An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Breech presentation.
Caron J. Gray ; Meaghan M. Shanahan .
Affiliations
Last Update: November 6, 2022 .
- Continuing Education Activity
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. This activity reviews the cause and pathophysiology of breech presentation and highlights the role of the interprofessional team in its management.
- Describe the pathophysiology of breech presentation.
- Review the physical exam of a patient with a breech presentation.
- Summarize the treatment options for breech presentation.
- Explain the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by breech presentation.
- Introduction
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the fetus sitting with flexion of both hips and both legs in a tuck position. Finally, the incomplete breech can have any combination of one or both hips extended, also known as footling (one leg extended) breech, or double footling breech (both legs extended). [1] [2] [3]
Clinical conditions associated with breech presentation include those that may increase or decrease fetal motility, or affect the vertical polarity of the uterine cavity. Prematurity, multiple gestations, aneuploidies, congenital anomalies, Mullerian anomalies, uterine leiomyoma, and placental polarity as in placenta previa are most commonly associated with a breech presentation. Also, a previous history of breech presentation at term increases the risk of repeat breech presentation at term in subsequent pregnancies. [4] [5] These are discussed in more detail in the pathophysiology section.
- Epidemiology
Breech presentation occurs in 3% to 4% of all term pregnancies. A higher percentage of breech presentations occurs with less advanced gestational age. At 32 weeks, 7% of fetuses are breech, and 28 weeks or less, 25% are breech.
Specifically, following one breech delivery, the recurrence rate for the second pregnancy was nearly 10%, and for a subsequent third pregnancy, it was 27%. Prior cesarean delivery has also been described by some to increase the incidence of breech presentation two-fold.
- Pathophysiology
As mentioned previously, the most common clinical conditions or disease processes that result in the breech presentation are those that affect fetal motility or the vertical polarity of the uterine cavity. [6] [7]
Conditions that change the vertical polarity or the uterine cavity, or affect the ease or ability of the fetus to turn into the vertex presentation in the third trimester include:
- Mullerian anomalies: Septate uterus, bicornuate uterus, and didelphys uterus
- Placentation: Placenta previa as the placenta is occupying the inferior portion of the uterine cavity. Therefore, the presenting part cannot engage
- Uterine leiomyoma: Mainly larger myomas located in the lower uterine segment, often intramural or submucosal, that prevent engagement of the presenting part.
- Prematurity
- Aneuploidies and fetal neuromuscular disorders commonly cause hypotonia of the fetus, inability to move effectively
- Congenital anomalies: Fetal sacrococcygeal teratoma, fetal thyroid goiter
- Polyhydramnios: Fetus is often in unstable lie, unable to engage
- Oligohydramnios: Fetus is unable to turn to vertex due to lack of fluid
- Laxity of the maternal abdominal wall: Uterus falls forward, the fetus is unable to engage in the pelvis.
The risk of cord prolapse varies depending on the type of breech. Incomplete or footling breech carries the highest risk of cord prolapse at 15% to 18%, while complete breech is lower at 4% to 6%, and frank breech is uncommon at 0.5%.
- History and Physical
During the physical exam, using the Leopold maneuvers, palpation of a hard, round, mobile structure at the fundus and the inability to palpate a presenting part in the lower abdomen superior to the pubic bone or the engaged breech in the same area, should raise suspicion of a breech presentation.
During a cervical exam, findings may include the lack of a palpable presenting part, palpation of a lower extremity, usually a foot, or for the engaged breech, palpation of the soft tissue of the fetal buttocks may be noted. If the patient has been laboring, caution is warranted as the soft tissue of the fetal buttocks may be interpreted as caput of the fetal vertex.
Any of these findings should raise suspicion and ultrasound should be performed.
Diagnosis of a breech presentation can be accomplished through abdominal exam using the Leopold maneuvers in combination with the cervical exam. Ultrasound should confirm the diagnosis.
On ultrasound, the fetal lie and presenting part should be visualized and documented. If breech presentation is diagnosed, specific information including the specific type of breech, the degree of flexion of the fetal head, estimated fetal weight, amniotic fluid volume, placental location, and fetal anatomy review (if not already done previously) should be documented.
- Treatment / Management
Expertise in the delivery of the vaginal breech baby is becoming less common due to fewer vaginal breech deliveries being offered throughout the United States and in most industrialized countries. The Term Breech Trial (TBT), a well-designed, multicenter, international, randomized controlled trial published in 2000 compared planned vaginal delivery to planned cesarean delivery for the term breech infant. The investigators reported that delivery by planned cesarean resulted in significantly lower perinatal mortality, neonatal mortality, and serious neonatal morbidity. Also, there was no significant difference in maternal morbidity or mortality between the two groups. Since that time, the rate of term breech infants delivered by planned cesarean has increased dramatically. Follow-up studies to the TBT have been published looking at maternal morbidity and outcomes of the children at two years. Although these reports did not show any significant difference in the risk of death and neurodevelopmental, these studies were felt to be underpowered. [8] [9] [10] [11]
Since the TBT, many authors since have argued that there are still some specific situations that vaginal breech delivery is a potential, safe alternative to planned cesarean. Many smaller retrospective studies have reported no difference in neonatal morbidity or mortality using these specific criteria.
The initial criteria used in these reports were similar: gestational age greater than 37 weeks, frank or complete breech presentation, no fetal anomalies on ultrasound examination, adequate maternal pelvis, and estimated fetal weight between 2500 g and 4000 g. In addition, the protocol presented by one report required documentation of fetal head flexion and adequate amniotic fluid volume, defined as a 3-cm vertical pocket. Oxytocin induction or augmentation was not offered, and strict criteria were established for normal labor progress. CT pelvimetry did determine an adequate maternal pelvis.
Despite debate on both sides, the current recommendation for the breech presentation at term includes offering external cephalic version (ECV) to those patients that meet criteria, and for those whom are not candidates or decline external cephalic version, a planned cesarean section for delivery sometime after 39 weeks.
Regarding the premature breech, gestational age will determine the mode of delivery. Before 26 weeks, there is a lack of quality clinical evidence to guide mode of delivery. One large retrospective cohort study recently concluded that from 28 to 31 6/7 weeks, there is a significant decrease in perinatal morbidity and mortality in a planned cesarean delivery versus intended vaginal delivery, while there is no difference in perinatal morbidity and mortality in gestational age 32 to 36 weeks. Of note, due to lack of recruitment, no prospective clinical trials are examining this issue.
- Differential Diagnosis
- Face and brow presentation
- Fetal anomalies
- Fetal death
- Grand multiparity
- Multiple pregnancies
- Oligohydramnios
- Pelvis Anatomy
- Preterm labor
- Primigravida
- Uterine anomalies
- Pearls and Other Issues
In light of the decrease in planned vaginal breech deliveries, thus the decrease in expertise in managing this clinical scenario, it is prudent that policies requiring simulation and instruction in the delivery technique for vaginal breech birth are established to care for the emergency breech vaginal delivery.
- Enhancing Healthcare Team Outcomes
A breech delivery is usually managed by an obstetrician, labor and delivery nurse, anesthesiologist and a neonatologist. The ultimate decison rests on the obstetrician. To prevent complications, today cesarean sections are performed and experienced with vaginal deliveries of breech presentation is limited. For healthcare workers including the midwife who has no experience with a breech delivery, it is vital to communicate with an obstetrician, otherwise one risks litigation if complications arise during delivery. [12] [13] [14]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Caron Gray declares no relevant financial relationships with ineligible companies.
Disclosure: Meaghan Shanahan declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Gray CJ, Shanahan MM. Breech Presentation. [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- [What effect does leg position in breech presentation have on mode of delivery and early neonatal morbidity?]. [Z Geburtshilfe Neonatol. 1997] [What effect does leg position in breech presentation have on mode of delivery and early neonatal morbidity?]. Krause M, Fischer T, Feige A. Z Geburtshilfe Neonatol. 1997 Jul-Aug; 201(4):128-35.
- The effect of intra-uterine breech position on postnatal motor functions of the lower limbs. [Early Hum Dev. 1993] The effect of intra-uterine breech position on postnatal motor functions of the lower limbs. Sival DA, Prechtl HF, Sonder GH, Touwen BC. Early Hum Dev. 1993 Mar; 32(2-3):161-76.
- The influence of the fetal leg position on the outcome in vaginally intended deliveries out of breech presentation at term - A FRABAT prospective cohort study. [PLoS One. 2019] The influence of the fetal leg position on the outcome in vaginally intended deliveries out of breech presentation at term - A FRABAT prospective cohort study. Jennewein L, Allert R, Möllmann CJ, Paul B, Kielland-Kaisen U, Raimann FJ, Brüggmann D, Louwen F. PLoS One. 2019; 14(12):e0225546. Epub 2019 Dec 2.
- Review Breech vaginal delivery at or near term. [Semin Perinatol. 2003] Review Breech vaginal delivery at or near term. Tunde-Byass MO, Hannah ME. Semin Perinatol. 2003 Feb; 27(1):34-45.
- Review [Breech Presentation: CNGOF Guidelines for Clinical Practice - Epidemiology, Risk Factors and Complications]. [Gynecol Obstet Fertil Senol. 2...] Review [Breech Presentation: CNGOF Guidelines for Clinical Practice - Epidemiology, Risk Factors and Complications]. Mattuizzi A. Gynecol Obstet Fertil Senol. 2020 Jan; 48(1):70-80. Epub 2019 Nov 1.
Recent Activity
- Breech Presentation - StatPearls Breech Presentation - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

- Pregnancy Classes

Breech Births
In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby’s buttocks, feet, or both are positioned to come out first during birth. This happens in 3–4% of full-term births.
What are the different types of breech birth presentations?
- Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
- Frank breech: In this position, the baby’s buttocks are aimed at the birth canal with its legs sticking straight up in front of his or her body and the feet near the head.
- Footling breech: In this position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What causes a breech presentation?
The causes of breech presentations are not fully understood. However, the data show that breech birth is more common when:
- You have been pregnant before
- In pregnancies of multiples
- When there is a history of premature delivery
- When the uterus has too much or too little amniotic fluid
- When there is an abnormally shaped uterus or a uterus with abnormal growths, such as fibroids
- The placenta covers all or part of the opening of the uterus placenta previa
How is a breech presentation diagnosed?
A few weeks prior to the due date, the health care provider will place her hands on the mother’s lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position. Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Can a breech presentation mean something is wrong?
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery.
Can a breech presentation be changed?
It is preferable to try to turn a breech baby between the 32nd and 37th weeks of pregnancy . The methods of turning a baby will vary and the success rate for each method can also vary. It is best to discuss the options with the health care provider to see which method she recommends.
Medical Techniques
External Cephalic Version (EVC) is a non-surgical technique to move the baby in the uterus. In this procedure, a medication is given to help relax the uterus. There might also be the use of an ultrasound to determine the position of the baby, the location of the placenta and the amount of amniotic fluid in the uterus.
Gentle pushing on the lower abdomen can turn the baby into the head-down position. Throughout the external version the baby’s heartbeat will be closely monitored so that if a problem develops, the health care provider will immediately stop the procedure. ECV usually is done near a delivery room so if a problem occurs, a cesarean delivery can be performed quickly. The external version has a high success rate and can be considered if you have had a previous cesarean delivery.
ECV will not be tried if:
- You are carrying more than one fetus
- There are concerns about the health of the fetus
- You have certain abnormalities of the reproductive system
- The placenta is in the wrong place
- The placenta has come away from the wall of the uterus ( placental abruption )
Complications of EVC include:
- Prelabor rupture of membranes
- Changes in the fetus’s heart rate
- Placental abruption
- Preterm labor
Vaginal delivery versus cesarean for breech birth?
Most health care providers do not believe in attempting a vaginal delivery for a breech position. However, some will delay making a final decision until the woman is in labor. The following conditions are considered necessary in order to attempt a vaginal birth:
- The baby is full-term and in the frank breech presentation
- The baby does not show signs of distress while its heart rate is closely monitored.
- The process of labor is smooth and steady with the cervix widening as the baby descends.
- The health care provider estimates that the baby is not too big or the mother’s pelvis too narrow for the baby to pass safely through the birth canal.
- Anesthesia is available and a cesarean delivery possible on short notice
What are the risks and complications of a vaginal delivery?
In a breech birth, the baby’s head is the last part of its body to emerge making it more difficult to ease it through the birth canal. Sometimes forceps are used to guide the baby’s head out of the birth canal. Another potential problem is cord prolapse . In this situation the umbilical cord is squeezed as the baby moves toward the birth canal, thus slowing the baby’s supply of oxygen and blood. In a vaginal breech delivery, electronic fetal monitoring will be used to monitor the baby’s heartbeat throughout the course of labor. Cesarean delivery may be an option if signs develop that the baby may be in distress.
When is a cesarean delivery used with a breech presentation?
Most health care providers recommend a cesarean delivery for all babies in a breech position, especially babies that are premature. Since premature babies are small and more fragile, and because the head of a premature baby is relatively larger in proportion to its body, the baby is unlikely to stretch the cervix as much as a full-term baby. This means that there might be less room for the head to emerge.
Want to Know More?
- Creating Your Birth Plan
- Labor & Birth Terms to Know
- Cesarean Birth After Care
Compiled using information from the following sources:
- ACOG: If Your Baby is Breech
- William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 24.
- Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R., et al, Ch. 21.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Episiotomy: Advantages & Complications

Retained Placenta

What is Dilation in Pregnancy?
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
This topic will focus on vaginal birth of breech singletons, with a brief discussion of breech delivery at cesarean. Choosing the best route of birth for the fetus in breech presentation and delivery of the breech first or second twin are reviewed separately.
● (See "Overview of breech presentation", section on 'Approach to management at or near term' .)
- Help & Feedback
- About epocrates
Breech presentation
Highlights & basics, diagnostic approach, risk factors, history & exam, differential diagnosis.
- Tx Approach
Emerging Tx
Complications.
PATIENT RESOURCES
Patient Instructions
Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head.
Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal mortality.
Incidence decreases as pregnancy progresses and by term occurs in 3% to 4% of singleton term pregnancies.
Treatment options include external cephalic version to increase the likelihood of vaginal birth or a planned cesarean section, the optimal gestation being 37 and 39 weeks, respectively.
Planned cesarean section is considered the safest form of delivery for infants with a persisting breech presentation at term.
Quick Reference
Key Factors
buttocks or feet as the presenting part
Fetal head under costal margin, fetal heartbeat above the maternal umbilicus.
Other Factors
subcostal tenderness
Pelvic or bladder pain.
Diagnostics Tests
1st Tests to Order
transabdominal/transvaginal ultrasound
Treatment options.
presumptive
<37 weeks' gestation
specialist evaluation
corticosteroid
magnesium sulfate
≥37 weeks' gestation not in labor
unsuccessful ECV with persistent breech
Classifications
Types of breech presentation
Baby's buttocks lead the way into the birth canal
Hips are flexed, knees are extended, and the feet are in close proximity to the head
65% to 70% of breech babies are in this position.
Baby presents with buttocks first
Both the hips and the knees are flexed; the baby may be sitting cross-legged.
One or both of the baby's feet lie below the breech so that the foot or knee is lowermost in the birth canal
This is rare at term but relatively common with premature fetuses.
Common Vignette
Other Presentations
Epidemiology
33% of births less than 28 weeks' gestation
14% of births at 29 to 32 weeks' gestation
9% of births at 33 to 36 weeks' gestation
6% of births at 37 to 40 weeks' gestation.
Pathophysiology
- Natasha Nassar, PhD
- Christine L. Roberts, MBBS, FAFPHM, DrPH
- Jonathan Morris, MBChB, FRANZCOG, PhD
- John W. Bachman, MD
- Rhona Hughes, MBChB
- Brian Peat, MD
- Lelia Duley, MBChB
- Justus Hofmeyr, MD

