- Second Opinion
Fetal Growth Restriction

What is fetal growth restriction (FGR)?
Fetal growth restriction (FGR) is a condition in which an unborn baby (fetus) is smaller than expected for the number of weeks of pregnancy (gestational age). It is often described as an estimated weight less than the 10th percentile. This means that the baby weighs less than 9 out of 10 babies of the same gestational age. Newborn babies with FGR may be called “small for gestational age.”
FGR can begin at any time during pregnancy. With FGR, the baby does not grow well. FGR may affect the overall size of the baby and the growth of organs, tissues, and cells. This can cause many problems. But many newborns who are small may just be small. They may not have any problems.
What causes FGR?
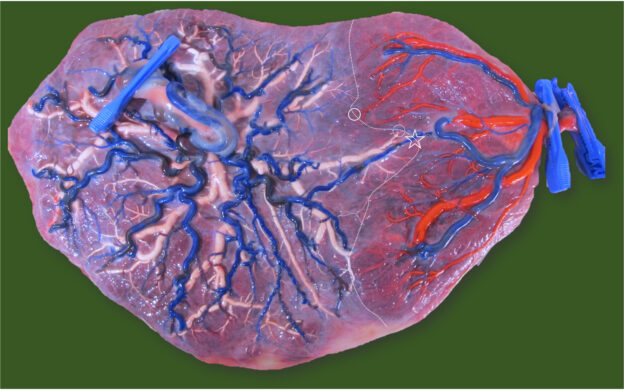
Many things increase the risk for FGR. These include problems with the placenta or umbilical cord. The placenta may not attach well. Or the blood flow through the umbilical cord may be limited. Factors in both the mother and the baby may cause FGR.
Factors in the mother that can cause FGR include:
High blood pressure or other heart and blood vessel disease
Too few red blood cells (anemia)
Long-term lung or kidney conditions
Autoimmune conditions such as lupus
Very low weight
A large amount of excess weight (obese)
Poor nutrition or weight gain
Alcohol or drug use
Cigarette smoking
Factors in the baby that can cause FGR include:
Being one of a twin or triplets
Birth defects, such as heart defects
Problem with genes or chromosomes
What are the symptoms of FGR?
A pregnant woman doesn’t have symptoms of FGR. But a baby with FGR may have certain signs after birth, such as:
Low birth weight
Low blood sugar levels
Lower body temperature
High level of red blood cells
Trouble fighting infections
How is FGR diagnosed?
One of the main reasons for regular prenatal exams is to make sure your baby is growing well. During pregnancy, the size of your baby is estimated in different ways, including:
Fundal height. To check fundal height, your healthcare provider measures from the top of your pubic bone to the top of your uterus (fundus). Fundal height, measured in centimeters (cm), is about the same as the number of weeks of pregnancy after the 20th week. For example, at 24 weeks gestation, your fundal height should be close to 24 cm. If the fundal height is less than expected, it may mean FGR.
If your healthcare provider thinks you have FGR, you will have other tests. These include:
Fetal ultrasound. Estimating fetal weight with ultrasound is the best way to find FGR. Ultrasound uses sound waves to create images of the baby in the womb. Sound waves will not harm you or the baby. Your healthcare provider or a technician will use the images to measure the baby. A diagnosis of FGR is based on the difference between actual and expected measurements at a certain gestational age.
Doppler ultrasound. You may also have this special type of ultrasound to diagnose FGR. Doppler ultrasound checks the blood flow to the placenta and through the umbilical cord to the baby. Decreased blood flow may mean your baby has FGR.
You may have repeat ultrasound exams, Doppler studies, and other tests.
How is FGR managed?
Management depends on how serious the FGR is. This is based on the ultrasound (estimated fetal weight) and Doppler ultrasound (blood flow to the baby), as well is risk factors and the number of weeks gestation.
Treatment may include:
Frequent monitoring. This means you will have prenatal visits more often, and ultrasound and Doppler ultrasound exams. You may have other tests.
Tracking fetal movements. Your healthcare provider may also ask you to keep track of fetal movements. If so, he or she will give you instructions.
Corticosteroid medicine
Hospital stay
Early delivery or emergency cesarean
What are possible complications of FGR?
FGR can cause many serious complications. Your baby may need to be delivered early and stay in the hospital. Your baby may have trouble breathing, infections, and other problems. Stillbirths and death may occur. As your child grows, he or she will be at higher risk for heart and blood vessel problems.
