Featured Topics
Featured series.
A series of random questions answered by Harvard experts.

Explore the Gazette
Read the latest.

Everything counts!

How do you read organization’s silence over rise of Nazism?

Got milk? Does it give you problems?
Photos by Stephanie Mitchell/Harvard Staff Photographer
Love, death, fear, guilt, pride, hope, friendship, alienation, and so much sorrow. Through it all, they kept showing up.
14 nurses on life and work during COVID
Colleen Walsh
Harvard Staff Writer
Since early 2020, when the pandemic exploded around the world, Massachusetts has seen nearly 19,000 COVID deaths and more than 840,000 cases. If a line graph of hospital admissions over the past 20 months looks like a series of peaks and valleys, the initial surge was Mount Everest for the state’s medical facilities, with patient loads and death rates that have not been matched since. To understand how the crisis has felt for frontline workers caring for the sick and dying, the Gazette reached out to 14 nurses at four Harvard-affiliated hospitals, many of whom work in intensive-care units. When the pandemic began, some had just started their careers, while others had been on the job for years. They risked their lives to stand by their patients, and their stories are marked by hope, heartbreak, and resilience.
“It’s never easy to witness my patients suffering, but I never gave up on any of them. I held out hope and prayed that each would survive.”
Afomia bekele.
Brigham & Women’s Hospital, Boston
I work on the gynecology surgical oncology inpatient floor, but during the pandemic, the entire floor converted into a COVID-19 inpatient unit. Working with these patients brought extraordinary challenges. First, I went through extreme anxiety and fear of being exposed to the virus and carrying it home to my family. In addition, the work was incredibly taxing. Nurses jumped in on many other job duties on the COVID floor in order to reduce the use of personal protective equipment. We fed patients, cleaned up after them, made video and audio calls with their loved ones. Through all this, seeing these patients deteriorate and having several heartbreaking discussions with family members was an emotional roller-coaster. The patients in this unit had low oxygen levels and could suddenly become critically ill. Of course, it’s never easy to witness my patients suffering, but I never gave up on any of them. I held out hope and prayed that each would survive. I cheered each patient that I discharged home, and seeing them reunite with a family member put a smile on my face. Most of all, I appreciated the support I received from my family. That encouraged me to keep going.
“The unknown was frightening, but the urgency the pandemic placed on health care workers all over the world didn’t allow us to sit in that fear or uncertainty for too long.”
Rachel bresilla.
Beth Israel Deaconess Medical Center, Boston
March 2020, my fast-paced medical-surgical unit came to an abrupt halt. John Ryan, our nursing director, informed us that our unit would be transitioning to a 36-bed COVID intensive-care unit. We were then whisked away to a four-hour crash course on “how to be a critical-care support nurse.” What I remember next is a unit filled with ventilated COVID patients. I vividly remember the fear that banded my co-workers and myself together and a sense of uncertainty that was felt throughout the medical center. The unknown was frightening, but the urgency the pandemic placed on health care workers all over the world didn’t allow us to sit in that fear or uncertainty for too long. Our patients needed us, their families were trusting us, and we were called to act, adapt, and help save as many of those precious lives we cared for as possible. I look back to that time with great pride. Pride in the devoted care we provided for each person in those hospital beds. Pride in how the Beth Israel Deaconess Medical Center community came together to support and encourage us in every way imaginable. Great pride in every hospital staff member who showed up every day despite the unknown. The year 2020 undoubtedly marked us all in a unique, defining way. For me, it’s the year I silenced fear, rose to the challenge, persevered, and embodied the year of the nurse.
“The intensive-care units were unrecognizable, with large numbers of very sick patients. … With all the personal protective equipment we were wearing, you could not identify who a person was or their role on the unit.”
Michelle covell.
Brigham & Women’s Hospital
As a medical intensive care unit nurse, I have been working through the pandemic in the same capacity from the start. The most stressful time was opening the first special pathogens unit (SPU). The intensive-care units were unrecognizable, with large numbers of very sick patients. Nurses, doctors, respiratory therapists, and physical therapists were pooled together from all over the hospital to help care for the patients. With all the personal protective equipment we were wearing, you could not identify who a person was or their role on the unit, so we put tape with our names and roles on our scrubs and instituted a shift huddle so people could briefly get to know each other and what was happening with their patients. As a charge nurse, I had to figure out who were the sickest patients needing the most support. I would try to keep morale going by assigning breaks and lunches. When my spouse, also a Brigham nurse, was deployed to the SPU, we worked opposite shifts so one of us could be home to manage remote learning for our eighth-grade twins. Members of our community wanted so desperately to help that a group of parents delivered dinners to our house three days a week for two months! Whether a homemade meal or just pizza delivery, it always arrived with a lovely note of support or some flowers, something positive and encouraging that helped us get through this time. These meals lifted a huge weight off our shoulders, and we are forever grateful to everyone for their support. The selfless acts that seem small but have a huge impact for the greater good are what bring me hope.
“We would go home to shower not just because we didn’t want to risk exposing loved ones, but to attempt to wash off trauma, wash away the guilt of wondering if we could do more.”
Grace defrank.
Mount Auburn Hospital, Cambridge
During the beginning of the pandemic there was no questioning — we showed up, we did what we had to do. We would go home to shower not just because we didn’t want to risk exposing loved ones, but to attempt to wash off trauma, wash away the guilt of wondering if we could do more and not spending quality time with our patients in their last moments. Death became commonplace. Nevertheless, sad and defeating. I had lost sight of myself as a nurse. If anything, the pandemic opened my eyes to how incredible health care workers are. We truly had each other’s backs and kept each other going. While working through COVID-19 will always affect me as a nurse, I refuse to let it define my nursing career. I’d like to think it pushed me into wanting more for myself in my career. I craved something new, something I hope to find more fulfilling. I am all of three shifts into a new job in the nursery and I can’t even try to explain how good it feels to hear, “Time of birth, 5:39 p.m.”
“The effects of the pandemic on the lives of mothers giving birth under these extreme conditions and the impact on their babies is something I still struggle to process.”
Sonya elenbaas.
Beth Israel Deaconess Medical Center
The pandemic shook our world, and the health care community in particular over these past 18 months. The effects of the pandemic on the lives of mothers giving birth under these extreme conditions and the impact on their babies is something I still struggle to process. As a neonatal intensive care unit (NICU) nurse at Beth Israel for the past 21 years, I have never experienced a crisis quite like this, despite the life-and-death nature of my job. There is a layer of complexity in treating moms and infants during a pandemic that necessitated the collaboration of clinicians from all areas of expertise in the NICU and labor and delivery units to minimize the risks of transmission of the virus and the potentially grave effects on our patients. My role as a nurse never felt more important or more valued than during this time. The innumerable gestures of gratitude from patients’ families, from our own families and friends, and from the world outside of the hospital were astounding and incredibly uplifting for all of us as health care workers. Reflecting on the past 18 months, I feel a sense of pride at having been part of a team of health care workers who found creative solutions to how we could safely care for high-risk infants born to COVID-positive mothers while not diminishing our responsibility to provide life-saving care. I see the progress that science and the understanding of the virus has brought to our level of care and the lives of our patients, and their families, and it gives me a feeling of relief as well as hope.
“These patients were parents, grandparents, sons, daughters, neighbors, and friends, all fighting this horrible virus alone in an isolated room.”
Michael ferrazzi.
I transferred to the medical intensive care unit from one of the medical step-down units during the beginning of the second surge back in the fall of 2020. I had no idea what I was getting myself into. To say I was overwhelmed and scared is an understatement. Seeing with my own eyes how critically ill with COVID-19 these patients were was truly eye-opening. These patients were parents, grandparents, sons, daughters, neighbors, and friends, all fighting this horrible virus alone in an isolated room. We utilized FaceTime and Zoom so our patients could see and communicate with their loved ones on a screen before we had to use a breathing tube to treat their deteriorating respiratory status. Unfortunately, for many this was the last time they saw their loved ones. Through all this hardship, I witnessed extraordinary teamwork with disciplines across the Brigham. Caregivers were working in unfamiliar areas with a common goal to care for and support these critical patients during an unprecedented time. I’m afraid we could experience another surge again, but I remain hopeful for a light at the end of this very dark tunnel.
“At first we were all fearful, worried about bringing COVID home to our families. But once we started taking care of these incredibly sick patients, we just did what needed to get done.”
Lisa mcneil.
Massachusetts General Hospital, Boston
I treated COVID-19 patients during both surges. I tried to make calls twice a day to update family members. In the beginning, we used our own phones to help them FaceTime, and later, the hospital was able to get a computer in every room, just so they could hear their voices. After 30 years in the intensive care unit, I’ve learned I’m here to help the patient, and the patient’s family. I lost my mother when I was young, and I’ve never forgotten how an incredible team of nurses and doctors helped me through. Their support ensured I wouldn’t carry that tragedy as a burden for the rest of my life. I try to bring that approach to the families I work with. Mass General has also supported us in every way. In the early days, volunteers from other parts of the hospital ensured we were putting on and taking off our protective equipment correctly to avoid any contamination. That was crucial in the beginning, and I am so grateful to them. I liken it to what the military must go through when something bad happens. Everyone just steps up to help. At first we were all fearful, worried about bringing COVID home to our families. But once we started taking care of these incredibly sick patients, we just did what needed to get done.
“To the family members who lost loved ones to COVID and were not able to be at their bedsides, please know they were not alone. We held their hands, we wiped their tears as we wiped our own, and we prayed for them as well as for you.”
Jane postizzi.
For most of my nursing career, I have worked on an intermediate medical unit that treats patients with a multitude of complex and chronic issues. These patients can become critically ill, and as medical professionals, we rely on our experience and education to help support them through such difficult times. It wasn’t until I worked directly with patients infected with COVID-19 in the special pathogens unit that I felt all that gained experience and intuition were essentially useless. I learned to accept the harsh unpredictability of COVID and harnessed my energy toward what I felt I could control: patient comfort and care. It was never lost on us that these patients were more alienated than the greater hospital population. The hospital provided means for patients to virtually communicate with their loved ones and, although this was deeply appreciated, it did not replace the importance of holding that person’s hand when it was needed most. We witnessed patients say goodbye to their families over Zoom and then we stayed by their sides. To the family members who lost loved ones to COVID and were not able to be at their bedsides, please know they were not alone. We held their hands, we wiped their tears as we wiped our own, and we prayed for them as well as for you.
“I never imagined I would begin my nursing career during a pandemic. Although I was excited to see what I could do as a nurse, I was also nervous as my floor became a COVID unit within a week.”
Madelin puleo.
Massachusetts General Hospital
I never imagined I would begin my nursing career during a pandemic. Although I was excited to see what I could do as a nurse, I was also nervous as my floor became a COVID unit within a week. One of the hardest things was seeing how quickly patients deteriorated. The worst part was that they could not have their loved ones at their bedsides. It was difficult to watch patients suffer physically and emotionally. Luckily, we were able to facilitate Zoom calls, allowing patients to see and speak to their families even if it was on a screen. In the beginning, we had little information about this disease. Hospitals saw a shortage of personal protective equipment and that terrified health care workers. We were afraid of getting COVID and spreading it to our loved ones. Months later this fear came true. I got sick with COVID despite having followed protocol. Luckily, I only experienced mild symptoms, and I got through it with the help of family and my husband, who was my rock. I am also extremely thankful for my co-workers’ support. From the beginning, everybody was so wonderful, teaching me how to become a great nurse, despite facing one of the scariest times in their careers. It was such a relief knowing no matter how unprepared I felt, they made sure I was ready to take care of these patients; I knew I was not alone in this fight. The year 2020 was not what any of us expected, but it taught me to be thankful for the small things and to appreciate life more.
“As we tackled this, we went from being hailed as heroes to being utterly overwhelmed by the constantly evolving policies, procedures, and guidelines that the pandemic created.”
Catie raftery.
Working as a nurse during a pandemic has been a humbling experience. What I presumed would be a smooth intro to intermediate medical nursing quickly shifted when the pandemic hit four months into my first hospital job. All of a sudden, we were immersed in this deadly pandemic, and a few months later, I was relocated to the COVID unit. There, our task was to treat patients with an illness marked by enigmatic spread and elusive cure, one which threatened to upend the lives of all those in its path. As we tackled this, we went from being hailed as heroes to being utterly overwhelmed by the constantly evolving policies, procedures, and guidelines that the pandemic created. In addition, we juggled comforting families only able to see their loved ones through the screens of iPads; holding the hands of those who feared for their lives; consciously deciding to spend additional time with patients who expressed feelings of loneliness and seclusion; and battling the constant fear and anxiety of exposing ourselves or our families. Although it may take years to process all these events, I know that every day I show up, give my all, and strive to bring hope, peace, comfort, and joy to every single person I encounter. It has been my greatest honor to be able to be a registered nurse in a time like this.
“These hard times have molded me into a more patient, caring, and empathetic person, both at my workplace and in my everyday life.”
Tatiana raufi.
Mount Auburn Hospital
I have been a nurse for two years now and over the last year alone, I have had experiences I never expected to have so early in my career. To put it bluntly, it’s been an emotional roller-coaster. I cannot emphasize enough how much I value the powerful bonds that I have created with my co-workers, my second family. Being at the bedside of those sick with COVID-19 has been psychologically and physically exhausting, but I’ve learned how critical my role as a nurse is in bridging a connection, with consistent communication with patients and their loved ones. There are many times I had to be the voice of my patient, whether it was relaying what was needed from the medical team or providing continuous updates to those they care about but who were unable to come into the hospital. These hard times have molded me into a more patient, caring, and empathetic person, both at my workplace and in my everyday life. Despite the tragedies I have witnessed, I am grateful for all I have learned and for who I have become.
“I had a 6-month-old at the time. Then, five days before our peak surge numbers in the hospital, I found out I was pregnant.”
Caitlin sullivan.
In my 12 years as a nurse, I never anticipated anything like this. Being scared and overwhelmed are the feelings that really stand out to me from March and April of 2020 — going to work every day not knowing if I was going to get sick or bring COVID-19 home. I had a 6-month-old at the time. Then, five days before our peak surge numbers in the hospital, I found out I was pregnant. I remember holding my son after a shift and thinking, “I can’t get this. I have to stay well for you.” I also remember the complete devastation the virus caused among our most vulnerable, and how ruthless it was. At first, we saw older patients with comorbidities. Then we started seeing people in their 40s and 50s who were otherwise healthy. Our most intensive therapies were no match for the virus. In the beginning, no families were allowed to visit, so we were the only ones with patients in their final moments, holding their hands. That stays with you. To cope, we relied on our co-workers. We cried together, supported each other, and just rallied together and found strength in one another because we shared that unique bond. The people I work with are truly incredible. We really couldn’t do what we do, or what we have done, without each other.
“How do I tell a neonatal intensive care unit nurse her assignment today is to hold the iPad for the family of a dying adult intensive-care unit patient so they can say goodbye?”
Mary tenney.
To the non-nursing community, I am the head nurse, the supervisor of nurses, the one who takes care of things like staffing and budgeting, but it’s actually so much more than that. On Feb. 28, 2020, I attended a hospital leadership meeting where we learned of a confirmed case of COVID-19 in California. My immediate thought was, “Just like Ebola, we’ll painstakingly make sure staff know how to use personal protective equipment but then never actually need it.” Within two weeks, I realized how naive that notion really was. To say supporting the nurses who reported to me was a challenge is a gross understatement. My job as their nurse manager is to make sure they are providing safe and quality care, but to also educate to protect them from harm. How do I teach them new ways of utilizing PPE, to extend the lifespan of their PPE? How do I tell a neonatal intensive care unit nurse her assignment today is to hold the iPad for the family of a dying adult intensive-care unit patient so they can say goodbye? I did it with empathy, encouragement, and positive reminders of why we all became nurses.
“The tears from my colleagues were real. The fear in their eyes was real. The compassionate care they provided to every patient coming into our emergency department was real. And the pride I have for my colleagues is real.”
Roxane white.
The end of 2019 was difficult, bringing us many challenges in the emergency department — and this was before COVID hit. While we were devising a plan to turn things around, 2020 reared its ugly head and brought us COVID. We didn’t know what to expect and were understandably afraid, however, it took a pandemic to help bring our team together. Every staff member in our department banded together to get through this thing together. We ensured each of us wore the proper personal protective equipment, despite the frequent changes to protocol. We listened to one another’s fears and raised each other’s spirits every day. We worked equally hard for the COVID patients who came in. The tears from my colleagues were real. The fear in their eyes was real. The compassionate care they provided to every patient coming into our emergency department was real. And the pride I have for my colleagues is real. This togetherness could be felt throughout the medical center, and it was a good feeling. Once you’ve been through a pandemic with your colleagues, you have a special bond that will last a lifetime.
Share this article
You might like.
New study finds step-count and time are equally valid in reducing health risks

Medical historians look to cultural context, work of peer publications in wrestling with case of New England Journal of Medicine

Biomolecular archaeologist looks at why most of world’s population has trouble digesting beverage that helped shape civilization
Glimpse of next-generation internet
Physicists demo first metro-area quantum computer network in Boston
Finding right mix on campus speech policies
Legal, political scholars discuss balancing personal safety, constitutional rights, academic freedom amid roiling protests, cultural shifts
‘The scientist is not in the business of following instructions.’
George Whitesides became a giant of chemistry by keeping it simple
How the COVID-19 Pandemic Changed the Role of Nurses

The COVID-19 pandemic has taught the world a harsh lesson about the fragility of the many systems we rely on each day and their interconnectedness. Health is the system most significantly impacted, and the COVID nurse roles and responsibilities within that system emerged as a lynchpin. Many people recognized for the first time why nurses and other health professionals are important not just to patient experience, but also to community health. The role of nurses and their experience shepherding patients through a pandemic will continue to be critical in rebuilding community health and preparing for the next health crisis—if and when one should arise.
“Nurses are leading in ways that are really quite similar to their usual work, but during a crisis, visibility and awareness of that work is higher,” Patricia Davidson , dean and professor at the Johns Hopkins School of Nursing in Baltimore, said in a recent interview. “The pandemic is heightening the need for team-based care, infection control, person-centered care and other skills that really speak to the strengths of nurses.”
Here are five reasons why nurses are important in today’s health care environment.
The Role of Nurses in Resource Management
The responsible management of health care resources—from people to technology to medicine and materials—has always been critical to the timely and effective delivery of high-quality health care. As the pandemic stretches health care facilities thin and shuts down critical industries that supply health care providers with necessary equipment, it has become apparent that resources as simple as gloves, gowns and masks—commonly referred to as personal protective equipment (PPE)—could make or break a health system’s ability to treat patients and preserve employee safety.
Even now that many manufacturing operations have come back online and supply chains are rebounding, the management of resources and preparation for future crises remains an important role of nurses. Nursing during a pandemic has given today’s nurses the once-in-a-generation experience of managing resources under the conditions of scarcity, and we celebrate them for the creativity and innovation they showed through the pandemic that will provide evidence-based strategies for the future.
According to research published in the Annals of Global Health , nurses play a crucial role in PPE management by minimizing the need for PPE. They do this by educating staff, coordinating PPE supply chains and leading efforts to reduce PPE use. “After the current crisis abates,” the researchers write, “nurses and other health professionals will need to work with government, health services and regulatory bodies to ensure that future stores of PPE are retained and fit for purpose and that PPE use is enveloped into the regularly evaluated core competencies of all health care workers.”
The Role of Nurses in Awareness and Public Education Campaigns
Nurses develop some of the strongest bonds with patients when compared with other health care providers in the continuum of care. The connections they forge make patients more receptive to their messaging—whether it be about medication compliance , self-care, health and wellness education, medical condition treatment compliance, preventive health or vaccination.
The role of nurses in building trust and educating people about the facts of the coronavirus and its variants cannot be overstated. Even as our grasp on controlling the pandemic has become firmer with vaccines and mitigation efforts, misinformation, politicization of information and skepticism remain as barriers to complete eradication of the virus. Because they are consistently ranked as the most trustworthy professionals , nurses are uniquely positioned to be effective educators who can dispel myths and help people weed through false or misleading information.
In the American Journal of Tropical Medicine and Hygiene , researchers write, “Nurses hold a vital function, as one of the most distinguished health service teams, in delivering public awareness regarding disease prevention and in decreasing the dissemination of myths regarding the epidemic. This involves countering myths, guiding people to available health services and supporting evidence-based patient management and infection reduction initiatives.” This was evident in late 2021 when the delta and omicron variants were wreaking havoc throughout the United States. Nurses went to various platforms including local and national news stations and social media to speak against the myths and educate the population on evidence-based health prevention and promotion.
This cultural and logistical shift in the delivery of care will undoubtedly require education, compassion and experience, three qualities that are also unique to nurses and position them to lead the transition.

The Role of Nurses in Government and Public Health Policymaking
The pandemic is revealing the many ways that various social determinants, such as education, financial stability, environment and access to health care influenced who was affected most by COVID-19. Many of these determinants can be affected by public policy, and attempts have been made in the past to address them with varying degrees of success. Nursing during the pandemic has exposed nurses to a real-world data set from which they can identify trends and propose solutions.
Nurses are also well-versed in the realm of policymaking, and have a history of advocating for their patients and themselves in the halls of Congress. Many nursing associations at state, local and national levels participate in letter-writing campaigns, awareness-raising and Congressional lobbying to inform legislators about the evolution of nursing practice and opportunities for improvement.
The role of nurses is well established in government, nonprofit and research institutions where they use their expertise to conduct research to solve real-world problems and provide a practitioner’s point of view on public health agendas.
“Nurses are predominantly depicted providing direct patient care,” write the authors of “ Nurse Expertise: A Critical Resource in the COVID-19 Pandemic Response ,” but they “are also well represented at every level of pandemic response from advising governments to leading research, coordinating public health teams and strategizing humanitarian responses to COVID-19. [...] Nurses with qualifications in infectious diseases, disaster management, public health and epidemiology are ideally placed to provide expert advice at governmental levels.”
Now that awareness has been raised about the many factors that can affect a person's susceptibility to outbreaks like the coronavirus and policymakers look to craft programs that can improve social determinants of health, nurses will be invaluable voices in the conversation about how our public health policy can evolve and improve.
The Role of Nurses in Population-based Medicine
The role of nurses in reimagining nursing practice will also be critical in the aftermath of the pandemic.
In their research, the authors of “Nurse Expertise” also found that “nurses worldwide have had to change their model of care to a population-based model with the rapid onset of this pandemic. [...] Nurses play key roles in many decentralized community health programs and population-level services. Health systems with a strong community focus that value preventive interventions and integrate community engagement and empowerment may have an advantage in pandemic response compared to the more traditional biomedical, hospital-centric systems. In community-centered settings, the acutely and chronically unwell do not need to congregate together over extended periods to receive health care in a single setting.”
The Role of Nurses in Training the Next Generation
Even before the pandemic, the need for nurses was projected to rise and outpace the output of nursing schools in the coming decade. Part of that imbalance is related to the number of current nurses who will be retiring soon—one of the trends in nursing for 2022 that will further increase demand for nurses throughout the United States.
A report from the American Nurses Association predicts more than 500,000 seasoned RNs anticipate retiring by 2022. The U.S. Bureau of Labor Statistics projects the need for 1.1 million new RNs for expansion and replacement of retirees, and to address the current nursing shortage.
In the current pandemic, nursing shortages are exacerbated by shifting infection surges that take down some working nurses and overwhelm others who are fortunate enough to remain healthy. In response nurses from across the country volunteer to join the ranks in COVID hotspots, and others have come out of retirement to offer their skills. Many of these nurses who parachuted into the crisis are doing so with a willingness to learn but without the most up-to-date knowledge on the methods specific to critical care.
This is confirmed by the “Nurse Expertise” authors, who write, “Experienced critical care nurses familiar with current practice and technology will supervise large numbers of returning and new nurses in ICUs, many of whom will be anxious about the extra responsibility and implementing unfamiliar practices, such as managing ventilated patients in the prone position, who are also highly infectious. Nurse practitioners and nurses in other advanced-care roles are likely to play a central role in training and mentoring. This new model of nursing care delivery calls for rapid critical care teaching and learning to prepare the new nursing workforce in a swift but robust manner to minimize risk, optimize patient safety and reduce the burden of supervision.”
After the pandemic wanes, there will still be patients dealing with long term effects from the COVID-19 virus who will need skilled nurses to help them recover and learn to manage their health. Nurses who worked through the pandemic will have the invaluable firsthand experience of treating the symptoms, complications and related illnesses of COVID-19 to help new and less-experienced nurses care for this population as their long-term outcomes continue to evolve and be studied.
Interested in Becoming a Nurse?
The importance of nurses has never been greater, and neither has the need. If you feel called to become a nurse, or even if you’re just curious, check out Elmhurst University’s distance Accelerated Bachelor of Science in Nursing (ABSN) . In just 16 months, you can be on the fast track to a rewarding career among the ranks of health care heroes.
Elmhurst University also offers an accelerated Master’s Entry in Nursing Practice (MENP) program, for students who already have a bachelor degree in another field but want to pursue a career in nursing. In 20 months you can achieve your Master of Science in Nursing (MSN) degree, while preparing to sit for the registered nurse licensure exam (NCLEX-RN) and clinical nurse leader (CNL) certification.
Learn whether the Accelerated BSN or MSN program is right for you .
Thank You For Your Interest
Unfortunately, your location is currently ineligible for our program but we’d like to help you continue your search. Visit OnlineABSNPrograms.com and enter your ZIP code to find a CCNE-accredited program near you.
Requirements Not Met
To proceed with either the BSN to MSN FNP or the BSN to DNP FNP, you are required to have a bachelor’s degree and hold your RN license.
If you don’t meet these requirements but would still like further information, please contact us .
To proceed with the EdD in Educational Leadership and Organizational Leadership, you are required to have a master’s degree.
If you don’t meet this requirement but would still like further information, please contact us .
X Close Box
© 2024 Elmhurst University • All Rights Reserved • Privacy Policy • California Privacy Notice
- Request Info
Cookie Acknowledgement
This website uses cookies to collect information to improve your browsing experience. Please review our Privacy Statement for more information.

- Office of the Provost
- Core Curriculum
- Academic Calendar
- Course Schedule
- Advisement Schedule
- Final Exam Schedule
- Visit Academics
- Check Application Status
- Undergraduate Admissions
- Graduate Admissions
- Pharmacy Admissions
- Veterinary Medicine Admissions
- Distance Ed
- Accepted Students
- Request Information
- Visit Admissions
- Public Service & Community Partnerships
- Professional & Continuing Education
- Youth Programs
- Government & Economic Development
- Osher Lifelong Learning Institute
- Faculty Engagement
- Outreach Global
- K-12 Outreach
- Visit Outreach
- Research Administration
- Work with Auburn Research
- Find Auburn Expertise
- Research Resources
- Centers & Institutes
- Graduate Research
- Undergraduate Research
- Auburn Research Magazine
- Research Symposia
- Visit Research
Pandemic highlights important role of nurses
Article body.
Since the days of Florence Nightingale during the Crimean War and Clara Barton during the Civil War, nurses have been an integral part of the care and treatment of the sick and wounded. The COVID-19 pandemic has shed a spotlight on nurses and reinforced the essential role they have in hospitals and clinics worldwide. Caralise Hunt, an associate professor and associate dean for academic affairs in Auburn’s School of Nursing, discusses the spotlight and what Auburn is doing to prepare young people for the future of health care.
How have nurses become heroes in this crisis?
Nurses are at the bedside with patients around the clock. They are prepared to assess patients’ conditions and make decisions about the type of care they need. Nurses implement the infectious disease prevention measures that control the spread of the virus. They spend a lot of time with patients, caring for them, listening to them, getting to know them. This is a scary time for patients; there are many unknowns related to coronavirus. Additionally, hospitals are limiting or prohibiting visitors so patients are in the hospital alone. Nurses are there for patients to advocate for them and provide the support they need and would normally get from their significant others.
When everyone else is trying to run away from danger, nurses walk toward it. They are making sacrifices to care for patients including staying in hotels so they don’t have to worry about taking the virus home to their family. They are placing themselves at risk for the good of their patients.
How will they continue to be looked to for help in the months/years to come?
As we move toward recovery from COVID-19, nurses will be providing health promotion/illness prevention education in our communities. They will dispel myths and provide evidence-based information about how to care for themselves and others during this pandemic.
How is Auburn preparing its nursing graduates to be ready to enter such a trying workforce?
We begin preparing our nursing students for the challenging health care environment from the moment they begin the nursing program. They are taught the foundational critical thinking and clinical judgment skills and we continue to develop those over the five semester baccalaureate program. We provide them with multiple interprofessional education experiences so they are prepared to work alongside other health care professionals to provide holistic, patient-centered care.
As Auburn’s School of Nursing transitioned to remote learning during the spring semester, faculty and staff prepared online simulation experiences for our students. These simulations were conducted using Zoom sessions with small student groups. They provided students the opportunity to think through next steps in care of a patient and make decisions about what should be done. We also incorporated several online resources, such as a personal protective equipment simulation.

