Article Contents
- < Previous

Case Study: The Implementation of Total Quality Management at the Charleston VA Medical Center's Dental Service
The views expressed in this article are those of the author and do not reflect the official policy or position of the U.S. Air Force, Department of Defense, or the Department of Veterans Affairs.
- Article contents
- Figures & tables
- Supplementary Data
Barry L. Matthews, Case Study: The Implementation of Total Quality Management at the Charleston VA Medical Center's Dental Service, Military Medicine , Volume 157, Issue 1, January 1992, Pages 21–24, https://doi.org/10.1093/milmed/157.1.21
- Permissions Icon Permissions
Total Quality Management (TQM) is an evolving management philosophy which has recently been introduced to the health care industry. TQM requires the use of a continuous process improvement methodology for delivered services. It was implemented at Charleston VAMC's Dental Service as a study to determine its effectiveness at the grassroots level. A modified Quality Circle was established within the clinical service under the guidance of Dr. Edward Deming's 14 principles. Top management support was not present. Many lessons were learned as process improvements were made. The overall success was limited due to the inability to address interdepartment process problems.
Email alerts
Citing articles via, looking for your next opportunity.
- Recommend to Your Librarian
Affiliations
- Online ISSN 1930-613X
- Print ISSN 0026-4075
- Copyright © 2024 The Society of Federal Health Professionals
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
The role of place on healthcare quality improvement: A qualitative case study of a teaching hospital
Affiliation.
- 1 Queen's Management School, Queen's University Belfast, Riddel Hall, 185 Stranmillis Road, Belfast, BT9 5EE, Northern Ireland, UK. Electronic address: [email protected].
- PMID: 29524869
- DOI: 10.1016/j.socscimed.2018.03.003
This article examines how the built environment impacts, and is impacted by, healthcare staff day to day practice, care outcomes and the design of new quality and patient safety (Q&PS) projects. It also explores how perceptions of the built environment affect inter-professional dynamics. In doing so, it contributes to the overlooked interplay between the physical, social, and symbolic dimensions associated with a hospital's place. The study draws on 46 in-depth semi-structured interviews conducted at a large teaching hospital in Portugal formed by two buildings. Interview transcripts were analysed inductively using thematic analysis. The major contribution of this study is to advance the understanding of the interactions among the different dimensions of place on Q&PS improvement. For example, findings indicate that some of the characteristics of the physical infrastructure of the hospital have a negative impact on the quality of care provided and/or significantly limit the initiatives that can be implemented to improve it, including refurbishment works. However, decisions on refurbishment works were also influenced by the characteristics of the patient population, hospital budget, etc. Likewise, clinicians' emotional reactions to the limitations of the buildings depended on their expectations of the buildings and the symbolic projections they attributed to them. Nevertheless, differences between clinicians' expectations regarding the physical infrastructure and its actual features influenced clinicians' views on Q&PS initiatives designed by non-clinicians.
Keywords: Case study; Healthcare quality management; Hospital; Patient safety; Place.
Copyright © 2018. Published by Elsevier Ltd.
Publication types
- Research Support, Non-U.S. Gov't
- Hospital Design and Construction*
- Hospitals, Teaching / statistics & numerical data*
- Organizational Case Studies
- Patient Safety
- Qualitative Research
- Quality Improvement / organization & administration*
To read this content please select one of the options below:
Please note you do not have access to teaching notes, integrated approach to healthcare quality management: a case study.
The TQM Magazine
ISSN : 0954-478X
Article publication date: 1 November 2006
The purpose of the paper is to develop an integrated quality management model, which identifies problems, suggests solutions, develops a framework for implementation and helps evaluate performance of health care services dynamically.
Design/methodology/approach
This paper uses logical framework analysis (LFA), a matrix approach to project planning for managing quality. This has been applied to three acute healthcare services (Operating room utilization, Accident and emergency, and Intensive care) in order to demonstrate its effectiveness.
The paper finds that LFA is an effective method of quality management of hospital‐based healthcare services.
Research limitations/implications
This paper shows LFA application in three service processes in one hospital. However, ideally this is required to be tested in several hospitals and other services as well.
Practical implications
In the paper the proposed model can be practised in hospital‐based healthcare services for improving performance.
Originality/value
The paper shows that quality improvement in healthcare services is a complex and multi‐dimensional task. Although various quality management tools are routinely deployed for identifying quality issues in health care delivery and corrective measures are taken for superior performance, there is an absence of an integrated approach, which can identify and analyze issues, provide solutions to resolve those issues, develop a project management framework (planning, monitoring, and evaluating) to implement those solutions in order to improve process performance. This study introduces an integrated and uniform quality management tool. It integrates operations with organizational strategies.
- Service operations
- Health services
- Quality management
Dey, P.K. and Hariharan, S. (2006), "Integrated approach to healthcare quality management: a case study", The TQM Magazine , Vol. 18 No. 6, pp. 583-605. https://doi.org/10.1108/09544780610707093
Emerald Group Publishing Limited
Copyright © 2006, Emerald Group Publishing Limited
Related articles
We’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here

An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Leading quality and safety on the frontline - a case study of department leaders in nursing homes.
