

15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)

Last updated on August 19th, 2023
Critical thinking is a powerful tool that nurses use to make informed decisions, provide top-notch care, and untangle complex problems.
Think of it as a toolbox filled with skills that let nurses dig deeper, understand better, and think smarter.
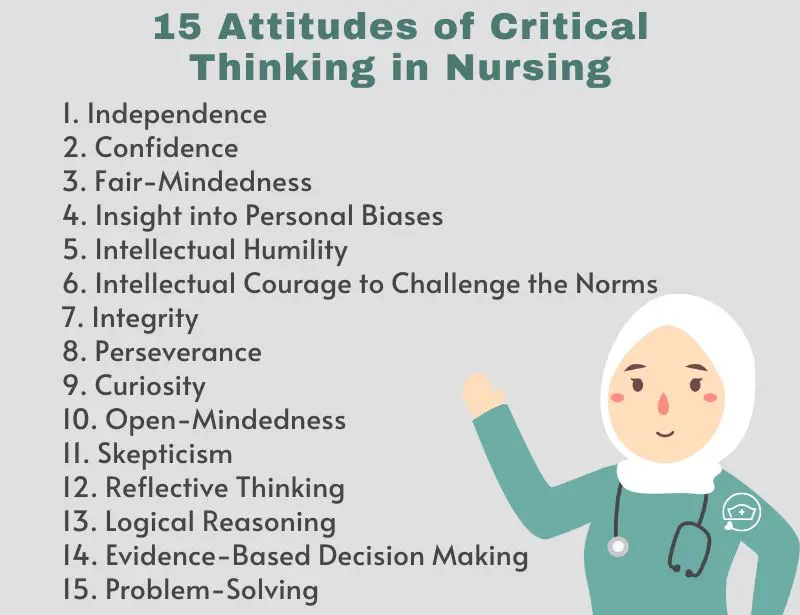
In this article, we’re going to explore the 15 super-important attitudes of critical thinking in nursing .
Each attitude is like a special key that helps nurses unlock the best care for their patients. Let’s dive in and learn about each attitude.
How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
15 Attitudes of Critical Thinking in Nursing
1. Independence
Independence is like thinking for yourself and making your own choices. Imagine you’re deciding what book to read, and you pick one that interests you, not just what others like – that’s being independent.
In nursing, independence means using your own judgment to provide the best care.
For, example, consider Rachel, a nurse, who considers various options to treat a patient’s pain, not just following what others do. Rachel’s independence helps her find solutions tailored to each patient’s needs.
Just like choosing your own book, independent nurses think critically and make decisions based on what’s best for their patients.
2. Confidence
Confidence is like believing in yourself and your abilities, even when faced with challenges. Imagine you’re trying a new activity, and you trust that you can learn and do well – that’s having confidence.
In nursing, confidence means having faith in your skills and judgment to provide excellent care. Example: For instance, think of Ava, a nurse, who remains composed when a patient’s condition suddenly worsens.
She knows she can handle the situation because of her training and experience. Ava’s confidence allows her to make quick and effective decisions during critical moments.
Just like trusting yourself in a new activity, confident nurses trust their expertise to deliver top-notch care to their patients.
3. Fair-Mindedness
Fair-mindedness is like treating everyone equally and making judgments based on facts, not personal feelings. Imagine you’re playing a game, and you give every player the same chance to win – that’s being fair-minded.
In nursing, fair-mindedness means being impartial and considering all viewpoints without bias.
For example, picture Liam, a nurse, who listens to both the patient and the family when making a decision about treatment.
He doesn’t let his own opinions influence his judgment. Liam’s fair-mindedness ensures that he provides balanced and patient-focused care.
Just like being fair in a game, fair-minded nurses make decisions that are just and unbiased, promoting the best outcomes for their patients.
4. Insight into Personal Biases
Insight into personal biases is like looking at yourself from the outside to see if your own feelings might affect your decisions. Imagine you have a favorite color, and you realize you tend to choose things in that color even if other options might be better – that’s being aware of your bias.
In nursing, insight into personal biases means being mindful of your own preferences and not letting them cloud your judgment.
For instance, think of Maya, a nurse, who knows she might prefer a particular treatment because it worked for her family member.
However, she steps back and considers what’s truly best for her patient’s situation. Maya’s insight helps her provide care that’s unbiased and patient-centered.
Just like being aware of your color preference, insight into personal biases helps nurses make decisions that are based on what’s right for their patients, not influenced by their own feelings.
5. Intellectual Humility
Intellectual humility is like knowing that you don’t have all the answers and being open to learning from others. Imagine you’re playing a video game, and you ask a friend for tips because they’re better at it – that’s being humble about your skills.
In nursing, intellectual humility means recognizing that you can always learn more and considering others’ expertise.
Picture James, a nurse, who seeks advice from experienced colleagues when faced with a complex case.
He knows that learning from others can lead to better patient care. James’s intellectual humility helps him grow as a nurse and keeps him open to new perspectives.
Just like seeking gaming tips, intellectual humility encourages nurses to value knowledge from various sources and continuously improve their practice.
6. Intellectual Courage to Challenge the Norms
Intellectual courage to challenge the norms is like having the bravery to question things that everyone believes are true. Imagine you’re playing a game with your friends, and everyone agrees on the rules – but you speak up and suggest a new way to play.
In nursing, intellectual courage means daring to question established practices and seeking innovative solutions.
For instance, think of Sarah, a nurse, who notices that a routine procedure might be improved for patient comfort.
Instead of staying silent, she speaks up and proposes a change, backed by research and careful thought. Sarah’s intellectual courage drives her to challenge the status quo for the sake of better patient care.
Just like suggesting a new game rule, nurses with this attitude challenge norms to advance healthcare practices and outcomes.
7. Integrity
Integrity is like being honest and doing the right thing, even when nobody’s watching. Imagine finding a lost wallet on the street – instead of keeping it, you return it to its owner because it’s the right thing to do.
In nursing, integrity means always acting ethically and responsibly, even in challenging situations.
Picture Emma, a nurse, who follows protocols and makes decisions based on what’s best for her patients, not personal gain.
Emma’s integrity shines when she prioritizes honesty, fairness, and patient well-being in every action she takes.
Just like returning that wallet, integrity is a nurse’s commitment to uphold high moral standards and maintain the trust placed in them by patients and their families.
8. Perseverance
Perseverance is like having a never-give-up attitude, even when things get tough. Imagine you’re trying to solve a challenging puzzle – even if it takes time and effort, you keep going until you find the solution.
In nursing, perseverance means facing obstacles and difficulties head-on without giving up.
For example, consider Mark, a nurse, who’s dealing with a complex patient case. Despite encountering roadblocks and uncertainties, Mark doesn’t lose hope.
He keeps researching, consulting colleagues, and trying different approaches until he finds the right solution for his patient.
Just like working through a tough puzzle, perseverance empowers nurses to keep pushing forward and find the answers that lead to the best care outcomes.
9. Curiosity
Curiosity is like having a hunger for knowledge that never goes away. Imagine you’re exploring a new place, and every corner seems to hide something interesting – you want to know what’s around the next bend.
In nursing, curiosity means having a strong desire to learn and discover.
Picture Anna, a nurse, who’s always asking questions like “Why?” and “How?” She’s not content with just knowing the basics; she wants to dive deeper and understand the “whys” behind patient conditions and treatments.
Anna’s curiosity drives her to stay updated with the latest research and innovative methods. Just like an explorer seeking new horizons, curious nurses seek new ways to provide better care for their patients.
10. Open-Mindedness
Open-mindedness is like having a door in your mind that’s always ready to welcome new ideas. Imagine you’re reading a book, and suddenly you come across a different way of thinking – instead of dismissing it, you consider it with interest.
In nursing, open-mindedness means being willing to listen to various viewpoints and explore different approaches.
For instance, think of Rachel, a nurse, who’s used to a specific way of treating wounds. But when a colleague suggests a new method, Rachel doesn’t shut the idea down.
Instead, she’s open to trying it out and seeing if it might work better for her patients. Just like being curious about new stories, open-minded nurses are curious about new ways to improve patient care.
11. Skepticism
Skepticism is like being a curious investigator who asks questions to make sure things are true. Imagine you hear about a magical potion that promises to make you fly – you might be skeptical and ask, “Is that really possible?”
In nursing, skepticism means not accepting things blindly but investigating to find the truth.
Picture Sarah, a nurse, who reads about a new treatment for pain relief. Instead of immediately believing it, she looks for evidence and checks if other experts agree.
Sarah’s skepticism helps her make sure that the treatments she uses are safe and effective for her patients.
Just like asking questions about that magical potion, nurses use skepticism to make informed decisions based on facts.
12. Reflective Thinking
Reflective thinking is like looking back at your day and thinking about what went well and what you could improve. Imagine you finished playing a game and you think about how you did – that’s reflective thinking!
In nursing, it’s when nurses take a moment to think about their actions, decisions, and interactions with patients.
For example, let’s say Jessica, a nurse, had a challenging day where she had to juggle multiple tasks. At the end of her shift, she takes a few minutes to reflect.
She thinks about what she did right, like comforting a worried patient, and what she could do better, like managing her time more efficiently.
This reflection helps Jessica learn from her experiences and become an even better nurse.
Just like looking in a mirror to see yourself, reflective thinking helps nurses see their actions and grow from them.
13. Logical Reasoning
Logical reasoning is like putting together the pieces of a puzzle to see the bigger picture. It’s about thinking step by step to reach a smart conclusion.
Imagine you have a math problem to solve. You start with the information you know and use logical steps to find the answer.
Similarly, nurses use logical reasoning to understand their patients’ situations
Let’s say Emily, a nurse, has a patient with a high fever and a sore throat. She gathers information about the symptoms, asks questions, and puts all the clues together.
By using logical steps, Emily figures out that the patient might have a throat infection and can recommend the right treatment.
Just like solving a puzzle, logical reasoning helps nurses connect the dots and make decisions that make sense for their patient’s health.
14. Evidence-Based Decision Making
Evidence-based decision-making is like being a detective who gathers clues before solving a mystery.
For instance, imagine Alex, a nurse, who wants to find the best way to help patients with diabetes manage their blood sugar levels.
Instead of guessing, he reads research studies and talks to experts in the field. Alex uses the facts he collects to choose treatments that are proven to work.
