time for the patients for receiving the laboratory reports.
Child clinicians frequently feel that there is little utility of health information systems in pediatrics because they tend to be structured for adult services ( Johnson, 2001 ). There are several functional areas, such as immunization records ( Smith, 1988 ), growth monitoring ( Rosenbloom et al. , 2006 ), drug dosing ( American Academy of Pediatrics, 2004 ), patient recognition ( Kuther, 2003 ) and decision support systems ( Miller et al. , 2001 ), which are so vital to the treatment of children and adolescents that their omission contributes to the system hindering quality pediatric care. In this case study, with the discussion with HMIS Nodal Officer, the pediatric department was able to design a customized module which had unique characteristics as compared to any adult-based systems. Drug dosage and calculations, immunizations and growth-monitoring systems were integrated successfully.
Literatures have shown that implementation of computerized blood bank inventory and emergency services ( Catassi and Petersen, 1967 ) and blood bag system ( Ali et al. , 2017 ) plays a significant part in hospital’s decision-making systems ( Li et al. , 2008 ). Similar results were observed in this case study also.
Mohapatra (2009) notes that combining in-patient, pathological and inventory management of hospital pharmaceutical stores enables to enhance the quality of service and efficiency while reducing operating costs. This economic benefits can be reflected in the price, which gives customers more good value. The use of HMIS has been proposed as a way to minimize prescription errors by increasing the readability, standardization and availability of information or providing automatic controls for possible drug-related issues, but the findings are inconsistent ( Huckvale et al. , 2010 ; McKibbon et al. , 2011 , 2012 ). In this case study, the findings suggested that the use of HMIS was helpful in inventory management once the employee got well trained in inventory modules and it generated profitability for the hospital.
Literature shows that during the process of automation, important performance variables involved in the phase of change management are organizational structure, technology infrastructure and implementation approach ( Galliers and Sutherland, 1991 ; Lubitz and Wickramasinghe, 2006 ; Nolan, Norton and CO, 1992 ). Emergent philosophy is more complex ( Markus and Robey, 1988 ) than imperative perspectives ( Robey and Boudreau, 1999 ), stressing a reciprocal instead of a one-way relationship involving technology and organization. Findings of this case study suggest that the management should have strategically thought about the change management perspectives in a visionary sense before taking the step for HMIS implementation. Most of the elder employees were resistant to change and found the system more complex. In terms of ease of use of HMIS, more than half of the employees were either neutral or disagreed in their responses.
Mumbai city map
Picture showing patient health card with UHID and bar coding
Discussion in the meeting conducted at Medical Superintendent’s office, Film City’s Hospital between authorities and the users on the HMIS challenges of blood bank
Progress of HMIS implementation at Film City’s Hospital up to February 2019
Digitization through electronic medical records (EMRs) at Film City’s Hospital
Table showing distribution of customized computer trolleys at Film City’s Hospital
Changes in key performance indicators (KPIs) at Film City’s Hospital after HMIS implementation
Average time spent per service
Average gain per unit volume of the services
Employees ( n = 75) responses for HMIS
Ali , R.S. , Hafez , T.F. , Ali , A.B. and Abd-Alsabour , N. ( 2017 ), “ Blood bag: a web application to manage all blood donation and transfusion processes ”, Paper presented at the 2017 International Conference on Wireless Communications, Signal Processing and Networking (WiSPNET) .
American Academy of Pediatrics ( 2004 ), “ Committee on fetus and newborn. Age terminology during the perinatal period. Pediatrics ”, Vol. 114 , pp. 1362 - 1364 .
Arreola , M. , Neiman , H.L. , Sugarman , A. , et al. ( 1997 ), “ Implementation of a radiology electronic imaging network: the community teaching hospital experience ”, Journal of Digital Imaging , Vol. 10 No. S1 , pp. 146 - 149 .
Ash , J.S. , Gorman , P.N. , Lavelle , M. , et al. , ( 2003 ), “ A Cross-Site qualitative study of physician order entry ”, Journal of American Medical Informatics Association ,
Azubuike , M.C. and Ehiri , J.E. ( 1999 ), “ Health information systems in developing countries: benefits, problems and prospects ”, Journal of the Royal Society for the Promotion of Health , Vol. 119 No. 3 , pp. 180 - 184 .
Bailey , J.E. and Pearson , S.W. ( 1983 ), “ Development of a tool for measuring and analyzing computer user satisfaction ”, Management Science , Vol. 29 No. 5 , pp. 530 - 545 .
Ball , M.J. ( 2003 ), “ Hospital information systems: Perspectives on problems and prospects ”, International Journal of Medical Informatics , Vol. 69 Nos 2/3 .
Bates , D.W. , Cohen , M. , Leape , L.L. , Overhage , J.M. , Shabot , M.M. and Sheridan , T. ( 2001 ), “ White paper – reducing the frequency of errors in medicine using information technology ”, Journal of the American Medical Informatics Association , Vol. 8 No. 4 , pp. 299 - 308 .
Benson , T. ( 2002 ), “ Why general practitioners use computers and hospital physicians do not – part 1: Incentives ”, British Medical Journal ,
Berg , M. ( 2001 ), “ Implementing information systems in health care organizations: myths and challenges ”, International Journal of Medical Informatics , Vol. 64 No. 2-3 .
Becich , M.J. , Gilbertson , J.R. , Gupta , D. , et al. ( 2004 ), “ Pathology and patient safety: the critical role of pathology informatics in error reduction and quality initiatives ”, Clinics in Laboratory Medicine , Vol. 24 No. 4 , pp. 913 - 943 .
Braa , J. , Heywood , A. and Shung King , M. ( 1997 ), “ District level information systems: two cases from South Africa ”, Methods of Information in Medicine , Vol. 36 No. 02 , pp. 115 - 121 .
Campbell , B. , Adjei , S. and Heywood , A. ( 1996 ), From Data to Decision Making in Health: The Evolution of a Health Management Information System , Royal Tropical Institute , Amsterdam .
Catassi , C.A. and Petersen , E.L. ( 1967 ), “ The blood inventory control SystemHelping blood bank management through computerized inventory control ”, Transfusion , Vol. 7 No. 1 , p. 196 .
Commission on Health Research for Development ( 1990 ), Health Research: essential Link to Equity in Development , Oxford University Press , New York, NY .
Cowan , D.F. ( 2005 ), “ Laboratory informatics and the laboratory information system ”, in Cowan , D.F. (Ed.), Informatics for the Clinical Laboratory , Springer , New York, NY , p. 1 - 20 .
Cummings , B.A. ( 1995 ), “ RIS integration strengthens PACS. PACS under managed care ”, Diagn Imaging , Vol. 17 , pp. 13 - 14 .
Degoulet , P. and Fieschi , M. ( 1997 ), Introduction to Clinical Informatics , Springer , New York, NY .
DeLone , W. and McLean , E. ( 1992 ), “ Information systems success: the quest for the dependent variable ”, Information Systems Research , Vol. 3 No. 1 , pp. 60 - 95 .
DNA ( 2019 ), “ HMIS delayed: Mumbaikars won't get rid of hospital queues soon ”, available at: www.dnaindia.com/mumbai/report-hmis-delayed-mumbaikars-won-t-get-rid-of-hospital-queues-soon-2710654 (accessed 7 March 2019 ).
Doll , W.J. and Torkzadeh , G. ( 1988 ), “ The measurement of end-user computing satisfaction ”, MIS Quarterly , Vol. 12 No. 2 , pp. 259 - 274 .
Eleveitch , F.R. and ( 2001 ), Spackman , KA. “ Clinical laboratory informatics ”, in Burtis , C.A. and Ashwood , E.R. (Eds), ( 2001 ), Tietz Fundamentals of Clinical Chemistry , 5th ed. , WB Saunders Company , pp. 262 - 271 .
Frere , J.J. ( 1987 ), Health and Management Information System for Child Survival Project in Pakistan , Technologies for Primary Health Care Project, United States Agency for International Development , Washington, DC , 1 - 23 .
Frisse , M.E. and Holmes , R.L. ( 2007 ), “ Estimated fi nancial savings associated with health information exchange and ambulatory care referral ”, Journal of Biomedical Informatics , Vol. 40 No. 6 , pp. S27 - 32 .
Galliers , R.D. and Sutherland , A.R. ( 1991 ), “ Information systems management and strategy formulation: the ‘stages of growth’ model revisited ”, Information Systems Journal , Vol. 1 No. 2 , pp. 89 - 114 .
Gay , S.B. , Sobel , A.H. , Young , L.Q. and Dwyer , S.J. ( 2002 ), “ Processes involved in reading imaging studies: workflow analysis and implications for workstation development ”, Journal of Digital Imaging , Vol. 15 No. 3 , pp. 171 - 177 .
Gibby , W.A. and Mciff , E.B. ( 1997 ), “ Lnformactics: Radiology networking fosters quality services: Diagn lmaging ”, Vol. 19 , pp. 145 - 159 .
Gladwin , J. ( 1999 ), “ An informational approach to health management in low-income countries ”, Ph.D. Thesis, University of Sheffield .
Hillestad , R. , Bigelow , J. , Bower , A. , Girosi , F. , Meili , R. , Scoville , R. , et al. ( 2005 ), “ Can electronic medical record systems transform health care? Potential health benefits, savings, and costs ”, Health Affairs) , Vol. 24 No. 5 , pp. 1103 - 1117 .
Huckvale , C. , Car , J. , Akiyama , M. , et al. ( 2010 ), “ Information technology for patient safety ”, Quality and Safety in Health Care , Vol. 19 No. S2 , pp. i25 - 33 .
Husein , K. , Adeyi , O. , Bryant , J. and Cara , N.B. ( 1993 ), “ Developing a primary health care management information system that supports the pursuit of equity, effectiveness and affordability ”, Social Science and Medicine (1982) , Vol. 36 No. 5 , pp. 585 - 596 .
Dudeck , J. , Blobel , B. and Lordieck , W. ( 1997 ), New Technologies in Hospital Information Systems , IOS Press .
Jayasuiriya , R. ( 1999 ), “ Managing information systems for health services in a developing country: a case study using a contextualist framework ”, International Journal of Information Management , Vol. 19 , pp. 335 - 349 .
Rodrigues , J. ( 2009 ), “ Health information systems: Concepts, methodologies, tools, and applications, volume 1. Medical information science reference ”,
Johnson , K.J. , Ravert , R.D. and Avertan , A. ( 2001 ), “ Hopkins teen central: assessment of an internet based support system for children with cystic fibrosis ”, PEDIATRICS , Vol. 107 No. 2 , pp. E24 .
Johnson , K.B. ( 2001 ), “ Barriers that impede the adoption of pediatric information technology ”, Archives of Pediatrics and Adolescent Medicine , Vol. 155 No. 12 , pp. 1374 - 1379 .
Kuruvilla , S. , Dzenowagis , J. , Pleasant , A. , Dwivedi , R. , Murthy , N. , Samuel , R. and Scholtz , M. ( 2004 ), “ Digital bridges need concrete foundations: lessons from the health internetwork India ”, BMJ , Vol. 328 No. 7449 , pp. 1193 - 1196 .
Kuther , T.L. ( 2003 ), “ Medical decision-making and minors: issues of consent and assent ”, Adolescence , Vol. 38 No. 150 , pp. 343 - 358 .
Levine , B. ( 1990 ), “ A tilo of interfaces pilots communication networks ”, Diagn Imaging Focus on PACS 12: I .
Li , B.N. , Chao , S. and Dong , M.C. ( 2007 ), “ SIBAS: a blood bank information system and its 5-year implementation at Macau ”, Computers in Biology and Medicine , Vol. 37 No. 5 , pp. 588 - 597 .
Li , B.N. , Dong , M.C. and Chao , S. ( 2008 ), “ On decision making support in blood bank information systems ”, Expert Systems with Applications , Vol. 34 No. 2 , pp. 1522 - 1532 .
Lifshitz , M.S. , Blank Ge . and Schexneider , K. ( 2007 ), “ Clinical laboratory informatics ”, in McPherson , R.A. and Pincus , M.R. (Eds), Henry’s Clinical Diagnosis and Management by Laboratory Methods , 21st ed. , WB Saunders Elsevier . pp. 112 - 121 .
Lippeveld , T.J. , Foltz , A. and Mahouri , Y.M. ( 1992 ), “ Transforming health facility-based reporting systems into management information systems: lessons from the Chad experience ”, Development Discussion Papers, No. 430 , Harvard Institute of International Development , Cambridge, MA , pp. 1 - 27 .
Lippeveld , T. , Sauerborn , R. and Bodart , C. ( 2000 ), Design and Implementation of Health Information Systems , World Health Organization , Geneva .
Little Johns , P. Wyatt , J.C. and Garvican , L. ( 2003 ), “ Evaluating computerized health information systems: Hard lessons still to be learnt ”, BMJ Publishing Group Ltd. BMJ.com .
Lubitz , D.V. and Wickramasinghe , N. ( 2006 ), “ Healthcare and technology: the doctrine of network centric healthcare ”, International Journal of Electronic Healthcare , Vol. 2 No. 4 , pp. 322 - 344 .
Lun , K.C. ( 1995 ), “ The role of information technology in health care cost containment ”, Singapore Med J , Vol. 36 No. 1 , pp. 32 - 34 .
Mariani , C. , Tronchi , A. , Oncini , L. , Pirani , O. and Murri , R. ( 2006 ), “ Analysis of the x-ray work flow in two diagnostic imaging departments with and without a RIS/PACS system ”, Journal of Digital Imaging , Vol. 19 , No. S1 , pp. 18 - 28 .
Markus , M.L. and Robey , D. ( 1988 ), “ Information technology and organizational change: causal structure in theory and research ”, Management Science , Vol. 34 No. 5 , pp. 583 - 598 .
McKibbon , K.A. , Lokker , C. , Handler , S.M. , et al. ( 2012 ), “ The effectiveness of integrated health information technologies across the phases of medication management: a systematic review of randomized controlled trials ”, Journal of the American Medical Informatics Association , Vol. 19 No. 1 , pp. 22 - 30 .
McKibbon , K.A. Lokker , C. Handler , S.M. et al. ( 2011 ),. “ Enabling medication management through health information technology (health IT) ”, Evid Rep Technol Assess (Full Rep) , 1 - 951 .
MCGM ( 2019 ), “ History of municipal corporation of greater mumbai ”, available at: https://portal.mcgm.gov.in/irj/portal/anonymous?NavigationTarget=navurl://e73b30fff440950441693f945ad3cba7 (accessed 7 March 2019 ).
MCGM Health Department ( 2019 ), “ Municipal corporation of greater Mumbai- Health department ”, available at: https://portal.mcgm.gov.in/irj/portal/anonymous?NavigationTarget=navurl://0a06009b86958aea412e367434b40c52 (accessed 7 March 2019 ).
MCGM IT Department ( 2019 ), “ Municipal corporation of greater Mumbai- Information technology department ”, available at: https://portal.mcgm.gov.in/irj/portal/anonymous/qlitdp?guest_user=english (accessed 7 March 2019 ).
MCGM RTI ( 2019 ), “ Municipal corporation of greater Mumbai- Citizen forum (right to information) department manuals ”, available at: https://portal.mcgm.gov.in/irj/portal/anonymous?NavigationTarget=navurl://14ebe3fd2ffb65c2dd97ceeda2158e11 (accessed 7 March 2019 ).
MCGM Bid Document ( 2018 ), “ Bid notification no.: 7100134255: Bid document for supply, installation, testing, commissioning and maintenance of hardware and network components for MCGM’s hospital management information system.’ law insider ”, available at: https://www.lawinsider.com/documents/lHp622wvpZJ (accessed 7 March 2019 ).
Miller , P.L. , Frawley , S.J. and Sayward , F.G. ( 2001 ), “ Issues in computer-based decision support in public health illustrated using projects involving childhood immunization ”, Journal of Public Health Management and Practice : Jphmp , Vol. 7 No. 6 , pp. 75 - 86 .
Mohapatra , S. ( 2009 ), Cases in Management Information System , PHI , New Delhi .
Mukul ( 2018 ), “ MCGM leveraging technology to boost healthcare delivery system ”, available at: https://ehealth.eletsonline.com/2019/02/mcgm-leveraging-technology-to-boost-healthcare-delivery-system/ (accessed 7 March 2019 ).
National Institutes of Health ( 2003 ), “ Committee on data standards for patient safety. Key capabilities of an electronic health record system: Letter report ”, National Academies Press , Washington, DC .
Nolan, Norton and CO ( 1992 ), Ondernemingsstrategie eninformatie technologie. (NNC and VSB) , The Hague .
Offenmuller , W. ( 1997 ), “ Expectations and solutions for HIS/R1S/PACS dataflow and workflow ”, J Digit Imaging , Vol. 10 , pp. 95 - 98 .
Pearson , S. , Balis , U.J. , Fuller , J. , et al. ( 2006 ), “ Managing and validating laboratory information systems; approved guideline ”, Clinical and Laboratory Standards Institute Document AUTO8-A , Vol. 26 No. 36 .
Ralston , M.D. , Coleman , R.M. , Beaulieu , D.M. , Scrutchfield , K. and Perkins , T. ( 2004 ), “ Progress toward paperless radiology in the digital environment: planning, implementation, and benefits ”, Journal of Digital Imaging , Vol. 17 No. 2 , pp. 134 - 143 .
Robey , D. and Boudreau , M.-C. ( 1999 ), “ Accounting for the contradictory organizational consequences of information technology: theoretical directions and methodological implications ”, Information Systems Research , Vol. 10 No. 2 , pp. 167 - 185 .
Robey , J.M. and Lee , S.H. ( 1990 ), “ Information system development in support of national health programme monitoring and evaluation: the case of the Philippines ”, World Health Statistical Quarterly , Vol. 43 , pp. 37 - 46 .
Rosenbloom , S.T. , Qi , X. , Riddle , W.R. , et al. ( 2006 ), “ Implementing pediatric growth charts into an electronic health record system ”, Journal of the American Medical Informatics Association , Vol. 13 No. 3 , pp. 302 - 308 .
Sandiford , P. , Annett , H. and Cibulskis , R. ( 1992 ), “ What can information systems do for primary health care? An international perspective ”, Social Science and Medicine , Vol. 34 No. 10 , pp. 1077 - 1087 .
Sapirie , S.A. and Orzeszyna , S. ( 1995 ), “ Selecting and defining national health indicators. Strengthening country health information unit, division of epidemiological surveillance and health situation and trend assessment ”, World Health Organization , Geneva , available at: www.who.int/healthservices-delivery/information/20000629d.htm
Shearer , S.O. , Miller , T. and Gillen , S. ( 1997 ), “ Picture archiving and communication system implementation: the practical considerations of adapting the technology to the real world of health care operations ”, Journal of Digital Imaging , Vol. 10 , No. S1 , pp. 158 - 160 .
Shekelle , P. Morton , S.C. and Keeler , E.B. ( 2006 ), “ Costs and benefits of health information technology ”, Rockville (MD): Agency for Healthcare Research and Quality (US); (Evidence Reports/Technology Assessments, No. 132) .
Sinard , J.H. and Morrow , J.S. ( 2001 ), “ Informatics and anatomic pathology: meeting challenges and charting the future ”, Human Pathology , Vol. 32 No. 2 , pp. 143 - 148 .
Sinard , J.H. ( 2006 ), “ Practical pathology informatics ”, Demystifying Informatics for the Practicing Anatomic Pathologist , Springer . New York, NY , pp. 1 - 380 .
Smith , D.L. , Hansen , H. , ( 1988 ), and., and Karim , M.S. “ Management information support for district health systems based on primary health care ”, in Wilson RG et al. (Eds), Management Information Systems and Microcomputers in Primary Health Care , Aga Khan Foundation , Geneva , 89 - 110 .
Smith , M.H. ( 1988 ), “ National childhood vaccine injury compensation act ”, Pediatrics , Vol. 82 No. 2 , pp. 264 - 269 .
Tamblyn , R. ( 2004 ), “ Improving patient safety through computerized drug management: the devil is in the details ”, HealthcarePapers , Vol. 5 No. 3 , pp. 52 - 68 .
The Hindu ( 2018 ), “ Dynacons systems bags contract worth ₹58 cr ”, available at: www.thehindubusinessline.com/markets/stock-markets/dynacons-systems-solutions/article24856706.ece (accessed 7 March 2019 ).
Twelfth Five year Plan Draft 2012 ( 2017 ), “ Social sectors, vol. 3.Govt. of India ”, available at: http://planningcommissiongov.in/plans/planrel/12thplan/welcome.html
Van Der Lei , J. , Duisterhout , J.S. , Westerhof , H. , Boon , W. , Cromme , P.V.M. and Van Bammel , J.H. ( 1993 ), “ The introduction of computer based patient records in The Netherlands ”, Annals of Internal Medicine , Vol. 119 No. 10 , pp. 1036 - 1041 .
Van Hartevelt , J.H.W. ( 1993 ), “ Information management in international development as an area for information services with a case in the field of health care in Ghana ”, International Forum on Information and Documentation , Vol. 18 , pp. 32 - 36 .
Veader , P.C. ( 1997 ), “ The missing links ”, February 16, 1997; Online: Peter C. Veader: Internet: August , Vol. 30, 1997
Wang , S.J. , Middleton , B. , Prosser , L.A. , Bardon , C.G. , Spurr , C.D. , Carchidi , P.J. , et al. ( 2003 ), “ A cost-benefit analysis of electronic medical records in primary care ”, The American Journal of Medicine , Vol. 114 No. 5 , pp. 397 - 402 .
White , K.S. ( 2005 ), “ Speech recognition implementation in radiology ”, Pediatric Radiology , Vol. 35 No. 9 , pp. 841 - 846 .
World Bank ( 1993 ), World Development Report 1993: Investing in Health , Oxford University Press , New York, NY .
World Bank ( 1999 ), World Development Indicators 1999 , The World Bank , Washington, DC .
Yasnoff , W.A. , O’Carroll Patrick , W. , Koo , D. , Linkins Robert , W. and Kilbourne , E.M. ( 2000 ), “ Public health informatics: Improving and transforming public health in the information age ”, Journal of Public Health Management and Practice : Jphmp , Vol. 6 No. 6 , pp. 67 - 75 .
Young , K.M. ( 2000 ), The World of Informatics: informatics for Healthcare Professionals , F.A. Davis Company , Philadelphia , p. 11 - 24 .
Further reading
Chaudhry , B. , Wang , J. , Wu , S. , Maglione , M. , Mojica , W. , Roth , E. , Morton , S.C. and Shekelle , P.G. ( 2006 ), “ Systematic review: Impact of health information technology on quality, efficiency and costs of medical care, improving patient care ”, Annals of Internal Medicine , Vol. 144 No. 10 , pp. 742 - 752 .
Connelly , D.P. , Sielaff , B.H. and Willard , K.E. ( 1996 ), “ The clinical workstation as the means of improving laboratory use ”, Clinica Chimica Acta , Vol. 248 No. 1 , pp. 51 - 64 .
Kallinikos , J. ( 2005 ), “ The order of technology: Complexity and control in a connected world ”, Information and Organization , Vol. 15 No. 3 , pp. 185 - 202 .
Kallinikos , J Contini and Lanzara , ( 2008 ), “ Institutional complexity and functional simplification: the case of money claim online service in England and Wales ”, in (Eds) ICT and Innovation in the Public Sector. European Studies in the Making of E-Governmen , Palgrave Macmillan , Basingstoke , pp. 174 - 210 .
Lanzara , G.F. ( 2008 ), “ Building digital institutions: ICT and the rise of assemblages in government ”, in Contini and Lanzara (Eds) , ICT and Innovation in the Public Sector. European Studies in the Making of E-Government , Palgrave Macmillan , Basingstoke , pp. 9 - 48 .
Margolis , C.Z. , Warshawsky , S.S. , Goldman , L. , Dagan , O. , Wirtschafter , T. and Pliskin , J.S. ( 1992 ), “ Computerized algorithms and pediatricians management of common problems in a community clinic ”, Acad Med , Vol. 67 , pp. 282 - 284 .
Schoenbaum , S.C. and Barnett , G.O. ( 1992 ), “ Automated ambulatory medical records systems: an orphan technology ”, International Journal of Technology Assessment in Health Care , Vol. 8 No. 4 , pp. 598 - 609 .
Schriger , D.L. , Baraff , L.J. , Buller , K. , et al. ( 2000 ), “ Implementation of clinical guidelines via a computer charting system: effect on the care of febrile children less than three years of age ”, Journal of the American Medical Informatics Association , Vol. 7 No. 2 , pp. 186 - 195 .
Scott , J.C. ( 1988 ), Seeing like a State: How Certain Schemes to Improve the Human Condition Have Failed , Yale University Press .
Corresponding author
Related articles, we’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
How Digital Transformation Can Improve Hospitals’ Operational Decisions
- Song-Hee Kim

