- Open access
- Published: 28 September 2018

Posttraumatic stress disorder: from diagnosis to prevention
- Xue-Rong Miao ORCID: orcid.org/0000-0002-0665-8271 1 ,
- Qian-Bo Chen 1 ,
- Kai Wei 1 ,
- Kun-Ming Tao 1 &
- Zhi-Jie Lu 1
Military Medical Research volume 5 , Article number: 32 ( 2018 ) Cite this article
54k Accesses
43 Citations
18 Altmetric
Metrics details
Posttraumatic stress disorder (PTSD) is a chronic impairment disorder that occurs after exposure to traumatic events. This disorder can result in a disturbance to individual and family functioning, causing significant medical, financial, and social problems. This study is a selective review of literature aiming to provide a general outlook of the current understanding of PTSD. There are several diagnostic guidelines for PTSD, with the most recent editions of the DSM-5 and ICD-11 being best accepted. Generally, PTSD is diagnosed according to several clusters of symptoms occurring after exposure to extreme stressors. Its pathogenesis is multifactorial, including the activation of the hypothalamic–pituitary–adrenal (HPA) axis, immune response, or even genetic discrepancy. The morphological alternation of subcortical brain structures may also correlate with PTSD symptoms. Prevention and treatment methods for PTSD vary from psychological interventions to pharmacological medications. Overall, the findings of pertinent studies are difficult to generalize because of heterogeneous patient groups, different traumatic events, diagnostic criteria, and study designs. Future investigations are needed to determine which guideline or inspection method is the best for early diagnosis and which strategies might prevent the development of PTSD.
Posttraumatic stress disorder (PTSD) is a recognized clinical phenomenon that often occurs as a result of exposure to severe stressors, such as combat, natural disaster, or other events [ 1 ]. The diagnosis of PTSD was first introduced in the 3rd edition of the Diagnostic and Statistical Manual (DSM) (American Psychiatric Association) in 1980 [ 2 ].
PTSD is a potentially chronic impairing disorder that is characterized by re-experience and avoidance symptoms as well as negative alternations in cognition and arousal. This disease first raised public concerns during and after the military operations of the United States in Afghanistan and Iraq, and to date, a large number of research studies report progress in this field. However, both the underlying mechanism and specific treatment for the disease remain unclear. Considering the significant medical, social and financial problems, PTSD represents both to nations and to individuals, all persons caring for patients suffering from this disease or under traumatic exposure should know about the risks of PTSD.
The aim of this review article is to present the current understanding of PTSD related to military injury to foster interdisciplinary dialog. This article is a selective review of pertinent literature retrieved by a search in PubMed, using the following keywords: “PTSD[Mesh] AND military personnel”. The search yielded 3000 publications. The ones cited here are those that, in the authors’ view, make a substantial contribution to the interdisciplinary understanding of PTSD.
Definition and differential diagnosis
Posttraumatic stress disorder is a prevalent and typically debilitating psychiatric syndrome with a significant functional disturbance in various domains. Both the manifestation and etiology of it are complex, which has caused difficulty in defining and diagnosing the condition. The 3rd edition of the DSM introduced the diagnosis of PTSD with 17 symptoms divided into three clusters in 1980. After several decades of research, this diagnosis was refined and improved several times. In the most recent version of the DSM-5 [ 3 ], PTSD is classified into 20 symptoms within four clusters: intrusion, active avoidance, negative alterations in cognitions and mood as well as marked alterations in arousal and reactivity. The diagnosis requirement can be summarized as an exposure to a stressor that is accompanied by at least one intrusion symptom, one avoidance symptom, two negative alterations in cognitions and mood symptoms, and two arousal and reactivity turbulence symptoms, persisting for at least one month, with functional impairment. Interestingly, in the DSM-5, PTSD has been moved from the anxiety disorder group to a new category of ‘trauma- and stressor-related disorders’, which reflects the cognizance alternation of PTSD. In contrast to the DSM versions, the World Health Organization’s (WHO) International Classification of Diseases (ICD) has proposed a substantially different approach to diagnosing PTSD in the most recent ICD-11 version [ 4 ], which simplified the symptoms into six under three clusters, including constant re-experiencing of the traumatic event, avoidance of traumatic reminders and a sense of threat. The diagnosis requires at least one symptom from each cluster which persists for several weeks after exposure to extreme stressors. Both diagnostic guidelines emphasize the exposure to traumatic events and time of duration, which differentiate PTSD from some diseases with similar symptoms, including adjustment disorder, anxiety disorder, obsessive-compulsive disorder, and personality disorder. Patients with the major depressive disorder (MDD) may or may not have experienced traumatic events, but generally do not have the invasive symptoms or other typical symptoms that PTSD presents. In terms of traumatic brain injury (TBI), neurocognitive responses such as persistent disorientation and confusion are more specific symptoms. It is worth mentioning that some dissociative reactions in PTSD (e.g., flashback symptoms) should be recognized separately from the delusions, hallucinations, and other perceptual impairments that appear in psychotic disorders since they are based on actual experiences. The ICD-11 also recognizes a sibling disorder, complex PTSD (CPTSD), composed of symptoms including dysregulation, negative self-concept, and difficulties in relationships based on the diagnosis of PTSD. The core CPTSD symptom is PTSD with disturbances in self-organization (DSO).
In consideration of the practical applicability of the PTSD diagnosis, Brewin et al. conducted a study to investigate the requirement differences, prevalence, comorbidity, and validity of the DSM-5 and ICD-11 for PTSD criteria. According to their study, diagnostic standards for symptoms of re-experiencing are higher in the ICD-11 than the DSM, whereas the standards for avoidance are less strict in the ICD-11 than in the DSM-IV [ 5 ]. It seems that in adult subjects, the prevalence of PTSD using the ICD-11 is considerably lower compared to the DSM-5. Notably, evidence suggested that patients identified with the ICD-11 and DSM-5 were quite different with only partially overlapping cases; this means each diagnostic system appears to find cases that would not be diagnosed using the other. In consideration of comorbidity, research comparing these two criteria show diverse outcomes, as well as equal severity and quality of life. In terms of children, only very preliminary evidence exists suggesting no significant difference between the two. Notably, the diagnosis of young children (age ≤ 6 years) depends more on the situation in consideration of their physical and psychological development according to the DSM-5.
Despite numerous investigations and multiple revisions of the diagnostic criteria for PTSD, it remains unclear which type and what extent of stress are capable of inducing PTSD. Fear responses, especially those related to combat injury, are considered to be sufficient enough to trigger symptoms of PTSD. However, a number of other types of stressors were found to correlate with PTSD, including shame and guilt, which represent moral injury resulting from transgressions during a war in military personnel with deeply held moral and ethical beliefs. In addition, military spouses and children may be as vulnerable to moral injury as military service members [ 6 ]. A research study on Canadian Armed Forces personnel showed that exposure to moral injury during deployments is common among military personnel and represents an independent risk factor for past-year PTSD and MDD [ 7 ]. Unfortunately, it seems that pre- and post-deployment mental health education was insufficient to moderate the relationship between exposure to moral injury and adverse mental health outcomes.
In general, a large number of studies are focusing on the definition and diagnostic criteria of PTSD and provide considerable indicators for understanding and verifying the disease. However, some possible limitations or discrepancies continue to exist in current research studies. One is that although the diagnostic criteria for a thorough examination of the symptoms were explicit and accessible, the formal diagnosis of PTSD using structured clinical interviews was relatively rare. In contrast, self-rating scales, such as the Posttraumatic Diagnostic Scale (PDS) [ 8 ] and the Impact of Events Scale (IES) [ 9 ], were used frequently. It is also noteworthy that focusing on PTSD explicitly could be a limitation as well. The complexity of traumatic experiences and the responses to them urge comprehensive investigations covering all aspects of physical and psychological maladaptive changes.
Prevalence and importance
Posttraumatic stress disorder generally results in poor individual-level outcomes, including co-occurring disorders such as depression and substance use, and physical health problems. According to the DSM-5 reporting, more than 80% of PTSD patients share one or more comorbidities; for instance, the morbidity of PTSD with concurrent mild TBI is 48% [ 8 ]. Moreover, cognitive impairment has been identified frequently in PTSD. The reported incidence rate for PTSD ranges from 5.4 to 16.8% in military service members and veterans [ 10 , 11 , 12 , 13 , 14 ], which is almost double those in the general population. The estimated prevalence of PTSD varies depending on the group of patients studied, the traumatic events occurred, and the measurement method used (Table 1 ). However, it still reflects the profound effect of this mental disease, especially with the rise in global terrorism and military conflict in recent years. While PTSD can arise at any life stage in any population, most research in recent decades has focused on returned veterans; this means most knowledge regarding PTSD has come from the military population. Meanwhile, the impact of this disease on children has received scant attention.
The discrepancy of PTSD prevalence in males and females is controversial. In a large study of OEF/OIF veterans, the prevalence of PTSD in males and females was similar, although statistically more prevalent in men versus women (13% vs. 11%) [ 15 ]. Another study on the Navy and Marine Corps showed a slightly higher incidence for PTSD in the women compared to men (6.6% vs. 5.3%) [ 12 ]. However, the importance of combat exposure is unclear. Despite a lower level of combat exposure than male military personnel, females generally have considerably higher rates of military sexual trauma, which is significantly associated with the development of PTSD [ 16 ].
It is reported that 44–72% of veterans suffer high levels of stress after returning to civilian life. Many returned veterans with PTSD show emotion regulation problems, including emotion identification, expression troubles and self-control issues. Nevertheless, a meta-analytic investigation of 34 studies consistently found that the severity of PTSD symptoms was significantly associated with anger, especially in military samples [ 17 ]. Not surprisingly, high levels of PTSD and emotional regulation troubles frequently lead to poor family functioning or even domestic violence in veterans. According to some reports, parenting difficulties in veteran families were associated with three PTSD symptom clusters. Evans et al. [ 18 ] conducted a survey to evaluate the impact of PTSD symptom clusters on family functioning. According to their analysis, avoidance symptoms directly affected family functioning, whereas hyperarousal symptoms had an indirect association with family functioning. Re-experience symptoms were not found to impact family functioning. Notably, recent epidemiologic studies using data from the Veterans Health Administration (VHA) reported that veterans with PTSD were linked to suicide ideations and behaviors [ 19 ] (e.g., non-suicidal self-injury, NSSI), in which depression as well as other mood disruptions, often serve as mediating factors.
Previously, there was a controversial attitude toward the vulnerability of young children to PTSD. However, growing evidence suggests that severe and persistent trauma could result in stress responses worse than expected as well as other mental and physical sequelae in child development. The most prevalent traumatic exposures for young children above the age of 1 year were interpersonal trauma, mostly related to or derived from their caregivers, including witnessing intimate partner violence (IPV) and maltreatment [ 20 ]. Unfortunately, because of the crucial role that caregivers play in early child development, these types of traumatic events are especially harmful and have been associated with developmental maladaptation in early childhood. Maladaptation commonly represents a departure from normal development and has even been linked to more severe effects and psychopathology. In addition, the presence of psychopathology may interfere with the developmental competence of young children. Research studies have also broadened the investigation to sequelae of PTSD on family relationships. It is proposed that the children of parents with symptoms of PTSD are easily deregulated or distressed and appear to face more difficulties in their psychosocial development in later times compared to children of parents without. Meanwhile, PTSD veterans described both emotional (e.g., hurt, confusion, frustration, fear) and behavioral (e.g., withdrawal, mimicking parents’ behavior) disruption in their children [ 21 ]. Despite the increasing emphasis on the effects of PTSD on young children, only a limited number of studies examined the dominant factors that influence responses to early trauma exposures, and only a few prospective research studies have observed the internal relations between early PTSD and developmental competence. Moreover, whether exposure to both trauma types in early life is associated with more severe PTSD symptoms than exposure to one type remains an outstanding question.
Molecular mechanism and predictive factors
The mechanisms leading to posttraumatic stress disorder have not yet been fully elucidated. Recent literature suggests that both the neuroendocrine and immune systems are involved in the formulation and development of PTSD [ 22 , 23 ]. After traumatic exposures, the stress response pathways of the hypothalamic–pituitary–adrenal (HPA) axis and sympathetic nervous system are activated and lead to the abnormal release of glucocorticoids (GC) and catecholamines. GCs have downstream effects on immunosuppression, metabolism enhancement, and negative feedback inhibition of the HPA axis by binding to the GC receptor (GR), thus connecting the neuroendocrine modulation with immune disturbance and inflammatory response. A recent meta-analysis of 20 studies found increased plasma levels of proinflammatory cytokines tumor necrosis factor-alpha (TNF-a), interleukin-1beta (IL-1b), and interleukin-6 (IL-6) in individuals with PTSD compared to healthy controls [ 24 ]. In addition, some other studies speculate that there is a prospective association of C-reactive protein (CRP) and mitogen with the development of PTSD [ 25 ]. These findings suggest that neuroendocrine and inflammatory changes, rather than being a consequence of PTSD, may in fact act as a biological basis and preexisting vulnerability for developing PTSD after trauma. In addition, it is reported that elevated levels of terminally differentiated T cells and an altered Th1/Th2 balance may also predispose an individual to PTSD.
Evidence indicates that the development of PTSD is also affected by genetic factors. Research has found that genetic and epigenetic factors account for up to 70% of the individual differences in PTSD development, with PTSD heritability estimated at 30% [ 26 ]. While aiming to integrate genetic studies for PTSD and build a PTSD gene database, Zhang et al. [ 27 ] summarized the landscape and new perspective of PTSD genetic studies and increased the overall candidate genes for future investigations. Generally, the polymorphisms moderating HPA-axis reactivity and catecholamines have been extensively studied, such as FKBP5 and catechol-O-methyl-transferase (COMT). Other potential candidates for PTSD such as AKT, a critical mediator of growth factor-induced neuronal survival, were also explored. Genetic research has also made progress in other fields. For example, researchers have found that DNA methylation in multiple genes is highly correlated with PTSD development. Additional studies have found that stress exposure may even affect gene expression in offspring by epigenetic mechanisms, thus causing lasting risks. However, some existing problems in the current research of this field should be noted. In PTSD genetic studies, variations in population or gender difference, a wide range of traumatic events and diversity of diagnostic criteria all may attribute to inconsistency, thus leading to a low replication rate among similar studies. Furthermore, PTSD genes may overlap with other mental disorders such as depression, schizophrenia, and bipolar disorder. All of these factors indicate an urgent need for a large-scale genome-wide study of PTSD and its underlying epidemiologic mechanisms.
It is generally acknowledged that some mental diseases, such as major depressive disorder (MDD), bipolar disorder, and schizophrenia, are associated with massive subcortical volume change. Recently, numerous studies have examined the relationship between the morphology changes of subcortical structures and PTSD. One corrected analysis revealed that patients with PTSD show a pattern of lower white matter integrity in their brains [ 28 ]. Prior studies typically found that a reduced volume of the hippocampus, amygdala, rostral ventromedial prefrontal cortex (rvPFC), dorsal anterior cingulate cortex (dACC), and the caudate nucleus may have a relationship with PTSD patients. Logue et al. [ 29 ] conducted a large neuroimaging study of PTSD that compared eight subcortical structure volumes (nucleus accumbens, amygdala, caudate, hippocampus, pallidum, putamen, thalamus, and lateral ventricle) between PTSD patients and controls. They found that smaller hippocampi were particularly associated with PTSD, while smaller amygdalae did not show a significant correlation. Overall, rigorous and longitudinal research using new technologies, such as magnetoencephalography, functional MRI, and susceptibility-weighted imaging, are needed for further investigation and identification of morphological changes in the brain after a traumatic exposure.
Psychological and pharmacological strategies for prevention and treatment
Current approaches to PTSD prevention span a variety of psychological and pharmacological categories, which can be divided into three subgroups: primary prevention (before the traumatic event, including prevention of the event itself), secondary prevention (between the traumatic event and the development of PTSD), and tertiary prevention (after the first symptoms of PTSD become apparent). The secondary and tertiary prevention of PTSD has abundant methods, including different forms of debriefing, treatments for Acute Stress Disorder (ASD) or acute PTSD, and targeted intervention strategies. Meanwhile, the process of primary prevention is still in its infancy and faces several challenges.
Based on current research on the primary prevention of post-trauma pathology, psychological and pharmacological interventions for particular groups or individuals (e.g., military personnel, firefighters, etc.) with a high risk of traumatic event exposure were applicable and acceptable for PTSD sufferers. Of the studies that reported possible psychological prevention effects, training generally included a psychoeducational component and a skills-based component relating to stress responses, anxiety reducing and relaxation techniques, coping strategies and identifying thoughts, emotion and body tension, choosing how to act, attentional control, emotion control and regulation [ 30 , 31 , 32 ]. However, efficiency for these training has not been evaluated yet due to a lack of high-level evidence-based studies. Pharmacological options have targeted the influence of stress on memory formation, including drugs relating to the hypothalamic-pituitary-adrenal (HPA) axis, the autonomic nerve system (especially the sympathetic nerve system), and opiates. Evidence has suggested that pharmacological prevention is most effective when started before and early after the traumatic event, and it seems that sympatholytic drugs (alpha and beta-blockers) have the highest potential for primary prevention of PTSD [ 33 ]. However, one main difficulty limiting the exploration in this field is related to rigorous and complex ethical issues, as the application of pre-medication for special populations and the study of such options in hazardous circumstances possibly touches upon questions of life and death. Significantly, those drugs may have potential side effects.
There are several treatment guidelines for patients with PTSD produced by different organizations, including the American Psychiatric Association (APA), the United Kingdom’s National Institute for Health and Clinical Excellence (NICE), the International Society for Traumatic Stress Studies (ISTSS), the Institute of Medicine (IOM), the Australian National Health and Medical Research Council, and the Department of Veterans Affairs and Department of Defense (VA, DoD) [ 34 , 35 , 36 , 37 , 38 ]. Additionally, a large number of research studies are aiming to evaluate an effective treatment method for PTSD. According to these guidelines and research, treatment approaches can be classified as psychological interventions and pharmacological treatments (Fig. 1 ); most of the studies provide varying degrees of improvement in individual outcomes after standard interventions, including PTSD symptom reduction or remission, loss of diagnosis, release or reduction of comorbid medical or psychiatric conditions, quality of life, disability or functional impairment, return to work or to active duty, and adverse events.
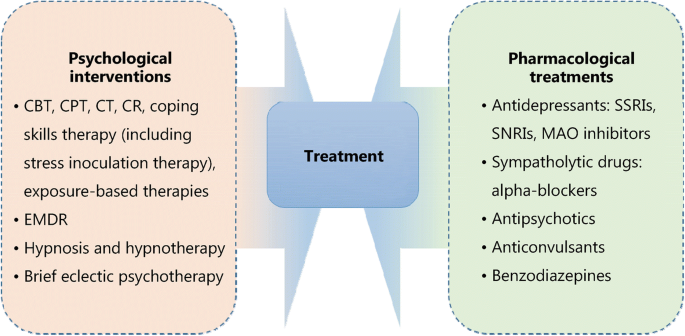
Psychological and pharmacological strategies for treatment of PTSD. CBT. Cognitive behavioral therapy; CPT. Cognitive processing therapy; CT. Cognitive therapy; CR. Cognitive restructuring; EMDR. Eye movement desensitization and reprocessing; SSRIs. Selective serotonin reuptake inhibitors; SNRIs. Serotonin and norepinephrine reuptake inhibitors; MAO. Monoamine oxidase
Most guidelines identify trauma-focused psychological interventions as first-line treatment options [ 39 ], including cognitive behavioral therapy (CBT), cognitive processing therapy (CPT), cognitive therapy (CT), cognitive restructuring (CR), coping skills therapy (including stress inoculation therapy), exposure-based therapies, eye movement desensitization and reprocessing (EMDR), hypnosis and hypnotherapy, and brief eclectic psychotherapy. These treatments are delivered predominantly to individuals, but some can also be conducted in family or group settings. However, the recommendation of current guidelines seems to be projected empirically as research on the comparison of outcomes of different treatments is limited. Jonas et al. [ 40 ] performed a systematic review and network meta-analysis of the evidence for treatment of PTSD. The study suggested that all psychological treatments showed efficacy for improving PTSD symptoms and achieving the loss of PTSD diagnosis in the acute phase, and exposure-based treatments exhibited the strongest evidence of efficacy with high strength of evidence (SOE). Furthermore, Kline et al. [ 41 ] conducted a meta-analysis evaluating the long-term effects of in-person psychotherapy for PTSD in 32 randomized controlled trials (RCTs) including 2935 patients with long-term follow-ups of at least 6 months. The data suggested that all studied treatments led to lasting improvements in individual outcomes, and exposure therapies demonstrated a significant therapeutic effect as well with larger effect sizes compared to other treatments.
Pharmacological treatments for PTSD include antidepressants such as selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), and monoamine oxidase (MAO) inhibitors, sympatholytic drugs such as alpha-blockers, antipsychotics, anticonvulsants, and benzodiazepines. Among these medications, fluoxetine, paroxetine, sertraline, topiramate, risperidone, and venlafaxine have been identified as efficacious in treatment. Moreover, in the Jonas network meta-analysis of 28 trials (4817 subjects), they found paroxetine and topiramate to be more effective for reducing PTSD symptoms than most other medications, whereas evidence was insufficient for some other medications as research was limited [ 40 ]. It is worth mentioning that in these studies, efficacy for the outcomes, unlike the studies of psychological treatments, was mostly reported as a remission in PTSD or depression symptoms; other outcomes, including loss of PTSD diagnosis, were rarely reported in studies.
As for the comparative evidence of psychological with pharmacological treatments or combinations of psychological treatments and pharmacological treatments with other treatments, evidence was insufficient to draw any firm conclusions [ 40 ]. Additionally, reports on adverse events such as mortality, suicidal behaviors, self-harmful behaviors, and withdrawal of treatment were relatively rare.
PTSD is a high-profile clinical phenomenon with a complicated psychological and physical basis. The development of PTSD is associated with various factors, such as traumatic events and their severity, gender, genetic and epigenetic factors. Pertinent studies have shown that PTSD is a chronic impairing disorder harmful to individuals both psychologically and physically. It brings individual suffering, family functioning disorders, and social hazards. The definition and diagnostic criteria for PTSD remain complex and ambiguous to some extent, which may be attributed to the complicated nature of PTSD and insufficient research on it. The underlying mechanisms of PTSD involve changes in different levels of psychological and molecular modulations. Thus, research targeting the basic mechanisms of PTSD using standard clinical guidelines and controlled interference factors is needed. In terms of treatment, psychological and pharmacological interventions could relief PTSD symptoms to different degrees. However, it is necessary to develop systemic treatment as well as symptom-specific therapeutic methods. Future research could focus on predictive factors and physiological indicators to determine effective prevention methods for PTSD, thereby reducing its prevalence and preventing more individuals and families from struggling with this disorder.
Abbreviations
American Psychiatric Association
Acute stress disorder
Cognitive behavioral therapy
Catechol-O-methyl-transferase
Cognitive processing therapy
Complex posttraumatic stress disorder
Cognitive restructuring
C-reactive protein
Cognitive therapy
Dorsal anterior cingulate cortex
Diagnostic and Statistical Manual
Disturbances in self-organization
Eye movement desensitization and reprocessing
Glucocorticoids
Glucocorticoids receptor
Hypothalamic–pituitary–adrenal axis
International classification of diseases
Impact of events scale
Interleukin-1beta
Interleukin-6
Institute of Medicine
Intimate partner violence
International Society for Traumatic Stress Studies
Monoamine oxidase
Major depressive disorder
United Kingdom’s National Institute for Health and Clinical Excellence
Non-suicidal self-injury
Posttraumatic diagnostic scale
Posttraumatic stress disorder
Randomized controlled trials
Rostral ventromedial prefrontal cortex
Serotonin and norepinephrine reuptake inhibitors;
Strength of evidence
Selective serotonin reuptake inhibitors
Tumor necrosis factor-alpha
DoD Department of Veterans Affairs and Department of Defense
Veterans Health Administration
World Health Organization
White J, Pearce J, Morrison S, Dunstan F, Bisson JI, Fone DL. Risk of post-traumatic stress disorder following traumatic events in a community sample. Epidemiol Psychiatr Sci. 2015;24(3):1–9.
Article Google Scholar
Kendell RE. Diagnostic and statistical manual of mental disorders, 3rd ed., revised (DSM-III-R). America J Psychiatry. 1980;145(10):1301–2.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM-5. America J Psychiatry. 2013. doi: https://doi.org/10.1176/appi.books.9780890425596.744053 .
Maercker A, Brewin CR, Bryant RA, Cloitre M, Reed GM, Van OM, et al. Proposals for mental disorders specifically associated with stress in the international classification of Diseases-11. Lancet. 2013;381(9878):1683–5.
Brewin CR, Cloitre M, Hyland P, Shevlin M, Maercker A, Bryant RA, et al. A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clin Psychol Rev. 2017;58(1): 1–15.
Google Scholar
Nash WP, Litz BT. Moral injury: a mechanism for war-related psychological trauma in military family members. Clin Child Fam Psychol Rev. 2013;16(4):365–75.
Nazarov A, Fikretoglu D, Liu A, Thompson M, Zamorski MA. Greater prevalence of post-traumatic stress disorder and depression in deployed Canadian Armed Forces personnel at risk for moral injury. Acta Psychiatr Scand. 2018;137(4):342–54.
Article CAS Google Scholar
Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: the posttraumatic diagnostic scale. Psychol Assess. 1997;9(9):445–51.
Gnanavel S, Robert RS. Diagnostic and statistical manual of mental disorders (5th edit) and the impact of events scale-revised. Chest. 2013;144(6):1974–5.
Reijnen A, Rademaker AR, Vermetten E, Geuze E. Prevalence of mental health symptoms in Dutch military personnel returning from deployment to Afghanistan: a 2-year longitudinal analysis. Eur Psychiatry. 2015;30(2):341–6.
Sundin J, Herrell RK, Hoge CW, Fear NT, Adler AB, Greenberg N, et al. Mental health outcomes in US and UK military personnel returning from Iraq. Br J Psychiatry. 2014;204(3):200–7.
Macera CA, Aralis HJ, Highfill-McRoy R, Rauh MJ. Posttraumatic stress disorder after combat zone deployment among navy and marine corps men and women. J Women's Health (Larchmt). 2014;23(6):499–505.
Macgregor AJ, Tang JJ, Dougherty AL, Galarneau MR. Deployment-related injury and posttraumatic stress disorder in US military personnel. Injury. 2013;44(11):1458–64.
Sandweiss DA, Slymen DJ, Leardmann CA, Smith B, White MR, Boyko EJ, et al. Preinjury psychiatric status, injury severity, and postdeployment posttraumatic stress disorder. Arch Gen Psychiatry. 2011;68(5):496–504.
Seal KH, Bertenthal D, Maguen S, Gima K, Chu A, Marmar CR. Getting beyond "Don't ask; don't tell": an evaluation of US veterans administration postdeployment mental health screening of veterans returning from Iraq and Afghanistan. Am J Public Health. 2008;98(4):714–20.
Street AE, Rosellini AJ, Ursano RJ, Heeringa SG, Hill ED, Monahan J, et al. Developing a risk model to target high-risk preventive interventions for sexual assault victimization among female U.S. army soldiers. Clin Psychol Sci. 2016;4(6):939–56.
Olatunji BO, Ciesielski BG, Tolin DF. Fear and loathing: a meta-analytic review of the specificity of anger in PTSD. Behav Ther. 2010;41(1):93–105.
Evans L, Cowlishaw S, Hopwood M. Family functioning predicts outcomes for veterans in treatment for chronic posttraumatic stress disorder. J Fam Psychol. 2009;23(4):531–9.
Mckinney JM, Hirsch JK, Britton PC. PTSD symptoms and suicide risk in veterans: serial indirect effects via depression and anger. J Affect Disord. 2017;214(1):100–7.
Briggsgowan MJ, Carter AS, Ford JD. Parsing the effects violence exposure in early childhood: modeling developmental pathways. J Pediatric Psychol. 2012;37(1):11–22.
Enlow MB, Blood E, Egeland B. Sociodemographic risk, developmental competence, and PTSD symptoms in young children exposed to interpersonal trauma in early life. J Trauma Stress. 2013;26(6):686–94.
Newport DJ, Nemeroff CB. Neurobiology of posttraumatic stress disorder. Curr Opin eurobiol. 2009;14(1 Suppl 1):13.