Just like a detective uses evidence to solve a case, Alex uses evidence to make informed decisions that lead to better patient outcomes.
15. Problem-Solving
Problem-solving is like being a detective on a mission. Think of it like when you have to figure out how to fix a broken toy.
For instance, Linda, a nurse, faces a challenge when a patient’s pain medication isn’t working well. Instead of giving up, she gathers information, talks to the patient, and works with the medical team to find a better solution.
Linda’s problem-solving skills help her piece together the right treatment plan, just like solving a tricky puzzle.
- What is Critical Thinking in Nursing? (Explained W/ Examples)
- What is the “5 Whys” Technique?
- What Are Socratic Questions?
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
Critical thinking is a powerful tool that nurses use every day. These 15 attitudes are like a treasure map that guides nurses through the world of healthcare.
From being independent thinkers to having the courage to challenge norms, these attitudes help nurses provide the best care possible.
Comments are closed.
Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.

Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Critical Thinking and Decision-Making Skills
Chapter 4 Critical Thinking and Decision-Making Skills Betsy Frank http://evolve.elsevier.com/Huber/leadership/ In an era of changing reimbursements, value based purchasing, and expanded roles for nursing in the health care delivery system, critical thinking and decision making are important skills for nurses caring for patients and for nurse leaders and managers. Both the American Nurses Association’s (2009) and American Association of Nurse Executives’ (2005) standards for practice for nurse administrators and executives support the fact that in a fast-paced health care delivery environment, staff nurses, leaders, and managers must be able to analyze and synthesize a large array of information, use critical thinking and decision making skills to deliver effective day to day patient care, and solve complex problems that occur in complex health care delivery systems (see Figure 4-1 ). Furthermore, the Magnet Hospital initiative and the Institute of Medicine’s ( Committee on the Robert Wood Johnson Foundation, 2011 ) Future of Nursing report highlight the need for nurses to be able to be fully involved and even take the lead in decision making from the unit level to the larger health care delivery system. FIGURE 4-1 Differences and interactions among critical thinking, problem solving, and decision making. Nurses are a cadre of knowledge workers within the health care system. As such, they need information, resources, and support from their environment. In fact, the nurse manager’s expertise in critical thinking and shared decision making are essential for creating healthy work environments where quality and effective care can be delivered ( Kramer et al., 2010 ; Zori et al., 2010 ). Critical thinking and decision-making competences include analytical skills as well as intuition. Just as intuition is part of expert clinical practice ( Benner, 1984 ), intuition plays an important role in developing managerial and leadership expertise (Shirey, 2007). DEFINITIONS Critical thinking can be defined as a set of cognitive skills including “interpretation, analysis, evaluation, inference, explanation, and self-regulation” ( Facione, 2007 , p. 1). Using these skills, nurses in direct patient care and leaders and managers can reflect analytically, reconceptualize events, and avoid the tendency to make decisions and problem solve hastily or on the basis of inadequate information. Facione also pointed out that critical thinking is not only a skill but also a disposition that is grounded in a strong ethical component. Critical thinking in nursing can be defined as “purposeful, informed, outcomes focused thinking…[that] applies logic, intuition, creativity and is grounded in specific knowledge, skills, and experience” ( Alfaro-LeFevre, 2009 , p. 7). Alfaro-LeFevre noted that outcomes-focused thinking helps to prevent, control, and solve problems. Tanner (2000) noted that critical thinking is much more than just the five steps of the nursing process. Problem solving involves moving from an undesirable to a desirable state ( Chambers, 2009 ). Problem solving occurs in a variety of nursing contexts, including direct client care, team-level leadership, and systems-level leadership. Nurses and nurse managers are challenged to move from step-by-step problem-solving techniques to incorporating creative thinking, which involves considering the context when meeting current and future challenges in health care delivery ( Chambers, 2009 ; Rubenfeld & Scheffer, 2006 ). Decision making is the process of making choices that will provide maximum benefit ( Drummond, 2001 ). Decision making can also be defined as a behavior exhibited in selecting and implementing a course of action from alternative courses of action for dealing with a situation or problem. It may or may not be the result of an immediate problem. Critical thinking and effective decision making are the foundation of effective problem solving. If problems require urgent action, then decisions must be made rapidly; if solutions do not need to be identified immediately, decision making can occur in a more deliberative way. Because problems change over time, decisions made at one point in time may need to be changed ( Choo, 2006 ). For example, decisions about how to staff a unit when a nurse calls in sick have to be made immediately. However, if a unit is chronically short-staffed, a decision regarding long-term solutions will have to be made. The process of selecting one course of action from alternatives forms the basic core of the definition of decision making. Choo (2006) noted that all decisions are bounded by cognitive and mental limits, how much information is processed, and values and assumptions. In other words, no matter the decision-making process, all decisions are limited by a variety of known and unknown factors. In a chaotic health care delivery environment, where regulations and standards of care are always changing, any decision may cause an unanticipated future problem. BACKGROUND Critical Thinking Critical thinking is both an attitude toward handling issues and a reasoning process. Critical thinking is not synonymous with problem solving and decision making ( Figure 4-1 ), but it is the foundation for effective decision making that helps to solve problems ( Fioratou et al., 2011 ). Figure 4-2 illustrates the way obstacles such as poor judgment or biased thinking create detours to good judgment and effective decision making. Critical thinking helps overcome these obstacles. Critical thinking skills may not come naturally. The nurse who is a critical thinker has to be open-minded and have the ability to reflect on present and past actions and to analyze complex information. Nurses who are critical thinkers also have a keen awareness of their surroundings ( Fioratou et al., 2011 ). FIGURE 4-2 Decision-making maze. Critical thinking is a skill that is developed for clarity of thought and improvement in decision-making effectiveness. The roots of the concept of critical thinking can be traced to Socrates, who developed a method of questioning as a way of thinking more clearly and with greater logical consistency. He demonstrated that people often cannot rationally justify confident claims to knowledge. Confused meanings, inadequate evidence, or self-contradictory beliefs may lie below the surface of rhetoric. Therefore it is important to ask deep questions and probe into thinking sequences, seek evidence, closely examine reasoning and assumptions, analyze basic concepts, and trace out implications. Other thinkers, such as Plato, Aristotle, Thomas Aquinas, Francis Bacon, and Descartes, emphasized the importance of systematic critical thinking and the need for a systematic disciplining of the mind to guide it in clarity and precision of thinking. In the early 1900s, Dewey equated critical thinking with reflective thought ( The Critical Thinking Community, 2008 ). Critical thinking, then, is characterized by thinking that has a purpose, is systematic, considers alternative viewpoints, occurs within a frame of reference, and is grounded in information ( The Critical Thinking Community, 2008 ). Questioning is implicit in the critical thinking process. The following are some of the questions to be asked when thinking critically about a problem or issue ( Elder & Paul, n.d. ): • What is the question being asked? • Is this the right question? • Is there another question that must be answered first? • What information is needed? • Given the information, what conclusions are justified? • Are there alternative viewpoints? No matter what questions are asked, critical thinkers need to know the “why” of the thinking, the mode of reasoning (inductive or deductive), what the source and accuracy of the information is, what the underlying assumptions and concepts are, and what might be the outcome of the thinking ( The Critical Thinking Community, 2008 ). Critical Thinking in Nursing Nurses in clinical practice continually make judgments and decisions based on the assessment and diagnosis of client needs and practice problems or situations. Clinical judgment is a complex skill grounded in critical thinking. Clinical judgment results in nursing actions directed toward achieving health outcomes ( Alfaro-LeFevre, 2009 ). Scheffer and Rubenfeld (2000) have stated that habits of the mind that are characteristic of critical thinking by nurses include confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, open-mindedness, perseverance, and reflection. Emphasizing the value of expert experience and holistic judgment ability, Benner (2003) cautioned that clinical judgments must not rely too heavily on technology and that the economic incentives to use technology must not come at the expense of human critical thinking and reasoning in individual cases. Critical thinkers have been distinguished from traditional thinkers in nursing. A traditional thinker, thought to be the norm in nursing, preserves status quo. Critical thinkers go beyond the step-by-step processes outlined in the nursing process and traditional problem solving. A critical thinker challenges and questions the norm and considers in the context of decision making potential unintended consequences. Unlike traditional thinkers, critical thinkers are creative in their thinking and anticipate the consequences of their thinking ( Rubenfeld & Scheffer, 2006 ). Creativity is necessary to deal with the complex twenty-first century health care delivery environment. Nurse leaders and managers have an obligation to create care delivery climates that promote critical thinking, which leads to innovative solutions to problems within the system of care ( Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing, at the Institute of Medicine; Institute of Medicine, 2011 ; Porter-O’Grady, 2011 ). Such a climate encourages deep reflection, especially so that nurses feel safe to learn from mistakes, and encourages nurses to ask questions and consider a variety of viewpoints and alternative solutions to problems. What specific strategies can be used to promote a climate in which critical thinking is fostered? First and foremost, the nurse manager/leader, in the role of mentor, coach, or preceptor, should encourage questions such as “Is what you are doing or proposing based on sound evidence?” ( Ignatavicius, 2008 ). However, Snowden and Boone (2007) cautioned that “best practice, by definition is past practice” (p. 71). Therefore use of best practices needs to be examined carefully in order to use them appropriately. Staff nurses and managers must use critical thinking skills in order to determine the appropriateness of implementing recommended practice protocols. As managers, allowing staff and self “think time” is essential for reflection and is a key component of critical thinking ( Zori & Morrison, 2009 ). Nurse managers’ critical thinking abilities promotes a positive practice environment which can lead to better patient outcomes ( Zori, Nosek, & Musil, 2010 ). Coaching new and experienced nurses to develop expertise in clinical judgment is critically important. Many new nurses, in particular, need to further develop their critical thinking skills ( Fero et al., 2008 ; Forneris & Peden-McAlpine, 2009 ). In addition to having preceptors and others ask questions of new nurses, nurse managers and leaders can use other strategies to enhance critical thinking in nursing staff. Developing concept maps is another useful strategy to promote critical thinking. Although typically used in prelicensure programs ( Ellermann et al., 2006 ), nurse managers can encourage their preceptors to use concept maps with orientees ( Toofany, 2008 ). Developing concept maps in concert with others further develops a nurse’s critical thinking through the process of dialogue. Simulations also promote critical thinking or “thinking like a nurse” ( Tanner, 2006 ). According to Tanner, simulations can promote clinical reasoning, which leads to making conclusions in the form of clinical judgments and, thus, effective problem solving. The use of human patient simulators is well known in educational settings. Simulators may also be useful in orienting new graduates to the acute care setting ( Leigh, 2011 ). Pulman and colleagues (2009) have reported on the use of simulators to promote critical thinking role development in inter-professional