It can help with patient flow, staffing, scheduling, and supply-chain management.
The use of digital technologies in clinical decision-making has received the most attention. But they also have the potential to help hospitals make better decisions in many areas of operations. Research and hospitals’ experiences show that they can make a big difference in such areas as the management of the patient flow, staffing, scheduling, and the supply chain. The result can be improvements in the quality and efficiency of care and patients’ access to it.
Many companies are interested in digital transformation — using digital technologies to create or modify business processes, culture, and customer experiences — to grow and stay ahead of the competition, and hospitals are no exception.
- Song-Hee Kim is an associate professor of operations management at the SNU Business School at Seoul National University. Her research focuses on data-driven decision-making within health care systems, especially how to design human-algorithm interactions to improve quality, efficiency, and access to care in hospitals.
- Hummy Song is an assistant professor of operations, information, and decisions at the University of Pennsylvania’s Wharton School. Her research focuses on how operations can be designed to help health care providers work more efficiently and effectively.
Partner Center

Healthcare Case Studies
Smart hospitals powered by vizzia.


Vizzia RTLS Solutions Case Studies
Piedmont healthcare saves $2 million with system-wide asset tracking and management, case study: piedmont healthcare, greater atlanta and north georgia.
With Vizzia’s RTLS deployed in multiple hospitals, Piedmont Healthcare is innovating in equipment management, including an in-house equipment rental service and $2 million saved throughout the health system.
Piedmont Healthcare is the largest healthcare provider in Georgia, serving more than 3 million patients across 1,400 locations. This includes 19 hospitals, 57 Piedmont Urgent Care centers, 25 QuickCare locations, and 1,875 Piedmont Clinic locations.

The Grady Health System in Atlanta, Georgia is one of the largest safety net health systems in the U.S., consisting of the 953-bed Grady Memorial Hospital, six neighborhood health centers, and the Marcus Stroke and Neuroscience Center.
Premier Level 1 trauma & stroke center leverages Vizzia RTLS solutions
Case study: grady health system, atlanta, georgia, topic: rtls asset management, environmental monitoring, stroke patient workflow.
Hospital clinicians closely collaborated with Vizzia to enhance their asset management, environmental monitoring, and stroke patient workflow procedures, saving the hospital time and money.
Mission Hospital saves $600,000 per year with Vizzia RTLS
Case study: mission hospital, mission viejo, california.
In the first year of Mission’s nine-year-and-counting partnership with Vizzia, lost or stolen equipment decreased from 14% to 0%, and the hospital started saving $600,000 per year.
As the only trauma center and the only designated pediatric healthcare center in south Orange County, California, Mission Hospital provides critical services to the community.

Emory Decatur Hospital had a problem. Nurses at the Atlanta-area hospital were spending 11,000 hours each year searching for and cleaning equipment—hours that could have gone to patient care.
Emory Decatur Hospital lowers capital costs with Vizzia RTLS
Case study: emory decatur hospital, decatur, georgia.
Soon after deploying Vizzia’s real-time location systems (RTLS), Emory Decatur Hospital was renting less equipment and reducing expenses by purchasing 150 fewer pumps than planned—a savings of $600,000.
Top-Ranked Biomedical Engineering Program Improves Automated Lab Monitoring with Vizzia
Case study: emory university school of medicine, atlanta, georgia, topic: rtls environmental monitoring.
Emory engaged with Vizzia Technologies to launch a robust environmental monitoring solution to improve automatic monitor temperature, humidity, and other environmental conditions of key rooms and refrigerators in their labs.

Emory University School of Medicine is one of the top-ranked institutions for NIH research funding. The Department of Biomedical Engineering is ranked number one for best undergraduate biomedical engineering programs by U.S. News and World Report.