How can FGR be prevented?
FGR can happen in any pregnancy. But some factors, like cigarette smoking or alcohol or medicine use, increase the risk for FGR. Regular and early prenatal care and a healthy diet and steady weight gain help to prevent FGR and other problems.
When should I call my healthcare provider?
Make sure your healthcare provider knows your health history. If you are counting fetal movements and find that the number has decreased, let your healthcare provider know. And if you notice other changes or if you have concerns about your pregnancy, call your healthcare provider.
Key points about fetal growth restriction
FGR is a condition in which the baby is smaller than expected for gestational age.
Many factors increase the risk for FGR. They may be related to the placenta, mother, or baby.
Estimating fetal weight with ultrasound is the best way to identify FGR.
If FGR is diagnosed, you will need to be closely monitored.
Tips to help you get the most from a visit to your healthcare provider:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your provider tells you.
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your provider if you have questions.
Related Links
- Johnson Center
- Fetal and Pregnancy Health
- Small for Gestational Age
- Large for Gestational Age
- Gestational Age Assessment
Related Topics
Care of the Baby in the Delivery Room
Connect with us:
Download our App:
- Leadership Team
- Vision, Mission & Values
- The Stanford Advantage
- Government and Community Relations
- Get Involved
- Volunteer Services
- Auxiliaries & Affiliates
© 123 Stanford Medicine Children’s Health
Selective Fetal Growth Restriction: What We Know and What We Don’t
Please note:.
This course may contain imagery and/or video of surgical procedures.
In this session, learners will be able to identify maternal and fetal indications for various fetal interventions and associated maternal-fetal outcomes and discuss prenatal counseling, obstetrical management, fetal therapy options, fetal surveillance and delivery planning for fetuses with select fetal anomalies. Learners will also be able to understand ongoing research endeavors related to maternal-fetal health and childhood outcomes.
- Nahla Khalek, MD, MPH, FACOG, MSEd
- Shelly Soni, MD
- Juliana Gebb, MD
This seminar focuses on fetal diagnosis and treatment and was delivered at a virtual event titled, “Selective Fetal Growth Restriction: What We Know and What We Don’t” on December 8, 2023.
Additional CHOP Resources:
- Richard D. Wood Jr. Center for Fetal Diagnosis and Treatment
- Upcoming Healthcare Professionals Events
Content Disclaimer
The Terms of Use and Privacy Policy set forth on the website of The Children’s Hospital of Philadelphia apply to any and all uses of and access to this site and the content found here.
The work presented in the presentations, videos, and other content on this site (“Presentations”) includes publicly available medical evidence, a consensus of medical practitioners, and/or opinions of individual practitioners that may differ from consensus opinions. These Presentations are intended only to provide general information and need to be adapted for each specific patient based on the practitioner’s professional judgment, consideration of any unique circumstances, the needs of each patient and their family, the availability of various resources at the health care institution where the patient is located, and other factors. The Presentations are not intended to constitute medical advice or treatment, nor should they be relied upon as such. The Presentations are not intended to create a doctor-patient relationship between/among The Children’s Hospital of Philadelphia, its physicians and the individual patients in question. The information contained in these Presentations are general in nature, and do not and are not intended to refer to specific patients.
CHOP, The Children’s Hospital of Philadelphia Foundation and its or their affiliates, the authors, presenters, practitioners, editors, and others associated with the creation of the Presentations (“CHOP”) are not responsible for errors or omissions in the Presentations; for any outcomes a patient might experience where a clinician reviewed one or more such Presentations in connection with providing care for that patient; and/or for any and all third party content on the site or in the Presentations. CHOP makes no warranty, expressed or implied, with respect to the currency, completeness, applicability or accuracy of the Presentations. Application of the information in or to a particular situation remains the professional responsibility of the practitioner who is directly treating the patient.
To the extent that the Presentations include information regarding drug dosing, in view of ongoing research, changes in government regulations and the constant flow of information relating to drug therapy and drug reactions, the viewer should not rely on the Presentation content, but rather is urged to check the package insert for each drug for indications, dosage, warnings and precautions.
Some drugs and medical devices presented in the Presentations have United States Food and Drug Administration (FDA) clearance for limited use in restricted research settings. It is the responsibility of the practitioner to ascertain the FDA status of each drug or device planned for use in their clinical practice.
