Username or email *
Password *
Forgotten password?
[email protected]
+44 (0)20 8834 4579

Medicine Personal Statement Examples
Get some inspiration to start writing your Medicine Personal Statement with these successful examples from current Medical School students. We've got Medicine Personal Statements which were successful for universities including Imperial, UCL, King's, Bristol, Edinburgh and more.
Personal Statement Examples
- Read successful Personal Statements for Medicine
- Pay attention to the structure and the content
- Get inspiration to plan your Personal Statement
Personal Statement Example 1
Check out this Medicine Personal Statement which was successful for Imperial, UCL, QMUL and King's.
Personal Statement Example 2
This Personal Statement comes from a student who received Medicine offers from Bristol and Plymouth - and also got an interview at Cambridge.
Personal Statement Example 3
Have a look at this Medicine Personal Statement which was successful for Imperial, Edinburgh, Dundee and Newcastle.
Personal Statement Example 4
Take a look at this Medicine Personal Statement which was successful for King's, Newcastle, Bristol and Sheffield.
Personal Statement Example 5
Pick up tips from this Medicine Personal Statement which was successful for Imperial, Birmingham and Manchester.
Personal Statement Example 6
This Personal Statement comes from a student who got into Graduate Entry Medicine at King's - and also had interviews for Undergraduate Medicine at King's, QMUL and Exeter.
Loading More Content

