Problem solving
Worrying is a natural response to life's problems. But when it takes over and we can start to feel overwhelmed, it can really help to take a step back and break things down.
Learning new ways to work through your problems can make them feel more manageable, and improve your mental and physical wellbeing.

Video: Problem solving
The tips in this video can help you to find strategies and solutions for tackling the problems that can be solved, and learning how to manage and cope with those that cannot.
Steps and strategies to help you solve problems
1. focus on your values.
Feeling like you have lots of problems to solve in different areas of your life can make it difficult to know how and where to start.
A great way to focus is to write down a few areas of your life that are most important to you right now – for example, a relationship, finances or a long-term goal like studying or developing your career.
This can make it easier to prioritise which problems to tackle.
2. Tackle problems with possible solutions first
It's important to work out if your problem can be solved or is a "hypothetical worry" – things that are out of your control even though you might think about them often.
They might be based on something that happened in the past that cannot be changed or a worry about the future that starts with "what if…".
Ask yourself whether a problem can be dealt with by doing something practical. If the answer is no, it's a hypothetical worry.
Make a list of your problems, and work out which are solvable and which are hypothetical.
3. Set aside time to work through solvable problems
Set aside 5 or 10 minutes to think about possible solutions for one of your solvable problems.
Try to be as open-minded as you can, even if some ideas feel silly. Thinking broadly and creatively is often when the best solutions come to mind.
It may feel difficult at first but, over time, this approach can start to feel easier.
Once you have some ideas, think through or write down:
- the pros and cons of each solution
- whether it's likely to work
- if you have everything you need to try it
4. Make a plan
The next step is to choose a solution you want to try and make a plan for putting it into action. Try to be specific:
- What are you going to do?
- Do you need the support of anybody else?
- How much time do you need?
- When will you do it?
5. Try 'worry time'
Not all of our problems can be solved right away, but it can be difficult to switch off and stop ourselves from dwelling on them.
Using the "worry time" technique to stick to a short set time – say 10 to 15 minutes in the evening – for worrying can make this much easier to manage.
You can learn more about the worry time technique on tackling your worries .
6. Find time to relax
Worrying about our problems can make it harder to relax, but there are lots of things you can try to help you clear your mind and feel calmer.
The most important thing is to find what works for you. It might be getting active, spending time on an existing hobby or trying a new one, or techniques like mindfulness, meditation or our progressive muscle relaxation exercise.
Video: Progressive muscle relaxation
This video will guide you through an exercise to help you recognise when you're starting to get tense, and relax your body and mind.
7. Review and reflect
Once you start trying new approaches to solving and managing problems, consider setting aside time to review what went well with your solutions or anything else you noticed.
Make notes of the problems you face and any strategies you use to overcome them. This can come in handy later on and also be a good reminder of what works best for you.
Ticking off on a checklist any problems you manage to solve is a great way to recognise your achievements and boost your confidence.
8. Give journaling a go
Sometimes getting our thoughts out of our head – and down onto paper, our phones or anything else – is a great way to stop our worries and "what ifs" from spiralling out of control.
Expressing ourselves in this way can also make it easier to spot when our thoughts are unhelpful and we may benefit from a more balanced outlook. Give it a go to see if this works for you.
More self-help CBT techniques you can try
Bouncing back from life's challenges.
Taking steps to stay on top of your mental wellbeing and build resilience can really help you deal with problems when times are tougher. Learn more, and see tips and techniques you can use.

Tackling your worries

Facing your fears

Staying on top of things
Find more ideas to try in self-help CBT techniques

Cognitive Behavioral Therapy
Solving problems the cognitive-behavioral way, problem solving is another part of behavioral therapy..
Posted February 2, 2022 | Reviewed by Ekua Hagan
- What Is Cognitive Behavioral Therapy?
- Find a therapist who practices CBT
- Problem-solving is one technique used on the behavioral side of cognitive-behavioral therapy.
- The problem-solving technique is an iterative, five-step process that requires one to identify the problem and test different solutions.
- The technique differs from ad-hoc problem-solving in its suspension of judgment and evaluation of each solution.
As I have mentioned in previous posts, cognitive behavioral therapy is more than challenging negative, automatic thoughts. There is a whole behavioral piece of this therapy that focuses on what people do and how to change their actions to support their mental health. In this post, I’ll talk about the problem-solving technique from cognitive behavioral therapy and what makes it unique.
The problem-solving technique
While there are many different variations of this technique, I am going to describe the version I typically use, and which includes the main components of the technique:
The first step is to clearly define the problem. Sometimes, this includes answering a series of questions to make sure the problem is described in detail. Sometimes, the client is able to define the problem pretty clearly on their own. Sometimes, a discussion is needed to clearly outline the problem.
The next step is generating solutions without judgment. The "without judgment" part is crucial: Often when people are solving problems on their own, they will reject each potential solution as soon as they or someone else suggests it. This can lead to feeling helpless and also discarding solutions that would work.
The third step is evaluating the advantages and disadvantages of each solution. This is the step where judgment comes back.
Fourth, the client picks the most feasible solution that is most likely to work and they try it out.
The fifth step is evaluating whether the chosen solution worked, and if not, going back to step two or three to find another option. For step five, enough time has to pass for the solution to have made a difference.
This process is iterative, meaning the client and therapist always go back to the beginning to make sure the problem is resolved and if not, identify what needs to change.

Advantages of the problem-solving technique
The problem-solving technique might differ from ad hoc problem-solving in several ways. The most obvious is the suspension of judgment when coming up with solutions. We sometimes need to withhold judgment and see the solution (or problem) from a different perspective. Deliberately deciding not to judge solutions until later can help trigger that mindset change.
Another difference is the explicit evaluation of whether the solution worked. When people usually try to solve problems, they don’t go back and check whether the solution worked. It’s only if something goes very wrong that they try again. The problem-solving technique specifically includes evaluating the solution.
Lastly, the problem-solving technique starts with a specific definition of the problem instead of just jumping to solutions. To figure out where you are going, you have to know where you are.
One benefit of the cognitive behavioral therapy approach is the behavioral side. The behavioral part of therapy is a wide umbrella that includes problem-solving techniques among other techniques. Accessing multiple techniques means one is more likely to address the client’s main concern.

Salene M. W. Jones, Ph.D., is a clinical psychologist in Washington State.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
- Provide Psychosocial Skills Training and Cognitive Behavioral Interventions
What to Know
Psychosocial skills training and cognitive behavioral interventions teach specific skills to students to help them cope with challenging situations, set goals, understand their thoughts, and change behaviors using problem-solving strategies.
Psychosocial skills training asks students to explore whether their behaviors align with their personal values. Cognitive behavioral interventions teach students to identify their own unhelpful thoughts and replace them with thoughts that are more helpful. Students might practice helpful coping behaviors and find positive activities to try. Doing these things can improve their mood and other symptoms of mental distress.
Districts and schools can deliver interventions in one-on-one settings, small groups, and classrooms. Some interventions focus on concepts that are also taught in social skill and emotional development programs, like self-control and decision-making. A counselor or therapist can lead these programs.
What Can Schools Do?
Promote acceptance and commitment to change.
Schools can help promote acceptance and positive behavior change for students through psychosocial skills training and dialectical behavior therapy. Psychosocial skills training asks students to explore whether their behaviors align with their personal values. Students who see that their behavior does not match their values can decide to make behavior changes. These trainings also help students accept what they cannot change and focus on what they can change. Dialectical behavior therapy teaches mindfulness, acceptance, and commitment skills.
Approaches using acceptance and commitment to change are associated with increases in students’ coping skills and decreases in depression and physical symptoms of depression.
Provide Cognitive Behavioral Interventions
Cognitive behavioral interventions for schools often include multiple sessions. They can be used for one student or a small group. Sessions often follow a standardized manual of activities to help students examine their own thoughts and behaviors. The interventions can include asking students to share what they learn about their thoughts and behaviors with their parents and other people. In some interventions, session leaders focus on a specific topic. Other interventions target mental health symptoms, like depression, anxiety, or post-traumatic stress.
Cognitive behavioral interventions can improve students’ mental health in many ways, including decreasing anxiety, depression, and symptoms related to post-traumatic stress.
- LARS & LISA
- Tools for Getting Along Curriculum—Behavior Management Resource Guide
- Cognitive Behavioral Intervention for Trauma in Schools (CBITS )
- Bounce Back
- Brief Intervention for School Clinicians
- Skills for Academic and Social Success
- Building Confidence
Engage Students in Coping Skills Training Groups
Coping skills training groups use principles of cognitive behavioral intervention to teach students skills to help them handle specific problems. Students can also use these skills to help them cope when their lives are changing. Similar to social, emotional, and behavioral learning programs, coping skills training often focuses on building resilience, or being able to “bounce back” when bad things happen. Students can practice skills outside of the small group, like they would with social skills and emotional development lessons.
Coping skills training groups can increase coping skills for students and decrease anxiety and depression.
- Journey of Hope
- High School Transition Program
Focus on Equity
Students who have been exposed to trauma may receive trauma-focused or trauma-informed interventions in school. Cognitive behavioral interventions that are trauma-informed meet the unique needs of students exposed to traumatic experiences. These interventions teach problem-solving and relaxation techniques and help reduce trauma-related symptoms, including behavioral challenges. Trauma-informed interventions can also improve students’ coping strategies.
Implementation Tips
Cognitive behavioral interventions and psychosocial skills training help with many kinds of student needs. They can be used at multiple grade levels. Leaders can:
- Work with school mental health staff to find ways for students to practice their new behaviors and coping skills.
- Use the Multitiered Systems of Support (MTSS) framework to ensure that students are appropriately matched with classroom, small-group, or individual interventions that meet their needs.
Want to Learn More?
For more details on MTSS and providing psychosocial skills training and cognitive behavioral interventions, see Promoting Mental Health and Well-Being in Schools: An Action Guide for School Administrators [PDF - 3 MB]
- Increase Students’ Mental Health Literacy
- Promote Mindfulness
- Promote Social, Emotional, and Behavioral Learning
- Enhance Connectedness Among Students, Staff, and Families
- Support Staff Well-Being
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
22 Best Counseling Interventions & Strategies for Therapists

Counseling is highly beneficial, with “far-reaching effects in life functioning” (Cochran & Cochran, 2015, p. 7).
While therapeutic relationships are vital to a positive outcome, so too are the selection and use of psychological interventions targeting the clients’ capability, opportunity, motivation, and behavior (Michie et al., 2014).
This article introduces some of the best interventions while identifying the situations where they are likely to create value for the client, helping their journey toward meaningful, value-driven goals.
Before you continue, we thought you might like to download our three Goal Achievement Exercises for free . These detailed, science-based exercises will help you or your clients create actionable goals and master techniques to create lasting behavior change.
This Article Contains:
What is a counseling intervention, list of popular therapeutic interventions, how to craft a treatment plan 101, 13 helpful therapy strategies, interventions & strategies for career counseling, 2 best interventions for group counselors, resources from positivepsychology.com, a take-home message.
“Changing ingrained behavior patterns can be challenging” and must avoid or at least reduce the risk of reverting (Michie et al., 2014, p. 11).
The American Psychological Association (n.d., para. 1) describes an intervention as “any action intended to interfere with and stop or modify a process, as in treatment undertaken to halt, manage, or alter the course of the pathological process of a disease or disorder.”
Interventions are intentional behaviors or “change strategies” introduced by the counselor to help clients implement problem management and move toward goals (Nelson-Jones, 2014):
- Counselor-centered interventions are where the counselor does something to or for the client, such as providing advice.
- Client-centered interventions empower the client, helping them develop their capacity to intervene in their own problems (for example, monitoring and replacing unhelpful thinking).
Creating or choosing the most appropriate intervention requires a thorough assessment of the client’s behavioral targets, what is needed, and how best to achieve them (Michie et al., 2014).
The selection of the intervention is guided by the:
- Nature of the problem
- Therapeutic orientation of the counselor
- Willingness and ability of the client to proceed
During counseling, various interventions are likely to be needed at different times. For that reason, counselors will require a broad range of techniques that fit the client’s needs, values, and culture (Corey, 2013).
In recent years, an increased focus has been on the use of evidence-based practice, where the choice and use of interventions is based on the best available research to make a difference in the lives of clients (Corey, 2013).

“Clients are hypothesis makers and testers” who have the reflective capacity to think about how they think (Nelson-Jones, 2014, p. 261).
Helping clients attend to their thoughts and learn how to instruct themselves more effectively can help them break repetitive patterns of insufficiently strong mind skills while positively influencing their feelings.
The following list includes some of the most popular interventions used in a variety of therapeutic settings (modified from Magyar-Moe et al., 2015; Sommers-Flanagan & Sommers-Flanagan, 2015; Cochran & Cochran, 2015; Corey, 2013):
Detecting and disputing demanding rules
Rigid, demanding thinking is identified by ‘musts,’ ‘oughts,’ and ‘shoulds’ and is usually unhelpful to the client.
For example:
I must do well in this test, or I am useless. People must treat me in the way I want; otherwise, they are awful.
Clients can be helped to dispute such thinking using “reason, logic, and facts to support, negate or amend their rules” (Nelson-Jones, 2014, p. 265).
Such interventions include:
- Functional disputing Pointing out to clients that their thinking may stand in the way of achieving their goals
- Empirical disputing Encouraging clients to evaluate the facts behind their thoughts
- Logical disputing Highlighting the illogical jumps in their thinking from preferences to demands
- Philosophical disputing Exploring clients’ meaning and satisfaction outside of life issues
Identifying automatic perceptions
Our perceptions greatly influence how we think. Clients can benefit from recognizing they have choices in how they perceive things and avoiding jumping to conclusions.
- Creating self-talk Self-talk can be helpful for most clients and can target anger management, stress handling, and improving confidence. For example:
This is not the end of the world. I’ve done this before; I can do it well again.
- Creating visual perceptions Building on the client’s existing visual images can be helpful in understanding and working through problematic situations (and their solutions).
One simple exercise to help clients see the strong relationship between visualizing and feeling involves asking clients to think of someone they love. Almost always, they form a mental image along with a host of feelings.
Visual relaxation is a powerful self-helping skill involving clients taking time out of their busy life to find calm through vividly picturing a real or imagined relaxing scene.
Creating better expectations
Clients’ explanatory styles (such as expecting to fail) can create self-fulfilling prophecies. Interventions can help by:
- Assessing the likelihood of risks or rewards
- Increasing confidence in the potential for success
- Identifying coping skills and support factors
- Time projection Imagery can help by enabling the client to step into a possible future where they manage and overcome difficult times or worrying situations.
For example, the client can imagine rolling forward to a time when they are successful in a new role at work or a developing relationship.
Creating realistic goals
Goals can motivate clients to improve performance and transition from where they are now to where they would like to be. However, it is essential to make sure they are realistic, or they risk causing undue pressure and compromising wellbeing.
The following interventions can help (Nelson-Jones, 2014):
- Stating clear goals The following questions are helpful when clients are setting goals :
Does the goal reflect your values? Is the goal realistic and achievable? Is the goal specific? Is the goal measurable? Does the goal have a timeframe?
Helping clients to experience feelings
Counseling can influence clients’ emotions and their physical reactions to emotions by helping them (Nelson-Jones, 2014):
- Experience feelings
- Express feelings
- Manage feelings
- Empty chair dialogue This practical intervention involves the client engaging in an imaginary conversation with another person; it helps “clients experience feelings both of unresolved anger and also of weakness and victimization” (Nelson-Jones, 2014, p. 347).
The client may be asked to shift to the empty chair and play the other person’s part to explore conflict, interactions, and emotions more fully (Corey, 2013).
Download 3 Free Goals Exercises (PDF)
These detailed, science-based exercises will help you or your clients create actionable goals and master techniques for lasting behavior change.
Download 3 Free Goals Pack (PDF)
By filling out your name and email address below.
- Email Address *
- Your Expertise * Your expertise Therapy Coaching Education Counseling Business Healthcare Other
- Phone This field is for validation purposes and should be left unchanged.
“Counselors and counseling trainees make choices both concerning specific interventions and about interventions used in combination” (Nelson-Jones, 2014, p. 223).
Through early and continued engagement with the client throughout the counseling approach , the counselor and client set specific, measurable, and achievable goals and create a treatment plan with a defined intervention strategy (Dobson, 2010).
The treatment plan becomes a map, combining interventions to reach client goals and overcome problems – to get from where they are now to where they want to be. However, no plan should be too fixed or risk preventing the client’s progress in their ‘wished-for’ direction. Rather, it must be open for regular revisit and modification (Nelson-Jones, 2014).
Counseling and therapeutic treatment plans vary according to the approaches used and the client’s specific needs but should be strength-based and collaborative. Most treatment plans typically consider the following points (modified from GoodTherapy, 2019):
- History and assessment – E.g., psychosocial history, symptom onset, past and present diagnoses, and treatment history
- Present concerns – The current concerns and issues that led the client to counseling
- Counseling contract – A summary of goals and desired changes, responsibility, and the counseling approach adopted
- Summary of strengths – It can be helpful to summarize the client’s strengths, empowering them for goal achievement.
- Goals – Measurable treatment goals are vital to the treatment plan.
- Objectives – Goals are broken down into smaller, achievable outcomes that support achievement during counseling.
- Interventions – Interventions should be planned early to support objectives and overall goals.
- Tracking progress and outcomes – Regular treatment plan review should include updating progress toward goals.
While a vital aspect of the counseling process is to ensure that treatment takes an appropriate direction for the client, it is also valuable and helpful for clients and insurance companies to understand likely timescales.

“Depression is one of the most common mental health disorders with a high burden of disease and the leading cause of years of life lost due to disability” (Hu et al., 2020, p. 1).
- Exercise interventions Research has shown that even low-to-moderate levels of exercise can help manage and treat depression (Hu et al., 2020).
- Gratitude Practicing gratitude can profoundly affect how we see our lives and those around us. Completing gratitude journals and reviewing three positive things that have happened at the end of the day have been shown to decrease depression and promote wellbeing (Shapiro, 2020).
- Behavioral activation Scheduling activities that result in positive emotions can help manage and overcome depression (Behavioral Activation for Depression, n.d.).
Anxiety can stop clients from living their lives fully and experiencing positive emotions. Many interventions can help, including:
- Understanding your anxiety triggers Interoceptive exposure techniques focus on reproducing sensations associated with anxiety and other difficult emotions. Clients benefit from learning to identify anxiety triggers, behavioral changes, and associated bodily sensations (Boettcher et al., 2016).
- Using a building image Clients are asked to form a mental image of themselves as a building. Their description of its state of repair and quality of foundation provides helpful insight into the client’s wellbeing and degree of anxiety (Thomas, 2016).
Grief therapy
Grief therapy helps clients accept reality, process the pain, and adjust to a new world following the loss of a loved one. Several techniques can help, including (modified from (Worden, 2018):
- Creating memory books Compiling a memory book containing photographs, memorabilia, stories, and poems can help families come together, share their grief, and reminisce.
- Directed imagery Like the ‘empty chair’ technique, through imagining the missing loved one in front of them, the grieving person is given the opportunity to talk to them.
Substance abuse
“There has been significant progress and expansion in the development of evidence-based psychosocial treatments for substance abuse and dependence” (Jhanjee, 2014, p. 1). Psychological interventions play a growing role in disorder treatment programs; they include:
- Brief optimistic interventions Brief advice is delivered following screening and assessment to at-risk individuals to reduce drinking and other harmful activities.
- Motivational interviewing This technique involves using targeted questioning while expressing empathy through reflective listening to resolve client ambivalence about their substance abuse.
Marriage therapy
Interventions are a vital aspect of marriage therapy , often targeting communication skills, problem-solving, and taking responsibility (Williams, 2012).
They can include the following interventions:
- Taking responsibility It is vital that clients take responsibility for their actions within a relationship. The counselor will work with the couple, asking the following questions, as required (modified from Williams, 2012):
How have you contributed to the relationship’s problems? What changes are needed to improve the relationship? Are you willing to make the changes needed?
- Create an action plan Once the couple agrees, the changes will be combined into a plan, with specific actions to help them achieve their goal.
Helping cancer patients
“There is no evidence to suggest that having counseling will help treat or cure your cancer”; however, it may help with coping, relationship issues, and dealing with practical problems (Cancer Research UK, 2019, para. 16).
Several counseling interventions that have proven helpful with the psychological burden include (Guo et al., 2013):
- Psychoeducation Sharing the importance of mental wellbeing and coping with the client and involving them in their cancer treatment can reduce anxiety and improve confidence.
- Cognitive-Behavioral Therapy Replacing incorrect or unhelpful beliefs can help the client achieve a more positive outlook regarding the treatment.
Career counselors help individuals or groups cope more effectively with career concerns, including (Niles & Harris-Bowlsbey, 2017):
- Career choice
- Managing career changes and transitions
- Job-related stress
- Looking for a job
While there are many interventions and strategies, the following are insightful and effective:
- Creating narratives Working with clients to build personal career narratives can help them see their movement through life with more meaning and coherence and better understand their decisions. Such an intervention can be valuable in looking forward and choosing the next steps.
- Group counseling Multiple group sessions can be arranged to cover different aspects of career-related issues and related emotional issues. They may include role-play or open discussion around specific topics.

The ultimate goals are usually to “help group members respond to each other with a combination of therapeutic attending, and sharing their own reactions and related experiences” (Cochran & Cochran, 2015, p. 329).
Examples of group interventions include:
- Circle of friends This group intervention involves gathering a child’s peers into a circle of friendly support to encourage and help them with problem-solving. The intervention has led to increased social acceptance of children with special needs (Magyar-Moe et al., 2015).
- Group mindfulness Mindfulness in group settings has been shown to be physically and mentally beneficial (Shapiro, 2020). New members may start by performing a body-scan meditation where they bring awareness to each part of their body before turning their attention to their breathing.
17 Tools To Increase Motivation and Goal Achievement
These 17 Motivation & Goal Achievement Exercises [PDF] contain all you need to help others set meaningful goals, increase self-drive, and experience greater accomplishment and life satisfaction.
Created by Experts. 100% Science-based.
We have many free interventions, using various approaches and mediums, that support the counseling process and client goal achievement.
- Nudge Interventions in Groups The group provides a valuable setting for exploring the potential of ‘nudges’ to alter behavior in a predictable way.
- Developing Interoceptive Exposure Therapy Interventions This worksheet explores the sensations behind panic attacks and phobias.
- Therapist Interoceptive Exposure Record Use this helpful log to track interoceptive exposure interventions.
- Motivational Interviewing This template uses the five stages of change to consider the client’s readiness for change and the appropriate interventions to use.
- Breaking Out of the Comfort Zone Making changes typically requires clients to step out of their comfort zone. This worksheet identifies opportunities to embrace new challenges.
More extensive versions of the following tools are available with a subscription to the Positive Psychology Toolkit© , but they are described briefly below:
- Benefit finding
Psychological research has identified long-term benefits to using benefit finding, with individuals reporting new appreciation for their strengths and building resilience (e.g., Affleck & Tennen, 1996; Davis et al., 1998; McMillen et al., 1997).
- Begin by talking about a traumatic event.
- Focus on the positive aspects of the experience.
- Consider what the experience has taught you.
- Identify how the experience has helped you grow
- Self-compassion box
Self-compassion is a crucial aspect of our psychological wellbeing, made up of showing ourselves kindness, accepting imperfection, and paying attention to personal suffering with clarity and objectivity.
- Step one – Begin by recognizing the uncompassionate self.
- Step two – Select self-compassion reminders.
- Step three – Redirect attention to self-compassion.
- Step four – Reflect on creating more self-compassion in life.
Over time, the client should see the gaps closing between where they are now and where they want to be.
If you’re looking for more science-based ways to help others reach their goals, check out this collection of 17 validated motivation & goal achievement tools for practitioners. Use them to help others turn their dreams into reality by applying the latest science-based behavioral change techniques.
Counseling uses interventions to create positive change in clients’ lives. They can be performed individually but typically form part of a treatment or intervention plan developed with the client.
Each intervention helps the client work toward their goals, strengthen their capabilities, identify opportunities, increase motivation, and modify behavior.
They aim to create sufficient momentum to support change and avoid the risk of the client reverting, transitioning the client (often one small step at a time) from where they are now to where they want to be.
While some interventions have value in multiple settings – individual, group, career, couples, family – others are specific and purposeful. Many interventions target unhelpful, repetitive thinking patterns and aim to replace harmful thoughts, unrealistic expectations, or biased thinking. Others create a possible future where the client can engage with what might be or could happen , coming to terms with change or their own negative emotions.
Use this article to explore the range of interventions available to counselors in sessions or as homework. Try them out in different settings, working with the client to identify their value or potential for modification.
We hope you enjoyed reading this article. Don’t forget to download our three Goal Achievement Exercises for free .
- Affleck, G., & Tennen, H. (1996). Construing benefits from adversity: Adaptational significance and dispositional underpinnings. Journal of Personality , 64 , 899–922.
- American Psychological Association. (n.d.). Intervention. In APA dictionary of psychology . Retrieved February 27, 2022, from https://dictionary.apa.org/intervention
- Behavioral Activation for Depression. (n.d.). Retrieved February 16, 2022, from https://medicine.umich.edu/sites/default/files/content/downloads/Behavioral-Activation-for-Depression.pdf
- Boettcher, H., Brake, C. A., & Barlow, D. H. (2016). Origins and outlook of interoceptive exposure. Journal of Behavior Therapy and Experimental Psychiatry , 53 , 41–51.
- Cancer Research UK. (2019). How counselling can help . Retrieved February 28, 2022, from https://www.cancerresearchuk.org/about-cancer/coping/emotionally/talking-about-cancer/counselling/how-counselling-can-help
- Cochran, J. L., & Cochran, N. H. (2015). The heart of counseling: Counseling skills through therapeutic relationships . Routledge, Taylor & Francis Group.
- Corey, G. (2013). Theory and practice of counseling and psychotherapy . Cengage.
- Davis, C. G., Nolen-Hoeksema, S., & Larson, J. (1998). Making sense of loss and benefiting from the experience: Two construals of meaning. Journal of Personality and Social Psychology , 75 , 561–574.
- Dobson, K. S. (Ed.) (2010). Handbook of cognitive-behavioral therapies (3rd ed.). Guilford Press.
- Guo, Z., Tang, H. Y., Li, H., Tan, S. K., Feng, K. H., Huang, Y. C., Bu, Q., & Jiang, W. (2013). The benefits of psychosocial interventions for cancer patients undergoing radiotherapy. Health and Quality of Life Outcomes , 11 (1), 1–12.
- GoodTherapy. (2019, September 25). Treatment plan . Retrieved February 27, 2022, from https://www.goodtherapy.org/blog/psychpedia/treatment-plan
- Hu, M. X., Turner, D., Generaal, E., Bos, D., Ikram, M. K., Ikram, M. A., Cuijpers, P., & Penninx, B. W. J. H. (2020). Exercise interventions for the prevention of depression: a systematic review of meta-analyses. BMC Public Health , 20 (1), 1255.
- Jhanjee, S. (2014). Evidence-based psychosocial interventions in substance use. Indian Journal of Psychological Medicine , 36 (2), 112–118.
- Magyar-Moe, J. L., Owens, R. L., & Conoley, C. W. (2015). Positive psychological interventions in counseling. The Counseling Psychologist , 43 (4), 508–557.
- McMillen, J. C., Smith, E. M., & Fisher, R. H. (1997). Perceived benefit and mental health after three types of disaster. Journal of Consulting and Clinical Psychology , 65 , 733–739.
- Michie, S., Atkins, L., & West, R. (2014). The behaviour change wheel: A guide to designing interventions . Silverback.
- Nelson-Jones, R. (2014). Practical counselling and helping skills . Sage.
- Niles, S. G., & Harris-Bowlsbey, J. (2017). Career development interventions . Pearson.
- Shapiro, S. L. (2020). Rewire your mind: Discover the science + practice of mindfulness . Aster.
- Sommers-Flanagan, J., & Sommers-Flanagan, R. (2015). Study guide for counseling and psychotherapy theories in context and practice: Skills, strategies, and techniques (2nd ed.). Wiley.
- Thomas, V. (2016). Using mental imagery in counselling and psychotherapy: A guide to more inclusive theory and practice . Routledge.
- Williams, M. (2012). Couples counseling: A step by step guide for therapists . Viale.
- Worden, J. W. (2018). Grief counseling and grief therapy: A handbook for the mental health practitioner . Springer.
Share this article:
Article feedback
What our readers think.
Hello wonderful staff members, I do hope you are well. I wanted to convey my sincerest gratitude for your free informative resource of brilliant information. I am an adult online psychology first year student as well as a sex therapy student, apart from my brilliant instructors with my sex therapy professors . I am on my own to teach myself with my psychology your resource have been my salvation as an independent psychology learning student. Your articles are all life enhancing written with comprehension and depth while not fraught with verbosity and complex language. I want you to know that your company’s generosity in making these articles free are the missing link in all students who would like to advance their academic careers. With profound appreciation Michelle
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

Youth Counseling: 17 Courses & Activities for Helping Teens
From a maturing body and brain to developing life skills and values, the teen years can be challenging, and mental health concerns may arise. Teens [...]

