An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Vivek Podder ; Valerie Lew ; Sassan Ghassemzadeh .
Affiliations
Last Update: August 28, 2023 .
- Introduction
The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers. The SOAP note is a way for healthcare workers to document in a structured and organized way. [1] [2] [3]
This widely adopted structural SOAP note was theorized by Larry Weed almost 50 years ago. It reminds clinicians of specific tasks while providing a framework for evaluating information. It also provides a cognitive framework for clinical reasoning. The SOAP note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the information provided by them. SOAP notes are an essential piece of information about the health status of the patient as well as a communication document between health professionals. The structure of documentation is a checklist that serves as a cognitive aid and a potential index to retrieve information for learning from the record. [4] [5] [6]
The 4 headings of a SOAP note are Subjective, Objective, Assessment and Plan. Each heading is described below.
This is the first heading of the SOAP note. Documentation under this heading comes from the “subjective” experiences, personal views or feelings of a patient or someone close to them. In the inpatient setting, interim information is included here. This section provides context for the Assessment and Plan.
Chief Complaint (CC)
The CC or presenting problem is reported by the patient. This can be a symptom, condition, previous diagnosis or another short statement that describes why the patient is presenting today. The CC is similar to the title of a paper, allowing the reader to get a sense of what the rest of the document will entail.
- Examples: chest pain, decreased appetite, shortness of breath.
However, a patient may have multiple CC’s, and their first complaint may not be the most significant one. Thus, physicians should encourage patients to state all of their problems, while paying attention to detail to discover the most compelling problem. Identifying the main problem must occur to perform effective and efficient diagnosis.
History of Present Illness (HPI)
The HPI begins with a simple one line opening statement including the patient's age, sex and reason for the visit.
- Example: 47-year old female presenting with abdominal pain.
This is the section where the patient can elaborate on their chief complaint. An acronym often used to organize the HPI is termed “OLDCARTS”:
- Onset: When did the CC begin?
- Location: Where is the CC located?
- Duration: How long has the CC been going on for?
- Characterization: How does the patient describe the CC?
- Alleviating and Aggravating factors: What makes the CC better? Worse?
- Radiation: Does the CC move or stay in one location?
- Temporal factor: Is the CC worse (or better) at a certain time of the day?
- Severity: Using a scale of 1 to 10, 1 being the least, 10 being the worst, how does the patient rate the CC?
It is important for clinicians to focus on the quality and clarity of their patient's notes, rather than include excessive detail.
- Medical history: Pertinent current or past medical conditions
- Surgical history: Try to include the year of the surgery and surgeon if possible.
- Family history: Include pertinent family history. Avoid documenting the medical history of every person in the patient's family.
- Social History: An acronym that may be used here is HEADSS which stands for Home and Environment; Education, Employment, Eating; Activities; Drugs; Sexuality; and Suicide/Depression.
Review of Systems (ROS)
This is a system based list of questions that help uncover symptoms not otherwise mentioned by the patient.
- General: Weight loss, decreased appetite
- Gastrointestinal: Abdominal pain, hematochezia
- Musculoskeletal: Toe pain, decreased right shoulder range of motion
Current Medications, Allergies
Current medications and allergies may be listed under the Subjective or Objective sections. However, it is important that with any medication documented, to include the medication name, dose, route, and how often.
- Example: Motrin 600 mg orally every 4 to 6 hours for 5 days
This section documents the objective data from the patient encounter. This includes:
- Vital signs
- Physical exam findings
- Laboratory data
- Imaging results
- Other diagnostic data
- Recognition and review of the documentation of other clinicians.
A common mistake is distinguishing between symptoms and signs. Symptoms are the patient's subjective description and should be documented under the subjective heading, while a sign is an objective finding related to the associated symptom reported by the patient. An example of this is a patient stating he has “stomach pain,” which is a symptom, documented under the subjective heading. Versus “abdominal tenderness to palpation,” an objective sign documented under the objective heading.
This section documents the synthesis of “subjective” and “objective” evidence to arrive at a diagnosis. This is the assessment of the patient’s status through analysis of the problem, possible interaction of the problems, and changes in the status of the problems. Elements include the following.
List the problem list in order of importance. A problem is often known as a diagnosis.
Differential Diagnosis
This is a list of the different possible diagnosis, from most to least likely, and the thought process behind this list. This is where the decision-making process is explained in depth. Included should be the possibility of other diagnoses that may harm the patient, but are less likely.
- Example: Problem 1, Differential Diagnoses, Discussion, Plan for problem 1 (described in the plan below). Repeat for additional problems
This section details the need for additional testing and consultation with other clinicians to address the patient's illnesses. It also addresses any additional steps being taken to treat the patient. This section helps future physicians understand what needs to be done next. For each problem:
- State which testing is needed and the rationale for choosing each test to resolve diagnostic ambiguities; ideally what the next step would be if positive or negative
- Therapy needed (medications)
- Specialist referral(s) or consults
- Patient education, counseling
A comprehensive SOAP note has to take into account all subjective and objective information, and accurately assess it to create the patient-specific assessment and plan.
- Issues of Concern
The order in which a medical note is written has been a topic of discussion. While a SOAP note follows the order Subjective, Objective, Assessment, and Plan, it is possible, and often beneficial, to rearrange the order. For instance, rearranging the order to form APSO (Assessment, Plan, Subjective, Objective) provides the information most relevant to ongoing care at the beginning of the note, where it can be found quickly, shortening the time required for the clinician to find a colleague's assessment and plan. One study found that the APSO order was better than the typical SOAP note order in terms of speed, task success (accuracy), and usability for physician users acquiring information needed for a typical chronic disease visit in primary care. Re-ordering into the APSO note is only an effort to streamline communication, not eliminate the vital relationship of S to O to A to P.
A weakness of the SOAP note is the inability to document changes over time. In many clinical situations, evidence changes over time, requiring providers to reconsider diagnoses and treatments. An important gap in the SOAP model is that it does not explicitly integrate time into its cognitive framework. Extensions to the SOAP model to include this gap are acronyms such as SOAPE, with the letter E as an explicit reminder to assess how well the plan has worked. [7] [8] [9] [10]
- Clinical Significance
Medical documentation now serves multiple needs and, as a result, medical notes have expanded in both length and breadth compared to fifty years ago. Medical notes have evolved into electronic documentation to accommodate these needs. However, an unintended consequence of electronic documentation is the ability to incorporate large volumes of data easily. These data-filled notes risk burdening a busy clinician if the data are not useful. As importantly, the patient may be harmed if the information is inaccurate. It is essential to make the most clinically relevant data in the medical record easier to find and more immediately available. The advantage of a SOAP note is to organize this information such that it is located in easy to find places. The more succinct yet thorough a SOAP note is, the easier it is for clinicians to follow.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Vivek Podder declares no relevant financial relationships with ineligible companies.
Disclosure: Valerie Lew declares no relevant financial relationships with ineligible companies.
Disclosure: Sassan Ghassemzadeh declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Podder V, Lew V, Ghassemzadeh S. SOAP Notes. [Updated 2023 Aug 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- SOAP Methodology in General Practice/Family Medicine Teaching in Practical Context. [Acta Med Port. 2016] SOAP Methodology in General Practice/Family Medicine Teaching in Practical Context. Santiago LM, Neto I. Acta Med Port. 2016 Dec 30; 29(12):854-859. Epub 2016 Dec 30.
- Toward Medical Documentation That Enhances Situational Awareness Learning. [AMIA Annu Symp Proc. 2016] Toward Medical Documentation That Enhances Situational Awareness Learning. Lenert LA. AMIA Annu Symp Proc. 2016; 2016:763-771. Epub 2017 Feb 10.
- Shifting from SOAP Notes to Consult Notes for Clinical Documentation by Pharmacy Students. [Am J Pharm Educ. 2022] Shifting from SOAP Notes to Consult Notes for Clinical Documentation by Pharmacy Students. Bradley CL, Wieder K, Schwartz SE. Am J Pharm Educ. 2022 Oct; 86(7):8781. Epub 2021 Dec 2.
- Review The essential SOAP note in an EHR age. [Nurse Pract. 2016] Review The essential SOAP note in an EHR age. Pearce PF, Ferguson LA, George GS, Langford CA. Nurse Pract. 2016 Feb 18; 41(2):29-36.
- Review Your note, your way: how to write an inpatient progress note accurately and efficiently as an intern. [Postgrad Med J. 2023] Review Your note, your way: how to write an inpatient progress note accurately and efficiently as an intern. Wei M, Salgado E, Girard CE, Santoro JD, Lepore N. Postgrad Med J. 2023 Jun 8; 99(1171):492-497.
Recent Activity
- SOAP Notes - StatPearls SOAP Notes - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
15 SOAP Note Examples and Templates in 2024

