

Nursing: How to Write a Literature Review
- Traditional or Narrative Literature Review
Getting started
1. start with your research question, 2. search the literature, 3. read & evaluate, 4. finalize results, 5. write & revise, brainfuse online tutoring and writing review.
- RESEARCH HELP
The best way to approach your literature review is to break it down into steps. Remember, research is an iterative process, not a linear one. You will revisit steps and revise along the way. Get started with the handout, information, and tips from various university Writing Centers below that provides an excellent overview. Then move on to the specific steps recommended on this page.
- UNC- Chapel Hill Writing Center Literature Review Handout, from the University of North Carolina at Chapel Hill.
- University of Wisconsin-Madison Writing Center Learn how to write a review of literature, from the University of Wisconsin-Madison.
- University of Toronto-- Writing Advice The Literature Review: A few tips on conducting it, from the University of Toronto.
- Begin with a topic.
- Understand the topic.
- Familiarize yourself with the terminology. Note what words are being used and keep track of these for use as database search keywords.
- See what research has been done on this topic before you commit to the topic. Review articles can be helpful to understand what research has been done .
- Develop your research question. (see handout below)
- How comprehensive should it be?
- Is it for a course assignment or a dissertation?
- How many years should it cover?
- Developing a good nursing research question Handout. Reviews PICO method and provides search tips.
Your next step is to construct a search strategy and then locate & retrieve articles.
- There are often 2-4 key concepts in a research question.
- Search for primary sources (original research articles.)
- These are based on the key concepts in your research question.
- Remember to consider synonyms and related terms.
- Which databases to search?
- What limiters should be applied (peer-reviewed, publication date, geographic location, etc.)?
Review articles (secondary sources)
Use to identify literature on your topic, the way you would use a bibliography. Then locate and retrieve the original studies discussed in the review article. Review articles are considered secondary sources.
- Once you have some relevant articles, review reference lists to see if there are any useful articles.
- Which articles were written later and have cited some of your useful articles? Are these, in turn, articles that will be useful to you?
- Keep track of what terms you used and what databases you searched.
- Use database tools such as save search history in EBSCO to help.
- Keep track of the citations for the articles you will be using in your literature review.
- Use RefWorks or another method of tracking this information.
- Database Search Strategy Worksheet Handout. How to construct a search.
- TUTORIAL: How to do a search based on your research question This is a self-paced, interactive tutorial that reviews how to construct and perform a database search in CINAHL.
The next step is to read, review, and understand the articles.
- Start by reviewing abstracts.
- Make sure you are selecting primary sources (original research articles).
- Note any keywords authors report using when searching for prior studies.
- You will need to evaluate and critique them and write a synthesis related to your research question.
- Consider using a matrix to organize and compare and contrast the articles .
- Which authors are conducting research in this area? Search by author.
- Are there certain authors’ whose work is cited in many of your articles? Did they write an early, seminal article that is often cited?
- Searching is a cyclical process where you will run searches, review results, modify searches, run again, review again, etc.
- Critique articles. Keep or exclude based on whether they are relevant to your research question.
- When you have done a thorough search using several databases plus Google Scholar, using appropriate keywords or subject terms, plus author’s names, and you begin to find the same articles over and over.
- Remember to consider the scope of your project and the length of your paper. A dissertation will have a more exhaustive literature review than an 8 page paper, for example.
- What are common findings among each group or where do they disagree?
- Identify common themes. Identify controversial or problematic areas in the research.
- Use your matrix to organize this.
- Once you have read and re-read your articles and organized your findings, you are ready to begin the process of writing the literature review.
2. Synthesize. (see handout below)
- Include a synthesis of the articles you have chosen for your literature review.
- A literature review is NOT a list or a summary of what has been written on a particular topic.
- It analyzes the articles in terms of how they relate to your research question.
- While reading, look for similarities and differences (compare and contrast) among the articles. You will create your synthesis from this.
- Synthesis Examples Handout. Sample excerpts that illustrate synthesis.
Regis Online students have access to Brainfuse. Brainfuse is an online tutoring service available through a link in Moodle. Meet with a tutor in a live session or submit your paper for review.
- Brainfuse Tutoring and Writing Assistance for Regis Online Students by Tricia Reinhart Last Updated Oct 26, 2023 81 views this year
- << Previous: Traditional or Narrative Literature Review
- Next: eBooks >>
- Last Updated: Feb 21, 2024 12:05 PM
- URL: https://libguides.regiscollege.edu/nursing_litreview
Nursing: Literature Review
- Required Texts
- Writing Assistance and Organizing & Citing References
- NCLEX Resources
- Literature Review
- MSN Students
- Physical Examination
- Drug Information
- Professional Organizations
- Mobile Apps
- Evidence-based Medicine
- Certifications
- Recommended Nursing Textbooks
- DNP Students
- Conducting Research
- Scoping Reviews
- Systematic Reviews
- Distance Education Students
- Ordering from your Home Library
Good Place to Start: Citation Databases
Interdisciplinary Citation Databases:
A good place to start your research is to search a research citation database to view the scope of literature available on your topic.
TIP #1: SEED ARTICLE Begin your research with a "seed article" - an article that strongly supports your research topic. Then use a citation database to follow the studies published by finding articles which have cited that article, either because they support it or because they disagree with it.
TIP #2: SNOWBALLING Snowballing is the process where researchers will begin with a select number of articles they have identified relevant/strongly supports their topic and then search each articles' references reviewing the studies cited to determine if they are relevant to your research.
BONUS POINTS: This process also helps identify key highly cited authors within a topic to help establish the "experts" in the field.
Begin by constructing a focused research question to help you then convert it into an effective search strategy.
- Identify keywords or synonyms
- Type of study/resources
- Which database(s) to search
- Asking a Good Question (PICO)
- PICO - AHRQ
- PICO - Worksheet
- What Is a PICOT Question?
Seminal Works: Search Key Indexing/Citation Databases
- Google Scholar
- Web of Science
TIP – How to Locate Seminal Works
- DO NOT: Limit by date range or you might overlook the seminal works
- DO: Look at highly cited references (Seminal articles are frequently referred to “cited” in the research)
- DO: Search citation databases like Scopus, Web of Science and Google Scholar
Web Resources
What is a literature review?
A literature review is a comprehensive and up-to-date overview of published information on a subject area. Conducting a literature review demands a careful examination of a body of literature that has been published that helps answer your research question (See PICO). Literature reviewed includes scholarly journals, scholarly books, authoritative databases, primary sources and grey literature.
A literature review attempts to answer the following:
- What is known about the subject?
- What is the chronology of knowledge about my subject?
- Are there any gaps in the literature?
- Is there a consensus/debate on issues?
- Create a clear research question/statement
- Define the scope of the review include limitations (i.e. gender, age, location, nationality...)
- Search existing literature including classic works on your topic and grey literature
- Evaluate results and the evidence (Avoid discounting information that contradicts your research)
- Track and organize references
- How to conduct an effective literature search.
- Social Work Literature Review Guidelines (OWL Purdue Online Writing Lab)
What is PICO?
The PICO model can help you formulate a good clinical question. Sometimes it's referred to as PICO-T, containing an optional 5th factor.
Search Example

- << Previous: NCLEX Resources
- Next: MSN Students >>

- Last Updated: Apr 9, 2024 1:30 PM
- URL: https://guides.himmelfarb.gwu.edu/Nursing

- Himmelfarb Intranet
- Privacy Notice
- Terms of Use
- GW is committed to digital accessibility. If you experience a barrier that affects your ability to access content on this page, let us know via the Accessibility Feedback Form .
- Himmelfarb Health Sciences Library
- 2300 Eye St., NW, Washington, DC 20037
- Phone: (202) 994-2850
- [email protected]
- https://himmelfarb.gwu.edu
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Bashir Y, Conlon KC. Step by step guide to do a systematic review and meta-analysis for medical professionals. Ir J Med Sci. 2018; 187:(2)447-452 https://doi.org/10.1007/s11845-017-1663-3
Bettany-Saltikov J. How to do a systematic literature review in nursing: a step-by-step guide.Maidenhead: Open University Press; 2012
Bowers D, House A, Owens D. Getting started in health research.Oxford: Wiley-Blackwell; 2011
Hierarchies of evidence. 2016. http://cjblunt.com/hierarchies-evidence (accessed 23 July 2019)
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2008; 3:(2)37-41 https://doi.org/10.1191/1478088706qp063oa
Developing a framework for critiquing health research. 2005. https://tinyurl.com/y3nulqms (accessed 22 July 2019)
Cognetti G, Grossi L, Lucon A, Solimini R. Information retrieval for the Cochrane systematic reviews: the case of breast cancer surgery. Ann Ist Super Sanita. 2015; 51:(1)34-39 https://doi.org/10.4415/ANN_15_01_07
Dixon-Woods M, Cavers D, Agarwal S Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006; 6:(1) https://doi.org/10.1186/1471-2288-6-35
Guyatt GH, Sackett DL, Sinclair JC Users' guides to the medical literature IX. A method for grading health care recommendations. JAMA. 1995; 274:(22)1800-1804 https://doi.org/10.1001/jama.1995.03530220066035
Hanley T, Cutts LA. What is a systematic review? Counselling Psychology Review. 2013; 28:(4)3-6
Cochrane handbook for systematic reviews of interventions. Version 5.1.0. 2011. https://handbook-5-1.cochrane.org (accessed 23 July 2019)
Jahan N, Naveed S, Zeshan M, Tahir MA. How to conduct a systematic review: a narrative literature review. Cureus. 2016; 8:(11) https://doi.org/10.7759/cureus.864
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1997; 33:(1)159-174
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 2014; 14:(1) https://doi.org/10.1186/s12913-014-0579-0
Moher D, Liberati A, Tetzlaff J, Altman DG Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6:(7) https://doi.org/10.1371/journal.pmed.1000097
Mueller J, Jay C, Harper S, Davies A, Vega J, Todd C. Web use for symptom appraisal of physical health conditions: a systematic review. J Med Internet Res. 2017; 19:(6) https://doi.org/10.2196/jmir.6755
Murad MH, Asi N, Alsawas M, Alahdab F. New evidence pyramid. Evid Based Med. 2016; 21:(4)125-127 https://doi.org/10.1136/ebmed-2016-110401
National Institute for Health and Care Excellence. Methods for the development of NICE public health guidance. 2012. http://nice.org.uk/process/pmg4 (accessed 22 July 2019)
Sambunjak D, Franic M. Steps in the undertaking of a systematic review in orthopaedic surgery. Int Orthop. 2012; 36:(3)477-484 https://doi.org/10.1007/s00264-011-1460-y
Siddaway AP, Wood AM, Hedges LV. How to do a systematic review: a best practice guide for conducting and reporting narrative reviews, meta-analyses, and meta-syntheses. Annu Rev Psychol. 2019; 70:747-770 https://doi.org/0.1146/annurev-psych-010418-102803
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008; 8:(1) https://doi.org/10.1186/1471-2288-8-45
Wallace J, Nwosu B, Clarke M. Barriers to the uptake of evidence from systematic reviews and meta-analyses: a systematic review of decision makers' perceptions. BMJ Open. 2012; 2:(5) https://doi.org/10.1136/bmjopen-2012-001220
Carrying out systematic literature reviews: an introduction
Alan Davies
Lecturer in Health Data Science, School of Health Sciences, University of Manchester, Manchester
View articles · Email Alan
Systematic reviews provide a synthesis of evidence for a specific topic of interest, summarising the results of multiple studies to aid in clinical decisions and resource allocation. They remain among the best forms of evidence, and reduce the bias inherent in other methods. A solid understanding of the systematic review process can be of benefit to nurses that carry out such reviews, and for those who make decisions based on them. An overview of the main steps involved in carrying out a systematic review is presented, including some of the common tools and frameworks utilised in this area. This should provide a good starting point for those that are considering embarking on such work, and to aid readers of such reviews in their understanding of the main review components, in order to appraise the quality of a review that may be used to inform subsequent clinical decision making.
Since their inception in the late 1970s, systematic reviews have gained influence in the health professions ( Hanley and Cutts, 2013 ). Systematic reviews and meta-analyses are considered to be the most credible and authoritative sources of evidence available ( Cognetti et al, 2015 ) and are regarded as the pinnacle of evidence in the various ‘hierarchies of evidence’. Reviews published in the Cochrane Library ( https://www.cochranelibrary.com) are widely considered to be the ‘gold’ standard. Since Guyatt et al (1995) presented a users' guide to medical literature for the Evidence-Based Medicine Working Group, various hierarchies of evidence have been proposed. Figure 1 illustrates an example.
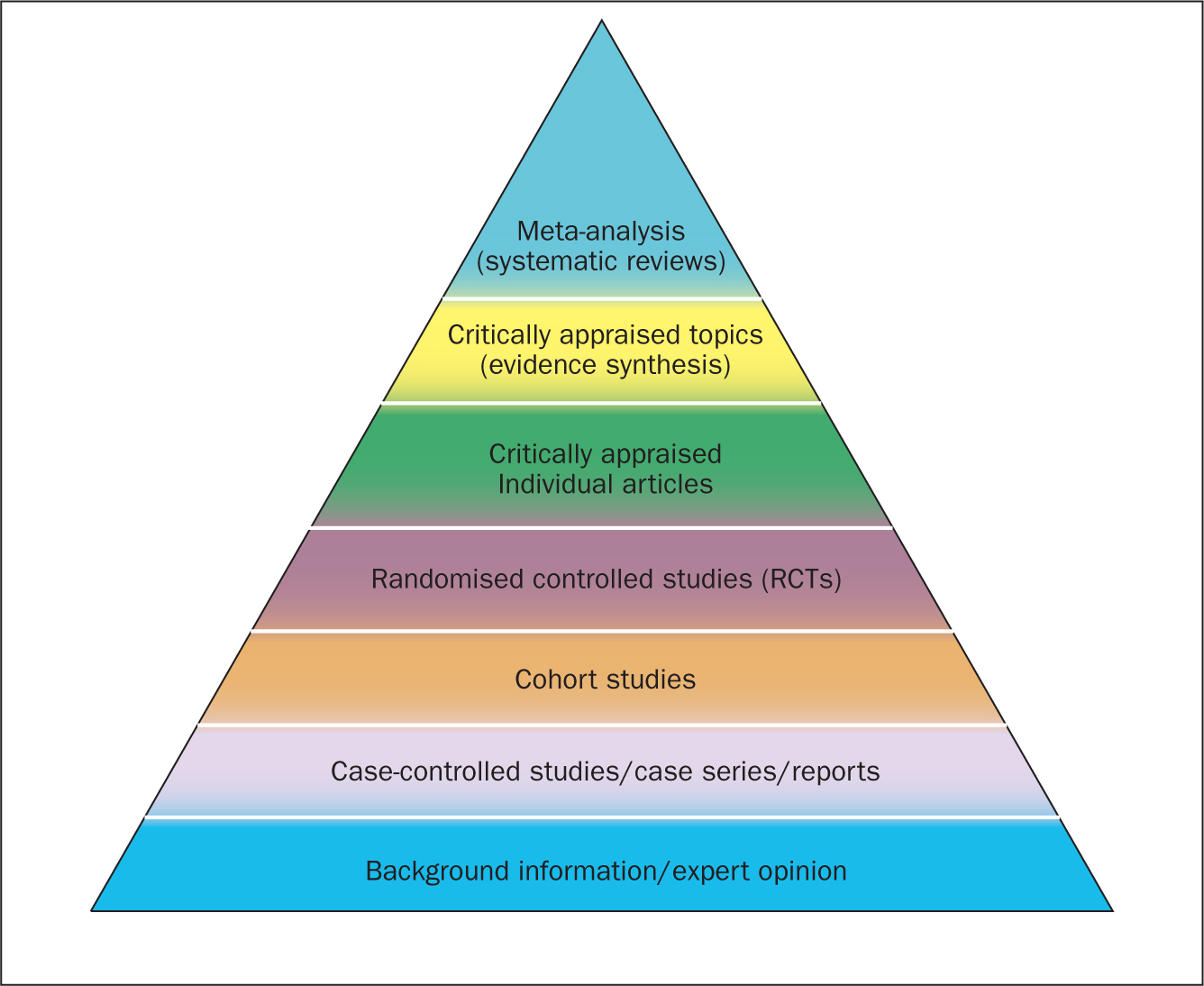
Systematic reviews can be qualitative or quantitative. One of the criticisms levelled at hierarchies such as these is that qualitative research is often positioned towards or even is at the bottom of the pyramid, thus implying that it is of little evidential value. This may be because of traditional issues concerning the quality of some qualitative work, although it is now widely recognised that both quantitative and qualitative research methodologies have a valuable part to play in answering research questions, which is reflected by the National Institute for Health and Care Excellence (NICE) information concerning methods for developing public health guidance. The NICE (2012) guidance highlights how both qualitative and quantitative study designs can be used to answer different research questions. In a revised version of the hierarchy-of-evidence pyramid, the systematic review is considered as the lens through which the evidence is viewed, rather than being at the top of the pyramid ( Murad et al, 2016 ).
Both quantitative and qualitative research methodologies are sometimes combined in a single review. According to the Cochrane review handbook ( Higgins and Green, 2011 ), regardless of type, reviews should contain certain features, including:
- Clearly stated objectives
- Predefined eligibility criteria for inclusion or exclusion of studies in the review
- A reproducible and clearly stated methodology
- Validity assessment of included studies (eg quality, risk, bias etc).
The main stages of carrying out a systematic review are summarised in Box 1 .
Formulating the research question
Before undertaking a systemic review, a research question should first be formulated ( Bashir and Conlon, 2018 ). There are a number of tools/frameworks ( Table 1 ) to support this process, including the PICO/PICOS, PEO and SPIDER criteria ( Bowers et al, 2011 ). These frameworks are designed to help break down the question into relevant subcomponents and map them to concepts, in order to derive a formalised search criterion ( Methley et al, 2014 ). This stage is essential for finding literature relevant to the question ( Jahan et al, 2016 ).
It is advisable to first check that the review you plan to carry out has not already been undertaken. You can optionally register your review with an international register of prospective reviews called PROSPERO, although this is not essential for publication. This is done to help you and others to locate work and see what reviews have already been carried out in the same area. It also prevents needless duplication and instead encourages building on existing work ( Bashir and Conlon, 2018 ).
A study ( Methley et al, 2014 ) that compared PICO, PICOS and SPIDER in relation to sensitivity and specificity recommended that the PICO tool be used for a comprehensive search and the PICOS tool when time/resources are limited.
The use of the SPIDER tool was not recommended due to the risk of missing relevant papers. It was, however, found to increase specificity.
These tools/frameworks can help those carrying out reviews to structure research questions and define key concepts in order to efficiently identify relevant literature and summarise the main objective of the review ( Jahan et al, 2016 ). A possible research question could be: Is paracetamol of benefit to people who have just had an operation? The following examples highlight how using a framework may help to refine the question:
- What form of paracetamol? (eg, oral/intravenous/suppository)
- Is the dosage important?
- What is the patient population? (eg, children, adults, Europeans)
- What type of operation? (eg, tonsillectomy, appendectomy)
- What does benefit mean? (eg, reduce post-operative pyrexia, analgesia).
An example of a more refined research question could be: Is oral paracetamol effective in reducing pain following cardiac surgery for adult patients? A number of concepts for each element will need to be specified. There will also be a number of synonyms for these concepts ( Table 2 ).
Table 2 shows an example of concepts used to define a search strategy using the PICO statement. It is easy to see even with this dummy example that there are many concepts that require mapping and much thought required to capture ‘good’ search criteria. Consideration should be given to the various terms to describe the heart, such as cardiac, cardiothoracic, myocardial, myocardium, etc, and the different names used for drugs, such as the equivalent name used for paracetamol in other countries and regions, as well as the various brand names. Defining good search criteria is an important skill that requires a lot of practice. A high-quality review gives details of the search criteria that enables the reader to understand how the authors came up with the criteria. A specific, well-defined search criterion also aids in the reproducibility of a review.
Search criteria
Before the search for papers and other documents can begin it is important to explicitly define the eligibility criteria to determine whether a source is relevant to the review ( Hanley and Cutts, 2013 ). There are a number of database sources that are searched for medical/health literature including those shown in Table 3 .
The various databases can be searched using common Boolean operators to combine or exclude search terms (ie AND, OR, NOT) ( Figure 2 ).
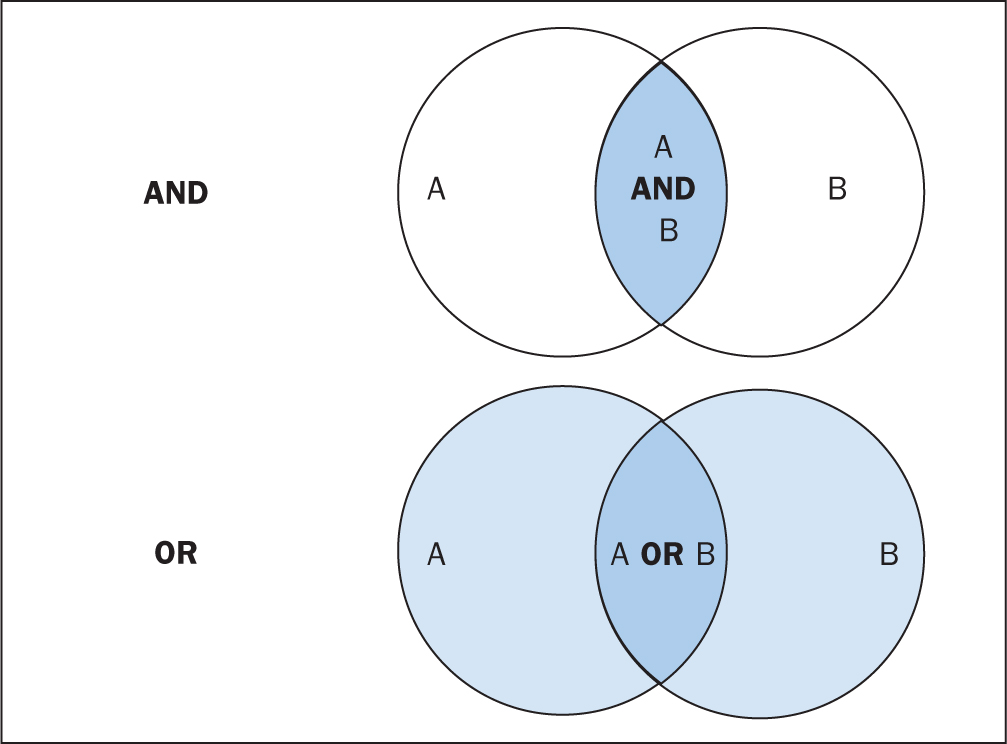
Although most literature databases use similar operators, it is necessary to view the individual database guides, because there are key differences between some of them. Table 4 details some of the common operators and wildcards used in the databases for searching. When developing a search criteria, it is a good idea to check concepts against synonyms, as well as abbreviations, acronyms and plural and singular variations ( Cognetti et al, 2015 ). Reading some key papers in the area and paying attention to the key words they use and other terms used in the abstract, and looking through the reference lists/bibliographies of papers, can also help to ensure that you incorporate relevant terms. Medical Subject Headings (MeSH) that are used by the National Library of Medicine (NLM) ( https://www.nlm.nih.gov/mesh/meshhome.html) to provide hierarchical biomedical index terms for NLM databases (Medline and PubMed) should also be explored and included in relevant search strategies.
Searching the ‘grey literature’ is also an important factor in reducing publication bias. It is often the case that only studies with positive results and statistical significance are published. This creates a certain bias inherent in the published literature. This bias can, to some degree, be mitigated by the inclusion of results from the so-called grey literature, including unpublished work, abstracts, conference proceedings and PhD theses ( Higgins and Green, 2011 ; Bettany-Saltikov, 2012 ; Cognetti et al, 2015 ). Biases in a systematic review can lead to overestimating or underestimating the results ( Jahan et al, 2016 ).
An example search strategy from a published review looking at web use for the appraisal of physical health conditions can be seen in Box 2 . High-quality reviews usually detail which databases were searched and the number of items retrieved from each.
A balance between high recall and high precision is often required in order to produce the best results. An oversensitive search, or one prone to including too much noise, can mean missing important studies or producing too many search results ( Cognetti et al, 2015 ). Following a search, the exported citations can be added to citation management software (such as Mendeley or Endnote) and duplicates removed.
Title and abstract screening
Initial screening begins with the title and abstracts of articles being read and included or excluded from the review based on their relevance. This is usually carried out by at least two researchers to reduce bias ( Bashir and Conlon, 2018 ). After screening any discrepancies in agreement should be resolved by discussion, or by an additional researcher casting the deciding vote ( Bashir and Conlon, 2018 ). Statistics for inter-rater reliability exist and can be reported, such as percentage of agreement or Cohen's kappa ( Box 3 ) for two reviewers and Fleiss' kappa for more than two reviewers. Agreement can depend on the background and knowledge of the researchers and the clarity of the inclusion and exclusion criteria. This highlights the importance of providing clear, well-defined criteria for inclusion that are easy for other researchers to follow.
Full-text review
Following title and abstract screening, the remaining articles/sources are screened in the same way, but this time the full texts are read in their entirety and included or excluded based on their relevance. Reasons for exclusion are usually recorded and reported. Extraction of the specific details of the studies can begin once the final set of papers is determined.
Data extraction
At this stage, the full-text papers are read and compared against the inclusion criteria of the review. Data extraction sheets are forms that are created to extract specific data about a study (12 Jahan et al, 2016 ) and ensure that data are extracted in a uniform and structured manner. Extraction sheets can differ between quantitative and qualitative reviews. For quantitative reviews they normally include details of the study's population, design, sample size, intervention, comparisons and outcomes ( Bettany-Saltikov, 2012 ; Mueller et al, 2017 ).
Quality appraisal
The quality of the studies used in the review should also be appraised. Caldwell et al (2005) discussed the need for a health research evaluation framework that could be used to evaluate both qualitative and quantitative work. The framework produced uses features common to both research methodologies, as well as those that differ ( Caldwell et al, 2005 ; Dixon-Woods et al, 2006 ). Figure 3 details the research critique framework. Other quality appraisal methods do exist, such as those presented in Box 4 . Quality appraisal can also be used to weight the evidence from studies. For example, more emphasis can be placed on the results of large randomised controlled trials (RCT) than one with a small sample size. The quality of a review can also be used as a factor for exclusion and can be specified in inclusion/exclusion criteria. Quality appraisal is an important step that needs to be undertaken before conclusions about the body of evidence can be made ( Sambunjak and Franic, 2012 ). It is also important to note that there is a difference between the quality of the research carried out in the studies and the quality of how those studies were reported ( Sambunjak and Franic, 2012 ).
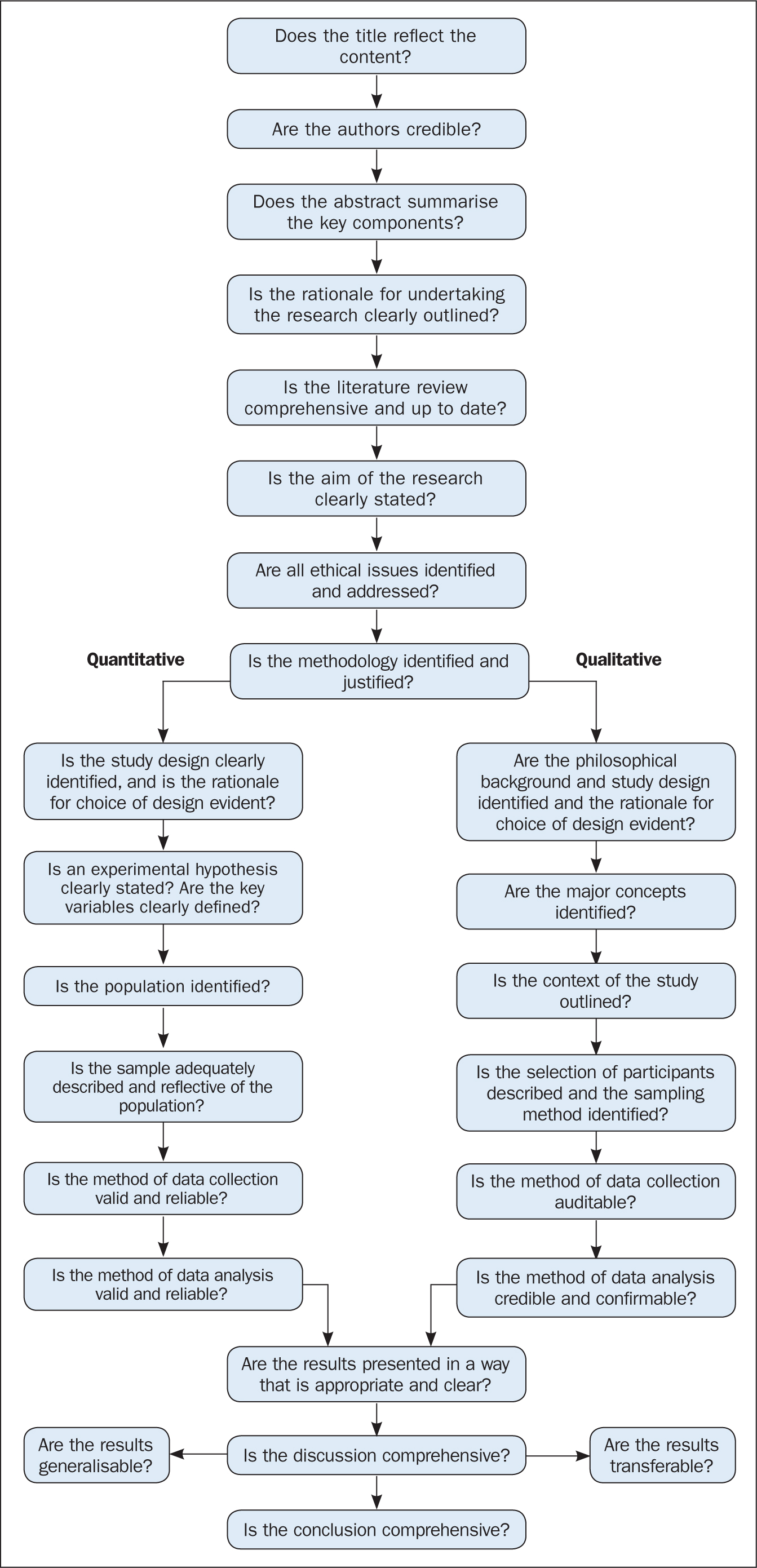
The quality appraisal is different for qualitative and quantitative studies. With quantitative studies this usually focuses on their internal and external validity, such as how well the study has been designed and analysed, and the generalisability of its findings. Qualitative work, on the other hand, is often evaluated in terms of trustworthiness and authenticity, as well as how transferable the findings may be ( Bettany-Saltikov, 2012 ; Bashir and Conlon, 2018 ; Siddaway et al, 2019 ).
