- Office of the Deputy Dean
- MD Admissions Committee
- Progress Committee
- EPCC Committee Minutes
- Thesis Chair Committee
- Curriculum Mapping Documents
- PreClerkship Policies
- Clerkship & ATP Policies
- University Policy Links
- Self-Study Task Force
- You said . . . We did . . .
- Faculty Training
- Renovation & Expansion of Student Space
- Faculty Mentor Responsibilities and Resources
- Departmental Thesis Chairs
- First-Year Summer Research
- Short-term Research
- One-year Fellowships
- Travel Info & Reimbursement
- Research Didactics
- START Summer Program
- Master of Health Science
- Student Research Day
- Forms, Deadlines & Funding
- Student Research Team
- Research Tradition
- The Yale System
- How to Apply
- Dates and Deadlines
- Fee Waivers
- Pre-medical Requirements
- Admissions Team
- Electives & Subinternships
- Staying for a Fifth Year
- Academic Advisors
- Performance Improvement
- Residency Applications
- Meet our Staff & Make an Appointment
- Wellness Programming: Upcoming Events
- Peer Advocate Program
- Day in the life of Med student
- Hear our Experiences
- Student Affairs Team
- Application Process
- International Students
- 2024-2025 Budget
- 2023-2024 Budget
- 2022-2023 Budget
- 2021-2022 Budget
- 2020-2021 Budget
- 2019-2020 Budget
- 2018-2019 Budget
- 2017-2018 Budget
- 2016-2017 Budget
- 2015-2016 Budget
- 2014-2015 Budget
- Research Funding, Extended Study and Financial Aid
- Frequently Asked Questions
- PA Online Student Budget
- FAFSA Application
- CSS Profile Application
- How to Avoid Common Errors
- Student Billing Information
- Financial Literacy Information
- External Scholarships
- Financial Aid Team
- Certificate in Global Medicine
- Topics in Global Medicine and Health
- Global Health Seminar
- Summer Research Abroad
- Electives at Other Yale Graduate Schools
- About the Course
- South Africa
- Connecticut
- Dominican Republic
- Lectures, Series, & Conferences
- Community & Advocacy Opportunities
- Faculty Advisors & Mentors
- Global Health Team
- Services & Facilities
- Program & Faculty Development
- Education & Research
- Simulated Participants
- Simulation Academy at Yale – Youth Entering Science (SAY-YES!)
- Faculty & Staff
- Advisory Board
- HAVEN Free Clinic
- Neighborhood Health Project
- Humanities in Medicine
- Biomedical Ethics
- Yale Journal of Biology & Medicine
- University Engagement Opportunities
- Community Engagement Opportunities
- Competencies
- Guiding Principles
- Graduation Requirements
- Year 1 Curriculum
- Year 2 Curriculum
- Introduction to the Profession (iPro)
- Scientific Foundations
- Genes and Development
- Attacks and Defenses
- Homeostasis
- Energy and Metabolism
- Connection to the World
- Across the Lifespan
- Professional Responsibility
- Scientific Inquiry
- Populations & Methods
- Biochemistry
- Cell Biology
- Diagnostic Methods
- Health Equity
- Pharmacology
- Communications Skills
- Clinical Reasoning
- Palliative Care
- Physical Examination
- Point of Care Ultrasound
- Early Clinical Experiences
- Emergency Medicine
- Primary Care
- Internal Medicine
- Recommended Readings
- Online Learning
- Interprofessional Educational
- Anesthesiology
- Child Study Center
- Clinical Longitudinal Elective
- Definitions
- Dermatology
- Diagnostic Imaging
- Family Medicine
- Interventional Radiology
- Laboratory Medicine
- Neurosurgery
- Obstetrics, Gynecology & Reproductive Sciences
- Ophthalmology and Visual Science
- Orthopaedics and Rehabilitation
- Therapeutic Radiology
- Elective Dates
- WEC Faculty
- Non-Clinical Electives
- Coaching Program
- Patient-Centered Language
- Race & Ethnicity
- Sex & Gender
- Full Glossary of Terms
- About The Inclusive Language Initiative
- Glossary Bibliography
- Curriculum Team
- Faculty Attestation
- Visiting Student Scholarship Program
- International Student FAQs
INFORMATION FOR
- Residents & Fellows
- Researchers

Formal MD Thesis Requirement
All students at Yale School of Medicine engage in research and are required to write an MD thesis during medical school. The only exceptions are students who have earned a PhD degree in the health sciences before matriculation and students enrolled in Yale’s MD/PhD program. The YSM MD Thesis is under the governance of the EPCC, which meets regularly to recommend rules, regulations, and deadlines.
Deadlines/Important Dates
Thesis approval process, thesis awards, required formatting and components of the md thesis, examples for reference section formatting, avoiding the risk of copyright violation and liability when submitting your md thesis, instructions for submitting a thesis to the yale medicine thesis digital library, thesis depositors declaration form, evaluations of advisor, student evaluation of thesis advisor.
- Yale School of Medicine Digital Thesis Depositor’s Declaration Form
- Thesis Deadline Extension Request Form
Thesis Deadlines for the 2023-2024 Academic Year
Md students:.
The Office of Student Research, in conjunction with the Dean’s Office, has established the following deadlines for theses submitted in partial fulfillment of the requirements for graduation in May 2024. The deadlines ensure that (1) students have sufficient time to complete their theses; (2) that there is sufficient time for rigorous departmental review and subsequent revision by students before final approval. These deadlines are strictly followed. Students are strongly encouraged to submit their theses well before the Class of 2024 Thesis Deadlines provided below. This timeliness will provide students, advisors, and sponsoring departments sufficient time for useful review and revision. It should be recognized by all concerned that the integrity of the thesis requirement and effective, rigorous review requires adherence to these deadlines. OSR will hold periodic “Thesis Check-in Sessions” via zoom for the Class of 2024 and will send periodic reminder emails with more detailed instructions as these deadlines approach.
*Students missing the August 4th, January 19th, and/or March 29th deadlines will be referred to the Progress Committee to ensure they receive adequate support to make progress towards this graduation requirement. Students missing the January 19th and/or March 29th deadlines will be ineligible for thesis prizes at graduation.
Extensions beyond the above thesis deadlines will be granted only for special circumstances and must have the approval of the student’s thesis mentor/advisor, academic advisor, and the Departmental Thesis Chairperson . Students seeking an extension for the January 19, 2024, deadline must submit a Thesis Deadline Extension Request Form to their Academic Advisor, and the Departmental Thesis Chair, for approval. Students missing the August 4th, January 19th, and/or March 29th deadlines will be referred to the Progress Committee to ensure they receive adequate support to make progress towards this graduation requirement. In the event of an extension, if granted, the following ABSOLUTE Class of 2024 Thesis Extension Deadlines will apply:
*All late theses require an extension. The student must submit the Thesis Deadline Extension Request Form before January 19, 2024.
MD/MHS Students:
Consistent with degree requirements, MD/MHS students must present their thesis to their three-person committee prior to the January 19th deadline. Students are encouraged to start arranging the date of this committee meeting in the fall to avoid unanticipated delays.
MD/PhD Students:
A different process applies to students in the MD/PhD program. For students enrolled in the combined MD/PhD Program, the dissertation submitted to and approved by the Graduate School will satisfy the MD thesis requirement. Therefore, MD/PhD students who have already defended their dissertation and received their PhD should provide this information to OSR via email as soon as possible.
To ensure compliance with YSM graduation deadlines, MD/PhD students in the class of 2024 who have not defended and submitted their dissertation to the Graduate School by the October 1, 2023, deadline will need to submit a copy of their dissertation directly to OSR via the MD/PhD Box Upload Link by March 15, 2024. OSR will convene a committee to review the dissertation, obtain feedback, and provide approval for graduation. Please note that MD/PhD students must also defend and submit their dissertation to the Graduate School no later than March 15, 2024, to meet the Graduate School spring degree deadline for conferral of the PhD degree. MD/PhD students who have not yet defended their dissertation should provide this information to OSR. If there are any questions about the process, please contact the MD/PhD Office.
Financial support is not provided for writing the thesis.
Thesis Preparation and Approval
Preparation for thesis submission begins in the summer of the fourth year with the OSR leadership. At this time, timeline and practices are distributed via email and reviewed with students in class meetings. Because thesis approval is a lengthy process involving three levels of review, students are encouraged to manage their time well and start writing their first draft early in the fall semester of their final year of medical school. A suggested timeline is provided below.
July : Thesis deadlines are distributed via email to all students in the graduating class and an informational session is held. Students should be on track to complete their thesis research by mid-fall. Any student anticipating a challenge in this regard should contact the OSR as soon as possible. All students expecting to graduate in May of a given year must, provide the OSR with information regarding their thesis title and mentor/advisor. Students will receive an email from the OSR containing a Medtrics link requesting this information. The OSR will contact all thesis mentors/advisors to confirm this role and to provide information and expectations regarding the thesis process.
August – December : Students should be finalizing research and writing their thesis draft. As the semester progresses, activities should shift from the data generation/analysis to the writing of the actual thesis. Students should do their best to complete the first draft of the thesis by mid-late December. Because students are also involved in the residency application and interview process, they are discouraged from starting new projects at this time.
December – January : This period is devoted to reviewing and editing of thesis draft that is ultimately approved by their thesis mentor/advisor and submitted by the student to the Thesis Chair of their sponsoring department. The YSM thesis mentor/advisor will be asked to complete a thesis assessment that evaluates the student’s mastery of YSM’s research-related educational objectives and provides formative summative feedback to the student.
January – March : The Departmental Thesis Chair coordinates thesis review by external reviewers. An “external reviewer” is defined as an individual who is not directly involved in the project. This individual may be a Yale faculty member internal or external to YSM or may hold a faculty appointment at an outside institution. This reviewer is required to complete a thesis assessment and provide formative summative feedback, as well as recommendations for any required changes, to the thesis. Departmental Thesis Chairs review assessments, notify students of departmental approval, and transmit these approvals to the OSR.
March : Theses and their associated assessments undergo school-level review by the OSR. Students receive YSM approval of their thesis along with summative feedback obtained during the review process. Students incorporate any required changes into their thesis and upload to the Yale Medicine Digital Thesis Library/Eli Scholar via the ProQuest platform (see below).
April : The OSR confirms that theses have been deposited into the Yale Medicine Digital Thesis Library and the registrar receives the names of students who have completed the thesis requirement.
The central role of the medical student thesis is to assess student’s performance on the YSM’s research-related educational objectives. As such, all students are expected to produce an excellent piece of scholarly work. In recognition of these achievements, the OSR has worked to develop an award process that celebrates the wonderful research being done by our students without creating a competitive atmosphere surrounding the thesis. Hence, thesis awards are based on competency-based assessments submitted by thesis mentors/advisors and reviewers during the approval process, and internal review of the final thesis that was deposited into the Yale Medicine Digital Thesis Library. Consistent with all other graduation prizes, YSM MD Thesis Awards will remain confidential until they are announced in the YSM Commencement Program on May 20, 2024. While some departments may elect to confer thesis “honors” based upon their own internal review, this recognition is distinct from YSM graduation prizes and is not under OSR’s purview.
Read about the required formatting and components for the thesis .
See helpful examples for reference section formatting.
Read about avoiding the risk of copyright violation and liability when submitting your MD Thesis.
Learn more about submitting a thesis to the Yale Medicine Thesis Digital Library .
Learn more about the Thesis Depositors Declaration Form.
Learn more about evaluating your experience with your thesis advisor .
Apply for a Thesis Extension
Read about the required formatting and components for the thesis.
Yale Journal of Biology and Medicine
Learn more about the journal or submit a manuscript.
- Bibliography
- More Referencing guides Blog Automated transliteration Relevant bibliographies by topics
- Automated transliteration
- Relevant bibliographies by topics
- Referencing guides
Dissertations / Theses on the topic 'Medical education – Aims and objectives'
Create a spot-on reference in apa, mla, chicago, harvard, and other styles.
Consult the top 50 dissertations / theses for your research on the topic 'Medical education – Aims and objectives.'
Next to every source in the list of references, there is an 'Add to bibliography' button. Press on it, and we will generate automatically the bibliographic reference to the chosen work in the citation style you need: APA, MLA, Harvard, Chicago, Vancouver, etc.
You can also download the full text of the academic publication as pdf and read online its abstract whenever available in the metadata.
Browse dissertations / theses on a wide variety of disciplines and organise your bibliography correctly.
Wasserman, Elizabeth. "Implementation evaluation as a dimension of the quality assurance of a new programme for medical education and training." Thesis, Stellenbosch : University of Stellenbosch, 2004. http://hdl.handle.net/10019.1/16079.
Machado, Durvalino Vieira. "Taxonomia de Bloom como ferramenta para avaliação da aprendizagem em um curso de medicina que utiliza métodos ativos de aprendizagem." Pontifícia Universidade Católica de São Paulo, 2018. https://tede2.pucsp.br/handle/handle/21630.
Speyer, Elizabeth C. "Teacher evaluation systems in four school boards." Thesis, McGill University, 1988. http://digitool.Library.McGill.CA:80/R/?func=dbin-jump-full&object_id=63876.
Bardis, Jim N. D. "Ex pede Parmenidem : an inquiry into bottomless things." Thesis, McGill University, 1994. http://digitool.Library.McGill.CA:80/R/?func=dbin-jump-full&object_id=22559.
Bosch, Marieke M. "Living the great mythic questions : an exploration of the inspirited school where narrative and authenticity intersect." Thesis, McGill University, 2002. http://digitool.Library.McGill.CA:80/R/?func=dbin-jump-full&object_id=29495.
Killingsworth, Scott Adamson. "Learning orientation : college climate antecedents, development-related outcomes, and malleability." Thesis, Georgia Institute of Technology, 2000. http://hdl.handle.net/1853/28981.
Coombs, Charlotte Rosalind Compton. "Toward a conception of educational leadership." Thesis, University of British Columbia, 1988. http://hdl.handle.net/2429/29233.
Fung, Tak-chuen Daniel, and 馮德全. "Using indicators in evaluating the implementation of educational aims: a case study." Thesis, The University of Hong Kong (Pokfulam, Hong Kong), 1996. http://hub.hku.hk/bib/B31958655.
Halwachi, Abdul Jalil Hassan. "Higher education institutions in the Arab states : a study of objectives and their achievement." Thesis, University of Stirling, 1985. http://hdl.handle.net/1893/1914.
Teoli, Roberto. "Myth, the body and wholeness : towards a more holistic conception of education." Thesis, McGill University, 2002. http://digitool.Library.McGill.CA:80/R/?func=dbin-jump-full&object_id=29523.
Felix, Alan Alistair. "Dominant pedagogies used in three rural geography primary school classrooms in the west coast district." Thesis, Cape Peninsula University of Technology, 2015. http://hdl.handle.net/20.500.11838/2133.
Goldie, J. G. "Impak van die verlengde graadprogramme aan die Universiteit van Stellenbosch : 'n evalueringstudie." Thesis, Stellenbosch : Stellenbosch University, 2013. http://hdl.handle.net/10019.1/97400.
Wilson, Fuge Blythe Ariana. "Confluent education: Curriculum developed to create connections for students." CSUSB ScholarWorks, 2008. https://scholarworks.lib.csusb.edu/etd-project/3334.
Bean, Maynard K. "Factors that affected the 1986 report of the Commission on Excellence in Education." Diss., This resource online, 1990. http://scholar.lib.vt.edu/theses/available/etd-09162005-115039/.
Chow, Kwok-wai Terry, and 周國偉. "The dialectic of utopia and ideology in education: the implications of the critical hermeneutic of PaulRicoeur." Thesis, The University of Hong Kong (Pokfulam, Hong Kong), 1992. http://hub.hku.hk/bib/B31233053.
St, Clair Sean William. "The Instructional Objective Writing Assistant (IOWA) : addressing the need for learning objectives in the engineering classroom." Thesis, Georgia Institute of Technology, 2000. http://hdl.handle.net/1853/19325.
Kayitankore, Bernard Narcisse. "Foreign training of academic staff and capacity building in higher education institutions in Rwanda." Thesis, University of the Western Cape, 2006. http://etd.uwc.ac.za/index.php?module=etd&action=viewtitle&id=gen8Srv25Nme4_8864_1182227521.
During the 1994 genocide in Rwanda, not only physical assets were eroded but more importantly, human capital were destroyed and left the country living hardly on qualified personnel at almost all levels of the economy to play a meaningful development role. While capacity building is needed in many sectors of the economy, it is especially important in the education sector. This study focuses on one particular issue namely to what extent sending academic staff for training in foreign countries can effectively contribute to capacity building in Rwandan higher education institutions (HEI). Various options exist to improve a strategy to build capacities in higher education institutions amongst others is the training of human resource which is the most important of all.
In order to investigate the above, both qualitative and quantitative methods were used. Techniques such as documentation, semi-structured interview, questionnaire and direct observation were also used in order to reach the research objectives. With regard to the main question of this study, findings reveal that funding academic staff for foreign training is believed to effectively contribute to capacity building in Rwandan higher education. As respondents explain, academic staff sent for training in foreign countries acquires new knowledge that is needed to build the country. This gained knowledge is spread all over the country through teaching at universities where most sectors of the country find their human resources. Being open minded, trained academic staff will be able to update his knowledge and therefore train in turn his students accordingly. However, findings inform also that Rwandan HEI are faced with multiple problems amongst others the problem of defining the real institutional needs for appropriate training. In this regard, findings suggest that for the training to be effective in Rwandan HEI there is a need of putting in place appropriate mechanisms and assessing institutional needs before training a person and training according to those specific needs in order to help the process of capacity building being more effective.
Beerman, Susan E. "Indiana "high schools that work" school improvement pilot sites : effects of programmatic change on administrative roles and responsibilities." Virtual Press, 1996. http://liblink.bsu.edu/uhtbin/catkey/1027092.
Arendse, Abraham John. "Die vestiging van 'n leerkultuur in 'n kinderhuisskool." Thesis, Stellenbosch : Stellenbosch University, 2002. http://hdl.handle.net/10019.1/52801.
陸嘉文. "澳門學校之校長與教師在教學理念與評估之調查研究." Thesis, University of Macau, 2007. http://umaclib3.umac.mo/record=b1637057.
Paul, Stephen John. "Aesthetic Justifications for Music Education: a Theoretical Examination of Their Usefulness." Thesis, University of North Texas, 1988. https://digital.library.unt.edu/ark:/67531/metadc331148/.
Sujjanun, Jintana. "A Study of the Perceptions of Students, Teachers, and Administrators of Actual and Ideal Educational Goals in Level Four Adult- Continuing Education Programs in Bangkok, Thailand." Thesis, North Texas State University, 1987. https://digital.library.unt.edu/ark:/67531/metadc330993/.
Rudhumbu, Norman. "The role of academic middle managers in the planning and implementation of curriculum change in private higher education institutions in Botswana." Thesis, University of Fort Hare, 2015. http://hdl.handle.net/10353/2979.
Spillman, Nancy Joan. "Higher education: An elixir for the retiree thus a tonic to society." CSUSB ScholarWorks, 2000. https://scholarworks.lib.csusb.edu/etd-project/1756.
Potjiri, Elizabeth Tello. "Free and compulsory primary education in Lesotho : democratic or not?" Thesis, Stellenbosch : Stellenbosch University, 2004. http://hdl.handle.net/10019.1/49968.
Escobar, Virginia Lizette. "Lessons in Character Development." CSUSB ScholarWorks, 2005. https://scholarworks.lib.csusb.edu/etd-project/2863.
Sharma, Seetal. "Globalisation and postcolonial identity." Thesis, Hong Kong : University of Hong Kong, 2002. http://sunzi.lib.hku.hk/hkuto/record.jsp?B25262348.
Giovannini, Eugene Vincent. "An analysis of existing and preferred goals for Virginia community colleges." Diss., This resource online, 1990. http://scholar.lib.vt.edu/theses/available/etd-08252008-162157/.
Yu, Kuang-Chao. "A comparison of program goals emphasized in technology education among selected groups of professionals in the state of Virginia." Diss., Virginia Tech, 1991. http://hdl.handle.net/10919/37290.
Thompson, Margie W. "The identification of change in school practice: a study of participant response from the 1983 and 1984 National Fellows Program." Diss., Virginia Polytechnic Institute and State University, 1985. http://hdl.handle.net/10919/49942.
Leasure, Debbie Dietrich. "The necessity of good writing criteria to the testing of writing." Thesis, Kansas State University, 1986. http://hdl.handle.net/2097/9927.
Gerber, Linda Ann. "A Study of Community College Instructional Stakeholder Attitudes Toward Student Outcome Goals." PDXScholar, 1994. https://pdxscholar.library.pdx.edu/open_access_etds/1275.
Smylie, Lana Rae. "Talking about tales: Creating a culture of stories for moral engagement." CSUSB ScholarWorks, 1998. https://scholarworks.lib.csusb.edu/etd-project/1511.
Dodd, Patricia M. "Assessing the Efficacy of Learning Communities at Four North Texas Community Colleges." Thesis, University of North Texas, 2002. https://digital.library.unt.edu/ark:/67531/metadc3255/.
Chan, Wing-kwong, and 陳榮光. "A study of the development of quality indicator systems in Hong Kong primary schools: a case study." Thesis, The University of Hong Kong (Pokfulam, Hong Kong), 1998. http://hub.hku.hk/bib/B31960017.
Jeffrey, Dennis Gordon. "Identifying the roadblocks: What impedes the transition of secondary seriously emotionally disturbed students?" CSUSB ScholarWorks, 1996. https://scholarworks.lib.csusb.edu/etd-project/1201.
Lozano, Albert Steven. "Science education at an elementary school: Teaching the scientific processes to English language learners." CSUSB ScholarWorks, 1996. https://scholarworks.lib.csusb.edu/etd-project/1246.
Gonzalez, Eduardo David. "Is there a difference between teacher perceptions about computer lab use in developing higher order thinking skills and actual computer lab practices?" CSUSB ScholarWorks, 2003. https://scholarworks.lib.csusb.edu/etd-project/2415.
Gammie, Robert Peter. "Psychological contracts in a business school context." Thesis, University of Stirling, 2006. http://hdl.handle.net/1893/228.
Hairston, Joe Allen. "Development of a process for Maryland school districts to assess implementation of the National Education Goals and Maryland's School for Success Goals." Diss., This resource online, 1993. http://scholar.lib.vt.edu/theses/available/etd-05042006-164532/.
Ontong, Krystle. "'n Ondersoek na 'n sin van plek en 'n pedagogie van plek in 'n Wes-Kaapse skool." Thesis, Stellenbosch : Stellenbosch University, 2013. http://hdl.handle.net/10019.1/85593.
Thompson, Lisa Anne. "Bloom's taxonomy goes high tech: A software review." CSUSB ScholarWorks, 2001. https://scholarworks.lib.csusb.edu/etd-project/3017.
Watson, James Richard. "Organizational change and reform in middle grade education: A California middle school case study." CSUSB ScholarWorks, 1996. https://scholarworks.lib.csusb.edu/etd-project/1140.
Slamat, Jerome Albert. "Teachers, assessment and outcomes-based education: a philosophical enquiry." Thesis, Stellenbosch : University of Stellenbosch, 2009. http://hdl.handle.net/10019.1/1131.