By Jamie Frew on Apr 25, 2024.
Fact Checked by Nate Lacson.
Introduction
SOAP notes are a helpful method of documentation designed to assist medical and mental health professionals in streamlining their clinical notes . Using a template such as SOAP notes means that you can capture, store, and interpret your client's information consistently over time.
You probably already know this, but SOAP is an acronym that stands for subjective, objective, assessment, and plan. Each letter refers to the different components of a soap note and helps outline the information you need to include and where to put it.
Even though SOAP notes are a simple way to record your progress notes , having an example or template is still helpful. That's why we've taken the time to collate some SOAP note examples we think will help you write more detailed and concise SOAP notes.
SOAP Note acronym
- Subjective (S): The client's perspective regarding their experience and perceptions of symptoms, needs, and progress toward treatment goals. This section often includes direct quotes from the client/ patient, vital signs, and other physical data.
- Objective (O): Your observed perspective as the practitioner, i.e., objective data ("facts") regarding the client, like elements of a mental status exam or other screening tools, historical information, medications prescribed, x-rays results, or vital signs.
- Assessment (A): Your clinical assessment of the available subjective and objective information. The assessment summarizes the client's status and progress toward measurable treatment plan goals.
- Plan (P): The actions that the client and the practitioner have agreed upon to be taken due to the clinician's assessment of the client's current status, such as assessments, follow-up activities, referrals, and changes in the treatment.
How to write a SOAP note
Although every practitioner will have their preferred methods for writing SOAP notes, there are helpful ways to ensure you cover all the correct information. We've already covered the type of information that should be covered in each section of a SOAP note, but here are some additional ways to guarantee this is done well.
The subjective section covers how the patient feels and what they report about their symptoms. The main topic, symptom, or issue that the patient describes is known as the Chief Complaint (CC). There may be more than one CC, and the primary CC may not be what the patient initially reports on. As their physician, you need to ask them as many questions as possible so you can identify the appropriate CC.
A History of Present Illness (HPI) also belongs in this section. This includes questions like:
- When did the symptoms begin?
- When did you first notice the CC?
- Where is the CC located?
- What makes the CC better?
- What makes the CC worse?
Pro tip #1 : It is a good idea to include direct quotes from the patient in this section.
Pro tip #2: Writing the subjective section needs to be concise. This may mean compacting the information the patient has given you to get the information across succinctly.
The objective section includes the data that you have obtained during the session. This may include:
- Vital signs
- Laboratory results
- X-ray results
- Physical exam
Based on the subjective information that the patient has given you and the nature of their CC, you will respond appropriately and obtain objective data that indicates the signs of the CC.
In addition to gathering test/lab results and vital signs, the objective section will include your observations about how the patient presents. This has their behavior, effect, engagement, conversational skills, and orientation.
Pro tip #3 : Confusion between symptoms and signs is common. The patient's symptoms should be included in the subjective section. In contrast, signs refer to quantifiable measurements or objective observations you have gathered indicating the presence of the CC.
It can help to think of the assessment section of a SOAP note as the synthesis between the subjective and objective information you have gathered. Using your knowledge of the patient's symptoms and the signs you have identified will lead to a diagnosis or informed treatment plan.
If there are several different CCs, you may want to list them as ‘Problems,' as well as the responding assessments. Practitioners frequently use the assessment section to compare their patients' progress between sessions, so you want to ensure this information is as comprehensive as possible while remaining concise.
Pro tip #4 : Although the assessment plan synthesizes information you've already gathered, you should never repeat yourself. Don't just copy what you've written in the subjective and objective sections.
The final section of a SOAP note covers the patient's treatment plan in detail based on the assessment section. You want to include immediate goals, the date of the next session (where applicable), and what the patient wants to achieve between their appointments.
In future sessions, you can use the plan to identify the patient's progress and judge whether the treatment plan requires changing.
The plan section may also include:
- Referrals to specialists
- Patient education
- Medications
- If further testing is required
- Progression or regression made by the client
15 SOAP note examples and templates
Although the above sections help outline the requirements of each SOAP notes section , having an example in front of you can be beneficial. That's why we've taken the time to collate some examples and SOAP note templates we think will help you write more detailed and concise SOAP notes.
SOAP note example for nurses or Nurse practitioners
John reports that he is feeling 'tired' and that he 'can't seem to get out of bed in the morning.' John is 'struggling to get to work' and says that he 'constantly finds his mind wandering to negative thoughts.' John stated that his sleep had been broken and he does not wake feeling rested. He reports that he does not feel as though the medication is making any difference and thinks he is getting worse.
John was unable to come into the practice and so has been seen at home. John's personal hygiene does not appear to be intact; he was unshaven and dressed in track pants and a hooded jumper which is unusual as he typically takes excellent care in his appearance. John appears to be tired; he is pale in complexion and has large circles under his eyes.
John's compliance with his new medication is good, and he appears to have retained his food intake. Weight is stable and unchanged.
John presents with symptoms consistent with a major depressive episode. This is evidenced by his low mood, slowed speech rate and reduced volume, depressed body language, and facial expression. However, it's important to note that this assessment is based on the information presented and a full diagnosis can only be confirmed by a qualified mental health professional.
Further exploration is needed to understand the duration and severity of these symptoms, as well as any potential contributing factors such as life stressors, medical conditions, or personal history. Additionally, while suicidal ideation is currently denied, it is crucial to monitor for any changes and ensure appropriate safety measures are in place.
Diagnosis: Major Depressive Disorder, Recurrent, Severe (F33.1 ICD-10) - Active
Problem: Depressed Mood
Rationale: John's depressed mood, evidenced by ongoing symptoms consistent with Major Depressive Disorder, significantly impacts his daily life and requires continued intervention.
Long-term goal: John will develop skills to recognize and manage his depression effectively.
Short-term goals and interventions:
- Maintain treatment engagement: Continue attending weekly individual therapy sessions to address negative thinking patterns, build coping mechanisms, and monitor progress.
- Optimize medication: Collaborate with the prescribing physician to continue titration of the SSRI fluoxetine as needed, ensuring optimal symptom control.
- Engage in daily physical activity: Encourage participation in structured physical activity, such as walking Jingo once a day, to improve mood and energy levels.
- Implement a safety plan: Develop a collaborative safety plan with John outlining clear steps and resources he can access in moments of suicidal ideation, ensuring his safety and well-being.
SOAP note example for psychotherapists
Stacey reports that she is 'feeling good' and enjoying her time away. Stacey reports she has been compliant with her medication and using her meditation app whenever she feels her anxiety.
Stacey was unable to attend her session as she is on a family holiday this week. She was able to touch base with me over the phone and was willing and able to make the phone call at the set time. Stacey appeared to be calm and positive over the phone.
Stacey presented this afternoon with a relaxed mood. Her speech was normal in rate, tone, and volume. Stacey was able to articulate her thoughts and feelings coherently.
Stacey did not present with any signs of hallucinations or delusions. Insight and judgment are good. No sign of substance use was present.
Plan to meet again in person at 2 pm next Tuesday, 25th May. Stacey will continue on her current medication and has given her family copies of her safety plan should she need it.
SOAP note example for pediatricians
Mrs. Jones states that Julia is "doing okay." Mrs. Jones said her daughter seems to be engaging with other children in her class. Mrs. Jones said Julia is still struggling to get to sleep and that "she may need to recommence the magnesium." Despite this, Mrs. Jones states she is "not too concerned about Julia's depressive symptomatology.
Mrs. Jones thinks Julia's condition has improved.
Julia will require ongoing treatment.
Plan to meet with Julia and Mrs. Jones next week to review mx. To continue to meet with Julia.
SOAP note example for social workers
Martin reports experiencing a worsening of his depressive symptoms, describing them as "more frequent and more intense" compared to previous experiences. He feels the depressive state is constantly present, with no improvement in anhedonia, and a significant decrease in energy levels compared to the previous month. He describes feeling constantly fatigued, both mentally and physically, and reports difficulty concentrating and increased irritability.
Importantly, Martin also shared experiencing daily thoughts of suicide, although he denies having a specific plan or intention to act on them.
Martin denies any hallucinations, delusions, or other psychotic-related symptomatology. His compliance with medication is good. He appears to have gained better control over his impulsive behavior as they are being observed less frequently. Martin appears to have lost weight and reports a diminished interest in food and a decreased intake.
Martin presents with significant symptoms consistent with Major Depressive Disorder, including worsening mood, anhedonia, fatigue, difficulty concentrating, and daily thoughts of suicide. His verbal and cognitive functioning appears intact, with no signs of psychosis. He demonstrates some insight into his depression and denies any current plan or intent to act on his suicidal thoughts.
However, his nonverbal presentation paints a concerning picture, with listlessness, distractedness, slow physical movement, and depressed body language reflecting the severity of his depressive episode. It is crucial to monitor his safety closely and address the suicidal ideation with appropriate interventions, despite the lack of an immediate plan.
Therefore, continuing therapy sessions with a focus on developing coping mechanisms, managing suicidal ideation, and exploring potential contributing factors is highly recommended.
Diagnosis: Major Depressive Disorder (MDD) - Active
Rationale: Martin's ongoing symptoms of depression, including daily suicidal ideation and significant functional impairment, necessitate continued intervention and support.
- Increase treatment frequency: Schedule follow-up therapy session in two days, on Friday, May 20th, to provide immediate support and monitor safety.
- Reinforce safety plan: Review and reinforce Martin's existing safety plan, ensuring he understands and has accessible resources to address suicidal thoughts.
- Encourage communication with family: Discuss the importance of informing a trusted family member about his current state of mind and seeking their support, while respecting Martin's autonomy concerning disclosure.
Additional considerations:
- Potential for medication management: Explore the potential benefits and risks of medication management, such as anti-depressants, in consultation with a physician, considering the severity and duration of symptoms.
- Collaboration with support systems: Consider involving other healthcare providers, such as Martin's primary care physician, in a coordinated care approach, if deemed necessary.
SOAP note example for psychiatrists
Ms. M. describes her current state as "doing okay" with a slight improvement in her depressive symptoms. While she still experiences persistent sadness, she acknowledges slight progress. Her sleep patterns remain disrupted, although she reports improved sleep quality and manages to get "4 hours sleep per night."
During the session, Ms. M. expressed discomfort with my note-taking, causing her anxiety. Additionally, she mentioned occasional shortness of breath and a general anxiety related to healthcare providers. Interestingly, she expressed concern about the location of her medical records.
Ms. M. is alert. Her mood is unstable but improved slightly, and she is improving her ability to regulate her emotions.
Ms. M. has a major depressive disorder.
Ms. M. will continue taking 20 milligrams of sertraline per day. If her symptoms do not improve in two weeks, the clinician will consider titrating the dose up to 40 mg. Ms. M. will continue outpatient counseling and patient education and handout. Comprehensive assessment and plan to be completed by Ms. M's case manager.
The SOAP note could include data such as Ms. M vital signs, patient's chart, HPI, and lab work under the Objective section to monitor his medication's effects.
SOAP note example for therapists
"I'm tired of being overlooked for promotions. I don't know how to make them see what I can do." Frasier's chief complaint is feeling "misunderstood" by her colleagues.
Frasier is seated, her posture is rigid, eye contact is minimal. Frasier appears to be presented with a differential diagnosis.
Frasier is seeking practical ways of communicating her needs to her boss, asking for more responsibility, and how she could track her contributions.
Book in for a follow-up appointment. Work through some strategies to overcome communication difficulties and lack of insight. Request GP or other appropriate healthcare professionals to conduct a physical examination.
SOAP note example for counselors
David states that he continues to experience cravings for heroin. He desperately wants to drop out of his methadone program and revert to what he was doing. David is motivated to stay sober by his daughter and states that he is "sober, but still experiencing terrible withdrawals" He stated that [he] "dreams about heroin all the time, and constantly wakes in the night drenched in sweat."
David arrived promptly for his appointment, completing his patient information sheet in the waiting room while exhibiting a pleasant demeanor during the session. He displayed no signs of intoxication.
While David still exhibits heightened arousal and some distractibility, his ability to focus has improved. This was evident during his sustained engagement in a fifteen-minute discussion about his partner and his capacity for self-reflection. Additionally, David demonstrated a marked improvement in personal hygiene and self-care. His recent physical exam also revealed a weight gain of 3 pounds.
David demonstrates encouraging progress in his treatment journey. He actively utilizes coping mechanisms, ranging from control techniques to exercises, resulting in a decrease in his cravings, dropping from "constant" to "a few times an hour." This signifies his active engagement and positive response to treatment.
However, it is crucial to acknowledge that David still experiences regular cravings, indicative of his ongoing struggle. Coupled with his history of five years of heroin use, it underscores the need for further support. To consolidate his gains and progress towards sustainable recovery, David would benefit from acquiring and implementing additional coping skills.
Therefore, considering both his current progress and the underlying factors related to his substance use, David would likely benefit from the addition of Cognitive Behavioral Therapy (CBT) alongside his current methadone treatment. Integrating CBT can equip him with valuable tools for managing triggers, challenging negative thoughts, and developing healthy coping mechanisms, ultimately enhancing his long-term recovery potential.
David has received a significant amount of psychoeducation within his therapy session. The therapist will begin to use dialectical behavioral therapy techniques to address David's emotion dysregulation. David also agreed to continue to hold family therapy sessions with his wife. Staff will continue to monitor David regularly in the interest of patient care and his past medical history.
SOAP note example for occupational therapists
Ruby stated that she feels 'energized' and 'happy.' She states that getting out of bed in the morning is markedly easier and she feels 'motivated to find work.' She has also stated that her 'eating and sleeping has improved,' but that she is concerned, she is 'overeating.'
Ruby attended her session and was dressed in a matching pink tracksuit. Her personal hygiene was good, and she had taken great care to apply her makeup and paint her nails. Ruby appeared fresh and lively. Her compliance with her medication is good, and she has been able to complete her jobseekers form.
Ruby presented this morning with markedly improved affect and mood. Her speech was normal in rate and pitch and appeared to flow easily. Her thoughts were coherent, and her conversation was appropriate. Ruby's appearance and posture were different from what they were in our last session. Ruby's medication appears to be assisting her mental health significantly.
- Follow-up appointment: Schedule a follow-up session with Ruby in one week to monitor her progress and address any emerging concerns.
- Open communication: Encourage Ruby to maintain open communication with me and contact me for any assistance or questions regarding her job search process. This fosters a collaborative approach and ensures timely support.
- Medication adherence: Collaborate with Ruby to ensure continued adherence to her prescribed medication regimen, emphasizing its importance in managing her condition.
- Multidisciplinary team (MDT) review: Share this latest session's information with Dr. Smith for review within the MDT meeting. This facilitates collaborative analysis, discussion of potential diagnoses, and formulation of a comprehensive treatment plan.
- Exploring potential vocational support: Depending on Ruby's needs and the MDT's recommendations, exploration of additional vocational support services might prove beneficial. This could include career counseling, interview preparation workshops, or specialized job search resources tailored to her specific situation.
- Addressing underlying factors: Further assessment is essential to identify any underlying factors contributing to Ruby's presentation, such as anxiety or depression, that might require additional interventions tailored to address them.
SOAP note example for dentists
Chief complaint: A 56-year-old woman presents with a chief complaint of "painful upper right back jaw for the past week or so."
History of present illness: The patient reports experiencing pain in her upper right back jaw for approximately one week. She describes the pain as [insert patient's description of the pain, e.g., sharp, dull, throbbing, aching]. She states that the pain is [insert patient's description of pain characteristics, e.g., constant, intermittent, worse with specific activities]. She denies any history of fever, chills, facial swelling, difficulty swallowing, or earache.
Past medical history: The patient denies any significant past medical history.
Medications: The patient denies taking any current medications.
Allergies: The patient reports an allergy to paracetamol.
Social history: The patient reports a history of [insert details of tobacco use, e.g., smoking cigarettes for 30 years, one pack per day] and [insert details of alcohol consumption, e.g., occasional social drinking].
- Blood pressure: 133/91 mmHg
- Heart rate: 87 beats per minute
- Temperature: 98.7 °F (37.1 °C)
Clinical Examination:
- No signs of swelling, asymmetry, pain, redness (erythema), numbness (paraesthesia), or tenderness to palpation (TMI) were observed in the external facial and jaw areas.
- Tooth #17 (FDI #27) is supra-erupted and contacting (occluding) the pericoronal tissues (gum tissue surrounding the crown) of tooth #16.
- Tooth #16 is partially erupted and exhibits:
- Red, inflamed gum tissue (erythematous gingiva)
- Presence of discharge (exudate)
- Pain upon palpation
- Pending - X-rays (including periapical (PA) and panoramic (Pano) views, or possibly a CT scan) are recommended to further evaluate the underlying anatomy and identify any potential bone involvement.
- Pericoronitis: The patient exhibits clinical signs consistent with pericoronitis affecting tooth #16. This includes the presence of: Partial eruption of the tooth Inflamed gum tissue (erythema) Discharge (exudate) around the tooth Pain upon palpation * Supra-eruption of the opposing tooth (#17) and its contact with the affected tissue
- Contributing factors: While a definitive cause cannot be established without further investigation, the patient's smoking history (one pack per week) could potentially contribute to the development of pericoronitis by compromising the immune response and increasing the risk of infection.
- Additional considerations: Further information is necessary to fully understand the underlying factors. Pending X-rays (PA and panoramic) will provide valuable insights into the bone structure and identify any potential complications, such as impaction or bone loss.
Therefore, a definitive diagnosis and comprehensive treatment plan will be determined following the completion of the X-ray studies and considering the patient's full medical history and any additional information gathered.
- Pain management: OTC pain meds (consider allergy) & warm compresses (10-15 min, several times/day).
- Definitive treatment: Schedule extraction of #17 after X-ray review.
- Antibiotics (pending): Consider 5-7 day course of amoxicillin based on X-ray and severity.
- Follow-up: See patient in 3-5 days (healing, post-op concerns, oral hygiene).
- Oral hygiene education: Instruct on proper brushing/flossing, gentle cleaning of affected area.
- Smoking cessation: Encourage quitting to improve healing and reduce infection risk.
SOAP note example for speech therapists
Jenny's mother stated, "Jenny's teacher can understand her better now" Jenny's mother is "stoked with Jenny's progress" and can "see the improvement is helpful for Jenny's confidence."
Jenny was able to produce /I/ in the final position of words with 80% accuracy.
Jenny's pronunciation has improved 20% since the last session with visual cues of tongue placement. Jenny has made marked improvements throughout the previous 3 sessions.
Jenny continues to improve with /I/ in the final position and is reaching the goal of /I/ in the initial position. Our next session will focus on discharge.
SOAP note example for Physical Therapists
At the time of the initial assessment, Bobby complained of dull aching in his upper back at the level of 3-4 on a scale of 10. Bobby stated that the "pain increases at the end of the day to a 6 or 7". Bobby confirmed he uses heat at home and finds that a "heat pack helps a lot."
The cervical spine range of motion is within functional limit with pain to the upper thoracic with flexion and extension. Cervical spine strength is 4/5. The right lateral upper extremity range of motion is within the functional limit, and strength is 5/5. Palpation is positive over paraspinal muscles at the level of C6 through to T4, with the right side being less than the left. The sensation is within normal limits.
Bobby is suffering from pain in the upper thoracic back.
To meet with Bobby on a weekly basis for modalities, including moist heat packs, ultrasound, and therapeutic exercises. The goal will be to decrease pain to a 0 and improve functionality.
SOAP note example for medical practitioners
66-year-old Darleene presents for a follow-up appointment regarding her hypertension. She reports feeling well, denying any dizziness, headaches, or fatigue.
Medical history: Darleene has no significant past medical history beyond hypertension. Her current medication regimen consists solely of HCTZ 25mg daily.
Lifestyle: Over the past three months, Darleene has successfully lost 53 pounds by implementing a low-fat diet and incorporating daily 10-minute walks. Notably, she also acknowledges consuming two glasses of wine nightly. Darleene denies using any over-the-counter medications like cold remedies or herbal supplements.
- Vital signs:
- BP: 153/80 mmHg
- Pulse: 76 beats per minute
- Weight: 155 lbs
- Height: 55 inches
- General appearance: Well-nourished, no acute distress.
- HEENT: Normocephalic, atraumatic, atraumatic, atraumatic (head, eyes, ears, nose, throat - all normal).
- Neck: Supple, no jugular venous distention (JVD).
- Lungs: Clear to auscultation bilaterally.
- Heart: Regular rate and rhythm, no murmurs.
- Abdomen: Soft, non-tender, no organomegaly.
- Extremities: No edema.
Darleene is here for a follow-up of her hypertension. It is not well-controlled since blood pressure is above the goal of 135/85. A possible trigger to her poor control of HTN may be her alcohol use or the presence of obesity.
1. Lifestyle modifications:
- Continue low-fat diet and exercise: Encourage Darleene to maintain her current healthy diet.
- Increase physical activity: Recommend gradually increasing walking duration to 20-30 minutes daily to further support weight loss and overall health.
- Moderate alcohol intake: Discuss the potential negative impact of excessive alcohol consumption on blood pressure control. Darleene agrees to limit her wine intake to weekend evenings only as a trial to assess its effect on her BP.
2. Monitoring and follow-up:
- Home blood pressure (BP) monitoring: Instruct Darleene to monitor her BP regularly at home and maintain a diary to document the readings.
- Potassium level check: Schedule a blood test to assess her potassium level due to the potential electrolyte imbalance associated with diuretic use.
- Follow-up appointment: Schedule a follow-up clinic visit in one month. At this visit, Darleene should bring her BP diary for review. Based on her progress, blood pressure readings, and overall evaluation, the addition of an ACE inhibitor medication might be considered if BP remains uncontrolled.
SOAP note example for massage therapists
Fred stated that it had been about one month since his last treatment. Fred stated that he "has been spending a lot more time on his computer" and attributes his increased tension in his upper back and neck to this. Currently, Fred experiences a dull aching 4/10 in his left trapezius area. He "would like a relaxation massage with a focus on my neck and shoulders."
Tenderness at the left superior angle of the scapula. Gross BUE and cervical strength. A full body massage was provided. TrPs at right upper traps and scapula. Provided client with education on posture when at the computer. Issued handouts and instructed on exercises. All treatment kept within Pt.
Fred reported 1/10 pain following treatment. Good understanding, return demonstration of stretches and exercises—no adverse reactions to treatment.
To continue DT and TRP work on upper back and neck as required. Reassess posture and sitting at the next visit.
Benefits of using a SOAP note template
Using a SOAP note template will lead to many benefits for you and your practice. These include:
- Consistency : If you use a SOAP note template, your progress notes will have a consistent format. In addition to simplifying your writing process, using compatible templates will make it easier for other providers to read your notes.
- Accuracy : SOAP note templates haven't just been created to make things easier for practitioners and aim to improve the quality of your documentation. Separating your notes into four sections ensures you cover all the correct information and don't forget any crucial details.
- Save time: Using SOAP note templates will also save you much time. Your documentation is already formatted well; you must fill in the missing information.
SOAP note downloadable templates
Now you know the benefits of using a SOAP note template, here are some downloadable options for you to choose from:
- Basic SOAP note template : Sometimes, simple is best. This SOAP note template separates the page into four relevant sections so you can lay out your information appropriately.
- SOAP note template with a diagram : Perfect for physiotherapists and massage therapists, this SOAP note template includes a body diagram so practitioners can be as specific with their information as possible.
Why go digital with SOAP Notes?
The healthcare landscape is changing, and technology offers clinicians exciting options. Software specifically designed for SOAP medical notes simplifies documentation, improves efficiency, and offers several key benefits:
- Effortless templates: Access and customize pre-built SOAP templates to save time and ensure consistent formatting.
- Secure storage: Ditch overflowing cabinets! SOAP note software offers secure, cloud-based storage solutions, keeping patient records readily accessible.
- Streamlined compliance: Navigate HIPAA regulations with confidence. The right software handles data security and privacy protocols for you.
- Time savings: Focus on what matters most—your patients. Streamline documentation and free up valuable time for patient care.
By adopting SOAP note software, you can modernize your practice, enhance efficiency, and ultimately, prioritize patient care.
Top 5 software solutions to write SOAP Notes
Many different software options are available for healthcare practitioners, and sometimes, it can be hard to know where to look. We've done some research and identified what we think to be the top 5 software solutions for writing SOAP notes.
1. Carepatron
Carepatron is our number one when it comes to healthcare software. Integrated with extensive progress note templates, clinical documentation resources, and storage capabilities, Carepatron is your one-stop shop.
The platform offers additional practice management tools, including:
- Appointment scheduling
- Appointment reminders
- Medical billing
- Client portal
- Dictation software
And most importantly, everything is HIPAA-compliant!
Carepatron has a free plan that is perfect for smaller businesses or start-up practices. If you want additional features, the Professional Plan is $12/month, and the Organization Plan is $19/month.
2. TherapyNotes
TherapyNotes is a platform that offers documentation templates, including SOAP, to healthcare practitioners. The system integrates with a documentation library, allowing clinicians to store all their progress notes safely. Due to their practical progress note tools, TherapyNotes facilitates effective communication and coordination of care across a client's providers.
- Solo Plan: $49/month
- Group Plan: $59/month
3. TheraNest
TheraNest's software gives clinicians unlimited group and individual therapy note templates. These notes are customizable and integrated with helpful tools like drop-down bars and DSM 5 codes.
- Up to 30 clients: $39/month
- Up to 40 clients: $50/month
- Up to 50 clients: $60/month
- Up to 80 clients: $90/month
Tebra is a widespread practice management software integrated with SOAP note templates. It allows clinicians to streamline documentation with valuable features, including autosave and drop-down options.
If you are interested in pricing, you should contact Tebra directly.
5. Simple Practice
Simple Practice is our final recommendation if you are looking for documentation software. Simple Practice offers a comprehensive selection of fully customizable note templates. Integrated with Wiley Treatment Planners, the platform allows you to choose from a wide range of pre-written treatment goals, objectives, and interventions.
- Starter Plan: $29/month
- Essential Plan: $69/month
- Plus Plan: $99/month
Drive your SOAP Note success with Carepatron
Empower your practice with Carepatron, the all-in-one solution for efficient and secure SOAP note management!
Carepatron's user-friendly software simplifies note-taking, saving precious time while ensuring precise and consistent documentation. Leverage pre-built templates, secure cloud storage, and built-in compliance features to streamline workflow and prioritize patient care.
Ready to experience the difference? Sign up for your free Carepatron trial today and see how easy SOAP notes can be!
Further reading:
- SOAP Notes for Physical Therapy
- 10 Quick Tips for Chiropractors Writing SOAP Notes
- SOAP Note - Example
- Making Psychology SOAP Notes More Efficient

Related Articles
Ethical Dilemmas in Counseling
Explore vital ethical dilemmas in counseling and learn how Carepatron's software ensures compliance and enhances decision-making in our comprehensive guide.

