An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List


Traditional Indigenous medicine in North America: A scoping review
Nicole redvers.
1 Department of Family & Community Medicine, School of Medicine and Health Sciences, University of North Dakota, Grand Forks, North Dakota, United States of America
2 Arctic Indigenous Wellness Foundation, Yellowknife, Northwest Territories, Canada
Be’sha Blondin
Associated data.
All relevant data are within the manuscript and its Supporting Information files.
Despite the documented continued use of traditional healing methods, modalities and its associated practitioners by Indigenous groups across North America, it is presumed that widespread knowledge is elusive amongst most Western trained health professionals and systems. This despite that the approximately 7.5 million Indigenous peoples who currently reside in Canada and the United States (US) are most often served by Western systems of medicine. A state of the literature is currently needed in this area to provide an accessible resource tool for medical practitioners, scholars, and communities to better understand Indigenous traditional medicine in the context of current clinical care delivery and future policy making.
A systematic search of multiple databases was performed utilizing an established scoping review framework. A consequent title and abstract review of articles published on traditional Indigenous medicine in the North American context was completed.
Of the 4,277 published studies identified, 249 met the inclusion criteria divided into the following five categorical themes: General traditional medicine, integration of traditional and Western medicine systems, ceremonial practice for healing, usage of traditional medicine, and traditional healer perspectives.
Conclusions
This scoping review was an attempt to catalogue the wide array of published research in the peer-reviewed and online grey literature on traditional Indigenous medicine in North America in order to provide an accessible database for medical practitioners, scholars, and communities to better inform practice, policymaking, and research in Indigenous communities.
Introduction
The United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP) was a pivotal document for the world’s Indigenous Peoples [ 1 ]. In addition to being quoted in numerous policy, research, and community initiatives since it was adopted, the declaration is now being used to evaluate the adequacy of national laws; for interpreting state obligations at the global level; and by some corporations, lending agencies, and investors in regards to resource and development opposition on Indigenous lands [ 2 ]. Article 24 of the declaration states that “Indigenous peoples have the right to their traditional medicines and to maintain their health practices, including the conservation of their vital medicinal plants, animals, and minerals” (UN document A/RES/61/295). The World Trade Organization has stated that “traditional medicine contributes significantly to the health status of many communities and is increasingly used within certain communities in developed countries. Appropriate recognition of traditional medicine is an important element of national health policy” [ 3 ].
The United Nation’s Economic and Social Council President in 2009, Sylvie Lucas, stated that “[t]he potential of traditional medicine should be fostered. … ‘We cannot ignore the potential of traditional medicine’ in the race to achieve the Millennium Development Goals and renew primary health care for those who lacked access to it … traditional medicine [is] a field in which the knowledge and know-how of developing countries was ‘enormous’—and that was a source of hope for improving the world’s health-care situation” [ 4 ].
In November 2008, member states of the World Health Organization (WHO) adopted the Beijing Declaration [ 5 ], where they recognized the role of traditional medicine in the improvement of public health and supported its integration into national health systems where appropriate [ 6 ]. The declaration also promotes improved education, research, and clinical inquiry into traditional medicine, as well as improved communication among health-care providers [ 6 ].
Research into some types of complementary and alternative medicine (CAM) practices has received large amounts of funding. For example, the US National Institute of Health has a division called the National Center for Complementary and Alternative Medicine (NCCAM), which in 2010 had a budget of US$128.8 million dollars [ 7 ]. Before the Beijing Declaration, sixty-two countries had national institutes for traditional medicine as of 2007, up from twelve in 1970 [ 4 ]. Despite this, there has been a complete lack of acknowledgement of the Indigenous traditional knowledge (TK) currently being used in many CAM professions. In some cases, there has been direct cultural appropriation of traditional medicine and practices by CAM or other biomedical groups in North America [ 8 ]. Although outdated, given the lack of scholarship in this area, a 1993 estimate put the total world sales of products derived from traditional medicines as high as US$43 billion [ 9 ]; however, only a tiny fraction of the profits were and are being returned to the Indigenous peoples and local communities from where these medicines were derived. In the early 1990s, it was estimated that “less than 0.001 per cent of profits from drugs developed from natural products and traditional knowledge accrue to the traditional people who provided technical leads for research” [ 10 ].
So, despite some progress on a global level in CAM research and practice, many Indigenous medicine systems around the world are still often given the back seat when it comes to both acknowledgement and practice within the conventional medical-care setting. The terms and attributes used for traditional medicine, such as ‘alternative’, translates into an epistemological discomfort regarding the identity of these medicines [ 11 ] that automatically sets a power differential from conventional care. In 2007, The Lancet published an article in which the authors stated, “[w]e now call on all health professionals to act in accordance with this important UN declaration of [I]ndigenous rights—in the ways in which we work as scientists with [I]ndigenous communities; in the ways in which we support [I]ndigenous peoples to protect and develop their traditional medicines and health practices; in our support and development of [I]ndigenous peoples’ rights to appropriate health services; and most importantly in listening, and in supporting [I]ndigenous peoples’ self-determination over their health, wellbeing, and development” [ 12 ].
In his 2008 dissertation, (Gus) Louis Paul Hill noted that there is a paucity of literature on Indigenous approaches to healing within Canada specifically, and little documentation and discussion of Indigenous healing methods in general [ 13 ]. With this, there is currently no formal Canadian (or US based) Indigenous health policy framework or national adopted policy on Indigenous traditional medicine [ 14 , 15 ], and no broad application and endorsement of Indigenous ways of achieving wellness markers that are self-determined in an already marginalized community (demonstrated by a lack of funding and accessibility to these services generally).
Despite this being an emerging scholarship area, with a clear lack of reflected national health policy, there is increasing evidence on the use of traditional Indigenous medicine in certain areas of need such as in substance abuse and addictions treatment [ 16 – 21 ]. When Canadian Indigenous communities were asked about the challenges currently facing their communities, 82.6% stated that the most common issue was alcohol and drug abuse [ 22 ] and that traditional medicine itself is a critically important part of Indigenous health [ 23 ], including in the support of addictions. Due to the often upstream, structural, and socio-political [ 24 ] factors driving substance abuse in addition to other health ailments in Indigenous communities, advancing co-production of treatment options such as utilizing traditional medicine that already fits into an Indigenous paradigm may ensure four key steps to wellness occur: decolonization, mobilization, transformation, and healing [ 25 ].
The present study
Despite the documented continued use of traditional healing methods, modalities, and their associated practitioners by Indigenous groups across North America, widespread knowledge of this domain is presumed elusive among most Western-trained health professionals and systems. This despite the fact that the approximately 7.5 million Indigenous peoples who currently reside in Canada and the United States (US) are most often served by Western systems of medicine. There is current exploration in the literature on how cultural competency and safety impacts health disparities across diverse populations; however, there is little attention to how traditional Indigenous medicine systems fit into this practice area. Therefore, an account of the state of the literature is currently needed in this area of traditional Indigenous medicine to provide an accessible resource tool for medical practitioners, scholars, and communities in the North American context to better understand Indigenous traditional medicine in the context of current clinical care delivery and future policy making. In addition, having baseline literature on this topic area available for use in cultural safety training, and diversity and inclusion training on or off reservations, is warranted and in need.
Considering the paucity of accessible information on traditional Indigenous medicine, in addition to the lack of cohesive understanding on what traditional healing is within the Western context, the purpose of this present study is–
- to catalogue the current state of the peer-reviewed and online grey literature on traditional medicine in the North American context by identifying the types and sources of evidence available, and
- to provide an evidence-informed resource guide for medical practitioners, scholars, and communities to better inform “practice, policymaking, and research [ 26 ]” in Indigenous communities.
The methodology for this scoping review was a mixed-methods approach (Western-Indigenous). The first four steps of the scoping review were conducted within a Western methodological approach as outlined by Pham et al. [ 27 ] and based on the framework outlined by Arksey and O’Malley [ 28 ] with subsequent recommendations made by Levac et al. [ 29 ] (i.e., (1) combining a broad research question with a clearly articulated scope of inquiry, (2) identifying relevant studies, (3) study selection, and (4) charting the data). For the fifth step, as outlined by Arksey and O’Malley [ 28 ], (i.e., (5) collating, summarizing, and reporting the results), we utilized a dominant Indigenous methodology that places a focus on personal research preparations with purpose, self-location, decolonization and the lens of benefiting the community [ 30 – 32 ]. Although this research process did include the Western conceptions of collating, summarizing, and reporting the results as per outlined and described by Arksey and O’Malley [ 28 ], there was a very clear intent of identifying ourselves, the authors, as being rooted within Indigenous communities, and within an Indigenous worldview. This meant that we were not able to critique or provide commentary to contradictory evidence found in the scoping review process, as it is not culturally appropriate to provide this type of analysis within the topic area of traditional medicine through an Indigenous worldview. As Saini points out, utilizing self-determined Indigenous methodologies is “critical to ensure Aboriginal research designs are not marginalized due to perceptions that they are somehow less valid or sophisticated than their counterparts” [ 33 ] at the community or systems level.
The sixth methodologic step in our scoping review, as advanced by Levac et al. [ 29 ], incorporates a consultation exercise involving key stakeholders to inform and validate study findings [ 26 ] and was done in parallel to all steps of the work. This was another mixed-method bridging step, where one Indigenous Elder who is considered a content expert in their respective community was utilized to ensure placement of the research in the Indigenous context despite the use of Western metrics for the data-collection portion of the work (as opposed to an academic or other institutional stakeholder). It must be noted that Indigenous Elders’ engagement with research is often solely for the purpose of benefiting their community [ 30 – 32 ]. This therefore creates a unique stakeholder engagement process that roots the research not to a specific Western-defined method or process but to a set of traditional Indigenous protocols (unwritten community directives defined through an Indigenous worldview) that must be followed to ensure uptake and acceptance of the work by Indigenous communities themselves. In essence, the ‘validation of study findings’ (as outlined by Levac et al. in their sixth methodologic step [ 29 ]) is not culturally malleable and needed to be changed to a process of reviewing the rules and parameters (i.e., traditional protocols) around how traditional medicine should be talked about in the context of research. The authors are both immersed in work with Indigenous communities and peoples and understands the importance of Indigenous research processes to move away from the conformity of Western notions of the scientific deductive process of new knowledge development, and instead to work towards providing space for the translational voices within Indigenous communities and peoples [ 34 ]. The review methodology was defined a priori.
Eligibility criteria, procedures, and search terms
Only articles published in peer-reviewed academic journals or easily accessible online reputable organizational documents and dissertation works that were formally published (i.e., online grey literature) were included. No limits were put on the type of research conducted, whether qualitative, quantitative, commentary, or otherwise given the specific nature of the topic and the assumed limited studies available for review. Studies were included if they made reference to traditional medicine, or if they noted specific traditional medicine interventions or practitioners (i.e., sweat lodge, traditional healers, etc.). Ethnobotanical, plant physiology, and reviews of specific Indigenous plants were excluded from this scoping review as they were most often not based on the context of traditional medicine but the function and action of the plant itself. All studies up until June 29, 2020 were included in the review.
The authors did not specify a definition for ‘traditional medicine’ before selecting studies for this review, which was purposeful. There is currently a vast array of traditional medicine modalities, practices, and people across North America who may have varying definitions or interpretations of the terms and practice. This therefore required a broad inductive and immersive approach to allow the community of researchers in this area to provide their own definitions regionally, which therefore made an impact on the breadth of articles found. All the variants of the words for traditional medicine that were used to include articles were based on existing knowledge, a pre-screen of the available literature, and consultation with an Elder (see S1 Table and ‘title and abstract relevance screening’ section).
No restrictions were put on language for the initial search; however, only English language articles were considered for inclusion. This was also due to a complete lack of peer-reviewed articles written in an Indigenous language being noted in prior work, in addition to the prospective difficulties and budget needed to attain translation support. With a multitude of Indigenous languages in North America, there is an unfortunate lack of access to translators for projects such as these. Articles that were outside of the continental US and Canada were also excluded (i.e., Pacific Islanders, etc.), in addition to those from Mexico despite the proximity of traditional lands within and to the US. This was due to differences in traditional medicine practice and agents in those areas. Books and book reviews were not included due to the difficulty in verifying their content. North American Indigenous was defined to be First Nations, Inuit, Métis, American Indian, Alaskan Native or the respective Bands and Tribes within the region. As demographic terminology changes depending on the region of the continent, it was important to ensure complete capture of the eligible literature by utilizing both Canadian and US Indigenous terminologies. A two-stage screening process was used to assess the relevance of studies identified in the search as further outlined below.
The scoping review process and search terms were developed with the aid of a medical librarian (D.O) in discussion with the lead author (N.R.). The search was created in PubMed using a combination of key terms and index headings related to North American Indigenous peoples and traditional medicine (see S1 Table ). The search was completed between December 27, 2018 and June 29, 2020 by searching the following databases with no limits on the start date, language, subject, or type: PubMed, EMBASE, PsycInfo, Elsevier’s Scopus, PROSPERO, and Dartmouth College’s Biomedical Library database due to the breadth of databases available in this library. In addition, manual searches of the following websites were completed: Indigenous Studies Portal, University of Saskatchewan [ 35 ]; National Collaborating Centre for Aboriginal Health [ 36 ]; the Aboriginal Healing Foundation’s archived website documents [ 37 ]; and the International Journal of Indigenous Health, which includes archives from the Journal of Aboriginal Health . Google Scholar was searched by inspecting the first two pages of results and then subsequently screening the next two pages if results were identified until no more relevant results had been found. The reference lists of randomly selected articles were manually searched with a “snowball” technique utilized to identify any further literature that may have been missed in the first search round until saturation of the search had been reached.
Title and abstract relevance screening
A title and abstract relevance form was developed by the author (N.R) in a session during the Elder consultation (B.B), mainly by the a priori identification of the search terms used and as listed in the S1 Table . As the goal was to capture as much available literature on the subject as possible, the title and abstract review were non-restrictive other than the stated eligibility criteria and search terms noted above. The reviewer was not masked to the article authors or journal names as this was not a results-based review. Some article titles did not have an abstract available for review and were therefore included in the subsequent full review to better characterize the content relevance to the topic area. If there was a question on the relevance of an article for inclusion, the Elder was brought into the discussion (B.B) as the final authority for the decision on whether to proceed with inclusion.
Data characterization, summary, and synthesis
After title and abstract screening, all the citations that were deemed relevant to the topic were kept in the scoping review database ( S2 Table ). All full text articles were obtained once identified as eligible; however, as the intent was not to provide critical review of the articles, they were not catalogued based on the completion of a full text article review. Instead, all articles were kept in the database from the title and abstract screening alone for the categorization process, ensuring that no judgement was placed on traditional medicine topics in keeping with an Indigenous methodological paradigm. Therefore a quality assessment procedure was not performed on the articles included in this scoping review as noted (e.g., Critical appraisal of qualitative research [ 38 ]) for a few reasons:
- The purpose of this review was to map the existing state of the literature on this topic and not to analyze the results of the included articles, and
- The vast array of formats and methodologies used in the Indigenous traditional medicine literature make the dominant Western metrics of validity simply not applicable to the current research purpose.
All citations found were compiled in a single Microsoft Excel 365 ProPlus spreadsheet. Coding of articles was done based on title and abstract review alone, with an Elder advisor to aid identification of categorical themes. Themes were based and developed by way of traditional knowledge (TK); however, it was noted in the synthesis process that there was often substantial overlap between themes. In these cases, a priority category was given for the ease of database creation which means that the categorical themes cannot be looked at as being black and white. Traditional Indigenous medicine is often very complex in its practice; however, an attempt was done to ease classification by assessing for the most discussed or most focused research topic(s) in each article.
Due to the substantial overlap of search terms used for traditional medicine in other disciplines (i.e., traditional medicine can be the term used from the Indigenous perspective or from the Western perspective), the initial search yielded thousands of articles.
Based on a review of the title and abstracts, 249 articles met the criteria for inclusion (see S2 Table for the full database of articles included). A full article review was conducted when the initial screen left questions about the relevance of the research for inclusion. Broad inclusion was purposeful, as by ensuring a wide capture of the literature was categorized, future research and program needs have a more complete database to pull information from. Articles ranged in date from the earliest year of publication, being in 1888, to the most recent publication, being in 2020 ( Fig 1 ). Sixty two percent of the articles were published prior to 2009 (n = 154) with the average year of publication being 2001.

There were five overlapping categorical themes that emerged in the review including: General traditional medicine, integration of traditional and Western medicine systems, ceremonial practice for healing, usage of traditional medicine, and traditional healer perspectives. Fig 2 summarizes the selection process and findings.

