Dopamine Function in the Brain
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
Learn about our Editorial Process
Karina Ascunce González
PhD Neuroscience Student, Yale University
Neuroscience B.A. (Hons), Harvard University
PhD Student at the Yale Biological & Biomedical Sciences' Interdepartmental Neuroscience Program interested in neurodegeneration, stem cell culture, and bioethics. AB in Neuroscience with a Secondary in Global Health & Health Policy from Harvard University. Karina has been published in peer reviewed journals.
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
On This Page:
Dopamine is a neurotransmitter that serves as a chemical messenger in the brain. It can function as both an excitatory and inhibitory neurotransmitter, leading to diverse effects on the brain, body, and behavior.

Dopamine is primarily known to be associated with feelings of pleasure and rewards . This chemical can also contribute to feelings of:
Dopamine is released when the brain is anticipating a reward. The flood of dopamine to the brain when experiencing a pleasurable stimulus (e.g., delicious food, video games, sex) can reinforce wanting to engage with this stimulus more due to the pleasurable feeling it causes.
This is a cycle of motivation, reward, and reinforcement. When associating a certain activity with pleasure, sometimes even mere anticipation may be enough to raise dopamine levels.
Dopamine is also implicated in learning, planning, and productivity. For instance, if someone has been working hard on a project for a long time, they can experience a surge of dopamine activity when it is finally completed.

Function of Dopamine
Dopamine is a neurotransmitter in the brain associated with pleasure, reward, motivation, and motor control. In psychology, it’s linked to feelings of gratification and is implicated in mood disorders, addiction, and certain behaviors when its levels are imbalanced.
Whilst strongly involved in pleasure and rewards, dopamine is also involved in other functions:
Motor function and movement
Mood regulation
Executive functioning
Memory and focus
Stress response
Digestion and blood flow
It is important to note that dopamine does not act in isolation. It works with other neurotransmitters and hormones, such as serotonin and adrenaline, to perform a variety of functions.
Dopamine is a catecholamine, a class of neurotransmitter which also includes epinephrine and norepinephrine. It was believed to be first identified in the brain by Kathleen Montagu in her 1957 paper demonstrating findings on key neurotransmitters.
As part of her research, she examined the quantities of norepinephrine, epinephrine, and 3-hydroxytryramine from extracted brain tissues of several species.
Montagu speculated that there might be an additional catecholamine similar to hydroxytyramine, which she later confirmed to be what is known as dopamine. Arvid Carlsson published research in the same year that confirmed dopamine was a neurotransmitter in the brain, as opposed to another precursor molecule.
Dopamine is highly concentrated in areas of the brain called the substantia nigra and the ventral tegmental area (VTA) in the midbrain. Other brain areas where dopamine can be made are the hypothalamus and the olfactory bulb.
There are dopamine pathways that can be triggered when exposed to a stimulus that is rewarding, resulting in increased amounts of dopamine circulating around brain areas.
Role Of Dopamine On Learning And Motivation
Reward system.
Dopamine plays a key role in the brain’s reward system . This neurotransmitter helps to reinforce certain behaviors that result in a reward.
In classical studies of rats, a surge of dopamine prompts the animal to press a lever to get a pellet of food repeatedly.
This works similarly in humans, for instance, when choosing to eat more pleasurable food, such as another slice of cake, because we have enjoyed the rewarding feeling the food has given us.
Reward Prediction
Some lines of study have found that midbrain dopamine neurons can be activated by proximal contact (touch, taste) with unexpected rewards.
When such events became predictable, the neurons were found to respond to the more distal (visual or auditory) stimuli that precede and predict the availability of the reward.
The neurons would then stop responding to the proximal contact with the reward (Romo & Schultz, 1990; Schultz et al., 1992).
This may be an oversimplification as the neurons that are no longer reactive to the proximal reward stimuli have been found to still be responsive to the lack of the reward.
When the expected proximal contact does not occur, the dopamine neurons become inhibited. So, although dopamine release is triggered by the earliest reliable predictor of reward, midbrain dopamine remains sensitive to the receipt or lack of reward.
The anticipation of expecting a reward was studied by researchers in a game of chance.
In the anticipation phase, where participants were told they might win money, blood flow was found in the amygdala and frontal cortex, indicating activity in the nucleus accumbens and the hypothalamus, all rich in dopamine receptors.
The bigger the potential reward, the greater dopamine-led brain activity was found.
Conditioned reinforcement
By allowing dopamine to affect choices, it can bias towards choosing the stimulus that was learned from the amount of positive or negative reinforcement the stimulus received.
Reward-associated motivational stimuli can serve as conditioned reinforcers when given after a response.
For instance, in a study on rats, when they were thirsty, they learned to work for the presentation of a light that was previously paired with water.
In this test, injections of amphetamine into the nucleus accumbens (a reward area of the brain) caused dopamine release. They enhanced response to the light (Taylor & Robbins, 1984), whereas dopamine-selective lesions of the nucleus accumbens reduced this response (Taylor & Robbins, 1986).
Therefore, dopamine can modulate the expression of conditioned reinforcement as well as is essential for the establishment of conditioned reinforcers.
What Dopamine Does In The Brain
Within the brain are dopamine receptors which are proteins found in the brain and other neurons throughout the body. As a dopamine signal approaches a nearby neuron, it binds to that neuron’s receptor.
The receptor and neurotransmitter work like a lock and key. The dopamine attaches to the dopamine receptor, delivering its chemical message by causing changes to occur in the neuron that received the signal.
Through the use of dopamine receptors, the effects of dopamine, such as movement coordination, pleasure, and cognition, can take effect.
Where is dopamine produced?
Dopamine is produced in several areas of the brain, including the ventral tegmental area (VTA: a dopamine-rich nucleus located within the midbrain) and the substantia nigra.
Once produced in the VTA, dopamine is transported to other areas of the brain through different dopamine pathways, the two main ones being the mesolimbic and the mesocorticol pathways. Other pathways include the nigrostriatal and tuberoinfundibular pathways.
Dopamine pathways are neuronal connections in which dopamine travels to areas of the brain and body to convey important information such as executive thinking, cognition, feelings of reward and pleasure, and voluntary movement.