How To Plan Your Counseling Session: 6 Examples
Planning is crucial in a counseling session to ensure that time inside–and outside–therapy sessions is well spent, with the client achieving a successful outcome within [...]

Applied Positive Psychology in Therapy: Your Ultimate Guide
Without a doubt, this is an exciting time for positive psychology in therapy. Many academics and therapists now recognize the value of this fascinating, evolving [...]
Read other articles by their category
- Body & Brain (49)
- Coaching & Application (57)
- Compassion (26)
- Counseling (51)
- Emotional Intelligence (24)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (20)
- Mindfulness (45)
- Motivation & Goals (45)
- Optimism & Mindset (34)
- Positive CBT (28)
- Positive Communication (20)
- Positive Education (47)
- Positive Emotions (32)
- Positive Leadership (17)
- Positive Parenting (3)
- Positive Psychology (33)
- Positive Workplace (37)
- Productivity (16)
- Relationships (46)
- Resilience & Coping (36)
- Self Awareness (21)
- Self Esteem (37)
- Strengths & Virtues (31)
- Stress & Burnout Prevention (34)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 07 October 2021
Young people’s mental health is finally getting the attention it needs
You have full access to this article via your institution.

A kite-flying festival in a refugee camp near Syria’s border with Turkey. The event was organized in July 2020 to support the health and well-being of children fleeing violence in Syria. Credit: Muhammed Said/Anadolu Agency/Getty
Worldwide, at least 13% of people between the ages of 10 and 19 live with a diagnosed mental-health disorder, according to the latest State of the World’s Children report , published this week by the United Nations children’s charity UNICEF. It’s the first time in the organization’s history that this flagship report has tackled the challenges in and opportunities for preventing and treating mental-health problems among young people. It reveals that adolescent mental health is highly complex, understudied — and underfunded. These findings are echoed in a parallel collection of review articles published this week in a number of Springer Nature journals.
Anxiety and depression constitute more than 40% of mental-health disorders among young people (those aged 10–19). UNICEF also reports that, worldwide, suicide is the fourth most-common cause of death (after road injuries, tuberculosis and interpersonal violence) among adolescents (aged 15–19). In eastern Europe and central Asia, suicide is the leading cause of death for young people in that age group — and it’s the second-highest cause in western Europe and North America.

Collection: Promoting youth mental health
Sadly, psychological distress among young people seems to be rising. One study found that rates of depression among a nationally representative sample of US adolescents (aged 12 to 17) increased from 8.5% of young adults to 13.2% between 2005 and 2017 1 . There’s also initial evidence that the coronavirus pandemic is exacerbating this trend in some countries. For example, in a nationwide study 2 from Iceland, adolescents (aged 13–18) reported significantly more symptoms of mental ill health during the pandemic than did their peers before it. And girls were more likely to experience these symptoms than were boys.
Although most mental-health disorders arise during adolescence, UNICEF says that only one-third of investment in mental-health research is targeted towards young people. Moreover, the research itself suffers from fragmentation — scientists involved tend to work inside some key disciplines, such as psychiatry, paediatrics, psychology and epidemiology, and the links between research and health-care services are often poor. This means that effective forms of prevention and treatment are limited, and lack a solid understanding of what works, in which context and why.
This week’s collection of review articles dives deep into the state of knowledge of interventions — those that work and those that don’t — for preventing and treating anxiety and depression in young people aged 14–24. In some of the projects, young people with lived experience of anxiety and depression were co-investigators, involved in both the design and implementation of the reviews, as well as in interpretation of the findings.
Quest for new therapies
Worldwide, the most common treatment for anxiety and depression is a class of drug called selective serotonin reuptake inhibitors, which increase serotonin levels in the brain and are intended to enhance emotion and mood. But their modest efficacy and substantial side effects 3 have spurred the study of alternative physiological mechanisms that could be involved in youth depression and anxiety, so that new therapeutics can be developed.

Mental health: build predictive models to steer policy
For example, researchers have been investigating potential links between depression and inflammatory disorders — such as asthma, cardiovascular disease and inflammatory bowel disease. This is because, in many cases, adults with depression also experience such disorders. Moreover, there’s evidence that, in mice, changes to the gut microbiota during development reduce behaviours similar to those linked to anxiety and depression in people 4 . That suggests that targeting the gut microbiome during adolescence could be a promising avenue for reducing anxiety in young people. Kathrin Cohen Kadosh at the University of Surrey in Guildford, UK, and colleagues reviewed existing reports of interventions in which diets were changed to target the gut microbiome. These were found to have had minimal effect on youth anxiety 5 . However, the authors urge caution before such a conclusion can be confirmed, citing methodological limitations (including small sample sizes) among the studies they reviewed. They say the next crop of studies will need to involve larger-scale clinical trials.
By contrast, researchers have found that improving young people’s cognitive and interpersonal skills can be more effective in preventing and treating anxiety and depression under certain circumstances — although the reason for this is not known. For instance, a concept known as ‘decentring’ or ‘psychological distancing’ (that is, encouraging a person to adopt an objective perspective on negative thoughts and feelings) can help both to prevent and to alleviate depression and anxiety, report Marc Bennett at the University of Cambridge, UK, and colleagues 6 , although the underlying neurobiological mechanisms are unclear.
In addition, Alexander Daros at the Campbell Family Mental Health Institute in Toronto, Canada, and colleagues report a meta-analysis of 90 randomized controlled trials. They found that helping young people to improve their emotion-regulation skills, which are needed to control emotional responses to difficult situations, enables them to cope better with anxiety and depression 7 . However, it is still unclear whether better regulation of emotions is the cause or the effect of these improvements.
Co-production is essential
It’s uncommon — but increasingly seen as essential — that researchers working on treatments and interventions are directly involving young people who’ve experienced mental ill health. These young people need to be involved in all aspects of the research process, from conceptualizing to and designing a study, to conducting it and interpreting the results. Such an approach will lead to more-useful science, and will lessen the risk of developing irrelevant or inappropriate interventions.

Science careers and mental health
Two such young people are co-authors in a review from Karolin Krause at the Centre for Addiction and Mental Health in Toronto, Canada, and colleagues. The review explored whether training in problem solving helps to alleviate depressive symptoms 8 . The two youth partners, in turn, convened a panel of 12 other youth advisers, and together they provided input on shaping how the review of the evidence was carried out and on interpreting and contextualizing the findings. The study concluded that, although problem-solving training could help with personal challenges when combined with other treatments, it doesn’t on its own measurably reduce depressive symptoms.
The overarching message that emerges from these reviews is that there is no ‘silver bullet’ for preventing and treating anxiety and depression in young people — rather, prevention and treatment will need to rely on a combination of interventions that take into account individual needs and circumstances. Higher-quality evidence is also needed, such as large-scale trials using established protocols.
Along with the UNICEF report, the studies underscore the transformational part that funders must urgently play, and why researchers, clinicians and communities must work together on more studies that genuinely involve young people as co-investigators. Together, we can all do better to create a brighter, healthier future for a generation of young people facing more challenges than ever before.
Nature 598 , 235-236 (2021)
doi: https://doi.org/10.1038/d41586-021-02690-5
Twenge, J. M., Cooper, A. B., Joiner, T. E., Duffy, M. E. & Binau, S. G. J. Abnorm. Psychol. 128 , 185–199 (2019).
Article PubMed Google Scholar
Thorisdottir, I. E. et al. Lancet Psychiatr. 8 , 663–672 (2021).
Article Google Scholar
Murphy, S. E. et al. Lancet Psychiatr. 8 , 824–835 (2021).
Murray, E. et al. Brain Behav. Immun. 81 , 198–212 (2019).
Cohen Kadosh, K. et al. Transl. Psychiatr. 11 , 352 (2021).
Bennett, M. P. et al. Transl Psychiatr. 11 , 288 (2021).
Daros, A. R. et al. Nature Hum. Behav . https://doi.org/10.1038/s41562-021-01191-9 (2021).
Krause, K. R. et al. BMC Psychiatr. 21 , 397 (2021).
Download references
Reprints and permissions
Related Articles

- Psychiatric disorders
- Public health

The rise of eco-anxiety: scientists wake up to the mental-health toll of climate change
News Feature 10 APR 24
Use fines from EU social-media act to fund research on adolescent mental health
Correspondence 09 APR 24

‘Without these tools, I’d be lost’: how generative AI aids in accessibility
Technology Feature 08 APR 24

Lethal dust storms blanket Asia every spring — now AI could help predict them
News 15 APR 24

Bird flu outbreak in US cows: why scientists are concerned
News Explainer 08 APR 24
Adopt universal standards for study adaptation to boost health, education and social-science research
Correspondence 02 APR 24

India is booming — but there are worries ahead for basic science
News 10 APR 24
How to break big tech’s stranglehold on AI in academia
Brazil’s postgraduate funding model is about rectifying past inequalities
Junior Group Leader Position at IMBA - Institute of Molecular Biotechnology
The Institute of Molecular Biotechnology (IMBA) is one of Europe’s leading institutes for basic research in the life sciences. IMBA is located on t...
Austria (AT)
IMBA - Institute of Molecular Biotechnology
Research Group Head, BeiGene Institute
A cross-disciplinary research organization where cutting-edge science and technology drive the discovery of impactful Insights
Pudong New Area, Shanghai
BeiGene Institute
Open Rank Faculty, Center for Public Health Genomics
Center for Public Health Genomics & UVA Comprehensive Cancer Center seek 2 tenure-track faculty members in Cancer Precision Medicine/Precision Health.
Charlottesville, Virginia
Center for Public Health Genomics at the University of Virginia
Husbandry Technician I
Memphis, Tennessee
St. Jude Children's Research Hospital (St. Jude)
Lead Researcher – Department of Bone Marrow Transplantation & Cellular Therapy
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Research article
- Open access
- Published: 26 October 2011
Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV
- Dixon Chibanda 1 ,
- Petra Mesu 2 ,
- Lazarus Kajawu 1 , 2 ,
- Frances Cowan 3 , 4 ,
- Ricardo Araya 5 &
- Melanie A Abas 6
BMC Public Health volume 11 , Article number: 828 ( 2011 ) Cite this article
27k Accesses
204 Citations
172 Altmetric
Metrics details
There is limited evidence that interventions for depression and other common mental disorders (CMD) can be integrated sustainably into primary health care in Africa. We aimed to pilot a low-cost multi-component 'Friendship Bench Intervention' for CMD, locally adapted from problem-solving therapy and delivered by trained and supervised female lay workers to learn if was feasible and possibly effective as well as how best to implement it on a larger scale.
We trained lay workers for 8 days in screening and monitoring CMD and in delivering the intervention. Ten lay workers screened consecutive adult attenders who either were referred or self-referred to the Friendship Bench between July and December 2007. Those scoring above the validated cut-point of the Shona Symptom Questionnaire (SSQ) for CMD were potentially eligible. Exclusions were suicide risk or very severe depression. All others were offered 6 sessions of problem-solving therapy (PST) enhanced with a component of activity scheduling. Weekly nurse-led group supervision and monthly supervision from a mental health specialist were provided. Data on SSQ scores at 6 weeks after entering the study were collected by an independent research nurse. Lay workers completed a brief evaluation on their experiences of delivering the intervention.
Of 395 potentially eligible, 33 (8%) were excluded due to high risk. Of the 362 left, 2% (7) declined and 10% (35) were lost to follow-up leaving an 88% response rate (n = 320). Over half (n = 166, 52%) had presented with an HIV-related problem. Mean SSQ score fell from 11.3 (sd 1.4) before treatment to 6.5 (sd 2.4) after 3-6 sessions. The drop in SSQ scores was proportional to the number of sessions attended. Nine of the ten lay workers rated themselves as very able to deliver the PST intervention.
We have found preliminary evidence of a clinically meaningful improvement in CMD associated with locally adapted problem-solving therapy delivered by lay health workers through routine primary health care in an African setting. There is a need to test the effectiveness of this task-shifting mental health intervention in an appropriately powered randomised controlled trial.
Trial registration
ISRCTN: ISRCTN25476759
Peer Review reports
Mental disorders cause considerable suffering, disability and social exclusion in Africa, and are poorly recognised and undertreated [ 1 , 2 ]. In Zimbabwe, common mental disorders, such as depression mixed with anxiety, are found in over 25% of those attending primary health care services or maternal services, and in up to 30% of females in the community [ 3 – 5 ]. In the Zimbabwean Shona language, thinking too much ( kufungisisa ), along with deep sadness ( kusuwisisa ), and painful heart (moyo unorwadza) are terms in common use for emotional distress being close to European and American categories of common forms of depression and anxiety [ 3 , 6 ]
There is increasing evidence, mainly from other world regions but also rapidly growing evidence from within low income countries, that improving mental health is a low cost approach to improve quality of life and reduce disability [ 7 , 8 ]. Very little of this evidence, however, is from Africa. In Chile, low intensity low-cost treatments for depression have been integrated into primary health care [ 9 ]. These include, for example, psycho education, problem-solving therapy and self-help approaches [ 10 , 11 ]. Problem-solving therapy has been shown to be effective for depression and common mental health problems [ 12 , 13 ]. Previous attempts to deliver care for common mental disorders through primary care clinics in Zimbabwe although promising in the short-term had shown little long-term success due to reliance on overstretched nursing staff and lack of supervision [ 14 ]. In 2005, a government operation in Mbare , a township in Harare, resulted in many people becoming homeless or losing their livelihoods [ 15 ] and was perceived by the Mbare community to lead to high rate of emotional distress. Local stakeholders identified the need for a community mental health intervention. This had to be at no extra cost to the primary health care clinic, to utilise space outside the overcrowded clinic rooms, and to use methods already tested locally. A pilot intervention based on a problem-solving approach was identified [ 16 ]. It was suggested this be delivered by lay health workers via a 'Friendship Bench' ( Chigaro Chekupanamazano ) placed in the clinic grounds, and that a system of supervision and stepped care be part of the package. A team comprising psychologists, a primary care nurse and a psychiatrist adapted existing training materials on problem solving therapy [ 16 , 17 ] in the light of experience working with lay workers and general nurses in primary care. Adaptations included at least one home visit by the lay workers early in the therapy given it is normal practice for lay workers to visit clients in their homes, and encouraging clients to schedule some positive activities that really mattered to them to make life more rewarding. The training and the intervention were pre-tested in 5 lay workers and 143 primary care clients and found to be acceptable to them and to the lay workers. The aim of this pilot was to gather preliminary data on the effectiveness of this intervention and to see if the intervention would be feasible, and if so to gather ideas about how best to implement it on a larger scale.
Mbare is a high density suburb or township in the south of Harare. It is characterized by ethnic diversity and high unemployment with most residents relying on informal trading. The literacy rate is estimated to be over 90%. There are three government run Primary Health Care (PHC) clinics, staffed almost exclusively by general nurses, for a population of approximately 200 000. The study took place in all three clinics.
Twenty lay workers, locally termed health promoters, support the nurses at these three clinics. The lay workers are a respected group of primary health care providers, commonly referred to as ambuya utano (grandmother health provider) (Figure 1 ). In Mbare , all lay workers are female, literate, have at least primary school education, and have lived locally for at least 15 years. Their mean age is 58 years. Their main role is in community health outreach, which includes supporting people living with HIV/AIDS and Tuberculosis by providing individual and family support (practical, psychological and spiritual) and encouraging medication adherence. They also deliver community health education and promotion e.g. through encouraging immunisation and methods to control disease outbreaks. Lay workers report weekly to the environmental health officer and a nurse-manager. The lay workers cover geographical patches, which are sections of the community demarcated by the City of Harare according to street grids. Each geographical patch has approximately 3000 inhabitants. Ten lay workers were selected at random for this pilot: three from two of the clinics and four from the largest clinic.