Clinical exam
Palpation of the abdomen to determine the position of the baby's head
Palpation of the abdomen to confirm the position of the fetal spine on one side and fetal extremities on the other
Palpation of the area above the symphysis pubis to locate the fetal presenting part
Palpation of the presenting part to confirm presentation, to determine how far the fetus has descended and whether the fetus is engaged.
Ultrasound examination
Premature fetus.
Prematurity is consistently associated with breech presentation. [ 6 ] [ 9 ] This may be due to the smaller size of preterm infants, who are more likely to change their in utero position.
Increasing duration of pregnancy may allow breech-presenting fetuses time to grow, turn spontaneously or by external cephalic version, and remain cephalic-presenting.
Larger fetuses may be forced into a cephalic presentation in late pregnancy due to space or alignment constraints within the uterus.
small for gestational age fetus
Low birth-weight is a risk factor for breech presentation. [ 9 ] [ 11 ] [ 12 ] [ 13 ] [ 14 ] Term breech births are associated with a smaller fetal size for gestational age, highlighting the association with low birth-weight rather than prematurity. [ 6 ]
nulliparity
Women having a first birth have increased rates of breech presentation, probably due to the increased likelihood of smaller fetal size. [ 6 ] [ 9 ]
Relaxation of the uterine wall in multiparous women may reduce the odds of breech birth and contribute to a higher spontaneous or external cephalic version rate. [ 10 ]
fetal congenital anomalies
Congenital anomalies in the fetus may result in a small fetal size or inappropriate fetal growth. [ 9 ] [ 12 ] [ 14 ] [ 15 ]
Anencephaly, hydrocephaly, Down syndrome, and fetal neuromuscular dysfunction are associated with breech presentation, the latter due to its effect on the quality of fetal movements. [ 9 ] [ 14 ]
previous breech delivery
The risk of recurrent breech delivery is 8%, the risk increasing from 4% after one breech delivery to 28% after three. [ 16 ]
The effects of recurrence may be due to recurring specific causal factors, either genetic or environmental in origin.
uterine abnormalities
Women with uterine abnormalities have a high incidence of breech presentation. [ 14 ] [ 17 ] [ 18 ] [ 19 ]
female fetus
Fifty-four percent of breech-presenting fetuses are female. [ 14 ]
abnormal amniotic fluid volume
Both oligohydramnios and polyhydramnios are associated with breech presentation. [ 1 ] [ 12 ] [ 14 ]
Low amniotic fluid volume decreases the likelihood of a fetus turning to a cephalic position; an increased amniotic fluid volume may facilitate frequent change in position.
placental abnormalities
An association between placental implantation in the cornual-fundal region and breech presentation has been reported, although some studies have not found it a risk factor. [ 8 ] [ 20 ] [ 21 ] [ 22 ] [ 10 ] [ 14 ]
The association with placenta previa is also inconsistent. [ 8 ] [ 9 ] [ 22 ] Placenta previa is associated with preterm birth and may be an indirect risk factor.
Pelvic or vaginal examination reveals the buttocks and/or feet, felt as a yielding, irregular mass, as the presenting part. [ 26 ] In cephalic presentation, a hard, round, regular fetal head can be palpated. [ 26 ]
The Leopold maneuver on examination suggests breech position by palpation of the fetal head under the costal margin. [ 26 ]
The baby's heartbeat should be auscultated using a Pinard stethoscope or a hand-held Doppler to indicate the position of the fetus. The fetal heartbeat lies above the maternal umbilicus in breech presentation. [ 1 ]
Tenderness under one or other costal margin as a result of pressure by the harder fetal head.
Pain due to fetal kicks in the maternal pelvis or bladder.
breech position
Visualizes the fetus and reveals its position.
Used to confirm a clinically suspected breech presentation. [ 28 ]
Should be performed by practitioners with appropriate skills in obstetric ultrasound.
Establishes the type of breech presentation by imaging the fetal femurs and their relationship to the distal bones.
Transverse lie
Differentiating Signs/Symptoms
Fetus lies horizontally across the uterus with the shoulder as the presenting part.
Similar predisposing factors such as placenta previa, abnormal amniotic fluid volume, and uterine anomalies, although more common in multiparity. [ 1 ] [ 2 ] [ 29 ]
Differentiating Tests
Clinical examination and fetal auscultation may be indicative.
Ultrasound confirms presentation.
Treatment Approach
Breech presentation <37 weeks' gestation.
The UK Royal College of Obstetricians and Gynaecologists (RCOG) recommends that corticosteroids should be offered to women between 24 and 34+6 weeks' gestation, in whom imminent preterm birth is anticipated. Corticosteroids should only be considered after discussion of risks/benefits at 35 to 36+6 weeks. Given within 7 days of preterm birth, corticosteroids may reduce perinatal and neonatal death and respiratory distress syndrome. [ 32 ] The American College of Obstetricians and Gynecologists (ACOG) recommends a single course of corticosteroids for pregnant women between 24 and 33+6 weeks' gestation who are at risk of preterm delivery within 7 days, including those with ruptured membranes and multiple gestations. It may also be considered for pregnant women starting at 23 weeks' gestation who are at risk of preterm delivery within 7 days. A single course of betamethasone is recommended for pregnant women between 34 and 36+6 weeks' gestation at risk of preterm birth within 7 days, and who have not received a previous course of prenatal corticosteroids. Regularly scheduled repeat courses or serial courses (more than two) are not currently recommended. A single repeat course of prenatal corticosteroids should be considered in women who are less than 34 weeks' gestation, who are at risk of preterm delivery within 7 days, and whose prior course of prenatal corticosteroids was administered more than 14 days previously. Rescue course corticosteroids could be provided as early as 7 days from the prior dose, if indicated by the clinical scenario. [ 33 ]
Magnesium sulfate given before anticipated early preterm birth reduces the risk of cerebral palsy in surviving infants. Physicians electing to use magnesium sulfate for fetal neuroprotection should develop specific guidelines regarding inclusion criteria, treatment regimens, and concurrent tocolysis. [ 34 ]
Breech presentation from 37 weeks' gestation, before labor
ECV is the initial treatment for a breech presentation at term when the patient is not in labor. It involves turning a fetus presenting by the breech to a cephalic (head-down) presentation to increase the likelihood of vaginal birth. [ 35 ] [ 36 ] Where available, it should be offered to all women in late pregnancy, by an experienced clinician, in hospitals with facilities for emergency delivery, and no contraindications to the procedure. [ 35 ] There is no upper time limit on the appropriate gestation for ECV, with success reported at 42 weeks.
There is no general consensus on contraindications to ECV. Contraindications include multiple pregnancy (except after delivery of a first twin), ruptured membranes, current or recent (<1 week) vaginal bleeding, rhesus isoimmunization, other indications for cesarean section (e.g., placenta previa or uterine malformation), or abnormal electronic fetal monitoring. [ 35 ] One systematic review of relative contraindications for ECV highlighted that most contraindications do not have clear empirical evidence. Exceptions include placental abruption, severe preeclampsia/HELLP syndrome, or signs of fetal distress (abnormal cardiotocography and/or Doppler flow). [ 36 ]
The procedure involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
The overall ECV success rate varies but, in a large series, 47% of women following an ECV attempt had a cephalic presentation at birth. [ 35 ] [ 38 ] Various factors influence the success rate. One systematic review found ECV success rates to be 68% overall, with the rate significantly higher for women from African countries (89%) compared with women from non-African countries (62%), and higher among multiparous (78%) than nulliparous women (48%). [ 39 ] Overall, the ECV success rates for nulliparous and multiparous non-African women were 43% and 73%, respectively, while for nulliparous and multiparous African women rates were 79% and 91%, respectively. Another study reported no difference in success rate or rate of cesarean section among women with previous cesarean section undergoing ECV compared with women with previous vaginal birth. However, numbers were small and further studies in this regard are required. [ 40 ]
Women's preference for vaginal delivery is a major contributing factor in their decision for ECV. However, studies suggest women with a breech presentation at term may not receive complete and/or evidence-based information about the benefits and risks of ECV. [ 41 ] [ 42 ] Although up to 60% of women reported ECV to be painful, the majority highlighted the benefits outweigh the risks (71%) and would recommend ECV to their friends or be willing to repeat for themselves (84%). [ 41 ] [ 42 ]
Cardiotocography and ultrasound should be performed before and after the procedure. Tocolysis should be used to facilitate the maneuver, and Rho(D) immune globulin should be administered to women who are Rhesus negative. [ 35 ] Tocolytic agents include adrenergic beta-2 receptor stimulants such as albuterol, terbutaline, or ritodrine (widely used with ECV in some countries, but not yet available in the US). One Cochrane review of tocolytic beta stimulants demonstrates that these are less likely to be associated with failed ECV, and are effective in increasing cephalic presentation and reducing cesarean section. [ 43 ] There is no current evidence to recommend one beta-2 adrenergic receptor agonist over another. Until these data are available, adherence to a local protocol for tocolysis is recommended. The Food and Drug Administration has issued a warning against using injectable terbutaline beyond 48 to 72 hours, or acute or prolonged treatment with oral terbutaline, in pregnant women for the prevention or prolonged treatment of preterm labor, due to potential serious maternal cardiac adverse effects and death. [ 44 ] Whether this warning applies to the subcutaneous administration of terbutaline in ECV is still unclear; however, studies currently support this use. The European Medicines Agency (EMA) recommends that injectable beta agonists should be used for up to 48 hours between the 22nd and 37th week of pregnancy only. They should be used under specialist supervision with continuous monitoring of the mother and unborn baby owing to the risk of adverse cardiovascular effects in both the mother and baby. The EMA no longer recommends oral or rectal formulations for obstetric indications. [ 45 ]
If ECV is successful, pregnancy care should continue as usual for any cephalic presentation. One systematic review assessing the mode of delivery after a successful ECV found that these women were at increased risk for cesarean section and instrumental vaginal delivery compared with women with spontaneous cephalic pregnancies. However, they still had a lower rate of cesarean section following ECV (i.e., 47%) compared with the cesarean section rate for those with a persisting breech (i.e., 85%). With a number needed to treat of three, ECV is still considered to be an effective means of preventing the need for cesarean section. [ 46 ]
Planned cesarean section should be offered as the safest mode of delivery for the baby, even though it carries a small increase in serious immediate maternal complications compared with vaginal birth. [ 24 ] [ 25 ] [ 31 ] In the US, most unsuccessful ECV with persistent breech will be delivered via cesarean section.
A vaginal mode of delivery may be considered by some clinicians as an option, particularly when maternal request is provided, senior and experienced staff are available, there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]