You shall indemnify, defend and hold harmless CHOP, The Children’s Hospital of Philadelphia Foundation, and its/their current and former employees, officers, and agents, trustees, and their respective successors, heirs and assigns (“Indemnitees”) against any claims, liability, damage, loss or expenses (including attorneys’ fees and expenses of litigation) in connection with any claims, suits, actions, demands or judgments arising directly or indirectly out of your reference to or use of the Presentations.
The Presentations are protected by copyright laws and in some cases patent laws, and all rights are reserved under such laws. No part of the Presentations may be reproduced in any form by any means, or utilized in any other way, absent prior written permission from the copyright owner.
By starting this module, you agree to our Content Disclaimer and Terms of Service.
Course Content
Course Includes
- Course Certificate
CHOP Employee? Log In Here
Username or Email Address
Forgot Password?
Remember Me
Fetal Growth Restriction: A Comprehensive Review of Major Guidelines
Affiliations.
- 1 Resident.
- 2 Assistant Professor.
- 3 Professor.
- 4 Associate Professor.
- 5 Assistant Professor, Third Department of Obstetrics and Gynaecology, School of Medicine, Faculty of Health Sciences, Aristotle University of Thessaloniki, Greece.
- PMID: 38134339
- DOI: 10.1097/OGX.0000000000001203
Importance: Fetal growth restriction (FGR) is a common pregnancy complication and a significant contributor of fetal and neonatal morbidity and mortality, mainly due to the lack of effective screening, prevention, and management policies.
Objective: The aim of this study was to review and compare the most recently published influential guidelines on the management of pregnancies complicated by FGR.
Evidence acquisition: A descriptive review of guidelines from the American College of Obstetricians and Gynecologists (ACOG), the Society for Maternal-Fetal Medicine, the International Federation of Gynecology and Obstetrics, the International Society of Ultrasound in Obstetrics and Gynecology, the Royal College of Obstetricians and Gynecologists, the Society of Obstetricians and Gynecologists of Canada (SOGC), the Perinatal Society of Australia and New Zealand, the Royal College of Physicians of Ireland, the French College of Gynecologists and Obstetricians (FCGO), and the German Society of Gynecology and Obstetrics on FGR was carried out.
Results: Several discrepancies were identified regarding the definition of FGR and small-for-gestational-age fetuses, the diagnostic criteria, and the need of testing for congenital infections. On the contrary, there is an overall agreement among the reviewed guidelines regarding the importance of early universal risk stratification for FGR to accordingly modify the surveillance protocols. Low-risk pregnancies should unanimously be evaluated by serial symphysis fundal height measurement, whereas the high-risk ones warrant increased sonographic surveillance. Following FGR diagnosis, all medical societies agree that umbilical artery Doppler assessment is required to further guide management, whereas amniotic fluid volume evaluation is also recommended by the ACOG, the SOGC, the Perinatal Society of Australia and New Zealand, the FCGO, and the German Society of Gynecology and Obstetrics. In case of early, severe FGR or FGR accompanied by structural abnormalities, the ACOG, the Society for Maternal-Fetal Medicine, the International Federation of Gynecology and Obstetrics, the Royal College of Obstetricians and Gynecologists, the SOGC, and the FCGO support the performance of prenatal diagnostic testing. Consistent protocols also exist on the optimal timing and mode of delivery, the importance of continuous fetal heart rate monitoring during labor, and the need for histopathological examination of the placenta after delivery. On the other hand, guidelines concerning the frequency of fetal growth and Doppler velocimetry evaluation lack uniformity, although most of the reviewed medical societies recommend an average interval of 2 weeks, reduced to weekly or less when umbilical artery abnormalities are detected. Moreover, there is a discrepancy on the appropriate timing for corticosteroids and magnesium sulfate administration, as well as the administration of aspirin as a preventive measure. Cessation of smoking, alcohol consumption, and illicit drug use are proposed as preventive measures to reduce the incidence of FGR.
Conclusions: Fetal growth restriction is a clinical entity associated with numerous adverse antenatal and postnatal events, but currently, it has no definitive cure apart from delivery. Thus, the development of uniform international protocols for the early recognition, the adequate surveillance, and the optimal management of growth-restricted fetuses seem of paramount importance to safely guide clinical practice, thereby improving perinatal outcomes of such pregnancies.
