- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- Effectiveness of...
Effectiveness of weight management interventions for adults delivered in primary care: systematic review and meta-analysis of randomised controlled trials
- Related content
- Peer review
- Claire D Madigan , senior research associate 1 ,
- Henrietta E Graham , doctoral candidate 1 ,
- Elizabeth Sturgiss , NHMRC investigator 2 ,
- Victoria E Kettle , research associate 1 ,
- Kajal Gokal , senior research associate 1 ,
- Greg Biddle , research associate 1 ,
- Gemma M J Taylor , reader 3 ,
- Amanda J Daley , professor of behavioural medicine 1
- 1 Centre for Lifestyle Medicine and Behaviour (CLiMB), The School of Sport, Exercise and Health Sciences, Loughborough University, Loughborough LE11 3TU, UK
- 2 School of Primary and Allied Health Care, Monash University, Melbourne, Australia
- 3 Department of Psychology, Addiction and Mental Health Group, University of Bath, Bath, UK
- Correspondence to: C D Madigan c.madigan{at}lboro.ac.uk (or @claire_wm and @lboroclimb on Twitter)
- Accepted 26 April 2022
Objective To examine the effectiveness of behavioural weight management interventions for adults with obesity delivered in primary care.
Design Systematic review and meta-analysis of randomised controlled trials.
Eligibility criteria for selection of studies Randomised controlled trials of behavioural weight management interventions for adults with a body mass index ≥25 delivered in primary care compared with no treatment, attention control, or minimal intervention and weight change at ≥12 months follow-up.
Data sources Trials from a previous systematic review were extracted and the search completed using the Cochrane Central Register of Controlled Trials, Medline, PubMed, and PsychINFO from 1 January 2018 to 19 August 2021.
Data extraction and synthesis Two reviewers independently identified eligible studies, extracted data, and assessed risk of bias using the Cochrane risk of bias tool. Meta-analyses were conducted with random effects models, and a pooled mean difference for both weight (kg) and waist circumference (cm) were calculated.
Main outcome measures Primary outcome was weight change from baseline to 12 months. Secondary outcome was weight change from baseline to ≥24 months. Change in waist circumference was assessed at 12 months.
Results 34 trials were included: 14 were additional, from a previous review. 27 trials (n=8000) were included in the primary outcome of weight change at 12 month follow-up. The mean difference between the intervention and comparator groups at 12 months was −2.3 kg (95% confidence interval −3.0 to −1.6 kg, I 2 =88%, P<0.001), favouring the intervention group. At ≥24 months (13 trials, n=5011) the mean difference in weight change was −1.8 kg (−2.8 to −0.8 kg, I 2 =88%, P<0.001) favouring the intervention. The mean difference in waist circumference (18 trials, n=5288) was −2.5 cm (−3.2 to −1.8 cm, I 2 =69%, P<0.001) in favour of the intervention at 12 months.
Conclusions Behavioural weight management interventions for adults with obesity delivered in primary care are effective for weight loss and could be offered to members of the public.
Systematic review registration PROSPERO CRD42021275529.
Introduction
Obesity is associated with an increased risk of diseases such as cancer, type 2 diabetes, and heart disease, leading to early mortality. 1 2 3 More recently, obesity is a risk factor for worse outcomes with covid-19. 4 5 Because of this increased risk, health agencies and governments worldwide are focused on finding effective ways to help people lose weight. 6
Primary care is an ideal setting for delivering weight management services, and international guidelines recommend that doctors should opportunistically screen and encourage patients to lose weight. 7 8 On average, most people consult a primary care doctor four times yearly, providing opportunities for weight management interventions. 9 10 A systematic review of randomised controlled trials by LeBlanc et al identified behavioural interventions that could potentially be delivered in primary care, or involved referral of patients by primary care professionals, were effective for weight loss at 12-18 months follow-up (−2.4 kg, 95% confidence interval −2.9 to−1.9 kg). 11 However, this review included trials with interventions that the review authors considered directly transferrable to primary care, but not all interventions involved primary care practitioners. The review included interventions that were entirely delivered by university research employees, meaning implementation of these interventions might differ if offered in primary care, as has been the case in other implementation research of weight management interventions, where effects were smaller. 12 As many similar trials have been published after this review, an updated review would be useful to guide health policy.
We examined the effectiveness of weight loss interventions delivered in primary care on measures of body composition (weight and waist circumference). We also identified characteristics of effective weight management programmes for policy makers to consider.
This systematic review was registered on PROSPERO and is reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement. 13 14
Eligibility criteria
We considered studies to be eligible for inclusion if they were randomised controlled trials, comprised adult participants (≥18 years), and evaluated behavioural weight management interventions delivered in primary care that focused on weight loss. A primary care setting was broadly defined as the first point of contact with the healthcare system, providing accessible, continued, comprehensive, and coordinated care, focused on long term health. 15 Delivery in primary care was defined as the majority of the intervention being delivered by medical and non-medical clinicians within the primary care setting. Table 1 lists the inclusion and exclusion criteria.
Study inclusion and exclusion criteria
- View inline
We extracted studies from the systematic review by LeBlanc et al that met our inclusion criteria. 11 We also searched the exclusions in this review because the researchers excluded interventions specifically for diabetes management, low quality trials, and only included studies from an Organisation for Economic Co-operation and Development country, limiting the scope of the findings.
We searched for studies in the Cochrane Central Register of Controlled Trials, Medline, PubMed, and PsychINFO from 1 January 2018 to 19 August 2021 (see supplementary file 1). Reference lists of previous reviews 16 17 18 19 20 21 and included trials were hand searched.
Data extraction
Results were uploaded to Covidence, 22 a software platform used for screening, and duplicates removed. Two independent reviewers screened study titles, abstracts, and full texts. Disagreements were discussed and resolved by a third reviewer. All decisions were recorded in Covidence, and reviewers were blinded to each other’s decisions. Covidence calculates proportionate agreement as a measure of inter-rater reliability, and data are reported separately by title or abstract screening and full text screening. One reviewer extracted data on study characteristics (see supplementary table 1) and two authors independently extracted data on weight outcomes. We contacted the authors of four included trials (from the updated search) for further information. 23 24 25 26
Outcomes, summary measures, and synthesis of results
The primary outcome was weight change from baseline to 12 months. Secondary outcomes were weight change from baseline to ≥24 months and from baseline to last follow-up (to include as many trials as possible), and waist circumference from baseline to 12 months. Supplementary file 2 details the prespecified subgroup analysis that we were unable to complete. The prespecified subgroup analyses that could be completed were type of healthcare professional who delivered the intervention, country, intensity of the intervention, and risk of bias rating.
Healthcare professional delivering intervention —From the data we were able to compare subgroups by type of healthcare professional: nurses, 24 26 27 28 general practitioners, 23 29 30 31 and non-medical practitioners (eg, health coaches). 32 33 34 35 36 37 38 39 Some of the interventions delivered by non-medical practitioners were supported, but not predominantly delivered, by GPs. Other interventions were delivered by a combination of several different practitioners—for example, it was not possible to determine whether a nurse or dietitian delivered the intervention. In the subgroup analysis of practitioner delivery, we refer to this group as “other.”
Country —We explored the effectiveness of interventions by country. Only countries with three or more trials were included in subgroup analyses (United Kingdom, United States, and Spain).
Intensity of interventions —As the median number of contacts was 12, we categorised intervention groups according to whether ≤11 or ≥12 contacts were required.
Risk of bias rating —Studies were classified as being at low, unclear, and high risk of bias. Risk of bias was explored as a potential influence on the results.
Meta-analyses
Meta-analyses were conducted using Review Manager 5.4. 40 As we expected the treatment effects to differ because of the diversity of intervention components and comparator conditions, we used random effects models. A pooled mean difference was calculated for each analysis, and variance in heterogeneity between studies was compared using the I 2 and τ 2 statistics. We generated funnel plots to evaluate small study effects. If more than two intervention groups existed, we divided the number of participants in the comparator group by the number of intervention groups and analysed each individually. Nine trials were cluster randomised controlled trials. The trials had adjusted their results for clustering, or adjustment had been made in the previous systematic review by LeBlanc et al. 11 One trial did not report change in weight by group. 26 We calculated the mean weight change and standard deviation using a standard formula, which imputes a correlation for the baseline and follow-up weights. 41 42 In a non-prespecified analysis, we conducted univariate and multivariable metaregression (in Stata) using a random effects model to examine the association between number of sessions and type of interventionalist on study effect estimates.
Risk of bias
Two authors independently assessed the risk of bias using the Cochrane risk of bias tool v2. 43 For incomplete outcome data we defined a high risk of bias as ≥20% attrition. Disagreements were resolved by discussion or consultation with a third author.
Patient and public involvement
The study idea was discussed with patients and members of the public. They were not, however, included in discussions about the design or conduct of the study.
The search identified 11 609 unique study titles or abstracts after duplicates were removed ( fig 1 ). After screening, 97 full text articles were assessed for eligibility. The proportionate agreement ranged from 0.94 to 1.0 for screening of titles or abstracts and was 0.84 for full text screening. Fourteen new trials met the inclusion criteria. Twenty one studies from the review by LeBlanc et al met our eligibility criteria and one study from another systematic review was considered eligible and included. 44 Some studies had follow-up studies (ie, two publications) that were found in both the second and the first search; hence the total number of trials was 34 and not 36. Of the 34 trials, 27 (n=8000 participants) were included in the primary outcome meta-analysis of weight change from baseline to 12 months, 13 (n=5011) in the secondary outcome from baseline to ≥24 months, and 30 (n=8938) in the secondary outcome for weight change from baseline to last follow-up. Baseline weight was accounted for in 18 of these trials, but in 14 24 26 29 30 31 32 44 45 46 47 48 49 50 51 it was unclear or the trials did not consider baseline weight. Eighteen trials (n=5288) were included in the analysis of change in waist circumference at 12 months.

Studies included in systematic review of effectiveness of behavioural weight management interventions in primary care. *Studies were merged in Covidence if they were from same trial
- Download figure
- Open in new tab
- Download powerpoint
Study characteristics
Included trials (see supplementary table 1) were individual randomised controlled trials (n=25) 24 25 26 27 28 29 32 33 34 35 38 39 41 44 45 46 47 50 51 52 53 54 55 56 59 or cluster randomised controlled trials (n=9). 23 30 31 36 37 48 49 57 58 Most were conducted in the US (n=14), 29 30 31 32 33 34 35 36 37 45 48 51 54 55 UK (n=7), 27 28 38 41 47 57 58 and Spain (n=4). 25 44 46 49 The median number of participants was 276 (range 50-864).
Four trials included only women (average 65.9% of women). 31 48 51 59 The mean BMI at baseline was 35.2 (SD 4.2) and mean age was 48 (SD 9.7) years. The interventions lasted between one session (with participants subsequently following the programme unassisted for three months) and several sessions over three years (median 12 months). The follow-up period ranged from 12 months to three years (median 12 months). Most trials excluded participants who had lost weight in the past six months and were taking drugs that affected weight.
Meta-analysis
Overall, 27 trials were included in the primary meta-analysis of weight change from baseline to 12 months. Three trials could not be included in the primary analysis as data on weight were only available at two and three years and not 12 months follow-up, but we included these trials in the secondary analyses of last follow-up and ≥24 months follow-up. 26 44 50 Four trials could not be included in the meta-analysis as they did not present data in a way that could be synthesised (ie, measures of dispersion). 25 52 53 58 The mean difference was −2.3 kg (95% confidence interval −3.0 to −1.6 kg, I 2 =88%, τ 2 =3.38; P<0.001) in favour of the intervention group ( fig 2 ). We found no evidence of publication bias (see supplementary fig 1). Absolute weight change was −3.7 (SD 6.1) kg in the intervention group and −1.4 (SD 5.5) kg in the comparator group.

Mean difference in weight at 12 months by weight management programme in primary care (intervention) or no treatment, different content, or minimal intervention (control). SD=standard deviation
Supplementary file 2 provides a summary of the main subgroup analyses.
Weight change
The mean difference in weight change at the last follow-up was −1.9 kg (95% confidence interval −2.5 to −1.3 kg, I 2 =81%, τ 2 =2.15; P<0.001). Absolute weight change was −3.2 (SD 6.4) kg in the intervention group and −1.2 (SD 6.0) kg in the comparator group (see supplementary figs 2 and 3).
At the 24 month follow-up the mean difference in weight change was −1.8 kg (−2.8 to −0.8 kg, I 2 =88%, τ 2 =3.13; P<0.001) (see supplementary fig 4). As the weight change data did not differ between the last follow-up and ≥24 months, we used the weight data from the last follow-up in subgroup analyses.
In subgroup analyses of type of interventionalist, differences were significant (P=0.005) between non-medical practitioners, GPs, nurses, and other people who delivered interventions (see supplementary fig 2).
Participants who had ≥12 contacts during interventions lost significantly more weight than those with fewer contacts (see supplementary fig 6). The association remained after adjustment for type of interventionalist.
Waist circumference
The mean difference in waist circumference was −2.5 cm (95% confidence interval −3.2 to −1.8 cm, I 2 =69%, τ 2 =1.73; P<0.001) in favour of the intervention at 12 months ( fig 3 ). Absolute changes were −3.7 cm (SD 7.8 cm) in the intervention group and −1.3 cm (SD 7.3) in the comparator group.

Mean difference in waist circumference at 12 months. SD=standard deviation
Risk of bias was considered to be low in nine trials, 24 33 34 35 39 41 47 55 56 unclear in 12 trials, 25 27 28 29 32 45 46 50 51 52 54 59 and high in 13 trials 23 26 30 31 36 37 38 44 48 49 53 57 58 ( fig 4 ). No significant (P=0.65) differences were found in subgroup analyses according to level of risk of bias from baseline to 12 months (see supplementary fig 7).

Risk of bias in included studies
Worldwide, governments are trying to find the most effective services to help people lose weight to improve the health of populations. We found weight management interventions delivered by primary care practitioners result in effective weight loss and reduction in waist circumference and these interventions should be considered part of the services offered to help people manage their weight. A greater number of contacts between patients and healthcare professionals led to more weight loss, and interventions should be designed to include at least 12 contacts (face-to-face or by telephone, or both). Evidence suggests that interventions delivered by non-medical practitioners were as effective as those delivered by GPs (both showed statistically significant weight loss). It is also possible that more contacts were made with non-medical interventionalists, which might partially explain this result, although the metaregression analysis suggested the effect remained after adjustment for type of interventionalist. Because most comparator groups had fewer contacts than intervention groups, it is not known whether the effects of the interventions are related to contact with interventionalists or to the content of the intervention itself.
Although we did not determine the costs of the programme, it is likely that interventions delivered by non-medical practitioners would be cheaper than GP and nurse led programmes. 41 Most of the interventions delivered by non-medical practitioners involved endorsement and supervision from GPs (ie, a recommendation or checking in to see how patients were progressing), and these should be considered when implementing these types of weight management interventions in primary care settings. Our findings suggest that a combination of practitioners would be most effective because GPs might not have the time for 12 consultations to support weight management.
Although the 2.3 kg greater weight loss in the intervention group may seem modest, just 2-5% in weight loss is associated with improvements in systolic blood pressure and glucose and triglyceride levels. 60 The confidence intervals suggest a potential range of weight loss and that these interventions might not provide as much benefit to those with a higher BMI. Patients might not find an average weight loss of 3.7 kg attractive, as many would prefer to lose more weight; explaining to patients the benefits of small weight losses to health would be important.
Strengths and limitations of this review
Our conclusions are based on a large sample of about 8000 participants, and 12 of these trials were published since 2018. It was occasionally difficult to distinguish who delivered the interventions and how they were implemented. We therefore made some assumptions at the screening stage about whether the interventionalists were primary care practitioners or if most of the interventions were delivered in primary care. These discussions were resolved by consensus. All included trials measured weight, and we excluded those that used self-reported data. Dropout rates are important in weight management interventions as those who do less well are less likely to be followed-up. We found that participants in trials with an attrition rate of 20% or more lost less weight and we are confident that those with high attrition rates have not inflated the results. Trials were mainly conducted in socially economic developed countries, so our findings might not be applicable to all countries. The meta-analyses showed statistically significant heterogeneity, and our prespecified subgroups analysis explained some, but not all, of the variance.
Comparison with other studies
The mean difference of −2.3 kg in favour of the intervention group at 12 months is similar to the findings in the review by LeBlanc et al, who reported a reduction of −2.4 kg in participants who received a weight management intervention in a range of settings, including primary care, universities, and the community. 11 61 This is important because the review by LeBlanc et al included interventions that were not exclusively conducted in primary care or by primary care practitioners. Trials conducted in university or hospital settings are not typically representative of primary care populations and are often more intensive than trials conducted in primary care as a result of less constraints on time. Thus, our review provides encouraging findings for the implementation of weight management interventions delivered in primary care. The findings are of a similar magnitude to those found in a trial by Ahern et al that tested primary care referral to a commercial programme, with a difference of −2.7 kg (95% confidence interval −3.9 to −1.5 kg) reported at 12 month follow-up. 62 The trial by Ahern et al also found a difference in waist circumference of −4.1 cm (95% confidence interval −5.5 to −2.3 cm) in favour of the intervention group at 12 months. Our finding was smaller at −2.5 cm (95% confidence interval −3.2 to −1.8 cm). Some evidence suggests clinical benefits from a reduction of 3 cm in waist circumference, particularly in decreased glucose levels, and the intervention groups showed a 3.7 cm absolute change in waist circumference. 63
Policy implications and conclusions
Weight management interventions delivered in primary care are effective and should be part of services offered to members of the public to help them manage weight. As about 39% of the world’s population is living with obesity, helping people to manage their weight is an enormous task. 64 Primary care offers good reach into the community as the first point of contact in the healthcare system and the remit to provide whole person care across the life course. 65 When developing weight management interventions, it is important to reflect on resource availability within primary care settings to ensure patients’ needs can be met within existing healthcare systems. 66
We did not examine the equity of interventions, but primary care interventions may offer an additional service and potentially help those who would not attend a programme delivered outside of primary care. Interventions should consist of 12 or more contacts, and these findings are based on a mixture of telephone and face-to-face sessions. Previous evidence suggests that GPs find it difficult to raise the issue of weight with patients and are pessimistic about the success of weight loss interventions. 67 Therefore, interventions should be implemented with appropriate training for primary care practitioners so that they feel confident about helping patients to manage their weight. 68
Unanswered questions and future research
A range of effective interventions are available in primary care settings to help people manage their weight, but we found substantial heterogeneity. It was beyond the scope of this systematic review to examine the specific components of the interventions that may be associated with greater weight loss, but this could be investigated by future research. We do not know whether these interventions are universally suitable and will decrease or increase health inequalities. As the data are most likely collected in trials, an individual patient meta-analysis is now needed to explore characteristics or factors that might explain the variance. Most of the interventions excluded people prescribed drugs that affect weight gain, such as antipsychotics, glucocorticoids, and some antidepressants. This population might benefit from help with managing their weight owing to the side effects of these drug classes on weight gain, although we do not know whether the weight management interventions we investigated would be effective in this population. 69
What is already known on this topic
Referral by primary care to behavioural weight management programmes is effective, but the effectiveness of weight management interventions delivered by primary care is not known
Systematic reviews have provided evidence for weight management interventions, but the latest review of primary care delivered interventions was published in 2014
Factors such as intensity and delivery mechanisms have not been investigated and could influence the effectiveness of weight management interventions delivered by primary care
What this study adds
Weight management interventions delivered by primary care are effective and can help patients to better manage their weight
At least 12 contacts (telephone or face to face) are needed to deliver weight management programmes in primary care
Some evidence suggests that weight loss after weight management interventions delivered by non-medical practitioners in primary care (often endorsed and supervised by doctors) is similar to that delivered by clinician led programmes
Ethics statements
Ethical approval.
Not required.
Data availability statement
Additional data are available in the supplementary files.
Contributors: CDM and AJD conceived the study, with support from ES. CDM conducted the search with support from HEG. CDM, AJD, ES, HEG, KG, GB, and VEK completed the screening and full text identification. CDM and VEK completed the risk of bias assessment. CDM extracted data for the primary outcome and study characteristics. HEJ, GB, and KG extracted primary outcome data. CDM completed the analysis in RevMan, and GMJT completed the metaregression analysis in Stata. CDM drafted the paper with AJD. All authors provided comments on the paper. CDM acts as guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: AJD is supported by a National Institute for Health and Care Research (NIHR) research professorship award. This research was supported by the NIHR Leicester Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care. ES’s salary is supported by an investigator grant (National Health and Medical Research Council, Australia). GT is supported by a Cancer Research UK fellowship. The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: This research was supported by the National Institute for Health and Care Research Leicester Biomedical Research Centre; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work.
The lead author (CDM) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported, and that no important aspects of the study have been omitted.
Dissemination to participants and related patient and public communities: We plan to disseminate these research findings to a wider community through press releases, featuring on the Centre for Lifestyle Medicine and Behaviour website ( www.lboro.ac.uk/research/climb/ ) via our policy networks, through social media platforms, and presentation at conferences.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/ .
- Renehan AG ,
- Heller RF ,
- Bansback N ,
- Birmingham CL ,
- Abdullah A ,
- Peeters A ,
- de Courten M ,
- Stoelwinder J
- Aghili SMM ,
- Ebrahimpur M ,
- Arjmand B ,
- KETLAK Study Group
- ↵ Department of Health and Social Care. New specialised support to help those living with obesity to lose weight UK2021. www.gov.uk/government/news/new-specialised-support-to-help-those-living-with-obesity-to-lose-weight [accessed 08/02/2021].
- U.S. Preventive Services Task Force
- ↵ National Institute for Health and Care Excellence. Maintaining a Healthy Weight and Preventing Excess Weight Gain in Children and Adults. Cost Effectiveness Considerations from a Population Modelling Viewpoint. 2014, NICE. www.nice.org.uk/guidance/ng7/evidence/evidence-review-2-qualitative-evidence-review-of-the-most-acceptable-ways-to-communicate-information-about-individually-modifiable-behaviours-to-help-maintain-a-healthy-weight-or-prevent-excess-weigh-8733713.
- ↵ The Health Foundation. Use of primary care during the COVID-19 pandemic. 17/09/2020: The Health Foundation, 2020.
- ↵ Australian Bureau of Statistics. Patient Experiences in Australia: Summary of Findings, 2017-18. 2019 ed. Canberra, Australia, 2018. www.abs.gov.au/AUSSTATS/[email protected]/Lookup/4839.0Main+Features12017-18?OpenDocument.
- LeBlanc ES ,
- Patnode CD ,
- Webber EM ,
- Redmond N ,
- Rushkin M ,
- O’Connor EA
- Damschroder LJ ,
- Liberati A ,
- Tetzlaff J ,
- Altman DG ,
- PRISMA Group
- McKenzie JE ,
- Bossuyt PM ,
- ↵ WHO. Main terminology: World Health Organization; 2004. www.euro.who.int/en/health-topics/Health-systems/primary-health-care/main-terminology [accessed 09.12.21].
- Aceves-Martins M ,
- Robertson C ,
- REBALANCE team
- Glasziou P ,
- Isenring E ,
- Chisholm A ,
- Wakayama LN ,
- Kettle VE ,
- Madigan CD ,
- ↵ Covidence [program]. Melbourne, 2021.
- Welzel FD ,
- Carrington MJ ,
- Fernández-Ruiz VE ,
- Ramos-Morcillo AJ ,
- Solé-Agustí M ,
- Paniagua-Urbano JA ,
- Armero-Barranco D
- Bräutigam-Ewe M ,
- Hildingh C ,
- Yardley L ,
- Christian JG ,
- Bessesen DH ,
- Christian KK ,
- Goldstein MG ,
- Martin PD ,
- Dutton GR ,
- Horswell RL ,
- Brantley PJ
- Wadden TA ,
- Rogers MA ,
- Berkowitz RI ,
- Kumanyika SK ,
- Morales KH ,
- Allison KC ,
- Rozenblum R ,
- De La Cruz BA ,
- Katzmarzyk PT ,
- Martin CK ,
- Newton RL Jr . ,
- Nanchahal K ,
- Holdsworth E ,
- ↵ RevMan [program]. 5.4 version: Copenhagen, 2014.
- Sterne JAC ,
- Savović J ,
- Gomez-Huelgas R ,
- Jansen-Chaparro S ,
- Baca-Osorio AJ ,
- Mancera-Romero J ,
- Tinahones FJ ,
- Bernal-López MR
- Delahanty LM ,
- Tárraga Marcos ML ,
- Panisello Royo JM ,
- Carbayo Herencia JA ,
- Beeken RJ ,
- Leurent B ,
- Vickerstaff V ,
- Hagobian T ,
- Brannen A ,
- Rodriguez-Cristobal JJ ,
- Alonso-Villaverde C ,
- Panisello JM ,
- Conroy MB ,
- Spadaro KC ,
- Takasawa N ,
- Mashiyama Y ,
- Pritchard DA ,
- Hyndman J ,
- Jarjoura D ,
- Smucker W ,
- Baughman K ,
- Bennett GG ,
- Steinberg D ,
- Zaghloul H ,
- Chagoury O ,
- Leslie WS ,
- Barnes AC ,
- Summerbell CD ,
- Greenwood DC ,
- Huseinovic E ,
- Leu Agelii M ,
- Hellebö Johansson E ,
- Winkvist A ,
- Look AHEAD Research Group
- LeBlanc EL ,
- Wheeler GM ,
- Aveyard P ,
- de Koning L ,
- Chiuve SE ,
- Willett WC ,
- ↵ World Health Organization. Obesity and Overweight, 2021, www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Starfield B ,
- Sturgiss E ,
- Dewhurst A ,
- Devereux-Fitzgerald A ,
- Haesler E ,
- van Weel C ,
- Gulliford MC
- Fassbender JE ,
- Sarwer DB ,
- Brekke HK ,
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 27 January 2020
Epidemiology and Population Health
Evidence from big data in obesity research: international case studies
- Emma Wilkins 1 ,
- Ariadni Aravani 1 ,
- Amy Downing 1 ,
- Adam Drewnowski 2 ,
- Claire Griffiths 3 ,
- Stephen Zwolinsky 3 ,
- Mark Birkin 4 ,
- Seraphim Alvanides 5 , 6 &
- Michelle A. Morris ORCID: orcid.org/0000-0002-9325-619X 1
International Journal of Obesity volume 44 , pages 1028–1040 ( 2020 ) Cite this article
948 Accesses
4 Citations
8 Altmetric
Metrics details
- Risk factors
- Signs and symptoms
Background/objective
Obesity is thought to be the product of over 100 different factors, interacting as a complex system over multiple levels. Understanding the drivers of obesity requires considerable data, which are challenging, costly and time-consuming to collect through traditional means. Use of ‘big data’ presents a potential solution to this challenge. Big data is defined by Delphi consensus as: always digital , has a large sample size, and a large volume or variety or velocity of variables that require additional computing power (Vogel et al. Int J Obes. 2019). ‘Additional computing power’ introduces the concept of big data analytics. The aim of this paper is to showcase international research case studies presented during a seminar series held by the Economic and Social Research Council (ESRC) Strategic Network for Obesity in the UK. These are intended to provide an in-depth view of how big data can be used in obesity research, and the specific benefits, limitations and challenges encountered.