Breech presentation from 37 weeks' gestation, during labor
The first option should be a planned cesarean section.
There is a small increase in the risk of serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
The long-term risks include potential compromise of future obstetric performance, increased risk of repeat cesarean section, infertility, uterine rupture, placenta accreta, placental abruption, and emergency hysterectomy. [ 60 ] [ 61 ] [ 62 ] [ 63 ]
Planned cesarean section is safer for babies, but is associated with increased neonatal respiratory distress. The risk is reduced when the section is performed at 39 weeks' gestation. [ 64 ] [ 65 ] [ 66 ] For women undergoing a planned cesarean section, RCOG recommends an informed discussion about the potential risks and benefits of a course of prenatal corticosteroids between 37 and 38+6 weeks' gestation. Although prenatal corticosteroids may reduce admission to the neonatal unit for respiratory morbidity, it is uncertain if there is any reduction in respiratory distress syndrome, transient tachypnea of the newborn, or neonatal unit admission overall. In addition, prenatal corticosteroids may result in harm to the neonate, including hypoglycemia and potential developmental delay. [ 32 ] ACOG does not recommend corticosteroids in women >37 weeks' gestation. [ 33 ]
Undiagnosed breech in labor generally results in cesarean section after the onset of labor, higher rates of emergency cesarean section associated with the least favorable maternal outcomes, a greater likelihood of cord prolapse, and other poor infant outcomes. [ 23 ] [ 67 ] [ 49 ] [ 68 ] [ 69 ] [ 70 ] [ 71 ]
This mode of delivery may be considered by some clinicians as an option for women who are in labor, particularly when delivery is imminent. Vaginal breech delivery may also be considered, where suitable, when delivery is not imminent, maternal request is provided, senior and experienced staff are available, there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
Findings from one systematic review of 27 observational studies revealed that the absolute risks of perinatal mortality, fetal neurologic morbidity, birth trauma, 5-minute Apgar score <7, and neonatal asphyxia in the planned vaginal delivery group were low at 0.3%, 0.7%, 0.7%, 2.4%, and 3.3%, respectively. However, the relative risks of perinatal mortality and morbidity were 2- to 5-fold higher in the planned vaginal than in the planned cesarean delivery group. Authors recommend ongoing judicious decision-making for vaginal breech delivery for selected singleton, term breech babies. [ 72 ]
ECV may also be considered an option for women with breech presentation in early labor, when delivery is not imminent, provided that the membranes are intact.
A woman presenting with a breech presentation <37 weeks is an area of clinical controversy. Optimal mode of delivery for preterm breech has not been fully evaluated in clinical trials, and the relative risks for the preterm infant and mother remain unclear. In the absence of good evidence, if diagnosis of breech presentation prior to 37 weeks' gestation is made, prematurity and clinical circumstances should determine management and mode of delivery.
Primary Options
12 mg intramuscularly every 24 hours for 2 doses
6 mg intramuscularly every 12 hours for 4 doses
The UK Royal College of Obstetricians and Gynaecologists recommends that corticosteroids should be offered to women between 24 and 34+6 weeks' gestation, in whom imminent preterm birth is anticipated. Corticosteroids should only be considered after discussion of risks/benefits at 35 to 36+6 weeks. Given within 7 days of preterm birth, corticosteroids may reduce perinatal and neonatal death and respiratory distress syndrome. [ 32 ]
The American College of Obstetricians and Gynecologists recommends a single course of corticosteroids for pregnant women between 24 and 33+6 weeks' gestation who are at risk of preterm delivery within 7 days, including those with ruptured membranes and multiple gestations. It may also be considered for pregnant women starting at 23 weeks' gestation who are at risk of preterm delivery within 7 days. A single course of betamethasone is recommended for pregnant women between 34 and 36+6 weeks' gestation at risk of preterm birth within 7 days, and who have not received a previous course of prenatal corticosteroids. Regularly scheduled repeat courses or serial courses (more than two) are not currently recommended. A single repeat course of prenatal corticosteroids should be considered in women who are less than 34 weeks' gestation, who are at risk of preterm delivery within 7 days, and whose prior course of prenatal corticosteroids was administered more than 14 days previously. Rescue course corticosteroids could be provided as early as 7 days from the prior dose, if indicated by the clinical scenario. [ 33 ]
consult specialist for guidance on dose
external cephalic version (ECV)
There is no upper time limit on the appropriate gestation for ECV; it should be offered to all women in late pregnancy by an experienced clinician in hospitals with facilities for emergency delivery and no contraindications to the procedure. [ 35 ] [ 36 ]
ECV involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
There is no general consensus on contraindications to ECV. Contraindications include multiple pregnancy (except after delivery of a first twin), ruptured membranes, current or recent (<1 week) vaginal bleeding, rhesus isoimmunization, other indications for cesarean section (e.g., placenta previa or uterine malformation), or abnormal electronic fetal monitoring. [ 35 ] One systematic review of relative contraindications for ECV highlighted that most contraindications do not have clear empirical evidence. Exceptions include placental abruption, severe preeclampsia/HELLP syndrome, or signs of fetal distress (abnormal cardiotocography and/or Doppler flow). [ 36 ]
Cardiotocography and ultrasound should be performed before and after the procedure.
If ECV is successful, pregnancy care should continue as usual for any cephalic presentation. A systematic review assessing the mode of delivery after a successful ECV found that these women were at increased risk for cesarean section and instrumental vaginal delivery compared with women with spontaneous cephalic pregnancies. However, they still had a lower rate of cesarean section following ECV (i.e., 47%) compared with the cesarean section rate for those with a persisting breech (i.e., 85%). With a number needed to treat of 3, ECV is still considered to be an effective means of preventing the need for cesarean section. [ 46 ]
tocolytic agents
see local specialist protocol for dosing guidelines
Tocolytic agents include adrenergic beta-2 receptor stimulants such as albuterol, terbutaline, or ritodrine (widely used with external cephalic version [ECV] in some countries, but not yet available in the US). They are used to delay or inhibit labor and increase the success rate of ECV. There is no current evidence to recommend one beta-2 adrenergic receptor agonist over another. Until these data are available, adherence to a local protocol for tocolysis is recommended.
The Food and Drug Administration has issued a warning against using injectable terbutaline beyond 48-72 hours, or acute or prolonged treatment with oral terbutaline, in pregnant women for the prevention or prolonged treatment of preterm labor, due to potential serious maternal cardiac adverse effects and death. [ 44 ] Whether this warning applies to the subcutaneous administration of terbutaline in ECV is still unclear; however, studies currently support this use. The European Medicines Agency (EMA) recommends that injectable beta agonists should be used for up to 48 hours between the 22nd and 37th week of pregnancy only. They should be used under specialist supervision with continuous monitoring of the mother and unborn baby owing to the risk of adverse cardiovascular effects in both the mother and baby. The EMA no longer recommends oral or rectal formulations for obstetric indications. [ 45 ]
A systematic review found there was no evidence to support the use of nifedipine for tocolysis. [ 73 ]
There is insufficient evidence to evaluate other interventions to help ECV, such as fetal acoustic stimulation in midline fetal spine positions, or epidural or spinal analgesia. [ 43 ]
Rho(D) immune globulin
300 micrograms intramuscularly as a single dose
Nonsensitized Rh-negative women should receive Rho(D) immune globulin. [ 35 ]
The indication for its administration is to prevent rhesus isoimmunization, which may affect subsequent pregnancy outcomes.
Rho(D) immune globulin needs to be given at the time of external cephalic version and should be given again postpartum to those women who give birth to an Rh-positive baby. [ 74 ]
It is best administered as soon as possible after the procedure, usually within 72 hours.
Dose depends on brand used. Dose given below pertains to most commonly used brands. Consult specialist for further guidance on dose.
elective cesarean section/vaginal breech delivery
Mode of delivery (cesarean section or vaginal breech delivery) should be based on the experience of the attending clinician, hospital policies, maternal request, and the presence or absence of complicating factors. In the US, most unsuccessful external cephalic version (ECV) with persistent breech will be delivered via cesarean section.
Cesarean section, at 39 weeks or greater, has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ] Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, bleeding, infection, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
Vaginal delivery may be considered by some clinicians as an option, particularly when maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
For women undergoing a planned cesarean section, the UK Royal College of Obstetricians and Gynaecologists recommends an informed discussion about the potential risks and benefits of a course of prenatal corticosteroids between 37 and 38+6 weeks' gestation. Although prenatal corticosteroids may reduce admission to the neonatal unit for respiratory morbidity, it is uncertain if there is any reduction in respiratory distress syndrome, transient tachypnea of the newborn, or neonatal unit admission overall. In addition, prenatal corticosteroids may result in harm to the neonate, including hypoglycemia and potential developmental delay. [ 32 ] The American College of Obstetricians and Gynecologists does not recommend corticosteroids in women >37 weeks' gestation. [ 33 ]
It is best administered as soon as possible after delivery, usually within 72 hours.
Administration of postpartum Rho (D) immune globulin should not be affected by previous routine prenatal prophylaxis or previous administration for a potentially sensitizing event. [ 74 ]
≥37 weeks' gestation in labor: no imminent delivery
planned cesarean section
For women with breech presentation in labor, planned cesarean section at 39 weeks or greater has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ]
Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
Continuous cardiotocography monitoring should continue until delivery. [ 24 ] [ 25 ]
vaginal breech delivery
Mode of delivery (cesarean section or vaginal breech delivery) should be based on the experience of the attending clinician, hospital policies, maternal request, and the presence or absence of complicating factors.
This mode of delivery may be considered by some clinicians as an option, particularly when maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
For women with persisting breech presentation, planned cesarean section has, however, been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ]
ECV may also be considered an option for women with breech presentation in early labor, provided that the membranes are intact.
There is no upper time limit on the appropriate gestation for ECV. [ 35 ]
Involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
Relative contraindications include placental abruption, severe preeclampsia/HELLP syndrome, and signs of fetal distress (abnormal cardiotocography and/or abnormal Doppler flow). [ 35 ] [ 36 ]
Rho(D) immune globulin needs to be given at the time of ECV and should be given again postpartum to those women who give birth to an Rh-positive baby. [ 74 ]
≥37 weeks' gestation in labor: imminent delivery
cesarean section
For women with persistent breech presentation, planned cesarean section has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ] Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
This mode of delivery may be considered by some clinicians as an option, particularly when delivery is imminent, maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
It is best administered as soon as possible after the delivery, usually within 72 hours.
External cephalic version before term
Moxibustion, postural management, follow-up overview, perinatal complications.
Compared with cephalic presentation, persistent breech presentation has increased frequency of cord prolapse, abruptio placentae, prelabor rupture of membranes, perinatal mortality, fetal distress (heart rate <100 bpm), preterm delivery, lower fetal weight. [ 10 ] [ 11 ] [ 67 ]
complications of cesarean section
There is a small increase in the risk of serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ]
The long-term risks include potential compromise of future obstetric performance, increased risk of repeat cesarean section, infertility, uterine rupture, placenta accreta, placental abruption, and emergency hysterectomy. [ 60 ] [ 61 ] [ 62 ] [ 63 ] The evidence suggests that using sutures, rather than staples, for wound closure after cesarean section reduces the incidence of wound dehiscence. [ 59 ]
Emergency cesarean section, compared with planned cesarean section, has demonstrated a higher risk of severe obstetric morbidity, intra-operative complications, postoperative complications, infection, blood loss >1500 mL, fever, pain, tiredness, and breast-feeding problems. [ 23 ] [ 48 ] [ 50 ] [ 70 ] [ 81 ]
Key Articles
Impey LWM, Murphy DJ, Griffiths M, et al; Royal College of Obstetricians and Gynaecologists. Management of breech presentation: green-top guideline no. 20b. BJOG. 2017 Jun;124(7):e151-77. [Full Text]
Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015 Jul 21;(7):CD000166. [Abstract] [Full Text]
Royal College of Obstetricians and Gynaecologists. External cephalic version and reducing the incidence of term breech presentation. March 2017 [internet publication]. [Full Text]
Cluver C, Gyte GM, Sinclair M, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb 9;(2):CD000184. [Abstract] [Full Text]
de Hundt M, Velzel J, de Groot CJ, et al. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014 Jun;123(6):1327-34. [Abstract]
Referenced Articles
1. Cunningham F, Gant N, Leveno K, et al. Williams obstetrics. 21st ed. New York: McGraw-Hill; 1997.
2. Kish K, Collea JV. Malpresentation and cord prolapse. In: DeCherney AH, Nathan L, eds. Current obstetric and gynecologic diagnosis and treatment. New York: McGraw-Hill Professional; 2002.
3. Scheer K, Nubar J. Variation of fetal presentation with gestational age. Am J Obstet Gynecol. 1976 May 15;125(2):269-70. [Abstract]
4. Nassar N, Roberts CL, Cameron CA, et al. Diagnostic accuracy of clinical examination for detection of non-cephalic presentation in late pregnancy: cross sectional analytic study. BMJ. 2006 Sep 16;333(7568):578-80. [Abstract] [Full Text]
5. Roberts CL, Peat B, Algert CS, et al. Term breech birth in New South Wales, 1990-1997. Aust N Z J Obstet Gynaecol. 2000 Feb;40(1):23-9. [Abstract]
6. Roberts CL, Algert CS, Peat B, et al. Small fetal size: a risk factor for breech birth at term. Int J Gynaecol Obstet. 1999 Oct;67(1):1-8. [Abstract]
7. Brar HS, Platt LD, DeVore GR, et al. Fetal umbilical velocimetry for the surveillance of pregnancies complicated by placenta previa. J Reprod Med. 1988 Sep;33(9):741-4. [Abstract]
8. Kian L. The role of the placental site in the aetiology of breech presentation. J Obstet Gynaecol Br Commonw. 1963 Oct;70:795-7. [Abstract]
9. Rayl J, Gibson PJ, Hickok DE. A population-based case-control study of risk factors for breech presentation. Am J Obstet Gynecol. 1996 Jan;174(1 Pt 1):28-32. [Abstract]
10. Westgren M, Edvall H, Nordstrom L, et al. Spontaneous cephalic version of breech presentation in the last trimester. Br J Obstet Gynaecol. 1985 Jan;92(1):19-22. [Abstract]
11. Brenner WE, Bruce RD, Hendricks CH. The characteristics and perils of breech presentation. Am J Obstet Gynecol. 1974 Mar 1;118(5):700-12. [Abstract]
12. Hall JE, Kohl S. Breech presentation. Am J Obstet Gynecol. 1956 Nov;72(5):977-90. [Abstract]
13. Morgan HS, Kane SH. An analysis of 16,327 breech births. JAMA. 1964 Jan 25;187:262-4. [Abstract]
14. Luterkort M, Persson P, Weldner B. Maternal and fetal factors in breech presentation. Obstet Gynecol. 1984 Jul;64(1):55-9. [Abstract]
15. Braun FH, Jones KL, Smith DW. Breech presentation as an indicator of fetal abnormality. J Pediatr. 1975 Mar;86(3):419-21. [Abstract]
16. Albrechtsen S, Rasmussen S, Dalaker K, et al. Reproductive career after breech presentation: subsequent pregnancy rates, interpregnancy interval, and recurrence. Obstet Gynecol. 1998 Sep;92(3):345-50. [Abstract]
17. Zlopasa G, Skrablin S, Kalafatić D, et al. Uterine anomalies and pregnancy outcome following resectoscope metroplasty. Int J Gynaecol Obstet. 2007 Aug;98(2):129-33. [Abstract]
18. Acién P. Breech presentation in Spain, 1992: a collaborative study. Eur J Obstet Gynecol Reprod Biol. 1995 Sep;62(1):19-24. [Abstract]
19. Michalas SP. Outcome of pregnancy in women with uterine malformation: evaluation of 62 cases. Int J Gynaecol Obstet. 1991 Jul;35(3):215-9. [Abstract]
20. Fianu S, Vaclavinkova V. The site of placental attachment as a factor in the aetiology of breech presentation. Acta Obstet Gynecol Scand. 1978;57(4):371-2. [Abstract]
21. Haruyama Y. Placental implantation as the cause of breech presentation [in Japanese]. Nihon Sanka Fujinka Gakkai Zasshi. 1987 Jan;39(1):92-8. [Abstract]
22. Filipov E, Borisov I, Kolarov G. Placental location and its influence on the position of the fetus in the uterus [in Bulgarian]. Akush Ginekol (Sofiia). 2000;40(4):11-2. [Abstract]
23. Waterstone M, Bewley S, Wolfe C. Incidence and predictors of severe obstetric morbidity: case-control study. BMJ. 2001 May 5;322(7294):1089-93. [Abstract] [Full Text]
24. Impey LWM, Murphy DJ, Griffiths M, et al; Royal College of Obstetricians and Gynaecologists. Management of breech presentation: green-top guideline no. 20b. BJOG. 2017 Jun;124(7):e151-77. [Full Text]
25. American College of Obstetricians and Gynecologists Committee on Obstetric Practice. ACOG committee opinion no. 745: mode of term singleton breech delivery. Obstet Gynecol. 2018 Aug;132(2):e60-3. [Abstract] [Full Text]
26. Beischer NA, Mackay EV, Colditz P, eds. Obstetrics and the newborn: an illustrated textbook. 3rd ed. London: W.B. Saunders; 1997.
27. Royal College of Obstetricians and Gynaecologists. Antepartum haemorrhage: green-top guideline no. 63. November 2011 [internet publication]. [Full Text]
28. American College of Obstetricians and Gynecologists. Practice bulletin no. 175: ultrasound in pregnancy. Obstet Gynecol. 2016 Dec;128(6):e241-56. [Abstract]
29. Enkin M, Keirse MJNC, Neilson J, et al. Guide to effective care in pregnancy and childbirth. 3rd ed. Oxford: Oxford University Press; 2000.
30. Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term. Cochrane Database Syst Rev. 2012 Oct 17;(10):CD000083. [Abstract] [Full Text]
31. Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015 Jul 21;(7):CD000166. [Abstract] [Full Text]
32. Stock SJ, Thomson AJ, Papworth S, et al. Antenatal corticosteroids to reduce neonatal morbidity and mortality: Green-top Guideline No. 74. BJOG. 2022 Jul;129(8):e35-60. [Abstract] [Full Text]
33. American College of Obstetricians and Gynaecologists Committee on Obstetric Practice. Committee opinion no. 713: antenatal corticosteroid therapy for fetal maturation. August 2017 (reaffirmed 2020) [internet publication]. [Full Text]
34. American College of Obstetricians and Gynecologists Committee on Obstetric Practice. Committee opinion no. 455: magnesium sulfate before anticipated preterm birth for neuroprotection. March 2010 (reaffirmed 2020) [internet publication]. [Full Text]
35. Royal College of Obstetricians and Gynaecologists. External cephalic version and reducing the incidence of term breech presentation. March 2017 [internet publication]. [Full Text]
36. Rosman AN, Guijt A, Vlemmix F, et al. Contraindications for external cephalic version in breech position at term: a systematic review. Acta Obstet Gynecol Scand. 2013 Feb;92(2):137-42. [Abstract]
37. Hofmeyr GJ. Effect of external cephalic version in late pregnancy on breech presentation and caesarean section rate: a controlled trial. Br J Obstet Gynaecol. 1983 May;90(5):392-9. [Abstract]
38. Beuckens A, Rijnders M, Verburgt-Doeleman GH, et al. An observational study of the success and complications of 2546 external cephalic versions in low-risk pregnant women performed by trained midwives. BJOG. 2016 Feb;123(3):415-23. [Abstract]
39. Nassar N, Roberts CL, Barratt A, et al. Systematic review of adverse outcomes of external cephalic version and persisting breech presentation at term. Paediatr Perinat Epidemiol. 2006 Mar;20(2):163-71. [Abstract]
40. Sela HY, Fiegenberg T, Ben-Meir A, et al. Safety and efficacy of external cephalic version for women with a previous cesarean delivery. Eur J Obstet Gynecol Reprod Biol. 2009 Feb;142(2):111-4. [Abstract]
41. Pichon M, Guittier MJ, Irion O, et al. External cephalic version in case of persisting breech presentation at term: motivations and women's experience of the intervention [in French]. Gynecol Obstet Fertil. 2013 Jul-Aug;41(7-8):427-32. [Abstract]
42. Nassar N, Roberts CL, Raynes-Greenow CH, et al. Evaluation of a decision aid for women with breech presentation at term: a randomised controlled trial [ISRCTN14570598]. BJOG. 2007 Mar;114(3):325-33. [Abstract] [Full Text]
43. Cluver C, Gyte GM, Sinclair M, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb 9;(2):CD000184. [Abstract] [Full Text]
44. US Food & Drug Administration. FDA Drug Safety Communication: new warnings against use of terbutaline to treat preterm labor. Feb 2011 [internet publication]. [Full Text]
45. European Medicines Agency. Restrictions on use of short-acting beta-agonists in obstetric indications - CMDh endorses PRAC recommendations. October 2013 [internet publication]. [Full Text]
46. de Hundt M, Velzel J, de Groot CJ, et al. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014 Jun;123(6):1327-34. [Abstract]
47. Lydon-Rochelle M, Holt VL, Martin DP, et al. Association between method of delivery and maternal rehospitalisation. JAMA. 2000 May 10;283(18):2411-6. [Abstract]
48. Yokoe DS, Christiansen CL, Johnson R, et al. Epidemiology of and surveillance for postpartum infections. Emerg Infect Dis. 2001 Sep-Oct;7(5):837-41. [Abstract]
49. van Ham MA, van Dongen PW, Mulder J. Maternal consequences of caesarean section. A retrospective study of intra-operative and postoperative maternal complications of caesarean section during a 10-year period. Eur J Obstet Gynecol Reprod Biol. 1997 Jul;74(1):1-6. [Abstract]
50. Murphy DJ, Liebling RE, Verity L, et al. Early maternal and neonatal morbidity associated with operative delivery in second stage of labour: a cohort study. Lancet. 2001 Oct 13;358(9289):1203-7. [Abstract]
51. Lydon-Rochelle MT, Holt VL, Martin DP. Delivery method and self-reported postpartum general health status among primiparous women. Paediatr Perinat Epidemiol. 2001 Jul;15(3):232-40. [Abstract]
52. Wilson PD, Herbison RM, Herbison GP. Obstetric practice and the prevalence of urinary incontinence three months after delivery. Br J Obstet Gynaecol. 1996 Feb;103(2):154-61. [Abstract]
53. Persson J, Wolner-Hanssen P, Rydhstroem H. Obstetric risk factors for stress urinary incontinence: a population-based study. Obstet Gynecol. 2000 Sep;96(3):440-5. [Abstract]
54. MacLennan AH, Taylor AW, Wilson DH, et al. The prevalence of pelvic disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000 Dec;107(12):1460-70. [Abstract]
55. Thompson JF, Roberts CL, Currie M, et al. Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth. 2002 Jun;29(2):83-94. [Abstract]
56. Australian Institute of Health and Welfare. Australia's mothers and babies 2015 - in brief. October 2017 [internet publication]. [Full Text]
57. Mutryn CS. Psychosocial impact of cesarean section on the family: a literature review. Soc Sci Med. 1993 Nov;37(10):1271-81. [Abstract]
58. DiMatteo MR, Morton SC, Lepper HS, et al. Cesarean childbirth and psychosocial outcomes: a meta-analysis. Health Psychol. 1996 Jul;15(4):303-14. [Abstract]
59. National Institute for Health and Care Excellence. Caesarean birth. Mar 2021 [internet publication]. [Full Text]
60. Greene R, Gardeit F, Turner MJ. Long-term implications of cesarean section. Am J Obstet Gynecol. 1997 Jan;176(1 Pt 1):254-5. [Abstract]
61. Coughlan C, Kearney R, Turner MJ. What are the implications for the next delivery in primigravidae who have an elective caesarean section for breech presentation? BJOG. 2002 Jun;109(6):624-6. [Abstract]
62. Hemminki E, Merilainen J. Long-term effects of cesarean sections: ectopic pregnancies and placental problems. Am J Obstet Gynecol. 1996 May;174(5):1569-74. [Abstract]
63. Gilliam M, Rosenberg D, Davis F. The likelihood of placenta previa with greater number of cesarean deliveries and higher parity. Obstet Gynecol. 2002 Jun;99(6):976-80. [Abstract]
64. Morrison JJ, Rennie JM, Milton PJ. Neonatal respiratory morbidity and mode of delivery at term: influence of timing of elective caesarean section. Br J Obstet Gynaecol. 1995 Feb;102(2):101-6. [Abstract]
65. Annibale DJ, Hulsey TC, Wagner CL, et al. Comparative neonatal morbidity of abdominal and vaginal deliveries after uncomplicated pregnancies. Arch Pediatr Adolesc Med. 1995 Aug;149(8):862-7. [Abstract]
66. Hook B, Kiwi R, Amini SB, et al. Neonatal morbidity after elective repeat cesarean section and trial of labor. Pediatrics. 1997 Sep;100(3 Pt 1):348-53. [Abstract]
67. Nassar N, Roberts CL, Cameron CA, et al. Outcomes of external cephalic version and breech presentation at term: an audit of deliveries at a Sydney tertiary obstetric hospital, 1997-2004. Acta Obstet Gynecol Scand. 2006;85(10):1231-8. [Abstract]
68. Nwosu EC, Walkinshaw S, Chia P, et al. Undiagnosed breech. Br J Obstet Gynaecol. 1993 Jun;100(6):531-5. [Abstract]
69. Flamm BL, Ruffini RM. Undetected breech presentation: impact on external version and cesarean rates. Am J Perinatol. 1998 May;15(5):287-9. [Abstract]
70. Cockburn J, Foong C, Cockburn P. Undiagnosed breech. Br J Obstet Gynaecol. 1994 Jul;101(7):648-9. [Abstract]
71. Leung WC, Pun TC, Wong WM. Undiagnosed breech revisited. Br J Obstet Gynaecol. 1999 Jul;106(7):638-41. [Abstract]
72. Berhan Y, Haileamlak A. The risks of planned vaginal breech delivery versus planned caesarean section for term breech birth: a meta-analysis including observational studies. BJOG. 2016 Jan;123(1):49-57. [Abstract] [Full Text]
73. Wilcox C, Nassar N, Roberts C. Effectiveness of nifedipine tocolysis to facilitate external cephalic version: a systematic review. BJOG. 2011 Mar;118(4):423-8. [Abstract]
74. Qureshi H, Massey E, Kirwan D, et al. BCSH guideline for the use of anti-D immunoglobulin for the prevention of haemolytic disease of the fetus and newborn. Transfus Med. 2014 Feb;24(1):8-20. [Abstract] [Full Text]
75. Hutton EK, Hofmeyr GJ, Dowswell T. External cephalic version for breech presentation before term. Cochrane Database Syst Rev. 2015 Jul 29;(7):CD000084. [Abstract] [Full Text]
76. Coyle ME, Smith CA, Peat B. Cephalic version by moxibustion for breech presentation. Cochrane Database Syst Rev. 2012 May 16;(5):CD003928. [Abstract] [Full Text]
77. Hofmeyr GJ, Kulier R. Cephalic version by postural management for breech presentation. Cochrane Database Syst Rev. 2012 Oct 17;(10):CD000051. [Abstract] [Full Text]
78. Hannah ME, Whyte H, Hannah WJ, et al. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004 Sep;191(3):917-27. [Abstract]
79. Eide MG, Oyen N, Skjaerven R, et al. Breech delivery and Intelligence: a population-based study of 8,738 breech infants. Obstet Gynecol. 2005 Jan;105(1):4-11. [Abstract]
80. Whyte H, Hannah ME, Saigal S, et al. Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004 Sep;191(3):864-71. [Abstract]
81. Brown S, Lumley J. Maternal health after childbirth: results of an Australian population based survey. Br J Obstet Gynaecol. 1998 Feb;105(2):156-61. [Abstract]
Published by
American College of Obstetricians and Gynecologists
2016 (reaffirmed 2022)
Royal College of Obstetricians and Gynaecologists (UK)
National Institute for Health and Care Excellence (UK)
Topic last updated: 2024-03-05
Natasha Nassar , PhD
Associate Professor
Menzies Centre for Health Policy
Sydney School of Public Health
University of Sydney
Christine L. Roberts , MBBS, FAFPHM, DrPH
Research Director
Clinical and Population Health Division
Perinatal Medicine Group
Kolling Institute of Medical Research
Jonathan Morris , MBChB, FRANZCOG, PhD
Professor of Obstetrics and Gynaecology and Head of Department
Peer Reviewers
John W. Bachman , MD
Consultant in Family Medicine
Department of Family Medicine
Mayo Clinic
Rhona Hughes , MBChB
Lead Obstetrician
Lothian Simpson Centre for Reproductive Health
The Royal Infirmary
Brian Peat , MD
Director of Obstetrics
Women's and Children's Hospital
North Adelaide
South Australia
Lelia Duley , MBChB
Professor of Obstetric Epidemiology
University of Leeds
Bradford Institute of Health Research
Temple Bank House
Bradford Royal Infirmary
Justus Hofmeyr , MD
Head of the Department of Obstetrics and Gynaecology
East London Private Hospital
East London
South Africa