Publication types
- Aspirin / therapeutic use
- Fetal Growth Retardation / diagnosis
- Fetal Growth Retardation / prevention & control
- Gynecology*
- Infant, Newborn
- Obstetrics*
- Prenatal Care

Intrauterine growth restriction
- Report problem with article
- View revision history

Citation, DOI, disclosures and article data
At the time the article was created Yuranga Weerakkody had no recorded disclosures.
At the time the article was last revised Karen Machang'a had no financial relationships to ineligible companies to disclose.
- Intrauterine growth restriction (IUGR)
- Intrauterine growth retardation
- Small for gestational age
- Small for gestational age (SGA)
- Intra uterine growth restriction
- Intra-uterine growth restriction (IUGR)
- Fetal growth restriction
- Fetal growth restriction (FGR)
- Intrauterine growth retardation (IUGR)
Intrauterine growth restriction (IUGR) or fetal growth restriction (FGR) is defined as an estimated fetal weight (EFW) and/or abdominal circumference (AC) at one point in time during pregnancy being below 3 rd percentile or EFW and/or AC below the 10 th percentile for gestational age with deranged Doppler parameters 14 .
An IUGR can be broadly divided into two main types:
type I: symmetrical intrauterine growth restriction
type II: asymmetrical intrauterine growth restriction
Some authors also enlist a third type termed: femur-sparing intrauterine growth restriction 10 .
On this page:
Clinical assessment, radiographic features, treatment and prognosis, differential diagnosis.
- Cases and figures
The symphysis fundal height (SFH) can be a commonly used crude measurement.
IUGR can result from a vast number of causes:
placental insufficiency (commonest cause overall)
abnormal uteroplacental circulation
abnormal fetoplacental circulation
maternal conditions
maternal narcotics/smoking
maternal alcohol use: fetal alcohol syndrome
maternal diabetes: when severe maternal diabetes, there can be a paradoxical IUGR as opposed to fetal macrosomia
maternal malnutrition/starvation
maternal vascular conditions
certain medications
other placental causes
increased incidence with a single umbilical artery
fetal conditions
multifetal pregnancy
intrauterine infections
chromosomal anomalies
triploidy (IUGR is of early-onset)
Down syndrome (not a dominant feature)
chromosome 4p deletion syndrome (Wolf-Hirschhorn syndrome)
chromosome 12p tetrasomy ( Pallister-Killian syndrome )
confined placental mosaicism (CPM) 13
other syndromic anomalies
Cornelia de Lange syndrome
Neu-Laxova syndrome
Pena Shokeir syndrome
Seckel syndrome
Silver-Russel syndrome
Smith-Lemli-Opitz syndrome
in utero substance exposure
e.g. fetal hydantoin syndrome
ADVERTISEMENT: Supporters see fewer/no ads
Antenatal ultrasound
Sonographic parameters include:
non-Doppler features
reduced abdominal circumference (AC) and/or EFW
AC and/or EFW <3 rd percentile
AC and/or EFW <10 th percentile with deranged Doppler parameters
presence of oligohydramnios without ruptured membranes
increased head circumference (HC) to abdominal circumference (AC) ratio (in asymmetrical type)
advanced placental grade
Doppler features (will require a chart to calculate absolute values)
umbilical artery Doppler assessment
increased PI above 95 th percentile
absent/reversed diastolic flow
umbilical venous Doppler assessment
presence of pulsatility
uterine arterial Doppler assessment
increased mean uterine artery PI above 95 th percentile
presence of notching in mid to late pregnancy
reduced below 5 th percentile
While there is no cure, management is reliant on a structured antenatal surveillance program with timely intervention in order to minimize fetal compromise.
