Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
The following is a scenario of a patient who experienced ruptured esophageal varices. The patient, Nora Allen, a 55-year-old female presented to the emergency department (ER) on May 5, 2017 just after 10:00 a.m., with complaints of two episodes of melena that morning.
Upon further assessment, her husband expressed concern that his wife had been drinking again because her behavior had seemed “strange”. He had these concerns because his wife had a 20-year history of alcohol abuse and was “under a lot of stress” due to the recent loss of her job. Nora has a history of alcoholism, cirrhosis of the liver, coronary artery disease (CAD) and anemia.
Upon assessment in the ER, her vital signs were 110/76, 85bpm, 95% on room air, 98.2ºF, 22 breaths/min. Neurologically, she was oriented to person, time and situation, but was confused as to where she was. Her pupils were 2mm and sluggish to light. She appeared anxious, was slurring her speech and had visible hand tremors. She reported nausea and melena, and had obvious ascites with a distended firm abdomen. An occult stool was positive and her skin was cool and clammy with poor skin turgor and weak pedal pulses. The remainder of her body systems were within normal limits.
While in the ER, 1 L normal saline (NS) bolus was administered, labs were drawn, a foley catheter was inserted. A blood glucose (finger stick) was taken. She was kept NPO for a scheduled endoscopy later that day.
At 1300, the patient began vomiting and was given an emesis bag. At 1310, Nora’s husband quickly informed the nurse that his wife was violently vomiting bright red blood. On reassessment, the patient’s BP was 94/63 and the HR was 98bpm. The patient was started on octreotide 50mcg bolus. She was intubated for airway protection and to prevent aspiration. She was administered 1 unit of packed red blood cells (PRBCs) and was taken immediately to the gastrointestinal lab for a STAT endoscopy for possible esophageal banding therapy.
The patient was diagnosed with ruptured esophageal varices and sent to the ICU for close observation and monitoring after successful placement of 12 esophageal bands. Overnight, the patient was administered another (1) unit of PRBC, to maintain a hemoglobin greater than 8 g/dL. The following morning at 10:45 a.m. Mrs. Allen was extubated after a successful sedation vacation and spontaneous breathing trial.
When the patient was stable, she was transferred to the medical-surgical floor for observation and case management. On the floor, the patient was educated regarding the reason for the ruptured esophageal varices and taught about her new prescription, propranolol, which, if taken correctly, should decrease the chance of a re-bleed. Lastly, although the patient was resistant to the cessation of alcohol consumption, she met with case management and was educated on alcohol cessation programs and support groups, such as alcoholics anonymous.
Discussion Questions
- If you were the case manager who was educating this unwilling patient about the various rehabilitation facilities, how would you have approached the situation?
- In this scenario, the patient’s vomiting caused the varix to rupture. What type of interventions or nursing assessment tools could have been utilized to prevent vomiting and subsequent rupture of the varix?
- During this scenario, the patient began to vomit large amounts of blood. How would you deal with family members who are in the room who may be shocked about this sudden change in the patient’s condition while also taking care of your patient?
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.

Share This Book
Patient Education Reference Center - Case Scenario #1 - Esophageal Varices
Nov 13, 2018 • knowledge, information.
Clinical Case Scenario #1
Health Education for a Male Inpatient with Esophageal Varices
Clinical Scenario
Forty five year old G.K. is admitted to the hospital’s Emergency Department. He is vomiting large amounts of blood. He is mildly intoxicated but alert. His pulse is fast and thready. An IV of normal saline 0.9% is started; he is given oxygen by mask, and is prepared to receive multiple units of packed red blood cells as needed (blood transfusions). He is transferred to the endoscopy lab for an immediate procedure to investigate the source of the bleeding.
In the Endoscopy lab it will be determined that he has bleeding esophageal varices, and a procedure will be performed to stop the bleeding. He will then be admitted to the hospital for observation.
Nursing goals include explanation of all procedures he is to undergo, given his level of comprehension, and written handouts for review later when fully conscious.
Searching in Patient Education Reference Center (PERC)
Esophageal varices: The nurse uses PERC to gather the handout she will need for Mr. K. From the Home page, she searches for esophageal varices She chooses the Conditions source type She reads #1: Esophageal varices and checks the paper to glean meaningful information to share with Mr. K. She prints the hospital-customized handout.
Blood transfusion: The nurse searches Procedures & Lab Tests and finds Blood Transfusion for Mr. K.
Endoscopy The nurse returns to the results list and chooses the Procedure source type. She prints Upper GI Endoscopy and shares the paper with Mr. K before he is sedated, answering his questions and providing reassurance.
The gastroenterologist performs the endoscopy and locates the bleeding site. He uses Endoscopic Band Ligation to stop the bleeding. M. K. recovers quickly and is returned to his room.
Mr. K. is visited by the hospital’s social worker to discuss the potentiality of alcoholism and is referred to a community services program for follow up. The Social worker uses PERC to search for alcoholism. She prints Alcoholism and Alcohol Abuse and reviews the paper with Mr. K.
Following his hospital stay, Mr. K is discharged home with Social Services support. The nurse chooses the Discharge Instructions source type and prints both Discharge Instructions for Upper GI endoscopy and Discharge Instructions for Endoscopic Band Ligation . She discusses his instructions which include important follow up instructions such as seeing his doctor within 2 days and avoiding alcohol.
Following Mr. K.’s discharge, the nurse adds all patient education papers to folders and their related subfolders in PERC, to make available to the other members of the multidisciplinary team.
Handouts for Acute Care Folders in PERC
Blood and Blood Products Blood transfusion GI : esophageal varices GI : Procedures Upper GI Endoscopy, Upper Band Ligation GI : Discharge info Discharge Instructions for Upper GI endoscopy, Discharge Instructions for Endoscopic Band Ligation. Psychosocial : Alcoholism


NurseStudy.Net
Nursing Education Site

Esophageal Varices Nursing Diagnosis and Care Plan
Last updated on February 20th, 2023 at 09:15 am
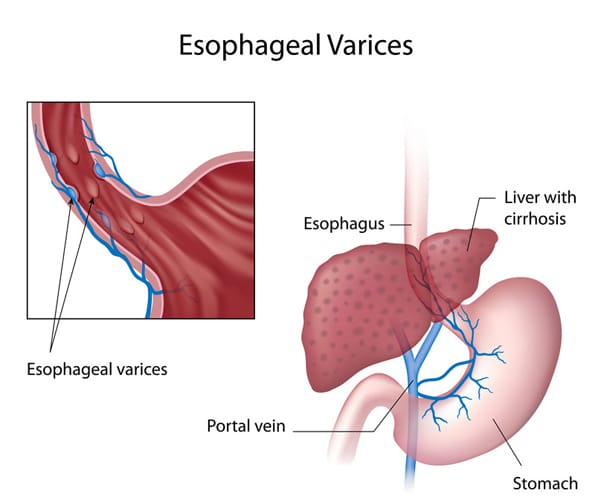
Esophageal varices are veins that are abnormally enlarged and are usually found on the lower two-thirds of the esophagus.
They arise from the blockage of the portal vein of the liver. Instead of flowing through the portal vein, the blood flows through the smaller blood vessels, which eventually causes venous enlargement, leakage, or even rupture.
The treatment plan for esophageal varices is mainly focused on the prevention or stoppage of their rupture and bleeding.
Signs and Symptoms of Esophageal Varices
Unless they are bleeding, esophageal varices may not present any signs or symptoms. A patient with bleeding esophageal varices may show:
- Hematemesis or vomiting large amounts of blood
- Black, tarry or bloody stools
- Lightheadedness
- Loss of consciousness due to severe bleeding
Esophageal varices related to liver disease may have the following symptoms:
- Jaundice or yellow coloration of eyes and skin
- Ascites or abdominal fluid buildup
- Getting easily bruised
Causes and Risk Factors of Esophageal Varices
Liver disease cause scarring of the liver tissue known as cirrhosis of the liver. The liver scar tissues facilitate the backing up of the blood flow, thus increasing the pressure in the liver’s portal vein.
This condition is known as portal hypertension. To compensation for the increased pressure, the blood is forced to flow in smaller veins, including those veins that are found in the esophagus’ lowest part.
Their small size means that they cannot accommodate a large volume of blood. The veins may balloon, rupture, and bleed in time.
Aside from liver cirrhosis, thrombosis or the formation of blood clot in the portal vein or splenic vein may cause esophageal varices.
Parasitic infection of the liver, such as schistosomiasis found in Asia, Africa, Caribbean countries, and South America, can cause liver damage and lead to the formation of esophageal varices.
Alcohol abuse may lead to the rupture and bleeding of esophageal varices.
Complications of Esophageal Varices
Bleeding is the most life-threatening complication of esophageal varices. Internal bleeding may result to shock due to loss of a significant amount of blood, and this is fatal.
Another complication of esophageal varices is the increased risk for another rupture and bleeding episode of other varices.
Diagnosis of Esophageal Varices
- Physical examination and history taking – to check for any hematemesis, black tarry or blood stools, as well as to explore any alcohol abuse or history of liver disease
- Endoscopy – to visualize the gastrointestinal system, looking for any dilation of veins and any presence of red spots or red streaks which may indicate a very high risk of rupture and bleeding. Treatment of bleeding esophageal varices can also be done during this exam.
- Capsule endoscopy – to perform endoscopy but with the use of a capsule that has a camera in it. The patient swallows this like a pill, and the camera takes images of the GI tract as it goes down. This is more expensive than the usual endoscopy, but can be helpful for those who cannot tolerate the endoscope tube
- Imaging – CT scan and ultrasound Doppler of the portal and splenic veins
Treatment of Esophageal Varices
- Portal vein drugs. Beta blockers such as propanolol and nadolol can help treat portal hypertension by lowering the blood pressure in the portal vein. These reduce the risk for esophageal varices rupture and bleeding. After a bleeding episode, drugs like vasopressin and octreotide can be prescribed for up to 5 days to reduce the blood flow in the portal vein.
- Endoscopic band ligation. This procedure can be done while the patient is undergoing endoscopic exam and the doctor finds out that there are esophageal varices that are bleeding, or at high risk of rupture and bleed in the future. The doctor uses an elastic band to tie off the veins that are bleeding.
- Balloon tamponade. To stop the bleeding, this procedure involves inflating a balloon temporarily (for up to 24 hours) in order to place pressure on the esophageal varices.
- Transjugular intrahepatic portosystemic shunt (TIPS). This procedure is used to create a diversion of the blood flow away from the portal vein by means of making a shunt or an opening between the hepatic vein and the portal vein.
Esophageal Varices Nursing Diagnosis
Nursing care plan for esophageal varices 1.
Nursing Diagnosis: Risk for Bleeding secondary to esophageal varices
Desired Outcome : The patient will be able to avoid having any frank or occult bleeding and will remain hemodynamically stable.
Nursing Care Plan for Esophageal Varices 2
Nursing Diagnosis: Imbalanced Nutrition: Less than Body Requirements related to digestive tract bleeding secondary to esophageal varices, as evidenced by hematemesis, weight loss, nausea and vomiting, loss of appetite and dizziness/ lightheadedness
Desired Outcome : The patient will be able to achieve a weight within his/her normal BMI range, demonstrating healthy eating patterns and choices.
Nursing Care Plan for Esophageal Varices 3
Risk for Decreased Cardiac Output
Nursing Diagnosis: Risk for Decreased Cardiac Output related to bleeding secondary to esophageal varices .
Desired Outcomes:
- The patient will exhibit adequate cardiac output after the bleeding is controlled as evidenced by stable vital signs, normal peripheral perfusion, adequate intake and output, warm and dry skin, absence of breathing difficulties, and normal level of consciousness.
- The patient will be able to demonstrate self-care activities to improve gastrointestinal and cardiac health.
Nursing Care Plan for Esophageal Varices 4
Risk for Deficient Fluid Volume
Nursing Diagnosis: Risk for Deficient Fluid Volume related to nausea and hematemesis secondary to esophageal varices.
- The patient will verbalize a decrease in the severity of nausea and vomiting.
- The patient will maintain adequate fluid volume while waiting for treatment as evidenced by stable vital signs, adequate skin perfusion, strong peripheral pulses, alert mental state, and urine output greater than 30ml per hour.
Nursing Care Plan for Esophageal Varices 5
Risk for Injury
Nursing Diagnosis: Risk for Injury related to lightheadedness secondary to bleeding esophageal varices.
- The patient will be able to prevent injury by doing activities within the parameters of limitation and modifying the environment to adapt to the patient’s capacity.
- The patient will be able to perform activities of daily living with minimal supervision and maintain a treatment regimen to regain balance and increase compliance.
More Esophageal Varices Nursing Diagnosis
- Risk for Shock
- Disturbed Body Image
- Deficient Knowledge
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care . St. Louis, MO: Elsevier. Buy on Amazon
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, & outcomes . St. Louis, MO: Elsevier. Buy on Amazon
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2020). Medical-surgical nursing: Concepts for interprofessional collaborative care . St. Louis, MO: Elsevier. Buy on Amazon
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination . St. Louis, MO: Elsevier. Buy on Amazon
Disclaimer:
Please follow your facilities guidelines and policies and procedures. The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes. This information is not intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.
Leave a Comment Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .

- Editorial Board
- Special Issues
- Submit Manuscript
- Articles in Press
- Current Issue
- Author Guidelines
- Indexing Completed
Esophageal varices incidences are increasing by nearly 5% every year. Esophageal varices are the causes of bleeding in approximately 18% of hospital admissions for upper GI bleeding.
Objective: The purpose of this study is to understand the cause, clinical manifestations and treatment course for esophageal varices.
Material and methods: Detailed clinical history and physical examination was done. All the pertinent investigations were studied thoroughly of the selected case.
Results: The esophageal varices is confirmed with the help of upper gastrointestinal gastroscopy and repaired by banding.
Conclusion: Esophageal varices usually go undiagnosed due to early common symptoms. Hematemesis is one of the suggestive of esophageal varices and OGD is only the confirmative diagnosis for it. The prognosis depends usually better if treatment received on time.
INTRODUCTION
Esophageal varices are abnormal, enlarged veins in the tube that connects the throat and stomach. Variceal rupture is governed by Laplace's law. Increased wall tension is the end result of increased intravariceal pressure, increased diameter of the varices and reduced wall thickness. The variceal wall thickness can be evaluated visually by the presence of red wale markings. These markings reflect areas where the wall is especially thin [1]. Variceal rupture often occurs at the level of the gastroesophageal junction, where the varices are very superficial and thus have thinner walls. Esophageal varices are the major complication of portal hypertension [2].
RISK FACTORS
· Large esophageal varices
· Red marks on the esophageal varices as seen on a lighted stomach scope (endoscopy)
· Portal hypertension
· Severe cirrhosis
· A bacterial infection
· Excessive alcohol use
· Excessive vomiting
· Constipation
· Severe coughing bouts
DIAGNOSTIC INVESTIGATIONS
· Blood tests
· Endoscopy
· Imaging tests, such as CT and MRI scans
ESOPHAGEAL VARICES SYMPTOMS
· Hematemesis
· Stomach pain
· Light-headedness or loss of consciousness
· Melena (black stools)
· Bloody stools (in severe cases)
· Shock (excessively low blood pressure due to blood loss that can lead to multiple organ damage)
Therapeutic approaches are variceal ligation (banding) and sclerotherapy. Banding is a medical procedure which uses elastic bands for constriction. Banding may be used to tie off blood vessels in order to stop bleeding, as in the treatment of bleeding esophageal varices. The band restricts blood flow to the ligated tissue, so that it eventually dies and sloughs away from the supporting tissue.
Sclerotherapy is a form of treatment where a doctor injects medicine into blood vessels or lymph vessels that causes them to shrink. It is commonly used to treat varicose veins or so-called spider veins. The procedure is non-surgical, requiring only an injection.
An 85 year old patient with known case of diabetes mellitus, hypertension since last 20 years and status post percutaneous transluminal coronary (2002, 2011 and 2015). Patient had no history of any bad habits like cigarette smoking, alcohol consumption or any other drug substance. Patient was found semiconscious at home at night suddenly and when aroused by relatives, patient had hematemesis of around 500 ml at home. Patient was brought to hospital. The patient had complaints of malena and acidity since one week. Patient was investigated in the form of alkaline phosphatase, alpha fetoprotein, serum glutamic pyruvic transaminase, SGOT, bilirubin, glucose, IgG, CBC, USG KUB, ABG, Electrocardiogram, APTT, ESR, USG whole abdomen.
CBC shows Hb less than 7 g/dl. USG whole abdomen was suggestive of reduced size of liver with diffusely altered echo texture and surface irregularity, suggestive of chronic liver parenchymal disease. Few small tortuous mesenteric venous collaterals, could be suggestive of portal hypertension.
Upper gastrointestinal gastroscopy was suggestive of esophageal varices. One band applied endoscopically and further, patient was managed with anti-diabetics, antacid, analgesic, antibiotic, beta blocker, statin and other supportive care.
Esophageal varices usually go undiagnosed until hematemesis occur. Hematemesis is a medical emergency and always occur due to upper GI tract bleeding. The color is usually bright red in color. The hematemesis is treated with somatostatin analogue (e.g. Octreotide) or vasopressin (e.g. Terlipressin); it helps to reduce splanchnic blood flow. The Glasgow-Blatch Ford Bleeding scoring system score is used to determine the risk. This scale is purely based on clinical and biochemical parameters. The warning signs of esophageal varices is dizziness even when awake, weight loss, low Hb level, complaints of acidity, heartburn, hematemesis and malena.
Patients with hypertension and diabetes have poor prognosis as medicines have adverse effects on liver which can lead to liver cirrhosis and portal hypertension as well. At advanced age, the banding is done for symptomatic treatment only as no other option is available at this age.
1. Hilzenrat N, Sherker AH (2012) Esophageal varices: Pathophysiology, approach and clinical dilemmas. Int J Hepatol 2012: 35-40.
2. Maruyama H, Yokosuka O (2012) Pathophysiology of portal hypertension and esophageal varices. Int J Hepatol 2012: 38-42.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
- SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Allergy Research (ISSN:2642-326X)
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Journal of Psychiatry and Psychology Research (ISSN:2640-6136)
- Journal of Rheumatology Research (ISSN:2641-6999)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Advance Research on Alzheimers and Parkinsons Disease
Newsletter signup