ANDREW S. COCO, M.D., M.S., AND STEPHANIE D. SILVERMAN, M.D.
Am Fam Physician. 1998;58(3):731-738
See related patient information handout on external cephalic version , written by the authors of this article.
External cephalic version is a procedure that externally rotates the fetus from a breech presentation to a vertex presentation. External version has made a resurgence in the past 15 years because of a strong safety record and a success rate of about 65 percent. Before the resurgence of the use of external version, the only choices for breech delivery were cesarean section or a trial of labor. It is preferable to wait until term (37 weeks of gestation) before external version is attempted because of an increased success rate and avoidance of preterm delivery if complications arise. After the fetal head is gently disengaged, the fetus is manipulated by a forward roll or back flip. If unsuccessful, the version can be reattempted at a later time. The procedure should only be performed in a facility equipped for emergency cesarean section. The use of external cephalic version can produce considerable cost savings in the management of the breech fetus at term. It is a skill easily acquired by family physicians and should be a routine part of obstetric practice.
The incidence of breech presentation at term is about 4 percent. 1 Multiple factors may cause a fetus to present breech instead of vertex, including placenta previa, multiple gestation, uterine anomalies, fetal anomalies, poor uterine tone and prematurity. The majority of cases have no apparent cause. Physicians performing external cephalic version (also referred to as external version) externally rotate the fetus from a breech presentation to a vertex presentation. Over the past 15 years, external cephalic version has become a valuable, although underused, option in the management of the breech fetus at term.
Before the resurgence of the use of external cephalic version, management of breech presentation consisted of either routine cesarean delivery or a selected trial of labor. However, over the past two decades, theoretically for safety concerns regarding the fetus, the rate of cesarean delivery for breech presentation increased from 14 percent in 1970 to the current rate of up to 100 percent at some institutions. 2 Very few trials of labor are being attempted. Approximately 12 percent of cesarean deliveries in the United States are performed for breech presentation. Breech presentation ranks as the third most frequent indication for cesarean section, following previous cesarean section and labor dystocia. 3 Routine use of external version could reduce the rate of cesarean delivery by about two thirds. 4
This article reviews the rationale for the use of external version and its technical aspects, including the currently accepted protocol and manual maneuvers, factors predicting success and cost-effectiveness.
History of External Cephalic Version
External version has apparently been practiced since the time of Aristotle (384 to 322 B.C.), who stated that many of his fellow authors advised midwives who were confronted with a breech presentation to “change the figure and place the head so that it may present at birth.” However, external version eventually fell out of favor as a result of several concerns: its high rate of spontaneous reversion (turning back to breech presentation) if performed before 36 weeks of gestation, possible fetal complications, and the assumption that an external version converts only those fetuses to vertex that would have converted spontaneously anyway.
The rebirth of the use of external version occurred in the early 1980s in the United States, after a protocol developed in Berlin was replicated with favorable results in several U.S. studies. 5 , 6 Consumer demands for more noninterventional birth experiences also played a role in its resurgence. Currently, external version is performed in many institutions, and the procedure is taught in most obstetric residency programs and in some family practice residency programs.
The safety of vaginal breech delivery has been a longstanding controversy. In a recent retrospective study, 7 investigators found that the risk of fetal morbidity and mortality is increased when vaginal delivery is attempted and concluded that cesarean section should be recommended routinely. In another study, 8 however, investigators reached an opposite conclusion. They calculated a corrected perinatal mortality of zero based on a series of 316 women undergoing a trial of labor.
Other studies have documented the success and safety of external version. The authors of a recent literature review 4 of 25 studies on the efficacy of external cephalic version calculated an overall success rate of 63.3 percent, with a range of 48 to 77 percent. Most of these studies used the currently accepted protocol that is discussed in this article. These studies documented minimal risks, including umbilical cord entanglement, abruptio placenta, preterm labor, premature rupture of the membranes (PROM) and severe maternal discomfort. Overall complication rates have ranged from about 1 to 2 percent since 1979. 4 In another study, 9 fetal heart rate changes occurred in 39 percent of fetuses during external version attempts, but these changes were transient and had no relationship to the final outcome. Importantly, the literature provides overwhelmingly reassuring evidence regarding the risk of fetal death. Before 1980, four fetal deaths from external cephalic version had been reported. All of these deaths occurred in association with attempts at external version using general anesthesia. 10 Since 1980, only two fetal deaths have been reported with external version. Both occurred without the use of fetal heart rate monitoring or ultrasonography in preterm infants in Zimbabwe. 11
A recent study 12 reported a success rate for external cephalic version of 69.5 percent. Noteworthy was the fact that among fetuses undergoing successful version, the incidence of intrapartum cesarean section was 16.9 percent, a figure that was 2.25 times higher than that in the control group. The high rate of cesarean delivery resulted from a significantly higher incidence of fetal distress and labor dystocia in the group receiving external version. Results of this study demonstrate that even after successful version, a higher rate of intrapartum abnormalities may occur.
Prospective, randomized trials regarding vaginal breech delivery are not available and are unlikely to be carried out because of liability concerns. A consensus in the obstetric literature is lacking, and the optimal rate of cesarean section is likely to remain elusive and controversial. A policy of routine cesarean section eliminates the fetal risks, but considerably increases the risks of maternal morbidity. Neither option addresses the primary problem of the breech presentation, which the external version can answer in selected situations.
Selection criteria for a safe attempt at vaginal breech delivery are listed in Table 1 . 13 When these criteria are applied, approximately 70 percent of women with a vaginal breech presentation will be candidates for attempted vaginal delivery. Of these, approximately two thirds will have a successful delivery. 8 If inclusion criteria are routinely used, the calculated success rate for vaginal delivery of a fetus in the breech position is just over 40 percent. Or, conversely, about 60 percent of fetuses presenting in the breech position will be delivered by cesarean section despite optimal attempts to achieve a vaginal delivery.
Not only does external cephalic version significantly reduce the number of breech presentations at term, its use also reduces the high rate of cesarean delivery for this indication. Any reduction in the primary rate of cesarean delivery has an additive effect on the overall rate by decreasing the number of women undergoing repeat cesarean delivery. The major benefits of external cephalic version are reduced maternal morbidity and mortality from surgery.
Timing of Breech Version at Term
External version has an 80 percent success rate when performed in preterm gestations. 14 Concomitantly, the spontaneous reversion rate is approximately 16 percent. It is surmised that the relatively small size of the preterm fetus is responsible for these high rates. A small fetus has more room to be turned and can revert on its own. At term (defined as 37 weeks or more of gestation), the success rate falls to 63 percent, but the reversion rate improves to 6 to 7 percent. 4 The same rationale (the larger fetus has less freedom of movement) is responsible for these reduced rates. The most important reason to wait until the fetus is at term is to avoid iatrogenic prematurity if complications arise. If an external version attempt results in active labor, ruptured membranes or fetal compromise that requires cesarean section, and the fetus is at term, delivery can proceed without concerns about complications of prematurity. Complications resulting from an external version attempt in a preterm fetus could result in increased fetal morbidity and mortality.
Because the incidence of PROM and pre-term labor is increased in breech presentations, it is crucial for the physician to diagnose the breech presentation as close to 37 weeks of gestation as possible and, ideally, by the 36th week. This early diagnosis allows lee-way for scheduling the external version and ultrasound examination. Otherwise, the opportunity to perform external version may be lost. Careful Leopold's maneuvers, followed by ultrasonography, must be diligently performed during third-trimester prenatal visits in order for diagnosis to be made early. An algorithm for external cephalic version is presented in Figure 1 .
Selection Criteria
In general, candidates for external version should be low-risk patients at 37 weeks of gestation or more, by good dating criteria. The type of breech (either frank, complete or footling) is not a factor in determining suitability. Studies support the safety of external version in women who are candidates for vaginal birth after cesarean delivery (VBAC) 15 and in women with a transverse lie. 16 (The latter study was actually conducted intrapartum.)
External version has been used successfully in VBAC candidates without any incidence of uterine rupture. 15 In a small study, 16 version was successfully performed on women presenting in labor with a transverse lie and intact membranes, reducing the cesarean section rate by 50 percent. External version has also been used safely and with very high success rates for the delivery of the second twin with non-vertex presentation, 17 although the experience in this setting is too limited to recommend it as the method of choice. A recent study on successful external version in preterm pregnancies 14 involving 110 patients demonstrated an overall success rate of 79 percent, with no increased incidence of PROM, preterm labor or adverse fetal effects. The protocol in this study included repeat external version if spontaneous reversion occurred. All repeat attempts were successful in the preterm group. Most study authors, however, feel that external version is too risky in the preterm patient for the reasons previously mentioned. Physicians must be aware of exclusion criteria when determining the appropriateness of external version ( Table 2 ) . 18
Protocol for External Cephalic Version
External version can be performed in an outpatient setting or on the maternity floor. An ultrasound machine and an experienced sonographer must be available. There must also be ready access to a facility equipped for cesarean delivery. Family physicians without privileges for cesarean section should only perform the procedure when obstetric backup is readily available. It is important that a formal protocol be followed in order to minimize the risk of complications. Table 3 outlines one of several protocols used for external cephalic version.
With the woman placed in the supine position, the abdomen is liberally coated with ultrasonic gel in order to decrease friction and lessen the chances of an overvigorous manipulation. External version can be performed by one or two persons experienced in the procedure. Initially, the degree of engagement of the presenting part should be determined and gentle disengagement performed if possible. This can be a key factor in achieving a successful outcome. It is actually the breech that is manipulated during the maneuver. The head is guided gently toward the pelvis as the breech is moved cephalad.
Physicians can begin with the classic forward roll or the “back flip.” 5 It probably does not matter which direction is chosen first, but most physicians tend to start with the forward roll ( Figures 2 through 4 ) . Some physicians, however, may base their preference on the position of the fetus. If the spine and head of the fetus are on the same side of the maternal midline, then the back flip may be attempted ( Figures 5 through 7 ) . If the spine and head are on opposite sides of the maternal midline, then the forward roll may be selected. If the first attempt is unsuccessful, a second attempt is usually made in the opposite direction. An alternative is to have a second person manipulate one of the fetal poles or elevate the breech through the vagina. In one study, 20 an acoustic stimulator has been shown to facilitate change of the fetal spine from midline to lateral, consequently improving the chances of success.
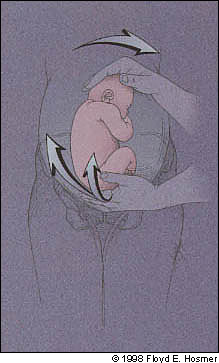
Emphasis should be on gentle persuasion of the fetus as opposed to forceful movements. Ranney, 21 one of the modern pioneers in the technique, states, “one should approach the gentle art of external cephalic version with a flexible attitude. The brain, nerves, muscles and fingers of the obstetrician should be sensitively elastic. This is no place for a hasty or domineering approach, which is futile, and possibly dangerous.”
Success is usually an all or nothing phenomenon and is attained quite easily if it is going to occur. In most recent studies, reports of successful version at term average about 65 percent. 4 It is important to monitor the fetal heart rate with the ultrasound probe during and after attempts at external version. Reasons to discontinue attempted version include excessive maternal discomfort, repeated failure or evidence of fetal compromise on monitoring. Most women do not find the procedure to be painful. If fetal bradycardia is detected after a successful version, it is recommended that the infant be returned to its previous breech presentation in hopes of reducing the risk of a tangled cord. If an attempt is unsuccessful and no evidence of fetal compromise is found, it is safe and cost-effective to repeat external version several days to one week later. 22
The risk of spontaneous reversion to a breech presentation following successful version is about 7 percent. However, one study 23 has shown that training women to make regular self-assessment of the presenting part after successful external version could improve the ultimate rate of vaginal delivery through use of prompt repeat external version when reversion is detected before labor. One case report 24 describes external version being performed successfully three times after spontaneous reversion, followed by induction of labor and a successful vaginal delivery.
Cost Effectiveness
Diagnostic and treatment algorithms are being established for many conditions, and it is becoming essential to document the cost-effectiveness of medical therapies. Several studies have focused on the cost-effectiveness of external cephalic version. A recent decision analysis 25 regarding the management of a breech pregnancy at term assumed a cost of $1,000 for external version based on California data. A strategy of routine external version for a breech presentation at term resulted in a savings of $1,473 per individual when compared with routine scheduling of a cesarean delivery. Another study 4 using different cost data concluded that the use of external version would result in a savings of 12.3 percent per birth if it were applied routinely.
Cruikshank DP. Breech presentation. Clin Obstet Gynecol. 1986;29:255-63.
Stafford RS. Recent trends in cesarean section use in California. West J Med. 1990;153:511-4.
Gabay M, Wolfe SM, eds. Unnecessary cesarean sections: curing a national epidemic. Washington, D.C.: Public Citizen Health Research Group, 1994.
Zhang J, Bowes WA, Fortney JA. Efficacy of external cephalic version: a review. Obstet Gynecol. 1993;82:306-12.
Saling E, Muller-Holve W. External cephalic version under tocolysis. J Perinat Med. 1975;3(2):115-22.
Van Dorsten JP, Schifrin BS, Wallace RL. Randomized control trial of external cephalic version with tocolysis in late pregnancy. Am J Obstet Gynecol. 1981;141:417-24.
Thorpe-Beeston JG, Banfield PJ, Saunders NJ. Outcome of breech delivery at term. BMJ. 1992;305:746-7.
Weiner CP. Vaginal breech delivery in the 1990s. Clin Obstet Gynecol. 1992;35:559-69.
Phelan JP, Stine LE, Mueller E, McCart D, Yeh S. Observations of fetal heart rate characteristics related to external cephalic version and tocolysis. Am J Obstet Gynecol. 1984;149:658-61.
Hofmeyr GJ. Effect of external cephalic version in late pregnancy on breech presentation and cesarean section rate: a controlled trial. Br J Obstet Gynaecol. 1983;90:392-9.
Kasule J, Chimbira TH, Brown IM. Controlled trial of external cephalic version. Br J Obstet Gynaecol. 1985;92:14-8.
Lau TK, Lo KW, Robers M. Pregnancy outcomes after successful external cephalic version for breech presentation at term. Am J Obstet Gynecol. 1997;176:218-23.
Eller DP, Van Dorsten JP. Breech presentation. Curr Opin Obstet Gynecol. 1993;5:664-8.
Kornman MT, Kimball KT, Reeves KO. Preterm external cephalic version in an outpatient environment. Am J Obstet Gynecol. 1995;172:1734-41.
Flamm BL, Fried MW, Lonky NM, Giles WS. External cephalic version after previous cesarean section. Am J Obstet Gynecol. 1991;165:370-2.
Phelan JP, Stine LE, Edwards NB, Clark SL, Horenstein J. The role of external version in the intra-partum management of the transverse lie presentation. Am J Obstet Gynecol. 1985;151:724-6.
Tchabo JG, Tomai BS. Selected intrapartum external cephalic version of the second twin. Obstet Gynecol. 1992;79:421-3.
American College of Obstetricians and Gynecologists. External cephalic version. ACOG practice patterns no. 4. Washington, D.C.: ACOG, 1997.
Stine LE, Phelan JP, Wallace R, Eglinton GS, van Dorsten JP, Schifrin BS. Update on external cephalic version performed at term. Obstet Gynecol. 1985;65:642-6.
Johnson RL, Elliot JP. Fetal acoustic stimulation, an adjunct to external cephalic version: a blinded randomized crossover study. Am J Obstet Gynecol. 1995;173:1369-72.
Ranney B. The gentle art of external cephalic version. Am J Obstet Gynecol. 1973;116:239-51.
Kilpatrick SJ, Safford KL. Repeat external cephalic version. Is it worth the effort?. J Reprod Med. 1995;40:775-8.
Bergstrom S. External cephalic version and daily post-versional maternal self-assessment of fetal presentation. A prospective study. Gynecol Obstet Invest. 1992;33:15-8.
Rosen DJ, Illeck JS, Greenspoon JS. Repeated external cephalic version at term. Am J Obstet Gynecol. 1992;167:508-9.
Gifford DS, Keeler E, Kahn KL. Reductions in cost and cesarean rate by routine use of external cephalic version: a decision analysis. Obstet Gynecol. 1995;85:930-6.
Continue Reading
More in afp, more in pubmed.
Copyright © 1998 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

