Appointments at Mayo Clinic
- Body donation at Mayo Clinic
- Making a donation
Mayo Clinic requires preregistration for whole-body donation. The prospective donor must sign the Consent for Mayo Clinic Body Donation form. Mayo Clinic no longer accepts power of attorney, next of kin, guardian, or conservator signatures on behalf of the potential donor. The donor authorizes the gift of whole-body donation before death, but the legal next of kin is responsible for carrying out the donor's wishes. If the next of kin opposes the donation, it will not occur. Mayo Clinic advises donors to notify their families of their intentions.
See initiating the donation process .

Body donation procedure
Mayo Clinic's procedure for accepting a whole-body donation begins with notification of a donor's death. A healthcare representative from the hospital, medical facility or hospice organization where the death occurs should contact Mayo Clinic's donor program coordinator.
The coordinator reviews the acceptance protocol to decide if the donation can be accepted. If the donation meets the acceptance criteria, the coordinator contacts the next of kin to determine if whole-body donation should proceed. Transportation of the body to Mayo Clinic is then be arranged.
If the death does not occur in a medical facility or under hospice care, local law enforcement personnel should be notified. The coroner or medical examiner determines if an autopsy is necessary. If no further investigation is required, Mayo Clinic is notified and proceeds with the acceptance procedure.
Typically, studies of donated bodies take 6 to 15 months. Mayo Clinic offers a type of cremation called biocremation as a means of final disposition. The biocremated remains can be returned to the family or interred in the Mayo Vault at Oakwood Cemetery in Rochester, Minnesota.
Mayo Clinic also provides traditional cremation as a means of final disposition. The cremated remains can be returned to the family or interred in the Mayo Vault at Oakwood Cemetery in Rochester, Minnesota. If burial of the body without cremation is the donor’s wish, the donor’s estate is responsible for all expenses.
Criteria and considerations for donation
Prospective donors should not consider themselves too old for whole-body donation. Unlike most organ donation programs, age is rarely a factor in whole-body donation.
Whole-body donation after organ donation
An individual is not eligible for whole-body donation after multiorgan or skin donation. Our program does allow eye donation. Mayo Clinic's donor program coordinator consults with the organ donation organization, for example, Lifesource or Lions Eye Bank, to evaluate the potential for whole-body donation acceptance.
Specific disease study
Mayo Clinic's Body Donation Program does not accept bodies donated for specific disease research.
Denial of a donation
Mayo Clinic makes every effort to accept all program-registered donors. Below are some reasons why the program might deny a donation:
- The potential donor had an infectious or contagious disease, such as HIV/AIDS, hepatitis B, hepatitis C, tuberculosis or prion diseases.
- The next of kin objects to the donation of the body, the family is not in agreement or there is family discord.
- The body is not acceptable for anatomical study due to, for example, being extremely emaciated, being extremely obese, or having an extensive medical or surgical history.
- The body has been autopsied or mutilated or is decomposed.
- The body is not able to be in the care of the Mayo Clinic Body Donation Program within 48 hours of death.
- The body was embalmed before arrival at Mayo Clinic's facility.
- Donations are not needed at the time.
Mayo Clinic encourages all potential donors to have an alternate plan in case the donation isn't accepted.
There is no payment for body donation, as explicitly stated by law in every state. Mayo Clinic has limited funds to reimburse transportation expenses for a whole-body donation. Any expenses beyond the fund limit are the responsibility of the donor's estate. If the donor dies out of state and the cost of transporting the body to Mayo Clinic is too expensive, the next of kin can contact a nearby medical school about making the donation there.
Body Donation Program
- Mayo Clinic
- Stabile Building 9-22 200 First St. SW Rochester, MN 55905
- Phone: 507-284-2693
- Email: [email protected]
- You may request an informational packet using this online form .
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Help Shape the Future of Medicine By Becoming a Body Donor
Medcure connects people wanting to donate their bodies to science – whole body donors – with the physicians and anatomical researchers who are uncovering tomorrow’s medical breakthroughs., donating your body to science, advancing the science of medicine with a priceless, no cost option.
Whole body donation is essential to our understanding of the human body and the development of new medical treatments. At MedCure, we help donors and their families connect with the physicians, surgeons, and researchers who are continuing this vital work. Thanks to their generosity and selflessness, we are able to live longer, healthier lives.
MedCure honors our donors by covering all expenses related to the donation process, including transportation, cremation, and a certified copy of the death certificate. We can accommodate the family’s wishes for the disposition of cremated remains, whether returned to them or placed in an ossuary. By request, we can also provide a family letter that shares information on how the donor contributed to medical science.
Connect with Us
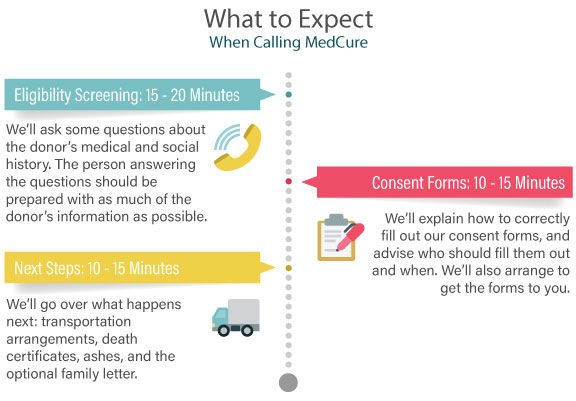
Donation Coordinators are available 24 hours a day to answer your questions and assist you with the donation process. Whether you are registering your future intent to be a body donor, you are currently receiving hospice care, or if your loved one has already passed, we can guide you through every step.
- Toll-free: +1-866-560-2525
- [email protected]
How It Works
Contact medcure.
We are available 24 hours a day to conduct a donor eligibility screening or to verify a donor pre-registration is on file.
Transportation
MedCure makes all of the transportation arrangements from the place of passing to one of our five US facilities at no cost to the donor or their caregivers.
Donor Matching
Donors are matched to institutions or projects according to medical history and current research needs. Family letters provide details on request.
Final Arrangements
Cremated remains are returned to the family within 5 months or may be placed in an ossuary. A certified death certificate is provided to the family or estate.
“I have always wanted to ‘give back’ and this is the perfect way. I was brought into this world via medical science and it is my choice to leave that way. MedCure and their representatives handled both my parents in the most kind and professional manner. They made me feel comfortable with my decisions and had such compassion for all my thoughts and questions.”
Betty Smith
Family Caregivers
MedCure offers a pre-screening program for patients who are receiving hospice care or who have been given a life expectancy of 6 months or less. While it isn’t necessary for your loved one to complete the screening ahead of time, it does make the call to MedCure at the time of passing much easier on the family. You can download our Hospice Patient Registry Kit to help guide you through each step of the process.
Registering Close To Passing
A donor's legal next of kin or Healthcare Power of Attorney can legally assist in arranging for body donation. A full and complete copy of the Healthcare Power of Attorney documents must be submitted with the body donation forms.
Contact MedCure To Start
A Donation Coordinator will ask screening questions to determine if an individual meets certain medical research criteria necessary for body donation.
Submit Body Donation Forms
Donation forms are available HERE . Completed documentation can be emailed to [email protected] or faxed to 503-257-9101.
Death Has Occured
MedCure should be called immediately to determine or review the donor's eligibility screening and to begin making transportation arrangements.
Hospice, Social Worker & Professional Caregivers: Click here for more information.
Body Donor Registry
If you or your loved one is close to passing, or if your loved one has just passed, please bypass pre-registry and call MedCure right away.
Registering for the Future
If you would like to register your intent to donate your body to science, please complete the pre-registry form and click the SEND button. After you register, we will mail you a welcome kit with additional information within two to three weeks. This kit explains the body donation process and includes a donor card for your wallet.
Our whole body donation program is open to most people, but there are some eligibility requirements. Please have a backup plan in case you are not eligible. See our eligibility notice below for more information.
Finally, please make sure you talk to your loved ones about your wish to donate. Donating yourself or a family member is a very personal decision, but one that should be shared with others who might be involved in the process.
If Your Loved One Has Passed
MedCure is your first call at the time of passing and will work with a local funeral home on your behalf. After donation, partial cremated remains will be returned to the family or may be placed in an ossuary. By request, MedCure will also send a family letter notifying family members how you or your loved one contributed to medical science.
- Download MedCure Whole Body Donation Form
- Call Us Now: +1-866-560-2525
Eligibility Notice
Most people who wish to donate can. There is no upper age limit and most disease processes are acceptable. In an effort to ensure that donations will ultimately be matched with medical professionals, certain standard acceptance criteria must be met at the time of passing.
The most common reasons for decline are a diagnosis of HIV/AIDS, hepatitis B or C, a history of intravenous (IV) drug use, recent incarceration or institutionalization, and being severely over or under weight at the time of death.
MedCure accepts donors from all states within the continental United States except Minnesota and North Dakota.
State (required) AL AK AZ AR CA CO CT DC DE FL GA HI ID IL IN IA KS KY LA ME MD MA MI MN MS MO MT NE NV NH NJ NM NY NC ND OH OK OR PA RI SC SD TN TX UT VT VA WA WV WI WY
I would like to receive the newsletter.
I am receiving hospice care.
How did you hear about us? (required) —Please choose an option— Internet-Google Internet-Other Funeral Home Other Donation Program Hospice Other Medical Professional Word of Mouth Other Media
Date of Birth (required)
I have read the eligibility notice.
How Do I Donate My Body to Research?

What happens to your body after you die is an extremely personal choice. From traditional burials to cremation to composting (yes, you read that right, you can compost your body when you die), there are more options than ever. There are also ways to donate your body, the most common being organ and tissue donation.
Less common, but just as impactful, is whole-body donation, when your remains are gifted to medical school training or research.
What is body donation?
The gift of your body to medicine is invaluable. As a whole-body donor, your body (cadaver) ensures future healthcare professionals understand the complexity of human anatomy.
“Anatomy is the language of doctors and they need to be fluent in that language,” says Catrin Pittack, associate teaching professor for Anatomy and the director of the Willed Body Program at the UW School of Medicine.
This is why body donation is essential to training the next generation of doctors and nurses. As good as the virtual anatomy models have become, they don’t allow students to learn how bodies differ between individuals nor understand the complex spatial relationships between the body’s tissues and organs, for example, how the nerves and arteries thread their way throughout the body.
Body donation helps more than just students. Healthcare professionals and researchers use cadavers for training, too.
For example, an orthopedic surgeon might need access to a cadaver to practice a new knee surgery technique, where the tissues need to be as realistic as possible. An otolaryngology resident might be learning how to do a cochlear implant, which would help patients with hearing loss.
It also allows medical researchers to contribute to life-saving care. Researchers might utilize the brains of donors who had Alzheimer's disease to study the pathology of the disease by using methods that are not possible in a living person, like taking slices of tissue to examine. Or they might be studying a specific type of cancer or a genetic disorder that increases a person’s risk of cancer.
What happens to a donated body?
It’s not as Edgar Allan Poe as it sounds.
When a registered donor dies, a health screening is completed to make sure the body is eligible for donation.
Unfortunately, not all bodies are accepted as donations. There are many reasons why a body could be ineligible , including severe trauma; infectious diseases like hepatitis, sepsis or COVID-19; skin conditions like extensive burns or ulcers; obesity or emaciation; jaundice; recent surgeries; and more. These rules and regulations are put in place to keep people safe when working with the cadavers.
If accepted into the program, a transport company brings the body to the morgue where there are trained funeral directors and embalmers.
From here, it’s a similar process as to what happens at a funeral home: The body is embalmed, replacing blood with embalming fluid to preserve the tissue.
“There is a slightly different ratio of embalming chemicals used in body donation programs as compared to a funeral home because the bodies need to remain preserved for up to three years,” says Pittack.
The embalming process itself takes three months before the body is preserved enough to be worked with in an anatomy lab. After embalming, the body could be in use for teaching or research from anywhere between two weeks up to three years.
Once the donation period is over, the body is cremated and either sent back to the family (if requested) or honored in a community burial ceremony.
“At UW, we have a service honoring the donors in a local chapel for family members. Some of the medical students talk, recite poems, or play instruments and it’s a really wonderful ceremony. We walk to the grave site together and offer our respects for the donor,” says Pittack.
Pittack works with donors regularly and has taught many students in anatomy labs throughout her career.
“The students are so grateful,” says Pittack. “They see the donor as their first teacher or patient — it’s an invaluable gift.”
What to consider before becoming a donor?
Deciding what to do with your body after death is a big decision. If you are considering becoming a whole-body donor, Pittack has some tips.
The first is to discuss the decision with your loved ones. In most willed-body programs, your remains might not be returned for up to three years, which is a big commitment when you’re talking about grief and closure.
“I would say talk it over with your loved ones and family members and make sure everyone is OK with it,” says Pittack. It’s important to be on the same page so your family knows what to expect and can be prepared, but ultimately, if you feel strongly about it, it’s your body and your final wish — so do what feels right.
It’s also essential to research the program you are thinking about donating to, adds Pittack.
“Do your research about the program and fill out the paperwork so there is a plan in advance,” she says.
Choosing what happens to your body when you die is a big choice, and one that you should feel informed and comfortable about when you make the final decision.
“Just know that it is an incredibly generous, selfless gift that you give,” says Pittack. “Our medical students couldn’t be learning about the complexities of the human body without these generous donations, and we are thankful and respectful of every donor who comes through our door.”
Recommended for you