Clinical Words to Use in Progress Notes
Explore a comprehensive guide to expand your clinical vocabulary and create effective progress notes.

Artificial Intelligence in Physical Therapy
Explore how AI transforms physical therapy with enhanced diagnostics, personalized treatments, and innovative technologies for better patient outcomes.

When to Stop Therapy
Explore key indicators for healthcare professionals on when to conclude therapy, ensuring effective patient management and therapeutic outcomes.
Psychoeducation
Empower patients with knowledge! Carepatron's guide explores psychoeducation in therapy & its benefits for mental health professionals.
Active Release Techniques
Discover the transformative power of Active Release Techniques (ART) for treating soft tissue disorders, enhancing mobility, and improving performance in healthcare.
Bowen Family Therapy
Explore Bowen Family Therapy with Carepatron! Our secure platform & features empower therapists to guide families & promote emotional well-being. Read here.
AI in Psychiatry
Explore the role of AI in psychiatry and its impact on diagnosing, treating, and managing mental health issues effectively. Learn more at Carepatron.
AI and Psychology
Explore how to maximize the power of AI in clinical practice while remaining ethical and effective.
9 Ways to Use AI in Nursing Practice
Discover how AI is transforming nursing! Explore 9 ways AI can improve patient care, ethical considerations, & how Carepatron empowers nurses.
How to Write an Email to a Patient: Tips for Success
Learn essential tips on how to craft effective patient emails that enhance communication and trust in healthcare. Try out our email templates here.

Physical Therapy Billing Units
Discover the importance of Physical Therapy Billing Units for successful healthcare reimbursement. Learn more now!

DBT Journal Prompts
Gain some inspiration to guide clients in practicing journaling and incorporating principles of DBT into their daily lives.
Art Therapy Group Activities
Explore art therapy & its benefits for healthcare professionals. Learn how Carepatron software empowers art therapists.
Physical Therapy CPT Codes
Learn about Physical Therapy CPT codes, including their significance, purpose, and utilization in inpatient billing.

When Can a Therapist Break Confidentiality?
Discover the crucial scenarios in which therapists may need to break confidentiality to ensure client safety and well-being. Learn more here.
30 Speech Therapy Games
Unleash the power of speech therapy! ️Our guide equips healthcare pros with everything they need to know: tips, strategies, & 30+ engaging speech therapy ideas & games!
Insights into Mental Health Crises: What you need to know
Explore the intricacies of a mental health crisis, understanding its signs, impacts, and intervention strategies for healthcare professionals.
Join 10,000+ teams using Carepatron to be more productive
- Therapy Tools
Writing SOAP Notes, Step-by-Step: Examples + Templates

Documentation is never the main draw of a helping profession, but progress notes are essential to great patient care. By providing a helpful template for therapists and healthcare providers, SOAP notes can reduce admin time while improving communication between all parties involved in a patient’s care.
In a few sections, we’ll give a clear overview of how therapy SOAP notes are written, along with helpful templates and software you can use to streamline the process even further. If you’re looking for a more efficient, concise way to document your telehealth sessions, this helpful guide will be of value.
How To Write Therapy SOAP Notes
Therapy SOAP notes follow a distinct structure that allows medical and mental health professionals to organize their progress notes precisely. [1]
As standardized documentation guidelines, they help practitioners assess, diagnose, and treat clients using information from their observations and interactions.
Importantly, therapy SOAP notes include vital information on a patient’s health status. This information can be shared with other stakeholders involved in their wellbeing for a more informed, collaborative approach to their care, as shown:

It’s critical to remember that digital SOAP notes must be shared securely and privately, using a HIPAA-compliant teletherapy platform . Here, we used Quenza.
The S.O.A.P Acronym
SOAP is an acronym for the 4 sections, or headings, that each progress note contains:
- Subjective: Where a client’s subjective experiences, feelings, or perspectives are recorded. This might include subjective information from a patient’s guardian or someone else involved in their care.
- Objective: For a more complete overview of a client’s health or mental status, Objective information must also be recorded. This section records substantive data, such as facts and details from the therapy session.
- Assessment: Practitioners use their clinical reasoning to record information here about a patient’s diagnosis or health status. A detailed Assessment section should integrate “subjective” and “objective” data in a professional interpretation of all the evidence thus far, and
- Plan: Where future actions are outlined. This section relates to a patient’s treatment plan and any amendments that might be made to it.
A well-completed SOAP note is a useful reference point within a patient’s health record. Like BIRP notes , the SOAP format itself is a useful checklist for clinicians while documenting a patient’s therapeutic progress.[REFERENCE ITEM=”Sando, K. R., Skoy, E., Bradley, C., Frenzel, J., Kirwin, J., & Urteaga, E. (2017). Assessment of SOAP note evaluation tools in colleges and schools of pharmacy. Currents in Pharmacy Teaching and Learning, 9 (4), 576.”]
In the next section, you’ll find an even more in-depth template for SOAP notes that can be used in a wide range of therapeutic sectors.
Therapy SOAP notes include vital information on a client’s health status; this can be shared with other stakeholders for more informed, collaborative patient care.
3 Helpful Templates and Formats
With a solid grasp of the SOAP acronym, you as a practitioner can improve the informative power of your P rogress Notes, as well as the speed with which you write them.
This generally translates into more one-on-one patient time, reduced misunderstandings, and improved health outcomes overall – so the table below should be useful.
SOAP Notes: A Step-By-Step Guide
Podder and colleagues give a great overview of the different subsections that a SOAP progress note can include. Based on their extensive article, we’ve created the following example that you can use as guidance in your work. [1]
Occupational Therapy SOAP Notes
In Occupational Therapy , a SOAP Progress Note might include the patient’s injuries and their severity, home exercises, and their effectiveness.
Based on observations and interaction with their client, an OT professional might adjust their treatment program accordingly. [2]
Laid out in the S, O, A, P format on therapy notes software , they might look like this:

Digital SOAP note tools like Quenza, which we’ve used here, will automatically create PDF copies for download, sharing, or HIPAA-compliant storage in a centralized place.

Because SOAP notes are best created while a session is still fresh in their minds, therapists might look for mobile-compatible software. This way, notes can be made on the spot from a tablet or smartphone.
Recommended: How to write Occupational Therapy SOAP Notes (+3 Examples)
Applied Behavior Analysis SOAP Notes
SOAP notes also play a valuable role in Applied Behavior Analysis , by allowing professionals to organize sessions better and communicate with a client’s other medical professionals. Legally, they may also accompany insurance claims to evidence the service being provided. [3]
It is important to remember that ABA SOAP notes , as psychotherapeutic documents, must be stored privately. They may form part of a client’s overall medical file other therapy notes.
These illustrative Occupational Therapy SOAP Notes and ABA SOAP Notes also exemplify how versatile SOAP notes can be. [4]
It’s why the framework is a commonly used standard in sectors such as Physical Therapy , Nursing, Rehabilitation, Speech Therapy , and more.
5 Examples of Effective Note-Taking
Many therapy software systems help to speed up the documentation of progress notes through in-built templates and diagnostic codes. At the end of the day, however, clinically valuable notes require careful thought and judgment when it comes to their content.
Effective notes are generally: [5]
- Written immediately following a therapy session. This way, a practitioner’s in-session time is spent focused on patient engagement and care ; writing notes immediately after helps minimize common mistakes such as forgetting details or recall bias.
- Professional. An important part of patient Electronic Health Records , SOAP notes should be legible and make use of professional jargon to serve as a common frame of reference. They should be written in the present tense.
- Concise and specific. Overly wordy progress notes unnecessarily complicate the decision-making process for other practitioners involved in a patient’s care. Brief, but pertinent information helps other providers reach conclusions more efficiently.
- Unbiased: In the Subjective section, particularly, there is little need for practitioners to use weighty statements, overly positive, negative, or otherwise judgmental language. SOAP notes are frequently used both as legal documents and in insurance claims.
- Utilize appropriate details, such as direct quotes: For a more comprehensive document that includes all the salient facts of an encounter.
An effective SOAP note is a useful reference point in a patient’s health record, helping improve patient satisfaction and quality of care.
3 Smart Software Solutions
In this section, we’ve reviewed three of the top practice management software systems offering helpful SOAP note functions.
These include SOAP note templates, discipline-specific codes, and treatment planning features that integrate with therapy progress notes.
Final Thoughts
With clear, consistent information on a patient’s health status and progress, therapists, psychiatrists, and counselors are much better equipped to manage their well-being. And while note-taking may not be glamorous, harnessing the right software can significantly reduce the time you spend on this vital part of healthcare .
SOAP notes play a pivotal role in streamlined, effective healthcare, and are a daily part of life for many practitioners. If you’ve tried and enjoyed using any particular templates, forms, or therapy notes solutions, let us know in a comment.
We hope this article has helped you streamline your note-taking. To put these tips into practice, don’t forget to try Quenza’s SOAP Notes tools for just $1 a month .
If you want to enhance the wellbeing of your clients more effectively, Quenza will give you everything you need to streamline your therapy notes, so you can focus on delivering the wellness results that matter.
- ^ Podder, V., Lew, V., & Ghassemzadeh, S. (2020). SOAP Notes. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482263/
- ^ Fusion Therapy. (2020). How To Write Therapy SOAP Notes.. Retrieved from: https://blog.fusionwebclinic.com/soap-notes-for-occupational-therapy
- ^ WebABA. (2020). Simple Guidelines for Writing SOAP Notes. Retrieved from https://webaba.com/2020/07/01/aba-practice-daily-simple-guidelines-for-writing-soap-notes/
- ^ Belden, J. L., Koopman, R. J., Patil, S. J., Lowrance, N. J., Petroski, G. F., & Smith, J. B. (2017). Dynamic electronic health record note prototype: seeing more by showing less. The Journal of the American Board of Family Medicine, 30 (6), 691.
- ^ Fusion Therapy. (2020). How To Write Therapy SOAP Notes. Retrieved from: https://blog.fusionwebclinic.com/soap-notes-for-occupational-therapy
thanks for info
Leave a reply Cancel
Your email address will not be published.

Download free guide (PDF)
Discover how to engage your clients on autopilot while radically scaling your coaching practice.
Coach, This Changes Everything (Free PDF)
Compliance and documentation
How to write soap notes.
Here’s how SOAP notes can help you write better, faster notes — and effectively document your work as a clinician.
Writing in a journal is easy: There are no rules, and it’s only for yourself. But progress notes come with a different kind of pressure.
While it might be intimidating to translate your care into a note, it’s simpler than it seems. Especially when you’re using a template like a SOAP note.
What is a SOAP note?
SOAP notes are a specific format for writing progress notes as a behavioral health clinician. They contain four primary sections, represented by its acronym: Subjective, Objective, Assessment, and Plan.
If you’re using a SOAP note template and filling out every section as directed, you should feel good about how your notes stack up to compliance expectations . Each section of a SOAP note is designed to help you document the most critical aspects of your session for compliance with insurance billing, including elements of a mental status exam and risk assessments.
A SOAP note’s holistic approach naturally encourages you as a provider to collect comprehensive insight about your client and their treatment. And because SOAP notes are widely recognized and used in many different healthcare settings, other care providers can easily recognize and review your mental healthcare records to provide continuity of care for your clients.
Headway’s built-in note template uses the SOAP note format, and includes one-click check boxes to help you fulfill the mental status exam and risk assessment on your notes.
As you sit down to write a SOAP note, reflect on your session and allow the four sections of the note template to guide you to document the most important aspects of your client’s current state and the progression of your treatment .
1. Subjective
The subjective section is where you document what your client is telling you about how they feel, their perceptions, and the symptoms.
It’s most important to document the things that relate to the client’s diagnosis. “For example, if your client is depressed, what’s telling you that they’re depressed?,” says Natalia Tague, LPC and Headway’s Clinical Engagement Lead. “The subjective section might include that the client says they've been crying every day, that they can't sleep, or that they've lost their appetite.”
Many providers elect to include a direct quote from the client in the subjective section of their SOAP notes, which helps demonstrate to insurers that the session was unique and veritable.
2. Objective
The objective section should include the therapist's observations, including measurable, observable data.
Consider what you’re seeing in the session that reflects what’s going on with the client in that moment.
“Literally: What are you seeing?,” says Natalia. “It’s things like: My patient's crying while we speak, they have trouble making eye contact, they seem disheveled, or they look like they haven't showered in a few days.”
3. Assessment
The assessment is the therapist's professional evaluation of the client’s condition, as captured in the subjective and objective sections. It should include their diagnosis, progress, risk assessment, formulation of the situation, and a review of the treatment plan.
In other words: This is where you should sum up the first two sections into a consideration of what’s going on with your client overall.
“The assessment is really just: What’s happening here?,” says Natalia. “What is all of this telling you about the bigger picture: Are they getting better? Are they getting worse? Has there been a drastic change?”
The plan section is where you document your intended actions moving forward. It includes treatment strategies, therapeutic goals, recommended interventions, and any necessary adjustments to the client's treatment plan.
It’s the future-looking piece of the care puzzle: The client has told you what’s going on. You’ve said what you’re observing. You put those two together into an assessment. And now it’s time to plan for the care you want to provide in future sessions.
“You might write that we’re going to meet weekly. Or we’re going to move to meet monthly because they seem to be doing okay. Another part of it might be saying: I think we need to process more of these triggers and build out some coping strategies,” says Natalia. “So the plan is just: Based on your assessment, where do you want to go next?”
SOAP note example
It’s important that SOAP notes, or notes in any template style follow the requirements of a progress note , such as including session details like the start and stop time and place of service.
Client Full Name: Connor Client Client Date of Birth: 2/2/1992 Date of Service: 7/10/2023 Exact start time and end time: 1:33 pm – 2:30 pm: 57 mins Session Location: 123 Serenity Lane, Miami, FL 33143 Diagnosis: (F32.1) Major depressive disorder, single episode, moderate) Subjective: During the session, the client, Connor, reported a significant improvement in his overall mood since our last meeting. He has been consistently utilizing coping mechanisms that were previously discussed and has been making an effort to engage in activities that he once found enjoyable. He expressed that his depressive symptoms have decreased in both intensity and frequency. Additionally, Connor mentioned a recent family gathering where he felt more engaged and connected with his loved ones. This positive experience provided him with a sense of social support, which he believes contributed to his improved mood. However, Connor expressed ongoing concerns about his sleep patterns, noting occasional difficulty falling asleep and early awakenings. Objective: Since our last session, Connor does not present a risk to self or others. His affect during the session was brighter and more animated compared to prior meetings. He actively participated in the session, showing improved eye contact and verbal expression. His body language suggested a decrease in overall tension compared to previous sessions. Connor's energy levels have improved, and he reported engaging in physical activities such as walking and jogging on a regular basis. His mood was calm, and his affect was appropriate for the course of the session. Assessment: Based on today's session, it is clear that Connor has made significant progress in managing his depressive symptoms. The combination of psychoeducation on coping strategies and increased engagement in pleasurable activities seems to be contributing positively to his overall well-being. His affect, mood, and verbal expression have all improved, indicating a positive response to therapy. However, Connor's ongoing concerns regarding his sleep patterns warrant further exploration. His difficulty falling asleep and early morning awakenings may indicate the presence of underlying stressors, which need to be identified and addressed. Plan: Moving forward, we will continue to reinforce and build upon effective coping strategies, such as mindfulness and behavioral activation. Additional attention will be given to Connor's sleep disturbances. We will explore potential triggers and stressors contributing to these issues and provide psychoeducation on sleep hygiene and relaxation techniques. The development of additional relaxation techniques to address his sleep concerns will also be considered. Connor's progress thus far is promising, and continued therapy sessions will aim to further improve his mood, manage his depressive symptoms, and address his sleep concerns.
This document is intended for educational purposes only. Examples are for purposes of illustration only. It is designed to facilitate compliance with payer requirements and applicable law, but please note that the applicable laws and requirements vary from payer to payer and state to state. Please check with your legal counsel or state licensing board for specific requirements.
Tips for writing SOAP notes
- A good rule of thumb is to plan for 5 to 7 minutes to write your progress notes. Try to fit them in between sessions as you’re able, so you don’t end every day with hours of catching up. “Learning how to write concise but accurate notes is such an important skill, just for your own self care as a provider,” says Natalia.
- Comprehensiveness is more important than length. “I’ve seen notes that are literally two sentences per section and they’re great, and then there are notes with four or five sentences for each and they still haven’t covered what they needed to cover,” says Natalia.
- Don’t stress about documenting every single thing that happened in session. For insurance purposes, focus on including the information that supports the client’s diagnosis, and substantiates the ongoing need for treatment and the approach you are using.
Use Headway’s progress note templates
While there are many options for documentation, Headway's in-product templates are designed to make note-taking fast and efficient, all while helping to take out the guesswork.
Plus, our templates are included at no additional cost for Headway providers.
Headway’s team and tools are here to make everything about working with insurance companies (including compliance!) as easy as possible.
How to write progress notes
Progress notes are the core piece of documentation a mental health care provider should write after each session with a client, but it’s more than just a record of what happened in the session.
Compliance— a Headway Guide
Navigating compliance can be time-consuming and stressful. We’re committed to changing that.

