Training to Teach in Medicine
This Harvard Medical School six-month, application-based certificate program aims to provide high-impact, evidence-based education for medical faculty and health care professionals.


Associated Schools

Harvard Medical School
What you'll learn.
Master evidence-based justifications for critical clinical education skill sets
Develop a framework to educate medical learners in practice through the study of educational theories
Learn and apply practical teaching skills to diverse groups of adult learners in bedside, ambulatory, classroom and other settings
Accelerate leadership and professional development in medical education pedagogies and teaching techniques
Course description
To successfully train the next generation of health care professionals, medical educators must utilize innovative teaching strategies and techniques in both classroom and clinical settings. Training to Teach in Medicine is an online program that integrates traditional and novel pedagogic methods, skills-based training, two live virtual workshops, online learning modules, individual and team projects, as well as a final capstone project to benefit your home institution.
Training to Teach in Medicine aims to develop skilled clinical educators who can apply educational theories and teaching best practices to instruct medical students and physicians-in-training, in turn equipping the future medical workforce for career success. Participants will graduate from the program with the skills, strategies and techniques required to educate medical students and adult learners in a variety of settings.
Participants will be eligible for Associate Alumni status upon successful completion of the program. Early tuition and need-based tuition reductions may be available.
Course Outline
Principles of Adult Learning
- Medical Education Pedagogy in the 21st Century
Application of Adult Learning and Theory to Teaching
- Enhancing Memory and Attention During Lectures
- Knowing Your Learner
Teaching Methods
- Flipped Classroom
- Strategies for Effective Teaching and Learning
Teaching on Wards and in Clinics
- Effective Teaching on the Wards and in the Clinic
- Microskills for Teaching in Clinical Settings
Contemporary Teaching Techniques
- Using Multimedia and Technology to Enhance Teaching
- Small Group Teaching
- Curriculum Development Steps
Assessment, Evaluation and Feedback
- Curriculum Development Steps- Selecting Assessment Tools
- The Use of Quizzes/Formative Assessments in Teaching and Learning
- How to Give and Get Effective Feedback
- Teaching and Assessment of Critical Thinking in Medicine
Physician Identify Formation and Life-Long Learning
- Promoting Lifelong Learning: Developing Curious Learners
- Reflection as a Teaching Tool in Medical Education
- Competence Assessment in Resident Training
- Leading Change in Academic Medicine
Medical Education Research
- Overview of Quantitative and Qualitative Methods
- Study Design in Medical Education Research
- Best Practices in Survey Design
Instructors

Jeremy Richards

Lauren Yang

Brian Persaud
You may also like.

Teachers Mentoring Teachers: Practices for Powerful Professional Communities
Explore mentoring relationships at different stages of a career in teaching, aiming to uncover practices that are specific to the teaching profession and to name what makes them so effective

Articulating the Intangibles of Teaching: Aligning Your Purpose and Practice for Instructional Leadership
Join a community of peers to excavate the intangibles of teaching, aligning mission, vision, methods, decisions, and student work in a comprehensive, personal language of practice.

Questions at the Core: Extending the Question Formulation Technique to Sustain an Inquiry-based Culture in Schools
Strengthen and refine your inquiry aptitude.
Medical Education
Make the AAMC your medical education home. Explore what we have to offer, from learning events, trainings, and professional development conferences to programs, initiatives, and scholarship on key and emerging topics. Get involved, advance your career, and help move the field of medical education forward.
Areas of Focus
Search form
- Advanced search
- Search responses
- Search blogs
- Effective teaching...
Effective teaching skills—how to become a better medical educator
- Related content
- Peer review
- Shvaita Ralhan , specialist registrar in care of the elderly and general internal medicine, Royal Devon and Exeter NHS Foundation Trust, Exeter, UK ,
- Paul Bhogal , interventional registrar, National Hospital for Neurology and Neurosurgery, London, UK ,
- Gauraang Bhatnagar , specialist registrar in clinical radiology, Peninsula Radiology Academy, Plymouth, UK ,
- Jane Young , consultant radiologist, Whittington Hospital NHS Trust, London, UK ,
- Matt Green , medical publisher director, BPP University College, London, UK
- mattgreen{at}bpp.com
Shvaita Ralhan , Paul Bhogal , Gauraang Bhatnagar , Jane Young , and Matt Green , authors of Effective Medical Teaching Skills , explore the importance of teaching in modern medicine and what steps you can take to enhance your teaching skills
In the past decade the principles of effective teaching for doctors have come of age. To earlier generations of doctors no training in specific teaching skills was provided. Teaching was a skill that you were expected to possess or acquire. Effective teaching techniques are now a requirement for doctors, as highlighted by the General Medical Council, 1 and can be learnt and perfected like any other medical skill. Every doctor is expected to deliver teaching, whether to medical students, allied health professionals, or postgraduate doctors. Furthermore, there is an expectation to show formal training in teaching methods. A passionate teacher will be an asset to any medical department. This, coupled with the personal satisfaction of being an effective teacher, is the motivation to become a better medical educator.
Skills required of an effective teacher
There are many skills that make a good medical educator. Figure 1 outlines some of these qualities. 2 ⇓ It is important to remember that most teachers do not begin their careers with a full complement of these skills; becoming an effective teacher is a process of continual refinement.

Fig 1 Characteristics of a good teacher 2
- Download figure
- Open in new tab
- Download powerpoint
How to improve your teaching skills
It is vital to have a basic grasp of how adults learn, the different learning styles, how to adapt your teaching to different situations, and an understanding of assessment. This can all be gained from self directed reading of general teaching texts; however, newer teaching manuals aimed specifically at teaching in medical education are often more digestible. A variety of medical education courses are also available, ranging from short focused training programmes that aim to provide doctors with the fundamentals of teaching to courses leading to a formal teaching qualification such as a certificate, diploma, or masters in medical education. Several of these can be undertaken through distance learning.
A great deal can also be learnt from observing and discussing teaching methods with experienced teachers. This can be taken further in the form of a mentor. The potential utilities of this role model are vast but can include advice, guidance, resource facilitation, and counselling about difficult teaching situations. The mentor is usually a senior colleague who can offer positive and negative feedback in a non-judgmental manner. The relationship may be a prolonged one, sometimes both professional and personal, and can be an asset to mentor and mentee.
Reflective practice and introspection help to develop a teaching philosophy to identify your personal approaches, objectives, and priorities. This process facilitates personal growth as a teacher and encourages you to incorporate new ideas regarding teaching.
Importance of providing feedback
Self improvement in any skill requires knowledge of how you are currently performing. It is well known that feedback improves performance. 3 Constructive feedback facilitates refinement and evolution of any teaching episode, whether it is a specific lecture or a whole curriculum. Appropriate feedback can be gained through several methods:
Feedback from students
Self (reflection)
Feedback from other teachers or colleagues.
They all have their own merits and drawbacks, but a combination of all three will result in the most reliable opinion.
Medical schools have embraced the importance of feedback; most now incorporate formalised feedback systems to ensure that the quality of teaching remains high. However, some more immediate forms of feedback, such as the Harvard one minute questionnaire, have the unique advantage of giving the teacher an opportunity to improve the particular episode for the very group of students providing the feedback. 4 Self feedback allows the teacher to build a portfolio of reflective logs that help to identify pearls, pitfalls, and specific strengths and weaknesses. Self feedback is the most consistent method and thus, in some ways, the most reliable. Feedback from colleagues is more difficult to obtain, and some people believe that the intrusive nature of direct observation falsifies the teaching environment and is unreliable. In these situations, indirect feedback (from video playback) is often a reasonable alternative. Feedback is at its most effective when several methods are used simultaneously and interpreted in a positive light.
Enlisting the help of modern technology
The past decade has seen an exponential increase in the use of modern technology in the field of medical education (fig 2). ⇓

Fig 2 Examples of modern technology in medical education
E-learning and webcasting are examples of educational strategies that have become commonplace in many medical institutions. More recently, interest has moved towards the use of mobile technologies to improve learning. Podcasts and vodcasts, audio and video files respectively, can be downloaded to portable computer devices such as an MP3 player. They are being increasingly used for lectures. Some of their many advantages include portability, facilitation of learning “on the go,” and encouragement of self directed learning. Selective replay to consolidate particular weaknesses can also be useful.
Wikis and blogs are websites that allow easy creation and editing of material (links to websites, uploading files), together with a record of continual dialogue by numerous individuals simultaneously. These can be used for students who are geographically separated and are propagating distance learning. They have been useful for creating virtual journal clubs, for example.
Interactive white boards combine the traditional flipchart, overhead projector, and white board. They are large touch sensitive surfaces that are connected to a computer and a digital projector. They can be useful in problem based learning when working with a small group. This technology promotes student interaction and collaboration within the learning environment.
Simulation based medical education allows the learner to use a variety of resources that aim to mimic real life situations. Simulation includes simplistic (low fidelity) procedural models that have been used for many years to assist individuals in task specific clinical skills—for example, genitourinary models for catheterisation. In recent years, new software and hardware have been developed to produce immersive high tech and high fidelity simulators for complex procedures such as laparoscopic surgery and endoscopy. The most sophisticated simulators are often in dedicated centres and can replicate tasks and environments simultaneously. In many of these the model can have heart sounds, breath sounds, and selectable electrocardiogram traces, and it can be possible to cannulate and intubate the same model. These simulators can be used to re-create a scenario in an operating theatre, for example. Audiovisual recording equipment is usually available to facilitate the valuable feedback process. Sophisticated simulators are ideal for group training and development of non-technical skills, such as teamwork, leadership, and delegation.
Simulation has important advantages. In a culture where the patient safety agenda is central, learners and teachers value the way that simulation provides a means of risk free learning. As organisational pressures increase, simulators allow trainees and trainers to engage in educational activities at a time convenient to them. The standardisation and repeatability of exact situations are useful in the assessment process. 5
The use of modern technology in education is not a passing trend but a powerful tool to supplement traditional teaching methods. The next generation of undergraduate students will automatically embrace these changes, and as teachers we must do the same to maximise the potential benefits and improve ourselves as medical educators.
Importance of research (and its challenges)
As in clinical medicine, evidence based practice in clinical education is paramount. As medical educators it is essential to ensure that the methods used, in which there is considerable national financial investment, are improving the practice of future doctors and therefore patients’ outcomes. The days of “see one, do one, teach one” are being replaced by teaching methods that are backed by research. High quality evidence is necessary to establish policy and practice of the highest standard and has resulted in the formation of specific organisations such as Best Evidence Medical Education.
Contemporary educational research faces numerous challenges. The traditional research methodologies that apply to trials of medical intervention do not necessarily suit educational research, and thus new research methodologies specific to educational practice are being developed. The difficulty in defining standardised outcomes can be further compounded by a lack of standardised and reliable assessment methods. Sometimes ethical difficulties arise. 6 All these challenges are slowly being tackled, and educational research is taking important steps in the right direction.
We can take heart from the progress that has been made over the preceding decades. We now have generations of students and doctors who consider training in teaching methods as part of the norm. Many students now have the opportunity to take formal qualifications and fellowships. Educational excellence, along with clinical excellence, is increasingly being recognised and rewarded appropriately. However, we cannot rest on our laurels and must continue to strive to improve how we teach and to embrace new ways of delivering teaching, while not losing sight of the main goal: to be better at treating patients and delivering high quality healthcare.
In times of limited resources and changes in delivery of services, we must also ensure that education is included, costed for, and not squeezed out.
Competing interests: All the authors are also authors of Effective Medical Teaching Skills , published by BPP Learning Media, of which MG is medical publishing director.
- ↵ General Medical Council. Tomorrow’s doctors. General Medical Council, 2003. www.gmc-org/education/undergraduate/undergraduate_policy/tomorrows_doctors.asp .
- ↵ Harden R M, Crosby J R. AMEE Education Guide No 20: The good teacher is more than a lecturer—the twelve roles of the teacher. Medical Teacher 2000 ; 22 : 334 -47. OpenUrl CrossRef Web of Science
- ↵ Ammons R. Effects of knowledge of performance: a survey and tentative theoretical formulation. J Gen Psychol 1956 ; 54 : 279 . OpenUrl CrossRef Web of Science
- ↵ Harvard University. 1-minute paper worksheet: a thinking-centered self-assessment tool. http://learnweb.harvard.edu/alps/thinking/docs/minute.htm .
- ↵ Bradley P. The history of simulation in medical education and possible future directions. Med Educ 2006 ; 40 : 254 -62. OpenUrl CrossRef PubMed Web of Science
- ↵ Murray E. Challenges in educational research. Med Educ 2002 ; 36 : 110 -2. OpenUrl CrossRef PubMed Web of Science
You are using an outdated browser. This website is best viewed in IE 9 and above. You may continue using the site in this browser. However, the site may not display properly and some features may not be supported. For a better experience using this site, we recommend upgrading your version of Internet Explorer or using another browser to view this website.
- Download the latest Internet Explorer - No thanks (close this window)
- Penn GSE Environmental Justice Statement
- Philadelphia Impact
- Global Initiatives
- Diversity & Inclusion
- Catalyst @ Penn GSE
- Penn GSE Leadership
- Program Finder
- Academic Divisions & Programs
- Professional Development & Continuing Education
- Teacher Programs & Certifications
- Undergraduates
- Dual and Joint Degrees
- Faculty Directory
- Research Centers, Projects & Initiatives
- Lectures & Colloquia
- Books & Publications
- Academic Journals
- Application Requirements & Deadlines
- Tuition & Financial Aid
- Campus Visits & Events
- International Students
- Options for Undergraduates
- Non-Degree Studies
- Contact Admissions / Request Information
- Life at Penn GSE
- Penn GSE Career Paths
- Living in Philadelphia
- DE&I Resources for Students
- Student Organizations
- Career & Professional Development
- News Archive
- Events Calendar
- The Educator's Playbook
- Find an Expert
- Race, Equity & Inclusion
- Counseling & Psychology
- Education Innovation & Entrepreneurship
- Education Policy & Analysis
- Higher Education
- Language, Literacy & Culture
- Teaching & Learning
- Support Penn GSE
- Contact Development & Alumni Relations
- Find a Program
- Request Info
- Make a Gift
- Current Students
- Staff & Faculty
Search form
Medical education, master of science in education (m.s.ed.), you are here, an innovative program for physicians and healthcare professionals who want to lead the way in medical education.
The Medical Education (Med Ed) master's program is a unique collaboration between physician educators and education experts. We provide a comprehensive, innovative curriculum designed for physicians and other healthcare professionals who want to pursue master-level training, evidence-based education, educational scholarship, and educational technologies. Our approach—brief on-site intensives paired with flexible distance learning—accommodates professionals from a broad geographic area and with a broad variety of professional roles and responsibilities.
What Sets Us Apart
About the program.
The Medical Education master’s program prepares healthcare professionals to be teachers of medical educators, educational scholars, and leaders who influence and inspire others to learn in undergraduate and graduate medical and healthcare programs. Our two-year program trains physicians and other healthcare professionals in the science of education while remaining solidly grounded in the medical environment. The executive format includes on-site classes over long weekends, independent study, and online sessions.
1 block per semester
Culminating experience Master's capstone
- Executive-Style
Participants complete four learning blocks over four semesters: Learning and Technology, Educational Research, Leadership, and Master’s Capstone. Virtual coaching clinics are coordinated with each of the program blocks. These clinics hone students’ online teaching abilities and collaborative learning skills, and help students complete their block assignments.
Prepare to teach medical educators : Gain an understanding of how adults learn, how to develop effective and efficient educational experiences in medical education, and how to teach others to do the same. Prepare to take on the many challenges facing medical educators, including assessment, curricular design, and integrating educational technologies into all types of learning experiences.
Become a medical education researcher : Gain the skills and knowledge to meet the growing need for research and innovation in medical education. Learn how to evaluate programs and publish your research in this area.
Grow into a leadership role at your healthcare organization or medical school : Influence and inspire others to learn. Develop the leadership competencies to plan, implement, and maintain successful, sustainable programs. Acquire leadership skills and tools that are highly relevant to medical education.
Admission to the Medical Education master’s program is offered every two years. The application for the Fall 2026 cohort will be available on September 1, 2025.
Our curriculum is designed to integrate the expertise of professional educators with the perspective of clinicians. Created for adult learners, the program is active, engaging, and experiential. We provide the newest thinking and scholarship in a variety of learning formats.
Our Master of Education (M.S.Ed.) requires completion of four blocks, each composed of on-site large-group and synchronous remote small-group sessions in the following areas:
- Learning and Technology: The Learning and Technology block introduces participants to theories of, and research on, learning, curriculum, instruction and technology in medical education. It connects the theories and research to learning and technology practices in the academic medical and healthcare contexts. In addition, participants will develop a deeper understanding of common educational challenges such as learner assessment, curricular development, and pedagogical techniques.
- Educational Research: Inquiry and investigation are central to refining and advancing education in medicine and healthcare. Leaders in medical education must also be skilled in program evaluation, which requires research. During the course of the Educational Research block, participants will become familiar with evaluation tools and techniques, qualitative and quantitative research methodologies, and pragmatic aspects of educational scholarship such as proposal development and publishing research.
- Leadership: The Leadership block provides an opportunity to explore concepts such as emotional intelligence, how to influence and motivate others, group and classroom dynamics, power dynamics, organizational change, and the impact of organizational culture on leading and learning in complex systems. Central to this block is the understanding that people with advanced training in education will be called upon to develop and administer programs, which requires leadership skills that few in medicine are ever taught.
- Master’s Capstone: The Master’s Capstone allows students to design their own paper and/or project based on needs in their individual workplaces. The project/paper structure is clearly outlined by program directors and supported through synchronous and asynchronous online sessions with faculty and students.
Virtual coaching clinics are coordinated with each of the four blocks of the program, and there are three or four clinics per block. The clinics hone students’ online teaching abilities and collaborative learning skills, and help students complete their block assignments. Clinic time is an essential part of teaching and learning in medical education, and coaching supports knowledge retention and skill acquisition. By harnessing technology, the Med Ed program provides students with small group teaching and learning experiences in the virtual world, overseen by experienced and trained coaches.
For information on courses and requirements, visit the Medical Education M.S.Ed. program in the University Catalog .
Cohort 2024-2026
Cohort 2022-2024, our faculty.