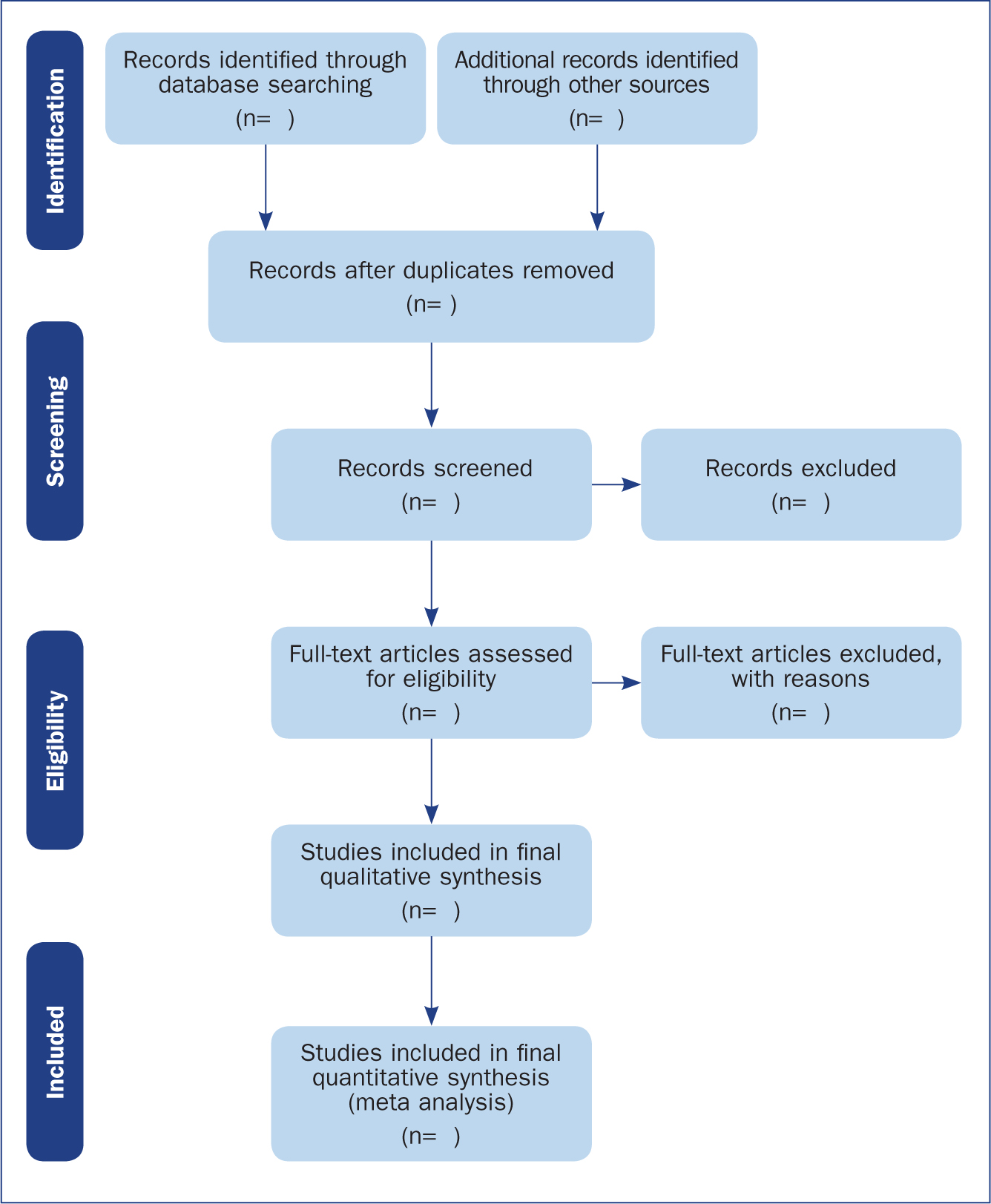
Reporting a review (the PRISMA statement)
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) provides a reporting structure for systematic reviews/meta-analysis, and consists of a checklist and diagram ( Figure 4 ). The stages of identifying potential papers/sources, screening by title and abstract, determining eligibility and final inclusion are detailed with the number of articles included/excluded at each stage. PRISMA diagrams are often included in systematic reviews to detail the number of papers included at each of the four main stages (identification, screening, eligibility and inclusion) of the review.
Data synthesis
The combined results of the screened studies can be analysed qualitatively by grouping them together under themes and subthemes, often referred to as meta-synthesis or meta-ethnography ( Siddaway et al, 2019 ). Sometimes this is not done and a summary of the literature found is presented instead. When the findings are synthesised, they are usually grouped into themes that were derived by noting commonality among the studies included. Inductive (bottom-up) thematic analysis is frequently used for such purposes and works by identifying themes (essentially repeating patterns) in the data, and can include a set of higher-level and related subthemes (Braun and Clarke, 2012). Thomas and Harden (2008) provide examples of the use of thematic synthesis in systematic reviews, and there is an excellent introduction to thematic analysis by Braun and Clarke (2012).
The results of the review should contain details on the search strategy used (including search terms), the databases searched (and the number of items retrieved), summaries of the studies included and an overall synthesis of the results ( Bettany-Saltikov, 2012 ). Finally, conclusions should be made about the results and the limitations of the studies included ( Jahan et al, 2016 ). Another method for synthesising data in a systematic review is a meta-analysis.
Limitations of systematic reviews
Apart from the many advantages and benefits to carrying out systematic reviews highlighted throughout this article, there remain a number of disadvantages. These include the fact that not all stages of the review process are followed rigorously or even at all in some cases. This can lead to poor quality reviews that are difficult or impossible to replicate. There also exist some barriers to the use of evidence produced by reviews, including ( Wallace et al, 2012 ):
- Lack of awareness and familiarity with reviews
- Lack of access
- Lack of direct usefulness/applicability.
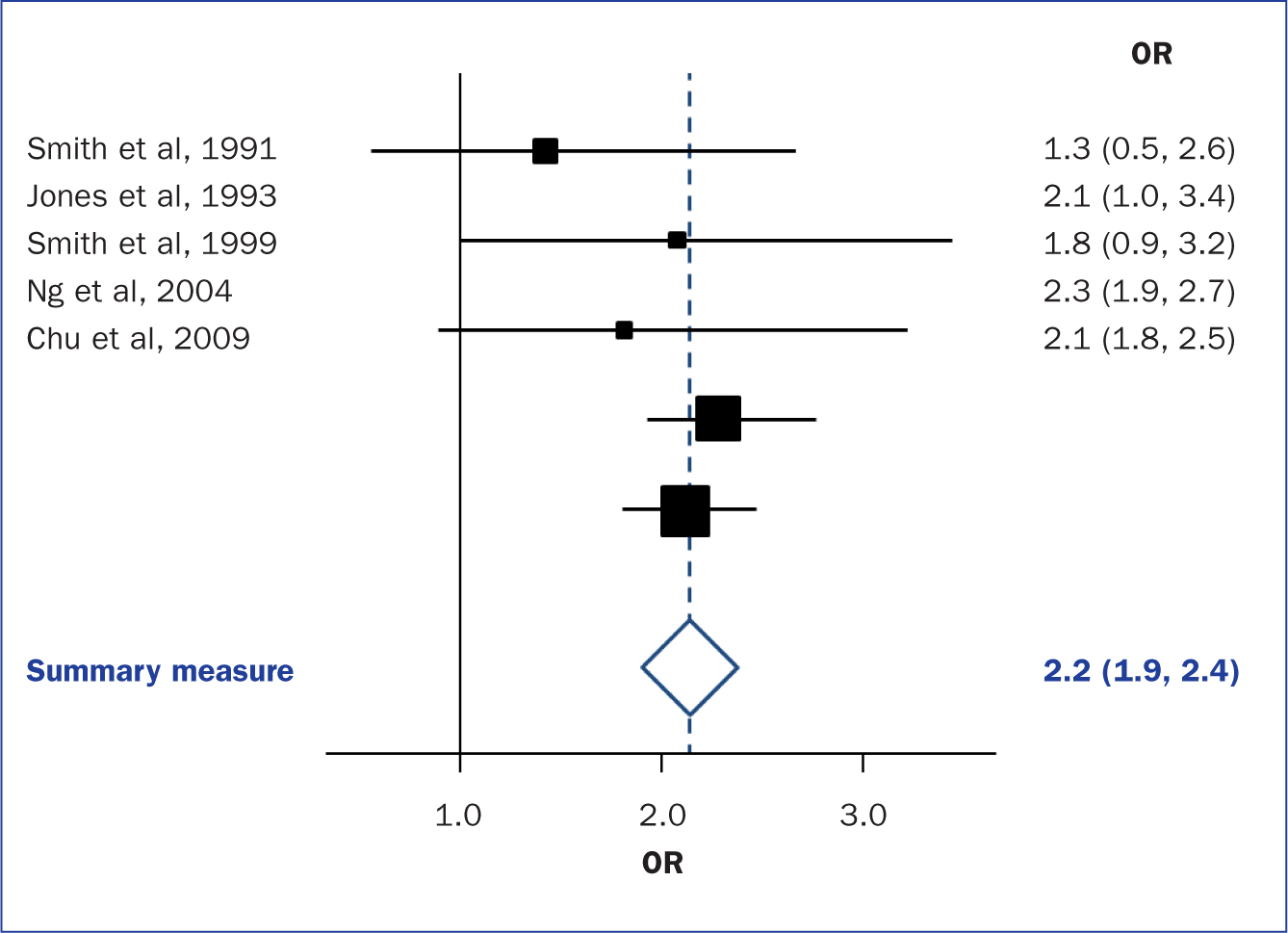
Meta-analysis
When the methods used and the analysis are similar or the same, such as in some RCTs, the results can be synthesised using a statistical approach called meta-analysis and presented using summary visualisations such as forest plots (or blobbograms) ( Figure 5 ). This can be done only if the results can be combined in a meaningful way.
Meta-analysis can be carried out using common statistical and data science software, such as the cross-platform ‘R’ ( https://www.r-project.org), or by using standalone software, such as Review Manager (RevMan) produced by the Cochrane community ( https://tinyurl.com/revman-5), which is currently developing a cross-platform version RevMan Web.
Carrying out a systematic review is a time-consuming process, that on average takes between 6 and 18 months and requires skill from those involved. Ideally, several reviewers will work on a review to reduce bias. Experts such as librarians should be consulted and included where possible in review teams to leverage their expertise.
Systematic reviews should present the state of the art (most recent/up-to-date developments) concerning a specific topic and aim to be systematic and reproducible. Reproducibility is aided by transparent reporting of the various stages of a review using reporting frameworks such as PRISMA for standardisation. A high-quality review should present a summary of a specific topic to a high standard upon which other professionals can base subsequent care decisions that increase the quality of evidence-based clinical practice.
- Systematic reviews remain one of the most trusted sources of high-quality information from which to make clinical decisions
- Understanding the components of a review will help practitioners to better assess their quality
- Many formal frameworks exist to help structure and report reviews, the use of which is recommended for reproducibility
- Experts such as librarians can be included in the review team to help with the review process and improve its quality
CPD reflective questions
- Where should high-quality qualitative research sit regarding the hierarchies of evidence?
- What background and expertise should those conducting a systematic review have, and who should ideally be included in the team?
- Consider to what extent inter-rater agreement is important in the screening process
Library Research Guides - University of Wisconsin Ebling Library
Uw-madison libraries research guides.
- Course Guides
- Subject Guides
- University of Wisconsin-Madison
- Research Guides
- Nursing Resources
- Conducting a Literature Review
Nursing Resources : Conducting a Literature Review
- Definitions of
- Professional Organizations
- Nursing Informatics
- Nursing Related Apps
- EBP Resources
- PICO-Clinical Question
- Types of PICO Question (D, T, P, E)
- Secondary & Guidelines
- Bedside--Point of Care
- Pre-processed Evidence
- Measurement Tools, Surveys, Scales
- Types of Studies
- Table of Evidence
- Qualitative vs Quantitative
- Types of Research within Qualitative and Quantitative
- Cohort vs Case studies
- Independent Variable VS Dependent Variable
- Sampling Methods and Statistics
- Systematic Reviews
- Review vs Systematic Review vs ETC...
- Standard, Guideline, Protocol, Policy
- Additional Guidelines Sources
- Peer Reviewed Articles
- Systematic Reviews and Meta-Analysis
- Writing a Research Paper or Poster
- Annotated Bibliographies
- Levels of Evidence (I-VII)
- Reliability
- Validity Threats
- Threats to Validity of Research Designs
- Nursing Theory
- Nursing Models
- PRISMA, RevMan, & GRADEPro
- ORCiD & NIH Submission System
- Understanding Predatory Journals
- Nursing Scope & Standards of Practice, 4th Ed
- Distance Ed & Scholarships
- Assess A Quantitative Study?
- Assess A Qualitative Study?
- Find Health Statistics?
- Choose A Citation Manager?
- Find Instruments, Measurements, and Tools
- Write a CV for a DNP or PhD?
- Find information about graduate programs?
- Learn more about Predatory Journals
- Get writing help?
- Choose a Citation Manager?
- Other questions you may have
- Search the Databases?
- Get Grad School information?
What is a Literature Review?
A literature review is an essay that surveys, summarizes, links together, and assesses research in a given field. It surveys the literature by reviewing a large body of work on a subject; it summarizes by noting the main conclusions and findings of the research; it links together works in the literature by showing how the information fits into the overall academic discussion and how the information relates to one another; it assesses the literature by noting areas of weakness, expansion, and contention. This is the essentials of literature review construction by discussing the major sectional elements, their purpose, how they are constructed, and how they all fit together.
All literature reviews have major sections:
- Introduction: that indicates the general state of the literature on a given topic;
- Methodology: an overview of how, where, and what subject terms used to conducted your search so it may be reproducable
- Findings: a summary of the major findings in that field;
- Discussion: a general progression from wider studies to smaller, more specifically-focused studies;
- Conclusion: for each major section that again notes the overall state of the research, albeit with a focus on the major synthesized conclusions, problems in the research, and even possible avenues of further research.
In Literature Reviews, it is Not Appropriate to:
- State your own opinions on the subject (unless you have evidence to support such claims).
- State what you think nurses should do (unless you have evidence to support such claims).
- Provide long descriptive accounts of your subject with no reference to research studies.
- Provide numerous definitions, signs/symptoms, treatment and complications of a particular illness without focusing on research studies to provide evidence and the primary purpose of the literature review.
- Discuss research studies in isolation from each other.
Remember, a literature review is not a book report. A literature review is focus, succinct, organized, and is free of personal beliefs or unsubstantiated tidbits.
- Types of Literature Reviews A detailed explanation of the different types of reviews and required citation retrieval numbers
Outline of a Literture Review

- << Previous: Peer Reviewed Articles
- Next: Systematic Reviews and Meta-Analysis >>
- Last Updated: Mar 19, 2024 10:39 AM
- URL: https://researchguides.library.wisc.edu/nursing
University Library
- Research Guides
- Literature Reviews
- Evidence-Based Practice
- Books & Media
What is a Literature Review?
Key questions for a literature review, examples of literature reviews, useful links, evidence matrix for literature reviews.
- Annotated Bibliographies
The Scholarly Conversation
A literature review provides an overview of previous research on a topic that critically evaluates, classifies, and compares what has already been published on a particular topic. It allows the author to synthesize and place into context the research and scholarly literature relevant to the topic. It helps map the different approaches to a given question and reveals patterns. It forms the foundation for the author’s subsequent research and justifies the significance of the new investigation.
A literature review can be a short introductory section of a research article or a report or policy paper that focuses on recent research. Or, in the case of dissertations, theses, and review articles, it can be an extensive review of all relevant research.
- The format is usually a bibliographic essay; sources are briefly cited within the body of the essay, with full bibliographic citations at the end.
- The introduction should define the topic and set the context for the literature review. It will include the author's perspective or point of view on the topic, how they have defined the scope of the topic (including what's not included), and how the review will be organized. It can point out overall trends, conflicts in methodology or conclusions, and gaps in the research.
- In the body of the review, the author should organize the research into major topics and subtopics. These groupings may be by subject, (e.g., globalization of clothing manufacturing), type of research (e.g., case studies), methodology (e.g., qualitative), genre, chronology, or other common characteristics. Within these groups, the author can then discuss the merits of each article and analyze and compare the importance of each article to similar ones.
- The conclusion will summarize the main findings, make clear how this review of the literature supports (or not) the research to follow, and may point the direction for further research.
- The list of references will include full citations for all of the items mentioned in the literature review.
A literature review should try to answer questions such as
- Who are the key researchers on this topic?
- What has been the focus of the research efforts so far and what is the current status?
- How have certain studies built on prior studies? Where are the connections? Are there new interpretations of the research?
- Have there been any controversies or debate about the research? Is there consensus? Are there any contradictions?
- Which areas have been identified as needing further research? Have any pathways been suggested?
- How will your topic uniquely contribute to this body of knowledge?
- Which methodologies have researchers used and which appear to be the most productive?
- What sources of information or data were identified that might be useful to you?
- How does your particular topic fit into the larger context of what has already been done?
- How has the research that has already been done help frame your current investigation ?
Example of a literature review at the beginning of an article: Forbes, C. C., Blanchard, C. M., Mummery, W. K., & Courneya, K. S. (2015, March). Prevalence and correlates of strength exercise among breast, prostate, and colorectal cancer survivors . Oncology Nursing Forum, 42(2), 118+. Retrieved from http://go.galegroup.com.sonoma.idm.oclc.org/ps/i.do?p=HRCA&sw=w&u=sonomacsu&v=2.1&it=r&id=GALE%7CA422059606&asid=27e45873fddc413ac1bebbc129f7649c Example of a comprehensive review of the literature: Wilson, J. L. (2016). An exploration of bullying behaviours in nursing: a review of the literature. British Journal Of Nursing , 25 (6), 303-306. For additional examples, see:
Galvan, J., Galvan, M., & ProQuest. (2017). Writing literature reviews: A guide for students of the social and behavioral sciences (Seventh ed.). [Electronic book]
Pan, M., & Lopez, M. (2008). Preparing literature reviews: Qualitative and quantitative approaches (3rd ed.). Glendale, CA: Pyrczak Pub. [ Q180.55.E9 P36 2008]
- Write a Literature Review (UCSC)
- Literature Reviews (Purdue)
- Literature Reviews: overview (UNC)
- Review of Literature (UW-Madison)
The Evidence Matrix can help you organize your research before writing your lit review. Use it to identify patterns and commonalities in the articles you have found--similar methodologies ? common theoretical frameworks ? It helps you make sure that all your major concepts covered. It also helps you see how your research fits into the context of the overall topic.
- Evidence Matrix Special thanks to Dr. Cindy Stearns, SSU Sociology Dept, for permission to use this Matrix as an example.
- << Previous: Misc
- Next: Annotated Bibliographies >>
- Last Updated: Jan 8, 2024 2:58 PM
- URL: https://libguides.sonoma.edu/nursing
- University of Detroit Mercy
- Health Professions
- Writing a Literature Review
- Find Articles (Databases)
- Evidence Based Nursing
- Searching Tips
- Books / eBooks
- Nursing Theory
- Adult-Gerontology Clinical Nurse Specialist
- Doctor of Nursing Practice
- NHL and CNL (Clinical Nurse Leader)
- Nurse Anesthesia
- Nursing Education
- Nurse Practitioner (FNP / ENP)
- Undergraduate Nursing - Clinical Reference Library
- General Writing Support
- Creating & Printing Posters
- Statistics: Health / Medical
- Health Measurement Instruments
- Streaming Video
- Anatomy Resources
- Database & Library Help
- Web Resources
- Evaluating Websites
- Medical / Nursing Apps & Mobile Sites
- Faculty Publications
Literature Review Overview
What is a Literature Review? Why Are They Important?
A literature review is important because it presents the "state of the science" or accumulated knowledge on a specific topic. It summarizes, analyzes, and compares the available research, reporting study strengths and weaknesses, results, gaps in the research, conclusions, and authors’ interpretations.
Tips and techniques for conducting a literature review are described more fully in the subsequent boxes:
- Literature review steps
- Strategies for organizing the information for your review
- Literature reviews sections
- In-depth resources to assist in writing a literature review
- Templates to start your review
- Literature review examples
Literature Review Steps

Graphic used with permission: Torres, E. Librarian, Hawai'i Pacific University
1. Choose a topic and define your research question
- Try to choose a topic of interest. You will be working with this subject for several weeks to months.
- Ideas for topics can be found by scanning medical news sources (e.g MedPage Today), journals / magazines, work experiences, interesting patient cases, or family or personal health issues.
- Do a bit of background reading on topic ideas to familiarize yourself with terminology and issues. Note the words and terms that are used.
- Develop a focused research question using PICO(T) or other framework (FINER, SPICE, etc - there are many options) to help guide you.
- Run a few sample database searches to make sure your research question is not too broad or too narrow.
- If possible, discuss your topic with your professor.
2. Determine the scope of your review
The scope of your review will be determined by your professor during your program. Check your assignment requirements for parameters for the Literature Review.
- How many studies will you need to include?
- How many years should it cover? (usually 5-7 depending on the professor)
- For the nurses, are you required to limit to nursing literature?
3. Develop a search plan
- Determine which databases to search. This will depend on your topic. If you are not sure, check your program specific library website (Physician Asst / Nursing / Health Services Admin) for recommendations.
- Create an initial search string using the main concepts from your research (PICO, etc) question. Include synonyms and related words connected by Boolean operators
- Contact your librarian for assistance, if needed.
4. Conduct searches and find relevant literature
- Keep notes as you search - tracking keywords and search strings used in each database in order to avoid wasting time duplicating a search that has already been tried
- Read abstracts and write down new terms to search as you find them
- Check MeSH or other subject headings listed in relevant articles for additional search terms
- Scan author provided keywords if available
- Check the references of relevant articles looking for other useful articles (ancestry searching)
- Check articles that have cited your relevant article for more useful articles (descendancy searching). Both PubMed and CINAHL offer Cited By links
- Revise the search to broaden or narrow your topic focus as you peruse the available literature
- Conducting a literature search is a repetitive process. Searches can be revised and re-run multiple times during the process.
- Track the citations for your relevant articles in a software citation manager such as RefWorks, Zotero, or Mendeley
5. Review the literature
- Read the full articles. Do not rely solely on the abstracts. Authors frequently cannot include all results within the confines of an abstract. Exclude articles that do not address your research question.
- While reading, note research findings relevant to your project and summarize. Are the findings conflicting? There are matrices available than can help with organization. See the Organizing Information box below.
- Critique / evaluate the quality of the articles, and record your findings in your matrix or summary table. Tools are available to prompt you what to look for. (See Resources for Appraising a Research Study box on the HSA, Nursing , and PA guides )
- You may need to revise your search and re-run it based on your findings.
6. Organize and synthesize
- Compile the findings and analysis from each resource into a single narrative.
- Using an outline can be helpful. Start broad, addressing the overall findings and then narrow, discussing each resource and how it relates to your question and to the other resources.
- Cite as you write to keep sources organized.
- Write in structured paragraphs using topic sentences and transition words to draw connections, comparisons, and contrasts.
- Don't present one study after another, but rather relate one study's findings to another. Speak to how the studies are connected and how they relate to your work.
Organizing Information
Options to assist in organizing sources and information :
1. Synthesis Matrix
- helps provide overview of the literature
- information from individual sources is entered into a grid to enable writers to discern patterns and themes
- article summary, analysis, or results
- thoughts, reflections, or issues
- each reference gets its own row
- mind maps, concept maps, flowcharts
- at top of page record PICO or research question
- record major concepts / themes from literature
- list concepts that branch out from major concepts underneath - keep going downward hierarchically, until most specific ideas are recorded
- enclose concepts in circles and connect the concept with lines - add brief explanation as needed
3. Summary Table
- information is recorded in a grid to help with recall and sorting information when writing
- allows comparing and contrasting individual studies easily
- purpose of study
- methodology (study population, data collection tool)
Efron, S. E., & Ravid, R. (2019). Writing the literature review : A practical guide . Guilford Press.
Literature Review Sections
- Lit reviews can be part of a larger paper / research study or they can be the focus of the paper
- Lit reviews focus on research studies to provide evidence
- New topics may not have much that has been published
* The sections included may depend on the purpose of the literature review (standalone paper or section within a research paper)
Standalone Literature Review (aka Narrative Review):
- presents your topic or PICO question
- includes the why of the literature review and your goals for the review.
- provides background for your the topic and previews the key points
- Narrative Reviews: tmay not have an explanation of methods.
- include where the search was conducted (which databases) what subject terms or keywords were used, and any limits or filters that were applied and why - this will help others re-create the search
- describe how studies were analyzed for inclusion or exclusion
- review the purpose and answer the research question
- thematically - using recurring themes in the literature
- chronologically - present the development of the topic over time
- methodological - compare and contrast findings based on various methodologies used to research the topic (e.g. qualitative vs quantitative, etc.)
- theoretical - organized content based on various theories
- provide an overview of the main points of each source then synthesize the findings into a coherent summary of the whole
- present common themes among the studies
- compare and contrast the various study results
- interpret the results and address the implications of the findings
- do the results support the original hypothesis or conflict with it
- provide your own analysis and interpretation (eg. discuss the significance of findings; evaluate the strengths and weaknesses of the studies, noting any problems)
- discuss common and unusual patterns and offer explanations
- stay away from opinions, personal biases and unsupported recommendations
- summarize the key findings and relate them back to your PICO/research question
- note gaps in the research and suggest areas for further research
- this section should not contain "new" information that had not been previously discussed in one of the sections above
- provide a list of all the studies and other sources used in proper APA 7
Literature Review as Part of a Research Study Manuscript:
- Compares the study with other research and includes how a study fills a gap in the research.
- Focus on the body of the review which includes the synthesized Findings and Discussion
Literature Reviews vs Systematic Reviews
Systematic Reviews are NOT the same as a Literature Review:
Literature Reviews:
- Literature reviews may or may not follow strict systematic methods to find, select, and analyze articles, but rather they selectively and broadly review the literature on a topic
- Research included in a Literature Review can be "cherry-picked" and therefore, can be very subjective
Systematic Reviews:
- Systemic reviews are designed to provide a comprehensive summary of the evidence for a focused research question
- rigorous and strictly structured, using standardized reporting guidelines (e.g. PRISMA, see link below)
- uses exhaustive, systematic searches of all relevant databases
- best practice dictates search strategies are peer reviewed
- uses predetermined study inclusion and exclusion criteria in order to minimize bias
- aims to capture and synthesize all literature (including unpublished research - grey literature) that meet the predefined criteria on a focused topic resulting in high quality evidence
Literature Review Examples
- Breastfeeding initiation and support: A literature review of what women value and the impact of early discharge (2017). Women and Birth : Journal of the Australian College of Midwives
- Community-based participatory research to promote healthy diet and nutrition and prevent and control obesity among African-Americans: A literature review (2017). Journal of Racial and Ethnic Health Disparities
- Vitamin D deficiency in individuals with a spinal cord injury: A literature review (2017). Spinal Cord
Resources for Writing a Literature Review
These sources have been used in developing this guide.
Resources Used on This Page
Aveyard, H. (2010). Doing a literature review in health and social care : A practical guide . McGraw-Hill Education.
Purdue Online Writing Lab. (n.d.). Writing a literature review . Purdue University. https://owl.purdue.edu/owl/research_and_citation/conducting_research/writing_a_literature_review.html
Torres, E. (2021, October 21). Nursing - graduate studies research guide: Literature review. Hawai'i Pacific University Libraries. Retrieved January 27, 2022, from https://hpu.libguides.com/c.php?g=543891&p=3727230
- << Previous: General Writing Support
- Next: Creating & Printing Posters >>
- Last Updated: Apr 19, 2024 3:11 PM
- URL: https://udmercy.libguides.com/nursing
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 21, Issue 2
- Reviewing the literature: choosing a review design
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Helen Noble 1 ,
- Joanna Smith 2
- 1 School of Nursing and Midwifery , Queen’s University Belfast , Belfast , UK
- 2 School of Healthcare , University of Leeds , Leeds , UK
- Correspondence to Dr Helen Noble, School of Nursing and Midwifery, Queen’s University Belfast, Belfast BT9 7BL, UK; helen.noble{at}qub.ac.uk
https://doi.org/10.1136/eb-2018-102895
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Many health professionals, students and academics including health researchers will have grappled with the challenges of undertaking a review of the literature and choosing a suitable design or framework to structure the review. For many undergraduate and master’s healthcare students their final year dissertation involves undertaking a review of the literature as a way of assessing their understanding and ability to critique and apply research findings to practice. For PhD and Master’s by Research students, a rigorous summary of research is usually expected to identify the state of knowledge and gaps in the evidence related to their topic focus and to provide justification for the empirical work they subsequently undertake. From discussions with students and colleagues, there appears to be much confusion about review designs and in particular the use and perhaps misuse of the term ‘systematic review’. For example, some quantitatively focused researchers subscribe to a ‘Cochrane’ approach as the only method to undertake a ‘systematic review’, with other researchers having a more pragmatic view, recognising the different purposes of a review and ways of applying systematic methods to undertake a review of the literature. Traditionally, systematic reviews have included only quantitative, experimental studies, usually randomised controlled trials. 1 More recently, systematic reviews of qualitative studies have emerged, 2 and integrative reviews which include both quantitative and qualitative studies. 3
In this article, we will build on a previous Research Made Simple article that outlined the key principles of undertaking a review of the literature in a structured and systemic way 4 by further exploring review designs and their key features to assist you in choosing an appropriate design. A reference to an example of each review outlined will be provided.
What is the purpose of undertaking a review of the evidence?
The purpose of a review of healthcare literature is primarily to summarise the knowledge around a specific question or topic, or to make recommendations that can support health professionals and organisations make decisions about a specific intervention or care issue. 5 In addition, reviews can highlight gaps in knowledge to guide future research. The most common approach to summarising, interpreting and making recommendations from synthesising the evidence in healthcare is a traditional systematic review of the literature to answer a specific clinical question. These reviews follow explicit, prespecified and reproducible methods in order to identify, evaluate and summarise the findings of all relevant individual studies. 6 Systematic reviews are typically associated with evaluating interventions, and therefore where appropriate, combine the results of several empirical studies to give a more reliable estimate of an intervention’s effectiveness than a single study. 6 However, over the past decade the range of approaches to reviewing the literature has expanded to reflect broader types of evidence/research designs and questions reflecting the increased complexity of healthcare. While this should be welcomed, this adds to the challenges in choosing the best review approach/design that meets the purpose of the review.
What approaches can be adopted to review the evidence?
- View inline
Key features of the common types of healthcare review
In summary, we have identified and described a variety of review designs and offered reasons for choosing a specific approach. Reviews are vital research methodology and help make sense of a body of research. They offer a succinct analysis which avoids the need for accessing individual research reports included in the review, increasingly vital for health professionals in light of the increasing vast amount of literature available. The field of reviews of the literature continues to change and while new approaches are emerging, ensuring methods are robust and remain paramount. This paper offers guidance to help direct choices when deciding on a review and provides an example of each approach.
- 5. ↵ Canadian Institutes of Health Research . Knowledge translation. Canadian Institutes of Health Research . 2008 . http://www.cihr.ca/e/29418.html ( accessed Jan 2018 ).
- 6. ↵ Centre for Reviews and Dissemination . Guidance for undertaking reviews in heathcare . 3rd ed . York University, York : CRD , 2009 .
- Buchwald H ,
- Braunwald E , et al
- Horvath M ,
- Massey K , et al
- Sheehan KJ ,
- Sobolev B ,
- Villán Villán YF , et al
- Christmals CD ,
- Whittemore R ,
- McInnes S ,
- Bonney A , et al
- Greenhalgh T ,
- Harvey G , et al
- Rycroft-Malone J ,
- McCormack B ,
- DeCorby K , et al
- Mitchison D ,
- 19. Joanna Briggs Institute Umbrella reviews . 2014 . http://joannabriggs.org/assets/docs/sumari/ReviewersManual-Methodology-JBI_Umbrella_Reviews-2014.pdf ( accessed Jan 2018 )
- van der Linde R , et al
Competing interests None declared.