Some of the lay health workers involved in the Friendship Bench project, sitting in front of one of the Benches .
Participants
Inclusion criteria: aged 18 and over; residents of geographical patches in Mbare , Harare, covered by the ten selected lay workers; score > 7 on Shona Symptom Questionnaire screen for common mental disorders. Exclusion criteria: requiring acute medical attention such that they cannot participate; severe psychiatric symptoms and/or risk to self or others requiring specialist referral as assessed by primary care research nurse
Ethical approval was obtained from the Medical Research Council of Zimbabwe and written informed consent was sought from all participants. The study was registered as a non-controlled trial http://www.controlled-trials.com/ISRCTN25476759
Recruitment
We aimed to recruit from the clinic staff, from the community, and from the lay workers themselves. The psychiatrist (DC) and psychologists (PM, KJ) presented to the clinic nursing staff and to all 20 lay workers the rationale for the project and referral methods to the friendship Bench. Notices written in the local vernacular language explaining the location and uses of the benches were placed at six different points within the entrance hall and waiting area of each clinic.
The lay workers introduced and publicised the Friendship Bench to the community through community stakeholders' meetings and during visits to people's homes, churches, schools and police stations. They introduced it as an adjunct to their normal daily community health outreach activity. They described the Friendship Bench approach as aimed at addressing common mental health issues such as kufungisisa (thinking too much) as a result of, among other things, HIV infection, AIDS, domestic violence, family sickness and poverty.
Clients were either referred or could self refer to the Friendship Bench, which was available Mon-Friday 9.00 am to 12.00 pm at each clinic. Those referred or who self-referred were directed by nursing or reception staff to sit on the Friendship Bench which in each clinic was a large wooden bench located under a tree within sight of the lay workers' office. One duty lay worker was responsible for the Bench each day on rotation and would approach the Bench after a potential client sat on it. The duty lay worker was responsible for collecting data on inclusion criteria including residential and basic demographic information and on psychological symptoms using the Shona Symptom Questionnaire (SSQ) [ 4 ]. She also gathered information on recent stressors using a brief life events screen based on one used previously in Harare [ 18 ]. Everyone was offered some education, advice and often sign-posted to support services. Those meeting inclusion criteria were referred to a research nurse for assessment of risk to self or to others (e.g. suicidal ideation, history of deliberate self harm, very severe symptoms). She referred those excluded on these grounds to the visiting psychiatrist (DC). She invited those meeting eligibility criteria to participate in the pilot and took written informed consent. She then referred them back to the lay worker who made arrangements for their first Friendship Bench session within 2-5 days with a lay worker that covered their geographical patch.
Outcome measure
The main outcome measure was the Shona Symptom Questionnaire (SSQ). The SSQ is a 14-item screening tool for common mental disorders, integrating local idioms and internationally recognised items for emotional distress. It was developed and validated in Zimbabwe using exemplary cross-cultural methods [ 4 ]. It is self-administered and has a reliable internal consistency (r = 0.85) and satisfactory sensitivity and specificity, with a score of > = 8 being the cut-point. It is based on a yes/no response and asks about symptoms such as thinking too much, failing to concentrate, work lagging behind, insomnia, suicidal ideation, unhappiness and so on, over a 1 week period. All participants were approached six to eight weeks after their first treatment session to complete a self-administered SSQ which was collected by the research nurse in the absence of the attending lay worker.
The Intervention
The intervention consisted of brief individual talking therapy based on problem-solving therapy delivered by a lay worker. Most sessions took place sitting on a bench termed "The Friendship Bench" ( Chigaro Chekupanamazano ). The Friendship Benches were made for the project by local craftsmen (see Figure 1 ). They are located within the grounds of each of the three participating clinics in a discrete area under the trees in the clinic gardens.
Table 1 shows the activities involved in the delivery of the Friendship Bench. The lay worker would initially explain to all participants how to self-administer the screening tool, the Shona Symptom Questionnaire. Problem-solving therapy (PST) included identification and exploration of problems, and identification and implementation of solutions, based on prior principles [ 19 ]. Our PST was a locally developed seven-step plan previously used in partnership with government, lay and traditional care providers [ 16 ]. Up to a maximum of 6 sessions on the Bench were offered with the second session taking place at the client's home and sometimes also one of the later sessions. Those most in financial need were referred to two local income-generating projects (peanut butter making; recycling). The problem solving therapy was enhanced with a component of activity scheduling in that clients were also encouraged to carry out activities that really mattered to them to make life more rewarding. Home visits included prayer. Prayer was already a well recognised part of the support provided by LW in their community health outreach role in Mbare , which has a 98% Christian population with more than 70 Christian faith groups. On average each prayer lasts 15-30 minutes and is delivered by one lay worker together with the family. The aim of the prayer is to comfort the sick and the family. The use of prayer in formal gatherings related to health is a common practice in Zimbabwe. The existing prayer format used prior to the introduction of the Friendship Bench was incorporated in the six sessions without any alterations.
Training, selection and supervision of facilitators
All 20 lay workers were trained.
We provided an 8-day training run by two clinical psychologists (PM and LK), a general nurse trained in systemic counselling (ST) and a psychiatrist (DC). This covered didactic lectures on common mental disorders (CMD), including kufungisisa (thinking too much) but particularly focussed on skills to identify CMD using the Shona Symptoms Questionnaire [ 4 ], and to manage CMD using simple psycho-education and problem-solving therapy [ 16 – 19 ]. Lay workers then took part in two days of pre-testing including screening, identification, and referral processes within the clinic, and referral of 'red flags' (critical case-situations such as suicidal risk). We made use of practise with clients on the Friendship Bench and in clients' homes'. We developed a client referral manual, which included a list of NGO's, private and public institutions, and church organizations to be used by lay workers or patients.
Ten lay workers were selected at random for the pilot: three from two of the clinics and four from the largest clinic.
A daily peer-support group for lay workers was introduced. The peer group meetings were facilitated by one of the lay workers who would then present during weekly group supervision where all lay workers participated. A clinic staff nurse trained in counseling provided weekly group supervision at the largest clinic. The clinical psychologist and the psychiatrist provided further supervision every fortnightly and monthly, respectively.
We developed a brief 6-item questionnaire with a 4-point Likert scale for the lay workers to evaluate the PST intervention. For instance, we asked them to rate the ease with which they had learned the problem-solving therapy approach, the ease with which they delivered the intervention and the proportion of clients who appeared to benefit from the PST approach. We asked the lay workers to complete this once 6 weeks after the study has begun. We also carried out one focus group with 6 of the 10 workers and asked them to describe their experiences of delivering the intervention. Their responses were recorded in writing and analysed for content and themes by two of the authors.
Data analysis
Descriptive statistics (means and standard deviations and proportions) were estimated for those who participated, who declines, who were lost to follow, and who were excluded due to psychiatric risk. We used t-tests and regression models to test changes in SSQ scores before and after completion of the treatment, adjusting for SSQ scores at baseline. Data were entered and analysed using EpiInfo 2002 and STATA 10.0 (Release 10, College Station, TX: Stata Corporation. 2003) after range checks and double entry of all questionnaires.
Recruitment and attrition at follow-up
Between July and November 2007, 948 persons visited the Bench. Of these 948 persons who visited the Bench, 395 (42%) scored above the cut-point of the Shona Symptom Questionnaire (SSQ). Among these, 33 (8%) with a mean SSQ score of 11.8 (sd 1.2) were excluded from the pilot study due to being severely depressed and/or suicidal and were referred to the psychologist or psychiatrist (see Figure 2 ). Of the 362 invited to take part, 2% (7) declined and 10% (35) were lost to follow-up leaving an 88% response rate (320 participants). Of the 395, 188 (48%) presented with an HIV-related problem of whom 166 (88%) participated.
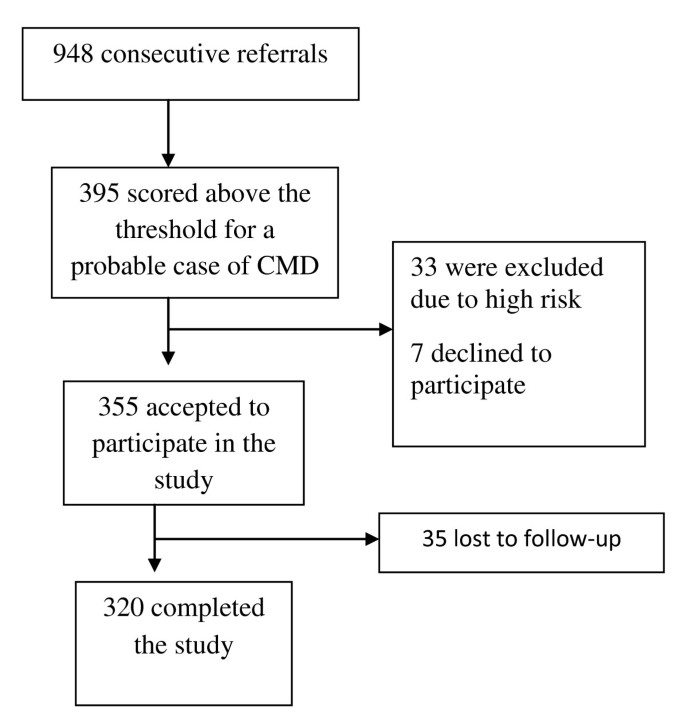
Flow diagram of recruitment into the study .
Table 2 shows the characteristics of the 395 who scored above the cut-point of the SSQ, according to whether or not they entered the study. Participants were more likely to be female. More of those who participated were female and married (70% female, 57% married) compared to those who declined (42% female, 43% married) or who were those lost to follow-up (40% female, 41% married). Those with less than eight years of education were more likely to be lost to follow-up than to participate. The primary reasons presented for visiting the Bench among those who participated were HIV-related, somatic complaints and domestic violence.
Most of those who participated were referred to the Friendship Bench by clinic staff (35%) and lay workers (24%). Other common forms of referral were: friend/relative (13%), self-referral (12%) or police (9%).
Psychological symptoms scores before and after the six-week intervention period
All participants completed a minimum of 3 sessions over a six week period with 20%, 30%, 21% and 30% completing 3, 4, 5 or 6 sessions respectively.
The mean SSQ score for the 320 cases was 11.3 (sd 1.4) before treatment. After receiving between 3 to 6 sessions the mean score dropped by 4.8 points to 6.5 (sd 2.4) [t = 13.6 (p = 0.0087)]. For those completing 3 or more sessions, 66% recovered to below case level on the SSQ at 6-8 weeks
Table 3 shows the drop in SSQ scores according to the number of sessions attended, adjusting for baseline SSQ score. The more sessions attended the larger the drop in SSQ scores with a drop of more than 3 points observed among those who attended all six sessions.
Lay workers evaluation
Nine of the ten lay workers rated themselves as very able to deliver the PST intervention. All of them rated at least half of their clients as benefiting from PST with 7/10 rating 'more than half' of their clients benefiting from the intervention. Themes emerging from the focus group suggested that the lay workers viewed effective ingredients of the Friendship Bench to include:
Their position of trust in the community-clients viewed them as wise and confidential. The clients viewed them as 'persons who would not gossip' which was 'reassuring in a small community'
Being able to visit clients in their homes which they felt instilled hope
Minimising stigma associated with having a mental health problem. The lay workers heard from their clients that as they were already connected with public health work (rather than psychiatry) and carried out home visits routinely as part of their work on public health promotion and that it was not stigmatising for clients with kufungisisa (thinking too much) to be visited.
The structured 'talk therapy' helped them to monitor the progress and challenges that clients were facing.
Breaking down the problems into specific and manageable steps
Giving feedback to clients.
In the focus group, the lay workers reported several case histories of their clients. These included the following:
A female client who had been to the bench with a score of 12/14 on the SSQ at baseline and subsequently received 2 home visits described the lay health workers as 'bringing peace' in her home, and 'less agitation' from her partner. Her score dropped to 7/14 after six sessions.
ii) A female client with an SSQ of 11/14 dropped to 6/14 after five sessions which included a home visit after she presented with being unable to come to terms with her HIV status.
iii) A female senior member of the local protestant church described the home visits as 'hope for those of us who are unable to open up in a church congregation about our HIV status'. Her score went down to 5/14 from 10/14 after 6 sessions.
This is the first example of lay health workers in Africa delivering a low intensity mental health intervention, using locally adapted tools, for common mental disorders in primary care. We have shown that it is feasible for lay workers to deliver this intervention for depression and common mental disorders, and that recruitment to the intervention from primary care, community agencies and self-referral was also feasible (Figure 2 ). The treatment appeared acceptable to the community and the lay workers were able to integrate the intervention into their routine work. Preliminary findings also show that the intervention is efficacious in reducing psychological morbidity, with a drop in score of nearly 5 points on the 14-item psychological outcome scale after 3-6 sessions, and efficacy proportional to the number of sessions attended. Over half of those who participated had presented with a problem related to HIV.
Chance does not seem a likely explanation for our finding as the significance value for the drop in score after 3-6 sessions was at p < 0.01 level. Bias may explain some of the results in that women and married participants were more likely to participate than to decline or to be lost to follow-up and those with lower education were more likely to be lost to follow-up than to participate. However, overall, the response rate of 88% was extremely high so it appears unlikely that bias is playing a major role in explaining the results. Measurement error is also unlikely to explain the findings. The Shona Symptom Questionnaire was developed using optimal cross-cultural methods and has been validated against an international diagnostic interview with most of those scoring at or above the recommended cut-off having mixed depression and anxiety or pure depression using ICD criteria [ 4 ].
We do not have a comparison group from the same study who did not receive the intervention. However, a prospective study in primary care in Harare showed that a mean drop in score of 4.7 (sd 6.3) on the SSQ was associated with recovery from 'case' to 'non-case' and with significantly less disability [ 20 ] (see Table 3 of the Patel paper). These authors further report that those who experienced a drop in score of 4 or more points on the SSQ were more likely to self-report an improvement in health than those who remained at case-level on the SSQ. Our crude mean drop in score of 4.8 points thus appears to represent a meaningful drop in score indicating efficacy of the Friendship Bench intervention. Furthermore, our finding that drop in score was significantly correlated with the number of sessions attended, even after adjusting for baseline SSQ score, adds weight to our assertion that the intervention appears to be efficacious. In our pilot, 34% remained cases at 6-8 weeks follow-up after the intervention, whereas in the Patel et al study [ 20 ], where there was no specific intervention, 48% of primary health care attenders remained cases.
The quantitative findings are supported by the lay workers evaluation. All of them rated at least half of their clients as benefiting from problem-solving therapy with 7/10 rating 'more than half' of their clients benefiting from the intervention. Themes that emerged from qualitative work support the argument that implementing this intervention through an existing public health intervention and by mature women with a position of trust in the community, helps explain its apparent efficacy. The lay workers-or 'grandmother health providers' are viewed as wise, confidential, authoritative and not prone to gossip. As the lay workers were already respected for their public health work, participants said they did not find it not stigmatising to be visited.
The intervention is theoretically closely linked to problem-solving therapy, which has been shown to be effective for depression and common mental health problems [ 12 , 13 ], together with an activity scheduling component [ 21 ]. It incorporates local adaptations that are integral to the routine work of the therapists who are culturally sanctioned lay health workers, known and respected as 'grandmother health providers'. For instance, the inclusion of Christian prayer for 15 minutes during 1 or 2 of the 6 sessions was part of the existing practice of the lay workers and it would have been inappropriate to remove that normal practice. While there is no evidence from randomised controlled trials that prayer is an effective treatment for depression in Christians, there is some suggestion from non-randomised studies with small samples that religious activities may benefit depression [ 22 ].
In 1994 we showed that major barriers to up-scaling mental health care in this setting include lack of supervision, and lack of recording systems for common mental disorders. We provided evidence that problems in improving primary mental health care may be less with the attitudes (or even the training) of primary care staff and more with bureaucratic limitations such as the inadequacy of the diagnostic codes, absence of mental health supervision, lack of protocol for following-up CMD patients, lack of medicines, and lack of incentives to see patients with CMD [ 23 ]. The Friendship Bench has managed to address some of these challenges, especially through making use of lay workers and providing a system for them of peer and nurse-led supervision, with an available step up to specialist care which has been used in less than 10% of cases screening positive for CMD. An emphasis on local concepts and terms helped to reduce stigma of mental disorders. The local knowledge of the lay workers facilitated linkage with two local income-generating projects (peanut butter making; recycling) for those in most financial need.
Our decision to use problem-solving therapy was anchored in earlier evidence that kufungisisa and common mental disorders were associated with everyday social and health problems [ 16 , 24 ], and that the community trusted the lay health workers to aid them in resolving these problems using culturally accepted methods, which sometimes included prayer. This is consistent with the traditionally accepted rationale for using problem-solving therapy [ 19 ]. We found that those who used a greater number of sessions benefited more. Thus in future work it will be important to optimise adherence to the intervention and to follow-up clients. Given the value found in Western settings of written materials for clients in low-intensity psychological treatments, we wish to develop these for clients in Zimbabwe, with the aim of increasing the efficacy of the therapy. We will also add training in more collaborative structured approaches to activity scheduling for clients who remain depressed despite problem-solving therapy.
Of the 320 participants in this pilot, just over half had presented with an HIV-related problem. There is need to evaluate whether treatment for depression might improve physical health outcomes such as medication adherence in those who have depression co-morbid with physical illness [ 25 ].
With the large treatment gap that currently exists in low and middle income countries for mental health care, lay workers may be able to play a pivotal role [ 26 ]. In Zimbabwe, earlier work has shown the feasibility of using lay workers to prevent mother to child transmission of HIV, and to screen for psychological morbidity [ 5 , 27 , 28 ]. While there is evidence supporting the effectiveness of task-shifting in HIV [ 29 ], immunization, malaria prevention, and management of upper respiratory infections [ 30 ], ours is an important study given the dearth of evidence on lay workers addressing depression and common mental health problems in Africa.
Limitations of the study include the short follow-up period of 6 weeks. Also, the observed drop in SSQ score after six sessions of problem-solving therapy was not controlled for potential confounding factors such as socio-economic position [ 31 ]. The fundamental limitation to this study is the absence of a comparison group receiving 'usual care' or a placebo intervention, if one could be found. Furthermore, the lay workers were not observed during the course of their work and what they did in practice could have differed from their training. The low level of attrition among the participants is unusual; however, this could be attributed to the short follow up period, the close proximity of participants to the local study area, and the ability of the lay workers and research nurse to physically follow up participants in the community, and is consistent with high follow-up rates found in previous research in Harare [ 20 ]. The City of Harare Health Department continued the Friendship Bench after the pilot. In the 14 months from January 2008 to February 2009, 2348 clients had visited the Friendship Bench with 973 having received the problem-solving intervention. In view of this it is imperative to rigorously test this intervention.
We have found preliminary evidence that lay primary health care workers can deliver locally adapted problem-solving therapy in Harare, Zimbabwe and that this can be associated with a meaningful reduction in symptoms of depression and common mental disorders. The problem solving therapy was integrated into the routine work load of the community based lay workers whose roles include supporting people living with HIV and carrying out health promotion activities. There is need to carry out appropriately powered randomised controlled trials to test if this task-shifting mental health intervention is effective compared to usual care in reducing psychological symptoms and also in improving physical health outcomes in those who have depression co-morbid with physical illness.
No external funding
Bolton P, et al: Group Interpersonal Psychotherapy for Depression in Rural Uganda: A Randomized Controlled Trial. Journal of the American Medical Association. 2003, 289 (23): 3117-10.1001/jama.289.23.3117.
Article PubMed Google Scholar
Saxena S, et al: Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007, 370 (9590): 878-89. 10.1016/S0140-6736(07)61239-2.
Abas MA, Broadhead JC: Depression and anxiety among women in an urban setting in Zimbabwe. Psychological Medicine. 1997, 27: 59-10.1017/S0033291796004163.
Article CAS PubMed Google Scholar
Patel V, et al: The Shona Symptom Questionnaire: the development of an indigenous measure of common mental disorders in Harare. Acta Psychiatrica Scandinavica. 1997, 95 (6): 469-10.1111/j.1600-0447.1997.tb10134.x.
Stranix-Chibanda L, et al: Screening for psychological morbidity in HIV-infected and HIV-uninfected pregnant women using community counselors in Zimbabwe. Journal of the International Association of Physicians in AIDS Care. 2005, 4 (4): 83-8. 10.1177/1545109706286555.
Patel V, et al: The explanatory models and phenomenology of common mental disorders in primary care in Harare. Psychological Medicine. 1995, 25: 1191-10.1017/S003329170003316X.
Lancet Global Mental Health Group, et al: Scale up services for mental disorders: a call for action. Lancet. 2007, 370 (9594): 1241-52.
Article Google Scholar
Hyman S, et al: Mental Disorders. Disease control priorities in Developing Countries). 2006, New York: Oxford University Press, 605-626.
Google Scholar
Araya R, et al: Treating depression in primary care in low-income women in Santiago, Chile: a randomised controlled trial. Lancet. 2003, 361 (9362): 995-1000. 10.1016/S0140-6736(03)12825-5.
Araya R, et al: Cost-effectiveness of a primary care treatment program for depression in low-income women in Santiago, Chile. American Journal of Psychiatry. 2006, 163 (8): 1379-87. 10.1176/appi.ajp.163.8.1379.
Richards DA, et al: Improving access to psychological therapies: phase IV prospective cohort study. British Journal of Clinical Psychology. 2009, 48 (Pt 4): 377-96.
Cuijpers P, et al: Problem Solving Therapies For Depression: A meta-analysis. European Psychiatry. 2007, 22 (1): 9-15. 10.1016/j.eurpsy.2006.11.001.
Malouff JM, et al: The efficacy of problem solving therapy in reducing mental and physical health problems: A meta-analysis. Clinical Psychology Review. 2007, 27 (1): 46-57. 10.1016/j.cpr.2005.12.005.
Abas M, et al: Primary care services for depression in Harare, Zimbabwe. Harvard Review of Psychiatry. 2003, 11 (3): 157-10.1080/10673220303952.
Tibaijuka AK: Report of the Fact-Finding Mission to Zimbabwe to assess the Scope and Impact of Operation Murambatsvina by the UN Special Envoy on Human Settlements Issues In Zimbabwe. UN Habitat. 2005
Abas M, et al: Defeating depression in the developing world: a Zimbabwean model. British Journal of Psychiatry. 1994, 164 (3): 293-10.1192/bjp.164.3.293.
Amani Trust: The Chiweshe Nurse-Counsellor Programme: Trainer's Manual (revised). Harare. 1994
Broadhead J, Abas M: Life events, difficulties and depression among women in an urban setting in Zimbabwe. Psychological Medicine. 1998, 28: 29-10.1017/S0033291797005618.
Mynors-Wallis L: Problem-solving treatment in general psychiatric practice. Advances in psychiatric treatment. 2001, 417-425.
Patel V, et al: Outcome of common mental disorders in Harare, Zimbabwe. British Journal of Psychiatry. 1998, 157: 53-57.
Mazzucchelli T, et al: Behavioral Activation Treatments for Depression in Adults: A Meta-analysis and Review. Clinical Psychology: Science and Practice. 16 (4): 383-411.
Townsend M, et al: Systematic Review of Clinical Trials Examining the Effects of Religion on Health. Southern Medical Journal. 2002, 95 (12): 142929-
Abas M, et al: Common mental disorders and primary health care: Current practice in low-income countries. Harvard Review of Psychiatry. 2003, 11 (3): 166-10.1080/10673220303954.
Patel V, et al: Women, poverty and common mental disorders in four restructuring societies. Social Science & Medicine. 1999, 49 (11): 1461-10.1016/S0277-9536(99)00208-7.
Article CAS Google Scholar
Sikkema K, et al: Mental Health Treatment to Reduce HIV transmission Risk Behaviour: A Positive Prevention Model. Aids and Behaviour. 2010, 14 (2): 252-10.1007/s10461-009-9650-y.
Patel V, et al: Improving the outcomes of primary care attenders with common mental disorders in developing countries: a cluster randomized controlled trial of a collaborative stepped care intervention in Goa, India. Trials. 2008, 9 (1): 4-10.1186/1745-6215-9-4.
Article PubMed PubMed Central Google Scholar
Shetty A, et al: The feasibility of preventing mother-to-child transmission of HIV using peer counselors in Zimbabwe. AIDS Research and Therapy. 2008, 5 (1): 17-10.1186/1742-6405-5-17.
Chibanda D, et al: Validation of the Edinburgh Postnatal Depression Scale among women in a high HIV prevalence area in urban Zimbabwe. Archives of Women's Mental Health. 2009
Zachariah N, et al: Task shifting in HIV/AIDS: opportunities, challenges and proposed actions for sub-Saharan Africa Royal Society of Tropical Medicine and Hygiene. 2009, 103: 549-558.
Lewin S, et al: Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database of Systematic Reviews. 2009, 3
Abas MA, et al: Socioeconomic Deprivation and Extended hospitalization in severe mental disorder; A two year follow-up study. Psychiatric Services. 2008, 59 (3): 322-325. 10.1176/appi.ps.59.3.322.
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2458/11/828/prepub
Download references
Acknowledgements
We thank Dr. F Lovemore Director of the Counselling Services Unit (CSU), and Dr. P Chonzi and Dr S Mungofa, Directors of The City of Harare Health Department, Harare hospital psychiatric unit and the Mbare community; Shirly Tshimanga (ST), nursing staff at the three clinics, Church groups, Local police, Schools, NGO's and the health promoters for their continued support of the Friendship Bench. Written consent was provided by the lay health workers for the photograph shown in Figure 1 .
Author information
Authors and affiliations.
Department of Psychiatry, University of Zimbabwe, Harare, Zimbabwe
Dixon Chibanda & Lazarus Kajawu
Counselling Services Unit, Harare, Zimbabwe
Petra Mesu & Lazarus Kajawu
Centre for Sexual Health and HIV Research, University College London, London, UK
Frances Cowan
Department of Community Medicine, University of Zimbabwe, Harare, Zimbabwe
School of Social and Community Medicine, Bristol, UK
Ricardo Araya
King's College London, Institute of Psychiatry, London, UK
Melanie A Abas
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Dixon Chibanda .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
DC was responsible for study design, data collection, writing manuscript and analysis of the data. PM and LK responsible for study design and review of second draft. FC reviewed second draft. RA assisted with analysing data and editing manuscripts.
MA developed Multiple Symptoms Card, made comments on first draft of manuscript, responsible for second draft of manuscript, contributed to revisions following referees comments and to writing of final draft. All authors read and approved the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, authors’ original file for figure 4, authors’ original file for figure 5, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Chibanda, D., Mesu, P., Kajawu, L. et al. Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV. BMC Public Health 11 , 828 (2011). https://doi.org/10.1186/1471-2458-11-828
Download citation
Received : 06 June 2010
Accepted : 26 October 2011
Published : 26 October 2011
DOI : https://doi.org/10.1186/1471-2458-11-828
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Primary Health Care
- Common Mental Disorder
- Common Mental Health Problem
- Primary Mental Health Care
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- COVID-19 and your mental health
Worries and anxiety about COVID-19 can be overwhelming. Learn ways to cope as COVID-19 spreads.
At the start of the COVID-19 pandemic, life for many people changed very quickly. Worry and concern were natural partners of all that change — getting used to new routines, loneliness and financial pressure, among other issues. Information overload, rumor and misinformation didn't help.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020.
Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19. And you're not alone if you've coped with the stress in less than healthy ways, such as substance use.
But healthier self-care choices can help you cope with COVID-19 or any other challenge you may face.
And knowing when to get help can be the most essential self-care action of all.
Recognize what's typical and what's not
Stress and worry are common during a crisis. But something like the COVID-19 pandemic can push people beyond their ability to cope.
In surveys, the most common symptoms reported were trouble sleeping and feeling anxiety or nervous. The number of people noting those symptoms went up and down in surveys given over time. Depression and loneliness were less common than nervousness or sleep problems, but more consistent across surveys given over time. Among adults, use of drugs, alcohol and other intoxicating substances has increased over time as well.
The first step is to notice how often you feel helpless, sad, angry, irritable, hopeless, anxious or afraid. Some people may feel numb.
Keep track of how often you have trouble focusing on daily tasks or doing routine chores. Are there things that you used to enjoy doing that you stopped doing because of how you feel? Note any big changes in appetite, any substance use, body aches and pains, and problems with sleep.
These feelings may come and go over time. But if these feelings don't go away or make it hard to do your daily tasks, it's time to ask for help.
Get help when you need it
If you're feeling suicidal or thinking of hurting yourself, seek help.
- Contact your healthcare professional or a mental health professional.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
If you are worried about yourself or someone else, contact your healthcare professional or mental health professional. Some may be able to see you in person or talk over the phone or online.
You also can reach out to a friend or loved one. Someone in your faith community also could help.
And you may be able to get counseling or a mental health appointment through an employer's employee assistance program.
Another option is information and treatment options from groups such as:
- National Alliance on Mental Illness (NAMI).
- Substance Abuse and Mental Health Services Administration (SAMHSA).
- Anxiety and Depression Association of America.
Self-care tips
Some people may use unhealthy ways to cope with anxiety around COVID-19. These unhealthy choices may include things such as misuse of medicines or legal drugs and use of illegal drugs. Unhealthy coping choices also can be things such as sleeping too much or too little, or overeating. It also can include avoiding other people and focusing on only one soothing thing, such as work, television or gaming.
Unhealthy coping methods can worsen mental and physical health. And that is particularly true if you're trying to manage or recover from COVID-19.
Self-care actions can help you restore a healthy balance in your life. They can lessen everyday stress or significant anxiety linked to events such as the COVID-19 pandemic. Self-care actions give your body and mind a chance to heal from the problems long-term stress can cause.
Take care of your body
Healthy self-care tips start with the basics. Give your body what it needs and avoid what it doesn't need. Some tips are:
- Get the right amount of sleep for you. A regular sleep schedule, when you go to bed and get up at similar times each day, can help avoid sleep problems.
- Move your body. Regular physical activity and exercise can help reduce anxiety and improve mood. Any activity you can do regularly is a good choice. That may be a scheduled workout, a walk or even dancing to your favorite music.
- Choose healthy food and drinks. Foods that are high in nutrients, such as protein, vitamins and minerals are healthy choices. Avoid food or drink with added sugar, fat or salt.
- Avoid tobacco, alcohol and drugs. If you smoke tobacco or if you vape, you're already at higher risk of lung disease. Because COVID-19 affects the lungs, your risk increases even more. Using alcohol to manage how you feel can make matters worse and reduce your coping skills. Avoid taking illegal drugs or misusing prescriptions to manage your feelings.
Take care of your mind
Healthy coping actions for your brain start with deciding how much news and social media is right for you. Staying informed, especially during a pandemic, helps you make the best choices but do it carefully.
Set aside a specific amount of time to find information in the news or on social media, stay limited to that time, and choose reliable sources. For example, give yourself up to 20 or 30 minutes a day of news and social media. That amount keeps people informed but not overwhelmed.
For COVID-19, consider reliable health sources. Examples are the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
Other healthy self-care tips are:
- Relax and recharge. Many people benefit from relaxation exercises such as mindfulness, deep breathing, meditation and yoga. Find an activity that helps you relax and try to do it every day at least for a short time. Fitting time in for hobbies or activities you enjoy can help manage feelings of stress too.
- Stick to your health routine. If you see a healthcare professional for mental health services, keep up with your appointments. And stay up to date with all your wellness tests and screenings.
- Stay in touch and connect with others. Family, friends and your community are part of a healthy mental outlook. Together, you form a healthy support network for concerns or challenges. Social interactions, over time, are linked to a healthier and longer life.
Avoid stigma and discrimination
Stigma can make people feel isolated and even abandoned. They may feel sad, hurt and angry when people in their community avoid them for fear of getting COVID-19. People who have experienced stigma related to COVID-19 include people of Asian descent, health care workers and people with COVID-19.
Treating people differently because of their medical condition, called medical discrimination, isn't new to the COVID-19 pandemic. Stigma has long been a problem for people with various conditions such as Hansen's disease (leprosy), HIV, diabetes and many mental illnesses.
People who experience stigma may be left out or shunned, treated differently, or denied job and school options. They also may be targets of verbal, emotional and physical abuse.
Communication can help end stigma or discrimination. You can address stigma when you:
- Get to know people as more than just an illness. Using respectful language can go a long way toward making people comfortable talking about a health issue.
- Get the facts about COVID-19 or other medical issues from reputable sources such as the CDC and WHO.
- Speak up if you hear or see myths about an illness or people with an illness.
COVID-19 and health
The virus that causes COVID-19 is still a concern for many people. By recognizing when to get help and taking time for your health, life challenges such as COVID-19 can be managed.
- Mental health during the COVID-19 pandemic. National Institutes of Health. https://covid19.nih.gov/covid-19-topics/mental-health. Accessed March 12, 2024.
- Mental Health and COVID-19: Early evidence of the pandemic's impact: Scientific brief, 2 March 2022. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1. Accessed March 12, 2024.
- Mental health and the pandemic: What U.S. surveys have found. Pew Research Center. https://www.pewresearch.org/short-reads/2023/03/02/mental-health-and-the-pandemic-what-u-s-surveys-have-found/. Accessed March 12, 2024.
- Taking care of your emotional health. Centers for Disease Control and Prevention. https://emergency.cdc.gov/coping/selfcare.asp. Accessed March 12, 2024.
- #HealthyAtHome—Mental health. World Health Organization. www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health. Accessed March 12, 2024.
- Coping with stress. Centers for Disease Control and Prevention. www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/. Accessed March 12, 2024.
- Manage stress. U.S. Department of Health and Human Services. https://health.gov/myhealthfinder/topics/health-conditions/heart-health/manage-stress. Accessed March 20, 2020.
- COVID-19 and substance abuse. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/covid-19-substance-use#health-outcomes. Accessed March 12, 2024.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed March 15, 2024.
- Negative coping and PTSD. U.S. Department of Veterans Affairs. https://www.ptsd.va.gov/gethelp/negative_coping.asp. Accessed March 15, 2024.
- Health effects of cigarette smoking. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm#respiratory. Accessed March 15, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed March 15, 2024.
- Your healthiest self: Emotional wellness toolkit. National Institutes of Health. https://www.nih.gov/health-information/emotional-wellness-toolkit. Accessed March 15, 2024.
- World leprosy day: Bust the myths, learn the facts. Centers for Disease Control and Prevention. https://www.cdc.gov/leprosy/world-leprosy-day/. Accessed March 15, 2024.
- HIV stigma and discrimination. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/hiv-stigma/. Accessed March 15, 2024.
- Diabetes stigma: Learn about it, recognize it, reduce it. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes_stigma.html. Accessed March 15, 2024.
- Phelan SM, et al. Patient and health care professional perspectives on stigma in integrated behavioral health: Barriers and recommendations. Annals of Family Medicine. 2023; doi:10.1370/afm.2924.
- Stigma reduction. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/od2a/case-studies/stigma-reduction.html. Accessed March 15, 2024.
- Nyblade L, et al. Stigma in health facilities: Why it matters and how we can change it. BMC Medicine. 2019; doi:10.1186/s12916-019-1256-2.
- Combating bias and stigma related to COVID-19. American Psychological Association. https://www.apa.org/topics/covid-19-bias. Accessed March 15, 2024.
- Yashadhana A, et al. Pandemic-related racial discrimination and its health impact among non-Indigenous racially minoritized peoples in high-income contexts: A systematic review. Health Promotion International. 2021; doi:10.1093/heapro/daab144.
- Sawchuk CN (expert opinion). Mayo Clinic. March 25, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and coronavirus
- COVID-19 and pets
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- COVID-19 drugs: Are there any that work?
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Mental health: What's normal, what's not - Related information Mental health: What's normal, what's not
- Mental illness - Related information Mental illness
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

Morning Carpool
21 Mental Shifts to Boost Problem-Solving Skills and Become More Strategic
Posted: February 10, 2024 | Last updated: February 10, 2024

Discover transformative mental shifts to supercharge your problem-solving skills. From embracing uncertainty to the power of daydreaming, prepare to change the way you tackle challenges forever!