Neigh GN, Ali FF. Co-morbidity of PTSD and immune system dysfunction: opportunities for treatment. Curr Opin Pharmacol. 2016;29:104–10.
Passos IC, Vasconcelos-Moreno MP, Costa LG, Kunz M, Brietzke E, Quevedo J, et al. Inflammatory markers in post-traumatic stress disorder: a systematic review, meta-analysis, and meta-regression. Lancet Psychiatry. 2015;2(11):1002.
Eraly SA, Nievergelt CM, Maihofer AX, Barkauskas DA, Biswas N, Agorastos A, et al. Assessment of plasma C-reactive protein as a biomarker of posttraumatic stress disorder risk. JAMA Psychiatry. 2014;71(4):423.
Lebois LA, Wolff JD, Ressler KJ. Neuroimaging genetic approaches to posttraumatic stress disorder. Exp Neurol. 2016;284(Pt B):141–52.
Zhang K, Qu S, Chang S, Li G, Cao C, Fang K, et al. An overview of posttraumatic stress disorder genetic studies by analyzing and integrating genetic data into genetic database PTSD gene. Neurosci Biobehav Rev. 2017;83(1):647–56.
Bolzenius JD, Velez CS, Lewis JD, Bigler ED, Wade BSC, Cooper DB, et al. Diffusion imaging findings in US service members with mild traumatic brain injury and posttraumatic stress disorder. J Head Trauma Rehabil. 2018. https://doi.org/10.1097/HTR.0000000000000378 [Epub ahead of print].
Logue MW, Rooij SJHV, Dennis EL, Davis SL, Hayes JP, Stevens JS, et al. Smaller hippocampal volume in posttraumatic stress disorder: a multi-site ENIGMA-PGC study. Biol. Psychiatry . 2018;83(3):244–53.
Sijaric-Voloder S, Capin D. Application of cognitive behavior therapeutic techniques for prevention of psychological disorders in police officers. Health Med. 2008;2(4):288–92.
Deahl M, Srinivasan M, Jones N, Thomas J, Neblett C, Jolly A. Preventing psychological trauma in soldiers: the role of operational stress training and psychological debriefing. Brit J Med Psychol. 2000;73(1):77–85.
Wolmer L, Hamiel D, Laor N. Preventing children's posttraumatic stress after disaster with teacher-based intervention: a controlled study. J Am Acad Child Adolesc Psychiatry. 2011;50(4):340–8 348.e1–2.
Skeffington PM, Rees CS, Kane R. The primary prevention of PTSD: a systematic review. J Trauma Dissociation. 2013;14(4):404–22.
Jaques H. Introducing the national institute for health and clinical excellence. Eur Heart J. 2012;33(17):2111–2.
PubMed Google Scholar
Schnyder U. International Society for Traumatic Stress Studies (ISTSS). Psychosomatik Und Konsiliarpsychiatrie. 2008;2(4):261.
Bulger RE. The institute of medicine. Kennedy Inst Ethics J. 1992;2(1):73–7.
Anderle R, Brown DC, Cyran E. Department of Defense[C]. African Studies Association. 2011;2011:340–2.
Feussner JR, Maklan CW. Department of Veterans Affairs[J]. Med Care. 1998;36(3):254–6.
Sripada RK, Rauch SA, Liberzon I. Psychological mechanisms of PTSD and its treatment. Curr Psychiatry Rep. 2016;18(11):99.
Jonas DE, Cusack K, Forneris CA, Wilkins TM, Sonis J, Middleton JC, et al. Psychological and pharmacological treatments for adults with posttraumatic stress disorder (PTSD). Agency Healthcare Res Quality (AHRQ). 2013;4(1):1–760.
Kline AC, Cooper AA, Rytwinksi NK, Feeny NC. Long-term efficacy of psychotherapy for posttraumatic stress disorder: a meta-analysis of randomized controlled trials. Clin Psychol Rev. 2018;59:30–40.
Download references
Acknowledgments
We thank Jamie Bono for providing professional writing suggestions.
This work was supported by the National Natural Science Foundation of China (31371084 and 31171013 by ZJL), and the National Natural Science Foundation of China (81100276 by XRM).
Author information
Authors and affiliations.
Department of Anesthesiology and Intensive Care, Third Affiliated Hospital of Second Military Medical University, Shanghai, China
Xue-Rong Miao, Qian-Bo Chen, Kai Wei, Kun-Ming Tao & Zhi-Jie Lu
You can also search for this author in PubMed Google Scholar
Contributions
ZJL and XRM conceived the project. QBC, KW and KMT conducted the article search and acquisition. XRM and QBC analyzed the data. XRM wrote the manuscript. All the authors read and discussed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Xue-Rong Miao .
Ethics declarations
Ethics approval and consent to participate.
Not Applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Miao, XR., Chen, QB., Wei, K. et al. Posttraumatic stress disorder: from diagnosis to prevention. Military Med Res 5 , 32 (2018). https://doi.org/10.1186/s40779-018-0179-0
Download citation
Received : 20 March 2018
Accepted : 10 September 2018
Published : 28 September 2018
DOI : https://doi.org/10.1186/s40779-018-0179-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cognitive impairment
- Psychological interventions
- Neuroendocrine
Military Medical Research
ISSN: 2054-9369
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 20 September 2021
Prefrontal cortex, amygdala, and threat processing: implications for PTSD
- M. Alexandra Kredlow 1 na1 ,
- Robert J. Fenster 2 na1 ,
- Emma S. Laurent ORCID: orcid.org/0000-0002-4820-8332 1 ,
- Kerry J. Ressler ORCID: orcid.org/0000-0002-5158-1103 2 &
- Elizabeth A. Phelps ORCID: orcid.org/0000-0002-6215-8159 1
Neuropsychopharmacology volume 47 , pages 247–259 ( 2022 ) Cite this article
41k Accesses
78 Citations
61 Altmetric
Metrics details
- Human behaviour
Posttraumatic stress disorder can be viewed as a disorder of fear dysregulation. An abundance of research suggests that the prefrontal cortex is central to fear processing—that is, how fears are acquired and strategies to regulate or diminish fear responses. The current review covers foundational research on threat or fear acquisition and extinction in nonhuman animals, healthy humans, and patients with posttraumatic stress disorder, through the lens of the involvement of the prefrontal cortex in these processes. Research harnessing advances in technology to further probe the role of the prefrontal cortex in these processes, such as the use of optogenetics in rodents and brain stimulation in humans, will be highlighted, as well other fear regulation approaches that are relevant to the treatment of posttraumatic stress disorder and involve the prefrontal cortex, namely cognitive regulation and avoidance/active coping. Despite the large body of translational research, many questions remain unanswered and posttraumatic stress disorder remains difficult to treat. We conclude by outlining future research directions related to the role of the prefrontal cortex in fear processing and implications for the treatment of posttraumatic stress disorder.
Similar content being viewed by others

Post-traumatic stress disorder: clinical and translational neuroscience from cells to circuits
Kerry. J. Ressler, Sabina Berretta, … William A. Carlezon Jr
Prefrontal-hippocampal interactions supporting the extinction of emotional memories: the retrieval stopping model
Michael C. Anderson & Stan B. Floresco

Sex differences in auditory fear discrimination are associated with altered medial prefrontal cortex function
Harriet L. L. Day, Sopapun Suwansawang, … Carl W. Stevenson
Introduction
Post-traumatic stress disorder (PTSD) is a maladaptive and debilitating psychiatric disorder typically accompanied by an extreme sense of fear at the time of trauma occurrence, with characteristic re-experiencing, avoidance, and hyperarousal symptoms in the months and years following the trauma. PTSD has a prevalence of ~6% but can occur in 25–35% of individuals who have experienced severe psychological trauma, such as combat veterans, refugees, and assault victims [ 1 , 2 , 3 ]. The differential risk determining those who do versus those who do not develop PTSD is multifactorial [ 4 , 5 , 6 , 7 ]. It is in part genetic, with at least 30–40% risk heritability for PTSD following trauma [ 8 , 9 , 10 ], and in part depends on past personal history, including adult and childhood trauma and psychological factors which may differentially mediate fear and emotion regulation. Additionally, considerable evidence now supports a model in which PTSD can be viewed, in part, as a disorder of fear dysregulation. This is advantageous because the neural circuitry underlying threat and fear-related behaviors in mammals, including the amygdala–hippocampus–medial prefrontal circuit, is among the most well-understood behavioral circuits in neuroscience [ 11 , 12 , 13 , 14 ]. Further, the study of threat behavior and its underlying circuitry has led to some of the most rapid progress in understanding learning and memory processes.
Although the amygdala and other subcortical regions are perhaps best understood with relationship to threat processing across species, burgeoning evidence has provided substantial support for the role of different regions of the prefrontal cortex (PFC) in particular in regulating the encoding of threat-related behaviors across species and the emotion of fear in humans. Furthermore, the PFC has a critical role in threat inhibition and extinction, as well as in processes such as emotion regulation and avoidance.
In contrast to the promise of current scientific approaches, in the clinic PTSD remains very difficult to treat [ 15 , 16 ]. The best current treatments are in the form of exposure-based cognitive-behavioral therapies, which are thought to act on the neurocircuitry of threat extinction, in particular through the PFC. The medication treatments for PTSD are primarily limited to traditional serotonin and norepinephrine reuptake inhibitors, which are used for a broad range of depression and anxiety disorders. Advances in understanding the neural circuit of regulation of threat, fear, and PTSD symptoms may lead to novel and more robust treatment approaches.
This review aims to synthesize our current understanding of the role of the PFC in threat behaviors and threat-related emotional processing, and the role of multiple PFC subregions in PTSD. As acknowledged, this line of research is relevant to the treatment of disorders characterized by fear, such as PTSD. However, in line with the two-system view of fear and anxiety [ 17 ] and in order to not make assumptions about emotional states, the term “threat” will be used when referring to the behavioral, psychophysiological, or neural outcomes of conditioning research. The term “fear” will be reserved for describing studies in which the subjective emotion of fear was assessed or discussing the emotion more generally.
Nonhuman animal research on threat processing
The medial prefrontal cortex (mPFC) of the rodent regulates a balance between goal-oriented and habitual behaviors [ 18 , 19 ]. The mPFC receives massive inputs from subcortical structures, including the amygdala, hippocampus, ventral striatum, hypothalamus, periaqueductal gray, and cerebellum, among others, that allow it to integrate the behavioral state of the animal and adjust behavioral decisions on a moment-to-moment basis. One of the most important mPFC functions is to integrate information about potential threats in the environment with other organismal drives to determine behavioral outputs [ 20 ].
Decades of basic research on the mPFC in rodents indicate that it plays a key role in the expression and storage of the Pavlovian threat response and the establishment of threat-related extinction memories [ 21 ]. Technological advances have evolved from lesion and pharmacologic studies to experiments utilizing circuit-perturbing and single-cell approaches, which are beginning to provide data at the cell-type resolution for the role of this critical structure in the threat response. Below, we will briefly review the anatomy of the rodent mPFC, the data implicating mPFC circuitry in the threat response and in threat extinction, molecular changes in mPFC cell types with threat acquisition and extinction, and future steps in these lines of research.
Anatomy of rodent mPFC
Like most cortical regions, the mPFC is a multi-layered structure of heterogeneous cell types, composed of excitatory pyramidal neurons, inhibitory interneurons, and support cells. Beginning with Brodmann, there have been debates about the existence and location of the mPFC in rodents due to the lack of a prominent granular layer [ 22 ; see Preuss and Wise, this issue]. Cross-species comparisons can be more easily made with respect to connectivity patterns [ 23 ]. The rodent mPFC is generally considered to consist of the medial precentral area (Fr2), the dorsal anterior cingulate cortex (dACC), prelimbic cortex (PL), and infralimbic cortex (IL) [ 24 ] (see Fig. 1a ).
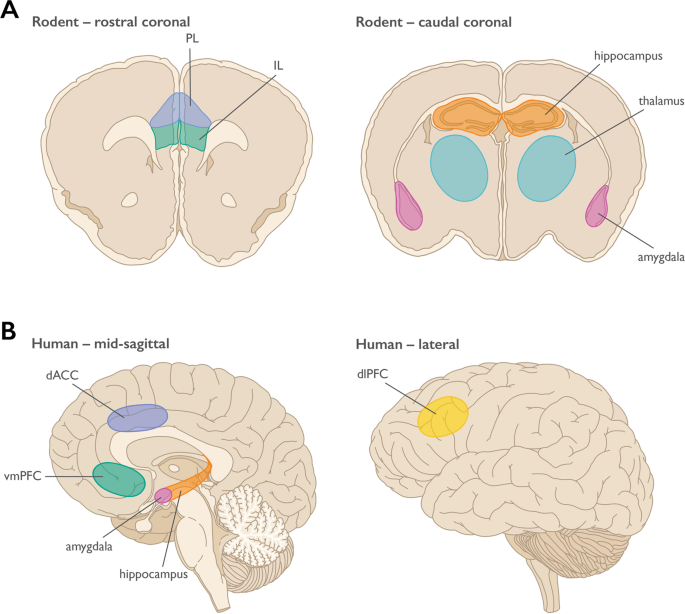
a Rodent anatomy highlighting regions involved in threat learning, extinction, avoidance, and the contextual modulation of threat expression; b Human anatomy highlighting regions involved in threat learning, extinction, avoidance, cognitive regulation, and the contextual modulation of threat expression. PL = prelimbic cortex, IL = infralimbic cortex; dACC = dorsal anterior cingulate cortex, vmPFC = ventromedial prefrontal cortex, dlPFC = dorsolateral prefrontal cortex.
For the purposes of this review, we will focus on rodent PL and IL, although recent work has implicated dACC in observational threat pathways, which may be relevant to PTSD from witnessed trauma [ 25 ]. Histologically in the mouse, PL and IL differ in the thickness of layer II/III and the prominence of layer separations between superficial II/III and layer V; however, this boundary is not easily demarcated [ 26 , 27 ]. Both PL and IL receive cortical input, as well as unidirectional projections from the hippocampus, mainly CA1 and subiculum [ 24 ]. Projections to the amygdala are bidirectional, although there are differences in the projection patterns of PL and IL to the amygdaloid complex, and there is some controversy about whether PL and IL synapse onto functionally different cell types [ 28 , 29 ]. Although there is some overlap in projection patterns, IL projects most heavily to lateral septum, bed nucleus of the stria terminalis, amygdala, hypothalamus, and brainstem, while PL sends more projections to insular cortex, nucleus accumbens, thalamus, and raphe nuclei [ 29 ]. The differences in these projection patterns suggest diverging functional roles for these adjacent structures.
Evidence for PL/IL distinction
For the past 20 years, there has been an extensive, although debated, literature showing differential roles for PL and IL in threat conditioning and threat extinction [ 21 ]. The first study to demonstrate a role for the rodent ventromedial prefrontal cortex (vmPFC) came from Morgan et al., who lesioned the mPFC [ 30 ]. A follow-up study demonstrated that more dorsal areas of the mPFC affected threat learning, while more ventral mPFC was required for threat extinction [ 31 ]. Quirk et al. supported this result when they [ 32 ] performed electrolytic lesions of the rat vmPFC and assessed threat extinction memory. They found that lesions that included caudal IL ablated threat extinction memories, while those that excluded the area had no effect. Pharmacological inactivation of PL and IL with agents such as the GABA agonist muscimol further suggested opposing roles for these structures in threat conditioning and threat extinction, respectively [ 33 ]. However, these results have not been universally reproduced [ 34 , 35 ]. More recent studies from the Quirk laboratory have used optogenetics to drive or inhibit activity in excitatory IL neurons during threat extinction. These data suggest that IL neurons are necessary for encoding threat extinction memories but may not be necessary for threat extinction memory storage or retention [ 36 ]. These findings also suggest that the threat extinction memory trace may be represented by different cell populations over time. Indeed, it has been known that the threat memory is likely constituted by a distributed network of cells across a range of brain regions. Inputs to the mPFC likely help to drive evolution of the memory trace over time.
Modulation of mPFC by subcortical structures
Because the mPFC must guide behavior on a moment-to-moment basis, it needs to receive a constant stream of information from subcortical structures and send out a coordinated response. The mPFC receives dense innervation from many subcortical structures, but we will focus here upon three crucial inputs: the hippocampus, amygdala, and thalamus. The canonical role of the hippocampus in threat circuitry is to encode context-specific information of a threat trace, as it is crucial for an organism to be able to distinguish threats as belonging to a particular context. The hippocampus itself appears to have a dorsal-ventral functional gradient, with the dorsal hippocampus encoding context more specifically, while the ventral hippocampus (vHPC) includes affective information as well [ 37 ].
The vHPC sends dense direct projections to the mPFC from CA1, but also bidirectional disynaptic indirect connections to the mPFC through the reuniens nucleus of the thalamus and the perirhinal cortex [ 38 ]. Lesion studies of the hippocampus suggest a critical role in context processing [ 39 ]. Reversible inactivation of the dorsal hippocampus, through either pharmacologic or chemogenetic means, interferes with context-specific information of a threat memory [ 40 , 41 ]. Inhibition of double-projecting vHPC neurons to the mPFC and basolateral amygdala (BLA) interferes with contextual threat recall [ 42 ] and disconnection of the vHPC from the mPFC interferes with renewal of threat memories, a context-dependent process [ 43 ]. Activity-tagging coupled with optogenetic inhibition suggests that threat conditioning and extinction memories exist in separate populations of neurons within the hippocampus [ 44 ], and the hippocampus may influence mPFC activity through feed-forward inhibition mechanisms through parvalbumin interneurons [ 45 ]. In return, the mPFC appears to suppress expression of erroneous contexts in a “top-down” manner through a disynaptic pathway through the reuniens nucleus of the thalamus [ 46 ]. In addition, there may be more routes of information flow from the PFC to the hippocampus, including direct routes from the nearby anterior cingulate [ 47 ].
The amygdala communicates the salience of the threat cue to the mPFC (see Murray and Fellows, this issue, for further discussion of amygdala-PFC interactions). For thirty years, the amygdala has been implicated in both threat learning [ 48 ] and threat extinction [ 49 ] processes. The BLA sends bidirectional projections to the mPFC [ 50 ]. There is evidence to suggest that there is a dorso-ventral topographic segregation of BLA input to the mPFC; more dorsal projections (to PL) encode threat-stimulating information while more ventral projections (to IL) encode threat extinction-related information [ 51 ]. Synaptic connections between PL neurons and BLA inputs also strengthen in response to stress, in part through endocannabinoid-mediated mechanisms [ 52 ]. Projection neurons within the BLA exhibit plasticity when conditioned stimulus-unconditioned stimulus pairings occur and convey this information to the mPFC.
Finally, nuclei within the thalamus help bind threat memories to context and facilitate shifts in the mPFC threat memory trace over time. The reuniens nucleus of the thalamus coordinates oscillatory synchrony between the mPFC and the vHPC, which is necessary for proper contextual representation of threat memories [ 46 , 53 ]. The paraventricular nucleus of the thalamus plays a crucial role in the encoding of threat memories over time [ 54 ] and appears to be necessary in shifting the temporal nature of how the mPFC encodes threat memories [ 55 ].
Molecular pathways in rodent mPFC
At the molecular level, threat conditioning and extinction are associated with epigenetic, transcriptional, and translational changes that likely modify synaptic weights and cell firing properties that persistently alter circuit function. Introduction of the translational inhibitor anisomycin, either intraventricularly or into the mPFC, causes a failure to retain threat extinction memories. This suggests that translation of new protein is necessary for the formation of a novel threat extinction memory [ 56 ]. Threat conditioning and threat recall are associated with unique, cell-type-specific transcriptional changes that persist for weeks after initial training [ 57 ]. Threat extinction also requires transcriptional processes within IL: injection of an inhibitor of PARP-1, a gene involved in ADP-ribosylaton that is necessary for transcription, into mPFC impairs contextual threat extinction [ 58 ].
The BDNF-TrkB neurotrophic factor pathway has also been extensively studied with regards to mPFC and memory formation in mPFC. Expression of Bdnf in PL is necessary for consolidation of cued threat conditioning [ 59 ], while infusion of Bdnf into IL after threat acquisition is sufficient to diminish threat responses in the absence of extinction training [ 60 ]. Threat extinction is also associated with epigenetic modification. In the IL, threat extinction is associated with acetylation of histones near the Bdnf locus [ 61 ], changes to the p300/CBP complex (PCAF) [ 62 ], as well as deposition of DNA-modification marks such as 5-hydroxymethylcytosine and N6-methyl-2’deoxyadenosine (m6dA) near loci of activity-dependent genes such as Bdnf .
Additionally, inhibition of PCAF in IL was shown to interfere with threat extinction [ 62 ]. Recently, Li et al. [ 63 ], have shown that knockdown of N6amt1 , the gene responsible for m6dA deposition, within IL, blocks changes to the m6dA mark at the Bdnf promoter in vivo and impairs threat extinction retention. These findings suggest that alterations in m6dA deposition are necessary for the formation of threat extinction memories within IL [ 63 ]. These findings also strongly support the hypothesis that threat extinction memory requires epigenetic changes within IL. Our understanding of the molecular changes that occur within the mPFC during threat-related processes are still in their infancy. Gene expression changes are unique to cell type, and cell-type-specific investigations of mPFC in threat conditioning and extinction are just beginning.
Stress and threat reactions
One potential factor that alters the ability to control emotional responses via altering PFC function is stress (for review, see 64,65, Kalin and Barbas, this issue). Studies in animal models have shown that acute stress leads to changes in neuronal signaling that impair function in the dlPFC [ 64 ] and IL cortex [ 66 ]. These changes are proposed to be due to the impact of increased catecholamines, in particular noradrenergic and dopaminergic signaling, on PFC neuronal activity with even relatively mild acute stress exposure [ 64 , 65 , 67 ]. Stress also impacts signaling within the amygdala. Noradrenergic signaling from the locus coeruleus to the amygdala was recently shown to be necessary to produce the immediate extinction deficit, an impairment in extinction learning that occurs soon after fear learning and is thought to be related to the stress of the fear learning process [ 68 ]. Activity of CRF-expressing neurons within the CeA was also recently shown to contribute to this phenomenon [ 69 ]. In rodents, chronic stress also impacts neural activity in both PL and IL cortex [ 70 ] and leads to structural changes in IL cortex [ 71 ]. One consequence of stress-related PFC impairment is enhanced threat learning and impaired extinction retention in rodent models [ 66 , 70 ].
In the next section we will explore the role of PFC in human threat processing research, from acquisition and encoding of threat, to its extinction and extinction recall. We will also further integrate additional findings with regards to other threat and avoidance behaviors in response to threat stimuli and the impact of stress on the PFC. Finally, we will examine how these different brain regions and behaviors are dysregulated in threat-related disorders such as PTSD.
Preclinical human threat processing research
Threat learning.
Perhaps it is not surprising, given the extensive research with nonhuman animals, that research in humans confirms a role for the amygdala and PFC in threat learning (see Fig. 1b and Fig. 2a ). The role of the amygdala was first demonstrated in patients with amygdala damage. Relative to healthy controls, both bilateral [ 72 ] and unilateral [ 73 ] amygdala damage resulted in impaired conditioned responses, as measured by the skin conductance response (SCR). However, these patients were able to verbally report the contingency between the conditioned stimulus and shock after the procedure, which was impaired in patients with hippocampal damage whose amygdala was intact [ 72 , 74 ]. These findings suggest that the amygdala is only critical for the implicit, physiological expression of threat learning in humans, with conscious knowledge about the threatening nature of stimuli in the environment remaining intact, despite amygdala lesions. Furthermore, these findings demonstrate that there are additional brain regions that are critical for the expression of the subjective fear and threat responses, including PFC areas that are discussed in more detail below.

a Healthy Threat Circuit. Regions involved in threat learning and the control of threat reactions via extinction, context, avoidance, or cognitive regulation. In healthy individuals the coordination of this circuit enables adaptive threat expression. b PTSD Threat Circuit. The dlPFC, vmPFC/IL, and hippocampus show impaired functioning with PTSD, whereas the amygdala and dACC/PL are enhanced. Disrupted connections between regions are indicated by dashed lines. The disrupted threat circuit with PTSD results in maladaptive threat expression. Prefrontal cortex regions are highlighted within the beige circle. Terms for animal/human homologous regions are in the same circles. PL = prelimbic cortex, IL = infralimbic cortex, dACC = dorsal anterior cingulate cortex, vmPFC = ventromedial prefrontal cortex, dlPFC = dorsolateral prefrontal cortex.
Consistent with these early patient studies, functional magnetic resonance imaging (fMRI) studies soon followed that showed increased blood oxygenation level dependent (BOLD) signal in the amygdala to a conditioned stimulus (relative to stimulus never paired with shock) [ 75 , 76 ], and the magnitude of this BOLD response was correlated with the strength of the conditioned response [ 76 ]. Interestingly, this differential amygdala BOLD response was only apparent in the early stages of threat conditioning. This finding is somewhat surprising given rodent research showing long-lasting changes in the amygdala lateral nucleus with threat learning. However, there is electrophysiological evidence in rodents showing that a subset of lateral nucleus amygdala neurons respond preferentially during initial learning [ 77 ], and there is greater responding overall at this time. It may be the case that BOLD changes in the amygdala can only be observed at time windows when there are larger populations of neurons responding, such as initial learning. One major limitation of fMRI for investigations of amygdala function in humans is that it is a relatively coarse measurement. Although the spatial resolution of standard BOLD imaging is generally 3 mm, in practice, with spatial smoothing and group averaging, the actual resolution is greater than 10 mm, which covers a substantial portion of the amygdala (which is slightly more than 1000 mm 3 in humans) and makes it very difficult to detect discrete responses in amygdala subnuclei. The challenges of using BOLD imaging to study the human amygdala is reflected in recent meta-analyses of fMRI threat learning studies, which fail to find BOLD changes in the amygdala [ 78 ], in spite of its critical role in threat learning in rodent models and patient studies.
In contrast to difficulties in detecting BOLD changes in the amygdala during threat learning, meta-analyses and individual studies reliably show activation in a number of other brain regions, including the insula cortex, which is linked to physiological arousal responses [ 79 ], the striatum, and the dACC (e.g., [ 76 , 78 , 80 ]). The dACC is a prefrontal region that is proposed to be the human homolog of the PL cortex in rodents [ 80 ]. As discussed earlier, the PL in rodents has been suggested to play a role in the expression of threat learning via projections to the basolateral amygdala, with stimulation of this region increasing conditioned freezing and inactivation reducing it.
In rodents, the PL and IL cortex are located adjacent to one another in the mPFC. In primate models, however, the PL and IL are farther apart. The primate PL cortex is thought to be divided into rostral and caudal regions with different connectivity patterns. The rostral region is thought to be more similar to the PL in rodents, with the dACC being the human homologue for that region [ 23 , 81 ]. Consistent with this suggestion, Milad et al. [ 80 ] found that both cortical thickness, and BOLD response magnitude to a conditioned stimulus in this region, were correlated with the strength of the conditioned response as measured with SCR in humans.
Although the basic circuitry of threat learning seems to be preserved across species, a primary difference between humans and other animals is that humans, more often than not, learn about threats in the environment via social interactions. For example, children learn to fear germs by being told about their existence and observing others engaging in actions attempting to avoid them. This ability is adaptive in that humans do not need to be physically harmed to learn about threats in the environment. It can also be maladaptive in that we can develop robust fears for events that are imagined and anticipated but never actually experienced, contributing greatly to human anxiety and fear-related disorders. To what extent do the brain systems involved in threat learning from direct experience, that have been investigated in rodent models, map onto socially acquired, imagined threats in humans?
To address this question, brain imaging and patient studies have examined threat learning through verbal instruction (e.g., being told a blue square predicts a shock, and then being shown a blue square) or observation (e.g., watching someone else receive a shock paired with a blue square, and then being shown a blue square). Consistent with Pavlovian threat conditioning, fMRI studies of both instructed and observational threat learning show activation in the amygdala, dACC, and insula [ 82 ]. For instructed learning, the amygdala BOLD response is left-lateralized [ 83 ], and only patients with left, but not right, amygdala damage show impaired physiological evidence of threat learning, perhaps because of the verbally mediated nature of this learning [ 84 ]. In contrast, observational learning results in increased bilateral BOLD signal in the amygdala, both when observing someone else receiving a shock paired with a conditioned stimulus (learning), and when viewing the conditioned stimulus afterwards (test). In addition, during observational learning, activation in a rostral mPFC region that has been implicated in mentalizing about others is correlated with the strength of the learned threat response as measured by SCR [ 85 ], and learning is stronger with greater empathy for the person being observed [ 86 ]. These results suggest that while the social learning of threat may engage unique neural circuitry due to the nature of the learning, it also takes advantage of the phylogenetically older mechanisms of Pavlovian threat conditioning for threat expression.