Great Medical School Personal Statement Examples (2024-2025) Insider’s Guide
A physician and former medical school admissions officer teaches you how to write your medical school personal statement, step by step. Read several full-length medical school personal statement examples for inspiration.
In this article, a former medical school admissions officer explains exactly how to write a stand-out medical school personal statement!
Our goal is to empower you to write a medical school personal statement that reflects your individuality, truest aspirations and genuine motivations.
This guide also includes:
- Real life medical school personal statement examples
- Medical school personal statement inventory template and outline exercise
- AMCAS, TMDSAS, and AACOMAS personal statement prompts
- Advanced strategies to ensure you address everything admissions committees want to know
- The secret to writing a great medical school personal statement
So, if you want your medical school personal statement to earn more more medical school interviews, you will love this informative guide.
Let’s dive right in.
Table of Contents
Medical School Personal Statement Fundamentals
If you are getting ready to write your medical school personal statement for the 2024-2025 application year, you may already know that almost 60% of medical school applicants are not accepted every year . You have most likely also completed all of your medical school requirements and have scoured the internet for worthy medical school personal statement examples and guidance.
You know the medical school personal statement offers a crucial opportunity to show medical schools who you are beyond your GPA and MCAT score .
It provides an opportunity to express who you are as an individual, the major influences and background that have shaped your interests and values, what inspired you to pursue medicine, and what kind of a physician you envision yourself becoming.
However, with so much information online, you are not sure who to trust. We are happy you have found us!
Because the vast majority of people offering guidance are not former admissions officers or doctors , you must be careful when searching online.
We are real medical school admissions insiders and know what goes on behind closed doors and how to ensure your medical school personal statement has broad appeal while highlighting your most crucial accomplishments, perspectives, and insights.
With tight limits on space, it can be tough trying to decide what to include in your medical school personal statement to make sure you stand out. You must think strategically about how you want to present your personal “big picture” while showing you possess the preprofessional competencies med schools are seeking.
When a medical school admissions reviewer finishes reading your medical school personal statement, ask yourself:
- What are the most important things you want that person to remember about you?
- Does your medical school personal statement sum up your personality, interests, and talents?
- Does your medical school personal statement sound as if it’s written from the heart?
It’s pretty obvious to most admissions reviewers when applicants are trying too hard to impress them. Being authentic and upfront about who you are is the best way to be a memorable applicant.
The Biggest Medical School Personal Statement Mistakes
The most common medical school personal statement mistake we see students make is that they write about:
- What they have accomplished
- How they have accomplished it
By including details on what you have accomplished and how, you will make yourself sound like every other medical school applicant.
Most medical school applicants are involved in similar activities: research, clinical work, service, and social justice work.
To stand out, you must write from the heart making it clear you haven’t marched through your premedical years and checking boxes.
We also strongly discourage applicants from using ChatGPT or any AI bot to write their medical school personal statement. Writing in your own voice is essential and using anything automated will undermine success.
The Medical School Personal Statement Secret
MedEdits students stand out in the medical school personal statement because in their personal statements they address:
WHY they have accomplished what they have.
In other words, they write in more detail about their passions, interests, and what is genuinely important to them.
It sounds simple, we know, but by writing in a natural way, really zeroing in on WHY YOU DO WHAT YOU DO, you will appeal to a wide variety of people in a humanistic way.
MedEdits students have done extremely well in the most recent medical school admissions cycle. Many of these applicants have below average “stats” for the medical schools from which they are receiving interviews and acceptances.
Why? How is that possible? They all have a few things in common:
- They write a narrative that is authentic and distinctive to them.
- They write a medical school personal statement with broad appeal (many different types of people will be evaluating your application; most are not physicians).
- They don’t try too hard to impress; instead they write about the most impactful experiences they have had on their path to medical school.
- They demonstrate they are humble, intellectual, compassionate, and committed to a career in medicine all at the same time.
Keep reading for a step by step approach to write your medical school personal statement.
“After sitting on a medical school admissions committee for many years, I can tell you, think strategically about how you want to present your personal “big picture.” We want to know who you are as a human being.”
As physicians, former medical school faculty, and medical school admissions committee members, this article will offer a step by step guide to simplify the medical school personal statement brainstorming and writing process.
By following the proven strategies outlined in this article, you will be and to write a personal statement that will earn you more medical school interviews . This proven approach has helped hundreds of medical school applicants get in to medical school the first time they apply!
Learn the 2024-2025 Medical School Personal Statement Prompts ( AMCAS , TMDSAS , AACOMAS )
The personal statement is the major essay portion of your primary application process. In it, you should describe yourself and your background, as well as any important early exposures to medicine, how and why medicine first piqued your interest, what you have done as a pre med, your personal experiences, and how you became increasingly fascinated with it. It’s also key to explain why medicine is the right career for you, in terms of both personal and intellectual fulfillment, and to show your commitment has continued to deepen as you learned more about the field.
The personal statement also offers you the opportunity to express who you are outside of medicine. What are your other interests? Where did you grow up? What did you enjoy about college? Figuring out what aspects of your background to highlight is important since this is one of your only chances to express to the med school admissions committee before your interview what is important to you and why.
However, it is important to consider the actual personal statement prompt for each system through which you will apply, AMCAS, AACOMAS, and TMDSAS, since each is slightly different.
Getting into a medical school has never been more competitive. Let the experts at MedEdits help you with your medical school application materials. We’ve worked with more than 5,000 students and 94% have been admitted to medical school.
Need help with your Personal Statement?
Schedule a free 15 Minute Consultation with a MedEdits expert.
2024 AMCAS Personal Statement Prompt
The AMCAS personal statement instructions are as follows:
Use the Personal Comments Essay as an opportunity to distinguish yourself from other applicants. Consider and write your Personal Comments Essay carefully; many admissions committees place significant weight on the essay. Here are some questions that you may want to consider while writing the essay:
- Why have you selected the field of medicine?
- What motivates you to learn more about medicine?
- What do you want medical schools to know about you that hasn’t been disclosed in other sections of the application?
In addition, you may wish to include information such as:
- Unique hardships, challenges, or obstacles that may have influenced your educational pursuits
- Comments on significant fluctuations in your academic record that are not explained elsewhere in your application
As you can see, these prompts are not vague; there are fundamental questions that admissions committees want you to answer when writing your personal statement. While the content of your statement should be focused on medicine, answering the open ended third question is a bit trickier.
The AMCAS personal statement length is 5,300 characters with spaces maximum.
2024 TMDSAS Personal Statement Prompt
The TMDSAS personal statement is one of the most important pieces of your medical school application.
The TMDSAS personal statement prompt is as follows:
Explain your motivation to seek a career in medicine. Be sure to include the value of your experiences that prepare you to be a physician.
This TMDSAS prompt is very similar to the AMCAS personal statement prompt. The TMDSAS personal statement length is 5,000 characters with spaces whereas the AMCAS personal statement length is 5,300 characters with spaces. Most students use the same essay (with very minor modifications, if necessary) for both application systems.
You’ve been working hard on your med school application, reading medical school personal statement examples, editing, revising, editing and revising. Make sure you know where you’re sending your personal statement and application. Watch this important medical school admissions statistics video.
2024 AACOMAS Personal Statement Prompt
The AACOMAS personal statement is for osteopathic medical schools specifically. As with the AMCAS statement, you need to lay out your journey to medicine as chronologically as possible in 5,300 characters with spaces or less. So you essentially have the same story map as for an AMCAS statement. Most important, you must show you are interested in osteopathy specifically. Therefore, when trying to decide what to include or leave out, prioritize any osteopathy experiences you have had, or those that are in line with the osteopathic philosophy of the mind-body connection, the body as self-healing, and other tenets.
Medical School Application Timeline and When to Write your Personal Statement
If you’re applying to both allopathic and osteopathic schools, you can most likely use the same medical school personal statement for both AMCAS and AACOMAS. In fact, this is why AACOMAS changed the personal statement length to match the AMCAS length several years ago.
Most medical school personal statements can be used for AMCAS and AACOMAS.
Know the Required Medical School Personal Statement Length
Below are the medical schools personal statement length limits for each application system. As you can see, they are all very similar. When you start brainstorming and writing your personal statement, keep these limits in mind.
AMCAS Personal Statement Length : 5,300 characters with spaces.
As per the AAMC website : “The available space for this essay is 5,300 characters (spaces are counted as characters), or approximately one page. You will receive an error message if you exceed the available space.”
AACOMAS Personal Statement Length : 5,300 characters with spaces
TMDSAS Personal Statement Length : 5,000 characters with spaces
As per the TMDSAS Website (Page 36): “The personal essay asks you to explain your motivation to seek a career in medicine. You are asked to include the value of your experiences that prepare you to be a physician. The essay is limited to 5000 characters, including spaces.”
Demonstrate Required Preprofessional Competencies
Next, your want to be aware of the nine preprofessional core competencies as outlined by the Association of American Medical Colleges . Medical school admissions committees want to see, as evidenced by your medical school personal statement and application, that you possess these qualities and characteristics. Now, don’t worry, medical school admissions committees don’t expect you to demonstrate all of them, but, you should demonstrate some.
- Service Orientation
- Social Skills
- Cultural Competence
- Oral Communication
- Ethical Responsibility to Self and Others
- Reliability and Dependability
- Resilience and Adaptability
- Capacity for Improvement
In your personal statement, you might be able to also demonstrate the four thinking and reasoning competencies:
- Critical Thinking
- Quantitative Reasoning
- Written Communication
- Scientific Inquiry
So, let’s think about how to address the personal statement prompts in a slightly different way while ensuring you demonstrate the preprofessional competencies. When writing your personal statement, be sure it answers the four questions that follow and you will “hit” most of the core competencies listed above.
1. What have you done that supports your interest in becoming a doctor?
I always advise applicants to practice “evidence based admissions.” The reader of your essay wants to see the “evidence” that you have done what is necessary to understand the practice of medicine. This includes clinical exposure, research, and community service, among other activities.
2. Why do you want to be a doctor?
This may seem pretty basic – and it is – but admissions officers need to know WHY you want to practice medicine. Many applicants make the mistake of simply listing what they have done without offering insights about those experiences that answer the question, “Why medicine?” Your reasons for wanting to be a doctor may overlap with those of other applicants. This is okay because the experiences in which you participated, the stories you can tell about those experiences, and the wisdom you gained are completely distinct—because they are only yours.
“In admissions committee meetings we were always interested in WHY you wanted to earn a medical degree and how you would contribute to the medical school community.”
Medical school admissions committees want to know that you have explored your interest deeply and that you can reflect on the significance of these clinical experiences and volunteer work. But writing only that you “want to help people” does not support a sincere desire to become a physician; you must indicate why the medical profession in particular—rather than social work, teaching, or another “helping” profession—is your goal.
3. How have your experiences influenced you?
It is important to show how your experiences are linked and how they have influenced you. How did your experiences motivate you? How did they affect what else you did in your life? How did your experiences shape your future goals? Medical school admissions committees like to see a sensible progression of involvements. While not every activity needs to be logically “connected” with another, the evolution of your interests and how your experiences have nurtured your future goals and ambitions show that you are motivated and committed.
4. Who are you as a person? What are your values and ideals?
Medical school admissions committees want to know about you as an individual beyond your interests in medicine, too. This is where answering that third open ended question in the prompt becomes so important. What was interesting about your background, youth, and home life? What did you enjoy most about college? Do you have any distinctive passions or interests? They want to be convinced that you are a good person beyond your experiences. Write about those topics that are unlikely to appear elsewhere in your statement that will offer depth and interest to your work and illustrate the qualities and characteristics you possess.
Related Articles:
- How to Get into Stanford Medical School
- How to Get into NYU Medical School
- How To Get Into Columbia Medical School
- How To Get Into UT Southwestern Medical School
- How To Get Into Harvard Medical School
Complete Your Personal Inventory and Outline (Example Below)
The bulk of your essay should be about your most valuable experiences, personal, academic, scholarly, clinical, academic and extracurricular activities that have impacted your path to medical school and through which you have learned about the practice of medicine. The best personal statements cover several topics and are not narrow in scope. Why is this important? Many different people with a variety of backgrounds, interests, and ideas of what makes a great medical student will be reading your essay. You want to make sure you essay has broad appeal.
The following exercise will help you to determine what experiences you should highlight in your personal statement.
When composing your personal statement, keep in mind that you are writing, in effect, a “story” of how you arrived at this point in your life. But, unlike a “story” in the creative sense, yours must also offer convincing evidence for your decision to apply to medical school. Before starting your personal statement, create an experience- based personal inventory:
- Write down a list of the most important experiences in your life and your development. The list should be all inclusive and comprise those experiences that had the most impact on you. Put the list, which should consist of personal, extracurricular, and academic events, in chronological order.
- From this list, determine which experiences you consider the most important in helping you decide to pursue a career in medicine. This “experience oriented” approach will allow you to determine which experiences best illustrate the personal competencies admissions committees look for in your written documents. Remember that you must provide evidence for your interest in medicine and for most of the personal qualities and characteristics that medical school admissions committees want to see.
- After making your list, think about why each “most important” experience was influential and write that down. What did you observe? What did you learn? What insights did you gain? How did the experience influence your path and choices?
- Then think of a story or illustration for why each experience was important.
- After doing this exercise, evaluate each experience for its significance and influence and for its “story” value. Choose to write about those experiences that not only were influential but that also will provide interesting reading, keeping in mind that your goal is to weave the pertinent experiences together into a compelling story. In making your choices, think about how you will link each experience and transition from one topic to the next.
- Decide which of your listed experiences you will use for your introduction first (see below for more about your introduction). Then decide which experiences you will include in the body of your personal statement, create a general outline, and get writing!
Remember, you will also have your work and activities entries and your secondary applications to write in more detail about your experiences. Therefore, don’t feel you must pack everything in to your statement!
Craft a Compelling Personal Statement Introduction and Body
You hear conflicting advice about application essays. Some tell you not to open with a story. Others tell you to always begin with a story. Regardless of the advice you receive, be sure to do three things:
- Be true to yourself. Everyone will have an opinion regarding what you should and should not write. Follow your own instincts. Your personal statement should be a reflection of you, and only you.
- Start your personal statement with something catchy. Think about the list of potential topics above.
- Don’t rush your work. Composing thoughtful documents takes time and you don’t want your writing and ideas to be sloppy and underdeveloped.
Most important is to begin with something that engages your reader. A narrative, a “story,” an anecdote written in the first or third person, is ideal. Whatever your approach, your first paragraph must grab your reader’s attention and motivate him to want to continue reading. I encourage applicants to start their personal statement by describing an experience that was especially influential in setting them on their path to medical school. This can be a personal or scholarly experience or an extracurricular one. Remember to avoid clichés and quotes and to be honest and authentic in your writing. Don’t try to be someone who you are not by trying to imitate personal statement examples you have read online or “tell them what you think they want to hear”; consistency is key and your interviewer is going to make sure that you are who you say you are!
When deciding what experiences to include in the body of your personal statement, go back to your personal inventory and identify those experiences that have been the most influential in your personal path and your path to medical school. Keep in mind that the reader wants to have an idea of who you are as a human being so don’t write your personal statement as a glorified resume. Include some information about your background and personal experiences that can give a picture of who you are as a person outside of the classroom or laboratory.
Ideally, you should choose two or three experiences to highlight in the body of your personal statement. You don’t want to write about all of your accomplishments; that is what your application entries are for!
Write Your Personal Statement Conclusion
In your conclusion, it is customary to “go full circle” by coming back to the topic—or anecdote—you introduced in the introduction, but this is not a must. Summarize why you want to be a doctor and address what you hope to achieve and your goals for medical school. Write a conclusion that is compelling and will leave the reader wanting to meet you.
Complete Personal Statement Checklist
When reading your medical school personal statement be sure it:
Shows insight and introspection
The best medical school personal statements tell a great deal about what you have learned through your experiences and the insights you have gained.
You want to tell your story by highlighting those experiences that have been the most influential on your path to medical school and to give a clear sense of chronology. You want your statement always to be logical and never to confuse your reader.
Is interesting and engaging
The best personal statements engage the reader. This doesn’t mean you must use big words or be a literary prize winner. Write in your own language and voice, but really think about your journey to medical school and the most intriguing experiences you have had.
Gives the reader a mental image of who you are
You want the reader to be able to envision you as a caregiver and a medical professional. You want to convey that you would be a compassionate provider at the bedside – someone who could cope well with crisis and adversity.
Illustrates your passion for, and commitment to, medicine
Your reader must be convinced that you are excited about and committed to a career in medicine!
Above all, your personal statement should be about you. Explain to your reader what you have done and why you want to be a doctor with insight, compassion, and understanding.
Medical School Personal Statement Myths
Also keep in mind some common myths about personal statements that I hear quite often:
My personal statement must have a theme.
Not true. The vast majority of personal statements do not have themes. In fact, most are somewhat autobiographical and are just as interesting as those statements that are woven around a “theme.” It is only the very talented writer who can creatively write a personal statement around a theme, and this approach often backfires since the applicant fails to answer the three questions above.
My personal statement must be no longer than one page.
Not true. This advice is antiquated and dates back to the days of the written application when admissions committees flipped through pages. If your personal statement is interesting and compelling, it is fine to use the entire allotted space. The application systems have incorporated limits for exactly this reason! Many students, depending on their unique circumstances, can actually undermine their success by limiting their personal statement to a page. That said, never max out a space just for the sake of doing so. Quality writing and perspectives are preferable to quantity.
My personal statement should not describe patient encounters or my personal medical experiences.
Not true. Again, the actual topics on which you focus in your personal statement are less important than the understanding you gained from those experiences. I have successful clients who have written extremely powerful and compelling personal statements that included information about clinical encounters – both personal and professional. Write about whichever experiences were the most important on your path to medicine. It’s always best, however, to avoid spending too much space on childhood and high school activities. Focus instead on those that are more current.
In my personal statement I need to sell myself.
Not exactly true. You never want to boast in your personal statement. Let your experiences, insights, and observations speak for themselves. You want your reader to draw the conclusion – on his or her own – that you have the qualities and characteristics the medical school seeks. Never tell what qualities and characteristics you possess; let readers draw these conclusions on their own based on what you write.
Medical School Personal Statement Examples and Analysis for Inspiration
Below are examples of actual medical school personal statements. You can also likely find medical school personal statements on Reddit.
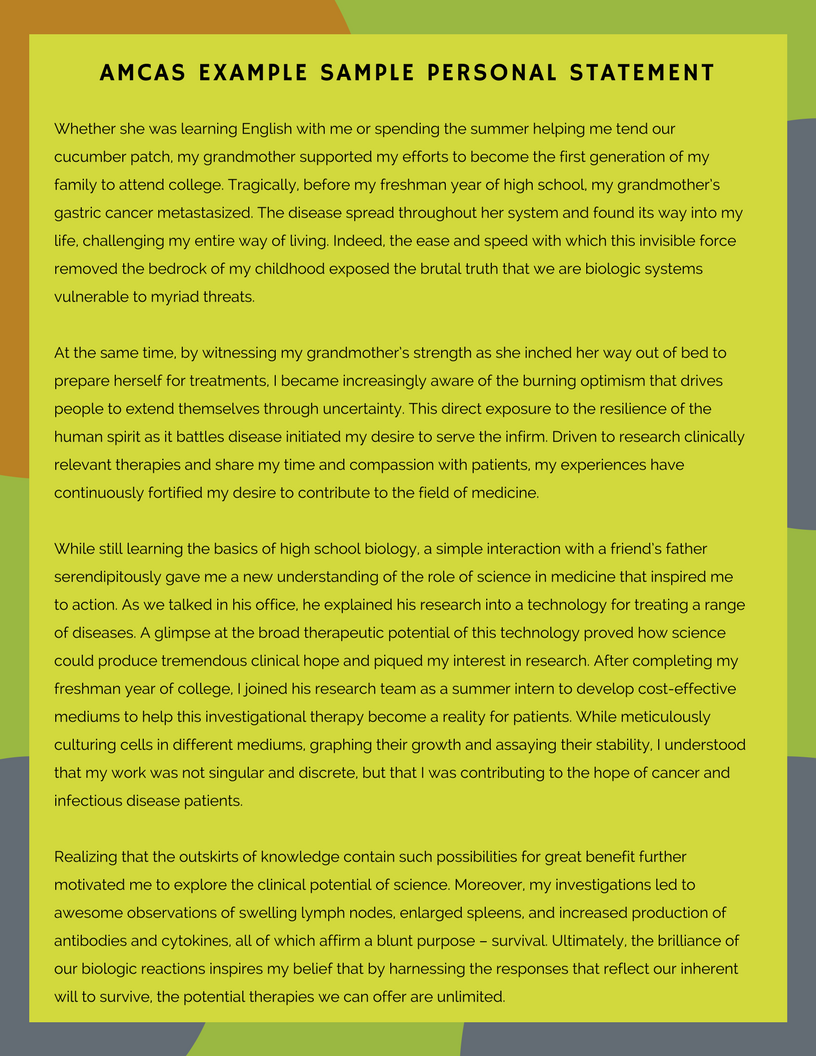
AMCAS Medical School Personal Statement Example and Analysis #1 with Personal Inventory
We will use Amy to illustrate the general process of writing an application to medical school, along with providing the resulting documents. Amy will first list those experiences, personal, extracurricular, and scholarly, that have been most influential in two areas: her life in general and her path to medical school. She will put this personal inventory in chronologic order for use in composing her personal statement.
She will then select those experiences that were the most significant to her and will reflect and think about why they were important. For her application entries, Amy will write about each experience, including those that she considers influential in her life but not in her choice of medicine, in her application entries. Experiences that Amy will not write about in her activity entries or her personal statement are those that she does not consider most influential in either her life or in her choice of medicine.
Amy’s personal inventory (from oldest to most recent)
- Going with my mom to work. She is a surgeon — I was very curious about what she did. I was intrigued by the relationships she had with patients and how much they valued her efforts. I also loved seeing her as “a doctor” since, to me, she was just “mom.”
- I loved biology in high school. I started to think seriously about medicine then. It was during high school that I became fascinated with biology and how the human body worked. I would say that was when I thought, “Hmm, maybe I should be a doctor.”
- Grandmother’s death, senior year of high school. My grandmother’s death was tragic. It was the first time I had ever seen someone close to me suffer. It was one of the most devastating experiences in my life.
- Global Health Trip to Guatemala my freshman year of college. I realized after going to Guatemala that I had always taken my access to health care for granted. Here I saw children who didn’t have basic health care. This made me want to become a physician so I could give more to people like those I met in Guatemala.
- Sorority involvement. Even though sorority life might seem trivial, I loved it. I learned to work with different types of people and gained some really valuable leadership experience.
- Poor grades in college science classes. I still regret that I did badly in my science classes. I think I was immature and was also too involved in other activities and didn’t have the focus I needed to do well. I had a 3.4 undergraduate GPA.
- Teaching and tutoring Jose, a child from Honduras. In a way, meeting Jose in a college tutoring program brought my Guatemala experience to my home. Jose struggled academically, and his parents were immigrants and spoke only Spanish, so they had their own challenges. I tried to help Jose as much as I could. I saw that because he lacked resources, he was at a tremendous disadvantage.
- Volunteering at Excellent Medical Center. Shadowing physicians at the medical center gave me a really broad view of medicine. I learned about different specialties, met many different patients, and saw both great and not-so-great physician role models. Counselor at Ronald McDonald House. Working with sick kids made me appreciate my health. I tried to make them happy and was so impressed with their resilience. It made me realize that good health is everything.
- Oncology research. Understanding what happens behind the scenes in research was fascinating. Not only did I gain some valuable research experience, but I learned how research is done.
- Peer health counselor. Communicating with my peers about really important medical tests gave me an idea of the tremendous responsibility that doctors have. I also learned that it is important to be sensitive, to listen, and to be open-minded when working with others.
- Clinical Summer Program. This gave me an entirely new view of medicine. I worked with the forensics department, and visiting scenes of deaths was entirely new to me. This experience added a completely new dimension to my understanding of medicine and how illness and death affect loved ones.
- Emergency department internship. Here I learned so much about how things worked in the hospital. I realized how important it was that people who worked in the clinical department were involved in creating hospital policies. This made me understand, in practical terms, how an MPH would give me the foundation to make even more change in the future.
- Master’s in public health. I decided to get an MPH for two reasons. First of all, I knew my undergraduate science GPA was an issue so I figured that graduate level courses in which I performed well would boost my record. I don’t think I will write this on my application, but I also thought the degree would give me other skills if I didn’t get into medical school, and I knew it would also give me something on which I could build during medical school and in my career since I was interested in policy work.
As you can see from Amy’s personal inventory list, she has many accomplishments that are important to her and influenced her path. The most influential personal experience that motivated her to practice medicine was her mother’s career as a practicing physician, but Amy was also motivated by watching her mother’s career evolve. Even though the death of her grandmother was devastating for Amy, she did not consider this experience especially influential in her choice to attend medical school so she didn’t write about it in her personal statement.
Amy wrote an experience-based personal statement, rich with anecdotes and detailed descriptions, to illustrate the evolution of her interest in medicine and how this motivated her to also earn a master’s in public health.
Amy’s Medical School Personal Statement Example:
She was sprawled across the floor of her apartment. Scattered trash, decaying food, alcohol bottles, medication vials, and cigarette butts covered the floor. I had just graduated from college, and this was my first day on rotation with the forensic pathology department as a Summer Scholar, one of my most valuable activities on the path to medical school. As the coroner deputy scanned the scene for clues to what caused this woman’s death, I saw her distraught husband. I did not know what to say other than “I am so sorry.” I listened intently as he repeated the same stories about his wife and his dismay that he never got to say goodbye. The next day, alongside the coroner as he performed the autopsy, I could not stop thinking about the grieving man.
Discerning a cause of death was not something I had previously associated with the practice of medicine. As a child, I often spent Saturday mornings with my mother, a surgeon, as she rounded on patients. I witnessed the results of her actions, as she provided her patients a renewed chance at life. I grew to honor and respect my mother’s profession. Witnessing the immense gratitude of her patients and their families, I quickly came to admire the impact she was able to make in the lives of her patients and their loved ones.
I knew I wanted to pursue a career in medicine as my mother had, and throughout high school and college I sought out clinical, research, and volunteer opportunities to gain a deeper understanding of medicine. After volunteering with cancer survivors at Camp Ronald McDonald, I was inspired to further understand this disease. Through my oncology research, I learned about therapeutic processes for treatment development. Further, following my experience administering HIV tests, I completed research on point-of-care HIV testing, to be instituted throughout 26 hospitals and clinics. I realized that research often served as a basis for change in policy and medical practice and sought out opportunities to learn more about both.
All of my medically related experiences demonstrated that people who were ‘behind the scenes’ and had limited or no clinical background made many of the decisions in health care. Witnessing the evolution of my mother’s career further underscored the impact of policy change on the practice of medicine. In particular, the limits legislation imposed on the care she could provide influenced my perspective and future goals. Patients whom my mother had successfully treated for more than a decade, and with whom she had long-standing, trusting relationships, were no longer able to see her, because of policy coverage changes. Some patients, frustrated by these limitations, simply stopped seeking the care they needed. As a senior in college, I wanted to understand how policy transformations came about and gain the tools I would need to help effect administrative and policy changes in the future as a physician. It was with this goal in mind that I decided to complete a master’s in public health program before applying to medical school.
As an MPH candidate, I am gaining insight into the theories and practices behind the complex interconnections of the healthcare system; I am learning about economics, operations, management, ethics, policy, finance, and technology and how these entities converge to impact delivery of care. A holistic understanding of this diverse, highly competitive, market-driven system will allow me, as a clinician, to find solutions to policy, public health, and administration issues. I believe that change can be more effective if those who actually practice medicine also decide where improvements need to be made.
For example, as the sole intern for the emergency department at County Medical Center, I worked to increase efficiency in the ED by evaluating and mapping patient flow. I tracked patients from point of entry to point of discharge and found that the discharge process took up nearly 35% of patients’ time. By analyzing the reasons for this situation, in collaboration with nurses and physicians who worked in the ED and had an intimate understanding of what took place in the clinical area, I was able to make practical recommendations to decrease throughput time. The medical center has already implemented these suggestions, resulting in decreased length of stays. This example illustrates the benefit of having clinicians who work ‘behind the scenes’ establish policies and procedures, impacting operational change and improving patient care. I will also apply what I have learned through this project as the business development intern at Another Local Medical Center this summer, where I will assist in strategic planning, financial analysis, and program reviews for various clinical departments.
Through my mother’s career and my own medical experiences, I have become aware of the need for clinician administrators and policymakers. My primary goal as a physician will be to care for patients, but with the knowledge and experience I have gained through my MPH, I also hope to effect positive public policy and administrative changes.
What’s Good About Amy’s Medical School Personal Statement:
Paragraphs 1 and 2: Amy started her personal statement by illustrating a powerful experience she had when she realized that medical caregivers often feel impotent, and how this contrasted with her understanding of medicine as a little girl going with her mother to work. Recognition of this intense contrast also highlights Amy’s maturity.
Paragraph 3: Amy then “lists” a few experiences that were important to her.
Paragraph 4: Amy describes the commonality in some of her experiences and how her observations were substantiated by watching the evolution of her mother’s practice. She then explains how this motivated her to earn an MPH so she could create change more effectively as a physician than as a layman.
Paragraph 5: Amy then explains how her graduate degree is helping her to better understand the “issues in medicine” that she observed.
Paragraph 6: Amy then describes one exceptional accomplishment she had that highlights what she has learned and how she has applied it.
Paragraph 7: Finally, Amy effectively concludes her personal statement and summarizes the major topics addressed in her essay.
As you can see, Amy’s statement has excellent flow, is captivating and unusual, and illustrates her understanding of, and commitment to, medicine. She also exhibits, throughout her application entries and statement, the personal competencies, characteristics, and qualities that medical school admissions officers are seeking. Her application also has broad appeal; reviewers who are focused on research, cultural awareness, working with the underserved, health administration and policy, teaching, or clinical medicine would all find it of interest.
med school personal statement examples
Osteopathic Medical School Personal Statement Example and Analysis #2
Medical School Personal Statement Example Background: This is a nontraditional applicant who applied to osteopathic medical schools. With a 500 and a 504 on the MCAT , he needed to showcase how his former career and what he learned through his work made him an asset. He also needed to convey why osteopathic medicine was an ideal fit for him. The student does an excellent job illustrating his commitment to medicine and explaining why and how he made the well-informed decision to leave his former career to pursue a career in osteopathic medicine.
What’s Good About It: A nontraditional student with a former career, this applicant does a great job outlining how and why he decided to pursue a career in medicine. Clearly dedicated to service, he also does a great job making it clear he is a good fit for osteopathic medical school and understands this distinctions of osteopathic practice..
Working as a police officer, one comes to expect the unexpected, but sometimes, when the unexpected happens, one can’t help but be surprised. In November 20XX, I had been a police officer for two years when my partner and I happened to be nearby when a man had a cardiac emergency in Einstein Bagels. Entering the restaurant, I was caught off guard by the lifeless figure on the floor, surrounded by spilled food. Time paused as my partner and I began performing CPR, and my heart raced as I watched color return to the man’s pale face.
Luckily, paramedics arrived within minutes to transport him to a local hospital. Later, I watched as the family thanked the doctors who gave their loved one a renewed chance at life. That day, in the “unexpected,” I confirmed that I wanted to become a physician, something that had attracted me since childhood.
I have always been enthralled by the science of medicine and eager to help those in need but, due to life events, my path to achieving this dream has been long. My journey began following high school when I joined the U.S. Army. I was immature and needed structure, and I knew the military was an opportunity to pursue my medical ambitions. I trained as a combat medic and requested work in an emergency room of an army hospital. At the hospital, I started IVs, ran EKGs, collected vital signs, and assisted with codes. I loved every minute as I was directly involved in patient care and observed physicians methodically investigating their patients’ signs and symptoms until they reached a diagnosis. Even when dealing with difficult patients, the physicians I worked with maintained composure, showing patience and understanding while educating patients about their diseases. I observed physicians not only as clinicians but also as teachers. As a medic, I learned that I loved working with patients and being part of the healthcare team, and I gained an understanding of acute care and hospital operations.
Following my discharge in 20XX, I transferred to an army reserve hospital and continued as a combat medic until 20XX. Working as a medic at several hospitals and clinics in the area, I was exposed to osteopathic medicine and the whole body approach to patient care. I was influenced by the D.O.s’ hands-on treatment and their use of manipulative medicine as a form of therapy. I learned that the body cannot function properly if there is dysfunction in the musculoskeletal system.
In 20XX, I became a police officer to support myself as I finished my undergraduate degree and premed courses. While working the streets, I continued my patient care experiences by being the first to care for victims of gunshot wounds, stab wounds, car accidents, and other medical emergencies. In addition, I investigated many unknown causes of death with the medical examiner’s office. I often found signs of drug and alcohol abuse and learned the dangers and power of addiction. In 20XX, I finished my undergraduate degree in education and in 20XX, I completed my premed courses.
Wanting to learn more about primary care medicine, in 20XX I volunteered at a community health clinic that treats underserved populations. Shadowing a family physician, I learned about the physical exam as I looked into ears and listened to the hearts and lungs of patients with her guidance. I paid close attention as she expressed the need for more PCPs and the important roles they play in preventing disease and reducing ER visits by treating and educating patients early in the disease process. This was evident as numerous patients were treated for high cholesterol, elevated blood pressure, and diabetes, all conditions that can be resolved or improved by lifestyle changes. I learned that these changes are not always easy for many in underserved populations as healthier food is often more expensive and sometimes money for prescriptions is not available. This experience opened my eyes to the challenges of being a physician in an underserved area.
The idea of disease prevention stayed with me as I thought about the man who needed CPR. Could early detection and education about heart disease have prevented his “unexpected” cardiac event? My experiences in health care and law enforcement have confirmed my desire to be an osteopathic physician and to treat the patients of the local area. I want to eliminate as many medical surprises as I can.
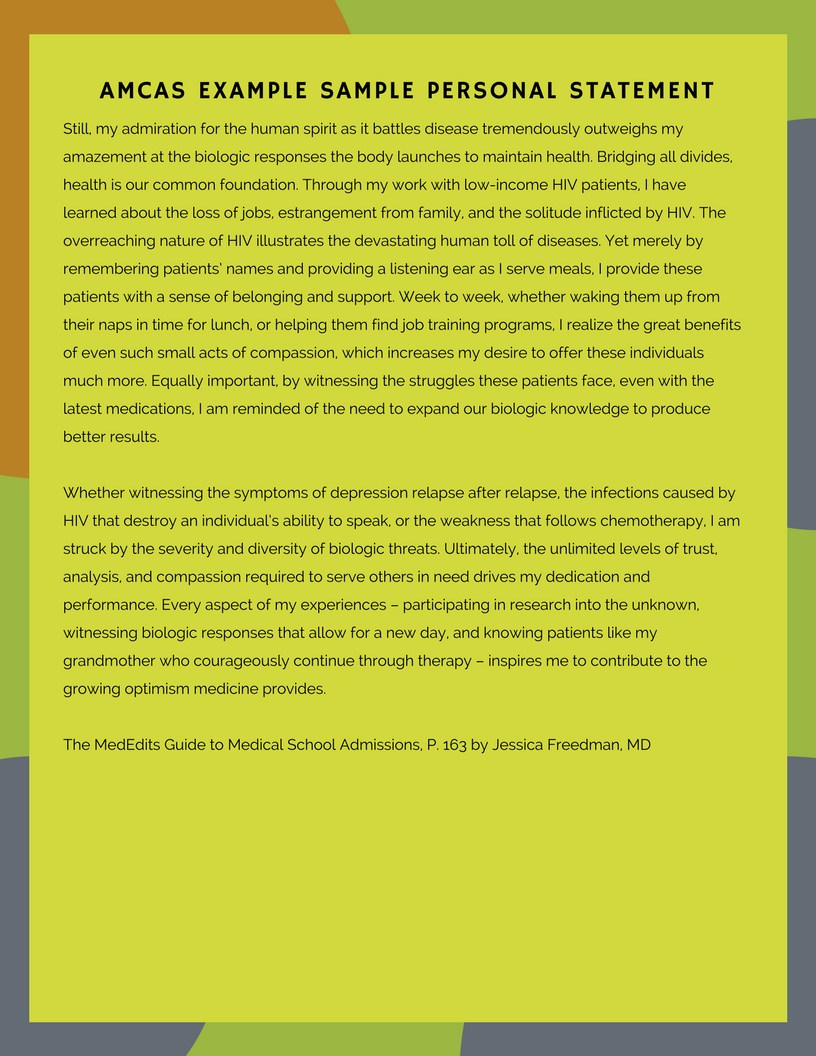
Texas Medical School Personal Statement Example and Analysis #3
Medical School Personal Statement Example Background: This applicant, who grew up with modest means, should be an inspiration to us all. Rather than allowing limited resources to stand in his way, he took advantage of everything that was available to him. He commuted to college from home and had a part-time job so he was stretched thin, and his initial college performance suffered. However, he worked hard and his grades improved. Most medical school admissions committees seek out applicants like this because, by overcoming adversity and succeeding with limited resources, they demonstrate exceptional perseverance, maturity, and dedication. His accomplishments are, by themselves, impressive and he does an outstanding job of detailing his path, challenges, and commitment to medicine. He received multiple acceptances to top medical schools and was offered scholarships.
What’s Good About It: This student does a great job opening his personal statement with a beautifully written introduction that immediately takes the reader to Central America. He then explains his path, why he did poorly early in college, and goes on to discuss his academic interests and pursuits. He is also clearly invested in research and articulates that he is intellectually curious, motivated, hard working, compassionate and committed to a career in medicine by explaining his experiences using interesting language and details. This is an intriguing statement that makes clear the applicant is worthy of an interview invitation. Finally, the student expresses his interest in attending medical school in Texas.
They were learning the basics of carpentry and agriculture. The air was muggy and hot, but these young boys seemed unaffected, though I and my fellow college students sweated and often complained. As time passed, I started to have a greater appreciation for the challenges these boys faced. These orphans, whom I met and trained in rural Central America as a member of The Project, had little. They dreamed of using these basic skills to earn a living wage. Abandoned by their families, they knew this was their only opportunity to re-enter society as self- sufficient individuals. I stood by them in the fields and tutored them after class. And while I tried my best to instill in them a strong work ethic, it was the boys who instilled in me a desire to help those in need. They gave me a new perspective on my decision to become a doctor.
I don’t know exactly when I decided to become a physician; I have had this goal for a long time. I grew up in the inner city of A City, in Texas and attended magnet schools. My family knew little about higher education, and I learned to seek out my own opportunities and advice. I attended The University with the goal of gaining admission to medical school. When I started college, I lacked the maturity to focus on academics and performed poorly. Then I traveled to Central America. Since I was one of the few students who spoke Spanish, many of the boys felt comfortable talking with me. They saw me as a role model.
The boys worked hard so that they could learn trades that would help them to be productive members of society. It was then I realized that my grandparents, who immigrated to the US so I would have access to greater opportunities, had done the same. I felt like I was wasting what they had sacrificed for me. When I returned to University in the fall, I made academics my priority and committed myself to learn more about medicine .
Through my major in neuroscience, I strengthened my understanding of how we perceive and experience life. In systems neurobiology, I learned the physiology of the nervous system. Teaching everything from basic neural circuits to complex sensory pathways, Professor X provided me with the knowledge necessary to conduct research in Parkinson’s disease. My research focused on the ability of antioxidants to prevent the onset of Parkinson’s, and while my project was only a pilot study at the time, Professor X encouraged me to present it at the National Research Conference. During my senior year, I developed the study into a formal research project, recruiting the help of professors of statistics and biochemistry.
Working at the School of Medicine reinforced my analytical skills. I spent my summer in the department of emergency medicine, working with the department chair, Dr. Excellent. Through Dr. Excellent’s mentorship, I participated in a retrospective study analyzing patient charts to determine the efficacy of D-dimer assays in predicting blood clots. The direct clinical relevance of my research strengthened my commitment and motivated my decision to seek out more clinical research opportunities.
A growing awareness of the role of human compassion in healing has also influenced my choice to pursue a career in medicine. It is something no animal model or cell culture can ever duplicate or rival. Working in clinical research has allowed me to see the selflessness of many physicians and patients and their mutual desire to help others. As a research study assistant in the department of surgery, I educate and enroll patients in clinical trials. One such study examines the role of pre-operative substance administration in tumor progression. Patients enrolled in this study underwent six weeks of therapy before having the affected organ surgically excised. Observing how patients were willing to participate in this research to benefit others helped me understand the resiliency of the human spirit.
Working in clinical trials has enabled me to further explore my passion for science, while helping others. Through my undergraduate coursework and participation in volunteer groups I have had many opportunities to solidify my goal to become a physician. As I am working, I sometimes think about my second summer in Central America. I recall how one day, after I had turned countless rows of soil in scorching heat, one of the boys told me that I was a trabajador verdadero—a true worker. I paused as I realized the significance of this comment. While the boy may not have been able to articulate it, he knew I could identify with him. What the boy didn’t know, however, was that had my grandparents not decided to immigrate to the US, I would not have the great privilege of seizing opportunities in this country and writing this essay today. I look forward to the next step of my education and hope to return home to Texas where I look forward to serving the communities I call home.
Final Thoughts
Above all, and as stated in this article numerous times, your personal statement should be authentic and genuine. Write about your path and and journey to this point in your life using anecdotes and observations to intrigue the reader and illustrate what is and was important to you. Good luck!
Medical School Personal Statement Help & Consulting
If all this information has you staring at your screen like a deer in the headlights, you’re not alone. Writing a superb medical school personal statement can be a daunting task, and many applicants find it difficult to get started writing, or to express everything they want to say succinctly. That’s where MedEdits can help. You don’t have to have the best writing skills to compose a stand-out statement. From personal-statement editing alone to comprehensive packages for all your medical school application needs, we offer extensive support and expertise developed from working with thousands of successful medical school applicants. We can’t promise applying to medical school will be stress-free, but most clients tell us it’s a huge relief not to have to go it alone.
MedEdits offers personal statement consulting and editing. Our goal when working with students is to draw out what makes each student distinctive. How do we do this? We will explore your background and upbringing, interests and ideals as well as your accomplishments and activities. By helping you identify the most distinguishing aspects of who you are, you will then be able to compose an authentic and genuine personal statement in your own voice to capture the admissions committee’s attention so you are invited for a medical school interview. Our unique brainstorming methodology has helped hundreds of aspiring premeds gain acceptance to medical school.
Sample Medical School Personal Statement
Example Medical School Personal Statement
- Website Disclaimer
- Terms and Conditions
- MedEdits Privacy Policy
- Medical School Application
Medical School Personal Statement Examples That Got 6 Acceptances
Featured Admissions Expert: Dr. Monica Taneja, MD
These 30 exemplary medical school personal statement examples come from our students who enrolled in one of our application review programs. Most of these examples led to multiple acceptance for our students. For instance, the first example got our student accepted into SIX medical schools. Here's what you'll find in this article: We'll first go over 30 medical school personal statement samples, then we'll provide you a step-by-step guide for composing your own outstanding statement from scratch. If you follow this strategy, you're going to have a stellar statement whether you apply to the most competitive or the easiest medical schools to get into .
>> Want us to help you get accepted? Schedule a free strategy call here . <<
Listen to the blog!
Article Contents 36 min read
Stellar medical school personal statement examples that got multiple acceptances, medical school personal statement example #1.
I made my way to Hillary’s house after hearing about her alcoholic father’s incarceration. Seeing her tearfulness and at a loss for words, I took her hand and held it, hoping to make things more bearable. She squeezed back gently in reply, “thank you.” My silent gesture seemed to confer a soundless message of comfort, encouragement and support.
Through mentoring, I have developed meaningful relationships with individuals of all ages, including seven-year-old Hillary. Many of my mentees come from disadvantaged backgrounds; working with them has challenged me to become more understanding and compassionate. Although Hillary was not able to control her father’s alcoholism and I had no immediate solution to her problems, I felt truly fortunate to be able to comfort her with my presence. Though not always tangible, my small victories, such as the support I offered Hillary, hold great personal meaning. Similarly, medicine encompasses more than an understanding of tangible entities such as the science of disease and treatment—to be an excellent physician requires empathy, dedication, curiosity and love of problem solving. These are skills I have developed through my experiences both teaching and shadowing inspiring physicians.
Medicine encompasses more than hard science. My experience as a teaching assistant nurtured my passion for medicine; I found that helping students required more than knowledge of organic chemistry. Rather, I was only able to address their difficulties when I sought out their underlying fears and feelings. One student, Azra, struggled despite regularly attending office hours. She approached me, asking for help. As we worked together, I noticed that her frustration stemmed from how intimidated she was by problems. I helped her by listening to her as a fellow student and normalizing her struggles. “I remember doing badly on my first organic chem test, despite studying really hard,” I said to Azra while working on a problem. “Really? You’re a TA, shouldn’t you be perfect?” I looked up and explained that I had improved my grades through hard work. I could tell she instantly felt more hopeful, she said, “If you could do it, then I can too!” When she passed, receiving a B+;I felt as if I had passed too. That B+ meant so much: it was a tangible result of Azra’s hard work, but it was also symbol of our dedication to one another and the bond we forged working together.
My passion for teaching others and sharing knowledge emanates from my curiosity and love for learning. My shadowing experiences in particular have stimulated my curiosity and desire to learn more about the world around me. How does platelet rich plasma stimulate tissue growth? How does diabetes affect the proximal convoluted tubule? My questions never stopped. I wanted to know everything and it felt very satisfying to apply my knowledge to clinical problems.
Shadowing physicians further taught me that medicine not only fuels my curiosity; it also challenges my problem solving skills. I enjoy the connections found in medicine, how things learned in one area can aid in coming up with a solution in another. For instance, while shadowing Dr. Steel I was asked, “What causes varicose veins and what are the complications?” I thought to myself, what could it be? I knew that veins have valves and thought back to my shadowing experience with Dr. Smith in the operating room. She had amputated a patient’s foot due to ulcers obstructing the venous circulation. I replied, “veins have valves and valve problems could lead to ulcers.” Dr. Steel smiled, “you’re right, but it doesn’t end there!” Medicine is not disconnected; it is not about interventional cardiology or orthopedic surgery. In fact, medicine is intertwined and collaborative. The ability to gather knowledge from many specialties and put seemingly distinct concepts together to form a coherent picture truly attracts me to medicine.
It is hard to separate science from medicine; in fact, medicine is science. However, medicine is also about people—their feelings, struggles and concerns. Humans are not pre-programmed robots that all face the same problems. Humans deserve sensitive and understanding physicians. Humans deserve doctors who are infinitely curious, constantly questioning new advents in medicine. They deserve someone who loves the challenge of problem solving and coming up with innovative individualized solutions. I want to be that physician. I want to be able to approach each case as a unique entity and incorporate my strengths into providing personalized care for my patients. Until that time, I may be found Friday mornings in the operating room, peering over shoulders, dreaming about the day I get to hold the drill.
Let's take a step back to consider what this medical school personal statement example does, not just what it says. It begins with an engaging hook in the first paragraph and ends with a compelling conclusion. The introduction draws you in, making the essay almost impossible to put down, while the conclusion paints a picture of someone who is both passionate and dedicated to the profession. In between the introduction and conclusion, this student makes excellent use of personal narrative. The anecdotes chosen demonstrate this individual's response to the common question, " Why do you want to be a doctor ?" while simultaneously making them come across as compassionate, curious, and reflective. The essay articulates a number of key qualities and competencies, which go far beyond the common trope, I want to be a doctor because I want to help people.
This person is clearly a talented writer, but this was the result of several rounds of edits with one of our medical school admissions consulting team members and a lot of hard work on the student's part. If your essay is not quite there yet, or if you're just getting started, don't sweat it. Do take note that writing a good personal essay takes advanced planning and significant effort.
I was one of those kids who always wanted to be doctor. I didn’t understand the responsibilities and heartbreaks, the difficult decisions, and the years of study and training that go with the title, but I did understand that the person in the white coat stood for knowledge, professionalism, and compassion. As a child, visits to the pediatrician were important events. I’d attend to my hair and clothes, and travel to the appointment in anticipation. I loved the interaction with my doctor. I loved that whoever I was in the larger world, I could enter the safe space of the doctor’s office, and for a moment my concerns were heard and evaluated. I listened as my mother communicated with the doctor. I’d be asked questions, respectfully examined, treatments and options would be weighed, and we would be on our way. My mother had been supported in her efforts to raise a well child, and I’d had a meaningful interaction with an adult who cared for my body and development. I understood medicine as an act of service, which aligned with my values, and became a dream.
I was hospitalized for several months as a teenager and was inspired by the experience, despite the illness. In the time of diagnosis, treatment and recovery, I met truly sick children. Children who were much more ill than me. Children who wouldn’t recover. We shared a four-bed room, and we shared our medical stories. Because of the old hospital building, there was little privacy in our room, and we couldn’t help but listen-in during rounds, learning the medical details, becoming “experts” in our four distinct cases. I had more mobility than some of the patients, and when the medical team and family members were unavailable, I’d run simple errands for my roommates, liaise informally with staff, and attend to needs. To bring physical relief, a cold compress, a warmed blanket, a message to a nurse, filled me with such an intense joy and sense of purpose that I applied for a volunteer position at the hospital even before my release.
I have since been volunteering in emergency departments, out-patient clinics, and long term care facilities. While the depth of human suffering is at times shocking and the iterations of illness astounding, it is in the long-term care facility that I had the most meaningful experiences by virtue of my responsibilities and the nature of the patients’ illnesses. Charles was 55 when he died. He had early onset Parkinson’s Disease with dementia that revealed itself with a small tremor when he was in his late twenties. Charles had a wife and three daughters who visited regularly, but whom he didn’t often remember. Over four years as a volunteer, my role with the family was to fill in the spaces left by Charles’ periodic inability to project his voice as well as his growing cognitive lapses. I would tell the family of his activities between their visits, and I would remind him of their visits and their news. This was a hard experience for me. I watched as 3 daughters, around my own age, incrementally lost their father. I became angry, and then I grew even more determined.
In the summer of third year of my Health Sciences degree, I was chosen to participate in an undergraduate research fellowship in biomedical research at my university. As part of this experience, I worked alongside graduate students, postdoctoral fellows, medical students, physicians, and faculty in Alzheimer’s research into biomarkers that might predict future disease. We collaborated in teams, and by way of the principal investigator’s careful leadership, I learned wherever one falls in terms of rank, each contribution is vital to the outcome. None of the work is in isolation. For instance, I was closely mentored by Will, a graduate student who had been in my role the previous summer. He, in turn, collaborated with post docs and medical students, turning to faculty when roadblocks were met. While one person’s knowledge and skill may be deeper than another’s, individual efforts make up the whole. Working in this team, aside from developing research skills, I realized that practicing medicine is not an individual pursuit, but a collaborative commitment to excellence in scholarship and leadership, which all begins with mentorship.
Building on this experience with teamwork in the lab, I participated in a global health initiative in Nepal for four months, where I worked alongside nurses, doctors, and translators. I worked in mobile rural health camps that offered tuberculosis care, monitored the health and development of babies and children under 5, and tended to minor injuries. We worked 11-hour days helping hundreds of people in the 3 days we spent in each location. Patients would already be in line before we woke each morning. I spent each day recording basic demographic information, blood pressure, pulse, temperature, weight, height, as well as random blood sugar levels, for each patient, before they lined up to see a doctor. Each day was exhausting and satisfying. We helped so many people. But this satisfaction was quickly displaced by a developing understanding of issues in health equity.
My desire to be doctor as a young person was not misguided, but simply naïve. I’ve since learned the role of empathy and compassion through my experiences as a patient and volunteer. I’ve broadened my contextual understanding of medicine in the lab and in Nepal. My purpose hasn’t changed, but what has developed is my understanding that to be a physician is to help people live healthy, dignified lives by practicing both medicine and social justice.
28 More Medical School Personal Statement Examples That Got Accepted
What my sister went through pushed me to strengthen my knowledge in medical education, patient care, and research. These events have influenced who I am today and helped me determine my own passions. I aspire to be a doctor because I want to make miracles, like my sister, happen. Life is something to cherish; it would not be the same if I did not have one of my four sisters to spend it with. As all stories have endings, I hope that mine ends with me fulfilling my dream of being a doctor, which has been the sole focus of my life to this point. I would love nothing more than to dedicate myself to such a rewarding career, where I achieve what those doctors did for my family. Their expertise allowed my sister to get all the care she needed for her heart, eyes, lungs, and overall growth. Those physicians gave me more than just my little sister, they gave me the determination and focus needed to succeed in the medical field, and for that, I am forever grateful. ","label":"Medical School Personal Statement Example #3","title":"Medical School Personal Statement Example #3"}]" code="tab4" template="BlogArticle">