Embrace Uncertainty
Accept that not all answers are immediately clear. Uncertainty can be a powerful motivator rather than a source of stress. By embracing the unknown, we open ourselves up to a broader range of possibilities and solutions.

Seek Diverse Perspectives
Look beyond your own experiences. Different perspectives can provide unique insights and spark innovative solutions. Engaging with people from various backgrounds allows you to see problems through a new lens and discover paths you might not have considered.

Simplify the Complex
Break down big problems into smaller, manageable parts. When faced with a complex issue, deconstruct it to understand its fundamental components. This approach makes the problem less daunting and easier to tackle, leading to clearer, more effective solutions.

Adopt a Growth Mindset
Believe in your ability to learn and grow. A growth mindset encourages resilience and the pursuit of knowledge. Challenges are just undiscovered opportunities with potential for personal and professional development.

Question Assumptions
Challenge the status quo. The barriers to solving a problem are often based on outdated or incorrect assumptions. By questioning the basis of your thinking, you can uncover new paths and innovative solutions.

Think in Reverse
Start with the desired outcome and work backward. This reverse-engineering approach forces you to think differently and can reveal insights you might have missed when approaching the problem linearly.

Embrace Failure as a Teacher
Learn from mistakes and change your perspective. Nobody likes to fail, but each failure provides valuable lessons that can guide future decisions and strategies. Failure isn’t the end but the beginning of understanding.

Harness the Power of Daydreaming
Let your mind wander. Sometimes, the best ideas come when you’re not actively trying to solve a problem. Allowing your mind to drift can lead to creative breakthroughs and unexpected solutions.

Practice Empathy
Understand others’ perspectives and needs. By putting yourself in someone else’s shoes, you can gain insights into the emotional and practical aspects of a problem, leading to more compassionate and effective solutions.

Set Clear Goals
Define what success looks like. Clear goals provide direction and focus, making identifying the steps needed to solve a problem easier. They also help measure progress and keep you motivated.

Stay Curious
Ask questions and seek knowledge. A curious mind is always looking for new information and ideas, which can lead to innovative problem-solving strategies. Curiosity is the engine of achievement.


Use Analogies
Draw parallels from different areas. Analogies can help clarify complex problems by relating them to something more familiar. This can simplify the problem-solving process and spark creative solutions.

Focus on the Process, Not Just the Outcome
Enjoy the journey of problem-solving. Focusing too much on the end result can lead to frustration and missed opportunities. By valuing the process, you can learn and adapt as you go, leading to more sustainable solutions.

Prioritize Effectively
Set deadlines for achieving your goals. Know what matters most. Not all aspects of a problem are equally important. By prioritizing the key factors, you can allocate your time and resources more effectively and achieve better results.

Build Resilience
Give yourself time to recover, then bounce back from setbacks. Resilience is crucial for problem-solving, as it allows you to keep going despite challenges and failures. Resilience turns problems into opportunities.

Cultivate Patience
Give solutions time to unfold. Sometimes, the best solutions emerge over time, and immediate answers aren’t always the best. Patience allows you to thoroughly explore options and make more considered decisions.

Practice Reflection
Don’t overlook the power of self-reflection. Take time to think about what you’ve learned. Reflecting on your experiences and the outcomes of your problem-solving efforts can provide valuable insights and improve future strategies.

Encourage Collaboration
Work with others to find solutions and share goals. Collaborating with a team can bring in a range of skills and perspectives that enhance the problem-solving process and lead to more effective solutions.

Visualize Success
Imagine the desired outcome. Visualization can be a powerful motivator to enhance your performance and guide your actions toward achieving your goals. Focusing on the end result in your mind’s eye can make it a reality.

Adapt and Evolve
Be willing to change your approach. The most effective problem-solvers are flexible and open to new methods and ideas. Adapting your strategy in response to new information or challenges can lead to better solutions.

Maintain a Positive Attitude
Stay optimistic and focused. A positive outlook can keep you motivated and open to new ideas. An optimistic mindset can also make the problem-solving process more enjoyable and less daunting.
More for You
Ryan Gosling, 'SNL' Cast Barely Keep It Together In 'Beavis And Butt-Head' Sketch
Donald Trump Makes Bold Claim About Iranian Attack on Israel
Former undercover agent recalls infiltrating the Hells Angels: 'A dangerous game to play'
Famous figures who had Titanic tickets but didn't make it on board
Helicopters race to rescue over 170 people trapped in cable car
Masters 2024: Tiger Woods shares touching final handshake with Verne Lundquist on 16th hole
RFK Jr. says he has ruled out Libertarian run for president
Common over-the-counter medicine linked to increased dementia risk
Mike Tyson fires off warning shot to Jake Paul in latest sparring session months before fight
Tax Day deals 2024: Score discounts, freebies at Krispy Kreme, Hooters, Potbelly, more
I tutor the children of some of Dubai's richest people. One of them paid me $3,000 to do his homework.
Bread Recalled After Threat-to-Life Warning Issued
Masters 2024: Low amateur's press conference ends with super awkward exchange regarding Tiger Woods
Top 10 Times Bill Hader Broke The SNL Cast
16 Compliments You Didn’t Realize Are Actually Pretty Insulting
Doctor shares what happens to our bodies moments before we die
Eric Moody, British Airways pilot who kept his cool when an ash cloud cut all four engines – obituary
Indiana Fever picks first in star-studded WNBA draft with Caitlin Clark. See full draft order
Use this 2-word phrase when your boss asks you to do more work than you have time to do, according to a therapist
I Lost White Friends When I Finally Spoke Out

Problem-Solving Courts/Specialty Courts
Know the warning signs.
Learn the common signs of mental illness in adults and adolescents.
Mental health conditions
Learn more about common mental health conditions that affect millions.
Find Your Local NAMI
Call the NAMI Helpline at
800-950-6264
Or text "HelpLine" to 62640
Where We Stand:
NAMI believes in minimizing justice-system response to people with mental illness, while ensuring that any interactions preserve health, well-being and dignity. NAMI supports the use of problem-solving courts as part of a broad strategy to reduce incarceration and promote diversion from further involvement in the criminal justice system for people with mental illness.
Why We Care:
People with mental illness and substance use disorders (SUDs) are overrepresented in our nation’s jails and prisons. An estimated 44% of people in jails and 37% of people in prisons have a mental illness, and an estimated 65% of people in prisons have an underlying SUD. In the veterans’ community, 55% of the nearly 50,000 veterans incarcerated in local jails report experiencing a mental illness.
Mental illness is not a crime, but untreated symptoms and limited access to care lead many to involvement with the criminal justice system. Many of these individuals are held for committing non-violent, minor offenses and misdemeanors resulting from the symptoms of untreated illness (disorderly conduct, loitering, trespassing, disturbing the peace) or for offenses like shoplifting and petty theft.
Problem-solving courts (also known as specialty courts) are specialized dockets within the criminal justice system that seek to address underlying mental health or SUD that contribute to the commission of certain criminal offenses in many cases, often providing treatment rather than punishment. The most common types of problem-solving courts are drug treatment, mental health and veterans treatment courts, although there are other specialty court dockets that may vary by state or county. Through these problem-solving courts, judges, prosecutors, defense attorneys, mental health providers and community partners collaborate to provide treatment in the community as an alternative to being charged and possibly convicted of a criminal offense that could result in incarceration.
As of 2020, there are an estimated 477 adult mental health courts and 56 juvenile mental health courts , along with approximately 3,500 drug treatment courts and 461 veterans treatment courts in the U.S. Most programs are only for those who face misdemeanor or nonviolent felony charges, but more recently, jurisdictions have explored courts for additional charges.
Problem-solving courts can be life changing for people with mental illness or SUDs who become involved in the criminal justice system. Veterans courts and drug courts show similar outcomes for participants. Mental health courts have been associated with reduced recidivism and incarceration, and can even improve mental health outcomes. There is some evidence that including case management and connection to services, such as housing and employment, increase the likelihood of success for participants of specialty courts.
How We Talk About It:
- People with mental illness and substance use disorders (SUDs) deserve help, not handcuffs. Yet, people with mental illness and SUDs are overrepresented in the criminal justice system.
- About 2 in 5 people who are incarcerated have a history of mental illness, resulting in jails and prisons becoming unintended mental health facilities where they are often limited access to effective treatment.
- NAMI is opposed to the continued criminalization of people with mental illness and believes that communities should invest in evidence-based solutions that help people with mental illness get on a path of recovery.
- Specialty courts, like mental health treatment courts and veterans courts, are an evidence-based tool that can reduce the number of people with mental illness in our nation’s jails and prisons and focus on treatment instead of punishment.
- As with all mental health treatment, specialty courts should work to engage the individual in their treatment so that it leads to long-term recovery beyond the period that the court is involved.
- Funding and other resources should be available to support the operations of specialty court programs, especially services and supports like housing and employment programs, that are central to these courts successfully helping individuals.
- NAMI believes that public policies should focus on investments in early intervention, comprehensive community mental health services, robust crisis response systems and justice diversion strategies to decriminalize people with mental illness and connect people to care.
- Specialty courts are an important tool in helping people with mental illness while focusing on their health and preserving their dignity. Communities should invest in these courts to better meet the needs of people with mental illness.
What We’ve Done:
- NAMI supports the Stepping Up Initiative which works with counties and other stakeholders to reduce the number of people with mental illness in jails.
- NAMI letter to House and Senate leadership advocating for the reauthorization of the Mentally Ill Offender Treatment and Crime Reduction Act (MIOTCRA), which funds mental health courts.
- NAMI letter to the House and Senate Appropriations leadership advocating for increased funding for MIOTCRA.
Print this Page
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Prev Med
- v.4(11); 2013 Nov
Social Problem Solving Ability Predicts Mental Health Among Undergraduate Students
Mansour ranjbar.
Mazandaran University of Medical Sciences, Sarri Mazandaran Province, Iran
Ali Asghar Bayani
1 Department of Psychology, Azadshahr Branch, Islamic Azad Universty, Azadshahr, Iran
Background:
The main objective of this study was predicting student's mental health using social problem solving- ability.
In this correlational. descriptive study, 369 (208 female and 161 male) from, Mazandaran University of Medical Science were selected through stratified random sampling method. In order to collect the data, the social problem solving inventory-revised and general health questionnaire were used. Data were analyzed through SPSS-19, Pearson's correlation, t test, and stepwise regression analysis.
Data analysis showed significant relationship between social problem solving ability and mental health ( P < 0.01). Social problem solving ability was significantly associated with the somatic symptoms, anxiety and insomnia, social dysfunction and severe depression ( P < 0.01).
Conclusions:
The results of our study demonstrated that there is a significant correlation between social problem solving ability and mental health.
INTRODUCTION
The definition and measurement of health is conceptually problematic and evolving.[ 1 ] The meaning of health has dramatically changed during the last 150 years.[ 2 ] According to World Health Organization (WHO), health is defined as the state of physical, mental, and social well-being and does not refer solely to the absence of a disease.[ 3 ]
With increasing understanding of health concept, the importance of mental health becomes more apparent[ 4 ] because health provides effective functionality of individuals, families, and society.[ 5 ] In order to enhance health, many different approaches such as biologic, behavior-therapy, psychodynamics, and many models such as medical, empowerment, behavioral change, educational, and social change have been introduced.[ 6 ] One recent concept considered effective in reduction of the psychological disorders is the social problem- solving ability.
Social problem solving refers to the process of problem solving within real world.[ 7 ] In this definition the word “social” is indicative of factors affecting coping behaviors of a person in the social environment.[ 8 ] Most of the researches about social problem- solving are influenced by the social problem solving model. The problem solving therapy (PST) approach, based on this model,[ 9 ] has been utilized as an intervention modality in depression, suicide,[ 10 ] reduction of problems related to mental and physical health,[ 11 ] and anxiety.[ 12 ] The social inefficiency is common among people with personality disorders, and the primary goal of the PST approach is to enhance social sufficiency.[ 13 ]
The impact of social problem solving on depression, anxiety and personality disorders has been reported in numerous studies by Marx et al ., Haago et al ., Kant et al ., Becker-Weidman et al ., and Bray et al .[ 14 , 15 , 16 , 17 , 18 ] According to diagnostic and statistical manual of mental disorders (DSM-IV), evaluation of personality disorders requires theoretical models for guiding diagnosis and treatment. Based on this definition, McMurran et al ., evaluated the relation between personality disorders and social problem solving and acknowledged the social problem solving as the theoretical basis of their research.[ 19 ]
Several studies have implicated the prevalence of mental disorders and high- risk behavior among university students.[ 20 , 21 , 22 , 23 ] This is partly because of rapid development of physical, psychological, and social functions in the adolescence in comparison to childhood, which prone them to emotional disturbances.[ 24 ] In addition to outcomes related to growth, these individuals are afflicted by educational concerns, living apart from family, college expenditures, and the change of living environment; all of these are important parameters in the makeup of behavioral dysfunctions.[ 25 ]
Planning efficient models in prevention and treatment of psychological disorders in adolescents and young adults is of utmost value. Based on this essentiality, we conducted a research in order to evaluate the role of social problem- solving ability in the prediction of undergraduate mental health.
Participants
This is a descriptive- correlational study. We randomly selected 369 undergraduate students (161 male, 208 female) from the Mazandaran University Medical Science, based on stratified randomized sampling. The mean age of the examinees was 22 years, of which 107 were married and 262 were single. They were selected from students of human studies, agriculture, engineering, and arts and had freely agreed to participate.
Instruments
The instruments for data collection are the following:
Social problem-solving inventory-revised
This is a 52-item, self-report questionnaire devised according to D’Zurilla et al .[ 26 ] The subscales of SPSI-R include: Positive problem orientation (PPO), negative problem orientation (NPO), rational problem solving (RPS), impulsivity/carelessness style (ICS), and avoidance style (AS).[ 27 ] Siu and Shek reported Cronbach coefficient alphas of SPSI-R ranged from 0.64 (PPO) to 0.98 (AS).[ 28 ]
General health questionnaire
The original general health questionnaire was designed by Goldberg in 1972.[ 29 ] We used GHQ-28 comprising of 4 subscale covering the physical symptoms, anxiety and insomnia, social functioning, and depression. Test-retest reliability coefficient of Farsi version of GHQ was 0.85.[ 30 ]
We used SPSS 19 to analyze data using Pierson's correlation coefficient, independent t -test, and stepwise regression analysis.
Mean and standard deviation for social problem solving and general health scores are presented in Table 1 . The correlation of the social problem solving abilities and its sub- scale with the general health questionnaire are presented in Table 2 . There is significant correlation between general health and the social problem solving abilities ( P < 0.01). The social problem solving abilities were significantly correlated with the physical symptoms, anxiety and insomnia, social dysfunction, and depression ( P < 0.01).
Mean and standard deviations of scales by sex

Significant Pearson correlation matrixes for total scores

Stepwise multiple regression analysis for the entire sample was used to determine the combination of variables that best predicts general mental health [ Table 3 ]. The variance of negative problem orientation accounted for 21.5% of the variance of general health score. Adding the impulsivity/carelessness style to this analysis, raised the value to 24.5%. These two variables were thus negatively correlated with the general health.
Summary of stepwise regression analysis for predicting students’ mental health

Studies performed about the status of mental health in college students imply mental disorders being prevalent.[ 31 ] These disorders lead to devastating individual and social outcomes and require preventive and treatment approaches. This study was done with the aim of evaluating the value of parameters related to social problem solving capabilities in the prediction of students’ mental health.
The results of our study demonstrate that there is a significant correlation between social problem- solving ability and mental health. Social problem- solving ability are significantly related to physical symptoms, anxiety and insomnia, social dysfunction, and depression. This is in concert with the results of the Nezu and Nezu and Ronan findings.[ 32 , 33 ] Marx et al .,[ 14 ] Haaga et al .,[ 15 ] D’Zurill et al .,[ 34 ] Baker and Williams[ 35 ] and Becker-Weidman et al .,[ 17 ] have also reported similar results.
Our study showed that almost 21.5% of the variance in general health variable may be related to predictive variable of negative problem orientation and that it is increased to 24.5% if the impulsivity/carelessness style is added. This finding is in agreement with the results of Nezu[ 12 ] and D’Zurilla et al .[ 34 ]
The results of our study demonstrate that social problem solving ability are significantly correlated with the mental health and may predict it. We recommend that colleges prepare plans in order to enhance the social problem solving skills among their population.
Our study is limited by its conduct over a single group of students. We recommend a larger multicenter study with various age groups and questionnaires.
Source of Support: Nil
Conflict of Interest: None declared.
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
Share Podcast

