Practical foundations of machine learning for addiction research. Part I. Methods and techniques
Affiliations.
- 1 Instituto de Cálculo, FCEyN, Universidad de Buenos Aires - CONICET, Buenos Aires, Argentina.
- 2 FaMAF, Universidad Nacional de Córdoba, Córdoba, Argentina.
- 3 Department of Psychiatry, University of Iowa, Iowa City, IA, USA.
- PMID: 35389305
- DOI: 10.1080/00952990.2021.1995739
Machine learning assembles a broad set of methods and techniques to solve a wide range of problems, such as identifying individuals with substance use disorders (SUD), finding patterns in neuroimages, understanding SUD prognostic factors and their association, or determining addiction genetic underpinnings. However, the addiction research field underuses machine learning. This two-part narrative review focuses on machine learning tools and concepts, providing an introductory insight into their capabilities to facilitate their understanding and acquisition by addiction researchers. This first part presents supervised and unsupervised methods such as linear models, naive Bayes, support vector machines, artificial neural networks, and k-means. We illustrate each technique with examples of its use in current addiction research. We also present some open-source programming tools and methodological good practices that facilitate using these techniques. Throughout this work, we emphasize a continuum between applied statistics and machine learning, we show their commonalities, and provide sources for further reading to deepen the understanding of these methods. This two-part review is a primer for the next generation of addiction researchers incorporating machine learning in their projects. Researchers will find a bridge between applied statistics and machine learning, ways to expand their analytical toolkit, recommendations to incorporate well-established good practices in addiction data analysis (e.g., stating the rationale for using newer analytical tools, calculating sample size, improving reproducibility), and the vocabulary to enhance collaboration between researchers who do not conduct data analyses and those who do.
Keywords: Machine learning; addiction; adicciones; aprendizaje automatico; artificial intelligence; ciencia de datos; data science; inteligencia artificial; métodos estadísticos; statistical methods.

Publication types
- Bayes Theorem
- Behavior, Addictive* / diagnosis
- Machine Learning
- Reproducibility of Results
- Substance-Related Disorders*
- Support Vector Machine
Investigating Digital Addiction in the Context of Machine Learning Based System Design
- Conference paper
- First Online: 28 March 2023
- Cite this conference paper

- Geetika Johar 14 &
- Ravindra Patel 15
Part of the book series: Lecture Notes in Networks and Systems ((LNNS,volume 649))
Included in the following conference series:
- International Conference on Innovations in Bio-Inspired Computing and Applications
469 Accesses
In recent years popularity and availability of digital content are increased due to low-cost internet and the availability of smartphones. The suitable and appropriate use of smartphones will help us in our daily personal and professional life. On the other hand, excessive and extreme use of smartphones may invite different kinds of physical and mental disorders. In this context, we proposed to review recent literature about digital addiction. First, we collected 20 recent research articles about different kinds of addictions and the current state of research trends. Then the role of machine learning in order to deal with addiction has been studied. Further some articles are explored for locating the suitable dataset used, techniques of data collection, machine learning algorithms being applied, area of employment, feature selected, and consequences of the articles. Finally based on the collected experiences of the recent efforts we proposed a Smartphone Addiction (SA) prediction and support framework using the Machine Learning (ML) technique. Finally, the conclusion has been made and future plan has also been discussed.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Cash, H., Rae, C.D., Steel, A.H., Winkler, A.: Internet addiction: a brief summary of research and practice. Current Psychiatry Rev. 8 (292–298), 292 (2012)
Article Google Scholar
Montag, C., Wegmann, E., Sariyska, R., Demetrovics, Z., Brand, M.: How to overcome taxonomical problems in the study of Internet use disorders and what to do with smartphone addiction. J. Behav. Addict. 9 (4), 908–914 (2020)
Noë, B., Turner, L.D., Linden, D.E.J., Allen, S.M., Winkens, B., Whitaker, R.M.: Identifying indicators of smartphone addiction through user-app interaction. Comput. Hum. Behav. 99 , 56–65 (2019)
Panova, T., Carbonell, X.: Is smartphone addiction really an addiction. J. Behav. Addict. 7 (2), 252–259 (2018)
Sunday, O.J., Adesope, O.O., Maarhuis, P.L.: The effects of smartphone addiction on learning: a meta-analysis. Comput. Hum. Behav. Rep. 4 , 100114 (2021)
Elhai, J.D., Levine, J.C., Hall, B.J.: Problematic smartphone use and mental health problems: current state of research and future directions. Dusunen Adam J. Psychiatry Neurological Sci. 32 , 1–3 (2019)
Google Scholar
Cha, S.S., Seo, B.K.: Smartphone use and smartphone addiction in middle school students in Korea: prevalence, social networking service, and game use. Health Psychol. Open 5 , 1–15 (2018)
Yu, S., Sussman, S.: Does smartphone addiction fall on a continuum of addictive behaviors? Int. J. Environ. Res. Public Health 17 , 422 (2020)
Tateno, M., Kim, D.J., Teo, A.R., Skokauskas, N., Guerrero, A.P.S., Kato, T.A.: Smartphone addiction in Japanese college students: usefulness of the Japanese version of the smartphone addiction scale as a screening tool for a new form of internet addiction. Psychiatry Investing 16 (2), 115–120 (2019)
Gökçearslan, Ş, Uluyol, Ç., Şahin, S.: Smartphone addiction, cyberloafing, stress and social support among university students: a path analysis. Child Youth Serv. Rev. 91 , 47–54 (2018)
Durak, H.Y.: Investigation of nomophobia and smartphone addiction predictors among adolescents in Turkey: demographic variables and academic performance, The Social Science Journal (2017)
Masud, M.T., Mamun, M.A., Thapa, K., Lee, D.H., Griffiths, M.D., Yang, S.H.: Unobtrusive monitoring of behavior and movement patterns to detect clinical depression severity level via smartphone. J. Biomed. Inform. 103 , 103371 (2020)
Mishra, S.: Learning from usage analysis of mobile devices. Procedia Comput. Sci. 167 , 1648–1655 (2020)
Ji, H.M., Chen, L.Y., Hsiao, T.C.: Real-Time Detection of Internet Addiction Using Reinforcement Learning System. In: GECCO ’19 Companion. Czech Republic, Association for Computing Machinery, Prague (2019)
Book Google Scholar
Hasegawa, T., Koshino, M.: Representation learning by convolutional neural network for smartphone sensor based activity recognition. In: CIIS 2019, Bangkok, Thailand (2019)
Chikersal, P., et al.: Detecting depression and predicting its onset using longitudinal symptoms captured by passive sensing: a machine learning approach with robust feature selection. ACM Trans. Comput.-Hum. Interact. 28 (1), Article 3, January 2021
Lee, M.S., Han, M.M.C., Pak, J.G.: Analysis of behavioral characteristics of smartphone addiction using data mining. Appl. Sci. 8 , 1191 (2018)
Sağbaş, E.A., Korukoglu, S., Balli, S.: Stress detection via keyboard typing behaviors by using smartphone sensors and machine learning techniques. J. Med. Syst. 44 (4), 1–12 (2020). https://doi.org/10.1007/s10916-020-1530-z
Elhai, J.D., Yang, H., Rozgonjuk, D., Montag, C.: Using machine learning to model problematic smartphone use severity: the significant role of fear of missing out. Addict. Behav. 103 , 106261 (2020)
Park, J., Jeong, J.E., Park, S.Y., Rho, M.J.: Development of the smartphone addiction risk rating score for a smartphone addiction management application. Front. Public Health 8 , 485 (2020)
Download references
Author information
Authors and affiliations.
Department of Computer Science and Engineering, UIT, RGPV, Bhopal, India
Geetika Johar
Department of Computer Applications, UIT, RGPV, Bhopal, India
Ravindra Patel
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Geetika Johar .
Editor information
Editors and affiliations.
Faculty of Computing and Data Science, Flame University, Pune, Maharashtra, India
Ajith Abraham
Computer Science and Engineering Department, Thapar Institute of Engineering and Technology, Patiala, Punjab, India
Scientific Network for Innovation and Research Excellence, Machine Intelligence Research Labs, Auburn, WA, USA
Niketa Gandhi
Interdisciplinary Studies Research Center (ISRC), Institute of Engineering, Polytechnique of Porto (ISEP/P.PORTO), INOV (Institute for Systems and Computer Engineering, Technology and Science), Porto, Portugal
Ana Maria Madureira
Department of Industrial Engineering, Istanbul Technical University, Istanbul, Türkiye
Cengiz Kahraman
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper.
Johar, G., Patel, R. (2023). Investigating Digital Addiction in the Context of Machine Learning Based System Design. In: Abraham, A., Bajaj, A., Gandhi, N., Madureira, A.M., Kahraman, C. (eds) Innovations in Bio-Inspired Computing and Applications. IBICA 2022. Lecture Notes in Networks and Systems, vol 649. Springer, Cham. https://doi.org/10.1007/978-3-031-27499-2_9
Download citation
DOI : https://doi.org/10.1007/978-3-031-27499-2_9
Published : 28 March 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-27498-5
Online ISBN : 978-3-031-27499-2
eBook Packages : Intelligent Technologies and Robotics Intelligent Technologies and Robotics (R0)
Share this paper
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Frontiers in Psychology
- Cognitive Science
- Research Topics
Machine Learning Approaches in Addiction Research
Total Downloads
Total Views and Downloads
About this Research Topic
Addiction is a brain disorder characterized by repeated use of drugs, or repetitive engagement in behavior such as gambling, despite harm to self and others. It can be also classified into substance and non-substance addiction (e.g., behavioral addiction) and both types of addiction are associated with severe ...
Keywords : • Addiction, Machine learning, Classification, Clustering, Multivariate pattern analysis
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.
Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password

Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Substance Use Disorders and Addiction: Mechanisms, Trends, and Treatment Implications
- Ned H. Kalin , M.D.
Search for more papers by this author
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health ( 1 ) suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol. When considering other substances, the report estimated that 4.4 million individuals had a marijuana use disorder and that 2 million people suffered from an opiate use disorder. It is well known that stress is associated with an increase in the use of alcohol and other substances, and this is particularly relevant today in relation to the chronic uncertainty and distress associated with the COVID-19 pandemic along with the traumatic effects of racism and social injustice. In part related to stress, substance use disorders are highly comorbid with other psychiatric illnesses: 9.2 million adults were estimated to have a 1-year prevalence of both a mental illness and at least one substance use disorder. Although they may not necessarily meet criteria for a substance use disorder, it is well known that psychiatric patients have increased usage of alcohol, cigarettes, and other illicit substances. As an example, the survey estimated that over the preceding month, 37.2% of individuals with serious mental illnesses were cigarette smokers, compared with 16.3% of individuals without mental illnesses. Substance use frequently accompanies suicide and suicide attempts, and substance use disorders are associated with a long-term increased risk of suicide.