Threat extinction
Much like threat learning, neuroimaging studies of threat extinction in humans have identified brain regions that parallel those involved in extinction in rodents (see Figs. 1b and 2a ). The vmPFC is proposed to be the homologue for the IL in rodents [ 87 ] and serves to inhibit threat responses produced by the amygdala. There is consistent evidence of increases in BOLD signal in the vmPFC during extinction learning [ 88 , 89 , 90 ] and recall [ 89 , 90 , 91 , 92 ] (for review, see [ 93 , 94 , 95 ]). Further, the degree of activation of the vmPFC has been shown to be positively correlated with the degree of extinction, or extinction retention, as measured by SCR [ 89 , 90 ], consistent with the suggested role of the IL in extinction in rodent models.
Brain morphology studies also point to the human vmPFC being involved in extinction. Milad et al. [ 96 ] found vmPFC thickness to be positively correlated with extinction recall. Specifically, greater thickness was associated with smaller SCR to the conditioned stimulus during extinction recall, suggestive of better extinction recall (see also [ 97 ]). Subsequently, Winkelman et al. [ 98 ] examined the relationship between vmPFC thickness and extinction learning, rather than recall, and found similar results. Greater vmPFC thickness was associated with smaller differential SCR during early extinction learning, suggestive of better extinction learning.
Targeting extinction with neuromodulation, neuroplasticity, and context modulation
One drawback of these MRI studies, however, is that they are correlational in nature. Unlike research conducted in rodents, specific brain regions in humans cannot be lesioned or tagged, nor can regions that are not on the surface of the brain be disrupted. Researchers are able, however, to stimulate or disrupt surface frontal regions of the brain in humans using non-invasive devices. For example, transcranial direct current stimulation (tDCS) applies a low-intensity current through two electrodes attached to the scalp, and transcranial magnetic stimulation (TMS) delivers an electric current through a coiled wire placed on the scalp, creating a magnetic field across the skull. Both of these strategies are thought to modulate neuronal activity in the human brain.
Using these techniques, a few recent brain stimulation studies [ 99 , 100 , 101 , 102 , 103 ] have been conducted in humans to probe the role of the vmPFC in extinction. For example, Dittert et al. [ 100 ] administered tDCS via bitemporal electrodes aimed at the vmPFC prior to and during extinction and found that tDCS, relative to sham, stimulation resulted in faster early extinction learning. Similarly, Raij et al. [ 102 ] found that TMS, during extinction learning, to an area of the frontal cortex functionally connected to the vmPFC (i.e., the left lateral PFC), but not to an area of the frontal cortex thought to be unconnected to the vmPFC, led to enhanced extinction recall. Although these studies provide some insight into the role of the vmPFC in extinction, given the location of the vmPFC and the fact that tDCS and TMS are applied externally, it is difficult to be certain that the vmPFC in particular was stimulated in these studies.
Consistent with animal models of extinction circuitry, the vmPFC interacts with other regions such as the amygdala and hippocampus to modulate threat responses during extinction. From rodent research showing that intra-amygdala infusion of the NMDA receptor agonist d-cycloserine, which enhances NMDA-dependent plasticity, facilitates extinction learning, and successful translation of this work to humans (see [ 104 ] for review), we know that the human amygdala plays a role in extinction learning. Human imaging studies, however, have been less consistent with finding changes in BOLD signal in the amygdala during extinction [ 76 , 88 , 90 , 95 , 105 ]. Much like with threat acquisition, it may be that the involvement of the amygdala in extinction is more subtle and difficult to detect using standard fMRI techniques [ 106 ]. Nonetheless, imaging research does point to changes in the relationship between the PFC and amygdala during extinction. Connectivity analyses have demonstrated functional coupling between the mPFC and amygdala during extinction learning [ 107 ], and vmPFC and amygdala during extinction recall [ 89 , 108 ].
Also consistent with animal models (e.g., [ 40 ]), research suggests that the hippocampus is involved in contextual modulation of extinction and works in concert with the PFC during contextual extinction learning. One of the first studies demonstrating hippocampal involvement in extinction showed that patients with damage to the hippocampus failed to show contextually modulated reinstatement of conditioned responses following extinction [ 74 ]. Brain imaging studies of the contextual modulation of extinction typically manipulate the visual background during extinction and report hippocampal activation during extinction recall [ 89 , 91 , 92 ]. Importantly, functional connectivity analyses also suggest coupling of the PFC and hippocampus during contextual extinction learning [ 107 ] and recall [ 89 ].
Sleep is another factor that has been shown to modulate threat control in humans. Sleep has been shown to enhance both threat learning, and the generalization of extinction learning in humans and other animals. The documented role for sleep in memory consolidation is proposed to extend to both threat memories and extinction memories. Which of these competing memory representations is selectively strengthened depends on contextual factors such a recency of learning and replay [ 109 ]. Because of evidence for sleep’s modulation of extinction learning across species, it has been suggested that disruptions of sleep following acute trauma, or predating the traumatic experience, may contribute to the etiology or perpetuation of PTSD [ 110 ].
Avoidance/active coping
Another method of reducing conditioned threat reactions is through active avoidance or coping. Initial rodent research on the neural circuitry of active avoidance found that while the passive expression of conditioned threat responses engages a pathway from the lateral nucleus to the central nucleus, when the animal engages in an action to avoid the unconditioned stimulus, projections from the lateral nucleus to the basal nucleus to the nucleus accumbens are involved. However, in order for the animal to produce an avoidance action, conditioned freezing must be inhibited which requires the IL cortex, much like in the expression of extinction (see [ 111 ] for a review).
One benefit of avoidance learning over extinction for controlling threat reactions is that avoidance learning results in a persistent reduction in the passive conditioned response, even when the avoidance action is no longer available [ 112 ]. This is in contrast to extinction in which the conditioned response often returns through spontaneous recovery, renewal, or reinstatement. Both the acquisition of avoidance, and the reduction of the persistent conditioned threat reaction following avoidance learning, are blocked by the injection of protein synthesis inhibitors into the IL. This indicates that plasticity in the IL is critical for the persistent reduction of conditioned responses with avoidance [ 112 ]. Mirroring these findings, studies have shown that previous history with escapable shock results in a lasting reduction of the conditioned response, and this effect is eliminated with IL inactivation [ 113 ].
In humans, there is evidence that both avoidance learning and history with escapable shock can persistently reduce conditioned threat actions as measured with SCR, even when no avoidance action is available [ 114 , 115 ]. However, in order to persistently diminish threat conditioned responses in humans, avoidance actions need to be learned through trial and error and there needs to be a subjective sense of control over the unconditioned stimulus during learning [ 115 ]. Simply providing the option of an action to avoid the unconditioned stimulus yields no lasting reduction of conditioned responses when the avoidance action is no longer available, and in fact can increase them by preventing extinction learning (called “protection from extinction”, [ 116 ]). Consistent with the circuity of avoidance learning detailed in rodent models, trial-by-trial avoidance learning yields increased BOLD activation in the vmPFC and ventral striatum, relative to standard extinction [ 114 ], suggesting the brain mechanisms of active coping are preserved across species.
Emotion regulation
Although extinction and active coping can be investigated across species, humans have the unique ability to use cognitive strategies to alter emotional responses, such as responses to fear provoking stimuli (for review, [ 117 ]). One common emotion regulation strategy is cognitive reappraisal. This strategy involves reframing thoughts (also called “appraisals”) about a stimulus in order to change the emotional response that that stimulus evokes. Emotion regulation strategies can be employed with the goal of either upregulating (i.e., increasing) or downregulating (i.e., decreasing) emotions. Here, the primary focus is on data related to downregulating negative emotions, fear in particular, as these data are most relevant to PTSD and its treatment. We highlight reappraisal, which is proposed to be similar to cognitive restructuring in clinic. Neuroimaging research has provided insight into the brain regions involved in emotion regulation in humans. Studies to date suggest that emotion regulation strategies aimed at downregulating negative emotions engage cognitive control regions of the PFC, which then modulate the amygdala via various potential pathways to influence negative emotional responses.
The most recent meta-analysis of fMRI studies of emotion regulation [ 118 ] found that all strategies aimed at downregulating negative emotions were collectively associated with increased BOLD signal in the following areas: ventrolateral prefrontal cortex (vlPFC), dorsolateral prefrontal cortex (dlPFC), and dorsomedial prefrontal cortex (dmPFC). While these were the largest areas of convergence, activation was also found in other areas (i.e., the bilateral inferior parietal lobule, supplementary motor area, pre-supplementary motor area, left middle temporal gyrus, and posterior cingulate gyrus). These findings were relatively consistent with a prior meta-analysis [ 119 ], with the exception that the prior meta-analysis also found decreased BOLD signal in the amygdala and parahippocampal gyrus, consistent with the notion that cognitive control regions of the PFC modulate amygdala activity during emotion regulation. One potential reason for differing results across these two meta-analyses may be differences in the studies examined and proportions of various emotion regulation strategies included. There is some evidence that different emotion regulation strategies may recruit distinct brain regions. For example, Dörfel et al. [ 120 ] found that some emotion regulation strategies are associated with reduced activity in the amygdala, whereas others are not.
Nonetheless, the majority of imaging research to date on emotion regulation focuses on the strategy of cognitive reappraisal. Meta-analyses of cognitive reappraisal alone have consistently found increased BOLD signal in the dlPFC, vlPFC, and dmPFC [ 93 , 121 , 122 ] and decreased BOLD signal in the amygdala [ 93 , 121 ]. The dlPFC is thought to be an important driver of emotion regulation and hypothesized to be involved in the manipulation of appraisals of stimuli in working memory [ 121 , 122 , 123 ]. The vlPFC is hypothesized to support choosing and inhibiting appraisals of stimuli [ 121 , 124 , 125 ] or potentially may signal salience and the need to reappraise [ 122 ]. Finally, the dmPFC is hypothesized to support abstracting affective meaning of stimuli or the processes of self-reflecting and identifying one’s own affective reactions to stimuli [ 121 , 126 , 127 , 128 , 129 , 130 ].
Two hypotheses have been proposed for how these cognitive control regions of the PFC (i.e., the dlPFC, vlPFC, and dmPFC) influence the amygdala: (1) that they engage the vmPFC which then modulates the amygdala, similar to the neurocircuitry of extinction [ 93 , 131 , 132 ], and (2) that they modulate lateral temporal areas associated with semantic and perceptual representations, which then indirectly influence the amygdala [ 121 ].
In support of the first hypothesis, anatomical research in nonhuman primates shows that connections between the lateral PFC and amygdala are sparse relative to the vmPFC and amygdala (e.g., [ 133 , 134 ]). Additionally, a study of cognitive reappraisal of threat conditioned stimuli by Delgado et al. [ 131 ] demonstrated increased BOLD signal in the dlPFC and decreased BOLD signal in the amygdala, but also changes in vmPFC activity that mirror those that occur during extinction. Specifically, increased BOLD signal in the vmPFC after successful cognitive reappraisal was observed. Further, connectivity analyses [ 131 , 132 ], a meta-analysis conducted by Diekhof et al. in 2011, and more recent dynamic causal modeling of cognitive reappraisal data [ 135 ], also support this hypothesis.
In contrast, two more recent meta-analyses favor the second hypothesis [ 121 , 122 ]. Specifically, in addition to increased activation of the cognitive control regions of the PFC mentioned above and modulation of the amygdala, Buhle et al. [ 121 ] report increased activation of the lateral temporal cortex during cognitive reappraisal. Notably, they did not observe increased activation of the vmPFC. There are many possible reasons for these differences in findings (see [ 121 , 136 , 137 ] for discussion), however, one possibility is that it has to do with the type of cognitive reappraisal procedure used. The study by Delgado etv al. [ 131 ] involved cognitive reappraisal of threat conditioned stimuli, whereas most of the studies included in the Buhle et al. [ 121 ] meta-analysis involved cognitive reappraisal of negatively-valenced photos. It could also be that the vmPFC is involved in cognitive reappraisal for some individuals more so than others. For example, the nature of vmPFC involvement during cognitive reappraisal has been observed to vary as a function of psychiatric symptoms [ 138 , 139 ].
To date, the majority of studies on brain regions involved in emotion regulation have examined fMRI data. To our knowledge, only one study has examined brain morphometry in relation to cognitive reappraisal task performance [ 97 ] and this study did not find a relationship between success of reappraisal and dlPFC, vlPFC, or vmPFC cortical thickness. Although there do not seem to be structural changes related to the successful cognitive reappraisal, there is one lesion study [ 140 ] that supports a role of the dlPFC in cognitive reappraisal. This study examined individuals with dlPFC lesions and found that they showed impaired ability to reappraise threat conditioned stimuli as indexed by poorer subjective fear outcomes, compared to matched controls. Additionally, a few brain stimulation studies have been conducted to probe the role of the PFC in emotion regulation. In this case, given the lateral location of the cognitive control regions of the PFC implicated in emotion regulation, tDCS or TMS can be used to target these regions. However, results of these studies have been inconsistent. While some studies have found that tDCS over the dlPFC or vlPFC enhances cognitive reappraisal [ 141 , 142 , 143 ], others have not [ 143 , 144 ].
Stress and threat control
As the discussion above indicates, there are several techniques that can be used to control learned threat reactions in humans when they are no longer adaptive. However, as outlined earlier, stress, both chronic and acute, can impact the function of PFC and subcortical regions implicated in threat control. In humans, experimental studies of chronic stress are not possible due to ethical concerns; however, there is evidence that a history of childhood abuse is correlated with reduced gray matter volume in PFC regions, including the vmPFC and orbital frontal cortex [ 145 ]. In addition, mild acute stress in humans impairs the efficacy of previously acquired cognitive reappraisal strategies in reducing conditioned threat and subjective fear [ 146 ] and results in enhanced spontaneous recovery following extinction training [ 147 ]. These latter findings suggest that even when threat control techniques are successfully learned, relatively mild acute stress may impair the ability to express this learning by impacting the function of PFC inhibitory circuits.
Role of PFC in PTSD
The above evidence suggests that stress, in particular, is associated with altered PFC function and its role in regulating subcortical emotional responses. PTSD is among the most well-understood, prevalent, and medically significant stress-related disorders. A fairly large set of studies now supports a clear role for altered PFC structure and function in PTSD and related disorders (see Fig. 2b ).
Structural imaging in PFC and PTSD
Related to stress exposure, independent of PTSD, a number of studies have identified smaller volumes in PFC and decreased structural connectivity between PFC and subcortical areas as a function of violence and trauma exposure. In a prospective study of Israeli soldiers, Admon et al. [ 148 ] used diffusion tensor imaging (DTI) pre- and post-military service, reporting that soldiers with decreased hippocampal structural connectivity with the vmPFC had a more maladaptive response to stressful military service. In a small study of victims of urban violence, Rocha-Rego et al. [ 149 ] found significant reductions in gray matter volume in the ventral premotor cortex and in the pregenual ACC as a function of civilian violence. Furthermore, in a moderately large sample of post-9/11 veterans, Clausen et al. [ 150 ] found that higher combat exposure uniquely related to lower cortical thickness in the left prefrontal lobe; and that, overall, combat exposure, PTSD, and head injuries differentially relate to alterations in cortical thickness.
A number of studies have also found decreased gray matter volumes related to traumatic stress symptoms. In development, with a study of ~50 youth, Keding and Herringa [ 151 ] found that those with PTSD had reduced gray matter volume in anterior vmPFC, which inversely correlated with PTSD duration. They suggest that pediatric PTSD is associated with abnormal structure of the vmPFC, possibly related to disrupted extinction and contextual gating of fear. Similarly, in a study of over 100 participants, it was found that maltreated youth with PTSD demonstrated decreased right vmPFC volumes compared to both maltreated youth without PTSD and nonmaltreated healthy controls [ 152 ]. Similar findings have been found in adult samples. A study of 85 veterans suggested decreased structural volumes of vmPFC and ACC in those with PTSD compared to controls [ 153 ] and a smaller study of 28 veterans found smaller subgenual cingulate volumes compared to controls, in addition to a number of other limbic region structural abnormalities [ 154 ].
A number of studies have also examined structural integrity of white matter tracts, including connections to and from the PFC. Koch et al. [ 155 ] used DTI to show decreased integrity of the uncinate fasciculus tract, connecting the vmPFC to multiple subcortical, limbic regions including the amygdala, in patients with PTSD. In addition, using DTI, Fani et al. [ 156 ] found that civilians with PTSD had decreased structural connectivity via the cingulum bundle, which supports the hippocampus-dACC pathway. They suggest that altered hippocampus-ACC connectivity may represent a highly salient intermediate neural phenotype for PTSD. Further analyses of this cohort found that individuals with the “risk” allele of the FKBP5 genetic biomarker, associated with childhood maltreatment and PTSD risk, also had decreased cingulum structural integrity.
Some of these structural changes may occur quite rapidly in the aftermath of trauma—or may be preexisting and predispose some individuals to a greater risk of PTSD following trauma. Using DTI and structural imaging in the weeks following trauma exposure, research has shown that reduced fractional anisotropy of the uncinate fasciculus at around the time of trauma predicted greater PTSD symptoms (in particular posttraumatic anhedonia) at 12 months post-trauma. Furthermore, as the traumatized participants were followed over time, increased gray matter volume of the vmPFC was also associated with reduced trauma-related symptoms over the 12 months following trauma [ 157 ]. In another study recruiting patients after trauma exposure with mild traumatic brain injury, smaller cortical volumes of superior frontal cortex and rostral and caudal cingulate at 2 weeks after trauma exposure contributed to the prediction of increased likelihood of 3-month PTSD diagnosis in multivariable models incorporating other established risk factors [ 158 ].
As with many other types of human data, sample size often limits interpretation, as small sample sizes are subject to both false positive and false negative biases. Therefore, as more studies have been performed of PTSD and structural imaging, much larger analyses can be performed via meta-analyses of multiple datasets. A recent meta-analysis confirmed, using voxel-based morphometry, that there were prominent volumetric reductions in the mPFC, including the ACC, when examining over 80 different MRI studies in PTSD compared to depression [ 159 ].
In addition, one of the largest meta-analyses to date of structural cortical volumes from the ENIGMA-PGC-PTSD workgroup, compared 1379 PTSD patients to 2192 controls without PTSD. A primary finding was that volumes of left and right lateral orbitofrontal gyri were significantly smaller in PTSD patients than controls and were negatively correlated with symptom severity. Together, these findings indicate that cortical volumes in PTSD patients are smaller in prefrontal regulatory regions, consistent with preclinical work suggesting a critical role for orbital frontal PFC regions in recovery and extinction of threat behaviors [ 160 ].
Functional imaging in PFC and PTSD
It is thought that fMRI, including both emotional and cognitive task-based MRI, as well as resting state MRI may be more sensitive to pathology-related functional activity. However, it can also be criticized as there are many processing steps and the data are essentially subtractions and comparisons between different tasks, timepoints, and individuals, making interpretation often more complex than structural MRI. Nonetheless, many of the same themes with regards to the role of PFC in PTSD are found with fMRI, complementing the above structural MRI findings as well as the healthy human and preclinical data.
While many fMRI studies of PTSD have had quite limited sample sizes, some are particularly informative. Script-driven imagery with participants reading or listening to scripts of their prior trauma experiences or other stressful vignettes has been a powerful probe for determining differential brain activity in PTSD. For example, in a case-control twin study with 26 male identical twin pairs (12 PTSD; 14 non-PTSD) discordant for PTSD and combat, script-driven imagery fMRI revealed diminished activation in the mPFC during stressful versus neutral imagery in PTSD patients relative to others [ 161 ].
Another powerful method for observing brain activity is using a masked emotional probe. In this design, participants are presented with an emotional stimulus for a very brief period of time (i.e., milliseconds) and then it is replaced by a non-emotional stimulus. This minimizes explicit awareness of the emotional stimulus, while still engaging emotional perception and the associated neutral structures. For example, Killgore et al. [ 162 ] used a masked emotional probe task and compared adults with anxiety or PTSD to healthy controls. Patients (all groups combined) showed greater amygdala and reduced vmPFC activation compared to controls during the masked fearful faces. Additionally, in a prospective emergency department study following patients longitudinally, Stevens et al. [ 163 ] used an unmasked fearful faces design to demonstrate that dorsal ACC activity during presentation of fearful faces predicts ongoing symptom maintenance in the aftermath of acute trauma in civilians. These findings are consistent with some of the findings of Milad et al. [ 164 , 165 , 166 ] related to impaired extinction recall, discussed in the next section.
A number of studies have also examined the role of activity within the PFC related to prediction of treatment response. Fonzo et al. [ 167 ] reported on fMRI task-based assessment while completing three tasks assessing emotional reactivity and regulation prior to prolonged exposure psychotherapy for PTSD. At baseline, individuals with the greatest symptom improvement with therapy showed, among other findings, greater dorsal PFC and vmPFC activation during emotional conflict regulation. They interpreted these findings to suggest that participants who are most likely to benefit from exposure therapy demonstrate spontaneous activity of PFC when superficially processing threat and adapting to emotional interference. Further analysis of this study suggested that psychotherapy increased lateral frontopolar cortex activity and connectivity with the vmPFC [ 168 ]. Additionally, greater increases in frontopolar activation were associated with improvements in hyperarousal symptoms and psychological well-being. Given these findings, the authors argue that frontopolar connectivity with ventromedial regions during emotion regulation is a possible key mechanism of psychotherapeutic improvement in PTSD.
In addition, in a mindfulness-based exposure therapy intervention with a small sample size, King et al. [ 169 ] found that posterior cingulate cortex (PCC)-dlPFC functional connectivity was correlated with improvement in PTSD avoidance and hyperarousal symptoms. Overall, they surmised that increased connectivity between PCC-dlPFC brain regions could be related to attentional control and symptom improvement.
It is important to note that the “standard” observation of hyperarousal-related PTSD with increased amygdala activation and decreased mPFC activation during stressful cues seems to be reversed when subjects with PTSD have high levels of dissociative symptoms. Hooper et al. have reported increased mPFC activation in the presence of PTSD with significant dissociative symptoms (e.g., [ 170 ]). Dynamic causal modeling has been used to interpret some level of causal and temporal relationship between functionally active brain networks. Nicholson et al. [ 171 ] found that PTSD without dissociation was characterized primarily by ‘bottom-up connectivity’ from the amygdala to the vmPFC, whereas PTSD with dissociation had predominant ‘top-down connectivity’ from the vmPFC to the amygdala. The authors suggest that this provides further data supporting a model of enhanced top-down, emotional over-regulation with significant dissociation, in contrast to decreased emotion regulation in the majority of PTSD cases.
Overall, these studies suggest that, in general, decreased vmPFC and dlPFC functional activation to stressful and trauma-related cues, often accompanied by increased dACC activation to such cues, are associated with greater PTSD symptoms and decreased responses to exposure-based therapies. Successful treatment appears to be accompanied by increased activation and functional connectivity of vmPFC/dlPFC regions with other cortical and subcortical areas. Notably, PTSD with significant dissociation seems to have differential connectivity patterns, as recently further demonstrated by Jovanovic et al. [ 172 ], and may benefit from distinct approaches to treatment and recovery.
PFC, threat extinction, behavioral inhibition
Work that has done the most to connect neuroimaging findings in PTSD with both healthy human neuroimaging work and preclinical work on threat acquisition and extinction includes neuroimaging studies specifically focused on extinction of threat cues in PTSD as well as inhibitory learning processes. Milad et al. initially demonstrated some of these effects in PTSD through optimization of a within-scanner threat conditioning and extinction protocol. They found that during extinction recall there was decreased activation of vmPFC and greater activation in dACC in PTSD relative to healthy trauma-exposed participants, which was associated with impaired physiological measures of extinction recall [ 165 ]. These data suggest that impairments in PTSD recovery may result, in part, from altered PFC regulation of threat extinction recall. Increased dACC activation during threat expression and extinction and decreased vmPFC activation with extinction recall were replicated in another study by this group examining context modulation in PTSD [ 166 ]. The dACC also appears to be associated with more PTSD symptoms at rest. Marin et al. [ 164 ] found that dACC resting activity positively correlated with PTSD symptom severity and predicted increased dACC activations during extinction recall.
In addition, Helpman et al. [ 173 ] examined threat conditioning and extinction in an fMRI task before and after a course of prolonged exposure treatment for PTSD. They found that PTSD patients had pre- to post-treatment reductions in rostral ACC (rACC) activation during extinction recall, and increases in functional coherence between rACC, vmPFC, and sgACC, suggesting these circuits are modified.
In another approach to this issue, Jovanovic et al. [ 174 ] found lower vmPFC activation during a simple stop signal (or “Go/No-go”) task related to behavioral inhibition in civilians with PTSD. Inhibition in this task correlated with a physiological measure of threat extinction in a fear-potentiated startle paradigm outside of the scanner. These data suggested that the same circuits involved in behavioral inhibition appear to be involved in fear inhibition processes during differential threat conditioning and extinction. A follow-up study with a larger sample size suggested that the effects of vmPFC/rACC on behavioral inhibition are moderated by childhood maltreatment effects in participants with PTSD [ 175 ].
Conclusions and future directions
Considerable progress has been made in understanding the role that the PFC plays in rodent threat learning and threat extinction, in healthy human studies of regulation of threat and fear emotion processing, and in the ways these areas may be dysregulated in threat-related disorders such as PTSD. Still, many questions remain. Much data supports a heuristic in which PL and IL play opposing roles in the rodent threat response, the former driving threat expression, the latter threat extinction. Similarly, in human studies, the dACC and Brodmann 32-related mPFC areas appear to support threat responses and are hyperactive in PTSD associated with hyperarousal and threat emotional dysregulation. Furthermore, human data support subgenual and Brodmann 25-related mPFC areas (i.e., the vmPFC) in regulating/suppressing threat responses, supporting extinction of threat behaviors and fear emotions, and in providing top-down emotional control over amygdala and other subcortical regions.
However, there are other data to suggest that, more generally, PL encodes for the learning of rules, while IL allows for rule reversal [ 18 ]. Thus, the precise role for the mPFC is not yet entirely clear. The lens through which the “fear and threat” neuroscientists see these areas needs to become more aligned with how the “appetitive and addiction” and “cognitive control” neuroscientists view them. This will help obtain a more comprehensive overall perspective on these regions, aid in understanding their normal function, and provide better treatment approaches for a large number of disorders associated with their dysfunction. The integration of elegant and powerful circuit tools, from intersectional optogenetic and chemogenetic circuit dissection to cellular and genetically driven in vivo calcium imaging combined with behavior, are providing remarkable cell- and circuit-level appreciation of basic behavioral functions in rodents. In humans, new tools such as fMRI-guided TMS, as one example, are beginning to allow relatively rapid translation of circuit function to targeted, precision-medicine approaches for individually guided care.
Furthermore, as we have learned with subcortical structures, different cell types residing within the same brain structure may have dramatically different, sometimes opposing, functions. The mPFC has immense cellular heterogeneity, and we may expect, functional complexity. Future cell-type specific studies that dissect the circuit- and molecular-adaptations to threat learning within the mPFC will reveal additional layers of complexity to this system, and, hopefully, new therapeutic targets for PTSD. Tools, such as single cell RNA sequencing, are now being used across species from rodent to post-mortem human brain, allowing for molecular dissections to complement the above functional circuit dissections. Their translation across species will support both a scientific understanding of conservation of molecules and circuits across evolution for specific survival-related behaviors, as well as provide much more powerful targets for pharmacological and biological intervention using animal model systems targeting known conserved molecules and cell types for human therapeutic development.
In summary, while much remains to be learned, it is an extraordinarily exciting time for the field in which a great deal of convergence and replication has resulted in a fairly robust understanding of threat processing and its regulation by the PFC. How these areas encode and express threat memories over time is rapidly being dissected and integrating these data into our understanding of pathology in disorders such as PTSD is occurring. Integrating translational research in the coming years promises exciting new discoveries and approaches which may both greatly expand our knowledge of how the brain encodes behavior and also drive development of novel and robust new treatment approaches.