Caralise Hunt is an associate professor and associate dean for academic affairs in Auburn University’s School of Nursing.

Auburn University is a nationally ranked land grant institution recognized for its commitment to world-class scholarship, interdisciplinary research with an elite, top-tier Carnegie R1 classification, life-changing outreach with Carnegie’s Community Engagement designation and an undergraduate education experience second to none. Auburn is home to more than 30,000 students, and its faculty and research partners collaborate to develop and deliver meaningful scholarship, science and technology-based advancements that meet pressing regional, national and global needs. Auburn’s commitment to active student engagement, professional success and public/private partnership drives a growing reputation for outreach and extension that delivers broad economic, health and societal impact.

- Auburn, Alabama 36849
- (334) 844-4000
- Website Feedback
- Auburn University at Montgomery
- Alabama Cooperative Extension System
- Alabama Agricultural Experiment Station
- Visitors Guide to Campus
- Campus Safety/Emergency Preparedness
- Distance and Continuing Education
- Office of Information Technology
- Diversity, Equity & Inclusion
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 24, Issue 4
- COVID-19: reflections on its impact on nursing
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-4308-4219 David Barrett 1 ,
- http://orcid.org/0000-0003-2221-1573 Roberta Heale 2
- 1 Faculty of Health Sciences , University of Hull , Hull , UK
- 2 School of Nursing , Laurentian University , Sudbury , Ontario , Canada
- Correspondence to Dr David Barrett, Faculty of Health Sciences, University of Hull, Hull HU6 7RX, UK; D.I.Barrett{at}hull.ac.uk
https://doi.org/10.1136/ebnurs-2021-103464
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
- nursing staff
- nurses- international
One of the characteristics of the COVID-19 pandemic is that much of what is published about it quickly becomes outdated. Such is the rate of change in the pandemic’s course—whether due to the roll-out of the vaccine program globally or the evolution of new variants—that the context in which articles are written may be very different by the time of publication.
Given that, it’s perhaps important to ‘time-stamp’ this editorial and outline the context at the time of writing. We’re writing this in the late summer of 2021; the UK is experiencing a third wave of the pandemic, while simultaneously removing almost all COVID-19 restrictions (such as limits on public gatherings), having fully vaccinated three-quarters of the adult population and partially vaccinated almost 9 out of 10 adults. Although there are differences, the situation is similar within other countries in Europe and North America, with vaccines seemingly weakening the link between infection, serious illness and death, thereby allowing for loosening of social restrictions.
Though the situation at the time you are reading this will no doubt be different, there are some things of which we can be sure. First, COVID-19 has already ‘ … killed millions, affected billions and cost trillions.’ 1 impacting all parts of the globe over a prolonged period. Second, the impact on healthcare services has been immense, whether through the acute pressures on hospital capacity during each wave of the pandemic, the need to redesign service delivery in order to minimise face-to-face interaction, or the long-term consequences of reduced elective and preventative services.
There has also been a personal toll on nurses and other healthcare professionals. The WHO estimates that as of May 2021, approximately 115 000 healthcare workers have died from COVID-19. 2 The impact of the pandemic on the mental health and well-being on practitioners has been well-documented, with anxiety, depression and post-traumatic stress disorder being reported in nurses, 3 along with increased risk of burnout and emotional exhaustion. 4 Some healthcare workers, including nurses, have also been subject to bullying and stigma, partly due to the perception that they are more likely to contract and spread COVID-19. 5
In the short-term then, the nursing profession’s focus must be on supporting its members’ well-being as we hopefully (given the roll-out of vaccinations globally) move into final stages of the pandemic. But what will the legacy of COVID-19 be for nurses and nursing in the years to come?
The delivery of healthcare has changed irreversibly during COVID-19, and nursing will need to adapt accordingly. The rapid shift to technology-mediated healthcare, such as virtual primary care consultations, will require nurses to ensure that they possess not only the technological skills required to manage these new approaches to providing care, but also the communication skills necessary to assess and support patients via different media (eg, videoconferencing; telephone). Critically, nurses must also be aware of the potential risk that certain groups of the population, such as older people or those facing digital poverty, may be uncomfortable with—or excluded by—the move to technology-mediated care. 6 As advocates for their patients, nurses must ensure that not only is the care they deliver person-centred, but that the modality through which care is provided is adapted according to the patients’ characteristics, abilities and preferences.
Complacency with infection control measures and gaps in public health policies and processes quickly became apparent during the pandemic. This is one area where nursing really showed its worth. Throughout the pandemic, nurses have used their extensive knowledge and skills on infection control measures, such as the effective use of PPE, to enhance the safety of staff and patients. Moving forward, nurses need to further define their role in infection control and ensure that they are centrally involved in related policy development and decision-making. 7
The public and media profile of nursing has never been higher. Across the globe, we have seen nurses and other practitioners applauded, praised and honoured for their work during the pandemic. There is no question that the contribution of nurses, along with other healthcare professionals and key workers, should be acknowledged by wider society. However, the raised and changed profile of the nursing profession within society is something of a double-edged sword.
One benefit may be that as nursing continues to face a workforce crisis, the public awareness of the profession will increase recruitment to nurse education courses. There are already indications that this could be occurring—in the UK, for example, 2021 saw a 32% year-on-year increase in applications to commence nursing courses (with a 39% increase in applications from the over-35s). 8 There are two important caveats with these data. First, it is impossible to know exactly what drives this increase or whether it is a long-term or short-term trend. For example, it may be due in part to the economic downturn and job insecurity linked to societal lockdowns, so could represent a transient increase in interest in nursing as a profession. Second, any benefit from increased student nurse recruitment may be offset by nurses leaving the profession due to the psychological and physical impact of COVID-19. The International Council of Nurses has highlighted that one-in-five National Nurses Associations report increased numbers of nurses leaving the profession in 2020, with many more reporting higher rates of intention-to-leave. 9
The enhanced profile of nurses has led to some concerns being raised regarding the nature of the profession’s portrayal in the media and among the public. This particularly relates to the ‘angels and heroes’ narrative, where nurses are viewed as self-sacrificing, brave and quasi-superhuman. Though this narrative is well-meaning and representative of the public’s gratitude towards nurses, it also risks the high-level skills and knowledge demonstrated by nurses being overlooked, potentially serving to ‘…undermine the professionalism of the nursing workforce, and reinforce the perception that nursing is an innately feminine, nurturing role . ’. 10 Over the coming years then, nursing needs to shape its profile in such a way that the complexity and skill involved in providing high quality care are at the forefront, while still acknowledging and celebrating the public trust and gratitude demonstrated during the pandemic.
There will come a time when we speak of COVID-19 in the past tense; when it will be subject to retrospective analysis and debate, rather than being something we continue to live through. However, the pandemic’s repercussions will be felt for years to come in society, in healthcare and in nursing. As a profession, there has never been a more important time to demonstrate resilience, to adapt to the changed context of care and to highlight nurses’ skills, knowledge and expertise. EBN journal will be focusing on this during October 2021 when the weekly blogs will explore the impact of COVID-19 on nurses, nursing and health.
Ethics statements
Patient consent for publication.
Not required.
- World Health Organization
- Heesakkers H ,
- van Mol MMC , et al
- Bruyneel A ,
- Tack J , et al
- Alcantara L ,
- Siddiqi S , et al
- Kronish I ,
- Fleck E , et al
- University and Colleges Admissions Service
- International Council of Nurses
- Stokes-Parish J ,
- Elliott R ,
- Rolls K , et al
Twitter @barrett1972, @robertaheale
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Provenance and peer review Commissioned; internally peer reviewed.
Read the full text or download the PDF:
Pandemic's Impact on the Nursing Profession
Nurses continue to experience effects on their health, morale and careers.
This article is based on reporting that features expert sources.
How Pandemic Impacts Nursing Profession
The COVID-19 pandemic made an immediate impact on the nursing profession. Some nurses suffered devastating health consequences. Many nurses dealt with excessive on-the-job stress, well-founded fears of becoming infected and grief over seeing patients succumb to COVID-19 while isolated from their families.

Getty Images
Workplaces became risky and fraught with shortages of adequate personal protective equipment like masks. Hospital jobs abruptly changed, and nurses found themselves caring for patients outside their realms of expertise, often with minimal training.
Even as the pandemic begins to wane unevenly across the U.S., long-term fallout on the nursing profession is likely. Burnout may linger even after the situation returns to "normal." For some nurses, conditions under which they worked may be the last straw that drives them away from bedside nursing. Yet, nursing schools are drawing more applicants.
Other positive glimmers – such as increased professional autonomy , leadership opportunities and career growth potential – have resulted from pandemic-based health care needs.
Below, nurses share their insights on the negative, positive and as-yet-unknown effects of COVID-19 on their professional peers.
First-Wave Effects
New York City was at the epicenter of the pandemic when COVID-19 first hit the U.S. There, nurses caring for patients during this first wave experienced depression, anxiety and illness, according to a study published April 5, 2021, in the journal Nursing Outlook.
About one-quarter of nurses reported anxiety and 17% reported depression among nearly 2,500 nurses surveyed working in four hospitals in the NYU Langone Health system, according to researchers at NYU Rory Meyers College of Nursing. Anxiety and depression increased the more that individual nurses cared for patients with COVID-19 . Younger nurses and nurses working in intensive care units were more likely to experience these mental health issues.
In addition, 13% of nurses reported having become infected with COVID-19. Nearly half of nurses had to self-isolate and nearly 20% lived in temporary housing that the hospital provided. Professional development and training, particularly in proper use of PPE, was one of the top helpful factors for caring for patients with COVID-19, according to study authors. Having a sense of mastery at work was the most protective against depression and anxiety.
Unfortunately, in many hospitals throughout the country, nurses often felt under-educated and under-trained to take care of COVID-19 patients. In numerous cases, the issue wasn't just knowing how to safely put on and remove PPE – it was not having enough PPE to safely take care of patients.
To reduce the spread of COVID-19, hospitals severely limited nonessential or nonemergency treatment, shutting down clinics and many services. As hospitals rapidly created new ICUs and shifted specialty units to focus on patients with COVID-19, many nurses were abruptly thrust into unfamiliar patient care settings and roles – like pediatric nurses suddenly required to take care of adult ICU patients. And, of course, nobody was experienced in giving care to patients infected with the novel coronavirus.
"Just-in-time training" is used in fields like disaster medicine to rapidly get health care providers up to speed, in the moment and at their location, in basic principles, skills, procedures and safety measures to take care of patients in a crisis.
But instead of "just in time," it was more a case of "too little, too late" when it came to COVID-19 preparation by health and hospital administrations, suggests Gerard Brogan, a registered nurse and director of nursing practice for the California Nurses Association/National Nurses United.
"In the American health care system there's just-in-time staffing, just-in-time procurement of supplies," Brogan says. "Well, what did that lead to? A paucity of personal protective equipment. That's been one of the biggest stories of the year."
The U.S. had plenty of advance warning about the pandemic, Brogan says. "Within the medical community, it's been known for decades there will be a pandemic," he says. "It's never been a question of 'if.' It was always a question of 'when.' And, certainly those who make these decisions aren't paying the price, of course. It's the frontline workers who are doing that."
Ernest Grant, president of the American Nurses Association, says PPE shortages represent the most immediate impact on the nursing profession. "It's hard to believe, but it's been over a year and nurses are still reporting that they're having difficulty getting their PPE, or personal protective equipment, such as masks," he says.
The necessity to reuse and resterilize face masks intended for disposal after a single use is a particular pandemic sore spot. Ongoing controversy as to whether it's truly safe to repeatedly wear these masks – especially when working with known or potentially infected patients – has sown fear, anger and mistrust among some frontline health care providers.
Brogan recalls one of the many discussions he's had with nurses over the issue: "This is absurd – a year ago, if I had reused an N95 mask, I literally would have been disciplined," the nurse told him. "Now, I'm being disciplined if I don't reuse an N95."
To address the situation, nursing organizations have advocated for improved distribution chains and use of the Defense Production Act . The DPA is law giving the president emergency authorization to control domestic industries. Most recently, it has been used to maximize production of N95 respirator masks and speed up vaccine production in the U.S. to alleviate shortages.
Health Consequences
Nurses who died of COVID-19 represent an irreversible loss from the pandemic. Whatever happens moving forward, their lives can never be replaced. Of the more than 3,600 health care workers who lost their lives to COVID-19 in the first year of the pandemic, nurses were the occupation most affected, accounting for 32% of those deaths, according to the Lost on the Frontline investigation, a joint effort of Kaiser Health News and The Guardian.
In October 2020, the Centers for Disease Control and Prevention broke down COVID-19-associated hospitalizations among health care personnel by specific occupation. Nursing-related occupations represented the largest proportion (36%) of health care personnel hospitalized with COVID-19, according to the CDC.
A new study focused on persistent effects. This research found that long COVID syndrome affected about 10% of health care workers, even some with initially mild symptoms. The study of previously healthy Swedish health care workers was published April 7 in JAMA. Symptoms included loss of taste and smell, fatigue and breathing problems which negatively affected their work, personal lives or both, months after being infected. Similar studies of U.S. health care workers are ongoing.
Ripe for Burnout
Nursing burnout and stress was already a problem before the pandemic. "Increasingly, nurses are having more and more tasks added to their to-do lists daily in hospitals," says Jacqueline Nikpour, a graduating PhD candidate at Duke University School of Nursing and an incoming postdoctoral fellow at the University of Pennsylvania School of Nursing's Center for Health Outcomes and Policy Research. "Then you just add the massive uncertainty – it goes beyond workload because you're working in survival mode with COVID for months on end." With cases decreasing, she says, "what you're starting to see is more of a prolonged burnout."
Early public support and gratitude expressed for nurses and other frontline health care workers may have eroded as the pandemic dragged on, Nikpour suggests. "Now, with the political debates about masks and vaccination, and people who are going out in large groups, nurses are saying, 'COVID cases are still happening – I'm still seeing these patients every day,'" she says. "And there's a lot of backlash from the public. Rather than it being, 'Oh, you're the health care heroes' like it was a year ago, now it's more, 'This is what you signed up for.'"
In a nationwide survey of more than 9,200 registered nurses released in March 2021, conducted by National Nurses United, participants reported these mental health and emotional issues a year into the pandemic:
- Of hospital RNs, 43% have more trouble sleeping than before the pandemic.
- More than 61% feel more stressed.
- Anxiety has increased for 57% of these nurses.
- About half feel more sad or depressed.
- Nearly 60% say they fear they'll contract COVID-19 and infect a family member.
Personal as well as professional lives have been strained, points out Robyn Begley, CEO of the American Organization for Nursing Leadership and chief nursing officer/senior vice president of workforce for the American Hospital Association.
"Throughout the pandemic, nurses have worked long hours while trying to simultaneously manage their personal lives at home, such as arranging child or elder care," Begley says. "Many nurses shared concerns over bringing the virus home to their families."
Job-related stress could have long-term as well as immediate effects, Begley adds. "We are concerned about the mental health and well-being of the nursing workforce," she says. "Nurses have worked tirelessly caring for critically ill dying patients without having the time to grieve or practice self-care. We are particularly concerned about the number of nurses who may leave their current roles providing direct patient care or exit the nursing profession entirely."
In the pandemic's wake, the preexisting nationwide nursing shortage could get worse. Nikpour currently works on a research team at the Sheps Center for Health Services Research at the University of North Carolina at Chapel Hill, as part of a partnership with the North Carolina Board of Nursing.
The team has created a supply-and-demand project of the state's nursing workforce over the next 10 to 15 years. "We're going to be releasing a model that demonstrates a shortage of up to and above 10,000 nurses across the state by 2033," Nikpour says. "That's pretty substantial. Now, you hope that things will be done to offset that by then."
Nationwide, the shortage of registered nurses is expected to intensify with baby boomers aging and health care needs increasing, according to the AACN website.
Silver Linings
The pandemic has produced some positives for the nursing profession. " There is greater recognition of the critical role that nurses play in fighting the pandemic – caring for patients while protecting and promoting the health of communities," Begley says. "Nurses have taken on leadership roles in this work, while utilizing innovative strategies to promote health such as telehealth technology, which allows patients to receive care from the safety and convenience of their home."
Rather than pushing students away from nursing careers, a recent survey showed an increase in applications to nursing schools, Begley notes.
Student enrollment in bachelor's and graduate-level nursing programs all increased in 2020, according to data released on April 1 by the American Association of Colleges of Nursing . For bachelor's programs to prepare new registered nurses, enrollment increased by nearly 6%.
However, there's a downside: With persistent shortages of nursing faculty to teach students and of clinical sites for training, thousands of qualified applicants are being turned away from nursing programs at four-year colleges and universities, the AACN survey found. For example, more than 65,000 applicants were denied enrollment into entry-level nursing programs last year.
Yet, nurses are needed more than ever. The pandemic could represent an opportunity for nurses to move to career paths beyond inpatient hospital units, and expand their presence in outpatient care and more broadly in public health, Nikpour says.
Nurses are taking major roles in efforts to reduce disparities in health care access, delivery and outcomes that are related to social determinants of health . For example, Nikpour says, North Carolina has been rolling out a state referral program called NCCARE 360. The program aims to address root causes of health problems – such as meeting the unmet social needs of a mother living in older housing with lead paint, affecting her child who has asthma. Rather than accepting the status quo of the child requiring periodic emergency visits for asthma attacks, the program would tackle the toxic environment in which the family lives, refer the child to preventive care and improve his or her health.
"Nurses are really going to need to be a part of these programs," Nikpour says. "Now, with increased focus on health equity, we're starting to see some of those opportunities emerge as nurses are looking for employment in other settings."
In light of the pandemic, advanced practice nurses realized an increase in their autonomy, with more ability to practice independently to meet the health care crisis.
"When the pandemic occurred, there was an emergency situation declared, which allowed more of what we call full-practice authority for the advanced practice nurses – nurse practitioners and clinical nurse specialists – to be able to do telehealth and telemedicine across state lines without fear of retribution," Grant says.
Some states which had required nurse practitioners to practice in collaborative agreements with supervising physicians temporarily suspended those requirements, notes an August 2020 article in the American Journal of Nursing . In addition, the Centers for Medicare and Medicaid Services granted nurse practitioners approval to provide certain medical services in long-term care settings that previously were only provided by physicians, according to the AJN piece.
It will be difficult to unring the bell after the pandemic has passed, Grant suggests. "We're not going to go back when this is over," he says. "Because we've proven that we can do this stuff. And this is an emergency situation – imagine what we could do in a quote-unquote normal situation to really be able to advocate for your patients."
People with chronic illnesses such as diabetes, arthritis and heart disease will continue with needs that must be met, Grant notes. "We've been able to achieve that through telehealth, telemedicine and other initiatives that have the public or the consumer feeling much more appreciative of the actions that nurses have been doing," he says. "So I feel pretty certain that once this pandemic is declared over and nurses begin to want to declare more full-practice authority, the public will be behind us. Because we have proven that we can do it. So we should be able to move forward."
Nurses Shine on Multiple Front Lines

The U.S. News Health team delivers accurate information about health, nutrition and fitness, as well as in-depth medical condition guides. All of our stories rely on multiple, independent sources and experts in the field, such as medical doctors and licensed nutritionists. To learn more about how we keep our content accurate and trustworthy, read our editorial guidelines .
Begley is CEO of the American Organization for Nursing Leadership and chief nursing officer, senior vice president of workforce for the American Hospital Association.
Brogan is a registered nurse and director of nursing practice for the California Nurses Association/National Nurses United.
Grant is president of the American Nurses Association.
Nikpour is a graduating PhD candidate at Duke University School of Nursing and an incoming postdoctoral fellow at the University of Pennsylvania School of Nursing’s Center for Health Outcomes and Policy Research.
Tags: nurses , Coronavirus , hospitals
Most Popular

Patient Advice

health disclaimer »
Disclaimer and a note about your health ».

Your Health
A guide to nutrition and wellness from the health team at U.S. News & World Report.
You May Also Like
Having a baby after cancer.
Christine Comizio May 21, 2024
10 Signs of Strep Throat
Elaine K. Howley May 20, 2024
Pregnancy Checklist
Payton Sy May 17, 2024
Early Pregnancy Signs
Vanessa Caceres May 17, 2024
Prostate Cancer: Questions to Ask
Ruben Castaneda and Payton Sy May 16, 2024

Does Medicare Cover the RSV Vaccine?
Paul Wynn May 16, 2024
5 Types of Primary Care Doctors
Elaine K. Howley May 15, 2024

How to Tell You Have a Hernia?
Claire Wolters May 14, 2024

How to Treat Seasonal Allergies
Shanley Chien May 13, 2024

Questions to Ask About Diabetes
Toby Smithson and Elaine K. Howley May 13, 2024

Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Nurses’ perspectives of taking care of patients with Coronavirus disease 2019: A phenomenological study
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Nursing, Faculty of Allied Health Sciences, University of Peradeniya, Peradeniya, Sri Lanka
Roles Formal analysis, Methodology, Writing – review & editing
Affiliation Department of Paediatrics, Faculty of Medicine, University of Peradeniya, Peradeniya, Sri Lanka
Affiliation School of Nursing, Kandy, Sri Lanka
- Sarath Rathnayake,
- Damayanthi Dasanayake,
- Sujeewa Dilhani Maithreepala,
- Ramya Ekanayake,
- Pradeepa Lakmali Basnayake