Affiliated Faculty
Patti Adelman Vice President, Center for Learning and Innovation & Physician Leadership Institute, Northwell Health Ed.D., University of Pennsylvania
Anthony R. Artino, Jr. Professor, The George Washington University School of Medicine and Health Sciences Ph.D., University of Connecticut
Dorene Balmer Director of Research on Pediatric Education at The Children’s Hospital Philadelphia Ph.D., Temple University
Quinn Bauriedel Co-Artistic Director, Pig Iron Theatre Company Diploma, Theatre, Ecole Jacques Lecoq
Robbin Chapman Adjunct Associate Professor Ph.D., Massachusetts Institute of Technology
Constance Filling Chief Learning Officer, Association of American Medical Colleges Ed.D., University of Pennsylvania
Pam Grossman Professor of Education Ph.D., Stanford University
Eric S. Holmboe Chief Research, Milestone Development, and Evaluation Officer, ACGME M.D., University of Rochester School of Medicine
Fran Johnston Founder and CEO, Teleos Leadership Institute Ph.D., Temple University
Rachel K. Miller Associate Professor, Division of Geriatrics, Perelman School of Medicine M.D., University of Medicine and Dentistry of New Jersey; M.S.Ed., University of Pennsylvania
Jennifer Moyer Executive Coach and Leadership Development Consultant, JSMoyer Consulting M.Ed., University of Virginia
Leslie K. Nabors Olah Adjunct Associate Professor Ed.D., Harvard University
Kristi Pintar Vice President, Change Leadership and Organizational Development, Christiana Care Health System Ed.D., University of Pennsylvania
Rosemary Carol Polomano Associate Dean for Practice, Penn Nursing Ph.D., University of Maryland
Sharon M. Ravitch Professor of Practice Ph.D., University of Pennsylvania
Abby Reisman Associate Professor Ph.D., Stanford University
Matthew Riggan Co-Founder and Executive Director, The Workshop School Ph.D., University of Pennsylvania
Gretchen Schmelzer Senior Associate, Teleos Leadership Institute Ph.D., Northeastern University
Corrie A. Stankiewicz Clinical Associate Professor of Medicine, Perelman School of Medicine M.D., University of Pennsylvania; M.S.Ed., University of Pennsylvania
Howard C. Stevenson Constance Clayton Professor of Urban Education Ph.D., Fuller Graduate School of Psychology
James K. Stoller Professor and Chairman, Education Institute, Cleveland Clinic M.D., Yale University
Greg Urban Arthur Hobson Quinn Professor of Anthropology, Penn Arts & Sciences Ph.D., University of Chicago
Michael Yudell Professor, Dornsife School of Public Health, Drexel University Ph.D./M.P.H., Columbia University
Program Directors & Staff
Kandi Wiens, M.B.A., Ed.D. Co-Director
Donald Boyer, M.D., M.S.Ed. Co-Director
Nyssa Levy Associate Director [email protected]
Jessica Hall Administrative Coordinator [email protected]
April Coleman Administrative Assistant [email protected]
"I wanted to make myself the best teacher and clinician I could be."
Sean P. Harbison, MD
Our graduates.
The Medical Education master's program is designed for physicians and other healthcare professionals who have, or are interested in pursuing, positions in educational leadership, such as:
- program directors
- fellowship directors
- clerkship directors
- positions with responsibilities in undergraduate or graduate medical education or faculty development
In addition, the program is tailored to meet the needs of healthcare professionals interested in a specific facet of medical education, such as simulation, research and scholarship, program evaluation, learner assessment, or leading learning efforts in complex systems. Our program strongly emphasizes equipping graduates to serve as leaders and resources within their institutions.
Alumni Careers
- Associate Professor of Anesthesia, Harvard Medical School
- Vice Chief of Medical Oncology, Cancer Treatment Centers of America (CTCA)
- Chief Resident in Family Medicine, University of British Columbia
- Associate Professor of Clinical Medicine, Hospital of the University of Pennsylvania
- Director, Faculty Resources, Nemours/A.I. duPont Hospital for Children
- Associate Professor of Clinical Pediatrics, University of Pennsylvania
- Associate Professor of Pediatrics, Medical University of South Carolina
- Pediatric Cardiologist, A.I. DuPont Hospital for Children
- Professor of Nutrition/Associate Dean of Education, University of Pennsylvania
- Program Director of the Emergency Medicine Residency, SUNY Downstate/Kings County Hospital
- Residency Program Director, University of Pennsylvania
Admissions & Financial Aid
Please visit our Admissions and Financial Aid pages for specific information on the application requirements , as well as information on tuition, fees, financial aid, scholarships, and fellowships.
Contact us if you have any questions about the program.
Graduate School of Education University of Pennsylvania 3700 Walnut Street Philadelphia, PA 19104 (215) 898-6415 [email protected] [email protected]
Nyssa Levy Associate Director (215) 573-0591 [email protected]
Please view information from our Admissions and Financial Aid Office for specific information on the cost of this program.
Most students in this program fund their degree through a combination of personal resources, employer benefits, and student loans.
A Unique Synergy
The Medical Education master’s program offers a unique synergy between the educational and academic medical realms. The University of Pennsylvania Graduate School of Education, the University of Pennsylvania Perelman School of Medicine, and Children’s Hospital of Philadelphia have come together to provide program participants access to educational expertise centered in the medical context.
The University of Pennsylvania Graduate School of Education is one of three Ivy League graduate schools of education and is a national leader in education research and the preparation of skilled education professionals.
Perelman School of Medicine
The University of Pennsylvania is the oldest and one of the finest medical schools in the United States. Penn is rich in tradition and heritage and at the same time consistently at the forefront of new developments and innovations in medical education and research.
Children's Hospital of Philadelphia
Since its start in 1855 as the nation's first hospital devoted exclusively to caring for children, The Children's Hospital of Philadelphia has been the birthplace for many dramatic firsts in pediatric medicine.
Related News & Research
Karen weaver analyzes division iii college closures in “forbes”.

Laura Perna cites trust issues in the FAFSA overhaul for “The Atlantic”

IES Predoctoral Training Program accepting applications for 2024–2025 academic year

New books by Penn GSE faculty tackle burnout immunity, fostering community-based research
You may be interested in, related programs.
- Penn Chief Learning Officer Ed.D.
- Executive Doctorate in Higher Education Management Ed.D.
Related Topics

MSc in Medical Education
- Entry requirements
- Funding and Costs
College preference
- How to Apply
About the course
This is a professional development course aimed at medical and healthcare education professionals. It focuses on the history, contemporary issues and development of the field, as well as research methods, and design and evaluation of research in medical education.
This part-time course is aimed at medical professionals and allied health professionals who are involved, or intend to be involved, in educating future health professionals. These professionals may include not only postgraduate physicians but also a range of graduate allied health science practitioners involved in the care of patients and in the education of future healthcare workforce.
The part-time MSc in Medical Education will be offered jointly by the Department of Education in the Social Sciences Division and the Medical School in the Medical Sciences Division, with formal responsibility for the programme resting with the Department of Education. Interdisciplinarity is endemic in education and medicine, and team-teaching capitalises upon the distinctive knowledge and skills of academics within the two departments.
In the first year of the course, you will be required to attend six teaching weekends at the Department of Education in Oxford over a Friday afternoon and Saturday. The Friday afternoon and Saturday morning sessions will consist of interactive lectures and workshops. Additional teaching and online support will be provided through the University’s Virtual Learning Environment (Canvas). Teaching will cover the following topics:
- Patients, learners and teachers
- Curriculum and pedagogy
- Assessment issues and practices
- Educational theory and philosophy
- Work-based learning and skill development
- Educational research methods
- Equity, diversity and belonging
In the second year, you will undertake a research and development project under the supervision of a member of academic staff culminating in a dissertation.
Supervision
The allocation of graduate supervision for this course is the responsibility of the Department of Education and the Medical School and it is not always possible to accommodate the preferences of incoming graduate students to work with a particular member of staff. Under exceptional circumstances a supervisor may be found outside of the Department of Education and the Medical School.
During the first year, supervision will consist primarily of online tutor and community feedback, with some face-to-face meetings during the teaching weekends. In the second year, you will have at least six hours of supervision hours where tutors will provide formative comments once on a draft thesis. You will have at least one online or in-person meeting with your supervisor in each of the three terms, in which you will report formally on your progress and be provided with feedback on specific issues.
Assessments will be structured progressively, with a range of formative and summative assessment pertaining to the modules. The formative assessments will be in the form of tasks undertaken in preparation for a session or after a session. The summative assessment will be through two examined assignments. In the second year, you will work individually on a research and development project producing a dissertation.
Graduate destinations
It is expected that the course will provide alumni with the skills they need to progress to education leadership positions in the medical field or in academia.
Changes to this course and your supervision
The University will seek to deliver this course in accordance with the description set out in this course page. However, there may be situations in which it is desirable or necessary for the University to make changes in course provision, either before or after registration. The safety of students, staff and visitors is paramount and major changes to delivery or services may have to be made in circumstances of a pandemic, epidemic or local health emergency. In addition, in certain circumstances, for example due to visa difficulties or because the health needs of students cannot be met, it may be necessary to make adjustments to course requirements for international study.
Where possible your academic supervisor will not change for the duration of your course. However, it may be necessary to assign a new academic supervisor during the course of study or before registration for reasons which might include illness, sabbatical leave, parental leave or change in employment.
For further information please see our page on changes to courses and the provisions of the student contract regarding changes to courses.
Entry requirements for entry in 2024-25
Proven and potential academic excellence.
The requirements described below are specific to this course and apply only in the year of entry that is shown. You can use our interactive tool to help you evaluate whether your application is likely to be competitive .
Please be aware that any studentships that are linked to this course may have different or additional requirements and you should read any studentship information carefully before applying.
Degree-level qualifications
As a minimum, applicants should hold or be predicted to achieve the following UK qualifications or their equivalent:
- a first-class or strong upper second-class undergraduate degree with honours in any medically related subject area.
Applicants who do not hold a relevant subject degree but have sufficient professional experience in a relevant working environment will be considered .
For applicants with a degree from the USA, the minimum GPA sought is 3.6 out of 4.0.
If your degree is not from the UK or another country specified above, visit our International Qualifications page for guidance on the qualifications and grades that would usually be considered to meet the University’s minimum entry requirements.
GRE General Test scores
No Graduate Record Examination (GRE) or GMAT scores are sought.
Other qualifications, evidence of excellence and relevant experience
- Evidence of your employer's support is required.
- Publications are not expected.
Further guidance
Successful applicants will be expected to demonstrate the ability to undertake part-time study, which may include evidence of support from an employer.
English language proficiency
This course requires proficiency in English at the University's higher level . If your first language is not English, you may need to provide evidence that you meet this requirement. The minimum scores required to meet the University's higher level are detailed in the table below.
*Previously known as the Cambridge Certificate of Advanced English or Cambridge English: Advanced (CAE) † Previously known as the Cambridge Certificate of Proficiency in English or Cambridge English: Proficiency (CPE)
Your test must have been taken no more than two years before the start date of your course. Our Application Guide provides further information about the English language test requirement .
Declaring extenuating circumstances
If your ability to meet the entry requirements has been affected by the COVID-19 pandemic (eg you were awarded an unclassified/ungraded degree) or any other exceptional personal circumstance (eg other illness or bereavement), please refer to the guidance on extenuating circumstances in the Application Guide for information about how to declare this so that your application can be considered appropriately.
You will need to register three referees who can give an informed view of your academic ability and suitability for the course. The How to apply section of this page provides details of the types of reference that are required in support of your application for this course and how these will be assessed.
Supporting documents
You will be required to supply supporting documents with your application. The How to apply section of this page provides details of the supporting documents that are required as part of your application for this course and how these will be assessed.
Performance at interview
Interviews are normally held as part of the admissions process.
Applicants meeting the selection criteria are interviewed by an admissions panel which include experts in the subject. Applicants will be notified of the opportunity to attend interview as soon as their application has been reviewed.
The interviews are normally held in person, however, there will be opportunity to attend an interview online. The admissions panel will assess the applicant's suitability for the course, covering professional experience and their desire to contribute to the field of assessment in terms of research or practice.
How your application is assessed
Your application will be assessed purely on your proven and potential academic excellence and other entry requirements described under that heading.
References and supporting documents submitted as part of your application, and your performance at interview (if interviews are held) will be considered as part of the assessment process. Whether or not you have secured funding will not be taken into consideration when your application is assessed.
An overview of the shortlisting and selection process is provided below. Our ' After you apply ' pages provide more information about how applications are assessed .
Shortlisting and selection
Students are considered for shortlisting and selected for admission without regard to age, disability, gender reassignment, marital or civil partnership status, pregnancy and maternity, race (including colour, nationality and ethnic or national origins), religion or belief (including lack of belief), sex, sexual orientation, as well as other relevant circumstances including parental or caring responsibilities or social background. However, please note the following:
- socio-economic information may be taken into account in the selection of applicants and award of scholarships for courses that are part of the University’s pilot selection procedure and for scholarships aimed at under-represented groups ;
- country of ordinary residence may be taken into account in the awarding of certain scholarships; and
- protected characteristics may be taken into account during shortlisting for interview or the award of scholarships where the University has approved a positive action case under the Equality Act 2010.
Processing your data for shortlisting and selection
Information about processing special category data for the purposes of positive action and using your data to assess your eligibility for funding , can be found in our Postgraduate Applicant Privacy Policy.
Admissions panels and assessors
All recommendations to admit a student involve the judgement of at least two members of the academic staff with relevant experience and expertise, and must also be approved by the Director of Graduate Studies or Admissions Committee (or equivalent within the department).
Admissions panels or committees will always include at least one member of academic staff who has undertaken appropriate training.
Other factors governing whether places can be offered
The following factors will also govern whether candidates can be offered places:
- the ability of the University to provide the appropriate supervision for your studies, as outlined under the 'Supervision' heading in the About section of this page;
- the ability of the University to provide appropriate support for your studies (eg through the provision of facilities, resources, teaching and/or research opportunities); and
- minimum and maximum limits to the numbers of students who may be admitted to the University's taught and research programmes.
Offer conditions for successful applications
If you receive an offer of a place at Oxford, your offer will outline any conditions that you need to satisfy and any actions you need to take, together with any associated deadlines. These may include academic conditions, such as achieving a specific final grade in your current degree course. These conditions will usually depend on your individual academic circumstances and may vary between applicants. Our ' After you apply ' pages provide more information about offers and conditions .
In addition to any academic conditions which are set, you will also be required to meet the following requirements:
Financial Declaration
If you are offered a place, you will be required to complete a Financial Declaration in order to meet your financial condition of admission.
Disclosure of criminal convictions
In accordance with the University’s obligations towards students and staff, we will ask you to declare any relevant, unspent criminal convictions before you can take up a place at Oxford.
As the MSc is a part-time course for researchers and professionals, the department takes pride in providing high quality IT support for your learning when you are away from Oxford. This includes a dedicated web-based virtual learning environment, which you will use to liaise with your supervisor and to exchange ideas with other students. If you wish to work in the department when you are visiting Oxford, there is a computer room with desks which also has points for personal laptop computers.
The Department of Education has been making a major contribution to the field of education for over 100 years and the department has a world class reputation for research, for teacher education and for its master's and doctoral programmes. The Department of Education combines international standing as a research-intensive department with the highest quality teaching.
In the 2021 evaluation of research quality in UK universities, the Research Excellence Framework (REF), Oxford University Department of Education had the highest overall percentage of research judged to be 4* (ie world-leading in terms of originality, significance and rigour) in Education in the UK. The department has ESRC recognition for its graduate training, and its teacher training was rated ‘outstanding’ by the Office for Standards in Education (OfSTED) in its most recent inspection in 2019.
Research in the department is organised around three major themes:
- Language, Cognition and Development
- Policy, Economy and Society
- Learning: Pedagogy, Learning and Knowledge.
Within each of these themes there are several research groups and centres. All staff and doctoral students belong to one or more of these research groups, each of which has its own seminar programme to which graduate students often contribute. In addition, the department as a whole sponsors regular seminars and public lectures which attract distinguished national and international speakers.
The Bodleian Education Library, located at the centre of the Department of Education, specialises in material on education and related fields. As well as a print collection of books, journals and statistics, the library provides access to a wide range of electronic resources. The library also houses a collection of teaching resources, primarily in support of subjects covered by the department's secondary PGCE course. The Social Sciences Library provides valuable additional resource to students pursuing programmes in the Department of Education.
Oxford has been a major contributor to the field of education for over 100 years and today the University’s Department of Education has a world class reputation for research, for teacher education and for its graduate courses.
The department offers one of the strongest graduate studies programmes in the UK with a range of full- and part-time MSc courses and a lively doctoral programme (DPhil) which is recognised for national funding by the ESRC.
The department's masters' courses are delivered by academics and research experts, the majority of whom are permanent staff engaged in their fields of research. The department's DPhil in Education has excellent facilities for the large number of full-time research students who are well integrated into the research of the department.
The department has an outstanding research profile. In the 2021 evaluation of research quality in UK universities, the Research Excellence Framework (REF), Oxford University Department of Education had the highest overall percentage of research judged to be 4* (ie world-leading in terms of originality, significance and rigour) in Education in the UK. A wide range of funded research projects are based in the department and many of these projects have had a major impact on national policy.
Oxford’s PGCE course has an international reputation for the quality of its work, undertaken in close collaboration with local Oxfordshire secondary schools. Over many years, it has consistently received the highest possible designation (Outstanding) from Ofsted in inspections.
View all courses View taught courses View research courses
The University expects to be able to offer over 1,000 full or partial graduate scholarships across the collegiate University in 2024-25. You will be automatically considered for the majority of Oxford scholarships , if you fulfil the eligibility criteria and submit your graduate application by the relevant December or January deadline. Most scholarships are awarded on the basis of academic merit and/or potential.
For further details about searching for funding as a graduate student visit our dedicated Funding pages, which contain information about how to apply for Oxford scholarships requiring an additional application, details of external funding, loan schemes and other funding sources.
Please ensure that you visit individual college websites for details of any college-specific funding opportunities using the links provided on our college pages or below:
Please note that not all the colleges listed above may accept students on this course. For details of those which do, please refer to the College preference section of this page.
Further information about funding opportunities for this course can be found on the faculty's website.
Annual fees for entry in 2024-25
Further details about fee status eligibility can be found on the fee status webpage.
Information about course fees
Course fees are payable each year, for the duration of your fee liability (your fee liability is the length of time for which you are required to pay course fees). For courses lasting longer than one year, please be aware that fees will usually increase annually. For details, please see our guidance on changes to fees and charges .
Course fees cover your teaching as well as other academic services and facilities provided to support your studies. Unless specified in the additional information section below, course fees do not cover your accommodation, residential costs or other living costs. They also don’t cover any additional costs and charges that are outlined in the additional information below.
Where can I find further information about fees?
The Fees and Funding section of this website provides further information about course fees , including information about fee status and eligibility and your length of fee liability .
Additional information
Please note that this course requires that you attend in Oxford for teaching, and you may incur additional travel and accommodation expenses for this. Further, as part of your course requirements, you will need to choose a dissertation topic. Depending on your choice of topic and the research required to complete it, you may incur additional expenses, such as travel expenses, research expenses, and field trips. You will need to meet these additional costs, although you may be able to apply for small grants from your department and/or college to help you cover some of these expenses.
Living costs
In addition to your course fees, you will need to ensure that you have adequate funds to support your living costs for the duration of your course.
For the 2024-25 academic year, the range of likely living costs for full-time study is between c. £1,345 and £1,955 for each month spent in Oxford. Full information, including a breakdown of likely living costs in Oxford for items such as food, accommodation and study costs, is available on our living costs page. The current economic climate and high national rate of inflation make it very hard to estimate potential changes to the cost of living over the next few years. When planning your finances for any future years of study in Oxford beyond 2024-25, it is suggested that you allow for potential increases in living expenses of around 5% each year – although this rate may vary depending on the national economic situation. UK inflationary increases will be kept under review and this page updated.
If you are studying part-time your living costs may vary depending on your personal circumstances but you must still ensure that you will have sufficient funding to meet these costs for the duration of your course.
Students enrolled on this course will belong to both a department/faculty and a college. Please note that ‘college’ and ‘colleges’ refers to all 43 of the University’s colleges, including those designated as societies and permanent private halls (PPHs).
If you apply for a place on this course you will have the option to express a preference for one of the colleges listed below, or you can ask us to find a college for you. Before deciding, we suggest that you read our brief introduction to the college system at Oxford and our advice about expressing a college preference . For some courses, the department may have provided some additional advice below to help you decide.
The following colleges accept students on the MSc in Medical Education:
- Balliol College
- Green Templeton College
- Harris Manchester College
- Jesus College
- Pembroke College
- Reuben College
- St Hilda's College
- Wolfson College
- Wycliffe Hall
Before you apply
Our guide to getting started provides general advice on how to prepare for and start your application. You can use our interactive tool to help you evaluate whether your application is likely to be competitive .
If it's important for you to have your application considered under a particular deadline – eg under a December or January deadline in order to be considered for Oxford scholarships – we recommend that you aim to complete and submit your application at least two weeks in advance . Check the deadlines on this page and the information about deadlines and when to apply in our Application Guide.
Application fee waivers
An application fee of £75 is payable per course application. Application fee waivers are available for the following applicants who meet the eligibility criteria:
- applicants from low-income countries;
- refugees and displaced persons;
- UK applicants from low-income backgrounds; and
- applicants who applied for our Graduate Access Programmes in the past two years and met the eligibility criteria.
You are encouraged to check whether you're eligible for an application fee waiver before you apply.
Do I need to contact anyone before I apply?
You do not need to make contact with the department before you apply but you are encouraged to visit the relevant departmental webpages to read any further information about your chosen course.
Completing your application
You should refer to the information below when completing the application form, paying attention to the specific requirements for the supporting documents .
For this course, the application form will include questions that collect information that would usually be included in a CV/résumé. You should not upload a separate document. If a separate CV/résumé is uploaded, it will be removed from your application .
If any document does not meet the specification, including the stipulated word count, your application may be considered incomplete and not assessed by the academic department. Expand each section to show further details.
Referees: Three overall, academic and/or professional
Whilst you must register three referees, the department may start the assessment of your application if two of the three references are submitted by the course deadline and your application is otherwise complete. Please note that you may still be required to ensure your third referee supplies a reference for consideration.
Your references will support intellectual ability, academic achievement, motivation and interest in the course and subject area, and ability to work effectively in a group and independently.
Official transcript(s)
Your transcripts should give detailed information of the individual grades received in your university-level qualifications to date. You should only upload official documents issued by your institution and any transcript not in English should be accompanied by a certified translation.
More information about the transcript requirement is available in the Application Guide.
Statement of purpose: A maximum of 1,000 words
Your statement should be written in English and explain your motivation for applying for the course at Oxford, your relevant experience and education, and the specific areas of the course that interest you and/or you intend to specialise in.
If possible, please ensure that the word count is clearly displayed on the document.
This will be assessed for:
- your reasons for applying
- your ability to present a coherent case in proficient English
- your commitment to the subject, beyond the requirements of the degree course
- your preliminary knowledge of the subject area and research techniques
- your capacity for sustained and intense work
- reasoning ability
- ability to absorb new ideas, often presented abstractly, at a rapid pace.
Written work: Two pieces of written work, a maximum of 7,000 words in total, or one long piece, a maximum of 7,000 words
Academic essays or other writing samples from your most recent qualification, typed and written in English, are required. Extracts of the requisite length from longer work are also permitted if prefaced by a note that puts them in context. The written work should be related to the subject you propose to study. The word count does not need to include any bibliography or brief footnotes.
Your written work will be assessed for:
- a comprehensive understanding of the subject area, including problems and developments in the subject
- your ability to construct and defend an argument
- your aptitude for analysis and expression
- your ability to present a reasoned case in proficient academic English.
Instructions for submitting one long piece of work instead of two short pieces
To submit one longer piece of work in your application instead of two shorter pieces, you should upload this document in the first 'Written work' slot on the 'Supporting Documents' tab of the Application Form. In the second 'Written work' slot, you should upload a PDF document with the following statement:
' I have included one long essay in lieu of two short essays. I have checked the course page to confirm this is permitted for this course. '
Start or continue your application
You can start or return to an application using the relevant link below. As you complete the form, please refer to the requirements above and consult our Application Guide for advice . You'll find the answers to most common queries in our FAQs.
Application Guide Apply
ADMISSION STATUS
Closed to applications for entry in 2024-25
Register to be notified via email when the next application cycle opens (for entry in 2025-26)
12:00 midday UK time on:
Friday 5 January 2024 Latest deadline for most Oxford scholarships
Friday 1 March 2024 Applications may remain open after this deadline if places are still available - see below
A later deadline shown under 'Admission status' If places are still available, applications may be accepted after 1 March . The 'Admissions status' (above) will provide notice of any later deadline.
*Three-year average (applications for entry in 2021-22 to 2023-24)
Further information and enquiries
This course is offered jointly by the Department of Education and the Medical Sciences Division
- Course page on the lead department's website
- Funding information from the department
- Academic and research staff
- Department research and divisional research
- Postgraduate applicant privacy policy