Stroke has become more common in younger adults under age 49.

- Load more stories

Benefits Of Whole Body Donation
Whole Body Donation Saves Lives.
You Can Benefit Humanity. We Can Help.
The Research For Life whole body donor program connects donors with medical researchers and educators who require human tissue for their essential work. Through this powerful gift, each donor has taken that monumental first step towards benefiting humanity and providing hope to future generations.
Donors allow medical students to get the training they need to become doctors. They also allow doctors to maintain their surgical and medical skills and assist medical device organizations in developing new implantable devices such as hips, knees, and other joints. Donor organ tissue samples help anatomical researchers develop breakthroughs in the treatment options for conditions like cancer, dementia, diabetes, Alzheimer’s disease, and so much more.
The experience and education gained using human tissue is far superior to any learning provided by artificial substitutes and textbooks. Human body donation after death makes the medical advancements possible that we see today and improves the quality of life for generations to come.
An End-of-Life Option for Almost Everyone.
Research For Life makes every effort possible to educate and help families through this deeply personal decision. The most common misconception we encounter is people believing that they would not be accepted as a donor. Who can donate? Almost everyone is eligible for whole body donation, even at the time of passing. There is no upper age limit restriction, and we accept donors who have or have had cancer or other diseases that would disqualify them from certain types of transplant donations. There are many myths about whole body donation; read our article on Understanding Whole Body Donation.
We believe it is important to know your options and be able to accurately compare whole body donation to other forms of final arrangements. Research For Life complies with the highest standards available throughout the donation process to honor the donor’s selfless gift. Our donation program is provided at no cost to the donor or the donor’s family.
A No-Cost Alternative for Final Arrangements.
As a part of our whole body donation program, Research For Life provides transportation from the location of the passing and cremation at no cost. When you donate your body to science, we make the process simple and helpful for your family members. Saving your family money is important, but saving them peace of mind is priceless.
What happens to the cremated remains is up to you. We provide several options to all our donors:
- Spread Ashes at Sea (a.k.a. Burial at Sea)
- “No Return” Option
If you choose to have the cremains spread at sea, there are some things you should know:
- Ashes are spread at an appropriate distance off the coast of California.
- Families or next of kin receive a “Spread at Sea Certificate” complete with witness details, dates, and coordinates of spreading location, including longitude and latitude.
- Families cannot attend the spreading; space does not allow for families
- We spread the ashes annually.
Anatomical donation plays a significant role in advancing medicine.
It is the donation of one’s remains – not for transplant, but for scientific research and medical education that has the power to impact the quality of medical care and breakthroughs that improve the quality of life for millions.
Have a Question?

Company Info
Phone: (800) 229-3244 Email: [email protected]
Licenses And Accreditations

Arizona Location
Phoenix, Arizona Office 2230 East Magnolia Street Phoenix, AZ 85034 P: 480.940.1310 F: 480.471.5177
California Location
Temecula, California Office 41743 Enterprise Cir N, Ste 104 Temecula, CA 92590 P: 951.719.3334 F: 951.823.5480
Useful links

- Become a Donor
- Donate a Loved One
- Research and Advancement

Give with Your Whole Being.
Anatomy Gifts Registry provides an alternative to traditional final arrangement options, including nearly free cremation services. By donating your body to science, individuals have a real and lasting way to support medical research advancements that impact the lives of future generations for decades to come. Through the benefits of whole body donation, medical communities are able to continue to discover cures and therapies for many diseases and conditions currently afflicting patients across the world.
LEARN MORE
Living Testimonials.
We were first introduced to Anatomy Gifts Registry (AGR) by our father who, upon being diagnosed with stage four colon cancer, registered with AGR. Like an old friend with experience and wisdom who knows just what to say, AGR comforted us through their kindness and professionalism.
Even when I just needed to talk to someone they were there to listen or lend a shoulder to cry on. And for that I will be forever grateful.
Both Stefanie and Kristin were kind, compassionate, responsive, and informative-they were incredibly helpful and caring at a very difficult time for the family.
Everyone was very considerate, kind, and reassuring that my mother would be lovingly taken care of.
It meant the world to my uncle that he could be a donor like his mother was. He was so proud and told everyone he made that decision.
Thanks so much for taking one of the more difficult aspects of death off our shoulders in a way that helps others so importantly.

Advancing Opportunities.
Anatomy Gifts Registry utilizes whole body donations to facilitate many studies that would otherwise be impossible, including: Anatomy and Physiology Student Education and Labs, Alzheimer’s, Dementia, and Parkinson’s Research, Drug Therapy, Emergency First Responder Training, Medical Resident Training, Minimally-Invasive Surgical Technology, Neurosurgery, Orthopedic Device Technology, Pain Management, Robotic Cardiac and Thoracic Surgical Training, Sports Medicine Surgeon and Physician Technique Development and more.
LEARN MORE ABOUT OUR PROCESS
Where do I start? Where can I find more information? What are some reliable resources?
Make a commitment to get organized! Finding a place to start can feel really overwhelming and incredibly challenging. At Anatomy Gifts Registry our expertly trained and compassionate staff put donors and donor families first. We make it a strict priority to ensure everyone considering donation have all the facts to make an informed decision. We also work ...
Breaking Body Donation Myths.
Facts not Fear or Fiction Over the years we’ve encountered individuals who have done their fair share of research on whole body donation, yet somewhere in the process information can still be misunderstood regarding final arrangements. If you have talked to your family and friends about your decision to donate, we sincerely thank and applaud you! If you ...
Who should have End-of-Life planning conversations & when?
Almost everyone. Sooner, rather than later. The reality is that even today, for most cultures and communities, a discussion about death is still considered one of the least comfortable conversations to have. The vast majority of people don’t want to think about it, let alone talk about it. Oftentimes this leaves loved ones responsible for ...
COVID-19 NOTICE
During this period, AGR has, for the most part, resumed routine operations. However, it is important to note that under all circumstances, the acceptance of any deceased person is contingent upon meeting AGR’s current donor safety and suitability criteria at the time of death (whether already enrolled in the registry or not). Donor acceptance criteria are subject to change. There may be additional considerations for donor eligibility during unprecedented times, such as this period with the current COVID-19 pandemic. For example, past or present infection with COVID-19, or possessing symptoms related to the disease, may impact a donor’s eligibility.
Please contact our Donor & Family Services Department at 1-800-300-5433 for the most comprehensive, up-to-date information.
Hide this message

- Privacy Overview
- Strictly Necessary Cookies
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.

Donate Your Body to Science & Give Hope to Future Generations
Why choose body donation to science.
Science Care donors have made countless contributions to medical research and education in areas such as cancer, heart disease, Alzheimer’s, and orthopedics to name a few.

Can I donate my body for medical research and education?
Do i have the option to be both an organ donor and a body donor for science.
Download free information packet
Learn how to donate your body to science, how to ensure your wishes are known, and how your ultimate gift gives hope to future generations.

More than 25,000 people join the Science Care Registry every year. State your intent now and let your wishes be known.

HOPE® Program for terminally ill patients
For those under hospice or palliative care, you can begin the screening process today for peace of mind for you and your loved ones.
More Information
Proactive planning, end-of-life options.
Explore the differences between burial, direct cremation, body donation to science, university donation, and more.
Ensuring Your Wishes Are Known
About 40% of those who register to donate never become donors. Here’s what you can do to ensure your wishes are honored.
More about Science Care
the science care process: how body donation works.
Learn about no-cost cremation, important forms to complete, and our commitment to honor each donor’s wish.
How You May Be Able to Advance Medical Research
96% of Science Care accepted donations are placed with medical education or research initiatives, helping donors leave a lasting legacy.
Newsletter Signup
Stay up-to-date with Science Care, medical research, and health and wellness tips.
Connect with Science Care
Body donation.
- How to Donate
- Your Wishes
- Medical Research Programs
- HOPE® Program
- Registration Checklist
- Cremation Services
- Types of Cremation
Educate a Patient
- Healthcare Workers
- HOPE® Enrollment
- End of Life Options
- Request Guidance
Researchers
- Researchers & Educators
- Specimen Procurement
- Scanning Options
- SC Facility Events
- Non-SC Facility Events
- Compliance & Safety
- Specimen Provider
- Resources Overview
- FAQ: Body Donation
- FAQ: Researchers
- FAQ: Healthcare Workers
- Newsletters
- Donor Memorial Tributes
- Body Donation by State
- About Science Care
- Memory in Nature
- Social Responsibility
Willed Body Program