environments. Decision Making Decision making is the essence of leadership and management. It is what leaders and managers are expected to do ( Keynes, 2008 ). Thus decisions are visible outcomes of the leadership and management process. The effectiveness of decision making is one criterion for evaluating a leader or manager. Yet staff nurses and nurse managers and leaders must make decisions in uncertain and complex environments ( Clancy & Delaney, 2005 ). Within a climate of uncertainty and complexity, nurse managers and leaders must also understand that all decision making involves high-stakes risk taking ( Clancy & Delaney, 2005 ; Keynes, 2008 ). If poor decisions are made, progress can be impeded, resources wasted, harm caused, and a career adversely affected. The results of poor decisions may be subtle and not appear until years later. Take, for instance, a decision to reduce expenses by decreasing the ratio of registered nurses to nurses’ aides. There may be a short-term cost savings, but if not implemented appropriately, this tactic may result in the gradual erosion of patient care over time (Kane et al., 2007). Unintended effects may include higher turnover of experienced nurses, increased adverse events such as medication errors, decreased staff morale, and lower patient satisfaction scores. The long-term outcome of this decision may actually result in increased expenses not reduced expenses. Thus it is vital for nurses to understand decision making and explore styles and strategies to enhance decision-making skills. Decision making, like traditional problem solving, has been traditionally thought of as a process with identifiable steps yet influenced by the context and by whether there is an intuitive grasp of the situation. However, Effken and colleagues (2010) stated that decision making is much more. Expert decision making is a constructive process in which the outcomes are not preplanned or simply pulled out of a memory bank. Instead, expert decision-making activities are creative, innovative, and adapted to uncertainty and the context of the current problem, using learning from prior experience (p. 189). Nurses make decisions in personal, clinical, and organizational situations and under conditions of certainty, uncertainty, and risk. Various decision-making models and strategies exist. Nurses’ control over decision making may vary as to amount of control and where in the process they can influence decisions. Although decision-making is more than a step-by-step process as noted by Effken and colleagues (2010) , awareness of the components, process, and strategies of decision making contributes to effectiveness in nursing leadership and management decision making. The basic elements of decision making, which enhances day to day activities, contributes to strategic planning and solves problems can be summarized into the following two parts: (1) identifying the goal for decision-making, and (2) making the decision. According to Guo (2008, p. 120) , the steps of the decision-making process can be illustrated as follows, using DECIDE: • D efine the problem and determine why anything should be done about it and explore what could be happening. • E stablish desirable criteria for what you want to accomplish. What should stay the same and what can be done to avoid future problems? • C onsider all possible alternative choices that will accomplish the desired goal or criteria for problem solution. • I dentify the best choice or alternative based on experience, intuition, experimentation. • D evelop and implement an action plan for problem solution. • E valuate decision through monitoring, troubleshooting, and feedback. Notice how these steps are analogous to the traditional problem-solving process or nursing process well-known by nurses and nurse managers. Thus decision making is used to solve problems. However, decision making is more than just problem solving. Decision making may also be the result of opportunities, challenges, or more long-term leadership initiatives as opposed to being triggered by an immediate problem. In any case, the processes are virtually the same, but their purposes may be slightly different. Nurse managers use decision making in managing resources and the environment of care delivery. Decision making involves an evaluation of the effectiveness of the outcomes that result from the decision-making process itself. Whether nurse managers are the sole decision makers or facilitate group decision making, all the factors that influence the problem-solving process also impact how decisions are made: who owns the problem that will result in a decision, what is the context of the decision to be made, and what lenses or perspectives influence the decision to be made? For example, the chief executive officer may frame issues as a competitive struggle not unlike a sports event. The marketing staff may interpret problems as military battles that need to be won. Nurse executives may view concerns from a care or family frame that emphasizes collaboration and working together. Learning and understanding which analogies and perspectives offer the best view of a problem or issue are vital to effective decision making. It may be necessary for nurse managers to expand their frame of reference and be willing to consider even the most outlandish ideas. Obviously, it is important to begin the goal definition phase with staff members who are closest to the issue. That includes staff nurses in concert with their managers. Often, decisions can originate within the confines of the shared governance system that may be in place within an organization ( Dunbar et al., 2007 ). It is wise, also, to consider adding individuals who have no connection with the issue whatsoever. Often it is these “unconnected” staff members who bring new decision frames to the meeting and have the most unbiased view of the problem. One of the core competencies for all health professionals is working in interprofessional teams ( Interprofessional Education Collaborative Expert Panel, 2011 ). Therefore using interprofessional teams for problem solving and decision making can be assumed to be more effective than working in disciplinary silos. No matter who is involved in the decision-making process, the basic steps to arrive at a decision to resolve problems remain the same. One critical aspect to note, however, is that in making decisions, nurse managers must have situational awareness ( Sharma & Ivancevic, 2010 ). That is, decision makers must always consider the context in which the outcome of the decision is to occur. A decision that leads to a desired outcome on one patient care unit may lead to undesirable outcomes on another unit because the patient care environment and personnel are different. DECISION OUTCOMES When looking at outcomes, one critical aspect of decision making is to determine the desired outcome. The desired outcome may vary, according to Guo (2008) , from an ideal or short-term resolution to covering up a situation. What is desired may be (1) for a problem to go away forever, (2) to make sure that all involved in this problem are satisfied with the solution and gain some benefit from it, or (3) to obtain an ideal solution. Sometimes a quick decision is desired, and researching different aspects of the problem or allowing for participation in decision making is not appropriate. For example, in disaster management, the nurse leader will use predetermined procedures for determining roles of the various personnel involved (Coyle et al., 2007). Desired decisions can be categorized into two end points: minimal and optimal. A minimal decision results in an outcome that is sufficient, satisfies basic requirements, and minimally meets desired objectives. This is sometimes called a “satisficing” decision . An optimizing decision includes comparing all possible solutions with desired objectives and then selecting the optimal solution that best meets objectives ( Choo, 2006 ; Guo, 2008 ). In addition to these two strategies, Layman (2011) drawing from Etzioni (1986) , discussed two other strategies: mixed scanning and incrementalism. Incrementalism is slow progress toward an optimal course of action. Mixed scanning combines the stringent rationalism of optimizing with the “muddling through” approach of incrementalism to form substrategies. Optimizing has the goal of selecting the course of action with the highest payoff (maximization). Limitations of time, money, or people may prevent the decision maker from selecting the more deliberative and slower process of optimizing. Still, the decision maker needs to focus on techniques that will enhance effectiveness in decision-making situations. Barriers to effective decision making exist and, once identified, can lead to going back through the decision-making process. Flaws in thinking can create hidden traps in decision making. These are common psychological tendencies that create barriers or biases in cognitive reflection and appraisal. Six common distortions are as follows ( Hammond et al., 1998 ; 2006 ): 1. Anchoring trap: When a decision is being considered, the mind gives a disproportionate weight to the first information it receives. Past events, trends, and numbers outweigh current and future realities. All individuals have preconceived notions and biases that influence decisions in a variety of ways. For instance the Institute of Medicine (IOM, 2001) endorsed the use of c omputerized p hysician o rder e ntry (CPOE) as one solution to reduce medication errors. Furthermore, The Centers for Medicare and Medicaid Services has set forth meaningful use criteria for implementation of CPOE as well as electronic health records (EHR). Despite incentive payments for implementing EHR ( HFMA P & P Board, 2012 ), the financial costs involved, human-factor errors and work-flow issues can hamper successful implementation ( Campbell et al., 2006 ). 2. Status-quo trap: Decision makers display a strong bias toward alternatives that perpetuate the status quo. In the face or rapid change in the environment, past practices that exhibit any sense of permanence provide managers with a feeling of security. 3. Sunk-cost trap: Past decisions become sunk costs, and new choices are often made in a way that justifies past choices. This may result in becoming trapped by an escalation of commitment. Because of rapid, ongoing advances in medical technology, managers are frequently pressured to replace existing equipment before it is fully depreciated. If the new equipment provides a higher level of quality at a lower cost, the sunk cost of the existing equipment is irrelevant to the decision-making process. However, managers may delay purchasing new equipment and forgo subsequent savings because the equipment has yet to reach the end of its useful life. 4. Confirming-evidence trap: Kahneman and colleagues (2011) noted that decision makers also fall into the trap of confirmation bias where contradictory data are ignored. This bias leads people to seek out information that supports an existing instinct or point of view while avoiding contradictory evidence. A typical example is favoring new technology over less glamorous alternatives. A decision maker may become so enamored by technological solutions (and slick vendor demonstrations) that he or she may unconsciously decide in favor of these systems even though strong evidence supports implementing less costly solutions first. 5. Framing trap: The way a problem is initially framed profoundly influences the choices made. Different framing of the same problem can lead to different decision responses. A decision frame can be viewed as a window into the varied reasons a problem exists. As implied by the word frame , individuals may perceive problems only within the boundaries of their own frame. The human resources director may perceive a staffing shortage as a compensation problem, the chief financial officer as an insurance reimbursement issue, the director of education as a training issue, and the chief nursing officer as a work environment problem. Obviously all these issues may contribute, in part, to the problem; however, each person, in looking through his or her individual frame, sees only that portion with which he or she is most familiar ( Layman, 2011 ). 