- Published: September 3, 2021
- https://doi.org/10.1371/journal.pone.0257064
- Reader Comments
The pandemic of Coronavirus disease 2019 (COVID-19) has brought significant pressure on nurses globally as they are the frontline of care. This study aimed to explore the experiences and challenges of nurses who worked with hospitalised patients with COVID-19. In this qualitative study, a purposive sample of 14 nurses participated in in-depth telephone interviews. Data were analysed using Colaizzi’s phenomenological method. Five key themes emerged: (1) physical and psychological distress of nurses, (2) willingness to work, (3) the essential role of support mechanisms, (4) educational and informational needs of nurses and (5) the role of modern technology in COVID-19 care. Although the provision of care led to physical and psychological distress among nurses, with their commitment and professional obligation, it is a new experience that leads to personal satisfaction. Guilty feeling related to inefficiency of care, witnessing the suffering of patients, discomfort associated with wearing personal protective equipment (PPE), work-related issues (e.g., long hour shifts), negative impact to the family and rejection by others are the leading distress factors. Religious beliefs, including keeping trust in good and bad merits, have become a strong coping mechanism. Addressing distress among nurses is essential. The reported learning needs of nurses included skills related to donning and doffing PPE, skills in performing nursing procedures and breaking bad news. Nurse managers need to pay special attention to expanding training opportunities as well as support mechanisms, for example, welfare, appreciations and counselling services for nurses. Modern technology, particularly robots and telecommunication, can perform an essential role in COVID-19 care. The establishment of timely policies and strategies to protect health workers during a national disaster like COVID-19 is needed.
Citation: Rathnayake S, Dasanayake D, Maithreepala SD, Ekanayake R, Basnayake PL (2021) Nurses’ perspectives of taking care of patients with Coronavirus disease 2019: A phenomenological study. PLoS ONE 16(9): e0257064. https://doi.org/10.1371/journal.pone.0257064
Editor: Harald Gündel, University Hospital Of Ulm, GERMANY
Received: November 16, 2020; Accepted: August 21, 2021; Published: September 3, 2021
Copyright: © 2021 Rathnayake et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All files are available from the OSF database (DOI 10.17605/OSF.IO/PHX43 ).
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Coronavirus disease 2019 (COVID-19) is a respiratory infectious disease caused by a newly identified coronavirus named SARS‐CoV‐2 [ 1 , 2 ]. Health workers, especially nurses, have to play a significant role in combating this health problem on both preventive and curative sides. A recent systematic review identified that nurses have a pivotal role in healthcare when responding to infectious disease pandemics and epidemics [ 3 ]. Koh et al. [ 4 ] report that facing emerging respiratory diseases is an unavoidable health hazard for nurses who are in the frontline of care as nurses have to live, experience and accept this risk. Caring for patients with COVID-19 demands more knowledge and training [ 5 ]; however, the literature supports that nurses provide this care without adequate expertise [ 6 ]. Moreover, several studies have explored that nurses experience extra pressure, burden and psychological problems during global respiratory outbreaks (e.g. Severe Acute Respiratory Syndrome [SARS], H1N1 influenza, Human Swine Influenza and Middle East Respiratory Syndrome [MERS]) [ 7 – 13 ]. Therefore, nurses need continuous support and training to improve their preparedness and efficacy of crisis management as well as to cope with psychological problems and safeguard their well-being [ 3 , 6 ].
However, there is limited evidence related to nurses’ experiences concerning caring for patients with COVID-19 globally. The available studies have mainly focused on exploring physical and psychological distress [ 5 , 6 , 14 ]. Liu et al. [ 6 ] have reported that health workers, including nurses dedicated to combating this pandemic while they experienced physical and emotional stress. There is a study that examined the overall perception of nurses towards COVID-19 care, and it identified challenges faced by nurses, for example, feeling of inefficiency, stress, fatigue, dilemma concerning care delivery and problems associated with using personal protective equipment (PPE) [ 15 ]. In a crisis like COVID-19, it is difficult to formulate a well-established evaluation plan; therefore, post hoc reflection of health workers helps to manage future crises effectively [ 9 ]. Therefore, further exploration of experiences, particularly the overall experiences of nurses who cared for patients with COVID-19, is essential. This study aimed to explore the experiences of nurses who cared for patients diagnosed with COVID-19 during the initial period of the crisis in Sri Lanka.
Materials and methods
Study design.
This qualitative study employed Colaizzi’s phenomenological approach [ 16 ].
Participants and recruitment.
Participants were nurses who took care of patients with COVID-19 in public hospitals for COVID-19 patients in Sri Lanka. A purposive sample of nurses was initially recruited through social media (i.e. Facebook). Then, the snowballing sampling method was applied to recruit potential participants. Data saturation was considered to determine the sample size [ 17 ]. Nurses who cared for at least one patient diagnosed with COVID-19 in public sector hospitals, who could speak in Sinhala, volunteers who were willing to participate in this study, and who were able to articulate their experiences were included. Nurses who worked in the private sector were excluded.
Data collection procedure.
In-depth telephone interviews were conducted by the first researcher during June 2020, using an interview guide developed by the research team based on the literature and aim of this study ( Table 1 ). The telephone method helped to collect data during the curfew period with travel restriction. After identifying the potential participants, we distributed written information sheets and consent forms via electronic media (i.e., email and WhatsApp). Possible time for both parties was set. Interviews were digitally recorded with prior permission from the participants. The duration of the interviews was ranged from 50 minutes to 75 minutes.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0257064.t001
Ethical considerations.
We obtained ethical approval for this study from the Ethical Review Committee, Faculty of Allied Health Sciences, University of Peradeniya, Sri Lanka. Verbal informed consent was sorted before data collection and recorded as a part of the telephone interviews.
Data analysis.
Three members of the research team transcribed digital audio files. All personal identifiers were removed from the transcripts. Participants received the transcripts to check their accuracy and resonance with their experiences [ 18 ]. Based on Colaizzi’s phenomenological approach [ 16 ], relevant themes were identified. When writing the detailed description, relevant quotes were translated into English from the Sinhala language by two researchers and the consensus was achieved. In the reporting of this study, we followed the consolidated criteria for reporting qualitative research (COREQ) checklist (S1 Appendix) [ 19 ].
The trustworthiness of the study.
The four-dimensional criteria were applied to ensure the trustworthiness of this study [ 20 , 21 ]. To achieve Credibility , participants received a copy of the transcription for member checking. Persistent observation of data was ensured by identifying themes and sub-themes, including reading and re-reading data and identifying statements and meanings relevant to nurses’ experiences. Additionally, participants received a summary report based on findings to check whether the analysis captures their experiences. For example, P13 said that results are a representation of the experiences and challenges they experienced during providing COVID-19 care. Transferability was assured by providing adequate contextual information (setting, sample, sample size, sample strategy, socio-demographics, inclusion and exclusion criteria and interview procedure). Dependability was achieved by using accepted standards i.e., Colaizzi phenomenological approach [ 16 ] in data analysis. To assure conformability , the first researcher identified the potential statements and meanings for the first transcription, and these meanings were discussed with other researchers for consensus. A continuous discussion was endured for new meanings. The first and second researchers categorised meanings and identified themes and sub-themes. A consensus was achieved for the final themes among team members.
Demographic characteristics
Table 2 shows the demographic characteristics of the participants. The sample consisted of one male and 13 female nurses.
https://doi.org/10.1371/journal.pone.0257064.t002
Five key themes and their attended sub-themes were identified ( Table 3 ). Nurses were de-identified in reporting (e.g., P1).
https://doi.org/10.1371/journal.pone.0257064.t003
Theme 1: Physical and psychological distress among nurses
This theme discusses the physical and psychological distress experienced by nurses.
Fear towards COVID-19.
Participants identified COVID-19 as a frightening disease. They stated that they were at increased risk of getting the infection; this risk was unavoidable, which led to increased fear of exposure to the virus. “Really, it is a risk. No matter how many safety precautions we take. If there is a slight mistake, we need to be afraid.” (P13). One nurse said that she heard several deaths due to COVID-19 among health workers around the world, and it worsened her feeling of scared. Some participants said that they were panicked when they heard the first diagnosed patient was coming to the unit and showed extreme fear when admitting the first patient. One participant said that she had a hallucination like feeling after the provision of care. “… Sometimes it’s like hallucination while on duty in the ward…sore throat. When I go home, I just feel like that… hurts a lot” (P2). Participants stated that they followed precautionary measures to maintain their health and to prevent from COVID-19. The reported measures were regular hand washing, regular temperature checking, drinking hot water, using traditional remedies like coriander and ginger mixed water, taking cod-liver oil, taking a high dose of Vitamin C, taking anti-histamine, having hot water baths and steam inhalation.
The negative impact on the family.
The majority of participants showed a feeling of fear related to being a potential carrier for family members. “I was a little scared that it would happen to me, but I scared, I would give this terrible disease to my husband, then to his family, the mother is too old…” (P6). They said that their family members were too scared, and dealing with those suffering was intolerable. Returning home and living with family members in the same house, living in hospital accommodations and looking after kids were some other issues reported. Participants reported that separation from family members, especially from their kids, was intolerable. “At that time, I came home, and my two babies were next door with my sister. I’m over here. I stand in the yard looking at my two children. How they are in that yard. It’s really hard to remember” (P14).
Social stigma and discriminations.
Participants said that they were rejected by peers, co-workers, family members, neighbours and society, making them frustrated. One participant said that when she worked in the COVID-19 unit, others looked at her like a patient with COVID-19 positive. “At that time, others looked at me; it was just like corona to me…” (P14). Another participant said that not only the general public, health staff also rejected them. “..Oh. Really sad. So when the health staff does the same. You don’t need to talk about ordinary people” (P13). Moreover, few participants said that they and their families were rejected by the neighbours, shops, and taxi drivers. “After this hospital was named as a corona hospital, there were rejections from the shops around” (P11). The majority stated that they did not tell others that they were working in COVID-19 units, and this condition led to limited social interactions and self-isolation. Some participants noted that rejection might be attributed to social stigma and the frightening nature of COVID-19.
Work-related physical and psychological discomfort.
Work-related factors, including lack of staff, working long hour shifts, increased workload, and inadequate rest time, were other main factors that led to physical tiredness and psychological burden. “In some shifts, the workload is too much for a single nurse; then, there was no time, we didn’t even have water or cup of tea” (P13). “There were only two nurses for 15 patients in this ward, but we had to work for about 50 patients. It was very difficult for us and tired. When we finished our duty, we were exhausted” (P2). Therefore, they highlighted that they require adequate rest time to improve their immunity.
Additionally, wearing PPE is one of the main factors that led to the physical and psychological burden. Reported physiological discomfort included difficulty breathing, excessive sweating, headache, back pain, skin damage and pressure on the nasal bridge due to strips of goggles, vomiting, fainting and visual disturbances. “…that goggle.., put on a cap.., it’s too much to bear, the day before I had a headache for a day and a half or two… and back pain, we walked in boots …, It’s hard.., there is a big discomfort in the body…” (P3). Participants further reported mist due to facemask and googles made difficulties in cannulation and drawing blood. In terms of psychological burden, one participant stated that wearing a PPE first time was a frightening experience. “I was so scared. I mean, it was hard to breathe when I put on an N95 mask. I felt very restless for a while. Then, I thought for a while, and that feeling went away a bit. Then, I went to collect blood…” (P12). They further said that they had an uncertainty related to protection received from PPE. They said that they had to take additional measures before donning PPE, for example, eating and drinking adequate water and going to washrooms, adding emotional discomfort. Moreover, all participants identified removing PPE as a very relaxing experience. One participant said that it might be due to physical relaxation or releasing from the risk of contact with patients. Another participant stated this experience as ‘like attaining Nirvana’, (i.e., a Sinhalese saying related to a feeling of sheer relaxation). “…after removing the PPE…, like going to Nirvana. Um… .it’s like going to Nirvana…” (P2).
Witnessing patients experiences.
Participants said that they witnessed the suffering of patients, including their fear of death. “…the fear in the heart of the patient when he was admitted. This is a fatal disease. All those patients told the story; we will die or what will happen to us…” (P12). They further stated that patients were very anxious, and some patients reported depressive symptoms, especially when they received positive PCR results. “…those guys… . yes, psychologically really upset. Let’s assume that when a patient is discharged, from the same set, if one patient cannot go home, that means he is the only positive, they mourned… like in a funeral…” (P8). They further said that older people and people with chronic diseases were terrified, and older people were helpless in the wards as nurses could not reach them all the time. Several participants stated that informing negative results to patients was the happiest experience for the patients and nurses. “He is 27 years old boy…I said, brother, your report is negative, now you can go, I really said ‘brother’… that boy was so worried. He cried when I told him that his PCR was negative, that’s happiness…” (P14). “I told the patient that your report is negative and you can go home in the evening. This is the best, happiest last moments out there…” (P2).
Guilty feeling related to inefficiency of care.
Although they were empathetic towards patients, participants stated that they had to limit care due to strict guidelines imposed. This situation caused a reduction in direct care time that led to the inefficiency of care. For instance, one participant stated, “... I did only whatever works need to do. We can’t go inside always without PPE…” (P11). Many participants said that wearing PPE limited the establishment of a good nurse-patient relationship. “…poor people. I meant they don’t see us. Really, they don’t know who we are. They know we’re nurses because we say we’re nurses.” (P2). They further stated that the provision of care with these limitations led to a guilty feeling as they were unable to provide adequate care compared to usual care. “Those people are terrified. We are less likely to get too close to a patient, even to reassure, when that happened, I felt sad when I couldn’t do that” (P11).
Coping mechanisms.
Many nurses highlighted that they believed their religion and followed religious activities before and after their duty shifts. “I am a Buddhist, of any religion, everyone is bound to give nursing care by their religion. I think my religion has taught me a lot about this. If we do something good, our parents and we will get something good. I really believe this” (P11). Some nurses believed that everything happened according to ‘good’ and ‘bad’ merits, and if they did a fair job, they would re-paid it as a prevention from COVID-19. “No matter what we do, you get it as good or bad merit whether you are a Catholic, a Muslim, a Buddhist or whatever. Although the way of saying ‘good and bad merit’ in each religion has changed, the way of receiving is the same”(P2). As reported by nurses, the main group who shared their suffering were nursing peers and friends. “We all talk together… we can’t go home. Sometimes in the quarters, talking to two or three people, (laughing)… and sharing our grief” (P3). Other reported methods were crying, trying to hiding uncomfortable thoughts (i.e., repression) and rationalisation. “…at the same time… No, it will not happen. He was also wearing a mask; I was also wearing a mask. This did not happen…” (P1).
Theme 2: Willingness to work
This theme highlights nurses’ willingness to provide care, including their sense of professional obligation.
Sense of professional obligation.
Nurses highlighted a sense of obligation for work. Some participants reported that they should provide this care because they were nurses. “It is not right to leave this time due to personal matters… . I am a nurse. I get paid” (P1). They showed their dedication and professional commitment to providing care. One participant said that her fellow nurse ran to a patient without completing PPE donning when the patient self-remove her endotracheal tube. “The patient self-removed the tube. The saturation of the monitor is dropping. Monitors are alarming. Now, she was half-dressed…, this nurse suddenly ran without goggles and boots” (P 14). Participants stated that this was an opportunity to serve the community and mother country that everyone cannot do. “I think I was able to do something better than others. We were able to do a lot for patients’ happiness… (P9). “…I had a feeling that I also participated in that national mission…” (P6).
Provision of care is a new experience.
As COVID-19 care is a newly emerged area, some participants stated about their motivation to provide care. They were curious and had a desire to work with patients. “Actually, I had to see how she (patient) was…, how we could deal with her…?” (P3). “It was a different experience … that’s why… at that time, it felt like to do something… that means I felt to go to COVID care unit” (P 7). Participants further viewed that it was a new experience for their professional life and an opportunity to learn and test new care strategies and protocols. “Everything is a new procedure and a new experience” (P12). “As a staff member, I tried my best to reduce patients’ stress. It feels like weird nursing care, not normal nursing. Did it in a new way. We had to adapt to the problems that arose” (P11). One participant noted that it was the best experience she had in her nursing life.
Personal satisfaction of nurses.
Although the provision of care was a terrible experience for them, many participants stated that they were delighted with the given care at the end of their placements. They used the words “happy”, “pleasure”, or “proud” to explain their satisfaction. “It’s nice to be involved with something like this. It’s a pleasure. Everyone is scared. We, as nurses, are directly involved. Proud of it. Glad to be able to do something as a nurse that not everyone can do…” (P6). One participant said that she felt like a ‘hero’ when she first cared for a patient. Moreover, they stated that they were happy as mass media promoted and highlighted their contribution to the COVID-19 crisis.
Theme 3: Educational and information needs of nurses
This theme encapsulates the educational and informational needs of nurses who cared for patients with COVID-19.
Need for prior training and education.
All participants highlighted the need for prior training and education to provide care for patients with COVID-19. Few participants said that previous experiences related to providing care for H1N1 influenza and MERS were beneficial to provide successful care. “…When H1N1 was there, I was on duty in that ward. With that experience, I was not scared. I have even taken blood samples from H1N1 positive patients” (P2). Although some nurses had participated in related training programmes, some reported on inadequate or no prior training opportunities, and it increased their fear of patients and care. “We placed there; we had to do everything. But I didn’t have any training. I always felt I would contaminate because I didn’t know how to do” (P14). “It was a little training. To wear PPE and how to do the cleaning. But, when I went to the ward, I thought, it was not enough” (P10). One nurse stated that only demonstration was not adequate for wearing PPE, and nurses should have even one opportunity to wear a PPE kit before the actual practice. They highlighted that the basic nursing curriculum needs to address these aspects, and a sufficient number of nurses should be trained to confront future challenges in a crisis like COVID-19.
Learning needs of nurses.
How to maintain safety during COVID-19 care, including donning and doffing of PPE, and performing nursing procedures, including collecting samples for PCR and disinfection, were the main care-related learning needs. “I did not even know how to wear the kit. N95 masks were not even in the ward (i.e. usual workplace). So, I was embarrassed because I did not know how to do” (P14). The other prioritised learning need was breaking bad news. Participants highlighted the challenges faced during informing positive PCR results to patients. “If we did fourteen PCRs, we say how many negatives and how many positives to patients. Only a few of these people were negative. Others were positive. We had people from different countries as well as from the Navy. It may vary from country to country” (P11). One participant said that they informed results to all patients as a group, while another stated that some patients wanted total confidentiality on positive PCR reports.
Learning strategies of nurses.
Participants further explored various learning strategies that they used during this period. Some nurses have participated in the planned training programmes conducted at the National Institute of Infectious Disease (NIID), Angoda, and they said that it was beneficial in providing care. Some hospitals have arranged institutional-based in-service programmes before opening new units. The majority noted that peers, especially experienced and trained nurses, helped them to learn wearing PPE and other care. “There were nurses who were trained. I asked them and did the same” (P7). According to participants, self-directed learning was a robust method, and the internet and the media helped improve their knowledge of COVID-19 care. Additionally, participants highly valued the availability of care guidelines and protocols and receiving timely information enabled them to get new knowledge and provide safe care.
Theme 4: Essential role in support mechanisms
This theme highlights the importance of support mechanisms, including workplace support and personal support networks for nurses.
Need for adequate resources
Participants emphasised that a comfortable work environment was paramount in providing adequate care, and they highly valued the availability of sufficient human resources, other facilities and equipment. They highlighted that a pre-plan is essential when establishing units for people affected with COVID-19. One participant stressed that they had a sufficient number of supportive staff, and it was very helpful. “While there were positive patients, there was a larger group of minor staff than us. They gave good support in our works” (P13). Participants said that the availability of facilities, particularly adequate protective measures, cleaning facilities and bathing facilities, are essential to ensure their safety and occupational preparedness. “…to get the maximum care from us, we need to have adequate protection. If we do not receive those things, we are also afraid, and it is difficult to give good care” (P11). However, some nurses reported inadequacy of facilities and equipment; for example, inadequate PPE, poorly arranged patient and staff areas, lack of restrooms, lack of facilities for cleaning and bath, and inadequate facilities to communicate with patients.
Need for welfare during frightening health crises.
The majority of the participants highlighted the need for welfare facilities, especially foods, transport and accommodation during a crisis. “We could have provided more facilities, food, transport, accommodation. We returned home daily. It’s hard. No problem, because none of us was COVID positive. If we came home while we were COVID positive…what will happen?” (P12). As reported by nurses, imposing curfew, travel restriction, lack of public transport, and limited shopping opportunities have limited their day-to-day life. Many emphasised that closing schools have created an additional burden to them as they had to look after their children while dedicating themselves to provide continuous care during this crisis. Some participants reported that managers of some hospitals paid attention to nurses’ welfare but expanding was essential.
Need for appreciation and incentives.
Nurses highlighted a lack of appreciation for their tireless efforts in caring for patients from managers and administrators. However, they identified patients as the main appreciators. One nurse said that patients’ feedback and appreciations were stuck on the door and window glasses as poems. “When patients leave, they stuck poems on the glasses. They have written, they were very scared when they came. But they were treated well. Felt like they were at home, and they had everything they needed” (P10). Although few hospital directors and nurse managers appreciated them, the majority highlighted a lack of appreciations from authorities. “They said, they will send a letter, but, still I did not receive” (P12). The lack of incentives (e.g. additional allowances and risk allowances) was another important point highlighted by nurses. Moreover, some participants said they had economic issues and did not receive payment for their overtime duties. “We were labelled as health heroes. We know we worked. Although labelled, we did not receive our overtime and public holiday payment even” (P2). They said that this situation demotivated them.
Need for professional counselling services.
Although some nurse managers supported to relieve the psychological stresses of nurses, many participants stated a lack of professional counselling services for both patients and staff who were in need during this situation. One participant said that she was depressed due to changing her workplace and placing her in a COVID-19 unit, but she did not receive any support to cope with her psychological concerns. Another nurse said that the establishment of counselling needs to be initiated at the very beginning. “I think it would be nice to have counselling for nurses at the very beginning. We had nurses who did not come for the duty” (P8).
The support network of nurses.
Participants identified the support received from peers, co-workers, family, friends and neighbours as the main branches of their support network. Many junior nurses said that their senior nurses helped them in decision making. They appreciated the help received from the care assistants and junior staff who worked in the same units. However, participants said that staff who worked outside the COVID-19 care units had expressed extreme fear of COVID-19, and it has led to difficulties in getting their service done. The majority of nurses highly valued the support received from the family in terms of psychological and other supports. Some nurses said that family members encouraged them to go to work. “My husband always said you have gone to do good to people where many people are reluctant to go. You go. You do not go to do any wrong. Do not be afraid” (P14). Many participants said that family members and relatives looked after their kids during this challenging period. However, one participant reported a negative experience. “I live in my husband’s house. My husband’s mother left the house when I said I am working in COVID hospital” (P7). Some participants said that their friends and neighbours helped them bring food and other stuff to their houses, manage household works, and provide transport.
Role of nurse managers and administrators.
Participants highlighted that hospital administration and nurse managers have a central role in COVID-19 care, particularly ensuring support for nurses. Nurses highly valued nurse managers’ positive leadership roles. Some participants identified nurse managers as experts because they used their prior experiences related to crisis management in organising COVID-19 care. The activities led by nurse managers, for example, doing basic risk assessment among nurses before placing to COVID-19 units, the arrangement of training programmes, granting leaves, arranging progress meetings, and arranging welfare, were highly appreciated. “Really, they are good. They helped us. They looked after patients as well as us. They asked what the problems are and what the shortcomings are. They arranged meetings to talk” (P9). However, some participants highlighted poor support received from and weak leadership qualities of nurse managers. They expected strong leadership qualities from nurse managers. One nurse said that when more patients come, nurse managers made decisions that benefited the institution than the staff. “Some of their answers, sometimes, to the advantage of the institution. Yes. Sometimes, they do not think about us at all. If not, they give the timely answers” (P2). Other main problems reported related to nurse managers’ role were placing nurses to COVID-19 units without asking their willingness or informing them, selecting only junior nurses, changing duty roster without informing, placing both husband and wife to COVID-19 care units, inadequate supervision, understaffing, and poor communication and coordination. One participant said that training was given to other nurses, but she had to work in the COVID-19 care unit without training. “At that time, I was really angry with the management. Others took the training, but we had to work” (P14). Many participants reported that they did not receive an opportunity to check PCR or did not receive a quarantine period, and they directly placed to the previous workplaces just after completion of duty at COVID-19 units.
Need for timely policies.
Participants further highlighted the need for timely policies in managing the COVID-19 crisis. These policy concerns included government, institutional and unit-level policies, including pre-planning before opening hospital and units, recruitment and duty delegation, resource allocation, policies related to infection control, testing PCR and providing facilities and welfare. One participant said that there was a plan for quarantine for nurses where necessary. Another one said that there was an excellent discharge policy in the hospital. “We did not discharge a patient until three consecutive PCRs are ‘negative’. Only after three were negative, the patient was discharged” (P8). However, many participants reported that there was no good plan to place the nurses in COVID-19 units, and one participant said that immediate calling is not a successful method.
Theme 5: Role of modern technology in COVID-19 care
This theme highlights the uses of modern technology in COVID-19 care.
Robots in direct patient care.
Participants stated that they used robots to deliver foods, medicines and other stuff to patients. Participants said that using robots in direct patient care reduced contact time with patients, which was a big help for nurses. “That means we do not always collide with the patients. We had a robot. He is the one who sends all the foods to the patient. We only collide directly with the patient when we take blood. That’s why we have to go very rarely” (P7). “We did not have much contact. We went to the patient when we wanted to collect blood and PCR. All the foods and medicines were sent to patients through the robot. So, having a robot was a big help” (P12). However, one participant said that there was a guilty feeling when introducing robots to COVID-19 care as it limited the nurse-patients interactions. To escape this guilty feeling, this nurse further noted that she maintained communication at an optimal level when she went to collect blood from the patient. “There, we just had an upset. That means we can’t go to the patient. Then, when we went to collect blood, we definitely talked to the patient. That means we were talking to the patient rather than over the phone or robot at that time. The relationship was well maintained” (P12).
Telecommunication in patient care.
Participants stated that modern communication methods, such as mobile phones, intercom system, and video camera systems, were used to improve nurse-patient communication, which helped to minimise exposure time to patients. “Most of the time, the patient and we communicated over the phone. So, we were not exposed. Besides, there was a video cam. We can talk to the patient even when robot went to the patient” (P2). One nurse highlighted the need for modern technology to improve communication with patients. “If there is a way to keep communication, a camera system, there is a way to talk about their problems and know their needs” (P4). One nurse stated that video records that included health education used to educate patients about COVID-19 and prevention. Additionally, nurses said that smart technologies, mainly smartphones, were promoted to patients as a way of communicating with their loved ones via video call.
Modern technology in information seeking.
Participants stated that the internet was one of the main sources of information seeking. They said that websites and YouTube were used to acquire not only knowledge but also in learning the necessary skills required. One nurse who did not receive prior training stated that she used videos available on YouTube to know how to provide care for patients with COVID-19. “With the support of others, I found out by watching the videos on YouTube.” (P7). NIID has developed a video related to COVID-19 care, and many nurses have used it to learn the required skills. “I watched the video by IDH (i.e., a short name for NIID). How this should be treated. How to wear PPE…How to remove PPE” (P1). Additionally, social media has been used to share and receive information. One nurse said that when she was appointed to the newly established care unit, she contacted a nurse who worked in NIID through Facebook and got the necessary information and knowledge related to caring for patients with COVID-19. “A nurse at IDH, which means, I’m not her friend. I made her my friend on my Facebook. (Laughing). I asked details from her, how is the patient cared for?” (P2).
This study explored the experiences of nurses who cared for patients with COVID-419 in Sri Lanka, especially in the initial period of the crisis. To the authors’ knowledge, this study is one of the first studies to examine the overall experiences of nurses as the recent studies related to caring for patients with COVID-19 have focused mainly on physical and psychological distress [ 5 , 6 , 14 , 22 ].
In line with recent studies related to COVID-19 care, this study reported a higher level of physical and psychological distress among nurses [ 5 , 6 , 14 , 15 , 22 ]. Fear towards COVID-19 has become one of the top reasons for their psychological distress. Recent studies report an extreme fear of COVID-19 among the general public [ 23 ] and health workers [ 6 , 15 ]. Consistent with our findings, Kim [ 10 ] reported fear among nurses towards contagious respiratory diseases is inevitable. The highly infectious nature, the high morbidity and mortality rates, the nature of the novelty of disease [ 24 ], and the non-availability of drug or vaccine [ 14 ] have increased this fear. Similar to our study, fear of contact and transmission of the disease is a significant issue confronted by nurses during respiratory disease outbreak [ 6 , 8 ]. In our study, nurses have paid special attention to maintain their health, and they have followed different measures to prevent the infection. This result is consistent with a recent study [ 14 ]. Extreme fear towards disease affects not only the psychological health of nurses but also patient care. To minimise the fear of COVID-19 among nurses, expanding education and training opportunities to improve knowledge and skills related to COVID-19 care is essential. Managers need to ensure a safe work environment for nurses in COVID-19 care units.
Similar to the findings of a recent study [ 15 ], this study reports fear of disease among nurses has been aggravated by being a carrier for the family members. Due to this situation, family members have shown extreme fear as they work in COVID-19 care units. Authorities need to ensure adequate precautions for nurses when they return to families. Additionally, the most reported causes for psychological stresses were separation from family members for an extended period and the inability to physically present to the family during this difficult time. Similar findings can be found in other studies [ 5 , 22 ]. Improving resiliency among nurses is essential. Support networks for families of health workers who are in the frontline of COVID-19 care need to be expanded.
Consistent with the findings of a previous study [ 25 ], facing social stigma and discrimination, mainly rejection by others related to COVID-19 care found in this study, are common issues for nurses worldwide [ 26 ]. Stigma has led to label nurses as ‘disease carriers’ [ 24 ] and limited social interaction and isolation among nurses. The stigma associated with COVID-19 is a predictor of compassion satisfaction, burnout, and compassion fatigue among health workers [ 25 ]. The present study reported not only the behaviour of the general public but also the behaviour of staff who did not work in the COVID-19 frontline contributed to stigmatisation and discrimination. To minimise the possible stigma and discrimination, improving public awareness needs to be expanded.
Moreover, this study reports sadness, worries and feeling of guilt related to care provision among nurses. Sadness and worries are mainly attributed to witnessing patients’ suffering, and recent studies on COVID-19 care also reported a similar phenomenon [ 6 , 15 , 22 ]). COVID-19 signifies with rapid progression of symptoms with high mortality and often leads to death [ 27 ]. Evidence indicates that witnessing patients’ sufferings, especially the painful end of a patient, is one of the main sources of psychological pressure among nurses [ 22 ]. Moreover, this situation has increased by the guilty feeling of nurses because they have to provide limited care compared to usual care due to strict care guidelines imposed; for example, wearing PPE before contact with patients. Similar to the present study, the feeling of the inefficiency of care has been explored in a recent study [ 15 ]. These negative consequences are associated with burnout, compassion fatigue and reduced well-being of nurses [ 28 ]. Improving psychological resilience is essential to cope with these issues [ 24 , 29 ], and psychological counselling for nurses are recommended [ 15 ].
Consistent with recent studies, this study further reported that understaffing, long working hours, shift work, and increased workload were associated with physical and psychological distress among nurses [ 5 , 6 ]. World Health Organisation (WHO) [ 30 ] highlights that work-related factors are positively related to the development of fatigue, staff burnout, increased psychological distress and reduced mental health among nurses who cared for patients with COVID-19. Paying attention to improving work conditions for nurses is essential. Moreover, discomfort related to PPE was found to be one of the significant sources of physical and psychological stress of nurses in this study, coinciding with the recent findings concerning COVID-19 care [ 6 , 14 ]. Difficulty in breathing, excessive sweating, headache, back pain, pressure on the nasal bridge due to strips of goggles, feeling of vomiting and fainting, and visual disturbances were the main problems identified. This study further identified that discomfort is increasing due to prolong usage of PPE, and a recent scoping review reported that prolonged use of PPE led to severe physiological discomfort; for example, skin breakdown among nurses [ 31 ]. To minimise the negative consequences of wearing PPE, nurse managers need to establish strategies for ensuring the safety of staff members by minimising the time required to wear PPE.
This study further explored the coping mechanisms used by nurses during this period. Interestingly, religious beliefs and practices and keeping trust in good and bad merits have become a powerful coping strategy among nurses. These beliefs help people to manage their stresses effectively compared to those who do not have religious practices [ 32 ]. Other reported coping strategies were sharing with peers, crying, repression and rationalisation. Among nurses on the front lines of COVID-19, strategies for coping with stress must be strengthened.
Although COVID-19 is a very frightening disease that led to physiological and psychological burden among nurses, similar to previous findings, this study reports the professional obligation, motivation and dedication of nurses who provide care for patients with COVID-19 [ 5 , 15 ]. The commitment of nurses has been reported in previous respiratory outbreaks, for example, SARS [ 9 ] and swine flu [ 11 ]. Sun et al. [ 5 ] highlight that negative emotions are dominant in the early stage of the crisis, but positive emotions appear gradually in the later stage. Similar to this phenomenon, this study says that nurses view COVID-19 care as a new experience and leads to personal satisfaction at the end of their duty placements. Provision of care for patients with COVID-19 is a great opportunity for the professional growth of nurses that include honour and respect [ 5 ]. The present study reports that mass media portrays nursing positively, and nurses’ contribution has been highly valued globally. Consequently, authorities need to appreciate and promote nurses’ invaluable contribution; then, nurses can continue this care efficiently.
Similar to recent studies [ 5 , 14 ], this study reports the importance of prior education and training for nurses during pandemics. Lack of knowledge is one of the main reasons for insecurity, and providing education on prevention and control of COVID-19 can reduce the psychological burden and insecurity among nurses [ 14 ]. This study reports inadequate or no prior training opportunities for nurses, and this situation leads to increasing fear and psychological distress related to providing COVID-19 care. Donning and doffing PPE, performing nursing procedures and breaking bad news were identified as prioritised educational needs of nurses. Especially, breaking bad news has been identified as a core component of communication concerning COVID-19 care, and demand for resources and support for effective bad news conversations is highlighted [ 33 ]. Education and training opportunities are needed to be expanded for nurses concerning the above learning needs in the Sri Lankan Context. This study further highlights the need for adding this content into basic curricula; therefore, nurse educators need to modify basic nursing curricula in Sri Lanka.
In addition to the availability of formal training programmes, peer learning, availability of care guidelines and protocols, self-directed learning, including the use of the internet and videos, such as a video developed by NIID, are the main learning strategies used by nurses. Promoting peer learning and ensuring timely care guidelines and protocols are essential. Self-directive knowledge has a promising role in health profession education [ 34 ], especially in emerging pandemic like COVID-19. Ensuring the availability of self-directive learning materials and providing facilities, for example, the internet and computers can promote nurses’ motivation for learning during health crises.
This study further highlights the support mechanisms available for nurses in the workplace and their personal life. Available support mechanisms of the workplace include the availability of adequate resources that ensure a safe work environment, welfare facilities, appreciations and incentives, and counselling facilities. WHO [ 30 ] also highlights the need for a healthy, safe and decent working environment for all health workers who provide care during the COVID-19 pandemic. Similar to previous studies, this study highlights the need for adequate resources, such as human resources, physical facilities, equipment, and PPE, to ensure a comfortable work environment [ 5 ]. This study further highlighted the role of the administrators and the need for timely policies in addressing the above aspects. Nurse leaders have an essential role in ensuring the safety of nurses [ 35 ]; therefore, the strong leadership qualities of nurse managers are crucial. Clinical leaders can be introduced to current practice settings in Sri Lanka.
In line with previous studies [ 5 , 6 , 14 ], this study identified the importance of support networks, including support from managers, peers, co-workers, family, friends and neighbours. The absence of sufficient support during infectious pandemics brings short-term and long term impact on nurses’ mental health [ 36 ]. Hence, authorities and media need to pay special attention to highlight the need for support for health workers during this crisis and strengthening the available support networks. Additionally, weaknesses in support strategies, especially welfare facilities for nurses, including accommodations, transport and meal facilities, were reported. Society has been limited due to curfew and lockdown, travel restrictions, closing shopping and limited transport. Therefore, expanding welfare for nurses should be prioritised. Moreover, our study reported a lack of appreciations, including incentives for nurses. In comprehensive workforce planning and development, appreciations and incentives are crucial to attract, retain and motivate health workers [ 37 ]. Establishing policies and strategies is essential to appreciate nurses’ hard work in the Sri Lankan context.
This study further explores the use of modern technology in COVID-19 care. One of the uses is telepresence robots. To the authors’ knowledge, this is the first experience of using robots to provide direct nursing care by nurses in the Sri Lankan context. Robotic systems can significantly reduce the transmission risks of infectious diseases for frontline workers because robots can provide care from a safe distance [ 38 ]. Nurses reported that robots were primarily used in serving foods and medicine. But, robots can be effectively used in other areas, for example, disinfection, measuring vital signs and assisting border controls in COVID-19 care [ 39 ]. Although nurses viewed that the use of robots in care helped to reduce direct contact time with patients, it led to a guilty feeling. With possible advantages, changing nurses’ perception towards robotic interventions in delivering care for frightening diseases like COVID-19 may be beneficial. More studies are recommended to examine user acceptance towards telepresence robots in direct nursing care in low-income countries like Sri Lanka.
Additionally, modern ICT, including internet, mobile technology, telephone, video technology with conferencing, internet-based education and videos, and social media, has been used in direct nursing care, informal education and information seeking. This study highlights the importance of those technologies in maintaining patient care while minimising possible contact. The literature emphasises the importance of modern technology in patient communication, workplace-based learning and increasing public awareness concerning COVID-19 care [ 40 ]. Therefore, nurses must be provided with the necessary support and facilities to use virtual technologies effectively. Skills training, including assessing patient’s non-verbal cues, emotional states and their understandings through virtual technologies, is essential [ 40 ].
Limitations
We conducted telephone interviews. The absence of visual cues, the potential for the distraction of interviewees by environmental disturbances and technological issues related to telephones are some limitations in telephone interviews [ 41 ].
This phenomenological study provides an insight into the experiences of a sample of nurses who took care of patients with COVID-19 in Sri Lanka. Although COVID-19 is a frightening disease with many negative impacts on nurses and their families, with their commitment and professional obligation, taking care of patients with COVID-19 is a new experience that leads to personal satisfaction among nurses. Physical and psychological distress among nurses is a common phenomenon due to worries related to witnessing the suffering of patients, guilty feeling related to limitations of care, work-related factors, discomfort associated with wearing PPE, negative impact to family and stigma and discrimination. Addressing psychological distress among nurses is a priority need. Hospital administrators and nurse managers have a significant role in making a comfortable work environment for nurses, including creating timely policies, providing adequate resources, training opportunities, comfortable shift methods, welfare, appreciation methods and incentives for nurses. Main support networks include the support received from management, peers, co-workers, family, friends, and neighbours. Strengthening these support mechanisms is essential. Previous education and training, as well as proper guidelines, are necessary to provide adequate care for patients with COVID-19. The main learning needs of nurses include donning and doffing of PPE, breaking bad news and performing nursing procedures. Expanding learning opportunities and revision of basic curricula have emerged. Moreover, modern technology, particularly robotic interventions and modern ICT can be integrated into patient care and nurses’ education. To face future challenges, the establishment of new care models, training programmes, nursing specialities and favourable policies related to COVID-19 care is crucial in the Sri Lankan context.
Supporting information
S1 checklist. coreq checklist in s1 appendix..
https://doi.org/10.1371/journal.pone.0257064.s001
Acknowledgments
The authors would like to thank all nurses who participated in this study.
- View Article
- PubMed/NCBI
- Google Scholar
- 2. World Health Organisation. Coronavirus. 2020. https://www.who.int/health-topics/coronavirus#tab=tab_1
- 16. Colaizzi P. Phenomenologic research as the phenomenologist views it. Existential Alternatives for Psychology. New York, NY: Oxford University Press; 1978.
- 17. Dworkin SL. Sample size policy for qualitative studies using in-depth interviews. Springer; 2012. https://doi.org/10.1007/s10508-012-0016-6
- 30. World Health Organisation. WHO calls for healthy, safe and decent working conditions for all health workers, amidst COVID-19 pandemic. 2020. https://www.who.int/news-room/detail/28-04-2020-who-calls-for-healthy-safe-and-decent-working-conditions-for-all-health-workers-amidst-covid-19-pandemic
News and views for the UB community
- Stories >
The role of nurses in the COVID-19 pandemic
By charles anzalone.
Published April 10, 2020