Magerøy M, Braut GS, Macrae C, et al. Leading quality and safety on the frontline - a case study of department leaders in nursing homes. J Healthc Leadersh. 2024;16:193-208. doi:10.2147/jhl.s454109.
Nursing homes face serious, ongoing patient safety challenges. This qualitative data analysis identified challenges and facilitators that are experienced by nursing home leaders in Norway as they manage the dual responsibilities of Health, Safety and Environment (HSE) and Quality and Patient Safety (QPS). The analysis identified four themes – temporal capacity, relational capacity, professional competence , and organizational structure – highlighting the importance of adequate resources , teamwork, and strong organizational safety culture .
Healthcare leaders' and elected politicians' approach to support-systems and requirements for complying with quality and safety regulation in nursing homes - a case study. September 13, 2023
Managing patient safety and staff safety in nursing homes: exploring how leaders of nursing homes negotiate their dual responsibilities- a case study. February 28, 2024
Investigating hospital supervision: a case study of regulatory inspectors' roles as potential co-creators of resilience. April 14, 2021
Resilience from a stakeholder perspective: the role of next of kin in cancer care. September 23, 2020
Positive deviance: a different approach to achieving patient safety. August 20, 2014
Determination of health-care teamwork training competencies: a Delphi study. December 2, 2009
Naming the "baby" or the "beast"? The importance of concepts and labels in healthcare safety investigation. April 5, 2023
Issues and complexities in safety culture assessment in healthcare. July 19, 2023
The patient died: what about involvement in the investigation process? June 24, 2020
Tools for establishing a sustainable safety culture within maternity services: a retrospective case study. April 26, 2023
Using the WHO International Classification of patient safety framework to identify incident characteristics and contributing factors for medical or surgical complication deaths October 2, 2019
Back to basics: checklists in aviation and healthcare. June 17, 2015
Results of a medication reconciliation survey from the 2006 Society of Hospital Medicine national meeting. January 14, 2009
Patient safety risks associated with telecare: a systematic review and narrative synthesis of the literature. January 7, 2015
Designing and pilot testing of a leadership intervention to improve quality and safety in nursing homes and home care (the SAFE-LEAD intervention). August 14, 2019
Prospects for comparing European hospitals in terms of quality and safety: lessons from a comparative study in five countries. March 27, 2013
Linking transformational leadership, patient safety culture and work engagement in home care services. January 29, 2020
How does the WHO Surgical Safety Checklist fit with existing perioperative risk management strategies? An ethnographic study across surgical specialties. March 18, 2020
Exploring challenges in quality and safety work in nursing homes and home care - a case study as basis for theory development. April 29, 2020
Family perceptions of medication administration at school: errors, risk factors, and consequences. April 16, 2008
Remembering to learn: the overlooked role of remembrance in safety improvement. December 7, 2016
Delivering high reliability in maternity care: in situ simulation as a source of organisational resilience. July 10, 2019
Learning from failure: the need for independent safety investigation in healthcare. November 19, 2014
The problem with incident reporting. October 28, 2015
Investigating for improvement? Five strategies to ensure national patient safety investigations improve patient safety. June 5, 2019
Can we import improvements from industry to healthcare? May 1, 2019
Governing the safety of artificial intelligence in healthcare. May 8, 2019
The harm susceptibility model: a method to prioritise risks identified in patient safety reporting systems. June 9, 2010
Early warnings, weak signals and learning from healthcare disasters. April 9, 2014
Imitating incidents: how simulation can improve safety investigation and learning from adverse events. June 27, 2018
Measurement and monitoring of safety: impact and challenges of putting a conceptual framework into practice. April 11, 2018
Safety analysis over time: seven major changes to adverse event investigation. January 24, 2018
Learning from patient safety incidents: creating participative risk regulation in healthcare. February 27, 2008
Communication and information deficits in patients discharged to rehabilitation facilities: an evaluation of five acute care hospitals. October 28, 2009
Deficits in discharge documentation in patients transferred to rehabilitation facilities on anticoagulation: results of a systemwide evaluation. August 6, 2008
Transformational improvement in quality care and health systems: the next decade. November 25, 2020
"Time is of the essence": relationship between hospital staff perceptions of time, safety attitudes and staff wellbeing. December 8, 2021
Dimensions of safety culture: a systematic review of quantitative, qualitative and mixed methods for assessing safety culture in hospitals. September 1, 2021
Unsafe care in residential settings for older adults. A content analysis of accreditation reports. December 13, 2023
Improving patient safety governance and systems through learning from successes and failures: qualitative surveys and interviews with international experts. December 6, 2023
Predictors of response rates of safety culture questionnaires in healthcare: a systematic review and analysis. October 26, 2022
Comparing rates of adverse events detected in incident reporting and the Global Trigger Tool: a systematic review. August 16, 2023
COVID-19: patient safety and quality improvement skills to deploy during the surge. June 24, 2020
A qualitative content analysis of retained surgical items: learning from root cause analysis investigations. May 27, 2020
Disentangling quality and safety indicator data: a longitudinal, comparative study of hand hygiene compliance and accreditation outcomes in 96 Australian hospitals. October 8, 2014
