Editor's Choice: JAMA Pediatrics —The Year in Review, 2023

Ilana Levene, BM, BCh; Nurul Husna Mohd Shukri, PhD; Frances O’Brien, MB, BS; et al
Original Investigation | May 6, 2024

Just Published
- Relaxation Therapy and Human Milk Feeding Outcomes Ilana Levene, BM, BCh; et al. Original Investigation online first open access Ilana Levene, BM, BCh; et al.
- Mandatory Child Protective Services Reporting for Substance-Exposed Newborns and Peripartum Outcomes Rohan Khazanchi, MD, MPH; et al. Research Letter online first Rohan Khazanchi, MD, MPH; et al.
- Long-Term Cardiovascular Outcomes in Children and Adolescents With Hypertension Cal H. Robinson, MD; et al. Original Investigation online first free access Cal H. Robinson, MD; et al.
- Certificates of Confidentiality and Mandatory Reporting Leslie E. Wolf, JD, MPH; et al. Viewpoint online first Leslie E. Wolf, JD, MPH; et al.
- Implications of Health Equity for Children With Disabilities Kara B. Ayers, PhD; et al. Viewpoint online first Kara B. Ayers, PhD; et al.
- Implications of a Biological Poverty Line for Infants Joan L. Luby, MD; et al. Viewpoint online first Joan L. Luby, MD; et al.
- Consensus Statement on Radiological Screening of Children With Suspected Physical Abuse Kshitij Mankad, MD; et al. Special Communication has active quiz Kshitij Mankad, MD; et al.
- Psychometric Properties of Screening Instruments for Social Network Use Disorder in Children and Adolescents Samantha Schlossarek, MSc; et al. Review has active quiz Samantha Schlossarek, MSc; et al.
- Inclusion of Non–English-Speaking Participants in Pediatric Health Research Annie Chen, BS; et al. Review has active quiz Annie Chen, BS; et al.
- 9,406 Views Screen Time Exposure at Age 1 Year and Developmental Delay at Ages 2 and 4 Years
- 7,335 Views Screen Time and Parent-Child Talk During the Early Years
- 5,555 Views Association of Screen Time and Depression in Adolescence
- 5,125 Views Eating Family Meals Together at Home
- 5,113 Views Associations Between Screen Use and Child Language Skills
- 5,083 Views Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19
- 4,854 Views Influence of Eat, Sleep, and Console on Infants Pharmacologically Treated for Opioid Withdrawal
- 4,597 Views Global Proportion of Disordered Eating in Children and Adolescents
- 3,902 Views Association of Habitual Checking Behaviors on Social Media With Functional Brain Development
- 3,302 Views Associations Between Screen Use and White Matter Integrity in Preschoolers
- 1,015 Citations Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19
- 745 Citations Maternal and Neonatal Morbidity and Mortality Among Pregnant Women With and Without COVID-19 Infection
- 281 Citations School Closures During Social Lockdown and Health and Well-being of Children and Adolescents During COVID-19
- 188 Citations Trends in Distribution of US Children With Multisystem Inflammatory Syndrome During the COVID-19 Pandemic
- 175 Citations Assessment of Maternal and Neonatal Cord Blood SARS-CoV-2 Antibodies and Placental Transfer Ratios
- 118 Citations Early Intervention for Children Aged 0 to 2 Years With or at High Risk of Cerebral Palsy
- 112 Citations Neurodevelopmental Status in Infants With and Without In Utero Exposure to SARS-CoV-2
- 107 Citations Global, Regional, and National Incidence and Mortality of Neonatal Preterm Birth, 1990-2019
- 104 Citations Screen Time Use Among US Adolescents During the COVID-19 Pandemic
- 103 Citations Prevalence of SARS-CoV-2 Infection in Children and Their Parents in Southwest Germany
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Internet Explorer Alert
It appears you are using Internet Explorer as your web browser. Please note, Internet Explorer is no longer up-to-date and can cause problems in how this website functions This site functions best using the latest versions of any of the following browsers: Edge, Firefox, Chrome, Opera, or Safari . You can find the latest versions of these browsers at https://browsehappy.com
- Publications
- HealthyChildren.org
Shopping cart
Order Subtotal
Your cart is empty.
Looks like you haven't added anything to your cart.
- Career Resources
- Philanthropy
- About the AAP
- Confidentiality in the Care of Adolescents: Policy Statement
- Confidentiality in the Care of Adolescents: Technical Report
- AAP Policy Offers Recommendations to Safeguard Teens’ Health Information
- One-on-One Time with the Pediatrician
- American Academy of Pediatrics Releases Guidance on Maintaining Confidentiality in Care of Adolescents
- News Releases
- Policy Collections
- The State of Children in 2020
- Healthy Children
- Secure Families
- Strong Communities
- A Leading Nation for Youth
- Transition Plan: Advancing Child Health in the Biden-Harris Administration
- Health Care Access & Coverage
- Immigrant Child Health
- Gun Violence Prevention
- Tobacco & E-Cigarettes
- Child Nutrition
- Assault Weapons Bans
- Childhood Immunizations
- E-Cigarette and Tobacco Products
- Children’s Health Care Coverage Fact Sheets
- Opioid Fact Sheets
- Advocacy Training Modules
- Subspecialty Advocacy Report
- AAP Washington Office Internship
- Online Courses
- Live and Virtual Activities
- National Conference and Exhibition
- Prep®- Pediatric Review and Education Programs
- Journals and Publications
- NRP LMS Login
- Patient Care
- Practice Management
- AAP Committees
- AAP Councils
- AAP Sections
- Volunteer Network
- Join a Chapter
- Chapter Websites
- Chapter Executive Directors
- District Map
- Create Account
- News from the AAP
- Latest Studies in Pediatrics
- Pediatrics OnCall Podcast
- AAP Voices Blog
- Campaigns and Toolkits
- Spokesperson Resources
- Join the AAP
- Exclusive for Members
- Membership FAQs
- AAP Membership Directory
- Member Advantage Programs
- Red Book Member Benefit
- My Membership
- Join a Council
- Join a Section
- National Election Center
- Medical Students
- Pediatric Residents
- Fellowship Trainees
- Planning Your Career
- Conducting Your Job Search
- Making Career Transitions
- COVID-19 State-Level Data Reports
- Children and COVID-19 Vaccination Trends
- Practice Research in the Office Setting (PROS)
Pediatrician Life and Career Experience Study (PLACES)
Periodic survey, annual survey of graduating residents.
- Child Population Characteristics Trends
- Child Health Trends
- Child Health Care Trends
- Friends of Children Fund
- Tomorrow’s Children Endowment
- Disaster Recovery Fund
- Monthly Giving Plans
- Honor a Person You Care About
- Donor-Advised Funds
- AAP in Your Will
- Become a Corporate Partner
- Employment Opportunities
- Equity and Inclusion Efforts
- RFP Opportunities
- Board of Directors
- Senior Leadership Team
- Constitution & By-Laws
- Strategic Plan

Advancing Pediatric Research
The AAP addresses important questions regarding pediatric practice and the health and well being of children by developing original research including practice-based network research.
Practice-Based Research in Office Settings (PROS)
Our programs, our priorities, get involved, pediatrician surveys.
The AAP has collected survey data from national samples of pediatricians for 35 years across 3 original research programs.
Child Health Data Trends
Child population characteristics, child health, child health care, child cases, hospitalizations, and mortality, child vaccination, research findings, aap news research updates.
AAP Research articles published in AAP News.
Research Journal Articles
AAP Research articles published in peer reviewed journals.
Pediatric Academic Societies Abstracts
AAP Research abstracts presented at Pediatric Academic Societies meetings.
Research Resources
Childstats.gov, children and clinical studies, children's health survey for asthma, committee on pediatric research, financial conflicts of interest policy and report, resident research grants, research networks, delivery room intervention and evaluation (drive) network.
- Open access
- Published: 04 May 2024
Changes in the epidemiology and clinical characteristics of viral gastroenteritis among hospitalized children in the Mainland of China: a retrospective study from 2016 to 2020
- Lingyun Guo 2 ,
- Yiliang Fu 1 ,
- Luci Huang 1 ,
- Guoshuang Feng 3 ,
- Gang Liu 2 ,
- Xiangpeng Chen 1 &
- Zhengde Xie 1
BMC Pediatrics volume 24 , Article number: 303 ( 2024 ) Cite this article
92 Accesses
1 Altmetric
Metrics details
Acute gastroenteritis (AGE) causes significant morbidity in children worldwide; however, the disease burden of children hospitalized with viral gastroenteritis in China has been rarely described. Through this study, we analyzed the data of hospitalized children with viral gastroenteritis to explore the changes in the epidemiology and clinical characteristics of viral gastroenteritis in the mainland of China.
Data were extracted from Futang Children's Medical Development Research Center (FRCPD), between 2016 and 2020, across 27 hospitals in 7 regions. The demographics, geographic distribution, pathogenic examination results, complications, hospital admission date, length of hospital stays, hospitalization charges and outcomes were collected and analyzed.
Viral etiological agents included rotavirus (RV), adenovirus (ADV), norovirus (NV) and coxsackievirus (CV) that were detected in 25,274 (89.6%), 1,047 (3.7%), 441 (1.5%) and 83 (0.3%) cases. There was a higher prevalence of RV and NV infection among children younger than 3 years of age. RV and NV had the highest detection rates in winter, while ADV in summer. Children with viral gastroenteritis were often accompanied by other diseases, such as myocardial diseases (10.98–31.04%), upper respiratory tract diseases (1.20–20.15%), and seizures (2.41–14.51%). Among those cases, the co-infection rate with other pathogens was 6.28%, with Mycoplasma pneumoniae ( M. pneumoniae ), Epstein-Barr virus (EBV), and influenza virus (FLU) being the most common pathogens. The median length of stay was 5 days, and the median cost of hospitalization corresponded to587 US dollars.
Conclusions
This finding suggests that viral gastroenteritis, especially those caused by RV, is a prevalent illness among younger children. Co-infections and the presence of other diseases are common. The seasonality and regional variation of viral etiological agents highlight the need for targeted prevention and control measures. Although viral gastroenteritis rarely leads to death, it also results in a significant economic burden on healthcare systems.
Peer Review reports
Acute gastroenteritis is a common disease that affects people of all ages, leading to serious complications in young children and the elderly [ 1 , 2 , 3 , 4 ]. In China, infectious diarrhea (excluding cholera, dysentery and enteric fever) has been classified as a class C infectious disease according to the national notifiable infectious diseases reporting system. Enteric viral pathogens are gradually becoming the leading pathogens of gastroenteritis which is also known as infectious diarrhea, due to the improved the quality of drinking water and the frequent use of antibiotics. Clinical manifestations of viral gastroenteritis include fever, abdominal pain, watery diarrhea, nausea and vomiting. Viral gastroenteritis is usually a self-limiting illness, requiring mainly supportive therapy, which usually resolves within 2–5 days. Viral pathogens include rotavirus (RV), norovirus (NV), astrovirus (AV) and adenovirus (ADV). NV infection affects people of all ages, while RV mainly infects children, particularly those under five years of age [ 5 , 6 , 7 , 8 ].
The implementation of RV vaccination has reduced RV problems to some extent, but the contribution of RV to pediatric acute gastroenteritis has not been replaced by other pathogens [ 3 , 6 , 9 ]. Vaccination has helped to reduce RV hospitalization, as well as change the epidemiology of RV disease in the United States and Spain [ 10 , 11 ]. RV vaccine is part of the National Immunization Programs (NIPs) in many countries, but it has not been included in China’s NIPs. The epidemiology and distribution of common pathogens causing infectious gastroenteritis, particularly viruses, are unclear in developing countries including China.
In China, there are few multicenter studies on the clinical epidemiological characteristics and disease burden of viral gastroenteritis in children. By using the hospitals’ electronic medical record management system, the medical data generated during the hospitalization of patients can be summarized into face sheet of discharge medical records (FSMRs). This study aimed to summarize and provide relevant data on the clinical epidemiology and disease burden of viral gastroenteritis in hospitalized children in China.
Study design and participants
In China, Futang Children's Medical Development Research Center (FRCPD) is the first non-profit social service organization established to care for children's lives and health and engage in children’s development research [ 12 ], supervised and managed by the Ministry of Civil Affairs of the People’s Republic of China and led by the Children’s Medical Center. The center currently consists of 47 provincial and municipal medical institutions and has established a nationwide children health service network [ 13 ]. In Dec 2015, FRCPD began to collect the data of FSMRs from its member hospitals. The National Center for Children's Health (Beijing), Beijing Children’s Hospital, Capital Medical University collected the data of the hospitalized children’s medical records from Jan 1st, 2016 to Dec 31st, 2020 in 27 tertiary children's hospitals under the FRCDP (Supplementary Material 1 ).
We designed this study to collect basic medical information of children hospitalized with viral gastroenteritis in the FUTang Updating medical REcords (FUTURE) database from 2016 to 2020, and extracted relevant information from the system based on the tenth revision of the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) code for children diagnosed with viral gastroenteritis (Fig. 1 ). The demographic information isdisplayed in Table 1 . Subgroups were divided according to the sex, age, region, and time of hospitalization status. All hospitals were divided into seven geographic regions. According to different ages, hospitalized children with viral gastroenteritis were divided into six groups, including neonate (≤ 28 days), infant (28 days < ~ ≤ 1 year old, neonate were excluded), toddler (1 < ~ ≤ 3 years old), preschooler (3 < ~ ≤ 6 years old), school–age children (6 < ~ ≤ 12 years old), adolescence (12 < ~ < 18 years old).