Course-related enquiries
Advice about contacting the department can be found in the How to apply section of this page
✉ [email protected]
Application-process enquiries
See the application guide
Visa eligibility for part-time study
We are unable to sponsor student visas for part-time study on this course. Part-time students may be able to attend on a visitor visa for short blocks of time only (and leave after each visit) and will need to remain based outside the UK.
Medical Education

The mission of the Master of Medical Science in Medical Education is to give those who already excel in one of the health sciences disciplines an opportunity to turn their specialized knowledge and skill towards the advancement of health professions education. Through research, skill building, and innovation, this master’s program seeks to transform health professions education in the service of advancing the health sciences and healthcare nationally and internationally. Graduates of our program will be well positioned to lead progress and make transformative change.

What Is Competency-Based Medical Education?

What is Competency-Based Medical Education (CBME)? Think flexible, lifelong learning, with knowledge and/or skills assessed throughout a continuum of learning. In a competency-based educational program, you don’t just acquire knowledge and then spit it back at the time of a final exam. Instead, the method of assessment is formative rather than summative, and you are evaluated on how you apply your knowledge to clinical situations that physicians often face. While summative exams, such as certification exams, play an important role in gauging levels of acquired knowledge, formative assessments are equally important.
Competency-based assessments are used to distinguish between the skills and knowledge that you already have and those for which you need more education and training. In contrast to time-based educational methods, CBME is a learner-centered, active, and lifelong experience that incorporates feedback between the teacher and the learner to fulfill the desired competency outcomes.
Adoption of the Competency-Based Medical Education Construct
The concept of competency-based training began in the 1920s, when U.S. industry and businesses started researching ways of teaching their employees the specific knowledge and skills needed to create a specific product in a standardized manner. However, in the 1960s, a movement to de-emphasize basic skills in education arose. The resulting decline in traditional scores of achievement eventually sparked a demand for the renewal of minimum standards and performance competencies.
The design of a competency-based system of education can be approached using the following steps:
- Identify the desired outcomes
- Define the level of performance for each competency
- Develop a framework for assessing competencies
- Evaluate the program on a continuous basis to be sure that the desired outcomes are being achieved
In 1999, the Accreditation Council for Graduate Medical Education (ACGME) and the American Board of Medical Specialties (ABMS) endorsed six domains of core competencies , and the outcome initiative (the Outcome Project) was soon launched.
The six ACGME Core Competencies are:
- Patient Care
- Medical Knowledge
- Professionalism
- Interpersonal and Communication Skills
- Practice-Based Learning and Improvement
- Systems-Based Practice
Even though there was standardized language around the core competencies of medical education, there were still no standardized assessment methods to determine whether or not a learner had achieved all of the core competencies prior to completion of residency training. This deficiency ultimately led to the creation of milestones to operationalize and implement the competencies. These milestones described the performance levels residents and fellows are expected to demonstrate for skills, knowledge, and behaviors in the six clinical competency domains and are significant points in development that are unique to each specialty.
In 2014, the ACGME required the reporting of milestones as part of the Next Accreditation System (NAS) for all ACGME-accredited residency and fellowship programs. In undergraduate medical education, there are two AAMC-defined performance levels: novice performance and performance expected of a graduating MD. In graduate medical education, there are five performance levels for each competency: novice, advanced beginner, competent individual, proficient individual, and expert physician.
The Next Goal
The Core Competencies are now the basic language for defining physician competence and are also the principles used in the training of physicians. The next goal of CBME is to link education in the competencies to improved quality of patient care. This ambitious step will require standardized methods to securely collect patient data and stratify for various clinical variables including disease specificity, overall patient health, and the multitude of health care professionals who care for each patient.
The shift to CBME was an important transition that allowed residents and fellows to be active agents in their own learning by comparing their milestone assessment and feedback data to their personal learning plans. However, the future of CBME is just being realized and offers many exciting opportunities moving forward.
You can read more about CBME here:
- Association of American Medical Colleges (AAMC) Core Competencies for Entering Medical Students
- Advancing Competency-Based Medical Education: A Charter for Clinician-Educators.
Share This Post!
21 comments.
The CBME is the basic and strong infrastructure of the excellent education . Thank you for your unbelievable inspiration .
The excellent medical education is capable of eliminating CVD/CAD, T2DM, and Cancer today’s growing epidemics. This will be realized when physicians will know CVD/CAD, T2DM and Cancer Inherited Real Risk, bedside diagnosed from birth and removed by unexpensive Quantum Therapy, rather than the CBME.
biology and the medical essay is interesting to read and your blog gives provide the diagnosed point, medical education tips of safety should know to every person.
The CBME is better & excellent education system. Very helpful, thanks for this.
Great information! Thanks for sharing. I would share this article at https://qanda.typicalstudent.org/ a platform for students, teachers and other related people to discuss their thoughts and experiences on learning and other topics.
Thanks a lot for allow me comment here
Over the last two decades, competency‐based frameworks have been internationally adopted as the primary educational approach in medicine. Yet competency‐based medical education (CBME) remains contested in the academic literature. We look broadly at the nature of this debate to explore how it may shape scholars’ understanding of CBME, and its implications for medical education research and practice. In doing so, we deconstruct unarticulated discourses and assumptions embedded in the CBME literature. Its really hard to garb a Government jobs with this competency.
After reading your article, I’m compelling to share your points on this topic. You have done a very good job with your attention to detail you put into this article.
Very helpful, thanks for this.
This will be realized when physicians will know CVD/CAD, T2DM and Cancer Inherited Real Risk, bedside diagnosed from birth and removed by unexpensive Quantum Therapy, rather than the CBME.
Great post, like’d your thoughts, thanks for sharing 🙂
I found this article good, interesting thoughts have been explained. keep it up, thanks for sharing
This is a very informative post for the blog writers and readers. Thanks for the sharing your concerned openly.
Great and Insightful post, Learnt a lot, for medical aspirants it is a must read. Keep posting such content.
have you developed curriculum for competence based learning .,or planning on the lines of Problem based learning.
After reading your article, I’m compelling to share your points on this topic.
The point of imparting medical education is to prepare graduates to effectively deal with the health needs of the general public. The present therapeutic training framework depends on an educational programs that is subject-focused and time based.
Great Article, i am reading your i gain lot of knowledge from this article keep post such content
In competency-based education, students work to ace abilities before they are introduced with new ideas. This gives students the opportunity to move at their own pace and take control of their education.
Some ideas of making this ingrained in knowledge: repetively teach, practice and test.from M1 to M4 the top 20 most urgent/import/deadly topic adding complexity to each year of Med Ed. Get MD input. For example:.
Top 20 most deadly diseases ie MI, Sepsis, Pulm Emboli, early Cancer detection Top 20 missed diagnoses Top 20 interpersonal physician-patient challenging discussions Top 20 ways to increase professionalism and stop being defensive Top 20 required for Boards or AACM/LCME in recognizing sings of uncommon diseases to refer to subspec. Every year do weekly practice and end of year Proficiency that the next higher medical students could teach and test with M4s being taguht and tested by either residents of MDs. Make it very straightforward, competency is goal, not trying to trick anyone. 100% to pass since so very practical and practiced and needed. Then residency and hospitals could continue adding complexity prn. Good luck and thank you!
Comments are closed.