- Open Access
- A-Z Journals
- Editor in Chiefs
Journal Groups
- Engineering
- Life Sciences


The Royal Children's Hospital Melbourne
- My RCH Portal

- Health Professionals
- Patients and Families
- Departments and Services
- Health Professionals
- Departments and Services
- Patients and Families
- Research
Nursing guidelines
- About nursing guidelines
- Nursing guidelines index
- Developing and revising nursing guidelines
- Other useful clinical resources
- Nursing guideline disclaimer
- Contact nursing guidelines
In this section
Acute management of an oesophageal variceal bleed
Introduction
Oesophageal varices (and indeed any varices) are a rare but serious complication of portal hypertension. Portal hypertension is defined by an increase in pressure within the portal circulatory system and is caused by an increase in vascular resistance in blood flow through the liver. In RCH’s patient population, portal hypertension is frequently a result of biliary atresia, but it can also be a manifestation of post-hepatic, pre-hepatic (e.g. portal vein obstruction), or other intra-hepatic problems such as cystic fibrosis, congenital hepatic fibrosis or other cirrhosis. With increased resistance in the portal vascular system, blood begins to shunt through collateral systemic vessels to return to the vena cava. Prolonged elevation in portal vein pressure causes dilatation of the collateral vessels, which can form internal varices in the rectum and varices in the gastro-oesophageal veins. Oesophageal variceal bleeds occur when the variceal wall tension exceeds the wall strength and subsequently rupture. Children with liver disease also have liver dysfunction, which results in clotting cascade problems and a deficit in Vitamin K-dependent factors. This increases the risk of significant haemorrhage in this patient group.
In several large studies of children with portal hypertension, approximately two thirds presented with haematemesis (vomiting blood) or melaena (blood in stool/dark stools caused by upper GI bleeds), usually from rupture of an oesophageal varix. Twenty to thirty percent of children with biliary atresia have variceal bleeds and tend to develop varices early, with an estimated risk of bleeding of fifteen percent before the age of two. Mortality rates associated with large bleeds range from zero to fifteen percent.
The aim of this guideline is to assist nurses and other health professionals in the management of infants and children with oesophageal varices to minimise risk of variceal bleeding. This guideline will also outline the management of an acute oesophageal variceal bleed.
Definition of Terms
- GI - gastrointestinal
- NGT – Nasogastric tube
- PPIs – Proton pump inhibitors (e.g., omeprazole, pantoprazole)
Assessment of Patients with Known or Suspected Varices
- Complete primary assessment as per Clinical Guidelines (Nursing) : Nursing assessment
- Routine observations as per Clinical Guidelines (Nursing): Observation and Continuous Monitoring
- Monitor for signs of hypovolaemia: e.g. tachycardia, hypotension.
- Investigations: FBE, UEC, VBG, Coagulation Screen, Group & hold, blood cultures, BGL, ammonia, see specimen collection .
- Monitor for upper GI bleeding (e.g. haematemesis or coffee ground vomit)
- Monitor for melaena or fresh blood in stools.
- Capture clinical images of melaena & haematemesis to guide volumes of blood loss.
- Monitor for abdominal distension or protruding umbilical veins, especially when seen in combination with other listed symptoms.
- Assess coagulation screen for risk of bleeding.
- Maintain strict fluid balance including measurement or estimation of losses, including urine output.
- Monitor for neurological changes.
Management of Children with Known or Suspected Varices
- Stylet should be removed.
- Insertion should be carried out by senior staff members or medical personnel in high-risk patients. Eg those who have had previous GI bleeds, those with significant coagulopathies, those with high grades varices as identified by treating team.
- NGT should not have a gastric aspirate taken from the tube. Instead, position should be confirmed by x-ray.
- Ensure patient has valid blood product consent on file (see Consent- Informed Procedure )
- Family should be provided with education on varices and at home emergency management plan by Liver & Intestinal Transplant Clinical Nurses Consultants or Gastroenterology team members.
- Patients should have routine surveillance gastroscopies to monitor status and progression of varices. Banding or sclerotherapy can be undertaken as required. Frequency of gastroscopies is dictated by treating gastroenterologist.
- Patients should have the following investigations prior to gastroscopies: FBE, UEC, coagulation screen, group & hold.
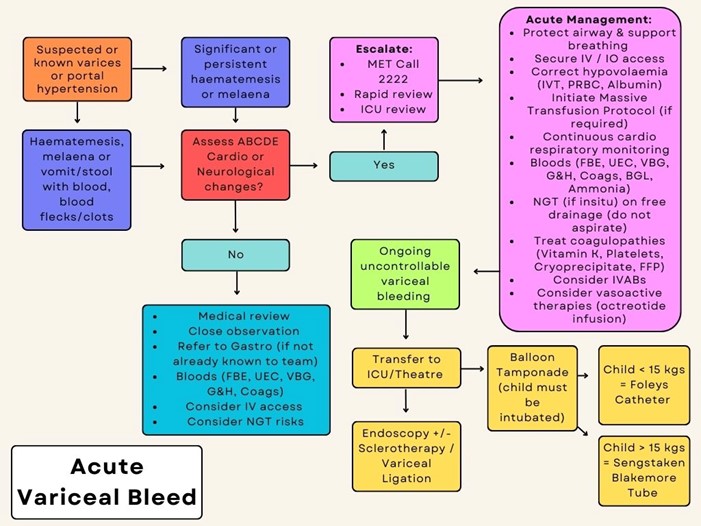
Acute Management of Variceal Bleed (refer to algorithm overleaf)
- Seek urgent medical/ ICU review/ MET (ext. 2222).
- Protect airway, support breathing as required (see Resuscitation guidelines ). Give oxygen to patients with significant circulatory impairment or shock.
- Secure large bore IV access.
- Consider need to activate Massive Haemorrhage and Critical Bleeding Procedure .
- No more than 20mL/kg NaCl bolus. Albumin should also be given if further fluid administration is required.
- RBCs if Hb <70g/L.
- Maintain strict fluid balance.
- Octreotide, IV bolus followed by IV infusion. Refer to Medication Guideline: Octreotide for dosing
- Always discuss with a gastroenterology fellow or consultant before commencing vasoactive therapy.
- Once bleeding controlled, slow wean of octreotide as per Octreotide Medication Guideline
- Monitor BGL 6 hourly whilst on octreotide infusion due to risk of hypoglycaemia and/or hyperglycaemia – escalate any abnormal results to treating team
- Continuous cardiorespiratory monitoring (see Clinical Guidelines (Nursing): Observation and Continuous Monitoring ).
- If NGT in situ, place on free drainage. Do NOT aspirate NGT . NGT should only be inserted under endoscopic guidance or with gastroenterologist consent.
- Consider treating coagulopathies (vitamin K, platelets, cryoprecipitate and FFP).
- If bleeding is ongoing and uncontrollable, patient will require Balloon Tamponade (Foleys Catheter if child <15kg or Sengstaken Blakemore tube if child>15kg). This will ideally be performed in the ICU or theatre environment.
- Transfer to ICU or theatre for management as clinically appropriate
- Consider prophylactic intravenous antibiotics.
- Patient should be kept nil by mouth (NBM) until bleeding controlled and medically cleared for oral intake.
- Whilst NBM, all regular medications should be given IV.
- Consider use of PPI: IV whilst NBM followed by oral once cleared for oral intake.
Management of Patients with Recent Variceal Bleeding/Banding
- Patients should remain nil by mouth (NBM) post variceal bleeding or banding and grade up diet as directed by treating gastroenterologist.
- Ensure patient has a valid group and hold in case requires transfusion.
- Maintain IV access.
- Ensure foley catheter is at bedside in case of re-bleed. If leaving the ward, patient must take catheter with them.
Special considerations
- For CVAD management (see Central Venous Access Device )
- Blood transfusion safety adherence (see Blood Transfusion Procedure ).
- Massive Transfusion Protocol (see Massive Haemorrhage and Critical Bleeding Procedure ).
- If body fluid splash (see Procedure Needlestick Injuries and Blood-Body Fluid Exposures ).
Algorithm for Management of Acute Variceal Bleed
- PICU Guidelines: Liver Protocols
- RCH Liver Transplant Protocol
- RCH Enteral Feeding and Medication Administration CPG
Clinician websites
- American College of Gastroenterology Practice Guideline
- British Society of Gastroenterology Guidelines
- The National Institute for Health and Care Excellence Clinical Guideline
- World Gastroenterology Guideline
- NICE Guideline: Stent Insertion for Bleeding Oesophageal Varices
Information for parents
- Children’s Liver Disease Foundation
- Starship Parent Guide to Portal Hypertension
- Starship Parent Guide to Liver Transplant
*Please remember to read the disclaimer .
The development of this nursing guideline was coordinated by Rachel Horn, CNC, Gastroenterology, and Laura Davies, CNS, Cockatoo, approved by the Nursing Clinical Effectiveness Committee. Updated December 2023.
Evidence table
- Pre-Nursing
- Nursing School
- After Graduation
Esophageal Varices: Patho, Manifestations, & Diagnostics

Jump to Sections
- What is a Varice?
Esophageal Varices Causes
Signs and symptoms of esophageal varices, esophageal varices assessment & diagnostics, esophageal varices nclex question.
Esophageal varices are complications due to liver diseases or dysfunctions. It’s important to identify and treat the underlying cause of them to prevent complications such as bleeding and improve patient outcomes.
You can think of esophageal varices as the result of having a plumbing backup.
What is a Varice? (The Septic Tank Analogy)
Associating esophageal varices with having a backup of septic tank content is helpful since you can compare the liver to the body’s septic tank. If the septic tank becomes clogged or has hardened, there will be an immediate backup from the system.
Toilets and sinks will have a backflow of waste products – water will not drain properly from the shower.
The Liver: The Body’s Septic Tank
As food is chewed inside the mouth, it goes down the esophagus, then into the stomach to be broken down by gastric juices. Digested food now goes inside the duodenum, the first part of the small intestine.
After the duodenum , the contents are sucked into the portal vein that goes through the pancreas. This process is referred to as the first-pass phenomenon concerning medications.
Hardening of the Liver
When the liver hardens due to some type of scarring, for instance:
- Cirrhosis that’s basically the production of scar tissue in the liver
Whatever the condition is, the backing up of blood into the portal vein is the main cause of esophageal varices.
Esophageal varices are primarily caused by increased pressure in the portal vein system, which can result from various underlying medical conditions. Some common causes of esophageal varices include:
- Cirrhosis : Cirrhosis scarring can obstruct blood flow through the liver, leading to increased pressure in the portal vein system.
- Hepatitis : Chronic hepatitis, a viral infection that causes inflammation and scarring of the liver, can also lead to esophageal varices.
- Congenital disorders : Rare genetic disorders, such as Budd-Chiari syndrome or portal vein thrombosis, can obstruct the portal vein and lead to increased pressure in the portal vein system.
- Thrombosis : Blood clots in the portal vein or its branches can cause portal hypertension and lead to the development of esophageal varices.
- Schistosomiasis : A parasitic infection common in parts of Africa and South America, schistosomiasis can cause liver damage and develop esophageal varices.
Since there is the backing up of blood or fluid inside the esophagus, the following manifestations will occur:
- Esophageal bleeding
- Vomiting with blood
- Bloody stools
- Decreased blood pressure (due to decreased volume caused by bleeding)
- A skyrocketing heart rate. Due to the decreased hemoglobin, the heart will compensate by pumping faster to distribute oxygen to the body’s different systems.
- Tachycardia
One of the main diagnostic procedures for patients with esophageal varices is esophagogastroduodenoscopy (EGD) . With EGD, a tube with a camera is inserted to visualize the inside of the esophagus.
Liver function tests are also done to check the status of the liver through abnormalities with alanine transaminase (ALT) and aspartate aminotransferase (AST).
The hemoglobin and hematocrit levels are also tested because if there is bleeding anywhere in the body, the lab results for H&H will be low.
When a patient comes in with perfused bleeding from his mouth, should you do an EGD?
Answer: No . The airway is the priority in any situation. In this case, if the patient is vomiting blood, stopping the bleeding is paramount.
The first thing to do is to relieve the patient of the blood by suctioning its mouth, and once the bleeding ceases, that’s when an EGD is done.
Aside from suctioning, there are other procedures done to stop the bleeding, namely:
- Medications
- Inserting a balloon catheter into the esophagus
Study More in Less Time
Using a study tool can help you keep engaged and at a steady pace when studying conditions like esophageal varices.
SimpleNursing is trusted by nursing students to retain more nursing school material while cutting down on study hours. We have adaptive exams to tailor the learning experience to each individual learner’s needs, interests, and abilities.
Get a better understanding of your nursing material .
Want to ace Nursing School Exams & the NCLEX?
Make topics click with easy-to-understand videos & more. We've helped over 1,000,000 students & we can help you too.
Share this post
Nursing students trust simplenursing.

SimpleNursing Student Testimonial
Most recent posts.