Harnessing implementation science to improve care quality and patient safety: a systematic review of targeted literature. May 21, 2014
'Between the flags': implementing a rapid response system at scale. May 14, 2014
Health service accreditation as a predictor of clinical and organisational performance: a blinded, random, stratified study. March 24, 2010
Improving patient safety: the comparative views of patient-safety specialists, workforce staff and managers. January 30, 2005
Learning from disasters to improve patient safety: applying the generic disaster pathway to health system errors. February 9, 2011
Beyond patient safety Flatland. June 30, 2010
Cultural and associated enablers of, and barriers to, adverse incident reporting. June 23, 2010
Nurses' workarounds in acute healthcare settings: a scoping review. June 19, 2013
Investigating patient safety culture across a health system: multilevel modelling of differences associated with service types and staff demographics. July 25, 2012
Analysis of Australian newspaper coverage of medication errors. January 25, 2012
Health professional networks as a vector for improving healthcare quality and safety: a systematic review. January 11, 2012
Effects of two commercial electronic prescribing systems on prescribing error rates in hospital in-patients: a before and after study. February 15, 2012
'Broken hospital windows': debating the theory of spreading disorder and its application to healthcare organizations. May 9, 2018
Changing how we think about healthcare improvement. June 13, 2018
Association between organisational and workplace cultures, and patient outcomes: systematic review. January 17, 2018
The application of the Global Trigger Tool: a systematic review. October 26, 2016
False dawns and new horizons in patient safety research and practice. December 20, 2017
Implementation of a patient safety incident management system as viewed by doctors, nurses and allied health professionals. May 6, 2009
A root cause analysis of clinical error: confronting the disjunction between formal rules and situated clinical activity. May 31, 2006
Attitudes toward the large-scale implementation of an incident reporting system. April 9, 2008
Experiences of health professionals who conducted root cause analyses after undergoing a safety improvement programme. December 20, 2006
Turning the medical gaze in upon itself: root cause analysis and the investigation of clinical error. October 26, 2005
The effect of physicians' long-term use of CPOE on their test management work practices. September 27, 2006
Incidence, origins and avoidable harm of missed opportunities in diagnosis: longitudinal patient record review in 21 English general practices. June 30, 2021
Educational levels of hospital nurses and surgical patient mortality. April 3, 2005
A systematic narrative review of coroners’ Prevention of Future Deaths reports (PFDs): a tool for patient safety in hospitals. November 1, 2023
Quality gaps identified through mortality review. February 1, 2017
Assessing the impact of teaching patient safety principles to medical students during surgical clerkships. July 20, 2011
Medical errors: mandatory reporting, voluntary reporting, or both? August 10, 2005
Journal Article
Implementation of a medication reconciliation risk stratification tool integrated within an electronic health record: a case series of three academic medical centers.
Effects of a refined evidence-based toolkit and mentored implementation on medication reconciliation at 18 hospitals: results of the MARQUIS2 study. May 19, 2021
What works in medication reconciliation: an on-treatment and site analysis of the MARQUIS2 study. April 12, 2023
Handoff practices in emergency medicine: are we making progress? March 23, 2016
Preventability and causes of readmissions in a national cohort of general medicine patients. May 4, 2016
Project BOOST implementation: lessons learned. September 10, 2014
Making inpatient medication reconciliation patient centered, clinically relevant and implementable: a consensus statement on key principles and necessary first steps. October 27, 2010
Process changes to increase compliance with the Universal Protocol for bedside procedures. June 1, 2011
Single-parameter early warning criteria to predict life-threatening adverse events. June 23, 2010
Impact of an automated email notification system for results of tests pending at discharge: a cluster-randomized controlled trial. November 27, 2013
Effect of a pharmacist intervention on clinically important medication errors after hospital discharge: a randomized trial. July 18, 2012
Effects of an online personal health record on medication accuracy and safety: a cluster-randomized trial. May 23, 2012
Project BOOST: effectiveness of a multihospital effort to reduce rehospitalization. August 21, 2013
A toolkit to disseminate best practices in inpatient medication reconciliation: Multi-Center Medication Reconciliation Quality Improvement Study (MARQUIS). July 31, 2013
Design and implementation of an automated email notification system for results of tests pending at discharge. February 29, 2012
The impact of automated notification on follow-up of actionable tests pending at discharge: a cluster-randomized controlled trial. April 11, 2018
Curriculum development and implementation of a national interprofessional fellowship in patient safety. September 5, 2018
Readiness of US general surgery residents for independent practice. October 4, 2017
The HOSPITAL score predicts potentially preventable 30-day readmissions in conditions targeted by the Hospital Readmissions Reduction Program. June 14, 2017
Medication safety in a psychiatric hospital. March 21, 2007
A controlled trial of a rapid response system in an academic medical center. June 25, 2008
Adverse events related to accidental unintentional ingestions from cough and cold medications in children. August 26, 2020
Evaluation of older persons' medications: a critical incident technique study exploring healthcare professionals' experiences and actions. June 23, 2021