- Medical Education and Training
Explore the latest in medical education and training, new educational approaches and technologies, CME, work duty hours, and more.
Publication
Article type.
- Excavating the Truth About Medical Racism From the American Medical Directory—Spinning Dross Into Gold JAMA Network Open Opinion May 10, 2024 Equity, Diversity, and Inclusion Academic Medicine Health Care Workforce Health Policy Medical Education Full Text | pdf link PDF open access
This cross-sectional study examines state- and county-level patterns related to the training and availability of Black physicians using data from the first edition of the American Medical Directory.
This cohort study examines the factors associated with variation in decision-making confidence of clinical competency committees for entrustable professional activity decisions in surgery.
This systematic review investigates the prevalence of harassment, including sexual harassment, bullying, and abuse, among obstetrics and gynecology medical students and clinicians.
This cross-sectional study assesses variations in accommodations for oral certifying examinations among Accreditation Council for Graduate Medical Education–specialties.
This study examines the association between physicians’ milestone ratings and certification examination scores and hospital outcomes for their patients.
In this narrative medicine essay, a medical ethicist discusses the complexity of juggling the interests of members in online forums dedicated to rare diseases after being blocked upon disclosing her affiliation with a medical school, thus barring her from the support and information she needed to manage her daughter’s rare disease.
This Viewpoint shares the experience of a single Otolaryngology−Head & Neck Surgery residency program that faced the scheduling challenges of having nearly a quarter of its residents expecting a child and on parental leave.
This Viewpoint advocates for the addition of clozapine prescribing as a milestone in psychiatric education.
This essay describes the author’s experience of improved patient care and collaboration the day the the electronic medical records system went down.
- New Rules Require Explicit Consent for Students to Perform Sensitive Exams JAMA News April 26, 2024 Shared Decision Making and Communication Ethics Health Care Economics, Insurance, Payment Anesthesiology Reproductive Health Full Text | pdf link PDF free
This essay reflects on the author’s approach to interviewing applicants for medical residency in the otolaryngology department.
When a resident announced that “the patient has no chance of surviving,” a medical student, in this narrative medicine essay, has pondered for years how her mother could have been so reduced and advocates using patients’ names when summarizing their conditions.
This Viewpoint makes the case for academic health systems to lead the way on climate change action in the US, including planning to reduce greenhouse gas emissions, educating current and future clinicians, and communicating with their patients and communities.
This cohort study assesses match rates of US applicants with and without disability into specialty residence programs.
This essay describes the author’s experience with the line between life and death and what the fragility of life means for patients and their medical teams.
This study examines the association between taking a leave of absence from medical school and placement into graduate medical education (GME) by race and ethnicity.
This survey study of US general surgery residents investigated which factors are associated with surgical trainees’ perceptions of meaningful mentorship, assessed associations of mentorship with resident education and wellness, and evaluated programmatic variation in mentorship.
- Ensuring Equitable Mentorship—We All Have a Role JAMA Surgery Opinion April 3, 2024 Surgery Full Text | pdf link PDF
This cross-sectional study assesses the ability of a large language model to process medical data and display clinical reasoning compared with the ability of attending physicians and residents.
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Career Feature
- Published: 16 March 2022
CAREER FEATURE
Integrating innovation as a core objective in medical training
- Okechi Boms ORCID: orcid.org/0000-0002-8887-5287 1 , 2 na1 ,
- Zhuo Shi 1 , 2 na1 ,
- Nathan Mallipeddi 1 , 2 ,
- Janice J. Chung ORCID: orcid.org/0000-0002-2941-0287 1 , 2 ,
- William H. Marks 2 , 3 ,
- David C. Whitehead ORCID: orcid.org/0000-0002-3132-5292 1 , 4 &
- Marc D. Succi 1 , 2 , 5
Nature Biotechnology volume 40 , pages 434–437 ( 2022 ) Cite this article
6418 Accesses
13 Citations
69 Altmetric
Metrics details
As innovations in the biotechnology sector continue to proliferate, the traditional education of medical students, residents and fellows will need to change to incorporate innovation as a core tenet of training.
The COVID-19 pandemic uncovered pressing needs for improved healthcare access, affordability and quality 1 . Rising to the challenge, individuals in the biotechnology sector embarked on collaborative ventures to design and implement innovative solutions to pandemic demands, which in many ways were masking inefficiencies in how care was delivered in general 2 , 3 , 4 , 5 , 6 . In parallel, the challenges posed by the pandemic spurred medical training programs to re-evaluate the goals and structures of the traditional medical curriculum 7 , 8 , 9 . Didactics and simulations transitioned into remote formats for medical students, and programs strove to reduce the cognitive load for residents and fellows in the setting of a pandemic 10 , 11 , 12 . Yet developments in medical training thus far still focus on the delivery and format of the curriculum, including flipped classroom and case-based models, as opposed to teaching innovation 13 , 14 . At this critical juncture, we propose the incorporation of innovation itself as a core tenet of medical training, as the importance of real-time medical innovations in biotechnology cannot be denied.
As the role of the healthcare professional continues to expand, and as healthcare reimbursement increasingly prioritizes value over quantity, acquiring the skill set of an innovator has become more vital and pertinent to all stages of medical training. Innovation in healthcare is defined as the implementation of a novel idea in the advancement of care delivery and health outcomes 15 . Our previous work demonstrated successful integration of innovation education into ACGME (Accreditation Council for Graduate Medical Education)-accredited residency programs and hospital departments 16 , 17 . Here, we delve further into innovation training: the skill sets in demand, potential barriers and opportunities to develop an infrastructure for innovation in medical training. Seizing these opportunities to address the needs of current healthcare trainees may enhance the development of change-markers in the field of biotechnology.
Innovation: a trained skill set
The pandemic placed a spotlight on the impact of innovation generated by healthcare professionals. Trainees are uniquely positioned within care teams to generate ground-level ideas for innovative care. Historically, the novel perspectives of trainees have contributed significantly to several landmark discoveries, from the description of pancreatic islet cells to the extraction of heparin 18 . Such opportunities are often inspired by trainees’ roles serving as a team’s interface with patients and with the electronic medical system through their administrative responsibilities. However, to a certain extent, current clinical training actively suppresses innovation because established principles and protocols are often promoted as the ‘right’ and the only way (i.e., look for horses, not zebras). The key issue is therefore training professionals to know when and how to innovate. Trainees equipped with the proper skill sets and resources have significant potential to identify, validate and devise solutions to current unmet needs, develop new gold standards of clinical care and reduce potential future problems. Additionally, embedding healthcare innovation programs directly within the academic setting may decrease the risk of premature technology transfer into an industry where the technical, clinical and/or biological expertise may not be fully realized. These risks are notable, as increased internal validation correlates with future commercial value 19 .
Targeted education is necessary to equip future generations of medical professionals with the ability to innovate efficiently and effectively. Although tangible tools and resources are important, the skill set to use them effectively will serve as the lifelong foundation for innovation. Learning the foundational steps of identifying problems, prototyping and researching the market in conjunction with experiential learning can provide trainees with a blueprint for innovation. From an industry standpoint, key components to successful innovations include establishing product–market fit, understanding the end-user and determining value drivers. The ACGME currently does not mandate any level of innovation-specific training in medical training and education. We believe that a high-quality education in this fundamental skill set of innovation can be incorporated into the training of medical professionals of all levels, regardless of the extent of tangible resources at the training institutions.
To analyze the current state of innovation education at the medical trainee level, we sent a preliminary survey (see Supplementary Note ) to readers of 2 Minute Medicine , a free open-source medical media and news organization 20 . The survey was created to assess trainees’ perception of innovation across three domains: understanding and participation in innovation, barriers to pursuing innovation and tools needed to pursue innovation. Trainees, including medical students, residents and fellows, answered questions in these domains according to Likert-type scales of 1–5 (such as Unimportant, Slightly Important, Moderately Important, Important and Very Important).
We received 51 responses from medical trainees, who included medical students, residents and fellows (response rate 51/1,142). Women made up 27% of respondents. Thirty percent of respondents described their learning environment as rural or suburban, and 26% of respondents were Hispanic or African-American (Table 1 ).
Present medical trainees’ perception of innovation
Even before the COVID-19 pandemic, the role of the medical professional has been expanding. Physicians have strived to influence healthcare beyond the walls of hospitals, leading to increasing numbers of trainees seeking additional degrees in fields such as business and administration, public health and public policy 21 . Aside from pursuing additional degrees, many trainees have channeled their efforts into social justice activism and government. In such a setting, medical innovation remains an underdeveloped area of training.
A central question for respondents was, “Do you consider yourself an innovator?” Thirty-one percent of respondents considered themselves innovators, 35% did not consider themselves innovators and 33% were unsure (Fig. 1 ). A traditional view of an innovator conjures images of a failed maverick seeking to create an intervention, or a social media prodigy changing human connection with a few strokes on a keyboard 22 . In all of these depictions, innovation is sought as an intrinsic quality, yet this fails to describe reality. Innovation requires a backbone of methodical research, as well as skilled execution to translate an idea from inception to a finished product. Even more, those images fail to account for the multidisciplinary approach required to change care. For trainees interested in innovation, these notions can act as mental and process blocks.
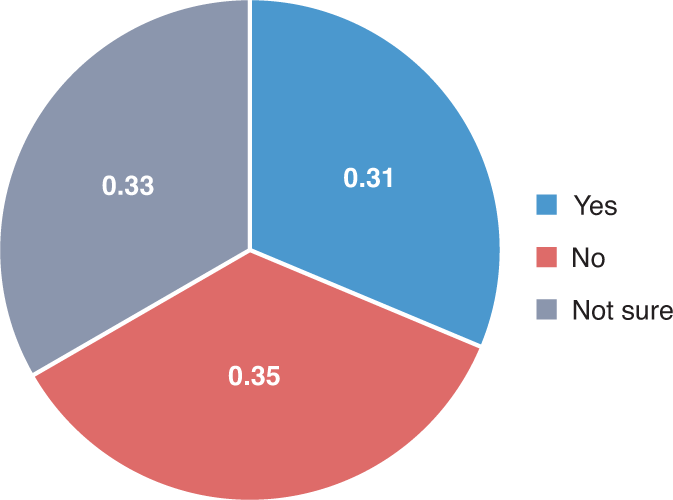
Chart shows 51 answers to a central question: “Do you consider yourself an innovator?”.
Barriers to healthcare innovation at the trainee level
There are various barriers to medical innovation, including technical-level barriers, public policy barriers, and political and economic barriers 23 . These range from a lack of understanding of disease processes to lack of education and exposure to the fundamental domains of healthcare innovation, as well as regulatory barriers to technology implementation.
From our survey, we noted the current level of participation, barriers and necessary tools to encourage innovation for medical trainees:
Participation: Trainees had relatively low participation across different forms of innovation. The three activities in which respondents reported the highest participation were improving disease specific outcomes (18%), healthcare delivery and access (16%) and workflow efficiencies (16%). The activities with the lowest participation, 8% in each case, were medical device development, drug development and improving pharmaceutical adherence. Trainees also rated themselves as having lower confidence relative to their stated level of understanding across areas of innovation in Fig. 2 .
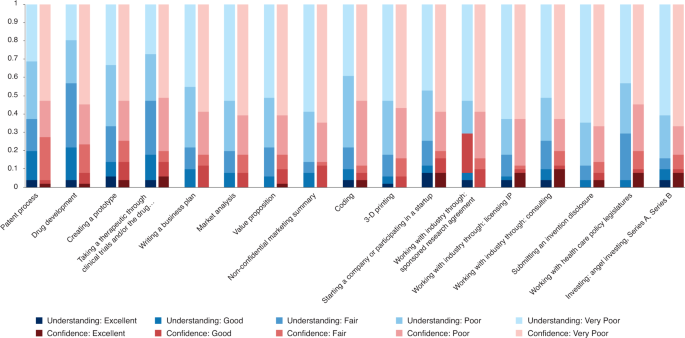
Bar chart illustrates the segmentation of understanding and confidence across various domains of innovation.
Barriers: Trainees ranked perceived barriers to innovation using the scale described above. The barriers most commonly noted as “Most Important” on the Likert scale included limited time and energy (43%), lack of physical resources (35%) and lack of expertise (31%).
Tools: The most beneficial tools for trainees were dedicated time (61%), financial support via grants and start-up funding (49%) and partnership with mentors (47%).
Opportunities for innovation integration in medical training programs
These responses indicate the innovation areas in which trainees are interested, the potential barriers and the tools that would help advance their pursuits. Trainees reported a generally low level of confidence in pursuing innovative activities despite relatively higher levels of understanding, which indicates a gap in the ability to translate ideas into skilled practice. As a result, integrated, hands-on programs as previously implemented may be a way to bridge the gap between knowing and building 16 , 17 . We recognize that institutions have various levels of resources and participants may seek different intensities of training. Hence, we present three thematic innovation programs, ranging from regimented innovation tracks to supplementary innovation programs that are amenable to integration into medical training.
Innovation tracks
For the most streamlined and direct approach, we advocate for longitudinal learning that provides in-depth teaching and protects time for trainees to pursue ventures. Medical schools and residency programs have incorporated specialty tracks into their curriculum, which have traditionally focused on training in global health, management, urban studies and policy. A longitudinal ‘innovation’ track would provide the time and resources for trainees to pursue ideas and collaborate with other departments and companies. A blueprint for such programs was previously published by the Medically Engineered Solutions in Healthcare (MESH) Incubator, wherein innovation bootcamps are taught in the same structure as traditional medical rotations for residents and fellows throughout the academic year, as well as the MESH Incubator Innovation Teams biodesign program, which integrates traditional multidisciplinary biodesign (medical, engineers, business personnel) into an integrated part-time program in which full-time trainees can participate without the need to step away from their ACGME training. Additional programs that may require dedicated time away from residency or training include the Stanford Biodesign Program, the University of Texas Austin’s Distinction Program for Care Transformation and Emory University’s Medical Innovation Track. These are 10-month to 2-year programs that bring together medical trainees, business personnel and scientists to learn and collaborate on innovative solutions 24 , 25 , 26 , 27 .
Workshop series
Residency programs and hospitals are also increasingly recognizing the importance of innovation programs. Short, intensive programs in technology development, including classes on intellectual property, have proven to be a venue for innovation training. Massachusetts General Hospital pioneered the first healthcare innovation rotation integrated into an ACGME residency program 16 . This 1-week rotation is taught to all trainees in all specialties and teaches the basics of artificial intelligence, 3-D printing, prototyping, intellectual property, commercialization, venture funding and much more, with documented outcomes demonstrating effectiveness 17 . These programs can be adapted and interwoven into the medical curriculum, especially during break and summer months.
Targeted skills
In addition to innovation tracks and workshops, short-term targeted programs can enhance specific trainee skills. The American Medical Association created the Accelerating Change in Medical Education Consortium with 37 medical schools that enroll nearly 24,000 students to bring about a platform for sharing pioneering ideas and solutions 28 . These schools include New York University, which created the NYU Health Care by the Numbers Curriculum to train medical students in using big data to improve healthcare quality, and Stanford Medical School, which has integrated virtual reality technology to improve educational experiences and promote diversity. Additionally, the creation of virtual innovative spaces in response to crisis, such as the Mass General Brigham COVID Innovation Center 29 , brings together trainee innovators and experienced investigators, and creates opportunities and fosters connections for trainees in technology, business and life sciences. These groups are low cost and high yield for hospitals and medical schools that have a more moderate level of resources, faculty time and funding.
Conclusions
The modern practice of medicine has extended beyond the examination room to the integration of basic science, innovation and biotechnology research at the bedside at a faster pace than ever before. Physicians, equipped with clinical knowledge, can both identify and address current and emerging gaps in quality healthcare. Our broad survey reveals that trainees interested in medical innovation lack the skills and resources to pursue such ventures. We acknowledge the limitations of our preliminary survey, which include low response rates. Additionally, our respondents might be trainees who routinely consume medical news and might not be representative of all medical trainees. However, using the survey as a soundboard, we can gain insight into the personal and professional barriers that trainees face when pursuing innovative solutions. We examined current pilot methods of incorporating innovation into the medical trainee curriculum. We propose a variety of models for institutions seeking to incorporate innovation into their curriculum, including innovation tracks, workshop groups and targeted skills. Each of these models provides mentorship, education and resources for trainees while accounting for time and financial restraints. The range in intensity, resources and stewardship of these programs allow medical and residency programs to tailor their innovation education models based on their students’ needs and institutional resources. An early introduction to constructive questioning can help train agile thinkers and change-makers in the field of biotechnology. The practice of problem-solving requires trainees to practice the fundamental skills of gathering information, building a diverse team, organizing a strategy and taking a risk to address the problem 30 . These transferable skills, once honed, extend to patient care within the wards and beyond.
Demeke, H. B. et al. MMWR Morb. Mortal. Wkly. Rep. 70 , 240–244 (2021).
Article CAS Google Scholar
Woolliscroft, J. O. Acad. Med. 95 , 1140–1142 (2020).
Article Google Scholar
Lee, S. M. & Trimi, S. J. Bus. Res. 123 , 14–22 (2021).
Chonde, D. B. et al. J. Am. Coll. Radiol. 18 , 1000–1008 (2021).
Sapoval, M. et al. Diagn. Interv. Imaging 101 , 413–415 (2020).
Imbrie-Moore, A. M. et al. Health Care (Don Mills) 8 , 225 (2020).
Google Scholar
Sabzwari, S. MedEdPublish 9 , 80 (2020).
Gaur, U. et al. Clin. Med. (Lond.) 2 , 1992–1997 (2020).
CAS Google Scholar
Chan, A. K., Wu, C., Cheung, A. & Succi, M. D. J. Med. Internet Res. 23 , e26666 (2021).
Hartsough, E. M., Arries, C., Amin, K. & Powell, D. Acad. Pathol. 8 , 23742895211010265 (2021).
Asselin, M. et al. MedEdPORTAL 17 , 11134 (2021).
Sukumar, S. et al. MedEdPORTAL 17 , 11106 (2021).
McLean, S. F. J. Med. Educ. Curric. Dev. 3 , JMECD.S20377 (2016).
Hew, K. F. & Lo, C. K. BMC Med. Educ. 18 , 38 (2018).
Kimble, L. E. & Massoud, E. M. J. EMJ Innov. 1 , 89–91 (2017).
Succi, M. D. et al. J. Am. Coll. Radiol. 17 , 1329–1333 (2020).
Succi, M. D., Uppot, R. N., Gee, M. S., McLoud, T. C. & Brink, J. A. J. Am. Coll. Radiol. 15 , 892–896 (2018).
Bettany, K. Br. Med. J. 348 , g2138 (2014).
Toner, M. & Tompkins, R. G. Surgery 143 , 168–171 (2008).
2 Minute Medicine ; https://www.2minutemedicine.com/
Brill, J. V. Gastroenterology 144 , 655 (2013).
Jeske, M. Engag. Sci. Technol. Soc. 6 , 306 (2020).
Aspden, P. (ed.). Medical Innovation in the Changing Healthcare Marketplace: Conference Summary (National Academies Press, 2002).
Augustin, D. A. et al. Surgery 167 , 535–539 (2020).
The University of Texas at Austin–Dell Medical School. Advancing Care Transformation ; https://dellmed.utexas.edu/education/academics/graduate-medical-education/distinction-program-for-care-transformation
Harvard University. Harvard HealthTech Innovation in Healthcare ; https://projects.iq.harvard.edu/healthtechfellowship/home
Emory University School of Medicine. Medical Innovation Track ; https://www.med.emory.edu/education/gme/housestaff/residency-tracks/medical-innovation.html
Members of the Accelerating Change in Medical Education Consortium. Accelerating Change in Medical Education ; https://www.ama-assn.org/education/accelerating-change-medical-education/member-schools-consortium
Center for COVID Innovation; https://covidinnovation.partners.org/
Green, M. J. et al. J. Med. Humanit. 37 , 475–483 (2016).
Download references
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors. It was approved with exemption by the Institutional Review Board of Massachusetts General Brigham.
Author information
These authors contributed equally: Okechi Boms, Zhuo Shi
Authors and Affiliations
Harvard Medical School, Boston, MA, USA
Okechi Boms, Zhuo Shi, Nathan Mallipeddi, Janice J. Chung, David C. Whitehead & Marc D. Succi
Medically Engineered Solutions in Healthcare (MESH) Incubator, Massachusetts General Hospital, Boston, MA, USA
Okechi Boms, Zhuo Shi, Nathan Mallipeddi, Janice J. Chung, William H. Marks & Marc D. Succi
Seismic Therapeutic, Watertown, MA, USA
William H. Marks
Department of Emergency Medicine, Massachusetts General Hospital, Boston, MA, USA
David C. Whitehead
Department of Radiology, Massachusetts General Hospital, Boston, MA, USA
- Marc D. Succi
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Marc D. Succi .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Supplementary information
Supplementary information.
Survey sent to 1,000 medical trainees
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Boms, O., Shi, Z., Mallipeddi, N. et al. Integrating innovation as a core objective in medical training. Nat Biotechnol 40 , 434–437 (2022). https://doi.org/10.1038/s41587-022-01253-x
Download citation
Published : 16 March 2022
Issue Date : March 2022
DOI : https://doi.org/10.1038/s41587-022-01253-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Integrating a healthcare innovation bootcamp into an international medical conference to democratize innovation learning.
- Debby Cheng
- James A. Brink
Nature Biotechnology (2023)
A strategy to incentivize innovation in the health care system: the innovation RVU
- Nathan V. Mallipeddi
- Jay Chandra
The need for need-finding in medical education
- Sainiteesh Maddineni
- Wasan Kumar
Innovating on innovation training with the Virtual Magic Wand (VMW) program: a qualitative study
- A. Davis Rebekah
- C. Lee Kachiu
- Lilit Garibyan
Archives of Dermatological Research (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Adv Med Educ Pract
Healthcare Simulation: A Key to the Future of Medical Education – A Review
1 Aga Khan University Medical College, Karachi, Sindh, Pakistan
Faisal Wasim Ismail
2 Department of Medicine, Aga Khan University Hospital, Karachi, Pakistan
Simulation originates from its application in the military and aviation. It is implemented at various levels of healthcare education and certification today. However, its use remains unevenly distributed across the globe due to misconception regarding its cost and complexity and to lack of evidence for its consistency and validity. Implementation may also be hindered by an array of factors unique to the locale and its norms. Resource-poor settings may benefit from diverting external funds for short-term simulation projects towards collaboration with local experts and local material sourcing to reduce the overall cost and achieve long-term benefits. The recent shift of focus towards patient safety and calls for reduction in training duration have burdened educators with providing adequate quantity and quality of clinical exposure to students and residents in a short time. Furthermore, the COVID-19 pandemic has severely hindered clinical education to curb the spread of illness. Simulation may be beneficial in these circumstances and improve learner confidence. We undertook a literature search on MEDLINE using MeSH terms to obtain relevant information on simulation-based medical education and how to best apply it. Integration of simulation into curricula is an essential step of its implementation. With allocations for deliberate practice and mastery learning under supervision of qualified facilitators, this technology is becoming essential in medical education.
To review the adaptation, spectrum of use, importance, and resource challenges of simulation in medical education and how best to implement it according to learning theories and best practice guides.
Simulation offers students and residents with adequate opportunities to practice their clinical skills in a risk-free environment. Unprecedented global catastrophes provide opportunities to explore simulation as a viable training tool. Future research should focus on sustainability of simulation-based medical education in LMICs.
Introduction
Simulation is defined as “the imitative representation of the functioning of one system or process by means of the functioning of another”. 1 It is an activity that mimics natural phenomena without the added risk of sustaining expected consequences. The degree to which a simulation resembles reality is termed fidelity. 2 Modern day simulation is used by a wide spectrum of generalist and specialist occupations for the purpose of training and certification. 3 However, simulation finds its historical and utilitarian roots in the fields of military and aviation. 3
Military application of simulation has long been observed in the form of war games. 4 Although the cost of purchasing and maintaining sophisticated simulators in the military has grown, their advantages far outweigh their liability. 5 Edward Link introduced simulation into aviation with his “Blue box” flight trainer. 6 Within 50 years, simulators were formally incorporated into civil aviation to be used to certify and license pilots. 3 One of many notable contributions to flight simulation is the National Aeronautics and Space Administration’s (NASA) Cockpit Resource Management principles. 3 These have been adopted in healthcare to benefit intensive care, anesthesia and surgical residents today. 3
Up until the 20th century, traditional apprenticeship was standard for clinical education. 7 It is still used as a primary delivery vehicle in some parts of the developing world. 7 Although simulation has long been established in medicine by means of anatomical models and preserved cadaveric tissue, Bradley defined three movements that paved the way for its modernization: the resuscitation movement, introduction of anesthetic simulators, and medical education reform. 7 Laerdal’s Resusci-Anne, Gaba’s CASE 1.2, and Good and Gravenstein’s GAS serve as predecessors to the modern human-patient simulator. 8 Medical simulators have continued to evolve rapidly in the past few decades. 8
Simulation has been adopted by medical educators throughout most of the developed world. 9 Although its advantages are comparable between resource contrasted settings, developing countries still struggle to employ it into mainstream use. 10 This stems from misconceptions regarding its availability, range and cost, and ambiguity related to its consistency and validity. 11 Because of the SARS-CoV-2 pandemic, patient interaction has been limited for students and residents to prevent spread of the disease. 12 This has created a unique opportunity to help galvanize momentum towards simulation in low- to middle-income countries (LMICs). 13
The aim of this literature review is to provide relevant and comprehensive information regarding the utility of simulation in medical education and use knowledge theories to determine how to best implement it in under and postgraduate medical education. We undertook a literature search on MEDLINE using MeSH terms: undergraduate medical education, postgraduate medical education, review, guidelines and simulation. Only articles in written in English were selected for further review, and preference was given to research published within the last 10 years.
The Spectrum of Healthcare Simulation (HS) in Medical Education
Gaba described 11 dimensions of the application of simulation in medical education. 14 Dimension 8 categorizes simulation technology based on complexity. 14 The five components of that dimension are role playing, standardized patients (SP), part-task trainers, the computer patient, and the electronic patient/virtual reality (VR). 14 SPs are trained individuals who can provide a concise medical history and portray relevant physical findings for their scenario. 8 They are popularly employed by medical educators throughout the globe because no technology is needed for the set-up. 8 SPs can also effectively simulate a vast array of medical and ethical scenarios. 8 Their validity and reliability in clinical skills assessment has led to the incorporation of SPs in examinations for licensure in Canada and the United States. 11 , 15–17
Part-task trainers comprise a representation of only a component of the human body. 7 These are frequented by subspecialties that recognize the benefit of deliberate practice to obtain mastery in technical, procedural, or psychomotor skills. 7 High-fidelity simulators can exhibit multiple clinical scenarios, and they are interactive and reactive. 18 Advanced part-task trainers with haptic feedback (ie, creating an experience of touch by applying force, vibration or movement in response to user operation) are being increasingly accepted in interventional and surgical training specialties such as ophthalmology and orthopedics. 11 Table 1 summarises the progress of medical simulators over time.
The Progress of Medical Simulators
Initial resistance to the implementation of simulation stemmed from the financial burden of training staff and maintenance of expensive technology. 19 Development of simulation centers is bridging the tricky gap between educator needs and access to equipment. 11 Despite the recent contributions to the gamut of simulation fidelity and cost-reduction, issues regarding its consistency and validity are the primary reason for the delay in global application. 11 However, evidence for the transition of the medical training enterprise towards simulation has gathered volume in the past 2 decades. 20 This is, in part, due to the growing emphasis on patient safety rather than bedside teaching. 20
The Imperative to Incorporate HS in Medical Education
Medical education is intensive and extensive. 21 Medical professionals are expected to be proficient and effective. 21 With a rapidly changing pattern of healthcare delivery, medical students and residents face an added challenge to keep up to date with the most recent standards of care. 22 , 23 Calls to reduce the duration of professional training and time constraints throughout the education process have the adverse effect of limiting exposure of students and residents to an adequate quality and quantity of clinical exposure. 24 , 25
This is where simulation may flourish. It can provide all learners with an acceptable variety and number of clinical scenarios. Furthermore, exposing all participants to the same scenarios and uncommon clinical cases might allow a more standard approach to clinical curricula. 2 This might also be useful downstream in potentially confronting the inadequacy and lack of preparedness felt by medical students and novice physicians in recent years. 26–31
It is important to correct the perception of simulation as a universally expensive commodity. Low-fidelity simulators like SPs and part-task trainers are readily available, inexpensive, and easily implemented. 8 This can ease incorporation into continued education and recertification programs without substantial impact on financial resources. 2
Most medical care is now delivered by teams, and simulation is integral in improving patient safety by means of Crisis Resource Management and team training techniques. 14 , 32 Real team training has the advantage over improvised team training because it allows for better observational learning, verbal persuasion, and heightened physiological responses borne out of member familiarity. 33 , 34 Moreover, testing team simulation in-situ yields far more constructive results than conducting the exercise at a simulation center. 33
It is also important to address the misconception that simulation is meant only to improve psychomotor skills. Studies show that simulation improves participant affective interpersonal communication and yields more empathic and adept professionals entering the workforce. 35–37
The utility of simulation is in allowing participants to revisit clinical scenarios and practice skills individually and collectively as a team until competence is achieved. A new model of medical education is thus required that has patient safety at its core, avoids the flaws of a purely apprenticeship training model, and provides unlimited opportunities to practice and perfect skills in a risk-free environment.
The Challenge for Low- to Middle-Income Countries (LMICs)
HS has already become the gold standard for medical education in a vast majority of the developed world. 9 The benefits of simulation-based medical education (SBME) are comparable between resource poor and resource abundant settings. 10 However, the need for these benefits is far more pronounced in developing countries due to inadequate access of care. 10 Using SBME to train entry-level providers, educate community workers, and bridge the gaps of understanding between healthcare providers and local populations who mistrust modern medicine may enhance the overall impact of HS. 10 It may also lower the rate of preventable adverse events that are already underreported in LMICs. 38
A recent literature review done by Martinerie et al showed that most studies investigating SMBE in LMICs were conducted in collaboration with international organizations. 9 Indeed, most quality improvement projects launched in LMICs are reliant on external funding. 38 Unit cost and operator expertise remain notable areas of concern regarding SBME implementation in resource poor settings. 9 This is worsened by inadequate cost reporting in SBME research. 39 Nevertheless, the availability of modern low-cost simulators could promote self-reliance in LMICs. 9 This is important as it will prevent unnecessary disruptions in the continuity of SBME due to bureaucratic tribulations. 40
Simulation may also be conducted online or virtually where the use of the internet or computer programs can help eliminate costs related to purchasing expensive equipment for on-site training. 41–43 A study by Okrainec et al demonstrated effective use of laparoscopic telesimulation in Botswana where resident training took place through Skype TM . 42 In another study, Adhikari et al used immersive virtual reality to conduct a sepsis game for pre-registered nurses. 43 Virtual reality provides three-dimensional environment that closely resembles real life. 43 The experience may be enhanced with haptics that provide real-time force feedback. 44 They reported a significant improvement in self-confidence and reduction in anxiety faced by the participants. 43 In addition to cost reduction, these courses can be taught over several weeks using a more dispersed strategy as opposed to short intensive modules. 42 However, there are limitations to these initiatives such as availability of technology, a stable internet connection, and digital literacy and confidence of users. 42 , 43
Another challenge for LMICs is the adaptability of SBME. 40 SBME is only effective if the simulations mimic realistic and relevant scenarios that account for resource limitations and disease distribution in the target setting. 40 If the simulation involves rare scenarios or clinical management that is not in common practice, the overall impact of the educational activity is lost. 40 Additionally, vital learner feedback during the process may be hindered by hierarchy in training structures, social and cultural norms, gender implications or language barriers. 40 Since each LMIC faces different challenges, dedicated time from experts and educators is required to define clear learning objectives, establish effective delivery of feedback and evaluate the type of SBME modality to use. 40
LMICs may also benefit from collaboration of local experts, institutions and manufacturers to develop and implement SBME. 40 A recent study by Gheza et al has shown that overall cost of expensive medical equipment can be effectively controlled using locally sourced materials and readily available devices while yielding comparable outcomes to patented products. 45 These efforts not only improve accessibility but also help increase market share for the products. 46
Sound Educational Andragogy
Bioscience, sociocultural, and learning theories have been used to design frameworks that are core to HS education strategies. 47 Kolb’s learning cycle is the most prominent among these theories and has been commonly used as a conceptual framework for simulation programs involving team training. 48 Kolb emphasizes that transformation of experience is essential in creation of knowledge. 49 His theory consists of four parts: concrete experience, reflective observation, abstract conceptualization, and active experimentation. 49 Participants undergo concrete experience as they complete the simulation scenario. 49 This is followed by debriefing where they reflect upon the experience and draw generalizations and conclusions from their observations to form abstract concepts. 49 These concepts are then actively used to influence actions in repeat simulations. 49 Active experimentation is an important but neglected step in the simulator learning process in most programs. 33 This is partly due to time and resource constraints. 33
Knowles’ adult learning principles of prior experience and response to problem-centered learning as opposed to content-centered learning, and Dewey’s theory of reflective thought argue that learners exhibit increased internal motivation to reflect on their performance when faced with difficult and relevant scenarios. 49–51 Debriefing in a group of participants where critique is offered under the observation of trained facilitators creates an environment for individuals to reflect on their own conceptual framework (innate beliefs that guide their thinking and actions). 33 According to Schön, this kind of reflection is more beneficial than reflecting-in-action during the simulation or reflecting-on-action after the simulation, which individuals usually do on their own and without peer input. 52
The convergence of the behavioral, constructivist, and social cognitive learning theories makes a strong case for HS to be incorporated into medical education curricula in both developed and developing countries. 53
COVID-19 and the Case for Simulation
The SARS-CoV-2 pandemic has negatively impacted the education of undergraduate and postgraduate trainees globally. 12 In response to isolation and preventative requirements issued by governments worldwide, there has been a unanimous shift towards technology-based education. Medical teaching employs a two-pronged approach: learning and practice. 54 Learning has been effectively delivered using online platforms during the pandemic, however the transition to a virtual setup presents its own problems. 54 These include time management, lack of infrastructure and resources, poor communication, negative attitudes and student engagement. 54 The opportunity for students to practice their clinical skills remains an area of concern. 54 , 55 While the gradual transition to telemedicine and the use of prerecorded clinical encounters have been helpful, they do not provide a viable substitute for physical examinations and direct observation of skills for feedback. 55 This is particularly pronounced with surgical/procedural training due to rationing of personal protective equipment and limiting of non-essential staff in operating rooms. 55 With access to patients being limited, elective surgical procedures being cancelled or reduced, and a limited number of students and residents allowed to engage in care to maintain standard operating procedures, it has become evident that simulation can fill a very important niche during this unprecedented time. 13 It will allow students and residents adequate exposure, time, and opportunity to learn and hone their skills. 13 This may be the best time for institutions to adopt HS as a medical education strategy and prepare for future contingencies. 13
The COVID-19 pandemic has also disproportionately affected vulnerable medical students such as those from developing countries and those with financially disadvantaged backgrounds. 56 Although the use of technology has been effective in these developing circumstances, students in LMICs may not have access to appropriate equipment and a stable internet connection to run them. 56 It is in part because of these issues that online learning is met with a poor response in the developing world. 56 This makes it more important to dispel the misconception of simulation as an expensive commodity and promote the use of local manufacturing and low-cost simulation.
Implementation of HS in Medical Education
Incorporation of HS as a teaching strategy in undergraduate and postgraduate medical education curricula requires a stepwise approach. 57 , 58 The first step is the assembly of human capital. 59 Simulation, as a teaching method, requires properly trained facilitators. 59 Improperly executed simulation can lead to unaccomplished objectives, poor to no learning, and disengaged or even psychologically impacted participants. 2 , 60–63 It is extremely important for medical institutions to recognize this and provide their faculty with adequate training in the operation of healthcare simulators before planning for induction and implementation of simulation as an education strategy. Adherence to best practices during the pre-brief, the simulation itself, and the debrief (including skill sign-off) is essential in the long-term success of a simulation program. 64
The next step is integration of simulation into the standard curriculum of a teaching program. 57 This can be done via amalgamation of this modality into an existing curriculum or through development of new curricula. 57 The process is carried out by a collaboration of the program director, content expert, and simulation expert in four phases: planning, implementation, evaluation, and revision. 57 Curricular integration has the advantage of using simulators to achieve learning objectives instead of ad hoc use that only adds to the course load, without achieving palpable benefit. 57
Once part of the curriculum, there should be provisions for deliberate practice. 57 Coined by Ericsson in 2004, deliberate practice is the repetition of psychomotor or cognitive skills to achieve defined goals in a controlled setting. 65 It is designed to provide feedback for error correction in subsequent practice until the participant displays competence and advances onto the next skill. 65 Deliberate practice is a more powerful predictor of superior expert performance than clinical aptitude. 66 It is also particularly useful in training for rarely performed procedures. 65 Simulation is versatile in the ability to not only expand on psychomotor skills but also assist in refining trainee confidence and self-sufficiency. 35–37 , 67
Deliberate practice is crucial in mastery learning. 57 The objective of mastery learning is to achieve performance on a level higher than basic competence. 57 Residents take different times to achieve mastery as they have dissimilar strengths and weaknesses. 57 Each participant must meet a set standard to progress through educational units of increasing difficulty. 57 Once mastery is achieved for a skill, range of difficulty and clinical variation in simulation training is increased in the case mix. 57 Both need to be adjusted according to the needs of the training program. 57
True learning occurs when participants are given time to achieve goals at a pace that is complementary to their learning capability. Desired outcomes can be accomplished by integrating simulation into curricula with the support of trained facilitators.
It is imperative that HS is adopted in undergraduate and postgraduate medical education globally. The evidence for its efficacy in adult learning is overwhelming, yet its use remains variable and opportunistic. Medical education needs to produce proficient and poised doctors for the future. Therefore, students and residents need to be provided with opportunities to practice and perfect their skills before real patient encounters. Future research priorities should focus on sustainability of simulation in LMICs and prioritize adequate and informative cost reporting. Foreign funds invested in limited and short-term simulation initiatives in developing countries should be redirected in collaboration with local experts towards more attainable and long-term projects. Unprecedented times when global healthcare is operating under extreme pressure (eg, during the COVID-19 pandemic) where patient interaction is limited provide unique opportunities to explore these areas. Strategic and integrated use of simulation is the way forward.
Funding Statement
The authors have received no funding for this article.
The authors report no conflicts of interest in this work.
AI in Medical Education: Global situation, effects and challenges
- Published: 10 July 2023
- Volume 29 , pages 4611–4633, ( 2024 )
Cite this article