Provenance and peer review Commissioned; internally peer reviewed.
Read the full text or download the PDF:
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 33, Issue 5
- Equitable and accessible informed healthcare consent process for people with intellectual disability: a systematic literature review
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-8498-7329 Manjekah Dunn 1 , 2 ,
- Iva Strnadová 3 , 4 , 5 ,
- Jackie Leach Scully 4 ,
- Jennifer Hansen 3 ,
- Julie Loblinzk 3 , 5 ,
- Skie Sarfaraz 5 ,
- Chloe Molnar 1 ,
- Elizabeth Emma Palmer 1 , 2
- 1 Faculty of Medicine & Health , University of New South Wales , Sydney , New South Wales , Australia
- 2 The Sydney Children's Hospitals Network , Sydney , New South Wales , Australia
- 3 School of Education , University of New South Wales , Sydney , New South Wales , Australia
- 4 Disability Innovation Institute , University of New South Wales , Sydney , New South Wales , Australia
- 5 Self Advocacy Sydney , Sydney , New South Wales , Australia
- Correspondence to Dr Manjekah Dunn, Paediatrics & Child Health, University of New South Wales Medicine & Health, Sydney, New South Wales, Australia; manjekah.dunn{at}unsw.edu.au
Objective To identify factors acting as barriers or enablers to the process of healthcare consent for people with intellectual disability and to understand how to make this process equitable and accessible.
Data sources Databases: Embase, MEDLINE, PsychINFO, PubMed, SCOPUS, Web of Science and CINAHL. Additional articles were obtained from an ancestral search and hand-searching three journals.
Eligibility criteria Peer-reviewed original research about the consent process for healthcare interventions, published after 1990, involving adult participants with intellectual disability.
Synthesis of results Inductive thematic analysis was used to identify factors affecting informed consent. The findings were reviewed by co-researchers with intellectual disability to ensure they reflected lived experiences, and an easy read summary was created.
Results Twenty-three studies were included (1999 to 2020), with a mix of qualitative (n=14), quantitative (n=6) and mixed-methods (n=3) studies. Participant numbers ranged from 9 to 604 people (median 21) and included people with intellectual disability, health professionals, carers and support people, and others working with people with intellectual disability. Six themes were identified: (1) health professionals’ attitudes and lack of education, (2) inadequate accessible health information, (3) involvement of support people, (4) systemic constraints, (5) person-centred informed consent and (6) effective communication between health professionals and patients. Themes were barriers (themes 1, 2 and 4), enablers (themes 5 and 6) or both (theme 3).
Conclusions Multiple reasons contribute to poor consent practices for people with intellectual disability in current health systems. Recommendations include addressing health professionals’ attitudes and lack of education in informed consent with clinician training, the co-production of accessible information resources and further inclusive research into informed consent for people with intellectual disability.
PROSPERO registration CRD42021290548.
- Decision making
- Healthcare quality improvement
- Patient-centred care
- Quality improvement
- Standards of care
Data availability statement
Data are available upon reasonable request. Additional data and materials such as data collection forms, data extraction and analysis templates and QualSyst assessment data can be obtained by contacting the corresponding author.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjqs-2023-016113
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
What is already known on this topic
People with intellectual disability are frequently excluded from decision-making processes and not provided equal opportunity for informed consent, despite protections outlined in the United Nations Convention on the Rights of Persons with Disabilities.
People with intellectual disability have the capacity and desire to make informed medical decisions, which can improve their well-being, health satisfaction and health outcomes.
What this review study adds
Health professionals lack adequate training in valid informed consent and making reasonable adjustments for people with intellectual disability, and continue to perpetuate assumptions of incapacity.
Health information provided to people with intellectual disability is often inaccessible and insufficient for them to make informed decisions about healthcare.
The role of support people, systemic constraints, a person-centred approach and ineffective healthcare communication also affect informed consent.
How this review might affect research, practice or policy
Health professionals need additional training on how to provide a valid informed consent process for people with intellectual disability, specifically in using accessible health information, making reasonable adjustments (e.g., longer/multiple appointments, options of a support person attending or not, using plain English), involving the individual in discussions, and communicating effectively with them.
Inclusive research is needed to hear the voices and opinions of people with intellectual disability about healthcare decision-making and about informed consent practices in specific healthcare settings.
Introduction
Approximately 1% of the world’s population have intellectual disability. 1 Intellectual disability is medically defined as a group of neurodevelopmental conditions beginning in childhood, with below average cognitive functioning and adaptive behaviour, including limitations in conceptual, social and practical skills. 2 People with intellectual disability prefer an alternative strength-based definition, reflected in the comment by Robert Strike OAM (Order of Australia Medal): ‘We can learn if the way of teaching matches how the person learns’, 3 reinforcing the importance of providing information tailored to the needs of a person with intellectual disability. A diagnosis of intellectual disability is associated with significant disparities in health outcomes. 4–7 Person-centred decision-making and better communication have been shown to improve patient satisfaction, 8 9 the physician–patient relationship 10 and overall health outcomes 11 for the wider population. Ensuring people with intellectual disability experience informed decision-making and accessible healthcare can help address the ongoing health disparities and facilitate equal access to healthcare.
Bodily autonomy is an individual’s power and agency to make decisions about their own body. 12 Informed consent for healthcare enables a person to practice bodily autonomy and is protected, for example, by the National Safety and Quality Health Service Standards (Australia), 13 Mental Capacity Act (UK) 14 and the Joint Commission Standards (USA). 15 In this article, we define informed consent according to three requirements: (1) the person is provided with information they understand, (2) the decision is free of coercion and (3) the person must have capacity. 16 For informed consent to be valid, this process must be suited to the individual’s needs so that they can understand and communicate effectively. Capacity is the ability to give informed consent for a medical intervention, 17 18 and the Mental Capacity Act outlines that ‘a person must be assumed to have capacity unless it is established that he lacks capacity’ and that incapacity can only be established if ‘all practicable steps’ to support capacity have been attempted without success. 14 These assumptions of capacity are also decision-specific, meaning an individual’s ability to consent can change depending on the situation, the choice itself and other factors. 17
Systemic issues with healthcare delivery systems have resulted in access barriers for people with intellectual disability, 19 despite the disability discrimination legislation in many countries who are signatories to the United Nations (UN) Convention on the Rights of Persons with Disabilities. 20 Patients with intellectual disability are not provided the reasonable adjustments that would enable them to give informed consent for medical procedures or interventions, 21 22 despite evidence that many people with intellectual disability have both the capacity and the desire to make their own healthcare decisions. 21 23
To support people with intellectual disability to make independent health decisions, an equitable and accessible informed consent process is needed. 24 However, current health systems have consistently failed to provide this. 21 25 To address this gap, we must first understand the factors that contribute to inequitable and inaccessible consent. To the best of our knowledge, the only current review of informed consent for people with intellectual disability is an integrative review by Goldsmith et al . 26 Many of the included articles focused on assessment of capacity 27–29 and research consent. 30–32 The review’s conclusion supported the functional approach to assess capacity, with minimal focus on how the informed consent processes can be improved. More recently, there has been a move towards ensuring that the consent process is accessible for all individuals, including elderly patients 33 and people with aphasia. 34 However, there remains a paucity of literature about the informed consent process for people with intellectual disability, with no systematic reviews summarising the factors influencing the healthcare consent process for people with intellectual disability.
To identify barriers to and enablers of the informed healthcare consent process for people with intellectual disability, and to understand how this can be made equitable and accessible.
A systematic literature review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P) systematic literature review protocol. 35 The PRISMA 2020 checklist 36 and ENhancing Transparency in REporting the synthesis of Qualitative research (ENTREQ) reporting guidelines were also followed. 37 The full study protocol is included in online supplemental appendix 1 .
Supplemental material
No patients or members of the public were involved in this research for this manuscript.
Search strategy
A search strategy was developed to identify articles about intellectual disability, consent and healthcare interventions, described in online supplemental appendix 2 . Multiple databases were searched for articles published between January 1990 to January 2022 (Embase, MEDLINE, PsychINFO, PubMed, SCOPUS, Web of Science and CINAHL). These databases include healthcare and psychology databases that best capture relevant literature on this topic, including medical, nursing, social sciences and bioethical literature. The search was limited to studies published from 1990 as understandings of consent have changed since then. 38 39 This yielded 4853 unique papers which were imported into Covidence, a specialised programme for conducting systematic reviews. 40
Study selection
Citation screening by abstract and titles was completed by two independent researchers (MD and EEP). Included articles had to:
Examine the informed consent process for a healthcare intervention for people with intellectual disability.
Have collected more than 50% of its data from relevant stakeholders, including adults with intellectual disability, families or carers of a person with intellectual disability, and professionals who engage with people with intellectual disability.
Report empirical data from primary research methodology.
Be published in a peer-reviewed journal after January 1990.
Be available in English.
Full text screening was completed by two independent researchers (MD and EEP). Articles were excluded if consent was only briefly discussed or if it focused on consent for research, capacity assessment, or participant knowledge or comprehension. Any conflicts were resolved through discussion with an independent third researcher (IS).
Additional studies were identified through an ancestral search and by hand-searching three major journals relevant to intellectual disability research. Journals were selected if they had published more than one included article for this review or in previous literature reviews conducted by the research team.
Quality assessment
Two independent researchers (MD and IS) assessed study quality with the QualSyst tool, 41 which can assess both qualitative and quantitative research papers. After evaluating the distribution of scores, a threshold value of 55% was used, as suggested by QualSyst 41 to exclude poor-quality studies but capture enough studies overall. Any conflicts between the quality assessment scores were resolved by a third researcher (EEP). For mixed-method studies, both qualitative and quantitative quality scores were calculated, and the higher value used.
Data collection
Two independent researchers (MD and JH) reviewed each study and extracted relevant details, including study size, participant demographics, year, country of publication, study design, data analysis and major outcomes reported. Researchers used standardised data collection forms designed, with input from senior researchers with expertise in qualitative research (IS and EEP), to extract data relevant to the review’s research aims. The form was piloted on one study, and a second iteration made based on feedback. These forms captured data on study design, methods, participants, any factors affecting the process of informed consent and study limitations. Data included descriptions and paragraphs outlining key findings, the healthcare context, verbatim participant quotes and any quantitative analyses or statistics. Missing or unclear data were noted.
Data analysis
A pilot literature search showed significant heterogeneity in methodology of studies, limiting the applicability of traditional quantitative analysis (ie, meta-analysis). Instead, inductive thematic analysis was chosen as an alternative methodology 42 43 that has been used in recent systematic reviews examining barriers and enablers of other health processes. 44 45 The six-phase approach described by Braun and Clarke was used. 46 47 A researcher (MD) independently coded the extracted data of each study line-by-line, with subsequent data grouped into pre-existing codes or new concepts when necessary. Codes were reviewed iteratively and grouped into categories, subthemes and themes framed around the research question. Another independent researcher (JH) collated and analysed the data on study demographics, methods and limitations. The themes were reviewed by two senior researchers (EEP and IS).
Qualitative methods of effect size calculations have been described in the literature, 48 49 which was captured in this review by the number of studies that identified each subtheme, with an assigned frequency rating to compare their relative significance. Subthemes were given a frequency rating of A, B, C or D if they were identified by >10, 7–9, 4–6 or <3 articles, respectively. The overall significance of each theme was estimated by the number of studies that mentioned it and the GRADE framework, a stepwise approach to quality assessment using a four-tier rating system. Each study was evaluated for risk of bias, inconsistency, indirectness, imprecision and publication bias. 50 51 Study sensitivity was assessed by counting the number of distinct subthemes included. 52 The quality of findings was designated high, moderate or low depending on the frequency ratings, the QualSyst score and the GRADE scores of studies supporting the finding. Finally, the relative contributions of each study were evaluated by the number of subthemes described, guided by previously reported methods for qualitative reviews. 52
Co-research
The findings were reviewed by two co-researchers with intellectual disability (JL and SS), with over 30 years combined experience as members and employees of a self-advocacy organisation. Guidance on the findings and an easy read summary was produced in line with best-practice inclusive research 53 54 over multiple discussions. Input from two health professional researchers (MD and EEP) provided data triangulation and sense-checking of findings.
Twenty-three articles were identified ( figure 1 ): 14 qualitative, 6 quantitative and 3 mixed-methods. Two papers included the same population of study participants: McCarthy 55 and McCarthy, 56 but had different research questions. Fovargue et al 57 was excluded due to a quality score of 35%. Common quality limitations were a lack of verification procedures to establish credibility and limited researcher reflexivity. No studies were excluded due to language requirements (as all were in English) or age restrictions (all studies had majority adult participants).
- Download figure
- Open in new tab
- Download powerpoint
PRISMA 2020 flowchart for the systematic review. 36
Studies were published from 1999 to 2020 and involved participant populations from the UK (n=18), USA (n=3), Sweden (n=1) and Ireland (n=1). Participant numbers ranged from 9 to 604 (median 21), and participants included people with intellectual disability (n=817), health professionals (n=272), carers and support people (n=48), and other professionals that work with people with intellectual disability (n=137, community service agency directors, social workers, administrative staff and care home staff). Ages of participants ranged from 8 to 84 years, though only Aman et al 58 included participants <18 years of age. This study was included as the article states very few children were included. Studies examined consent in different contexts, including contraception and sexual health (6/23 articles), 58–60 medications (5/23 articles), 58–62 emergency healthcare, 63 cervical screening, 64 community referrals, 58–61 65 mental health, 66 hydrotherapy, 64 blood collection 67 and broad decision-making consent without a specific context. 65 68–71 A detailed breakdown of each study is included in online supplemental appendix 3 .
Six major themes were identified from the studies, summarised in figure 2 . An overview of included studies showing study sensitivity, effect size, QualSyst and GRADE scores is given in online supplemental appendix 4 . Studies with higher QualSyst and GRADE scores contributed more to this review’s findings and tended to include more subthemes; specifically, Rogers et al , 66 Sowney and Barr, 63 Höglund and Larsson, 72 and McCarthy 55 and McCarthy. 56 Figure 3 gives the easy read version of theme 1, with the full easy read summary in online supplemental appendix 5 .
Summary of the identified six themes and subthemes.
Theme 1 of the easy read summary.
Theme 1—Health professionals’ attitudes and lack of education about informed consent
Health professionals’ attitudes and practices were frequently (18/21) identified as factors affecting the informed consent process, with substantial evidence supporting this theme. Studies noted the lack of training for health professionals in supporting informed consent for people with intellectual disability, their desire for further education, and stereotypes and discrimination perpetuated by health professionals.
Lack of health professional education on informed consent and disability discrimination legislation
Multiple studies reported inconsistent informed consent practices, for various reasons: some reported that health professionals ‘forgot’ to or ‘did not realise consent was necessary’, 63 73 but inconsistent consent practices were also attributed to healthcare providers’ unfamiliarity with consent guidelines and poor education on this topic. Carlson et al 73 reported that only 44% of general practitioners (GPs) were aware of consent guidelines, and there was the misconception that consent was unnecessary for people with intellectual disability. Similarly, studies of psychologists 66 and nurses 63 found that many were unfamiliar with their obligations to obtain consent, despite the existence of anti-discrimination legislation. People with intellectual disability describe feeling discriminated against by health professionals, reflected in comments such as ‘I can tell, my doctor just thinks I’m stupid – I'm nothing to him’. 74 Poor consent practices by health professionals were observed in Goldsmith et al , 67 while health professionals surveyed by McCarthy 56 were unaware of their responsibility to provide accessible health information to women with intellectual disability. Improving health professional education and training was suggested by multiple studies as a way to remove this barrier. 63 65–67 69 73
Lack of training on best practices for health professions caring for people with intellectual disability
A lack of training in caring for and communicating with people with intellectual disability was also described by midwives, 72 psychologists, 66 nurses, 63 pharmacists 61 and GPs. 56 72 75 Health professionals lacked knowledge about best practice approaches to providing equitable healthcare consent processes through reasonable adjustments such as accessible health information, 56 60 66 longer appointments times, 60 72 simple English 62 67 and flexible approaches to patient needs. 63 72
Health professionals’ stereotyping and assumptions of incapacity
Underlying stereotypes contributed to some health professionals’ (including nurses, 63 GPs 56 and physiotherapists 64 ) belief that people with intellectual disability lack capacity and therefore, do not require opportunities for informed consent. 56 64 In a survey of professionals referring people with intellectual disability to a disability service, the second most common reason for not obtaining consent was ‘patient unable to understand’. 73
Proxy consent as an inappropriate alternative
People with intellectual disability are rarely the final decision-maker in their medical choices, with many health providers seeking proxy consent from carers, support workers and family members, despite its legal invalidity. In McCarthy’s study (2010), 18/23 women with intellectual disability said the decision to start contraception was made by someone else. Many GPs appeared unaware that proxy consent is invalid in the UK. 56 Similar reports came from people with intellectual disability, 55 56 60 64 69 76 health professionals (nurses, doctors, allied health, psychologists), 56 63 64 66 77 support people 64 77 and non-medical professionals, 65 73 and capacity was rarely documented. 56 62 77
Exclusion of people with intellectual disability from decision-making discussions
Studies described instances where health professionals made decisions for their patients with intellectual disability or coerced patients into a choice. 55 72 74 76 77 In Ledger et al 77 , only 62% of women with intellectual disability were involved in the discussion about contraception, and only 38% made the final decision, and others stated in Wiseman and Ferrie 74 : ‘I was not given the opportunity to explore the different options. I was told what one I should take’. Three papers outlined instances where the choices of people with intellectual disability were ignored despite possessing capacity 65 66 69 and when a procedure continued despite them withdrawing consent. 69
Theme 2—Inadequate accessible health information
Lack of accessible health information.
The lack of accessible health information was the most frequently identified subtheme (16/23 studies). Some studies reported that health professionals provided information to carers instead, 60 avoided providing easy read information due to concerns about ‘offending’ patients 75 or only provided verbal information. 56 67 Informed consent was supported when health professionals recognised the importance of providing medical information 64 and when it was provided in an accessible format. 60 Alternative approaches to health information were explored, including virtual reality 68 and in-person education sessions, 59 with varying results. Overall, the need to provide information in different formats tailored to an individual’s communication needs, rather than a ‘one size fits all’ approach, was emphasised by both people with intellectual disability 60 and health professionals. 66
Insufficient information provided
Studies described situations where insufficient information was provided to people with intellectual disability to make informed decisions. For example, some people felt the information from their GP was often too basic to be helpful (Fish et al 60 ) and wanted additional information on consent forms (Rose et al 78 ).
Theme 3—The involvement of support people
Support people (including carers, family members and group home staff) were identified in 11 articles as both enablers of and barriers to informed consent. The antagonistic nature of these findings and lower frequency of subthemes are reflected in the lower quality assessments of evidence.
Support people facilitated communication with health professionals
Some studies reported carers bridging communication barriers with health to support informed consent. 63 64 McCarthy 56 found 21/23 of women with intellectual disability preferred to see doctors with a support person due to perceived benefits: ‘Sometimes I don’t understand it, so they have to explain it to my carer, so they can explain it to me easier’. Most GPs in this study (93%) also agreed that support people aided communication.
Support people helped people with intellectual disability make decisions
By advocating for people with intellectual disability, carers encouraged decision-making, 64 74 provided health information, 74 77 emotional support 76 and assisted with reading or remembering health information. 55 58 76 Some people with intellectual disability explicitly appreciated their support person’s involvement, 60 such as in McCarthy’s 55 study where 18/23 participants felt supported and safer when a support person was involved.
Support people impeded individual autonomy
The study by Wiseman and Ferrie 74 found that while younger participants with intellectual disability felt family members empowered their decision-making, older women felt family members impaired their ability to give informed consent. This was reflected in interviews with carers who questioned the capacity of the person with intellectual disability they supported and stated they would guide them to pick the ‘best choice’ or even over-ride their choices. 64 Studies of psychologists and community service directors described instances where the decision of family or carers was prioritised over the wishes of the person with intellectual disability. 65 66 Some women with intellectual disability in McCarthy’s studies (2010, 2009) 55 56 appeared to have been coerced into using contraception by parental pressures or fear of losing group home support.
Theme 4—Systemic constraints within healthcare systems
Time restraints affect informed consent and accessible healthcare.
Resource limitations create time constraints that impair the consent process and have been identified as a barrier by psychologists, 66 GPs, 56 hospital nurses 63 and community disability workers. 73 Rogers et al 66 highlighted that a personalised approach that could improve informed decision-making is restricted by inflexible medical models. Only two studies described flexible patient-centred approaches to consent. 60 72 A survey of primary care practices in 2007 reported that most did not modify their cervical screening information for patients with intellectual disability because it was not practical. 75
Inflexible models of consent
Both people with intellectual disability 76 and health professionals 66 recognised that consent is traditionally obtained through one-off interactions prior to an intervention. Yet, for people with intellectual disability, consent should ideally be an ongoing process that begins before an appointment and continues between subsequent ones. Other studies have tended to describe one-off interactions where decision-making was not revisited at subsequent appointments. 56 60 72 76
Lack of systemic supports
In one survey, self-advocates highlighted a lack of information on medication for people with intellectual disability and suggested a telephone helpline and a centralised source of information to support consent. 60 Health professionals also want greater systemic support, such as a health professional specialised in intellectual disability care to support other staff, 72 or a pharmacist specifically to help patients with intellectual disability. 61 Studies highlighted a lack of guidelines about healthcare needs of people with intellectual disabilities such as contraceptive counselling 72 or primary care. 75
Theme 5—Person-centred informed consent
Ten studies identified factors related to a person-centred approach to informed consent, grouped below into three subthemes. Health professionals should tailor their practice when obtaining informed consent from people with intellectual disability by considering how these subthemes relate to the individual. Each subtheme was described five times in the literature with a relative frequency rating of ‘C’, contributing to overall lower quality scores.
Previous experience with decision-making
Arscott et al 71 found that the ability of people with intellectual disability to consent changed with their verbal and memory skills and in different clinical vignettes, supporting the view of ‘functional’ capacity specific to the context of the medical decision. Although previous experiences with decision-making did not influence informed consent in this paper, other studies suggest that people with intellectual disability accustomed to independent decision-making were more able to make informed medical decisions, 66 70 and those who live independently were more likely to make independent healthcare decisions. 56 Health professionals should be aware that their patients with intellectual disability will have variable experience with decision-making and provide individualised support to meet their needs.
Variable awareness about healthcare rights
Consent processes should be tailored to the health literacy of patients, including emphasising available choices and the option to refuse treatment. In some studies, medical decisions were not presented to people with intellectual disability as a choice, 64 and people with intellectual disability were not informed of their legal right to accessible health information. 56
Power differences and acquiescence
Acquiescence by people with intellectual disability due to common and repeated experiences of trauma—that is, their tendency to agree with suggestions made by carers and health professionals, often to avoid upsetting others—was identified as an ongoing barrier. In McCarthy’s (2009) interviews with women with intellectual disability, some participants implicitly rejected the idea that they might make their own healthcare decisions: ‘They’re the carers, they have responsibility for me’. Others appeared to have made decisions to appease their carers: ‘I have the jab (contraceptive injection) so I can’t be blamed for getting pregnant’. 55 Two studies highlighted that health professionals need to be mindful of power imbalances when discussing consent with people with intellectual disability to ensure the choices are truly autonomous. 61 66
Theme 6—Effective communication between health professionals and patients
Implementation of reasonable adjustments for verbal and written information.
Simple language was always preferred by people with intellectual disability. 60 67 Other communication aids used in decision-making included repetition, short sentences, models, pictures and easy read brochures. 72 Another reasonable adjustment is providing the opportunity to ask questions, which women with intellectual disability in McCarthy’s (2009) study reported did not occur. 55
Tailored communication methods including non-verbal communication
Midwives noted that continuity of care allows them to develop rapport and understand the communication preferences of people with intellectual disability. 72 This is not always possible; for emergency nurses, the lack of background information about patients with intellectual disability made it challenging to understand their communication preferences. 63 The use of non-verbal communication, such as body language, was noted as underutilised 62 66 and people with intellectual disability supported the use of hearing loops, braille and sign language. 60
To the best of our knowledge, this is the first systematic review investigating the barriers and enablers of the informed consent process for healthcare procedures for people with intellectual disability. The integrative review by Goldsmith et al 26 examined capacity assessment and shares only three articles with this systematic review. 69 71 73 Since the 2000s, there has been a paradigm shift in which capacity is no longer considered a fixed ability that only some individuals possess 38 39 but instead as ‘functional’: a flexible ability that changes over time and in different contexts, 79 reflected in Goldsmith’s review. An individual’s capacity can be supported through various measures, including how information is communicated and how the decision-making process is approached. 18 80 By recognising the barriers and enablers identified in this review, physicians can help ensure the consent process for their patients with intellectual disability is both valid and truly informed. This review has highlighted the problems of inaccessible health information, insufficient clinical education on how to make reasonable adjustments and lack of person-centred trauma-informed care.
Recommendations
Health professionals require training in the informed consent process for people with intellectual disability, particularly in effective and respectful communication, reasonable adjustments and trauma-informed care. Reasonable adjustments include offering longer or multiple appointments, using accessible resources (such as easy read information or shared decision-making tools) and allowing patient choices (such as to record a consultation or involve a support person). Co-researchers reported that many people with intellectual disability prefer to go without a support person because they find it difficult to challenge their decisions and feel ignored if the health professional only talks to the support person. People with intellectual disability also feel they cannot seek second opinions before making medical decisions or feel pressured to provide consent, raising the possibility of coercion. These experiences contribute to healthcare trauma. Co-researchers raised the importance of building rapport with the person with intellectual disability and of making reasonable adjustments, such as actively advocating for the person’s autonomy, clearly stating all options including the choice to refuse treatment, providing opportunities to contribute to discussions and multiple appointments to ask questions and understand information. They felt that without these efforts to support consent, health professionals can reinforce traumatic healthcare experiences for people with intellectual disability. Co-researchers noted instances where choices were made by doctors without discussion and where they were only given a choice after requesting one and expressed concern that these barriers are greater for those with higher support needs.
Co-researchers showed how these experiences contributed to mistrust of health professionals and poorer health outcomes. In one situation, a co-researcher was not informed of a medication’s withdrawal effects, resulting in significant side-effects when it was ceased. Many people with intellectual disability describe a poor relationship with their health professionals, finding it difficult to trust health information provided due to previous traumatic experiences of disrespect, coercion, lack of choice and inadequate support. Many feel they cannot speak up due to the power imbalance and fear of retaliation. Poor consent practices and lack of reasonable adjustments directly harm therapeutic alliances by reducing trust, contribute to healthcare trauma and lead to poorer health outcomes for people with intellectual disability.
Additional education and training for health professionals is urgently needed in the areas of informed consent, reasonable adjustments and effective communication with people with intellectual disability. The experiences of health professionals within the research team confirmed that there is limited training in providing high-quality healthcare for people with intellectual disability, including reasonable adjustments and accessible health information. Co-researchers also suggested that education should be provided to carers and support people to help them better advocate for people with intellectual disability.
Health information should be provided in a multimodal format, including written easy read information. Many countries have regulation protecting the right to accessible health information and communication support to make an informed choice, such as UK’s Accessible Information Standard, 81 and Australia’s Charter of Health Care Rights, 24 yet these are rarely observed. Steps to facilitate this include routinely asking patients about information requirements, system alerts for an individual’s needs or routinely providing reasonable adjustments. 82 Co-researchers agreed that there is a lack of accessible health information, particularly about medications, and that diagrams and illustrations are underutilised. There is a critical need for more inclusive and accessible resources to help health professionals support informed consent in a safe and high-quality health system. These resources should be created through methods of inclusive research, such as co-production, actively involving people with intellectual disability in the planning, creation, and feedback process. 53
Strengths and limitations
This systematic review involved two co-researchers with intellectual disability in sense-checking findings and co-creating the easy read summary. Two co-authors who are health professionals provided additional sense-checking of findings from a different stakeholder perspective. In future research, this could be extended by involving people with intellectual disability in the design and planning of the study as per recommendations for best-practice inclusive research. 53 83
The current literature is limited by low use of inclusive research practices in research involving people with intellectual disability, increasing vulnerability to external biases (eg, inaccessible questionnaires, involvement of carers in data collection, overcompliance or acquiescence and absence of researcher reflexivity). Advisory groups or co-research with people with intellectual disability were only used in five studies. 58 60 68 74 76 Other limitations include unclear selection criteria, low sample sizes, missing data, using gatekeepers in patient selection and predominance of UK-based studies—increasing the risk of bias and reducing transferability. Nine studies (out of 15 involving people with intellectual disability) explicitly excluded those with severe or profound intellectual disability, reflecting a selection bias; only one study specifically focused on people with intellectual disability with higher support needs. Studies were limited to a few healthcare contexts, with a focus on consent about sexual health, contraception and medications.
The heterogeneity and qualitative nature of studies made it challenging to apply traditional meta-analysis. However, to promote consistency in qualitative research, the PRISMA and ENTREQ guidelines were followed. 36 37 Although no meta-analyses occurred, the duplication of study populations in McCarthy 2009 and 2010 likely contributed to increased significance of findings reported in both studies. Most included studies (13/23) were published over 10 years ago, reducing the current relevance of this review’s findings. Nonetheless, the major findings reflect underlying systemic issues within the health system, which are unlikely to have been resolved since the articles were published, as the just-released final report of the Australian Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability highlights. 84 There is an urgent need for more inclusive studies to explore the recommendations and preferences of people with intellectual disability about healthcare choices.
Informed consent processes for people with intellectual disability should include accessible information and reasonable adjustments, be tailored to individuals’ needs and comply with consent and disability legislation. Resources, guidelines and healthcare education are needed and should cover how to involve carers and support people, address systemic healthcare problems, promote a person-centred approach and ensure effective communication. These resources and future research must use principles of inclusive co-production—involving people with intellectual disability at all stages. Additionally, research is needed on people with higher support needs and in specific contexts where informed consent is vital but under-researched, such as cancer screening, palliative care, prenatal and newborn screening, surgical procedures, genetic medicine and advanced therapeutics such as gene-based therapies.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
- Maulik PK ,
- Mascarenhas MN ,
- Mathers CD , et al
- World Health Organisation
- Council for Intellectual Disability
- Emerson E ,
- Shogren KA ,
- Wehmeyer ML ,
- Reese RM , et al
- Cordasco KM
- Hallock JL ,
- Jordens CFC ,
- McGrath C , et al
- Brenner LH ,
- Brenner AT ,
- United Nations Population Fund
- Australian Commission on Safety and Quality in Health Care
- The Joint Commission
- Beauchamp TL ,
- Childress JF
- New South Wales Attorney General
- United Nations General Assembly
- Strnadová I ,
- Loblinzk J ,
- Scully JL , et al
- MacPhail C ,
- McKay K , et al
- Keywood K ,
- Fovargue S ,
- Goldsmith L ,
- Skirton H ,
- Cash J , et al
- Morris CD ,
- Niederbuhl JM ,
- Arscott K ,
- Fisher CB ,
- Davidson PW , et al
- Giampieri M
- Shamseer L ,
- Clarke M , et al
- McKenzie JE ,
- Bossuyt PM , et al
- Flemming K ,
- McInnes E , et al
- Appelbaum PS
- ↵ Covidence systematic review software . Melbourne, Australia ,
- Proudfoot K
- Papadopoulos I ,
- Koulouglioti C ,
- Lazzarino R , et al
- Onwuegbuzie AJ
- BMJ Best Practice
- Guyatt GH ,
- Vist GE , et al
- Garcia-Lee B
- Brimblecombe J , et al
- Benson BA ,
- Farmer CA , et al
- Ferguson L ,
- Graham YNH ,
- Gerrard D ,
- Laight S , et al
- Huneke NTM ,
- Halder N , et al
- Ferguson M ,
- Jarrett D ,
- McGuire BE , et al
- Woodward V ,
- Jackson L , et al
- Conboy-Hill S ,
- Leafman J ,
- Nehrenz GM , et al
- Höglund B ,
- Carlson T ,
- English S , et al
- Wiseman P ,
- Walmsley J ,
- Tilley E , et al
- Khatkar HS , et al
- Holland AJ , et al
- Beauchamp TL
- England National Health Service
- National Health Service England
- Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
- Data supplement 3
- Data supplement 4
- Data supplement 5
Contributors MD, EEP and IS conceived the idea for the systematic review. MD drafted the search strategy which was refined by EEP and IS. MD and EEP completed article screening. MD and IS completed quality assessments of included articles. MD and JH completed data extraction. MD drafted the original manuscript. JL and SS were co-researchers who sense-checked findings and were consulted to formulate dissemination plans. JL and SS co-produced the easy read summary with MD, CM, JH, EEP and IS. MD, JLS, EEP and IS reviewed manuscript wording. All authors critically reviewed the manuscript and approved it for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. MD is the guarantor responsible for the overall content of this manuscript.