Mesolimbic pathways
This dopamine pathway is highly involved in the functions of pleasure and reward. Beginning at the VTA, dopamine produced here projects to the nucleus accumbens.
When here, dopamine primarily mediates feelings of pleasure and reward. For instance, if someone eats a food they enjoy, dopamine is released from the VTA to the nucleus accumbens which then creates positive feelings that reinforce the behavior.
Sometimes stimuli can create intense feelings of euphoria.
The nucleus accumbens is found in the ventral striatum and is part of a complex circuit involving the amygdala and the hippocampus. The activation of the mesolimbic dopamine pathway communicates that it wants to repeat what just happened to feel the rewarding sensation again.
Since the nucleus accumbens has connections to the amygdala, a region of the limbic system associated with emotions, this attributes feelings towards the experienced reward.
Likewise, connections to the hippocampus, an area associated with memory, can attribute memories of pleasure to the experience to reinforce this sensation to happen again.
Stimulating the nucleus accumbens is important for daily activities, but over-stimulation can result in cravings for the stimulus which stimulates it.
Mesocorticol pathways
As with the mesolimbic pathways, the mesocortical pathway starts with dopamine projections originating from the VTA. From the VTA, signals are sent to the prefrontal cortex, an area involved in cognition, working memory, and decision-making.
Thus, activation of this pathway brings about the conscious experience of the pleasure and reward being experienced. Attention, concentration, and decisions can be made as a result of pleasure and reward.
Dysfunction in this pathway can therefore result in poor concentration and an inability to make decisions.
Nigrostriatal pathways
This dopamine pathway is involved in motor planning. The dopamine projections start in the substantia nigra, a basal ganglia structure located in the midbrain.
These projections go to the caudate and putamen, which are also parts of the basal ganglia. The neurons in this pathway stimulate purposeful movement and contain about 80% of the dopamine in the brain.
If there are reductions in the number of dopamine neurons in this pathway, this can result in motor control impairments, including movement disorders such as Parkinson’s disease.
Symptoms of dysfunction in this pathway may include spasms, contractions, tremors, and motor restlessness.
Tuberoinfundibular pathways
The dopamine neurons in this pathway originate in the hypothalamus, an area that plays a role in hormone production and helps to stimulate many important processes in the body.
Specifically, the neurons are in the arcuate and periventricular nuclei of the hypothalamus. These then project to the infundibular region of the hypothalamus. In this pathway, dopamine is released into the portal circulation that connects this region to the pituitary gland.
Here, dopamine functions to inhibit prolactin release. Prolactin is a protein secreted by the pituitary gland that enables milk production and has important functions in metabolism, sexual satisfaction, and the immune system.
Dopamine Hypothesis In Schizophrenia
The dopamine hypothesis for schizophrenia suggests that some of the symptoms of schizophrenia involve excess dopamine activity.
The dopamine hypothesis of schizophrenia was derived from observations in the 1960s where the effects of amphetamines resembled schizophrenia. Amphetamines increase dopamine function (Seeman et al., 1976).
Dopamine appears to play a big role in the activity of the frontal and temporal lobes, particularly parts of the cerebral cortex of these lobes that play a role in the cognitive, emotional, and perceptual functions that are often abnormal in schizophrenia.
However, inconsistencies in post-mortem findings and debates on whether certain changes were due to drugs or the disease made it challenging to pinpoint schizophrenia’s exact link with dopamine. Yet, imaging studies revealed that schizophrenic patients release more dopamine than healthy individuals in response to certain scenarios (Laruelle et al., 1996).
The discovery of organic changes in the brains of schizophrenic patients through imaging techniques shifted the focus to viewing schizophrenia as a neurodevelopmental disorder.
This suggested that schizophrenia might stem from reduced dopamine function in the prefrontal cortex, leading to increased dopamine in other areas (mesolimbic). Potential treatments now consider balancing these levels, exemplified by drugs like aripiprazole (Carlsson, 1988).
There appear to be abnormalities in the mesocortical and mesolimbic pathways that carry dopamine from the VTA to areas of the cerebral cortex.
Disruptions in the parts of the cerebral cortex are believed to cause many of the cognitive symptoms of schizophrenia, such as disorganized thinking, difficulty integrating thoughts, and poor concentration.
Abnormal activity of dopamine pathways in the limbic system is believed to be responsible for many of the negative symptoms of schizophrenia, such as lack of motivation and social withdrawal.
Also, dopamine abnormalities in the temporal and prefrontal areas of the brain are believed to be overactive in those with schizophrenia and thus can lead to some of the positive symptoms of the condition, such as hallucinations and delusions .
This hypothesis aligns with the use of some antipsychotic drug medications, which work to block dopamine receptor in the brain appear to be effective in treating the positive symptoms of schizophrenia.
Likewise, the effects of dopamine-enhancing drugs such as methamphetamine and cocaine, over repeated exposure, may gradually induce paranoid psychosis in non-schizophrenic people.
This well-documented observation shows that sustained increases in dopamine activity can cause some of the similar symptoms of schizophrenia.
However, the dopamine hypothesis for schizophrenia may be an oversimplification as there may be many other neuronal network abnormalities and neurotransmitter systems involved in causing the condition.
Research since the dopamine hypothesis has indicated that glutamate, GABA, acetylcholine, and serotonin alterations are also involved in the pathology of schizophrenia, so it may not be dopamine alone which affects this condition.
What about the future?
We know a lot about two types of dopamine receptors in the brain, but less about three others. Using mice in research , scientists discovered the importance of the D5 receptor in male and female sexual behaviors. Also, some research shows mice might like sugar even if they can’t produce dopamine.
Notably, there’s a growing consensus that studying dopamine should not be in isolation but in conjunction with other transmitter systems. This integrated approach recognizes the broader neuronal organization and connectivity in the brain.
Even though dopamine neurons comprise less than 1% of brain neurons, alterations in dopamine levels or functions can significantly influence behavior.
This underscores the idea that dopamine’s primary role might be integrating information pertinent to biologically significant stimuli rather than transmitting specific data.
What happens if dopamine is depleted?
Low dopamine levels may result in some of the following symptoms:
– Reduced alertness – Difficulty concentrating – A lack of motivation – Poor coordination – Movement difficulties – Inability to feel pleasure
In more extreme cases, a lack of dopamine could result in conditions such as Parkinson’s disease, dopamine transporter deficiency syndrome, or depression.
Although dopamine alone may not directly cause depression, low levels of dopamine have been suggested to cause specific symptoms associated with this condition, such as motivational issues, feeling hopeless and helpful, and a loss of interest in previously enjoyed activities.
It’s suggested that these symptoms may be linked to a dysfunction in the dopamine systems of the brain. A main trigger for these dysfunctions could be due to stress, pain, lack of sleep, or trauma.
A physiological explanation is that there may be a diminished dopamine release from the presynaptic neurons and/or impairment in signal transduction, possibly due to changes in the number of dopamine receptors.
Attention deficit hyperactivity disorder (ADHD) is a condition that is also associated with low levels of dopamine.
Symptoms of ADHD include difficulties with concentration and attention, impulsiveness and finding it difficult to remain still.
Since people with ADHD have lowered dopamine levels, they are more likely to carry out behaviors in order to obtain more dopamine.
What are the symptoms of high dopamine?
High levels of dopamine can make people feel euphoric in the short term; however, over time, it can be detrimental. In excess, dopamine can be a contributing factor in mania , hallucinations, and delusions.
A surplus of dopamine can result in more competitive behaviors, aggression, poor control over impulses, gambling behaviors, and addiction.
As such, addictive drugs can increase levels of dopamine, encouraging the individual to continue to use these drugs to reach that pleasurable feeling of reward.
This does not just have to be an addiction to drugs; people can be addicted to anything which gives them a surge of dopamine, such as video games, food, and social media use.
How do I get my dopamine levels back to normal?
Depending on whether dopamine levels are too high or low will determine what techniques to take. If wanting to increase dopamine levels, some ways can include:
– Establishing a good sleep schedule – Less screen time (e.g., television, phone), especially before bed – Learning to meditate or undertaking mindfulness training – Exercising regularly – Changes in diet to increase levels of vitamin D and essential fatty acids – Physical therapy for muscle stiffness and movement problems
Dopamine agonists – a class of drugs that bind to and activate dopamine receptors in the brain, mimicking the action of naturally-occurring dopamine in the brain.
For those with too much dopamine, such as individuals with schizophrenia, dopamine antagonists are usually recommended.
These are a class of drugs that bind to and block dopamine receptors, turning down the dopamine activity.
Many antipsychotic drugs are dopamine antagonists, including Chlorpromazine (Thorazine), Risperidone (Risperdal), and Clozapine (Clozaril).
What happens when you ‘dopamine fast’?
Dopamine fasting is a recent trend where people strive to ‘reset’ their dopamine levels by completely abstaining from anything that brings them pleasure. This can include phone use, social media, video games, delicious food, sex, and social interaction.
Taking breaks from behaviors that trigger strong amounts of dopamine release could allow the brain to recover and restore itself, being an antidote to the age of overstimulation we live in.
Kent Berridge, a professor of psychology and neuroscience, suggests that taking a break from a stimulating activity (or all of them) will not reset dopamine levels, but it can stop the dopamine system from turning on constantly.
Dopamine fast is not believed to be something that can reduce dopamine, but having breaks from one or two pleasurable activities at a time can help in reducing impulsive behaviors.
In addition, a specific study showed that dopamine fasting from the social media platform Facebook for a week helped students regain 13.3 hours of their time and significantly reduced depressive symptoms by 17%, which allowed them to engage in more healthy behaviors instead (Mosquere et al., 2019).
Brisch, R., Saniotis, A., Wolf, R., Bielau, H., Bernstein, H. G., Steiner, J., Bogerts, B., Braun, K., Jankowski, Z., Kumaratilake, J., Henneberg, M. & Gos, T. (2014). The role of dopamine in schizophrenia from a neurobiological and evolutionary perspective: old fashioned, but still in vogue. Frontiers in psychiatry , 5, 47.
Bridges, N. (2016, November 25). Dopamine Pathways. Sanesco. https://sanescohealth.com/blog/dopamine-pathways/
Cannon, C. M., Scannell, C. A., & Palmiter, R. D. (2005). Mice lacking dopamine D1 receptors express normal lithium chloride‐induced conditioned taste aversion for salt but not sucrose. European Journal of Neuroscience , 21 (9), 2600-2604.
Carlsson, A. (1988). The current status of the dopamine hypothesis of schizophrenia. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology, 1 (3), 179-186.
Conrad, B. (n.d.). The Role of Dopamine as a Neurotransmitter in the Human Brain. Enzo. Retrieved 2021, November 5, from: https://www.enzolifesciences.com/science-center/technotes/2018/november/the-role-of-dopamine-as-a-neurotransmitter-in-the-human-brain/
Laruelle, M., Abi-Dargham, A., Van Dyck, C. H., Gil, R., D’Souza, C. D., Erdos, J., … & Innis, R. (1996). Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects. Proceedings of the National Academy of Sciences , 93 (17), 9235-9240.
Mosquera, R., Odunowo, M., McNamara, T., Guo, X., & Petrie, R. (2020). The economic effects of Facebook. Experimental Economics, 23(2), 575-602.
Pietrangelo, A. (2019, November 5). How Does Dopamine Affect the Body? Healthline. https://www.healthline.com/health/dopamine-effects
Romo, R., & Schultz, W. (1990). Dopamine neurons of the monkey midbrain: contingencies of responses to active touch during self-initiated arm movements. Journal of neurophysiology, 63 (3), 592-606.
Schultz, W., Apicella, P., Scarnati, E., & Ljungberg, T. (1992). Neuronal activity in monkey ventral striatum related to the expectation of reward. Journal of Neuroscience, 12(12), 4595-4610.
Seeman, P., Lee, T., Chau-Wong, M., & Wong, K. (1976). Antipsychotic drug doses and neuroleptic/dopamine receptors. Nature , 261 (5562), 717-719.
Sepah, C. (2019, August 7). The Definitive Guide to Dopamine Fasting 2.0 – The Hot Silicon Valley Trend. LinkedIn. https://www.linkedin.com/pulse/dopamine-fasting-new-silicon-valley-trend-dr-cameron-sepah/
Taylor, J. R., & Robbins, T. W. (1984). Enhanced behavioural control by conditioned reinforcers following microinjections of d-amphetamine into the nucleus accumbens. Psychopharmacology, 84( 3), 405-412.
Taylor, J. R., & Robbins, T. W. (1986). 6-Hydroxydopamine lesions of the nucleus accumbens, but not of the caudate nucleus, attenuate enhanced responding with reward-related stimuli produced by intra-accumbens d-amphetamine. Psychopharmacology, 90(3), 390-397.
Wise, R. A. (2004). Dopamine, learning and motivation. Nature Reviews Neuroscience, 5 (6), 483-494.
Further Reading
- Volkow, N. D., Wang, G. J., Kollins, S. H., Wigal, T. L., Newcorn, J. H., Telang, F., … & Swanson, J. M. (2009). Evaluating Dopamine Reward Pathway in ADHD. JAMA, 302 (10), 1084-1091.
- Belujon, P., & Grace, A. A. (2017). Dopamine System Dysregulation in Major Depressive Disorders. International Journal of Neuropsychopharmacology, 20( 12), 1036-1046.

Reviewed by Psychology Today Staff
Dopamine is known as the feel-good neurotransmitter—a chemical that ferries information between neurons. The brain releases it when we eat food that we crave or while we have sex , contributing to feelings of pleasure and satisfaction as part of the reward system. This important neurochemical boosts mood, motivation , and attention , and helps regulate movement, learning, and emotional responses.
- Dopamine and Behavior
- Dopamine and the Brain
- How to Increase Dopamine

In lab experiments, dopamine prompts a rat to press a lever for food again and again. This is no different in humans; it’s the reason why we partake in more than one helping of cake. This press-the-lever action applies to addiction as well. People with low levels of dopamine may be more prone to addiction; a person seeking pleasure via drugs or alcohol or food needs higher and higher levels of dopamine.
Dopamine causes you to want, desire, seek out, and search. It increases your general level of arousal and your goal-directed behavior. Dopamine makes you curious about ideas and fuels your search for information. Dopamine creates reward-seeking loops in the sense that people will repeat pleasurable behavior, from checking Instagram to taking drugs.
A person with high levels of dopamine, whether due to temperament or to a transient—perhaps chemically induced state—can be described as a sensation seeker. The upside of sensation seeking is that people see potential stressors as challenges to be overcome rather than threats that might crush them. This mindset is a buffer against the stress of life. It increases their hardiness and r esilience in the long term.
The release of dopamine creates a reward circuit in the brain. This circuit registers an intense experience (such as getting high) as "important" and creates lasting memories of it as pleasurable. Dopamine changes the brain on a cellular level, commanding the brain to do it again.

Swedish pharmacologist and neuroscientist Arvid Carlsson won the Nobel prize in 2000 for his research on dopamine, showing its importance in brain function. He helped show that the neurotransmitter is heavily involved in the motor system. When the brain fails to produce enough dopamine, it can result in Parkinson’s disease. The primary treatment for Parkinson’s disease is a drug called L-dopa, which spurs the production of dopamine.
Dopamine has also been implicated in schizophrenia and ADHD ; the brain systems underlying these conditions (as well as substance abuse disorder) are complex. The activity of the dopamine system depends on the state of one’s dopamine receptors, and in people with these conditions, the chemical interacts with other factors in ways that have yet to be explained.
It is no exaggeration to say that dopamine makes us human. Beginning in infant development, dopamine levels are critical, and mental disabilities can arise if dopamine is not present in sufficient quantities. Dopamine is implicated in genetic conditions like congenital hypothyroidism. Dopamine deficiency is also implicated in other conditions such as Alzheimer's, depressive disorders, binge-eating, addiction, and gambling.
Drugs currently used to treat ADHD do indeed increase the effectiveness of dopamine. This helps patients with ADHD focus and pay better attention to one thing at a time. How exactly more dopamine translates into better concentration and focus is not yet understood.
In this neurodegenerative disorder, the decline begins with the dopamine-producing cells in the brain where movement is coordinated. As these cells degrade, motor function is compromised , which includes tremors, rigidity, bradykinesia or slowed movement, as well as changes in speech and gait.

Scientists who study neurological and psychiatric disorders have long been interested in how dopamine works and how relatively high or low levels of dopamine in the brain relate to behavioral challenges and disability.
There are ways to up one's dopamine levels naturally, and basic self-care is the place to start. A night of fitful sleep, for one, can reduce dopamine drastically. Here are some tips to boost levels:
- Eat foods rich in tyrosine including cheese, meats, fish, dairy, soy, seeds, nuts, beans, lentils, among others. While tyrosine supplements are available, consuming foods is preferred.
- Up magnesium intake with foods such as seeds, nuts, soy, beans, whole grains, among others.
- Avoid processed foods, high-fats, sugar, caffeine.
- Proper sleep hygiene is mandatory, as it fuels dopamine production.
- Exercise daily.
- Avoid stress, apply techniques such as meditation , visualization , breathing exercises.
- Consider the use of natural nootropics including L-Tyrosine and L-theanine.

Discover how challenges that are not fun in the moment—but rewarding in retrospect—can grow resilience, deepen life satisfaction, and lead to transformative personal growth.

Deciding how we are going to eat is not a matter of free will. Our bodies and brains have their own agenda.

We all have our own personalities, preferences, and quirks, and they should all be reflected in our styles. Finding your style can lead to increased self-esteem and confidence.

More than 21 million Americans—celebrities and "regular" folks among them— have both a substance use disorder and a serious psychiatric problem. What do we know about this issue?
Capitalizing on your motivation or eliminating apathy and inaction means keen awareness of the powerful role of rewards and your unique dopamine production.

Oxytocin fuels maternal instincts, tells us who brings us the most joy, helps us make friends, and is associated with the development of empathy but also hatred and prejudice.

Discover how non-alcoholic beverages might impact alcohol recovery; Could they be the key to controlling cravings, or do they pose unseen risks?