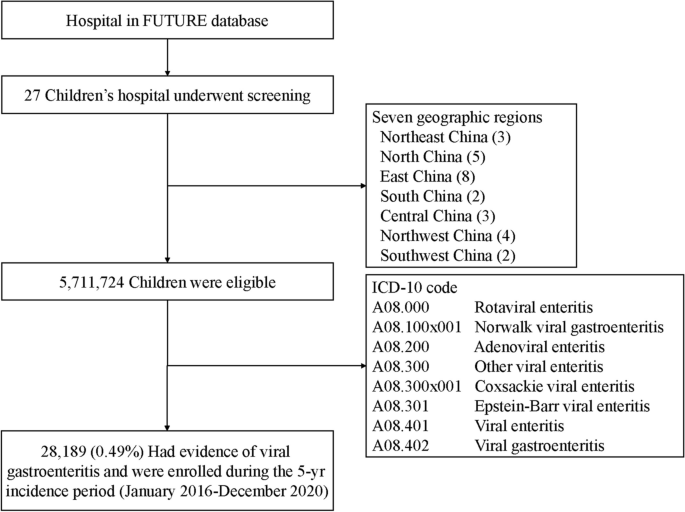
Screening, eligibility, and enrollment of children with viral gastroenteritis. A total of 28,189 children had the clinical and etiological diagnosis that met the inclusion criteria of viral gastroenteritis
Inclusion and exclusion criteria
This retrospective study included only children under the age of 18 who were hospitalized for viral gastroenteritis based on the classification of viral gastroenteritis according to ICD-10 codes, we collected basic medical information from the FUTURE database. Children were diagnosed with viral gastroenteritis according to the clinical and etiological diagnosis [ 3 , 4 ]. Data of children with unknown sex, age, region or resident condition were excluded.
Statistical analysis
Continuous variables were presented as mean ± standard deviation (SD) and compared between groups by Student’s t-test when normally distributed. For not normally distributed variables, the data were expressed as median (interquartile range, IQR), and Kruskal–Wallis test as well as Steel–Dwass test (for multiple comparisons) were performed to compare the difference among groups. Categorical variables were expressed as number (%) or proportions and compared between/among groups by χ2 or Fisher’s exact tests, when appropriate. IBM SPSS Statistics 23.0 software (SPSS Inc., USA) was used for data analysis. P value < 0.05 was considered statistically significant.
Prevalence of viral gastroenteritis in children
During 2016–2020, a total of 28,189 hospitalized children with viral gastroenteritis were enrolled in the FUTang Updating medical Records (FUTURE) database, which accounted for 0.5% (28,189/5,711,724) of all hospitalized cases, with 60.6% male (17,099) and 39.3% female (11,096) (Table 1 ). In different month and admission years, the proportions of male were higher compared to female (Fig. 2 ). The information on sex, age, year, season, regions and outcomes is shown in Table 1 .
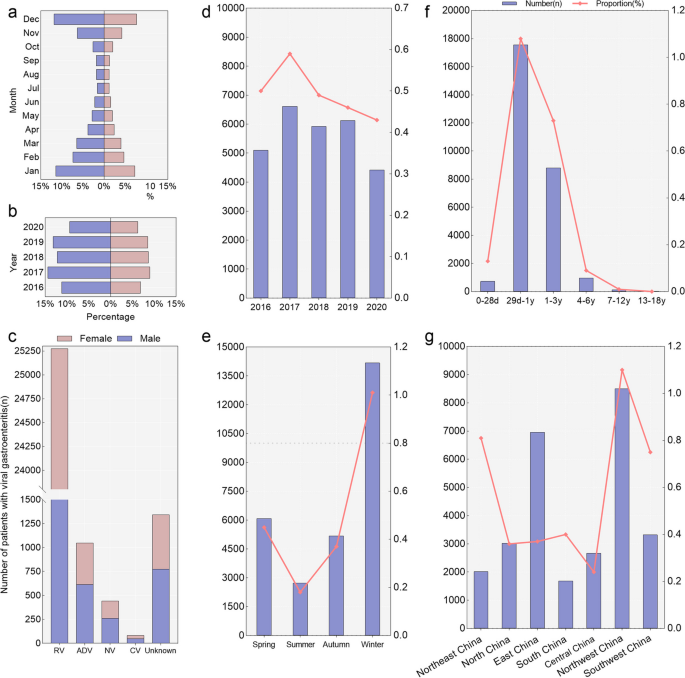
The proportion of children hospitalized for viral gastroenteritis by different gender, years, ages and regions. Panel a - c show the proportion of different years, months and pathogens according to gender. Panel d - g show the number and proportion in different years, age groups, seasons and regions of China, the left Y axis (the bars) is the number, while the right Y axis (the line plots) is the proportion of hospitalized children with viral gastroenteritis. The definition of "unknown" is that children with viral gastroenteritis were for an unspecified viral cause
In different genders, years, regions, and age groups, we evaluated the proportion of viral gastroenteritis hospitalizations to total hospitalization (Table 1 , Fig. 2 ). Females had a higher proportion of children with viral gastroenteritis than males ( P < 0.001 ), with the rates of 0.5% (11,090/2,179,388) and 0.5% (17,099/3,532,336), respectively (Table 1 ). The rate of viral gastroenteritis in the age group from 29 days to 1 year old was significantly higher than those in other age groups (Table 1 ) ( P < 0.001 ). The proportion of viral gastroenteritis hospitalizations to total hospitalization also differed with seasonal variability, which was higher in winter and lower in summer (Table 1 ) ( P < 0.001 ). Northwest China had the highest proportion (1.1%, 8,505/775,561) and Central China had the lowest proportion (0.2%, 2,671/1,098,999) ( P < 0.001 ).
Viral gastroenteritis characterized by different viral pathogens
Among those admitted to the hospital with a diagnosis of viral gastroenteritis, 95.2% (26,845/28,189) cases were positive for viral infection (RV, NV, CV and ADV) (Table 2 , Fig. 3 ). RV had the highest positive proportion (89.7%) than the other viruses ( P < 0.001 ). RV, NV, CV and ADV had the highest positive rate in the 28 days < ~ ≤ 1 year group than other age groups ( P < 0.001 ). RV and NV had the highest detection rate in winter compared with other seasons, while ADV had the highest detection rate in summer ( P < 0.001 ). RV showed high detection rates in Northwest China and East China (28.3% and 25.4%), while NV had a high detection rate in North China, CV in East China and ADV in Northwest China (46.9%, 94.0% and 61.5%) compared to other regions ( P < 0.001 ) (Table 2 ).
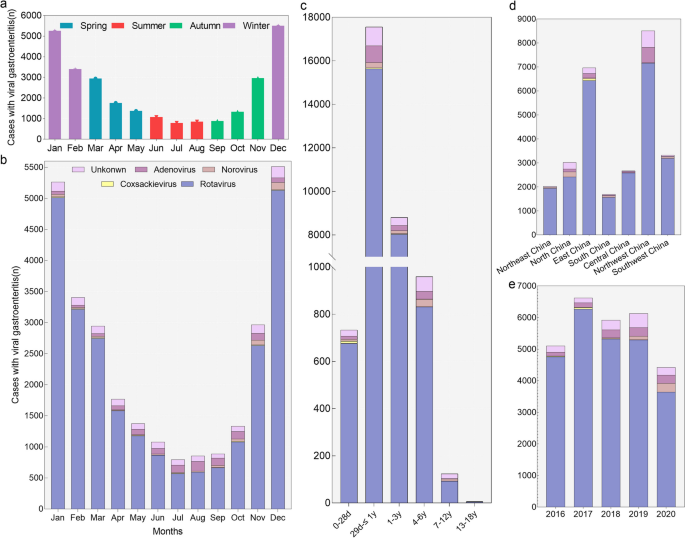
Pathogens detected in children with viral gastroenteritis requiring hospitalization. Panel a show the number of hospitalized children with viral gastroenteritis in different seasons. Panel b show the pathogens distribution in different months. Seasons were based on months as follows: winter, January through March; spring, April through June; summer, July through September; fall, October through December. Panel c - e show the pathogens distribution in in different age groups, years and regions of China. The definition of "unknown" is that children with viral gastroenteritis were for an unspecified viral cause
Viral gastroenteritis combined with other diseases
Children hospitalized with viral gastroenteritis were often presented with one or more coexisting diseases. Among the 25,274 cases of RV-positive children, they had various other diseases. Specifically, 31.04% had myocardial diseases, 14.41% had upper respiratory tract diseases, 11.83% had bronchitis, and 6.92% had bronchopneumonia. Meantime, myocardial diseases and upper respiratory tract diseases are also common in children infected with CV, NV and ADV (Table 3 ). Among positive cases of CV (23 cases), RV (7845 cases), NV (75 cases), and ADV (115 cases) with myocardial diseases, myocardial injury rates were highest for cases of myocardial impairment, with 100.00% (23 cases), 78.88% (6188 cases), 95.0% (72 cases), and 73.04% (84 cases), respectively. Nervous system diseases such as seizure accounted for 14.51% of children with NV, 6.02% with ADV, 5.60% with RV and 2.41% with CV. Among RV-positive children with seizures, there were 14 cases of febrile seizures (0.99%), 31 cases of benign convulsions with gastroenteritis (2.19%), and 218 cases of benign infantile convulsions (15.41%). Moreover, other diseases were relatively low, such as urogenital diseases, and nutritional diseases (Table 3 ).
Coinfection with other pathogens
For 26,845 viral gastroenteritis cases with RV, CV, NV or ADV, the co-infection rate was 6.28% (1686/26845): viruses in 792 (2.95%), bacteria in 176 (0.66%), fungi and atypical pathogens in 718 (2.67%). The most commonly co-infection pathogens were Mycoplasma pneumoniae ( M. pneumoniae ) (1.95%, 523 cases), Epstein-Barr virus (EBV) (0.98%, 262 cases), influenza virus (FLU) (0.67%, 181 cases), cytomegalovirus (CMV) (0.53%, 141 cases), candida albicans ( C. albicans ) (0.48%, 129 cases), and respiratory syncytial virus (RSV) (0.41%, 110 cases) (Table 4 ). M. pneumoniae was detected more commonly in viral gastroenteritis children infected with RV or NV than with CV or ADV (2.01–2.27% vs. 0–0.57%). EBV (1.00%, 253/25274) and RSV (0.42%, 107/25274) were more commonly co-infected with RV in children with viral gastroenteritis, while CMV more commonly with CV (1.20%, 1/83) and FLU with NV (0.91%, 4/441) (Table 4 ).
Complications
Complications of viral gastroenteritis included dehydration, acidosis, electrolyte disorders and shock (Table 5 ). Children aged 28 days < ~ ≤ 1 year were most likely to suffer from acidosis, while those aged 6 < ~ ≤ 12 years old were most likely to suffer from dehydration ( P < 0.001 ). Dehydration was more common in children with NV infection, while electrolyte disturbances were more prevalent in children with RV infection, and acidosis with ADV infection ( P < 0.001 ).
LOS, hospitalization expense, discharge and outcome
The median length of stay (LOS) for hospitalized viral gastroenteritis patients was 5 days (IQR: 3–6 days), and the median expense was 587 USD (541–642 USD) (Table 6 ). The LOS was shortest for children aged 1 < ~ ≤ 3 years and longest for children aged 28 days < ~ ≤ 1 year. Total costs were highest among hospitalized patients aged ≤ 28 days( P < 0.001 ). Children with RV gastroenteritis had the longest LOS ( P < 0.001 ). The hospital cost was the highest with ADV gastroenteritis (642 US$) and lowest with RV gastroenteritis (541 US$). The majority of hospitalized patients recovered and were able to be discharged within a few days, in which the percentage of discharge by patient with medical advice was 93.5% (26,363 cases) (Table 1 ). Fortunately, there were no deaths in our study.
This study summarized and analyzed the FSMRs data of 28,189 hospitalized children with viral gastroenteritis from 2016 to 2020 in the mainland of China to provide further evidence for the role of gastrointestinal viral infections in this most common gastrointestinal emergency in children. We found that the burden of viral gastroenteritis related hospitalization was the highest among children younger than 3 years of age. RV, CV, ADV and NV accounted for 95.2% of the children with viral gastroenteritis. We demonstrated that the coexistence rates of viral gastroenteritis with upper respiratory tract diseases, myocardial diseases, or seizure were high, and the co-occurrence of other viral, bacterial or atypical pathogen infections was common in pediatric patients hospitalized with viral gastroenteritis, such as M. pneumoniae , EBV and CMV.