- Cerebral Palsy
- Erb's Palsy
- Brain Damage
- Delivery Complications
- Prenatal Problems
- Birth Injury Stories

- Breech Position
Not all babies move into the normal head-first presentation before delivery. Instead, a certain percentage of babies do not reposition and end up with their butt and/or feet downwards towards the birth canal with the head up.
This referred to as the "breech" position or breech presentation. Breech position is not normal and consider a pregnancy complication. The occurrence rate of breech position is around 5% or 1 out of every 25 babies in full-term pregnancies. The occurrence rate for breach presentation is significantly higher, however, in preterm pregnancies.
Normally in the last few weeks of a pregnancy the baby will gradually reposition itself in the head down presentation in preparation for birth. Head first is the normal presentation because it is the optimal position to safely and effectively facilitate vaginal delivery. When in the head first position the crown of the baby's skull functions like a spear head which pushes into and through the birth canal.
Breech presentation generally includes any presentation in which the baby's butt or feet are pointing down towards the birth canal. However, there are several different recognized subtypes of breech presentation depending on the specifics and extent of the baby's abnormal position and the positioning of the legs:
- Frank Breech : the butt is still facing down toward the birth canal (same as with complete breech) instead of the legs being bent at the knees and tucked in the fetal position the baby's legs at straight at the knees and facing upwards so that the feet are basically in front of the face. Frank breech is the most common type of breech in full-terms babies and accounts for anywhere from 50-70% of all breech presentations.
- Footling Breech : in a footling breech presentation the baby's feet are actually pointing downward and will enter first into the birth canal ahead of the butt. Footling breech is more common in premature babies. Fooling has the second highest occurrence rate of all breech positions.
- Complete Breech : in complete breech presentation the butt is aimed down towards the birth canal entrance and the baby is in the traditional "fetal" position with knees bent and pulled up to the chest and feet near the butt. Complete breech is rarest of all types of breech presentation. Less than 10% of breech birth are classified as complete breech.
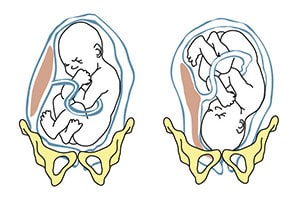
- Pregnancy with twins or multiples
- Mother has had prior pregnancies
- Maternal history of premature delivery
- Too much amniotic fluid ( polyhydramnios )
- Placenta previa
- Abnormally shaped uterus or abnormal uterine growths (fibroids)
The occurrence of any of these complications during pregnancy can significantly increase the chances of breech presentation occurring. However, breech presentation can occur in a normal pregnancy without complications.
Breech presentation is something that gets diagnosed towards the very end of a full term pregnancy. A formal diagnosis of breech presentation is not made until at least the 35 th week of pregnancy because before week 35 it is perfectly normal for a baby to be positioned head-up or sideways. Repositioning is something that the baby is supposed to naturally do on their own in the final few weeks before birth.
Diagnosis of breech presentation will start in a prenatal examination occurring at or sometime after the 35 th week of gestation. The doctor will initially perform a manual abdominal exam to gently feel around and identify the apparent position of the baby's head, butt and feet. If the baby doesn't seem to be in the expected position an ultrasound will usually be done to confirm the diagnosis of breech presentation. If ultrasound imaging is not enough there are also special prenatal X-rays that can be done to give doctors a more accurate image of the baby's presentation.
When a baby is in breech position attempting a vaginal delivery can be very dangerous and most OB/GYNs will automatically plan to deliver the baby via C-section. There are several reasons why vaginal delivery of a breech baby is so hazardous.
For starters, breech presentation makes the basic mechanics of vaginal delivery much more difficult. The baby's head is the largest part of their body so it is the most difficult to push through the birth canal. This is why brachial plexus palsy is the most common injury in a vaginal breech delivery. In a normal, head-first delivery the crown of the baby's head sort of spears its way into and through the birth canal. Getting the head safely through the birth canal in the reverse direction is much more difficult and potentially dangerous.
Another major reason why vaginal delivery from breech position is so hazardous is because there is a much higher risk of a delivery complication called umbilical cord prolapse . Umbilical cord prolapse is one of the most dangerous events that can occur during childbirth. It occurs when the umbilical cord (the baby's lifeline to the mother) drops down into the birth canal in front of the baby (instead of behind like in a normal delivery). When the cord goes first and the baby comes through the birth canal after the umbilical cord gets squeezed and compressed against the walls of the birth canal by the baby's head and body. This can severely restrict or even cut off oxygen supply to the baby and cause major brain injuries or even death from perinatal asphyxia.
Attempting a vaginal delivery when the baby is in breech position can greatly increase the risk of a birth injury. Although there is currently a major push towards doing less C-sections, breech presentation is a situation where a planned C-section is simply the most sensible option. This is particularly true for premature babies that are more fragile.
Further Reading
Athiel, Y., et al. (2022). Association Between Hospitals' Cesarean Delivery Rates For Breech Presentation And Their Success Rates For External Cephalic Version. European Journal of Obstetrics & Gynecology and Reproductive Biology, 270 , 156-163.
This article looked at the association between a hospital’s C-section and external cephalic version rates. The researchers found that the ECV success rates correlated with C-section rates for persistent breech presentations.
Benmessaoud, I., et al. (2022). Analysis of spontaneous labor progression of breech presentation at term. PloS one, 17 (3), e0262002.
This article looked at the labor progression pattern in breech presentation patients and determined whether the breech type or parity affected cervical dilation speed. The researchers found that the labor progression’s first stage in breech presentation involved latent and active phases. They also found that labor progression should be interpreted based on parity and breech type did not seem to influence the cervical dilation rate when adequately managed.
Claire, G., et al. (2022). Neonatal morbidity and mortality for preterm in breech presentation regarding the onset mode of labor. Archives of Gynecology and Obstetrics , 1-10.
This study compared the neonatal mortality and morbidity rates in preterm breech deliveries involving induced labor and spontaneous labor. The researchers found that both groups had similar neonatal mortality and morbidity rates. They concluded that the onset mode of labor did not seem to affect neonatal mortality and morbidity in breech presentation cases.
Coskun, B., et al. (2020). Comparison of Emergency and Elective Cesarean Sections in the Breech Presentation: A Case-Control Study.
This study compared outcomes in breech presentation pregnancies that underwent an emergency C-section and those that underwent an elective C-section. The researchers found that the emergency C-section group had lower Apgar scores and postoperative hemoglobin levels. They also found that cervical dilations of two centimeters and above in emergency C-sections were associated with lower hemoglobin counts, increased blood transfusion needs, and NICU transfers. The researchers concluded that healthcare providers should use caution when considering emergency C-sections and avoid iatrogenic preterm births.
Lallemant, M., et al. (2021). Asymmetric pelvis and term breech presentation: is planned vaginal delivery still a safe option? Archives of Gynecology and Obstetrics, 304 , 919-927.
This study looked at whether planned vaginal deliveries were safe for term breech presentations involving asymmetric pelvises. The researchers found higher vaginal delivery rates in the asymmetric pelvis group compared to the symmetric group. They also found no statistical differences in neonatal and maternal complications. The researchers concluded that breech presentation births were “not an indication for” an elective C-section.
Gunay, T., et al. (2020). Comparison of maternal and fetal complications in pregnant women with breech presentation undergoing spontaneous or induced vaginal delivery, or cesarean delivery. Taiwanese Journal of Obstetrics and Gynecology, 59 (3), 392-397.
This study compared and contrasted complications in spontaneous, induced, or C-section deliveries that involved breech presentation. The researchers found that induced vaginal deliveries had the highest complication rate, while C-sections had the lowest. They concluded that healthcare providers should consider specific delivery types’ risks and benefits when handling breech presentation pregnancies.
Martel-Santiago, C.R., et al. (2020). Delivery in breech presentation: Perinatal outcome and neurodevelopmental evaluation at 18 months of life. European Journal of Obstetrics & Gynecology and Reproductive Biology, 255 , 147-153.
This study compared the outcomes of cephalic and breech deliveries. The researchers found that C-sections involving breech presentations had lower Apgar scores than cephalic presentations. They also found that vaginal concluded that healthcare providers should implement specific protocols in certain breech presentation pregnancies to achieve similar outcomes as cephalic presentation ones.
Toijonen, A.E., et al. (2020). A comparison of risk factors for breech presentation in preterm and term labor: a nationwide, population-based case-control study. Archives of Gynecology and Obstetrics, 301 , 393-403.
This study looked at whether breech presentation’s common risks in term labor were present in preterm labor. The researchers found that breech presentation-associated factors in preterm breech deliveries were similar to factors in term pregnancies. By contrast, they found that exceptionally preterm breech births had comparable risks to cephalic presentations.
- Birth Defects
- Cerebral Palsy Birth Injuries
- Infant Brain Damage
- Amniotic Fluid Embolism
- Cephalopelvic Disproportion
- Cervical Dystonia in Infants
- Epidurals and Birth Injuries
- Episiotomy Complications and Side Effects
- Fetal Monitoring During Childbirth
- Forceps Delivery & Birth Injuries
- Fundal Pressure
- Herpes and Infants
- Meconium Aspiration Syndrome
- Most Dangerous Delivery Room Complications
- Newborn Resuscitation and Birth Injuries
- Pitocin and Birth Injuries
- Retained Placenta
- Shoulder Dystocia
- Subconjunctival Hemorrhage
- The History of Childbirth
- Umbilical Cord Prolapse
- Ruptured Uterus
- Vacuum Assisted Delivery and Birth Injuries
- Vaginal Tears
- Help Center