Methods and results
Three case studies are presented. The first investigated the influence of the built environment on physical activity. It used spatial data on green spaces and exercise facilities alongside individual-level data on physical activity and swipe card entry to leisure centres, collected as part of a local authority exercise class initiative. The second used a variety of linked electronic health datasets to investigate associations between obesity surgery and the risk of developing cancer. The third used data on tax parcel values alongside data from the Seattle Obesity Study to investigate sociodemographic determinants of obesity in Seattle.
Conclusions
The case studies demonstrated how big data could be used to augment traditional data to capture a broader range of variables in the obesity system. They also showed that big data can present improvements over traditional data in relation to size, coverage, temporality, and objectivity of measures. However, the case studies also encountered challenges or limitations; particularly in relation to hidden/unforeseen biases and lack of contextual information. Overall, despite challenges, big data presents a relatively untapped resource that shows promise in helping to understand drivers of obesity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Non-traditional data sources in obesity research: a systematic review of their use in the study of obesogenic environments
Julia Mariel Wirtz Baker, Sonia Alejandra Pou, … Laura Rosana Aballay
Trends in the prevalence of adult overweight and obesity in Australia, and its association with geographic remoteness
Syed Afroz Keramat, Khorshed Alam, … Rubayyat Hashmi
Best practices for analyzing large-scale health data from wearables and smartphone apps
Jennifer L. Hicks, Tim Althoff, … Scott L. Delp
Davison KK, Birch LL. Childhood overweight: a contextual model and recommendations for future research. Obes Rev. 2001;2:159–71.
Article CAS PubMed PubMed Central Google Scholar
Egger G, Swinburn B. An “ecological” approach to the obesity pandemic. BMJ. 1997;315:477–80.
Harrison K, Bost KK, McBride BA, Donovan SM, Grigsby-Toussaint DS, Kim J, et al. Toward a developmental conceptualization of contributors to overweight and obesity in childhood: the six-Cs model. Child Dev Perspect. 2011;5:50–8.
Article Google Scholar
Butland B, Jebb S, Kopelman P, McPherson K, Thomas S, Mardell J et al. Foresight. Tackling obesities: future choices—project report. Government Office for Science; 2007.
Rutter HR, Bes-Rastrollo M, de Henauw S, Lahti-Koski M, Lehtinen-Jacks S, Mullerova D, et al. Balancing upstream and downstream measures to tackle the obesity epidemic: a position statement from the European association for the study of obesity. Obes Facts. 2017;10:61–3.
Article PubMed PubMed Central Google Scholar
Mittelstadt BD, Floridi L. The ethics of big data: current and foreseeable issues in biomedical contexts. Sci Eng Ethics. 2016;22:303–41.
Article PubMed Google Scholar
Kaisler S, Armour F, Espinosa JA, Money W. Big data: issues and challenges moving forward. In: Proceedings of the 46th Hawaii International Conference on System Sciences. Association for Computing Machinery Digital Library; 2013. p. 995–1004.
Herland M, Khoshgoftaar TM, Wald R. A review of data mining using big data in health informatics. J Big Data. 2014;1: https://doi.org/10.1186/2196-1115-1-2 .
Vogel C, Zwolinsky S, Griffiths C, Hobbs M, Henderson E, Wilkins E. A Delphi study to build consensus on the definition and use of big data in obesity research. Int J Obes. 2019. https://doi.org/10.1038/s41366-018-0313-9 .
Morris M, Birkin M. The ESRC strategic network for obesity: tackling obesity with big data. Int J Obes. 2018;42:1948–50.
Timmins K, Green M, Radley D, Morris M, Pearce J. How has big data contributed to obesity research? A review of the literature. Int J Obes. 2018;42:1951–62.
Monsivais P, Francis O, Lovelace R, Chang M, Strachan E, Burgoine T. Data visualisation to support obesity policy: case studies of data tools for planning and transport policy in the UK. Int J Obes. 2018;42:1977–86.
Morris M, Wilkins E, Timmins K, Bryant M, Birkin M, Griffiths C. Can big data solve a big problem? Reporting the obesity data landscape in line with the Foresight obesity system map. Int J Obes. 2018;42:1963–76.
Vayena E, Salathé M, Madoff LC, Brownstein JS. Ethical challenges of big data in public health. PLOS Comput Biol. 2015;11:e1003904.
Article PubMed PubMed Central CAS Google Scholar
Silver LD, Ng SW, Ryan-Ibarra S, Taillie LS, Induni M, Miles DR, et al. Changes in prices, sales, consumer spending, and beverage consumption one year after a tax on sugar-sweetened beverages in Berkeley, California, US: a before-and-after study. PLoS Med. 2017;14:e1002283.
Gore RJ, Diallo S, Padilla J. You are what you tweet: connecting the geographic variation in america’s obesity rate to Twitter content. PLoS ONE. 2015;10:e0133505.
Nguyen QC, Li D, Meng H-W, Kath S, Nsoesie E, Li F, et al. Building a national neighborhood dataset from geotagged Twitter data for indicators of happiness, diet, and physical activity. JMIR Public Health Surveill. 2016;2:e158.
Hirsch JA, James P, Robinson JR, Eastman KM, Conley KD, Evenson KR, et al. Using MapMyFitness to place physical activity into neighborhood context. Front Public Health. 2014;2:1–9.
Althoff T, Hicks JL, King AC, Delp SL, Leskovec J. Large-scale physical activity data reveal worldwide activity inequality. Nature. 2017;547:336–9.
Kerr NL. HARKing: hypothesizing after the results are known. Pers Soc Psychol Rev. 1998;2:196–217.
Article CAS PubMed Google Scholar
Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380:219–29.
Bennett JE, Li G, Foreman K, Best N, Kontis V, Pearson C, et al. The future of life expectancy and life expectancy inequalities in England and Wales: Bayesian spatiotemporal forecasting. Lancet. 2015;386:163–70.
World Health Organisation. Report of the Commission on ending childhood obesity. Geneva, Switzerland: World Health Organisation; 2016.
Centers for Disease Control and Prevention. Recommended community strategies and measurements to prevent obesity in the United States. Atlanta, GA, U.S.: Centers for Disease Control and Prevention; 2009.
Local Government Association. Building the foundations: tackling obesity through planning and development. London, UK: Local Government Association; 2016.
Burgoine T, Alvanides S, Lake AA. Creating ‘obesogenic realities’; Do our methodological choices make a difference when measuring the food environment? Int J Health Geogr. 2013;12. https://doi.org/10.1186/1476-072X-12-33 .
Wilkins E, Morris M, Radley D, Griffiths C. Methods of measuring associations between the Retail Food Environment and weight status: Importance of classifications and metrics. SSM Popul Health. 2019. https://doi.org/10.1016/j.ssmph.2019.100404 .
Bardou M, Barkun AN, Martel M. Obesity and colorectal cancer. Gut. 2013;62:933–47.
Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin. 2014;64:104–17.
Derogar M, Hull MA, Kant P, Östlund M, Lu Y, Lagergren J. Increased risk of colorectal cancer after obesity surgery. Ann Surg. 2013;258:983–8.
Kant P, Hull MA. Excess body weight and obesity—the link with gastrointestinal and hepatobiliary cancer. Nat Rev Gastroenterol Hepatol. 2011;8:224–38.
Östlund MP, Lu Y, Lagergren J. Risk of obesity-related cancer after obesity surgery in a population-based cohort study. Ann Surg. 2010;252:972–6.
Sainsbury A, Goodlad RA, Perry SL, Pollard SG, Robins GG, Hull MA. Increased colorectal epithelial cell proliferation and crypt fission associated with obesity and roux-en-Y gastric bypass. Cancer Epidemiol Biomark Prev. 2008;17:1401–10.
Article CAS Google Scholar
Aravani A, Downing A, Thomas JD, Lagergren J, Morris EJA, Hull MA. Obesity surgery and risk of colorectal and other obesity-related cancers: an English population-based cohort study. Cancer Epidemiol. 2018;53:99–104.
Openshaw S. The modifiable areal unit problem. In: Concepts and techniques in modern geography. Norwich: Geo Books; 1984. p. 1–41.
Kwan M-P. The uncertain geographic context problem. Ann Assoc Am Geogr. 2012;102:958–68.
Di Zhu X, Yang Y, Liu X. The importance of housing to the accumulation of household net wealth. Harvard, USA: Joint Center for Housing Studies, Harvard University; 2003.
Rehm CD, Moudon AV, Hurvitz PM, Drewnowski A. Residential property values are associated with obesity among women in King County, WA, USA. Soc Sci Med. 2012;75:491–5.
Drewnowski A, Buszkiewicz J, Aggarwal A. Soda, salad, and socioeconomic status: findings from the Seattle Obesity Study (SOS). SSM Popul Health. 2019;7:e100339.
Birkin M, Morris MA, Birkin TM, Lovelace R. Using census data in microsimulation modelling. In: Stillwell J, Duke-Williams O, editors. The Routledge handbook of census resources, methods and applications. 1st ed. Routledge: IJO publication; 2018.
Jiao J, Drewnowski A, Moudon AV, Aggarwal A, Oppert J-M, Charreire H, et al. The impact of area residential property values on self-rated health: a cross-sectional comparative study of Seattle and Paris. Prev Med Rep. 2016;4:68–74.
Nguyen DM, El-Serag HB. The epidemiology of obesity. Gastroenterol Clinics. 2010;39:1–7.
Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Commun Health. 2001;55:111–22.
Timperio A, Salmon J, Telford A, Crawford D. Perceptions of local neighbourhood environments and their relationship to childhood overweight and obesity. Int J Obes. 2005;29:170–5.
Roda C, Charreire H, Feuillet T, Mackenbach JD, Compernolle S, Glonti K, et al. Mismatch between perceived and objectively measured environmental obesogenic features in European neighbourhoods. Obes Rev. 2016;17 S1:31–41.
Drewnowski A, Arterburn D, Zane J, Aggarwal A, Gupta S, Hurvitz PM, et al. The Moving to Health (M2H) approach to natural experiment research: a paradigm shift for studies on built environment and health. SSM Popul Health. 2019;7:100345.
Bourassa SC, Cantoni E, Hoesli M. Predicting house prices with spatial dependence a comparison of alternative methods. J Real Estate Res. 2010;32:139–60.
Google Scholar
Wilkins EL, Radley D, Morris MA, Griffiths C. Examining the validity and utility of two secondary sources of food environment data against street audits in England. Nutr J. 2017;16:1–13.
Nevalainen J, Erkkola M, Saarijarvi H, Nappila T, Fogelholm M. Large-scale loyalty card data in health research. Digit Health. 2018;4:2055207618816898.
PubMed PubMed Central Google Scholar
Aiello L, Schifanello R, Quercia D, Del Prete L. Large-scale and high-resolution analysis of food purchases and health outcomes. EPJ Data Sci. 2019;8:14.
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Zwolinsky S, McKenna J, Pringle A, Widdop P, Griffiths C, Mellis M, et al. Physical activity and sedentary behavior clustering: segmentation to optimize active lifestyles. J Phys Act Health. 2016;13:921–8.
Bauman A, Ainsworth BE, Sallis JF, Hagströmer M, Craig CL, Bull FC, et al. The descriptive epidemiology of sitting: a 20-country comparison using the International Physical Activity Questionnaire (IPAQ). Am J Prev Med. 2011;41:228–35.
Guerin PB, Diiriye RO, Corrigan C, Guerin B. Physical activity programs for refugee somali women: working out in a new country. Women & Health. 2003;38:83–99.
Pope L, Harvey J. The efficacy of incentives to motivate continued fitness-center attendance in college first-year students: a randomized controlled trial. J Am Coll Health. 2014;62:81–90.
Cetateanu A, Jones A. Understanding the relationship between food environments, deprivation and childhood overweight and obesity: evidence from a cross sectional England-wide study. Health Place. 2014;27:68–76.
Harrison F, Burgoine T, Corder K, van Sluijs EM, Jones A. How well do modelled routes to school record the environments children are exposed to? A cross-sectional comparison of GIS-modelled and GPS-measured routes to school. Int J Health Geogr. 2014;13:5.
Ells LJ, Macknight N, Wilkinson JR. Obesity surgery in England: an examination of the health episode statistics 1996–2005. Obes Surg. 2007;17:400–5.
Nielsen JDJ, Laverty AA, Millett C, Mainous AG, Majeed A, Saxena S. Rising obesity-related hospital admissions among children and young people in England: National time trends study. PLoS ONE. 2013;8:e65764.
Smittenaar C, Petersen K, Stewart K, Moitt N. Cancer incidence and mortality projections in the UK until 2035. Br J Cancer. 2016;115:1147–55.
Wallington M, Saxon EB, Bomb M, Smittenaar R, Wickenden M, McPhail S, et al. 30-day mortality after systemic anticancer treatment for breast and lung cancer in England: a population-based, observational study. The Lancet Oncol. 2016;17:1203–16.
Smolina K, Wright FL, Rayner M, Goldacre MJ. Determinants of the decline in mortality from acute myocardial infarction in England between 2002 and 2010: Linked national database study. BMJ. 2012;344:d8059.
Hanratty B, Lowson E, Grande G, Payne S, Addington-Hall J, Valtorta N, et al. Transitions at the end of life for older adults–patient, carer and professional perspectives: A mixed-methods study. Health Serv Deliv Res. 2014. https://doi.org/10.3310/hsdr02170 .
Aggarwal A, Monsivais P, Cook AJ, Drewnowski A. Does diet cost mediate the relation between socioeconomic position and diet quality? Eur J Clin Nutr. 2011;65:1059–66.
Drewnowski A, Aggarwal A, Tang W, Moudon AV. Residential property values predict prevalent obesity but do not predict 1-year weight change. Obesity. 2015;23:671–6.
Download references
Acknowledgements
The ESRC Strategic Network for Obesity was funded via ESRC grant number ES/N00941X/1. The authors would like to thank all of the network investigators ( https://www.cdrc.ac.uk/research/obesity/investigators/ ) and members ( https://www.cdrc.ac.uk/research/obesity/network-members/ ) for their participation in network meetings and discussion which contributed to the development of this paper.
Author information
Authors and affiliations.
Leeds Institute for Data Analytics and School of Medicine, University of Leeds, Leeds, UK
Emma Wilkins, Ariadni Aravani, Amy Downing & Michelle A. Morris
Center for Public Health Nutrition, University of Washington, Seattle, WA, USA
Adam Drewnowski
School of Sport, Leeds Beckett University, Leeds, UK
Claire Griffiths & Stephen Zwolinsky
Leeds Institute for Data Analytics and School of Geography, University of Leeds, Leeds, UK
- Mark Birkin
Engineering and Environment, Northumbria University, Newcastle, UK
Seraphim Alvanides
GESIS—Leibniz Institute for the Social Sciences, Cologne, Germany
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Michelle A. Morris .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Wilkins, E., Aravani, A., Downing, A. et al. Evidence from big data in obesity research: international case studies. Int J Obes 44 , 1028–1040 (2020). https://doi.org/10.1038/s41366-020-0532-8
Download citation
Received : 23 May 2019
Revised : 20 December 2019
Accepted : 07 January 2020
Published : 27 January 2020
Issue Date : May 2020
DOI : https://doi.org/10.1038/s41366-020-0532-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
- Julia Mariel Wirtz Baker
- Sonia Alejandra Pou
- Laura Rosana Aballay
International Journal of Obesity (2023)
Creating a long-term future for big data in obesity research
- Emma Wilkins
- Michelle A. Morris
International Journal of Obesity (2019)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Research article
- Open access
- Published: 02 May 2019
Enhancing knowledge and coordination in obesity treatment: a case study of an innovative educational program
- Tonje C. Osmundsen ORCID: orcid.org/0000-0002-5776-6694 1 ,
- Unni Dahl 2 &
- Bård Kulseng 3 , 4
BMC Health Services Research volume 19 , Article number: 278 ( 2019 ) Cite this article
4380 Accesses
7 Citations
1 Altmetric
Metrics details
Currently, there is a lack of knowledge, organisation and structure in modern health care systems to counter the global trend of obesity, which has become a major risk factor for noncommunicable diseases. Obesity increases the risk of diabetes, cardiovascular diseases, musculoskeletal disorders and cancer. There is a need to strengthen integrated care between primary and secondary health care and to enhance care delivery suited for patients with complex, long-term problems such as obesity. This study aimed to explore how an educational program for General Practitioners (GPs) can contribute to increased knowledge and improved coordination between primary and secondary care in obesity treatment, and reports on these impacts as perceived by the informants.
In 2010, an educational program for the specialist training of GPs was launched at three hospitals in Central Norway opting for improved care delivery for patients with obesity. In contrast to the usual programs, this educational program was tailored to the needs of GPs by offering practice and training with a large number of patients with obesity and type 2 diabetes for an extended period of time. In order to investigate the outcomes of the program, a qualitative design was applied involving interviews with 13 GPs, head physicians and staff at the hospitals and in one municipality.
Through the program, participants strengthened care delivery by building knowledge and competence. They developed relations between primary and secondary care providers and established shared understanding and practices. The program also demonstrated improvement opportunities, especially concerning the involvement of municipalities.
Conclusions
The educational program promoted integrated care between primary and secondary care by establishing formal and informal relations, by improving service delivery through increased competence and by fostering shared understanding and practices between care levels. The educational program illustrates the combination of advanced high-quality training with the development of integrated care.
Peer Review reports
Obesity and diabetes are grave international health problems [ 1 , 2 ] and the economic burden for both patients and national economies is significant [ 3 ]. Obesity is a complex condition often involving several other chronic and serious diseases requiring lifelong follow-up [ 4 , 5 , 6 ]. It often affects whole families and intervention is needed at multiple levels, including social and psychological dimensions. Treatment is therefore complex and time-consuming and poses a challenge for the organisation of health care services [ 7 , 8 ]. Currently, there is a lack of well-established integrated approaches for prevention and treatment across health care levels.
Treatment offerings
To tackle these challenges, the coordination of services needs to be improved [ 7 , 9 , 10 ]. In Norway, the Coordination Reform was launched in 2010 [ 11 ]. Here, as in other countries [ 12 ], integrated care is accompanied by goals for moving patients from secondary health care to primary care, increasing focus on prevention and health-promoting activities and patient involvement. Obese and overweight patients with related diseases have traditionally been offered treatment in primary care, but in recent years the number of patients with severe obesity and complications has increased and consequently, so has the number of patients referred to secondary health care. To counter such a development, primary and secondary health care providers should jointly develop integrated care based on an understanding of the disease’s complexity. In addition, knowledge and capacity at the primary health care level must be improved and services targeted at prevention and cure must be made available.
Although health care workers are key players in the effort to stop the obesity trend in the population and to prevent the complications of obesity, international research suggests that obese patients do not receive adequate help for their health problems. Studies have shown that health care providers’ treatment and attitude towards overweight and obese patients are governed by poor knowledge and inconsistencies [ 13 , 14 ] and have a strong weight bias, indicating stigma [ 15 , 16 ]. A mapping in Central Norway showed a lack of knowledge and tools for how to treat and prevent overweight and obesity [ 17 ]. Less than half of the obese patients who sought medical help for their lifestyle problems were advised to lose weight by their GP [ 18 ] or given exercise counselling [ 19 ], and while research has shown that such advice and counselling may have an effect on weight loss, it is inadequate [ 20 ]. Limited treatment contact is thought to be the main reason why modest weight loss is achieved [ 20 ]. There are available treatment guidelines for primary care, but there are currently few sufficiently effective established treatment offerings available to children and adults struggling with overweight and obesity within primary health care [ 21 ]. More extensive treatment in primary care is often randomly organised, at times by local enthusiasts. Treatment is difficult to establish in primary care because of the complexity involved in treating obesity, and while GPs are competent to diagnose obesity, there is a general lack in knowledge about treating the disease [ 13 , 14 ] and available time [ 20 ]. Furthermore, considering coordination between primary and secondary health care providers, integrated care for patients with obesity is underdeveloped [ 4 , 14 , 22 , 23 , 24 ]. In Norway, obese patients are normally referred to secondary health care when they have a Body Mass Index (BMI) ≥ 40 or BMI ≥ 35 kg/m 2 with complications of obesity, while children should have an iso-BMI > 35 or iso-BMI > 30 kg/m2 with complications of obesity [ 25 ]. However, until a patient reaches this stage in the development of the disease, few treatments are available, and when a patient is referred to secondary health care, a lack of coordination and cooperation between primary and secondary care leads to treatments that may be limited in scope and time.
Education of GP specialists in the health care system in Norway
The health care system in Norway is primarily a public system organised in two levels. Secondary healthcare services are owned and financed by the Ministry of Health and Care Services and managed through four regional health authorities. The primary care level includes general practitioners (GPs), nursing homes, home care services, maternal and child health centres and out-of-hours services. Primary care is organised and financed by the local authorities (municipalities). Even though GPs are organised as a part of the primary care level, GPs are private contractors and not organised in a shared formal organisation that can instruct GPs or act as a partner on behalf of GPs [ 26 ].
The educational program for becoming a GP specialist in Norway includes 1 year of practice at a hospital. Currently, there are no positions targeted at GPs’ educational needs, so a GP seeking specialization must apply for a regular specialist training position at a hospital. In most of these positions, the doctor is enrolled in the rota system. This means that candidates will often spend time in emergency admissions on evening and night shifts that are compensated by time off. This leaves little time to attend in-house patients and perform routine follow-up of patients, both of which are relevant for their practice as GPs.
Theoretical basis
Mur-Veeman et al. [ 27 ] have shown that organizational and financial splits between health care providers, such as those present in Norway between primary and secondary health care, hinder integrated care development and delivery. Organizational divides are closely linked to contradictory interests, separate professional cultures, power relations and mistrust between health care providers. Martinussen [ 28 ] has shown that the interaction between GPs and hospital physicians has improvement potential, and weak collaboration between GPs and hospitals has been the focus of several studies [ 29 , 30 , 31 ]. Delayed or inaccurate communication can have substantial implications for the quality of care, which is especially apparent when patients need lifelong follow-up. Efforts to strengthen integrated care can counteract such inadequate treatment at the interstices between providers. In this paper, integrated care is defined as “[ ] a coherent set of methods and models on the funding, administrative, organizational, service delivery and clinical levels designed to create connectivity, alignment and collaboration within and between the cure and care sectors” [ 32 ].
There are many strategies available to foster integrated care. It is found that different commitments, goals and tasks can be major obstacles for collaboration between care levels [ 33 ]. Thus, defining roles and having a shared purpose is essential to achieve successful interorganizational collaboration [ 34 ]. Other approaches include training of medical staff, a focus on how they perform their responsibilities and tasks, and how they work together with colleagues and patients [ 32 ]. Face-to-face interaction is well known to foster trust and collaborative relations. This has also earlier been shown to apply to the relationships between GPs and hospital specialists [ 28 , 35 ]. Networking and collaboration both horizontally and vertically across health care providers promotes integrated care, as well as a “Shared understanding of patient needs, common professional language and criteria, the use of specific, agreed-upon practices and standards throughout the lifecycle of a particular disease or condition…” [ 32 ].
Fruitful integration between care levels is dependent on communication between primary and secondary health care providers [ 36 ], and this collaboration becomes even more important for patients with multiple complex conditions and needs [ 37 ]. Efforts to improve integration should aim to understand the perspectives of clinicians in each setting and implement strategies that engage both groups by way of shared communication through direct access to each other, interpersonal relations, shared electronic medical records and clearly defined accountability [ 31 ]. However, organizational and financial splits between these two parts of the health care system impede such collaboration. The lack of a common hierarchy and governance structure necessitates professionals to create combined responsibilities for shared accountability and decision making to deliver integrated care [ 38 ]. There is therefore a need for models and methods that may enhance care delivery suited for patients with complex, long term problems that cut across multiple care providers and settings. Such models should combine the clinical expertise of the specialist and the ability of GPs to bridge the gap between medical and social problems [ 39 ] to allow for continuity of care over time. The development of agreed care pathways has the potential to align clinical, management and service user interests across primary and secondary care [ 40 ] but has been shown to be most effective in contexts where patient care trajectories are predictable [ 41 ]. When pathways are more variable, this is a demanding intervention that requires comprehensive and prolonged efforts by health care professionals in the involved organizations [ 42 ].