Joann Sands, clinical assistant professor in the School of Nursing, is well-acquainted with disasters and emergencies.
Declaring a “passion” for disaster and emergency response management, Sands’ expertise includes disaster preparedness and response, resiliency after a disaster, disaster epidemiology and more areas all too familiar in this COVID-19 pandemic.
“Nurses play a very important role both locally and globally. They are on the front lines caring for these patients day in and day out,” says Sands, who has been a volunteer firefighter/EMT for the past 12 years.
“ They are able to see what is working, as well as things that can be done differently to provide more effective and efficient care, and offer suggestions for improvement.”
Given her expertise – and also to observe the World Health Organization designation of 2020 as the Year of the Nurse and Midwife – Sands talks to UBNow about the role of nurses in disaster preparedness and response.
Given your background in disaster and emergency response education, what advice would you give everyday people dealing with the COVID-19 pandemic? Any message for health care workers??
Please stay home. I understand it can be very difficult, but if you are not an essential employee that must leave to go to work, stay home. Limit trips to the grocery store to when you absolutely need to. Now is not the time to be strolling through the aisles of Target, touching all products, shopping for new home décor, or having small talk with other customers. Get your essential items and go home. Also, keep washing your hands and avoid touching your face. Although you shouldn’t be going to visit all of your family members and friends, it is still important to keep in contact with them. Call them or video chat. Check to make sure they are doing OK and keep that connection.
For health care workers, just a message you are doing everything you can in a situation you probably never imagined yourself being in. Take a deep breath, lean on each other for support, reach out if you need someone to talk to, and find healthy ways to decompress. You are important, brave and very much appreciated for all of the hard work you are doing!
What roles do nurses play in mitigating the spread of infectious diseases? Why and how are they important in managing a health crisis such as a pandemic?
Mitigating the spread of infectious diseases is so important because one of the main things we want to try to accomplish is reducing patient deaths and slowing the spread of the disease so we are able to handle the numbers of patients when the surge hits.
Nurses are important in managing a health crisis because they are a vital link between the patient and the rest of the health care team. They are with their patients for their whole shift, and through assessment and critical thinking are able to notice subtle changes in their patients that could indicate they are decompensating or getting worse, or getting better. They are able to determine the human response to the medical problem. Nurses relay their assessment findings to providers, they are able to determine if respiratory therapy needs to be called, they are able to assess the patient’s response to medical treatments, and they educate the patients, along with providing a listening ear or a calming touch.
What have you heard from your fellow nurses working in hospitals about their workload and expectations?
The patients they are seeing are sick, very, very sick. This virus is impacting everyone. Many of the patients they are caring for are younger patients and they are just as sick, requiring ICU care and intubation.
Why is it important for health care workers, especially nurses, to have education and training in disaster preparedness and emergency response?
As nurses comprise the largest component of the health care workforce, should a disaster occur, it is inevitable that nurses will be caring for those victims and patients. It is important that they are trained and have the knowledge and skills to respond, whether they are caring for someone on the front lines of the disaster or in a hospital.
What can they do to protect themselves against risk?
One of the first things is having enough proper PPE to use while working. Health care workers are implementing other strategies to help protect themselves against risk, including changing out of their work attire before entering their homes, showering as soon as they get home, and many health care providers are also isolating themselves into a separate room of their home, away from other family members to try to protect their family members as best they can. And of course, meticulous handwashing!
What advice would you give people trying their best to live their lives and at the same time trying to stay safe?
The best thing is staying home, frequent handwashing, and keeping frequently touched surfaces clean. Everyone is trying to adjust to a new way of living, along with likely feeling overwhelmed. It is important to remember to take care of your mental health. Some ways to help cope with stress include developing a schedule, frequent breaks, staying active, getting enough sleep, staying hydrated and eating healthy, well-balanced meals. Be informed, but also limit your time in front of the news coverage. As our county executive keeps reiterating, it is important to stay physically distant, but that does not mean you need to be socially distant.
Covid-19: Ethical Challenges for Nurses
- PMID: 32410225
- PMCID: PMC7272859
- DOI: 10.1002/hast.1110
The Covid-19 pandemic has highlighted many of the difficult ethical issues that health care professionals confront in caring for patients and families. The decisions such workers face on the front lines are fraught with uncertainty for all stakeholders. Our focus is on the implications for nurses, who are the largest global health care workforce but whose perspectives are not always fully considered. This essay discusses three overarching ethical issues that create a myriad of concerns and will likely affect nurses globally in unique ways: the safety of nurses, patients, colleagues, and families; the allocation of scarce resources; and the changing nature of nurses' relationships with patients and families. We urge policy-makers to ensure that nurses' voices and perspectives are integrated into both local and global decision-making so as to minimize the structural injustices many nurses have faced to date. Finally, we urge nurses to seek sources of support throughout this pandemic.
Keywords: Covid-19 pandemic; allocation of scarce resources; crisis standards of care; moral distress; nurse-patient-family relationship; nursing ethics; safety of nurses.
© 2020 The Hastings Center.
- Betacoronavirus
- Coronavirus Infections / nursing*
- Ethics, Nursing*
- Health Care Rationing / ethics
- Nurse-Patient Relations / ethics
- Pneumonia, Viral / nursing*
- Safety Management / ethics
- Stress, Psychological / epidemiology
Fear, frustration, compassion and shame: What nurses are dealing with during the pandemic
Nurses share stories of arduous work that is emotionally draining, a risk to their health.
The nurses on the front lines of COVID-19
Social sharing.
(WARNING: This story contains graphic descriptions that may disturb or offend some readers.)
There are close to 450,000 nurses in Canada. Some work in hospitals, some in long-term care homes, some are privately hired, but they all share one commonality. Since the beginning of COVID-19, they have been on the front lines of an international pandemic that has taken more than 1.4 million lives worldwide , including 12,000 in this country.
The work they've done has been arduous and a risk to their personal safety and health, but they have persevered. The National talked to three nurses in three different provinces about their experiences, and these are their stories.
Clarice Shen, Toronto

Clarice Shen, 25, is an acute care nurse at Toronto's Sunnybrook Health Sciences Centre. In January, just a year out of nursing school, she was caring for a patient who was exhibiting symptoms of a virus that didn't even have a name yet.
He turned out to be the first patient to test positive with COVID-19 in Canada.
"There was a lot of uncertainty, but as a team, we kind of came together and supported ourselves," Shen said.
When it became clear the hospital needed to expand the intensive care unit, Shen volunteered to work in the ICU to support the staff there. She's been on 12-hour shifts in the ICU ever since.
A number of the things she has experienced when dealing with COVID-19 patients were new to her.
"From a nursing standpoint, the fact that a lot of patients with the virus get sick really, really fast — they can present to the hospital with very mild symptoms, and they can progress very, very quickly to the point where mechanical ventilation is needed — I was really taken aback. Because it is really traumatic to be put on a ventilator," Shen said.
In her time in the ICU, Shen has helped care for dozens of COVID-19 patients and says most people don't realize how hard it is to be intubated.
"I was caring for a patient on a ventilator and he had this thing where his body just on and off twitched, where his teeth would bite down on the ventilator. And his teeth were actually coming out, like, he bit off part of his tongue and his teeth were coming out, and there was blood everywhere," Shen said.
I never imagined that I'd be in a position to tell someone 'you can't visit your loved one in the hospital.' - Clarice Shen
As hospital rules changed, Shen has had to tell the families of seriously ill patients that they could no longer visit, or that they must cut visits short. She says she's tried to address the frustration she deals with daily by maintaining compassion.
"I never imagined that I'd be in a position to tell someone 'you can't visit your loved one in the hospital,'" Shen said.
"I try to help them understand what it is that we're trying to do … helping them feel that I'm on their side, even though the situation might be really challenging."
And Shen has held the hands of many patients in the ICU while they passed. Too many times, she says, a patient's condition has worsened and they've succumbed to COVID-19 so quickly that their families couldn't get there in time.


Clarice Shen
One recent instance sticks in her mind, when she was at the bedside of a woman who died before her two daughters could get to the hospital. Shen was covering a break for the nurse who was the patient's primary care provider, so she didn't know the patient very well.
"All I could really tell her is that I loved the colour of her nails, and that her hair was beautiful, and that her daughters loved her. So I eventually just told her over and over again that her daughters wished that they could be here," Shen said.
"It's important she didn't feel alone. I mean, it's an honour and a privilege that I can be there for patients in their final moments."
As cases reach record highs in Toronto and the city finds itself in a second lockdown, Shen says she wishes people could see what she sees in one shift in the ICU. She thinks it would scare them as much as it does her, and help keep them vigilant against contracting or spreading the virus.
"You know, last week you had two COVID patients in the hospital. And this week you have 15, and two waiting in the ER, and you have no beds in the ICU. And then you're trying to get people out of the ICU who would benefit, potentially, from a few more days of staying there, because you need that bed. So, that is scary for me," Shen said.
Meaghan Thumath, Vancouver

Meaghan Thumath is a registered nurse who wears many hats.
She works with homeless and marginalized communities in Vancouver's notorious downtown East side. She also teaches nursing, does clinical research, and participates in international deployments with The World Health Organization that have included work on Ebola and other outbreaks overseas.
Since the outbreak of COVID-19, Thumath has been harnessing her experience to care for patients in Vancouver who are largely without other options.
"Sometimes that can look like a homeless camp. Sometimes it's a single-room occupancy building that's owned by a private owner. Sometimes it's a homeless shelter, and sometimes it's a supported-housing facility," Thumath said. "We find people where they are."
I think if you can treat people with dignity, and be trauma-informed and understand sometimes people might be scared, generally people are extremely grateful. - Meaghan Thumath
Thumath's patients are often dealing with many more issues than just possible exposure to COVID-19.
"So we are seeing a sort of twinning of the overdose crisis as well as COVID-19. And then on top of that, people are still struggling with HIV, and Hepatitis C, and other infections," Thumath said.
She points out that asking homeless people to self-isolate or quarantine when they are exposed to COVID-19 presents added challenges that most Canadians with a place to live can't begin to understand.
Part of her job is also training shelter workers in best practices for when people with symptoms show up on their doorsteps.
Thumath says she does the work, and takes the personal risks associated with it, because of how rewarding it is.
"It's a huge honour, because people are so grateful for your help. I think if you can treat people with dignity, and be trauma-informed and understand sometimes people might be scared, generally people are extremely grateful," she said.

Meaghan Thumath
The personal risks she takes are significant. Thumath recently returned from a trip with the World Health Organization to South Africa, assisting with the pandemic response there.
She was also part of the team that helped repatriate people from Wuhan, China, to Canadian Forces Base Trenton in the spring this year. It was on that assignment that Thumath contracted the virus herself.
She says that experience helps her better understand what her patients are facing.
The toll her work has had on her family is something that weighs on her as well. Thumath is married and has two children. She writes goodbye letters to them every time she is deployed somewhere in case she doesn't return.
"I'm grateful to my husband for being supportive, but it does weigh on me," she says. "That's the hardest thing — a drawer full of letters to them just in case I don't come back."
Shaye Fleming, Calgary

Shaye Fleming has been off work since September. That's when the 29-year-old caught COVID-19 while on a regular shift as a cardiac nurse at Calgary's Foothills Medical Centre.
"It's been over two months now, and I'm just starting to feel a little bit back to normal," she said.
"I still get quite short of breath, and this isn't like me, you know? I usually can run, walk, like, usually I'm quite active."
The ongoing impact of the virus has left Fleming frustrated, and feeling another emotion she says she wasn't expecting.
"I've been experiencing a lot of anxiety with it as well. When you're young you think you'll be fine, and I was one of those people that wasn't worried about getting it. And so the fact that it has been a prolonged recovery period, and I'm lacking a lot of that stamina that I once had, yeah, it's been hard for sure," she said.
Fleming has tried to return to work twice, but was unable to both times. Her symptoms have continued to be too debilitating.
... That shame of not being able to go back to work when I felt like I should have been OK, that makes you feel pretty shameful as well. - Shaye Fleming
She hopes to try again this week. Not being able to go back to work has only added to her stress, she said.
"I haven't been able to be there, and be a support for my co-workers and my colleagues," Fleming said. "So, you know, that shame of not being able to go back to work when I felt like I should have been OK, that makes you feel pretty shameful as well."
As cases spike in Alberta and around the country, Fleming says she hopes people heed social distancing requirements and listen to public health officials. But she adds that regardless of how people approach the pandemic, nurses will always be there to care for them if they fall ill, even though providing that care means a risk to their own health.
"We will care for your loved ones and for you, regardless of what you believe in and what you value at the moment during this pandemic," she said. "Nurses will always be there for you."

Shaye Fleming
About the author.
Producer, The National
Perlita Stroh is a producer with The National at CBC News. She works on news and current affairs stories and is based in Toronto.
With files from David Common
Related Stories
- Point of View Pandemic Perspectives: What it's like studying to become a nurse during COVID-19
- Front-line workers sound the alarm on burnout as they battle the pandemic's second wave
- University of Alberta study examines COVID-19 toll on health-care workers
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 21, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Study shows excessive patient loads were the greatest cause of moral distress among health personnel during pandemic
by University of Córdoba
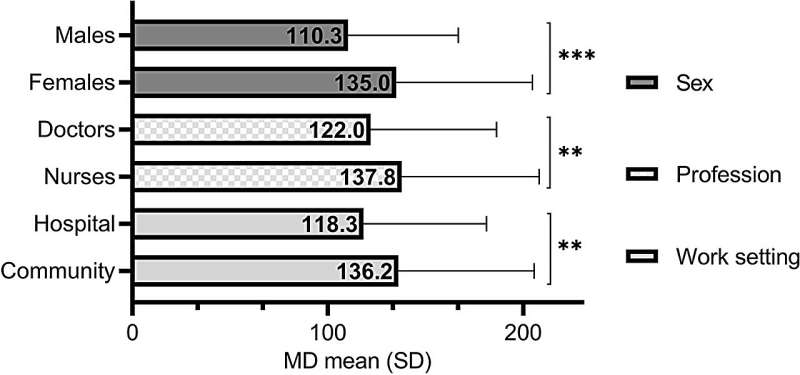
Being a woman, a nursing professional, and working in the community sphere increased the risk of moral distress (MD), according to a study by the University of Cordoba carried out among more than 500 professionals with the Public Health Service of Andalusia in a period immediately after the COVID-19 pandemic.
Moral distress is the psychological harm that arises when people are forced to witness or perform actions that clash with their moral values. It is a problem that affects health care professionals , who are often exposed to hardships, long shifts, stress, and high levels of responsibility. During the pandemic, while society saw them as heroes, these professionals suffered high levels of moral distress .
"Worryingly high" levels of moral stress are recorded in the recent work published by Eloy Girela, Cristina Beltrán and Manuel Romero, researchers at the University of Cordoba who evaluated the prevalence of this problem among professionals in different areas of the Public Health Service of Andalusia during the early post-pandemic period.
The study is published in the journal BMC Medical Ethics .
"Our most significant findings were that women, nurses and those who work in the community sphere ( primary care and emergency community services) face a higher risk of moral stress," explained Eloy Girela, a researcher in the Legal and Forensic Medicine Area.
The study was carried out with a sample of 566 professionals spanning Primary Care, Palliative Care, Intensive Care, Internal Medicine, Pulmonology and ER, services that apparently "featured more moral conflicts during the pandemic because there was a scarcity of resources to care for patients, so they had to make decisions entailing great responsibility," says Girela.
To evaluate the level of moral stress suffered by these professionals, and obtain the predictors associated with this problem, the team validated and used the MMD-HP-SPA (Measure of Moral Distress for Health care Professionals), developed in 2019 and which has 27 items corresponding to situations experienced by these workers.
"We obtained a significantly higher level of moral distress than in other similar studies, an aspect that we found worrisome," said Manuel Romero, a researcher with the Department of Nursing, Pharmacology and Physiotherapy.
Being a woman, working in Nursing, and being dedicated to community services increases the risk of suffering from it, but so does a lack of health care resources.
"Having to care for more patients than I can, safely," "a lack of resources, equipment, or beds," and "seeing patient care suffer from a lack of continuous care" were the three factors that generated the most moral distress in participants, according to the study.
This situation not only affects the physical and mental health of health personnel, but also that of patients as well. "The institutional response is fundamental," say the authors of this study, who see institutional organization and greater funding for services as solutions to the situations of excessive patient loads and scant resources suffered by the health personnel.
"Training, the existence of protocols, a more ethical climate, work-life balance strategies, and actions more focused on each service," proposes Legal and Forensic Medicine researcher Cristina Beltrán.
With this study, almost simultaneously with another published by a Galician team (Rodríguez-Ruiz et al. 2022), the MMD-HP-SPA scale was validated in Spain.
Ascertaining why being a woman is a risk factor, and the relationship between moral distress and burnout, are among the lines of study that the research team will explore to address this problem affecting society's health.
Explore further
Feedback to editors

Regular fish oil supplement use might increase first-time heart disease and stroke risk
5 hours ago

Pedestrians may be twice as likely to be hit by electric/hybrid cars as petrol/diesel ones

Study finds jaboticaba peel reduces inflammation and controls blood sugar in people with metabolic syndrome
6 hours ago

Study reveals how extremely rare immune cells predict how well treatments work for recurrent hives
7 hours ago

Researchers find connection between PFAS exposure in men and the health of their offspring

Researchers develop new tool for better classification of inherited disease-causing variants

Specialized weight navigation program shows higher use of evidence-based treatments, more weight lost than usual care

Exercise bouts could improve efficacy of cancer drug
8 hours ago

Drug-like inhibitor shows promise in preventing flu

Scientists discover a novel way of activating muscle cells' natural defenses against cancer using magnetic pulses
Related stories.

Pediatric critical care professionals experiencing moral distress
Nov 1, 2021

New tool measures moral distress in pandemic nursing care
Aug 4, 2022

Learning about nurses' moral distress during crisis care
Aug 25, 2021

Survey measures causes of and counters to moral distress in radiology
Mar 22, 2023

Majority of clinicians in US safety net practices report 'moral distress' during COVID-19 pandemic
Aug 26, 2022

Moral distress and moral strength among clinicians in health care systems
Sep 23, 2019
Recommended for you

Heart rate synchrony predicts effective group decision-making, research suggests
11 hours ago

Study models how ketamine's molecular action leads to its effects on the brain
12 hours ago

Study shows exercise spurs neuron growth and rewires the brain, helping mice forget traumatic and addictive memories
May 20, 2024

Researchers discover top-down signals in brain circuits regulating depression

Yoga and meditation-induced altered states of consciousness are common in the general population, study says

Researchers uncover biological trigger of early puberty
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
North Carolina grapples with growing nursing shortage

Need a job? Nurses are more in need now than ever
Job fairs aim to ease nursing shortage within cape fear valley health system, carolina panthers unveil plans, renderings of proposed charlotte practice facility near bank of america stadium, lamelo ball sued by woman who says he hit her son with his car, buyer pays $925,000 for highest-selling michael jordan rookie card, report says, acc votes to accept settlements in antitrust lawsuits against ncaa, canes collapse, the panthers paint and a nascar fight in the sports moments of the week.

WRAL Late News

WRAL WeatherCenter Forecast

Evening Pick 3 Pick 4 and Cash 5

Mega Millions Drawing

Daytime Pick 3 and Pick 4 Drawing
- Public Service That Makes a Difference ®
New England Public Policy Center Regional Briefs
Nursing home closures in new england: impact on long-term care, labor markets.