The University of Washington's Willed Body Program is a whole-body donation program for donors from Washington State. The gift of your body to the UW School of Medicine is an invaluable contribution to the education of future healthcare providers, enabling them to study and understand the complexity of the human body in a way that is not possible by any other means.
In addition to helping students in the health professions master complex anatomy, your donation will allow medical researchers to develop and maximize important tools to help patients. The University of Washington is one of the foremost medical research institutions in the world, conducting studies that will not only further develop the body of knowledge within the field of medicine, but eventually alleviate human suffering.
We are deeply grateful for your consideration of this extraordinary gift. Donating your body is a significant decision, and we understand there are complex questions that arise when considering it. We have prepared a letter that answers many of the questions potential donors have asked us over the years, and also includes legal and medical reasons that a donation may be declined. In order to fully benefit from the exceptional gift you are providing, it is important that you, your family and the University of Washington have a mutual understanding and agreement about the donor process. This letter is prepared in the spirit of promoting this understanding.
Donation resources
Program information, contact information.
Main Phone Number: 206.543.1860 Email: [email protected] Office Hours: 9am-2pm Monday thru Friday, excluding holidays. Available by phone 24/7 to report death of a potential donor.
If you are calling during our office hours to report a recent death, please call our main number and one of our staff will assist you.
If you are calling after hours to report a recent death, please call our main number and follow the voice message prompts to reach an after-hours technician.
If you wish to receive information about our program and a donor registration form via mail, or if you would like to speak with one of our staff about the program, please call our main number during business hours or leave a voice message with your contact information. For any other non-urgent questions or to receive information electronically, please use our email address. We respond to emails and phone calls within one business day.
Catrin Pittack, Ph.D. Willed Body Program Director Shawn Kamke Embalmer and Operations Manager Jessica Lacy Anatomical Embalmer
Information about COVID and donation
For the safety of our staff, we do not accept donors - registered or unregistered - who are COVID positive at the time of death or who have tested positive within 10 days of death. The only exception is if the decedent tested negative five days after a positive test and was free of COVID symptoms at the time of death. Please call our office at 206.543.1860 , if you have any questions regarding this policy.
Annual Memorial and Burial Ceremony
Thanks to the family and friends who joined us in celebrating and honoring the generous donors in our program at our annual memorial service. It was such a pleasure meeting all the family members and friends of our donors. We especially enjoyed hearing all the wonderful stories from you about your loved ones' lives. It's a reminder that they live on in all your hearts. Please feel free to visit our community plot at Evergreen-Washelli Memorial Park anytime and enjoy a restful time on our memorial bench. Call Evergreen-Washelli business office at 206-362-5200 if you need directions to our plot. If you are interested in engraving your loved one's name on the UW plaque, contact the Evergreen-Washelli business office for more information. Note that the Willed Body Program does not cover the cost of engraving. If you missed this year's donor ceremony, you are welcome to join us in the Fall of 2024. Check this page in September for more information. A special thanks to all who participated in this year’s program! What wonderful gifts you all shared. Thank you again for joining us. In Peace, Catrin Pittack, PhD Director, Willed Body Program Shawn Kamke Program Operations Specialist, Willed Body Program Jessica Lacy Anatomical Embalmer, Willed Body Program Lucas West Anatomical Embalmer, Willed Body Program Ceremony Date and Time: Friday, October 13, 2023, 10:00 a.m. Website: www.uwmedicine.org/willedbody Email: [email protected] Phone: 206.543.1860 (M-F, 9am-2pm)
How do I get to Evergreen-Washelli Funeral Home & Cemetery Chapel?
For driving directions to the ceremony, please contact the Evergreen-Washelli Funeral Home & Cemetery business office 206.362.5200 . Address: 11111 Aurora Avenue N. Seattle, WA 98133.
Do I need to RSVP?
Will we witness the burial of my loved one’s cremated remains.
No. If your loved one chose to be buried in our communal plot at Evergreen Washelli, the actual burial will take place a few days before the ceremony.

Will you be reading the names of individual donors during the ceremony?
Our ceremony is a service intended to express our sincerest gratitude for the donors and their families, but we will not be reading the individual names of donors during the ceremony.
Will my loved one's name be engraved on the University of Washington plaque?
If you would like your loved one's name engraved on the UW plaque, please contact the Evergreen-Washelli business office at 2063625200 for more information. Please note that the Evergreen-Washelli business office does not have the names of individual donors in our program; these records are with the UW Willed Body Program only. Engraving consists of first and last name, year of birth and year of death. Also note that the UW does not cover the cost of engraving.
How many donor's family members can attend?
We welcome any family members and friends but ask you to be mindful of the fact that there is limited space in the chapel.
Will there be refreshments?
Yes, light refreshments including coffee, tea, and water will be available.
Are there restrooms at the chapel?
Is there parking near the chapel.
Yes, plenty and it's free.
The Willed Body Program is a resource for the following Research Programs:
- Genetic Anatomy: genome sequencing in modern human anatomy
- Alzheimer's Disease Research Program
- Prostate Cancer Research Program
- Cardiovascular Research and Education
- Neurological Surgery: catheter guidance system to improve patient safety during brain surgery
- Structural Informatics: spatial and symbolic representations of human structure
Publications
1. A Kumar, M Dougherty, GM Findlay, M Geisheker, J Klein, J Lazar, H Machkovech, J Resnick, R Resnick, AI Salter, F Talebi-Liasi, C Arakawa, J Baudin, A Bogaard, R Salesky, Q Zhou, K Smith, JI Clark, J Shendure, MS Horwitz. (2014) Genome Sequencing of Idiopathic Pulmonary Fibrosis in Conjunction with Medical School Human Anatomy PLOS One 9(9): e106744; doi:10.1371/journal.pone.010674
2. CL Fligner, JI Clark, JM Clark, LW Larson & JE Poole (2018) Surgical Anatomy for the Implanting Physician. in Surgical Implantation of Cardiac Rhythm Devices, 1st Edition by JE Poole & LW Larson. Elsevier. Philadelphia PA.”
UW School of Medicine international ranking
UW Anatomy was ranked tenth in the world, and fourth in the USA (behind Harvard, Vanderbilt and Utah) by the Center for World University Rankings (CWUR). CWUR reviewed academic programs in 26,000 educational institutions in sixty countries. The Willed Body Program is essential for the success of Anatomical research and education at the University of Washington.

CSS Adjustments
- About UW Medicine
- Harborview Medical Center
- UW Medical Center – Montlake
- UW Medical Center – Northwest
- UW Medicine Primary Care Clinics
- Medical Conditions Directory
- Patient Resources
- UW School of Medicine
- UW Medicine Research
- UW Physicians
- UW Medicine Newsroom
- Price Transparency
- UW Medicine Fact Book
- Right as Rain Health Blog
- Fred Hutchinson Cancer Center
- The Huddle - for employees
- Airlift Northwest
- Employee Resources
- Valley Medical Center
- Give Website Feedback
- Online Privacy Statement
- Policies and Notices
- Copyright And Healthcare Disclaimer
- Website Terms And Conditions Of Use
- Medical Education & Research
- Whole Body Donation
- Charitable Support
Looking to donate?
What is Whole Body Donation: A Comprehensive Guide
Whole body donation is a crucial yet often misunderstood aspect of medical science. It involves donating one’s entire body after death for the purpose of medical research and education. Unlike organ donation, which is primarily focused on saving or improving lives through transplantation, whole body donation provides an invaluable resource for medical students and researchers. This guide aims to demystify whole body donation, showing its importance and the ethical considerations involved.
Defining Whole Body Donation
At its core, whole body donation is the gift of one’s entire body for medical advancement post-mortem . This process is distinct from organ donation, as it supports a broader scope of medical research and training. Whole body donations are invaluable in teaching anatomy, practicing surgical techniques, and conducting research that leads to medical breakthroughs.
The practice is governed by strict legal and ethical standards to ensure that donations are made willingly and used responsibly. At MERI, adherence to these standards is a main concern, ensuring that each donation is treated with the dignity and respect it deserves, while contributing significantly to the advancement of medical knowledge.
Why People Choose to Donate
The decision to donate one’s body to science is a deeply personal and inspiring choice, often rooted in a desire to contribute to something greater than oneself. For many, it’s a profound expression of altruism, a way to leave an indelible mark on the world that extends far beyond their lifetime. Donors are often driven by a desire to advance medical research, knowing that their contribution could play a crucial role in medical breakthroughs and the betterment of future healthcare.
Environmental considerations also influence the decision to donate. In an era where ecological consciousness is growing, whole body donation presents an eco-friendly alternative to traditional burial methods. It aligns with the values of those who seek to leave the earth better than they found it, offering a sustainable choice that benefits the planet.
Each donor’s story is unique, but the underlying theme is a shared commitment to improving life for others. Whether motivated by personal experiences with medical conditions, a desire to aid in the education of future medical professionals, or environmental concerns, the choice to donate one’s body to science is a profound expression of generosity and hope for the future.
History of Body Donation
The history of body donation is as old as medicine itself, with its roots tracing back to ancient civilizations where the study of human anatomy began. This practice dates back to prehistoric times when voluntary body donations for anatomical studies were viewed as noble deeds. These early contributions laid the groundwork for understanding the human body in ways that observation alone could never achieve.
By the third century, the school of Greek medicine in Alexandria began using cadavers to further human anatomy education, marking a significant advancement in medical science. This practice, however, faced its share of challenges. Over time, unethical practices concerning body donation led many societies to view these acts with skepticism or even disdain.
It wasn’t until the mid-1950s that a significant shift occurred. Formal body donation programs began to emerge, replacing the reliance on anatomy acts that previously supplied medical schools with the bodies of the deceased. This change marked a move towards more ethical and respectful practices in the use of human bodies for medical education.
By the mid-1980s, a new era in body donation had firmly taken root. Nearly all American medical schools relied on voluntary anatomical gifts, showing us a growing recognition of the dignity and value of the human body, even in death. At MERI, we are proud to be part of this ongoing tradition, upholding the highest standards of respect and ethical practice in body donation. Our work not only honors the generosity of our donors but also contributes significantly to the advancement of medical education and research, ensuring that their legacy continues to benefit future generations.
How to Donate Your Body to Science: The Donation Process Explained
The process of donating your body to science is governed by specific protocols and ethical guidelines, designed to ensure that each donation is handled with the utmost respect and care. From the initial decision to the final handling of the donated body, every step is taken with consideration for the donor’s wishes and the needs of the medical community.
Pre-donation
The first step in becoming a whole body donor is registering with a reputable donation program, such as MERI’s Genesis Whole Body Donation Program . This involves completing necessary documentation, which typically includes a consent form and a detailed medical history. It’s important to inform your family or legal representatives of your decision, as they will be involved in the donation process after your passing.
Posthumous handling
After a donor’s passing, the donation program takes over to ensure respectful and dignified handling of the body. This includes transportation of the body to the facility and preparation for its use in medical education and research. At MERI, we place a strong emphasis on safety and dignity throughout the donation process. Our procedures are designed to maintain the highest standards of care, respecting the donor’s contribution and ensuring their legacy is honored.
The role MERI plays
MERI plays a critical role in facilitating whole body donations, adhering to ethical guidelines and treating each donation with the care and respect it deserves. Each donated body is treated with the highest level of respect and dignity, ensuring that it plays an important role in advancing medical research and training. Our approach is centered on preserving the honor and legacy of the donor, while facilitating significant advancements in medical science.
Contributions to Medical Science
Breakthroughs in medical science have been propelled by the generous contributions of body donations. These selfless acts have revolutionized cancer research, providing invaluable insights into disease progression and innovative treatments. Moreover, neurological studies, specifically relating to conditions such as Parkinson’s and Alzheimer’s , have reaped immense benefits from donated bodies, offering critical knowledge and potential therapies. Furthermore, these contributions have significantly advanced our understanding of mental health conditions in psychiatry, leading to the creation of more effective treatment options.
Each donation plants seeds of knowledge that grow into the medical advancements of tomorrow, changing lives far and wide.
The Legacy Left Behind
Whole body donation creates a legacy that extends far beyond the life of the donor. Personal stories from families who have chosen this path often speak of a profound sense of pride and comfort, knowing their loved ones continue to contribute to society even after passing. These tributes show us not just the emotional significance of the decision but also its tangible impact on medical advancements. The research facilitated by these donations has the potential to affect countless lives, shaping the future of medical care and treatment for generations to come.
This legacy is about more than just medical education; it’s a lasting contribution to the betterment of society. Families often find solace in the thought that their loved one’s donation is helping to train the next generation of healthcare professionals and is instrumental in medical breakthroughs that could one day save lives.
Reflecting on the Gift of Life and Knowledge
Whole body donation represents a cycle of life and knowledge, a selfless act that contributes to the ongoing pursuit of medical understanding and innovation. It’s a decision that has far-reaching implications, impacting not just the medical community but society as a whole. Through each donation, the donor imparts a gift of knowledge that continues to grow and evolve, influencing medical practices and treatments for years to come.
At MERI, we are deeply committed to advancing medical science through respectful and ethical practices. We recognize the invaluable contribution of each donor and are dedicated to ensuring that their gift is honored and utilized to its fullest potential. Our approach is rooted in a profound respect for life and the pursuit of knowledge, and we are continually inspired by the generosity of our donors.
To learn more about the impact of whole body donation and how you can contribute to this vital work, we invite you to explore our donor resources . If you are considering becoming a donor and wish to leave a lasting legacy in the field of medical science, please contact us. Your decision to donate could be the key to unlocking new medical breakthroughs and enhancing healthcare for future generations.
MERI: (901) 722-8001 (800) 360-6374
Genesis: (901) 278-7841 (877)-288-4483 (GIVE)
44 South Cleveland Memphis, TN 38104
If you require additional assistance, don’t hesitate to reach out to our team for more help. Please fill out the form below for further assistance and we will get back with you as soon as possible.
Anatomical Gift Program