10 insurer requirements commonly missing from notes
Based on our conversations with insurers, here are 10 of the items most commonly missing from charting documentation, including examples of what it takes to meet the requirements for each.
Accurate Clinical Documentation: Exploring SOAP Notes
Effortless clinical notes with speech recognition AI
Maintaining accurate clinical documentation, including SOAP notes, is fundamental to a thriving healthcare practice. As the medical landscape progresses, our methods for managing clinical records, such as the SOAP note format, must evolve in tandem. This article is a comprehensive guide aimed at enhancing clinical documentation skills, including understanding the SOAP acronym medical and the SOAP notes meaning, at any stage of your medical career.
The Rationale Behind Clinical Documentation
Often perceived as a tedious task within the bustling healthcare environment, clinical documentation, especially maintaining patient records, should be recognized for its importance. Medical records are a critical component, transcending a mere checkbox on your list of responsibilities.
Communication
A patient’s record, or patient note, is a vital tool for communication among healthcare providers. Thorough documentation provides subsequent providers, including yourself, with insights into the patient’s condition and the logic underpinning the chosen treatment plan, thereby ensuring continuity of high-quality patient care.
Legal Consideration
Medical records not only facilitate patient care but also act as legal documents, meeting regulatory requirements and subject to close examination in the face of a malpractice lawsuit. Precise documentation of sensitive conversations about treatment decisions, care limitations, and prognosis is imperative.
Reimbursement
Clinical notes, or clinic notes, are not just records but also service documents. The precision of these notes is pivotal for securing reimbursement, which in turn impacts the cost and revenue aspects of your healthcare business or the institution you represent.
Setting the Context Right
Prior to delving into the substance of a clinical note, such as a SOAP note, it’s essential to set the correct context. Confirm that you’re documenting in the appropriate patient chart, ensure the date and time are precise, and make it clear to future readers who is the author of the note.
Ensuring the accuracy of the patient’s name, date/time, heading, and signature in the SOAP note is crucial to avoid significant time loss and adverse health outcomes. It’s essential that these basic aspects of the SOAP note are clearly stated and correct to maintain the integrity of the soap note documentation.

SOAP Method for Clinical Note Writing
Begin your clinical note with a summary of the main presenting issues, followed by the SOAP method for documentation that is both clear and consistent. This approach, often referred to as the soap note format, helps in maintaining a structured clinical note and is integral to the soap acronym medical documentation process.
The patient’s account of their condition, often detailed in the HPI (History of Present Illness) section of a SOAP note, should be expressed in their own words. It’s important to include the chronology, quality, and severity of the symptoms, as well as details on the onset, to accurately reflect the hpi and history of present illness.
In the Objective section of your SOAP documentation, record measurable facts about the patient’s status, such as vital signs, observations, results from the physical exam findings, and any pertinent lab results. These objective data are critical for a comprehensive clinical assessment.
Your primary medical diagnosis or interpretation of the data should be included in the Assessment section, based on the subjective and objective information gathered. This is a critical part of clinical reasoning and diagnoses, which informs the subsequent steps in patient care.
Finally, outline a specific treatment plan in your SOAP note documentation, detailing the actions taken or to be taken following the consultation, which may include medications, procedures, referral, or education. This treatment plan is essential for guiding patient care and ensuring continuity.
Road to better Clinical Documentation
Although the SOAP note structure provides a helpful framework for a clinical note, it does not ensure perfection. Here are some additional recommendations to enhance your soap note documentation and ensure it meets the highest standards of medical record-keeping.
- Document as soon as possible after providing care
- Be thorough yet brief
- Be clear and avoid ambiguous terms
Legal Aspects of Clinical Documentation
Strict regulatory requirements govern the management of clinical records to ensure their accuracy, legibility, and uphold data protection, while also facilitating patient access to their own medical records.
Accuracy and Legibility
From a legal perspective, it’s crucial to document relevant clinical findings, detail the record of decisions made, actions agreed upon, and outline the proposed treatment plan, all of which are often encapsulated in consult notes.
Confidentiality and Data Protection
In the digital age, confidentiality involves not only refraining from sharing patient data without consent but also implementing necessary measures to safeguard that data against unauthorized access.
Patient Access to Medical Records
Patients are entitled to patient access to their medical records, a right that is increasingly safeguarded by law to ensure transparency and patient empowerment.
Making Clinical Notes Open and Accessible
Under the 2021 Cures Rule , all U.S. hospitals and clinicians are mandated to ensure clinical notes are promptly accessible to patients, prompting some to revise their documentation content or tone to enhance patient access and understanding. Specifically, the rule requires that hospitals enable patients to easily access their full electronic health record, including physician notes, online without delays or fees. This aims to give patients more control over their health data to promote patient empowerment and care coordination. However, some clinicians worry that open access may require removing technical jargon, subjective remarks, or sensitive topics from notes to prevent confusion or distress. Ultimately though, transparency and health literacy are vital – striking an appropriate balance will likely require ongoing clinician training plus clear communication with patients on interpreting content.
Augnito: Revolutionizing SOAP Notes
Introducing Augnito , an AI-powered ambient clinical intelligence platform that streamlines the SOAP note-taking process. Augnito allows physicians to dictate patient encounters and assessments, which are then automatically documented in the EMR as a SOAP note.
Augnito integrates seamlessly with existing EMR systems, offering high transcription accuracy and coding accuracy without the need for infrastructure upgrades, thereby reducing errors and saving time otherwise spent on proofreading and ensuring data integrity.
Keeping Clinical Documentation Efficient
Efficiency is paramount in clinical documentation efficiency. Here are seven tips for ensuring your clinical notes are completed promptly and accurately:
- Leverage the skills of your team members
- Complete most documentation in the room
- Know the E/M documentation guidelines
- Use essential EHR functions
- Perfect clinical notes won’t be perfect
- Forget the “opus”
- Time yourself
In conclusion, impeccable clinical notes, including SOAP notes, not only fulfill fundamental clinical and legal standards but also harmonize with your EHR workflow. As healthcare progresses, it’s vital to evolve your approach to documentation, embracing the SOAP format and comprehending the significance of what SOAP stands for in medical terms. Regularly reviewing your SOAP documentation practices and making the necessary updates is crucial to remain aligned with the evolving SOAP notes meaning and best practices.
Table of Contents
Featured Posts

Imran Shaikh
Top 10 AI Contributions to Cancer Research and Treatment
May 10, 2024

Voices of Augnito – feat Anuj Dua, Senior Manager, Sales
May 2, 2024

AI in Healthcare : Top 7 Ways AI Has and Will Continue to Impact
May 1, 2024
5 Perfect Nursing SOAP Note Examples + How to Write

One of the most important parts of a nurse’s job is documentation, and there are several types of nurses' notes used in nursing care today. Nursing notes are the way healthcare providers communicate and promote continuity of care. In this article, we will discuss one type of nursing notes, SOAP nursing notes. I will answer the question, “What is a nursing SOAP note?” I will also share the steps to writing a good SOAP nursing note and provide you with 5 perfect nursing SOAP note examples + how to write them.
WHAT IS A NURSING SOAP NOTE?
Who developed nursing soap notes, what is the purpose of writing a nursing soap note, what is the difference between a nursing soap note and a nursing progress note, 4 advantages of nursing soap notes, advantage #1: nursing soap notes facilitate clinical reasoning., advantage #2: soap nursing notes promote active listening., advantage #3: soap nursing notes help create a detailed medical history., advantage #4: nursing soap notes help facilitate communication between nurses and doctors., 3 disadvantages of nursing soap notes, disadvantage #1: many nurses and healthcare providers question the order of the soap nursing note format., disadvantage #2: patients may have several complaints that must be addressed., disadvantage #3: gathering information to determine patient progress can be time-consuming with soap nursing notes., what elements should be included in a nursing soap note, 1. subjective data (s):, 2. objective data (o):, 3. assessment findings (a):, 4. plan of care (p):, what elements should not be included in a nursing soap note, 1. information that is irrelevant to the patient’s current condition:, 2. speculations about the patient’s symptoms or feelings:, 3. confusing pronouns:, 4. avoid judgmental statements:, 5. avoid using slang terms or unprofessional phrases:, how to write a perfect nursing soap note, what are the perfect examples of nursing soap notes, 5 most common mistakes to avoid while writing nursing soap notes, mistake #1: not naming the source of information, about the mistake:, how to avoid:, mistake #2: not providing supporting objective data, mistake #3: repeating subjective and objective data in the assessment section, mistake #4: rewriting the whole treatment plan, mistake #5: assuming the first complaint is the “chief” complaint, bonus 5 expert tips for writing nursing soap notes faster, tip #1: write your note at an appropriate time., tip #2: use direct statements, avoiding overly wordy content., tip #3: be specific and to the point., tip #4: document each patient encounter as soon as possible., tip #5: connect interventions with your diagnosis., my final thoughts, frequently asked questions answered by our expert, 1. who can write a nursing soap note, 2. when to write a nursing soap note, 3. do nurses write soap notes every shift, 4. ideally, how long should nursing soap notes be, 5. what’s the most important part of a nursing soap note, 6. can i use abbreviations in a nursing soap note, 7. what tense do i write a nursing soap note, 8. are nursing soap notes handwritten or printed, 9. how to sign off a nursing soap note, 10. what happens if i forget to write a soap note on the time it should have been written, 11. can a nursing student write a nursing soap note.