- Privacy Policy
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Please do not include any confidential or sensitive information in a contact form, text message, or voicemail. The contact form sends information by non-encrypted email, which is not secure. Submitting a contact form, sending a text message, making a phone call, or leaving a voicemail does not create an attorney-client relationship.

Rebecca Dekker
The Evidence on: Breech Version
Originally published on October 11, 2012 and updated on March 29, 2021. All Rights Reserved. Please read our Disclaimer and Terms of Use . For a printer-friendly PDF, become a Professional Member to access our complete library.
How common is the breech position?
Breech position (bottom first) is present in 3% to 4% of term pregnancies. Breech positioning is common prior to term—25% are breech before 28 weeks, but by 32 weeks only 7% of babies are breech. The vast majority of breech babies in the United States (U.S.) are now born by planned Cesarean (Table 1). The use of a safe procedure to help turn breech babies into a head-down position (aka cephalic position) may help to lower the Cesarean rate (ACOG 2020).
What is an external cephalic version?
External = from the outside, cephalic = head first, version = turning
An external cephalic version is when a care provider puts their hands on the outside of your belly and turns the baby, using either a forward or backward roll, into a cephalic (head-down) position. This is also called an ECV, version, or “hands to belly” procedure (ACOG 2020).
We compiled some statistics from the Centers for Disease Control (Table 1). There were 150,678 breech babies in the U.S. during the year 2019, or 4% of all babies. Of these, 93.8% were born by Cesarean. The number of known breech births made up 11.8% of all Cesareans in 2019.

How many pregnant people with breech babies have a version?
We contacted the CDC for the most recent data in the U.S. (Table 2). In 2019, only 10,783 people (0.2%) underwent an external cephalic version (ECV) procedure, compared to 11,158 (0.3%) in 2016. As you can see in the table below, the success rate decreased from 55.8% in 2016 to 48.5% in 2019. Of the people who had successful ECVs in 2019, 71.9% went on to have spontaneous vaginal births. On the other hand, the 2019 failure rate of ECVs was 51.5%, and 91.3% of those with failed ECVs went on to have Cesarean births.