I came to America, leaving my parents and friends behind, to grasp my chance at a better future. I believe this chance is now in front of me. Medicine is the only path I truly desire because it satisfies my curiosity about the human body and it allows me to directly interact with patients. I do not want to miss this chance to further hone my skills and knowledge, in order to provide better care for my patients. ","label":"Medical School Personal Statement #4","title":"Medical School Personal Statement #4"}]" code="tab5" template="BlogArticle">
The time I have spent in various medical settings has confirmed my love for the field. Regardless of the environment, I am drawn to patients and their stories, like that scared young boy at AMC. I am aware that medicine is a constantly changing landscape; however, one thing that has remained steadfast over the years is putting the patient first, and I plan on doing this as a physician. All of my experiences have taught me a great deal about patient interaction and global health, however, I am left wanting more. I crave more knowledge to help patients and become more useful in the healthcare sector. I am certain medical school is the path that will help me reach my goal. One day, I hope to use my experiences to become an amazing doctor like the doctors that treated my sister, so I can help other children like her. ","label":"Medical School Personal Statement Example #5","title":"Medical School Personal Statement Example #5"}]" code="tab6" template="BlogArticle">
My interest in the field of medicine has developed overtime, with a common theme surrounding the importance of personal health and wellness. Through my journey in sports, travelling, and meeting some incredible individuals such as Michael, I have shifted my focus from thinking solely about the physical well-being, to understanding the importance of mental, spiritual, and social health as well. Being part of a profession that emphasizes continuous education, and application of knowledge to help people is very rewarding, and I will bring compassion, a hard work ethic and an attitude that is always focused on bettering patient outcomes. ","label":"Medical School Personal Statement Example # 7","title":"Medical School Personal Statement Example # 7"}]" code="tab8" template="BlogArticle">
Medicine embodies a hard science, but it is ultimately a profession that treats people. I have seen firsthand that medicine is not a \u201cone-treatment-fits-all\u201d practice, as an effective physician takes a holistic approach. This is the type of physician I aspire to be: one who refuses to shy away from the humanity of patients and their social context, and one who uses research and innovation to improve the human condition. So, when I rethink \u201cwhy medicine?\u201d, I know it\u2019s for me \u2013 because it is a holistic discipline, because it demands all of me, because I am ready to absorb the fascinating knowledge and science that dictates human life, and engage with humanity in a way no other profession allows for. Until the day that I dawn the coveted white coat, you can find me in inpatient units, comforting the many John\u2019s to come, or perhaps at the back of an operating room observing a mitral valve repair \u2013 dreaming of the day the puck is in my zone. ","label":"Medical School Personal Statement Example #8","title":"Medical School Personal Statement Example #8"}]" code="tab9" template="BlogArticle">
When I signed up to be a live DJ, I didn't know that the oral skills I practiced on-air would influence all aspects of my life, let alone lead me to consider a career in the art of healing. I see now, though, the importance of these key events in my life that have allowed me to develop excellent communication skills--whether that be empathic listening, reading and giving non-verbal cues, or verbal communication. I realize I have always been on a path towards medicine. Ultimately, I aim to continue to strengthen my skills as I establish my role as a medical student and leader: trusting my choices, effectively communicating, and taking action for people in need. ","label":"Medical School Personal Statement Example #9","title":"Medical School Personal Statement Example #9"}]" code="tab10" template="BlogArticle">
\u201cWhy didn\u2019t I pursue medicine sooner?\u201d Is the question that now occupies my mind. Leila made me aware of the unprofessional treatment delivered by some doctors. My subsequent activities confirmed my desire to become a doctor who cares deeply for his patients and provides the highest quality care. My passion for research fuels my scientific curiosity. I will continue to advocate for patient equality and fairness. Combining these qualities will allow me to succeed as a physician. ","label":"Medical School Personal Statement Example #10","title":"Medical School Personal Statement Example #10"}]" code="tab11" template="BlogArticle">
Medical school personal statement example: #11
Medical school personal statement example: #12, medical school personal statement example: #13, medical school personal statement example: #14, medical school personal statement example: #15, medical school personal statement example: #16, medical school personal statement example: #17, medical school personal statement example: #18, medical school personal statement example: #19, medical school personal statement example: #20, medical school personal statement example: #21, medical school personal statement example: #22, medical school personal statement example: #23, medical school personal statement example: #24, medical school personal statement example: #25, medical school personal statement example: #26, medical school personal statement example: #27, medical school personal statement example: #28, medical school personal statement example: #29, medical school personal statement example: #30.
Please note that all personal statements are the property of the students who wrote them, re-printed with permission. Names and identifying characteristics have been changed. Plagiarism detection software is used when evaluating personal statements. Plagiarism is grounds for disqualification from the application. ","label":"NOTE","title":"NOTE"}]" code="tab2" template="BlogArticle">
As one of the most important medical school requirements , the personal statement tells your story of why you decided to pursue the medical profession. Keep in mind that personal statements are one of the key factors that affect medical school acceptance rates . This is why it's important to write a stellar essay!
“Personal statements are often emphasized in your application to medical school as this singular crucial factor that distinguishes you from every other applicant. Demonstrating the uniqueness of my qualities is precisely how I found myself getting multiple interviews and offers into medical school.” – Dr. Vincent Adeyemi, MD, Emory University school of Medicine
But this is easier said than done. In fact, medical school personal statements remain one of the most challenging parts of students' journeys to medical school. Here's our student Melissa sharing her experience of working on her personal statement:
"I struggled making my personal statement personal... I couldn't incorporate my feelings, motives and life stories that inspired me to pursue medicine into my personal statement" -Melissa, BeMo Student
Our student Rishi, who is now a student at the Carver College of Medicine , learned about the importance of the medical school personal statement the hard way:
"If you're a reapplicant like me, you know we all dread it but you have to get ready to answer what has changed about your application that we should accept you this time. I had an existing personal statement that did not get me in the first time so there was definitely work to be done." - Rishi, BeMo Student, current student at the Carver College of Medicine
The importance of the medical school personal statement can actually increase if you are applying to medical school with any red flags or setbacks, as our student Kannan did:
"I got 511 on my second MCAT try... My goal was anything over median of 510 so anything over that was honestly good with me because it's just about [creating] a good personal statement at that point... I read online about how important the personal statement [is]... making sure [it's] really polished and so that's when I decided to get some professional help." - Kannan, BeMo Student, current student at the Schulich School of Medicine
As you can see from these testimonials, your medical school personal statement can really make a difference. So we are here to help you get started writing your own personal statement. Let's approach this step-by-step. Below you will see how we will outline the steps to creating your very best personal statement. And don't forget that if you need to see more examples, you can also check out our AMCAS personal statement examples, AACOMAS personal statement examples and TMDSAS personal statement examples to further inspire you!
Here's a quick run-down of what we'll cover in the article:
Now let's dive in deeper!
#1 Understanding the Qualities of a Strong Med School Personal Statement
Before discussing how to write a strong medical school personal statement, we first need to understand the qualities of a strong essay. Similar to crafting strong medical school secondary essays , writing a strong personal statement is a challenging, yet extremely important, part of your MD or MD-PhD programs applications. Your AMCAS Work and Activities section may show the reader what you have done, but the personal statement explains why. This is how Dr. Neel Mistry, MD and our admissions expert, prepared for his medical school personal statement writing:
"The personal statement is an opportunity for you to shine and really impress the committee to invite you for an interview. The personal statement is your chance to be reflective and go beyond what is stated on your CV and [activities]. In order to stand out, it is important to answer the main questions [of medical school personal statements] well: a bit about yourself and what led you to medicine, why you would make an ideal medical student and future physician, what attracts you to [medicine], and what sets you apart from the other candidates. The key here is answering the last two questions well. Most candidates simply highlight what they have done, but do not reflect on it or mention how what they have done has prepared them for a future medical career." - Dr. Neel Mistry, MD
“my essay also focused on volunteering in the local health clinic during the many summer breaks. volunteering was more than just another activity to tick off my bucket list for my medical school … i volunteered because i wanted to view medical practice through the lenses of already qualified doctors, not because i needed a reason to be a doctor. i understood that the admissions committee would be more interested in how i was motivated.” – dr. vincent adeyemi..
A personal statement should be deeply personal, giving the admissions committee insight into your passions and your ultimate decision to pursue a career in medicine. A compelling and introspective personal statement can make the difference between getting an interview and facing medical school rejection . Review our blogs to find out how to prepare for med school interviews and learn the most common medical school interview questions .
As you contemplate the task in front of you, you may be wondering what composing an essay has to do with entering the field of medicine. Many of our students were surprised to learn that medical school personal statements are so valued by med schools. The two things are more closely related than you think. A compelling personal statement demonstrates your written communication skills and highlights your accomplishments, passions, and aspirations. The ability to communicate a complex idea in a short space is an important skill as a physician. You should demonstrate your communication skills by writing a concise and meaningful statement that illustrates your best attributes. Leaving a lasting impression on your reader is what will lead to interview invitations.
A quick note: if you are applying to schools that do not require the formal medical school personal statement, such as medical schools in Canada , you should still learn how to write such essays. Many medical schools in Ontario , for example, ask for short essays for supplementary questionnaires. These are very similar to the personal statement. Knowing how to brainstorm, write, and format your answers is key to your success!!!
You want to give yourself as much time as possible to write your statement. Do not think you can do this in an evening or even in a week. Some statements take months. My best statement took almost a year to get right. Allow yourself time and start early to avoid added stress. Think of the ideas you want to include and brainstorm possible ways to highlight these ideas. Ask your friends for ideas or even brainstorm your ideas with people you trust. Get some feedback early to make sure you are headed in the right direction.
“I wrote scores of essays at my desk in those few weeks leading up to application submission. I needed it to be perfect. Do not let anyone tell you to settle. There was no moment when I had this shining light from the sky filtering into my room to motivate me. The ultimate trick is to keep writing. It is impossible to get that perfect essay on the first try, and you may not even get it on your fifteenth attempt, but the goal is to keep at it, keep making those edits, and never back down.” – Dr. Vincent Adeyemi
All personal statements for medical school, often start by explaining why medicine is awesome; the admission committee already knows that. You should explain why you want a career in medicine. What is it about the practice of medicine that resonates with who you are? Naturally, this takes a lot of reflection around who you are. Here are some additional questions you can consider as you go about brainstorming for your essay:
- What motivates you to learn more about medicine?
- What is something you want them to know about you that isn't in your application?
- Where were you born, how did you grow up, and what type of childhood did you have growing up (perhaps including interesting stories about your siblings, parents, grandparents)?
- What kinds of early exposure to the medical field left an impression on you as a child?
- Did you become familiar with and interested in the field of medicine at an early stage of your life? If so, why?
- What are your key strengths, and how have you developed these?
- What steps did you take to familiarize yourself with the medical profession?
- Did you shadow a physician? Did you volunteer or work in a clinical setting? Did you get involved in medical research?
- What challenges have you faced? Have these made an impact on what you chose to study?
- What are your favorite activities?
- What kinds of extracurriculars for medical school or volunteer work have you done, and how have these shaped who you are, your priorities, and or your perspectives on a career in medicine?
- What was your "Aha!" moment?
- When did your desire to become a doctor solidify?
- How did you make the decision to apply to medical school?
You shouldn't try to answer all of these in your essay. Try only a few main points that will carry over into the final draft. Use these to brainstorm and gather ideas. Start developing your narrative by prioritizing the most impactful responses to these prompts and the ideas that are most relevant to your own experiences and goals. The perfect personal statement not only shows the admissions committee that you have refined communication skills, but also conveys maturity and professionalism. It should also display your motivation and suitability for medical practice. Here's how our student Alison, who was a non-traditional applicant with a serious red flag in her application, used her brainstorming sessions with our admissions experts to get a theme going in her medical school personal statement and her overall application package:
"I think it was during my brainstorming session that we really started talking about... what the theme [was] going to be for my application. And I think that was really helpful in and of itself. Just [reflecting] 'Hey, what's your focus going to be like? How are we going to write this? What's the style going to be?' Just to create an element of consistency throughout..." Alison, BeMo Student, current student at Dell Medical School
After brainstorming, you should be able to clearly see a few key ideas, skills, qualities, and intersections that you want to write about. Once you've isolated the elements you want to explore in your essay (usually 2-4 key ideas), you can begin building your outline. In terms of structure, this should follow the standard academic format, with an introduction, body paragraphs, and a conclusion.
As you begin thinking about what to include in your personal essay, remember that you are writing for a specific audience with specific expectations. Your evaluator will be familiar with the key qualities desired by medical schools, as informed by the standards of the profession. But keep in mind that they too are human, and they respond well to well-crafted, engaging essays that tell a story. Here's what our student Alison had to share about keeping your audience in mind when writing your personal statement:
"Make it easy for the reader to be able to work [their] way through [your personal statement]. Because, at the end of the day, I think one thing that helped me a lot was being able to think about who was going to be reading this application and it's going to be these people that are sitting around a desk or sitting at a table and [go] through massive numbers of applications every single day. And the easier and more digestible that you can make it for them, gives you a little bit of a win." - Alison, BeMo student, current student at Dell Medical School
The admissions committee will be examining your essay through the lens of their particular school's mission, values, and priorities. You should think about your experiences with reference to the AAMC Core Competencies and to each school's mission statement so that you're working toward your narrative with the institution and broader discipline in mind.
Review AAMC Core Competencies : The AAMC Core Competencies are the key characteristics and skills sought by U.S. medical schools. These are separated into three general categories:
You are not expected to have mastered all of these competencies at this stage of your education. Display those that are relevant to your experiences will help demonstrate your commitment to the medical profession.
Review the school's mission statement: Educational institutions put a lot of time and care into drafting their school's vision. The mission statement will articulate the overall values and priorities of each university, giving you insight into what they might seek in candidates, and thus what you should try to display in your personal statement. Echoing the values of the university helps illustrate that you are a good fit for their intellectual culture. The mission statement may help you identify other priorities of the university, for example, whether they prioritize research-based or experiential-based education. All this research into your chosen medical schools will help you tremendously not only when you write you personal statement, but also the rest of your medical school application components, including your medical school letter of intent if you ever need to write one later.
Just like the personal statement is, in essence, a prompt without a prompt. They give you free rein to write your own prompt to tell your story. This is often difficult for students as they find it hard to get started without having a true direction. Below is a list of ideas to get your creative juices flowing. Use these prompts as a starting point for your essay. Also, they are a great way of addressing why you want to be a doctor without saying something generic.
- The moment your passion for medicine crystallized
- The events that led you toward this path
- Specific instances in which you experienced opportunities
- Challenges that helped shape your worldview
- Your compassion, resilience, or enthusiastic collaboration
- Demonstrate your commitment to others
- Your dependability
- Your leadership skills
- Your ability to problem-solve or to resolve a conflict
These are personal, impactful experiences that only you have had. Focus on the personal, and connect that to the values of your future profession. Do that and you will avoid writing the same essay as everyone else. Dr. Monica Taneja, MD and our admissions expert, shares her tip that got her accepted to the University of Maryland School of Medicine :
"I focused on my journey to medicine and opportunities that I sought out along the way. Everyone’s path and validation is unique, so walking the reader through your growth to the point of application will naturally be different, but that's what I wanted to share in my personal statement." - Dr. Monica Taneja, MD
“the essay is not about what you have been through; it's about who it made you into.” – dr. vincent adeyemi.
Admissions committees don't want your resumé in narrative form. The most boring essays are those of applicants listing their accomplishments. Remember, all that stuff is already in the activities section of the application. This is where you should discuss interesting or important life events that shaped you and your interest in medicine (a service trip to rural Guatemala, a death in the family, a personal experience as a patient). One suggestion is to have an overarching theme to your essay to tie everything together, starting with an anecdote. Alternatively, you can use one big metaphor or analogy through the essay. Dr. Jaime Cazes, MD and experienced admissions committee member of the University of Toronto Faculty of Medicine, encourages you to be creative when it comes to the theme of your personal statement:
"It is very easy to make the “cookie cutter” personal statement. To a reviewer who is reading tens of these at a time it can become quite boring. What I did was [tell] a story. Like any good novel, the stories' first lines are meant to hook the reader. This can be about anything if you can bring it back and relate it to your application. It could be about the time your friend was smashed up against the boards in hockey and you, with your limited first aid experience helped to treat him. It is important that the story be REAL." - Dr. Jaime Cazes, MD
Your personal statement must be well-organized, showing a clear, logical progression, as well as connections between ideas. It is generally best to use a chronological progression since this mirrors your progression into a mature adult and gives you the opportunity to illustrate how you learned from early mistakes later on. Carry the theme throughout the statement to achieve continuity and cohesion. Use the theme to links ideas from each paragraph to the next and to unite your piece.
Medical School Personal Statement Structure
When working toward the initial draft of your essay, it is important to keep the following in mind: The essay should read like a chronological narrative and have good structure and flow. Just like any academic essay, it will need an introduction, body content, and a conclusion. If you're wondering whether a medical school advisor can help you with your medical school application, check out our blog for the answer.
Check out our video to learn how to create a killer introduction to your medical school personal statement:
Introduction
The introductory paragraph and, even more importantly, the introductory sentence of your essay, will most certainly make or break your overall statement. Ensure that you have a creative and captivating opening sentence that draws the reader in. This is your first and only chance to make a first impression and really capture the attention of the committee. Starting with an event or an Aha! moment that inspired your decision to pursue a medical profession is one way to grab their attention. The kinds of things that inspire or motivate you can say a lot about who you are as a person.
The broader introductory paragraph itself should serve several functions. First, it must draw your reader in with an eye-catching first line and an engaging hook or anecdote. It should point toward the qualities that most effectively demonstrate your desire and suitability for becoming a physician (you will discuss these qualities further in the body paragraphs). The thesis of the introduction is that you have certain skills, experiences, and characteristics and that these skills, experiences, and characteristics will lead you to thrive in the field of medicine. Finally, it must also serve as a roadmap to the reader, allowing them to understand where the remainder of the story is headed.
That is a lot of work for a single paragraph to do. To better help you envision what this looks like in practice, here is a sample introduction that hits these main points.
I was convinced I was going to grow up to be a professional chef. This was not just another far-fetched idealistic childhood dream that many of us had growing up. There was a sense of certainty about this dream that motivated me to devote countless hours to its practice. It was mostly the wonder that it brought to others and the way they were left in awe after they tried a dish that I recall enjoying the most creating as a young chef. But, when I was 13, my grandfather was diagnosed with stage four lung cancer, and I realized that sometimes cooking is not enough, as I quickly learned about the vital role physicians play in the life of everyday people like my family and myself. Although my grandfather ended up passing away from his illness, the impact that the healthcare team had on him, my family, and I will always serve as the initial starting point of my fascination with the medical profession. Since that time, I have spent years learning more about the human sciences through my undergraduate studies and research, have developed a deeper understanding of the demands and challenges of the medical profession through my various volunteer and extra-curricular experiences, and although it has been difficult along the way, I have continued to forge a more intimate fascination with the medical field that has motivated me to apply to medical school at this juncture of my life. ","label":"Sample Introduction","title":"Sample Introduction"}]" code="tab3" template="BlogArticle">
In the body of your essay, you essentially want to elaborate on the ideas that you have introduced in your opening paragraph by drawing on your personal experiences to provide evidence. Major points from the above sample introduction could be: dedication and resilience (practicing cooking for hours, and devoting years to undergraduate studies in human sciences), passion and emotional connection (being able to create something that inspired awe in others, and personally connecting with the work of the grandfather's healthcare team), motivation and drive (being inspired by the role physicians play in their patients' lives, participating in volunteer work and extracurriculars, and an enduring fascination with the field of medicine). Depending on the details, a selection of volunteer and extra-curricular experiences might also be discussed in more detail, in order to emphasize other traits like collaboration, teamwork, perseverance, or a sense of social responsibility – all key characteristics sought by medical schools. Just like an academic essay, you will devote one paragraph to each major point, explaining this in detail, supporting your claims with experiences from your life, and reflecting on the meaning of each plot point in your personal narrative, with reference to why you want to pursue a medical career.
Your final statement should not be a simple summary of the things you have discussed. It should be insightful, captivating, and leave the reader with a lasting impression. Although you want to re-emphasize the major ideas of your essay, you should try to be creative and captivating, much like your opening paragraph. Sometimes if you can link your opening idea to your last paragraph it will really tie the whole essay together. The conclusion is just as important as the introduction. It is your last chance to express your medical aspirations. You want to impress the reader while also leaving them wanting more. In this case, more would mean getting an interview so they can learn more about who you are! Leave them thinking I have got to meet this person.
The narrative you construct should display some of your most tightly held values, principles, or ethical positions, along with key accomplishments and activities. If you see yourself as someone who is committed to community service, and you have a track record of such service, your story should feature this and provide insight into why you care about your community and what you learned from your experiences. Saying that you value community service when you've never volunteered a day in your life is pointless. Stating that your family is one where we support each other through challenge and loss (if this is indeed true), is excellent because it lays the groundwork for telling a story while showing that you are orientated towards close relationships. You would then go on to offer a brief anecdote that supports this. You are showing how you live such principles, rather than just telling your reader that you have such principles:
"Remember to use specific personal examples throughout your statement to make it more impactful and memorable for the readers. Often, painting a picture in the reader’s mind in the form of a story helps with this." - Dr. Neel Mistry, MD
A lot of students make the mistake of verbalizing their personal attributes with a bunch of adjectives, such as, "This experience taught me to be a self-reliant leader, with excellent communication skills, and empathy for others..." In reality, this does nothing to convey these qualities. It's a mistake to simply list your skills or characteristics without showing the reader an example of a time you used them to solve a problem. If you simply list your skills or characteristics (telling), without demonstrating the ways you have applied them (showing), you risk coming across as arrogant. The person reading the essay may not believe you, as you've not really given them a way to see such values in your actions. It is better to construct a narrative to show the reader that you possess the traits that medical schools are looking for, rather than explicitly stating that you are an empathetic individual or capable of deep self-reflection. Instead of listing adjectives, tell your personal story and allow the admissions committee to paint the picture for themselves. This step is very challenging for many students, but it's one of the most important strategies used in successful essays. Writing this way will absolutely make your statement stand out from the rest.
While it may be tempting to write in a high academic tone, using terminology or jargon that is often complex or discipline-specific, requiring a specialized vocabulary for comprehension. You should actually aim to write for a non-specialist audience. Remember, in the world of medicine, describing a complex, clinical condition to a patient requires using specific but clear words. This is why your personal statement should show that you can do the same thing. Using large words in unwieldy ways makes you sound like you are compensating for poor communication skills. Use words that you believe most people understand. Read your personal statement back to a 14-year-old, and then again to someone for whom English is not their first language, to see if you're on the right path.
Ultimately, fancy words do not make you a good communicator; listening and ensuring reader comprehension makes you a good communicator. Instead of using complex terminology to tell the admissions committee that you have strong communication skills, show them your communication skills through clear, accessible prose, written with non-specialists in mind. A common refrain among writing instructors is, never use a $10 word where a $2 word will suffice. If you can say it in plain, accessible language, then this is what you should do.
Display Professionalism
Professionalism may seem like a difficult quality to display when only composing a personal statement. After all, the reader can't see your mannerisms, your personal style, or any of those little qualities that allow someone to appear professional. Professionalism is about respect for the experience of others on your team or in your workplace. It is displayed when you are able to step back from your own individual position and think about what is best for your colleagues and peers, considering their needs alongside your own. If a story is relevant to why you want to be a physician and demonstrates an example of how you were professional in a workplace setting, then it is appropriate to include in your essay.
One easy way to destroy a sense of professionalism is to act in a judgmental way towards others, particularly if you perceived and ultimately resolved an error on someone else's part. Sometimes students blame another medical professional for something that went wrong with a patient.
They might say something to the effect of, "The nurse kept brushing off the patient's concerns, refusing to ask the attending to increase her pain medications. Luckily, being the empathetic individual that I am, I took the time to listen to sit with the patient, eventually bringing her concerns to the attending physician, who thanked me for letting him know."
There are a couple of things wrong with this example. It seems like this person is putting down someone else in an attempt to make themselves look better. They come across as un-empathetic and judgmental of the nurse. Maybe she was having a busy day, or maybe the attending had just seen the patient for this issue and the patient didn't really need re-assessment. Reading this kind of account in a personal statement makes the reader question the maturity of the applicant and their ability to move past blaming others and resolve problems in a meaningful way. Instead of allocating blame, identify what the problem was for the patient and then focus on what you did to resolve it and reflect on what you learned from the whole experience.
One last note on professionalism: Being professional does not mean being overly stoic, hiding your emotions, or cultivating a bland personality. A lot of students are afraid to talk about how a situation made them feel in their personal statement. They worry that discussing feelings is inappropriate and will appear unprofessional. Unfortunately for these students, emotional intelligence is hugely important to the practice of medicine. In order to be a good doctor, one must be aware of their own emotions as well as those of their patients. Good doctors are able to quickly identify their own emotions and understand how their emotional reactions may inform their actions, and the ability to deliver appropriate care, in a given situation. Someone who is incapable of identifying their emotions is also incapable of managing them effectively and will likely struggle to identify the emotions of others. So, when writing your personal statement, think about how each experience made you feel, and what you learned from those feelings and that experience.
How to Write About Discrepancies and Common Mistakes to Avoid
Part of your essay's body can include a discussion of any discrepancies or gaps in your education, or disruptions in your academic performance. If you had to take time off, or if you had a term or course with low grades, or if you had any other extenuating circumstances that impacted your education, you can take time to address these here. It is very important to address these strategically. Do not approach this section as space to plead your case. Offer a brief summary of the situation, and then emphasize what you learned from such hardships. Always focus on the positive, illustrating how such difficulties made you stronger, more resilient, or more compassionate. Connect your experiences to the qualities desired by medical schools. Here's how I student Alison address an academic discrepancy in her application:
I had an academic dishonesty during undergrad, which, at the time, ended up being this big misunderstanding. But I was going to appeal this and get it off my record. I was supposed to start nursing school two weeks after this whole ordeal had gone down and, at our university, if you try to appeal your academic dishonesty then you'd have to take an incomplete in that class and I needed this class in order to start nursing school. So I wasn't able to [appeal]. So when I talked with the people at the nursing school they were like ‘it's no big deal, it's fine’. [But] it came back and it haunted me very much. When I was applying [to medical school] I started looking online [to see] how big of a deal is it to have this ‘red flag’ on my application. I started reading all of these horror stories on Student Doctor Network and all of these other forums about how if you have an academic dishonesty you shouldn't even bother applying, that you'll never get in. Schools will blacklist you and I was [wondering] what am I going do. [My advisor suggested I use the essay to talk about my discrepancy].
First off, if anyone out there has an academic violation don't read student doctor network. don't listen to anybody. you absolutely are still a potential medical student and schools are not going to blacklist you just because of one mistake that you made. that's all lies. don't listen to them. i don't even think it came up a single time during any of my interviews. i think a lot of that came back to how i wrote that essay and the biggest advice that i can give that i got from the [bemo] team is explain what happened… just give the facts. be very objective about it. in the last two thirds [of the essay] you want to focus on what you learned from it and how it made you a better person and how it's going to make you a better physician.” – alison, bemo student, current student at dell medical school.
We hope many of you find a peace of mind when you read Alison's story. Because it shows that with the right approach to your medical school personal statement, you can overcome even red flags or setbacks that made you dread the application process. Use your personal statement to emphasize your ability to persevere through it all but do so in a positive way. Most of all, if you feel like you have to explain yourself, take accountability for the situation. State that it is unfortunate and then redirect it to what you learned and how it will make you a better doctor. Always focus on being positive and do not lament on the negative situation too much.
Additional Mistakes to Avoid in Personal Statements:
Check out this video on the top 5 errors to avoid in your personal statement!
Step 3: Writing Your First Draft
As you can see, there is a LOT of planning and consideration to be done before actually starting your first draft. Properly brainstorming, outlining, and considering the content and style of your essay prior to beginning the essay will make the writing process much smoother than it would be you to try to jump right to the draft-writing stage. Now, you're not just staring at a blank page wondering what you could possibly write to impress the admissions committee. Instead, you've researched what the school desires from its students and what the medical profession prioritizes in terms of personal characteristics, you've sketched out some key moments from your life that exemplify those traits, and you have a detailed outline that just needs filling in.
As you're getting started, focus on getting content on the page, filling in your outline and getting your ideas arranged on the page. Your essay will go through multiple drafts and re-writes, so the first step is to free write and start articulating connections between your experiences and the characteristics you're highlighting. You can worry about flow, transitions, and perfect grammar in later drafts. The first draft is always a working draft, written with the understanding that its purpose is to act as a starting point, not an ending point. Once you've completed a draft, you can begin the revising process. The next section will break down what to do once you have your first draft completed.
You can also begin looking at things like style, voice, transitions, and overall theme. The best way to do this is to read your essay aloud. This may sound strange, but it is one of the single most impactful bits of writing advice a student can receive. When we're reading in our heads (and particularly when we're reading our own words), it is easy to skip over parts that may be awkwardly worded, or where the grammar is off. As our brains process information differently, depending on whether we're taking in visual or auditory information, this can also help you understand where the connections between ideas aren't as evident as you would like. Reading the essay aloud will help you begin internalizing the narrative you've crafted, so that you can come to more easily express this both formally in writing and informally in conversation (for example, in an interview).
#1 Did You Distinguish Yourself From Others?
Does your narrative sound unique? Is it different than your peers or did you write in a generic manner? Our admissions expert Dr. Monica Taneja, MD, shares how she got the attention of the admissions committee with her personal statement:
"I also found it helpful to give schools a 'punch-line'. As in I wanted them to remember 1-2 things about me that are my differentiators and I reiterated those throughout [the personal statement]." - Dr. Monica Taneja, MD
Use your narrative to provide a compelling picture of who you are as a person, as a learner, as an advocate, and as a future medical professional. What can you offer? Remember, you will be getting a lot out of your med school experience, but the school will be getting a lot out of you, as well. You will be contributing your research efforts to your department, you will be participating in the academic community, and as you go on to become a successful medical professional you will impact the perception of your school's prestige. This is a mutually beneficial relationship, so use this opportunity to highlight what you bring to the table, and what you will contribute as a student at their institution. Let them know what it is about you that is an attribute to their program. Make them see you as a stand out from the crowd.
#2 Does My Essay Flow and is it Comprehensible?
Personal statements are a blessing and a curse for admission committees. They give them a better glimpse of who the applicant is than simple scores. Also, they are long and time-consuming to read. And often, they sound exactly alike. On occasion, a personal statement really makes an applicant shine. After reading page after page of redundant, cookie-cutter essays, an essay comes along with fluid prose and a compelling narrative, the reader snaps out of that feeling of monotony and gladly extends their enthusiastic attention.
Frankly, if the statement is pleasant to read, it will get read with more attention and appreciation. Flow is easier to craft through narrative, which is why you should root the statement in a story that demonstrates characteristics desirable to medical schools. Fluidity takes time to build, though, so your statement should be etched out through many drafts and should also be based on an outline. You need to brainstorm, then outline, then draft and re-draft, and then bring in editors and listeners for feedback (Note: You need someone to proofread your work. Bestselling authors have editors. Top scholars have editors. I need an editor. You need an editor. Everyone needs an editor). Then, check and double-check and fix anything that needs fixing. Then check again. Then submit. You want this to be a statement that captures the reader's interest by creating a fluid, comprehensible piece that leads the reader to not only read each paragraph but want to continue to the next sentence.
#3 Did You Check Your Grammar?
If you give yourself more than one night to write your statement, the chances of grammatical errors will decrease considerably. If you are pressed for time, upload your file into an online grammar website. Use the grammar checker on your word processor, but know that this, in itself, isn't enough. Use the eyes and ears of other people to check and double-check your grammar, punctuation, and syntax. Read your statement out loud to yourself and you will almost certainly find an error (and likely several errors). Use fresh eyes to review the statement several times before you actually submit it, by walking away from it for a day or so and then re-reading it. Start your essay early, so that you actually have time to do this. This step can make or break your essay. Do not waste all the effort you have put into writing, to only be discarded by the committee for using incorrect grammar and syntax.
#4 Did You Gather Feedback From Other People?
The most important tip in writing a strong application essay is this getting someone else to read your work. While the tips above are all very useful for writing a strong draft, nothing will benefit you more than getting an outside appraisal of your work. For example, it's very easy to overlook your own spelling or grammatical errors. You know your own story and you may think that your narrative and it's meaning make sense to your reader. You won't know that for sure without having someone else actually read it. This may sound obvious, but it's still an absolute necessity.
“It was very helpful for two of my mentors to review my statements before submitting my application. Ensure you trust the judgement and skills of the person to whom you would be giving your personal statement for review.” – Dr. Vincent Adeyemi
Have someone you trust to read the essay and ask them what they thought of it. What was their impression of you after reading it? Did it make sense? Was it confusing? Do they have any questions? What was the tone of the essay? Do they see the connections you're trying to make? What were their takeaways from your essay, and do these align with your intended takeaways for your reader? Ideally, this person should have some knowledge of the application process or the medical profession, so that they can say whether you were successful in demonstrating that you are a suitable candidate for medical school. However, any external reader is better than no external reader at all.
Avoid having people too close to you read your work. They may refrain from being too critical in an effort to spare your feelings. This is the time to get brutal, honest feedback. If you know someone who is an editor but do not feel that they can be objective, try and find someone else.
Want more examples? Check out our video below:
FAQs and Final Notes
Your personal statement should tell your story and highlight specific experiences or aspects of your journey that have led you to medicine. If your first exposure or interest in the medical field was sparked from your own medical struggles, then you can certainly include this in your statement. What is most important is that you write about what factors or experiences attributed to you deciding that medicine is the right career path for you.
Sometimes students shy away from including their own personal struggles and describing how they felt during difficult times but this is a great way for admissions committees to gain perspective into who you are as a person and where your motivations lie. Remember, this is your story, not someone else's, so your statement should revolve around you. If you choose to discuss a personal hardship, what's most important is that you don't cast yourself as the victim and that you discuss what the experience taught you. Also, medical schools are not allowed to discriminate against students for discussing medical issues, so it is not looked at as a red flag unless you are talking about an issue inappropriately. For example, making yourself appear as the victim or not taking responsibility.
All US medical schools require the completion of a personal statement with your AMCAS, TMDSAS or AACOMAS applications.
Medical schools in Canada on the other hand, do not require or accept personal statements. In lieu of the personal statement, a few of these schools may require you to address a prompt in the form of an essay, or allow you to submit an explanation essay to describe any extenuating circumstances, but this is not the same as the US personal statement. For example, when applying through OMSAS , the University of Toronto medical school requires applicants to complete four short, 250 words or less, personal essays.
Many students struggle with whether or not they should address an unfavorable grade in their personal statement. What one student does isn't necessarily the right decision for you.
To help you decide, think about whether or not that bad grade might reflect on your poorly. If you think it will, then it's best to address the academic misstep head-on instead of having admissions committees dwell on possible areas of concern. If you're addressing a poor evaluation, ensure that you take responsibility for your grade, discuss what you learned and how your performance will be improved in the future - then move on. It's important that you don't play the victim and you must always reflect on what lessons you've learned moving forward.
Of course not, just because you didn't wake up one morning and notice a lightbulb flashing the words medicine, doesn't mean that your experiences and journey to medicine are inferior to those who did. Students arrive to medicine in all sorts of ways, some change career paths later in life, some always knew they wanted to pursue medicine, and others slowly became interested in medicine through their life interactions and experiences. Your personal statement should address your own unique story to how you first became interested in medicine and when and how that interest turned to a concrete desire.
While your entire statement is important, the opening sentence can often make or break your statement. This is because admission committee members are reviewing hundreds, if not thousands of personal statements. If your opening sentence is not eye-catching, interesting, and memorable, you risk your statement blending in with the large pile of other statements. Have a look at our video above for tips and strategies for creating a fantastic opening sentence.
Having your statement reviewed by family and friends can be a good place to start, but unfortunately, it's near-impossible for them to provide you with unbiased feedback. Often, friends and family members are going to support us and rave about our achievements. Even if they may truly think your statement needs work, they may feel uncomfortable giving you their honest feedback at the risk of hurting your feelings.
In addition, family and friends don't know exactly what admission committee members are looking for in a personal statement, nor do they have years of experience reviewing personal statements and helping students put the best version of themselves forward. For these reasons, many students choose to seek the help of a professional medical school advisor to make sure they have the absolute best chances of acceptance to medical school the first time around.
If you have enough time set aside to write your statement without juggling multiple other commitments, it normally takes at least four weeks to write your statement. If you are working, in school, or volunteering and have other commitments, be prepared to spend 6-8 weeks.
Your conclusion should have a summary of the main points you have made in your essay, but it should not just be a summary. You should also end with something that makes the reader want to learn more about you (i.e. call you for an interview). A good way to do this is to include a call-back to your opening anecdote: how have you grown or matured since then? How are you more prepared now to begin medical school?
The goal is to show as many of them as you can in the WHOLE application: this includes your personal statement, sketch, reference letters, secondary essays, and even your GPA and MCAT (which show critical thinking and reasoning already). So, it’s not an issue to focus on only a few select experiences and competencies in the personal statement.
Yes, you can. However, if you used an experience as a most meaningful entry, pick something else to talk about in your essay. Remember, you want to highlight as many core competencies across your whole application). Or, if you do pick the same experience: pick a different specific encounter or project with a different lesson learned.
Once your essay is in good shape, it's best to submit to ensure your application is reviewed as soon as possible. Remember, with rolling admissions, as more time passes before you submit your application, your chances of acceptance decreases. Nerves are normal and wanting to tinker is also normal, but over-analyzing and constant adjustments can actually weaken your essay.
So, if you're thinking about making more changes, it's important to really reflect and think about WHY you want to change something and if it will actually make the essay stronger. If not your changes won't actually make the essay stronger or if it's a very minor change you're thinking of making, then you should likely leave it as is.
The reality is, medical school admission is an extremely competitive process. In order to have the best chance of success, every part of your application must be stellar. Also, every year some students get in whose GPAs or MCAT scores are below the median. How? Simply because they must have stood out in other parts of the application, such as the personal statement.
The ones that honestly made the most impact on you. You'll need to reflect on your whole life and think about which experiences helped you grow and pushed you to pursue medicine. Ideally, experiences that show commitment and progression are better than one-off or short-term activities, as they usually contribute more to growth.
Final Notes
This Ultimate Guide has demonstrated all the work that needs to be done to compose a successful, engaging personal statement for your medical school application. While it would be wonderful if there was an easy way to write your personal statement in a day, the reality is that this kind of composition takes a lot of work. As daunting as this may seem, this guide lays out a clear path. In summary, the following 5 steps are the basis of what you should take away from this guide. These 5 steps are your guide and sort of cheat sheet to writing your best personal statement.
5 Main Takeaways For Personal Statement Writing:
- Brainstorming
- Content and Theme
- Multiple Drafts
- Revision With Attention to Grammar
While a strong personal statement alone will not guarantee admission to medical school, it could absolutely squeeze you onto a medical school waitlist , off the waitlist, and onto the offer list, or give someone on the admissions committee a reason to go to battle for your candidacy. Use this as an opportunity to highlight the incredible skills you've worked and studied to refine, the remarkable life experiences you've had, and the key qualities you possess in your own unique way. Show the admissions committee that you are someone they want to meet. Remember, in this context, wanting to meet you means wanting to bring you in for an interview!
Dr. Lauren Prufer is an admissions expert at BeMo. Dr. Prufer is also a medical resident at McMaster University. Her medical degree is from the Schulich School of Medicine and Dentistry. During her time in medical school, she developed a passion for sharing her knowledge with others through medical writing, research, and peer mentoring.
To your success,
Your friends at BeMo
BeMo Academic Consulting
Want more free tips? Subscribe to our channels for more free and useful content!
Apple Podcasts
Like our blog? Write for us ! >>
Have a question ask our admissions experts below and we'll answer your questions.
Jack Weaver
I have been reading posts regarding this topic and this post is one of the most interesting and informative one I have read. Thank you for this!
Hello Jack! Thank you very much for your comment. We glad you find this helpful!
Get Started Now
Talk to one of our admissions experts
Our site uses cookies. By using our website, you agree with our cookie policy .
FREE Training Webinar: How To Make Your Med School Application Stand Out
(and avoid the top 5 reasons that get 90% of applicants rejected).
Time Sensitive. Limited Spots Available:
We guarantee your acceptance to med school or you don't pay.
Swipe up to see a great offer!
- Undergraduates
- Ph.Ds & Postdocs
- Prospective Students & Guests
- What is a Community?
- Student Athletes
- First Generation and/or Low Income Students
- International Students
- LGBTQ Students
- Students of Color
- Students with Disabilities
- Student Veterans
- Exploring Careers
- Advertising, Marketing & PR
- Finance, Insurance & Real Estate
- General Management & Leadership Development Programs
- Law & Legal Services
- Startups, Entrepreneurship & Freelance Work
- Environment, Sustainability & Energy
- Media & Communications
- Policy & Think Tanks
- Engineering
- Healthcare, Biotech & Global Public Health
- Life & Physical Sciences
- Programming & Data Science
- Graduate School
- Health Professions
- Business School
- Meet with OCS
- Student Organizations Workshop Request
- OCS Podcast Series
- Office of Fellowships
- Navigating AI in the Job Search Process
- Cover Letters & Correspondence
- Job Market Insights
- Professional Conduct & Etiquette
- Professional Online Identity
- Interview Preparation
- Resource Database
- Yale Career Link
- Jobs, Internships & Other Experiences
- Gap Year & Short-Term Opportunities
- Planning an International Internship
- Funding Your Experience
- Career Fairs/Networking Events
- On-Campus Recruiting
- Job Offers & Salary Negotiation
- Informational Interviewing
- Peer Networking Lists
- Building Your LinkedIn Profile
- YC First Destinations
- YC Four-Year Out
- GSAS Program Statistics
- Statistics & Reports
- Contact OCS
- OCS Mission & Policies
- Additional Yale Career Offices
Writing the Personal Statement for Health Professions Applications
- Share This: Share Writing the Personal Statement for Health Professions Applications on Facebook Share Writing the Personal Statement for Health Professions Applications on LinkedIn Share Writing the Personal Statement for Health Professions Applications on X
🎥 Watch this short video
The personal statement gives you the opportunity to present a compelling snapshot of who you are and perhaps why you want to be a doctor. Use your personal statement to say what others can’t. The personal statement can be a tricky genre to master. On the one hand, you want to give the admissions committee a sense of your personality and who you are. On the other hand, you must sound focused and professional, which sounds like it might impede your ability to capture your personality.
But this does not have to be the case. What you need to do is figure out how to say what drives you to want to become a healthcare professional in as specific a way as possible. The more specific you can be, the more the admissions committee will feel as if they have a sense of who you are.
You don’t need gimmicks, jokes, artificial drama, or hyperbole to express who you are or why you would make a good medical student or doctor. All you need are carefully selected details that you can craft into a unique and compelling story that conveys a sense of purpose and motivation.
What Makes a Good Personal Statement?
- There is no exact template for an effective personal statement. Often, however, strong personal statements combine a concise description of a personal experience with reflection on how this experience either led the writer to pursue medicine or indicates the writer’s character or commitment.
- Good personal statements often have a strong sense of narrative. This does not mean that they read like short stories, though they can relate a few scenes or anecdotes from your life. They have a strong sense of narrative, rather, in how they convey the writer’s sense of dedication to medicine. Strong personal statements often give readers an idea of how applicants see their experiences as leading to the decision to pursue medicine.
How to Get Started
The personal statement is an exercise in self-reflection. Questions to consider:
- Who are you? I am driven to… I have learned to… I believe…
- What are your most passionate interests or concerns? What problem(s) most occupy your thinking and your efforts?
- How did you develop those interests? (Not just the story, but what drives you.)
- What errors or regrets have taught you something important about yourself?
- When does time disappear for you? What does this tell you about your passions, your values?
- What ideas, books, courses, events have had a profound impact on you? How so?
- To what extent do your current commitments reflect your most strongly held values?
- When have you changed? Consider yourself before and after; what does this change mean?
- How do your interests and who you are relate to your goals in medical school and as a doctor?
Start a “shoebox”; a place to keep random notes for your personal statement; be ready to write at any time. Review these items occasionally; let them tell you more about what you want your personal statement to say. Start writing drafts, experiments; you will know when a paragraph begins to gel.
A Suggested Writing Process
Everyone writes differently, so these are potential strategies rather than rules.
- Make a list of some of your most defining experiences – extracurricular activities, specific classes, volunteer work, research, hobbies, etc. Try not to include overly personal experiences (breakups, trouble with parents, illnesses in the family, and so on). It’s difficult to write about such things without being sentimental or cliché. You want experiences in which you did something and had to make a choice.
- From this list, try to select an experience that particularly demonstrates your intellectual curiosity, your dedication to service, your composure under pressure, your leadership ability, or any other personal trait that you think is particularly relevant to your case that you would make a good doctor or medical student.
- Start writing a draft based on this experience. You want to be specific, but don’t get bogged down with an abundance of anecdotes or minutiae. Try to use your draft to craft a succinct story that demonstrates your character and your motivations.
- Set the draft aside for some time (a number of days or weeks), and then revisit it with fresh eyes. Be as honest with yourself as you can be: What works in this draft? What doesn’t work? What sounds cliché or unspecific? Would a reader who doesn’t know me at all get a sense of my personal character and dedication?
- Revise, revise, revise: tighten the structure, add new things to make your point clearer, take away sentences or sections that now seem unnecessary, use the active voice as much as possible, and anything else that needs to be done. If what you have just doesn’t seem to be coming together, do not be afraid to start over.
- Solicit feedback from a couple of trusted readers and revise again based on the suggestions that you find most useful. Don’t solicit feedback from too many people though – too many responses can be overwhelming.
- Edit your work for grammatical mistakes, typos, clumsy repetitions, and so on. Make your prose impeccable before you submit your statement. Asking help from other readers can be especially helpful with editing, as sometimes it gets difficult to read your work with fresh eyes.
Things to Do
- Use the experience that you describe to tell a story of personal progress, particularly progress towards your commitment to medicine.
- Write with active verbs as much as possible.
- Strive for concision.
- Sound humble but also confident.
Things Not to Do – Common Pitfalls
- Don’t talk in hyperbolic terms about how passionate you are. Everyone applying to medical school can say they are passionate. Instead, show your readers something you have done that indicates your passion.
- Don’t adopt an overly confessional or sentimental tone. You need to sound professional.
- Don’t treat the personal statement like a piece of creative writing.
- Don’t put your resume in narrative form.
- Don’t use jargon, abbreviations, slang, etc.
- Don’t use too many qualifiers: very, quite, rather, really, interesting…
- Don’t write in overly flowery language that you would normally never use.
- Don’t include famous quotations. If you must quote, use something that shows significant knowledge.
- Don’t write about yourself in an overly glorifying or overly self-effacing manner.
What to Remember
- They are read by non-specialists, so write for an intelligent non-medical audience.
- Actions sometimes speaks louder than words so give examples of experiences rather than describing them.
- All information must be accurate – don’t pad, but don’t be falsely modest either.
- The personal statement, in part, serves as a test of your communication skills. How well you write it is as important as the content.
Writing Resources
- AAMC: 7 Tips for Writing your AMCAS Personal Statement
- Graduate Admission Essays: What Works, What Doesn’t and Why , Donald Asher, Ten Speed Press
- On Writing Well , William Zinsser
- Elements of Style , Strunk and White, Macmillan
- Article : 2 Med School Essays that Admissions Officers Loved
- Guidance for Writing Personal Statements, Work & Activities Section, Secondary Applications
Office of Career Strategy
Visiting yale.
Check your email to book a FREE call with an expert advisor
- Medical Schools
- Study Guides
- Student Life
- Visit Main Website
How To Write The Perfect Medical School Personal Statement