Children with viral gastroenteritis under 18 years of age have a ratio of 1.54 to1 between males and females. The result coincided with previous research in China, which showed the ratio was 1.68:1 for children under 5 years of age with gastroenteritis in western China from 2015 to 2019 [ 14 ]. Our data suggests that children bearing the greatest burden of hospitalization associated with AGE especially infected with RV were children younger than 3 years (96.3%). In comparison with other studies worldwide [ 15 , 16 , 17 ], there is a significant difference in the detection rate of rotavirus and norovirus. This may be attributed to the involvement of multiple hospitals in this study, each of which adopted different diagnostic methods. Additionally, RV infection often results in fever, vomiting, dehydration, and severe diarrhea compared to NV infection, increasing the likelihood of hospitalization [ 18 , 19 , 20 ]. This study specifically focused on hospitalized patients with viral gastroenteritis, rather than the entire population or patients with diarrhea. It’s important to consider that hospitalized patients usually have more severe conditions than outpatients, which may explain the significantly higher detection rate of RV compared to NV. This study clearly showed the seasonal characteristics of the hospitalized cases in children with viral gastroenteritis over the past five years. The fluctuation of the total number and rate were mainly caused by the change in RV, and the infection of rotavirus mainly occurs from November to March, which is in accordance with previous studies from other countries and other regions of China [ 9 , 21 , 22 , 23 ].
In China, the Lanzhou lamb rotavirus (LLR) vaccine was licensed and has been available since 2000 in China, RotaTeq (RV5) in 2018, and Lanzhou lamb reassortant rotavirus vaccine, live, oral, trivalent (Vero cell) (LLR3) in 2023. Even they have not been included in NIPs, the number of rotavirus vaccine doses produced and administered in China has been increasing [ 24 , 25 ]. RV showed the smallest number and lowest proportion in 2020, which can demonstrate that the contribution of RV to pediatric acute gastroenteritis will gradually decrease as the application of vaccine. Moreover, the COVID-19 (coronavirus disease 2019) pandemic may have altered the epidemiological landscape of various pathogens. In response to COVID-19, control strategies such as social distancing, lockdowns, and enhanced personal hygiene standards were implemented, affecting the transmission of pathogens [ 26 , 27 , 28 , 29 ]. A retrospective study on Chinese Taiwan children revealed that RV hospitalization rates among children < 5 years of age significantly declined by 24.0% in post-vaccine compared to pre-vaccine rotavirus seasons [ 30 ]. A multicenter study in China from 2003 to 2012 showed a 70% decrease in the mortality rate of rotavirus gastroenteritis (RVGE) in 2012 compared to 2003 [ 2 ]. So, the increasing use of rotavirus vaccines can diminish the burden and change the epidemiology of rotavirus disease worldwide especially in developing countries, as Shim et al. showed that vaccines had a protective effect for hospitalized children with acute gastroenteritis [ 31 ]. Advancements in the medical infectious disease reporting system, pathogen detection technology, and awareness about sending specimens for testing for pathogens have resulted in the detection of more positive cases. The first-dose RV vaccine coverage in China was 20.3%, with only 1.8% coverage for the third dose; consequently, despite a decrease in hospitalization and mortality rates for RVGE in China, the disease burden persists [ 32 ].
Viral gastroenteritis combined with myocardial diseases refers to the condition where viral infection leads to myocardial damage and myocarditis [ 33 , 34 ]. In this study, the proportion of viral gastroenteritis combined with myocarditis was high, ranging from 10.98% to 31.04%, in which over 70% of cases were diagnosed with myocardial injuries. Cioc et al. revealed that among 13 cases of sudden cardiac arrest patients, 5 cases of CV and 4 cases of RV in myocardial tissue samples, and a number of case reports have described especially myocarditis of RV infection [ 35 , 36 ]. Viral gastroenteritis can also be associated with central nervous system (CNS) diseases, known as encephalitis or meningitis. This study found that the proportion of cases with seizures was from 2.41–14.51%, in which benign infantile convulsions had the highest proportion, and benign convulsions with gastroenteritis only accounted for 0–21.88% of cases with seizures, similar to other reports [ 37 , 38 , 39 ]. There have been numerous cases with respiratory diseases, including 60 cases (6.59%) of ADV-associated pneumonia and bronchopneumonia. According to previous studies, ADV is more commonly cause gastrointestinal diseases by serotypes 40 or 41 [ 40 , 41 ]. Therefore, for children hospitalized with viral gastroenteritis, we should pay attention to the possibility of concurrent other systemic diseases and remain vigilant for the occurrence of severe cases.
In terms of the co-infection with other pathogens, M. pneumoniae , EBV, FLU, and CMV were the main pathogens of viral gastroenteritis in hospitalized children. M. pneumoniae and FLU infections usually cause respiratory diseases, such as Mycoplasma pneumoniae pneumonia and viral pneumonia, which aligned with the high proportion of respiratory diseases among children with viral gastroenteritis that were mentioned earlier. In this study EBV-positive cases included infectious mononucleosis, EBV viremia, and other EBV-related diseases. It is important to note that a positive result does not necessarily indicate that EBV infection will result in disease or symptoms, because most patients may have latent EBV infection [ 42 ]. Similar to EBV, CMV is typically asymptomatic in the majority of individuals. However, in children with compromised immune function who are hospitalized with viral gastroenteritis, CMV infection can cause clinical symptoms and complications, such as hepatitis, pneumonia, and impairment of the brain and visual system. For children with viral gastroenteritis, properly controlling infections caused by other pathogens is crucial to immunocompromised patients, including immune deficiencies, hematopoietic stem cell transplantation or liver transplantation [ 43 , 44 ].
AGE is generally a self-limiting condition and resolves within one week, which is most commonly associated with viral infection [ 45 , 46 , 47 ]. There were no fatal cases in our study, as a result of viral gastroenteritis, patients usually suffered from complications, such as dehydration, electrolyte disorders, and acidosis. Our study showed there was more dehydration in children with NV infections, electrolyte disturbances in children with RV infections, and electrolyte disorders with ADV infections. LOS and hospitalization expense of children with viral gastroenteritis were associated with age, region and pathogens in children.
Our study has some limitations. The most frequently seen patients with viral gastroenteritis are outpatients, while our database only contains the data generated from hospitalized children, so little is known regarding the total incidence of viral gastroenteritis. Meanwhile, various detection methods for pathogens in different hospitals lead to the effectiveness of the detection method for the same pathogen is diverse, so we are unable to make comparisons between different pathogens. In this study, no follow-up information was available for the children with viral gastroenteritis, especially patients who had been transferred to other hospitals. Due to a lack of clear information regarding the patient's RV vaccination status, it is hard to assess the protective effect of RV vaccination in viral gastroenteritis.
Rotavirus was detected in nearly 90% of children with viral gastroenteritis among hospitalized children in the mainland of China. Most cases occurred among children younger 3 years during the winter months. Children with viral gastroenteritis were often accompanied by other diseases and pathogens, with myocardial diseases the most common disease and M. pneumoniae the most common pathogen. Continuous surveillance is needed to monitor the prevalence of viral gastroenteritis, and the immunization schedule of rotavirus is essential for adequate management of viral gastroenteritis.
Availability of data and materials
The dataset used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Acute gastroenteritis
Futang Children's Medical Development Research Center
Coxsackievirus
Enterovirus
Mycoplasma pneumoniae
Epstein-Barr virus
Influenza virus
National Immunization Programs
Face sheet of discharge medical records
International Statistical Classification of Diseases and Related Health Problems 10th Revision
Interquartile range
Cytomegalovirus
Candida albicans
Respiratory syncytial virus
Length of stay
World Health Organization
Lanzhou lamb rotavirus
Lanzhou lamb reassortant rotavirus vaccine, live, oral, trivalent (Vero cell)
Rotavirus gastroenteritis
Central nervous system
Reiner RC Jr, Graetz N, Casey DC, Troeger C, Garcia GM, Mosser JF, et al. Variation in childhood diarrheal morbidity and mortality in Africa, 2000–2015. N Engl J Med. 2018;379(12):1128–38.
Article PubMed Google Scholar
Zhang J, Duan Z, Payne DC, Yen C, Pan X, Chang Z, et al. Rotavirus-specific and overall diarrhea mortality in chinese children younger than 5 years: 2003 to 2012. Pediatr Infect Dis J. 2015;34(10):e233–7.
Article PubMed PubMed Central Google Scholar
Meier JL. Viral acute gastroenteritis in special populations. Gastroenterol Clin North Am. 2021;50(2):305–22.
Hartman S, Brown E, Loomis E, Russell HA. Gastroenteritis in children. Am Fam Physician. 2019;99(3):159–65.
PubMed Google Scholar
Collaborators GDaI. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the global burden of disease study 2016. Lancet Infect Dis. 2018;18(11):1211–28.
Article Google Scholar
Yang L, Shi S, Na C, Li B, Zhao Z, Yang T, et al. Rotavirus and norovirus infections in children under 5 years old with acute gastroenteritis in Southwestern China, 2018–2020. J Epidemiol Glob Health. 2022;12(3):292–303.
Article CAS PubMed PubMed Central Google Scholar
Pitkänen O, Markkula J, Hemming-Harlo M. A major decrease in viral acute gastroenteritis in hospitalized finnish children as rotavirus returns as the most detected pathogen. Int J Infect Dis. 2022;114:273–8.
Öner SZ, Kaleli İ, Demi RM, Mete E, Çalişkan A. Rotavirus and adenovirus prevalence in patients with acute viral gastroenteritis in Denizli, Turkey, 2017–2021. J Med Virol. 2022;94(8):3857–62.
Paternina-Caicedo A, Parashar U, Garcia-Calavaro C, de Oliveira LH, Alvis-Guzman N, De la Hoz-Restrepo F. Diarrheal deaths after the introduction of rotavirus vaccination in 4 countries. Pediatrics. 2021;147(1):e20193167.
Burke RM, Tate JE, Han GS, Quenelle R, Gautam R, Wadford DA, et al. Rotavirus vaccination coverage during a rotavirus outbreak resulting in a fatality at a subacute care facility. J Pediatric Infect Dis Soc. 2020;9(3):287–92.
Article CAS PubMed Google Scholar
Hallowell BD, Parashar UD, Curns A, DeGroote NP, Tate JE. Trends in the laboratory detection of rotavirus before and after implementation of routine rotavirus vaccination - United States, 2000–2018. MMWR Morb Mortal Wkly Rep. 2019;68(24):539–43.
Feng G, Zeng Y, Tian J, Wang X, Tai J, Song F, et al. Disease spectrum analysis of hospitalized children in China: a study of 18 tertiary children’s hospitals. Pediatr Investig. 2019;3(3):159–64.
Guo K, Wang XY, Feng GS, Tian J, Zeng YP, Ma SX, et al. The epidemiology of blood transfusion in hospitalized children: a national cross-sectional study in China. Transl Pediatr. 2021;10(4):1055–62.
Cao RR, Ma XZ, Li WY, Wang BN, Yang Y, Wang HR, et al. Epidemiology of norovirus gastroenteritis in hospitalized children under five years old in western China, 2015–2019. J Microbiol Immunol Infect. 2021;54(5):918–25.
Amodio E, De Grazia S, Genovese D, Bonura F, Filizzolo C, Collura A, et al. Clinical and epidemiologic features of viral gastroenteritis in hospitalized children: an 11-year surveillance in palermo (Sicily). Viruses. 2022;15(1):41.
Calduch EN, Cattaert T, Verstraeten T. Model estimates of hospitalization discharge rates for norovirus gastroenteritis in Europe, 2004–2015. BMC Infect Dis. 2021;21(1):757.
Aliabadi N, Antoni S, Mwenda JM, Weldegebriel G, Biey JNM, Cheikh D, et al. Global impact of rotavirus vaccine introduction on rotavirus hospitalisations among children under 5 years of age, 2008–16: findings from the global rotavirus surveillance network. Lancet Glob Health. 2019;7(7):e893–903.
Zhang J, Yang F. Correlation between infection with rotavirus and norovirus and acute gastroenteritis in children. Endemic Dis Bull (in Chinese). 2018;33(03):74–6.
Google Scholar
Cui X, Feng G, Jln F, Xu X. Investigation and clinical analysis of norovirus and rotavirus infection in 942 children with acute diarrhea. Chin J Practical Pediatr (in Chinese). 2016;31(08):603–7.
Wei K, Liu X, Liu D, Chang Q, Xiang J, Wang P. Investigation on the prevalence of group A rotavirus and norovirus in hospitalized children with diarrhea in Wuwei area, Gansu province. Chin J Viral Dis (in Chinese). 2014;4(02):137–40.
Sharma P, Katewa S, Meel SK, Katewa V, Bishnoi A, Verma VK, et al. Clinicoepidemiological profile and genetic characterization of circulating rotavirus strain among children < 5 years hospitalized for acute gastroenteritis in Western Rajasthan. India Indian J Pediatr. 2021;88(Suppl 1):97–104.
Lu W, Li J, Li J, Ai D, Song H, Duan Z, et al. Short-term impacts of meteorology, air pollution, and internet search data on viral diarrhea infection among children in Jilin Province, China. Int J Environ Res Public Health. 2021;18(21):11615.
Nan X, Jinyuan W, Yan Z, Maosheng S, Hongjun L. Epidemiological and clinical studies of rotavirus-induced diarrhea in China from 1994–2013. Hum Vaccin Immunother. 2014;10(12):3672–80.