Addiction is the key process that underlies substance use disorders, and research using animal models and humans has revealed important insights into the neural circuits and molecules that mediate addiction. More specifically, research has shed light onto mechanisms underlying the critical components of addiction and relapse: reinforcement and reward, tolerance, withdrawal, negative affect, craving, and stress sensitization. In addition, clinical research has been instrumental in developing an evidence base for the use of pharmacological agents in the treatment of substance use disorders, which, in combination with psychosocial approaches, can provide effective treatments. However, despite the existence of therapeutic tools, relapse is common, and substance use disorders remain grossly undertreated. For example, whether at an inpatient hospital treatment facility or at a drug or alcohol rehabilitation program, it was estimated that only 11% of individuals needing treatment for substance use received appropriate care in 2018. Additionally, it is worth emphasizing that current practice frequently does not effectively integrate dual diagnosis treatment approaches, which is important because psychiatric and substance use disorders are highly comorbid. The barriers to receiving treatment are numerous and directly interact with existing health care inequities. It is imperative that as a field we overcome the obstacles to treatment, including the lack of resources at the individual level, a dearth of trained providers and appropriate treatment facilities, racial biases, and the marked stigmatization that is focused on individuals with addictions.
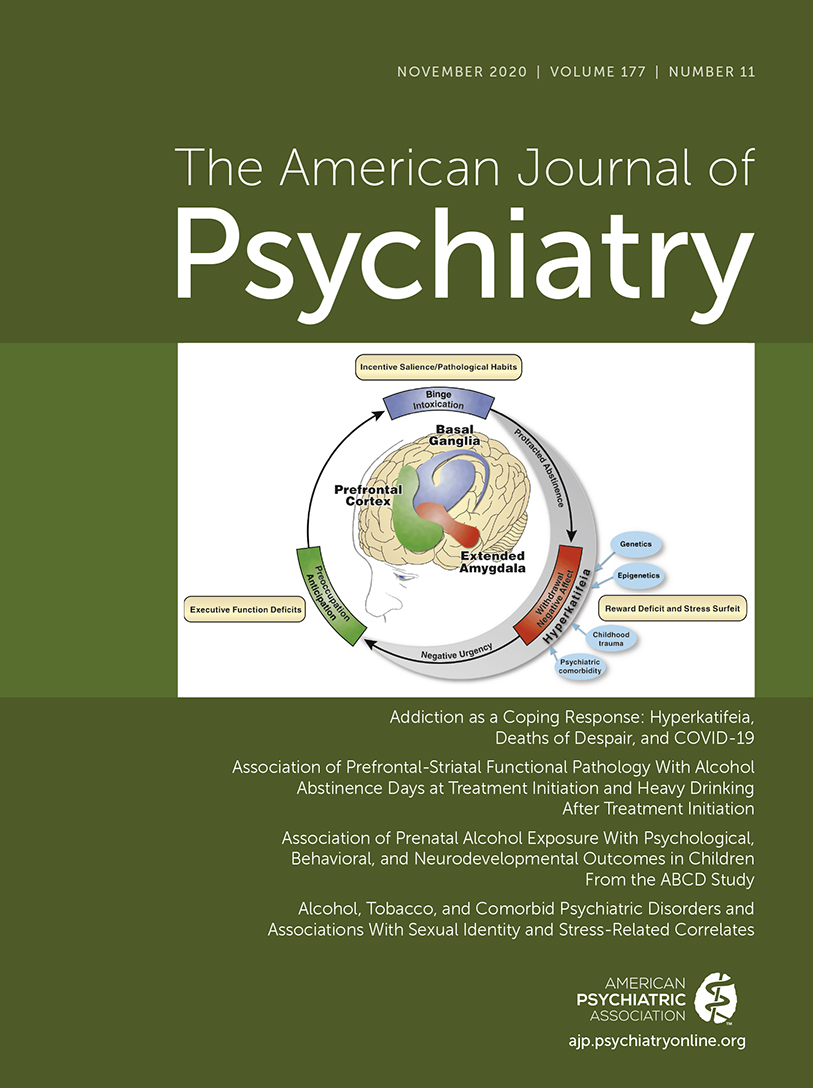
This issue of the Journal is focused on understanding factors contributing to substance use disorders and their comorbidity with psychiatric disorders, the effects of prenatal alcohol use on preadolescents, and brain mechanisms that are associated with addiction and relapse. An important theme that emerges from this issue is the necessity for understanding maladaptive substance use and its treatment in relation to health care inequities. This highlights the imperative to focus resources and treatment efforts on underprivileged and marginalized populations. The centerpiece of this issue is an overview on addiction written by Dr. George Koob, the director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and coauthors Drs. Patricia Powell (NIAAA deputy director) and Aaron White ( 2 ). This outstanding article will serve as a foundational knowledge base for those interested in understanding the complex factors that mediate drug addiction. Of particular interest to the practice of psychiatry is the emphasis on the negative affect state “hyperkatifeia” as a major driver of addictive behavior and relapse. This places the dysphoria and psychological distress that are associated with prolonged withdrawal at the heart of treatment and underscores the importance of treating not only maladaptive drug-related behaviors but also the prolonged dysphoria and negative affect associated with addiction. It also speaks to why it is crucial to concurrently treat psychiatric comorbidities that commonly accompany substance use disorders.
Insights Into Mechanisms Related to Cocaine Addiction Using a Novel Imaging Method for Dopamine Neurons
Cassidy et al. ( 3 ) introduce a relatively new imaging technique that allows for an estimation of dopamine integrity and function in the substantia nigra, the site of origin of dopamine neurons that project to the striatum. Capitalizing on the high levels of neuromelanin that are found in substantia nigra dopamine neurons and the interaction between neuromelanin and intracellular iron, this MRI technique, termed neuromelanin-sensitive MRI (NM-MRI), shows promise in studying the involvement of substantia nigra dopamine neurons in neurodegenerative diseases and psychiatric illnesses. The authors used this technique to assess dopamine function in active cocaine users with the aim of exploring the hypothesis that cocaine use disorder is associated with blunted presynaptic striatal dopamine function that would be reflected in decreased “integrity” of the substantia nigra dopamine system. Surprisingly, NM-MRI revealed evidence for increased dopamine in the substantia nigra of individuals using cocaine. The authors suggest that this finding, in conjunction with prior work suggesting a blunted dopamine response, points to the possibility that cocaine use is associated with an altered intracellular distribution of dopamine. Specifically, the idea is that dopamine is shifted from being concentrated in releasable, functional vesicles at the synapse to a nonreleasable cytosolic pool. In addition to providing an intriguing alternative hypothesis underlying the cocaine-related alterations observed in substantia nigra dopamine function, this article highlights an innovative imaging method that can be used in further investigations involving the role of substantia nigra dopamine systems in neuropsychiatric disorders. Dr. Charles Bradberry, chief of the Preclinical Pharmacology Section at the National Institute on Drug Abuse, contributes an editorial that further explains the use of NM-MRI and discusses the theoretical implications of these unexpected findings in relation to cocaine use ( 4 ).
Treatment Implications of Understanding Brain Function During Early Abstinence in Patients With Alcohol Use Disorder
Developing a better understanding of the neural processes that are associated with substance use disorders is critical for conceptualizing improved treatment approaches. Blaine et al. ( 5 ) present neuroimaging data collected during early abstinence in patients with alcohol use disorder and link these data to relapses occurring during treatment. Of note, the findings from this study dovetail with the neural circuit schema Koob et al. provide in this issue’s overview on addiction ( 2 ). The first study in the Blaine et al. article uses 44 patients and 43 control subjects to demonstrate that patients with alcohol use disorder have a blunted neural response to the presentation of stress- and alcohol-related cues. This blunting was observed mainly in the ventromedial prefrontal cortex, a key prefrontal regulatory region, as well as in subcortical regions associated with reward processing, specifically the ventral striatum. Importantly, this finding was replicated in a second study in which 69 patients were studied in relation to their length of abstinence prior to treatment and treatment outcomes. The results demonstrated that individuals with the shortest abstinence times had greater alterations in neural responses to stress and alcohol cues. The authors also found that an individual’s length of abstinence prior to treatment, independent of the number of days of abstinence, was a predictor of relapse and that the magnitude of an individual’s neural alterations predicted the amount of heavy drinking occurring early in treatment. Although relapse is an all too common outcome in patients with substance use disorders, this study highlights an approach that has the potential to refine and develop new treatments that are based on addiction- and abstinence-related brain changes. In her thoughtful editorial, Dr. Edith Sullivan from Stanford University comments on the details of the study, the value of studying patients during early abstinence, and the implications of these findings for new treatment development ( 6 ).
Relatively Low Amounts of Alcohol Intake During Pregnancy Are Associated With Subtle Neurodevelopmental Effects in Preadolescent Offspring
Excessive substance use not only affects the user and their immediate family but also has transgenerational effects that can be mediated in utero. Lees et al. ( 7 ) present data suggesting that even the consumption of relatively low amounts of alcohol by expectant mothers can affect brain development, cognition, and emotion in their offspring. The researchers used data from the Adolescent Brain Cognitive Development Study, a large national community-based study, which allowed them to assess brain structure and function as well as behavioral, cognitive, and psychological outcomes in 9,719 preadolescents. The mothers of 2,518 of the subjects in this study reported some alcohol use during pregnancy, albeit at relatively low levels (0 to 80 drinks throughout pregnancy). Interestingly, and opposite of that expected in relation to data from individuals with fetal alcohol spectrum disorders, increases in brain volume and surface area were found in offspring of mothers who consumed the relatively low amounts of alcohol. Notably, any prenatal alcohol exposure was associated with small but significant increases in psychological problems that included increases in separation anxiety disorder and oppositional defiant disorder. Additionally, a dose-response effect was found for internalizing psychopathology, somatic complaints, and attentional deficits. While subtle, these findings point to neurodevelopmental alterations that may be mediated by even small amounts of prenatal alcohol consumption. Drs. Clare McCormack and Catherine Monk from Columbia University contribute an editorial that provides an in-depth assessment of these findings in relation to other studies, including those assessing severe deficits in individuals with fetal alcohol syndrome ( 8 ). McCormack and Monk emphasize that the behavioral and psychological effects reported in the Lees et al. article would not be clinically meaningful. However, it is feasible that the influences of these low amounts of alcohol could interact with other predisposing factors that might lead to more substantial negative outcomes.