“In nothing do men more nearly approach the gods, than in giving health to men” Marcus Tullius Cicero (106 - 43 BCE)
You have already chosen to commit yourself to study medicine in Europe , and we want to help you every step of the way. Many future students don’t know how to write their medicine personal statement. Every day we get asked questions such as:
- What is a personal statement for a medical university?
- How to write one?
- What should I include in it?
- What is the purpose of the medical personal statement?
Based on years of experience and our expert advisor’s guidelines, this article will provide the best tips and examples for writing your personal statement.
This post will assist you whether you haven't even considered what to include in your personal statement or have written it and want to double-check that you're on the right track.
Table of Contents
- 1 What is a medical personal statement?
- 2 What is the difference between a personal statement and a motivation letter?
- 3 What is the length of a personal statement?
- 4 What role do personal statements play in medical schools?
- 5 What do medical universities want to see in your personal statement?
- 6 Which medical schools in Europe should you apply to with a personal statement?
- 7 Why is a personal statement so important?
- 8 What should I include in my personal statement?
- 9 How to structure a medical personal statement?
- 10.1.1 Step 1. Create a list of the qualities that you want to demonstrate
- 10.1.2 Step 2. Think about a situation when you have shown these qualities
- 10.1.3 Step 3. Present your experience as a captivating story
- 10.1.4 Step 4. Show, don’t tell
- 11 How to create great body paragraphs in a medicine personal statement?
- 12 How to end a personal statement in a meaningful way?
- 13.2 DON’TS:
- 14 Checklist for your MD personal statement
What is a medical personal statement?
More than 100 medical schools in Europe teach medicine, dentistry, veterinary, and pharmacy in English. Each university has its entry requirements . Some may require you to sit an entrance exam in Chemistry, Biology, Physics, or Mathematics. Others have no entrance exam but just an interview.
As part of the application process, some medical schools will ask for additional materials such as CVs ( application resume ), recommendations, and, more often, medicine personal statements or motivation letters.
A medical personal statement is a kind of essay. You get the chance to tell your personal story of why you have chosen medicine as a career. It is the first opportunity for admissions tutors to evaluate you as a person rather than a collection of grades and achievements. Therefore you must create a strong first impression. You have to think of it not as a burdensome part of the application process but as an excellent opportunity to shine among the other applicants.
What is the difference between a personal statement and a motivation letter?
As we mentioned, some schools require a personal statement and another motivation letter. It is essential to know the difference between them.
A personal statement is more about self-promotion . You should explain why you are the best candidate for a particular course and want to become a doctor. It is more about your personality traits and skills to help you achieve your dream career.
A motivation letter is more about your future study ambitions and how the programme you're applying to will assist you in achieving your objectives. In other words, why and how will studying medicine help you in the future .
What is the length of a personal statement?
Every medical university has its requirements regarding the length of the personal statement. Therefore, before you start writing it, you must check the specific guidelines of the university you are applying to.
However, often it will have to be around 500 words . Yes, it must be short, accurate, and straightforward.
What role do personal statements play in medical schools?
There are a few ways that medical schools will use your personal statement.
- It may not play a role in the selection process at all.
- It will be read but not evaluated . However, if you manage to prepare an excellent essay, it will demonstrate your passion for medicine and will certainly not harm you in the long run.
- It is used to aid in decision-making between two candidates with identical academic results. An essay can be a turning point in your path to becoming a doctor.
- Usually, medical universities use students' personal statements before interviews to prepare a few questions you will be asked during the interview. This is another reason many schools ask for this kind of essay. They use it as a starting point in discussions. As a result, it's a good idea to write about things you'd be willing to expand on if requested.
What do medical universities want to see in your personal statement?
Medical universities know that to be a good doctor, you need skills such as:
- Self-reflection
- Prioritising
- Good time management
- Working under pressure
- Critical thinking
- Attention to detail
- Problem-solving skills
- Willingness to accept accountability for your actions
- Soft skills
Keep these things in mind when you draft your essay. You shouldn’t just say, “I am empathetic”. Rather than that, you have to give an example and write about a situation when you demonstrated these skills.
Which medical schools in Europe should you apply to with a personal statement?
Some of the medical universities in Europe that require a medical student personal statement as part of the application process are:
- European University In Tbilisi (Georgia)
- Poznan University of Medical Science (Poland)
- Pavol Jozef Šafárik University in Kosice (Slovakia)
Why is a personal statement so important?
It's one thing to demonstrate academic success and another to present yourself positively as an individual. Striking a balance between the two is crucial. So take your time and carefully consider what you want to include and how you will present it.
The top 3 reasons why a medicine personal statement is so important are:
- It allows you to show your best qualities
- It can help you stand out from your competition
- It is a great way to prepare for your medical school interview
What should I include in my personal statement?
Let’s make it clear one more time. A personal statement is about YOU, and your personal skills that make you an ideal applicant to study medicine in Europe. Hence, medical schools are looking to know more about:
- What motivated you to study medicine? ( Motivation )
- Why in this country? Why in this particular university? ( Motivation and exploration )
- What steps have you taken to get knowledge about it? ( Exploration )
- Why do you think you'd be a good fit for medicine? ( Suitability )
Describe your passion for medicine and the reason for making your statement unique. Learn more about the country's history, and find things that you can name as an advantage for studying there. Read about the university's history and the city where it is located. Find prominent people who have studied and contributed to science development at a given university. Show originality.
Make sure to include a line about your hobbies/interests outside of school and reflect on past experiences that taught you something valuable like commitment, the ability to work in a team, and the importance of helping those in need.
How to structure a medical personal statement?
In general, medicine personal statement structure can be divided into 3 parts:
- Introduction - motivation
In this paragraph, your main goal is to make the reader want to read more and tell what made you choose medicine as a career.
- Main body - exploration and suitability
This is where you have to tell your story and how your qualities make you a perfect applicant. It is the ideal place to write about the knowledge you gained while shadowing a doctor , for example.
- Conclusion - motivation
Bring everything together.
How to write a strong medical personal statement introduction?
Ensure you have an original and intriguing starting phrase that will entice the reader to continue reading. This is your only chance to leave a lasting impression and grab the admissions tutors' attention.
One method to get their attention is to start with an incident or an “Aha!” moment that inspired your decision to pursue a career in medicine. What inspires or motivates you will reveal a lot about your personality. But from our experience, we know that very few students have such a moment.
Many applicants have known they wanted to be a doctor since childhood or have developed an interest in medicine.
If you are one of them, the simple truth is that you can’t start your essay with a fascinating experience or life-changing story. And that’s okay.
What to do, then?
Step-by-step guide on how to start writing a personal statement for medicine:
Step 1. create a list of the qualities that you want to demonstrate.
Take a piece of paper and write down the traits and abilities you want to reveal to the reader. There is no need to create a long list. Just think of 10 qualities that will help you become a great doctor. Some examples include:
- Effective communication skills
- Knowledge-seeking
- Understanding
- Team worker
We have all heard the phrase “Quality over Quantity”. This seeing relates to your writing too. If you try to include all 10 points on your list, you will end up with an inconsistent and uninfluential opening of your essay. Therefore you have to revise your list and pick up only 2 or 3 qualities . Please don’t waste time figuring out which ones are ideal because they don’t exist. Here the trick is to choose those that describe you best and that you can actually write about.
Step 2. Think about a situation when you have shown these qualities
This step is self-explanatory, but here are some guidelines that you can follow to pick the perfect event to write about.
Choose a story you can share in a few sentences (5 or 6). A good option is an event that comes from shadowing doctors, working in a clinic, volunteering, and extracurricular activity related to medicine.
Suppose you want to be original. Connect a travel story or work experience with the abilities you have chosen to highlight. This will guarantee a unique story that will impress the admissions committee.
Step 3. Present your experience as a captivating story
If you are worried about the story you picked, let us tell you a secret. It is not about choosing the perfect topic but presenting it engagingly. Remember that one event can be written in both dull and intriguing ways. Strive for the second!
Step 4. Show, don’t tell
Maybe this is the most crucial step of writing a medical personal statement. Don’t tell: “I have great communication skills.” Show it with your compelling story! The key is to demonstrate your qualities.
How to create great body paragraphs in a medicine personal statement?
In the body of your essay, you essentially want to expand the concepts stated in your introduction paragraph by using personal experiences as proof.
You have already written about why you want to study medicine. So it's time to dive in. Write in detail about the experiences that helped you grow and led to your decision to study medicine. Each key point should be given its own paragraph.
Here are a few steps that you can follow to write the best medicine personal statement ever:
- Explain why you wanted to participate in the experience you are writing about.
- Describe how you felt during the event.
- Describe your accomplishments and lessons learned.
- What impact did your experience have on you and the environment around you?
- Explain how your experience influenced your desire to apply to medical school.
How to end a personal statement in a meaningful way?
Your medical personal statement conclusion should be like your introduction: showing your interest in studying medicine. You have to wrap everything together and leave the reader wanting to learn more about you.
You should re-emphasise your essay's main points and highlight these 3 things one more time:
- Qualities that will make you one of the best doctors
- Knowledge gained as a result of your formative experiences
- Your sincere passion for being a medical student