Do You Understand the Problem You’re Trying to Solve?
To solve tough problems at work, first ask these questions.
- Apple Podcasts
- Google Podcasts
Problem solving skills are invaluable in any job. But all too often, we jump to find solutions to a problem without taking time to really understand the dilemma we face, according to Thomas Wedell-Wedellsborg , an expert in innovation and the author of the book, What’s Your Problem?: To Solve Your Toughest Problems, Change the Problems You Solve .
In this episode, you’ll learn how to reframe tough problems by asking questions that reveal all the factors and assumptions that contribute to the situation. You’ll also learn why searching for just one root cause can be misleading.
Key episode topics include: leadership, decision making and problem solving, power and influence, business management.
HBR On Leadership curates the best case studies and conversations with the world’s top business and management experts, to help you unlock the best in those around you. New episodes every week.
- Listen to the original HBR IdeaCast episode: The Secret to Better Problem Solving (2016)
- Find more episodes of HBR IdeaCast
- Discover 100 years of Harvard Business Review articles, case studies, podcasts, and more at HBR.org .
HANNAH BATES: Welcome to HBR on Leadership , case studies and conversations with the world’s top business and management experts, hand-selected to help you unlock the best in those around you.
Problem solving skills are invaluable in any job. But even the most experienced among us can fall into the trap of solving the wrong problem.
Thomas Wedell-Wedellsborg says that all too often, we jump to find solutions to a problem – without taking time to really understand what we’re facing.
He’s an expert in innovation, and he’s the author of the book, What’s Your Problem?: To Solve Your Toughest Problems, Change the Problems You Solve .
In this episode, you’ll learn how to reframe tough problems, by asking questions that reveal all the factors and assumptions that contribute to the situation. You’ll also learn why searching for one root cause can be misleading. And you’ll learn how to use experimentation and rapid prototyping as problem-solving tools.
This episode originally aired on HBR IdeaCast in December 2016. Here it is.
SARAH GREEN CARMICHAEL: Welcome to the HBR IdeaCast from Harvard Business Review. I’m Sarah Green Carmichael.
Problem solving is popular. People put it on their resumes. Managers believe they excel at it. Companies count it as a key proficiency. We solve customers’ problems.
The problem is we often solve the wrong problems. Albert Einstein and Peter Drucker alike have discussed the difficulty of effective diagnosis. There are great frameworks for getting teams to attack true problems, but they’re often hard to do daily and on the fly. That’s where our guest comes in.
Thomas Wedell-Wedellsborg is a consultant who helps companies and managers reframe their problems so they can come up with an effective solution faster. He asks the question “Are You Solving The Right Problems?” in the January-February 2017 issue of Harvard Business Review. Thomas, thank you so much for coming on the HBR IdeaCast .
THOMAS WEDELL-WEDELLSBORG: Thanks for inviting me.
SARAH GREEN CARMICHAEL: So, I thought maybe we could start by talking about the problem of talking about problem reframing. What is that exactly?
THOMAS WEDELL-WEDELLSBORG: Basically, when people face a problem, they tend to jump into solution mode to rapidly, and very often that means that they don’t really understand, necessarily, the problem they’re trying to solve. And so, reframing is really a– at heart, it’s a method that helps you avoid that by taking a second to go in and ask two questions, basically saying, first of all, wait. What is the problem we’re trying to solve? And then crucially asking, is there a different way to think about what the problem actually is?
SARAH GREEN CARMICHAEL: So, I feel like so often when this comes up in meetings, you know, someone says that, and maybe they throw out the Einstein quote about you spend an hour of problem solving, you spend 55 minutes to find the problem. And then everyone else in the room kind of gets irritated. So, maybe just give us an example of maybe how this would work in practice in a way that would not, sort of, set people’s teeth on edge, like oh, here Sarah goes again, reframing the whole problem instead of just solving it.
THOMAS WEDELL-WEDELLSBORG: I mean, you’re bringing up something that’s, I think is crucial, which is to create legitimacy for the method. So, one of the reasons why I put out the article is to give people a tool to say actually, this thing is still important, and we need to do it. But I think the really critical thing in order to make this work in a meeting is actually to learn how to do it fast, because if you have the idea that you need to spend 30 minutes in a meeting delving deeply into the problem, I mean, that’s going to be uphill for most problems. So, the critical thing here is really to try to make it a practice you can implement very, very rapidly.
There’s an example that I would suggest memorizing. This is the example that I use to explain very rapidly what it is. And it’s basically, I call it the slow elevator problem. You imagine that you are the owner of an office building, and that your tenants are complaining that the elevator’s slow.
Now, if you take that problem framing for granted, you’re going to start thinking creatively around how do we make the elevator faster. Do we install a new motor? Do we have to buy a new lift somewhere?
The thing is, though, if you ask people who actually work with facilities management, well, they’re going to have a different solution for you, which is put up a mirror next to the elevator. That’s what happens is, of course, that people go oh, I’m busy. I’m busy. I’m– oh, a mirror. Oh, that’s beautiful.
And then they forget time. What’s interesting about that example is that the idea with a mirror is actually a solution to a different problem than the one you first proposed. And so, the whole idea here is once you get good at using reframing, you can quickly identify other aspects of the problem that might be much better to try to solve than the original one you found. It’s not necessarily that the first one is wrong. It’s just that there might be better problems out there to attack that we can, means we can do things much faster, cheaper, or better.
SARAH GREEN CARMICHAEL: So, in that example, I can understand how A, it’s probably expensive to make the elevator faster, so it’s much cheaper just to put up a mirror. And B, maybe the real problem people are actually feeling, even though they’re not articulating it right, is like, I hate waiting for the elevator. But if you let them sort of fix their hair or check their teeth, they’re suddenly distracted and don’t notice.
But if you have, this is sort of a pedestrian example, but say you have a roommate or a spouse who doesn’t clean up the kitchen. Facing that problem and not having your elegant solution already there to highlight the contrast between the perceived problem and the real problem, how would you take a problem like that and attack it using this method so that you can see what some of the other options might be?
THOMAS WEDELL-WEDELLSBORG: Right. So, I mean, let’s say it’s you who have that problem. I would go in and say, first of all, what would you say the problem is? Like, if you were to describe your view of the problem, what would that be?
SARAH GREEN CARMICHAEL: I hate cleaning the kitchen, and I want someone else to clean it up.
THOMAS WEDELL-WEDELLSBORG: OK. So, my first observation, you know, that somebody else might not necessarily be your spouse. So, already there, there’s an inbuilt assumption in your question around oh, it has to be my husband who does the cleaning. So, it might actually be worth, already there to say, is that really the only problem you have? That you hate cleaning the kitchen, and you want to avoid it? Or might there be something around, as well, getting a better relationship in terms of how you solve problems in general or establishing a better way to handle small problems when dealing with your spouse?
SARAH GREEN CARMICHAEL: Or maybe, now that I’m thinking that, maybe the problem is that you just can’t find the stuff in the kitchen when you need to find it.
THOMAS WEDELL-WEDELLSBORG: Right, and so that’s an example of a reframing, that actually why is it a problem that the kitchen is not clean? Is it only because you hate the act of cleaning, or does it actually mean that it just takes you a lot longer and gets a lot messier to actually use the kitchen, which is a different problem. The way you describe this problem now, is there anything that’s missing from that description?
SARAH GREEN CARMICHAEL: That is a really good question.
THOMAS WEDELL-WEDELLSBORG: Other, basically asking other factors that we are not talking about right now, and I say those because people tend to, when given a problem, they tend to delve deeper into the detail. What often is missing is actually an element outside of the initial description of the problem that might be really relevant to what’s going on. Like, why does the kitchen get messy in the first place? Is it something about the way you use it or your cooking habits? Is it because the neighbor’s kids, kind of, use it all the time?
There might, very often, there might be issues that you’re not really thinking about when you first describe the problem that actually has a big effect on it.
SARAH GREEN CARMICHAEL: I think at this point it would be helpful to maybe get another business example, and I’m wondering if you could tell us the story of the dog adoption problem.
THOMAS WEDELL-WEDELLSBORG: Yeah. This is a big problem in the US. If you work in the shelter industry, basically because dogs are so popular, more than 3 million dogs every year enter a shelter, and currently only about half of those actually find a new home and get adopted. And so, this is a problem that has persisted. It’s been, like, a structural problem for decades in this space. In the last three years, where people found new ways to address it.
So a woman called Lori Weise who runs a rescue organization in South LA, and she actually went in and challenged the very idea of what we were trying to do. She said, no, no. The problem we’re trying to solve is not about how to get more people to adopt dogs. It is about keeping the dogs with their first family so they never enter the shelter system in the first place.
In 2013, she started what’s called a Shelter Intervention Program that basically works like this. If a family comes and wants to hand over their dog, these are called owner surrenders. It’s about 30% of all dogs that come into a shelter. All they would do is go up and ask, if you could, would you like to keep your animal? And if they said yes, they would try to fix whatever helped them fix the problem, but that made them turn over this.
And sometimes that might be that they moved into a new building. The landlord required a deposit, and they simply didn’t have the money to put down a deposit. Or the dog might need a $10 rabies shot, but they didn’t know how to get access to a vet.
And so, by instigating that program, just in the first year, she took her, basically the amount of dollars they spent per animal they helped went from something like $85 down to around $60. Just an immediate impact, and her program now is being rolled out, is being supported by the ASPCA, which is one of the big animal welfare stations, and it’s being rolled out to various other places.
And I think what really struck me with that example was this was not dependent on having the internet. This was not, oh, we needed to have everybody mobile before we could come up with this. This, conceivably, we could have done 20 years ago. Only, it only happened when somebody, like in this case Lori, went in and actually rethought what the problem they were trying to solve was in the first place.
SARAH GREEN CARMICHAEL: So, what I also think is so interesting about that example is that when you talk about it, it doesn’t sound like the kind of thing that would have been thought of through other kinds of problem solving methods. There wasn’t necessarily an After Action Review or a 5 Whys exercise or a Six Sigma type intervention. I don’t want to throw those other methods under the bus, but how can you get such powerful results with such a very simple way of thinking about something?
THOMAS WEDELL-WEDELLSBORG: That was something that struck me as well. This, in a way, reframing and the idea of the problem diagnosis is important is something we’ve known for a long, long time. And we’ve actually have built some tools to help out. If you worked with us professionally, you are familiar with, like, Six Sigma, TRIZ, and so on. You mentioned 5 Whys. A root cause analysis is another one that a lot of people are familiar with.
Those are our good tools, and they’re definitely better than nothing. But what I notice when I work with the companies applying those was those tools tend to make you dig deeper into the first understanding of the problem we have. If it’s the elevator example, people start asking, well, is that the cable strength, or is the capacity of the elevator? That they kind of get caught by the details.
That, in a way, is a bad way to work on problems because it really assumes that there’s like a, you can almost hear it, a root cause. That you have to dig down and find the one true problem, and everything else was just symptoms. That’s a bad way to think about problems because problems tend to be multicausal.
There tend to be lots of causes or levers you can potentially press to address a problem. And if you think there’s only one, if that’s the right problem, that’s actually a dangerous way. And so I think that’s why, that this is a method I’ve worked with over the last five years, trying to basically refine how to make people better at this, and the key tends to be this thing about shifting out and saying, is there a totally different way of thinking about the problem versus getting too caught up in the mechanistic details of what happens.
SARAH GREEN CARMICHAEL: What about experimentation? Because that’s another method that’s become really popular with the rise of Lean Startup and lots of other innovation methodologies. Why wouldn’t it have worked to, say, experiment with many different types of fixing the dog adoption problem, and then just pick the one that works the best?
THOMAS WEDELL-WEDELLSBORG: You could say in the dog space, that’s what’s been going on. I mean, there is, in this industry and a lot of, it’s largely volunteer driven. People have experimented, and they found different ways of trying to cope. And that has definitely made the problem better. So, I wouldn’t say that experimentation is bad, quite the contrary. Rapid prototyping, quickly putting something out into the world and learning from it, that’s a fantastic way to learn more and to move forward.
My point is, though, that I feel we’ve come to rely too much on that. There’s like, if you look at the start up space, the wisdom is now just to put something quickly into the market, and then if it doesn’t work, pivot and just do more stuff. What reframing really is, I think of it as the cognitive counterpoint to prototyping. So, this is really a way of seeing very quickly, like not just working on the solution, but also working on our understanding of the problem and trying to see is there a different way to think about that.
If you only stick with experimentation, again, you tend to sometimes stay too much in the same space trying minute variations of something instead of taking a step back and saying, wait a minute. What is this telling us about what the real issue is?
SARAH GREEN CARMICHAEL: So, to go back to something that we touched on earlier, when we were talking about the completely hypothetical example of a spouse who does not clean the kitchen–
THOMAS WEDELL-WEDELLSBORG: Completely, completely hypothetical.
SARAH GREEN CARMICHAEL: Yes. For the record, my husband is a great kitchen cleaner.
You started asking me some questions that I could see immediately were helping me rethink that problem. Is that kind of the key, just having a checklist of questions to ask yourself? How do you really start to put this into practice?
THOMAS WEDELL-WEDELLSBORG: I think there are two steps in that. The first one is just to make yourself better at the method. Yes, you should kind of work with a checklist. In the article, I kind of outlined seven practices that you can use to do this.
But importantly, I would say you have to consider that as, basically, a set of training wheels. I think there’s a big, big danger in getting caught in a checklist. This is something I work with.
My co-author Paddy Miller, it’s one of his insights. That if you start giving people a checklist for things like this, they start following it. And that’s actually a problem, because what you really want them to do is start challenging their thinking.
So the way to handle this is to get some practice using it. Do use the checklist initially, but then try to step away from it and try to see if you can organically make– it’s almost a habit of mind. When you run into a colleague in the hallway and she has a problem and you have five minutes, like, delving in and just starting asking some of those questions and using your intuition to say, wait, how is she talking about this problem? And is there a question or two I can ask her about the problem that can help her rethink it?
SARAH GREEN CARMICHAEL: Well, that is also just a very different approach, because I think in that situation, most of us can’t go 30 seconds without jumping in and offering solutions.
THOMAS WEDELL-WEDELLSBORG: Very true. The drive toward solutions is very strong. And to be clear, I mean, there’s nothing wrong with that if the solutions work. So, many problems are just solved by oh, you know, oh, here’s the way to do that. Great.
But this is really a powerful method for those problems where either it’s something we’ve been banging our heads against tons of times without making progress, or when you need to come up with a really creative solution. When you’re facing a competitor with a much bigger budget, and you know, if you solve the same problem later, you’re not going to win. So, that basic idea of taking that approach to problems can often help you move forward in a different way than just like, oh, I have a solution.
I would say there’s also, there’s some interesting psychological stuff going on, right? Where you may have tried this, but if somebody tries to serve up a solution to a problem I have, I’m often resistant towards them. Kind if like, no, no, no, no, no, no. That solution is not going to work in my world. Whereas if you get them to discuss and analyze what the problem really is, you might actually dig something up.
Let’s go back to the kitchen example. One powerful question is just to say, what’s your own part in creating this problem? It’s very often, like, people, they describe problems as if it’s something that’s inflicted upon them from the external world, and they are innocent bystanders in that.
SARAH GREEN CARMICHAEL: Right, or crazy customers with unreasonable demands.
THOMAS WEDELL-WEDELLSBORG: Exactly, right. I don’t think I’ve ever met an agency or consultancy that didn’t, like, gossip about their customers. Oh, my god, they’re horrible. That, you know, classic thing, why don’t they want to take more risk? Well, risk is bad.
It’s their business that’s on the line, not the consultancy’s, right? So, absolutely, that’s one of the things when you step into a different mindset and kind of, wait. Oh yeah, maybe I actually am part of creating this problem in a sense, as well. That tends to open some new doors for you to move forward, in a way, with stuff that you may have been struggling with for years.
SARAH GREEN CARMICHAEL: So, we’ve surfaced a couple of questions that are useful. I’m curious to know, what are some of the other questions that you find yourself asking in these situations, given that you have made this sort of mental habit that you do? What are the questions that people seem to find really useful?
THOMAS WEDELL-WEDELLSBORG: One easy one is just to ask if there are any positive exceptions to the problem. So, was there day where your kitchen was actually spotlessly clean? And then asking, what was different about that day? Like, what happened there that didn’t happen the other days? That can very often point people towards a factor that they hadn’t considered previously.
SARAH GREEN CARMICHAEL: We got take-out.
THOMAS WEDELL-WEDELLSBORG: S,o that is your solution. Take-out from [INAUDIBLE]. That might have other problems.
Another good question, and this is a little bit more high level. It’s actually more making an observation about labeling how that person thinks about the problem. And what I mean with that is, we have problem categories in our head. So, if I say, let’s say that you describe a problem to me and say, well, we have a really great product and are, it’s much better than our previous product, but people aren’t buying it. I think we need to put more marketing dollars into this.
Now you can go in and say, that’s interesting. This sounds like you’re thinking of this as a communications problem. Is there a different way of thinking about that? Because you can almost tell how, when the second you say communications, there are some ideas about how do you solve a communications problem. Typically with more communication.
And what you might do is go in and suggest, well, have you considered that it might be, say, an incentive problem? Are there incentives on behalf of the purchasing manager at your clients that are obstructing you? Might there be incentive issues with your own sales force that makes them want to sell the old product instead of the new one?
So literally, just identifying what type of problem does this person think about, and is there different potential way of thinking about it? Might it be an emotional problem, a timing problem, an expectations management problem? Thinking about what label of what type of problem that person is kind of thinking as it of.
SARAH GREEN CARMICHAEL: That’s really interesting, too, because I think so many of us get requests for advice that we’re really not qualified to give. So, maybe the next time that happens, instead of muddying my way through, I will just ask some of those questions that we talked about instead.
THOMAS WEDELL-WEDELLSBORG: That sounds like a good idea.
SARAH GREEN CARMICHAEL: So, Thomas, this has really helped me reframe the way I think about a couple of problems in my own life, and I’m just wondering. I know you do this professionally, but is there a problem in your life that thinking this way has helped you solve?
THOMAS WEDELL-WEDELLSBORG: I’ve, of course, I’ve been swallowing my own medicine on this, too, and I think I have, well, maybe two different examples, and in one case somebody else did the reframing for me. But in one case, when I was younger, I often kind of struggled a little bit. I mean, this is my teenage years, kind of hanging out with my parents. I thought they were pretty annoying people. That’s not really fair, because they’re quite wonderful, but that’s what life is when you’re a teenager.
And one of the things that struck me, suddenly, and this was kind of the positive exception was, there was actually an evening where we really had a good time, and there wasn’t a conflict. And the core thing was, I wasn’t just seeing them in their old house where I grew up. It was, actually, we were at a restaurant. And it suddenly struck me that so much of the sometimes, kind of, a little bit, you love them but they’re annoying kind of dynamic, is tied to the place, is tied to the setting you are in.
And of course, if– you know, I live abroad now, if I visit my parents and I stay in my old bedroom, you know, my mother comes in and wants to wake me up in the morning. Stuff like that, right? And it just struck me so, so clearly that it’s– when I change this setting, if I go out and have dinner with them at a different place, that the dynamic, just that dynamic disappears.
SARAH GREEN CARMICHAEL: Well, Thomas, this has been really, really helpful. Thank you for talking with me today.
THOMAS WEDELL-WEDELLSBORG: Thank you, Sarah.
HANNAH BATES: That was Thomas Wedell-Wedellsborg in conversation with Sarah Green Carmichael on the HBR IdeaCast. He’s an expert in problem solving and innovation, and he’s the author of the book, What’s Your Problem?: To Solve Your Toughest Problems, Change the Problems You Solve .
We’ll be back next Wednesday with another hand-picked conversation about leadership from the Harvard Business Review. If you found this episode helpful, share it with your friends and colleagues, and follow our show on Apple Podcasts, Spotify, or wherever you get your podcasts. While you’re there, be sure to leave us a review.
We’re a production of Harvard Business Review. If you want more podcasts, articles, case studies, books, and videos like this, find it all at HBR dot org.
This episode was produced by Anne Saini, and me, Hannah Bates. Ian Fox is our editor. Music by Coma Media. Special thanks to Maureen Hoch, Adi Ignatius, Karen Player, Ramsey Khabbaz, Nicole Smith, Anne Bartholomew, and you – our listener.
See you next week.
- Subscribe On:
Latest in this series
This article is about leadership.
- Decision making and problem solving
- Power and influence
- Business management
Partner Center
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
- What Does Depression Feel Like?
- Identify Your Emotions
- Cope With Your Emotions
- When You Feel Lonely
- When You Feel Emotional
- When You Feel Unappreciated
- When You Feel a Loss of Interest
- When You Feel Irritable
- When You Feel Tired
- When You Feel Worthless
- When You Feel Anxious
- When You Feel Unhappy
- When You Feel Helpless
- When You Feel Hopeless
Healthy Coping Skills for Uncomfortable Emotions
Emotion-Focused and Problem-Focused Strategies
Amy Morin, LCSW, is a psychotherapist and international bestselling author. Her books, including "13 Things Mentally Strong People Don't Do," have been translated into more than 40 languages. Her TEDx talk, "The Secret of Becoming Mentally Strong," is one of the most viewed talks of all time.
:max_bytes(150000):strip_icc():format(webp)/VW-MIND-Amy-2b338105f1ee493f94d7e333e410fa76.jpg)
Rachel Goldman, PhD FTOS, is a licensed psychologist, clinical assistant professor, speaker, wellness expert specializing in eating behaviors, stress management, and health behavior change.
:max_bytes(150000):strip_icc():format(webp)/Rachel-Goldman-1000-a42451caacb6423abecbe6b74e628042.jpg)
- Emotion-Focused Skills
Healthy Problem-Focused Coping Skills
- Unhealthy Coping Skills
Proactive Coping Skills
- Find What Works
- Next in Small Ways to Feel Better When You're Depressed Guide 10 Things to Do When You Feel Alone
Whether you’ve been dumped by your date or you’ve had a rough day at the office, having healthy coping skills can be key to getting through tough times. Coping skills help you tolerate, minimize, and deal with stressful situations in life.
Coping skills are the tactics that people use to deal with stressful situations. Managing your stress well can help you feel better physically and psychologically and impact your ability to perform your best.
But not all coping skills are created equal. Sometimes, it’s tempting to engage in strategies that will give quick relief but might create bigger problems for you down the road. It’s important to establish healthy coping skills that will help you reduce your emotional distress or rid yourself of the stressful situations you face. Examples of healthy coping skills include:
- Establishing and maintaining boundaries
- Practicing relaxation strategies such as deep breathing, meditation, and mindfulness
- Getting regular physical activity
- Making to-do lists and setting goals
This article explores coping skills that can help you manage stress and challenges. Learn more about how different strategies, including problem-focused and emotion-focused skills, can be most helpful.
Verywell / Emily Roberts
Problem-Based vs. Emotion-Based
The five main types of coping skills are: problem-focused coping, emotion-focused coping, religious coping, meaning-making, and social support.
Two of the main types of coping skills are problem-based coping and emotion-based coping. Understanding how they differ can help you determine the best coping strategy for you.
- Problem-based coping is helpful when you need to change your situation, perhaps by removing a stressful thing from your life. For example, if you’re in an unhealthy relationship, your anxiety and sadness might be best resolved by ending the relationship (as opposed to soothing your emotions).
- Emotion-based coping is helpful when you need to take care of your feelings when you either don’t want to change your situation or when circumstances are out of your control. For example, if you are grieving the loss of a loved one, it’d be important to take care of your feelings in a healthy way (since you can’t change the circumstance).
There isn’t always one best way to proceed. Instead, it’s up to you to decide which type of coping skill is likely to work best for you in your particular circumstance. The following are examples of stressful situations and how each approach could be used.
Reading Your Performance Review
You open your email to find your annual performance review. The review states that you are below average in several areas and you’re surprised by this because you thought you were performing well. You feel anxious and frustrated.
- Problem-focused coping : You go to the boss and talk about what you can do to improve your performance. You develop a clear plan that will help you do better and you start to feel more confident about your ability to succeed.
- Emotion-focused coping : You spend your lunch break reading a book to distract yourself from catastrophic predictions that you’re going to be fired. After work, you exercise and clean the house as a way to help you feel better so you can think about the situation more clearly.
Getting a Teenager to Clean
You have told your teenager he needs to clean his bedroom. But it’s been a week and clothes and trash seem to be piling up. Before heading out the door in the morning, you told him he has to clean his room after school "or else." You arrive home from work to find him playing videos in his messy room.
- Problem-focused coping : You sit your teenager down and tell him that he’s going to be grounded until his room is clean. You take away his electronics and put him on restriction. In the meantime, you shut the door to his room so you don’t have to look at the mess.
- Emotion-focused coping : You decide to run some bathwater because a hot bath always helps you feel better. You know a bath will help you calm down so you don’t yell at him or overreact.
Giving a Presentation
You’ve been invited to give a presentation in front of a large group. You were so flattered and surprised by the invitation that you agreed to do it. But as the event approaches, your anxiety skyrockets because you hate public speaking .
- Problem-focused coping : You decide to hire a public speaking coach to help you learn how to write a good speech and how to deliver it confidently. You practice giving your speech in front of a few friends and family members so you will feel better prepared to step on stage.
- Emotion-focused coping : You tell yourself that you can do this. You practice relaxation exercises whenever you start to panic. And you remind yourself that even if you’re nervous, no one else is even likely to notice.
Problem-based coping skills focus on changing the situation, while emotional-based coping skills are centered on changing how you feel. Knowing which approach is right for a specific situation can help you deal with stress more effectively.
Get Advice From The Verywell Mind Podcast
Hosted by therapist Amy Morin, LCSW, this episode of The Verywell Mind Podcast shares how to face uncomfortable emotions, featuring comedian Paul Gilmartin.
Follow Now : Apple Podcasts / Spotify / Google Podcasts
Healthy Emotion-Focused Coping Skills
Whether you’re feeling lonely , nervous, sad, or angry , emotion-focused coping skills can help you deal with your feelings in a healthy way. Healthy coping strategies may soothe you, temporarily distract you, or help you tolerate your distress.
Sometimes it’s helpful to face your emotions head-on. For example, feeling sad after the death of a loved one can help you honor your loss.
So while it would be important to use coping skills to help relieve some of your distress, coping strategies shouldn’t be about constantly distracting you from reality.
Other times, coping skills may help you change your mood. If you’ve had a bad day at work, playing with your kids or watching a funny movie might cheer you up. Or, if you’re angry about something someone said, a healthy coping strategy might help you calm down before you say something you might regret.
Other examples of healthy ways to cope with emotions include:
- Care for yourself : Put on lotion that smells good, spend time in nature, take a bath, drink tea, or take care of your body in a way that makes you feel good such as painting your nails, doing your hair, putting on a face mask.
- Engage in a hobby : Do something you enjoy such as coloring, drawing, or listening to music .
- Exercise : Do yoga, go for a walk, take a hike, or engage in a recreational sport.
- Focus on a task : Clean the house (or a closet, drawer, or area), cook a meal, garden, or read a book.
- Practice mindfulness : List the things you feel grateful for, meditate , picture your "happy place," or look at pictures to remind you of the people, places, and things that bring joy.
- Use relaxation strategies : Play with a pet, practice breathing exercises, squeeze a stress ball, use a relaxation app, enjoy some aromatherapy, try progressive muscle relaxation , or write in a journal.
There are many ways you might decide to tackle a problem head-on and eliminate the source of your stress. In some cases, that may mean changing your behavior or creating a plan that helps you know what action you’re going to take.
In other situations, problem-focused coping may involve more drastic measures, like changing jobs or ending a relationship. Here are some examples of positive problem-focused coping skills:
- Ask for support from a friend or a professional.
- Create a to-do list.
- Engage in problem-solving.
- Establish healthy boundaries .
- Walk away and leave a situation that is causing you stress.
- Work on managing your time better.
Whether emotion-focused or problem-focused, healthy coping skills should help calm stress without avoiding the issue. The right coping skill often depends on the situation and your specific needs in the moment.
Unhealthy Coping Skills to Avoid
Just because a strategy helps you endure emotional pain, it doesn’t mean it’s healthy. Some coping skills could create bigger problems in your life. Here are some examples of unhealthy coping skills:
- Drinking alcohol or using drugs : Substances may temporarily numb your pain, but they won’t resolve your issues. Substances are likely to introduce new problems into your life. Alcohol, for example, is a depressant that can make you feel worse. Using substances to cope also puts you at risk for developing a substance use disorder and it may create health, legal, financial problems, and social problems.
- Overeating : Food is a common coping strategy. But, trying to "stuff your feelings" with food can lead to an unhealthy relationship with food and health issues. Sometimes people go to the other extreme and restrict their eating (because it makes them feel more in control) and clearly, that can be just as unhealthy.
- Sleeping too much : Whether you take a nap when you’re stressed out or you sleep late to avoid facing the day, sleeping offers a temporary escape from your problems. However, when you wake up, the problem will still be there.
- Venting to others : Talking about your problems so that you can gain support, develop a solution, or see a problem in a different way can be healthy. But studies show repeatedly venting to people about how bad your situation is or how terrible you feel is more likely to keep you stuck in a place of pain.
- Overspending : While many people say they enjoy retail therapy as a way to feel better, shopping can become unhealthy. Owning too many possessions can add stress to your life. Also, spending more than you can afford will only backfire in the end and cause more stress.
- Avoiding : Even “healthy” coping strategies can become unhealthy if you’re using them to avoid the problem. For example, if you are stressed about your financial situation, you might be tempted to spend time with friends or watch TV because that’s less anxiety-provoking than creating a budget. But if you never resolve your financial issues, your coping strategies are only masking the problem.
Unhealthy coping techniques—such as drinking or avoiding the problem—may offer some temporary relief, but they tend to make things worse in the long run. These unhealthy tactics can also lead to other problems that create more stress and make coping more difficult.
Coping skills are usually discussed as a reactive strategy: When you feel bad, you do something to cope. But, research shows that proactive coping strategies can effectively manage the future obstacles you’re likely to face.
For example, if you have worked hard to lose weight, proactive coping strategies could help you maintain your weight after your weight loss program has ended. You might plan for circumstances that might derail you—like the holiday season or dinner invitations from friends—to help you cope. You also might plan for how you will cope with emotions that previously caused you to snack, like boredom or loneliness.
Proactive coping can also help people deal with unexpected life changes, such as a major change in health. A 2014 study found that people who engaged with proactive coping were better able to deal with the changes they encountered after having a stroke.
Another study found that people who engaged in proactive coping were better equipped to manage their type 2 diabetes. Participants who planned ahead and set realistic goals enjoyed better psychological well-being.
So, if you are facing a stressful life event or you’ve undergone a major change, try planning ahead. Consider the skills you can use to cope with the challenges you’re likely to face. When you have a toolbox ready to go, you’ll know what to do. And that could help you to feel better equipped to face the challenges ahead.
Proactive coping has been found to be an effective way to help people deal with both predictable changes like a decline in income during retirement, as well as unpredictable life changes such as the onset of a chronic health condition.
Find What Works for You
The coping strategies that work for someone else might not work for you. Going for a walk might help your partner calm down. But you might find going for a walk when you’re angry causes you to think more about why you’re mad—and it fuels your angry feelings. So you might decide watching a funny video for a few minutes helps you relax.
You might find that certain coping strategies work best for specific issues or emotions. For example, engaging in a hobby may be an effective way to unwind after a long day at work. But, going for a walk in nature might be the best approach when you’re feeling sad.
When it comes to coping skills, there’s always room for improvement. So, assess what other tools and resources you can use and consider how you might continue to sharpen your skills in the future.
It's important to develop your own toolkit of coping skills that you’ll find useful. You may need to experiment with a variety of coping strategies to help you discover which ones work best for you.
A Word From Verywell
Healthy coping skills can help protect you from distress and face problems before they become more serious. By understanding the two main types of coping skills, you can better select strategies that are suited to different types of stress.
If you are struggling to practice healthy coping skills or find yourself relying on unhealthy ones instead, talking to a mental health professional can be helpful. A therapist can work with you to develop new skills that will serve your mental well-being for years to come.
Get Help Now
We've tried, tested, and written unbiased reviews of the best online therapy programs including Talkspace, BetterHelp, and ReGain. Find out which option is the best for you.
Aldwin CM, Yancura LA. Coping . In: Encyclopedia of Applied Psychology . Elsevier; 2004:507-510. doi:10.1016/B0-12-657410-3/00126-4
Byrd-Craven J, Geary DC, Rose AJ, Ponzi D. Co-ruminating increases stress hormone levels in women . Horm Behav . 2008;53(3):489-92. doi:10.1016/j.yhbeh.2007.12.002
Drummond S, Brough P. Proactive coping and preventive coping: Evidence for two distinct constructs? . Personality and Individual Differences . 2016;92:123-127. doi:10.1016/j.paid.2015.12.029.
Tielemans NS, Visser-Meily JM, Schepers VP, Post MW, van Heugten CM. Proactive coping poststroke: Psychometric properties of the Utrecht Proactive Coping Competence Scale . Arch Phys Med Rehabil. 2014;95(4):670-5. doi:10.1016/j.apmr.2013.11.010
By Amy Morin, LCSW Amy Morin, LCSW, is a psychotherapist and international bestselling author. Her books, including "13 Things Mentally Strong People Don't Do," have been translated into more than 40 languages. Her TEDx talk, "The Secret of Becoming Mentally Strong," is one of the most viewed talks of all time.
- Open access
- Published: 07 April 2024
Efficacy of a virtual nursing simulation-based education to provide psychological support for patients affected by infectious disease disasters: a randomized controlled trial
- Eunjung Ko 1 &
- Yun-Jung Choi 1
BMC Nursing volume 23 , Article number: 230 ( 2024 ) Cite this article
163 Accesses
1 Altmetric
Metrics details
Virtual simulation-based education for healthcare professionals has emerged as a strategy for dealing with infectious disease disasters, particularly when training at clinical sites is restricted due to the risk of infection and a lack of personal protective equipment. This research evaluated a virtual simulation-based education program intended to increase nurses’ perceived competence in providing psychological support to patients affected by infectious disease disasters.
The efficacy of the program was evaluated via a randomized controlled trial. We recruited 104 nurses for participation in the study and allocated them randomly and evenly to an experimental group and a control group. The experimental group was given a web address through which they could access the program, whereas the control group was provided with a web address that directed them to text-based education materials. Data were then collected through an online survey of competence in addressing disaster mental health, after which the data were analyzed using the Statistical Package for the Social Sciences(version 23.0).
The analysis showed that the experimental group’s disaster mental health competence (F = 5.149, p =.026), problem solving process (t = 3.024, p =.003), self-leadership (t = 2.063, p =.042), learning self-efficacy (t = 3.450, p =.001), and transfer motivation (t = 2.095, p =.039) significantly statistically differed from those of the control group.
Conclusions
A virtual nursing simulation-based education program for psychological support can overcome limitations of time and space. The program would also be an effective learning resource during infectious disease outbreaks.
Clinical trial registration
This Korean clinical trial was retrospectively registered (21/11/2023) in the Clinical Research Information Service ( https://cris.nih.go.kr ) with trial registration number KCT0008965.
Peer Review reports
The last two decades have confronted the world with a variety of infectious diseases, such as severe acute respiratory syndrome, which first occurred in Asia in 2003 before spreading worldwide, including Korea, in only a few months. Since then, infectious disease outbreaks began to be recognized as severe disasters. Other examples include the 2009 H1N1 influenza outbreak, which caused more than 10,000 deaths worldwide and 140 deaths in Korea; the proliferation of the Ebola virus, which resulted in a fatality rate of more than 90% in Africa in 2014; and the outbreak of Middle East respiratory syndrome in 2015, Zika virus disease in 2016, and coronavirus disease (COVID-19) in 2019 [ 1 ]. The COVID-19 pandemic, in particular, has caused infections among approximately 64 million people and the deaths of 1.5 million individuals as of December 2020 [ 2 ].
Direct victims of infectious disease disasters, infected patients, and quarantined individuals suffer from a fear of stigma or social blame and guilt, but even people who are unexposed to sources of infection experience psychological distress from anxiety and fear of disease or possible death [ 3 ]. They also blame infected people and harbor hatred toward them [ 3 ]. This assertion is supported by an examination of web search behaviors and infodemic attitudes toward COVID-19, which identified superficial and racist attitudes [ 4 ]. Additionally, in research using a health stigma and discrimination framework related to communicable diseases, the authors found that people exhibit negative stereotypes, biases, and discriminatory conduct toward infected groups owing to fears of contagion, concerns about potential harm, and perceptions that individuals violate central values [ 5 ]. Stigmatized individuals experience adverse effects on their health because of both the stress induced by stigma and the decreased use of available services [ 5 ].
Severe and prolonged anxiety, fear, blame, and aggression can lead to mental health problems, including depression, anxiety, panic attacks, somatic symptoms, post-traumatic stress disorder, psychosis, and even suicide and life-threatening behaviors [ 6 ]. Therefore, recovery from the psychological trauma caused by a disaster should be regarded as equally necessary as physical recovery, with emphasis placed on psychological support activities that prevent the deterioration of mental health [ 7 ].
Disasters pose a significant threat to mental health support systems, wherein the lack of healthcare professionals or psychologists trained to address these conditions exacerbates the psychological distress and psychopathological risk experienced by society [ 8 ]. When training at clinical sites is restricted due to infection risks and a lack of personal protective equipment (PPE), an emerging solution is virtual simulation [ 9 ].
A virtual simulation is a simulation modality developed on the basis of video or graphic recordings featuring virtual patients and delivered via either a static or mobile device. It replicates real-world clinical situations and affords learners an interactive experience [ 10 ]. Virtual simulation-based education provides an immersive clinical environment, as virtual patients respond to a learner’s assessments and interventions [ 11 , 12 ]. It enables two-way communication, and allows medical professionals to practice making clinical decisions [ 10 ]. Virtual patients are equipped with voice, intonation, and expressions that reinforce the educational narrative within the virtual environment, thereby enhancing the effectiveness of the learning experience [ 13 ]. One of the primary advantages of virtual simulation-based education is its provision of a safe and non-threatening environment in which learners can practice. It also offers flexible and reproducible learning experiences, thus catering to the diverse needs of learners [ 14 ].
Self-assessment is the most commonly used competence evaluation tool, as it is cost-effective and helps nurses improve their practice by identifying their strengths and weaknesses for development [ 15 ]. Self-assessed competence is also related to the quality of patient care because nurses promote continuous learning by determining educational needs through such evaluations [ 16 ]. The competence perceived by a nurse is inherently subjective given its self-reported nature and poses a challenge in establishing a direct correlation with the actual care of patients [ 17 , 18 ]. However, studies have indicated that increased levels of self-perceived competence are associated with a significant increase in core competencies related to patient care and frequent use of clinical skills [ 19 , 20 ]. Perceived competence likewise influences the job satisfaction and organizational citizenship behavior of nurses and is significantly related to absenteeism, one of the deterrents to the delivery of quality care [ 21 , 22 ].
Competence refers to the possession of qualifications and abilities to satisfy professional standards, as well as the capability to perform tasks and duties in a suitable and effective manner [ 23 ]. Competencies for disaster mental health are crucial for enhancing disaster response capabilities. These competencies encompass a range of skills, knowledge, and attitudes necessary for mental health professionals to effectively support individuals and communities affected by disasters [ 24 ]. Such competencies and how they are affected by simulation-based training have been explored in some studies, which reported a significant increase in competence after exposure to the aforementioned education [ 25 , 26 ].
The simulation education defined in mock training designs based on real situations provides opportunities to exercise problem-solving through various strategies. Problem-solving process is considered key competency through which learners are expected to enhance their relevant knowledge and clinical performance abilities [ 27 ]. In particular, problem-solving processes for identifying and assessing problems and finding solutions are psychological strategies that help people cope and recover after a disaster [ 28 ]. A scoping review on the effect of simulation-based education on the problem-solving process indicated that out of 32 studies reviewed, 21 demonstrated statistically significant improvement in people’s ability to resolve problems [ 29 ].
Simulation training can also address self-leadership, which is an essential self-learning quality that aids individuals in staying motivated and focused on their learning goals. It is also required as a basic qualification of professional nurses, who must be able to take initiative and make responsible decisions [ 30 , 31 ]. Previous studies have reported statistically significant improvements in self-leadership following simulation training [ 32 , 33 ].
Another aspect that benefits from simulation-driven education is learning self-efficacy, which plays a crucial role in predicting learners’ levels of engagement and academic success in online education. It reflects learners’ confidence in their ability to manage their own learning process. It is a significant predictor of both learners’ participation levels and their academic achievements in online education settings [ 34 , 35 ]. Several studies have demonstrated virtual simulation- or online education-induced significant improvements in learning self-efficacy [ 36 , 37 ]. Finally, virtual simulation-based education can also improve the motivation to transfer new knowledge and skills learned through education to clinical practice [ 38 ]. This motivation is considered an essential measure of effective learning for nurses working in the clinical field [ 38 ]. A previous study reported that psychiatric nursing simulation training combined with post-course debriefing significantly increases participants’ level of motivation to transfer [ 38 ].
On the basis of the discussion above, this study evaluated a virtual nursing simulation-based education program on disaster psychology designed to provide psychological support to patients affected by infectious disease disasters.
Study design
This study conducted a randomized controlled trial (RCT) to test the virtual nursing simulation-based education program of interest. The RCT protocol used was based on CONSORT guidelines.
Participants
We recruited nurses working at general hospitals in South Korea. With permission from the nurse managers of these hospitals, a participation notice was posted on the institutions’ internet bulletin boards for nurses for a week. The two-sided test criterion, with a significance level (α) of 0.05, a power (1-β) of 0.80, and a medium effect size of 0.6, dictates that the minimum number of participants per group be 90. The effect size was based on a virtual simulation intervention study conducted by Kim and Choi [ 36 ]. Taking the dropout rate into consideration, we recruited 104 nurses, who were assigned to an experimental group and a control group using the random sampling functionality of the Statistical Package for the Social Sciences (SPSS version 23.0). Out of the initial sample, 11 participants were excluded because they were on vacation, could not be contacted, or provided incomplete responses during data collection (Fig. 1 ).
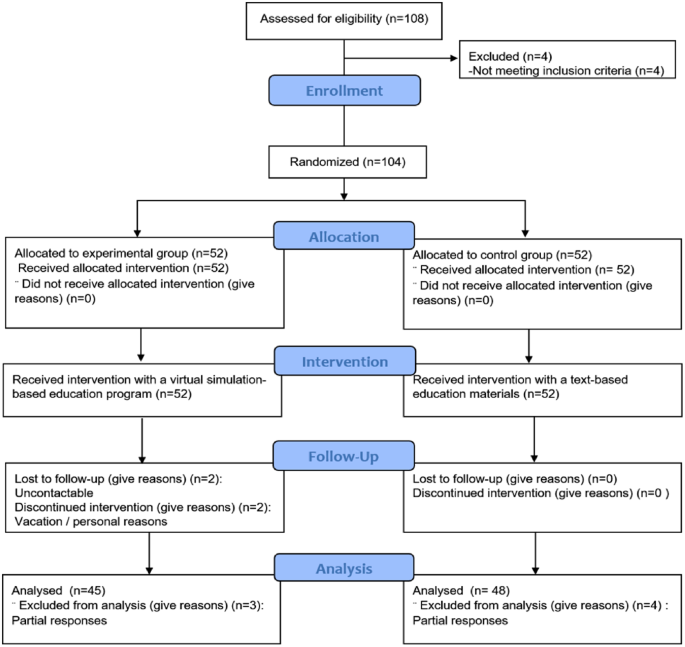
Flowchart of the randomized controlled trial
The virtual nursing simulation-based education program
This study probed into the virtual nursing simulation-based education program developed by Ko [ 39 ]. The program is implemented using an e-learning development platform, Articulate Storyline, whose operating environment is compatible with all web browsers (Internet Explorer, Microsoft Edge, Firefox, Google Chrome, etc.). It is a mobile-friendly application that can run in devices with Android and iOS operating systems. When an individual uses their smartphone or personal computer to access the server via the web address corresponding to the education program, the content functions execute. Ko’s [ 39 ] program involves five stages of learning completed in 100 min: (1) preparatory learning (30 min), (2) pre-test (5 min), (3) pre-briefing (5 min), (4) simulation game (30 min), and (5) structured self-debriefing (30 min) (Fig. 2 ).
Preparatory learning comes with lecture materials on guidelines for providing psychological support to victims of infectious disease disasters, administering psychological first aid, donning and doffing PPE, and exercising mindfulness through videos and pictures. In the pretest stage, a learner answers five questions and can immediately check the correct responses, which come with detailed explanations. In the prebriefing stage, an overview of a nursing simulation scenario, patient information, learning objectives, and instructions on using the virtual simulation are provided. During the simulation game, a video of the simulation is presented. It starts with a 39-year-old female, a standardized patient who is age- and gender-matched to the scenario, confirmed to have contracted COVID-19 and transferred to a negative pressure isolation room. The patient presents with extreme anxiety and feeling of tightness in her chest. During the game, learners are expected to complete 12 quizzes. In the debriefing stage, a summary of the simulation quiz results and self-debriefing questions are provided, and the comments made by learners are saved in the Naver cloud platform.
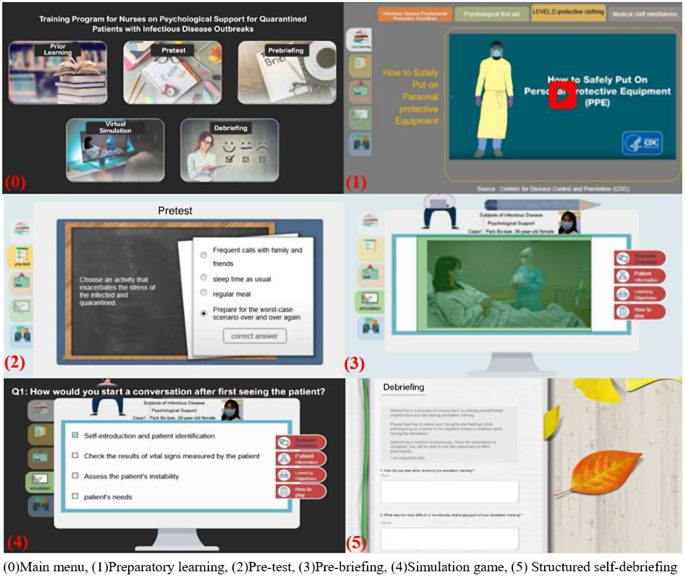
The evaluated virtual nursing simulation-based education program (examples are our own work)
Measurements
Disaster mental health competence.
Disaster mental health competence was measured using the perceived competence scale for disaster mental health workforce (PCS-DMHW), which was developed by Yoon and Choi [ 40 ]. This tool consists of 24 questions related to knowledge (6 questions), attitudes (9 questions), and skills (9 questions). Each item is rated using a five-point Likert scale (0 = strongly disagree, 4 = strongly agree), and the responses are summed. The higher the score, the greater the perception of competence in a relevant area [ 40 ]. The Cronbach’s α values of the PCS-DMHW were 0.95 and 0.94 at the time of tool development and the present study, respectively.
Problem solving process
Problem solving process was determined using a tool modified and supplemented by Park and Woo [ 41 ] on the grounds of the problem solving process and behavior survey developed by Lee [ 42 ]. This tool is composed of 25 questions on five factors, namely, problem discovery, problem definition, problem solution design, problem solution execution, and problem solving review [ 41 ]. The reliability of the tool was 0.89 at the time of development [ 41 ], but the Cronbach’s α found in the current research was 0.94.
Self-leadership
Self-leadership was measured using a tool developed by Manz [ 43 ] and modified by Kim [ 44 ]. The tool consists of 18 questions distributed over six factors (three questions each): self-defense, rehearsal, goal setting, self-compensation, self-expense edition, and constructive thinking. The reliability of the tool at the time of development and the present research was (Cronbach’s α) 0.87 and 0.82, respectively.
Learning self-efficacy
To ascertain learning self-efficacy, we used the tool developed by Ayres [45] and translated by Park and Kweon [ 38 ]. This tool consists of 10 questions, and it had a reliability (Cronbach’s ⍺) of 0.94 and 0.93 at the time of development and the current study, respectively.
Motivation to transfer
We used Ayres’s [45] motivation to transfer scale, which was translated by Park and Kweon [ 38 ]. Its reliability at the time of development and the present research was (Cronbach’s ⍺) 0.80 and 0.93, respectively.
Data collection
The experimental and control groups were administered a pretest through an online survey. The web address through which the evaluated virtual simulation-based education program could be accessed was provided to the experimental group, whereas text-based education materials on psychological support for victims of infectious disease disasters were given to the control group. The groups were simultaneously sent the program’s instruction manual, and their inquiries were answered through chat. After the interventions, each participant was administered a posttest through another online survey.
Data analysis
The collected data were analyzed using SPSS version 23.0. The homogeneity test for general characteristics between the experimental and control groups was analyzed using a t-test, a chi-square test, and Fisher’s exact test. The normality of the dependent variables was analyzed using the Kolmogorov-Smirnov test. Changes in the dependent variables between the pretest and posttest were analyzed using a paired t-test. Differences in the dependent variables before and after the groups’ use of the interventions were examined via a t-test and ANCOVA.
Ethical considerations
We completed education in bioethics law prior to the research and obtained approval of the research proposal and questionnaire from the Institutional Review Board of the affiliated university (IRB approval number 1041078-202003-HRSB-070-01CC). A signed consent form was also obtained from each participant after the purpose and methods of the research, the confidentiality of personal information, and the voluntary nature of participation or their right to withdraw from the study were explained to them. All collected data were kept in a lockable cabinet, and electronic data were encrypted and stored. These data are to be discarded after three years.
A total of 93 participants (45 in the experimental group and 48 in the control group) were left after the exclusion of unsuitable respondents. of the between-group comparisons of the subjects indicated no significant differences between them (5% significance level) in terms of general characteristics, such as gender, age, work unit, and clinical experience (Table 1 ).
The score of the experimental group on disaster mental health competence increased from 48.13 in the pretest to 70.51 in the posttest (+ 22.38), whereas that of the control group increased from 53.33 in the pretest to 68.38 in the posttest (+ 15.04). These findings reflect a statistically significant difference in competence between the groups (F = 5.149, p =.026). The scores of the experimental and control groups on problem solving process increased from 73.07 in the pretest to 88.24 in the posttest (+ 15.18) and from 75.75 in the pretest to 83.77 in the posttest (+ 8.02), respectively. As with the competence findings, these point to a significant difference between the groups in terms of the ability to resolve problems (t = 3.024, p =.003) (Table 2 ).
The score of the experimental group on self-leadership increased from 54.87 in the pretest to 59.58 in the posttest (+ 4.71), and that of the control group increased from 57.48 in the pretest to 60.10 in the posttest (+ 2.63). These results denote a statistically significant difference in this ability between the groups (t = 2.063, p =.042). The scores of the experimental and control participants on learning self-rose from 55.40 in the pretest to 58.84 in the posttest (+ 3.44) and from 56.81 in the pretest to 57.13 in the posttest (+ 0.31), respectively. Again, a statistically significant difference was found between the groups (t = 3.450, p =.001). Their scores on motivation to transfer rose from 49.31 in the pretest to 54.29 in the posttest (+ 4.98) (experimental group) and the score increased from 50.50 in the pretest to 51.85 in the posttest (+ 1.35) (control group), pointing to a significant difference between the groups (t = 2.095, p =.039).
As previously stated, this research was evaluated a virtual nursing simulation-based education program designed to provide psychological support to patients affected by infectious disease disasters. The results showed statistically significant increases in the experimental group’s pretest and posttest scores on disaster mental health competence, problem solving process, self-leadership, learning self-efficacy, and motivation to transfer.
The experimental group achieved more statistically significant improvements in disaster mental health competence than did the control group. This finding is similar to the statistically significant increase in the average disaster mental health competence shown by providers of disaster mental health services providers and non-expert groups after PFA training involving lecture and practice [ 46 ]. It is also consistent with the significant increase in the scores of school counselors on disaster mental health competence after a lecture and simulation on PFA [ 25 ]. In their study on disaster relief workers, Kang and Choi [ 26 ] measured the participants’ performance competence in PFA after the delivery of a lecture and simulation-based education using a standardized patient. The authors found a significant increase in PFA performance competence, consistent with the present research. Since there are currently no other virtual simulation-based education programs for disaster psychological support available, we compared the effectiveness of various PFA training methods with the program assessed in the present work.
In the current research, the posttest scores of the experimental group on problem solving process significantly increased, similar to the results of Kim et al.’s study on virtual simulation- and blended simulation-based education on asthmatic child nursing [ 47 ]. Both the control and experimental groups (virtual simulation only and blended simulation featuring high-fidelity and virtual simulations, respectively) showed an increase in their problem solving process scores. These results and those derived in the present work are similar because reading and pretest phases were incorporated into the design of the previous study. Given that researchers have used commercial virtual simulations featuring avatars rather than standardized patient videos available through English-based platforms, user experiences may differ, thus requiring a qualitative analysis to identify differences. However, Kim et al. [ 47 ] did not implement a debriefing after the virtual simulation program, rendering comparison impossible. Another research reported that a multimodality simulation education that combines such methods as virtual simulation, the use of mannequins, and part-task training increase increased the scores of hospital nurses’ on problem solving process [ 48 ].