General traditional medicine
There were 126 articles identified for this category with the majority of the publications being from 2009 and earlier (75%, n = 95). Thirty-three of the articles were based in Canada, one was based in both Canada and the US, and the remaining ninety-two were based in the US alone. The publication dates for articles spanned a wide time period between 1888 and 2020 (average year of publication was 1997), with the majority being commentary or qualitative in nature.
In the review of this category, it became clearly evident that the terms or conceptualizations applied to traditional medicine or its variants (i.e., traditional healing, Native American healing, etc.) were very generalized. Specifically, the general research topics ranged from trying to answer the question of what is traditional medicine [ 13 , 39 – 41 ], to asking questions on the efficacy and acceptance of traditional medicine [ 42 – 44 ], to the applicability of traditional medicine with specific disease states [ 45 – 47 ], in addition to stories of healing by recipients of traditional medicine practice or approaches [ 48 , 49 ].
According to Alvord and Van Pelt, traditional medicine is described in the Navajo culture as a medicine that is performed by a hataalii , which is someone who sees a person not simply as a body, but as a whole being with body, mind, and spirit seen to be connected to other people, to families, to communities, and even to the planet and universe [ 50 ]. In helping to clarify the intent and purpose for utilizing a traditional Indigenous medicine approach, Hill describes it as “the journey toward self-awareness, self-knowledge, spiritual attunement and oneness with Creation” and “the lifelong process of understanding one’s gifts from the Creator and the embodiment of life’s teaching that [an] individual has received” [ 13 ]. The traditional medicine practitioner’s role in the healing process has been described as their being an instrument, a helper, the worker, the preparer, the doer in the healing process with the work using the “medicines” being slow, careful, respectful, and embodying a sense of humility [ 51 ].
Also of note in this section of articles, was the subtle distinction between the terms ‘traditional healing’ compared to the actual using of ‘traditional medicines’. The core of ‘traditional healing’ was said to be or attaining spiritual ‘connectedness’, in which there were many stated ways for developing this in order to have a strong physical body and mind [ 52 ]. In essence, this ‘connectedness’ could be with or without the actual use of what we would call a ‘medicine’ in Western terms achieved instead through being in harmony with the natural environment, through fasting, prayer, or meditation, or through the use of actual ‘traditional medicines’ that could include plant- and herb-based medicines [ 52 ].
Quantitative data analysis within the general traditional medicine category of articles was rarely performed. When quantitative analysis was performed, it was usually done in a mixed method format that utilized survey tools alongside qualitative approaches (e.g., interviews, focus groups) [ 53 – 55 ]. For example, a mixed methods study by Mainguy et al., found that the level of spiritual transformation achieved through interaction with traditional healers was associated with a subsequent improvement in medical illness in 134 of 155 people ( P < .0001), and that this association exhibited a dose-response relationship [ 55 ]. In another mixed-methods study by Marsh et al., a 13-week intervention with “Indigenous Healing and Seeking Safety” in 17 participants demonstrated improvement in trauma symptoms, as measured by the TSC-40, with a mean decrease of 23.9 (SD = 6.4, p = 0.001) points, representing a 55% improvement from baseline [ 53 ]. Furthermore, in this study all six TSC-40 subscales demonstrated a significant decrease (i.e., anxiety, depression, sexual abuse trauma index, sleep disturbance, dissociation, and sexual problems) [ 53 ].
It was clear from the review of articles in this category that a large number of the articles were written from an observational or commentary perspective by non-Indigenous scholars (e.g., anthropologic perspectives) [ 42 , 56 ]. Those written more than twenty years ago often had titles or content that would not be considered culturally appropriate in today’s scholarly work. For example, an article by Walter Vanast from 1992 was titled, “‘Ignorant of any Rational Method’: European Assessments of Indigenous Healing Practices in the North American Arctic” [ 57 ]. Considerations for the issue of quality and accuracy in this body of literature will be addressed in the discussion section of this paper.
Integration of traditional and Western medicine systems
A total of 61 articles in this category were reviewed, with publication dates ranging from the year 1974 to the year 2019 (average year of publication was 2006). Sixteen percent (n = 10) of these articles were from nursing journals, and 39% (n = 24) were articles from mental health and/or substance abuse journals. Of the total number of articles in this section, 61% (n = 37) were based in the US, with the remaining being from Canada (n = 24).
Articles in this category fell into overlapping subsets within the overarching theme of the integration of traditional Indigenous medicine systems with Western medicine systems. There were articles specifically calling for physicians and other healthcare providers to better collaborate with traditional healers [ 58 , 59 ], and also calls for health “systems” to better coordinate and work with Indigenous medicine systems and associated practitioners [ 60 – 62 ]. Some of the articles focused on cultural accommodations, and awareness and attitudes in medical settings towards traditional medicine and healers [ 63 – 65 ]. Lastly, a number of articles reviewed existing medical environments, practitioners, and facilities that had either piloted or fully integrated traditional and Western medical care under the same roof or practice [ 24 , 66 – 69 ].
The integration of traditional medicine into existing medical education environments was showcased through a residency training program as described by Kessler et al. [ 70 ]. In 2011, the University of New Mexico Public Health department and their General Preventive Medicine Residency Program in the United States started to integrate traditional healing into the resident training curriculum with full implementation completed by 2015. An innovative approach was used in the teaching delivery by utilizing a compendium of training methods, which included learning directly from traditional healers and direct participation in healing practices by residents [ 70 ]. The “incorporation of this residency curriculum resulted in a means to produce physicians well trained in approaching patient care and population health with knowledge of culturally based health practices in order to facilitate healthy patients and communities” [ 70 ].
Other articles in this section described the role of nurses in advocating for Indigenous healing programs and treatment. In research by Hunter et al., healing holistically can be said to match the time-honored values seen in the nursing profession: caring, sharing, and empowering clients [ 71 ]. Participant observations demonstrated that health centers could support progression along a cultural path by providing traditional healing with transcultural nurses acting as lobbyists for culturally sensitive health programs directed by Indigenous peoples [ 71 ]. This need for advocacy and awareness building on traditional ways of healing were emphasized throughout this category of articles.
According to Joseph Gone, “Lakota doctoring [traditional healing] remains highly relevant for wellness interventions and healthcare services even though it is not amenable in principle to scientific evaluation” [ 72 ]. In reference to Indigenous healing practices in general, Gone states that in Indigenous settings “we already know what works in our communities” and this claim seems “to reflect the vaunted authority of personal experience within Indigenous knowledge systems [ 72 ].
Some scholars noted the potential harms of not moving towards a respectful dialogue between the two systems of medicine (i.e., Western and Indigenous). A noted article by David Baines, an Indigenous physician from the Tlingit/Tsimshian tribe in Southeast Alaska, describes one of his patients who had metastatic lung cancer [ 73 ]. The patient had an oncologist but also went to a traditional healer to help deal with the pain she was having [ 73 ]. When the patient told the oncologist she was seeing a traditional healer, the oncologist got angry and wanted to know why she wanted to see a “witch doctor” [ 73 ]. The patient was offended and angry and refused to go back to the oncologist. She ended up dying a very painful death. Dr. Baines noted that it is important to remember we have the same goal—a healthy patient [ 73 ].
Ceremonial practice for healing
Thirty articles were identified for this category. Important sub-categories became apparent in the review, including sweat lodge ceremonies (n = 15), traditional tobacco ceremonies and use (n = 6), birth and birthplace as a ceremony (n = 2), puberty ceremonies (n = 4), and using ceremony as a model for healing from a relative’s death or from trauma (n = 3). There were only eight Canadian studies published in this category, with the majority being based in the US (n = 22).
Sweat lodge ceremonies (SLC) have been practiced by many Indigenous nations since ancient times. SLCs are used as a process of honoring transformation and healing that is central to many Indigenous traditionalisms [ 74 ]. Gossage et al. examined the role of SLCs in the treatment for alcohol use disorder in incarcerated people [ 75 ]. The Dine Center for Substance Abuse Treatment staff utilized SLCs as a specific modality for jail-based treatment and analyzed its effect on a number of parameters. Experiential data was collected from 123 inmates after SLCs with several cultural variables showing improvement [ 75 ]. Gossage et al. also reported results from a similar prior study that analysed data for 100 inmates who participated in SLCs [ 75 ]. The research found that incarceration recidivism rates for those SLC participants was only 7% compared with an estimated 30–40% for other inmates who did not participate in such ceremonies [ 75 ]. Another study by Marsh et al., gathered qualitative evidence about the impact of the SLC on participants in a trauma and substance-abuse program and reported an increase in spiritual and emotional well-being that participants said was directly attributable to the ceremony [ 76 ].
Much of the existing literature on ceremonial tobacco focuses on either the perception of usage or the usage in general by Indigenous peoples in the region examined. In research done by Struthers and Hodge, six Ojibwe traditional healers and spiritual leaders described the sacred use of tobacco [ 77 ]. Interviews with these traditional healers confirmed that “sacred tobacco continues to play a paramount role in the community and provides a foundation for the American Indian Anishinabe or Ojibwe culture. They reiterated that using tobacco in the sacred way is vital for the Anishinabe culture [as] tobacco holds everything together and completes the circle. If tobacco is not used in a sacred manner, the circle is broken and a disconnect occurs in relation to the culture” [ 77 ].
The exploration of ceremonies surrounding birth and the relationship that is created through birth practices were outlined in a few studies reviewed for this category [ 78 , 79 ]. Ceremony was referred to in this context as the practice of what can be considered “rituals of healing”, noting that pregnancy itself “is carrying sacred water” [ 78 ]. As Rachel Olson points out, “[b]ringing people “back” to practicing ceremonial ways is seen as a healing process from the trauma encountered by First Nations peoples in Canada, as well as a way to both maintain our connection to the land and water, and to keep that same land and water safe for future generations. The implication in this is that by restoring our connection to the land through ceremony, other structural issues will again come into balance” [ 78 ].
Usage of traditional medicine
Data collection was completed in reservation and urban Indigenous communities to determine the usage rates of traditional medicine by Indigenous peoples. There was a total of 14 articles published on this topic, which included over 650 participants combined who completed surveys or interviews. Five studies were completed in Canada, and the remaining were completed in the United States (n = 9). Seventy-nine percent of the studies were published prior to 2009 (n = 11). The average year of publication was 2002 with publication dates ranging from 1988 to 2017. Rates of usage of both traditional medicines and traditional healers varied per region. Relevant findings are summarized in Table 1 .
Overall, the perception of traditional medicine amongst Indigenous people were positive. Several studies noted that access was an issue for many respondents who had the stated desire to use traditional medicine or see a traditional healer but did not know where to go for this support or treatment.
Traditional healer perspectives
The viewpoints of traditional healers themselves are an important contribution to this research topic. There were 18 studies that elicited the perspectives from Elders and traditional healers ranging in dates of publication between 1993 and 2019 (average year of publication was 2011). Twelve studies were either fully or partially based in the US, with nine articles published in either nursing or mental health related journals.
Moorehead et al. describe discussions held with a group of traditional healers on the possibilities and challenges of collaboration between Indigenous and conventional biomedical therapeutic approaches [ 93 ]. The participants recommended the implementation of cultural programming, the observance of mutuality and respect, the importance of clear and honest communication, and the need for awareness of cultural differences as a unique challenge that must be collaboratively overcome for collaboration [ 93 ].
It is not culturally acceptable to alter the words or provide an interpretation of the words of traditional healers. The following are some notable excerpts from traditional healer interviews that occurred in the literature reviewed:
The doctors and nurses at a local hospital asked me to speak to them on natural medicines . So I did . You could tell the doctors have a hard time trying to understand traditional healing and the use of plants to heal…it is hard for them to understand . Some of them got up and left when I started to talk about how you have to develop a relationship with the plant world…They sometimes have a hard time if things are not done their way…I respect the medicine , I just wish Western medical persons would understand [ 94 ] … When we gather medicine…the plant has a spirit in it…and…the spirit of those plants stays in the medicine…Every individual is different…every remedy is different…because specific things work for specific people…We’re made up of four parts…physical , mental , emotional , and spiritual . Sometimes sickness can be caused by imbalance within a person . When we do Indian healing…it goes to the source of the problem…not to the symptoms [ 94 ]. It’s a very powerful gift that we’ve been given…I am not a healer…I am only an instrument in that whole process . I am the helper and the worker , the preparer , and the doer . The healing ultimately comes from the Creator…With the lighting of that smudge , holding that eagle feather while we pray…these sacred medicines , these sacred pipes , and everything that we carry in our bundles . That’s where the strength comes from…from those medicines , from Mother Earth , and from the Creator … You are a part of creation , you’re a part of everything…there is this interrelatedness of all things , of all creation , and everything has life…we’re a whole family . And we’re related to all living things and all beings and all people [ 95 ]. I’ve been saying it for years . We need more medicine people . We need more Native healers…male and female [ 96 ].
It was apparent throughout the articles reviewed for this category that many traditional healers were not opposed to Western medicine; however, many had voiced concerns that Western medicine seemed to not respect them (i.e., didn’t respect their way of thinking or disregarded their knowledge base). Overall, a deep understanding and appreciation for the long-standing colonial injury felt in many Indigenous communities demonstrated through the cumulative effects of trauma ‘snowballing’ across generations [ 94 ] has become a platform for much of the traditional healers’ work in their home communities. To work with these present and historical harms, there was a clear advocacy among many of the traditional healers interviewed for ensuring the availability of therapeutic talk within cultural settings in addition to ceremonial participation to help facilitate healing and the revival of traditional spiritual beliefs [ 97 ].
This scoping review identified 249 articles that were predominately qualitative in nature, pertaining to traditional Indigenous medicine in the North American context. Although there was broad coverage of the topic area, it became apparent that many of the published articles were written from an ‘outsider’ perspective (i.e., observational research by scholars outside of the Indigenous communities themselves). With this, there was a slight shift noted in the type of research that was completed on traditional medicine around the 2000s. Prior to this date, it became apparent by the writing style used by many authors (i.e., they, them, etc.) that the articles were very much written “about” Indigenous people and their traditional medicine practice(s). Although post-2000 there was still quite a large volume of articles written by non-Indigenous scholars, there was an increasing presence of articles authored or co-authored by Indigenous people themselves [ 13 , 60 , 68 , 72 , 76 ]. The significance in this regard is notable as the presentation of Indigenous medicine by outside researchers often misses key cultural nuances, sometimes uses inappropriate or even insulting terminology, has a tendency to make assumptions that are not always correct (implicit bias), and presents an application or integrationist perspective that comes from what is often perceived to be a dominant Western knowledge system. As this type of ‘outsider’ scholarship serves as the foundational academic and clinical knowledge base for many of the current assumptions around traditional medicine, it was important to catalogue where some of the noted bias comes from.
Although it can be culturally inappropriate to assume there are pan-Indigenous ways of looking at traditional medicine and its practice (due to often stark differences in the practice of traditional medicine regionally), similar sentiments were expressed throughout many of the published articles. One was the assumed dominance of conventional medicine over traditional medicine practice, presented sometimes unconsciously through Western providers’ or researchers’ accounts of the subject and the language used. One possible consideration in this respect is that Indigenous-based interventions were often defined by a Western methodological approach and governance structure, which could be said to constrain and change the descriptions or programs themselves into something they were not actually meant to be. One solution to this issue would be to utilize an Indigenous methodological approach, governance structure, and reporting approach for these interventions, and then adapt the Western system to this approach and structure instead [ 58 ]. This would better ensure the centering of an Indigenous worldview and knowledge system through a truly self-determined Indigenous model with a potentially higher degree of success.
There is often a misperception that Indigenous peoples are in need of Westernized science in order to ‘legitimize’ our knowledge and healing systems [ 98 ]. It was clear from the literature reviewed on traditional healer perspectives that there was great opportunity for Western medicine and providers to learn about other ways of looking at health and disease in a form of respectful cooperation with Elders and Indigenous communities. This is consistent with the work of Berbman in 1973 who tells a story about a psychiatrist who brought some Navajo medicine men into his practice to demonstrate some of the things that he does in his practice [ 99 ] (i.e., the psychiatrist’s intent was to teach the medicine men). The psychiatrist demonstrated putting a Navajo woman under hypnosis for the medicine men.
One of the medicine men stated, “I’m not surprised to see something like this happen because we do things like this, but I am surprised that a white man should know anything so worthwhile… they [then] asked that my subject … diagnose something [while under hypnosis]. I objected, saying that neither she nor I knew how to do this and that it was too serious a matter to play with. They insisted that we try, however, and finally we decided that a weather prediction was not too dangerous to attempt. …When my subject was in a deep trance, I instructed her to visualize the weather for the next six months. She predicted light rain within the week, followed by a dry spell of several months and finally by a good rainy season in late summer. I make no claim other than the truthful reporting of facts: She was precisely correct” [ 99 ].
It was also evident through the articles reviewed that many Indigenous peoples using traditional medicine do not disclose this use to their Western healthcare providers. This reflects on the importance of developing culturally safe health systems and healthcare providers with strong communication skills for diverse patient settings. The story told by David Baines about the oncologist calling the patient’s traditional healer a “witch doctor” was a clear example of a lack of respect for utilizing a shared decision-making methodology for best outcomes in a clinical setting [ 73 ]. Implicit as well as overt bias against medical pluralism in diverse settings needs to be acknowledged and addressed in often authoritarian institutional settings [ 100 , 101 ] for best patient outcomes.
Overall, there has been a recent push with somewhat more acceptance in certain conventional medical settings towards supporting traditional Indigenous medicine interventions as demonstrated in some of the literature in this scoping review; however, the question remains whether or not “these efforts tend to represent political achievements more so than bona fide epistemological reconciliation” [ 72 ]. With continuing and significant health disparities existing in Indigenous populations in North America [ 102 ], a broader concerted effort needs to be mobilized and operationalized to ensure that Indigenous self-determined ways of knowing in relation to health and delivery of care is prioritized. Initial outcomes are promising in regard to traditional medicine’s benefit for Indigenous peoples in self-determined healthcare environments and settings. This has been clearly demonstrated by some of the literature reviewed here, yet, without more formalized support from all levels of the healthcare system, it will be difficult to expand these benefits and health outcomes to all Indigenous peoples who desire this type of care. This review and database ( S2 Table ) will hopefully serve as a repository for a portion of the academic literature contributing to practice, policy making, and research on this topic. This effort is aligned with Article 24 of the United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP):
Indigenous peoples have the right to their traditional medicines and to maintain their health practices, including the conservation of their vital medicinal plants, animals, and minerals [ 1 ].
Limitations
This scoping review was an attempt to catalogue the literature in the area of traditional Indigenous medicine in the North American context. The use of defined categories may give the impression of distinct traditional medicine themes unrelated to each other; however, due to the wholistic nature of traditional medicine, there will always be substantial overlap between concepts given the interconnected nature of all aspects of Indigenous healing practices. Categorical themes were used to help create some organization of the large body of literature aiding with delineating future research needs as well as for the ease of pulling for programmatic and policy needs.
It is possible, due to the substantial overlapping terminology with other fields, that some articles may have been missed in the search strategy. With this, an effective search strategy in this field would require the searcher to be familiar with how Indigenous medicine terminology is commonly used and applied in academia to be able to correctly select and screen articles from a very large databases of mixed disciplines. Traditional medicine terminology can be complex and can be referenced using other languages or simply geographic location. Due to this, any published articles that used unique ways of referencing traditional medicine or were described using an Indigenous language term could have caused additional articles to be missed; however, due to saturation being reached in the methods review, we feel the literature was well represented in our database. Regardless, this comprehensive database ( S2 Table ) of the available literature should not be considered exhaustive of all available material on this topic.
From an Indigenous worldview, culture and cultural practices can be looked at and examined as being a form of medicine. Even traditional language can be considered a form of cultural medicine [ 103 ]. This review excluded studies to this effect due to the variation in interpretations that are possible in this area; however, this exclusion was not intended to degrade or minimize the importance of culture as a healing strategy in any way. Due to the need to capture one defined area of this topic on traditional medicine and healing as a first step, further research can now build upon this work by evolving the scholarship area to be inclusive of all facets of Indigenous healing.
Traditionally within Indigenous communities, knowledge on traditional healing or the medicines themselves was and is passed down through a strong oral tradition that often involves deep ceremonial practice. As knowledge transmission in the North American context most often does not include a written record, historical and present-day information on community practice in this area is rightfully held within Indigenous communities themselves. This form of knowledge needs to be recognized, honored, and respected in the context of the traditional protocols that the respective community follows under the guidance of their Elders. This knowledge is the true knowledge that is most often not reflected in written academic scholarship. Some Indigenous communities have become more engaged with research as you will have seen throughout this review; however, some choose not to engage in this form of knowledge transmission for a variety of important reasons. This review, although detailed, is therefore only a small snapshot of the vast knowledge that exists within Indigenous communities in North America.
A critical review of the retained full text articles was not completed as the intent was to provide a representative and complete database on this topic. In addition, the vast array of formats and methodologies used in the Indigenous traditional medicine literature make the dominant Western metrics of validity simply not applicable to the current research purpose. Because it is not culturally acceptable to critique traditional Indigenous medicine, an Indigenous methodology was honored. Using an inclusive framework for this topic, several articles that were not written by Indigenous peoples or communities were included, which in some cases portrayed gross stereotypes from ‘outside’ observations of traditional medicine practice(s). The reader is therefore advised to exercise caution when utilizing information from ‘outside’ observational and older studies that may not be reflective of actual and current Indigenous community perspectives on the topic discussed. To this end, we highly recommend prioritizing the respectful engagement of Indigenous scholars and/or their scholarship, community members, and local knowledge holders to better ensure the concepts and resources presented here will be grounded and relevant within any local or cultural context.
This scoping review identified 249 articles pertaining to traditional Indigenous medicine in the North American context with the following categorical themes being identified: General Traditional Medicine, Integration of Traditional and Western Medicine Systems, Ceremonial Practice for Healing, Usage of Traditional Medicine, and Traditional Healer Perspectives.
Although effort has been made to better accommodate Indigenous ways of knowing and healing into healthcare settings and delivery models, self-determined options for traditional Indigenous healing are still lacking in Western institutions. This scoping review underscores the crucial need to further examine the dynamics of healthcare relations in a post-colonial context, with more open spaces for dialogue surrounding the use of Indigenous traditional healing often desired in racially diverse medical settings. The prerequisite to move closer to transformative practice in this area involves prioritizing further research and communication on this topic with a focus on applied self-determined interventions and programming.
Supporting information
S1 checklist, acknowledgments.
A very heartfelt thank you to all of the Indigenous Elders and communities who have shared their stories and perspectives throughout this body of literature. Special thanks to Margo Greenwood, PhD, at the National Collaborating Center for Indigenous Health (NCCIH) for her helpful guidance on this project in addition to Daisy Goodman, CNM, DNP, MPH, for her ongoing support and helpful recommendations with the writing process. Thank you also to Devon Olson of Library Sciences at the University of North Dakota for aid in the search term development process.
Funding Statement
The author(s) received no specific funding for this work.
Data Availability
Traditional Indigenous medicine in North America: A scoping review
Affiliations.
- 1 Department of Family & Community Medicine, School of Medicine and Health Sciences, University of North Dakota, Grand Forks, North Dakota, United States of America.
- 2 Arctic Indigenous Wellness Foundation, Yellowknife, Northwest Territories, Canada.
- PMID: 32790714
- PMCID: PMC7425891
- DOI: 10.1371/journal.pone.0237531
Background: Despite the documented continued use of traditional healing methods, modalities and its associated practitioners by Indigenous groups across North America, it is presumed that widespread knowledge is elusive amongst most Western trained health professionals and systems. This despite that the approximately 7.5 million Indigenous peoples who currently reside in Canada and the United States (US) are most often served by Western systems of medicine. A state of the literature is currently needed in this area to provide an accessible resource tool for medical practitioners, scholars, and communities to better understand Indigenous traditional medicine in the context of current clinical care delivery and future policy making.
Methods: A systematic search of multiple databases was performed utilizing an established scoping review framework. A consequent title and abstract review of articles published on traditional Indigenous medicine in the North American context was completed.
Findings: Of the 4,277 published studies identified, 249 met the inclusion criteria divided into the following five categorical themes: General traditional medicine, integration of traditional and Western medicine systems, ceremonial practice for healing, usage of traditional medicine, and traditional healer perspectives.
Conclusions: This scoping review was an attempt to catalogue the wide array of published research in the peer-reviewed and online grey literature on traditional Indigenous medicine in North America in order to provide an accessible database for medical practitioners, scholars, and communities to better inform practice, policymaking, and research in Indigenous communities.
Publication types
- Delivery of Health Care / methods
- Delivery of Health Care / organization & administration*
- Medicine, Traditional / methods*
- Medicine, Traditional / statistics & numerical data*
- North America
Grants and funding
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 09 November 2023
Coproducing health research with Indigenous peoples
- Chris Cunningham ORCID: orcid.org/0000-0001-7083-9088 1 &
- Monica Mercury 2
Nature Medicine volume 29 , pages 2722–2730 ( 2023 ) Cite this article
2078 Accesses
20 Altmetric
Metrics details
- Health care
- Translational research
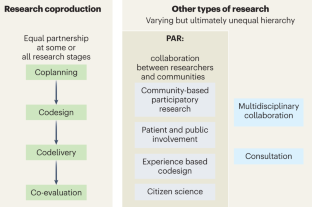
The coproduction of health research represents an important advance in the realm of participatory methodologies, which have evolved over the past five decades. This transition to a collaborative approach emphasizes shared control between academic researchers and their partners, fostering a more balanced influence on the research process. This shift not only enhances the quality of the research and the evidence generated, but also increases the likelihood of successful implementation. For Indigenous peoples, coproduced research represents a critical development, enabling a shift from being mere ‘subjects’ of research to being active controllers of the process—including addressing the extractive and oppressive practices of the past. In this Review, we explore how research coproduction with Indigenous peoples is evolving. An ‘Indigenous turn’ embraces the concept of shared control while also considering the principles of reciprocity, the incommensurability of Western and Indigenous knowledge systems, divergent ethical standards, strategic and political differences, and the broader impact of processes and outcomes. To illustrate these ideas, we present examples involving New Zealand’s Māori communities and offer recommendations for further progress.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Mapping the community: use of research evidence in policy and practice
Elizabeth N. Farley-Ripple, Kathryn Oliver & Annette Boaz