We have witnessed many efforts to foster integrated care in the past decade, and this topic has received substantial political interest [ 11 , 27 ]. However, there are few reports on how educational programs for care providers can contribute. A noteworthy exception is Hirsh et al. [ 43 ], who studied how a clerkship model may provide undergraduate students with training relevant for the continuity of care. Concerning the specialist training of GPs, there are few examples of similar discussions. Surveying former research in the area revealed that specialist training is rarely debated, and when it is, the discussion concerns evaluation forms, attendance and curricula. We did find a few examples of case studies in which GPs visited local hospitals for knowledge exchange [ 44 , 45 ]. Such cases have been reported as beneficial for integrated care and mutual learning between GPs and hospital staff, but collaboration lasts a short time, does not involve GPs practising at the hospital and does not demand much involvement between GPs and hospital staff. In response to the challenges described above, the Centre for Obesity Research (ObeCe) at St. Olavs Hospital, Trondheim University Hospital wanted to develop an educational program fostering integrated care. Thus, in 2010, an educational program for the specialization of GPs was established at three regional hospitals in Norway to enhance the exchange of knowledge and strengthen coordination between primary and secondary healthcare providers.
The research question addressed in this paper is thus: what are the main outcomes of the educational program relevant for care delivery to obese patients, as experienced by the participants?
In this study, we investigated how an educational program for GPs in one region in Norway, including one university hospital and two general hospitals, could contribute to enhancing the continuation of care across health care providers. This educational program provides a case study of how educational measures may be designed to promote integrated care. To evaluate the program, understand its potential contribution to integrated care and reveal how it may be improved, a qualitative study [ 46 ] was undertaken. Central documents concerning the establishment and organization of the program were read and analysed, and 13 informants were interviewed. All participants in the program, as well as their closest collaborators at the hospitals and a representative from one municipality, were interviewed.
Research setting
The program was initiated in November 2010 by the management of the Centre for Obesity Research (ObeCe). ObeCe was established in 2005 in line with national and regional health policies [ 47 , 48 ] and is a research and development centre that has carried out several projects to promote collaboration between primary and secondary health care regarding overweight and diabetes. ObeCe does not have patient treatment as its main concern. This allows the unit the freedom and mandate to create new practices like the educational program for GPs [ 49 ]. By June 2014, eight GPs had participated or were currently participating in the project.
The program was designed by ObeCe to provide GPs with relevant training and education for their general practice and to strengthen the connection between primary and secondary care. It was also geared towards providing primary health care providers with competence concerning a grave public health problem, as it focused on subject areas relevant for the prevention and treatment of overweight and obesity. The GPs received extensive training with the same patient groups that they meet in their general practice and which they considered challenging. The costs of the educational program were limited to salary expenses for the involved GPs, in addition, they contributed financially to their respective departments by treating patients.
The GPs were employed in educational positions on temporary contracts limited to one-year full time. They had the possibility to work part time, leaving them the opportunity to continue with their own practice. During the program, the GPs participated both in clinical practice and theoretical studies. They were part of multidisciplinary teams at different departments at the hospital. The program was designed to provide the GPs with knowledge and training in four main areas: clinical practices, theoretical studies, research and the development of integrated care. However, the informants emphasized that the balance between these four areas could be adjusted to allow for individual interests and needs. A tutor supported them during the course of the program.
The GPs worked at three different departments to gain clinical practice: the Multidisciplinary Outpatient Clinic for Obesity, the Department of Endocrinology and ObeCE. The multidisciplinary Outpatient Clinic for Obesity is a clinic with health professionals such as surgeons, psychologists, nutritional experts, physiotherapists and endocrinologists that receives children, adults and families, and has a broad perspective on obesity-related issues similar to the perspective of a GP. The GPs did not participate in the rota system, so they had fixed days each week at the different departments: three days at the Department of Endocrinology, one day at the Multidisciplinary Outpatient Clinic for Obesity and one day at ObeCe. They were given their own list of patients to follow for an extended period.
They were involved in patient care at the clinics and in preparing obese patients for operations and for self-management. They also received training in treating patients with type 2 diabetes at the Department of Endocrinology. The GPs evaluated referrals to the hospital from other GPs, conducted physical examinations, reviewed medical histories, provided diagnoses and followed up with tests. These examinations provided the basis to determine the severity of the disease and to create a treatment plan for the patient. They followed patients long enough to observe the effects of the treatments and the patients’ experiences.
The educational program was devised to give the GPs access to theoretical studies and they participated in courses, both initiated by the hospital in general and available at each clinic. Internal courses at the hospital (two hours each week) are required for any specialist under training, but in this program, the GPs also attended lectures at each clinic for one hour each week. In addition, they contributed themselves by holding lectures for the staff at the clinics and at ObeCe. They were also given leeway and encouraged to take initiative in areas they felt they could improve and contribute to.
The GPs had 20% of their time dedicated to research and were encouraged to contribute to the professional development of the field of obesity and overweight. They were expected to update themselves on the latest research results, and as a requirement of the program, the GPs participated in on-going research projects within one month of their employment. The GPs who participated in the program received their formal qualifications as specialists and re-certification in line with the purpose of the program.
Participants
All those involved or related to the program at the time of the study and available for interviews were asked to participate, and all accepted. Those interviewed included five GPs who were enrolled in the program, two nurses, one research assistant, four head physicians and one manager from the local municipality, thereby covering those informants most involved and familiar with the project. Interviews were conducted in two rounds: in April 2012 and in September 2013. The methodological approach was deemed appropriate, as the study was exploratory and aimed to uncover respondents’ experiences and opinions. Each interview lasted from one to two hours. Participation was voluntary.
Data collection and analysis
As a basis for the interviews, a semi-structured guide was developed reflecting the research questions of the study and sent to each informant before the interview (see Additional file 1 , Interview guide). Informants were asked how they experienced the program, in particular about the effects of the program on their own knowledge, expertise and ability to provide quality of care, as well as the results for the various clinics at the hospital and the primary health care services. Informants were also asked whether they saw the program as useful for the particular patient group and society at large, and if so, in what ways. The guide was flexible and allowed the informants to include any new themes they found relevant to describe the program and their experience. All interviews were taped and later transcribed. The data was systematically categorised and coded. The analytical process focused on identifying and differentiating the concepts and topics the informants described, both those introduced by the interview guide and those provided by the informants themselves. Concrete examples of integrated care practices and other examples of results from the program were noted. Similarities and differences between each informant and the informant’s group were coded and compared. The analytical approach was inductive and exploratory, focusing on the concepts and categories as described by the informants.
In interviews, both GPs and their collaborators at the hospital emphasized three main areas they saw as important outcomes of the program: (1) the establishment of relations and networks which breached the organizational divide between primary and secondary care; (2) increased knowledge and competence both at the primary care level and at the hospital; and (3) the development of shared practices and the use of shared standards. In addition, the informants also identified shortcomings, mainly related to the weak integration the GPs experienced with their own municipalities.
Establishing relations and networks
Through the program, GPs and hospital staff became acquainted and formed collaborative relations, both during the time the GPs were at the hospital and after. Since the GPs worked in three different departments at the hospital, they were able to establish relations with several colleagues at the hospital, both doctors and nurses. Both GPs and hospital staff emphasised in interviews the value of the personal relations and networks they had been able to build through the program. One of the GPs stated:
“The most important thing is the increased competence and the network of contacts you get. It becomes so much simpler. And that is a part of the point, that it becomes seamless and that it should work like this” (GP3).
The GPs were encouraged to contribute to areas they felt they could improve and, as a result, they established the first formal arena for knowledge exchange between staff at the ObeCe and the Outpatient Clinic for Obesity so that employees from the two departments can meet at regular intervals for lectures and research updates. This was made possible because the GPs worked fixed days at both departments and were, unlike their colleagues at the hospital, not in the rota system. The rota system affords less individual predictability, as it is not known well in advance which person will occupy which shift. The GPs would know months in advance where they would work each day, so it was easier to plan ahead and take responsibility to schedule activities for knowledge exchange with their hospital colleagues.
The program aided in forming new relations and networks. The GPs emphasised in interviews how this was made possible because they were met by informed and positive colleagues at the hospital. Respect and trust characterised the relations that were established and laid the grounds for open discussions and mutual learning.
Increased knowledge and competence
The program offered several opportunities for training, both through formal courses initiated at the hospital and through the time specified for research. The interviewed GPs explained that they had increased their knowledge of overweight and obese patients, and related diseases such as diabetes, through participating in the program.
According to the informants, the professional environment of the hospital, the time set aside for research and the tutoring they received during the program gave room for investigations that the GPs rarely had time for in their general practice.
The program also provided knowledge and competence that extends beyond those of a formal qualification in overweight and obesity treatment. In an interview, one of the participating GPs explained how the program had changed her attitude towards the patient group and increased her understanding of the complexity of the field of overweight and obesity:
“It is easy to have prejudices concerning this patient group, and there is much stigmatisation. I notice that with colleagues and others who are not familiar with the field. It is easy to conclude, as with other lifestyle related diseases, that it is self-inflicted and weak individuals who are not capable of changing their own situation. It is of course not so simple” (GP1).
The GPs also stated they had an increased sense of confidence in treating obese and overweight patients with related diseases such as diabetes when returning to their medical practices. During their time at the hospital, they were able to see a large number of patients with type 2 diabetes, which increased their confidence in their ability to treat this patient group. Earlier, they would have referred type 2 diabetes patients to secondary health care because they did not feel confident enough to treat them themselves. As explained by GP2:
“My attitude changes while I am here [at the hospital]. I see possibilities for all that can be done in my general practice. Before, I would think that ‘now I have tried with this patient for half a year, and nothing happens, we won’t get any further.’ Now, with new knowledge, I believe there is more we can do” (GP2).
There was a mutual exchange of knowledge between the GPs and medical personnel at the hospital, especially concerning care delivery. A head physician at one of the clinics where the GPs worked said:
“Professionally, it has been very positive for our clinic that they have brought with them the GPs’ views into treatment for diabetes. We are able to discuss what is feasible to do in a general practice, and what we need to continue to do here” (Head Physician).
Shared practices and use of shared standards
It was stated in the objectives of the program that the GPs were to contribute to increased cooperation between the primary and secondary health care levels. The program had thus allocated funds for arranging conferences and meetings between the GPs and their respective municipalities.
The program resulted in the dissemination of knowledge not only to the participating GPs, but also to health personnel at the primary care level. Several of the GPs initiated training courses and lectures for fellow GPs in their municipalities that occurred at their own medical centres, in larger conferences and in permanent colloquium groups where a smaller number of GPs met regularly for research updates and discussions. One of the projects in which the GPs were involved investigated how an intermediate care service at the primary health care level could assume the postoperative follow-up of obese patients in collaboration with local GPs.
An internet course qualifying GPs for their specialisation was developed by one of the GPs in the program and launched nationwide. Also, general information leaflets were developed, providing information to GPs concerning the treatment of patients who have undergone gastric bypass operations. This included a document listing the short- and long-term side effects of gastric bypass. The involvement of the GPs at ObeCe also resulted in several international publications written by them and their colleagues at the hospital, thus disseminating knowledge to a broader international audience.
In the clinical domain, the program resulted in improved shared understanding and practices between the primary and secondary health care levels. This was achieved by the close involvement of the GPs at different departments in the hospital, and through the activities the GPs initiated at their own medical centres and in primary care in general. The GPs said they had realised that through their knowledge and experience of both primary and secondary health care, they could play an important role in creating shared practices across care providers.
Shared practices between primary and secondary care were developed and continuously improved because of the program. These measures allowed for the increased involvement of and information to GPs when their patients were at the hospital. One of the nurses summed up the new practices for the GPs’ strengthened involvement:
“[GP1] has done much for communications with the GPs. Patients receive a letter, and the GPs get notified that the patient is in a post-operative group. Patients receive a form they need to fill out. This didn’t exist before [GP1] and the other GPs were here” (Nurse 1).
Also, specific procedures for follow-up of patients who had undergone gastric bypass were amended, as they did not function properly. Patients had earlier failed to attend their appointments at the hospital and the patients’ GPs were not involved. Also, in the case of diabetes patients, the primary care level was not actively involved. Alternate consultations between the hospitals and respective GPs were therefore initiated as a result of the program. This was seen as a way to enable the primary health care level to be more involved in follow-up care. In addition, the program resulted in initiatives to improve horizontal integration across health services, social services and other care providers.
Both physicians and nurses said they gained much knowledge through the close contact with GPs. They emphasised having an increased understanding of the GPs’ opportunities and constraints when attending patients in their general practices. Hospital staff also claimed that they now recognised the need to collaborate more closely with GPs while their respective patients were receiving treatment at the hospital and after, and that they understood more of how to improve the collaboration between primary and secondary health services. Some also said they had changed their practices as a result of what they learned from the GPs.
The informants perceived that the educational program had immediate value for those involved in enabling and supporting the development of integrated care. It provided high quality training for GPs while meeting the national and local challenges of achieving integrated care. One of the GPs concluded:
“The project has been successful, because we have become a part of the work at ObeCe, meaning integrated care in practice, because we are GPs playing on the same field as the secondary health care services” (GP5).
Shortcomings
However, the program also had shortcomings. These concerned the relationship and collaboration between the GPs and their respective municipalities. One of the reasons given by the respondents was that the organisation of the municipalities’ services and the decision-making process is fragmented. The interviewed GPs were unsure of who they could present ideas to at the municipality to initiate projects they believed could improve health care services and did not know whether their ideas would be in line with current plans and budgets. One stated:
“Yes, I am sitting here and I want to make things happen in my municipality, but it is not so easy when there are no systems or frameworks for it. You have to make it happen yourself, and nobody expects anything” (GP2).
The GPs found it difficult to know whom to approach at the municipalities and how they could work to realise their ideas. The informants suggested that the educational program should include clear expectations for how the GPs could establish plans for their work in the municipalities while under training, because when they returned to their general practices, there would be less time to plan and think about new projects.
Outcomes of the program
The educational program incorporated several strategies earlier identified as beneficial for fostering integrated care in three important domains: organisational, service delivery and clinical practice [ 32 ]. Central to the development of integrated care is vertical integration between primary and secondary health care through formal and informal relations, networks and collaboration , which breaches the organizational divide between the two systems [ 27 ]. High quality service delivery hinges on the knowledge and competence of medical staff both at the primary and secondary health care levels, and is not only related to the specific disease(s), but also to care delivery [ 32 ]. In the clinical domain, a shared understanding of patient needs and use of shared practices and standards between providers is essential [ 37 ]. Interviews with personnel involved in the program indicate that the program showed results in these directions, even though there were also shortcomings. For example, the interviewed GPs did not know whom to approach in their respective municipalities to realize new ideas and changes in care delivery.
The educational program has been shown to be able to foster relations between hospital staff and GPs, which are lacking in the existent health care system. This is important for a patient group that will continuously be in need for care to avoid serious complications and that has the risk of becoming revolving-door patients due to a fragmented and poorly integrated health care system. As Tricco et al. found [ 50 ], multidisciplinary care is needed for chronic patients with complex conditions, and improving care for this group is effective at reducing readmissions. Care needs to be provided in a continuous interplay between primary and secondary care by health professionals who have defined roles and responsibilities and a shared purpose [ 31 , 33 , 34 ]. This corresponds to earlier recommendations for care delivery for patients with complex care needs [ 37 ], that shows that their need for care is best met by close interaction and collaboration between primary and secondary health care providers.
The educational program contributes to integrated care for obese patients by combining the expertise of specialists from the hospital with the broader and more holistic experience and competence of GPs [ 39 ]. Obesity is a condition that requires caregivers to bridge medical and social problems. With the increased prevalence of complex conditions, hospitals cannot simply discharge patients to primary health care without themselves offering to share their knowledge and expertise. Secondary health care has experienced a strong increase in referrals for patients suffering from obesity and related conditions. To reduce this burden, secondary health care providers need to engage with care givers in primary care to strengthen their ability and capacity to treat this patient group. Also, medical staff at secondary health care institutions need to gain an understanding of how obesity and subsequent treatment are intertwined with broader issues such as work, family life and social problems, as well as the framework conditions of the patients’ local communities. A Cochrane review [ 51 ] concluded that audit and feedback strategies can be important to improve professional practice, but this improvement depend on how the feedback is provided and by whom. Creating a learning environment, as in this educational program where health professionals openly discuss practices and alternative approaches, can thus be a potential strategy for enhancing quality of care.
Through collaboration and direct dialogue, the GPs and specialists involved in the educational program create and shape shared understanding and practices. Patient’s awareness of such dialogues between the GP and specialists from the hospital has earlier been suggested to strengthen patients’ sense of security [ 52 ]. Collaboration between caregivers from primary and secondary health care services is important both for the quality of care that is given to this patient group and to ensure continuity of care. Other strategies, such as developing agreed care pathways, could provide stronger alignment between primary and secondary health care providers, but it might also demand much efforts and prolonged engagement to implement [ 42 ], especially when patient pathways are variable [ 41 ], as in the case of obesity.
The educational model thus promises to compensate for some of the problems of the current organization of the health care system [ 27 ]. The artificial division between clinical specialists at hospitals and GPs in primary care has earlier been shown to lead to weak communication, which affects the continuity and quality of care [ 28 , 29 , 30 , 31 ]. A doctoral thesis concluded that integration depends on the collaborative partners’ ability to develop all-embracing objectives and view their services and work as a part of the total chain of care. Integration depends on sufficient communication and interorganisational teamwork, a learning environment, common perspectives and clarified roles [ 36 ]. Through developing relations, enhancing knowledge and competence and shared understanding and practices, the educational program studied here promises to breach obstacles to continuity of care for patients suffering from obesity. There are many different strategies that have been shown to be conducive to enhancing quality of care, both within and across primary and secondary care. However, as Grol and Grimshaw [ 53 ] argue, approaches should be fit for purpose and adapted to the barriers and facilitators to change in each situation. The approach chosen here answered a perceived need to strengthen knowledge in primary care. The program continues and is now in use at several departments at St. Olavs Hospital. It should be considered a step towards strengthening integrated care between primary and secondary care.
In Central Norway, since 2010, the educational program has gradually been instituted as a permanent program that is offered to a number of departments at St. Olavs Hospital. As of today, 35 GPs have been employed at seven different departments (Department of Ophthalmology, Department of Ear, Nose and Throat, Head and Neck Surgery, Child Department, Department of Endocrinology, Department of Neurology, Department of Clinical Pharmacology and Department of Gynaecology) at St. Olavs Hospital, Trondheim University Hospital, and in three different departments (Department of Geriatrics, Child Department and Department of Surgery) at Namsos Hospital. According to the Director of Integrated Healthcare at St. Olavs, the experiences from these departments are univocally positive (Personal communication, email to author BK, 6.1.2018). In sum, these experiences reflect this study’s findings. The departments found it useful to interact with GPs to learn more about the expertise in general practice and the GPs increased their knowledge, which in turn was transferred to their colleagues in primary care. Increased knowledge and competence in primary care resulted in fewer referrals to the hospital. Finally, the capacities of the different departments at the hospital increased with the aid of the GPs.
The educational program did not seek to alter the organizational divides between primary and secondary care, but focused on strengthening connectivity and collaboration across these divides by involving GPs in secondary care for a defined time period. According to the informants, this had positive impacts for both primary and secondary care, as discussed above. This was considered a necessary first step to demonstrate the usefulness and feasibility of the program, considering the large number (47) of municipalities in this region, all with highly diversified tasks and structures. An important lesson learnt from this program is that while obesity and diabetes are a growing concern in Norwegian municipalities, it is important to designate funding of assigned positions directed towards such illnesses as a cost-sharing scheme across several municipalities. The continuation of the program now (2018) shows that groups of municipalities are engaging with secondary health care providers to incorporate the increased knowledge and experience of the GPs in municipal structures.
Limitations and future research
The empirical basis for this article is limited, with 13 respondents and one case, although it was carried out in three hospitals. The results are indicative of how such an educational program may contribute to integrated care, but a more extensive program and more studies are needed to reach findings that can be considered representative. The strength of the study is its reporting of a novel model that may foster integrated care and strengthen the expertise of primary care while reducing the burden on the acute sector.
Revising educational programs in line with the model described here may be an affordable and feasible approach to dealing with some of the organizational splits between health care providers. The costs of the program were limited to salary expenses for the participating GPs, and their work at the hospital contributed financially to the respective departments. However, further research should also assess the costs of the intervention and compare these to other strategies for integration. Nevertheless, there is a need for more systematic knowledge of how educational programs may contribute to integrated care and how such programs may have long-term effects on the collaboration between primary and secondary health care providers. Further research should study the effects of such programs, and especially seek to assess how patients experience strengthened interactions and collaboration between GPs and hospital staff.
The educational program illustrates how one may combine high quality training with integrated care. It constitutes a promising path for both increased medical competence and improved integrated patient care because it involves health care personnel from both primary and secondary care who together develop practices that are implemented across care providers. The program is applicable to different professional domains, especially those where patients can benefit from coordinated health services and where health personnel can collaborate to develop practices that merge competences and approaches from both primary and secondary health care services.
Important challenges remain in engaging more municipalities to incorporate the increased knowledge of GPs into municipal structures and to disseminate the lessons learnt from this program to other regions.
Abbreviations
Body Mass Index
General practitioner
Centre for Obesity Research
Yach D, Stuckler D, Brownell KD. Epidemiologic and economic consequences of the global epidemics of obesity and diabetes. Nat Med. 2006;12(1):62–6.
Article CAS Google Scholar
James PT, Leach R, Kalamara E, Shayeghi M. The worldwide obesity epidemic. Obes Res. 2001;9(Suppl 4):228–33.
Article Google Scholar
Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011;12(2):131–41.
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. 2000;WHO Tech Report 894. http://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ . Accessed 10 Apr 2017.
World Health Organization. Global strategy on diet, nutrition, and the prevention of chronic diseases. 2003;WHO Tech Report 916. http://apps.who.int/iris/bitstream/10665/42665/1/WHO_TRS_916.pdf . Accessed 10 Apr 2017.
Rivenes AC, Harvey SB, Mykletun A. The relationship between abdominal fat, obesity, and common mental disorders: results from the HUNT study. J Psychosom Res. 2009;66(4):269–75.
Truswell AS, Hiddink GJ, Green LW, Roberts R, van Weel C. Practice-based evidence for weight management: alliance between primary care and public health. Fam Pract. 2012;29(Suppl 1):6–9.
Seidell JC, Halberstadt J, Noordam H, Niemer S. An integrated health care standard for the management and prevention of obesity in the Netherlands. Fam Pract. 2012;29(Suppl 1):153–6.
McDonald J, Jayasuriya R, Harris MF. The influence of power dynamics and trust on multidisciplinary collaboration: a qualitative case study of type 2 diabetes mellitus. BMC Health Serv Res. 2012. https://doi.org/10.1186/1472-6963-12-63 .
Berendsen AJ, Benneker WH, Jong BM, Klazinga NS, Schuling J. Motives and preferences of general practitioners for new collaboration models with medical specialists: a qualitative study. BMC Health Serv Res. 2007. https://doi.org/10.1186/1472-6963-7-4 .
Norwegian Ministry of Health and Care Services. The Coordination Reform. Proper treatment - at the right place and right time. Oslo: Norwegian Ministry of Health and Care Services; Report No. 47 (2008–2009) to the Storting. [Summary in English, full version in Norwegian].
Mur-Veeman I, van Raak A, Paulus A. Comparing integrated care policy in Europe: does policy matter? Health Policy. 2008;85(2):172–83.
Vetter ML, Herring SJ, Sood M, Shah NR, Kalet AL. What do resident physicians know about nutrition? An evaluation of attitudes, self-perceived proficiency and knowledge. J Am Coll Nutr. 2008;27(2):287–98.
Kirk SFL, Price SL, Penney TL, Rehman L, Lyons RF, Piccinini-Vallis H, et al. Blame, shame, and lack of support: a multilevel study on obesity management. Qual Health Res. 2014;24(6):790–800.
Schwartz MB, Chambliss HO, Brownell KD, Blair SN, Billington C. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11(9):1033–9.
McVey GL, Walker KS, Beyers J, Harrison HL, Simkins SW, Russell-Mayhew S. Integrating weight bias awareness and mental health promotion into obesity prevention delivery: a public health pilot study. Prev Chronic Dis. 2013;10:120185.
Kulseng B, Ødegård R, Følling I. En evalueringsrapport av prosjektet ‘Overvekt og Folkehelse’ – modell for samhandling mellom første og andrelinjetjenesten. [an evaluation report of the ‘obesity and public health project’ – a model for coordination between primary and secondary health care.]. Regionalt senter for sykelig overvekt, St. Olavs Hospital; 2012. [in Norwegian].
Foster GD, Wadden TA, Makris AP, Davidson D, Sanderson RS, Allison DB, Kessler A. Primary care physicians’ attitudes about obesity and its treatment. Obes Res. 2003;11(10):1168–77.
Lobelo F, Duperly J, Frank E. Physical activity habits of doctors and medical students influence their counselling practices. Br J Sports Med. 2009;43(2):89–92.
Wadden TA, Volger S, Sarwer DB, Vetter ML, Tsai AG, Berkowitz RI, et al. A two-year randomized trial of obesity treatment in primary care practice. N Engl J Med. 2011;365:1969–79.
Mazur A, Matusik P, Revert K, Nyankovskyy S, Socha P, Binkowska-Bury M, et al. Childhood obesity: knowledge, attitudes, and practices of European pediatric care providers. Pediatrics. 2013;132(1):100–8.
Eger K, Gleichweit S, Rieder A, Stein KV. Prioritising integrated care initiatives on a national level. Experiences from Austria. Int J Integr Care. 2009;9(3).
Nguyen N, Champion JK, Ponce J, Quebbemann B, Patterson E, Pham B, et al. A review of unmet needs in obesity management. Obes Surg. 2012;22(6):956–66.
Mühlbacher A, Bethge S. Preferences of overweight and obese patients for weight loss programs: a discrete-choice experiment. Int J Integr Care. 2013;13(3).
Helsedirektoratet. Nasjonal faglig retningslinje for forebygging, utredning og behandling av overvekt og fedme hos barn og unge. [National standard for prevention, examination and treatment of obesity and overweight in children and adolescents in Norwegian]. 2010. https://helsedirektoratet.no/retningslinjer/nasjonal-faglig-retningslinje-for-forebygging-utredning-og-behandling-av-overvekt-og-fedme-hos-barn-og-unge . Accessed 10 Apr 2017.