Nurses' experience with presenteeism and the potential consequences on patient safety: a qualitative study among nurses at out-of-hours emergency primary care facilities. January 10, 2024
Medication dosage calculation among nursing students: does digital technology make a difference? A literature review. September 14, 2022
Clinical efficacy of combined surgical patient safety system and the World Health Organization's checklists in surgery: a nonrandomized clinical trial. June 3, 2020
Patient Safety Primers
Long-term Care and Patient Safety
Annual Perspective
Special Section: IEA Health Care 2021. February 28, 2024
Patient safety in nursing homes from an ecological perspective: an integrated review. January 17, 2024
National Healthcare Quality and Disparities Reports. January 9, 2024
Nurses' perspectives on medication errors and prevention strategies in residential aged care facilities through a national survey. December 20, 2023
The relationship between nursing home staffing and resident safety outcomes: a systematic review of reviews. December 6, 2023
Innovative approaches to analysing aged care falls incident data: International Classification for Patient Safety and correspondence analysis. November 8, 2023
Early identification and evaluation of severe pressure injuries. October 18, 2023
Exploring medication safety structures and processes in nursing homes: a cross-sectional study. August 30, 2023
Reimagining Healthcare Teams: Leveraging the Patient-Clinician-AI Triad To Improve Diagnostic Safety. August 16, 2023
Long-term care healthcare-associated infections in 2022: an analysis of 20,216 reports. May 24, 2023
WebM&M Cases
Efforts to improve the safety culture of the elderly in nursing homes: a qualitative study. April 19, 2023
Factors differentiating nursing homes with strong resident safety climate: a qualitative study of leadership and staff perspectives. February 15, 2023
New AHRQ SOPS Workplace Safety Supplemental Item Set for Nursing Homes. February 15, 2023
Surveys on Patient Safety Culture Nursing Home Survey: 2023 User Database Report. February 8, 2023
Nursing home patient safety culture perceptions among licensed practical nurses. February 1, 2023
Interventions to increase patient safety in long-term care facilities-umbrella review. January 25, 2023
Patient safety measurement tools used in nursing homes: a systematic literature review. December 7, 2022
Patient safety culture in assisted living: staff perceptions and association with state regulations. November 30, 2022
Reinforcing the Value and Roles of Nurses in Diagnostic Safety: Pragmatic Recommendations for Nurse Leaders and Educators. October 5, 2022
Nursing Home Survey on Patient Safety Culture. August 31, 2022
Accuracy of pressure ulcer events in US nursing home ratings. August 24, 2022
Using health information technology in residential aged care homes: an integrative review to identify service and quality outcomes. August 17, 2022
Communication disparities between nursing home team members. July 20, 2022
Long-term care healthcare-associated infections in 2021: an analysis of 17,971 reports. July 13, 2022
Supplemental Item Set for Nursing Home SOPS: Call for Pilot Participants. July 6, 2022

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
Sign up for the newsletter
Digital editions.

Total quality management: three case studies from around the world
With organisations to run and big orders to fill, it’s easy to see how some ceos inadvertently sacrifice quality for quantity. by integrating a system of total quality management it’s possible to have both.

Top 5 ways to manage the board during turbulent times Top 5 ways to create a family-friendly work culture Top 5 tips for a successful joint venture Top 5 ways managers can support ethnic minority workers Top 5 ways to encourage gender diversity in the workplace Top 5 ways CEOs can create an ethical company culture Top 5 tips for going into business with your spouse Top 5 ways to promote a healthy workforce Top 5 ways to survive a recession Top 5 tips for avoiding the ‘conference vortex’ Top 5 ways to maximise new parents’ work-life balance with technology Top 5 ways to build psychological safety in the workplace Top 5 ways to prepare your workforce for the AI revolution Top 5 ways to tackle innovation stress in the workplace Top 5 tips for recruiting Millennials
There are few boardrooms in the world whose inhabitants don’t salivate at the thought of engaging in a little aggressive expansion. After all, there’s little room in a contemporary, fast-paced business environment for any firm whose leaders don’t subscribe to ambitions of bigger factories, healthier accounts and stronger turnarounds. Yet too often such tales of excess go hand-in-hand with complaints of a severe drop in quality.
Food and entertainment markets are riddled with cautionary tales, but service sectors such as health and education aren’t immune to the disappointing by-products of unsustainable growth either. As always, the first steps in avoiding a catastrophic forsaking of quality begins with good management.
There are plenty of methods and models geared at managing the quality of a particular company’s goods or services. Yet very few of those models take into consideration the widely held belief that any company is only as strong as its weakest link. With that in mind, management consultant William Deming developed an entirely new set of methods with which to address quality.
Deming, whose managerial work revolutionised the titanic Japanese manufacturing industry, perceived quality management to be more of a philosophy than anything else. Top-to-bottom improvement, he reckoned, required uninterrupted participation of all key employees and stakeholders. Thus, the total quality management (TQM) approach was born.
All in Similar to the Six Sigma improvement process, TQM ensures long-term success by enforcing all-encompassing internal guidelines and process standards to reduce errors. By way of serious, in-depth auditing – as well as some well-orchestrated soul-searching – TQM ensures firms meet stakeholder needs and expectations efficiently and effectively, without forsaking ethical values.