There is general agreement in the U.s. that the Cesarean rate is higher than necessary, and changes should be made to safely bring it down. For this reason, there is renewed interest in both ECV and vaginal breech birth. As the rate of successful ECVs and vaginal breech birth goes up, the Cesarean rate goes down (ACOG 2020).
Unfortunately, the ECV is an underused procedure. In the U.S., ACOG (2020) states that as many as 20-30% of people who are eligible for ECV are not offered it, even though attempting ECV lowers their chance of Cesarean.
In an Australian study, only 66% of pregnant people had ever heard of an ECV, and most of them (87%) had learned about version from books or family/friends—not from care providers. Only 39% of participants said they would choose an ECV if they had a breech baby, and 22% were undecided. The participants who did not want a version said that they had concerns about effectiveness and safety for the baby (Raynes-Greenow et al. 2004).
In 2017, another Australian study looked at over 32,000 people who had singleton breech pregnancies of ≥36 weeks between 2002 and 2012 (Bin et al. 2017). Only 10.5% of the group attempted an ECV. As many as 67.2% did not attempt an ECV even though they were considered to be good candidates for the procedure according to Australian practice guidelines. The practice guidelines identified 22.3% of the group as too high risk for the procedure. The authors note that it is not clear whether the low rate of ECV attempts is related to care providers failing to offer it or pregnant people declining the procedure.
In a Dutch study, investigators estimated that less than half of people in the Netherlands with a breech baby at term had an ECV. Approximately 20-30% of them refused an ECV and decided to have a planned Cesarean instead. It was estimated that anywhere from 4% to 33% of pregnant people are not given the option of a having an ECV by their care providers (Vlemmix et al. 2010).
In the U.S., it could be that care providers aren’t offering versions as readily because health insurance plans (including Medicaid) consider it to be a part of regular, routine prenatal care (Personal correspondence, Johannson, 2017)– thus preventing hospitals and clinics from being adequately reimbursed for an ECV. An ECV takes time and resources, especially considering the potential need for medications (and in some cases, an epidural), and the need for pre- and post- procedure tests and monitoring for wellbeing.
Are external cephalic versions effective for reducing the risk of Cesarean?
Many people believe that the U.S. Cesarean rate is higher than necessary and that we should explore ways to bring the overall rate down. Since breech babies are almost always born by Cesarean, there is a renewed interest in attempting ECV to increase the chance of vaginal birth (ACOG, 2020). Also, versions are cost-effective when compared to a scheduled Cesarean (Tan et al. 2010).
In a 2015 Cochrane review, Hofmeyr et al. (2015) combined the results from eight randomized, controlled trials with 1,308 participants who were randomly assigned to either ECV or no treatment. The quality of the studies was mixed. In order to control for quality of the studies, the researchers looked at the results both with and without the poorer quality studies. When they did so, the results stayed the same.
Overall, the researchers found that attempting an ECV at term decreased the relative risk of breech birth by 58% and decreased the relative risk of Cesarean by 43%. There were no differences in any other outcomes, including Apgar scores, neonatal admission, or infant deaths. The studies did not look at maternal satisfaction (Hofmeyr et al. 2015).
It is important to note that five of the eight studies in this review took place between 1981 and 1991, a time when breech vaginal births were more common. Since the publication of the “Term Breech Trial” in 2000, breech vaginal births have become extremely rare, and most breech babies are born by planned Cesarean. Therefore, it is possible that if these randomized trials were replicated today, having an ECV might result in an even larger reduction in the risk of Cesarean.
In a different systematic review published in 2020, Devold Pay et al. reviewed two randomized trials (conducted in 1981 and 1984) and seven observational studies (carried out between 1985 and 2014) comparing the effects of ECV or no ECV on more than 184,000 pregnant people who were eligible for an ECV at ≥ 36 weeks. Altogether, the review included 7,091 attempted ECVs. Studies were conducted in high-resource settings in northern, western, and central Europe, the U.S., Canada, Australia, and New Zealand. When the review authors combined the data, they found that attempted ECV was linked to a significant reduction in Cesarean and non-cephalic presentation at birth. They estimated that a policy of attempted ECV (compared to no attempted ECVs) would probably result in between 320 to 710 fewer non-cephalic presentations at birth and 271 to 376 fewer Cesareans per 1,000 labors.
The authors also found that ECV attempts were linked to a slightly increased rate of Apgar score < 7 at 5 minutes compared to no ECV attempt (24 vs. 19 per 1,000). They estimated that attempted ECV would probably result in 2 to 10 more low Apgar scores at. 5 minutes per 1,000 labors. Attempted ECV had no effect on low Apgar scores at 1-minute, perinatal death, or NICU admission.
This review was limited by unclear risk of bias for the 2 RCTs and serious risk of bias for the 7 observational studies. The largest study in the review had serious risk of bias, largely due to its reliance on U.S. birth certificate data from 2006 (Balayla et al., 2014). Devold Pay et al. concluded that more high-quality research is needed, but the available evidence suggests that when ECV is attempted at or near term, there is a substantially reduced risk of Cesarean and a slightly increased risk of low Apgar score at 5 minutes.
A separate observational study published in 2016 (Weiniger et al.) found several additional benefits to ECV. This study examined data from a U.S. healthcare utilization database and was not included in either the Cochrane review or the Devold Pay et al. review. Researchers compared 56,409 people who had a successful ECV with 1,023,166 people who had a persistent breech baby at the time of birth. The Cesarean rate was 20.2% in the successful ECV group vs. 94.9% in the persistent breech group. The researchers also found that people with successful ECV also had overall better maternal outcomes including lower rates of infection (endometritis and sepsis), shorter hospital stays, lower hospital charges, but higher rates of inflammation of the membranes (chorioamnionitis).
Overall, a successful ECV can have important personal benefits for an individual by helping someone avoid major abdominal surgery. Versions can also have population-level benefits by lowering the overall Cesarean rate. If everyone with a breech baby at term attempted an ECV, then about half would be successful. Of those with successful ECVs, about three quarters would eventually give birth vaginally. This means that more than a third of people with term breech pregnancies could avoid a Cesarean if everyone attempted an ECV. Given that 3% to 4% of all term pregnancies are breech, the overall Cesarean rate would come down by 1% to 2%. Obviously not all people with breech pregnancies at term are good candidates for the procedure, and some would refuse the procedure, so the real reduction in the Cesarean rate may not be as large. But it’s important to understand that the real benefit in reducing the number of Cesareans from breech pregnancies comes later on, in subsequent pregnancies– since many of those would result in repeat Cesareans, which carry additional risks.
Are there any other risks of an ECV?
The sample sizes from the previously mentioned reviews were too small to give an accurate picture of rare risks of an ECV. In order to look at risks, we need to look at a study with a larger number of ECV procedures.
In 2008, Grootscholten et al. combined the results of 84 studies that included 12,955 participants who experienced an attempted ECV. They only included studies that reported on complications from attempted versions on single babies done after 36 weeks of pregnancy. The average success rate for turning a baby out of the breech position was 58%. The overall complication rate was 6%, and the rate of serious complications (placenta abruption or stillbirth) was 0.24%. There were 12 stillbirths out of the 12,955 cases, and two of these deaths were related to the ECV. The other deaths were un-related to the ECV or unexplained. The unexplained stillbirths were diagnosed 10 to 31 days after the version. Placenta abruption occurred in 0.18% of participants (11 abruptions out of 12,955 ECVs), and 10 of these abruptions resulted in an emergency Cesarean (Grootscholten et al. 2008).
Other complications included cord prolapse (0.18%), temporary abnormal fetal heart rate patterns (4.7%), vaginal bleeding (0.34%), and water breaking (0.22%). There was one urgent Cesarean for every 286 ECVs. In summary, researchers found that ECV is safe, but they recommended that a version should take place in a setting where an urgent Cesarean could be performed if necessary.
Is an ECV painful?
The potential pain or discomfort from an ECV may discourage some people from attempting the procedure. Several studies have asked mothers about their experiences during and after an attempted ECV. Researchers at a large teaching hospital in the Netherlands conducted a study of 249 people attempting an ECV (Truijens et al. 2014). Before the ECV attempt, researchers spent about 30 minutes interviewing participants about symptoms of depression and fear of the ECV. Immediately after the procedure, a different researcher (who was blind to the earlier interview) assessed each participant’s pain perception.
They found that the most important factor influencing pain perception was whether the ECV was successful at turning the baby or not. To put it another way, people who had successful ECVs reported significantly less pain than people with failed ECV attempts. The average ECV attempt lasted just under four minutes, and ranged from less than a minute to 16 minutes. As would be expected, the people who underwent longer procedures reported more pain. The important takeaway, however, is that the length of the procedure—or any other factor for that matter—didn’t totally explain why people with failed ECV attempts reported more pain. It appears that the negative emotions that follow a disappointing outcome independently influence how much pain a person recalls. Data from the pre-ECV interviews showed that depression and fear also independently influence pain perception. This means that people who have signs of depression or expect the procedure to be painful are more likely to actually find it painful compared to people without signs or depression or fear going into the procedure.
In Australia, researchers interviewed 16 first-time mothers and six experienced mothers who had attempted an ECV but it did not successfully turn the baby (Watts et al. 2016). The mothers went on to have either planned Cesareans (45%) or planned vaginal breech births (55%). When asked how they felt about the attempted ECV, the majority of people replied that the procedure was painful. Some people reported pain that lasted for a while after they were home. Nearly half of the people interviewed (46%) said that they would not attempt a version in a future pregnancy. It’s important to remember that the people being interviewed did not have successful ECVs, and as we saw in the study from the Netherlands, an attempted ECV’s outcome can greatly influence your pain perception. The authors concluded that attempting an ECV should be only one of multiple options that pregnant people with term breech can consider—other options include planned Cesarean or vaginal breech birth.
- To learn more about vaginal breech birth, visit our podcast interview with Breech Without Borders, available here [Coming soon!]
- To learn more about family-friendly Cesareans, visit our Signature Article here .
Pain management during an ECV
Some therapies can be used to reduce the discomfort of a breech version attempt. A study in Spain compared 300 people who received nitrous oxide, or laughing gas (a 50:50 mix of nitrous and oxygen) starting three minutes before attempting an ECV with 150 people who did not receive gas with the procedure (Burgos et al. 3013). There were no differences in the rate of complications, the Cesarean rate, or the success rate of the ECV, but people who received gas were 49% less likely to report severe pain from the procedure.
A study in China randomly assigned 72 people to intravenous (IV) remifentanil and 72 people to a saline IV solution (placebo) during an attempted ECV (Wang et al. 2017). All of the people in this study were giving birth for the first time. Remifentanil is a synthetic opioid that is sometimes used to manage pain during labor. The researchers found that the people who received the remifentanil reported less pain immediately after the procedure and more satisfaction when asked 10 minutes after the ECV. They also found a difference in the success rate of the version between groups—the people who received remifentanil had a success rate of 57% and the placebo group had a success rate of 39%. There were no differences as far as complications. Earlier studies have also found that remifentanil decreases pain during ECV attempts, but findings are conflicting regarding whether it increases the success rate of the version or not.
A review paper found that people who receive epidurals, spinals, or a combination of both report less pain and discomfort during an ECV than those who do not (1.2% versus 9.3%) (Magro-Malosso et al. 2016). An additional benefit to epidurals, spinals, or combination epidural-spinal pain management is that researchers have found these methods may increase the success rate of the version (discussed further below). It’s thought that epidurals, spinals, and combined spinal-epidurals help keep your abdominal muscles relaxed, which may allow the care provider to more easily rotate the baby (Carvalho & Bateman 2017).
When is the best time to have an ECV?
You can choose to have an ECV before term (34 to 37 weeks), at term (>37 weeks), or even during labor.
In the largest randomized controlled trial to compare ECVs before term and at term, researchers found that doing an ECV before term increases the chance that the baby will be head down at birth (59% versus 51%). However, they also found that having an early ECV does not lower the risk of having a Cesarean. There was also evidence that doing an ECV before term may increase the risk of premature birth (Hutton et al. 2011). In a later analysis of the data, the researchers found that lower gestational age was a predictor of success during an ECV among people who had given birth before, but that a more important predictor of success was if the baby was still floating above the pelvis (had not yet descended into the pelvis) (Hutton et al. 2017).
A Cochrane review from 2015 combined five trials to study ECVs attempted before term. The review was dominated by the large Hutton et al. (2011) trial, so not surprisingly the results are consistent with that trial’s results. The Cochrane reviewers concluded that an ECV done between 34 and 36 weeks does result in more babies that are head-down at the time of birth compared with an ECV at gestational age ≥ 37 weeks. However, the decrease in breech presentation at birth did not lead to an overall lowering of the Cesarean rate. Based on these findings, the first attempt at a version is usually scheduled at gestational age ≥ 37 weeks (Lim & Lucero 2017). People should discuss the potential benefits and risks of an early ECV with their care providers— weighing the greater likelihood of successful ECV before 37 weeks against the rare complication of birthing a preterm infant.
Finally, for people who discover that they are pregnant with a breech baby during labor, there is some evidence showing that ECV can be successful when performed during early labor. In a study that used U.S. data from 1998 to 2011, the ECV success rate was 65% when it was attempted during hospital admission for birth. People with successful ECV in early labor were significantly less likely to have a Cesarean or have a hospital stay greater than 7 days compared to people who remained with breech presentation at the time of birth (Weiniger et al. 2016).
Are there any techniques that increase the likelihood of a successful ECV?
Researchers have studied several techniques that could increase the chance of success with a breech version. So far, the most helpful technique seems to be using drugs to prevent labor contractions (also known as tocolysis). In a Cochrane review, researchers combined the results of 28 studies with more than 2,700 participants who were randomly assigned to receive an ECV alone or ECV with an additional technique, such as tocolysis or having an epidural ( Cluver et al. 2015 ). The participants who were randomly assigned to receive tocolytic drugs (drugs to prevent contractions) during the version were 23% less likely to have an eventual Cesarean for breech positioning compared to those who did not receive tocolysis. Participants who received tocolysis were also 68% more likely to have babies with head-first positioning at the start of labor.
In the Cochrane review, the participants who were randomly assigned to have an epidural or spinal (in combination with tocolysis) during the ECV were 39% more likely to have a successful ECV ( Cluver et al. 2015 ). There were no differences in any of the other outcomes between participants with and without epidurals, such as cephalic presentation at the start of labor or rate of Cesareans, but the number of participants in the study (279 people) may not have been large enough to find an effect.
The use of anesthesia during ECV is still controversial and should be considered on an individual basis. One meta-analysis of nine randomized trials (934 people) found that the participants who received an epidural, spinal, or combination spinal-epidural had a higher rate of successful ECV compared to the participants who received IV pain medications or no treatment (58% versus 43%). The epidural/spinal group also had a higher rate of cephalic presentation at the start of labor (55% versus 40%) and a higher vaginal birth rate (54% versus 45%). The participants in both groups also received tocolysis. There were no differences in the rate of complications between groups (Magro-Malosso et al. 2016).
However, a different meta-analysis that included 18 RCTs and 1 quasi-randomized trial (2,296 people) did not find evidence that using anesthesia during ECV increased the vaginal birth rate (Hao et al. 2020). Using epidural, spinal, or spinal-epidural significantly increased the success rate of ECV, but did not reduce the risk of Cesarean.
Some care providers recommend against epidurals and spinals for ECV attempts because it makes for a much longer and more complicated procedure. And even though epidural/spinal anesthesia is the most effective medication for a successful ECV, pregnant people report more satisfaction with intravenous and inhalation anesthesia (Hao et al. 2020).
One small study found that vibroacoustic stimulation (applying sound to the abdomen) resulted in successful ECVs in 86% of participants (19 of 22) compared to 8% of participants (one of 12) in the placebo group that only received sound into the nurse’s arm (Johnson & Elliott 1995). The current evidence is too weak to draw conclusions about the effectiveness of this technique. However, it deserves further research in larger studies since it is inexpensive, noninvasive, and has no known side effects.
Some people recommend using moxibustion, a type of Chinese medicine, to help turn a breech baby. To learn more about the evidence on moxibustion, you can find the Cochrane review on that subject here .
Are there any other factors that may influence the ECV success rate?
One of our physician reviewers has found in his experience that there are three important factors for a successful version procedure (Personal correspondence, Morris, 2017):
- A physician who believes in the benefits of the procedure and is skilled at performing it
- A well-informed patient who is also motivated to avoid a first and therefore subsequent Cesarean
- A willingness by the physician to abandon the procedure if requires more than the normal amount of manipulation or the baby does not tolerate the procedure
One U.S. study found that there is an inverse relationship between the rate of successful ECV and a hospital’s Cesarean rate. In other words, the higher the hospital’s Cesarean rate, the lower their ECV success rate (Weiniger et al. 2016). It’s not clear why this is the case– perhaps hospitals with high Cesarean rates are not following best practices for ECV success, or perhaps this relationship has to do with the type of patients who are seeking care at hospitals with high Cesarean rates.
Researchers have also looked at factors specific to the individual and the pregnancy that may influence the success rate of versions. The researchers that conducted the randomized trial comparing early versus late ECV used the data from that trial (and an earlier pilot trial) to study the factors that influence the success rate of ECVs (Hutton et al. 2017). Of the 1,253 people who had an ECV, 742 were giving birth for the first time and 511 were people who had given birth before. The ECV was considered to be successful— meaning that the baby immediately turned and was still cephalic at the time of birth— in 33% of the people who were giving birth for the first time and 61% of those who had given birth before. Overall, 11% of the participants attempted more than one ECV. Note that it is not standard practice in the U.S. to attempt another version on a later day after a failed version attempt (Personal correspondence, Johannson, 2017).
Hutton et al. (2017) found that the following factors are strongly linked to higher ECV success rates:
- Having given birth to previous children
- If the baby is not engaged in the pelvis (described as floating or dipping)
- If the care provider can easily feel the baby’s head on palpation (related to the baby’s position as well as maternal body fat)
Other factors that increase the likelihood of an ECV’s success to a lesser extent are:
- If the placenta is posterior (on the back side of the uterus) (Hutton et al. 2017)
- If the birthing person’s BMI is less than 32.7 (Hutton et al. 2017)
- If there are normal levels of amniotic fluid (an Amniotic Fluid Index >10) (Lim & Lucero 2017)
- If the waters are intact (Lim & Lucero 2017)
- If the uterus is normally shaped (Lim & Lucero 2017)
- If the abdominal wall muscles are relaxed (Lim & Lucero 2017)
- Non-frank breech presentation (Lim & Lucero 2017)
Another way to look at it is that certain factors make an ECV less likely to work. People should have an honest discussion with their care provider before deciding to attempt a version. If someone has one or more of these factors then they should know that they have a lower chance of success—not to be discouraged, but to have realistic expectations about the outcome.
This is not a complete list, but some factors that decrease the success rate of an ECV are (Ehrenberg-Buchner & Van De Ven 2015):
- First time giving birth
- The baby has already descended into the pelvis (engaged)
- The care provider can not easily feel the baby’s head on palpation
- Maternal body mass index ≥ 32.7
- The baby is small for gestational age
- The placenta is on the front, side, or top of the uterus
- Amniotic fluid volume is higher or lower than normal
- Abdominal muscles and/or uterus firm and tense
- Waters have already broken
- The baby’s spine is located towards the back
- Frank breech presentation
Hutton et al. (2017) also found that gestational age of <37 weeks was linked to successful ECVs in people who had given birth before. However, they recommend that care providers focus on the individual baby’s descent rather than use a standard gestational age cut-off, so that an ECV can be planned before the baby becomes engaged in the pelvis while still doing as much as possible to avoid influencing preterm birth.
Are there any reasons why someone cannot have an ECV?
Different guidelines list different reasons why certain people should not have an ECV. Whenever there is a reason not to do something, that reason is called a “contraindication.” In 2012, researchers did a systematic review to determine which contraindications are based on research evidence ( Rosman et al. 2012 ). It’s important to be clear that the failure to find research evidence to support a contraindication does not mean that there is evidence showing the factor to be safe. Rather, it means that there is a lack of evidence—we can’t say that the factor is contraindicated but we also can’t say that it is not.
For the 39 different contraindications listed in international guidelines, the researchers could only find research evidence for six of these. In other words, 33 of the 39 contraindications were based on clinical opinion alone. Of the six contraindications that had research evidence, five of these lacked strong evidence that they were, in fact, contraindications. The research evidence does not support these contraindications for an ECV: having had a previous Cesarean, fetal growth restriction, suspected big baby, low amniotic fluid, and high amniotic fluid.
The authors concluded that there is good evidence—based on both research and physiology— that people should NOT have an ECV if they have a history of placenta abruption or if placenta abruption is suspected, if there is a diagnosis of severe pre-eclampsia, or if there are signs of fetal distress. Also, if vaginal birth is considered to be contraindicated, then an ECV would also be contraindicated.
Again, it is important to note that although there may be little research evidence to back up some contraindications, many factors haven’t been well studied, and some care providers may use their expert opinion to recommend against an ECV in certain circumstances. A care provider may anticipate a difficult version, a low likelihood of success, or perhaps that the benefits do not outweigh the risks. For example, a care provider may not want to perform an ECV on someone with very low amniotic fluid because that increases the difficulty of the procedure. Other care providers might not want to perform an ECV if the baby has the umbilical cord wrapped around the neck. Although there is no solid research on these topics, the care provider may base their clinical opinion on previous experience or the mechanism (means) by which the factor could affect the version procedure—and find it to be too difficult, or that the risks of the procedure outweigh the benefits.
The American College of Obstetricians and Gynecologists (ACOG) recommends that:
“Because the risk of an adverse event occurring as a result of external cephalic version is small and the cesarean delivery rate is significantly lower among women who have undergone successful external cephalic version, all women who are near term with breech presentations should be offered an external cephalic version attempt if there are no contraindications.”
Since the data have yet to establish clear contraindications, they recommend that care providers should consider each patient individually as a potential candidate for an ECV. The expert medical opinion is that care providers should assess contractions and fetal well-being before and after the attempted version and that ECV should only be attempted in settings where Cesareans are immediately available.
ACOG recently updated their guidelines to recommend consideration of the use of epidurals or spinals in combination with tocolytic therapy (medications used to suppress premature labor) to increase the ECV success rate (Level B – based on limited or inconsistent scientific evidence). People with this combination treatment had a higher rate of successful ECV, were more likely to have a head-down baby in labor, and had a higher rate of vaginal birth after successful ECV in some studies. ACOG stated that the data were insufficient to favor spinal versus epidural, or to evaluate the benefits of epidurals/spinals without tocolysis.
Can someone with a previous Cesarean have an ECV?
The 2017 Australian study of over 32,000 people with breech pregnancies found that a previous Cesarean was the most common reason that people were told they were too high risk to attempt an ECV (Bin et al. 2017). However, as we’ve stated, there is little research evidence that a previous Cesarean should be considered a contraindication for a version (Rosman et al. 2012). In fact, the available evidence suggests that the risks of an ECV and the chance that it will be successful are similar between people who have had a prior Cesarean and those who have not.
The most recent and largest study on this topic was a systematic review published by Homafar et al. in 2020. The authors identified 8 observational studies with 14,515 participants who had an ECV– 1,215 had a prior Cesarean (almost all of them only had one prior Cesarean), and 13,300 did not have a prior Cesarean. All 8 studies were rated as being at low risk of bias.
The researchers found that the median ECV success rate among people with a prior Cesarean was 74%, which was similar to those who did not have a prior Cesarean birth. Approximately 75% of people who had a successful ECV and a history of prior Cesarean went on to have a vaginal birth. The researchers estimated that for every 1.7 ECVs that are attempted in someone with a prior Cesarean, one subsequent Cesarean birth would be avoided.
In terms of side effects, 7 of the 8 studies reported on uterine rupture, and there were no cases of uterine rupture during ECV among people with or without a prior Cesarean. Other rare adverse effects included temporary fetal heart rate abnormalities (0.6%) and urgent Cesarean (0.2%).
The authors concluded the majority of people with a prior Cesarean who have a successful ECV will go on to have a vaginal birth after Cesarean.
In summary, the evidence shows that:
- Attempting one or more ECVs will result in a baby who is head-down at the time of birth in 33% of first-time birthing people and 61% of people who have given birth before
- Having a history of prior Cesarean does not mean you should not be offered an ECV
- An ECV can be painful for many people, but it’s less painful if the procedure is successful, and there are medications that can be used to manage pain
- Tocolytic drugs that prevent labor contractions have been shown to improve the success of ECV
- Benefits of the ECV include a significant decrease in the risk of Cesarean, a decrease in breech positioning at birth, and a decrease in the risk of needing repeat Cesareans with future pregnancies
- The most common risk is a temporary change in the infant’s heart rate (highest rates reported in the research are 4.7%); serious complications requiring urgent Cesarean are rare (0.24%)
EBB 310 – Doulas & Nurses Advocating Together for Positive Shifts in Birth Culture with Joyce Dykema, EBB Instructor & Brianna Fields, RN
Don't miss an episode! Subscribe to our podcast and leave a review! iTunes | Spotify | YouTube Dr. Rebecca Dekker is joined by Joyce Dykema, doula and EBB Instructor, and Brianna Fields, a labor and delivery nurse, to discuss advocating for positive shifts in...