Speedballing, combining fentanyl with cocaine or methamphetamine, is the fourth wave of the opioid crisis in the U.S.

How your brain responds to reward matters more than the power of positive emotion.

Exploring dopamine's role in addiction and consumer behavior helps us understand how it shapes our motivations and influences decision-making.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

Dopamine (DA) Hypothesis
The Dopamine (DA) Hypothesis proposes that imbalances in the neurotransmitter dopamine are responsible for the development and symptoms of certain psychiatric conditions, particularly schizophrenia and bipolar disorder.
Neurotransmitter: Dopamine
Dopamine is a chemical messenger (neurotransmitter) in the brain that plays a crucial role in various physiological and psychological functions. It is involved in regulating movement, motivation, cognition, reward, pleasure, and emotional responses.
Overview of the Hypothesis
The Dopamine Hypothesis suggests that abnormalities in the functioning of dopamine systems within the brain contribute to the development and manifestation of psychiatric disorders. It proposes that an excess or dysregulation of dopamine transmission can result in the characteristic symptoms observed in certain conditions.
Schizophrenia
In the context of schizophrenia, the DA Hypothesis suggests that an increase in dopamine activity in specific brain regions, such as the mesolimbic pathway, contributes to the positive symptoms of the disorder, including hallucinations and delusions. Medications that block dopamine receptors, known as antipsychotics, are commonly used in the treatment of schizophrenia.
Bipolar Disorder
Regarding bipolar disorder, the DA Hypothesis proposes that there is an imbalance in dopamine levels between manic and depressive episodes. During manic episodes, there is a surge in dopamine activity, leading to heightened energy, euphoria, and impulsivity. In contrast, reduced dopamine levels during depressive episodes may contribute to the lack of motivation and pleasure commonly experienced by individuals with bipolar disorder.
Limitations and ongoing research
The DA Hypothesis has provided valuable insights into the understanding and treatment of schizophrenia and bipolar disorder. However, it is important to note that the hypothesis does not fully explain the complexity of these disorders, as multiple neurotransmitters and brain systems are involved. Ongoing research aims to refine the Dopamine Hypothesis and explore other contributing factors, such as glutamate and serotonin, to gain a more comprehensive understanding of these conditions.
- Architecture and Design
- Asian and Pacific Studies
- Business and Economics
- Classical and Ancient Near Eastern Studies
- Computer Sciences
- Cultural Studies
- Engineering
- General Interest
- Geosciences
- Industrial Chemistry
- Islamic and Middle Eastern Studies
- Jewish Studies
- Library and Information Science, Book Studies
- Life Sciences
- Linguistics and Semiotics
- Literary Studies
- Materials Sciences
- Mathematics
- Social Sciences
- Sports and Recreation
- Theology and Religion
- Publish your article
- The role of authors
- Promoting your article
- Abstracting & indexing
- Publishing Ethics
- Why publish with De Gruyter
- How to publish with De Gruyter
- Our book series
- Our subject areas
- Your digital product at De Gruyter
- Contribute to our reference works
- Product information
- Tools & resources
- Product Information
- Promotional Materials
- Orders and Inquiries
- FAQ for Library Suppliers and Book Sellers
- Repository Policy
- Free access policy
- Open Access agreements
- Database portals
- For Authors
- Customer service
- People + Culture
- Journal Management
- How to join us
- Working at De Gruyter
- Mission & Vision
- De Gruyter Foundation
- De Gruyter Ebound
- Our Responsibility
- Partner publishers

Your purchase has been completed. Your documents are now available to view.
Does the dopamine hypothesis explain schizophrenia?
Chi-Ieong David Lau is a Consultant Neurologist whose research interests focus on the cognitive neuroscience underpinning neurological diseases. His recent work includes the investigation of the visual system in migraine, as well as the modulation of slow-wave-sleep-related memory consolidation using a variety of methods, including EEG, neuroimaging, brain stimulation, and genetics. He completed his medical degree and neurology training in Taiwan and postgraduate studies at the University College London and the University of Oxford, supported by the British Chevening Scholarship.
Han-Cheng Wang is a Consultant Neurologist at Shin Kong Wu Ho-Su Memorial Hospital, with specialist clinics for Parkinson’s disease and movement disorders. He is Assistant Professor of Neurology at the College of Medicine, National Taiwan University. He is the former President and present Standing Member of the Executive Board of Taiwan Movement Disorder Society. His research interests include understanding basic neurophysiology underlying human movements and movement disorders. He is interested in linking clinical features with functional connectivity of the brain, reflected in his recent works correlating regional cerebral blood flow (CBF) changes and tract-specific abnormalities with severity of Parkinsonism.
Jung-Lung Hsu is a Clinical Neurologist. He is interested in behavioral/cognitive neuroscience. His main study is focused on brain structural change and human behavior. He is also participating in the event-related potential (ERP) study (P50 and MMN) of schizophrenia patients.
Mu-En Liu’s research interests include biological psychiatry and geriatric psychiatry. Some of the study topics are novel in the genetic study of cognitive ageing. Recently, he examined genetic effects on age-related morphologic changes in the brain. His researches may clarify the underlying molecular mechanisms of brain aging.
The dopamine hypothesis has been the cornerstone in the research and clinical practice of schizophrenia. With the initial emphasis on the role of excessive dopamine, the hypothesis has evolved to a concept of combining prefrontal hypodopaminergia and striatal hyperdopaminergia, and subsequently to the present aberrant salience hypothesis. This article provides a brief overview of the development and evidence of the dopamine hypothesis. It will argue that the current model of aberrant salience explains psychosis in schizophrenia and provides a plausible linkage between the pharmacological and cognitive aspects of the disease. Despite the privileged role of dopamine hypothesis in psychosis, its pathophysiological rather than etiological basis, its limitations in defining symptoms other than psychosis, as well as the evidence of other neurotransmitters such as glutamate and adenosine, prompt us to a wider perspective of the disease. Finally, dopamine does explain the pathophysiology of schizophrenia, but not necessarily the cause per se. Rather, dopamine acts as the common final pathway of a wide variety of predisposing factors, either environmental, genetic, or both, that lead to the disease. Other neurotransmitters, such as glutamate and adenosine, may also collaborate with dopamine to give rise to the entire picture of schizophrenia.
About the authors