Breslau N. The epidemiology of posttraumatic stress disorder: what is the extent of the problem? J Clin Psychiatry. 2001;62:16–22.
PubMed Google Scholar
Bromet E, Sonnega A, Kessler RC. Risk factors for DSM-III-R posttraumatic stress disorder: findings from the National Comorbidity Survey. Am J Epidemiol. 1998;147:353–61.
Article CAS PubMed Google Scholar
McLaughlin KA, Koenen KC, Friedman MJ, Ruscio AM, Karam EG, Shahly V, et al. Subthreshold posttraumatic stress disorder in the world health organization world mental health surveys. Biol Psychiatry. 2015;77:375–84.
Article PubMed Google Scholar
Jovanovic T, Ressler KJ. How the neurocircuitry and genetics of fear inhibition may inform our understanding of PTSD. Am J Psychiatry. 2010;167:648–62.
Article PubMed PubMed Central Google Scholar
Morgan Iii C, Grillon C, Southwick SM, Davis M, Charney DS. Fear-potentiated startle in posttraumatic stress disorder. Biol Psychiatry. 1995;38:378–85.
Article Google Scholar
Rauch SL, Shin LM, Phelps EA. Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research—past, present, and future. Biol Psychiatry. 2006;60:376–82.
Yehuda R, LeDoux J. Response variation following trauma: a translational neuroscience approach to understanding PTSD. Neuron. 2007;56:19–32.
Duncan LE, Ratanatharathorn A, Aiello AE, Almli LM, Amstadter AB, Ashley-Koch AE, et al. Largest GWAS of PTSD (N = 20 070) yields genetic overlap with schizophrenia and sex differences in heritability. Mol Psychiatry. 2018;23:666–73.
Gelernter J, Sun N, Polimanti R, Pietrzak R, Levey DF, Bryois J, et al. Genome-wide association study of post-traumatic stress disorder reexperiencing symptoms in> 165,000 US veterans. Nat Neurosci. 2019;22:1394–401.
Article CAS PubMed PubMed Central Google Scholar
Nievergelt CM, Maihofer AX, Klengel T, Atkinson EG, Chen C-Y, Choi KW, et al. International meta-analysis of PTSD genome-wide association studies identifies sex-and ancestry-specific genetic risk loci. Nat Commun. 2019;10:1–16.
Article CAS Google Scholar
Davis M, Walker DL, Myers KM. Role of the amygdala in fear extinction measured with potentiated startle. Ann NY Acad Sci. 2003;985:218–32.
LeDoux J. Fear and the brain: where have we been, and where are we going? Biol Psychiatry. 1998;44:1229–38.
Phelps EA, LeDoux JE. Contributions of the amygdala to emotion processing: from animal models to human behavior. Neuron. 2005;48:175–87.
Shin LM, Liberzon I. The neurocircuitry of fear, stress, and anxiety disorders. Neuropsychopharmacology. 2010;35:169–91.
Abdallah CG, Averill LA, Akiki TJ, Raza M, Averill CL, Gomaa H, et al. The neurobiology and pharmacotherapy of posttraumatic stress disorder. Annu Rev Pharm Toxicol. 2019;59:171–89.
Krystal JH, Davis LL, Neylan TC, Raskind MA, Schnurr PP, Stein MB, et al. It is time to address the crisis in the pharmacotherapy of posttraumatic stress disorder: a consensus statement of the PTSD psychopharmacology working group. Biol Psychiatry. 2017;82:e51–e59.
LeDoux JE, Pine DS. Using neuroscience to help understand fear and anxiety: a two-system framework. Am J Psychiatry. 2016;173:1083–93.
Gourley SL, Taylor JR. Going and stopping: Dichotomies in behavioral control by the prefrontal cortex. Nat Neurosci. 2016;19:656–64.
Woon EP, Sequeira MK, Barbee BR, Gourley SL. Involvement of the rodent prelimbic and medial orbitofrontal cortices in goal-directed action: a brief review. J Neurosci Res. 2020;98:1020–30.
Miller EK. The prefrontal cortex and cognitive control. Nat Rev Neurosci. 2000;1:59–65.
Giustino TF, Maren S. The role of the medial prefrontal cortex in the conditioning and extinction of fear. Front Behav Neurosci. 2015;9:298.
Ongür D, Price JL. The organization of networks within the orbital and medial prefrontal cortex of rats, monkeys and humans. Cereb Cortex. 2000;10:206–19.
Heilbronner SR, Rodriguez-Romaguera J, Quirk GJ, Groenewegen HJ, Haber SN. Circuit-based corticostriatal homologies between rat and primate. Biol Psychiatry. 2016;80:509–21.
Heidbreder CA, Groenewegen HJ. The medial prefrontal cortex in the rat: evidence for a dorso-ventral distinction based upon functional and anatomical characteristics. Neurosci Biobehav Rev. 2003;27:555–79.
Allsop SA, Wichmann R, Mills F, Burgos-Robles A, Chang CJ, Felix-Ortiz AC, et al. Corticoamygdala transfer of socially derived information gates observational learning. Cell. 2018;173:1329–42.e18.
Van De Werd HJ, Uylings HB. Comparison of (stereotactic) parcellations in mouse prefrontal cortex. Brain Struct Funct. 2014;219:433–59.
Van De Werd HJ, Rajkowska G, Evers P, Uylings HB. Cytoarchitectonic and chemoarchitectonic characterization of the prefrontal cortical areas in the mouse. Brain Struct Funct. 2010;214:339–53.
Strobel C, Marek R, Gooch HM, Sullivan RKP, Sah P. Prefrontal and auditory input to intercalated neurons of the amygdala. Cell Rep. 2015;10:1435–42.
Vertes RP. Differential projections of the infralimbic and prelimbic cortex in the rat. Synap. 2004;51:32–58.
Morgan MA, Romanski LM, LeDoux JE. Extinction of emotional learning: contribution of medial prefrontal cortex. Neurosci Lett. 1993;163:109–13.
Morgan MA, LeDoux JE. Differential contribution of dorsal and ventral medial prefrontal cortex to the acquisition and extinction of conditioned fear in rats. Behav Neurosci. 1995;109:681–8.
Quirk GJ, Russo GK, Barron JL, Lebron K. The role of ventromedial prefrontal cortex in the recovery of extinguished fear. J Neurosci. 2000;20:6225–31.
Sierra-Mercado D, Padilla-Coreano N, Quirk GJ. Dissociable roles of prelimbic and infralimbic cortices, ventral hippocampus, and basolateral amygdala in the expression and extinction of conditioned fear. Neuropsychopharmacology. 2011;36:529–38.
Cho JH, Deisseroth K, Bolshakov VY. Synaptic encoding of fear extinction in mPFC-amygdala circuits. Neuron. 2013;80:1491–507.
Garcia R, Chang CH, Maren S. Electrolytic lesions of the medial prefrontal cortex do not interfere with long-term memory of extinction of conditioned fear. Learn Mem. 2006;13:14–7.
Do-Monte FH, Manzano-Nieves G, Quinones-Laracuente K, Ramos-Medina L, Quirk GJ. Revisiting the role of infralimbic cortex in fear extinction with optogenetics. J Neurosci. 2015;35:3607–15.
Kheirbek MA, Drew LJ, Burghardt NS, Costantini DO, Tannenholz L, Ahmari SE, et al. Differential control of learning and anxiety along the dorsoventral axis of the dentate gyrus. Neuron. 2013;77:955–68.
Eichenbaum H. Prefrontal-hippocampal interactions in episodic memory. Nat Rev Neurosci. 2017;18:547–58.
Phillips RG, LeDoux JE. Differential contribution of amygdala and hippocampus to cued and contextual fear conditioning. Behav Neurosci. 1992;106:274–85.
Corcoran KA, Maren S. Hippocampal inactivation disrupts contextual retrieval of fear memory after extinction. J Neurosci. 2001;21:1720–6.
Hallock HL, Quillian HM, Maynard KR, Mai Y, Chen HY, et al. Molecularly defined hippocampal inputs regulate population dynamics in the prelimbic cortex to suppress context fear memory retrieval. Biol Psychiatry. 2020;88:554–65.
Kim WB, Cho JH. Synaptic targeting of double-projecting ventral CA1 hippocampal neurons to the medial prefrontal cortex and basal amygdala. J Neurosci. 2017;37:4868–82.
Orsini CA, Kim JH, Knapska E, Maren S. Hippocampal and prefrontal projections to the basal amygdala mediate contextual regulation of fear after extinction. J Neurosci. 2011;31:17269–77.
Lacagnina AF, Brockway ET, Crovetti CR, Shue F, McCarty MJ, Sattler KP, et al. Distinct hippocampal engrams control extinction and relapse of fear memory. Nat Neurosci. 2019;22:753–61.
Marek R, Jin J, Goode TD, Giustino TF, Wang Q, Acca GM, et al. Hippocampus-driven feed-forward inhibition of the prefrontal cortex mediates relapse of extinguished fear. Nat Neurosci. 2018;21:384–92.
Ramanathan KR, Jin J, Giustino TF, Payne MR, Maren S. Prefrontal projections to the thalamic nucleus reuniens mediate fear extinction. Nat Commun. 2018;9:4527.
Rajasethupathy P, Sankaran S, Marshel JH, Kim CK, Ferenczi E, Lee SY, et al. Projections from neocortex mediate top-down control of memory retrieval. Nature. 2015;526:653–9.
LeDoux JE, Iwata J, Cicchetti P, Reis DJ. Different projections of the central amygdaloid nucleus mediate autonomic and behavioral correlates of conditioned fear. J Neurosci. 1988;8:2517–29.
Falls WA, Davis M. Lesions of the central nucleus of the amygdala block conditioned excitation, but not conditioned inhibition of fear as measured with the fear-potentiated startle effect. Behav Neurosci. 1995;109:379–87.
Burgos-Robles A, Kimchi EY, Izadmehr EM, Porzenheim MJ, Ramos-Guasp WA, Nieh EH, et al. Amygdala inputs to prefrontal cortex guide behavior amid conflicting cues of reward and punishment. Nat Neurosci. 2017;20:824–35.
Senn V, Wolff SB, Herry C, Grenier F, Ehrlich I, Gründemann J, et al. Long-range connectivity defines behavioral specificity of amygdala neurons. Neuron. 2014;81:428–37.
Marcus DJ, Bedse G, Gaulden AD, Ryan JD, Kondev V, Winters ND, et al. Endocannabinoid signaling collapse mediates stress-induced amygdalo-cortical strengthening. Neuron. 2020;105:1062–76.e6.
Xu W, Südhof TC. A neural circuit for memory specificity and generalization. Science. 2013;339:1290–5.
Padilla-Coreano N, Do-Monte FH, Quirk GJ. A time-dependent role of midline thalamic nuclei in the retrieval of fear memory. Neuropharmacology. 2012;62:457–63.
Do-Monte FH, Quinones-Laracuente K, Quirk GJ. A temporal shift in the circuits mediating retrieval of fear memory. Nature. 2015;519:460–3.
Santini E, Ge H, Ren K, Pena de Ortiz S, Quirk GJ. Consolidation of fear extinction requires protein synthesis in the medial prefrontal cortex. J Neurosci. 2004;24:5704–10.
Chen MB, Jiang X, Quake SR, Südhof TC. Persistent transcriptional programmes are associated with remote memory. Nature. 2020;587:437–42.
Inaba H, Tsukagoshi A, Kida S. PARP-1 activity is required for the reconsolidation and extinction of contextual fear memory. Mol Brain. 2015;8:63.
Choi DC, Maguschak KA, Ye K, Jang SW, Myers KM, Ressler KJ. Prelimbic cortical BDNF is required for memory of learned fear but not extinction or innate fear. Proc Natl Acad Sci USA. 2010;107:2675–80.
Peters J, Dieppa-Perea LM, Melendez LM, Quirk GJ. Induction of fear extinction with hippocampal-infralimbic BDNF. Science. 2010;328:1288–90.
Bredy TW, Wu H, Crego C, Zellhoefer J, Sun YE, Barad M. Histone modifications around individual BDNF gene promoters in prefrontal cortex are associated with extinction of conditioned fear. Learn Mem. 2007;14:268–76.
Wei W, Coelho CM, Li X, Marek R, Yan S, Anderson S, et al. p300/CBP-associated factor selectively regulates the extinction of conditioned fear. J Neurosci. 2012;32:11930–41.
Li X, Zhao Q, Wei W, Lin Q, Magnan C, Emami MR, et al. The DNA modification N6-methyl-2’-deoxyadenosine (m6dA) drives activity-induced gene expression and is required for fear extinction. Nat Neurosci. 2019;22:534–44.
Arnsten AF. Stress signalling pathways that impair prefrontal cortex structure and function. Nat Rev Neurosci. 2009;10:410–22.
Arnsten AF, Raskind MA, Taylor FB, Connor DF. The effects of stress exposure on prefrontal cortex: Translating basic research into successful treatments for post-traumatic stress disorder. Neurobiol Stress. 2015;1:89–99.
Izquierdo A, Wellman CL, Holmes A. Brief uncontrollable stress causes dendritic retraction in infralimbic cortex and resistance to fear extinction in mice. J Neurosci. 2006;26:5733–8.
Fitzgerald PJ, Giustino TF, Seemann JR, Maren S. Noradrenergic blockade stabilizes prefrontal activity and enables fear extinction under stress. Proc Natl Acad Sci USA. 2015;112:E3729–37.
Giustino TF, Ramanathan KR, Totty MS, Miles OW, Maren S. Locus coeruleus norepinephrine drives stress-induced increases in basolateral amygdala firing and impairs extinction learning. J Neurosci. 2020;40:907–16.
Jo YS, Namboodiri VMK, Stuber GD, Zweifel LS. Persistent activation of central amygdala CRF neurons helps drive the immediate fear extinction deficit. Nat Commun. 2020;11:422.
Wilber AA, Walker AG, Southwood CJ, Farrell MR, Lin GL, Rebec GV, et al. Chronic stress alters neural activity in medial prefrontal cortex during retrieval of extinction. Neuroscience. 2011;174:115–31.
Shansky RM, Hamo C, Hof PR, McEwen BS, Morrison JH. Stress-induced dendritic remodeling in the prefrontal cortex is circuit specific. Cereb Cortex. 2009;19:2479–84.
Bechara A, Tranel D, Damasio H, Adolphs R, Rockland C, Damasio AR. Double dissociation of conditioning and declarative knowledge relative to the amygdala and hippocampus in humans. Science. 1995;269:1115–8.
LaBar KS, LeDoux JE, Spencer DD, Phelps EA. Impaired fear conditioning following unilateral temporal lobectomy in humans. J Neurosci. 1995;15:6846–55.
LaBar KS, Phelps EA. Reinstatement of conditioned fear in humans is context dependent and impaired in amnesia. Behav Neurosci. 2005;119:677.
Büchel C, Morris J, Dolan RJ, Friston KJ. Brain systems mediating aversive conditioning: an event-related fMRI study. Neuron. 1998;20:947–57.
LaBar KS, Gatenby JC, Gore JC, LeDoux JE, Phelps EA. Human amygdala activation during conditioned fear acquisition and extinction: a mixed-trial fMRI study. Neuron. 1998;20:937–45.
Repa JC, Muller J, Apergis J, Desrochers TM, Zhou Y, LeDoux JE. Two different lateral amygdala cell populations contribute to the initiation and storage of memory. Nat Neurosci. 2001;4:724–31.
Fullana M, Harrison B, Soriano-Mas C, Vervliet B, Cardoner N, Àvila-Parcet A, et al. Neural signatures of human fear conditioning: an updated and extended meta-analysis of fMRI studies. Mol Psychiatry. 2016;21:500–08.
MacNamara A, Rabinak CA, Fitzgerald DA, Zhou XJ, Shankman SA, Milad MR, et al. Neural correlates of individual differences in fear learning. Behav Brain Res. 2015;287:34–41.
Milad MR, Quirk GJ, Pitman RK, Orr SP, Fischl B, Rauch SL. A role for the human dorsal anterior cingulate cortex in fear expression. Biol Psychiatry. 2007;62:1191–4.
Roberts AC, Clarke HF. Why we need nonhuman primates to study the role of ventromedial prefrontal cortex in the regulation of threat-and reward-elicited responses. Proc Natl Acad Sci USA. 2019;116:26297–304.
Article CAS PubMed Central Google Scholar
Olsson A, Phelps EA. Social learning of fear. Nat Neurosci. 2007;10:1095–102.
Phelps EA, O’Connor KJ, Gatenby JC, Gore JC, Grillon C, Davis M. Activation of the left amygdala to a cognitive representation of fear. Nat Neurosci. 2001;4:437–41.
Funayama ES, Grillon C, Davis M, Phelps EA. A double dissociation in the affective modulation of startle in humans: effects of unilateral temporal lobectomy. J Cogn Neurosci. 2001;13:721–9.
Olsson A, Nearing KI, Phelps EA. Learning fears by observing others: the neural systems of social fear transmission. Soc Cogn Affect Neurosci. 2007;2:3–11.
Olsson A, McMahon K, Papenberg G, Zaki J, Bolger N, Ochsner KN. Vicarious fear learning depends on empathic appraisals and trait empathy. Psychol Sci. 2016;27:25–33.
Milad MR, Quirk GJ. Fear extinction as a model for translational neuroscience: ten years of progress. Annu Rev Psychol. 2012;63:129–51.
Gottfried JA, Dolan RJ. Human orbitofrontal cortex mediates extinction learning while accessing conditioned representations of value. Nat Neurosci. 2004;7:1144–52.
Milad MR, Wright CI, Orr SP, Pitman RK, Quirk GJ, Rauch SL. Recall of fear extinction in humans activates the ventromedial prefrontal cortex and hippocampus in concert. Biol Psychiatry. 2007;62:446–54.
Phelps EA, Delgado MR, Nearing KI, LeDoux JE. Extinction learning in humans: role of the amygdala and vmPFC. Neuron. 2004;43:897–905.
Kalisch R, Korenfeld E, Stephan KE, Weiskopf N, Seymour B, Dolan RJ. Context-dependent human extinction memory is mediated by a ventromedial prefrontal and hippocampal network. J Neurosci. 2006;26:9503–11.
Lonsdorf TB, Haaker J, Kalisch R. Long-term expression of human contextual fear and extinction memories involves amygdala, hippocampus and ventromedial prefrontal cortex: a reinstatement study in two independent samples. Soc Cogn Affect Neurosci. 2014;9:1973–83.
Diekhof EK, Geier K, Falkai P, Gruber O. Fear is only as deep as the mind allows: a coordinate-based meta-analysis of neuroimaging studies on the regulation of negative affect. Neuroimage. 2011;58:275–85.
Menz MM, Rihm JS, Büchel C. REM sleep is causal to successful consolidation of dangerous and safety stimuli and reduces return of fear after extinction. J Neurosci. 2016;36:2148–60.
Fullana MA, Albajes-Eizagirre A, Soriano-Mas C, Vervliet B, Cardoner N, Benet O, et al. Fear extinction in the human brain: a meta-analysis of fMRI studies in healthy participants. Neurosci Biobehav Rev. 2018;88:16–25.
Milad MR, Quinn BT, Pitman RK, Orr SP, Fischl B, Rauch SL. Thickness of ventromedial prefrontal cortex in humans is correlated with extinction memory. Proc Natl Acad Sci USA. 2005;102:10706–11.
Hartley CA, Fischl B, Phelps EA. Brain structure correlates of individual differences in the acquisition and inhibition of conditioned fear. Cereb Cortex. 2011;21:1954–62.
Winkelmann T, Grimm O, Pohlack ST, Nees F, Cacciaglia R, Dinu-Biringer R, et al. Brain morphology correlates of interindividual differences in conditioned fear acquisition and extinction learning. Brain Struct Funct. 2016;221:1927–37.
Abend R, Jalon I, Gurevitch G, Sar-El R, Shechner T, Pine D, et al. Modulation of fear extinction processes using transcranial electrical stimulation. Transl Psychiatry. 2016;6:e913–e13.
Dittert N, Hüttner S, Polak T, Herrmann MJ. Augmentation of fear extinction by transcranial direct current stimulation (tDCS). Front Behav Neurosci. 2018;12:76.
Ganho-Ávila A, Gonçalves ÓF, Guiomar R, Boggio PS, Asthana MK, Krypotos A-M, et al. The effect of cathodal tDCS on fear extinction: a cross-measures study. PLoS One. 2019;14:e0221282.
Raij T, Nummenmaa A, Marin M-F, Porter D, Furtak S, Setsompop K, et al. Prefrontal cortex stimulation enhances fear extinction memory in humans. Biol Psychiatry. 2018;84:129–37.
van’t Wout M, Mariano TY, Garnaat SL, Reddy MK, Rasmussen SA, Greenberg BD. Can transcranial direct current stimulation augment extinction of conditioned fear? Brain Stimul. 2016;9:529–36.
Norberg MM, Krystal JH, Tolin DF. A meta-analysis of D-cycloserine and the facilitation of fear extinction and exposure therapy. Biol Psychiatry. 2008;63:1118–26.
Knight DC, Smith CN, Cheng DT, Stein EA, Helmstetter FJ. Amygdala and hippocampal activity during acquisition and extinction of human fear conditioning. Cogn Affect Behav Neurosci. 2004;4:317–25.
Morriss J, Hoare S, van Reekum CM. It’s time: a commentary on fear extinction in the human brain using fMRI. Neurosci Biobehav Rev. 2018;94:321–2.
Lang S, Kroll A, Lipinski SJ, Wessa M, Ridder S, Christmann C, et al. Context conditioning and extinction in humans: differential contribution of the hippocampus, amygdala and prefrontal cortex. Eur J Neurosci. 2009;29:823–32.
Ganella DE, Barendse ME, Kim JH, Whittle S. Prefrontal-amygdala connectivity and state anxiety during fear extinction recall in adolescents. Front Hum Neurosci. 2017;11:587.
Pace-Schott EF, Germain A, Milad MR. Effects of sleep on memory for conditioned fear and fear extinction. Psychol Bull. 2015;141:835–57.
Pace-Schott EF, Germain A, Milad MR. Sleep and REM sleep disturbance in the pathophysiology of PTSD: the role of extinction memory. Biol Mood Anxiety Disord. 2015;5:3.
LeDoux JE, Moscarello J, Sears R, Campese V. The birth, death and resurrection of avoidance: a reconceptualization of a troubled paradigm. Mol Psychiatry. 2017;22:24–36.
Moscarello JM, LeDoux JE. Active avoidance learning requires prefrontal suppression of amygdala-mediated defensive reactions. J Neurosci. 2013;33:3815–23.
Baratta MV, Lucero TR, Amat J, Watkins LR, Maier SF. Role of the ventral medial prefrontal cortex in mediating behavioral control-induced reduction of later conditioned fear. Learn Mem. 2008;15:84–7.
Boeke EA, Moscarello JM, LeDoux JE, Phelps EA, Hartley CA. Active avoidance: neural mechanisms and attenuation of Pavlovian conditioned responding. J Neurosci. 2017;37:4808–18.
Hartley CA, Gorun A, Reddan MC, Ramirez F, Phelps EA. Stressor controllability modulates fear extinction in humans. Neurobiol Learn Mem. 2014;113:149–56.
Lovibond PF, Davis NR, O’Flaherty AS. Protection from extinction in human fear conditioning. Behav Res Ther. 2000;38:967–83.
Gross JJ. Emotion regulation: current status and future prospects. Psychol Inq. 2015;26:1–26.
Morawetz C, Bode S, Derntl B, Heekeren HR. The effect of strategies, goals and stimulus material on the neural mechanisms of emotion regulation: a meta-analysis of fMRI studies. Neurosci Biobehav Rev. 2017;72:111–28.
Frank D, Dewitt M, Hudgens-Haney M, Schaeffer D, Ball B, Schwarz N, et al. Emotion regulation: quantitative meta-analysis of functional activation and deactivation. Neurosci Biobehav Rev. 2014;45:202–11.
Dörfel D, Lamke J-P, Hummel F, Wagner U, Erk S, Walter H. Common and differential neural networks of emotion regulation by detachment, reinterpretation, distraction, and expressive suppression: a comparative fMRI investigation. Neuroimage 2014;101:298–309.
Buhle JT, Silvers JA, Wager TD, Lopez R, Onyemekwu C, Kober H, et al. Cognitive reappraisal of emotion: a meta-analysis of human neuroimaging studies. Cereb Cortex. 2014;24:2981–90.
Kohn N, Eickhoff SB, Scheller M, Laird AR, Fox PT, Habel U. Neural network of cognitive emotion regulation—an ALE meta-analysis and MACM analysis. Neuroimage. 2014;87:345–55.
Wager TD, Smith EE. Neuroimaging studies of working memory. Cogn Affect Behav Neurosci. 2003;3:255–74.
Robbins TW. Shifting and stopping: fronto-striatal substrates, neurochemical modulation and clinical implications. Philos Trans R Soc Lond Biol Sci. 2007;362:917–32.
Simmonds DJ, Pekar JJ, Mostofsky SH. Meta-analysis of Go/No-go tasks demonstrating that fMRI activation associated with response inhibition is task-dependent. Neuropsychologia. 2008;46:224–32.
Amodio DM, Frith CD. Meeting of minds: the medial frontal cortex and social cognition. Nat Rev Neurosci. 2006;7:268–77.
Binder JR, Desai RH, Graves WW, Conant LL. Where is the semantic system? A critical review and meta-analysis of 120 functional neuroimaging studies. Cereb Cortex. 2009;19:2767–96.
Cato MA, Crosson B, Gökçay D, Soltysik D, Wierenga C, Gopinath K, et al. Processing words with emotional connotation: an FMRI study of time course and laterality in rostral frontal and retrosplenial cortices. J Cogn Neurosci. 2004;16:167–77.
Crosson B, Cato MA, Sadek JR, Gökçay D, Bauer RM, Fischler IS, et al. Semantic monitoring of words with emotional connotation during fMRI: contribution of anterior left frontal cortex. J Int Neuropsychol Soc. 2002;8:607–22.
Olsson A, Ochsner KN. The role of social cognition in emotion. Trends Cogn Sci. 2008;12:65–71.
Delgado MR, Nearing KI, LeDoux JE, Phelps EA. Neural circuitry underlying the regulation of conditioned fear and its relation to extinction. Neuron. 2008;59:829–38.
Schiller D, Delgado MR. Overlapping neural systems mediating extinction, reversal and regulation of fear. Trends Cogn Sci. 2010;14:268–76.
Ghashghaei HT, Barbas H. Pathways for emotion: interactions of prefrontal and anterior temporal pathways in the amygdala of the rhesus monkey. Neuroscience. 2002;115:1261–79.
Ghashghaei H, Hilgetag CC, Barbas H. Sequence of information processing for emotions based on the anatomic dialogue between prefrontal cortex and amygdala. Neuroimage. 2007;34:905–23.
Steward T, Davey CG, Jamieson AJ, Stephanou K, Soriano-Mas C, Felmingham KL, et al. Dynamic neural interactions supporting the cognitive reappraisal of emotion. Cereb Cortex. 2021;31:961–73.
Berboth S, Morawetz C. Amygdala-prefrontal connectivity during emotion regulation: a meta-analysis of psychophysiological interactions. Neuropsychologia 2021;153:107767.
Morawetz C, Riedel MC, Salo T, Berboth S, Eickhoff S, Laird AR, et al. Multiple large-scale neural networks underlying emotion regulation. Neurosci Biobehav Rev. 2020;116:382–95.
Erk S, Mikschl A, Stier S, Ciaramidaro A, Gapp V, Weber B, et al. Acute and sustained effects of cognitive emotion regulation in major depression. J Neurosci. 2010;30:15726–34.
Johnstone T, Van Reekum CM, Urry HL, Kalin NH, Davidson RJ. Failure to regulate: counterproductive recruitment of top-down prefrontal-subcortical circuitry in major depression. J Neurosci. 2007;27:8877–84.
Kroes MC, Dunsmoor JE, Hakimi M, Oosterwaal S, collaboration NP, Meager MR, et al. Patients with dorsolateral prefrontal cortex lesions are capable of discriminatory threat learning but appear impaired in cognitive regulation of subjective fear. Soc Cogn Affect Neurosci. 2019;14:601–12.