In the present work, the experimental group’s self-leadership scores increased after they used the program, and these scores were higher [ 49 , 50 ]. This difference can be explained by the fact that our respondents voluntarily participated in our research given their interest in self-learning programs for disaster psychological support; even in the comparison studies, participants with stronger interest in leadership education typically exhibited heightened degrees of self-leadership [ 51 ]. The increase in self-leadership scores in the current research is consistent with a previous study involving a two-hour simulation education about PPE donning and doffing, medication administration, and medical specimen treatment in a scenario of patients suspected of having infectious diseases [ 32 ]. Another research showed that simulation education on high-risk pregnancy enhances nursing students’ problem-solving processes and self-leadership [ 52 ].
Learning self-efficacy is a key variable that enables the prediction of learners’ degrees of participation in online education and the prediction of their academic achievements, as it points to the ability to manage their learning processes [ 34 , 53 ]. The results of the current research in this regard are consistent with those of a study on the online practice of basic nursing skills, which increased participants’ learning self-efficacy [ 54 ]. The researchers included an online quiz about basic nursing skills and feedback sections for learners’ self-evaluations of their performance as avenues through which to encourage autonomy in learning. A similar approach was used in the present study, which involved both a pretest for self-evaluation, direct feedback on the virtual simulation, and a self-debriefing session, enabling the participants to reflect on their simulation experiences while reviewing other participants’ answers during self-debriefing. These functions of the evaluated program were expected to factor importantly in the significant increase in the participants’ learning self-efficacy scores.
Many studies on practice education have examined participants’ motivations to transfer knowledge and skills alongside their learning self-efficacies. In the current research, the motivation to transfer scores of the experimental increased, and the difference between the two groups was statistically meaningful. This result is consistent with the findings of Park and Kweon on the simulation education about psychiatric nursing, during which post-course debriefing increased the participants’ average scores on motivation to transfer and learning self-efficacy [ 38 ]. Conversely, Kang and Kim found that a six-week simulation program for alcoholic patient care did not generate a significant increase in the participants’ motivation to transfer and learning self-efficacy scores [ 55 ]. This finding was attributed to the unfamiliarity of the local community scenario used in the research to the participants, who were in their senior year of nursing school [ 55 ]. This limitation was overcome in the current research by administering a qualitative survey of nurses’ actual demand for education on psychological support for infectious disease patients. That is, the survey presented scenarios that the participants needed.
As with other studies, the present research was encumbered by several limitations. First, the self-assessment measures used in this study may be unreliable, because they are based on individuals’ subjective perceptions and interpretations of their abilities. There is also the possibility of respondent fatigue given that the participants were compelled to answer numerous questions. Future studies should incorporate both subjective and objective measures into data collection and consider as concise an evaluation method as possible to prevent respondent fatigue. Second, this study did not establish a direct link between the obtained results and actual changes in practice or improvements in patient outcomes. We propose a follow-up study to investigate the impact of the education program examined in this study on either the mental health of patients or the quality of patient care. Third, simulation-based education tends to be accompanied with more guidance than text-based program because the former has diverse components, including quiz games, and participants are predisposed to allocate more time to simulation-based education. These may potentially influence the results. In the future, we propose to conduct research by modifying education under the same time and guided condition.
This study proposed that a well-designed virtual nursing simulation-based education program can be an effective modality with which to satisfy the educational needs of nurses in the context of infectious disease outbreaks. Such programs can be easily used by nurses anywhere and anytime before they are deployed to provide psychological support to patients with infectious diseases. They are also expected to contribute to enhancing competence in addressing disaster mental health and improving the quality of care of patients afflicted with infectious diseases.
Data availability
The datasets used and/or analyzed in this study are available from the corresponding author upon reasonable request.
Abbreviations
Coronavirus disease 2019
Randomized controlled trial
Personal protective equipment
Statistical Package for the Social Sciences
Analysis of covariance
Psychological first aid
World Health Organization. WHO coronavirus disease (COVID-19) dashboard. 2020.
Oh EG, Yu SH, Kang JH, Oh YJ, Cha KI, Jeon YH, et al. Perspectives on nursing profession for a post-COVID-19 new normal. Korean J Adult Nurs. 2020;32(3):221–2.
Article Google Scholar
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. Rapid review. Lancet. 2020;395:912–20.
Article CAS PubMed PubMed Central Google Scholar
Çalışkan C, Özsezer G, Pay M, Demir G, Çelebi I, Koçak H. Web search behaviors and infodemic attitudes regarding COVID-19 in Turkey: a framework study for improving response and informing policy on the COVID-19 infodemic. Front Public Health. 2022;10:948478.
Article PubMed PubMed Central Google Scholar
Stangl AL, Earnshaw VA, Logie CH, Van Brakel WC, Simbayi L, Barré I, et al. The health stigma and discrimination Framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019;17:1–13.
Tucci V, Moukaddam N, Meadows J, Shah S, Galwankar SC, Kapur GB. The forgotten plague: psychiatric manifestations of Ebola, Zika, and emerging infectious diseases. J Global Infect Dis. 2017;9(4):151.
Korea Mental Health Technology R&D Project. (2017). Korean Disaster and Mental Health Support Guidelines.
Zhang J, Wu W, Zhao X, Zhang W. Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: a model of West China Hospital. Precision Clin Med. 2020;3(1):3–8.
Liu W. The effects of virtual simulation on undergraduate nursing students’ mental health literacy: a prospective cohort study. Issues Ment Health Nurs. 2020:1–10.
Cant R, Cooper S, Sussex R, Bogossian F. What’s in a name? Clarifying the nomenclature of virtual simulation. Clin Simul Nurs. 2019;27:26–30.
Foronda C, Bauman EB. Strategies to incorporate virtual simulation in nurse education. Clin Simul Nurs. 2014;10(8):412–812.
Berman NB, Durning SJ, Fischer MR, Huwendiek S, Triola MM. The role for virtual patients in the future of medical education. Acad Med. 2016;91(9):1217–22.
Article PubMed Google Scholar
Verkuyl M, Hughes M, Tsui J, Betts L, St-Amant O, Lapum JL. Virtual gaming simulation in nursing education: a focus group study. J Nurs Educ. 2017;56(5):274–80.
Cobbett S, Snelgrove-Clarke E. Virtual versus face-to-face clinical simulation in relation to student knowledge, anxiety, and self-confidence in maternal-newborn nursing: a randomized controlled trial. Nurse Educ Today. 2016;45:179–84.
Bahreini M, Shahamat S, Hayatdavoudi P, Mirzaei M. Comparison of the clinical competence of nurses working in two university hospitals in Iran. Nurs Health Sci. 2011;13(3):282–8.
Goliroshan S, Babanataj R, Aziznejadroshan P. Investigating the self-assessment of clinical competency of nurses working in Babol University of Medical Sciences hospitals. Middle East J Family Med. 2018;7(10):279.
Google Scholar
Bam V, Diji AKA, Asante E, Lomotey AY, Adade P, Akyeampong BA. Self-assessed competencies of nurses at an emergency department in Ghana. Afr J Emerg Med. 2020;10(1):8–12.
O’Leary J. Comparison of self-assessed competence and experience among critical care nurses. J Nurs Adm Manag. 2012;20(5):607–14. https://doi.org/10.1111/j.1365-2834.2012.01394.x .
Kim KM, Choi JS. Self-perceived competency of infection control nurses based on Benner’s framework: a nationwide survey in Korea. Appl Nurs Res. 2015;28(2):175–9.
Hassankhani H, Hasanzadeh F, Powers KA, Dadash Zadeh A, Rajaie R. Clinical skills performed by Iranian emergency nurses: perceived competency levels and attitudes toward expanding professional roles. J Emerg Nurs. 2018;44(2):156–63. https://doi.org/10.1016/j.jen.2017.06.007 .
Biagioli V, Prandi C, Nyatanga B, Fida R. The role of professional competency in influencing job satisfaction and organizational citizenship behavior among palliative care nurses. J Hospice Palliat Nurs. 2018;20(4):377–84.
Alreshidi NM, Alaseeri R, Garcia M. Factors influencing absenteeism among nursing staff in the primary health care centers in hail: a preliminary study for enhancing staff commitment. Health Sci J. 2019;13(3):658–1.
Rodolfa E, Bent R, Eisman E, Nelson P, Rehm L, Ritchie P. A cube model for competency development: implications for psychology educators and regulators. Prof Psychology: Res Pract. 2005;36(4):347.
King RV, Burkle FM, Walsh LE, North CS. Competencies for disaster mental health. Curr Psychiatry Rep. 2015;17(3).
Lee JS, You S, Choi YK, Youn Hy SH. A preliminary evaluation of the training effects of a didactic and simulation-based psychological first aid program in students and school counselors in South Korea. PLoS ONE. 2017;12(7):e0181271.
Kang JY, Choi YJ. Effects of a psychological first aid simulated training for pregnant flood victims on disaster relief worker’s knowledge, competence, and self-efficacy. Appl Nurs Res. 2020:1513.
Park S, Kim S. The effects of team-based simulation education on problem solving process. Korean J Health Communication. 2019;14(2):165–72.
Australian Psychological Society. Useful skills for disaster recovery: Problem solving. 2016.
Lim A, Song Y. A scoping review of instruments for measuring problem-solving ability in simulation nursing education in Korea: a focus on process behavior survey. J Korean Acad Fundamentals Nurs. 2022;29(3):269–83.
Lee M, Lee M, Kim S. A study on nursing students’ self-leadership and their perception of learning. J Korean Acad Soc Nurs Educ. 2015;21(3):417–25. https://doi.org/10.5977/jkasne.2015.21.3.417 .
Goldsby E, Goldsby M, Neck CB, Neck CP. Under pressure: time management, self-leadership, and the nurse manager. Administrative Sci. 2020;10(3):38.
Kim JK, Song MS. Effects of respiratory infectious disease simulation-based education on nursing students of clinical competency, self-leadership and critical thinking. J Korea Academia-Industrial Cooperation Soc. 2019;20(8):93–101.
Cho GY, Seo MK. Influencing factors of learning flow, self-leadership and debriefing satisfaction on problem solving ability of nursing students in simulation learning. J Fisheries Mar Sci Educ. 2020;32(2):409–19.
Artino AR. Motivational beliefs and perceptions of instructional quality: Predicting satisfaction with online training. J Comput Assist Learn. 2008;24(3):260–70.
Yu BM, Jeon JC, Park HJ. The effects on learning motivation and self-efficacy according to the type of reflection. J Educational Inform Media. 2013;19(4):837–59.
Kim KA, Choi DW. The effect of virtual simulation in nursing education: an application of care for acute heart disease patients. J Korean Soc Simul Nurs. 2018;6(2):1–13.
Sapiano AB, Sammut R, Trapani J. The effectiveness of virtual simulation in improving student nurses’ knowledge and performance during patient deterioration: a pre and post test design. Nurse Educ Today. 2018;62:128–33.
Park SY, Kweon YR. The effect of using standardized patients in psychiatric nursing practical training for nursing college students. J Korean Acad Psychiatric Mental Health Nurs. 2012;21(1):79–88.
Ko E. Development of a virtual simulation-based nurse education program to provide psychological support for patients affected by infectious disease disasters [dissertation]. [Seoul, Korea]: Chung-Ang University.
Yoon HY, Choi YK. The development and validation of the perceived competence scale for disaster mental health workforce. Psychiatry Invest. 2019;16(11):816.
Park JW, Woo OH. The effects of PBL (problem-based learning) on problem solving process by learner’s metacognitive level. J Educational Technol. 1999;15(3):55–81.
Lee JS. The effects of process behaviors on problem-solving performance in various tests. Dissertation Abstracts International Section A: Humanities and Social Sciences. 1978;39(4-A):2149.
Manz CC. The art of self-leadership: strategies for personal effectiveness in your life and work. Prentice-Hall; 1983.44. Kim HS. The relationship between self-leadership and job satisfaction of middle school teacher [master’s thesis]. [Seoul]: Soongsil University; 2003. 83 p. 45. Ayres HW. Factors related to motivation to learn and motivation to transfer learning in a nursing population [dissertation]. [Raleigh]: North Carolina State University.
Kim HS. The relationship between self-leadership and job satisfaction of middle school teacher [master?s thesis]. [Seoul]: Soongsil University; 2003. 83 p.
Ayres HW. Factors related to motivation to learn and motivation to transfer learning in a nursing population [dissertation]. [Raleigh]: North Carolina State University.
Park H, Choi S, Choi Y, Park S, You S, Baik M, et al. Effect of Korean version of psychological first aid training program on training disaster mental health service provider. J Korean Neuropsychiatric Association. 2020;59(2):123–35.
Kim M, Kim S, Lee WS. Effects of a virtual reality simulation and a blended simulation of care for pediatric patient with asthma. Child Health Nurs Res. 2019;25(4):496–506.
Noh J, Oh EG, Kim SS, Jang YS, Chung HS, Lee O. Development and evaluation of a multimodality simulation disaster education and training program for hospital nurses. Int J Nurs Pract. 2020:e12810.
Cho JL. The effect of self-leadership and communication barriers on nursing performance in hospital nurses. J Convergence Cult Technol. 2019;5(2):239–46.
Kwon SN, Park HJ. Effects of nurses’ positive psychological capital, self-leadership, and relational bonds on organizational commitment. J Korean Acad Nurs Adm. 2020;26(3):241–50.
Yoo JY, Lee YH, Ha YK. A convergence study on the effects of self-leadership and job satisfaction on nursing performance in general hospital nurses. J Convergence Inform Technol. 2019;9(10):28–38.
Park SY, Shim CS. Effects of a simulator-based delivery education on the major satisfaction, nursing professionalism and clinical competence of the nursing students. J Korea Entertainment Ind Association (JKEIA). 2018;12(5):199.
Jeon JC. The effects on learning motivation and self-efficacy according to the type of reflection. J Educational Inform Media. 2013;19(4):837–59.
Kim S, Cho Y. Proliferation of online learning and the implications for teaching and learning in future university education. J Lifelong Learn Soc. 2018;14(4):51–78.
Kang GS, Kim Y. Development and application of integrated-simulation practice program using standardized patients: caring for alcoholism with diabetes mellitus in the community. J Korea Academia-Industrial Cooperation Soc. 2016;17(8):662–72.
Download references
Acknowledgements
The authors would like to thank Eun-Joo Choi and Dong-Hee Cho for their contributions to the development of the simulation program.
This work was supported by the National Research Foundation of Korea (NRF) through a grant funded by the Korean government (Ministry of Science and ICT) (NRF-2020R1A2B5B0100208).
Author information
Authors and affiliations.
Chung-Ang University, Red Cross College of Nursing, Seoul, South Korea
Eunjung Ko & Yun-Jung Choi
You can also search for this author in PubMed Google Scholar
Contributions
K.E. and Y.C. wrote the design, collected data, data analysis, results, discussion, and conclusion.
Corresponding author
Correspondence to Yun-Jung Choi .
Ethics declarations
Ethics approval and consent to participate.
This study was conducted in accordance with the Declaration of Helsinki (Association World Medical, 2013) and was part of a larger study. It was approved by the Institutional Review Board of Chung-Ang University (IRB approval number 1041078-202003-HRSB-070-01CC) and retrospectively registered (21/11/2023) in the Clinical Research Information Service ( https://cris.nih.go.kr ) with trial registration number KCT0008965. All the participants provided written informed consent and were informed of the right to withdraw from participation at any time during the research until publication. Data confidentiality was ensured, and the results were provided to the participants at their request.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ko, E., Choi, YJ. Efficacy of a virtual nursing simulation-based education to provide psychological support for patients affected by infectious disease disasters: a randomized controlled trial. BMC Nurs 23 , 230 (2024). https://doi.org/10.1186/s12912-024-01901-4
Download citation
Received : 01 November 2023
Accepted : 29 March 2024
Published : 07 April 2024
DOI : https://doi.org/10.1186/s12912-024-01901-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Virtual simulation
- Psychological support
- Infectious diseases disaster
- Nursing education
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
2024 Global Health Equity Challenge
Mental Health Education, Intuitive and Resonating Coaching and Therapy
Princess Mae Bartolome
Our Organization
What is the name of your solution, provide a one-line summary of your solution..
Rebooting Psychotherapy (Mental Health Education) to Prevent and Cure Depression and Anxiety & for Individuation (Self-Healers)
In what city, town, or region is your solution team headquartered?
In what country is your solution team headquartered.
- Philippines
What type of organization is your solution team?
Hybrid of for-profit and nonprofit
Film your elevator pitch.
What specific problem are you solving.
One of the moving stories, such as "I'm 28 and I'm Scheduled to Die in May," sheds light on the tough truth of euthanasia linked to mental health challenges, urging for early mental health interventions. Kalinga emerges as a beacon of hope, pioneering revolutionary mental health treatment. Through the fusion of problem-solving therapy with AI-backed support, Kalinga guarantees convenient access to mental health services. This initiative tackles the escalating mental health emergency characterized by rising suicide rates and diminishing wellness.
For many years, Cognitive Behavioral Therapy (CBT) has been a popular treatment for mental health problems. However, its effectiveness is now being questioned due to the changing nature of mental health issues and the gap between research findings and patient experiences. Therefore, there is a need for new and flexible solutions that can better meet the needs of individuals dealing with mental health challenges.
The crisis is a global problem, not just limited to the United States. In the Philippines, mental health is a crucial but frequently overlooked part of public health. An article on Rappler called "Breaking down barriers to mental health rights" highlights the difficulties Filipinos face in getting mental health services. Cultural taboos, scarce resources, and a lack of awareness about mental health all play a part in discouraging people from seeking help, despite the resilience ingrained in Filipino culture.
The Philippines still struggles with the stigma surrounding mental health, despite efforts by the government to promote education and awareness. Many people continue to see mental illness as a weakness or moral flaw, which results in discriminatory attitudes towards those seeking help. This stigma causes individuals to stay silent and feel ashamed, making it difficult for them to seek the support they need and worsening their suffering.
In addition, the Philippines faces a lack of mental health professionals and facilities, especially in disadvantaged regions. This shortage hinders people in smaller communities from getting the mental health care they need in a timely manner. With insufficient government funding for mental health services, the current system is finding it difficult to keep up with the increasing need for assistance and therapy.
Despite the challenges we face, projects such as Kalinga provide a ray of hope by promoting novel methods for mental health treatment, influenced by the admirable trait of Philippine Indigenous Culture, "caring for community." Through the use of technology and community-centered efforts, Kalinga aims to address barriers to access and offer assistance to those who require it. By utilizing online tools and mobile apps, Kalinga strives to enhance the availability of mental health resources and reduce the stigma surrounding seeking help for mental health issues.
To sum up, it is clear that there is a pressing demand for a transformation in mental health services in the United States and the Philippines, which reflects the global concern for mental health. Efforts such as Kalinga are working to break down the barriers and stereotypes related to mental health, with the aim of creating a more inclusive and empathetic approach to mental health care.
What is your solution?
Kalinga believes that it is important to listen to patients' feedback in the field of mental health care. They promote innovative and holistic strategies to address the complex challenges that individuals encounter. By making significant changes to therapist training, therapy techniques, education, and healing methods, Kalinga aims to transform mental health care and enhance outcomes for individuals dealing with mental health issues.
Kalinga's approach includes incorporating medical intuition into therapist training. This helps therapists better understand the underlying causes of mental health issues. For instance, a therapist with medical intuition might identify that a client's anxiety is linked to a past trauma and upbringing, leading to more precise and successful interventions.
Additionally, Kalinga promotes a problem-solving therapy that is intuitive and impactful. This therapy has shown promise in enhancing psychological well-being, as evidenced by a study which found that "MPST could be beneficial in reducing depressive symptoms and enhancing positive coping in older adults in nursing homes" (Virág, Zábó., Anna, Csiszar., Zoltan, Ungvari., György, Purebl, 2023). This approach to therapy focuses on intuitive insights and emotional connections, allowing therapists to form deeper bonds with their clients. By incorporating intuition, therapists can assist clients in uncovering underlying issues and developing more meaningful solutions through a collaborative effort between the patient and the healer.
Additionally, Kalinga believes in the importance of individuation and self-actualization, guiding people on a path to self-discovery, authenticity, and personal development. This approach helps clients tap into their full potential and build resilience for a greater sense of fulfillment. With a focus on promoting individuation, Kalinga empowers clients to prioritize their mental well-being and make meaningful improvements in their lives.
Kalinga not only provides training for therapists and therapy techniques but also offers mental health education for independent healers. With resources like books plus coaching programs, Kalinga gives aspiring healers the knowledge and skills to help others on their mental health path. By empowering individuals to be independent healers, Kalinga broadens the access to mental health support and fosters a culture of compassion and empathy.
Finally, Kalinga emphasizes transpersonal trauma and nervous system healing techniques, which address trauma and promote healing on a holistic level encompassing mind, body, and spirit. This integrative approach recognizes the interconnectedness of individuation and psychological well-being, offering comprehensive support for individuals experiencing trauma-related mental health challenges. By addressing trauma on multiple levels, Kalinga helps clients heal and reclaim their sense of wholeness.
There will be also parenting programs where parents will learn how shower unconditional love to their children as a way to Rebooting Psychotherapy.
After all, Kalinga focuses on addressing deep-seated trauma and nurturing the nervous system through healing methods that cater to the whole individual - mind, body, and spirit. This all-encompassing tactic acknowledges how personal growth and mental wellness are closely linked, providing thorough assistance to those grappling with trauma-induced mental health issues. By tackling trauma from various angles, Kalinga aids in the restoration of clients' well-being and self-completeness.
Who does your solution serve, and in what ways will the solution impact their lives?
Kalinga is leading the way in transforming mental health care in the Philippines. They are taking a unique approach that is inclusive, empowering, and focuses on healing. With the belief that mental health is a common issue that impacts people from all walks of life, Kalinga is dedicated to serving everyone, no matter their social standing, ethnicity, or where they live.
Kalinga's main goal is to help individuals become their true selves (individuation/self-actualization) and overcome suffering. By encouraging people to explore who they are and embrace their individuality, Kalinga hopes to promote authenticity and alignment with their life's purpose. This journey towards self-discovery is coupled with a desire to reach higher levels of consciousness and break free from limitations. Kalinga uses methods like mindfulness, meditation, and progressive therapies to guide people towards personal growth and achieving their full potential.
In addition, Kalinga emphasizes the importance of living without trauma for maintaining good mental health. Understanding how past events and current worries can deeply affect mental well-being, Kalinga places a strong emphasis on providing trauma-informed care and assistance for healing and moving forward. By acknowledging and working through emotional scars and promoting resilience, Kalinga cultivates a supportive atmosphere for personal growth and well-being.
Kalinga's main focus is on helping people reach their maximum potential. This means supporting them in addressing mental health issues and empowering them to overcome hurdles and utilize their natural abilities. By providing personalized interventions and comprehensive assistance, Kalinga helps individuals thrive and make positive contributions to a more lively and healthy society.
Kalinga offers specialized services for various demographics and needs. Indigenous Peoples receive Spiritual Healing based on cultural practices, promoting a sense of belonging and cultural understanding. Teenagers benefit from Problem Solving Therapy and unique programs such as Psychological Academic Coaching and Gap Year Programs to help with academic success and personal development.
Individuals from lower socioeconomic backgrounds can benefit from Kalinga's approach, which involves Problem Solving Therapy along with practical skills training through Holistic Entrepreneurial Classes and Apprenticeships. This helps to break cycles of poverty and despair. In underserved areas, Kalinga also works towards bridging the digital divide by offering specialized gadgets and apps for remote access to mental health resources and support.
Kalinga now provides enhanced support for people at risk of suicide by pairing Hotline services with Problem Solving Therapy and Urgent Trauma Healing Therapy Sessions for quick assistance. To combat high dropout rates in mental health initiatives, Kalinga offers Medical Intuition Training for professionals to improve their skills and support abilities. This involves introducing more psychology courses at universities and establishing an afterschool training program for psychologists.
In schools and workplaces, Kalinga supports holistic health programs that focus on preventing and addressing issues early on. Through promoting empathy, understanding, and unity, Kalinga dreams of a world where all individuals can succeed with love and support.
Kalinga aims to help people and communities reach their full potential, fostering a society marked by strength, empowerment, and overall well-being through its comprehensive approach.
How are you and your team well-positioned to deliver this solution?
I may not have a psychology degree required for the startup, but I offer a valuable perspective and firsthand experience of overcoming autism, as confirmed by my psychiatrist.
I have successfully dealt with my own mental health issues using unconventional methods. By applying Problem Solving Therapy to myself and listening to my intuition, I was able to heal my nervous system in unique ways. I am familiar with the difficulties and obstacles that people encounter in their healing process. My personal battle with mental health problems gives me a deep understanding of our clients' struggles, allowing me to provide customized services to meet their individual needs.
Furthermore, my choice to advance my education in transpersonal psychology at CIIS shows my dedication to advancing my career and gaining the essential expertise to assist our clients efficiently. Transpersonal psychology provides a comprehensive method to mental well-being that coincides with our objective at Kalinga, highlighting the interconnection of mind, body, and spirit in the healing process.
While having credentials is essential, I firmly believe that genuine expertise in the mental health field extends beyond academic qualifications. It involves having empathy, a deep understanding, and a sincere commitment to positively impact people's lives. The team I work with is well-equipped to fulfill these criteria. At Kalinga, our team exemplifies these traits, bringing a wide range of backgrounds and experiences to provide empathetic and efficient assistance to individuals requiring help.
To sum it up, even though I don't hold a psychology degree, my personal experiences, continuous learning, and commitment to our goal equip me and our team to provide our solution with genuine care, compassion, and a profound grasp of the difficulties our clients encounter. Together, we are devoted to making a groundbreaking difference in the lives of those grappling with mental health challenges.
Which dimension of the Challenge does your solution most closely address?
Which of the un sustainable development goals does your solution address.
- 1. No Poverty
- 3. Good Health and Well-Being
- 4. Quality Education
- 8. Decent Work and Economic Growth
What is your solution’s stage of development?
Please share details about why you selected the stage above..
I have created and tested a new form of problem-solving therapy that aims to revolutionize mental health care. Drawing from my personal experiences and research in psychology and spirituality, I have developed a unique approach to addressing the underlying issues behind mental health challenges and promoting overall healing.
Throughout the testing phase, I held a number of pilot sessions where I engaged with individuals from different backgrounds who were dealing with various mental health challenges. This gave them a sense of optimism and support in dealing with their own struggles. Although my main focus was on assessing the success of my approach on myself, these sessions offered valuable perspectives on how my methodology could make a difference.
In the pilot sessions, I have noticed some positive outcomes that align with my personal experiences:
- Improved understanding of my emotions and thoughts: I now have a better grasp of my own feelings, thoughts, and actions, which has allowed me to have a clearer understanding of the challenges I face in terms of mental health.
- Stronger ability to handle stress and bounce back: I have developed better coping mechanisms and resilience to deal with stress, overcome difficulties, and build stronger relationships with others, ultimately leading to genuine happiness.
- Increased sense of empowerment and control: I have felt more empowered to take proactive steps towards my recovery journey, regaining a sense of control and power over my own life.
I have been primarily focused on testing my own methods, but these initial results show promising potential for their effectiveness. Despite only testing them on myself so far, the observations and findings I've gathered lay a strong groundwork for developing and expanding this new mental health care approach.
In the future, I will keep working on improving and growing my methodology by learning from my experiences and getting input from colleagues and experts in the field. I want to build on what I've already learned and share my approach to help improve mental health care for others.
Why are you applying to Solve?
Kalinga faces numerous obstacles in its efforts to improve mental health services, including financial, technical, legal, cultural, and market barriers that make it difficult to provide personalized and accessible support.
Financial Challenges:
Securing adequate funding is a major hurdle for Kalinga as it strives to support its initiatives. Conducting psychological research involves significant financial costs, including data collection, analysis, publication, and dissemination. Furthermore, establishing and growing a mental health startup requires substantial investments in infrastructure, technology development, and operational expenses. Solve has the potential to greatly help in overcoming these financial barriers by offering grant funding, investment opportunities, and financial expertise to improve resource allocation and sustainability strategies.
Legal Barriers:
It is crucial for a mental health startup like Kalinga to understand and comply with legal frameworks and regulations. Navigating licensing requirements, protecting intellectual property, and ensuring compliance with healthcare regulations are key aspects of running a successful operation. Solve can provide valuable legal guidance to help manage these challenges. They can offer support on regulatory compliance, assist with contract negotiations, and provide advice on intellectual property management. This can help mitigate legal risks and support the sustainable growth of the organization.
Cultural Barriers:
When it comes to mental health, cultural beliefs and values play a big role in how people perceive and approach the topic. This can make it difficult to reduce stigma and provide culturally sensitive services. Kalinga is working on creating interventions that are tailored to the specific needs of indigenous and marginalized groups. By collaborating with experts and community leaders, Solve can help bridge the gap between different cultures and create solutions that are relevant and accepted by the community.
Market Barriers:
Creating partnerships and collaborations is crucial for increasing reach, maximizing impact, and ensuring long-term revenue. Kalinga is aiming to establish partnerships with government bodies, healthcare providers, non-governmental organizations (NGOs), and businesses in order to extend its reach and improve its service delivery. Solve can help facilitate networking events, strategic partnerships, and initiatives to build capacity, enabling Kalinga to form valuable partnerships and utilize shared resources for a bigger social impact.
Hands-On Mentorship:
Mentors play a crucial role in the growth and development of organizations. Kalinga seeks experienced mentors to provide strategic advice, practical knowledge, and networking opportunities to improve its impact and sustainability. Solve will facilitate connections between Kalinga and mentors from diverse fields, establishing mentorship programs and leadership development initiatives to empower the team and achieve success.
We are seeking guidance to enhance our existing connections with stakeholders like the local government, NGOs, and private partners in order to discover more opportunities for collaboration. In addition, we plan to reach out to MIT Solve for assistance in growing our network and forming important partnerships that are in line with our goals.
In which of the following areas do you most need partners or support?
- Business Model (e.g. product-market fit, strategy & development)
- Financial (e.g. accounting practices, pitching to investors)
- Human Capital (e.g. sourcing talent, board development)
- Legal or Regulatory Matters
- Monitoring & Evaluation (e.g. collecting/using data, measuring impact)
- Product / Service Distribution (e.g. delivery, logistics, expanding client base)
- Public Relations (e.g. branding/marketing strategy, social and global media)
- Technology (e.g. software or hardware, web development/design)
Who is the Team Lead for your solution?
What makes your solution innovative.
In our approach to mental health, we draw on a variety of sources such as advanced research and innovative techniques. One important influence is Alan Kazdin's study "Rebooting Psychotherapy," which emphasizes the importance of individuals taking control of their own healing. Our new method focuses on empowering individuals through education on self-discovery and personal growth. We believe in the importance of preventing and treating mental health issues independently, without constant therapist supervision.
The blending of personal philosophies with mental health care is a key aspect of our innovative approach. While Kazdin advocates for evidence-based treatment options, we emphasize the importance of personalized and holistic care. Individuation involves recognizing individuals as unique while considering their specific needs and experiences.
We aim to enhance the effectiveness of interventions by incorporating individuation into our approach, ultimately revolutionizing mental health care through tailored solutions aligned with each individual's journey to wellness.
Bringing gut feelings into Problem-Solving Therapy (PST) is important as it is a practical and outcome-oriented approach to overcoming challenges. Although PST typically emphasizes logical problem-solving methods, our new approach recognizes the valuable perspective and knowledge that intuition can bring to therapy. By merging intuition (I) with PST, individuals benefit from more personalized and successful therapeutic outcomes. This also empowers them to utilize their intuition in making informed choices about their mental well-being.
Moreover, our method utilizes technology to eliminate barriers to access and enhance the expandability of mental health services. Currently, we utilize teletherapy and application platforms to deliver mental health services from a distance, as well as online and telephone tutorial services to reach out to those seeking support. This integration of technology allows for increased empowerment, connection, and personalized care, revolutionizing the delivery of mental health services.
In our strategy, we prioritize inclusion and cultural relevance. We understand the significance of honoring, preserving, and respecting the different experiences and histories of cultural communities. Drawing inspiration from indigenous healing practices and cultural traditions, we develop interventions that are culturally sensitive and promote cooperation and understanding among diverse communities. By prioritizing cultural competency and inclusivity, our goal is to create a more equitable, cooperative, and comprehensive mental health system that benefits all individuals.
In brief, our method stands out for valuing individuality, intuition, technology, and cultural impact, while also being informed by the latest research and methods like those of Alan Kazdin. Our proposal for crafting a unique mental health care policy involves integrating these factors. Our goal is to utilize them to explore new possibilities and guide individuals towards emotional wellness.
Describe in simple terms how and why you expect your solution to have an impact on the problem.
"Our solution aims to tackle mental health challenges by putting into practice a Theory of Change that emphasizes problem-solving, enhanced wellbeing, individual growth, holistic development, and societal innovation.
First and foremost, our focus is on Problem Solving, in both personal and professional aspects. We recognize that people encounter different challenges and pressures in their lives that can harm their mental well-being. Our goal is to offer practical and efficient problem-solving techniques and assistance to help individuals tackle obstacles and handle stress more efficiently. This proactive strategy doesn't just ease current struggles but also equips individuals with essential skills to face future challenges, ultimately promoting a sense of empowerment and control.
As people enhance their problem-solving and coping abilities, we expect to see an increase in their overall well-being. Enhanced well-being includes mental health, physical health, emotional stability, and social connections. By approaching mental health challenges in a comprehensive and holistic manner, our solution encourages a well-rounded and satisfying lifestyle, marked by increased resilience, positivity, and contentment. This positive change in well-being not only helps individuals personally, but also helps create healthier communities and societies as a whole.
Our solution focuses on the importance of self-discovery and personal growth, emphasizing the concept of Individuation or Self-Actualization. We recognize that each individual is unique, with their own professional skills, values, and aspirations. By creating an environment that promotes self-exploration and authenticity, our solution enables individuals to be true to themselves, follow their passions, and live according to their values. In addition to enhancing individual dignity and self-worth, the process of individuation also leads to self-realization, enthusiasm, and a sense of purpose in life.
Moreover, our approach acknowledges the significance of harnessing Holistic Potential, covering every aspect of a person's existence - physical, emotional, mental, and spiritual. By integrating holistic methods into mental health support such as mindfulness practices, self-care routines, and holistic therapies, our approach enables individuals struggling with mental disorders to regain their mental well-being and live an ordinary life. This holistic viewpoint not only tackles symptoms but also examines root causes and encourages sustained wellness and growth.
Finally, as we aim to support social innovation, we focus on fostering a culture of creativity, collaboration, and social welfare. Through the promotion of new methods in mental health care, including technological solutions, community projects, and culturally appropriate practices, our approach sparks wider societal changes. This philosophy impacts not only individual well-being but also shapes how mental health is viewed by society, influences institutional practices, and informs policy decisions, ultimately creating a more inclusive, supportive, and resilient environment for everyone.
To sum up, our Theory of Change presents a journey from addressing problems to enhancing overall well-being, individual growth, achieving one's full potential, and fostering innovation within society. Addressing mental health issues and stagnation can be tackled by implementing forward-thinking, comprehensive, and creative approaches. It is firmly believed that these approaches will empower individuals, revitalize communities, and lead to enduring positive transformations in society.
What are your impact goals for your solution and how are you measuring your progress towards them?
Our impact goals for our solution are centered around promoting holistic wellbeing, enhancing life satisfaction, and facilitating psychological assessments for individuation, ultimately leading to actualized lives. Community initiatives regarded as the source of fruits of the work of HealthyGamerGG serve as the basis for the long-term outcome. The ultimate goal is to improve the state of the society. To measure our progress towards these impact goals, we employ a range of specific indicators that reflect key dimensions of wellbeing, satisfaction, and personal growth. These indicators stay as quantitative and qualitative measures to ensure that the solution we are proposing is effective over the long run. One of our primary indicators is the measurement of holistic wellbeing, which encompasses physical, emotional, mental, and spiritual dimensions. We employ complementary evaluation methods, like the WHO-5 Well-being Index and the PERMA Profiler, to provide means for measuring the aggregate wellbeing in a society that adopts our solution.By regularly administering these assessments, we can track improvements in key areas such as positive emotions, life satisfaction, and sense of purpose. Along with life quality, our other crucial goal is to assess and measure changes in life satisfaction, as well.We employ standardized scales such as the Satisfaction with Life Scale (SWLS) to evaluate subjective perceptions of life satisfaction and fulfillment among our target population. Employing survey and interviews on a longitudinal basis, we record participants' experiences in terms of the quality of their lives and check whether there is any correlation between our solution and the positive outcomes in this sphere. Furthermore, our impact goals include facilitating psychological assessments for individuation, inspired by the work of HealthyGamerGG. We employ such tools as the Myers-Briggs Type Indicator (MBTI), the Big Five Personality Inventory, and narrative based assessments to equip people with knowledge that will help them understand their strengths, concepts of their values and personality traits. By conducting pre- and post-assessments, we measure changes in self-awareness, self-acceptance, and personal growth, reflecting progress towards individuation and actualization. To complete the quantitative parameters, we also obtain qualitative data from participants feedback, testimonials as well as success stories.These narratives provide rich insights into the lived experiences of individuals engaging with our solution, capturing the nuances of their personal journeys, challenges overcome, and aspirations achieved. The utilization of qualitative data lets us see the playing role of our solution in the patients’ recovery and the system’s overall improvement. Thereafter, we can make room for improvements and innovativeness. Overall, our approach to measuring progress towards our impact goals combines quantitative assessments of wellbeing and life satisfaction with qualitative insights into personal growth and self-discovery. Our evaluation framework will incorporate a multi-dimensional scale in order to convey the value for our solution of improved life of individuals as well the ultimate goal of a widespread wellbeing and true living.
Describe the core technology that powers your solution.
To enhance the effectiveness and accessibility of our solution at Kalinga, we leverage a combination of core technologies that empower individuals to embark on their mental health journey with confidence and convenience. We put in our effort where we are breaking our notions so as to include people from all cultural backgrounds and do so acknowledging the fact that our clients are not all from a homogenous income background. Here's how our core technologies support our mission:Here's how our core technologies support our mission:
User-Friendly App and Accesible Hotline and Specialized Cellphone/Kindle for Mental Health Education: What we do, we are proud of that is the extensive mobile application for mental health support and empowerment, which we have designed to be user-friendly and uplifting, with the aim of improving mood and enthusiasm. Through our support platform, we have taken care of all classes and types of people and we continue to bring effective and comprehensive support (in all Philippine languages). Accessible via smartphones or specialized devices like Kindles, our app provides a wealth of resources, including guided meditation sessions, self-help articles, interactive exercises, and real-time crisis intervention tools. This technology guarantees that people are able to seek crucial mental health resources from either personal or family members even with the limited traditional psychological services. Additionally, our focus on specialized devices ensures compatibility with lower-cost options, making it accessible to those with limited financial means. What makes our approach different is our individualized intervention for everyone to cater to everyone's individual concerns and needs. Library of Books: The downstreaming of this consciousness is what will drive our organization and the belief in the transformative role of knowledge and education is foundational.Through our extensive library of digital books, individuals can explore a wide range of topics related to mental health, personal development, and holistic healing, translated in Filipino languages. Starting with self-help guides and affirming memoirs, our selected collection presents different voices and mentors to accompany you towards the recovery end point.By providing access to these resources, we empower individuals to take an active role in their mental health and personal growth, regardless of their socioeconomic status.
Which of the following categories best describes your solution?
A new application of an existing technology
Please select the technologies currently used in your solution:
- Internet of Things
- Software and Mobile Applications
In which countries do you currently operate?
How many people work on your solution team.
Founder: Princess Mae Bartolome
Co-Founder: Winslet Anne Bartolome
How long have you been working on your solution?
The team is working within 5 months, starting in November 2023. The conceptualization started in October 2023.
Tell us about how you ensure that your team is diverse, minimizes barriers to opportunity for staff, and provides a welcoming and inclusive environment for all team members.
Ensuring diversity, minimizing barriers to opportunity, and fostering a welcoming and inclusive environment are foundational principles at KALINGA. We recognize the value of diverse perspectives, experiences, and backgrounds in driving innovation and creating positive social impact. Here's how we prioritize these principles within our team:
Indigenous Empowerment:
- KALINGA is committed to promoting indigenous ways of healing that are rooted in cultural traditions and supported by scientific research. We actively seek to incorporate indigenous healing practices into our services, recognizing their efficacy and relevance in addressing mental health challenges.
- To ensure indigenous representation within our team, we actively recruit and collaborate with indigenous healers, practitioners, and community leaders. We provide opportunities for their voices to be heard and respected, empowering them to contribute their expertise to our initiatives.
- Additionally, we invest in research and development to bridge the gap between traditional healing practices and modern science, ensuring that indigenous knowledge is recognized and integrated into evidence-based approaches to mental health care.
Apprenticeship Programs:
- KALINGA's apprenticeship programs are designed to provide opportunities for individuals from all socioeconomic backgrounds to develop skills and expertise in mental health care. These programs are open to anyone with a passion for healing and a commitment to making a positive impact in their communities.
- We collaborate with partners across various sectors, including Korean entertainment companies, to offer apprenticeship opportunities that expose participants to diverse perspectives and experiences. By leveraging partnerships with industry leaders, we ensure that our apprentices gain valuable insights and hands-on training in a supportive and inclusive environment.
- Our apprenticeship programs prioritize accessibility and affordability, minimizing financial barriers to participation through scholarships, stipends, and other forms of support. Through the active outreach to individuals from distinct marginalized communities and diverse backgrounds, we are building a system by which people formerly in these communities can rise and enter into the careers of mental health care professionals.
At Kalinga, diversity is not just a goal but a core value that informs everything we do. We welcome a diversity in perspectives and uplift the culture which encourages all members to be involved, equally valued and to freely contribute with the individual talents they possess.We prioritize equity and fairness in recruitment, hiring, and promotion practices, ensuring that opportunities for advancement are accessible to everyone regardless of race, ethnicity, gender, sexual orientation, disability, or socioeconomic status. Not only that, we offer them ongoing training and professional development programs to fasten careers and raise the overall level of performance as well.We offer cultural competency training, unconscious bias awareness workshops, and inclusive leadership programs to foster a culture of understanding, empathy, and collaboration. On the whole, Kalinga pledges to the formation of a different, fairer and kinder workplace for people of different sex, people with disabilities, LGBTQ+ community and other groups to reach their full potential.
What is your business model?
A business model targeting low-income clients focuses on providing affordable or free treatment to those in need. The goal is to break down barriers to mental health care for marginalized communities, such as those with limited financial resources, by offering services at lower costs or using different payment methods. This strategy can be integrated into the various business model options for a social enterprise mental health startup mentioned earlier.
- Subscription-Based Model: Some individuals with limited incomes may benefit from a subscription model that offers reduced-cost services, possibly with a combination of a Freemium model for those in extreme poverty. This structure allows for payment on a sliding scale according to income level, making mental health support more accessible to those who might not otherwise be able to afford traditional therapy services.
- Freemium Model: The freemium model in mental health offers basic tools and support for free, funded by ads on the app. Premium features and counseling sessions are available at a reduced cost for those with limited income. This ensures access to necessary services without financial obstacles, while also offering further support as needed.
- Pay-Per-Session Model: Under the Pay-Per-Session Model, individuals with lower income can receive mental health sessions at reduced rates or through various funding sources such as endowments from society, PhilHealth, and philanthropic donations. This allows them to access the support they need without financial barriers.
- Corporate Wellness Programs to Prevent Mental Illness: When working with companies to provide mental health services for their employees, the business model for low-income clients may include bargaining for reduced rates or funded services for employees who do not have access to full mental health coverage through their employer's insurance plan, in accordance with the Mental Health Law in the Philippines.
- Philanthropic and PhilHealth Funding: Philanthropic funding is essential for social enterprises that cater to low-income clients, as it helps sustain operations and keeps services affordable and accessible. Grants and donations from foundations or individual donors, such as the community pantries in the Philippines in 2021, play a vital role in providing subsidized services for those in need.
To summarize, the business model aimed at low-income clients in a social enterprise mental health startup involves strategies to make mental health services affordable, accessible, and inclusive for underserved communities. Through discounted rates, sliding-scale pricing, subsidized services, and financial assistance options, social enterprises can address mental health disparities and improve access to care for all.
Do you primarily provide products or services directly to individuals, to other organizations, or to the government?
What is your plan for becoming financially sustainable, and what evidence can you provide that this plan has been successful so far.
Our approach to building Kalinga's financial sustainability goes beyond the norm, guaranteeing a dynamic business model that not only thrives but also advances our goal of providing easily accessible mental health support. An exclusive look at our creative tactics can be found here:
Diversified Revenue Streams:
To expand our reach in the Philippines, we plan to partner with various organizations and individuals like Senator Risa Hontiveros and PhilHealth. These collaborations will involve working with government agencies, NGOs such as Youth For Mental Health Coalition and KadaKareer, and private sector entities to amplify the effects of our solution. We also aim to seek assistance from international organizations like United Nation's Youth Co:Lab and philanthropic groups such as Open Philanthropy to support our nationwide expansion. Through strategic partnerships and resource utilization, we aim to have a significant impact on mental health issues at a broader level.
Technology Integration:
We have integrated cutting-edge technology into our service delivery, embracing the digital era. Utilizing technology not only boosts our ability to grow but also creates opportunities for generating revenue through premium digital services and collaborations with tech firms. This has allowed us to extend our reach to underserved areas and disadvantaged families. Our accessibility has improved with the use of teletherapy and remote mental health centers, AI-powered mental health evaluations, and virtual support communities. By anticipating the future evolution of the digital landscape, we can ensure that our services remain effective within our existing framework.
Initiatives for Community Engagement:
We believe that a thriving community relies heavily on mental well-being. As such, we have prioritized our resources towards community engagement initiatives, reflecting the spirit of the Philippine tradition of 'bayanihan', rather than traditional clinical services. These initiatives, spanning from grassroots advocacy efforts to mental health workshops in educational institutions, not only educate the public but also cultivate a loyal and supportive community. Our approach aims to not only increase financial stability but also nurture a strong sense of belonging and personal and professional development among community members.
Evidence of Success:
During our prototype stage, we have seen positive results from our strategies inspired by successful models used in other businesses. One example is partnerships with insurance programs, like PhilHealth for Physical Ailments, which have boosted revenue and services for other healthcare organizations. Our unique pricing models have also proven effective in attracting users and generating income in various industries, giving us confidence in their potential success for Kalinga..
Overall, Kalinga has multiple sources of income and valuable partnerships that set us up for financial stability in the long run as we work towards our goal of supporting mental health and wellness for everyone. By constantly assessing and improving our strategies, we are dedicated to reaching our objectives and creating a significant difference in the realm of mental health services.
Solution Team
The Solve team will review your report and remove any inappropriate content.
Why is this item inappropriate?
We use cookies.
We use cookies and other tracking technologies to improve your browsing experience on our website and to understand where our visitors are coming from. By browsing our website, you consent to our use of cookies and other tracking technologies.
Unpacking associations among children's spatial skills, mathematics, and arithmetic strategies: decomposition matters
Affiliations.
- 1 Faculty of Psychology, Department of Psychology, University of Basel, Missionsstrasse 62, 4055, Basel, Switzerland. [email protected].
- 2 Department of Educational and Health Psychology, University of Education Schwäbisch Gmünd, Schwäbisch Gmünd, Germany. [email protected].
- 3 Faculty of Psychology, Department of Psychology, University of Basel, Missionsstrasse 62, 4055, Basel, Switzerland.
- 4 Institute of Psychology, Faculty of Social Sciences, The John Paul II Catholic University of Lublin, Lublin, Poland.
- PMID: 38613569
- DOI: 10.1007/s00426-024-01952-x
Several studies revealed links between mental rotation and mathematical tasks, but the intervening processes in this connection remain rather unexplored. Here, we aimed to investigate whether children's mental rotation skills relate to their accuracy in solving arithmetic problems via their usage of decomposition strategies, thus probing one potential intervening process. To this end, we examined a sample of 6- to 8-year-olds (N = 183) with a chronometric mental rotation task, and asked children to solve several arithmetic problems while assessing their solution strategies. After each arithmetic problem, children were asked about their strategy to solve the respective arithmetic problem and these were classified as either counting, decomposition, or retrieval strategies. Analyses were controlled for age, sex, fluid and verbal reasoning. Results indicated that children's response times and accuracy in the mental rotation task were best explained by linear functions of rotation angle, suggesting the usage of dynamic mental transformation strategies. A multiple mediation model revealed that children with higher mental rotation skills were more inclined to use higher-level mental strategies such as decomposition which in turn increased their accuracy of solving arithmetic problems. None of the other arithmetic strategies revealed significant indirect effects. These findings suggest that children with higher mental rotation skills may profit from visualizing and flexibly transforming numerical magnitudes, increasing the frequency of decomposition strategies. Overall, decomposition may play a unique role in the connection between children's mental rotation and arithmetic skills, which is an essential information for planning future training and experimental studies.
© 2024. The Author(s).
Grants and funding
- 100014L_192206/Schweizerischer Nationalfonds zur Förderung der Wissenschaftlichen Forschung
- 2019/01/Y/HS6/00049/National Science Centre in Poland
ORIGINAL RESEARCH article
Environmental measurement study of double-aging neighborhoods under the epa-s model in china provisionally accepted.