What Is Mean Arterial Pressure?
Today, we dissect a topic that’s vital — quite literally — to the lifeblood of…

PQRST EKG Wave
Imagine your heart telling a story, not with words, but with waves — rhythmic, dynamic,…

How to Easily Find a Vein When Starting an Intravenous Access (IV)
Ask any nurse or health care professional about how to find a vein when starting…

Comprehensive Overview of Anatomy Regions, Planes, and Parts
If asked to drop what you’re doing right now and take a quiz on anatomy,…
Find what you are interested in
- Patient Care & Health Information
- Diseases & Conditions
- Esophageal varices
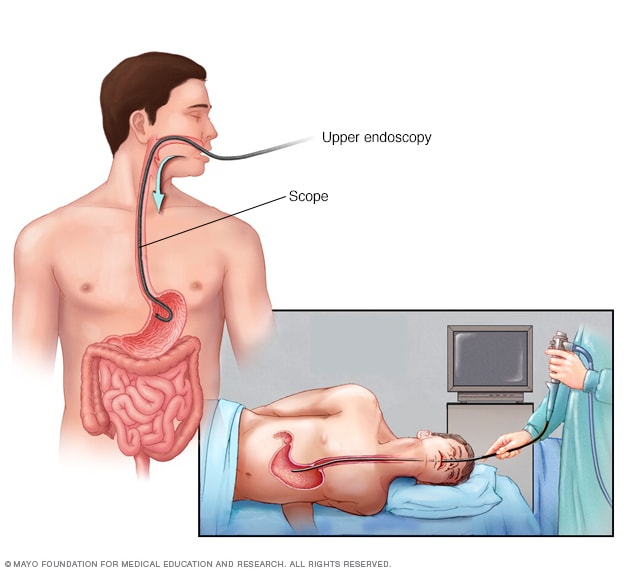
- Upper endoscopy
An upper endoscopy procedure involves inserting a long, flexible tube called an endoscope down your throat and into your esophagus. A tiny camera on the end of the endoscope allows views of your esophagus, stomach and the beginning of your small intestine, called the duodenum.
If you have cirrhosis, your health care provider typically screens you for esophageal varices when you're diagnosed. How often you'll have screening tests depends on your condition. Main tests used to diagnose esophageal varices are:
Endoscopic exam. A procedure called upper gastrointestinal endoscopy is the preferred method of screening for esophageal varices. An endoscopy involves inserting a flexible, lighted tube called an endoscope down the throat and into the esophagus. A tiny camera on the end of the endoscope lets your doctor examine your esophagus, stomach and the beginning of your small intestine, called the duodenum.
The provider looks for dilated veins. If found, the enlarged veins are measured and checked for red streaks and red spots, which usually indicate a significant risk of bleeding. Treatment can be performed during the exam.
- Imaging tests. Both abdominal CT scans and Doppler ultrasounds of the splenic and portal veins can suggest the presence of esophageal varices. An ultrasound test called transient elastography may be used to measure scarring in the liver. This can help your provider determine if you have portal hypertension, which may lead to esophageal varices.
More Information
- Capsule endoscopy
The primary aim in treating esophageal varices is to prevent bleeding. Bleeding esophageal varices are life-threatening. If bleeding occurs, treatments are available to try to stop the bleeding.
Treatment to prevent bleeding
Treatments to lower blood pressure in the portal vein may reduce the risk of bleeding esophageal varices. Treatments may include:
- Medicines to reduce pressure in the portal vein. A type of blood pressure drug called a beta blocker may help reduce blood pressure in your portal vein. This can decrease the likelihood of bleeding. Beta blocker medicines include propranolol (Inderal, Innopran XL) and nadolol (Corgard).
Using elastic bands to tie off bleeding veins. If your esophageal varices appear to have a high risk of bleeding, or if you've had bleeding from varices before, your health care provider might recommend a procedure called endoscopic band ligation.
Using an endoscope, the provider uses suction to pull the varices into a chamber at the end of the scope and wraps them with an elastic band. This essentially "strangles" the veins so that they can't bleed. Endoscopic band ligation carries a small risk of complications, such as bleeding and scarring of the esophagus.
Treatment if you're bleeding
Bleeding esophageal varices are life-threatening, and immediate treatment is essential. Treatments used to stop bleeding and reverse the effects of blood loss include:
- Using elastic bands to tie off bleeding veins. Your provider may wrap elastic bands around the esophageal varices during an endoscopy.
- Taking medicines to slow blood flow into the portal vein. Medicines such as octreotide (Sandostatin) and vasopressin (Vasostrict) slow the flow of blood to the portal vein. Medicine is usually continued for up to five days after a bleeding episode.
Diverting blood flow away from the portal vein. If medicine and endoscopy treatments don't stop the bleeding, your provider might recommend a procedure called transjugular intrahepatic portosystemic shunt (TIPS).
The shunt is an opening that is created between the portal vein and the hepatic vein, which carries blood from your liver to your heart. The shunt reduces pressure in the portal vein and often stops bleeding from esophageal varices.
But TIPS can cause serious complications, including liver failure and mental confusion. These symptoms can develop when toxins that the liver normally would filter are passed through the shunt directly into the bloodstream.
TIPS is mainly used when all other treatments have failed or as a temporary measure in people awaiting a liver transplant.
Placing pressure on varices to stop bleeding. If medicine and endoscopy treatments don't work, your provider may try to stop bleeding by applying pressure to the esophageal varices. One way to temporarily stop bleeding is by inflating a balloon to put pressure on the varices for up to 24 hours, a procedure called balloon tamponade. Balloon tamponade is a temporary measure before other treatments can be performed, such as TIPS .
This procedure carries a high risk of bleeding recurrence after the balloon is deflated. Balloon tamponade also may cause serious complications, including a rupture in the esophagus, which can lead to death.
- Restoring blood volume. You might be given a transfusion to replace lost blood and a clotting factor to stop bleeding.
- Preventing infection. There is an increased risk of infection with bleeding, so you'll likely be given an antibiotic to prevent infection.
- Replacing the diseased liver with a healthy one. Liver transplant is an option for people with severe liver disease or those who experience recurrent bleeding of esophageal varices. Although liver transplantation is often successful, the number of people awaiting transplants far outnumbers the available organs.
Re-bleeding
There is a high risk that bleeding might recur in people who've had bleeding from esophageal varices. Beta blockers and endoscopic band ligation are the recommended treatments to help prevent re-bleeding.
After initial banding treatment, your provider typically repeats your upper endoscopy at regular intervals. If necessary, more banding may be done until the esophageal varices are gone or are small enough to reduce the risk of further bleeding.
Potential future treatment
Researchers are exploring an experimental emergency therapy to stop bleeding from esophageal varices that involves spraying an adhesive powder. The hemostatic powder is given through a catheter during an endoscopy. When sprayed on the esophagus, hemostatic powder sticks to the varices and may stop bleeding.
Another potential way to stop bleeding when all other measures fail is to use self-expanding metal stents (SEMS). SEMS can be placed during an endoscopy and stop bleeding by placing pressure on the bleeding esophageal varices.
However, SEMS could damage tissue and can migrate after being placed. The stent is typically removed within seven days and bleeding could recur. This option is experimental and isn't yet widely available.
- Blood transfusion
- Liver transplant
Preparing for your appointment
You might start by seeing your primary health care provider. Or you may be referred immediately to a provider who specializes in digestive disorders, called a gastroenterologist. If you're having symptoms of internal bleeding, call 911 or your local emergency number to be taken to the hospital for urgent care.
Here's some information to help you get ready for an appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before a specific test. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment.
- Key personal information, including major stresses, recent life changes or recent travels, family and personal medical history, and your alcohol use.
- All medications, vitamins or other supplements you take, including doses.
- Questions to ask your doctor.
Take a family member or friend along, if possible, to help you remember information you're given.
For esophageal varices, questions to ask include:
- What's likely causing my symptoms?
- What other possible causes are there?
- What tests do I need?
- What's the best course of action?
- What are the side effects of the treatments?
- Are my symptoms likely to recur, and what can I do to prevent that?
- I have other health conditions. How can I best manage them together?
- Are there restrictions that I need to follow?
- Should I see a specialist?
- Are there brochures or other printed materials I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your provider is likely to ask you questions, such as:
- When did your symptoms begin?
- Have your symptoms stayed the same or gotten worse?
- How severe are your symptoms?
- Have you had signs of bleeding, such as blood in your stools or vomit?
- Have you had hepatitis or yellowing of your eyes or skin (jaundice)?
- Have you traveled recently? Where?
- If you drink alcohol, when did you start and how much do you drink?
What you can do in the meantime
If you develop bloody vomit or stools while you're waiting for your appointment, call 911 or your local emergency number or go to an emergency room immediately.
- Sanyal AJ. Overview of the management of patients with variceal bleeding. https://www.uptodate.com/contents/search. Accessed Jan. 11, 2023.
- Varices. Merck Manual Professional Version. https://www.merckmanuals.com/professional/gastrointestinal-disorders/gastrointestinal-bleeding/varices/?autoredirectid=1083. Accessed Jan. 11, 2023.
- Ferri FF. Esophageal varices. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed Jan. 17, 2023.
- Rockey DC. Causes of upper gastrointestinal bleeding in adults. https://www.uptodate.com/contents/search. Accessed Jan. 11, 2023.
- Sanyal AJ, et al. Prediction of variceal hemorrhage in patients with cirrhosis. https://www.uptodate.com/contents/search. Accessed Jan. 11, 2023.
- 13 ways to a healthy liver. American Liver Foundation. https://liverfoundation.org/resource-center/blog/13-ways-to-a-healthy-liver/. Accessed Jan. 17, 2023.
- AskMayoExpert. Esophageal and gastric varices. Mayo Clinic; 2022.
- Zuckerman MJ, et al. Endoscopic treatment of esophageal varices. Clinical Liver Disease. 2022; doi:10.1016/j.cld.2021.08.003.
Associated Procedures
Products & services.
- A Book: Mayo Clinic on Digestive Health
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
VIDEO LIBRARY
Nursing Care Plan For Esophageal Varices
Introduction:.
Esophageal varices are a critical and potentially life-threatening medical condition often associated with underlying liver disease. These enlarged, fragile veins in the lower esophagus pose a significant risk of bleeding and require vigilant care and management. This nursing care plan is designed to provide a structured approach to assess, intervene, and educate both patients and healthcare professionals regarding esophageal varices and their associated complications.
Esophageal varices develop as a result of portal hypertension, a condition characterized by increased pressure in the portal vein, typically due to liver disease. The fragility of these engorged blood vessels makes them susceptible to bleeding, which can be life-threatening. Nurses play a pivotal role in the early detection of esophageal varices, managing their associated risks, and providing patient education to minimize complications.
In this nursing care plan, we will outline a systematic approach to assess patients at risk for or diagnosed with esophageal varices, manage potential complications, and educate patients and their families about the condition, treatment options, and preventive measures. By addressing the multifaceted aspects of care required for esophageal varices, we aim to improve patient outcomes and reduce the risk of life-threatening bleeding episodes.
Recognizing that patients with esophageal varices often have complex healthcare needs, our care plan emphasizes early detection, monitoring for bleeding risk, and interventions to manage and prevent complications. We also stress the importance of patient education to empower individuals to participate actively in their care and take measures to safeguard their health.
In summary, this nursing care plan for esophageal varices seeks to provide patients and healthcare professionals with the knowledge, skills, and support needed to manage this challenging condition effectively. Through comprehensive assessment, proactive interventions, and education, nurses can play a significant role in enhancing the well-being and safety of individuals with esophageal varices.
Nursing Assessment for Esophageal Varices:
A thorough nursing assessment for esophageal varices is vital in detecting and managing this high-risk condition effectively. The assessment should encompass a range of physical, psychological, and laboratory evaluations. Here is a comprehensive nursing assessment for esophageal varices:
1. Patient Identification and Introduction:
- Introduce yourself to the patient and establish a trusting and empathetic rapport.
- Verify the patient’s identity using two identifiers (e.g., name and date of birth) and cross-reference with their medical records.
2. Chief Complaint and History of Present Illness (HPI):
- Begin by asking the patient about their chief complaint and specific symptoms related to esophageal varices, such as hematemesis (vomiting blood), melena (black, tarry stools), or signs of gastrointestinal bleeding.
- Explore the duration, severity, and any factors that exacerbate or alleviate symptoms.
3. Medical History:
- Gather information about the patient’s medical history, particularly any underlying liver disease or conditions predisposing to esophageal varices, such as cirrhosis or portal hypertension.
- Document any prior history of gastrointestinal bleeding, endoscopic procedures, or treatments for liver disease.
4. Medications and Allergies:
- Document the patient’s current medications, dosages, and adherence to prescribed treatments.
- Inquire about allergies or sensitivities to medications, including nonsteroidal anti-inflammatory drugs (NSAIDs) and blood thinners.
5. Alcohol and Substance Use:
- Assess the patient’s history of alcohol consumption, recreational drug use, or exposure to hepatotoxins, which can contribute to liver disease and esophageal varices.
- Inquire about current or past smoking habits.
6. Nutritional Status:
- Evaluate the patient’s nutritional status, weight changes, and dietary habits, as malnutrition is common in patients with advanced liver disease.
- Document the presence of jaundice or ascites, which may indicate liver dysfunction.
7. Bleeding Risk Assessment:
- Assess for risk factors associated with bleeding from esophageal varices, such as the presence of varices on imaging studies, the severity of liver disease, and platelet count.
- Monitor for signs of active bleeding or shock, such as hemodynamic instability, rapid heart rate, and low blood pressure.
8. Psychosocial Assessment:
- Evaluate the patient’s emotional and psychological well-being, particularly regarding the diagnosis and implications of esophageal varices.
- Inquire about the patient’s social support system, stressors, and coping mechanisms.
9. Physical Examination:
- Perform a thorough physical examination, including an assessment of vital signs (blood pressure, heart rate, respiratory rate, temperature).
- Examine for signs of liver disease, such as hepatomegaly, splenomegaly, and ascites.
10. Mental Status Examination:
- Assess the patient’s cognitive function, orientation, mood, and affect.
- Monitor for signs of confusion, encephalopathy, or hepatic encephalopathy, which may indicate advanced liver disease.
11. Laboratory and Diagnostic Tests:
- Review laboratory results, including liver function tests (e.g., liver enzymes, bilirubin, albumin, INR), platelet count, and complete blood count (CBC).
- Evaluate coagulation profile, including prothrombin time (PT) and activated partial thromboplastin time (aPTT).
- Consider imaging studies, such as abdominal ultrasound, CT scan, or endoscopy, to assess the presence and severity of varices.
This comprehensive nursing assessment for esophageal varices serves as the foundation for developing an individualized care plan, facilitating early detection and intervention, and addressing the physical and emotional needs of the patient. Early recognition of risk factors, ongoing monitoring for bleeding, and collaboration with the healthcare team are crucial for optimizing patient outcomes in individuals at risk for esophageal varices.
Nursing Diagnoses for Esophageal Varices:
1. risk for gastrointestinal bleeding related to the presence of esophageal varices..
- Esophageal varices are fragile, enlarged veins in the lower esophagus, which pose a high risk of bleeding. This diagnosis emphasizes the need for preventive measures to minimize the risk of bleeding.
2. Imbalanced Nutrition: Less than Body Requirements related to difficulty swallowing and risk of gastrointestinal bleeding.
- Patients with esophageal varices may experience dysphagia and dietary restrictions, leading to inadequate nutritional intake. This diagnosis addresses the risk of malnutrition.
3. Impaired Liver Function related to underlying liver disease, such as cirrhosis or hepatitis.
- Liver diseases, such as cirrhosis or hepatitis, are common underlying causes of esophageal varices. This diagnosis focuses on monitoring and addressing impaired liver function.
4. Risk for Aspiration related to difficulty swallowing and the potential for vomiting blood.
- Patients with bleeding esophageal varices are at risk of aspirating blood into the airway. This diagnosis addresses the need to prevent aspiration and its complications.
5. Risk for Infection related to the potential for gastrointestinal bleeding and compromised immune function.
- Gastrointestinal bleeding can lead to an increased risk of infection. This diagnosis emphasizes infection prevention measures in patients with esophageal varices.
6. Risk for Bleeding related to fragile esophageal varices.
- Esophageal varices are prone to bleeding, and patients are at risk of experiencing bleeding episodes. This diagnosis focuses on interventions to prevent and manage bleeding.
7. Disturbed Body Image related to visible abdominal ascites or other signs of liver disease.
- The presence of ascites and other signs of liver disease can impact a patient’s body image. This diagnosis addresses body image concerns.
8. Knowledge Deficit related to esophageal varices, complications, and self-care management.
- Patients and their families may lack knowledge about esophageal varices and their management. This diagnosis emphasizes the need for patient and family education.
9. Anxiety related to the diagnosis of esophageal varices and associated complications.
- The diagnosis of esophageal varices and the risk of bleeding can lead to significant anxiety. This diagnosis addresses the patient’s emotional response to the condition.
10. Ineffective Coping related to the challenges posed by esophageal varices and associated liver disease.
- Coping with the diagnosis and management of esophageal varices can be challenging. This diagnosis focuses on the patient’s coping strategies and support needs.
These nursing diagnoses for esophageal varices provide a foundation for developing a patient-centered care plan, emphasizing preventive measures, risk management, and support for patients and their families. The selection of specific nursing diagnoses should be based on a comprehensive assessment and tailored to the patient’s unique needs and circumstances.