Romøren TI, Torjesen DO, Landmark B. Promoting coordination in Norwegian health care. Int J Integr Care. 2011;11.
Mur-Veeman I, Hardy B, Steenbergen M, Wistow G. Development of integrated care in England and the Netherlands: managing across public-private boundaries. Health Policy. 2003;65:227–41.
Martinussen PE. Hospital physicians’ assessments of their interaction with GPs: the role of physician and community characteristic. Health Policy. 2013;(1):14–21.
Garasen H, Johnsen R. The quality of communication about older patients between hospital physicians and general practitioners: a panel study assessment. BMC Health Serv Res. 2007;7:133.
Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297:831–41.
Jones CD, Vu MB, O’Donnell CM, Anderson ME, Patel S, Wald HL, et al. A failure to communicate: a qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations. J Gen Intern Med. 2015;30:417. https://doi.org/10.1007/s11606-014-3056-x .
Article PubMed Google Scholar
Kodner DL, Spreeuwenberg C. Integrated care: meaning, logic, applications, and implications - a discussion paper. Int J Integr Care. 2002;2.
Johannessen A-K, Lurås H, Steihaug S. The role of an intermediate unit in a clinical pathway. Int J Integr Care 2013;13(1). http://www.ijic.org/articles/abstract/10.5334/ijic.859/ , accessed 19 June 2018.
Olson CA, Balmer JT. Factors contributing to successful Interorganizational collaboration: the case of CS2day. J Contin Educ Heal Prof. 2011;31(Suppl 1):S3–12.
Tjerbo T, Kjekshus LE. Coordinating health care: lessons from Norway. Int J Integr Care. 2005;5.
Dahl U. The impact of an Intermediate Care Hospital on the chain of care for hospitalized elderly people. PhD thesis. Norwegian University of Science and Technology, Faculty of Medicine, Dep. of Public Health and General Practice. 2015.
Coleman EA, Fox PD. One patient, many places: managing health care transitions part II: practitioner skills and patient and caregiver preparation. Ann Longterm Care. 2004;12:34–9.
Google Scholar
Valentijn PP, Schepman SM, Opheij W, Bruijnzeels MA. Understanding integrated care: a comprehensive conceptual framework based on the integrative functions of primary care. International Journal of Integrated Care. 2013;13(1):None.
McWhinney I. A textbook of family medicine. New York: Oxford University Press; 1997.
Allen D. From boundary concept to boundary object: the practice and politics of care pathway development. Soc Sci Med. 2009;69(3):354–61.
Allen D. Systematic review of the effectiveness of integrated care pathways: what works, for whom, in which circumstances. Int J Evid Based Healthcare. 2009;7:61–74.
Røsstad T, Garåsen H, Steinsbekk A, et al. Implementing a care pathway for elderly patients, a comparative qualitative process evaluation in primary care. BMC Health Serv Res. 2015;15:86.
Hirsh DA, Ogur B, Thibault GE, Cox M. ‘Continuity’ as an organizing principle for clinical education reform. N Engl J Med. 2007;356(8):858–66.
Frydenberg K, Nylehn P. General practice consultants at all Norwegian hospitals. Tidsskrift for Norsk Laegeforening. 2003;123:2481 [in Norwegian].
Senanayake S, Bowden F, Ironside J, Robertson T. A teaching ward round in infectious diseases - a pilot module. Aust Fam Physician. 2006;35:357–8.
PubMed Google Scholar
Silverman D. Doing qualitative research. 3rd ed. London: SAGE Publications Ltd; 2009.
Helse- og omsorgsdepartementet. [Ministry of Health Care Services]. Styringsdokument 2004. [Governing document 2004]. https://www.regjeringen.no/globalassets/upload/hod/bestillerdokumnet/styringsdokument-helse-midt-norge.pdf . [in Norwegian]. Accessed 10 Apr 2017.
Helse Midt Norge RHF Styret. Styresak 59/08 HMN RHF. [Central Norway health authority board item 59/08 HMN RHF]. 2008. https://ekstranett.helse-midt.no/1001/Sakspapirer/sak%2059-08%20Behandlingstilbud%20til%20personer%20med%20sykelig%20overvekt%20vedl%201%20Utredn%20og%20beh%20av%20sykelig%20overvekt%20i%20speshelsetj%20-voksne.pdf . [in Norwegian]. Accessed 10 Apr 2017.
Mørk BE, Hoholm T, Maaninen-Olsson E, Aanestad M. Changing practice through boundary organizing: a case from medical R&D. Hum Relat. 2012;65(2):263–88.
Tricco AC, Antony J, Ivers NM, et al. Effectiveness of quality improvement strategies for coordination of care to reduce use of health care services: a systematic review and meta-analysis. CMAJ. 2014;186:568–78.
Ivers N, Jamtvedt G. Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. In The Cochrane library. John Wiley & Sons, Ltd.; 2012 http://cochranelibrary-wiley.com/doi/10.1002/14651858.CD000259.pub3/full , accessed June 20, 2018.
Osmundsen TC, Jaatun EA, Heggem GF, Kulseng B. Service innovation from the edges – enhanced by telemedicine decision support. PUC. 2015;19(3):699–708.
Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet. 2003;362(9391):1225–30.
Download references
Acknowledgements
The authors are grateful to Central Norway Regional Health Authority for supporting the research, and to the informants at St. Olavs Hospital, Trondheim University Hospital, Namsos Hospital, Ålesund Hospital and an anonymous municipality who willingly contributed with their opinions and experiences.
The ObeCe covered the costs of data collection unrestrictedly. The writing of this paper was partly financed through the SPIS project (Norwegian Research Council, grant number 220553).
Availability of data and materials
The data from the qualitative interviews is not made publicly available in order to fully protect the informants’ anonymity.
Author information
Authors and affiliations.
NTNU Social Research, Dragvoll Allé 38b, N-7491, Trondheim, Norway
Tonje C. Osmundsen
Norwegian Hospital Construction Agency, Klæbuveien 118, 7031, Trondheim, Norway
Centre for Obesity Research (ObeCe), Clinic of Surgery, St. Olavs University Hospital, 7006, Trondheim, Norway
Bård Kulseng
Department of Cancer Research and Molecular Medicine, Norwegian University of Science and Technology, N-7489, Trondheim, Norway
You can also search for this author in PubMed Google Scholar
Contributions
Each author has read and approved the final version and all made important contributions. TCO: Conception and design, data collection, analysis and interpretation, writing the article, critical revision of the article, final approaval. UD: Analysis and interpretation, writing the article, critical revision of the article, final approval. BK: Initiation of the study, analysis and interpretation, writing the article, critical revision of the article, final approval.
Corresponding author
Correspondence to Tonje C. Osmundsen .
Ethics declarations
Ethics approval and consent to participate.
The project received approval from the Ombudsman for Research and Social Science Data Service in Norway, which serves as an ethics committee for Norwegian Research Institutes. We received informed consent for the interviews and for recording of the interviews by e-mail. This information was repeated verbally to the informants before the interviews started. All data has been treated and presented to preserve anonymity and confidentiality.
Consent for publication
The informants involved in this study gave consent for direct quotes from their interviews to be used in this manuscript.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Additional file
Additional file 1:.
Interview guide. (DOCX 24 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Osmundsen, T.C., Dahl, U. & Kulseng, B. Enhancing knowledge and coordination in obesity treatment: a case study of an innovative educational program. BMC Health Serv Res 19 , 278 (2019). https://doi.org/10.1186/s12913-019-4119-9
Download citation
Received : 30 May 2017
Accepted : 24 April 2019
Published : 02 May 2019
DOI : https://doi.org/10.1186/s12913-019-4119-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Integrated care
- General practitioners
- Specialist training
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- MEMBER DIRECTORY
- Member Login
- Publications
- Clinician Well-Being
- Culture of Health and Health Equity
- Fellowships and Leadership Programs
- Future of Nursing
- U.S. Health Policy and System Improvement
- Healthy Longevity
- Human Gene Editing
- U.S. Opioid Epidemic
- Staff Directory
- Opportunities
- Action Collaborative on Decarbonizing the U.S. Health Sector
- Climate Communities Network
- Communicating About Climate Change & Health
- Research and Innovation
- Culture of Health
- Fellowships
- Emerging Leaders in Health & Medicine
- Culture & Inclusiveness
- Digital Health
- Evidence Mobilization
- Value Incentives & Systems
- Substance Use & Opioid Crises
- Reproductive Health, Equity, & Society
- Credible Sources of Health Information
- Emerging Science, Technology, & Innovation
- Pandemic & Seasonal Influenza Vaccine Preparedness and Response
- Preventing Firearm-Related Injuries and Deaths
- Vital Directions for Health & Health Care
- NAM Perspectives
- All Publications
- Upcoming Events
- Past Events
- MEMBER HOME

An Innovative Approach to Employer-Provided Benefits for Obesity Care: A Case Report on H-E-B’s Healthier Lifestyle Choices Program
The clinical and economic impact of obesity.
Obesity presents a formidable challenge to health care financing systems. According to the 2017-2018 National Health and Nutrition Survey (NHANES), rates of obesity among U.S. adults have now climbed to 42.8% (Hales et al., 2020). The problem of this high prevalence of obesity has been particularly highlighted during the COVID-19 pandemic, when individuals with obesity were shown to have increased risk for adverse outcomes of COVID-19, including hospitalization, admission to the intensive care unit, mechanical ventilation, or death (Kompaniyets et al., 2021). In addition, the increase in obesity rates has also led to an increase in the burden of other obesity-driven chronic diseases, such as heart disease, cancer, chronic lung disease, stroke, diabetes, Alzheimer’s disease, and chronic kidney disease. According to the Centers for Disease Control and Prevention (CDC), six in ten American adults have at least one chronic disease and four in ten have two or more (NCCDPHP, 2022).
Given this connection between obesity and chronic disease, the impact of obesity on medical care costs is alarming. According to a recent study, aggregate medical costs in 2016 due to obesity among U.S. adults were $260.6 billion (Cawley et al., 2021). Adults with obesity (BMI > 30 kg/m²) incurred $2,505 more in annual medical costs, double the medical expenditures of those with BMI between 18.5 and 25 kg/m² (Cawley et al., 2021). Patients with obesity had higher costs in every category of care, including inpatient and outpatient expenses, as well as prescription drug expenses. Further, costs were shown to increase significantly with class of obesity, with class 1 (BMI 30<35 kg/m²), class 2 (BMI 35<40 kg/m²), and class 3 (BMI > 40 kg/m²) categories demonstrating ascending costs. For those whose insurance was funded by public programs, annual medical expenditures were more ($2,868) as compared to those with privately funded health insurance ($2,058) (Cawley et al., 2021).
Obesity also has economic implications beyond direct health care costs, including productivity costs (absenteeism, presenteeism, disability, premature mortality), transportation costs, and human capital costs (Hammond and Levine, 2010). This commentary explores a case study of one large employer, H-E-B, LP, that developed and implemented an employer-provided benefits program as an attempt to tackle the clinical and economic impacts of obesity among their workforce.
The Problem: Lack of Health Care Provider Engagement and Financial Disincentives
Given the adverse clinical and economic impacts of obesity, prevention and remediation of obesity and its health complications are of great importance for public health. Medical and surgical approaches to obesity treatment have made distinct progress in producing safe and sustainable weight loss with resultant health benefits, but low rates of obesity diagnoses hinder this progress (Bray et al., 2016). A 2019 U.S.-based study of primary care providers (PCPs) in 15 health systems found that obesity was diagnosed in only 45% of patients with obesity and only 70% of patients with severe obesity (Ciemins et al., 2020). When obesity was diagnosed, however, 17% of patients lost more than 5% of body weight and 6% of patients lost more than 10% (Ciemins et al., 2020). Still, even successful diagnoses are difficult to follow through on: for example, follow-up appointments are scheduled less than 25% of the time (Kaplan et al., 2018). There is a disconnect between what health professionals know can be done to produce clinically meaningful weight loss and what they are able to implement on a broad scale.
The barriers to successful obesity intervention in real-world medicine are numerous (Hite et al., 2019). One such barrier, highlighted in the development of obesity Standards of Care and Obesity Competencies, is the lack of a trained workforce (Dietz and Gallagher, 2019; Kushner et al., 2019). Another commonly cited barrier is the lack of reimbursement: more than 50% of PCPs have indicated that improvements in the reimbursement process “would improve their ability to counsel patients with obesity” (Petrin et al., 2017). In 2016-2017, only 21 state Medicaid programs reimbursed providers for nutritional counseling, 16 programs covered pharmacotherapy, and 49 programs covered bariatric surgery (Jannah et al., 2018). It is clear that providers cannot provide obesity care without financial support.
Businesses as Part of the Solution: The Importance of Employer-Based Obesity Benefit Plans
There are many health benefits of reducing body weight in persons with obesity. The benefits begin with weight loss of about 5% over one or two years, and expand with greater weight loss (Ryan and Yockey, 2017). Thus, weight reduction should be associated with direct medical cost savings and, if intervention costs can be minimized, even a return on investment. The economic case for bariatric surgery is especially strong. Bariatric surgery produces sustainable, clinically significant weight loss; reduction in cardiovascular events and mortality; and reduction in health care costs (Lopes et al., 2015). When combined with clinical interventions, lifestyle intervention counseling has also shown improved treatment engagement and economic benefits (Wadden et al., 2020). For example, when provided to more than 52,000 employees as a wellness benefit, an online digital weight loss program administered over one year demonstrated 2.8% average body weight loss, with 23% of this population achieving 5% or more weight loss at one year (Horstman et al., 2018). In a sub study of that benefit, the 4,790 participants studied had $3,693,090 of total medical costs savings in the three years following the intervention (with total program costs of $1,639,961), a 2.3:1 return on investment (Horstman et al., 2021). The Diabetes Prevention Program also successfully reduced medical costs compared to the control group (Diabetes Prevention Program Research Group, 2012). While there is some emerging evidence from integration of large electronic health record data sets of the cost savings of non-surgical weight loss, more real-world studies of the costs are needed, as well as the cost-effectiveness of such treatments, including medications (Ding et al., 2021). Clearly, both payers and providers must have a shared understanding that obesity is a chronic disease for which treatments can produce sustained weight reduction, remediation of obesity complications, and even reduction in health care costs.
Businesses can also play a valuable role in supporting their employees with obesity and providing benefits that reach at-risk populations. Just as there has been a change in scientific knowledge about the biologic basis of obesity – an understanding that obesity is not caused by a lack of willpower and is indeed a disease – there is an emerging change in attitudes among human resource managers, who are beginning to see that it is appropriate to include medical and surgical management of obesity in employee health benefits. Understanding the biologic basis of obesity means that medical management is essential and education in nutrition and physical activity is not sufficient as a health benefit. Incorporating medications into the benefit plan, which is compatible with a medical approach to chronic disease management, is included in the case study below.
Case Study: H-E-B, LP
H-E-B, LP (H-E-B) is a family-owned grocery retailer, manufacturer, and transportation company, operating for 117 years with a footprint in Texas and Mexico and powered by more than 130,000 employees, referred to as “Partners.” H-E-B views its culture as a source of pride and attributes that culture and the reputation of the company to its Partners.
H-E-B’s commitment to its Partners includes providing opportunities for Partners to make healthier lifestyle choices through a robust, value-based benefits plan design. More than 10 years ago, H-E-B began tracking a cohort of Partners’ biometric results as part of a corporate health and wellness program (Partners in this cohort were screened every year from 2010-2019, excluding 2017). Over the past 10 years, H-E-B’s incentive program has rewarded participants with a reduced Partner premium contribution. Partners who improve upon their biometric results earn a larger reduction on their weekly premium. The most prevalent risk factor within the H-E-B Partner population is overweight and obesity, as defined by body mass index (BMI). Recognizing that Partners have a need for weight reduction, H-E-B implemented value-based benefits that support Partners seeking reduction in body weight and BMI through a variety of treatment options which can be selected by Partners with the advice of health care providers.
The value-based plan design components of the H-E-B benefits include:
- Digital therapeutics to help Partners monitor important health metrics and consult with telehealth providers when needed;
- Near-worksite employee primary care clinics;
- Three free Registered Dietitian (RD) consultations annually, and, once exhausted, RD visits that are covered by a low Partner co-pay;
- Network of Employee Assistance Program counselors that are trained in behavior change and motivational interviewing (an approach to behavior change that includes a guiding style of communication, patient empowerment, and respect for patient autonomy) (Miller and Rollnick, 2013);
- Coverage of obesity medications with a custom prior authorization process managed by H-E-B pharmacists; and
- Coverage for bariatric surgery (all Partners must engage with the H-E-B BlueCross BlueShield of Texas [BCBSTX] Partner Care Team prior to surgery).
In 2019, one year after implementing an outcomes-based incentive requirement and supporting Partners with new benefit offerings, H-E-B recognized measured improvement in the prevalence of overweight and obesity (via BMI measurements) of the cohort population, which it has screened every year since 2010.
Learnings and Best Practices
H-E-B’s approach to population health has evolved over time. Each evolution occurred after a thorough analysis of the data and consideration of how a change might impact company culture. Obesity medication coverage, for example, relied on a strategy to educate company leaders and overcome stigma about obesity medication to garner support. Company leaders were briefed to ensure they understood the data and recognized the need for coverage. The company built a financial model around medications, considering co-pays and use of generic medications. While progress is incremental, going forward, H-E-B’s leaders will consider other plan designs marketed as incentives, taking into consideration overall plan costs. Options under discussion include changes in bariatric surgery plan coverage, other preventive health improvement program options, such as those noted above, and the use of telehealth services and devices.
Can the H-E-B Experience Inform National Efforts?
H-E-B is proud to have included obesity care in its benefits package and has made it accessible for all its Partners. The decision to cover obesity medications is particularly noteworthy. What makes the H-E-B model especially innovative is the care with which the company approached the design of benefits and the way it used its own data for decision making. Other companies might consider gathering data describing their employees’ health from their insurance carriers, interviewing companies providing health promotion interventions, and surveying their employees to identify health care priorities and needs. These measures might support the adoption of core components of obesity care (meaningful lifestyle intervention programs, and medical and surgical management provision). These surveys and above-mentioned data gathering efforts would help define the scope and severity of the problem and the types of obesity treatment services which ought to be covered. Employers, in partnership with scientists, doctors, point solution companies, and insurance carriers, have an opportunity to identify evidence-based obesity treatment modalities that can support clinically significant weight loss among persons with obesity, define the economic consequences of those treatment approaches, and determine the best ways for employees to access the defined solutions.
Among government programs, comprehensive obesity benefits are becoming more common: as of 2023, federal employees, active-duty military, and veterans will all have access to the full continuum of care. Under current law, Medicare does not cover anti-obesity medications (Bodenheimer, 2022). In Congress, bipartisan and bicameral efforts are underway to provide Medicare beneficiaries access to the full continuum of coverage for weight management (117th Congress, 2021). While a modern approach to weight management in the nation’s largest insurance program would be a critical step forward, obesity coverage is required in order to achieve a meaningful reduction in obesity prevalence and its concomitant chronic disease burden. The H-E-B case study provided above is one approach. Other employers will also need to understand the financial, social, and personal benefits of including obesity care in their benefits packages to begin to make significant progress in caring for people who are overweight or have obesity.
Join the conversation!
D ownload the graphics below and share them on social media!

- 117th 2021. Treat and Reduce Obesity Act of 2021, H.R. 1577. Available at: https://www.congress.gov/bill/117th-congress/house-bill/1577/text (accessed June 8, 2022).
- Bodenheimer, Laurie. 2022. Subject: Federal Employees Health Benefits Program Call Letter. Available at: https://www.opm.gov/healthcare-insurance/healthcare/carriers/2022/2022-03.pdf (accessed July 26, 2022)
- Bray, G. A., G. Frühbeck, D. H. Ryan, and J. P. Wilding. 2016. Management of obesity. Lancet 387(10031):1947-56. https://doi.org/ 1016/S0140-6736(16)00271-3.
- Cawley, J., A. Biener, C. Meyerhoefer, Y. Ding, T. Zvenyach, B. G. Smolarz, and A. Ramasamy. 2021. Direct medical costs of obesity in the United States and the most populous states. Journal of Managed Care & Specialty Pharmacy 27(3):354-366. https://doi.org/10.18553/jmcp.2021.20410.
- Ciemins, E. L., V. Joshi, J. K. Cuddeback, R. F. Kushner, D. B. Horn, and W. T. Garvey. 2020. Diagnosing obesity as a first step to weight loss: An observational study. Obesity (Silver Spring) 28(12):2305-9. https://doi.org/10.1002/oby.22954.
- Diabetes Prevention Program Research Group. 2012. The 10-year cost-effectiveness of lifestyle intervention or metformin for diabetes prevention: an intent-to-treat analysis of the DPP/DPPOS. Diabetes Care 35(4):723-30. https://doi.org/10.2337/dc11-1468.
- Dietz, W. H., C. and Gallagher. 2019. A Proposed Standard of Obesity Care for All Providers and Payers. Obesity (Silver Spring) 27(7):1059-1062. https://doi.org/10.1002/oby.22507.
- Ding, Y., X. Fan, C. M. Blanchette, B. G. Smolarz, W. Weng, and A. Ramasamy. 2021. Economic value of nonsurgical weight loss in adults with obesity. Journal of Managed Care & Specialty Pharmacy 27(1):37-50. https://doi.org/10.18553/jmcp.2020.20036.
- Hales, C. M., M. D. Carroll, C. D. Fryar, and C. L. Ogden. 2020. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief (360): 1-8. Available at: https://www.cdc.gov/nchs/data/databriefs/db360-h.pdf (accessed June 8, 2022).
- Hammond R. A., and R. Levine. 2010. The economic impact of obesity in the United States. Diabetes, Metabolic Syndrome and Obesity 3:285-295. https://doi.org/10.2147/DMSOTT.S7384.
- Hite, A., D. Victorson, R. Elue, and B. A. Plunkett. 2019. An exploration of barriers facing physicians in diagnosing and treating obesity. American Journal of Health Promotion 33(2):217-24. https://doi.org/10.1177/0890117118784227.
- Horstman, C. M., D. H. Ryan, L. J. Aronne, C. M. Apovian, J. P. Foreyt, H. M. Tuttle, and D. A. Williamson. 2021. Return on investment: Medical savings of an employer-sponsored digital intensive lifestyle intervention for weight loss. Obesity (Silver Spring) 29:654-661. https://doi.org/ 1002/oby.23117.
- Horstman, C., Aronne, L., Wing, R., Ryan, D.H. and Johnson, W.D. 2018. Implementing an online weight-management intervention to an employee population: Initial experience with real appeal. Obesity 26: 1704-1708. https://doi.org/10.1002/oby.22309.
- Jannah, N., J. Hild, C. Gallagher, and W. H. Dietz. 2018. Coverage for obesity prevention and treatment services: Analysis of Medicaid and state employee health insurance programs. Obesity (Silver Spring) 26(12):1834-1840. https://doi.org/10.1002/oby.22307.
- Kaplan, L. M., A. Golden, K. Jinnett, R. L. Kolotkin, T. K. Kyle, M. Look, J. Nadglowski, P. M. O’Neil, T. Parry, K. J. Tomaszewski, B. Stevenin, S. K. Lilleøre, and N. V. Dhurandhar. 2018. Perceptions of barriers to effective obesity care: Results from the national ACTION study. Obesity (Silver Spring) 26(1):61-9. https://doi.org/10.1002/oby.22054.
- Kompaniyets, L., A. B. Goodman, B. Belay, D. S. Freedman, M. S. Sucosky, S. J. Lange, A. V. Gundlapalli, T. K. Boehmer, and H. M. Blanck. 2021. Body mass index and risk for COVID-19-related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death – United States, March-December 2020. Morbidity and Mortality Weekly Report 70(10):355-361. https://doi.org/ 15585/mmwr.mm7010e4.
- Kushner, R. F., D. B. Horn, W. S. Butsch, J. D. Brown, K. Duncan, C. S. Fugate, C. Gorney, E. L. Grunvald, L. I. Igel, M. Pasarica, N. Pennings, T. Soleymani, and A. Velazquez. 2019. Development of obesity competencies for medical education: A report from the obesity medicine education collaborative. Obesity (Silver Spring) 27(7):1063-1067. https://doi.org/10.1002/oby.22471.
- Lopes, E. C., I. Heineck, G. Athaydes, N. G., Meinhardt, K. E. Souto, and A. T. Stein. 2015. Is bariatric surgery effective in reducing comorbidities and drug costs? A systematic review and meta-analysis. Obesity Surgery 25(9):1741-49. https://doi.or/10.1007/s11695-015-1777-5.
- Miller, W. R. and S. Rollnick. 2013. Motivational interviewing: Helping people to change . 3rd edition. Guillford Press.
- National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP). 2022. Chronic diseases in America . Available at: https://www.cdc.gov/chronicdisease/resources/infographic/chronic-diseases.htm (accessed December 29, 2021).
- Petrin, C., S. Kahan, M. Turner, C. Gallagher, and W. H. Dietz. 2017. Current attitudes and practices of obesity counselling by health care providers. Obesity Research & Clinical Practice 11(3):352-9. https://doi.org/10.1016/j.orcp.2016.08.005.
- Ryan, D. H., and S. R. Yockey. 2017. Weight loss and improvement in comorbidity: Differences at 5%, 10%, 15%, and over. Current Obesity Reports . 6(2):187-194. https://doi.org/10.1007/s13679-017-0262-y.
- Wadden, T. A., J. S. Tronieri, and M. L. Butryn. 2020. Lifestyle modification approaches for the treatment of obesity in adults. The American Psychologist 75(2):235–251. https://doi.org/10.1037/amp0000517.
https://doi.org/10.31478/202209a
Suggested Citation
Ammerman, A. and D. H. Ryan. 2022. An Innovative Approach to Employer-Provider Benefits for Obesity Care: A Case Report on H-E-B’s Healthier Lifestyle Choices Program. NAM Perspectives. Commentary, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/202209a .