- Open access
- Published: 24 May 2023
Comparing oral case presentation formats on internal medicine inpatient rounds: a survey study
- Brendan Appold 1 ,
- Sanjay Saint 1 , 2 ,
- David Ratz 2 &
- Ashwin Gupta 1 , 2
BMC Medical Education volume 23 , Article number: 377 ( 2023 ) Cite this article
2796 Accesses
11 Altmetric
Metrics details
Oral case presentations – structured verbal reports of clinical cases – are fundamental to patient care and learner education. Despite their continued importance in a modernized medical landscape, their structure has remained largely unchanged since the 1960s, based on the traditional Subjective, Objective, Assessment, Plan (SOAP) format developed for medical records. We developed a problem-based alternative known as Events, Assessment, Plan (EAP) to understand the perceived efficacy of EAP compared to SOAP among learners.
We surveyed (Qualtrics, via email) all third- and fourth-year medical students and internal medicine residents at a large, academic, tertiary care hospital and associated Veterans Affairs medical center. The primary outcome was trainee preference in oral case presentation format. The secondary outcome was comparing EAP and SOAP on 10 functionality domains assessed via a 5-point Likert scale. We used descriptive statistics (proportion and mean) to describe the results.
The response rate was 21% (118/563). Of the 59 respondents with exposure to both the EAP and SOAP formats, 69% ( n = 41) preferred the EAP format as compared to 19% ( n = 11) who preferred SOAP ( p < 0.001). EAP outperformed SOAP in 8 out of 10 of the domains assessed, including advancing patient care, learning from patients, and time efficiency.
Conclusions
Our findings suggest that trainees prefer the EAP format over SOAP and that EAP may facilitate clearer and more efficient communication on rounds, which in turn may enhance patient care and learner education. A broader, multi-center study of the EAP oral case presentation will help to better understand preferences, outcomes, and barriers to implementation.
Peer Review reports
Excellent inter-physician communication is fundamental to both providing high-quality patient care and promoting learner education [ 1 ], and has been recognized as an important educational goal by the Clerkship Directors in Internal Medicine, the Association of American Medical Colleges, and the Accreditation Council for Graduate Medical Education [ 2 ]. Oral case presentations, structured verbal reports of clinical cases [ 3 ], have been referred to as the “currency with which clinicians communicate” [ 4 ]. Oral case presentations are a key element of experiential learning in clinical medicine, requiring learners to synthesize, assess, and convey pertinent patient information and to formulate care plans. Furthermore, oral case presentations allow supervising clinicians to identify gaps in knowledge or clinical reasoning and enable team members to learn from one another. Despite modernization in much of medicine, oral case presentation formats have remained largely unchanged, based on the traditional Subjective, Objective, Assessment, Plan (SOAP) format developed by Dr. Lawrence Weed in his Problem Oriented Medical Record in 1968 [ 5 ].
Given that the goals of a medical record are different than those of oral case presentations, it should not be assumed that they should share the same format. While Dr. Weed sought to make the medical record as “complete as possible,” [ 6 ] internal medicine education leaders have expressed desire for oral case presentations that are succinct, with an emphasis on select relevant details [ 2 ]. Using a common SOAP format between the medical record and oral case presentations risks conflating the distinct goals for each of these communication methods. Indeed, in studying how learners gain oral case presentation skills, Haber and Lingard [ 7 ] found differences in understanding of the fundamental purpose of oral case presentations between medical students and experienced physicians. While students believed the purpose of oral case presentations was to organize the large amount of data they collected about their patients, experienced physicians saw oral case presentations as a method of telling a story to make an argument for a particular conclusion [ 7 ].
In accordance with Dr. Weed’s “problem-oriented approach to data organization,” [ 6 ] but with an eye toward optimizing for oral case presentations, we developed an alternative to SOAP known as the Events, Assessment, Plan (EAP) format. The EAP format is used for patients who are already known to the inpatient team, and may also be utilized for newly admitted patients for whom the attending physician already has context (e.g., via handoff or review of an admission note). As the EAP approach is utilized by a subset of attending physicians at our academic hospital, we sought to understand the perceived effectiveness of the EAP format in comparison to the traditional SOAP format among learners (i.e., medical students and resident physicians).
EAP is a problem-based format used at the discretion of the attending physician. In line with suggested best practices [ 8 ], the EAP structure aims to facilitate transmission of data integrated within the context of clinical problem solving. In this format, significant interval events are discussed first (e.g., a fall, new-onset abdominal pain), followed by a prioritized assessment and plan for each relevant active problem. Subjective and objective findings are integrated into the assessment and plan as relevant to a particular problem. This integration of subjective and objective findings by problem is distinct from SOAP, where subjective and objective findings are presented separately as their own sections, with each section often containing information that is relevant to several problems (Fig. 1 , Additional file 1 : Appendix A).
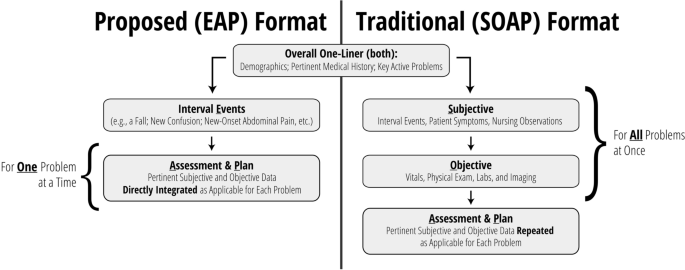
Overview: comparing EAP to SOAP
Settings and participants
We surveyed third- and fourth-year medical students, and first- through fourth-year internal medicine and internal medicine-pediatrics residents, caring for patients at a large, academic, tertiary care hospital and an affiliated Veterans Affairs medical center. Internal medicine is a 12-week core clerkship for all medical students in their second year, with 8 weeks spent on the inpatient wards. All student participants had completed their internal medicine clerkship rotation at the time of the survey. We did not conduct a sample size calculation at the outset of this study.
Data collection methods and processes
An anonymous, electronic survey (Qualtrics, Provo, UT) was created to assess student and resident experience with and preference between EAP and SOAP oral case presentation formats during inpatient internal medicine rounds (Additional file 2 : Appendix B). Ten domains were assessed via 5-point Likert scale (1 [strongly disagree] to 5 [strongly agree]), including the ability of the format to incorporate the patient’s subjective experience, the extent to which the format encouraged distillation and integration of information, the extent to which the format focused on the assessment and plan, the format’s ability to help trainees learn from their own patients and those of their peers, time efficiency, and ease of use. Duration of exposure to each format was also assessed, as were basic demographic data for the purposes of understanding outcome differences among respondents (e.g., students versus residents). For those who had experienced both formats, preference between formats was recorded as a binary choice. Participants additionally had the opportunity to provide explanation via free text. For participants with experience in both formats, the order of evaluation of EAP and SOAP formats were randomized by participant. For questions comparing EAP and SOAP formats directly, choice order was randomized.
The survey was distributed via official medical school email in October 2021 and was available to be completed for 20 days. Email reminders were distributed approximately one week after distribution and again 48 h prior to survey conclusion.
The primary outcome was trainee preference in oral case presentation format. Secondary outcomes included comparison between EAP and SOAP on content inclusion/focus, data integration, learning, time efficiency, and ease of use.
Statistical analyses
Descriptive statistics were used to describe the results (proportion and mean). For comparative analysis between EAP and SOAP, responses from respondents who had experience with both formats were compared using the Wilcoxon Signed Rank Test to evaluate differences. All statistical analyses were done using SAS V9.4 (SAS Institute, Cary, NC). We considered p < 0.05 to be statistically significant.
The overall response rate was 21% (118/563). The response rate was 14% ( n = 62/441) among medical students and 46% ( n = 56/122) among residents. Respondents were 61% ( n = 72) female. A total of 98% ( n = 116) and 52% ( n = 61) of respondents reported experience with SOAP and EAP formats, respectively. Among medical students, 60% ( n = 37) reported experience with SOAP only while 39% ( n = 24) had experience with both formats. Among residents, 36% ( n = 20) and 63% ( n = 35) had experience with SOAP only and both formats, respectively (Table 1 ). Most students (93%) and residents (96%) reported > 8 weeks of exposure to the SOAP format. Duration of exposure to the EAP format varied (0 to 2 weeks [32% of students, 17% of residents], 2 to 4 weeks [36% of students, 47% of residents], 4 to 8 weeks [16% of students, 25% of residents], and > 8 weeks [16% of students, 11% of residents]).
Of the 59 respondents with exposure to both the SOAP and EAP formats, 69% ( n = 41) preferred the EAP format as compared to 19% ( n = 11) preferring SOAP ( p < 0.001). The remainder ( n = 7, 12%) indicated either no preference between formats or indicated another preference. Among residents, 66% ( n = 23) favored EAP, whereas 20% ( n = 7) and 14% ( n = 5) preferred SOAP or had no preference, respectively ( p < 0.001). Among students, 75% ( n = 18) favored EAP, whereas 17% ( n = 4) and 8% ( n = 2) favored SOAP or had no preference, respectively ( p < 0.001).
Likert scale ratings for domains assessed by trainees who had experience in either format are shown in Table 2 . In general, scores for each domain were higher for EAP than SOAP, with the exception of perceived ease of use among students. Among those with experience using both formats, EAP outperformed SOAP most prominently in time efficiency (mean 4.39 vs 2.59, p < 0.001) and encouragement to: focus on assessment and plan (4.64 vs 3.05, p < 0.001), distill pertinent information (4.63 vs 3.17, p < 0.001), and integrate data (4.58 vs 3.31, p < 0.001) (Table 3 ). Respondents also ranked EAP higher in its effectiveness at advancing patient care (4.31 vs 3.71, p < 0.001), its capacity to convey one’s thinking (4.53 vs 3.95, p < 0.001), and its ability to facilitate learning from peers (4.10 vs 3.58, p < 0.001) and one’s own patients (4.24 vs 3.78, p = 0.003). There were no significant differences in the amount of time allotted for discussing the patient’s subjective experience or in ease of use.
Evaluation of trainee free text responses regarding oral case presentation preference revealed several general themes (Table 4 ). First, respondents generally felt that EAP was more time efficient and less repetitive, allowing for additional time to be spent discussing pertinent patient care decisions. Second, several respondents indicated that EAP aligns well with how trainees consider problems naturally (as a single problem in completion). Finally, respondents generally believed that EAP allowed learners to effectively communicate their thinking and demonstrate their knowledge. Those preferring SOAP most often cited format familiarity and the difficulty in switching between formats in describing their preference, though some also believed SOAP was more effective in describing a patient’s current status.
Our single site survey comparing 2 oral case presentation formats revealed a preference among respondents for EAP over SOAP for those medical students and internal medicine residents who had experience with both formats. Furthermore, EAP outperformed SOAP in 8 out of 10 of the functionality domains assessed, including areas such as advancing patient care, learning from patients, and, particularly, time efficiency. Such a constellation of findings implies that EAP may not only be a more effective means to accomplish the key goals of oral case presentations, but it may also provide an opportunity to save time in the process. In line with SOAP’s current de facto status as an oral case presentation format, almost all respondents reported exposure to the SOAP format. Still, indicative of EAP’s growing presence at our academic system, more than one third of medical students and more than one half of residents also reported having experience with the EAP format.
While limited data exist that compare alternative oral case presentations to SOAP on inpatient medicine rounds, such alternatives have been previously trialed in other clinical venues. One such format, the multiple mini-SOAP, developed for complex outpatient visits, encourages each problem to be addressed “in its entirety” before presenting subsequent problems, and emphasizes prioritization by problem pertinency [ 9 ]. The creators suggest that this approach encourages more active trainee participation in formulating the assessment and plan for each problem, by helping the trainee to avoid getting lost in an “undifferentiated jumble of problems and possibilities” [ 9 ] that accumulate when multiple problems are presented all at once. On the receiving end, the multiple mini-SOAP enables faculty to assess student understanding of specific clinical problems one at a time and facilitates focused teaching accordingly.
Another approach has been assessed in the emergency department. Specifically, Maddow and colleagues explored assessment-oriented oral case presentations to increase efficiency in communication between residents and faculty at the University of Chicago [ 10 ]. In the assessment-oriented format, instead of being presented in a stylized order, pertinent information was integrated into the analysis. The authors found that assessment-oriented oral case presentations were about 40% faster than traditional presentations without significant differences in case presentation effectiveness.
Prior to our study, the nature of the format for inpatient medicine oral case presentations had thus far escaped scrutiny. This is despite the fact that oral case presentations are time (and therefore resource) intensive, and that they play an integral role in patient care and learner education. Our study demonstrates that learners favor the EAP format, which has the potential to increase both the effectiveness and efficiency of rounding.
Still, it should be noted that a transition to EAP does present challenges. Implementing this problem-based presentation format requires a conscious effort to ensure a continued holistic approach to patient care: active problems should be defined and addressed in accordance with patient preferences, and the patient’s subjective experience should be meaningfully incorporated into the assessment and plan for each problem. During initial implementation, attending physicians and learners must internalize this new format, often through trial and error.
From there, on an ongoing basis, EAP may require more upfront preparation by attending physicians as compared to SOAP. While chart review by attendings in advance of rounding is useful regardless of the format utilized, this practice is especially important for the EAP format, where trainees are empowered to interpret and distill – rather than simply report a complete set of – information. Therefore, the attending physician must be aware of pertinent data prior to rounds to ensure that key information is not neglected. Specifically, attendings should pre-orient themselves with laboratory values, imaging, and other studies completed, and new suggestions from consultants. More extensive pre-work may be required if teams wish to employ the EAP format for newly admitted patients, as attending physicians must also familiarize themselves with a patient’s medical history and their current presentation prior to initial team rounds.
Our findings should be interpreted within the context of specific limitations. First, low response rates may have led to selection bias within our surveyed population. For instance, learners who desired change in the oral case presentation format may have been more motivated to engage with our survey. Second, there could be unmeasured confounding variables that could have skewed our results in favor of the EAP format. For example, attendings who utilized the EAP format may have been more likely to innovate in other ways to create a more positive experience for learners, which may have influenced the scoring of the oral case presentation format. Third, our findings were largely based on subjective experience. Objective measurement (e.g., duration of rounds, patient care outcomes) may lend additional credibility to our findings. Lastly, our study included only a single site, limiting our ability to generalize our findings.
Our study also had several strengths. Our learner participant pool was broad and included all third- and fourth-year medical students and all internal medicine residents at a major academic hospital. Participation was encouraged regardless of the nature of a participant’s prior exposure to different oral case presentation formats. Our survey was anonymous with randomization to mitigate order bias, and we focused our comparison analysis on those who had exposure to both the EAP and SOAP formats. We collected data to compare EAP with SOAP in 2 distinct ways: head-to-head preference and numeric ratings amongst key domains. Both of these methods demonstrated a significant preference for EAP among learners in aggregate, as well as for students and residents analyzed independently.
Our findings suggest a preference for the EAP format over SOAP, and that EAP may facilitate clearer and more efficient communication on rounds. These improvements may in turn enhance patient care and learner education. While our preliminary data are compelling, a broader, multi-center study of the EAP oral case presentation is necessary to better understand preferences, outcomes, and barriers to implementation. Further studies should seek to improve response rates, for the data to represent a larger proportion of trainees. One potential strategy to improve response rates among medical students and residents is to survey them directly at the end of each internal medicine clerkship period or rotation, respectively. Ultimately, EAP may prove to be a much-needed update to the “currency with which clinicians communicate.”
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, AG, upon reasonable request.
Kihm JT, Brown JT, Divine GW, Linzer M. Quantitative analysis of the outpatient oral case presentation: piloting a method. J Gen Intern Med. 1991;6(3):233–6.
Article Google Scholar
Green EH, Durning SJ, DeCherrie L, Fagan MJ, Sharpe B, Hershman W. Expectations for oral case presentations for clinical clerks: opinions of internal medicine clerkship directors. J Gen Intern Med. 2009;24(3):370–3.
Daniel M, Rencic J, Durning SJ, Holmboe E, Santen SA, Lang V, et al. Clinical Reasoning Assessment Methods: A Scoping Review and Practical Guidance. Acad Med. 2019;94(6):902–12.
Lewin LO, Beraho L, Dolan S, Millstein L, Bowman D. Interrater reliability of an oral case presentation rating tool in a pediatric clerkship. Teach Learn Med. 2013;25(1):31–8.
Wright A, Sittig DF, McGowan J, Ash JS, Weed LL. Bringing science to medicine: an interview with Larry Weed, inventor of the problem-oriented medical record. J Am Med Inform Assoc. 2014;21(6):964–8.
Weed LL. Medical records that guide and teach. New Engl J Med. 1968;278(12):652–7.
Haber RJ, Lingard LA. Learning oral presentation skills: a rhetorical analysis with pedagogical and professional implications. J Gen Intern Med. 2001;16(5):308–14.
Wiese J, Saint S, Tierney LM. Using clinical reasoning to improve skills in oral case presentation. Semin Med Pract. 2002;5(3):29–36.
Google Scholar
Schillinger E, LeBaron S. The multiple mini-SOAP format for student presentations of complex patients. Fam Med. 2003;35(1):13–4.
Maddow CL, Shah MN, Olsen J, Cook S, Howes DS. Efficient communication: assessment-oriented oral case presentation. Acad Emerg Med. 2003;10(8):842–7.
Download references
Acknowledgements
The authors would like to thank Jason M. Engle, MPH, who helped edit, prepare, format, and submit this manuscript and supporting files.
Author information
Authors and affiliations.
University of Michigan Medical School, Ann Arbor, MI, USA
Brendan Appold, Sanjay Saint & Ashwin Gupta
VA Ann Arbor Healthcare System, 2215 Fuller Road, Ann Arbor, MI, 48105, USA
Sanjay Saint, David Ratz & Ashwin Gupta
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: BA SS AG. Data curation: BA DR AG. Formal Analysis: BA SS DR AG. Funding acquisition: SS AG. Investigation: BA SS AG. Methodology: BA SS AG. Project administration: BA SS AG. Resources: SS AG. Software: DR. Supervision: SS AG. Validation: BA SS DR AG. Visualization: BA SS DR AG. Writing – original draft: BA AG. Writing – review & editing: BA SS DR AG. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Ashwin Gupta .
Ethics declarations
Ethics approval and consent to participate.
All methods were carried out in accordance with relevant guidelines and regulations. The need for ethical approval was waived by the ethics committee/Institutional Review Board of the University of Michigan Medical School. The need for informed consent was waived by the ethics committee/Institutional Review Board of the University of Michigan Medical School.
Consent for publication
Not applicable.
Competing interests
Dr. Saint, Mr. Ratz, and Dr. Gupta are employed by the US Department of Veterans Affairs. Dr. Saint reports receiving grants from the Department of Veterans Affairs and personal fees from ISMIE Mutual Insurance Company, Jvion, and Doximity. Dr. Appold, Mr. Ratz, and Dr. Gupta report no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Appendix A. Exemplar Transcripts (EAP, SOAP).
Additional file 2:
Appendix B. Survey Instrument.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Appold, B., Saint, S., Ratz, D. et al. Comparing oral case presentation formats on internal medicine inpatient rounds: a survey study. BMC Med Educ 23 , 377 (2023). https://doi.org/10.1186/s12909-023-04292-3
Download citation
Received : 24 August 2022
Accepted : 22 April 2023
Published : 24 May 2023
DOI : https://doi.org/10.1186/s12909-023-04292-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Oral case presentations
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Community Health Worker Curriculum
Documentation skills for chws: writing useful case notes.
At the end of this unit, participants will be able to:
- Create documentation using the SOAP note format
- Identify the purpose and common elements of good case notes
- Identify the challenges associated with completing case notes in an effective manner
- Identify best practices and what you as a CHW bring to the process
- Practice writing a progress note based on a case study
DOWNLOAD MATERIALS:
Lesson plan and handouts (PDF)
PowerPoint slides (PPT)
SOAP Note Case Study
Subjective section, objective analysis, assessment analysis, nursing theorist.
R.A is a 16-year-old female with type 1diabetes first diagnosed 5 years ago. She is also obese and has hypothyroidism. She was binge drinking, but quit 2 years ago upon being advised that alcohol could worsen her health condition.
Unless when she has an emergency, she usually comes to the hospital for follow-up every month. Today, she has come for routine follow-up. Although she is asymptomatic, her blood pressure is 170/99 mmHg. She does not report any episodes or symptoms of hypoglycemia. She was using insulin, but stopped 8 months ago after she improved her condition.
R.A has a healthy appearance and she is not characterized by signs of acute distress. Upon being physically examined, it is shown that she has a height of 165cm, weight of 90kg and a pulse rate of 86 beats per minute. The physical examination also reveals that she has a blood pressure of 170/99 mmHg. She does not present with retinopathy or thyromegaly (the retina is healthy and the thyroid glands are not inflamed). Also, she does not have diabetic foot ulcers that are common in diabetic patients.
Laboratory tests show that she has proteinuria, a cholesterol level of 230mg/dL, normal TSH levels, Hb level of 9.5%, creatinine level of 1.7mg/dL, glucose level of 190mg/dL, HDL and LDL of 134 and 35mg/dL respectively. Also, laboratory results reveal that she has normal electrolytes.
Related complications
These are complications with which the patient presents. They are the following:
- Hypertension
- Dyslipidemia
- Nephropathy that is confirmed by proteins in the blood. It is an indication that kidney nephrons are not functioning well to ultra-filter blood. Thus, excreted urine has traces of proteins (Ludvigsson et al., 2008).
Risk factors
Risk factors could worsen type 1 diabetes in the patient. They are the following factors:
- Obesity, which is indicated by a body mass index (BMI) of greater than 25.
- Kidney malfunction (indicated by a high creatinine value of 1.7mg/dL).
- Hypertension (readings are greater than 140/90 mmHg).
- A1C>/= 5.7%.
Therapeutic goals
- Clinical efforts should focus on controlling glycemia to A1C level less than 7%. (However, caution should be taken so that hypoglycemia cannot be caused in the process of controlling blood sugar).
- It should be a goal to prevent cardiovascular disease from occurring in the patient (This could be a serious complication).
- Reduce blood pressure to values lower than 130/80 mmHg. This is the recommended upper limit of blood pressure for diabetic patients (Ludvigsson et al., 2008).
- Cardiovascular disease risks should be reduced by encouraging the patient to feed on food that helps to maintain healthy cholesterol levels. For healthy persons, the low density lipoprotein (LDL) should not exceed 100 (Ludvigsson et al., 2008).
Current medication
R.A says that she is not on medications. A treatment should be initiated to lower A1C and help to control symptoms associated with type 1diabetes and other conditions. Other therapies may also be started to help to prevent complications that are foreseeable in the near future (Bergenstal et al., 2010).
Further laboratory tests and work-up
- Tests to assess liver functions. Biochemical liver tests determine levels of biochemical compounds crucial in regulating normal physiological functions. Elevated levels of biochemical in the liver would indicate that liver functions are altered.
- In order to confirm that the patient has hypertension, blood pressure test would be repeated. If found to be normal, then the test will have to be conducted by many laboratories to determine the true values (Ludvigsson et al., 2008, Bergenstal et al., 2010).
- CBC should be conducted so that infections can be ruled out or monitored. It is important to rule out infections in the patient because they could lead to worsening of her condition. Also, it is important to manage the infections with the right medications.
- List of effective and failed medications.
- A detailed family history to establish whether there are any relatives who have suffered from the same condition (type 1 diabetes) and the time of onset.
- Immunizations received in the past and their clinical implications. A review would be done to assess whether previous immunizations could have interfered with the normal immune system of the patient.
- Trends of adhering to medications offered in the past and barriers that hindered the patient from adhering to the medications. The medical history will help to select the best therapies to provide and ways of addressing barriers that could make the patient not take medications as prescribed (Ludvigsson et al., 2008).
Treatment recommendations
The diabetic patient will be put on insulin. In addition, she needs to adopt a healthy lifestyle that will involve feeding on a balanced diet characterized by significant amounts of carbohydrates. Also, body exercises will greatly help the patient to live a healthy life (Chase et al., 2008). Her blood pressure problem could be addressed by taking lisinopril 10mg daily.
- Insulin use requires routine monitoring of blood glucose levels (Bergenstal et al., 2010).
- Carbohydrate and fat dietary intake should be monitored. Total fat dietary intake should not be greater than 7% of the total number of sources of calories (Bergenstal et al., 2010).
Health education
Educational approaches should aim to inform the patient about ways of using medications so that they could improve her condition. Also, she will be taught how to maintain a healthy lifestyle. Healthy lifestyle changes will involve a healthy diet and aerobic exercises like walking and running (Chase et al., 2008; Bergenstal et al., 2010).
Follow-up and referrals
- A1C should be routinely monitored for a period of 3 months.
- Hypertension should be assessed at every routine visit.
- LDL follow-up assessments could be done every 1-2 years.
- Referrals will be recommended when her conditions worsen. They would involve being referred to physicians or healthcare facilities dealing with specific health conditions.
Cultural interventions
No cultural interventions are recommended for this patient.
The care, core and cure nursing theory would be used to offer care to the diabetic patient. The nursing theory was formulated by Lydia E. Hall and it asserts that a patient should set his or her goals (George, 2010). If the patient in the case study sets her goals, then she would work toward achieving them, and she would be influenced by her feelings and value system. The nursing theory would greatly impact the patient to improve her condition.
Bergenstal, R. M., Tamborlane, W. V., Ahmann, A., Buse, J. B., Dailey, G., Davis, S. N…. & Wood, M. A. (2010). Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes. New England Journal of Medicine, 363 (4), 311-320.
Chase, H. P., Fiallo-Scharer, R., Messer, L., Gage, V., Burdick, P., Laffel, L…. & Xing, D. (2008). Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med, 359 (14), 1464-76.
George, J. B. (2010). Nursing theories . Upper Saddle River, NJ: Prentice Hall.
Ludvigsson, J., Faresjö, M., Hjorth, M., Axelsson, S., Chéramy, M., Pihl, M…. & Casas, R. (2008). GAD treatment and insulin secretion in recent-onset type 1 diabetes. New England Journal of Medicine, 359 (18), 1909-1920.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, January 16). SOAP Note. https://ivypanda.com/essays/soap-note-case-study/
"SOAP Note." IvyPanda , 16 Jan. 2024, ivypanda.com/essays/soap-note-case-study/.
IvyPanda . (2024) 'SOAP Note'. 16 January.
IvyPanda . 2024. "SOAP Note." January 16, 2024. https://ivypanda.com/essays/soap-note-case-study/.
1. IvyPanda . "SOAP Note." January 16, 2024. https://ivypanda.com/essays/soap-note-case-study/.
Bibliography
IvyPanda . "SOAP Note." January 16, 2024. https://ivypanda.com/essays/soap-note-case-study/.
- The Problem of Diabetes Among African Americans
- Stress Management in Rheumatoid Arthritis Patients
- Diabetic Scenario: Dealing With High Blood Pressure
- A Career in Dentistry
- Dental Hygienist: Reasons for Choosing This Career
- Drug and Alcohol Testing
- Family Tree and Its Importance
- Hemoglobin A1C Test for Diabetes
Effect of high-risk pregnancy on prenatal stress level: a prospective case-control study
- Open access
- Published: 11 May 2024
Cite this article
You have full access to this open access article