Nursing Interventions for Esophageal Varices:
1. gastrointestinal bleeding prevention:.
- Monitor vital signs and assess for signs of gastrointestinal bleeding, such as melena, hematemesis, or hematochezia.
- Administer prescribed medications, such as non-selective beta-blockers or vasoconstrictors, to reduce the risk of bleeding by decreasing portal pressure.
2. Nutritional Support:
- Collaborate with a registered dietitian to develop a nutrition plan that ensures adequate caloric and protein intake while avoiding foods that may exacerbate variceal bleeding.
- Consider enteral nutrition (e.g., nasogastric or gastrostomy tube) if the patient is unable to maintain oral nutrition.
3. Medication Management:
- Administer medications as ordered, such as proton pump inhibitors (PPIs), to reduce gastric acid secretion and decrease the risk of ulceration and bleeding.
- Educate the patient about the importance of medication compliance and potential side effects.
4. Hemorrhage Control:
- Maintain a patent intravenous (IV) line and have blood products (packed red blood cells, fresh frozen plasma, platelets) readily available in case of acute bleeding.
- Prepare for endoscopic procedures, such as band ligation or sclerotherapy, to manage active bleeding.
5. Bleeding Precautions:
- Instruct the patient to avoid activities that may increase intra-abdominal pressure, such as heavy lifting or straining during bowel movements.
- Teach the patient to report any signs of bleeding, including blood in vomit or stools, immediately.
6. Liver Function Monitoring:
- Regularly assess liver function with laboratory tests, including liver enzymes, bilirubin, albumin, INR, and ammonia levels.
- Collaborate with the healthcare team to address complications of liver disease, such as hepatic encephalopathy or ascites.
7. Ascites Management:
- Implement strategies to manage ascites, such as sodium restriction, diuretics, and paracentesis, to relieve abdominal discomfort and reduce the risk of infection.
- Monitor for signs of infection in patients with ascites, such as fever, abdominal pain, or altered mental status.
8. Psychological Support:
- Provide emotional support and counseling to help the patient cope with the diagnosis of esophageal varices and the associated risks.
- Encourage the patient to seek support from family, support groups, or mental health professionals if needed.
9. Patient and Family Education:
- Educate the patient and family about esophageal varices, their causes, complications, and preventive measures.
- Emphasize the importance of medication adherence, dietary restrictions, and the need for regular follow-up appointments.
10. Advance Care Planning:
- Initiate discussions about advance care planning, including the patient’s preferences for resuscitation, end-of-life care, and the designation of a healthcare proxy if desired.
- Assist the patient in documenting their wishes and communicating them to their healthcare team.
These nursing interventions for esophageal varices aim to manage the condition effectively, reduce the risk of bleeding, and provide holistic care for patients. Individualized care plans should be developed based on the patient’s specific condition, comorbidities, and preferences. Collaborative efforts with the healthcare team, timely assessment, and continuous patient education are essential for achieving positive outcomes and enhancing the patient’s quality of life.
Conclusion :
In conclusion, the nursing care plan developed for patients with esophageal varices underscores the critical role of nursing in the early detection, management, and prevention of this high-risk condition. Esophageal varices represent a challenging medical condition, often arising from underlying liver disease, and pose a significant risk of gastrointestinal bleeding. The care plan is designed to address the multifaceted aspects of care, from risk assessment to interventions and patient education.
Throughout this care plan, we have emphasized the importance of a thorough nursing assessment, individualized interventions, and proactive education. The assessment phase focused on identifying risk factors, assessing for gastrointestinal bleeding, and understanding the patient’s physical and emotional condition. This information serves as the basis for a tailored care plan that aims to reduce the risk of bleeding, manage complications, and improve the patient’s overall well-being.
The nursing diagnoses selected in the care plan reflect the diverse challenges posed by esophageal varices, encompassing the need for bleeding prevention, nutritional support, liver function management, and emotional support. These diagnoses guide the selection of interventions aimed at addressing the unique needs of each patient.
Bleeding prevention strategies are a cornerstone of the care plan, including medication management and measures to decrease portal pressure. Nutritional support and medication management are crucial for ensuring the patient’s nutritional well-being and preventing complications. Hemorrhage control and bleeding precautions are essential in managing acute bleeding episodes, with a focus on early intervention.
Patient and family education is central to this care plan, empowering individuals to actively participate in their care, understand the condition, and take preventive measures. By educating patients and their families, we aim to enhance their ability to make informed decisions and actively manage their health.
It is important to acknowledge that patients with esophageal varices often have complex healthcare needs, requiring collaboration with various healthcare professionals, including hepatologists, gastroenterologists, and dietitians. A multidisciplinary approach is crucial to address the diverse facets of care comprehensively.
In conclusion, our nursing care plan for esophageal varices is rooted in principles of patient safety, prevention, and evidence-based practice. Through the implementation of this plan, we aim to reduce the risk of bleeding, improve patient outcomes, and support individuals in managing this challenging condition effectively. By combining ongoing assessment, collaboration, and education, we contribute to enhancing the patient’s overall well-being and quality of life.
Nursing Assessment for Esophageal Varices Nursing Diagnoses for Esophageal Varices Nursing Interventions for Esophageal Varices
Leave a Reply
Your email address will not be published. Required fields are marked *
- Mycobacterium Leprae : Deciphering the Mysteries of Leprosy
- Leptospira Interrogans: The Bacterium Behind Leptospirosis
- Haemophilus Influenzae: A Versatile Bacterial Pathogen
- Mycoplasma Pneumoniae: Exploring Atypical Pneumonia
- Treponema Pallidum – The Bacterium Behind Syphilis
TERMS OF SERVICE
PRIVACY POLICY
Made For Medical
Copyrights © 2024. All rights reserved.
🌟Calling all Doctors, Nurses, and Physician Assistants! 🩺✨
🚀Supercharge your medical knowledge with our exclusive video lectures tailored for YOU!! 🚀 Unlock expert insights, earn FREE CME/CE credits, and learn at your own pace! 📚💡

Esophageal Varices Nursing Management
- Bleeding esophageal varices are hemorrhagic processes involving dialted, tortuous veins in the submucosa of the lower esophagus. .
Risk Factors
- Portal hypertension resulting from obstructed portal venous circulation
Pathophysiology
- In portal hypertension, collateral circulation develops in the lower esophagus as venous blood, which is diverted from the GI tract and spleen because of portal obstruction, seeks an outlet.
- Because of excessive intraluminal pressure, these collateral veins become tortuous, dilated, and fragile. They are particularly prone to ulceration and hemorrhage. Rupture of esophageal varices is the most common cause of death of clients with hepatic cirrhosis.
image by : hepatitisc.uw.edu
Assessment/Clinical Manifestations/Signs And Symptoms
- Hematemesis and melena, if ulcerated massive hemorrhage occurs
- Signs of hepatic encephalopathy
- Dilated abdominal veins
Laboratory and diagnostic study findings
- Endoscopy identifies the cause and site of bleeding
- Ultrasound and computed tomography assist in identifying the site of bleeding
Medical Management
Non-surgical treatment is preferred because of the high mortality associated with emergency surgery to control bleeding from esophageal varices and because of the poor physical condition of most of these patients.
Nonsurgical measures include:
- Pharmacologic therapy: somatostatin, vasopressin, beta-blocker and nitrates
- Balloon tamponade, saline lavage, endoscopic sclerotherapy
- Transjugular intrahepatic portosystemic shunting (TIPS)
- Esophageal banding therapy, variceal band ligation
If necessary, surgery may involve:
- Bypass procedures (e.g. portacaval shunts, splenorenal shunt, mesocaval shunt)
- Devascularization and transaction
Aggressive medical care includes evaluation of extent of bleeding and continuous monitoring of vital signs when hematemesis and melena are present.
Signs of potential hypovolemia are noted; blood volume is monitored with a central venous pressure or arterial catheter.
Oxygen is administered to prevent hypoxia and maintain adequate blood oxygenation, and intravenous fluids and volume expanders are administered to restore fluid volume and replace electrolytes.
Need for blood transfusion is assessed, and intake and output (insert indwelling catheter) are monitored.
Nursing Diagnosis
- Risk for bleeding
- Imbalanced nutrition: less than body requirements
Nursing Management
Provide ongoing assessment.
- Assess for ecchymosis, epistaxis, petechiae, and bleeding gums
- Monitor level of consciousness, vital signs, and urinary output to evaluate fluid balance.
- Monitor the client during blood transfusion administration if prescribed.
Institute measure to address bleeding.
- Use small-gauge needles, and apply pressure or cold for bleeding.
Provide nursing care for the client undergoing a prescribed balloon tamponade to control bleeding.
- Explain the procedure to the client to reduce fear and enhance cooperation with insertion and maintenance of the esophageal tamponade tube.
- Monitor the client closely to prevent accidental removal or displacement of the tube with resultant airway obstruction.
Provide nursing intervention for the client undergoing a prescribed iced saline lavage.
- Ensure nasogastric tube patency to prevent aspiration
- Observe gastric aspirate for evidence of bleeding.
- Protect the client from chilling.
After injection sclerotherapy, assess for:
- Esophageal perforation
- Continued bleeding
After portal-systemic surgical intervention, monitor for complications.
- Development of systemic encephalopathy
- Liver failure
Administer prescribed medications, which may include vasopressin and vitamin K.
Related posts, acid-base imbalances nursing care plan & management, herniorrhaphy ii, degenerative joint disease (osteoarthritis) nursing management.
You are using an outdated browser. Please upgrade your browser to improve your experience.
- About Journal

Asian Journal of Nursing Education and Research
2349-2996 (Online) 2231-1149 (Print)
Esophageal Varices: A Case Study
Author(s): Neha Abhishek Sharma
Email(s): [email protected]

Address: Neha Abhishek Sharma Ambaji Nursing College, Ganeshpura. *Corresponding Author
Published In: Volume - 10 , Issue - 3 , Year - 2020

ABSTRACT: Esophageal varices incidences are increasing by nearly 5% every year. Esophageal varices are the causes of bleeding in approximately 18% of hospital admissions for upper GI bleeding. Objective: The purpose of this study to understand the cause, clinical manifestations and treatment course for esophageal varices. Material and methods: detailed clinical history and physical examination was done. All the pertinent investigations were studied thoroughly of the selected case. Results: the esophageal varices is confirmed with the help of Upper gastrointestinal gastroscopy and repaired by banding. Conclusion: Esophageal varices is usually goes undiagnosed due to early common symptoms. Hematemesis is one of thesuggestive of esophageal varices and OGD is only the confirmative diagnosis for it. The prognosis is depend usually better if treatment received on time.
- esophageal varices
- portal hypertension
- hematemesis

Cite this article: Neha Abhishek Sharma. Esophageal Varices: A Case Study. Asian J. Nursing Education and Research. 2020; 10(3): 321-322. doi: 10.5958/2349-2996.2020.00067.1 Cite(Electronic): Neha Abhishek Sharma. Esophageal Varices: A Case Study. Asian J. Nursing Education and Research. 2020; 10(3): 321-322. doi: 10.5958/2349-2996.2020.00067.1 Available on: https://ajner.com/AbstractView.aspx?PID=2020-10-3-15
Recomonded Articles:

Asian Journal of Nursing Education and Research (AJNER) is an international, peer-reviewed journal devoted to nursing sciences....... Read more >>>
Quick Links
- Submit Article
- Author's Guidelines
- Paper Template
- Copyright Form
- Cert. of Conflict of Intrest
- Processing Charges
- Indexing Information

Latest Issues
Popular articles, recent articles.