The gift of an anatomical donation is an altruistic act that immeasurably benefits our students, our faculty and--ultimately--society at large.
Anatomical gift donations create an indispensable pathway for expanding our students' knowledge in the study of anatomy, which is one of the most essential courses in the education of future physicians, dentists, nurses and other health-care professionals. What's more, these gifts support our faculty's trailblazing research, enabling new therapies for illness and disease so we can live live longer, healthier lives.
The Anatomical Gift Program is a non-profit funded by the University at Buffalo and operated for the benefit of the Western New York community. Individuals who would like to donate their bodies can do so at no cost to them or their estate. We are grateful to all of those who wish to donate their bodies for anatomical education and medical research.
If you have any questions that this website does not answer, please feel free to contact us directly.
Phone : (716) 829-2913 Email : [email protected]
Our program's next scheduled closure for equipment maintenance will be from 12:00pm July 18 2024 until 9:00am July 29 2024. If your loved one passes away during a closure, a backup plan will be needed. We cannot accept donations during a closure. Any deaths that occur on a day we are closed will NOT be accepted. The 48 hour notification does not apply when the program is closed. We apologize for any inconvenience and appreciate your understanding.
The office is open Monday - Friday from 9 a.m. - 4 p.m for general program inquiries. An answering service is always available for calls to report a death and will contact our staff immediately.
Memorial Services
The Anatomical Gift Program holds memorial services in honor of those who have donated their bodies to our program. To accommodate families who cannot be present the day of the ceremony, we make these services available via Zoom and Youtube. For more details about these services, please visit the Memorial Services page.

If you are interested in becoming a donor in the Anatomical Gift Program, contact the office or follow "Be a Donor" for more information.

Request or print Anatomical Gift Program forms for consent, emergency contact, disposition, change of address and next of kin.
For the Family