- Wei Zhang 1 ,
- Mingxuan Cai 1 ,
- Hong Joo Lee 2 ,
- Richard Evans 3 ,
- Chengyan Zhu 4 &
- Chenghan Ming 5
2471 Accesses
5 Citations
Explore all metrics
Artificial Intelligence (AI) is transforming healthcare and shows considerable promise for the delivery of medical education. This systematic review provides a comprehensive analysis of the global situation, effects, and challenges associated with applying AI at the different stages of medical education.
This review followed the PRISMA guidelines, and retrieved studies published on Web of Science, PubMed, Scopus, and IEEE Xplore, from 1990 to 2022. After duplicates were removed (n = 1407) from the 6371 identified records, the full text of 179 records were screened. In total, 42 records were eligible.
It revealed three teaching stages where AI can be applied in medical education (n = 39), including teaching implementation (n = 24), teaching evaluation (n = 10), and teaching feedback (n = 5). Many studies explored the effectiveness of AI adoption with questionnaire survey and control experiment. The challenges are performance improvement, effectiveness verification, AI training data sample and AI algorithms.
Conclusions
AI provides real-time feedback and accurate evaluation, and can be used to monitor teaching quality. A possible reason why AI has not yet been applied widely to practical teaching may be the disciplinary gap between developers and end-user, it is necessary to strengthen the theoretical guidance of medical education that synchronizes with the rapid development of AI. Medical educators are expected to maintain a balance between AI and teacher-led teaching, and medical students need to think independently and critically. It is also highly demanded for research teams with a wide range of disciplines to ensure the applicability of AI in medical education.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
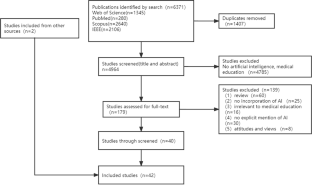
Similar content being viewed by others