Van, Wyk Berte. "A conceptual analysis of transformation at three South African universities in relation to the national plan for higher education." Thesis, Stellenbosch : Stellenbosch University, 2004. http://hdl.handle.net/10019.1/49812.
Ferreira, Flávio Batista 1981. "Regulação local da política de expansão do ensino superior público paulista : diferentes concepções de universidade no projeto do novo campus da Unicamp em Limeira." [s.n.], 2013. http://repositorio.unicamp.br/jspui/handle/REPOSIP/250837.
Ashworth, Phyllis Corbett. "An examination of goals for Virginia's community colleges as perceived by members of the Virginia Senate and community college presidents." Diss., Virginia Polytechnic Institute and State University, 1989. http://hdl.handle.net/10919/54761.
Niven, Penelope Mary. "Narrating emergence in the curious terrain of academic development research: a realist perspective." Thesis, Rhodes University, 2012. http://hdl.handle.net/10962/d1003558.
Erbstoesser, Richard James. "Student motivation: instilling a desire to learn in middle school students." CSUSB ScholarWorks, 1997. https://scholarworks.lib.csusb.edu/etd-project/1302.
Venter, Antoinette. "Cognitive preparation of NCS (grades 10-12) accounting learners for studies at a University of Technology." Thesis, Cape Peninsula University of Technology, 2016. http://hdl.handle.net/20.500.11838/2367.
AI in Medical Education: Global situation, effects and challenges
- Published: 10 July 2023
- Volume 29 , pages 4611–4633, ( 2024 )
Cite this article
- Wei Zhang 1 ,
- Mingxuan Cai 1 ,
- Hong Joo Lee 2 ,
- Richard Evans 3 ,
- Chengyan Zhu 4 &
- Chenghan Ming 5
2032 Accesses
4 Citations
Explore all metrics
Artificial Intelligence (AI) is transforming healthcare and shows considerable promise for the delivery of medical education. This systematic review provides a comprehensive analysis of the global situation, effects, and challenges associated with applying AI at the different stages of medical education.
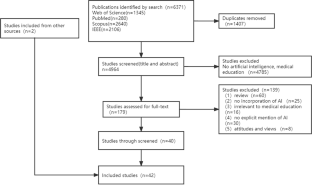
This review followed the PRISMA guidelines, and retrieved studies published on Web of Science, PubMed, Scopus, and IEEE Xplore, from 1990 to 2022. After duplicates were removed (n = 1407) from the 6371 identified records, the full text of 179 records were screened. In total, 42 records were eligible.
It revealed three teaching stages where AI can be applied in medical education (n = 39), including teaching implementation (n = 24), teaching evaluation (n = 10), and teaching feedback (n = 5). Many studies explored the effectiveness of AI adoption with questionnaire survey and control experiment. The challenges are performance improvement, effectiveness verification, AI training data sample and AI algorithms.
Conclusions
AI provides real-time feedback and accurate evaluation, and can be used to monitor teaching quality. A possible reason why AI has not yet been applied widely to practical teaching may be the disciplinary gap between developers and end-user, it is necessary to strengthen the theoretical guidance of medical education that synchronizes with the rapid development of AI. Medical educators are expected to maintain a balance between AI and teacher-led teaching, and medical students need to think independently and critically. It is also highly demanded for research teams with a wide range of disciplines to ensure the applicability of AI in medical education.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

AIM in Medical Education

AI’s Role and Application in Education: Systematic Review
Data availability.
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Aldeman, N. L. S., de SáUrtigaAita, K. M., Machado, V. P., da Mata Sousa, L. C. D., Coelho, A. G. B., da Silva, A. S., Silva Mendes, A. P., de Oliveira Neres, F. J., & do Monte, S. J. H. (2021). Smartpathk: A platform for teaching glomerulopathies using machine learning. BMC Medical Education, 21 (1), 248. https://doi.org/10.1186/s12909-021-02680-1
Article PubMed PubMed Central Google Scholar
Alonso-Silverio, G. A., Pérez-Escamirosa, F., Bruno-Sanchez, R., Ortiz-Simon, J. L., Muñoz-Guerrero, R., Minor-Martinez, A., & Alarcón-Paredes, A. (2018). Development of a Laparoscopic Box Trainer Based on Open Source Hardware and Artificial Intelligence for Objective Assessment of Surgical Psychomotor Skills. Surgical Innovation, 25 (4), 380–388. https://doi.org/10.1177/1553350618777045
Article PubMed Google Scholar
Baloul, M. S., Yeh, V.J.-H., Mukhtar, F., Ramachandran, D., Traynor, M. D., Shaikh, N., Rivera, M., & Farley, D. R. (2022). Video Commentary & Machine Learning: Tell Me What You See, I Tell You Who You Are. Journal of Surgical Education, 79 (6), e263–e272. https://doi.org/10.1016/j.jsurg.2020.09.022
Bienstock, J. L., Katz, N. T., Cox, S. M., Hueppchen, N., Erickson, S., & Puscheck, E. E. (2007). To the point: Medical education reviews—providing feedback. American Journal of Obstetrics and Gynecology, 196 (6), 508–513. https://doi.org/10.1016/j.ajog.2006.08.021
Bing-You, R., Hayes, V., Varaklis, K., Trowbridge, R., Kemp, H., & McKelvy, D. (2017). Feedback for Learners in Medical Education: What Is Known? A Scoping Review . Wolters Kluwer. https://doi.org/10.1097/ACM.0000000000001578
Bissonnette, V., Mirchi, N., Ledwos, N., Alsidieri, G., Winkler-Schwartz, A., Del Maestro, R. F., Yilmaz, R., Siyar, S., Azarnoush, H., Karlik, B., Sawaya, R., Alotaibi, F. E., Bugdadi, A., Bajunaid, K., Ouellet, J., & Berry, G. (2019). Artificial Intelligence Distinguishes Surgical Training Levels in a Virtual Reality Spinal Task. Journal of Bone and Joint Surgery-American, 101 (23), e127. https://doi.org/10.2106/JBJS.18.01197
Article Google Scholar
Borakati, A. (2021). Evaluation of an international medical E-learning course with natural language processing and machine learning. BMC Medical Education, 21 (1), 181. https://doi.org/10.1186/s12909-021-02609-8
Chan, H.-P., Samala, R. K., Hadjiiski, L. M., & Zhou, C. (2020). Deep Learning in Medical Image Analysis. In G. Lee & H. Fujita ( Ed.), Deep Learning in Medical Image Analysis: Challenges and Applications (pp. 3–21). Springer International Publishing. https://doi.org/10.1007/978-3-030-33128-3_1
Chan, K. S., & Zary, N. (2019). Applications and Challenges of Implementing Artificial Intelligence in Medical Education: Integrative Review. JMIR Medical Education, 5 (1), e13930. https://doi.org/10.2196/13930
Chen, C.-K. (2010). Curriculum Assessment Using Artificial Neural Network and Support Vector Machine Modeling Approaches: A Case Study. IR Applications. Volume 29. In Association for Institutional Research (NJ1) . Association for Institutional Research. https://eric.ed.gov/?id=ED524832
Chen, L., Chen, P., & Lin, Z. (2020). Artificial Intelligence in Education: A Review. Ieee Access, 8 , 75264–75278. https://doi.org/10.1109/ACCESS.2020.2988510
Cheng, C.-T., Chen, C.-C., Fu, C.-Y., Chaou, C.-H., Wu, Y.-T., Hsu, C.-P., Chang, C.-C., Chung, I.-F., Hsieh, C.-H., Hsieh, M.-J., & Liao, C.-H. (2020). Artificial intelligence-based education assists medical students’ interpretation of hip fracture. Insights into Imaging, 11 (1), 119. https://doi.org/10.1186/s13244-020-00932-0
de Lima, R. M., de Medeiros Santos, A., Mendes Neto, F. M., de Sousa, F., Neto, A., Leão, F. C. P., de Macedo, F. T., & de Paula Canuto, A. M. (2016). A 3D serious game for medical students training in clinical cases. IEEE International Conference on Serious Games and Applications for Health (SeGAH), 2016 , 1–9. https://doi.org/10.1109/SeGAH.2016.7586255
Dharmasaroja, P., & Kingkaew, N. (2016). Application of artificial neural networks for prediction of learning performances. 2016 12th International Conference on Natural Computation, Fuzzy Systems and Knowledge Discovery (ICNC-FSKD) , 745–751. https://doi.org/10.1109/FSKD.2016.7603268
Estai, M., & Bunt, S. (2016). Best teaching practices in anatomy education: A critical review. Annals of Anatomy - Anatomischer Anzeiger, 208 , 151–157. https://doi.org/10.1016/j.aanat.2016.02.010
Fajrianti, E. D., Sukaridhoto, S., Rasyid, M. U. H. A., Suwito, B. E., Budiarti, R. P. N., Hafidz, I. A. A., Satrio, N. A., & Haz, A. L. (2022). Application of Augmented Intelligence Technology with Human Body Tracking for Human Anatomy Education. IJIET: International Journal of Information and Education Technology , 12 (6), Article 6.
Fang, Z., Xu, Z., He, X., & Han, W. (2022).Artificial intelligence-based pathologic myopia identification system in the ophthalmology residency training program. Frontiers in Cell and Developmental Biology , 10 . https://doi.org/10.3389/fcell.2022.1053079
Fazlollahi, A. M., Bakhaidar, M., Alsayegh, A., Yilmaz, R., Winkler-Schwartz, A., Mirchi, N., Langleben, I., Ledwos, N., Sabbagh, A. J., Bajunaid, K., Harley, J. M., & Del Maestro, R. F. (2022). Effect of Artificial Intelligence Tutoring vs Expert Instruction on Learning Simulated Surgical Skills Among Medical Students: A Randomized Clinical Trial. JAMA Network Open, 5 (2), e2149008. https://doi.org/10.1001/jamanetworkopen.2021.49008
Fernández-Alemán, J. L., López-González, L., González-Sequeros, O., Jayne, C., López-Jiménez, J. J., & Toval, A. (2016). The evaluation of i-SIDRA – a tool for intelligent feedback – in a course on the anatomy of the locomotor system. International Journal of Medical Informatics, 94 , 172–181. https://doi.org/10.1016/j.ijmedinf.2016.07.008
Foss, C. L. (1987). Learning from errors in ALGEBRALAND . Institute for Research on Learning.
Furlan, R., Gatti, M., Menè, R., Shiffer, D., Marchiori, C., Levra, A. G., Saturnino, V., Brunetta, E., & Dipaola, F. (2021). A Natural Language Processing-Based Virtual Patient Simulator and Intelligent Tutoring System for the Clinical Diagnostic Process: Simulator Development and Case Study. JMIR Medical Informatics, 9 (4), e24073. https://doi.org/10.2196/24073
Gendia, A. (2022). Cloud Based AI-Driven Video Analytics (CAVs) in Laparoscopic Surgery: A Step Closer to a Virtual Portfolio. Cureus , 14 (9). https://doi.org/10.7759/cureus.29087
Gil, D. H., Heins, M., & Jones, P. B. (1984). Perceptions of medical school faculty members and students on clinical clerkship feedback. Academic Medicine, 59 (11), 856.
Article CAS Google Scholar
Goh, P. S. (2021). The vision of transformation in medical education after the COVID-19 pandemic. Korean Journal of Medical Education, 33 (3), 171–174. https://doi.org/10.3946/kjme.2021.197
Article MathSciNet PubMed PubMed Central Google Scholar
Gorospe-Sarasúa, L., Munoz-Olmedo, J. M., Sendra-Portero, F., & de Luis-García, R. (2022a). Challenges of Radiology education in the era of artificial intelligence . 6.
Gorospe-Sarasúa, L., Muñoz-Olmedo, J. M., Sendra-Portero, F., & de Luis-García, R. (2022b). Challenges of Radiology education in the era of artificial intelligence. Radiología (english Edition), 64 (1), 54–59. https://doi.org/10.1016/j.rxeng.2020.10.012
Han, R., Yu, W., Chen, H., & Chen, Y. (2022). Using artificial intelligence reading label system in diabetic retinopathy grading training of junior ophthalmology residents and medical students. BMC Medical Education , 22 (1), Article 1. https://doi.org/10.1186/s12909-022-03272-3
Hattie, J., & Timperley, H. (2007). The power of feedback. Review of educational research, 77 (1), 81–112. https://doi.org/10.3102/003465430298487
Hedderich, D. M., Keicher, M., Wiestler, B., Gruber, M. J., Burwinkel, H., Hinterwimmer, F., Czempiel, T., Spiro, J. E., Pinto dos Santos, D., Heim, D., Zimmer, C., Rückert, D., Kirschke, J. S., & Navab, N. (2021). AI for Doctors—A Course to Educate Medical Professionals in Artificial Intelligence for Medical Imaging. Healthcare , 9 (10), Article 10. https://doi.org/10.3390/healthcare9101278
Hewson, M. G., & Little, M. L. (1998). Giving Feedback in Medical Education. Journal of General Internal Medicine, 13 (2), 111–116. https://doi.org/10.1046/j.1525-1497.1998.00027.x
Article CAS PubMed PubMed Central Google Scholar
Hisan, U. K., & Amri, M. M. (2023). ChatGPT and Medical Education: A Double-Edged Sword. Journal of Pedagogy and Education Science , 2 (01), Article 01. https://doi.org/10.56741/jpes.v2i01.302
Hisey, R., Camire, D., Erb, J., Howes, D., Fichtinger, G., & Ungi, T. (2022). System for Central Venous Catheterization Training Using Computer Vision-Based Workflow Feedback. IEEE Transactions on Biomedical Engineering, 69 (5), 1630–1638. https://doi.org/10.1109/TBME.2021.3124422
Hosny, A., Parmar, C., Quackenbush, J., Schwartz, L. H., & Aerts, H. J. W. L. (2018). Artificial intelligence in radiology. Nature Reviews Cancer , 18 (8), Article 8. https://doi.org/10.1038/s41568-018-0016-5
Hu, H., Li, J., Lei, X., Qin, P., & Chen, Q. (2019). Design of health statistics intelligent education system based on Internet +. Journal of Physics: Conference Series, 1168 (6), 062003. https://doi.org/10.1088/1742-6596/1168/6/062003
Hwang, G.-J., Xie, H., Wah, B. W., & Gašević, D. (2020). Vision, challenges, roles and research issues of Artificial Intelligence in Education. Computers and Education: Artificial Intelligence, 1 , 100001. https://doi.org/10.1016/j.caeai.2020.100001
Islam, G., Kahol, K., Li, B., Smith, M., & Patel, V. L. (2016). Affordable, web-based surgical skill training and evaluation tool. Journal of Biomedical Informatics, 59 , 102–114. https://doi.org/10.1016/j.jbi.2015.11.002
Karambakhsh, A., Kamel, A., Sheng, B., Li, P., Yang, P., & Feng, D. D. (2019). Deep gesture interaction for augmented anatomy learning. International Journal of Information Management, 45 , 328–336. https://doi.org/10.1016/j.ijinfomgt.2018.03.004
Kirubarajan, A., Young, D., Khan, S., Crasto, N., Sobel, M., & Sussman, D. (2022). Artificial Intelligence and Surgical Education: A Systematic Scoping Review of Interventions. Journal of Surgical Education, 79 (2), 500–515. https://doi.org/10.1016/j.jsurg.2021.09.012
Klar, R., & Bayer, U. (1990). Computer-assisted teaching and learning in medicine. International Journal of Bio-Medical Computing, 26 (1–2), 7–27. https://doi.org/10.1016/0020-7101(90)90016-N
Article CAS PubMed Google Scholar
Kurniawan, M. H., Suharjito, Diana, & Witjaksono, G. (2018). Human Anatomy Learning Systems Using Augmented Reality on Mobile Application . 135 , 80–88. https://doi.org/10.1016/j.procs.2018.08.152
Lam, A., Lam, L., Blacketer, C., Parnis, R., Franke, K., Wagner, M., Wang, D., Tan, Y., Oakden-Rayner, L., Gallagher, S., Perry, S. W., Licinio, J., Symonds, I., Thomas, J., Duggan, P., & Bacchi, S. (2022a). Professionalism and clinical short answer question marking with machine learning. Internal Medicine Journal, 52 (7), 1268–1271. https://doi.org/10.1111/imj.15839
Lam, K., Chen, J., Wang, Z., Iqbal, F. M., Darzi, A., Lo, B., Purkayastha, S., & Kinross, J. M. (2022b). Machine learning for technical skill assessment in surgery: A systematic review. Npj Digital Medicine , 5(1), Article 1. https://doi.org/10.1038/s41746-022-00566-0
Lazarus, M. D., Truong, M., Douglas, P., & Selwyn, N. (2022). Artificial intelligence and clinical anatomical education: Promises and perils. Anatomical Sciences Education , n/a (n/a). https://doi.org/10.1002/ase.2221
Lee, J., Wu, A. S., Li, D., Kulasegaram, K., & (Mahan). (2021). Artificial Intelligence in Undergraduate Medical Education: A Scoping Review. Academic Medicine, 96 (11S), S62. https://doi.org/10.1097/ACM.0000000000004291
Lee, L. S., Aluwee, S. A. Z. S., Meng, G. C., Palanisamy, P., & Subramaniam, R. (2020). Interactive Tool Using Augmented Reality (AR) for Learning Knee and Foot Anatomy Based on CT Images 3D Reconstruction. 2020 International Conference on Computational Intelligence (ICCI) , 281–286. https://doi.org/10.1109/ICCI51257.2020.9247820
Li, Y., Bai, C., & Reddy, C. K. (2016). A distributed ensemble approach for mining healthcare data under privacy constraints. Information Sciences, 330 , 245–259. https://doi.org/10.1016/j.ins.2015.10.011
Li, Y. S., Lam, C. S. N., & See, C. (2021). Using a Machine Learning Architecture to Create an AI-Powered Chatbot for Anatomy Education. Medical Science Educator, 31 (6), 1729–1730. https://doi.org/10.1007/s40670-021-01405-9
Luan, H., Geczy, P., Lai, H., Gobert, J., Yang, S. J. H., Ogata, H., Baltes, J., Guerra, R., Li, P., & Tsai, C.-C. (2020). Challenges and Future Directions of Big Data and Artificial Intelligence in Education. Frontiers in Psychology , 11 . https://doi.org/10.3389/fpsyg.2020.580820
Martin, J. A., Regehr, G., Reznick, R., Macrae, H., Murnaghan, J., Hutchison, C., & Brown, M. (1997). Objective structured assessment of technical skill (OSATS) for surgical residents. BJS (british Journal of Surgery), 84 (2), 273–278. https://doi.org/10.1046/j.1365-2168.1997.02502.x
Mirchi, N., Bissonnette, V., Yilmaz, R., Ledwos, N., Winkler-Schwartz, A., & Del Maestro, R. F. (2020). The Virtual Operative Assistant: An explainable artificial intelligence tool for simulation-based training in surgery and medicine. Plos One, 15 (2), e0229596. https://doi.org/10.1371/journal.pone.0229596
Muller, S. (1984). Physicians for the twenty-first century: Report of the project panel on the general professional education of the physician and college preparation for medicine. Journal of Medical Education, 59 , 1–208.
Google Scholar
Nagaraj, M. B., Namazi, B., Sankaranarayanan, G., & Scott, D. J. (2023). Developing artificial intelligence models for medical student suturing and knot-tying video-based assessment and coaching. Surgical Endoscopy, 37 (1), 402–411. https://doi.org/10.1007/s00464-022-09509-y
Nakawala, H., Ferrigno, G., & De Momi, E. (2018). Development of an intelligent surgical training system for Thoracentesis. Artificial Intelligence in Medicine, 84 , 50–63. https://doi.org/10.1016/j.artmed.2017.10.004
Neves, S. E., Chen, M. J., Ku, C. M., Karan, S., DiLorenzo, A. N., Schell, R. M., Lee, D. E., Diachun, C. A. B., Jones, S. B., & Mitchell, J. D. (2021). Using Machine Learning to Evaluate Attending Feedback on Resident Performance. Anesthesia & Analgesia, 132 (2), 545–555. https://doi.org/10.1213/ANE.0000000000005265
Niitsu, H., Hirabayashi, N., Yoshimitsu, M., Mimura, T., Taomoto, J., Sugiyama, Y., Murakami, S., Saeki, S., Mukaida, H., & Takiyama, W. (2013). Using the Objective Structured Assessment of Technical Skills (OSATS) global rating scale to evaluate the skills of surgical trainees in the operating room. Surgery Today, 43 (3), 271–275. https://doi.org/10.1007/s00595-012-0313-7
Ötles, E., Kendrick, D. E., Solano, Q. P., Schuller, M., Ahle, S. L., Eskender, M. H., Carnes, E., & George, B. C. (2021). Using Natural Language Processing to Automatically Assess Feedback Quality: Findings From 3 Surgical Residencies. Academic Medicine, 96 (10), 1457. https://doi.org/10.1097/ACM.0000000000004153
Ouyang, F., Zheng, L., & Jiao, P. (2022). Artificial intelligence in online higher education: A systematic review of empirical research from 2011 to 2020. Education and Information Technologies . https://doi.org/10.1007/s10639-022-10925-9
Peter, H., & Goodridge, W. (2004). Integrating Two Artificial Intelligence Theories in a Medical Diagnosis Application. In M. Bramer & V. Devedzic ( Ed.), Artificial Intelligence Applications and Innovations (pp. 11–23). Springer US. https://doi.org/10.1007/1-4020-8151-0_2
Qian, X., Jingying, H., Xian, S., Yuqing, Z., Lili, W., Baorui, C., Wei, G., Yefeng, Z., Qiang, Z., Chunyan, C., Cheng, B., Kai, M., & Yi, Q. (2022). The effectiveness of artificial intelligence-based automated grading and training system in education of manual detection of diabetic retinopathy. Frontiers in Public Health, 10 , 1025271. https://doi.org/10.3389/fpubh.2022.1025271
Razzak, M. I., Naz, S., & Zaib, A. (2018). Deep Learning for Medical Image Processing: Overview, Challenges and the Future. In N. Dey, A. S. Ashour, & S. Borra ( Ed.), Classification in BioApps: Automation of Decision Making (pp. 323–350). Springer International Publishing. https://doi.org/10.1007/978-3-319-65981-7_12
Sadeghi Esfahlani, S., Izsof, V., Minter, S., Kordzadeh, A., Shirvani, H., & Esfahlani, K. S. (2020). Development of an Interactive Virtual Reality for Medical Skills Training Supervised by Artificial Neural Network. In Y. Bi, R. Bhatia, & S. Kapoor ( Ed.), Intelligent Systems and Applications (pp. 473–482). Springer International Publishing. https://doi.org/10.1007/978-3-030-29513-4_34
Shiang, T., Garwood, E., & Debenedectis, C. M. (2022). Artificial intelligence-based decision support system (AI-DSS) implementation in radiology residency: Introducing residents to AI in the clinical setting. Clinical Imaging, 92 , 32–37. https://doi.org/10.1016/j.clinimag.2022.09.003
Siyar, S., Azarnoush, H., Rashidi, S., Winkler-Schwartz, A., Bissonnette, V., Ponnudurai, N., & Del Maestro, R. F. (2020). Machine learning distinguishes neurosurgical skill levels in a virtual reality tumor resection task. Medical and Biological Engineering and Computing, 58 (6), 1357–1367. https://doi.org/10.1007/s11517-020-02155-3
Solano, Q. P., Hayward, L., Chopra, Z., Quanstrom, K., Kendrick, D., Abbott, K. L., Kunzmann, M., Ahle, S., Schuller, M., Ötleş, E., & George, B. C. (2021). Natural Language Processing and Assessment of Resident Feedback Quality. Journal of Surgical Education, 78 (6), e72–e77. https://doi.org/10.1016/j.jsurg.2021.05.012
Stephens, G. C., Rees, C. E., & Lazarus, M. D. (2021). Exploring the impact of education on preclinical medical students’ tolerance of uncertainty: A qualitative longitudinal study. Advances in Health Sciences Education, 26 (1), 53–77. https://doi.org/10.1007/s10459-020-09971-0
Sqalli, M. T., Al-Thani, D., Elshazly, M. B., & Al-Hijji, M. (2022). A Blueprint for an AI & AR-Based Eye Tracking System to Train Cardiology Professionals Better Interpret Electrocardiograms. In N. Baghaei, J. Vassileva, R. Ali, & K. Oyibo ( Ed.), Persuasive Technology (pp. 221–229). Springer International Publishing. https://doi.org/10.1007/978-3-030-98438-0_17
Szasz, P., Louridas, M., Harris, K. A., Aggarwal, R., & Grantcharov, T. P. (2015). Assessing Technical Competence in Surgical Trainees: A Systematic Review. Annals of Surgery, 261 (6), 1046. https://doi.org/10.1097/SLA.0000000000000866
Torre, D. M., Sebastian, J. L., & Simpson, D. E. (2003). Learning Activities and High-Quality Teaching: Perceptions of Third-Year IM Clerkship Students. Academic Medicine, 78 (8), 812.