The authors would like to thank Miss Frankie Wing See Tam for her valuable comments on the manuscript.
Conflicts of interest: The authors have no conflicts of interest relevant to this article.
Abbott, C.C., Jaramillo, A., Wilcox, C.E., and Hamilton, D.A. (2013). Antipsychotic drug effects in schizophrenia: a review of longitudinal FMRI investigations and neural interpretations. Curr. Med. Chem. 20 , 428–437. Search in Google Scholar
Abi-Dargham, A. (2003). Probing cortical dopamine function in schizophrenia: what can D1 receptors tell us? World Psychiatry 2 , 166–171. Search in Google Scholar
Abi-Dargham, A. and Moore, H. (2003). Prefrontal DA transmission at D1 receptors and the pathology of schizophrenia. Neuroscientist 9 , 404–416. 10.1177/1073858403252674 Search in Google Scholar
Abi-Dargham, A., Gil, R., Krystal, J., Baldwin, R.M., Seibyl, J.P., Bowers, M., van Dyck, C.H., Charney, D.S., Innis, R.B., and Laruelle, M. (1998). Increased striatal dopamine transmission in schizophrenia: confirmation in a second cohort. Am. J. Psychiatry 155 , 761–767. Search in Google Scholar
Abi-Dargham, A., Mawlawi, O., Lombardo, I., Gil, R., Martinez, D., Huang, Y., Hwang, D.R., Keilp, J., Kochan, L., Van Heertum, R., et al. (2002). Prefrontal dopamine D1 receptors and working memory in schizophrenia. J. Neurosci. 22 , 3708–3719. 10.1523/JNEUROSCI.22-09-03708.2002 Search in Google Scholar
Abi-Dargham, A., Xu, X., Thompson, J.L., Gil, R., Kegeles, L.S., Urban, N.B., Narendran, R., Hwang, D., Laruelle, M., and Slifstein, M. (2012). Increased prefrontal cortical D(1) receptors in drug naive patients with schizophrenia: a PET study with [(1)(1)C]NNC112. J. Psychopharmacol. 26 , 794–805. 10.1177/0269881111409265 Search in Google Scholar
Agid, O., Seeman, P., and Kapur, S. (2006). The “delayed onset” of antipsychotic action–an idea whose time has come and gone. J. Psychiatry Neurosci. 31 , 93–100. Search in Google Scholar
Akil, M., Pierri, J.N., Whitehead, R.E., Edgar, C.L., Mohila, C., Sampson, A.R., and Lewis, D.A. (1999). Lamina-specific alterations in the dopamine innervation of the prefrontal cortex in schizophrenic subjects. Am. J. Psychiatry 156 , 1580–1589. 10.1176/ajp.156.10.1580 Search in Google Scholar
Allen, N.C., Bagade, S., McQueen, M.B., Ioannidis, J.P., Kavvoura, F.K., Khoury, M.J., Tanzi, R.E., and Bertram, L. (2008). Systematic meta-analyses and field synopsis of genetic association studies in schizophrenia: the SzGene database. Nat. Genet. 40 , 827–834. 10.1038/ng.171 Search in Google Scholar
Andreasen, N.C. (1982). Negative symptoms in schizophrenia. Definition and reliability. Arch. Gen. Psychiatry 39 , 784–788. 10.1001/archpsyc.1982.04290070020005 Search in Google Scholar
Barch, D.M. and Ceaser, A. (2012). Cognition in schizophrenia: core psychological and neural mechanisms. Trends Cognit. Sci. 16 , 27–34. 10.1016/j.tics.2011.11.015 Search in Google Scholar
Barch, D.M., Carter, C.S., Braver, T.S., Sabb, F.W., MacDonald, A. 3rd., Noll, D.C., and Cohen, J.D. (2001). Selective deficits in prefrontal cortex function in medication-naive patients with schizophrenia. Arch. Gen. Psychiatry 58 , 280–288. 10.1001/archpsyc.58.3.280 Search in Google Scholar
Berridge, K.C. and Robinson, T.E. (1998). What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res. Brain Res. Rev. 28 , 309–369. 10.1016/S0165-0173(98)00019-8 Search in Google Scholar
Berton, O., McClung, C.A., DiLeone, R.J., Krishnan, V., Renthal, W., Russo, S.J., Graham, D., Tsankova, N.M., Bolanos, C.A., Rios, M., et al. (2006). Essential role of BDNF in the mesolimbic dopamine pathway in social defeat stress. Science 311 , 864–868. 10.1126/science.1120972 Search in Google Scholar PubMed
Boison, D., Singer, P., Shen, H.Y., Feldon, J., and Yee, B.K. (2013). Adenosine hypothesis of schizophrenia – opportunities for pharmacotherapy. Neuropharmacology 62 , 1527–1543. 10.1016/j.neuropharm.2011.01.048 Search in Google Scholar
Boksa, P. and El-Khodor, B.F. (2003). Birth insult interacts with stress at adulthood to alter dopaminergic function in animal models: possible implications for schizophrenia and other disorders. Neurosci. Biobehav. Rev. 27 , 91–101. 10.1016/S0149-7634(03)00012-5 Search in Google Scholar
Bossong, M.G., van Berckel, B.N., Boellaard, R., Zuurman, L., Schuit, R.C., Windhorst, A.D., van Gerven, J.M., Ramsey, N.F., Lammertsma, A.A., and Kahn, R.S. (2009). Delta 9-tetrahydrocannabinol induces dopamine release in the human striatum. Neuropsychopharmacology 34 , 759–766. 10.1038/npp.2008.138 Search in Google Scholar PubMed
Breier, A., Su, T.P., and Pickar, D. (1997). Schizophrenia is associated with elevated amphetamine-induced synaptic dopamine concentrations: evidence from a novel positron emission tomography method. Proc. Natl. Acad. Sci. USA 94 , 2569–2574. 10.1073/pnas.94.6.2569 Search in Google Scholar PubMed PubMed Central
Brody, A.L., Olmstead, R.E., London, E.D., Farahi, J., Meyer, J.H., Grossman, P., Lee, G.S., Huang, J., Hahn, E.L., and Mandelkern, M.A. (2004). Smoking-induced ventral striatum dopamine release. Am. J. Psychiatry. 161 , 1211–1218. 10.1176/appi.ajp.161.7.1211 Search in Google Scholar PubMed
Butwell, M., Jamieson, E., Leese, M., and Taylor, P. (2000). Trends in special (high-security) hospitals. 2: Residency and discharge episodes, 1986–1995. Br. J. Psychiatry 176 , 260–265. 10.1192/bjp.176.3.260 Search in Google Scholar PubMed
Carlsson, A. and Lindqvist, M. (1963). Effect of chlorpromazine or haloperidol on formation of 3methoxytyramine and normetanephrine in mouse brain. Acta Pharmacol. Toxicol. 20 , 140–144. 10.1111/j.1600-0773.1963.tb01730.x Search in Google Scholar PubMed
Caspi, A., Moffitt, T.E., Cannon, M., McClay, J., Murray, R., Harrington, H., Taylor, A., Arseneault, L., Williams, B., Braithwaite, A., et al. (2005). Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biol. Psychiatry 57 , 1117–1127. 10.1016/j.biopsych.2005.01.026 Search in Google Scholar PubMed
Catafau, A.M., Corripio, I., Pérez, V., Martin, J.C., Schotte, A., Carrió, I., and Alvarez, E. (2006). Dopamine D2 receptor occupancy by risperidone: implications for the timing and magnitude of clinical response. Psychiatry Res. 148 , 175–183. 10.1016/j.pscychresns.2006.02.001 Search in Google Scholar PubMed
Coyle, J.T. (2006). Glutamate and schizophrenia: beyond the dopamine hypothesis. Cell. Mol. Neurobiol. 26 , 365–384. 10.1007/s10571-006-9062-8 Search in Google Scholar PubMed
Crawley, J.C., Owens, D.G., Crow, T.J., Poulter, M., Johnstone, E.C., Smith, T., Oldland, S.R., Veall, N., Owen, F., Zanelli. G.D. (1986). Dopamine D2 receptors in schizophrenia studied in vivo. Lancet 2 , 224–225. 10.1016/S0140-6736(86)92525-0 Search in Google Scholar
da Silva Alves, F., Figee, M., van Avamelsvoort, T., Veltman, D., and de Haan, L. (2008). The revised dopamine hypothesis of schizophrenia: evidence from pharmacological MRI studies with atypical antipsychotic medication. Psychopharmacol. Bull. 41 , 121–132. Search in Google Scholar
Davis, K.L., Kahn, R.S., Ko, G., and Davidson, M. (1991). Dopamine in schizophrenia: a review and reconceptualization. Am. J. Psychiatry 148 , 1474–1486. 10.1176/ajp.148.11.1474 Search in Google Scholar PubMed
Dold, M., Li, C., Tardy, M., Khorsand, V., Gillies, D., and Leucht, S. (2012). Benzodiazepines for schizophrenia. Cochrane Database Syst. Rev. 11, CD006391. 10.1002/14651858.CD006391.pub2 Search in Google Scholar PubMed PubMed Central
Fusar-Poli, P., Howes, O.D., Allen, P., Broome, M., Valli, I., Asselin, M.C., Grasby, P.M., and McGuire, P.K. (2010). Abnormal frontostriatal interactions in people with prodromal signs of psychosis: a multimodal imaging study. Arch. Gen. Psychiatry 67 , 683–691. 10.1001/archgenpsychiatry.2010.77 Search in Google Scholar PubMed
Fusar-Poli, P. and Meyer-Lindenberg, A. (2013). Striatal presynaptic dopamine in schizophrenia, part I: meta-analysis of dopamine active transporter (DAT) density. Schizophr. Bull. 39 , 22–32. 10.1093/schbul/sbr111 Search in Google Scholar PubMed PubMed Central
Goldman-Rakic, P.S. and Selemon, L.D. (1997). Functional and anatomical aspects of prefrontal pathology in schizophrenia. Schizophr. Bull. 23 , 437–458. 10.1093/schbul/23.3.437 Search in Google Scholar PubMed
Gordon, J.A. (2010). Testing the glutamate hypothesis of schizophrenia. Nat. Neurosci. 13 , 2–4. 10.1038/nn0110-2 Search in Google Scholar PubMed
Guo, N., Hwang, D.R., Lo, E.S., Huang, Y.Y., Laruelle, M., and Abi-Dargham, A. (2003). Dopamine depletion and in vivo binding of PET D1 receptor radioligands: implications for imaging studies in schizophrenia. Neuropsychopharmacology 28 , 1703–1711. 10.1038/sj.npp.1300224 Search in Google Scholar PubMed
Heinrichs, R.W. (2007). Cognitive improvement in response to antipsychotic drugs: neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE Trial. Arch. Gen. Psychiatry 64 , 631–632. 10.1001/archpsyc.64.6.631 Search in Google Scholar PubMed
Honey, G.D., Bullmore, E.T., Soni, W., Varatheesan, M., Williams, S.C.R., and Sharma, T. (1999). Differences in frontal cortical activation by a working memory task after substitution of risperidone for typical antipsychotic drugs in patients with schizophrenia. Proc. Natl. Acad. Sci. USA 96 , 13432–13437. 10.1073/pnas.96.23.13432 Search in Google Scholar PubMed PubMed Central
Howes, O.D., Egerton, A., Allan, V., McGuire, P., Stokes, P., and Kapur, S. (2009a). Mechanisms underlying psychosis and antipsychotic treatment response in schizophrenia: insights from PET and SPECT imaging. Curr. Pharm. Des. 15 , 2550–2559. 10.2174/138161209788957528 Search in Google Scholar
Howes, O.D., Montgomery, A.J., Asselin, M.C., Murray, R.M., Valli, I., Tabraham, P., Bramon-Bosch, E., Valmaggia, L., Johns, L., Broome, M., et al. (2009b). Elevated striatal dopamine function linked to prodromal signs of schizophrenia. Arch. Gen. Psychiatry 66 , 13–20. 10.1001/archgenpsychiatry.2008.514 Search in Google Scholar
Huttunen, J., Heinimaa, M., Svirskis, T., Nyman, M., Kajander, J., Forsback, S., Solin, O., Ilonen, T., Korkeila, J., Ristkari, T., et al. (2008). Striatal dopamine synthesis in first-degree relatives of patients with schizophrenia. Biol. Psychiatry 63 , 114–117. 10.1016/j.biopsych.2007.04.017 Search in Google Scholar
Isaac, S.O. and Berridge, C.W. (2003). Wake-promoting actions of dopamine D1 and D2 receptor stimulation. J. Pharmacol. Exp. Ther. 307 , 386–394. 10.1124/jpet.103.053918 Search in Google Scholar
Jones, H.M., Brammer, M.J., O′Toole, M., Taylor, T., Ohlsen, R.I., Brown, R.G., Purvis, R., Williams, S., and Pilowsky, L.S. (2004). Cortical effects of quetiapine in first-episode schizophrenia: a preliminary functional magnetic resonance imaging study. Biol. Psychiatry 56 , 938–942. 10.1016/j.biopsych.2004.08.006 Search in Google Scholar
Kahn, R.S., Harvey, P.D., Davidson, M., Keefe, R.S., Apter, S., Neale, J.M., Mohs, R.C., and Davis, K.L. (1994). Neuropsychological correlates of central monoamine function in chronic schizophrenia: relationship between CSF metabolites and cognitive function. Schizophr. Res. 11 , 217–224. 10.1016/0920-9964(94)90015-9 Search in Google Scholar
Kapur, S. (2003). Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia. Am. J. Psychiatry 160 , 13–23. 10.1176/appi.ajp.160.1.13 Search in Google Scholar PubMed
Kapur, S., Zipursky, R.B., and Remington, G. (1999). Clinical and theoretical implications of 5-HT2 and D2 receptor occupancy of clozapine, risperidone, and olanzapine in schizophrenia. Am. J. Psychiatry 156 , 286–293. 10.1176/ajp.156.2.286 Search in Google Scholar
Karlsson, P., Farde, L., Halldin, C., and Sedvall, G. (2002). PET study of D(1) dopamine receptor binding in neuroleptic-naive patients with schizophrenia. Am. J. Psychiatry 159 , 761–767. 10.1176/appi.ajp.159.5.761 Search in Google Scholar PubMed
Kebabian, J.W. and Calne, D.B. (1979). Multiple receptors for dopamine. Nature 277 , 93–96. 10.1038/277093a0 Search in Google Scholar PubMed
Kestler, L.P., Walker, E., and Vega, E.M. (2001). Dopamine receptors in the brains of schizophrenia patients: a meta-analysis of the findings. Behav. Pharmacol. 12 , 355–371. 10.1097/00008877-200109000-00007 Search in Google Scholar PubMed
King, M.V., Seeman, P., Marsden, C.A., and Fone, K.C. (2009). Increased dopamine D2High receptors in rats reared in social isolation. Synapse 63 , 476–483. 10.1002/syn.20624 Search in Google Scholar
Kirsch, P., Ronshausen, S., Mier, D., and Gallhofer, B. (2007). The influence of antipsychotic treatment on brain reward system reactivity in schizophrenia patients. Pharmacopsychiatry 40 , 196–198. 10.1055/s-2007-984463 Search in Google Scholar
Knable, M.B., Hyde, T.M., Herman, M.M, Carter, J.M, Bigelow, L., and Kleinman, J.E. (1994). Quantitative autoradiography of dopamine-D1 receptors, D2 receptors, and dopamine uptake sites in postmortem striatal specimens from schizophrenic patients. Biol. Psychiatry 36 , 827–835. 10.1016/0006-3223(94)90593-2 Search in Google Scholar
Knable, M.B., Hyde, T.M., Murray, A.M., Herman, M.M., and Kleinman, J.E. (1996). A postmortem study of frontal cortical dopamine D1 receptors in schizophrenics, psychiatric controls, and normal controls. Biol. Psychiatry 40 , 1191–1199. 10.1016/S0006-3223(96)00116-3 Search in Google Scholar
Kosaka, J., Takahashi, H., Ito, H., Takano, A., Fujimura, Y., Matsumoto, R., Nozaki, S., Yasuno, F., Okubo, Y., Kishimoto, T., et al. (2010). Decreased binding of [11C]NNC112 and [11C]SCH23390 in patients with chronic schizophrenia. Life Sci. 86 , 814–818. 10.1016/j.lfs.2010.03.018 Search in Google Scholar
Kraguljac, N.V., Reid, M., White, D., Jones, R., den Hollander, J., Lowman, D., and Lahti, A.C. (2012). Neurometabolites in schizophrenia and bipolar disorder – a systematic review and meta-analysis. Psychiatry Res. 203 , 111–125. 10.1016/j.pscychresns.2012.02.003 Search in Google Scholar
Laruelle, M. (2000). The role of endogenous sensitization in the pathophysiology of schizophrenia: implications from recent brain imaging studies. Brain Res. Brain Res. Rev. 31 , 371–384. 10.1016/S0165-0173(99)00054-5 Search in Google Scholar
Laruelle, M., Abi-Dargham, A., Gil, R., Kegeles, L., and Innis, R. (1999). Increased dopamine transmission in schizophrenia: relationship to illness phases. Biol. Psychiatry 46, 56–72. 10.1016/S0006-3223(99)00067-0 Search in Google Scholar
Laruelle, M., Abi-Dargham, A., van Dyck, C.H., Gil, R., D’Souza, C.D., Erdos, J., McCance, E., Rosenblatt, W., Fingado, C., Zoghbi, S.S., et al. (1996). Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects. Proc. Natl. Acad. Sci. USA 93 , 9235–9240. 10.1073/pnas.93.17.9235 Search in Google Scholar PubMed PubMed Central
Leucht, S., Busch, R., Hamann, J., Kissling, W., and Kane, J.M. (2005). Early-onset hypothesis of antipsychotic drug action: a hypothesis tested, confirmed and extended. Biol. Psychiatry 57 , 1543–1549. 10.1016/j.biopsych.2005.02.023 Search in Google Scholar PubMed
Lewis, R., Kapur, S., Jones, C., DaSilva, J., Brown, G.M., Wilson, A.A., Houle, S., and Zipursky, R.B. (1999). Serotonin 5-HT2 receptors in schizophrenia: a PET study using [18F]setoperone in neuroleptic-naive patients and normal subjects. Am. J. Psychiatry 156 , 72–78. 10.1176/ajp.156.1.72 Search in Google Scholar
Lund, A., Kroken, R., Thomsen, T., Hugdahl, K., Smievoll, A.I., Barndon, R., Iversen, J., Landrø, N.I., Sundet, K., Rund, B.R., et al. (2002). “Normalization” of brain activation in schizophrenia. An fMRI study. Schizophr. Res. 58 , 333–335. 10.1016/S0920-9964(01)00369-3 Search in Google Scholar
Martinot, J.L., Paillere-Martinot, M.L., Loc′h, C., Hardy, P., Poirier, M.F., Mazoyer, B., Beaufils, B., Mazière, B., Allilaire, J.F., and Syrota, A. (1991). The estimated density of D2 striatal receptors in schizophrenia. A study with positron emission tomography and 76Br-bromolisuride. Br. J. Psychiatry 158 , 346–350. 10.1192/bjp.158.3.346 Search in Google Scholar PubMed
Martinot, J.L., Paillere-Martinot, M.L., Loc′h, C., Lecrubier, Y., Dao-Castellana, M.H., Aubin, F., Allilaire, J.F., Mazoyer, B., Mazière, B., and Syrota, A. (1994). Central D2 receptors and negative symptoms of schizophrenia. Br. J. Psychiatry 164, 27–34. 10.1192/bjp.164.1.27 Search in Google Scholar PubMed
McClelland, G.R., Cooper, S.M., and Pilgrim, A.J. (1990). A comparison of the central nervous system effects of haloperidol, chlorpromazine and sulpiride in normal volunteers. Br. J. Clin. Pharmacol. 30 , 795–803. 10.1111/j.1365-2125.1990.tb05444.x Search in Google Scholar PubMed PubMed Central
McGowan, S., Lawrence, A.D., Sales, T., Quested, D., and Grasby, P. (2004). Presynaptic dopaminergic dysfunction in schizophrenia: a positron emission tomographic [18F]fluorodopa study. Arch. Gen. Psychiatry 61 , 134–142. 10.1001/archpsyc.61.2.134 Search in Google Scholar PubMed
Meisenzahl, E.M., Scheuerecker, J., Zipse, M., Ufer, S., Wiesmann, M., Frodl, T., Koutsouleris, N., Zetzsche, T., Schmitt, G., Riedel, M., et al (2006). Effects of treatment with the atypical neuroleptic quetiapine on working memory function: a functional MRI follow-up investigation. Eur. Arch. Psychiatry Clin. Neurosci. 256 , 522–531. 10.1007/s00406-006-0687-x Search in Google Scholar PubMed
Meltzer, H.Y. (1979). Clinical evidence for multiple dopamine receptors in man. Commun. Psychopharmacol. 3 , 457–470. Search in Google Scholar
Meltzer, H.Y. (1989). Clinical studies on the mechanism of action of clozapine: the dopamine-serotonin hypothesis of schizophrenia. Psychopharmacology 99 Suppl , S18–S27. 10.1007/BF00442554 Search in Google Scholar PubMed
Meltzer, H.Y., Sommers, A.A., and Luchins, D.J. (1986). The effect of neuroleptics and other psychotropic drugs on negative symptoms in schizophrenia. J. Clin. Psychopharmacol. 6 , 329–338. 10.1097/00004714-198612000-00002 Search in Google Scholar
Meyer, U. and Feldon, J. (2009). Prenatal exposure to infection: a primary mechanism for abnormal dopaminergic development in schizophrenia. Psychopharmacology 206 , 587–602. 10.1007/s00213-009-1504-9 Search in Google Scholar PubMed
Monchi, O., Taylor, J.G., and Dagher, A. (2000). A neural model of working memory processes in normal subjects, Parkinson’s disease and schizophrenia for fMRI design and predictions. Neural Networks 13 , 953–973. 10.1016/S0893-6080(00)00058-7 Search in Google Scholar
Moncrieff, J. (2009). A critique of the dopamine hypothesis of schizophrenia and psychosis. Harv. Rev. Psychiatry 17 , 214–225. 10.1080/10673220902979896 Search in Google Scholar PubMed
Nieratschker, V., Nothen, M.M., and Rietschel, M. (2010). New genetic findings in schizophrenia: Is there still room for the dopamine hypothesis of schizophrenia? Front Behav. Neurosci. 4 , 1–10. doi: 10.3389/fnbeh.2010.00023. 10.3389/fnbeh.2010.00023 Search in Google Scholar PubMed PubMed Central
Nikolaus, S., Antke, C., and Müller, H.W. (2009). In vivo imaging of synaptic function in the central nervous system: II. Mental and affective disorders. Behav. Brain Res. 204 , 32–66. 10.1016/j.bbr.2009.06.009 Search in Google Scholar PubMed
Ogawa, S. and Lee, T.M. (1990). Magnetic resonance imaging of blood vessels at high fields: in vivo and in vitro measurements and image simulation. Magn. Reson. Med. 16 , 9–18. 10.1002/mrm.1910160103 Search in Google Scholar PubMed
Okubo, Y., Suhara, T., Suzuki, K., Kobayashi, K., Inoue, O., Terasaki, O., Someya, Y., Sassa, T., Sudo, Y., Matsushima, E., et al. (1997). Decreased prefrontal dopamine D1 receptors in schizophrenia revealed by PET. Nature 385 , 634–636. 10.1038/385634a0 Search in Google Scholar PubMed
Patil, S. T., Zhang, L., Martenyi, F., Lowe, S.L., Jackson, K.A., Andreev, B.V, Avedisova, A.S, Bardenstein, L.M, Gurovich, I.Y., Morozova, M.A., et al. (2007). Activation of mGlu2/3 receptors as a new approach to treat schizophrenia: a randomized Phase 2 clinical trial. Nat. Med. 13 , 1102–1107. 10.1038/nm1632 Search in Google Scholar PubMed
Pearce, R.K., Seeman, P., Jellinger, K., and Tourtellotte, W.W. (1990). Dopamine uptake sites and dopamine receptors in Parkinson’s disease and schizophrenia. Eur. Neurol. 30 Suppl 1 , 9–14. 10.1159/000117168 Search in Google Scholar PubMed
Pearlson, G.D., Tune, L.E., Wong, D.F., Aylward, E.H., Barta, P.E., Powers, R.E., Tien, A.Y., Chase, G.A., Harris, G.J., Rabins, P.V. (1993). Quantitative D2 dopamine receptor PET and structural MRI changes in late-onset schizophrenia. Schizophr. Bull. 19 , 783–795. 10.1093/schbul/19.4.783 Search in Google Scholar PubMed
Pilowsky, L.S., Bressan, R.A., Stone, J.M., Erlandsson, K., Mulligan, R.S., Krystal, J.H., and Ell, P.J. (2006). First in vivo evidence of an NMDA receptor deficit in medication-free schizophrenic patients. Mol. Psychiatry 11 , 118–119. 10.1038/sj.mp.4001751 Search in Google Scholar PubMed
Pilowsky, L.S., Costa, D.C., Ell, P.J., Murray, R.M., Verhoeff, N.P., and Kerwin, R.W. (1992). Clozapine, single photon emission tomography, and the D2 dopamine receptor blockade hypothesis of schizophrenia. Lancet 340 , 199–202. 10.1016/0140-6736(92)90467-H Search in Google Scholar
Pilowsky, L.S., Costa, D.C., Ell, P.J., Murray, R.M., Verhoeff, N.P., and Kerwin, R.W. (1993). Antipsychotic medication, D2 dopamine receptor blockade and clinical response: a 123I IBZM SPET (single photon emission tomography) study. Psychol. Med. 23 , 791–797. 10.1017/S0033291700025575 Search in Google Scholar
Port, J.D. and Agarwal, N. (2011). MR spectroscopy in schizophrenia. J. Magn. Reson. Imaging 34 , 1251–1261. 10.1002/jmri.22787 Search in Google Scholar
Pruessner, J.C., Champagne, F., Meaney, M.J., and Dagher, A. (2004). Dopamine release in response to a psychological stress in humans and its relationship to early life maternal care: a positron emission tomography study using [ 11 C]raclopride. J. Neurosci. 24 , 2825–2831. 10.1523/JNEUROSCI.3422-03.2004 Search in Google Scholar
Remington, G. and Kapur, S. (1999). D2 and 5-HT2 receptor effects of antipsychotics: bridging basic and clinical findings using PET. J. Clin. Psychiatry 60 (Suppl 10) , 15–19. Search in Google Scholar
Roiser, J.P., Stephan, K.E., and Joyce, E.M. (2009). Do patients with schizophrenia exhibit aberrant salience? Psychol. Med. 39, 199–209. Search in Google Scholar
Rothman, R.B., Baumann, M.H., Dersch, C.M., Romero, D.V., Rice, K.C., Carroll, F.I., and Partilla, J.S. (2001). Amphetamine-type central nervous system stimulants release norepinephrine more potently than they release dopamine and serotonin. Synapse 39 , 32–41. 10.1002/1098-2396(20010101)39:1<32::AID-SYN5>3.0.CO;2-3 Search in Google Scholar
Rowland, L.M., Kontson, K., West, J., Edden, R.A., Zhu, H., Wijtenburg, S.A., Holcomb, H.H., and Barker, P.B. (2012). In vivo measurements of glutamate, GABA, and NAAG in schizophrenia. Schizophr. Bull. Oct 18. [Epub ahead of print]. 10.1016/S0920-9964(12)70871-X Search in Google Scholar
Rzanny, R., Klemm, S., Reichenbach, J.R., Pfleiderer, S.O., Schmidt, B., Volz, H.P., Blanz, B., and Kaiser, W.A. (2003). 31P-MR spectroscopy in children and adolescents with a familial risk of schizophrenia. Eur. Radiol. 13 , 763–770. 10.1007/s00330-002-1565-1 Search in Google Scholar
Seeman, P. and Lee, T. (1975). Antipsychotic drugs: direct correlation between clinical potency and presynaptic action on dopamine neurons. Science 188 , 1217–1219. 10.1126/science.1145194 Search in Google Scholar
Snitz, B.E., MacDonald, A. 3rd, Cohen, J.D., Cho, R.Y., Becker, T., and Carter, C.S. (2005). Lateral and medial hypofrontality in first-episode schizophrenia: functional activity in a medication-naive state and effects of short-term atypical antipsychotic treatment. Am. J. Psychiatry 162 , 2322–2329. 10.1176/appi.ajp.162.12.2322 Search in Google Scholar
Stanley, J.A., Williamson, P.C., Drost, D.J., Carr, T.J., Rylett, R.J., Morrison-Stewart, S., and Thompson, R.T. (1994). Membrane phospholipid metabolism and schizophrenia. An in vivo 31P-MR spectroscopy study. Schizophr. Res. 13 , 209–215. 10.1016/0920-9964(94)90044-2 Search in Google Scholar
Stefanis, N.C., Henquet, C., Avramopoulos, D., Smyrnis, N., Evdokimidis, I., Myin-Germeys, I., Stefanis, C.N., and Van Os, J. (2007). COMT Val158Met moderation of stress-induced psychosis. Psychol. Med. 37 , 1651–1656. 10.1017/S0033291707001080 Search in Google Scholar
Taylor, D.M. and Duncan-McConnell, D. (2000). Refractory schizophrenia and atypical antipsychotics. J. Psychopharmacol. 14 , 409–418. 10.1177/026988110001400411 Search in Google Scholar
Taylor, K.I., Zach, P., and Brugger, P. (2002). Why is magical ideation related to leftward deviation on an implicit line bisection task? Cortex 38 , 247–252. 10.1016/S0010-9452(08)70653-1 Search in Google Scholar
Taylor, S.F., Koeppe, R.A., Tandon, R., Zubieta, J.K., and Frey, K.A. (2000). In vivo measurement of the vesicular monoamine transporter in schizophrenia. Neuropsychopharmacology 23 , 667–675. 10.1016/S0893-133X(00)00165-2 Search in Google Scholar
Thomas, M.A., Ke, Y., Levitt, J., Caplan, R., Curran, J., Asarnow, R., and McCracken, J. (1998). Preliminary study of frontal lobe 1H MR spectroscopy in childhood-onset schizophrenia. J. Magn. Reson. Imaging 8 , 841–846. 10.1002/jmri.1880080413 Search in Google Scholar
Tune, L., Barta, P., Wong, D., Powers, R.E., Pearlson, G., Tien, A.Y., and Wagner, H.N. (1996). Striatal dopamine D2 receptor quantification and superior temporal gyrus: volume determination in 14 chronic schizophrenic subjects. Psychiatry Res. 67 , 155–158. 10.1016/0925-4927(96)02728-X Search in Google Scholar
Ujike, H. (2002). Stimulant-induced psychosis and schizophrenia: the role of sensitization. Curr. Psychiatry Rep. 4 , 177–184. 10.1007/s11920-002-0024-7 Search in Google Scholar
van Os, J. (2009). A salience dysregulation syndrome. Br. J. Psychiatry 194 , 101–103. 10.1192/bjp.bp.108.054254 Search in Google Scholar
van Os, J., Rutten, B.P., and Poulton, R. (2008). Gene-environment interactions in schizophrenia: review of epidemiological findings and future directions. Schizophr. Bull. 34 , 1066–1082. 10.1093/schbul/sbn117 Search in Google Scholar
Vollenweider, F.X., Vontobel, P., Oye, I., Hell, D., and Leenders, K.L. (2000). Effects of (S)-ketamine on striatal dopamine: a [11C]raclopride PET study of a model psychosis in humans. J. Psychiatr. Res. 34 , 35–43. 10.1016/S0022-3956(99)00031-X Search in Google Scholar
Waddington, J.L., O’Callaghan, E., Buckley, P., Larkin, C., Redmond, O., Stack, J., and Ennis, J.T. (1992). MR imaging and spectroscopy in schizophrenia in relation to the neurodevelopmental hypothesis. Clin. Neuropharmacol. 15 Suppl 1 Pt A , 118A–119A. 10.1097/00002826-199201001-00064 Search in Google Scholar
Walsh, E., Leese, M., Taylor, P., Johnston, I., Burns, T., Creed, F., Higgit, A., and Murray, R. (2002). Psychosis in high-security and general psychiatric services: report from the UK700 and special hospitals’ treatment resistant schizophrenia groups. Br. J. Psychiatry 180 , 351–357. 10.1192/bjp.180.4.351 Search in Google Scholar
Walter, H., Heckers, S., Kassubek, J., Erk, S., Frasch, K., and Abler, B. (2010). Further evidence for aberrant prefrontal salience coding in schizophrenia. Front. Behav. Neurosci. 3, 1–9. doi: 10.3389/neuro.08.062.2009. 10.3389/neuro.08.062.2009 Search in Google Scholar
Walter, H., Kammerer, H., Frasch, K., Spitzer, M., and Abler, B. (2009). Altered reward functions in patients on atypical antipsychotic medication in line with the revised dopamine hypothesis of schizophrenia. Psychopharmacology 206 , 121–132. 10.1007/s00213-009-1586-4 Search in Google Scholar
Weiss, E.M., Siedentopf, C., Golaszewski, S., Mottaghy, F.M., Hofer, A., Kremser, C., Felber, S., and Fleischhacker, W.W. (2007). Brain activation patterns during a selective attention test–a functional MRI study in healthy volunteers and unmedicated patients during an acute episode of schizophrenia. Psychiatry Res. 154 , 31–40. 10.1016/j.pscychresns.2006.04.009 Search in Google Scholar
Wise, R.A., Spindler, J., deWit, H., and Gerberg, G.J. (1978). Neuroleptic-induced “anhedonia” in rats: pimozide blocks reward quality of food. Science 201 , 262–264. 10.1126/science.566469 Search in Google Scholar
Wolf, R.C., Vasic, N., Höse, A., Spitzer, M., and Walter, H.. (2007). Changes over time in frontotemporal activation during a working memory task in patients with schizophrenia. Schizophr. Res. 91 , 141–150. 10.1016/j.schres.2006.12.001 Search in Google Scholar
Wong, D.F., Wagner, H.N. Jr., Tune, L.E., Dannals, R.F., Pearlson, G.D., Links, J.M., Tamminga, C.A., Broussolle, E.P., Ravert, H.T., Wilson, A.A, et al. (1986). Positron emission tomography reveals elevated D2 dopamine receptors in drug-naive schizophrenics. Science 234 , 1558–1563. 10.1126/science.2878495 Search in Google Scholar
Yamasue, H., Fukui, T., Fukuda, R., Yamada, H., Yamasaki, S., Kuroki, N., Abe, O., Kasai, K., Tsujii, K., Iwanami, A., et al. (2002). 1H-MR spectroscopy and gray matter volume of the anterior cingulate cortex in schizophrenia. Neuroreport 13 , 2133–2137. 10.1097/00001756-200211150-00029 Search in Google Scholar
Zakzanis, K.K. and Hansen, K.T. (1998). Dopamine D2 densities and the schizophrenic brain. Schizophr. Res. 32 , 201–206. 10.1016/S0920-9964(98)00041-3 Search in Google Scholar
©2013 by Walter de Gruyter Berlin Boston
- X / Twitter
Supplementary Materials
Please login or register with De Gruyter to order this product.
Journal and Issue
Articles in the same issue.
Find Study Materials for
- Business Studies
- Combined Science
- Computer Science
- Engineering
- English Literature
- Environmental Science
- Human Geography
- Macroeconomics
- Microeconomics
- Social Studies
- Browse all subjects
- Read our Magazine
Create Study Materials
Often called the ‘feel-good’ hormone, dopamine is in charge of making you feel happy, satisfied, and motivated. When you feel good because you have accomplished something, your brain experiences a dopamine spike. What occurs, though, when there is an imbalance? Could this imbalance play a role in the development of schizophrenia ? This is where the dopamine hypothesis of schizophrenia enters the picture, examining how the imbalance of dopamine levels and the abundance of dopamine receptors contributes to schizophrenia.
Explore our app and discover over 50 million learning materials for free.
- The Dopamine Hypothesis
- Explanations
- StudySmarter AI
- Textbook Solutions
- Approaches in Psychology
- Basic Psychology
- Biological Bases of Behavior
- Biopsychology
- Careers in Psychology
- Clinical Psychology
- Cognition and Development
- Cognitive Psychology
- Data Handling and Analysis
- Developmental Psychology
- Eating Behaviour
- Emotion and Motivation
- Famous Psychologists
- Forensic Psychology
- Health Psychology
- Individual Differences Psychology
- Issues and Debates in Psychology
- Personality in Psychology
- Psychological Treatment
- Relationships
- Research Methods in Psychology
- Biological Explanations for Schizophrenia
- Cognitive Behavioural Therapy
- Cognitive Explanations for Schizophrenia
- Diagnosis and Classification of Schizophrenia
- Dysfunctional Family
- Family Therapy
- Interactionist Approach Schizophrenia
- Neural Correlates
- Psychological Explanations for Schizophrenia
- Psychological Therapies for Schizophrenia
- Reliability and Validity in Diagnosis and Classification of Schizophrenia
- Role Of Cannabis
- Schizophrenia Genetics
- Token Economy
- Treatment and Therapies for Schizophrenia
- Typical and Atypical Antipsychotics
- Ventricular Size
- Scientific Foundations of Psychology
- Scientific Investigation
- Sensation and Perception
- Social Context of Behaviour
- Social Psychology
Lerne mit deinen Freunden und bleibe auf dem richtigen Kurs mit deinen persönlichen Lernstatistiken
Nie wieder prokastinieren mit unseren Lernerinnerungen.
- We will discuss the dopamine hypothesis of schizophrenia .
- First, we will provide a dopamine hypothesis psychology definition.
- Then, we explore the various aspects of the biological explanations of the schizophrenia dopamine hypothesis. including the dopamine hypothesis of psychosis.
- Finally, we will examine the d opamine hypothesis's strengths and weaknesses through an evaluation of the dopamine hypothesis.