PIH Health in Southern California is a regional healthcare delivery network serving more than 3 million residents in Los Angeles County, Orange County, and the San Gabriel Valley. The fully integrated network is comprised of 3 acute care hospitals with 1,130 beds.
Top-15 U.S. Hospital System Benefits From Vizzia Fully Managed RTLS
Case study: pih health whittier, california, topics: rtls asset management optimization.
PIH had a legacy asset tracking and temperature monitoring system that was not well utilized or maintained. Vizzia partnered closely with hospital leadership to deliver a fully managed RTLS solution that provided significant operational benefits.

RTLS Industry Success

Healthcare IT News is part of HIMSS Media and the industry’s authortative source covering the people, policy, and technology driving next-generation healthcare.
Rtls saves wake forest baptist health $3.5m in medical equipment expenses and reduced wait times by 50%. (article), rtls saves adventist health white memorial $1m per year and reduced hospital staff expenses by $498,000. (article), rtls saves texas health presbyterian dallas hospital $412,000 in the first year and 80% reduction in repairs. (article), rtls increases patient revenue $351,000 in a year at christus santa rosa hospital and saves workflow time. (article), rtls reduces patient wait times by 75% at oregon medical group and increases clinical patient care by 50%. (article), rtls users report gains: 85% data visibility; 65% patient safety; 59% process efficiency; 41% financial return. (article), rtls users rank providers: all vizzia tech customers strongly rate their reporting tools and automated alerts. (article), rtls protects against infections for 8k staff and patients at wake forest baptist health with contact tracing. (article), rtls reduces contact tracing from 2 weeks down to 5-10 minutes at methodist hospital southern california. (article), rtls provides a cost-effective staff duress solution that can protect healthcare workers and reduce burnout. (article), rtls has a higher 60% sensitivity in covid contact tracing cases compared to conventional tracing method. (article), rtls improves care quality, patient experience, clinician wellbeing and expenses at commonsprit in colorado. (article), rtls installed in new tech-intensive hospital to enhance the patient experience at valley health in new jersey. (article), rtls to optimize nursing efficiency and enhance patient care, saving nurses 1 hour searching for equipment. (article).
Contact Vizzia Today!
Call: 1-855-849-9421 Email: [email protected]

- First Name *
- Name This field is for validation purposes and should be left unchanged.

About Vizzia
Vizzia is a leading provider of fully managed Real-Time Location Systems (RTLS), helping hospitals reduce costs, streamline processes and improve patient care.
RTLS Solutions
- Asset Management
- Contact Tracing
- Environmental Monitoring
- Hand Hygiene Compliance
- Hospital Wayfinding
- Infant Security
- Patient Workflow
- Reports & Analytics
- Staff Duress
- Case Studies
- Industry Articles
- Savings Calculator
- White Papers
- Privacy Policy
Vizzia Technologies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Integr Care
- v.22(1); Jan-Mar 2022

Case Management Programs for Improving Integrated Care for Frequent Users of Healthcare Services: An Implementation Analysis
Dr. catherine hudon.
1 Département de médecine de famille et de médecine d’urgence, Université de Sherbrooke, 3001, 12e Avenue Nord, Sherbrooke, QC, Canada
2 Centre de recherche du CHUS, 12e Avenue Nord Porte 6, Sherbrooke, QC, Canada
Maud-Christine Chouinard
3 Faculté des sciences infirmières, Université de Montréal, Pavillon Marguerite-d’Youville, 2375 Chemin de la Côte-Sainte-Catherine, Montreal, QC, Canada
Mathieu Bisson
Astrid brousselle.
4 School of Public Administration, University of Victoria, Public Administration, HSD building, Room A302, Victoria, BC, Canada
Mireille Lambert
5 Centre intégré universitaire de santé et services sociaux du Saguenay–Lac-Saint-Jean, 930 rue Jacques-Cartier E, Chicoutimi, QC, Canada
Alya Danish
Charo rodriguez.
6 Department of Family Medicine, McGill University, 5858, Chemin de la Côte-des-Neiges, Montreal, QC, Canada
Véronique Sabourin
7 Patient partner, CA
Introduction:
Case management programs (CMP) for frequent users of healthcare services presenting complex healthcare needs constitute an effective strategy to improve patient experience of integrated care and to decrease healthcare overuse and cost. This study sought to identify characteristics of these programs, and their implementation contexts, that help to improve patient self-management, experience of integrated care, and healthcare services use.
A mixed methods multiple embedded case study design was conducted, with six CMP implemented in six hospitals of a region of Quebec (Canada).
Within-case analysis describes the structural, environmental, organizational, practitioner, patient, and innovation level characteristics of each CMP and their services integration outcomes based on patient experience, self-management and healthcare services use. Cross-case analysis suggests that the skills, leadership and experience of the case manager, providers’ access to the individualized services plan, consideration of the needs of the patient and family members, their participation in decision-making, and the self-management approach, impact integrated care and healthcare services use.
Conclusion and discussion:
This study underscores the necessity of an experienced, knowledgeable and well-trained case manager with interpersonal skills to optimize CMP implementation such that patients are more proactive in their care and their outcomes improve.
Introduction
Individuals with chronic conditions sometimes have complex healthcare needs, due to mental health comorbidities and/or social vulnerabilities [ 1 ] and become frequent users of healthcare services [ 2 , 3 , 4 ]. Organizing services to improve care for these patients with complex needs is a priority for healthcare systems [ 4 ] and requires an integration of clinical services offered by health and social care professionals, as well as community-based ones [ 5 ]. Models of integrated care such as case management [ 6 ] improve the quality of care, patient satisfaction, access to care, and care transitions [ 7 , 8 ], and reduce the probability of hospitalization, when compared with usual care [ 9 ].
Case management programs (CMP) for frequent users of healthcare services with complex needs constitute an effective strategy to improve patient experience of integrated care and to decrease healthcare overuse and cost [ 10 , 11 , 12 ]. Case management is a dynamic, systematic and collaborative approach used to ensure, coordinate, and integrate care and services for a clientele. The case manager is a key practitioner or navigator (often a nurse or a social worker) who evaluates, plans, implements, coordinates, and prioritizes services based on individuals’ needs, and offers self-management support in close collaboration with health, social and community partners [ 13 ].
A majority of studies have reported the effectiveness of CMP with indicators such as improvement in patient satisfaction and quality of life, and reduction of healthcare services use, ED visits, hospitalization rates, and cost [ 10 , 11 , 12 ]. Although the evidence in support of CMP is strong, there remains a paucity of evidence about the implementation process that lead to these outcomes in local contexts [ 14 ]. The aim of this study was to identify characteristics of CMP, and the contexts where they are implemented, that help to improve patient self-management, experience of integrated care, and healthcare services use.
Methodology
Design of the study.
This was a case study, more specifically a multiple embedded case study with a mixed-methods design [ 15 ]. Such a methodology appears the most appropriate for an implementation analysis in a complex system, and to study cases, with varied contexts, as they evolve over time [ 15 , 16 ]. In addition to allowing for an in-depth analysis of each case, the analysis strategies used in this design help to systematically compare trends observed between cases. It is recommended that four to ten cases be considered [ 17 ] in the multiple case study logic of theoretical replication [ 15 ]. This study included six cases, where each case was the CMP implemented in each hospital. The three different units of analysis that were interwoven to obtain an in depth understanding of each case were: 1) the hospital (organizational ‘macro’ level); 2) the CMP itself for frequent users of services (‘meso’ level) and 3) the individual (‘micro’ level), more particularly patients who are frequent users.
Context of the study
The study was realized in the Saguenay-Lac-Saint-Jean region of Quebec, a province in Canada. This region is the third largest territory in Quebec and has a very low average population density of 2.9 inhabitants per square kilometre. Much of the population is French-speaking and less than 1% are immigrants. Compared to the whole Quebec population, the residents of the Saguenay-Lac-Saint-Jean region have lower educational attainment and experience more mental health conditions [ 18 ]. In the province of Quebec, regions are divided into administrative sectors referred to as County Regional Municipalities (CRM). In the Saguenay subregion, one of these CRM is served by three hospitals, and in the Lac-Saint-Jean subregion, three of these CRM are each served by a hospital.
Case management program
In 2008, the Saguenay-Lac-Saint-Jean health and social services agency mandated the six hospitals of its territory to implement CMP for frequent users of healthcare services. Between 2009 and 2015, six CMP, the cases included in this study, were deployed by stakeholders’ committees made up of a coordinator, managers, services coordinators and case managers. CMP aimed to improve self-management support and integrated care, and decrease ED use, hospitalizations as well as healthcare cost. Case managers (a nurse or a social worker or both in dyad) in each of the six hospitals were recruited and trained to the case management approach. The training enabled the case managers to identify patients with complex care needs, assess their specific needs, and develop the individualized service plans (ISP) to respond to those needs in collaboration with the patient, their relatives and other actors involved in the implementation of the ISP, including nurses, social workers, family physicians, pharmacists, and representatives of community organizations.
In 2015, during the data collection of the study, the government of Quebec reorganized the healthcare system by merging local hospitals into larger regional entities in order to centralize health and social services. This resulted in an effort from a single CMP committee made up of a coordinator, a manager, a performance improvement consultant and case managers to standardize the program offered by the six hospitals. Members of the committee also discussed challenges and facilitators to the implementation of the CMP in this new context, as well as factors at the healthcare system level that could influence the case managers’ work. Criteria for enrolment were standardized, targeting patients with more than six ED visits or three hospitalizations in the previous year. Frequent users were identified electronically through hospital admissions and ED records. The provincial healthcare system reorganization had major impacts on clinical, professional, administrative, management and governance aspects of the healthcare system. For example, there was staff turnover at the case manager and manager level, which affected the implantation of CMP in many cases.
Conceptual framework
Two conceptual frameworks guided this study. First, given that we were interested in the implementation of CMP, we used Chaudoir et al. [ 19 ] which proposes five broad categories of factors to consider when evaluating the implementation of an innovation, namely: 1) structural and environmental-level factors; 2) organizational-level factors; 3) practitioner-level factors; 4) patient–level factors, and 5) innovation-level factors. Second, to examine patient experience of integrated care, the model proposed by the National Collaboration in Integrated Care and Support was used [ 20 ]. It consists of six dimensions of care integration based on patient experience: 1) consideration of patient and family needs, 2) communication with the patient and between practitioners, 3) access to information, 4) patient involvement in decision-making, 5) care planning, and 6) transitions between various professionals.
Participants
Key informants involved in the six CMP and healthcare services used by patients with complex health needs were recruited through purposeful sampling [ 21 ] in each hospital. Patients recruited were frequent users of hospital services, who had six visits to the ED or more, or three hospitalizations or more in the previous year.
Data collection
An implementation analysis strategy [ 22 ] guided the three methods of qualitative data collection and the method of quantitative data collection. While qualitative methods were used to inform self-management and patient experience of integrated care, quantitative data collection methods allowed the measurement of ED services use.
Qualitative data
Individual interviews and focus groups.
Semi-structured individual interviews (n = 56) and focus groups (n = 11) were conducted between December 2014 and May 2018 with 24 patients, 12 case managers and intermediate managers, 8 senior managers, 12 family physicians, 25 community stakeholders and 6 pharmacists, with interview guides, adapted for each type of actor, and addressed the five main categories of factors of the Chaudoir et al. framework of innovation implementation [ 19 ], and the six dimensions of patient experience [ 20 ]. Data saturation was not the goal for each group, but the diversity of actors engaged provided a complete representation of each case [ 23 ]. All individual interviews and focus groups were audio recorded and transcribed verbatim.
Participant observation
A member of the research team performed participant observation during one case management training session, individual case manager activities (n = 6) (e.g. evaluation of targeted patient needs, contacts with patients and their healthcare providers, ISP meetings), and quarterly meetings of the CMP committee of each of the six hospitals (n = 11). The member of the research team was invited to attend all committee meetings and share updates about the research project. These meetings were also an opportunity to consult committee members on how the research project could provide new knowledge that would help them. Data were collected using field notes [ 21 ].
Document analysis
Minutes of the CMP committee meetings were collected as they provided insight into the characteristics of the CMP and the CMP implementation, including challenges and means to overcome them [ 24 ].
Quantitative data
Clinical and administrative data.
Using the hospitals’ Magic Chronique computer software [ 25 ], the number of frequent users of ED was recorded monthly for each hospital beginning in December 2012 (the year preceding the start date of the study) and ending on May 2018. Data quality was controlled using an integrated model of information quality and a series of validation algorithms.
For each case, all qualitative data were analysed together as one data corpus using a deductive (themes based on the conceptual frameworks [ 19 , 20 ] and inductive (themes emerging from the data) thematic analysis [ 26 ]. All data sources were examined to identify characteristics of CMP, and their contexts that can be related (positively or negatively) to the examined outcomes, i.e. patient self-management, experience of integrated care, and healthcare services use. Qualitative data were managed by two authors who used NVivo V.11 server software (QSR International Pty). Other authors, including an experienced patient partner, participated in the analysis. Persistent observation, and methodological and investigator triangulation were used to ensure credibility [ 27 ].
The number of ED frequent users (six visits or more in the previous year) was tabulated for each hospital and represented in one graph to allow for visual comparison.
Integration of qualitative and quantitative data
Qualitative and quantitative results were compared for each case [ 28 ]. Qualitative data was analysed first, quantitative data second, then cross-analyses merged the two corpora of data [ 15 ]. A case history was written for each case ( Table 2 ) to summarize merged data [ 26 ]. To compare the six case records, three analytic techniques used in case study research were used, namely pattern comparison, search for competing explanations and construction of explanations [ 15 ]. Management, data reduction and cross case comparisons were conducted with NVivo V.11 software using matrix queries.
Case management program (CMP) implementation in each setting: case stories.
The study was approved by the ethics committee of the Centre for integrated health and social services of Saguenay-Lac-Saint-Jean (2014–015).
Table 1 provides the descriptive characteristics of each of the six CMP.
Characteristics of the six case management programs.
CMP: case management program; CRM: County regional municipality; ED: Emergency department; ISP: Individual service plan.
Figure 1 illustrates the evolution of the number of ED frequent users during the implementation of the CMP. While the number of frequent users increased considerably in the case A and increased slightly in the case D, an important decrease was observed for the case C and a slight decrease in the case F. These last two cases are considered “success stories”. The cases B and E remain relatively stable.