Author Information
Abigail Ammerman, MPH, is Sr. Manager of Benefits Programs at H-E-B, LP. Donna H. Ryan, MD, is Professor Emerita at Pennington Biomedical Research Center.
Acknowledgments
The authors would like to acknowledge Cypress Lynx, MPH, of the National Academies of Science, Engineering, and Medicine for her valuable contributions to this paper.
Conflict-of-Interest Disclosures
Abigail Ammerman is a full-time employee of H-E-B, LP and is president of the San Antonio Business Group on Health. Donna H. Ryan is a scientific advisor to Novo Nordisk, Wondr Health, Calibrate, Gila Therapeutics, Real Appeal, Epitomee, Xeno Bioscience, Roman, Lilly, Zealand, Amgen, Altimmune and Ysopia; receives honoraria for lectures from Novo Nordisk, and IFA Celtic. She serves on a Data Safety Monitoring Board for Rhythm and a study Steering Committee for Novo Nordisk and is a stock option holder in Epitomee, Calibrate, Roman, and Scientific Intake.
Correspondence
Questions or comments should be directed to Abigail Ammerman at [email protected].
The views expressed in this paper are those of the authors and not necessarily of the authors’ organizations, the National Academy of Medicine (NAM), or the National Academies of Sciences, Engineering, and Medicine (the National Academies). The paper is intended to help inform and stimulate discussion. It is not a report of the NAM or the National Academies. Copyright by the National Academy of Sciences. All rights reserved.
Join Our Community
Sign up for nam email updates.
- Open access
- Published: 13 November 2023
How are people with obesity managed in primary care? – results of a qualitative, exploratory study in Germany 2022
- Julian Wangler 1 &
- Michael Jansky 1
Archives of Public Health volume 81 , Article number: 196 ( 2023 ) Cite this article
780 Accesses
1 Altmetric
Metrics details
Counselling and management of overweight and obesity are tasks for which general practitioners possess favourable qualifications. Based on a long-term doctor-patient relationship, GPs have various options for actions to deal with overweight problems. To date, however, there is only little evidence on the experiences which people with obesity have made with the primary physician model and the care needs and wishes they actually address to their GPs. This study investigated what experiences people with obesity have had with GP care and what care needs and wishes they communicated to their GPs. The results will be used to derive starting points for optimising the primary healthcare setting.
A total of 32 individuals affected by obesity were recruited over 24 online health forums. With them, we conducted qualitative interviews in the time between April and October 2022.
The respondents considered the primary care physician to be the central contact person when they sought advice and support with weight problems. The advice of the GP was associated with an increased willingness to deal with reducing one’s own weight. Despite this positive perception, widespread drawbacks existed from the perspective of the respondents: (1) incidental or late discovery of obesity, (2) absence of continuous weight counselling, (3) no agreement on specific weight reduction goals, (4) no referrals to help and support services, (5) insensitive discussion. Only some of the respondents who have recently been able to reduce their weight sustainably attributed their success primarily to the support they received from their GP.
GPs should be encouraged to address obesity consistently and promptly. In addition, concrete recommendations and realistic goals for weight loss should be formulated. Continuous and motivating discussions are crucial in this regard. A focus on nutrition and exercise counselling in the GP’s office should also be encouraged. GPs should be strengthened in their role as mediators by integrating their patients into a network of further assistance as needed. The development of care structures for obesity management should be promoted.
Peer Review reports
In recent years, obesity has received increased attention as a chronic disease [ 1 , 2 ]. Current figures for Germany indicate that 53% of adults are overweight (BMI 25-29.9 kg/m²) and of these 17% are obese (BMI > 30 kg/m²) [ 1 , 2 , 3 ]. For Europe, obesity is thought to be significantly involved in the development of approximately 80% of incident cases of type 2 diabetes mellitus, approximately 35% of all ischaemic heart diseases, and approximately 55% of all hypertensive diseases [ 4 ]. In addition, the clinical picture is associated with considerable mental distress [ 5 , 6 , 7 ]. A large meta-study of evidence-based international guidelines for the treatment of people with weight problems revealed that most guidelines come to the conclusion that overweight and obesity should be treated in a multidisciplinary manner like a chronic disease [ 8 ]. In this context, BMI should be included as a routine indicator. A multifactorial, comprehensive lifestyle programme that comprises reduced caloric intake, increased physical activity, and measures supporting a behavioural change for at least 6 to 12 months is recommended [ 9 ]. After weight loss, long-term weight maintenance interventions will be required. In summary, there was considerable agreement in the evidence-based international guidelines that overweight and obesity management should be implemented as an elementary constituent of medical healthcare.
When it comes to counselling and managing people with obesity, primary care is particularly significant [ 10 ]. GPs often have a long history of familiarity with their patients, hence it is likely that the good relationship of personal trust between physician and patient might have a positive impact on treatment when dealing with a sensitive issue such as obesity [ 11 , 12 ].
Apart from counselling and support, GPs have several options at their disposal that serve the purpose of effecting weight reduction based on lifestyle changes [ 13 ]. This may include dietary and exercise therapy counselling, therapeutic interventions, or a referral to external help services. Patients in need of special psychosocial stabilisation might benefit from psychological intervention. Medication and surgical therapy options may also be taken into consideration [ 1 , 2 ].
Previous international studies indicated that GPs are aware of the importance of primary care in overweight and obesity management [ 14 ]. However, they often have negative attitudes towards people with obesity (e.g., insinuation of lacking willpower) [ 15 , 16 , 17 ]. Self-report research suggests that many GPs hold severely biassed and incongruent views about the aetiology of obesity, about people with overweight and obesity [ 18 , 19 , 20 ]. In a representative survey of over 600 GPs in southeastern France, Bocquier et al. have shown that approximately a third of respondents had (very) negative attitudes towards people with obesity; 57% were pessimistic about patients’ ability to lose weight [ 14 ]. Schwenke et al. were able to identify stigmatising attitudes towards patients with obesity in a clinical study with 47 GPs using the Fat Phobia Scale (FPS) [ 21 ]. Younger GP age, male gender and a lower number of referrals to specialists were associated with higher levels of stigmatising attitudes. A qualitative study by Teixeira et al. was also able to show that GPs tend to regard people with obesity as being unmotivated and non-compliant [ 22 ]. Correspondingly, a lack of belief in the efficacy of nutrition or exercise therapies was found among a subset of GPs. As a result of subliminal stereotyping, insensitive and inconsistent communication on behalf of the physician might occur in cases of obesity [ 11 ]. Often, GPs seem to prefer assuming a more passive attitude and regard the patient to be primarily responsible for his (or her) weight loss [ 23 , 24 ]. Along with this, treatment plans for weight loss are highly individualised [ 25 ]. A lack of adequate structures and programmes is discussed as another reason for the reservation of GPs in obesity management [ 26 – 28 ].
The results of previous studies vary widely with regard to the willingness of people with obesity to seek advice and, if necessary, therapeutic support from their GPs. Surveys conducted in Australian and Israeli practices, for example, showed that patients who attributed an important mediating role to their GPs in terms of weight management, welcomed regular GP advice on dietary issues and physical activity, and showed a high willingness to accept lifestyle changes [ 28 , 29 , 30 ]. Several papers stated that overweight individuals who had received advice regarding their weight from their GPs often made greater efforts to lose weight [ 13 , 31 ].
On the other hand, surveys in the USA showed that patients had little interest in counselling services and that the physicians’ attempts to initiate lifestyle changes were often not accepted [ 32 ]. Patients often did not raise the issue of obesity on their own initiative during consultations, but expected appropriate advice from their attending physician [ 33 ]. Other studies found that people with obesity were often dissatisfied with the support they received from their GP. In many cases, the diagnosis of overweight and obesity was not accompanied by specific advice or instructions on diets or physical activity [ 34 , 35 ].
Beyond individual international findings, there is a lack of current studies for German-speaking countries that focus on overweight and obesity management by GPs. In particular, the experiences and care needs of the patients have hardly been examined. The present study investigates how people with obesity experience the support provided by GPs and what their needs and wishes with regard to obesity management are. The results will be used to determine starting points for an optimisation of primary care.
Guidelines and recruitment
In order to address the research interest, we developed a semi-structured interview guide. It was based both on a relevant literature search and a preliminary study [ 36 ]. The topics were the importance of the GP in obesity prevention, the content and form of the GP’s consultation, the effect and assessment of the consultation, potential therapies, general care needs, and possibilities for improving the GP’s care.
The respondents were recruited on 24 online health forums focusing on obesity as their main topic. For this purpose, a call was launched to provide information about the general topic. Individuals who were willing to partake in an interview (no incentives) could contact us via a specified email address.
Subsequent to the voluntary recall of the interested persons (a total of 42 persons from eight of the twelve forums), height, weight, age, gender and living environment (based on the number of inhabitants; general differentiation according to the categories of large city, medium-sized city, small town and rural community) were collected in advance. The criterion to be fulfilled for inclusion was that the individuals to be recruited had been diagnosed with significant overweight (defined as BMI > 25 kg/m²) by a physician or other healthcare professional during the last two years.
In summary, we selected 32 subjects with the highest reported body weight from the abovementioned pool of 42 interested test subjects and recruited them for the study. Choosing the subjects with the highest reported weight was a pragmatic decision, as we felt the likelihood of obtaining valuable information on the topic at hand was greatest. Correspondingly, we had a preference for obese and severely overweight patients according to the focus of the study. The limitation to 32 interviews was, first, due to the nature of the qualitative-exploratory study; secondly, the resources in the project were limited; thirdly, the pool of available subjects was also comparatively small.
Procedure and sample
All interviews were conducted in rotation by the authors in the time between April and October 2022. In addition to one telephone interview, the option of conducting an interview via chat was also offered. The idea was that, overweight and obesity being a socially sensitive topic, respondents would be more willing to provide truthful information about their situation and experiences with medical care when guarded by the greater anonymity provided by a chat interview. Ultimately, 20 individuals chose in favour of a telephone interview, whereas in 12 cases interviews were conducted via chat. The interviews lasted between 35 and 65 min.
In advance, the respondents were informed about the topic of the interview and received an informed consent form. The latter included the assurance of strict pseudonymisation as well as deletion of the conversation recordings or chat protocols after completion of the evaluation.
Table 1 shows the sample obtained:
Ethics approval and consent to participate
During this study, no patient data was gathered or clinical tests performed. All 32 individual interviews were strictly pseudonymised. The Ethics Commission of the State of Rhineland-Palatinate, Germany, informed us that approval by an ethics committee was not necessary for a study that does not involve patient data.
Written informed consent for participation and the recording was obtained from all participants before the start of the study.
Data analysis
The transcripts created after data collection were evaluated in teamwork by applying a qualitative content analysis according to Mayring [ 37 ] (using MAXQDA software). First, we elaborated the meaningful basic statements, then we further abstracted and summarised them until a system of categories was finally created which was closely oriented to the guideline. It was repeatedly checked and, if necessary, modified as the evaluation progressed. Our focus was set on a logical categorisation of the different experiences, perspectives and needs. COREQ was used as the reporting statement [ 38 ].
The category system we created is divided into five main categories (subcategories in brackets):
Role of the GP in the care and treatment of patients with obesity problems (a) competences of the GP; b) readiness to accept and implement the recommendations given by the GP).
Experiences with care provided by the GP (a) reason for weight counselling; b) initiator of weight counselling; c) interval or regularity of weight counselling)
Subjects of weight counselling: (a) identification of causes; b) information about overweight consequences; c) agreement on weight-loss goals/strategies; d) therapy plan and success criteria; e) dietary counselling; f) exercise counselling; g) other services or assistance)
Satisfaction with care provided by the GP (a) assessment of behaviour and communication; b) assessment of time commitment; c) consideration of the patient’s own ideas; d) assessment of the weight loss concept; e) physician responses and goal adjustment; f) implications for the patient’s own motivation; g) implementation and success of weight loss)
Articulation of care needs (a) focus and nature of primary care physician support; b) starting points for improvement; c) promotion of physician-patient relationship and motivation).
Theoretical saturation became apparent after 24 interviews. Regardless, we had set the condition that all arranged 32 interviews should be carried out.
Role of general practitioners in the care and treatment of obesity
In principle, all respondents considered the GP to be the right contact person to advise patients in matters of prevention of overweight and related risk factors, and the one to take therapeutic measures if necessary. Many respondents emphasised that the GP is in the best position to “pick up patients at their own situation” (I-2 m) and to support them in their overweight management on the basis of an established relationship of trust in the long term.
“I believe that the general practitioner is the best possible authority to turn to, for only he/she knows me well enough and is aware of the problems I have. He/she is who I trust most.” (I-10f) .
In the opinion of most respondents (24), the advice and assistance given by their GPs was of greater importance than the recommendations of other physicians or health professionals when it came to achieving weight loss and promoting a healthy lifestyle.
Experiences with general practitioners
In the course of the interviews, we identified several problem areas of GP care provision of people with obesity (see Fig. 1 ).
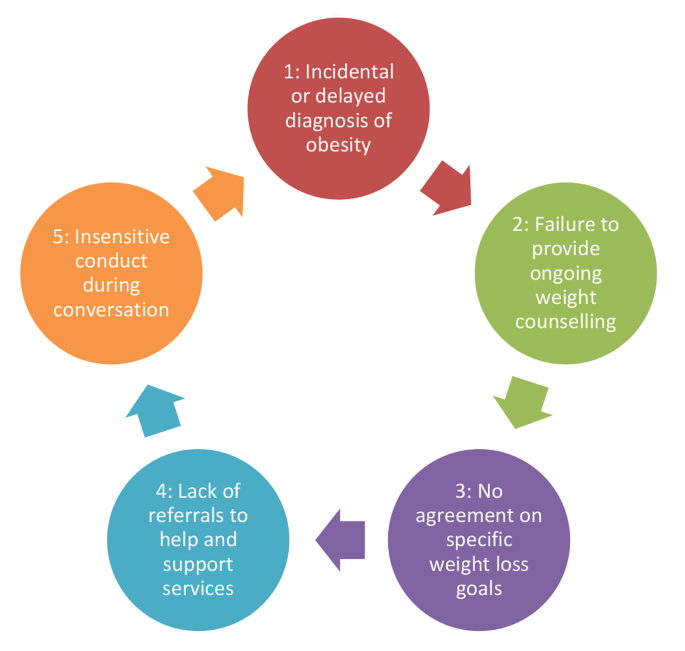
Identified problem areas of obesity care provided by general practitioners
30 of the 32 respondents stated that they had already discussed their weight with their current or a previous GP. In some cases, check-up examinations were mentioned as occasions for weight counselling, participation in a disease management programme or a treatment of diabetes were also mentioned in individual cases. The majority, however, stated that there had been no specific reason and that weight had been discussed rather casually (see Fig. 1 , point 1).
“The fact that we came to talk about my overweight was more or less coincidental. It was not actively controlled now.“ (I-18f) .
18 respondents stated that the doctor originally had taken the initiative and brought up the subject of obesity; whereas 12 other persons had consulted the GP.
“I have been consulting my general practitioner for a long time, but he has never approached me openly about the subject. […] We just stumbled upon it at some point.“ (I-22f) .
According to statements made by 12 persons, weight counselling took place once, for 6 persons more often than once, and 12 respondents stated that overweight issues had become a recurring topic of conversation since it had been brought up the first time. However, a majority (20) admitted that conversations about the weight situation had taken place earlier or very irregularly and that it often had not been foreseeable for them when the topic would come up again (see Fig. 1 , point 2).
Issues of weight counselling
In almost all cases (28), the GPs emphasised the negative consequences of obesity. After the overweight had been identified, some of the physicians (14) were also concerned to find out possible causes so that individual needs could be better addressed.
“No, he didn’t ask more specifics on that. He then very quickly moved on to the recommendation.“ (I-18f) .
Based on the agreement between physician and patient that weight reduction should be aimed for, a majority (22) described that a moderate reduction in weight was recommended with the goal of maintaining the new weight. However, only 6 individuals reported that specific goals were agreed upon. Most often. the time frame in which progress should be made also remained an open question (see Fig. 1 , point 3).
Twenty-four respondents stated that general dietary counselling had been provided. The physicians frequently had recommended a low-calorie diet and given specific advice such as avoiding certain foods or substituting certain products (“lots of vegetables, little meat”). Other patients had been advised to reduce the amount of food they ate and change their eating rhythm (“regular eating habits”), or even their ‘eating culture’ (“conscious eating”). In individual cases (6), the GP would hand out a diet plan. In two cases, an app specifically for dietary change had been recommended. Beyond the actual consultation and isolated measures such as diet plans, the physicians rather rarely recommended additional help and support services. 6 persons mentioned referrals to dietary counselling, health insurance offers, self-help groups, special cooking courses or spa stays.
While nutrition was addressed comparatively often, only a smaller number of respondents recalled exercise counselling. Beyond general references to the importance of regular exercise, 10 respondents described suggestions for physical activities (e.g., getting an exercise bike, joining a cardiac sports group, swimming, walking). Hardly any concrete suggestions were made concerning the frequency and intensity of physical activities. 4 persons stated that the GP had referred them to concrete offers of help (e.g., health fitness centres, courses offered by community colleges).
Satisfaction with general practitioner care
Most respondents (18) positively rated that the GP had principally signalled their willingness to help, had pointed out the risk factors of being too overweight and had responded to queries. In addition, a partnership-like relationship was praised (16).
“The trust level is just very high, yes. So the preconditions are already fulfilled.“ (I-6 m) .
However, many respondents criticised the care which their GPs actually provided. In particular, they strongly expressed that no continuous guidance had taken place; often one or two relatively short conversations on the subject of overweight was all they had (see Fig. 1 , point 2).
“ It was kind of like this: ‘Once and then never again.‘ It just didn’t amount to much that way. There was nothing like continuous care worth mentioning.“ (I-14 m) .
Another widespread point of criticism, also voiced by those respondents for whom the GP had suggested specific measures for weight reduction, had to do with the absence of success criteria. Since there had been no goals to be achieved beyond general recommendations, they had lacked an orientation benchmark and a motivating element (see Fig. 1 , point 3).
“ It would have helped me a lot if I had known when to achieve what. I mean goals that are set specifically for you.“ (I-24 m) . “In what time should I achieve what and how? These questions have not been clarified exactly. And if you lack that, then you don’t have a compass when you lose weight. […] Then the whole thing is quickly doomed to failure.“ (I-28f) .
According to their own statements, ten respondents had been successful in reducing their weight noticeably and sustainably in recent years or months. This is attributed to the support of the GP by 4 persons. A huge number of the respondents (18) refer to what they see as a lack of therapeutic support. Apart from general counselling, there had been a “lack of a coherent, clear concept [of] how the pounds should fall off” (I-2 m).
“You can’t call it therapy. Just a ‘you should do this and could do that’” (I-30m).
In addition, from the point of view of a majority of the respondents (20), the GPs made too few complementary offers in the process of care as to what help and support options were available for continuous weight loss and an increase in fitness in the local vicinity (see Fig. 1 , point 4).
“No, there was far too little coming. It seemed to me that he didn’t know much about such courses either, like what kind of possibilities existed.“ (I-18f) . “I felt a bit fobbed off. ‘Take some kind of course’. Which one? What? Where is there something here?“ (I-30 m) .
Ten respondents mentioned that they felt that there had occasionally been a lack of empathy on the part of GPs when dealing with the weight situation (see Fig. 1 , point 5). Situations were described in which rude, arrogant or insulting behaviour on the part of the physicians became apparent. In two cases, this stigmatising behaviour resulted in the termination of the physician-patient relationship.
“I felt that he was cracking little jokes on me, saying something like: everything will soon collapse under you should you go on like this.“ (I-20f) .
In addition, a widespread passivity of physicians has been described (14), which had led to patients feeling left alone with their weight problem. This is partly associated with negative attitudes of practitioners towards people with obesity (6).
“Patients like us have experienced this before […]: Physicians who do not give us much credit. The fat ones can’t get it together, they just can’t stop eating.“ (I-14 m) .
Regardless of the care actually experienced, the majority of the respondents favoured a proactive approach by GPs when dealing with overweight patients. An open but polite and sensitive approach was advocated.
Central to almost all interviewees are continuous discussions that serve to provide ongoing advice and, not least, motivation. The intervals should ideally be a few weeks in order, for example, to be able to analyse reasons for failure in good time and to try out new approaches.
“If there are no such deadlines, then you quickly lose sight of it and let things slide. You have to keep at it regularly to overcome your weaker self.“ (I-10f) .
The respondents attached great importance to agreeing on tangible goals (weight to be reduced, time periods) and measures. In doing so, action steps should be chosen to accommodate patients’ sensitivities and interests.
“I would like to enrol in a structured diet or exercise programme, teaching me how to lose weight slowly but surely. And also goals that I can measure myself against.“ (I- 28f) .
Respondents articulated a desire for referrals or referrals to help, whether it be health insurance options, fitness classes, or support groups. The GP is seen as a good platform from which to raise awareness of such flanking offers.
“If my GP recommended such a course to me, I would definitely be much more likely to accept it than if I had heard about it somewhere else.“ (I-30 m) .
Main findings and comparison with prior work
The interviews revealed that people with obesity and overweight consider GPs as key contacts in matters of advice, support and therapy. GPs are associated with the potential to appropriately and continuously address the individual needs of appropriate patients. Based on these assumptions, a considerable proportion of respondents signalled an increased willingness to lose weight when the GP provided counselling, motivation, and referrals [ 13 , 30 , 31 ]. Based on the agreement between GP and patient that weight reduction should be aimed for, a majority described that a moderate reduction in weight was recommended with the goal of maintaining the new weight. Overall, there are no significant differences in our sample between key socio-demographic characteristics such as gender, age or living environment.
Despite these fundamentally positive perceptions of the role of GPs, the study results reveal a number of deficiencies. For example, problems of obesity are often identified rather casually or are addressed with a delay. In addition, many patients experience it as problematic that there is hardly any regular exchange about their own weight situation and that GPs often limit themselves to giving a quite generalised advice on diet and/or exercise. In many cases, the fact that no specific weight loss goals have been agreed upon was perceived as a considerable deficit affecting the patient’s own orientation and motivation. In addition, people with obesity were referred to existing support services in a rather situation-dependent manner. In individual cases, the physician-patient relationship was encumbered by the insensitive behaviour of some physicians, which induced the patients concerned to assume that their physicians doubted that their patients could muster the necessary discipline. Of those respondents who stated that they had recently been able to reduce their weight sustainably, only a small number attributed this success mainly to the support they had received from their GP.
The results fit into the body of evidence that obesity is a polarising condition among physicians and varying degrees of willingness to provide care can be encountered [ 6 , 10 , 11 , 27 , 28 ]. Previous studies have indicated that GPs often shy away from assuming an active role in obesity management. Reasons for this are seen to exist in a lack of time and resources, but a lack of patient motivation is also assumed [ 25 , 36 ]. Also of importance is that many GPs feel left to their own devices in a task as comprehensive and long-term as obesity care. Various studies revealed that GPs complain about a deficit of existing structures, which results in a lack of individualisable therapy concepts in which patients can be continuously supported by the GP in the process of their lifestyle change [ 15 , 26 , 32 , 34 ]. In addition, it has been shown that knowledge of locally available help and support services to which referrals can be made is often limited, and only a smaller proportion of physicians make consistent use of them, for example, by referring to fitness and exercise providers or psychotherapists [ 32 , 33 ].
It is noticeable that these are largely conservative therapeutic approaches that GPs take or recommend.In this context, it could be discussed why main causes related to eating and physical activity were addressed. Obesity is a complex disease, often characterized by comorbidities, that should be treated multidisciplinary [ 9 , 10 , 11 ]. Various studies and scoping reviews provide evidence that the focus of GPs on nutrition and exercise therapies may have something to do with the (latent) stigmatisation of people with obesity as mentioned in the introduction [ 6 , 14 , 20 ]. Within the sample, best practice examples can be found for motivational consultation and the effort to engage with patients in their personal situation. Such behavioural treatment strategies can play a central role in long-term treatment outcomes [ 33 , 34 ]. Nevertheless, the doctors’ prescribing behavior implies that, from their perspective, it is almost exclusively about patients working on themselves, whereas more complex interactions between health and social factors tend to be ignored [ 17 , 21 ]. In this respect, it would be advisable to sensitize GPs so that they are as open as possible to complex causes of obesity and, accordingly, to multi-perspective solutions.
Recent studies emphasised the great value and indispensability of primary care for weight problems in order to effectively encounter the global spread of overweight and obesity [ 39 ]. This was accompanied by a greater inclusion of patient needs, interests, and experiences, which can contribute to greater activation, self-determination, and longer-term weight loss success [ 40 ]. It seems particularly important that weight loss goals are realistic and achievable [ 20 ].
Implications
From the results of the present study and in connection with further studies, various implications for future research and interventions can be derived. The goal is to specifically optimise primary care support for people with obesity.
Some GPs tend to see the causes of obesity in the patient’s personality. Therefore, it seems advisable to raise awareness among GPs that obesity can have as complex background involving factors such as life circumstances and pre-existing conditions [ 2 , 3 , 5 ].
GPs should be encouraged in their role as mediators by referring their patients to an extended healthcare network including psychotherapists or dietary assistants [ 41 ]. For example, health authorities often provide a useful guide to the local training and consultation services available.
Accordingly, developing structured care programmes for obesity management seems sensible. These programmes should not only aim towards improving patient care but also training for GPs and their practice staff. International model projects may provide guidance and could be adapted to suit the specific situation [ 41 – 44 ].
Ideally, GPs should be placed in a position where they can fulfil two main tasks – individual consultation and treatment as well as coordination within a multidisciplinary obesity care network [ 41 , 45 ].
Strengths and weaknesses
A qualitative survey has several limitations that should be taken into consideration.
This study was based on self-reported height and weight (BMI), so that incorrect information cannot be ruled out.
The investigation carried out was a non-representative study with a small sample that is not representative of the entirety of primary care patients with a severe degree of obesity. Accordingly, the weakness of this study is the small sample of the population surveyed and with a low degree of obesity since the majority of the population surveyed is overweight.