Complications
There are many including:
antepartum
iatrogenic prematurity
perinatal stroke
intrapartum
abnormal fetal status (fetal heart rate tracing)
emergency Cesarean section
need for active neonatal resuscitation
hypothermia
hypoglycemia
hypocalcemia
polycythemia
coagulopathy
hepatocellular dysfunction
respiratory distress syndrome
necrotizing enterocolitis
intraventricular hemorrhage, especially in premature IUGR neonates <750 g
hypoxic-ischemic encephalopathy
increased risk of:
short stature
cerebral palsy
developmental delay
behavioral and emotional problems
lower IQ scores
chronic lung disease
future cardiovascular disease and hypertension
General considerations include:
incorrect dates
small for dates fetus
Quiz questions
- 1. Grant EG, Tessler FN, Perrella RR. Clinical Doppler imaging. AJR Am J Roentgenol. 1989;152 (4): 707-17. AJR Am J Roentgenol (citation) - Pubmed citation
- 2. Smith-bindman R, Chu PW, Ecker JL et-al. US evaluation of fetal growth: prediction of neonatal outcomes. Radiology. 2002;223 (1): 153-61. doi:10.1148/radiol.2231010876 - Pubmed citation
- 3. Altman DG, Hytten FE. Intrauterine growth retardation: let's be clear about it. Br J Obstet Gynaecol. 1989;96 (10): 1127-32. - Pubmed citation
- 4. Ott WJ. The diagnosis of altered fetal growth. Obstet. Gynecol. Clin. North Am. 1988;15 (2): 237-63. - Pubmed citation
- 5. Botsis D, Vrachnis N, Christodoulakos G. Doppler assessment of the intrauterine growth-restricted fetus. Ann. N. Y. Acad. Sci. 2006;1092 : 297-303. doi:10.1196/annals.1365.027 - Pubmed citation
- 6. Mandruzzato G, Antsaklis A, Botet F et-al. Intrauterine restriction (IUGR). J Perinat Med. 2008;36 (4): 277-81. doi:10.1515/JPM.2008.050 - Pubmed citation
- 7. Gerber S, Hohlfeld P, Viquerat F et-al. Intrauterine growth restriction and absent or reverse end-diastolic blood flow in umbilical artery (Doppler class II or III): A retrospective study of short- and long-term fetal morbidity and mortality. Eur. J. Obstet. Gynecol. Reprod. Biol. 2006;126 (1): 20-6. doi:10.1016/j.ejogrb.2005.07.008 - Pubmed citation
- 8. Baschat AA. Fetal growth restriction - from observation to intervention. J Perinat Med. 2010;38 (3): 239-46. doi:10.1515/JPM.2010.041 - Pubmed citation
- 9. Galan HL, Ferrazzi E, Hobbins JC. Intrauterine growth restriction (IUGR): biometric and Doppler assessment. Prenat. Diagn. 2002;22 (4): 331-7. doi:10.1002/pd.311 - Pubmed citation
- 10. Sanders RC, Winter TC. Clinical sonography, a practical guide. Lippincott Williams & Wilkins. (2006) ISBN:0781748690. Read it at Google Books - Find it at Amazon
- 11. Bamfo JE, Odibo AO. Diagnosis and management of fetal growth restriction. J Pregnancy. 2011;2011 : 640715. doi:10.1155/2011/640715 - Free text at pubmed - Pubmed citation
- 12. Merz E, Bahlmann F. Ultrasound in obstetrics and gynecology. Thieme Medical Publishers. (2005) ISBN:1588901475. Read it at Google Books - Find it at Amazon
- 13. Lestou VS, Kalousek DK. Confined placental mosaicism and intrauterine fetal growth. Arch. Dis. Child. Fetal Neonatal Ed. 1998;79 (3): F223-6. Arch. Dis. Child. Fetal Neonatal Ed. (link) - Free text at pubmed - Pubmed citation
- 14. L.J. Salomon, Z. Alfirevic, F. Da Silva Costa et-al. ISUOG Practice Guidelines: ultrasound assessment of fetal biometry and growth. (2019) Ultrasound in Obstetrics & Gynecology. 53 (6): 715. doi:10.1002/uog.20272 - Pubmed
Incoming Links
- Turner syndrome
- Placental calcification
- Reversal of umbilical arterial end diastolic flow
- Fetal hydantoin syndrome
- Pregnancy-associated plasma protein-A
- Uterine artery flow notching
- Fetal transverse cerebellar diameter
- Placenta membranacea
- Intravenous drug user
- Edwards syndrome
- Congenital rubella syndrome
- Symphyseal fundal height
- Placental insufficiency
- Barth syndrome
- Wharton jelly
- Oesophageal atresia
- Placental thickness
- Patau syndrome
- Fetal IUGR - severe haemodynamic adaptation
- Single umbilical artery
- Asymmetrical intrauterine growth restriction with fetal distress
- Severe IUGR with critical dopplers
- Early onset IUGR with critical Dopplers
- Intrauterine growth restriction - symmetrical
- Intra-uterine growth restriction
- Question 1861
- Question 1680
Promoted articles (advertising)
By section:.