By opting to reframe the way employees think about the company’s goals and processes, TQM allows CEOs to make sure certain things are done right from day one. According to Teresa Whitacre, of international consulting firm ASQ , proper quality management also boosts a company’s profitability.
“Total quality management allows the company to look at their management system as a whole entity — not just an output of the quality department,” she says. “Total quality means the organisation looks at all inputs, human resources, engineering, production, service, distribution, sales, finance, all functions, and their impact on the quality of all products or services of the organisation. TQM can improve a company’s processes and bottom line.”
Embracing the entire process sees companies strive to improve in several core areas, including: customer focus, total employee involvement, process-centred thinking, systematic approaches, good communication and leadership and integrated systems. Yet Whitacre is quick to point out that companies stand to gain very little from TQM unless they’re willing to go all-in.
“Companies need to consider the inputs of each department and determine which inputs relate to its governance system. Then, the company needs to look at the same inputs and determine if those inputs are yielding the desired results,” she says. “For example, ISO 9001 requires management reviews occur at least annually. Aside from minimum standard requirements, the company is free to review what they feel is best for them. While implementing TQM, they can add to their management review the most critical metrics for their business, such as customer complaints, returns, cost of products, and more.”
The customer knows best: AtlantiCare TQM isn’t an easy management strategy to introduce into a business; in fact, many attempts tend to fall flat. More often than not, it’s because firms maintain natural barriers to full involvement. Middle managers, for example, tend to complain their authority is being challenged when boots on the ground are encouraged to speak up in the early stages of TQM. Yet in a culture of constant quality enhancement, the views of any given workforce are invaluable.
AtlantiCare in numbers
5,000 Employees
$280m Profits before quality improvement strategy was implemented
$650m Profits after quality improvement strategy
One firm that’s proven the merit of TQM is New Jersey-based healthcare provider AtlantiCare . Managing 5,000 employees at 25 locations, AtlantiCare is a serious business that’s boasted a respectable turnaround for nearly two decades. Yet in order to increase that margin further still, managers wanted to implement improvements across the board. Because patient satisfaction is the single-most important aspect of the healthcare industry, engaging in a renewed campaign of TQM proved a natural fit. The firm chose to adopt a ‘plan-do-check-act’ cycle, revealing gaps in staff communication – which subsequently meant longer patient waiting times and more complaints. To tackle this, managers explored a sideways method of internal communications. Instead of information trickling down from top-to-bottom, all of the company’s employees were given freedom to provide vital feedback at each and every level.
AtlantiCare decided to ensure all new employees understood this quality culture from the onset. At orientation, staff now receive a crash course in the company’s performance excellence framework – a management system that organises the firm’s processes into five key areas: quality, customer service, people and workplace, growth and financial performance. As employees rise through the ranks, this emphasis on improvement follows, so managers can operate within the company’s tight-loose-tight process management style.
After creating benchmark goals for employees to achieve at all levels – including better engagement at the point of delivery, increasing clinical communication and identifying and prioritising service opportunities – AtlantiCare was able to thrive. The number of repeat customers at the firm tripled, and its market share hit a six-year high. Profits unsurprisingly followed. The firm’s revenues shot up from $280m to $650m after implementing the quality improvement strategies, and the number of patients being serviced dwarfed state numbers.
Hitting the right notes: Santa Cruz Guitar Co For companies further removed from the long-term satisfaction of customers, it’s easier to let quality control slide. Yet there are plenty of ways in which growing manufacturers can pursue both quality and sales volumes simultaneously. Artisan instrument makers the Santa Cruz Guitar Co (SCGC) prove a salient example. Although the California-based company is still a small-scale manufacturing operation, SCGC has grown in recent years from a basement operation to a serious business.
SCGC in numbers
14 Craftsmen employed by SCGC
800 Custom guitars produced each year
Owner Dan Roberts now employs 14 expert craftsmen, who create over 800 custom guitars each year. In order to ensure the continued quality of his instruments, Roberts has created an environment that improves with each sale. To keep things efficient (as TQM must), the shop floor is divided into six workstations in which guitars are partially assembled and then moved to the next station. Each bench is manned by a senior craftsman, and no guitar leaves that builder’s station until he is 100 percent happy with its quality. This product quality is akin to a traditional assembly line; however, unlike a traditional, top-to-bottom factory, Roberts is intimately involved in all phases of instrument construction.
Utilising this doting method of quality management, it’s difficult to see how customers wouldn’t be satisfied with the artists’ work. Yet even if there were issues, Roberts and other senior management also spend much of their days personally answering web queries about the instruments. According to the managers, customers tend to be pleasantly surprised to find the company’s senior leaders are the ones answering their technical questions and concerns. While Roberts has no intentions of taking his manufacturing company to industrial heights, the quality of his instruments and high levels of customer satisfaction speak for themselves; the company currently boasts one lengthy backlog of orders.
A quality education: Ramaiah Institute of Management Studies Although it may appear easier to find success with TQM at a boutique-sized endeavour, the philosophy’s principles hold true in virtually every sector. Educational institutions, for example, have utilised quality management in much the same way – albeit to tackle decidedly different problems.