Increased Comorbidity Between Substance Use and Psychiatric Disorders in Sexual Identity Minorities
There is no question that victims of societal marginalization experience disproportionate adversity and stress. Evans-Polce et al. ( 9 ) focus on this concern in relation to individuals who identify as sexual minorities by comparing their incidence of comorbid substance use and psychiatric disorders with that of individuals who identify as heterosexual. By using 2012−2013 data from 36,309 participants in the National Epidemiologic Study on Alcohol and Related Conditions–III, the authors examine the incidence of comorbid alcohol and tobacco use disorders with anxiety, mood disorders, and posttraumatic stress disorder (PTSD). The findings demonstrate increased incidences of substance use and psychiatric disorders in individuals who identified as bisexual or as gay or lesbian compared with those who identified as heterosexual. For example, a fourfold increase in the prevalence of PTSD was found in bisexual individuals compared with heterosexual individuals. In addition, the authors found an increased prevalence of substance use and psychiatric comorbidities in individuals who identified as bisexual and as gay or lesbian compared with individuals who identified as heterosexual. This was most prominent in women who identified as bisexual. For example, of the bisexual women who had an alcohol use disorder, 60.5% also had a psychiatric comorbidity, compared with 44.6% of heterosexual women. Additionally, the amount of reported sexual orientation discrimination and number of lifetime stressful events were associated with a greater likelihood of having comorbid substance use and psychiatric disorders. These findings are important but not surprising, as sexual minority individuals have a history of increased early-life trauma and throughout their lives may experience the painful and unwarranted consequences of bias and denigration. Nonetheless, these findings underscore the strong negative societal impacts experienced by minority groups and should sensitize providers to the additional needs of these individuals.
Trends in Nicotine Use and Dependence From 2001–2002 to 2012–2013
Although considerable efforts over earlier years have curbed the use of tobacco and nicotine, the use of these substances continues to be a significant public health problem. As noted above, individuals with psychiatric disorders are particularly vulnerable. Grant et al. ( 10 ) use data from the National Epidemiologic Survey on Alcohol and Related Conditions collected from a very large cohort to characterize trends in nicotine use and dependence over time. Results from their analysis support the so-called hardening hypothesis, which posits that although intervention-related reductions in nicotine use may have occurred over time, the impact of these interventions is less potent in individuals with more severe addictive behavior (i.e., nicotine dependence). When adjusted for sociodemographic factors, the results demonstrated a small but significant increase in nicotine use from 2001–2002 to 2012–2013. However, a much greater increase in nicotine dependence (46.1% to 52%) was observed over this time frame in individuals who had used nicotine during the preceding 12 months. The increases in nicotine use and dependence were associated with factors related to socioeconomic status, such as lower income and lower educational attainment. The authors interpret these findings as evidence for the hardening hypothesis, suggesting that despite the impression that nicotine use has plateaued, there is a growing number of highly dependent nicotine users who would benefit from nicotine dependence intervention programs. Dr. Kathleen Brady, from the Medical University of South Carolina, provides an editorial ( 11 ) that reviews the consequences of tobacco use and the history of the public measures that were initially taken to combat its use. Importantly, her editorial emphasizes the need to address health care inequity issues that affect individuals of lower socioeconomic status by devoting resources to develop and deploy effective smoking cessation interventions for at-risk and underresourced populations.
Conclusions
Maladaptive substance use and substance use disorders are highly prevalent and are among the most significant public health problems. Substance use is commonly comorbid with psychiatric disorders, and treatment efforts need to concurrently address both. The papers in this issue highlight new findings that are directly relevant to understanding, treating, and developing policies to better serve those afflicted with addictions. While treatments exist, the need for more effective treatments is clear, especially those focused on decreasing relapse rates. The negative affective state, hyperkatifeia, that accompanies longer-term abstinence is an important treatment target that should be emphasized in current practice as well as in new treatment development. In addition to developing a better understanding of the neurobiology of addictions and abstinence, it is necessary to ensure that there is equitable access to currently available treatments and treatment programs. Additional resources must be allocated to this cause. This depends on the recognition that health care inequities and societal barriers are major contributors to the continued high prevalence of substance use disorders, the individual suffering they inflict, and the huge toll that they incur at a societal level.
Disclosures of Editors’ financial relationships appear in the April 2020 issue of the Journal .
1 US Department of Health and Human Services: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality: National Survey on Drug Use and Health 2018. Rockville, Md, SAMHSA, 2019 ( https://www.samhsa.gov/data/nsduh/reports-detailed-tables-2018-NSDUH ) Google Scholar
2 Koob GF, Powell P, White A : Addiction as a coping response: hyperkatifeia, deaths of despair, and COVID-19 . Am J Psychiatry 2020 ; 177:1031–1037 Link , Google Scholar
3 Cassidy CM, Carpenter KM, Konova AB, et al. : Evidence for dopamine abnormalities in the substantia nigra in cocaine addiction revealed by neuromelanin-sensitive MRI . Am J Psychiatry 2020 ; 177:1038–1047 Link , Google Scholar
4 Bradberry CW : Neuromelanin MRI: dark substance shines a light on dopamine dysfunction and cocaine use (editorial). Am J Psychiatry 2020 ; 177:1019–1021 Abstract , Google Scholar
5 Blaine SK, Wemm S, Fogelman N, et al. : Association of prefrontal-striatal functional pathology with alcohol abstinence days at treatment initiation and heavy drinking after treatment initiation . Am J Psychiatry 2020 ; 177:1048–1059 Link , Google Scholar
6 Sullivan EV : Why timing matters in alcohol use disorder recovery (editorial). Am J Psychiatry 2020 ; 177:1022–1024 Abstract , Google Scholar
7 Lees B, Mewton L, Jacobus J, et al. : Association of prenatal alcohol exposure with psychological, behavioral, and neurodevelopmental outcomes in children from the Adolescent Brain Cognitive Development Study . Am J Psychiatry 2020 ; 177:1060–1072 Link , Google Scholar
8 McCormack C, Monk C : Considering prenatal alcohol exposure in a developmental origins of health and disease framework (editorial). Am J Psychiatry 2020 ; 177:1025–1028 Abstract , Google Scholar
9 Evans-Polce RJ, Kcomt L, Veliz PT, et al. : Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates . Am J Psychiatry 2020 ; 177:1073–1081 Abstract , Google Scholar
10 Grant BF, Shmulewitz D, Compton WM : Nicotine use and DSM-IV nicotine dependence in the United States, 2001–2002 and 2012–2013 . Am J Psychiatry 2020 ; 177:1082–1090 Link , Google Scholar
11 Brady KT : Social determinants of health and smoking cessation: a challenge (editorial). Am J Psychiatry 2020 ; 177:1029–1030 Abstract , Google Scholar
- Cited by None
- Substance-Related and Addictive Disorders
- Addiction Psychiatry
- Transgender (LGBT) Issues
Analysis and Prediction of Drugs using Machine Learning Techniques
Ieee account.
- Change Username/Password
- Update Address
Purchase Details
- Payment Options
- Order History
- View Purchased Documents
Profile Information
- Communications Preferences
- Profession and Education
- Technical Interests
- US & Canada: +1 800 678 4333
- Worldwide: +1 732 981 0060
- Contact & Support
- About IEEE Xplore
- Accessibility
- Terms of Use
- Nondiscrimination Policy
- Privacy & Opting Out of Cookies
A not-for-profit organization, IEEE is the world's largest technical professional organization dedicated to advancing technology for the benefit of humanity. © Copyright 2024 IEEE - All rights reserved. Use of this web site signifies your agreement to the terms and conditions.
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

EFFECTS OF MOBILE GAMES (MOBILE LEGENDS) TO THE BEHAVIOR AND HEALTH OF A SHS STUDENTS

Related Papers
Int. J. of Aquatic Science
Bharath Yuvaraj
WSEAS Transactions on …
Idayu Sabri
Asian Journal of Clinical Pediatrics and Neonatology
Academia I N T E R N A T I O N A L Journals
Background: The present research study was design to investigate the factors affecting academic performance as well as physical performance of school going children of schools of Indore district. The variable under consideration were academic performance and physical performance as a dependent variable and gender, age, residential area (rural/urban),accommodation, study hours, sleep hours ,time spend on mobile and electronic gaming were independent variables. Subjects and Methods: The data was collected from 670 students of age group 11-15years of different school of Indore using simple random sampling technique.378 student were found to have access to mobile gaming/electronic gaming with more than 2 hour of routing access. Results: For analysis Chi-square was used. The finding revealed that school performance regarding physical activity, academic performance, & psychomotor effect in the class had declined with repetitive use of mobile phone and electronic gaming. Conclusion: A linear model was also proposed that will be helpful to improve the performance of school going Teenagers.
Eduardo Edu C . Cornillez Jr. , Jessie Richie De los Santos , Vicente D. Carillo, Jr
Abstract: The increasing number of students who are hooked on playing online mobile games (OMG) is alarming. As such, this study was realized to address the problem. This study assessed the gaming profile towards OMG and its relation to the academic performance of the engineering students of Eastern Visayas State University Tanauan Campus (EVSUTC). Specifically, the study investigated the correlation between student's number of hours spent on playing OMG (at school and home), commonly played OMG (at school and home), reasons for playing OMG and attitudes on playing OMG with academic performance utilizing Eta and Pearson r correlation analyses. A random sample of 134 student respondents were selected through purposive sampling of those who are playing OMG using their mobile phones. Descriptive correlational research design was utilized and a validated survey instrument was employed to gather the needed information. The findings revealed that majority of the students played mobile legends and spent mostly 2 hours playing OMG for a reason of boredom. The overall attitudes of the students on playing OMG were interpreted as Less Favorable (M=2.58, SD=1.13). Out of the independent variables being set in the study, the number of hours spent on playing OMG at home (r=-0.188, p=0.039) and commonly played OMG at school (r=0.203, p=0.045) were found significantly correlated with student's academic performance. Hence, the students' time spent on playing OMG at home and the type of games that students played at school have significant bearing to their academic performance. As such, delimiting student's usage of internet can be made to address the problem.
Jurnal Basicedu
Faizatul Husna
Research into mobile game addiction has increased over the previous two decades. The purpose of this study was to investigate the association between on-line mobile gaming and academic performances among adolescent students in Aceh's elementary schools. The study revealed that boys are more of a player compared to girls who often play games and those who play online games are around 11-12 years old have an average playing time 3-5 hours/day. The research population consisted of elementary students from Aceh, with a sample size of 55 pupils. Included in the study was the Game Addiction Scale (Lemmens et al., 2009). Then, using regression analysis, the hypothesis was tested. From the finding, we can conclude that academic performance was found to be negatively associated with online gaming. This is owing to the fact that playing games for long periods of time reduces their ability to focus on academic tasks. This study can serve as a reference to adolescents online gaming habits, ...
International Journal Of Community Medicine And Public Health
Balaji Arumugam
Background: Nowadays the teens playing outdoor games are difficult to be seen and of course, they play all these games not in reality but in a screen using video games. The biggest revolution in electronic world has put our teens more addicted towards video games which not only affect their academic performance but also have impact on their behaviour and health. The objectives of the study were to assess the pattern of video game usage among the study population; to determine the influence of video game in behaviour of the study population.Methods: The study was conducted as a cross sectional study during January and February 2018, among medical students of tertiary care hospital, Chennai. The data was collected using preformed pretested questionnaire. Data were analyzed using SPSS 21.Results: Out of 211 study participants, majority 168 (80%) were males. Around, 97 (45.9%) participants, liked to play during night hours and most 114 (54.1%) of them preferred adventure and racing game...