Information on the memorial services that UB holds for family members, and testimonials from grateful medical students.
Frequently Asked Questions
We understand that you may have questions about our program or the process of donating your body to the program. Find answers here.
How You Can Help Medical Research: Donating Your Blood, Tissue, and Other Samples
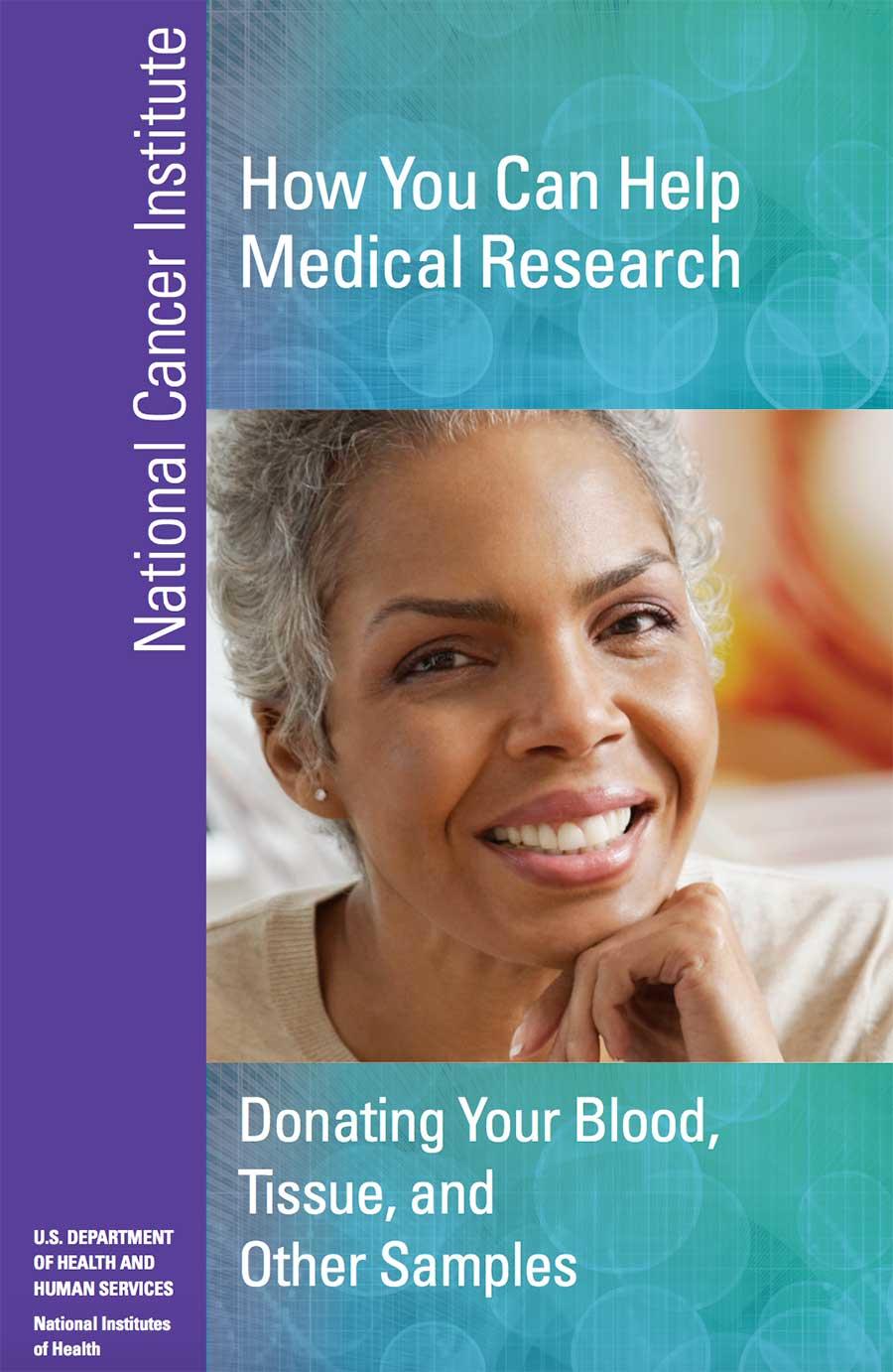
How You Can Help Medical Research: Donating Your Blood, Tissue, and Other Samples covers the importance of tissue donation for advancing medical research.
This booklet:
- Explains what tissue samples are
- Explains why it’s important for people to donate tissue
- Discusses how and where to donate
- Responds to many common questions and concerns
By understanding all that is involved in tissue donation, this booklet can help you talk with your doctor and loved ones and make a decision that works for you.
This booklet was printed in August 2012.
Medical School
- MD Students
- Residents & Fellows
- Faculty & Staff
- Duluth Campus Leadership
- Department Heads
- Dean's Distinguished Research Lectureship
- Dean's Tribute to Excellence in Research
- Dean’s Tribute to Excellence in Education
- Twin Cities Campus
- Office of the Regional Dean
- Office of Research Support, Duluth Campus
- CentraCare Regional Campus St. Cloud
- Office of Diversity, Equity & Inclusion
- Office of Faculty Affairs
- Grant Support
- Medical Student Research Opportunities
- The Whiteside Institute for Clinical Research
- Office of Research, Medical School
- Graduate Medical Education Office
- Office of Graduate and Postdoctoral Studies
- Departments
- Centers & Institutes
- Dr. James E. Rubin Medical Memorial Award
- Fisch Art of Medicine Student Awards
- Graduating Medical Student Research Award
- Veneziale-Steer Award
- Dr. Marvin and Hadassah Bacaner Research Awards
- Excellence in Geriatric Scholarship
- Distinguished Mentoring Award
- Distinguished Teaching Awards
- Cecil J. Watson Award
- Exceptional Affiliate Faculty Teaching Award
- Exceptional Primary Care Community Faculty Teaching Award
- Herz Faculty Teaching Development Awards
- The Leonard Tow Humanism in Medicine Awards
- Year 1+2 Educational Innovative Award
- Alumni Philanthropy and Service Award
- Distinguished Alumni Award
- Early Distinguished Career Alumni Award
- Harold S. Diehl Award
- Nomination Requirements
- Duluth Scholarships & Awards
- Account Management
- Fundraising Assistance
- Research & Equipment Grants
- Medical School Scholarships
- Student Research Grants
- Board members
- Alumni Celebration & Reunions
- Alumni Relations - Office of Alumni Relations
- Maximizing Medical Practice Series
- Diversity & Inclusion
- The Bob Allison Ataxia Research Center
- Children's Health
- Orthopaedics
- Regenerative Medicine
- Scholarships
- Transplantation
- MD Student Virtual Tour
- Why Minnesota?
- Facts & Figures
- Annika Tureson
- Caryn Wolter
- Crystal Chang
- Emily Stock
- Himal Purani
- Jamie Stang
- Jordan Ammons
- Julia Klein
- Julia Meyer
- Kirsten Snook
- Madison Sundlof
- Rashika K Shetty
- Rishi Sharma
- Savannah Maynard
- Prerequisite Courses
- Student National Medical Association Mentor Program
- Minority Association of Pre-Med Students
- Twin Cities Entering Class
- Next Steps: Accepted Students
- Degrees Offered
- Preceptor Resources (MD)
- Doctor of Physical Therapy (DPT)
- Message from the Director
- Clinical Training
- Curriculum & Timeline
- Integrated Physician Scientist Training
- MSTP Student Mentoring and Career Development
- External Fellowships
- Student Directory
- Student Advisory Committee
- Staff Directory
- Steering Committee
- Alumni Directory
- MSTP Student First Author Papers
- Thesis Defense
- MSTP Graduate Residency Match Information
- MSTP Code of Ethics
- Research Experience
- International Applicants
- Prerequisites
- Applicant Evaluation
- The Interview Process
- Application Process
- Financial Support
- Pre-MSTP Summer Research Program
- MSTP Virtual Tour
- Physician Scientist Training Programs
- Students with Disabilities
- Clinical Continuity & Mentoring Program
- Mental Health and Well-Being
- Leadership in Diversity Fellowship
- M1 and M2 Research Meeting
- Monthly Student Meetings
- MSTP Annual Retreat
- Preparation
- Women in Science & Medicine
- Graduate Programs/Institute Activities & Seminars
- CTSI Translational Research Development Program (TRDP)
- Grant Opportunities
- Graduate Programs
- Residencies & Fellowships
- Individualized Pathways
- Continuing Professional Development
- CQI Initiative
- Improvement Summary
- Quality Improvement Communication
- Student Involvement
- Student Voice
- Contact the Medical School Research Office
- Research Support
- Training Grants
- Veteran's Affairs (VA)
- ALPS COVID For Patients
- 3D/Virtual Reality Procedural Training
- Addressing Social Determinants of Health in the Age of COVID-19
- Augmented Reality Remote Procedural Training and Proctoring
- COVID19: Outbreaks and the Media
- Foundations in Health Equity
- Global Medicine in a Changing Educational World
- INMD 7013: COVID-19 Crisis Innovation Lab A course examining the COVID-19 crisis
- Intentional Observational Exercises - Virtual Critical Care Curriculum
- Live Suture Sessions for EMMD7500
- M Simulation to Provide PPE training for UMN students returning to clinical environments
- Medical Student Elective course: COVID-19 Contact Tracing with MDH
- Medical Students in the M Health Fairview System Operations Center
- Telehealth Management in Pandemics
- Telemedicine Acting Internship in Pediatrics
- The Wisdom of Literature in a Time of Plague
- Virtual Simulations for EMMD7500 Students
- COVID-19 Publications
- Blood & Marrow Transplant
- Genome Engineering
- Immunology & Infectious Disease
- Magnetic Resonance Imaging
- News & Events
- Support the Institute
- Lung Health
- Medical Discovery Team on Addiction Faculty
- Impact on Education
- Meet Our Staff
- Donation Criteria
- Health Care Directive Information
- Inquiry Form
- Other Donation Organizations
- Death Certificate Information
- Social Security Administration Notification and Death Benefit Information
- Grief Support
- Deceased Do Not Contact Registration and Preventing Identity Theft
- Service of Gratitude
- For Educators and Researchers
- Research Ethics
- Clinical Repository
- Patient Care
- Blue Ridge Research Rankings
- Where Discovery Creates Hope
What Is Whole Body Donation?
Whole body donation.
Whole body donation is a form of non-transplant anatomical donation made under the Darlene Luther Uniform Anatomical Gift Act. Typically, donation authorization is completed prior to death on behalf of the individual. At the time of death or immediately following a funeral, the deceased’s remains are received by the Anatomy Bequest Program and used for educational and research purposes. The donation lasts 2-18 months and the donor’s remains are either cremated or buried after the donation process. More information on the donation process is available on the How to Donate page.
Donation costs
Typically, donation to the Anatomy Bequest Program has no associated costs to the donor's next-of-kin/authorizing person. However, if the donor’s next-of-kin/authorizing person chooses to have a funeral before donation or have the donor’s body buried after donation there will be funeral home expenses associated with the donation. These expenses are the responsibility of the donor’s family or estate.
Frequently asked questions
+ can i be both an organ and a whole body donor.
Yes. We encourage you to sign up for any donor program that interests you. At the time of death, we work with other donor organizations and the next of kin/authorizing person to facilitate any and all donations possible. A list of other donor organizations may be found here: Lions Gift of Sight , LifeSource , American Donor Services
+ Upon my death, can I donate tissue for specific disease research and still donate my body to your program?
The best time to bring up this option is prior to the donor's death. It is recommended that individuals interested in supporting specific disease research, contact the Anatomy Bequest Program in order to discuss the options and complete all necessary paperwork.
It is important to note that the Program cannot guarantee research outcomes.
+ Can I receive a report on the findings pertaining to the studies?
No, at this time this option is not available. The Program's core mission is to support anatomical education for the University of Minnesota Medical School. Anatomical education is the foundation of a student's medical knowledge and is the first course they take during their first year of Medical School. Therefore, the students are not knowledgeable enough at this time to diagnose or recognize diseases and conditions. Rather, they use this knowledge as they go forward in other curriculum courses such as pathology.
The Anatomy Bequest Program does not perform autopsies.
+ Can the University of Minnesota decline my body even if I have completed donation forms?
Yes. The Program must reserve the right to decline individuals for a number of reasons.
- The individual has a disease such as HIV/AIDS, hepatitis B, hepatitis C, tuberculosis or a Prion disease
- The individual is morbidly obese as determined by the Program
- There is significant family discord at the time of death or immediately thereafter
- The condition or pathology of the remains precludes adequate and/or safe preparation, storage or study
If the Program declines to accept the donation at the time of death, it becomes the responsibility of the next of kin/authorizing person to make final arrangements.
+ How does the Anatomy Bequest Program protect the dignity of the donors?
The Anatomy Bequest Program has instituted a number of safeguards to make sure program donors are handled with dignity and respect.
All access to human donors has to be approved by the Anatomy Bequest Program Proposal Review Committee. The Committee reviews proposals in order to ensure that each proposed study has scientific merit, is consistent with the donor’s consent, and has controls in place to protect the donor’s identity and dignity.
Each anatomy student is required to review a standardized orientation presentation which reviews the Program’s policies. The Program requires all individuals who have access to donors to conduct themselves in accordance with established policies. The Program prohibits the use of cellular phones in the anatomy laboratories as a way to prevent unauthorized images of the donors from being taken. The Program also restricts access to the laboratories and only registered students, faculty, or researchers are permitted to have access to the human donors.
The Program, through policy creation, education, and outreach, works to create a culture that protects, values, and honors the individuals who have made anatomical gifts for the benefit of medical education and research.
+ What if I die outside of Minnesota?
Effective October 1, 2023, Anatomy Bequest Program will no longer accept the body donations of individuals who die outside of the state of Minnesota.
When a death occurs outside of the state of Minnesota, the donor’s next of kin or authorizing person is responsible for contacting a donation program in the state where the death occurred or making alternate final disposition arrangements.
If you are a part time resident of the state of Minnesota, you may wish to register for whole body donation in more than one state. We encourage you to visit the following website for a list of academic institutions in the United States that have whole body donation programs: https://anatbd.acb.med.ufl.edu/usprograms/
+ Why do the studies last as long as 18 months?
The director of the Program understands that they are asking grieving family members for a long period of commitment. We hope that family members understand that they have the opportunity to have a funeral, with their loved one's remains present, prior to the donation process. We do not want to delay or postpone the grieving process.
Before a donor's remains can be used to educate health care practitioners, the donor's remains need to be anatomically prepared. The anatomical preparation process currently recommended requires arterial preservation. After arterial preservation, the donor's remains are isolated for a period of time to better eliminate the possibility of transmitting harmful microorganisms to students, staff, or researchers.
After isolation, the donor's remains are used for study in semester or yearlong courses. The course assigned depends on the time of year.
+ How is our program different from others?
We are one of the largest body donation programs in the U.S. and have significantly more staff and resources, as well as oversight, than most.
+ What protections are in place to ensure donor wishes are respected?
- Internally, we have strict procedures, as well as checks and balances, to ensure ethical and compliant practices throughout our program.
- We have a dedicated quality assurance staff member who audits our internal processes on both an assigned and random basis. She also performs vendor audits of our transportation and cremation vendors, which include unannounced site visits and inspections.
- We regularly undergo external audits and University-level review to ensure that all donor remains are accounted for.
- We routinely re-evaluate our processes to identify and mitigate any potential weaknesses.
- We have an Anatomy Bequest Program Proposal Review Committee, which serves as an institutional review committee and must approve all proposals before any study or course can be supported.
+ Is there federal or state regulation of whole body donation?
At this time there is no federal oversight of whole body donation. The director of our Anatomy Bequest Program, Angela McArthur , has been an outspoken advocate for more state and federal regulatory oversight of non-transplant anatomical donation for 20 years. She is also nationally recognized as a leader in both the ethics and accreditation processes of non-transplant donation.
Anatomy Bequest Program
- How to Donate
- What to Expect After a Loved One Has Died
CONTACT ANATOMY BEQUEST PROGRAM
Phone: 612-625-1111 Fax: 612-625-1688
Email: [email protected]
Address: 3-102 Nils Hasselmo Hall, 312 Church Street SE, Minneapolis, MN 55455
The Anatomical Education Program was created in 1903 by the Indiana General Assembly to ensure the quality of education for medical, dental and allied health students across the state of Indiana. This program is administered by Indiana University School of Medicine and is authorized to provide for the acquisition, distribution and standards of use of donated human remains.
At the time of an enrolled donor’s passing, a health care professional should simply call the Anatomical Education Program at 317-274-7450 to report the death and go through a brief telephone screening. Upon acceptance of the donor, the Anatomical Education Program provides transportation and embalming, notifies Social Security, and assists in filing paperwork (such as death certificates and other necessary forms). Following use of the body for teaching, the remains are cremated and either inurned in Crown Hill Cemetery in Indianapolis or, upon request, returned to the family.
Make a Donation
Human bodies used for medical education are obtained entirely through donations, and an adequate number of donors allow the schools to maintain high standards of health science education and health care in Indiana. Those who decide to bequeath bodies to the health sciences make a significant contribution that benefits the quality of life and care of the living.
Enrollment Forms
Service of Gratitude
An annual service honors those who have made this generous final gift to medical education.
Frequently Asked Questions
- Who may bequeath their body to medical science in Indiana? Any person 18 years of age or over may donate their body to medical science in Indiana. No upper age limit applies.
- How do I enroll to donate my body to the Anatomical Education Program? Simply complete the Certificate of Bequeathal and Biographical Information forms and return the signed original documents to the Anatomical Education Program office. Body donors must be pre- registered with the program prior to death. Persons holding Power of Attorney or Health Care Representative may sign the bequeathal form on behalf of the donor if the donor is unable to sign.
- Who may sign as a witness on my Certificate of Bequeathal? Any adult family member or friend may witness a donor’s signature. It is not necessary to have the Certificate notarized.
- How much does the Anatomical Education Program pay for bodies? No money is paid for procurement of bodies for anatomical studies. All human material utilized in teaching is acquired by donation only.
- How much will it cost for me to donate my body to the program? If an individual donates directly to the Anatomical Education Program, no costs are associated with the donation. The Anatomical Education Program will provide transportation and embalming as well as assistance in filing paperwork (e.g., burial permit, death certificate and other necessary forms) at no cost to the donor or their family. However, the family must pay directly for newspaper charges for obituaries and county health department fees for certified death certificates.
- May I have a funeral service or use a funeral home for the services listed above? If a donor or family elects to use a local funeral home, a healthcare professional must still call at the time of death to provide information for the medical screening to determine acceptance to the Anatomical Education Program. If accepted, the family may elect to have a funeral service with the donor’s body present, after which the body is brought to the Anatomical Education Program. Some families choose a traditional funeral service, while most donate directly to the Anatomical Education Program and hold a memorial service with no remains present at a church or funeral home, or wait until the cremains are returned (up to 24 months after death) to hold a service. A funeral director will charge for their services, and the donor or their family will be responsible for all funeral home fees.
- What procedure should be followed upon my death? A nurse or doctor involved in the donor’s healthcare should call the Anatomical Education Program at 317-274-7450. IU School of Medicine has a contract mortuary service available to receive reports of a donor’s passing outside of normal business hours. A medical screening will be conducted over the phone to determine if the remains can be accepted.
- What could prevent my body from being accepted? The cause or manner of death could prevent use of a body for medical education. A body cannot be accepted if an infectious or communicable disease (including COVID-19) is present or if there is trauma to the body that renders it unusable for teaching. Ostomies/stomas, amputations, recent surgeries, or excessive height and/or weight could also prevent acceptance. The Anatomical Education Program is unable to accept donors measuring over 6’1” tall or weighing more than 225 lbs; the maximum acceptable BMI for any donor is 30.
- May an autopsy or post-mortem examination be conducted on a body that is intended for donation to medical education? No, the Anatomical Education Program cannot accept autopsied bodies.
- How will my body be used by this program? All donations are used for the purpose of advancing medical education.
- What happens if my body is not accepted by the Anatomical Education Program? The Anatomical Education Program at the IU School of Medicine makes every effort to accept all donations. However, if a body is unable to be accepted, the donor’s family will be notified at the time of the telephone medical screening and will be advised to call a funeral home to arrange an alternative form of disposition.
- What happens to my body after the studies are complete? Bodies donated to the Anatomical Education Program are individually cremated. The program usually requires 18 to 24 months before the cremains may be claimed or inurned.
- Who pays for the cremation? The Anatomical Education Program of Indiana University School of Medicine pays cremation costs.
- Can my family receive a report of your findings? Typically, no reports are provided to families. Because donors are utilized for education, bodies are studied by medical students who are not yet qualified to provide an assessment about causes of death or medical conditions. Donor bodies are studied to gain an in-depth understanding of human anatomy; research into specific diseases or conditions are not conducted.
- Can my remains be returned to my family? Yes, most families choose this option. The donor may stipulate on the Certificate of Bequeathal a wish to have cremains returned to the family. Following cremation, the family will be notified by a Final Disposition Letter and may confirm in writing to instruct the Program to return the cremains by certified, insured, express mail.
- What if I do not want my cremains returned? A portion of Crown Hill Cemetery in Indianapolis has been set aside for burial of those who gave their bodies to benefit medical education. The cemetery area is marked with a memorial wall and path that can be personalized at a family’s request and expense. Inurnment in Crown Hill Cemetery requires written permission from the family.
- Can a ‘keepsake’ portion of my remains be returned to my family if I choose inurnment at Crown Hill Cemetery? No. If the donor or their family requests that the Anatomical Education Program assume responsibility for inurnment, cremated remains will not be divided before being laid to rest in Crown Hill Cemetery.
The Anatomical Education Program annually hosts both a Service of Gratitude to honor all whole body donors and a graveside service for those who have chosen inurnment in Crown Hill Cemetery. The Service of Gratitude is held each spring and is open to all. The student-led Service of Gratitude includes a reading of the names of all donors from the previous calendar year. This service is an opportunity for students, faculty and staff to express thanks and it is not intended to replace a family’s personalized memorial for their loved one.
Families whose loved ones' names will be read will receive an invitation in the mail. The graveside service at Crown Hill Cemetery is held each autumn. Families whose loved ones will be laid to rest in Crown Hill Cemetery will receive an invitation in the mail.
- What if I die in a different state? The Anatomical Education Program cannot accept the bodies of donors who die outside the State of Indiana. For information about whole body donation programs at other accredited institutions please visit: https://anatbd.acb.med.ufl.edu/usprograms/
- Will the Anatomical Education Program accept my body if I donate my eyes and/or other organs or tissues for transplant? A donor may donate their eyes through Donate Life Indiana, the Indiana Lions Eye Bank, Vision First, or another agency. Eye donation is the only type of tissue donation that may be performed; the donation of other tissues or organs would render the body unacceptable to the Anatomical Education Program.
- Where can I get information on the donation of eyes organs and other tissue? To register as an organ or tissue donor in Indiana, contact Donate Life Indiana – Lindsey Johnson, Director – 3760 Guion Rd., Indianapolis, IN 46222; 317-222-3414.
- Should the bequeathal of my body be made a provision in my will? It may be, but this is not necessary. If this provision is made only in a donor’s will, the body may not be accepted, as there is usually a considerable delay before a will is probated. The Anatomical Education Program requests that the Certificate of Bequeathal be signed by the donor and two competent witnesses. It is not necessary to include a copy of a will.
- May I pay the expenses that the Anatomical Education Program incurs with my body donation? Yes. The Anatomical Education Program does accept monetary donations to help offset expenses associated with medical, dental and health professions education within the State of Indiana. Such donations qualify for an Indiana College Credit on state tax forms and also qualify for an itemized deduction on Federal tax forms.
- Where can I find answers to additional questions I may have? If you have additional questions about bequeathal procedures or the Anatomical Education Program, call 317-274-7450 or email [email protected] .
Please enter both an email address and a password.
Account login
- Show/Hide Password Show password Hide password
- Reset Password
Need to reset your password? Enter the email address which you used to register on this site (or your membership/contact number) and we'll email you a link to reset it. You must complete the process within 2hrs of receiving the link.
We've sent you an email.
An email has been sent to Simply follow the link provided in the email to reset your password. If you can't find the email please check your junk or spam folder and add [email protected] to your address book.
- About RCS England