Participatory action research
Flora Cornish, Nancy Breton, … Darrin Hodgetts

Negotiating the ethical-political dimensions of research methods: a key competency in mixed methods, inter- and transdisciplinary, and co-production research
Simon West & Caroline Schill
Durose, C., Perry, B. & Richardson, L. Is co-production a ‘good’ concept? Three responses. Futures 142 , 102999 (2022).
Article Google Scholar
Laursen, S. et al. Collaboration across worldviews: managers and scientists on Hawai’i Island utilize knowledge coproduction to facilitate climate change adaptation. Environ. Manag. 62 , 619–630 (2018).
Farr, M. et al. Co-producing knowledge in health and social care research: reflections on the challenges and ways to enable more equal relationships. Humanit. Soc. Sci. Commun. 8 , 105 (2021).
Cornish, F. et al. Participatory action research. Nat. Rev. Methods Primers 3 , 34 (2023).
Article CAS Google Scholar
Masterson, D., Areskoug Josefsson, K., Robert, G., Nylander, E. & Kjellstrom, S. Mapping definitions of co-production and co-design in health and social care: a systematic scoping review providing lessons for the future. Health Expect. 25 , 902–913 (2022).
Article PubMed PubMed Central Google Scholar
Halvorsrud, K. et al. Identifying evidence of effectiveness in the co-creation of research: a systematic review and meta-analysis of the international healthcare literature. J. Public Health 43 , 197–208 (2021).
Osborne, S. P., Radnor, Z. & Strokosch, K. Co-production and the co-creation of value in public services: a suitable case for treatment? Public Manag. Rev. 18 , 639–653 (2016).
Oliver, K., Kothari, A. & Mays, N. The dark side of coproduction: do the costs outweigh the benefits for health research? Health Res. Policy Syst. 17 , 33 (2019).
Ortiz-Prado, E. et al. Potential research ethics violations against an indigenous tribe in Ecuador: a mixed methods approach. BMC Med. Ethics 21 , 100 (2020).
McKenzie, D., Whiu, T. A., Matahaere-Atariki, D., Goldsmith, K. & Te Puni Kōkiri. Co-production in a Māori context. Soc. Policy J. N. Z. 33 , 32–46 (2008)
Latulippe, N. & Klenk, N. Making room and moving over: knowledge co-production, Indigenous knowledge sovereignty and the politics of global environmental change decision-making. Curr. Opin. Environ. Sustain. 42 , 7–14 (2020).
Yua, E., Raymond-Yakoubian, J., Daniel, R. A. & Behe, C. A framework for co-production of knowledge in the context of Arctic research. Ecol. Soc. 27 , 34 (2022).
Manuel-Navarrete, D., Buzinde, C. N. & Swanson, T. Fostering horizontal knowledge co-production with Indigenous people by leveraging researchers’ transdisciplinary intentions. Ecol. Soc. 26 , 22 (2021).
Haines, J., Du, J. T., Geursen, G., Gao, J., & Trevorrow, E. Understanding Elders’ knowledge creation to strengthen Indigenous ethical knowledge sharing. In Proc. RAILS - Research Applications, Information and Library Studies, 2016, School of Information Management, Victoria University of Wellington, New Zealand, 6-8 December, 2016; http://InformationR.net/ir/22-4/rails/rails1607.html (2017).
Wilson, S. Research is Ceremony: Indigenous Research Methods (Fernwood Publishing, 2008).
Google Scholar
Durie, M. Whaiora: Māori Health Development (Oxford Univ. Press, 1998).
Maher, P. A review of ‘traditional’ aboriginal health beliefs. Aust. J. Rural Health 7 , 229–236 (1999).
Article CAS PubMed Google Scholar
Martin, K. & Mirraboopa, B. Ways of knowing, being and doing: a theoretical framework and methods for indigenous and indigenist re‐search. J. Aust. Stud. 27 , 203–214 (2003).
Gee, G., Dudgeon, P., Schultz, C., Hart, A. & Kelly, K. Healing Models and Programmes in Working Together: Aboriginal and Torres Strait Islander Mental Health and Wellbeing Principles and Practice (eds Dudgeon P, Milroy H and Walker R) Part 6, 417–532 (Commonwealth of Australia, 2014).
Chino, M. & Debruyn, L. Building true capacity: indigenous models for indigenous communities. Am. J. Public Health 96 , 596–599 (2006).
Napoli, M. Holistic health care for native women: an integrated model. Am. J. Public Health 92 , 1573–1575 (2002).
Pulotu-Endemann, F. K. Strategic Directions for the Mental Health Services for Pacific Islands People, 1–7 (Ministry of Health, 1995).
Richmond, C. A. M., Ross, N. A. & Bernier, J. in Moving Forward, Making a Difference (eds. White, J. P. et al.) 4 , 1–15 (Aboriginal Policy Research Consortium International, 2007).
Hamalainen, S., Musial, F., Salamonsen, A., Graff, O. & Olsen, T. A. Sami yoik, Sami history, Sami health: a narrative review. Int. J. Circumpolar Health 77 , 1454784 (2018).
Smith, L. Thought space Wānanga—a Kaupapa Māori decolonizing approach to research translation. Genealogy 3 , 74 (2019).
Smith, L. T. Decolonizing Methodologies: Research and Indigenous Peoples (Zed Books, 2012).
Smith, G. H. The Development of Kaupapa Maori: Theory and Praxis . PhD thesis, Univ. Auckland (1997).
Smith, L. T. in Kaupapa Rangahau A Reader: A Collection of Readings from the Kaupapa Maori Research Workshop Series (eds. Pihama, L. & South, K.) 47–52 (Te Kotahi Research Institute, 2015).
Cunningham, C. A framework for addressing Maori knowledge in research, science and technology. Pac. Health Dialog. 7 , 62–69 (2000).
CAS PubMed Google Scholar
Greenaway, A. et al. Methodological sensitivities for co-producing knowledge through enduring trustful partnerships. Sustain. Sci. 17 , 433–447 (2021).
Waldegrave, C., Cunningham, C., Love, C. & Nguyen, G. Co-creating culturally nuanced measures of loneliness with Māori elders. Innov. Aging 4 , 610 (2020).
Article PubMed Central Google Scholar
King, P. T., Cormack, D., Edwards, R., Harris, R. & Paine, S. J. Co-design for indigenous and other children and young people from priority social groups: a systematic review. SSM Popul. Health 18 , 101077 (2022).
Rolleston, A. K., Korohina, E. & McDonald, M. Navigating the space between co-design and mahitahi: building bridges between knowledge systems on behalf of communities. Aust. J. Rural Health 30 , 830–835 (2022).
Ullrich, J. S., Demientieff, L. X. & Elliott, E. Storying and re-storying: co-creating indigenous well-being through relational knowledge exchange. Am. Rev. Can. Stud. 52 , 247–259 (2022).
Minoi, J.-L. et al. A participatory co‑creation model to drive community engagement in rural Indigenous schools: a case study in Sarawak. Electron. J. e-Learn. 17 , 157–167 (2019).
Zurba, M. et al. Learning from knowledge co-production research and practice in the twenty-first century: global lessons and what they mean for collaborative research in Nunatsiavut. Sustain. Sci. 17 , 449–467 (2021).
Koster, R., Baccar, K. & Lemelin, R. H. Moving from research ON, to research WITH and FOR Indigenous communities: a critical reflection on community-based participatory research. Can. Geogr. 56 , 195–210 (2012).
Peters, D. et al. Participation is not enough. In Proc. 30th Australian Conference on Computer–Human Interaction (eds Buchanan, G. & Stevenson, D.) 97–101 (Association for Computing Machinery, 2018).
Bryant, J. et al. Beyond deficit: ‘strengths-based approaches’ in Indigenous health research. Sociol. Health Illn. 43 , 1405–1421 (2021).
Article PubMed Google Scholar
Goodyear-Smith, F. & Ashton, T. New Zealand health system: universalism struggles with persisting inequities. Lancet 394 , 432–442 (2019).
Maclean, K. et al. Decolonising knowledge co-production: examining the role of positionality and partnerships to support Indigenous-led bush product enterprises in northern Australia. Sustain. Sci. 17 , 333–350 (2021).
Johnson, J. T. & Murton, B. Re/placing native science: indigenous voices in contemporary constructions of nature. Geogr. Res. 45 , 121–129 (2007).
Morton Ninomiya, M. E. et al. Knowledge translation approaches and practices in Indigenous health research: a systematic review. Soc. Sci. Med. 301 , 114898 (2022).
Martel, R., Shepherd, M. & Goodyear-Smith, F. He awa whiria—a ‘braided river’: an Indigenous Māori approach to mixed methods research. J. Mix. Methods Res. 16 , 17–33 (2022).
Pitama, S. et al. Meihana model: a clinical assessment framework. N.Z. J. Psychol. 36 , 118–125 (2007).
Wright, A. L., Gabel, C., Ballantyne, M., Jack, S. M. & Wahoush, O. Using two-eyed seeing in research with Indigenous people: an integrative review. Int. J. Qual. Methods 18 , 160940691986969 (2019).
Bandola-Gill, J., Arthur, M. & Leng, R. I. What is co-production? Conceptualising and understanding co-production of knowledge and policy across different theoretical perspectives. Evid. Policy 19 , 275–298 (2023).
Pain, R. et al. Mapping Alternative Impact—Alternative Approaches to Impact from Co-produced Research . Project report (Durham Univ., 2015).
Carroll, S. R. et al. The CARE principles for Indigenous data governance. Data Sci. J. 19 , 1–12 (2020).
Baum, F., MacDougall, C. & Smith, D. Participatory action research. J. Epidemiol. Commun. Health 60 , 854–857 (2006).
Kemmis, S. & McTaggart, R. in The Sage Handbook of Qualitative Research (eds. Denzin, N. & Lincoln, Y.) 559–604 (Sage, 2005).
Siffels, L. E., Sharon, T. & Hoffman, A. S. The participatory turn in health and medicine: the rise of the civic and the need to ‘give back’ in data-intensive medical research. Humanit. Soc. Sci. Commun. 8 , 306 (2021).
Israel, B., Eng, E., Schultz, A. & Parker, E. Methods in Community-Based Participatory Research (Jossey-Bass, 2005).
Williams, O., Robert, G., Martin, G. P., Hanna, E. & O’Hara, J. in Decentring Health and Care Networks (eds. Bevir, M. & Waring, J.) 213–237 (Springer, 2020).
Liabo, K., Boddy, K., Burchmore, H., Cockcroft, E. & Britten, N. Clarifying the roles of patients in research. Br. Med. J. 361 , k1463 (2018).
Tanay, M. A. L. et al. Co-designing a cancer care intervention: reflections of participants and a doctoral researcher on roles and contributions. Res. Involv. Engagem. 8 , 36 (2022).
Craig, E. et al. in Handbook of Social Sciences and Global Public Health (ed. Liamputtong, P.) 1–15 (Springer, 2023).
Cohn, J. P. Citizen science: can volunteers do real research? BioScience 58 , 192–197 (2008).
Dickinson, J. L., Zuckerberg, B. & Bonter, D. N. Citizen science as an ecological research tool: challenges and benefits. Annu. Rev. Ecol. Evol. Syst. 41 , 149–172 (2010).
Morales, M. P. E. Participatory action research (PAR) cum action research (AR) in teacher professional development: a literature review. Int. J. Res. Educ. Sci. 2 , 156–165 (2016).
Méndez, V., Caswell, M., Gliessman, S. & Cohen, R. Integrating agroecology and participatory action research (PAR): lessons from Central America. Sustainability 9 , 705 (2017).
Rodriguez, L. F. & Brown, T. M. From voice to agency: guiding principles for participatory action research with youth. New Dir. Youth Dev. 2009 , 19–34 (2009).
Gatenby, B. & Humphries, M. Feminist participatory action research: methodological and ethical issues. Women’s Stud. Int. Forum 23 , 89–105 (2000).
Fine, M. & Torre, M. E. Critical participatory action research: a feminist project for validity and solidarity. Psychol. Women Q. 43 , 433–444 (2019).
Reid, C., Tom, A. & Frisby, W. Finding the ‘action’ in feminist participatory action research. Action Res. 4 , 315–332 (2016).
Dadich, A., Moore, L. & Eapen, V. What does it mean to conduct participatory research with Indigenous peoples? A lexical review. BMC Public Health 19 , 1388 (2019).
Dudgeon, P., Bray, A., Darlaston-Jones, D. & Walker, R. Aboriginal Participatory Action Research: An Indigenous Research Methodology Strengthening Decolonisation and Social and Emotional Wellbeing—Discussion Document (Lowitja Institute, 2020).
Peltier, C. An application of two-eyed seeing: Indigenous research methods with participatory action research. Int. J. Qual. Methods 17 , 160940691881234 (2018).
Datta, R. et al. Participatory action research and researcher’s responsibilities: an experience with an Indigenous community. Int. J. Soc. Res. Methodol. 18 , 581–599 (2014).
Aika, L. & Greenwood, J. in Education, Participatory Action Research, and Social Change: International Perspectives (eds. Kapoor, D. & Jordan, S.) 59–72 (Palgrave Macmillan, 2009).
Smylie, J. et al. Knowledge translation and indigenous knowledge. Int. J. Circumpolar Health 63 , 139–143 (2004).
Agrawai, A. Dismantling the divide between Indigenous and scientific knowledge. Dev. Change 23 , 413–439 (1995).
Durie, M. Understanding health and illness: research at the interface between science and Indigenous knowledge. Int. J. Epidemiol. 33 , 1138–1143 (2004).
Ermine, W. J. The ethical space of engagement. Indigenous Law J. 6 , 193–203 (2007).
Ellison, C. Indigenous Knowledge and Knowledge Synthesis Translation and Exchange (KSTE) (National Collaborating Centre for Indigenous Health, 2014).
Download references
Acknowledgements
We acknowledge funding support from the Ageing Well National Science Challenge for the Tai Kaumātuatanga Older Māori Wellbeing and Participation: Present and Future Focus (1903R) project and team members C. Love and C. T. Waldegrave.
Author information
Authors and affiliations.
Research Centre for Hauora & Health (RCHH), Massey University, Wellington, New Zealand
Chris Cunningham
The Family Centre Social Policy Research Unit, Lower Hutt, New Zealand
Monica Mercury
You can also search for this author in PubMed Google Scholar
Contributions
Positionality statement. Both authors identify as Māori, the Indigenous people of Aotearoa New Zealand. C.C. is a member of the Ngāti Raukawa, Ngāti Toa, Te Ātiawa and Te Ātihaunui-a-Pāparangi iwi (tribes) and also claims Anglo-European ancestry. A scientist by training, he holds a PhD in chemistry (1988) and has worked as a Māori health researcher since 1996 and as a professor since 2001. He is a director of a Treaty of Waitangi-led research center in a New Zealand university. M.M. identifies as Te Iwi Mōrehu, Ngāti Kahungunu ki Te Wairarapa and ki Te Wairoa through her Māori father and is of Chinese descent through her mother. She is a trained educator (MEd) and community-based health researcher working in the nongovernmental sector.
Corresponding author
Correspondence to Chris Cunningham .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Medicine thanks Jeneile Luebke, Jacquie Kidd and Malcolm King for their contribution to the peer review of this work. Primary Handling Editor: Karen O’Leary, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Cunningham, C., Mercury, M. Coproducing health research with Indigenous peoples. Nat Med 29 , 2722–2730 (2023). https://doi.org/10.1038/s41591-023-02588-x
Download citation
Received : 11 June 2023
Accepted : 13 September 2023
Published : 09 November 2023
Issue Date : November 2023
DOI : https://doi.org/10.1038/s41591-023-02588-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
- Open access
- Published: 14 December 2015
Integrating traditional indigenous medicine and western biomedicine into health systems: a review of Nicaraguan health policies and miskitu health services
- Heather Carrie 1 , 2 ,
- Tim K. Mackey 3 , 4 , 5 &
- Sloane N. Laird 6
International Journal for Equity in Health volume 14 , Article number: 129 ( 2015 ) Cite this article
24k Accesses
21 Citations
3 Altmetric
Metrics details
An Erratum to this article was published on 03 February 2016
Throughout the world, indigenous peoples have advocated for the right to retain their cultural beliefs and traditional medicine practices. In 2007, the more than 370 million people representing 5000 distinct groups throughout the world received global recognition with the adoption of the United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP). UNDRIP Article 24 affirms the rights of indigenous peoples to their traditional medicines and health practices, and to all social and health services. Although not a legally binding agreement, UNDRIP encourages nation states to comply and implement measures to support and uphold its provisions. Within the context of indigenous health and human rights, Nicaragua serves as a unique case study for examining implementation of UNDRIP Article 24 provisions due to the changes in the Nicaraguan Constitution that strive for the overarching goal of affirming an equal right to health for all Nicaraguans and supporting the integration of traditional medicine and biomedicine at a national and regional level. To explore this subject further, we conducted a review of the policy impact of UNDRIP on health services accessible to the Miskitu indigenous peoples of the North Atlantic Autonomous Region (RAAN). We found that although measures to create therapeutic cooperation are woven into Nicaraguan health plans at the national and regional level, in practice, the delivery of integrated health services has been implemented with varying results. Our review suggests that the method of policy implementation and efforts to foster intercultural collaborative approaches involving respectful community engagement are important factors when attempting to assess the effectiveness of UNDRIP implementation into national health policy and promoting traditional medicine access. In response, more study and close monitoring of legislation that acts to implement or align with UNDRIP Article 24 is necessary to ensure adequate promotion and access to traditional medicines and health services for indigenous populations in Nicaragua and beyond.
Introduction
There are more than 370 million people representing 5000 distinct indigenous peoples throughout the world [ 1 ]. Within this diverse global community, a strong and growing movement continues to advocate for self-determination with the right to regain and retain traditional indigenous cultural practices. A steady rise of united influence emerged in the late 1970s and continues to gain momentum with the passing of international declarations and national laws [ 1 ]. Included in some of these international, national, and regional policies, are provisions calling for ensuring and protecting the rights of indigenous peoples to their traditional medicine. These policies are written with the intention of supporting both the traditional indigenous medicine healers in offering their services and for the indigenous individuals in accessing traditional medicines and practices [ 2 ].
In 2007, in a landmark moment following more than two decades of negotiation, 143 member states adopted the United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP) reflecting widespread recognition by the international community to the individual and collective rights of indigenous peoples. UNDRIP Article 24 specifically affirms the fundamental rights of indigenous peoples to their traditional medicines and health practices, and to all social and health services. Although not a legally binding instrument, UNDRIP represents an important step forward in developing a framework of internationally agreed upon norms and principles specifically reaffirming the unique human right to health for indigenous peoples [ 2 ]. Though the UNDRIP was designed to promote a set of international standards and obligations to be adopted by member states and potentially translated into national policy making, there is a general lack of research examining its effectiveness and influence in the context of health policy.
Hence, this review seeks to determine if the principles enshrined in UNDRIP have been successfully translated and implemented into national health policy in Nicaragua, a country home to a Native American indigenous population known as the Miskitu peoples of the North Atlantic Autonomous Region (RAAN) [ 3 ]. In the latest population census conducted by the Nicaragua National Institute of Information Development (INIDE) in 2005, Miskitus were found mainly living in the northeast corner of Nicaragua in a province known as the RAAN, with a population of more than 120,000 – nearly 45,000 urban and 75,000 rural [ 4 ]. The Miskitu peoples of Nicaragua were chosen as a focal point for this review because they are affected by both national and regional policies that include provisions for supporting the rights of indigenous peoples to their traditional medicine. The Miskitu possess a unique history in gaining semi-autonomy from the central government of Nicaragua after indigenous insurgency efforts against the Sandinista government led to the Autonomy Statute of 1987 (Law 28) initiated in hopes of bringing peace to the region. Although Law 28 recognizes the rights to self-determination for the Atlantic Coast people (mostly Miskitu), the Nicaraguan central government maintains influence in regional policy implementation - including those policies affecting health service accessibility [ 5 ].
In this review we specifically set out to assess whether Nicaragua’s national and regional health plans positively influence the integration of traditional indigenous medicine and western Biomedicine; how these policies impact the health services being accessed, delivered, and used by the Miskitu; and whether these policies could serve as a global health policy model for other indigenous populations who wish to promote their right to health as recognized by UNDRIP. To accomplish this, we conducted a literature review and analysis of documents related to Nicaraguan indigenous health, Nicaragua’s national health policy and laws, and health provisions of the UNDRIP. The inclusion criteria for documents reviewed in this study comprised of: peer-reviewed literature; reports published by NGOs and other civil society actors; and reports and policy documents issued by local, national, regional or international organizations discussing Nicaraguan indigenous health policy. In retrieving these documents we used a combination of online Google searches for keywords associated with Nicaraguan indigenous health, searched for literature on the subject from PubMed/Medline and Academic Search Complete databases, and also searched for documents in both English and Spanish on websites of international and regional organizations as well as from Nicaraguan government agencies. Document extraction and review was conducted from October to December, 2014.
Our review begins with a brief summary of global health governance for indigenous peoples' right to health and Nicaragua’s own national and regional health plans to discover how traditional knowledge and indigenous peoples practices are included as policy to be implemented in health care settings. We then examine the health services accessible to the Miskitu peoples and seek to understand how traditional practices and biomedicines are used separately or together to provide care for specific conditions. In addition, we examine what training exists for health care providers in this community to support inter-cultural respect for both traditional knowledge and medical empirical evidence. Lastly, we assess whether Nicaragua’s national and regional health plans meet the standards set forth under UNDRIP Article 24 and provide recommendations for future policy implementation.
Brief history of global health governance for indigenous peoples’ right to health
It is important to examine other international policy instruments that have been adopted and that have provided critical foundational support for the right to health for Indigenous populations that preceded the adoption of the UNDRIP. In 1989, The International Labour Organization Convention, (No. 169) was the first contemporary international policy guaranteeing rights to indigenous peoples and specifically declares a right to health services for indigenous and tribal peoples in independent countries. In addition, the Convention calls for government responsibility in providing community-based, culturally appropriate care, preferably from health care providers employed from the local community, with input from the community [ 6 ].
In 1993 and 1997 , the Pan American Health Organization (PAHO) passed resolutions to promote the right to health and the access to health care for indigenous peoples in the Americas [ 7 ]. Resolutions CD37.R5 and CD40.R6: Health of Indigenous Peoples Initiative acknowledges the inequities in the status of health and lack of access to basic health services [ 7 ]. These resolutions consist of provisions to support the right to self-determination and respect for cultural values regarding health care along with the right to alternative models of care to deal with “insufficient coverage, inadequate access, and the lack of acceptability of health services on the part of indigenous populations” [ 7 ]. It also urges member governments to establish mechanisms that allow for representation of indigenous peoples in the development of health care services for their own populations [ 7 ]. The PAHO resolutions served to guide the health measures framework for indigenous peoples residing in the Americas [ 7 ].
In 2007, after a decade of additional PAHO resolutions and increased social and political activism to have indigenous peoples' rights acknowledged internationally, the United Nations drafted and adopted a Declaration on the Rights of Indigenous Peoples (UNDRIP) (143 states affirming, 4 voting against [Australia, Canada, New Zealand and the United States], and 11 abstentions). In this declaration, the right to health is clearly stated in Article 24, Section One by affirming the right to traditional medicine within indigenous health care practices and access to other health care services without discrimination and in Section Two by affirming the right to the highest level of mental and physical health with governmental support in obtaining this goal [ 2 ]. These rights are in accordance with the World Health Organization (WHO) Constitution’s declaration of health as a fundamental human right and the United Nations Economic and Social Council (ECOSOC) function to promote respect for human rights [ 8 , 9 ].
Nicaragua’s national health laws and indigenous health policy
Nicaragua’s national and regional laws closely parallel the trajectory of the body of international declarations and principles concerning indigenous peoples. However, the first Nicaraguan national law with provisions for indigenous peoples' rights was initiated two decades before UNDRIP with the adoption of the Nicaragua Constitution of 1987. Even preceding the 1987 Constitution, Nicaragua’s Ministry of Health created a program in 1985 to “revitalize popular and traditional medicine” [ 10 ] as a necessary response to the wartime high costs of imported pharmaceutical materials [ 10 ]. The Nicaragua Constitution Article 5 expresses that “the State recognizes the existence of indigenous peoples who enjoy the rights, … and guarantees … their identity and culture, to have their own forms of social organization and administer their local affairs, as well as to preserve the communal forms of land property…” [ 11 ]. Article 180 reinstates this idea by giving the communities of the Atlantic Coast, where most of the Miskitu reside, the right to live and create organizations based upon their cultural traditions [ 11 ].
Additionally, Article 89 of the Nicaragua Constitution supports the communities of the Atlantic Coast in the right to maintain and cultivate their own cultural identities, as well as to manage their local affairs within their traditions and historical customs. This article also demands that the state recognize a communal form of land-ownership within the Atlantic Coast. Thus, the Mistiku peoples living in the Atlantic Coast region have a form of land ownership to enable them to maintain and support conservation of traditional plants, animals and mineral medicines [ 11 ]. Hence, the right to manage and access their traditional medicines is also affirmed in Article 24 of the UNDRIP along with the right to self-determination at the state level [ 2 ].
To further revitalize access and promotion of traditional medicine, the Ministry of Health created the National Centre of Popular and Traditional Medicine in 1989 with the objectives of: organizing traditional medicine research; training health care providers in traditional medicine practices; and commercializing the production of medicinal plants. In 1991, the Centre separated from the Ministry of Health to become its own non-profit foundation with new objectives to recover and preserve traditional practices; promote the use of medicinal plants, and create a medicinal plant distribution network through pharmacies in the health system [ 10 ].
Although health care services for the indigenous peoples of Nicaragua initially were managed at the national level, this changed when the federal government developed the National Health Plan of 2004–2015, which started to decentralize medical services and resources from the national level to regional authorities. This decentralization of health care was influenced by international organizations calling for a sector-wide health care services delivery development approach. The plan also included provisions to allow for non-government organizations (NGOs) and health care foundations to set up programs within the country, as well as for the privatization of some health care services. Additionally, an aim of the policy was to incorporate or integrate the “cosmovision” of the communities into practice, to define the cultural-specific meaning of full wellness and complete health. The cosmovision approach originally began as a concept started in 1996 as part of Nicaragua’s health plan for the RAAN region to foster therapeutic cooperation in equal terms between traditional medicine practices and western biomedicine [ 3 ].
To further support the cosmovision of indigenous communities, Nicaragua’s General Health Law of 2005 calls for indigenous peoples within the Atlantic Coast regions to be enabled to develop health methods that are consistent with their traditions and communities. Specifically, provisions state that the RAAN region may define and implement through regulations models of health care according to their traditions and customs of medicine and designate health authorities by methods they adopt [ 5 ]. This law is consistent with the PAHO initiatives, which demands the respect for indigenous peoples values and social organizations [ 7 ].
With the 2007 national election, a change in government guided health policy into a different direction. The decentralization remained, but the new health plan moved away from privatization and toward a policy based on the concept of universal care with ideas of free access to basic services. This new direction in health policy was based on concepts of equity and solidarity, with the idea of citizen responsibility and participation in their health care [ 12 ]. The policy was deemed to be community-based, which is a provision of the International Labour Organization (ILO) Convention 169, for indigenous and tribal peoples, and was ratified by Nicaragua in 2010 [ 6 ]. The plan also placed an emphasis on families. In 2009, the Modelo de Salud Familiar y Comunitario (MOSAFC), (Model of Family and Community Health) supported the idea that health care should incorporate the concept of an integrated approach with a focus on the promotion of health that addresses the differences within health determinants by including traditional medicine with western biomedicine [ 12 ]. This concept of integrating health care is nation-based, as it does not consider global policies, but tries to address local issues of the Atlantic Coast region and the multiple communities that have developed overtime with an emphasis on their unique customs and cultures.
In 2011, Nicaragua enacted Ley No. 759, Ley de Medicina Tradicional Ancestral (Law No. 759, Law of Traditional Ancestral Medicine), which specifically addresses equity and access to traditional and ancestral medicine [ 13 ]. The law also reestablished coordination between regions of indigenous peoples, updated a project plan for construction of an alternative medicine center, and has led to coordination between the Ministry of Health to incorporate intercultural concepts into health care models [ 13 ].
Recently, in 2014, Nicaragua adopted Ley No. 774, Ley de Medicina Natural, Terapias, Complementarias Y Productos Naturales En Nicargaua (Law No.774, Law of Natural and Complementary Medicine, Therapies, and Natural Products), which establishes provisions to promote access and use of natural medicine that includes traditional medicine practices, products and health services. Additionally, Law 774 declares the right of choice in therapeutic care to the Nicaraguan people and outlines regulatory procedures to oversee health care providers, products, and services [ 14 ]. Articles 23 and 24 specifically address safety in the use of medicinal plants with a cautionary protocol for toxic botanicals and guidelines for regulation of use. Finally, the law supports both the integration of natural medicine into the national health system and appointment of representatives of natural medicine organizations into the National Health Council [ 14 ].
Gaps in translation and implementation of international law and domestic Nicaraguan indigenous health policies
In reviewing Nicaragua’s national and regional laws pertaining to health and health care services, the provisions appear to generally align with the standards set forth in UNDRIP, but nevertheless introduce significant policy gaps and challenges that require further examination. Specifically, actual health care accessibility and health services delivery for indigenous communities in Nicaragua appears to be deficient, indicating that translation of UNDRIP into national health policy exists, but actual implementation to ensure indigenous health care rights and use of traditional medicine has not yet been adequately effectuated in these communities.
Under the Nicaraguan health system, accessing basic health services, a provision under UNDRIP Article 24 and included in the national health plan, remains difficult for Mistiku communities due to lack of public infrastructure (i.e. roads and affordable public transportation in the region) as well as a lack of sufficient health care workers to cover services needed to ensure access to hospitals and other treatment facilities [ 3 ]. Most health care services targeted towards these populations are delivered by health posts that consist of limited health care staff coverage (e.g. only one doctor and two nurses) [ 3 ]. Another method to deliver health care services to the Mistiku, which was developed under the community-based plan, allows for medical brigadistas (also known as independent health volunteers) to serve the rural areas of the Atlantic Coast, in order to promote public health interventions. Yet, these health care providers may not have the cultural knowledge or experience to appropriately deliver health care services or critical health behavior-related information, including inability to speak or understand the Mistiku language. Despite these challenges, in the context of basic access to health care, this indigenous community is able to access medical services at the two hospitals located in the autonomous regions or in other regions of the country, though the delivery of such services may not integrate indigenous medicine [ 15 ].
Another provision of the UNDRIP Article 24, Section One, calls for the conservation of plants, animals, and minerals used in traditional medicine [ 2 ]. As previously described, the Nicaraguan Constitution includes provisions for these protections in the form of communal land-ownership rights, which was included in the country’s Constitution as a means to enable indigenous peoples to protect their land, property and resources [ 11 ]. However, the Constitution nor the national laws that implement these principles, do not specifically create an adequate mechanism (whether a legal process, dispute resolution system, or other form of due process) to sufficiently protect these resources from outside sources or the government itself, essentially leaving the Miskitu and others without the appropriate means to exercise their rights and protect their resources either for the use of traditional medicine or for conservation purposes.
Integration effort: traditional medicine and western biomedicine
Although the intention to create therapeutic cooperation between indigenous traditional healers and western biomedical health care providers is woven into Nicaraguan health plans at the national and regional level, in practice integrated health services delivery has been implemented for the RAAN Miskitu with varying efforts and results [ 3 , 16 ]. The more successful integration efforts foster intercultural cooperation and a “from the community and for the community” [ 16 ] approach whereas the less successful integration efforts treat traditional medicine as mostly a supplementary or last resort resource.
In a 2009 study, Wedel reviewed existing literature that examined the collaborative efforts of traditional healers and biomedical health care providers serving the RAAN Miskitu population, noting that the biomedical providers often had an advantage over traditional healers in their authority and use of treatments [ 3 ]. He found traditional medicine care was primarily used at the discretion of biomedical health care providers as part of their own therapeutic treatment or alternatively by a traditional healer called in only to care for those who suffered with ailments outside of the general scope of biomedicine [ 3 ]. With illnesses deemed “spiritual” or “cultural,” Wedel found a willing transfer of medical authority from the biomedical providers to the traditional healers for therapeutic treatment; that Miskitu healers were used as a marginalized complement mostly when biomedicine failed [ 3 ].
This last-resort use of traditional medicine undermines the essence of a collaborative approach in integrating health services for therapeutic cooperation, and instead positions the western biomedical health provider as the medical authority acting as a gatekeeper to the traditional healers. When interviewed by Wedel, many Miskitu traditional healers expressed an openness to working with the western biomedical community to share in the care and clinical management of patients. Some also expressed a frustration with those western physicians who completely dismiss the value of traditional medicine and refuse to consult with the local healers, especially when the illness shows signs of being rooted in sorcery or of a spiritual nature [ 3 ]. When interviewing biomedical providers, Wedel found that those who were born in the RAAN region or were of Miskitu origin were more open to traditional medicine, and that western nurses were more accepting of the traditional practices than western doctors [ 3 ].
Barriers to implementing integration efforts
The most evident barrier to implementing integration efforts is the vastly different belief systems of western biomedical practitioners and their traditional indigenous healer counterparts in regards to illness, health and healing. Much of the Miskitu health beliefs involve a connection between spirit entities and illness [ 3 ]. Hence, those western biomedical practitioners unfamiliar with Miskitu culture or skeptical of these beliefs, may discount the value of traditional healers. Likewise, traditional healers who may have attained most of their medicinal knowledge through apprenticeship or non-university training, may not comprehend or believe in the western health care model. These divergent educational backgrounds and belief systems can be further complicated by potential language barriers inhibiting the success of working together and collaboratively on behalf of shared patients [ 3 ].
Additionally, funding for traditional medicines can be limited and can hamper integration efforts. Specifically, regional Health Ministries often claim that there is significant difficulty in planning and budgeting for some health services provided by traditional healers who offer an individualized approach to treatment that can require varying remedies and fees in contrast to standardized health services offered by western biomedical personnel covered by the Health Ministry as basic health services [ 3 ]. With funds being distributed so unevenly between the health providers, biomedical practitioners may have more access to health systems financing in addition to their general advantage of authority in clinical decision-making [ 3 ]. In this sense, though the overall cost of delivery for traditional medicines may be lower than the price of modern medicine, lack of sufficient funding and coverage to enable access may limit the use of traditional medicine in communities where it is desired. Further, there is also the need to better integrate traditional medicine and modern medicine in order to address broader public health and patient safety concerns that may arise from their uncoordinated use - such as the problems of abuse/overdose, toxicity or poison risk, potential for adverse events, medication interaction, overlap of active ingredient and need for appropriate dosaging - that have not been fully explored for potential benefit.
Efforts to foster therapeutic cooperation
In spite of these barriers, efforts to foster therapeutic cooperation and collaboration between health care providers continues through inter-cultural training, integrated participation in therapeutic encounters, third party links and increasing the number of Miskitu health care providers with an education in biomedicine. As an example, the local university URACCAN (Universidad de las Regiones Autónomas de la Costa Caribe de Nicaragua) hosts the Institute of Traditional Medicine and Community Development (IMTRADEC) serving as a link between the national health policy plan, traditional healers and the Health Ministry by organizing educational workshops and multidisciplinary health brigades [ 3 ]. These workshops focus on inter-cultural exchange with courses on traditional medicine and discussions on health policies. Those working for IMTRADEC also facilitate opportunities for biomedical practitioners and traditional healers to work directly together in the provisioning of health care and sharing knowledge for the benefit of their shared patients.
Working more closely with local communities, Acción Médica Cristiana (AMC), a Nicaraguan ecumenical non-governmental health and development agency is attempting to effectively address social determinants of health directly with community members through a method of Participatory Action Research (PAR). This process requires community members to prioritize their own needs for addressing the determinant of health problems such as disease outbreak, food security, safety, and health impacts of natural disasters in order to effectively create a community health system based on the cultural values of the community [ 16 ]. In this collaborative approach, AMC workers learn more about traditional medicine practices and the cultural views of the community to successfully work in therapeutic cooperation with empowered community members [ 16 ]. Hence, efforts by the AMC represent an example of successful community engagement that results in a community based approach to addressing the social determinants of health and a more collaborative integration of traditional medicine and biomedicine health services delivery.
At the international level, the WHO Traditional Medicine Strategy 2014–2023 outlines strategic objectives for Member States to further the integration of traditional medicine into national health systems and to protect consumers of care through the regulation of products, practices and practitioners. Strategic Objective 4.2.1 specifically addresses the need for creating a regulatory model to ensure the safety and effectiveness of products and services. With a goal to support diverse Member States in creating unique regulatory frameworks to “meet the health needs and choices of their people”, [ 17 ] WHO encourages collaborative partnerships between regional and local stakeholders in addition to setting international standards to guide national policy [ 17 ].
In summary, our review indicates that although Nicaragua has embarked on a health policy strategy that includes core principles of the UNDRIP with the intention to recognize the fundamental right to health for indigenous communities such as the Miskitu, full implementation of the UNDRIP and the ability to ensure effective therapeutic cooperation between indigenous traditional healers and western biomedical health care providers remains challenging for a variety of different reasons. As of 2009, IMTRADEC appeared to be the only organization devoted to the implementation of the national and regional plans to support the Miskitu indigenous peoples in securing their right to their traditional medicines and fostering the integration of health services. This may have been influenced by a continuing dominance of western biomedicine over traditional medicine in Miskitu health care practice settings and health systems financing. Lack of policy implementation and prioritization is occurring despite the fact that Nicaragua had taken significant steps to translate the general principles of UNDRIP into national and regional health policy, though more progressive constitutional amendments supporting equality of all health care providers would likely be helpful. In response, more robust efforts to fully support integration of health care practices and establishment of an adequately funded inter-cultural training program for all health care providers and healers must continually be implemented to create a blended health care service system and cross cultural therapeutic cooperation. Further, international development assistance within the health sector needs to recognize the importance of supporting therapeutic cooperation and community cosmovision as an integral part of implementing international indigenous health rights that can also lead to better health care access and outcomes. In this sense, the future of Nicaragua’s national indigenous health policies is critical to the current discourse of indigenous global health governance, policy, and international human rights law requiring further study, advocacy and support in order to ensure the realization of internationally agreed upon principles respecting traditional medicine and the right of indigenous peoples to the highest level of mental and physical health.
Data availability
We reviewed publicly available data that is available per the references included in this study.
Abbreviations
Acción Médica Cristiana
United Nations Economic and Social Council
International Labour Organization
Institute of Traditional Medicine and Community Development
Community and Family Health Model
Non-Government Organizations
Pan American Health Organization
Participatory Action Research
North Atlantic Autonomous Region
United Nations Declaration on the Rights of Indigenous Peoples
Universidad de las Regiones Autónomas de la Costa Caribe de Nicaragua
World Health Organization
Internationational Work Group for Indigenous Affairs (IWGIA). The Indigenous World 2014. Edited by Mikkelsen C. New Jersey: Transaction Publishers; 2014:93–100. [ http://www.iwgia.org/iwgia_files_publications_files/0671_I2014eb.pdf ].
United Nations General Assembly. United Nations Declaration on the Rights of Indigenous Peoples: resolution / adopted by the General Assembly, 2 October 2007. [ http://www.un.org/esa/socdev/unpfii/documents/DRIPS_en.pdf ].
Wedel J. Bridging the Gap between western and indigenous medicine in eastern Nicaragua. Anthropological Notebooks. 2009;15:49–64.
Gobierno do Nicaragua: Censo 2005 VIII Censo do Poblaciòn y IV de Vivienda. 2006:41[ http://www.inide.gob.ni/censos2005/resumencensal/resumen2.pdf ].
Campbell Bush SC. The intercultural health model of the North Autonomous Atlantic Region of Nicaragua: A model based on the rights and cosmovision of Afrodescendants, Indigenous and Mestizos people. A comparative study to enhance health with identity. Master's thesis. Oslo University College, Social Science Department; 2011:8–46.
International Labour Organization (ILO). Indigenous and Tribal Peoples Convention,1989:C169 art 25. [ http://www.ilo.org/dyn/normlex/en/f?p=NORMLEXPUB:12100:0::NO::P12100_INSTRUMENT_ID:312314 ].
Pan American Health Organization (PAHO). Health of the Indigenous Peoples Initiative-Strategic Directions and Plan of Action 2003–2007. Washington, DC: PAHO; 2003. [ http://www1.paho.org/hq/dmdocuments/2009/50-Eng%20Plan2003-2007.pdf ].
World Health Organization (WHO). World Health Organization Constitution. Geneva: World Health Organization; 2006:Preamble.
United Nations. Charter of the United Nations and Statute of the International Court of Justice. New York: United Nations, Office of Public Information; 1945: art 55.
World Health Organization (WHO). Bulletin of the World Health Organization. Regulatory Situation of Herbal Medicines- A Worldwide View. Geneva: World Health Organization;1998:8–9. [ http://apps.who.int/medicinedocs/en/d/Jwhozip57e/ ].
Nicaragua’s Constitution of 1987 with Amendments through 2005 [ https://www.constituteproject.org/constitution/Nicaragua_2005.pdf ].
Barten F. Quality of Care in Nicaragua. Exploring experiences, challenges and opportunities. Report commissioned by the Policy and Operations Evaluation Department (IOB) of the Ministry of Foreign Affairs. Netherlands; 2009:1–28. [ https://www.government.nl/documents/reports/2010/09/01/iob-quality-of-care-in-nicaragua-exploringexperiences-challenges-and-opportunities ].
Pan American Health Organization (PAHO): Nicaragua. In Health in the Americas. 2012 Edition, Country Volume. Pan American Health Organization; 2012:477–488. [ http://www.paho.org/saludenlasamericas/index.php?option=com_docman&task=doc_view&gid=140&Itemid= ].
Gobierno de Reconciliación y Unidad Nacional Unida Nicaragua Triunfa: Reglamento de La Ley No. 774. 2014.[ http://legislacion.asamblea.gob.ni/normaweb.nsf/b92aaea87dac762406257265005d21f7/dd7cde1b9616253a06257cf4004ca2eb?OpenDocument ].
Sequeira M, Espinoza H, Amador JJ, Domingo G, Quintanilla M, de los Santos T. The Nicaraguan Health System. Seattle, Washington: Program for Appropriate Technology in Health (PATH); 2011:1–33. [ http://www.path.org/publications/files/TSnicaragua-health-system-rpt.pdf ].
Forbes B, Gutiérrez G. Chapter 6 Nicaragua II. In Building Partnerships in the Americas: A Guide for Global Health Workers. Edited by Krasnoff MJ. Hanover, New Hampshire: Dartmouth College Press; 2013:152–185.
World Health Organization (WHO). WHO Traditional Medicine Strategy. Geneva: World Health Organization; 2013:44-52.[ http://www.who.int/medicines/publications/traditional/trm_strategy14_23/en/ ].
Download references
Acknowledgments
This research was supported by the Joint Masters Program in Health Policy and Law Capstone Student Scholarship and authors greatly acknowledge this support.
Author information
Authors and affiliations.
Center for Health Policy and Leadership, Bastyr University, 14500 Juanita Drive NE, Kenmore, WA, 98028, USA
Heather Carrie
University of California, San Diego – California Western School of Law, San Diego, USA
Department of Anesthesiology, University of California, San Diego School of Medicine, San Diego, USA
Tim K. Mackey
Division of Global Public Health, Department of Medicine, University of California, San Diego School of Medicine, San Diego, USA
Global Health Policy Institute, San Diego, California, USAᅟ
University of California, San Diego – Extension, San Diego, USA
Sloane N. Laird
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Heather Carrie .
Additional information
Competing interests.
All authors report no conflicts of interest associated with this manuscript.
Authors’ contributions
We note that with respect to author contributions, Heather Carrie (HC), Tim K Mackey (TM), and Sloane Laird (SL) jointly conceived, drafted, edited and finalized this manuscript. All authors have reviewed and approved its content. All authors have read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Carrie, H., Mackey, T.K. & Laird, S. Integrating traditional indigenous medicine and western biomedicine into health systems: a review of Nicaraguan health policies and miskitu health services. Int J Equity Health 14 , 129 (2015). https://doi.org/10.1186/s12939-015-0260-1
Download citation
Received : 02 June 2015
Accepted : 27 October 2015
Published : 14 December 2015
DOI : https://doi.org/10.1186/s12939-015-0260-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Indigenous health
- Traditional medicine
- Health and human rights
- Miskitu people
- Global health governance
- Nicaragua health policy
International Journal for Equity in Health
ISSN: 1475-9276
- General enquiries: [email protected]
- Open access
- Published: 24 March 2022