Psychology and Education: A Multidisciplinary Journal
Psychology and Education
A descriptive cross-sectional study enabled the researchers to explore the level of mobile game dependency among the students enrolled in Telesforo and Natividad Alfonso High School (TNAHS) for the school year 2022-2023. This method also allowed the assessment of the social effects of mobile game dependency, which was also the objective of this study. This study employed a quantitative research design with the purposive sampling procedure applied as the sampling technique for data selection and printed self-questionnaires that were provided by the researchers as the research instrument. A total of 123 respondents participated in this study, comprising both junior high and senior high school students. The findings show that the respondents agreed with mobile game dependency. Thus, it shows that the level of mobile game dependency among TNAHS students was found to be quite high. Finally, the relationship between the level of mobile dependency and socialization of high school students was found to be significant and positive.
Research Square (Research Square)
Orawan Keeratisiroj
Ramazan Yılmaz
Digital games are becoming more and more popular among today's students. Digital games are used directly or indirectly in many areas such as marketing and communication. In terms of of education, digital games allow students to socialize and also provides stundents with the development of motivation and self-regulation skills. Digital games have become an important pedogogical tool thanks to such benefits. It is important to know the habits and preferences of the students who play digital games to get the best benefit in education. Because the habits and preferences of individuals playing digital games are seen as a cultural phenomenon. So it is necessary to know the preferences and the habits of learners in the target culture. The aim of this research is to analyze the digital gaming habits of high school students. This study is based on survey model. It was conducted in a province in Western Black Sea Region. It was carried out an Anatolian High School students. Participants of this research consist of 418 high school students. The survey was conducted by means of a questionnaire developed by researchers. This questionnaire contains questions about the demographic information of students and determination of the habits of playing digital games. In the analysis phase the percentage, frequency, mean and standart deviation were used. 49.2% of male students and 50.8% of female students participated in the research. 97.3% of the students have a smartphone but 2.7% of the students do not have a smartphone. Also 81.8% of the students have the smartphones with internet connection. When it comes to the frequency of playing digital games 33.7% of the students play digital games everyday, 14.1% play digital games three or four days a week, 25.3% play digital games one day or two days a week, 16.2% play digital games a few times a month. When it comes to the frequency of daily digital gaming 20.5% of students play digital games less than an hour, 21.7% of students play one or two hours, 9.6% of students play three or four hours, 1.2% of students play for five or six hours and 1.2% of students play 7 hours and more. When students are asked where to play their digital games, 50% of students play their digital games on the smartphone, 3.3% of students play digital games on tablet, 3.3% of students play digital games on game console, 6.2% of students play digital games on PC, 34.4% of students play on their laptops. 72.2% students who play digital games say that they play single-user digital game. 27.3% of students say that they play multiuser digital games. When it comes to multiuser digital games, 0.7% of students say that they play with their parents, 23.4% of students say that they play with their friends, 75.9% of students say that they play with unfamiliar people on the internet. 19.1% of students say that they go to the internet cafe to play digital games. When the findings obtained from research are
James Ryan Paredes
Online video games are video games played online via a mobile device, and are particularly popular when downloaded for free (e.g., “freemium game” – games played for free and where customers can pay for extra features), and can be single-player or multiplayer games (Su, Chiang, Lee, & Chang, 2016). It is also one of the main entertainment features on smartphones, and this could be potentially problematic in terms of dependent use among the students. Moreover, the purpose of this study is to enlighten the students and increase consciousness regarding the effect of mobile game addiction and to advocate prevention towards this problem. Comprehending the gathered data, the researcher decided to conduct this study to find out the effect on the students. In addition, it also aims to suggest possible solutions and preventions to the rapidly increasing of too much usage of online video games that may lead to addiction.
A Review of Alprazolam Use, Misuse, and Withdrawal
Alprazolam is one of the most widely prescribed benzodiazepines for the treatment of generalized anxiety disorder and panic disorder. Its clinical use has been a point of contention as most addiction specialists consider it to be highly addictive, given its unique psychodynamic properties which limit its clinical usefulness, whereas many primary care physicians continue to prescribe it for longer periods than recommended. Clinical research data has not fully shed light on its “abuse liability,” yet it is one of the most frequently prescribed benzodiazepines. “Abuse liability” is the degree to which a psychoactive drug has properties that facilitate people misusing it, or becoming addicted to it, and is commonly used in the literature. We have replaced it in our manuscript with “misuse liability” as it reflects a more updated terminology consistent with the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). In this paper, we have reviewed alprazolam’s indications for use, its effect on pregnant women, misuse liability, withdrawal syndrome, pharmacodynamic properties, and suggest better clinical prescription practice of alprazolam by presenting an indepth theory of its clinical effects with use and withdrawal.
Alprazolam is not only the most commonly prescribed benzodiazepine, but it is the most commonly prescribed psychotropic medication in the United States, accounting for more than 48 million prescriptions dispensed in 2013 ( Grohol, 2016 ). This persists despite the fact that many prescribers consider alprazolam to have high misuse liability and it is shown to result in a more severe withdrawal syndrome than other benzodiazepines, even when tapered according to manufacturer guidelines ( Browne and Hauge, 1986 ; Kantor, 1986 ). Based on national emergency department (ED) visit data, alprazolam is the second most common prescription medication and the most common benzodiazepine to be involved in ED visits related to drug misuse ( SAMHSA, 2013 ).
Benzodiazepines are implicated in approximately one-third of intentional overdoses or suicide attempts ( Henderson et al., 1993 ). A database review of poisoning admissions to a regional toxicology service revealed that when alprazolam was involved, the median length of stay (LOS) was 19 hours, which was 1.27 (95% confidence interval [CI] 1.04, 1.54) times longer compared with other benzodiazepines, and patients were 2.06 (95% CI 1.27, 3.33) times more likely to be admitted to the intensive care unit (ICU) compared with other benzodiazepines after multivariate analysis adjusting for age, dose, sex, time to ingestion, and co-ingested drugs ( Isbister et al., 2004 ). In a longitudinal cohort study between July 1, 2011, and June 30, 2012, more than half of the patients who visited hospital and “community practice-based research network” received benzodiazepine prescriptions at least once from their primary care physician (PCP). Those clinicians were found to prescribe benzodiazepines disproportionately to patients with at least some known risk factors for benzodiazepine-related adverse events including increased age, pulmonary diseases, and other substance use disorders ( Kroll et al., 2016 ).
There are significant discrepancies between prescribing habits and risk associated with the use of benzodiazepines, including alprazolam, largely due to the lack of important data informing clinicians on best clinical practice. While more recent research studies involving benzodiazepines are scant, the subject of alprazolam misuse continues to be a reality with which many providers struggle and should continue to be addressed. We have performed an indepth review of the alprazolam literature, summarizing older and newer publications, in an attempt to provide a better understanding of how alprazolam’s unique pharmacokinetic and pharmacodynamic properties affect its misuse liability and offer some prescription guidelines for its safe and effective use.
INDICATIONS FOR USE AND EFFICACY
Alprazolam is a high-potency triazolobenzodiazepine that is US Food and Drug Administration (FDA)-approved for the treatment of anxiety and panic disorders. Alprazolam is biotransformed by hepatic microsomal oxidation, yielding 4 and α-hydroxyalprazolam as its principal metabolites, and is metabolized by cytochrome P450 (CYP) 3A4 ( Greenblatt and Wright, 1993 ).
The US FDA’s approval for alprazolam came after 2 large, randomized, clinical trials that demonstrated short-term efficacy and clinically acceptable tolerability versus placebo ( Ballenger et al., 1988 ; Klerman, 1988 ). A plasma concentration range between 20 and 40 ng/mL has been suggested for targeting symptoms of panic disorder, with higher concentrations being associated with more significant central nervous system depressant effects. The side effects of alprazolam tablets are likely to be an extension of its pharmacological activity, and most commonly include drowsiness, dizziness, fatigue, dysarthria, headache, memory impairment, and depression.
In a review of its efficacy as monotherapy for the treatment of anxiety, panic disorder, and depression, Jonas and Cohon (1993) reviewed 84 studies of alprazolam versus active-drug comparators and/or placebo. They found that alprazolam was superior to placebo and as effective or superior to all comparator benzodiazepines, including diazepam, lorazepam, and bromazepam; all comparator antidepressants, including amitriptyline, imipramine, and dothiepin (or dosulepin, a tricyclic antidepressant not approved for use in the United States); and buspirone for the treatment of anxiety disorder, as measured by reductions in the Hamilton Rating Scale for Anxiety (HAM-A). The review found that the onset of the anxiolytic effect was significantly more rapid for alprazolam compared with amitriptyline, and its antipanic effect was significantly more rapid compared with propranolol and imipramine. However, a 2011 meta-analysis of all single or double-blind, randomized controlled trials comparing alprazolam with other benzodiazepines in the treatment of panic disorder found no significant differences on any of the outcomes of clinical efficacy, including mean panic attack frequency, improvement in HAM-A score, and proportion of patients free of panic attacks at the final evaluation ( Moylan et al., 2011 ). Alprazolam is relatively more toxic than other benzodiazepines in overdose. Alprazolam has been consistently found to approximate the magnitude of anxiolytic effect of other comparable benzodiazepines.
Alprazolam has also been used off-label for the treatment of depression, but its antidepressant effects have not been systematically evaluated. In a review of 25 studies ( Jonas and Cohon, 1993 ) (n = 2643), alprazolam was found to be superior to placebo, and as effective as all comparator anti-depressants, including amitriptyline, clomipramine, desipramine, dothiepin, doxepin, and imipramine, for the treatment of “neurotic” or moderate depression, whereas the comparator antidepressants were perhaps superior to alprazolam for the treatment of severe depression. The diagnosis of “neurotic depression” was mostly reflecting depressive symptoms associated with major personality disorders. According to the review, data from several studies showed the onset of antidepressant effect was significantly more rapid for alprazolam compared with the antidepressants, and alprazolam was just as well-tolerated as all comparator medications. A Cochrane review of alprazolam’s efficacy as antidepressant monotherapy evaluated 21 more recent randomized controlled trials and found that alprazolam was superior to placebo, and as effective as the tricyclic antidepressants, including amitriptyline, desipramine, dothiepin, doxepin, and imipramine, and the heterocyclic antidepressant mianserin, for the treatment of depression in adults, as measured by reductions in the Hamilton Rating Scale for Depression (HAM-D) ( van Marwijk et al., 2012 ). However, the authors concluded that the studies included in the review were heterogeneous, of poor quality, and only addressed short-term effects, thus limiting the significance of the findings. Additionally, it was not clear if the clinical effect of alprazolam was due to a unique antidepressant effect or rather a nonspecific effect on co-occurring anxiety and sleep-related issues. The authors also questioned the funding sources of the trials and the possibility of interpretation bias favoring alprazolam, as no other trial involving other benzodiazepines has been conducted for this indication.