Top tips for medicine personal statement from our expert advisors:
- Connect your extracurricular activities to how they will help you become a better doctor
- Tell a story
- Always double-check for grammar and spelling mistakes
- Show professionalism
- Use clear, direct language
- Ask your family for an opinion
- Don’t lie, be true to yourself
- Don’t try to cover everything
- Don’t use cliches
- Don't forget about the proper structure
Checklist for your MD personal statement
Before sending your medical personal statement, make sure you cover the following:
- Is your first paragraph clear about why you want to be a doctor?
- Have you thought about what you learned from each of the situations you've mentioned?
- Is there a phrase or two regarding your hobbies or outside interests?
- Is your grammar correct?
- Do you show that you possess the qualities necessary for this profession?
- Do you indicate that you understand the reality of a career in medicine?
- Is your final paragraph a summary of why you believe you are well-suited for the medicine course and career?
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
About Medlink Students
Leading international recruitment company for medical students in Europe. British Council certified. 10+ years of experience and more than 10,000 students advised.

Related Posts

Get Advice on Studying Abroad
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Grad Med Educ
- v.14(5); 2022 Oct
Ten Steps for Writing an Exceptional Personal Statement
Danielle jones.
All authors are with Emory University School of Medicine
Danielle Jones, MD, is Associate Professor of Medicine, Associate Section Chief of the Division of General Internal Medicine Grady Section, and Associate Program Director, Internal Medicine Residency
J. Richard Pittman, Jr
J. Richard Pittman Jr, MD, is Associate Professor of Medicine, and Program Director, Fourth Year Internal Medicine Sub-Internship
Kimberly D. Manning
Kimberly D. Manning, MD, FACP, FAAP, is Professor of Medicine, and Associate Vice Chair, Diversity, Equity, and Inclusion, Department of Medicine
The personal statement is an important requirement for residency and fellowship applications that many applicants find daunting. Beyond the cognitive challenge of writing an essay, time limitations for busy senior residents on clinical rotations present added pressure. Objective measures such as scores and evaluations paint only a partial picture of clinical and academic performance, leaving gaps in a candidate's full portrait. 1 , 2 Applicants, seemingly similar on paper, may have striking differences in experiences and distances traveled that would not be captured without a personal narrative. 2 , 3 We recommend, therefore, reframing personal statements as the way to best highlight applicants' greatest strengths and accomplishments. A well-written personal statement may be the tipping point for a residency or fellowship interview invitation, 4 , 5 which is particularly important given the heightened competition for slots due to increased participation on virtual platforms. Data show that 74% to 78% of residency programs use personal statements in their interview selection process, and 48% to 54% use them in the final rank. 6 , 7 With our combined 50 years of experience as clerkship and residency program directors (PDs) we value the personal statement and strongly encourage our trainees to seize the opportunity to feature themselves in their words.
Our residency and medical school leadership roles position us to edit and review numerous resident and student personal statements annually. This collective experience has helped us identify patterns of struggle for trainees: trouble starting, difficulty organizing a cogent narrative, losing the “personal” in the statement, and failing to display unique or notable attributes. While a bland personal statement may not hurt an applicant, it is a missed opportunity. 4 , 8 We also have distinguished helpful personal statement elements that allow PDs to establish candidates' “fit” with their desired residency or fellowship. A recent study supports that PDs find unique applicant information from personal statements helpful to determine fit. 4 Personal statement information also helps programs curate individualized interview days (eg, pair interviewers, guide conversations, highlight desirable curricula). Through our work with learners, we developed the structured approach presented here ( Figure 1 ). Applicants can use our approach to minimize typical struggles and efficiently craft personal statements that help them stand out. Busy residents, particularly, have minimal time to complete fellowship applications. We acknowledge there is no gold standard or objective measures for effective personal statement preparation. 9 Our approach, however, combined with a practical tool ( Figure 2 ), has streamlined the process for many of our mentees. Moreover, faculty advisors and program leaders, already challenged by time constraints, can use this tool to enhance their coaching and save time, effort, and cognitive energy.