- differentiation
- Care giver satisfaction
- Nursing care services
- Care givers.
- self-administered
- confidentiality
- hospitalization
- Individuals
- Prevention strategies.
- Cardiovascular
- disease-causing
- cardiovascular
- community-based
- cardio-vascular
- socio-demographic
- Younger Adults
- Rashtriya Bal Swasthya Karyakram
- District Early Intervention Centre
- Menstrual Cup
- Nursing Students.
- transformative
- revolutionized
- administrative
- AI based technology
- Nursing Education
- Nursing Practice.
- Mental Health
- Counselling
- Counsellor.
- immunotherapeutic
- Radiation therapy
- Chemotherapy
- Targeted therapy
- Immunotherapy
- Precision medicine
- Drug resistance.
- transplantation
- life-threatening
- complicationsthat
- helpindividuals
- Alport syndrome
- Type IV collagen
- Genetic mutation
- Basement membrane
- Genetic counseling.
- considerations
- multidisciplinary
- medical/forensic
- Forensic nursing
- Global Anti-violence.
- microenvironment
- biomarker-guided
- Drug resistance
- CAR-T therapy
- immune system.
- abnormalities”
- Early detection
- Urinary abnormalities
- Urine dip-strip analysis
- Chronic kidney disease.
- Non-probability
- self-structured
- Early Marriage
- Determinants
- Psychosocial Factors
- Married Women.
- implementation
- institution-developed
- Curriculum development
- Kern’s six-step approach
- Orientation training program learning outcomes
- Simulation.
- semi-structured
- non-vegetarian
- Heart Attack
- Preventive Measures
- Industries.
- infrastructure
- culture-specific
- non-probability
- inconsistencies
- Recommendations:
- Online education
- Epidemiological
- Implementation
- Structured teaching program – behavioural and emotional disorders with onset usually occurring in childhood and adolescence (f-90-f-98).
- socio-economic
- schistosomiasis
- Worm infestation
- Effectiveness
- Knowledge and planned teaching programme.
- Taichi exercise
- staff nurses
- perceived Stress scale.
- cross-sectional
- descriptive-comparative
- illness-Singapore
- restrictiveness
- tolerance/support
- Nursing students
- Mental illness.
Hepatic Cirrhosis
- Hepatic cirrhosis is a chronic hepatic disease characterized by diffuse destruction and fibrotic regeneration of hepatic cells.
Table of Contents
- What is Hepatic Cirrhosis?
Classification
Pathophysiology, statistics and incidences, clinical manifestations, complications, assessment and diagnostic findings, pharmacologic therapy, surgical management, nursing assessment, nursing diagnosis, nursing care planning & goals, nursing interventions, discharge and home care guidelines, documentation guidelines, practice quiz: hepatic cirrhosis, what is hepatic cirrhosis.
The end-stage of liver disease is called cirrhosis.
- As necrotic tissue yields to fibrosis, this disease alters liver structure and normal vasculature, impairs blood and lymph flow, and ultimately causes hepatic insufficiency.
- The prognosis is better in noncirrhotic forms of hepatic fibrosis, which cause minimal hepatic dysfunction and don’t destroy liver cells.
These clinical types of cirrhosis reflect its diverse etiology:
- Laennec’s cirrhosis. The most common type, this occurs in 30% to 50% of cirrhotic patients, up to 90% of whom have a history of alcoholism.
- Biliary cirrhosis. Biliary cirrhosis results in injury or prolonged obstruction.
- Postnecrotic cirrhosis. Postnecrotic cirrhosis stems from various types of hepatitis .
- Pigment cirrhosis. Pigment cirrhosis may result from disorders such as hemochromatosis.
- Cardiac cirrhosis. Cardiac cirrhosis refers to cirrhosis caused by right-sided heart failure .
- Idiopathic cirrhosis. Idiopathic cirrhosis has no known cause.
Although several factors have been implicated in the etiology of cirrhosis, alcohol consumption is considered the major causative factor.
- Necrosis. Cirrhosis is characterized by episodes of necrosis involving the liver cells.
- Scar tissue. The destroyed liver cells are gradually replaced with a scar tissue.
- Fibrosis. There is diffuse destruction and fibrotic regeneration of hepatic cells.
- Alteration. As necrotic tissue yields to fibrosis, the disease alters the liver structure and normal vasculature, impairs blood and lymph flow, and ultimately causes hepatic insufficiency.
Various types of cirrhosis may occur in different types of individuals.
- The most common, Laennec’s cirrhosis, occurs in 30% to 50% of cirrhotic patients.
- Biliary cirrhosis occurs in 15% to 20% of patients.
- Postnecrotic cirrhosis occurs in 10% to 30% of patients.
- Pigment cirrhosis occurs in 5% to 10% of patients.
- Idiopathic cirrhosis occurs in about 10% of patients.
Different types of cirrhosis have different causes.
- Excessive alcohol consumption. Too much alcohol intake is the most common cause of cirrhosis as liver damage is associated with chronic alcohol consumption.
- Injury. Injury or prolonged obstruction causes biliary cirrhosis.
- Hepatitis. The different types of hepatitis can cause postnecrotic cirrhosis.
- Other diseases. Diseases such as hemochromatosis causes pigment cirrhosis.
- Right-sided heart failure. Cardiac cirrhosis, a rare kind of cirrhosis, is caused by right-sided heart failure.
Clinical manifestations of the different types of cirrhosis are similar, regardless of the cause.
- GI system. Early indicators usually involve gastrointestinal signs and symptoms such as anorexia , indigestion, nausea , vomiting constipation , or diarrhea .
- Respiratory system . Respiratory symptoms occur late as a result of hepatic insufficiency and portal hypertension , such as pleural effusion and limited thoracic expansion due to abdominal ascites, interfering with efficient gas exchange leading to hypoxia.
- Central nervous system . Signs of hepatic encephalopathy also occur as a late sign, and these are lethargy, mental changes, slurred speech, asterixis (flapping tremor), peripheral neuritis, paranoia, hallucinations, extreme obtundation, and ultimately, coma.
- Hematologic. The patient experiences bleeding tendencies and anemia .
- Endocrine. The male patient experiences testicular atrophies, while the female patient may have menstrual irregularities, and gynecomastia and loss of chest and axillary hair .
- Skin. There is severe pruritus, extreme dryness, poor tissue turgor, abnormal pigmentation, spider angiomas, palmar erythema, and possibly jaundice .
- Hepatic. Cirrhosis causes jaundice, ascites, hepatomegaly, edema of the legs, hepatic encephalopathy, and hepatic renal syndrome.
The complications of hepatic cirrhosis include the following:
- Portal hypertension . Portal hypertension is the elevation of pressure in the portal vein that occurs when blood flow meets increased resistance.
- Esophageal varices. Esophageal varices are dilated tortuous veins in submucosa of the lower esophagus.
- Hepatic encephalopathy. Hepatic encephalopathy may manifest as deteriorating mental status and dementia or as physical signs such as abnormal involuntary and voluntary movements.
- Fluid volume excess . Fluid volume excess occurs due to an increased cardiac output and decreased peripheral vascular resistance.
Laboratory findings and imaging studies that are characteristic of cirrhosis include:
- Liver scan. Liver scan shows abnormal thickening and a liver mass.
- Liver biopsy . Liver biopsy is the definitive test for cirrhosis as it detects destruction and fibrosis of the hepatic tissue.
- Liver imaging. Computed tomography scan , ultrasound, and magnetic resonance imaging may confirm the diagnosis of cirrhosis through visualization of masses, abnormal growths, metastases, ans venous malformations.
- Cholecystography and cholangiography. These two visualize the gallbladder and the biliary duct system.
- Splenoportal venography. Splenoportal venography visualizes the portal venous system.
- Percutaneous transhepatic cholangiography. This test differentiates intrahepatic from extrahepatic obstructive jaundice and discloses hepatic pathology and the presence of gallstones .
- Complete blood count . There is decreased white blood cell count, hemoglobin level and hematocrit, albumin, or platelets.
Medical Management
Treatment is designed to remove or alleviate the underlying cause of cirrhosis.
- Diet . The patient may benefit from a high-calorie and a medium to high protein diet , as developing hepatic encephalopathy mandates restricted protein intake.
- Sodium restriction. is usually restricted to 2g/day .
- Fluid restriction. Fluids are restricted to 1 to 1.5 liters/day .
- Activity. Rest and moderate exercise is essential.
- Paracentesis. Paracentesis may help alleviate ascites.
- Sengstaken-Blakemore or Minnesota tube. The Sengstaken-Blakemore or Minnesota tube may also help control hemorrhage by applying pressure on the bleeding site.
Drug therapy requires special caution because the cirrhotic liver cannot detoxify harmful agents effectively.
- Octreotide . If required, octreotide may be prescribed for esophageal varices.
- Diuretics . Diuretics may be given for edema, however, they require careful monitoring because fluid and electrolyte imbalance may precipitate hepatic encephalopathy.
- Lactulose. Encephalopathy is treated with lactulose.
- Antibiotics . Antibiotics are used to decrease intestinal bacteria and reduce ammonia production, one of the causes of encephalopathy.
Surgical procedures for management of hepatic cirrhosis include:
- Transjugular intrahepatic portosystemic shunt (TIPS) procedure. The TIPS procedure is used for the treatment of varices by upper endoscopy with banding to relieve portal hypertension.
Nursing Management
Nursing management for the patient with cirrhosis of the liver should focus on promoting rest, improving nutritional status, providing skin care, reducing risk of injury, and monitoring and managing complications.
Assessment of the patient with cirrhosis should include assessing for:
- Bleeding. Check the patient’s skin, gums, stools, and vomitus for bleeding.
- Fluid retention. To assess for fluid retention, weigh the patient and measure abdominal girth at least once daily.
- Mentation. Assess the patient’s level of consciousness often and observe closely for changes in behavior or personality.
Based on the assessment data, the major nursing diagnosis for the patient are:
- Activity intolerance related to fatigue , lethargy, and malaise.
- Imbalanced nutrition : less than body requirements related to abdominal distention and discomfort and anorexia.
- Impaired skin integrity related to pruritus from jaundice and edema.
- High risk for injury related to altered clotting mechanisms and altered level of consciousness.
- Disturbed body image related to changes in appearance, sexual dysfunction , and role function.
- Chronic pain and discomfort related to enlarged liver and ascites.
- Fluid volume excess related ascites and edema formation.
- Disturbed thought processes and potential for mental deterioration related to abnormal liver function and increased serum ammonia level.
- Ineffective breathing pattern related to ascites and restriction of thoracic excursion secondary to ascites, abdominal distention, and fluid in the thoracic cavity.
Main Article: 8 Liver Cirrhosis Nursing Care Plans
The major goals for a patient with cirrhosis are:
- Report decrease in fatigue and increased ability to participate in activities.
- Maintain a positive nitrogen balance, no further loss of muscle mass, and meet nutritional requirements.
- Decrease potential for pressure ulcer development and breaks in skin integrity .
- Reduce the risk of injury.
- Verbalize feelings consistent with improvement of body image and self-esteem.
- Increase level of comfort.
- Restore normal fluid volume.
- Improve mental status, maintain safety, and ability to cope with cognitive and behavioral changes.
- Improve respiratory status.
The patient with cirrhosis needs close observation, first-class supportive care, and sound nutrition counseling.
Promoting Rest
- Position bed for maximal respiratory efficiency; provide oxygen if needed.
- Initiate efforts to prevent respiratory, circulatory, and vascular disturbances.
- Encourage patient to increase activity gradually and plan rest with activity and mild exercise.
Improving Nutritional Status
- Provide a nutritious, high-protein diet supplemented by B-complex vitamins and others, including A, C, and K.
- Encourage patient to eat: Provide small, frequent meals, consider patient preferences, and provide protein supplements, if indicated.
- Provide nutrients by feeding tube or total PN if needed.
- Provide patients who have fatty stools (steatorrhea) with water-soluble forms of fat-soluble vitamins A, D, and E, and give folic acid and iron to prevent anemia .
- Provide a low-protein diet temporarily if patient shows signs of impending or advancing coma; restrict sodium if needed.
Providing Skin Care
- Change patient’s position frequently.
- Avoid using irritating soaps and adhesive tape.
- Provide lotion to soothe irritated skin; take measures to prevent patient from scratching the skin.
Reducing Risk of Injury
- Use padded side rails if patient becomes agitated or restless.
- Orient to time, place, and procedures to minimize agitation.
- Instruct patient to ask for assistance to get out of bed.
- Carefully evaluate any injury because of the possibility of internal bleeding.
- Provide safety measures to prevent injury or cuts (electric razor, soft toothbrush).
- Apply pressure to venipuncture sites to minimize bleeding.
Monitoring and Managing Complications
- Monitor for bleeding and hemorrhage .
- Monitor the patient’s mental status closely and report changes so that treatment of encephalopathy can be initiated promptly.
- Carefully monitor serum electrolyte levels are and correct if abnormal.
- Administer oxygen if oxygen desaturation occurs; monitor for fever or abdominal pain , which may signal the onset of bacterial peritonitis or other infection .
- Assess cardiovascular and respiratory status; administer diuretics, implement fluid restrictions, and enhance patient positioning , if needed.
- Monitor intake and output , daily weight changes, changes in abdominal girth, and edema formation.
- Monitor for nocturia and, later, for oliguria, because these states indicate increasing severity of liver dysfunction.
Home Management
- Prepare for discharge by providing dietary instruction, including exclusion of alcohol.
- Refer to Alcoholics Anonymous , psychiatric care, counseling, or spiritual advisor if indicated.
- Continue sodium restriction; stress avoidance of raw shellfish.
- Provide written instructions, teaching, support, and reinforcement to patient and family.
- Encourage rest and probably a change in lifestyle (adequate,well-balanced diet and elimination of alcohol).
- Instruct family about symptoms of impending encephalopathy and possibility of bleeding tendencies and infection.
- Offer support and encouragement to the patient and provide positive feedback when the patient experiences successes.
- Refer patient to home care nurse , and assist in transition from hospital to home.
Expected patient outcomes include:
- Reported decrease in fatigue and increased ability to participate in activities.
- Maintained a positive nitrogen balance, no further loss of muscle mass, and meet nutritional requirements.
- Decreased potential for pressure ulcer development and breaks in skin integrity.
- Reduced the risk of injury.
- Verbalized feelings consistent with improvement of body image and self-esteem.
- Increased level of comfort.
- Restored normal fluid volume.
- Improved mental status, maintain safety, and ability to cope with cognitive and behavioral changes.
- Improved respiratory status.
The focus of discharge education is dietary instructions.
- Alcohol restriction. Of greatest importance is the exclusion of alcohol from the diet, so the patient may need referral to Alcoholics Anonymous, psychiatric care, or counseling.
- Sodium restriction. Sodium restriction will continue for considerable time, if not permanently.
- Complication education. The nurse also instructs the patient and family about symptoms of impending encephalopathy, possible bleeding tendencies, and susceptibility to infection.
The focus of documentation may include:
- Level of activity.
- Causative or precipitating factors.
- Vital signs before, during, and following activity.
- Plan of care.
- Response to interventions, teaching, and actions performed.
- Teaching plan.
- Changes to plan of care.
- Attainment or progress toward desired outcome.
- Caloric intake.
- Individual cultural or religious restrictions, personal preferences.
- Availability and use of resources.
- Duration of the problem.
- Perceptio of pain, effects on lifestyle, and expectations of therapeutic regimen .
- Results of laboratory tests, diagnostic studies, and mental status and cognitive evaluation .
Here are some practice questions for this study guide .Please visit our nursing test bank page for more NCLEX practice questions .
1. Which assessment finding indicates that lactulose is effective in decreasing the ammonia level in the client with hepatic encephalopathy?
A. Passage of two or three soft stools daily. B. Evidence of watery diarrhea . C. Daily deterioration in the client’s handwriting. D. Appearance of frothy, foul-smelling stools.
1. Correct Answer: A. Passage of two or three soft stools daily.
- A: Two or three soft stools daily indicate effectiveness of the drug.
- B: Watery diarrhea indicates overdose.
- C: Daily deterioration in the client’s handwriting indicates an increase in the ammonia level and worsening of hepatic encephalopathy.
- D: Frothy, foul-smelling stools indicate steatorrhea, caused by impaired fat digestion.
2. For a client with hepatic cirrhosis who has altered clotting mechanisms, which intervention would be most important?
A. Allowing complete independence of mobility . B. Applying pressure to injection sites. C. Administering antibiotics as prescribed. D. Increasing nutritional intake.
2. Correct Answer: B. Applying pressure to injection sites.
- B: Prolonged application of pressure to injection or bleeding sites is important.
- A: Complete independence may increase the client’s potential for injury, because an unsupervised client may injure himself and bleed excessively.
- C&D: Antibiotics and good nutrition are important to promote liver regeneration.
3. A client with advanced cirrhosis has been diagnosed with hepatic encephalopathy. The nurse expects to assess for:
A. Malaise. B. Stomatitis. C. Hand tremors. D. Weight loss.
3. Correct Answer: C. Hand tremors.
- C: Flapping of the hands (asterixis), changes in mentation, agitation, and confusion are common.
- A&B: Malaise and stomatitis are not related to neurological involvement.
- D: These clients typically have ascites and edema so experience weight gain.
4. A client diagnosed with chronic cirrhosis who has ascites and pitting peripheral edema also has hepatic encephalopathy. Which of the following nursing interventions are appropriate to prevent skin breakdown?
A. Range of motion every 4 hours. B. Turn and reposition every 2 hours. C. Abdominal and foot massages every 2 hours. D. Sit in chair for 30 minutes each shift.
4. Correct Answer: B. Turn and reposition every 2 hours.
- B: Careful repositioning can prevent skin breakdown.
- A: Range of motion exercises preserve joint function but do not prevent skin breakdown.
- C: Abdominal or foot massage will not prevent skin breakdown but must be cleansed carefully to prevent breaks in skin integrity.
- D: The feet should be kept at the level of heart or higher so Fowler’s position should be employed.
5. The nurse must be alert for complications with Sengstaken-Blakemore intubation including:
A. Pulmonary obstruction. B. Pericardiectomy syndrome. C. Pulmonary embolization. D. Cor pulmonale.
5. Correct Answer: A. Pulmonary obstruction.
- A: Rupture or deflation of the balloon could result in upper airway obstruction .
- B, C, D: The other choices are not related to the tube.
Other posts from the site you may like:
- 8 Liver Cirrhosis Nursing Care Plans
- 7 Hepatitis Nursing Care Plans
- Bile Duct Stones (Choledocholithiasis)
Leave a Comment Cancel reply
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- World J Gastrointest Pharmacol Ther
- v.10(1); 2019 Jan 21
Update on the management of gastrointestinal varices
Umesha boregowda.
Department of Gastroenterology and Hepatology, University of California San Francisco, Fresno, CA 93721, United States
Chandraprakash Umapathy
Nasir halim, madhav desai.
Department of Gastroenterology and Hepatology, Kansas University Medical Center, Kansas City, KS 66160, United States
Arpitha Nanjappa
Subramanyeswara arekapudi.
Department of Medicine, VA Central California Healthcare System, Fresno, CA 93703, United States
Thimmaiah Theethira
Department of Gastroenterology and Hepatology, VA Central California Healthcare System, Fresno, CA 93703, United States
Marina Roytman
Shreyas saligram.
Department of Gastroenterology and Hepatology, VA Central California Healthcare System, Fresno, CA 93703, United States. ude.fscu.onserf@margilass
Corresponding author: Shreyas Saligram MD, MRCP, Assistant Professor, Director, Doctor, Department of Gastroenterology and Hepatology, University of California San Francisco, 2823 Fresno Street, Fresno, CA 93721, United States. ude.fscu.onserf@margilass
Telephone: +1-559-4593821 Fax: +1-559-4593887
Cirrhosis of liver is a major problem in the western world. Portal hypertension is a complication of cirrhosis and can lead to a myriad of pathology of which include the development of porto-systemic collaterals. Gastrointestinal varices are dilated submucosal veins, which often develop at sites near the formation of gastroesophageal collateral circulation. The incidence of varices is on the rise due to alcohol and obesity. The most significant complication of portal hypertension is life-threatening bleeding from gastrointestinal varices, which is associated with substantial morbidity and mortality. In addition, this can cause a significant burden on the health care facility. Gastrointestinal varices can happen in esophagus, stomach or ectopic varices. There has been considerable progress made in the understanding of the natural history, pathophysiology and etiology of portal hypertension. Despite the development of endoscopic and medical treatments, early mortality due to variceal bleeding remains high due to significant illness of the patient. Recurrent variceal bleed is common and in some cases, there is refractory variceal bleed. This article aims to provide a comprehensive review of the management of gastrointestinal varices with an emphasis on endoscopic interventions, strategies to handle refractory variceal bleed and newer endoscopic treatment modalities. Early treatment and improved endoscopic techniques can help in improving morbidity and mortality.
Core tip: Cirrhosis of liver can lead to gastrointestinal varices. Gastrointestinal bleed from varices can be debilitating and can cause morbidity and mortality if not well controlled. This is a detailed review on the endoscopic management of variceal bleed and gives an insight into some of the new endoscopic techniques that can be helpful in treating variceal bleed.
INTRODUCTION
Less than 1% of the United States population have cirrhosis of liver[ 1 ]. In the western world, the most common etiology of portal hypertension is cirrhosis due to alcoholic liver disease, nonalcoholic steatohepatitis (NASH), and hepatitis C infection[ 2 ]. According to a recent estimate 15 million people in the United States have alcohol abuse disorder, nearly 88000 people die annually due to alcohol, and 10%-15% of people with alcoholism develop cirrhosis[ 3 ]. Another 3 million people have chronic hepatitis C infection[ 4 ], and 25%-28% of these patients go on to develop cirrhosis[ 5 , 6 ]. Nonalcoholic fatty liver disease (NAFLD) is a spectrum of chronic liver disease consisting of mild to an advanced form of fatty degeneration of the liver described as NASH. Prevalence of NASH is estimated to be around 3%-8% of the general population, and 10%-25% of these patients progress to cirrhosis[ 7 ]. Moreover, the rate of NASH is rising due to the increasing prevalence of obesity, insulin resistance, and diabetes. NASH is the second most common cause among patients with cirrhosis who are currently waiting for liver transplant. Recent trends have indicated that NAFLD is expected to overtake hepatitis C and alcohol as the most common etiology of liver cirrhosis and indication for liver transplants in the western countries by year 2030[ 8 , 9 ]. Therefore, in order to reduce morbidity and mortality, as well as the overall burden on healthcare, it is essential to develop cost-effective screening and management strategies for portal hypertension related to cirrhosis.
NATURAL HISTORY OF GASTROINTESTINAL VARICES
Gastrointestinal varices are abnormally dilated submucosal veins in the digestive tract due to portal hypertension and can potentially cause life-threatening bleeding. Prevalence of varices increases with the severity of liver disease (Child-Pugh class A 42.7%, class B 70.7% and class C 75.5%)[ 2 , 10 ]. The Child-Pugh score is described in Table Table1. 1 . The incidence of esophageal varices in cirrhotic patients is around 5% at the end of one year and 28% at the end of three years. Small varices progress to large varices at a rate of 10% to 12% annually[ 11 ]. Approximately 50% of all patients with a new diagnosis of cirrhosis have gastrointestinal varices[ 2 ]. Annual risk of variceal bleeding among small and large varices is 5% and 15% respectively[ 12 ]. The six-week mortality rate among patients with index variceal bleeding is approximately 20%[ 13 ]. Risk of rebleeding without endoscopic intervention is almost 60% with an increased mortality rate (33%)[ 14 ].
Child-Pugh scoring and classification
Class A (score 5-6), class B (score 7-9), and class C (score 10-15). PT/INR: Prothrombin time/international standardized ratio.
PATHOPHYSIOLOGY
The development of portal hypertension in cirrhosis is a multifactorial process with changes in both the portal and systemic circulation. This is shown in Figure Figure1. 1 . The majority of patients in western countries with portal hypertension have underlying cirrhosis. Non-cirrhotic portal hypertension is typically less common and encompasses a broad range of pathology, typically vascular in origin[ 15 ]. Portal hypertension is defined as hepatic vein pressure gradient (HVPG) more than 5 mmHg. The HVPG is a surrogate means to measure pressure in the portal veins. Normal HVPG (= hepatic vein wedge pressure - free hepatic vein pressure) is around 3-5 mmHg. Varices usually develop when patients have HVPG >10 mmHg and presence of HVPG > 12 mmHg is a risk factor for variceal bleeding. Reduction in HVPG to less than 12 mmHg or by ≥ 20% from baseline reduces the risk of initial bleeding, and other complications of portal hypertension (ascites, encephalopathy)[ 14 ].