AIM in Medical Education

AI’s Role and Application in Education: Systematic Review
Data availability.
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Aldeman, N. L. S., de SáUrtigaAita, K. M., Machado, V. P., da Mata Sousa, L. C. D., Coelho, A. G. B., da Silva, A. S., Silva Mendes, A. P., de Oliveira Neres, F. J., & do Monte, S. J. H. (2021). Smartpathk: A platform for teaching glomerulopathies using machine learning. BMC Medical Education, 21 (1), 248. https://doi.org/10.1186/s12909-021-02680-1
Article PubMed PubMed Central Google Scholar
Alonso-Silverio, G. A., Pérez-Escamirosa, F., Bruno-Sanchez, R., Ortiz-Simon, J. L., Muñoz-Guerrero, R., Minor-Martinez, A., & Alarcón-Paredes, A. (2018). Development of a Laparoscopic Box Trainer Based on Open Source Hardware and Artificial Intelligence for Objective Assessment of Surgical Psychomotor Skills. Surgical Innovation, 25 (4), 380–388. https://doi.org/10.1177/1553350618777045
Article PubMed Google Scholar
Baloul, M. S., Yeh, V.J.-H., Mukhtar, F., Ramachandran, D., Traynor, M. D., Shaikh, N., Rivera, M., & Farley, D. R. (2022). Video Commentary & Machine Learning: Tell Me What You See, I Tell You Who You Are. Journal of Surgical Education, 79 (6), e263–e272. https://doi.org/10.1016/j.jsurg.2020.09.022
Bienstock, J. L., Katz, N. T., Cox, S. M., Hueppchen, N., Erickson, S., & Puscheck, E. E. (2007). To the point: Medical education reviews—providing feedback. American Journal of Obstetrics and Gynecology, 196 (6), 508–513. https://doi.org/10.1016/j.ajog.2006.08.021
Bing-You, R., Hayes, V., Varaklis, K., Trowbridge, R., Kemp, H., & McKelvy, D. (2017). Feedback for Learners in Medical Education: What Is Known? A Scoping Review . Wolters Kluwer. https://doi.org/10.1097/ACM.0000000000001578
Bissonnette, V., Mirchi, N., Ledwos, N., Alsidieri, G., Winkler-Schwartz, A., Del Maestro, R. F., Yilmaz, R., Siyar, S., Azarnoush, H., Karlik, B., Sawaya, R., Alotaibi, F. E., Bugdadi, A., Bajunaid, K., Ouellet, J., & Berry, G. (2019). Artificial Intelligence Distinguishes Surgical Training Levels in a Virtual Reality Spinal Task. Journal of Bone and Joint Surgery-American, 101 (23), e127. https://doi.org/10.2106/JBJS.18.01197
Article Google Scholar
Borakati, A. (2021). Evaluation of an international medical E-learning course with natural language processing and machine learning. BMC Medical Education, 21 (1), 181. https://doi.org/10.1186/s12909-021-02609-8
Chan, H.-P., Samala, R. K., Hadjiiski, L. M., & Zhou, C. (2020). Deep Learning in Medical Image Analysis. In G. Lee & H. Fujita ( Ed.), Deep Learning in Medical Image Analysis: Challenges and Applications (pp. 3–21). Springer International Publishing. https://doi.org/10.1007/978-3-030-33128-3_1
Chan, K. S., & Zary, N. (2019). Applications and Challenges of Implementing Artificial Intelligence in Medical Education: Integrative Review. JMIR Medical Education, 5 (1), e13930. https://doi.org/10.2196/13930
Chen, C.-K. (2010). Curriculum Assessment Using Artificial Neural Network and Support Vector Machine Modeling Approaches: A Case Study. IR Applications. Volume 29. In Association for Institutional Research (NJ1) . Association for Institutional Research. https://eric.ed.gov/?id=ED524832
Chen, L., Chen, P., & Lin, Z. (2020). Artificial Intelligence in Education: A Review. Ieee Access, 8 , 75264–75278. https://doi.org/10.1109/ACCESS.2020.2988510
Cheng, C.-T., Chen, C.-C., Fu, C.-Y., Chaou, C.-H., Wu, Y.-T., Hsu, C.-P., Chang, C.-C., Chung, I.-F., Hsieh, C.-H., Hsieh, M.-J., & Liao, C.-H. (2020). Artificial intelligence-based education assists medical students’ interpretation of hip fracture. Insights into Imaging, 11 (1), 119. https://doi.org/10.1186/s13244-020-00932-0
de Lima, R. M., de Medeiros Santos, A., Mendes Neto, F. M., de Sousa, F., Neto, A., Leão, F. C. P., de Macedo, F. T., & de Paula Canuto, A. M. (2016). A 3D serious game for medical students training in clinical cases. IEEE International Conference on Serious Games and Applications for Health (SeGAH), 2016 , 1–9. https://doi.org/10.1109/SeGAH.2016.7586255
Dharmasaroja, P., & Kingkaew, N. (2016). Application of artificial neural networks for prediction of learning performances. 2016 12th International Conference on Natural Computation, Fuzzy Systems and Knowledge Discovery (ICNC-FSKD) , 745–751. https://doi.org/10.1109/FSKD.2016.7603268
Estai, M., & Bunt, S. (2016). Best teaching practices in anatomy education: A critical review. Annals of Anatomy - Anatomischer Anzeiger, 208 , 151–157. https://doi.org/10.1016/j.aanat.2016.02.010
Fajrianti, E. D., Sukaridhoto, S., Rasyid, M. U. H. A., Suwito, B. E., Budiarti, R. P. N., Hafidz, I. A. A., Satrio, N. A., & Haz, A. L. (2022). Application of Augmented Intelligence Technology with Human Body Tracking for Human Anatomy Education. IJIET: International Journal of Information and Education Technology , 12 (6), Article 6.
Fang, Z., Xu, Z., He, X., & Han, W. (2022).Artificial intelligence-based pathologic myopia identification system in the ophthalmology residency training program. Frontiers in Cell and Developmental Biology , 10 . https://doi.org/10.3389/fcell.2022.1053079
Fazlollahi, A. M., Bakhaidar, M., Alsayegh, A., Yilmaz, R., Winkler-Schwartz, A., Mirchi, N., Langleben, I., Ledwos, N., Sabbagh, A. J., Bajunaid, K., Harley, J. M., & Del Maestro, R. F. (2022). Effect of Artificial Intelligence Tutoring vs Expert Instruction on Learning Simulated Surgical Skills Among Medical Students: A Randomized Clinical Trial. JAMA Network Open, 5 (2), e2149008. https://doi.org/10.1001/jamanetworkopen.2021.49008
Fernández-Alemán, J. L., López-González, L., González-Sequeros, O., Jayne, C., López-Jiménez, J. J., & Toval, A. (2016). The evaluation of i-SIDRA – a tool for intelligent feedback – in a course on the anatomy of the locomotor system. International Journal of Medical Informatics, 94 , 172–181. https://doi.org/10.1016/j.ijmedinf.2016.07.008
Foss, C. L. (1987). Learning from errors in ALGEBRALAND . Institute for Research on Learning.
Furlan, R., Gatti, M., Menè, R., Shiffer, D., Marchiori, C., Levra, A. G., Saturnino, V., Brunetta, E., & Dipaola, F. (2021). A Natural Language Processing-Based Virtual Patient Simulator and Intelligent Tutoring System for the Clinical Diagnostic Process: Simulator Development and Case Study. JMIR Medical Informatics, 9 (4), e24073. https://doi.org/10.2196/24073
Gendia, A. (2022). Cloud Based AI-Driven Video Analytics (CAVs) in Laparoscopic Surgery: A Step Closer to a Virtual Portfolio. Cureus , 14 (9). https://doi.org/10.7759/cureus.29087
Gil, D. H., Heins, M., & Jones, P. B. (1984). Perceptions of medical school faculty members and students on clinical clerkship feedback. Academic Medicine, 59 (11), 856.
Article CAS Google Scholar
Goh, P. S. (2021). The vision of transformation in medical education after the COVID-19 pandemic. Korean Journal of Medical Education, 33 (3), 171–174. https://doi.org/10.3946/kjme.2021.197
Article MathSciNet PubMed PubMed Central Google Scholar
Gorospe-Sarasúa, L., Munoz-Olmedo, J. M., Sendra-Portero, F., & de Luis-García, R. (2022a). Challenges of Radiology education in the era of artificial intelligence . 6.
Gorospe-Sarasúa, L., Muñoz-Olmedo, J. M., Sendra-Portero, F., & de Luis-García, R. (2022b). Challenges of Radiology education in the era of artificial intelligence. Radiología (english Edition), 64 (1), 54–59. https://doi.org/10.1016/j.rxeng.2020.10.012
Han, R., Yu, W., Chen, H., & Chen, Y. (2022). Using artificial intelligence reading label system in diabetic retinopathy grading training of junior ophthalmology residents and medical students. BMC Medical Education , 22 (1), Article 1. https://doi.org/10.1186/s12909-022-03272-3
Hattie, J., & Timperley, H. (2007). The power of feedback. Review of educational research, 77 (1), 81–112. https://doi.org/10.3102/003465430298487
Hedderich, D. M., Keicher, M., Wiestler, B., Gruber, M. J., Burwinkel, H., Hinterwimmer, F., Czempiel, T., Spiro, J. E., Pinto dos Santos, D., Heim, D., Zimmer, C., Rückert, D., Kirschke, J. S., & Navab, N. (2021). AI for Doctors—A Course to Educate Medical Professionals in Artificial Intelligence for Medical Imaging. Healthcare , 9 (10), Article 10. https://doi.org/10.3390/healthcare9101278
Hewson, M. G., & Little, M. L. (1998). Giving Feedback in Medical Education. Journal of General Internal Medicine, 13 (2), 111–116. https://doi.org/10.1046/j.1525-1497.1998.00027.x
Article CAS PubMed PubMed Central Google Scholar
Hisan, U. K., & Amri, M. M. (2023). ChatGPT and Medical Education: A Double-Edged Sword. Journal of Pedagogy and Education Science , 2 (01), Article 01. https://doi.org/10.56741/jpes.v2i01.302
Hisey, R., Camire, D., Erb, J., Howes, D., Fichtinger, G., & Ungi, T. (2022). System for Central Venous Catheterization Training Using Computer Vision-Based Workflow Feedback. IEEE Transactions on Biomedical Engineering, 69 (5), 1630–1638. https://doi.org/10.1109/TBME.2021.3124422
Hosny, A., Parmar, C., Quackenbush, J., Schwartz, L. H., & Aerts, H. J. W. L. (2018). Artificial intelligence in radiology. Nature Reviews Cancer , 18 (8), Article 8. https://doi.org/10.1038/s41568-018-0016-5
Hu, H., Li, J., Lei, X., Qin, P., & Chen, Q. (2019). Design of health statistics intelligent education system based on Internet +. Journal of Physics: Conference Series, 1168 (6), 062003. https://doi.org/10.1088/1742-6596/1168/6/062003
Hwang, G.-J., Xie, H., Wah, B. W., & Gašević, D. (2020). Vision, challenges, roles and research issues of Artificial Intelligence in Education. Computers and Education: Artificial Intelligence, 1 , 100001. https://doi.org/10.1016/j.caeai.2020.100001
Islam, G., Kahol, K., Li, B., Smith, M., & Patel, V. L. (2016). Affordable, web-based surgical skill training and evaluation tool. Journal of Biomedical Informatics, 59 , 102–114. https://doi.org/10.1016/j.jbi.2015.11.002
Karambakhsh, A., Kamel, A., Sheng, B., Li, P., Yang, P., & Feng, D. D. (2019). Deep gesture interaction for augmented anatomy learning. International Journal of Information Management, 45 , 328–336. https://doi.org/10.1016/j.ijinfomgt.2018.03.004
Kirubarajan, A., Young, D., Khan, S., Crasto, N., Sobel, M., & Sussman, D. (2022). Artificial Intelligence and Surgical Education: A Systematic Scoping Review of Interventions. Journal of Surgical Education, 79 (2), 500–515. https://doi.org/10.1016/j.jsurg.2021.09.012
Klar, R., & Bayer, U. (1990). Computer-assisted teaching and learning in medicine. International Journal of Bio-Medical Computing, 26 (1–2), 7–27. https://doi.org/10.1016/0020-7101(90)90016-N
Article CAS PubMed Google Scholar
Kurniawan, M. H., Suharjito, Diana, & Witjaksono, G. (2018). Human Anatomy Learning Systems Using Augmented Reality on Mobile Application . 135 , 80–88. https://doi.org/10.1016/j.procs.2018.08.152
Lam, A., Lam, L., Blacketer, C., Parnis, R., Franke, K., Wagner, M., Wang, D., Tan, Y., Oakden-Rayner, L., Gallagher, S., Perry, S. W., Licinio, J., Symonds, I., Thomas, J., Duggan, P., & Bacchi, S. (2022a). Professionalism and clinical short answer question marking with machine learning. Internal Medicine Journal, 52 (7), 1268–1271. https://doi.org/10.1111/imj.15839
Lam, K., Chen, J., Wang, Z., Iqbal, F. M., Darzi, A., Lo, B., Purkayastha, S., & Kinross, J. M. (2022b). Machine learning for technical skill assessment in surgery: A systematic review. Npj Digital Medicine , 5(1), Article 1. https://doi.org/10.1038/s41746-022-00566-0
Lazarus, M. D., Truong, M., Douglas, P., & Selwyn, N. (2022). Artificial intelligence and clinical anatomical education: Promises and perils. Anatomical Sciences Education , n/a (n/a). https://doi.org/10.1002/ase.2221
Lee, J., Wu, A. S., Li, D., Kulasegaram, K., & (Mahan). (2021). Artificial Intelligence in Undergraduate Medical Education: A Scoping Review. Academic Medicine, 96 (11S), S62. https://doi.org/10.1097/ACM.0000000000004291
Lee, L. S., Aluwee, S. A. Z. S., Meng, G. C., Palanisamy, P., & Subramaniam, R. (2020). Interactive Tool Using Augmented Reality (AR) for Learning Knee and Foot Anatomy Based on CT Images 3D Reconstruction. 2020 International Conference on Computational Intelligence (ICCI) , 281–286. https://doi.org/10.1109/ICCI51257.2020.9247820
Li, Y., Bai, C., & Reddy, C. K. (2016). A distributed ensemble approach for mining healthcare data under privacy constraints. Information Sciences, 330 , 245–259. https://doi.org/10.1016/j.ins.2015.10.011
Li, Y. S., Lam, C. S. N., & See, C. (2021). Using a Machine Learning Architecture to Create an AI-Powered Chatbot for Anatomy Education. Medical Science Educator, 31 (6), 1729–1730. https://doi.org/10.1007/s40670-021-01405-9
Luan, H., Geczy, P., Lai, H., Gobert, J., Yang, S. J. H., Ogata, H., Baltes, J., Guerra, R., Li, P., & Tsai, C.-C. (2020). Challenges and Future Directions of Big Data and Artificial Intelligence in Education. Frontiers in Psychology , 11 . https://doi.org/10.3389/fpsyg.2020.580820
Martin, J. A., Regehr, G., Reznick, R., Macrae, H., Murnaghan, J., Hutchison, C., & Brown, M. (1997). Objective structured assessment of technical skill (OSATS) for surgical residents. BJS (british Journal of Surgery), 84 (2), 273–278. https://doi.org/10.1046/j.1365-2168.1997.02502.x
Mirchi, N., Bissonnette, V., Yilmaz, R., Ledwos, N., Winkler-Schwartz, A., & Del Maestro, R. F. (2020). The Virtual Operative Assistant: An explainable artificial intelligence tool for simulation-based training in surgery and medicine. Plos One, 15 (2), e0229596. https://doi.org/10.1371/journal.pone.0229596
Muller, S. (1984). Physicians for the twenty-first century: Report of the project panel on the general professional education of the physician and college preparation for medicine. Journal of Medical Education, 59 , 1–208.
Google Scholar
Nagaraj, M. B., Namazi, B., Sankaranarayanan, G., & Scott, D. J. (2023). Developing artificial intelligence models for medical student suturing and knot-tying video-based assessment and coaching. Surgical Endoscopy, 37 (1), 402–411. https://doi.org/10.1007/s00464-022-09509-y
Nakawala, H., Ferrigno, G., & De Momi, E. (2018). Development of an intelligent surgical training system for Thoracentesis. Artificial Intelligence in Medicine, 84 , 50–63. https://doi.org/10.1016/j.artmed.2017.10.004
Neves, S. E., Chen, M. J., Ku, C. M., Karan, S., DiLorenzo, A. N., Schell, R. M., Lee, D. E., Diachun, C. A. B., Jones, S. B., & Mitchell, J. D. (2021). Using Machine Learning to Evaluate Attending Feedback on Resident Performance. Anesthesia & Analgesia, 132 (2), 545–555. https://doi.org/10.1213/ANE.0000000000005265
Niitsu, H., Hirabayashi, N., Yoshimitsu, M., Mimura, T., Taomoto, J., Sugiyama, Y., Murakami, S., Saeki, S., Mukaida, H., & Takiyama, W. (2013). Using the Objective Structured Assessment of Technical Skills (OSATS) global rating scale to evaluate the skills of surgical trainees in the operating room. Surgery Today, 43 (3), 271–275. https://doi.org/10.1007/s00595-012-0313-7
Ötles, E., Kendrick, D. E., Solano, Q. P., Schuller, M., Ahle, S. L., Eskender, M. H., Carnes, E., & George, B. C. (2021). Using Natural Language Processing to Automatically Assess Feedback Quality: Findings From 3 Surgical Residencies. Academic Medicine, 96 (10), 1457. https://doi.org/10.1097/ACM.0000000000004153
Ouyang, F., Zheng, L., & Jiao, P. (2022). Artificial intelligence in online higher education: A systematic review of empirical research from 2011 to 2020. Education and Information Technologies . https://doi.org/10.1007/s10639-022-10925-9
Peter, H., & Goodridge, W. (2004). Integrating Two Artificial Intelligence Theories in a Medical Diagnosis Application. In M. Bramer & V. Devedzic ( Ed.), Artificial Intelligence Applications and Innovations (pp. 11–23). Springer US. https://doi.org/10.1007/1-4020-8151-0_2
Qian, X., Jingying, H., Xian, S., Yuqing, Z., Lili, W., Baorui, C., Wei, G., Yefeng, Z., Qiang, Z., Chunyan, C., Cheng, B., Kai, M., & Yi, Q. (2022). The effectiveness of artificial intelligence-based automated grading and training system in education of manual detection of diabetic retinopathy. Frontiers in Public Health, 10 , 1025271. https://doi.org/10.3389/fpubh.2022.1025271
Razzak, M. I., Naz, S., & Zaib, A. (2018). Deep Learning for Medical Image Processing: Overview, Challenges and the Future. In N. Dey, A. S. Ashour, & S. Borra ( Ed.), Classification in BioApps: Automation of Decision Making (pp. 323–350). Springer International Publishing. https://doi.org/10.1007/978-3-319-65981-7_12
Sadeghi Esfahlani, S., Izsof, V., Minter, S., Kordzadeh, A., Shirvani, H., & Esfahlani, K. S. (2020). Development of an Interactive Virtual Reality for Medical Skills Training Supervised by Artificial Neural Network. In Y. Bi, R. Bhatia, & S. Kapoor ( Ed.), Intelligent Systems and Applications (pp. 473–482). Springer International Publishing. https://doi.org/10.1007/978-3-030-29513-4_34
Shiang, T., Garwood, E., & Debenedectis, C. M. (2022). Artificial intelligence-based decision support system (AI-DSS) implementation in radiology residency: Introducing residents to AI in the clinical setting. Clinical Imaging, 92 , 32–37. https://doi.org/10.1016/j.clinimag.2022.09.003
Siyar, S., Azarnoush, H., Rashidi, S., Winkler-Schwartz, A., Bissonnette, V., Ponnudurai, N., & Del Maestro, R. F. (2020). Machine learning distinguishes neurosurgical skill levels in a virtual reality tumor resection task. Medical and Biological Engineering and Computing, 58 (6), 1357–1367. https://doi.org/10.1007/s11517-020-02155-3
Solano, Q. P., Hayward, L., Chopra, Z., Quanstrom, K., Kendrick, D., Abbott, K. L., Kunzmann, M., Ahle, S., Schuller, M., Ötleş, E., & George, B. C. (2021). Natural Language Processing and Assessment of Resident Feedback Quality. Journal of Surgical Education, 78 (6), e72–e77. https://doi.org/10.1016/j.jsurg.2021.05.012
Stephens, G. C., Rees, C. E., & Lazarus, M. D. (2021). Exploring the impact of education on preclinical medical students’ tolerance of uncertainty: A qualitative longitudinal study. Advances in Health Sciences Education, 26 (1), 53–77. https://doi.org/10.1007/s10459-020-09971-0
Sqalli, M. T., Al-Thani, D., Elshazly, M. B., & Al-Hijji, M. (2022). A Blueprint for an AI & AR-Based Eye Tracking System to Train Cardiology Professionals Better Interpret Electrocardiograms. In N. Baghaei, J. Vassileva, R. Ali, & K. Oyibo ( Ed.), Persuasive Technology (pp. 221–229). Springer International Publishing. https://doi.org/10.1007/978-3-030-98438-0_17
Szasz, P., Louridas, M., Harris, K. A., Aggarwal, R., & Grantcharov, T. P. (2015). Assessing Technical Competence in Surgical Trainees: A Systematic Review. Annals of Surgery, 261 (6), 1046. https://doi.org/10.1097/SLA.0000000000000866
Torre, D. M., Sebastian, J. L., & Simpson, D. E. (2003). Learning Activities and High-Quality Teaching: Perceptions of Third-Year IM Clerkship Students. Academic Medicine, 78 (8), 812.
Vayena, E., & Blasimme, A. (2017). Biomedical Big Data: New Models of Control Over Access, Use and Governance. Journal of Bioethical Inquiry, 14 (4), 501–513. https://doi.org/10.1007/s11673-017-9809-6
Voss, G., Bockholt, U., Los Arcos, J. L., Müller, W., Oppelt, P., & Stähler, J. (2000). Lahystotrain. Studies in Health Technology and Informatics, 70 , 359–364. https://doi.org/10.3233/978-1-60750-914-1-359
Wang, M., Sun, Z., Jia, M., Wang, Y., Wang, H., Zhu, X., Chen, L., & Ji, H. (2022). Intelligent virtual case learning system based on real medical records and natural language processing. BMC Medical Informatics and Decision Making, 22 (1), 60. https://doi.org/10.1186/s12911-022-01797-7
Willan, P. L. T., & Humpherson, J. R. (1999). Concepts of variation and normality in morphology: Important issues at risk of neglect in modern undergraduate medical courses. Clinical Anatomy, 12 (3), 186–190. https://doi.org/10.1002/(SICI)1098-2353(1999)12:3%3c186::AID-CA7%3e3.0.CO;2-6
Wolverton, S. E., & Bosworth, M. F. (1985). A survey of resident perceptions of effective teaching behaviors. Family Medicine, 17 (3), 106–108.
CAS PubMed Google Scholar
Wood, B. P. (2000). Feedback: A Key Feature of Medical Training. Radiology, 215 (1), 17–19. https://doi.org/10.1148/radiology.215.1.r00ap5917
Article MathSciNet CAS PubMed Google Scholar
Yang, W., Hebert, D., Kim, S., & Kang, B. (2019). MCRDR Knowledge-Based 3D Dialogue Simulation in Clinical Training and Assessment. Journal of Medical Systems, 43 (7), 200. https://doi.org/10.1007/s10916-019-1262-0
Yilmaz, Y., Nunez, A. J., Ariaeinejad, A., Lee, M., Sherbino, J., & Chan, T. M. (2022). Harnessing Natural Language Processing to Support Decisions Around Workplace-Based Assessment: Machine Learning Study of Competency-Based Medical Education. JMIR Medical Education, 8 (2), e30537. https://doi.org/10.2196/30537
Yilmaz-Recai, Winkler-Schwartz, A., Mirchi, N., Reich, A., Christie, S., Tran, D. H., Ledwos, N., Fazlollahi, A. M., Santaguida, C., Sabbagh, A. J., Bajunaid, K., & Del Maestro, R. (2022). Continuous monitoring of surgical bimanual expertise using deep neural networks in virtual reality simulation. Npj Digital Medicine , 5 (1), Article 1. https://doi.org/10.1038/s41746-022-00596-8
Zahiri, M., Booton, R., Siu, K.-C., & Nelson, C. A. (2016). Design and Evaluation of a Portable Laparoscopic Training System Using Virtual Reality. Journal of Medical Devices , 11(1). https://doi.org/10.1115/1.4034881
Zhao, S., Zhang, X., Jin, F., & Hahn, J. (2021). An Auxiliary Tasks Based Framework for Automated Medical Skill Assessment with Limited Data. 2021 43rd Annual International Conference of the IEEE Engineering in Medicine Biology Society (EMBC) , 1613–1617. https://doi.org/10.1109/EMBC46164.2021.9630498
Download references
This paper is supported by National Natural Science Foundation of China (Project No. 72104087, 72004070) and University-Industry Collaborative Education Program supported by Ministry of Education in China (220505084312449).
Author information
Authors and affiliations.
School of Medicine and Health Management, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Wei Zhang & Mingxuan Cai
Department of Business Administration, The Catholic University of Korea, Seoul, Korea
Hong Joo Lee
Faulty of Computer Science, Dalhousie University, Halifax, Canada
Richard Evans
School of Political Science and Public Administration, Wuhan University, Wuhan, China
Chengyan Zhu
College of Public Administration and Law, Hunan Agricultural University, Changsha, China
Chenghan Ming
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Chengyan Zhu .
Ethics declarations
Conflict of interest, additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 13 KB)
Supplementary file2 (docx 60 kb), rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Zhang, W., Cai, M., Lee, H.J. et al. AI in Medical Education: Global situation, effects and challenges. Educ Inf Technol 29 , 4611–4633 (2024). https://doi.org/10.1007/s10639-023-12009-8
Download citation
Received : 11 March 2023
Accepted : 26 June 2023
Published : 10 July 2023
Issue Date : March 2024
DOI : https://doi.org/10.1007/s10639-023-12009-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Artificial intelligence
- Applications of AIMED
- Effectiveness of AIMED
- Challenges of AIMED
- Find a journal
- Publish with us
- Track your research

Groundbreaking held for UC Merced's new Medical Education Building
A groundbreaking ceremony was held for UC Merced's new Medical Education Building on Wednesday.
The four-story building will feature more than 200-thousand square feet of instructional, academic office, and research space.
The new facility will be home to UC Merced's medical education pathway, which was developed in partnership with UCSF and UCSF Fresno
Since the university opened in 2005, the need for more local medical professionals has only grown, especially with the 2022 closure of Madera Community Hospital.
"This is obviously one of the most medically underserved regions in the state of California. Very few specialties, many people have to travel south to Los Angeles, the Bay Area, UCSF," explained UC Merced Chancellor Juan Sanchez Munoz.
Munoz says UC Merced is committed to improving access to high-quality healthcare in the Central Valley.
The new building will house the university's 'B.S. to M.D. Pathway' program, as well as the departments of psychology and public health and the Health Sciences Research Institute.
"This is the groundbreaking for a significant facility that will serve as a foundation for medical training and eventually the school of medicine independently accredited here at UC Merced," said Munoz.
Current pre-med students are excited to have improved medical training right in their own community.
The $300 million dollar is being funded by a combination of state general fund appropriations, the school's budget and donations.
The school says the project will eventually help churn out locally raised and educated doctors who will care for the region.
Now that the ground has been broken, the medical education building is expected to open in Fall of 2026.
For news updates, follow Nic Garcia on Facebook , Twitter and Instagram .