Fu C, Dong Z, Shen J, Yang Z, Liao Y, Hu W, et al. Rotavirus gastroenteritis infection among children vaccinated and unvaccinated with rotavirus vaccine in Southern China: a population-based assessment. JAMA Netw Open. 2018;1(4):e181382.
Zhang H, Lai X, Mak J, Sriudomporn S, Zhang H, Fang H, et al. Coverage and equity of childhood vaccines in China. JAMA Netw Open. 2022;5(12):e2246005.
Steens A, Knol MJ, Freudenburg-de Graaf W, de Melker HE, van der Ende A, van Sorge NM. Pathogen- and type-specific changes in invasive bacterial disease epidemiology during the first year of the COVID-19 pandemic in The Netherlands. Microorganisms. 2022;10(5):972.
Lamrani Hanchi A, Guennouni M, Ben Houmich T, Echchakery M, Draiss G, Rada N, et al. Changes in the epidemiology of respiratory pathogens in children during the COVID-19 pandemic. Pathogens. 2022;11(12):1542.
Luciani L, Ninove L, Zandotti C, Nougairède A. COVID-19 pandemic and its consequences disrupt epidemiology of enterovirus meningitis. South-East France J Med Virol. 2021;93(4):1929–31.
Kies KD, Thomas AS, Binnicker MJ, Bashynski KL, Patel R. Decrease in enteroviral meningitis: an unexpected benefit of coronavirus disease 2019 (COVID-19) mitigation? Clin Infect Dis. 2021;73(9):e2807–9.
Burke RM, Shih S, Hsiung CA, Yen C, Jiang B, Parashar UD, et al. Impact of rotavirus vaccination on rotavirus hospitalizations in Taiwanese children. Vaccine. 2021;39(49):7135–9.
Shim JO, Chang JY, Shin S, Moon JS, Ko JS. Changing distribution of age, clinical severity, and genotypes of rotavirus gastroenteritis in hospitalized children after the introduction of vaccination: a single center study in Seoul between 2011 and 2014. BMC Infect Dis. 2016;16:287.
Luo HM, Ran L, Meng L, Lian YY, Wang LP. Analysis of epidemiological characteristics of report cases of rotavirus diarrhea in children under 5 years old in China, 2005–2018. Zhonghua Yu Fang Yi Xue Za Zhi. 2020;54(2):181–6.
CAS PubMed Google Scholar
Rauff B, Malik A, Bhatti YA, Chudhary SA, Fatima K, Rafiq S, et al. Association of viruses in the development of cardiovascular diseases. Curr Pharm Des. 2021;27(37):3913–23.
Ammirati E, Frigerio M, Adler ED, Basso C, Birnie DH, Brambatti M, et al. Management of acute myocarditis and chronic inflammatory cardiomyopathy: an expert consensus document. Circ Heart Fail. 2020;13(11):e007405.
Dian Z, Sun Y, Zhang G, Xu Y, Fan X, Yang X, et al. Rotavirus-related systemic diseases: clinical manifestation, evidence and pathogenesis. Crit Rev Microbiol. 2021;47(5):580–95.
Cioc AM, Nuovo GJ. Histologic and in situ viral findings in the myocardium in cases of sudden, unexpected death. Mod Pathol. 2002;15(9):914–22.
Ogawa C, Kidokoro H, Ishihara N, Tsuji T, Kurahashi H, Hattori A, et al. Splenial lesions in benign convulsions with gastroenteritis associated with rotavirus infection. Pediatr Neurol. 2020;109:79–84.
Wang D, Jiang Y, Hong S, Ma J, Liao S, Cheng M, et al. Prognostic factors for the recurrence of afebrile seizures after benign convulsions associated with mild gastroenteritis. Epilepsia. 2021;62(12):3068–75.
Hungerford DJ, French N, Iturriza-Gómara M, Read JM, Cunliffe NA, Vivancos R. Reduction in hospitalisations for acute gastroenteritis-associated childhood seizures since introduction of rotavirus vaccination: a time-series and change-point analysis of hospital admissions in England. J Epidemiol Community Health. 2019;73(11):1020–5.
Sdiri-Loulizi K, Gharbi-Khelifi H, de Rougemont A, Hassine M, Chouchane S, Sakly N, et al. Molecular epidemiology of human astrovirus and adenovirus serotypes 40/41 strains related to acute diarrhea in Tunisian children. J Med Virol. 2009;81(11):1895–902.
Dey RS, Ghosh S, Chawla-Sarkar M, Panchalingam S, Nataro JP, Sur D, et al. Circulation of a novel pattern of infections by enteric adenovirus serotype 41 among children below 5 years of age in Kolkata. India J Clin Microbiol. 2011;49(2):500–5.
Cohen JI. Epstein-Barr virus infection. N Engl J Med. 2000;343(7):481–92.
Kohli R, Cortes M, Heaton ND, Dhawan A. Liver transplantation in children: state of the art and future perspectives. Arch Dis Child. 2018;103(2):192–8.
Bateman CM, Kesson A, Powys M, Wong M, Blyth E. Cytomegalovirus Infections in children with primary and secondary immune deficiencies. Viruses. 2021;13(10):2001.
Posovszky C, Buderus S, Classen M, Lawrenz B, Keller KM, Koletzko S. Acute infectious gastroenteritis in infancy and childhood. Dtsch Arztebl Int. 2020;117(37):615–24.
PubMed PubMed Central Google Scholar
Lee B, Damon CF, Platts-Mills JA. Pediatric acute gastroenteritis associated with adenovirus 40/41 in low-income and middle-income countries. Curr Opin Infect Dis. 2020;33(5):398–403.
Bányai K, Estes MK, Martella V, Parashar UD. Viral gastroenteritis. Lancet. 2018;392(10142):175–86.
Download references
Acknowledgements
We are grateful to investigators from members of the Futang Research Center of Pediatric Development (FRCPD).
This work was supported by the National Natural Science Foundation of China (grant number 82172245 and 81971922); Beijing Natural Science Foundation (grant number L192014); CAMS Innovation Fund for Medical Sciences (grant number 2019-I2M-5–026); and Beijing Excellent Talents Training Program (grant number 2018000021469G274).
Author information
Authors and affiliations.
Beijing Key Laboratory of Pediatric Respiratory Infection Diseases, Key Laboratory of Major Diseases in Children, Ministry of Education, National Clinical Research Center for Respiratory Diseases, Research Unit of Critical Infection in Children, Chinese Academy of Medical Sciences, 2019RU016, Laboratory of Infection and Virology, Beijing Pediatric Research Institute, Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, Beijing, China
Fei Li, Qi Li, Yiliang Fu, Luci Huang, Xiangpeng Chen & Zhengde Xie
Department of Infectious Disease, National Center for Children’s Health, Key Laboratory of Major Diseases in Children, Ministry of Education, Beijing Children’s Hospital, Capital Medical University, Beijing, China
Lingyun Guo & Gang Liu
Big Data and Engineering Research Center, Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, Beijing, China
Hui Xu & Guoshuang Feng
You can also search for this author in PubMed Google Scholar
Contributions
XPC and ZDX conceptualized and designed the study, reviewed and revised the final manuscript. FL collected clinical data, analyzed the results, and drafted the initial manuscript. LYG, QL, HX and GSF analyzed the results and provided clinical context for study methods; YLF, LCH, and GL critically contributed to the final manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Correspondence to Xiangpeng Chen .
Ethics declarations
Ethics approval and consent to participate.
The study protocol was approved by the medical ethics committee of the Beijing Children’s Hospital, Capital Medical University. The ethics committee approved the waiver of informed consent from parents/guardians of the minors, because the present study was a retrospective analysis of clinical data and all methods were performed in accordance with the ethical guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Li, F., Guo, L., Li, Q. et al. Changes in the epidemiology and clinical characteristics of viral gastroenteritis among hospitalized children in the Mainland of China: a retrospective study from 2016 to 2020. BMC Pediatr 24 , 303 (2024). https://doi.org/10.1186/s12887-024-04776-1
Download citation
Received : 06 October 2023
Accepted : 18 April 2024
Published : 04 May 2024
DOI : https://doi.org/10.1186/s12887-024-04776-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Epidemiology
- Viral gastroenteritis
- Co-infection

BMC Pediatrics
ISSN: 1471-2431
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Share full article
Advertisement
Supported by
Physical Fitness Linked to Better Mental Health in Young People
A new study bolsters existing research suggesting that exercise can protect against anxiety, depression and attention challenges.

By Matt Richtel
Physical fitness among children and adolescents may protect against developing depressive symptoms, anxiety and attention deficit hyperactivity disorder, according to a study published on Monday in JAMA Pediatrics.
The study also found that better performance in cardiovascular activities, strength and muscular endurance were each associated with greater protection against such mental health conditions. The researchers deemed this linkage “dose-dependent,” suggesting that a child or adolescent who is more fit may be accordingly less likely to experience the onset of a mental health disorder.
These findings come amid a surge of mental health diagnoses among children and adolescents, in the United States and abroad, that have prompted efforts to understand and curb the problem.

The new study, conducted by researchers in Taiwan, compared data from two large data sets: the Taiwan National Student Fitness Tests, which measures student fitness performance in schools, and the National Insurance Research Databases, which records medical claims, diagnoses prescriptions and other medical information. The researchers did not have access to the students’ names but were able to use the anonymized data to compare the students’ physical fitness and mental health results.
The risk of mental health disorder was weighted against three metrics for physical fitness: cardio fitness, as measured by a student’s time in an 800-meter run; muscle endurance, indicated by the number of situps performed; and muscle power, measured by the standing broad jump.
Improved performance in each activity was linked with a lower risk of mental health disorder. For instance, a 30-second decrease in 800-meter time was associated, in girls, with a lower risk of anxiety, depression and A.D.H.D. In boys, it was associated with lower anxiety and risk of the disorder.
An increase of five situps per minute was associated with lower anxiety and risk of the disorder in boys, and with decreased risk of depression and anxiety in girls.
“These findings suggest the potential of cardiorespiratory and muscular fitness as protective factors in mitigating the onset of mental health disorders among children and adolescents,” the researchers wrote in the journal article.
Physical and mental health were already assumed to be linked , they added, but previous research had relied largely on questionnaires and self-reports, whereas the new study drew from independent assessments and objective standards.
The Big Picture
The surgeon general, Dr. Vivek H. Murthy, has called mental health “the defining public health crisis of our time,” and he has made adolescent mental health central to his mission. In 2021 he issued a rare public advisory on the topic. Statistics at the time revealed alarming trends: From 2001 to 2019, the suicide rate for Americans ages 10 to 19 rose 40 percent, and emergency visits related to self-harm rose 88 percent.
Some policymakers and researchers have blamed the sharp increase on the heavy use of social media, but research has been limited and the findings sometimes contradictory. Other experts theorize that heavy screen use has affected adolescent mental health by displacing sleep, exercise and in-person activity, all of which are considered vital to healthy development. The new study appeared to support the link between physical fitness and mental health.
“The finding underscores the need for further research into targeted physical fitness programs,” its authors concluded. Such programs, they added, “hold significant potential as primary preventative interventions against mental disorders in children and adolescents.”
Matt Richtel is a health and science reporter for The Times, based in Boulder, Colo. More about Matt Richtel
Understanding A.D.H.D.
The challenges faced by those with attention deficit hyperactivity disorder can be daunting. but people who are diagnosed with it can still thrive..
Millions of children in the United States have received a diagnosis of A.D.H.D . Here is how their families can support them .
The condition is also being recognized more in adults . These are some of the behaviors that might be associated with adult A.D.H.D.
Since a nationwide Adderall shortage started, some people with A.D.H.D. have said their medication no longer helps with their symptoms. But there could be other factors at play .
Everyone has bouts of distraction and forgetfulness. Here is when psychiatrists diagnose it as something clinical .
The disorder can put a strain on relationships. But there are ways to cope .
Though meditation can be beneficial to those with A.D.H.D., sitting still and focusing on breathing can be hard for them. These tips can help .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Journal Information
On this page: Aims and scope of journal | Journal metrics | Abstracted/indexed in | ISSN and eISSN | Benefits of publishing with PR | Newsfeeds
Aims and scope of journal
Pediatric Research publishes original translational research papers, invited reviews, and commentaries on the etiologies and treatment of diseases of children and disorders of development, extending from basic science to epidemiology and quality improvement.
Topic Areas Adolescent Medicine, Allergy, Anesthesia, Behavior, Bioethics/Palliative Care, Cardiology, Cardiometabolic Disorders, Clinical Research/Methodology, Controversies, Critical Care, Development, Developmental Biology, Diversity, Equity and Inclusion, Emergency Medicine, Endocrinology, Environmental Health, Epidemiology, Fetus & Pregnancy, Gastroenterology, General Pediatrics, Genetics & Epigenetics, Global Health, Health Equity, Health Services Research, Hematology, Hyperbilirubinemia, Immunology, Infectious Disease, Kawasaki Disease, Microbiome, Neonatal Neurology, Neonatology, Nephrology, Neuroimaging, Neurology, Nutrition, Obesity, Oncology, Patient Safety, Pharmacology, Precision Medicine, Public Health, Pulmonology, Quality Improvement, Regenerative Biology, Rheumatology, Stem Cells, Substance Abuse, Transplantation, Toxicology.