Vayena, E., & Blasimme, A. (2017). Biomedical Big Data: New Models of Control Over Access, Use and Governance. Journal of Bioethical Inquiry, 14 (4), 501–513. https://doi.org/10.1007/s11673-017-9809-6
Voss, G., Bockholt, U., Los Arcos, J. L., Müller, W., Oppelt, P., & Stähler, J. (2000). Lahystotrain. Studies in Health Technology and Informatics, 70 , 359–364. https://doi.org/10.3233/978-1-60750-914-1-359
Wang, M., Sun, Z., Jia, M., Wang, Y., Wang, H., Zhu, X., Chen, L., & Ji, H. (2022). Intelligent virtual case learning system based on real medical records and natural language processing. BMC Medical Informatics and Decision Making, 22 (1), 60. https://doi.org/10.1186/s12911-022-01797-7
Willan, P. L. T., & Humpherson, J. R. (1999). Concepts of variation and normality in morphology: Important issues at risk of neglect in modern undergraduate medical courses. Clinical Anatomy, 12 (3), 186–190. https://doi.org/10.1002/(SICI)1098-2353(1999)12:3%3c186::AID-CA7%3e3.0.CO;2-6
Wolverton, S. E., & Bosworth, M. F. (1985). A survey of resident perceptions of effective teaching behaviors. Family Medicine, 17 (3), 106–108.
CAS PubMed Google Scholar
Wood, B. P. (2000). Feedback: A Key Feature of Medical Training. Radiology, 215 (1), 17–19. https://doi.org/10.1148/radiology.215.1.r00ap5917
Article MathSciNet CAS PubMed Google Scholar
Yang, W., Hebert, D., Kim, S., & Kang, B. (2019). MCRDR Knowledge-Based 3D Dialogue Simulation in Clinical Training and Assessment. Journal of Medical Systems, 43 (7), 200. https://doi.org/10.1007/s10916-019-1262-0
Yilmaz, Y., Nunez, A. J., Ariaeinejad, A., Lee, M., Sherbino, J., & Chan, T. M. (2022). Harnessing Natural Language Processing to Support Decisions Around Workplace-Based Assessment: Machine Learning Study of Competency-Based Medical Education. JMIR Medical Education, 8 (2), e30537. https://doi.org/10.2196/30537
Yilmaz-Recai, Winkler-Schwartz, A., Mirchi, N., Reich, A., Christie, S., Tran, D. H., Ledwos, N., Fazlollahi, A. M., Santaguida, C., Sabbagh, A. J., Bajunaid, K., & Del Maestro, R. (2022). Continuous monitoring of surgical bimanual expertise using deep neural networks in virtual reality simulation. Npj Digital Medicine , 5 (1), Article 1. https://doi.org/10.1038/s41746-022-00596-8
Zahiri, M., Booton, R., Siu, K.-C., & Nelson, C. A. (2016). Design and Evaluation of a Portable Laparoscopic Training System Using Virtual Reality. Journal of Medical Devices , 11(1). https://doi.org/10.1115/1.4034881
Zhao, S., Zhang, X., Jin, F., & Hahn, J. (2021). An Auxiliary Tasks Based Framework for Automated Medical Skill Assessment with Limited Data. 2021 43rd Annual International Conference of the IEEE Engineering in Medicine Biology Society (EMBC) , 1613–1617. https://doi.org/10.1109/EMBC46164.2021.9630498
Download references
This paper is supported by National Natural Science Foundation of China (Project No. 72104087, 72004070) and University-Industry Collaborative Education Program supported by Ministry of Education in China (220505084312449).
Author information
Authors and affiliations.
School of Medicine and Health Management, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Wei Zhang & Mingxuan Cai
Department of Business Administration, The Catholic University of Korea, Seoul, Korea
Hong Joo Lee
Faulty of Computer Science, Dalhousie University, Halifax, Canada
Richard Evans
School of Political Science and Public Administration, Wuhan University, Wuhan, China
Chengyan Zhu
College of Public Administration and Law, Hunan Agricultural University, Changsha, China
Chenghan Ming
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Chengyan Zhu .
Ethics declarations
Conflict of interest, additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 13 KB)
Supplementary file2 (docx 60 kb), rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Zhang, W., Cai, M., Lee, H.J. et al. AI in Medical Education: Global situation, effects and challenges. Educ Inf Technol 29 , 4611–4633 (2024). https://doi.org/10.1007/s10639-023-12009-8
Download citation
Received : 11 March 2023
Accepted : 26 June 2023
Published : 10 July 2023
Issue Date : March 2024
DOI : https://doi.org/10.1007/s10639-023-12009-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Artificial intelligence
- Applications of AIMED
- Effectiveness of AIMED
- Challenges of AIMED
- Find a journal
- Publish with us
- Track your research
A vision of the use of technology in medical education after the COVID-19 pandemic
This article was migrated. The article was marked as recommended.
Medical education across the world has experienced a major disruptive change as a consequence of the COVID-19 pandemic and technology has been rapidly and innovatively used to maintain teaching and learning. The future of medical education is uncertain after the pandemic resolves but several potential future scenarios are discussed to inform current decision-making about the future provision of teaching and learning. The use of emergent technology for education, such as artificial intelligence for adaptive learning and virtual reality, are highly likely to be essential components of the transformative change and the future of medical education. The benefits and challenges of the use of technology in medical education are discussed with the intention of informing all providers on how the changes after the pandemic can have a positive impact on both educators and students across the world.
technology, medical education, transformative change, coronavirus, COVID-19
Introduction
The purpose of this Personal View is to offer a vision of the use of technology in medical education after the COVID-19 pandemic begins to resolve. Both authors have a keen interest in the innovative use of technology in medical education and an awareness of the current and future trends in the use of technology to enhance teaching and learning. We will begin by a reflection on the current increased use of technology as a major factor in enabling the continuation of medical education during the pandemic. This reflection will be followed by a discussion of several potential future scenarios that are based on the emergent trends in the use of technology but also an understanding of how complex social systems respond over time to the trigger of major events. We will also discuss the benefits and challenges of the future use of technology in medical education after the pandemic resolves.
A transformative change in the current approach to medical education across the world is inevitable and although the full extent is unknown at the current time it is essential to consider potential future scenarios to begin the process of preparing for the future ( Chermack, 2004 ). We fully appreciate the difficulty that many medical educators will experience in considering the future at a time when most educators across the world are deeply engaged in responding to the current enormous challenges, both personal and professional as clinicians and educators. However, it is essential that all educational policy makers, curriculum planners and educators across the continuum of medical education, from basic to continuing, can begin to critically reflect on the present situation and make appropriate decisions about the future of medical education for when the pandemic resolves.
The impact of the COVID-19 pandemic
The pandemic has resulted in the widespread disruption of medical education and professional training ( Ahmed et al. , 2020 ; Murphy, 2020 ). Examples include reduced teaching with redeployment of medical educators to clinical care and the quarantine and impact of illness on medical educators and students. Measures to ensure social distancing have included closure of medical schools and working from home for both educators and students. Local and international travel, and attendance at training programs has been halted. Physical attendance at workshops and symposia, conferences, clinical attachments and visiting fellowships has ceased. Tragically, there have also been an increasing number of deaths that include doctors and other healthcare professionals.
The current response to the COVID-19 pandemic
Overall, the current response to the pandemic has been the increased awareness and adoption of currently available technologies in medical education, and also in the wider education sector ( Iwai, 2020 ). These changes across the continuum of medical education have been mainly to replace existing approaches for the provision of medical education, driven by the urgency to implement a feasible and practical solution to the crises, with educators using familiar technology.
Medical schools and other medical education providers, including commercial organizations and professional bodies, have rapidly scaled up the provision of educational content and training online, as well as faculty development in the use of technology, especially by online courses. Large group in-person lectures have been replaced by streamed online lectures, using technologies for screen capture and online dissemination. Small group sessions and tutorials have been replaced with interactive Webinars using web conferencing platforms. All of these learning resources can be easily accessed from mobile devices.
A major challenge for medical educators at the present time has been to replicate the experience of clinical encounters. These encounters range from clinic and ward rounds to interactive patient sessions to training in interpersonal and inter professional communication and clinical skills. Currently available technology, such as videos, podcasts, simple virtual reality, computer simulations and serious games, are beginning to be used to assist educators and facilitate student learning and training in these areas. Simple online platforms, such as websites and blogs, can provide basic information but also offer opportunities to host videos for demonstrating essential skills, such as procedural clinical skills and communication ( Dong and Goh, 2015 ). Medical educators can remotely coach students with real time mobile video tools and apps.
The increasing trends of competency based medical education (CBME) and programmatic assessment require regular assessments of student achievement. Medical schools have creatively responded to the challenge of a lack of opportunities to observe student performance or to hold large scale examinations. Formative and summative assessments for core knowledge have started to use a variety of online tools and platforms. The range is from websites, discussions forums and online discussion spaces to real-time online chat and communication apps. Feedback on performance and the assessment of skills acquisition has similarly started to maximize the ubiquitous availability of video and audio on mobile devices to enable assessment in authentic contexts, either clinical or simulated. These assessments should be ideally based on high quality evidence and theory informed assessment and evaluation strategies ( Martin et al ., 2019 ).
We are heartened to see greater national collaboration between medical schools to share educational and training resources (PIVOT MedEd, 2020 ). Commercial providers are also increasing their engagement and collaboration with medical schools.
The future after the COVID-19 pandemic
We consider that it will be highly unlikely that there will be a return to the previous approach to the provision of medical education as existed before the pandemic, especially the contribution of technology for enhancing teaching and learning. The change will be transformative, with a major change in how individuals and the wider social system within which each individual lives and works. The uncertainty at the current time is around the extent of this transformation since it is dependent on the complex interaction between several major factors that are difficult, and some observers would say almost impossible, to predict. These conversion factors are mainly related to the length of time that the pandemic is disruptive, since a long disruption is likely to produce significant alteration in several of the factors. The factors include the number and availability of educators, economic constraints and the need to rapidly expand the clinical workforce. All of these factors will have a major impact on the future way that educators and their institutions will provide medical education.
Understanding the transformation
Our framework to understand transformative change is Normalisation Process Theory (NPT). This sociological theoretical framework has been increasingly used to understand how a new practice, such as the use of technology, becomes embedded within a social system (“normalisation”) through an active process, both individually and collectively, that occurs over a period of time ( Scantlebury et al ., 2017 ). The new practice becomes embedded when it is routinely incorporated in the everyday work of individuals and groups. The key phases of this dynamic interactive process between individuals and others in the social system begin with the development of a shared understanding of the benefits and importance of the change to be achieved, and this is followed by the building and sustaining of individual and collective commitment around an intervention. Finally, there is ongoing resolution of any issues around differences in opinions about the new practice and there is increased allocation of resources to enable the new practice to become embedded. Once the practice is embedded it is considered both individually and collectively as the usual way of working and the new practice is unlikely to revert back to the original practice, especially if there have been major conversion factors that have initiated the transformation.
The NPT framework suggests at the present time that the process of transformation in the increased use of technology in medical education is within the early phases, with what appears to be a rapid and progressive individual and collective acceptance and commitment to the use of technology to enhance teaching and learning. The extent to which the transformation leads to embedding of technology will be variable across different providers of medical education but one future potential future scenario is that only minor transformative change will occur, with increased use of current technology, especially with a greater emphasis on online learning and mobile devices to replace face to face group teaching and meetings.
However, another potential future scenario is that of major transformative change in medical education, especially if there has been a major disruptive influence on the way that we all live and work after the pandemic resolves. If there is a major disruptive challenge to medical education, such as a vastly reduced number of educators and the need to rapidly expand the education of the future workforce across the continuum of medical education, the variety of current technology being used to augment medical education will be inefficient and inappropriate to meet the high demand. Educators will need to develop and implement innovative solutions in response to this high demand and an awareness of future trends in the use of technology is invaluable in beginning to prepare for the future.
Understanding the emergent technology
The Horizon 2020 Teaching and Learning report was produced by an expert panel to highlight how emergent technology has the potential to transform future provision of higher education ( Brown et al ., 2020 ). There are two main envisaged changes; adaptive learning and extended reality.
The introduction of adaptive learning offers a personalized approach to enable all students to access a wide range of learning resources and to provide information to educators about how students are learning from their experience. Essential for adaptive learning is the integrated application of two types of emergent technology: artificial intelligence (AI) and learning analytics ( Chan and Zary, 2019 ; Wartman and Combs, 2019 ). The application of artificial intelligence creates “thinking machines” to provide learning content and assessments that can adaptively interact with students using text and voice. These applications range from learning anatomy to complex clinical diagnostic and management challenges. Robotic tutors that are adaptive to problem-solving have been used alongside school children to facilitate their individual self-regulated learning ( Jones and Castellano, 2018 ). Learning analytics collect information about the process and outcomes of learning that are essential to inform educators about the progress and trajectory of both individual and groups of students. The learning potential of these new approaches is that students can obtain personalized learning that is tailored to their individual needs and there is also the opportunity to reduce the time for the development of individual competence and to decrease the time required for face to face interaction with educators and patients.
Extended reality (XR) provides students with learning experiences that either blends physical and virtual elements (augmented reality or AR) or provides a totally virtual immersive experience (virtual reality or VR) ( Zweifach and Triola, 2019 ). The immersive experience has the intention to replicate a real-life experience and this can be delivered through headsets or mobile devices. An emergent trend in technology is haptic simulation which replicates the physical sensations of a real-life experience, such as touch. The learning potential is that these sophisticated experiences can be applied to a range of clinical topics, from communication and clinical skills to deliberate practice of surgical procedures, and also they can be integrated with adaptive learning to realize additional benefits.
The middle ground future scenario
The potential future scenario for medical education and the contribution of technology to enhance teaching and learning after the resolution of the pandemic is likely to be in the middle ground between the two extreme ends of the spectrum that we have presented in the two previous scenarios. It is highly likely that the use of technology will increase and this also includes an accelerated application of many of the newer types of emergent technology that have been described in the Horizon 2020 report. However, the extent to which these types of emergent technology have become, and continue to be, embedded will be dependent on the complex mix of factors within a particular context. These factors include the length of time of disruption to previous approaches to medical education and the available resources, including support from learning technologists and access to the emergent technology. Overall, an integrated approach that combines elements of both technology and face to face teaching and learning experiences is likely to characterise the future scenario.
The benefits of change after the COVID-19 pandemic
Whatever the change and extent of transformation in medical education after the pandemic it is inevitable that there will increased individual and collective awareness and acceptance of the innovative potential that technology, including emergent technology, can offer to enhance teaching and learning across the continuum of medical education ( Goh, 2016 ). The ‘anytime anywhere’ aspect of using technology offers new opportunities for specific groups of students, such as increasing access and participation to part-time students and providing shortened programmes for gifted or talented students.
It will be interesting to see if the current increased spirit of national collaboration of medical educators to freely create, share and curate learning content will continue. There is the exciting opportunity for these collaborations to spread and include educators from across the world. The benefits in meeting the World Health Organisation goals to provide universal health coverage through an urgent and rapid increase in trained workforce cannot be underestimated (World Health Organisation, 2015). However, the digital divide between countries, especially between high and low and middle income countries, is potentially a major challenge to these ventures. Technology that is appropriate to the local contexts, with lower bandwidth cellular and online networks, will need to be considered and international collaboration between medical schools will need to be developed.
The challenges of change after the COVID-19 pandemic
We have presented several potential future scenarios of the use of technology, including emergent technology, in medical education after the pandemic resolves and our overall vision has been positive, with a discussion of the advantages for teaching and learning. However, it is important to consider the challenges that will need to be addressed if the expected potential transformative changes are to continue to be embedded and further evolve over time.
The effective of use of technology for enhancing teaching and learning has been discussed earlier but achieving the desired outcome and impact will only be realised by continuing to develop all medical educators in how to skillfully align the various contributory factors, including the learner, the learning objectives, the learning content, the instructional design, the technology and the context ( Zaharias and Poylymenakou, 2009 ). The Horizon 2020 report also highlights the essential need to implement ‘learning engineering’ if an emergent technology, such as more sophisticated virtual reality, is being considered for use in teaching and learning. The components of this approach includes design thinking, agile and iterative development, user experience evaluation and the application of learning science to craft the learning experience ( Badwan et al. , 2018 ). Many educators are likely to require further development and training in the effective use of technology for enhancing teaching and learning.
The development of emergent technology, especially when specifically for teaching and learning, is often costly and requires a range of different expertise. However, the Horizon 2020 report also highlights the increasing trend for open educational resources (OER) that are available without restriction, including financial cost, to both educators and students across the world. We consider that the opportunity for all medical education providers to offer OER has never been more appropriate and we urge all providers to continue their current collaborative ventures.
Finally, at this time of transformative change in the use of technology in medical education, we recommend that the opportunity is grasped to increase the development of an educational scholarship related to the use of technology and to increase the implementation of global benchmarking standards ( Goh and Sandars, 2019 ). Both of these ventures have the future potential to ensure that the transformative change continues to benefit medical education across the world.
Take Home Messages
The COVID-19 pandemic has been a major disruptive change to medical education across the world and the use of technology has been rapidly and innovatively used in an attempt to maintain teaching and learning. When the pandemic resolves, transformative change is likely to occur in the way that technology will be used in medical education, especially with the integration of emergent technology. There are significant benefits to this transformative change but there are important challenges that need to be addressed if the future and continuing use of technology in medical education is to be effective and have a positive impact on both educators and students across the world.
Notes On Contributors
Poh Sun Goh, MBBS, FRCR, FAMS, MHPE, FAMEE, is an Associate Professor and Senior Consultant Radiologist at the Yong Loo Lin School of Medicine, National University of Singapore, and National University Hospital, Singapore. He is a graduate of the Maastricht MHPE program, a member of the AMEE TEL committee, and a Fellow of AMEE. ORCiD: https://orcid.org/0000-0002-1531-2053
John Sandars MB ChB (Hons), MSc, MD, MRCP, MRCGP, FAcadMEd, CertEd, FHEA is Professor of Medical Education at Edge Hill University Medical School, Ormskirk, UK, and is Co-Chair of the AMEE Technology Enhanced Learning Committee. ORCiD: https://orcid.org/0000-0003-3930-387X
Declarations
The author has declared that there are no conflicts of interest.
Ethics Statement
This is a Personal Opinion piece and does not require Ethics Approval.
External Funding
This article has not had any External Funding
Bibliography/References
- Ahmed H., Allaf M., Elghazaly H. (2020) COVID-19 and medical education.The Lancet.Online First. Published: March 23, 2020. https://doi.org/10.1016/S1473-3099(20)30226-7
- Badwan B., Bothara R., Latijnhouwers M., Smithies A., et al. (2018) The importance of design thinking in medical education.Medical Teacher. 40 (4), pp. 425–426. https://doi.org/10.1080/0142159X.2017.1399203
- Brown M., McCormack M., Reeves J., Brook D. C., et al. (2020) 2020 Educause Horizon Report Teaching and Learning Edition.Louisville, EDUCAUSE. Available at: https://library.educause.edu/resources/2020/3/2020-educause-horizon-report-teaching-and-learning-edition#materials (Accessed:24 March 2020).
- Chan K. S., Zary N. (2019) Applications and Challenges of Implementing Artificial Intelligence in Medical Education: Integrative Review.JMIR medical education. 5 (1), e13930. https://doi.org/10.2196/13930
- Chermack T. J. (2004) Improving decision-making with scenario planning.Futures. 36 (3), pp. 295–309. https://doi.org/10.1016/S0016-3287(03)00156-3
- Dong C., Goh P. S. (2015) Twelve tips for the effective use of videos in medical education.Medical Teacher. 37 (2), pp. 140–5. https://doi.org/10.3109/0142159X.2014.943709
- Goh P. S., Sandars J. (2019) Digital Scholarship - rethinking educational scholarship in the digital world.MedEdPublish. 8 (2), 15. https://doi.org/10.15694/mep.2019.000085.1
- Goh P. S. (2016) eLearning or Technology enhanced learning in medical education - Hope, not Hype.Medical Teacher. 38 (9), pp.957–958. https://doi.org/10.3109/0142159X.2016.1147538
- Iwai Y. (2020) Online Learning during the COVID-19 Pandemic: What do we gain and what do we lose when classrooms go virtual?Scientific American.Published on March 13, 2020. Available at: https://blogs.scientificamerican.com/observations/online-learning-during-the-covid-19-pandemic/ (Accessed:24 March 2020).
- Jones A., Castellano G.(2018) Adaptive robotic tutors that support self-regulated learning: A longer-term investigation with primary school children.International Journal of Social Robotics. 10 (3), pp.357–370. https://doi.org/10.1007/s12369-017-0458-z
- Martin F., Ritzhaupt A., Kumar S., Budhrani K. (2019) Award-winning faculty online teaching practices: Course design, assessment and evaluation, and facilitation.The Internet and Higher Education. 42 , pp.34–43. https://doi.org/10.1016/j.iheduc.2019.04.001
- Murphy B. (2020) COVID-19: How the virus is impacting medical schools.Published March 18, 2020. Available at: https://www.ama-assn.org/delivering-care/public-health/covid-19-how-virus-impacting-medical-schools (Accessed:24 March 2020).
- PIVOT MedEd (2020) PIVOT Med Ed.Available at: https://sites.google.com/view/pivotmeded/home (Accessed: 24 March 2020).