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers

Screening for Late-Onset Fetal Growth Restriction in Antepartum Fetal Monitoring Using Deep Forest and SHAP
- Conference paper
- First Online: 11 May 2024
- Cite this conference paper

- Jianhong Huo 6 ,
- Guohua Li 6 ,
- Chongwen Li 6 ,
- Guiqing Liu 8 ,
- Qinqun Chen 6 ,
- Jialu Li 6 ,
- Yuexing Hao 9 &
- Hang Wei 10
Part of the book series: Lecture Notes on Data Engineering and Communications Technologies ((LNDECT,volume 207))
Included in the following conference series:
- International Conference on Fuzzy Information & Engineering
Fetal growth restriction (FGR) is the second leading cause of perinatal death, of which late-onset fetal growth restriction (LFGR) accounts for 70%–80% and has a low detection rate. Cardiotocography (CTG) is a routine tool for antepartum fetal monitoring, continuously recording fetal heart rate (FHR) to assess the development of the fetus. Therefore, in this paper, we proposed a hybrid DF-SHAP model that screens LFGR in routine CTG monitoring using deep forest (DF) and Shapley Additive Explanation (SHAP). Firstly, principal component analysis, spearman correlation analysis and logistic regression analysis were implemented to explore significant FHR features for LFGR. After data preprocessing, deep forest multi-granularity scanning was introduced to probe the connection among the features. Then the cascade forest phase, which was designed to integrate random forest, extra trees, logistic regression and extreme gradient boosting as the basic classifiers, iteratively generated new layers and finally got the best performance model. Finally, SHAP was introduced to enhance the interpretability of DF and to interpret the impact of each feature on the predicted value. The experimental results showed that the proposed DF-SHAP model outperformed the state-of-the-art LFGR recognition models using CTG data and had good interpretability. This indicates that the DF-SHAP model is feasible for screening LFGR in antepartum fetal monitoring.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Crovetto, F., et al.: First-trimester screening with specific algorithms for early-and late-onset fetal growth restriction. Ultrasound Obstet. Gynecol. 48 (3), 340–348 (2016)
Article Google Scholar
Feng, Y., Zheng, H., Fang, D., Mei, S., Zhong, W., Zhang, G.: Prediction of late-onset fetal growth restriction using a combined first- and second-trimester screening model. J. Gynecol. Obstet. Hum. Reprod. 51 (2), 102273 (2022)
Google Scholar
Lundberg, S.M., Lee, S.I.: A unified approach to interpreting model predictions. In: Advances in Neural Information Processing Systems, vol. 30 (2017)
Oros, D., Figueras, F., Cruz-Martinez, R., Meler, E., Gratacos, E.: Longitudinal changes in uterine, umbilical and fetal cerebral doppler indices in late-onset small-for-gestational age fetuses. Ultrasound Obstet. Gynecol. 37 (2), 191–195 (2011)
Pini, N., et al.: A machine learning approach to monitor the emergence of late intrauterine growth restriction. Front. Artif. Intell. 4 , 622616 (2021)
Qi, T.I., Sun, Y.L.: Clinical analysis of prenatal stressless fetal heart monitor combined with electronic fetal heart monitor. Chin. J. Fam. Plann. Gynecotokology 11 (1), 73–76 (2019)
Savchev, S., et al.: Evaluation of an optimal gestational age cut-off for the definition of early- and late-onset fetal growth restriction. Fetal Diagn. Ther. 36 (2), 99–105 (2014)
Signorini, M.G., Pini, N., Malovini, A., Bellazzi, R., Magenes, G.: Integrating machine learning techniques and physiology based heart rate features for antepartum fetal monitoring. Comput. Methods Programs Biomed. 185 , 105015 (2020)
Zhou, Z.H., Feng, J.: Deep forest: towards an alternative to deep neural networks. In: IJCAI, pp. 3553–3559 (2017)
Download references
Acknowledgement
This work is supported by Natural Science Foundation of China No.61976052 and No.71804031, Medical Scientific Research Foundation of Guangdong Province No. A2019428 and National Undergraduate Innovation and Venture Training Project No. 202210572005.
Recommender: Associate Professor Bo Xu, Guangdong University of Finance and Economics in China.
Author information
Authors and affiliations.
School of Medical Information Engineering, Guangzhou University of Chinese Medicine, Guangzhou, China
Jianhong Huo, Guohua Li, Chongwen Li, Qinqun Chen & Jialu Li
The Second Affiliated Hospital, Guangzhou Medical University, Guangzhou, China
The First Affiliated Hospital, Guangzhou University of Chinese Medicine, Guangzhou, China
Guiqing Liu
Department of Human Centered Design, Cornell University, Ithaca, NY, USA
Yuexing Hao
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Hang Wei .