It is also worth noting that the number of clinical trials involving alprazolam significantly decreased circa the advent of newer antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), and that there are no clinical trials directly comparing alprazolam or any other benzodiazepines with SSRIs or other newer antidepressants as monotherapy for anxiety disorder, panic disorder, or depression. However, while the available data show that alprazolam monotherapy is as effective as other benzodiazepines for the treatment of anxiety and panic disorders, this must be considered along with its propensity for tolerance, dependence, and rebound anxiety.
ALPRAZOLAM AND PREGNANCY
The US FDA has identified alprazolam and other benzodiazepines as pregnancy category D, which indicates prior evidence of human fetal risk. Twenty-one to 33% of pregnant females are estimated to receive psychotropic drugs ( Levenson, 2011 ), and often these medications are prescribed to treat psychiatric symptoms that predate the pregnancy. Despite the risks, benzodiazepines are often used during pregnancy to manage symptoms of anxiety. In some cases, they are continued throughout the pregnancy, even when they are no longer clinically indicated, because the pregnant mother is physically dependent and discontinuation could harm the fetus due to increased risk of withdrawal symptoms, including seizures. Data from a systematic review that included 9 observational studies with more than one million subjects suggested that benzodiazepines are not associated with an increased risk of teratogenicity ( NICE, 2014 ). However, dysmorphism and mental retardation resembling those observed with fetal alcohol syndrome have been reported in 8 Swedish children born of mothers who had taken high doses of benzodiazepines regularly throughout pregnancy ( Laegreid et al., 1989 ). Other retrospective studies also suggest that benzodiazepines or hypnotic benzodiazepine receptor agonists could be associated with congenital malformations ( Altshuler and Cohen, 1997 ; ACOG, 2007 ). To the extent that benzodiazepines are associated with teratogenic effects, many experts consider the absolute increase to be small ( Dolovich et al., 1998 ; Yonkers et al., 2004 ).
Alprazolam and its 2 hydroxylated metabolites are known to cross the placenta. Retrospective studies evaluating pregnancy outcomes of women exposed to alprazolam during the first trimester of pregnancy found conflicting results of congenital anomalies ( Iqbal et al., 2002 ). Positive studies reported the occurrence of cleft lip, inguinal hernia, hypospadias, cryptorchidism, tracheoesophageal fistula, microcephaly, strabismus, congenital hip dislocation, and neonatal withdrawal syndrome, although no clear relationship was found between the use of alprazolam and the congenital malformations ( Iqbal et al., 2002 ).
Alprazolam is also excreted into breast milk in low concentrations. There are few case reports of alprazolam causing neonatal withdrawal syndrome and mild drowsiness in nursing infants ( Iqbal et al., 2002 ).
Given the significant concerns of potential risk, but conflicting reports of causation of teratogenic effects, a careful risk-benefit analysis and informed consent is critical when considering prescribing alprazolam for pregnant or breastfeeding women.
MISUSE LIABILITY
All experiments using double-blind, placebo-controlled human laboratory designs have demonstrated that benzodiazepines, as a class, produce reinforcing effects indicating misuse liability in subjects with histories of drug misuse ( Griffiths and Wolf, 1990 ). Head-to-head benzodiazepine comparison studies in general have been scant. Two clinical studies of participants with benzodiazepine dependence revealed a significant preference for alprazolam over diazepam in equipotent doses ( Schmauss et al., 1988 , 1989 ). However, in another study of recreational drug users without physical dependence, alprazolam was found to have less misuse liability than diazepam ( Orzack et al., 1988 ). Most prescribers with experience in addiction medicine consider alprazolam to have high misuse liability, especially when prescribed to individuals with a history of some type of substance use disorder ( Griffiths and Wolf, 1990 ). Another study suggested that individuals with a history of alcohol or opiate use prefer alprazolam to other benzodiazepines (eg, chlordiazepoxide and oxazepam) as they found it to be more rewarding ( Ciraulo et al., 1997 ; Iguchi et al., 1989 ; Wolf et al., 1989 ). Similarly, in a small double-blind study of 14 inpatients with a history of benzodiazepine dependence who were undergoing benzodiazepine withdrawal, alprazolam was preferred to equipotent doses of diazepam in a drug choice test ( Apelt et al., 1990 ). Not surprisingly, the national ED visit data and national prescription data show that alprazolam is related to more ED visits related to drug misuse per prescription (1 in 311) than the next 3 most commonly prescribed benzodiazepines—lorazepam (1 in 540), diazepam (1 in 517), and clonazepam (1 in 321) ( SAMHSA, 2013 ; Grohol, 2016 ). CDC prescription death rate data reveal that between 2003 and 2009, alprazolam had the highest death rate increase of all benzodiazepines and second highest overall at 234%, compared with 168% for benzodiazepines as a class (CDC, 2011).
Alprazolam’s misuse potential stems from its unique pharmacokinetic properties of rapid absorption, low lipophilicity, and short half-life ( t 1/2 ), and pharmacodynamic properties of high potency and more severe withdrawal symptoms occurring after a shorter period of use. Compared with diazepam, alprazolam is less lipophilic, thus having a smaller volume of distribution, and is less protein-bound at 68%, compared with 98% for diazepam, meaning its faster metabolism and shorter duration of action would increase its abuse liability more so than that of diazepam. The half-life of diazepam in healthy young volunteers is 22 to 72 hours and is oxidatively metabolized to desmethyldiazepam ( t 1/2 = 30–300 hours). The half-life of alprazolam is much shorter (8–16 hours), with no accumulation of oxidative metabolites. Diazepam and its metabolites accumulate in the body, followed by a slow washout once the drug is discontinued, thus triggering fewer withdrawal symptoms than the more rapidly eliminated alprazolam. Additionally, alprazolam—a triazolobenzodiazepine—is a more potent benzodiazepine than diazepam, with a 1 mg alprazolam being equipotent to 10 mg of diazepam ( NICE, 2014 ). There is no clear evidence suggesting the increased potency of the triazole moiety is increasing its potential for dependence or addiction, though it is hypothesized that the triazole moiety may have unique receptor-binding effects which are not fully known ( Juergens, 1991 ). The triazole ring may also play a role in the metabolism of alprazolam. Compounds with a triazole ring or a fused imidazole ring, such as midazolam, are metabolized rapidly by α-hydroxylation of the methyl substituent on the triazole or imidazole ring. The resulting active α-hydroxylated metabolite is quickly inactivated by glucuronidation, making the drug short-acting.
In addition to its pharmacological properties which may contribute to its increased misuse potential, alprazolam uniquely affects the dopaminergic function in the striatum similarly to stimulants. Administration of alprazolam, and not lorazepam, has been found to elicit a significant increase in extracellular dopamine concentrations in the striatum and a marked trend towards increased levels of serotonin, which induced behavioral stimulatory effects on animals ( Bentue-Ferrer et al., 2001 ). The striatum is a heterogeneous structure connected to dopaminergic reward circuitry, receiving input from the prefrontal cortex and ventral tegmental area to guide behavioral output, including motor planning, decision-making, motivation, and reward. Most drugs involved in misuse or addiction consistently lead to dopamine release in the striatum ( Di Chiara and Imperato, 1988 ; White and Kalivas, 1998 ; Willuhn et al., 2010 ; Vander Weele et al., 2014 ).
Most studies conducted to assess benzodiazepines misuse liability in head-to-head comparisons are more than 20 years old. With the approval of the long-acting formulation, some would argue that the risks, and several of alprazolam unfavorable pharmacokinetic properties, including rapid absorption and short half-life, would be mitigated when alprazolam is prescribed in its extended-release formulation (alprazolam-XR).
In a study of 14 outpatients with a history of sedative misuse, alprazolam immediate-release (IR) at 2 and 1 mg doses increased all 6 measures of positive drug effects, including ratings of “liking,” “good effects,” and “strength.” Alprazolam-XR at a dose of 2 mg per day did not increase any of the same 6 measures of positive drug effects, but 3 mg per day increased 3 of the 6 measures, mainly “liking” and “good effects.” Participants were willing to pay more money to retake alprazolam compared with placebo for both immediate and extended-release formulations ( Mumford et al., 1995 ). While the data for this small human laboratory study may seem to suggest that the extended-release alprazolam may have less misuse potential, there is a clear dose effect with the extended-release form, with the higher dose being associated with more positive drug effects. The recommended dose for the extended-release formulation ranges between 3 and 6 mg daily, and therefore higher doses within the recommended range could be associated with a similar degree of misuse potential as the IR formulation.
THE TOLERANCE PHENOMENON
Long-term use of benzodiazepine in general is controversial and not recommended, although commonly practiced. Interestingly, tolerance was found to develop relatively quickly for the hypnotic, sedative, and anticonvulsant actions of all benzodiazepines, whereas results on tolerance to anxiolytic and amnesic effects have not been consistent across studies or molecules tested ( Lucki and Rickels, 1986 ; Lucki et al., 1986 ; Curran et al., 1994 ). It is important to note that physical dependence, usually defined by withdrawal symptoms including seizures, does not require the presence of clinical tolerance, and conversely tolerance may develop without any signs of physical dependence. Furthermore, the degree of cognitive recovery that may take place after a benzodiazepine taper is unclear, with compelling evidence not supporting full restitution of cognitive function, at least in the first 6 months after cessation, and suggestion that there may be some permanent deficits in comparison to controls ( Barker et al., 2004 ). In a controlled longitudinal study of alprazolam for the treatment of panic disorder with agoraphobia, alprazolam produced pronounced impairments on a word recall task at baseline and at the 24-week medication-free follow-up ( Curran et al., 1994 ).
In another study of patients with panic disorder, neither anxiolytic tolerance nor daily dose increase was observed after 8 weeks of alprazolam treatment, with continued efficacy at 6 months ( Schweizer et al., 1993 ). There is a subpopulation of patients exposed to benzodiazepines that is more likely to escalate their dose, mainly those with coexisting drug or alcohol use problem ( Griffiths and Wolf, 1990 ; NICE, 2014 ). Most would agree that tolerance is a multifactorial process that occurs at different rates for different patients, and also depends on the profile of the benzodiazepine used. In general, available data have been inconsistent with large variance between studies highlighting the need of well-designed long-term clinical trials addressing the question of tolerance with all benzodiazepines including alprazolam.