- Scantlebury A., Sheard L., Watt I., Cairns P., et al. (2017) Exploring the implementation of an electronic record into a maternity unit: a qualitative study using Normalisation Process Theory.BMC Med Inform Decis Mak. 17 (4), pp. 1–10. https://doi.org/10.1186/s12911-016-0406-0
- Wartman S., Combs C. (2019) Reimagining Medical Education in the Age of AI.AMA Journal of Ethics. 21 (2):E146–E152. https://doi.org/10.1001/amajethics.2019.146
- World Health Organization (2015). Health workforce 2030: towards a global strategy on human resources for health.Available at: https://apps.who.int/iris/bitstream/handle/10665/330092/9789241508629-eng.pdf (Accessed:24 March 2020).
- Zaharias P., Poylymenakou A (2009) Developing a usability evaluation method for e-learning applications: Beyond functional usability.Intl. Journal of Human-Computer Interaction. 25 (1), pp. 75–98. https://doi.org/10.1080/10447310802546716
- Zweifach S. M., Triola M. M. (2019) Extended Reality in Medical Education: Driving Adoption through Provider-Centered Design.Digital Biomarkers. 3 , pp. 14–21. https://doi.org/10.1159/000498923
Comments on this article Comments (0)
Open peer review.
This review has been migrated. The reviewer awarded 4 stars out of 5
The article is a combination of a status analysis post COVID pandemic and a projection into the future of what is to come after the situation is over. I likes a lit the framework and think it is useful in documenting the situation but i believe more insight into the future sustainable gains if this chaos is needed
Competing Interests: No conflicts of interest were disclosed.
- Respond or Comment
- COMMENT ON THIS REPORT
This review has been migrated. The reviewer awarded 5 stars out of 5
I read this article by two experts in TEL with interest and found the framework very helpful indeed. It veered around a bit from being an opinion piece to a position paper with recommendations, and I think defining the focus and structure a bit more clearly would help.However, this is just my view and I thought it was excellent with some good signposting to helpful resources as well. There’s lots more literature on change management such as transition curves, etc and the leadership literature on collaboration etc that might be considered too.I also agree with other reviewers and the authors about Impact of the length of the lockdowns on the normalisation. At the moment we’re still a bit in the excited crisis management stage and we need to shift along the curve so all this learning and potential innovation and transformation isn’t lost A great paper, thank you
This is an interesting article on the use of technology in medical education after the COVID-19 pandemic. As mentioned by the authors the duration and extent of the disruption can influence the possible scenario of medical education. Emergent technology is becoming cheaper and more widely available and today most can be accessed using a smartphone or a tablet. One of the important issues will be the cost of the created content and what may be considered as a fair price for the developers. If it become too high then many educators in developing nations may not be able to access the same. This is another in a series of manuscripts in MedEdPublish on the COVID-19 pandemic and its effects on different aspects of medical education.
Interesting opinion on the use of technology in medical education after the COVID-19 pandemic with rich examples and data! It enlightens us to think deeply about the impact of the COVID-19 pandemic on medical education.
Note on Abstract and IntroductionThe abstract stated the thesis statement of the initiated work except explaining the design of the paper though the very last clause of the abstract “The benefits and challenges of the use of technology in medical education are discussed with the intention of informing all providers on how the changes after the pandemic can have a positive impact on both educators and students across the world” provided the trajectory of constructions of the paper.Introduction should initiate a thesis statement along with the explanation of the scope of ‘technology use’, ‘medical education’, ‘covid-19’ and ‘the vision’ on all these progress and trajectory.The Body of DiscussionThe opinion writing is argumentative and is constructed with examples and researched data. The authors have been tailored to make this conception convincing across the continuum of medical education by providing recent references.Note on Benefits and Challenges of changes:The paper has been neutrally justified with the address of benefits and challenges of the envisaged trajectory of distribution of medical education. But the later portions of both the paragraphs have introduced recommendation; for example, the following statement “Technology that is appropriate to the local contexts, with lower bandwidth cellular and online networks, will need to be considered and international collaboration between medical schools will need to be developed” should have been superimposed at the place of recommendation. Note on Take Home messages and ConclusionThe paper has not directly introduced any discussion on conclusion where the thesis statement of the paper becomes iterative and approved. This paper supposes to fail in this case; Take home messages has been concluding remarks of the paper and that’s why; the recommendation is underestimated. But irrespective of these constructional pitfalls, the introduced idea is constructive, adoptable and it claims novelty. The theme is clear and convincing.
This is an excellent article outlining trends in technology in medical education and how the covid 19 pandemic will affect these trends. The authors are very likely to be right that things will not go back to the way they were before. But how things will change is hard to predict. Technology enhanced learning has been becoming normalised for some time now – it is just another way for students and doctors to learn. Students and doctors often say they use online resources to stay updated. But the pace of change of the knowledge base around covid 19 has been unprecedented. Learners cannot read all of it or stay across all of it. Point of care learning will be needed as a result. This will be especially important for those final year students who are now rapidly preparing for actual practice. It would be interesting to hear the views of the authors and others about technology enhanced learning and a rapidly changing knowledge base.
The authors have aptly putforth their views in the present article about the aid by technology in medical education. In the coming months, with a great hope of positivity, we can believe that medical education and the whole aim of equipping medical personels for the future can be achieved more prominently.The spread of the COVID-19 has brought a stark reality to the human kind that change is constant. And this should spring us back in action with better ways of teaching, learning and treating our patients. The ubiquitous availability of video and audio accessories in all our techologies including laptops, mobile phones has eased this difficult phase.Indeed, it is essential to assimilate and plan a new way of reaching out to all the concerned individuals.
If anything good can come out of the Covid-19 pandemic it is the change that will occur in health professions education ( and education in general) and the emergence of technology -enhanced learning, in all its forms. As someone whose children call a digital dinosaur when it comes to IT, I found this paper very easy to read and an excellent review of both the present and potential future situations re TEL.I strongly recommend it to all those involved in curriculum planning.
An interesting opinion piece from two authors with a major interest and understanding of the area of technology supporting learning. It would be useful to situate this paper with others where the current COVID situation has meant that educators have used technology in practice to over come difficulties for example the recent piece by Judy McKimm and colleagues: Manuscript ID: 2936Article title: Health Professions' Educators' Adaptation to Rapidly Changing Circumstances: The Ottawa 2020 Conference Experience
Reviewer Status
Alongside their report, reviewers assign a status to the article:
Reviewer Reports
- Manish Khazane , SRM UNIVERSITY,RAMAPURAM,CHENNAI.
- Trevor Gibbs , AMEE
- Trudie Roberts , Leeds Institute of Medical Education
- Kieran Walsh , BMJ
- Shaoting Feng , The First Affiliated Hospital of Sun Yat-sen University
- P Ravi Shankar , American International Medical University
- Judy McKimm , Swansea University
- Samar Ahmed , Ain Shams University Faculty of Medicine
Comments on this article
All Comments (0)
Competing Interests Policy
Provide sufficient details of any financial or non-financial competing interests to enable users to assess whether your comments might lead a reasonable person to question your impartiality. Consider the following examples, but note that this is not an exhaustive list:
- Within the past 4 years, you have held joint grants, published or collaborated with any of the authors of the selected paper.
- You have a close personal relationship (e.g. parent, spouse, sibling, or domestic partner) with any of the authors.
- You are a close professional associate of any of the authors (e.g. scientific mentor, recent student).
- You work at the same institute as any of the authors.
- You hope/expect to benefit (e.g. favour or employment) as a result of your submission.
- You are an Editor for the journal in which the article is published.
- You expect to receive, or in the past 4 years have received, any of the following from any commercial organisation that may gain financially from your submission: a salary, fees, funding, reimbursements.
- You expect to receive, or in the past 4 years have received, shared grant support or other funding with any of the authors.
- You hold, or are currently applying for, any patents or significant stocks/shares relating to the subject matter of the paper you are commenting on.
Stay Updated
Sign up for content alerts and receive a weekly or monthly email with all newly published articles
Register with MedEdPublish
Already registered? Sign in
Not now, thanks
Stay Informed
Sign up for information about developments, publishing and publications from MedEdPublish.
We'll keep you updated on any major new updates to MedEdPublish
The email address should be the one you originally registered with F1000.
You registered with F1000 via Google, so we cannot reset your password.
To sign in, please click here .
If you still need help with your Google account password, please click here .
You registered with F1000 via Facebook, so we cannot reset your password.
If you still need help with your Facebook account password, please click here .
If your email address is registered with us, we will email you instructions to reset your password.
If you think you should have received this email but it has not arrived, please check your spam filters and/or contact for further assistance.
- Harvard Medical School
HMS Theses and Dissertations
- Communities & Collections
- By Issue Date
- FAS Department
- Quick submit
- Waiver Generator
- Lin, Yan (2)
- Aboelsaad, Iman Ahmed Fathalla (1)
- Acar, Utkucan (1)
- Acharya, Shree (1)
- Afari, Henrietta (1)
- Afinogenova, Yuliya (1)
- Agrawal, Vishesh (1)
- Akabane, Andressa Lumi (1)
- Akinwunmi, Babatunde Olayode (1)
- Al Qureshah, Fahd (1)
- ... View More
- Medicine (79)
- Immunology (60)
- Education (14)
- Neurosciences (14)
- Health sciences (13)
- Oncology (12)
- Bioinformatics (10)
- Biology (8)
- Health education (6)
- Medical Personnel (6)
- Scholarly Project (2)
- Honors in a Special Field (1)
- Master of Medical Sciences in Biomedical Informatics (1)
- Master’s Program in Clinical Investigation (1)
- DASH Stories
- Accessibility
- COVID-related Research
- Terms of Use
- Privacy Policy
- By Collections
- By Departments
Recent Submissions
Adaptive expertise in plastic surgery: the plastic surgeon experience of developing, maintaining and teaching adaptive expertise , klf6 mediates de novo ornithine synthesis and polyamine production in pancreatic ductal adenocarcinoma , integration of decision support algorithm and genomic mutational analysis for enhanced diagnosis and characterization of hematological diseases .
- Open access
- Published: 16 April 2019
Medical education today: all that glitters is not gold
- L. Maximilian Buja ORCID: orcid.org/0000-0001-8386-7029 1
BMC Medical Education volume 19 , Article number: 110 ( 2019 ) Cite this article
50k Accesses
111 Citations
23 Altmetric
Metrics details
The medical education system based on principles advocated by Flexner and Osler has produced generations of scientifically grounded and clinically skilled physicians whose collective experiences and contributions have served medicine and patients well. Yet sweeping changes launched around the turn of the millennium have constituted a revolution in medical education. In this article, a critique is presented of the new undergraduate medical education (UME) curricula in relationship to graduate medical education (GME) and clinical practice.
Medical education has changed and will continue to change in response to scientific advances and societal needs. However, enthusiasm for reform needs to be tempered by a more measured approach to avoid unintended consequences. Movement from novice to master in medicine cannot be rushed. An argument is made for a shoring up of biomedical science in revised curricula with the beneficiaries being nascent practitioners, developing physician-scientists --and the public.
Unless there is further modification, the new integrated curricula are at risk of produce graduates deficient in the characteristics that have set physicians apart from other healthcare professionals, namely high-level clinical expertise based on a deep grounding in biomedical science and understanding of the pathologic basis of disease. The challenges for education of the best possible physicians are great but the benefits to medicine and society are enormous.
Peer Review reports
Introduction
The traditional medical education system widely adopted throughout most of the twentieth century has produced generations of scientifically grounded and clinically skilled physicians who have served medicine and society well. Yet sweeping changes launched around the turn of the millennium have constituted a revolution in undergraduate medical education (UME) and graduate medical education (GME) [ 1 , 2 , 3 ]. While continual assessment leading to measured adaptation is essential for the enduring value of a system, simultaneous and multifaceted change such as that occurring in the traditional medical education system qualifies as disruptive innovation [ 4 ]. The purpose of this article is to offer a critique and express a major concern by a physician-scientist, pathologist and medical educator that the contemporary medical education system is being subject to the downside of disruptive innovation with unintended and potentially detrimental long-term outcomes for academic medicine and clinical practice.
The past century in medical education
The education of a physician has developed to encompass pre-medical preparation, a course of study in a medical school which is typically a major component of an academic medical center (AHC), and medical specialty training in residency and fellowship programs, UME and GME, respectively [ 5 , 6 ]. This education provides the basis for a professional career enhanced by continuing medical education and life-long learning. Early in the twentieth century, medical education became guided by principles articulated by Abraham Flexner and William Osler. Flexner recommended that medical schools should be university based, have minimum admission requirements, implement a rigorous curriculum with applied laboratory and clinical science content, and have faculty actively engaged in research [ 5 , 7 ]. Osler championed bedside teaching, bringing medical students into direct contact with patients, and learning medicine from these direct experiences under the guidance of faculty clinicians [ 7 , 8 ]. The result was the establishment of two key components or pillars of medical education, namely, the basic or foundational sciences and the clinical sciences [ 2 ]. The two-pillar model of medical education provided the conceptual basis for a four-year UME curriculum comprising biomedical science courses in the pre-clinical years and clinical clerkships in the clinical years. Medical schools utilizing this construct produced scientifically grounded physicians capable of a high level of clinical practice as well as a subset who pursued highly successful careers as physician-scientists and academicians [ 9 ].
AHCs and healthcare system
A fundamental element in the achievement of medical schools in the twentieth century was the development of medical education as a public trust and social contract between the medical schools and society [ 5 ]. However, in-depth analysis of the history of medical education has shown that it is inextricably intertwined with healthcare delivery and broader societal norms [ 5 , 6 , 7 ]. UME and much of GME take place in academic health centers (AHC), which must function in the world of healthcare delivery [ 10 ], and are subject to the complexities of the associated health care system in which they operate, including the fragmented American healthcare system [ 11 , 12 , 13 , 14 ].
Calls for curriculum reform and restructuring
In this context, discontent among academics and professional organizations concerning the traditional medical education construct has accelerated in recent years [ 1 , 2 , 3 , 15 , 16 , 17 , 18 , 19 , 20 , 21 ]. Both the teaching methodology and the content of the established curriculum have come under severe criticism. Calls have been made repeatedly for the cultivation of a different type of physician more attuned to and equipped for practice in the current healthcare scene [ 15 , 16 , 17 , 18 , 19 , 20 ].
Reform movement and integrated curriculum
To promote more active learning and less passive learning, curriculum developers have introduced a variety of approaches, including small group sessions, problem-based learning, self-directed learning, team-based learning, and flipped classrooms as replacements for the traditional lecture format [ 21 ]. However, many in the reform movement consider that pedagogical reform, while necessary, must be joined by content reform to develop the requisite skill set in future practitioners of medicine [ 15 , 16 , 17 , 18 , 19 , 20 ]. As a result, there has been a movement in mass toward adoption of a radically redesigned curriculum as a third wave, post-Flexnerian approach to medical education [ 1 , 2 ]. A major goal of the curriculum reformers is to produce physicians who can deliver an individualized plan of care that reflects the physician’s mastery of basic physiology, awareness of the best current evidence, skillful patient communication, and shared decision-making [ 20 ].
The ideal of the post-Flexnerian third wave is a fully integrated curriculum in place of the traditional curriculum comprised of a distinct pre-clinical component with subject-based courses and a subsequent clinical component [ 22 ]. Initial implementation involves partial integration comprising horizontal integration defined as integration across disciplines but within a finite period of time and vertical integration representing integration across time with breakdown of the traditional barrier between basic and clinical sciences. A fully integrated curriculum is characterized by spiral integration encompassing both horizontal and vertical integration combining integration across time and across disciplines [ 22 ].
This revised design also includes added content addressing broader issues constituting “Health Systems Science” as a third pillar of medical education co-equal with basic and clinical medical sciences [ 23 , 24 , 25 , 26 ]. Topics include population health, health policy, healthcare delivery systems, and interdisciplinary care. A correlate is the replacement of the biomedical model of health and disease with a broader biopsychosocial model of health, disease and the patient-physician relationship [ 23 , 27 ].
A related development is the implementation of the new MCAT that aims to balance testing in the natural sciences with testing in the social and behavioral sciences and assessing critical analysis and reasoning skills. The redesign is based on the premise that tomorrow’s physicians need broader skills and knowledge than in the past [ 28 ]. Medical education reform also includes heavy emphasis on professionalism and professional identity development [ 29 ]. The reforms also are aimed at achieving a more coherent continuum of medical education [ 30 ]. My institution, McGovern Medical School of The University of Texas Health Science Center at Houston, embarked on the path of curriculum restructuring in 2013 and has instituted such a redesigned curriculum beginning in 2016 [ 31 ].

Influence of oversight bodies
Advances in medical care and technology have been driving forces behind these curriculum changes. In the United States, a major impetus for such curriculum changes has come from the Liaison Committee for Medical Education (LCME), and its sponsoring institutions, the American Association of Medical Colleges (AAMC) and the American Medical Association (AMA), and the Accreditation Council for Graduate Medical Education (ACGME) (more accurately, thought leaders in these organizations) [ 32 ]. Regulatory bodies in other countries have had similar roles [ 22 ]. Curriculum reformers have used the imperative of actual and perceived expectations of the LCME as a driver of curriculum revision.
Characteristics of Today’s medical students
A major consideration in any discussion of education is the profile of the students. Analysis of today’s students is that they score higher on assertiveness, self-liking, narcissistic traits, high expectations, and some measures of stress, anxiety and poor mental health, and also lower on self-reliance [ 33 , 34 , 35 ]. These generational characteristics are rooted in shifts in culture and reflect changes in society. These character traits are clearly established by the time students enter medical school.
Notable individual exceptions reinforce the average characteristics of today’s students which have definite positive aspects, such as the focus on the individual, but also some negative consequences [ 33 , 34 , 35 ]. Motivation can become dysfunctional so that high levels of dedication to a previously enjoyed activity can result in burnout. Burnout is alarmingly high among today’s medical students and residents [ 36 , 37 ]. Burnout is a psychosocial syndrome that is associated with motivational, performance and psychological difficulties. Perfectionism, defined as a combination of high standards and high self-criticism, is also on the rise [ 38 , 39 ]. The two may compound each other.
The characteristics of today’s medical students including their strengths and vulnerabilities, present special challenges for faculty engaged in their education [ 40 , 41 , 42 , 43 ]. Notably, while these students have high I.Q.s, they typically show little desire to read long texts [ 33 ]. The implication for educational design (pedagogy) is that these students likely benefit from a structured but also more interactive learning experience and that instruction may need to be delivered in shorter segments and perhaps incorporate more material in media such as videos and an interactive format. But, even when the classroom hour is used for so-called active learning approaches, such as the flipped classroom, attendance is still often poor. There has been a proliferation of commercial products, including First Aid, Firecracker, Osmosis and Pathoma, that attract students with shortcut approaches, including flashcards and videos, for passing standardized tests [ 44 ]. These products cater to the study habits of many of today’s students. Many of today’s medical students are opting for elective perusal online of previously recorded lectures and the use of various previously mentioned study aids while minimizing direct classroom interaction with professors [ 45 ].
General critique
While apparently accepting the practices of today’s medical students as a fait accompli , a key tenant of the reform movement is that the traditional subject-based and lecture-based curriculum has failed to accomplish the desired outcome of producing physicians for the twenty-first century [ 20 ]. Content reformers favor a repeal of major parts of the traditional UME curriculum to make room for the lessons that are aimed at allowing students to develop skills in modern clinical reasoning and decision-making. Major goals of integration are to break down barriers between the basic and clinical sciences and to promote retention of knowledge and acquisition of skills through repetitive and progressive development of concepts and their applications [ 22 ].
Reformers recognize that implementation of the new curriculum requires trade-offs and hard choices. They have clearly articulated that topics such as clinical decision-making, comparative effectiveness and other Health Systems Science topics must take priority over the depth of basic science content presented in traditional courses [ 20 ]. The argument is made that major revamping of basic science in the curriculum is acceptable because of perceived major overlap and repetition among traditional basic science courses. There also is the often unstated but implied view that traditional basic science courses burden medical students with excessive and unnecessary detail. While strong emphasis is placed on integrating basic science courses and providing clinical experiences early in the curriculum, the extension of basic science content into the clinical years has been identified as a major challenge and a major shortcoming of integrated curricula [ 22 , 46 ].
The first two years of the UME curriculum is the only time in the entire professional career of a physician when the fundamentals of biomedical science and the clinical skills of history taking and physical examination intersect coherently, and are formally taught and learned. A background in factual knowledge and relationships among facts is crucial for critical thinking and evidence-based decision-making in medicine [ 46 , 47 , 48 , 49 ]. Studies have shown that factual knowledge of medical science is essential for the development of clinical skill [ 46 , 47 , 48 , 49 , 50 ]. Clinical knowledge is gained from the integration of conceptual knowledge (facts, “what” information), strategic knowledge (“how” information) and conditional knowledge (“why” information) [ 49 ]. There is no short cut here; a certain amount of memorization and with some repetition is required. It is counterproductive to dilute the learning experience of the core material in the pre-clinical years by substituting other topics that are best learned after a foundation is laid and its strength tested through the crucible of clinical practice.
Competency-based education: time-based versus competency-based medical education and accelerated medical education
Momentum has continued to grow for demonstration of a set of competencies rather than cognitive knowledge alone as the primary outcome of UME as well as GME. The movement toward outcomes and competency-based education in UME was presaged by a focus on innovation in GME, which led to the introduction by the Accreditation Council for Graduate Medical Education (ACGME) of the six competencies as key elements in residency training programs [ 51 , 52 ]. Change in the world of GME was compounded by the introduction of the duty hour requirements at about the same time [ 53 ]. The ACGME has moved further along the path of competency-based training with the introduction of milestones as a focus of the new accreditation system (NAS) [ 54 , 55 ]. Competencies also have been linked to Entrustable Professional Activities [ 56 ].
Some are taking the competency construct further by promoting time variable criteria for the granting of the medical degree as well as certification in medical specialties following a period of graduate training [ 57 , 58 , 59 , 60 , 61 , 62 ]. Others are promoting an accelerated three-year UME program [ 63 ].
All would agree that the goal of medical education is to produce competent physicians. However, the educational approach embodied in competence-based curricula for highly skilled professions including medicine versus lower level occupations has been found to be philosophically questionable, methodologically complex and highly controversial [ 64 , 65 ]. The logistics of implementing such programs are daunting and represent another major draw on faculty time to provide evaluation of the ascertainment of the set of competencies and entrustable professional activities (EPAs) of the learners [ 56 , 66 ]. A more feasible approach would be to maintain fixed time programs but allow accelerated advancement coupled with opportunities for dual degrees, pursuit of research, and other projects [ 67 ].
Arguments in favor of reduction of UME to a 3 year program include increased production of physicians to meet the shortage and reduction of student debt. The current interest in some quarters for a 3 year program represents the third time in the last century this idea has been promoted [ 64 ]. This third wave will have to face many of the same issues that affected the previous two attempts.
Impact of student evaluation systems
How students function in an educational program is inextricably linked to how they are evaluated. Recurrent movements to abolish grades, exams and honor societies to mitigate undue competiveness, stress and general malaise is the present educational zeitgeist [ 68 , 69 , 70 , 71 , 72 ]. For many years, the standard system of student evaluation was based on numerical grades in every course and led to a cumulative numerical score and class ranking. As a component of disruptive innovation, some medical schools have completely abolished grades and implemented pass-fail systems. However, most medical schools, including some who have tried the purely pass-fail approach, have arrived at a system of Honors, High Pass, Pass, Marginal Pass and Fail -- essentially the A through F system used in K-12 education [ 73 ].