6. Estimating and forecasting traps: People make estimates or forecasts about uncertain events, but their minds are not calibrated for making estimates in the face of uncertainty. The notion that experience is the parent of wisdom suggests that mature managers, over the course of their careers, learn from their mistakes. It is reasonable to assume that the knowledge gained from a manager’s failed projects would be applied to future decisions. Whether right or wrong, humans tend to take credit for successful projects and find ways to blame external factors on failed ones. Unfortunately, this form of overconfidence often results in overly optimistic projections in project planning. This optimism is usually buried in the analysis done before ranking alternatives and recommendations. Conversely, excessive cautiousness or prudence may also result in faulty decisions. This is called aversion bias ( Kahneman et al., 2011 ). Dramatic events may overly influence decisions because of recall and memory, exaggerating the probability of rare but catastrophic occurrences. It is important that managers objectively examine project planning assumptions in the decision-making process to ensure accurate projections. Because misperceptions, biases, and flaws in thinking can influence choices, actions related to awareness, testing, and mental discipline can be employed to ferret out errors in thinking before the stage of decision making ( Hammond et al., 1998 ). Data-driven decision making is important ( Dexter et al., 2011 ; Lamont, 2010 ; Mick, 2011 ). The electronic health record can be mined for valuable data, upon which fiscal, human resource, and patient care decisions can be made. However, the data derived can be overwhelming and cause decision makers to make less than optimal decisions. Shared decision making can help ameliorate decision traps ( Kahneman et al., 2011 ) because dissent within the group may help those accountable for the decision to prevent errors that are “motivated by self-interest” (p. 54). More alternatives can be generated by a group and more data can be gathered upon which to base the decision, rather than just using data that is more readily apparent. DECISION-MAKING SITUATIONS The situations in which decisions are made may be personal, clinical, or organizational ( Figure 4-3 ). Personal decision making is a familiar part of everyday life. Personal decisions range from multiple small daily choices to time management and career or life choices. FIGURE 4-3 Decision-making situations. Clinical decision making in nursing relates to quality of care and competency issues. According to Tanner (2006) , decision making in the clinical arena is called clinical judgment . In nursing, as with all health professions, clinical judgments should be patient-centered, use available evidence from research and other sources, and use available informatics tools (IOM, 2003). These crucial judgments should take place within the context of interprofessional collaboration. Within a hospital or other health care agency, a social network forms that is interprofessional ( Tan et al., 2005 ). This social network has to collaborate for positive change within the organization and to make clinical decisions of the highest quality. Nurses manage care and make decisions under conditions of certainty, uncertainty, and risk. For example, if research has shown that, under prescribed conditions, the selection of a specific nursing intervention is highly likely to produce a certain outcome, then the nurse in that situation faces a condition of relative certainty. An example would be the prevention of decubitus ulcers by frequent repositioning. If little knowledge is available or if the specific situation is more complex or variant from the usual, then the nurse faces uncertainty. Risk situations occur when a threat of harm to patients exists. Conditions of risk occur commonly relative to the administration of medications, crisis events, infection control, invasive procedures, and the use of technology in nursing practice. Furthermore, these conditions also apply to the administration of nursing care delivery, in which decision making is a critical function. Conditions of uncertainty and complexity are common in nursing care management. Over time, the complexity of health care processes has increased as a natural outgrowth of innovation and new technology. With computerized integration of billing, physician ordering, results of diagnostic tests, information about medications and their actions and side effects, and critical pathways and computerized charting, complexity increases more. Trying to integrate so many data points in care delivery can overwhelm the care provider who is making clinical judgments. As a result, subtle failures in any part of the information system can go unnoticed and have catastrophic outcomes. For example, if the computer system in the emergency room cannot “talk” to the system in the operating room, then errors in care management, such as giving cephalexin to patient who has an allergy can occur. If a provider fails to input critical information, such as a medication that a patient is taking, a fatal drug interaction could occur when another provider prescribes a new medication. Ready access to the Internet and online library sources can further create complexity in the decision-making process as care providers have access to more information upon which to make decisions. Readily accessible information related to evidence-based practice and information gleaned from human resources records and clinical systems can overwhelm nurse managers and leaders. Nurse leaders are coming to understand that innovation and new technology are the driving forces behind the discovery of new knowledge and improvements in patient care. Overlapping, unclear, and changing roles for nurses as a result of new technology and services create complex decision-making situations and impact the quality of care delivered (IOM, 2003). In addition, workflow interruptions can inhibit critical thinking, particularly in a chaotic environment ( Cornell et al., 2011 ; Sitterding et al., 2012 ). ADMINISTRATIVE AND ORGANIZATIONAL DECISION MAKING According to Choo (2006) , organizations use information to “make decisions that commit resources and capabilities to purposeful action” (p. 1). Nurse managers, for example, make staffing decisions and thus commit financial resources for the purpose of delivering patient care. Hospital administrators may decide to add additional services to keep up with external forces. These decisions subsequently have financial implications related to reimbursement, staffing, and the like. Etzioni (1989) noted that the traditional model for business decisions was rationalism. However, he further asserted that as information flow became more complex and faster-paced, a new decision-making model based on the use of partial information that has not been fully analyzed had begun to evolve. He called this model “humble decision making.” This approach arises in response to the need to make a decision when the amount of data exceeds the time available to analyze it. For instance, predicting the outcome of clinical and administrative decisions in health care is problematic because such processes are collectively defined as c omplex a daptive s ystems (CASs). A CAS is characterized by groups of individuals who act in unpredictable, nonlinear (not cause and effect) ways, such that one person’s actions affect all the others ( Holden, 2005 ). In CASs, humans do behave in unpredictable ways ( Tan et al., 2005 ). Critical thinking can help all health care personnel to examine these complex systems, wherein groups solve problems through complex, continually altering interactions between the environment and all involved in the decision making ( Fioratou et al., 2011 ). Situations within the environment constantly change and decision makers need to reframe their thinking as they broaden their awareness of the context of their decisions ( Sharma & Ivancevic, 2010 ). Having situation awareness is a must ( Fioratou et al., 2011 ; Sitterding et al., 2012 ). Decision makers need to make every effort to forecast unanticipated consequences of their decisions. For example if staffing is cut, what adverse events might occur (Kane et al., 2007)? Decision making is also influenced by the manager’s leadership style. A democratic/collaborative style of leadership and decision making works best in a complex adaptive system, such as a hospital, which is characterized by a large array of social relationships that can have an economic impact on an organization. Staff nurses who are not engaged in shared decision making may experience less job satisfaction and subsequently may leave an organization, leading to loss of expertise in patient care ( Gromley, 2011 ). However, the full array of leadership styles may at some time be used in the decision-making process. Vroom and Yetton (1973) proposed a classic managerial decision-making model that identified five managerial decision styles on a continuum from minimal subordinate involvement to delegation. Their model uses a contingency approach, which assumes that situational variables and personal attributes of the leader influence leader behavior and thus can affect organizational effectiveness. To diagnose the situation, the decision maker examines the following seven problem attributes: 1. The importance of the quality of the decision 2. Whether there is sufficient information/expertise 3. The amount of structure to the problem 4. The extent to which acceptance/commitment of followers is critical to implementation 5. The probability that an autocratic decision will be accepted 6. The motivation of followers to achieve organizational goals 7. The extent to which conflict over preferred solutions is likely
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Legal and Ethical Issues
- Change and Innovation
- Data Management and Clinical Informatics
- Power and Conflict
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Emerg Med

Major challenges and barriers in clinical decision-making as perceived by emergency medical services personnel: a qualitative content analysis
Mostafa bijani.
1 Department of Medical Surgical Nursing, Fasa University of Medical Sciences, Fasa, 81936-13119 Iran
Saeed Abedi
Shahnaz karimi, banafsheh tehranineshat.
2 Community-based Psychiatric Care Research Center, Department of Nursing, School of Nursing and Midwifery, Shiraz University of Medical Sciences, Shiraz, Iran

Associated Data
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Having to work in unpredictable and critical conditions, emergency care services (EMS) personnel experience complicated situations at the scene of accidents which, inevitably, influence their clinical decisions. There is a lack of research into the challenges which these professionals encounter. Accordingly, the present study aims to explore the major challenges and barriers which affect clinical decision-making from the perspective of EMS personnel.
The present study is a qualitative work with a content analysis approach. Selected via purposeful sampling, the subjects were 25 members of the EMS personnel in Iran who met the inclusion criteria. The study lasted from December 2019 to July 2020. Sampling was maintained to the point of data saturation. Data were collected using semi-structured, in-depth, individual interviews. The collected data were analyzed via qualitative content analysis.
The results of data analysis were categorized into four themes and eight categories. The main themes were professional capabilities, occupational and environmental factors, inefficient organizational management, and ethical issues.
The results of the present study show that clinical knowledge, experience, and skills contribute to emergency care personnel’s professional capabilities in making clinical decisions. Good teamwork skills and time management can prevent feelings of confusion when the number of the injured to be attended to is large. Effective clinical decision-making skills can not only help the personnel make the right decision, but enhances their resilience and enables them to adapt to hard and unpredictable conditions. Professional factors, organizational management, and ethical matters constitute the other major factors which influence the clinical decision-making of emergency care personnel at the scene of accidents and determine the quality of their clinical performance. Thus, it is essential that pre-hospital emergency care managers improve the quality of EMS personnel’s clinical decision-making skill.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12873-021-00408-4.
In most societies today, quality pre-hospital emergency care is an essential component of caring for patients in need of emergency care [ 1 ]. Pre-hospital emergency care consists of all the emergency medical services which are provided to patients outside the hospital before they are transferred to the nearest medical center [ 2 ]. In pre-hospital emergency care, seconds and minutes can mean the difference between life and death, between suffering a serious disability and living a normal life. In order for EMS personnel to provide timely care and evaluate patients’ status in the shortest possible time, it is necessary that they be equipped with effective clinical decision-making skills and be able to make the right decision for a patient in unpredictable conditions [ 3 , 4 ]. Clinical decision-making, an important process in which the best action to achieve the desired goals is chosen, largely determines the quality of care, patient safety, and the possibility of future complications [ 5 ]. As an essential part of the professional duties of the medical personnel, clinical decision-making consists of analysis of information, making decisions, and taking action based on those decisions to accomplish the desired objective [ 6 ]. According to Emergency Nurses Association, clinical decision-making is one of the most important professional capabilities in emergency care personnel which can significantly improve the efficacy and quality of care provided [ 7 ].
The work environment in pre-hospital emergency care is complicated and unpredictable. At times, the EMS personnel should provide care to patients whose conditions are critical and unstable and who are in a life-threatening situation. Obviously, in order to make an appropriate response to quick changes in a patient’s conditions, EMS personnel should be able to decide quickly: they should know how to perform a quick evaluation of a patient’s status, determine the clinical priorities, and implement the correct intervention accordingly [ 8 , 9 ]. If EMS personnel do not have good decision-making skills, they cannot make good clinical decisions and make the right intervention, which can make a patient’s condition more critical or, in some cases, even cause permanent injuries or death [ 10 ].