ALPRAZOLAM WITHDRAWAL SYNDROME
Alprazolam and alprazolam-XR carry the same general risk of withdrawal as other benzodiazepines. The manufacturer recommends a taper not to exceed 0.5 mg every 3 days ( Kantor, 1986 ). Alprazolam use for merely 1 week produces discontinuation symptoms in mice ( Galpern et al., 1991 ), and the withdrawal syndrome associated with its discontinuation is generally regarded as being more severe than other benzodiazepine withdrawal syndromes, even when alprazolam is tapered according to manufacturer guidelines ( Browne and Hauge, 1986 ; Kantor, 1986 ). Specifically, alprazolam withdrawal syndrome has been described as involving a more complicated and, in some aspects, unique rebound anxiety compared with other benzodiazepine withdrawal syndromes ( Browne and Hauge, 1986 ). One study reported that of 17 patients with panic disorder treated with alprazolam, 15 patients had recurrence or an increase in their panic attacks, and 9 had significant new somatic symptoms, such as malaise, weakness, insomnia, tachycardia, and dizziness, after alprazolam discontinuation, despite a taper over 4 weeks ( Fyer et al., 1987 ). Another study reported that of 126 patients with panic disorder treated with alprazolam, 27% of patients had rebound anxiety that was more severe than pretreatment anxiety, and 35% of patients had new somatic symptoms after alprazolam discontinuation, despite a taper over 4 weeks ( Pecknold et al., 1988 ). In a case series of 8 patients with combat-induced post-traumatic stress disorder (PTSD) treated with alprazolam at an average dose of 4.9 mg per day, all 8 patients developed worsening anxiety, sleep disturbance, and nightmares, 7 patients had irritability and hyperalertness, 6 patients had rage reactions and homicidal ideation, and 4 patients developed dissociative reactions and suicidal ideation upon alprazolam discontinuation, despite a taper over an average of 8.4 weeks ( Risse et al., 1990 ). Another study demonstrated that alprazolam withdrawal causes more frequent and severe sleep disturbances compared with diazepam withdrawal ( Kales et al., 1988 ).
Alprazolam withdrawal syndrome may also feature unique clinical symptoms compared with other benzodiazepine withdrawal syndromes. There are several case reports of delirium and psychosis caused by alprazolam withdrawal, whereas there are scant reports of these symptoms in cases of other benzodiazepine withdrawal ( Zipursky et al., 1985 ; Freiberger and Marsicano, 1991 ; Zalsman et al., 1997 ; McKenzie et al., 2014 ). There are several case reports of hyperadrenergic states caused by alprazolam withdrawal ( Páll et al., 2014 ), with the most impressive example describing a pseudo-pheochromocytoma, characterized by intermittent episodes of hypertensive crisis with sinus tachycardia, some so severe as to require ICU admission. Interestingly, despite ICU care and administration of beta-blockers and alpha-blockers, the pseudo-pheochromocytoma was only successfully treated by alprazolam re-instatement ( Orzack et al., 1988 ).
The use of other benzodiazepines in treating alprazolam withdrawal is quite common, yet not fully investigated. Often switching to a long-acting benzodiazepine with inherent accumulation of metabolites, followed by a gradual dose taper, are effective strategies resulting in a safe and smoother detoxification for most cases. However, interestingly, both chlordiazepoxide and diazepam were found to be ineffective in preventing alprazolam withdrawal symptoms in 2 separate cases ( Schweizer et al., 1993 ; Sachdev et al., 2014 ). Lorazepam was also found to be ineffective in controlling alprazalom-induced withdrawal symptoms in a critically ill patient who was admitted to the ICU ( Risse et al., 1990 ). This lack of response has been consistent when switching from a triazolobenzodiazepines, such as alprazolam and triazolam, to a benzodiazepine with no triazole moiety. The triazole ring may have a unique binding affinity for a subgroup of benzodiazepine receptors that are not generally affected by other benzodiazepines ( Albeck, 1987 ), making substituting alprazolam with another benzodiazepine less effective in preventing rebound anxiety and withdrawal symptoms. There are published data on open-label clinical observations of 37 alprazolam-dependent patients who were successfully tapered from alprazolam using clonazepam substitution, with only 2 patients experiencing rebound panic symptoms, and no patients experiencing any other withdrawal symptoms ( Patterson, 1990 ). Clonazepam is usually chosen because it has an intermediate to long half-life, ranging from 17 to 60 hours, and is associated with less rebound anxiety and withdrawal symptoms in comparison with shorter-acting agents. One should be mindful that longer-acting drugs have shorter durations of action when given acutely because of their pharmacokinetic properties, requiring a few days to a week to reach steady state. It is therefore recommended that for the first week, the substitution should be given on a twice or 3 times per day schedule.
Perhaps even more interestingly, there are reports of successful treatment of the alprazolam withdrawal syndrome using carbamazepine ( Klein et al., 1986 ) and clonidine, neither of which has appreciable affinity for benzodiazepine receptors ( Vinogradov et al., 1986 ; Fyer et al., 1988 ). The mechanism of action of carbamazepine remains unknown, but there is limited evidence suggesting that carbamazepine can increase gamma-aminobutyric acid (GABA) concentrations, possibly by decreasing turnover and inhibiting sodium channel-mediated neuroexcitation ( Galpern et al., 1991 ). Carbamazepine is also known to enhance catecholamine function and therefore may improve symptoms of sleep disturbance, anxiety, and mood instability, which are common in withdrawal. This explains its positive effects in general for the treatment of benzodiazepine withdrawal syndrome. It is also consistent with open-label reports and a double-blind study supporting the use of carbamazepine in benzodiazepine withdrawal ( Björkqvist et al., 1976 ). In contrast to other benzodiazepines, alprazolam activates alpha-2 adrenoceptors, which could account for its reported enhanced effectiveness in the treatment of panic disorder, but also the hyperadrenergic state seen with its discontinuation ( Eriksson et al., 1986 ). Rebound anxiety is common and is often severe with alprazolam discontinuation because of its short half-life and the unique alpha-2 adrenergic effect. Both carbamazepine and clonidine act at the alpha-2 adrenoceptors level and could counteract the hyperadrenergic state that has been reported during discontinuation of alprazolam. Both drugs were also found to act synergistically via carbamazepine induced super-sensitivity of the alpha-2-adrenergic receptors through which clonidine exerts its primary effect ( Dilsaver et al., 1993 ), although, to our knowledge, this combination has not been used to treat the alprazolam withdrawal syndrome. Conversely, there are reports of withdrawal from carbamazepine and clonidine with symptoms similar to those seen in alprazolam withdrawal, including psychosis ( Adler et al., 1982 ; Heh et al., 1988 ) and hyperadrenergic states ( Tollefson, 1981 ). Thus, alprazolam likely has unique pharmacodynamic properties that contribute to its distinctive withdrawal syndrome, would theoretically prohibit complete cross-tolerance between alprazolam and other benzodiazepines, and may be related to the putative pharmacodynamic properties of carbamazepine and clonidine. Carbamazepine is metabolized by CYP3A4, and interactions with other drugs that induce, inhibit, or compete for CYP3A4 are relatively common, which may limit its use. Clonidine acts exclusively at the alpha-2 adrenoceptors levels and lacks carbamazepine’s GABAergic function and mood stabilization, thus leaving patients to experience all the other withdrawal symptoms if used alone for detoxification.
There are also encouraging case reports and case series with the use of other antiseizure medications to help alleviate symptoms of benzodiazepine withdrawal. There are 3 case reports suggesting that valproate may be effective for the treatment of sedative-hypnotic withdrawal, but a double-blind, placebo-controlled study failed to replicate the results ( Rickels et al., 1999 ). When gabapentin, an antiseizure medication with high affinity for voltage-gated calcium channels was added to a structured withdrawal regimen in patients with benzodiazepines use disorder for rapid inpatient withdrawal (less than a week); patients experienced minimal discomfort and the added benefit of reduced cravings for benzodiazepines ( Penders, 2015 ).
CONCLUSIONS
Alprazolam is the most widely prescribed and misused benzodiazepine in the United States. It can be used safely and effectively when prescribed appropriately, after thoroughly evaluating the risks and benefits of treatment. Side effects are common, but often downplayed by patients, given its rapid onset of therapeutic action and unique reinforcing properties. Common complaints reported with varying frequency by patients treated with alprazolam include sedation, fatigue, ataxia, amnesia, slurred speech, poor concentration, hypersensitivity, and irritability.
All benzodiazepines carry a risk of misuse, diversion, tolerance, and physical dependence. Misuse and diversion are more frequently seen in patients with a personal or family history of alcohol or drug misuse ( Ciraulo et al., 1997 ). Withdrawal symptoms associated with alprazolam discontinuation seem to be more severe than with other benzodiazepines probably due to its shorter half-life, high potency causing severe rebound anxiety, and it is affinity to the alpha-2 adreno-receptors. Some of the risks listed above could be mitigated with the use of alprazolam-XR, although little is known about the long-acting formulation, except for one small human laboratory study indicating that lower doses were not as reinforcing as the IR formulation.
Alprazolam has been reported to cause withdrawal and sedation in the newborn and should be avoided during pregnancy and lactation. As a general rule, exposure to any type of benzodiazepine during the first trimester should be avoided.
Alprazolam is significantly more toxic than other benzodiazepines in cases of overdoses and should be avoided in patients at increased risk of suicide, or who are using alcohol, opioids, or other sedating drugs. Generally, SSRIs or serotonin-norepinephrine reuptake inhibitors (SNRIs) are considered first-line pharmacological treatment for anxiety disorders ( Baldwin and Polkinghorn, 2005 ; Bandelow et al., 2008 ), but it usually takes few weeks to reach therapeutic effects, and therefore benzodiazepine use may have a role in alleviating acute symptoms of anxiety and distress early in treatment ( Nutt, 2005 ). Alprazolam should be prescribed primarily in its extended-release formulation for a short duration to minimize misuse liability and only to those with no prior substance use history. Prescribers should take measures to ensure patients taking alprazolam are not co-ingesting other CYP3A4 substrates, especially opioids, to minimize morbidity and mortality associated with co-ingested substances. The use of benzodiazepines with opioids doubles the risk of respiratory depression and death, and should be avoided. In the rare instance that patients require both an opioid and benzodiazepine, or during the tapering phase, patients should be alerted to the risk of death and offered a prescription of the opioid antagonist naloxone. Grapefruit and grapefruit juice should also be avoided, as they contain furanocoumarins that inhibit CYP3A4 and therefore cause blood levels of alprazolam to increase. This may be accomplished by fostering open communication about diet and substance use with patients, regularly checking prescription monitoring databases, and perhaps randomly checking urine drug screens. Alprazolam should be discontinued much more slowly than the manufacturer guidelines suggest. A reasonable guideline ( Pecknold et al., 1988 ) is to not to exceed 0.125 mg weekly and over a period of at least 8 weeks ( Risse et al., 1990 ). It could be substituted with a faster taper of a longer-acting benzodiazepine such as clonazepam, using clonidine and/or carbamazepine augmentation. Gabapentin is another option that should be considered during alprazolam discontinuation to prevent rebound anxiety, cravings, and other withdrawal symptoms.