- Donate Your Body to Medical Science
Donating your body, brain or tissue to a medical school or research establishment is a valuable gift - your donation will become an important resource for training healthcare professionals or for research, and such donations are highly valued by staff and students alike.
If you are interested in donating your body, you need to contact your local medical school who can answer specific enquiries and provide consent forms. The minimum age for donation is 17 and you will need to make your wishes known in writing (and witnessed) prior to death. Consent cannot be given by anyone else after your death.
A list of frequently asked questions are available on the Human Tissue Authority website or you can view their donation pack online .
Share this page:
- Support our work
- Global Appeal 2023 - Fill in the GAPS
- Conserve our Collections Appeal 2022: Revive the Age of Enlightenment & Rediscover our Stories
- Image Bank Appeal 2022 - Help us recognise every body
- Winter appeal 2020: Support pioneering research to beat COVID-19
- Christmas appeal 2019: help us improve access to surgical care for children with inguinal hernia in Nepal
- Ways to Donate
- Leave a gift in your will
- Fundraising Events
- Our Fundraising Promise
Body Donation Program
The decision to donate your body to WMed upon your death represents the ultimate gift to the world of medical education and a tremendous opportunity for the students who will become exceptional clinicians, leaders, educators, advocates, and researchers of tomorrow.
Once you register to become a donor, the Body Donation Program keeps your name and contact information on file. Upon your death, a caregiver or family member must contact us right away (within 24 hours of death). We take calls 24 hours a day, 365 days a year at 1.844.366.9633 . If within 50 miles of WMed, we will arrange for a licensed transporter to transport your body to the medical school, where it may be used to teach students and physicians about the structure of the human body, and for the purpose of conducting medical research.
The length of donation is specified by the donor or donor’s representative at the time of registration for a period of four years, six years, or forever. Once study of the body is complete, we either arrange for cremation or the donor may continue to contribute to education and research as part of the WMed Skeletal Research Collection. The donor form also asks whether the cremated remains shall be returned to the family or buried at the WMed memorial.
The Body Donation Program recognizes the substantial gift of each donated body and treats each with the utmost care and respect. You are encouraged to share the information with your family so they are familiar with the program and fulfill your wishes upon your death. It is also suggested that an alternate burial plan be considered in the event your body is not able to be accepted for donation.
There is no cost to the next-of-kin or estate for transport of the body to WMed for deaths within 50 miles, cremation of the remains, or shipping of the cremated remains within the continental United States.
In February 2018, the Body Donation Program was featured in a two-part series on Kalamazoo’s WWMT NewsChannel 3 . The story featured interviews with second-year student Dan Ferman, as well as faculty and staff from WMed.
1.844.366.9633 [email protected]
© 2024 Western Michigan University Homer Stryker M.D. School of Medicine 300 Portage Street, Kalamazoo, MI 49007
“Lord Knows What’s Being Done with My Blood!”: Black Women’s Perceptions of Biospecimen Donation for Clinical Research in the United States
- Published: 07 May 2024
Cite this article

- Kyrah K. Brown ORCID: orcid.org/0000-0002-7028-6791 1 ,
- Shameka Poetry Thomas ORCID: orcid.org/0000-0002-5225-0090 2 ,
- R. Mathew Brothers ORCID: orcid.org/0000-0002-3281-5277 1 &
- Yue Liao ORCID: orcid.org/0000-0002-9384-336X 1
56 Accesses
Explore all metrics
Black women are underrepresented in clinical research and clinical trials. Knowledge gaps lead to biased clinical practice and care. There is a small but growing body of literature on Black women’s perceptions about participation when biospecimen donation is sought by researchers. This is the first known study to investigate willingness to participate in clinical research involving biospecimen donation among Black women of reproductive age in the United States.
This cross-sectional study recruited 496 Black women (ages 18–49) from a research crowdsourcing platform. Participants completed a 46-item online survey which asked about their willingness to provide blood samples for clinical health research and reasons for their willingness or for any unwillingness. Descriptive statistics and thematic analysis method were used to analyze the data.
Less than half (44%) of participants reported willingness to provide blood samples for clinical research. The most common concerns of those expressing unwillingness to provide samples were “fear of blood sample being misused” and “distrust with the health researchers handling the samples.” We identified six qualitative themes from the analysis of participants’ open-ended responses. The most important factors include a desire for integrity and transparency in research, institutional racism contributing to mistrust, and adequate compensation and clearly defined benefits to participation.
Conclusions
The recruitment and engagement of Black women in clinical biospecimen research should involve transparent, trustworthy, and anti-racist practices and informed respect for Black women’s autonomy. There is a need to address Black women’s concerns about exploitative profits and mistrust of academic and medical institutions.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
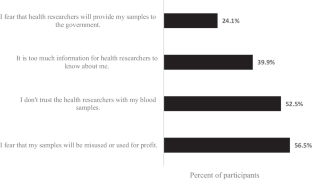
Similar content being viewed by others