Feeser M, Prehn K, Kazzer P, Mungee A, Bajbouj M. Transcranial direct current stimulation enhances cognitive control during emotion regulation. Brain Stimul. 2014;7:105–12.
He Z, Lin Y, Xia L, Liu Z, Zhang D, Elliott R. Critical role of the right VLPFC in emotional regulation of social exclusion: a tDCS study. Soc Cogn Affect Neurosci. 2018;13:357–66.
Marques LM, Morello LY, Boggio PS. Ventrolateral but not dorsolateral prefrontal cortex tDCS effectively impact emotion reappraisal–effects on emotional experience and interbeat interval. Sci Rep. 2018;8:1–12.
Vieira L, Marques D, Melo L, Marques RC, Monte-Silva K, Cantilino A. Transcranial direct current stimulation effects on cognitive reappraisal: an unexpected result? Brain Stimul. 2020;13:650–2.
Gold AL, Sheridan MA, Peverill M, Busso DS, Lambert HK, Alves S, et al. Childhood abuse and reduced cortical thickness in brain regions involved in emotional processing. J Child Psychol Psychiatry. 2016;57:1154–64.
Raio CM, Orederu TA, Palazzolo L, Shurick AA, Phelps EA. Cognitive emotion regulation fails the stress test. Proc Natl Acad Sci USA. 2013;110:15139–44.
Raio CM, Brignoni-Perez E, Goldman R, Phelps EA. Acute stress impairs the retrieval of extinction memory in humans. Neurobiol Learn Mem. 2014;112:212–21.
Admon R, Leykin D, Lubin G, Engert V, Andrews J, Pruessner J, et al. Stress‐induced reduction in hippocampal volume and connectivity with the ventromedial prefrontal cortex are related to maladaptive responses to stressful military service. Hum Brain Mapp. 2013;34:2808–16.
Rocha-Rego V, Pereira MG, Oliveira L, Mendlowicz MV, Fiszman A, Marques-Portella C, et al. Decreased premotor cortex volume in victims of urban violence with posttraumatic stress disorder. PLoS One. 2012;7:e42560.
Clausen AN, Clarke E, Phillips RD, Haswell C, Morey RA. Combat exposure, posttraumatic stress disorder, and head injuries differentially relate to alterations in cortical thickness in military veterans. Neuropsychopharmacology. 2020;45:491–98.
Keding TJ, Herringa RJ. Abnormal structure of fear circuitry in pediatric post-traumatic stress disorder. Neuropsychopharmacology. 2015;40:537–45.
Morey RA, Haswell CC, Hooper SR, De Bellis MD. Amygdala, hippocampus, and ventral medial prefrontal cortex volumes differ in maltreated youth with and without chronic posttraumatic stress disorder. Neuropsychopharmacology. 2016;41:791–801.
Mueller SG, Ng P, Neylan T, Mackin S, Wolkowitz O, Mellon S, et al. Evidence for disrupted gray matter structural connectivity in posttraumatic stress disorder. Psychiatry Res Neuroimaging. 2015;234:194–201.
Herringa R, Phillips M, Almeida J, Insana S, Germain A. Post-traumatic stress symptoms correlate with smaller subgenual cingulate, caudate, and insula volumes in unmedicated combat veterans. Psychiatry Res: Neuroimaging. 2012;203:139–45.
Koch SB, Van Zuiden M, Nawijn L, Frijling JL, Veltman DJ, Olff M. Decreased uncinate fasciculus tract integrity in male and female patients with PTSD: a diffusion tensor imaging study. J Psychiatry Neurosci. 2017;42:331.
Fani N, King TZ, Shin J, Srivastava A, Brewster RC, Jovanovic T, et al. Structural and functional connectivity in posttraumatic stress disorder: associations with FKBP5. Depress Anxiety. 2016;33:300–07.
Harnett NG, Stevens JS, van Rooij SJ, Ely TD, Michopoulos V, Hudak L, et al. Multimodal structural neuroimaging markers of risk and recovery from posttrauma anhedonia: a prospective investigation. Depress Anxiety. 2021;38:79–88.
Stein MB, Yuh E, Jain S, Okonkwo DO, Mac Donald CL, Levin H, et al. Smaller regional brain volumes predict posttraumatic stress disorder at 3 months after mild traumatic brain injury. Biol Psychiatry. 2021;6:352–9.
Google Scholar
Bromis K, Calem M, Reinders AA, Williams SC, Kempton MJ. Meta-analysis of 89 structural MRI studies in posttraumatic stress disorder and comparison with major depressive disorder. Am J Psychiatry. 2018;175:989–98.
Zimmermann KS, Li C-C, Rainnie DG, Ressler, et al. Memory retention involves the ventrolateral orbitofrontal cortex: comparison with the basolateral amygdala. Neuropsychopharmacology. 2018;43:373–83.
Dahlgren MK, Laifer LM, VanElzakker MB, Offringa R, Hughes KC, Staples-Bradley LK, et al. Diminished medial prefrontal cortex activation during the recollection of stressful events is an acquired characteristic of PTSD. Psychol Med. 2018;48:1128.
Killgore WD, Britton JC, Schwab ZJ, Price LM, Weiner MR, Gold AL, et al. Cortico‐limbic responses to masked affective faces across ptsd, panic disorder, and specific phobia. Depress Anxiety. 2014;31:150–9.
Stevens JS, Kim YJ, Galatzer-Levy IR, Reddy R, Ely TD, Nemeroff CB, et al. Amygdala reactivity and anterior cingulate habituation predict posttraumatic stress disorder symptom maintenance after acute civilian trauma. Biol Psychiatry. 2017;81:1023–9.
Marin M-F, Song H, VanElzakker MB, Staples-Bradley LK, Linnman C, Pace-Schott EF, et al. Association of resting metabolism in the fear neural network with extinction recall activations and clinical measures in trauma-exposed individuals. Am J Psychiatry. 2016;173:930–8.
Milad MR, Pitman RK, Ellis CB, Gold AL, Shin LM, Lasko NB, et al. Neurobiological basis of failure to recall extinction memory in posttraumatic stress disorder. Biol Psychiatry. 2009;66:1075–82.
Rougemont‐Bücking A, Linnman C, Zeffiro TA, Zeidan MA, Lebron‐Milad K, Rodriguez‐Romaguera J, et al. Altered processing of contextual information during fear extinction in PTSD: an fMRI study. CNS Neurosci Ther. 2011;17:227–36.
Fonzo GA, Goodkind MS, Oathes DJ, Zaiko YV, Harvey M, Peng KK, et al. PTSD psychotherapy outcome predicted by brain activation during emotional reactivity and regulation. Am J Psychiatry. 2017;174:1163–74.
Fonzo GA, Goodkind MS, Oathes DJ, Zaiko YV, Harvey M, Peng KK, et al. Selective effects of psychotherapy on frontopolar cortical function in PTSD. Am J Psychiatry. 2017;174:1175–84.
King AP, Block SR, Sripada RK, Rauch S, Giardino N, Favorite T, et al. Altered default mode network (DMN) resting state functional connectivity following a mindfulness‐based exposure therapy for posttraumatic stress disorder (PTSD) in combat veterans of Afghanistan and Iraq. Depress Anxiety. 2016;33:289–99.
Hopper JW, Frewen PA, van der Kolk BA, Lanius RA. Neural correlates of reexperiencing, avoidance, and dissociation in PTSD: Symptom dimensions and emotion dysregulation in responses to script‐driven trauma imagery. J Trauma Stress. 2007;20:713–25.
Nicholson AA, Friston KJ, Zeidman P, Harricharan S, McKinnon MC, Densmore M, et al. Dynamic causal modeling in PTSD and its dissociative subtype: Bottom–up versus top–down processing within fear and emotion regulation circuitry. Hum Brain Mapp. 2017;38:5551–61.
Lebois LA, Li M, Baker JT, Wolff JD, Wang D, Lambros AM, et al. Large-scale functional brain network architecture changes associated with trauma-related dissociation. Am J Psychiatry. 2021;178:165–73.
Helpman L, Marin M-F, Papini S, Zhu X, Sullivan GM, Schneier F, et al. Neural changes in extinction recall following prolonged exposure treatment for PTSD: a longitudinal fMRI study. Neuroimage Clin. 2016;12:715–23.
Jovanovic T, Ely T, Fani N, Glover EM, Gutman D, Tone EB, et al. Reduced neural activation during an inhibition task is associated with impaired fear inhibition in a traumatized civilian sample. Cortex. 2013;49:1884–91.
Stevens JS, Ely TD, Sawamura T, Guzman D, Bradley B, Ressler KJ, et al. Childhood maltreatment predicts reduced inhibition‐related activity in the rostral anterior cingulate in PTSD, but not trauma‐exposed controls. Depress Anxiety. 2016;33:614–22.
Download references
KJR has received consulting income from Alkermes and Takeda, research support from NIH, Genomind, and Brainsway, and he is on scientific advisory boards for Janssen and Verily, all of which are unrelated to the present work. This work was supported by NIH (KJR: P50-MH115874, R01-MH108665; EAP: RO1- DA042855), the Frazier Institute at McLean Hospital (KJR), and the James S. McDonnell Foundation (EAP). EAP, MAK, RJF, and ESL have nothing to disclose.
Author information
These authors contributed equally: M. Alexandra Kredlow, Robert J. Fenster.
Authors and Affiliations
Department of Psychology, Harvard University, Cambridge, MA, USA
M. Alexandra Kredlow, Emma S. Laurent & Elizabeth A. Phelps
Division of Depression and Anxiety, McLean Hospital; Department of Psychiatry, Harvard Medical School, Cambridge, MA, USA
Robert J. Fenster & Kerry J. Ressler
You can also search for this author in PubMed Google Scholar
Contributions
EAP, RJF, MAK, ESL and KJR conceptualized, wrote, and edited the manuscript. ESL made the figures.
Corresponding authors
Correspondence to Kerry J. Ressler or Elizabeth A. Phelps .
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Alexandra Kredlow, M., Fenster, R.J., Laurent, E.S. et al. Prefrontal cortex, amygdala, and threat processing: implications for PTSD. Neuropsychopharmacol. 47 , 247–259 (2022). https://doi.org/10.1038/s41386-021-01155-7
Download citation
Received : 16 April 2021
Revised : 03 August 2021
Accepted : 06 August 2021
Published : 20 September 2021
Issue Date : January 2022
DOI : https://doi.org/10.1038/s41386-021-01155-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Basolateral amygdala neuropeptide y system modulates binge ethanol consumption.
- Stacey L. Robinson
- Sophie C. Bendrath
- Todd E. Thiele
Neuropsychopharmacology (2024)
Therapeutic mechanisms of psychedelics and entactogens
- Boris D. Heifets
- David E. Olson
Distributed neural representations of conditioned threat in the human brain
- Edward F. Pace-Schott
- Mohammed R. Milad
Nature Communications (2024)
Anxiety and dysautonomia symptoms in patients with a NaV1.7 mutation and the potential benefits of low-dose short-acting guanfacine
- Rita de Cássia Collaço
- Maxime Lammens
- Frank Bosmans
Clinical Autonomic Research (2024)
Functional changes in neural mechanisms underlying post-traumatic stress disorder in World Trade Center responders
- Azzurra Invernizzi
- Elza Rechtman
- Megan K. Horton
Translational Psychiatry (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Trauma, Resilience, Anxiety Disorders, and PTSD
- Ned H. Kalin , M.D.
Search for more papers by this author
Stress and trauma are well known to be critical factors in the development and maintenance of psychopathology. In some stress-related disorders, such as anxiety and depression, stress can play an etiological role, whereas in other disorders like schizophrenia, stress can precipitate and exacerbate symptoms. Stress occurring early in life in the form of traumatic events is a transdiagnostic risk factor for developing psychopathology, whereas posttraumatic stress disorder (PTSD) is a disorder that is specifically defined as a maladaptive response to traumatic events. In the midst of the COVID-19 pandemic, and certainly to no one’s liking, we currently are involved in a naturalistic experiment linking stress to mental suffering and psychopathology.
Most of us have never experienced stressors of the magnitude and length associated with the global COVID-19 pandemic. Because the pandemic has been so prolonged, and in part as a way to cope, many of us have become inured to its catastrophic effects. It is mind boggling that we have begun to accept as commonplace the fact that 3,000 Americans per day are dying from COVID-19 or that the economic consequences are so dire that 16% of adults with children report not having sufficient food ( 1 ). Although it may be obvious, it is important to enumerate why the COVID-19 pandemic represents the perfect storm of stressors and traumatic events:
A long-term sense of uncertainty about the future coupled with a sense of uncontrollability.
Concerns about contracting COVID-19, becoming gravely ill, and dying.
Worries about losing loved ones and friends, and the grief associated with real losses.
The trauma associated with being gravely ill with COVID-19.
Prolonged physical separation and social isolation from family and friends.
Disruption of regular routines, including work and school for children.
Losses of jobs, business failures, and the profound economic consequences.
Lack of trust in leadership to effectively deal with the crisis.
As mental health care providers, we are in the uniquely challenging position of both personally experiencing the disruptive influences of chronic stress associated with the pandemic and working with patients and other vulnerable individuals to mitigate the consequences of the stress and tragedies that they are experiencing. It is critical to underscore the need to provide additional resources to underprivileged and marginalized individuals, as they are particularly vulnerable to the direct and indirect consequences of the COVID-19 pandemic. For example, Black and Latino households are twice as likely as White households to experience food insufficiency during the pandemic.
The focus of this issue of the Journal is highly relevant, as it provides new insights into the neural alterations associated with trauma, resilience, anxiety disorders, and PTSD as well as insights into new, promising treatment strategies. Dr. Yuval Neria, a PTSD expert from Columbia University, reviews neuroimaging findings in relation to PTSD and addresses how they may relate to the heterogeneity of PTSD symptom presentation and inform selective treatment approaches ( 2 ). Dr. Yair Bar-Haim from Tel Aviv University and his colleagues present a thought-provoking commentary suggesting that symptoms associated with the intrusive reexperiencing of traumatic events should be prioritized as a focus of research efforts to elaborate mechanisms underlying responses to trauma and PTSD ( 3 ). Dr. Dylan Gee and Paola Odriozola from Yale University coauthor a review that uses a translational neuroscience approach to discuss learning mechanisms relevant to the maladaptive regulation of fear and anxiety. In addition to considering conditioned fear learning and extinction, this review emphasizes the importance of safety signal learning, describes its underlying mechanisms, and speculates about the potential utility of using safety signal learning approaches in treating youths with anxiety disorders ( 4 ).
Is Inducing Anxiety in Healthy Individuals a Valid Approach for Understanding Pathophysiological Processes in Patients With Anxiety Disorder?
Numerous studies in healthy individuals have used threat-related paradigms in combination with neuroimaging to characterize the neural correlates of adaptive anxiety responses. The findings from these studies have frequently been used to draw inferences about alterations in neural activation that are associated with maladaptive anxiety responses in individuals with anxiety disorders. Chavanne and Robinson focus on determining whether studying healthy individuals under conditions of threat is a valid approach for understanding brain processes relevant to psychopathology ( 5 ). In their study, the authors first performed a meta-analysis on neuroimaging findings from studies in which patients with anxiety disorders were compared with control subjects when exposed to emotion-related paradigms. The results of this analysis were further compared with a meta-analysis of imaging findings assessing neural responses induced by unpredictable threat paradigms in healthy individuals. Across healthy individuals and those with anxiety disorders, increased activation was found in the insula, cingulate cortex, medial prefrontal cortex, and periaqueductal gray. There were also some differences between individuals with specific disorders and healthy control subjects. Similarities in neural activation between healthy individuals exposed to threat and individuals with anxiety disorders appeared to be greatest for individuals with specific phobias and were least similar for those with generalized anxiety disorder. In an editorial, Dr. Alexander Shackman from the University of Maryland and Dr. Andrew Fox from the University of California, Davis, discuss these findings in relation to the validity of using healthy subjects to understand pathophysiological processes in patients with anxiety disorders. They also point to additional work that needs to be done with animal models and humans to further develop an understanding of the mechanisms underlying pathological anxiety ( 6 ).
Using Brain Network Connectivity to Estimate the Severity of Dissociative Symptoms
Dissociative symptoms are a hallmark of PTSD and can be very disabling. The study by Lebois et al. ( 7 ) presents data demonstrating the capacity to use machine learning with functional connectivity MRI data to modestly estimate individual differences in dissociative symptoms in women with PTSD. In their study involving 65 women, the authors demonstrated that they could estimate about 24% of the variance in an individual’s dissociative symptom severity by using the functional connectivity data. Hyperconnectivity between regions of the default mode network and the frontoparietal network appeared to contribute most to this prediction. Of importance, this brain network connectivity–based estimate controlled for childhood trauma and PTSD symptom severity, suggesting that the connectivity patterns identified to be associated with dissociative symptoms involved distinct neural alterations. In addition to providing a better understanding of the neural underpinnings of dissociative symptoms, the results of this study suggest that in the future it may be plausible to use brain-based neural connectivity measurements as an objective proxy for subjective reports of dissociative symptoms. In his insightful editorial, Dr. Vinod Menon from Stanford University discusses how the functions of the default mode network and frontoparietal network, and their interactions, may relate to the subjective experience of dissociation ( 8 ). In addition, he suggests that interventions aimed at components of the salience network, such as the anterior cingulate cortex, may ameliorate dissociative symptoms by affecting interactions between the default mode and frontoparietal networks.
Patterns of Cortical Thinning Are Shared Across Individuals With Internalizing, Externalizing, and Thought Disorder–Related Symptoms
Brain structural alterations are commonly reported in patients across various psychiatric diagnoses. Romer and colleagues ( 9 ) present data demonstrating overlapping patterns of reduced cortical thickness in individuals with internalizing symptoms (e.g., depression and anxiety), externalizing symptoms (e.g., substance abuse and antisocial behavior), and thought disorder–related symptoms (e.g., delusions and hallucinations). This study used structural imaging data to assess cortical thickness and cortical surface area from 45-year-old individuals who were part of the longitudinally studied Dunedin Cohort. In addition to demonstrating cortical thinning across diagnostic domains, patterns of cortical thinning were related to the general psychopathology dimensional score known as the p factor. It is important to keep in mind that these relations do not address issues of causality. Based on these data, the authors argue that the transdiagnostic nature of pervasive cortical thinning further supports the value of a broad and general approach to study the relations between psychopathology and brain alterations.
Resilience During Pregnancy Is Associated With Increased Telomere Length in Newborns
Telomeres are strands of nucleotides at the ends of chromosomes that have various functions, including protecting the chromosome from degradation. In general, shortened telomeres have been associated with stress exposure, various illnesses, and aging. Verner and colleagues ( 10 ) studied 656 mother-infant dyad pairs and, by using multiple behavioral measures collected during pregnancy, computed factors associated with stress and positivity. Telomere length was assessed in leukocytes collected from cord blood at birth. The findings demonstrate an association between individual differences in pregnant mothers’ stress factor and shorter telomere length in newborns. In contrast, individual differences in the positivity factor during pregnancy were associated with increased telomere length. By statistically accounting for the effects of positivity on stress, the authors derived what they considered to be a measure of resilience, and by using this measure, they demonstrate that maternal resilience is associated with increased telomere length in newborns. The findings from this study are exciting as they suggest that resilience during pregnancy has important implications at the cellular and molecular level for newborns and for their development. In her editorial, Dr. Stacy Drury from Tulane University further discusses the relevance of telomere length and function in relation to health and disease. She also presents possible mechanisms by which stress during pregnancy might affect offspring telomeres ( 11 ).
Ketamine Treatment for PTSD
New and effective treatments are needed for patients with PTSD. Feder et al. ( 12 ) report findings from a randomized clinical trial examining the effects of repeated intravenous ketamine infusions on symptoms in PTSD patients. Ketamine is an N -methyl- d -aspartate receptor antagonist with effects on numerous other systems, including opiate receptors, and when administered in subanesthetic doses, it is effective in rapidly decreasing depressive symptoms. The authors of the present study previously reported that a single dose of ketamine had positive short-term effects in PTSD patients, and they now extend this work by assessing the effects of repeated ketamine administration as a means to provide longer-term efficacy. In the study, 30 chronically ill PTSD patients were randomly assigned to receive, over a 2-week period, either six infusions of ketamine (0.5 mg/kg) or midazolam (0.045 mg/kg) as an active placebo. In the 29 individuals who completed the study, 15 received ketamine. The findings demonstrated rapid responses to ketamine. When assessed at 1 and 2 weeks, ketamine was significantly and robustly more effective in reducing symptoms compared with midazolam. It is important to note that although the repeated ketamine infusions were highly effective, the median time to the loss of the ketamine response was 27.5 days. In their editorial, Dr. Murray Stein from the University of California, San Diego, and Dr. Naomi Simon from New York University emphasize the need to develop more effective treatments for PTSD. They also comment on the renewed interest in psychedelic drugs as therapeutic agents and the possible mechanisms by which ketamine may work in relation to modifying the recall of traumatic memories associated with PTSD ( 13 ).
Conclusions
The imperative to understand how stress and trauma increase the vulnerability to develop psychiatric illnesses could not be more relevant and timelier as the world’s population is experiencing unprecedented levels of stress, trauma, fear, anxiety, and grief. It is also extremely important to focus on, and understand, the factors that promote resilience, as we witness the remarkable capacities of individuals to endure, cope with, and overcome the adversity and challenges presented by the pandemic.
This issue of the Journal provides a comprehensive focus on new research findings relevant to these issues. Highlights from the reports in this issue include findings that there is evidence supporting the dimensionality of anxiety, as there is shared activation of anxiety-related neural circuitry between healthy individuals and those with anxiety disorders; that resilience during pregnancy is associated with greater “healthier” telomere length in newborns; that focusing on safety learning may be a fruitful treatment approach for anxiety disorders, especially for children; that machine learning methods can be employed with imaging data to predict the severity of dissociative symptoms in PTSD patients; and that repeated ketamine administration over a 2-week period robustly decreases PTSD symptoms.
Disclosures of Editors’ financial relationships appear in the April 2020 issue of the Journal .
1 Center on Budget and Policy Priorities: Tracking the COVID-19 recession’s effects on food, housing, and employment hardships. https://www.cbpp.org/sites/default/files/atoms/files/8-13-20pov.pdf Google Scholar
2 Neria Y : Functional neuroimaging in PTSD: from discovery of underlying mechanisms to addressing diagnostic heterogeneity . Am J Psychiatry 2021 ; 178:128–135 Abstract , Google Scholar
3 Bar-Haim Y, Stein MB, Bryant RA, et al. : Intrusive traumatic reexperiencing: pathognomonic of the psychological response to traumatic stress . Am J Psychiatry 2021 ; 178:119–122 Link , Google Scholar
4 Odriozola P, Gee DG : Learning about safety: conditioned inhibition as a novel approach to fear reduction targeting the developing brain . Am J Psychiatry 2021 ; 178:136–155 Link , Google Scholar
5 Chavanne AV, Robinson OJ : The overlapping neurobiology of induced and pathological anxiety: a meta-analysis of functional neural activation . Am J Psychiatry 2021 ; 178:156–164 Link , Google Scholar
6 Shackman AJ, Fox AS : Two decades of anxiety neuroimaging research: new insights and a look to the future (editorial). Am J Psychiatry 2021 ; 178:106–109 Link , Google Scholar
7 Lebois LAM, Li M, Baker JT, et al. : Large-scale functional brain network architecture changes associated with trauma-related dissociation . Am J Psychiatry 2021 ; 178:165–173 Link , Google Scholar
8 Menon V : Dissociation by network integration (editorial). Am J Psychiatry 2021 ; 178:110–112 Abstract , Google Scholar
9 Romer AL, Elliott ML, Knodt AR, et al. : Pervasively thinner neocortex as a transdiagnostic feature of general psychopathology . Am J Psychiatry 2021 ; 178:174–182 Abstract , Google Scholar
10 Verner G, Epel E, Lahti-Pulkkinen M, et al. : Maternal psychological resilience during pregnancy and newborn telomere length: a prospective study . Am J Psychiatry 2021 ; 178:183–192 Abstract , Google Scholar
11 Drury SS : Building resilience for generations: the tip of the chromosome (editorial). Am J Psychiatry 2021 ; 178:113–115 Abstract , Google Scholar
12 Feder A, Costi S, Rutter SB, et al. : A randomized controlled trial of repeated ketamine administration for chronic posttraumatic stress disorder . Am J Psychiatry 2021 ; 178:193–202 Link , Google Scholar
13 Stein MB, Simon NM : Ketamine for PTSD: well, isn’t that special (editorial). Am J Psychiatry 2021 ; 178:116–118 Abstract , Google Scholar
- Cited by None
- Posttraumatic Stress Disorder (PTSD)
- Coronavirus/COVID-19
- Anxiety Disorders
Breakthrough Study on Post-Traumatic Stress Disorder
A collaboration of researchers, institutions and databases makes advances on the understanding of the genetic component of ptsd.
- Joseph McClain - [email protected]
Media contact:
- Miles Martin - [email protected]
Published Date
Share this:, article content.
The Psychiatric Genetics Consortium (PGC), a consortium of researchers led by scientists at University of California San Diego School of Medicine has made significant advancements in the understanding of the neurobiology of post-traumatic stress disorder (PTSD), a condition the World Health Organization says affects some 250 million people around the world.
The group recently announced their findings from a genome-wide association study of 1,222,822 people in a paper recently published in the journal Nature Genetics .
Caroline M. Nievergelt, Ph.D., professor of psychiatry at UC San Diego School of Medicine, is the co-first author on the paper, together with Adam X. Maihofer, PhD., an assistant project scientist in Nievergelt’s lab. PGC-PTSD co-chair Murray B. Stein M.D., M.P.H., professor of psychiatry and public health at UC San Diego is also a co-author of the study.
Nievergelt explained that the work confirmed previous neurobiological studies of PTSD and built upon them, identifying 95 loci — positions of genes on a chromosome — significant to PTSD, including 80 new loci.
“As the number of samples has increased, we have gained a better understanding of the genetic factors that contribute to PTSD risk,” Stein said.
The paper underscores the importance of heritability in PTSD risk and notes that the identified genes influence processes related to PTSD symptoms such as stress, fear and threat responses. She said their findings also point to possible associations among PTSD and other mental and physical disorders.
The PGC was formed in 2007, dedicated to finding genes that predispose an individual to psychiatric disorders, such as bipolar disorder or schizophrenia, Nievergelt said. She added that each disorder is addressed by one of 11 working groups, one of which is the PGC for PTSD, which she chairs.
Nievergelt explained that the benefits of research by a consortium extend beyond the hive-mind input of numerous collaborators working toward a common goal. A genome-wide association study (GWAS) examines and compares genomes of a large number of people in a search for genetic markers associated with a specific condition. A GWAS for polygenic disorders such as PTSD necessarily requires an enormous sample size, she noted.
“And no one PI (principal investigator) is able to get nearly enough subjects for a genome-wide association study, so through the consortium we have a large number of collaborators combining data from all over the world,” Nievergelt said.
The PCG for PTSD consortium includes researchers from a wide number of research institutions and universities worldwide. Notable participants include co-chairs Karestan Koenen, Ph.D., from the Harvard Chan School of Public Health and the Broad Institute of MIT, and Kerry Ressler, M.D., Ph.D., of Harvard Medical School and McLean Hospital.
{/exp:typographee}
The brain, DNA, and a fractured glass effect as a PTSD metaphor. Photo by Adobe AI.
The consortium’s database was assembled from various sources, representing a variety of causes and levels of trauma. Nievergelt said the sources included the Marine Resiliency Study, in which U.S. Marine Corps members were assessed before and after going to war, and Army STARRS, a longitudinal study of U.S. Army soldiers. Another is the Grady Trauma Project that includes victims of violent crime, mostly African American individuals from inner cities. Other datasets incorporated into the PGC for PTSD megadata list came from Electronic Health Records (EHRs) and the VA Million Veterans Program. The consortium also incorporated data from Europe and Latin America.
At an appropriate stage, the consortium members agree on a data freeze and begin their examination, seeking to identify specific genes likely to be associated with PTSD. The paper represents “a milestone” in the understanding of the genetic component of PTSD, Nievergelt said.
“It’s the first time that we actually have a very strong genetic signal,” said Maihofer, who analyzed the data. The genetic signal — essentially a mapping of RNA or DNA activity relevant to PTSD — allowed the consortium to pinpoint specific genes and analyze pathways of gene expression for future research or even for eventual treatment strategies, Maihofer explained.