By John M. Barry
Mr. Barry, a scholar at the Tulane University School of Public Health and Tropical Medicine, is the author of “The Great Influenza: The Story of the Deadliest Pandemic in History.”
In 1918, an influenza virus jumped from birds to humans and killed an estimated 50 million to 100 million people in a world with less than a quarter of today’s population. Dozens of mammals also became infected.
Now we are seeing another onslaught of avian influenza. For years it has been devastating bird populations worldwide and more recently has begun infecting mammals , including cattle, a transmission never seen before. In another first, the virus almost certainly jumped recently from a cow to at least one human — fortunately, a mild case.
While much would still have to happen for this virus to ignite another human pandemic, these events provide another reason — as if one were needed — for governments and public health authorities to prepare for the next pandemic. As they do, they must be cautious about the lessons they might think Covid-19 left behind. We need to be prepared to fight the next war, not the last one.
Two assumptions based on our Covid experience would be especially dangerous and could cause tremendous damage, even if policymakers realized their mistake and adjusted quickly.
The first involves who is most likely to die from a pandemic virus. Covid primarily killed people 65 years and older , but Covid was an anomaly. The five previous pandemics we have reliable data about all killed much younger populations.
The 1889 pandemic most resembles Covid (and some scientists believe a coronavirus caused it). Young children escaped almost untouched and it killed mostly older people, but people ages 15 to 24 suffered the most excess mortality , or deaths above normal. Influenza caused the other pandemics, but unlike deaths from seasonal influenza, which usually kills older adults, in the 1957, 1968 and 2009 outbreaks, half or more deaths occurred in people younger than 65. The catastrophic 1918 pandemic was the complete reverse of Covid: Well over 90 percent of the excess mortality occurred in people younger than 65. Children under 10 were the most vulnerable, and those ages 25 to 29 followed.
Any presumption that older people would be the chief victims of the next pandemic — as they were in Covid — is wrong, and any policy so premised could leave healthy young adults and children exposed to a lethal virus.
The second dangerous assumption is that public health measures like school and business closings and masking had little impact. That is incorrect.
Australia, Germany and Switzerland are among the countries that demonstrated those interventions can succeed. Even the experience of the United States provides overwhelming, if indirect, evidence of the success of those public health measures.
The evidence comes from influenza, which transmits like Covid, with nearly one-third of cases transmitted by asymptomatic people. The winter before Covid, influenza killed an estimated 25,000 here ; in that first pandemic winter, influenza deaths were under 800. The public health steps taken to slow Covid contributed significantly to this decline, and those same measures no doubt affected Covid as well.
So the question isn’t whether those measures work. They do. It’s whether their benefits outweigh their social and economic costs. This will be a continuing calculation.
Such measures can moderate transmission, but they cannot be sustained indefinitely. And even the most extreme interventions cannot eliminate a pathogen that escapes initial containment if, like influenza or the virus that causes Covid-19, it is both airborne and transmitted by people showing no symptoms. Yet such interventions can achieve two important goals.
The first is preventing hospitals from being overrun. Achieving this outcome could require a cycle of imposing, lifting and reimposing public health measures to slow the spread of the virus. But the public should accept that because the goal is understandable, narrow and well defined.
The second objective is to slow transmission to buy time for identifying, manufacturing and distributing therapeutics and vaccines and for clinicians to learn how to manage care with the resources at hand. Artificial intelligence will perhaps be able to extrapolate from mountains of data which restrictions deliver the most benefits — whether, for example, just closing bars would be enough to significantly dampen spread — and which impose the greatest cost. A.I. should also speed drug development. And wastewater monitoring can track the pathogen’s movements and may make it possible to limit the locations where interventions are needed.
Still, what’s achievable will depend on the pathogen’s severity and transmissibility, and, as we sadly learned in the United States, how well — or poorly — leaders communicate the goals and the reasons behind them.
Specifically, officials will confront whether to impose the two most contentious interventions, school closings and mask mandates. What should they do?
Children are generally superspreaders of respiratory disease and can have disproportionate impact. Indeed, vaccinating children against pneumococcal pneumonia can cut the disease by 87 percent in people 50 and older. And schools were central to spreading the pandemics of 1957, 1968 and 2009. So there was good reason to think closing schools during Covid would save many lives.
In fact, closing schools did reduce Covid’s spread, yet the consensus view is that any gain was not worth the societal disruption and damage to children’s social and educational development. But that tells us nothing about the future. What if the next pandemic is deadlier than 1957’s but as in 1957, 48 percent of excess deaths are among those younger than 15 and schools are central to spread? Would it make sense to close schools then?
Masks present a much simpler question. They work. We’ve known they work since 1917, when they helped protect soldiers from a measles epidemic. A century later, all the data on Covid have actually demonstrated significant benefits from masks.
But whether to mandate masks is a difficult call. Too many people wear poorly fitted masks or wear them incorrectly. So even without adding in the complexities of politics, compliance is a problem. Whether government mask mandates will be worth the resistance they foment will depend on the severity of the virus.
That does not mean that institutions and businesses can’t or shouldn’t require masks. Nor does it mean we can’t increase the use of masks with better messaging. People accept smoking bans because they understand long-term exposure to secondhand smoke can cause cancer. A few minutes of exposure to Covid can kill. Messaging that combines self-protection with communitarian values could dent resistance significantly.
Individuals should want to protect themselves, given the long-term threat to their health. An estimated 7 percent of Americans have been affected by long Covid of varying severity, and a re-infection can still set it off in those who have so far avoided it. The 1918 pandemic also caused neurological and cardiovascular problems lasting decades, and children exposed in utero suffered worse health and higher mortality than their siblings. We can expect the same from the next pandemic.
What should we learn from the past? Every pandemic we have good information about was unique. That makes information itself the most valuable commodity. We must gather it, analyze it, act upon it and communicate it.
Epidemiological information can answer the biggest question: whether to deploy society-wide public health interventions at all. But the epidemiology of the virus is hardly the only information that matters. Before Covid vaccines were available, the single drug that saved the most lives was dexamethasone. Health officials in Britain discovered its effectiveness because the country has a shared data system that enabled them to analyze the efficacy of treatments being tried around the country. We have no comparable system in the United States. We need one.
Perhaps most important, government officials and health care experts must communicate to the public effectively. The United States failed dismally at this. There was no organized effort to counter social media disinformation, and experts damaged their own credibility by reversing their advice several times. They could have avoided these self-inflicted wounds by setting public expectations properly. The public should have been told that scientists had never seen this virus before, that they were giving their best advice based on their knowledge at the time and that their advice could — and probably would — change as more information came in. Had they done this, they probably would have retained more of the public’s confidence.
Trust matters. A pre-Covid analysis of the pandemic readiness of countries around the world rated the United States first because of its resources. Yet America had the second-worst rate of infections of any high-income country.
A pandemic analysis of 177 countries published in 2022 found that resources did not correlate with infections. Trust in government and fellow citizens did. That’s the lesson we really need to remember for the next time.
John M. Barry, a scholar at the Tulane University School of Public Health and Tropical Medicine, is the author of “The Great Influenza: The Story of the Deadliest Pandemic in History.”
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
Republish This Story
Nursing Homes Wield Pandemic Immunity Laws To Duck Wrongful Death Suits

In early 2020, with reports of covid-19 outbreaks making dire headlines, Trever Schapers worried about her father’s safety in a nursing home in Queens.
She had delighted in watching her dad, John Schapers, blow out the candles on his 90th birthday cake that February at the West Lawrence Care Center in the New York City borough. Then the home went into lockdown.
Soon her father was dead. The former union painter spiked a fever and was transferred to a hospital, where he tested positive for covid, his daughter said, and after two weeks on a ventilator, he died in May 2020.
But when Trever Schapers sued the nursing home for negligence and wrongful death in 2022, a judge dismissed the case, citing a New York state law hastily passed early in the pandemic. It granted immunity to medical providers for “harm or damages” from an “act or omission” in treating or arranging care for covid. She is appealing the decision.
“I feel that families are being ignored by judges and courts not recognizing that something needs to be done and changed,” said Schapers, 48, who works in the medical field. “There needs to be accountability.”

The nursing home did not return calls seeking comment. In a court filing, the home argued that Schapers offered no evidence that the home was “grossly negligent” in treating her father.
More than four years after covid first raged through many U.S. nursing homes, hundreds of lawsuits blaming patient deaths on negligent care have been tossed out or languished in the courts amid contentious legal battles.
Even some nursing homes that were shut down by health officials for violating safety standards have claimed immunity against such suits, court records show. And some families that allege homes kept them in the dark about the health of their loved ones, even denying there were cases of covid in the building, have had their cases dismissed.
Schapers alleged in a complaint to state health officials that the nursing home failed to advise her that it had admitted covid-positive patients from a nearby hospital in March 2020. In early April, she received a call telling her the facility had some covid-positive residents.
“The call I received was very alarming, and they refused to answer any of my questions,” she said.
About two weeks later, a social worker called to say that her father had a fever, but the staff did not test him to confirm covid, according to Schapers’ complaint.
The industry says federal health officials and lawmakers in most states granted medical providers broad protection from lawsuits for good faith actions during the health emergency. Rachel Reeves, a senior vice president with the American Health Care Association, an industry trade group, called covid “an unprecedented public health crisis brought on by a vicious virus that uniquely targeted our population.”
In scores of lawsuits, however, family members allege that nursing homes failed to secure enough protective gear or tests for staffers or residents, haphazardly mixed covid-positive patients with other residents, failed to follow strict infection control protocols, and brazenly misled frightened families about the severity of covid outbreaks among patients and staff.
“They trusted these facilities to take care of loved ones, and that trust was betrayed,” said Florida attorney Lindsey Gale, who has represented several families suing over covid-related deaths.
“The grieving process people had to go through was horrible,” Gale said.
Email Sign-Up
Subscribe to KFF Health News' free Weekly Edition.
A Deadly Toll
KFF Health News found that more than 1,100 covid-related lawsuits, most alleging wrongful death or other negligent care, were filed against nursing homes from March 2020 through March of this year.
While there’s no full accounting of the outcomes, court filings show that judges have dismissed some suits outright, citing state or federal immunity provisions, while other cases have been settled under confidential terms. And many cases have stalled due to lengthy and costly arguments and appeals to hash out limits, if any, of immunity protection.
In their defense, nursing homes initially cited the federal Public Readiness and Emergency Preparedness Act , which Congress passed in December 2005. The law grants liability protection from claims for deaths or injuries tied to vaccines or “medical countermeasures” taken to prevent or treat a disease during national emergencies.
The PREP Act steps in once the secretary of Health and Human Services declares a “ public health emergency ,” which happened with covid on March 17, 2020 . The emergency order expired on May 11, 2023.
The law carved out an exception for “willful misconduct,” but proving it occurred can be daunting for families — even when nursing homes have long histories of violating safety standards, including infection controls.
Governors of at least 38 states issued covid executive orders, or their legislatures passed laws, granting medical providers at least some degree of immunity , according to one consumer group’s tally. Just how much legal protection was intended is at the crux of the skirmishes.
Nursing homes answered many negligence lawsuits by getting them removed from state courts into the federal judicial system and asking for dismissal under the PREP Act.
For the most part, that didn’t work because federal judges declined to hear the cases. Some judges ruled that the PREP Act was not intended to shield medical providers from negligence caused by inaction, such as failing to protect patients from the coronavirus. These rulings and appeals sent cases back to state courts, often after long delays that left families in legal limbo.
“These delays have been devastating,” said Jeffrey Guzman, a New York City attorney who represents Schapers and other families. He said the industry has fought “tooth and nail” trying to “fight these people getting their day in court.”

Empire State Epicenter
New York, where covid hit early and hard, is ground zero for court battles over nursing home immunity.
Relatives of residents have filed more than 750 negligence or wrongful death cases in New York counties since the start of the pandemic, according to court data KFF Health News compiled using the judicial reporting service Courthouse News Service. No other area comes close. Chicago’s Cook County, a jurisdiction where private lawyers for years have aggressively sued nursing homes alleging poor infection control , recorded 121 covid-related cases.
Plaintiffs in hundreds of New York cases argue that nursing homes knew early in 2020 that covid would pose a deadly threat but largely failed to gird for its impact. Many suits cite inspection reports detailing chronic violations of infection control standards in the years preceding the pandemic, court records show. Responses to this strategy vary.
“Different judges take different views,” said Joseph Ciaccio, a New York lawyer who has filed hundreds of such cases. “It’s been very mixed.”
Lawyers for nursing homes counter that most lawsuits rely on vague allegations of wrongdoing and “boilerplate” claims that, even if true, don’t demonstrate the kind of gross negligence that would override an immunity claim.
New York lawmakers added another wrinkle by repealing the immunity statute in April 2021 after Attorney General Letitia James noted the law could give nursing homes a free pass to make “financially motivated decisions” to cut costs and put patients at risk.
So far, appeals courts have ruled lawmakers didn’t specify that the repeal should be made retroactive, thus stymying many negligence cases.
“So these cases are all wasting the courts’ time and preventing cases that aren’t barred by immunity statutes from being resolved sooner and clogging up the court system that was already backlogged from COVID,” said attorney Anna Borea, who represents nursing homes.
Troubled Homes Deflect Suits
Some nursing homes that paid hefty fines or were ordered by health officials to shut down at least temporarily because of their inadequate response to covid have claimed immunity against suits, court records show.
Among them is Andover Subacute and Rehabilitation nursing home in New Jersey, which made national headlines when authorities found 17 bodies stacked in a makeshift morgue in April 2020.
Federal health officials fined the facility $220,235 after issuing a critical 36-page report on covid violations and other deficiencies, and the state halted admissions in February 2022.
Yet the home has won court pauses in at least three negligence lawsuits as it appeals lower court rulings denying immunity under the federal PREP Act, court records show. The operators of the home could not be reached for comment. In court filings, they denied any wrongdoing.
In Oregon, health officials suspended operations at Healthcare at Foster Creek, calling the Portland nursing home “a serious danger to the public health and safety.” The May 2020 order cited the home’s “consistent inability to adhere to basic infection control standards.”
Bonnie Richardson, a Portland lawyer, sued the facility on behalf of the family of Judith Jones, 75, who had dementia and died in April 2020. Jones’ was among dozens of covid-related deaths at that home.
“It was a very hard-fought battle,” said Richardson, who has since settled the case under confidential terms. Although the nursing home claimed immunity, her clients “wanted to know what happened and to understand why.” The owners of the nursing home provided no comment.
No Covid Here
Many families believe nursing homes misled them about covid’s relentless spread. They often had to settle for window visits to connect with their loved ones.
Relatives of five patients who died in 2020 at the Sapphire Center for Rehabilitation and Nursing in the Flushing neighborhood in Queens filed lawsuits accusing the home’s operators of keeping them in the dark.
When they phoned to check on elderly parents, they either couldn’t get through or were told there was “no COVID-19 in the building,” according to one court affidavit.

One woman grew alarmed after visiting in February 2020 and seeing nurses wearing masks “below their noses or under their chin,” according to a court affidavit.
The woman was shocked when the home relayed that her mother had died in April 2020 from unknown causes, perhaps “from depression and not eating,” according to her affidavit.
A short time later, news media reported that dozens of Sapphire Center residents had died from the virus — her 85-year-old mother among them, she argued in a lawsuit.
The nursing home denied liability and won dismissal of all five lawsuits after citing the New York immunity law. Several families are appealing. The nursing home’s administrator declined to comment.
Broadening Immunity
Nursing home operators also have cited immunity to foil negligence lawsuits based on falls or other allegations of substandard care, such as bedsores, with little obvious connection to the pandemic, court records show.
The family of Marilyn Kearney, an 89-year-old with a “history of dementia and falls,” sued the Watrous Nursing Center in Madison, Connecticut, for negligence. Days after she was admitted in June 2020, she fell in her room, fracturing her right hip and requiring surgery, according to court filings.
She died at a local hospital on Sept. 16, 2020, from sepsis attributed to dehydration and malnutrition, according to the suit.
Her family argued that the 45-bed nursing home failed to assess her risk of falling and develop a plan to prevent that. But Watrous fired back by citing an April 2020 declaration by Connecticut Gov. Ned Lamont, a Democrat, granting health care professionals or facilities immunity from “any injury or death alleged to have been sustained because of the individual’s or health care facility’s acts or omissions undertaken in good faith while providing health care services in support of the state’s COVID-19 response.”
Watrous denied liability and, in a motion to dismiss the case, cited Lamont’s executive order and affidavits that argued the home did its best in the throes of a “public health crisis, the likes of which had never been seen before.” The operators of the nursing home, which closed in July 2021 because of covid, did not respond to a request for comment. The case is pending.
Attorney Wendi Kowarik, who represents Kearney’s family, said courts are wrestling with how much protection to afford nursing homes.
“We’re just beginning to get some guidelines,” she said.
One pending Connecticut case alleges that an 88-year-old man died in October 2020 after experiencing multiple falls, sustaining bedsores, and dropping more than 30 pounds in the two months he lived at a nursing home, court records state. The nursing home denied liability and contends it is entitled to immunity.
So do the owners of a Connecticut facility that cared for a 75-year-old woman with obesity who required a lift to get out of bed. She fell on April 26, 2020, smashing several teeth and fracturing bones. She later died from her injuries, according to the suit, which is pending.
“I think it is really repugnant that providers are arguing that they should not be held accountable for falls, pressure sores, and other outcomes of gross neglect,” said Richard Mollot, executive director of the Long Term Care Community Coalition, which advocates for patients.
“The government did not declare open season on nursing home residents when it implemented COVID policies,” he said.
Protecting the Vulnerable
Since early 2020, U.S. nursing homes have reported more than 172,000 residents’ deaths, according to Centers for Medicare & Medicaid Services data. That’s about 1 in 7 of all recorded U.S. covid deaths.
As it battles covid lawsuits, the nursing home industry says it is “struggling to recover due to ongoing labor shortages, inflation, and chronic government underfunding,” according to Reeves, the trade association executive.
She said the American Health Care Association has advocated for “reasonable, limited liability protections that defend staff and providers for their good faith efforts” during the pandemic.
“Caregivers were doing everything they could,” Reeves said, “often with limited resources and ever-changing information, in an effort to protect and care for residents.”
But patients’ advocates remain wary of policies that might bar the courthouse door against grieving families.
“I don’t think we want to continue to enact laws that reward nursing homes for bad care,” said Sam Brooks, of the Coalition for the Protection of Residents of Long-Term Care Facilities, a patient advocacy group.
“We need to keep that in mind if, God forbid, we have another pandemic,” Brooks said.
Bill Hammond, a senior fellow at the Empire Center for Public Policy, a nonpartisan New York think tank, said policymakers should focus on better strategies to protect patients from infectious outbreaks, rather than leaving it up to the courts to sort out liability years later.
“There is no serious effort to have that conversation,” Hammond said. “I think that’s crazy.”
Related Topics
- Public Health
- Connecticut
- Nursing Homes
Copy And Paste To Republish This Story
By Fred Schulte May 14, 2024
In early 2020, with reports of covid-19 outbreaks making dire headlines, Trever Schapers worried about her father’s safety in a nursing home in Queens.
But when Trever Schapers sued the nursing home for negligence and wrongful death in 2022, a judge dismissed the case, citing a New York state law hastily passed early in the pandemic. It granted immunity to medical providers for “harm or damages” from an “act or omission” in treating or arranging care for covid. She is appealing the decision.
“I feel that families are being ignored by judges and courts not recognizing that something needs to be done and changed,” said Schapers, 48, who works in the medical field. “There needs to be accountability.”
“The call I received was very alarming, and they refused to answer any of my questions,” she said.
About two weeks later, a social worker called to say that her father had a fever, but the staff did not test him to confirm covid, according to Schapers’ complaint.
The industry says federal health officials and lawmakers in most states granted medical providers broad protection from lawsuits for good faith actions during the health emergency. Rachel Reeves, a senior vice president with the American Health Care Association, an industry trade group, called covid “an unprecedented public health crisis brought on by a vicious virus that uniquely targeted our population.”
“They trusted these facilities to take care of loved ones, and that trust was betrayed,” said Florida attorney Lindsey Gale, who has represented several families suing over covid-related deaths.
“The grieving process people had to go through was horrible,” Gale said.
While there’s no full accounting of the outcomes, court filings show that judges have dismissed some suits outright, citing state or federal immunity provisions, while other cases have been settled under confidential terms. And many cases have stalled due to lengthy and costly arguments and appeals to hash out limits, if any, of immunity protection.
In their defense, nursing homes initially cited the federal Public Readiness and Emergency Preparedness Act , which Congress passed in December 2005. The law grants liability protection from claims for deaths or injuries tied to vaccines or “medical countermeasures” taken to prevent or treat a disease during national emergencies.
The PREP Act steps in once the secretary of Health and Human Services declares a “ public health emergency ,” which happened with covid on March 17, 2020 . The emergency order expired on May 11, 2023.
The law carved out an exception for “willful misconduct,” but proving it occurred can be daunting for families — even when nursing homes have long histories of violating safety standards, including infection controls.
Governors of at least 38 states issued covid executive orders, or their legislatures passed laws, granting medical providers at least some degree of immunity , according to one consumer group’s tally. Just how much legal protection was intended is at the crux of the skirmishes.
For the most part, that didn’t work because federal judges declined to hear the cases. Some judges ruled that the PREP Act was not intended to shield medical providers from negligence caused by inaction, such as failing to protect patients from the coronavirus. These rulings and appeals sent cases back to state courts, often after long delays that left families in legal limbo.
“These delays have been devastating,” said Jeffrey Guzman, a New York City attorney who represents Schapers and other families. He said the industry has fought “tooth and nail” trying to “fight these people getting their day in court.”
Relatives of residents have filed more than 750 negligence or wrongful death cases in New York counties since the start of the pandemic, according to court data KFF Health News compiled using the judicial reporting service Courthouse News Service. No other area comes close. Chicago’s Cook County, a jurisdiction where private lawyers for years have aggressively sued nursing homes alleging poor infection control , recorded 121 covid-related cases.
“Different judges take different views,” said Joseph Ciaccio, a New York lawyer who has filed hundreds of such cases. “It’s been very mixed.”
Lawyers for nursing homes counter that most lawsuits rely on vague allegations of wrongdoing and “boilerplate” claims that, even if true, don’t demonstrate the kind of gross negligence that would override an immunity claim.
New York lawmakers added another wrinkle by repealing the immunity statute in April 2021 after Attorney General Letitia James noted the law could give nursing homes a free pass to make “financially motivated decisions” to cut costs and put patients at risk.
So far, appeals courts have ruled lawmakers didn’t specify that the repeal should be made retroactive, thus stymying many negligence cases.
“So these cases are all wasting the courts’ time and preventing cases that aren’t barred by immunity statutes from being resolved sooner and clogging up the court system that was already backlogged from COVID,” said attorney Anna Borea, who represents nursing homes.
In Oregon, health officials suspended operations at Healthcare at Foster Creek, calling the Portland nursing home “a serious danger to the public health and safety.” The May 2020 order cited the home’s “consistent inability to adhere to basic infection control standards.”
Bonnie Richardson, a Portland lawyer, sued the facility on behalf of the family of Judith Jones, 75, who had dementia and died in April 2020. Jones’ was among dozens of covid-related deaths at that home.
“It was a very hard-fought battle,” said Richardson, who has since settled the case under confidential terms. Although the nursing home claimed immunity, her clients “wanted to know what happened and to understand why.” The owners of the nursing home provided no comment.
Many families believe nursing homes misled them about covid’s relentless spread. They often had to settle for window visits to connect with their loved ones.
Relatives of five patients who died in 2020 at the Sapphire Center for Rehabilitation and Nursing in the Flushing neighborhood in Queens filed lawsuits accusing the home’s operators of keeping them in the dark.
When they phoned to check on elderly parents, they either couldn’t get through or were told there was “no COVID-19 in the building,” according to one court affidavit.
One woman grew alarmed after visiting in February 2020 and seeing nurses wearing masks “below their noses or under their chin,” according to a court affidavit.
The woman was shocked when the home relayed that her mother had died in April 2020 from unknown causes, perhaps “from depression and not eating,” according to her affidavit.
The nursing home denied liability and won dismissal of all five lawsuits after citing the New York immunity law. Several families are appealing. The nursing home’s administrator declined to comment.
The family of Marilyn Kearney, an 89-year-old with a “history of dementia and falls,” sued the Watrous Nursing Center in Madison, Connecticut, for negligence. Days after she was admitted in June 2020, she fell in her room, fracturing her right hip and requiring surgery, according to court filings.
Her family argued that the 45-bed nursing home failed to assess her risk of falling and develop a plan to prevent that. But Watrous fired back by citing an April 2020 declaration by Connecticut Gov. Ned Lamont, a Democrat, granting health care professionals or facilities immunity from “any injury or death alleged to have been sustained because of the individual’s or health care facility’s acts or omissions undertaken in good faith while providing health care services in support of the state’s COVID-19 response.”
Watrous denied liability and, in a motion to dismiss the case, cited Lamont’s executive order and affidavits that argued the home did its best in the throes of a “public health crisis, the likes of which had never been seen before.” The operators of the nursing home, which closed in July 2021 because of covid, did not respond to a request for comment. The case is pending.
Attorney Wendi Kowarik, who represents Kearney’s family, said courts are wrestling with how much protection to afford nursing homes.
“We’re just beginning to get some guidelines,” she said.
“I think it is really repugnant that providers are arguing that they should not be held accountable for falls, pressure sores, and other outcomes of gross neglect,” said Richard Mollot, executive director of the Long Term Care Community Coalition, which advocates for patients.
“The government did not declare open season on nursing home residents when it implemented COVID policies,” he said.
Since early 2020, U.S. nursing homes have reported more than 172,000 residents’ deaths, according to Centers for Medicare & Medicaid Services data. That’s about 1 in 7 of all recorded U.S. covid deaths.
As it battles covid lawsuits, the nursing home industry says it is “struggling to recover due to ongoing labor shortages, inflation, and chronic government underfunding,” according to Reeves, the trade association executive.
She said the American Health Care Association has advocated for “reasonable, limited liability protections that defend staff and providers for their good faith efforts” during the pandemic.
“Caregivers were doing everything they could,” Reeves said, “often with limited resources and ever-changing information, in an effort to protect and care for residents.”
But patients’ advocates remain wary of policies that might bar the courthouse door against grieving families.
“I don’t think we want to continue to enact laws that reward nursing homes for bad care,” said Sam Brooks, of the Coalition for the Protection of Residents of Long-Term Care Facilities, a patient advocacy group.
“We need to keep that in mind if, God forbid, we have another pandemic,” Brooks said.
“There is no serious effort to have that conversation,” Hammond said. “I think that’s crazy.”
We encourage organizations to republish our content, free of charge. Here’s what we ask:
You must credit us as the original publisher, with a hyperlink to our kffhealthnews.org site. If possible, please include the original author(s) and KFF Health News” in the byline. Please preserve the hyperlinks in the story.
It’s important to note, not everything on kffhealthnews.org is available for republishing. If a story is labeled “All Rights Reserved,” we cannot grant permission to republish that item.
Have questions? Let us know at KHNHelp@kff.org
More From KFF Health News

Exclusive: Senator Urges Biden Administration To Thwart Fraudulent Obamacare Enrollments

High Price of Popular Diabetes Drugs Deprives Low-Income People of Effective Treatment

Listen to the Latest ‘KFF Health News Minute’

Biden Leans Into Health Care, Asking Voters To Trust Him Over Trump
Thank you for your interest in supporting Kaiser Health News (KHN), the nation’s leading nonprofit newsroom focused on health and health policy. We distribute our journalism for free and without advertising through media partners of all sizes and in communities large and small. We appreciate all forms of engagement from our readers and listeners, and welcome your support.
KHN is an editorially independent program of KFF (Kaiser Family Foundation). You can support KHN by making a contribution to KFF, a non-profit charitable organization that is not associated with Kaiser Permanente.
Click the button below to go to KFF’s donation page which will provide more information and FAQs. Thank you!

Sign up for the Health News Florida newsletter

Nursing homes wield pandemic immunity laws to duck wrongful death suits

More than 172,000 nursing home residents died of covid. In lawsuits, some families who lost loved ones say they were misled about safety measures or told that COVID wasn’t a danger in their facilities.
In early 2020, with reports of COVID-19 outbreaks making dire headlines, Trever Schapers worried about her father’s safety in a nursing home in Queens.
She had delighted in watching her dad, John Schapers, blow out the candles on his 90th birthday cake that February at the West Lawrence Care Center in the New York City borough. Then the home went into lockdown.
Soon her father was dead. The former union painter spiked a fever and was transferred to a hospital, where he tested positive for COVID, his daughter said, and after two weeks on a ventilator, he died in May 2020.
But when Trever Schapers sued the nursing home for negligence and wrongful death in 2022, a judge dismissed the case, citing a New York state law hastily passed early in the pandemic. It granted immunity to medical providers for “harm or damages” from an “act or omission” in treating or arranging care for COVID. She is appealing the decision.
“I feel that families are being ignored by judges and courts not recognizing that something needs to be done and changed,” said Schapers, 48, who works in the medical field. “There needs to be accountability.”
The nursing home did not return calls seeking comment. In a court filing, the home argued that Schapers offered no evidence that the home was “grossly negligent” in treating her father.
More than four years after COVID first raged through many U.S. nursing homes, hundreds of lawsuits blaming patient deaths on negligent care have been tossed out or languished in the courts amid contentious legal battles.