Differences in preferences for models of consent for biobanks between Black and White women
Promoting inclusive recruitment: a qualitative study of black adults’ decision to participate in genetic research, biobanking in israel 2016–17; expressed perceptions versus real life enrollment, data availability.
The data presented in this study are available on reasonable request from the corresponding author.
Powell-Wiley TM, Baumer Y, Baah FO, Baez AS, Farmer N, Mahlobo CT, et al. Social determinants of cardiovascular disease. Circul Res. 2022;130:782–99.
Article CAS Google Scholar
Forrester S, Jacobs D, Zmora R, Schreiner P, Roger V, Kiefe CI. Racial differences in weathering and its associations with psychosocial stress: the CARDIA study. SSM - Popul Health. 2019;7:100319.
Article Google Scholar
Geronimus AT, Hicken M, Keene D, Bound J. Weathering and age patterns of allostatic load scores among Blacks and Whites in the United States. Am J Public Health. 2006;96:826–33.
Article PubMed PubMed Central Google Scholar
Akins JD, Martin ZT, Patik JC, Curtis BM, Campbell JC, Olvera G, et al. Young, non-hispanic black men and women exhibit divergent peripheral and cerebral vascular reactivity. Exp Physiol. 2022;107:450–61.
Article PubMed Google Scholar
Allen AM, Wang Y, Chae DH, Price MM, Powell W, Steed TC, et al. Racial discrimination, the superwoman schema, and allostatic load: exploring an integrative stress-coping model among African American women. Ann N Y Acad Sci. 2019;1457:104–27.
Martin ZT, Al-daas IO, Cardenas N, Vu J, Brown KK, Brothers R. Conduit artery and forearm microvascular reactivity in Black and White females: examining the role of Greater Superwoman Schema endorsement. FASEB J. https://faseb.onlinelibrary.wiley.com/doi/abs/10.1096/fasebj.2022.36.S1.R4850 .
National Cancer Institute, Division of Cancer Treatment and Diagnosis. Frequently asked questions (FAQs) [Internet]. [cited 2023 Oct 8]. https://biospecimens.cancer.gov/patientcorner/faq.asp#q2 .
Bowen DJ, Penchaszadeh VB. Special issue: enhancing minority recruitment into genetics research. Community Genet. 2008;11:189–190.
Branson RD, Davis K, Butler KL. African Americans’ participation in clinical research: importance, barriers, and solutions. Am J Surg. 2007;193:32–9. discussion 40.
Compadre AJ, Simonson ME, Gray K, Runnells G, Kadlubar S, Zorn KK. Challenges in recruiting African-American women for a breast cancer genetics study. Hered Cancer Clin Pract. 2018;16:8.
Gorelick PB, Harris Y, Burnett B, Bonecutter FJ. The recruitment triangle: reasons why African Americans enroll, refuse to enroll, or voluntarily withdraw from a clinical trial. An interim report from the African-American Antiplatelet Stroke Prevention Study (AAASPS). J Natl Med Assoc. 1998;90:141–5.
CAS PubMed PubMed Central Google Scholar
Hughes C, Peterson SK, Ramirez A, Gallion KJ, McDonald PG, Skinner CS, et al. Minority recruitment in hereditary breast cancer research. Cancer Epidemiol Biomarkers Prev. 2004;13:1146–55.
Spruill IJ. Enhancing recruitment of African-American families into genetic research: lessons learned from Project SuGar. J Community Genet. 2010;1:125–32.
Wujcik D, Wolff SN. Recruitment of African Americans to National Oncology Clinical Trials through a clinical trial shared resource. J Health Care Poor Underserved. 2010;21:38–50.
Ambrosone CB, Zirpoli G, Ruszczyk M, Shankar J, Hong C-C, McIlwain D, et al. Parity and breastfeeding among African-American women: differential effects on breast cancer risk by estrogen receptor status in the women’s Circle of Health Study. Cancer Causes Control. 2014;25:259–65.
Bekash A, Saini J, Fan X, Hooke J, Mural R, Shriver C, et al. Differential benign breast disease co-occurrence with cancer in Caucasian and African American women. Cancer Res. 2009;69:3066.
Conti DV, Darst BF, Moss LC, Saunders EJ, Sheng X, Chou A, et al. Trans-ancestry genome-wide association meta-analysis of prostate cancer identifies new susceptibility loci and informs genetic risk prediction. Nat Genet. 2021;53:65–75.
Article CAS PubMed PubMed Central Google Scholar
Manrai AK, Funke BH, Rehm HL, Olesen MS, Maron BA, Szolovits P, et al. Genetic misdiagnoses and the potential for health disparities. N Engl J Med. 2016;375:655–65.
Rebbeck TR, Bridges JFP, Mack JW, Gray SW, Trent JM, George S, et al. A framework for promoting diversity, equity, and inclusion in genetics and genomics research. JAMA Health Forum. 2022;3:e220603.
Adams-Campbell LL, Dash C, Palmer JR, Wiedemeier MV, Russell CW, Rosenberg L, et al. Predictors of biospecimen donation in the Black women’s Health Study. Cancer Causes Control. 2016;27:797–803.
Barber LE, Palmer JR, Bertrand KA, Wang C. Abstract C040: predictors of blood biospecimen provision among African American women. Cancer Epidemiol Biomarkers Prev. 2020;29:C040–040.
Radecki Breitkopf C, Williams KP, Ridgeway JL, Parker MW, Strong-Simmons A, Hayes SN, et al. Linking education to action: a program to increase research participation among African American Women. J Women’s Health. 2018;27:1242–1249.
Ridley-Merriweather KE, Head KJ. African American women’s perspectives on donating healthy breast tissue for research: implications for recruitment. Health Commun. 2017;32:1571–1580.
Smith YR, Johnson AM, Newman LA, Greene A, Johnson TRB, Rogers JL. Perceptions of clinical research participation among African American women. J Womens Health (Larchmt). 2007;16:423–8.
Sheppard VB, Hurtado-de-Mendoza A, Zheng Y-L, Wang Y, Graves KD, Lobo T, et al. Biospecimen donation among Black and White breast cancer survivors: opportunities to promote precision medicine. J Cancer Surviv. 2018;12:74–81.
Yen GP, Davey A, Ma GX. Factors that affect willingness to donate blood for the purpose of biospecimen research in the Korean American community. Biopreserv Biobank. 2015;13:107–13.
Scherr CL, Ramesh S, Marshall-Fricker C, Perera MA. A review of African Americans’ beliefs and attitudes about genomic studies: opportunities for message design. Front Genet. 2019 [cited 2021 May 30];10. https://www.frontiersin.org/articles/ https://doi.org/10.3389/fgene.2019.00548/full .
Liao Y, Brown KK. Usage of digital health tools and perception of mHealth intervention for physical activity and sleep in Black women. Int J Environ Res Public Health. 2022;19:1557.
Centers for Disease Control and Prevention. About chronic health diseases [Internet]. [Cited 9 September 2023]. National Center for Chronic Disease Prevention and Health Promotion. 2022. https://www.cdc.gov/chronicdisease/about/index.htm .
Braun V, Clarke V. Thematic analysis. In: Cooper H, Camic PM, Long DL, Panter AT, Rindskopf D, Sher KJ, editors. APA handbook of research methods in psychology, vol 2: research designs: quantitative, qualitative, neuropsychological, and biological. Washington, DC, US: American Psychological Association; 2012. p. 57–71.
Chapter Google Scholar
Royal C, Baffoe-Bonnie A, Kittles R, Powell I, Bennett J, Hoke G, et al. Recruitment experience in the first phase of the African American Hereditary Prostate Cancer (AAHPC) study. Ann Epidemiol. 2000;10:S68–77.
Article CAS PubMed Google Scholar
Shavers VL, Lynch CF, Burmeister LF. Racial differences in factors that influence the willingness to participate in medical research studies. Ann Epidemiol. 2002;12:248–56.
Shavers-Hornaday VL, Lynch CF, Burmeister LF, Torner JC. Why are African Americans under-represented in medical research studies? Impediments to participation. Ethn Health. 1997;2:31–45.
Tong EK, Fung L-C, Stewart SL, Paterniti DA, Dang JHT, Chen MS Jr. Impact of a biospecimen collection seminar on willingness to donate biospecimens among Chinese Americans: results from a randomized, controlled community-based trial. Cancer Epidemiol Biomarkers Prev. 2014;23:392–401.
Raines-Milenkov A, Felini M, Baker E, Acharya R, Diese EL, Onsa S et al. Willingness of a multiethnic immigrant population to donate biospecimens for research purposes. J Immigrant Minority Health [Internet]. 2021 [cited 2022 Jan 23]; https://doi.org/10.1007/s10903-021-01241-4 .
Scott EA, Schlumpf KS, Mathew SM, Mast AE, Busch MP, Gottschall JL, et al. Biospecimen repositories: are blood donors willing to participate? Transfusion. 2010;50:1943–1950.
Dash C, Wallington SF, Muthra S, Dodson E, Mandelblatt J, Adams-Campbell LL. Disparities in knowledge and willingness to donate research biospecimens: a mixed-methods study in an underserved urban community. J Community Genet. 2014;5:329–336.
Hagiwara N, Berry-Bobovski L, Francis C, Ramsey L, Chapman RA, Albrecht TL. Unexpected findings in the exploration of African American underrepresentation in biospecimen collection and biobanks. J Canc Educ. 2014;29:580–7.
Hinton EC. Black American millennials coping with the myth of a post-racist society. Dissertation [Internet]. Minnesota, United States: Walden University; 2020 [cited 2024 Apr 3]. https://www.proquest.com/docview/2386924967/abstract/F3D47F93F35B442CPQ/1 .
Jones-Eversley S, Adedoyin AC, Robinson MA, Moore SE. Protesting Black inequality: a commentary on the Civil Rights Movement and Black Lives Matter. J Community Pract. 2017;25:309–24.
Luckerson V. Why millenials can’t afford to be colorblind. Time [Internet]. 2015 Jul 6 [cited 2024 Apr 3]; https://time.com/3944697/millennials-race-confederate-flag/ .
Merdad L, Aldakhil L, Gadi R, Assidi M, Saddick SY, Abuzenadah A, et al. Assessment of knowledge about biobanking among healthcare students and their willingness to donate biospecimens. BMC Med Ethics. 2017;18:32.
Henderson C, Scott T, Schinder B, Hager E, Friedman FS, Miller E, et al. Shifting the paradigm from participant mistrust to researcher and institutional trustworthiness: a qualitative study of researchers’ perspectives on building trustworthiness with Black communities. Community Health Equity Res Policy. 2022. https://doi.org/10.1177/0272684X221117710 .
Thomas SP. Trust also means centering Black women’s reproductive health narratives. Hastings Cent Rep. 2022;52:S18–21.
Wilson Y. Is trust enough? Anti-Black racism and the perception of Black vaccine “hesitancy.” Hastings Cent Rep. 2022;52(Suppl 1):S12–7.
PubMed Google Scholar
Dang JHT, Rodriguez EM, Luque JS, Erwin DO, Meade CD, Chen MS. Engaging diverse populations about biospecimen donation for cancer research. J Community Genet. 2014;5:313–327.
Griffith DM, Jaeger EC, Bergner EM, Stallings S, Wilkins CH. Determinants of trustworthiness to conduct medical research: findings from focus groups conducted with racially and ethnically diverse adults. J Gen Intern Med. 2020;35:2969–75.
Association of American Medical Colleges. The principles of trustworthiness [Internet]. Center For Health Justice. 2022 [cited 2022 Jun 22]. https://www.aamchealthjustice.org/resources/trustworthiness-toolkit .
Thomas SP, Amini K, Floyd KJ, Willard R, Wossenseged F, Keller M, et al. Cultivating diversity as an ethos with an anti-racism approach in the scientific enterprise. HGG Adv. 2021;2:100052.
PubMed PubMed Central Google Scholar
Ford CL, Airhihenbuwa CO. The public health critical race methodology: praxis for antiracism research. Soc Sci Med. 2010;71:1390–8.
Goings TC, Belgrave FZ, Mosavel M, Evans CBR. An antiracist research framework: principles, challenges, and recommendations for dismantling racism through research. J Soc Social Work Res. 2023;14:101–28.
Ross LJ. Reproductive justice as intersectional feminist activism. Souls. 2017;19:286–314.
ten Have H. Patrão Neves M do C. Respect for autonomy. In: ten Have H, Patrão Neves M do C, editors. Dictionary of global bioethics [Internet]. Cham: Springer International Publishing; 2021 [cited 2023 Aug 2]. pp. 913–913. https://doi.org/10.1007/978-3-030-54161-3_450 .
Davis D-A. Obstetric racism: the racial politics of pregnancy, Labor, and Birthing. Med Anthropol. 2019;38:560–73.
Roberts D. Killing the Black body: race, reproduction, and the meaning of liberty. Knopf Doubleday Publishing Group; 2014.
Google Scholar
Wilson WD, Jackson FH, Harrell JR. Framework for ethical community engagement (ECE) with underserved populations in the rural south: a help for bioethics and healthcare promotion. J Health Care Poor Underserved. 2019;30:91–104.
Erwin DO, Moysich K, Kiviniemi MT, Saad-Harfouche FG, Davis W, Clark-Hargrave N, et al. Community-based partnership to identify keys to biospecimen research participation. J Canc Educ. 2013;28:43–51.
Veseli B, Sandner S, Studte S, Clement M. The impact of COVID-19 on blood donations. PLoS ONE. 2022;17:e0265171.
Behar-Horenstein L, Warren R, Setiawan VW, Perkins C, Schmittgen TD. Enhancing African American participation in biospecimens: a case in point for pancreatic cancer. CHD [Internet]. 2020 [cited 2021 May 30]; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8294622/ .
Beskow LM. Lessons from HeLa cells: the ethics and policy of biospecimens. Annu Rev Genom Hum Genet. 2016;17:395–417.
Beskow LM, Friedman JY, Hardy NC, Lin L, Weinfurt KP. Developing a simplified consent form for biobanking. PLoS ONE. 2010;5:e13302.
Clark US, Hurd YL. Addressing racism and disparities in the biomedical sciences. Nat Hum Behav. 2020;4:774–7.
Flory J, Emanuel E. Interventions to improve research participants’ understanding in informed consent for research: a systematic review. JAMA. 2004;292:1593–601.
Kim EJ, Kim SH. Simplification improves understanding of informed consent information in clinical trials regardless of health literacy level. Clin Trails. 2015;12:232–6.
Page SA, Manhas KP, Muruve DA. A survey of patient perspectives on the research use of health information and biospecimens. BMC Med Ethics. 2016;17:48.
Spector-Bagdady K. Hospitals should act now to notify patients about research use of their data and biospecimens. Nat Med. 2020;26:306–308.
Rodriguez EM, Saad-Harfouche FG, Miller A, Mahoney MC, Ambrosone CB, Morrison CD, et al. Engaging diverse populations in biospecimen donation: results from the Hoy Y Mañana study. J Community Genet. 2016;7:271–277.
Download references
This research study was supported by startup funds awarded to Dr. Yue Liao from the University of Texas at Arlington.
Author information
Authors and affiliations.
Department of Kinesiology, University of Texas at Arlington, 500 W. Nedderman Drive, Arlington, TX, 76019, USA
Kyrah K. Brown, R. Mathew Brothers & Yue Liao
School of Public Health, Harvard University, Boston, MA, USA
Shameka Poetry Thomas
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization, K.K.B and Y.L.; methodology, Y.L. and K.K.B.; formal analysis, K.K.B and Y.L.; writing—original draft preparation, K.K.B.; writing—review and editing, Y.L., S.P.T., R.M.B; funding acquisition, Y.L. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Kyrah K. Brown .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics Approval
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of the University of Texas at Arlington (protocol number 2021−0207) on 1 February 2021.
Consent to Participate
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Brown, K.K., Thomas, S.P., Brothers, R.M. et al. “Lord Knows What’s Being Done with My Blood!”: Black Women’s Perceptions of Biospecimen Donation for Clinical Research in the United States. J. Racial and Ethnic Health Disparities (2024). https://doi.org/10.1007/s40615-024-02015-y
Download citation
Received : 05 November 2023
Revised : 06 April 2024
Accepted : 28 April 2024
Published : 07 May 2024
DOI : https://doi.org/10.1007/s40615-024-02015-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Biospecimen
- Patient preference
- Black or African American
- Health inequities
- Women’s health
- Find a journal
- Publish with us
- Track your research