Funding This systematic literature review was funded by the National Health & Medical Research Council (NHMRC), Targeted Call for Research (TCR) into Improving health of people with intellectual disability. Research grant title "GeneEQUAL: equitable and accessible genomic healthcare for people with intellectual disability". NHMRC application ID: 2022/GNT2015753.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Linked Articles
- Editorial It is up to healthcare professionals to talk to us in a way that we can understand: informed consent processes in people with an intellectual disability Jonathon Ding Richard Keagan-Bull Irene Tuffrey-Wijne BMJ Quality & Safety 2024; 33 277-279 Published Online First: 30 Jan 2024. doi: 10.1136/bmjqs-2023-016830

Read the full text or download the PDF:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Grad Med Educ
- v.8(3); 2016 Jul
The Literature Review: A Foundation for High-Quality Medical Education Research
a These are subscription resources. Researchers should check with their librarian to determine their access rights.
Despite a surge in published scholarship in medical education 1 and rapid growth in journals that publish educational research, manuscript acceptance rates continue to fall. 2 Failure to conduct a thorough, accurate, and up-to-date literature review identifying an important problem and placing the study in context is consistently identified as one of the top reasons for rejection. 3 , 4 The purpose of this editorial is to provide a road map and practical recommendations for planning a literature review. By understanding the goals of a literature review and following a few basic processes, authors can enhance both the quality of their educational research and the likelihood of publication in the Journal of Graduate Medical Education ( JGME ) and in other journals.
The Literature Review Defined
In medical education, no organization has articulated a formal definition of a literature review for a research paper; thus, a literature review can take a number of forms. Depending on the type of article, target journal, and specific topic, these forms will vary in methodology, rigor, and depth. Several organizations have published guidelines for conducting an intensive literature search intended for formal systematic reviews, both broadly (eg, PRISMA) 5 and within medical education, 6 and there are excellent commentaries to guide authors of systematic reviews. 7 , 8
- A literature review forms the basis for high-quality medical education research and helps maximize relevance, originality, generalizability, and impact.
- A literature review provides context, informs methodology, maximizes innovation, avoids duplicative research, and ensures that professional standards are met.
- Literature reviews take time, are iterative, and should continue throughout the research process.
- Researchers should maximize the use of human resources (librarians, colleagues), search tools (databases/search engines), and existing literature (related articles).
- Keeping organized is critical.
Such work is outside the scope of this article, which focuses on literature reviews to inform reports of original medical education research. We define such a literature review as a synthetic review and summary of what is known and unknown regarding the topic of a scholarly body of work, including the current work's place within the existing knowledge . While this type of literature review may not require the intensive search processes mandated by systematic reviews, it merits a thoughtful and rigorous approach.
Purpose and Importance of the Literature Review
An understanding of the current literature is critical for all phases of a research study. Lingard 9 recently invoked the “journal-as-conversation” metaphor as a way of understanding how one's research fits into the larger medical education conversation. As she described it: “Imagine yourself joining a conversation at a social event. After you hang about eavesdropping to get the drift of what's being said (the conversational equivalent of the literature review), you join the conversation with a contribution that signals your shared interest in the topic, your knowledge of what's already been said, and your intention.” 9
The literature review helps any researcher “join the conversation” by providing context, informing methodology, identifying innovation, minimizing duplicative research, and ensuring that professional standards are met. Understanding the current literature also promotes scholarship, as proposed by Boyer, 10 by contributing to 5 of the 6 standards by which scholarly work should be evaluated. 11 Specifically, the review helps the researcher (1) articulate clear goals, (2) show evidence of adequate preparation, (3) select appropriate methods, (4) communicate relevant results, and (5) engage in reflective critique.
Failure to conduct a high-quality literature review is associated with several problems identified in the medical education literature, including studies that are repetitive, not grounded in theory, methodologically weak, and fail to expand knowledge beyond a single setting. 12 Indeed, medical education scholars complain that many studies repeat work already published and contribute little new knowledge—a likely cause of which is failure to conduct a proper literature review. 3 , 4
Likewise, studies that lack theoretical grounding or a conceptual framework make study design and interpretation difficult. 13 When theory is used in medical education studies, it is often invoked at a superficial level. As Norman 14 noted, when theory is used appropriately, it helps articulate variables that might be linked together and why, and it allows the researcher to make hypotheses and define a study's context and scope. Ultimately, a proper literature review is a first critical step toward identifying relevant conceptual frameworks.
Another problem is that many medical education studies are methodologically weak. 12 Good research requires trained investigators who can articulate relevant research questions, operationally define variables of interest, and choose the best method for specific research questions. Conducting a proper literature review helps both novice and experienced researchers select rigorous research methodologies.
Finally, many studies in medical education are “one-offs,” that is, single studies undertaken because the opportunity presented itself locally. Such studies frequently are not oriented toward progressive knowledge building and generalization to other settings. A firm grasp of the literature can encourage a programmatic approach to research.
Approaching the Literature Review
Considering these issues, journals have a responsibility to demand from authors a thoughtful synthesis of their study's position within the field, and it is the authors' responsibility to provide such a synthesis, based on a literature review. The aforementioned purposes of the literature review mandate that the review occurs throughout all phases of a study, from conception and design, to implementation and analysis, to manuscript preparation and submission.
Planning the literature review requires understanding of journal requirements, which vary greatly by journal ( table 1 ). Authors are advised to take note of common problems with reporting results of the literature review. Table 2 lists the most common problems that we have encountered as authors, reviewers, and editors.
Sample of Journals' Author Instructions for Literature Reviews Conducted as Part of Original Research Article a

Common Problem Areas for Reporting Literature Reviews in the Context of Scholarly Articles

Locating and Organizing the Literature
Three resources may facilitate identifying relevant literature: human resources, search tools, and related literature. As the process requires time, it is important to begin searching for literature early in the process (ie, the study design phase). Identifying and understanding relevant studies will increase the likelihood of designing a relevant, adaptable, generalizable, and novel study that is based on educational or learning theory and can maximize impact.
Human Resources
A medical librarian can help translate research interests into an effective search strategy, familiarize researchers with available information resources, provide information on organizing information, and introduce strategies for keeping current with emerging research. Often, librarians are also aware of research across their institutions and may be able to connect researchers with similar interests. Reaching out to colleagues for suggestions may help researchers quickly locate resources that would not otherwise be on their radar.
During this process, researchers will likely identify other researchers writing on aspects of their topic. Researchers should consider searching for the publications of these relevant researchers (see table 3 for search strategies). Additionally, institutional websites may include curriculum vitae of such relevant faculty with access to their entire publication record, including difficult to locate publications, such as book chapters, dissertations, and technical reports.
Strategies for Finding Related Researcher Publications in Databases and Search Engines

Search Tools and Related Literature
Researchers will locate the majority of needed information using databases and search engines. Excellent resources are available to guide researchers in the mechanics of literature searches. 15 , 16
Because medical education research draws on a variety of disciplines, researchers should include search tools with coverage beyond medicine (eg, psychology, nursing, education, and anthropology) and that cover several publication types, such as reports, standards, conference abstracts, and book chapters (see the box for several information resources). Many search tools include options for viewing citations of selected articles. Examining cited references provides additional articles for review and a sense of the influence of the selected article on its field.
Box Information Resources
- Web of Science a
- Education Resource Information Center (ERIC)
- Cumulative Index of Nursing & Allied Health (CINAHL) a
- Google Scholar
Once relevant articles are located, it is useful to mine those articles for additional citations. One strategy is to examine references of key articles, especially review articles, for relevant citations.
Getting Organized
As the aforementioned resources will likely provide a tremendous amount of information, organization is crucial. Researchers should determine which details are most important to their study (eg, participants, setting, methods, and outcomes) and generate a strategy for keeping those details organized and accessible. Increasingly, researchers utilize digital tools, such as Evernote, to capture such information, which enables accessibility across digital workspaces and search capabilities. Use of citation managers can also be helpful as they store citations and, in some cases, can generate bibliographies ( table 4 ).
Citation Managers

Knowing When to Say When
Researchers often ask how to know when they have located enough citations. Unfortunately, there is no magic or ideal number of citations to collect. One strategy for checking coverage of the literature is to inspect references of relevant articles. As researchers review references they will start noticing a repetition of the same articles with few new articles appearing. This can indicate that the researcher has covered the literature base on a particular topic.
Putting It All Together
In preparing to write a research paper, it is important to consider which citations to include and how they will inform the introduction and discussion sections. The “Instructions to Authors” for the targeted journal will often provide guidance on structuring the literature review (or introduction) and the number of total citations permitted for each article category. Reviewing articles of similar type published in the targeted journal can also provide guidance regarding structure and average lengths of the introduction and discussion sections.
When selecting references for the introduction consider those that illustrate core background theoretical and methodological concepts, as well as recent relevant studies. The introduction should be brief and present references not as a laundry list or narrative of available literature, but rather as a synthesized summary to provide context for the current study and to identify the gap in the literature that the study intends to fill. For the discussion, citations should be thoughtfully selected to compare and contrast the present study's findings with the current literature and to indicate how the present study moves the field forward.
To facilitate writing a literature review, journals are increasingly providing helpful features to guide authors. For example, the resources available through JGME include several articles on writing. 17 The journal Perspectives on Medical Education recently launched “The Writer's Craft,” which is intended to help medical educators improve their writing. Additionally, many institutions have writing centers that provide web-based materials on writing a literature review, and some even have writing coaches.
The literature review is a vital part of medical education research and should occur throughout the research process to help researchers design a strong study and effectively communicate study results and importance. To achieve these goals, researchers are advised to plan and execute the literature review carefully. The guidance in this editorial provides considerations and recommendations that may improve the quality of literature reviews.
- Open access
- Published: 24 April 2024
Breast cancer screening motivation and behaviours of women aged over 75 years: a scoping review
- Virginia Dickson-Swift 1 ,
- Joanne Adams 1 ,
- Evelien Spelten 1 ,
- Irene Blackberry 2 ,
- Carlene Wilson 3 , 4 , 5 &
- Eva Yuen 3 , 6 , 7 , 8
BMC Women's Health volume 24 , Article number: 256 ( 2024 ) Cite this article
159 Accesses
Metrics details
This scoping review aimed to identify and present the evidence describing key motivations for breast cancer screening among women aged ≥ 75 years. Few of the internationally available guidelines recommend continued biennial screening for this age group. Some suggest ongoing screening is unnecessary or should be determined on individual health status and life expectancy. Recent research has shown that despite recommendations regarding screening, older women continue to hold positive attitudes to breast screening and participate when the opportunity is available.
All original research articles that address motivation, intention and/or participation in screening for breast cancer among women aged ≥ 75 years were considered for inclusion. These included articles reporting on women who use public and private breast cancer screening services and those who do not use screening services (i.e., non-screeners).
The Joanna Briggs Institute (JBI) methodology for scoping reviews was used to guide this review. A comprehensive search strategy was developed with the assistance of a specialist librarian to access selected databases including: the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline, Web of Science and PsychInfo. The review was restricted to original research studies published since 2009, available in English and focusing on high-income countries (as defined by the World Bank). Title and abstract screening, followed by an assessment of full-text studies against the inclusion criteria was completed by at least two reviewers. Data relating to key motivations, screening intention and behaviour were extracted, and a thematic analysis of study findings undertaken.
A total of fourteen (14) studies were included in the review. Thematic analysis resulted in identification of three themes from included studies highlighting that decisions about screening were influenced by: knowledge of the benefits and harms of screening and their relationship to age; underlying attitudes to the importance of cancer screening in women's lives; and use of decision aids to improve knowledge and guide decision-making.
The results of this review provide a comprehensive overview of current knowledge regarding the motivations and screening behaviour of older women about breast cancer screening which may inform policy development.
Peer Review reports
Introduction
Breast cancer is now the most commonly diagnosed cancer in the world overtaking lung cancer in 2021 [ 1 ]. Across the globe, breast cancer contributed to 25.8% of the total number of new cases of cancer diagnosed in 2020 [ 2 ] and accounts for a high disease burden for women [ 3 ]. Screening for breast cancer is an effective means of detecting early-stage cancer and has been shown to significantly improve survival rates [ 4 ]. A recent systematic review of international screening guidelines found that most countries recommend that women have biennial mammograms between the ages of 40–70 years [ 5 ] with some recommending that there should be no upper age limit [ 6 , 7 , 8 , 9 , 10 , 11 , 12 ] and others suggesting that benefits of continued screening for women over 75 are not clear [ 13 , 14 , 15 ].
Some guidelines suggest that the decision to end screening should be determined based on the individual health status of the woman, their life expectancy and current health issues [ 5 , 16 , 17 ]. This is because the benefits of mammography screening may be limited after 7 years due to existing comorbidities and limited life expectancy [ 18 , 19 , 20 , 21 ], with some jurisdictions recommending breast cancer screening for women ≥ 75 years only when life expectancy is estimated as at least 7–10 years [ 22 ]. Others have argued that decisions about continuing with screening mammography should depend on individual patient risk and health management preferences [ 23 ]. This decision is likely facilitated by a discussion between a health care provider and patient about the harms and benefits of screening outside the recommended ages [ 24 , 25 ]. While mammography may enable early detection of breast cancer, it is clear that false-positive results and overdiagnosis Footnote 1 may occur. Studies have estimated that up to 25% of breast cancer cases in the general population may be over diagnosed [ 26 , 27 , 28 ].
The risk of being diagnosed with breast cancer increases with age and approximately 80% of new cases of breast cancer in high-income countries are in women over the age of 50 [ 29 ]. The average age of first diagnosis of breast cancer in high income countries is comparable to that of Australian women which is now 61 years [ 2 , 4 , 29 ]. Studies show that women aged ≥ 75 years generally have positive attitudes to mammography screening and report high levels of perceived benefits including early detection of breast cancer and a desire to stay healthy as they age [ 21 , 30 , 31 , 32 ]. Some women aged over 74 participate, or plan to participate, in screening despite recommendations from health professionals and government guidelines advising against it [ 33 ]. Results of a recent review found that knowledge of the recommended guidelines and the potential harms of screening are limited and many older women believed that the benefits of continued screening outweighed the risks [ 30 ].
Very few studies have been undertaken to understand the motivations of women to screen or to establish screening participation rates among women aged ≥ 75 and older. This is surprising given that increasing age is recognised as a key risk factor for the development of breast cancer, and that screening is offered in many locations around the world every two years up until 74 years. The importance of this topic is high given the ambiguity around best practice for participation beyond 74 years. A preliminary search of Open Science Framework, PROSPERO, Cochrane Database of Systematic Reviews and JBI Evidence Synthesis in May 2022 did not locate any reviews on this topic.
This scoping review has allowed for the mapping of a broad range of research to explore the breadth and depth of the literature, summarize the evidence and identify knowledge gaps [ 34 , 35 ]. This information has supported the development of a comprehensive overview of current knowledge of motivations of women to screen and screening participation rates among women outside the targeted age of many international screening programs.
Materials and methods
Research question.
The research question for this scoping review was developed by applying the Population—Concept—Context (PCC) framework [ 36 ]. The current review addresses the research question “What research has been undertaken in high-income countries (context) exploring the key motivations to screen for breast cancer and screening participation (concepts) among women ≥ 75 years of age (population)?
Eligibility criteria
Participants.
Women aged ≥ 75 years were the key population. Specifically, motivations to screen and screening intention and behaviour and the variables that discriminate those who screen from those who do not (non-screeners) were utilised as the key predictors and outcomes respectively.
From a conceptual perspective it was considered that motivation led to behaviour, therefore articles that described motivation and corresponding behaviour were considered. These included articles reporting on women who use public (government funded) and private (fee for service) breast cancer screening services and those who do not use screening services (i.e., non-screeners).
The scope included high-income countries using the World Bank definition [ 37 ]. These countries have broadly similar health systems and opportunities for breast cancer screening in both public and private settings.
Types of sources
All studies reporting original research in peer-reviewed journals from January 2009 were eligible for inclusion, regardless of design. This date was selected due to an evaluation undertaken for BreastScreen Australia recommending expansion of the age group to include 70–74-year-old women [ 38 ]. This date was also indicative of international debate regarding breast cancer screening effectiveness at this time [ 39 , 40 ]. Reviews were also included, regardless of type—scoping, systematic, or narrative. Only sources published in English and available through the University’s extensive research holdings were eligible for inclusion. Ineligible materials were conference abstracts, letters to the editor, editorials, opinion pieces, commentaries, newspaper articles, dissertations and theses.
This scoping review was registered with the Open Science Framework database ( https://osf.io/fd3eh ) and followed Joanna Briggs Institute (JBI) methodology for scoping reviews [ 35 , 36 ]. Although ethics approval is not required for scoping reviews the broader study was approved by the University Ethics Committee (approval number HEC 21249).
Search strategy
A pilot search strategy was developed in consultation with an expert health librarian and tested in MEDLINE (OVID) and conducted on 3 June 2022. Articles from this pilot search were compared with seminal articles previously identified by the members of the team and used to refine the search terms. The search terms were then searched as both keywords and subject headings (e.g., MeSH) in the titles and abstracts and Boolean operators employed. A full MEDLINE search was then carried out by the librarian (see Table 1 ). This search strategy was adapted for use in each of the following databases: Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medical Literature Analysis and Retrieval System Online (MEDLINE), Web of Science and PsychInfo databases. The references of included studies have been hand-searched to identify any additional evidence sources.
Study/source of evidence selection
Following the search, all identified citations were collated and uploaded into EndNote v.X20 (Clarivate Analytics, PA, USA) and duplicates removed. The resulting articles were then imported into Covidence – Cochrane’s systematic review management software [ 41 ]. Duplicates were removed once importation was complete, and title and abstract screening was undertaken against the eligibility criteria. A sample of 25 articles were assessed by all reviewers to ensure reliability in the application of the inclusion and exclusion criteria. Team discussion was used to ensure consistent application. The Covidence software supports blind reviewing with two reviewers required at each screening phase. Potentially relevant sources were retrieved in full text and were assessed against the inclusion criteria by two independent reviewers. Conflicts were flagged within the software which allows the team to discuss those that have disagreements until a consensus was reached. Reasons for exclusion of studies at full text were recorded and reported in the scoping review. The Preferred Reporting Items of Systematic Reviews extension for scoping reviews (PRISMA-ScR) checklist was used to guide the reporting of the review [ 42 ] and all stages were documented using the PRISMA-ScR flow chart [ 42 ].
Data extraction
A data extraction form was created in Covidence and used to extract study characteristics and to confirm the study’s relevance. This included specific details such as article author/s, title, year of publication, country, aim, population, setting, data collection methods and key findings relevant to the review question. The draft extraction form was modified as needed during the data extraction process.
Data analysis and presentation
Extracted data were summarised in tabular format (see Table 2 ). Consistent with the guidelines for the effective reporting of scoping reviews [ 43 ] and the JBI framework [ 35 ] the final stage of the review included thematic analysis of the key findings of the included studies. Study findings were imported into QSR NVivo with coding of each line of text. Descriptive codes reflected key aspects of the included studies related to the motivations and behaviours of women > 75 years about breast cancer screening.
In line with the reporting requirements for scoping reviews the search results for this review are presented in Fig. 1 [ 44 ].
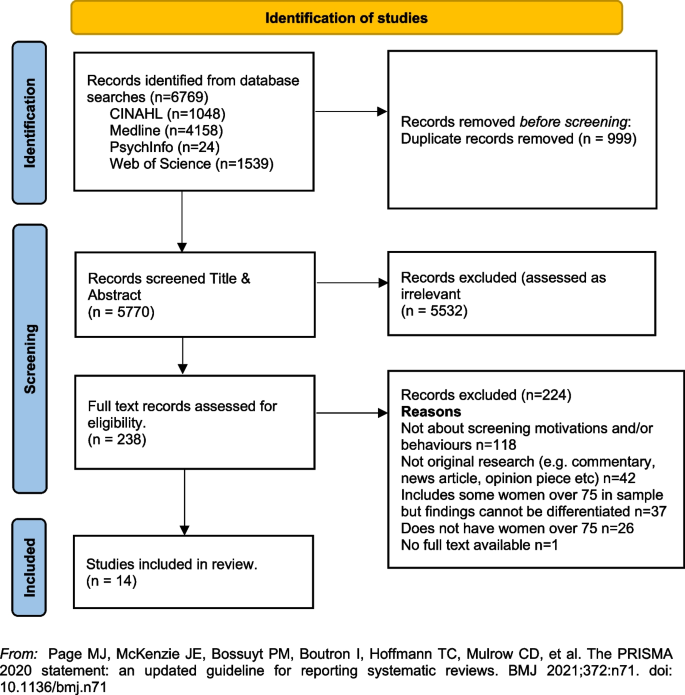
PRISMA Flowchart. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71
A total of fourteen [ 14 ] studies were included in the review with studies from the following countries, US n = 12 [ 33 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 ], UK n = 1 [ 23 ] and France n = 1 [ 56 ]. Sample sizes varied, with most containing fewer than 50 women ( n = 8) [ 33 , 45 , 46 , 48 , 51 , 52 , 55 ]. Two had larger samples including a French study with 136 women (a sub-set of a larger sample) [ 56 ], and one mixed method study in the UK with a sample of 26 women undertaking interviews and 479 women completing surveys [ 23 ]. One study did not report exact numbers [ 50 ]. Three studies [ 47 , 53 , 54 ] were undertaken by a group of researchers based in the US utilising the same sample of women, however each of the papers focused on different primary outcomes. The samples in the included studies were recruited from a range of locations including primary medical care clinics, specialist medical clinics, University affiliated medical clinics, community-based health centres and community outreach clinics [ 47 , 53 , 54 ].
Data collection methods varied and included: quantitative ( n = 8), qualitative ( n = 5) and mixed methods ( n = 1). A range of data collection tools and research designs were utilised; pre/post, pilot and cross-sectional surveys, interviews, and secondary analysis of existing data sets. Seven studies focused on the use of a Decision Aids (DAs), either in original or modified form, developed by Schonberg et al. [ 55 ] as a tool to increase knowledge about the harms and benefits of screening for older women [ 45 , 47 , 48 , 49 , 52 , 54 , 55 ]. Three studies focused on intention to screen [ 33 , 53 , 56 ], two on knowledge of, and attitudes to, screening [ 23 , 46 ], one on information needs relating to risks and benefits of screening discontinuation [ 51 ], and one on perceptions about discontinuation of screening and impact of social interactions on screening [ 50 ].
The three themes developed from the analysis of the included studies highlighted that decisions about screening were primarily influenced by: (1) knowledge of the benefits and harms of screening and their relationship to age; (2) underlying attitudes to the importance of cancer screening in women's lives; and (3) exposure to decision aids designed to facilitate informed decision-making. Each of these themes will be presented below drawing on the key findings of the appropriate studies. The full dataset of extracted data can be found in Table 2 .
Knowledge of the benefits and harms of screening ≥ 75 years
The decision to participate in routine mammography is influenced by individual differences in cognition and affect, interpersonal relationships, provider characteristics, and healthcare system variables. Women typically perceive mammograms as a positive, beneficial and routine component of care [ 46 ] and an important aspect of taking care of themselves [ 23 , 46 , 49 ]. One qualitative study undertaken in the US showed that few women had discussed mammography cessation or the potential harms of screening with their health care providers and some women reported they would insist on receiving mammography even without a provider recommendation to continue screening [ 46 ].
Studies suggested that ageing itself, and even poor health, were not seen as reasonable reasons for screening cessation. For many women, guidance from a health care provider was deemed the most important influence on decision-making [ 46 ]. Preferences for communication about risk and benefits were varied with one study reporting women would like to learn more about harms and risks and recommended that this information be communicated via physicians or other healthcare providers, included in brochures/pamphlets, and presented outside of clinical settings (e.g., in community-based seniors groups) [ 51 ]. Others reported that women were sometimes sceptical of expert and government recommendations [ 33 ] although some were happy to participate in discussions with health educators or care providers about breast cancer screening harms and benefits and potential cessation [ 52 ].
Underlying attitudes to the importance of cancer screening at and beyond 75 years
Included studies varied in describing the importance of screening, with some attitudes based on past attendance and some based on future intentions to screen. Three studies reported findings indicating that some women intended to continue screening after 75 years of age [ 23 , 45 , 46 ], with one study in the UK reporting that women supported an extension of the automatic recall indefinitely, regardless of age or health status. In this study, failure to invite older women to screen was interpreted as age discrimination [ 23 ]. The desire to continue screening beyond 75 was also highlighted in a study from France that found that 60% of the women ( n = 136 aged ≥ 75) intended to pursue screening in the future, and 27 women aged ≥ 75, who had never undergone mammography previously (36%), intended to do so in the future [ 56 ]. In this same study, intentions to screen varied significantly [ 56 ]. There were no sociodemographic differences observed between screened and unscreened women with regard to level of education, income, health risk behaviour (smoking, alcohol consumption), knowledge about the importance and the process of screening, or psychological features (fear of the test, fear of the results, fear of the disease, trust in screening impact) [ 56 ]. Further analysis showed that three items were statistically correlated with a higher rate of attendance at screening: (1) screening was initiated by a physician; (2) the women had a consultation with a gynaecologist during the past 12 months; and (3) the women had already undergone at least five screening mammograms. Analysis highlighted that although average income, level of education, psychological features or other types of health risk behaviours did not impact screening intention, having a mammogram previously impacted likelihood of ongoing screening. There was no information provided that explained why women who had not previously undergone screening might do so in the future.
A mixed methods study in the UK reported similar findings [ 23 ]. Utilising interviews ( n = 26) and questionnaires ( n = 479) with women ≥ 70 years (median age 75 years) the overwhelming result (90.1%) was that breast screening should be offered to all women indefinitely regardless of age, health status or fitness [ 23 ], and that many older women were keen to continue screening. Both the interview and survey data confirmed women were uncertain about eligibility for breast screening. The survey data showed that just over half the women (52.9%) were unaware that they could request mammography or knew how to access it. Key reasons for screening discontinuation were not being invited for screening (52.1%) and not knowing about self-referral (35.1%).
Women reported that not being invited to continue screening sent messages that screening was no longer important or required for this age group [ 23 ]. Almost two thirds of the women completing the survey (61.6%) said they would forget to attend screening without an invitation. Other reasons for screening discontinuation included transport difficulties (25%) and not wishing to burden family members (24.7%). By contrast, other studies have reported that women do not endorse discontinuation of screening mammography due to advancing age or poor health, but some may be receptive to reducing screening frequency on recommendation from their health care provider [ 46 , 51 ].
Use of Decision Aids (DAs) to improve knowledge and guide screening decision-making
Many women reported poor knowledge about the harms and benefits of screening with studies identifying an important role for DAs. These aids have been shown to be effective in improving knowledge of the harms and benefits of screening [ 45 , 54 , 55 ] including for women with low educational attainment; as compared to women with high educational attainment [ 47 ]. DAs can increase knowledge about screening [ 47 , 49 ] and may decrease the intention to continue screening after the recommended age [ 45 , 52 , 54 ]. They can be used by primary care providers to support a conversation about breast screening intention and reasons for discontinuing screening. In one pilot study undertaken in the US using a DA, 5 of the 8 women (62.5%) indicated they intended to continue to receive mammography; however, 3 participants planned to get them less often [ 45 ]. When asked whether they thought their physician would want them to get a mammogram, 80% said “yes” on pre-test; this figure decreased to 62.5% after exposure to the DA. This pilot study suggests that the use of a decision-aid may result in fewer women ≥ 75 years old continuing to screen for breast cancer [ 45 ].
Similar findings were evident in two studies drawing on the same data undertaken in the US [ 48 , 53 ]. Using a larger sample ( n = 283), women’s intentions to screen prior to a visit with their primary care provider and then again after exposure to the DA were compared. Results showed that 21.7% of women reduced their intention to be screened, 7.9% increased their intentions to be screened, and 70.4% did not change. Compared to those who had no change or increased their screening intentions, women who had a decrease in screening intention were significantly less likely to receive screening after 18 months. Generally, studies have shown that women aged 75 and older find DAs acceptable and helpful [ 47 , 48 , 49 , 55 ] and using them had the potential to impact on a women’s intention to screen [ 55 ].
Cadet and colleagues [ 49 ] explored the impact of educational attainment on the use of DAs. Results highlight that education moderates the utility of these aids; women with lower educational attainment were less likely to understand all the DA’s content (46.3% vs 67.5%; P < 0.001); had less knowledge of the benefits and harms of mammography (adjusted mean ± standard error knowledge score, 7.1 ± 0.3 vs 8.1 ± 0.3; p < 0.001); and were less likely to have their screening intentions impacted (adjusted percentage, 11.4% vs 19.4%; p = 0.01).
This scoping review summarises current knowledge regarding motivations and screening behaviours of women over 75 years. The findings suggest that awareness of the importance of breast cancer screening among women aged ≥ 75 years is high [ 23 , 46 , 49 ] and that many women wish to continue screening regardless of perceived health status or age. This highlights the importance of focusing on motivation and screening behaviours and the multiple factors that influence ongoing participation in breast screening programs.
The generally high regard attributed to screening among women aged ≥ 75 years presents a complex challenge for health professionals who are focused on potential harm (from available national and international guidelines) in ongoing screening for women beyond age 75 [ 18 , 20 , 57 ]. Included studies highlight that many women relied on the advice of health care providers regarding the benefits and harms when making the decision to continue breast screening [ 46 , 51 , 52 ], however there were some that did not [ 33 ]. Having a previous pattern of screening was noted as being more significant to ongoing intention than any other identified socio-demographic feature [ 56 ]. This is perhaps because women will not readily forgo health care practices that they have always considered important and that retain ongoing importance for the broader population.
For those women who had discontinued screening after the age of 74 it was apparent that the rationale for doing so was not often based on choice or receipt of information, but rather on factors that impact decision-making in relation to screening. These included no longer receiving an invitation to attend, transport difficulties and not wanting to be a burden on relatives or friends [ 23 , 46 , 51 ]. Ongoing receipt of invitations to screen was an important aspect of maintaining a capacity to choose [ 23 ]. This was particularly important for those women who had been regular screeners.