Pediatric Research 's mission statement
Optimize children's health by publishing and communicating peer reviewed science and to foster the development of future pediatric researchers.
Journal Metrics
Article metrics such as number of downloads, citations and online attention are available from each article page, and provide an overview of the attention received by a paper.
2022 Citation Metrics
2-year Impact Factor*: 3.6 5-year Impact Factor*: 3.7 Immediacy index*: 0.6 Eigenfactor® score*: 0.01624 Article influence score*: 1.1 Journal Citation Indicator*: 1.22 SNIP**: 1.273 SJR***: 1.040
*2022 Journal Citation Reports® Science Edition (Clarivate Analytics, 2023) **Source-normalized Impact per Paper (Scopus) ***SCImago Journal Rank (Scopus)
2023 Usage Metrics
Downloads: 4,039,474 Altmetric mentions: 6,427
Abstracted/indexed in
Crossref PubMed British Library CAS Copyright Clearance Center EBSCO ExLibris GNM Healthcare Clarivate Analytics (Web of Science) PORTICO Scopus ProQuest Yewno UNSILO
ISSN and eISSN
The international standard serial number (ISSN) for Pediatric Research is 0031-3998 and the electronic international standard serial number (eISSN) is 1530-0447.
Benefits of publishing with PR
- We are the official publication of the American Pediatric Society, the European Society for Paediatric Research, and the Society for Pediatric Research.
- We publish original translational research papers, invited reviews, and commentaries on the etiologies and treatment of diseases of children and disorders of development, extending from basic science to epidemiology and quality improvement.
- We have an established reputation built up over 50 years with wide visibility on nature.com and in print.
Publishing with PR and Springer Nature provides an author with a wide range of benefits:
License to Publish
The International Pediatric Research Foundation does not require authors of original research papers to assign copyright of their published contributions. Authors grant the International Pediatric Research Foundation an exclusive license to publish, in return for which they can re-use their papers in their future printed work.
In addition, authors are encouraged to archive their version of the manuscript in their institution's repositories (as well as on their personal web sites), six months after the original publication. Authors should cite the publication reference and doi number on any deposited version, and provide a link from it to the published article on the Springer Nature website. This policy complements the policies of the US National Institutes of Health, the Wellcome Trust and other research funding bodies around the world. Springer Nature recognizes the efforts of funding bodies to increase access of the research they fund, and strongly encourages authors to participate in such efforts.
Daily publication online
New articles in PR , as in all Springer Nature journals, are published daily online ahead of the archival print issue, ensuring the research is made publicly available and can be cited as soon as possible after acceptance for publication. The online publication is a preliminary, unedited version, available on average less than a week after receipt by production.
Supplementary online material
Authors are invited to submit additional supporting material such as data sets or video for publication in the online version of the journal. Online supplementary material makes the most of the Web as a delivery platform and can often give articles greater depth, making them more useful to readers.
Authors who choose to publish in any Springer Nature journal can be assured that its staff's publishing, editorial and production skills are committed to maintaining the highest possible quality and standards.
Exposure - widest possible readership
All Springer Nature journals including PR , are available online via site licenses to academic, corporate and government institutions and consortia. Journals are available to members of these institutions at the click of a mouse, adding speed and visibility to authors' research papers.
Regular free e-mail alerts
Content published in PR has the potential to reach scientists around the world who have signed up for Springer Nature's free table of contents e-alerts, ensuring additional exposure to authors. These e-alerts allow recipients to click through to the full article if they subscribe or work at an institution with a site license, or click through to the article's abstract for other readers.
Focused subject areas on nature.com
From immunology to physics, genetics to materials, subject-specific areas provide a focused environment for readers, providing a monthly updated focus for a particular field.
Abstracting and indexing
PR is included in the leading abstracting and indexing services including ISI, MEDLINE, EMBASE and BIOSIS. Extensive reference linking to MEDLINE, ISI, Chemport and others via services such as Crossref and DOI numbers provide seamless online linking between articles and databases.
Media coverage
The Springer Nature press office provides information about exceptionally interesting papers published throughout Springer Nature. More than 2,000 journalists and media organizations worldwide subscribe to the press service, ensuring that papers receive maximum exposure in the world's most important media channels including newspapers, magazines, radio and television.
Extending science further - global collaborations
Springer Nature and PR support some projects aimed at making current research available to a broader community of scientists and practitioners.
All Springer Nature journals, including PR , are in WHO's HINARI (Health InterNetwork Access to Research Initiative) program, which provides free access to public institutions in developing countries.
Pediatric Research now provides its latest table of contents as an RSS web feed. This allows users with an RSS reader to receive automatic updates whenever new content is added to these pages.
Receive Pediatric Research' s current issue table of contents.
Find out more about RSS feeds , how to download an RSS reader and see all the news feeds offered by Springer Nature.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
Practice Gap
Epidemiology and etiology, uti pathogenesis, risk factors for uti, young infants, anatomic disorders of the urinary tract, bowel and bladder dysfunction, sexual activity, clinical manifestations, decision to test, urine testing, making the diagnosis, uncertainties in diagnosis, decision to treat empirically versus wait for culture, empirical antibiotics, definitive antibiotic treatment, duration of treatment, kidney and urinary tract imaging, kidney and bladder ultrasonography, voiding cystourethrogram, uti prevention, antibiotic-conserving approaches to prevent uti, surgical approaches to prevent uti, viral and fungal uti, conclusions, urinary tract infections in children.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Melanie C. Marsh , Guillermo Yepes Junquera , Emily Stonebrook , John David Spencer , Joshua R. Watson; Urinary Tract Infections in Children. Pediatr Rev May 2024; 45 (5): 260–270. https://doi.org/10.1542/pir.2023-006017
Download citation file:
- Ris (Zotero)
- Reference Manager
Despite the American Academy of Pediatrics guidelines for the evaluation, treatment, and management of urinary tract infections (UTIs), UTI diagnosis and management remains challenging for clinicians. Challenges with acute UTI management stem from vague presenting signs and symptoms, diagnostic uncertainty, limitations in laboratory testing, and selecting appropriate antibiotic therapy in an era with increasing rates of antibiotic-resistant uropathogens. Recurrent UTI management remains difficult due to an incomplete understanding of the factors contributing to UTI, when to assess a child with repeated infections for kidney and urinary tract anomalies, and limited prevention strategies. To help reduce these uncertainties, this review provides a comprehensive overview of UTI epidemiology, risk factors, diagnosis, treatment, and prevention strategies that may help pediatricians overcome the challenges associated with acute and recurrent UTI management.
Recognizing and reducing risk of initial and recurrent urinary tract infections (UTIs) are important given the disease burden associated with UTI to patients, families, and the health-care system. Prompt and accurate UTI diagnosis and thoughtful antibiotic management help ameliorate antimicrobial resistance. Reducing recurrent UTI risk includes evaluating a child for factors that augment UTI susceptibility, such as bowel and bladder dysfunction or anatomic kidney or urinary tract disorders.
Appropriately diagnose urinary tract infections in children based on clinical manifestations and laboratory testing.
Manage urinary tract infections, including optimal antibiotic choice and duration as well as imaging studies.
Identify and mitigate risk factors for recurrent urinary tract infections.
Urinary tract infection (UTI) is a common infection occurring in childhood. In the United States, pediatric UTI accounts for approximately 1.5 million ambulatory visits and 50,000 hospital inpatient admissions annually. ( 1 )( 2 ) UTI prevalence varies by sex, age, and circumcision status. Females account for 80% to 90% of pediatric UTIs overall. ( 1 )( 3 ) Among males, uncircumcised infants experience the highest UTI prevalence. ( 4 ) An estimated 7% to 8% of females and 1% to 2% of males will have at least 1 UTI by age 6 to 7 years. ( 5 )( 6 )
UTIs are primarily caused by bacteria, and uropathogenic Escherichia coli (UPEC) is the most common pathogen, accounting for approximately 80% of UTIs in children. Table 1 displays the relative frequencies of the 6 most common uropathogens encountered among children in a national surveillance database. ( 7 ) Less commonly, other enteric gram-negative bacilli such as Citrobacter species and Serratia marcescens are implicated. Among gram-positive bacteria, enterococci are the most common, but Staphylococcus saprophyticus should be considered in female adolescents. ( 8 ) In addition, group B streptococcus, Staphylococcus aureus , and coagulase-negative staphylococci may be seen in neonates. ( 9 )( 10 ) Viruses and fungi are less common UTI pathogens and are briefly discussed at the end of this review.
Most Common Uropathogens among Children from a Large US Surveillance Network
Data from Edlin et al. ( 7 )
To establish a UTI, uropathogenic bacteria originate from the enteric and vaginal tracts, spread across the perineum, ascend the urethra, and invade the bladder. Our understanding of UTI pathogenesis has been advanced by studying UPEC-associated infections in preclinical models and in clinical settings. To initiate cystitis (ie, infection restricted to the bladder), UPEC produce adhesive organelles called type 1 pili that bind and promote invasion of the superficial bladder urothelium. After internalization, UPEC enter a cytosolic niche called an intracellular bacterial community (IBC). ( 11 )( 12 )( 13 ) IBCs develop from a single bacterium and consist of an estimated 10 5 organisms encased in a highly organized matrix. In the IBC, UPEC develop filaments that extrude from the infected cell. Filamentous UPEC attach to adjacent epithelial cells, reinvade the urothelium, and create additional IBCs. ( 14 )( 15 ) To limit infection, the host exfoliates infected bladder cells into the urinary stream. After exfoliation, UPEC may invade the underlying basal urothelium and establish a quiescent intracellular reservoir (QIR). In the absence of bacterial replication, QIRs can persist for weeks and are protected from host immune mechanisms and antibiotics. Although the QIR population is small, it is considered a source of recurrent cystitis. ( 15 )( 16 )
To establish pyelonephritis (ie, kidney infection), uropathogens ascend the ureters and invade the kidney. Specifically, UPEC bind to epithelial cells in the kidney’s collecting tubules. Binding to these kidney epithelia depends on the ability of UPEC to produce type 1 pili or P-pili. After binding to kidney tubular cells, cytolytic UPEC strains trigger apoptosis, which facilitates their invasion into the kidney interstitium, promotes kidney inflammation, and impairs kidney functions. ( 11 )( 13 )
As pathogens ascend the urinary tract, they encounter mechanical and physiologic barriers that limit infection. These factors include the unidirectional flow of urine, changes in urine osmolarity and pH, soluble IgA and Tamm-Horsfall protein, iron-chelating siderophores, and antimicrobial peptides. If pathogens invade the bladder urothelium or attach to kidney epithelial cells, they initiate host responses that exfoliate urothelial cells to promote bacterial clearance or engage pattern recognition receptors, including toll-like receptors, to elicit inflammatory chemokines and cytokines that recruit immune cells to eradicate bacteria. ( 17 )
Although all children are susceptible to UTI, select populations have increased UTI susceptibility.
Neonates and young infants have increased UTI susceptibility because an immature immune system can facilitate bacterial colonization and adhesion to the urothelium. In addition, elevated androgen levels in males younger than 6 months may heighten UTI risk. ( 18 ) In the first year after birth, uncircumcised male children are at increased risk for UTI due to increased concentrations of uropathogens around the external urethral meatus that can potentially colonize the urinary tract and lead to infection. ( 19 )( 20 )
Patients with congenital kidney and urinary tract anomalies or inappropriate bladder emptying are at increased risk for UTI. Bladder emptying can be impaired by a functional or anatomic obstruction that occurs with a neurogenic bladder or posterior urethral valves. Impaired bladder drainage facilitates urinary stasis and bacterial replication. Moreover, the need to perform bladder catheterization can heighten UTI risk. ( 21 ) Kidney anomalies such as cystic kidney disease or nephrolithiasis may increase UTI risk. Vesicoureteral reflux (VUR) is a UTI risk factor that has been studied extensively. ( 22 ) VUR results in urine passing up 1 or both ureters in a retrograde fashion often to the kidneys. The clinical significance of VUR is based on the premise that it predisposes children to acute pyelonephritis by transporting bacteria from the bladder to the kidney, which may lead to kidney injury.
Bowel and bladder dysfunction (BBD) describes a group of lower urinary tract symptoms combined with bowel disorders, including functional constipation, that prevent appropriate peristalsis and compromise bladder emptying. ( 23 ) The most common signs and symptoms of BBD in toilet-trained children are urinary urgency, withholding maneuvers (eg, crossing legs or squatting down to use the heel to apply pressure to the perineum), and daytime wetting. ( 24 ) BBD is more common among children with a UTI compared with the general population. As a risk factor for recurrent UTI, BBD disproportionately influences incidence in children with VUR.
Sexual activity and the use of spermicides and diaphragms are also UTI risk factors. Intercourse augments UTI by facilitating the transfer of uropathogens from the perineum and genital tract into the urethral meatus. ( 25 )( 26 )
Children with a UTI may present with a variety of signs and symptoms, which may be affected by age and development ( Table 2 ). In verbal children, the presence of lower urinary tract symptoms alone suggests cystitis. In contrast, fever, vomiting, or flank pain suggests upper tract involvement, and pyelonephritis is presumed. Infants, preverbal children, and some medically complex youth are unable to report urinary tract symptoms. In those cases, suspicion for UTI is often triggered by a fever without an apparent focus. In addition, jaundice from direct and/or indirect hyperbilirubinemia that is not explained by another etiology may be a clue in some neonates and young infants with UTI, including those without fever or other signs of illness. ( 27 )( 28 )( 29 )( 30 )( 31 ) Many other conditions may present with signs and symptoms similar to a UTI, as discussed later herein.