The recruitment via online forums made it likely that a specific group with needs of specific information and discussion had been recruited for the sample. According to the authors’ impression, the ultimately recruited group showed an overall high interest in being systematically attended and medically advised by their GPs. At the same time, this type of recruitment was a good way to obtain patients who were willing to talk as openly as possible about their problems of overweight and obesity care as provided by GPs.
More than one-third of the interviews were not conducted by telephone, but by chat. It seems obvious that contributions in chat communication do not allow for the same possibilities of articulation and interaction as oral interviews do. In this respect, it should be considered that information might have been lost or simplified here.
Conclusions
Despite the favourable conditions of the primary care setting, the interviews provide evidence that the potential of primary care for overweight and obesity management is currently not being fully exploited. The following starting points for optimisation therefore seem advisable:
Overweight problems should be addressed systematically, consistently and promptly in primary care. Useful occasions are, for example, medical check-ups.
The identification of severe overweight or obesity should be linked to concrete recommendations for action and realistic, individually coordinated targets. Here, existing guidelines provide further assistance and orientation [ 42 ].
Focused nutrition and physical activity counselling in primary care practices appears to be a useful contribution to support obesity prevention. Good practice examples and models have already been presented in this regard [ 46 ]. Practice staff could be involved in a supportive manner and receive targeted further training, so that GPs can be relieved by delegation.
Regular, binding discussions and efforts to ‘pick up’ patients from their personal situation (behaviour-oriented treatment strategies) and to motivate them continuously are important prerequisites for the long-term success of obesity management [ 47 ].
It seems advisable to raise awareness among family physicians that obesity can have complex backgrounds, in which not only the individual lifestyle, but also life circumstances, genetic predisposition and pre-existing conditions are effective.
Family physicians should be encouraged in their role as mediators by integrating people with obesity into further help networks as needed. Almost all statutory health insurers offer prevention programmes; the same applies to health offices, which often have a good overview of courses and counselling offers in the district [ 27 ]. Municipal cooperation networks for health promotion could account for great added value in providing GPs with an overview of existing health services and in referring patients in a targeted manner [ 47 , 48 ].
The development of structured, GP-based care programmes for obesity management seems to make sense.
Data availability
Data from this research are not publicly available because participants did not give permission for recordings or transcripts to be released to other researchers.
Abbreviations
General Practitioner
The GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27. https://doi.org/10.1056/NEJMoa1614362 .
Article Google Scholar
Klein S, Krupka S, Behrendt S, et al. editors. Weißbuch Adipositas – Versorgungssituation in Deutschland (White paper on obesity - the health care situation in Germany). Berlin: MVG; 2016.
Google Scholar
Mensink GB, Lampert T, Bergmann E. Overweight and obesity in Germany 1984–2003. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2005;48(12):1348–56. https://doi.org/10.1007/s00103-005-1163-x .
Article CAS PubMed Google Scholar
Prospective Studies Collaboration. Body-Mass-Index and cause specific mortality in 900000 adults: collaborative analysis of 57 prospective studies. Lancet. 2009;373(9669):1083–96. https://doi.org/10.1016/S0140-6736(09)60318-4 .
Article PubMed Central Google Scholar
Anderson DA, Wadden TA. Treating the obese patient. Suggestions for primary care practice. Arch Fam Med. 1999;8(2):156–67. https://doi.org/10.1001/archfami.8.2.156 .
Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17(5):1–24. https://doi.org/10.1038/oby.2008.636 .
WHO Europe. The challenge of obesity in the WHO European Region and strategies for response. Kopenhagen; 2007.
Semlitsch T, Stigler F, Jeitler K, et al. Management of overweight and obesity in primary care-A systematic overview of international evidence-based guidelines. Obes Rev. 2019;20(9):1218–30. https://doi.org/10.1111/obr.12889 .
Durrer Schutz D, Busetto L, Dicker D, et al. European practical and patient-centred guidelines for adult obesity management in primary care. Obes Facts. 2019;12(1):40–66. https://doi.org/10.1159/000496183 .
Article PubMed PubMed Central Google Scholar
Whitlock EP, Orleans CT, Pender N, et al. Evaluating primary care behavioral counseling interventions. Am J Prev Med. 2002;22(4):267–84. https://doi.org/10.1016/s0749-3797(02)00415-4 .
Brown I, Thompson J, Tod A, et al. Primary care support for tackling obesity: a qualitative study of the perceptions of obese patients. Br J Gen Pract. 2006;56(530):666–72.
PubMed PubMed Central Google Scholar
van Dijk L, Otters HB, Schuit AJ. Moderately overweight and obese patients in general practice: a population based survey. BMC Fam Pract. 2006;7:43. https://doi.org/10.1186/1471-2296-7-43 .
Loureiro ML, Nayga RM. Obesity, weight loss and physician‘s advice. Soc Sci Med. 2006;62(10):2458–68. https://doi.org/10.1016/j.socscimed.2005.11.011 .
Article PubMed Google Scholar
Bocquier A, Verger P, Basdevant A, et al. Overweight and obesity: knowledge, attitudes, and practices of general practitioners in France. Obes Res. 2005;13(4):787–95. https://doi.org/10.1038/oby.2005.89 .
Brotons C, Ciurana R, Pineiro R, et al. Dietary advice in clinical practice: the views of general practitioners in Europe. Am J Clin Nutr. 2003;77(4 Suppl):1048S–51. https://doi.org/10.1093/ajcn/77.4.1048S .
Huang J, Yu H, Marin E, et al. Physicians‘ weight loss counseling in two public hospital primary care clinics. Acad Med. 2004;79(2):156–61. https://doi.org/10.1097/00001888-200402000-00012 .
Jay M, Kalet A, Ark T, et al. Physicians’ attitudes about obesity and their associations with competency and specialty: a cross-sectional study. BMC Health Serv Res. 2009;9:106. https://doi.org/10.1186/1472-6963-9-106 .
Al-Ghawi A, Uauy R. Study of the knowledge, attitudes and practices of physicians towards obesity management in primary health care in Bahrain. Public Health Nutr. 2009;12(10):1791–8. https://doi.org/10.1017/S1368980008004564 .
Brown I, Thompson J. Primary care nurses’ attitudes, beliefs and own body size in relation to obesity management. J Adv Nurs. 2007;60(5):535–43. https://doi.org/10.1111/j.1365-2648.2007.04450.x .
Rathomi H, Dale T, Mavaddat N, et al. General Practitioners‘ knowledge, attitudes, and Practices of Dietary Advice for Weight Control in their overweight patients: a scoping review. Nutrients. 2023;15(13):2920. https://doi.org/10.3390/nu15132920 .
Schwenke M, Luppa M, Pabst A, et al. Attitudes and treatment practice of general practitioners towards patients with obesity in primary care. BMC Fam Pract. 2020;21(1):169. https://doi.org/10.1186/s12875-020-01239-122 .
Teixeira FV, Pais-Ribeiro JL, Maia A. A qualitative study of GPs’ views towards obesity: are they fighting or giving up? Public Health. 2015;129(3):218–25. https://doi.org/10.1016/j.puhe.2015.01.004 .
Ogden J, Baig S, Earnshaw G, et al. What is health? GPs and patients worlds collide. Patient Educ Couns. 2001;45(4):265–9. https://doi.org/10.1016/s0738-3991(01)00128-8 .
Ogden J, Flanagan Z. Beliefs of the causes and solutions of obesity: A comparison of GPs and lay people. Patient Educ Couns 2008; 71(1): 72–78. DOI: 0.1016/j.pec.2007.11.022.
Sonntag U, Brink A, Renneberg B, et al. GPs‘ attitudes, objectives and barriers in counselling for obesity – a qualitative study. Eur J Gen Pract. 2011;18(1):9–14. https://doi.org/10.3109/13814788.2011.627424 .
Ärzte Zeitung. Krankenkassen fordern mehr strukturierte Behandlungsprogramme (Health insurance companies are demanding more structured treatment programs). 2018. https://www.aerztezeitung.de/medizin/krankheiten/adipositas/article/955042/adipositas-krankenkassen-fordern-strukturierte-behandlungsprogramme.html . Accessed 21 March 2023.
Herbers J. Der Hausarzt als ‚Abnehm-Coach‘ (The general practitioner as a ‘weight loss coach’) 2013. https://www.allgemeinarzt-online.de/archiv/a/der-hausarzt-als-abnehm-coach-1571807 . Accessed 21 March 2023.
Metz U, Welke J, Esch T, et al. Perception of stress and quality of life in overweight and obese people – implications for preventive consultancies in primary care. Med Sci Monit. 2009;15(1):1–6.
Fogelman Y, Vinker S, Lachter J, et al. Managing obesity. A survey of attitudes and practices among Israeli primary care physicians. Int J Obes Relat Metab Disord. 2002;26(10):1393–7. https://doi.org/10.1038/sj.ijo.0802063 .
Article CAS Google Scholar
Tan D, Zwar NA, Dennis SM, et al. Weight management in general practice: what do patients want? Med J Aust. 2006;185(2):73–5. https://doi.org/10.5694/j.1326-5377.2006.tb00474.x .
Klumbiene J, Petkeviciene J, Vaislavavicius V, et al. Advising overweight patients about diet and physical activity in primary health care: Lithuanian health behaviour monitoring study. BMC Public Health. 2006;6:30–6. https://doi.org/10.1186/1471-2458-6-30 .
Ruelaz A, Diefenbach P, Simon B, et al. Perceived barriers to weight management in primary care- perspectives of patients and providers. J Intern Med. 2007;22(4):518–22. https://doi.org/10.1007/s11606-007-0125-4 .
Tham M, Young D. The role of the General Practitioner in weight management in primary care – a cross sectional study in General Practice. BMC Fam Pract. 2008;9:66. https://doi.org/10.1186/1471-2296-9-66 .
Greiner KA, Born W, Hall S, et al. Discussing weight with obese primary care patients: physicians and patient perceptions. J Gen Intern Med. 2008;23(5):581–7. https://doi.org/10.1007/s11606-008-0553-9 .
Simkin-Silverman LR, Gleason KA, King WC, et al. Predictors of weight control advice in primary care practices: patient health and psychosocial characteristics. Prev Med. 2005;40(1):71–82. https://doi.org/10.1016/j.ypmed.2004.05.012 .
Wangler J, Jansky M. Einstellungen Von Hausärzten Zum Adipositasmanagement – Ergebnisse Einer Qualitativen Interviewreihe in Rheinland-Pfalz und Hessen (attitudes of general practitioners towards obesity management – results of a qualitative interview series in Rhineland-Palatinate and Hesse). Z Allg Med. 2020;96(4):159–65. https://doi.org/10.3238/zfa.2020.0159-0165 .
Mayring P. Qualitative inhaltsanalyse. Grundlagen Und Techniken. Weinheim: Beltz; 2010.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health C. 2007;19(6):249–357. https://doi.org/10.1093/intqhc/mzm042 .
Jansen S, Desbrow B, Ball L. Obesity management by general practitioners: the unavoidable necessity. Aust J Prim Health. 2015;21(4):366–8. https://doi.org/10.1071/PY15018 .
Sturgiss E, Jay M, Dampbell-Scherer D, et al. Challenging assumptions in obesity research. BMJ. 2017;359:j5303. https://doi.org/10.1136/bmj.j5303 .
Gstettner A, Holzapfel C, Stoll J, et al. Weight reduction: evaluation of options in primary care and patient satisfaction. Dtsch Med Wochenschr. 2013;138(19):989–94. https://doi.org/10.1055/s-0033-1343164 .
Wadden TA, Volger S, Sarwer DB, et al. A two-year randomized trial of obesity treatment in primary care practice. N Engl J Med. 2011;365(21):1969–79. https://doi.org/10.1056/NEJMoa1109220 .
Article CAS PubMed PubMed Central Google Scholar
Osmundsen TC, Dahl U, Kulseng B. Enhancing knowledge and coordination in obesity treatment: a case study of an innovative educational program 2019. BMC Health Serv Res. 2019;19(1):278. https://doi.org/10.1186/s12913-019-4119-9 .
Sturgiss E, Haesler EM, Elmitt N, et al. Increasing general practitioners’ confidence and self-efficacy in managing obesity: a mixed methods study. BMJ Open. 2017;7(1):e014314. https://doi.org/10.1136/bmjopen-2016-014314 .
Holmberg C, Sarganas G, Mittring N, et al. Primary prevention in general practice - views of German general practitioners: a mixed-methods study. BMC Fam Pract. 2014;15(1):103. https://doi.org/10.1186/1471-2296-15-103 .
Lau D, Klein R, Steinkohl M. Prevention through focused nutritional advice in general practice. Z Allg Med. 2003;79(5):234–7.
Wiesemann A, Barlet J, Engeser P, et al. Verhaltensorientierte Beratungsstrategien für die Hausarztpraxis (Behavior-oriented counseling strategies for general practitioners). Z Allg Med. 2006;82(3):103–7.
Prüfer F, Joos S, Milksch A. Die Rolle Des Hausarztes in Der Kommunalen Gesundheitsförderung (the role of the general practitioner in community health promotion). Prävention Und Gesundheitsförderung. 2015;10(2):180–5. https://doi.org/10.1007/s11553-015-0486-1 .
Download references
Acknowledgements
Not applicable.
This research was not funded.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
University Medical Center of the Johannes Gutenberg University Mainz, Centre for General Medicine and Geriatrics – Mainz, Mainz, Germany
Julian Wangler & Michael Jansky
You can also search for this author in PubMed Google Scholar
Contributions
The authors alone are responsible for the content and the writing of the paper.JW prepared, coordinated and implemented the project. Both JW and MJ contributed to the project design, analysis of transcripts and drafting of the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Julian Wangler .
Ethics declarations
During this study, no patient data was gathered or clinical tests performed. All 32 individual interviews were strictly pseudonymised. The Ethics Commission of the State of Rhineland-Palatinate, Germany, informed us that approval by an ethics committee was not necessary for a study that does not involve patient data. Written informed consent for participation and the recording was obtained from all participants before the start of the study.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wangler, J., Jansky, M. How are people with obesity managed in primary care? – results of a qualitative, exploratory study in Germany 2022. Arch Public Health 81 , 196 (2023). https://doi.org/10.1186/s13690-023-01214-z
Download citation
Received : 06 April 2023
Accepted : 03 November 2023
Published : 13 November 2023
DOI : https://doi.org/10.1186/s13690-023-01214-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- General practitioner
Archives of Public Health
ISSN: 2049-3258
- General enquiries: [email protected]
Data and case studies
Resources Policy Dossiers Obesity & COVID-19 Data and case studies
- Sugar-Sweetened Beverage Tax
- Digital Marketing
- School-based interventions
- Community-level interventions
- Pregnancy & Obesity
- Childhood Obesity Treatment
- Front-of-pack nutrition labelling
- Obesity & COVID-19
- Physical Activity
- Food Systems
- Weight Stigma
World Obesity have collated some of the recent data and case studies available looking pertaining to obesity and the current outbreak of COVID-19.
Researchers at Johns Hopkins University in the US examined 265 patients to determine if younger patients hospitalised with COVID-19 were more likely to be living with overweight and obesity. They found a correlation, which they hypothesise may be due to physiologic changes from obesity. Other comorbidities these patients may have had were not reported. Read the full study here .
Chinese researchers identified 66 patients with COVID-19 and fatty liver disease and compared the outcomes for those with and without obesity. They found obesity was a significant risk factor for severe illness in this population after accounting for other factors (age, gender, smoking, diabetes, high blood pressure, and dyslipidaemia). Read the full study here .
The global rise in the prevalence of obesity and type 2 diabetes can be partially explained by a rise in diets high in fats, sugars and refined carbohydrates. Diets high in saturated fatty acids cause inflammation and immune disfunction, which may explain why minority groups (who experience disproportionate rates of diseases linked to nutrition, such as obesity and diabetes) are also hospitalised with COVID-19 at higher rates. Read the full study here .
MicroRNAs (abbreviated miRNAs) are produced in human cells to regulate gene expression. Some research has suggested that these may also defend against viruses. These researchers identified 848 miRNAs that are may be effective against SARS and 873 that could target COVID-19 using genome sequences of each of these viruses. Previous studies have suggested that the elderly and those with underlying conditions (including obesity) may produce less of these miRNAs, possibly explaining why these groups are at increased risk of severe illness from COVID-19. However, trials in human and animal subjects are needed to verify these theoretical results. Read the full study here .
Given the importance of determining the risk factors for morbidity and mortality related to COVID-19, this retrospective study analysed the frequency and outcomes of COVID-19 patients in critical care who are living with overweight or obesity. “Of the 3,615 individuals who tested positive for COVID-19, 775 (21%) had a body mass index (BMI) 30-34, and 595 (16% of the total cohort) had a BMI >35.” While patients were separated into elderly (over 60) and younger (under 60) groups, it was not reported if the study controlled for other variables that may affect the course of COVID-19. Read the full study here .
This piece describes two patients with obesity that experienced damage to their airways while being intubated due to severe illness from COVID-19. The authors recommend videolaryngoscopy for intubation to protect both patients and healthcare workers. Read the full study here .
These researchers chose to specifically examine how many COVID-19 patients living with obesity or overweight were placed on ventilators. Based in Lille, France, the study included 124 patients, 68.8% of whom ultimately required ventilation. They established a dose-response relationship- increasing body max index (BMI) increased the risk of needing ventilation. This study found that BMI seemed to be associated with ventilator treatments independently of age, diabetes or high blood pressure. However, further research must be conducted before this relationship is proven. Read the full study here .
Researchers obtained medical records of 16,749 people hospitalised for COVID-19 to determine what were some of the factors that made patients more likely to experience severe cases of the illness. Slightly over half of patients had at least one underlying condition (including obesity) and these patients were more likely to die from COVID-19. The study found that obesity is linked to mortality, independently of age, gender and other associated conditions. Read the full study here .
Using a very large sample size of 17,425,455, this cohort study aimed to identify risk factors associated with mortality due to COVID-19 across the general population. Among the comorbidities, most of them were associated with increased risk, including obesity. Furthermore, deprivation was also identified as a major risk factor. Specifically, for patients with overweight and obesity, as their body mass index increased, so did their risk of dying from COVID-19. Read the full study here .
This study included 48 critically ill patients with COVID-19 treated with invasive ventilation in Spain. Of this population, 48% were living with obesity, 44% with hypertension, and 38% with chronic lung disease. Symptoms and patient outcomes were also described. Read the full study here .
This study examined the correlation between severe disease and body mass index (BMI) among 357 patients in France. People diagnosed with severe COVID-19 were 1.35 times more likely to also be living with obesity and people in critical care with COVID-19 were 1.89 times more likely to be living with obesity than the general public. This study adjusted for age and gender of patients but no other cofounding factors. Read the full study here .
Previous research has demonstrated that children tend to gain weight during when school is not in session, so experts have been concerned about the impact of lockdowns due to coronavirus on childhood obesity rates. This study observed lifestyle behaviours in 41 children living with obesity at baseline and then three weeks into quarantine. Scientists found that children reported eating more meals, as well as more potato chips, red meat, and sugar-sweetened beverages. They slept more, exercised less and spent much more time looking at screens. As a result, researchers recommend that lifestyle interventions be delivered through telemedicine while the lockdown lasts. Read the full study here .
A recent study from France examined 1317 COVID-19 patients living with diabetes. Of these, more than 10% passed away and almost 33% needed to be placed on a ventilator within a week of admission to the hospital. Obesity was found to be an independent risk factor for poor outcomes when other cofounding factors were accounted for. Read the full study here .
This study found that, of 5700 patients admitted to 12 selected New York hospitals with COVID-19, 56.6% had hypertension (high blood pressure), 41.7% were living with obesity and 33.8% had diabetes. It also reported data on patient outcomes. Read the full study here .
Wuhan city, the capital of Hubei province in China, was for a long time the epicentre of the COVID-19 outbreak. This study presents information of patients admitted to two Wuhan hospitals with laboratory-confirmed COVID-19. 191 patients were included in order to determine what risk factors lead to fatalities, describe Covid-19 symptoms over time, determine how long patients are infectious after they recover and record what treatments were tried. It should be noted that almost half of patients had underlying health conditions such as hypertension or heart disease, although obesity was not measured. Read the full study here .
This study examined 24 adults to determine which populations in the Seattle area were hospitalised with severe illness from COVID-19, what underlying conditions they had, the results of medical imaging tests and whether they recovered. Patients had an average body mass index of 33.2 (give or take 7.2 units) and over half (58%) of patients were diagnosed with diabetes. Scientists concluded that “patients with coexisting conditions and older age are at risk for severe disease and poor outcomes after ICU [intensive care unit] admission.” Read the full study here .
Looking at 383 patients in Shenzen, China, this study was the first to directly examine the correlation between obesity and severe illness from coronavirus. For this study, a person with a body mass index (BMI) between 24.0 - 27.9 was considered overweight and a person with a BMI greater than 28 was considered to be living with obesity. While people living with obesity generally experienced the same length of illness, they were significantly more likely to develop severe pneumonia, even when accounting for other risk factors. Read the full study here .
Based on a sample of 4,103 New York City residents, this paper evaluates what characteristics make people more likely to be admitted to the hospital and critical care. Overall, it was observed that 39.8% of people living with obesity were hospitalised, compared to 14.5% without. Scientists found “particularly strong associations of older age, obesity, heart failure and chronic kidney disease with hospitalization risk, with much less influence of race, smoking status, chronic pulmonary disease and other forms of heart disease.” Read the full study here .
In order to ensure the proper monitoring of COVID-19-related hospitalisations across the United States, the COVID-19-Associated Hospitalization Surveillance Network (COVID-NET) was developed. This report “presents age-stratified COVID-19-associated hospitalisation rates for patients admitted during March 1-28, 2020, and clinical data on patients admitted during March 1-30, 2020.” Among the 1,482 patients diagnosed and hospitalised with COVID-19, 90% had at least one comorbidity and 42% were living with obesity, with African Americans and the elderly disproportionately affected. Read the full study here .
This report examined demographic information of patients hospitalised with COVID-19 in China. Of these, older patients, diabetics and those living with obesity were significantly more likely to be considered “severely ill.” The study also looked at symptoms during admission at admission and treatment options. Read the full study here .
In this study, researchers used data from 103 consecutive patients hospitalized in the USA. There were two major findings- a correlation between critical care admissions due to COVID-19 and a body mass index greater than 35 in general, and a correlation between needing invasive mechanical ventilation and having both heart disease and obesity. These findings were adjusted for age, sex, and race. Read the full study here .
This article examined how SARS- CoV-2 impacts pregnancy using 46 patients in the USA. Almost all patients who developed severe disease were living with overweight and obesity. After diagnosis, 16% of patients were admitted to the hospital and 2% were placed in intensive care. Researchers believe this, along with the need to induce labour prematurely in some patients to improve breathing, may suggest that pregnant women should be classified as a vulnerable group. Read the full study here .
School and recreational space closures due to COVID-19 have reduced physical activity among children. Researchers used modeling software to simulate the following scenarios:
- No school closures (control)
- Schools closed for two months
- Schools closed for two months and 10% reduction in physical activity over the summer break
- Schools closed for four months (April through May and September through October) and 10% reduction in physical activity over the summer break
- Schools closed for six months (April through May and September through December) and 10% reduction in physical activity over the summer break
Overall, the pandemic is projected to increase mean standardised body mass index (BMI) between 0.056 (two-month closure) and 0.198 (six-month closure) units. It may also increase the percentage of children living with obesity in the USA by up to 2.373 percentage points. Read the full study here .
This study was conducted to examine the characteristics and course of disease in 50 New York children (under 21 years of age) hospitalised with COVID-19. Of the study population, 11 patients had obesity and 8 had overweight. Obesity was found to be a significant risk factor for both severe disease and mechanical ventilation while immunosuppression was not. Read the full study here .
Researchers at the University of Chicago Medical Center found that patients hospitalized with COVID-19 were more likely to die if they were also living with obesity, even when accounting for age, sex, and underlying conditions. 238 patients were included within the study. These researchers did not find a significant connection with admission to critical care units or mechanical ventilation in patients with obesity. Limitations included the makeup of the study population, as the sample size was small and the vast majority were African American, so the results may not be representative of all people. Read the full study here.
This meta-analysis and systematic review found nine separate articles regarding the link between COVID-19, obesity and more severe diseases. Between all studies, 1817 patients were examined. Researchers found an odds ratio of 1.89 for poor outcomes in patients with obesity, especially among younger patients, which indicates that obesity increases the risk of severe diseases. Read the full study here .
A meta-analysis concluded that people living with obesity were more likely to have worse outcomes if they also contracted COVID-19. Researchers identified nine articles (six of which were retrospective case-control studies, four of which were retrospective cohort studies, and one of which used both methods) and extracted data from each. Limitations included heterogeneity in study design (particularly regarding the definition of obesity), lack of comorbidity reporting, and low quantity of studies used. Read the full study here .
As almost 75% of American adults over the age of 20 are living with overweight or obesity, this disease should be considered a public health priority, especially given the increased likelihood of poor outcomes in COVID-19 patients with obesity. The paper outlines several mechanisms explaining why obesity may lead to more severe disease, including having more of the receptor the virus uses to enter cells, reduced lung function, chronic inflammation, endothelial disfunction, changes in blood clotting, and physiological changes related to common comorbidities of obesity. Finally, several compelling studies linking obesity to increased risk of complications are included. Read the full study here .
Evidence shows that the impact of COVID-19 tends to be more serious in specific vulnerable groups, including people living with obesity. Furthermore, the pandemic also seems to have a number of indirect repercussions including on eating behaviour patterns among people with obesity. The objective of this study was “to examine the impact of the COVID-19 pandemic on patronage to unhealthy eating establishments in populations with obesity.”