Background in Iran
Pre-hospital emergency care in Iran dates back to 1975 when the first emergency care department was founded in the capital city of Tehran. After that, pre-hospital emergency care departments were gradually formed in the other provinces of Iran. These departments consist of urban centers and road centers. Pre-hospital emergency care personnel have an associate or bachelor’s degree in emergency care. Also, nurses who have a bachelor’s or master’s degree may be employed in pre-hospital emergency care. Two staff members must be present in every shift. Due to lack of staff, the shifts are on a 24-h basis and each staff member should work three 24-h shifts a week. Moreover, currently, only males are employed in pre-hospital emergency care and there is not any female staff. In pre-hospital emergency care departments, there is not a single set of clinical guidelines for the personnel and, in certain cases, the personnel act according to the internal regulations laid down by their mangers, which limits their freedom and independence.
Not many qualitative studies have addressed the factors which affect the clinical decision-making of emergency care personnel. However, a qualitative approach can result in an in-depth understanding of the concept in question and help determine its various aspects. Qualitative studies allow for determining the dimensions of a concept in a cultural context from the viewpoint of individuals who have been involved with the concept in question for a long time [ 11 ]. In addition, a qualitative approach can prove useful in identifying the barriers to clinical decision-making by emergency care personnel and achieving a deeper understanding of their experiences and challenges. In order for the quality of pre-hospital care to be improved, the rich experiences of the personnel with regard to the challenges of clinical decision-making need to be addressed. Without an understanding of the feelings and challenges which emergency care personnel experience during clinical decision-making at the scene of accidents, it is not possible to develop their professional capabilities and improve the quality of pre-hospital emergency care. Accordingly, the present study is a qualitative attempt at investigating the leading challenges and barriers in EMS personnel’s clinical decision-making.
The present study is a qualitative work of research with a content analysis approach. Conventional content analysis in qualitative research is applied when there is a lack of knowledge about the concept under study. Since the body of literature on the leading challenges and barriers in EMS personnel’s clinical decision-making is quite small, the researchers used the above-mentioned approach for their study [ 12 ]. Twenty-five members of pre-hospital emergency care personnel were selected via purposeful sampling and invited to participate in the study. Purposeful sampling is one of the frequently-used methods in qualitative studies. In purposeful sampling, the subjects are selected by the researcher. The subjects who are selected have rich and in-depth knowledge and experience of the concept under study and can provide a detailed insight into it [ 13 ]. Thus, the researchers selected individuals with extensive experience or knowledge of the subject of the study. After consulting the emergency care mangers, the researchers selected one of the personnel who could interact better and provide rich information for the initial interview. Then the first participant was asked to name a colleague who had rich knowledge and experience of the subject under study. In this manner, based on the information provided by the mangers and the participants chosen earlier, more participants who had a good understanding of the subject of the study were selected. Sampling was maintained to the point of data saturation. Data saturation was achieved when no new data could be collected and no new categories or sub-categories could be extracted [ 14 ]. In this study, data saturation was reached after 23 interviews, and two further interviews were done to ensure no new data was available.
Yet, to ensure that the data was saturated, the researchers conducted two additional interviews. The inclusion criteria were having at least 1 year’s experience of work in pre-hospital emergency care, being willing to participate in the study, and being able to provide extensive and rich information about the challenges and barriers in clinical decision-making.
Data were collected through semi-structured, individual interviews, in the interval between December 2019 and July 2020. All the interviews were conducted by the first author (MB) in the conference room of the emergency department after prior arrangements with the head of the emergency department and the participants. Each interview lasted from 45 to 60 min.
The interview guide was developed according to the views of the research team and the available literature. The face and content validity of the questionnaire was examined and verified by 10 members of the emergency care personnel and 4 pre-hospital emergency care experts and professors. Accordingly, the face validity of the interview guide was determined based on the results of three initial interviews with the participants and some minor changes were made to make the questions more comprehensible. The content of the three interviews was not included in the final analysis. The focuses of interview questions were based on your experiences; what factors can influence clinical decision-making?” What skills do you need to make the right clinical decision? (Additional file 1 : Interview Guide and Question).
At the end of each interview, the participants were thanked for their cooperation and were asked for their phone numbers in case the interviewer had any other questions, needed the participants to confirm their statements, or had to interview a participant again. Immediately after completion, each interview was transcribed. To maintain confidentiality with regard to the information acquired from the participants by phone or in interviews, the researchers assured the participants that their information would be used for research purposes only and would remain confidential throughout the study and after in the process of collecting and analyzing the data.
The collected data were analyzed using Graneheim and Lundman’s approach to content analysis (2004): initially, to immerse in the data and to achieve a general idea of it, the researchers read each transcript several times. Next, the words, sentences, or paragraphs which carried significance were selected as meaning units. The meaning units were assigned codes which showed a summary of the meaning of the unit and then the texts were codified. Afterwards, the codes were compared in terms of their similarities and differences, the similar codes were merged, and the codes and texts were reviewed again. Based on their similarities, the meaning units were categorized. To ensure the reliability of the codes, the researchers reviewed the categories and compared them against the data again. The themes were identified after deep reflection and comparison of the categories with each other. In this regard we try to use both manifest and latent analysis [ 15 ]. Accordingly, after completion, each interview was immediately transcribed by the first author (MB). Subsequently, the first author read and re-read the transcripts and, after obtaining a general understanding of the content, analyzed the data inductively. When the transcripts were being read, significant paragraphs and sentences were marked. The words, sentences, and paragraphs which contained a significant point about the challenges of clinical decision-making were selected as semantic units. Each significant paragraph or phrase was assigned a code. In the next stage, the third author (SK) reviewed the transcripts and verified the semantic units and open codes. Possible disagreements over the semantic units and codes were resolved in meetings attended by all the research team members (MB, SK, SA, and BT). The research team also verified the quality of data analysis. Based on the similarities and compatibilities between them, the codes were classified and categories were developed. To ensure the reliability of the codes, the researchers reviewed the categories and compared them with the data again. Eventually, in consecutive, joint meetings, the research team extracted the main themes after careful consideration and comparison of the categories. The collected data were analyzed in MAXQDA v. 2007 (Table 1 , Example of data analysis process).
An example of coding and development of categories and themes
To ensure the trustworthiness of the results, the researchers applied Lincoln and Guba’s criteria [ 16 ]. Accordingly, to ensure credibility, the researchers applied prolonged engagement with data, member checking, and peer debriefing. For member-checking, 2 of the pre-hospital emergency care personnel were presented with a copy of the encoded interviews which was confirmed. To perform peer-checking, the researchers had four experts analyze and observe the process of data analysis and validate the codes and categories. The dependability of the study results was enhanced through describing the methods used to code the concepts and themes, as well as presenting textual and audio data. Also, two members of the research team examined the findings individually and then discussed them to resolve any possible disagreements to ensure dependability. To ensure that the results were confirmable, the researchers showed the encoded data to the participants to verify the accuracy of the extracted categories and subcategories. The conditions of the respondents and how they were interviewed were clearly described to add to the transferability of the study results. The researchers also tried to select the study subjects solely based on the objectives of the study and free of bias. Data were analyzed as soon as they were collected to help the researcher be aware of the principles of the research. Transferability was ensured by providing a comprehensive description of the subject of the study, the participants’ characteristics, and methods of data collection and data analysis, along with documented examples of the participants’ quotes.
In the process of collecting and analyzing the data, the researchers applied bracketing. Bracketing is a method used in qualitative research to minimize the potential threats of prejudgment which can adversely affect the research process [ 17 ]. Thus, the researchers tried to ignore their own personal knowledge, beliefs, values, and experiences in order to accurately describe the emergency care personnel’s views on the challenges of clinical decision-making. The researchers did not judge the data and accepted it as it was.
Ethical considerations
All participants gave written informed consent to participate in the study. The present study was conducted in accordance with the principles of the revised Declaration of Helsinki, a statement of ethical principles which directs physicians and other participants in medical research involving human subjects. Moreover, the study was approved by the local Ethics Committee of Fasa University of Medical Sciences, Fasa, Iran (IR.FUMS.REC.1398.168).
This study recruited a total of 25 subjects. The mean and standard deviation of the participants’ ages was 33.52 ± 5.89 years. The personal characteristics of the participants are shown in Table 2 . Based on the participants’ experiences, as a major professional capability which emergency care personnel should be skilled at, clinical decision-making is comprised of clinical knowledge, skills, experience, and judgment for identifying patients’ problems, analyzing their conditions, making the right decision, and taking effective measures based on that decision. From the participants’ point of view, clinical decision-making is influenced by a wide variety of factors. Analyses of the qualitative data yielded four themes and eight categories (Table 3 ).
Individual characteristics of the participants
Themes and categories extracted from content analysis
Professional capabilities
“Professional capabilities” was the most noticeable theme extracted from the participants’ experiences. This theme consists of the following categories: Clinical Competence and Psychological empowerment consists of emotional stability and resilience.
Clinical competence
Clinical Competence consists of clinical knowledge, clinical experience, clinical skills, teamwork skills, time management skills and clinical judgment skills.