Clinical Manifestations of Urinary Tract Infections in Children
Given the nonspecific nature of UTI in children, decisions around testing must consider risk factors for UTI, number and severity of signs and symptoms, and the presence or absence of a clinically apparent alternative explanation. For febrile children aged 2 to 23 months in whom UTI is considered, the free, online UTICalc ( https://uticalc.pitt.edu ) is an excellent resource that incorporates demographic and clinical information to guide decisions about urine testing (and subsequently, empirical treatment). ( 32 )( 33 ) For other groups of children, validated decision support tools are not available, and thus the decision to test is based on clinical suspicion.
Once the decision to test for a UTI is made, collecting a urine sample is the next step. Clinicians have several options for urine collection depending on the age and development of the child. To collect a urine sample from infants and young children who are incontinent, the American Academy of Pediatrics (AAP) guidelines provide 2 options. ( 34 ) Option 1 is to collect urine via catheterization or suprapubic aspiration for urinalysis and culture. Option 2 is to collect urine by noninvasive means (eg, urine bag) for urinalysis; if the results show pyuria, nitrite, or bacteriuria, then a second sample obtained via catheterization or suprapubic aspiration must be obtained for urinalysis and culture. One emergency department showed that by implementing option 2, many children avoided an invasive procedure without prolonging length of stay. ( 35 ) Importantly, urine samples collected via bag should not be used for culture because of higher rates of contamination. ( 36 )( 37 ) Likewise, urine collected via cotton balls in neonates should not be cultured. In toilet-trained children, a mid-stream, clean-catch method is recommended.
Hallmarks of a UTI are pyuria, urinary nitrite, and bacteriuria. ( 34 )( 38 ) Pyuria is defined by urine microscopy with at least 5 white blood cells (WBCs) per high-power field from centrifuged urine or at least 10 WBC/mm 3 from noncentrifuged urine, or detection of leukocyte esterase (as a surrogate marker for pyuria) on urine dipstick analysis. Nitrite is detected when bacteria capable of reducing urinary nitrate to nitrite have incubated in the urine for at least 4 hours. ( 39 ) Enteric gram-negative bacteria, Pseudomonas , and some staphylococcal species reduce nitrate, whereas streptococci and enterococci do not. Significant bacteriuria may be demonstrated on urine microscopy and ultimately confirmed by growth of a uropathogen in urine culture. In many ambulatory settings, urine microscopy is not available at the point of care, precluding an immediate assessment for WBCs or bacteria.
Many studies have evaluated the test characteristics of urinalysis (dipstick and/or microscopy) for diagnosing UTI, or more accurately, for predicting a positive urine culture. Sensitivity and specificity depend on the population tested (age, sex, comorbidities), urine collection method, urinalysis method used, threshold for positivity of the urinalysis component, and definition of a positive urine culture. Summary data from 3 meta-analyses and 1 large study are shown in Table 3 . ( 40 )( 41 )( 42 )( 43 ) Enhanced urinalysis, which consists of a urine Gram-stain plus hemocytometer WBC count from uncentrifuged urine, performs better than standard urinalysis but requires additional time and expertise compared with standard urinalysis. ( 44 ) Urine Gram-stain is particularly helpful when the child has received antibiotics before obtaining urine for culture.
Summary of Urinalysis Test Characteristics
+LR=positive likelihood ratio, −LR=negative likelihood ratio.
Data derived from Downs et al, ( 40 ) Gorelick and Shaw, ( 41 ) Kazi et al, ( 42 ) and Williams et al. ( 43 ).
In febrile children aged 2 to 24 months, the AAP guidelines define UTI as both a urinalysis suggesting infection (pyuria or bacteriuria) and a urine culture that yields at least 50,000 colony forming units (CFU)/mL of a uropathogen. ( 34 ) In toilet-trained children, a UTI diagnosis is made in the presence of urinary signs and symptoms, urinalysis suggesting infection, and positive urine culture. A threshold of 50,000 or 100,000 CFU/mL is typically used to define significant bacteriuria from clean-catch specimens.
Several factors make the diagnosis of UTI challenging. First, UTI signs and symptoms can be nondescript and overlap with other clinical conditions. A meta-analysis of studies examining signs and symptoms of pediatric UTI found that among preverbal children, fever (temperature >102.2°F [>39°C] and especially >104°F [>40°C]), fever duration longer than 24 hours, and suprapubic tenderness increased the probability of UTI, whereas vomiting, diarrhea, poor feeding, and irritability were of little diagnostic value. ( 45 ) Among verbal children, abdominal pain, back pain, dysuria, frequency, and new-onset enuresis were helpful, whereas offensive urine odor had no effect on UTI probability. The absence of any individual symptom was insufficient to exclude a UTI.
Second, pyuria may be caused by many conditions other than UTI, including urethritis, vulvovaginitis, sexually transmitted infections, appendicitis, other acute febrile illnesses, crystalluria or nephrolithiasis, intrinsic kidney disease, and others. ( 46 ) The common scenario of a symptomatic child whose urine dipstick is positive for leukocyte esterase but negative for nitrite leads to diagnostic uncertainty.
Third, diagnosing UTI in the absence of pyuria is the subject of debate. The AAP guidelines emphasize the necessity of pyuria, stating that pyuria is the key to distinguishing true UTI from asymptomatic bacteriuria or culture contamination in young, febrile children. ( 38 ) Despite historical concerns that young infants up to 2 to 3 months old do not reliably demonstrate pyuria, recent studies showed high sensitivity of pyuria in this age group. ( 9 )( 47 ) However, some experts have challenged the inclusion of pyuria in the definition of UTI based on a meta-analysis showing the point prevalence of asymptomatic bacteriuria to be less than 0.5% and a study showing that pyuria was absent in 13% of symptomatic children with positive urine culture results. ( 38 )( 48 )( 49 ) In addition, compared with UPEC, non– E coli pathogens are less likely to result in pyuria. ( 49 )
Fourth, the definition of a positive urine culture is unclear. The AAP guidelines’ threshold of 50,000 CFU/mL from catheterized specimens is based on the cutoff point above which most cultures yield a single uropathogen rather than contaminants. ( 50 ) However, some studies suggest that the culture threshold defining UTI should be lower than 50,000 CFU/mL. ( 51 )( 52 ) The AAP guidelines point out reasons for low colony counts in some patients (eg, short incubation time in the bladder in infants) and describes the culture threshold as “operational and not absolute.” ( 34 ) In febrile infants with pyuria, cultures yielding at least 10,000 CFU/mL may be indicative of a UTI. ( 53 )
Fifth, distinguishing between cystitis and pyelonephritis is not clear-cut. When upper urinary tract signs or symptoms are present ( Table 2 ), clinicians typically presume that the patient has pyelonephritis for subsequent management decisions. Fever is considered an upper urinary tract symptom because studies have shown that most children with a febrile UTI have evidence of pyelonephritis on technetium-99m dimercaptosuccinic acid scan, the previous gold standard imaging modality for pyelonephritis that is no longer in clinical use. ( 54 )( 55 ) In addition, serum inflammatory markers have not proved to be of sufficient diagnostic value for pyelonephritis. ( 56 )
Finally, although beyond the scope of this review, assessment of symptoms and test results is even more challenging in children with immunocompromise or anatomic disorders of the urinary tract. Pyuria is often absent in febrile neutropenic children with a UTI. ( 57 ) Children with neurogenic bladders are at increased for UTI but also have high rates of asymptomatic pyuria and bacteriuria. ( 58 )( 59 ) Standard criteria to optimally identify those with true infection are lacking.
To minimize diagnostic uncertainty, an expert panel on diagnostic stewardship for UTI recently recommended that ideal reporting of urine culture results should inform clinicians that colony counts greater than 100,000 CFU/mL may not represent a true infection in the absence of symptoms and that treatment for mixed flora or asymptomatic bacteriuria is unnecessary. ( 60 ) In addition, culture reports should differentiate between contaminants and typical uropathogens. Finally, identification and testing of isolates should not be automatically reported when more than 2 unique bacterial isolates are present in culture. Implementation of strategies such as these may guide clinicians in not only UTI diagnosis but also appropriate treatment.
During the past 3 decades, E coli have developed mechanisms to evade the bactericidal mechanisms of antibiotics routinely prescribed to treat UTIs, such as β-lactams, fluoroquinolones, and aminoglycosides. Up to 90% of E coli strains are now resistant to at least 1 unique antibiotic, and E coli infections now account for half the estimated global burden of antibiotic resistance. Antibiotic overuse and misuse have accelerated the prevalence of antibiotic resistance among UPEC. ( 61 )
Because it takes approximately 24 hours to receive initial urine culture results, clinical signs and symptoms and urinalysis results are often used to make a presumptive diagnosis of UTI. Studies have shown that among children diagnosed as having a UTI based on symptoms and urinalysis results, almost half have a resultant negative urine culture. ( 62 )( 63 ) If a child with suspected cystitis is well-appearing and does not have fever or other signs of systemic illness, it is reasonable to wait for the culture result before initiating antibiotic therapy. This is particularly pertinent in the current climate of antibiotic overuse and may curtail emerging antimicrobial resistance. ( 64 ) However, it is important that reliable follow-up is available, which may include having the patient’s or guardian’s contact information, identifying the primary care provider, or establishing outpatient follow-up in their medical home.
In children with suspected UTI associated with fever or other upper urinary tract symptoms, prompt empirical antibiotic should be provided while awaiting culture results. Prolonged fever before initiation of antibiotic therapy may increase risk of kidney scar formation. ( 65 )( 66 ) Although previously this relationship has been controversial and potentially confounded by age, recurrent UTI, ethnicity, or BBD, there does seem to be an association when controlling for these factors. ( 66 ) Risk of scar increases most steeply after 48 to 72 hours of delay from fever onset to antibiotic initiation. However, 1 study found that for every hour that antibiotics were delayed, the odds of new scarring increased by 0.8%. ( 66 )
When considering empirical therapy for UTI treatment, it is important to review local antibiogram data (ie, antibiotic susceptibility patterns) for common uropathogens, as well as any previous urine culture and susceptibility data specific to the child if there is a history of UTI. ( 38 ) Given the predominance of UPEC, even in children without nitrite on urinalysis, it is probably unnecessary to cover for Enterococcus species empirically. ( 67 ) There are several reasonable oral empirical antibiotic options. Nitrofurantoin is a targeted UTI antibiotic that is an excellent empirical choice for treating cystitis in adolescents, where the monohydrate/macrocrystal formulation may be given via a capsule twice daily. However, nitrofurantoin oral suspension for younger children is a less attractive option given poor palatability, the 6-hour dosing interval, and higher cost. Furthermore, nitrofurantoin should not be used to treat suspected pyelonephritis because it does not achieve adequate serum or kidney tissue concentrations. Cephalexin is another narrow-spectrum antibiotic with high UPEC susceptibility in many geographic locations. If local antibiogram data are favorable, cephalexin may be given for children with cystitis or pyelonephritis, at appropriate doses for the indication. ( 68 )
Other empirical options suggested in AAP guidelines include amoxicillin-clavulanate, oral third-generation cephalosporins, and trimethoprim-sulfamethoxazole (TMP-SMX). Amoxicillin alone is usually a poor choice for empirical treatment because of high rates of UPEC resistance, but it may be used for definitive treatment if appropriate based on culture and susceptibility results. Although oral third-generation cephalosporins (cefdinir, cefixime, cefpodoxime) do have a role in UTI treatment, they are broader in spectrum and have less favorable pharmacokinetic properties compared with cephalexin. ( 69 ) In addition, clinicians sometimes erroneously assume that susceptibility of urine isolates to intravenous (IV) third-generation cephalosporins (ceftriaxone, cefotaxime) predicts susceptibility to oral third-generation agents, but this is not reliably true. TMP-SMX was previously a commonly used empirical antibiotic for UTI, but resistance among UPEC has increased over time and exceeds 20% in many areas of the United States. ( 7 ) Ciprofloxacin is not a wise antibiotic choice for most children. Similar to TMP-SMX, ciprofloxacin resistance is increasing. ( 7 ) Furthermore, given concerns regarding its adverse effects, ciprofloxacin should be reserved for treatment of infections for which no reasonable oral alternative exists. ( 70 ) In addition, children who are receiving prophylactic antibiotics may have increased risk of resistant organisms, and previous urine cultures should be reviewed when choosing antimicrobial coverage in this population. ( 71 )( 72 )
For those unable to tolerate enteral agents, IV and intramuscular options can be considered. If a child is otherwise stable to be discharged home, a single dose of intramuscular ceftriaxone 50 mg/kg may be given, followed by an oral antibiotic prescription and close outpatient follow-up. Although there are no clear-cut guidelines on when children require hospital admission for the monitoring and treatment of a UTI, factors for consideration are listed in Table 4 . For children hospitalized for IV treatment, appropriate options include cefazolin, ceftriaxone, or dual therapy with ampicillin plus gentamicin. Cefazolin is preferred as a narrow-spectrum empirical option if local susceptibility patterns are favorable.