When prescribing alprazolam, clinicians should discuss the treatment plan or consider using a formalized written treatment agreement, which both educates patients about the risks of benzodiazepines use and clarifies expectations, including the short-term nature of the prescription. Many providers feel pressurized by their patients to continue prescribing as they try to wean them off benzodiazepines, and more-so with alprazolam, given the positive subjective drug effects. Alprazolam should not be prescribed at a higher dose than is US FDA-recommended, and providers should consider discontinuation if patients are requesting higher doses, as it may signal therapeutic tolerance and/or misuse.
Well-designed human studies addressing alprazolam’s reinforcing effects and the discontinuation syndrome are needed, and must consider important issues such as selection of appropriate comparison drug, dose, formulation, and population. Future research should also further investigate the misuse liability of alprazolam XR, and should attempt to clarify the role of carbamazepine, clonidine, other anticonvulsant drugs, and related compounds in the treatment of the alprazolam withdrawal syndrome.
The authors report no conflicts of interest.
- ACOG. American College of Obstetricians and Gynecologists Practice Bulletin No. 87 November 2007: Use of psychiatric medications during pregnancy and lactation. Obstet Gynecol. 2007; 110 :1179. [ PubMed ] [ Google Scholar ]
- Adler LE, Bell J, Kirch D, et al. Psychosis associated with clonidine withdrawal. Am J Psychiatry. 1982; 139 :110–112. [ PubMed ] [ Google Scholar ]
- Albeck JH. Withdrawal and detoxification from benzodiazepine dependence: a potential role for clonazepam. J Clin Psychiatry. 1987; 48 (Suppl):43–48. [ PubMed ] [ Google Scholar ]
- Altshuler L, Cohen L. Pharmacologic management of psychiatric illness during pregnancy: dilemmas and guidelines. Year Book Psychiatry Appl Mental Health. 1997; 1997 :491. [ PubMed ] [ Google Scholar ]
- Apelt S, Schmauss C, Emrich H. Preference for alprazolam as opposed to diazepam in benzodiazepine-dependent psychiatric inpatients. Pharmacopsychiatry. 1990; 23 :70–75. [ PubMed ] [ Google Scholar ]
- Baldwin DS, Polkinghorn C. Evidence-based pharmacotherapy of generalized anxiety disorder. Int J Neuropsychopharmacol. 2005; 8 :293–302. [ PubMed ] [ Google Scholar ]
- Ballenger JC, Burrows GD, DuPont RL, et al. Alprazolam in panic disorder and agoraphobia: Results from a multicenter trial: I. Efficacy in short-term treatment Arch Gen Psychiatry. 1988; 45 :413–422. [ PubMed ] [ Google Scholar ]
- Bandelow B, Zohar J, Hollander E, et al. WFSBP Task Force on Treatment Guidelines for Anxiety, Obsessive-Compulsive and Post-Traumatic Stress Disorders. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive-compulsive and post-traumatic stress disorders. World J Biol Psychiatry. 2008; 9 :248–312. [ PubMed ] [ Google Scholar ]
- Barker MJ, Greenwood KM, Jackson M, et al. Persistence of cognitive effects after withdrawal from long-term benzodiazepine use: a meta-analysis. Arch Clin Neuropsychol. 2004; 19 :437–454. [ PubMed ] [ Google Scholar ]
- Bentue-Ferrer D, Reymann J, Tribut O, et al. Role of dopaminergic and serotonergic systems on behavioral stimulatory effects of low-dose alprazolam and lorazepam. Eur Neuropsychopharmacol. 2001; 11 :41–50. [ PubMed ] [ Google Scholar ]
- Björkqvist SE, Isohanni M, Mäkelä R, et al. Ambulant treatment of alcohol withdrawal symptoms with carbamazepine: a formal multicentre double-blind comparison with placebo. Acta Psychiatr Scand. 1976; 53 :333–342. [ PubMed ] [ Google Scholar ]
- Browne J, Hauge K. A review of alprazolam withdrawal. Drug Intelligence Clin Pharm. 1986; 20 :837–841. [ PubMed ] [ Google Scholar ]
- Centers for Disease Control and Prevention. Drug overdose deaths: Florida, 2003–2009. MMWR. 2011; 60 :869–872. [ PubMed ] [ Google Scholar ]
- Ciraulo DA, Barnhill JG, Ciraulo AM, et al. Alterations in pharmacodynamics of anxiolytics in abstinent alcoholic men: subjective responses, abuse liability, and electroencephalographic effects of alprazolam, diazepam, and buspirone. J Clin Pharmacol. 1997; 37 :64–73. [ PubMed ] [ Google Scholar ]
- Curran HV, Bond A, O’Sullivan G, et al. Memory functions, alprazolam and exposure therapy: a controlled longitudinal study of agoraphobia with panic disorder. Psychol Med. 1994; 24 :969–976. [ PubMed ] [ Google Scholar ]
- Di Chiara G, Imperato A. Drugs abused by humans preferentially increase synaptic dopamine concentrations in the mesolimbic system of freely moving rats. Proc Natl Acad Sci USA. 1988; 85 :5274–5278. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dilsaver SC, Peck JA, Traumata D, et al. Treatment with carbamazepine may enhance ( 2-noradrenergic autoreceptor sensitivity. Biol Psychiatry. 1993; 34 :551–557. [ PubMed ] [ Google Scholar ]
- Dolovich LR, Addis A, Vaillancourt JR, et al. Benzodiazepine use in pregnancy and major malformations or oral cleft: meta-analysis of cohort and case-control studies. BMJ. 1998; 317 :839–843. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Eriksson E, Carlsson M, Nilsson C, et al. Does alprazolam, in contrast to diazepam, activate alpha2-adrenoceptors involved in the regulation of rat growth hormone secretion? Life Sci. 1986; 38 :1491–1498. [ PubMed ] [ Google Scholar ]
- Freiberger JJ, Marsicano TH. Alprazolam withdrawal presenting as delirium after cardiac surgery. J Cardiothorac Vasc Anesth. 1991; 5 :150–152. [ PubMed ] [ Google Scholar ]
- Fyer AJ, Liebowitz MR, Gorman JM, et al. Discontinuation of alprazolam treatment in panic patients. Am J Psychiatry. 1987; 144 :303–308. [ PubMed ] [ Google Scholar ]
- Fyer AJ, Liebowitz MR, Gorman JM, et al. Effects of clonidine on alprazolam discontinuation in panic patients: a pilot study. J Clin Psychopharmacol. 1988; 8 :270–274. [ PubMed ] [ Google Scholar ]
- Galpern WR, Miller LG, Szabo GK, et al. Chronic benzodiazepine administration: IX. Attenuation of alprazolam discontinuation effects by carbamazepine. Biochem Pharmacol. 1991; 42 :99–104. [ PubMed ] [ Google Scholar ]
- Greenblatt DJ, Wright CE. Clinical pharmacokinetics of alprazolam. Clin Pharmacokinet. 1993; 24 :453–471. [ PubMed ] [ Google Scholar ]
- Griffiths RR, Wolf B. Relative abuse liability of different benzodiazepines in drug abusers. J Clin Psychopharmacol. 1990; 10 :237–243. [ PubMed ] [ Google Scholar ]
- Grohol J. Top 25 Psychiatric Medication Prescriptions for 2013. 2016 Available at: https://psychcentral.com/lib/top-25-psychiatric-medication-prescriptions-for-2013/
- Heh CW, Sramek J, Herrera J, et al. Exacerbation of psychosis after discontinuation of carbamazepine treatment. Am J Psychiatry. 1988; 145 :878–879. [ PubMed ] [ Google Scholar ]
- Henderson A, Wright M, Pond S. Experience with 732 acute overdose patients admitted to an intensive care unit over six years. Med J Australia. 1993; 158 :28–30. [ PubMed ] [ Google Scholar ]
- Iguchi MY, Griffiths RR, Bickel WK, et al. Relative abuse liability of benzodiazepines in methadone maintained populations in three cities. NIDA Res Monograph. 1989; 95 :364–365. [ PubMed ] [ Google Scholar ]
- Iqbal MM, Sobhan T, Ryals T. Effects of commonly used benzodiazepines on the fetus, the neonate, and the nursing infant. Psychiatr Serv. 2002; 53 :39–49. [ PubMed ] [ Google Scholar ]
- Isbister GK, O’regan L, Sibbritt D, et al. Alprazolam is relatively more toxic than other benzodiazepines in overdose. Br J Clin Pharmacol. 2004; 58 :88–95. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jonas JM, Cohon MS. A comparison of the safety and efficacy of alprazolam versus other agents in the treatment of anxiety, panic, and depression: a review of the literature. J Clin Psychiatry. 1993; 54 (Suppl 25–45):46–48. [ PubMed ] [ Google Scholar ]
- Juergens S. Alprazolam and diazepam: addiction potential. J Subst Abuse Treatment. 1991; 8 :43–51. [ PubMed ] [ Google Scholar ]
- Kales A, Soldatos CR, Bixler EO, et al. Diazepam: effects on sleep and withdrawal phenomena. J Clin Psychopharmacol. 1988; 8 :340–346. [ PubMed ] [ Google Scholar ]
- Kantor SJ. A difficult alprazolam withdrawal. J Clin Psychopharmacol. 1986; 6 :124–125. [ PubMed ] [ Google Scholar ]
- Klein E, Uhde TW, Post RM. Preliminary evidence for the utility of carbamazepine in alprazolam withdrawal. Am J Psychiatry. 1986; 143 :235–236. [ PubMed ] [ Google Scholar ]
- Klerman GL. Overview of the cross-national collaborative panic study: I. efficacy in short-term treatment. Arch Gen Psychiatry. 1988; 45 :407–412. [ PubMed ] [ Google Scholar ]
- Kroll DS, Nieva HR, Barsky AJ, et al. Benzodiazepines are prescribed more frequently to patients already at risk for benzodiazepine-related adverse events in primary care. J Gen Intern Med. 2016; 31 (9):1027–1034. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Laegreid L, Olegrd R, Walström J, et al. Teratogenic effects of benzodiazepine use during pregnancy. J Pediatr. 1989; 114 :126–131. [ PubMed ] [ Google Scholar ]
- Levenson JL. The American Psychiatric Publishing Textbook of Psychosomatic Medicine: Psychiatric Care of the Medically Ill. 2. Arlington, Virginia: American Psychiatric Pub; 2011. [ Google Scholar ]
- Lucki I, Rickels K. The behavioral effects of benzodiazepines following long-term use. Psychopharmacol Bull. 1986; 22 :424. [ PubMed ] [ Google Scholar ]
- Lucki I, Rickels K, Geller AM. Chronic use of benzodiazepines and psycho-motor and cognitive test performance. Psychopharmacology. 1986; 88 :426–433. [ PubMed ] [ Google Scholar ]
- McKenzie RR, Jr, Madadi P, Sharma TR. Alprazolam withdrawal delirium and brief reversible psychosis: a case report. Prim Care Companion CNS Disord. 2014:16. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Moylan S, Staples J, Ward SA, et al. The efficacy and safety of alprazolam versus other benzodiazepines in the treatment of panic disorder. J Clin Psychopharmacol. 2011; 31 :647–652. [ PubMed ] [ Google Scholar ]
- Mumford G, Evans S, Fleishaker J, et al. Alprazolam absorption kinetics affects abuse liability. Clin Pharmacol Therapeut. 1995; 57 :356–365. [ PubMed ] [ Google Scholar ]
- National Collaborating Centre for Mental Health. NICE guideline (CG192) London, UK: British Psychological Society and The Royal College of Psychiatrists; 2014. Antenatal and postnatal mental health: clinical management and service guidance—updated edition. [ PubMed ] [ Google Scholar ]
- Nutt DJ. Overview of diagnosis and drug treatments of anxiety disorders. CNS Spectrums. 2005; 10 :49–56. [ PubMed ] [ Google Scholar ]
- Orzack MH, Friedman L, Dessain E, et al. Comparative study of the abuse liability of alprazolam, lorazepam, diazepam, methaqualone, and placebo. Int J Addict. 1988; 23 :449–467. [ PubMed ] [ Google Scholar ]
- Páll A, Becs G, Erdei A, et al. Pseudopheochromocytoma induced by anxiolytic withdrawal. Eur J Med Res. 2014; 19 :53. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Patterson JF. Withdrawal from alprazolam dependency using clonazepam: clinical observations. J Clin Psychiatry. 1990; 51 (5, Suppl):47–49. [ PubMed ] [ Google Scholar ]