ETV Bharat / state
Uttar Pradesh: BHEL DGM Fulfills Father's Last Wish, Donates His Body to Medical College in Jhansi

By ETV Bharat English Team
Published : May 12, 2024, 11:39 AM IST
Updated : May 12, 2024, 12:28 PM IST
Children of a man who had wished that his body be used for medical research after his death donated his body to a medical college in Uttar Pradesh's Jhansi. The deceased Krishna Kumar Soni had served as a deputy manager in the telecommunications department before retiring in 2006. He died on May 10 at 78. His elder son Anand, who works as a Senior Deputy General Manager (DGM) in BHEL, spoke to ETV Bharat about his father's wish.
Jhansi (Uttar Pradesh): Fulfilling their father's last wish, the children of a former telecommunication department Deputy Manager who died on Friday donated his body to a medical college in Uttar Pradesh's Jhansi.
The deceased Krishna Kumar Soni died a natural death. He was 78 and served in several posts in the telecommunication department for decades before retiring as Deputy Manager from Jabalpur in 2006.
Soni had asked his children to donate his body after his death so that the medical students could learn from it. Abiding by his wish, Soni's eldest son Anand, younger one Anupam, and his daughter Anuradha donated the body to the medical college.
Anand, who works as Senior Deputy General Manager (DGM) in BHEL, told ETV Bharat that his father had made a wish that his body be donated so that it could be used for learning and progress in medical science. "He wanted his body to be used in medical science and that the students benefit and learn from it. He had decided several years ago and had informed us about the same," Anand said.
More About Body Donation
Body Donation, also called Deh Dan in India, is the donation of the whole body after death for medical research and education. According to Organ Receiving & Giving Awareness Network (ORGAN), an NGO at the forefront of organ donation, Deh Dan is important for helping medical students and researchers understand the human body, and for the advancement of science.
How to pledge
ORGAN says that any person wishing to donate their body can make prior arrangements with the local medical college, hospital, or an NGO, before death. Individuals may request a consent form from a medical institution or an NGO, which will then give information about policies and procedures followed after the potential donor is deceased. However, signing a prior consent form is not compulsory but is preferable so that your family is aware of your decision and the role they need to play in fulfilling your wish.
Some renowned Indians who donated their body for medical research include Jurist Leila Seth, CPI (M) leader Somnath Chatterji, Former West Bengal Chief Minister Jyoti Basu, and Jana Sangh leader Nanaji Deshmukh.
Bhubaneswar: Parents Donate Organs of Their 8-Year-Old Brain Dead Son In first bilateral hand transplant in north India, dying patient saves four lives Women outnumber men while signing up on portal for organ donation
Quick Links / Policies
- PRIVACY POLICY
- CODE OF ETHICS
- TERMS & CONDITIONS
Please write to us, for media partnership and Ad-sales inquiries. Email: [email protected]
Jaipur's Himmat Singh Lives Up to His Name, Climbs 70,679 Stairs To Have A Crack at Guinness World Record
Mother's day 2024: five last-minute gift ideas to surprise your mom, as summers simmer, here's how you can protect yourself from heat wave, with artificial intelligence, researchers find where greek philosopher plato was buried.

Copyright © 2024 Ushodaya Enterprises Pvt. Ltd., All Rights Reserved.

IMAGES
VIDEO
COMMENTS
Body donation procedure. Mayo Clinic's procedure for accepting a whole-body donation begins with notification of a donor's death. A healthcare representative from the hospital, medical facility or hospice organization where the death occurs should contact Mayo Clinic's donor program coordinator. The coordinator reviews the acceptance protocol ...
Body donation for medical education and disease research impacts everyone's quality of life. Research For Life is a Whole Body donation organization working to bridge the gap between donors, medical educators, and disease researchers developing solutions for a more advanced "tomorrow.". Through our work, we have helped to change the lives ...
Body donation significantly impacts advancements in medical research, development, and education every day. MedCure acts as a bridge between whole-body donors and the medical professionals who rely on those donations to help shape the future of medicine. Together, these donors and medical professionals make lasting impacts on the future of ...
The gift of body donation allows medical researchers and educators to practice, learn, and create new techniques that continue to improve and save lives. ... Stay up-to-date with Science Care, medical research, and health and wellness tips. Your Email Address: I consent to having Science Care collect my email address.* Thank you! Your ...
Donation Coordinators are available 24 hours a day to answer your questions and assist you with the donation process. Whether you are registering your future intent to be a body donor, you are currently receiving hospice care, or if your loved one has already passed, we can guide you through every step. Toll-free: +1-866-560-2525.
Whole-body donation is the act of gifting your body to medical education or research when you die. Body donation allows future healthcare professionals to master complex anatomy. It also helps medical researchers contribute to life-saving care for current and future patients. What happens to your body after you die is an extremely personal choice.
Research For Life connects whole body donors to the educators and researchers who use human tissue to advance medicine. We have worked with thousands of families through the Research For Life Donor Program. This program provides a no-cost alternative to traditional funeral arrangements that includes transportation, cremation, and options for the final disposition of the cremains. Pre ...
Whole Body Donation Saves Lives. You Can Benefit Humanity. We Can Help. The Research For Life whole body donor program connects donors with medical researchers and educators who require human tissue for their essential work. Through this powerful gift, each donor has taken that monumental first step towards benefiting humanity and providing hope to future generations.
By donating your body to science, individuals have a real and lasting way to support medical research advancements that impact the lives of. 800-300-5433 . Toggle navigation . Navigation. About Us ... Through the benefits of whole body donation, medical communities are able to continue to discover cures and therapies for many diseases and ...
The Science Care Process: How Body Donation Works. Learn about no-cost cremation, important forms to complete, and our commitment to honor each donor's wish. How You May Be Able to Advance Medical Research. 96% of Science Care accepted donations are placed with medical education or research initiatives, helping donors leave a lasting legacy.
The Medical Education and Research Institute (MERI) in Memphis, TN is the non-profit organization that supports the Genesis Whole Body Donation Program. Donors make critical education and training possible through their selfless and generous gift for physicians, surgeons, nurses, EMTs, and other medical professionals from around the world.
The Body Donation Program is fundamental, not just to the education of our medical students, but it's also pivotal in the advancements of medical research and surgical training. Real human donors offer an unparalleled resource for learning and practice.
Willed Body Program. The University of Washington's Willed Body Program is a whole-body donation program for donors from Washington State. The gift of your body to the UW School of Medicine is an invaluable contribution to the education of future healthcare providers, enabling them to study and understand the complexity of the human body in a ...
Defining Whole Body Donation. At its core, whole body donation is the gift of one's entire body for medical advancement post-mortem. This process is distinct from organ donation, as it supports a broader scope of medical research and training. Whole body donations are invaluable in teaching anatomy, practicing surgical techniques, and ...
We are grateful to all of those who wish to donate their bodies for anatomical education and medical research. If you have any questions that this website does not answer, please feel free to contact us directly. Phone: (716) 829-2913. Email : [email protected].
PDF. How You Can Help Medical Research: Donating Your Blood, Tissue, and Other Samples covers the importance of tissue donation for advancing medical research. This booklet: Explains what tissue samples are. Explains why it's important for people to donate tissue. Discusses how and where to donate. Responds to many common questions and concerns.
Whole body donation is a form of non-transplant anatomical donation made under the Darlene Luther Uniform Anatomical Gift Act. Typically, donation authorization is completed prior to death on behalf of the individual. At the time of death or immediately following a funeral, the deceased's remains are received by the Anatomy Bequest Program ...
Body Donation Program. 216.444.6870. Register. Contact Us. Due to COVID-19, we cannot accept body donations of individuals who had, or tested positive for, COVID-19 within 30 days prior to death. Read More About Our Conditions of Acceptance.
Anatomical Donations Program. 3767 Medical Science Building II. 1137 Catherine St. Ann Arbor, MI 48109-5608. 734-764-4359. [email protected].
Body Donation. The Anatomical Education Program was created in 1903 by the Indiana General Assembly to ensure the quality of education for medical, dental and allied health students across the state of Indiana. This program is administered by Indiana University School of Medicine and is authorized to provide for the acquisition, distribution ...
Donating your body, brain or tissue to a medical school or research establishment is a valuable gift - your donation will become an important resource for training healthcare professionals or for research, and such donations are highly valued by staff and students alike.
Once you register to become a donor, the Body Donation Program keeps your name and contact information on file. Upon your death, a caregiver or family member must contact us right away (within 24 hours of death). We take calls 24 hours a day, 365 days a year at 1.844.366.9633.
Purpose Black women are underrepresented in clinical research and clinical trials. Knowledge gaps lead to biased clinical practice and care. There is a small but growing body of literature on Black women's perceptions about participation when biospecimen donation is sought by researchers. This is the first known study to investigate willingness to participate in clinical research involving ...
Body Donation, also called Deh Dan in India, is the donation of the whole body after death for medical research and education. According to Organ Receiving & Giving Awareness Network (ORGAN), an NGO at the forefront of organ donation, Deh Dan is important for helping medical students and researchers understand the human body, and for the ...