Ethnomedicinal study of medicinal plants used by Mizo tribes in Champhai district of Mizoram, India
- T. B. C. Laldingliani 1 ,
- Nurpen Meitei Thangjam 1 ,
- R. Zomuanawma 2 ,
- Laldingngheti Bawitlung 1 ,
- Anirban Pal 3 &
- Awadhesh Kumar ORCID: orcid.org/0000-0003-4751-1142 1
Journal of Ethnobiology and Ethnomedicine volume 18 , Article number: 22 ( 2022 ) Cite this article
10k Accesses
10 Citations
8 Altmetric
Metrics details
Medicinal plants have been used countless times for curing diseases mainly in developing countries. They are easily available with little to no side effects when compared to modern medicine. This manuscript encompasses information on ethnomedicinal plants in Champhai district, located in the North East Region (NER) of India. The region lies within Indo-Burma biodiversity hotspot. This study will be the first quantitative report on the ethnomedicinal plants used by the local tribes of this region. Knowledge of medicinal plants is mostly acquired by word of mouth, and the knowledge is dying among the local youths with the prevalence of modern medicine. Hence, there is urgency in deciphering and recording such information.
Information was gathered through interviews with 200 informants across 15 villages of the Champhai district. From the data obtained, we evaluate indices such as used report (UR), frequency of citation (FC), informant consensus factor ( F ic ), cultural values (CVs) and relative importance (RI) for all the plant species. Secondary data were obtained from scientific databases such as Pubmed, Sci Finder and Science Direct. The scientific name of the plants was matched and arranged in consultation with the working list of all plant species ( http://www.theplantlist.org ).
Totally, 93 plant species from 53 families and 85 genera were recorded. The most common families are Euphorbiaceae and Asteraceae with six and five species representatives, respectively. Leaves were the most frequently used part of a plant and were usually used in the form of decoction. Curcuma longa has the most cultural value (27.28 CVs) with the highest used report (136 FC), and the highest RI value was Phyllanthus emblica . The main illness categories as per Frequency of citation were muscle/bone problem (0.962 F ic ), gastro-intestinal disease (0.956 F ic ) and skin care (0.953 F ic ).
The people of Mizoram living in the Champhai district have an immense knowledge of ethnomedicinal plants. There were no side effects recorded for consuming ethnomedicinal plants. We observed that there is a scope of scientific validation of 10 plant species for their pharmacological activity and 13 species for the phytochemical characterisation or isolation of the phytochemicals. This might pave the path for developing a scientifically validated botanical or lead to semisyntheic derivatives intended for modern medicine.
Plants have been known to be a major source of diverse chemical compounds possessing both medicinal properties and commercial value. There have been several reports on medicinal plants as a source for drug discovery. However, new diseases will likely continue to emerge along with drug-resistant pathogens. This dynamic nature of pathogens has constantly challenged researchers to look for alternatives. The past few decades have witnessed the surge in ethnomedicinal plant research [ 1 ], one of the reasons being that the natural products have played an important role in the development of drugs, contributing more than 50% of clinical drugs in the pharmaceutical industry [ 2 ]. Further, the rapid growth in human population has raised the demand which in turn has increased the quest for novel plant resources, triggering a threat to natural resources [ 3 ].
Traditional knowledge and practices of herbal remedies have been passed on to new generations over the centuries and will continue to do so, with some variations taking place every generation. Plants have been the essential source for therapeutic regimes since ages, and traditional practices are proved to have little known side effects besides their low cost and easy availability. India has been well known worldwide for its indigenous traditional pieces of knowledge and practices from ancient times, through different systems of medicine such as Ayurveda, Siddha and Unani [ 4 ]. Although more than 427 tribal communities are having vast diversity of ancient traditions, still there has been criticism of ethnomedicines due to regional variation, political and socio-economic challenges [ 5 ]. Reports are stating that several plants have been increasingly utilised by the indigenous people of India [ 1 ]. Generally, in India, it was estimated that 6,000 species are used in traditional and herbal medicine which represent about 75% of the needs of the third world, and meanwhile, 3,000 plants were officially acknowledged due to their medicinal values [ 6 ].
The healthcare system of India witnesses a wide variation encompassing urban and rural populations which rely on both modern and traditional systems of medicine. The recently implemented Ayushman Bharat Pradhan Mantri Jan Arogya Yojana from the Commonwealth Fund enables cashless secondary and tertiary care at private facilities [ 7 ]. Besides, health insurance schemes also exist for institutions and factories. Catering to the huge population has its limitations, and thus, many of the ailments are treated either by traditional healers or through traditional knowledge and practices, especially in remote areas. One such state in the North-Eastern part of India is Mizoram.
Although some researchers [ 8 , 9 , 10 , 11 , 12 , 13 ] have documented and identified several ethnomedicinal plants of Mizoram mentioning their mode of preparation, usage, distribution and habitat, they mostly reported from the core areas of the cities. Their studies highlighted the qualitative data. However, there are no in-depth ethnobotanical studies recorded in Champhai district. Therefore, the present study aims to carry out a quantitative study using different cultural importance indices to assess the most valued plants and document the ethnomedicinal practices involving medicinal plants of the Champhai district of Mizoram, India. Their practical knowledge has been established based on more than a century of credence and observation.
Description of the study area
Mizoram lies within the Indo-Burma biodiversity hotspot region and shares two international borders with Bangladesh in the west and Myanmar in the east. According to Champion and Seth (1968), Mizoram forests are classified into Tropical semi-evergreen forests, tropical wet evergreen forests and mountain sub-tropical pine forests [ 14 ]. The study area, i.e. the Champhai district, is classified as a rural area where healthcare facilities are relatively poor which drives the people to rely on traditional medicines. The traditional healers using medicinal plant-based formulations for various ailments indicate that traditional medicines are still one of the mainstays in their contemporary health care. It is felt that prospection and research on the medicinal plants that play such an important role in the health care of Mizo tribes need a more intensified effort.
Champhai is one of the 8 districts in Mizoram, amidst the North-East Region of India. It is located in the eastern part of Mizoram, internationally bordered by Myanmar and therefore becoming the main gate of trading for India and Myanmar. It lies between 23.456° N latitude and 93.328°E longitude. The average annual rainfall is approximately 1814 mm, and the temperature remains around 18.6 °C which is slightly colder than the rest of the state during winter. The total land area is 3185.83 sq kilometres at an elevation around 1678 m above sea level, population density is 10 per sq kilometres (32,734). According to an official Census (2011), Champhai reported a population of 1,26,000, of which male and female were 62,357 and 63,388, respectively [ 15 ]. The study area was divided into 15 village council areas (Vengthlang, Vengthlang North, Venglai, Vengsang, Electric veng, Kanan, Kahrawt, Bethel, New Champhai, Zotlang, Hmunhmeltha, Tualcheng, Ngopa, Khawzawl and East Lungdar) for extensive data collection (Fig. 1 ). The majority of people living in this area are Mizo tribe and use the Mizo dialect in common.
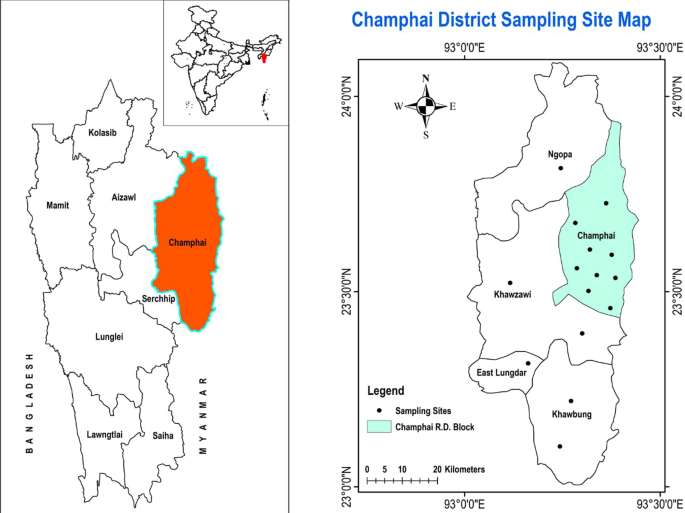
Location of the present study area: Champhai district, Mizoram, India
Investigative method
In the field study, formal questionnaires were distributed to each participant while having face to face interviews at their residence. At least 16 people were interviewed in each village council area. Only those people who have knowledge in the art of preparing medicines either for their families or their neighbourhood were considered for the interaction. The interactions primarily focussed on their experience, type of dosage form, duration of usage, any adverse effects observed and the source of their knowledge about the plant and their parts used. This information was then correlated with the scientific data curated from related databases (Pubmed, SciFinder and Science Direct). In most of the cases, the voucher specimens were deposited (Herbarium, Mizoram University, Aizawl, Mizoram, India) for their authentication and archiving.
Characteristics of demographic data
This demonstrated the socio-economic information of the informant including qualities like age, sex, education level and occupation. Using random sampling method, 200 people (12–14 individuals from each village) in the ages group of 18–71 years were interviewed, of which 112 and 82 were males and females, respectively. Respondents belonged to various professions while some were students. Most of the informants do not engage in full-time ethnomedicinal practice or as a profession. The feature of demographical characteristics obtained in the study is tabulated below (Table 1 ).
Quantitative analysis
Frequency of citation
Frequency of citation was used to further examine the primary data by finding the sum of total citations/usage reports for a particular species. The usage report is the quotation of one plant by an informant [ 16 ].
Use value or UV is used to express the correlative importance of each particular plant species locally known and was calculated by the following equation [ 17 ].
where ‘ U i ’ represents the number of citations of each species by the informants and ‘ n ’ represents the total number of informants in the study area. The larger the number of citations, the greater is the use-value.
Informant consensus factor
F ic or ICF is used to represent the consistency of the information among the informants, indicating whether there were shared knowledge and concurrence in the use of plants for treating the ailment category among the plant’s users in the study area. It was calculated by the following equation [ 18 ].
where ‘ N ur ’ refers to the number of users reports in each illness category and ‘ N t ’ refers to the number of plant species used for a particular illness category by all the informants.
Further, F ic value with 1 or either close to 1 indicates that a large number of informants had agreed on using few plants for curing an illness category while low F ic value signified that there was an argument on using medicinal plants to treat illness amidst the category.
Relative importance
When calculating RI, both the informants who mentioned the useful plant species and their various kinds of uses are considered. So, it was calculated by the following equation [ 19 ].
where ‘NUC’ refers to the number of illnesses use category of each species divided by the total number of most use categories among the species and ‘NT’ refers to the number of illness types of uses of each species divided by the total number of most types of uses among the species.
Cultural values
In this index, the use category is taken into account and it was calculated by using the following equation [ 20 ].
where ‘UCs’ is the number of the used reports for each species divided by the total number of use categories of that species. ‘ICs’ is the number of informants who mention each plant as effective divided by the total number of informants, and ∑IUCs is the number of informants who report the use of each species divided by the total number of informants.
Demographic characteristics
All the 200 respondents were randomly selected from 15 village council areas interviewing at least 16 persons in each area with no equal separation of male–female ratio. Amongst them, the elderly in their seventies and above occupied 6.5% only, while people between 31 and 50 years old occupied 34.5%. The average age among the informants was 54 years. Mizoram is the second most literate state in the country (2011 census), and all the informants were literate having at least primary school level education. Out of the total informants, 32.5% were engaged in government jobs like teachers, officers, while 35% were self-employed like farmers, carpenters, skilled workers, small businesses and the rest 32.5% of the informants were unemployed including students and housewives (Table 1 ).
Taxonomy identification
In the present study, 93 medicinal plant species belonging to 53 families and 85 genera have been reported for treating various kinds of ailments. The most prominent families were Euphorbiaceae with 6 plant species followed by Asteraceae with 5 plant species and 4 species each among Cucurbitaceae and Zingiberaceae. Liliaceae, Fabaceae, Verbenaceae, Solanaceae, Rutaceae, Anacardiaceae are with 3 species each while Orchidaceae, Combrethaceae Theaceae, Arecaceae, Apocynaceae, Musaceae, Rubiaceae, Scrophulariaceae, Lamiaceace, Mimosaceae, Smilacaceae are with 2 species each and other 34 families with one species each as shown in Table 2 . The high usage report of this large family like Euphorbiaceae (6 species), Asteraceae (5 species) and Zingiberaceae (4 species) occupied 10.8%, 9.2% and 8.35% of the total used report, respectively, indicating that most people in the study area are inclined to use plants that are easily available and abundant around them (Table 2 ).
Frequency of usage of parts of plants
The most commonly used medicinal plants fell under herbs (35.5%) followed by trees (33.3%), shurbs (18.3%) and creepers (12.9%) as shown in (Fig. 2 ). Among the parts, leaves, fruits and barks were mainly utilised by the informants (Fig. 3 ). A detailed analysis concluded that leaves (47%) followed by fruits (14%), barks (11%), seeds (10%), rhizomes (6%), stems (4%), young shoot (2%), oil (1%) and in some cases the whole plant (3%) were used for ethnomedicinal purposes.
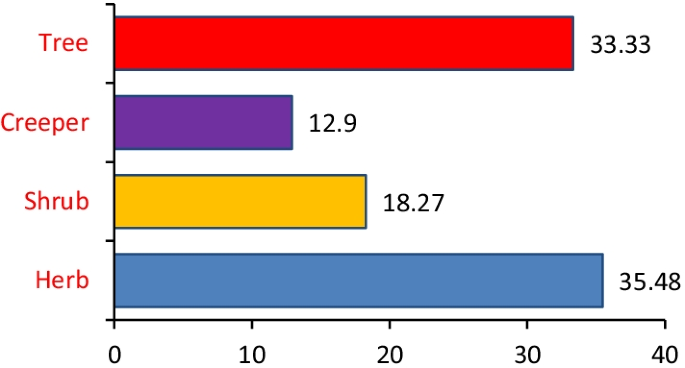
Percentage of plants habit