Nievergelt says there are several directions the consortium wants to take in terms of next steps. One is to increase and diversify the sample size. She said the group has received funding from the National Institute of Mental Health to go to Africa and enroll African people in the genetics study, an effort lead by co-chair Koenen. “That will help us improve risk prediction for other people of African ancestry, a group that has been relatively neglected in earlier studies,” Nievergelt noted.
UC San Diego co-authors
Authors affiliated with the University of California San Diego School of Medicine Department of Psychiatry, in addition to first authors Caroline M. Nievergelt and Adam X. Maihofer, are: Dewleen G. Baker, Carol E. Franz, William S. Kremen, Elizabeth A. Mikita, Sonya B. Norman, Matthew S. Panizzon and Murray B. Stein, also affiliated with the UCSD Herbert Wertheim School of Public Health and Human Longevity Science. Other UC San Diego authors are Anders M. Dale, of the Department of Radiology, Department of Neurosciences, and Wesley K. Thompson, of the Herbert Wertheim School of Public Health and Human Longevity Science.
Other noteworthy participants in the study
PGC-PTSD co-chairs:
Kerry J. Ressler, of the Department of Psychiatry at Harvard Medical School; McLean Hospital, and Department of Medicine (Biomedical Genetics), Boston University Chobanian & Avedisian School of Medicine; as well as Karestan C. Koenen, of the Department of Epidemiology at the Harvard T.H. Chan School of Public Health, the Broad Institute of MIT and Harvard, the Stanley Center for Psychiatric Research; and McLean Hospital Developmental Biopsychiatry Research Program.
Writing group members are:
Elizabeth G. Atkinson, Department of Molecular and Human Genetics, Baylor College of Medicine; Chia-Yen Chen, Biogen Inc.,Translational Sciences; Karmel W. Choi, Department of Epidemiology, Harvard T.H. Chan School of Public Health, and the Department of Psychiatry at Massachusetts General Hospital; Jonathan R. I. Coleman, King’s College London, National Institute for Health and Care Research Maudsley Biomedical Research Centre, and King’s College London, Social, Genetic and Developmental Psychiatry Centre, Institute of Psychiatry, Psychology and Neuroscience; Nikolaos P. Daskalakis, Broad Institute of MIT and Harvard, and the Stanley Center for Psychiatric Research in the Department of Psychiatry of Harvard Medical School, and the McLean Hospital, Center of Excellence in Depression and Anxiety Disorders; Laramie E. Duncan, Department of Psychiatry and Behavioral Sciences, Stanford University; Renato Polimanti, VA Connecticut Healthcare Center, and the Department of Psychiatry of Yale University School of Medicine.
Competing interest
Murray B. Stein has in the past three years received consulting income from Aptinyx, atai Life Sciences, BigHealth, Biogen, Bionomics, Boehringer Ingelheim, Delix Therapeutics, EmpowerPharm, Engrail Therapeutics, Janssen, Jazz Pharmaceuticals, Karuna Therapeutics, NeuroTrauma Sciences, Otsuka US, PureTech Health, Sage Therapeutics, and Roche/Genentech. He also has stock options in Oxeia Biopharmaceuticals and EpiVario. Anders M. Dale holds equity in CorTechs Labs and serves on the Scientific Advisory Board of Human Longevity and the Mohn Medical Imaging and Visualization Center, and also receives funding through research grants with General Electric Healthcare. Other authors associated with UCSD declare no competing interests.
Support and funding
Major financial support for the PGC-PTSD was provided by the National Institute of Mental Health (NIMH) grants R01MH106595 and R01MH124847, by the Cohen Veterans Bioscience and by the Stanley Center for Psychiatric Research at the Broad Institute.
Full lists of authors and their affiliations and competing interests, funding/support sources are available on the paper.
"No one PI (principal investigator) is able to get together nearly enough subjects for a genome-wide association study, so through the consortium we have a large number of collaborators combining data from all over the world."
You May Also Like
Creating a “greener,” more connected society, electronic health records unlock genetics of tobacco use disorder, following cellular lineage, stay in the know.
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.
You have been successfully subscribed to the UC San Diego Today Newsletter.
Campus & Community
Arts & culture, visual storytelling.
- Media Resources & Contacts
Signup to get the latest UC San Diego newsletters delivered to your inbox.
Award-winning publication highlighting the distinction, prestige and global impact of UC San Diego.
Popular Searches: Covid-19 Ukraine Campus & Community Arts & Culture Voices
PTSD Research Paper

This sample PTSD research paper features: 6100 words (approx. 20 pages), an outline, and a bibliography with 13 sources. Browse other research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.

Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code, i. reactions to traumatic events, a. acute reactions, b. posttraumatic stress disorder, c. course of ptsd, ii. measures of ptsd, a. interviews, b. self-report measures, iii. prevalence of ptsd, iv. vulnerability and resiliency factors in ptsd, v. concomitant problems following trauma, vi. theories on the development and maintenance of ptsd, a. psychoanalytic theories, b. cognitive and behavioral theories, c. psychobiological approaches, vii. psychological and pharmacological interventions in ptsd, a. early interventions, b. cognitive-behavioral therapies, 1. prolonged exposure (pe), 2. stress inoculation training (sit), 3. cognitive therapy, 4. cognitive processing therapy (cpt), 5. eye movement desensitization and reprocessing (emdr), c. pharmacotherapy, d. hypnotherapy and psychodynamic psychotherapy.
VIII. Bibliography
Psychologists and physicians have long been interested in vulnerability and resilience factors in reaction to extreme stress. Earlier accounts of posttrauma reactions focused on descriptions of cases. Spurred by inclusion of Post-traumatic Stress Disorder (PTSD) in the psychiatric diagnosis nomenclature in 1980, experimental research has examined many facets of the phenomenon.
In the Diagnostic and Statistical Manual (DSM-IV) published by the American Psychiatric Association in 1994, a trauma is defined as an experienced or witnessed event that involves threat of death or serious injury, and which evokes feelings of terror, horror, or helplessness. Thus, events such as anticipated death of a loved one, job loss, or divorce would not qualify as a trauma in this formulation. The International Classification of Diseases (ICD-10), published by the World Health Organization in 1992, describes a traumatic event as having an exceptionally threatening or catastrophic nature, which would be likely to cause pervasive distress in almost anyone.
The most common traumas studied are combat, sexual assault, sexual abuse in childhood, criminal victimization, torture, accidents, and natural disasters. Larger-scale traumas, such as mass migration, refugee camp experiences, and holocausts, have not yet been thoroughly researched. Clearly, such mass traumas would be expected to have considerable impact on those individuals directly affected as well as on their children, communities, and cultures.
A number of physical and psychological symptoms are considered common reactions immediately after a traumatic experience. Many trauma victims report being disoriented and anxious after a trauma and have difficulty sleeping and concentrating. Victims are often reluctant to talk about the trauma or deliberately contemplate it; nevertheless the traumatic memory intrudes on their thoughts quite frequently. In recognition of the severe distress and psychological dysfunction that often occur immediately after a trauma, a new diagnostic classification called Acute Stress Disorder (ASD) was adopted in the DSM-IV in 1994. The focus of this disorder is on dissociative features, and, consequently, the symptom criteria include at least three of the following: a sense of numbing, detachment, or lack of emotional responsiveness, a reduction in awareness of surroundings (e.g., being in a daze), derealization, depersonalization, and dissociative amnesia. Reexperiencing of the trauma, avoidance, and arousal, as defined in the criteria for PTSD, must also exist. A diagnosis of Acute Stress Disorder is warranted when such symptoms last between 2 days and 1 month, occur within 1 month of the trauma, and interfere significantly with daily functioning.
Posttraumatic Stress Disorder, as described in DSM-IV, is a set of symptoms that begins after a trauma and persists for at least 1 month. The symptoms fall into three clusters. First, the individual must reexperience the trauma in one of the following ways: nightmares, flashbacks, or intrusive and distressing thoughts about the event; or intense emotional distress or physiological reactivity when reminded of the event. Second, the individual must have three of the following avoidance symptoms: avoidance of thoughts or feelings related to the trauma, avoidance of trauma reminders, psychogenic amnesia, emotional numbing, detachment or estrangement from others, decreased interest in leisure activities, or a sense of foreshortened future. Third, the individual must experience two of the following arousal symptoms: difficulty falling or staying asleep, difficulty concentrating, irritability or outbursts of anger, hypervigilance, or an exaggerated startle response. To meet diagnostic criteria for PTSD, the symptoms must cause significant impairment in daily functioning. These criteria provide a good operational definition of PTSD, as they describe the symptoms seen in most cases. However, the three categories of symptoms are not empirically validated as distinct symptom clusters. For instance, it is not clear that the symptoms of behavioral avoidance and emotional numbing are similar and belong in the same category.
The ICD-IO criteria for PTSD also include some reexperiencing symptoms (nightmares, flashbacks, distress on exposure to reminders), actual or preferred avoidance of trauma reminders, and either an inability to recall important aspects of the trauma or sustained psychological sensitivity and arousal (sleep disturbance, hypervigilance, difficulty concentrating). These three criteria must all be met within 6 months of the traumatic event for a diagnosis to be given.
Several differences between the two definitions can be identified. First, the DSM-IV specifies a minimal number of symptoms that need to be observed to receive the diagnosis, whereas the ICD-IO leaves more freedom for clinical judgment. The advantage of the former approach is its utility in clearly operationalizing the concept of PTSD. The disadvantage is its rigidity and the possibility that one symptom can determine diagnostic membership. Second, the ICD-IO does not recognize the numbing symptoms, which together with flashbacks and nightmares are thought to be cardinal features of PTSD. Third, arousal symptoms are optional in the ICD-IO but are required in the DSM-IE Clinical observation and theoretical accounts of PTSD support the importance of these symptoms and render the ICD-IO diagnostic criteria less satisfactory.
The course of PTSD is variable. For the majority of individuals, symptoms begin immediately after the trauma, although some appear to have a delayed reaction. During the first 3 months after the trauma, the individual is said to have acute PTSD, whereas chronic PTSD is defined as symptoms persisting beyond 3 months. Symptoms can fluctuate over time between diagnosis of PTSD, subthreshold symptoms, and few or no symptoms. Recovery is affected by a number of factors, including perception of oneself and one’s surroundings, actual social support, life stress, coping style, and personality.
A number of measures have been developed to assess PTSD, including clinical interviews and self-report instruments. These measures vary widely in terms of the target symptoms, administration time, and the samples used for ascertaining psychometric properties. Adult assessment tools are reviewed in the next section. Although some measures have also been developed for children, they are outside the scope of this paper.
The Structured Clinical Interview for DSM (SCID) is believed to be the most widely used diagnostic interview. Its major disadvantage, however, is that it does not provide a measure of symptom severity. Several other interviews that provide information of both diagnostic status and symptom severity are available. Two interviews are becoming quite widely used in PTSD research. The first is the Clinician-Administered PTSD Scale (CAPS) that yields separate scores for frequency and intensity for each symptom. Disadvantages of this interview include a long administration time and validation on military veterans only. The second interview, the PTSD Symptom Scale Interview (PSS-I), includes a combined frequency/severity rating for each of the 17 PTSD symptoms in the DSM-IV and thus yields both a diagnosis and a continuous severity rating. Unlike the CAPS, the PSS-I takes only about 15 to 20 minutes to administer and was validated on female assault victims.
Several self-report scales have been developed to assess symptoms of PTSD. The first was the Revised Impact of Events Scale (RIES), which yields two factors: intrusion and avoidance. A revised version of the RIES added hyperarousal items, but has shown mixed results in reliability studies and, like its predecessor, does not correspond fully to the DSM-IV PTSD symptoms. Two scales, the Mississippi Scale and the Penn Inventory, have excellent psychometric properties in veteran samples but do not provide information about diagnostic status because they do not fully correspond to the DSM-IV defining symptoms.
The PTSD Symptom Scale-Self-Report (PSS-SR) and its successor, the PTSD Diagnostic Scale (PDS), provide information about each of the 17 DSM-IV symptoms, yielding both diagnostic and severity information. The PDS is the only self-report instrument that assesses all DSM-IV criteria, including information about the nature of the traumatic event and the level of functional interference, in addition to information about PTSD diagnosis and symptom severity. It was validated in a sample of victims of a wide range of traumas and evidenced sound psychometric properties, and thus can be used in studies of various trauma populations.
Lifetime prevalence of PTSD in the general population is estimated at 9%, with up to a third of these cases having chronic PTSD. Among trauma victims, the rate is much higher, estimated at 24 %. However, the rates of PTSD tend to vary considerably among different types of trauma. For instance, estimates of the lifetime prevalence of PTSD in Vietnam War veterans range from 27 to 65%; in civilian populations exposed to terrorism and torture, prevalence ranges from 33 to 54%. Between 35% and 94% of victims of violent assaults manifest PTSD. In contrast, accidents and natural disasters appear to produce lower rates of PTSD, 4.6 to 59%, depending on the event studied and the degree of exposure. Even individuals with little or no direct exposure to the trauma can develop PTSD; this phenomenon has been referred to as the “ripples outward” effect. Importantly, certain occupations are at risk for PTSD by virtue of increased probability of repeated direct exposure to trauma; between 9% and 26% of professionals such as police, nurses, and firefighters develop PTSD in reaction to stressors experienced on the job.
Prevalence in certain vulnerable populations is much higher than in the general population, presumably because individuals in these groups have been exposed to more traumatic experiences. These include populations seeking outpatient psychotherapy and those in substance abuse clinics. Women appear to be somewhat more likely than men to develop PTSD after trauma, 10.4 % versus 5 %, respectively. As noted earlier, the prevalence of emotional difficulties after mass traumas, such as refugee camp experiences or holocausts, has not been systematically studied.
Factors implicated in posttrauma reactions can be divided into three categories: pretrauma variables, variables related to the trauma itself, and posttrauma variables.
Research on pretrauma demographic variables has not identified reliable predictors of who will develop chronic PTSD with one exception: women are somewhat more likely to manifest PTSD than men after experiencing a similar trauma. In contrast, it appears that poor psychological and social functioning prior to the trauma renders the individual vulnerable to developing chronic symptoms. For instance, prior hospitalization and a history of drug abuse were found to be associated with a more severe posttrauma reaction. Also, a history of traumatic events in childhood or adulthood predicts a more severe response to a new trauma.
The nature of the trauma itself also appears to affect recovery. First, traumas differ in their likelihood of producing PTSD; rape, for example, is more likely to produce persistent symptoms than a natural disaster. Second, given a specific trauma (e.g., rape), injury and perceived threat of death produce more severe and persistent reactions.
Several posttrauma factors have been found to exacerbate symptoms. It appears that dissociation (emotional numbing, amnesia, depersonalization) shortly after a trauma hinders recovery. Also, on average, assault victims who exhibit more severe initial reactions to the trauma also show more symptoms later on. Thus, individuals seem to differ in how strongly they are affected by a similar trauma, and their initial reaction is associated with later psychopathology.
Evidence on the role of social support as facilitating or hindering recovery is equivocal. It seems that negative reactions from others, such as blame, increase posttrauma psychopathology, but, unfortunately, positive reactions do not show the expected positive effects. Excessive anger or guilt after the trauma also appears to block readjustment. Additional longitudinal research on the factors that promote resilience to trauma are clearly needed.
Traumatized individuals not only exhibit ASD or PTSD symptoms, but also depression, substance abuse, anxiety, dissociation, and physical health problems.
The rate of use and abuse of drugs and alcohol, including nicotine, in traumatized individuals is higher than in the general population. There are at least two explanations for this finding. First, traumatized individuals may choose to cope with their symptoms by increasing substance use. Second, substance abuse may increase the risk of being exposed to a traumatic experience.
Many individuals report symptoms of depression after a traumatic event, such as sadness, lack of energy, diminished interest in leisure activities, hopelessness, sleeplessness, and eating disturbances. Although some of these symptoms overlap with the defining symptoms of PTSD (e.g., markedly diminished interest in activities), the two disorders are separate entities and both can develop independently as a response to a traumatic experience.
The incidence of comorbid anxiety disorders is also elevated among individuals with PTSD. For example, lifetime comorbidity of panic disorder in Vietnam veterans with PTSD was 21% in females and 8% in males, versus 1.5 to 3.5% in the general population. The lifetime prevalence of obsessive-compulsive disorder was found to be 13% in females and 10% in males, as compared with 2.5 % in the general population.
There is a greater frequency of physical health problems among trauma victims than in the general population, especially among those who develop chronic PTSD. Trauma victims have higher rates of gastrointestinal disorders and pelvic or abdominal pain, and visit the doctor more often than the general population. In the aftermath of rape and child sexual abuse, gynecological and psychosexual problems such as vaginal discharge, dysmennorhea, dyspareunia, vaginismus, and pelvic pain have also been noted.
Reactions to trauma have long captured the interest of theorists of psychopathology. Janet’s 1889 theory of reactions to trauma has influenced both early and contemporary conceptualizations. Janet proposed that when confronted with a traumatic event that besieges the victim with an overabundance of intense thoughts and feelings, too numerous or intense to integrate, some individuals selectively attend away from the trauma to trauma-irrelevant thoughts and feelings. Thus, ideas related to the trauma remain split off or dissociated from normal consciousness and become “fixed.” Although out of consciousness, these “fixed ideas” remain part of the victim’s ideational content, and therefore continue to exert influence over his or her thought, mood, and behavior in the form of fragmented reliving of the trauma such as visual images, somatic states, emotional conditions, or behavioral reenactment.
Freud wrestled with understanding the influence of traumatic experiences on the individual’s psyche. In early writings, he was influenced by Janet’s theory on the strength of the emotional reactions that are produced by a traumatic experience and that force the victim to become fixated on the trauma. Later, Freud abandoned the dissociation view and proposed that the persistence of trauma reactions reflects an association between the traumatic event and childhood repressed conflicts, ideas, or impulses, and the efforts to prevent conscious awareness of them. He also coined the concept of “repetition compulsion” to explain trauma reexperiencing, proposing that because of the need to keep it away from consciousness, the individual is forced to repeat aspects of the trauma as a contemporary experience rather than as a memory of it. Influenced by World War I experiences, Freud refocused on the external reality, and, in the spirit of Janet, viewed the emotional upheaval generated by the trauma as the source of traumatic neurosis. He suggested that the intensity of the trauma, the inability to find conscious expressions for it, and the unpreparedness of the individual cause a breach to the stimulus barrier and overwhelm the defense mechanisms. More recent theorists have proposed that the developmental level and ego resources available to the victim are central to the manner in which the trauma is experienced and to the production of symptoms. For instance, a young child, easily overwhelmed and flooded with emotion, may experience complete helplessness in the face of trauma, whereas a mature adult would be more likely to respond through emotional numbing and cognitive constriction. Psychoanalytic theorists and practitioners focus on the need to help the victim acknowledge and bear the trauma and the resulting psychic damage, and develop coping mechanisms such that the memories of the trauma are incorporated into his or her current experience.
Several schools of thought inspired cognitive-behavioral theories of PTSD. The first is learning theory, which explains PTSD symptoms in terms of instrumental and classical conditioning. The learning model that most directly influenced cognitive-behavioral treatments (CBT) aimed at anxiety reduction was Mowrer’s two-factor theory. First, Mowrer proposed that fear is acquired through classical conditioning, where a neutral stimulus comes to evoke fear through its pairing with an aversive stimulus. Applying this theory to explain PTSD symptoms, neutral stimuli (e.g., supermarket) that were present during the trauma are presumed to acquire the ability to elicit fear through their associations with the danger stimuli (e.g., gun). Through the processes of generalization and second-order conditioning, stimuli similar to those present during the trauma also come to evoke fear. For instance, the stimuli all men, being alone, and the word rape can all acquire the capacity to cause anxiety. In Mowrer’s second stage, avoidance behavior is established through the process of operant conditioning. That is, an individual learns to reduce trauma-related anxiety through avoidance of, or escape from, the feared stimuli. Escape and avoidance behaviors are negatively reinforced because avoidance diminishes the aversive fear state.
Cognitive-behavioral therapy of PTSD has also been influenced by cognitive theory. Cognitive theory assumes that the interpretation of events, rather than events themselves, underlies emotional reactions. Accordingly, an event can be interpreted in different ways and consequently can evoke different emotions. Aaron Beck and colleagues suggest that trauma victims who manifest chronic persistent anxiety are unable to discriminate between safe and unsafe signals, and consequently their thinking is dominated by the perception of danger. They also suggest that traumatic fear can be maintained through a sense of incompetence to handle stressful events.
Other cognitive theorists have postulated that cognitive schemas are disrupted after victimization. A schema is a meaning structure that guides the perception, organization, and interpretation of incoming information. Common to these theories is the supposition that a traumatic experience requires cognitive modification and that such modification is accomplished by assimilation and accommodation. Accordingly, the victim must either assimilate the traumatic experience into preexisting schemas, or, more often, change schemas to accommodate the traumatic experience. In her 1992 book, Janoff-Bulman took the position that people in general hold the assumptions: “the world is benevolent, the world is meaningful, and self is worthy,” and these assumptions are incompatible with a traumatic experience. Building on Janoff-Bulman’s ideas, other theorists suggest that the following areas are of particular relevance: safety, dependency/trust of self and others, power, esteem, intimacy, and independence.
Coming from the psychoanalytic tradition, Horowitz integrated psychoanalytical and information processing notions in his 1986 book, suggesting that people have a basic need to match trauma-related information with their “inner models based on old information.” The process of recovery entails the repeated revision of both trauma-related information and the inner models until they agree, which Horowitz referred to as the “completion tendency.”
Foa and Kozak integrated cognitive and learning theories to explain the development and maintenance of pathological anxiety in what they called emotional processing theory. In their 1986 paper, fear is conceived as a cognitive structure or a program for escaping danger which includes representations of fear stimuli, fear responses, and their meaning. Pathological fear, they suggested, is distinguished from normal fear in that it includes erroneous associations and evaluations. Emotional processing theory views anxiety disorders as representing distinctive fear structures in memory, and the persistence of anxiety symptoms is conceived as reflecting impairment in emotional processing. Accordingly, PTSD is construed as reflecting a fear memory that contains erroneous associations and evaluations, whereas a normal trauma memory reflects associations and evaluations that better match reality. First, a pathological PTSD structure contains excessive response representations that are reflected in the PTSD symptoms. Second, this structure includes erroneous stimulus-stimulus associations that do not accurately represent the world. For example, the pathological fear structure of a woman who was raped at gunpoint by a bald man would contain an association between “bald men” and “gun.” In reality, however, bald men are not more likely to carry guns or to rape than men with a full head of hair. Third, the structure also includes erroneous associations between harmless stimuli such as “bald,” “home, …. suburbs,” and the meaning of “dangerous.” Being raped one time while at home in the suburbs does not tangibly increase the chance of encountering violence in that environment. Fourth, the structure includes erroneous associations between harmless stimuli and escape or avoidance responses. For example, the victim who was raped by the bald man would tend to run away from such men. In reality, however, running away from “bald men” is not likely to enhance safety. These erroneous associations would lead to mistakenly interpreting the world as entirely dangerous.
Another set of erroneous associations and evaluations is the interpretation of the victim’s response representations. It is thought that the victim’s responses during and after the trauma, and in particular the PTSD symptoms, are interpreted to mean self-incompetence. In summary, emotional processing theory hypothesizes that two major pathological concepts underlie PTSD: the world as entirely dangerous, and the self as entirely inept.
Psychophysiological, neurohormonal, neuroanatomical, and immunological changes have been observed in animals exposed to extreme stress and in trauma victims who developed PTSD (van der Kolk, McFarlane, & Weisaeth, 1996). These changes have been hypothesized to disregulate responses to incoming information and to inhibit successful processing of traumatic memories.
The normal stress response upon exposure to a high-magnitude stressor is a complex neurohormonal response, including the release of catecholamines (e.g., epinephrine and norepinephrine), serotonin, endogenous opioids, and hormones of the hypothalamus, pituitary, or adrenal gland (e.g., cortisol, vasopressin, oxytocin). Normally, the introduction of a stressor produces intense and rapid stress responses, and these dissipate quickly after the removal of the stressor. However, after prolonged exposure to stress, the stress responses become disregulated.
Theorists propose that PTSD reflects a failure to regulate autonomic reactions to stimuli such that the individual either experiences hyperreactivity or “shutting down” and emotional numbing. Individuals with PTSD show hyperreactivity, as measured by heart rate, skin conductance, and blood pressure, in reaction to reminders of traumatic events. This disregulation of the emotional and physiological responsiveness occurs with specific reminders of the trauma as well as in reaction to intense but neutral stimuli, signifying a loss of stimulus discrimination. In addition, the individual may come to fear his or her emotional reactions because of being able to do little to control them.
Neurohormonal changes in individuals with PTSD have also been found. First, prolonged stress causes depletion of the noradrenergic system, such that receptors become hypersensitive to any new release of norepinephrine. This noradrenergic hyperreactivity is linked to the increased arousal and startle of PTSD. The high levels of norepinephrine are proposed to inhibit the release of corticotrophin-releasing hormone and thereby inhibit the entire hypothalamic-pituitaryadrenocortical axis. This inhibition, in turn, produces a deficiency in endogenous opioids. Some theories postulate that the reexperiencing symptoms of PTSD cause a burst in the release of endogenous opioids and therefore make up for this deficiency. These endogenous opioids are thought to produce an artificial numbing or calmness, another hallmark of PTSD. Additional theories propose that cortisol responses are lowered in retraumatized individuals and that serotonin levels may decrease in response to prolonged inescapable stress.
In addition to psychophysiological and neurohormonal factors, specific brain abnormalities have recently been detected in individuals with PTSD. One system that is implicated in the disorder is the limbic system, which is thought to function in memory and in emotional reactions to incoming stimuli. One area in the limbic system, the hippocampus, is presumed to record spatial and temporal aspects of experiences in memory. Researchers have noted decreased hippocampal volume in trauma victims with PTSD compared with those without PTSD. One possible explanation for this finding is that individuals with smaller hippocampuses are more likely to develop PTSD; a more likely interpretation of these results is that increased cortisol activity causes shrinkage, because cortisol is toxic to the hippocampus.
A second area in the limbic system, the amygdala, also appears to be altered in individuals with PTSD. The amygdala is thought to assign meaning to incoming stimulation by integrating memory images with emotional experiences associated with those memories, guiding emotional behavior. A single intense stimulation of the amygdala appears to alter the limbic physiology such that a “kindling” effect occurs. That is, the behavior that follows may be predominantly either “fight” or “flight,” and a pattern of conditioned behavior is set up such that there is limited processing of incoming information before the response is initiated.
Several psychological interventions have been used with trauma victims, including supportive counseling individually or in groups, brief dynamic psychotherapy, hypnotherapy, pharmacotherapy, and cognitivebehavioral therapy. As recently reviewed by Foa and Meadows, although a variety of psychological interventions are used routinely with trauma victims, controlled outcome studies have tended to focus on cognitive-behavioral treatments such as systematic desensitization, exposure, and anxiety management. Nevertheless, hypnotherapy and psychodynamic therapy have also shown promise in the few studies examining their efficacy.
The popular supposition among trauma theories is that for recovery to occur after a traumatic experience, special processing efforts should take place. This view has prompted the development of early intervention programs. These programs have focused on education, debriefing after trauma, and training professionals at risk (e.g., police). Usually, “critical incident stress debriefing” is conducted in groups, such as emergency workers, and focuses on education about common reactions to traumatic experiences, encouraging trauma victims to process their experiences in a group setting. Although such programs have become routine in many places, little is known about their efficacy. In fact, some experts have raised concerns that such programs could interfere with rather than facilitate the natural recovery process.
The recognition that victims who exhibit severe reactions immediately after the trauma are more likely to develop chronic dysfunction has prompted researchers to implement interventions that aim to prevent chronic PTSD. Foa and colleagues conducted a study to compare PTSD severity of female assault victims, who received a brief prevention program (four individual therapy sessions), to that of victims who underwent an assessment procedure. Victims who received the brief prevention program had less severe PTSD and depressive symptoms 2 months after the assault. Clearly, more studies of this type are needed before confidence in prevention efforts can be established.
Currently, five cognitive-behavioral interventions are in use for PTSD: Prolonged Exposure, cognitive therapy, Stress Inoculation Training, Cognitive Processing Therapy, and Eye Movement Desensitization and Reprocessing.