This has led to the rise of the exaggerated importance of United States Medical Licensing Exam (USMLE) scores, particularly, USMLE Step 1 scores, as the major or sole objective evaluation of cognitive achievement of medical students. Proponents argue that the new curricula are successful because students are performing at least as well on USMLE Step 1 as they did in the old curricula, and that they do as well in pass-fail systems as in systems with grades [ 68 , 69 , 70 , 71 , 72 ]. However, these advocates, in essence, are contributing to the perpetuation of the undue importance of USMLE Step 1.
An undue emphasis on a single high stakes summative evaluation creates a dilemma for medical educators and students [ 73 ]. An excessive focus develops on preparing students for the USMLE Step 1 examination and “teaching to the test” [ 20 , 74 ]. This milieu is counterproductive to in depth assimilation of subject matter in the biomedical sciences. Unintended consequences in multiple domains include conflict with holistic undergraduate medical education admission practices, student well-being, and medical curricula.
Medical students have become increasingly aware of the “USMLE issue.” In an Invited Commentary, medical students from various institutions across the country have reflected on their shared experiences and have postulated that the emphasis on USMLE Step 1 for residency selection has fundamentally altered the preclinical learning environment, creating a “Step 1 climate” [ 44 ]. They have commented on how the Step 1 climate negatively impacts education, diversity, and student well-being, and they have urged a national conversation on the elimination of reporting Step 1 numeric scores. Educators also have articulated similar recommendations regarding making the USMLE results reporting as pass/fail [ 75 , 76 ]. But concern has also been voiced that pass/fail can be a disincentive to motivation for broad knowledge acquisition. Also, the development of an alternate, more holistic standardized metric by which to compare students’ applications for residency positions has been proposed but is currently not operative [ 74 ].
The movement away from meaningful grades for medical school courses also has led to an increasingly elaborate subjective evaluation in “dean’s letters” [ 77 , 78 ]. The AAMC has introduced the Medical Student Performance Evaluation (MSPE) as a refinement of the “dean’s letter.” Approaches to evaluation of student performance generally involve formative and summative exams in the pre-clinical years, and subject exams coupled with faculty assessment of performance, in the clinical clerkships. Then, these evaluations (honors, high pass, pass, etc.) are integrated into lengthy MSPEs or dean’s letters that provide commentary and largely subjective impressions. In spite of the AAMC guidelines of comparative information about applicants be included, dean’s letters or MSPEs often continue to lack specificity regarding student performance [ 77 , 78 ]. Major emphasis continues to rest on USMLE scores for the granting of interviews and ranking of applicants by residency program selection committees [ 74 ].
A second influential criterion relied upon in resident candidate ranking and selection is election to the Alpha Omega Alpha (AOA) Honor Society from the top one-sixth of the class. Election into AOA has long been a motivator for student performance. A relationship between AOA membership and selection into highly competitive residencies is well known [ 79 ]. AOA is receiving criticism that membership is not reflecting the balance of diversity of the student body [ 80 , 81 ]. But, I hold that AOA must maintain a focus on excellence [ 82 ].
The grade abolition movement misses the reality of competition in human affairs. I think that the dilemmas about the “USMLE issue” can be diffused by a return to providing meaningful grades for medical school courses and an overall summative evaluation for the four years of medical school. (My definition of meaningful grades encompasses either numerical or letter grade equivalents which reflect actual performance relative to other students and objective norms.) Students must compete and excel to gain admittance into medical school. This shouldn’t be any different when students are training to be physicians. Safeguards can be put in place to deal with excess competition [ 33 ]. Nevertheless, competition within bounds promotes excellence. I strongly concur with the view that medicine is based on being a meritocracy and needs to remain a meritocracy [ 82 , 83 ].
Impact on medical educators
Over the years, medical educators, including basic biomedical science educators and clinician educators, have had to adapt to changes in curriculum [ 84 , 85 , 86 ]. Many medical educators have experienced significant challenges in the implementation of the new curriculum [ 87 ]. Competing demands on faculty time are causing stress and burnout among faculty as well as learners. A curriculum heavily geared to small group teaching places further considerable demand on faculty time. A significant inverse relationship has been found between faculty members’ readiness to change teaching approaches and their severity of burnout [ 87 ].
The educational mission itself can be enhanced by the recognition of foundational principles for teaching and education [ 88 ]. At Johns Hopkins University School of Medicine, a formal review process has led to the articulation of 10 foundational principles or characteristics of a medical educator [ 88 ]. Each principle addresses an important theme in the educational mission. These principles include specific recognition of the importance of being a role model and the responsibility to develop the next generation of physicians (Table 1 ).
Ethics, professionalism and inter-professionalism in the curriculum
A major goal of the new curriculum is the development of holistic, ethical physicians with clear communication skills imbued with empathy and compassion for patients [ 29 ]. These goals are not new but are imbedded in the ideals of the medical profession which are intrinsic to its code of ethics [ 89 ]. There is a longstanding consensus that professionalism and professional identity formation need to be key elements of medical education [ 29 ]. However, a unifying theoretical or practical model to integrate the teaching of professionalism into the medical curriculum has not emerged [ 90 , 91 ]. Nevertheless, role modeling and personal reflections -- ideally guided by faculty -- rather than blocks of time devoted to didactic exercises -- are widely held to be the most effective techniques for developing professionalism [ 90 , 91 ]. Inter-professional education, another major contemporary thrust, also is best addressed after a foundation in the biomedical sciences is developed [ 92 ].
Regarding the issue of classroom attendance, medical student and teaching faculty attitudes have been found to differ regarding the importance of classroom attendance and its relationship to professionalism, findings that were at least partially explained by differing expectations of the purpose of the preclinical classroom experience [ 45 ]. Students tended to view class-going primarily as a tool for learning factual material, whereas many faculty viewed it as serving important functions in the professional socialization process [ 45 ]. Rather than dealing with practical solutions to enhancing the value of lectures, other formats are promoted which place inordinate demands on faculty time. This scenario is off-kilter. It sends the wrong messages to students regarding personal responsibility and professionalism. A practical approach to dealing with differing expectations and to effectively instill professionalism is to provide students, residents and staff with a written list of expected behaviors coupled with teaching and role modeling, assessment and remediation [ 93 ].
Impact on pathology
Pathology is uniquely both a medical science and a clinical discipline [ 94 , 95 , 96 , 97 , 98 , 99 ]. In the analogy of the tree of medicine, the trunk is general pathology, which draws from all the basic biomedical sciences to elucidate general principles of regulation and dysregulation of homeostasis, and divides into the many branches of special pathology (organ system pathology); each one of these branches supports a specialized field of clinical medicine [ 95 ]. Thus, the place of pathology in the curriculum is seminally important in linking the basic biomedical sciences to clinical medicine and providing an understanding of the pathobiological basis of disease. The Association of Pathology Chairs has put forward a position paper on pathology competencies for medical education [ 99 ]. Since a solid understanding of pathology is core to the practice of medicine in any specialty, the position paper posits that all medical students must learn the basic mechanisms of disease, their manifestations in major organ systems, and how to apply that knowledge to clinical practice for diagnosis and management of patients. However, the place given to the pathobiological basis of disease in the new curriculum models is diminished.
Although a traditional curriculum includes a formal pathology course, pathology has been disadvantaged by the fact that students generally have little exposure to pathology or pathologists in the professionally formative clerkship years [ 100 , 101 , 102 ]. However, a distinction needs to be made between student perceptions of pathology as a career and pathology as a critically important medical science. The task of grounding medical students in principles of pathology, including pathogenesis and pathophysiology of disease, has been made considerably more difficult by the design of the new integrated, modular curriculum. The resultant discontinuance of pathology courses and their replacement by elements of pathology scattered episodically in the pre-clinical years likely has resulted in the dilution of core scientific principles and has contributed to a reduced understanding and interest in pathology [ 100 , 101 , 102 ].
Initiatives to increase the exposure and understanding of pathology and the autopsy are necessarily going to be tailored to the local environment operative at each institution [ 100 , 101 , 102 , 103 , 104 , 105 ]. While these approaches cannot fully substitute for the coherent presentation of the pathobiological basis of disease in a pathology course, it is imperative that pathology educators make this effort.
Nevertheless, exposure of medical students to the autopsy is a casualty of the current environment [ 106 , 107 , 108 , 109 ]. As a consequence, it is disconcerting but hardly surprising that physicians now in residency training and clinical practice have little understanding or appreciation for the autopsy, and, therefore, have little motivation for or experience with discussion of the autopsy with next of kin of the deceased. This state of affairs is contributing to the decline of the autopsy, which remains a uniquely important procedure for quality assurance in medicine [ 108 , 109 ].
Another correlate of the current undergraduate medical educational environment is that pathology now has the lowest percentage of residency positions filled by U.S. seniors in the National Residency Matching Program [ 110 , 111 ]. Furthermore, pathology residency programs have joined other medical specialties in conducting “boot camps” for incoming trainees [ 112 , 113 , 114 ]. The boot camps are aimed at providing the basics of a necessary foundation in pathology-specific medical science and in introducing basic skills and processes required for practice of anatomic pathology and laboratory medicine [ 112 ]. The assessment of pathology educators is that the new LCME-driven curriculum is producing a medical graduate who may think differently, but certainly lacks subject-specific knowledge for a variety of medical specialties. A putatively superior curriculum should not present a need for remedial learning for its graduates. Hopefully, boot camps for pathology trainees will be more effective than appears to be the case for bootcamps for trainees in surgical specialties [ 114 ].
Impact on physician-scientists
Physician-scientists of various stripes have a unique and important role in translating basic science discoveries into advances in clinical medicine [ 115 , 116 ]. Their numbers are small and their development is under threat. In some institutions, tailored curricula are being implemented to promote the development of clinician scientists [ 117 , 118 ]. Nevertheless, there is a legitimate concern that the diminished position of basic science in the new curriculum is detrimental to the future maturation of physician-scientists [ 119 ].
Early predictors of career achievement in academic medicine have been identified as: 1) membership in AOA, 2) rank in the top third of the graduating class, and 3) research experience in medical school [ 9 ]. These three factors were of crucial importance in launching my career as was the seminal importance of a faculty mentor [ 120 , 121 ]. The new curricula need to ensure that such opportunities are available for motivated medical students.
Complexities and proposed solutions
Reformers contend that changes in the healthcare system and in medical practice in the clinic and hospital have outpaced those in the classroom, resulting in a declining relevance of the traditional curriculum and a growing urgency for a paradigm shift in medical education. Three barriers to the implementation of evidence-based curriculum reform have been identified [ 20 ]. First, curriculum revision must take place within a certain time frame, making it a zero-sum game. Second, transitioning from a few basic scientists lecturing entire classes from the podium to numerous small groups often tutored by clinical faculty dramatically increases the teaching demands on all faculty and especially faculty clinicians. Third, an inevitable tension is created between a holistic educational approach and the imperative to prepare students for USMLE Step 1.
Regarding the first point, reformers contend that reduction and revamping of the basic science content is warranted and can be achieved by elimination of perceived redundancy in the old curriculum. But the reality is that biomedical science, both in terms of curriculum time and emphasis, has been diminished in the new curricula [ 102 , 118 , 119 ]. Further negative pressure on the basic sciences is coming from the initiative to incorporate Health Systems Science into the curriculum with associated need to develop faculty with skills in teaching this material [ 23 , 24 , 25 , 26 , 27 ].
Pertinent to the second point, there are special challenges for faculty in educating the current generation of medical students in the Information Age [ 33 , 40 , 41 , 42 ]. Certainly faculty educators need to recognize the characteristics of today’s students and take this into consideration in implementation of the curriculum. However, rather than taking a laissez faire approach, faculty educators need to set expectations regarding standards of performance [ 93 ]. In medical education, it is vital that faculty and staff temper overconfidence and excessive risk-taking [ 33 ]. Pedagogical approaches can be modified to meet the learning pattern of today’s medical students, for example, by blending lecture and non-lecture formats [ 43 ]. Nevertheless, standards for content and learning should remain the same; educators cannot compromise on the material that must be learned [ 33 ]. Also, medical students need to be taught and experience functioning and decision making in the face of inevitable uncertainties in life and medical practice [ 122 , 123 ].
Regarding the third point, neo-curriculum advocates contend that solutions to the dilemma of the usurpation of the curriculum by the USMLE lie outside the control of undergraduate medical educators [ 20 ]. These advocates say that solutions require creativity and action from residency selection committees and the USMLE’s sponsors, the Federation of State Medical Boards and the National Board of Medical Examiners, because of the implementation of the new UME curriculum. But those in control of the UME curriculum can ensure that meaningful objective summative assessments of students in both pre-clinical and clinical courses are included in dean’s letters so that the USMLE is not the sole or primary objective assessment presented to residency selection committees.
In spite of the complexities, I contend that rebalancing the position of medical science in the medical educational curriculum has paramount importance [ 46 , 47 , 48 , 49 , 50 , 102 , 119 ]. This is to be achieved by providing the necessary amount of unencumbered space freed of major competing priorities. Different schools may use different approaches. Nevertheless, I favor restoration of subject-based courses, including a pathology course. Appropriate coordination of subject matter among the courses is essential, but this does not require the modular integration approach. Optimal ways of integrating topics in Health Systems Science during the multiyear curriculum need to be developed such as not to unduly compete with education in the core medical sciences.
Trends in American healthcare, academic medical centers and academic medicine
Contemporaneous with restructuring of medical education, medical practice has undergone a fundamental transformation, dominated by a fixation on increasing efficiency in the delivery of care with quality of care a secondary consideration [ 124 , 125 ]. The standard for the medical product has become good enough rather than excellent.
Regarding academic medicine, from 1985 to 2008, the percentage of active doctors engaged in teaching, research or administration decreased from 9 to 5.5%, and the number of teachers and mentors per US medical graduate declined from 0.11 to 0.07 [ 124 , 125 ]. During the decade prior to 2004, biomedical research funding from all sources in America increased at an annual rate of 6.3%, and the United States funded more than half of all biomedical research conducted throughout the world. Since 2004, the growth rate for research funding has decreased to 0.8%, and the U.S.’ share of the world’s research investment has decreased to 44%. From 1996 to 2014, the percent of Nobel laureates in medicine or physiology who were at US institutions at the time of the award decreased from 80 to 45% [ 124 , 125 ].
These very disturbing trends underscore some of the final words of the noted astrophysicist, Stephen Hawking, who warned that education and science around the world are “in danger now more than ever before” [ 126 ].
As eloquently stated by Brigham and Johns, the essence of excellence in medicine is more than doing what we know to do well, but must include a commitment to discovering what will make the better possible, and a dedication to perpetuating the best of the profession [ 125 ]. I content that countering the very disturbing trends just described is going to require a major multifaceted effort including a renewed commitment to advocacy for education and science and the rigorous education of new scientifically grounded physicians and physician-scientists who can carry the torch forward.
The essence of a physician
As articulated over 100 years ago, the characteristics of the ideal physician extend to personal life, professional life and public life [ 127 ]. There is a broad consensus that the good doctor manifests a combination of humanistic and scientific attributes and capabilities [ 128 , 129 ]. Seven key roles of the ideal doctor have been identified as communicator, collaborator, manager, health advocate, scholar, professional, and the integrating role of medical expert. Importantly all the roles overlap equally to create the ‘Medical Expert’ [ 130 , 131 ]. Movement from novice to master in medicine (medical expert) cannot be rushed. Time, experience –and yes, repetition -- is necessary for maturation. This maturation needs to be built on a solid foundation in biomedical science and the pathobiology of disease. The time and place to inculcate the core of this foundation is the first two years of the UME. There are many years for learning and perfecting clinical skills and evidence-based medicine. This will not happen effectively without a sound foundation in biomedical science. A byproduct of a restoration of a strong medical science curriculum will be a boost to the development of future generations of physician-scientists. Conversely, the combination of educational deficiencies coupled with lifestyle preferences carries the risk of diminishing the status of future physicians [ 33 ].
Enthusiasm for reform needs to be tempered by a more cautious and realistic approach. Unless there is modulation, the new curriculum is at risk of producing graduates deficient in the characteristic which have set physicians apart from other healthcare professionals, namely superior clinical expertise based on a deep grounding in biomedical science and understanding of the pathobiology of disease. Physicians need to remain the preeminent medical experts who strongly rely on understanding of basic mechanisms, particularly in dealing with difficult cases [ 47 , 48 , 49 ].
The overarching goal of medical education is the imparting of the highest principles, knowledge and skills in the nascent physician -- not bending medical education to follow prevalent but counterproductive personal and cultural trends. Our society requires physicians who will not just fit into the current dysfunctional American healthcare system but rather work to change it [ 11 , 12 , 13 , 14 ].
Medicine is a field that attracts people who want to have an impact, and this desire can be harnessed to improve medical education. The character traits of today’s medical students can potentially be harnessed to good ends, such as helping others through medicine. Good medical education resembles evolution in that it advances by ensuring the advancement of the fittest, including the fittest of the current generation of medical students just as the fittest of previous generations have succeeded in the past [ 33 , 82 , 83 ]. The challenges for education of the best possible physicians are great but the benefits for medicine and society are enormous.
Into the future, medical education Quo Vadis?
Abbreviations
American Association of Medical Colleges
Accreditation Council for Graduate Medical Education
Academic health center
American Medical Association
Alpha omega alpha honor medical society
Entrustable professional activity
- Graduate medical education
Liaison Committee for Medical Education
Medical college aptitude test
Medical Student Performance Evaluation
New accreditation system
- Undergraduate medical education
United States Medical Licensing Examination
Gutierrez CM, Cox SM, Dalrymple JL. The revolution in medical education. Texas Med. 2016;112:58–61.
Google Scholar
Samarasekera DD, Goh PS, Lee SS, Gwee MCE. The clarion call for a third wave in medical education to optimize healthcare in the twenty-first century. Med Teach. 2018;40:982–85. https://doi.org/10.1080/0142159X.2018.1500973 . [Epub ahead of print].
Article Google Scholar
Shelton PG, Corral I, Kyle B. Advances in undergraduate medical education: meeting the challenges of an evolving world of education, healthcare and technology. Psychiatr Q. 2017;88:225–34.
Neem JN. Let’s not rush into disruptive innovation. Inside Higher Ed. March 16, 2017 ( insidehighered.com ).
Ludmerer KM. Time to heal. American medical education from the turn of the century to the era of managed care. New York: Oxford University Press; 1999. p. 514.
Ludmerer KM. Let me heal. The opportunity to preserve excellence in American medicine. New York: Oxford University Press; 2015. p. 431.
Norman G. Medical education: past, present and future. Perspect Med Educ. 2012;1:6–14.
Ryan TJ. Osler and his teaching: relevant today. Postgrad Med J. 2015;91(1080):540–1.
Brancati FL, Mead LA, Levine DM, Martin D, Margolis S, Klag MJ. Early predictors of career achievement in academic medicine. JAMA. 1992;267:1372–1.
Lee TH. Discovering strategy: a key challenge for academic health centers. Trans Am Clin Climatol Assn. 2016;127:300–12.
Richmond JB, Fein R. The health care mess: how we got into it and what it will take to get out. Cambridge, Massachusetts: Harvard University Press; 2005. 308 pp
Book Google Scholar
Clifton GL Flatlined. Resuscitating American Medicine. New Brunswick: Rutgers University Press; 2009. p. 322.
Relman AS. A second opinion: rescuing America’s health care. Cambridge, MA: The Century Foundation; 2007. p. 205.
LeFanu J. The rise and fall of modern medicine. Revised Edition. New York: Basic Books, 2012, 590 pp.
Cooke M, Irby DM, Sullivan W, Ludmerer KM. American medical education 100 years after the Flexner report. N Engl J Med 2006;355:1339–1344.
Irby CM, O’Brien BC. Calls for reform of medical education by the Carnegie Foundation for the Advancement of Teaching: 1910 and 2010. Acad Med. 2010;85:220–7.
Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, Fineberg H, Garcia P, Ke Y, Kelley P, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–58.
Weisberg DF. Science in the service of patients: lessons from the past in the moral battle for the future of medical education. Yale J Biol Med. 2014;87:79–89.
Wartman SA, Combs CD. Medical education must move from the information age to the age of artificial intelligence. Acad Med. 2018;93:107–9.
Stevens CD. Repeal and replace? A note of caution for medical school curriculum reformers. Acad Med. 2018:1425–7.
Schwartzstein RM, Roberts DH. Saying goodbye to lectures in medical school – paradigm shift or passing fad? N Engl J Med. 2017;377:605–7.
Brauer DG, Ferguson KJ. The integrated curriculum in medical education: AMEE guide no. 96. Med Teacher. 2015;37:312–22.
Skochelak SE, Hawkins RE, Lawson JE, Starr SR, Borkan JM, Gonzalo JD. Health systems science. Philadelphia: Elsevier; 2017. p. 228.
Fred H, Gonzalo JD. Reframing medical education. Texas Heart Inst J. 2018;45:123–5.
Gonzalo JD, Caverzagie KJ, Hawkins RE, Lawson L, Wolpaw DR, Chang A. Concerns and responses for integrating health systems science into medical education. Acad Med. 2018;93:843–9.
Gonzalo JD, Chang A, Wolpaw DR. New educator roles for health systems science: implications of new physician competencies for U.S. medical school faculty. Acad Med. 2019;94:501–6.
Engel GL. The clinical application of the biopsychosocial model. Am J Psychiatry. 1980;137:535–44.
Kirch DG, Mitchell K, Ast C. The new 2015 MCAT: testing competencies. JAMA. 2013;310:2243–4.
Kirch DG, Gusic ME, Ast C. Undergraduate medical education and the foundation of physician professionalism. JAMA. 2015;313:1797–8.
Aschenbrener CA, Ast C, Kirch DG. Graduate Medical Education: Its Role in Achieving a True Medical Education Continuum. Acad Med. 2015;90:1203–9.
Curriculum/Office of Educational Programs/. McGovern Medical School. https://med.uth.edu/oep/medical-education/curriculum/ .
LCME FUNCTIONS AND STRUCTURE OF A MEDICAL SCHOOL: Standards for accreditation of medical education programs leading to the MD degree, March 2017 ( www.lcme.org/publications/#standards ).
Twenge JM. Generational changes and their impact in the classroom: teaching generation me. Med Educ. 2009;43:398–405.
Twenge J. Generation Me. Why Today's Young Americans are more confident, assertive, entitled - and more miserable than ever before: Atria Books; 2014. Simon and Schuster, Inc. New York; 2014.
Twenge JM. IGen - why Today's super-connected kids are growing up les rebellious, more tolerant, less happy - and completely unprepared for adulthood: Atria Books. Simon and Schuster, Inc. New York 2017.
Rodrigues H, Cobucci R, Oliveira A, Cabral JV, Medeiros L, Gurgel K, Souza T, Goncalves AK. Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS One. 2018;13:e0206840. https://doi.org/10.1371/journal.pone.0206840 .
Frajerman A, Morvan Y, Krebs MO, Gorwood P, Chaumette B. Burnout in medical students before residency: a systematic review and meta-analysis. European Psych. 2019;55:36–42.
Hill AP, Curran T. Multidimensional perfectionism and burnout: a meta-analysis. Personal Soc Psychol Rev. 2016;20:269–88.
Curran T, Hill AP. Perfectionism is increasing over time: a meta-analysis ofBirth cohort differences from 1989 to 2016. Psychol Bull. 2019;145:410–29.