Number of ED frequent users* for each hospital.
* FU: 6 ED visits or more in the previous year.
Intra-case results
Table 2 merged qualitative and quantitative data to present case stories.
Cross-case results
Tables 3 , ,4, 4 , ,5 5 present the cross-case results. The outcomes (see the legend) are identified according to the five categories of Chaudoir et al. framework.
Structural, environmental, and organizational characteristics influencing integrated care, self-management and health services use for each case.
ISP: Individualized services plan.
Practitioner and patient characteristics influencing integrated care, self-management and health services use for each case.
CT: care trajectory; ED: emergency department.
Characteristics of the innovation (the CMP) influencing integrated care, self-management and health services use for each case.
Legend for Tables 3 , ,4 4 and 5 5
Outcomes associated with each CMP characteristic
- 1.1 Consideration of patient and family needs
- 1.2 Communication with the patient and between practitioners
- 1.3 Access to information
- 1.4 Patient involvement in decision-making
- 1.5 Care planning
- 1.6 Transitions between various health professionals and practitioners
- 2 Self-management
- 3 Health services use
In the tables, the arrows represent an increase (↑), a decrease (↓), or an effect on another outcome (→), while the + and – signs represent contextual factors having a positive or negative impact on the implantation of CMPs.
Cross-Case Synthesis
The skills, leadership and experience of the case manager seem to be the characteristics of the CMP that have the most positive influence on patient experience of integrated care, self-management and healthcare services use. The case manager’s leadership was critical in both successful cases (C and F), i.e. where we observed a decrease of ED visits. Their coordination, communication and networking skills improved integrated care by facilitating collaboration among professionals and also the transitions between health services, for which information access was a key. These improvements were also observed when the case manager was experienced, well-known in his/her workplace (C and F) and located near the providers (cases D, E, F).
Regarding the other characteristics of the CMP, four stand out from our cross-case analysis: 1) the individualized services plan (all cases), 2) patient and family needs assessment (all cases), 3) patient and family participation in decision-making (all cases), and 4) the self-management approach (cases C, D and F).
Our results suggest that where staff turnover and thus, health care team instability, was present due to organizational issues and the health system reorganization (cases B, D and E), negative impacts on care integration, especially regarding communication and care transitions, were observed. However, when case managers were well supported by their managers (cases B, E and F), they had the opportunity to create more personalized care trajectories. Therefore, patient transition through care pathways was optimized and their use of services was more appropriate. Reassurance of patients by their case manager appears to be particularly important for those with anxiety as it seems to have contributed to a reduction in their ED visits.
This study underscores the necessity of an experienced, knowledgeable, and well-trained case manager with strong interpersonal skills to optimize CMP implementation such that patients are more proactive in their care and their outcomes improve. These qualities improve care coordination which is one of the main components of CMP [ 30 , 31 ]. Similarly, Ross et al. pointed out that the case manager skills such as ability to develop good interpersonal relationships, problem-solving, negotiation and brokerage, prescribing qualifications play a key role to facilitate CMP implementation and improve outcomes [ 32 ]. Case manager training could include a focus on these skills. Indeed, a qualitative systematic review by Joo et al. revealed that insufficient training was a barrier to the case manager’s role [ 33 ]. Likewise, our results also underscored the importance of adequate training, but also that it can be challenging to ensure such training when there is a high turnover of case managers. Hong et al. provide a potential solution to this by suggesting that all care team members receive training, in order to build a relationship of trust with the patient [ 31 ].
To improve integrated care, although coordination by a skilled case manager is the core of case management, self-management support is important for CMP as a whole [ 14 , 34 , 35 ]. Self-management support seeks to improve patients’ knowledge and awareness of their care plan, self-efficacy, sense of control over their condition, and motivation to take more responsibility for their health [ 36 , 37 ]. To effectively provide this support, case managers should adopt an approach that is relevant, meaningful and centred on patient needs [ 32 ]. When the patient and caregiver manage the patient’s care adequately, their use of healthcare services is more appropriate and reduced rates of readmission are observed [ 38 ]. Furthermore, encouraging patients and their families to participate in decisions regarding the ISP better meets patient needs, promotes patient and family involvement in patient care and leads to fewer ED visits [ 35 , 39 , 40 ].
It could be argued that in-depth descriptions of the six CMP settings studied would be helpful to judge whether the results of this study are transferable to similar healthcare system settings [ 41 ]. However, given that the six CMP are heterogenous in terms of the populations they serve, their urban and rural environments, their size, the types of providers, among other key features (see Table 1 ), this aspect increases the theoretical transferability of the results. That said, this study’s findings should be considered in light of some limitations that could be addressed in future research. First, only one source of quantitative data (ED visits) was used to measure CMP efficacy. Second, the qualitative data did not provide much insight into the factors linked to the ‘patient’ category of outcomes outlined in the Chaudoir et al. conceptual framework. Third, the qualitative results are relevant to many contextual factors in the other five categories of outcomes, but only those regarding the outcomes of interest (i.e., patient experience of integrated care and integrated care) are reported. Fourth, the case managers’ activities were not measured and evaluated. To further increase the credibility of the results, survey studies could be conducted with validated questionnaires that assess the impact of CMP on patients and the results could be triangulated with those presented herein. Finally, exploring system or organization level outcomes could complete the picture of the impact of CMP on frequent users’ health outcomes.
Studying CMP as they unfold is crucial to building the knowledge base regarding the components of CMP and the roll-out required to improve integrated care. This study is one of few that explore the implementation of CMP for frequent users of ED services in hospital settings. Additional implementation studies conducted in differing contexts or healthcare systems would be useful to confirm and further enrich the findings. In this regard, Malebranche et al. recently suggested that further research was needed to better understand the advantages and disadvantages of implementing case management as primary care program versus predominantly ED or hospital-based one [ 42 ]. Teper et al.’s systematic review of CMP implementation in primary care settings identified common facilitators and barriers of CMP implementation in hospital settings including case managers’ skills, training, and relationship building and team communication practices [ 43 ]. In a systematic mixed studies review on the barriers of CMP implementation for people with dementia in community-based primary health care, Khanassov et al. also reported the importance of communication between case managers and other professionals and services [ 44 ]. Identifying contextual barriers to CMP implementation can help to select more effective implementation strategies resulting in increased positive outcomes [ 44 , 45 ].
Based on the results of the study, recommendations can be made to senior and intermediate managers and clinicians for the planning and implementation of CMP. Senior managers should ensure ongoing support for the implementation of CMP and information sharing among health professionals. They should ensure stability in the health and social care teams, especially to maintain an experienced case manager. They also have a responsibility to promote the culture of a person-centred approach, i.e. one that encourages the consideration of patients’ needs and shared decision-making. Intermediate managers should facilitate the skills, leadership and experience of the case manager, as well as his/her proximity to providers. They will need to focus on the case manager’s skills during the hiring process and provide quality training in case management with frequent users. In addition, intermediate managers should foster professional development by, for example, allowing time for the case manager to participate in a community of practice or co-development activities. Clinicians must consider the needs of patients and their families when implementing the CMP. They should also provide support to patients and encourage their autonomy and involve them and their families in decision-making.
This study underscores the necessity of an experienced, knowledgeable and well-trained case manager with interpersonal skills to optimize CMP implementation such that patients are more proactive in their care and their outcomes improve. Providers’ access to the individualized services plan, consideration of the needs of the patient and family members, their participation in decision-making, and the self-management approach, also impact patient experience of integrated care, self-management and services use.
Acknowledgements
We would like to thank the following intermediate and senior managers (Myriam-Nicole Bilodeau, Martine Couture, Julie Labbé, Jean Morneau, Sylvie Massé, Mélanie Paradis, Caroline Savard and Marc Villeneuve), patient partners (Claude Spence, Gilles Gauthier), and clinicians (Marie-Ève Bergeron, Marc Bolduc, Audrey Corneau, Sylvain Gagnon, Julie Godbout and Cécilia Ruiz) who participated in the governance of this study and made valuable contributions. We also thank Paula L. Bush, PhD, for her substantive and editorial comments and revisions to a previous version of this manuscript.
Adelaide Belo, Senior Consultant – Internal Medicine, Coordinator of Integrated Care Team – Unidade Local de Saúde do Litoral Alentejano – Portugal and President of the Portuguese Association for Integrated Care -PAFIC.
One anonymous reviewer.
Competing Interests
The authors have no competing interests to declare.
Hospital Case Management: A Review: 2019-2022
Affiliations.
- 1 Mary McLaughlin Davis, DNP, MSN, ACNS-BC, NEA-BC, CCM, is a certified case manager, clinical nurse specialist, and senior director for Case Management Cleveland Clinic Main Campus and Akron General Hospital. She served as an executive board member of the Case Management Society of America from 2013 to 2019 and president from 2016 to 2018.
- 2 Colleen Morley, DNP, RN, CCM, CMC, CMCN, ACM-RN, FCM, is a certified case manager and the associate chief clinical operations officer, Care Continuum, University of Illinois Health System. She is president of Chicago Case Management Society of America, served on the national executive board of directors from 2019 to the present and is the national president elect.
- PMID: 35901252
- DOI: 10.1097/NCM.0000000000000565
Purpose/objectives: In June 2019, a Case Management Society of America (CMSA) task force published "The Practice of Hospital Case Management: A White Paper." This was an important first step to outline the value of hospital case managers (HCMs) and to put forward recommendations for how to operationalize a major change in most hospitals for how case managers can practice.The SARS-CoV2 (COVID-19) pandemic drastically changed the practice of all interdisciplinary work within hospitals. The White Paper recommended that HCMs follow a select patient population through the hospital. Hospital case manager leaders realized that HCMs can work remotely and communicate with patients because meeting them in person was not an option. Hospital case managers are still resistant to leaving the hospital unit-based model, even after they experienced the value of this concept during the height of the pandemic.
Primary practice setting: Acute care hospitals.
Findings/conclusions: The White Paper recommended separating HCMs from utilization management. One unintended consequence is the loss of necessary knowledge and competencies. These are related to compliance with the Centers for Medicare & Medicaid Services Conditions of Participation and regulatory mandates that can affect patient care and financial well-being. Hospital case manager leaders must stay current with these government requirements for hospitals and for all levels of care and keep the case managers informed, proficient, and fluent when coordinating the care of patients.
Implications for case management practice: Hospital case manager practice is evolving; change is the single constant in health care. This review of the CMSA Hospital Case Management Whitepaper demonstrates that in just three short years, the landscape of health care can change dramatically.Today's HCM leader must proactively address a multigenerational workforce, lack of title protection, and the COVID-19-induced "Great Resignation." The value of the HCM has never been more apparent as during the pandemic as the need to "empty beds" is critical, and the HCM is the professional who has the skill to provide efficient and patient-centered care coordination. The HCM leader practices positive leadership techniques that benefit the leader, the HCM, and most importantly the patient.
Copyright © 2022 Wolters Kluwer Health, Inc. All rights reserved.
Publication types
- Case Management
- United States
Advertisement
Improving Health Care Management in Hospitals Through a Productivity Dashboard
- Systems-Level Quality Improvement
- Published: 12 March 2020
- Volume 44 , article number 87 , ( 2020 )
Cite this article
- Miguel Pestana 1 ,
- Ruben Pereira ORCID: orcid.org/0000-0002-3001-5911 1 &
- Sérgio Moro 1
3475 Accesses
19 Citations
Explore all metrics
Health information systems have been developed to help hospital managers steer daily operations, including key performance indicators (KPIs) for monitoring on a time-aggregated basis. Yet, current literature lacks in proposals of productivity dashboards to assist hospitals stakeholders. This research focuses on two related problems: (1) hospital organizations need access to productivity information to improve access to services; and (2) managers need productivity information to optimize resource allocation. This research consists in the development of dashboards to monitor information obtained from a hospital organization to support decision makers. To develop and evaluate the productivity dashboard, the Design Science Research (DSR) methodology was adopted. The dashboard was evaluated by stakeholders of a large Portuguese hospital who contributed to iteratively improving its design toward a useful decision support tool. Additionally, it was ascertained that monitoring productivity needs more study and that the dashboards on these themes are valuable assets at a monitoring level and subsequent decision-making process.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

The algorithm journey map: a tangible approach to implementing AI solutions in healthcare
William Boag, Alifia Hasan, … Mark Sendak

Artificial intelligence and HRM: identifying future research Agenda using systematic literature review and bibliometric analysis
Neelam Kaushal, Rahul Pratap Singh Kaurav, … Neeraj Kaushik