Indications for Hospitalization of Children with a Urinary Tract Infection
Once urine culture and susceptibility data are available, antibiotic treatment should be tailored to the most narrow-spectrum agent effective for the infection. In hospitalized children, transition from IV to oral antibiotics should be considered as soon as children are tolerating medications and fluids by mouth. Oral antibiotics are equally as efficacious as IV antibiotics in most children. ( 73 )( 74 ) An approach to guide clinicians on antibiotic administration includes “cascade reporting” of antibiotic susceptibility. When antibiotic susceptibility testing is finalized in a positive urine culture, the cascade reporting preferentially lists antibiotics recommended by the local antimicrobial stewardship program or national societies. This strategy promotes antimicrobial stewardship and may reduce antibiotic misuse or overuse. ( 60 )
For cystitis, national US guidelines for treatment duration are lacking, but an antibiotic course of 3 to 4 days seems to be equivalent to longer courses and is endorsed by multiple international organizations. ( 75 )( 76 )( 77 )( 78 )( 79 ) For febrile UTI/pyelonephritis, courses as short as 7 days are supported by comparative effectiveness data and are consistent with AAP guidelines. ( 34 )( 80 ) The recently published Short-Course Therapy for Urinary Tract Infections in Children (SCOUT) randomized clinical trial evaluated 5-day versus 10-day treatment durations for children 2 months to 10 years old meeting strict UTI criteria, 38% of whom were febrile at presentation (94% of those aged 2–23 months). ( 81 ) For the primary outcome of treatment failure (occurrence of UTI at or before the day 11–14 follow-up visit), short-course treatment failed noninferiority criteria. However, the low rates of treatment failure overall (4.2% in the short-course group) were encouraging, and 67 children would need to be treated with the longer duration to prevent 1 febrile UTI. A favorable response to treatment is indicated by improvement, and ultimately resolution, of symptoms. Obtaining a urine culture after completing antibiotic therapy as a proof of cure is not recommended. ( 82 )
AAP guidelines recommend kidney and bladder ultrasonography (KBUS) in all infants aged 2 to 24 months with a febrile UTI. ( 34 ) In most cases, the KBUS may be performed after the acute UTI process has resolved to minimize transient findings caused by inflammation. Early imaging is recommended to evaluate for a kidney/perinephric abscess or obstructive uropathy if the course is unusually severe or clinical improvement does not occur after 48 hours of appropriate antibiotic therapy. The goal of KBUS is to evaluate for urinary tract anomalies such as obstruction, nephrolithiasis, abdominal mass, or structural kidney anomalies. Although findings such as ureteral dilation and hydronephrosis may suggest VUR, it is not a sensitive imaging modality for VUR diagnosis. ( 54 ) KBUS should also be considered in older children with recurrent UTIs, non– E coli pathogens, unusually severe presentations, and acute kidney injury, and in male patients ( Fig ).

Suggested management for children with repeated urinary tract infections (UTIs). Stepwise investigation and screening strategies are outlined in the orange boxes, and management strategies are shown in the blue boxes. *A voiding cystourethrogram should be considered if kidney and bladder ultrasonography shows evidence of uroepithelial thickening, hydronephrosis, or hydroureter. + A referral to pediatric urology should be considered for a child with high-grade vesicoureteral reflux (VUR), ureterocele, bladder diverticulum, solitary kidney, horseshoe kidney, kidney size discrepancy greater than 1 cm, kidney cysts, or kidney scarring. Adapted from Khan et al. ( 83 )
Historical AAP guidelines recommended a voiding cystourethrogram (VCUG) for all children aged 2 to 24 months after their first febrile UTI to accurately identify VUR. Studies after these guidelines were published showed that less than 30% of children undergoing VCUG had VUR and only 10% of those had dilating VUR. ( 84 )( 85 ) As a result, the AAP guidelines were amended and now recommend a VCUG after a febrile UTI in children 2 to 24 months old with an abnormal KBUS, atypical uropathogens or clinical course, known kidney scarring, or family history of structural kidney disease. ( 34 ) VCUG should also be obtained, even in the setting of normal KBUS, if a child has recurrent UTI given the limited sensitivity of KBUS to detect VUR as noted previously herein ( Fig ).
Antibiotics should be used sparingly for UTI prevention. A major concern of using long-term antibiotic prophylaxis for prevention of recurrent UTI is the development of antibiotic resistance. ( 86 )( 87 ) In the Randomized Intervention for Children with Vesicoureteral Reflux (RIVUR) study, 76% of recurrent UTIs in children receiving TMP-SMX prophylaxis were due to antibiotic-resistant pathogens compared with 28% in the placebo group. ( 88 ) Although the RIVUR study demonstrated a 50% reduction in recurrent UTI for those receiving daily TMP-SMX prophylaxis, this equates to 8 children with VUR being treated with antibiotic prophylaxis for a single child to benefit. ( 89 ) Furthermore, these results have not been consistent in other studies or in systematic reviews and meta-analyses. ( 89 )( 90 ) Thus, pediatricians should be highly selective in terms of which patient populations to place on daily antibiotic prophylaxis. Before doing so, they should also consider addressing other variables that can promote UTI ( Fig ).
Clinicians can use standardized questionnaires for diagnosing BBD in a primary care setting. These include the Dysfunctional Voiding Scoring System and the Vancouver Symptom Score for Dysfunctional Elimination Syndrome, which can be accessed online or in the following references. ( 91 )( 92 ) Both surveys quantitatively and qualitatively assess constipation, daytime and nighttime wetting, urinary urgency, and difficulty in voiding or stooling. If a child with UTI is suspected of having BBD, pediatricians can recommend a voiding and stooling diary to document frequency of voiding and defecation, volume voided, incontinence, stool characteristics, and fluid intake. An objective measurement of stool can be made using the modified Bristol stool chart for children, available online or in the following reference. ( 93 )
BBD treatment can include managing constipation with hydration, increased fiber intake, and stool softeners. If there is concern for withholding urine or an overactive bladder contributing to UTI, these conditions can be managed with biofeedback or behavioral modifications such as timed voiding (voiding on schedule every 2–3 hours). ( 23 ) Oxybutynin, an anticholinergic agent, can be used in children with an overactive bladder. ( 94 ) Referral to a pediatric urology practice for evaluation or treatment of voiding disorders may also be considered ( Fig ). ( 83 )
Due to rising antibiotic resistance rates, antibiotic-sparing options to prevent UTI are needed. There are several approaches that have been investigated, but none of them are recommended as front-line approaches to prevent UTI. The role of hydration in preventing UTI has been tested in several small, historical observational studies. Findings from these studies have recently been summarized in a systematic review in adults and children. ( 95 ) However, because of mixed methods and results of the included studies, drawing firm conclusions about the role of hydration in UTI prevention is not possible.
Cranberry-based products are popular, with the active ingredient proanthocyanidin preventing UPEC adhesion to bladder epithelial cells or reducing the formation of bacterial biofilms. Pediatric clinical trials suggest that cranberry products modestly reduce the incidence of UTI in youth with normal urinary tract anatomy. A review of 8 trials using cranberry juice or cranberry extract for UTI prevention concluded that 4 trials had a reduced incidence of UTI with cranberry-based therapy. ( 96 ) However, definitive conclusions cannot be made from these trials about the utility of cranberry products in UTI prevention given their differences in cranberry formulations and dosing. Larger, well-designed trials are needed. The value of cranberry in UTI prevention has recently been reviewed. ( 97 )
Probiotics comprising Lactobacillus species also show promise in UTI prevention. Probiotics boost endogenous immune defenses, scavenge nutrients needed by bacteria for replication, reduce pH to suppress uropathogen growth, and prevent UPEC binding to urothelial cells. ( 61 )( 98 )( 99 ) During the past 2 decades, several studies have tested the effects of probiotics on UTI prevention with or without antibiotics. ( 100 )( 101 )( 102 ) Given the mixed outcomes in these studies, the utility of probiotics for UTI prevention in children is unclear.
D-mannose is a monosaccharide that competitively inhibits UPEC binding to urothelial cells. Given promising preclinical data, synthetic mannosides are now being developed and tested. ( 103 ) To date, there are few clinical studies of D-mannose in pediatric UTI prevention. Thus, we can only speculate about the benefits of D-mannose from adult data that show efficacy. However, given the variations in design among different studies, the clinical benefits of D-mannose remain unclear. ( 97 )( 104 )( 105 )
Vaccinations are also being developed to prevent UTI. Four vaccines have recently shown promise in randomized controlled trials. The immunogens on which these vaccines are based include whole cell heat-killed bacteria, bacterial cell wall components, nutrient acquisition proteins, and proteins facilitating bacterial adhesion. ( 106 )( 107 )( 108 )
Male circumcision decreases UTI risk, specifically among neonates, and the AAP supports the benefits of circumcision for UTI risk reduction. ( 19 )( 109 ) In older children, high-grade or dilating VUR surgical correction can reduce UTI susceptibility. Clinical trials comparing medical versus surgical management for recurrent UTI show comparable decreases in UTI incidence and kidney scarring. ( 110 )( 111 ) Thus, surgery is reserved for children whose VUR is unlikely to spontaneously resolve, those with higher risk for pyelonephritis, a history of kidney scarring, or impaired kidney function. Surgical correction is not recommended for children with low-grade VUR given the high likelihood of spontaneous resolution and low risk of kidney scarring. ( 83 )
Adenovirus can cause UTIs in immunocompetent hosts, including urethritis, hemorrhagic cystitis, and nephritis. Treatment is supportive. In hematopoietic stem cell recipients, adenovirus, BK virus, and cytomegalovirus can cause hemorrhagic cystitis. In kidney transplant recipients, BK virus reactivation is associated with nephropathy. Management of these infections in immunocompromised hosts is often multifaceted and beyond the scope of this review. ( 112 )( 113 ) When Candida is isolated in urine culture, it may indicate a UTI or colonization. In asymptomatic patients with an indwelling bladder catheter, removal of the catheter without antifungal therapy is typically sufficient. ( 114 ) However, for patients who are very-low-birthweight infants, neutropenic, or undergoing a urologic procedure, treatment of asymptomatic candiduria is recommended. Those with symptoms suggesting cystitis or pyelonephritis may also be treated, and fluconazole is the drug of choice for susceptible organisms. Additional evaluation and management recommendations for UTI due to Candida in specific patient populations are provided in national guidelines. ( 114 )
UTI continues to challenge pediatric medical providers. Prompt and accurate diagnosis is important to minimize UTI symptoms, reduce UTI-associated sequelae, and minimize the inappropriate use of antibiotics. With a better understanding of the etiology, pathogenesis, diagnosis, and treatment of UTI, clinicians will be better prepared to manage this common clinical infection.
Uropathogenic Escherichia coli is the most common cause of urinary tract infection (UTI), followed by other enteric gram-negative bacilli and Enterococcus species. (Based on strong research evidence) ( 7 )
UTICalc is an excellent decision support tool that clinicians may use when considering a UTI in a febrile infant or young child (2–23 months of age). The tool calculates pre-test and post-test probabilities of UTI and guides decisions regarding whether to test and empirically treat for UTI. (Based on strong research evidence) ( 32 )( 33 )
A UTI is best defined by the presence of symptoms with inflammation evidenced by pyuria and a urine culture with at least 50,000 colony-forming units per milliliter of a uropathogen. However, challenges surrounding UTI diagnosis include signs and symptoms that are nonspecific, debate around the necessity of pyuria, and uncertainty regarding the optimal culture threshold to define significant bacteriuria. (Based on some research evidence as well as consensus) ( 34 )( 38 )( 53 )
Cephalexin and nitrofurantoin are recommended empirical oral antibiotic choices for UTI (if supported by local antibiotic susceptibility data), usually for 3 to 4 days for uncomplicated cystitis and 7 days for febrile UTI/pyelonephritis. (Based on some research evidence as well as consensus) ( 75 )( 80 )
After a first febrile UTI in an infant or young child, clinicians should obtain kidney and bladder ultrasonography (KBUS) to evaluate for urinary tract anomalies. A voiding cystourethrogram is indicated if the KBUS is abnormal or if the child experiences a second febrile UTI. (Based on some research evidence as well as consensus) ( 34 )
Clinicians should strive to identify and mitigate modifiable risk factors for UTI and recurrence, including bowel and bladder dysfunction (BBD). Assessment for BBD via validated questionnaires, initiation of behavior interventions, and treatment of constipation can begin in the medical home, with referral to specialists in cases refractory to initial interventions. (Based on some research evidence as well as consensus) ( 23 )( 24 )
Drs Spencer and Watson supervised the drafting and finalizing of the manuscript and are co–senior authors.
AUTHOR DISCLOSURES: Drs Marsh, Junquera, Stonebrook, Spencer, and Watson have disclosed no financial relationships relevant to this article. This commentary does not contain a discussion of an unapproved/investigative use of a commercial product/device. Dr. Marsh receives ongoing research funding for her work with UTI from the Livewell Grant through Advocate Aurora Research Institute (AARI). This grant did not fund any work directly related to the manuscript.