Even some nursing homes that were shut down by health officials for violating safety standards have claimed immunity against such suits, court records show. And some families that allege homes kept them in the dark about the health of their loved ones, even denying there were cases of COVID in the building, have had their cases dismissed.
Schapers alleged in a complaint to state health officials that the nursing home failed to advise her that it had admitted COVID-positive patients from a nearby hospital in March 2020. In early April, she received a call telling her the facility had some COVID-positive residents.
“The call I received was very alarming, and they refused to answer any of my questions,” she said.
About two weeks later, a social worker called to say that her father had a fever, but the staff did not test him to confirm COVID, according to Schapers’ complaint.
The industry says federal health officials and lawmakers in most states granted medical providers broad protection from lawsuits for good faith actions during the health emergency. Rachel Reeves, a senior vice president with the American Health Care Association, an industry trade group, called COVID “an unprecedented public health crisis brought on by a vicious virus that uniquely targeted our population.”
In scores of lawsuits, however, family members allege that nursing homes failed to secure enough protective gear or tests for staffers or residents, haphazardly mixed COVID-positive patients with other residents, failed to follow strict infection control protocols, and brazenly misled frightened families about the severity of COVID outbreaks among patients and staff.
“They trusted these facilities to take care of loved ones, and that trust was betrayed,” said Florida attorney Lindsey Gale, who has represented several families suing over COVID-related deaths.
“The grieving process people had to go through was horrible,” Gale said.
A Deadly Toll
KFF Health News found that more than 1,100 COVID-related lawsuits, most alleging wrongful death or other negligent care, were filed against nursing homes from March 2020 through March of this year.
While there’s no full accounting of the outcomes, court filings show that judges have dismissed some suits outright, citing state or federal immunity provisions, while other cases have been settled under confidential terms. And many cases have stalled due to lengthy and costly arguments and appeals to hash out limits, if any, of immunity protection.
In their defense, nursing homes initially cited the federal Public Readiness and Emergency Preparedness Act , which Congress passed in December 2005. The law grants liability protection from claims for deaths or injuries tied to vaccines or “medical countermeasures” taken to prevent or treat a disease during national emergencies.
The PREP Act steps in once the secretary of Health and Human Services declares a “ public health emergency ,” which happened with COVID on March 17, 2020 . The emergency order expired on May 11, 2023.
The law carved out an exception for “willful misconduct,” but proving it occurred can be daunting for families — even when nursing homes have long histories of violating safety standards, including infection controls.
Governors of at least 38 states issued COVID executive orders, or their legislatures passed laws, granting medical providers at least some degree of immunity , according to one consumer group’s tally. Just how much legal protection was intended is at the crux of the skirmishes.
Nursing homes answered many negligence lawsuits by getting them removed from state courts into the federal judicial system and asking for dismissal under the PREP Act.
For the most part, that didn’t work because federal judges declined to hear the cases. Some judges ruled that the PREP Act was not intended to shield medical providers from negligence caused by inaction, such as failing to protect patients from the coronavirus. These rulings and appeals sent cases back to state courts, often after long delays that left families in legal limbo.
“These delays have been devastating,” said Jeffrey Guzman, a New York City attorney who represents Schapers and other families. He said the industry has fought “tooth and nail” trying to “fight these people getting their day in court.”
Empire State Epicenter
New York, where COVID hit early and hard, is ground zero for court battles over nursing home immunity.
Relatives of residents have filed more than 750 negligence or wrongful death cases in New York counties since the start of the pandemic, according to court data KFF Health News compiled using the judicial reporting service Courthouse News Service. No other area comes close. Chicago’s Cook County, a jurisdiction where private lawyers for years have aggressively sued nursing homes alleging poor infection control , recorded 121 COVID-related cases.
Plaintiffs in hundreds of New York cases argue that nursing homes knew early in 2020 that COVID would pose a deadly threat but largely failed to gird for its impact. Many suits cite inspection reports detailing chronic violations of infection control standards in the years preceding the pandemic, court records show. Responses to this strategy vary.
“Different judges take different views,” said Joseph Ciaccio, a New York lawyer who has filed hundreds of such cases. “It’s been very mixed.”
Lawyers for nursing homes counter that most lawsuits rely on vague allegations of wrongdoing and “boilerplate” claims that, even if true, don’t demonstrate the kind of gross negligence that would override an immunity claim.
New York lawmakers added another wrinkle by repealing the immunity statute in April 2021 after Attorney General Letitia James noted the law could give nursing homes a free pass to make “financially motivated decisions” to cut costs and put patients at risk.
So far, appeals courts have ruled lawmakers didn’t specify that the repeal should be made retroactive, thus stymying many negligence cases.
“So these cases are all wasting the courts’ time and preventing cases that aren’t barred by immunity statutes from being resolved sooner and clogging up the court system that was already backlogged from COVID,” said attorney Anna Borea, who represents nursing homes.
Troubled Homes Deflect Suits
Some nursing homes that paid hefty fines or were ordered by health officials to shut down at least temporarily because of their inadequate response to COVID have claimed immunity against suits, court records show.
Among them is Andover Subacute and Rehabilitation nursing home in New Jersey, which made national headlines when authorities found 17 bodies stacked in a makeshift morgue in April 2020.
Federal health officials fined the facility $220,235 after issuing a critical 36-page report on COVID violations and other deficiencies, and the state halted admissions in February 2022.
Yet the home has won court pauses in at least three negligence lawsuits as it appeals lower court rulings denying immunity under the federal PREP Act, court records show. The operators of the home could not be reached for comment. In court filings, they denied any wrongdoing.
In Oregon, health officials suspended operations at Healthcare at Foster Creek, calling the Portland nursing home “a serious danger to the public health and safety.” The May 2020 order cited the home’s “consistent inability to adhere to basic infection control standards.”
Bonnie Richardson, a Portland lawyer, sued the facility on behalf of the family of Judith Jones, 75, who had dementia and died in April 2020. Jones’ was among dozens of COVID-related deaths at that home.
“It was a very hard-fought battle,” said Richardson, who has since settled the case under confidential terms. Although the nursing home claimed immunity, her clients “wanted to know what happened and to understand why.” The owners of the nursing home provided no comment.
No COVID Here
Many families believe nursing homes misled them about COVID’s relentless spread. They often had to settle for window visits to connect with their loved ones.
Relatives of five patients who died in 2020 at the Sapphire Center for Rehabilitation and Nursing in the Flushing neighborhood in Queens filed lawsuits accusing the home’s operators of keeping them in the dark.
When they phoned to check on elderly parents, they either couldn’t get through or were told there was “no COVID-19 in the building,” according to one court affidavit.
One woman grew alarmed after visiting in February 2020 and seeing nurses wearing masks “below their noses or under their chin,” according to a court affidavit.
The woman was shocked when the home relayed that her mother had died in April 2020 from unknown causes, perhaps “from depression and not eating,” according to her affidavit.
A short time later, news media reported that dozens of Sapphire Center residents had died from the virus — her 85-year-old mother among them, she argued in a lawsuit.
The nursing home denied liability and won dismissal of all five lawsuits after citing the New York immunity law. Several families are appealing. The nursing home’s administrator declined to comment.
Broadening Immunity
Nursing home operators also have cited immunity to foil negligence lawsuits based on falls or other allegations of substandard care, such as bedsores, with little obvious connection to the pandemic, court records show.
The family of Marilyn Kearney, an 89-year-old with a “history of dementia and falls,” sued the Watrous Nursing Center in Madison, Connecticut, for negligence. Days after she was admitted in June 2020, she fell in her room, fracturing her right hip and requiring surgery, according to court filings.
She died at a local hospital on Sept. 16, 2020, from sepsis attributed to dehydration and malnutrition, according to the suit.
Her family argued that the 45-bed nursing home failed to assess her risk of falling and develop a plan to prevent that. But Watrous fired back by citing an April 2020 declaration by Connecticut Gov. Ned Lamont, a Democrat, granting health care professionals or facilities immunity from “any injury or death alleged to have been sustained because of the individual’s or health care facility’s acts or omissions undertaken in good faith while providing health care services in support of the state’s COVID-19 response.”
Watrous denied liability and, in a motion to dismiss the case, cited Lamont’s executive order and affidavits that argued the home did its best in the throes of a “public health crisis, the likes of which had never been seen before.” The operators of the nursing home, which closed in July 2021 because of COVID, did not respond to a request for comment. The case is pending.
Attorney Wendi Kowarik, who represents Kearney’s family, said courts are wrestling with how much protection to afford nursing homes.
“We’re just beginning to get some guidelines,” she said.
One pending Connecticut case alleges that an 88-year-old man died in October 2020 after experiencing multiple falls, sustaining bedsores, and dropping more than 30 pounds in the two months he lived at a nursing home, court records state. The nursing home denied liability and contends it is entitled to immunity.
So do the owners of a Connecticut facility that cared for a 75-year-old woman with obesity who required a lift to get out of bed. She fell on April 26, 2020, smashing several teeth and fracturing bones. She later died from her injuries, according to the suit, which is pending.
“I think it is really repugnant that providers are arguing that they should not be held accountable for falls, pressure sores, and other outcomes of gross neglect,” said Richard Mollot, executive director of the Long Term Care Community Coalition, which advocates for patients.
“The government did not declare open season on nursing home residents when it implemented COVID policies,” he said.
Protecting the Vulnerable
Since early 2020, U.S. nursing homes have reported more than 172,000 residents’ deaths, according to Centers for Medicare & Medicaid Services data. That’s about 1 in 7 of all recorded U.S. COVID deaths.
As it battles COVID lawsuits, the nursing home industry says it is “struggling to recover due to ongoing labor shortages, inflation, and chronic government underfunding,” according to Reeves, the trade association executive.
She said the American Health Care Association has advocated for “reasonable, limited liability protections that defend staff and providers for their good faith efforts” during the pandemic.
“Caregivers were doing everything they could,” Reeves said, “often with limited resources and ever-changing information, in an effort to protect and care for residents.”
But patients’ advocates remain wary of policies that might bar the courthouse door against grieving families.
“I don’t think we want to continue to enact laws that reward nursing homes for bad care,” said Sam Brooks, of the Coalition for the Protection of Residents of Long-Term Care Facilities, a patient advocacy group.
“We need to keep that in mind if, God forbid, we have another pandemic,” Brooks said.
Bill Hammond, a senior fellow at the Empire Center for Public Policy, a nonpartisan New York think tank, said policymakers should focus on better strategies to protect patients from infectious outbreaks, rather than leaving it up to the courts to sort out liability years later.
“There is no serious effort to have that conversation,” Hammond said. “I think that’s crazy.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — an independent source of health policy research, polling, and journalism. Learn more about KFF .


Laura Santhanam Laura Santhanam
Leave your feedback
- Copy URL https://www.pbs.org/newshour/health/how-bird-flu-puts-workers-on-farms-and-in-food-processing-plants-at-higher-risk
How bird flu puts workers on farms and in food processing plants at higher risk
Outside a farm in Michigan in early May, an RV pulled up and parked. Registered nurse Aracely Nerio and others helped set up a canopy, where nearby farmworkers could find shade or bottles of water, and check their blood pressure and glucose levels. Health care is often out of reach for these laborers.
Those quick check-ins “are the 10 minutes that this person has with you, and that’s all they’re going to have for the next year” to learn how ro stay healthy and on the job, said Nerio, whose own migrant family moved from Texas to Michigan for a better life.
“They’re going to work through colds,” she said. “They’re going to work through all this stuff until they are exhausted or basically can’t.”
This season, health care workers like Nerio are focused on how these patients will be affected by one emerging concern specifically: H5N1, also known as highly pathogenic avian flu or bird flu, which has been confirmed in multiple outbreaks among wild and domesticated animals in the United States. People who work closely with those animals or at food processing plants face higher exposure to risk of infection. And migrant workers face disproportionate risk, compared to the general population. According to Amy Liebman, chief program officer for workers, environment and climate at the Migrant Clinicians Network, these workers make up the bulk of the agricultural and food processing industries. They also are more likely to lack affordable access to health care , and may hesitate to report symptoms if it means not working.
“Worker health and safety is a public health issue, and it needs to be treated that way,” Liebman said.
In the United States, other strains of bird flu began to circulate among poultry in 2020 – the height of the COVID pandemic, when public health experts were already overwhelmed. Meanwhile, H5N1 started to spread in Europe and to several other continents before the first cases in the U.S. were detected in wild birds in 2022. More than 90 million birds in the U.S. alone have been affected by this strain.
In the last two years, this flu has jumped from birds to cows and been confirmed twice in humans in the U.S., most recently in a Texas dairy worker in March . Public health officials, veterinarians and epidemiologists have worried for two decades that something like this – the jump from bird to mammal to human – could happen, and eventually explode into another full-on pandemic.
The virus is extremely dangerous for birds (and the business of poultry farmers by extension), but infected cows have typically regained health within two weeks. Continued testing has shown that pasteurization of dairy products is effective at eliminating risk of infection to this heat-sensitive virus, despite the presence of viral fragments even in commercially available milk.
But the workers on the front lines may be handling animals and food products before they have been treated. And each exposure to the virus carries the possibility of transmission, which allows it to mutate, evolving for its own survival.
“The more this virus circulates, the more there is a chance for mutations,” said Dr. Jennifer Nuzzo, a professor of epidemiology who directs the Pandemic Center at the Brown University School of Public Health. And more mutations could mean a bigger risk of the virus becoming highly infectious among more people.
Some 70 dairy farm workers in Colorado alone were being monitored this month for symptoms and possible illness, CBS News recently reported .
So far, the Centers for Disease Control and Prevention says it has identified no unusual patterns in new flu infections based on available data. Health Secretary Xavier Becerra urged at-risk workers this month to “pay attention to how you feel,” and to look for symptoms that include coughing, fever, sore throat, muscle aches, shortness of breath or eye redness or irritation for 10 days after contact with an animal.
Working at their own risk
Each year in Michigan , where farmland makes up a quarter of the entire state , migrant laborers come to harvest the food that ends up on tables nationwide – no matter what it takes. Farmworkers often wake at 5 a.m. to prune cherry branches, pluck strawberries or milk cows, Nerio said of the patients she typically sees through her work with InterCare Community Health Network, headquartered in Bangor, Michigan.
Sixteen-hour work days are common. By 9 p.m., many workers return from farms to modest camps where entire families may crowd into a single room and share bathrooms. They chase the growing seasons in Michigan, Florida, Texas and beyond, keeping enough of their earnings to pay for food, rent and fuel while sending the rest of their money home. Homemade remedies, like cinnamon tea, along with ibuprofen and Vicks VapoRub amount to health care for many workers when they feel unwell.
Despite lessons the nation learned during the COVID pandemic, there is no paid sick leave option for these essential workers, Liebman said. When pandemic dollars that had once funded public health awareness campaigns dried up, outreach about how to stay healthy during a pandemic grew more haphazard.
On April 5, the CDC issued a health alert to clinicians to look for people with symptoms of respiratory illness, eye irritation and exposure history, as well as how to diagnose and treat people with the virus. The Texas patient had presented doctors with what appeared to be severe conjunctivitis, and further testing showed he was sick with bird flu.
With those realities in mind and a virus at risk of infecting more humans, the Biden administration on May 10 offered up to $28,000 per affected facility over the next four months to buy personal protective equipment , cover expenses to launder uniforms for workers, pay for shipping costs for animal testing samples, and provide funding to heat-treat milk products. These measures are part of a $101 million package dedicated to H5N1 response.
Dr. Nirav Shah from the CDC said they would compensate farm workers who agree to nasal swabs, blood samples and an interview, all in an effort to understand what makes someone more susceptible to developing symptoms of this type of flu.
“We’re building trust in the only way it has ever been built, which is one conversation at a time,” Shah told journalists during a briefing.
What remains unclear is whether health officials have enough time to build that trust before the situation worses.
What public health experts want to see
As the federal government’s response gains momentum (along with efforts by more state and local authorities, commercial farms and businesses), public health officials are hoping for a more coordinated network of resources to support farmworkers and their employers – without stirring unnecessary alarm or fear-mongering. More needs to be done to create clear communication, build relationships and relay updates about the virus through trusted messengers in affected communities, Liebman said.
The CDC is tracking influenza data collected through wastewater surveillance to gauge how H5N1 is developing, and its public dashboard is expected to be available online this week. That is a step in the right direction, said Dr. Marcus Plescia, chief medical officer with the Association of State and Territorial Health Officials.
“It’s a tool that could help us know if we’re moving in the right direction,” he said, but its data should be interpreted with other factors, including more widespread testing.
Availability of rapid testing needs to be prioritized to allow public health officials to pinpoint where these outbreaks are happening with greater nuance, Nuzzo said, but also to allow workers to return to work when they are well. More widespread testing also would help the public assess the threat that H5N1 poses to humans, she said. “If a lot of people are infected and don’t have a serious infection, that would be important information to know.”
Nuzzo added that farmworkers and workers in food processing plants need incentives to come forward, especially if doing so could potentially cost them in lost wages or their jobs.
In Michigan, Nerio said she is going to keep showing up for workers, telling them what she and other health workers learn about H5N1 and the risk it poses to humans. Right now, education is her most effective tool to help people working to make a better life in this country.
“If we empower the farmworker to care about their own health, that’s going to go a long way.”
Even after COVID, the nation’s pandemic response is hobbled by inconsistent financial support and fickle political will, said Dr. Shira Doron with the Infectious Diseases Society of America. when “we need a constant stream of funding.”
“Resources get put into pandemic preparedness when there’s a clear and present threat and get pulled back when the threat recedes,” she said.
Looking across decades of crises in public health, a version of this story has been told with frightening repetition. H5N1 is just the latest edition.
Laura Santhanam is the Health Reporter and Coordinating Producer for Polling for the PBS NewsHour, where she has also worked as the Data Producer. Follow @LauraSanthanam
Support Provided By: Learn more
Educate your inbox
Subscribe to Here’s the Deal, our politics newsletter for analysis you won’t find anywhere else.
Thank you. Please check your inbox to confirm.

The Role and Impact of Presidential Leadership in Modern Democracies
This essay about the role and impact of presidential leadership in modern democracies examines the essential attributes of presidents, including their ability to inspire through vision, manage crises effectively, and shape international relations. It discusses how presidents can influence both national stability and global politics, while also highlighting the potential risks associated with the concentration of power, such as authoritarian tendencies and ethical failures. The piece emphasizes the profound and complex influence of presidential leadership on both political and societal realms.
How it works
In contemporary democracies, the influence and responsibilities of presidential leadership are profoundly impactful and diverse. From the hallowed halls of government to the vibrant public squares, the presidency represents both supreme authority and immense responsibility. This essay explores the essence of presidential leadership in modern democratic states and its effects on both political landscapes and societal norms.
At its core, presidential leadership combines a variety of attributes including vision, charisma, strategic insight, and adept management of both domestic and international affairs.
The modern presidency goes beyond simple administration; it represents a nexus of power and accountability, where the actions of one can reverberate globally and be remembered throughout history.
A key element of effective presidential leadership is the capacity to present a unifying and inspiring vision. Presidents who articulate an inspiring vision can mobilize hope, foster unity, and set a path toward shared goals. For instance, Franklin D. Roosevelt’s New Deal significantly altered the U.S. during the Great Depression, much as Nelson Mandela’s advocacy for unity reshaped post-apartheid South Africa. These leaders demonstrate how visionary leadership can ignite progress in challenging times.
Beyond rhetoric, presidential leadership deeply influences crisis management. During times of economic crises, natural disasters, or global health emergencies like the COVID-19 pandemic, presidential decisions are crucial in steering the nation from turmoil to recovery and reassurance. The effectiveness with which a president manages these crises can determine the balance between disorder and recovery.
Internationally, presidents play critical roles in shaping foreign policy and global interactions. Their ability to handle international relations, forge alliances, and manage conflicts is essential. The diplomatic skills of leaders like John F. Kennedy during the Cuban Missile Crisis or Angela Merkel within the European Union highlight how presidents influence international politics and national interests abroad.
Moreover, presidential leadership involves connecting with citizens on a personal level, understanding their needs, and addressing their concerns. The empathy and compassion a president shows can soothe national distress and promote social healing. This is evident in how leaders respond to national tragedies or advocate for marginalized groups, bridging societal gaps and fostering recovery.
However, presidential power also comes with risks. The centralization of power might lead to authoritarian tendencies, undermining democratic values and trust in public institutions. The rise of populist leaders has highlighted the dangers of charismatic yet divisive leadership that can intensify societal divides and weaken democratic structures.
Additionally, personal failures and ethical violations of presidents can have lasting adverse effects on governance and public perception. Scandals and incompetence can diminish trust and tarnish a presidency, as seen in the historical examples of Richard Nixon’s Watergate scandal and Bill Clinton’s impeachment.
In conclusion, presidential leadership in modern democracies is complex and pivotal. It encompasses crafting visions, managing crises, and influencing global affairs. True leadership is tested not by the wielding of power but by the ability to inspire and elevate society. As we move forward in the 21st century, the character and decisions of presidents will crucially shape the futures of their nations and mark their places in history.
Cite this page
The Role and Impact of Presidential Leadership in Modern Democracies. (2024, May 21). Retrieved from https://papersowl.com/examples/the-role-and-impact-of-presidential-leadership-in-modern-democracies/
"The Role and Impact of Presidential Leadership in Modern Democracies." PapersOwl.com , 21 May 2024, https://papersowl.com/examples/the-role-and-impact-of-presidential-leadership-in-modern-democracies/
PapersOwl.com. (2024). The Role and Impact of Presidential Leadership in Modern Democracies . [Online]. Available at: https://papersowl.com/examples/the-role-and-impact-of-presidential-leadership-in-modern-democracies/ [Accessed: 22 May. 2024]
"The Role and Impact of Presidential Leadership in Modern Democracies." PapersOwl.com, May 21, 2024. Accessed May 22, 2024. https://papersowl.com/examples/the-role-and-impact-of-presidential-leadership-in-modern-democracies/
"The Role and Impact of Presidential Leadership in Modern Democracies," PapersOwl.com , 21-May-2024. [Online]. Available: https://papersowl.com/examples/the-role-and-impact-of-presidential-leadership-in-modern-democracies/. [Accessed: 22-May-2024]
PapersOwl.com. (2024). The Role and Impact of Presidential Leadership in Modern Democracies . [Online]. Available at: https://papersowl.com/examples/the-role-and-impact-of-presidential-leadership-in-modern-democracies/ [Accessed: 22-May-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley - PMC COVID-19 Collection