Structured Approach to Writing a Personal Statement

Ten Steps for Writing an Exceptional Personal Statement: Digital Tool
Note: Use the QR code to download the digital tool and follow the 10 steps highlighted in Figure 1.
Given word count and space limitations, deciding what to include in a personal statement can be challenging. An initial brainstorm helps applicants recall personal attributes and experiences that best underscore key strengths (Step 1). 10 Writing explicit self-affirmations is challenging, so we recommend pairing with a near peer who may offer insight. Useful prompts include:
- ▪ What 3 words best encapsulate me?
- ▪ What accomplishments make me proud?
- ▪ What should every program know about me?
Reflecting on these questions (Step 2) helps elucidate the foundations of the narrative, 10 including strengths, accomplishments, and unique elements to be included. Additionally, the preparation steps help uncover the “thread” that connects the story sequentially. While not all agree that personal or patient stories are necessary, they are commonly included. 5 One genre analysis showed that 97% of applicants to residency programs in internal medicine, family medicine, and surgery used an opening that included either a personal narrative (66%) and/or a decision to enter medicine (54%) or the specialty of choice (72%). 9 Radiology PDs ranked personal attributes as the second most important component in personal statements behind choice of specialty. 9 Further, a descriptive study of anesthesia applicants' personal statements ranked those that included elements such as discussion of a family's or friend's illness or a patient case as more original. 3 We feel that personal and patient stories often provide an interesting hook to engage readers, as well as a mechanism to highlight (1) personal characteristics, (2) journey to and/or enthusiasm for desired discipline, and (3) professional growth, all without giving the impression of being boastful. Sketching these Step 2 fundamentals prepares applicants to begin writing with intention.
Writing and Structuring
Once key elements are identified, the next steps assist with the actual writing. Utilizing information gleaned from the “Preparing” steps, start with a freewriting exercise (Step 3), an unrestricted association of ideas aimed at answering, “What experiences have cultivated my strong interest in pursuing [______]?” At this stage, ignore spelling and grammar. Just write, even if the product is the roughest, rough draft imaginable. 10 Setting a timer for 10 to 15 minutes establishes a less intimidating window to start. Freewriting generates the essential initial content that typically will require multiple revisions. 10
Next, we recommend structuring the freewriting content into suggested paragraphs (Step 4), using the following framework to configure the first draft:
- ▪ Introductory paragraph: A compelling story, experience, or something that introduces the applicant and makes the reader want to know more (the hook). If related to a patient or other person, it should underscore the writer's qualities.
- ▪ Paragraph 2: Essential details that a program must know about the applicant and their proudest accomplishments.
- ▪ Paragraph(s) 3-4: Specific strengths related to the specialty of choice and leadership experiences.
- ▪ Closing paragraph: What the applicant values in a training program and what they believe they can contribute.
Evaluate what has been written and ensure that, after the engaging hook, the body incorporates the best pieces identified during the preparation steps (Step 5). A final paragraph affords ample space for a solid conclusion to the thread. Occasionally the narrative flows better with separate strengths and leadership paragraphs for a total of 5, but we strongly recommend the final statement not exceed 1 single-spaced page to reduce cognitive load on the reader.
This part of the process involves revising the piece into a final polished personal statement. Before an early draft is shared with others, it should be evaluated for several important factors by returning to the initial questions and then asking (Step 6):
“Does this personal statement…”
- Amplify my strengths, highlight my proudest accomplishments, and emphasize what a program must know about me?
- Have a logical flow?
- Accurately attribute content and avoid plagiarism?
- Use proper grammar and avoid slang or profanity?
While not as challenging as the other steps, optimization takes time. 10 At this stage, “resting” the draft for 1 week minimum (Step 7) puts a helpful distance between the writer and their work before returning, reading, and editing. 10 Writers can edit their own work to a point, but they often benefit by enlisting a trusted peer or advisor for critiques. Hearing their draft read aloud by a peer or advisor allows the applicant to evaluate the work from another perspective while noting how well it meets the criteria from the tool (provided as online supplementary data).
A virtual or in-person meeting between applicant and mentor ultimately saves time and advances the writer to a final product more quickly than an email exchange. Sending the personal statement in advance helps facilitate the meeting. Invite the advisor to candidly comment on the tool's criteria to yield the most useful feedback (Step 8). When done effectively, edits can be made in real time with the mentor's input.
We bring closure to the process by focusing on spelling and grammar checks (Step 9). Clarity, conciseness, and the use of proper English were rated as extremely important by PDs. 3 , 9 Grammatical errors distract readers, highlight inattention to detail, and detract from the personal statement. 3 , 9 Once more, we recommend resting the draft before calling it final (Step 10). If the piece required starting over or significant rewriting based on feedback received, we also suggest seeking additional feedback on this draft, ideally from someone in the desired residency or fellowship discipline. If only minor edits (eg, flow, language) were incorporated, the personal statement can be considered complete at this time.
Writing a personal statement represents a unique opportunity for residency and fellowship applicants to amplify their ERAS application beyond the confines of its objective components. 3 Using this stepwise approach encourages each personal statement to be truly personal and streamlines the process for applicants and reviewers alike. All stakeholders benefit: applicants, regardless of their scores and academic metrics, can arm themselves with powerful means for self-advocacy; PDs gain a clearer idea of individual applicants, allowing them to augment the selection process and curate the individual interview day; and faculty mentors can offer concrete direction to every mentee seeking their help.
We use cookies to enhance our website for you. Proceed if you agree to this policy or learn more about it.
- Essay Database >
- Essays Samples >
- Essay Types >
- Personal Statement Example
Cardiology Personal Statements Samples For Students
14 samples of this type
Do you feel the need to check out some previously written Personal Statements on Cardiology before you start writing an own piece? In this free database of Cardiology Personal Statement examples, you are given a fascinating opportunity to discover meaningful topics, content structuring techniques, text flow, formatting styles, and other academically acclaimed writing practices. Implementing them while crafting your own Cardiology Personal Statement will surely allow you to finalize the piece faster.
Presenting the finest samples isn't the only way our free essays service can aid students in their writing efforts – our authors can also create from point zero a fully customized Personal Statement on Cardiology that would make a strong foundation for your own academic work.
Free Personal Statement About Fellowship
Cardiology fellowship program personal statement sample, cardiology personal statement sample.
Don't waste your time searching for a sample.
Get your personal statement done by professional writers!
Just from $10/page
Free Personal Statement On Cardiology
Personal statement, cardiology fellowship personal statement examples, personal statement on jjt md cardiovascular medicine 11057627, example of personal statement on cardiology fellowship.
Despite enjoying my current job as a faculty in an academic hospital medicine program, my enthusiasm for Cardiology has continued to grow. I did not succeed in obtaining a cardiology fellowship position during my internal medicine residency but this interest of mine led me to study Nuclear Medicine as I was particularly attracted to Nuclear Cardiology.
Cardiology Fellowship Personal Statement Example
I graduated from the American University of the Caribbean School of Medicine in 2009 and have been working as a doctor since then. I have thoroughly enjoyed this time and I am now keen to complete a fellowship in Cardiology. This field of medicine in the reason I decided to train as a doctor; I have a huge interest in cardiology and, in particular, cardiovascular diseases, and am keen to pursue a lifelong career in the field.
Example Of Personal Statement On Job Application
Organization, wayne state university personal statement examples, personal statement, personal statement on application for cardiology fellowship, application for cardiology fellowship, example of personal statement on degree objective, admission essay, fellowship in vascular diagnostics and intervention personal statement sample.
For the last four years I have been working as an Intervention Cardiologist. I have thoroughly enjoyed my time working in this field and I am now keen to undertake additional training in Vascular Diagnostics and Intervention. I would like to apply for the fellowship at Massachusetts General Hospital as I believe I have the skills, experience and enthusiasm required to excel in the program.
Cardiology Fellowship Application Personal Statement
From childhood, it has been my dream to be a doctor and it has been a great source of pride in me to have been able to realise this dream in the last few years. Furthermore, my professional medical experience has enabled me to realise that I am fascinated by the human heart and its inner-mechanics. As a result, it is my honour to request that I be accepted on to the Cardiology Fellowship and I wish to do so in Canada as it is my understanding that its cardiology training is amongst the best in the world.
Password recovery email has been sent to [email protected]
Use your new password to log in
You are not register!
By clicking Register, you agree to our Terms of Service and that you have read our Privacy Policy .
Now you can download documents directly to your device!
Check your email! An email with your password has already been sent to you! Now you can download documents directly to your device.
or Use the QR code to Save this Paper to Your Phone
The sample is NOT original!
Short on a deadline?
Don't waste time. Get help with 11% off using code - GETWOWED
No, thanks! I'm fine with missing my deadline
- Text or Call Us 917-994-0765

- Medical School Personal Statement Examples
Your Personal Statement for Medical School will arguably be the most important essay you’ll ever write…So no pressure, right?
Our team has the honor of helping applicants craft their story in an impactful way. Below are a few of those effective personal statement essays from recently accepted medical students.
Please note that these are final drafts. It took multiple rounds of revisions to reach the draft you are about to read.

Read Courtney’s Personal Statement
Read Matt’s Personal Statement
Read Alex’s Personal Statement
Read Suzy’s Personal Statement
Medical school personal statement Sample #1
I stood shoulder to shoulder with choir members, hundreds of eyes in our direction, each seated in the great hall known as the Dallas Myerson Symphony Center. The countless rehearsals, rhythms, and lyrics danced through my mind as I watched the conductor raise his arms, and eagerly awaited his signal. His baton came crashing down and within seconds, the room was filled with the sound of musicians whose every note, melody, and harmony were married together to form an exquisite synchrony. We sang the words of the great poet William Ernest Henley who emphasized resilience in the face of suffering as well as bravery in the face of adversity. I could physically see the impact of our voices on those in the room, particularly evident when beginning an ascent to an emotionally salient crescendo. It was through this experience that I recognized the unifying and healing power of music as well as the importance of holistic healing. This was a theme that has been at the forefront of my growth and empowerment as I faced some of the hardest years of my life in search of my own emotional healing. In a manner similar to music’s impact, I am motivated to become a physician to heal those around me through a holistic approach, advocacy, and continual evolvement along a journey of lifelong learning and growth.
I still remember my mother frantically waking my brother and I to tell us that our, then, dad was in the hospital, which left us searching for holistic healing ourselves. It was not until later that I learned he had suffered an aortic dissection. I was seven years old and struck with worry though simultaneously grateful for the miracle performed by the cardiothoracic surgeons. This was the initial spark that led me to uncover my passion for science as well as interest in medicine. Three years later, he carefully told me that for most of his life he felt as if he has been living in the wrong body. I remember the confusion, lack of comprehension, and most importantly, the newly surfaced and seemingly infinite compassion I felt towards both my mom and my now transgender father. This was a situation far from simple and many times, I was left amongst familial dissension, shadows of lost friends, and fear. Regardless, I remained resilient and found solace in my faith and music. Each provided an outlet to transform sadness and fear into something beautiful and face my emotions head-on with the help of those who loyally surrounded me. In stumbling upon this emotional healing, I saw correlations between the emotional and spiritual healing that our bodies demand to be physically well and later recognized that this was a significant aspect of what drew me to medicine. In the future, I long to bring comfort and peace to patients who trust in me during their most vulnerable times and when they are most afraid, as so many have done for me.
In the words of William Ernest Henley, having been through the trials of my circumstances, I continue to “find myself unafraid” and able to overcome challenges. I think I ultimately learned this perseverance and endurance from my mother, who never gave up even when she had to start over to provide for my brother and I. Simultaneously, I felt the pain my dad faced and saw my mother defy all odds to overcome our situation. My experiences are what pushes me to want to make a difference in a world that can be so cruel to so many. I remember the judgement and lack of compassion I faced when I was with my dad as well as the deliberate marginalization my dad faced as a transgender woman. This incited a sense of advocacy in me and prompted me to become part of a non-profit organization dedicated to serving a similarly marginalized community, the homeless. I have been able to work alongside college students to cultivate change and provide supplies to those in need. I see the ability to reiterate and continue this spirit through a career in medicine. For physicians are the listeners, the branches that extend across communities and through diverse populations, ultimately the advocates for their patients and deliverers of holistic care. I long to begin this journey, even if just as a budding twig among hundreds of branches, on the path to making a difference.
Much as a choir performance is dependent upon each component, pursuing a standard of holistic healing is also far from an individual endeavor. It takes a comprehensive team to meet the needs of a patient and their family, a reoccurring theme that I have been exposed to countless times. For this is a career that requires traversing a path that is no easy feat, but one that will procure undoubtable fulfillment and beauty. This is a place in my life I might never have expected I would be, but one that I welcome with open arms. I have found myself ready to face my journey of endless growth and possibility as I am certain I want to become a physician and certain that I am capable because I have faced adversity and have only grown stronger as a result.
Are you Struggling with your personal statement?
Watch a free 30 minute workshop to learn how to overcome writer’s block and finish writing your personal statement.
Medical school personal statement Sample #2
Reading through mission statements of various medical schools, I have discovered an enthralling question: Is medicine science or art? I find this discourse of disparate viewpoints interesting because of a similar battle that has played out in my own mind between the head and the heart. Medicine is where I belong as it provides an avenue between these two raging forces unique to any other field I have found. A career as a clinician is precisely the symphony of problem solving I crave and the opportunity to love humanity I long for, making it the perfect life for me.
My initial attraction to medicine during high school came from my inquisitive nature, a desire to solve puzzles. I enjoy the thrill of mastering a topic, and then either revealing how the pieces fit to others, or using my newfound expertise in the application of solving new problems. Thus, it’s no wonder that I found medicine invigorating. It provides an endless depth of knowledge to plunder, and the opportunity to utilize that material in new situations.
Previously, I saw the human machine as something I could solve and repair if I knew enough. This has driven me to seek out opportunities to understand the deep mechanistic nature of the body. I wanted, and still want, to understand medicine at its most basic level, and then apply that knowledge to fixing diseases. Because of this desire, I have continued to seek out medical knowledge in my own time, through reading and research at school.
Admittedly, this first attraction to medicine was misguided and born of selfishness. I saw my future self as a medical Sherlock Holmes-the smartest person in the room disseminating my own cleverness from on high to solve a medical problem. I had only a mild interest in the artful, human, side of medicine. This intense passion to solve problems I now see is not itself inherently wrong and will indeed serve me well in medical school, but such a desire must be tempered by the heart.
When I arrived at college, my concept of the world, and with it medicine, was completely rearranged. Living in close community, I soon realized a simple, but important Truth: Life is not about you. It isn’t even about each other on an individual level. It’s about how people connect and intersect on the whole and effect change for their fellow man. This perspective shift drastically changed how I lived at school. Now I had a desire to serve others and participate in my activities precisely to do so.
I also shifted how I understood medicine. Medicine, it seemed, was not the cold calculation of Holmesian deduction to fix diseases as I once believed, but the art of understanding, navigating, and mitigating human pain in whatever form-physical, emotional, psychological- via the conduit of scientific understanding. While the science of medicine first attracted me to the field, it is the desire to practice the art of medicine that has continued to propel me towards a career as a physician.
My understanding of medicine as an art and a science and my desire to pursue both have only grown stronger as I have become a patient myself. Last summer, I became very ill, and spent most of my summer asleep, in the bathroom, or at the clinic, only being diagnosed with ulcerative colitis at the end of July. In such a vulnerable position, I experienced first-hand that importance and impact of medicine as art and science. Dr. Hallak, my gastroenterologist, treated not just my illness, but the fear and pain I possessed, and for that I am forever grateful (and fortunately, also healthy).
Likewise, Dr. Hallak graciously taught me about my disease on a mechanistic level, demonstrating that he understood the science of medicine as deeply as I had hoped a clinician would. Thus, I was assured that a career as a clinician could sate my scientific hunger as well. In Dr. Hallak I clearly saw that I did not have to compromise between my desire to understand the human body as a machine, and my need to serve others and effect change in their lives. When I think of the type of physician I want to be, I know that I want to follow Dr. Hallak’s example and live a life using science to not simply fix disease, but to heal human pain.
Because of these experiences, I believe that medicine is precisely this: the application of knowledge of both humankind- our hearts, souls, minds, and bodies- and human disease towards the eradication of human pain. In this definition, I have found a means to navigate the tricky space between medicine as science and art, between my inquisitiveness and the earnest longing to benefit others, between the head and the heart. I am confident that in my future career as a physician I will be able to fulfill these two desires.
Furthermore, I believe that my perspective on medicine, one that unifies art and science, is necessary for the evolving landscape of medicine. With the advent of new technologies, future physicians will be called to new roles. It is only by understanding and synthesizing the disparate halves of medicine that we as future physicians can fulfill these new, unknown roles. It is my hope that I might bring a fresh perspective to the field of medicine, and bring a positive impact not simply for my own sake, but for all the patients I will have in the future.
Interested in viewing an in-depth personal statement review?
Medical school personal statement Sample #3
I gripped the kitchen phone and listened to a voice utter words that even at six years old, I could never forget: “your father is cured.” A sigh of relief escaped my lips as I realized that the invisible monsters that plagued my father’s body, ones much scarier than the Boogeyman hidden under my bed, were finally gone. My resilient father was no longer infected with hepatitis B and C. During his fight against those invisible monsters, I was far too young to understand the etiology of his ailments, much less the pharmacodynamics of his medications. However, there was one thing that at six years old I undisputedly understood; these monsters were making my father weak despite costly treatments. Seeing the physical and emotional pain my father bore and the constant havoc it wreaked on my family, I desperately scrambled to educate myself, naively using the computer as leverage to find a remedy. Each search was met with medical jargon my juvenile mind could not decode. However, after years of searching, “Dr. S,” my father’s gastroenterologist, accomplished what I had been naively trying to do: find a cure. Dr. S’s holistic understanding of my father and his heroic ability to help planted a seed of motivation inside me to become a physician, like him. One that is dedicated to curing others of the monsters that plague their bodies.
Growing up, various questions flooded my mind regarding my father’s illness. Why did he have hepatitis? Why did it take so long to find a cure? Slowly, answers emerged as I educated myself on healthcare in underdeveloped countries. My father, who was from a village outside X, was unknowingly infected with hepatitis. His life back home was simple, but the unsanitary health practices, lack of infrastructure, smoke-polluted air, contaminated water, and minimal health education or preventative medicine produced a suboptimal environment for sustaining a healthy lifestyle. As a result of these conditions and the insufficiency of available physicians, many individuals were beset by disease and mortality. This predisposition is, unfortunately, a reality that my father and millions of others living in underdeveloped countries or marginalized communities in the United States unjustly face. Learning about these roadblocks to healthcare subsequently made my passion to become a physician even more deeply rooted. My mission has now evolved into becoming a physician dedicated to implementing preventative medicine for underserved individuals.
While immersing myself in clinical experiences as an emergency medical technician (EMT), I became aware of prevailing healthcare inequalities, similar to what my father endured. While sitting on the edge of a blue seat in the ambulance, I watched my patient, “Max,” clutch his abdomen as he sat on the stretcher. “Max, do you have stomach pain?” though was not met with a response. “Max, ¿tiene dolor?” As the words left my mouth, all eyes turned to me. Max sluggishly nodded. “¿Max, dónde le duele?” He slowly pointed to his stomach. I continued to speak to Max in Spanish, which allowed me to further my assessment and obtain vitals. The time I spent caring for Max during transport underscored the importance of being adaptable to linguistic and cultural differences, as equitable patient care is dependent on the ability to acknowledge and cater to these differences. Being an EMT has allowed me to mitigate barriers to healthcare within my community, though I am left with the urge to do more. As a physician, I will be able to provide longitudinal care and make seeking primary care more accessible for marginalized individuals, such as my father and Max.
While becoming a physician for marginalized communities is part of my goal, it was not until my health promotion class that I realized how these populations can benefit from both preventative and osteopathic medicine. For these individuals, imbalances in internal and external stressors, whether they be environmental, social, emotional, or biological, may result in illness, such as my father’s. Rather than advocating for costly or invasive symptomatic treatment, A.T. Still’s philosophy on the mind, body, and spirit has demonstrated that as an osteopathic physician, I can holistically treat or even prevent disease by restoring these imbalances. Moreover, the second tenant of osteopathic medicine surrounding self-regulation and self-healing would allow me to help marginalized individuals realize that they have the innate tools necessary to maintain optimal health and overcome disease. Altogether, this outlook would enable these individuals, who often cannot afford costly treatment, to feel empowered and capable of controlling their own health narratives. Although my introduction to osteopathic medicine was brief, the impact it has made on my journey to medicine is long-lasting.
Never would I have thought that four simple words would lead me down a path towards becoming an osteopathic physician. Yet, the story behind them inadvertently ignited a fire within me. Regardless of cultural differences or even language barriers, I now know that with an osteopathic outlook, I can be the hope in medicine for underserved communities and deliver the life-changing words that I once received.
Need help writing your personal statement?
Be memorable. claim an interview spot. get accepted..

Medical school personal statement Sample #4
One 40-minute bus ride and three wrong turns later, I arrived at Dr. C’s cardiology clinic in X. After climbing the stairs to the clinic doors, a volunteer coordinator welcomed me and gestured to a waiting room brimming with restless patients. “We’re behind schedule today. Here’s the first patient’s chart. You’ll learn on the go.” He ushered me quickly into the nearest patient room, where I found myself standing in front of a confused elderly woman. I took a deep breath and introduced myself. Then, listening carefully, I began to update her medical chart as she described her sharp chest pain. As I reviewed her family and social history, she inhaled shallowly: her only daughter had passed away a few weeks earlier. She crumpled the medication list in her lap, her gaze downcast. I acknowledged her pain, handed her a box of tissues as well as a glass of water and listened to her as she shared fond memories of her daughter. Once we finished our session, I brought her over to Dr. C, who warmly squeezed her hand. I observed as he listened and patiently attended to each of her concerns while he simultaneously interpreted her electrocardiogram results and prescribed a regimen of beta-blockers. As I watched her leave the office with a renewed sense of calm, I immediately recognized the significance of a patient-physician relationship defined by curiosity, compassion, and communication.
My interest in medicine began as a child living with X, my exuberant autistic brother with a fierce sweet tooth. As I watched childhood friends take part in friendly sibling rivalries, I could not help but wonder if I would ever be able to do the same. With his speech limited to a handful of utterances and with his aversion to physical touch, I had to learn how to connect with X in other ways. Despite my short stature as a child, I remember tenaciously balancing myself upon a kitchen stool, foraging through the top cupboards, and sneaking away with a box of cookies so that my brother and I could eat together in contented silence. Yet this shared silence led me to so many questions: Would I ever know what X was thinking? How did this happen? My love for my brother grew alongside the puzzling nature of his diagnosis. This acted as the initial push into an education in the sciences and into a desire to uncover the intricacies of the human body.
Armed with a background in biochemistry, my pursuit of knowledge propelled me through an undergraduate senior thesis in Dr. K’s lab. Enlightened by the scientific method and curious about the molecular processes underlying complex illnesses, I decided to examine the regulation of transcription factors involved in renal fibrosis, a pathological marker of chronic kidney disease. This laborious but rewarding process allowed me to correlate the presence of the cav-1 gene to the lowered expression of the SP1 transcription factor and the decreased production of follistatin, a protein that neutralizes pro-inflammatory pathways and protects against renal fibrosis. Though I was thrilled by my findings, I was still left unsatisfied. I had originally set out to seek answers, but I realized that what I wanted even more was to be reassured in the face of the unknown. More than that, I wanted to offer assurance to those in similarly ambiguous situations through experiences in clinical and community settings.
For the better part of a decade, I offered assurance in the emergency department (ED) at X. There, I formed strong relationships and gained experience working alongside accomplished and dedicated physicians. However, the ED, for most patients, is often a place of distress. I remember one particular patient crying relentlessly while her mother spoke to me about a research study that we were conducting at the hospital. She mentioned that her daughter loved to draw, but in their haste to the hospital, she had forgotten to bring drawing supplies. As her mother read over the consent form that I presented to her, I excused myself to find paper and crayons. When I returned, I sat next to the child as she drew her favorite cartoons. I complimented her artistic skills. She laughed relentlessly, engrossing herself further in her evolving artwork. This scene continues to replay in my mind – the reprieve that art offered, the child’s pure joy, and her mother mouthing “Thank You” from her seat. While not a technical part of my role as a clinical research project assistant, this small act brought tranquility to a stressful environment. Being willing to exceed beyond expectations for others in a compassion-led approach is essential for connecting with and advocating for patients.
While the silence between my brother and me prompted questions, it equally taught me lessons that no one else could. From him, I learned about the individuality in human connection and the power of kindness. My experiences combined with a penchant for scientific inquiry have both established and continuously reaffirmed my desire to become a physician. Whether it is following up with a distressed cardiology patient or connecting with distraught families in the ED, I want to improve the lives of others and provide a place of solace for all that I meet.
- 917-994-0765
- [email protected]
- Medical School Admissions
- Residency Application
- The PreMed App
- MCAT Vitals
- Meet Our Team
- Testimonials
- Join the Team
© 2024 Motivate MD

- All-In-One Packages
- Personal Statement Editing
- Essay Brainstorming Session
- Activities Section Editing
- Secondary Essays Editing
- Admissions Consulting
- Interview Preparation
- CASPer Test Prep
- ERAS Common Application Editing
- Interview Prep
- Essay Editing
- MCAT Question of the Day
- List of Medical Schools
- Medical School Map
- Tools for Applying to Medical School
- Medical School Application Timeline
- Medical School Secondary Essays Examples
- FAQs about Medical School Interviews
- Medical School Interview Common Questions & Answers
- Motivate MD Team
- Free Consultation

Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps
Feature | Maintaining Professionalism and Ethics in Cardiovascular Care
Cardiology magazine.

Addressing the "practical management of professional and ethical behavior of cardiovascular clinicians and scientists" is at the center of a new ACC and American Heart Association (AHA) report based on the proceedings of a joint 2020 Consensus Conference on Professionalism and Ethics.
The report, which was published in the Journal of the American College of Cardiology and Circulation on May 11, provides specific recommendations regarding important and timely topics, such as diversity, equity, inclusion and belonging; racial, ethnic and gender inequities; conflicts of interest; clinician well-being; data privacy; social justice; and modern health care delivery systems. It updates previous guidance issued by the ACC and AHA in 2004.
"There is no better time than now to review, evaluate and take a fresh perspective on medical ethics and professionalism," says Conference Co-chair C. Michael Valentine, MD, MACC , ACC past president and professor of medicine at the Heart and Vascular Center at the University of Virginia in Charlottesville. "We hope this report will provide cardiovascular professionals and health systems with the recommendations and tools they need to address conflicts of interest, racial, ethnic and gender inequities and improve diversity, inclusion and wellness among our workforce."
The Conference report was developed by a diverse group of cardiologists, internists and associated health care professionals and laypersons. The group was organized into five separate task forces charged with making specific recommendations in the following areas:
- Task Force 1: Conflicts of interest
- Task Force 2: Diversity, equity, inclusion and belonging
- Task Force 3: Clinician well-being
- Task Force 4: Patient autonomy, privacy and social justice in health care
- Task Force 5: Modern health care delivery
Members of Task Force 1 specifically address conflicts of interest a health care practitioner, a researcher or other health care professional might face due to relationships with industry, academic institutions, health care systems, professional organizations, research institutions, advisory bodies, etc. The task force makes specific recommendations related to association and intellectual interests; research and publication; and disclosure of relationships with industry in educational activities and scientific publications. It also offers guidance for external assessments of interests, peer review and grant study, and providing expert testimony and opinions.
The work of Task Force 2 builds on the ACC's Code of Ethics and Diversity and Inclusion Governance Principles, as well as AHA's Code of Ethics and Nondiscrimination Policy and provides a roadmap for achieving diversity, equity, inclusion and belonging (DEIB). Specifically, the task force provides guidance on eradicating bias, harassment, structural racism and sexism, and outlines specific accountabilities for clinicians, hospitals and health systems, and specialty societies, noting that these entities "must be held accountable for institutional culture and for visibly championing, working toward, and achieving DEIB."
When it comes to enhancing clinician well-being, Task Force 3 recommendations focus on organizational strategies, as well as strategies for improving the efficiency of health information technology – a key factor in clinician burnout. Additionally, recommendations are included to improve the well-being of trainees and researchers, and to identify and assist physicians with impaired and disruptive behaviors. "The stigma of seeking mental health help in the United States is highly prevalent, is especially pervasive in medicine, and is associated with barriers to seeking help," the report states. "Clinicians and team members must be taught to recognize a potentially impaired physician and to understand the process for confidential reporting of concerns."
Recommendations from Task Force 4 focus on three specific areas, including patient autonomy, especially as it relates to clinical decision-making; privacy, data access and transparency; and social justice in medical education and clinical practice. "As much as 80% of a person's health is determined by the social and economic conditions of their environment," says Conference Co-chair Ivor J. Benjamin, MD, FACC , former AHA president and director of the cardiovascular center, co-director of the NIH T32 Postdoctoral Fellowship in Cardiovascular Sciences and professor of medicine at the Medical College of Wisconsin in Milwaukee. "To achieve social justice and mitigate health disparities, we must go to the margins and shift our discussions to be inclusive of populations such as rural and marginalized groups from the perspective of a health equity lens for all."
C. Michael Valentine, MD, MACC
Modern health care delivery and overcoming challenges related to new care delivery systems are the focus of Task Force 5. The group offers guidance for addressing potential conflicts of interest when designing and engaging in these new models, as well as defines medical professionalism for the employed clinician. "The majority of our members are now employed and must be engaged as the leaders for change in cardiovascular care," says Valentine.
The task force also addresses ethical challenges and professionalism related to billing, coding, documentation and electronic health records. "The transformation of care delivery models and the complexities of new technologies mandate increased attention and careful introspection in relationship to professionalism and ethics," the report states. "Evolving employment and payment models, rapidly changing delivery sites of care, and the documentation of care require maintenance of standards that are beyond reproach and representative of the trust placed in all physicians and clinicians. It is the responsibility of each individual, as well as our professional communities, to continually evaluate the degree to which such standards are maintained and met."
Representatives from the Heart Failure Society of America, Preventive Cardiology Nurses Association, American College of Preventive Medicine, American Association for Thoracic Surgery, American College of Physicians and industry provided feedback and review of the new report.
Click here for the complete report, including a complete list of committee members and co-authors. The recommendations set forth in this report do not necessarily reflect the official policy of the AHA and the ACC.
Details and recommendations from the Conference Report are presented and discussed as part of an ACC.21 session titled "Diversity and Equity: The Means to Expand Inclusion and Belonging," available on demand starting May 15 at 8 a.m. ET (ACC.21 registration is required). Hear from Valentine, Benjamin and other committee members and co-authors on topics ranging from avoiding biased decision-making to balancing change and professionalism. Click here for more information.
Over the years, the ACC has developed educational programs and tools to help inform the next generation of cardiovascular professionals about the importance of professionalism. Member Sections like the Women in Cardiology Section have held focused webinars, while podcasts like Practice Made Perfect have served as important mediums for discussions on professionalism and related issues. In addition, ACC meetings like the Annual Scientific Session and Cardiovascular Summit also provide forums for helping cardiovascular clinicians understand and value professionalism.
Most recently, the ACC has updated its Professionalism Module to coincide with the release of the Conference Report. The free, case-based online module allows participants to earn up to 1.5 MOC points by answering multiple-choice questions on the topic of medical professionalism, including integrity and accountability, fair and ethical use of health care resources, self-regulation and commitment to excellence. "Our hope is that clinicians can use this module to grow their knowledge and understanding of medical professionalism and be able to apply it in real-life interactions with colleagues, patients and others," says William J. Oetgen, MD, MBA, MACC .
Visit ACC.org/Education to access the updated Professionalism Module and learn more about upcoming events.
The ACC's Code of Ethics sets standards and provides guidance for members in their clinical practice, and in their professional activities, generally. The Code delineates requirements for relationships with patients, other professionals, the ACC, and requirements for members' relationship to the community and government. The Code of Ethics also outlines training and continuing medical education responsibilities, guidelines for the provision of expert witness testimony, and obligations to disclose conflicts of interest. Adherence to the Code of Ethics is a condition of ACC membership and any violations of the Code are addressed pursuant to the Professional Conduct Program Procedures included in the Code of Ethics. Click here to access the Code of Ethics.
Both the ACC and AHA have long histories of formally addressing issues related to medical ethics and professionalism, ranging from joint Bethesda Conferences and Consensus Conferences starting in 1989 to ongoing ratification and adoption of the Medical Professionalism in the New Millennium: A Physician Charter . Professionalism is also embedded in the ACC's Core Values.
"The Charter, published in 2002, is the standard for a document expressing the tenets of medical professionalism and has been adopted by more than 100 medical societies and medical specialty societies around the world," says William J. Oetgen, MD, MBA, MACC , a member of the 2020 Conference Executive Committee and co-editor of the ACC's newly updated Professionalism Module. According to Oetgen, the Charter and its tenets served as the foundation from which the 2020 Conference Task Force members crafted their respective recommendations included in the new report.
Click here to read the 1989 JACC President's Page from then ACC President C. Richard Conti, MD, MACC , on the first Bethesda Conference.
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, Heart Failure and Cardiomyopathies, Acute Heart Failure
Keywords: ACC Publications, Cardiology Magazine, Advisory Committees, American Heart Association, Cardiology, Codes of Ethics, Conflict of Interest, Committee Membership, Constitution and Bylaws, Delivery of Health Care, Disclosure, Documentation, Decision Making, Education, Medical, Education, Medical, Continuing, Educational Status, Employment, Electronic Health Records, Ethics, Professional, Ethics, Medical, Expert Testimony, Family Characteristics, Fellowships and Scholarships, Feedback, Government, Heart Failure, Maintenance, Hospitals, Medical Informatics, Medicine, Mental Health, Policy, Peer Review, Privacy, Racism, Reference Standards, Sexism, Social Justice, Social Responsibility, Societies, Societies, Medical, Thoracic Surgery, Trust, Wisconsin, Health Workforce
You must be logged in to save to your library.
Jacc journals on acc.org.
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Email: [email protected]
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- ACC.org Quick Start Guide
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
Cardiovascular Research Personal Statement
Sample Cardiovascular Research Personal Statement
Over the course of completing a BSc in Physiology at the University of Glasgow, I feel I successfully made a transition from seeing the sciences as subjects to be learnt through textbooks and supervised laboratory work to viewing them as constantly evolving disciplines, characterised by near-limitless unanswered research questions. The basis of my love of science has therefore shifted from a desire to learn to a wish to help push the boundaries of scientific knowledge. Having developed a solid interest in cardiovascular biology, I now wish to take the first step in embarking upon a career in scientific research through studying for an MSc in Cardiovascular Research.
My BSc has provided me with both a well-rounded understanding of the science behind the human bodyand a firm foundation of knowledge and research skills in cardiovascular research, upon which I hope to build through completing the MSc. In my final year I developed a very strong interest in vascular biology, generated initially by taught modules, andsubsequently strengthened through completing a research project in this area, for which I was awarded the Undergraduate Prize for Physiology by the university. My interest in this area has endured due to the engrossing experience of carrying out this research and my recognition of the crucial role that vascular biology research has played – and will continue to play – in creating therapies for vascular diseases.
My undergraduate research project was entitled “The role of anandamide and GPR55 in modulating vascular neuroeffector transmission in the rat tail artery”. Although I recognise that there is a large gulf between undergraduate research projects and professional research, the fact that the project corroborated other research that suggest that a greater understanding of cannabinoids could contribute to advances in creating new therapeutic approaches for diseases such as hypertension was a great reward to me. Moreover, I enjoyed all aspects of carrying out the project, and valued the experience and knowledge it gave me, not just of current research in vascular biology, but also of how to devise, execute, analyse and present a research project.
The possibility of gaining a much greater level of competence in these areas attracts me to the MSc. I wish to follow up masters-level study with carrying out PhD research – and hopefully beyond that a postdoctoral research career – and as a result I see it as vital that I gain a thorough grounding in research skills and methods associated with vascular biology. I am equally enthusiastic about the prospect of studying taught courses that focus explicitly on cardiovascular research. Above all, I look forward to applying the theoretical and practical grounding that I gain to carrying out research in the latter part of the masters.
My interest in cardiovascular research is the key component of a broader interest in health care that I have built on through carrying out work placements in the healthcare sector. Most recently, I worked as an assistant to a dental surgeon based in St. Lucia. The placement helped me to make a greater mental connection between scientific research and the day-to-day delivery of healthcare. After learning about an oral health campaign that was being run in St. Lucia, for example, I became interested in research relating to oral health care and other types of disease, and was fascinated to learn of research that indicates a link between oral health care and heart disease. Such potential discoveries further stimulate my interest in scientific research. Indeed, quite apart from my deep intellectual interest in vascular biology, the fact that cardiovascular diseases continue to be the biggest cause of death is, in my view, a highly compelling reason to be involved in this area. I hope, upon completion of the MSc, to carry out doctoral research, and ultimately contribute to human wellbeing through working as a postdoctoral researcher in the field.
We hope this sample Cardiovascular Research Personal Statement is a helpful guide for relevant content and structure for writing your own statement.
Personal Statement
- The Application Process
- UCAS Criteria
- Choosing a Degree
- Why is a Good Personal Statement Important?
- Your Personal Statement
- Example Personal Statements
- Personal Statement Help
- Personal Statement Format
- Points to Remember
- The UK Tuition Fees System
- Student Loans
- Student Finance
- Full Subjects List
- Disabled UCAS Applicants
- A-Level Results Day
- A Guide to Results Day
- Clearing & A Level Results Day
- A Guide to Clearing
- Visas to study in the UK
- Missed the January UCAS deadline?
- No University Offers…What Next?
- Interview Skills
- PGCE Interviews
- Applying to Oxbridge
- Before you go to University
- University Checklist
- Studying Abroad
- Applying to University Overseas
- Apply to study Internationally
- Preparing for Studying Abroad
- Benefits of Studying Abroad
- Taking a Gap Year
- Should You Take A Gap Year?
- Study Independently
- Choosing Accommodation
ADVERTISEMENTS
- Louisville.edu
- Health Sciences Center
- PeopleSoft HR
- PeopleSoft Campus Solutions
- PeopleSoft Financials
- Business Ops
- Cardinal Careers
Office of Faculty Affairs and Advancement
- Faculty Affairs /
- Letter Templates /
Personal Statement Template

