By Michelle Stephenson, Contributing Editor

Treating Floaters: The Pros, Cons and Techniques
Some retinal surgeons are modifying their stance on treating floaters in certain symptomatic patients..
F loaters are a common complaint of patients of all ages, often caused by myopia in younger patients, and posterior vitreous detachment in older people. Until recently, vitreous floaters weren’t viewed as something to be treated, and patients just had to cope with them as best as they could. Here, retina specialists discuss the sometimes controversial topic of actually treating these annoying, but sometimes debilitating, opacities.
Changing Attitudes
“Historically, floaters were dismissed by ophthalmologists, and I was one of those doctors for a very long time,” says Jerry Sebag, MD, FACS, senior scientist at the Doheny Eye Institute/UCLA in Pasadena. “This stemmed from a lack of understanding of the origin of patient complaints and a lack of the ability to clinically measure things to characterize the condition as mild, moderate or severe. We didn’t have those tools and were therefore left to determine whether an individual claiming disturbance by floaters was justified or overreacting. About 15 years ago, I started listening to these patients, and I started to believe them.”
“I realized that we need to begin considering floaters a disease in some people,” Dr. Sebag adds. “Many people have floaters that are inconsequential, but there are also many people who are debilitated by the opacities that induce floaters. ‘Floaters’ is a term that’s misused. It’s mistakenly used to refer to structures within the eye, but floaters are not structures. They’re a visual phenomenon that is created by opacities within the vitreous. When you use ultrasound to image the structures within the eye that cause the visual phenomenon of floaters, we use the term ‘echodensity,’ ” he adds.
To further clarify things, Dr. Sebag coined the term “vision degrading myodesopsia” to refer to patients who have clinically significant vitreous floaters. 1 “This term doesn’t roll off your tongue easily, but it sure sounds like a disease. And that’s what’s needed to stimulate the paradigm shift in our perception that must occur if we’re going to help those people who are afflicted, in many cases severely,” Dr. Sebag says.
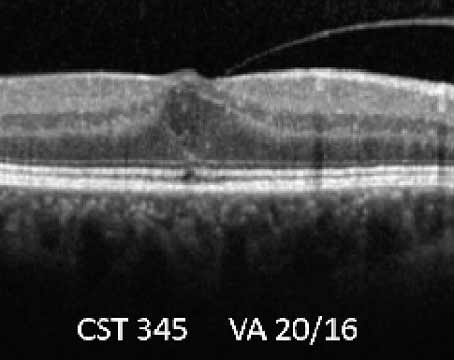
In collaboration with acoustic engineers in New York, and with Dr. Alfredo Sadun at the Doheny Eye Institute in Pasadena, Dr. Sebag developed metrics that he now uses on a routine basis to evaluate patients who complain of floaters. The first metric measures the density of vitreous using quantitative ultrasonography. 2 “Ultrasound used to be a mainstay in evaluating the eye, but ever since optical coherence tomography came along, people tend to default to that rather than use ultrasound to image the structures within the eye. OCT is excellent for the retina, but it’s poor to evaluate vitreous, and so ultrasound has filled that void. We worked with acoustic engineers and developed ways to quantify ultrasound imaging to assess the severity of the structural changes within the vitreous body that cause the visual phenomenon of floaters,” he adds.
The other useful metric was to measure contrast sensitivity. 3,4 “While this has been available for many years, ophthalmologists tend not to routinely do that test. Instead, we rely on visual acuity as a measure of the person’s ocular health. While that’s useful for evaluating some diseases, it’s not good in evaluating the visual impact of vitreous opacities. Contrast sensitivity, however, is a very useful way to measure the impact of vitreous opacities on vision and to explain why people are so unhappy,” Dr. Sebag describes.
According to Jennifer I. Lim, MD, director of the Retina Service at University of Illinois Health, there are two schools of thought on how to surgically treat floaters. First is a core vitrectomy where the vitreous gel and any visible opacities are removed centrally. Second is the complete vitrectomy with creation of a PVD. “I perform complete vitrectomies, and I induce a PVD if there’s not one already,” she says.
Dr. Lim mentions that floaters originate in some patients who are very nearsighted or have other vitreous abnormalities, from vitreous degeneration and liquefaction. “In the other group of patients, where the PVD has occurred, the floaters result from collapse of the vitreous gel and opacities within the gel,” she says. “Floaters may result from liberated tissue/blood/pigment as the vitreous separates from the underlying retina and can also result from a retinal tear, or from a retinal detachment if it occurs during the patient’s PVD. Of course, the risks of inducing a retinal tear are higher while you create a PVD surgically especially in highly myopic eyes with thin retinas. However, if you don’t induce a PVD, over the course of time, that patient will eventually develop a PVD, and when he or she does, that patient will develop floaters, in addition to being at risk for a retinal tear or a retinal detachment at that time. Thus, I like to create the PVD in the operating room where it’s very controlled, and then not have to worry about the patient undergoing a PVD in the future and getting floaters back again.”
Dr. Sebag has studied this and found that it occurs in only 14.1 percent of individuals who have undergone limited vitrectomy without intraoperative PVD induction. 5 None of those cases developed retinal tears or detachments.