The D opamine Hypothesis of Schizophrenia: Definition
The dopamine hypothesis, first proposed by Van Rossum in 1967, is the theory that too much dopamine in the subcortical and limbic regions of the brain may cause positive schizophrenic symptoms . According to the dopamine hypothesis, negative symptoms are associated with less dopamine in the prefrontal cortex .
The dopamine hypothesis was later revised as research revealed schizophrenic patients might also have too many dopamine receptors.
Dopamine is a neurotransmitter that helps the brain send messages to specific body parts. Neurotransmitters are chemical messengers within the brain .
Neurotransmitters bind to receptors in nerve cells after they cross a small gap between them called the synapse. Dopamine is a neurotransmitter involved in our brain’s pleasure and reward systems. The receptors of dopamine are implicated in the dopamine hypothesis of schizophrenia, in that some researchers theorise too many receptors contribute to the overactivity of dopamine in the brain and any subsequent schizophrenic developments.
Biological Explanations of Schizophrenia: Dopamine Hypothesis
The dopamine hypothesis is a biological explanation of schizophrenia, so how does it work? What parts of the brain are involved in the dopamine hypothesis?
- Dopamine is produced in different areas of the brain, and for schizophrenia, we are concerned with the substantia nigra and the ventral tegmental area .
The dopamine produced in the substantia nigra helps us trigger physical movements, including the parts of the face and mouth needed for speech. Problems with this may be responsible for some symptoms of schizophrenia , such as alogia (lack of speech) and psychomotor disturbances.
Damage to dopaminergic neurons in the substantia nigra is correlated with the development of Parkinson's.
Dopamine produced in the ventral tegmental area is released when we expect or receive a reward. This helps both animals and humans modify their behaviour to be more likely to result in a reward or positive experience. An excess of dopamine can lead to hallucinations and delusional or confused thinking, all of which are symptoms of schizophrenia .