These researchers combined GPS data with known obesity rates to determine how many people with obesity entered unhealthy restaurants during the COVID-19 pandemic (December 2019- April 2020). Prior to lockdowns, more people in areas with high obesity rates entered fast food restaurants; in March, fewer people did across all areas; however, the numbers of patrons steadily increased during April, at a faster rate in areas with higher obesity rates. While informative, a number of limitations were observed, including the fact that not all consumers exactly match the demographics of the area they live in and that more variables may contribute to restaurant traffic than accounted for here. Read the full study here .
Various studies over the past few months have linked obesity to a more serious course of illness from COVID-19. It is therefore essential that we improve our understanding of the possible reasons for the link and what it means for those living with obesity. This systematic review looks at the influence of obesity on COVID-19 outcomes and proposes biological mechanisms as to why a more severe courseof illness can occur. It also discusses the implications of COVID-19 for those living with obesity. Read the full study here .
Both COVID-19 and childhood obesity are pandemics raging across America today. Obesity is an independent risk factor for the severity of COVID-19, suggesting that children with obesity could see a more severe course of illness due to COVID-19. The stay-at-home mandates and physical distancing preventative measures have resulted in a lack of access to nutritious foods, physical activity, routines and social interactions, all of which could negatively impact children -especially those living with obesity. Read the full study here .
Obesity has been suggested as a risk factor for poor outcome in those with COVID-19. Studies show that patients with obesity are more likely to require mechanical ventilation. In fact, multiorgan failure in patients with COVID-19 and obesity could be dueto the chronic metabolic inflammation and predisposition to the “enhanced release of cytokines-pathophysiology accompanying severe obesity”. However, the association between body mass index (BMI) and COVID-19 outcomes has yet to be fully explored. This study intends to address that gap. Read the full study here .
Emerging evidence suggests that the severity of COVID-19 in a patient is associated with overweight and obesity. Patients with obesity are at risk for a number of other non-communicable diseases, including cardiovascular dysfunction and hypertension and diabetes. In individuals living with overweight and obesity, macronutrient excess in adipose tissue stimulates adipocytes “to release tumour necrosis factor α(TNF-α), interleukin-6 (IL-6) and other pro-inflammatory mediators and to reduce production of the anti-inflammatory adiponectin, thus predisposing to a proinflammatory state and oxidative stress”. Obesity also impairs immune responses; it has a negative impact on pathogen defences within the body. Therefore, the acceleration of viral inflammatory responses in COVID-19 and more unfavourable prognoses are associated with individuals living with obesity. Read the full study here .
Obesity has been identified as a comorbidity for severe outcomes in patients with COVID-19. In this study, comorbidities associated with increased risk of COVID-19 were determined in a population-based analysis of Mexicans with at least one comorbidity. Data was obtained from the COVID-19 database of the publicly available Mexican Ministry of Health “Dirección General de Epidemiología”. Variables of the patients’ heath were all noted, such as age, gender, smoking status, history of COVID-19 contact, comorbidities, etc. Patients with missing information were excluded in the analysis. To determine the independent effect of each comorbidityon COVID-19 and separate the effect of two or more, “analysis was limited to patients reporting only one comorbidity." Read the full study here .
Obesity has arisen as a major complication for the COVID-19 pandemic, which has been caused by the novel SARS-CoV-2 virus. The former is a major health concern due to its side-effects on human health and association with morbidity and mortality. Evidence points out that obesity can worsen patient prognosis due to COVID-19 infection. There may be a “pathophysiological link that could explain the fact that obese patients are prone to present with SARS-CoV-2 complications”. The authors present mechanistic obesity-related issues that aggravate the SARS-CoV-2 infection in patients living with obesity and the possible molecular links between obesity and SARS-CoV-2 infection. Read the full study here .
The highly infectious serious acute respiratory syndrome COVID-19 has caused high morbidity and mortality all over the world. It has been suggested that SARS-CoV-2, the pathogen of COVID-19, uses angiotensin-converting enzyme 2 (ACE2) as a cell receptor. This receptor is found in the lungs but also many other organs, including the adipose tissue, heart, and oral epithelium. Previous studies have identified obesity as a critical factor in the prognoses of COVID-19 patients, and that, in patients with COVID-19, non-survivors had a higher body mass index (BMI) than survivors. This study intended to “investigate the association between obesity and poor outcomes of COVID-19 patients." Read the full study here .
Approximately 45% of individuals worldwide have overweight or obesity. Obesity is characterized by its pro-inflammatory condition. The excess visceral and omental adiposity seen in individuals with obesity are linked with an increase in pro-inflammatory cytokines that affect systemic cellular processes. Importantly, they “change the nature and frequency of immune cells infiltration”. When a high percentage of a population have obesity, more virulent viral strains tend to develop, and the reach of a virus is wider. Furthermore, the state of obesity is correlated to the presence of comorbidities that are dangerous to human health, such as type 2 diabetes and hypertension. This systematic review includes articles from a myriad of databases in order to address how living with obesity impacts one’s reaction to the SARS-CoV-2 virus and course of COVID-19. Read the full study here .
The psychological impact of COVID-19 lockdown and quarantine on children has been documented to cause “anxiety, worrying, irritability, depressive symptoms, and even post-traumatic stress disorder symptoms”. In particular, children living with severe obesity may struggle with anxieties about the possibility of obesogenic issues that can arise during the course of illness due to COVID-19. In this study, 75 families (one child interviewed per family) were interviewed on anxiety that their child with severe obesity may have, and on what specific type anxieties they are. 24 of 75 children reported having COVID-19 related anxieties. Read the full study here .
In this multi-centre study focused on retrospective observational data from eight hospitals throughout Greece, the data on 90 critically ill patients positive for COVID-19 is analysed. Those hospitalised due to COVID-19 reflect critically ill patients whodeveloped extremely severe acute respiratory syndrome (SARS) in elderly patients with COVID-19-related pneumonia and/or underlying chronic diseases. Many underlying chronic diseases have been identified as risk factors for developing more severe COVID-19. These include type-2 diabetes, cardiovascular diseases, and hypertension. Obesity has also been associated with disease severity. In this study the relation of comorbidities such as obesity and type-2 diabetes and COVID-19 disease severity is explored. Read the full study here .
According to the World Health Organisation, physical inactivity is the fourth leading cause of death, and increases the risk of a person contracting a “metabolic disease, including obesity and type 2 diabetes (T2D).” This article points out that those seeking treatment for obesity or T2D may find difficulty in doing so during the COVID-19 pandemic due to lockdowns. As it has been found that sedentary behaviour increases one's risk for many chronic diseases, the authors wished to explore hypothetical immunopathologyof COVID-19 in patients living with obesity and how the immune defences against COVID-19 may be related to the “immuno-metabolic dysregulations'' characterised by it. Furthermore, they explore the possibility of exercise as a counteractive measure due to its anti-inflammatory properties. Read the full study here .
Obesity has been linked to a less-efficient immune response in the human body as well as poorer outcomes for respiratory diseases. In this article, researchers hypothesised that a higher Body Mass Index is a risk factor for a more severe course of illness for COVID-19. They followed all patients hospitalised from 11 January to 16 February 2020 until March 26 2020 at the Third People’s Hospital of Shenzhen (China), which was dedicated to COVID-19 treatment. Read the full study here .
As reported by the World Health Organization, the global prevalence of obesity is still on the rise both across high-income as well as low-and middle-income countries. Obesity has been associated with an increase in mortality for patients fighting COVID-19. The authors suggest that the inflammatory profile associated with patients with obesity is conducive to a more severe course of illness in patients with COVID-19. Read the full study here .
Researchers studying COVID-19, the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), have concluded that obesity, diabetes, hypertension or cardiovascular disease is correlated to an increased severity of illness due to COVID-19. Obesity has been associated with SARS-CoV-2 due to the “cytokine storm” of the latter; a number of the pro-inflammatory cytokines released in the “storm” which are detrimental to organ function are also found contributing to the chronic low-grade inflammation in patients with obesity. The authors wished to study a Middle Eastern population and assess the outcome of COVID-19 in relation to obesity. They observed clinical data from patients in the Al Kuwait Hospital in Dubai, UAE, to study the correlation between obesity and poor clinical outcomes of COVID-19. Read the full study here .
In many previous studies, underlying conditions such as obesity, hypertension and diabetes have been found to be correlated with an increased rate of hospitalisation and death due to SARS-CoV-2. Obesity is a non-communicable disease marked by an imbalanced energy state due to hypertrophy and hyperplasia of adipose tissue. Increased secretion of various cytokines and hormones, such as interleukin-6, tumour necrosis factor alpha and leptin, establishes a low-grade inflammatory state in patients with obesity. These pro-inflammatory cytokines predispose individuals “to increased risk for infection and adverse outcomes”. The metabolic disorders that are associated with obesity are numerous, including diabetes, hypertension and cardiovascular diseases. Most are associated with an increased risk of severe COVID-19. Due to this link, obesity is “an important factor in determining the morbidity and mortality risk in SARS CoV 2 patients” as well as the need for mechanical ventilation. Read the full study here .
Pulmonary consolidation is the most common complication of COVID-19. A high percentageof COVID-19 related pulmonary consolidationis due to extensive pulmonary fibrosis (PF). Viral infections have been shown to be a risk factor for PF, and both viral infections and aging were“strongly associated cofactors” for PF in this study. Infection with SARS-CoV-2, the virus responsible for COVID-19,suppresses the angiotensin-converting enzyme 1 (ACE2), which is a receptor exploited by the virus for cell entry; this receptor is “a negative regulator of” PF, which therefore links the virus to the progression of PF. Read the full study here .
Elevated body mass index has been marked as a risk factor for COVID-19 severity, hospital admissions and mortality. Diabetes and hypertension have also been associated with severe and fatal cases of COVID-19. Mendelian randomisation (MR) analyses the causal effect of an exposure risk factor on an outcome using genetic variants as instruments of estimation. In this study, the causal relationship between obesity traits (such as elevated BMI and metabolic disorders) and quantitative cardiometabolic biomarkers and COVID-19 susceptibility was examined by MR. Data was obtained from the UK Biobank. 1,211 individuals who had tested positive for COVID-19 and 387,079 individuals who were negativeor untestedwere analysed. Read the full study here .
Obesity and diabetes have both been identified in epidemiological reports as comorbidities “frequently associated with severe forms of COVID-19”. Both have also been identified as an independent risk factor for the severity of COVID-19 in a patient. The presence of these diseases is associated with each other; therefore, they could “confer a particularly high risk of severe COVID-19”. In previous analysis of the CORONAvirus-SARS-CoV-2 and Diabetes Outcomes (CORONADO) Study, it was shown “that body mass index (BMI) was positively and independently associated with severe COVID-19-related outcomes ... in patients with diabetes hospitalised for COVID-19”. In this analysis of the CORONADO data, the course of COVID-19 and its relationship to obesity in patients with type 2 diabetes hospitalised for this disease is explored. The influence of age on BMI and COVID-19 prognosis is also addressed due to the heightened impact of COVID-19 on the elderly population. Read the full study here .
Share this page
Training & Events
SCOPE E-Learning
We offer the only internationally recognised course on obesity management. Read more here.
Global Obesity Observatory
We offer various statistics, maps and key data around the topic of obesity. You can find all that and more here.
Policy & Advocacy
Our Policy Priorities
We have developed five key areas of policy that are a priority to us. Want to know more? Check them out here!
- Our Members
- Partnerships
- Patient Portal
- Membership Application Form
- Member Benefits
- Finance Committee
- Annual Report and Financials
- Prevalence of Obesity
- Causes of Obesity
- Obesity Classification
- Prevention of Obesity
- Obesity as a disease
- Commercial determinants of obesity
- Childhood Obesity
- Obesity in Universal Health Coverage
- The ROOTS of Obesity
- World Obesity Day
- Healthy Venues
- Reinventing the Food System: A Report
- The Spotlight Project
- SCOPE Examination
- Guide to SCOPE Certification
- SCOPE Schools
- Accreditation
- SCOPE Fellows
- Leadership Programme
- SCOPE Pricing
- SCOPE Accredited Events
- Event Archive
- International Congress on Obesity
Sign up for notifications
Obesity and harmful alcohol consumption are predictors for advanced liver disease in the disease management program for type 2 diabetes
Affiliations.
- 1 Metabolic Liver Research Program, I. Department of Medicine, University Medical Centre Mainz, Mainz, Germany.
- 2 I. Department of Medicine, University Medical Centre Mainz, Mainz, Germany.
- 3 Diabetology Practice Mainz, Mainz, Germany.
- 4 Diabetology and Family Practice, Bad Kreuznach, Germany.
- 5 Department of Internal Medicine II, Saarland University Medical Centre, Homburg, Germany.
- 6 University of the Saarland, Saarbrücken, Germany.
- PMID: 38206118
- PMCID: PMC10859704
- DOI: 10.1002/ueg2.12511
Background: Type 2 diabetes mellitus (T2DM) is a major risk factor for advanced liver disease. The aim of this prospective cohort study was to assess the prevalence and associated risk factors of liver fibrosis and cirrhosis in primary care centers participating in the diabetes disease management program (DMP) in Germany.
Methods: A total of 175 participants with the diagnosis of T2DM were enrolled in two primary care centers. Steatotic liver disease (SLD; hepatic steatosis, ≥275 dB/m), fibrosis (≥8 kPa), and cirrhosis (≥15 kPa) were assessed non-invasively using vibration-controlled transient elastography. Multivariable logistic regression analysis was performed to identify clinical predictors of fibrosis and cirrhosis. The AUDIT questionnaire was used to screen for alcohol consumption, and a score ≥8 was considered harmful alcohol consumption.
Results: The majority of participants were male (62%), and the median age was 66 years (interquartile range 59; 71). The median body mass index was 31.1 kg/m 2 , with 58.9% of the participants being obese. Harmful alcohol consumption was prevalent in 8.0% and 20.0% of the entire cohort and in those with cirrhosis, respectively. The prevalence of SLD, fibrosis, and cirrhosis was 77.1%, 42.3%, and 12.0%, respectively. In multivariable logistic regression analysis, obesity, and harmful alcohol consumption were associated with the highest odds of fibrosis (odds ratio [OR] 5.198, 95% confidence interval [CI] 2.269-11.908) and cirrhosis (OR 5.615, 95% CI 1.274-24.756), respectively.
Conclusion: The prevalence of fibrosis and cirrhosis in patients seen in the diabetes DMP in Germany is high. Obesity and harmful alcohol consumption increase the risk of fibrosis and cirrhosis in people with T2DM. Screening for advanced liver disease and associated risk factors within the DMP program may reduce the liver disease burden in this high-risk population.
Keywords: VCTE; alcohol consumption; cirrhosis; liver fibrosis; obesity; steatotic liver disease; type 2 diabetes.
© 2024 The Authors. United European Gastroenterology Journal published by Wiley Periodicals LLC on behalf of United European Gastroenterology.
- Alcohol Drinking / adverse effects
- Alcohol Drinking / epidemiology
- Alcoholism* / complications
- Diabetes Mellitus, Type 2* / diagnosis
- Diabetes Mellitus, Type 2* / epidemiology
- Disease Management
- Liver Cirrhosis / diagnosis
- Liver Cirrhosis / epidemiology
- Liver Cirrhosis / etiology
- Obesity / complications
- Obesity / diagnosis
- Obesity / epidemiology
- Prospective Studies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Obesity and Cardiovascular Disease
A 43-year-old man with a long history of obesity presented to our Weight Management Center 5 years after being disabled in a motor vehicle accident and gaining weight to a lifetime high of 269 kg and body mass index (BMI) of 85 kg/m 2 . His comorbidities were hypertension, obstructive sleep apnea, gastroesophageal reflux disease, gout, and osteoarthritis, and he had recently developed type 2 diabetes mellitus. Medications used included metformin, glyburide, losartan, hydrochlorothiazide, and diltiazem. He was motivated and met criteria for weight loss via a surgical intervention. Preoperatively, he was placed on a high-protein diet plus an appetite suppressant (phentermine) to achieve 10% weight loss. His weight declined, but he developed new-onset atrial fibrillation 3 weeks later, which was thought to be related to phentermine use and was cardioverted back to sinus rhythm.
Several months later, the patient underwent gastric bypass bariatric surgery with a preoperative weight of 252 kg. His type 2 diabetes mellitus resolved immediately after surgery, as did his gastroesophageal reflux and hypertension. Ten months after surgery, his weight was down to 177 kg (BMI=56 kg/m 2 ) with hemoglobin A1c of 5.9%, fasting blood glucose of 82 mg/dL, and blood pressure of 137/ 82 mm Hg, and he was no longer taking any medication.
Obesity: Relationship to Cardiovascular Disease
Although there are multiple long-term deleterious health effects of excess weight, obesity as defined by BMI ≥30 kg/m 2 is associated with premature atherosclerosis, increased risk of myocardial infarction and heart failure, and decreased survival, largely because of cardiovascular deaths, particularly in extreme weight categories. 1 , 2 Factors that contribute to cardiovascular disease in obesity are multifactorial and include metabolic dysregulation with increased prevalence of atherogenic risk factors, including insulin resistance, hypertension, and dyslipidemia; adverse cardiac remodeling characterized by hypertrophy, chamber enlargement, and impaired ventricular systolic and diastolic function; vascular endothelial dysfunction; premature coronary artery disease; increased sympathetic tone; pulmonary hypertension with right-sided heart strain; and arrhythmias. 3 Additionally, obesity is linked to a chronic state of inflammation evidenced by increased circulating levels of proinflammatory cytokines, derived largely from hepatic and adipose sources that may play roles in mechanisms of insulin resistance, plaque activation, myocardial hypertrophy, and cardiovascular disease progression. We recently observed that inflammatory changes in fat tissue are linked to systemic arterial dysfunction and abnormal clinical phenotypes, which suggests the possibility of a pathogenic adipose-cardiovascular axis. 4 Although BMI is useful in predicting overall risk, other factors, including adiposity distribution, degree of visceral or ectopic fat burden, percent body fat, genetic factors, sex, and possibly qualitative features of adipose tissue, may be germane to clinical disease expression. 5 , 6
Treatment of Obesity: Surgery and Pharmacotherapy
The case illustrated in this clinician update provides an example of the risks and benefits of various kinds of obesity treatments and highlights how potential options should be chosen with the patient’s medical history in mind.
Weight control is the cornerstone of therapy for both primary and secondary prevention of cardiovascular disease. Standard diets and exercise strategies have had limited efficacy because of low rates of long-term success in sustaining weight losses of 5% to 10% of initial body weight beyond 6 months. The use of appetite suppressants, which typically work on the hypothalamus, to decrease food intake can potentiate weight loss as long as treatment is sustained; however, weight is quickly regained on cessation of the agent. These drugs are also fraught with side effects such as blood pressure and pulse elevations, anxiety, and insomnia and thus can be extremely difficult to use, especially in patients with cardiovascular disease or risk factors. With a high BMI (class V obesity) and comorbidities such as hypertension, sleep apnea, and type 2 diabetes mellitus, the patient in this Clinician Update is certainly at increased cardiovascular risk. One of his prescribed medications, phentermine, acts primarily as a norepinephrine-releasing agent and centrally suppresses appetite in the hypothalamus. Because of its amphetamine-like actions, it also exerts peripheral effects of pulse and blood pressure elevation. In a patient with this degree of obesity, it is likely that the combination of sleep apnea, possibly right-sided heart overload, and phentermine effects triggered atrial fibrillation.
The medical and surgical treatments for obesity have a core of behavioral approaches in common: diet and exercise modification. These modalities need to be included concomitantly with medical or surgical options, likely lifelong, for successful outcomes.
This patient was unable to tolerate one of the pharmacotherapeutic options for obesity treatment because of its common sympathomimetic cardiovascular side effects. Unfortunately, many of the medications for obesity have undergone intense scrutiny because of potential cardiovascular and other side effects and have come up short when evaluated for health risk versus benefit. Phentermine was approved for weight loss by the Food and Drug Administration (FDA) in 1959 for short-term (12 weeks) treatment of obesity; long-term studies are unavailable. 7 It was combined with fenfluramine in a popular combination termed “phen-fen” until concerns about valvulopathy prompted the FDA to withdraw fenfluramine from the market in 1997. Another agent for obesity, sibutramine, approved in 1997 for long-term use, was withdrawn from the market recently after a study of subjects with preexisting cardiovascular disease, type 2 diabetes mellitus, or both showed increased risk of nonfatal myocardial infarction and stroke with treatment for a mean duration of 3.4 years. 8
Currently, the only centrally acting appetite suppressants on the market for obesity treatment are phentermine and diethylpropion, both of which are sympathomimetics with potential cardiovascular side effects. Orlistat, a peripherally acting agent, is a pancreatic and gastric lipase inhibitor that blocks 25% to 30% of fat calories from absorption in the gastrointestinal tract. Its actions are considered mild compared with appetite suppressants, with those who take it achieving less than a 5% weight loss compared with placebo. 9 The FDA guidance for industry for weight loss drugs recommends that drugs brought through the approval process show for efficacy a difference in mean weight loss between product and placebo groups of at least 5% or that the proportion of subjects undergoing active treatment who lose ≥5% of baseline body weight be at least 35%.
Other agents that did not achieve FDA approval for obesity treatment recently for safety reasons include rimonabant, a cannabinoid receptor antagonist; lorcaserin, a 5-hydroxytryptamine (serotonin) 2C receptor agonist; and the combination drugs topiramate/ phentermine and naltrexone/bupropion. Concerns about side effects were again the predominant reason for non-approval status, including anxiety and depression for rimonabant, breast tumors in rat models for lorcaserin, cardiovascular effects and teratogenicity for topiramate/phentermine, and elevations in blood pressure for naltrexone/ bupropion. These drugs did meet the FDA efficacy recommendations listed above. The approval bar for obesity agents in the United States is high because of the number of Americans who would be eligible for these agents (33.8% of the population was considered obese in the United States as of 2008).
Table 1 summarizes recent pharmacological agents used for obesity treatment. 10 – 12 The National Institutes of Health/National Heart, Lung, and Blood Institute guidelines on the assessment and treatment of obesity recommend that pharmacotherapy for obesity be considered for those patients with a BMI ≥30 kg/m 2 or ≥27 kg/m 2 with at least 1 serious comorbidity. All pharmacotherapeutic options for obesity should be adjuncts to dietary and physical activity recommendations. 13 Newer medical approaches to obesity management may include the addition of incretin hormones, the blood levels of which are altered after gastric bypass surgery. GLP-1 (glucagon-like peptide 1) agonists such as exenatide and liraglutide have been shown to promote weight loss in both diabetic and nondiabetic patients. Other experimental approaches include combinations of injectable agents plus leptin, a hormone secreted by adipose tissue that signals satiety in the hypothalamus. These approaches are considered an off-label use of approved agents in the case of GLP-1 agonists and experimental in the case of leptin in combination with other agents. Table 2 summarizes the recent activity of newer pharmaceutical obesity agents in the FDA approval process. 14
Current and Recent Pharmacotherapy for Obesity in the United States 10 – 12
5HT indicates 5-hydroxytryptamine (serotonin); BP, blood pressure; MI, myocardial infarction; OTC, over-the-counter; and FDA, Food and Drug Administration.
Newer Agents for Obesity 14
NA indicates not available; GABA, γ -aminobutyric acid; BP, blood pressure; FDA, Food and Drug Administration; 5HT2C, 5-hydroxytryptamine (serotonin) 2C receptor; and GLP-1, glucagon-like peptide 1.
Given the limited efficacy of anti-obesity medications and behavioral interventions, bariatric operations have provided an alternative yet durable approach to combat obesity and its comorbidities. Bariatric surgery has increased exponentially in the United States and has evolved to become one of the safer surgical operations performed in the United States, with a 30-day mortality rate of 0.3% and an early complication rate of 4.1%. 15 Bariatric surgery encompasses several different procedures: Roux-en-Y gastric bypass, laparoscopic adjustable gastric band, and the biliopancreatic diversion and biliopancreatic diversion with duodenal switch ( Figure ). The 2 most commonly performed in the United States are the Roux-en-Y gastric bypass and laparoscopic adjustable gastric band. These procedures are recommended for patients with BMI ≥40 kg/m 2 or ≥35 kg/m 2 with at least 1 serious comorbidity. One type of laparoscopic adjustable gastric band was recently approved by the FDA (2011) for a lower BMI indication, BMI ≥35 kg/m 2 or ≥30 kg/m 2 with a serious comorbidity.

Surgical treatments for obesity. A , Laparoscopic adjustable gastric band (LAGB). B , Biliopancreatic diversion (BPD). C , Roux-en-Y gastric bypass (RYGB). D , Biliopancreatic diversion with duodenal switch (BPDDS).
Cardiovascular Benefits of Weight Loss
Studies have shown the benefits of a modest 5% to 10% weight loss on cardiovascular risk factors, most notably the Diabetes Prevention Program, in which an average 7% weight loss with an intensive lifestyle intervention of diet and exercise delayed the progression to type 2 diabetes mellitus in those with prediabetes. 16
Our patient underwent the Roux-en-Y gastric bypass, which resolved most of his comorbidities, including type 2 diabetes mellitus, hypertension, reflux disease, and osteoarthritis. The Roux-en-Y gastric bypass can produce on average a 25% weight loss by 9 to 12 months after the procedure. There is robust literature highlighting the immediate and consistent amelioration of metabolic abnormalities after bariatric surgery, in many cases much before major weight loss begins. This improvement, in the case of type 2 diabetes mellitus, may occur immediately and results from alterations in the secretion of several gut-derived hormones, notably GLP-1, GIP (gastric inhibitory polypeptide), PYY (peptide YY), and ghrelin, with endocrine functions that modulate insulin sensitivity and glucose utilization. 17
Data suggest that gastric bypass has more profound effects on the gut milieu than restrictive operations such as laparoscopic adjustable gastric banding. The immediate change in insulin sensitivity also does not occur with medical weight loss alone, which suggests that gastric bypass surgery alters specific aspects of the gastrointestinal hormonal environment that are presently incompletely understood. Improvements in other cardiac risk factors, such as normalization of blood pressure and lipids, also occur in conjunction with laparoscopic adjustable gastric band and/or medical weight loss and tend to be apparent after a 5% to 10% change of initial body weight.