Dr. Lim adds that, “Once you navigate the psychosocial and physical exam aspects of it, it’s a reasonable procedure to do. I’m quite pleased that my patients are doing well. This includes both the older patients who have the PVD, as well as the younger ones who just have the liquified vitreous and are very bothered by the floaters. Some of them—who have floaters in both eyes—after they have one eye done, want the other eye done as well because they’re so happy to be free of floaters. I have patients who are several years out from surgery, and they’re quite pleased with their outcome.”
If a patient has a cataract and vitreous floaters, she performs a combined case and has an anterior segment surgeon remove the cataract. Then, she performs the vitrectomy for the floaters.
Dr. Sebag’s procedure of choice is a limited vitrectomy. “I leave 3 or 4 mm of gel vitreous behind the lens intact to mitigate against cataract formation, and if the patient doesn’t have a PVD, I don’t induce one surgically, to minimize the risks of retinal tears and detachments but also to limit the increase of intravitreal oxygen levels that occurs following vitrectomy,” he says. “It’s the increase of O 2 in vitreous that causes the changes in the lens that result in cataract formation. So, limited vitrectomy was developed in recognition of the fact that doing vitrectomy for floaters needed to be as safe as possible. To increase the safety profile, I avoided inducing a PVD and hoped that, as a result, the incidence of retinal tears and detachments would be lower. It turns out that this only occurs 1.5 percent of the time, meaning that limited vitrectomy is 98.5-percent safe,” he says.
In 2018, he published a study of 195 subjects who were treated with limited vitrectomy. 6 This study had a high success rate as determined by quantitative ultrasonography and by measuring contrast sensitivity. “Concerning the latter,” says Dr. Sebag, “in 139 consecutive cases who preoperatively had an average degradation in contrast sensitivity of 91 percent in comparison to controls, contrast sensitivity was normal in each case within a week of limited vitrectomy, and that was sustained for months and years thereafter. Cataract surgery was required in only 16.9 percent of cases, and retinal detachments only occurred in 1.5 percent of cases.
“Moreover, the patients were extremely happy, and we also documented that quantitative ultrasonography was significantly better in this series of patients,” Dr. Sebag adds. “The complication rates were very acceptable. This study showed that limited vitrectomy was highly effective and safe.”
Studies have also shown that, after limited vitrectomy in patients who are unhappy after cataract surgery with multifocal IOL implantation, contrast sensitivity improved, in spite of the multifocal intraocular lens. 7 Dr. Sebag therefore recommends vitreous evaluation in patients who are unhappy with multifocal pseudophakia and that there be consideration of limited vitrectomy for these unhappy patients.
He has performed more than 300 limited vitrectomies on all types of patients. “So far, limited vitrectomy has been found to be more cost effective than amblyopia therapy, cataract surgery, and retinal detachment repair,” 8 he says.
YAG laser vitreolysis (YLV) is an alternative to vitrectomy, because surgery isn’t for everyone. “In spite of being highly skeptical of YLV in the past, I’ve opened my mind to the possibility that YLV has a role in certain cases,” says Dr. Sebag. “Whereas YLV has been done for years all over the world, it hasn’t been embraced by the vitreoretinal surgery community. It’s being done by general ophthalmologists, and I wonder whether it might be embraced by the vitreoretinal community and perhaps be done with greater precision and efficacy if it could be shown to be effective in a subgroup of individuals.”
He believes that YLV will be somewhat successful, but not in all patients. “The reason is that there’s more than one cause for vision-degrading myodesopsia and vitreous floaters,” he notes. “The leading cause is a PVD, which tends to be the case in older individuals. I think that in those individuals, it will turn out that YAG laser isn’t effective, except for the subset of people who have a disturbing Weiss ring or a particularly prominent central vitreous opacity in whom YLV might be effective, at least subjectively by questionnaire evaluation and perhaps also by contrast sensitivity measurements.”
He believes that patients with myopic vitreopathy, which is the second leading cause for vitreous floaters and vision-degrading myodysopsia, 9 may be good candidates for YAG laser treatment. “These people tend to be younger and don’t have a PVD, so those may be the individuals who should be treated with YAG laser. We’re currently conducting a prospective clinical trial of YLV and hope to report the results in the not-too-distant future,” he says.