Pandemic perspectives from the frontline—The nursing stories
Elizabeth l. polinard.
1 Ascension Texas, Austin Texas, USA
Tiffany N. Ricks
Ellen stoetzner duke, kimberly a. lewis.
2 University of California, San Francisco California, USA
3 The University of Texas at Austin, Austin Texas, USA
Associated Data
Data available on request due to privacy/ethical restrictions.
To describe the experiences of registered nurses working in a US healthcare system during the COVID‐19 pandemic.
This qualitative thematic analysis study is a secondary analysis of stories submitted by nurses to a repository established by the parent study.
Registered nurses working in various roles in a healthcare system submitted stories ( N = 45) to open‐ended prompts via an online repository between June 2020 and February 2021. A team of three nurse scientists coded the stories using Dedoose software. Initial codes were then reviewed by the team to synthesize initial coding into themes. The COREQ checklist was used to ensure research reporting guidelines were met.
Thematic analysis revealed three themes in a global theme of COVID‐19 pandemic‐related personal and professional evolution: (1) The art and science of pandemic nursing, (2) Persisting despite challenges; and (3) Learning as we went. Each of the three organizing themes were supported by basic themes.
Conclusions
Identified themes affirm some of nursing's long‐standing core values, such as the central role of human connectedness in restoring health, but findings also reflect new evolutionary processes of moral identity formation that occurred among nurses and the nursing profession during the COVID‐19 pandemic.
Findings from this study describe the processes by which nurses' moral identity evolved during a segment of the COVID‐19 pandemic. Collectively, these evolutions represent important shifts in the nursing profession. Using findings from this study, nurse educators, nurse managers and healthcare administrators will be able to implement effective, sustainable policies and processes that meet the needs of both the community and the workforce.
No Patient or Public Contribution
This study was designed to capture the experiences of nurses employed by one healthcare organization. However, it was not conducted using input or suggestions from the public or the patient population served by the organization.
1. INTRODUCTION
With the onset of the COVID‐19 pandemic, a global spotlight was focused on healthcare workers and their response to a healthcare crisis, the likes of which has not been seen since the devastating flu pandemic of 1918 (Kolawole, 2010 ). The World Health Organization's (WHO) designation of 2020 as The Year of the Nurse (Yazdi, 2019 ) proved to be a prescient action; nowhere is this light more intently focused than on nursing. The successful evolution of the state of global healthcare involves identifying opportunities for transformation and growth inherent in any healthcare crisis. Consequently, documenting experiences of the COVID‐19 pandemic is crucial for understanding the personal and professional experiences and changes occurring as a consequence of this pandemic. Quality nursing care is essential for effective healthcare (Catton & Iro, 2021 ), thus the experiences of nurses are vital to informing how to advance and adapt to an irrevocably changed healthcare landscape. Engaging the voices of the largest group of frontline workers allows us to capture and to preserve this unprecedented moment in history as it unfolds .
In 1850 Emerson ( 1903 ) once wrote, “All things are engaged in writing their history …” Humans are a species for whom stories have historically helped us not only record but make sense of events influencing our development and advancement. As such, qualitative research with its emphasis on lived experiences is a tool widely used by nurse researchers to explore the effects of the current global pandemic on nursing and patient experiences as evidenced by the numerous publications devoted to this topic. We would argue that more is necessary. Hence, our study provides insight into the unique experiences of nurses involved in caring for communities across the nation; it is these stories that will allow both bearing witness and being witnessed, and that will ultimately allow healthcare entities to participate in making meaning of this upending, world‐changing and ongoing event.
This study, involving associates from a national healthcare system, was initiated to first establish a repository for the stories of healthcare workers' personal and professional experiences of the pandemic. Then, the stories submitted to the repository by nurses were systematically analysed and synthesized into themes. The purpose of this study is to give a voice to nurses by describing the experiences and impact of the COVID‐19 pandemic in nurses' own words. We found that the experiences of nurses during the pandemic were rich and diverse, but also contained some commonalities. These commonalities can be used to inform policies and practises to effectively support nurses and ensure their voices are heard as the pandemic continues, subsequently driving a more strategic and empowering transformation of the nursing profession.
2. BACKGROUND
Nurses have experienced profound positive and negative effects of the current pandemic in both their personal and professional lives. Many describe being changed physically, emotionally or spiritually (Foli et al., 2021 ; Moretti et al., 2021 ). The psychological trauma associated with witnessing the traumatic experiences of others while experiencing your own trauma is well documented (Schuster & Dwyer, 2020 ). In many ways, the COVID‐19 pandemic has affirmed long‐standing, virtuous characteristics attributed to the nursing profession; stories about nurses' heroism, selflessness, courage, faith, patriotism and compassion were, and still are, abundant in the news (Halberg et al., 2021 ; Ke et al., 2021 ).
However, as the pandemic persists, nurses are experiencing negative effects, too. As of May 2021, an estimated 115,000 healthcare workers have died from COVID‐19, although reporting is scant and the exact number is unknown (WHO, 2021 ). Nurses who identify as racial and ethnic minorities have been disproportionately affected, with a higher death rate from COVID‐19 (Qureshi et al., 2021 ). Many nurses who are COVID‐19 survivors are experiencing enduring physical, cognitive and psychosocial symptoms for several months after the initial illness (Henneghan et al., 2022 ). The cognitive impact on executive function was greatest among the 28–33‐year‐old age group in one study by Henneghan et al. The mental health of nurses and their families has also been affected (Kellogg et al., 2021 ; Li et al., 2021 ; Nestor et al., 2021 ; Norman et al., 2021 ). The physical and mental effects are impacting workforce retention, resulting in nurses intending to leave their jobs and the profession in greater numbers than were reported pre‐pandemic (Mirzaei et al., 2021 ; Nashwan et al., 2021 ).
Despite the depth of the impact, in the frenzy of healthcare systems to address the COVID‐19 pandemic, it can be difficult to ‘hear’ or discern the collective voice of the nursing workforce. This is in part because nurse voices are underrepresented at the highest levels of leadership and often missing from the media, even though nurses make up the largest segment of the healthcare workforce (Mason et al., 2018 ). In 2018, only 4% of hospital boards of directors, the group of leaders responsible for organizational decision‐making, included a nurse (Van Dyke et al., 2019 ). Globally, 60–74% of WHO member countries have a government‐level chief nursing officer responsible for a national nursing strategy, but the United States is not one of those countries (WHO, 2015 ; WHO, 2020 ). One consequence of this absence is that there is not a designated person at the national level who is responsible for identifying the needs of the nursing workforce, and for ensuring that those needs are met. Yet at the local level, we witnessed numerous signs of courageous nursing leadership and advocacy, manifesting in both traditional and novel ways, and felt that their stories deserved to be told and their voices amplified.
Evidence is building about nurses' experiences during the COVID‐19 pandemic, and the impact on both the individual, as well as the nursing profession. Robinson and Stinson ( 2021 ) studied the ‘lived experiences’ of 14 nurses working in a variety of units caring for COVID‐19 patients across facilities in the United States (U.S.). One of three major themes that emerged from their study via semi‐structured telephone interviews and verbatim transcription was ‘the human connection.’ Subthemes were identified and revealed the immeasurable disruptions in those human connections, and the struggles, compassion and resilience of the nurses to face those challenges. There is qualitative evidence describing why nurses report to duty during a pandemic, the psychosocial impact of working during a pandemic and the implications of the hero narrative. Throughout the past year, several repositories of frontline healthcare worker stories have been created, but to the best of our knowledge, this is the first to report a systematic, qualitative synthesis of the stories submitted to an open‐ended prompt by nurses at any level or role in a U.S. national healthcare system (American Hospital Association, 2021 ; Bennett et al., 2020 ; Loresto Jr et al., 2021 ; National Institutes of Health, 2020 ; Xu et al., 2021 ).
The impact of the pandemic on nursing and nurses is too complex and multifaceted to be captured solely by surveys and quantitative research. In her book, Bylander ( 2020 ) reminds us of the importance of using clinician experiences to “frame a new paradigm of care” (p. 76) that maximizes health equity. Historically, the stories of healthcare workers' experiences during a pandemic have not only provided insights into the political and social climate of the time but have also served to inform subsequent advancements in social justice as well as changes in healthcare policies and practises (Corless, et al., 2018 ; D'Antonio, 2019 ; Jones & Saines, 2019 ; Kolawole, 2010 ). For example, using archived stories and interviews, Jones and Saines ( 2019 ) made the compelling case that the hardwon inclusion of 18 Black nurses in the U.S. Army during the influenza pandemic of 1918–1919, was a catalyst for the advancement of civil rights in the Army Nurse Corps and the Red Cross.
3. THE STUDY
The primary aim of this study was to gain an in‐depth understanding of nurses' personal and professional experiences throughout the COVID‐19 pandemic. Using audio and audiovisual recorded and written stories in response to question prompts, we aimed to capture the experiences of nurses through the participants' own words and voices. Hence, the research question guiding this study was: How are nurses working in any role of a national U.S. healthcare system experiencing the COVID‐19 pandemic?
3.2. Design
This qualitative thematic analysis study is a secondary analysis of stories submitted by nurses to an Institutional Review Board (IRB) approved study repository established by the parent study.
3.3. Sample/participants
The parent study involved recruiting interdisciplinary healthcare workers who had been directly involved in one or more aspects of COVID‐19 pandemic patient care, education or planning. Healthcare workers were recruited from across multiple clinical settings throughout the U.S. Participants were required to identify their role in healthcare (e.g. nurse, physician, surgical technician, etc.). Those associates employed in non‐clinical roles such as environmental services, food services or maintenance were also invited to submit stories.
3.4. Data collection
Repository stories examined in this study were collected prior to the availability of vaccines between June 2020 and February 2021 using audio, audiovisual and/or written methods. Advertised via posted informational fliers, a QR code was used to access a secure, internally facing web platform developed in REDCap, a web application in which surveys can be created, data captured and databases managed. The Pandemic Perspectives protocol contained instructions (including the directive to maintain HIPAA compliance), prompts and a link to upload recordings or written stories. Story prompts included questions like “Without including any identifying information, please discuss a patient experience you've had during this time that was significant to you” and “Think about your shifts at work right now. How are things different from work before COVID‐19?”
In appreciation of the collaborative nature of healthcare, the option to record with a peer was made available as well. Clinicians were encouraged to share their story with another colleague in more of a conversational format. The data collection platform provided a checkbox to indicate a peer‐to‐peer recording. If checked, two consents and two demographic sections were opened for the peers to access and complete before being given the option to upload their written story or recording. Otherwise, participants were asked to complete one consent and demographic form. Demographics included age, self‐identified sex (male, female, non‐binary, transgender or other), self‐identified race and ethnicity, tenure as a nurse at the organization, and professional role. See Table 1 .
Characteristics of nurse participants ( N = 45)
3.5. Ethical considerations
This study received full approval from the IRB of the organization. All participants provided electronic informed consent.
3.6. Data analysis
Consistent with the analysis process outlined by Braun and Clarke ( 2006 , 2019 ), an inductive thematic analysis was used to explore the personal and professional experiences of nurses during the COVID‐19 pandemic. A six‐step method of qualitative data analysis, the process is both a reflexive and a recursive one. At the time of our analysis, the repository included 45 stories from nurses, 43 of which were written submissions and two of which were audio recordings that were transcribed by the principal investigator. Data immersion occurred with extensive reading and documentation of preliminary patterns and potential codes. Additionally, the team met weekly to discuss all aspects of the analytic process. Meeting minutes were kept for reflexive review and as an essential part of the audit trail.
Using the Dedoose software program ( 2021 ), the research team identified relevant excerpts from the stories as codes of data. The stories were divided equally among individual team members for initial code determination. The use of Dedoose enabled the team to collectively review each code extracted by an individual team member, thus enhancing the credibility of the analysis process.
All potentially significant themes were then identified and included in a Google spreadsheet with relevant codes listed with each theme. Subsequently, thematic maps were created to assist us in visualizing the themes as independently significant while allowing us to consider ways they were connected or linked. Our culminating thematic map not only reflected the entire data set but also provided a visual representation of the answer to our research question. Both the spreadsheet and the maps are elements of the audit trail.
Furthermore, our analysis involved comprehensive discussions of each theme, how these themes were defined, the stories and excerpts that best represented these themes, and finally, the names for each theme. Personal insights were contributed by each team member as the data were repeatedly examined and as this process evolved to reinforce the integrity of our findings.
3.7. Validity and reliability/Rigour
Unlike quantitative data analysis, qualitative analysis requires the researcher themself to act as the mechanism for analysis as they engage with the data (Norwell et al., 2017 ), thus making the establishment of rigour and trustworthiness imperative. Key trustworthiness criteria as identified by Whittemore et al. ( 2001 ) include credibility (participants' meanings are accurately interpreted and reflected), authenticity (a variety of voices are heard), criticality (the research is critically assessed) and integrity (the investigators are self‐reflexive).
3.7.1. Credibility
Credibility was firmly established and enhanced in several ways, beginning with our team's rigorous and sustained engagement with the data. All nursing stories gathered in the indicated time frame were identified, uploaded to the Dedoose platform and read repeatedly throughout the data analysis process. Due to the volume of the data, after the initial reading by team members the stories were divided equally among us for preliminary code production. Codes were then systematically cross checked and validated by the entire team during weekly meetings. Our collaborative approach ultimately resulted in the generation of resonant and nuanced themes while reinforcing the credibility of the analysis process (Braun & Clarke, 2019 ; Norwell et al., 2017 ). Additionally, the use of the Dedoose software program allowed us to work efficiently with a significant amount of content, subsequently expediting an in‐depth, rich and complex analysis.
The aforementioned weekly research team meetings were held throughout the entire analysis process during which we refined codes and themes, discussed evolving ideas and developed items such as the theme map that are integrated into our audit trail. Meeting minutes and personal notes were kept illustrating both the reflexive and the recursive nature of the team's process.
Finally, we were fortunate enough to present our preliminary findings to several groups of frontline and executive nurses. This external check essentially allowed us to assess resonance with and recognition of the experiences reflected in the findings. Responses tended to be very moving as nurses verified seeing themselves and/or their colleagues in the data.
3.7.2. Authenticity
Authenticity was realized in the very nature of the study itself. Establishing a national repository for an entire healthcare system allowed frontline nurses and those nurses in executive positions from multiple sites in many areas of the country to participate, thus ensuring that a variety of voices were heard.
3.7.3. Criticality
As discussed previously, criticality was achieved by the assessments done during our weekly team meetings, the nursing peer and leadership debriefings and the development of our audit trail. Notably, the leadership debriefings included nurse research scientists whose feedback contributed to the critical appraisal of our research.
3.7.4. Integrity
Self‐reflexivity was practised by all team members as demonstrated by our manuscript notes, weekly meetings and thoughtful dialoguing. Likewise, personal self‐reflective notes were recorded by the PI throughout the research process, including after every peer and leadership debriefing, frequently involving personal correspondence between the PI and those frontline nurses and nurse leaders who attended these debriefings.
4. FINDINGS
In total, 45 registered nurses participated in this study. Sample characteristics are detailed in Table 1 . A majority identified as female (91.3%) and white (78.3%). Participants had a mean of 12.1 ± 12.0 years of experience in their current role (range 2 months to 38 years), and the mean age was 42.9 ± 13.2 years. Most stories were submitted by nurses working in Midwestern and Southern U.S. locations. Although additional gender identity options were made available for participants (e.g. non‐binary and transgender), all participants identified as either ‘male’ or ‘female’.
Data synthesis identified a global overarching theme with three organizing themes describing pandemic‐related personal and professional evolutions in perspectives, nursing care and patient engagement, moral identity and values. Each organizing theme was further supported by basic themes. Basic themes reflect the grouping of similar concepts, phenomena and relevant topics. These basic themes were then connected and used to support the creation of organizing themes. Although the stories were as individual as the experiences of each professional nurse, they also revealed some common elements that spanned location, practice specialty, nurse characteristics and nursing roles. Hence, the thematic analysis process yielded themes that affirm values long‐attributed to nurses and nursing, but they also described the occurrence of both an individual and collective evolution. These evolutionary experiences reflected transformations in thought, identity, coping mechanisms, perspective about the art and science of nursing, roles and clinical practice. This shift in how nurses viewed themselves was supported with the following organizational themes: “The Art and Science of Nursing During a Pandemic,” “Persisting Despite Challenges,” and “Learning as We Went.” Table 2 provides additional details about each of the themes.
Pandemic perspectives: theme table
4.1. The art and science of nursing during a pandemic
It is common to hear nursing described as both an art and a science. The symbiotic nature of the relationship between the two skill sets has emerged as the foundation of nursing practice; likewise, it often informs the meaning that nurses associate with their work (Peplau, 1988 ). This organizing theme was further organized into four basic themes: moral identity disruption, wholeness, meaning making of the patient experience and acknowledging the loss.
4.1.1. Moral identity disruption
As nursing core values such as autonomy and honesty (Chitty & Black, 2007 ) are learned and practised, they become integrated with personal and organizational values to create a nursing moral identity (Fowler, 2015 ). The unique, dynamic dimensions of nursing practice can profoundly affect nurses' construction of moral identity—both professionally and personally—in different ways. For example, when the sacrosanct mandate of “first do no harm” is perceived as compromised, moral injury may result (Williamson et al., 2020 ) leading to a disruption in moral identity. Moral identity disruption became evident when nurses described how their practice and the potential impact of their care had changed since the pandemic started. A frontline RN with 25 years' experience offered the following perspective:
The main issue I have is that I am a very friendly, smile all the time at every one, and like to have physical contact (touch, hold or shake a hand, or give a hug, when appropriate) when someone is having a difficult time or given some life changing news. I like to sit near them, be interactive, and use a tender touch. The time period I went through nursing, touch was encouraged. Now that social distancing is the only way to be around people, I feel empathy and tenderness have been removed, to a certain degree. If a nurse doesn't get creative, the care given seems cold and distant. I look forward to the going back to the time of being "present" in all the sense of the word .
The inability to provide care and interact with colleagues in ways that align with personal perceptions of nurses and nursing , was found to trigger feelings of uncertainty, conflict and disappointment.
Being ostracised by others, especially other health care workers, because we were perceived as "unclean" was devastating on our psyche. We went from loving being nurses to questioning why we were in this profession. I have been a nurse for 34 years and have never experienced anything like this. Not with Ebola, not with H1N1, not with SARS. The mistrust of each other, the raging over mask mandates, the uncivility [sic] of people with each other . (Frontline RN with 34 years of experience)
4.1.2. Wholeness
Appreciating the multifaceted nature of the nursing experience lends itself to the concept of ‘wholeness’. In their attempt to remain physically, emotionally, mentally and socially ‘whole’, many nurses shared insights into how their initial focus on self‐preservation evolved into self‐care as they considered implications for the future state of self—both in and outside of the nursing profession.
I lost my daily routine. I stopped reading, meditating, working out, and eating healthy. One day it hit me that I needed to get back to my routine, make the best of each day and focus less on not knowing what the next day would bring but be grateful for the moment. I started doing yoga, running, reaching out to old friends, reading, meditating, facetiming my family and going to bed early regularly. Quickly my perspective on covid changed. Maybe this was the change I needed, maybe this was the reminder that I needed to appreciate the small things and stop focusing on what the future will bring . (Frontline RN with 3 years of experience)
4.1.3. Meaning making of the patient experience
Participants routinely shared personal perspectives of patient experiences and how those experiences, having been shaped by evolving policies and procedures related to the pandemic, affected their practice, specifically their ability to fulfil roles they seemed to associate with the art and science of nursing. These experiences and range of interactions influenced perceptions of themselves and their care. A frontline nurse with 1 year of experience said, “A mask, gown, shield and gloves have put a damper on one of the most fundamental aspects of being human. A patient with long term [ sic ] HIV told me it was the 80's [ sic ] all over again. On the other side of the shield, I wept.” The idea of compassionate care would likely most closely align with the art of nursing. However, compassionate care should not only apply to how nurses care for people, but also how they care for themselves.
4.1.4. Acknowledging the loss
The notion of self‐care being an aspect of the art of nursing was highlighted in the grief experiences shared by participants. Their grief experiences were shaped by both personal and collective experiences of pain and suffering. Most participants expressed a sense of profound loss associated with frequent deaths of patients, family members and friends, unmet expectations and abrupt changes in professional roles. A majority indicated that they had not experienced this level of loss during their professional careers, and in an effort to bear witness to these experiences, they acknowledged the suffering and pain of their patients, colleagues and themselves. It was this self‐compassion and care that seemed to help these nurses overcome feelings of helplessness and hopelessness. As one frontline nurse said, “If death teaches us anything it'd be the importance of cherishing life and the people around us, to find joy in the small things and to not leave things unfinished. By doing so and by giving and receiving more love than I ever have before, I think I'll be able to recover and heal” (Frontline RN with less than 1 year of experience).
4.2. Persisting despite challenges
Nurses described the process of persisting despite the potentially overwhelming emotional and logistical challenges created by the COVID‐19 pandemic. Nurses in our sample described three basic tools that they relied on to fulfil their perceived duty to their patients: teamwork, gratitude and spirituality (Table 2 ). Strong emotions such as extraordinary fear, stress and anxiety, uncertainty, grief and loss, and feelings of isolation were mentioned to some degree by all participants. Nurses shared stories rife with fear of the unknown and of stress related to managing nursing practice, specifically long‐held beliefs about the art and science of nursing, in completely new ways. A frontline nurse with 6 years' experience said, “There is no doubt that this has been the most difficult time in health care for my time [ sic ]. Stress, anxiety, fear… are all things that we have overcome to continue to deliver care to our patients.”
4.2.1. Teamwork
The theme ‘persisting despite challenges’ was reflected in the collective desire among nurses to continue ‘showing up’ both for their colleagues, as well as their patients and the community at large. Participants expressed a desire to provide the best care possible despite the abundance of challenges associated with caring for a community reeling from the novel coronavirus. Participants identified that the key component in achieving this common goal of persistence was teamwork and support from their colleagues. Teamwork was deemed crucial in encouraging one another, sharing best practises and information, as well as creating workplace efficiencies. Teamwork appears to have helped associates remain committed to their work despite adversity.
What will remain with me forever is the excellence of our nursing team, who each day give it their all to help those under their care. The positive attitude of our nurses and PCTs (patient care technicians) and entire team as they continue to meet the daily challenges presented to them on a daily and minute by minute basis . (Non‐frontline nurse with 35 years of experience)
4.2.2. Gratitude
The sustained commitment and sense of duty to continue working were also framed and grounded in gratitude. Even in the context of uncertainty and stressful experiences, participants consistently reported an intentional focus on gratitude as a means of fatigue and burnout mitigation. For a majority of participants, the appreciation for family, community and organizational support, connectedness to coworkers and positive patient outcomes helped foster feelings of mental well‐being and counter anxiety in stressful work situations. A unit manager with 10 years' experience shared, “But the experience in general, very much life‐changing and we're just grateful to be alive and proud of our care ‐ I couldn't be more proud of the facility I work for because I trusted the people that took care of my husband, and I trust them to take care of everybody else as well.” Another non‐frontline nurse with 19 years of experience declared, “I am so grateful for such a fulfilling career as a nurse and all the wonderful people who support me at work daily.”
4.2.3. Spirituality
Many participants spoke about the importance of spirituality and religious faith in their ability to persevere through moments of uncertainty and distress. For them, a deliberate focus on faith and prayer was a strategy they often utilized to remain hopeful, as well as to renew or reinforce their sense of purpose. In reference to her team, a nurse with 5 years of experience as a manager and 17 as an RN asserted, “By the morning we were proud of the work we had done. We followed our Christian values and prayed for the community at the end of our shift.” Many reported finding comfort and a sense of optimism associated with their religion. “My faith continues to comfort me as we wait for this pandemic to become [ sic ] under control,” was stressed by a non‐frontline RN (with 36 years of nursing experience) in the early stages of the pandemic.
4.3. Learning as we went
The skilful adaptation to the progression of the COVID‐19 pandemic is reflected in the theme of ‘learning as we went’, supported by two basic themes of the new registered nurse and the organizational response. This process was shaped and affected by the organizational response to resource allocation, perceived support (e.g. additional orientation time), as well as years of experience and tenure. It is imperative to frame this process of learning as one with both positive and negative repercussions. To be sure, these instances were sometimes considered opportunities for personal growth, but most participants expressed an overall sense of fear and exhaustion that were associated with constant change.
We were unfamiliar with the virus, the incubation period, the extreme contagious nature of it and what to do about it. We were changing processes daily, sometimes hourly as we moved through the beginning phases. We really knew so little . (5 years experience as a nurse manager, 17 as a nurse)
4.3.1. New registered nurse
Embarking on a new career in nursing requires tenacity, courage, flexibility and dedication. Nursing can, at times, be overwhelming, yet satisfying. The adaptive nature of nursing practice in the context of the COVID‐19 pandemic has been maximized. Newly licensed nurses experienced a profound challenge as they entered the nursing profession. They were challenged to transition into a new profession while simultaneously being expected quickly to: develop new skill sets; manage stress, anxiety and exhaustion; absorb and adhere to frequent policy and practice changes; and care for people with a complex, unknown condition.
I am a part of a new nurse residency cohort. I had been on my own as a nurse on my floor for about a month before our unit became strictly COVID patients. I remember how we started with less than 10 patients with COVID. I also remember coming to work and suddenly being told I was taking care of COVID patients of my own … .[ sic ] as a brand new nurse. I was completely taken off guard and unprepared. I was terrified. I held in tears as I got report from the day‐shift nurses . (RN with less than 1 year experience)
As the pandemic abated, many newly licensed frontline nurses reported feeling lost as they transitioned from practising on newly created COVID‐19 units back into the specialty they were initially hired (e.g. postpartum).
So when we went back to our "normal", I was still a baby nurse who had only been on my own for one month before going into full on COVID. I had to relearn and adjust again. I am still adjusting. I deal with anxiety a lot and go to work overwhelmed most days. I try my best. I know COVID had an effect on us all. It definitely had an effect on me as a brand new nurse. I am proud I got to serve in this Pandemic, but no one can prepare you for it and the aftermath . (Frontline nurse with less than 1 year experience)
4.3.2. Organizational response
The COVID‐19 pandemic created a multitude of challenges for healthcare entities. Nurses acknowledged that organizations were also ‘learning as they went’ while simultaneously doing what they believed was best for their workforce and community. This dynamic learning and adaptive process was apparent in resource utilization and allocation (e.g. personal protective equipment), as well as frequently changing policies and procedures (e.g. visitor guidelines). There was a consensus among participants that organizational leadership response to supply shortages, care complexities and uncertainties influenced their ability to adapt to these changes.
Supplies that we took for granted in the context of “they are always there and always will be” now were gone, fit testing upon fit testing occurs as levels of supplies dwindle; gowns that we are used to, no longer exist. Re‐using supplies and bundling of care for the safety of all now occurs … creative staff with positive demeanors … they smile and are proud to be here to continue the remarkable work they have always done, just now in a different way. I'm grateful for the support of our management team . (Non‐frontline nurse with 35 years of experience)
5. DISCUSSION
Our study highlights the various ways in which the COVID‐19 pandemic impacted nurses through the overarching theme of the process of personal and professional evolution supported by three main themes: the art and science of nursing during a pandemic, persisting despite challenges and learning as we went. Although some aspects of the themes are reported in other studies—for example, the idea of learning as we went (LoGiudice & Bartos, 2021 )—the personal and professional evolutionary process as revealed throughout the three main themes has not been previously described in the literature. The nurses in our study found themselves learning and evolving in real time, without specific frameworks for patient safety or self‐care, or direct evidence to guide practice structure. This dynamic process of evolution was not only enlightening and challenging at times, but it was also devastating when personal safety and patient care delivery were perceived as compromised.
Because nursing schools are tasked with educating nurses to become proficient in caring for people in the most vulnerable moments of their lives, nursing is undergirded by professional values and ethical principles that pervade all aspects of practice. These core values (e.g. altruism and integrity) and principles are a starting point for ethical behaviour and personal integrity (Chitty & Black, 2007 ). In other words, nurses use a combination of their personal and professional values and experiences to formulate what they believe to be the characteristics of a ‘good nurse’. Discourse between moral identity and the professional duties and obligations of nurses is likely to arise when internal and external situations and factors occur that evoke uncertainty, fear and vulnerability. According to Schmidt ( 2011 ), (discourse) “requires agents who articulate and communicate their ideas in exchanges that may involve discussion, deliberation, negotiation, and contestation.”
Along with strong core principles and values bolstered by effective discourse, it is important to consider the contextual factors that influence the moral identity of nurses. Peter et al. ( 2018 ) suggest that there tends to be a reciprocal relationship between the strength of nurses' moral identity and their feeling like the care they are providing is having a positive impact on the health and well‐being of their patients and community. According to Chrisinger (2021, p. 10), “Trauma is trauma. Viewed through a less clinical and more philosophical lens, these sorts of trauma might best be described as events that split life into two. Before the event, there is wholeness. After the event, there is fracture. Where there was once some semblance of safety and security, dignity and peace, there is now fear and hopelessness, pain and grief.” It is this process that healthcare entities and organizations must recognize, accept and adapt to create a workplace that supports the mental and emotional well‐being of its staff in effective, sustainable ways.
Understandably, the pandemic evoked a gamut of emotions evident in our study, including pride, fear, anxiety, grief and gratitude—emotions that nurses describe having to manage both personally and professionally. Coping with extreme emotions and adapting to new, untested models of care and workflow while interacting with patients in the ‘COVID reality’ affected both the art and science of nursing. Therefore, evidence of moral identity disruption is apparent in many of the narratives submitted, particularly those submitted by newer RNs. However, even experienced RNs expressed grappling with changes in patient care that demanded compromise of established practice and professional values.