Studies of amphetamines given to people without a history of schizophrenia showed that the effect of high levels of dopamine the drug had induced led to symptoms very similar to those of paranoid schizophrenia.
Later revisions of the hypothesis stated that possibly an excess of dopamine in the mesolimbic areas of the brain contributes to positive symptoms, and a low level of dopamine in the brain’s prefrontal cortex contributes to negative symptoms.
Dopamine Hypothesis of Psychosis: Development of the Dopamine Hypothesis
In the 1960s and 1970s, research was conducted into the use of amphetamine drugs and their effect on dopamine levels within the brain. The researchers found that psychotic symptoms increased when these drugs were consumed, sparking the idea that dopamine may help us understand how psychotic symptoms in schizophrenia patients may come to be.
The Dopamine Hypothesis: Strengths and Weaknesses
The dopamine hypothesis has been around for close to 60 years, and has gone through a series of developments alongside facing scrutiny in research. Let's evaluate the dopamine hypothesis of schizophrenia and examine its strengths and weaknesses.
Weaknesses of the Dopamine Hypothesis
The dopamine hypothesis, like any other, has its weaknesses.
- Cause and Effect: One problem with this explanation is that it is not certain whether a dopamine imbalance causes schizophrenia or whether schizophrenia causes a dopamine imbalance. Since the causal nature of the argument is unclear, it is crucial to be careful in determining cause and effect in the development of schizophrenia.
- Farde et al. (1990): Farde et al. (1990) found no difference between the dopamine receptor (D2) levels of schizophrenia patients and control patients. Farde et al.'s (1990) finding suggests that the dopamine hypothesis may not apply to all patients with schizophrenia.
- Determinism: The dopamine hypothesis can be considered deterministic (the belief that factors beyond our control determine human behaviour) because it assumes that the development of schizophrenia depends on the amount of dopamine or dopamine receptors in our brains, which does not correspond to psychological explanations of schizophrenia. It ignores how the environment affects the development of the disorder.Deterministic theories have their limitations, as they are not compatible with societal notions of responsibility, free will and self-control, on which many of our legal and moral norms are based.
Strengths of the Dopamine Hypothesis
On the other hand, some studies are sympathetic to the role dopamine plays in the development of schizophrenia.
- Parkinson's Disease and Levodopa (L-Dopa): Some patients are given levodopa when treating Parkinson’s disease, a drug that increases dopamine levels in the brain. These patients are reported to experience psychotic side effects similar to schizophrenia symptoms, such as hallucinations and dyskinesia. The dopamine aspect supports the role that dopamine plays in the development of schizophrenic symptoms.
- Abi-Dargham et al. (2000): Abi-Dargham et al. (2000) investigated whether there was a true increased level of dopamine and dopamine 2 (D2) receptors within the brain for schizophrenic people compared to controls, accounting for the effects of patients taking antipsychotics and artificially elevating their levels. They found that their results indicated, that for the levels to match up, schizophrenic patients must have an increased level of both dopamine and dopamine receptors compared to controls.