Mechanism of portal hypertension and the development of gastrointestinal varices. VEGF: Vascular endothelial growth factor; PDGF: Platelet-derived growth factor; NO: Nitric oxide; HVPG: Hepatic venous pressure gradient.
Porto-systemic shunting due to portal hypertension causes diversion of the portal blood into systemic circulation and results in variceal formation. Presence of ongoing liver injury due to alcohol, viral hepatitis (hepatitis B and C), or NASH can lead to increase in the size of the varices, whereas elimination of etiological factor can lead to decrease in the size or disappearance of varices in patients with alcoholic cirrhosis[ 16 , 17 ].
Intrahepatic hemodynamics
Architectural distortion : Hepatocellular injury causes transformation of hepatic stellate cells into myofibroblasts. Increased expression of pro-inflammatory genes and fibrotic activity, as a result, promotes neoangiogenesis and interstitial collagen deposition resulting in distortion of the hepatic sinusoidal architecture[ 18 , 19 ]. Architectural damage and regenerative nodules are responsible for nearly 2 nd /3 rd of the increase in intrahepatic resistance.
Increased vascular resistance : In addition to the known anatomical disruption in the sinusoidal architecture, it is now understood that there are changes in the neurohormonal regulation of vascular tone within the portal circulation. The hepatic injury causes increased production of vasoconstrictors (endothelin 1[ 20 , 21 ] and thromboxane A2[ 22 , 23 ]) and reduction in nitric oxide (NO) synthesis due to sinusoidal endothelial dysfunction[ 24 ]. The imbalance in the production of vasoconstrictors and vasodilators causes impaired vasomotor control leading to further increase in resistance and is responsible for approximately 1 st /3 rd of the increase in intrahepatic resistance[ 25 , 26 ].
Extrahepatic hemodynamics
Portal hypertension induces neurohormonal changes in the splanchnic circulation as well. Overproduction of NO from splanchnic endothelium leads to reduced splanchnic and systemic vascular resistance[ 27 - 29 ]. Furthermore, a compensatory activation of the renin-angiotensin mechanism leads to increased cardiac output and hepatic blood flow. Increased portal pressure is also suspected to result in overproduction of angiogenic factors such as vascular endothelial growth factor, platelet-derived growth factor at the microcirculatory level, contributing to angiogenesis and collateral formation resulting in varices[ 30 , 31 ].
Gastrointestinal varices develop as a consequence of portal hypertension. Most common etiology of portal hypertension in the United States is cirrhosis due to alcohol, NASH, and hepatitis C. The exact prevalence of portal hypertension is not known. Causes of portal hypertension are classified as below.
Presinusoidal
Extrahepatic : Portal vein thrombosis, splenic vein thrombosis.
Intrahepatic : Schistosomiasis, congenital hepatic fibrosis, and sarcoidosis. (1) Sinusoidal: Cirrhosis due to viral hepatitis (hepatitis B and C), NASH, alcohol, primary biliary cirrhosis, primary sclerosing cholangitis, hemochromatosis, Wilson’s disease, and cytotoxic drugs; and (2) Postsinusoidal: Budd-Chiari syndrome, caval web, constrictive pericarditis, and veno-occlusive disorders.
MECHANISM OF VARICEAL BLEEDING
Increased blood flow through the portosystemic collaterals due to portal hypertension causes dilation of the submucosal venous plexus resulting in elevated intravariceal pressure and wall tension. The mechanism of variceal rupture can be explained by Frank’s modified Laplace’s law[ 32 ]. This is shown in Figure Figure2 2 .

Mechanism of variceal bleeding. P: Pressure; R: Radius; WT: Wall thickness.
Wall tension (T) = [Transmural pressure (Pvarices-Plumen) × variceal radius (R)]/[Variceal wall thickness (WT)].
RISK STRATIFICATION FOR VARICEAL BLEEDING
Hvpg > 12 mmhg.
Rise in portal pressure causes increased flow through the varices and thus increased intravariceal pressure. In a randomized control trial (RCT) patients with HVPG < 12 mmHg did not develop variceal bleeding[ 33 ], and presence of HVPG > 20 mmHg was associated with high risk of failed hemostasis and death[ 34 ]. Whereas, a decrease in HVPG > 20% from the baseline reduces complications of portal hypertension including bleeding, ascites, encephalopathy, and death[ 35 - 37 ].
Variceal size
Large varices (> 5 mm) have a higher tendency to bleed due to increased wall tension as explained above.
Wall tension
Increased wall tension and the presence of ‘red wale sign’ (dilated capillaries on the variceal wall) indicate a high risk for bleeding.
Other factors
Presence of coagulopathy, infection, and decompensated cirrhosis are other risk factors for variceal bleeding.
DIAGNOSTIC TESTS FOR GASTROINTESTINAL VARICES
Esophago-gastro duodenoscopy (EGD) is the gold standard procedure used in the diagnosis of gastroesophageal varices (GOVs). Based on the endoscopic assessment, GOVs are classified into small (< 5 mm), and large varices(> 5 mm)[ 38 ] for clinical management. Disadvantages of endoscopy include the risk of sedation, higher cost, bleeding and risk of aspiration.
Endoscopic ultrasound
Endoscopic ultrasound (EUS) has been evaluated as a diagnostic tool in assessing GOVs. EUS is better than EGD in detecting gastric varices (GVs), and its ability to evaluate the anatomy of collateral and perforating veins makes it an excellent choice in monitoring treatment response to endoscopic variceal ligation (EVL) and predicting recurrence[ 39 - 41 ]. Currently, EUS is not considered as a primary diagnostic modality due to limited availability of local expertise.
Capsule endoscopy
A recent meta-analysis reviewed the use of capsule endoscopy for the diagnosis and grading of esophageal varices and noted a diagnostic accuracy of 90% with a pooled sensitivity and specificity of 83% and 85%, respectively[ 42 ]. The inability of capsule endoscopy to detect GVs is a significant drawback. Even though capsule endoscopy is relatively less invasive and does not require sedation, the diagnostic sensitivity is not adequate to advocate for index surveillance. It may be a consideration for a select subgroup of high-risk patients who are unwilling to undergo more invasive traditional endoscopic evaluation[ 43 , 44 ]. One study showed that 97% of the patients preferred capsule endoscopy over endoscopy with or without sedation[ 44 ].
Noninvasive testing
Various clinical findings, laboratory tests, and imaging studies have been considered as predictors of clinically significant portal hypertension (CSPH) (HVPG > 12 mmHg); however, they are not accurate enough to either reliably diagnose or exclude CSPH. Specifically, transient elastography, platelet count, spleen size, magnetic resonance elastography, and splenic stiffness are the most commonly used parameters to predict the presence of CSPH and varices in patients with cirrhosis. The presence of portosystemic collaterals on ultrasound, computed tomography, or magnetic resonance imaging is indicative of CSPH and necessitate screening endoscopy[ 38 ]. Liver stiffness measured by transient elastography in combination with platelet count can rule out presence high-risk varices[ 45 ]. A liver stiffness < 20 kPa and platelet count > 150000/μL indicate < 5% chance of having high-risk varices, and screening endoscopy can be safely deferred as long as ongoing clinical monitoring can be assured[ 46 ].
ESOPHAGEAL VARICES
Epidemiology.
Esophageal varices are the most common type of gastrointestinal varices, and their prevalence in Child-Pugh class A is 42.7%, around 70.7% in class B, and 75.5% in class C[ 2 ]. The bleeding risk for small varices and large varices is around 5% and 15% per year respectively. Early mortality rate (6 wk) is approximately 20%[ 47 ] in esophageal varices after index bleeding.
Venous drainage from the sub-mucosal venous plexus of the esophagus drains into the collateral veins around the esophagus. The interconnected collateral venous plexus runs longitudinally along the esophagus and communicates with submucosal venous plexus through perforating veins in the palisading area. The cervical esophagus drains into inferior thyroid vein, the thoracic esophagus drains to azygous, hemizygous, intercostal, and bronchial veins, whereas the abdominal portion of the esophagus drains into the left gastric vein, which in turn empties into the portal vein. Portal hypertension leads to shunting of blood from the portal circulation into these low pressure, thin-walled submucosal systemic veins and manifest as varices.
Modified Paquet classification
Grade I : Varices extending just above the mucosal level.
Grade II : Varices projecting by one-third of the luminal diameter that cannot be compressed with air insufflation.
Grade III : Varices projecting up to 50% of the luminal diameter and in contact with each other.
Screening and surveillance EGD for esophageal VARICES
Shown in Figure Figure3. 3 . All patients who are newly diagnosed with cirrhosis should be screened for esophageal varices. Patients with compensated cirrhosis without varices in the absence of ongoing liver injury, endoscopy should be done every three years. Those who have compensated cirrhosis without varices, but have an ongoing liver injury (alcohol abuse, hepatitis C) and/or other cofactor diseases (alcohol/obesity) screening endoscopy should be repeated every two years.

Screening endoscopy for esophageal varices per practice society guidelines[ 38 , 48 ]. NSBBs: Nonselective beta-blockers; EVL: Endoscopic variceal ligation; EGD: Esophago-gastro duodenoscopy; LS: Liver stiffness; PLT: Platelet.
Patients with small varices without ongoing liver injury or cofactor disease endoscopy is recommended every two years, and every year if either ongoing liver injury or cofactor disease is present. Patients with medium and large size varices should be started on nonselective beta-blockers or considered for EVL. If the patient is on nonselective beta blockers, no further surveillance endoscopy is needed.
On the other hand, if EVL is considered for primary prophylaxis endoscopy should be done every 1-2 wk until eradication and then repeated every 6-12 mo.
Management of patients with esophageal varices that have not bled
Either nonselective beta blockers or EVL (Figure (Figure4) 4 ) can be used as primary prophylaxis of variceal hemorrhage in patients with medium/large esophageal varices. Only approved nonselective beta-blockers are propranolol, nadolol, and carvedilol[ 38 , 48 - 52 ]. The choice should be made based on the cost, contraindications, availability, and patient preference. Nonselective beta-blockers are preferred over EVL due to their low cost, easy availability, ability to reduce the HVPG. Nonselective beta-blockers reduce the risk of hemorrhage and other complications (ascites, encephalopathy, and death) of portal hypertension[ 37 ]. Based on the currently available data, beta-blockers do not prevent the development of varices or their progression from small to large varices, although there is some reported benefit of reduction in risk of bleeding.

Endoscopic variceal ligation for primary prophylaxis. A: Esophageal varices before banding; B: Esophageal varix post banding.
The effect of nadolol on the progression of variceal size was studied in a prospective randomized study. A total of 161 patients were randomized into nadolol ( n = 83) and placebo ( n = 78) groups. All patients had yearly screening endoscopy and with a mean follow up of 36 mo. The cumulative probability of bleeding and progression of small varices was lower in nadolol group (20%) when compared to placebo (51%) ( P < 0.001) (absolute risk difference: 31%; 95%CI: 17%-45%)[ 53 ]. However, this benefit has not been proven in other studies.
In a recent meta-analysis of 6 RCTs, the effect of nonselective beta-blockers in cirrhotic patients with no or small varices was analyzed. The incidence of large varices (OR = 1.05, 95%CI: 0.25-4.36; P = 0.95), first variceal bleeding (OR = 0.59, 95%CI: 0.24-1.47; P = 0.26) and death (OR = 0.70, 95%CI: 0.45-1.10; P = 0.12) were similar in both nonselective beta-blocker group and placebo group. However, the incidence of adverse events in the nonselective beta-blockers group was significantly higher than the placebo group. Notably, nonselective beta-blockers did not reduce the incidence of large varices or prevent the progression of small varices to large varices[ 54 ].
On the other hand, when compared to nonselective beta blockers, EVL has a higher rate of recurrence of varices, lacks the benefit of HVPG reduction, and needs further endoscopic surveillance. EVL has lower but more severe side effects (bleeding, ulcers, and strictures) compared to nonselective beta-blockers (weakness, tiredness, shortness of breath). However, there is no significant difference in the mortality rate between the two[ 46 ].
In a prospective randomized study, the combination of EVL and propranolol was compared to EVL alone among high-risk patients. One hundred forty-four patients in total were randomized into EVL + propranolol ( n = 72) group and EVL alone ( n = 72) group respectively. Addition of propranolol to EVL did not reduce the risk of first variceal bleed (7% vs 11%, P = 0.72) or death (8% vs 15%, P = 0.37). However, the combination group had significant adverse effects due to propranolol in 22% of the patients. Combination of nonselective beta-blockers and EVL is not recommended as primary prophylaxis due to a higher rate of side effects. However, the recurrence of varices was significantly lower when propranolol was added ( P = 0.03)[ 55 ]. Recent practice society guidelines suggest the use of nonselective beta-blockers as a recommended therapy for primary prophylaxis for small varices with high-risk features (presence of ‘red wale’ signs or decompensated cirrhosis)[ 38 , 46 ].
Isosorbide mononitrate, sclerotherapy, glue injection, and transjugular intrahepatic portosystemic stent (TIPS) shunt are not used as primary prophylaxis due to a higher rate of side effects without mortality benefit.
Use of nonselective beta-blockers among patients who have cirrhosis with refractory ascites is controversial. A prospective case study showed that the use of nonselective beta-blockers in this patient group was associated with increased mortality[ 56 ]. Another study also showed the increased risk of renal injury, hospital stay and mortality with the use of nonselective beta-blockers with spontaneous bacterial peritonitis due to post-paracentesis circulatory dysfunction[ 57 ]. However, a meta-analysis of 3 RCTs and 13 observational studies ( n = 8279) showed no significant difference in mortality or incidence of hepatorenal syndrome and spontaneous bacterial peritonitis among cirrhosis patients with refractory ascites, when treated with nonselective beta blockers[ 58 ]. Due to concern for possible deleterious effects in patients with advanced cirrhosis, many physicians now prefer EVL over nonselective beta blockers. Larger RCTs are required before nonselective beta-blockers are considered as a contraindication in this subgroup.
Management of acute esophageal variceal bleeding
General measures: All patients with acute variceal bleeding should be resuscitated at an early stage to protect the airway and achieve hemodynamic stability, preferably in a medical intensive care unit. Prognostic indicators for early mortality due to acute variceal bleeding are HVPG, Child-Pugh score, and model for end-stage liver disease (MELD) score. A MELD score of > 19 showed 20% mortality due to index variceal bleeding[ 34 , 47 , 59 ]. When measured within 24 h of acute bleeding, HVPG > 20 mmHg predicts a high risk of early rebleeding and death[ 38 , 48 , 60 ]. The Child-Pugh score is also a significant predictor of early mortality and can help guide patient risk stratification[ 61 ]. Medical management with vasoactive agents, antibiotics, blood transfusion, combined with EVL is the standard of care in treating acute variceal bleeding.
Restrictive transfusion strategy: All patients with Hb ≤ 7 g/dL should get packed red blood cells to maintain hemoglobin at 7-8 g/dL. Previous RCTs have shown a survival benefit, reduced need for blood transfusion, and a lower rate of adverse events with a restrictive strategy when compared to liberal transfusion[ 62 ].
Most patients with acute variceal bleeding have elevated HVPG (> 12 mmHg). Further elevation of HVPG due to liberal transfusion can increase the risk of rebleeding. In a recent meta-analysis, the incidence of death (OR = 0.52, 95%CI: 0.31-0.87, P = 0.01), blood transfusion requirement (standard mean difference: -0.74, 95%CI: -1.15--0.32, P = 0.0005) and hospital stay (standard mean difference: -0.17, 95%CI: -0.30--0.04, P = 0.009) were significantly lower in the restrictive transfusion group compared to the liberal transfusion group[ 63 ].
Therefore, a restrictive transfusion strategy should be employed in managing patients with acute variceal bleeding. The current practice society guidelines do not recommend routine use of plasma products and platelet transfusion in this setting due to inconsistent data on the use of plasma products and reliability of prothrombin time (PT)/international normalized ratio (INR) in patients with cirrhosis[ 38 , 46 ]. However, platelet and plasma transfusion can be done in select patients who are hemodynamically unstable with active variceal bleeding (goal: platelet count > 50000/ μL and INR < 1.5)[ 47 ].
Vasoactive agents: Vasoactive agents such as octreotide, terlipressin, somatostatin, and vasopressin cause splanchnic vasoconstriction and thus reduce portal pressure. All patients with confirmed or suspected variceal bleeding should be started on vasoactive agents as early as possible and should be continued for 2-5 d. They can be stopped early if the patient undergoes a TIPS procedure.
Terlipressin is a synthetic analog of vasopressin. The role of terlipressin in acute variceal bleeding was analyzed in a meta-analysis involving 1609 patients from 22 studies. Among those 22 studies, seven studies (443 patients) compared the effect of terlipressin to a placebo group. Terlipressin group was noted to have a statistically significant reduction in all-cause mortality (relative risk = 0.66, 95%CI: 0.49-0.88). Remaining studies compared terlipressin to somatostatin, octreotide, vasopressin or balloon tamponade. There was no significant difference in mortality or adverse events between the groups[ 64 , 65 ].
Use of vasoactive agents has been shown to reduce acute bleeding, need for transfusion, and seven-day all-cause mortality[ 66 ]. There was no significant difference in their efficacy or benefits noted between these agents[ 67 ].
Antibiotics: Short-term antibiotics should be started in all patients with suspected or confirmed variceal bleeding to reduce bacterial infection, recurrent bleeding, and mortality[ 38 , 48 , 68 , 69 ]. Bacterial infection is also considered to be an independent risk factor for variceal rupture. Choice of antibiotics should be based on local resistance pattern. However, third-generation cephalosporins with gram-negative coverage are commonly used. Intravenous ceftriaxone 1 g, every 24 h for a maximum of 7 d is preferred over oral fluroquinolones[ 38 , 46 ].
Other considerations: Most patients with variceal bleeding have loss of intravascular volume, and it is paramount to prevent hypotension. Due to the risk of hypotension and hemodynamic deterioration, nonselective beta-blockers should not be started during acute variceal bleeding and should be discontinued if the patient is already taking. However, nonselective beta-blockers should be restarted after the acute event, once hemostasis is achieved and vasoactive agents are discontinued.
Endoscopic management
Endoscopic intervention should be performed as early as possible but should be within 12 h from the time of presentation as per practice society guidelines. The diagnosis of variceal bleeding as the etiology of acute upper gastrointestinal bleeding is made when any of the following is noted on upper endoscopy: (1) Actively bleeding varices (Figure (Figure5); 5 ); (2) Signs of recent bleeding noted on varices or high-risk stigmata; e.g ., telangiectasia, red color signs, platelet-fibrin plug (white nipple sign), red wale marking or varices on varices (Figure (Figure6); 6 ); (3) Presence of varices and blood is noted in the stomach, with no other source of bleeding noted.