Although a favorable reduction in proatherogenic metabolic profiles occurs within weeks to months, long-term data from the Swedish Obese Subjects (SOS) study demonstrate substantial and sustained benefit, with >10-year rates of recovery from diabetes, sleep apnea, hypertension, hypertriglyceridemia, and hyperuricemia after bariatric surgery, which is remarkable. Importantly, these alterations are associated with reduced risk of myocardial infarction and prolonged cardiovascular survival. 18 In addition to improving metabolic dysfunction, weight reduction is associated with decreases in circulating cytokines such as interleukin 6, tumor necrosis factor- α , and C-reactive protein and upregulation of vasculoprotective factors such as adiponectin. Beneficial physiological and structural changes also become manifest with weight loss. For example, our group has shown that vascular endothelial function improves significantly within 3 months after bariatric surgery and is sustained at 12 months. 19 , 20 Cardiac geometry and myocardial performance also improve after weight intervention.
In the Utah Obesity Study, marked weight reduction 2 years after gastric bypass induced regression of left ventricular hypertrophy and ventricular enlargement and improved biventricular systolic function. These occurred in parallel with improved left ventricular diastolic relaxation and tissue Doppler parameters that correlated with improved exercise capacity. 21 Additionally, electrophysiological properties may change, with several studies demonstrating correction of abnormal QTc intervals, heart rate recovery, and autonomic tone.
In summary, targeted weight loss reverses many aspects of abnormal cardiovascular function, and clinical data demonstrate long-term survival benefit, in particular with bariatric surgical intervention. The treatment decision for a given obese individual must be tailored on the basis of patient preference and eligibility, comorbidity burden, and the risk-benefit ratio of potential medical and surgical options. Future research may unravel additional beneficial mechanisms of different weight loss strategies and potentially pave the way for safer and more effective dietary or medical options for obesity treatment. The goal of future research into antiobesity agents is to induce a “medical gastric bypass” with perhaps a combination of incretin hormones and appetite suppressants.
Acknowledgments
Sources of Funding
Dr Apovian is supported by National Institutes of Health grants 5P30DK046200-19, R21 HD061311-01A1, R01 AG037547-01, R01 HL084213, and P01 HL081587; Dr Gokce is supported by National Institutes of Health grants R01 HL084213 and P01 HL081587.
Disclosures
Dr Apovian participates on advisory boards for Allergan, Amylin, Orexigen, Merck, Johnson and Johnson, Arena, and Sanofiaventis. Dr Gokce reports no conflicts.
Follow us on :

Take a look at the Recent articles
A case study: obesity and the metabolic syndrome. a three-pronged program, targeting education, close follow-up and a dietary supplement, significantly decrease body weight and body fat, grethe s birketvedt.
Medical Center for Obesity and Research, Baerum, Oslo, Norway
E-mail : [email protected]
Carl Fredrik Schou
Teres Colosseum, Oslo, Norway
Erling Thom
ETC Research and Development, Oslo, Norway
DOI: 10.15761/IOD.1000143
A 38-year old woman with a body fat content of 52.2% and a BMI of 48.2 kg/m 2 was seeking medical treatment in an outpatient obesity clinic in Oslo, Norway. She suffered from a severe abdominal hernia and was not qualified for surgery of this condition until her BMI was under 30 kg/m 2 . Additionally, she was severely challenged in terms of mobility as she was born with cerebral palsy and required either a wheel chair or crutches to get around. Over the years she had sought several treatment options to control her obesity but with no success. She did not qualify for bariatric surgery and was severely depressed when she came to the clinic. After examination and diagnosis, the decision was made to begin a multi-pronged treatment using a natural dietary supplement, combined with the customized educational program called “The Body in the Brain”, and a close medical follow-up with regular appointments to the outpatient clinic. After twenty-three months of treatment, the woman had lost 38 kg of bodyweight and had normalized fat percentage for her age and gender. In conclusion, it is possible to successfully treat severe obesity and return a patient to a normal body fat percentage with the combination of a natural dietary supplement, a designed diet composition and a weight loss behavioral program.
obesity, weight loss, metabolic syndrome
Introduction
Obesity and the metabolic syndrome are linked together [1]. When an individual gets severely obese, insulin resistance, hypertension and increased abdominal circumference follow as a natural cause due to the excess fat in the body. Obesity and the metabolic syndrome has been extensively researched and today clinical evidence implicates intra-abdominal adiposity as a powerful driving force for elevated cardio metabolic risk [2]. This association appears to arise directly, via secretion of adipokines, and indirectly, through promotion of insulin resistance.
The most important therapeutic intervention effective in subjects with the metabolic syndrome should focus on weight reduction and regular daily physical activities. Health experts agree that making lifestyle changes, including following a healthy eating pattern, reducing caloric intake, and engaging in physical activity, are the basis for achieving long-term weight loss [3,4]. However, weight-loss and weight-management regimens have frequently been ineffective. Therefore, effective medical interventions to manage weight gain and slow or prevent progression to obesity are needed. Control of diet and exercise are cornerstones of the management of excess weight. A number of nutritional approaches and diets with different proportions of lipids, proteins and carbohydrates have been prescribed for weight loss. Initial guidance on weight loss was earlier years a restriction in saturated fats that unfortunately did not necessarily result in weight loss. Recently, a shift towards a reduction in refined carbohydrates has been a new approach to lose weight.
Several studies have indicated that fiber-rich foods and fiber supplements have moderate weight reducing effects, and may also improve the lipid profile in overweight and obese individuals [5,6]. There are hundreds of weight loss products sold over the counter today. Typically, these OTC supplements have not been clinically tested, can have significant unwanted side effects and not yield successful results in helping people to lose weight.
The natural product, used in this case study is supplement that consists of a unique combination of three natural ingredients: white kidney bean extract, locust bean gum extract and green tea extract that affect weight loss with little to no side effects. The white kidney bean extract is phaseolus vulgaris, a bean extract containing phaseolamin. Phaseolamin is a glycoprotein found mainly in white and red kidney beans and is an effective alfa-amylase inhibitor [7]. The extract of locust bean gum, is a seed-coat extract that decreases ghrelin [8], the hunger hormone and make you feel faster satiated and will postpone the hunger sensation after a meal. Locust bean gum has also shown lipid lowering effects in several studies [9]. The third ingredient is a green tea extract [10-12], Camellia sinensis with anti-inflammatory and antioxidant properties with a small increase in the energy expenditure.
Aim of study
The aim of this study was to investigate whether a dietary supplement with white kidney bean extract, locust bean gum extract and green tea extract in combination with a program with lifestyle changes would enhance weight loss and fat loss and improve the metabolic parameters in a severe obese patient with the metabolic syndrome.
A 38 year old woman with a history of obesity, diabetes type 2 and hypertension was seeking treatment in an out-patient clinic in Oslo, Norway for medical weight loss management. She was well aware of the link between obesity, diabetes and cardiovascular disease and felt this appointment she had asked for was her last chance in getting help with her health problems.
She had been normal weight as a child and adolescent, but do to a dependency of crutches and a wheelchair she had gradually put on weight in her twenties. She was married with two young children and she increased in weight after each child birth. She suffered a severe abdominal hernia that stressed her, but she had been refused surgery due to her heavy weight.
She had in her childhood and teens always been of normal weight, active and healthy in spite of her physical disabilities. When she got married, she gradually gained weight and the weight culminated after her second child was born. She had developed diabetes type 2 and hypertension after her children were born, and was medicated with antihypertensive and antidiabetics. Her primary care physician had not really been interested in her weight and had several times suggested higher doses of medications or insulin injections. The patient was not interested in insulin injections as she was afraid of gaining more weight.
Our patient had been sedentary the last 5 years due to the abdominal hernia. She had tried many weight loss efforts on her own, had started working with a personal trainer and had weekly sessions with a physical therapist. Her diet had been high in fat and calories although she was very well educated in nutritious food. However, she admitted to overeating, and periods of binging. She drunk about 2.5 liter of diet soda a day including diet juice. She was very conscious about eating habits when it came to her two kids, and they were both healthy and in normal weight. She had a university education and was well informed of her health situation. But she was under much stress in her daily life and struggled daily to get help from health authorities.
Her initial anthropometric measurements included a weight of 125kg with a height of 1.61m, a body mass index (BMI) of 48.2kg/m 2 which classified her as morbidly obese. Her fat % was 52.2% with 65 kg fat mass measured by bioelectrical impedance analysis (BIA)[13] (Tanita Body Composition Analyzer BC-418) for analyzing the composition of the body, such as weight, lean body mass (LBM), total body water(TBW), fat free mass (FFM) and basal metabolic rate (BMR). Her HbA1c had the last 2 months ranged from 11.7% till 8.8% and her hypertension was 160/95 mm Hg.
Informed consent
The patient has signed and approved the consent form.
On the first visit to our clinic, the patient was advised of which food items of simple carbohydrates she should try to avoid in her daily diet. She was given restrictions in caloric content and a diet plan, specifically designed for her health situation with emphasis on her hypertension and diabetes type 2. She was also advised to drink water with a slice of lime instead of diet sodas and diet juice. One of her main goals was to be able to not require medications for control of her hypertension that would then improve her diabetes type 2 and simultaneously decrease her weight. It was extremely important for the treating physician to give her food compositions that targeted the ability to relieve stress in the gut-brain axis.
Her resting metabolic rate (RMR) was measured to 1828 kcal and the physician designed a diet in the range of 1200kcal to 1600 kcal. In that way, she at least could have a deficit of about 400 kcal a day taking into account her limited physical activity level. In a two week period this regimen would theoretically allow her approximately a 0.5 kg loss in weight. Due to her decrease in simple carbohydrates she was advised to check her blood sugar 3 times per day and write the recordings down until next meeting. She was instructed on how to decrease her diabetes medication based on her blood sugar levels.
The weight management program at our clinic was continuing with bi-weekly visits by the patient for the next six weeks, and then monthly visits after that time. Furthermore, the patient was advised after six weeks to additionally take one capsule of the dietary supplement twenty minutes before each of the main meals, breakfast, lunch and dinner.
On a monthly basis, her weight and body fat percentage were recorded with BIA at the doctor visits. Moreover, she was given 1 hour consultation with behavioral modification with advise to lifestyle changes according to a program entitled the “Body in the Brain”, a recently published book in Norway, targeting education on how the brain and the body work together in hormonal harmony when the right diet is introduced for the right person. The patient was allowed to eat whatever she wanted in the diet plan restricted to 1200-1600 kcal, excluded from the carbohydrate list were white breads and pasta, cookies, cake, candy, sugar-sweetened sodas and drinks as well as diet sodas and diet juice. She followed the educational program related to the “Body in the Brain”[14] where she each month was given new insight into how the body and the brain worked together in a hormonally balanced way. She was also gradually introduced to healthier foods, e.g., food that was rich in tryptophan, an essential amino acid that target serotonin in the brain and indirectly impact insulin levels. In her diet plan was a list of tryptophan rich food such as e.g.salmon, chicken, cod, tuna, apricots, broccoli, sprouts, whole grain, skimmed milk and almonds, food that was known as comfort food or mood food. The list was extended each visit and the food the patient did not like was replaced with other food items.
In her first two weeks of treatment she lost only one pound, but she reported that her blood sugar had not spiked as much as prior times after she had tried to avoid sugar and other simple carbohydrates. She admitted it was difficult to avoid these foods as she always had had a sweet tooth. On her second visit she was educated in how the body relates to the brain in a hormonal way when certain food items are ingested. She was introduced to the amino acid tryptophan and how the tryptophan rich food would create more harmony in the gut-brain axis, increase serotonin levels and decrease cortisol and thereby improve insulin sensitivity. The education went on for 22 months and at each visit the biochemistry of food were addressed. How the food she ingested had an impact on her body and brain was a favorite topic of the visits to come.
Over the next four weeks she had lost only 1.2 kg. The visit two weeks later showed a decrease of an additional 0.7 kg, however the fat percentage in her body had not changed. Until this time, the fat lost was attributable to pure lean body mass. She was then introduced to the patented supplement consisting of Green tea extract, White kidney bean extract and Locust bean gum extract, a supplement that was sold over the counter in Norway, approved by the Norwegian Medicines Agency and also recently the ingredients were approved by the FDA in the US. She gradually lost weight each month with a simultaneous loss in fat percentage. 12 months later she had lost 21 kg of which 85% was loss in fat mass. She became less depressed, her energy level had improved, and she was still very motivated for further weight loss.
By the end of the 23 month treatment period she had lost 38 kg and the fat percentage in the body had decreased to 31.9% which was within normal limits for her age. Her blood sugar was under control. However, she was still on antidiabetics, however, her blood sugar and HbA1c was within normal limits and her hypertension was well regulated. Six months later, she was accepted for the surgery of her abdominal hernia as her fat mass was within normal range in spite of a BMI>30kg/m 2 .
The patented diet supplement with white kidney bean extract, locust bean gum and green tea extract in combination with an education program (The Body in The Brain) consisting of twenty-six outpatient clinic sessions, resulted in a very significant weight loss, improvement in fat percentage, hypertension and blood sugar levels in an obese woman following this program. In terms of the weight loss observed in this patient, fat was more than 75% of the total weight lost indicating a qualitative weight reduction where less than one quart of the weight lost was lean body mass[15]. The patient lost 25% more body fat of her weight lost than would predicted with lifestyle changes alone. The special designed diet program was modified accordingly in subsequent visits due to changes in the BMR. Her caloric intake was never changed to lesser than her BMR. The reason why her energy level increased and her mood improved, can very well be caused by the change in diet.,At each meal, she ate primarily foods rich in tryptophan combined with complex carbohydrates and thereby increased her serotonin levels. Several studies have shown that increased serotonin levels are related to mood elevations [16,17]. However, her improved mood and higher energy in this patient, may also be caused by the fat lost relieving the stress in the gut-brain axis.
The amount of fat mass lost of weight lost was far more than reported in earlier studies. This is in accordance with earlier unpublished pilot studies with the diet supplement used in this case report. We believe that adding this specific supplement to this combined treatment enhanced fat loss and thereby normalized parameters associated with the metabolic syndrome. Earlier studies have shown that in severe obese individuals it is almost impossible to reach normal fat mass with lifestyle changes and behavioral modification alone. We believe that our natural supplement had both carbohydrate and lipid lowering effects on fat metabolism and also increased the fat expenditure. Moreover, we believe that the education program, The Body in the Brain used in this three-pronged program, enhanced the weight loss. The patient understood the mechanisms in her body related to the food she ate, which increased her motivation for weight loss and prevented weight gain again as in earlier reports. Moreover, an encouraging physician at each visit may also be important for the patient to reach her goals. We cannot neglect the fact that obese patients are very sensitive to the knowledge of the physician and the way she is being encouraged on her road to weight loss.
A program like this can be a valuable method in the treatment of obesity in the future.
A three-pronged treatment paradigm that includes close physician follow-up, a well designed education program, and the addition of a dietary supplement consisting of an extract of white kidney bean, an extract of locust bean gum and an extract of green tea extract gave a substantial weight loss and a loss in fat mass towards a normal fat percentage in a severe obese person with the metabolic syndrome.
- Després JP, Lemieux I (2006) Abdominal obesity and metabolic syndrome. Nature 444: 881-887. [ Crossref ]
- Scheen AJ (2004) Management of the metabolic syndrome. Minerva Endocrinol 29: 31-45. [ Crossref ]
- Pittler MH, Ernst E (2004) Dietary supplements for body-weight reduction: a systematic review. Am J ClinNutr 79: 529-536. [ Crossref ]
- Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, et al. (2013) AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation : 1- 63.
- Birketvedt GS, Aaseth J, Florholmen JR, Ryttig K (2000) Long-term effect of fibre supplement and reduced energy intake on body weight and blood lipids in overweight subjects. ActaMedica (Hradec Kralove) 43: 129-132. [ Crossref ]
- Birketvedt GS, Langbakk B, Florholmen J (2004)A Dietary Supplement with Bean Extract Decreases Body Weight, Body Fat, Waist Circumference and Blood Pressure in Overweight and Obese Subjects. Current Topics in Nutraceutical Research 3:137-142.
- Preuss HG (2009) Bean amylase inhibitor and other carbohydrate absorption blockers: effects on diabesity and general health. J Am CollNutr 28: 266-276. [ Crossref ]
- Gruendel S, Garcia AL, Otto B, Mueller C, Steiniger J, et al. (2006) Carob pulp preparation rich in insoluble dietary fiber and polyphenols enhances lipid oxidation and lowers postprandial acylated ghrelin in humans. J Nutr 136:1533-1538. [ Crossref ]
- Zavoral JH, Hannan P, Fields DJ, Hanson MN, Frantz ID, et al. (1983) Thehypolipidemic effect of locust bean gum food products in familial hypercholesterolemic adults and children. Am J ClinNutr 38: 285-294. [ Crossref ]
- Toda (1989) Green tea extract has been shown to decrease weight in overweight subjects. Nippon SaikingakuZasshi 44: 669-672.
- Dulloo AG, Duret C, Rohrer D, Girardier L, Mensi N, et al. (1999) Efficacy of a green tea extract rich in catechin polyphenols and caffeine in increasing 24-h energy expenditure and fat oxidation in humans. Am J ClinNutr 70: 1040-1045. [ Crossref ]
- Wolfram S (2007) Effects of green tea and EGCG on cardiovascular and metabolic health. J Am CollNutr 26: 373S-388S. [ Crossref ]
- Böhm A, Heitmann BL (2013) The use of bioelectrical impedance analysis for body composition in epidemiological studies. Eur J ClinNutr 67 Suppl 1: S79-85. [ Crossref ]
- Birketvedt GS (2008) The Body in the Brain. Editor XLibriz, Norway. 280 p Norwegian language. In press for English translation.
- Heymsfield SB, Gonzalez MC, Shen W, Redman L, Thomas D (2014) Weight loss composition is one-fourth fat-free mass: a critical review and critique of this widely cited rule. Obes Rev 15: 310-321. [ Crossref ]
- Benton D, Donohoe RT (1999) The effects of nutrients on mood. Public Health Nutr 2: 403-409. [ Crossref ]
- Ottley C (2000) Food and mood. Nurs Stand 15: 46-52. [ Crossref ]
Editorial Information
Editor-in-chief.
Sharma S Prabhakar Texas Tech University Health Sciences Center
Article Type
Publication history.
Received: January12, 2016 Accepted: February08, 2016 Published: February 11, 2016
©2016Birketvedt GS.This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Birketvedt GS, Schou CF, Thom E(2016) A case study: Obesity and the metabolic syndrome. A threepronged program, targeting education, close follow-up and a dietary supplement, significantly decrease body weight and body fat. Integr ObesityDiabetes. 2:doi: 10.15761/IOD.1000143
Corresponding author
Medical Center for Obesity and Research, Baerum, Oslo, Norway.
Journal Home
- Article Info
- Author Info
- Figures & Data
- Privacy Policy
- Terms & conditions
© 2018 Copyright OAT. All rights reserved.

IMAGES
VIDEO
COMMENTS
naltrexone-bupropion. Class: Obesity. Action: naltrexone, an opioid antagonist, and bupropion, an antidepressant - might help with cravings. Dosing: 8/90mg, 1 tab po qam titrating to max of 2 tabs po q am and 1 tab po q pm. Pregnancy: X. Monitoring: Cr at baseline, BP, HR, depression/suicide.
Introduction. Obesity is associated with an increased risk of diseases such as cancer, type 2 diabetes, and heart disease, leading to early mortality.1 2 3 More recently, obesity is a risk factor for worse outcomes with covid-19.4 5 Because of this increased risk, health agencies and governments worldwide are focused on finding effective ways to help people lose weight.6
Introduction. Obesity is an increasing, global public health issue. Patients with obesity are at major risk for developing a range of comorbid conditions, including cardiovascular disease (CVD), gastrointestinal disorders, type 2 diabetes (T2D), joint and muscular disorders, respiratory problems, and psychological issues, which may significantly affect their daily lives as well as increasing ...
Obesity is a complex chronic disease in which abnormal or excess body fat (adiposity) impairs health, increases the risk of long-term medical complications and reduces lifespan. 1 Epidemiologic studies define obesity using the body mass index (BMI; weight/height 2), which can stratify obesity-related health risks at the population level.Obesity is operationally defined as a BMI exceeding 30 kg ...
Coronary heart disease. A case-control study involving 27,000 participants from 52 countries demonstrated that WHR was the strongest predictor of myocardial infarction (MI), independent of age, gender, ethnicity, smoking status or CVD risk factors (hypertension, diabetes, dyslipidaemia). ... Screening for and management of obesity in adults: U ...
The number of Americans having weight loss surgery increased by 804% between 1998 and 2004, which appears to be a driver for the recent development of obesity disease management and bariatric surgery case management programs. Implications for case management practice: Although the immaturity and lack of studies citing outcomes of obesity ...
Indeed, in a negative control analysis, Case Study 2 found a higher incidence of lung cancer among those with obesity, and particularly those undergoing obesity treatment, compared with the ...
An integrated health care standard for the management and prevention of obesity in the Netherlands. Fam Pract. 2012;29(Suppl 1):153-6. Article Google Scholar McDonald J, Jayasuriya R, Harris MF. The influence of power dynamics and trust on multidisciplinary collaboration: a qualitative case study of type 2 diabetes mellitus.
The Role of Individualized Exercise Prescription in Obesity Management-Case Study Int J Environ Res Public Health . 2021 Nov 16;18(22):12028. doi: 10.3390/ijerph182212028.
4 Primary Care and Community Health Centers There is an alarming trend toward overweight and obesity in America. Nearly two-thirds of the population is overweight, with 34 percent considered medically obese.1 At the front lines of this epidemic are primary care providers and CHCs that see a great number of patients who
This report presents the discussion on the potential impact of defining obesity as a disease on the patient, the healthcare system, the economy, and the wider society. ... a case-control study of 105 patients. Obes Surg. 2022; 32: ... National and local strategies in The Netherlands for obesity prevention and management in children and ...
In the present case study, a 65-year-old male patient with body mass index (BMI) 43.8 kg/m 2 (obesity class III), hypertonia, prediabetes, hyperlipidemia, and knee arthrosis started a supervised and complex lifestyle medicine program. The patient was an elite football player in his twenties and, after that, exercised sparsely or not at all.
While a modern approach to weight management in the nation's largest insurance program would be a critical step forward, obesity coverage is required in order to achieve a meaningful reduction in obesity prevalence and its concomitant chronic disease burden. The H-E-B case study provided above is one approach.
In recent years, obesity has received increased attention as a chronic disease [1, 2].Current figures for Germany indicate that 53% of adults are overweight (BMI 25-29.9 kg/m²) and of these 17% are obese (BMI > 30 kg/m²) [1,2,3].For Europe, obesity is thought to be significantly involved in the development of approximately 80% of incident cases of type 2 diabetes mellitus, approximately 35% ...
The management of youth with severe obesity is strongly impacted by social determinants of health and family dynamics. We present case studies of three patients seen in our tertiary care obesity treatment clinic as examples of the challenges faced by these patients and their families, as well as by the medical team.
World Obesity have collated some of the recent data and case studies available looking pertaining to obesity and the current outbreak of COVID-19. ... As almost 75% of American adults over the age of 20 are living with overweight or obesity, this disease should be considered a public health priority, especially given the increased likelihood of ...
At Lilly, we want to help people living with excess weight access care that is based on research. The first step is to help the public to see obesity as a long-term disease rather than a lifestyle choice. By taking part in a clinical research study focused on chronic weight management, you can help to make a difference. Click here to find a trial.
A 38 year old woman with a history of obesity, diabetes type 2 and hypertension was seeking treatment in an out-patient clinic in Oslo, Norway for medical weight loss management. She was well aware of the link between obesity, diabetes and cardiovascular disease and felt this appointment she had asked for was her last chance in getting help
classified obesity as a disease. In India, the prevalence of overweight increased from 9.7% ... pur, for further management. History of Past illness History of Past illness doesn't reveal any ... (Obesity) A Success Story- A Case Study IAMJ: OCTOBER, 2017 3984 Details of Snehapana procedure Sneha Matra, Jaranakala etc are illustrated in
Introduction. Obesity has been identified as a prime candidate for cardiovascular diseases, type II diabetes mellitus (T2DM), dyslipidemias, and a host of related complications.[] According to the World Health Organization (WHO), more than 1.9 billion adults worldwide were overweight, with 650 million obese adults in 2016, and this number will increase if no remedial strategies are taken.
Background: Type 2 diabetes mellitus (T2DM) is a major risk factor for advanced liver disease. The aim of this prospective cohort study was to assess the prevalence and associated risk factors of liver fibrosis and cirrhosis in primary care centers participating in the diabetes disease management program (DMP) in Germany.
A small study of eight patients with morbid obesity on a very low-carbohydrate diet observed benefits on symptoms and esophageal acid exposure in pH probe testing.
For example, among 1093 adults with type 1 diabetes but no known heart disease, the rate of incident major adverse cardiovascular events after 6.3 years was 41 per 1000 person-years for an N ...
Case study. A 43-year-old man with a long history of obesity presented to our Weight Management Center 5 years after being disabled in a motor vehicle accident and gaining weight to a lifetime high of 269 kg and body mass index (BMI) of 85 kg/m 2.His comorbidities were hypertension, obstructive sleep apnea, gastroesophageal reflux disease, gout, and osteoarthritis, and he had recently ...
the worldwide prevalence of obesity nearly tripled. from 1975 to 2016. Overweight and obesity kill. most of the people of the world 2 then underweight. About 13% of the world's adult population ...
Abstract. A 38-year old woman with a body fat content of 52.2% and a BMI of 48.2 kg/m 2 was seeking medical treatment in an outpatient obesity clinic in Oslo, Norway. She suffered from a severe abdominal hernia and was not qualified for surgery of this condition until her BMI was under 30 kg/m 2.Additionally, she was severely challenged in terms of mobility as she was born with cerebral palsy ...