Practical Applications of the Dopamine Hypothesis
Now that we have gained some insight into the dopamine hypothesis’s theoretical aspects, let us look at how it is applied in practice.
Typical Antipsychotic Drugs: First Generation
The dopamine hypothesis has contributed to the development of antipsychotics for schizophrenia and several other disorders in which sufferers experience psychosis.
Typical antipsychotic drugs work by blocking D2 receptors in the brain, limiting dopamine activity. Blocking dopamine receptors can help reduce positive symptoms such as hallucinations
Typical antipsychotics tend to block dopamine in all areas of the brain, not just those that cause schizophrenic symptoms, which can lead to harmful side effects.
Examples of typical antipsychotics include chlorpromazine and haloperidol .
Atypical Antipsychotic Drugs: Second Generation
Atypical antipsychotic s are newer drugs that usually do not have as severe side effects as typical antipsychotics.
Atypical antipsychotics only inhibit dopamine receptors in the limbic system rather than throughout the brain.
They help control the symptoms of schizophrenia without interfering with other systems and potentially causing the same side effects as the previous generation of medications.Atypical antipsychotics bind to dopamine receptors and act on glutamate (an excitatory neurotransmitter) and serotonin. This means that these drugs can help with positive symptoms and reduce negative symptoms such as low mood and impaired cognitive function.
Because of their effect on serotonin, these antipsychotics can also help treat some comorbidities associated with schizophrenia, such as anxiety and depression .
Evaluating Practical Applications of the Dopamine Hypothesis
Considering the practical applications of the dopamine hypothesis affect patients, it's important we evaluate it thoroughly before moving forwards.
Drug treatments such as antipsychotics, developed based on the dopamine hypothesis, help patients manage their daily lives and quality of life. These drugs are relatively easy to make and administer and can positively impact healthcare providers and the economy. This is because they help people with schizophrenia to leave treatment and return to their daily lives, such as their jobs, allowing more people to be treated.
While these drugs help with schizophrenic symptoms, it is essential to point out that they cannot cure schizophrenia. This means that we need more research to find a long-term solution to the disease.
There are some ethical questions about these drugs. In some hospitals, antipsychotic medications may be used to benefit staff rather than patients to make it easier to work with patients.
Antipsychotic medications can have serious side effects, such as tardive dyskinesia, a condition that involves involuntary facial ‘tics’ such as rapid blinking, chewing movements, or rolling of the tongue. Sometimes the side effects can be worse than the initial symptoms of schizophrenia.
The Dopamine Hypothesis - Key takeaways
- The dopamine hypothesis, first proposed by Van Rossum in 1967, is the theory that high dopamine levels may cause schizophrenic symptoms.
- In the 1960s and 70s, researchers studied amphetamines and their effect on dopamine levels in the brain. Researchers found that psychotic symptoms increased when these drugs were used. This finding gave us the idea that this could help us understand the cause of psychotic symptoms in schizophrenia patients.
- Problems with dopamine production and imbalances in dopamine in the substantia nigra and ventral tegmental area may be responsible for the symptoms of schizophrenia, such as alogia, hallucinations, and psychomotor disturbances.
- It is difficult to establish cause and effect in the dopamine hypothesis, however, many studies support the evidence that imbalances in the brain concerning dopamine are related to psychotic and negative symptoms. More research is needed to identify what causes schizophrenia.
Frequently Asked Questions about The Dopamine Hypothesis
--> what is the dopamine hypothesis of schizophrenia in psychology.
The dopamine hypothesis, first proposed by Van Rossum in 1967, is the theory that high or low levels of dopamine may cause schizophrenic symptoms.
--> What is the role of dopamine in schizophrenia?
The dopamine hypothesis suggests dopamine level imbalances and too many dopamine receptors play a role in the development of symptoms of schizophrenia. However, the dopamine hypothesis does not fully explain how the disorder develops. Newer antipsychotics that are generally more effective than previous drug treatments target more neurotransmitters than just dopamine, suggesting that it may not exclusively be dopamine that causes schizophrenia.
--> What is the original dopamine hypothesis of schizophrenia?
The original dopamine hypothesis states that too much dopamine within an individual's brain causes the onset of schizophrenic symptoms, such as hallucinations.
--> Do people with schizophrenia have low levels of dopamine?
Schizophrenic people may have low levels of dopamine. The dopamine hypothesis suggests both low and high levels of dopamine in certain areas of the brain may be responsible for schizophrenic symptoms. Low levels of dopamine, for instance, may result in negative symptoms.
Test your knowledge with multiple choice flashcards
What did Farde et al. (1990) find in their study into the dopamine hypothesis?
True or False: The dopamine hypothesis was later revised as research revealed schizophrenic patients may also have too many dopamine receptors, which can also contribute to the disorder.
Excess dopamine in the mesolimbic pathway (ventral tegmental area and nucleus accumbens) contributes to ________ symptoms of schizophrenia.
Your score:
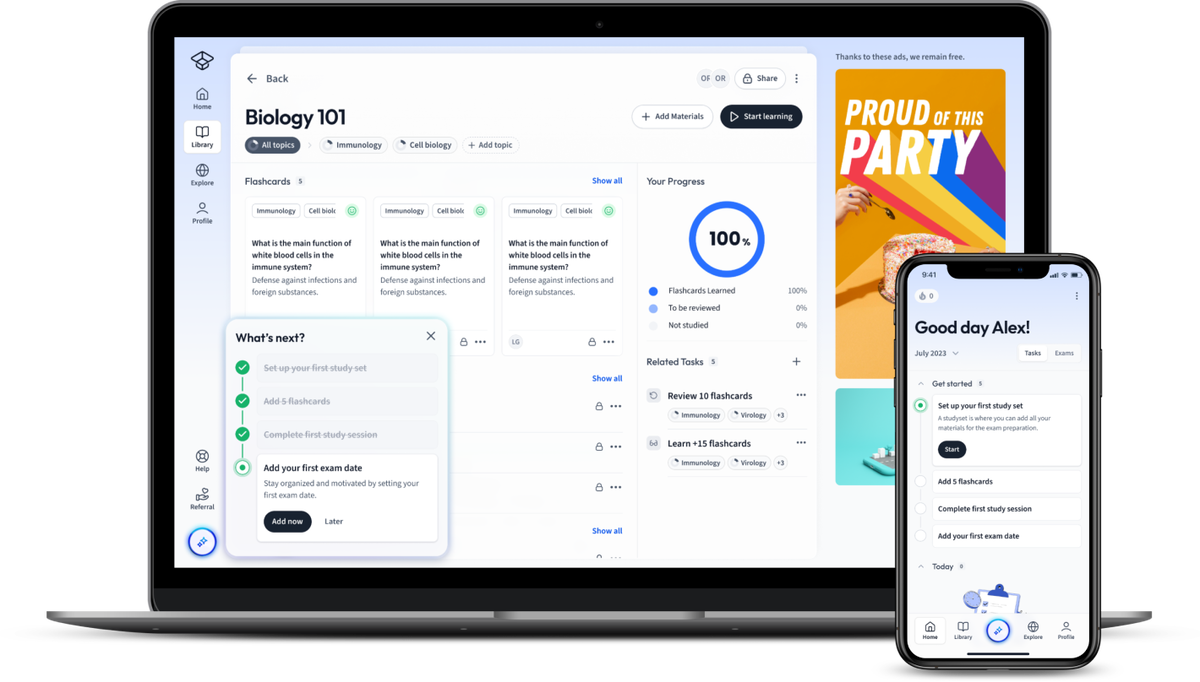
Join the StudySmarter App and learn efficiently with millions of flashcards and more!
Learn with 13 the dopamine hypothesis flashcards in the free studysmarter app.
Already have an account? Log in
What is dopamine?
A neurotransmitter associated with the rewards system of our brains.
What is a synapse?
A small gap between neurons across which messages are fired through neurotransmitters.
Issues with dopamine production in the ________ nigra contributes to symptoms of schizophrenia.
substantia.
No difference in dopamine (D2) receptor levels between schizophrenic and non-schizophrenic participants.
The dopamine hypothesis is a deterministic theory. Why is this a limitation?
Deterministic theories have their limitations, as they are not compatible with societal notions of responsibility and self-control, on which many of our legal and moral norms are based.
How does Parkinson's treatment, L-Dopa, support the dopamine hypothesis?
Some patients are given levodopa (L-Dopa) when treating Parkinson’s disease, a drug that increases dopamine levels in the brain. These patients are reported to experience psychotic side effects similar to schizophrenia symptoms. This supports the role that dopamine plays in the development of schizophrenic symptoms.
of the users don't pass the The Dopamine Hypothesis quiz! Will you pass the quiz?
How would you like to learn this content?
Free psychology cheat sheet!
Everything you need to know on . A perfect summary so you can easily remember everything.
Join over 22 million students in learning with our StudySmarter App
The first learning app that truly has everything you need to ace your exams in one place
- Flashcards & Quizzes
- AI Study Assistant
- Study Planner
- Smart Note-Taking

Sign up to highlight and take notes. It’s 100% free.
This is still free to read, it's not a paywall.
You need to register to keep reading, create a free account to save this explanation..
Save explanations to your personalised space and access them anytime, anywhere!
By signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Entdecke Lernmaterial in der StudySmarter-App
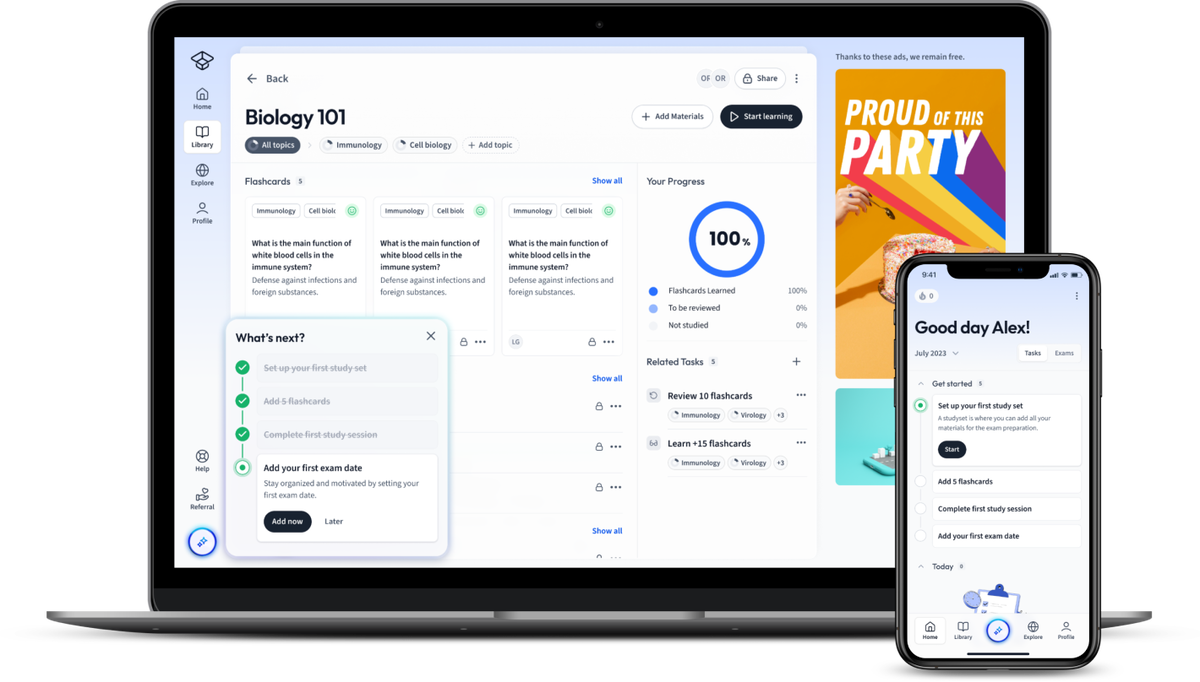
Does the dopamine hypothesis explain schizophrenia?
- PMID: 23843581
- DOI: 10.1515/revneuro-2013-0011
The dopamine hypothesis has been the cornerstone in the research and clinical practice of schizophrenia. With the initial emphasis on the role of excessive dopamine, the hypothesis has evolved to a concept of combining prefrontal hypodopaminergia and striatal hyperdopaminergia, and subsequently to the present aberrant salience hypothesis. This article provides a brief overview of the development and evidence of the dopamine hypothesis. It will argue that the current model of aberrant salience explains psychosis in schizophrenia and provides a plausible linkage between the pharmacological and cognitive aspects of the disease. Despite the privileged role of dopamine hypothesis in psychosis, its pathophysiological rather than etiological basis, its limitations in defining symptoms other than psychosis, as well as the evidence of other neurotransmitters such as glutamate and adenosine, prompt us to a wider perspective of the disease. Finally, dopamine does explain the pathophysiology of schizophrenia, but not necessarily the cause per se. Rather, dopamine acts as the common final pathway of a wide variety of predisposing factors, either environmental, genetic, or both, that lead to the disease. Other neurotransmitters, such as glutamate and adenosine, may also collaborate with dopamine to give rise to the entire picture of schizophrenia.
Publication types
- Brain / diagnostic imaging
- Brain / metabolism*
- Brain / pathology
- Dopamine / genetics
- Dopamine / metabolism*
- Models, Biological*
- Neuroimaging
- Radionuclide Imaging
- Schizophrenia / etiology*
- Schizophrenia / metabolism*
- Schizophrenia / pathology