Percentage of parts used
Mode of preparation and administration
The mode of formulation preparation or administration was observed to be in the form of decoction (44.2%) followed by paste (23%), raw (19.5%), juice (9.73%), powder (1.77%) and others like maceration and oil (1.77%) (Fig. 4 .).
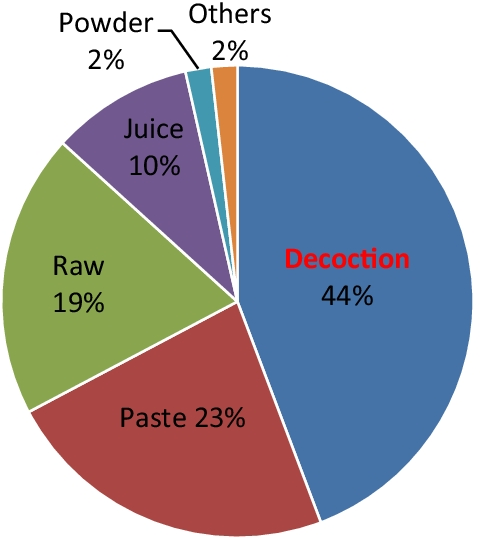
Distribution of formulation usage
Usage analysis based on the treatment of ailments
The total number of user reports documented in this study was 2717, in which all different illnesses were categorised into 16 groups using International Classification of Primary Care (ICPC) with a slight modification. Among the illness category, the gastro-intestinal disease has the highest usage report (940) followed by skincare (259) cardiovascular (222), kidney disease (196), hyperglycaemia (175), ENT (159), genito-urinary disease (139) and so on as shown in Table 3 .
Data analysis
Among the total number of user reports (UR) cited, Curcuma longa L. (136 FC), Flueggea virosa (Roxb. ex Willd.) Royle (126 FC), Psidium guajava L. (98 FC), Chromolaena odorata (L.) R.M. King & H. Rob. (87 FC), Mikania micrantha Kunth. (82 FC), Citrus limon (L.) Osbeck (68 FC), Carica papaya L. (53 FC), Ananas comosus (L.) Merr. (49 FC), Sarcococca pruniformis Lindl. (49 FC), Phyllanthus emblica L. (48 FC), Rhus chinensis Mill. (45 FC), Clerodendrum glandulosum Lindl. (44 FC), Senecio scandens Buch- Ham. ex D. Don (43 FC) were those species having the highest FC (Table 4 ).
Plant use value
From the UV value evaluation, Curcuma longa L. (0.68), Flueggea virosa (Roxb. ex Willd.) Royle (0.63), Psidium guajava L. (0.49), Chromolaena odorata (L.) R.M. King & H. Rob. (0.43), Mikania micrantha Kunth. (0.41), Citrus limon (L.) Osbeck (0.34), Carica papaya L. (0.26), Ananas comosus (L.) Merr. (0.24), Sarcococca pruniformis Lindl. (0.24), Phyllanthus emblica L. (0.24), Clerodendrum glandulosum Lindl. (0.22), Rhus chinensis Mill. (0.22), Senecio scandens Buch- Ham. ex D. Don (0.21) were reported to have the highest use value (UV).
We calculated the informant consensus factor by categorising the reported illness into 16 ailment groups along with the number of users report and taxa (Table 5 ). In our study, F ic values ranged from 0.866 to 0.962 which were all close to 1.
Relative importance and cultural value
Results of top-ranking species in terms of both indices of relative importance and cultural value are given in Table 6 . This study elucidates the highest cultural valued species and relative importance species utilised by the inhabitants of the study area. In general, the evaluated values were quite high in case of CVs and an average value of RI (0.607 ± 0.38) clarified that the versatile species, i.e. Phyllanthus emblica (RI = 2) was 3.3 times more relevant than the rest of the listed species.
Correlation and validation studies
An attempt was made to compare the use of all the medicinal plants reported by the informants with the previous papers published for their biological activity or ethnomedicines (Table 4 ). According to the studies conducted by Cakilcioglu et al., 2011, it was stated that if a medicinal plant has been reported for similar use in other parts of the world, its pharmacological effect could be more easily known [ 209 ].
The use of crude juice of Allium cepa L. showed a significantly higher hair growth rate than tap water when applied twice a day for two months which corroborated the present report of hair regrowth [ 22 ]. Metallothionein, an antioxidant protein present in Aloe vera (L.) gel, has been reported to have a protective effect against UV and gamma radiation damage to the skin. It scavenges free radicals by preventing the suppression of glutathione peroxidase and superoxide dismutase in the skin [ 30 ]. So, this validated the used of A. vera for skin care and burning by the Mizo tribes. In the present study, Betula alnoides Buch- Ham. ex D. Don has been used as toothpaste for whitening teeth while it was proved that 80% methanolic bark extract had the potential α-glucosidase inhibitory effect that prevent the (98.4%) at 40 µg/mL concentration [ 2 ]. Cajanus cajan (L.) Millsp is used effectively in Champhai district to treat jaundice and intestinal worms. To certify this, the methanolic extracts showed hepatoprotective activity in Swiss albino mice by inducing carbon tetrachloride (CCl 4 ) that cause liver damage. It lowers the serum levels of glutamate pyruvate transaminase (SGPT), or alanine aminotransferase (ALT) aspartate aminotransferase (AST) or serum glutamate oxaloacetate transaminase (SGOT) significantly [ 58 ].
When the aqueous extracts of Carica papaya L. and Ananas comosus L. were given to Spraque Dawley rats orally at doses of 5 and 10 mg/kg, both possessed mild to strong diuretic activity. Careful measure should be taken when using these plants as increase in the level of urinary K + , serum BUN and creatinine were mentioned [ 71 ]. This validated the used of C. papaya and A. comosus in kidney disease and urinary infection. The contemporary reports showed that Drymaria cordata (L.) was used as an instant pain killer for rheumatism; meanwhile, the scientific study also demonstrated that the aqueous whole plant extract exhibited analgesic and antipyretic properties at doses of 100, 200, and 400 mg/kg p.o mediated through peripheral and central mechanisms [ 210 ]. The latex water-soluble fraction of Euphorbia royleana Boiss. showed dose-dependent anti-arthritic and anti-inflammatory effects in rats and mice administered through gavage at doses of 50–200 mg/kg having more than 1500 mg/kg oral LD 50 in both [ 135 ]. Dose-dependent and significant decline in the number of abdominal constrictions induced by intraperitoneal administration of acetic acid was observed in methanol extract of Lablab purpureus (L.) Sweet. at a dose of 200 mg and 400 mg exhibited far better analgesic activity than 200 mg aspirin per kg of body weight [ 211 ].
Colocasia esculenta (L.) Schott and Elaeagnus caudata Schltdl. ex Momiy. were declared to use to discharge placenta after birth and to treat vaginal discharge (Lochia) for women in present study. Besides this record, in Cachar hills district of Assam, India, 5 ml of Elaeagnus caudata fresh root extract diluted in 10 ml of fresh water was also administered orally once a week to prevent miscarriage during pregnancy although there is no scientific study to backup this claim [ 118 ]. Apart from present report in Jamaica, Mikania micrantha Kunth. was most popularly used too for wound healing and its extract showed anti-inflammatory and antimicrobial activity against common pathogens, namely Escherichia coli , Staphylococcus aureus and Streptococcus sp. [ 212 ]. The decoction of Psidium guajava leaf was effectively used for diarrhoea which already proved to have antidiarrhoeal and protein conservative effects in diarrhoeal rats at a dose of 50 and 100 mg/kg of body weight. It increased the kidney weight and concentration of sodium, potassium and chloride significantly [ 213 ]. In the animal study of anti-urolithialic activity of Solanum nigrum , the fruit hydroalcoholic extract elicited potent activity against calcium oxalate urolithiasis effected by ethylene glycol through tumour necrosis factor adiponectin stimulation and alpha inhibition, also maintained the balance between stone promoter and inhibitor such as calcium and magnesium, respectively [ 214 ]. Thus, this authenticated the used of S. nigrum for removing kidney stone by the Mizo tribes in India.
Anoectochilus brevilabris Lindl. , Begonia inflata C.B. Clark , Dysoxylum excelsum Blume , Embelia vestita Roxb , Ensete glaucum (Roxb.) Cheesman , Gomphogyne cissiformis Griff. , Helicia robusta (Roxb.) R. Br. ex Blume , Laurocerasus undulata (Buch- Ham. ex D. Don) M. Roem. and Lobelia angulata G. Forst., Sarcococca pruniformis Lindl. were the plants that did not have biological activity reported previously which means that there is no scientific validation to support their application. Therefore, these plants were especially recommended in carrying out further investigation.
In addition, we compiled the secondary metabolite isolated chemical constituents done by several researchers for all the documented plants in the present study. Further investigation revealed that secondary metabolites from 13 plant species that have neither less nor none chemical compound isolated or identified— Anoectochilus brevilabris Lindl., Begonia inflata C. B. Clark., Castanopsis tribuloides (Sm.) A. DC., Combretum wallichii DC, Elaeagnus caudata Schltdl. ex Momiy., Embelia vestita Roxb., Ensete glaucum (Roxb.) Cheesman, Gomphogyne cissiformis Griff., Helicia robusta (Roxb.) R. Br. ex Blume, Laurocerasus undulata (Buch- Ham. ex D. Don) M. Roem., Lobelia angulata G. Forst., Pandanus odorifer (Forssk.) Kuntze, Sarcococca pruniformis Lindl. (Table 4 ) which will surely have great potent on ethnopharmacological study.
According to our findings, women practitioners (44%) were less than men (56%) which may be explained partly by the low sex ratio of the district; however, it can be assumed that women play lesser role in ethnomedicinal practices [ 215 , 216 ]. Among self-employed, farmers account for 58.5%, business persons 34.2% and carpenters were 21.4%. Farmers represented the highest percentage as they often lack access to modern healthcare facilities due to various issues ranging from financial, transportation and higher education. These issues forced them to rely on traditional medicines, cultivating and utilising them more regularly than others and somehow playing a big role in conservation too. Through this study, we observed that young informants like students around 18 to 25 years old have little expertise in practicing ethnomedicine and utilised them rarely as compared to elder informants. This may be due to change in mentality brought by education to rely only on prescribed medicines. Further, the results of the usage of plants dominated by the families were followed and confirmed the work done by some researchers stating that greater the plants grew in the study area the more it will be favourably and commonly used [ 217 ]. This supports the non-random plant selection hypothesis by Moerman 1979 [ 218 ]. Large families such as Asteraceae and Euphorbiaceae were most utilised while Orchidaceae and Poaceae were underutilised (low used report). However, due to non-random selection, small families like Cucurbitaceae and Zingiberaceae became over-represented (high used report). Thus, this implies that medicinal plants are not selected randomly by the inhabitants of Champhai district but are utilised based on their cultural and traditional knowledge [ 219 ]. In the present study, we laid out the only accepted botanical names by ‘The Plant List’ and their family, local name, habit, mode of preparation and ailments as illustrated in Table 4 .
Out of 93 species, 40 were cultivated species, whereas 53 were found in the wild. There were also 6 invasive alien species most notably Chromolaena odorata and Mikania micrantha which were commonly used to treat wounds topically. This is because wounds are the most common form of injury and these two species can be found almost everywhere [ 219 ]. The frequent use of herbaceous plants as medicines among the informants was due to their richness, abundance as well as their ability to grow easily in nature. Meanwhile, many parts of the world have been commonly using herbs as their medicinal ingredients due to their wide range of medicinal properties [ 220 ]. Leaves are the most utilised part of the plants due to their ease off collection as compared to their underground part. It is also the active site of photosynthesis accompanied by the production of metabolites [ 1 , 221 ]. In addition, leaves can be easily prepared and stored. It can be dried quickly under the sun in lesser amount of time than other parts like stem, bark and rhizome.
Similarly, it is also reported that decoction was the most common preparation method for herbal medicine while in some other tribal community [ 3 ], preparation of paste was the most common method applied [ 1 , 216 , 222 ]. For decoction the plant part was washed thoroughly and boiled with water administering the juice orally, whereas for paste the materials were crushed or rubbed within palms and applied topically. To make fine powder plant parts were shade dried and ground. Intake of oral administration and external topical formulation were the main mode of administration used in traditional herbal medicines which has also been previously reported [ 215 , 223 ]. Regarding the duration of consumption of herbal medicine, it depends on the illness whether it was short term or long term. For instance, short-term illness like cold, flu, stomach upset and skin problem, the consumption period did not last more than 1 week. On the contrary, the long-term illness like diabetes, kidney failure and heart diseases, the consumption period of plants (e.g., Flueggea virosa ) was much longer and last more than a month and so on.
The inhabitants of the study area extensively exploited medicinal plants to treat various illnesses and other needs which have not been previously reported. For instance, Anoetochilus brevilabris was used for pile treatments, Betula alnoides as toothpaste, Capsicum annuum to soothe and prevent scars from skin burns. Colocasia esculenta to expel lochia, Euphorbia milii as antidiarrhoea, Lablab purpureus as a pain reliever, Mussaenda macrophylla to stop internal bleeding and Parkia timoriana for treating baby umbilical cord. From this study it was clear that among the informants, stomach problems like ulcer, indigestion, diabetes, hypertension and kidney problems were common illness resulting in high user rate of consuming herbal medicines and similar record was reported by Mahwasane et al., [ 224 ]. Further, skin problem like dermatitis which was the second highest usage report was the highest ailment in most other tribal communities like Malda district in West Bengal reported by Saha et al. [ 225 ].
Generally, majority of the informants did not consume the medicines prescribed by the Doctor’s prescribed medicines along with their herbal medicine and claimed that many plants like Sarcococca pruniformis (tonsil), Psidium guajava (diarrhoea), Mikania micrantha (cut/wound), Flueggea virosa (chicken pox), Elaeagnus caudata (veginal discharge) were really effective and most importantly, none of them reported any adverse effect such as vomiting, headache, nausea, allergic reactions and/or skin rashes. Moreover, regarding the expenditure on buying medicines, 38% of the informants usually purchased their herbal medicines either in raw form ( Allium sativum, Allium cepa, Beta vulgaris ) or in processed form like juice ( Citrus limon, Phyllanthus emblica, Citrus aurantiifolia ), fruits ( Punica granatum, Phyllanthus emblica, Cucumis sativus ), and powder ( Curcuma longa ). Concerned about the source of their knowledge, all the informants reported that they have heard and learned some of their information from their elders, family and/or acquaintances. Besides these, 30% of the informants have also gathered additional information through social media and 10% through books, magazines and newspapers. This documentation clearly showed that knowledge and cultural practices of herbal medicines had been shared through the indigenous community through word of mouth.
Frequency of citation showed the sociocultural importance of medicinal plants to identify their therapeutic value [ 16 ]. The FC value is directly proportional to the use value (UV), the more FC value will increase the used value significantly.
Curcuma longa L. is one of the main commercially grown as seasoning plants in India. In Southeast Asia including India and China, turmeric powder has been used extensively for spice and colouring food material. It had a wide range of medicinal value that curcumin was the main bioactive chemical constituents [ 226 ]. C. longa was a mandatory spice that each and every household kept it that’s why the reason used report (UR) for medicinal value and cultural value (CVs) were high among the informants. In case of CVs, the high value was due to a greater number of the used report with lesser-used categories. The informants in present study reported that Flueggea virosa have a prominent effectiveness against diabetes (59 UR) and chickenpox (50 UR). The Mizo tribes extensively used F. virosa and Embelia vestita Roxb. plant to treat chickenpox and measles by bathing once a day with the decoction of leaf mixed with water. Apart from the degree of the used report, this index also attributed to the effectiveness of their use and importance.
Higher in the UV value indicates the more rate of agreeing and sharing their knowledges and practices of the medicinal plants among the informants [ 216 ]. Among the Terai forest of western Nepal Curcuma longa L. was also reported as the highest used value [ 227 ] similar to this result.
The plants with low UV value were Colocasia esculenta (L.) Schott, Eulophia nuda Lindl. and Ocimum americanum L., Maesa indica (Roxb.) A. DC, Morus macroura Miq, Tectona grandis L.f., Hibiscus sinensis Mill, Elaeis guineensis Jacq, Smilax perfoliata Lour with less than 0.05 UV as shown in Table 4 . Tectona grandis L.f. was also described with very low UV value by Ayyanar and Ignacimuthu as relevant to this result [ 1 ]. According to Chaudhary et al. 2006, the plants with low used value were in at risk of misrecollecting and passing on to the young generation which might be gradually disappearing [ 228 ]. On the other hand, the relevance of knowing the plant used value was for the convenience of pharmacological study and their used reliability [ 229 ].
However, Rajakumar and Shivanna had mentioned that the value of F ic depends on the accessibility of the taxa for the treatment of various diseases in the study area. Muscle/Bone problem with 81 UR have the highest F ic value of 0.962 followed by gastro-intestinal disease (GID) with 940 UR and skin care (SC) with 259 UR (Table 5 ). The lowest F ic value in the present study was the General Health (GH) category (Cold, fever, immunity boost) with 0.887 which was still more than the previous maximum F ic value report in Shimoga district, Karnataka, India i.e. 0.77 in Liver complaints [ 230 ]. Most RI value ( Phyllanthus emblica ) is considered to be versatile on its uses which would also increase the importance of the plant when it is used to treat more illnesses. The high RI values of some species may be attributed to their abundance and availability in the study area [ 19 ].
Overall, the quantitative analysis revealed that Curcuma longa was the most relevant species with the highest used value, frequency of citation and cultural value except in relative importance. This is due to the fact that the RI value is independent of the number of informants used report. On the conflict of these report, our study indicated that there was high consistency of the indigenous informant knowledge in the practices of ethnomedicines and utilised the same plants to treat it.
Conclusions
The present study concluded that the native people in the study area have their unique way of utilising medicinal plants to treat different kinds of ailments. We documented 93 valuable medicinal plants belonging to 55 families and 85 genera in which Euphorbiaceae and Asteraceae family were the most widely used in the area. This study supported the non-random selection of medicinal plants hypothesis. Among the plants part, leaves were the most commonly used. No new medicinal taxa were reported, but this study is a first quantitative report of ethnomedicine in this region and no informant had reported an adverse effect of herbal medicines. Their traditional pieces of knowledge had been passed on from their elders mostly through word of mouth. This study also revealed that younger generations between the ages of 18 and 30 have little to no knowledge of preparation of herbal medicines and their use as compared to the older age groups. This is mostly due to the availability of modern clinical drugs in the villages. Therefore, the traditional knowledge and practices of medicinal plants in the study area are somehow at risk of dying. This is why it is important to document the valuable knowledge as well as for conservation of the taxa.
The use of quantitative indices was essential in the field of ethnobotany to determine the most valuable plants along with their role played in a particular culture and to develop conservation initiatives. The plants which have high usage report and frequency of citation were known to possess numerous phytochemical compounds. The calculated informant consensus factor was extremely high, which means that the acquired data can be used as reference and reliable for ethnopharmacological study in the future. Even though the remedial value of many high cited plants has already been verified, there are still some plants that need to be validated. Hence, they are strongly recommended for further studies to develop alternative drugs.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
Used reports
Whole plants
Young shoot
Ayyanara M, Ignacimuthub S. Ethnobotanical survey of medicinal plants commonly used by Kani tribals in Tirunelveli hills of Western Ghats, India. J Ethnopharmacol. 2011;134:851–64. https://doi.org/10.1016/j.jep.2011.01.029 .
Article Google Scholar
Ghimire BK, Tamang JP, Yu CY, Jung SJ, Chung IM. Antioxidant, antimicrobial activity and inhibition of α-glucosidase activity by Betula alnoides Buch. bark extract and their relationship with polyphenolic compounds concentration. Immunopharmacol Immunotoxicol. 2012;34:824–31. https://doi.org/10.3109/08923973.2012.661739 .
Article PubMed Google Scholar
Simbo DJ. An ethnobotanical survey of medicinal plants in Babungo, Northwest Region, Cameroon. J Ethnobiol Ethnomed. 2010;6:8. https://doi.org/10.1186/1746-4269-6-8 .
Article PubMed PubMed Central Google Scholar
Fabricant DS, Farnsworth NR. The value of plants used in traditional medicine for drug discovery. Environ Health Perspect. 2001;109:69–75. https://doi.org/10.1289/ehp.01109s169 .
Article CAS PubMed PubMed Central Google Scholar
Kadhirvel K, Ramya S, Sudha TS, Ravi AV, Rajasekaran C, Selvi RV, Jayakumararaj R. Ethnomedicinal survey on plants used by tribals in Chitteri Hills. Environ We Int J Sci Tech. 2010;5:35–46.
Google Scholar
Rai PK, Lalramnghinglova H. Ethnomedicinal plant resources of Mizoram, India: Implication of traditional knowledge in health care system. Ethnobot Leafl. 2010;3:6.
Tikkanen R, Osborn R, Mossialos E, Djordjevic A, Wharton GA. International Health Care System Profiles, India. The Commonwealth Fund. 2020 https://www.commonwealthfund.org/international-health-policy-enter/countries/india. Accessed 21 June 2021.
Lalramnghinglova H, Jha LK. Ethnomedicine from Mizoram—North East India. Ethnobotany. 1997;9:105–11.
Lalnundanga, Sahoo UK, Jha LK. Ethnobotanical flora in the humid sub-tropical semi-evergreen forest of Mizoram. In: Proceedings national conference on healthcare and developments of herbal medicines, Raipur. 1997.
Sharma HK, Chhangte L, Dolui AK. Traditional medicinal plants in Mizoram, India. Fitoterapia. 2001;72(2):146–61. https://doi.org/10.1016/S0367-326X(00)00278-1 .
Article CAS PubMed Google Scholar
Lalramnghinglova H. Ethno-medicinal plants of mizoram. Bishen Singh Mahendra, Pal Singh, Dehradun, India; 2003.
Singh NP, Singh KP, Singh DK. Flora of Mizoram. Botanical Survey of India. Ministry of Environment and Forest. Government of India, Kolkata; 2002.
Sawmliana M. The Book of mizoram plants. Zakhuma P, Aizawl, Mizoram; 2003.
Champion GH, Seth SK. A revised survey of the forest types of India. Dehradun: Natraj Publishers; 1968.
Champhai district. Government of Mizoram, India. 2021. https://champhai.nic.in/about-district/ . Accessed 03 Jan 2021.
Khajuria AK, Manhas RK, Kumar H, Bisht NS. Ethnobotanical study of traditionally used medicinal plants of Pauri District of Uttarakhand, India. J Ethnopharmacol. 2021;276: 114204. https://doi.org/10.1016/j.jep.2021.114204 .
Gazzaneo LRS, Lucena RFP, Albuquerque UP. Knowledge and use of medicinal plants by local specialists in a region of Atlantic Forest in the state of Pernambuco. J Ethnobiol Ethnomed. 2005;1:9. https://doi.org/10.1186/1746-4269-1-9 .
Heinrich M, Ankli A, Frei B, Weimann C, Sticher O. Medicinal plants in Mexico: healers’ consensus and cultural importance. Soc Sci Med. 1998;47:1859–71. https://doi.org/10.1016/S0277-9536(98)00181-6 .
Albuquerque UP, Lucena RF, Monteiro JM, Florentino AT, Cecília de Fátima CB. Evaluating two quantitative ethnobotanical techniques. Ethnobot. Res. Appl. 2006;4:051–60. https://ethnobotanyjournal.org/index.php/era/article/view/101.
Sujarwo W, Caneva G. Using quantitative indices to evaluate the cultural importance of food and nutraceutical plants: comparative data from the Island of Bali (Indonesia). J Cult Herit. 2016;18:342–8. https://doi.org/10.1016/j.culher.2015.06.006 .
Kundan SB, Anupam S. Phytoconstituents and therapeutic potential of Allium cepa Linn—a review. Phcog Rev. 2009;3(5):170–80.
Sharquie KE, Al-Obaidi HK. Onion juice ( Allium cepa L.), a new topical treatment for alopecia areata. J Dermatol. 2002;29:343–6. https://doi.org/10.1111/j.1346-8138.2002.tb00277.x .
Teshika JD, Zakariyyah AM, Zaynab T, Zengin G, Rengasamy KR, Pandian SK, Fawzi MM. Traditional and modern uses of onion bulb ( Allium cepa L.): a systematic review. Crit Rev Food Sci Nutr. 2019;59(1):39–70. https://doi.org/10.1080/10408398.2018.1499074 .
Article CAS Google Scholar
Batiha GES, Beshbishy AM, Elewa Y, Taha A. Chemical constituents and pharmacological activities of garlic ( Allium sativum L.): a review. Nutrients. 2020;12:872. https://doi.org/10.3390/nu12030872 .
Miron T, Rabinkov A, Mirelman D, Wilchek M, Weiner L. The mode of action of allicin: its ready permeability through phospholipid membranes may contribute to its biological activity. Biochim Biophys Acta. 2000;1463:20–30. https://doi.org/10.1016/S0005-2736(99)00174-1 .
Harris JC, Cottrell SL, Plummer S, Lloyd D. Antimicrobial properties of Allium sativum (garlic). Appl Microbial Biotechnol. 2001;57:282–6. https://doi.org/10.1007/s002530100722 .
Ishtiaq M, Hanif W, Khan MA, Ashraf M, Butt AM. An ethnomedicinal survey and documentation of important medicinal folklore food phytonims of Flora of Samahni Valley, (Azad Kashmir) Pakistan. Pakistan J Biol Sci. 2007;10:2241–56. https://doi.org/10.3923/pjbs.2007.2241.2256 .
Singh VK, Singh DK. Pharmacological effects of garlic ( Allium sativum L.). Annu Rev Biomed Sci. 2008;10:6–26.
Arunkumar S, Muthuselvam M. Analysis of phytochemical constituents and antimicrobial activities of Aloe vera L. against clinical pathogens. World J Agric Sci. 2009;5:572–6.
CAS Google Scholar
Christaki E, Florou-Paneri PC. Aloe vera: a plant for many uses. J Food Agric Environ. 2010;8:245–9.
Sahu PK, Giri DD, Singh R, Pandey P, Gupta S, Shrivastava AK, Kumar A, Pandey KD. Therapeutic and medicinal uses of Aloe vera : a review. J Pharm Pharmacol. 2013;4:599–610. https://doi.org/10.4236/pp.2013.48086 .
Kalaria P, Gheewala P, Chakraborty M, Kamath J. A phytopharmacological review of Alstonia scholaris : a panoramic herbal medicine. Int J Res Ayurveda Pharm. 2012;3:367–71.
Arulmozhi S, Mazumder PM, Ashok P, Narayanan LS. Pharmacological activities of Alstonia scholaris Linn. (Apocynaceae)—a review. Pharmacogn Rev. 2007;1:163–70.
Baliga MS. Review of the phytochemical, pharmacological and toxicological properties of Alstonia scholaris Linn. R. Br (Saptaparna). Chin J Integr Med. 2012. https://doi.org/10.1007/s11655-011-0947-0 .
Huang XJ, Chen WH, Ji MH, Guo FY, Shu HM, Zheng CJ. Chemical constituents from leaves of Ananas comosus and their biological activities. Zhong Cao Yao. 2015;46:949–54. https://doi.org/10.7501/j.issn.0253-2670.2015.07.002 .
Pavan R, Jain S, Kumar A. Properties and therapeutic application of bromelain: a review. Biotechnol Res Int. 2012;6: 976203. https://doi.org/10.1155/2012/976203 .
Rathnavelu V, Alitheen NB, Sohila S, Kanagesan S, Ramesh R. Potential role of bromelain in clinical and therapeutic applications. Biomed Rep. 2016;3:283–8. https://doi.org/10.3892/br.2016.720 .
Lin TC, Tanaka T, Nonaka G, Nishioka I, Young TJ. Isolation and characterization of novel complex tannins (Flavano-ellagitannins). Anogeissinin and Anogeissusin-B, from Anogeissus acuminata (Roxb ex Dc) Guill et Perr var Lanccolata Wall ex Clarke. Chem Pharm Bull. 1991;39:1144–7. https://doi.org/10.1248/cpb.39.1144 .
Monali PM, Padhy R. Antibacterial activity of green silver nanoparticles synthesized from Anogeissus acuminata against multidrug resistant urinary tract infecting bacteria in vitro and host-toxicity testing. J Appl Biomed. 2018;16:120–5. https://doi.org/10.1016/j.jab.2017.11.003 .
Panda SK, Laxmipriya P, Pieter L, Maoxuan L, Johan N, Walter L. Antimicrobial anthelmintic, and antiviral activity of plants traditionally used for treating infectious disease in the Similipal Biosphere Reserve, Odisha, India. Front Pharmacol. 2017;8:658. https://doi.org/10.3389/fphar.2017.00658 .
Panda SS, Girgis AS, Prakash A, Khanna L, Khanna P, Shalaby EM, Fawzy NG, Jain SC. Protective effects of Aporosa octandra bark extract against d -galactose induced cognitive impairment and oxidative stress in mice. Heliyon. 2018. https://doi.org/10.1016/j.heliyon.2018.e00951 .
Sahu BP, Gouda P, Patnaik C. Aporosa octandra , a Less studied plant species with potential drug activities-I: identification of a new compound from aqueous ethanolic extract of its stem bark. Int J Adv Res Sci Eng Tech. 2016;3:2219–24.
Vabeiryureilai M, Lalrinzuali K, Rosangkima G, Jagetia GC. Qualitative phytochemical analysis and antioxidant activity of Aporosa octandra (Buch-Ham. ex D. Don) extracts. Int J Pharmacol Res. 2014;6:68–73.
Siddiqui BS, Ali ST, Rasheed M, Kardar MN. Chemical constituents of the flowers of Azadirachta indica . Helv Chim Acta. 2003;86:2787–96. https://doi.org/10.1002/hlca.200390229 .
Biswas K, Chattopadhyay I, Banerjee RK, Bandyopadhyay U. Biological activities and medicinal properties of neem ( Azadirachta indica ). Curr Sci. 2002;82:1336–45.
Doshi GM, Nalawade VV, Mukadam AS, Chaskar PK, Zine SP, Somani RR, Une HD. Structural elucidation of chemical constituents from Benincasa hispida seeds and Carissa congesta roots by gas chromatography: mass spectroscopy. Pharmacogn Res. 2015;7(3):282–93.
Al-Snafi AE. The pharmacological importance of Benincasa hispida . A review. Int J Pharm Sci Res. 2013;4:165–70.
Qadrie ZL, Hawisa NT, Khan MA, Samuel M, Anandan R. Antinociceptive and anti-pyretic activity of Benincasa hispida (Thunb.) cogn. in wistar albino rats. Pak J Pharm Sci. 2009;22:287–90.
PubMed Google Scholar
El-Hawary SS, Hammouda FM, Tawfik WA, Kassem HA, Abdelshafeek KA, El-Shamy SS. Investigation of some chemical constituents, cytotoxicity and antioxidant activities of Beta vulgaris var. altissima cultivated in Egypt. Rasayan J Chem. 2017;10:1391–401. https://doi.org/10.7324/RJC.2017.1041936 .
El-Beltagi HS, Mohamed HI, Megahed BHM, Gamal M, Safwat G. Evaluation of some chemical constituents, antioxidant, antibacterial and anticancer activities of Beta vulgaris L. root. Fresenius Environ Bull. 2018;27:6369–78.
Ninfali P, Angelino D. Nutritional and functional potential of Beta vulgaris cicla and rubra. Fitoterapia. 2013;89:188–99. https://doi.org/10.1016/j.fitote.2013.06.004 .
Dũng NX, Mõi LD, Leclercq PA. Constituents of the bark oil of Betula alnoides Ham ex. D. Don from Vietnam. J Essent Oil Res. 1995;7:565–6. https://doi.org/10.1080/10412905.1995.9698589 .
Thu NB, Trung TN, Ha DT, Khoi NM, Hung TV, Hien TT, Yim NH, Bae KH. Screening of Vietnamese medicinal plants for cytotoxic activity. Nat Prod Sci. 2010;16:43–9.
Yang DS, Yang YP, Yong-hong Y, Xiao-li L. Chemical constituents of Bischofia javanica . Nat Prod Res Dev. 2013;25:1056–9. https://doi.org/10.3969/j.issn.1001-6880.2013.08.009 .
Khan MR, Kihara M, Domoloso A. Anti-microbial activity of Bidens pilosa , Bischofia javanica, Elmerillia papuana and Sigesbekia orientalis . Fitoterapia. 2001;72:662–5. https://doi.org/10.1016/S0367-326X(01)00261-1 .
Lingadurai S, Roy S, Joseph RV, Nath LK. Antileukemic activity of the leaf extract of Bischofia javanica blume on human leukemic cell lines. Indian J Pharmacol. 2011;43:143–9.
Anadebe VC, Okafor NA, Ezeugo JO, Amanjide IJ, Ogide BC. GC-MS analysis of phytochemical compounds in Cajanus cajan leaf. J Chem Pharm Res. 2017;9:360–3.
Pal D, Mishra P, Sachan N, Ghosh AK. Biological activities and medicinal properties of Cajanus cajan (L) Millsp. J Adv Pharm Technol Res. 2011;2:207–14.
Tu Y, Sun L, Guo M, Chen W. The medicinal uses of Callicarpa L. in traditional Chinese medicine: an ethnopharmacological, phytochemical and pharmacological review. J Ethnopharmacol. 2013;146:465–81. https://doi.org/10.1016/j.jep.2012.12.051 .
Zhu HB, Li BM, Liu C, Chen RY. Chemical constituents of Camellia sinensis var. assamica. Zhongguo Zhong yao za. 2013;38:1386–9. https://doi.org/10.4268/cjcmm20130925 .
Sarangi AB. Medicinal and therapeutic potentialities of tea ( Camellia sinensis L.)—a review. Food Res Int. 2009;42:529–35. https://doi.org/10.1016/j.foodres.2009.01.007 .
Hamilton-Miller JM. Antimicrobial properties of tea ( Camellia sinensis L.) antimicrobe. Agents Chemother. 1995;39:2375–7.
Grutenherman F, Russo E. Cannabis and cannabinoids, pharmacology, toxicology and therapeutic potential. New York: The Howarth Integrative Healing Press; 2002.
Nuutinen T. Medicinal properties of terpenes found in Cannabis sativa and Humulus lupulus . Eur J Med Chem. 2018;157:198–228. https://doi.org/10.1016/j.ejmech.2018.07.076 .
Siddiqui BS, Aslam H, Ali ST, Khan S, Begum S. Chemical constituents of Centella asiatica . J Asian Nat Prod Res. 2007;9:407–14. https://doi.org/10.1080/10286020600782454 .
Kalshetty P, Aswar U, Bodhankar S, Sinnathambi A, Mohan V, Thakurdesai P. Antidepressant effects of standardized extract of Centella asiatica L. in olfactory bulbectomy model. Biomed Aging Pathol. 2012;2:48–53. https://doi.org/10.1016/j.biomag.2012.03.005 .
Punturee K, Wild CP, Kasinrerk W, Vinitketkumnuen U. Immunomodulatory activities of Centella asiatica and Rhinacanthus nasutus extracts. Asian Pac J Cancer Prev. 2005;6:396–400.
Marin A, Ferreres F, Tomás-Barberán FA, Gil MI. Characterization and quantitation of antioxidant constituents of sweet pepper ( Capsicum annuum L.). J Agric Food Chem. 2004;52:3861–9. https://doi.org/10.1021/jf0497915 .
Khan FA, Mahmood T, Ali M, Saeed A, Maalik A. Pharmacological importance of an ethnobotanical plant: Capsicum annuum L. Nat Prod Res. 2014;28:1267–74. https://doi.org/10.1080/14786419.2014.895723 .
Yogiraj V, Goyal PK, Chauhan CS, Goyal A, Vyas B. Carica papaya Linn: an overview. Int J Herbal Med. 2014;2:1–8.
Adam Y, Nasaruddin AA, Zuraini A, Arifah AK, Zakaria MOFZ, Somchit MN. Diuretic activity of roots from Carica papaya L. and Ananas comosus L. Int J Pharm Sci Rev Res. 2013;23:163–7.
Krishna KL, Paridhavi M, Patel KL. Review on nutritional, medicinal and pharmacological properties of Papaya ( Carica papaya Linn.). Nat Prod Radiance. 2008;7:364–73. http://nopr.niscair.res.in/handle/123456789/5695
Prakash D, Upadhyay G, Gupta C, Pushpangadan P, Singh KK. Antioxidant and free radical scavenging activities of some promising wild edible fruits. Int Food Res J. 2012;19:1109–16.
Ferreres F, Pereira DM, Valentão P, Andrade PB, Seabra RM, Sottomayor M. New Phenolic compounds and antioxidant potential of Catharanthus roseus . J Agric Food Chem. 2008;56:9967–74.
Aslam J, Khan SH, Siddiqui ZH, Fatima Z, Maqsood M, Bhat MA, Nasim SA, Ilah A, Ahmad IZ, Khan SA, Mujib A. Catharanthus roseus (L.) G. Don. An important drug: it’s applications and production. Pharmacie Globale. 2010;4:1–16.
Gajalakshmi S, Vijayalakshmi SD, Rajeswari V. Pharmacological activities of Catharanthus roseus : a perspective review. Int J Pharm Bio Sci. 2013;4:431–9.
Hassan HM, Eldesoky AM, Al-Rashdi A, Ahmed HM. Green corrosion electrochemistry: Cheilocostus speciosus extract (CSE) investigated electro-analytically as a potential green corrosion inhibitor for copper within acidic solution. Int J Emerg Trends Eng Develop. 2016;7:72–98.
Ayam VS, Gogoi P. Evaluation of antioxidant activity of the selected frequently used traditional wild medicinal plants from Lakhimpur, Assam (India). Pleione. 2018;12:187–92. https://doi.org/10.26679/Pleione.12.2.2018 .
Benelli G, Govindarajan M, Rajeswary M, Vaseeharan B, Alyahya SA, Alharbi NS, Kadaikunnan S, Khaled JM, Maggi F. Insecticidal activity of camphene, zerumbone and α-humulene from Cheilocostus speciosus rhizome essential oil against the Old-World bollworm Helicoverpa armigera . Ecotoxicol Environ Saf. 2018;148:781–6. https://doi.org/10.1016/j.ecoenv.2017.11.044 .
Owolabi MS, Ogundajo A, Yusuf KO, Lajide L, Villanueva HE, Tuten JA, Setzer WN. Chemical composition and bioactivity of the essential oil of Chromolaena odorata from Nigeria. Rec Nat Prod. 2010;4:72–8.
Taiwo OB, Olajide OA, Soyannwo OO, Makinde JM. Anti-inflammatory, antipyretic and antispasmodic properties of Chromolaena Odorata . Pharm Biol. 2000;38:367–70. https://doi.org/10.1076/phbi.38.5.367.5970 .
Vaisakh MN, Pandey A. The invasive weed with healing properties: a review on Chromolaena odorata . Int J Pharm Sci Res. 2012;3:80–3.
Abyaneh M, Shams-Ghahfarokhi M, Rezaee MB, Jaimand K, Alinezhad S, Saberi R, Yoshinari T. Chemical composition and antiaflatoxigenic activity of Carum carvi L., Thymus vulgaris and Citrus aurantifolia essential oils. Food Control. 2009;20:1018–24. https://doi.org/10.1016/j.foodcont.2008.12.007 .
Pathan RK, Gali PR, Pathan P, Gowtham T, Pasupuleti S. In vitro antimicrobial activity of Citrus aurantifolia and its phytochemical screening. Asian Pac J Trop Dis. 2012;2:328–31. https://doi.org/10.1016/S2222-1808(12)60176-5 .
Taur DJ, Kulkarni VB, Patil RY, Patil RN. Anthelmintic activity of Ocimum sanctum and Citrus aurantifolia oils. Pharmacologyonline. 2009;3:495–9.
Xu YR, Zhang KF, Xie QJ, Lin JX, Huan KX, Liao Y. Chemical constituents from young fruits of Citrus maxima cv. Shatian. Zhong Yao Cai. 2015;38:1879–81.
CAS PubMed Google Scholar
Abirami A, Nagarani G, Siddhuraju P. Antimicrobial activity of crude extract of Citrus hystrix and Citrus maxima . Int J Pharm Sci. 2013;4:1–5.
Shivananda A, Rao DM, Jayaveera KN. Analgesic and anti-inflammatory activities of Citrus maxima (J. Burm) Merr in animal models. Res J Pharm Biol Chem Sci. 2013;4:1800–10. http://rjpbcs.com/pdf/2013_4(2 )/
Kefford JF. The chemical constituents of citrus fruits. Adv Food Res. 1960;2016(9):285–372. https://doi.org/10.1016/S0065-2628(08)60278-5 .
Szczykutowicz MK, Szopa A, Ekiert H. Citrus limon (Lemon) phenomenon—a review of the chemistry, pharmacological properties, applications in the modern pharmaceutical, food, and cosmetics industries, and biotechnological studies. Plants. 2020;9:119. https://doi.org/10.3390/plants9010119 .
Jadeja RN, Thounaojam MC, Singh TB, Devkar RV, Ramachandran AV. Traditional uses, phytochemistry and pharmacology of Clerodendron glandulosum Coleb—a review. Asian Pac J Trop Med. 2012;5:1–6. https://doi.org/10.1016/S1995-7645(11)60236-8 .
Prajapati R, Kalariya M, Umbarkar R, Parmar S, Sheth N. Colocasia esculenta : a potent indigenous plant. Int J Nutr Pharmacol Neurol Dis. 2011;1:90–6. http://www.ijnpnd.com/text.asp?2011/1/2/90/84188
Agyare C, Boakye YD, Apenteng JA, Dapaah SO, Appiah T, Adow A. Antimicrobial and anti-inflammatory properties of Anchomanes difformis (Bl.) Engl. and Colocasia esculenta (L.) Schott. Biochem Pharmacol. 2016;5:1. https://doi.org/10.4172/2167-0501.1000201.
Kubde MS, Khadabadi SS, Farooqui IA, Deore SL. In-vitro anthelmintic activity of Colocasia esculenta . Der Pharma Lett. 2010;2:82–5.
Patil BR, Ageely HM. Antihepatotoxic activity of Colocasia esculenta leaf juice. Int J Adv Biotech Res. 2011;2:296–304.
Koné WM, Vargas M, Keiser J. Anthelmintic activity of medicinal plants used in Côte d’Ivoire for treating parasitic diseases. Parasitol Res. 2012;110:2351–62. https://doi.org/10.1007/s00436-011-2771-z .
Joshi RK. Study on essential oil composition of the roots of Crassocephalum crepidioides (Benth.) S. Moore. J Chil Chem Soc. 2014;59:2363–5. https://doi.org/10.4067/S0717-97072014000100025 .
Tomimori K, Nakama S, Kimura R, Tamaki K, Ishikawa C, Mori N. Antitumor activity and macrophage nitric oxide producing action of medicinal herb Crassocephalum crepidioides . BMC Complement Altern Med. 2012;12:1–11. https://doi.org/10.1186/1472-6882-12-78 .
Bahar E, Akter KM, Lee GH, Lee HY, Rashid HO, Choi MK, Bhattarai KR, Hossain MMM, Ara J, Mazumder K, Raihan O. β-Cell protection and antidiabetic activities of Crassocephalum crepidioides (Asteraceae) Benth. S. Moore extract against alloxan-induced oxidative stress via regulation of apoptosis and reactive oxygen species (ROS). BMC Complement Altern Med. 2017;17:179. https://doi.org/10.1186/s12906-017-1697-0 .
Rezig L, Chouaibi M, Msaada K, Hamdi H. Chemical composition and profile characterisation of pumpkin ( Cucurbita maxima ) seed oil. Ind Crops Prod. 2012;37:82–7. https://doi.org/10.1016/j.indcrop.2011.12.004 .
Md PM, Md TK. Overview on Cucurbita maxima seed. J Dent Med Sci. 2017;16:29–33. https://doi.org/10.9790/0853-1603132933 .
Borah A. Chemical composition, antioxidant, anti-inflammatory, anti-microbial and in-vitro cytotoxic efficacy of essential oil of Curcuma caesia Roxb. leaves: an endangered medicinal plant of North East India. Ind Crops Prod. 2019;129:448–54. https://doi.org/10.1016/j.indcrop.2018.12.035 .
Baghel SS, Baghel RS, Sharma K, Sikarwar I. Pharmacological activities of Curcuma caesia . Int J Green Pharm. 2013;7:1–5. https://doi.org/10.22377/ijgp.v7i1.287 .
Lateef EA. Bioactive chemical constituents of Curcuma longa L. rhizomes extract inhibit the growth of human hepatoma cell line (HepG2). Acta Pharm. 2016;66:387–98. https://doi.org/10.1515/acph-2016-0028 .
Krup V, Prakash LH, Harini A. Pharmacological activities of turmeric ( Curcuma longa Linn): a review. J Homeop Ayurv Med. 2013;2:133. https://doi.org/10.4172/2167-1206.1000133 .
Wu XY, Chao ZM, Wang C, Tan ZG, Sun W. Chemical constituents contained in fatty oil from seeds of Cucumis sativus . Zhongguo Zhong Yao Za Zhi. 2012;37:3252–5.
Saeedi R, Sultana A, Rahman K. Ethnomedicinal uses and pharmacological activities of different parts of Cucumis sativus Linn: an update. Int J Pharm Sci Res. 2020;11:1549–56. https://doi.org/10.13040/IJPSR.0975-8232.11,4,1549-56 .
Zhu SH, Zhang QJ, Chen Q, Zhou T, Yao RJ. Study on the chemical constituents of Dichrocephala integrifolia . Zhong Yao Cai. 2010;33:53–5.
Emégam NK, Nguepi MSD, Lambou AF, Okomolo FCM, Sotoing GT, Bougolla DP, Pale S, Kameni JSN, Bum EN. Antioxidant properties of Dichrocephala integrifolia (Asteraceae) in a mouse model of monosodium glutamate-induced neurotoxicity. Afr J Tradit Complement Altern Med. 2017;14:147–55.
Kouémou NE, Taiwe GS, Moto FC, Pale S, Ngoupaye GT, Njapdounke JS, Nkantchoua GC, Pahaye DB, Bum EN. Nootropic and neuroprotective effects of Dichrocephala integrifolia on scopolamine mouse model of Alheimer’s disease. Front Pharmacol. 2017. https://doi.org/10.3389/fphar.2017.00847 .
Lee CL, Yen MH, Hwang TL, Yang JC, Peng CY, Chen CJ, Chang WY, Wu YC. Anti-inflammatory and cytotoxic component from Dichrocephala integrifolia . Phytochem Lett. 2015;12:237–42. https://doi.org/10.1016/j.phytol.2015.04.012 .
Gandhi D, Mehta P. Dillenia indica Linn. and Dillenia pentagyna Roxb.: pharmacognostic, phytochemical and therapeutic aspects. J App Pharm Sci. 2013;3:134–42. https://doi.org/10.7324/JAPS.2013.31124 .
Cheng WY, Kuo YH, Huang CJ. Isolation and identification of novel estrogenic compounds in Yam Tuber ( Dioscorea alata Cv. Tainung No. 2). J Agric Food Chem. 2007;55:7350–8. https://doi.org/10.1021/jf0711690 .
Das A, Chaudhuri D, Chatterjee A. Study of antioxidant and reactive oxygen species scavenging activity of the edible tuber of “Greater Yam” ( Dioscorea alata L.) from North-east India. Asian J Pharm Clin Res. 2012;5:74–84.
Maithili V, Dhanabal SP, Mahendran S, Vadivelan R. Antidiabetic activity of ethanolic extract of tubers of Dioscorea alata in alloxan induced diabetic rats. Indian J Pharmacol. 2011;43:455–9.
Nono NR, Nzowa KL, Barboni L, Tapondjou AL. Drymaria cordata (Linn.) willd (caryophyllaceae): ethnobotany, pharmacology and phytochemistry. Adv Biol Chem. 2014;4:160–7. https://doi.org/10.4236/abc.2014.42020 .
Liu HB, Zhang CR, Dong SH, Yang SP, Sun Q, Geng MY, Yue JM. Sesquiterpenes from Dysoxylum oliganthum and Dysoxylum excelsum . J Asian Nat Prod Res. 2012;14:224–34. https://doi.org/10.1080/10286020.2011.645810 .
Jayashree R, Albert S, Minaram N. Medicinal plants of North Cachar Hills district of Assam used by the Dimasa tribe. Indian J Tradit Knowl. 2012;11:520–7. http://nopr.niscair.res.in/handle/123456789/14395.
Sharma BK, Ramashanker SG, Rahaman L, Nath N, Kaipeng DL. Plant based folk treatments from North East India for jaundice (an overview). J Med Plants Stud. 2016;4:234–47.
Lasekan O, Buettner A, Christlbauer M. Investigation of important odorants of palm wine ( Elaeis guineensis ). Food Chem. 2007;105:15–23. https://doi.org/10.1016/j.foodchem.2006.12.052 .
Owoyele BV, Owolabi GO. Traditional oil palm (Elaeis guineensis Jacq.) and its medicinal uses: a review. Tang Human Med. 2014. https://doi.org/10.5667/tang.2014.0004 .
Yin NGS, Abdullah S, Phin CK. Phytochemical constituents from leaves of Elaeis guineensis and their antioxidant and antimicrobial activities. Int J Pharm Pharm Sci. 2013;5:137–40.
Shivprasad M, Varsha J. GC-MS screening of some bioactive compounds from methanolic extract of medicinally relevant wild edible plant parts. Int J Sci Res Sci Tech. 2018;4:49–56.
Sethiya NK, Brahmbhat K, Chauhan B, Mishra SH. Pharmacognostic and phytochemical investigation of Ensete superbum (Roxb.) Cheesman pseudostem. Indian J Nat Prod Resour. 2016;7:51–8. http://nopr.niscair.res.in/handle/123456789/34105.
Akter K, Barnes EC, Loa-Kum-Cheung WL, Yin P, Kichu M, Brophy JJ, Barrow RA, Imchen I, Vemulpad SR, Jamie JF. Antimicrobial and antioxidant activity and chemical characterisation of Erythrina stricta Roxb. (Fabaceae). J Ethnopharmacol. 2016;185:171–81. https://doi.org/10.1016/j.jep.2016.03.011 .
Araújo-Júnior JX, de Oliveira MS, Aquino PG, Alexandre-Moreira MS, Sant’Ana AE. A phytochemical and ethnopharmacological review of the genus Erythrina in Phytochemicals. In: Rao V, editors. A global perspective of their role in nutrition and health. London: InTech; 2012. p. 327–49.
Subhashini N, Purnima S, Devi JA, Thirupathi AT, Lavanya N. Anti-inflammatory activity of Erythrina stricta Roxb. in albino rats. Int J Pharm Tech Res. 2011;3:1014–8.
Hada S, Yadav DK, Roat P, Kumari N. Eulophia Nuda : a review of its traditional uses, phytochemistry and pharmacology. Pharm Chem J. 2020;54:40–5. https://doi.org/10.1007/s11094-020-02152-8 .
Jain JB, Kumane SC, Bhattacharya S. Medicinal flora of Madhya Pradesh and Chattisgarh—a review. Indian J Tradit Knowl. 2006;5:237–42. http://nopr.niscair.res.in/handle/123456789/6845.
Pascal OA, Bertrand AEV, Esaïe T, Sylvie HAM, Eloi AY. A review of the ethnomedical uses, phytochemistry and pharmacology of the Euphorbia genus. J Pharm Innov. 2017;6:34–9.
Rauf A, Muhammad N, Qaisar M, Uddin G, Hussain I. Preliminary antinociceptive studies of methanol extract of Euphorbia milli . Middle-East J Med Plants Res. 2012;1:68–70. https://doi.org/10.5829/idosi.mejmpr.2011.1.3.1115 .
Saleem H, Zengin G, Locatelli M, Mollica A, Ahmad I, Mahomoodally FM, Abidin SAZ, Ahemad N. In vitro biological propensities and chemical profiling of Euphorbia milii Des Moul (Euphorbiaceae): a novel source for bioactive agents. Ind Crops Prod. 2019;130:9–15. https://doi.org/10.1016/j.indcrop.2018.12.062 .
Wang P, Xie C, An L, Yang X, Xi Y, Yuan S, Zhang C, Tuerhong M, Jin DQ, Lee D, Zhang J. Bioactive diterpenoids from the stems of Euphorbia royleana . J Nat Prod. 2019;82:183–93. https://doi.org/10.1021/acs.jnatprod.8b00493 .
Ashraf A, Sarfraz RA, Rashid MA, Shahi M. Antioxidant, antimicrobial, antitumor, and cytotoxic activities of an important medicinal plant ( Euphorbia royleana ) from Pakistan. J Food Drug Anal. 2015;23:109–15. https://doi.org/10.1016/j.jfda.2014.05.007 .
Bani S, Kaul A, Jaggi BS, Suri KA, Suri OP, Sharma OP. Anti-inflammatory activity of the hydrosoluble fraction of Euphorbia royleana latex. Fitoterapia. 2000;71:655–62. https://doi.org/10.1016/S0367-326X(00)00225-2 .
Wang GC, Liang JP, Wang Y, Li Q, Ye WC. Chemical constituents from Flueggea virosa . Chin J Nat Med. 2008;6:251–3. https://doi.org/10.1016/S1875-5364(09)60022-4 .
Chao CH, Cheng JC, Shen DY, Huang HC, Wu YC, Wu TS. Terpenoids from Flueggea virosa and their anti-hepatitis C virus activity. Phytochemistry. 2016;128:60–70. https://doi.org/10.1016/j.phytochem.2016.04.003 .
Ezeonwumelu JOC, Omar AN, Ajayi AM, Okoruwa AG, Tanayen JK, Kiplagat DM, Okpanachi OA, Abba S, Ezekiel I, Onchweri AN, Okonkwo CO. Phytochemical screening, acute toxicity, anti-inflammatory and anti-pyretic studies of aqueous extract of the root of Flueggea virosa (Roxb. ex Willd.) in rats. Int J Pharm Biomed Sci. 2012;3:128–35.
Wang GC, Li T, Deng FY, Li YL, Ye WC. Five new phenolic glycosides from Hedyotis scandens . Bioorganic Med Chem Lett. 2013;5:1379–82. https://doi.org/10.1016/j.bmcl.2012.12.077 .
Rahman MA, Uddin SB, Wilcock CC. Medicinal plants used by Chakma tribe in Hill Tracts districts of Bangladesh. Indian J Tradit Knowl. 2007;6:508–17. http://nopr.niscair.res.in/handle/123456789/991
Subba B, Basne P. Antimicrobial activity of some medicinal plants from east and central part of Nepal. Int J Appl Sci Biotechnol. 2014;2:88–92. https://doi.org/10.3126/ijasbt.v2i1.9697 .
Jadhav VM, Thorat RM, Kadam VJ, Sathe NS. Hibiscus rosa sinensis Linn – ‘“Rudrapuspa”’: a review. J Pharm Res. 2009;2:1168–73.
Mak YM, Chuah LO, Ahmad R, Bhat R. Antioxidant and antibacterial activities of hibiscus ( Hibiscus rosa-sinensis L.) and Cassia ( Senna bicapsularis L.) flower extracts. J King Saud Univ Sci. 2013;25(4):275–82. https://doi.org/10.1016/j.jksus.2012.12.003 .
Fu J, Dai L, Lin Z, Lu H. Houttuynia cordata Thunb: a review of phytochemistry and pharmacology and quality control. Chinese Med. 2013;4:101–23. https://doi.org/10.4236/cm.2013.43015 .
Mohanraj R, Sivasankar S. Sweet potato ( Ipomoea batatas [L.] Lam)—a valuable medicinal food: a review. J Med Food. 2014;17:733–41. https://doi.org/10.1089/jmf.2013.2818 .
Hossain S, Ahmed R, Bhowmick S, Al Mamun A, Hashimoto M. Proximate composition and fatty acid analysis of Lablab purpureus (L.) legume seed: implicates to both protein and essential fatty acid supplementation. Springer Plus. 2016;5:1899. https://doi.org/10.1186/s40064-016-3587-1 .
Al-Snafi AE. The pharmacology and medical importance of Dolichos lablab ( Lablab purpureus )—a review. IOSR J Pharm. 2017;7:22–30.
Wei JC, Wang PC, Zhou XI. The caffeoyl phenylethanoid glycosides from Lindernia ruellioides and their anti-HBV effects. J Asian Nat Prod Res. 2018;20:757–62. https://doi.org/10.1080/10286020.2017.1357549 .
Das AK, Nongmaithem R. Phytochemical study of selected medicinal plants used by the maring tribe of Chandel district, Manipur. India J Pharmacogn Phytochem. 2019;8:2155–60.
Kuruvilla GR, Neeraja M, Srikrishna A, Rao SGRS. A new quinone from Maesa indica ( Roxb) A DC, (Myrsinaceae). Indian J Chem Sect B. 2010;49:1637–41.
Patil A, Jadhav V, Arvindekar A, More T. Antidiabetic activity of Maesa indica (Roxb). stem bark in Streptozotoc in induced diabetic rats. American J Phytomed Clin Ther. 2014;2:957–62.
Wei L, Wee W, Siong J, Syamsumir D. Characterization of antimicrobial, antioxidant, anticancer property and chemical composition of Michelia champaca seed and flower extracts. Stamford J Pharm Sci. 2011;4:19–24. https://doi.org/10.3329/sjps.v4i1.8862 .
Vimala R, Nagarajan S, Alam M, Susan T, Joy S. Anti-inflammatory and antipyretic activity of Michelia champaca Linn., (White variety), Ixora Brachiata Roxb. and Rhynchosia Cana (Willd.) D.C. flower extract. Indian J Exp Biol. 1997;35:1310–4.
Dan GD, Yi Z, Wei LE, Tao W, Min HL. Chemical constituents of Mangifera indica leaves (I). Zhong Cao Yao. 2011;42:428–31. http://www.ceps.com.tw/ec/ecJnlIntro.aspx?Jnliid=2790.
Parvez GMM. Pharmacological activities of mango ( Mangifera indica ): a review. J Pharmacogn Phytochem. 2016;5:1–7.
Pandey AK, Rai MK, Acharya D. Chemical composition and antimycotic activity of the essential oils of corn mint ( Mentha arvensis ) and lemon grass ( Cymbopogon flexuosus ) against human pathogenic fungi. Pharm Biol. 2003;41:421–5. https://doi.org/10.1076/phbi.41.6.421.17825 .
Thawkar BS, Jawarkar AG, Kalamkar PV, Pawar KP, Kale MK. Phytochemical and pharmacological review of Mentha arvensis . Int J Green Pharm. 2016;10:2. https://doi.org/10.22377/ijgp.v10i2.643 .
Chow YL, Quon HH. Chemical constituents of the heartwood of Mesua ferrea . Phytochemistry. 1968;7:1871–4. https://doi.org/10.1016/S0031-9422(00)86662-5 .
Chahar MK, Sanjaya KDS, Geetha L, Lokesh T, Manohara KP. Mesua ferrea L.: a review of the medical evidence for its phytochemistry and pharmacological actions. Afr J Pharm Pharmacol. 2013;7:211–9. https://doi.org/10.5897/AJPP12.895 .
Shao H, Nan P, Peng S, Zhang C. Study of chemical constituents of essential oil from flowers of Mikania micrantha . Zhong Yao Cai. 2001;24:341–2.
Dev UK, Md Hossain T, Md IZ. Phytochemical investigation, antioxidant activity and antihelmintic activity of Mikania micrantha leaves. World J Pharma Res. 2015;4:121–33.
Lentz DL, Clark AM, Hufford CD, Meurer-Grimes B, Passreiter CM, Cordero J, Ibrahimi O, Okunade AL. Antimicrobial properties of Honduran medicinal plants. J Ethnopharmacol. 1998;63:253–63. https://doi.org/10.1016/S0378-8741(98)00100-7 .
Yuan K, Lü JL, Yin MW. Chemical constituents of C-glycosylflavones from Mimosa pudica . Yao Xue Xue Bao. 2006;41:435–8.
Joseph B, George J, Mohan J. Pharmacology and traditional uses of Mimosa pudica . Int J Pharma Sci Drug Res. 2013;5:41–4.
Farrag EK, Kassem MES, Bayoumi D, Shaker SE, Afifi MS. Phytochemical study, phenolic profile and antigastric ulcer activity of Morus macroura Miq. fruits extract. J Appl Pharm Sci. 2017;7:152–60. https://doi.org/10.7324/JAPS.2017.70527 .
Sidhu JS, Zafar TA. Bioactive compounds in banana fruits and their health benefits. Food Qual Saf. 2018;2:183–8. https://doi.org/10.1093/fqsafe/fyy019 .
Jyothirmayi N, Rao NM. Banana medicinal uses. J Med Sci Tech. 2015;4:152–60.
Mathew NS, Negi PS. Traditional uses, phytochemistry and pharmacology of wild banana ( Musa acuminata Colla): a review. J Ethnopharmacol. 2017;196:124–40. https://doi.org/10.1016/j.jep.2016.12.009 .
Kim NC, Desjardins AE, Wu CD, Kinghorn AD. Activity of triterpenoid glycosides from the root bark of Mussaenda macrophylla against two oral pathogens. J Nat Prod. 1999;62:1379–84. https://doi.org/10.1021/np9901579 .
Chowdhury SR, Akter S, Sharmin T, Islam F, Quadery TM. Antimicrobial activity of five medicinal plants of Bangladesh. J Pharmacogn Phytochem. 2013;2:164–70.
Shadia E, El-Aziz A, Omer EA, Sabra AS. Chemical composition of Ocimum americanum essential oil and its biological effects against, agrotis ipsilon, (Lepidoptera: Noctuidae). Res J Agric Biol Sci. 2007;3:740–7.
Hakkim FL, Arivazhagan G, Boopathy R. Antioxidant property of selected Ocimum species and their secondary metabolite content. J Med Plant Res. 2008;2:250–7.
Thaweboon S, Thaweboon B. In vitro antimicrobial activity of Ocimum americanum L. essential oil against oral microorganisms. Southeast Asian J Trop Med Public Health. 2009;40:1025–33.
Ahad A, Ganai AA, Sareer O, Najm MZ, Kausar MA, Mujeeb M, Siddiqui WA. Therapeutic potential of oroxylum indicum : a review. J Pharma Res Opinion. 2012;2:163–72.
Singh HV, Chaudhary AK. A review on the taxonomy, ethnobotany, chemistry and pharmacology of Oroxylum indicum Vent. Indian J Pharm Sci. 2011;73:483–90.
Hussain A, Oves M, Alajmi MF, Hussain I, Amir S, Ahmed J, Rehman MT, El-Seedi HR, Ali I. Biogenesis of ZnO nanoparticles using Pandanus odorifer leaf extract: anticancer and antimicrobial activities. RSC Adv. 2019;9:15357–69. https://doi.org/10.1039/C9RA01659G .
Angami T, Bhagawati R, Touthang L, Makdoh B, Bharati KA, Silambarasan R, Ayyanar M. Traditional uses, phytochemistry and biological activities of Parkia timoriana (DC.) Merr., an underutilized multipurpose tree bean: a review. Genet Resour Crop Evol. 2018;65:679–92. https://doi.org/10.1007/s10722-017-0595-0 .
Gaire BP, Subedi L. Phytochemistry, pharmacology and medicinal properties of Phyllanthus emblica Linn. Chin J Integr Med. 2014. https://doi.org/10.1007/s11655-014-1984-2 .
Lin HY, Yuan CY, Xin WY, Peng LD, Juan CW, Lei LJ, Lai LF. Chemical constituents of Picria fel-terrae . Guangxi Zhiwu Guihaia. 2010;30:887–90.
Kumarasingha R, Karpe AV, Preston S, Yeo TC, Lim DS, Tu CL, Luu J, Simpson KJ, Shaw JM, Gasser RB, Beale DJ. Metabolic profiling and in vitro assessment of anthelmintic fractions of Picria fel-terrae Lour. Int J Parasitol Drugs Drug Resist. 2016;6:171–8. https://doi.org/10.1016/j.ijpddr.2016.08.002 .
Satria D, Silalahi J, Haro G, Ilyas S, Hsb PAZ. Antioxidant and antiproliferative activities of an ethylacetate fraction of Picria fel-terrae Lour. Herbs. Asian Pac J Cancer Prev. 2017;18:399–403.
PubMed PubMed Central Google Scholar
Samuelsen AB. The traditional uses, chemical constituents and biological activities of Plantago major L. a review. J Ethnopharmacol. 2000;71:1–21. https://doi.org/10.13040/IJPSR.0975-8232.11(4).1549-56 .
Begum S, Hassan SI, Ali SN, Siddiqui BS. Chemical constituents from the leaves of Psidium guajava . Nat Prod Res. 2004;18:135–40. https://doi.org/10.1080/14786410310001608019 .
Martha R, Gutiérrez P, Mitchell S, Solis RS. Psidium guajava : a review of its traditional uses, phytochemistry and pharmacology. J Ethnopharmacol. 2008;117:1–27. https://doi.org/10.1016/j.jep.2008.01.025 .
Tai Z, Zhang F, Cai L, Shi J, Cao Q, Ding Z. Flavonol glycosides of Pseudodrynaria coronans and their antioxidant activity. Chem Nat Compd. 2012;48:221–4. https://doi.org/10.1007/s10600-012-0209-1 .
Jasuja ND, Saxena R, Chandra S, Sharma R. Pharmacological characterization and beneficial uses of Punica granatum . Asain J Plant Sci. 2012;11:251–67.
Djakpo O, Yao W. Rhus chinensis and Galla chinensis—Folklore to modern evidence: review. Phytother Res. 2010;24:1739–47. https://doi.org/10.1002/ptr.3215 .
Rishi P, Bimala S. Extraction and isolation of chemical constituents from Schima wallichii Bark. Int J Eng Sci Res Tech. 2014;3:175–80.
Das S, Ghosh LK. Evaluation of analgesic, antipyretic and anti-inflammatory activity of different fractions of Schima wallichii barks. Pharmacologia. 2013;4:400–3. https://doi.org/10.5567/pharmacologia.2013.400.403 .
Sarbadhikary SB, Bhowmik S, Datta BK, Mandal NC. Antimicrobial and antioxidant activity of leaf extracts of two indigenous angiosperm species of Tripura. Int J Curr Microbiol Appl Sci. 2015;4:643–55.
Wang D, Huang L, Chen S. Senecio scandens Buch-Ham.: a review on its ethnopharmacology, phytochemistry, pharmacology, and toxicity. J Ethnopharmacol. 2013;149:1–23. https://doi.org/10.1016/j.jep.2013.05.048 .
Hua S, Zhang Y, Liu J, Dong L, Huang J, Lin D, Fu X. Ethnomedicine, phytochemistry and pharmacology of Smilax glabra : an important traditional Chinese medicine. Am J Chin Med. 2018;46:261–97. https://doi.org/10.1142/S0192415X18500143 .
Biao CY, Ming ZD, Shan YS. Chemical constituents of Smilax perfoliata . Acta Bot Sin. 2004;46:618–20.
Borkataky M. Antimcrobial and antioxidant activity of Smilax perfoliate Lour. Der Pharm Lett. 2014;6:246–50.
Zhao Y, Liu F, Lou HX. Studies on the chemical constituents of Solanum nigrum . Zhong Yao Cai. 2010;33:555–6.
Hameed HI, Calixto CMR, Yahya HM. A review: Solanum nigrum L. antimicrobial, antioxidant properties, hepatoprotective effects and analysis of bioactive natural compounds. Res J Pharm Tech. 2017;10:4063–8. https://doi.org/10.5958/0974-360X.2017.00737.5 .
Jain RAS, Gupta SSPI, Gabrani R. Solanum nigrum : current perspectives on therapeutic properties. Altern Med Rev. 2011;16:78–85.
Chang FR, Yen CT, El-Shazly M, Yu CY, Yen MH, Cheng YB, Chen SL, Wu YC. Spirostanoids with 1,4-dien-3-one or 3β,7α-diol-5,6-ene moieties from Solanum violaceum . Bioorg Med Chem Lett. 2013;23:2738–42. https://doi.org/10.1016/j.bmcl.2013.02.060 .
Karim A, Islam B, Tareq SM, Islam MT. Antinociceptive and antipyretic activities of Solanum violaceum Ortega. Int J Med. 2017;5:90–3. https://doi.org/10.14419/ijm.v5i1.7282 .
Mahaldar K, SaifuzMahaldar K, Saifuzzaman M, Irin T, Barman AK, Islam MK, Rahman MM, Islam MA. Analgesic, anthelmintic and toxicity studies of Solanum violaceum Linn. leaves. Orient Pharm Exp Med. 2016;16:147–52. https://doi.org/10.1007/s13596-016-0227-9 .
Bora NS, Kakoti BB, Gogoi B, Goswami AK. Ethno-medicinal claims, phytochemistry and pharmacology of Spondias pinnata : a review. Int J pharm Sci Res. 2014;5:1138–45. https://doi.org/10.13040/IJPSR.0975-8232.5(4) .
Goswami DV, Nirmal SA, Patil MJ, Dighe NS, Laware NS, Patta SR. An overview of Tectona grandis : chemistry and pharmacological profile. Phcog Rev. 2009;3:181–5.
Vyas P, Yadav DK, Khandelwal P. Tectona grandis (Teak)—a review on its phytochemical and therapeutic potential. Nat Prod Res. 2019;33:2338–54.
El-Ghorab A, El-Massry KF, Shibamoto T. Chemical composition of the volatile extract and antioxidant activities of the volatile and nonvolatile extracts of egyptian corn silk ( Zea mays L.). J Agric Food Chem. 2007;55:9124–7. https://doi.org/10.1021/jf071646e .
Mendoza-Díaz S, del Carmen Ortiz-Valerio M, Castaño-Tostado E, de Dios Figueroa-Cardenas J, Reynoso-Camacho R, Ramos-Gómez M, Campos-Vega R, Loarca-Piña G. Antioxidant capacity and antimutagenic activity of anthocyanin and carotenoid extracts from nixtamalized pigmented creole maize races ( Zea mays L.). Plant Foods Hum Nutr. 2012;67:442–9. https://doi.org/10.1007/s11130-012-0326-9 .
Nessa F, Ismail Z, Mohamed N. Antimicrobial activities of extracts and flavonoid glycosides of corn silk ( Zea mays L.). Int J Biotechnol Wellness Ind. 2012;1:115–21.
Gupta SK, Sharma A. Medicinal properties of Zingiber officinale Roscoe—a review. IOSR J Pharm Biol Sci. 2011;5:124–9.
Rehman R, Akram M, Akhtar N, Jabeen Q, Shah SA, Ahmed K, Shaheen G, Asif HM. Zingiber officinale Roscoe (Parmacological activity). J Med Plants Res. 2011;5:344–8.
Çakılcıoğlu U, Khatun S, Türkoğlu I, Hayta S. Ethnopharmacological survey of medicinal plants in Maden (Elazığ–Turkey). J Ethnopharmacol. 2011;137:469–86. https://doi.org/10.1016/j.jep.2011.05.046 .
Akindele AJ, Ibe IF, Adeyemi OO. Analgesic and antipyretic activities of Drymaria cordata (Linn.) Willd (Caryophyllaceae) extract. Afr J Tradit Complement Altern Med. 2012;9:25–35.
Proma JJ, Faruque MO, Rahman S, Bashar ABMA, Rahmatullah M. Analgesic potential and phytochemical screening of Lablab purpureus aerial parts. World J Pharm Pharmaceut Sci. 2014;3:165–73.
Bakir M, Facey PC, Hassan I, Mulder WH, Porter RB. Mikanolide from Jamaican Mikania micrantha . Acta Crystallogr C. 2004;6:11. https://doi.org/10.1107/S0108270104017809 .
Koriem KM, Arbid MS, Saleh HN. Antidiarrheal and protein conservative activities of Psidium guajava in diarrheal rats. J Integr Med. 2019;17:57–65. https://doi.org/10.1016/j.joim.2018.12.001 .
Salama AA, El-Kassaby MI, Hassan A. Anti-urolithiatic activity of Solanum nigrum hydroalcoholic extract in ethylene glycol-induced urolithiasis in rats. Egypt Pharmaceut J. 2019;18:311. https://www.epj.eg.net/text.asp?2019/18/4/311/272269 .
Yirga G, Teferi M, Gidey G, Zerabruk S. An ethnoveterinary survey of medicinal plants used to treat livestock diseases in Seharti-Samre district, Northern Ethiopia. Afr J Plant Sci. 2012;6:113–9. https://doi.org/10.5897/AJPS11.242 .
Parthiban R, Vijayakumar S, Prabhu S, Gnanaselvam J, Yabesh EM. Quantitative traditional knowledge of medicinal plants used to treat livestock diseases from Kudavasal taluk of Thiruvarur district, Tamil Nadu, India. Rev Bras Farmacogn. 2016;26:109–21. https://doi.org/10.1016/j.bjp.2015.07.016 .
Jadid N, Kurniawan E, Himayani CES, Prasetyowati I, Purwani KI, Muslihatin W, Hidayati D, Tjahjaningrum ITD. An ethnobotanical study of medicinal plants used by the Tengger tribe in Ngadisari village, Indonesia. PLoS ONE. 2020;15:7. https://doi.org/10.1371/journal.pone.0235886 .
Moerman DE. Symbols and selectivity: a statistical analysis of native American medical ethnobotany. J Ethnopharmacol. 1979;1:111–9. https://doi.org/10.1016/0378-8741(79)90002-3 .
Kutal DH, Kunwar RM, Uprety Y, Adhikari YP, Bhattarai S, Adhikari B, Kunwar LM, Bhatt MD, Bussmann RW. Selection of medicinal plants for traditional medicines in Nepal. J Eethnobiol Ethnomed. 2021;17(1):1–11. https://doi.org/10.1186/s13002-021-00486-5 .
Addo-Fordjour P, Kofi Anning A, Durosimi Belford EJ, Akonnor D. Diversity and conservation of medicinal plants in the Bomaa community of the Brong Ahafo region, Ghana. J Med Plants Res. 2008;2:226–33.
Ghorbani A. Studies on pharmaceutical ethnobotany in the region of Turkmen Sahra, north of Iran (Part 1): general results. J Ethnopharmacol. 2005;102:58–68. https://doi.org/10.1016/j.jep.2005.05.035 .
Poonam K, Singh GS. Ethnobotanical study of medicinal plants used by the Taungya community in Terai Arc Landscape, India. J Ethnopharmacol. 2009;123:167–76. https://doi.org/10.1016/j.jep.2009.02.037 .
Luseba D, Tshisikhawe MP. Medicinal plants used in the treatment of live-stock diseases in Vhembe region, Limpopo province. S Afr J Med Plants Res. 2014;7:593–601. https://doi.org/10.5897/JMPR12.1213 .
Mahwasane ST, Middleton L, Boaduo N. An ethnobotanical survey of indigenous knowledge on medicinal plants used by the traditional healers of the Lwamondo area, Limpopo province, South Africa. S Afr J Bot. 2013;88:69–75. https://doi.org/10.1016/j.sajb.2013.05.004 .
Saha MR, Sarker DD, Sen A. Ethnoveterinary practices among the tribal community of Malda district of West Bengal, India. Indian J Tradit Knowl. 2014;13: 359–67. http://nopr.niscair.res.in/handle/123456789/27931
Verma RK, Kumari P, Maurya RK, Kumar V, Verma RB, Singh RK. Medicinal properties of turmeric ( Curcuma longa L.): a review. Int J Chem Stud. 2018;6(4):1354–7.
Singh AG, Kumar A, Tewari DD. An ethnobotanical survey of medicinal plants used in Terai forest of western Nepal. J Ethnobiol Ethnomedicine. 2012;8:19. https://doi.org/10.1186/1746-4269-8-19 .
Chaudhary MI, He Q, Cheng YY, Xiao PG. Ethnobotany of medicinal plants from Tian Mu Shan biosphere reserve, Zhejiang-Province, China. Asian J Plant Sci. 2006;5:646–53.
Çakılcıoğlu U, Türkoğlu I. An ethnobotanical survey of medicinal plants in Sivrice (Elazığ-Turkey). J Ethnopharmacol. 2010;132:165–75. https://doi.org/10.1016/j.jep.2010.08.017 .
Rajakumar N, Shivanna MB. Ethnomedicinal application of plants in the eastern region of Shimoga District, Karnataka. India J Ethnopharmacol. 2009;126:64–73. https://doi.org/10.1016/j.jep.2009.08.010 .
Download references
Acknowledgements
The authors were thankful to the department of Horticulture, Aromatic and Medicinal Plant, Mizoram University, for providing the necessary facilities to complete our work. We also offer our heartfelt gratitude to all the local people of Champhai district, Mizoram, who shared their valuable knowledge and precious time for this research.
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Horticulture, Aromatic and Medicinal Plants, School of Earth Sciences and Natural Resources Management, Mizoram University, Aizawl, 796004, India
T. B. C. Laldingliani, Nurpen Meitei Thangjam, Laldingngheti Bawitlung & Awadhesh Kumar
Department of Botany, School of Life Science, Mizoram University, Aizawl, 796004, India
R. Zomuanawma
Bioprospection and Product Development, CSIR-Central Institute of Medicinal and Aromatic Plants, CIMAP, Lucknow, 226015, India
Anirban Pal
You can also search for this author in PubMed Google Scholar
Contributions
TBCL and AK carry out ethnobotanical survey, write the manuscript and analyse the data; TBCL, NMT, RZ, LB and AK were study proposer, design the questionnaire and revise the manuscript; NMT and AP design the graphical abstract; RZ and AP were proof reader. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Awadhesh Kumar .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Laldingliani, T.B.C., Thangjam, N.M., Zomuanawma, R. et al. Ethnomedicinal study of medicinal plants used by Mizo tribes in Champhai district of Mizoram, India. J Ethnobiology Ethnomedicine 18 , 22 (2022). https://doi.org/10.1186/s13002-022-00520-0
Download citation
Received : 26 October 2021
Accepted : 14 March 2022
Published : 24 March 2022
DOI : https://doi.org/10.1186/s13002-022-00520-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ethnomedicinal
- Indo-Burma hotspot
Journal of Ethnobiology and Ethnomedicine
ISSN: 1746-4269
- General enquiries: [email protected]
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- The Cass review: an...
The Cass review: an opportunity to unite behind evidence informed care in gender medicine
- Related content
- Peer review
- Kamran Abbasi , editor in chief
- kabbasi{at}bmj.com
- Follow Kamran on Twitter @KamranAbbasi
At the heart of Hilary Cass’s review of gender identity services in the NHS is a concern for the welfare of “children and young people” (doi: 10.1136/bmj.q820 ). 1 Her stated ambition is to ensure that those experiencing gender dysphoria receive a high standard of care. This will be disputed, of course, by people and lobbying groups angered by her recommendations, but it is a theme running through the review. Cass, a past president of the UK’s Royal College of Paediatrics and Child Health, seeks to provide better care for children and adolescents on one of the defining issues of our age. Her conclusion is alarming for anybody who genuinely cares for child welfare: gender medicine is “built on shaky foundations” (doi: 10.1136/bmj.q814 ). 2
That verdict is supported by a series of review papers published in Archives of Disease in Childhood , a journal published by BMJ and the Royal College of Paediatrics and Child Health (doi: 10.1136/archdischild-2023-326669 doi: 10.1136/archdischild-2023-326670 doi: 10.1136/archdischild-2023-326499 doi: 10.1136/archdischild-2023-326500 ). 3 4 5 6 The evidence base for interventions in gender medicine is threadbare, whichever research question you wish to consider—from social transition to hormone treatment.
For example, of more than 100 studies examining the role of puberty blockers and hormone treatment for gender transition only two were of passable quality. To be clear, intervention studies—particularly of drug and surgical interventions—should include an appropriate control group, ideally be randomised, ensure concealment of treatment allocation (although open label studies are sometimes acceptable), and be designed to evaluate relevant outcomes with adequate follow-up.
One emerging criticism of the Cass review is that it set the methodological bar too high for research to be included in its analysis and discarded too many studies on the basis of quality. In fact, the reality is different: studies in gender medicine fall woefully short in terms of methodological rigour; the methodological bar for gender medicine studies was set too low, generating research findings that are therefore hard to interpret. The methodological quality of research matters because a drug efficacy study in humans with an inappropriate or no control group is a potential breach of research ethics. Offering treatments without an adequate understanding of benefits and harms is unethical. All of this matters even more when the treatments are not trivial; puberty blockers and hormone therapies are major, life altering interventions. Yet this inconclusive and unacceptable evidence base was used to inform influential clinical guidelines, such as those of the World Professional Association for Transgender Health (WPATH), which themselves were cascaded into the development of subsequent guidelines internationally (doi: 10.1136/bmj.q794 ). 7
The Cass review attempted to work with the Gender Identity Development Service (GIDS) and the NHS adult gender services to “fill some of the gaps in follow-up data for the approximately 9000 young people who have been through GIDS to develop a stronger evidence base.” However, despite encouragement from NHS England, “the necessary cooperation was not forthcoming.” Professionals withholding data from a national inquiry seems hard to imagine, but it is what happened.
A spiralling interventionist approach, in the context of an evidence void, amounted to overmedicalising care for vulnerable young people. A too narrow focus on gender dysphoria, says Cass, neglected other presenting features and failed to provide a holistic model of care. Gender care became superspecialised when a more general, multidisciplinary approach was required. In a broader sense, this failure is indicative of a societal failure in child and adolescent health (doi: 10.1136/bmj.q802 doi: 10.1136/bmj-2022-073448 ). 8 9 The review’s recommendations, which include confining prescription of puberty blockers and hormonal treatments to a research setting (doi: 10.1136/bmj.q660 ), now place the NHS firmly in line with emerging practice internationally, such as in Scandinavia (doi: 10.1136/bmj.p553 ). 10 11
Cass proposes a future model of regional multidisciplinary centres that provide better access and, importantly, standardised care for gender dysphoria, including a smoother transition between adolescent and adult services. Staff will need training. All children and young people embarking on a care pathway will be included in research to begin to rectify the problems with the evidence base, with long term outcomes being an important area of focus. An already stretched workforce will need to extend itself further (doi: 10.1136/bmj.q795 doi: 10.1136/bmj-2024-079474 ). 12 13 In the meantime, some children and young people will turn to the private sector or online providers to meet their needs. The dangers in this moment of service transition are apparent.
But it’s also a moment of opportunity. Families, carers, advocates, and clinicians—acting in the best interests of children and adolescents—face a clear choice whether to allow the Cass review to deepen division or use it as a driver of better care. The message from the evidence reviews in Archives of Disease in Childhood is as unequivocal as it could be. Cass’s review is independent and listened to people with lived experience. Without doubt, the advocacy and clinical practice for medical treatment of gender dysphoria had moved ahead of the evidence—a recipe for harm.
People who are gender non-conforming experience stigmatisation, marginalisation, and harassment in every society. They are vulnerable, particularly during childhood and adolescence. The best way to support them, however, is not with advocacy and activism based on substandard evidence. The Cass review is an opportunity to pause, recalibrate, and place evidence informed care at the heart of gender medicine. It is an opportunity not to be missed for the sake of the health of children and young people. It is an opportunity for unity.
- Mitchell A ,
- Langton T ,
- Heathcote C ,
- Hewitt CE ,
- Hardiman L ,
- Wilkinson E
- Dixon-Woods M ,
- Summers C ,
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Traditional Indigenous medicine in North America: A scoping review