The hospital of the future: rethinking architectural design to enable new patient-centered treatment concepts
Carlos Amato, Leslie McCanne, … Lukas Bernhard
Rahimi, H., Kavosi, Z., Shojaei, P., and Kharazmi, E., Key performance indicators in hospital based on balanced scorecard model. J. Heal. Manag. Informatics 4(1):17–24, 2016.
Google Scholar
McDermott, C., and Stock, G. N., Hospital operations and length of stay performance. Int. J. Oper. Prod. Manag. 27(9):1020–1042, 2007.
Article Google Scholar
Koumpouros, Y., Balanced scorecard: Application in the general Panarcadian Hospital of Tripolis, Greece. Int. J. Health Care Qual. Assur. 26(4):286–307, 2013.
Poba-Nzaou, P., Uwizeyemungu, S., Raymond, L., and Paré, G., Motivations underlying the adoption of ERP systems in healthcare organizations: Insights from online stories. Inf. Syst. Front. 16(4):591–605, 2014.
Sun, J., and Qu, Z., Understanding health information technology adoption: A synthesis of literature from an activity perspective. Inf. Syst. Front. 17(5):1177–1190, 2015.
Moro, S., Cortez, P., and Rita, P., Business intelligence in banking: A literature analysis from 2002 to 2013 using text mining and latent Dirichlet allocation. Expert Syst. Appl. 42(3):1314–1324, 2015.
Ghazisaeidi, M., Safdari, R., Torabi, M., Mirzaee, M., Farzi, J., and Goodini, A., Development of performance dashboards in healthcare sector: Key practical issues. Acta Inform. Medica 23(5):317–321, 2015.
T. Knabke and S. Olbrich, “The impact of in-memory technology on the agility of data warehouse-based business intelligence systems - a preliminary study among experts,” Proc. der 12. Int. Tagung Wirtschaftsinformatik (WI 2015 ) , no. Paper 44, pp. 645–659, 2015.
Forsman, J., Anani, N., Eghdam, A., Falkenhav, M., and Koch, S., Integrated information visualization to support decision making for use of antibiotics in intensive care: Design and usability evaluation. Informatics Heal. Soc. Care 38(4):330–353, 2013.
Baskett, L., LeRouge, C., and Tremblay, M. C., Using the dashboard technology properly. Health Prog. 89(5):16–23, 2008.
PubMed Google Scholar
J. Ryan, B. Doster, S. Daily, and C. Lewis, “Key Performance Indicators across the Perioperative Process: Holistic Opportunities for Improvement via Business Process Management,” pp. 3479–3488, 2017.
Eckerson, W. W., Performance dashboards: Measuring, monitoring, and managing your business. John Wiley & Sons, 2010.
Pauwels, K. et al., Dashboards as a service: Why, what, how, and what research is needed? J. Serv. Res. 12(2):175–189, 2009.
Berler, A., Pavlopoulos, S., and Koutsouris, D., Using key performance indicators as knowledge-management tools at a regional health-care authority level. IEEE Trans. Inf. Technol. Biomed. 9(2):184–192, 2005.
M. Linna, “Benchmarking hospital productivity,” no. 7, pp. 1–5, 2006.
Nguyen, B. V., Burstein, F., and Fisher, J., Improving service of online health information provision: A case of usage-driven design for health information portals. Inf. Syst. Front. 17(3):493–511, Jun. 2015.
Black, N., Browne, J., and Cairns, J., Health care productivity. BMJ 333(7563):312–313, Aug. 2006.
A. Sharpe, H. Messinger, and C. Bradley, “The measurement of output and productivity in the health care sector in Canada: An overview,” 2007.
Henkel, M., Johannesson, P., and Perjons, E., Value and goal modelling in healthcare. Management:1–14, 2007.
Ashrafi, N., Kelleher, L., and Kuilboer, J.-P., The impact of business intelligence on healthcare delivery in the USA. Interdiscip. J. Inf. 9(9):117–130, 2014.
Kawamura, T., Kimura, T., and Tsumoto, S., Estimation of service quality of a hospital information system using a service log. Rev. Socionetwork Strateg. 8(2):53–68, 2014.
Mettler, T., and Vimarlund, V., Understanding business intelligence in the context of healthcare. Health Informatics J. 15(3):254–264, 2009.
Stadler, J. G., Donlon, K., Siewert, J. D., Franken, T., and Lewis, N. E., Improving the efficiency and ease of healthcare analysis through use of data visualization dashboards. Big Data 4(2):129–135, 2016.
S. Al-Hajj, I. Pike, and B. Fisher, “Interactive Dashboards: Using Visual Analytics for knowledge Transfer and Decision Support,” 2013 Work. Vis. Anal. Healthc. , pp. 37–40, 2013.
H. Providers and G. S. Nelson, “The Healthcare Performance Dashboard : Linking Strategy to Metrics Table of Contents SAS Global Forum 2010,” pp. 1–10, 2010.
Park, K. W., Smaltz, D., McFadden, D., and Souba, W., The operating room dashboard. J. Surg. Res. 164(2):294–300, 2010.
Prevedello, L. M., Andriole, K. P., Hanson, R., Kelly, P., and Khorasani, R., Business intelligence tools for radiology: Creating a prototype model using open-source tools. J. Digit. Imaging 23(2):133–141, 2010.
E. R. Mahendrawathi, D. Pranantha, and J. D. Utomo, “Development of dashboard for hospital logistics management,” ICOS 2010 –2010 IEEE Conf. Open Syst. , no. Icos, pp. 86–90, 2010.
Martin, N., Bergs, J., Eerdekens, D., Depaire, B., and Verelst, S., Developing an emergency department crowding dashboard: A design science approach. Int. Emerg Nurs 39:68–76, 2018.
Ward, M. J., Marsolo, K. A., and Froehle, C. M., Applications of business analytics in healthcare. Bus. Horiz. 57(5):571–582, 2014.
Gordon, J., and Richardson, E., Continuous improvement in the Management of Hospital Wards: The use of operational dashboards. Int. J. Manag. 30(4):414–417, 2013.
R. Shailam, A. Botwin, M. Stout, and M. S. Gee, “Real-time electronic dashboard technology and its use to improve pediatric radiology workflow,” Curr Probl. Diagnostic Radiol . , 2017.
S. Al-Hajj, I. Pike, B. E. Riecke, and B. Fisher, “Visual analytics for public health: Supporting knowledge construction and decision-making,” Proc. Annu. Hawaii Int. Conf. Syst. Sci . , 2013.
Franklin, A., Gantela, S., Shifarraw, S., Johnson, T. R., Robinson, D. J., King, B. R., Mehta, A. M., Maddow, C. L., Hoot, N. R., Nguyen, V., Rubio, A., Zhang, J., and Okafor, N. G., Dashboard visualizations: Supporting real-time throughput decision-making. J. Biomed. Inform. 71:211–221, 2017.
Hill, H. M., Measuring productivity in bioanalysis. Bioanalysis 4(19):2317–2319, 2012.
Article CAS Google Scholar
Zhang, X., Gallagher, K., and Goh, S., BI application: Dashboards for healthcare. 17th Am. Conf. Inf. Syst. 2011, AMCIS 2011 5:3898–3902, 2011.
Hain, P. D., Daru, J., Robbins, E., Bode, R., Brands, C., Garber, M., Gosdin, C., Marks, M., Percelay, J., Terferi, S., and Tobey, D., A proposed dashboard for pediatric hospital medicine groups. Hosp. Pediatr. 2(2):59–68, 2012.
M. Barrento, “Admissão da Business Intelligence às Urgências Hospitalares Business Intelligence admission to Hospital emergency,” 2013.
W. Presthus and I. Bergum, “Business Intelligence to the People. A Case Study of Dashboard Adoption in the Health Care sector,” Nor. Konf. Organ. bruk av IT , vol. 23, no. 1, 2015.
Daley, K., Richardson, J., James, I., Chambers, A., and Corbett, D., Clinical dashboard: Use in older adult mental health wards. Psychiatrist 37(3):85–88, 2013.
Donaldson, N., Brown, D. S., Aydin, C. E., Bolton, M. L. B., and Rutledge, D. N., Leveraging nurse-related dashboard benchmarks to expedite performance improvement and document excellence. J. Nurs. Adm. 35(4):163–172, 2005.
Miniati, R., Frosini, F., Cecconi, G., Dori, F., Iadanza, E., Biffi Gentili, G., Belardinelli A, “Development of Web-Based Operating Theatre Dashboard for Activity Monitoring and Planning in Hospitals,” Proc. IEEE-EMBS Int. Conf. Biomed. Heal. Informatics (BHI 2014 ) , vol. 50139, p. IN PRESS, 2014.
McLeod, B., Zaver, F., Avery, C., Martin, D. P., Wang, D., Jessen, K., and Lang, E. S., Matching capacity to demand: A regional dashboard reduces ambulance avoidance and improves accessibility of receiving hospitals. Acad. Emerg. Med. 17(12):1383–1389, 2010.
J. P. McGlothlin, S. Vedire, E. Crawford, J. Pappas, B. Bruneau, and L. Obregon, “Improving patient care through analytics,” 2016 4th Int. Symp. Comput. Bus. Intell. , pp. 94–100, 2016.
Ryan, J., Doster, B., Daily, S., and Lewis, C., A balanced perspective to perioperative process management aligned to hospital strategy. Int. J Heal. Inf Syst. Informatics 9(4):1–19, 2014.
S. Al-Hajj, I. Pike, and B. Fisher, “Visual analytics to support medical decision-making process,” XXIV Conf. Eur. Fed. Med. Inf. Qual. life through Qual. Information., pp. 1–3, 2012.
L. A. Mallak, “DPM and DFID: Interactive tools for evidence-based decision making,” PICMET Portl. Int. Cent. Manag. Eng. Technol. Proc., pp. 642–649, 2009.
Arinze, B., A model for delivering smart healthcare using patient-facing dashboards, clinical DSS and electronic health records. Can. Conf. Electr. Comput. Eng.:1–4, 2014.
Mattingly, W. A. et al., Real-time enrollment dashboard for multisite clinical trials. Contemp. Clin. Trials Commun. 1:17–21, 2015.
Egan, M., Clinical dashboards. Crit. Care Nurs. Q. 29(4):354–361, 2006.
Jha, A., and Epstein, A., Hospital governance and the quality of care. Health Aff. 29(1):182–187, 2010.
Perron, C. E., Bachur, R. G., and Stack, A. M., Development, implementation, and use of an emergency physician performance dashboard. Clin. Pediatr. Emerg. Med. 18(2):115–123, 2017.
Dixon, B. E., Jabour, A. M., Phillips, E. O. K., and Marrero, D. G., An informatics approach to medication adherence assessment and improvement using clinical, billing, and patient-entered data. J. Am. Med. Informatics Assoc. 21(3):517–521, 2014.
A. Koronios and J. Gao, “Data Quality for Emergency Department BI Dashboard,” Adv. Intell. Syst. Res. , no. 2001, pp. 301–309, 2010.
P. Silva et al. , “Hospital database workload and fault forecasting,” 2012 IEEE-EMBS Conf. Biomed. Eng. Sci. IECBES 2012 , no. December, pp. 63–68, 2012.
R. Alharbey, “Predictive Analytics Dashboard for Monitoring Patients in Advanced Stages of COPD,” 2016 49th Hawaii Int. Conf. Syst. Sci. , pp. 3455–3461, 2016.
M. Y. Santos, “A data-driven analytics approach in the study of pneumonia ’ s fatalities,” 2015.
J. Ryan, B. Doster, S. Daily, and C. Lewis, “Key performance indicators across the perioperative process: Holistic opportunities for improvement via business process management,” in Proceedings of the 50th Hawaii international conference on system sciences, 2017.
M. Barrento, “European Benchmarking in Healthcare Analysis by Country with highlight on Portugal,” pp. 1–4, 2017.
V. Georgiana, D. Kartawiguna, and Indrajani, “Evaluation of radiology data warehouse implementation on education, research, and quality assurance,” Proc. 2016 Int. Conf. Inf. Manag. Technol. ICIMTech 2016 , no. November, pp. 277–280, 2017.
Hevner, A. R., March, S. T., Park, J., and Ram, S., Design science in information systems research. MIS Q. 28(1):75–105, 2004.
S. Few, “Information dashboard design,” 2006.
C. N. Knaflic, Storytelling with data: A data visualization guide for business professionals . John Wiley & Sons, 2015.
Nogueira, Paulo; Martins, José; Rita, Francisco; Fatela L., “Dashboards da saúde: passado, presente e futuro. Uma Perspetiva Da Evolução Em Portugal.,” pp. 1–9, 2017.
Karami, M., Langarizadeh, M., and Fatehi, M., Evaluation of effective dashboards: Key concepts and criteria. Open Med Inform J 11(1):52–57, 2017.
C. A. Wexler, Steve, Shaffer Jeffrey, The big book of dashboards: visualizing your data using real-world business scenarios. Wiley, 2017.
Voelker, K. E., Rakich, J. S., and French, G. R., The balanced scorecard in healthcare organizations: A performance measurement and strategic planning methodology. Hosp. Top. 79(3):13–24, 2001.
Download references
Author information
Authors and affiliations.
DCTI, ISCTE-Instituto Universitário de Lisboa, Line 1: Av. das Forças Armadas, 1649-026, Lisbon, Portugal
Miguel Pestana, Ruben Pereira & Sérgio Moro
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ruben Pereira .
Ethics declarations
Conflict of interest.
The authors declare that they do not have conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Systems-Level Quality Improvement
Rights and permissions
Reprints and permissions
About this article
Pestana, M., Pereira, R. & Moro, S. Improving Health Care Management in Hospitals Through a Productivity Dashboard. J Med Syst 44 , 87 (2020). https://doi.org/10.1007/s10916-020-01546-1
Download citation
Received : 21 January 2019
Accepted : 18 February 2020
Published : 12 March 2020
DOI : https://doi.org/10.1007/s10916-020-01546-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health information systems
- Business intelligence
- Hospital management
- Find a journal
- Publish with us
- Track your research