The global financial crisis hit higher education harder than many might have expected, and nowhere have the odds stacked higher than in India. The nation plays home to one of the world’s fastest-growing markets for business education. Yet over recent years, the relevance of business education in India has come into question. A report by one recruiter recently asserted just one in four Indian MBAs were adequately prepared for the business world.
RIMS in numbers
9% Increase in test scores post total quality management strategy
22% Increase in number of recruiters hiring from the school
20,000 Increase in the salary offered to graduates
50,000 Rise in placement revenue
At the Ramaiah Institute of Management Studies (RIMS) in Bangalore, recruiters and accreditation bodies specifically called into question the quality of students’ educations. Although the relatively small school has always struggled to compete with India’s renowned Xavier Labour Research Institute, the faculty finally began to notice clear hindrances in the success of graduates. The RIMS board decided it was time for a serious reassessment of quality management.
The school nominated Chief Academic Advisor Dr Krishnamurthy to head a volunteer team that would audit, analyse and implement process changes that would improve quality throughout (all in a particularly academic fashion). The team was tasked with looking at three key dimensions: assurance of learning, research and productivity, and quality of placements. Each member underwent extensive training to learn about action plans, quality auditing skills and continuous improvement tools – such as the ‘plan-do-study-act’ cycle.
Once faculty members were trained, the team’s first task was to identify the school’s key stakeholders, processes and their importance at the institute. Unsurprisingly, the most vital processes were identified as student intake, research, knowledge dissemination, outcomes evaluation and recruiter acceptance. From there, Krishnamurthy’s team used a fishbone diagram to help identify potential root causes of the issues plaguing these vital processes. To illustrate just how bad things were at the school, the team selected control groups and administered domain-based knowledge tests.
The deficits were disappointing. A RIMS students’ knowledge base was rated at just 36 percent, while students at Harvard rated 95 percent. Likewise, students’ critical thinking abilities rated nine percent, versus 93 percent at MIT. Worse yet, the mean salaries of graduating students averaged $36,000, versus $150,000 for students from Kellogg. Krishnamurthy’s team had their work cut out.
To tackle these issues, Krishnamurthy created an employability team, developed strategic architecture and designed pilot studies to improve the school’s curriculum and make it more competitive. In order to do so, he needed absolutely every employee and student on board – and there was some resistance at the onset. Yet the educator asserted it didn’t actually take long to convince the school’s stakeholders the changes were extremely beneficial.
“Once students started seeing the results, buy-in became complete and unconditional,” he says. Acceptance was also achieved by maintaining clearer levels of communication with stakeholders. The school actually started to provide shareholders with detailed plans and projections. Then, it proceeded with a variety of new methods, such as incorporating case studies into the curriculum, which increased general test scores by almost 10 percent. Administrators also introduced a mandate saying students must be certified in English by the British Council – increasing scores from 42 percent to 51 percent.
By improving those test scores, the perceived quality of RIMS skyrocketed. The number of top 100 businesses recruiting from the school shot up by 22 percent, while the average salary offers graduates were receiving increased by $20,000. Placement revenue rose by an impressive $50,000, and RIMS has since skyrocketed up domestic and international education tables.
No matter the business, total quality management can and will work. Yet this philosophical take on quality control will only impact firms that are in it for the long haul. Every employee must be in tune with the company’s ideologies and desires to improve, and customer satisfaction must reign supreme.
Contributors
- Industry Outlook

- Kindle Store
- Kindle eBooks
- Medical eBooks
Promotions apply when you purchase
These promotions will be applied to this item:
Some promotions may be combined; others are not eligible to be combined with other offers. For details, please see the Terms & Conditions associated with these promotions.
- Highlight, take notes, and search in the book
- In this edition, page numbers are just like the physical edition
- Create digital flashcards instantly
Rent $49.00
Today through selected date:
Rental price is determined by end date.
Buy for others
Buying and sending ebooks to others.
- Select quantity
- Buy and send eBooks
- Recipients can read on any device
These ebooks can only be redeemed by recipients in the US. Redemption links and eBooks cannot be resold.

Download the free Kindle app and start reading Kindle books instantly on your smartphone, tablet, or computer - no Kindle device required .
Read instantly on your browser with Kindle for Web.
Using your mobile phone camera - scan the code below and download the Kindle app.

Image Unavailable

- To view this video download Flash Player
Healthcare Quality Management: A Case Study Approach 1st Edition, Kindle Edition
Healthcare Quality Management: A Case Study Approach is the first comprehensive case-based text combining essential quality management knowledge with real-world scenarios. With in-depth healthcare quality management case studies, tools, activities, and discussion questions, the text helps build the competencies needed to succeed in quality management.
Written in an easy-to-read style, Part One of the textbook introduces students to the fundamentals of quality management, including history, culture, and different quality management philosophies, such as Lean and Six Sigma. Part One additionally explains the A3 problem-solving template used to follow the Plan-Do-Study-Act (PDSA) or Define, Measure, Analyze, Improve, and Control (DMAIC) cycles, that guides your completion of the problem-solving exercises found in Part Two. The bulk of the textbook includes realistic and engaging case studies featuring common quality management problems encountered in a variety of healthcare settings. The case studies feature engaging scenarios, descriptions, opinions, charts, and data, covering such contemporary topics as provider burnout, artificial intelligence, the opioid overdose epidemic, among many more.