Women over 75 require more information to make decisions regarding screening [ 23 , 52 , 54 , 55 ], however health care providers must also be aware that the element of choice is important for older women. Having a capacity to choose avoids any notion of discrimination based on age, health status, gender or sociodemographic difference and acknowledges the importance of women retaining control over their health [ 23 ]. It was apparent that some women would choose to continue screening at a reduced frequency if this option was available and that women should have access to information facilitating self-referral [ 23 , 45 , 46 , 51 , 56 ].
Decision-making regarding ongoing breast cancer screening has been facilitated via the use of Decision Aids (DAs) within clinical settings [ 54 , 55 ]. While some studies suggest that women will make a decision regardless of health status, the use of DAs has impacted women’s decision to screen. While this may have limited benefit for those of lower educational attainment [ 48 ] they have been effective in improving knowledge relating to harms and benefits of screening particularly where they have been used to support a conversation with women about the value of screening [ 54 , 55 , 56 ].
Women have identified challenges in engaging in conversations with health care providers regarding ongoing screening, because providers frequently draw on projections of life expectancy and over-diagnosis [ 17 , 51 ]. As a result, these conversations about screening after age 75 years often do not occur [ 46 ]. It is likely that health providers may need more support and guidance in leading these conversations. This may be through the use of DAs or standardised checklists. It may be possible to incorporate these within existing health preventive measures for this age group. The potential for advice regarding ongoing breast cancer screening to be available outside of clinical settings may provide important pathways for conversations with women regarding health choices. Provision of information and advice in settings such as community based seniors groups [ 51 ] offers a potential platform to broaden conversations and align sources of information, not only with health professionals but amongst women themselves. This may help to address any misconception regarding eligibility and access to services [ 23 ]. It may also be aligned with other health promotion and lifestyle messages provided to this age group.
Limitations of the review
The searches that formed the basis of this review were carried in June 2022. Although the search was comprehensive, we have only captured those studies that were published in the included databases from 2009. There may have been other studies published outside of these periods. We also limited the search to studies published in English with full-text availability.
The emphasis of a scoping review is on comprehensive coverage and synthesis of the key findings, rather than on a particular standard of evidence and, consequently a quality assessment of the included studies was not undertaken. This has resulted in the inclusion of a wide range of study designs and data collection methods. It is important to note that three studies included in the review drew on the same sample of women (283 over > 75)[ 49 , 53 , 54 ]. The results of this review provide valuable insights into motivations and behaviours for breast cancer screening for older women, however they should be interpreted with caution given the specific methodological and geographical limitations.
Conclusion and recommendations
This scoping review highlighted a range of key motivations and behaviours in relation to breast cancer screening for women ≥ 75 years of age. The results provide some insight into how decisions about screening continuation after 74 are made and how informed decision-making can be supported. Specifically, this review supports the following suggestions for further research and policy direction:
Further research regarding breast cancer screening motivations and behaviours for women over 75 would provide valuable insight for health providers delivering services to women in this age group.
Health providers may benefit from the broader use of decision aids or structured checklists to guide conversations with women over 75 regarding ongoing health promotion/preventive measures.
Providing health-based information in non-clinical settings frequented by women in this age group may provide a broader reach of information and facilitate choices. This may help to reduce any perception of discrimination based on age, health status or socio-demographic factors.
Availability of data and materials
All data generated or analysed during this study is included in this published article (see Table 2 above).
Cancer Australia, in their 2014 position statement, define “overdiagnosis” in the following way. ‘’Overdiagnosis’ from breast screening does not refer to error or misdiagnosis, but rather refers to breast cancer diagnosed by screening that would not otherwise have been diagnosed during a woman’s lifetime. “Overdiagnosis” includes all instances where cancers detected through screening (ductal carcinoma in situ or invasive breast cancer) might never have progressed to become symptomatic during a woman’s life, i.e., cancer that would not have been detected in the absence of screening. It is not possible to precisely predict at diagnosis, to which cancers overdiagnosis would apply.” (accessed 22. nd August 2022; https://www.canceraustralia.gov.au/resources/position-statements/overdiagnosis-mammographic-screening ).
World Health Organization. Breast Cancer Geneva: WHO; 2021 [Available from: https://www.who.int/news-room/fact-sheets/detail/breast-cancer#:~:text=Reducing%20global%20breast%20cancer%20mortality,and%20comprehensive%20breast%20cancer%20management .
International Agency for Research on Cancer (IARC). IARC Handbooks on Cancer Screening: Volume 15 Breast Cancer Geneva: IARC; 2016 [Available from: https://publications.iarc.fr/Book-And-Report-Series/Iarc-Handbooks-Of-Cancer-Prevention/Breast-Cancer-Screening-2016 .
Australian Institute of Health and Welfare. Cancer in Australia 2021 [Available from: https://www.canceraustralia.gov.au/cancer-types/breast-cancer/statistics .
Breast Cancer Network Australia. Current breast cancer statistics in Australia 2020 [Available from: https://www.bcna.org.au/media/7111/bcna-2019-current-breast-cancer-statistics-in-australia-11jan2019.pdf .
Ren W, Chen M, Qiao Y, Zhao F. Global guidelines for breast cancer screening: A systematic review. The Breast. 2022;64:85–99.
Article PubMed PubMed Central Google Scholar
Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, et al. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30(8):1194–220.
Article CAS PubMed Google Scholar
Hamashima C, Hattori M, Honjo S, Kasahara Y, Katayama T, Nakai M, et al. The Japanese guidelines for breast cancer screening. Jpn J Clin Oncol. 2016;46(5):482–92.
Article PubMed Google Scholar
Bevers TB, Helvie M, Bonaccio E, Calhoun KE, Daly MB, Farrar WB, et al. Breast cancer screening and diagnosis, version 3.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Net. 2018;16(11):1362–89.
Article Google Scholar
He J, Chen W, Li N, Shen H, Li J, Wang Y, et al. China guideline for the screening and early detection of female breast cancer (2021, Beijing). Zhonghua Zhong liu za zhi [Chinese Journal of Oncology]. 2021;43(4):357–82.
CAS PubMed Google Scholar
Cancer Australia. Early detection of breast cancer 2021 [cited 2022 25 July]. Available from: https://www.canceraustralia.gov.au/resources/position-statements/early-detection-breast-cancer .
Schünemann HJ, Lerda D, Quinn C, Follmann M, Alonso-Coello P, Rossi PG, et al. Breast Cancer Screening and Diagnosis: A Synopsis of the European Breast Guidelines. Ann Intern Med. 2019;172(1):46–56.
World Health Organization. WHO Position Paper on Mammography Screening Geneva WHO. 2016.
Google Scholar
Lansdorp-Vogelaar I, Gulati R, Mariotto AB. Personalizing age of cancer screening cessation based on comorbid conditions: model estimates of harms and benefits. Ann Intern Med. 2014;161:104.
Lee CS, Moy L, Joe BN, Sickles EA, Niell BL. Screening for Breast Cancer in Women Age 75 Years and Older. Am J Roentgenol. 2017;210(2):256–63.
Broeders M, Moss S, Nystrom L. The impact of mammographic screening on breast cancer mortality in Europe: a review of observational studies. J Med Screen. 2012;19(suppl 1):14.
Oeffinger KC, Fontham ETH, Etzioni R, Herzig A, Michaelson JS, Shih YCT, et al. Breast cancer screening for women at average risk: 2015 Guideline update from the American cancer society. JAMA - Journal of the American Medical Association. 2015;314(15):1599–614.
Walter LC, Schonberg MA. Screening mammography in older women: a review. JAMA. 2014;311:1336.
Article CAS PubMed PubMed Central Google Scholar
Braithwaite D, Walter LC, Izano M, Kerlikowske K. Benefits and harms of screening mammography by comorbidity and age: a qualitative synthesis of observational studies and decision analyses. J Gen Intern Med. 2016;31:561.
Braithwaite D, Mandelblatt JS, Kerlikowske K. To screen or not to screen older women for breast cancer: a conundrum. Future Oncol. 2013;9(6):763–6.
Demb J, Abraham L, Miglioretti DL, Sprague BL, O’Meara ES, Advani S, et al. Screening Mammography Outcomes: Risk of Breast Cancer and Mortality by Comorbidity Score and Age. Jnci-Journal of the National Cancer Institute. 2020;112(6):599–606.
Demb J, Akinyemiju T, Allen I, Onega T, Hiatt RA, Braithwaite D. Screening mammography use in older women according to health status: a systematic review and meta-analysis. Clin Interv Aging. 2018;13:1987–97.
Qaseem A, Lin JS, Mustafa RA, Horwitch CA, Wilt TJ. Screening for Breast Cancer in Average-Risk Women: A Guidance Statement From the American College of Physicians. Ann Intern Med. 2019;170(8):547–60.
Collins K, Winslow M, Reed MW, Walters SJ, Robinson T, Madan J, et al. The views of older women towards mammographic screening: a qualitative and quantitative study. Br J Cancer. 2010;102(10):1461–7.
Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst. 2010;102(9):605–13.
Hersch J, Jansen J, Barratt A, Irwig L, Houssami N, Howard K, et al. Women’s views on overdiagnosis in breast cancer screening: a qualitative study. BMJ : British Medical Journal. 2013;346:f158.
De Gelder R, Heijnsdijk EAM, Van Ravesteyn NT, Fracheboud J, Draisma G, De Koning HJ. Interpreting overdiagnosis estimates in population-based mammography screening. Epidemiol Rev. 2011;33(1):111–21.
Monticciolo DL, Helvie MA, Edward HR. Current issues in the overdiagnosis and overtreatment of breast cancer. Am J Roentgenol. 2018;210(2):285–91.
Shepardson LB, Dean L. Current controversies in breast cancer screening. Semin Oncol. 2020;47(4):177–81.
National Cancer Control Centre. Cancer incidence in Australia 2022 [Available from: https://ncci.canceraustralia.gov.au/diagnosis/cancer-incidence/cancer-incidence .
Austin JD, Shelton RC, Lee Argov EJ, Tehranifar P. Older Women’s Perspectives Driving Mammography Screening Use and Overuse: a Narrative Review of Mixed-Methods Studies. Current Epidemiology Reports. 2020;7(4):274–89.
Austin JD, Tehranifar P, Rodriguez CB, Brotzman L, Agovino M, Ziazadeh D, et al. A mixed-methods study of multi-level factors influencing mammography overuse among an older ethnically diverse screening population: implications for de-implementation. Implementation Science Communications. 2021;2(1):110.
Demb J, Allen I, Braithwaite D. Utilization of screening mammography in older women according to comorbidity and age: protocol for a systematic review. Syst Rev. 2016;5(1):168.
Housten AJ, Pappadis MR, Krishnan S, Weller SC, Giordano SH, Bevers TB, et al. Resistance to discontinuing breast cancer screening in older women: A qualitative study. Psychooncology. 2018;27(6):1635–41.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Peters M, Godfrey C, McInerney P, Munn Z, Tricco A, Khalil HAE, et al. Chapter 11: Scoping reviews. JBI Manual for Evidence Synthesis 2020 [Available from: https://jbi-global-wiki.refined.site/space/MANUAL .
Peters MD, Godfrey C, McInerney P, Khalil H, Larsen P, Marnie C, et al. Best practice guidance and reporting items for the development of scoping review protocols. JBI evidence synthesis. 2022;20(4):953–68.
Fantom NJ, Serajuddin U. The World Bank’s classification of countries by income. World Bank Policy Research Working Paper; 2016.
Book Google Scholar
BreastScreen Australia Evaluation Taskforce. BreastScreen Australia Evaluation. Evaluation final report: Screening Monograph No 1/2009. Canberra; Australia Australian Government Department of Health and Ageing; 2009.
Nelson HD, Cantor A, Humphrey L. Screening for breast cancer: a systematic review to update the 2009 U.S. Preventive Services Task Force recommendation2016.
Woolf SH. The 2009 breast cancer screening recommendations of the US Preventive Services Task Force. JAMA. 2010;303(2):162–3.
Covidence systematic review software. [Internet]. Veritas-Health-Innovation 2020. Available from: https://www.covidence.org/ .
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73.
Tricco AC, Lillie E, Zarin W, O’Brien K, Colquhoun H, Kastner M, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16(1):15.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Beckmeyer A, Smith RM, Miles L, Schonberg MA, Toland AE, Hirsch H. Pilot Evaluation of Patient-centered Survey Tools for Breast Cancer Screening Decision-making in Women 75 and Older. Health Behavior and Policy Review. 2020;7(1):13–8.
Brotzman LE, Shelton RC, Austin JD, Rodriguez CB, Agovino M, Moise N, et al. “It’s something I’ll do until I die”: A qualitative examination into why older women in the U.S. continue screening mammography. Canc Med. 2022;11(20):3854–62.
Article CAS Google Scholar
Cadet T, Pinheiro A, Karamourtopoulos M, Jacobson AR, Aliberti GM, Kistler CE, et al. Effects by educational attainment of a mammography screening patient decision aid for women aged 75 years and older. Cancer. 2021;127(23):4455–63.
Cadet T, Aliberti G, Karamourtopoulos M, Jacobson A, Gilliam EA, Primeau S, et al. Evaluation of a mammography decision aid for women 75 and older at risk for lower health literacy in a pretest-posttest trial. Patient Educ Couns. 2021;104(9):2344–50.
Cadet T, Aliberti G, Karamourtopoulos M, Jacobson A, Siska M, Schonberg MA. Modifying a mammography decision aid for older adult women with risk factors for low health literacy. Health Lit Res Prac. 2021;5(2):e78–90.
Gray N, Picone G. Evidence of Large-Scale Social Interactions in Mammography in the United States. Atl Econ J. 2018;46(4):441–57.
Hoover DS, Pappadis MR, Housten AJ, Krishnan S, Weller SC, Giordano SH, et al. Preferences for Communicating about Breast Cancer Screening Among Racially/Ethnically Diverse Older Women. Health Commun. 2019;34(7):702–6.
Salzman B, Bistline A, Cunningham A, Silverio A, Sifri R. Breast Cancer Screening Shared Decision-Making in Older African-American Women. J Natl Med Assoc. 2020;112(5):556–60.
PubMed Google Scholar
Schoenborn NL, Pinheiro A, Kistler CE, Schonberg MA. Association between Breast Cancer Screening Intention and Behavior in the Context of Screening Cessation in Older Women. Med Decis Making. 2021;41(2):240–4.
Schonberg MA, Kistler CE, Pinheiro A, Jacobson AR, Aliberti GM, Karamourtopoulos M, et al. Effect of a Mammography Screening Decision Aid for Women 75 Years and Older: A Cluster Randomized Clinical Trial. JAMA Intern Med. 2020;180(6):831–42.
Schonberg MA, Hamel MB, Davis RB. Development and evaluation of a decision aid on mammography screening for women 75 years and older. JAMA Intern Med. 2014;174:417.
Eisinger F, Viguier J, Blay J-Y, Morère J-F, Coscas Y, Roussel C, et al. Uptake of breast cancer screening in women aged over 75years: a controversy to come? Eur J Cancer Prev. 2011;20(Suppl 1):S13-5.
Schonberg MA, Breslau ES, McCarthy EP. Targeting of Mammography Screening According to Life Expectancy in Women Aged 75 and Older. J Am Geriatr Soc. 2013;61(3):388–95.
Download references
Acknowledgements
We would like to acknowledge Ange Hayden-Johns (expert librarian) who assisted with the development of the search criteria and undertook the relevant searches and Tejashree Kangutkar who assisted with some of the Covidence work.
This work was supported by funding from the Australian Government Department of Health and Aged Care (ID: Health/20–21/E21-10463).
Author information
Authors and affiliations.
Violet Vines Centre for Rural Health Research, La Trobe Rural Health School, La Trobe University, P.O. Box 199, Bendigo, VIC, 3552, Australia
Virginia Dickson-Swift, Joanne Adams & Evelien Spelten
Care Economy Research Institute, La Trobe University, Wodonga, Australia
Irene Blackberry
Olivia Newton-John Cancer Wellness and Research Centre, Austin Health, Melbourne, Australia
Carlene Wilson & Eva Yuen
Melbourne School of Population and Global Health, Melbourne University, Melbourne, Australia
Carlene Wilson
School of Psychology and Public Health, La Trobe University, Bundoora, Australia
Institute for Health Transformation, Deakin University, Burwood, Australia
Centre for Quality and Patient Safety, Monash Health Partnership, Monash Health, Clayton, Australia
You can also search for this author in PubMed Google Scholar
Contributions
VDS conceived and designed the scoping review. VDS & JA developed the search strategy with librarian support, and all authors (VDS, JA, ES, IB, CW, EY) participated in the screening and data extraction stages and assisted with writing the review. All authors provided editorial support and read and approved the final manuscript prior to submission.
Corresponding author
Correspondence to Joanne Adams .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
Ethics approval and consent to participate was not required for this study.
Consent for publication
Consent for publication was not required for this study.
Competing interest
The authors declare they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Dickson-Swift, V., Adams, J., Spelten, E. et al. Breast cancer screening motivation and behaviours of women aged over 75 years: a scoping review. BMC Women's Health 24 , 256 (2024). https://doi.org/10.1186/s12905-024-03094-z
Download citation
Received : 06 September 2023
Accepted : 15 April 2024
Published : 24 April 2024
DOI : https://doi.org/10.1186/s12905-024-03094-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breast cancer
- Mammography
- Older women
- Scoping review
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Should I do a synthesis (i.e. literature review)?
- Questions & Quandaries
- Published: 18 April 2024
Cite this article

- H. Carrie Chen 1 ,
- Ayelet Kuper 2 , 3 , 4 ,
- Jennifer Cleland 5 &
- Patricia O’Sullivan 6
272 Accesses
1 Altmetric
Explore all metrics
This column is intended to address the kinds of knotty problems and dilemmas with which many scholars grapple in studying health professions education. In this article, the authors address the question of whether one should conduct a literature review or knowledge synthesis, considering the why, when, and how, as well as its potential pitfalls. The goal is to guide supervisors and students who are considering whether to embark on a literature review in education research.
Avoid common mistakes on your manuscript.
Two junior colleagues come to you to ask your advice about carrying out a literature review on a particular topic. “Should they?” immediately pops into your mind, followed closely by, if yes, then what kind of literature review is appropriate? Our experience is that colleagues often come to suggest a literature review to “kick start” their research (in fact, some academic programs require them as part of degree requirements), without a full understanding of the work involved, the different types of literature review, and what type of literature review might be most suitable for their research question. In this Questions and Quandaries, we address the question of literature reviews in education research, considering the why, when, and how, as well as potential pitfalls.
First, what is meant by literature review? The term literature review has been used to refer to both a review of the literature and a knowledge synthesis (Maggio et al., 2018 ; Siddaway et al., 2019 ). For our purposes, we employ the term as commonly used to refer to a knowledge synthesis , which is a formal comprehensive review of the existing body of literature on a topic. It is a research approach that critically integrates and synthesizes available evidence from multiple studies to provide insight and allow the drawing of conclusions. It is an example of Boyer’s scholarship of integration (Boyer, 1990 ). In contrast, a review of the literature is a relatively casual and expedient method for attaining a general overview of the state of knowledge on a given topic to make the argument that a new study is needed. In this interpretation, a literature review serves as a key starting point for anyone conducting research by identifying gaps in the literature, informing the study question, and situating one’s study in the field.
Whether a formal knowledge synthesis should be done depends on if a review is needed and what the rationale is for the review. The first question to consider is whether a literature review already exists. If no, is there enough literature published on the topic to warrant a review? If yes, does the previous review need updating? How long has it been since the last review and has the literature expanded so much or are there important new studies that need integrating to justify an updated review? Or were there flaws in the previous review that one intends to address with a new review? Or does one intend to address a different question than the focus of the previous review?
If the knowledge synthesis is to be done, it should be driven by a research question. What is the research question? Can it be answered by a review? What is the purpose of the synthesis? There are two main purposes for knowledge synthesis– knowledge support and decision support. Knowledge support summarizes the evidence while decision support takes additional analytical steps to allow for decision-making in particular contexts (Mays et al., 2005 ).
If the purpose is to provide knowledge support, then the question is how or what will the knowledge synthesis add to the literature? Will it establish the state of knowledge in an area, identify gaps in the literature/knowledge base, and/or map opportunities for future research? Cornett et al., performed a scoping review of the literature on professional identity, focusing on how professional identity is described, why the studies where done, and what constructs of identity were used. Their findings advanced understanding of the state of knowledge by indicating that professional identity studies were driven primarily by the desire to examine the impact of political, social and healthcare reforms and advances, and that the various constructs of professional identity across the literature could be categorized into five themes (Cornett et al., 2023 ).
If, on the other hand, the purpose of the knowledge synthesis is to provide decision support, for whom will the synthesis be relevant and how will it improve practice? Will the synthesis result in tools such as guidelines or recommendations for practitioners and policymakers? An example of a knowledge synthesis for decision support is a systematic review conducted by Spencer and colleagues to examine the validity evidence for use of the Ottawa Surgical Competency Operating Room Evaluation (OSCORE) assessment tool. The authors summarized their findings with recommendations for educational practice– namely supporting the use of the OSCORE for in-the-moment entrustment decisions by frontline supervisors in surgical fields but cautioning about the limited evidence for support of its use in summative promotions decisions or non-surgical contexts (Spencer et al., 2022 ).
If a knowledge synthesis is indeed appropriate, its methodology should be informed by its research question and purpose. We do not have the space to discuss the various types of knowledge synthesis except to say that several types have been described in the literature. The five most common types in health professions education are narrative reviews, systematic reviews, umbrella reviews (meta-syntheses), scoping reviews, and realist reviews (Maggio et al., 2018 ). These represent different epistemologies, serve different review purposes, use different methods, and result in different review outcomes (Gordon, 2016 ).
Each type of review lends itself best to answering a certain type of research question. For instance, narrative reviews generally describe what is known about a topic without necessarily answering a specific empirical question (Maggio et al., 2018 ). A recent example of a narrative review focused on schoolwide wellbeing programs, describing what is known about the key characteristics and mediating factors that influence student support and identifying critical tensions around confidentiality that could make or break programs (Tan et al., 2023 ). Umbrella reviews, on the other hand, synthesize evidence from multiple reviews or meta-analyses and can illuminate agreement, inconsistencies, or evolution of evidence on a topic. For example, an umbrella review on problem-based learning highlighted the shift in research focus over time from does it work, to how does it work, to how does it work in different contexts, and pointed to directions for new research (Hung et al., 2019 ).
Practical questions for those considering a literature review include whether one has the time required and an appropriate team to conduct a high-quality knowledge synthesis. Regardless of the type of knowledge synthesis and use of quantitative or qualitative methods, all require rigorous and clear methods that allow for reproducibility. This can take time, up to 12–18 months. A high-quality knowledge synthesis also requires a team whose members have expertise not only in the content matter, but also in knowledge synthesis methodology and in literature searches (i.e. a librarian). A team with multiple reviewers with a variety of perspectives can also help manage the volume of large reviews, minimize potential biases, and strengthen the critical analysis.
Finally, a pitfall one should be careful to avoid is merely summarizing everything in the literature without critical evaluation and integration of the information. A knowledge synthesis that merely bean counts or presents a collection of unconnected information that has not been reflected upon or critically analyzed does not truly advance knowledge or decision-making. Rather, it leads us back to our original question of whether it should have been done in the first place.
Boyer, E. L. (1990). Scholarship reconsidered: Priorities of the professoriate (pp. 18–21). Princeton University Press.
Cornett, M., Palermo, C., & Ash, S. (2023). Professional identity research in the health professions—a scoping review. Advances in Health Sciences Education , 28 (2), 589–642.
Article Google Scholar
Gordon, M. (2016). Are we talking the same paradigm? Considering methodological choices in health education systematic review. Medical Teacher , 38 (7), 746–750.
Hung, W., Dolmans, D. H. J. M., & van Merrienboer, J. J. G. (2019). A review to identify key perspectives in PBL meta-analyses and reviews: Trends, gaps and future research directions. Advances in Health Sciences Education , 24 , 943–957.
Maggio, L. A., Thomas, A., & Durning, S. J. (2018). Knowledge synthesis. In T. Swanwick, K. Forrest, & B. C. O’Brien (Eds.), Understanding Medical Education: Evidence, theory, and practice (pp. 457–469). Wiley.
Mays, N., Pope, C., & Popay, J. (2005). Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. Journal of Health Services Research & Policy , 10 (1_suppl), 6–20.
Siddaway, A. P., Wood, A. M., & Hedges, L. V. (2019). How to do a systematic review: A best practice guide for conducting and reporting narrative reviews, meta-analyses, and meta-syntheses. Annual Review of Psychology , 70 , 747–770.
Spencer, M., Sherbino, J., & Hatala, R. (2022). Examining the validity argument for the Ottawa Surgical Competency operating room evaluation (OSCORE): A systematic review and narrative synthesis. Advances in Health Sciences Education , 27 , 659–689.
Tan, E., Frambach, J., Driessen, E., & Cleland, J. (2023). Opening the black box of school-wide student wellbeing programmes: A critical narrative review informed by activity theory. Advances in Health Sciences Education . https://doi.org/10.1007/s10459-023-10261-8 . Epub ahead of print 02 July 2023.
Download references
Author information
Authors and affiliations.
Georgetown University School of Medicine, Washington, DC, USA
H. Carrie Chen
Wilson Centre for Research in Education, University Health Network, University of Toronto, Toronto, Canada
Ayelet Kuper
Division of General Internal Medicine, Sunnybrook Health Sciences Center, Toronto, Canada
Department of Medicine, University of Toronto, Toronto, Canada
Lee Kong Chian School of Medicine, Nanyang Technological University Singapore, Singapore, Singapore
Jennifer Cleland
University of California San Francisco School of Medicine, San Francisco, CA, USA
Patricia O’Sullivan
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to H. Carrie Chen .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Chen, H.C., Kuper, A., Cleland, J. et al. Should I do a synthesis (i.e. literature review)?. Adv in Health Sci Educ (2024). https://doi.org/10.1007/s10459-024-10335-1
Download citation
Published : 18 April 2024
DOI : https://doi.org/10.1007/s10459-024-10335-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 25 April 2024
A scoping review of academic and grey literature on migrant health research conducted in Scotland
- G. Petrie 1 ,
- K. Angus 2 &
- R. O’Donnell 2
BMC Public Health volume 24 , Article number: 1156 ( 2024 ) Cite this article
151 Accesses
8 Altmetric
Metrics details
Migration to Scotland has increased since 2002 with an increase in European residents and participation in the Asylum dispersal scheme. Scotland has become more ethnically diverse, and 10% of the current population were born abroad. Migration and ethnicity are determinants of health, and information on the health status of migrants to Scotland and their access to and barriers to care facilitates the planning and delivery of equitable health services. This study aimed to scope existing peer-reviewed research and grey literature to identify gaps in evidence regarding the health of migrants in Scotland.
A scoping review on the health of migrants in Scotland was carried out for dates January 2002 to March 2023, inclusive of peer-reviewed journals and grey literature. CINAHL/ Web of Science/SocIndex and Medline databases were systematically searched along with government and third-sector websites. The searches identified 2166 journal articles and 170 grey literature documents for screening. Included articles were categorised according to the World Health Organisation’s 2016 Strategy and Action Plan for Refugee and Migrant Health in the European region. This approach builds on a previously published literature review on Migrant Health in the Republic of Ireland.
Seventy-one peer reviewed journal articles and 29 grey literature documents were included in the review. 66% were carried out from 2013 onwards and the majority focused on asylum seekers or unspecified migrant groups. Most research identified was on the World Health Organisation’s strategic areas of right to health of refugees, social determinants of health and public health planning and strengthening health systems. There were fewer studies on the strategic areas of frameworks for collaborative action, preventing communicable disease, preventing non-communicable disease, health screening and assessment and improving health information and communication.
While research on migrant health in Scotland has increased in recent years significant gaps remain. Future priorities should include studies of undocumented migrants, migrant workers, and additional research is required on the issue of improving health information and communication.
Peer Review reports
The term migrant is defined by the International Organisation for Migration as “ a person who moves away from his or her place of usual residence, whether within a country or across an international border, temporarily or permanently, and for a variety of reasons. The term includes several well-defined legal categories of people, including migrant workers; persons whose particular types of movements are legally-defined, such as smuggled migrants; as well as those whose status are not specifically defined under international law, such as international students.” [ 1 ] Internationally there are an estimated 281 million migrants – 3.6% of the world population, including 26.4 million refugees and 4.1 million asylum seekers – the highest number ever recorded [ 2 ]. The UN Refugee Society defines the term refugee as “ someone who has been forced to flee his or her country because of persecution, war or violence…most likely, they cannot return home or are afraid to do so .” The term asylum-seeker is defined as “someone whose request for sanctuary has yet to be processed.” [ 3 ].
Net-migration to Europe was negative in the 19th century due to higher levels of emigration, however in the mid-20th century immigration began to rise, because of an increase in migrant workers and following conflicts in the Middle East and North Africa [ 4 ]. Current migration drivers include conflicts alongside world-wide economic instability, exacerbated by the Covid-19 pandemic [ 5 ]. Environmental damage due to climate change is expected to inflate the number of asylum seekers entering Europe in future [ 6 ]. The increase in migration to Europe is not a short-term influx but a long-term phenomenon, and European nations must adapt and find solutions to resulting financial, safeguarding and health challenges [ 7 ].
Data on healthcare use by migrants in Europe is variable, which means cross-country comparisons are inadequate [ 8 ]. Many countries do not record migration information within health records and all use disparate criteria to classify migrant status. The lack of comparative data hinders public health surveillance and effective interventions [ 9 ]. Even where information is available, results can be contradictory due to the multifarious migrant population. Migrants have a wide range of origin countries, socio-economic position, age and journeys undertaken which can affect health status [ 10 ].
Migrants initially may have better health than the general population, known as the ‘Healthy Migrant effect’ [ 11 ]. However, health declines with increasing length of residence [ 12 ] and over time to levels comparable with the general population [ 13 ]. Second generation immigrants may have higher mortality than average [ 14 ]. The process of acculturation to the host country, with adoption of unhealthy lifestyle and behaviours, increases the risk for chronic disease [ 15 ]. In addition, inequalities in health of migrants compared to host populations has been confirmed by wide-ranging research [ 16 ].
Host countries may limit healthcare access, with undocumented migrants sometimes only entitled to emergency care [ 17 ]. Even when access is granted, inequitable services can affect quality of care due to language barriers and cultural factors [ 18 ]. Poor working/living conditions and discrimination can exacerbate health inequalities [ 12 ]. Processing facilities for asylum seekers are frequently overpopulated, stressful environments [ 19 ] and threat of deportation, lack of citizenship rights and integration can negatively affect health and access to care [ 20 ]. Undocumented workers are unprotected by health and safety legislation leading to dangerous working conditions and injuries [ 15 ].
A systematic review of migrant health in the European Union (EU) found migrants have worse self-perceived health than the general population [ 21 ]. Research evidence indicates increased prevalence of cardiovascular disease, diabetes, mental health disorders and adverse pregnancy outcomes. Exposure to conflict, harsh travel conditions and suboptimal vaccine programmes can mean higher risk of communicable disease [ 22 ]. Scoping reviews have also been conducted to describe trends within migration health research in the United Kingdom (UK) [ 23 ] and identify gaps for future research agendas in the UK [ 23 ] and in the Republic of Ireland [ 24 ].
Almost three-quarters (73%) of published migration health research in the UK has been conducted in England, focusing primarily on infectious diseases and mental health. There is limited evidence on the social determinants of health, access to and use of healthcare and structural and behavioural factors behaviours that influence migrant health in the UK [ 23 ]. By contrast, a large amount of the migration research conducted in the Republic of Ireland has focused on the social determinants of health, and on health system adaptations, with a paucity of research focusing on improving health information systems [ 24 ].