DOPAMINE HYPOTHESIS
The theory that schizophrenia is caused by an excess of dopamine in the brain. See glutamate hypothesis .

Leave a Reply
Your email address will not be published. Required fields are marked *
Latest Posts

The Future Of Education: Can You Earn A Psychology Degree Online?

Insomnia & Mental Illness: What is the Correlation?

Stop Guessing: Here Are 3 Steps to Data-Driven Psychological Decisions

Getting Help with Grief: Understanding Therapy & How It Can Help

Exploring the Psychology of Risk and Reward

Understanding ADHD in Women: Symptoms, Treatment & Support

Meeting the Milestones: A Guide to Piaget's Child Developmental Stages

Counseling, Therapy, and Psychology: What Is The Difference?
The Psychology of Metaphysical Belief Systems

4 Key Considerations When Supporting a Loved One Through a Legal Battle for Justice

Finding Balance: The Psychological Benefits of Staying Active

The Psychology of Winning: Case Studies and Analysis from the World of Sports
Popular psychology terms, medical model, hypermnesia, affirmation, brainwashing, backup reinforcer, message-learning approach, affiliative behavior, basic anxiety, gender coding, confederate.
Find over 25,000 psychological definitions
dopamine hypothesis
Browse dictionary by letter, psychology term of the day.
May 7th 2024
developmental measure

DOPAMINE HYPOTHESIS
The Dopamine Hypothesis has been a prominent area of study in the field of neuroscience for several decades. It is the idea that the neurotransmitter dopamine plays a central role in the pathology of schizophrenia. This hypothesis was first proposed by Carlsson and Lindqvist in 1963, and since then it has been the subject of much research and debate.
A key component of the dopamine hypothesis is that dopamine is involved in the development of psychotic symptoms, such as hallucinations and delusions. It is thought that an imbalance in the dopamine system, either too much or too little dopamine in certain areas of the brain, can lead to the symptoms of schizophrenia. This is because dopamine plays an important role in regulating certain cognitive processes, such as memory, learning, and attention.
Several lines of evidence support the dopamine hypothesis. Neuroimaging studies have shown differences in dopamine levels in the brains of people with schizophrenia, compared to those without the disorder. Pharmacological studies have also shown that antipsychotic medications, which work by blocking the effects of dopamine, can reduce psychotic symptoms. Additionally, genetic studies have identified several genes that are associated with an increased risk of schizophrenia, and many of these genes are involved in the dopamine system.
Despite the evidence for the dopamine hypothesis, it is still an area of active research and debate. Many studies have suggested that other neurotransmitters, such as glutamate, may also be involved in the development of schizophrenia. Additionally, it is still unclear exactly how dopamine imbalances lead to the symptoms of schizophrenia, and how these imbalances can be treated.
In conclusion, the dopamine hypothesis is a widely accepted theory that is supported by a large body of evidence. However, further research is needed to fully understand the role of dopamine in schizophrenia and to develop effective treatments for this disorder.
Carlsson, A., & Lindqvist, M. (1963). Effect of chlorpromazine or haloperidol on the formation of 3-methoxytyramine and normetanephrine in mouse brain. Acta Pharmacologica et Toxicologica, 20(2), 140–144.
Howes, O., & Kapur, S. (2009). The dopamine hypothesis of schizophrenia: Version III—the final common pathway. Schizophrenia Bulletin, 35(3), 549–562.
Lam, D. H., & Weickert, C. S. (2008). The dopamine hypothesis of schizophrenia: Making sense of the data. Schizophrenia Research, 102(1–3), 1–11.
Yolken, R. H., & Fatemi, S. H. (2012). Neurodevelopment in schizophrenia: From genes to environment. Neuroscience & Biobehavioral Reviews, 36(1), 131–145.
Related terms
Dehydration, delay of gratification, demonstration experiment.

IMAGES
VIDEO
COMMENTS
Dopamine is a neurotransmitter that serves as a chemical messenger in the brain. It can function as both an excitatory and inhibitory neurotransmitter, leading to diverse effects on the brain, body, and behavior. Dopamine is transferred between neurons in the brain through a process called synaptic transmission, where dopamine molecules are ...
Dopamine hypothesis. The dopamine hypothesis of ADHD is based on the facts: (1) that symptoms of ADHD are reduced by stimulant treatment which blocks the dopamine reuptake mechanism in the striatum; and (2) that some patients with ADHD have abnormalities in genes responsible for dopamine regulation. However, this hypothesis has been questioned.
dopamine hypothesis. Updated on 04/19/2018. the influential theory that schizophrenia is caused by an excess of dopamine in the brain, due either to an overproduction of dopamine or a deficiency of the enzyme needed to convert dopamine to norepinephrine (adrenaline). There is some supporting pharmacological and biochemical evidence for this ...
Dopamine. Dopamine is known as the feel-good neurotransmitter—a chemical that ferries information between neurons. The brain releases it when we eat food that we crave or while we have sex ...
The Dopamine Hypothesis: Version II. In 1991, Davis et al 10 published a landmark article describing what they called "a modified dopamine hypothesis of schizophrenia" that reconceptualized the dopamine hypothesis in the light of the findings available at the time. The main advance was the addition of regional specificity into the hypothesis to account for the available postmortem and ...
The dopamine hypothesis is the oldest neurochemical theory of the pathophysiology of psychosis. Established in the last century based on clinical observations, the theory received considerable scientific attention in past decades. Over the years, the integration of new empirical evidence resulted in a constant refinement of its neurobiological ...
The dopamine hypothesis of how antipsychotic drugs exert their beneficial effect in psychotic illness has an interesting history that dates back to 1950. This hypothesis is not to be confused with the dopamine hypothesis of schizophrenia; the aim of the latter is to explain the etiology of schizophrenia. The present review does not deal with ...
The dopamine hypothesis of schizophrenia or the dopamine hypothesis of psychosis is a model that attributes the positive symptoms of schizophrenia to a disturbed and hyperactive dopaminergic signal transduction. The model draws evidence from the observation that a large number of antipsychotics have dopamine-receptor antagonistic effects. The ...
The dopamine (DA) hypothesis of schizophrenia (DHS) has, since its inception over 30 years ago, been among the most prominent etiologic theories in psychiatry. This essay begins by summarizing the history of its emergence and efforts to empirically test it through the examination of (i) cerebrospinal fluid DA metabolites, (ii) neuroendocrine measures, (iii) clinical response to ...
The Dopamine Hypothesis suggests that abnormalities in the functioning of dopamine systems within the brain contribute to the development and manifestation of psychiatric disorders. It proposes that an excess or dysregulation of dopamine transmission can result in the characteristic symptoms observed in certain conditions.
The dopamine hypothesis has been the cornerstone in the research and clinical practice of schizophrenia. With the initial emphasis on the role of excessive dopamine, the hypothesis has evolved to a concept of combining prefrontal hypodopaminergia and striatal hyperdopaminergia, and subsequently to the present aberrant salience hypothesis. This article provides a brief overview of the ...
The dopamine hypothesis, first proposed by Van Rossum in 1967, is the theory that high dopamine levels may cause schizophrenic symptoms. In the 1960s and 70s, researchers studied amphetamines and their effect on dopamine levels in the brain. Researchers found that psychotic symptoms increased when these drugs were used.
The dopamine hypothesis of schizophrenia postulates that an excess of dopamine subcortically is associated with the positive symptoms. At the same time, the negative and cognitive symptoms of schizophrenia are thought to arise from a deficit of dopamine in the cortex. Evidence for the co-existence of subcortical dopamine excess and cortical ...
dopamine (DA) n. a catecholamine neurotransmitter that has an important role in motor behavior and is implicated in numerous mental conditions and emotional states (see catecholamine hypothesis; dopamine hypothesis ). It is found in dopaminergic neurons in the brain and elsewhere. It is synthesized from the dietary amino acid tyrosine, which in ...
The dopamine hypothesis has been the cornerstone in the research and clinical practice of schizophrenia. With the initial emphasis on the role of excessive dopamine, the hypothesis has evolved to a concept of combining prefrontal hypodopaminergia and striatal hyperdopaminergia, and subsequently to the present aberrant salience hypothesis.
The dopamine hypothesis of schizophrenia. The ' dopamine hypothesis of schizophrenia ', simply stated, postulates that certain dopaminergic pathways are overactive in schizophrenia and so cause the symptoms of an acute schizophrenic episode. Clinical studies indicate that drugs like L-dopa or amphetamine, which potentiate dopaminergic ...
Dopamine (DA) Hypothesis. The dopamine (DA) hypothesis is a theory that proposes a biological cause of schizophrenia. This is the oldest theory about the cause of schizophrenia and was first presented in the 1960s. It suggests that schizophrenia is caused by too much DA transmission in the brain. Pharmacological evidence exists for this theory ...
The dopamine hypothesis of schizophrenia is a prime example. Many things contribute to your defining characteristics. Childhood experiences, genetics, and the level of chemicals in your brain all ...
Psychology Definition of DOPAMINE HYPOTHESIS: The theory that schizophrenia is caused by an excess of dopamine in the brain. See glutamate hypothesis.
Dopamine is a neurotransmitter made in your brain. It plays a role as a "reward center" and in many body functions, including memory, movement, motivation, mood, attention and more. High or low dopamine levels are associated with diseases including Parkinson's disease, restless legs syndrome and attention deficit hyperactivity disorder ...
dopamine hypothesis the influential theory that schizophrenia is caused by an excess of dopamine in the brain, due either to an overproduction of dopamine or a deficiency of the enzyme needed to convert dopamine to norepinephrine (adrenaline). ... Psychology term of the day. April 21st 2024. cued speech. cued speech speech that is supplemented ...
The Dopamine Hypothesis has been a prominent area of study in the field of neuroscience for several decades. It is the idea that the neurotransmitter dopamine plays a central role in the pathology of schizophrenia. This hypothesis was first proposed by Carlsson and Lindqvist in 1963, and since then it has been the subject of much research and ...