This is a set of procedures that involves confrontation with feared stimuli, either in vivo or in imagination. With PTSD, exposure therapy typically includes repeated reliving of the traumatic event in imagination and actual confrontation with feared situations and objects that have been avoided because they are reminders of the trauma but are not intrinsically dangerous.
As discussed earlier, the theoretical basis of PE lies in learning and emotional-processing theories. Foa and Kozak have proposed that successful therapy involves correcting the pathological elements of the fear structure, and that this corrective process is the essence of emotional processing. They further suggest that regardless of the type of therapeutic intervention used, two conditions are required for fear reduction. First, the fear structure must be activated through introduction of fear-relevant information. If the fear structure is not activated (fear is not evoked), the structure would not be available for modification. Second, during exposure, information that is incompatible with the existing pathological elements (e.g., fear reduction) must be provided so that the pathological fear structure can be corrected. Specifically, exposure researchers hypothesize that repeated reliving promotes several cognitive changes. First, it promotes habituation of anxiety associated with the trauma memory, and this habituation disconfirms the victim’s erroneous belief that anxiety will stay forever and therefore lead to disastrous consequences. Second, reliving promotes discrimination between “remembering” the trauma and “encountering” it again, thus reinforcing the realization that remembering itself is not dangerous. Third, repeated exposure promotes differentiation between the trauma and similar but safe situations, disconfirming the idea that the world is extremely dangerous. Fourth, it promotes the association between PTSD symptoms and a sense of mastery, rather than incompetence. Finally, repeated recounting of the trauma narrative helps to organize the narrative and thereby to facilitate the integration of the trauma memory.
Several controlled studies on exposure have shown their usefulness in treating PTSD. Whereas studies on veterans showed only modest improvement, two studies with female rape victims showed more improvement. Foa and colleagues found that exposure (imaginal and in vivo) was effective in eliminating PTSD in 55% of rape victims with chronic PTSD compared with 45% of those who received supportive counseling. Superior results were found in a second study: about 70% of victims who received Prolonged Exposure lost their PTSD diagnosis, and none of the women in a wait-list group lost their diagnosis. These treatment effects were maintained at 6-month follow-up.
This intervention consists of training victims to handle anxiety with several skills for anxiety management: relaxation, thought stopping, assertiveness, cognitive therapy, coping self-statements, and guided imagery. Although the direct goal of anxiety management techniques is to teach patients techniques to manage their anxiety, the successful acquisition of such techniques can have indirect effects on the victim’s schemas of self and the world. Specifically, the victim’s experience of being able to control the anxiety fosters a more positive self-image and thereby modifies the perception of the world as overwhelmingly dangerous. Several studies point to the efficacy of this program used alone or in combination with other techniques. For example, the two studies on rape victims reported earlier found that SIT significantly reduced PTSD, to a degree comparable to that of exposure.
Researchers believed that if PE and SIT are quite, but not completely, successful in ameliorating PTSD symptoms, a program that combined these two treatments would yield superior results. However, research does not support this view: combined programs were helpful for female assault victims, but not more than exposure or stress inoculation alone.
Cognitive techniques are often incorporated into anxiety management programs that teach patients to examine and change systematically maladaptive thoughts that can lead to negative responses. Cognitive therapy involves the use of discourse, in which the patient is taught to identify the beliefs underlying the fear, to examine whether they are distorted or accurately reflect reality, and to replace mistaken or dysfunctional beliefs with more realistic, functional ideas about the ability of the patient to cope with stress and the dangerousness of the world. One possible benefit of cognitive restructuring is that it addresses directly beliefs underlying emotions other than fear, such as anger and guilt. Early investigations of this technique revealed some promise in the use of this therapy to reduce symptoms of PTSD in rape victims.
Another cognitive-behavioral program called Cognitive Processing Therapy is described in Resick and Schnicke’s 1992 book. It involves cognitive restructuring and exposure through writing about the trauma. The cognitive therapy is geared toward correcting maladaptive cognitions associated with rape, such as power, safety, and esteem. In one study, on the average, victims who received CPT reported 40% symptom reduction, and these gains were maintained over time. More studies are needed to establish the efficacy of this relatively new treatment.
This therapy, described by Shapiro in 1995, is a form of exposure with a cognitive emphasis, accompanied by guided eye movements. The studies that have evaluated the efficacy of this treatment produced equivocal results. Some show good results, but others show no improvement. Because these studies have many methodological problems, it is difficult to determine the validity of the findings. Further well-controlled studies are needed before a definite conclusion about the value of EMDR can be made.
Many medications have been used for the treatment of PTSD, but only a few have been systematically studied. Most of these have used male combat veterans, and thus the efficacy of pharmacotherapy for other traumatized populations is largely unknown. Tricyclic antidepressants have been used in an attempt to reduce locus coeruleus overactivity and noradrenergic disregulation found in PTSD, with equivocal results. Amitriptyline and imipramine have shown modest reductions in PTSD symptoms in comparison with placebo in double-blind studies with male veterans. In contrast, desipramine failed to show efficacy. One study of fluoxetine, a selective serotonin reuptake inhibitor used to regulate serotonergic dysfunction in individuals with PTSD, found it to be effective in reducing symptoms of PTSD, especially in trauma victims other than Vietnam veterans.
Other medications that have been tested include anticonvulsants such as carbamazepine and valproic acid; but no double-blind studies have been conducted to date. Beta-adrenergic blockers such as propanolol have shown promise in reducing aggressivity and arousal symptoms in open studies, and alpha2-adrenergic agonists, such as clonidine, appear to be effective through their suppression of locus coeruleus activity.
Finally, benzodiazepines have been widely used to suppress anxiety and are believed to reduce PTSD symptoms by reducing limbic system kindling and reversing neurochemical changes in the locus coeruleus and hypothalamus. However, the rebound anxiety and withdrawal symptoms associated with benzodiazepines can be problematic.
In summary, most of our knowledge about efficacy of pharmacotherapy for PTSD is confounded by the restricted samples used in existing studies. Most were conducted on Vietnam veterans, whose symptoms are particularly resistant to all types of treatments, and therefore the present results may underestimate the efficacy of this treatment.
Hypnotherapy uses heightened concentration and focused attention to facilitate treatment related to trauma. It is based on the supposition that individuals with PTSD are unknowingly entering trance states when they reexperience the trauma and that hypnotherapy can help them learn how to control their trance states and digest the dissociated traumatic experience in a controlled manner. One study found hypnosis to be as effective as psychodynamic psychotherapy and a type of exposure called systematic desensitization. More studies of this technique are needed before conclusions can be drawn about the usefulness of hypnotherapy.
Psychodynamic psychotherapy has also been used to help individuals recover from trauma. It focuses on intrapsychic conflict about the trauma rather than on resolution of specific symptoms of PTSD. The methods used are in some respects similar to those used in cognitive-behavioral therapy, as these interventions focus on helping the victims process the traumatic experience and on teaching them how to tolerate anxiety. Both individual and group therapies have been used, and some preliminary studies suggest the utility of these interventions.
Bibliography:
- American Psychiatric Association. (1994). Diagnostic and statistical manual (4th ed.). Washington, DC: American Psychiatric Press.
- Davidson, J. R. T., & Foa, E. B. (Eds.). (1993). Post-traumatic stress disorder: DSM-IV and beyond. Washington, DC: American Psychiatric Press.
- Foa, E. B., & Kozak, M. J. (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99, 20-35.
- Foa, E. B., & Meadows, E. A. (1997). Psychosocial treatments for post-traumatic stress disorder: A critical review. In J. Spence (Ed.), Annual review of psychology. Palo Alto, CA: Annual Reviews, Inc.
- Foa, E. B., & Riggs, D. S. (1993). Post-traumatic stress disorder in rape victims. In J. Oldham, M. B. Riba, & A. Tasman (Eds.), American psychiatric press review of psychiatry (Vol. 12, pp. 273-303). Washington, DC: American Psychiatric Press.
- Horowitz, M. J. (1986). Stress response syndromes (2nd edition). Northvale, NJ: Jason Aronson, Inc.
- Janet, P. (1889). L’Automatisme psychologique. Paris: Felix Alcan. (Reprinted 1973, Paris, Societe Pierre Janet.)
- Janoff-Bulman, R. (1992). Shattered assumptions: Towards a new psychology of trauma. New York: Free Press.
- Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Post-traumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048-1060.
- Resick, P. A., & Schnicke, M. K. (1992). Cognitive processing therapy for sexual assault survivors: A treatment manual. Newbury Park, CA: Sage.
- Shapiro, F. (1995). Eye movement desensitization and reprocessing: Basic principles, protocols, and procedures. New York: Guilford Press.
- van der Kolk, B. A., McFarlane, A. C., & Weisaeth, L. (Eds.). (1996). Traumatic stress: The effect of overwhelming experience on mind, body, and society. New York: Guilford Press.
- World Health Organization. (1993). ICD- I O: The ICD- IO classification of mental and behavioural disorders: Diagnostic criteria for research. Geneva, Switzerland: Author.
ORDER HIGH QUALITY CUSTOM PAPER

112 PTSD Essay Topic Ideas & Examples
🏆 best ptsd topic ideas & essay examples, 👍 good essay topics on ptsd, ⭐ simple & easy ptsd essay titles, ❓ ptsd research questions examples.
- PTSD in Charlie of “The Perks of Being a Wallflower” As an example of the latter, this paper focuses on the analysis of Charlie Kelmeckis, the protagonist of Stephen Chbosky’s novel The Perks of Being a Wallflower, and his PTSD.
- Post-Traumatic Stress Disorder: Case Conceptualization Samuel, an 8-year-old black male, lives in an adopted white family consisting of the father, incarcerated for domestic violence charges, the mother, the primary caretaker and the only home provider, and the older sibling. We will write a custom essay specifically for you by our professional experts 808 writers online Learn More
- Post Traumatic Stress Disorder (PTSD) as a Health Issue in the Society The treatment is aimed at relieving the symptoms that the patient seems to be experiencing so that the individual can be able to deal with the traumatic experience.
- Zaccari et al. (2020). “Yoga for Veterans With PTSD”: Content, Strength, and Weaknesses This discussion reviews the strengths and weaknesses of the method, sampling, and validity of Zaccari et al.research. The assertions reported in the article are supported by cited and referenced scientific studies, which enhances the validity […]
- Living With Post Traumatic Stress Disorder This can be achieved by making efforts to keep away from the people and also the places that act as a reminder of the events.
- Post-Traumatic Stress Disorder Assets and Facilities It was easy to detect PTSD assets and facilities in the area, as the society and the government are currently establishing a vast amount of amenities for this disorder.
- Aspects of the Posttraumatic Stress Disorder They include direct or indirect exposure to stressors, intrusion symptoms, the persistent avoidance of trauma-related stressors, negative alterations in mood and the development of mental health comorbidities, aggression, and self-destructive behavior, the duration for not […]
- The Importance of PTSD for Master Leaders Course in the Army The multiplicity of this manifestation and presentation of PTSD creates a research question focusing on the need for research into the main types of disorder and the support.
- Self-Reported PTSD (Posttraumatic Stress) Symptoms and Social Support At the same time, multiple authors prove that social support and connectedness with family members, relatives, friends, and other members of the community contribute to PTG and the minimization of the signs of PTSD in […]
- The Traumas from Post Traumatic Stress Disorder Measuring the prevalence and incidence of PTSD requires excellent knowledge of epidemiology and biostatistics. The prevalence and incidence of PTSD have increased since 2000.
- Post-Traumatic Stress Disorder: Preliminary Care Coordination The personal character of trauma and how the patient reacts to it justifies the need to design patient-centered interventions to address this healthcare problem.
- Post-Traumatic Stress Disorder: Causes and Symptoms The article by Smith entitled Posttraumatic Stress Disorder is valuable because it offers important information on the causes and symptoms of PTSD and ways of recognizing and treating the condition.
- Major Depressive Disorder and Post-Traumatic Stress Disorder Her sleep is turbulent, she has rape nightmares, her mood is depressed, and her affect is congruent and constrained. Her mental process is rational and linear, and her mental faculties are largely intact.
- Posttraumatic Stress Disorder: Case Presentation Report Date of initial assessment: N/A PSEUDO Name: Ana Ana is a self-referred and re-occurring client who entered counseling after the case of domestic violence. As a result, Ana expressed feelings of anxiety and fear […]
- The DSM-5 Criteria for Posttraumatic Stress Disorder The inference is backed by the fact that Victor’s traumatic situation is persistently manifesting intrusion symptoms such as nightmares, flashbacks, unwanted upsetting memories, and a lack of willingness to share previous hurtful events. Victor displays […]
- Posttraumatic Stress Disorder Treatment Research Therefore, the advantage of qualitative research, in this case, relates to the ability to investigate patients’ PTSD treatment experiences and uncover their meanings.
- Post-Traumatic Stress Disorder Misapprehension A significant proportion of civilians are affected by post-traumatic stress but ignore the symptoms and fail to seek early interventions influenced by misconceptions about how PTSD develops and its symptoms.
- Post-Traumatic Stress Disorder and Opioid Use in Veterans This study examined the proportion of United States veterans who had PTSD and engaged in the use of illegal opioids to cope with it or had done so in the past.
- Post Traumatic Stress Disorder in A Journal for Jordan Considering the loss of her husband in the war, Dana had not recovered, and the expression of irate reaction is a symptom of PTSD.
- Post-Traumatic Stress Disorder Development Avoidance of objects that remind you of the traumatic incident is another symptom of PTSD. Identifying erroneous and unreasonable beliefs about the incident and replacing them with a more balanced image is also part of […]
- Sexual Aversion and Post-Traumatic Stress Disorder This aspect causes difficulties in prescribing therapy, since the latter requires a thorough study of the psychological nature of the problems. In the treatment of sexual aversion disorder, a doctor needs to investigate a complex […]
- Secondary Post Traumatic Stress Disorder in Children The relationship between parents’ experiences and interactions with the onset of PTSD in children will be explored. There is vast information on the management of treatment and prevention of PTSD in children.
- Aspects of Secondary PTSD in Children They constantly contact and interact with each other, and the latter inadvertently affects the mental health of the former, which leads to the development of secondary PTSD.
- Post-Traumatic Stress Disorder and Parenting Style On a scale of 1 to 10, with 1 being lowest and 10 being highest, how much do you believe that kids need to learn early who the boss is in the family?
- Psychiatry: PTSD Following Refugee Trauma The psychiatrists finally recognized PTSD in the first version of the Diagnostic and Statistical Manual of Mental Disorders after the mass occurrence of similar symptoms in Vietnam veterans.
- 35-Year-Old Man With PTSD: Case Study In such a case, it is recommended this is precisely a recommendation, not a requirement to do an MRI, which would allow a better study of the patient’s body.
- PTSD Dual Representation Theory Use in Military Personnel However, it is the position of this paper that this is mere gender stereotyping and the real cause of trauma among women veterans has to do with sexual harassment.
- Post-Traumatic Stress Disorder and Substance Use Disorder The hypothesis of self-medication is one of the mechanisms that can expound the comorbidity between post-traumatic stress disorder and anxiety illness.
- Substance Abuse Disorders and PTSD The concept indicates that people who have PTSD are at higher risk of substance abuse and consequently substance disorders due to the tendency to consume alcohol and use drugs to deal with stress.
- “Mindfulness Interventions in the Treatment of PTSD” by Williston The primary purpose of that article is to conduct a survey of meta-analyses related to the efficiency of cognitive behavioral therapy.
- “Experiences of Military Spouses of Veterans With Combat-Related PTSD” by Yambo Spouses living with PTSD veterans are unprepared and struggling to deal with issues that their husbands experience.
- Post-Traumatic Stress Disorder Pathophysiology Sakellariou and Stefanatou, further link threat responsiveness and fear regulation with the signalling of 5-HT within the amygdala; this is an area within the brain deemed essential in comprehending the reaction to fear and aetiology […]
- The Fiction Character`s PTSD Diagnosis: Rambo According to the American Psychiatric Association, experiencing traumatic events, witnessing the events, learning that a traumatic event occurred to a close person, and is exposed to aversive details of events are the triggers of PTSD.
- IL-6: Predicting the Development of PTSD Therefore, it is important to understand and define the biological underpinnings of immune dysregulation in PTSD as it also plays a crucial role in helping us to understand the nature of the associations between PTSD […]
- Cognitive Processing Therapy and Evidence Based Interventions for Veterans Diagnosed With PTSD According to the evidence attained, comprehensive and extensive evidence is crucial in providing a clear correlation of the benefits accrued from CPT in comparison to other forms of treatment.
- Effective Use of Prazosin for Posttraumatic Stress Disorder All the traditional agents have shown to have several side effects and cannot be fully relied on in treatment of PTSD.
- Post-Traumatic Stress Disorder Diagnostics and Screening Do you observe a headache from the early morning? Do you have a headache when you sleep well?
- PTSD Mental Disorder: Triggers, Clinical Manifestations, and Treatment PTSD is normally characterized as a mental disorder that is a direct result of anxiety-related syndromes that came about as a direct result of a traumatic event.
- Posttraumatic Stress Disorder The study seeks to find out the prevalence of TBI/PTSD and the variations in the prevalence based on the severity of TBI, as well as other related variables.
- Post-Traumatic Stress Disorder (PTSD) Among Vets One of the integral components of this concept is the problem of traumatic stressors, as is customary in international classifications, the issue of post-traumatic stress disorder.
- Post-Traumatic Stress Disorder: Overview The overall process of evaluation and analysis of the film was done correctly and adhered to the standard principles of counseling.
- Post-Traumatic Stress Disorder Treatment in Intellectually Disabled Patients: The Promise of Eye Movement Desensitization and Reprocessing Therapy The use and application of findings that shed light on current research gaps related to the effectiveness of EMDR in PTSD patients with IDs may contribute to improvements in this population’s quality of life and […]
- Client Diagnosis: Posttraumatic Stress Disorder As for the PTSD itself, the client meets criterion A because she reported car accident involving death of the other passenger.
- Disaster Crisis: Post-Traumatic Stress Disorder Symptoms Since the account of the incidence, almost a month, she lost interest in work and concentration on activities relating to work at her place of work.
- Posttraumatic Stress Disorder After Rape Attempt During the treatment of the patient, the Target Memory is the day the girl was attacked. In her treatment, it is necessary to eliminate the feeling of guilt for the accident.
- Post Traumatic Stress Disorder: Causes and Consequences An interesting finding from the interview is that Abby and her husband had faced the accident together, however, the reactions of the two to the accident were radically different.
- Post Traumatic Stress Disorder: German Researches The other objective of the study was to identify the specific features a traumatic event could influence PTSP in the solders.
- Posttraumatic Stress Disorder in Veteran Community The creation of special programs for the rehabilitation of veterans helped alleviate the problem of PTSD during the wars in Iraq and Afghanistan and facilitated the development of a support system that is currently used.
- “Emotional Freedom Technique and Post-Traumatic Stress Disorder” by Rebecca L. Fahey The author considers a special method of influencing military veterans who experience the effects of PTSD and feel acute bouts of depression.
- Post-Traumatic Stress Disorder and Treatment Effectiveness In the final section, the effectiveness of all the explored interventions will be discussed to summarize the results of the present literature review.
- Post-Traumatic Stress Disorder in Missouri Veterans Unfortunately, the implemented policies have failed to meet the needs of different veterans, such as the Welcome Back Veterans, the Veterans Health Administration, and the Military Health System. Louis has several policies and programs aimed […]
- Posttraumatic Stress Disorder Management in Children The purpose of this paper is to determine whether the application of the perspective of clinical psychology as the platform for treating PTSD in children will have better effects than the adoption of the methods […]
- Racial Disparities in Posttraumatic Stress Disorder Treatment Within the framework of this submission, the author is going to discuss several components that may critically impact the complexity of psychological traumas received by African American soldiers and provide a conceptualized policy that will […]
- Posttraumatic Stress Disorder in Hispanic Teenager Family dynamics and social withdrawal do not seem to have affected the client’s academic history; her grades are good and she has no history of behavioral problems.
- Posttraumatic Stress Disorder Treatment in Soldier Within the framework of the reviewed case, one of the key needs of the soldier is to be able to cope with anger and irritation.
- Cognitive Behavioral Therapy in Treating PTSD The chosen case is the case of Ivan S, who is a war veteran who suffers from a variety of psychological symptoms that affect his relationships with his family and loved ones. Secondly, Ivan shows […]
- Posttraumatic Stress Disorder: Modality Treatment Plan With the problem of nightmares and the related lack of sleep, the unmet need of psychological stability results in the interruption of sleep because of traumatic thoughts and nightmares.
- Post-Traumatic Stress Disorder and Its Theories The study by Bandelow et al.showed that the development of PTSD is associated with the dysregulation of the hypothalamic-pituitary-adrenal axis and the impaired sympathoadrenal medullary system as part of immunity.
- Emotion Regulation and Posttraumatic Stress Disorder This choice can be attributed to the positive role of the family in the emotional and cognitive function of a sufferer. The proposed intervention is to be in the form of a workshop for families […]
- PTSD as the Primary Factor Causing Infant Death The lack of studies on the issue of expecting mothers and their subgroups needs to be mentioned among the primary issues that hamper the process of addressing the problem concerning high infant death rates.
- Kant’s and Mill’s Ideas for Post-Traumatic Stress Disorder From this review, the fourth section of the paper outlines the more compelling view, which is that Kant’s vision of a good life is more superior to Mill’s vision of the same.
- Post Traumatic Stress Disorder or Combat Fatigue According to Walser, the use of acceptance and commitment therapy is effective in treating a case of post-traumatic stress disorder, which entails the patients to experience positive and negative events without treating them as reality.
- Post Traumatic Stress Disorder: Caucasian Girl’ Case In Mary’s case, the medical practitioner will listen and encourage her to talk about the events when she feels ready. As a result, she will be in a better position to cope with the problem.
- “One Family’s Fight Against PTSD” by Shawn Gourley It was a counselor, who precipitated the harmony in the family explaining both husband and spouse the fact that their life could not be the same as before.
- Post-Traumatic Stress Disorder in Soldiers With the help of the course materials, I was able to understand that Huerta had a panic attack just from its description. It is critical to be honest with oneself and to accept the problem.
- Post-Traumatic Stress Disorder: Gender Variations In this regard, the aim of the current research is to provide evidence that women have the same probability of getting PTSD as men.
- Post Traumatic Stress Disorder: Joseph Wolpe Treatment Theory This is similar to the concept of phobias wherein a person is presented with an animal that he is irrationally afraid of and the result is fear or in the case of an inanimate object […]
- SNOMED-CT and PTSD Terminologies Based on the research questions described in the foregoing discussions, the researchers mapped a total of 153 PTSD-specific concepts and terms to the SNOMED-CT controlled medical terminologies and concept codes.
- Post-Traumatic Stress Disorder – Psychology Post-traumatic stress disorder is thought to be as a result of either corporeal disturbance or emotional disturbance, or more often a mishmash of both.
- Post Traumatic Stress Disorder Principles and Types The affected areas of the body include the nervous system, the brain and hormonal system. A number of issues are to be taken into consideration as for the treatment of the PDST.
- Post-Traumatic Stress Disorder in Veterans Patient education is important in order to eradicate any form of misconception that the patients may have about PTSD, and enhance the levels of understanding of the patients, along with an improvement on their ability […]
- Post-Traumatic Stress Disorder: Causes, Symptoms and Treatments One who is trying to numb and avoid remembrance of the event is likely to avoid thoughts, activities, places and even feelings that may associate with the trauma, have a feeling of detachment from others […]
- Critical Review of a Mental Disorder: The Post Traumatic Stress Disorder in DSM-IV-TR However, the risk to contracting the condition is always determined by the resilience of the personnel to these exposures, past unsettled concerns in their life history, and the quantity as well as intensity of depiction […]
- Post Traumatic Stress Disorder and Its Treatment In this case a person constantly relieves the event through any of the following exposure to a situation that is similar to the event, vivid memories of the event, perceptions, and sometimes through dreams.
- Comparison of the Etiology, Diagnosis, and Treatment of DID and PTSD Individuals who were exposed to acts of violence in the past are likely to try and expose others to similar conditions. The inability to diagnose is attributed to the fact that the effects of these […]
- Post-Traumatic Stress Disorder and Abused Women In most cases, these incidences of women abuse occur within the confine of a family set up or relationship where one partner tends to mistreat, mishandle, abuse and assaults the other partner and in most […]
- Post Traumatic Stress Disorder: History and Symptoms This essay looks into the history, the symptoms of posttraumatic stress disorder, and the individuals who are likely to suffer from this condition, psychological problems associated with this condition and the treatment of the disorder.
- Earthquakes as a Cause of the Post Traumatic Stress Disorder Although earthquake is a major cause of the post traumatic stress disorder, there are other factors that determine the development of the same.
- Post Traumatic Stress Disorder Developed in Repeated War Zones Deployment Most of the combatants, usually, tailored a war awareness state to manage the consistent pressure of battle duty. Majority of the combat soldiers that were repeatedly deployed to war zones suffered post traumatic stress disorders.
- Effects of PTSD and Correlation between Diagnosis and Violence It is also worth noting that there is a correlation between PTSD and violence, though this has been cited to be of minimal significance.
- Abnormal Psychology: Posttraumatic Stress Disorder In addition, some of this research indicates that the differences in the degree of the disorder are due to the varying nature of the trauma experienced by that individual.
- Post Traumatic Stress Disorder: Assessment and Treatment Strategies If PTSD is ignored and fails to be treated, it can lead to disturbing consequences which widely affects not only the PTSD victim but also the relationships of the victim with his family and the […]
- The Effects of PTSD on Families of Veterans Drug abuse may result from the inadequacies in the coping abilities of family members as they try to come into terms with the suffering of their fellow family member.
- Post Traumatic Stress Disorder in Veterans and How Family Relationships Are Affected Both qualitative and quantitative data shall be used with numbers being used to provide evidence of the occurrence and magnitude of the effects of the condition on the population.
- Characteristics and Treatments of Post Traumatic Stress Disorder For in-depth understanding of the background of PTSD is, this paper will adopt a specific definition of abnormality that relates to the disorder itself. The category of the syndrome will also determine the type of […]
- Analysis of Posttraumatic Stress Disorder in Military Personnel The experiences that military personnel undergo determine the nature and extent of the posttraumatic stress disorder they develop during and after their deployment. However, Ramirez had resilience factors that helped him to cope and manage […]
- How PTSD Affects Veteran Soldiers’ Families The effects are even worse to the partner who is left behind; whether wife or husband because they are required to care for the children and the thought of being the sole bread winner makes […]
- What Are the Signs of PTSD?
- How Dogs Can Help Veterans Overcome PTSD?
- What Is PTSD Usually Caused By?
- How Do People Deal With PTSD?
- What Are the Symptoms of PTSD?
- What’s the Difference Between PTSD and TBI?
- How the Cherokee Nation Can Overcome Generational PTSD?
- Why Are People With PTSD Angry?
- Does PTSD Change Personality?
- What Happens if PTSD Is Untreated?
- How Does PTSD Effect Veterans?
- What Is the Diagnostic Criteria for Post-traumatic Stress Disorder?
- Is PTSD a Permanent Disorder?
- What Type of Mental Disorder Is PTSD?
- Can PTSD Cause Mental Breakdown?
- What Are PTSD Triggers?
- Are People With PTSD Mentally Ill?
- How Do Doctors Test for PTSD?
- Can PTSD Be Mistaken for Bipolar?
- What Are the Causes and Psychological Consequences of Post-traumatic Stress Disorder?
- What Do PTSD Episodes Look Like?
- What’s It Like Living With Someone With PTSD?
- Can PTSD Cause Jealousy?
- Does PTSD Affect Intimacy?
- Can PTSD Cause Emotional Detachment?
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, March 1). 112 PTSD Essay Topic Ideas & Examples. https://ivypanda.com/essays/topic/ptsd-essay-topics/
"112 PTSD Essay Topic Ideas & Examples." IvyPanda , 1 Mar. 2024, ivypanda.com/essays/topic/ptsd-essay-topics/.
IvyPanda . (2024) '112 PTSD Essay Topic Ideas & Examples'. 1 March.
IvyPanda . 2024. "112 PTSD Essay Topic Ideas & Examples." March 1, 2024. https://ivypanda.com/essays/topic/ptsd-essay-topics/.