2020, PLOS ONE
Background Despite the documented continued use of traditional healing methods, modalities and its associated practitioners by Indigenous groups across North America, it is presumed that widespread knowledge is elusive amongst most Western trained health professionals and systems. This despite that the approximately 7.5 million Indigenous peoples who currently reside in Canada and the United States (US) are most often served by Western systems of medicine. A state of the literature is currently needed in this area to provide an accessible resource tool for medical practitioners, scholars, and communities to better understand Indigenous traditional medicine in the context of current clinical care delivery and future policy making. Methods A systematic search of multiple databases was performed utilizing an established scoping review framework. A consequent title and abstract review of articles published on traditional Indigenous medicine in the North American context was completed. Findings Of the 4,277 published studies identified, 249 met the inclusion criteria divided into the following five categorical themes: General traditional medicine, integration of traditional and Western medicine systems, ceremonial practice for healing, usage of traditional medicine, and traditional healer perspectives. Conclusions This scoping review was an attempt to catalogue the wide array of published research in the peer-reviewed and online grey literature on traditional Indigenous medicine in North America in order to provide an accessible database for medical practitioners, scholars, and communities to better inform practice, policymaking, and research in Indigenous communities
Related Papers
Complementary therapies in nursing & midwifery
Valerie Eschiti
Traditional indigenous healing is widely used today, as it has been since time immemorial. This article describes the following areas in regards to traditional healing: (a) an explanation of indigenous peoples, (b) a definition of traditional indigenous healing, (c) a portrayal of traditional healers, (d) health within indigenous culture, (e) traditional healing techniques, (f) utilization of traditional healing, (g) how to find a traditional healer, and (h) comparing traditional healing principles with mainstream ways. It is important to have knowledge about this method of holistic healing so health care providers and nurses can integrate it into the health care for individuals and/or families that choose traditional indigenous healing.
From the research, there appears to be very few minor similarities between indigenous healing methods and Western medicine. Look at our current Western systems of health, with its clinics and hospitals, general practitioners, and a myriad of specialists. Similarly, for your North American indigenous peoples, one could equate sacred ceremonial sites to hospitals, or how they have an equally specialized and broad set of individuals at their disposal for their health and healing, such as diagnosis specialist, spiritualist, herbalist, or medicine man/woman (Robbins & Dewar, 2011).
International Journal of Disability, Development and Education
Tarrell Portman
Social science & medicine (1982)
Janice Morse
In this article, Cree Indian methods of treating disease are compared with the treatment process and procedures used in the Western health Care system. Ethnographic data permitted the identification of the five components of Cree healing: the ritual, contract, treatment, didactic, and closure components. These components are compared with equivalent phases in the physician-patient and nurse-patient relationship. In particular, the process of comparison permits the identification of incongruities that the Cree may encounter when using the Western system. These include the inability to identify one's own state of health and abnormalities; a passive, rather than a participatory role in healing; the incomprehensible notion of "silent" diseases and preventative treatment; the specialization of the caring, curing, and counselling roles of practitioners and the limited perspective of "holism" in health care.
Journal of Integrative and Complementary Medicine
Nadine Ijaz
Tommy K. Begay
National Native Health Research Training Conference Indigenous Research: Native Approaches to Sustainable Health Mystic Lake Center Prior Lake, Minnesota August 8-10, 2018 Traditional Medicine Plenary Speaker: Thursday, August 9th, 11:00 – 12:00pm, Waconia I Tommy K. Begay, PhD, MPH Clinical Assistant Professor Faculty Affiliate: Social, Cognitive, and Affective Neuroscience Laboratory Department of Psychiatry College of Medicine University of Arizona Title: Researching Sacred Wisdom: A Clash of Paradigms In documenting the effectiveness of Traditional Medicine, researchers face unique challenges in methodology, data collection, and the interpretation of results. For the most part, these challenges stem from rigid methods, protocols, and thought processes associated with both: Traditional Medicine and scientific research – each having distinct paradigms. Research methodology consists of a series of rigid, objective steps that have a tendency to impinge upon processes that constitute Traditional Medicine. In general, the processes associated with Traditional Medicine rely upon a commitment to a philosophy that infuses mind, body, and spirit – what the presenter refers to as Sacred Wisdom. As a result, changes to physiology and affect may be difficult to obtain, code, and utilize. Understanding these challenges becomes important in the pursuit, acquisition, and utilization of funding for programs associated with effective, culturally relevant, interventions associated with Native concepts of health, wellness, and healing. Furthermore, the acquisition of funding for such interventions may be required to be “evidence based”. By understanding the parameters of these two paradigms, researchers may incorporate methods of inquiry that provide a more legitimate assessment, and evaluation of the changes in health and wellness associated with Traditional Medicine.
International Journal of Disability Development and Education
Lisa Lopez Levers
In this article, I review five articles selected for this Special Issue of the International Journal of Disability, Development and Education on indigenous healing. I have considered the various traditions of indigenous healing, and I situate my analysis within the context of disability, development, and education. Such an analysis reflects the conundrum involving professional identity politics and the elusiveness of intentionality. In response to the five articles, I offer commentary on the social constructions of health, illness, healing, and disability, as these constructs vary across cultures. I suggest that the ability of professionals to inspire trust among clients is potentially a practitioner marker of efficacy across medical paradigms, and is a dynamic that is often misunderstood. I illuminate the healing process as a dynamic of reciprocity and engagement. Finally, I discuss and emphasise the need for developing collaborative programming and integrative service delivery models.
Integrating Traditional Healing Practices into Counseling and Psychotherapy
International Journal of Circumpolar Health
Nicole Redvers
In this commentary, we argue that Indigenous patients in the Northwest Territories (NWT) have a right to access traditional medicine and related practitioners as a part of the continuum of medical care. Indigenous people make up over half of the NWT population, spread over vast geographic areas with representation from First Nations, Inuit and Métis (FNIM) people. Ensuring barrier-free access to traditional medicine and providers in a culturally respectful environment is a challenge that requires structural transformation in the territorial health system. The ongoing transmission of knowledge about Indigenous traditional medicine in Northern Canada and the collective survival of Northern peoples is a testament to the applicability of traditional medicines in a self-determined wellness system. Through a discussion of the barriers to policy development and implementation, this commentary aims to elevate Indigenous perspectives and offer recommendations for integrating traditional medicines into Northern health systems. ARTICLE HISTORY
Family Medicine and Community Health
ObjectivesChronic conditions represent an important source of major health issues among Indigenous People. The same applies to those, who live off-reserve and in urban areas. However, very few healthcare services are considered culturally safe, resulting in some avoidance of the public healthcare system. Our goal was to review the literature on culturally safe practices available to urban Indigenous People who suffer from chronic diseases.DesignWe conducted a scoping review to determine what culturally safe healthcare services are currently offered for the management of chronic conditions in urban Indigenous populations, to contribute to a tailored, holistic and safe space in mainstream healthcare systems.Eligibility criteriaPeer-reviewed original research articles had to be published by 27 October 2020, in English or French.Information source: In October 2020, we searched five academic databases (EBSCO, PsycArticles, SocINDEX, MEDLINE and PsycINFO) and also reviewed grey literature...
RELATED PAPERS
Physical Review Letters
Jorge José
IEEE Internet Computing
Carlos Carballo Rodríguez
osman metalla
Tlatemoani: Revista Académica de Investigación
Diana Zavala Cuevas
Limoges, Lambert-Lucas, coll. « Linguistique »
Sylvie Patron
Guillermo Schinella
nebrija.com
Andrea Menegotto
Language, Cognition, and Mind
Carla Umbach
Curtis's Botanical Magazine
Richard Wilford
Revista Triângulo
Patrícia Marcoccia
Journal of Business Research - Turk
Sinan Saracli
Data in Brief
Marcelo Maraschin
Muhammad Nur
ANAIS DO VI SIMPOSIO BRASILEIRO DE QUALIDADE DO PROJETO NO AMBIENTE CONSTRUIDO
Silvio Burattino Melhado
MATEC Web of Conferences
Nazirah Ahmad
Applied Thermal Engineering
Shoaib Ahmed
Dementia and geriatric cognitive disorders extra
Øyvind Kirkevold
Vii Connepi Congresso Norte Nordeste De Pesquisa E Inovacao
Manuella Macedo Barbosa
Journal of Marine Science and Technology
sakine mashjoor
Prof.Dr. Ferit izci
Iranian Journal of Insurance Research
Basic Hepatology
Letters in Applied Microbiology
Food Quality and Preference
Agnieszka Rybowska
Dr. Charlotte Stephens
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- Introduction
- Article Information
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Grubbs JB , Kraus SW. Binge Drinking Among Sports Gamblers. JAMA Netw Open. 2024;7(4):e245473. doi:10.1001/jamanetworkopen.2024.5473
Manage citations:
© 2024
- Permissions
Binge Drinking Among Sports Gamblers
- 1 Department of Psychology, Center on Alcohol, Substance use, And Addictions, University of New Mexico, Albuquerque
- 2 Department of Psychology, University of Nevada, Las Vegas
Over the past 6 years, sports wagering has become accessible to most individuals in the US via mobile applications or websites. 1 Increasing evidence suggests that sports wagering is associated with greater substance use and misuse, particularly alcohol, and symptoms of alcohol use disorder. 2 - 4 Alcohol consumption is higher among sports gamblers, 3 and sports gamblers often use substances while gambling. 5 Sports gamblers tend to be more inclined toward risk taking, suggesting that sports gambling may be associated with more risky alcohol use behaviors. 4 - 6 Accordingly, we examined whether individuals who wager on sports in the US are at greater risk of binge use of alcohol.
This survey study was approved by the Bowling Green State University Institutional Review Board; informed consent was obtained from all participants. The study followed the AAPOR reporting guideline.
From March 17 to April 6, 2022, we collected a census-matched sample of US adults with an oversample of adults who wager on sports. Full information about this survey is available elsewhere. 1 Race and ethnicity data were collected because they are potential factors in sports gambling likelihood and binge drinking habits. Among those reporting any past year alcohol use, binge drinking was assessed via the National Institute on Drug Abuse Quick Screen, version 1.0, which asks how often respondents consumed an excess of alcohol at a single time (≥5 drinks for men; ≥4 for women). Participants responded on a scale of 1 (never) to 5 (daily or more). Sports betting status was assessed by asking participants whether they had placed bets on sporting events or esports or participated in daily fantasy sports over the past 12 months.
Statistical analyses were conducted in SPSS, version 28. We conducted 2-tailed χ 2 analyses for distributions of past year binge drinking frequency, followed by multinomial logistic regressions estimating binge drinking frequency; P < .05 was considered statistically significant.
A total of 4363 respondents were included (51.4% men, 46.4% women, and 2.2% nonbinary or other; mean [SD] age, 49.6 [16.2] years) ( Table 1 ). The national census-matched survey consisted of 2806 participants (mean [SD] age, 48.9 [17.2] years; 1365 [48.6%] men and 1441 [51.4%] women; response rate, 2806 of 3203 [87.6%]). The oversample of sports gamblers consisted of 1557 participants (mean [SD] age, 41.7 [15.3] years; 1043 [67.0%] men and 514 [33.0%] women; response rate, 1557 of 1978 [78.7%]), of whom 1474 reported past year sports betting. Additionally, in the national sample, 338 respondents (12.0%) indicated they had gambled on sports in the past 12 months, resulting in a total of 1812 sports gamblers ( Table 1 ). Sports gamblers were disproportionally likely to be men and younger. In these combined samples, 3267 respondents (74.9%) reported past year alcohol use.
Sports wagerers were disproportionately more likely to report binge drinking at monthly or greater frequency over the past 12 months and were also disproportionately less likely to report no binge drinking episodes in the past 12 months ( Table 1 ). Multinomial logistic regressions adjusted for age and race and ethnicity showed that sports gamblers were substantially more likely to report higher levels of binge drinking ( Table 2 ), suggesting that elevated risky drinking episodes among sports gamblers are not due to demographic differences.
In this survey study, binge drinking in both men and women was reported at greater frequency among sports wagering individuals compared with nongamblers and non–sports gamblers. This study is limited by its cross-sectional design and use of nonprobability polling methods. Regardless, with past research showing that sports gamblers are more likely to report symptoms of alcohol use disorder, our results suggest that individuals who wager on sports use alcohol in particularly risky ways. Given the rapid spread of sports wagering in the US over recent years, this finding highlights an immense need for ongoing research, particularly to examine how novel gambling technologies influence the prevalence, presentation, and prevention of alcohol use disorders and related harms.
Accepted for Publication: February 9, 2024.
Published: April 1, 2024. doi:10.1001/jamanetworkopen.2024.5473
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Grubbs JB et al. JAMA Network Open .
Corresponding Author: Joshua B. Grubbs, PhD, Center for Alcohol, Substance Use, and Addiction, University of New Mexico, 2650 Yale Blvd SE, Albuquerque, NM 87106 ( [email protected] ).
Author Contributions: Drs Grubbs and Kraus had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Both authors.
Acquisition, analysis, or interpretation of data: Both authors.
Drafting of the manuscript: Both authors.
Critical review of the manuscript for important intellectual content: Both authors.
Statistical analysis: Both authors.
Obtained funding: Both authors.
Administrative, technical, or material support: Grubbs.
Conflict of Interest Disclosures: Dr Grubbs reported receiving research grant funding from the Problem Gambling Network of Ohio outside the submitted work. Dr Kraus reported receiving personal fees from New York Council on Problem Gambling, the International Center for Responsible Gaming, the California Council on Problem Gambling, and Massachusetts General Hospital Psychiatry Academy, serving as editor-in-chief for Taylor & Francis journals, and receiving Summer research support from the Nevada Project on Problem Gambling during the conduct of the study. No other disclosures were reported.
Funding/Support: This study was supported by grants from the International Center for Responsible Gaming, the Kindbridge Research Institute, and the Problem Gambling Network of Ohio.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See the Supplement .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- International edition
- Australia edition
- Europe edition