EBB 308 – The Intersection of Environmental Justice and Midwifery Care with Dr. Tanya Khemet Taiwo
Don't miss an episode! Subscribe to our podcast and leave a review! iTunes | Spotify | YouTube Curious which toxins should be most avoided for people of reproductive age and their children? In this episode, Dr. Tanya Khemet Taiwo, LM, CPM, MPH, PhD unravels the...
EBB 307 – Unexplained Infertility, Endometriosis, and a Birth Center Birth Story with Ellora La Shier, EBB Childbirth Class Graduate
Don't miss an episode! Subscribe to our podcast and leave a review! iTunes | Spotify | GoogleIn this episode, Ellora La Shier, graduate of the EBB Childbirth Class, shares about her struggle with six years of unexplained infertility and how it impacted her...
Pin It on Pinterest
- https://www.facebook.com/EvidenceBasedBirth/
- https://plus.google.com/106146540771436369846?hl=en
- https://www.pinterest.com/ebbirth/pins/
- https://www.linkedin.com/in/rebecca-dekker-8b3b3b22/
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Original Article
- Published: 24 October 2013
Breech presentation at delivery: a marker for congenital anomaly?
- D Mostello 1 ,
- J J Chang 2 ,
- C Guild 4 ,
- K Stamps 2 &
- T L Leet 2 na1
Journal of Perinatology volume 34 , pages 11–15 ( 2014 ) Cite this article
19k Accesses
21 Citations
17 Altmetric
Metrics details
- Paediatrics
- Pregnancy outcome
To determine whether congenital anomalies are associated with breech presentation at the time of birth.
Study Design:
A population-based, retrospective cohort study was conducted among 460 147 women with singleton live births using the Missouri Birth Defects Registry, which includes all defects diagnosed during the first year of life. Maternal and obstetric characteristics and outcomes between breech and cephalic presentation groups were compared using χ 2 -square statistic and Student’s t -test. Multivariable binary logistic regression analysis was used to estimate adjusted odds ratios (aORs) and 95% confidence intervals (CIs).
At least one congenital anomaly was more likely present among infants breech at birth (11.7%) than in those with cephalic presentation (5.1%), whether full-term (9.4 vs 4.6%) or preterm (20.1 vs 11.6%). The relationship between breech presentation and congenital anomaly was stronger among full-term births (aOR 2.09, CI 1.96, 2.23, term vs 1.40, CI 1.26, 1.55, preterm), but not in all categories of anomalies.
Conclusion:
Breech presentation at delivery is a marker for the presence of congenital anomaly. Infants delivered breech deserve special scrutiny for the presence of malformation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
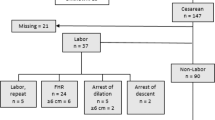
Maternal and neonatal factors associated with cesarean delivery in a cohort of pregnancies complicated by prenatally diagnosed congenital heart disease

Congenital anomalies among newborn babies in Felege-Hiwot Comprehensive Specialized Referral Hospital, Bahir Dar, Ethiopia
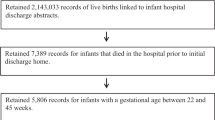
Understanding the relative contributions of prematurity and congenital anomalies to neonatal mortality
Cruikshank DP . Breech presentation. Clin Obstet Gynecol 1986; 29 : 255–263.
Article CAS Google Scholar
Braun FHT, Jones KL, Smith DW . Breech presentation as an indicator of fetal abnormality. J Pediatr 1975; 86 : 419–421.
Axelrod FB, Leistner HL, Porges RF . Breech presentation among infants with familial dysautonomia. J Pediatr 1974; 84 : 107–109.
Fianu S, Vaclavinkova V . The site of placental attachment as a factor in the aetiology of breech presentation. Acta Obstet Gynecol Scand 1978; 57 : 371–372.
Brenner WE, Bruce RD, Hendricks CH . The characteristics and perils of breech presentation. Am J Obstet Gynecol 1974; 118 : 700–712.
Luterkort M, Persson P, Weldner B . Maternal and fetal factors in breech presentation. Obstet Gynecol 1984; 64 : 55–59.
Rayl J, Gibson PJ, Hickok DE . A population-based case-control study of risk factors for breech presentation. Am J Obstet Gynecol 1996; 174 : 28–32.
Axelrod FB, Porges RF, Sein ME . Neonatal recognition of familial dysautonomia. J Pediatr 1987; 110 : 946–948.
Gimovsky ML, Paul RH . Singleton breech presentation in labor: experience in 1980. Am J Obstet Gynecol 1982; 143 : 733–739.
Berendes HW, Weiss W, Deutschberger J, Jackson E . Factors associated with breech delivery. Am J Public Health Health 1965; 55 : 708–719.
Mazor M, Hagay ZJ, Leiberman JR, Biale Y, Insler V . Fetal malformations associated with breech delivery. Implications for obstetric management. J Reprod Med 1985; 30 : 884–886.
CAS PubMed Google Scholar
Alexander GR, Kogan MD, Himes JH . 1994–1996 US singleton birth weight percentiles for gestational age by race, Hispanic origin, and gender. Matern Child Health J 1999; 3 : 225–231.
Sorensen T, Hasch E, Lange AP . Fetal presentation during pregnancy [Letter]. Lancet 1979; 2 : 477.
Mickey RM, Greenland S . The impact of confounder selection criteria on effect estimation. Am J Epidemiol 1989; 129 : 125–137.
Hall JE, Kohl SG, O’Brien F, Ginsberg M . Breech presentation and perinatal mortality. Am J Obstet Gynecol 1965; 91 : 665–683.
Kauppila O . The perinatal mortality in breech deliveries and observations on affecting factors: a retrospective study of 2227 cases. Acta Obstet Gynecol Scand (Suppl) 1975; 39 : 1–79.
CAS Google Scholar
Goldberg JD . Routine screening for fetal anomalies: expectations. Obstet Gynecol Clin N Am 2004; 31 : 35–50.
Article Google Scholar
Grandjean H, Larroque D, Levi S . Sensitivity of routine ultrasound screening of pregnancies in the Eurofetus database. The Eurofetus Team. Ann N Y Acad Sci 1998; 847 : 118–124.
Wren C, Reinhardt Z, Khawaja K . Twenty-year trends in diagnosis of life-threatening neonatal cardiovascular malformations. Arch Dis Child Fetal Neonatal Ed 2008; 93 : F33–F35.
Bower C, Rudy E, Callaghan A, Quick J, Nassar N . Age at diagnosis of birth defects. Birth Defects Res A Clin Mol Teratol 2010; 88 : 251–255.
Tanner JP, Salemi JL, Hauser KW, Correia JA, Watkins SM, Kirby RS . Birth defects surveillance in Florida: infant death certificates as a case ascertainment source. Birth Defects Res A Clin Mol Teratol 2010; 88 : 1017–1022.
Wang Y, Sharpe-Stimac M, Cross PK, Druschel CM, Hwang S . Improving case ascertainment of a population-based birth defects registry in New York state using hospital discharge data. Birth Defects Res A Clin Mol Teratol 2005; 73 : 663–668.
Salemi JL, Tanner JP, Kennedy S, Block S, Bailey M, Correia JA et al . A comparison of two surveillance strategies for selected birth defects in Florida. Public Health Rep 2012; 127 : 391–400.
Frost F, Starzyk P, George S, McLaughlin JF . Birth complication reporting: the effect of birth certificate design. Am J Public Health 1984; 74 : 505–506.
Zollinger TW, Przybylski MJ, Gamache RE . Reliability of Indiana birth certificate data compared to medical records. Ann Epidemiol 2006; 16 : 1–10.
Download references
Acknowledgements
Many thanks go to Gilad Gross, MD for his helpful advice on improving this manuscript. The authors also acknowledge the Missouri Department of Health and Senior Services, Section of Epidemiology for Public Health Practice as the original source of the data. The analysis, interpretations and conclusions in the present study are those of the authors and not the Missouri Department of Health and Senior Services, Section of Epidemiology for Public Health Practice.
Author information
T L Leet: Dr Leet is deceased.
Authors and Affiliations
Division of Maternal-Fetal Medicine, Department of Obstetrics, Gynecology and Women’s Health, School of Medicine, Saint Louis University, St Louis, MO, USA
Department of Epidemiology, School of Public Health, Saint Louis University, St Louis, MO, USA
J J Chang, F Bai, K Stamps & T L Leet
Department of Biostatistics, School of Public Health, Saint Louis University, St Louis, MO, USA
Department of Pediatrics and the Center for Outcomes Research, School of Medicine, Saint Louis University, St Louis, MO, USA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to D Mostello .
Ethics declarations
Competing interests.
The authors declare no conflict of interest.
Additional information
Presented at the 32nd Annual Meeting of the Society for Maternal-Fetal Medicine, February 6–11, 2012, Dallas, TX, USA.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Mostello, D., Chang, J., Bai, F. et al. Breech presentation at delivery: a marker for congenital anomaly?. J Perinatol 34 , 11–15 (2014). https://doi.org/10.1038/jp.2013.132
Download citation
Received : 01 May 2013
Revised : 01 September 2013
Accepted : 13 September 2013
Published : 24 October 2013
Issue Date : January 2014
DOI : https://doi.org/10.1038/jp.2013.132
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- congenital abnormalities
- labor presentation
- pregnancy outcome
This article is cited by
A comparison of risk factors for breech presentation in preterm and term labor: a nationwide, population-based case–control study.
- Anna E. Toijonen
- Seppo T. Heinonen
- Georg Macharey
Archives of Gynecology and Obstetrics (2020)
Outcome of small for gestational age-fetuses in breech presentation at term according to mode of delivery: a nationwide, population-based record linkage study
- Pia Hinnenberg
- Anna Toijonen
Archives of Gynecology and Obstetrics (2019)
Cesarean deliveries and maternal weight retention
- Kandice A. Kapinos
- Olga Yakusheva
- Marianne Weiss
BMC Pregnancy and Childbirth (2017)
Breech presentation at term and associated obstetric risks factors—a nationwide population based cohort study
- Mika Gissler
- Seppo Heinonen
Archives of Gynecology and Obstetrics (2017)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
UnitedHealth says hackers possibly stole large number of Americans' data
- Medium Text
Sign up here.
Reporting by Manas Mishra, Mariam Sunny and Sriparna Roy in Bengaluru; Editing by Krishna Chandra Eluri, Sriraj Kalluvila and Richard Chang
Our Standards: The Thomson Reuters Trust Principles. New Tab , opens new tab

Technology Chevron

In China, Elon Musk scores wins on the path to self-driving cars
Elon Musk made progress towards rolling out Tesla's advanced driver-assistance package in China on a whirlwind weekend trip to Beijing, sending the company's shares up by almost 18% on Monday.
Britain's track bike for the Paris Olympics pushes technological boundaries and will give the team the best chance of continuing its domination, according to one of the design partners for the new machine officially unveiled on Monday.

IMAGES
VIDEO
COMMENTS
Epidemiology. Breech presentation occurs in 3% to 4% of all term pregnancies. A higher percentage of breech presentations occurs with less advanced gestational age. At 32 weeks, 7% of fetuses are breech, and 28 weeks or less, 25% are breech. Specifically, following one breech delivery, the recurrence rate for the second pregnancy was nearly 10% ...
The main types of breech presentation are: Frank breech - Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term. Complete breech - Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
Overview. Breech presentation is defined as a fetus in a longitudinal lie with the buttocks or feet closest to the cervix. This occurs in 3-4% of all deliveries. The percentage of breech deliveries decreases with advancing gestational age from 22-25% of births prior to 28 weeks' gestation to 7-15% of births at 32 weeks' gestation to 3-4% of ...
A breech baby, or breech birth, is when your baby's feet or buttocks are positioned to come out of your vagina first. Your baby's head is up closest to your chest and its bottom is closest to your vagina. Most babies will naturally move so their head is positioned to come out of the vagina first during birth. Breech is common in early ...
In a breech presentation, the body comes out first, leaving the baby's head to be delivered last. The baby's body may not stretch the cervix enough to allow room for the baby's head to come out easily. There is a risk that the baby's head or shoulders may become wedged against the bones of the mother's pelvis.
Breech Births. In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby's buttocks, feet, or both are positioned to come out first during birth. This happens in 3-4% of full-term births.
Labour with a preterm breech should be managed as with a term breech. C. Where there is head entrapment, incisions in the cervix (vaginal birth) or vertical uterine D incision extension (caesarean section) may be used, with or without tocolysis. Evidence concerning the management of preterm labour with a breech presentation is lacking.
Almost 90% of breech presentations are born by C/S — no differentiation made between elective and non-elective C/S (3e). Planned VBB success rate of 70% (3d). Reports rate of in labour C/S for breech presentation to be 86.9% in 2002 (3e).
Women with a breech presentation at term should be offered external cephalic version (ECV) unless there is an absolute contraindication. ... Rate of adverse neonatal and maternal outcomes following planned and actual breech birth. Percentage of staff who have undergone training in vaginal breech delivery (100%). 12 Useful links and support ...
1. Background. The management of breech presentation continues to cause academic and clinical contention globally [[1], [2], [3]].In recent years, research has shown that if certain criteria are met, and appropriately experienced and skilled clinicians are available, Vaginal Breech Birth (VBB) is a safe option [[4], [5], [6]].However, with Caesarean Section (C/S) rates for breech presentation ...
…in nonfrank breech presentations and was the reason for cesarean birth in 5/63 (7.9 percent) complete or incomplete breech presentations versus 3/222 (1.4 percent) frank breech presentations.However, …
At full term, around 3%-4% of births are breech. The different types of breech presentations include: Complete: The fetus's knees are bent, and the buttocks are presenting first. Frank: The fetus's legs are stretched upward toward the head, and the buttocks are presenting first. Footling: The fetus's foot is showing first.
(See "Overview of breech presentation" and "External cephalic version".) For patients who present in labor with a breech fetus, cesarean birth is the preferred approach in many hospitals in the United States and elsewhere. Cesarean is performed for over 90 percent of breech presentations, and this rate has increased worldwide . However, even in ...
Baby's buttocks lead the way into the birth canal. Hips are flexed, knees are extended, and the feet are in close proximity to the head. 65% to 70% of breech babies are in this position. Complete breech. Baby presents with buttocks first. Both the hips and the knees are flexed; the baby may be sitting cross-legged.
Of 2526 women having a TOL, 1796 (71%) delivered vaginally for an overall vaginal birth rate of 22.5%. In North America, over 100 000 women have pregnancies that remain breech at term annually. With a success rate similar to that of the PREMODA study, some 25 000 could safely avoid Cesarean delivery. Breech presentation is increased with fetal ...
A total of 130 breech deliveries were matched with 130 cephalic deliveries. No perinatal mortality occurred in either group. The C-section percentage was greater in the breech presentation group compared with the cephalic delivery group (72.3 % vs. 14.6 %; p < 0.001). Children in the breech presentation had a threefold increased risk for Apgar scores <7 at 1 min (OR 3.2; 95 % CI: 1.2-8.4; p ...
A breech presentation at delivery occurs when the fetus does not turn to a cephalic presentation. ... Among frank breech babies the incidence is 0.5 percent, among complete breeches 5 percent, and among footling breeches 15 percent. Head entrapment is caused by the failure of the fetal head to negotiate the maternal midpelvis. At full term, the ...
Single-center retrospective study of women with trials of vaginal delivery of a singleton fetus in breech presentation at of after 37 weeks of gestation. ... (16.4 vs 12.6 %), which almost exactly matches the percentage of cord prolapse observed in that type of presentation (4.5 %). Among these studies, Jennewein and us are the only studies ...
The incidence of breech presentation at term is about 4 percent. 1 Multiple factors may cause a fetus to present breech instead of vertex, including placenta previa, multiple gestation, uterine ...
This referred to as the "breech" position or breech presentation. Breech position is not normal and consider a pregnancy complication. The occurrence rate of breech position is around 5% or 1 out of every 25 babies in full-term pregnancies. The occurrence rate for breach presentation is significantly higher, however, in preterm pregnancies.
Breech position (bottom first) is present in 3% to 4% of term pregnancies. Breech positioning is common prior to term—25% are breech before 28 weeks, but by 32 weeks only 7% of babies are breech. The vast majority of breech babies in the United States (U.S.) are now born by planned Cesarean (Table 1). The use of a safe procedure to help turn ...
At least one congenital anomaly was more likely to be present in infants in the breech presentation (11.7%) than those in cephalic presentation (5.1%) at birth. Table 2 shows the rates of ...
UnitedHealth Group said on Monday that hackers stole health and personal data of potentially a "substantial proportion" of Americans from its systems in February, as the largest U.S. health ...