- Open access
- Published: 10 May 2024
Importance of multimodal resident education curriculum for general surgeons: perspectives of trainers and trainees
- Jeeyeon Lee 1 na1 ,
- Hyung Jun Kwon 1 na1 ,
- Soo Yeon Park 1 &
- Jin Hyang Jung 1
BMC Medical Education volume 24 , Article number: 518 ( 2024 ) Cite this article
120 Accesses
Metrics details
Satisfaction should be prioritized to maximize the value of education for trainees. This study was conducted with professors, fellows, and surgical residents in the Department of general surgery (GS) to evaluate the importance of various educational modules to surgical residents.
A questionnaire was administered to professors ( n = 28), fellows ( n = 8), and surgical residents ( n = 14), and the responses of the three groups were compared. Four different categories of educational curricula were considered: instructor-led training, clinical education, self-paced learning, and hands-on training.
The majority of surgeons regarded attending scrubs as the most important educational module in the training of surgical residents. However, while professors identified assisting operators by participating in surgery as the most important, residents assessed the laparoscopic training module with animal models as the most beneficial.
Conclusions
The best educational training course for surgical residents was hands-on training, which would provide them with several opportunities to operate and perform surgical procedures themselves.
Peer Review reports
Introduction
Continuous, lifelong medical education should be provided because it is essential to training qualified specialists in every medical field [ 1 ]. Educational periods may be categorized as medical college, postgraduate, and specialist education. The residency training program is the most important part of postgraduate education. However, departments of general surgery (GS) in the United States and South Korea are seeing decreased demand for surgical residencies [ 2 , 3 , 4 ].
The decreasing demand for residencies in GS is critical because it results in a lack of specialists. The reasons for this demand reduction vary and include the fatigue accumulated from emergency surgeries, the deterioration of their quality of life, and the frequent stressful situations caused by handling vital organs [ 5 , 6 , 7 ]. Nevertheless, many physicians continue to choose surgical residency and might feel enthusiastic when they succeed in performing surgery, thus saving patients’ lives and improving patients’ odds of survival. Although a majority of surgical applicants apply with this intent, they experience frustration and often regret their decision when faced with the harsh reality of the field. In light of these problems, surgical residency training should pay attention to the mental and physical well-being of residents. In particular, unlike the trainers’ generation, residents of the twenty-first century prioritize work-life balance, technological proficiency, adaptability to pandemic situations, diversity, and inclusion [ 8 , 9 , 10 , 11 ]. These factors have gained even greater emphasis following the coronavirus pandemic. Given that residents in Korea tend to avoid challenging but essential medical care, motivation becomes even more critical for those applying to GS. Educational programs that fail to consider these specific characteristics may lead to decreased achievement and efficiency.
Experts agree that instructors must consider trainees’ satisfaction to maximize educational impact [ 12 , 13 ]. Each qualified specialist’s training involves numerous educational training modules, which should be accessible and tailored to the demands of surgery. Instructors should determine how to increase educational impact by verifying the degree of satisfaction of surgical residents and evaluating the efficacy of the educational curriculum. Educational programs are generally divided into instructor-led training (ILT) and self-paced learning (SPL), and the program should be structured to balance these two areas equally [ 14 , 15 , 16 , 17 , 18 ]. Moreover, in the education of doctors, each resident must receive not only theoretical education but also more detailed programs related to clinical and technical skills.
In this study, by evaluating the responses of professors, fellows, and surgical residents in a department of GS regarding trainee satisfaction and the importance of educational training modules, we identified the most appropriate educational curriculum for residents to establish better training courses toward cultivating specialists with higher qualifications.
The educational curricula for surgical residents were organized by the Education Committee of the department of surgery at Kyungpook National University Hospital, Daegu, Republic of Korea. The categories of educational curricula were classified into ILT, clinical education, SPL, hands-on training, and detailed training courses (Table 1 , Supplementary Fig. 1 ). ILT is defined as a training and learning program provided by instructors or teachers, whereas SPL is a student-driven learning design [ 18 , 19 , 20 ].
The importance of different categories of resident education was assessed on the basis of a cross-sectional questionnaire proffered via e-mails or text messages. Professors, fellows, and surgical residents responded to the survey. Academic faculty and clinical specialists comprised the group of professors. Fellows were defined as specialists who had completed their residency within the immediately preceding two years. The training system for medical residents in Korea consists of a three-year format, and accordingly, surgical residents consisted of first-year, second-year, and third-year residents following the curriculum of the Korean Surgical Society. All the professors and fellows, who have successfully completed their residency and obtained specialist qualifications, were regarded as educators. And only residents in their first to third years of training were considered as trainees.
The questionnaire comprised nine items, including the level of the surgeons; their self-estimated daily working hours; and the time they estimated to have devoted to the education of residents in a week, excluding routine jobs (Supplementary Table 1 ). The top three important education curricula among the 15 training courses constituting the educational curricula were further classified into the four categories.
Each complete response collected from professors, fellows, and residents was analyzed and presented in the form of bar graphs for convenient comparison.
Sociodemographic characteristics
In total, 50 surgeons responded to the questionnaires. Six of the respondents repeated their submissions because of incomplete forms. The mean ages of the groups of professors ( n = 28), fellows ( n = 8), and residents ( n = 14) were 47.3 years (SD, ± 15.1), 33.3 years (SD, ± 2.3), and 31.0 years (SD, ± 3.3), respectively.
Professors specialized in breast/thyroid (n = 7, 25.0%), colorectal ( n = 6, 21.4%), upper gastrointestinal ( n = 5, 17.9%), vascular ( n = 4, 14.3%), hepato-bilio-pancreatic ( n = 3, 10.7%), pediatric ( n = 1, 3.6%), trauma (n = 1, 3.6%), and critical care ( n = 1, 3.6%) surgeries. Fellows majored in vascular ( n = 3, 37.5%), colorectal ( n = 2, 25.0%), upper gastrointestinal ( n = 1, 12.5%), breast/thyroid ( n = 1, 12.5%), and critical care ( n = 1, 12.5%) surgeries. Fourteen residents from the first year ( n = 2, 14.3%), second year ( n = 4, 28.6%), and third year ( n = 8, 57.1%) participated (Supplementary Table 3 ).
Self-estimated daily working time and time devoted to the education of residents in a week.
Professors responded that they worked 8 h ( n = 8, 28.6%), 10 h ( n = 13, 46.4%), and more than 12 h ( n = 7, 25.0%) per day. However, a majority of fellows ( n = 6, 75.0%) and residents ( n = 12, 85.7%) responded that they worked for more than 12 h per day. Professors and residents spent approximately 2 h per week on the education of surgical residents, excluding routine jobs (Supplementary Table 2 ).
Most helpful educational category for the training of surgical residents.
Of the four different educational categories, clinical education was regarded as the most helpful educational course for surgical residents by all groups. A marginal majority of professors (by a slight margin) regarded the ILT course as the most helpful to education. While fellows selected clinical education and SPL as the most and least helpful courses, surgical residents identified hands-on training and SPL as the most and least helpful courses, respectively (Fig. 1 ).

Importance ratings of four major educational categories for surgical residency training indicate that clinical education was considered the most important (*) curriculum overall. However, each group, including professors, fellows, and residents, judged different curricula to be the most important
Top three important educational curricula for surgical residents
The identification of the three most important curricula among the 15 training courses covered in the four categories was performed by way of a featured survey question. As shown in Table 2 , each group selected attending scrubs as the most important program among the three most important courses.
Importance of training courses in the ILT category for the training of surgical residents
All the surgeons selected general lectures by professors as the most important curriculum in the ILT category for the training of surgical residents. Notably, fellows and residents considered this curriculum the most important course to a greater extent than professors did. By contrast, professors and residents considered residents’ participation in regular in-hospital conferences the least important in resident training, whereas fellows considered the Surgical Grand Rounds as less important than other curricula (Fig. 2 ).
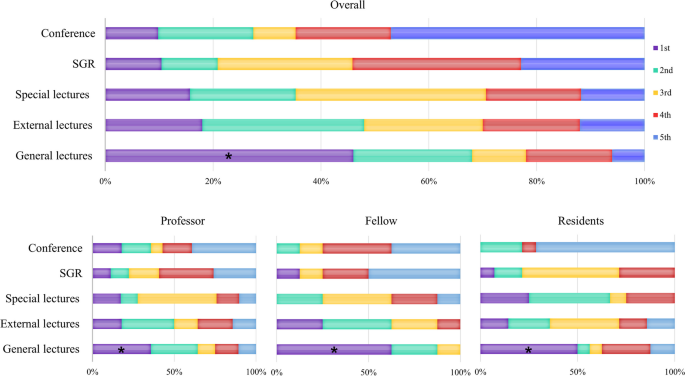
Importance ratings of instructor-led training (ILT) courses for surgical residency training indicate that general lectures were considered the most important (*) part of the curriculum overall. All groups consistently judged general lectures to be the most important educational program
Importance of the training course in the clinical education category of surgical residents’ training.
All groups responded that attending scrubs was the most important training method in clinical education. While the professor and resident groups ranked attending inpatient and outpatient clinics as second and third in importance, respectively, the fellow group rated the clinics with a similar degree of importance in clinical education (Fig. 3 ).
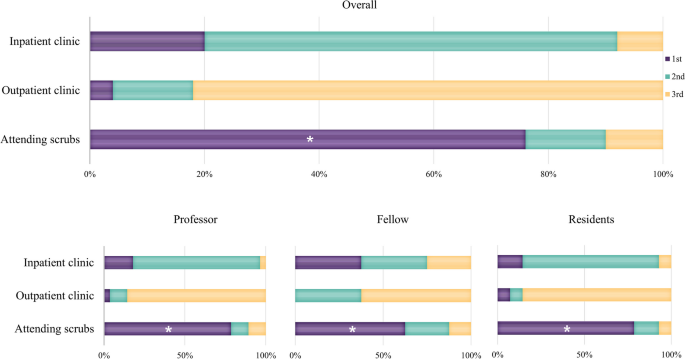
Importance ratings of courses within the clinical education category for surgical resident training indicate that attending scrubs are considered the most important, both overall and by each group
Importance of the training course in the SPL category for the training of surgical residents
All groups considered the regular journal club the most important training course in the SPL category. While the professor and fellow groups considered the manual for surgical residents less important than other curricula, residents regarded it as the third-most important course. Surgical residents considered collecting data and writing articles the least important (Fig. 4 ).
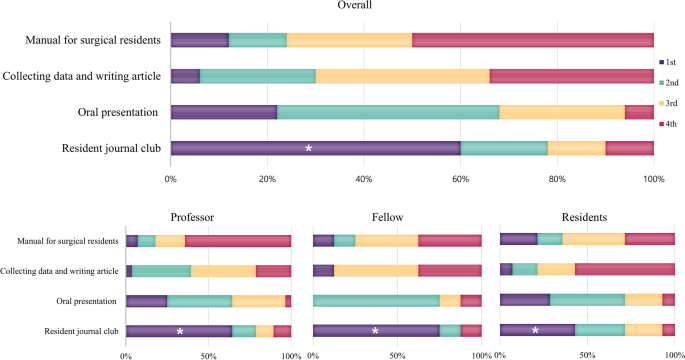
Importance ratings of self-paced learning (SPL) courses for surgical residency training indicate that resident journal club was considered the most important (*) part of the curriculum overall. And all groups consistently judged resident journal club to be the most important educational program
Importance of the training course in the hands-on training category for surgical residents’ training
In the hands-on category, the dry-lab laparoscopy training module within the hospital was deemed by professors as the most important training course for surgical residents, whereas the laparoscopic training module in the professional education center with animal models was perceived as most important by fellows and residents (Fig. 5 ).
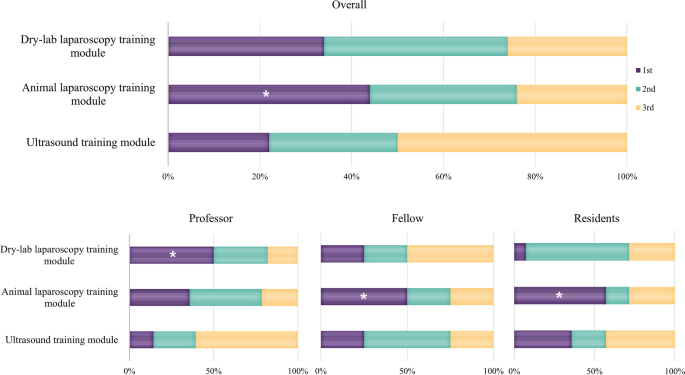
Importance rating of courses within the hands-on training category for the training of surgical residents. While the professor group judged that dry lab laparoscopy training module was the most important (*), the fellow and resident groups judged the animal laparoscopy training module to be more important
This study revealed that trainers and trainees differ in their criteria for evaluating the importance of educational components, with surgical residents particularly interested in hands-on training. Halsted emphasized the significance of clinical and practical training in the education of American surgeons [ 21 ]. Similarly, current GS professors and residents place a high value on practical and technical education. However, stringent ethical standards present challenges for residents practicing directly on cadavers or patients [ 22 , 23 , 24 , 25 , 26 ]. Consequently, professors typically offer thorough theoretical training before introducing practical skills to mitigate potential complications. The contemporary environment is causing divergent approaches between trainers and trainees. If an education system that closely simulates human conditions is developed, and a system where trainees can freely receive education within ethical boundaries is established, it could become the most efficient approach to education.
A series of educational courses must be provided to medical students, interns, residents, and fellows to ensure medical specialists’ optimal training. Although these training courses may be delivered at various levels depending on the knowledge and needs of trainees, instructors have predominantly solely developed the ILT curriculum. However, the actual effectiveness of training courses may differ from the instructors’ expectations; furthermore, considering the satisfaction of the trainees while planning the courses could improve the learning experience [ 12 , 13 , 27 ].
When designing curricula, it is crucial to consider that surgical residents apply for residencies because they are interested in surgery and are aspired to be surgeons. Some professors focus on teaching academic theory, while others contend that mastering the art of thesis writing is the most critical aspect of education. Nonetheless, the most basic desire of surgeons must be considered. In our current study, we found that the opinions of professors, fellows, and residents regarding the most important training courses for surgical residents were similar.
While the group of professors believed that watching many standardized surgeries is the most important training course needed by surgical residents to participate and assist in surgeries, residents considered having practical operating experience as the most important. Therefore, residents regarded the laparoscopic training module in the professional institute with animal models as the most important curriculum in the training of surgical residents. The responses from the group of fellows, who had completed their residency within the past two years, revealed a trend that intermediates between the views of professors and residents. Given their transitioning status from learners to educators, their opinions are considered very important. In fact, these opinions represented a compromise between the perspectives of professors and residents in their roles as educators.
Each of the different learning methodologies of ILT and SPL has advantages and disadvantages [ 15 , 16 , 17 ]. ILT offers detailed materials and immediate feedback but is limited by structured schedules and instructor variability. SPL allows flexibility in timing and location with the use of open-source materials, enabling repeated review of content, though it lacks the immediate feedback of ILT and may require more time for comprehension. Ultimately, trainees benefit most from actively engaging with the educational material and their learning process.
Although this study focused on resident education, only 14 residents were actually included which is a limitation of this study. However, unfortunately, this is the real-world situation in South Korea. Many doctors are avoiding essential medical services, such as internal medicine, GS, obstetrics and gynecology, and pediatrics. Instead, a majority prefer departments like plastic surgery, ophthalmology, and dermatology, which focus on cosmetic procedures or enhancing the quality of life. This is the reason why, despite being a fairly large-scale national university hospital, the number of residents was small. This situation underlines the importance of further improving the quality of education.
The responses in this study can help standardize the appropriate educational programs for surgical residents in GS departments. Based on these research findings, the authors' institution has decided to enhance technical education with theoretical support. It is currently developing and implementing education on ultrasound and biopsy techniques, laparoscopic bowel anastomosis, and robotic surgery. We established close cooperation with other departments so that in addition to surgical skills training, we could directly experience and learn other departments' techniques (intubation, ventilator manipulation, CPR, and so on.). Various colleagues and companies are supporting this training, viewing it as an investment in the future generation of surgeons. As demonstrated in the authors' study, it is necessary to verify and evaluate the educational programs of each institution for their rationality and efficiency. This approach will contribute to the training of better surgeons by enabling residents to engage more actively in the curriculum.
The educational impact of training materials and methods can be maximized when surgical residents engage in the preferred training resources that provide them with satisfaction. Therefore, the best educational training course for surgical residents would include providing them with many opportunities to operate and perform surgical procedures themselves. Although written materials and theories remain important, the effect of education is enhanced when the surgical residents’ satisfaction is increased through the provision of practical learning opportunities.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, JHJ, upon reasonable request.
Institute of Medicine (US) Committee on Optimizing Graduate Medical Trainee (Resident) Hours and Work Schedule to Improve Patient Safety. Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. Edited by Ulmer C, Miller Wolman D, Johns MME. Washington (DC): National Academies Press (US); 2009.
Kling SM, Raman S, Taylor GA, Philp MM, Poggio JL, Dauer ED, Oresanya LB, Ross HM, Kuo LE. Trends in general surgery resident experience with colorectal surgery: an analysis of the accreditation council for graduate medical education case logs. J Surg Educ. 2022;79(3):632–42.
Article Google Scholar
Ahn JS, Cho S, Park WJ. Changes in the health indicators of hospital medical residents during the four-year training period in Korea. J Korean Med Sci. 2022;37(25):e202.
Are C, Stoddard H, Carpenter LA, O’Holleran B, Thompson JS. Trends in the match rate and composition of candidates matching into categorical general surgery residency positions in the United States. Am J Surg. 2017;213(1):187–94.
Tracy TF Jr. Surgical fatigue-what dreams may come: comment on “surgeon fatigue.” Arch Surg. 2012;147(5):435–6.
Kiernan M, Civetta J, Bartus C, Walsh S. 24 hours on-call and acute fatigue no longer worsen resident mood under the 80-hour work week regulations. Curr Surg. 2006;63(3):237–41.
McCormick F, Kadzielski J, Landrigan CP, Evans B, Herndon JH, Rubash HE. Surgeon fatigue: a prospective analysis of the incidence, risk, and intervals of predicted fatigue-related impairment in residents. Arch Surg. 2012;147(5):430–5.
Malangoni MA, Biester TW, Jones AT, Klingensmith ME, Lewis FR Jr. Operative experience of surgery residents: trends and challenges. J Surg Educ. 2013;70(6):783–8.
Jarman BT, Cogbill TH, Mathiason MA, O’Heron CT, Foley EF, Martin RF, Weigelt JA, Brasel KJ, Webb TP. Factors correlated with surgery resident choice to practice general surgery in a rural area. J Surg Educ. 2009;66(6):319–24.
Cyr-Taro AE, Kotwall CA, Menon RP, Hamann MS, Nakayama DK. Employment and satisfaction trends among general surgery residents from a community hospital. J Surg Educ. 2008;65(1):43–9.
Rasmussen JM, Najarian MM, Ties JS, Borgert AJ, Kallies KJ, Jarman BT. Career satisfaction, gender bias, and work-life balance: a contemporary assessment of general surgeons. J Surg Educ. 2021;78(1):119–25.
Hou J, He Y, Zhao X, Thai J, Fan M, Feng Y, Huang L. The effects of job satisfaction and psychological resilience on job performance among residents of the standardized residency training: a nationwide study in China. Psychol Health Med. 2020;25(9):1106–18.
Waltz LA, Muñoz L, Weber Johnson H, Rodriguez T. Exploring job satisfaction and workplace engagement in millennial nurses. J Nurs Manag. 2020;28(3):673–81.
Chen BY, Kern DE, Kearns RM, Thomas PA, Hughes MT, Tackett S. From modules to MOOCs: application of the six-step approach to online curriculum development for medical education. Acad Med. 2019;94(5):678–85.
Vestergaard LD, Løfgren B, Jessen CL, Petersen CB, Wolff A, Nielsen HV, Krarup NH. A comparison of pediatric basic life support self-led and instructor-led training among nurses. Eur J Emerg Med. 2017;24(1):60–6.
Bylow H, Karlsson T, Claesson A, Lepp M, Lindqvist J, Herlitz J. Supplementary dataset to self-learning training compared with instructor-led training in basic life support. Data Brief. 2019;25:104064.
Bylow H, Karlsson T, Claesson A, Lepp M, Lindqvist J, Herlitz J. Self-learning training versus instructor-led training for basic life support: a cluster randomised trial. Resuscitation. 2019;139:122–32.
Hildebrandt GH, Belmont MA. Self-paced versus instructor-paced preclinical training in operative dentistry: a case study. J Dent Educ. 2018;82(11):1178–84.
Dhaliwal N, Simpson F, Kim-Sing A. Self-paced online learning modules for pharmacy practice educators: Development and preliminary evaluation. Curr Pharm Teach Learn. 2018;10(7):964–74.
Bengio Y, Courville A, Vincent P. Representation learning: a review and new perspectives. IEEE Trans Pattern Anal Mach Intell. 2013;35(8):1798–828.
Halsted WS. The Training of the Surgeon. Bulletin of the John Hopkins Hospital. 1904;15:267–75.
Google Scholar
Hoffman BD. Using self-determination theory to improve residency training: learning to make omelets without breaking eggs. Acad Med. 2015;90(4):408–10.
Nguyen VT, Losee JE. Time- versus competency-based residency training. Plast Reconstr Surg. 2016;138(2):527–31.
Cabar FR, Lacerda DCR, de Freitas GTS, Gorga ML. The need to standardize use of the newly deceased in medical trainings. Clinics (Sao Paulo). 2020;75:e2391.
Saber M, Enjoo SA, Mahboudi A, Tabei SZ. Using newly deceased patients in teaching clinical skills: its ethical and educational challenges. J Adv Med Educ Prof. 2018;6(2):78–85.
Rajagopal AS, Champney TH. Teaching without harm: the ethics of performing posthumous procedures on the newly deceased. Cureus. 2020;12(12):e11855.
Huang L, Caspari JH, Sun X, Thai J, Li Y, Chen FZ, Zhao XD. Risk and protective factors for burnout among physicians from standardized residency training programs in Shanghai: a cross-sectional study. BMC Health Serv Res. 2020;20(1):965.
Download references
Acknowledgements
The authors thank to Byeongju Kang, Byunghyuk Yu, Deokbi Hwang, Gyu-Seog Choi, Ho Yong Park, Ho Young Chung, Hye Jin Kim, Hyung Kee Kim, Ji Yeon Park, Jin Ho Chung, Jin Young Park, Jun Seok Park, Ki Bum Park, Kyoung Hoon Lim, Oh Kyoung Kwon, Sang Geol Kim, Seung Huh, Seung Soo Lee, Seung Ho Song, Sung-Min Lee, Wan Wook Kim, Woo Sung Yun, Yang Soo Lim, Yoon Jin Hwang, Dong-hee Na, Heejung Keum, Hui je Jeong, Hyeon Ju Kim, Jae Yeong Yang, Min Hye Jeong, Sue hyun Park, Young Hye Kim, Eunji Kim, Gunwoo Kim, Gyoyeong Chu, Hakyung Yoon, Hannah Kim, Hoyeon Kwon, Hyunjae Kang, Jeong Eon Suh, Ji Hyun Jung, Junhyun Park, Seokhyun Wi, Sujin Kang, Suyeong Hwang, Taewan Ku, all of whom participated in the survey of this study.
Not applicable.
Author information
Jeeyeon Lee and Hyung Jun Kwon contributed equally to this work.
Authors and Affiliations
Department of Surgery, Kyungpook National University Chilgok Hospital, Hoguk-Ro 807, Buk-Gu, 41404, Daegu, Republic of Korea
Jeeyeon Lee, Hyung Jun Kwon, Soo Yeon Park & Jin Hyang Jung
You can also search for this author in PubMed Google Scholar
Contributions
Guarantor of the integrity of the study: JL, Study concept: JL, JHJ, Study design: JL, JHJ, Definition of intellectual content: JL, SYP, HJK, Literature research: SYP, HJK, Data acquisition: JL, JHJ, HJK, Data analysis: JL, SYP, Manuscript preparation: JL, JHJ, Manuscript review: JHJ, Manuscript editing: JHJ, JL. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Jin Hyang Jung .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Institutional Review Board Committee of Kyungpook National University Chilgok Hospital, Daegu, Republic of Korea (KNUCH 2022–07-024–001). Informed consent was obtained from all subjects.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lee, J., Kwon, H.J., Park, S.Y. et al. Importance of multimodal resident education curriculum for general surgeons: perspectives of trainers and trainees. BMC Med Educ 24 , 518 (2024). https://doi.org/10.1186/s12909-024-05515-x
Download citation
Received : 08 October 2023
Accepted : 03 May 2024
Published : 10 May 2024
DOI : https://doi.org/10.1186/s12909-024-05515-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- History, Facts & Figures
- YSM Dean & Deputy Deans
- YSM Administration
- Department Chairs
- YSM Executive Group
- YSM Board of Permanent Officers
- FAC Documents
- Current FAC Members
- Appointments & Promotions Committees
- Ad Hoc Committees and Working Groups
- Chair Searches
- Leadership Searches
- Organization Charts
- Faculty Demographic Data
- Professionalism Reporting Data
- 2022 Diversity Engagement Survey
- State of the School Archive
- Faculty Climate Survey: YSM Results
- Strategic Planning
- Mission Statement & Process
- Beyond Sterling Hall
- COVID-19 Series Workshops
- Previous Workshops
- Departments & Centers
- Find People
- Biomedical Data Science
- Health Equity
- Inflammation
- Neuroscience
- Global Health
- Diabetes and Metabolism
- Policies & Procedures
- Media Relations
- A to Z YSM Lab Websites
- A-Z Faculty List
- A-Z Staff List
- A to Z Abbreviations
- Dept. Diversity Vice Chairs & Champions
- Dean’s Advisory Council on Lesbian, Gay, Bisexual, Transgender, Queer and Intersex Affairs Website
- Minority Organization for Retention and Expansion Website
- Office for Women in Medicine and Science
- Committee on the Status of Women in Medicine Website
- Director of Scientist Diversity and Inclusion
- Diversity Supplements
- Frequently Asked Questions
- Recruitment
- By Department & Program
- News & Events
- Executive Committee
- Aperture: Women in Medicine
- Self-Reflection
- Portraits of Strength
- Mindful: Mental Health Through Art
- Event Photo Galleries
- Additional Support
- MD-PhD Program
- PA Online Program
- Joint MD Programs
- How to Apply
- Advanced Health Sciences Research
- Clinical Informatics & Data Science
- Clinical Investigation
- Medical Education
- Visiting Student Programs
- Special Programs & Student Opportunities
- Residency & Fellowship Programs
- Center for Med Ed
- Organizational Chart
- Leadership & Staff
- Committee Procedural Info (Login Required)
- Faculty Affairs Department Teams
- Recent Appointments & Promotions
- Academic Clinician Track
- Clinician Educator-Scholar Track
- Clinican-Scientist Track
- Investigator Track
- Traditional Track
- Research Ranks
- Instructor/Lecturer
- Social Work Ranks
- Voluntary Ranks
- Adjunct Ranks
- Other Appt Types
- Appointments
- Reappointments
- Transfer of Track
- Term Extensions
- Timeline for A&P Processes
- Interfolio Faculty Search
- Interfolio A&P Processes
- Yale CV Part 1 (CV1)
- Yale CV Part 2 (CV2)
- Samples of Scholarship
- Teaching Evaluations
- Letters of Evaluation
- Dept A&P Narrative
- A&P Voting
- Faculty Affairs Staff Pages
- OAPD Faculty Workshops
- Leadership & Development Seminars
- List of Faculty Mentors
- Incoming Faculty Orientation
- Faculty Onboarding
- Past YSM Award Recipients
- Past PA Award Recipients
- Past YM Award Recipients
- International Award Recipients
- Nominations Calendar
- OAPD Newsletter
- Fostering a Shared Vision of Professionalism
- Academic Integrity
- Addressing Professionalism Concerns
- Consultation Support for Chairs & Section Chiefs
- Policies & Codes of Conduct
- First Fridays
- Fund for Physician-Scientist Mentorship
- Grant Library
- Grant Writing Course
- Mock Study Section
- Research Paper Writing
- Establishing a Thriving Research Program
- Funding Opportunities
- Join Our Voluntary Faculty
- Child Mental Health: Fostering Wellness in Children
- Faculty Resources
- Research by Keyword
- Research by Department
- Research by Global Location
- Translational Research
- Research Cores & Services
- Program for the Promotion of Interdisciplinary Team Science (POINTS)
- CEnR Steering Committee
- Experiential Learning Subcommittee
- Goals & Objectives
- Issues List
- Print Magazine PDFs
- Print Newsletter PDFs
- YSM Events Newsletter
- Social Media
- Patient Care
INFORMATION FOR
- Residents & Fellows
- Researchers
Building Capacity in Medical Students to Care for Transgender and Gender Diverse Patients
Part of the team who led the initiative.
A small group of Yale medical and public health students collaborated with faculty mentors to develop a clinical skills-based simulation session on caring for transgender and gender diverse patients, in which all MD students will participate in during their clinical year.
The initiative began in May 2022. As Yale School of Medicine (YSM) MD student Bassel Shanab explains, students were graduating “feeling uncomfortable in their ability to provide care to transgender and nonbinary patients.” Although, he says, there were pre-clinical lectures on the physiology of hormones in hormone replacement therapy, the negative and damaging effects of gender dysphoria, and societal discrimination, “we lacked the in-person clinical instruction that would ensure students can confidently serve such a marginalized group of patients."
MD student Ryan Bahar, who was involved with the initiative, adds, “Transgender and gender diverse (TGD) individuals experience alarming health disparities compared to their cisgender counterparts. While there are many reasons for this unacceptable status quo, from lack of insurance to outright discrimination, one is particularly important to grapple with in medical education: students are not sufficiently trained to provide adequate health care to TGD individuals.”
A group of students at YSM—led by MD-PhD student Kyle Gavulic—made developing curriculum to fill this gap a priority in the wake of various state-mandated restrictions on gender-affirming care. The students connected with Assistant Professor of Pediatrics Meredithe McNamara, MD, MS, and MD student Christine Lepore, who were working on evidence-based medico-legal responses to some of these bans. This led to brainstorming about enhancing YSM’s curriculum.
Creating curricular content
The group brought in John Encandela, PhD, executive director of evaluation & assessment, Center for Medical Education; Jaideep Talwalkar, MD, assistant dean for education and director of clinical skills; Beverley Sheares, MD, MS, Health Equity Thread (HET) leader; and Douglas Shenson, MD, MPH, MA, MS, HET deputy leader. The students completed a literature review of existing medical education curricula on gender-affirming care across the country, as well as a needs assessment of the YSM curricula, and developed a proposal for a "meta" curriculum, unique to YSM’s teaching model but derived from two validated curricula, on clinical skills in caring for transgender and gender diverse patients.
The group piloted the curriculum in January 2023, in partnership with HAVEN Free Clinic, training 13 medical, nursing, and PA student volunteers. The pilot demonstrated the curriculum was effective. (The project team presented their findings on a poster at YSM’s Medical Education Day in 2023.)
The conversation then shifted to where this training would fit best in the curriculum and which students would receive it. It was decided that all MD and MD-PhD clerkship students would participate during a precede, which is the orientation before each clerkship rotation. The first 40 MD students participated in the training in March 2024, and it received excellent reviews. The remaining students will participate later this year. Assuming the feedback remains positive, the training will become a permanent part of the precede curriculum.
Recruiting simulated participants
Simulated participants (SPs) are an important component of the training. Gavulic explains, “Our goal was to recruit from the local transgender and gender diverse community so that our actors possessed the lived experiences of the patient population we were aiming to empower health professional students to better care for.” Jillian Celentano, LMSW, an SP and a mentor and advocate for the trans community, “has been a very close and absolutely critical partner in this work,” Gavulic adds. “We really couldn't have pulled this off without her.” Celentano recruited all the volunteers for the pilot and was a key player in the recruitment effort to hire enough SPs to train all medical students, which was led by Barbara Hildebrand, BFA, assistant director of the Simulated Participant Program.
Hildebrand explains they were seeking individuals “to embody fictional patients with specific gender journeys authentically. This requires staying in character, adhering to case details, providing feedback, and repeating the portrayal multiple times within a two-hour workshop.”
Leveraging YSM’s existing SP community, which included eight people who identified as transgender or gender diverse, Hildebrand embarked on an innovative recruitment strategy, which resulted in six new SPs. Partnering with Program Coordinator A Gould, they created trans-friendly recruiting posters, and Hildebrand forged partnerships with local colleges and universities through their DEI offices. Hildebrand calls Gavulic and Celentano “invaluable” partners, who were “referring applicants and connecting me with gender affirming health care practices in CT to share the job posting.”
Celentano expects most new recruits will continue as SPs “because they realize the impact they are having,” and explains, “We are petrified to go to a new medical provider. We know there is a big gap with providers who are trained to engage with gender diverse patients.”
"It is immensely gratifying for our SP Program to play a pivotal role in delivering cutting-edge curriculum to our medical students,” says Hildebrand. She adds that the SPs’ “willingness to be vulnerable creates a safe environment for students to learn and practice essential skills, ultimately shaping them into compassionate health care providers for transgender and gender diverse patients. I am incredibly proud of the SPs’ courage and the profound impact they have on our educational mission."
Encandela says he is “certain that this workshop would not exist without the steady and patient efforts of a small group of students dedicated to making this happen. They saw the gap in the curriculum; did the necessary groundwork to identify necessary resources; conducted a proof-of-concept pilot; and worked with faculty and administrative leaders in getting the workshop into the regular clerkship curriculum.” He credits Gavulic for “spearheading the effort and remaining steadfast through the process of development to implementation.”
Reflecting on the initiative, Gavulic says, it “not only tremendously advanced YSM's undergraduate medical education on trans health care, but also promises to nourish generations of graduating YSM students in feeling competent enough to provide the same quality of care to the trans and gender diverse community and to counter the spread of disinformation. This dual-pronged aim is truly what this is all about so that trans and gender diverse patients can feel safe and affirmed while seeking health care.”
Echoing these points, McNamara notes, “Trans and gender-expansive people are more visible than ever and the evidence regarding the benefits of gender-affirming care has never been stronger.” Therefore, she continues, “this is a natural time to make sure that emerging physicians are fully equipped with clinical skills to provide welcoming, evidence-based and comprehensive care to gender diverse people.” Additionally, McNamara is concerned that “the misinformation climate regarding gender-affirming care is quite virulent now,” leading to policies that restrict access to care for trans and gender-expansive people. The medical community, she says, “including emerging physicians, are powerful and credible messengers who can dispel myths and protect marginalized people.”
In addition to those mentioned in the article, the project team would like to acknowledge MD student Shamik Bhat and MPH student Sujana Nelakanti for their invaluable contributions in developing and implementing the curriculum; Manager of Clinical Medical Education Programs Gina Franco and Clerkship Director Shefali Pathy, MD, MPH, for their unwavering support in implementing this into the Clerkship curriculum; and all the faculty champions for their expertise and generosity of their time to make this a success, including Anika Anam, MD, Iman Berrahou, MD, Susan Boulware, MD, Diane Bruessow, MPAS, PA-C, Joseph Canarie, MD, Mukta Dhond, MD, Barbara Gulanski, MD, MPH, Allister Hirschmann, PA-C, Nathan Levitt, FNP-BC, MSN, RN, MA, Nicolas Meade, PsyD, Christy Olezeski, PhD, Allura Ralston, PhD, Jenn Suski, APRN, and Tristan Marvin Uy, MD, MPH.
- Diversity and Inclusion
Featured in this article
- Anika K. Anam, MD
- Iman Berrahou, MD
- Shamik Bhat
- Susan D. Boulware, MD
- Diane Bruessow, MPAS, PA-C, DFAAPA
- Joseph Canarie, MD
- Mukta Dhond, MD
- John Encandela, PhD
- Gina Franco
- Kyle Gavulic
- Barbara Gulanski, MD, MPH
- Barbara Hildebrand, BFA
- Allister Hirschman, PA
- Nathan Levitt
- Meredithe McNamara, MD, MS, FAAP
- Nicolas Meade, PsyD
- Christy Olezeski, PhD
- Shefali Pathy, MD, MPH
- Allura Ralston
- Bassel Shanab
- Beverley Sheares, MD, MS
- Douglas Shenson, MD, MPH, MA, MS
- Jennifer Suski
- Jaideep S. Talwalkar, MD
- Tristan Marvin Uy