Gender medicine ‘built on shaky foundations’, Cass review finds
Analysis finds most research underpinning clinical guidelines, hormone treatments and puberty blockers to be low quality
Review of gender services has major implications for mental health services
The head of the world’s largest review into children’s care has said that gender medicine is “built on shaky foundations”.
Dr Hilary Cass, the paediatrician commissioned to conduct a review of the services provided by the NHS to children and young people questioning their gender identity, said that while doctors tended to be cautious in implementing new findings in emerging areas of medicine, “quite the reverse happened in the field of gender care for children”.
Cass commissioned the University of York to conduct a series of analyses as part of her review.
Two papers examined the quality and development of current guidelines and recommendations for managing gender dysphoria in children and young people. Most of the 23 clinical guidelines reviewed were not independent or evidence based, the researchers found.
A third paper on puberty blockers found that of 50 studies, only one was of high quality.
Similarly, of 53 studies included in a fourth paper on the use of hormone treatment, only one was of sufficiently high quality, with little or only inconsistent evidence on key outcomes.
Here are the main findings of the reviews:
Clinical guidelines
Increasing numbers of children and young people experiencing gender dysphoria are being referred to specialist gender services. There are various guidelines outlining approaches to the clinical care of these children and adolescents.
In the first two papers, the York researchers examined the quality and development of published guidelines or clinical guidance containing recommendations for managing gender dysphoria in children and young people up to the age of 18.
They studied a total of 23 guidelines published in different countries between 1998 and 2022. All but two were published after 2010.