Our sample of nurses described the compounding effect of overcoming logistical challenges in the presence of strong psychosocial emotions. The complexity of addressing the logistical challenges for nursing practice created by the COVID‐19 pandemic is consistent with findings from recent studies (Góes et al., 2020 ; Yuan et al., 2020 ). Themes like extraordinary fear (Góes et al., 2020 ), stress and anxiety (Chidiebere Okechukwu et al., 2020 ; González‐Gil et al., 2021 ), uncertainty (González‐Gil et al., 2021 ), grief and loss (Hofmeyer & Taylor, 2021 ; Nyatanga, 2020 ) and social isolation (Luo et al., 2020 ) are also consistent with previous work about healthcare workers during the pandemic. The nurses in our sample relied on teamwork, gratitude and spirituality to persist despite the potentially overwhelming circumstances. Even still, their stories contained beginning signs of moving beyond moral identity to moral identity disruption. This shift further illustrates the need for healthcare entities to create opportunities to influence moral identity development in ways that leave nurses ‘whole’ and able to care for themselves and the community effectively. Future work should also investigate how the presence of moral identity disruption has evolved as the pandemic endures.
The last of the organizing themes, ‘learning as we went’, featured prominently in the nurses' stories in our sample. Our findings echo the work of LoGiudice and Bartos ( 2021 ) in which two of their five overall themes are: “Theme 1: What's the Protocol Today? Where, Oh Where, Is the Research?”; and “Theme 2: Family Ties Broken: How Nurses Bridge the Gap” (p. 19). Nurses in our study repeatedly described their frustrations with the lack of and changing evidence during the pandemic together with their ethical and moral distress in delivering quality, compassionate management for their patients and their significant others.
Furthermore, some degree of real‐time adaptation was expected because of the novel nature of the virus. However, the prominence of this theme in our findings also reflects the need to increase two key roles in the hospital‐based nursing workforce: nurse educators and nurse scientists. This theme lays bare the consequences of healthcare systems operating with increasingly limited nurse education departments (Mlambo et al., 2021 ). It also exposes how few nurse scientists are both working in hospital systems and actively conducting nursing care delivery and/or workforce research. For example, fewer than 1% of U.S. nurses have a doctoral degree, and of those only an estimated 3% with a research‐focused doctoral training program work in a hospital as principal investigators in a nursing research‐based role (National Institutes of Health, 2018 ; Nursing Management, 2017 ; U.S. Department of Health and Human Services, Health Resources and Services Administration, 2010 ).
5.1. Implications for practice
As we emerge from the pandemic and look to the future, the nursing profession can take actions now to address the themes identified in our study. To support the pandemic‐related disruptions in the art and science of nursing, organizations, leaders and colleagues can begin by acknowledging the extensive grief and loss in local (e.g. daily huddles) and national venues (e.g. system‐wide initiatives). Grief can be complex and individualized, and as such a multi‐faceted approach may be most useful (Wallace et al., 2020 ). For example, organizations could provide direct access to a mental health worker (Shore et al., 2016 ; Wallace et al., 2020 ) via a hospital code (e.g. ‘Code Lavender’) which could deploy a chaplain or other mental health support team member to an area of the hospital to provide listening sessions and comfort supplies for acute distress (e.g. items that attend to the five senses such as snacks or beverages; essential oil patches, compresses, diffusers, soothing sounds, weighted blankets, etc.).
Apart from an individualized approach, the work environment can be adjusted to support coping with grief and loss (Gibson, 2017 ; Wallace et al., 2020 ). These adjustments include being adequately staffed to allow for break time to disconnect from the traumatic event; adequately preparing nurses for their response role via sufficient training and education; making nurses aware of local resources and services to refer patients and families for additional assistance; and having adequate supervision and peer support while facilitating patient care (Gibson, 2017 ; Wallace et al., 2020 ).
Leaders should look for evidence‐based strategies to promote teamwork (Lacerenza et al., 2018 ; Rosen et al., 2018 ), gratitude (Aryankhesal et al., 2019 ; Melnyk et al., 2020 ), and spirituality (Crane & Ward, 2016 ). One way to do so is to re‐evaluate the ‘scope creep’ that occurred early in the pandemic. Due to personal protective equipment preservation strategies, infection prevention strategies, and solutions to hospital‐wide staffing shortages, nurses were asked to shoulder additional tasks that previously were shared among the multi‐professional healthcare team (Centers for Disease Control and Prevention, 2020 ). Tasks such as cleaning and sanitizing patient rooms, delivering and removing patient trays, or phlebotomy can now be reassigned to their appropriate departments to relieve nurses of tasks that had not required skilled nursing care to complete.
Shortening or modifying new nurses' orientation periods was a necessary action for many hospitals during the pandemic, but this truncation has also contributed to increased turnover and burnout among our newest colleagues (Turale & Nantsupawat, 2021 ). Organizations need a solution that will nurture early and essential professional development while also addressing increased staffing needs. One possible solution is for hospitals and nursing schools to work in partnership to conditionally hire pre‐licensure students who are entering their capstone training hours. This strategy allows students to train as pre‐licensed in the unit in which they will be working post‐licensure, which will probably shorten orientation time for both the nurse and hospital post‐licensure.
Three actions may minimize the theme of ‘learning as we went’ in future pandemics. First, direct national and local efforts to increase the number of research‐focused, doctorally prepared nurses. Next, increase the number of nurse educators and nurse scientists working in hospital systems and involve them in leadership planning, strategizing and operational decision‐making. Because of their integrated roles in the healthcare system, clinical nurse scientists are best positioned to expediently produce care‐delivery and workforce evidence. Since they are familiar with the key stakeholders and the system's operations, clinical nurse scientists can operate efficiently and effectively to produce both retrospective and prospective research. Lastly, ensure that nurse scientists lead or support research‐related efforts in hospital systems. By doing so, hospital systems can ensure the production of high‐quality evidence to guide nursing care delivery and workforce decisions.
5.2. Limitations
The recruitment methods utilized in this study led to a sample that was predominantly female and non‐Hispanic white. As a result, some groups of nurses were underrepresented in our sample such as people who identify as male and those who identify as racial and ethnic minorities. It is unknown how their stories may be similar to or different from those in our sample. To ensure a representative sample, future research should incorporate targeted recruitment strategies. This study design did not involve contacting participants to ask follow‐up or probing questions, so findings are limited to the stories as‐submitted. However, these stories capture nurse perspectives in their own words, the content of which was determined by the participant at the time of submission. As such, they represent what the nurse perceived to be the most important narrative to offer at that moment. Finally, the nurse experience has evolved over time. This cross‐sectional collection of stories represents a snapshot of experiences at a particular moment in time, but it is unknown how these individuals' perspectives have evolved since their submissions. Future studies should examine the nurse experience through the arc of the pandemic.
6. CONCLUSION
Nurses are agents of change. As such, they occupy a unique position in the creation of formative, historical reflections, policies and processes for navigating the current and future pandemics. The Pandemic Perspectives program is vital for facilitating our understanding of the effects of the COVID‐19 pandemic on nurses' experiences, their practice and the experiences of their patients. Effective professional evolution—and, it can be argued, the evolution of healthcare—requires a re‐evaluation of how healthcare organizations acknowledge that nursing and nurses have changed. The knowledge gained from this program can be used for such a re‐evaluation and will enable us to inform policies, guide hospital management, anticipate long‐term health needs to allocate resources accordingly, identify lasting innovations and provide evidence‐based recommendations for management of future pandemics and other healthcare crises.
FUNDING INFORMATION
This research received no specific grant from any funding agency in the public, commercial or not‐for‐profit sectors.
CONFLICT OF INTEREST
The authors have no conflict of interest to declare.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/jan.15306 .
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the support from all the people who contributed to this project: Lori Alesia, Molly Amelse, Jeff Bothof, Victoria Boyce, James Brown, LeeAnn Christie, Terri Delgado‐Roulhac, Matthew French‐Bravo, Esmeralda Galvan, Lindsey Green, Toni Hamilton, Wendy Miller, Trisha Musich, Mary Sitterding, Charles Snodgrass, Rachelle Vick, Sarah Wasson and Amy Wilson.
APPENDIX A.
Pandemic perspectives: Prompts
- Talk about your shifts at work right now. How are things different from work before COVID‐19?
- What have you felt since the pandemic began? Think about your experiences mentally, emotionally and physically. What changes have you noticed?
- Have you noticed changes in any other areas of your life? Please talk a little bit about those changes.
- What has been the most difficult thing for you about the pandemic?
- Have you had any positive experiences?
- What have you learned about yourself that you did not already know?
- Has anything surprised you about working during this time?
- Think about things like keeping families connected, conserving use of PPE, supporting each other, connecting with patients or anything else that you and others have thought about or done.
What kinds of things have you or anyone you work with done to problem‐solve during this time? What are people doing to deal with things that are challenges during this time? How have these ideas been used and how did they work out?
- Without including any identifying information, please discuss a patient experience you have had during this time that was significant to you.
- How has your journey informed how you'll move forward?
- What will remain with you forever?
- How will you recover and heal?
- Is there anything else you want to talk about?
Polinard, E. L. , Ricks, T. N. , Duke, E. S. , & Lewis, K. A. (2022). Pandemic perspectives from the frontline—The nursing stories . Journal of Advanced Nursing , 00 , 1–14. 10.1111/jan.15306 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Elizabeth L. Polinard and Tiffany Ricks are considered joint first authors.
Contributor Information
Elizabeth L. Polinard, Email: gro.noisnecsa@dranilope .
Kimberly A. Lewis, @nurse_lewis .
DATA AVAILABILITY STATEMENT
- American Hospital Association . (2021). VacciNation: Inspiring stories on the national COVID‐19 vaccine rollout . Retrieved from https://www.aha.org/vaccine‐stories
- Aryankhesal, A. , Mohammadibakhsh, R. , Hamidi, Y. , Alidoost, S. , Behzadifar, M. , Sohrabi, R. , & Farhadi, Z. (2019). Interventions on reducing burnout in physicians and nurses: A systematic review . Medical Journal of the Islamic Republic of Iran , 33 , 77. 10.34171/mjiri.33.77 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bennett, P. , Noble, S. , Johnston, S. , Jones, D. , & Hunter, R. (2020). COVID‐19 confessions: A qualitative exploration of healthcare workers experiences of working with COVID‐19 . BMJ Open , 10 ( 12 ), e043949. 10.1136/bmjopen-2020-043949 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Braun, V. , & Clarke, V. (2006). Using thematic analysis in psychology . Qualitative Research in Psychology , 3 ( 2 ), 77–101. 10.1191/1478088706qp063oa [ CrossRef ] [ Google Scholar ]
- Braun, V. , & Clarke, V. (2019). Reflecting on reflexive thematic analysis . Qualitative Research in Sport, Exercise, and Health , 11 ( 4 ), 589–597. 10.1080/2159676X.2019.1628806 [ CrossRef ] [ Google Scholar ]
- Bylander, J. (2020). Narrative matters: Writing to change the health care system (2nd ed., pp. 1–301). Johns Hopkins University Press. [ Google Scholar ]
- Catton, H. , & Iro, E. (2021). How to reposition the nursing profession for a post‐covid age . BMJ , 373 , n1105. 10.1136/bmj.n1105 [ CrossRef ] [ Google Scholar ]
- Centers for Disease Control and Prevention . (2020). COVID1‐9 Summary for Healthcare Facilities: Strategies for Optimizing the Supply of PPE during Shortages . Retrieved from https://www.cdc.gov/coronavirus/2019‐ncov/hcp/ppe‐strategy/strategies‐optimize‐ppe‐shortages.html#print
- Chidiebere Okechukwu, E. , Tibaldi, L. , & La Torre, G. (2020). The impact of COVID‐19 pandemic on mental health of Nurses . La Clinica Terapeutica , 171 ( 5 ), e399–e400. 10.7417/CT.2020.2247 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chitty, K. K. , & Black, B. P. (2007). Professional nursing: Concepts and challenges (5th ed.). Saunders/Elsevier. [ Google Scholar ]
- Corless, I. B. , Nardi, D. , Milstead, J. A. , Larson, E. , Nokes, K. M. , Orsega, S. , Kurth, A. E. , Kirksey, K. M. , & Woith, W. (2018). Expanding nursing's role in responding to global pandemics 5/14/2018 . Nursing Outlook , 66 ( 4 ), 412–415. 10.1016/j.outlook.2018.06.003 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Crane, P. J. , & Ward, S. F. (2016). Self‐healing and self‐care for nurses . AORN Journal , 104 ( 5 ), 386–400. 10.1016/j.aorn.2016.09.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dedoose Version 8.0.35 , web application for managing, analyzing, and presenting qualitative and mixed method research data (2021). Los Angeles, CA: SocioCultural Research Consultants, LLC. https://www.dedoose.com/
- D’Antonio, P. (2019). The great flu and after: Why the nurses? American Journal of Public Health , 109 ( 6 ), 832–833. 10.2105/ajph.2019.305093 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Emerson, R. W. (1903). In Emerson E. W. (Ed.), The Complete Works (Vol. 12 ). Houghton Mifflin. [ Google Scholar ]
- Foli, K. J. , Forster, A. , Cheng, C. , Zhang, L. , & Chiu, Y. C. (2021). Voices from the COVID‐19 frontline: Nurses' trauma and coping . Journal of Advanced Nursing , 77 ( 9 ), 3853–3866. 10.1111/jan.14988 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fowler, M. D. M. (2015). Guide to the code of ethics for nurses: Development, application, and interpretation (2nd ed.). American Nurses Association. [ Google Scholar ]
- Gibson, A. (2017). An inquiry into older disaster responders' secondary traumatic stress . Paper presented at the 21st International Association of Gerontological Societies' World Congress of Gerontology and Geriatrics Meeting. San Francisco, CA.
- Góes, F. , Silva, A. , Santos, A. , Pereira‐Ávila, F. , Silva, L. , Silva, L. , & Goulart, M. (2020). Challenges faced by pediatric nursing workers in the face of the COVID‐19 pandemic . Revista Latino‐Americana de Enfermagem , 28 , e3367. 10.1590/1518-8345.4550.3367 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- González‐Gil, M. T. , González‐Blázquez, C. , Parro‐Moreno, A. I. , Pedraz‐Marcos, A. , Palmar‐Santos, A. , Otero‐García, L. , Navarta‐Sánchez, M. V. , Alcolea‐Cosín, M. T. , Argüello‐López, M. T. , Canalejas‐Pérez, C. , Carrillo‐Camacho, M. E. , Casillas‐Santana, M. L. , Díaz‐Martínez, M. L. , García‐González, A. , García‐Perea, E. , Martínez‐Marcos, M. , Martínez‐Martín, M. L. , Palazuelos‐Puerta, M. , Sellán‐Soto, C. , & Oter‐Quintana, C. (2021). Nurses' perceptions and demands regarding COVID‐19 care delivery in critical care units and hospital emergency services . Intensive & Critical Care Nursing , 62 , 102966. 10.1016/j.iccn.2020.102966 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Halberg, N. , Jensen, P. S. , & Larsen, T. S. (2021). We are not heroes —The flipside of the hero narrative amidst the COVID19‐pandemic: A Danish hospital ethnography . Journal of Advanced Nursing , 77 , 2429–2436. 10.1111/jan.14811 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Henneghan, A. M. , Lewis, K. A. , Gill, E. , Franco‐Rocha, O. Y. , Vela, R. D. , Medick, S. , & Kesler, S. R. (2022). Describing cognitive function and psychosocial outcomes of COVID‐19 survivors: A cross‐sectional analysis . Journal of the American Association of Nurse Practitioners , 34 ( 3 ), 499–508. 10.1097/jxx.0000000000000647 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hofmeyer, A. , & Taylor, R. (2021). Strategies and resources for nurse leaders to use to lead with empathy and prudence so they understand and address sources of anxiety among nurses practising in the era of COVID‐19 . Journal of Clinical Nursing , 30 ( 1–2 ), 298–305. 10.1111/jocn.15520 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jones, M. M. , & Saines, M. (2019). The eighteen of 1918‐1919: Black nurses and the great flu pandemic in the United States . The American Journal of Public Health , 109 , 877–884. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ke, Q. , Chan, S. W. , Kong, Y. , Fu, J. , Li, W. , Shen, Q. , & Zhu, J. (2021). Frontline nurses' willingness to work during the COVID‐19 pandemic: A mixed‐methods study . Journal of Advanced Nursing , 77 ( 9 ), 3880–3893. 10.1111/jan.14989 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kellogg, M. B. , Schierberl Scherr, A. E. , & Ayotte, B. J. (2021). "All of this was awful:" Exploring the experience of nurses caring for patients with COVID‐19 in the United States . Nursing Forum , 56 ( 4 ), 869–877. 10.1111/nuf.12633 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kolawole, B. (2010). Nursing and the 1918–1919 Spanish influenza epidemic . Journal of Community Nursing , 24 ( 6 ), 30–34. [ Google Scholar ]
- Lacerenza, C. N. , Marlow, S. L. , Tannenbaum, S. I. , & Salas, E. (2018). Team development interventions: Evidence‐based approaches for improving teamwork . The American Psychologist , 73 ( 4 ), 517–531. 10.1037/amp0000295 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Li, J. , Su, Q. , Li, X. , Peng, Y. , & Liu, Y. (2021). COVID‐19 negatively impacts on psychological and somatic status in frontline nurses . Journal of Affective Disorders , 294 , 279–285. 10.1016/j.jad.2021.07.031 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- LoGiudice, J. A. , & Bartos, S. (2021). Experiences of nurses during the COVID‐19 pandemic: A mixed‐methods study . AACN Advanced Critical Care , 32 ( 1 ), 14–26. 10.4037/aacnacc2021816 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Loresto, F. L., Jr. , Nunez, L. , Tarasenko, L. , Pierre, M. S. , Oja, K. , Mueller, M. , Switzer, B. , Marroquin, K. , & Kleiner, C. (2021). The nurse COVID and historical epidemics literature repository: Development, description, and summary . Nursing Outlook , 69 ( 3 ), 257–264. 10.1016/j.outlook.2020.12.017 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Luo, M. , Guo, L. , Yu, M. , Jiang, W. , & Wang, H. (2020). The psychological and mental impact of coronavirus disease 2019 (COVID‐19) on medical staff and general public ‐ A systematic review and meta‐analysis . Psychiatry Research , 291 , 113190. 10.1016/j.psychres.2020.113190 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mason, D. J. , Nixon, L. , Glickstein, B. , Han, S. , Westphaln, K. , & Carter, L. (2018). The Woodhull study revisited: Nurses' representation in health news media 20 years later . Journal of Nursing Scholarship , 50 ( 6 ), 695–704. 10.1111/jnu.12429 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Melnyk, B. M. , Kelly, S. A. , Stephens, J. , Dhakal, K. , McGovern, C. , Tucker, S. , Hoying, J. , McRae, K. , Ault, S. , Spurlock, E. , & Bird, S. B. (2020). Interventions to improve mental health, well‐being, physical health, and lifestyle behaviors in physicians and nurses: A systematic review . American Journal of Health Promotion , 34 ( 8 ), 929–941. 10.1177/0890117120920451 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mirzaei, A. , Rezakhani Moghaddam, H. , & Habibi Soola, A. (2021). Identifying the predictors of turnover intention based on psychosocial factors of nurses during the COVID‐19 outbreak . Nursing Open , 8 ( 6 ), 3469–3476. 10.1002/nop2.896 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mlambo, M. , Silén, C. , & McGrath, C. (2021). Lifelong learning and nurses' continuing professional development, a metasynthesis of the literature . BMC Nursing , 20 ( 1 ), 62. 10.1186/s12912-021-00579-2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moretti, C. , Ceccaroni, S. E. , Confortini, R. , Roncaglio, C. M. , Lionetto, V. , Ndocaj, K. , Festa, L. , Calderone, C. , Sarli, L. , & Artioli, G. (2021). Taking care. Nursing towards Covid‐19 patients during the pandemic emergency in Italy: A qualitative study . Acta Bio‐Medica , 92 ( S2 ), e2021025. 10.23750/abm.v92iS2.11944 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nashwan, A. J. , Abujaber, A. A. , Villar, R. C. , Nazarene, A. , Al‐Jabry, M. M. , & Fradelos, E. C. (2021). Comparing the impact of COVID‐19 on nurses' turnover intentions before and during the pandemic in Qatar . Journal of Personalized Medicine , 11 ( 6 ), 456. 10.3390/jpm11060456 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National Institutes of Health . (2018). The nurse scientist workforce . The Physician‐Scientist Workforce Report 2014. Retrieved from https://report.nih.gov/workforce/psw/nurse_scientist_workforce.aspx
- National Institutes of Health . (2020). Behind the mask: Real stories from NIH staff about life during the COVID‐19 pandemic . Retrieved from https://history.nih.gov/display/history/Behind+the+Mask
- Nestor, S. , O' Tuathaigh, C. , & O' Brien, T. (2021). Assessing the impact of COVID‐19 on healthcare staff at a combined elderly care and specialist palliative care facility: A cross‐sectional study . Palliative Medicine , 35 ( 8 ), 1492–1501. 10.1177/02692163211028065 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Norman, S. B. , Feingold, J. H. , Kaye‐Kauderer, H. , Kaplan, C. A. , Hurtado, A. , Kachadourian, L. , Feder, A. , Murrough, J. W. , Charney, D. , Southwick, S. M. , Ripp, J. , Peccoralo, L. , & Pietrzak, R. H. (2021). Moral distress in frontline healthcare workers in the initial epicenter of the COVID‐19 pandemic in the United States: Relationship to PTSD symptoms, burnout, and psychosocial functioning . Depression and Anxiety , 38 , 1007–1017. 10.1002/da.23205 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Norwell, L. S. , Norris, J. M. , White, D. E. , & Moules, N. J. (2017). Thematic analysis: Striving to meet trustworthiness criteria . International Journal of Qualitative Methods , 16 , 1–13. 10.1177/1609406917733847 [ CrossRef ] [ Google Scholar ]
- Nursing Management . (2017). Nurse scientists . Nursing Management (Springhouse) , 48 ( 2 ), 1. 10.1097/01.NUMA.0000512494.20590.32 [ CrossRef ] [ Google Scholar ]
- Nyatanga, B. (2020). Impact of COVID‐19 on loss and grief: a personal lens . British Journal of Community Nursing , 25 ( 6 ), 306–307. 10.12968/bjcn.2020.25.6.306 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peplau, H. E. (1988). The art and science of nursing: Similarities, differences, and relations . Nursing Science Quarterly , 1 ( 1 ), 8–15. 10.1177/089431848800100105 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peter, E. , Simmonds, A. , & Liaschenko, J. (2018). Nurses' narratives of moral identity: Making a difference and reciprocal holding . Nursing Ethics , 25 ( 3 ), 324–334. 10.1177/0969733016648206 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Qureshi, I. , Garcia, R. , Ali, N. , & Randhawa, G. (2021). Understanding the disproportionate effects of COVID‐19 on nurses from ethnic minority backgrounds . Nursing Standard. , 36 , 29–34. 10.7748/ns.2021.e11645 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Robinson, R. , & Stinson, C. K. (2021). The lived experiences of nurses working during the COVID‐19 pandemic . Dimensions of Critical Care Nursing , 40 ( 3 ), 156–163. https://pubmed.ncbi.nlm.nih.gov/33792274 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rosen, M. A. , Diaz Granados, D. , Dietz, A. S. , Benishek, L. E. , Thompson, D. , Pronovost, P. J. , & Weaver, S. J. (2018). Teamwork in healthcare: Key discoveries enabling safer, high‐quality care . The American Psychologist , 73 ( 4 ), 433–450. 10.1037/amp0000298 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schmidt, V. (2011). Speaking of change: Why discourse is key to the dynamics of policy transformation . Critical Policy Studies , 5 , 106–126. 10.1080/19460171.2011.576520 [ CrossRef ] [ Google Scholar ]
- Schuster, M. , & Dwyer, P. A. (2020). Post‐traumatic stress disorder in nurses: An integrative review . Journal of Clinical Nursing , 29 ( 15–16 ), 2769–2787. [ PubMed ] [ Google Scholar ]
- Shore, J. C. , Gelber, M. W. , Koch, L. , & Sower, E. (2016). Anticipatory grief . Journal of Hospice & Palliative Nursing , 18 ( 1 ), 15–19. https://www.deepdyve.com/lp/wolters‐kluwer‐health/anticipatory‐grief‐YxPSzf7gxk [ Google Scholar ]
- Turale, S. , & Nantsupawat, A. (2021). Clinician mental health, nursing shortages and the COVID‐19 pandemic: Crises within crises . International Nursing Review , 68 ( 1 ), 12–14. 10.1111/inr.12674 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- U.S. Department of Health and Human Services, Health Resources and Services Administration (2010). The registered nurse population: Findings from the 2008 national sample survey of registered nurses. Retrieved from https://data.hrsa.gov/DataDownload/NSSRN/GeneralPUF08/rnsurveyfinal.pdf
- Van Dyke, K. , Combes, J. , & Joshi, M. (2019). Percentage of hospital boards with RN members . American Hospital Association Healthcare Governance Survey Report. Retrieved from https://campaignforaction.org/resource/percentage‐hospital‐boards‐rn‐members/
- Wallace, C. L. , Wladkowski, S. P. , Gibson, A. , & White, P. (2020). Grief during the COVID‐19 pandemic: Considerations for palliative care providers . Journal of Pain and Symptom Management , 60 ( 1 ), e70–e76. 10.1016/j.jpainsymman.2020.04.012 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Whittemore, R. , Chase, S. K. , & Mandle, C. L. (2001). Validity in qualitative research . Qualitative Health Research , 11 , 522–537. 10.1177/104973201129119299 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Williamson, V. , Murphy, D. , & Greenberg, N. (2020). COVID‐19 and experiences of moral injury in front‐line key workers . Occupational Medicine , 70 , 317–319. 10.1093/occmed/kqaa052 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization . (2015). Roles and responsibilities of government chief nursing and midwifery officers: A capacity‐building manual . Retrieved from https://www.who.int/hrh/nursing_midwifery/15178_gcnmo.pdf
- World Health Organization . (2020). State of the World's Nursing 2020 . Retrieved from https://apps.who.int/iris/rest/bitstreams/1274201/retrieve
- World Health Organization . (2021). Director‐General's opening remarks at the World Health Assembly . Retrieved from https://www.who.int/director‐general/speeches/detail/director‐general‐s‐opening‐remarks‐at‐the‐world‐health‐assembly‐‐‐24‐may‐2021
- Xu, H. , Stjernswärd, S. , & Glasdam, S. (2021). Psychosocial experiences of frontline nurses working in hospital‐based settings during the COVID‐19 pandemic ‐ A qualitative systematic review . International Journal of Nursing Studies Advances , 100037. Advance online publication. doi: 10.1016/j.ijnsa.2021.100037, 3 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yazdi, M. (2019). 2020 is the ‘year of the nurse’ ‐ Here's what that means for nurses . Nurse.org. Retrieved from https://nurse.org/articles/2020‐the‐year‐of‐the‐nurse‐and‐midwife/
- Yuan, L. , Chen, S. , & Xu, Y. (2020). Donning and doffing of personal protective equipment protocol and key points of nursing care for patients with COVID‐19 in ICU . Stroke and Vascular Neurology , 5 ( 3 ), 302–307. 10.1136/svn-2020-000456 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
A global pandemic needs strong nursing staff engagement in clinical management, awareness and knowledge exchange, and public safety. The American Nurses Association's Code of Ethics for Nurses (2015) is the definitive professional conduct norm for the nursing field. Clause 2 of the code specifies that "the sole responsibility of the nurse ...
Life in the pandemic: Some reflections on nursing in the context of COVID‐19. In the unparalleled and extraordinary public health emergency in which we find ourselves, across the world nurses stand as we always do—at the front line. Nurses everywhere are staffing our clinics, hospital wards and units—in some situations, literally working ...
She decided to pursue a nursing career after taking a school trip to Costa Rica, where she found herself in need of hospital care. The nurse who cared for her inspired her to do the same for others. Stake wrote this essay to share her experience of the pandemic. Cleveland Clinic is a non-profit academic medical center.
14 nurses on life and work during COVID. Colleen Walsh. Harvard Staff Writer. November 2, 2021 long read. Since early 2020, when the pandemic exploded around the world, Massachusetts has seen nearly 19,000 COVID deaths and more than 840,000 cases. If a line graph of hospital admissions over the past 20 months looks like a series of peaks and ...
The U.S. Bureau of Labor Statistics projects the need for 1.1 million new RNs for expansion and replacement of retirees, and to address the current nursing shortage. In the current pandemic, nursing shortages are exacerbated by shifting infection surges that take down some working nurses and overwhelm others who are fortunate enough to remain ...
The COVID-19 pandemic has called nurses everywhere to have honest and transparent discussions about how our work in the crisis context, and the barriers that prevent us from effectively achieving our responsibilities, is distressing us as human beings. Burnout, trauma, emotional distress, professional grief, and moral suffering have all ...
During the COVID-19 pandemic, nurses have been the provider with the most prolonged face-to-face contact with patients and associated exposure to patient suffering and viral transmission.1 Nurses have experienced practice changes, fear for themselves and their families, and moral distress from the inability to provide optimal care.2-4 Throughout this time, it has been important for nurse ...
The COVID-19 pandemic has shed a spotlight on nurses and reinforced the essential role they have in hospitals and clinics worldwide. Caralise Hunt, an associate professor and associate dean for academic affairs in Auburn's School of Nursing, discusses the spotlight and what Auburn is doing to prepare young people for the future of health care
One of the characteristics of the COVID-19 pandemic is that much of what is published about it quickly becomes outdated. Such is the rate of change in the pandemic's course—whether due to the roll-out of the vaccine program globally or the evolution of new variants—that the context in which articles are written may be very different by the time of publication. Given that, it's perhaps ...
The more than 1,140 U.S. nurses who lost their lives in the first year of the pandemic knew the risks to themselves and their families. And yet they stayed in harm's way. They cared for their ...
More. The COVID-19 pandemic made an immediate impact on the nursing profession. Some nurses suffered devastating health consequences. Many nurses dealt with excessive on-the-job stress, well ...
The Executive Vice President and Chief Nursing Officer for CommonSpirit Health discusses challenges nurses are facing during the Covid-19 pandemic, predominantly in terms of staffing, burnout, and compassion fatigue and PTSD; how burnout has been a problem in nursing for decades; and involving nurses in the vision for the future of health care delivery.
The pandemic of Coronavirus disease 2019 (COVID-19) has brought significant pressure on nurses globally as they are the frontline of care. This study aimed to explore the experiences and challenges of nurses who worked with hospitalised patients with COVID-19. In this qualitative study, a purposive sample of 14 nurses participated in in-depth telephone interviews.
Joann Sands, clinical assistant professor in the School of Nursing, is well-acquainted with disasters and emergencies. Declaring a "passion" for disaster and emergency response management, Sands' expertise includes disaster preparedness and response, resiliency after a disaster, disaster epidemiology and more areas all too familiar in this COVID-19 pandemic.
Another role that nurses play during a pandemic is maintaining supplies of medical equipment and protective items such as masks, gloves, and hand sanitizer. These resources can easily become scarce during a crisis, and nurses play a vital role in safeguarding these supplies from theft or hoarding. For example, Wendy Shaw, a nurse in Washington ...
From nursing student to pandemic practitioner. Alicia Sgroi, BSN, RN began working as an RN on a medical-surgical unit in February 2020. At the time, she and her colleagues knew a new coronavirus was coming to the United States. ... At the end of her essay, Sgroi reflects that she is exactly where she is supposed to be, and that she feels an ...
The Covid-19 pandemic has highlighted many of the difficult ethical issues that health care professionals confront in caring for patients and families. The decisions such workers face on the front lines are fraught with uncertainty for all stakeholders. Our focus is on the implications for nurses, who are the largest global health care ...
A semi‐structured interview guide was developed based on the researchers' experiences as nursing educators and articles and essays that were regularly printed in lay publications, scholarly journals, or presented on television news reports about the COVID‐19 crisis. ... And as the pandemic grew, nurses were facing new challenges—working ...
There are close to 450,000 nurses in Canada. Some work in hospitals, some in long-term care homes, some are privately hired, but they all share one commonality. Since the beginning of COVID-19 ...
Nearly 30 percent of Singing River's 500 beds are empty. With 169 unfilled nursing positions, administrators must keep the beds empty. Nursing shortages have long vexed hospitals. But in the ...
New tool measures moral distress in pandemic nursing care. Aug 4, 2022. Learning about nurses' moral distress during crisis care. Aug 25, 2021 ...
Pandemic burnout builds on a pre-existing nursing shortage. But Triangle universities are expanding programs to train nurses to step into the gap. North Carolina grapples with growing nursing shortage
Nursing home closures can also have a direct impact on employment. Whereas most industries rebounded quickly from the spike in job losses at the onset of the COVID-19 pandemic, employment in nursing homes and residential care facilities has still not recovered. Figure 3 disaggregates the three industries comprising health services in New England.
226. By John M. Barry. Mr. Barry, a scholar at the Tulane University School of Public Health and Tropical Medicine, is the author of "The Great Influenza: The Story of the Deadliest Pandemic in ...
But when Trever Schapers sued the nursing home for negligence and wrongful death in 2022, a judge dismissed the case, citing a New York state law hastily passed early in the pandemic. It granted immunity to medical providers for "harm or damages" from an "act or omission" in treating or arranging care for covid. She is appealing the ...
But when Trever Schapers sued the nursing home for negligence and wrongful death in 2022, a judge dismissed the case, citing a New York state law hastily passed early in the pandemic. It granted immunity to medical providers for "harm or damages" from an "act or omission" in treating or arranging care for COVID. She is appealing the ...
Abstract. Nurses, as front-line care providers, strive to offer adequate care to their clients. They have acquired valuable experiences during the COVID-19 pandemic that enhance the nursing profession. This study aimed to explore nurses' caring experiences in the COVID-19 pandemic. This is a qualitative meta-aggregative systematic review.
Nuzzo added that farmworkers and workers in food processing plants need incentives to come forward, especially if doing so could potentially cost them in lost wages or their jobs. In Michigan ...
This essay explores the essence of presidential leadership in modern democratic states and its effects on both political landscapes and societal norms. At its core, presidential leadership combines a variety of attributes including vision, charisma, strategic insight, and adept management of both domestic and international affairs.
1. INTRODUCTION. With the onset of the COVID‐19 pandemic, a global spotlight was focused on healthcare workers and their response to a healthcare crisis, the likes of which has not been seen since the devastating flu pandemic of 1918 (Kolawole, 2010).The World Health Organization's (WHO) designation of 2020 as The Year of the Nurse (Yazdi, 2019) proved to be a prescient action; nowhere is ...