COMMENTS
High-Impact, Evidence-Based Education for Health Care ProfessionalsTo successfully train the next generation of health care professionals, medical educators must utilize innovative teaching strategies and techniques in both classroom and clinical settings. Training to Teach in Medicine is a six-month online certificate program taught by distinguished Harvard Medical School faculty for ...
Training to Teach in Medicine. This Harvard Medical School six-month, application-based certificate program aims to provide high-impact, evidence-based education for medical faculty and health care professionals. Learn More. November 7, 2024 - June 1, 2025. $7,900 - $8,900.
Make the AAMC your medical education home. Explore what we have to offer, from learning events, trainings, and professional development conferences to programs, initiatives, and scholarship on key and emerging topics. Get involved, advance your career, and help move the field of medical education forward.
A variety of medical education courses are also available, ranging from short focused training programmes that aim to provide doctors with the fundamentals of teaching to courses leading to a formal teaching qualification such as a certificate, diploma, or masters in medical education. Several of these can be undertaken through distance learning.
Training to Teach in Medicine develops essential skills while guiding learners in their exploration of modern medical education pedagogy and innovative teaching techniques. Our scholars, both early-career and seasoned educators, will enhance their knowledge of medical education. This blended-learning approach includes self-paced online lectures, interactive live webinars, focused symposia ...
Education is constant - from being the student to the teacher, medical professionals are ever present in the cycle of learning. With this course developed by the Stanford Faculty Development Center for Medical Teachers, you'll be able to establish a positive learning environment to reach a broad range of learners, in different settings, on different subject topics.
The Master of Medical Sciences in Medical Education is a two-year program with two primary goals: To give students a solid foundation in the theories and principles underpinning health professions education, such as the science of learning, strategies of curriculum development and education design, adult learning theories, integration of ...
The Medical Education (Med Ed) master's program is a unique collaboration between physician educators and education experts. We provide a comprehensive, innovative curriculum designed for physicians and other healthcare professionals who want to pursue master-level training, evidence-based education, educational scholarship, and educational ...
Make coaching an integral part of your physician training with practical resources from the AMA's handbook for learners. The webinar, "The AMA and medical education: How did we get here, and where are we going?," was produced by the AMA Accelerating Change in Medical Education initiative and featured speakers from the AMA's senior medical ...
Why you would like to be considered for the Training to Teach in Medicine program; An overview of your medical education and teaching experience(s) How this program will impact your career or professional development; Letter of recommendation: The recommender must be a department/division head/director/chair or supervisor. The letter should be ...
The part-time MSc in Medical Education will be offered jointly by the Department of Education in the Social Sciences Division and the Medical School in the Medical Sciences Division, with formal responsibility for the programme resting with the Department of Education. Interdisciplinarity is endemic in education and medicine, and team-teaching ...
Harvard Medical School. The mission of the Master of Medical Science in Medical Education is to give those who already excel in one of the health sciences disciplines an opportunity to turn their specialized knowledge and skill towards the advancement of health professions education. Through research, skill building, and innovation, this master ...
The Jackson Memorial Hospital (MJMH) complex in Miami, Florida, which serves as the primary teaching hospital for the Leonard M. Miller School of Medicine ((UMMSM) within the University of Miami (UM), is pictured in July 2010.. Medical education in the United States includes educational activities involved in the education and training of physicians in the country, with the overall process ...
In graduate medical education, there are five performance levels for each competency: novice, advanced beginner, competent individual, proficient individual, and expert physician. The Next Goal The Core Competencies are now the basic language for defining physician competence and are also the principles used in the training of physicians.
Teaching with real patients in the clinical setting lies at the heart of health professional education, providing an essential component to clinical training. This is true of all the health disciplines - particularly medicine, nursing, dentistry, physiotherapy, and dietetics. Clinical tutorials orientate students to the culture and social aspects of the healthcare environment, and shape ...
Medical Education and Training. Explore the latest in medical education and training, new educational approaches and technologies, CME, work duty hours, and more. This cross-sectional study examines state- and county-level patterns related to the training and availability of Black physicians using data from the first edition of the American ...
69 Altmetric. Metrics. As innovations in the biotechnology sector continue to proliferate, the traditional education of medical students, residents and fellows will need to change to incorporate ...
The education of a physician has developed to encompass pre-medical preparation, a course of study in a medical school which is typically a major component of an academic medical center (AHC), and medical specialty training in residency and fellowship programs, UME and GME, respectively [5, 6]. This education provides the basis for a ...
Training Programs. Cleveland Clinic offers training programs in internal/family medicine and a variety of specialties - and in several locations in Cleveland as well as in Florida. Call 216.444.5690. Request Training Verification.
The Spectrum of Healthcare Simulation (HS) in Medical Education. Gaba described 11 dimensions of the application of simulation in medical education. 14 Dimension 8 categorizes simulation technology based on complexity. 14 The five components of that dimension are role playing, standardized patients (SP), part-task trainers, the computer patient, and the electronic patient/virtual reality (VR ...
Purpose Artificial Intelligence (AI) is transforming healthcare and shows considerable promise for the delivery of medical education. This systematic review provides a comprehensive analysis of the global situation, effects, and challenges associated with applying AI at the different stages of medical education. Methods This review followed the PRISMA guidelines, and retrieved studies ...
Discover the many ways you can earn continuing medical education (CME) online and further your education in the medical field. American Medical Association members have the opportunity to explore free CME for physicians across various disciplines. Learn more about the online learning resources and free CME online for physicians with the AMA.
Current pre-med students are excited to have improved medical training right in their own community. The $300 million dollar is being funded by a combination of state general fund appropriations ...
Efforts to advance health equity in medical education have ranged from implicit-bias training to supplementary curricula in structural competency, cultural humility, and antiracism. 10-12 ...
Addressing the Lack of Legal Training in Medical Education. The Training to Teach in Medicine program provided Ferrada with a platform to channel her passion for education into actionable initiatives. Her capstone project focused on creating a court-based educational program on compliance with legal and ethical obligations following a patient ...
Continuous, lifelong medical education should be provided because it is essential to training qualified specialists in every medical field . Educational periods may be categorized as medical college, postgraduate, and specialist education. The residency training program is the most important part of postgraduate education.
The group piloted the curriculum in January 2023, in partnership with HAVEN Free Clinic, training 13 medical, nursing, and PA student volunteers. The pilot demonstrated the curriculum was effective. (The project team presented their findings on a poster at YSM's Medical Education Day in 2023.)
The fellows will participate in a curriculum to ensure a full education regarding the regulatory and financial aspects of serving as a Hospice Medical Director and a physician in long-term care. The fellows will be able to tailor their experience to provide more of one setting, as well as longitudinal care for specific patients, if they wish to ...