Serving as a powerful replacement to more theory-based quality management textbooks, Healthcare Quality Management provides context to challenging situations encountered by any healthcare manager, including the health administrator, nurse, physician, social worker, or allied health professional.
- 25 Realistic Case Studies–Explore challenging Process Improvement, Patient Experience, Patient Safety, and Performance Improvement quality management scenarios set in various healthcare settings
- Diverse Author Team–Combines the expertise and knowledge of a health management educator, a Chief Nursing Officer at a large regional hospital, and a health system-based Certified Lean Expert
- Podcasts–Listen to quality management experts share stories and secrets on how to succeed, work in teams, and apply tools to solve problems
- Quality Management Tools–Grow your quality management skill set with 25 separate quality management tools and approaches tied to the real-world case studies
- Competency-Based Education Support–Match case studies to professional competencies, such as analytical skills, community collaboration, and interpersonal relations, using case-to-competency crosswalks for health administration, nursing, medicine, and the interprofessional team
- Comprehensive Instructor’s Packet–Includes PPTs, extensive Excel data files, an Instructor’s Manual with completed A3 problem-solving solutions for each Case Application Exercise, and more!
- Student ancillaries–Includes data files and A3 template
- ISBN-13 978-0826145130
- Edition 1st
- Sticky notes On Kindle Scribe
- Publisher Springer Publishing Company
- Publication date February 28, 2020
- Language English
- File size 36513 KB
- See all details
- Kindle (5th Generation)
- Kindle Keyboard
- Kindle (2nd Generation)
- Kindle (1st Generation)
- Kindle Paperwhite
- Kindle Paperwhite (5th Generation)
- Kindle Touch
- Kindle Voyage
- Kindle Oasis
- Kindle Scribe (1st Generation)
- Kindle Fire HDX 8.9''
- Kindle Fire HDX
- Kindle Fire HD (3rd Generation)
- Fire HDX 8.9 Tablet
- Fire HD 7 Tablet
- Fire HD 6 Tablet
- Kindle Fire HD 8.9"
- Kindle Fire HD(1st Generation)
- Kindle Fire(2nd Generation)
- Kindle Fire(1st Generation)
- Kindle for Windows 8
- Kindle for Windows Phone
- Kindle for BlackBerry
- Kindle for Android Phones
- Kindle for Android Tablets
- Kindle for iPhone
- Kindle for iPod Touch
- Kindle for iPad
- Kindle for Mac
- Kindle for PC
- Kindle Cloud Reader
Customers who bought this item also bought

Editorial Reviews
About the author.
Zachary Pruitt, PhD, MHA, CPH, is assistant professor and director of community practice at the University of South Florida College of Public Health.
Candace S. Smith, PhD, RN, NEA-BC, is chief nursing officer at Manatee Memorial Hospital.
Eddie Pérez-Ruberté, MS, is senior Lean project manager at BayCare Health Systems who leads the deployment of the Lean management system and culture. Eddie is a certified Lean expert and a certified Six Sigma Black Belt from the American Society for Quality. He also helps organizations implement Lean programs through his consulting company, Areito Group. Eddie is an instructor for the Institute of Industrial and Systems Engineers where he teaches Lean and Six Sigma and certifies students in these methodologies at multiple universities and healthcare organizations across the United States.
Product details
- ASIN : B07YP7XC7V
- Publisher : Springer Publishing Company; 1st edition (February 28, 2020)
- Publication date : February 28, 2020
- Language : English
- File size : 36513 KB
- Text-to-Speech : Enabled
- Screen Reader : Supported
- Enhanced typesetting : Enabled
- X-Ray : Not Enabled
- Word Wise : Not Enabled
- Sticky notes : On Kindle Scribe
- Print length : 404 pages
- #43 in Health Care Administration
- #106 in Health Care Delivery (Kindle Store)
- #132 in Public Health (Kindle Store)
Customer reviews
Customer Reviews, including Product Star Ratings help customers to learn more about the product and decide whether it is the right product for them.
To calculate the overall star rating and percentage breakdown by star, we don’t use a simple average. Instead, our system considers things like how recent a review is and if the reviewer bought the item on Amazon. It also analyzed reviews to verify trustworthiness.
- Sort reviews by Top reviews Most recent Top reviews
Top reviews from the United States
There was a problem filtering reviews right now. please try again later..