- Hülya Türkmen ORCID: orcid.org/0000-0001-6187-9352 1 ,
- Bihter Akın ORCID: orcid.org/0000-0002-3591-3630 2 &
- Yasemin Erkal Aksoy ORCID: orcid.org/0000-0002-7453-1205 2
44 Accesses
Explore all metrics
The study aimed to determine the effects of high-risk pregnancy on prenatal stress levels. The study was conducted with a case-control design in Turkey in September-December 2019. The sample included pregnant women diagnosed with high-risk pregnancy and were at their 36th or later gestational weeks as the case group ( n = 121) and healthy pregnant women as the control group ( n = 245). The Antenatal Perceived Stress Inventory (APSI) and the Revised Prenatal Distress Questionnaire (NUPDQ-17 Item Version) were used to assess the stress levels of the participants in the study. It was determined that high-risk pregnancy was associated with higher rates of prenatal stress (APSI: p < 0.001, effect size = 0.388; NUPDQ: p = 0.002, effect size = 0.272) compared to the control group. The results of the linear regression analysis showed that high-risk pregnancy affected APSI (R 2 = 0.043, p < 0.001) and NUPDQ (R 2 = 0.033, p = 0.009) scores, but education levels, number of pregnancies, and number of abortions did not affect APSI and NUPDQ scores. According to the results of this study, high-risk pregnant women are in a risk group for stress. It is of great importance for the course of a pregnancy that healthcare professionals assess the stress levels of pregnant women in the high-risk pregnancy category and provide psychological support to pregnant women who have high stress levels or are hospitalized.
Avoid common mistakes on your manuscript.
Introduction
A high-risk pregnancy is a significant health problem that threatens the health of the pregnant woman, the health of her fetus, and ultimately the health of her newborn, increases the risk of morbidity and mortality, and has physiological, psychological, social, and economic aspects (Cincioğlu et al., 2020 ; Gözüyeşil & Düzgün, 2021 ; Sinaci et al., 2020 ). Chronic diseases existing before pregnancy and problems that arise during pregnancy can make a pregnancy risky. Pregnant women with gestational diabetes mellitus, preeclampsia/eclampsia, potential threat of preterm labor, cervical insufficiency, premature rupture of membranes, vaginal bleeding, Rh incompatibility, intrauterine growth retardation, and infections are in the high-risk category (Gözüyeşil & Düzgün, 2021 ; Sinaci et al., 2020 ; ACOG, 2019 ; Soğukpınar et al., 2018 ; Üzar-Özçetin & Erkan, 2019 ; ACOG, 2018 ).
Approximately 10% of all pregnancies in the world are considered to be in the high-risk category (Cincioğlu et al., 2020 ; Gourounti et al., 2015a , b ; Göüyeşil & Düzgün, 2021 ; Sinaci et al., 2020 ; Soğukpınar et al., 2018 ; Üzar-Özçetin & Erkan, 2019 ). According to Turkey Demographic and Health Survey (TNSA) 2018 data, 35% of pregnancies in Turkey are in the high-risk category (Hacettepe University Institute of Population Studies, 2019 ).
Good mental health during pregnancy is important for the health of both the pregnant woman and her fetus (Gümüşdaş et al., 2014 ). In a high-risk pregnancy, the normal outcome of the pregnancy and the birth of a healthy baby are threatened. These pregnant women have a variety of health needs that must be met. If these needs are not met, the mother may experience extreme stress and anxiety (Ölçer & Oskay, 2015 ). In the case of intense stress caused by the risks of pregnancy, the elevation of catecholamines such as cortisol and epinephrine may increase the possibility of pregnancy complications (e.g., preeclampsia) and adversely affect pregnancy outcomes (e.g., intrauterine growth retardation) (Atasever & Çelik, 2018 ; Cetin et al., 2017 ; Deshpande, 2016 ; Gözüyeşil & Düzgün, 2021 ; Riggin, 2020 ; Traylor et al., 2020 ; Yüksel et al., 2013 ). Moreover, newborns exposed to extreme stress during the intrauterine period may have permanent health problems later in their lives (Graignic-Philippe et al., 2014 ; MacKinnon et al., 2018 ; Van De Loo et al., 2016 ).
It is seen that distress in pregnancy has a high prevalence ranging between 11.9% and 63.5% in studies conducted in Turkey (Yüksel et al., 2013 ; Çapık et al., 2015 ; Gözüyeşil & Düzgün, 2021 ). It is very important that health professionals identify pregnant women at risk of stress to ensure a healthy pregnancy process and protect the fetus and newborn from the harmful effects of stress. This way, more careful monitoring of pregnant women at risk of stress can be ensured, and the negative consequences of stress can be prevented with appropriate interventions (Williamson et al., 2023 ; Atasever & Çelik, 2018 ; Pinar et al., 2022 ). It is reported in the international literature that mental problems such as anxiety and stress are more common in high-risk pregnancies than in healthy pregnancies (Byatt et al., 2014 ; Abedian et al., 2015 ; Gourounti et al., 2015a , b ). In Turkey, there are few studies examining the prenatal stress levels of high-risk pregnant women. However, in these studies, the prenatal stress levels of women with healthy and high-risk pregnancies were not compared, and only the stress levels of high-risk pregnancies were determined (Gözüyeşil & Düzgün, 2021 ; Üzar-Özçetin & Erkan, 2019 ). Current evidence indicates that studies describing the concept of prenatal stress in high-risk pregnancies with different diagnoses are needed to learn more about the complex aspects of prenatal stress and identify the sociodemographic and obstetric factors that may lead to high-risk pregnancies for early diagnosis (Pinar et al., 2022 ; Hung et al., 2021 ; Gözüyeşil & Düzgün, 2021 ; Mete et al., 2020 ; Üzar-Özçetin & Erkan, 2019 ; Atasever & Çelik, 2018 ). For this reason, it is thought that this study will guide healthcare professionals who provide care for women with high-risk pregnancies about the services they will provide.
This study aims to prospectively determine the effects of high-risk pregnancies on prenatal stress levels compared to healthy pregnant women, using two different measurement instruments.
Materials and methods
Research questions.
Does high-risk pregnancy have an impact on prenatal stress?
What are the factors affecting the prenatal distress levels of women diagnosed with high-risk pregnancy?
Is there a difference in prenatal stress levels among different high-risk pregnancy diagnoses?
Design and settings
This case-control study was conducted to determine the difference between the stress levels of women with healthy and high-risk pregnancies. In other words, it was aimed to determine the suspected causal effect of high-risk pregnancy on prenatal stress levels. This case-control study was carried out between September and December 2019 at the Obstetrics and Gynecology Inpatient and Outpatient Clinics of Atatürk City Hospital in the Balıkesir province of Turkey. The case and control groups included women who were selected from the same hospital.
The hospital where the study was conducted hosted a total of 4,152 deliveries in 2018. Approximately 10% of all pregnancies are considered to be in the high-risk category (Sinaci et al., 2020 ). The sample size required to conduct the study was calculated as 134 high-risk pregnant women using the Epi Info StatCalc program based on an assumed population size of 4152, prevalence of 10%, margin of error of 5%, and in a 95% confidence interval. The study was completed with a total of 384 pregnant women, including 134 high-risk pregnant women and 250 healthy pregnant women, who accepted to participate in the study and filled out the consent form. However, the data of 13 pregnant women in the case group and 5 pregnant women in the control group were excluded from the study because they filled out the data collection forms incompletely. For the case group ( n = 121), the post hoc power analysis (G*Power 3.1) revealed a medium effect size and a power of 0.421.
The inclusion criteria of the study were being in a gestational week further than 36 weeks, not having a psychiatric diagnosis, and being 18 years old or order. Pregnant women who were hospitalized in the Obstetrics and Gynecology Inpatient Clinic, were diagnosed with high-risk pregnancy by a physician, and met the inclusion criteria were included in the high-risk pregnancy group. In the control group, pregnant women who were healthy, were at or above their 36th gestational week, and visited the Outpatient Clinics were included. Women who wanted to leave the study or responded incompletely to the data collection forms were excluded. After those who met the inclusion criteria were included, no pregnant women withdrew from the study by their own accord. However, 18 pregnant women were excluded from the study because they filled out the forms incompletely.
High-risk pregnancies were defined as the presence of one or more of the following: pre-existing chronic diseases, preeclampsia, gestational diabetes mellitus (GDM), vaginal bleeding, placenta previa, threat of preterm labor, premature rupture of membranes, intrauterine growth retardation (IUGR), fetal anomaly/distress, multiple pregnancy, polyhydramnios/oligohydramnios, Rh incompatibility, and infectious diseases (Cincioğlu et al., 2020 ; Gözüyeşil & Düzgün, 2021 ; Sinaci et al., 2020 ; Üzar-Özçetin & Erkan, 2019 ).
Data collection
A Personal Information Form, the Antenatal Perceived Stress Inventory, and the Prenatal Distress Questionnaire were administered to the participants. The participants were informed about the study, the purpose of the study was explained to them, and their written consent was obtained. The data collection forms were administered to the participants by the first author. The data were collected based on the self-reports of the participants. The data collection period was between September and December 2019. The interviews lasted about 15 min for each participant.
Personal information form
The form which was prepared by the researchers in line with the literature consisted of a total of 20 questions on some characteristics of the participants, including their sociodemographic characteristics and obstetric history (Gözüyeşil & Düzgün, 2021 ; Mete et al., 2020 ; Üzar-Özçetin & Erkan, 2019 ; Atasever & Çelik, 2018 ).
Antenatal perceived stress inventory (APSI)
The Turkish validity and reliability study of the inventory developed by Razurel et al. ( 2014 ) to assess perceived stress in the prenatal period was performed by Atasever and Çelik ( 2018 ). The inventory is applied to pregnant women at the 36th -39th gestational weeks. It is a 5-point Likert-type scale (very much = 5 points, much = 4 points, quite = 3 points, a little = 2 points, none = 1 point) and consists of 12 items and 3 dimensions. Its dimensions are Medical and Obstetric Risks/Fetal Health, Psychosocial Changes during Pregnancy, and Prospect of Childbirth. The minimum and maximum scores that can be obtained from the inventory are 12 and 60. High scores indicate high levels of stress perceived by pregnant women. In the study conducted by Atasever and Çelik, Cronbach’s alpha internal consistency coefficient for APSI was found to be 0.70, while this coefficient was found as 0.81 in this study.
Revised prenatal distress questionnaire ((NUPDQ)-17 Item Version)
The questionnaire developed by Yali and Lobel ( 1999 ) to determine the levels of stress experienced by women regarding pregnancy-related issues was revised by Lobel ( 2008 ). The Turkish validity and reliability study of the questionnaire was performed by Yüksel et al. ( 2011 ). The questionnaire is in the form of a 3-point Likert-type scale (very much = 2 points, a little = 1 point, none = 0 point) and consists of 17 items. The questionnaire is unidimensional. The minimum and maximum scores that can be obtained from the questionnaire are 0 and 34. High scores indicate that pregnant women have high levels of prenatal distress. Cronbach’s alpha internal consistency coefficient for NUPDQ was found to be 0.85 in the study performed by Yüksel et al., while it was found as 0.82 in this study.
Statistical analysis
Frequency, percentage, mean, and standard deviation values were used in the data analyses. Whether the data had normal distribution was tested using the Kolmogorov-Smirnov test. The Chi-squared test and independent-samples t-test methods were used to identify the differences between groups in terms of the sociodemographic and obstetric information of the participants. The Mann-Whitney U Test was used to determine the differences between the case and control groups in terms of their total APSI, APSI subscale, and total NUPDQ scores. The Type I error level was accepted as p < 0.05. A Cohen’s d value of 0.20 is considered to indicate a small effect size, a value of 0.50 is considered to show a medium effect size, and a value of 0.80 or greater is interpreted as a large effect size (Özsoy & Özsoy, 2013 ). Since education, number of pregnancies, and number of miscarriages, which are thought to have an impact on stress levels, may be confounding factors, the linear regression analysis in this study was carried out to determine whether these factors or high-risk pregnancy affected the stress levels of the participants (Models 1 and 2). As a result of the Mann-Whitney U Test, a significant difference was found between high-risk pregnancies and healthy pregnancies in terms of “psychosocial changes during pregnancy” and “prospect of childbirth”. For this reason, APSI dimensions were collected in a single model, and a linear regression analysis was performed for the further analysis of the relationship between high-risk pregnancy and the APSI dimension scores of the participants (Model 3). The variable with the highest β coefficient was considered the relatively most significant independent variable. Multicollinearity was ignored in case of Tolerance > 0.20 and variance inflation factors (VIF) < 10. R 2 shows what percentage of the dependent variable is explained by the independent variables. According to Cohen, R 2 values of 0.0196, 0.1300, and 0.2600 are the lower thresholds for small, medium, and large effect sizes, respectively (Özsoy & Özsoy, 2013 ). One-Way MANOVA was also conducted to see whether there was a difference in stress levels during pregnancy between the case and control groups. The comparison of the stress levels of the participants in the case group based on their diagnoses was conducted with the Kruskal-Wallis test.
Ethical considerations
For the study to be carried out, approval was obtained from the Clinical Research Ethics Committee of the Faculty of Medicine of the University, and written permission was obtained from the institution where the study would be conducted (2019/123). The purpose of the study was explained to the pregnant women who agreed to participate, and they were informed that their identifying information would be kept confidential. The written consent of the participants was obtained with the Volunteer Information Form. The participants in both the case and control groups who were thought to need counseling were referred to a specialist for psychological support.
Table 1 shows the sociodemographic and obstetric characteristics of the participants. There was no significant difference between the women in the case and control groups in terms of age, whether they had an income-generating job, income status, place of residence, parity, number of living children, status of having a planned pregnancy, and smoking status ( p > 0.05). It was determined that the participants in the case group had significantly lower education levels than those in the control group ( p < 0.001). Moreover, the number of pregnancies ( p = 0.036) and the number of abortions ( p = 0.012) in the case group were found significantly higher than those in the control group. These results supported the hypothesis that some sociodemographic and obstetric characteristics of women are associated with high-risk pregnancies.
According to the Kolmogorov-Smirnov test results, the total APSI and NUPDQ scores of the participants were not normally distributed ( p < 0.001). Table 2 shows the stress levels of the participants compared based on their scale scores. The total APSI ( p < 0.001, Cohen’s d = 0.388) and total NUPDQ ( p = 0.002, Cohen’s d = 0.272) scores of the participants in the case group were significantly higher than those of the participants in the control group. The APSI Psychosocial Changes during Pregnancy ( p < 0.001, Cohen’s d = 0.473) and Prospect of Childbirth ( p < 0.001, Cohen’s d = 0.314) dimension scores of the participants in the case group were also significantly higher than those of the participants in the control group. These results supported the hypothesis that prenatal stress levels are higher in high-risk pregnancies than in healthy pregnancies.
Table 3 shows the stress levels of the participants with different diagnoses in the case group. In terms of risky pregnancies, the most frequently observed diagnoses were the threat of preterm labor in 37.2% of the participants in the case group, vaginal bleeding/placenta previa in 20.7%, and gestational diabetes mellitus in 10.7%. No statistically significant correlation was found between the diagnoses of the participants in the case group and their total APSI or NUPDQ scores ( p > 0.05). This result did not support the hypothesis that there is a difference in prenatal stress levels based on differences in high-risk pregnancy diagnoses.
In the linear regression analysis, Model 1 included APSI on education, gravidity, number of abortions, and high-risk pregnancy, and it was determined that there was a significant relationship between APSI and high-risk pregnancies, where the former explained 4.3% of the total variance in the latter (R 2 = 0.043) ( p < 0.001). Model 2 included NUPDQ on education, gravidity, number of abortions, and high-risk pregnancy, and it was determined that there was a significant relationship between NUPDQ and high-risk pregnancies, where the former explained 3.3% of the total variance in the latter (R 2 = 0.033) ( p = 0.009). Model 3 included APSI dimensions, and it was determined that there was a significant relationship between psychosocial changes during pregnancy and high-risk pregnancy, where the former explained 5.7% of the total variance in the latter ( R = 0.057) ( p < 0.001) (Table 4 ).
As a result of the MANOVA, it was determined that having a high-risk or a pregnancy was associated with significant differences in the combined set of dependent variables (APSI and NUPDQ total scores), F = 6.231, p = 0.002, Wilk’s Lambda = 0.967. There were significant differences between the case and control groups in terms of their APSI psychosocial changes during pregnancy and prospect of childbirth dimension scores, F = 7.258, p < 0.001, Pillai’s Trace = 0.057. (Table 5 ).
This study determined the stress levels of pregnant women with high-risk and healthy pregnancies. Stress experienced in high-risk pregnancies can have negative effects in terms of the pregnancy process and maternal and fetal health (Atasever & Çelik, 2018 ; Gözüyeşil & Düzgün, 2021 ; Riggin, 2020 ; Traylor et al., 2020 ; Yüksel et al., 2011 ). Therefore, it is thought that the results of this study will contribute to the literature.
It was determined in this study that the education levels of the high-risk pregnant women, who constituted the case group, were lower compared to the healthy pregnant women in the control group. Other studies in the literature have shown that risk factors in pregnancy are at higher rates in women with low educational levels (Annagür et al., 2014 ; Soğukpınar et al., 2018 ; Topalahmetoğlu et al., 2017 ; Türkmen, 2019 ). It is thought that as education levels increase, the knowledge levels of pregnant women about the management of risk factors in pregnancy increase, and these situations are intervened with in the early period. Moreover, high education levels can also prevent factors that may cause a high-risk pregnancy such as malnutrition, ill-advised exercise practices, and lack of antenatal care. For this reason, considering the results of our study, it is recommended that health professionals provide education to pregnant women with low education levels about prenatal care, proper nutrition, exercise, and antenatal follow-ups.
The numbers of pregnancies and abortions among the participants in the case group in this study were significantly higher compared to those in the control group. In the study by Orbay et al. ( 2017 ), the number of pregnancies among pregnant women with GDM was lower than the number of pregnancies among those without GDM. Cincioğlu et al. ( 2020 ) found the mean number of abortions among pregnant women with risky pregnancies to be 1.31 ± 0.71. As the number of pregnancies increases, the potential risks of pregnancy also increase. More frequent monitoring of pregnant women with a high number of abortions by health professionals and providing information about family planning methods to women with a high number of pregnancies will prevent high-risk pregnancies.
High-risk pregnancies consist of many obstetric pathologies including maternal chronic diseases. Every pathologic condition experienced during pregnancy can affect the women’s stress levels (Sinaci et al., 2020 ). In this study, two different scales were used to measure the stress levels of the participants, and the stress levels of the participants in the case group were found to be higher than the stress levels of those in the control group. Gözübebek and Düzgün (2021) stated that 63.5% of pregnant women diagnosed with risky pregnancies experienced distress. Üzar-Özçetin and Erkan ( 2019 ) reported high perceived stress levels in high-risk pregnant women. In their meta-analysis study, Amiri and Behnezhad ( 2019 ) revealed that diabetes during pregnancy was a risk factor for anxiety symptoms, and diabetes increased the risk of anxiety by up to 48%. Other studies in the literature have shown that high-risk pregnant women also have high anxiety levels (Byatt et al., 2014 ; Denis et al., 2012 ; Gourounti et al., 2015a , b ; McDonald et al., 2021 ; Orbay et al., 2017 ; Sinaci et al., 2020 ; Hung et al., 2021 ).
It was reported that low education levels, having a history of abortion, and a high number of pregnancies may cause prenatal stress (Atasever & Çelik, 2018 ). In this study, lower education levels and higher numbers of pregnancies and abortions were found in the case group than in the healthy control group. Since low education levels and high numbers of pregnancies and abortions were thought to be potential confounding factors in terms of prenatal stress, further analyses tests were performed, and it was determined that these factors did not affect stress levels to a significant extent. The research in this field may benefit from a more in-depth exploration of potential implications and confounding factors related to education.
In the studies performed by Üzar-Özçetin and Erkan ( 2019 ) and Yüksel et al. ( 2013 ), it was found that the stress levels of pregnant women who had experienced hospitalization due to any risk during pregnancy were high. It is considered that diagnosis methods, treatment methods, symptoms, complications, and their effects on the fetus for high-risk pregnancies cause great stress in pregnant women, and the fact that some pregnant women spend this process in the hospital increases their stress levels even further. For this reason, considering the results of our study, it is recommended that healthcare professionals inform the pregnant woman about her diagnosis and symptoms and explain each procedure to be performed, and that healthcare institutions provide more comfortable hospital rooms.
In this study, it was seen that the prenatal stress levels of the participants were high in terms of psychosocial changes during pregnancy. Intense stress can cause a sense of helplessness and hopelessness by depleting the energy of individuals, as well as negatively affecting their physical and mental health (Sharma & Rush, 2014 ). For this reason, healthcare professionals have an important role in the care of pregnant women with high-risk pregnancies. They should take an active role in the early diagnosis of at-risk pregnant women through qualified home visits and by initiating and continuing treatment. Advanced clinical guidelines and case management models should be developed for women having high-risk pregnancies.
In the study by Pinar et al. ( 2022 ), women with high-risk pregnancies were given training on stress management. After the training program, it was determined that 51.4% of the women in the intervention group and 75.7% in the control group experienced stress. Based on these results, it is recommended that healthcare professionals provide training, to ensure the active participation of the pregnant woman and her partner, on stress management to reduce the perceived stress, anxiety, and hopelessness levels of women in high-risk pregnancy cases. Additionally, these pregnant women should be provided with methods to cope with stress such as breathing exercises, relaxation exercises, appropriate physical exercises, visualization/yoga, massage therapy, music therapy, explanations about social support factors, and practices strengthening their spirituality (Ölçer & Oskay, 2015 ).
In this study, no significant difference was found in the prenatal stress levels of the participants in the case group based on their obstetric diagnoses of high-risk pregnancy. In the study by Byatt et al. ( 2014 ), no significant difference was identified between obstetric diagnoses in terms of anxiety levels in pregnant women. A high-risk pregnancy causes high stress levels in pregnant women due to similar diagnostic tests, treatment methods, hospitalization, complications, and fetal outcomes (Kent et al., 2015 ).
It is thought that high stress levels are not associated with obstetric diagnoses, and similar stress levels are experienced by all pregnant women aware of any risky situation during their pregnancies. Nevertheless, an increase in stress levels in risky pregnancies such as cases of preeclampsia may cause a further aggravation in the clinical status of women. Healthcare professionals should be aware of the higher stress levels of these pregnant women, they should help the pregnant woman express her feelings and thoughts by providing a reassuring communication environment, and plan appropriate consultancy, intervention, and care routines to help reduce their stress levels. These professionals can also coach high-risk pregnant women in terms of stress reduction and coping mechanisms. Pregnant women with high stress levels should be referred to a specialist for psychological support and therapy.
Strengths and limitations
The strength of this study was its prospective design with a control group. In this study, the use of two similar scales in terms of measuring the stress levels of pregnant women provided rigor and transparency compared to data obtained in previous studies. Since these scales were included in studies in Turkey only in the context of testing their validity and reliability in Turkish, it was decided to use them in the study as they measure stress levels in the prenatal period. A limitation of the study was that the pre-pregnancy stress levels of the participants, which would affect their present condition, were not measured in the study. Women with high stress levels before pregnancy have a higher risk of high-risk pregnancy. In other words, instead of high-risk pregnancy increasing stress levels, high stress levels may have affected the high-risk pregnancy statuses of the women. The results of the study also revealed a significant difference in education levels between the case and control groups. However, as a result of further analyses, it was determined that education did not affect prenatal stress levels.
In this study, it was determined that high-risk pregnancy affected prenatal stress. Moreover, it was found that the participants in the case group who had high-risk pregnancies had lower education levels and higher numbers of pregnancies and abortions compared to the participants in the control group with healthy pregnancies. This is why healthcare professionals are recommended to bear in mind that pregnant women with low education levels and a high number of pregnancies and abortions are at risk of high-risk pregnancies and monitor these pregnant women more frequently and carefully.
It is of great importance for the course of a pregnancy that healthcare professionals assess the stress levels of pregnant women in the high-risk pregnancy category, provide psychological support to pregnant women who have high stress levels or are hospitalized, offer them counseling and training opportunities (e.g., relaxation exercises, breathing exercises, practices strengthening their spirituality, music therapy), take appropriate precautions, and refer these pregnant women to specialists if needed. Moreover, since the stress levels of these pregnant women will increase even more during childbirth, alternative methods to reduce the fear of childbirth and childbirth pain should be explained.
It is recommended to organize educational programs such as trainings, seminars, and conferences on stress management during pregnancy for health professionals working in family health centers, community health centers, and gynecology departments.
Consequently, more studies with larger sample sizes are needed to compare diagnostic stress levels in high-risk pregnancies. In addition to prenatal stress and childbirth fear levels, future studies should also determine the stress levels of women before pregnancy for similar comparisons between high-risk and healthy pregnancies.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abedian, Z., Soltani, N., Mokhber, N., & Esmaily, H. (2015). Depression and anxiety in pregnancy and postpartum in women with mild and severe preeclampsia. Iranian Journal of Nursing and Midwifery Research , 20 , 454–459.
Article PubMed PubMed Central Google Scholar
ACOG (2018). Practice Bulletin 190 Summary: Gestational diabetes Mellitus. Obstetrics and Gynecology, 31 (2), 406–408.
Google Scholar
ACOG. (2019). American College of Obstetricians and gynecologists’ Committee on Practice bulletins-obstetrics and the Society for Maternal-Fetal Medicine. ACOG Practice Bulletin 204: Fetal growth restriction. Obstetrics and Gynecology , 133 (2), 97–109.
Amiri, S., & Behnezhad, S. (2019). Diabetes and anxiety symptoms: A systematic review and meta-analysis. The International Journal of Psychiatry in Medicine . https://doi.org/10.1177/0091217419837407
Article PubMed Google Scholar
Annagür, B. B., Kerimoğlu, Ö. S., Gündüz, Ş., & Tazegül, A. (2014). Are there any differences in psychiatric symptoms and eating attitudes between pregnant women with hyperemesis gravidarum and healthy pregnant women? Journal of Obstetrics and Gynaecology Research , 40 (4), 1009–1014.
Atasever, İ., & Çelik, A. S. (2018). The validity and reliability of the Antenatal Perceived stress inventory Turkish version: A methodological study. Health Care Women International , 39 (10), 1140–1151. https://doi.org/10.1080/07399332.2018.1469635
Article Google Scholar
Byatt, N., Hicks-Courant, K., Davidson, A., Levesque, R., Mick, E., Allison, J., et al. (2014). Depression and anxiety among high-risk pregnancy obstetric inpatients. General Hospital Psychiatry , 36 , 644–649.
Çapık, A., Apay, E., S., & Sakar, T. (2015). Determination of the level of distress in pregnant women. Journal of Anatolia Nursing and Health Science , 18 , 196–203.
Cetin, O., Guzel Ozdemir, P., Kurdoglu, Z., & Sahin, H. G. (2017). Investigation of maternal psychopathological symptoms, dream anxiety and insomnia in preeclampsia. The Journal of Maternal-Fetal & Neonatal Medicine , 30 (20), 2510–2515.
Cincioğlu, E., Durat, G., Öztürk, S., & Akbaş, H. (2020). Mental States and coping styles with stress of women in high-risk pregnancy. Health and Society , 20 (3), 148–157.
Denis, A., Michaux, P., & Callahan, S. (2012). Factors implicated in moderating the risk for depression and anxiety in high risk pregnancy. Journal of Reproductive and Infant Psychology , 30 (2), 124–134. https://doi.org/10.1080/02646838.2012.677020
Deshpande, J. (2016). The effect of selected aspect of Garbha Sanskar on stress, coping strategies and wellbeing of antenatal mothers. International Journal of - Science and Research , 5 (3), 588–591.
Gourounti, K., Karapanou, V., Karpathiotaki, N., & Vaslamatzis, G. (2015a). Anxiety and depression of high risk pregnant women hospitalized in two public hospital settings in Greece. International Archives of Internal Medicine , 8 (25), 1–6.
Gourounti, K., Karpathiotaki, N., & Vaslamatzis, G. (2015b). Psychosocial stress in high risk pregnancy. International Archives of Internal Medicine , 8 , 1–9.
Gözüyeşil, E., & Düzgün, A. A. (2021). Prenatal distress and the contributing factors in high-risk pregnant women. Journal of Education and Research in Nursing , 18 (2), 183–189.
Graignic-Philippe, R., Dayan, J., Chokron, S., Jacquet, A. Y., & Tordjman, S. (2014). Effects of prenatal stress on fetal and child development: A critical literature review. Neuroscience & Biobehavioral Reviews , 43 , 137–162.
Gümüşdaş, M., Apay, S. E., & Özorhan, E. Y. (2014). Comparison of Psycho-Social Health in pregnant women with and without risk. Journal of Health Science and Profession , 1 (2), 32–42.
Hacettepe University Institute of Population Studies 2018. (2019). Turkey demographic and health survey . Hacettepe University Institute of Population Studies, T.R. Presidency of Turkey Directorate of Strategy and Budget and TUBİTAK.
Hung, H. Y., Su, P. F., Wu, M. H., & Chang, Y. J. (2021). Status and related factors of depression, perceived stress, and distress of women at home rest with threatened preterm labor and women with healthy pregnancy in Taiwan. Journal of Affective Disorders , 280 (1), 156–166. https://doi.org/10.1016/j.jad.2020.10.062
Kent, R. A., Yazbek, M., Heyns, T., & Coetzee, I. (2015). The support needs of high-risk antenatal patients in prolonged hospitalization. Midwifery , 31 (1), 164–169.
Lobel, M. (2008). The Stony Brook pregnancy project: Revised prenatal distress questionnaire (NUPDQ): 17-Item version . NUPDQ2.DOC.
MacKinnon, N., Kingsbury, M., Mahedy, L., Evans, J., & Colman, I. (2018). The association between prenatal stress and externalizing symptoms in childhood: Evidence from the Avon Longitudinal Study of parents and children. Biological Psychiatry , 83 (2), 100–108.
McDonald, H. M., Sherman, K. A., & Kasparian, N. A. (2021). Factors associated with psychological distress among Australian women during pregnancy. Personality and Individual Differences , 172 , 1–9.
Mete, S., Fata, S., & Özberk, H. (2020). Comparison of stress levels in Risky and Non-risky pregnancies. Journal of Academic Research in Nursing , 6 (3), 554–560. https://doi.org/10.5222/jaren.2020.93898
Ölçer, Z., & Oskay, U. (2015). Stress in high-risk pregnancies and coping methods. Journal of Education and Research in Nursing , 12 (2), 85–92.
Orbay, E., Tüzün, S., Çınkıt, B., Ölmez, M. B., Tekin, S., Purut, E., et al. (2017). Antenatal anxiety in pregnant women with gestational diabetes Mellitus. Ankara Medical Journal , 2 , 111–118.
Özsoy, G., & Özsoy, S. (2013). Effect size reporting in educational research. Elementary Education Online , 12 (2), 334–346.
Pinar, S. E., Daglar, G., & Aksoy, O. D. (2022). The effect of stress management training on perceived stress, anxiety and hopelessness levels of women with high-risk pregnancy. Journal of Obstetrics and Gynaecology , 42 (1), 17–22. https://doi.org/10.1080/01443615.2020.1867970
Razurel, C., Kaiser, B., Dupuis, M., Antonietti, J. P., Citherlet, C., Epiney, M., & Sellenet, C. (2014). Validation of the antenatal perceived stress inventory. Journal of Health Psychology , 19 (4), 471–481.
Riggin, L. (2020). The assocation between gestational diabetes and mental illness: A scoping review. Canadian Journal of Diabetes , 44 (6), 566–571.
Sharma, M., & Rush, S. E. (2014). Mindfulness-based stress reduction as a stress management intervention for healthy individuals: A systematic review. Journal of Evidence-Based Integrative Medicine , 19 , 271–286.
Sinaci, S., Tokalioglu, E. Ö., Ocal, D., Atalay, A., Yilmaz, G., Keskin, H. L., et al. (2020). Does having a high-risk pregnancy influence anxiety level during the COVID-19 pandemic? European Journal of Obstetrics & Gynecology and Reproductive Biology , 255 , 190–196.
Soğukpınar, N., Akmeşe, Z. B., Hadimli, A., Balçik, M., & Akin, B. (2018). Risky pregnancy Profile in Maternity hospitals: Sample of Izmir Province. Journal of Academic Research in Nursing , 4 (1), 37–44. https://doi.org/10.5222/jaren.2018.037
Topalahmetoğlu, Y., Altay, M. M., Cırık, D. A., Tohma, Y. A., Çolak, E., Çoşkun, B., et al. (2017). Depression and anxiety disorder in hyperemesis gravidarum: A prospective case-control study. Turkish Journal of Obstetrics and Gynecology , 14 , 214–219. https://doi.org/10.4274/tjod.78477
Traylor, C. S., Johnson, J. D., Kimmel, M. C., & Manuck, T. A. (2020). Effects of psychological stress on adverse pregnancy outcomes and nonpharmacologic approaches for reduction: An expert review. American Journal of Obstetrics & Gynecology MFM , 2 (4), 100229. https://doi.org/10.1016/j.ajogmf.2020.100229
Türkmen, H. (2019). The effect of hyperemesis gravidarum on prenatal adaptation and quality of life: A prospective case–control study. Journal of Psychosomatic Obstetrics & Gynecology , 40 , 1–8. https://doi.org/10.1080/0167482x.2019.1678020
Üzar-Özçetin, Y. S., & Erkan, M. (2019). Resilience, perceived stress and psychosocial health of high-risk pregnant women. Cukurova Medical Journal , 44 (3), 1017–1026. https://doi.org/10.17826/cumj.502989
Van De Loo, K. F., Van Gelder, M. M., Roukema, J., Roeleveld, N., Merkus, P. J., & Verhaak, C. M. (2016). Prenatal maternal psychological stress and childhood asthma and wheezing: A meta-analysis. European Respiratory Journal , 47 (1), 133–146.
Williamson, S. P., Moffitt, R. L., Broadbent, J., Neumann, D. L., & Hamblin, P. S. (2023). Coping, wellbeing, and psychopathology during high-risk pregnancy: A systematic review. Midwifery , 116 , 1–11.
Yali, M. A., & Lobel, M. (1999). Coping and distress in pregnancy: An investigation of medically high risk women. Journal of Psychosomatic Obstetrics & Gynecology , 20 , 39–52.
Yüksel, F., Akın, S., & Durna, A. (2011). The Turkish adaptation of the revised prenatal distress questionnaire: A reliability/validity and factor analysis study. Journal of Education and Research in Nursing , 8 , 43–51.
Yüksel, F., Akin, S., & Durna, Z. (2013). Prenatal distress in Turkish pregnant women and factors associated with maternal prenatal distress. Journal of Clinical Nursing , 23 (1–2), 54–64.
PubMed Google Scholar
Download references
Acknowledgements
The authors express thanks to the mothers for participation in the study.
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK). No funding was received to conduct the study.
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and affiliations.
Department of Midwifery, Faculty of Health Sciences, Balıkesir University, Balıkesir, Turkey
Hülya Türkmen
Department of Midwifery, Faculty of Health Sciences, Selçuk University, Konya, Turkey
Bihter Akın & Yasemin Erkal Aksoy
You can also search for this author in PubMed Google Scholar
Contributions
Study conception and design: Hülya TÜRKMEN. Data collection: Hülya TÜRKMEN. Data analysis and interpretation: Hülya TÜRKMEN. Drafting of the article: Hülya TÜRKMEN, Bihter AKIN, Yasemin ERKAL AKSOY. Critical revision of the article: Hülya TÜRKMEN, Bihter AKIN, Yasemin ERKAL AKSOY.
Corresponding author
Correspondence to Hülya Türkmen .
Ethics declarations
For the study to be carried out, approval was obtained from the Clinical Research Ethics Committee of the Faculty of Medicine of the University, and written permission was obtained from the institution where the study would be conducted (2019/123).
Conflict of interest
No potential conflict of interest is reported by the authors.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Türkmen, H., Akın, B. & Erkal Aksoy, Y. Effect of high-risk pregnancy on prenatal stress level: a prospective case-control study. Curr Psychol (2024). https://doi.org/10.1007/s12144-024-05956-z
Download citation
Accepted : 28 March 2024
Published : 11 May 2024
DOI : https://doi.org/10.1007/s12144-024-05956-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- High-risk pregnancy
- Prenatal stress
- Psychosocial changes during pregnancy
- Find a journal
- Publish with us
- Track your research
- Share full article
Advertisement
Supported by
Study Suggests Genetics as a Cause, Not Just a Risk, for Some Alzheimer’s
People with two copies of the gene variant APOE4 are almost certain to get Alzheimer’s, say researchers, who proposed a framework under which such patients could be diagnosed years before symptoms.