Migration and Health in Scotland
Immigration to Scotland began to rise in 2003 with the expansion of the EU [ 25 ]. The population in Scotland increased from 5.11 million to 5.47 million between 2005 and 2020 and is predicted to continue rising until 2028 [ 26 ] despite low birth rates, with the increased population resulting from inward migration [ 27 ]. Scotland’s population is becoming more ethnically diverse [ 28 ] and susceptibility to different health conditions varies by ethnic group, which has implications for the planning and provision of health services [ 29 ]. 7% of the current Scottish population are non-UK nationals and 10% were born outside Britain. The commonest countries of origin were Poland, Ireland, Italy, Nigeria and India [ 30 ].
Within Scotland, linking health data to ethnicity is standard in order to monitor and improve health of minority groups [ 31 ]. Ethnic background can differ from country of birth which means migration status cannot be assumed [ 32 ], although health inequalities experienced by migrants often extend to affect all ethnic minority groups [ 33 ]. The Scottish Health and Ethnicity Linkage Study (SHELS) linked census data to health records of 91% of the population which has provided information on mortality and morbidity by ethnic group and country of birth [ 34 ]. SHELS research indicates that the white-Scottish population have a higher mortality rate than other ethnic groups. This may be consequent to the comparatively poor health of the Scottish population relative to other European nations: high mortality rates in the general population may cause a perception that the health of minorities is more advantageous than in reality [ 35 ].
Cezard et al’s [ 13 ] analysis of self-perceived health among people in Scotland found that being born abroad had a positive impact on health status. Health declined with increased length of residence, which may be explained by cultural convergence with the majority population. Allik et al. [ 36 ] compared health inequalities by ethnic background and found that with increasing age, health differences reduced thus people aged over 75 of all ethnicities had similar or worse health status than White-Scottish people. While working-age migrants appear to be healthier than the White Scottish population, it cannot be assumed that in future this would extend to older age groups.
Research has shown deprivation as a cause of heath inequalities among ethnic minority and migrant groups [ 37 ]. The socio-economic status of minority ethnic groups in Scotland is unusual, as most are of similar or higher status than the white-Scottish population [ 38 ]. Therefore, public health interventions targeting deprivation may not address risk-factors for ethnic minorities and migrants [ 36 ]. Further research on determinants of health in migrants can help with planning and design of inclusive policies.
The 2011 census indicated that 50% of immigrants lived in the cities of Edinburgh, Glasgow, and Aberdeen. Glasgow had a greater percentage of non-European immigrants due to participation in the Asylum dispersal programme [ 39 ]. 10% of UK asylum seekers are placed in Glasgow, but records are not kept following approval of asylum claims, therefore the size of the refugee population is unknown [ 40 ]. While immigration is controlled by the British government, in policy areas devolved to the Scottish government, refugees and asylum seekers have more rights than elsewhere in UK, including access to primary healthcare for undocumented migrants [ 40 ]. Despite the mitigating effect of Scottish policies, asylum seekers’ health is worsened by the asylum process and associated poverty, marginalisation, and discrimination [ 40 ]. Health deteriorates with increasing length of time in the asylum system [ 40 ] and asylum seekers and refugees have additional health needs and require enhanced support [ 41 ]. Research on the health needs of asylum seekers in Scotland is required to ensure adequate healthcare.
Aim and objectives
While scoping reviews on migrant health have been carried out in Europe [ 12 ], Ireland [ 24 ] and the UK [ 23 ] none are currently specific to the Scottish context. Given the devolved government of Scotland and demographics described above, a targeted review would help to clarify research priorities, with the aim of improving health and health care within the migrant community in Scotland. This work therefore builds on the published scoping review of migrant health in the Republic of Ireland [ 24 ]. The authors recommend replication of the study in other countries to facilitate cross-country comparison. Our aim was to scope peer-reviewed research and grey literature on migrant health conducted in Scotland and identify any gaps in the evidence. Our objectives were to: [1] understand the extent of the available research by topic area [2] summarise the types of research already conducted, populations studied, topics covered and approaches taken [3], map the existing research conducted in Scotland and [4] identify areas for future research based on any gaps in the evidence identified.
A scoping review was conducted as they can aid detection of evidence gaps [ 42 ] and allow incorporation of grey literature in topics with insufficient published research [ 43 ]. Arksey and O’Malley’s [ 44 ] five stage scoping review framework was used.
Stage 1: identifying the research question
Arskey and O’Malley [ 44 ] suggest maintaining a broad approach to identifying the research question, in order to generate breadth of coverage. On this basis, and in line with the research question identified in the Villarroel et al. [ 24 ] scoping review, our research question was framed as follows: What is the scope, main topics and gaps in evidence in the existing literature on health of international migrants living in Scotland? Arksey and O’Malley [ 44 ] highlight the importance of defining terminology at the outset of scoping reviews. For consistency, we used the broad definition of ‘migrant’ as per Villaroel et al. [ 24 ], from the International Organisation for Migration (IOM) [ 1 ]. References to refugees or asylum seekers followed the United Nations Refugee Agency definitions [ 3 ].
Stage 2: identifying relevant studies
Electronic database searches identified reports alongside a grey literature search, in line with Arskey and O’Malley’s [ 44 ] guidance to search for evidence via different sources. CINAHL, Web of Science, SocIndex and Medline academic databases were selected with input from co-authors. Search terms for the review were based upon those used by Villaroel et al. [ 24 ] with additional relevant terms from Hannigan et al. [ 9 ] The strategy combined three sets of terms for: Migrants (e.g., refugee, migrant, immigrant or newcomer), Scotland and Health. Both free text terms and index terms were used and adapted to the 4 academic databases and searches were run on 10th March 2023 (see Additional File 1 for database search strategies). Thirteen Government, University, and third-sector websites in Scotland were scoped for selection then hand-searched for grey literature (listed in Additional File 1 ).
Stage 3: study selection
Net-migration to Scotland increased in the 2000s [ 27 ] hence a date range of January 2002-March 2023 was used to identify evidence. The search was limited to English only. Inclusion/exclusion criteria for the studies were based on those used by Villaroel et al. [ 24 ] and expanded upon following discussion with co-authors (see Table 1 ). Reports were included if based on primary or secondary research on the health of international migrants in Scotland and used qualitative, quantitative or mixed methods research design. International or UK based reports were only included if Scottish results were documented separately. Reports on the health of ethnic minority groups in Scotland was included if place of birth was recorded. Research on internal (non-international) migrants within Scotland, either moving from one Scottish area to another or from another part of the United Kingdom to Scotland, were excluded.
Stage 4: data charting
All records were saved to RefWorks for screening. Records were first screened at title/abstract stage with 10% independently checked by the co-authors. The remaining reports were single screened using full text by the first author. Data from the included records was extracted and organised in tabular form under the following headings, which were agreed by team members: article type (peer-reviewed article or grey literature), publication date, geographical setting, study/intervention’s target population, funding, primary research focus on migrant health (y/n), study objective, data collection method, study design (qualitative/quantitative/mixed) and main finding. Reports were not critically appraised in this scoping review.
Stage 5: collating, summarising and reporting results
A report (either a peer-reviewed journal article or grey literature report) is used as our unit of analysis. In order to present the range of research identified, reports were grouped by the different headings in our data charting table and the outcomes considered for relevance to our scoping review’s aim. Our Results summarise the recency, focus, study designs and funding sources of the identified research, followed by the geographical settings and whether Scotland was included in international research reports. Reports were grouped by their study population and further sub-divided by publication type and geographical area for summarising. Finally, the WHO’s European strategy and action plan (SAAP) for refugee and migrant health [ 7 ] is a policy framework designed to help governments and other stakeholders monitor and improve migrant health in Europe. There are nine strategic areas in the WHO’s SAAP, which prioritise the most salient issues. In line with Villaroel et al’s [ 24 ] approach and in order to compare scoping review outcomes, these areas were used to categorise the findings of this review. Each report was matched to the most appropriate SAAP:
Establishing a Framework for Collaborative Action.
Advocating for the right to health of refugees.
Addressing the social determinants of health.
Achieving public health preparedness and ensuring an effective response.
Strengthening health systems and their resilience.
Preventing communicable disease.
Preventing and reducing the risks caused by non-communicable disease.
Ensuring ethical and effective health screening and assessment.
Improving health information and communication.
The primary focus (aims and objectives) of each report was used to identify the relevant SAAP area/areas. To improve reliability, results were compared using coding criteria used in Villaroel et al’s study (MacFarlane 2023, personal communication, 31st May). 10% of the reports were checked by one co-author to ensure consistent coding to SAAP categories. Any instances of uncertainty in mapping reports to the relevant SAAP area/areas were discussed and resolved by team members.
This scoping review of the literature on migrant health in Scotland identified 2166 records from academic literature databases, following duplicate removal, and 170 records from website searches (see Fig. 1 ). Following screening, a total of 71 peer-reviewed journal articles and 29 grey literature studies (totalling 100 reports) were included for analysis (Results table and reference list are presented in Additional File 2 ).
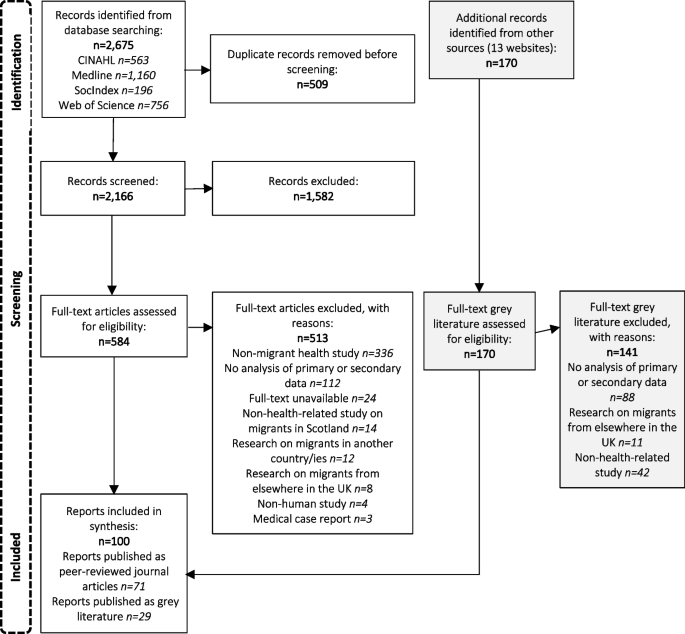
Flow chart illustrating the identification of sources of evidence included in the scoping review
Overall findings
The majority of reports were published between 2013 and 2022. Fifty-eight reports (58%) focused exclusively on migrant health [ 18 , 39 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 ]. 23 centred on health but included other populations in addition to migrants – for example research on ethnic minorities or other vulnerable groups [ 13 , 31 , 35 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 ]. Seventeen reports were included where the sample population were migrants, but the primary topic was not health – for example destitution, integration, and service needs [ 27 , 73 , 74 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 ]. Health data was reported as part of the wider subject matter. One report [ 136 ] looked at the social determinants of breastfeeding including migrant status and one [ 137 ] compared attitudes to aging and family support between countries.
Funding sources were not declared for 35 (35%) of reports. The Scottish Government funded 20 reports (20%) [ 13 , 27 , 32 , 39 , 45 , 46 , 47 , 66 , 77 , 88 , 99 , 100 , 101 , 102 , 113 , 116 , 119 , 121 , 129 , 134 ]. Other common sources of funding included Government funded public bodies ( n = 13) [ 45 , 48 , 49 , 50 , 51 , 52 , 53 , 104 , 107 , 113 , 116 , 131 , 136 ], the Scottish Health Service ( n = 18) (either the National Health Service (NHS) [ 13 , 54 , 56 , 57 , 58 , 59 , 102 , 113 , 116 ], local NHS trusts [ 45 , 60 , 61 , 77 , 102 , 103 , 112 ] or by Public Health Scotland [ 13 , 113 ]) Eleven reports (11%) were funded by Universities. The charity sector financed 15 (15%) reports [ 53 , 63 , 66 , 69 , 70 , 71 , 72 , 73 , 74 , 103 , 111 , 123 , 125 , 132 , 138 ] and the EU and Scottish local authorities funded four reports each [ 45 , 62 , 75 , 76 , 77 , 102 , 125 , 135 ]. Professional bodies financed one report [ 126 ] as did the Japanese government [ 64 ]. No reports received funding from the business sector. The biggest sources of funding for grey literature were Refugee charities (40%) and the Scottish government (30%) (see Fig. 2 ).
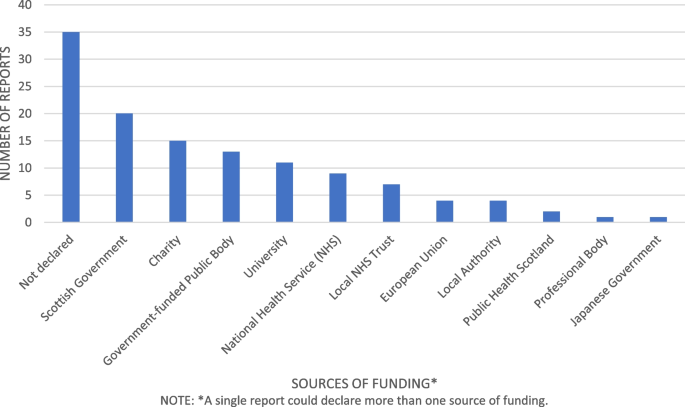
Sources of funding for migrant health research in Scotland
Research methods and data collection
52% of reports used qualitative research methods. Forty-five reports (86%) collected data using 1–1 interviews and 24 (46%) used focus groups. Other methods of data collection included questionnaires (six studies (11%)), workshops (two studies (3.85%)) and observation (two studies (3.85%)). Oral/written evidence, guided play sessions, family case studies and participatory activity sessions were used in one report each.
28% of reports used quantitative research methods, most commonly cross section design (ten studies (36%)) and cohort design (18 studies (64%)). Information was obtained from databases including medical records, Census data and national records in 21 reports (75%). Questionnaires were used in six reports (21%). Other methods including body measurements, food diaries, blood samples, interviews and case reviews were used in 1 report each.
20% of reports used mixed methods. The most common method of data collection was questionnaires in 14 reports (70%), interviews in ten reports (50%), focus groups in seven reports (35%), workshops in three reports (13.6%), and databases in three reports (13.6%). Other methods included literature review in two reports (10%), case note reviews in two reports (10%) and one reports each used mapping and school records.
Geographical areas of study
Ninety-one reports were situated in Scotland, of which 35 (38.5%) covered the whole country and 56 (61.5%) specified a city or area where research was undertaken. Some UK and international reports also specified the area of Scotland. The largest share of research within Scotland overall was in Glasgow with 36 reports, followed by Edinburgh with 16 reports, Lothian with six reports, Aberdeen with five reports and Grampian with three reports. The Northeast, Stirling, Highlands, Inverness, Lanarkshire, Motherwell and Selkirk had one report in each area.
There were seven international reports, three on mortality by country of birth [ 75 , 76 , 78 ], one on cross cultural communication [ 79 ], one on maternity care in Poland and Scotland [ 99 ], one comparing attitudes to aging in China and Scotland [ 137 ] and one on the link between birthweights and integration of migrants [ 64 ]. The remaining two reports were UK based, one on immunisation of Roma and traveller communities [ 117 ] and one on the link between ethnic diversity and mortality [ 104 ]. All the included international and UK reports documented the Scottish data separately within results.
Migrant population
Thirty-one reports included all migrants in the study population. The remaining reports included 30 studies on asylum seekers/refugees, 11 on Polish migrants, ten on Africans, six each on South Asians/Chinese/European, three on Arabs, and two on Roma populations (see Fig. 3 ). Most reports did not specify the country of origin for Asylum seekers and refugees - where country of birth was specified, reports were also included in the appropriate category.
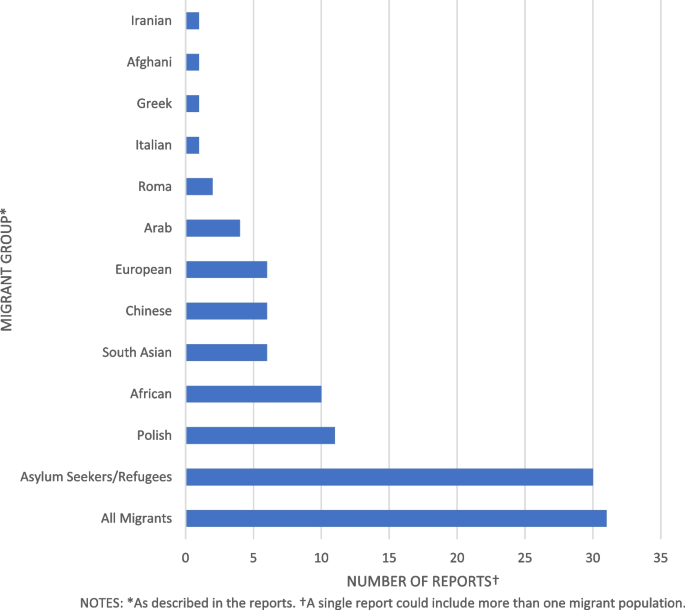
Migrant populations studied in health research in Scotland
Grey literature and peer-reviewed reports differed in population focus. The most common populations of interest in grey literature were asylum seekers/refugees consisting of 18 reports (62%) [ 27 , 47 , 54 , 55 , 59 , 63 , 70 , 71 , 72 , 73 , 74 , 123 , 125 , 127 , 128 , 132 , 134 , 138 ] while for peer-reviewed journals 24 reports (34%) focused on all migrants [ 13 , 35 , 45 , 48 , 64 , 76 , 78 , 79 , 80 , 81 , 104 , 105 , 108 , 109 , 113 , 114 , 115 , 116 , 118 , 120 , 121 , 122 , 136 ].
Migrant study population also differed by local area; Glasgow city, where the majority of research occurred, had 18 reports of 36 (50%) on Asylum seekers/refugees [ 47 , 48 , 52 , 53 , 54 , 55 , 58 , 63 , 70 , 71 , 72 , 82 , 83 , 127 , 128 , 130 , 138 , 139 ] eight reports (22%) on Africans [ 52 , 53 , 84 , 85 , 86 , 87 , 106 , 107 ], seven reports (19%) on all migrants [ 45 , 48 , 80 , 102 , 104 , 105 , 121 ] and two reports (5.5%) on Roma migrants [ 103 , 117 ]. Other populations had one reports each. In Edinburgh five reports of 16 (31%) were on the Polish population [ 56 , 67 , 68 , 89 , 90 ], and two reports (12.5%) on Asylum seekers/refugees [ 60 , 133 ], Chinese [ 62 , 137 ], South Asian [ 46 , 119 ], all migrants [ 105 , 121 ] and Africans [ 87 , 107 ]. The remaining migrant groups had one report each. Other areas of Scotland show no clear pattern with studies in disparate migrant population groups.
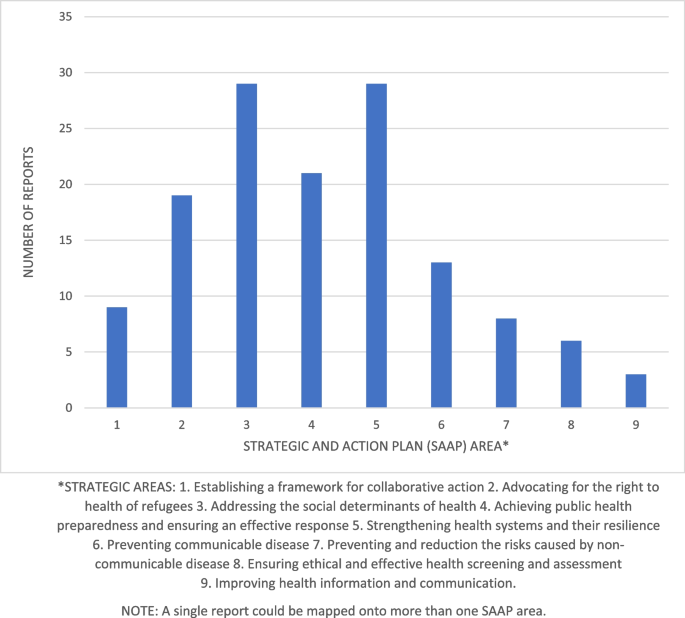
Number of reports per Strategic and Action Plan (SAAP) Area
SAAP Area mapping
1. establishing a framework for collaborative action.
Nine reports had a primary focus on collaborative action and were categorised under SAAP area 1 (see Fig. 4 ) [ 66 , 70 , 72 , 73 , 103 , 125 , 129 , 132 , 134 ]. Four reports (33%) used a mixed methods study design, the remaining five reports (67%) used a qualitative design. One report [ 66 ] focused on the epidemiology of female genital mutilation and a proposed intervention strategy. One report [ 66 ] focused on the epidemiology of female genital mutilation and a proposed intervention strategy. One report [ 103 ] evaluated service provision to the Roma community in Glasgow. The remaining reports focused on refugees and asylum seekers: four [ 73 , 125 , 132 , 134 ] evaluations of refugee integration projects, one [ 70 ] on services available to pregnant women, and one [ 72 ] an assessment of a peer-education service. One report [ 129 ] was a review of service provisions for migrants during the Covid-19 pandemic. All reports in SAAP area 1 were grey literature and three (37.5%) had a primary focus on migrant health while four (50%) focused on integration, one (11%) included data on ethnic minorities and one (11%) on services during the covid-19 pandemic. The majority (seven reports (78%)) were also categorised to another SAAP area most commonly area 2 (five studies (55%)) or area 5 (four studies (44%)).
2. Advocating for the right to health of refugees
Nineteen reports focused on SAAP area 2, advocating for the right to health of refugees (see Fig. 4 ) [ 47 , 52 , 53 , 54 , 55 , 63 , 70 , 71 , 83 , 103 , 123 , 124 , 125 , 127 , 128 , 129 , 134 , 138 , 140 ]. Sixteen reports (84%) had a qualitative study design and the remaining three (16%) reports used mixed methods. Nine reports (47%) focused on the health impact of the asylum system [ 52 , 55 , 71 , 74 , 123 , 127 , 128 , 129 , 138 ], five (26%) on health and access to care [ 47 , 54 , 83 , 103 , 124 ], two (10.5%) on maternity care [ 63 , 70 ], two (10.5%) on integration services [ 125 , 134 ] and one report on mental health in HIV positive migrants [ 53 ]. Nine reports (47%) had a primary focus on migrant health while the remaining 10 (53%) also involved wider social issues. The majority (15 (79%)) of reports were grey literature. All the articles in this group overlapped with another SAAP area. Area 3 is the most common joint category with ten reports (53%) followed by area 5 with seven reports (37%), area 1 shares five reports (26%), while areas 4 and 8 share one report each (5%).
3. Addressing the social determinants of health
Twenty-nine reports were categorised to SAAP area 3 – addressing the social determinants of health (see Fig. 4 ) [ 13 , 27 , 45 , 50 , 52 , 55 , 60 , 62 , 63 , 65 , 68 , 71 , 74 , 80 , 81 , 82 , 91 , 92 , 93 , 102 , 112 , 123 , 124 , 127 , 128 , 136 , 137 , 138 ]. The majority (14 (48%)) used a qualitative study method, eight (28%) used quantitative methodology and the remaining seven reports (24%) used mixed methods. Nineteen reports (65.5%) were peer-reviewed journals [ 13 , 45 , 50 , 52 , 60 , 62 , 63 , 65 , 68 , 80 , 81 , 82 , 91 , 92 , 93 , 104 , 112 , 124 , 136 , 137 ] and ten (34.5%) were grey literature [ 27 , 55 , 63 , 71 , 74 , 102 , 123 , 127 , 128 , 138 ]. Ten reports (34.5%) discussed the effects of the asylum system on health [ 27 , 52 , 63 , 71 , 74 , 123 , 124 , 127 , 128 , 137 ] and one (3.5%) migration and health [ 50 ]. Six reports (21%) focused on culture and ethnicity [ 82 , 92 , 102 , 104 , 112 , 137 ], five reports (17%) discussed economic and environmental determinants of health [ 13 , 45 , 67 , 81 , 93 ] and five reports (17%) the health impact of social activities [ 55 , 60 , 62 , 80 , 91 ]. Of the remaining reports, one [ 65 ] discussed Brexit and mental health of European migrants and one discussed the effect of coping strategies on wellbeing in Polish migrants [ 68 ]. Most reports, 18 (62%) had a primary focus on migrant health [ 45 , 50 , 52 , 55 , 60 , 62 , 63 , 65 , 67 , 68 , 71 , 80 , 81 , 82 , 91 , 92 , 93 , 102 ], six reports (21%) discussed wider social factors in addition to health [ 74 , 123 , 124 , 127 , 128 , 138 ]. Of the remaining reports three (10%) looked at ethnic background and country of birth [ 13 , 112 , 136 ], one [ 27 ] included other vulnerable groups and one [ 137 ] included people living in China and Chinese migrants to Scotland. Thirteen reports were also categorised to one or more additional SAAP area - ten (34%) were also applicable to area 2 [ 52 , 55 , 63 , 71 , 74 , 123 , 124 , 127 , 128 , 138 ], three (10%) to area 5 [ 63 , 82 , 92 ] and one (7%) to area 4 [ 27 ].
4. Achieving public health preparedness and ensuring an effective response
Twenty-one reports were assigned to SAAP area 4 (see Fig. 4 ) [ 27 , 31 , 35 , 39 , 47 , 57 , 64 , 75 , 76 , 77 , 78 , 94 , 104 , 108 , 109 , 111 , 113 , 114 , 116 , 120 , 135 ] of which fourteen (67%) used quantitative research methods, four (19%) mixed methods and three (14%) qualitative methods. Thirteen (62%) reports were peer-reviewed journals [ 35 , 59 , 64 , 75 , 78 , 104 , 108 , 109 , 111 , 113 , 114 , 116 , 120 ] and eight (38%) grey literature [ 27 , 31 , 39 , 47 , 57 , 77 , 94 , 135 ]. Most reports (12 (57%)) focused on morbidity and mortality in migrant populations [ 31 , 35 , 64 , 75 , 76 , 78 , 104 , 108 , 109 , 113 , 114 , 116 ]. Six (29%) investigated health status and healthcare needs in migrant groups in Scotland [ 39 , 47 , 57 , 77 , 94 , 135 ]. Two reports (9.5%) analysed the epidemiology of HIV infections [ 111 , 120 ] and the remaining report focused on the health needs of young people during the covid-19 pandemic [ 27 ]. Nine reports (43%) had a primary focus on migrant health [ 39 , 47 , 55 , 64 , 75 , 76 , 77 , 78 , 94 ] while eight (38%) also analysed data by ethnicity [ 31 , 35 , 104 , 108 , 109 , 113 , 114 , 116 ]. Of the remaining reports, three (14%) included other populations within Scotland [ 27 , 111 , 120 ] and one (5%) included other characteristics in addition to health information [ 135 ]. Ten reports (48%) were also categorised to another SAAP area; one to area 2 [ 47 ], one to area 3 [ 27 ], four to area 5 [ 47 , 57 , 77 , 135 ], two to area 6 [ 111 , 120 ] and two to area 9 [ 31 , 108 ].
5. Strengthening health systems and their resilience
Twenty-nine reports were assigned to SAAP area 5 (see Fig. 4 ) [ 18 , 47 , 48 , 49 , 54 , 57 , 63 , 69 , 70 , 72 , 77 , 79 , 82 , 83 , 92 , 95 , 96 , 97 , 99 , 101 , 103 , 118 , 119 , 126 , 129 , 131 , 133 , 135 , 141 ] of which 23 (79%) used qualitative research methods. Three reports used quantitative methods (10.3%) and the remaining three used mixed methods (10.3%). Twelve reports (41%) examined migrants needs and experiences of health care [ 47 , 49 , 54 , 57 , 58 , 77 , 83 , 95 , 103 , 119 , 129 , 135 ], eight (24%) focused on pregnancy and childcare [ 63 , 70 , 92 , 96 , 97 , 99 , 101 , 118 ] and two (7%) on barriers to healthcare access [ 48 , 131 ]. Two reports (7%) evaluated healthcare programmes [ 72 , 133 ] and two focused on communication in primary care [ 79 ] and maternity services [ 69 ]. The remaining three reports (10%) covered sexual health [ 82 ], health information needs of Syrian refugees [ 126 ] and general practitioner training [ 18 ]. Nineteen (65.5%) were peer reviewed journals [ 18 , 48 , 49 , 58 , 69 , 79 , 82 , 83 , 92 , 95 , 96 , 97 , 99 , 101 , 118 , 119 , 125 , 131 , 133 ] and ten (34.5%) were grey literature [ 47 , 54 , 57 , 63 , 70 , 72 , 77 , 103 , 129 , 135 ]. Twenty-one (72%) had a primary focus on migrant health [ 18 , 47 , 48 , 49 , 54 , 57 , 58 , 63 , 69 , 70 , 72 , 77 , 79 , 82 , 83 , 92 , 95 , 96 , 97 , 99 , 101 ]. Six reports (21%) included research on other characteristics or services [ 103 , 126 , 129 , 131 , 133 , 135 ]. The remaining two reports (7%) included ethnic groups as well as migrants in the data [ 118 , 119 ]. Nineteen reports (65.5%) were also assigned to one or more other category areas: five reports (17%) to area 1 [ 47 , 70 , 72 , 103 , 129 ], five reports (17%) to area 2 [ 54 , 63 , 83 , 103 , 129 ], three reports (10%) to area 3 [ 63 , 82 , 92 ], four reports (14%) to area 4 [ 47 , 57 , 77 , 135 ], one (3.5%) to area 7 [ 119 ] and one (3.5%) to area 9 [ 48 ].
6. Preventing communicable diseases
Fourteen reports were assigned to SAAP area 6 (see Fig. 4 ) [ 56 , 61 , 87 , 88 , 89 , 90 , 105 , 106 , 107 , 111 , 115 , 117 , 120 , 122 ] of which four (31%) used quantitative methods, five (38%) used qualitative methods and five (38%) used mixed methods. Five reports (38.5%) examined immunisation behaviour [ 56 , 61 , 89 , 90 , 117 ], five (38%) on epidemiology and treatment of HIV [ 106 , 107 , 111 , 120 , 122 ]. The remaining four reports (31%) focused on tuberculosis in healthcare workers [ 115 ], malaria [ 105 ] and sexual health services [ 87 , 88 ]. Only one reports was grey literature [ 88 ], the remainder were peer-reviewed journals. Six reports (46%) had a primary focus on migrant health [ 56 , 61 , 87 , 88 , 89 , 90 ] while seven reports (54%) also included other at-risk groups in the analysis. Four reports (31%) were also assigned to another SAAP category, two (15%) to area 4 [ 111 , 120 ] and two (15%) to area 8 [ 88 , 115 ].
7. Preventing and reducing the risks posed by non-communicable diseases
Eight reports were categorised to SAAP area 7 (see Fig. 4 ) [ 46 , 51 , 59 , 84 , 85 , 86 , 98 , 119 ] of which six (75%) used qualitative research methods, one (12.5%) used quantitative methods and one (12.5%) used mixed methods. Only one report (12.5%) was grey literature [ 59 ] the remaining seven reports (87.5%) were peer-reviewed journals [ 48 , 87 , 92 , 126 , 127 , 128 , 140 ]. Three reports (37.5%) focused on health behaviours [ 51 , 85 , 98 ], two (25%) on mental health, two (25%) on diabetes and one (12.5%) on chronic disease. Seven reports(87.5%) had a primary focus on migrant health [ 46 , 51 , 59 , 84 , 85 , 86 , 98 ], with the remaining report (12.5%) including ethnic minority groups [ 119 ]. One report (12.5%) was also assigned to SAAP area number 5 [ 119 ].