Roberts DH, Newman LR, Schwartzstein RM. Twelve tips for facilitating millennials’ learning. Med Teacher. 2012;34:274–8.
Hunter N, Smith CC, Reynolds EE. Become an effective resident teacher and team leader in 10 tried-and-true steps. J Grad Med Ed. 2018;10:488–90.
Maggio LA, Artino AR Jr. Staying up to date and managing information overload. J Grad Med Ed. 2018;10:597–8.
Liu Q, Peng W, Zhang F, Hu R, Li Y, Yan W. The effectiveness of blended learning in health professions: systematic review and meta-analysis. J Med Internet Res. 2016;18(1):e2.
Chen DR, Priest KC, Batten JN, Fragoso LE, Reinfield BI, Laitman BM. Student Perspectives on the "Step 1 Climate" in Preclinical Medical Education. Acad Med. 2019;94:302–4.
Zazulia AR, Goldhoff P. Faculty and medical student attitudes about preclinical classroom attendance. Teaching Learning Med. 2014;26:327–34.
Schmidt H. Integrating the teaching of basic sciences, clinical sciences, and biopsychosocial issues. Acad Med. 1998;73:S24–31.
Finnerty EP, Chauvin S, Bonaminio G, Andrews M, Carroll RG, Pangaro LN. Flexner revisited: the role and value of the basic sciences in medical education. Acad Med. 2010;85:349–55.
Pangaro L. The role and value of the basic sciences in medical education: the perspective of clinical education – students; progress from understanding to action. Med Sci Educ. 20(3). http://www/iamse.org/ .
Schmidmaier R, Eiber S, Ebersbach R, Schiller M, Hege I, Holzer M, fischer MR. Learning the facts in medical school is not enough: which factors predict successful application of procedural knowledge in a laboratory setting? BMC Med Educ. 2013;13:28.
Violato C, Gao H, O’Brien MC, Grier D, Shen E. How do physicians become medical experts? A test of three competing theories: distinct domains, independent influence and encapsulation models. Adv Health Sci Educ. 2018;23:249–63.
Leach DC. The ACGME competencies: substance or form? Accreditation Council for Graduate Medical Education. J Am Coll Surg. 2001;192:396–8.
Leach DC. Changing education to improve patient care. Postgrad Med J. 2008;84:437–41.
Greenberg WE, Borus JF. The impact of resident duty hour and supervision changes: a review. Harv Rev Psychiatry. 2016;24:69–76.
Byrne LM, Miller RS, Philibert I, Ling LJ, Potts JR 3rd, Lieh-Lai MW, Nasca TJ. Program performance in the next accreditation system (NAS): results of the 2015-2016 annual data review. J Grad Med Educ. 2017;9:406–10.
Wagner R, Weiss KB, Passiment ML, Nasca TJ. Pursuing E\excellence in clinical learning environments. J Grad Med Educ. 2016;8:124–7.
Englander R, Flynn T, Call S, Carraccio C, Cleary L, Fulton TB, Garrity MJ, Lieberman SA, Lindeman B, Lypson ML, Minter RM, Rosenfield J, Thomas J, Wilson MC, Aschenbrener CA. Toward defining the foundation of the MD degree: core entrustable professional activities for entering residency. Acad Med. 2016;91:1352–8.
Powell DE, Carriccio C. Toward competency based medical education. N Engl J Med. 2018;378:3–5.
Frank JR, Snell L, Englander R, Holmboe ES, ICBME Collaborators. Implementing competency-based medical education: moving forward. Med Teacher 2017;39:568–573.
Holmboe ES, Sherbino J, Englander R, Snell L, Frank JR. On behalf of the ICBME Collaborators a call to action: the controversy of and rationale for competency-based medical education. Medical Teacher. 2017;39:574–81.
Lucey CR, Thibault GE, Ten Cate O. Competency-based, time-variable education in the health professions: crossroads. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S1–5.
Murray KE, Lane JL, Carraccio C, Glasgow T, Long M, West DC, O’Connor M, Hobday P, Schwartz A, Englander R, Education in pediatrics across the continuum (EPAACA) study group. Crossing the gap: using competency-based assessment to determine whether learners are ready for the undergraduate-to-graduate transition. Acad Med. 2019;94:338–45.
Harris P, Bhanji F, Topps M, Ross S, Lieberman S, Frank JR, Snell L, Sherbino J, Collaborators ICBME. Evolving concepts of assessment in a competency-based world. Med Teach. 2017;39:603–8.
Leong SL, et al. Roadmap for creating an accelerated three-year medical educational program. Med Educ Online. 2017;22:1396172.
Schwartz CC, Ajjarapu AS, Stamy CD, Schwinn DA. Comprehensive history of 3-year and accelerated US medical school programs: a century in review. Medical Education Online. 2018;23:1530557. https://doi.org/10.1080/10872981.2018.1530557 .
Malone K, Supri S. A critical time for medical education: the perils of competence-based reform of the curriculum. Adv Health Sci Educ. 2012;17:241–6.
Lupi CS, Ownby AR, Jokela JA, Cutrer WB, Thompson-Busch AK, Catallozzi M, Noble JM, Amiel JM. Faculty development revisited: a systems-based view of stakeholder development to meet the demands of entrusable professional activity implementation. Acad Med. 2018;93:1472–9.
Frishman WE. Student research projects and theses: should they be a requirement for medical school graduation? Heart Dis. 2001;3:140–4.
Spring L, Robillard D, Gehlbach L, Moore Simas TA. Impact of pass/fail grading on medical students’ well-being and academic outcomes. Med Ed. 2011;45:867–77.
Robins JA, McInnes MD, Esmail K. What information is provided in transcripts and medical student performance records from Canadian medical schools? A retrospective cohort study. Med Ed Online. 2014;19:25181.
Ange B, Wood EA, Thomas A, Wallach PM. Differences in medical students’ academic performance between a pass/fail and tiered grading system. Southern Med J. 2018;111:683–7.
Wasson LT, Cusmano A, Meli L, Louh I, Falzon L, Hampsey M, Young G, Shaffer J, Davidson KW. Association between learning environment interventions and medical student well-being: a systematic review. JAMA. 2016;316:2237–52.
Pereira AG, Woods M, Olson APJ, van den Hoogenhof S, Duffy BL, Englander R. Criterion-based assessment in a norm-based world: how can we move past grades. Acad Med. 2018;93:560–4.
Schuman AD, Heisel CJ, Black KM, Matusko N, Gilbert CM, James CL, Reddy RM, et al. Student factors that influence clerkship grades and matching into a surgical residency. J Surg Educ. 2019;76:393–400.
Moynahan KF. The current use of United States medical licensing examination step 1 scores: holistic admissions and student well-being are in the balance. Acad Med. 2018;93:963–5.
Katsufrakis PJ, Chaudhry HJ. Improving residency selection requires close study and better understanding of stakeholder needs. Acad Med. 2019;94:305–8.
Andolsek KM. One small step for step 1. Acad Med. 2019;94:309–13.
Naidich JB, Grimaldi GM, Lombardi P, Davis LP, Naidich JJ. A program director's guide to the medical student performance evaluation (former dean's letter) with a database. J Am Coll Radiol. 2014;11:611–5.
Andolsek KM. Improving the medical student performance evaluation to facilitate resident selection. Acad Med. 2016;91:1475–9.
Grayson MS, Newton DA, Patrick PA, Smith L. Impact of AOA status and perceived lifestyle on career choices of medical school graduates. J Gen Intern Med. 2011;26:1434–40.
Wijesekera TP, Kim M, Moore EZ, Sorenson O, Ross DA. All other things being equal: exploring racial and gender disparities in medical school honor society induction. Acad Med. 2019;94:562–9.
Boatright D, Ross D, O'Connor P, Moore E, Nunez-Smith M. Racial disparities in medical student membership in the alpha omega alpha honor society. JAMA Intern Med. 2017;177:659–65.
Frishman WH, Alpert JS. Medicine as a meritocracy. Am J Med. 2019;132:401–2.
Polastri M, Truisi MC. Meritocracy? Ask yourself. J Intensive Care Soc. 2017. p. 276–8.
Greenberg L. The evolution of the clinician–educator in the United States and Canada: personal reflections over the last 45 years. Acad Med. 2018;93:1764–6.
Ibrahim H, Stadler DJ, Archuleta S, Shah NG, Bertram A, Chandrasekhar Nair S, Alkhal A, Al-Mohammed AA, Cofrancesco J. Clinician-educators in emerging graduate medical education systems: description, roles and perceptions. Postgrad Med J. 2016;92:14–20.
Stoddard HA, Brownfield ED. Clinician–educators as dual professionals: a contemporary reappraisal. Acad Med. 2016;91:921–4.
Arvandi Z, Emami A, Zarghi N, Alavinia SM, Shirazi M, Parikh SV. Linking medical faculty stress/burnout to willingness to implement medical school curriculum change: a preliminary investigation. J Eval Clin Practice. 2016;22:86–92.
Cofrancesco Jr J, Ziegelstein RC, Hellmann DB. Developing foundational principles for teaching and education for a school of medicine. The pharos/Spring 2018, pp. 43–46.
Riddick FA Jr. The code of ethics of the American Medical Association. Oschner J. 2003;5:6–10.
Birden H, Glass N, Wilson I, Harrison M, Usherwood T, Nass D. Teaching professionalism in medical education: a best evidence medical education (BEME) systematic review. BEME guide no. 25. Med Teach. 2013;35:e1252–66.
Al-Eraky MM. Twelve tips for teaching medical professionalism at all levels of medical education. Med Teach. 2015;37:1018–25.
Dow A, Thibault G. Interprofessional education - a foundation for a new approach to health care. N Engl J Med. 2017;377:803–5.
Kirk LM. Professionalism in medicine: definitions and considerations for teaching. Proc Baylor Univ Med Cent. 2007;20:13–6.
Kumar V, Abbas AK, Aster JC, editors. Robbins and Cotran pathologic basis of disease, ninth edition. Philadelphia: Saunders/Elsevier, 2015, 1391 pp.
Majno G, Joris I. Cells, Tissues, and Disease. Principles of General Pathology. Second Edition. Oxford and New York: Oxford University Press, 2004, 1005 pp. (see pp. vii-ix).
Buja LM, Krueger GRF. Netter’s illustrated human pathology. Teterboro, NJ: icon learning systems; 2005. Second edition: Elsevier; 2014. p. 528.
Krueger GRF, Buja LM, Chandrasekhar C, editors. Atlas of anatomic pathology with imaging. London: Springer; 2013. p. 821.
Buja LM, Butany J, editors. Cardiovascular pathology, 4 th edition. New York: Elsevier; December 2016. p. 814.
Association of Pathology Chairs Pathology Competencies for Med Educ (PCME). https://journals.sagepub.com/page/apc/pcme
Holland L, Bosch B. Medical students’ perceptions of pathology and the effect of the second-year pathology course. Human Pathol. 2006;37:1–8.
Magid MS, Cambor CL. The integration of pathology into the clinical years of undergraduate medical education: a survey and review of the literature. Human Pathol. 2012;43:567–76.
Mukundu Nagesh N, Chiva Giurca B, Lishman S. Innovating undergraduate pathology education through public engagement. Virchows Arch. 2018;472:853–63.
Knollmann-Ritschel BEC, Regula DP, Borowitz MJ, Conran R, Prystowsky MB. Pathology competencies for medical education and educational cases. Acad Pathol. 2017;4:1–36.
Knollmann-Ritschel BEC, Suarez E, Gilliland W, Conran R, Pock A. Pathology course director perspectives of a recent LCME experience: preparation in an integrated curriculum with the revised standards. Acad Pathol. 2017;4:1–7.
Weinstein R, Waer AL, Weinstein JB, Briehl MM, Holcomb MJ, Erps KA, Holtrust AL, Tomkins JM, Barker GP, Krupinski EA. Second Flexner century: the democracratization of medical knowledge: repurposing a general pathology course into multigrade-level “gateway” courses. Acad Pathol. 2017;4:2374289517718872. https://doi.org/10.1177/2374289517718872 .
Rhatigan RM. The autopsy in modern undergraduate medical education: a qualitative study of uses and curriculum considerations. Comparing the case materials available from a teaching hospital's autopsies in 1968 and 20 years later. Acad Med. 1991;66:158–61.
Talmon G. The use of autopsy in preclinical medical education: a survey of pathology educators. Arch Pathol Lab Med. 2010;134:1047–53.
Xiao J, Krueger GR, Buja LM, Covinsky M. The impact of declining clinical autopsy: need for revised healthcare policy. Am J Med Sci. 2009;377:41–6.
Buja LM, Barth R, Krueger GR, Brodsky SV, Hunter RL. The importance of the autopsy in medicine: perspectives of pathology colleagues. Acad Pathol. 2019;6:1–9. https://doi.org/10.1177/2374289519834041 .
Jajosky RP, Jajosky AN, Kleven DT, Singh G. Fewer seniors from United States allopathic medical schools are filling pathology residency positions in the Main residency match, 2008-2017. Hum Pathol. 2018;73:26–32.
Alexander CB. Pathology graduate medical education (overview from 2006-2010). Hum Pathol. 2011;42:763–9.
Naritoku WY, Vasovic L, Steinberg JJ, Prystowsky MB, Powell SZ. Anatomic and clinical pathology boot camps: filling pathology-specific gaps in undergraduate medical education. Arch Pathol Lab Med. 2014;138:316–21.
Yeh DH, Fung K, Malekzadeh S. Boot camps: preparing for residency. Otolaryngol Clin N Am. 2017;50:1003–13.
Neylan CJ, Nelson EF, Dumon KR, Morris JB, Williams NN, Dempsey DT, Kelz RR, Fisher CS, Allen SR. Medical school surgical boot camps: a systematic review. J Surg Educ. 2017;74:384–9.
Daye D, Patel CB, Ahn J, Nguyen FT. Challenges and opportunities for reinvigorating the physician-scientist pipeline. J Clin Invest. 2015;125:883–7.
Milewicz DM, Lorenz RG, Dermody TS, Brass LF. National Association of MD-PhD programs executive committee. Rescuing the physician-scientist workforce: the time for action is now. J Clin Invest. 2015;125:3742–7.
Hall AK, Sl M, Kay Lund P. Clinician–investigator training and the need to pilot new approaches to recruiting and retaining this workforce. Acad Med. 2017;92:1382–9.
Miller D, Thornton CS, Keough MB, Roberts JI, Yipp B, Hollenberg M, Bau JT, Peplowski MA, Beck PL. A prescription that addresses the decline of basic science education in medical school. Clin Invest Med. 2014;37:E284–91.
Catastrophic neglect of the basic sciences in medicine. Lancet. 2012;379:1273.
Ferrans VJ, Hibbs RG, Buja LM. Nucleoside phosphatase activity in atrial and ventricular myocardium of the rat: a light and electron microscopic study. Am J Anat. 1969;125:47–86.
Buja LM. In memoriam: Victor J. Ferrans, MD, PhD Circulation 2002;105:544–5.
Wray CM, Loo LK. The diagnosis, prognosis, and treatment of medical uncertainty. Grad Med Educ December. 2015. https://doi.org/10.4300/JGME-D-14-00638.1 .
Duke A. Thinking in bets. Making smarter decisions when you Don’t have all the facts. New York: Portfolio/Penguin; 2018. p. 276.
Johns ME, Niparko JK. Averaging excellence out? Arch Otolaryngol Head Neck Surg. 1996;122:1039–40.
Brigham K, Johns MME. Good enough medicine: are we “averaging excellence out”? The Pharos. 2018:32–4.
The Associated Press. Posted: Oct 15, 2018 1:55 PM ET | Last Updated: October 15, 2018.
Keen WW. The ideal physician. JAMA. 1900;XXXIV:1592–4.
Hurwitz S, Kelly B, Powis D, Smyth R, Lewin T. The desirable qualities of future doctors – a study of medical student perceptions. Med Teacher. 2013;35:e1332–9.
Steiner-Hofbauer V, Schrank B, Holzinger A. What makes a good doctor? Wien Med Wochenschr. 2018;168:398–405.
RCPSC. CanMEDS 2000: Extract from the CanMEDS 2000 societal needs working group report. Med Teach 2000;22:549–54.
RCPSC. CanMEDS [Online]. Ottawa: College of Physicians and Surgeons of Canada. http://www.royalcollege.ca/rcsite/canmeds/canmeds-framework-e .
Buja LM, Cox SM, Lieberman SA, MacClements J, Williams JF, Esterl RM Jr, Shine KI. A university system's approach to enhancing the educational mission of health science schools and institutions: the University of Texas Academy of Health Science Education. Med Educ Online. 2013;13:1–6. https://doi.org/10.3402/meo.v18i0.20540 .
Download references
Acknowledgements
Local funds only - from the author’s discretionary account including payments he receives from Elsevier for serving as the editor-in-chief of Cardiovascular Pathology, the official journal of the Society for Cardiovascular Pathology.
Availability of data and materials
Not applicable.
Author information
Authors and affiliations.
Department of Pathology and Laboratory Medicine, McGovern Medical School, The University of Texas Health Science Center at Houston (UTHealth), 6431 Fannin St., MSB2.276, Houston, TX, 77005, USA
L. Maximilian Buja
You can also search for this author in PubMed Google Scholar
Contributions
This is a single author paper.
Corresponding author
Correspondence to L. Maximilian Buja .
Ethics declarations
Author’s information.
The author is a physician-scientist who has had longstanding involvement in medical education with regular direct engagement with medical students, residents and fellows during the course of a long career in academic medicine. This career also has involved multiple leadership roles, including department chair (1989–1996), member of the Residency Review Committee for Pathology (1994–1999), member of the board of directors of the ACGME (2003–2009), Medical School dean who supervised a successful LCME accreditation review (1996–2003), Executive Vice President for Academic Affairs who supervised a successful reaffirmation of accreditation of the health science center by the Southern Association of Colleges and Schools (SACS) (2003–2009), director of the Texas Medical Center (TMC) Library (2009–2016), and founding president of a unique system-wide educational academy (2004) [ 132 ].
Ethics approval and consent to participate
Consent for publication, competing interests.
The author declares that he has no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Buja, L.M. Medical education today: all that glitters is not gold. BMC Med Educ 19 , 110 (2019). https://doi.org/10.1186/s12909-019-1535-9
Download citation
Received : 21 January 2019
Accepted : 27 March 2019
Published : 16 April 2019
DOI : https://doi.org/10.1186/s12909-019-1535-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical science
- pathology, physician-scientists.
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Dissertations & Theses
- Collections
Home > Medicine > Medicine Thesis Digital Library
Yale Medicine Thesis Digital Library
Starting with the Yale School of Medicine (YSM) graduating class of 2002, the Cushing/Whitney Medical Library and YSM Office of Student Research have collaborated on the Yale Medicine Thesis Digital Library (YMTDL) project, publishing the digitized full text of medical student theses on the web as a valuable byproduct of Yale student research efforts. The digital thesis deposit has been a graduation requirement since 2006. Starting in 2012, alumni of the Yale School of Medicine were invited to participate in the YMTDL project by granting scanning and hosting permission to the Cushing/Whitney Medical Library, which digitized the Library’s print copy of their thesis or dissertation. A grant from the Arcadia Fund in 2017 provided the means for digitizing over 1,000 additional theses. IF YOU ARE A MEMBER OF THE YALE COMMUNITY AND NEED ACCESS TO A THESIS RESTRICTED TO THE YALE NETWORK, PLEASE MAKE SURE YOUR VPN (VIRTUAL PRIVATE NETWORK) IS ON.