HospiNEXT - Acceptance & Satisfaction
Client: a leading hospital in johor.
The hospital was already using another application for managing all their administrative and clinical related activities. They were not satisfied with the performance and wanted to evaluate HospiNEXT. We conducted a case study for the same through exploring the influential factors that affect the acceptance and satisfaction levels among different healthcare professionals in the Hospital.
DSS developed an exclusive approach to
We conducted objective quantitative survey methods to collect data directly from different types of Hospital Information Management system users. The survey covered 5 sections:
- Demographic user information
- Assessment on existing Hospital Information Management system
- Accessibility and availability of computers
- Impact of using Hospital Information Management system on patient care
We found that the most influential factors are :
- Availability of computers (laptops & computers on wheels) - To facilitate direct and immediate data entry and information retrieval processes
- Slow performance and responsiveness
It is observed that main areas of potential improvement are:
System performance – Improving the performance of the Hospital Information Management system is achieved by -
- Increasing the availability of computers at the point of care
- Making the Application more user-friendly
- Defining new methods for data entry
- Improve the MIS reporting
Organizational support – A very crucial factor that can be achieved by providing training and dedicated time (during working hours) for users to learn and practice on the Hospital Information Management system.
Users' feedback – Better and more reliable channels of communication and feedback are needed to consider users' complaints, suggestions and contribution.
We understood the system functionality thoroughly, the need for changes and improvement. We implemented HospiNEXT in their hospital and appointed a dedicated 2-member team to maintain their information in the application. After 1-month, it is observed that there is a lot of improvement in the system performance with increased information quality. Also our team conducted the user trainings (weekly) and immediate support was provided for all the helpdesk tickets arised. Now we are proud to have this hospital as our permanent client.
- Top Courses
- Online Degrees
- Find your New Career
- Join for Free
What Is Case Management? Definition, Process, and Models
Case management is all about connecting patients with health care providers, designing treatment plans, and making sure it all gets done on time. Learn more about this project-oriented health care profession.
![case study hospital management system [Featured Image]: A case manager, wearing a blue uniform and a blue head covering, is sitting in front of three computer screens, looking at charts.](https://d3njjcbhbojbot.cloudfront.net/api/utilities/v1/imageproxy/https://images.ctfassets.net/wp1lcwdav1p1/74UCNQZ7eoX2IiTXBfxqlm/22e01be84083d62ce5b73fd342e8c6a1/GettyImages-108436364__1_.jpg?w=1500&h=680&q=60&fit=fill&f=faces&fm=jpg&fl=progressive&auto=format%2Ccompress&dpr=1&w=1000)
In health care, case management is a process that connects patients with health care providers, resources, and services. Directed toward ensuring that patients receive the best possible care, case management requires case managers to maneuver different health care systems and collaborate with stakeholders, including patients, medical professionals, and health insurers.
In this article, you will learn more about case management, its process, and explore some different case management models. At the end, you will find more articles and courses you can take to gain a fuller understanding of case management.
What is a case manager?
A case manager is a certified medical professional who connects patients with health care providers, coordinates appointments and treatment plans, and helps patients meet their optimum level of health.
Nurse case managers , for example, are registered nurses (RN) who use their medical expertise to help patients maneuver the health care system and health insurance to receive appropriate care.
What is case management?
Case management is a process that involves numerous stages and requires a unique intersection of health care knowledge and interpersonal skills. In this section, you’ll learn more about what you can expect from the case management process, the skills you’ll need to do it, and find an example of case management in action.
The case management process
Case management is a collaborative process in which a case manager works with clients to ensure they obtain the proper health care in the most cost-effective manner. This is what the process typically looks like:
1. Screening: The case manager reviews a client’s medical records, medical history, and current financial, living, and social support situation to understand client’s needs and current circumstances.
2. Assessment: The case manager conducts more in-depth research and meets with the client to assess their medical condition and circumstances. They might assess the client's health insurance, support systems, and treatment response history.
3. Risk evaluation: In this stage, the case manager evaluates the client's risk for particular ailments. Common factors that are evaluated include existing medical conditions, blood pressure, mental health, and finances.
4. Planning: The planning stage is when a case manager creates a plan of care for their client, which outlines their health objectives, self-care goals, health care options and services, care schedule, and any relevant resources.
5. Implementation: Once a plan has been devised, the case manager now helps the client implement it by guiding them in making sure they attend appointments and educating them about health care-related issues.
6. Follow-up: During the follow-up stage, the case manager sees how the client is progressing through their treatment plan by speaking with them, their health care providers, and their personal support network. If needed, the case manager might advise changing the treatment plan.
7. Evaluating outcomes: Finally, the case manager reviews the entire case and evaluates its outcomes, such as the client's well-being, finances, and whether they received appropriate care.
Build job-ready skills with a Coursera Plus subscription
- Get access to 7,000+ learning programs from world-class universities and companies, including Google, Yale, Salesforce, and more
- Try different courses and find your best fit at no additional cost
- Earn certificates for learning programs you complete
- A subscription price of $59/month, cancel anytime
Case management skills
Being a case manager requires both technical health care knowledge and strong interpersonal skills. Common skills that case managers should possess include:
Medical knowledge of a wide variety of ailments
Knowledge of the health care system, including different medical professionals, medical organizational structures, and health insurance providers
Project management and coordination
Communication
The ability to collaborate with others
Case management example
An elderly patient who recently suffered a stroke might be assigned a case manager at their hospital to ensure they get the ongoing care they need. In this situation, the case manager would act as a liaison between the patient and their health insurer. They would assess the patient’s current support network, suggest rehabilitation centers, and direct them toward additional resources. Over time, they would monitor the patient’s progress and make sure they attend their medical appointments and take any prescribed medication.
Case management models
There are three primary case management models used in health care. While they are all oriented toward getting clients the care they need, each has its own unique emphasis. A case manager might use a combination of these models depending on their client’s needs.
Brokerage case management model
The brokerage case management model involves a case manager assessing a client’s need and then acting as a broker that connects them with the relevant resources, services, and medical professionals. Typically, case managers in this system have little personal contact with the client, acting instead as a liaison to ensure they receive the care they need. This model places less emphasis on monitoring outcomes and more on connecting clients with the medical professionals who will.
Clinical case management model
The clinical case management model involves a case manager (often a therapist or counselor ) assigned by a clinical care provider. The case manager works directly with the client in a clinical capacity, providing care as well as coordinating and developing treatment plans. Such direct collaboration can increase the client’s health outcomes and encourage them to follow their care plan more directly.
Strengths-based clinical case management model
The strengths-based clinical case management model is oriented around empowering clients and their support networks so they can meet their health goals. In effect, this model encourages psychological and emotional empowerment by reframing internal narratives and social empowerment by changing environmental factors that could be holding clients back. Though initially developed for those with severe mental health problems, this model can be used for a variety of clients with unique needs.
Learn more about case management
As you plan your future career as a case manager, you might consider taking a flexible, cost-effective online course to gain critical job skills and deeper insight into the patient experience. The University of Houston’s Value-Based Care Specialization introduces course takers to the fundamentals of value-based care, such as the role of case management and the power of effective communication to improve health outcomes for both patients and health care professionals.
Keep reading
Coursera is the global online learning platform that offers anyone, anywhere access to online course...
This content has been made available for informational purposes only. Learners are advised to conduct additional research to ensure that courses and other credentials pursued meet their personal, professional, and financial goals.

Hospital Management System
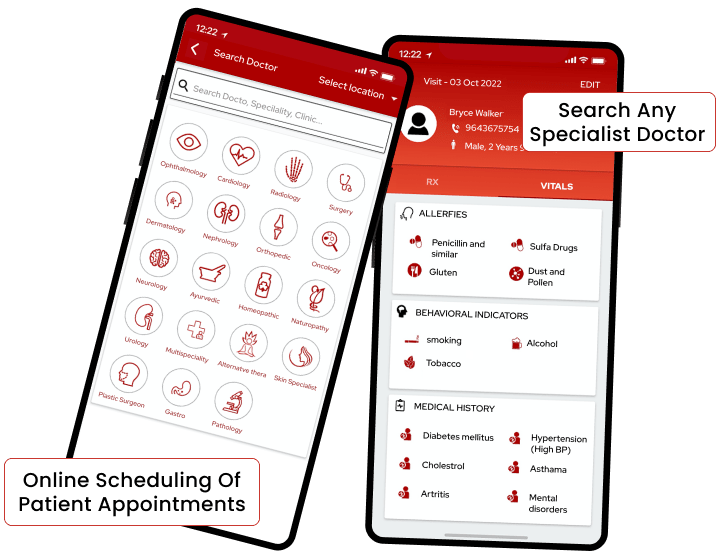
Customer Profile
A Texas-based clinical practice wanted to develop a secure mobile and web-based healthcare solution to modify their traditional healthcare practices and automate several routine tasks like managing the medical data, appointments, schedules of practitioners, etc.
Issue/Problem
Today, healthcare service providers come across various challenges – How to efficiently manage various routine operations? How to automate the appointment management process, improve communication with patients and save the medical records securely in digital format?
Our Healthcare Management System (HMS) has helped our client to manage the patients’ appointments, schedules of practitioners and other clinical operations. The accurate healthcare data saved the vital time of practitioners and they could utilize it to cater to more patients. Ultimately, this enhanced the patient experience, improved the productivity and efficiency of work. We understand your business. Discover how we can partner with you in your healthcare journey.
When developing an app, we focus on our client’s business objectives & specific requirements. Explore how partnering with us can help you to build a transformative Hospital Management Solution.

Technology has revolutionized the healthcare sector completely. Our Healthcare Management System (HMS) is a comprehensive solution to various challenges faced by the client’s clinical practice. The HMS integrates the medical data of the patients into the in-built Electronic Medical Record (EMR) system and makes the functioning paperless. The sensitive medical data remains safe and secure as the system is HIPAA compliant. List of all the practitioners can be saved in the system and they can check their appointments or schedule new ones. They can add their details (appointments, diagnostic notes, prescriptions, monthly schedules) and if needed, they can call the patients using this system. They can review the schedules of other practitioners as well.
Developmental Challenges
Our team came across some developmental challenges as mentioned below:
- Manual appointment scheduling consumed the important time of the staff and practitioners.
- Manual calling to patients resulted in mismanagement in case of rescheduling/canceling of appointments.
- If medical reports, prescriptions, etc. got misplaced or forgotten by the patients, affected the quality of treatment due to missing data.
- There wasn’t a proper platform for communicating with patients, if needed.
- Practitioners had to search for paper records to access the health information of their patients; it was time-consuming.
- Saving of administrative details of staff and practitioners were done manually. It was time-consuming and prone to errors.
HMS app developed by us overcame all the above operational challenges. HMS works as a patient scheduler system for booking the appointments conveniently. It saves the Electronic Medical Records (EMR) safely so that the patients need not worry about carrying the medical reports, prescriptions, etc. to the clinic every time. Practitioners can also provide e-prescriptions to the patients in case of an emergency. Using HMS resulted in increased patient satisfaction. Searching health records of patients became much easier. The documentation errors were also reduced. There was better control over the administrative operations of the practice. Eventually, it resulted in improved patient engagement while saving time and efforts of the staff. It helped in increasing profitability and improving the reputation of the practice.
Solution Highlights
- Appointment scheduling, audio and video consultation, calendar integration.
- Push Notifications.
- Payment Integration, transaction history.
- Integration with electronic medical records and electronic health records.
- Insurance claims.
- Bluetooth scanning & detecting the sensors.
- HIPAA compliant solution.
- E-Prescription.
- Hospital operations management, staff management and shift management.
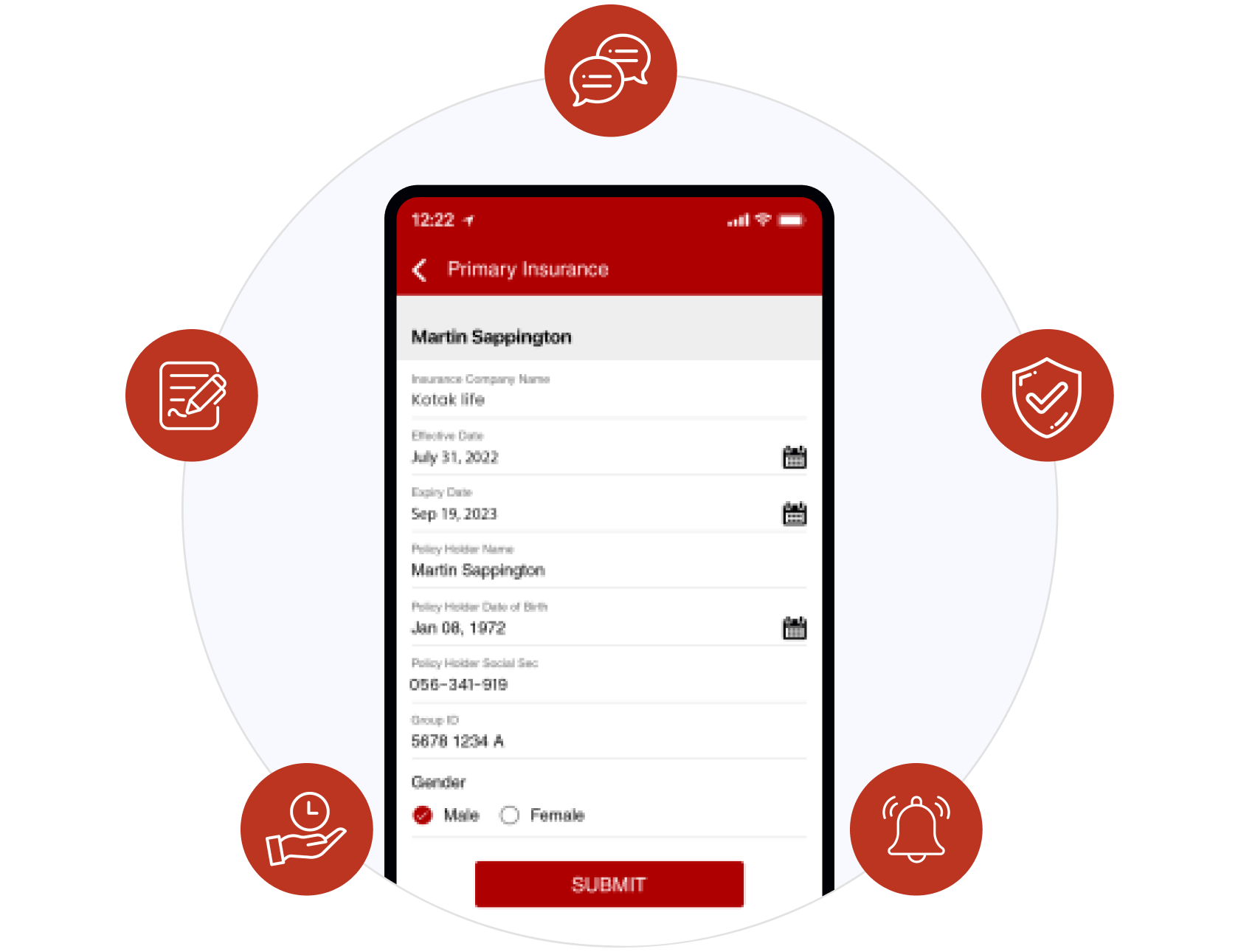
- Online scheduling of patient appointments by the staff or practitioners.
- Saving appointment details and medical history of the patients on a single system.
- Creating and editing the profile of the practitioners.
- Automatically sending reminders about the daily appointments, events, etc to the practitioners.
- Adding any notes, events, appointments or interests in the schedule by the practitioners.
- Rescheduling/cancelling of the appointments.
- Checking the weekly/monthly calendar of self or other practitioners.
- Calling and communicating with the patients.
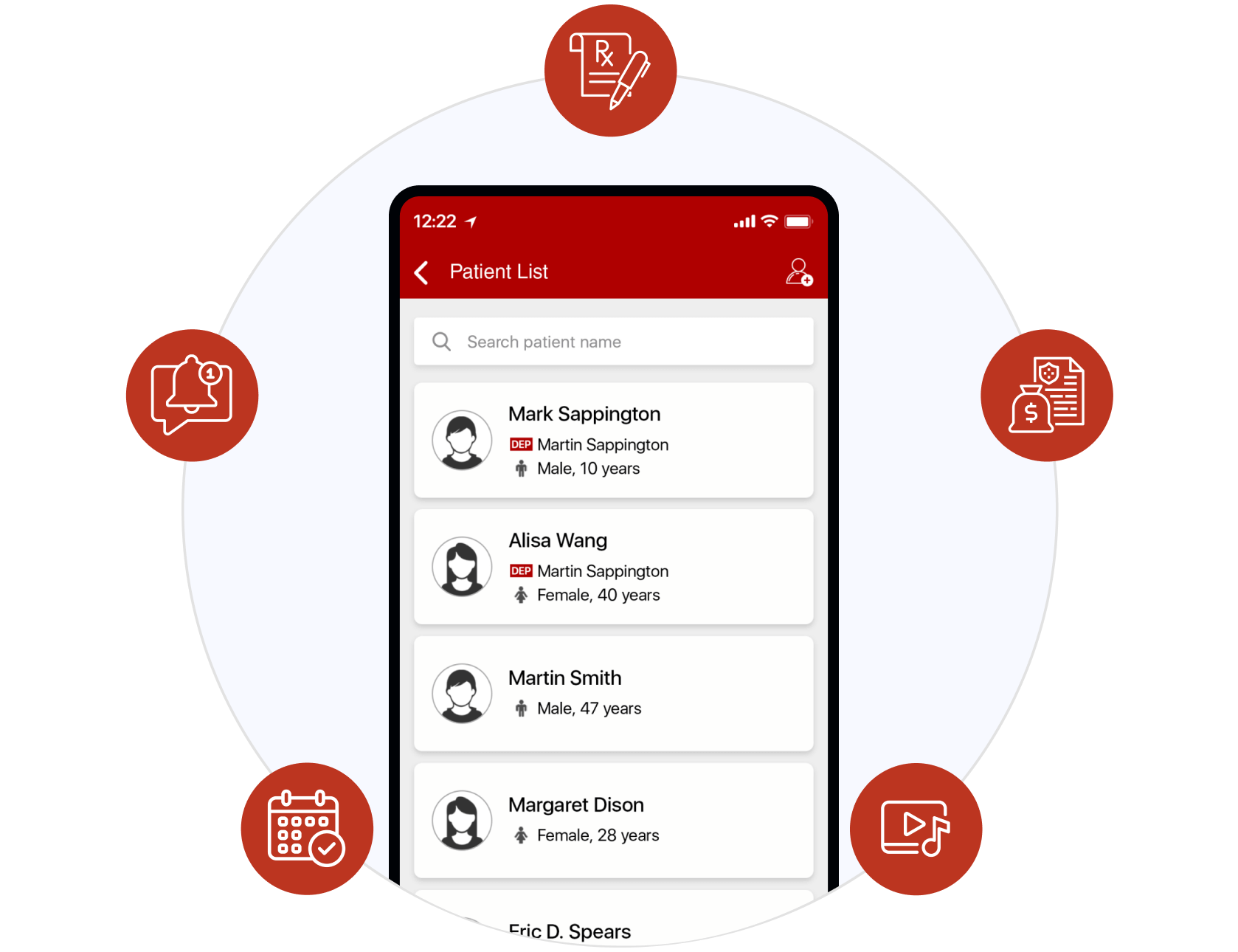
Let us help you right away!
If you are interested to know more about our success stories in healthcare sector, or looking for a similar kind of Healthcare solution, then please hit the button below to share scope and requirements of your project.
© 2024 Biz4Solutions - Mobile and Web App Development Services
Built with Enlightenment Theme and WordPress