By Pam Belluck
Scientists are proposing a new way of understanding the genetics of Alzheimer’s that would mean that up to a fifth of patients would be considered to have a genetically caused form of the disease.
Currently, the vast majority of Alzheimer’s cases do not have a clearly identified cause. The new designation, proposed in a study published Monday, could broaden the scope of efforts to develop treatments, including gene therapy, and affect the design of clinical trials.
It could also mean that hundreds of thousands of people in the United States alone could, if they chose, receive a diagnosis of Alzheimer’s before developing any symptoms of cognitive decline, although there currently are no treatments for people at that stage.
The new classification would make this type of Alzheimer’s one of the most common genetic disorders in the world, medical experts said.
“This reconceptualization that we’re proposing affects not a small minority of people,” said Dr. Juan Fortea, an author of the study and the director of the Sant Pau Memory Unit in Barcelona, Spain. “Sometimes we say that we don’t know the cause of Alzheimer’s disease,” but, he said, this would mean that about 15 to 20 percent of cases “can be tracked back to a cause, and the cause is in the genes.”
The idea involves a gene variant called APOE4. Scientists have long known that inheriting one copy of the variant increases the risk of developing Alzheimer’s, and that people with two copies, inherited from each parent, have vastly increased risk.
The new study , published in the journal Nature Medicine, analyzed data from over 500 people with two copies of APOE4, a significantly larger pool than in previous studies. The researchers found that almost all of those patients developed the biological pathology of Alzheimer’s, and the authors say that two copies of APOE4 should now be considered a cause of Alzheimer’s — not simply a risk factor.
The patients also developed Alzheimer’s pathology relatively young, the study found. By age 55, over 95 percent had biological markers associated with the disease. By 65, almost all had abnormal levels of a protein called amyloid that forms plaques in the brain, a hallmark of Alzheimer’s. And many started developing symptoms of cognitive decline at age 65, younger than most people without the APOE4 variant.
“The critical thing is that these individuals are often symptomatic 10 years earlier than other forms of Alzheimer’s disease,” said Dr. Reisa Sperling, a neurologist at Mass General Brigham in Boston and an author of the study.
She added, “By the time they are picked up and clinically diagnosed, because they’re often younger, they have more pathology.”
People with two copies, known as APOE4 homozygotes, make up 2 to 3 percent of the general population, but are an estimated 15 to 20 percent of people with Alzheimer’s dementia, experts said. People with one copy make up about 15 to 25 percent of the general population, and about 50 percent of Alzheimer’s dementia patients.
The most common variant is called APOE3, which seems to have a neutral effect on Alzheimer’s risk. About 75 percent of the general population has one copy of APOE3, and more than half of the general population has two copies.
Alzheimer’s experts not involved in the study said classifying the two-copy condition as genetically determined Alzheimer’s could have significant implications, including encouraging drug development beyond the field’s recent major focus on treatments that target and reduce amyloid.
Dr. Samuel Gandy, an Alzheimer’s researcher at Mount Sinai in New York, who was not involved in the study, said that patients with two copies of APOE4 faced much higher safety risks from anti-amyloid drugs.
When the Food and Drug Administration approved the anti-amyloid drug Leqembi last year, it required a black-box warning on the label saying that the medication can cause “serious and life-threatening events” such as swelling and bleeding in the brain, especially for people with two copies of APOE4. Some treatment centers decided not to offer Leqembi, an intravenous infusion, to such patients.
Dr. Gandy and other experts said that classifying these patients as having a distinct genetic form of Alzheimer’s would galvanize interest in developing drugs that are safe and effective for them and add urgency to current efforts to prevent cognitive decline in people who do not yet have symptoms.
“Rather than say we have nothing for you, let’s look for a trial,” Dr. Gandy said, adding that such patients should be included in trials at younger ages, given how early their pathology starts.
Besides trying to develop drugs, some researchers are exploring gene editing to transform APOE4 into a variant called APOE2, which appears to protect against Alzheimer’s. Another gene-therapy approach being studied involves injecting APOE2 into patients’ brains.
The new study had some limitations, including a lack of diversity that might make the findings less generalizable. Most patients in the study had European ancestry. While two copies of APOE4 also greatly increase Alzheimer’s risk in other ethnicities, the risk levels differ, said Dr. Michael Greicius, a neurologist at Stanford University School of Medicine who was not involved in the research.
“One important argument against their interpretation is that the risk of Alzheimer’s disease in APOE4 homozygotes varies substantially across different genetic ancestries,” said Dr. Greicius, who cowrote a study that found that white people with two copies of APOE4 had 13 times the risk of white people with two copies of APOE3, while Black people with two copies of APOE4 had 6.5 times the risk of Black people with two copies of APOE3.
“This has critical implications when counseling patients about their ancestry-informed genetic risk for Alzheimer’s disease,” he said, “and it also speaks to some yet-to-be-discovered genetics and biology that presumably drive this massive difference in risk.”
Under the current genetic understanding of Alzheimer’s, less than 2 percent of cases are considered genetically caused. Some of those patients inherited a mutation in one of three genes and can develop symptoms as early as their 30s or 40s. Others are people with Down syndrome, who have three copies of a chromosome containing a protein that often leads to what is called Down syndrome-associated Alzheimer’s disease .
Dr. Sperling said the genetic alterations in those cases are believed to fuel buildup of amyloid, while APOE4 is believed to interfere with clearing amyloid buildup.
Under the researchers’ proposal, having one copy of APOE4 would continue to be considered a risk factor, not enough to cause Alzheimer’s, Dr. Fortea said. It is unusual for diseases to follow that genetic pattern, called “semidominance,” with two copies of a variant causing the disease, but one copy only increasing risk, experts said.
The new recommendation will prompt questions about whether people should get tested to determine if they have the APOE4 variant.
Dr. Greicius said that until there were treatments for people with two copies of APOE4 or trials of therapies to prevent them from developing dementia, “My recommendation is if you don’t have symptoms, you should definitely not figure out your APOE status.”
He added, “It will only cause grief at this point.”
Finding ways to help these patients cannot come soon enough, Dr. Sperling said, adding, “These individuals are desperate, they’ve seen it in both of their parents often and really need therapies.”
Pam Belluck is a health and science reporter, covering a range of subjects, including reproductive health, long Covid, brain science, neurological disorders, mental health and genetics. More about Pam Belluck
The Fight Against Alzheimer’s Disease
Alzheimer’s is the most common form of dementia, but much remains unknown about this daunting disease..
How is Alzheimer’s diagnosed? What causes Alzheimer’s? We answered some common questions .
A study suggests that genetics can be a cause of Alzheimer’s , not just a risk, raising the prospect of diagnosis years before symptoms appear.
Determining whether someone has Alzheimer’s usually requires an extended diagnostic process . But new criteria could lead to a diagnosis on the basis of a simple blood test .
The F.D.A. has given full approval to the Alzheimer’s drug Leqembi. Here is what to know about i t.
Alzheimer’s can make communicating difficult. We asked experts for tips on how to talk to someone with the disease .