Office of Faculty Affairs
Abell Administration Building 323 East Chestnut Street, Room 408 Louisville, KY 40202
Office Hours
M-F 8:00 am to 4:00 pm
Director: (502) 852-6165
Vice Dean: (502) 852-6266
Faculty Affairs Contacts
Personal Statement for PhD Applicants
New section.
Your personal statement is your chance to shine, to stand out from among the hundreds of other PhD applicants.
The personal statement (or statement of purpose) is your introduction of yourself to the application reviewers. This brief statement (generally one to two pages) should communicate your abilities, accomplishments and goals. It must also show us your writing skills, including your ability to present yourself and your ideas concisely. It should show your commitment to and motivation for graduate school based on your history. It should have a positive tone, be honest, and professional.
This is your chance to shine, to stand out from among the hundreds of statements that the reviewer is reading.
It is crucial that you get some honest critiques on your statement before you submit it to the school. However, the voice of the statement should be yours. Remember, if you are invited for an interview, the school will expect to meet the person who wrote the statement. Although you should not have to rewrite your entire essay for each school/program you are applying to, it should be tailored for each program.
Patient-Centered Adult Cardiovascular Care: A Scientific Statement From the American Heart Association
- PMID: 38602110
- DOI: 10.1161/CIR.0000000000001233
Patient-centered care is gaining widespread acceptance by the medical and lay communities and is increasingly recognized as a goal of high-quality health care delivery. Patient-centered care is based on ethical principles and aims at establishing a partnership between the health care team and patient, family member, or both in the care planning and decision-making process. Patient-centered care involves providing respectful care by tailoring management decisions to patients' beliefs, preferences, and values. A collaborative care approach can enhance patient engagement, foster shared decision-making that aligns with patient values and goals, promote more personalized and effective cardiovascular care, and potentially improve patient outcomes. The objective of this scientific statement is to inform health care professionals and stakeholders about the role and impact of patient-centered care in adult cardiovascular medicine. This scientific statement describes the background and rationale for patient-centered care in cardiovascular medicine, provides insight into patient-oriented medication management and patient-reported outcome measures, highlights opportunities and strategies to overcome challenges in patient-centered care, and outlines knowledge gaps and future directions.
Keywords: AHA Scientific Statements; cardiovascular diseases; decision-making; patient-centered care; patient-reported outcomes; structural determinants of health.
Publication types
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- For authors
- New editors
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- Cardiorespiratory fitness is a strong and consistent predictor of morbidity and mortality among adults: an overview of meta-analyses representing over 20.9 million observations from 199 unique cohort studies
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-1768-319X Justin J Lang 1 , 2 , 3 ,
- http://orcid.org/0000-0001-6729-5649 Stephanie A Prince 1 , 2 ,
- Katherine Merucci 4 ,
- http://orcid.org/0000-0002-4513-9108 Cristina Cadenas-Sanchez 5 , 6 ,
- http://orcid.org/0000-0002-5607-5736 Jean-Philippe Chaput 2 , 7 , 8 ,
- http://orcid.org/0000-0002-1752-5431 Brooklyn J Fraser 3 , 9 ,
- http://orcid.org/0000-0001-5461-5981 Taru Manyanga 10 ,
- Ryan McGrath 3 , 11 , 12 , 13 ,
- http://orcid.org/0000-0003-2001-1121 Francisco B Ortega 5 , 14 ,
- http://orcid.org/0000-0002-7227-2406 Ben Singh 3 ,
- http://orcid.org/0000-0001-7601-9670 Grant R Tomkinson 3
- 1 Centre for Surveillance and Applied Research , Public Health Agency of Canada , Ottawa , Ontario , Canada
- 2 School of Epidemiology and Public Health, Faculty of Medicine , University of Ottawa , Ottawa , Ontario , Canada
- 3 Alliance for Research in Exercise, Nutrition and Activity (ARENA), Allied Health and Human Performance , University of South Australia , Adelaide , South Australia , Australia
- 4 Health Library , Health Canada , Ottawa , Ontario , Canada
- 5 Department of Physical Education and Sports, Faculty of Sport Sciences, Sport and Health University Research Institute (iMUDS) , University of Granada; CIBEROBN, ISCIII , Granada , Andalucía , Spain
- 6 Stanford University, Department of Cardiology; and Veterans Affair Palo Alto Health Care System , Palo Alto , California , USA
- 7 Children’s Hospital of Eastern Ontario Research Institute , Ottawa , Ontario , Canada
- 8 Department of Pediatrics, Faculty of Medicine , University of Ottawa , Ottawa , Ontario , Canada
- 9 Menzies Institute for Medical Research , University of Tasmania , Hobart , Tasmania , Australia
- 10 Division of Medical Sciences , University of Northern British Columbia , Prince George , British Columbia , Canada
- 11 Fargo VA Healthcare System , Fargo , North Dakota , USA
- 12 Department of Health, Nutrition, and Exercise Sciences , North Dakota State University , Fargo , North Dakota , USA
- 13 Department of Geriatrics , University of North Dakota , Grand Forks , North Dakota , USA
- 14 Faculty of Sport and Health Sciences , University of Jyväskylä , Jyväskylä , Finland
- Correspondence to Dr Justin J Lang, Public Health Agency of Canada, Ottawa, Canada; justin.lang{at}phac-aspc.gc.ca
Objective To examine and summarise evidence from meta-analyses of cohort studies that evaluated the predictive associations between baseline cardiorespiratory fitness (CRF) and health outcomes among adults.
Design Overview of systematic reviews.
Data source Five bibliographic databases were searched from January 2002 to March 2024.
Results From the 9062 papers identified, we included 26 systematic reviews. We found eight meta-analyses that described five unique mortality outcomes among general populations. CRF had the largest risk reduction for all-cause mortality when comparing high versus low CRF (HR=0.47; 95% CI 0.39 to 0.56). A dose–response relationship for every 1-metabolic equivalent of task (MET) higher level of CRF was associated with a 11%–17% reduction in all-cause mortality (HR=0.89; 95% CI 0.86 to 0.92, and HR=0.83; 95% CI 0.78 to 0.88). For incident outcomes, nine meta-analyses described 12 unique outcomes. CRF was associated with the largest risk reduction in incident heart failure when comparing high versus low CRF (HR=0.31; 95% CI 0.19 to 0.49). A dose–response relationship for every 1-MET higher level of CRF was associated with a 18% reduction in heart failure (HR=0.82; 95% CI 0.79 to 0.84). Among those living with chronic conditions, nine meta-analyses described four unique outcomes in nine patient groups. CRF was associated with the largest risk reduction for cardiovascular mortality among those living with cardiovascular disease when comparing high versus low CRF (HR=0.27; 95% CI 0.16 to 0.48). The certainty of the evidence across all studies ranged from very low-to-moderate according to Grading of Recommendations, Assessment, Development and Evaluations.
Conclusion We found consistent evidence that high CRF is strongly associated with lower risk for a variety of mortality and incident chronic conditions in general and clinical populations.
- Cardiovascular Diseases
- Cohort Studies
- Physical fitness
Data availability statement
Data are available on reasonable request.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bjsports-2023-107849
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Many systematic reviews have examined the prospective link between baseline cardiorespiratory fitness and health outcomes, but no study has compiled all the evidence to help identify important gaps in the literature.
WHAT THIS STUDY ADDS
This study identified 26 systematic reviews with meta-analysis representing over 20.9 million observations from 199 unique cohort studies. Cardiorespiratory fitness was strongly and consistently protective of a variety of incident chronic conditions and mortality-related outcomes.
Gaps in the literature continue to exist, with limited evidence available among women, and certain clinical populations. Several health outcomes could benefit from future meta-analyses, including specific cancer types, especially among women (eg, breast cancer) and mental health conditions beyond depression.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Given the strength of the predictive utility of cardiorespiratory fitness across many health outcomes, cardiorespiratory fitness would be a valuable risk stratification tool in clinical practice.
Introduction
Cardiorespiratory fitness (CRF) is a physical trait that reflects the integrated function of numerous bodily systems to deliver and use oxygen to support muscle activity during sustained, rhythmic, whole-body, large muscle physical activity. 1 CRF can be objectively measured using direct (usually by maximal exercise testing with concomitant gas exchange analysis) 2 or indirect (exercise predicted equations) 3 4 methods with a variety of maximal or submaximal protocols using different modalities (eg, stationary cycling, treadmill running/walking, bench stepping, field-based running/walking). Non-exercise prediction equations with reasonable validity are also available when direct CRF measurement is not feasible. 5 6 CRF is commonly expressed as the maximum or peak rate of oxygen consumption per kilogram of body mass (common units: mL/kg/min) or metabolic equivalents of task (METs). Nearly half of the variance in CRF is attributable to genetics, with the remainder modified primarily through habitual physical activity. 7 For example, brisk walking for approximately 150 min per week can result in large relative improvements in CRF among sedentary and unfit individuals. 8 9 Even those with severe chronic disease can improve CRF through well-planned aerobic physical activity programmes. 10
Low CRF is considered a strong chronic disease risk factor that is not routinely assessed in clinical practice. 11 Evidence suggests that the inclusion of CRF as a clinical vital sign would enhance patient management by improving the classification of those at high risk of adverse outcomes. 11 The evidence supporting CRF as an important risk factor has accumulated since the 1980s through large cohort studies that investigated the prospective risk of all-cause mortality and cardiovascular events associated with CRF. 12–14 Research has linked CRF to the incidence of some cancers (eg, colon/rectum, lung), 15 type 2 diabetes, 16 metabolic syndrome, 17 stroke 18 and depression. 19 Higher CRF may even improve the prognosis in those with chronic conditions such as cancer, 20 peripheral artery disease, 21 heart failure 22 and chronic kidney disease. 23
Given the mounting evidence supporting CRF as an important risk factor, numerous systematic reviews with meta-analyses summarising results of primary studies for various health outcomes have been published. Kodama et al 24 published the first meta-analysis on the health-related predictive validity of CRF and found that a 1-MET (3.5 mL/kg/min) higher level of CRF was associated with a 13% and 15% reduction in the risk of all-cause mortality and cardiovascular disease (CVD) events, respectively. This study helped to establish the meaningful clinically important difference (MCID) of 1-MET for exercise trials. Since Kodama’s study, there have been several systematic reviews with meta-analyses, with several published in recent years (ie, 2020+). Most systematic reviews have focused on a single health outcome. To date, there has not been a systematic synthesis of the relationships between CRF and a broad range of health outcomes. To help summarise the breadth of evidence, an overview of reviews provides a systematic method to examine evidence across a range of outcomes for a specific exposure. 25 Thus, the objective of this study was to conduct an overview of systematic reviews with meta-analyses from cohort studies that investigated relationships between CRF and prospective health-related outcomes among adults. We also aimed to assess the certainty of the evidence for each identified health outcome.
This overview followed the methods outlined in the Cochrane handbook, 25 and additional methods that were published elsewhere. 26 We adhered to both the Preferred Reporting Items for Overviews of Reviews statement 27 and the Meta-analyses of Observational Studies in Epidemiology reporting standards. 28 The overview was prospectively registered with the PROSPERO international prospective register of systematic reviews (#CRD42022370149). Here, we present a condensed methods section with the full methods available in online supplemental methods .
Supplemental material
Eligibility criteria.
Adult populations (≥18 years) including apparently healthy and clinical populations with diagnosed chronic conditions. Studies that focused on certain special populations were excluded (ie, those recovering from surgery, athletes, disease at birth, pregnant individuals).
The primary exposure was CRF measured using the following approaches: (1) maximal exercise testing with gas analysis (ie, directly measured V̇O 2max/peak ), (2) maximal or submaximal exercise testing without gas analysis, which used either exercise prediction equations to estimate CRF or the measured exercise performance (ie, indirect measures) or (3) non-exercise prediction equations for estimating CRF.
Any health-related outcome such as all-cause or cause-specific mortality, incident conditions related to physical risk factors, chronic conditions or mental health issues were included. Among populations with diagnosed chronic conditions, we included evidence on outcomes such as mortality or disease severity.
Study design
Only systematic reviews with meta-analyses that searched a minimum of two bibliographic databases and provided a sample search strategy were included. We also included meta-analyses that pooled data from primary prospective/retrospective cohort or case-control studies. These studies were the focus because of their ability to assess causality for observational research.
Publication status and language restriction
Only systematic reviews published in peer-reviewed journals in English, French or Spanish (based on authors’ language capacity) were eligible. Conference abstracts or papers, commentaries, editorials, dissertations or grey literature were ineligible.
Systematic reviews published during the past 20 years for the initial search.
Information sources
Five bibliographic databases, including OVID Medline, OVID Embase, Scopus, CINAHL and EBSCOhost SPORTDiscus, were searched from 1 January 2002 to 21 November 2022. The search was later updated from 1 November 2022 to 8 March 2024.
Search strategy
A research librarian (KM) created the search strategy in collaboration with the authorship team, and the final search was peer-reviewed by an independent research librarian using the Peer Review of Electronic Search Strategies guidelines. 29 The search strategies for each database are available in online supplemental appendix 1 . The reference lists of included papers were also searched for additional relevant systematic reviews.
Selection process
All records were imported into RefWorks where duplicates were removed using automated and manual methods. Records were imported into Covidence for further deduplication and record screening. Reviewers were not blinded to the study metadata when screening. The title and abstract from each record were screened by two of the following independent reviewers (JJL, SAP, CC-S, J-PC, BJF, TM, BS and GRT) against the inclusion criteria. Full-text papers were obtained for each record that met the inclusion criteria or provided insufficient evidence to make a conclusive decision at the title and abstract stage. Conflicts during title and abstract screening automatically advanced to full-text screening. Each full-text record was screened by two of the following independent reviewers (JJL, SAP, CC-S, J-PC, BJF, TM, BS and GRT) against the inclusion criteria. Conflicts at the full-text stage were resolved through discussion by two reviewers (JJL and SAP), with a third reviewer resolving disagreements (GRT).
Data collection process
Data extraction was completed in Covidence using a form that was piloted by the authorship group for accuracy. Data from the included studies were extracted by two of the following independent reviewers (JJL, SAP, CC-S, J-PC, BJF, TM, FBO, BS and GRT). Conflicts were resolved by one reviewer (JJL), who contacted the reviewers who extracted the data when necessary to resolve conflicts.
The data extraction form included several items related to the demographic characteristics of the primary studies, the meta-analyses effect estimates and related statistics, and details for risk of bias and subgroup analyses.
Review quality
We extracted the original risk of bias assessment for each primary study, as reported by the study authors. Most of the included studies used the Newcastle-Ottawa Scale (NOS) to assess risk of bias for cohort studies. 30 In the event that risk of bias was not assessed, a new assessment was conducted and verified by two reviewers using the NOS. We also assessed quality of the systematic reviews using the second edition of A MeaSurement Tool to Assess systematic Reviews 2 (AMSTAR2) checklist. 31 Two of the following independent reviewers (JJL, SAP, CC-S, J-PC, BJF, TM, FBO, BS and GRT) assessed review quality. Conflicts were resolved by one reviewer (JJL), with the reviewers who extracted the data contacted to resolve outstanding conflicts.
Effect measures
We presented pooled hazard ratios (HRs) or relative risks (RRs) for an incident event (ie, mortality or morbidity) across the included systematic reviews. We extracted data from models that compared high versus low CRF and those that examined the impact of a 1-MET higher level of CRF.
Synthesis of data
We followed an outcome-centric approach, as outlined by Kho et al . 26 Our goal was to identify systematic reviews with non-overlapping primary studies for each outcome to avoid double counting evidence. When more than one eligible systematic review was identified for a single outcome, we calculated the corrected covered area (CCA) to assess the degree of overlap in the primary studies. 32
Where, N is the total number of times a primary study appeared across reviews (inclusive of double counting), r is the number of unique primary studies and c is the number of systematic reviews included for the outcome.
The CCA was interpreted as slight (0%–5%), moderate (6%–10%), high (11%–15%) or very high (>15%). If the CCA was slight or moderate, we included multiple systematic reviews per outcome. If the CCA was high or very high, we selected the highest quality systematic review according to the AMSTAR2 assessment. We included the most recent systematic review when reviews of the same outcome were rated as equal in quality.
Synthesis of results
For each health outcome, we reported evidence for apparently healthy and clinical populations separately. We summarised results using a narrative synthesis approach using summary of findings tables. Results were reported as described by the systematic review authors. Meta-analytical results, including the effect, confidence limits, number of studies and number of participants, were presented by outcome using a forest plot to allow for easy comparison between studies. RR values were taken to approximate the HR. When comparing high versus low CRF, we inverted the scale when studies compared low versus high by taking the reciprocal (ie, HR=2.00 was changed to HR=0.50). Dose−response values were rescaled to a 1-MET higher level of CRF when more than 1-MET was used or if the unit increase was in VO 2 . We rescaled by taking the natural log of the HR, dividing or multiplying it to correspond with 1-MET, and exponentiating the result. Subgroup analyses for sex were described when available.
Certainty of the evidence assessment
For each outcome, the certainty of the evidence was assessed using a modified Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach. 33 Observational cohort evidence began at ‘high’ certainty because randomised controlled trials were deemed not feasible for our research question. 34 The certainty of the evidence could be rated down based on five domains (ie, risk of bias, imprecision, inconsistency, indirectness and publication bias). See online supplemental table 1 for a GRADE decision rules table.
Equity, diversity and inclusion statement
Our research team included diversity across genders with representation from researchers at all career stages. We stratified our results by sex which allowed use to identify the potential need for more diversity in this area of the literature. This stratification allowed us to discuss the overall generalisability of our results. The GRADE evaluation carried out in this study assessed the indirectness of the results. We downgraded evidence that did not demonstrate good global representation or did not provide a gender-balanced sample. Reducing indirectness is important for ensuring the results are representative of the target population.
We identified 9062 records after removing duplicates, assessed 199 full-text papers, and excluded 165 papers during full-text screening, and 8 papers because of high or very high overlap based on the CCA calculation (see figure 1 and online supplemental appendix 2 for full texts with reasons for exclusion). The proportion of agreement between reviewers for title and abstract screening ranged from 95% to 100% while the agreement for full-text screening ranged from 75% to 100%. We included 26 systematic reviews with meta-analyses representing over 20.9 million observations from 199 unique cohort studies, including 21 mortality or incident chronic disease outcomes. We identified CCA values in the high or very high range for sudden cardiac mortality (CCA=33%; n=2), incident heart failure (33%; n=2), incident depression (50%; n=2), incident type 2 diabetes (25%; n=4) and all-cause mortality among those living with heart failure (14%; n=3; see online supplemental appendix 2 for more details). We included multiple systematic reviews for all-cause mortality because the CCA was moderate (10%; n=3).
- Download figure
- Open in new tab
- Download powerpoint
PRISMA flow chart depicting the number of papers identified, screened and included in the overview. *A list of excluded studies with reasons are provided in online supplemental appendix 2 .
Tables 1–3 describe the study characteristics. We identified 8 systematic reviews that investigated mortality outcomes, with pooled data from 95 unique primary cohort studies. Nine systematic reviews investigated incident outcomes, pooling data from 63 unique primary cohort studies. The remaining 9 systematic reviews investigated health-related outcomes among populations living with chronic conditions, which represented data from 51 unique primary cohort studies. 11 reviews were of critically low quality, 4 were low, 8 were moderate and 3 were of high quality as assessed using the AMSTAR2 (see online supplemental table 2 ). See online supplemental table 3 for a detailed summary of findings with the certainty of the evidence for each outcome.
- View inline
Study characteristics for general populations without known disease at baseline and mortality outcomes
Study characteristics for general populations without known disease at baseline and incident outcomes
Study characteristics for clinical populations with diagnosed chronic disease at baseline and mortality outcomes
Figure 2 illustrates results for CRF as a predictor of mortality outcomes, which included all-cause, CVD, sudden cardiac, all cancer and lung cancer mortality. When comparing high versus low CRF across all outcomes, there was a 41% (HR for all-cause mortality 24 =0.59; 95% CI 0.52 to 0.66) to 53% (HR for all-cause mortality 35 =0.47; 95% CI 0.39 to 0.56) reduction in the risk of premature mortality. The certainty of the evidence was assessed as very low-to-moderate, mainly due to serious indirectness (ie, most studies only included male participants). In assessing the dose–response relationship, a 1-MET higher level of CRF was associated with a 7% (HR for all cancer mortality 35 =0.93; 95% CI 0.91 to 0.96) to 51% (HR for sudden cardiac mortality 36 =0.49; 95% CI 0.33 to 0.73) reduction in the risk of premature mortality. The certainty of the evidence ranged from very low-to-moderate, largely due to serious indirectness from a large proportion of male-only studies. Sex differences were similar between outcomes with larger CIs for females because of smaller samples (see online supplemental figure 1 ). For example, there were 1 858 274 male participants compared with 180 202 female participants for all-cause mortality.
HRs for each mortality outcome in apparently healthy populations at baseline for high versus low CRF and per 1-MET increase in CRF. Estimates from Laukkanen (2022), Han (2022), Kodama (2009) and Aune (2020) were reported as RR, the remaining studies were reported as HR. Qui (2021) reported estimates from self-reported CRF. Kodama (2009) reported low versus high CRF which were inverted for this study. CRF, cardiorespiratory fitness; CVD, cardiovascular disease; eCRF, estimated non-exercise cardiorespiratory fitness; GRADE, Grading of Recommendations, Assessment, Development and Evaluations; MET, metabolic equivalent of task; NA, not applicable; NR, not reported; RR, relative risk.
Figure 3 describes results for CRF as a predictor of newly diagnosed chronic conditions, including: hypertension, heart failure, stroke, atrial fibrillation, dementia, chronic kidney disease, depression and type 2 diabetes. Online supplemental figure 2 describes results for all cancer (male only), lung cancer (male only), colon/rectum cancer (male only) and prostate cancer. When comparing high versus low CRF, there was a 37% (HR for incident hypertension 37 =0.63; 95% CI 0.56 to 0.70) to 69% (HR for incident heart failure 38 =0.31; 95% CI 0.19 to 0.49) reduction in the risk of incident conditions. The certainty of this evidence was rated as very low-to-low largely due to inconsistency and indirectness (ie, high heterogeneity that could not be described by subgroup analysis and largely male populations). The dose–response relationship per 1-MET higher level of CRF was associated with a 3% (HR for incident stroke 39 =0.97; 95% CI 0.96 to 0.98) to 18% (HR for incident heart failure 38 =0.82; 95% CI 0.79 to 0.84) reduction in the risk of incident conditions. The certainty of the evidence ranged from very low-to-low due to inconsistency and indirectness. Only two studies reported results for females separately. High versus low CRF was more protective for incident stroke and type 2 diabetes among females compared with males ( online supplemental figure 2 ). Among men, there was a null association between high versus low CRF for prostate cancer (HR=1.15; 95% CI 1.00 to 1.30). 40
HRs for each incident outcome in apparently healthy populations at baseline for high versus low CRF and per 1-MET increase in CRF. Note: Estimates from Cheng (2022), Aune (2021), Wang (2020), Xue (2020), Tarp (2019) and Kunutsor (2023) were reported as RR, the remaining studies were reported as HR. Kandola (2019) reported estimates for low versus high which were inverted for this study. The estimates from Tarp (2019) are fully adjusted for adiposity. Aune (2021) was reported per 5-MET increase which we converted to 1-MET increase for this study. CRF, cardiorespiratory fitness; CVD, cardiovascular disease; GRADE, Grading of Recommendations, Assessment, Development and Evaluations; MET, metabolic equivalent of task; NA, not applicable; NR, not reported; RR, relative risk.
Figure 4 highlights results comparing high versus low CRF among individuals living with chronic conditions. There was a 19% (HR for adverse events among those living with pulmonary hypertension 41 =0.81; 95% CI 0.78 to 0.85) to 73% (HR for cardiovascular mortality among those living with CVD 42 =0.27; 95% CI 0.16 to 0.48) reduction in the risk of all-cause and type-specific mortality. Comparing delayed versus not delayed heart rate recovery was associated with an 83% reduced risk of adverse events among those living with coronary artery disease. The certainty of the evidence for mortality in those living with a chronic condition was rated as very low-to-low largely due to risk of bias, indirectness and imprecision (ie, low-quality studies, mainly male participants and small sample sizes). No evidence examining sex differences were available. See online supplemental table 3 for a detailed summary of findings.
HRs for health outcomes in patients living with chronic conditions at baseline for high versus low CRF and delayed versus not delayed HRR. Estimates from Morris (2014) were reported as RR, the remaining estimates were reported as HR. Yang (2023), Fuentes-Abolafio (2020), Morris (2014), Rocha (2022) and Lachman (2018) reported estimates as low versus high which were inverted for this study. Cantone (2023) was reported per 1-unit VO 2 increase which we converted to 1-MET increase for this study. Adverse events for Lachman (2018) were all-cause mortality, cardiovascular mortality and hospitalisations for congestive heart failure. CRF, cardiorespiratory fitness; CVD, cardiovascular disease; GRADE, Grading of Recommendations, Assessment, Development and Evaluations; HRR, heart rate recovery; MET, metabolic equivalent of task; NA, not applicable; NR, not reported; RR, relative risk.
This overview of systematic reviews demonstrated that CRF is a strong and consistent predictor of risk across many mortality outcomes in the adult general population. Among populations living with chronic conditions such as cancer, heart failure and CVD, this study showed better prognosis for those with higher CRF. We also demonstrated that low CRF is an important risk factor for developing future chronic conditions such as hypertension, heart failure, stoke, atrial fibrillation, dementia and depression. Given that we summarised evidence from cohort studies, and randomised controlled trials cannot be used in our investigation, the results of this study may signal a causal relationship between CRF and future health outcomes. We also found a significant dose–response effect showing protection for every 1-MET higher level of CRF. This evidence further supports 1-MET as an MCID for CRF and could be considered as a target for interventions. The strength and consistency of the evidence across a wide range of outcomes supports the importance of CRF for clinical assessment and public health surveillance.
Several studies have identified the need for the routine measurement of CRF in clinical and public health practice. 11 43 For instance, a scientific statement from the American Heart Association concluded that healthcare providers should assess CRF during annual routine clinical visits using submaximal tests (eg, treadmill, cycling or bench stepping tests) or self-report estimates and that patients living with chronic conditions should have CRF measured regularly using a symptom-limited direct measure. 11 There are several benefits to regular measurement of CRF in clinical practice. First, CRF is an important risk factor that provides additional information beyond traditional risk factors such as blood pressure, total cholesterol and smoking status. 44 Second, given the strong link with habitual physical activity, CRF could be a valuable tool to help guide exercise prescription. In those with low CRF (defined based on age, sex and health status), large relative improvements can be attained through additional moderate physical activity (ie, brisk walking at a heart rate of 50% of peakO 2 ). 45 The largest health benefits have been observed when individuals move from being unfit to fit. 46 Lastly, CRF measured using field-based tests are easy to implement with a variety of tests that could be adapted to suit space and time limitations.
Areas of future work
Applying the GRADE approach to evaluate the certainty of the evidence helped identify several important gaps in the literature. Nearly all the outcomes identified in this study were downgraded due to the evidence being generated largely from samples comprising males. Although an increase in female samples would help improve the certainty of the evidence, it likely would not impact the magnitude of the observed effects because the benefits of CRF were similar for males and females in our study (see online supplemental figures 1,2 ) and other large cohort studies. 47 There is also a need for higher-quality studies with larger samples sizes in clinical populations, as many of the outcomes were downgraded due to primary studies with high risk of bias, low sample sizes (<4000 participants), and inconsistencies in the measurement of CRF across studies. Improving the evidence for CRF in clinical populations remains an important research gap. For instance, outcomes in clinical populations with a serious or very serious risk of bias were often rated this way due to a lack of adequate control for confounding, including a lack of adjustment for age, sex, and body mass.
In addition to the need for higher-quality studies with greater samples in more diverse populations including females, we did not identify any systematic reviews that explored the association between CRF and breast cancer 48 or mental health outcomes beyond incident depression and dementia, as an example. These outcomes present important areas for future work. Finally, future studies would benefit from repeated longitudinal measures of CRF to further establish causality.
Implications for clinical practice
This study further demonstrates the importance of including CRF measurement in regular clinical practice. For every 1-MET (3.5 mL/kg/min) higher level of CRF, we identified substantial reductions in the risk of all-cause, CVD and cancer mortality. We also identified significant reductions in the risk of incident hypertension, heart failure, stroke, atrial fibrillation and type 2 diabetes per higher MET. For most, a 1-MET higher level of CRF is attainable through a regular aerobic exercise programme. For example, in a large population-based observational study of over 90 000 participants, nearly 30% were able to increase their CRF by 1-MET (median follow-up was 6.3 years) without intervention. 49 However, for some, improvements as small as 0.5-METs may substantially benefit health. 50 51
Given the strength of the predictive utility of CRF across many health outcomes, CRF would be a valuable risk stratification tool in clinical practice. Furthermore, the predictive strength of CRF is maintained regardless of age, sex and race. 47 Through regular CRF measurement, clinicians could better identify patients at greater risk of premature mortality, initiating the need for targeted exercise prescription. Improvements in CRF through regular physical activity results in a proportional reduction in mortality risk, regardless of the presence of other major risk factors such as higher body mass index, hypertension, type 2 diabetes, dyslipidaemia, or smoking. 49 There is an important need for clinical and public health guidelines around the assessment, interpretation of results and MCID of CRF across age, sex and clinical populations.
Strengths and limitations
Our paper has several strengths, including a focus on pooled meta-analyses from cohort studies, assessment of the certainty of the evidence using a modified GRADE, and an evaluation of the systematic review quality using AMSTAR2. Our study identifies gaps where new evidence is needed across a broad range of health outcomes. However, this study is not without limitations. As in any overview, the quality of the data is restricted to the included papers. In our case, heterogeneity was high for many of the included meta-analyses and was often not explained by subgroup analyses. We also identified low-to-very low certainty of the evidence for most outcomes, suggesting the need for higher-quality studies in this research area including adequate adjustment for confounding and greater representation of females. The evidence was also limited to studies examining associations between a single measure of CRF and prospective health outcomes.
Our findings showed that high CRF is strongly associated with lower risk of premature mortality, incident chronic conditions (ie, hypertension, heart failure, stroke, atrial fibrillation, dementia and depression), and poor prognosis in those with existing chronic conditions. The consistency of the evidence across a variety of health outcomes demonstrates the importance of CRF and the need to incorporate this measure in routine clinical and public health practice. Future studies should focus on outcomes with limited evidence and where the certainty of the evidence was rated as very low by improving study quality.
Ethics statements
Patient consent for publication.
Not applicable.
Acknowledgments
We would like to acknowledge the support of Valentine Ly, MLIS, Research Librarian at the University of Ottawa for her help with translating and conducting the search strategy in CINAHL and SPORTDiscus. We would also like to acknowledge the Health Library at Health Canada and the Public Health Agency of Canada for their support in constructing and carrying out the search strategy for MEDLINE, Embase and Scopus. The PRESS peer-review of the search strategy was carried out by Shannon Hayes, MLIS, research librarian, from the Health Library at Health Canada and the Public Health Agency of Canada. We would also like to thank Joses Robinson and Iryna Demchenko for their help with the paper.
- Caspersen CJ ,
- Powell KE ,
- Christenson GM
- Balady GJ ,
- Sietsema K , et al
- Pollock ML ,
- Schmidt D , et al
- Kaminsky LA ,
- Vatten LJ ,
- Nauman J , et al
- Sun Z , et al
- Bouchard C ,
- Rice T , et al
- Stofan JR ,
- DiPietro L ,
- Davis D , et al
- Garber CE ,
- Blissmer B ,
- Deschenes MR , et al
- Sandercock G ,
- Hurtado V ,
- Arena R , et al
- DeRouen TA ,
- Cumming GR ,
- Borysyk L , et al
- Paffenbarger RS , et al
- Robsahm TE ,
- Heir T , et al
- Sieverdes JC ,
- Lee D , et al
- Lee DC , et al
- Hooker SP ,
- Colabianchi N , et al
- Åberg MAI ,
- Nyberg J , et al
- Groarke JD ,
- Claggett B , et al
- Leeper NJ ,
- Zhou M , et al
- Ferreira JP ,
- Anker SD , et al
- Roshanravan B ,
- Robinson-Cohen C ,
- Patel KV , et al
- Tanaka S , et al
- Pollock M ,
- Fernandes RM ,
- Becker LA , et al
- Poitras VJ ,
- Janssen I , et al
- Pieper D , et al
- Brooke BS ,
- Schwartz TA ,
- McGowan J ,
- Sampson M ,
- Salzwedel DM , et al
- O’Connell D , et al
- Reeves BC ,
- Wells G , et al
- Antoine S-L ,
- Mathes T , et al
- Guyatt GH ,
- Vist GE , et al
- Spencer FA ,
- Falavigna M , et al
- Shi X , et al
- Schlesinger S ,
- Hamer M , et al
- Chen S , et al
- Leitzmann MF , et al
- Cheng Y , et al
- Pozuelo-Carrascosa DP ,
- Alvarez-Bueno C ,
- Cavero-Redondo I , et al
- Barbagelata L ,
- Bluro I , et al
- Ezzatvar Y ,
- Izquierdo M ,
- Núñez J , et al
- Kokkinos P ,
- Gander JC ,
- Hébert JR , et al
- Church TS ,
- Earnest CP ,
- Skinner JS , et al
- Barlow CE , et al
- Faselis C ,
- Samuel IBH , et al
- Katsaroli I ,
- Sidossis L ,
- Katsagoni C , et al
- Bonafiglia JT ,
- Preobrazenski N ,
- Islam H , et al
- Poirier P ,
- Norris CM , et al
- Beets MW , et al
- Caputo JL ,
- Laukkanen JA ,
- Isiozor NM ,
- Kunutsor SK
- Kandola A ,
- Ashdown-Franks G ,
- Stubbs B , et al
- Kunutsor SK ,
- Myers J , et al
- Blond K , et al
- Wu C , et al
- Cantone A ,
- Serenelli M ,
- Sanguettoli F , et al
- Ramírez-Vélez R ,
- Sáez de Asteasu ML , et al
- Fuentes-Abolafio IJ ,
- Pérez-Belmonte LM , et al
- Lachman S ,
- Terbraak MS ,
- Limpens J , et al
- Morris DR ,
- Rodriguez AJ ,
- Moxon JV , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
JJL and SAP are joint first authors.
X @JustinJLang, @SPrinceWare, @bensinghphd
Contributors JJL, GRT and SAP conceptualised and planned the study design. JJL and SAP led the study. JJL accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish. All coauthors contributed to article screening. JJL and SAP wrote the first draft of the article. All coauthors reviewed, revised and approved the final manuscript.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors. Dr. Ortega is supported by the Grant PID2020-120249RB-I00 funded by MCIN/AEI/10.13039/501100011033 and by the Andalusian Government (Junta de Andalucía, Plan Andaluz de Investigación, ref. P20_00124). Dr. Cadenas-Sanchez is supported by a grant from the European Union’s Horizon 2020 research and innovation programme under the Marie Sklodowska Curie grant agreement No 101028929. Dr. Fraser is supported by a National Heart Foundation of Australia Postdoctoral Fellowship (106588).
Disclaimer The content and views expressed in this articles are those of the authors and do not necessarily reflect those of the Government of Canada.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Integrating Specialist and Primary Care in Chronic Disease Management
- 1 Department of Epidemiology and Biostatistics, Schulich School of Medicine and Dentistry, Western University, London, Ontario, Canada
- 2 Department of Family Medicine, Schulich School of Medicine and Dentistry, Western University, London, Ontario, Canada
- 3 Department of Medicine, Schulich School of Medicine and Dentistry, Western University, London, Ontario, Canada
- 4 Lawson Health Research Institute, London Health Sciences Centre, London, Ontario, Canada
- 5 ICES, London, Ontario, Canada
- 6 Centre for Studies in Family Medicine, Schulich School of Medicine and Dentistry, Western University, London, Ontario, Canada
- Original Investigation Electronic Health Record Population Health Management for Chronic Kidney Disease Care Manisha Jhamb, MD, MPH; Melanie R. Weltman, PharmD; Susan M. Devaraj, PhD, MS, RD; Linda-Marie Ustaris Lavenburg, DO, MS; Zhuoheng Han, MS; Alaa A. Alghwiri, PhD; Gary S. Fischer, MD; Bruce L. Rollman, MD, MPH; Thomas D. Nolin, PharmD, PhD; Jonathan G. Yabes, PhD JAMA Internal Medicine
Alongside efforts to develop new strategies for the early diagnosis and delayed progression of chronic kidney disease (CKD), it remains critical to implement existing interventions effectively. Since the patients who might benefit are asymptomatic and undiagnosed, the tasks of early diagnosis and intervention naturally belong to the primary care practitioners (PCPs) who are in regular contact with these as-yet undiagnosed patients. 1 , 2 Despite PCPs’ familiarity with preventive measures, such as smoking cessation, blood pressure control, and diabetes control, both time constraints and the need to stay up to date with current CKD guidelines and manage competing clinical priorities often pose challenges in achieving optimal CKD outcomes. 3 This requires collaboration between specialists and PCPs, which has worked at small scale 4 but, to our knowledge, not been tried systemwide. 5
Read More About
Yazdani Y , Garg AX , Zwarenstein M. Integrating Specialist and Primary Care in Chronic Disease Management. JAMA Intern Med. Published online April 15, 2024. doi:10.1001/jamainternmed.2024.0873
Manage citations:
© 2024
Artificial Intelligence Resource Center
Best of JAMA Network 2022
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- Risk of cardiovascular disease with high-dose versus low-dose use of non-steroidal anti-inflammatory drugs in ankylosing spondylitis
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-0498-5762 Ji-Won Kim 1 ,
- Jun Sik Yoon 2 ,
- Sojeong Park 3 ,
- Hasung Kim 3 ,
- Ji Sung Lee 4 ,
- http://orcid.org/0000-0003-0957-0395 Jung-Yoon Choe 1
- 1 Division of Rheumatology, Department of Internal Medicine , Daegu Catholic University School of Medicine , Daegu , Korea (the Republic of)
- 2 Department of Internal Medicine , Busan Paik Hospital, Inje University College of Medicine , Busan , Korea (the Republic of)
- 3 Data Science Team , Hanmi Pharm Co Ltd , Seoul , Korea (the Republic of)
- 4 Department of Clinical Epidemiology and Biostatistics, Asan Medical Center , University of Ulsan College of Medicine , Seoul , Korea (the Republic of)
- Correspondence to Dr Ji-Won Kim, Division of Rheumatology, Department of Internal Medicine, Daegu Catholic University School of Medicine, Daegu, 42472, Korea (the Republic of); kimjw689{at}cu.ac.kr
Objective To investigate the risk of cardiovascular disease (CVD) associated with increasing dose of a non-steroidal anti-inflammatory drug (NSAID) in patients with ankylosing spondylitis (AS).
Methods Using the Korean National Health Insurance database, patients newly diagnosed with AS without prior CVD between 2010 and 2018 were included in this nationwide cohort study. The primary outcome was CVD, a composite outcome of ischaemic heart disease, stroke or congestive heart failure. Exposure to NSAIDs was evaluated using a time-varying approach. The dose of NSAIDs was considered in each exposure period. Cox proportional hazard regression was used to investigate the risk of CVD associated with NSAID use.
Results Of the 19 775 patients (mean age, 36 years; 75% were male), 19 706 received NSAID treatment. During follow-up period of 98 290 person-years, 1663 cases of CVD occurred including 1157 cases of ischaemic heart disease, 301 cases of stroke and 613 cases of congestive heart failure. Increasing dose of NSAIDs was associated with incident CVD after adjusting for confounders (adjusted HR (aHR) 1.10; 95% CI 1.08 to 1.13). Specifically, increasing dose of NSAIDs was associated with incident ischaemic heart disease (aHR 1.08; 95% CI 1.05 to 1.11), stroke (aHR 1.09; 95% CI 1.04 to 1.15) and congestive heart failure (aHR 1.12; 95% CI 1.08 to 1.16). The association between NSAID dose and higher CVD risk was consistent in different subgroups.
Conclusion In a real-world AS cohort, higher dose of NSAID treatment was associated with a higher risk of CVD, including ischaemic heart disease, stroke and congestive heart failure.
- Cardiovascular Diseases
- Spondylitis, Ankylosing
- Anti-Inflammatory Agents, Non-Steroidal
Data availability statement
Data are not available to the public because they are only accessible in an analysis centre with permission from the Korea National Health Insurance Sharing Service.
https://doi.org/10.1136/ard-2023-225406
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Non-steroidal anti-inflammatory drugs (NSAIDs) are the first-line treatment for ankylosing spondylitis (AS), but these drugs can increase the risk of vascular events and congestive heart failure in the general population.
Patients with AS are treated with NSAIDs continuously or on-demand according to their disease activity and comorbidities.
However, it is uncertain whether to treat patients with AS continuously or intermittently with NSAIDs from a cardiovascular disease (CVD) point of view.
WHAT THIS STUDY ADDS
Higher dose of NSAID treatment was associated with a higher risk of CVD, including ischaemic heart disease, stroke and congestive heart failure, in patients with AS compared with lower dose treatment.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This result may recommend the appropriate NSAID treatment strategies in patients with AS from a CVD point of view.
Introduction
Ankylosing spondylitis (AS) is a chronic inflammatory disease characterised by inflammation and radiographic damage of the axial skeleton. Because non-steroidal anti-inflammatory drugs (NSAIDs) can suppress inflammation and relieve pain, they are used as the first-line treatment for AS. Continuous treatment with NSAIDs is preferred over on-demand treatment in patients with active AS with an elevated disease activity. 1 In patients with high inflammatory burden, continuous NSAID treatment delayed radiographic progression compared with NSAIDs on-demand. 2 However, NSAID treatment involves some concerns regarding gastrointestinal and renal toxicities and cardiovascular disease (CVD). Whether to use NSAIDs continuously or on-demand is determined considering the risk and benefit ratio including patients’ disease activity and comorbid conditions.
Cardiovascular risk management is important in patients with AS because of the increased risk of CVD compared with the general population. 3 Although NSAID treatment is also related to increased cardiovascular risk, it seems to be less harmful in AS than in the general population. We recently examined the risk of CVD associated with long-term use of NSAIDs in both AS and non-AS cohorts and found a lower risk of CVD associated with long-term NSAID use in patients with AS than in non-AS individuals. 4 However, it is uncertain whether to treat patients with AS continuously or on-demand with NSAIDs from a CVD point of view. 5 Therefore, we examined the risk of CVD according to increasing dose of NSAIDs using a real-world AS cohort.
Study design and data source
This nationwide population-based cohort study was based on the Korean National Health Insurance database. South Korea has a universal healthcare system that provides medical insurance to the entire population by national health insurance and medical aid programmes. The Korean National Health Insurance database includes all medical claims covered by these programmes. The database contains demographic data; date of death; healthcare utilisation data such as diagnostic codes, details of prescription, medical procedures, treatments and costs; and medical check-up data including health behaviour data. The data between January 2002 and December 2019 were available at the time of analysis. Because all data were anonymised in the database, informed consent was waived.
Study participants
Patients with newly diagnosed AS between 1 January 2010 and 31 December 2018 were included in this study. AS was identified according to the International Classification of Diseases 10th revision (ICD-10) code-based definition: ≥2 claims of primary diagnostic code of AS (M45) without primary diagnostic code of rheumatoid arthritis (RA; M05) or systemic lupus erythematosus (M32). 6 To increase the validity of the ICD code-based diagnosis, the diagnosis was confirmed by registration in the rare intractable disease (RID) programme. The RID programme supports people with RIDs who should meet predefined criteria (eg, modified New York criteria for AS) to be included in the programme. The case definition for AS was validated by meticulous chart review performed by an expert rheumatologist, and the positive predictive value was 91.7% ( online supplemental table 1 ). Patients who had medical claims for AS between January 2002 and December 2009 were excluded to identify incident cases of AS. The date of AS diagnosis was determined as the index date. Patients were excluded if they were aged <18 years at the index visit, had a history of CVD between January 2002 and the index visit, developed CVD within 6 months from the index visit or had a follow-up duration <6 months. Finally, patients aged ≥18 years with newly diagnosed AS without prior or recent CVD with ≥6 months of follow-up were eligible to participate in the study.
Supplemental material
Outcome variable.
The primary outcome was the composite outcome of ischaemic heart disease, stroke or congestive heart failure. The secondary outcomes were specific cardiovascular outcomes such as ischaemic heart disease, stroke and congestive heart failure. The case definitions were ≥1 hospitalisation or outpatient clinic visit with ICD-10 codes of I20-I24 (for ischaemic heart disease); I60, I61, I63 or I64 (for stroke); and I50, I110, I130 or I132 (for congestive heart failure). 7–11
Exposure variable
All NSAIDs prescribed during the study period (including non-selective NSAIDs and selective COX-2 inhibitors) were examined. The list of prescribed NSAIDs is presented in online supplemental table 2 . The type and dose of NSAIDs and the days prescribed NSAIDs during the period of interest were collected from the Korean National Health Insurance database. Exposure to NSAIDs was evaluated using a time-varying approach by defining periods of NSAID use as ‘NSAID-exposed’ and periods longer than 1 month without NSAID use as ‘NSAID-unexposed.’ To consider the dose in the association between NSAID use and CVD, the defined daily dose (DDD) was determined for each NSAID exposure. The DDD is the assumed average maintenance dose per day for a drug used for its main indication in adults, as suggested by the WHO Collaborating Centre for Drug Statistics Methodology. 12 For example, the daily dose of aceclofenac 200 mg or meloxicam 15 mg is 1 DDD.
Other variables
Baseline data on age, sex (male or female), socioeconomic status (lower, middle or higher tertile), body mass index (BMI; <18.5, ≥18.5 to <25 or ≥25 kg/m 2 ), smoking status (never, former or current), hypertension (yes or no), diabetes (yes or no), hyperlipidaemia (yes or no), and prescription of tumour necrosis factor (TNF) inhibitors during follow-up was collected. At least 6 months of a prescription of any TNF inhibitors during the follow-up period was considered as use of TNF inhibitors. Definitions of hypertension, diabetes and hyperlipidaemia were based on combination of ICD-10 codes and medications as follows: at least one claim of ICD-10 codes I10–I15 with antihypertensive medications; at least one claim of ICD-10 codes E10–E14 with antidiabetic medications; and at least one claim of ICD-10 code E78 with statin use, respectively. 9
Statistical analysis
Descriptive statistics are presented as mean (SD) for continuous variables and number (percentage) for categorical variables. The study participants were followed up until outcomes, death, emigration or 31 December 2019. Those who died or emigrated before occurrence of outcomes were censored.
The study exposure was NSAID use, considered as a time-varying variable. We calculated HRs with 95% CIs for cardiovascular outcomes using Cox proportional hazards regression model with time-dependent covariates. Potential confounders of age, sex, socioeconomic status, BMI, smoking status, hypertension, diabetes, hyperlipidaemia and time-varying TNF inhibitor use were considered in a multivariable analysis. We conducted subgroup analyses of the cardiovascular outcomes based on age (<45 or ≥45 years), sex, hypertension, diabetes and hyperlipidaemia.
Additionally, among the NSAID-exposed periods, NSAID exposure ≥0.5 DDD was defined as a high-dose use of NSAIDs. The cumulative incidence of cardiovascular outcomes associated with high-dose use of NSAIDs was analysed by Kaplan-Meier method.
P values <0.05 were considered statistically significant. All statistical analyses were conducted using SAS V.9.4 (SAS, Cary, North Carolina, USA) and R V.4.0.3 (R Foundation for Statistical Computing, Vienna, Austria).
Patient and public involvement
Patients and the public were not involved in the design, conduct, reporting or dissemination plans of our research.
Patient characteristics
After excluding 5310 patients according to the predefined exclusion criteria, a total of 19 775 patients were eligible for this study ( figure 1 ). Baseline characteristics of study participants are presented in table 1 . Mean (SD) age was 36.1 (12.8) years and 14 836 (75%) patients were male. Of the 19 775 patients, 13.7%, 7.8% and 8.1% had underlying hypertension, diabetes and hyperlipidaemia at baseline, respectively. During the follow-up period, 99.7% received NSAID treatment and 30.2% received TNF inhibitor treatment.
- Download figure
- Open in new tab
- Download powerpoint
Selection of eligible study participants.
- View inline
Baseline characteristics of patients with AS
CVD associated with NSAID use
During the follow-up period of 98 290 person-years (median follow-up duration, 4.7 (IQR 2.7–7.0) years), 1663 cases of CVD (including 1157 cases of ischaemic heart disease, 301 cases of stroke and 613 cases of congestive heart failure) developed. The incidence rate of CVD was 16.9 per 1000 person-years. The cumulative incidence of CVD according to high-dose NSAID use was shown in figure 2 . Increasing dose of NSAIDs was associated with an increased risk of incident CVD after adjustments for age, sex, socioeconomic status, BMI, smoking status, hypertension, diabetes, hyperlipidaemia and TNF inhibitor use (adjusted HR (aHR) 1.10, 95% CI 1.08 to 1.13; table 2 ). Specifically, increasing dose of NSAIDs was associated with the risk of ischaemic heart disease (aHR 1.08, 95% CI 1.05 to 1.11), stroke (aHR 1.09, 95% CI 1.04 to 1.15) and congestive heart failure (aHR 1.12, 95% CI 1.08 to 1.16).
Cumulative incidence of (A) cardiovascular disease, (B) ischaemic heart disease, (C) stroke and (D) congestive heart failure associated with high-dose use of NSAIDs in patients with AS. High-dose and low-dose use were defined as NSAID exposure ≥0.5 DDD and <0.5 DDD among the NSAID-exposed periods, respectively. AS, ankylosing spondylitis; DDD, defined daily dose; NSAIDs, non-steroidal anti-inflammatory drugs.
Risk of cardiovascular outcomes associated with NSAID use
Stratified analyses were performed in different subgroups of age, sex, hypertension, diabetes and hyperlipidaemia ( table 3 ). Higher NSAID dose consistently increased the risk of incident CVD, as well as specific outcomes of ischaemic heart disease, stroke and congestive heart failure, in the different subgroups. The risk of CVD associated with NSAID use was higher in women than in men, which might be explained by a higher risk of stroke associated with NSAID use in women.
Risk of cardiovascular outcomes associated with NSAID use in subgroups of age, sex, hypertension, diabetes and hyperlipidaemia
Other factors associated with incident CVD
In addition to NSAID use, age (aHR 1.044, 95% CI 1.040 to 1.048), socioeconomic status (aHR 0.71, 95% CI 0.63 to 0.80), BMI ≥25 kg/m 2 (obesity; aHR 1.19, 95% CI 1.07 to 1.33), current smoking (aHR 1.28, 95% CI 1.11 to 1.48), hypertension (aHR 1.52, 95% CI 1.34 to 1.72) and hyperlipidaemia (aHR 1.27, 95% CI 1.10 to 1.46) were independent risk factors associated with CVD development in patients with AS ( online supplemental table 3 ). TNF inhibitor use tended to exert lower risk of CVD without statistical significance (aHR 0.92, 95% CI 0.81 to 1.05).
This nationwide population-based cohort study longitudinally followed up patients with AS to demonstrate the impact of NSAID use pattern on the occurrence of CVD. Higher dose treatment with NSAIDs increased the risk of CVD, including ischaemic heart disease, stroke and congestive heart failure, in patients with AS. The elevated cardiovascular risk associated with increasing NSAID dose was consistent across subgroups of age, sex, hypertension, diabetes and hyperlipidaemia.
NSAIDs can increase the risk of major vascular events (including myocardial infarction (MI) and stroke) and heart failure. 13 14 The underlying mechanism for increased vascular events by NSAIDs is imbalance between prothrombotic vasoconstrictive thromboxane A2 (induced by COX-1) and antithrombotic vasodilatory prostacyclin (induced by COX-2). 15 Although there might be some difference in cardiovascular risk between specific NSAIDs due to relative COX-2 inhibition compared with COX-1 inhibition, both traditional NSAIDs and selective COX-2 inhibitors can increase the risk. 16 Also, NSAIDs can cause sodium and water retention in addition to vasoconstriction, leading to blood pressure elevation and increased risk of heart failure.
While an increased risk of CVD related to NSAIDs has been found in the general population, the results from previous studies in the AS population are conflicting. 17–20 A case-control study in Taiwan reported that long-term (≥12 months) NSAID use did not increase the risk of CVD in patients with AS. 17 Another case-control study in Taiwan showed that celecoxib was negatively associated with coronary artery disease in patients with AS. 18 A French nationwide study found a lower risk of major cardiovascular events (such as MI and stroke) associated with NSAIDs in patients with AS, suggesting a cardiovascular protective effect of NSAIDs in such a population. 19 In contrast, a nested case-control study using the UK national health data showed that current NSAID use increased the risk of MI in patients with spondyloarthritis relative to remote NSAID use. 20 However, aforementioned studies did not consider the dose of NSAIDs in the association between NSAID use and cardiovascular risk. Because most patients with AS receive NSAID treatment, and the dose of NSAIDs can change according to disease activity and comorbid conditions, assessing cardiovascular risk according to the dose of NSAIDs is an important issue. By applying time-varying exposure of NSAIDs in the analysis, we demonstrated that higher dose NSAID treatment increases the risk of CVD in AS compared with lower dose treatment. Our results could be supported by a finding that continuous (high-dose) NSAID use was associated with incident hypertension in AS. 21
Patients with AS carry a higher risk of atherosclerotic CVD and congestive heart failure. 3 Consistently, our cohort also showed a higher risk of ischaemic heart disease, stroke and congestive heart failure in patients with AS compared with non-AS controls. 4 Chronic inflammation might explain the higher cardiovascular risk of an AS population compared with the general population. Inflammatory rheumatic disease and atherosclerotic CVD share inflammatory pathways, and controlling inflammation may attenuate the risk of atherosclerotic CVD in patients with AS. 22 Therefore, cardiovascular risk associated with NSAID use might be lower in patients with AS than in the general population. Our previous study showed that the risk of CVD associated with long-term NSAID use was lower in patients with AS than in non-AS controls. 4 This pattern was also found in patients with RA. The cardiovascular risk associated with NSAIDs was lower in patients with RA than in controls without RA based on the Danish national cohort study. 7 Taken together, these results suggest that increasing the dose of NSAIDs is associated with a higher cardiovascular risk in AS, but that the increased risk might be lower than that in the general population.
There are some limitations of the study. First, this study was conducted in a retrospective manner. However, it is challenging to conduct a prospective study by applying different treatment strategies to patients to observe the occurrence of CVD, which, by its nature requires, long periods of time. This large, nationwide cohort longitudinally monitored the development of CVD for a relatively long follow-up period. Second, levels of acute phase reactants or AS disease activity could not be considered in the study because the data were not included in the National Health Insurance database. TNFi use, which was considered as a confounder in multivariable analysis, might partially reflect the AS disease activity status. Third, the diagnosis of cardiovascular outcomes defined by ICD codes may not be accurate. For example, the validity of heart failure outcome should be confirmed to clarify the diagnosis of heart failure. Positive predictive values for ICD-10 code-based heart failure diagnoses were 0.75‒0.96 in the European Electronic Health Records. 23 Unfortunately, the cardiovascular outcome definitions by ICD code-based algorithms are not fully validated in the Korean National Insurance database. We adapted operational definitions commonly used in cardiovascular research using the Korean National Health Insurance database. 9–11 To overcome potential outcome misclassification, we performed another analysis by applying a stringent ICD-10 code-based diagnostic algorithm of heart failure. Elevated cardiovascular risk according to increasing NSAID dose was also found in the analysis (data not shown), which was in line with our main results. In addition, the aetiology and subtype of heart failure could not be determined in this study due to characteristics of administrative claims data. Fourth, there may be a gap between NSAID prescription and actual intake when using a medical claims database. However, we assumed that the gap between total prescription and actual intake of NSAIDs would be minimal in patients with AS from the Korean National Health Insurance database. Given that patients with AS take NSAIDs continuously or on-demand according to their disease activity status, the dose and duration of NSAID prescription are adjusted by the amount of the remaining drugs and actual NSAID intake when the patients have remaining NSAIDs during follow-up visits.
In conclusion, this large longitudinal cohort study compared the CVD risk between high-dose and low-dose users of NSAIDs in patients with AS. Higher dose treatment with NSAIDs was associated with a higher risk of CVD, including ischaemic heart disease, stroke and congestive heart failure, relative to lower dose treatment. We should be aware of the difference in cardiovascular risk between NSAID doses and should consider dose reduction of NSAIDs whenever disease activity is controlled in patients with AS.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
The study protocol was approved by the Institutional Review Board of the Daegu Catholic University Medical Center (CR-20-227).
- Deodhar A ,
- Gensler LS , et al
- Landewé R ,
- Dougados M , et al
- Rao SR , et al
- Park S , et al
- Heslinga SC ,
- Rollefstad S , et al
- Lindhardsen J ,
- Gislason GH ,
- Jacobsen S , et al
- Atiquzzaman M ,
- Kopec J , et al
- Cho M-C , et al
- Park S-J , et al
- WHO Collaborating Centre for Drug Statistics Methodology
- Emberson J , et al. , Coxib and traditional NSAID Trialists’ (CNT) Collaboration
- Cannon CP , et al
- Baraliakos X ,
- Dendukuri N ,
- Rich B , et al
- Yen J-H , et al
- Leong P-Y ,
- Yeo K-J , et al
- Desmarets M ,
- Martin B , et al
- Dubreuil M ,
- Louie-Gao Q ,
- Peloquin CE , et al
- Reveille JD , et al
- Davidson J ,
- Banerjee A ,
- Muzambi R , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Handling editor Josef S Smolen
Contributors Conceptualisation: J-WK. Methodology: J-WK and JSY. Formal analysis: J-WK, JSY, SP, HK and JSL. Funding acquisition: J-WK. Investigation: J-WK. Data curation: J-WK. Supervision: J-WK, JSY, JSL and J-YC. Writing—original draft preparation: J-WK. Writing—review and editing: J-WK, JSY, JSL and J-YC. J-WK is the guarantor who accepts full responsibility for the work and/or the conduct of the study, had access to the data and controlled the decision to publish.
Funding This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (Ministry of Science and ICT) (No. 2022R1F1A1073837).
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Recently Viewed
Listening...
Johnson & Johnson to Acquire Shockwave Medical
Enhances johnson & johnson’s ability to transform the treatment landscape for cardiovascular disease and continue to improve patient outcomes extends johnson & johnson medtech’s position in highest-growth, innovation-oriented segments of cardiovascular intervention accelerates sales growth and accretive to operating margin for both johnson & johnson and johnson & johnson medtech conference call at 8:30 a.m. et to discuss details of the transaction.
- Copy link Link copied
NEW BRUNSWICK, N.J. and SANTA CLARA, Calif., April 5, 2024 – Johnson & Johnson (NYSE: JNJ) and Shockwave Medical, Inc. (Nasdaq: SWAV) (“Shockwave”) today announced that they have entered into a definitive agreement under which Johnson & Johnson will acquire all outstanding shares of Shockwave for $335.00 per share in cash, corresponding to an enterprise value of approximately $13.1 billion including cash acquired. The transaction was approved by both companies’ boards of directors.
The acquisition of Shockwave further extends Johnson & Johnson MedTech’s position in cardiovascular intervention and accelerates its shift into higher-growth markets. Cardiovascular intervention is one of the fastest-growing global medtech markets, with significant unmet patient need. With the addition of Shockwave, Johnson & Johnson will expand its MedTech cardiovascular portfolio into two of the highest-growth, innovation-oriented segments of cardiovascular intervention – coronary artery disease (CAD) and peripheral artery disease (PAD). The transaction follows Johnson & Johnson MedTech’s successful acquisitions of Abiomed, a leader in heart recovery, and more recently Laminar, an innovator in left atrial appendage elimination for patients with non-valvular atrial fibrillation (AFib). These acquisitions complement and build on Johnson & Johnson’s established global leadership position in electrophysiology through the Biosense Webster portfolio. Following the close of the transaction, Johnson & Johnson MedTech will be a category leader in four high-growth cardiovascular segments.
Shockwave is a leading, first-to-market provider of innovative intravascular lithotripsy (IVL) technology for the treatment of calcified CAD and PAD. IVL is a minimally invasive, catheter-based treatment for calcified arterial lesions, which can reduce blood flow and cause pain or heart attack. IVL helps restore blood flow by cracking calcium lesions using sonic pressure waves and is used in both CAD and PAD, often in combination with stenting. Shockwave offers the only commercially available IVL technology and has safely, simply, and effectively treated approximately 400,000 patients globally. In addition to its leading IVL platform, Shockwave also recently acquired Neovasc Inc., a company that has developed the Reducer System, a novel product focused on symptom relief of refractory angina. The Reducer System has a growing commercial presence. It is currently undergoing clinical studies in the U.S. and is CE marked in the European Union and the United Kingdom. Joaquin Duato, Chairman and Chief Executive Officer of Johnson & Johnson, said, “With our focus on Innovative Medicine and MedTech, Johnson & Johnson has a long history of tackling cardiovascular disease – the leading cause of death globally. The acquisition of Shockwave and its leading IVL technology provides a unique opportunity to accelerate our impact in cardiovascular intervention and drive greater value for patients, shareholders and health systems.”
Tim Schmid, Executive Vice President and Worldwide Chairman of Johnson & Johnson MedTech, said, “Shockwave offers a truly differentiated opportunity to further enhance our leadership position in medtech, expand into additional high-growth segments, and ultimately transform the future of cardiovascular treatment. Shockwave’s IVL technology for treating CAD and PAD, and its strong pipeline, are in a class of their own. We look forward to bringing Shockwave’s solutions into Johnson & Johnson MedTech and the hands of more physicians around the world.”
“Shockwave has transformed the treatment of complex calcified arterial disease through the pioneering development of intravascular lithotripsy, and it is our mission to make this remarkable technology available to patients worldwide,” said Doug Godshall, President and CEO of Shockwave. “As part of a larger, more diverse organization, with broad expertise and a core focus on improving patient outcomes, we are confident we will be able to further solidify IVL as the global standard of care for patients. I am deeply grateful to our team members and colleagues whose efforts have made today’s milestone possible; their accomplishments and passion have been extraordinary. I could not think of a better partner and home than Johnson & Johnson as the Shockwave team prepares to write its next exciting chapter.”
Transaction Benefits
- Solidifies Johnson & Johnson MedTech’s leadership in cardiovascular intervention: IVL is the only technology that can treat both intimal and medial calcification, and Shockwave offers the first and only commercially available IVL platform for CAD and PAD. This acquisition will complement Johnson & Johnson MedTech’s leadership positions in heart recovery (Abiomed) and electrophysiology (Biosense Webster) to make it a category leader in four of the largest and highest-growth medtech markets within cardiovascular intervention.
- Enhances opportunity to serve patients worldwide through complementary fit with Johnson & Johnson: Shockwave’s IVL and Abiomed’s Impella ® heart pump platform play a critical role in complex percutaneous coronary intervention (PCI) procedures. Specifically, IVL is used in approximately 30% of high-risk PCI cases that also use Impella ® today. This clinical compatibility, combined with Johnson & Johnson MedTech’s established global commercial infrastructure, provides numerous opportunities to accelerate the adoption of these segment-leading technologies to patients in need.
- Provides robust pipeline for future growth in underpenetrated markets: Shockwave benefits from a strong pipeline focused on continued innovation and expansion of its product portfolio in CAD and PAD, and the potential use of IVL in new indications, including carotid artery disease and structural heart disease, over the coming years. Shockwave is also evaluating its Reducer System technology in clinical studies to treat patients with refractory angina.
- Accelerates sales growth: The acquisition of Shockwave accelerates Johnson & Johnson MedTech’s ongoing efforts to increase its presence in high-growth markets with unmet need, while expanding its reach and scale globally. The proposed transaction adds a high-performing business in an underpenetrated category with a strong pipeline and an attractive growth and margin profile. The transaction is expected to accelerate revenue growth for both Johnson & Johnson and Johnson & Johnson MedTech. Shockwave is ultimately expected to become Johnson & Johnson MedTech’s thirteenth priority platform, as defined by annual sales of at least $1 billion.
- Delivers immediate operational accretion: The transaction will be accretive to operating margin for both Johnson & Johnson and Johnson & Johnson MedTech. Johnson & Johnson expects the transaction to be operationally accretive upon closing, but considering the impact of financing costs, is expected to dilute adjusted earnings per share by approximately $0.10 in 2024 and approximately $0.17 in 2025.
Transaction Details and Path to Completion
Under the terms of the agreement, Johnson & Johnson will acquire all outstanding shares of Shockwave for $335.00 per share in cash through a merger of Shockwave with a wholly owned Johnson & Johnson subsidiary. Johnson & Johnson expects to fund the transaction through a combination of cash on hand and debt.
Johnson & Johnson expects to maintain a strong balance sheet and to continue to support its stated capital allocation priorities of R&D investment, competitive dividends, value-creating acquisitions and strategic share repurchases.
Following the completion of the transaction, Shockwave will operate as a business unit within Johnson & Johnson MedTech, and financials will be reported within Johnson & Johnson MedTech’s Cardiovascular portfolio, which was previously referred to as Interventional Solutions. In addition to his current responsibilities for Abiomed as the Global Head of Heart Recovery, Michael Bodner will assume responsibility for the business upon close. Isaac Zacharias, who has 6 years with Shockwave, most recently serving as President and Chief Commercial Officer, will transition to become Worldwide President of Shockwave, reporting to Michael Bodner. Doug Godshall, Shockwave’s President and Chief Executive Officer, will advise through the transition.
The closing of the transaction is expected to occur by mid-year 2024 subject to the receipt of Shockwave’s shareholder approval, as well as the receipt of applicable regulatory approvals and other customary closing conditions. Following completion of the transaction, Shockwave’s common stock will no longer be listed for trading on the Nasdaq Global Select Market.
Investor Conference Call
Johnson & Johnson and Shockwave will conduct a conference call with investors to discuss the transaction today, April 5, 2024, at 8:30 a.m. ET.
Participant Dial-In: 877-869-3847
Webcast: https://event.webcasts.com/starthere.jsp?ei=1664558&tp_key=36372427f7
A simultaneous webcast of the call for investors and other interested parties may be accessed by utilizing the link provided above. A replay will be available approximately two hours after the live webcast by visiting www.investor.jnj.com or https://ir.shockwavemedical.com .
As previously announced, Johnson & Johnson will also host a conference call for investors at 8:30 a.m. ET on Tuesday, April 16th to review first-quarter results.
In light of the joint conference call today, Shockwave has cancelled its conference call to discuss its financial results for the first quarter of fiscal year 2024, previously scheduled for May 6, 2024, 4:30 EST.
J.P. Morgan Securities LLC is serving as financial advisor to Johnson & Johnson and Freshfields Bruckhaus Deringer LLP is serving as legal advisor.
Perella Weinberg Partners is serving as financial advisor to Shockwave and Fenwick & West LLP is serving as legal advisor.
About Johnson & Johnson At Johnson & Johnson, we believe health is everything. Our strength in healthcare innovation empowers us to build a world where complex diseases are prevented, treated, and cured, where treatments are smarter and less invasive, and solutions are personal. Through our expertise in Innovative Medicine and MedTech, we are uniquely positioned to innovate across the full spectrum of healthcare solutions today to deliver the breakthroughs of tomorrow, and profoundly impact health for humanity. Learn more at https://www.jnj.com/ .
About Shockwave Medical, Inc.
Shockwave Medical is a leader in the development and commercialization of innovative products that are transforming the treatment of cardiovascular disease. Its first-of-its-kind Intravascular Lithotripsy (IVL) technology has transformed the treatment of atherosclerotic cardiovascular disease by safely using sonic pressure waves to disrupt challenging calcified plaque, resulting in significantly improved patient outcomes. Shockwave has also recently acquired the Reducer, which is under clinical investigation in the United States and is CE Marked in Europe. By redistributing blood flow within the heart, the Reducer is designed to provide relief to the millions of patients worldwide suffering from refractory angina. Learn more at www.shockwavemedical.com .
Additional Information and Where to Find It
This communication may be deemed to be solicitation material in respect of the proposed acquisition of Shockwave Medical by Johnson & Johnson.
In connection with the proposed transaction, Shockwave intends to file relevant materials with the U.S. Securities and Exchange Commission (“SEC”), including Shockwave’s proxy statement in preliminary and definitive form. Promptly after filing the definitive proxy statement, Shockwave will mail the definitive proxy statement and a proxy card to the security holders of Shockwave.
INVESTORS AND SECURITY HOLDERS OF SHOCKWAVE ARE URGED TO READ ALL RELEVANT DOCUMENTS FILED WITH THE SEC, INCLUDING SHOCKWAVE’S PROXY STATEMENT (WHEN THEY ARE AVAILABLE), BECAUSE THEY CONTAIN OR WILL CONTAIN IMPORTANT INFORMATION ABOUT THE PROPOSED TRANSACTION AND THE PARTIES TO THE PROPOSED TRANSACTION.
Investors and security holders of Shockwave are or will be able to obtain these documents (when they are available) free of charge from the SEC’s website at www.sec.gov or free of charge from Shockwave on Shockwave’s website at https://ir.shockwavemedical.com.
Participants in the Solicitation Johnson & Johnson and Shockwave and certain of their respective directors and executive officers, under SEC rules, may be deemed to be “participants” in the solicitation of proxies from security holders of Shockwave in connection with the proposed transaction. Information about Johnson & Johnson’s directors and executive officers is set forth in Johnson & Johnson’s Proxy Statement on Schedule 14A for its 2024 Annual Meeting of Shareholders, which was filed with the SEC on March 13, 2024, and Johnson & Johnson’s Annual Report on Form 10-K for the fiscal year ended December 31, 2023, which was filed with the SEC on February 16, 2024. Information about Shockwave’s directors and executive officers is set forth in Shockwave’s Proxy Statement on Schedule 14A for its 2023 Annual Meeting of Stockholders, which was filed with the SEC on April 21, 2023, and Shockwave’s Current Report on Form 8-K filed with the SEC on January 29, 2024. To the extent holdings of Johnson & Johnson’s or Shockwave’s securities by their respective directors or executive officers have changed since the amounts set forth in such 2024 or 2023 proxy statements, such changes have been or will be reflected on Initial Statements of Beneficial Ownership on Form 3 or Statements of Change in Ownership on Form 4 filed with the SEC. Investors and security holders of Shockwave are or will be able to obtain these documents free of charge from the SEC’s website at www.sec.gov, from Johnson & Johnson on Johnson & Johnson’s website at www.jnj.com, from Shockwave on Shockwave’s website at www.shockwavemedical.com/ or on request from Johnson & Johnson or Shockwave. Additional information concerning the interests of Shockwave’s participants in the solicitation, which may, in some cases, be different than those of Shockwave’s security holders generally, will be set forth in Shockwave’s proxy statement relating to the proposed transaction when it becomes available.
Cautions Concerning Forward-Looking Statements
- This communication contains “forward-looking statements” regarding the acquisition of Shockwave by Johnson & Johnson.
- The reader is cautioned not to rely on these forward-looking statements. These statements are based on current expectations of future events.
- If underlying assumptions prove inaccurate or known or unknown risks or uncertainties materialize, actual results could vary materially from the expectations and projections of Johnson & Johnson or Shockwave. Risks and uncertainties include, but are not limited to: the risk that the closing conditions for the acquisition will not be satisfied, including the risk that clearance under the Hart-Scott-Rodino Antitrust Improvements Act or other applicable antitrust laws will not be obtained; uncertainty as to the percentage of Shockwave security holders that will vote to approve the proposed transaction at the Shockwave stockholder meeting; the possibility that the transaction will not be completed in the expected timeframe or at all; potential adverse effects to the businesses of Johnson & Johnson or Shockwave during the pendency of the transaction, such as employee departures or distraction of management from business operations; the risk of security holder litigation relating to the transaction, including resulting expense or delay; the potential that the expected benefits and opportunities of the acquisition, if completed, may not be realized or may take longer to realize than expected; challenges inherent in product research and development, including uncertainty of clinical success and obtaining regulatory approvals; uncertainty of commercial success for new products; manufacturing difficulties and delays; product efficacy or safety concerns resulting in product recalls or regulatory action; economic conditions, including currency exchange and interest rate fluctuations; the risks associated with global operations; competition, including technological advances, new products and patents attained by competitors; challenges to patents; changes to applicable laws and regulations, including tax laws and global health care reforms; adverse litigation or government action; changes in behavior and spending patterns or financial distress of purchasers of health care services and products; and trends toward health care cost containment.
- In addition, there will be risks and uncertainties related to the ability of the Johnson & Johnson family of companies to successfully integrate the programs, products, technologies and employees/operations and clinical work of Shockwave. A further list and description of these risks, uncertainties and other factors and the general risks associated with the respective businesses of Johnson & Johnson and Shockwave can be found in Johnson & Johnson’s Annual Report on Form 10-K for the fiscal year ended December 31, 2023, filed with the SEC on February 16, 2024, including in the sections captioned “Cautionary Note Regarding Forward-Looking Statements” and “Item 1A. Risk Factors,” in Johnson & Johnson’s most recently filed Quarterly Report on Form 10-Q, in Johnson & Johnson’s subsequent filings with the SEC and in Shockwave’s Annual Report on Form 10-K for the fiscal year ended December 31, 2023, filed with the SEC on February 26, 2024, including in the sections captioned “Special Note Regarding Forward-Looking Statements” and “Item 1A. Risk Factors,” and in Shockwave’s subsequent filings with the SEC. Copies of these filings, as well as subsequent filings, are available online at www.sec.gov, www.jnj.com, www.shockwavemedical.com/ or on request from Johnson & Johnson or Shockwave. Neither Johnson & Johnson nor Shockwave undertakes to update any forward-looking statement as a result of new information or future events or developments, except as required by law.
Johnson & Johnson
Media Contact: Ryan Carbain [email protected]
Investor Contact: Tracy Menkowski investor-relations@it s .jnj.com
Shockwave Medical
Media Contact: Scott Shadiow +1.317.432.9210 [email protected]
Investor Contact: Debbie Kaster [email protected]