Other technologies are currently being considered for treating vitreous floaters. “Picosecond and femtosecond lasers may prove to be more effective than YAG laser, especially if the treatment can be localized with 3D imaging guidance of the laser energy,” says Dr. Sebag. “That would help YLV, as well, but with more powerful lasers, we will probably be able to ablate the opacities rather than just break them down, which is what’s occurring now with the YAG laser. Pharmacologic vitreolysis may also play an important role in chemically breaking down the aggregates of collagen that are in the vitreous body that cause the shadows that result in the visual phenomenon of floaters and degradation of contrast sensitivity. I’m very excited about the possibility of developing drugs and injecting them into the vitreous body to treat vitreous floaters and vision degrading myodesopsia.
“Following the recent anti-VEGF experience,” Dr. Sebag continues, “we’re all comfortable injecting drugs into the vitreous body, so it wouldn’t be that hard to get the community to accept pharmacologic vitreolysis as a treatment paradigm for vision degrading myodesopsia, but we need to develop the right drugs and use them at the right dose, so a lot of work needs to be done in that regard.”
Another approach is being developed at the University of Ghent in Belgium using nanoparticles that are specifically designed to adhere to the opacities within the vitreous body that are causing floaters and vision-degrading myodesopsia. 10 “After injecting the nanoparticles, a low-energy laser is used to treat the vitreous body, which doesn’t have to be targeted because the nanoparticles chemically adhere to the opacities and preferentially absorb the laser energy, creating localized nanobubbles that break up the membranes and aggregates of collagen that are causing the floaters and vision degrading myodesopsia,” explains Dr. Sebag. “This has been developed in vitro and has been tested in rabbits in vivo . 10 It’s been shown that the laser energy levels that are required are 1,000 times less than what’s currently being used for YLV. I would like to see it developed further for the treatment of patients with vitreous floaters.”
Then, there is an optical approach. “If we understood the optics and physics of how light is interacting with the structures within the vitreous body that are causing floaters and inducing vision-degrading myodesopsia, 11 perhaps that could be corrected with an optical apparatus that counteracts the untoward effects of light scattering, which degrade contrast sensitivity. If we neutralize that, maybe we could decrease the symptoms and lessen the impact by treating optically,” Dr. Sebag says.
Dr. Sebag concludes that, “It’s not often that you come across an unmet medical need, where simply opening your mind and heart not only opens new diagnostic and therapeutic avenues, but resonates with patients. They feel ignored, they feel dismissed, they sometimes even feel insulted by the approach that we’ve taken up until now. But, as is always the case with increased knowledge and good science, we become armed with the tools that will help us understand the plight of our patients and enable us to develop better ways to evaluate what’s happening to them, as well as more effective and safer ways to treat them.”
Dr. Lim has no financial interests to disclose. Dr. Sebag has IP interests in the patents for quantitative ultrasonography and Nanobubble therapy.
1. Sebag J. Vitreous and vision degrading myodesopsia. Prog Retinal Eye Res 2020;100847.
2. Mamou J, Wa CA, Yee KM, et al. Ultrasound-based quantification of vitreous floaters correlates with contrast sensitivity and quality of life. Invest Ophthalmol Vis Sci 2015;56:1611-1617.
3. Garcia G, Khoshnevis M, Yee KM, Nguyen-Cuu J, Nguyen JH, Sebag J. Degradation of contrast sensitivity following posterior vitreous detachment. Am J Ophthalmol 2016;172:7-12.
4. Garcia G, Khoshnevis M, Nguyen-Cuu J, et al. The effects of aging vitreous on contrast sensitivity function. Graefe’s Arch Clin Exp Ophthalmol 2018;256:919-925.
5. Boneva SK, Nguyen JH, Gui W, et al. Recurrent floaters following limited vitrectomy for vision degrading myodesopsia. Retina 2023;43:1114-1121.
6. Sebag J, Yee KMP, Nguyen JH, Nguyen-Cuu J. Long-term safety and efficacy of limited vitrectomy for vision degrading myodesopsia resulting from vitreous floaters. Ophthalmology Retina 2018;2:881-887.
7. Nguyen JH, Yee KMP, Nguyen-Cuu, et al. Vitrectomy improves contrast sensitivity in multifocal pseudophakia with vision degrading myodesopsia. Am J Ophthalmol 2022;244:196-204.
8. Rostami B, Nguyen-Cuu J, Brown G, et al. Cost-effectiveness of limited vitrectomy for vision degrading myodesopsia. Am J Ophthalmol 2019;204:1-6.
9. Nguyen JH, Nguyen-Cuu J, Mamou J, et al. Vitreous structure and visual function in myopic vitreopathy causing vision degrading myodesopsia. Am J Ophthalmol 2021;224:246-253.
10. Sauvage F, Nguyen VP, Li Y, et al. Laser-induced nanobubbles safely ablate vitreous opacities in vivo. Nature Nanotechnology 2022;17:552-559.
11. Paniagua-Diaz A, Nguyen JH, Artal P, Sebag J. Light scattering by vitreous of humans with Vision Degrading Myodesopsia from floaters. Invest Ophthalmol Vis Sci 2024 (In Press).
Related Articles
A new understanding of vitreous structure, buckling may be preferred in macula-off detachments.

The Impact of DRCR Protocol Studies
Lab-grown retinal cells may open door to restoring vision, distinguishing infection post-intravitreal injection, current issue.

Table of Contents
Read digital edition, read pdf edition, subscriptions.

Copyright © 2024 Jobson Medical Information LLC unless otherwise noted.
All rights reserved. Reproduction in whole or in part without permission is prohibited.

IMAGES
VIDEO