According to one of the participants:
One of the most important professional capabilities that emergency care personnel need to make quick and correct clinical decisions is clinical knowledge. Unfortunately, some of our colleagues here don’t have enough clinical knowledge. I mean, for example, they don’t know much about the physiopathology of diseases. How can you possibly make a good clinical decision and take effective clinical measures if you are ignorant about the causes and treatments of diseases? (P10, 18 years of experience)
Another participant stated that:
Some of our colleagues have a lot of clinical experience and can make a quick diagnosis at first glance at a patient and then make the right clinical decision accordingly. (P3, 16 years of experience)
Another subcategory of professional capabilities which was found to have an impact on clinical decision-making was clinical skills. One of the participants remarked:
There are people here who don’t have the required clinical skills. For instance, they can’t do a proper assessment of a patient’s status, or they don’t know how to use the equipment. On many occasions, when we were on a mission, one of my co-workers couldn’t use the cardiac monitoring device or the defibrillator the right way. If you can’t do a proper monitoring or assess your patients, how can you make the right clinical decision and do the right thing for them? (P7, 9 years of experience)
“Teamwork skills” was another component of professional capabilities referred to by many of the participants. Based on the participants’ experiences, having good teamwork skills can contribute to good decision-making and, as a result, providing quality care. Sometimes, the emergency care personnel encounter a large number of patients or casualties and need to possess satisfactory teamwork skills and time management skills to make good clinical decisions. According to one of the participants:
On some missions when we have to deal with a large number of casualties, my colleagues and I get confused and find it hard to make a good decision. In my experience, this is because we are not skilled enough in teamwork and time management. At the scene of accidents, everyone wants to be boss and tell the others what to do and that causes chaos which wastes our time and puts a patient’s life at risk. (P19, 12 years of experience)
Another aspect of professional capabilities with an impact on clinical decision-making is clinical judgment. From the participants’ experiences, good clinical judgment plays an important part in making correct and reasonable clinical decisions in all situations, especially in emergency situations where a quick diagnosis is necessary. As one of the participants pointed out:
A skillful and capable member of the emergency care personnel should be able to analyze and interpret the implicit and explicit symptoms of a patient and use that information to make a proper clinical judgment and clinical decision. (P12, 15 years of experience)
One of the major challenges and problems which I have repeatedly seen in the clinical decision-making of the emergency care personnel is poor clinical judgment. Some of my co-workers don’t have the necessary skills in this area and can’t come to a good conclusion and decision based on the status of a patient and analysis of their symptoms. And so they make mistakes in their decision-making and I’ve sometimes seen them put a patient’s life in danger. (P8, 10 years of experience)
Psychological empowerment
Resilience is another component part of Psychological empowerment which the participants’ experiences showed to affect clinical decision-making. From the participants’ point of view, resilience means that the emergency care personnel should be flexible, should be able to adapt to the hard and unpredictable conditions of work in pre-hospital emergency care, and should possess great tolerance. One of the participants stated that:
Having a high tolerance threshold is an essential quality in pre-hospital emergency care personnel. I’ve witnessed cases where some personnel with good professional knowledge and skills lost their patience in critical conditions or when the number of the injured was high. They couldn’t manage the scene of the accident and make a logical clinical decision. (P16,14 years of experience)
Another component of Psychological empowerment which has an impact on clinical decision-making is emotional stability. According to one of the participants:
Work conditions in pre-hospital emergency care are very complicated and unpredictable. So it is necessary for emergency care personnel to be emotionally stable so they can manage the scenes of accidents well, keep calm, make the right decision, and take effective clinical measures. (P25, 2 years of experience)
Another participant remarked that:
Unfortunately, some of my colleagues do not have emotional stability: they lose their temper easily and can’t manage their anger. Sometimes we come across patients who are very aggressive and irritable. If we don’t manage our feelings and emotions, we can’t make the right decision for them and may even put their lives in danger. (P2, 10 years of experience)
Occupational and environmental factors
Another theme of the major challenges and barriers which affect clinical decision-making is occupational and environmental factors. This theme consists of the following categories: Occupational factors and Environmental factors.
Occupational factors
Occupational factors consist of time of missions, location of missions, Fatigue and occupational burnout and patients’ status.
One of the occupational factors referred to by the participants is the time of missions. At times, pre-hospital emergency care personnel have to go on a mission at night and in complete darkness or in bad weather conditions, which circumstances can adversely affect the speed and accuracy of the personnel’s decision-making. According to one of the participants:
Many times, I’ve had to be present at the side of a patient in unstable weather conditions, in foggy weather, or at night. It is really hard to work in such circumstances and to judge the situation and make the right clinical decision quickly. I would rather go on a hundred missions in one shift at day time than get dispatched at night or in bad weather. (P5, 8 years of experience)
Another occupational factor from the participants’ perspective is the location of missions in pre-hospital emergency care. One of the participants mentioned that:
Serving in inter-city stations and rural areas is much harder and more stressful than working in stations located in the city. Since we have to drive long distances and it takes much time to get to urban medical centers, when patients’ conditions are critical, we really get confused and can’t make the right decision immediately and provide the necessary care. (P9, 8 years of experience)
Patients’ status and the conditions at the scene of accidents are other factors which affect clinical decision-making. According to one of the participants:
Sometimes, the scene of an accident is very unsafe and full of hazards and these conditions have a negative impact on our decision-making. For instance, I’ve occasionally had to appear at the scene of a murder or shooting incident, or where there was an ongoing fight, or where a house or a vehicle was on fire. Well, under such unsafe circumstances, how am I supposed to care for a patient when my own life is in danger? (P11, 5years of experience)
Patients’ status one another of the occupational factors which affect clinical decision-making is emergency care.
Our decisions are also affected by the clinical conditions of a patient. For example, sometimes, the patient is unconscious or the patient is deaf or speech-impaired and can’t communicate with us. At such times, it is not possible to acquire reliable data about a patient’s status and make the right decision. (P6, 7 years of experience)
Another of the occupational factors which affect clinical decision-making is emergency care personnel’s fatigue and occupational burnout. As one of the participants remarked:
Working in pre-hospital emergency care is really demanding and there are not many who can bear the pressure. Sometimes, I’ve had to go on about 30 missions in a 24-hour shift. Work overload and shortage of experienced staff have caused fatigue and burnout in the personnel and these have negative effects on our concentration, mental acuity, and decision-making. (P13, 4 years of experience)
Environmental factors
Environmental factors consist of conditions at the scene of accidents and spread of infectious diseases. According to one of the participants:
“Sometimes, the scene of an accident is very unsafe and full of hazards and these conditions have a negative impact on our decision-making. For instance, I’ve occasionally had to appear at the scene of a murder or shooting incident, or where there was an ongoing fight, or where a house or a vehicle was on fire. Well, under such unsafe circumstances, how am I supposed to care for a patient when my own life is in danger?” (P11, 5 years of experience)
Spread of infectious diseases is another dimension of the environmental factors. According to one of the participants:
When there is an outbreak of a dangerous infectious disease, like Ebola, H1N1, or COVID-19, sometimes there is a conflict between the emergency care personnel’s decisions and what the patients want. Even if we judge a patient’s condition to be critical and decide that he or she should be transferred to the hospital, the patient or the patient’s family don’t care about our decision and refuse to have the patient transferred because of their fear of the epidemic. (P15, 3 years of experience)
On a similar note, another participant stated that:
On a mission, I had to give care to a patient who had symptoms of sudden cardiac arrest. Even though I told the patient and his family that the patient’s condition was serious, they ignored my decision and said because of the spread of the coronavirus, they wouldn’t have their patient taken to the hospital. (P17, 5 years of experience)
Inefficient organizational management
Another theme of the major challenges and barriers in clinical decision-making is inefficient organizational management which consists of the following categories: Structural challenges, and challenges of human resources and medical equipment.
Structural challenges
Structural challenges consist of management’s failure to support the personnel in the case of errors in decision-making and legal troubles, inefficiency of the dispatch center, management’s failure to conduct root cause analysis and take corrective action in the case of errors in decision-making, conflicts in the regulations and lack of a clear operation manual.
Another component part of structural challenges from the participants’ perspective is the managers’ failure to support the personnel in the case of errors in decision-making and legal troubles. Many of the participants stated that they are not adequately supported by their mangers if legal issues arise and the patients press charges against the personnel. They also mentioned that the mangers do not take any effective measures toward analyzing the root causes of clinical errors and or take corrective action.
Unfortunately, in matters of legal issues and charges, the managers don’t support the personnel as much as they’re expected to. There are many cases in which, because of a clinical error, patients’ families have sued the personnel, but the management failed to give enough support. If you do a good job on a hundred tasks, they will tell you that you are just doing your duties. But if you make a single mistake, you’ll immediately get reprimanded. Out of this fear of being reprimanded or sued by patients, some of the personnel do not report the errors in their clinical decision-making. (P24, 11 years of experience)
Conflicts in the regulations and lack of a clear operations manual” was another issue referred by the participants. In this relation, one of the participants stated that:
There is not a clear manual which describes the responsibilities of the emergency care personnel. For instance, according to the internal codes, the pre-hospital emergency care personnel should not administer intravenous medications and if they do and their action puts a patient’s life in danger, they will be held liable. Sometimes, we really don’t know what the right decision is and what kind of action we should take. When a patient is having a seizure, should I administer diazepam to them or not? (P20, 15 years of experience)
Once, I had a 45-year old patient with severe chest pains. Based on his symptoms, my diagnosis was cardiac arrest and we transferred him to the hospital. In the triage unit, the emergency medicine doctor scolded me for not having given an intravenous nitroglycerin injection to the patient. He said all we know is how to transfer patients! I explained to him that we’re not allowed to administer medicine intravenously. (P1, 11 years of experience)
Inefficiency of the dispatch center is another aspect of the structural challenges referred by the participants. One of the participants’ comments in this relation is as follows :
The dispatch center is the brains and director of the operations in pre-hospital emergency care. Unfortunately, employment of individuals who lack the required knowledge and skills in this field disrupts the operations. For instance, one time, the personnel at the dispatch unit announced that a patient had signs of weakness and dizziness and could have hypoglycemia. When we got to the patient’s side, we realized he’d had cardiac arrest and that the dispatch center had suggested hypoglycemia by mistake. Misleading information from the dispatch unit can prevent the personnel from making the right diagnosis and, consequently, the right decision. (P4, 2 years of experience)
Challenges of human resources and medical equipment
Challenges of human resources and medical equipment consist of employment of inexperienced and inefficient personnel, shortage of equipment and not organizing workshops for the professional empowerment.
Employing personnel who don’t have the necessary expertise and skills in pre-hospital emergency care is another component part of challenges of human resources and medical equipment which the participants’ experiences showed to affect clinical decision-making.
One of the participants’ comments in this relation is as follows:
Employing personnel who don’t have the necessary expertise and skills in pre-hospital emergency care is actually gambling with people’s lives. Unfortunately, because of organizational benefits and lack of budget, the senior managers hire inexperienced individuals who don’t have the necessary knowledge and skills in pre-hospital emergency care. On many occasions, I’ve seen some of my colleagues who lack expertise in making a diagnosis make wrong decisions and put a patient’s life in danger. When we object to the mangers, they say the budget is limited and they can’t afford to hire skilled workforce. (P23, 17 years of experience).
Not organizing workshops for the professional empowerment is another component part of challenges of human resources and medical equipment which the participants’ experiences showed to affect clinical decision-making.