IMAGES
VIDEO
COMMENTS
The SOAP note is a way for healthcare workers to document in a structured and organized way.[1][2][3] ... One study found that the APSO order was better than the typical SOAP note order in terms of speed, task success (accuracy), and usability for physician users acquiring information needed for a typical chronic disease visit in primary care. ...
Introduction. SOAP notes are a helpful method of documentation designed to assist medical and mental health professionals in streamlining their clinical notes. Using a template such as SOAP notes means that you can capture, store, and interpret your client's information consistently over time. You probably already know this, but SOAP is an acronym that stands for subjective, objective ...
A well-completed SOAP note is a useful reference point within a patient's health record. Like BIRP notes, the SOAP format itself is a useful checklist for clinicians while documenting a patient's therapeutic progress.[REFERENCE ITEM="Sando, K. R., Skoy, E., Bradley, C., Frenzel, J., Kirwin, J., & Urteaga, E. (2017). Assessment of SOAP ...
SOAP note example. It's important that SOAP notes, or notes in any template style follow the requirements of a progress note, such as including session details like the start and stop time and place of service. Client Full Name: Connor Client. Client Date of Birth: 2/2/1992. Date of Service: 7/10/2023.
As the medical landscape progresses, our methods for managing clinical records, such as the SOAP note format, must evolve in tandem. This article is a comprehensive guide aimed at enhancing clinical documentation skills, including understanding the SOAP acronym medical and the SOAP notes meaning, at any stage of your medical career.
Not only does this format allow for thorough documentation, but it also assists the counselor in representing client concerns in a holistic framework, thus permitting practitioners, paraprofessionals, and case managers to better understand the concerns and needs of the client.
Facing SOAP oral presentations may cause a number of symptoms in the uninitiated M3: racing heart, rollercoaster gut, and sweaty palms. As with many first-time experiences you'll encounter in your third year, preparation goes a long way toward surviving SOAP oral presentations. But first, let's make sure we're clear on an important point.
This video shows How to make a perfect SOAP Format Case Presentation especially for PharmD students. From PharmD second yr onwards students need to collect a...
Not only does this format allow for thorough documentation, but it also assists the counselor in representing client concerns in a holistic framework, thus permitting practitioners, paraprofessionals, and case managers to better understand the concerns and needs of the client.
Page 1of 2. SOAP CASE NOTES GUIDE. The SOAP case note style can be used to document meetings with your client in a consistent manner. It may not be applicable for all clients or all sessions but it can be useful in guiding you when you write your case notes. SOAP notes can provide consistent documentation to monitor the client's progress and ...
36 likes • 20,132 views. A. Abel C. Mathew. He I present a case of Type 1 Diabetes mellitus with Pneumonia in standard SOAP format. Health & Medicine. 1 of 38. Download now. Case Presentation in SOAP Format - Download as a PDF or view online for free.
The format used for SOAP notes prompts the nurse to review all evidence, including subjective and objective data and information from the assessment, before reaching a nursing diagnosis. This is essential because if the nurse considers all the subjective and objective data while performing an assessment, they can develop a care plan based on ...
Narrative Format SOAP Format ADIME Format* Meal/snack pattern (FH-1.2.2.3) JO eats two meals and snacks throughout the day. Food intake (FH-1.2.2) includes most foods and has a high consumption of sugar based beverages during the day. Alcohol intake (FH-1.4.1) is limited to social occasions. Total energy intake
Oral case presentations - structured verbal reports of clinical cases - are fundamental to patient care and learner education. Despite their continued importance in a modernized medical landscape, their structure has remained largely unchanged since the 1960s, based on the traditional Subjective, Objective, Assessment, Plan (SOAP) format developed for medical records.
Pharmaceutical Care: WHO-FIP Model, Soap Analysis, and Illustrative Case Studies Download book PDF ... Selvaraj S, Karan A (2009) Deepening health insecurity in India: evidence from national sample surveys since 1980s. Econ Pol Wkly 44:55-60. Google Scholar Toklu HZ, Hussain A (2013) The changing face of pharmacy practice and the need for a ...
Case analysis in SOAP format. May 21, 2021 • Download as PPTX, PDF •. 2 likes • 1,750 views. A. Alida Vincent. SOAP notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible formats that could be used by a health professional. They are entered in the patients medical ...
SOAP Note and Case Summary. Sore Throat. COLLAPSE. Case: Mr. W is a 30-year-old man who complains of having a sore throat for 3 days. Mr. W's symptoms started abruptly 3 days ago when sore throat, pain with swallowing, fever, and headaches developed. He denies symptoms of cough, coryza, or rhinorrhea. Mr. W is otherwise healthy.
Create documentation using the SOAP note format; Identify the purpose and common elements of good case notes; Identify the challenges associated with completing case notes in an effective manner; Identify best practices and what you as a CHW bring to the process; Practice writing a progress note based on a case study; DOWNLOAD MATERIALS:
Unless when she has an emergency, she usually comes to the hospital for follow-up every month. Today, she has come for routine follow-up. Although she is asymptomatic, her blood pressure is 170/99 mmHg. She does not report any episodes or symptoms of hypoglycemia. She was using insulin, but stopped 8 months ago after she improved her condition.
1. NURS 223 Case Study/SOAPIE Note Problem-Oriented Charting The common charting format SOAPIE is ideal for a narrative client record of the nursing process.. SOAPIE, a systematic approach, details a goal-oriented nursing care plan in a note. SOAPIE Note S Subjective (report what the client states) O Objective (record what the nurse observes (also measurable - vital signs, physical ...
Apr 11, 2021 • Download as PPTX, PDF •. 8 likes • 2,605 views. V. varshawadnere. case presentation on osteoarthritis condition. Education. 1 of 13. Download now. Osteoarthritis case- SOAP FORMAT - Download as a PDF or view online for free.
The study aimed to determine the effects of high-risk pregnancy on prenatal stress levels. The study was conducted with a case-control design in Turkey in September-December 2019. The sample included pregnant women diagnosed with high-risk pregnancy and were at their 36th or later gestational weeks as the case group (n = 121) and healthy pregnant women as the control group (n = 245). The ...
Module 1 Case Study Notes Template EDUC 201 Teaching Profession Case Study Template Educational Record Your Name:Melissa Denton Chapter (No. And Title): 1 Case Study Student: Davon Age: Grade: Gender: Male Ethnicity: Category: Type of Person to Whom the Student Responds Notes: Davon responds to a teacher who provides structure within the classroom. The teacher needs to be consistent in every ...
68 likes • 25,548 views. Deepak Rx. Case presentation in SOAPME format highlighting the prescriptive role of a pharmacist in Critical and Ambulatory care. Health & Medicine. 1 of 46. Download now. Download to read offline. Case presentation - SOAP Format - Download as a PDF or view online for free.
May 6, 2024 Updated 12:19 p.m. ET. Scientists are proposing a new way of understanding the genetics of Alzheimer's that would mean that up to a fifth of patients would be considered to have a ...