Bleeding esophageal varices.

High-risk stigmata of bleeding from esophageal varices. A: Platelet-fibrin plug on esophageal varix (white nipple sign); B: Bleeding esophageal varix post banding.
EVL (Figure (Figure7) 7 ) was first proposed for the treatment of esophageal varices in 1988 by Van Stiegmann et al[ 70 ]. Currently, EVL is considered to be the first line of endoscopic treatment for the management of bleeding esophageal varices. EVL has better hemostasis, a lower rate of side effects (ulcer, stricture), a reduced rate of early rebleeding, and a lower rate of early mortality compared to sclerotherapy. Higher rebleeding in sclerotherapy is thought to be due to sustained elevation of HVPG, whereas HVPG returned to baseline with EVL[ 71 - 73 ]. The slightly higher rate of variceal recurrence after EVL, when compared to sclerotherapy is due to its inability to affect the blood flow through perforators and esophageal collateral veins.

Endoscopic variceal band ligation.
Treatment failure
Sengstaken-Blakemore tube : Whenever variceal bleeding is not controlled by EVL, temporary hemostatic measures should be used as a bridge to more definitive treatment, such as TIPS or variceal shunt surgery. Sengstaken-Blakemore tube is inserted through the mouth or nose and then distended to achieve hemostasis during active variceal bleeding by tamponading varices. The rate of hemostasis with Sengstaken-Blakemore tube varies (47%-80%). It is associated with a high rate of serious adverse events including aspiration, esophageal ulceration, and rarely esophageal rupture. Sengstaken-Blakemore tubes cannot be left in place for more than 24 h due to an increased risk of adverse events and a high rate of rebleeding (50%)[ 72 , 73 ].
Metal stents : Endoscopically placed self-expanding fully covered metal stents (Figure (Figure8) 8 ) can achieve hemostasis in most cases (80%-96%). The stents expand inside the esophagus and tamponade the varices to achieve hemostasis. They can be left in place for up to 2 wk and have a lower rate of serious adverse events and transfusion requirements when compared to balloon tamponade[ 74 , 75 ]. Adverse events associated with this modality of treatment include stent migration (28%), rebleeding (16%) and ulcers. However, there was no significant difference in mortality compared to balloon tamponade[ 76 , 77 ].

Metal stents for the treatment of bleeding esophageal varices. A: Bleeding esophageal varix before stenting; B: Esophageal varix after metal stent.
In a meta-analysis of 12 studies ( n = 155) hemostasis was achieved in 96% (95%CI: 0.90-1.00) of the patients within 24 h with 97% technical success (95%CI: 0.91-1.00). Adverse events (rebleeding, ulceration and stent migration) were noted in 36% (95%CI: 0.23-0.50) of the patients. Pooled susvival rate at 30 d and 60 d were 68% (95%CI: 0.56-0.80) and 64% (95%CI: 0.48-0.78) respectively[ 78 ]. Similar results were noted in another meta analsysis of 5 studies ( n = 80) with technical success of 96.7% (95%CI: 91.6%-99.5%) and hemostasis of 93.9% (95%CI: 82.2%-99.6%). Rebleeding was observed in 13.2% (95%CI: 1.8%-32.8%) and the overall mortality was 34.5% (95%CI: 24.8%-44.8%)[ 79 ].
Based on the above evidence, self-expanding metal stents are a better choice for bridge therapy in uncontrolled esophageal variceal bleeding and should be used whenever available.
Patients with uncontrolled variceal hemorrhage despite the combination of medical and endoscopic treatment should be considered for early TIPS within (24 h) with covered PTFE (polytetrafluoroethylene) stents. TIPS is a shunt created by placing a stent between the portal vein and hepatic vein to reduce the portal pressure and thereby portal hypertension. Also, early rebleeding (within five days of initial bleeding) can be treated with repeat endoscopic intervention or covered TIPS stent[ 38 , 46 , 48 ].
TIPS vs pharmacotherapy and endoscopic treatment
In a meta-analysis of six comparative studies, TIPS was compared with medical and endoscopic treatment for acute variceal bleeding. In this study, the survival rate (HR = 0.55; 95%CI: 0.38-0.812) was better in TIPS patients, and the incidence of bleeding-related death (OR = 0.19; 95%CI: 0.06-0.59) was lower compared to medical/endoscopic treatment. There was no significant increase in hepatic encephalopathy (OR = 1.37; 95%CI: 0.63-2.99) in TIPS patients. Although there was no significant difference in rebleeding rate between the two groups, it was evident that rebleeding in the high-risk patients was higher on subgroup analysis[ 80 ].
Early TIPS vs pharmacotherapy and endoscopy in high-risk patients
Patients with Child-Pugh class B with active bleeding and class C are considered high-risk due to increased risk of treatment failure and rebleeding.
In a 2010 study, early TIPS was compared with pharmacotherapy (vasoactive agents) and EVL in Child-Pugh class C patients and class B patients with a high risk of treatment failure. Sixty-two patients were randomized into the treatment group (early TIPS, n = 32), and control group (pharmacotherapy and EVL, n = 31). Rescue TIPS was used in control group as needed for treatment failure. Rebleeding or failure to control bleeding occurred in one patient in the early TIPS group and 14 patients in the control group ( P = 0.001). The one-year actuarial survival rate was 61% in the control group vs 86% in the early-TIPS group ( P < 0.001)[ 81 ].
In another international multicenter observational study (671 patients from 34 centers) patients who were admitted for acute variceal bleeding with Child-Pugh class C, and Child-Pugh class B with active bleeding were included in the study. Patients were treated with either pharmacotherapy and endoscopic interventions or preemptive TIPS. Preemptive TIPS was associated with significantly lower one-year mortality (22% vs 47%, P = 0.002), treatment failure and rebleeding (92% vs 74%, P = 0.017) when compared to patients treated with pharmacotherapy and endoscopic interventions. TIPS also prevented the development of new ascites or worsening of pre-existing ascites[ 82 ]. Even though these results are encouraging, it was an observational study, and patients were not randomized. Each center chose to treat the patient with either preemptive TIPS or medications and endoscopy at its discretion. Therefore, the results may not be generalized. However, large RCTs can determine the use of preemptive TIPS in this high-risk population[ 82 ].
Complications from TIPS include hepatic encephalopathy, heart failure, and stent stenosis. The incidence of hepatic encephalopathy is close to 50% without a significant difference in mortality[ 83 ]. Absolute contraindications for TIPS include heart failure, severe pulmonary hypertension, severe tricuspid valve regurgitation, sepsis, and unrelieved biliary obstruction. Relative contraindications are portal vein thrombosis, hepatoma, uncorrected coagulopathy, and severe thrombocytopenia (platelet count < 20000/μL).
Direct ultrasound-guided direct intrahepatic porto-caval shunt
Patients who failed TIPS, those who have altered anatomy due to previous surgery or congenital anomaly, or are otherwise not candidates for TIPS, can be treated with direct ultrasound-guided direct intrahepatic porto-caval shunt (DIPS)[ 84 ]. The DIPS is a modified TIPS procedure, and it involves percutaneous ultrasound-guided puncture from the inferior vena cava to the portal vein through the caudate lobe of the liver.
Porto-caval shunt surgeries
Surgical shunts are considered when all other treatment modalities fail. Portocaval surgery has a very high rate of encephalopathy but does have good bleeding control. Most patients who undergo portocaval shunt surgery already have high morbidity and surgery adds to it further[ 85 ]. In a recent RCT, emergency TIPS procedure was compared with emergency portocaval shunt surgery, and shunt surgery was noted to have superior bleeding control, long-term survival (10 years vs 1.99 years) and low rate of encephalopathy. However, this has not been replicated, and more evidence is required before using portocaval shunt surgery as a salvage procedure after failure of first-line treatment with medical therapy and EVL[ 86 ].
Secondary prophylaxis
Patients who were treated with EVL and medical therapy without TIPS are at high risk for rebleeding. Approximately 60% of patients will experience rebleeding during the first year and have a high mortality rate (up to 33%) with no further intervention. Combination therapy with nonselective beta blockers (propranolol and nadolol) and EVL is the first line of treatment for secondary prophylaxis with a goal to eradicate varices and prevent recurrent bleeding[ 87 ]. TIPS should be considered if patients do not tolerate or fail the combination of nonselective beta-blockers and EVL.
A multicenter RCT compared TIPS with the combination of EVL or glue injection and nonselective beta-blockers. Patients in the TIPS group had a significantly lower rebleeding rate (0%) compared to the EVL or glue injection and nonselective beta blockers group (29%) without a significant difference in survival benefit[ 88 ].
GASTRIC VARICES
GVs are less frequent compared to esophageal varices and are reported to be seen in 20% of the patients with portal hypertension[ 38 , 89 ]. Bleeding from GVs account for 20% of all variceal bleeding[ 48 ]. The annual bleeding rate in GVs, which have never bled before is reported to be as low as 16% per year. Sarin et al[ 90 ] classified GVs based on their location.
Sarin classification
Shown in Figure Figure9. 9 . Gastroesophageal varix type 1 (GOV1): Extension of esophageal varices along lesser curvature (most common 75% of GVs); GOV2: Extension of esophageal varices along the greater curvature; Isolated gastric varix type 1 (IGV1): Isolated varices seen in the fundus of the stomach; IGV2: Isolated varices in the stomach (body, pylorus, antrum).

Sarin classification of gastric varices. GOV1: Gastroesophageal varix type 1; GOV2: Gastroesophageal varix type 2; IGV1: Isolated gastric varix type 1; IGV2: Isolated gastric varix type 2.
Predictors of bleeding from GVs
Location (IGV1 > GOV2 > GOV1); The severity of liver disease; Stigmata of high-risk bleeding such as ‘red wale’ sign.
GVs bleed less frequently but have high mortality due to the severity of bleeding. Bleeding from IGV is associated with the highest risk of death[ 38 , 48 , 91 ].
GVs have complex anatomy and understanding the anatomy assists in the endoscopic management of GVs. The most common type of GVs are GOV1 and are usually associated with portal hypertension due to cirrhosis. They are a continuation of esophageal varices along the lesser curvature of the stomach. These are supplied by the esophageal collateral veins and are also treated similarly to esophageal varices.
On the other hand, GOV2 and IGV1 are supplied by the posterior and left gastric vein, which later drains into left renal vein due to porto-systemic shunting. Therefore GOV2 and IGV1 are together called cardiofundal varices[ 91 ]. Isolated IGV1 can be associated with splenic vein thrombosis in the setting of pancreatitis or malignancy.
Diagnosis of GVs
Diagnosis of GVs (Figure (Figure10) 10 ) is commonly done with endoscopy. However, the recent use of EUS has increased the sensitivity of detecting GVs. No guidelines are currently available regarding the use of endoscopy or EUS specifically to diagnose GVs.

Gastric varices.
Management of patients with GVs that have not bled
Primary prophylaxis for GVs is not well established. Currently, nonselective beta-blockers are the first line of treatment as per practice society guidelines, in large part due to their ability to prevent other complications of cirrhosis. The role of endoscopic glue (N-butyl-2-cyanoacrylate) injection and EVL in primary prophylaxis are not clear. One study has shown glue injection was associated with lower bleeding and mortality due to GVs when compared to nonselective beta blockers[ 92 ]. Prophylactic EUS guided injection has also shown to be equally beneficial, and further studies are required to evaluate its role in primary prophylaxis for GVs.
Management of acute gastric variceal bleeding
Medical management of suspected gastric variceal bleeding is similar to esophageal variceal bleeding as described above, including airway protection, admission to the intensive care unit, blood transfusion, vasoactive agents, and antibiotics (Figure (Figure11 11 ).