Unfortunately, the administration does not take any special measures to update the knowledge and skills of the personnel. Over the past there, not a single workshop has been held and the knowledge of most of the personnel is not up-to-date. We have repeatedly asked for training courses in basic and advanced CPR and trauma emergency care, but the administration says it doesn’t have any budget for workshops. How can the personnel make good clinical decisions and do the right thing for their patients when their knowledge and skills are not up-to-date? (P10, 18 years of experience)
Another issue under the category of challenges of human resources and medical equipment is shortage of equipment. One of the participants stated that:
Some of the ambulances in inter-city and rural emergency stations lack such medical devices as suction machines, cardiac monitors, pulse oximeter, and ventilators. Even now that we have to deal with the COVID-19 epidemic, we don’t have access to personal protective equipment, like masks, gloves, and special gowns, and our fear of getting the infection has a negative effect on our diagnoses and, in turn, our decisions and actions. (P24, 13 years of experience)
According to another participant:
When there is no heart monitor, pulse oximeter, or ventilator inside the ambulance, how am I supposed to diagnose a patient’s cardiac or respiratory problem and make a proper clinical decision that won’t be a threat to the patient’s life? (P18, 6 years of experience)
Ethical issues
The final theme of the major challenges and barriers in clinical decision-making is “ethical issues” which consists of categories of respect for patients’ physical privacy and respect for patients’ sexual privacy.
Respect for patients’ physical privacy
Regarding respect for patients’ physical privacy, in the Iranian culture, it is important that patients’ physical privacy be maintained and that their private parts not seen by caregivers, especially opposite-sex caregivers. According to a participant:
Sometimes, we must provide care to female patients, especially young females, who have palpitations or chest pains and are in need of immediate cardiac monitoring. It is not ethical for the patients or even for us who are in the Iranian culture to see the female patient’s body. It is really a tough job to make a decision at such times and the patients may get very uncomfortable. (P13, 4 years of experience)
Respect for patients’ sexual privacy
The participants also mentioned that, considering the dominant Islamic culture in Iran, showing respect for the sexual privacy of patients is very important to patients and their families. One of the participants stated that:
While we were transferring a pregnant woman, we realized she had broken her water and was in labor. The baby was coming and we had to help her deliver it. The poor woman seemed very embarrassed and uncomfortable. It is so hard to make a decision in such conditions. After all, we are Muslim and our ethical principles dictate that at such times, care should be given by a person of the same gender as the patient. But in Iran, there are no female staff members in the pre-hospital emergency care . (P21, 3 years of experience)
This study explored the major challenges and barriers which affect clinical decision-making from the perspective of EMS personnel. The analysis of the participants’ experiences showed that challenges and barriers of the participants’ clinical decision-making consisted of four areas: professional capabilities, occupational and environmental factors, inefficient organizational management, and ethical issues.
At the scene of accidents, the emergency care personnel encounter various clinical challenges which affect their clinical decision-making [ 18 ]. At the same time, it is the ethical and professional responsibility of emergency care personnel to provide quality care based on code of ethics to victims at the scene of accidents [ 19 ]. The findings of the present study concern pre-hospital emergency care personnel’s perception of the major challenges which affect clinical decision-making at the scene of accidents.
Professional capabilities, including clinical knowledge and skills, were found to play an important part in pre-hospital emergency care personnel decision-making. Similarly, in their study of the barriers to nurses’ clinical decision-making in the university hospitals of the south of Iran, Mousavi et al., report that having knowledge, clinical experience, and clinical skills are essential to making good clinical decisions—the clinical decision-making mean score of the nurses who had poor clinical knowledge, experience, and skills was unsatisfactory [ 20 ]. Another important component of professional capabilities which has a significant impact on clinical decision-making is clinical judgment. According to the study of Engebretsen et al., clinical judgment is a necessary skill for all nurses, especially pre-hospital emergency care nurses, as it enables them to make accurate diagnoses and make proper clinical decisions [ 21 ]. Likewise, the results of the study of Anderson et al., show that clinical judgment and critical thinking play a key role in making clinical decisions in all situations, in particular the critical and complicated conditions which prevail in pre-hospital emergency care [ 22 ]. In the present study, the participants stated that some of their colleagues do not have adequate clinical knowledge, skills, and experience and cannot, therefore, make the right decision for their patients. Similarly, the results of the study of Perona et al., show that clinical knowledge and skills and clinical experience are key factors in emergency care personnel’s clinical decision-making. Lack of those capabilities poses a challenge when the personnel should make clinical decisions and adversely affects the quality and safety of the care. Accordingly, it is necessary for pre-hospital emergency care administrators to take measures to improve the professional capabilities of their personnel [ 23 ]. Emergency Nurses Association (ENA) has always stressed that advances in technology, increase in professional knowledge, and work specialization mean that emergency care nurses’ clinical knowledge and performance need to be improved regularly. Since emergency care is an unpredictable area and, occasionally, the personnel have to deal with a large number of patients with various issues, it is necessary for the emergency care personnel to possess such professional capabilities as clinical knowledge and skills to be able to make the right clinical decision and provide safe and quality care accordingly [ 24 ]. The results of the study of Aloyce, et al. show that the emergency nurses who lack the required clinical knowledge and skills make mistakes in their clinical decision-making and triage [ 25 ].
In the present study, “teamwork skills” was found to be another important aspect of professional capabilities which affects clinical decision-making. In Grover’s qualitative-exploratory study of emergency nurses’ experiences of teamwork in a hospital in Australia, the participants stated that teamwork skills are among the essential clinical skills which emergency nurses must possess. The participants’ experiences showed that when the emergency department is busy and a large number of patients must be attended to, teamwork skills can significantly facilitate clinical decision-making. The personnel with poor teamwork skills get nervous and confused at such times and cannot make logical decisions for their patients [ 26 ].
Based on the participants’ experiences, the emergency care personnel occasionally have to provide care to patients who are very irritable and aggressive. If the personnel fail to manage their own feelings and emotions in such circumstances, they cannot make a good clinical decision for the patients and may even take actions which put the patients’ lives at risk. The results of the study of Lin et al., show that emergency nurses must possess high levels of resilience and tolerance so that they can employ their capabilities in the critical conditions of emergency situations and, by making quick and correct clinical decisions, implement effective clinical interventions [ 27 ]. Halpern, states that pre-hospital emergency is a complicated, unpredictable, and stressful environment. At times, patients or their companions, who are under considerable stress, may behave in violent and insulting ways. Therefore, it is essential for the emergency care personnel to possess such psychological qualities as resilience and emotional intelligence to be able to control their emotions and make the right clinical decision and, consequently, take effective clinical measures. By holding workshops, pre-hospital emergency care administrators can enhance the personnel’s psychological capabilities [ 28 ].. Similarly, Gunnarsson et al., report that emergency nurses must possess resilience and emotional stability to be able to use their professional abilities effectively and take proper clinical measures at the time of an emergency. Although such factors as fatigue from work overload, shortage of personnel, and stressful work conditions in emergency departments have an adverse effect on the performance of emergency care personnel, nurses who are resilient and can manage their emotions continue to provide high-quality care [ 29 ].
Occupational and environmental factors constitute another category of the major challenges and barriers which affect emergency care personnel’ clinical decision-making. According to the study of Li, et al. (2018), shortage of experienced nurses in emergency departments, increase in workload, and fatigue and burnout are the most significant occupational factors which adversely affect the personnel’ diagnoses and decision-making and lead to patients’ dissatisfaction and poor-quality care [ 30 ].
Another category of the major challenges which affect emergency care personnel’ clinical decision-making is inefficient organizational management. According to the study of Bijani et al., employment of inexperienced personnel who lack the required expertise, lack of facilities and equipment, inadequate support for the personnel, absence of clear instructions, conflicts in the regulations, and failure to hold workshops for the professional empowerment of emergency nurses are the most significant challenges which affect the quality of triage in emergency departments [ 31 ]. These findings are consistent with the results of the present study.
From the participants’ perspective, lack of an emergency doctor to consult and lack of a set of standard clinical guidelines are among the major barriers to satisfactory clinical decision-making. Thus, it is recommended that the senior management at emergency care departments set standard evidence-based clinical guidelines for the personnel to follow. Also, pre-hospital emergency care personnel should have access to the clinical consultation of an emergency doctor stationed at the emergency care center. Likewise, Bashiri et al. report that evidence-based clinical guidelines and instructions and having access to advice from a doctor in emergency care departments play a key role in improving the process of clinical decision-making by emergency care personnel and will result in higher quality care [ 32 ].
Another important category which was found to affect emergency care personnel’ clinical decision-making is ethical issues. Showing respect for the privacy of patients and maintaining their human dignity are among the most important ethical responsibilities of caregivers [ 33 ]. Accordingly, all caregivers are expected to maintain their patients’ privacy and dignity [ 34 ].
In the present study, too, the views of the interviewed pre-hospital emergency care personnel showed that one of the key factors which influence clinical decision-making is showing respect for the physical and sexual privacy of patients. The dominant religious-cultural beliefs and values in Iran dictate that the bodies of all individuals, especially women, should be covered, in particular their genitalia and breast area, and that there should not be any physical contact between men and women who are not related to each other. Thus, to respect the privacy of patients and accident victims, even in pre-hospital emergency care, it is necessary that patients receive care from same-gender caregivers. But the national laws of Iran forbid women from working in pre-hospital emergency care. Therefore, there is need for changes which will allow the employment of female personnel in emergency care. On a similar note, the results of the study of Torabi et al., show that, from the viewpoint of pre-hospital emergency care personnel, maintaining the physical and sexual privacy of patients is among the key aspects of clinical and ethical decision-making [ 35 ].
In pre-hospital emergency care, maintaining patients’ privacy according to the patient’s physical conditions, personal life, and lifestyle is essential. These rights apply to deceased victims, too [ 36 ]. In the study of Abelsson & Lindwall, the participants state that covering the body of a victim, e.g. keeping a patient’s body covered when electrodes are being attached, is essential to maintaining his/her privacy. Keeping a victim’s body covered in line with the victim’s values and beliefs while emergency care is being given to him/her at the scene is an ethical obligation [ 37 ]. Maintaining patient privacy and patient dignity are closely connected. Dignity is a social and cultural concept and individuals’ perceptions of maintaining privacy and dignity are influenced by their beliefs and values [ 38 ]. As a result of the dominant religious and cultural beliefs in Iran, women feel embarrassed when they remove their clothing to be examined by a male nurse or doctor and consider that situation to be unethical. Therefore, EMS male personnel in Iran feel uncomfortable when they should provide services to female victims at the scene of accidents, but try to give care based on their cultural and religious values and commitment to professional ethics.