8. Ensuring ethical and effective health screening and assessment
There were six reports assigned to category 8 (see Fig. 4 ) [ 53 , 88 , 100 , 110 , 115 , 121 ] of which two (33%) used a quantitative research method, three (50%) used a qualitative method and one used mixed methods. One report (14%) was grey literature [ 88 ] the remaining five reports (83%) were peer reviewed journals [ 53 , 100 , 110 , 115 , 121 ]. Three reports (50%) focused on cancer screening in migrant women [ 21 , 100 , 110 ], one (17%) analysed access to HIV testing among African migrants [ 53 ], one (17%) on T.B in healthcare workers [ 72 ] and one (17%) on sexual health [ 36 ]. Three reports (50%) had a primary focus on migrant health [ 53 , 88 , 100 ] while the remaining three reports (50%) included other at-risk groups in the analysis [ 110 , 115 , 121 ]. There were three reports which overlapped with other SAAP areas: one [ 53 ] (17%) was categorised to area 2 while two [ 88 , 115 ] (33%) were categorised to area 6.
9. Improving health information and communication
Three reports were assigned to SAAP area 9 (see Fig. 4 ) [ 31 , 108 , 130 ]. One of these (33%) used a qualitative approach, one (33%) used a quantitative approach and one (33%) used mixed methods. Two [ 108 , 130 ] (66%) were peer-reviewed journal articles and one [ 31 ] (33%) was grey literature. Two reports (66%) focused on improving migrant demographics and health information using databases [ 31 , 108 ] while one (33%) described an information-needs matrix for refugees and asylum seekers [ 130 ]. Two [ 31 , 108 ] included ethnicities in the data while one [ 130 ] had a primary focus on migrant health. Two reports [ 31 , 108 ] (66%) also applied to SAAP area 4 while one report [ 130 ] (33%) was in SAAP area 9 only.
To our knowledge this is the first scoping review conducted on migrant health in Scotland. A previous rapid literature review [ 94 ] found most research focused on health behaviours, mental health, communicable disease and use of and access to healthcare; however, the review limited migrant definition to those who had immigrated within five years and asylum seekers were not included.
In our review, the majority of reports were published from 2013 onwards, aligning with the expansion in migrant research internationally [ 142 ]. 52% used qualitative research methods, 28% used quantitative methods and 20% used mixed methods. 58% focused on migrant health: the remaining papers included other populations or health as part of a wider remit. Research funding was mostly provided by the Scottish Government, NHS, refugee charities and Universities. No studies received funding from the private sector, although this sector has the potential resource and capacity to play a key role in funding future research to improve migrant health in Scotland. Geographically, most studies took place in Glasgow (36%), nationwide (38.5%) or Edinburgh (16%) – other areas were under-represented including Aberdeen (5%), despite being the city with the largest migrant population [ 30 ]. There was a lack of studies in rural localities. These findings concur with a UK migrant health review by Burns et al. [ 23 ] where research was concentrated in larger cities and data was sparse in rural areas relative to the migrant population.
Half of the research identified that was conducted in Glasgow focused on asylum seekers/refugees. Glasgow was previously the only Scottish city to host asylum seekers [ 143 ] and currently supports the most asylum seekers of any local authority in the UK [ 29 ]. In April 2022, the UK government widened the Asylum dispersal scheme to all local authorities [ 144 ]. Around 70% of Scotland’s refugee support services are based in Glasgow and the South-west [ 145 ]. As reduced access to services may impact the health of asylum seekers, research in Glasgow may not be generalizable to other regions of Scotland.
Almost one-third (30%) of all reports focused on asylum seekers and refugees – an overrepresentation given that only 18% of migrants to the UK are asylum seekers [ 146 ] and as low as 2% of all migrants in Scotland [ 147 ]. Asylum seekers and refugees are at risk of poor health due to trauma, difficult journeys, overcrowded camps, poor nutrition and lack of access to healthcare [ 148 ]. They have worse maternity outcomes and increased rates of mental illness [ 149 ]. Increased research on health of asylum seekers and refugees is necessary due to their additional vulnerabilities [ 142 ]. However, asylum seeker’s country of origin was generally not specified. Asylum seekers have heterogenic backgrounds [ 150 ] and nationality and trauma experience affect health status [ 151 ]. Further research focused on specific nationalities of asylum seekers would enhance understanding of the health needs in this population.
Almost one-third (31%) of studies did not specify a migrant group. This concurs with a Norwegian migrant health study by Laue et al. [ 152 ] where 36% of research did not identify country of birth. Where nationality was identified, Polish, African and South Asian were most prevalent. Poles are the largest migrant group in Scotland, however for the other most common immigrant groups of Irish, Italian and Nigerian [ 30 ] there was an absence of research. No studies took place on Nigerian migrants – nine studies indicated African populations, but country of birth was not specified. Since March 2022, 23,000 Ukrainians have migrated to Scotland [ 153 ], however no studies on Ukrainians were identified currently. Research may be underway which is yet to be published.
Only one study explored the impact of Brexit on European migrants’ health despite 56% of migrants to Scotland being EU nationals [ 30 ]. Again, research may be taking place currently, which is yet to be published. No studies involved undocumented migrants despite this populations’ high rates of poor physical/mental health exacerbated by poor housing and working conditions [ 154 ]. An estimated 7.2–9.5% of the workforce in the UK are migrant workers who have higher risks of poor working conditions and injury [ 155 ]. Scotland depends on a migrant workforce for some industries such as agriculture [ 156 ] but only two research papers specified migrant workers.
Most research papers related to the right to health of refugees (SAAP 2), social determinants of health (SAAP 3), public health planning (SAAP 4) and strengthening health systems (SAAP 5). Areas with less research were frameworks for collaborative action (SAAP 1), preventing communicable disease (SAAP 6), preventing non-communicable disease (SAAP 7) and health screening and assessment (SAAP 8). Only three studies related to improving health information and communication (SAAP 9). Lebano et al. [ 12 ] conducted a literature review of migrant health in Europe and found data collection unreliable and disorganised. There is a lack of data on the numbers and types of migrants entering Scotland and research tends not to differentiate between ethnic minorities and migrants [ 94 ]. As poor-quality information hinders surveillance and planning of services SAAP area 9 is an important consideration for increased research.
Villarroel et al. [ 24 ] also found more research in SAAP areas 3 to 5 and less in areas 6 to 9. However, their study returned no results in category 1, collaborative action, or 2, the right to health of refugees, while this study assigned 9% of articles to category 1 and 19% to category 2. Most articles in our study relating to categories 1 and 2 were grey literature, which was excluded from the original Irish scoping review. This highlights a potential difference in the focus of peer-reviewed articles compared to government/refugee charity commissioned reports. Collaborative action and the right to health of refugees and asylum seekers are entwined in Scotland due to the complex policy environment; the social determinants of health such as housing, education, welfare rights and social integration are influenced by a variety of UK and Scottish statutory bodies as well as third sector organisations [ 157 ]. Despite this complexity, organisations work well together [ 158 ]. Further academic research in this area would enhance joint working practices and networks.
A scoping review in the UK [ 23 ] found similar quantities of research corresponding to SAAP areas 3, 2 and 9. However in Scotland areas 1, 5 and 8 were a combined 44% of included papers compared with 27.8% of results on health systems and structures in Burns et al’s [ 23 ] study. Almost half of the articles in SAAP areas 1,5 and 8 were grey literature, which was not included in Burns et al’s [ 23 ] review. Conversely, Burns et al. [ 23 ] found 81.9% of research in the UK related to epidemiology, equivalent to SAAP categories 4,6 and 7. In a Norwegian scoping review of migrant health [ 152 ] 65% of research was related to epidemiological data on health and disease. Only 42% of the research in this current study related to epidemiological data; the quantity of evidence was reduced by excluding combined research from the UK. As Scotland has higher mortality and morbidity than elsewhere in the UK [ 29 ] it is important to undertake further epidemiological research limited to Scotland.
Strengths and weaknesses
Strengths of this review include the use of the WHO’s SAAP categories [ 7 ] to classify data, in accordance with the Villarroel et al’s [ 24 ] study: this means results are linked to policy on migrant health and facilitates comparability to the Irish study results. Additionally results include data on migrant groups, locality, and funding of included papers; these highlight potential omissions for future research consideration. Results include diverse research methods and published and grey literature giving a wide overview of available evidence, reported using the Preferred Reporting Items for Systematic reviews and Meta-Analyses for Scoping Reviews (PRISMA-ScR) checklist (see Additional File 3 ) [ 159 ].
Limitations included the lack of an open-access protocol and search limitations of English language and selected databases. This means some relevant reports may be omitted. Due to time and resource limitations no quality appraisal was planned for included reports. Whilst we did not synthesise the findings for each topic area and migrant group, future systematic reviews could be undertaken to address this limitation and build on this work.
Conclusions
Immigration and ethnic diversity in Scotland have increased since 2002 which is reflected in the expansion of migrant health research. This review highlights evidence gaps including a lack of research in rural areas, undocumented migrants and migrant workers. There is a tendency to cluster asylum seekers together rather than differentiate between national groups. Within the SAAP areas there is less evidence relating to collaborative action, preventing communicable disease, preventing non-communicable disease and health screening and assessment. Further research is required on improving health information and communication for migrant populations in Scotland – a significant omission given the importance of accurate information for health service planning.
Availability of data and materials
All data analysed during this review comes from the papers listed in Additional file 2 .
Abbreviations
European Union
Human Immunodeficiency Virus
National Health Service
Strategy and Action Plan
The Scottish Health and Ethnicity Linkage Study
United Kingdom
World Health Organisation
International Organisation for Migration (IOM). IOM Definition of Migrant. 2024. Available from: https://www.iom.int/about-migration .Cited 2024 Feb 8.
International Organisation for Migration United Nations. World Migration Report. 2022. Available from: available: https://worldmigrationreport.iom.int/wmr-2022-interactive/ .
The United Nations Refugee Angency. Refugee facts: What is a refugee? 2024. Available from: https://www.unrefugees.org/refugee-facts/what-is-a-refugee/ . Cited 2024 Feb 8.
Migration Data Portal. Migration data in Europe. 2023. Available from: https://www.migrationdataportal.org/regional-data-overview/europe#past-and-present-trends . Cited 2023 Aug 22.
International Centre for Migration Policy Development. Migration Outlook 2022 Twelve migration issues to look out for in 2022 Origins, key events and priorities for Europe. 2022. Available from: https://www.icmpd.org/file/download/56783/file/ICMPD%2520Migration%2520Outlook%25202022.pdf .
European Parliament. Exploring migration causes: why people migrate. 2023. Available from: https://www.europarl.europa.eu/news/en/headlines/world/20200624STO81906/exploring-migration-causes-why-people-migrate .
World Health Organisation. Strategic plan: Strategy and Action Plan for Refugee and Migrant Health in the WHO European Region 2016–2022. 2016. Available from: https://www.who.int/publications/i/item/strategic-plan-strategy-and-action-plan-for-refugee-and-migrant-health-in-the-who-european-region-2016-2022 .
Graetz V, Rechel B, Groot W, Norredam M, Pavlova M. Utilization of health care services by migrants in Europe—a systematic literature review. Br Med Bull. 2017;121(1):5–18. Available from: https://www.academic.oup.com/bmb/article-lookup/doi/10.1093/bmb/ldw057 .
Article CAS PubMed Google Scholar
Hannigan A, O'Donnell P, O'Keeffe M, MacFarlane A. How do Variations in Definitions of “Migrant” and their Application Influence the Access of Migrants to Health Care Services? Copenhagen: WHO Regional Office for Europe; 2016. (Health Evidence Network Synthesis Report, No. 46.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK391032/ .
Rechel B, Mladovsky P, Ingleby D, Mackenbach JP, McKee M. Migration and health in an increasingly diverse Europe. Lancet. 2013;381(9873):1235–45. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673612620868 .
Article PubMed Google Scholar
Giannoni M, Franzini L, Masiero G. Migrant integration policies and health inequalities in Europe. BMC Public Health. 2016;16(1):463. Available from: http://www.bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-016-3095-9 .
Article PubMed PubMed Central Google Scholar
Lebano A, Hamed S, Bradby H, Gil-Salmerón A, Durá-Ferrandis E, Garcés-Ferrer J, et al. Migrants’ and refugees’ health status and healthcare in Europe: a scoping literature review. BMC Public Health. 2020;20(1):1039. Available from: https://www.bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-08749-8 .
Cézard G, Finney N, Kulu H, Marshall A. Ethnic differences in self-assessed health in Scotland: The role of socio-economic status and migrant generation. Popul Space Place. 2022;28(3):e2403. Available from: https://onlinelibrary.wiley.com/doi/10.1002/psp.2403 .
Article Google Scholar
Anson J. The migrant mortality advantage: a 70 month follow-up of the brussels population. Eur J Popul. 2004;20(3):191–218.
World Health Organisation. Health of refugees and migrants. WHO European Region. 2018. Available from: https://www.who.int/publications/i/item/health-of-refugees-and-migrants---who-european-region-(2018) .
Mladovsky P. A framework for analysing migrant health policies in Europe. Health Policy (New York). 2009;93(1):55–63. Available from: https://www.linkinghub.elsevier.com/retrieve/pii/S0168851009001444 .
De Vito E, de Waure C, Specchia ML, Parente P, Azzolini E, Frisicale EM, et al. Are undocumented migrants’ entitlements and barriers to healthcare a public health challenge for the European Union? Public Health Rev. 2016;37(1):13. Available from: http://publichealthreviews.biomedcentral.com/articles/10.1186/s40985-016-0026-3 .
Katikireddi SV, Bhopal R, Quickfall JA. GPs need training and funding in caring for refugees and asylum seekers. BMJ. 2004;328(7442):770.1. Available from: https://www.bmj.com/lookup/doi/10.1136/bmj.328.7442.770 .
Carballo M, Hargreaves S, Gudumac I, Maclean EC. Evolving migrant crisis in Europe: implications for health systems. Lancet Glob Heal. 2017;5(3):e252-253. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2214109X17300402 .
Juárez SP, Honkaniemi H, Dunlavy AC, Aldridge RW, Barreto ML, Katikireddi SV et al. Effects of non-health-targeted policies on migrant health: a systematic review and meta-analysis. Lancet Glob Heal. 2019;7(4):e420–35. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2214109X18305606 .
Nielsen SS, Krasnik A. Poorer self-perceived health among migrants and ethnic minorities versus the majority population in Europe: a systematic review. Int J Public Health. 2010;55(5):357–71. Available from: ( http://link.springer.com/10.1007/s00038-010-0145-4 ).
World Health Organsation. World report on the health of refugees and migrants. 2022. Available from: https://www.who.int/publications/i/item/9789240054462 .
Burns R, Zhang CX, Patel P, Eley I, Campos-Matos I, Aldridge RW. Migration health research in the United Kingdom: a scoping review. J Migr Heal. 2021;4:100061. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2666623521000283 .
Villarroel N, Hannigan A, Severoni S, Puthoopparambil S, MacFarlane A. Migrant health research in the Republic of Ireland: a scoping review. BMC Public Health. 2019;19(1):324. Available from: ( https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-6651-2 ).
Scottish Government. Demographic Change in Scotland. 2010. Available from: https://www.gov.scot/binaries/content/documents/govscot/publications/research-and-analysis/2010/11/demographic-change-scotland/documents/0108163-pdf/0108163-pdf/govscot%3Adocument/0108163.pdf .
National Records of Scotland. Projected Population of Scotland (Interim) 2020-based. 2022. Available from: https://www.nrscotland.gov.uk/files/statistics/population-projections/2020-based/pop-proj-2020-scot-nat-pub.pdf .
Scottish Government. Coronavirus (COVID-19) - experiences of vulnerable children, young people, and parents: research. 2021. Available from: https://www.gov.scot/publications/experiences-vulnerable-children-young-people-parents-during-covid-19-pandemic/ .
Scotland’s Census. Scotland’s Census: Ethnicity. 2011. Available from: https://www.scotlandscensus.gov.uk/census-results/at-a-glance/ethnicity/#:~:text=Scotland’spopulationwas96.0%25 .
Walsh D. The changing ethnic profiles of Glasgow and Scotland, and the implications for population health. 2017. Available from: https://www.gcph.co.uk/assets/0000/6255/The_changing_ethnic_profiles_of_Glasgow_and_Scotland.pdf .
National Records of Scotland. Migration Statistics Quarterly Summary for Scotland. 2021. Available from: https://www.nrscotland.gov.uk/files/statistics/migration/quarterly-summary/miration-statistics-quarterly-summary-february-2021.pdf .
The Scottish Ethnicity and Health Research Strategy Working Group. Health in our Multi-ethnic Scotland Future Research Priorities. 2009. Available from: https://www.healthscotland.scot/media/1842/health-in-our-multi-ethnic-scotland-full-report.pdf .
The Scottish Public Health Observatory. Ethnic minorities: defining ethnicity and race. 2023. Available from: https://www.scotpho.org.uk/population-groups/ethnic-minorities/defining-ethnicity-and-race/ . Cited 2023 Aug 22.
Krasnik A, Bhopal RS, Gruer L, Kumanyika SK. Advancing a unified, global effort to address health disadvantages associated with migration, ethnicity and race. Eur J Public Health. 2018;28(suppl_1). Available from: https://academic.oup.com/eurpub/article/doi/10.1093/eurpub/cky046/4956664 .
Bhopal R, Fischbacher C, Povey C, Chalmers J, Mueller G, Steiner M, et al. Cohort profile: scottish health and ethnicity linkage study of 4.65 million people exploring ethnic variations in disease in Scotland. Int J Epidemiol. 2011;40(5):1168–75. Available from: https://academic.oup.com/ije/article-lookup/doi/10.1093/ije/dyq118 .
Bhopal RS, Gruer L, Cezard G, Douglas A, Steiner MFC, Millard A, et al. Mortality, ethnicity, and country of birth on a national scale, 2001–2013: a retrospective cohort (Scottish Health and Ethnicity Linkage Study). Basu S, editor. Plos Med. 2018;15(3):e1002515. https://doi.org/10.1371/journal.pmed.1002515 . Basu S, editor.
Allik M, Brown D, Dundas R, Leyland AH. Differences in ill health and in socioeconomic inequalities in health by ethnic groups: a cross-sectional study using 2011 Scottish census. Ethn Health. 2022;27(1):190–208. https://doi.org/10.1080/13557858.2019.1643009 ( https://www.tandfonline.com/doi/full/ ).
Watkinson RE, Sutton M, Turner AJ. Ethnic inequalities in health-related quality of life among older adults in England: secondary analysis of a national cross-sectional survey. Lancet Public Hea. 2021;6(3):e145-154.
Fischbacher CM, Cezard G, Bhopal RS, Pearce J, Bansal N. Measures of socioeconomic position are not consistently associated with ethnic differences in cardiovascular disease in Scotland: methods from the Scottish Health and Ethnicity Linkage Study (SHELS). Int J Epidemiol. 2014;43(1):129–39. Available from: https://academic.oup.com/ije/article-lookup/doi/10.1093/ije/dyt237 .
Scottish Government. Characteristics of Recent and Established EEA and non-EEA migrants in Scotland: Analysis of the 2011 Census. 2015. Available from: https://www.gov.scot/publications/characteristics-recent-established-eea-non-eea-migrants-scotland-analysis-2011-census/ .
House of Lords Library. Refugees and asylum-seekers: UK policy. 2022. https://lordslibrary.parliament.uk/refugees-and-asylum-seekers-uk-policy/ .
British Medical Association. Refugee and asylum seeker patient health toolkit. Unique health challenges for refugees and asylum seekers. 2022. Available from: https://www.bma.org.uk/advice-and-support/ethics/refugees-overseas-visitors-and-vulnerable-migrants/refugee-and-asylum-seeker-patient-health-toolkit/unique-health-challenges-for-refugees-and-asylum-seekers .
Khalil H, Peters M, Godfrey CM, McInerney P, Soares CB, Parker D. An evidence-based approach to scoping reviews. Worldviews Evidence-Based Nurs. 2016;13(2):118–23. Available from: https://doi.org/10.1111/wvn.12144 .
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. Available from: ( http://implementationscience.biomedcentral.com/articles/10.1186/1748-5908-5-69 ).
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.Available from: http://www.tandfonline.com/doi/abs/10.1080/1364557032000119616 ).
Kearns A, Whitley E, Egan M, Tabbner C, Tannahill C. Healthy migrants in an unhealthy city? The Effects of time on the health of migrants living in deprived areas of glasgow. J Int Migr Integr. 2017;18(3):675–98. Available from: http://link.springer.com/10.1007/s12134-016-0497-6 .
PubMed Google Scholar
Porqueddu T. Herbal medicines for diabetes control among Indian and Pakistani migrants with diabetes. Anthropol Med. 2017;24(1):17–31. Available from: https://www.tandfonline.com/doi/full/10.1080/13648470.2016.1249338 .
Roshan N. Supporting new communities: a qualitative study of health needs among asylum seekers and refugee communities in North Glasgow final report. 2005. Available from: https://www.stor.scot.nhs.uk/handle/11289/579930 .
Piacentini T, O’Donnell C, Phipps A, Jackson I, Stack N. Moving beyond the ‘language problem’: developing an understanding of the intersections of health, language and immigration status in interpreter-mediated health encounters. Lang Intercult Commun. 2019;19(3):256–71. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1353829214001233 .
Sime D. ‘I think that Polish doctors are better’: Newly arrived migrant children and their parents׳ experiences and views of health services in Scotland. Health Place. 2014;30:86–93. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1353829214001233 .
Steven K, Munoz S, Migrants, Matter. Report of a Peer Researched Project on EU Migrant Health in the Highlands of Scotland. University of the Highlands and Islands. 2016. Available from: https://www.spiritadvocacy.org.uk/assets/Birchwood-Highland-HUG-Migrants-Matter-study-2015-2016.pdf .
Anderson AS, Bush H, Lean M, Bradby H, Williams R, Lea E. Evolution of atherogenic diets in South Asian and Italian women after migration to a higher risk region. J Hum Nutr Diet. 2005;18(1):33–43. Available from: ( https://onlinelibrary.wiley.com/doi/10.1111/j.1365-277X.2004.00584.x ).
Isaacs A, Burns N, Macdonald S, O’Donnell CA. ‘I don’t think there’s anything I can do which can keep me healthy’: how the UK immigration and asylum system shapes the health and wellbeing of refugees and asylum seekers in Scotland. Crit Public Health. 2022;32(3):422–32. Available from: https://www.tandfonline.com/doi/full/10.1080/09581596.2020.1853058 .
Palattiyil G, Sidhva D. Caught in a web of multiple jeopardy: post-traumatic stress disorder and HIV-positive asylum seekers in Scotland. Clin Soc Work J. 2015;43(4):362–74. Available from: http://link.springer.com/10.1007/s10615-015-0542-5 ).
Abdulkadir J, Azzudin A, Buick A, Curtice L, Dzingisai M, Easton D, et al. What do you mean, I have a right to health? Participatory action research on health and human rights. 2016. Available from: https://strathprints.strath.ac.uk/58209/1/Abdulkadir_etal_IPPI_2016_What_do_you_mean_I_have_a_right_to_health.pdf .
Strang A, Quinn N. Integration or isolation? Mapping social connections and well-being amongst refugees in Glasgow. 2014. Available from: https://eresearch.qmu.ac.uk/bitstream/handle/20.500.12289/4139/eResearch%25204139.pdf?sequence=1&isAllowed=y .
Gorman DR, Bielecki K, Larson HJ, Willocks LJ, Craig J, Pollock KG. Comparing vaccination hesitancy in polish migrant parents who accept or refuse nasal flu vaccination for their children. Vaccine. 2020;38(13):2795–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0264410X20302255 .
Love J, Vertigans S, Domaszk E, Zdeb K, Love A, Sutton P. Health & ethnicity in Aberdeenshire: a study of Polish in-migrants; a report for the Scottish Health Council. 2007. Available from: https://rgu-repository.worktribe.com/output/247667 .
O’Donnell CA, Higgins M, Chauhan R, Mullen K. Asylum seekers’ expectations of and trust in general practice: a qualitative study. Br J Gen Pract. 2008;58(557):e1-11. Available from: https://bjgp.org/lookup/doi/10.3399/bjgp08X376104 .
Quinn N, Shirjeel S, Siebelt L, Donnelly R, Pietka E. An evaluation of the sanctuary community conversation programme to address mental health stigma with asylum seekers and refugees in Glasgow. 2011. Available from: https://www.healthscotland.com/uploads/documents/5584-SanctuaryCommunityConversationEvaluation.pdf .
Ager A. Community contact and mental health amongst socially isolated refugees in Edinburgh. J Refug Stud. 2002;15(1):71–80. Available from: https://academic.oup.com/jrs/article-lookup/doi/10.1093/jrs/15.1.71 .
Sim JA, Ulanika AA, Katikireddi SV, Gorman D. Out of two bad choices, I took the slightly better one’: Vaccination dilemmas for Scottish and Polish migrant women during the H1N1 influenza pandemic. Public Health. 2011;125(8):505–11. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350611001697 .
Zhao S, Patuano A. International Chinese Students in the UK: association between use of green spaces and lower stress levels. Sustainability. 2021;4(1):89. Available from: https://www.mdpi.com/2071-1050/14/1/89 .
Da Lomba S, Murray N. Women and Children First? Refused asylum seekers’ access to and experiences of maternity care in Glasgow. 2014. Available from: https://strathprints.strath.ac.uk/58655/1/Lomba_Murray_SRC_2014_Women_and_Children_First_Refused_Asylum_Seekers_Access_to_and_Experiences.pdf .
Sørbye IK, Vangen S, Juarez SP, Bolumar F, Morisaki N, Gissler M, et al. Birthweight of babies born to migrant mothers - What role do integration policies play? SSM - Popul Heal. 2019;9:100503. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2352827319301971 .
Teodorowski P, Woods R, Czarnecka M, Kennedy C. Brexit, acculturative stress and mental health among EU citizens in Scotland. Popul Space Place. 2021;27(6). Available from: https://onlinelibrary.wiley.com/doi/10.1002/psp.2436 .
Baillot H, Murray N, Connelly E, Howard N. Tackling Female Genital Mutilation in Scotland: A Scottish model of intervention. 2014. Available from: https://www.celcis.org/application/files/8116/2185/5421/Tackling_Female_Genital_Mutilation_-_A_Scottish_Model_of_Intervention.pdf .
Weishaar HB. Consequences of international migration: a qualitative study on stress among Polish migrant workers in Scotland. Public Health. 2008;122(11):1250–6. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350608000942 .
Weishaar HB. You have to be flexible—coping among polish migrant workers in Scotland. Health Place. 2010;16(5):820–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1353829210000432 .
Crowther S, Lau A. Migrant polish women overcoming communication challenges in scottish maternity services: a qualitative descriptive study. Midwifery. 2019;72:30–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0266613819300361 .
Fassetta G, Da Lomba S, Quinn N. A healthy start? Experiences of pregnant refugee and asylum seeking women in Scotland. 2016. Available from: https://www.redcross.org.uk/-/media/documents/about-us/research-publications/refugee-support/a-healthy-start-report.pdf .
Positive Action in Housing. 12 months since the Park Inn Tragedy in Glasgow, one in three hotel asylum seekers say their mental health has deteriorated. 2021. Available from: https://www.paih.org/one-in-three-glasgow-asylum-seekers-suffering-depression-and-anxiety .
Strang A. Refugee Peer Education for Health and Well-being. Evaluation Report. 2015. Available from: https://www.scottishrefugeecouncil.org.uk/wp-content/uploads/2019/10/Peer-Education-Evaluation-Report.pdf .
Strang A, Marsden R, Mignard E. The Holistic Integration Service: Learning and Evaluation Year 1. 2014. Available from: https://www.scottishrefugeecouncil.org.uk/wp-content/uploads/2019/10/Holistic-Integration-Service-year-1-evaluation-report.pdf .
British Red Cross. How will we survive? Steps to preventing destitution in the asylum system. 2021. Available from: https://www.redcross.org.uk/-/media/documents/about-us/how-will-we-survive-preventing-destitution-in-the-asylum-system.pdf .
Bhopal RS, Rafnsson SB, Agyemang C, Fagot-Campagna A, Giampaoli S, Hammar N, et al. Mortality from circulatory diseases by specific country of birth across six European countries: test of concept. Eur J Public Health. 2012;22(3):353–9. Available from: https://academic.oup.com/eurpub/article-lookup/doi/10.1093/eurpub/ckr062 .
Rafnsson SB, Bhopal RS, Agyemang C, Fagot-Campagna A, Harding S, Hammar N, et al. Sizable variations in circulatory disease mortality by region and country of birth in six European countries. Eur J Public Health. 2013;23(4):594–605. Available from: https://academic.oup.com/eurpub/article-lookup/doi/10.1093/eurpub/ckt023 ).
de Lima P, Masud Chaudhry M, Whelton R, Arshad R. A study of migrant workers in Grampian. 2007. Available from: . http://www.communitiesscotland.gov.uk/stellent/groups/public/%0Adocuments/webpages/pubcs_019731.pdff .
Ikram UZ, Mackenbach JP, Harding S, Rey G, Bhopal RS, Regidor E, et al. All-cause and cause-specific mortality of different migrant populations in Europe. Eur J Epidemiol. 2016;31(7):655–65. Available from: http://link.springer.com/10.1007/s10654-015-0083-9 .
de Brún T, De-Brún MO, van Weel-Baumgarten E, van Weel C, Dowrick C, Lionis C, et al. Guidelines and training initiatives that support communication in cross-cultural primary-care settings: appraising their implementability using Normalization Process Theory. Fam Pract. 2015;cmv022. Available from: https://academic.oup.com/fampra/article-lookup/doi/10.1093/fampra/cmv022 .
García-Medrano S, Panhofer H. Improving migrant well-being: spontaneous movement as a way to increase the creativity, spontaneity and welfare of migrants in Glasgow. Body Mov Danc Psychother. 2020;15(3):189–203. Available from: https://www.tandfonline.com/doi/full/10.1080/17432979.2020.1767208 .
Jamil NA, Gray SR, Fraser WD, Fielding S, Macdonald HM. The relationship between vitamin D status and muscle strength in young healthy adults from sunny climate countries currently living in the northeast of Scotland. Osteoporos Int. 2017;28(4):1433–43. Available from: http://link.springer.com/10.1007/s00198-016-3901-3 .
Kaneoka M, Spence W. The cultural context of sexual and reproductive health support: an exploration of sexual and reproductive health literacy among female Asylum Seekers and Refugees in Glasgow. Int J Migr Heal Soc Care. 2019;16(1):46–64. Available from: https://www.emerald.com/insight/content/doi/10.1108/IJMHSC-01-2019-0002/full/html .
O’Donnell CA, Higgins M, Chauhan R, Mullen K. They think we’re OK and we know we’re not. A qualitative study of asylum seekers’ access, knowledge and views to health care in the UK. BMC Health Serv Res. 2007;7(1):75. Available from: https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-7-75 .
Cooper M, Harding S, Mullen K, O’Donnell C. ‘A chronic disease is a disease which keeps coming back … it is like the flu’: chronic disease risk perception and explanatory models among French- and Swahili-speaking African migrants. Ethn Health. 2012;17(6):597–613. Available from: http://www.tandfonline.com/doi/abs/10.1080/13557858.2012.740003 .