IMAGES
VIDEO
COMMENTS
Cardiology Personal Statement Example Three. My interest in the heart began in high school when I shadowed an echocardiographer at my local hospital. I became interested in the muscle after dissecting the heart of a frog and a pig in my AP biology class. I inquired about an opportunity to learn more, and my teacher referred me to someone she ...
Part 1: Introduction to the medical school personal statement. You probably know someone who achieved a solid GPA and MCAT score, conducted research, shadowed physicians, engaged in meaningful volunteer work, and met all the other medical school requirements, yet still got rejected by every school they applied to.. You may have even heard of someone who was rejected by over 30 medical schools ...
Personal Statement Example 6. This Personal Statement comes from a student who got into Graduate Entry Medicine at King's - and also had interviews for Undergraduate Medicine at King's, QMUL and Exeter. Get some inspiration for your Medicine Personal Statement with these successful examples from current Medical School students.
Medical School Personal Statement Fundamentals. If you are getting ready to write your medical school personal statement for the 2024-2025 application year, you may already know that almost 60% of medical school applicants are not accepted every year. You have most likely also completed all of your medical school requirements and have scoured the internet for worthy medical school personal ...
28 More Medical School Personal Statement Examples That Got Accepted. Medical School Personal Statement Example #3. Imagine holding a baby wearing doll clothes and a diaper made of gauze because she was too small. When I was 4 years old, my sister was born 4 months prematurely, weighing only 1 pound and 7 ounces.
Importantly, never make something up in your personal statement. Virani: The first pitfall is a personal statement that is too diffuse, such as those that list a lot of items but do not provide the reader with an understanding of how those items relate to an applicant's future in medicine or cardiology. The second pitfall is a personal ...
There is no exact template for an effective personal statement. Often, however, strong personal statements combine a concise description of a personal experience with reflection on how this experience either led the writer to pursue medicine or indicates the writer's character or commitment. Good personal statements often have a strong sense ...
Motivation refers to a student's ongoing preparation for the health profession and can include the initial inspiration.; Fit is determined through self-assessment of relevant values and personal qualities as they relate to the profession.; Capacity is demonstrated through holistically aligning with the competencies expected in the profession.; Vision relates to the impact you wish to make in ...
10.1 Step-by-step guide on how to start writing a personal statement for medicine: 10.1.1 Step 1. Create a list of the qualities that you want to demonstrate. 10.1.2 Step 2. Think about a situation when you have shown these qualities. 10.1.3 Step 3.
Given word count and space limitations, deciding what to include in a personal statement can be challenging. An initial brainstorm helps applicants recall personal attributes and experiences that best underscore key strengths (Step 1). 10 Writing explicit self-affirmations is challenging, so we recommend pairing with a near peer who may offer ...
Monday - Friday 8 a.m. - 5 p.m. Personal Statement Basics. The personal statement is submitted as part of the centralized application for most health professional schools. It is your only opportunity to "speak directly to the Admissions Committee" about your character, your motivations, your values. Your letters of recommendation and interview ...
The Power of Patient Stories to Inspire Us to Prevent Cardiovascular Disease and Death: Personal Reflections on the AHA's Scientific Sessions 2021 Donald M. Lloyd-Jones Correspondence to: Donald M. Lloyd-Jones, MD, ScM, Department of Preventive Medicine, Northwestern University Feinberg School of Medicine, 680 North Lake Shore Drive, Suite ...
Cardiovascular Science Personal Statement Sample. 851 Words4 Pages. PERSONAL STATEMENT (NURFATIN BT MOHD SHAH) I want to further my study in this course because it is thrilling and rapidly- moving subject area, that is highly pertinent to the problem facing by society today. As far as I concern, cardiovascular disease is one of the popular ...
Cardiology Fellowship Program Personal Statement Sample. In my third year of medicine school at Ross University on November 2008, I was intrigued by a class on open heart surgery of a patient suffering from myocardial infarction. The video documented of each step and explained the logic behind each incision of a heart vessel.
Medical school personal statement Sample #1. I stood shoulder to shoulder with choir members, hundreds of eyes in our direction, each seated in the great hall known as the Dallas Myerson Symphony Center. The countless rehearsals, rhythms, and lyrics danced through my mind as I watched the conductor raise his arms, and eagerly awaited his signal.
"As much as 80% of a person's health is determined by the social and economic conditions of their environment," says Conference Co-chair Ivor J. Benjamin, MD, FACC, former AHA president and director of the cardiovascular center, co-director of the NIH T32 Postdoctoral Fellowship in Cardiovascular Sciences and professor of medicine at the ...
Cardiology Fellowship Personal Statement Samples, Professional Writing. I have been inspired by the example of the early cardiologists who labored to identify and treat complex cardiac problems on ...
The cardiovascular system, which consists of the heart and blood vessels, is the circulatory systems in our body. The major function of the system is transportation; the heart is the system pump and the blood vessels are the delivery routes. The heart transport respiratory gases, nutrients, wastes, and other substances vital to the body's ...
Cardiovascular Physiology Personal Statement. 622 Words3 Pages. I was inspired to consider a career in cardiovascular physiology partly because my mother is a nurse and also because I enjoyed studying triple Science at school. I enjoyed the practical work undertaken as part of my GCSEs in the laboratory. I also have an interest in the Natural ...
Sample Cardiovascular Research Personal Statement. Over the course of completing a BSc in Physiology at the University of Glasgow, I feel I successfully made a transition from seeing the sciences as subjects to be learnt through textbooks and supervised laboratory work to viewing them as constantly evolving disciplines, characterised by near-limitless unanswered research questions.
Physician wellness in academic cardiovascular medicine: a scientific statement from the American Heart Association. Circulation. 2022;146:e229-e241. doi: 10.1161/CIR.0000000000001093 The expert peer review of AHA-commissioned documents (eg, scientific statements, clinical practice guidelines, systematic reviews) is conducted by the AHA Office ...
Pediatric Medicine. Cardiovascular Care. Ear, Nose, and Throat. Eye Care Specialists. Family Medicine. Geriatric Care. ... Louisville Women in Medicine & Science (L-WIMS) Committees. Faculty Wellness. Career Development. VIDEOS. Annual Work Plans and Performance Reviews. Letter Templates. Personal Statement Template; Personal Statement Template
SHARE: Your personal statement is your chance to shine, to stand out from among the hundreds of other PhD applicants. Highlight your research experience, interests, and career goals. The personal statement (or statement of purpose) is your introduction of yourself to the application reviewers. This brief statement (generally one to two pages ...
The objective of this scientific statement is to inform health care professionals and stakeholders about the role and impact of patient-centered care in adult cardiovascular medicine. This scientific statement describes the background and rationale for patient-centered care in cardiovascular medicine, provides insight into patient-oriented ...
The Indiana Technical School of Medicine in cooperation with the Cardiovascular Institute both CVI's research arm, the Krannert Cardiovascular Research Center, will launch a new cardiovascular fellowship this summer that will fuel innovation in cardiovascular medicine. An Anderson Cardiovascular Innovation Fellowship is a 12-month training program drafted to develop friends from novice ...
Objective To examine and summarise evidence from meta-analyses of cohort studies that evaluated the predictive associations between baseline cardiorespiratory fitness (CRF) and health outcomes among adults. Design Overview of systematic reviews. Data source Five bibliographic databases were searched from January 2002 to March 2024. Results From the 9062 papers identified, we included 26 ...
Complementary and Alternative Medicine; Consensus Statements; Coronavirus (COVID-19) Critical Care Medicine ... Economics, and Policy Promoting EDI in Genetics Research PTSD and Cardiovascular Disease Red Blood Cell Transfusion: 2023 AABB International Guidelines Reimagining Children's ... Create a free personal account. To register for email ...
Objective To investigate the risk of cardiovascular disease (CVD) associated with increasing dose of a non-steroidal anti-inflammatory drug (NSAID) in patients with ankylosing spondylitis (AS). Methods Using the Korean National Health Insurance database, patients newly diagnosed with AS without prior CVD between 2010 and 2018 were included in this nationwide cohort study.
Enhances Johnson & Johnson's Ability to Transform the Treatment Landscape for Cardiovascular Disease and Continue to Improve Patient Outcomes Extends Johnson & Johnson MedTech's Position in Highest-Growth, Innovation-Oriented Segments of Cardiovascular Intervention Accelerates Sales Growth and Accretive to Operating Margin for Both Johnson & Johnson and Johnson & Johnson MedTech Conference ...