Most of them lacked “an independent and evidence-based approach and information about how recommendations were developed”, the researchers said.
Few guidelines were informed by a systematic review of empirical evidence and they lack transparency about how their recommendations were developed. Only two reported consulting directly with children and young people during their development, the York academics found.
“Healthcare services and professionals should take into account the poor quality and interrelated nature of published guidance to support the management of children and adolescents experiencing gender dysphoria/incongruence,” the researchers wrote.
Writing in the British Medical Journal (BMJ) , Cass said that while medicine was usually based on the pillars of integrating the best available research evidence with clinical expertise, and patient values and preferences, she “found that in gender medicine those pillars are built on shaky foundations”.
She said the World Professional Association of Transgender Healthcare (WPATH) had been “highly influential in directing international practice, although its guidelines were found by the University of York’s appraisal to lack developmental rigour and transparency”.
In the foreword to her report, Cass said while doctors tended to be cautious in implementing new findings “quite the reverse happened in the field of gender care for children”.
In one example, she said a single Dutch medical study, “suggesting puberty blockers may improve psychological wellbeing for a narrowly defined group of children with gender incongruence”, had formed the basis for their use to “spread at pace to other countries”. Subsequently, there was a “greater readiness to start masculinising/feminising hormones in mid-teens”.
She added: “Some practitioners abandoned normal clinical approaches to holistic assessment, which has meant that this group of young people have been exceptionalised compared to other young people with similarly complex presentations. They deserve very much better.”
Both papers repeatedly pointed to a key problem in this area of medicine: a dearth of good data.
She said: “Filling this knowledge gap would be of great help to the young people wanting to make informed choices about their treatment.”
Cass said the NHS should put in place a “full programme of research” looking at the characteristics, interventions and outcomes of every young person presenting to gender services, with consent routinely sought for enrolment in a research study that followed them into adulthood.
Gender medicine was “an area of remarkably weak evidence”, her review found, with study results also “exaggerated or misrepresented by people on all sides of the debate to support their viewpoint”.
Alongside a puberty blocker trial, which could be in place by December, there should be research into psychosocial interventions and the use of the masculinising and feminising hormones testosterone and oestrogen, the review found.
Hormone treatment
Many trans people who seek medical intervention in their transition opt to take hormones to masculinise or feminise their body, an approach that has been used in transgender adults for decades.
“It is a well-established practice that has transformed the lives of many transgender people,” the Cass review notes, adding that while these drugs are not without long-term problems and side-effects, for many they are dramatically outweighed by the benefits.
For birth-registered females, the approach means taking testosterone, which brings about changes including the growth of facial hair and a deepening of the voice, while for birth-registered males, it involves taking hormones including oestrogen to promote changes including the growth of breasts and an increase in body fat. Some of these changes may be irreversible.
However, in recent years a growing proportion of adolescents have begun taking these cross-sex, or gender-affirming, hormones, with the vast majority who are prescribed puberty blockers subsequently moving on to such medication.
This growing take-up among young people has led to questions over the impact of these hormones in areas ranging from mental health to sexual functioning and fertility.
Now researchers at the University of York have carried out a review of the evidence, comprising an analysis of 53 previously published studies, in an attempt to set out what is known – and what is not – about the risks, benefits and possible side-effects of such hormones on young people.
All but one study, which looked at side-effects, were rated of moderate or low quality, with the researchers finding limited evidence for the impact of such hormones on trans adolescents with respect to outcomes, including gender dysphoria and body satisfaction.
The researchers noted inconsistent findings around the impact of such hormones on growth, height, bone health and cardiometabolic effects, such as BMI and cholesterol markers. In addition, they found no study assessed fertility in birth-registered females, and only one looked at fertility in birth-registered males.
“These findings add to other systematic reviews in concluding there is insufficient and/or inconsistent evidence about the risks and benefits of hormone interventions in this population,” the authors write.
However, the review did find some evidence that masculinising or feminising hormones might help with psychological health in young trans people. An analysis of five studies in the area suggested hormone treatment may improve depression, anxiety and other aspects of mental health in adolescents after 12 months of treatment, with three of four studies reporting an improvement around suicidality and/or self-harm (one reported no change).
But unpicking the precise role of such hormones is difficult. “Most studies included adolescents who received puberty suppression, making it difficult to determine the effects of hormones alone,” the authors write, adding that robust research on psychological health with long-term follow-up was needed.
The Cass review has recommended NHS England should review the current policy on masculinising or feminising hormones, advising that while there should be the option to provide such drugs from age 16, extreme caution was recommended, and there should be a clear clinical rationale for not waiting until an individual reached 18.
Puberty blockers
Treatments to suppress puberty in adolescents became available through routine clinical practice in the UK a decade ago.
While the drugs have long been used to treat precocious puberty – when children start puberty at an extremely young age – they have only been used off-label in children with gender dysphoria or incongruence since the late 1990s. The rationale for giving puberty blockers, which originated in the Netherlands, was to buy thinking time for young people and improve their ability to smooth their transition in later life.
Data from gender clinics reported in the Cass review showed the vast majority of people who started puberty suppression went on to have masculinising or feminising hormones, suggesting that puberty blockers did not buy people time to think.
To understand the broader effects of puberty blockers, researchers at the University of York identified 50 papers that reported on the effects of the drugs in adolescents with gender dysphoria or incongruence. According to their systematic review, only one of these studies was high quality, with a further 25 papers regarded as moderate quality. The remaining 24 were deemed too weak to be included in the analysis.
Many of the reports looked at how well puberty was suppressed and the treatment’s side-effects, but fewer looked at whether the drugs had their intended benefits.
Of two studies that investigated gender dysphoria and body satisfaction, neither found a change after receiving puberty blockers. The York team found “very limited” evidence that puberty blockers improved mental health.
Overall, the researchers said “no conclusions” could be drawn about the impact on gender dysphoria, mental and psychosocial health or cognitive development, though there was some evidence bone health and height may be compromised during treatment.
Based on the York work, the Cass review finds that puberty blockers offer no obvious benefit in helping transgender males to help their transition in later life, particularly if the drugs do not lead to an increase in height in adult life. For transgender females, the benefits of stopping irreversible changes such as a deeper voice and facial hair have to be weighed up against the need for penile growth should the person opt for vaginoplasty, the creation of a vagina and vulva.
In March, NHS England announced that children with gender dysphoria would no longer receive puberty blockers as routine practice. Instead, their use will be confined to a trial that the Cass review says should form part of a broader research programme into the effects of masculinising and feminising hormones.
- Transgender
- Young people

Veteran trans campaigner: ‘Cass review has potential for positive change’

Cass review must be used as ‘watershed moment’ for NHS gender services, says Streeting

‘This isn’t how good scientific debate happens’: academics on culture of fear in gender medicine research

Five thousand children with gender-related distress awaiting NHS care in England

Ban on children’s puberty blockers to be enforced in private sector in England

What Cass review says about surge in children seeking gender services

Adult transgender clinics in England face inquiry into patient care

‘Children are being used as a football’: Hilary Cass on her review of gender identity services

Thousands of children unsure of gender identity ‘let down by NHS’, report finds

Most viewed

VIDEO
COMMENTS
Introduction. The United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP) was a pivotal document for the world's Indigenous Peoples [].In addition to being quoted in numerous policy, research, and community initiatives since it was adopted, the declaration is now being used to evaluate the adequacy of national laws; for interpreting state obligations at the global level; and ...
The resurgence of Western psychedelic research and practice has led to increasing concerns from many Indigenous Nations regarding cultural appropriation, lack of recognition of the sacred cultural positioning of these medicines, exclusionary practices in research and praxis, and patenting of traditional medicines. Indigenous voices and leadership have been notably absent from the Western ...
Methods: A systematic search of multiple databases was performed utilizing an established scoping review framework. A consequent title and abstract review of articles published on traditional Indigenous medicine in the North American context was completed. Findings: Of the 4,277 published studies identified, 249 met the inclusion criteria ...
The persistence of colonial legacy shapes significant inequities in the physical, mental, and emotional health and well-being for marginalized groups, particularly for Indigenous Peoples globally (Gracey & King, 2009; Kirmayer et al., 2014; Nutton & Fast, 2015; Walters & Simoni, 2009).For example, in the United States, American Indians and Alaskan Natives have an estimated life expectancy that ...
An estimated 370 million Indigenous people reside in 90 countries, approximately 5% of the global population. Approximately 300 million Indigenous people live in extremely disadvantaged rural locations, constituting 15% of the global poor (United Nations, 2013, 2017).Indigenous people have suffered from historic injustices due to colonization and the dispossession of their lands, territories ...
Coproduced health research is a collaborative process that brings together researchers and a diverse range of nonacademic 'stakeholders' (some will prefer 'partners' or even 'knowledge ...
Throughout the world, indigenous peoples have advocated for the right to retain their cultural beliefs and traditional medicine practices. In 2007, the more than 370 million people representing 5000 distinct groups throughout the world received global recognition with the adoption of the United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP). UNDRIP Article 24 affirms the ...
Objective: This systematic review aimed to describe traditional, complementary and integrative medicine (TCIM) use among Indigenous peoples with diabetes from Australia, Canada, New Zealand and the United States (US).. Methods: A systematic search following the PRISMA (Preferred Reporting Items for Systematic Reviews and MetaAnalyses) statement guidelines was conducted.
Background Despite the documented continued use of traditional healing methods, modalities and its associated practitioners by Indigenous groups across North America, it is presumed that widespread knowledge is elusive amongst most Western trained health professionals and systems. This despite that the approximately 7.5 million Indigenous peoples who currently reside in Canada and the United ...
Education is an important value in human cultures. Goulet and Goulet (2014) identified three forms of the teaching-learning process conceptualized in the indigenous Cree language: "kiskinaumegahin (teaching another), kiskinaumasowin (teaching oneself), and kiskinaumatowin (teaching each other)" (p. 65). While teaching as a profession was necessitated by the increased complexities of modern ...
Traditional medicine among the Aboriginal peoples of the Canadian boreal forest is based on oral tradition transmitted through several generations [13, 47].It is a cultural phenomenon, dynamic and adaptive, like language and other cultural manifestations [].The holistic approach of Aboriginal healing systems involves spirituality and intimate connection with the natural environment [47, 48].
Conclusions. This scoping review was an attempt to catalogue the wide array of published research in the. peer-reviewed and online grey literature on traditional Indigenous medicine in North ...
Various research studies have indicated that the bioactivities of C. tuberculata might be due to the presence of certain classes of compounds including pregnane ... Bibi T, Khan MA, Ahmad M, Zafar M, Hina S. Indigenous knowledge of folk medicine by the women of Kalat and Khuzdar Regions of Balochistan, Pakistan. Pakistan J Bot. 2010;42(3):1465 ...
Dahlberg and Trygger, "Indigenous Medicine and Primary Healthcare," 8 9. 23 Konadu, I ndigenous Medicine and Knowledge , 159; Robert W. Wyllis, "Ghanaian Spiritu al
a. series. of. prescriptions handed down from generation to. generation over a period of 3,000 years. Indigenous Medical Practitioners historically. enjoyed a noble position in the soc ial ...
Ethical principles of traditional Indigenous medicine to guide western psychedelic research and practice Yuria Celidwen,a ,m* Nicole Redvers,bc Cicilia Githaiga,d Janeth Calambás,e,m Karen Añaños,f Miguel Evanjuanoy Chindoy, g,m Riccardo Vitale, Juan Nelson Rojas,h ,i mDelores Mondragón,j Yuniur Vázquez Rosalío,k,m and Angelina Sacbajál aUniversity of California, Berkeley, CA, USA
The results showed that 11% of the local population use traditional medicine, against 67% who use both traditional and modern medicine. The ethnomedicinal uses of 44 medicinal species representing 28 families were reported on. Lamiaceae were the most representative and include 32% of the identified species. The medicinal use revealed that ...
Background Medicinal plants have been used countless times for curing diseases mainly in developing countries. They are easily available with little to no side effects when compared to modern medicine. This manuscript encompasses information on ethnomedicinal plants in Champhai district, located in the North East Region (NER) of India. The region lies within Indo-Burma biodiversity hotspot ...
The need to classify disease and predict outcomes is as old as medicine itself. Nearly 50 years ago, the advantage of applying multivariable statistics to these problems became evident. 1 Since then, the increasing availability of databases containing often-complex clinical information from tens or even hundreds of millions of patients, combined with powerful statistical techniques and ...
The Cass review: an opportunity to unite behind evidence informed care in gender medicine. At the heart of Hilary Cass's review of gender identity services in the NHS is a concern for the welfare of "children and young people" (doi: 10.1136/bmj.q820 ). 1 Her stated ambition is to ensure that those experiencing gender dysphoria receive a ...
John W. Vinson (left) and an unnamed colleague dissect rats for research, Norway, March 18, 1959. From the John W. Vinson papers, 1923-1979 (inclusive), 1961-1979 (bulk), H MS c479. Harvard Medical Library, Francis A. Countway Library of Medicine, Boston, Mass.
A total of 1414 patients underwent randomization (701 to the TAVI group and 713 to the SAVR group). The mean (±SD) age of the patients was 74±4 years; 57% were men, and the median Society of ...
A total of 3260 patients were assigned to receive empagliflozin and 3262 to receive placebo. During a median follow-up of 17.9 months, a first hospitalization for heart failure or death from any ...
PLOS ONE RESEARCH ARTICLE Traditional Indigenous medicine in North America: A scoping review Nicole Redvers ID1,2*, Be'sha Blondin2 1 Department of Family & Community Medicine, School of Medicine and Health Sciences, University of North Dakota, Grand Forks, North Dakota, United States of America, 2 Arctic Indigenous Wellness Foundation ...
To help orient this consensus process more directly towards solutions, we further summarize in Table 2 additional recommended practical solutions within Western psychedelic research and practice. This consensus process emphasized that by continuing the extraction and commercialization of various traditional Indigenous medicines, Western institutions are destroying the core themes of Indigenous ...
Over the past 6 years, sports wagering has become accessible to most individuals in the US via mobile applications or websites. 1 Increasing evidence suggests that sports wagering is associated with greater substance use and misuse, particularly alcohol, and symptoms of alcohol use disorder. 2-4 Alcohol consumption is higher among sports gamblers, 3 and sports gamblers often use substances ...
medicine in the North American context by identifying the types and sources of evidence available, and b. to provide an evidence-informed resource guide for medical practitioners, scholars, and communities to better inform "practice, policymaking, and research [26]" in Indigenous communities. PLOS ONE Indigenous medicine in North America
Last modified on Wed 10 Apr 2024 01.00 EDT. The head of the world's largest review into children's care has said that gender medicine is "built on shaky foundations". Dr Hilary Cass, the ...