Strengths of the study
The present study is the first qualitative attempt at exploring the challenges which affect clinical decision-making from Iranian pre-hospital emergency care personnel’s point of view and can be regarded as a significant accomplishment. In addition, in the present study, a wide range of the factors which have an impact on pre-hospital emergency care personnel’s clinical decision-making were identified. These findings can be employed to improve the quality of pre-hospital emergency care services and the personnel’s clinical decision-making skills.
Limitations of the study
One of the limitations of the study is that it only addressed the views of pre-hospital emergency care personnel and the ideas of patients, as the beneficiaries of emergency care services, were not taken into account. Also, due to differences between the cultural, social, and economic conditions of Iran and those of other countries, the results may not be completely transferable and similar studies should be carried out in other countries.
In today’s healthcare systems, patients in critical conditions usually receive their first care from pre-hospital emergency care personnel. The more correctly, accurately, and quickly these professionals act, the lower will be the rate of fatalities and possible disabilities and the more trust people can place in the services provided by pre-hospital emergency care departments. The success of these departments depends on a variety of factors, one of the most important of them being the ability to make good clinical decision-making. Therefore, it is necessary that those challenges should be identified and addressed in order for the quality of emergency services to improve. The results of the present study show that clinical knowledge, experience, and skills contribute to emergency care personnel’s professional capabilities in making clinical decisions. Good teamwork skills and time management can prevent feelings of confusion when the number of the injured to be attended to is large. Effective clinical decision-making skills can not only help the personnel make the right decision, but enhances their resilience and enables them to adapt to hard and unpredictable conditions. Professional factors, organizational management, and ethical matters constitute the other major factors which influence the clinical decision-making of emergency care personnel at the scene of accidents and determine the quality of their clinical performance. Thus, it is essential that pre-hospital emergency care managers improve the quality of EMS personnel’s clinical decision-making skill.
Acknowledgements
This paper was extracted from a research project with the ethical code (IR.FUMS.REC.1398.168) in Fasa University of Medical Sciences, Fasa, Iran. The authors appreciate Fasa University of Medical Sciences for financially supporting this research and who Emergency Medical Services Personnel participated in the study.
Abbreviation
Authors’ contributions.
All authors (MB, SA, SK, and BT) have participated in the conception and design of the study. MB and SK, contributed the data collection and pre-pared the first draft of the manuscript. MB, SA and BT, critically revised and checked closely the proposal, the analysis and interpretation of the data and design the article. All authors read and approved the final manuscript.
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Availability of data and materials
Ethics approval and consent to participate.
All the participants gave written informed consent to participate in the study. The present study was conducted in terms of the principles of the revised Declaration of Helsinki, which is a statement of ethical principles that directs physicians and other participants in medical research involving human subjects. The participants were assured about their anonymity and confidentiality of their information. Moreover, the study was approved by the Institutional Research Ethics Committee of Fasa University of Medical Sciences, Fasa, Iran (ethical code: IR.FUMS.REC.1398.168).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mostafa Bijani, Email: moc.oohay@afatsom_inahzib .
Saeed Abedi, Email: moc.liamg@6891deeasideba .
Shahnaz Karimi, Email: moc.oohay@20022002rakhahs .
Banafsheh Tehranineshat, Email: moc.oohay@hehsfanabt .
[Clinical decision making and critical thinking in the nursing diagnostic process]
Affiliation.
- 1 Notfallzentrum Insel, Universitätsspital, Stettlerstrasse 15, CH-3006 Bern. [email protected]
- PMID: 17051512
- DOI: 10.1024/1012-5302.19.5.275
The daily routine requires complex thinking processes of nurses, but clinical decision making and critical thinking are underestimated in nursing. A great demand for educational measures in clinical judgement related with the diagnostic process was found in nurses. The German literature hardly describes nursing diagnoses as clinical judgements about human reactions on health problems / life processes. Critical thinking is described as an intellectual, disciplined process of active conceptualisation, application and synthesis of information. It is gained through observation, experience, reflection and communication and leads thinking and action. Critical thinking influences the aspects of clinical decision making a) diagnostic judgement, b) therapeutic reasoning and c) ethical decision making. Human reactions are complex processes and in their course, human behavior is interpreted in the focus of health. Therefore, more attention should be given to the nursing diagnostic process. This article presents the theoretical framework of the paper "Clinical decision making: Fostering critical thinking in the nursing diagnostic process through case studies".
Publication types
- English Abstract
- Decision Making
- Nursing Diagnosis*

COMMENTS
15 Attitudes of Critical Thinking in Nursing. 15 Attitudes of Critical Thinking in Nursing. 1. Independence. Independence is like thinking for yourself and making your own choices. Imagine you're deciding what book to read, and you pick one that interests you, not just what others like - that's being independent.
Critical thinking underlies independent and interdependent decision making. Critical thinking includes questioning, analysis, synthesis, interpretation, inference, inductive and deductive reasoning, intuition, application, and creativity 8 (p. 9). Course work or ethical experiences should provide the graduate with the knowledge and skills to:
These competencies were grouped into 5 components of critical thinking: problem recognition, clinical decision making, prioritization, clinical implementation, and reflection. The potential application of this tool may enable nurse leaders to identify critical thinking strengths and individualize learning activities based on the specific needs ...
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing ...
Chapter 15 Critical Thinking in Nursing Practice Objectives • Describe characteristics of a critical thinker. • Discuss the nurse's responsibility in making clinical decisions. • Discuss how reflection improves clinical decision making. • Describe the components of a critical thinking model for clinical decision making. • Discuss critical thinking skills used in nursing practice.
Go to: Improving clinical reasoning techniques is the right way to facilitate decision-making from prognostic, diagnostic, and therapeutic points of view. However, the process to do that is to fill knowledge gaps by studying and growing experience and knowing some cognitive aspects to raise the awareness of thinking mechanisms to avoid ...
another: critical thinking, clinical reasoning, clinical judgment, decision-making, problem-solving, and nursing process. 4. Identify four principles of the scientifi c method that are evident in CT. 5. Compare and contrast the terms problem-focused thinking and outcome-focused thinking. 6. Clarify the term critical thinking indicator (CTI). 7.
The literature review identified several gaps in the current knowledge about CT and clinical decision making among nurses. First, although it is evident that nurses use different decision processes in making clinical decisions, there are few comparisons of these processes or the role of factors that influence them.
BACKGROUND Critical Thinking. Critical thinking is both an attitude toward handling issues and a reasoning process. Critical thinking is not synonymous with problem solving and decision making (), but it is the foundation for effective decision making that helps to solve problems (Fioratou et al., 2011).Figure 4-2 illustrates the way obstacles such as poor judgment or biased thinking create ...
Consequently, Critical thinking is a collection of dispositions and skills that improve decision making processes through such cognitive abilities as analysis, implication, and assessment [5]. In ...
1. Explain the difference between critical thinking and clinical judgment. 2. Discuss why critical thinking and clinical judgment are essential in nursing. 3. Compare the nursing process to the clinical judgment process. 4. Describe attitudes of good critical thinkers. 5. Define vigilance. 6. Prioritize patient care activities based on the ...
Discuss the critical thinking attitudes used in clinical decision making. ... Critical Thinking Model for Clinical Decision Making. Models serve to explain concepts and help nurses make decisions and judgements about patients. Kataoka-Yahiro and Saylor (1994) devised the critical thinking model of nursing judgement. ...
The nursing schools should accept attitudes that encouraging critical thinking and mobilize the skills of clinical decision-making (Tønnessen et al., 2020). The World Health Organization (WHO) recommends, as the gold standard in professional nurse training, the development of clinical decision-making, problem-solving and critical thinking in ...
Discuss how reflection improves clinical decision making. Describe the components of a critical thinking model for clinical decision making. Discuss critical thinking skills used in nursing practice. Explain the relationship between clinical experience and critical thinking. Discuss the critical thinking attitudes used in clinical decision making.
Likewise, the results of the study of Anderson et al., show that clinical judgment and critical thinking play a key role in making clinical decisions in all situations, in particular the critical and complicated conditions which prevail in pre-hospital emergency care . In the present study, the participants stated that some of their colleagues ...
There are a multitude of definitions of critical thinking, but one that is simple, yet meaningful is: Critical thinking is the process of identifying and evaluating evidence to guide decision-making. (Paul & Elder, 2008) Riddell (2007) argues that the process of clinical thinking is not simple and requires an "explanation rather than a
Decision-Making vs. Clinical Reasoning . The medical literature mostly uses the . terms decision-making or clinical rea-soning, the latter being increasingly frequent in recent decades. Originally issued from research on the psychology of decision-making, decision theory is a model of idealized rationality, 2. a pre-
The daily routine requires complex thinking processes of nurses, but clinical decision making and critical thinking are underestimated in nursing. A great demand for educational measures in clinical judgement related with the diagnostic process was found in nurses. The German literature hardly descr …
Discuss the critical thinking attitudes used in clinical decision making. The use of intellectual standards during assessment ensures that you obtain a complete database of information. Professional standards for critical thinking refer to ethical criteria for nursing judgments, evidence-based criteria for evaluation, and criteria for ...
Discuss the critical thinking attitudes used in clinical decision making These define how a successful thinker approaches a problem, Knowing when information is misleading and recognizing your own limits are examples how attitudes guide thinking.
Objectives: • Describe characteristics of a critical thinker. • Discuss the nurse's responsibility in making clinical decisions. • Discuss how reflection improves clinical decision making. • Describe the components of a critical thinking model for clinical decision making. • Discuss critical thinking skills used in nursing practice.
This problem has been solved! You'll get a detailed solution that helps you learn core concepts. Question: Discuss the critical thinking attitudes used in clinical decision making. Here's the best way to solve it. Critical thinking is an essential attitudes used in clinical decision making. Critical thinking invo...
Ch. 15 foundations. Discuss a nurses responsibility in making clinical decisions. An Rn is responsible for making decisions on the bases if clinical information. she replies on knowledge and experience when deciding if a patient is having complications that call for notification of a health care provider or if a teaching plan for a patient is ...