Ezika EA. An exploration of smoking behavior of african male immigrants living in glasgow. Tob Use Insights. 2014;7:TUI .S13262. Available from: http://journals.sagepub.com/doi/10.4137/TUI.S13262 .
Karadzhov D, White R. Between the whispers of the devil and the revelation of the word : christian clergy’s mental health literacy and pastoral support for BME congregants. J Spiritual Ment Heal. 2020;22(2):147–72. Available from: https://www.tandfonline.com/doi/full/10.1080/19349637.2018.1537755 ).
Yakubu BD, Simkhada P, van Teijlingen E, Eboh W. Sexual health information and uptake of sexual health services by African women in Scotland: a pilot study. Int J Heal Promot Educ. 2010;48(3):79–84. Available from: http://www.tandfonline.com/doi/abs/10.1080/14635240.2010.10708186 .
Goff J, Kay K, Lima M, Shallangwa S, We All Have A. Different Consciousness About It: Exploring the Sexual Health Needs of People From African Communities in Scotland. 2021. Available from: https://www.waverleycare.org/wp-content/uploads/2023/05/We_All_Have_Different_Consciousness_About_It_Report.pdf .
Bielecki K, Craig J, Willocks LJ, Pollock KG, Gorman DR. Impact of an influenza information pamphlet on vaccination uptake among Polish pupils in Edinburgh, Scotland and the role of social media in parental decision making. BMC Public Health. 2020;20(1):1381. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-09481-z .
Article CAS PubMed PubMed Central Google Scholar
Gorman DR, Bielecki K, Willocks LJ, Pollock KG. A qualitative study of vaccination behaviour amongst female Polish migrants in Edinburgh, Scotland. Vaccine. 2019;37(20):2741–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0264410X19304220 .
Bak-Klimek A, Karatzias T, Elliott L, MacLean R. The determinants of well-being among polish economic immigrants. Testing the sustainable happiness model in migrant population. J Happiness Stud. 2018;19(6):1565–88. Available from: http://link.springer.com/10.1007/s10902-017-9877-7 .
Cheung NF. The cultural and social meanings of childbearing for Chinese and Scottish women in Scotland. Midwifery. 2002;18(4):279–95. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0266613802903281 .
Papadaki A, Scott J. The impact on eating habits of temporary translocation from a Mediterranean to a Northern European environment. Eur J Clin Nutr. 2002;56(5):455–61. Available from: https://www.nature.com/articles/1601337 .
McCann A, Mackie P. Improving the Health of Migrants to Scotland: An update for Scottish Directors of Public Health. 2016. Available from: https://www.scotphn.net/wp-content/uploads/2016/04/2016_03_23-Migrant-Health-Report-FINAL-1.pdf .
Ahmed A, Cameron S, Dickson C, Mountain K. Arabic-speaking students’ primary care experiences in Scotland. Community Pract J Community Pract Heal Visit Assoc. 2010;83(2):23–6.
Google Scholar
Bray J, Gorman D, Dundas K, Sim J. Obstetric care of New European migrants in Scotland: an audit of antenatal care, obstetric outcomes and communication. Scott Med J. 2010;55(3):26–31. Available from: ( http://journals.sagepub.com/doi/10.1258/rsmsmj.55.3.26 .
Cheung NF. Choice and control as experienced by Chinese and Scottish childbearing women in Scotland. Midwifery. 2002;18(3):200–13. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0266613802903153 .
Spence W, Zhu L. Perceptions of smoking cessation among Glasgow’s Chinese community. Tob Prev Cessat. 2017;3(October). Available from: http://www.journalssystem.com/tpc/Perceptions-of-smoking-cessation-among-Glasgow-s-Chinese-community,77942,0,2.html .
Gorman DR, Katikireddi SV, Morris C, Chalmers JWT, Sim J, Szamotulska K, et al. Ethnic variation in maternity care: a comparison of Polish and Scottish women delivering in Scotland 2004–2009. Public Health. 2014;128(3):262–7. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350613003910 .
Gorman DR, Porteous LA. Influences on Polish migrants’ breast screening uptake in Lothian, Scotland. Public Health. 2018;158:86–92. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350617304018 .
Hogg R, de Kok B, Netto G, Hanley J, Haycock-Stuart E. Supporting Pakistani and Chinese families with young children: perspectives of mothers and health visitors. Child Care Health Dev. 2015;41(3):416–23. Available from: https://onlinelibrary.wiley.com/doi/10.1111/cch.12154 .
Kearns A, Whitley E. Health, Wellbeing and Social Inclusion of Migrants in North Glasgow. 2010. Available from: https://www.gowellonline.com/assets/0000/0521/Health_Wellbeing_and_Social_Inclusion_of_Migrants_in_North_Glasgow.pdf .
Poole L, Adamson K. Report on the Situation of the Roma Community in Govanhill, Glasgow. 2008. Available from: https://www.bemis.org.uk/resources/gt/scotland/reportonthesituationoftheromacommunityingovanhill,Glasgow.pdf .
Schofield L, Walsh D, Feng Z, Buchanan D, Dibben C, Fischbacher C, et al. Does ethnic diversity explain intra-UK variation in mortality? A longitudinal cohort study. BMJ Open. 2019;9(3):e024563. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2018-024563 .
Unger HW, McCallum AD, Ukachukwu V, McGoldrick C, Perrow K, Latin G, et al. Imported malaria in Scotland – an overview of surveillance, reporting and trends. Travel Med Infect Dis. 2011;9(6):289–97. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1477893911001074 .
Young I, Flowers P, McDaid LM. Barriers to uptake and use of pre-exposure prophylaxis (PrEP) among communities most affected by HIV in the UK: findings from a qualitative study in Scotland. BMJ Open. 2014;4(11):e005717. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2014-005717 .
Young I, Flowers P, McDaid LM. Key factors in the acceptability of treatment as prevention (TasP) in Scotland: a qualitative study with communities affected by HIV. Sex Transm Infect. 2015;91(4):269–74. Available from: https://sti.bmj.com/lookup/doi/10.1136/sextrans-2014-051711 .
Bhopal R, Cm FI, Teiner SM, Halmers CJ, Ovey PC, Amieson J. Ethnicity and health in Scotland: Can we fill the information gap ? A demonstration project focusing on coronary heart disease and linkage of census and health records. Ethics. 2005. Available from: http://www.cphs.mvm.ed.ac.uk/docs/Retrocodingfinalreport.pdf .
Cezard GI, Bhopal RS, Ward HJT, Bansal N, Bhala N. Ethnic variations in upper gastrointestinal hospitalizations and deaths: the Scottish Health and Ethnicity Linkage Study. Eur J Public Health. 2016;26(2):254–60. Available from: https://academic.oup.com/eurpub/article-lookup/doi/10.1093/eurpub/ckv182 .
Christie-de Jong F, Kotzur M, Amiri R, Ling J, Mooney JD, Robb KA. Qualitative evaluation of a codesigned faith-based intervention for muslim women in Scotland to encourage uptake of breast, colorectal and cervical cancer screening. BMJ Open. 2022;12(5):e058739. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2021-058739 .
Cree VE, Sidhva D. Children and HIV in Scotland: findings from a cross-sector needs assessment of children and young people infected and affected by HIV in Scotland. Br J Soc Work. 2011;41(8):1586–603. Available from: https://academic.oup.com/bjsw/article-lookup/doi/10.1093/bjsw/bcr036 .
Gallimore A, Irshad T, Cooper M, Cameron S. Influence of culture, religion and experience on the decision of Pakistani women in Lothian, Scotland to use postnatal contraception: a qualitative study. BMJ Sex Reprod Heal. 2021;47(1):43–8. Available from: https://jfprhc.bmj.com/lookup/doi/10.1136/bmjsrh-2019-200497 .
Gruer LD, Cézard GI, Wallace LA, Hutchinson SJ, Douglas AF, Buchanan D, et al. Complex differences in infection rates between ethnic groups in Scotland: a retrospective, national census-linked cohort study of 1.65 million cases. J Public Health (Bangkok). 2022;44(1):60–9. Available from: https://academic.oup.com/jpubhealth/article/44/1/60/6106111 .
Article CAS Google Scholar
Bhala N, Cézard G, Ward HJT, Bansal N, Bhopal R. Ethnic variations in liver- and alcohol-related disease hospitalisations and mortality: the Scottish health and ethnicity linkage study. Alcohol Alcohol. 2016;51(5):593–601. Available from: https://academic.oup.com/alcalc/article-lookup/doi/10.1093/alcalc/agw018 .
Pollock KG, McDonald E, Smith-Palmer A, Johnston F, Ahmed S. Tuberculosis in healthcare workers, Scotland. Scott Med J. 2017;62(3):101–3. Available from: http://journals.sagepub.com/doi/10.1177/0036933017727963 .
Gruer LD, Millard AD, Williams LJ, Bhopal RS, Katikireddi SV, Cézard GI, et al. Differences in all-cause hospitalisation by ethnic group: a data linkage cohort study of 4.62 million people in Scotland, 2001–2013. Public Health. 2018;161:5–11. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350618301501 .
Jackson C, Bedford H, Cheater FM, Condon L, Emslie C, Ireland L, et al. Needles, Jabs and Jags: a qualitative exploration of barriers and facilitators to child and adult immunisation uptake among Gypsies, Travellers and Roma. BMC Public Health. 2017;17(1):254. Available from: http://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-017-4178-y .
John JR, Curry G, Cunningham-Burley S. Exploring ethnic minority women’s experiences of maternity care during the SARS-CoV-2 pandemic: a qualitative study. BMJ Open. 2021;11(9):e050666. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2021-050666 .
Lawton J, Ahmad N, Hanna L, Douglas M, Hallowell N. Diabetes service provision: a qualitative study of the experiences and views of Pakistani and Indian patients with Type 2 diabetes. Diabet Med. 2006;23(9):1003–7. Available from: https://onlinelibrary.wiley.com/doi/10.1111/j.1464-5491.2006.01922.x .
Livingston MR, Shaw LE, Codere G, Goldberg DJ. Human immunodeficiency virus acquired heterosexually abroad: expert panel assessment of the indigenous/nonindigenous to the united kingdom status of cases. J Travel Med. 2006;12(1):19–25. Available from: https://academic.oup.com/jtm/article-lookup/doi/10.2310/7060.2005.00005 .
Nelson M, Patton A, Robb K, Weller D, Sheikh A, Ragupathy K, et al. Experiences of cervical screening participation and non-participation in women from minority ethnic populations in Scotland. Heal Expect. 2021;24(4):1459–72. Available from: https://onlinelibrary.wiley.com/doi/10.1111/hex.13287 .
Noble G, Okpo E, Tonna I, Fielding S. Factors associated with late HIV diagnosis in North-East Scotland: a six-year retrospective study. Public Health. 2016;139:36–43. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0033350616301020 .
Gillespie M. Trapped: Destitution and Asylum in Scotland. 2012. Available from: http://www.rst.org.uk/wp-content/uploads/2012/11/Trapped-destitution-and-asylum-summary-final-compressed-pictures.pdf .
Hopkins P, Hill M. The needs and strengths of unaccompanied asylum-seeking children and young people in Scotland. Child Fam Soc Work. 2010;15(4):399–408. Available from: https://onlinelibrary.wiley.com/doi/10.1111/j.1365-2206.2010.00687.x .
Marsden R, Harris C. “We started life again”: Integration experiences of refugee families reuniting in Glasgow. 2015. Available from: https://www.refworld.org/docid/560cde294.html .
Martzoukou K, Burnett S. Exploring the everyday life information needs and the socio-cultural adaptation barriers of Syrian refugees in Scotland. J Doc. 2018;74(5):1104–32. Available from: https://www.emerald.com/insight/content/doi/10.1108/JD-10-2017-0142/full/html .
McKenna R. From pillar to post: Destitution among people refused asylum in Scotland. 2019; Available from: https://www.rst.org.uk/wp-content/uploads/2019/03/From-Pillar-to-Post-Feb-2019.pdf .
Independent Commission of Inquiry. Failings in the provision of care to New Scots during the Covid pandemic: Part 2. 2022. Available from: https://static1.squarespace.com/static/62af1289a666c80e00b17253/t/636b9190408f81778746eaa7/1667994032702/AIS+Phase+2+Report+Full.pdf .
Trevena P, Gawlewicz A, Wright S. Addressing the needs of Scotland’s migrant and minority ethnic populations under Covid-19: lessons for the future. 2022. Available from: https://migrantessentialworkers.com/wp-content/uploads/2022/11/SC-Migrant-C19-Innovations.pdf .
Oduntan O, Ruthven I. The information needs matrix: a navigational guide for refugee integration. Inf Process Manag. 2019;56(3):791–808. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0306457318306939 .
Sime D, Fox R, Migrant C. Social capital and access to services post-migration: transitions, negotiations and complex agencies. Child Soc. 2015;29(6):524–34. Available from: https://onlinelibrary.wiley.com/doi/10.1111/chso.12092 .
Strang A, Baillot H, Mignard E. Insights into integration pathways. New Scots and the Holistic Integration Service. A report drawing on year two of the Holistic Integration Service. 2015. Available from: https://scottishrefugeecouncil.org.uk/wp-content/uploads/2019/10/Holistic-Integration-Service-Year-2-report.pdf .
Weir KEA, Wilson SJ, Gorman DR. The Syrian vulnerable person resettlement programme: evaluation of Edinburgh’s reception arrangements. J Public Health (Bangkok). 2018;40(3):451–60. Available from: https://academic.oup.com/jpubhealth/article/40/3/451/4600209 .
Hammond CN. Scots 2- Engagement analysis of the New Scot Refugee Integration Strategy 2018–2022. 2018. Available from: https://www.gov.scot/binaries/content/documents/govscot/publications/research-and-analysis/2018/06/news-scots-2-engagement-analysis-new-scots-refugee-integration-strategy/documents/00537019-pdf/00537019-pdf/govscot%3Adocument/00537019.pdf .
Blake Stevenson. A8 Nationals in Glasgow. 2007. Available from: http://crosshillandgovanhill.org.uk/grindocs/A8NationalsinGlasgow.pdf .
Ajetunmobi O, Whyte B, Chalmers J, Fleming M, Stockton D, Wood R. Informing the ‘early years’ agenda in Scotland: understanding infant feeding patterns using linked datasets. J Epidemiol Community Health. 2014;68(1):83–92. Available from: https://jech.bmj.com/lookup/doi/10.1136/jech-2013-202718 .
Laidlaw K, Wang D, Coelho C, Power M. Attitudes to ageing and expectations for filial piety across Chinese and British cultures: a pilot exploratory evaluation. Aging Ment Health. 2010;14(3):283–92. Available from: http://www.tandfonline.com/doi/abs/10.1080/13607860903483060 .
Marsden R, Aldegheri E, Khan A, Lowe M, Strang A, Salinas E, et al. “What’s going on?” A study into destitution and poverty faced by asylum seekers and refugees in Scotland. 2005. Available from: http://www.rst.org.uk/wp-content/uploads/2012/11/Whats_going_on_A_study.pdf .
Quinn N. Participatory action research with asylum seekers and refugees experiencing stigma and discrimination: the experience from Scotland. Disabil Soc. 2014;29(1):58–70. Available from: http://www.tandfonline.com/doi/abs/10.1080/09687599.2013.769863 .
British Red Cross, Refugee Survival Trust. How will we survive? Steps to preventing destitution in the asylum system. 2021. Available from: https://mcusercontent.com/c17c136fc126588cb51e5471d/files/a35dd0e1-d785-f962-6a41-01e928493775/DASS_Research_Report_2021.pdf .
O’Donnell R, Angus K, McCulloch P, Amos A, Greaves L, Semple S. Fathers’ views and experiences of creating a smoke-free home: a scoping review. Int J Environ Res Public Health. 2019;16(24):5164. Available from: https://www.mdpi.com/1660-4601/16/24/5164 .
Sweileh WM, Wickramage K, Pottie K, Hui C, Roberts B, Sawalha AF, et al. Bibliometric analysis of global migration health research in peer-reviewed literature (2000–2016). BMC Public Health. 2018;18(1):777. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-018-5689-x .
Wren K. Supporting asylum seekers and refugees in glasgow: the role of multi-agency networks. J Refug Stud. 2007;20(3):391–413. Available from: https://academic.oup.com/jrs/article-lookup/doi/10.1093/jrs/fem006 .
UK Government Home Office. A Fairer Asylum Accommodation System. 2022. Available from: https://www.emcouncils.gov.uk/write/Migration/Asylum_Dispersal_Factsheet_PDF.pdf .
Scottish Refugee Council. Scotland’s Welcome: an analysis of community support for refugee integration. 2020. Available from https://scottishrefugeecouncil.org.uk/wp-content/uploads/2021/01/Community-support-analysis-2020.pdf .
Sturge G, UK Parliament House of Commons Library Asylum statistics Research Briefing. 2023. Available from: https://commonslibrary.parliament.uk/research-briefings/sn01403/#:~:text=IntheyearendingJune,ofimmigrantstotheUK .
The Migration Observatory. Where do migrants live in the UK? The Migration Observatory at the University of Oxford. 2022. Available from: https://migrationobservatory.ox.ac.uk/resources/briefings/where-do-migrants-live-in-the-uk .
Pavli A, Maltezou H. Health problems of newly arrived migrants and refugees in Europe. J Travel Med. 2017;24(4). Available from: http://academic.oup.com/jtm/article/doi/10.1093/jtm/tax016/3095987/Health-problems-of-newly-arrived-migrants-and .
Humphris R, Bradby H. Health Status of Refugees and Asylum Seekers in Europe. In: Oxford Research Encyclopedia of Global Public Health. Oxford University Press; 2017. Available from: https://oxfordre.com/publichealth/view/10.1093/acrefore/9780190632366.001.0001/acrefore-9780190632366-e-8 .
Bradby H, Humphris R, Newall D, Phillimore J. Public Health Aspects of Migrant Health: A Review of the Evidence on Health Status for Refugees and Asylum Seekers in the European Region. (Health Evidence Network Synthesis Report, No. 44.) ANNEX 2, DEFINITIONS OF REFUGEES, ASYLUM SEEKERS AND MIGRANTS IN THE LITERATURE. Copenhagen: Eerat; 2015. Available from: https://www.ncbi.nlm.nih.gov/books/NBK379415/ .
Gerritsen AAM, Bramsen I, Devillé W, van Willigen LHM, Hovens JE, van der Ploeg HM. Physical and mental health of Afghan, Iranian and Somali asylum seekers and refugees living in the Netherlands. Soc Psychiatry Psychiatr Epidemiol. 2006;41(1):18–26. Available from: http://link.springer.com/10.1007/s00127-005-0003-5 .
Laue J, Diaz E, Eriksen L, Risør T. Migration health research in Norway: a scoping review. Scand J Public Health. 2023;51(3):381–90. Available from: http://journals.sagepub.com/doi/10.1177/14034948211032494 .
Scottish Refugee Council. Ukraine response one year on. 2023. Available from: https://scottishrefugeecouncil.org.uk/ukraine-response-one-year-on/ . Cited 2023 Aug 26.
Woodward A, Howard N, Wolffers I. Health and access to care for undocumented migrants living in the European Union: a scoping review. Health Policy Plan. 2014;29(7):818–30. Available from: https://academic.oup.com/heapol/article-lookup/doi/10.1093/heapol/czt061 .
Simon J, Kiss N, Laszewska A, Mayer S. Public health aspects of migrant health: a review of the evidence on health status for labour migrants in the European Region. Health Evidence Network Synthesis Report 43. 2015. Available from: http://www.epgencms.europarl.europa.eu/cmsdata/upload/114f16b6-1667-44ab-802b-a5a83dd50af0/WHO-HEN-Report-A5-1-Labour-FINAL_EN.pdf .
Scottish Government. Seasonal migrant workers in Scottish agriculture: research report. 2023. Available from: https://www.gov.scot/publications/seasonal-migrant-workers-scottish-agriculture/pages/10/ .
Scottish Government. New Scots: refugee integration strategy 2018–2022. 2018. Available from: https://www.gov.scot/publications/new-scots-refugee-integration-strategy-2018-2022/pages/11/ .
Oliva A, Palavra V, Caloun J. Refugees in Scotland: understanding the policy domain. 2016. Available from: https://www.academia.edu/34097718/REFUGEES_IN_SCOTLAND_UNDERSTANDING_THE_POLICY_DOMAIN .
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. Available from: https://www.acpjournals.org/doi/10.7326/M18-0850 .
Download references
Acknowledgements
Thank-you to Professor Anne MacFarlane and PHD student Anne Cronin, of the University of Limerick, Ireland for sharing the coding guidelines currently used in an update to Villarroel et. al’s 2019 study on Migrant Health in the Republic of Ireland.
No funding was received for this work, which was undertaken as G. Petrie’s Master of Public Health dissertation module at the University of Stirling.
Author information
Authors and affiliations.
Caledonia House, NHS Greater Glasgow and Clyde, Glasgow, Scotland, UK
Institute for Social Marketing and Health, Faculty of Health Sciences and Sport, University of Stirling, Stirling, FK9 4LA, Scotland, UK
K. Angus & R. O’Donnell
You can also search for this author in PubMed Google Scholar
Contributions
KA, RO and GP finalised the study design collectively. GP conducted the searches, analysis and write up, with support from KA and RO. All three authors read and approved the manuscript prior to submission.
Corresponding author
Correspondence to R. O’Donnell .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Petrie, G., Angus, K. & O’Donnell, R. A scoping review of academic and grey literature on migrant health research conducted in Scotland. BMC Public Health 24 , 1156 (2024). https://doi.org/10.1186/s12889-024-18628-1
Download citation
Received : 04 September 2023
Accepted : 16 April 2024
Published : 25 April 2024
DOI : https://doi.org/10.1186/s12889-024-18628-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Asylum seekers
- Scoping review
- Research funding
- Immigration
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Bibliometric analysis of nursing education reviews
Affiliations.
- 1 Duke University School of Nursing, Durham, NC, USA. Electronic address: [email protected].
- 2 John Chambers College of Business and Economics, West Virginia University, Morgantown, WV, USA. Electronic address: [email protected].
- 3 West Virginia University, Morgantown, WV, USA. Electronic address: [email protected].
- 4 Liberty University, Lynchburg, VA, USA. Electronic address: [email protected].
- 5 Future of Privacy Forum, Washington, DC, USA. Electronic address: [email protected].
- 6 School of Nursing, Duke University Medical Center Library, Durham, NC, USA. Electronic address: [email protected].
- PMID: 38676961
- DOI: 10.1016/j.nedt.2024.106217
Background: While the number of reviews of nursing education research has increased over the years, bibliometric studies about these reviews are limited.
Objectives: The purposes were to: (1) examine the number of reviews of nursing education research published from 2018 through 2022, (2) identify journals publishing these reviews, (3) identify the types and topics of reviews in nursing education, and (4) analyze how these reviews are labeled (standard versus nonstandard).
Design: This was a bibliometric study of reviews in nursing education.
Methods: The search for reviews in nursing education was done using CINAHL Complete via the EBSCO host platform and was limited to articles published in peer reviewed journals. The results were imported into EndNote, and the title or abstract was used to identify the review type. The categorized reviews were then exported into Microsoft Excel. The titles and abstracts were searched to identify reviews in nursing education, resulting in 600 articles analyzed in this study. The topics of the reviews were identified via natural language processing techniques based on the Medical Subject Headings biomedical vocabulary in the manual tags with each article.
Results: The number of reviews has steadily increased over the years. The top journal in which reviews were published was Nurse Education Today (n = 197). Nearly a quarter (n = 149, 24.8 %) of the reviews were integrative, followed by systematic (n = 117, 19.5 %), scoping (n = 117, 19.5 %), and literature (n = 85, 14.2 %). There were 12 main topics: most reviews were on simulation, followed by critical thinking methods and the academic achievement of nursing students.
Conclusion: This study documented an increase in the number of reviews of nursing education research over the last five years. The most common type was an integrative review, followed by systematic, scoping, and literature. Reviews on simulation were most common.
Keywords: Bibliometric analysis; Evidence synthesis; Integrative review; Nursing education research; Reviews of research.
Copyright © 2024 Elsevier Ltd. All rights reserved.

IMAGES
VIDEO
COMMENTS
Implementing evidence into practice requires nurses to identify, critically appraise and synthesise research. This may require a comprehensive literature review: this article aims to outline the approaches and stages required and provides a working example of a published review. Literature reviews aim to answer focused questions to: inform professionals and patients of the best available ...
Once you have read and re-read your articles and organized your findings, you are ready to begin the process of writing the literature review. 2. Synthesize. (see handout below) Include a synthesis of the articles you have chosen for your literature review. A literature review is NOT a list or a summary of what has been written on a particular ...
A literature review is a comprehensive and up-to-date overview of published information on a subject area. Conducting a literature review demands a careful examination of a body of literature that has been published that helps answer your research question (See PICO). Literature reviewed includes scholarly journals, scholarly books ...
Background. A literature review is a critical analysis of published research literature based on a specified topic (Pluye et al., 2016).Literature reviews identify literature then examine its strengths and weaknesses to determine gaps in knowledge (Pluye et al. 2016).Literature reviews are an integral aspect of research projects; indeed, many reviews constitute a publication in themselves ...
Therefore, in this article, we provide a comprehensive guide to be used by health care and nursing scholars while choosing among 4 popular types of reviews (narrative, integrative, scoping, and ...
fi. taken is in uenced by the purpose of the review and. fl. resources available. However, the stages or methods used to undertake a review are similar across approaches and include: Formulating clear inclusion and exclusion criteria, for example, patient groups, ages, conditions/treat-ments, sources of evidence/research designs;
The purpose of a review of healthcare literature is primarily to summarise the knowledge around a specific question or topic, or to make recommendations that can support health professionals and organisations make decisions about a specific intervention or care issue.5 In addition, reviews can highlight gaps in knowledge to guide future research.
Abstract. Systematic reviews provide a synthesis of evidence for a specific topic of interest, summarising the results of multiple studies to aid in clinical decisions and resource allocation. They remain among the best forms of evidence, and reduce the bias inherent in other methods. A solid understanding of the systematic review process can ...
ong 4 popular types of reviews (narrative, integrative, scoping, and systematic review), including a descriptive discussion, critical analysis, and decision map tree. Although some review methodologies are more rigorous, it would be inaccurate to say that one is preferable over the others. Instead, each methodology is adequate for a certain type of investigation, nursing methodology research ...
A literature review is an essay that surveys, summarizes, links together, and assesses research in a given field. It surveys the literature by reviewing a large body of work on a subject; it summarizes by noting the main conclusions and findings of the research; it links together works in the literature by showing how the information fits into the overall academic discussion and how the ...
Systematic reviews that summarize the available information on a topic are an important part of evidence-based health care. There are both research and non-research reasons for undertaking a literature review. It is important to systematically review the literature when one would like to justify the need for a study, to update personal ...
A literature review can be a short introductory section of a research article or a report or policy paper that focuses on recent research. Or, in the case of dissertations, theses, and review articles, it can be an extensive review of all relevant research. The format is usually a bibliographic essay; sources are briefly cited within the body ...
Despite the availability of guidelines about the different types of review literature, the identification of the best approach is not always clear for nursing researchers. ... Reviews of Literature in Nursing Research: Methodological Considerations and Defining Characteristics ANS Adv Nurs Sci. 2022 Jul-Sep;45(3):197-208. doi: 10.1097/ANS ...
Nursing interventions can be evaluated qualitatively, as this method enhances the significance of clinical trials and emphasizes the distinctive work and outcomes of nursing care (Sandelowski, 1996 ). However, there are few examples of detailed methodological strategies for doing so (Schumacher et al., 2005 ).
A literature review is NOT an academic research paper, an annotated bibliography, or a report on original research. Unlike an academic research paper, the main focus of a literature review is not to develop a new argument. A literature review is an overview of a topic that shows the reader what research has been done on that subject.A literature review may build on an annotated bibliography ...
Run a few sample database searches to make sure your research question is not too broad or too narrow. If possible, discuss your topic with your professor. 2. Determine the scope of your review. The scope of your review will be determined by your professor during your program. Check your assignment requirements for parameters for the Literature ...
This review includes a systematic search, research review, and descriptive analysis of existing literature. Search strategy In September 2021, three databases, Web of Science, PubMed, and Child National Knowledge Infrastructure (CNKI), were searched using 'professional self-concept of nursing student' or 'nursing students' professional ...
Abstract. Aim: To identify and synthesize qualitative evaluation methods used in nursing interventions. Design: A systematic qualitative review with a content analysis. Four databases were used: MEDLINE, PsycINFO, Embase and CINAHL using pre-defined terms. The included papers were published from 2014-2018.
International Journal of Mental Health Nursing is a mental health journal examining trends and developments in mental health practice and research. Abstract This review examines factors associated with quality of life (QoL) in persons with young-onset dementia (YOD).
The purpose of a review of healthcare literature is primarily to summarise the knowledge around a specific question or topic, or to make recommendations that can support health professionals and organisations make decisions about a specific intervention or care issue. 5 In addition, reviews can highlight gaps in knowledge to guide future research.
Background. Mistreatment by patients is a detrimental phenomenon predominant in healthcare organizations. However, there is a lack of nursing literature regarding the underlying mechanisms and boundary conditions that exist between mistreatment by patients and its detrimental consequences.
A systematic literature review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P) systematic literature review protocol.35 The PRISMA 2020 checklist36 and ENhancing Transparency in REporting the synthesis of Qualitative research (ENTREQ) reporting guidelines were also followed.37 ...
There is therefore a clear need for systematic literature reviews to inform professionals' practice when identifying autistic children and when working with their parents during this process. There have been previous reviews on this topic (Boshoff et al., 2018; Legg & Tickle, 2019).
Nursing Research, Chapter 6, Literature Review. Review of Literature. Click the card to flip 👆. The process of finding relevant research reports, critically appraising the studies, and synthesizing the study results. The written description of the literature that results from the process is also called a review of literature.
Purpose and Importance of the Literature Review. An understanding of the current literature is critical for all phases of a research study. Lingard 9 recently invoked the "journal-as-conversation" metaphor as a way of understanding how one's research fits into the larger medical education conversation. As she described it: "Imagine yourself joining a conversation at a social event.
Hasnan Baber ([email protected]) is an Assistant Professor of management, strategy and entrepreneurship at the American University of Sharjah, Sharjah, UAE.He has received a PhD degree in management studies from Woosong University, Daejeon, South Korea, and two master's degrees in business administration and public administration.
The Joanna Briggs Institute (JBI) methodology for scoping reviews was used to guide this review. A comprehensive search strategy was developed with the assistance of a specialist librarian to access selected databases including: the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline, Web of Science and PsychInfo.
This column is intended to address the kinds of knotty problems and dilemmas with which many scholars grapple in studying health professions education. In this article, the authors address the question of whether one should conduct a literature review or knowledge synthesis, considering the why, when, and how, as well as its potential pitfalls. The goal is to guide supervisors and students who ...
This study aimed to scope existing peer-reviewed research and grey literature to identify gaps in evidence regarding the health of migrants in Scotland. A scoping review on the health of migrants in Scotland was carried out for dates January 2002 to March 2023, inclusive of peer-reviewed journals and grey literature.
Background: While the number of reviews of nursing education research has increased over the years, bibliometric studies about these reviews are limited. Objectives: The purposes were to: (1) examine the number of reviews of nursing education research published from 2018 through 2022, (2) identify journals publishing these reviews, (3) identify the types and topics of reviews in nursing ...