1. IvyPanda . "112 PTSD Essay Topic Ideas & Examples." March 1, 2024. https://ivypanda.com/essays/topic/ptsd-essay-topics/.
Bibliography
IvyPanda . "112 PTSD Essay Topic Ideas & Examples." March 1, 2024. https://ivypanda.com/essays/topic/ptsd-essay-topics/.
- Abnormal Psychology Paper Topics
- Cognitive Therapy Essay Topics
- Anxiety Essay Topics
- Evidence-Based Practice Titles
- Fear Questions
- Sexual Assault Essay Titles
- Mental Disorder Essay Topics
- Cognitive Behavioral Therapy Topics
- Slaughterhouse Five Titles
- Depression Essay Topics
- Psychopathology Paper Topics
- Mental Health Essay Ideas
- Stress Titles
- Medical Marijuana Topics
- Postpartum Depression Paper Topics
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can J Psychiatry
- v.59(9); 2014 Sep
Language: English | French
Posttraumatic Stress Disorder in Adults: Impact, Comorbidity, Risk Factors, and Treatment
Jitender sareen.
1 Professor of Psychiatry, Psychology, and Community Health Sciences, University of Manitoba, Winnipeg, Manitoba.
Associated Data
During the last 30 years, there has been a substantial increase in the study of posttraumatic stress disorder (PTSD). Several high-profile traumatic events, such as the wars in Afghanistan and Iraq, and the terrorist attacks of September 11 on the World Trade Center, have led to a greater public interest in the risk and protective factors for PTSD. In this In Review paper, I discuss some of the important advances in PTSD. The paper provides a concise review of the evolution of PTSD diagnosis in the Diagnostic and Statistical Manual of Mental Disorders, impact of PTSD in the community, an overview of the established risk factors for developing PTSD, and assessment and treatment. Throughout the paper, controversies and clinical implications are discussed.
Au cours des 30 dernières années, l’étude du trouble de stress post-traumatique (TSPT) a connu une croissance substantielle. Plusieurs événements traumatiques importants, comme la guerre en Afghanistan et en Irak, et les attaques terroristes du 11 septembre sur le World Trade Center ont suscité un plus grand intérêt du public pour le risque et les facteurs protecteurs du TSPT. Dans cet article d’In Review, je discute des importants progrès réalisés dans le TSPT. L’article offre un bref survol de l’évolution du diagnostic du TSPT dans le Manuel diagnostique et statistique des troubles mentaux, de l’impact du TSPT dans la communauté, d’un aperçu des facteurs de risque établis pour développer un TSPT, et de l’évaluation et du traitement. Les controverses et les implications cliniques sont discutées dans l’article.
Posttraumatic stress disorder is a prevalent mental health problem associated with substantial psychiatric morbidity. Although PTSD had been observed throughout history, PTSD was first introduced in the third edition of the DSM in 1980, and since, there has been a burgeoning amount of literature on this topic. More recently, there has been a rapid expansion in knowledge and interest in understanding risk factors for PTSD and its treatments. Several systematic reviews on the risk factors for development of PTSD have recently been written. In this paper, I will describe the changes in PTSD diagnosis in the DSM, the impact of PTSD in the community, and the most well-established risk and protective factors for PTSD. Throughout the paper, I will highlight clinical implications and controversies.
How Is PTSD Defined in DSM-5?
PTSD first appeared as a diagnosis in the third edition of the DSM. 1 Online eTable 1 describes the changes in criteria for PTSD during the course of different editions of the DSM. 2 – 5 There have been substantial changes in the criteria for PTSD in the DSM-5. PTSD has been removed from the “Anxiety Disorders” chapter and moved to a new chapter called “Trauma- and Stress-Related Disorders.” Although the exact definition of PTSD has varied across the different editions, 4 core features of PTSD have remained stable:
- experiencing or witnessing a stressful event;
- re-experiencing symptoms of the event that include nightmares and (or) flashbacks;
- efforts to avoid situations, places, and people that are reminders of the traumatic event; and
- hyperarousal symptoms, such as irritability, concentration problems, and sleep disturbances.
In DSM-5, an additional criterion of “negative alterations in cognitions and mood” 5, p 271 has been added. This criterion includes symptoms, such as persistent negative beliefs and expectations about oneself, persistent distorted blame of self or others, dissociative symptoms, feelings of detachment and constricted affect.
Clinical Pearls
As PTSD is highly comorbid with other mental disorders, aside from trauma exposure, what differentiates PTSD from other disorders is the re-experiencing symptoms (for example, nightmares and flashbacks). Many of the other symptoms of PTSD, such as hyperarousal, avoidance, and numbing, overlap with other mental disorders, such as generalized anxiety disorder, panic disorder, and depression. Thus it is important to delineate whether the person is re-experiencing symptoms in relation to a traumatic event.
It is also important to underscore that people who do not meet the full criteria for PTSD may have significant impairment that requires intervention. Many studies have demonstrated that people with subthreshold PTSD have intermediate levels of impairment between those with full PTSD and no symptoms. 6 , 7 Therefore, dimensional approaches to psychopathology are warranted.
Controversies
There has been substantial dispute about how to define traumatic events. 8 In earlier editions of the DSM, the external stressor was an event distressing to anyone and outside the range of so-called normal human experience. More recent editions of the DSM have included a broader range of traumatic events, with the inclusion of a criterion that the person’s response include intense fear, horror, and helplessness. 9 In DSM-5, there has been a substantial change to the stressor criterion from previous editions. The stressor criterion requires exposure to “death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence.” 5, p 271 A person’s response to the stressor, part of DSM-IV criterion for PTSD, has been removed for DSM-5.
Which Traumatic Events Are Most Likely to Be Associated With PTSD?
Epidemiologic studies from around the world have demonstrated that most people in the community have experienced traumatic events that would fulfill stressor criterion for PTSD. 10 – 14 In men, the following traumatic events are the most common: witnessing another person being killed or badly injured, being in a life-threatening accident, and being threatened with a weapon. Among women, the following traumatic events are the most common: experiencing a natural disaster, witnessing another person being killed or badly injured, and being in a life-threatening accident. 10 – 14
- Exposure to traumatic events and PTSD are prevalent in society.
- PTSD is associated with comorbidity with mental and physical health problems and elevates the risk for suicidal behaviour.
- Risk and protective factors for development of PTSD can be conceptualized based on pretraumatic, traumatic event, and posttraumatic factors.
- Psychological interventions are much more effective than pharmacologic interventions for reducing PTSD symptoms.
- Although the first-line pharmacological treatment of PTSD is antidepressants, many patients require additional medications to help with insomnia and nightmares (for example, prazosin).
Among men, the 2 types of traumatic events that have been studied extensively are combat exposure and injuries. Rape, childhood sexual abuse, and intimate partner violence have been studied extensively among women. Although the prevalence rates among different traumatized samples range widely, there is a dose–response relation between severity and duration of traumatic event and the risk for development of PTSD. Dohrenwend et al 15 demonstrated that there was a monotonic increase in the risk for development of PTSD in relation to increasing frequency of traumatic event exposure.
People presenting with PTSD symptoms are often exposed to multiple traumatic events. It is important to understand that the traumatic event that triggers PTSD may be an accumulation of multiple exposures to various traumatic events. Understanding the person’s trauma history and the meaning of the traumatic event on their sense of self and future is important in developing a treatment plan.
Delayed-onset PTSD is one of the controversial areas in the literature on PTSD and in clinical practice. 16 The usual course of symptoms is for a person to have the greatest number of symptoms immediately after the trauma and for the symptoms to diminish over time. A systematic review on this issue found that 25% of people with PTSD had delayed-onset PTSD (defined as symptoms met criteria for PTSD at least 6 months after the trauma). 16 The authors concluded that people with delayed-onset PTSD often have substhreshold symptoms after the traumatic event and then have an increase in symptoms that rise above threshold over time. In DSM-5, PTSD with “delayed expression” 5, 272 has been included when the full diagnosis of PTSD is not met until 6 months after the trauma(s).
How Common Is PTSD and What Is the Impact on Society?
A wide range of prevalence rates is found in PTSD across epidemiologic studies. For example, US and Canadian samples have found lifetime PTSD estimates to range between 6% and 9%, 10 , 17 – 19 whereas Australian samples have found lower rates (1% to 2%). 20 Table 2 shows the prevalence of PTSD in some of the nationally representative samples. 21 It remains unknown whether these differences are due to methodological issues in assessment or true differences across samples. The prevalence of PTSD among certain populations exposed to high rates of traumatic events, including physical injury, 22 combat exposure, 23 peacekeeping, disaster, 24 and rape, 25 have demonstrated much higher rates of PTSD than the general population (prevalence estimates range between 10% and 40%).
General population studies describing the prevalence of posttraumatic stress disorders
PTSD has substantial impact on the individual and society. There has been emerging evidence demonstrating that, among the anxiety disorders, PTSD is one of the most strongly associated with suicidal behaviour, even after adjusting for other axes I and II mental disorders. 26 – 28 Data from several cross-sectional and longitudinal studies have replicated this finding. 26 – 28 People with PTSD also struggle with interpersonal problems, parenting difficulties, and reductions in household income, 29 and have several mental and physical health comorbidities.
Comorbidity with mental disorders is common in PTSD. Epidemiologic samples have demonstrated that over 90% of people with PTSD have at least 1 lifetime comorbid mental disorder. 10 Some of the most prevalent comorbid conditions with PTSD are major depressive disorder, alcohol abuse and (or) dependence, and another anxiety disorder. Self-medication of PTSD symptoms with alcohol and illicit drugs has been demonstrated to be associated with comorbid alcohol or drug use disorders. 30 Among Axis II disorders, there has been increasing evidence that PTSD is associated with borderline personality disorder 31 and antisocial personality disorder. 32 It is possible that personality styles associated with impulsivity may put the person at risk of exposure to traumatic situations.
Studies in combat veterans 33 , 34 and in the general population have shown that PTSD is associated with several physical health conditions. Mild TBI has been shown to be an important risk factor for development of PTSD. 35 Our group demonstrated that, even after adjusting for other Axis I disorders, PTSD was associated with bone and joint disease, neurological conditions, cardiovascular conditions, respiratory conditions, and metabolic disease (odds ratios ranging between 1.5 and 3.0). 36 – 37 The mechanisms that underlie these associations between PTSD and physical health problems are not well understood. It is possible that PTSD increases the risk of developing physical health problems through sleep disturbances, physical symptoms, obesity, 38 or development of comorbid depression and substance use. Conversely, the sudden onset of a serious life-threatening illness, such as myocardial infarction, may trigger PTSD symptoms. Common factors, such as poverty, 39 , 40 environment, 41 and genetics, 42 , 43 may also play an important role in developing comorbidity.
PTSD is common in the community and clinical practice. People often present to physicians and mental health professionals with various physical symptoms, depression, and substance use. It is important to screen for a history of traumatic events and PTSD. In primary care, patients with PTSD often present with headaches, sleep disturbances, and pain. In mental health clinics, people with PTSD often present with depression, substance use, and self-harm.
A broad range of prevalence estimates exist for PTSD, depending on the type of sample that has been assessed. For example, North American nationally representative lifetime prevalence rates of PTSD range between 6% and 9%, whereas rates in nationally representative samples of Australians range between 1% and 2%. Similarly, in high-risk groups (for example, exposure to injuries or combat), estimates of PTSD have ranged widely between 1% and 40%. 22 It remains unknown whether these differences are due to methodological issues in assessment or true differences across samples.
Suicidal behaviour and comorbid mental and physical disorders are associated with PTSD and traumatic events. It remains unknown whether it is the trauma or the PTSD symptoms that drive the associations with suicidal behaviour. For example, Wilcox et al 27 demonstrated that suicidal behaviour was associated with PTSD, but not with exposure to traumatic events. However, other studies have demonstrated that childhood adversities and traumatic events are associated with suicidal behaviour. 44 Similar issues have been considered in understanding the comorbidity of PTSD with substance use 45 and physical illness. It seems that both stressful life events and PTSD are independently associated with comorbidity and with suicidal behaviour.
Risk Factors for Development of PTSD
There is a large body of literature on the risk factors for PTSD, and several published reviews of risk factors for PTSD. Two key meta-analyses of PTSD risk factors have been conducted by Brewin et al 46 and Ozer et al. 47 Figure 1 shows a summary of the empirically validated risk factors for PTSD that have been demonstrated across various samples.

Empirically-derived risk factors for development of posttraumatic stress disorder (PTSD)
Several pretrauma risk factors for PTSD have been identified in different populations. Females are at higher risk for PTSD than males. For most traumatic events, women showed greater risk for developing PTSD than men. Age, race, socioeconomic, and marital status have not been strongly associated with risk for PTSD. Cognitive vulnerabilities (for example, low IQ or previous history of head injury) are associated with increased vulnerability for PTSD. Exposure to life stressors (for example, childhood maltreatment or other adult life stressors) prior to the index trauma (trauma considered by the person as the inciting stressful event) has been associated with an increased risk for PTSD. A pretrauma history of mental disorders, especially mood and anxiety disorders and conduct disorder, is associated with PTSD. 48 – 50 Personality factors, such as neuroticism 51 and avoidance coping, 52 , 53 have been shown to be associated with increased risk for PTSD, while extraversion has been shown to be protective. There has been an expanding body of literature on the genetic risk factors associated with the development of PTSD. Many genetic markers are currently under investigation, including the serotonin transporter gene, 54 as well as genes associated with the hypothalamic–pituitary–adrenal axis. 55
Regarding trauma-related risk factors, many studies have examined the type and severity of trauma as a risk factor for development of PTSD. 22 , 56 Most studies have not found a relation between severity of injury 56 – 62 and risk for development of PTSD. Intentional or assaultive injury has shown to be a risk factor for onset of PTSD. 56 There has also been some evidence suggesting that TBI, especially mild TBI, is specifically linked to PTSD. 58 – 60 There has been some work suggesting that self-perceived fear of death during the traumatic event has been associated with PTSD. 61 Peritraumatic dissociation has also been shown to be a consistent risk factor for PTSD. 62
Numerous posttrauma risk factors for PTSD have been identified. Multiple studies have shown that a high heart rate (>95 bpm) at first presentation to an emergency department is a risk factor for PTSD among people with physical injury. 63 Acute high levels of pain have been linked to PTSD among patients with severe physical injury. 64 There is a substantial body of evidence that PTSD and pain are often comorbid through mutual maintenance. Asmundson et al 65 suggest that pain is a reminder of the traumatic event that triggers flashbacks. PTSD symptoms, such as insomnia, reduce the threshold for pain. 66 Further, although length of hospitalization has not been shown to be a strong predictor of mental health problems, 67 admission to an intensive care unit 67 has been indicated in one study to be a risk factor for PTSD. The level of physical disability and lack of ability to return to work have been shown to be associated with increased risk for PTSD. 68 – 72 Social supports during the posttrauma period have been shown to be a protective factor in PTSD. 71 Financial stress 56 and legal involvement owing to trauma have been shown to be important in risk for PTSD.
From a clinical perspective, posttrauma low social supports, and pain are strongly associated with PTSD. Interventions aimed at reducing pain 72 and improving social supports 73 lower the likelihood of PTSD. Understanding the nature of the trauma, appraisals of the risk of death associated with the trauma, and concerns about the meaning of the trauma on a person’s future capacity to work and function are important in the clinical assessment of people with PTSD.
There is substantial interest and controversy in the ability of DSM-IV acute stress disorder (symptoms of PTSD and dissociation within the first month of the traumatic event) to predict long-term PTSD symptoms. 74 However, the literature is largely mixed about the clinical utility of this diagnosis in predicting PTSD. 75 , 76 Other indicators of adjustment following traumatic experiences may be more powerful predictors of PTSD. Recently, a 10-item scale, the Post-Traumatic Adjustment Scale, has shown good sensitivity and specificity in predicting PTSD and depression in a sample of physically injured patients. 77 Future work needs to consider whether this measure can be used as a predictor of PTSD in noninjured samples. DSM-5 has made substantial changes to the acute stress disorder criteria. The mandatory need requirement of dissociative symptoms present in DSM-IV has been removed.
Literature Limitations on the Epidemiology and Risk Factors for PTSD Development
Although there has been expansion of our understanding of PTSD during the last 30 years, numerous questions remain about the epidemiology and risk factors for development of PTSD. Basic questions about how common PTSD is remain unanswered. Most of the studies on the prevalence of PTSD have used general population or military veteran samples. The prevalence of PTSD among vulnerable groups, such as children and adolescents, 78 elderly, ethnic minorities, refugees, and First Nations, Inuit, and Metis populations, has not been well established. Future work needs to address these important gaps. Although, there are numerous well-established, population-level risk factors for development of PTSD, the estimation of risk for PTSD at an individual level is lacking. Future studies should consider developing prediction algorithms for the development of PTSD among certain professions that have a high likelihood of exposure to traumatic events (for example, police officers, military personnel, and rescue workers). Such prediction algorithms have been developed for heart disease (for example, the Framingham Heart Study 79 , 80 ) and depression. 81 Further, the longitudinal course of PTSD has not been well established. One epidemiologic study of young adults found that 50% of people with a PTSD diagnosis continued to meet criteria 3 years later. 82 However, there is a need for longitudinal research on the course and predictors of chronic PTSD.
Clinical Assessment and Treatment of PTSD
There is an enormous body of literature and several practice guidelines on this topic. 83 – 88 Here, a general overview of assessment and treatment of PTSD is provided. A careful assessment of the person presenting with PTSD needs to be done in a sensitive manner. People suffering with PTSD symptoms often are reluctant to speak about the details of the traumatic event. The psychiatric assessment should carefully consider the impact of the PTSD symptoms on the person’s sleep patterns, relationships, and functioning. 83 – 86 A careful assessment of comorbid mental disorders and physical health problems at the time of presentation is required for planning appropriate treatment. The assessment of safety and suicide risk is important in the assessment and ongoing treatment. Inpatient, day program, and outpatient treatment settings should be considered based on the severity and comorbidity of the presentation. 83 – 86 To monitor progress in treatment, brief self-report measures of symptoms of PTSD should be routinely used. The 17-item PTSD Checklist, 89 and the Impact of Events Scale 90 are 2 commonly used scales for monitoring PTSD symptoms.
Similar to other common mental disorders, the treatment of PTSD usually requires a combination of psychological and pharmacological treatment. Psychological treatments for PTSD are considered first-line treatment for PTSD and have been shown to have larger effect sizes in RCTs than pharmacotherapy. 83 – 86 CBT, prolonged exposure, and eye movement desensitization and reprocessing therapy have all had multiple RCTs that have shown large reductions in PTSD symptoms. 83 – 86 However, for most patients with PTSD, access to evidence-based therapies is not easy owing to a limited number of trained therapists. There is an urgent need to consider novel ways to make CBT more accessible. Recently, a large US RCT in primary care demonstrated the effectiveness of delivering CBT for anxiety disorders by minimally trained clinicians. 91 The primary care clinicians had minimal training in CBT and delivered CBT with the assistance of a computer program. 91 These types of novel approaches for delivering evidence-based therapies to large populations require replication in Canadian settings.
Pharmacotherapy for PTSD
The pharmacotherapy trials in PTSD have shown smaller effect sizes (0.3 to 0.8) than psychological interventions (>1.0). Selective serotonin reuptake inhibitors, such as fluoxetine, sertraline, and paroxetine, and serotonin norepinephrine reuptake inhibitors, such as venlafaxine, have demonstrated efficacy in reducing PTSD symptoms and are considered first-line medication treatments for PTSD. 92 , 93 However, antidepressants alone are not usually effective in treating the insomnia and nightmares associated with PTSD. 93 There is often a need for additional medication that improves sleep. Prazosin, trazodone, zopiclone, and atypical antipsychotics are options in treating insomnia and nightmares associated with PTSD. Several studies have demonstrated the efficacy of prazosin (2 to 20 mg per day), an alpha one–adrenergic blocker in reducing nightmares, and hyperarousal related to PTSD. 94 , 95 Although there is less controlled evidence for the use of trazodone and zopiclone, these agents are often used by clinicians in treating PTSD and are recommended in practice guidelines. There are mixed findings on the use of atypical antipsychotics in the treatment of PTSD. The largest RCT in this area did not show beneficial effects of risperidone in treating PTSD. 96 Also, owing to the metabolic and extrapyramidal side effects associated with atypical antipsychotics, these agents should be used judiciously. If the symptoms of PTSD are refractory to other medications and comorbid borderline personality traits are present (for example, impulsivity and anger), atypical antipsychotics may be considered. Several other agents, such as valproic acid, lithium, and lamotrigine, are considered third-line treatments in PTSD. There is increasing awareness of the strong comorbidity between PTSD and alcohol and drug use disorders. 87 A recent large RCT demonstrated the effectiveness of naltrexone (an opioid receptor antagonist) in combination with prolonged exposure therapy in reducing PTSD symptoms and alcohol use among patients with PTSD and alcohol dependence. 97 Readers interested in a more comprehensive review of the treatment of PTSD are referred to the following articles. 83 – 87
Conclusions
In summary, PTSD is a common mental health problem that has a substantial impact on the individual and society. There is increasing evidence that PTSD is associated with suicidal behaviour and comorbidity with mental and physical health conditions. Finally, a large body of literature has distinguished the pretrauma, trauma, and posttrauma risk factors for PTSD. Clinicians and policy makers need to consider these factors in developing optimal interventions and maximizing clinical outcomes.
Acknowledgments
Dr Sareen is grateful to Julie Erickson, Sarah Maria Raposo, Cara Katz, and Daniel Palitsky for their thoughtful review of the manuscript. Preparation of this article was supported by a Manitoba Health Research Council Chair award to Dr Sareen.
The Canadian Psychiatric Association proudly supports the In Review series by providing an honorarium to the authors.
Abbreviations

IMAGES
VIDEO
COMMENTS
Search for more papers by this author. Richard A. Bryant, Richard A. Bryant. School of Psychology, University of New South Wales, Sydney, NSW, Australia ... Post-traumatic stress disorder (PTSD) is arguably the most common psychiatric disorder to arise after exposure to a traumatic event. ... A consistent pattern in PTSD research is that ...
Post-traumatic stress disorder (PTSD) is a chronic mental disorder resulting in a reduced quality of life and increased economic burden. Exposure to a traumatic stressor is the trigger for PTSD development . For that, a distinction between ordinary and traumatic stressors (those that have the potential to result in PTSD) is necessary.
Post-traumatic stress disorder (PTSD) is a psychiatric disorder that results from the experience or witnessing of traumatic or life-threatening events. PTSD has profound psychobiological correlates, which can impair the person's daily life and be life threatening. In light of current events (e.g. extended combat, terrorism, exposure to certain ...
Current treatment strategies for control of trauma-associated symptoms of Post Traumatic Stress Disorder (PTSD) have recently been updated by the Veterans Affairs (VA) and the Department of Defense (DoD, after over a decade of dedicated research. The most recent evidence is compelling that its use of trauma-focused therapies such as Cognitive ...
Posttraumatic stress disorder (PTSD) is a recognized clinical phenomenon that often occurs as a result of exposure to severe stressors, such as combat, natural disaster, or other events [].The diagnosis of PTSD was first introduced in the 3rd edition of the Diagnostic and Statistical Manual (DSM) (American Psychiatric Association) in 1980 [].PTSD is a potentially chronic impairing disorder ...
Introduction. Post-traumatic stress disorder (PTSD) is a possible psychopathological consequence of exposure to a traumatic event that threatens one's psychological and/or physical integrity Citation 1-3.Individuals with PTSD may recurrently experience memories, sensations, and emotions of a traumatic event through sensory flashbacks or nightmares, or experience avoidance, irritability ...
2. Articles in this issue. Early psychological interventions for adults exposed to trauma (Roberts, Kitchiner, Kenardy, Lewis, & Bisson, Citation 2020).This paper concludes that the quality of the evidence remains low but includes recommendations for cognitive behavioural therapy with a trauma focus (CBT-TF), cognitive therapy and eye movement desensitisation and reprocessing (EMDR) for early ...
Post-traumatic stress disorder (PTSD) is one of the few neuropsychiatric disorders for which the timing and cause of onset are understood, facilitating research into the underlying mechanisms. In ...
Abstract. Posttraumatic stress disorder can be viewed as a disorder of fear dysregulation. An abundance of research suggests that the prefrontal cortex is central to fear processing—that is, how ...
Dr. Yair Bar-Haim from Tel Aviv University and his colleagues present a thought-provoking commentary suggesting that symptoms associated with the intrusive reexperiencing of traumatic events should be prioritized as a focus of research efforts to elaborate mechanisms underlying responses to trauma and PTSD . Dr.
PGC-PTSD co-chair Murray B. Stein M.D., M.P.H., professor of psychiatry and public health at UC San Diego is also a co-author of the study. Nievergelt explained that the work confirmed previous neurobiological studies of PTSD and built upon them, identifying 95 loci — positions of genes on a chromosome — significant to PTSD, including 80 ...
Conclusions. This paper provided a literature review of PTSD with the focus on traumatic stress prevention form a public health perspective. A traumatic experience is an event that can pierce into the integrity of an individual or a group causing distress, feelings of helplessness, horror, or intense fear reaction.
Post-traumatic stress disorder (PTSD) is a psychiatric disorder that results. from the experie nce or witnessing of traumatic or life-threateni ng events. PTSD has profound psycho -. biological ...
A recent systematic review of complementary and alternative medicine for posttraumatic stress disorder (PTSD) found positive evidence for mindfulness-based interventions (MBIs). 1 To date, the literature mostly comprises cross-sectional analyses and prospective outcome studies that compare MBIs to treatment as usual (TAU) or wait-list control groups. 2-9 Randomized control trials (RCTs) are ...
Posttraumatic stress disorder (PTSD) is a common, chronic, and disabling condition in veteran and military populations (Forbes et al., 2019).Four decades of research established therapies that show clinically meaningful improvements in patients with PTSD (Bryant, 2019).However, nonresponse rates have been high, particularly in military and veteran populations, and around two thirds of treated ...
Posttraumatic Stress Disorder (PTSD) is an anxiety problem that develops in some people after extremely traumatic events, such as combat, crime, an accident, or natural disaster. This page showcases content from APA Publishing about PTSD. For more resources from APA, visit our Clinical Practice Guideline for the Treatment of Posttraumatic ...
Stigmas surrounding mental illness in the military have steadily decreased over time but remain high (Acosta et al., 2014).Reducing the stigmas associated with mental health within military populations is a current priority as research has shown that these stigmas may serve as a barrier to treatment for those returning from combat (Acosta et al., 2014; Blais et al., 2014).
Posttraumatic stress disorder (PTSD) is a chronic, often debilitating mental health disorder that may develop after a traumatic life event. Fortunately, effective psychological treatments for PTSD exist. In 2017, the Veterans Health Administration and Department of Defense (VA/DoD) and the American Psychological Association (APA) each published ...
Some people develop post-traumatic stress disorder (PTSD) after experiencing a shocking, scary, or dangerous event. It is natural to feel afraid during and after a traumatic situation. Fear is a part of the body's normal "fight-or-flight" response, which helps us avoid or respond to potential danger. People may experience a range of ...
PTSD Research Paper. This sample PTSD research paper features: 6100 words (approx. 20 pages), an outline, and a bibliography with 13 sources. Browse other research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help.
An Understanding of Post-Traumatic Stress Disorder. Elizabeth Mackey Grand Canyon University PSY 470 - Abnormal Psychology Lori Rice 10/8/ Most people who have experienced trauma inevitably recover from the shock, but there is a small number of individuals who continue to be in distress even long after the event has ended.
1. Introduction. Post-traumatic stress disorder (PTSD) is a debilitating mental condition that can significantly impact the sufferer's quality of life [1,2,3].A study by Rapaport et al. found that 59% of patients suffering from PTSD had severely impaired overall quality of life based on the Quality of Life Enjoyment and Satisfaction Questionnaire [].
Samuel, an 8-year-old black male, lives in an adopted white family consisting of the father, incarcerated for domestic violence charges, the mother, the primary caretaker and the only home provider, and the older sibling. We will write. a custom essay specifically for you by our professional experts. 809 writers online.
The paper provides a concise review of the evolution of PTSD diagnosis in the Diagnostic and Statistical Manual of Mental Disorders, impact of PTSD in the community, an overview of the established risk factors for developing PTSD, and assessment and treatment. Throughout the paper, controversies and clinical implications are discussed.