Theses/Dissertations from 2023 2023
Radiomics: A Methodological Guide And Its Applications To Acute Ischemic Stroke , Emily Avery
Characterization Of Cutaneous Immune-Related Adverse Events Due To Immune Checkpoint Inhibitors , Annika Belzer
An Investigation Of Novel Point Of Care 1-Tesla Mri Of Infants’ Brains In The Neonatal Icu , Elisa Rachel Berson
Understanding Perceptions Of New-Onset Type 1 Diabetes Education In A Pediatric Tertiary Care Center , Gabriel BetancurVelez
Effectiveness Of Acitretin For Skin Cancer Prevention In Immunosuppressed And Non-Immunosuppressed Patients , Shaman Bhullar
Adherence To Tumor Board Recommendations In Patients With Hepatocellular Carcinoma , Yueming Cao
Clinical Trials Related To The Spine & Shoulder/elbow: Rates, Predictors, & Reasons For Termination , Dennis Louis Caruana
Improving Delivery Of Immunomodulator Mpla With Biodegradable Nanoparticles , Jungsoo Chang
Sex Differences In Patients With Deep Vein Thrombosis , Shin Mei Chan
Incorporating Genomic Analysis In The Clinical Practice Of Hepatology , David Hun Chung
Emergency Medicine Resident Perceptions Of A Medical Wilderness Adventure Race (medwar) , Lake Crawford
Surgical Outcomes Following Posterior Spinal Fusion For Adolescent Idiopathic Scoliosis , Wyatt Benajmin David
Representing Cells As Sentences Enables Natural Language Processing For Single Cell Transcriptomics , Rahul M. Dhodapkar
Life Vs. Liberty And The Pursuit Of Happiness: Short-Term Involuntary Commitment Laws In All 50 US States , Sofia Dibich
Healthcare Disparities In Preoperative Risk Management For Total Joint Arthroplasty , Chloe Connolly Dlott
Toll-Like Receptors 2/4 Directly Co-Stimulate Arginase-1 Induction Critical For Macrophage-Mediated Renal Tubule Regeneration , Natnael Beyene Doilicho
Associations Of Atopic Dermatitis With Neuropsychiatric Comorbidities , Ryan Fan
International Academic Partnerships In Orthopaedic Surgery , Michael Jesse Flores
Young Adults With Adhd And Their Involvement In Online Communities: A Qualitative Study , Callie Marie Ginapp
Becoming A Doctor, Becoming A Monster: Medical Socialization And Desensitization In Nazi Germany And 21st Century USA , SimoneElise Stern Hasselmo
Comparative Efficacy Of Pharmacological Interventions For Borderline Personality Disorder: A Network Meta-Analysis , Olivia Dixon Herrington
An Examination Of Honor Society Membership, Mistreatment, And Discrimination By Medical Student Demographics , Katherine Ann Hill
Factors Influencing Decision For Contralateral Prophylactic Mastectomy Versus Unilateral Mastectomy , Julian Huang
Beta-Catenin Nuclear Transport In Wnt Signaling: Kap-Beta2/transportin Mediates Nuclear Import Of Beta-Catenin Via A Py-Nls Motif In A Ran Gtpase Dependent Manner , Woong Y. Hwang
Perspectives On Emergency Department-Initiated Buprenorphine Among Clinical Pharmacists , Marissa Justen
Examination For Independent Predictors Of Seasonality Of Birth Across Forty-Nine Low- And Middle-Income Countries: Analyses Of The United States Agency For International Development Demographic And Health Survey Data , Jehanzeb Kayani
Pediatricians, Social Identity, And The Law In The Early-Twentieth-Century United States , Christopher R. Keys
Single Neuronal Firing Dynamics In A Mouse Model For Absence Seizures , Waleed Khan
The Impact Of Cannabidiol In Patients With Early Psychosis: A Randomized Controlled Trial , Sreeja Kodali
Renalase Agonist Therapy And The Cardiac Response To Pressure Overload In Chronic Kidney Disease , Govind Krishna Kumar Nair
Sociodemographic And Insurance Disparities In Urologic Oncology Care Access And Surgical Outcomes , Folawiyo Laditi
How Ethics Committees Deliberate Resource Allocation For Undocumented Children, A Qualitative Analysis , YuKyung Lee
Mental Health Service Use Among Immigrant And U.S. Born Asian American Pacific Islanders , Hieronimus Loho
Severity And Operative Age In Metopic Synostosis: The Association With Neurocognitive Outcomes , Aaron Samuel Long
Comparison Of The Bone Bruise Patterns In Contact And Non-Contact Acute Anterior Cruciate Ligament Injuries , Jay Thomas Moran
Multi-Omic Differences Between Right And Left Sided Colorectal Cancer Liver Metastases , Montana Tremaine Morris
Almajiri Health; A Scoping Review On Disease, Health Literacy And Space For Participatory Research , Muzzammil Imran Muhammad
Investigating Effects Of Glycolysis Inhibition On Metabolism And Extracellular Ph In A Mouse Model Of Hepatocellular Carcinoma , David Nam
Applying Deep Learning To Identify Imaging Biomarkers To Predict Cardiac Outcomes In Cancer Patients , Aishwarya Kishore Nene
Incarcerated Patients Have Higher Mortality After Trauma: An Unreported Healthcare Disparity , Harry NewmanPlotnick
The Association Between Social Needs Care Coordination And Social Needs Status Amongst Patients In A Federally Qualified Health Center , Autumn Nobles
Diagnosis Of Polycystic Ovary Syndrome And Non-Hispanic Black Race Are Predictive Of Hypertension In Reproductive Age Women -Analysis Of Real World Electronic Medical Record Data , Nyerovwo Okifo
Utility Of Shear Wave Elastography In Breast Cancer Diagnosis: A Systematic Review And Meta-Analysis , Aishwarya Pillai
“I Was Reaching Out For Help And They Did Not Help Me”: Mental Healthcare In The Carceral State , Anna Grace Preston
Associations Of Frailty With Tumor Characteristics & Longitudinal Outcomes In Patients With Meningiomas , Hanya M. Qureshi
A Single Nucleotide Polymorphism In An Rgs6 Enhancer Regulates Heart Rate Variability And Parasympathetic Modulation , Namita Ravi
Firearm Injury Prevention Strategies In Children And Young Adults , Christopher Schenck
Assessing Quality Of Oral Cancer Care Across A Health System And Region: Opportunities To Improve Care , Hemali Parimal Shah
Single-Cell Transcriptomic Atlas Reveals Molecular Drivers Of Human Inner Ear Development , Amar H. Sheth
More Than Meets The Eye: Improving Recognition Of Child Abuse In Emergency Departments , May Shum
A Novel Smarcc1-Mutant Bafopathy Implicates Epigenetic Dysregulation Of Fetal Neural Progenitors In The Pathogenesis Of Congenital Hydrocephalus , Amrita K. Singh
Baseline Skin Cytokine Profiles Determined By Rna In Situ Hybridization Correlate With Response To Dupilumab In Patients With Eczematous Dermatitis , Katelyn Singh
Barriers To Identifying Learning Disabilities: A Qualitative Study Of Clinicians And Educators , Lauren Stone
"Come On. I Need An Answer." A Mixed-Methods Study Of Barriers And Disparities In Diagnostic Odysseys , Zeyu Tang
Cognitive Impairment And Long-Term Health Outcomes In Patients With Coronary Microvascular Dysfunction , Abriana Tasillo
Family Dyads, Emotional Labor, And The Theater Of The Clinical Encounter: Co-Constructive Patient Simulation As A Reflective Tool In Child And Adolescent Psychiatry Training , Isaiah Thomas
Comparative Effectiveness Of Digital Breast Tomosynthesis For Breast Cancer Screening In Older Women , Akhil Upneja
Analysis Of Prices And Outcomes For Common Hospitalized Conditions In 2021 , Lina Vadlamani
Recording Multiunit Activity Of The Locus Coeruleus In An Awake Mouse Model Of Focal Limbic Seizures , Marcus Valcarce-Aspegren
Improving Cancer Classification With Domain Adaptation Techniques , Juliana Veira
Soil-Transmitted Helminthiases And Deworming Response In School-Aged Children In Retalhuleu, Guatemala , Rebeca Esther Vergara Greeno
The Synergy Between Physiologic Dendritic Cells And Mrna-Loaded Lipid Nanoparticles And Its Potential As A Cellular Immunotherapy , Brian Myles Wei
Lipid Profiles Help Explain Protection From Atherosclerosis In Ascending Aortic Aneurysm Patients , Gabe Weininger
The Impact Of Peer Interventions On Physical Activity For Individuals Living With Mental Illness , Julia Wolfe
Perioperative Outcomes In Patients With Systemic Sclerosis: An Analysis Of A Large Case Series , Luying Yan
Engineering And Evaluating Biodegradable Bioadhesive Nanoparticle-Encapsulated Sunscreens , Beverly Xi Yu
Theses/Dissertations from 2022 2022
Contested Spaces, Stigmatized Treatment: Methadone In 1970s New York, Boston, And New Orleans , Zoe Miranda Adams
Comorbid Pad And Mvd: A Retrospective Nrd Analysis Of Trends, Outcomes, And Readmissions , Miguel Algara
Epidemiology Of Domestic Violence-Related Ocular Injuries Among Adult Patients , Joana E. Andoh
Longitudinal Modeling Of Early Hiv Burden In The Central Nervous System , Victor Diego Armengol
Generating Clinical Evidence Using Real World Data And Personal Digital Devices , Victoria L. Bartlett
Incidence And Prognosis Of Cranial Neuropathies In Children With Covid-19: A Systematic Review And Meta-Analysis , Priyanka Bisarya
A Deep Dive In Head & Neck Cancer: Machine Learning Applications In Diagnostic And Prognostic Evaluations , Alexandra Tan Bourdillon
A Serological Survey Of Sars-Cov-2 Infection In Casino Employees , Julian Campillo Luna
The Real Cause Of The Broken Rib: Developments In Pediatricians' Approach To Child Abuse; 1960 - 2020 , Sofia Charania
Identification Of A Novel Link Between Adiposity And Visuospatial Ability , Herbert Alexander Chen
Predictors Of Very Late Onset Infection In Kidney Transplant Recipients At Least Ten Years Post Transplant , Harry Cheung
Deep Learning Algorithms For Predicting Response To Neoadjuvant Chemotherapy For Breast Cancer , Rachel Choi
Testing Ictal Conscious Awareness: Responsiveness Versus Recall Of Experiences During Seizures , Violeta Contreras Ramirez
Mechanisms Of Progestin Resistance In Reproductive-Age Women With Atypical Endometrial Hyperplasia , Katherine Mcmaster Cooke
Biomarkers Of Egfr Decline After Pediatric Cardiac Surgery In The Assess-Aki Cohort , Christina Anne-Josiane De Fontnouvelle
Amd3100 Administration For The Treatment Of Asherman’s Syndrome In A Murine Model , Pablo Antonio Delis
Fracture Callus Evaluation In The Setting Of Breast Cancer Metastasis And Rescue Of Healing Via Inhibition Of Erk1/2 , Christopher Dussik
Primary Care Characteristics And Medication Management Among Patients Receiving Office Based Opioid Treatment With Buprenorphine , Xinxin Du
Factors Impacting Trauma-Specific Quality Of Life Following Injury: A Multi-Center Assessment In Lebanon , Ali Elreichouni
Consciousness: Mechanisms And Neuropsychiatric Outcomes , Isaac Gilbert Freedman
Investigation Of Outcomes Following Cervical Spine Surgery In Patients With Pre-Existing Non-Spinal Neurological Conditions , Anoop Raj Galivanche
Medical Students’ Experiences, Knowledge, And Perceptions Of Patients With Substance Use Disorder , Sophia Francesca Gamez
“people Fall Through The Cracks”: Prolonged Lengths Of Stay Beyond Medical Necessity , Lucy Gao
Housing As Healthcare: The Role Of Homelessness In Patient Characteristics And Retention In Outpatient Medication For Opioid Use Disorder Treatment , Marina Gaeta Gazzola
Sleep Apnea In Veterans With Schizophrenia: Estimating Prevalence And Impact On Cognition , Stephen Edward Ghazikhanian
Self-Injurious Behavior And Problematic Video Gaming In Adolescents With Problematic Shopping , Norman Robert Greenberg
Importance Of Social Support In Older Adults After Hospitalization For Acute Myocardial Infarction , Yaakov Green
In-Vivo Nanoparticle Delivery To Fetal Mouse Pancreas And Liver , Mary Elizabeth Guerra
Characteristics Of Inpatient Behavioral Health Services And Hormonal Treatment Decision-Making In Transgender/gender-Expansive Youth , Justin William Halloran
Preferential Utilization Of Resident Physicians To Care For Patients With Medicaid And Persons Of Color At Us Academic Health Centers , Samer Hassan
Atypical Presentation Of Hereditary Hypophosphatemic Rickets With Hypercalciuria Due To Digenic Mutations , Bryan Bo-Ran Ho
Gender Differences In Outcomes Of Coordinated Specialty Care For Early Psychosis , Seong Im Hong
Resident Physician Thriving And The Residency Experience During The Covid-19 Pandemic: A Qualitative Study , Joshua Hyman
Early Experience With The Fda’s Breakthrough Devices Program And Potential Payment Mechanisms , James Johnston
Page 1 of 31
Advanced Search
- Notify me via email or RSS
- Disciplines
- Researcher Profiles
- Author Help
Copyright, Publishing and Open Access
- Terms & Conditions
- Open Access at Yale
- Yale University Library
- Yale Law School Repository
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright

Home > MAHE Student Work > KMCMLR
Kasturba Medical College, Mangalore Theses and Dissertations
Theses/dissertations from 2021 2021.
“The Impact of Self-Stigma of Seeking Help and Perceived Social Support on Burnout among Clinical Psychologists” , Aavrita A
The impact of self-stigma of seeking help &percieved social support on burnout among clinical psychologists. , Aavrita .
Immediate Effects of Novel Hand Rehabilitation Board on Fine Motor Skills in Children with Cerebral Palsy. , Romita Fernandes. Abraham
"COMPARISON OF THREE SCORING CRITERIA TO ASSESS RECOVERY FROM GENERAL ANAESTHESIA IN THE POST-ANAESTHESIA CARE UNIT- A LONGITUDINAL OBSERVATIONAL STUDY " , Shagun Aggarwal
Comparative predictive validity of Alberta Infant Motor Scale and Infant Neurological International Battery in Low Birth Weight Infants- A Prospective Longitudinal Study. , Polisetti Siva Sai Anand
Antagonistic Asynchrony in Muscle Recruitment Pattern of Forward Reach Movement In Children With Cerebral Palsy. , Sanya Anklesaria
Muscle fatigue response of rotator cuff muscles in sitting and standing postures , Lisanne Aranha
Effectiveness of static weight bearing versus modified constraint induced movement therapy on improving hand function in hemiplegic cerebral palsy- A Randomized Clinical Trial. , Ruth Bavighar
How informed are our patients about generic medicines? – A study from coastal South India , Darshan BB
Morphological variants of the human spleen, a cadaveric study , Murlimanju BV
Association between cervical breast cancer and Diabtetes mellitus among women seeking health care in tertiary hospitals od south India: A cross sectional study , Pratik Kumar Chatterjee
Carcinoma Breast in among Women with Diabetes Mellitus: A Case Control Study , Pratik Kumar Chatterjee
Perception of Empathy among medical students: A cross sectional study , Pratik Kumar Chatterjee
CLINICOMYCOLOGICAL PROFILE OF DERMATOPHYTOSIS IN A TERTIARY CARE HOSPITAL IN SOUTH INDIA , Adyashree Dalai
Study of outcome of Ponseti technique of management for idiopathic clubfoot in a tertiary center in south India , Lulu Damsas
Comparative study of emotional labour &burnout on life satisfaction among school teachers across different educational settings , Meghana Dharampalan
“Comparative Study of Emotional Labor and Burnout on Life Satisfaction Among School Teachers Across Different Educational Settings” , Meghana V. Dharmapalan
“Relationship Between Sexual Fantasy, Sexual Communication, Personality Traits and Sexual Satisfaction in Married Individuals” , Rhea Dhir
Comparing the efficacy of USG guided supraclavicular brachial plexus block with or without intercostobrachial nerve block for forearm surgeries – an observational study , DIKSHA D’MELLO
Does Quality of Sitting influence Functional Mobility in Cerebral Palsy? A cross-sectional study , Kaiorisa N. Doctor
Factors effecting gait velocity in osteoarthritis knee-An observational study. , Lisha Gretal D’silva
Effect of Inspiratory Muscle Training on Pulmonary Function, Functional Capacity, Quality Of Life And Length Of Stay in individuals undergoing Cardiac Surgery , Fiona Verdine Dsouza
Relationship of Academic Resilience with Self-Efficacy, and Perceived Social Support; Among Civil Service Aspirants , Neha Eldho
EFFICACY, FEASIBILITY, AND SAFETY OF PERCUTANEOUS IMAGE-GUIDED CATHETER DRAINAGE OF THORACIC, ABDOMINAL, AND PELVIC FLUID COLLECTION , Aishwarya Gadwal
Comparison of efficacy of two different bolus doses of norepinephrine as prophylac-tic to prevent post-spinal hypotension during elective caesarean section , PRANATHI GARAPATI
Trends in Frailty and its Associated factors in Community Dwelling Elderly Indian Population during COVID-19 Pandemic- A Prospective Analytical Study , Karan Gautam
Speech Sound acquisition in some south Indian Dravidian languages: A systematic review , Jesica George
Comparison of Femoral nerve block with Dexmedetomidine and Adductor canal block with Dexmedetomidine for postoperative analgesia for Total Knee Arthroplasty . , NEHA GEORGE
Assessment Of Cardiovascular Risk Factors In Patients With Osteoarthritis Knee , Sagar Goel
Effectiveness of Intermittent Cervical Traction with and without Neural Mobilization in Discogenic Cervical Radiculopathy , Aditi Goyal
Study of maternal and cord blood vitamin B12 levels with anthropometry in term neonates born to normal and malnourished mothers: a hospital based cross sectional study , Sugapradha a. GR
Development of a Questionnaire to Determine the Intervention and Service Delivery Practices of Speech-Language Pathologists for Children with Speech Sound Disorders in India , Shaily Gupta
Relationship between Physical Activity, Objective Sleep Parameters and Circadian Rhythm in Patients with Head and Neck Cancer receiving Chemoradiotherapy- A Longitudinal Study , Rachita Gururaj
“Emotional Contagion, Perceived Stress and Coping Strategies Among Nurses” , Saumya Hariharan
Assessment of knowledge and belief about stuttering among undergraduate medical students , Anushree Harihar
Association of serum lipid levels and other systemic risk factors with retinal hard exudates in diabetic retinopathy patients. , Harshita Mukesh Hiran
Assessment of risk of Diabetes Mellitus by using Indian Diabetes Risk Score among Housekeeping staff , Ramesh Holla
“Emotional Intelligence, Self-compassion, and Life-Satisfaction In Clinical Psychologists” , Vania Jacob
UPPER-CROSSED SYNDROME AND DISABILITY IN SHOULDER ADHESIVE CAPSULITIS. , Aishwarya Jaideep
Study to assess the role of doppler ultrasound in evaluation of arteriovenous hemodialysis fistula and the complications of hemodialysis access , Ishank Jain
Relationship between burnout compassion fatigue, work environment & mindfulness in medical residents , Pranay Javeri
“Relationship Between Burnout, Compassion Fatigue, Work Environment and Mindfulness in Medical Residents” , Pranay Harichandra Javeri
“Dating Anxiety in Emerging Adults” , Jisha V. Jayaprakash
“Relationship Between Tolerance for Disagreement and Mindfulness in Married Males and Married Females” , Jahnavi Jha
Antibiotic usage and susceptibility patterns in Uncomplicated UTI in a Tertiary Hospital in South India , Christy John
Association of bed rise difficulty scale with trunk impairment and functional scales among stroke patients , Leena G. John
Is there a correlation between Pediatric Berg Balance Scale and Centre of Pressure Excursion measured through Dual Axis Static Force Plate™ to assess Balance in Children with Spastic Cerebral Palsy and Typically Developing? , Niharika Joshi
Comparison of Sensory Processing Responses in Cerebral Palsy Subtypes and Typically Developing Children (7-36 months): A Cross Sectional Study. , Archana Antony K
‘A study on the Role of Learned Helplessness, Selfefficacy and Perceived Social Support in Determining Resilience in Parents of Children with Neurodevelopmental Disorders’ , Benaisha Khurshed Katrak
A study of correlation of maternal serum zinc levels with breast milk and cord blood of late preterm neonates , Rashmi Katti
Correlation of histopathology and direct immunofluorescence findings in clinically diagnosed prurigo nodularis , Haritha K
Difference in proximal femur loading due to muscle activity during partial weight bearing and NWB standing- A cross-sectional study. , Smital Kshirsagar
Effect of Sesamol on neurobiochemical changes in diet induced (DIO) obesity model of Zebra fish (Danio rerio) , Rashmii K.S.
Importance of integration of medical ethics with undergraduate medical curriculum- Instructors and student’s perspectives. , Rashmii K.S.
Long-term potentiation (LTP): A simple yet powerful cellular process in learning and memory , Rashmii K.S.
Parkinson's Disease Overview: Alternative Potential Curcumin Treatment, Current Treatment and Prevalence Among Ethnic Groups , Rashmii K.S.
Smart brain of India vs. tricky drugs , Rashmii K.S.
The Role of Professionalism and Ethics Training: Instructor’s and Student’s perspectives in a medical College , Rashmii K.S.
Violence Against Doctors: A Qualitative Study On This Rising Predicament , Rashmii K.S.
Morphometric study of the gracilis muscle and its pedicles , Chettiar Ganesh Kumar
Comparative study of bed side tests to assess difficult airway in paediatric patients , S.Abinandha Kumar
Euphorbia thymifolia (Linn.)- A review on ethno pharmacological properties , Vasavi Kumblekar
COMPARISON OF KNOWLEDGE, ATTITUDE, AND PRACTICE TOWARDS THE USE OF SUNSCREEN IN DAILY LIFE BETWEEN FIRST -AND THIRD -YEAR MEDICAL STUDENTS , Aarushi Lall
‘Feminist Identity, Socio-cultural Attitude Towards Appearance, and Body Images issues in Emerging Adult Women’ , Sheena Lonappan
A novel approach to quantify the Dynamic Windlass Mechanism , Ishita Mahajan
METFORMIN VERSUS INSULIN IN THE MANAGEMENT OF GESTATIONAL DIABETES , Varikuti Manogna
Cognitive abilities among employed and unemployed middle-aged women – a systematic review , Aswini M
‘Emotional Intelligence, Job Satisfaction and Psychological Well-being Among Nurses’ , Chetna M
RELATIONSHIP OF COMPUTER AIDED DESIGN(CAD)-BASED PHOTOGRAMMETRY FOR FACIAL DYSFUNCTION WITH FACIAL GRADING SYSTEMS FOR BELL’S PALSY: A PROSPECTIVE OBSERVATIONAL STUDY , Ankita Mehendale
“Effect of Sensation Seeking and Anxious Traits on Suicidal Ideation Among Adults by Birth Order” , Haripriya G. M
Clinical & radiological assessment of intertrochanteric fractures treated with PFN A2 , Harish M
Effect of a home-based pulmonary rehabilitation programme on respiratory function, functional capacity, and quality of life in patients with chronic obstructive pulmonary disease , Vaibhavi Mhatre
Profiling Communication Characteristics of Individuals with Acquired Neuro-communication Disorder in a Tertiary Care Setup , Nikita Subudhi M
Relationship between weight bearing symmetry, trunk control and fear of fall amongst subjects with stroke: A cross sectional study , VIVIAN NEHAL MONIS
Lower extremity muscle recruitment pattern during sit to stand transfer in children with cerebral palsy as compared to typically developing children- a cross sectional study. , Kiran P. Nadgauda
Knowledge, attitudes and practices of Indian classical singers towards vocal healthcare , Raveena Muralidharan Nair
"Perspectives of Indian Speech Language Pathologists on Adolescent Language Assessment" , Rohana Muralidharan Nair
Effect Of Yoga On Perceived Stress And Pulmonary Function In High Stressed Postmenopausal Women , Vinodini NA
Refractory errors, blood groups & diabetes mellitus: A corrleative study in south Indian population , Vinodini NA
Comparison of Functional outcomes for displaced extra-articular distal radius fractures managed by Conservative versus Operative methods: A Prospective cohort study , Muhammed Ehsan Nazeer
COMPARATIVE STUDYOF THE EFFECTIVENESS OF VAPOCOOLANT SPRAY VERSUS EMLA®® CREAM IN REDUCING PAIN DURING INTRAVENOUS CANNULATION IN ADULT POPULATION , Sisla Nazer P
Assessment of attitude among public towards stuttering in a coastal city of Southern Karnataka , Prithvi N
"Severity assessment of acute pancreatitis using ct severity index and modified ct severity index: association with clinical outcomes and ranson’s criteria. " , GEETANJALI PARMAR
“The Effect of Culture Shock on Adjustment and Psychological Wellbeing Among College Going Students” , Akanksha Patra
‘Effect of Religiosity on Attitude Towards Euthanasia in Medical Students’ , Sumedha Pawar
Development Of A Questionnaire To Determine The Clinical Assessment Practices Of Speech-Language Pathologists For Children With Speech Sound Disorders In India , Prasila Elsa Philip
Correlation of oxidised LDL with oxidant and antioxidant enzymes in subjects with elevated LDL levels , Pooja p
Association of emotional intelligence of primigravida mothers with breastfeeding self efficacy in the early postpartum period and exclusive breastfeeding rates up to 6 months. , Priyanka Reddy p
Morphometric study of the Sartorius muscle and its vascular pedicles , M.D. Prameela
Comparison of the analgesic duration using ultrasound guided popliteal sciatic nerve block between diabetics with neuropathy and non-diabetics without neuropathy , GANESH PRASAD
Early follicular and Mid-luteal phase associated changes in Lower extremity Muscle strength , length and Agility in amateur female athletes – a Prospective Analytical study , Vishnu Priya
Assessment of mobile device based educational intervention on breastfeeding technique in multigravida mothers and its effect on early infant feeding pattern- A randomized controlled trial. , Keerthi Raj
THERMAL ULTRASOUND, MANIPULATION AND EXERCISE ON PAIN AND MOUTH OPENING IN CHRONIC TEMPOROMANDIBULAR JOINT DISORDER: A CASE REPORT , Suchita S. Rao
Correlation of Histopathology and Direct Immunofluorescence: Findings in clinically diagnosed Prurigo nodularis in a Tertiary care hospital , Haritha Reddy
EFFECT OF POSITIONING ON THE PAIN RESPONSE OF INFANTS VACCINATED WITH IPV AND PENTAVALENT (dtwp-HEPATITIS B-HEMOPHILUS INFLUENZA B) VACCINES , Sontosh Reddy
Assessment of the acceptable length of Right internal jugular central venous catheters. , Nivedhitha R
PRELEVANCE OF WORK RELATED DERMATOLOGICAL SYMPTOMS IN HEALTH CARE WORKERS IN COVID-19 ERA , Rana R
COMPARISON OF TWO ROUTINE FACIAL EXERCISE PROTCOLS FOR BELL’S PALSY- A RANDOMIZED CONTROLLED TRIAL , Stephanie Santiago
Profiling selected speech characteristics in individuals with Chronic Cough , Nawal Palakkal Sathar
Advanced Search
- Notify me via email or RSS
- Institutions
- Disciplines
Author Corner
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
Edinburgh Research Archive

- ERA Home
- Edinburgh Medical School
Edinburgh Medical School thesis and dissertation collection
By Issue Date Authors Titles Subjects Publication Type Sponsor Supervisors
Search within this Collection:
Edinburgh Medical School is one of two schools at the College of Medicine and Veterinary Medicine at the University of Edinburgh. The Edinburgh Medical School integrates research and teaching across our three Deaneries: Biomedical Sciences, Clinical Sciences and Molecular,Genetic and Population Health Sciences.