- App Value Calculator
- Project Planner
- Book a Meeting
By continuing to use this website you agree to our Cookie Policy. I Agree

Hospital Management System
- Back to Portfolio
Our South Africa based client is one of the leading providers of Healthcare management services who envisioned to design a solution with leading-edge medical technologies. The system they decided to develop needed to be able to successfully facilitate the complex challenges of the healthcare sector and provide seamless healthcare facilities. The client approached TatvaSoft with a goal to develop a cloud-based Medical Information System for both web and mobile-based platforms to deliver public health security with strategies to focus on medications, precise diagnosis, and organized health record management.
Client was more inclined towards providing revolutionary and intelligent medical facilities using a cloud-based system adhering to medical intelligence and healthcare standards. Moreover, they also wanted to create an application that would provide information about the patient to the doctor along with the records of past visits and past health issues.
Some of the primary requirements of the client were:
- A comprehensive mobile application and web interface with symptom-based predictions
- Provide a kiosk assisted solution
- Facilitate video calling services with medical experts for constant monitoring of the health condition in regular cases as well as in case of emergencies
- Centralized and secure database for patients records and interoperability with other healthcare providers
- Empowering the system with Artificial intelligence for symptom-based health predictions
- Multi-lingual supported web applications valid across different geographies of the world.
Tools & Technology
Laravel • PHP • KendoUI • Node.js • Electron • Socket.io • WebRTC
Experienced and proficient PHP developers at TatvaSoft have explored the nitty-gritty of the client’s requirements to develop a unified and robust application. This application was developed using an evolutionary approach where initial features of the application were developed and later with time expanded the features with refined development cycles, development feedback until a satisfactory product is developed. Thus, a requirement for utilizing the latest technology emerged which led us to use JavaScript based Node.JS for our project.
Some of our eminent features of the offering are
General Feature
- Adding basic information and the symptoms during registration in the kiosk-based system.
- This SaaS-based platform can help customers book an appointment from the web application.
- For a consultation, the users can also utilize the video calling option with doctors for precise and visual consultation.
- Doctors are intelligently categorized based on their field of expertise and accordingly, the patients are arrayed.
- For Doctors, they can store patients’ information prescribed in this kiosk system with the diagnosis report and medication prescribed.
Login Facilities
The application adheres to the standards of security and is enabled with Biometrics for users to log in
Symptom Prediction
This feature enables users to add or select disease and get predictions of it. The possibility or prediction of the disease is displayed in percentage format depending on how accurate are the symptoms.
Patients are allowed to use their GPS and search for a doctor or specialist and book an appointment using this application. This app will also notify and send a reminder before an hour before the appointment. Our Blockchain-based system stores and secures the database as a history to patient’s medical records for any future use.
Users and Accessibility Rights
The hospital management system application is designed specifically for three types of users and is intelligently bifurcated for accessibility between
1. Clerk account:
Once the patient arrives at the hospital, they have to check on their confirmation of the appointment with the clerks available. There are multiple clerks available for patient’s convenience.
The clerk has been assigned with two major rights
Register Patient
If the patient is new and has come for the first time then the clerks can assist them with registration for the first time. They can generate a print number after the initial registration process.
Validate Patient
If the patient is already registered then the clerk has to validate the details when the patient comes for the first time into the kiosk system. After Validation, they are assigned to the Nurse account’s queue.
2. Nurse account:
After the clerk prints the number, multiple nurses are working in the hospital who are assigned with a list of patients and based on the number of patients in the Nurse queue they are diverted towards the specialists.
In the nurse's system, there will be a patient queue where a list of patients will be displayed as per their appointment numbers. Nurses can click on patients and get all details about the patient profile and the patient’s past visit history. Nurses can capture the patient’s allergies, medical conditions, chronic medication, surgical history, family history, and lifestyle.
The nurse can also check the patient's vitals and add vital information to the patient’s current appointment. Later, the nurse can also assign that patient to the related department’s queue so that doctors of the ward can check the patient on time.
If a patient's health is critical then the Nurse can directly admit the patient to the emergency ward.
3. Doctor account:
Whenever a new doctor registers himself in the application, he has the option to select a list of departments he specializes in. After the selections have opted, the doctors are assigned to these specialized departments. Doctors can select patients from the queue and the assigned but cannot see patients of other doctors in the queue list of the same department.
Doctors have access to all the patient details. They can validate the records stored by the nurse and edit it if required. With an option to re-capture vitals. Doctors can also capture additional patient allergies, medical conditions, chronic medication, surgical history, family history, and lifestyle.
Doctors can do the below actions in the appointment.
1. Capture Soap:
- Add the subject in the text area for current appointments.
- Add the objective in the text area for current appointments.
- Select Diagnosis (It will have the doctor’s most commonly selected diagnoses as the first listed ones)
- Use order sets to order tests, create prescriptions, and choose treatment plans.
- Create a treatment plan and save it as a template and use the same template for diagnosis.
2. Create Prescriptions:
- Use already created templates or manually add items required
- The script can be printed or sent straight to the pharmacy
3. Order tests:
- They can choose either Pathology or Radiology sections and check the boxes of the tests that should be done, or use templates where the tests are already selected based on the template
4. Create Referrals:
- Create referral notes for the patient with a predefined page layout.
5. Create Sick Notes:
- Create a sick note for the patient with predefined page layout
- Confirm death of patients and fill out the required form, which the doctor prints and provides to the right person
- Discharge summary printed once the doctor has chosen to complete the consultation
Additional features
- Doctors and Nurses can chat or perform audio calling from the system. We have used socket.io library for text chat and audio calling functionality.
- The queues of nurses and doctors are managed by socket so the real-time appointment list and number will be displayed in the hospital's computer screens.
- This application is created with Electron js for compatibility with the desktop applications.
Collaboration with TatvaSoft, a web development company enabled the client access to benefits such as
- Access to a pool of specialists, doctors, and physicians.
- Doctors and patients can save their time by accessing the online platform
- 24*7 Flexibility and convenience to access doctors and hospital facilities
- Centralized platform for doctors to understand patients' demographics
- The client can sell the solution to different healthcare management companies and generate a new revenue stream
Filter Portfolios
By industries.
- Energy & Utility
- Health & Insurance
- Media & Entertainment
- Shipping, Transportation & Logistics
- Travel & Hospitality
- Government & Public Safety
- Retail & ecommerce
- Oil & Gas, Mining
By Technologies
- Microsoft .NET
- Mobile Apps
Related Case Studies

Organ Transplant Care

Doctors To You App

Medical Record Management System

Healthcare & Risk Management System
MBA Knowledge Base
Business • Management • Technology
Home » Management Case Studies » Case Study: Hospital Management System (HMS)
Case Study: Hospital Management System (HMS)
XO Hospital Management System
XO Infotech Ltd. has developed a core package — Hospital Management System that addresses all major functional areas of Hospital. The development environment ensures that XO HMS has the portability and connectivity to run on virtually all standard hardware platforms, with stringent data security and easy recovery in case of a system failure. XO HMS provides the benefits of streamlined operations, enhanced administration and control, improved response to patient care, cost control, and increased profitability.
Some of the Subsystem Modules in XO HMS:
Reception : The reception module handles various enquiries about the patient’s admission and discharge details, bed census, and the patient’s movements within the hospital. The system can also handle fixed-cost package deals for patients as well as Doctor Consultation and Scheduling, Doctor Consultancy Fees and Time Allocation.
OPD, IPD Registration and Admission : This module helps in registering information about patients and handling both IPD and OPD patient’s query. A unique ID is generated for each patient after registration. This helps in implementing customer relationship management and also maintains medical history of the patient.
Administration : This module handles all the master entry details for the hospital requirement such as consultation detail such as doctor specialization, consultancy fee, and service charges.
Security : This module handles multi level security of XO HMS so that every admission and transaction can be traced with the help of user ID.
Pharmacy Store : This module deals with all medical items. This module helps in maintaining Item Master Maintenance, Receipt of Drugs/consumables, issue handling of material return, generating retail bills, stock maintenance. It also helps in fulfilling the requirements of both IPD and OPD Pharmacy.
Purchase : This module helps in raising purchase orders, maintaining purchase details and other purchase related details.
Phlebotomy : This specific module caters in maintaining test requisitions, sample collection status and various procedures for collection of sample for the tests prescribed.
Laboratory : This module enables the maintenance of investigation requests by the patient and generation of test results for the various available services, such as clinical pathology, X-ray and ultrasound tests. Requests can be made from various points, including wards, billing, sample collection and the laboratory receiving point. The laboratory module is integrated with the in-patient/ outpatient registration, wards and billing modules.
Emergency : The development of this module keeps in mind the criticality of this department. Every care has been taken to ensure that minimum of time is taken to register the patient, so as to reduce the tension of the already stressed out relatives. Neither any detailed contact information of the patient is required nor any information about the payment type is solicited.
OT Management : This module deals with operation theatre activities such as equipment used detail, resource ordering, drug order, gynecology detail recording, laboratory order and reports transfer requisition, patient monitoring, blood request, new born baby detail and details of delivery.
Minor Surgery : This module is same in features as in OT management though the function is different. This module deals with the surgeries minor in nature, which does not require complete anesthesia.
Blood Bank : The blood bank module provides information on the collection and storage of blood, results of blood tests, cross-matching identifications, and transfusion reactions. It also enables the maintenance of donor mailing lists and donation ledgers. It would also provide online stock of blood available in three blood banks (GTB, LNJP and DDU
Ward Management : The ward management module takes care of medical equipment, doctor visit, vitals recording, patient case sheet, diet ordering, blood requisition, transfer intimation and discharge intimation etc. It also deals with the maintenance of the wards, inter- and intra-ward transfers.
OPD and IPD Billing : The billing module facilitates cashier and billing operations for different categories of patients and automatic posting of charges for different services such as lab tests, medicines supplied, consulting fees, food and beverage charges, etc. It enables credit party billing through integration with the financial accounting module.
Intensive Care Unit (ICU) : This module caters to scheduling, maintaining ICU Record, drug orders, consultant details, specific blood requests etc.
Food and Beverages : This module facilitates collection of information regarding various diet routines of patients and identifies the resources required to satisfy diet orders. Depending on the diet orders and other requests from canteen, the kitchen order plan can be prepared to decide the menu for the day. Analysis of the consumption patterns helps in better and efficient management of the kitchen.
Discharge Summary : The module helps in generating patient’s discharge summary, which includes patient’s health at the time of discharge, medical history, various diagnosis and drug prescriptions, history of present illness and course in hospital.
Financial Accounting : This module deals with cash/bank, receipts/payments, journal vouchers, etc. Various books of accounts, such as cashbook, bankbook and ledgers, can be generated and maintained using this module. It can also generate trial balance, balance sheet, and profit and loss statements.
Marketing Module : This module ensures that the hospital gets maximum exposure to the general public and vice versa. This module keeps track of the enquiries made at the reception and follows the lead.
Doctor’s Module : This module helps the doctors to keep a track of the entire medical history of a particular patient. Details such as the medicines prescribed, general medical records, previous consultations are all available to the doctor.
HR Management : Various MIS Reports are generated on the above modules for the smooth functioning of the hospital management so that checks can be made on any irregularity done in the hospital.
Questions :
1. Using tools of System Analysis elaborate any one of the subsystems of HMS in detail.
2. Draw any Patient registration form and any one sample MIS report.
3. Prepare the Data dictionary for the Doctors Master file.
4. Elucidate the conceptual plan for implementation of the Hospital Management System.
5. You are hired as a System Analyst , advice on the following :
(a) Networking requirements
(b) Database model requirements
Related Posts:
- The Concept of Systems
- ERP Process
- Electronic Data Interchange (EDI)
- CASE (Computer Aided Software Engineering) Tools
- Case Study of FedEx: Leveraging Information Technology to Grow Business
- Educational Management Information System (EMIS)
- ERP Tutorial
- ERP Planning
- Case Study of China Telecom: ERP Implementation
- The factors which lead to the success and failure of MIS in an organization
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Introduction to Database Systems by ITL Education Solutions Limited
Get full access to Introduction to Database Systems and 60K+ other titles, with a free 10-day trial of O'Reilly.
There are also live events, courses curated by job role, and more.
Case Study-1
Hospital management system.
XYZ hospital is a multi speciality hospital that includes a number of departments, rooms, doctors, nurses, compounders, and other staff working in the hospital. Patients having different kinds of ailments come to the hospital and get checkup done from the concerned doctors. If required they are admitted in the hospital and discharged after treatment.
The aim of this case study is to design and develop a database for the hospital to maintain the records of various departments, rooms, and doctors in the hospital. It also maintains records of the regular patients, patients admitted in the hospital, the check up of patients done by the doctors, the patients that have been operated, and patients discharged ...
Get Introduction to Database Systems now with the O’Reilly learning platform.
O’Reilly members experience books, live events, courses curated by job role, and more from O’Reilly and nearly 200 top publishers.
Don’t leave empty-handed
Get Mark Richards’s Software Architecture Patterns ebook to better understand how to design components—and how they should interact.
It’s yours, free.