American Academy of Pediatrics
bowel and bladder dysfunction
colony forming units
intracellular bacterial community
intravenous
kidney and bladder ultrasonography
quiescent intracellular reservoir
trimethoprim-sulfamethoxazole
uropathogenic Escherichia coli
urinary tract infection
voiding cystourethrogram
vesicoureteral reflux
Supplementary data
Advertising Disclaimer »
Citing articles via
Email alerts.
Affiliations
- Editorial Board
- ABP Content Spec Map
- Pediatrics On Call
- Online ISSN 1526-3347
- Print ISSN 0191-9601
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Spatial Variations of the Activity of 137 Cs and the Contents of Heavy Metals and Petroleum Products in the Polluted Soils of the City of Elektrostal
- DEGRADATION, REHABILITATION, AND CONSERVATION OF SOILS
- Open access
- Published: 15 June 2022
- Volume 55 , pages 840–848, ( 2022 )
Cite this article
You have full access to this open access article

- D. N. Lipatov 1 ,
- V. A. Varachenkov 1 ,
- D. V. Manakhov 1 ,
- M. M. Karpukhin 1 &
- S. V. Mamikhin 1
1466 Accesses
2 Citations
Explore all metrics
The levels of specific activity of 137 Cs and the contents of mobile forms (1 M ammonium acetate extraction) of heavy metals (Zn, Cu, Ni, Co, Cr, Pb) and petroleum products were studied in the upper soil horizon of urban landscapes of the city of Elektrostal under conditions of local radioactive and chemical contamination were studied. In the soils within a short radius (0–100 m) around the heavy engineering plant, the specific activity of 137 Cs and the contents of mobile forms of Pb, Cu, and Zn were increased. The lognormal distribution law of 137 Cs was found in the upper (0–10 cm) soil layer; five years after the radiation accident, the specific activity of 137 Cs varied from 6 to 4238 Bq/kg. The coefficients of variation increased with an increase in the degree of soil contamination in the following sequence: Co < Ni < petroleum products < Cr < 137 Cs < Zn < Pb < Cu ranging from 50 to 435%. Statistically significant direct correlation was found between the specific activity of 137 Cs and the contents of mobile forms of Pb, Cu, and Zn in the upper horizon of urban soils, and this fact indicated the spatial conjugacy of local spots of radioactive and polymetallic contamination in the studied area. It was shown that the specific activity of 137 Cs, as well as the content of heavy metals and petroleum products in the upper layer (0–10 cm) of the soils disturbed in the course of decontamination, earthwork and reclamation is reduced.
Similar content being viewed by others
Accumulation and migration of heavy metals in soils of the rostov region, south of russia.

Geographical Features of Pollution of the Territory of Yakutia With Cesium-137

Activity Concentration of Natural Radionuclides and Total Heavy Metals Content in Soils of Urban Agglomeration
Avoid common mistakes on your manuscript.
INTRODUCTION
Contaminants migrate and accumulate in urban ecosystems under the impact of both natural and technogenic factors. The processes of technogenic migration of 137 Cs are most pronounced in radioactively contaminated territories. It was found in urboecological studies that the intensity of sedimentation of aerosol particles containing radionuclides and heavy metals is determined by the types of the surfaces of roofs, walls, roads, lawns, and parks and by their position within the urban wind field [ 12 , 26 ]. Traffic in the cities results in significant transport of dust and associated contaminants and radionuclides [ 15 , 24 ]. During decontamination measures in the areas of Chernobyl radioactive trace, not only the decrease in the level of contamination but also the possibility of secondary radioactive contamination because of the transportation of contaminated soil particles by wind or water, or anthropogenic transfer of transferring of ground were observed [ 5 , 6 ]. Rainstorm runoff and hydrological transport of dissolved and colloidal forms of 137 Cs can result in the accumulation of this radionuclide in meso- and microdepressions, where sedimentation takes place [ 10 , 16 ]. Different spatial distribution patterns of 137 Cs in soils of particular urban landscapes were found in the city of Ozersk near the nuclear fuel cycle works [ 17 ]. Natural character of 137 Cs migration in soils of Moscow forest-parks and a decrease in its specific activity in industrial areas have been revealed [ 10 ]. Determination of the mean level and parameters of spatial variations of 137 Cs in soils is one of primary tasks of radioecological monitoring of cities, including both unpolluted (background) and contaminated territories.
Emissions and discharges from numerous sources of contamination can cause the accumulation of a wide range of toxicants in urban soils: heavy metals (HMs), oil products (OPs), polycyclic aromatic hydrocarbons (PAHs), and other chemical substances. Soil contamination by several groups of toxicants is often observed in urban landscapes [ 20 , 23 ] because of the common contamination source or close pathways of the migration of different contaminants. A comprehensive analysis of contamination of urban soils by radionuclides and heavy metals has been performed in some studies [ 21 , 25 ]. The determination of possible spatial interrelationships between radioactive and chemical contaminations in urban soils is an important problem in urban ecology.
A radiation accident took place in the Elektrostal heavy engineering works (EHEW) in April 2013: a capacious source of 137 Cs entered the smelt furnace, and emission of radioactive aerosols from the aerating duct into the urban environment took place. The activity of molten source was estimated at about 1000–7000 Ci [ 14 ]. The area of contamination in the territory of the plant reached 7500 m 2 . However, radioactive aerosols affected a much larger area around the EHEW, including Krasnaya and Pervomaiskaya streets, and reached Lenin Prospect.
Geochemical evaluation of contamination of the upper soil horizon in the city of Elektrostal was carried out in 1989–1991. This survey indicated the anomalies of concentrations of wolfram, nickel, molybdenum, chromium, and other heavy metals related to accumulation of alloying constituent and impurities of non-ferrous metals in the emissions of steelmaking works [ 19 ].
The aim of our work was to determine the levels of specific activity of 137 Cs, concentrations of mobile forms of heavy metals (Zn, Cu, Ni, Co, Cr, and Pb) and oil products in the upper soil horizons in different urban landscapes of the city of Elektrostal under the conditions of local radioactive and chemical contamination.
Author information
Authors and affiliations.
Lomonosov Moscow State University, 119991, Moscow, Russia
D. N. Lipatov, V. A. Varachenkov, D. V. Manakhov, M. M. Karpukhin & S. V. Mamikhin
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to D. N. Lipatov .
Ethics declarations
The authors declare that they have no conflicts of interest.
Additional information
Translated by T. Chicheva
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Lipatov, D.N., Varachenkov, V.A., Manakhov, D.V. et al. Spatial Variations of the Activity of 137 Cs and the Contents of Heavy Metals and Petroleum Products in the Polluted Soils of the City of Elektrostal. Eurasian Soil Sc. 55 , 840–848 (2022). https://doi.org/10.1134/S1064229322060072
Download citation
Received : 21 October 2021
Revised : 22 December 2021
Accepted : 30 December 2021
Published : 15 June 2022
Issue Date : June 2022
DOI : https://doi.org/10.1134/S1064229322060072
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- urban soils
- urban ecosystems
- radiation monitoring
- decontamination
- Urban Technosols
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
Child Health Needs and the Pediatric Hematology-Oncology Workforce: 2020-2040. Child Health and the US Pediatric Subspecialty Workforce: Planning for the Future. Child Health Needs and the Pediatric Endocrinology Workforce: 2020-2040. Child Health Needs and the Developmental-Behavioral Pediatrics Workforce Supply: 2020-2040. Browse All.
K. Kayentao and OthersN Engl J Med 2024;390:1549-1559. Malaria is a major cause of illness worldwide. In a phase 2 trial in Mali, one subcutaneous dose of L9LS, a monoclonal antibody targeting ...
BMC Pediatrics is an open access journal publishing peer-reviewed research articles in all aspects of health care in neonates, children and adolescents, as ...
From antibiotic prescribing to bronchiolitis, our editors have selected the most popular Pediatrics articles that had an important impact on our readers in 2021, including 5 COVID-19 articles. Happy reading and don't forget to share these important studies with your cohorts. Follow Pediatrics on Facebook so you don't miss the latest research as ...
Pediatric Research publishes original research papers, reviews, and commentaries on the etiologies and treatment of diseases of children and disorders of development, extending from basic science ...
Browse the archive of articles on Pediatric Research. All; 1996 Abstracts The American Pediatric Society and The Society for Pediatric Research (2354)
The Journal of Pediatrics is an international peer-reviewed journal that advances pediatric research and serves as a practical guide for pediatricians who manage health and diagnose and treat disorders in infants, children, and adolescents.The Journal publishes original work based on standards of excellence and expert review. The Journal seeks to publish high quality original articles that are ...
Subscribe to the JAMA Pediatrics journal. HomeNew OnlineIssuesFor Authors. Editor's Choice: JAMA Pediatrics—The Year in Review, 2023. Relaxation Therapy and Human Milk Feeding Outcomes. Ilana Levene, BM, BCh; Nurul Husna Mohd Shukri, PhD; Frances O'Brien, MB, BS; et al. Original Investigation | May 6, 2024. online.
All articles are open access until the end of January 2023. Happy reading and remember to share these important studies with your colleagues. Follow Pediatrics on Facebook and Twitter to stay up to date on the latest research, which is published daily. To purchase an individual subscription to Pediatrics, visit shopAAP.
This is an introduction to an article series devoted to the current state and future of pediatric research. The role of public-private partnerships, influencing factors, challenges, and recent ...
The Journal of Pediatrics is an international peer-reviewed journal that advances pediatric research and serves as a practical guide for pediatricians who manage health and diagnose and treat disorders in infants, children, and adolescents.The Journal publishes original work based on standards of excellence and expert review. The Journal seeks to publish high quality original articles that are ...
Impact. This is an introduction to an article series devoted to the current state and future of pediatric research. The role of public-private partnerships, influencing factors, challenges, and recent trends in pediatric research are described, with emphasis on funding, drug and device development, physician-scientist training, and diversity.
BMC Pediatrics is an open access journal publishing peer-reviewed research articles in all aspects of health care in neonates, children and adolescents, as well as related molecular genetics, pathophysiology, and epidemiology. Join the Board.
Pediatric Research in Office Settings (PROS), founded in 1986, is the practice-based research network of the AAP. Its mission is to improve the health of children and enhance primary care practice by conducting and fostering national collaborative-based research. ... AAP Research articles published in peer reviewed journals. Pediatric Academic ...
All articles are available for free until the end of January 2024. Happy reading, and please share these important studies with your colleagues. Stay up to date on the latest research by following Pediatrics on Facebook, Twitter, and Instagram to stay up to date on the latest research, which is published daily.
Study design and participants. In China, Futang Children's Medical Development Research Center (FRCPD) is the first non-profit social service organization established to care for children's lives and health and engage in children's development research [], supervised and managed by the Ministry of Civil Affairs of the People's Republic of China and led by the Children's Medical Center.
Clinical Research Article (1028) ESPR European Society for Pediatric Research, Siena, Italy August 31 2005 - September 3 2005 (430) ESPR European Society for Pediatric Research: Stockholm, Sweden ...
A new study bolsters existing research suggesting that exercise can protect against anxiety, depression and attention challenges. By Matt Richtel Physical fitness among children and adolescents ...
Partnership supports implementation of evidence-based strategies. After losing a young patient to suicide in early 2023, Dr. Edward Salzberg, a pediatrician at Roswell Pediatrics Center in Georgia, found himself looking for solutions. "I had a teenager who died by suicide within 30 minutes of leaving their wellness visit," Salzberg recalled.
The possibility of using furfurol for the production of ash-free high-strength active carbons with spheroidal particles as adsorbents and catalyst supports is substantiated. A single-stage process that incorporates the resinification of furfurol, the molding of a spherical product, and its hardening while allowing the process cycle time and the ...
New-type toroidally focused ultrasonic flaw detectors, whose application provides an appreciable increase in the flaw detection rate with retention of high sensitivity to flaws, are considered. The construction of a flaw detector is presented, the sizes of a gauge for the formation of the toroidal surface of a lens are given, and the technology of the manufacturing of a toroidal lens is described.
In this issue of Pediatric Research, Goodman et al. conducted a retrospective, observational cohort study to explore the relationship between a history of congenital anomalies and the severity of ...
Features of the macrostructure and microstructure of uranium dioxide powders are considered. Assumptions are made on the mechanisms of the behavior of powders of various natures during pelletizing. Experimental data that reflect the effect of these powders on the quality of fuel pellets, which is evaluated by modern procedures, are presented. To investigate the structure of the powders, modern ...
Aims and scope of journal. Pediatric Research publishes original translational research papers, invited reviews, and commentaries on the etiologies and treatment of diseases of children and ...
Despite the American Academy of Pediatrics guidelines for the evaluation, treatment, and management of urinary tract infections (UTIs), UTI diagnosis and management remains challenging for clinicians. Challenges with acute UTI management stem from vague presenting signs and symptoms, diagnostic uncertainty, limitations in laboratory testing, and selecting appropriate antibiotic therapy in an ...
Field research was carried out in the city of Elektrostal, Moscow oblast, in July 2018, i.e. 5 years and 3 months after the local fallout of 137 Cs in the result of radiation accident. The emission of 137 Cs from the chimney of steel melting plant spread to the west of heavy engineering works in April 2013 in the day of radiation accident [].The surveyed part of the city near the plant ...