- Pecknold JC, Swinson RP, Kuch K, et al. Alprazolam in panic disorder and agoraphobia: Results from a multicenter trial: III. Discontinuation effects. Arch Gen Psychiatry. 1988; 45 :429–436. [ PubMed ] [ Google Scholar ]
- Penders T. Gabapentin (Neurontin): an adjunct for benzodiazepine withdrawal. Ommega Internations. 2015; 1 :1–8. [ Google Scholar ]
- Rickels K, Schweizer E, Garcia Espana F, et al. Trazodone and valproate in patients discontinuing long-term benzodiazepine therapy: effects on withdrawal symptoms and taper outcome. Psychopharmacology. 1999; 141 :1–5. [ PubMed ] [ Google Scholar ]
- Risse SC, Whitters A, Burke J, et al. Severe withdrawal symptoms after discontinuation of alprazolam in eight patients with combat-induced posttraumatic stress disorder. J Clin Psychiatry. 1990; 51 :206–209. [ PubMed ] [ Google Scholar ]
- Sachdev G, Gesin G, Christmas AB, et al. Failure of lorazepam to treat alprazolam withdrawal in a critically ill patient. World J Crit Care Med. 2014; 3 :42. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- SAMHSA. Drug Abuse Warning Network, 2011: national estimates of drug-related emergency department visits. Subst Abuse Mental Health Serv Administr. 2013; 13 :4760. [ PubMed ] [ Google Scholar ]
- Schmauss C, Apelt S, Emrich H. The seeking and liking potentials of alprazolam. Am J Psychiatry. 1988; 145 :128a–128. [ PubMed ] [ Google Scholar ]
- Schmauss C, Apelt S, Emrich H. Preference for alprazolam over diazepam. Am J Psychiatry. 1989; 146 :408. [ PubMed ] [ Google Scholar ]
- Schweizer E, Rickels K, Weiss S, et al. Maintenance drug treatment of panic disorder: I. Results of a prospective, placebo-controlled comparison of alprazolam and imipramine. Arch Gen Psychiatry. 1993; 50 :51–60. [ PubMed ] [ Google Scholar ]
- Tollefson GD. Hyperadrenergic hypomania consequent to the abrupt cessation of clonidine. J Clin Psychopharmacol. 1981; 1 :93–95. [ PubMed ] [ Google Scholar ]
- van Marwijk H, Allick G, Wegman F, et al. Alprazolam for depression. Cochrane Database Syst Rev. 2012:CD007139. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Vander Weele CM, Porter-Stransky KA, Mabrouk OS, et al. Rapid dopamine transmission within the nucleus accumbens: dramatic difference between morphine and oxycodone delivery. Eur J Neurosci. 2014; 40 :3041–3054. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Vinogradov S, Reiss A, Csernansky J. Clonidine therapy in withdrawal from high-dose alprazolam treatment. Am J Psychiatry. 1986; 143 :1188. [ PubMed ] [ Google Scholar ]
- White FJ, Kalivas PW. Neuroadaptations involved in amphetamine and cocaine addiction. Drug Alcohol Depend. 1998; 51 :141–153. [ PubMed ] [ Google Scholar ]
- Willuhn I, Wanat MJ, Clark JJ, et al. Dopamine signaling in the nucleus accumbens of animals self-administering drugs of abuse. Behav Neurosci Drug Addict. 2010; 3 :29–71. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wolf B, Iguchi MY, Griffiths RR. Sedative/tranquilizer use and abuse in alcoholics currently in outpatient treatment: incidence, pattern and preference. NIDA Res Monograph. 1989; 95 :376–377. [ PubMed ] [ Google Scholar ]
- Yonkers KA, Wisner KL, Stowe Z, et al. Management of bipolar disorder during pregnancy and the postpartum period. Am J Psychiatry. 2004; 161 :608–620. [ PubMed ] [ Google Scholar ]
- Zalsman G, Hermesh H, Munitz H. Alprazolam withdrawal delirium: a case report. Clin Neuropharmacol. 1997; 21 :201–202. [ PubMed ] [ Google Scholar ]
- Zipursky RB, Baker RW, Zimmer B. Alprazolam withdrawal delirium unresponsive to diazepam: case report. J Clin Psychiatry. 1985; 46 :344–345. [ PubMed ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
As a result, clinical practices and tools were too distant from research areas for ML results to be interpreted. 7. Conclusions. This review summarizes EEG, brain imaging, behavioural, and kinematic studies on ML applications in addiction research. By employing well-defined inclusion and exclusion criteria, the authors avoided the review bias.
Abstract. This study aims to provide a systematic review of the applications of machine learning methods in addiction research. In this study, multiple searches on MEDLINE, Embase and the Cochrane Database of Systematic Reviews were performed. 23 full-text articles were assessed and 17 articles met the inclusion criteria for the final review ...
ML appraoches in addiction research ... in addiction research, however, the results and findings of. ... success 3/ recent papers to the past 4 years (2022,2021, 2020,
This review describes a workflow to guide the application of machine learning in addiction research, detailing study design, data collection, data pre-processing, modeling, and results communication. How to train, validate, and test a model, detect and characterize overfitting, and determine an adequate sample size are some of the key issues ...
success 3/ recent papers to the past 4 years (2022,2021, 2020, 2019), from the following well known publishers (Nature, ... Fig. 1. ML appraoches in addiction research where each hypothesis will ...
An updated review of the application of ML techniques for addiction disorders to provide strong evidence about the potential of ML methods to accelerate early prevention and intervention is presented, ultimately aiming to pave the way for further applications of ML approaches in this field. Constant contributions of Machine Learning (ML) technology in health sciences has extended to solve ...
Purpose of review: To provide an accessible overview of some of the most recent trends in the application of machine learning to the field of substance use disorders and their implications for future research and practice. Recent findings: Machine-learning (ML) techniques have recently been applied to substance use disorder (SUD) data for multiple predictive applications including detecting ...
Machine learning assembles a broad set of methods and techniques to solve a wide range of problems, such as identifying individuals with substance use disorders (SUD), finding patterns in neuroimages, understanding SUD prognostic factors and their association, or determining addiction genetic underpinnings. However, the addiction research field ...
2022. TLDR. An updated review of the application of ML techniques for addiction disorders to provide strong evidence about the potential of ML methods to accelerate early prevention and intervention is presented, ultimately aiming to pave the way for further applications of ML approaches in this field. Expand.
1 Center for Mental Health Education, School of Psychology, Southwest University, Chongqing, China; 2 Chongqing Youth and Vocational Technical College, Chongqing, China; As a new type of addictive behaviors and distinct from traditional internet game addiction on desktop computers, mobile game addiction has attracted researchers' attention due to its possible negative effects on mental health ...
In this context, we proposed to review recent literature about digital addiction. First, we collected 20 recent research articles about different kinds of addictions and the current state of research trends. Then the role of machine learning in order to deal with addiction has been studied.
Machine learning (ML) is the method to find patterns and make prediction from data. ... However, the addiction research field underuses machine learning. This two-part narrative review focuses on ...
This Research Topic will be served as a platform for researchers to share and discuss the applications of the machine learning framework in addiction research, with a focus on neuroimaging data. We expect this collection of articles to further advance our understanding of the neural mechanisms, etiology, objective diagnosis criteria, prevention ...
Abstract. This study aims to provide a systematic review of the applications of machine learning methods in addiction research. In this study, multiple searches on MEDLINE, Embase and the Cochrane Database of Systematic Reviews were performed. 23 full-text articles were assessed and 17 articles met the inclusion criteria for the final review ...
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
Relevant publications were obtained when the terms included in the search query appeared in the title, abstract, or keywords. We defined the search query of each topic based on prior research on ML, social media , and mental health . We excluded papers that were not written in English or were categorized as other document types (Figure 1). As a ...
In the era of increasing demand of data analytics in drug discovery domain, processing the complex high dimensional drug datasets is a challenging research area. High dimensionality refers to dataset having more number of columns than rows in which there may be irrelevant features that are futile. For reducing high dimensionality issue, feature selection techniques are widely adopted. Feature ...
Introduction. Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that "addiction is a brain disease", articulated a set of implications of this position, and outlined an agenda for realizing its promise [].The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the ...
Mobile Game Addiction and Depression. Internet game addiction is characterized by cognitive and emotional deficits. Previous studies have reported the co-occurrence of Internet addition and depression (13, 14).In addition, a longitudinal study found that Internet game addition/depression severity at an earlier time positively predicted the depression/Internet game addition severity at a later ...
It cause to addiction when must be exposed to playing. They are effected to family, financial, health, academic performance, and peers/friends when use excessively. This research aims to know the effects of Computer Games to Selected Information and Communications Technology (ICT)Students in San Jose National High School.
The system architecture of the prediction of addiction to drugs and alcohol We have evaluated the classifiers based on accuracy and other metrics like sensitivity, specificity, precision, recall ...
Academia.edu is a platform for academics to share research papers. EFFECTS OF MOBILE GAMES (MOBILE LEGENDS) TO THE BEHAVIOR AND HEALTH OF A SHS STUDENTS ... Research into mobile game addiction has increased over the previous two decades. ... Mobile Legends Players. The result of this study will help the ML players to know that there is a ...
Alprazolam is one of the most widely prescribed benzodiazepines for the treatment of generalized anxiety disorder and panic disorder. Its clinical use has been a point of contention as most addiction specialists consider it to be highly addictive, given its unique psychodynamic properties which limit its clinical usefulness, whereas many primary care physicians continue to prescribe it for ...