Check it out now on O’Reilly
Dive in for free with a 10-day trial of the O’Reilly learning platform—then explore all the other resources our members count on to build skills and solve problems every day.

Case Study: Redesigning the Inpatient Case Management Team

The discharge planning arm of a patient’s hospital journey primarily lies with the patient’s case manager, a nurse who helps evaluate the patient’s discharge needs and collaborates on the best plan for the patient after discharge. The process for most patients is straightforward: they either go to another facility or gain some temporary support at home and connect with outpatient clinics.
At Boston Medical Center (BMC), however, the discharge planning process is complicated by its complex patient population, who may not have insurance, citizenship, or homes to discharge to. Delays in creating a safe discharge plan can result in unnecessary days in the hospital even after patients are medically cleared for discharge, resulting in unnecessary costs to our healthcare system, unavailable beds for those who need them, and frustration across staff.
Finding solutions to appropriately reduce length of stay and facilitate better throughput is top of mind for clinical operations — at BMC, our average morning occupancy was 98% on our Medical Surgical floors, for example, versus an industry target of just 80%. Further, every week, we identified at least 30–40 patients “stuck” in the hospital. Freeing these beds and back-filling them with new patients creates a significant financial opportunity associated with reducing length of stay.
The hospital’s Central Flow Unit (a team of physician, nursing, and administrative leaders that oversee and improve patient flow) partnered with our case management department to evaluate opportunities to support the team given the complexity of our patient population. We examined three core questions in consultation with other hospitals.
Should our case managers be responsible for discharge planning and utilization management, or split the tasks? Case management departments typically support both the discharge planning process and the utilization management function, which ensures appropriate payor reimbursement given the clinical profile of the patient. In different environments, case managers do both tasks or divide the responsibilities over two groups. Is a team-based, unit-based, or hybrid case management model most appropriate for our hospital’s needs? Case management can be structured to follow either a set number of beds (e.g., beds 1 – 20 on a unit) or a physician team (e.g., general medicine team). Both models have pros and cons that need to be assessed for each environment. Whereas some hospitals localize physician teams to specific units, this alignment was not the case at Boston Medical Center. What is the appropriate number of patients for a case manager to support? Based on the design of the unit vs. team-based alignment, and the inclusion or exclusion of utilization management, a hospital must determine how many patients a case manager can effectively support.
As a result, we designed a new discharge planning structure that has shown early success in reducing length of stay.
Context: What drove the redesign
We historically followed a unit-based structure where each case manager followed a set of beds — a maximum of 18 beds on a Medical Surgical unit — which facilitated strong relationships with patients’ families and other unit-based teams such as nursing. In this model, case managers were responsible for both the discharge planning and utilization management process.
Our physician teams were scattered across many units, increasing the number of case managers each physician team had to interact with, and likewise the number of physician teams each case manager had to interact with. In fact, a review of our data showed that our highest-volume teams were interacting with eight to nine case managers on average. This model created huge inefficiencies, and as they interacted with more case managers, patient length of stay also increased.
Balancing discharge planning and utilization management
After evaluating our systems, we chose a hybrid case management model — pairing the physician teams that were the most scattered with a team-based case manager, and assigning specific beds for the other case managers. This model requires more day-to-day management from leadership to distribute patients among case managers, but provides relief to the physician teams and case managers who were struggling with a high number of interactions.
Pre-COVID, we had settled on keeping the discharge planning and utilization management tasks associated with patients to one case manager. This was our incumbent model. It had synergies across the tasks, and it was also a team structure supported by half the institutions we consulted.
However, COVID-19 response necessitated that our case management department internally split the tasks. A central team managing denials and appeals took on the utilization management tasks for all patients in house, benefiting from the fact that we primarily cared for one diagnosis: COVID-19.
Anecdotally, our floor case managers appreciated the bandwidth to focus on discharge planning afforded by the split of responsibilities. We are now striving to maintain this split given the staff satisfaction.
Appropriate case mangement case load
Our final question concerned how many patients per case manager was appropriate to facilitate efficient and high-quality throughput. Our inquiry into the caseloads per case manager at other institutions quickly highlighted that our case managers were caring for significantly more patients — an average of 17 patients at BMC while the average at other hospitals was 12, accounting for differences in structures.
In the end, with the shift to team-based case management we reduced the case load for the case managers assigned to these teams, accounting for the fact that they will be spread out, an additional challenge in its own right. We maintained the case load for the other case managers, appreciating that they now could focus on discharge planning exclusively, bringing their case load on par with other institutions who have split functions.
Conclusions from case management redesign
Our decisions related to the structure of case management were anchored in additional recommendations meant to strengthen the processes and data systems within the department to make the environment that our case managers work in effective for them. Underscoring these efforts is collaboration across disciplines and strong, on-the-ground leadership ensuring these changes work for the front-line teams. We are assessing the impact of these changes with both qualitative and quantitative metrics and are excited for the potential these changes have for our patients and our staff — initial findings of 0.7 day reduction in LOS for teams in this new program compared to a baseline of five months indicate we are on the right path.
Boston Medical Center is a 514-bed hospital and houses the busiest emergency department in New England. In January 2019, we created the Central Flow Unit (CFU) which oversees patient flow and is co-led by physician, nursing and administrative leaders. The CFU, in collaboration with many stakeholders, has worked to improve patient flow and problems many hospitals encounter. Along the way, we have turned to the literature and our peers across the country to learn more about the challenges and progress against them. In the spirit of collaborating across institutions, we are sharing an inside look at some of our biggest successes in improving inpatient operations and care. Don’t forget to check out our other results in The Hospital Playbook series.

Neha Gaur is the senior director of inpatient operations and cancer care at Boston Medical Center. She co-leads the Central Flow Unit with nursing and physician partners. She graduated from the University of Pennsylvania and the Wharton School of Business with a master's degree in biotechnology, as well as bachelor of science and bachelor of arts degrees.
THIS IS IN TOP OF TEMPLATE

IMAGES
VIDEO
COMMENTS
Hospital management software must help you keep hospital data safe and secure. You can limit the access to authorized personnel only. Make sure to look for HIPAA Compliant software for PHI security. 3. Improved access to patient data. You can have easy entry to all patient-related data on a system using an HMS.
A case study approach [ 47, 48] was adopted here to understand the deployment of a whole system change in the acute hospital along the four dimensions of STS outlined above. A case study is an approach that is used to generate an in-depth, multi-faceted understanding of a complex issue in its real-life context [ 49 ].
HOSPITAL MANAGEMENT CASE STUDIES. As a physician-owned organization, we value results. Enhancing the quality and efficiency of hospital management, while improving patient outcomes, is our goal. We continually measure real-life results to demonstrate success. Looking for information related to a specific measurement goal?
The successful case study of this hospital showcases the transformative power of HMS, highlighting its benefits, challenges, and lessons learned throughout the implementation process. As we look ahead, the future of HMS holds promising advancements, including artificial intelligence, cloud-based solutions, and interoperability with other systems.
Abstract. The vital importance of HospitalManagement Systems (HMS) in healthcareorganizations is examined in this review study.HMS is a complex software tool that combinespatient administration ...
CHAPTER FIVE DISCUSSION OF RESULTS 5.0 CONCLUSION The project Hospital Management System (HMS) is for computerizing the working in a hospital. It is a great improvement over the manual system. The computerization of the system has speed up the process. In the current system, the front office managing is very slow.
Onboarding the team. Our team will be ready and happy to work with you and bring your dream to life as soon as you sign off on it. Max. file size: 8 MB. Hospital management system working on AI technology is crucial for seamless operations. Read our case study on hospital management system.
For this initiative, hospital management information system (HMIS) has to be implemented across 400+ health facilities in the city.,A case study methodology was adopted to study HMIS implementation. Wave 1 of Phase 1 implementation of HMIS is carried out as a pilot project at Film City's Hospital, Mumbai, which "go-live" on 21st June 2018.
January 18, 2022. Andrew Brookes/Getty Images. Summary. The use of digital technologies in clinical decision-making has received the most attention. But they also have the potential to help ...
Piedmont Healthcare saves $2 million with system-wide asset tracking and management. Case study: Piedmont Healthcare, Greater Atlanta and North Georgia. With Vizzia's RTLS deployed in multiple hospitals, Piedmont Healthcare is innovating in equipment management, including an in-house equipment. rental service and $2 million saved throughout the.
Design of the study. This was a case study, more specifically a multiple embedded case study with a mixed-methods design . Such a methodology appears the most appropriate for an implementation analysis in a complex system, and to study cases, with varied contexts, as they evolve over time [15,16]. In addition to allowing for an in-depth ...
Our hospital management system puts the hospital's culture at a very high level; a hospital has no soul without culture, and we are committed to the idea that the hospital's cultural values can penetrate into the marrow of each employee. ... The impact of intersectionality on nursing leadership, empowerment and culture: a case study ...
Affiliations 1 Mary McLaughlin Davis, DNP, MSN, ACNS-BC, NEA-BC, CCM, is a certified case manager, clinical nurse specialist, and senior director for Case Management Cleveland Clinic Main Campus and Akron General Hospital. She served as an executive board member of the Case Management Society of America from 2013 to 2019 and president from 2016 to 2018.
Health information systems have been developed to help hospital managers steer daily operations, including key performance indicators (KPIs) for monitoring on a time-aggregated basis. Yet, current literature lacks in proposals of productivity dashboards to assist hospitals stakeholders. This research focuses on two related problems: (1) hospital organizations need access to productivity ...
Impact of using Hospital Information Management system on patient care. We found that the most influential factors are : Availability of computers (laptops & computers on wheels) - To facilitate direct and immediate data entry and information retrieval processes. Slow performance and responsiveness. It is observed that main areas of potential ...
Abstract and Figures. A Case Study on Hospital Management System. Figure2.1: A comparison between Agile and Waterfall models. Figure4.1: Example of GUI interface (View Test Results/ Using Graphics ...
The case management process. Case management is a collaborative process in which a case manager works with clients to ensure they obtain the proper health care in the most cost-effective manner. This is what the process typically looks like: 1. Screening: The case manager reviews a client's medical records, medical history, and current ...
Case Study. HMS. Hospital Management System. Industry. Hospital Management. Customer Profile. A Texas-based clinical practice wanted to develop a secure mobile and web-based healthcare solution to modify their traditional healthcare practices and automate several routine tasks like managing the medical data, appointments, schedules of ...
Hospital Case Management 4 Case Management Society of America©, June 2019 support system in managing their medical/social/mental health conditions more efficiently and effectively _ (AHRQ.gov, 2014). In a 1998 study, case management was defined as a ^means of
The hospital management system application is designed specifically for three types of users and is intelligently bifurcated for accessibility between. 1. Clerk account: Once the patient arrives at the hospital, they have to check on their confirmation of the appointment with the clerks available.
1. Using tools of System Analysis elaborate any one of the subsystems of HMS in detail. 2. Draw any Patient registration form and any one sample MIS report. 3. Prepare the Data dictionary for the Doctors Master file. 4. Elucidate the conceptual plan for implementation of the Hospital Management System. 5.
Case Study-1 Hospital Management System AIM. XYZ hospital is a multi speciality hospital that includes a number of departments, rooms, doctors, nurses, compounders, and other staff working in the hospital. Patients having different kinds of ailments come to the hospital and get checkup done from the concerned doctors. If required they are ...
Pre-COVID, we had settled on keeping the discharge planning and utilization management tasks associated with patients to one case manager. This was our incumbent model. It had synergies across the tasks, and it was also a team structure supported by half the institutions we consulted. However, COVID-19 response necessitated that our case ...
A Case Study on Hospital Management System. Maha. Mahmoud. Under the supervision of Dr Geetha Achuthan. Abstract. Nowadays, the IT system has made many changes in the medical field. Managing a multi-speciality hospital is a challenging task in this fast-paced world of medicine. Therefore, the need for a management type of organization is ...
Case Study 1 Hospital Management System Aim: XYZ hospital is a multi specialty hospital that includes a number of departments, rooms, doctors, nurses, compounders, and other staff working in the hospital. Patients having different. kinds of ailments come to the hospital and get checkup done from the concerned doctors. If.