Algorithm for the management of acute variceal bleed. ICU: Intensive care unit; EGD: Esophago-gastro duodenoscopy; NSBB: Nonselective beta blockers; EVL: Endoscopic variceal ligation; TIPS: Transjugular intrahepatic portosystemic shunt.
Endoscopic interventions
Diagnosis of gastric variceal bleeding can be made based on endoscopic findings. Most practice guidelines recommend endoscopic glue injection as the first line of treatment in the management of acute gastric variceal bleeding. However, glue injection comes with the risk of several complications including venous and systemic thromboembolism (pulmonary embolism, stroke), ulcers, protracted bleeding, splenic and portal vein thrombosis[ 93 ]. Portal vein thrombosis due to embolized glue can render a future plan for TIPS and liver transplantation ineffective. Embolized glue can also act as a nidus of infection and cause recurrent bacteremia[ 94 ]. Successful glue injection requires experience due to gastric anatomy. Because of the drawbacks mentioned above, many centers use TIPS as the first line of treatment in managing acute gastric variceal bleeding.
A RCT compared efficacy and complication of TIPS and glue injection in treating GVs. Rebleeding (11% vs 38%, P = 0.014; OR = 3.6, 95%CI: 1.2-11.1) and transfusion requirements were lower ( P < 0.01) in TIPS compared to endoscopic glue injection with similar initial hemostasis, side effects, and mortality[ 95 ].
Even though initial hemostasis in both glue injection and EVL is similar for GOV1 GVs, rebleeding is high in EVL. So EVL should be avoided[ 96 - 98 ]. Combination of sclerotherapy and EVL is currently not recommended due to a higher rate of complications, and adverse events without mortality benefit[ 99 ]. In a recent RCT, scleroligation (variceal ligation + sclerotherapy) compared to EVL alone, in the management of GOVs, the scleroligation group required a lower number of endoscopic procedures, transfusion, and bands used, without a significant difference in recurrence rate, major side effects, and mortality[ 100 ]. Further research is needed to prove the benefits of scleroligation.
The recent emergence of EUS guided glue and coil injection in treating GVs has shown a lower bleeding rate, transfusion requirements, and mortality when compared to glue injection. When EUS guided coil embolization alone was compared with EUS guided glue injection, both had similar hemostasis rates, but coil embolization had fewer adverse events and required a fewer number of endoscopies[ 101 ]. When these two techniques were combined (glue + coil), the mean number of coils used, mean volume of glue used, and the recurrence rate was lower compared to either of them alone[ 102 ].
Patients with uncontrolled gastric variceal bleeding despite endoscopic intervention should be managed with balloon tamponade with Sengstaken-Blakemore tube or Linton-Nachlas tube as a bridge to definitive treatment. In a controlled trial Sengstaken-Blakemore tube failed to control gastric variceal bleeding in all the cases, and 50% hemostasis was achieved by Linton-Nachlas tube. Types of GVs and their frequency between the two groups was not available[ 73 ]. This difference could be attributed to a larger gastric balloon (500 mL) when compared to smaller gastric balloon in the Sengstaken-Blakemore tube. Therefore, Linton-Nachlas tube should be used whenever possible.
Hemostatic powder
Hemostatic powder (TC 325 - hemospray) and similar products have been used as bridging therapy in controlling acute peptic ulcer bleeding in the past. The hemostatic powder when sprayed at the bleeding site, it absorbs water and creates a mechanical barrier to achieve hemostasis. Recently one study assessed its role in acute variceal bleeding. Hemostasis in the study group was better than the control group, with fewer study group patients requiring rescue endoscopy (12%). Rescue endoscopy was performed if initial hemostasis was not achieved within the first 12 h with hemospray. All patients were later treated with definitive endoscopic intervention after 24 h. Larger RCTs are required to evaluate the role of hemostasis powder, and currently not approved by Food and Drug Administration[ 103 , 104 ].
Patients with GVs who fail to respond to the endoscopic treatment will require TIPS or shunt surgery to control acute variceal bleeding. Recurrent bleeding is noted in 11%-30% of the patients who undergo TIPS.
Balloon-occluded retrograde transvenous obliteration
Patients with GVs and gastro-renal collaterals can be treated with balloon-occluded retrograde transvenous obliteration (BRTO). This procedure involves retrograde cannulation of the outflow channels which drain the GVs through the femoral or jugular vein, and obliteration of the varices and collaterals assisted by balloon occlusion and followed by coil and sclerosant. Various studies have evaluated its efficacy in treating GVs. A recent meta-analysis showed a success rate for obliteration was 97.3%, and 33.3% recurrence. BRTO can be considered as an alternative to TIPS in managing GVs. A retrospective review of 142 consecutive patients treated for acute gastric variceal bleeding comparing the efficacy of BRTO ( n = 95) and TIPS ( n = 47) showed significantly lower rebleeding rate in BRTO (8.6%) group compared to TIPS (19.8%)[ 105 ] at the end of the first year. There was no significant difference in mortality. BRTO is mostly done in Asian countries, but recently it is gaining popularity in the United States[ 38 , 48 , 106 ].
Risk of rebleeding among patients who are treated with glue injection for gastric variceal bleeding was noted to vary from 15%-72%[ 98 , 107 , 108 ]. TIPS is considered to be superior to endoscopic glue injection for secondary prophylaxis of GVs[ 38 ]. However, there is no significant mortality benefit when compared to glue injection. The role of nonselective beta-blockers is not evident in secondary prophylaxis of GVs. Data on EUS guided glue injection and coiling for primary and secondary prophylaxis is lacking. Larger multicenter RCTs will help in understanding the role of EUS in the management of GVs.
ECTOPIC GASTROINTESTINAL VARICES
Gastrointestinal varices can develop in the duodenum, rectum, colon, small bowel, gallbladder and the retroperitoneal areas. The prevalence of ectopic gastrointestinal varices is unknown. According to one estimate, among patients with cirrhosis and portal hypertension who underwent angiography, 40% of patients had duodenal varices. Ectopic varices are responsible for up to 1%-5% of all variceal bleeding. Understanding the complex anatomy of ectopic varices, and their anastomosis with mesenteric veins is essential in managing ectopic varices[ 91 , 109 ].
Duodenal varices
Duodenal varices are more commonly seen in noncirrhotic, extrahepatic portal hypertension ( e.g ., portal vein thrombosis, splenic vein thrombosis) and their prevalence is around 0.4%[ 109 ]. Duodenal varices form due to Porto-mesenteric and Porto-portal anastomosis. Duodenal varices are noted on endoscopy as submucosal dilated veins, usually arising from anastomosis between tributaries of the superior mesenteric vein and portal vein draining into inferior vena cava. EUS is notably superior in diagnosing duodenal varices compared to EGD[ 110 ]. Acute duodenal variceal bleeding is usually treated with endoscopic glue injection. There have been no RCTs evaluating the treatment strategies for duodenal varices owing to their rarity. In the largest case series involving ten patients with duodenal variceal glue injection, 4 out of the five patients who presented with acute bleeding were treated with endoscopic glue injection and had 100% hemostasis rate without recurrence[ 110 ]. Duodenal varices bleed at a lower hepatic venous pressure gradient, and therefore TIPS may not be sufficient to treat duodenal varices and need further definitive treatment with intravascular obliteration with glue injection, or embolization through BRTO. BRTO can also be used for patients who fail endoscopic therapy and are not candidates for TIPS[ 111 ].
Rectal varices
Rectal varices usually arise from portosystemic anastomosis between superior hemorrhoidal veins (a tributary of the inferior mesenteric vein) and the middle or inferior hemorrhoidal veins (tributaries of iliac or pudendal veins). Prevalence of rectal varices patients with portal hypertension varies from 28%-56% in cirrhotic patients[ 112 ], and are more common among patients with extrahepatic portal vein obstruction(up to 90%)[ 113 ]. EUS has a higher sensitivity to detect rectal varices compared to endoscopy. Risk of bleeding from rectal varices is 8%-38%[ 112 ]. Rectal varices bleed at the lower hepatic venous pressure gradient and may not disappear with TIPS. Endoscopic variceal band ligation is the preferred method of treatment for rectal varices compared to endoscopic sclerotherapy or glue injection, but the recurrence rate of rebleeding is high with Endoscopic variceal band ligation. Recurrent bleeding in endoscopic sclerotherapy (33%) was much lower compared to EVL (55.6%)[ 114 ] but not commonly used due to the occurrence of severe ulcers. Endoscopic glue injection can be useful in managing rectal varices, but nearly 0.5%-4.3% of these patients develop embolization. EUS guided coil and glue embolization is also considered useful in large rectal varices that are not amenable to variceal ligation[ 115 ]. Role of BRTO has been evaluated in small case series; no RCTs are available to compare its efficacy. Optimal management of rectal varices is not yet established.
Stomal varices
Stomal varices usually occur at the mucocutaneous junction of the stoma, due to portosystemic shunt between the portal circulation of the bowel and systemic circulation of the abdominal wall. Diagnosis of stomal varices is difficult, on physical exam, they appear as bluish discoloration of the skin. Visibly dilated veins and characteristic raspberry appearance of the stoma should prompt further evaluation for the cause of bleeding. Patients with stomal varices can be treated with a glue injection. Percutaneous sclerotherapy is not recommended due to increased risk of damaging the stoma. Gastrointestinal varices can also form in other parts of the gastrointestinal tract including jejunum, ileum, and colon as well. The actual prevalence of these varices is unknown but considered to be low.
In summary, development, and utilization of newer treatment modalities such as therapeutic EUS, BRTO, and hemospray in managing gastrointestinal varices will help to reduce further- the morbidity and mortality related to variceal bleeding. Further research in understanding the risk factors, mechanism of liver injury, and evaluation of antifibrotic agents to prevent architectural changes to the liver can revolutionize the management of portal hypertension and its complications.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: None of the authors have any conflicts of interest.
Peer-review started: August 27, 2018
First decision: October 5, 2018
Article in press: December 11, 2018
P- Reviewer: Lo GH, Qi XS S- Editor: Ma RY L- Editor: A E- Editor: Bian YN
Contributor Information
Umesha Boregowda, Department of Gastroenterology and Hepatology, University of California San Francisco, Fresno, CA 93721, United States.
Chandraprakash Umapathy, Department of Gastroenterology and Hepatology, University of California San Francisco, Fresno, CA 93721, United States.
Nasir Halim, Department of Gastroenterology and Hepatology, University of California San Francisco, Fresno, CA 93721, United States.
Madhav Desai, Department of Gastroenterology and Hepatology, Kansas University Medical Center, Kansas City, KS 66160, United States.
Arpitha Nanjappa, Department of Gastroenterology and Hepatology, University of California San Francisco, Fresno, CA 93721, United States.
Subramanyeswara Arekapudi, Department of Medicine, VA Central California Healthcare System, Fresno, CA 93703, United States.
Thimmaiah Theethira, Department of Gastroenterology and Hepatology, University of California San Francisco, Fresno, CA 93721, United States.
Helen Wong, Department of Gastroenterology and Hepatology, VA Central California Healthcare System, Fresno, CA 93703, United States.
Marina Roytman, Department of Gastroenterology and Hepatology, University of California San Francisco, Fresno, CA 93721, United States.
Shreyas Saligram, Department of Gastroenterology and Hepatology, University of California San Francisco, Fresno, CA 93721, United States. Department of Gastroenterology and Hepatology, VA Central California Healthcare System, Fresno, CA 93703, United States. ude.fscu.onserf@margilass .

IMAGES
VIDEO
COMMENTS
Nursing Case Studies by and for Student Nurses. 25. The following is a scenario of a patient who experienced ruptured esophageal varices. The patient, Nora Allen, a 55-year-old female presented to the emergency department (ER) on May 5, 2017 just after 10:00 a.m., with complaints of two episodes of melena that morning. ...
Nov 13, 2018 • Knowledge. Clinical Case Scenario #1. Health Education for a Male Inpatient with Esophageal Varices. Clinical Scenario. Forty five year old G.K. is admitted to the hospital's Emergency Department. He is vomiting large amounts of blood. He is mildly intoxicated but alert. His pulse is fast and thready.
Nursing Care Plan for Esophageal Varices 2. Nursing Diagnosis: Imbalanced Nutrition: Less than Body Requirements related to digestive tract bleeding secondary to esophageal varices, as evidenced by hematemesis, weight loss, nausea and vomiting, loss of appetite and dizziness/ lightheadedness.
CASE SUMMARY. A 46-year-old woman, who denied a history of liver disease, was admitted to our hospital on presentation of hematemesis. Laboratory examination revealed a hemoglobin level of 83 g/L, and a platelet count of 397 × 10 9 /L. The appearance of gastric and esophageal varices with red colored signs as displayed by an urgent endoscopy was followed by endoscopic variceal ligation and ...
Esophageal varices are dilated submucosal distal esophageal veins connecting the portal and systemic circulations. This happens due to portal hypertension (most commonly a result of cirrhosis), resistance to portal blood flow, and increased portal venous blood inflow. The most common fatal complication of cirrhosis is variceal rupture; the severity of liver disease correlates with the presence ...
Esophageal varices incidences are increasing by nearly 5% every year. Esophageal varices are the causes of bleeding in approximately 18% of hospital admissions for upper GI bleeding. Objective: The purpose of this study is to understand the cause, clinical manifestations and treatment course for esophageal varices.
Esophageal varices (EV) are one of the most common causes of acute upper gastrointestinal bleeding (UGIB) with varying prevalence worldwide [1,2]. They are the leading cause of death from UGIB. ... This case study validates the efficacy of the EUS coil/CYA in the treatment of GV. Coil placement, with or without CYA, can have unfavorable ...
The development of this nursing guideline was coordinated by Rachel Horn, CNC, Gastroenterology, and Laura Davies, CNS, Cockatoo, approved by the Nursing Clinical Effectiveness Committee. ... Some small case-series paediatric studies have been undertaken (421). ... Assessment of risk of bleeding from esophageal varices during management of ...
Esophageal varices are primarily caused by increased pressure in the portal vein system, which can result from various underlying medical conditions. ... Study More in Less Time. Using a study tool can help you keep engaged and at a steady pace when studying conditions like esophageal varices. SimpleNursing is trusted by nursing students to ...
Main tests used to diagnose esophageal varices are: Endoscopic exam. A procedure called upper gastrointestinal endoscopy is the preferred method of screening for esophageal varices. An endoscopy involves inserting a flexible, lighted tube called an endoscope down the throat and into the esophagus.
Esophageal varices are abnormal, enlarged veins in the tube that connects the throat and stomach. Variceal rupture is governed by Laplace's law. Increased wall tension is the end result of increased intravariceal pressure, increased diameter of the varices, and reduced wall thickness. The variceal wall thickness can be evaluated visually by the ...
Introduction: Esophageal varices are a critical and potentially life-threatening medical condition often associated with underlying liver disease. These enlarged, fragile veins in the lower esophagus pose a significant risk of bleeding and require vigilant care and management. This nursing care plan is designed to provide a structured approach ...
The rates of development and growth of EV are most likely related to the degree of hepatic dysfunction, and once varices develop, they typically increase in size. 1 The prevalence of esophageal varices is reported to be 42% in CTP-A, 71% in CTP-B, and 76% in CTP-C cirrhosis. 2 The risk of bleeding for small and large varices is estimated at 5% ...
Identify the diagnostic procedures and nursing implications for esophageal varices. 6. Compare and contrast the treatment options and nursing implications for esophageal varices. 7. Discuss the rationale for Mr. Hubert's vasopressin therapy, management of side effects, and nursing concerns. 8.
Definition Bleeding esophageal varices are hemorrhagic processes involving dialted, tortuous veins in the submucosa of the lower esophagus. . Risk Factors Portal hypertension resulting from obstructed portal venous circulation Pathophysiology In portal hypertension, collateral circulation develops in the lower esophagus as venous blood, which is diverted from the GI tract and spleen because of ...
Objectives To identify and understand Nursing care in patients with esophageal varices.; Methods to adopt while managing acute variceal bleeding.; Nurses role in prevention of secondary bleeding. Design: used for this article is to review method. Data sources are different types of Medical and Gastroenterology text books, Medical Journals and Medical Surgical Nursing Text Books.
All the pertinent investigations were studied thoroughly of the selected case. Results: the esophageal varices is confirmed with the help of Upper gastrointestinal gastroscopy and repaired by banding. Conclusion: Esophageal varices is usually goes undiagnosed due to early common symptoms. ... Esophageal Varices: A Case Study. Asian J. Nursing ...
JT Esophageal varices are caused by portal hypertension most commonly due to cirrhosis or to portal vein thrombosis. In patients with cirrhosis, the liver becomes fibrotic and hardened and the blood is unable to pass through the liver from the visceral veins. ... Call for Case Studies. We invite our readers to submit case studies for ...
CASE STUDY ESOPHAGEAL VARICES 23. For the Disease Summary for this case study, see the CD-ROM. 108 PART 3 GASTROINTESTINAL DISORDERS. Intravenous infusion with a solution of D 5 W and colloid was begun through a central line. Oxygen was started at 3 L/min. Octreotide was administered to help stop the bleeding. A physical examination was performed.
The end-stage of liver disease is called cirrhosis. Hepatic cirrhosis is a chronic hepatic disease characterized by diffuse destruction and fibrotic regeneration of hepatic cells. As necrotic tissue yields to fibrosis, this disease alters liver structure and normal vasculature, impairs blood and lymph flow, and ultimately causes hepatic ...
Abstract. Esophageal varices are about 10%-15% of UGIB. Over 90% of patients with cirrhosis develop portal hypertension (PHT), but not all patients with PHT and liver cirrhosis have esophageal varices. At the time of diagnosis, only 60% of patients with cirrhosis have esophageal varices. In the case of variceal bleeding suspects, vasoactive ...
CASE STUDY ESOPHAGEAL VARICES PATIENT PRESENTATION Chief Complaint "I've been throwing up blood, enough to fill my bathroom sink!" HPI Ethyl Johnson is a 55-year-old woman who presents to the ED with complaint of vomiting blood and bright red blood per rectum. She was in her usual state of health, until shortly after taking a dose of lactulose when she began to feel sick and subsequently ...
A prospective case study showed that the use of nonselective beta-blockers in this patient group was associated with increased mortality ... Smith C, Lieberman G. The natural history of esophageal varices; a study of 115 cirrhotic patients in whom varices were diagnosed prior to bleeding. Am J Med. 1959; 26:228-237. [Google Scholar] 17. ...