Recent Submissions
Phenotype of newly generated neurons following spinal cord injury in zebrafish , exploration of relationships between life course measures of socioeconomic status and structural brain changes linked with older life cognitive decline , high resolution analysis of the tumour microenvironment of high grade serous ovarian cancer (hgsoc) using single cell transcriptomics and quantitative histopathological examination , complications of portal hypertension: clinical studies , imaging of abdominal aortic aneurysm disease activity and implications for endovascular aneurysm repair , hallmarks of cotranslational protein complex assembly and its relationship with the dominant-negative effect , optimising islet transplantation therapy for the treatment of type 1 diabetes by targeting the liver niche with etanercept-loaded microparticles to promote the long term function of islets , developing a systematic, data-driven framework to identify, evaluate, and prioritise candidate drugs for clinical trials in motor neuron disease , investigating an arginase 1⁺ monocyte- macrophage population in driving fibrosis in chronic kidney disease. , in vivo investigation of component-specific functions of the hippo pathway , prevalence of female infertility in the uk armed forces , understanding colorectal cancer risk loci that alter transcriptional dynamics , behaviour change intervention for smokeless tobacco (st) cessation delivered by dentists in a dental setting: a feasibility study , dna methylation & its regulation in colorectal tumours , lesion reversibility in small vessel disease: understanding changes contributing to vascular dementia , effect of autologous macrophage therapy in cirrhosis in response to individual immune reparative pathways: developing a novel therapy , computational techniques to interpret the neural code underlying complex cognitive processes , identifying genomic and phenotypic risks factors for the clinical progression of depressive symptoms , investigating the essential extracellular invadolysin metalloprotease , defining novel regulators of inflammatory signalling in pancreatic cancer .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ind Psychiatry J
- v.32(1); Jan-Jun 2023
- PMC10236658
Selecting a thesis topic: A postgraduate’s dilemma
Rajiv k. saini.
Department of Psychiatry, Command Hospital (EC) Kolkata, West Bengal, India
Mohan Issac
1 Department of Psychiatry, The University of Western Australia, Perth, Australia
K. J. D. Kumar
2 Department of Psychiatry, Military Hospital, Pathankot, Punjab, India
Suprakash Chaudhury
3 Department of Psychiatry, D. Y. Patil Medical College, Dr. D. Y. Patil Vidyapeeth, Pimpri, Pune, Maharashtra, India
Rachit Sharma
4 Department of Psychiatry, Armed Forces Medical College, Pune, Maharashtra, India
Ankit Dangi
5 Department of Psychiatry, Command Hospital, Panchkula, Haryana, India
It is said that well begun is half done. Choosing a thesis topic and submitting a research protocol is an essential step in the life cycle of a postgraduate resident. National Medical Commission of India mandates that all postgraduate trainees must submit at least one original research work (dissertation), one oral paper, one poster, and one publication to be eligible for final year examination. It is the duty of the faculty to ensure that trainees take active interest and submit their theses on time. However, their journey is often marred by multiple challenges and hurdles. The literature was searched from year 2000 onwards till 2011 using Pubmed, ResearchGate, MEDLINE, and the Education Resources Information Centre databases with terms related to residency training, selecting thesis topic, challenges or hurdles, and conversion of thesis into journal article. Existing literature on the subject matter is sparse. Current article advocates promotion of ethical and original research during postgraduation and proposes a checklist for residents before submission of their proposals.
INTRODUCTION
Residency is an extremely important period in the life cycle of a modern medical graduate. During this period, a resident learns to practice and acquire proficiency in a subject under guidance of a teacher. Along with acquiring new skills, it is also expected that they learn to critically analyze clinical scenarios and reach a rational conclusion. They are also expected to formulate and conduct original research which is submitted in form of a dissertation or thesis. Research work by a postgraduate should eventually translate into a scientific publication in a peer-reviewed medical journal, which helps in dissemination of thesis findings to the community and scientists. It is essential toward furthering medical knowledge, clinical practice, and the progression of science.[ 1 ] The National Medical Commission has stated the aims of completing this task as “Writing the thesis is aimed at contributing to the development of a spirit of inquiry, besides exposing the candidate to the techniques of research, critical analysis, acquaintance with the latest advances in medical science and the manner of identifying and consulting available literature.”[ 2 ]
CHOOSING THE TOPIC
The most intriguing question while conducting research is “How do I choose the right topic and will I be able to find the right answer?” Starting off with fire in the belly gives the best chance of seeing one’s work through. So, it is important to choose something that entices one’s mind and promises a gratifying result. Existing literature on the topic suggests that the journey of choosing the right topic is often marred by multiple challenges and dilemmas at various stages of this tumultuous journey. There are constraints of time, availability of resources, and support network.[ 3 ]
Therefore, students must remain open to suggestions from within and outside their minds. It is also important to allow the research area to simmer inside their mind for some time so that they can analyze various facets of the chosen area. It is at deeper layer of learning where higher order thinking skills such as analysis, synthesis, and evaluation reside. This then justifies the longer period it takes to arrive at a meaningful thesis title as it represents the highest order of cognitive reasoning referred to as “create” stage.[ 2 ] Short of this, novice researchers operate at lower order and remain “copy-paste” type of researchers.[ 4 ]
Lord “Dhanwantri” also known Physician of Gods brought “ Amrit ” elixir of life after “Samudra Manthan,” which was the result of intensive deliberations.[ 5 ] A systematic stepwise approach for answering any research question offers the best chance of finding the right answer. Succeeding paragraphs in this article shall delve into an enriching scientific journey toward zeroing onto a suitable thesis title.
Area of interest
A journey into an area of one’s interest is bound to be fulfilling. It is a good idea to review one’s past works and experiences, which may be intriguing. A frank and one-to-one discussion with the guide further helps in unravelling novel ideas. Starting with an open and fertile mind promises novel ideas and helps to sustain long-term interest and enthusiasm.[ 6 ] Tendency to merely replicate similar studies should be avoided as they fail to ignite the zest for newer information.[ 7 ] Think about why you got into your field of study. Consider what you like to read about in your free time, especially things related to your field.
From general to specific
A dissertation topic in medicine needs to be captivating and must intrigue the reader to look closer into the research work.[ 8 ] At the outset, it is a good strategy to just define a broad area and a dissertation topic need not be very specific or restrictive. The defined general area must be studied thoroughly and all its facets analyzed in detail. Look for gaps in knowledge which offer an avenue for research. For example, while studying factors responsible for relapse in alcohol dependence, doing a research on employment status of the spouse may be a good idea as it may not have been studied as extensively as other factors. It is needless to say that the student must first be familiar with the disease and all the variables which define its long-term trajectory. Medical science is an evolving field . There are factors of significance that can crop up during course of the study. Therefore, some scope for minor modifications must be kept for unexpected spinoffs. Most of the institutional review board permit minor revision of the protocols though they adhere to their own standards to safeguard interests of the patients. Authors conducted a survey and found that out of 184 submitted, 96 (52%) received requests for minor revision of research protocols. The acceptance resulted in further refinements in research methodology and outcomes.[ 9 ] Therefore, while submitting any protocol, some scope for minor change with probable reasons must be endorsed so that there are no complications while submitting final draft. After discussion with the guide, a suitable title can be given to the research proposal. Selection of the title should be such that it reflects the gist of the whole research and must attract attention of the reader. The title has a long shelf life and may be the first (and many a times, also the only) part of an article that readers see or read. Based on their understanding of the title, readers decide if the article is relevant to them or not.[ 8 ]
Do not bite more than you can chew
The average time allotted for completion of the MD/MS/DNB thesis is 2 years. It may be further reduced due to administrative delays like allotment of thesis guides and selection of topic. It is safe to assume that it takes around 1 month to finalize and submit the protocol and 2 months to write, print, and submit the complete thesis. That leaves just around year and nine months for actual and adequate data collection. All these facts must be kept in mind to ensure genuineness of data.[ 10 ]
A bird in hand is worth two in the bush
Modern medical science thrives on multispecialty approach, and it is not uncommon that students may end up with a research topic involving more than one department or more than one facility of the institution. Studies conducted during Covid pandemic are perfect examples owing to multiple facets of the illness in terms of prevention, pathophysiology, and long-term sequele.[ 11 ] A realistic check for the available resources in terms of infrastructure, availability of study materials, and support from affiliated departments must be done before finalizing the research topic. It is highly unlikely that your thesis is the first or the last research work in a particular area. Negotiating with other department/institution to regularly avail their facilities is often challenging. It is because of the difference in timing, priorities, work culture, and administrative barriers. One way to deal with it is to have a co-guide from that facility/institution. Dissertation reviewers have noticed that students often select topics that become unmanageable during course of their study. It can lead to development of stress and uncertainty about findings at the time of analysis. It was found that institutional support in terms of guidance, access to other departments, and statistical guidance improved overall performance of students and led to timely submission of thesis for publication in journals.[ 12 ]
Avoid controversy
Getting into controversy during initial years of residency is bound to raise stress levels and may dissuade the worker from continuing the research work. Field of medicine is fast evolving on the wheels of technology. Moral and ethical boundaries are slowly getting blurred. Many a times, laws are not revised and many laws are land specific. Therefore, it is a sound practice to familiarize oneself with existing laws and to take care that they are not violated. Central Drug Standard and Control Organization is the regulatory authority responsible for clinical trial oversight, approval, and inspections in India. It functions under Director General of Health Servicesand part of Ministry of Health and Family Welfare. The information is available online on their website and it is updated regularly. It is a good idea to visit the website and familiarize oneself about the existing laws before undertaking any research work. The website also gives information about National Ethical Guidelines for biomedical and health research involving human participants. Similarly, informed consent needs to be spelt out quite clearly and should be devoid of incomplete information or concealment of vital health related information. It is now mandatory that all research proposals be vetted by institutional ethical committee prior to submission to the university.[ 13 - 15 ]
Conformation with national health policy
Young medical professionals can contribute immensely by their research designs and valuable inputs in ratifying existing health-related measures or to suggest further refinements. This concept must always be kept in mind while formulating any research designs. Researchers of today are planners for tomorrow and their work is reflection of their goal toward health of the nation. In a comprehensive report, it was found that merely 0.5% of the 4230 thesis citations were quoted in policy decision.[ 16 ] The figures may be even lower for this country. The figures are abysmal compared to the magnitude of the research undertaken in centers of higher learning. The success of National Iodine Deficiency Disorder Control Program in India owes credit to sound scientific inquiries beginning in 1956. Despite stiff opposition and cultural bias, the program gained strength and helped in significantly reducing burden of iodine deficiency disorders.[ 17 ] The findings led to significant policy change and legislation supporting sale of only iodized salt in the country.
Scope for publication
Any research work is considered futile if it does not reach the stage of publication in a reputed journal. A genuine research must eventually translate into a research article. It has become increasingly difficult to translate thesis into a scientific publication in an indexed journal due to stringent standards and peer review. In a retrospective analysis of 85 theses, it was found that the conversion rate to peer-reviewed publication was 32.5%. The most common reasons for not publishing were a lack of originality and poor design. The authors further encouraged publication of full length articles as it helped residents in long term.[ 18 ] Originality of research, sound methodology, and analysis of data besides cogency in manuscript writing have been defining factors that promote acceptance of an article in a reputed journal.[ 19 ] Lure of quick publishing in a predatory journal can be damaging in the long run. Young and inexperienced authors publishing in a predatory journal must be aware of the damage of their reputation, of inadequate peer-review processes and that these journals might get closed any time for variety of reasons. Such publishing harms the scientific community in the long run, and hence such an approach is best avoided.[ 20 ] It is prudent practice to check whether an intended journal is predatory or not from the https://predatoryjournals.com/journals/or Beall’s list (https://beallslist.net/). Similarly, increasing the score by “salami” publication is unethical and should be avoided.
Familiarization with research methodology
Imagine you are gifted a do-it-yourself kit to build a plane which can fly. It is meant for an age group of 18 years or more and should take 1 h to assemble. It has all the wheels, gears, levers, motors, wires, motherboard, etc., required to assemble it into a functioning plane. The kit also has a manual. How long should it take to assemble? 60 min? Now imagine trying to assemble without the manual. It may be extremely difficult if not impossible to assemble the plane and is surely bound to take much longer. Research methodology is exactly like a manual for research. A major confounding factor in medical research is student’s conceptual understanding and comfort level with research methodology.[ 21 ] Findings indicate that there were noticeable differences in perspectives regarding what constitutes research methodology and its utility at least during the first year of residency.[ 21 ] Familiarizing with basic research methods is now mandated for all the medical postgraduates before they submit their research proposals, and free certificate online courses are available on their website. Writing a thesis during MD/MS and DNB courses, without having a correct research methodology planning, is practically impossible. Some of the prominent causes of rejection of submitted manuscripts are poor methodology, small sample size, and poor statistical analysis.[ 22 ] Furthermore, postgraduate students choose research methodology based on a number of factors such as familiarity with a method, methodological orientation of the primary supervisor, the domain of study, and the nature of research problems pursued. Participants reported key challenges that they faced in understanding research methodology include framing research questions, understanding the theory or literature and its role in shaping research outcomes, and difficulties in performing data analysis.[ 23 ]
Motivation level of the researcher
Dr APJ Abdul Kalam, former president of India, quoted that “Dream is not that you see in sleep but it is something that doesn’t let you sleep.” No research work will reach its logical conclusion till the time a researcher has strong motivation to pursue it. Another factor that defines sustained interest in thesis topic is motivation. As described by David Langford, there exists a continuum from extrinsic to intrinsic motivation.[ 24 ] Extrinsic motivation basically refers to a situation wherein the students are ordered (to study). As we move along this continuum, the quality of learning improves consistently with the maturing of the relationship between teacher and student. The culmination of the relationship occurs when the teacher becomes an enabler while the student becomes an active self-learner (intrinsic motivation). The process involves a definitive element of mentorship. In traditional Indian context, Gurukul envisages a firm and enduring relationship between “Guru” (teacher) and “Shishya” (student). Vedas in ancient times were combined with prepared commentaries in the form of “Upanisads.” The term upanisad refers to “Sitting down near a teacher in order to learn.” Though many students have inherent intrinsic motivation, a dynamic “Guru” can really shape the “Shishya.” Though the concept is old, it still remains relevant in modern times because learning medical practice is both art and science and best habits are still passed on to the next generation by trained and experienced teachers.[ 25 ]
WHAT CAN HELP POSTGRADUATE THESIS SELECTION?
The authors of this article put their minds together to devise a questionnaire that can act as a checklist for the residents before they actually submit their draft proposal for submission [ Table 1 ]. The checklist contains 10 questions and the responses can be marked from strongly disagree to strongly agree on a five-point likert scale. The checklist can be self-administered and the responses will give an insight into the lacunae. The residents can gradually work on these lacunae so that they feel at ease during the fantastic journey of scientific research and publication.
Postgraduate thesis topic selection questionnaire
Note: Rate your responses after regular intervals while preparing your research proposal and work on areas that feel difficult
Choosing thesis topic and submitting the protocols is an important milestone in the career of a postgraduate resident. However, its importance cannot be undermined from the fact that it is usually the first scientific pursuit of a medical graduate. Challenges and hurdles are expected but can be overcome with sustained and systematic effort. The authors of this article reviewed the literature concerning this topic and found some key areas which a resident must familiarize with before finalizing their research topic. The postgraduate thesis selection questionnaire can further act as a checklist to facilitate the process.
Financial support and sponsorship
Minds United for Health Sciences & Humanity Trust, IToP STEPS program grant.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Minds United for Health Sciences & Humanity Trust, IToP STEPS program grant for financial support and motivation.

IMAGES
VIDEO
COMMENTS
The 1910 Flexner Report, officially titled "Medical Education in the United States and Canada," was a landmark document that brought about medical education reform in North America. Abraham Flexner, a research scholar at the Carnegie Foundation, visited all 155 medical schools in operation at the time to assess the state of medical education.
Medical education is a specialized discipline within education in general but still follows principles that apply to any learning culture. There are many important features to a medical education often conceptualized as the science (eg, genetics, biochemistry, pathology) and the social (eg, professionalism, team activity, human interaction ...
Dissertation writing in post graduate medical education. SS Harsoor, Mridul M Panditrao, 1 Sumesh Rao, 2 Sukhminder Jit Singh Bajwa, 3 Nishant Sahay, 4 ... University guidelines, but generally ranges between 150 to 300 words. Although it comes at the very beginning of the thesis, it is the last part one writes. It must not be a 'copy-paste ...
Arianne Teherani, Gaurab Basu. , Pages: 377-379. First Published: 07 December 2023. The authors issue a call to action to the medical education research community, encouraging each of us to lean into the important role we play in addressing the climate and health crisis. Abstract.
Abstract. Systems approach is a time tested, method of trying to understand the reality holistically, and resolving the issues by problem-solving method. It has resulted in enormous applications in almost every field of knowledge, science, technology, industries, agriculture, and health or education. The main essence of systems thinking lies in ...
Medical Education is the leading international journal for research about health professional education. As a pre-eminent medical education journal, we publish papers that are practically relevant and advance conceptual understanding of educational issues, reflecting worldwide or provocative issues and perspectives.
for the Degree of Master of Medical Sciences in Medical Education. Harvard University. Boston, Massachusetts. April 2019 Thesis Mentor: Dr. Amy Marie Sullivan. Tzu-Hung Liu. Understanding Medical Students' Self-Directed Learning in the Clinical Setting: A Cross-Cultural Qualitative Study in the U.S. and Taiwan.
Formal MD Thesis Requirement. All students at Yale School of Medicine engage in research and are required to write an MD thesis during medical school. The only exceptions are students who have earned a PhD degree in the health sciences before matriculation and students enrolled in Yale's MD/PhD program. The YSM MD Thesis is under the ...
Thesis (DPhil)--University of Stellenbosch, 2004. ENGLISH ABSTRACT: In this thesis, an 'alignment approach' to the quality assurance of medical curricula is developed and practically illustrated in the evaluation of a section of a new curriculum in undergraduate medical education and training instituted at the Faculty of Health Sciences of the University of Stellenbosch in 1999.
Alleviating human suffering around the world begins with effective medical educationOver the past several decades, the sciences informing general and health professions education have grown in prominence and potential such that master's programs in this field are now distinguishing components of leading universities. Further, the skills associated with this degree are increasingly viewed as ...
Medical education has a reputation for being demanding and stressful. However, longitudinal surveys across the whole course of study considering risks and resources are rare. For the evaluation of stress and coping we administered the standard instruments Perceived Medical School Stress Scale (PMSS), Hospital Anxiety and Depression Scale (HADS), Work-Related Behavior and Experience Patterns ...
August - Students must attend the HST Research Assistantship (RA) and Thesis meeting and turn in an I-9 form to MIT. December - Identify lab, complete RA paperwork. Includes filling out RA form, and completing online paperwork (W4, M4, direct deposit). Beginning in January - Turn in RA form to Laurie Ward, MIT (this can be delayed, but RA ...
To secure high standards in the quality of education in medical schools, peer-teaching programs should be accompanied by training and supervision [11, 17]. A strength of this research project is that it is a cross-section of all Dutch universities and all study years. Therefore, the results give a good picture of the opinion of Dutch medical ...
Distinct work Your thesis should be distinct from any prior or concurrent graduate-level thesis. Work submitted to fulfill program requirements for another graduate degree (e.g., masters or doctorate) at Harvard or any other university is NOT eligible. ... Harvard Medical School Tosteson Medical Education Center, Suite 347 260 Longwood Avenue ...
The teaching of scientific communication is an important part of basic medical education. Producing a thesis is an essential step for a student graduating from medical school [].It is also important that medical and dental undergraduate curricula should include the teaching of scientific thinking and the principles of scientific research [].In Finland, 10-20 weeks are reserved for advanced ...
Purpose Artificial Intelligence (AI) is transforming healthcare and shows considerable promise for the delivery of medical education. This systematic review provides a comprehensive analysis of the global situation, effects, and challenges associated with applying AI at the different stages of medical education. Methods This review followed the PRISMA guidelines, and retrieved studies ...
The impact of the COVID-19 pandemic. The pandemic has resulted in the widespread disruption of medical education and professional training (Ahmed et al., 2020; Murphy, 2020).Examples include reduced teaching with redeployment of medical educators to clinical care and the quarantine and impact of illness on medical educators and students.
Integration of Decision Support Algorithm and Genomic Mutational Analysis for Enhanced Diagnosis and Characterization of Hematological Diseases . The bone marrow can be a window into human disease, providing valuable insights into the underlying mechanisms of various conditions that disrupt normal hematopoiesis. Accompanying the bone marrow ...
The medical education system based on principles advocated by Flexner and Osler has produced generations of scientifically grounded and clinically skilled physicians whose collective experiences and contributions have served medicine and patients well. Yet sweeping changes launched around the turn of the millennium have constituted a revolution in medical education.
The digital thesis deposit has been a graduation requirement since 2006. Starting in 2012, alumni of the Yale School of Medicine were invited to participate in the YMTDL project by granting scanning and hosting permission to the Cushing/Whitney Medical Library, which digitized the Library's print copy of their thesis or dissertation.
Such a shift during the coronavirus disease 2019 (COVID-19) pandemic however resulted in interruption of the medical education even in the most successful medical training programs [1,2]. Besides the clinical activities, teaching, and training, producing a research paper or thesis is an essential step for a student graduating from medical ...
Perception of Empathy among medical students: A cross sectional study, Pratik Kumar Chatterjee. PDF. CLINICOMYCOLOGICAL PROFILE OF DERMATOPHYTOSIS IN A TERTIARY CARE HOSPITAL IN SOUTH INDIA, Adyashree Dalai. PDF. Study of outcome of Ponseti technique of management for idiopathic clubfoot in a tertiary center in south India, Lulu Damsas. PDF
Complications of portal hypertension: clinical studies . Dunne, Philip D. J. (The University of Edinburgh, 2024-03-28) INTRODUCTION: With over 1.32 million global liver cirrhosis related deaths annually, the burden of liver disease is still rising, predominantly due to alcohol and the metabolic syndrome.
Choosing thesis topic and submitting the protocols is an important milestone in the career of a postgraduate resident. However, its importance cannot be undermined from the fact that it is usually the first scientific pursuit of a medical graduate. Challenges and hurdles are expected but can be overcome with sustained and systematic effort.