Editor information
Editors and affiliations.
School of Mathematics and Information Sciences, Guangzhou University, Guangzhou, Guangdong, China
Bing-Yuan Cao
Pearl River Delta Regional Logistics Research Center, Guangdong Baiyun University, Guangzhou, China
Shu-Feng Wang
Department of Applied Mathematics, University of Mazandaran, Bābolsar, Iran
Hadi Nasseri
Yu-Bin Zhong
Rights and permissions
Reprints and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this paper
Cite this paper.
Huo, J. et al. (2024). Screening for Late-Onset Fetal Growth Restriction in Antepartum Fetal Monitoring Using Deep Forest and SHAP. In: Cao, BY., Wang, SF., Nasseri, H., Zhong, YB. (eds) Intelligent Systems and Computing. ICFIE 2022. Lecture Notes on Data Engineering and Communications Technologies, vol 207. Springer, Singapore. https://doi.org/10.1007/978-981-97-2891-6_29
Download citation
DOI : https://doi.org/10.1007/978-981-97-2891-6_29
Published : 11 May 2024
Publisher Name : Springer, Singapore
Print ISBN : 978-981-97-2890-9
Online ISBN : 978-981-97-2891-6
eBook Packages : Engineering Engineering (R0)
Share this paper
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

IMAGES
VIDEO
COMMENTS
Fetal growth restriction (FGR) affects about 3% to 7% of all pregnancies.[1] FGR is defined as a condition in which the fetus fails to attain the growth potential as determined by the genetic makeup. Ultrasonography-estimated fetal weight (EFW) of less than the 10th percentile for the specific gestational age (GA) is required for the diagnosis of FGR.[2] Some fetuses are constitutionally small ...
3. Guidelines for data collection, analysis and presentation of fetal growth restriction. It was the consensus of the Brighton Collaboration Fetal Growth Restriction Working Group to recommend the following guidelines to enable meaningful and standardized collection, analysis, and presentation of information about FGR. However, implementation ...
Fetal growth restriction, previously called intrauterine growth restriction, is a condition in which a fetus does not achieve its optimal growth potential. It impacts up to 10% of pregnancies and ...
ABSTRACT: Fetal growth restriction, also known as intrauterine growth restriction, is a common complication of pregnancy that has been associated with a variety of adverse perinatal outcomes. There is a lack of consensus regarding terminology, etiology, and diagnostic criteria for fetal growth restriction, with uncertainty surrounding the optimal management and timing of delivery for the ...
Fetal growth restriction (FGR) is a condition in which an unborn baby (fetus) is smaller than expected for the number of weeks of pregnancy (gestational age). It is often described as an estimated weight less than the 10th percentile. This means that the baby weighs less than 9 out of 10 babies of the same gestational age. Newborn babies with FGR may be called "small for gestational age."
Introduction. Fetal growth restriction (FGR) is the condition in which a fetus does not reach its intrinsic growth potential and in which the risk of severe complications in both the short- and the long term is increased. 1-12 FGR is a common complication of pregnancy that occurs in five to ten percent of all pregnancies. 13,14 The most common pathophysiological mechanism is placental ...
A fetus diagnosed to be small at ultrasound requires a structured diagnostic work-up in order to achieve an optimal ante- and perinatal management. Fetal or intrauterine growth restriction (FGR/IUGR) affects approximately 5 - 8% of all pregnancies and refers to a fetus not exploiting its genetically determined growth potential.
Investigations in Pregnancies with Suspected Fetal Growth Restriction. 11. Suspected fetal growth restriction should be systematically assessed by the health care provider with a detailed history, ... such as the detection of breech presentation or major fetal abnormalities, 78 that are beyond the scope of this guideline. ...
Fetal growth restriction, previously called intrauterine growth restriction, is a condition in which a fetus does not achieve its optimal growth potential. It impacts up to 10% of pregnancies
Both published in 2020, the guidelines of the Society for Maternal-Fetal Medicine (SMFM) 1 and those of the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) 2 on fetal growth restriction (FGR) make recommendations in respect of the diagnosis, monitoring and delivery timing of FGR pregnancies. The SMFM guidance 1, being a document aimed primarily at USA practitioners ...