- 1 Tianjin University, China
- 2 Tsinghua University, China
The final, formatted version of the article will be published soon.
The "double aging" problem of the aging population and the simultaneous aging of the community's physical environment will become a huge challenge in highly urbanized areas of the world, and China's performance is becoming more and more obvious, affecting the physical and mental health and quality of life of the elderly. Nowadays, the paradigm of solving the double aging problem with the concept of "active aging" is gaining international acceptance, which means the elderly are centered on the design and construction of a community environment that maintains their ability to live independently and promotes active social interaction in urban regeneration. However, existing research still has shortcomings in how to apply the perspective of active aging to establish an indicator system for evaluating the built environment of "double aging" neighborhoods and formulate action strategies. The study constructs a theoretical analysis framework of EPA-S (E-Environment supports, P-Personal abilities, A-Activity behaviors, S-State of healthy and active life) from the perspective of active aging and builds the model based on that. This observational study designed the survey content and collected sample data in four typical double-aging neighborhoods in Beijing for multi-layer linear regression analysis to verify the reliability of the model and the correlation between indicators. It found that the design of the "EPA-S" model has a certain degree of credibility. In addition to personal socioeconomic factors, active living abilities, and material environmental support also have a significant impact on the mental health and happiness of the elderly. Specifically, being more involved in community public affairs and collective cultural and recreational activities, and better improving the quality of public activity venues and service facilities within walking distance of the elderly are related to the elderly maintaining good physical and mental health. The "EPA-S" model established in this study can be used as a reference tool to evaluate the active aging level of "double-aging" neighborhoods. At the same time, the analysis results of each variable also provide important inspiration for formulating specific neighborhoods’ regeneration strategies.
Keywords: Double aging, Active aging, older neighborhoods, urban regeneration, China
Received: 06 Nov 2023; Accepted: 12 Apr 2024.
Copyright: © 2024 Chen, Gan and Bian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Mx. Lanchun Bian, Tsinghua University, Beijing, 100084, Beijing, China
People also looked at