This Clinical Opinion reviews the literature about the diagnosis, antepartum surveillance, and time of delivery of fetuses suspected to be small for gestational age or growth restricted. Several guidelines have been issued by major professional organizations, including the International Society of Ultrasound in Obstetrics and Gynecology and the Society for Maternal-Fetal Medicine. The ...
3.2.12 Clinical presentation and Antenatal Diagnosis of the Intrauterine Growth Restricted Foetus. Certainty of GA is key to the diagnosis of IUGR. Twenty to 40% of pregnant women are, however, unsure of their last menstrual periods. ... Barker DJP, Adult consequences of Fetal growth restriction, Clin Obstet Gynaecol, 2006;49(2):270-283. View ...
Fetal growth restriction. Sep 26, 2016 • Download as PPTX, PDF •. 59 likes • 15,286 views. Kirtan Vyas. Fetal Growth restriction includes definition, various types , diagnosis and management. Health & Medicine. Slideshow view. Download now. Fetal growth restriction - Download as a PDF or view online for free.
Intrauterine growth restriction (IUGR) is when the fetal weight is estimated to be below the 10th percentile for its gestational age. Causes range from chronic diseases or infections in the birthing parent to issues with the placenta and umbilical cord. Treatment includes frequent fetal monitoring and testing and, possibly, early delivery.
Fetal growth restriction, or FGR, is also known as intrauterine growth restriction, or IUGR; and is defined as a fetal weight or abdominal circumference below the 10th percentile for gestational age, as determined by ultrasound measurements.In contrast, small for gestational age, or SGA, refers to a term newborn with a birth weight less than the 10th percentile for gestational age.
The work presented in the presentations, videos, and other content on this site ("Presentations") includes publicly available medical evidence, a consensus of medical practitioners, and/or opinions of individual practitioners that may differ from consensus opinions. ... Selective Fetal Growth Restriction (sFGR) - Current Understanding and ...
Fetal growth restriction (FGR) refers to a fetus that has failed to achieve its genetically determined growth potential and affects up to 5-10% of pregnancies. ... Obviously, other obstetrical factors such as the gestational age, cervical status, fetal presentation, and maternal medical complications may influence the choice of delivery route ...
Importance: Fetal growth restriction (FGR) is a common pregnancy complication and a significant contributor of fetal and neonatal morbidity and mortality, mainly due to the lack of effective screening, prevention, and management policies. Objective: The aim of this study was to review and compare the most recently published influential guidelines on the management of pregnancies complicated by ...
collection, analysis, and presentation for fetal growth restriction as an adverse event following immunization Fetuses that fail to meet their growth potential in utero are at risk for adverse antenatal and postnatal events such as stillbirth, preterm birth, and adverse neonatal and long-term health out-comes [1-5].
New ISUOG Practice Guidelines provide definitions of fetal growth restriction and small-for-gestational age, and describe the best possible management options based on current data and knowledge. Read the free-access ISUOG Practice Guidelines.
Background: Fetal growth restriction is commonly defined using small for gestational age (SGA) birth (birthweight < 10th percentile) as a proxy, but this approach is problematic because most SGA infants are small but healthy. In this proof-of-concept study, we sought to develop a new approach for identifying fetal growth restriction at birth ...
Citation, DOI, disclosures and article data. Intrauterine growth restriction (IUGR) or fetal growth restriction (FGR) is defined as an estimated fetal weight (EFW) and/or abdominal circumference (AC) at one point in time during pregnancy being below 3 rd percentile or EFW and/or AC below the 10 th percentile for gestational age with deranged ...
Fetal growth restriction (FGR) is the second leading cause of perinatal death, of which late-onset fetal growth restriction (LFGR) accounts for 70%-80% and has a low detection rate. Cardiotocography (CTG) is a routine tool for antepartum fetal monitoring, continuously recording fetal heart rate (FHR) to assess the development of the fetus.
An increase in cesarean delivery (CD) is observed among women with epilepsy. This trend can be attributed to multiple factors including fetal growth restriction, fetal distress, hypertensive disorders of pregnancy, and seizures in pregnancy. We also found a similar increased risk of induced labor and spontaneous abortion in PWWE.
Intrauterine growth restriction (IUGR), a condition that occurs due to various reasons, is an important cause of fetal and neonatal morbidity and mortality. It has been defined as a rate of fetal growth that is less than normal in light of the growth potential of that specific infant. Usually, IUGR and small for gestational age (SGA) are used ...