IMAGES
VIDEO
COMMENTS
Problem-solving therapy is a short-term treatment used to help people who are experiencing depression, stress, PTSD, self-harm, suicidal ideation, and other mental health problems develop the tools they need to deal with challenges. This approach teaches people to identify problems, generate solutions, and implement those solutions.
Problem-Solving Therapy aims to reduce the incidence and impact of mental health disorders and improve wellbeing by helping clients face life's difficulties (Dobson, 2011). This article introduces Problem-Solving Therapy and offers techniques, activities, and worksheets that mental health professionals can use with clients.
In insight problem-solving, the cognitive processes that help you solve a problem happen outside your conscious awareness. 4. Working backward. Working backward is a problem-solving approach often ...
Problem solving. Worrying is a natural response to life's problems. But when it takes over and we can start to feel overwhelmed, it can really help to take a step back and break things down. Learning new ways to work through your problems can make them feel more manageable, and improve your mental and physical wellbeing.
Problem-solving is one technique used on the behavioral side of cognitive-behavioral therapy. The problem-solving technique is an iterative, five-step process that requires one to identify the ...
This self-help guide is intended for people with mild-to-moderate mental health issues. If you're feeling distressed, in a state of despair, suicidal or in need of emotional support you can phone NHS 24 on 111. For an emergency ambulance phone 999. It's easy to feel overwhelmed by problems, particularly if you're experiencing mental health ...
Problem-solving therapy aims to help individuals adopt a realistically optimistic view of coping, understand the role of emotions more effectively, and creatively develop an action plan geared to reduce psychological distress and enhance well-being. Interventions include psychoeducation, interactive problem-solving exercises, and motivational ...
In mental health conditions like depression, anxiety, substance use, phobias, and many others, ... The skills CBT often emphasizes, like problem-solving, personal interaction, and time management ...
Problem-Solving the Solution-Focused Way. In the past few decades, a strength-based movement has emerged in the field of mental health. It offers an alternative to problem-focused approaches that ...
Psychosocial skills training and cognitive behavioral interventions teach specific skills to students to help them cope with challenging situations, set goals, understand their thoughts, and change behaviors using problem-solving strategies. Psychosocial skills training asks students to explore whether their behaviors align with their personal ...
"Depression is one of the most common mental health disorders with a high burden of disease and the leading cause of years of life lost due to disability" (Hu et al., 2020, p. 1). ... Interventions are a vital aspect of marriage therapy, often targeting communication skills, problem-solving, and taking responsibility (Williams, 2012).
The aim of this study was to investigate the influence of problem solving therapy (PST) on effortful cognition in major depression (MD). ... All HCs had no personal history of mental disorders. Patients with MD were selected from Wuxi Mental Health Center Affiliated to Nanjing Medical University, No. 156 Qianrong Road, Rongxiang Street, Binhu ...
The review explored whether training in problem solving helps to alleviate depressive symptoms 8. The two youth partners, in turn, convened a panel of 12 other youth advisers, and together they ...
This review assessed the efficacy of problem-solving therapy (PST) in helping individuals to overcome any type of health problem. The authors concluded that there is strong evidence for the effectiveness of PST. The conclusion was derived from a meta-analysis of clinically and statistically variable data and there were a number of methodological concerns, therefore it may not be reliable.
Problem-Solving . Learning problem-solving skills during cognitive behavioral therapy can help you learn how to identify and solve problems that may arise from life stressors, both big and small. It can also help reduce the negative impact of psychological and physical illness.
Problem-solving therapy has been shown to be effective for depression and common mental health problems [12, 13]. Previous attempts to deliver care for common mental disorders through primary care clinics in Zimbabwe although promising in the short-term had shown little long-term success due to reliance on overstretched nursing staff and lack ...
Depression and loneliness were less common than nervousness or sleep problems, but more consistent across surveys given over time. Among adults, use of drugs, alcohol and other intoxicating substances has increased over time as well. ... Mental Health and COVID-19: Early evidence of the pandemic's impact: Scientific brief, 2 March 2022. World ...
Discover transformative mental shifts to supercharge your problem-solving skills. From embracing uncertainty to the power of daydreaming, prepare to change the way you tackle challenges forever!
Problem-solving courts (also known as specialty courts) are specialized dockets within the criminal justice system that seek to address underlying mental health or SUD that contribute to the commission of certain criminal offenses in many cases, often providing treatment rather than punishment. The most common types of problem-solving courts ...
Social problem solving ability was significantly associated with the somatic symptoms, anxiety and insomnia, social dysfunction and severe depression ( P < 0.01). The results of our study demonstrated that there is a significant correlation between social problem solving ability and mental health.
To solve tough problems at work, first ask these questions. Problem solving skills are invaluable in any job. But all too often, we jump to find solutions to a problem without taking time to ...
Substances are likely to introduce new problems into your life. Alcohol, for example, is a depressant that can make you feel worse. Using substances to cope also puts you at risk for developing a substance use disorder and it may create health, legal, financial problems, and social problems. Overeating: Food is a common coping strategy.
Severe and prolonged anxiety, fear, blame, and aggression can lead to mental health problems, including depression, anxiety, panic attacks, somatic symptoms, post-traumatic stress disorder, ... Park S, Kim S. The effects of team-based simulation education on problem solving process. Korean J Health Communication. 2019;14(2):165-72. Google Scholar
By incorporating medical intuition, intuitive problem-solving, and holistic healing techniques, Kalinga aims to revolutionize the way mental health challenges are understood and addressed. Through therapist training, therapy techniques, education, and healing modalities, Kalinga offers a transformative vision for mental health care that ...
Several studies revealed links between mental rotation and mathematical tasks, but the intervening processes in this connection remain rather unexplored. Here, we aimed to investigate whether children's mental rotation skills relate to their accuracy in solving arithmetic problems via their usage of …
The "double aging" problem of the aging population and the simultaneous aging of the community's physical environment will become a huge challenge in highly urbanized areas of the world, and China's performance is becoming more and more obvious, affecting the physical and mental health and quality of life of the elderly. Nowadays, the paradigm of solving the double aging problem with the ...