Report an issue
- Amazon Newsletter
- About Amazon
- Accessibility
- Sustainability
- Press Center
- Investor Relations
- Amazon Devices
- Amazon Science
- Sell on Amazon
- Sell apps on Amazon
- Supply to Amazon
- Protect & Build Your Brand
- Become an Affiliate
- Become a Delivery Driver
- Start a Package Delivery Business
- Advertise Your Products
- Self-Publish with Us
- Become an Amazon Hub Partner
- › See More Ways to Make Money
- Amazon Visa
- Amazon Store Card
- Amazon Secured Card
- Amazon Business Card
- Shop with Points
- Credit Card Marketplace
- Reload Your Balance
- Amazon Currency Converter
- Your Account
- Your Orders
- Shipping Rates & Policies
- Amazon Prime
- Returns & Replacements
- Manage Your Content and Devices
- Recalls and Product Safety Alerts
- Conditions of Use
- Privacy Notice
- Consumer Health Data Privacy Disclosure
- Your Ads Privacy Choices
- Open access
- Published: 13 May 2024
Nurse perceptions of practice environment, quality of care and patient safety across four hospital levels within the public health sector of South Africa
- Immaculate Sabelile Tenza 1 ,
- Alwiena J. Blignaut 1 ,
- Suria M. Ellis 2 &
- Siedine K. Coetzee 1
BMC Nursing volume 23 , Article number: 324 ( 2024 ) Cite this article
73 Accesses
Metrics details
Improving the practice environment, quality of care and patient safety are global health priorities. In South Africa, quality of care and patient safety are among the top goals of the National Department of Health; nevertheless, empirical data regarding the condition of the nursing practice environment, quality of care and patient safety in public hospitals is lacking.
This study examined nurses’ perceptions of the practice environment, quality of care and patient safety across four hospital levels (central, tertiary, provincial and district) within the public health sector of South Africa.
This was a cross-sectional survey design. We used multi-phase sampling to recruit all categories of nursing staff from central ( n = 408), tertiary ( n = 254), provincial ( n = 401) and district ( n = 244 [large n = 81; medium n = 83 and small n = 80]) public hospitals in all nine provinces of South Africa. After ethical approval, a self-reported questionnaire with subscales on the practice environment, quality of care and patient safety was administered. Data was collected from April 2021 to June 2022, with a response rate of 43.1%. ANOVA type Hierarchical Linear Modelling (HLM) was used to present the differences in nurses’ perceptions across four hospital levels.
Nurses rated the overall practice environment as poor (M = 2.46; SD = 0.65), especially with regard to the subscales of nurse participation in hospital affairs (M = 2.22; SD = 0.76), staffing and resource adequacy (M = 2.23; SD = 0.80), and nurse leadership, management, and support of nurses (M = 2.39; SD = 0.81). One-fifth (19.59%; n = 248) of nurses rated the overall grade of patient safety in their units as poor or failing, and more than one third (38.45%; n = 486) reported that the quality of care delivered to patient was fair or poor. Statistical and practical significant results indicated that central hospitals most often presented more positive perceptions of the practice environment, quality of care and patient safety, while small district hospitals often presented the most negative. The practice environment was most highly correlated with quality of care and patient safety outcomes.
There is a need to strengthen compliance with existing policies that enhance quality of care and patient safety. This includes the need to create positive practice environments in all public hospitals, but with an increased focus on smaller hospital settings.
Peer Review reports
Improving the nurse practice environment, quality of healthcare and patient safety has become a global priority [ 1 ]. This is because countries worldwide are striving to provide universal health coverage (UHC) to their citizens, and quality and safe care has been prioritised in the agenda to achieve UHC [ 2 , 3 ]. Recently there has been an increase in scholarly attention on the relationship between the nurse practice environment, quality of healthcare and patient safety, with global consensus that a positive nurse practice environment contributes positively to these [ 4 ].
The nurse practice environment is defined as the organisational characteristics of a work context that facilitate or constrain professional nursing practice [ 5 ]. Quality of care is the degree to which health services for individuals and populations increase the likelihood of the desired health outcomes [ 6 ], and patient safety is a dimension of quality of care and is defined as the avoidance of unintended or unexpected harm to people during the provision of healthcare [ 1 ].
Studies on the nurse practice environment have focused on nurse participation in organisational affairs, staffing and resource adequacy, and nurse leadership, management, and support of nurses, nurse-physician collegial relations, and foundations of quality of care [ 7 , 8 , 9 ]. A recent meta-analysis [ 10 ] found consistent and significant associations between the practice environment and quality of care and patient safety, based on data from 1,368,420 patients in 22 countries (including South Africa), 141 nursing units, 165,024 nurses, and 2677 hospitals. Ten years ago, a South African article—the only one from Africa included in this meta-analysis—showed the following trends: 52.3% of nurses assessed their practice environment as either poor or fair, 20.7% rated the quality of care as either poor or fair, and 5.5% rated patient safety as inadequate or failing [ 11 ]. In all cases, the public sector had worse outcomes than the private sector; and the study concluded that the nurse practice environment was significantly associated with better nurse and patient outcomes [ 11 ]. No national study has since followed this, with most studies focusing on small-scale or single-site qualitative and quantitative descriptive studies. Furthermore the variables of interest were explored separately from each other, such as the influence of the nurse practice environment on nurse outcomes [ 12 , 13 ], professional nurses’ understanding of quality nursing care [ 14 ], with a primary focus on patient safety culture [ 13 , 15 , 16 , 17 ]. Quality of care and patient safety studies in South Africa reported negative experiences of health providers, but these were not linked with the practice environment, even with ample evidence of its influence. One significant issue is the existence of policy documents that govern quality of care and patient safety in the nation. These include the following: the Patient Rights Charter, the Batho Pele principles, the National Core Standards framework [ 18 ], the National Guideline for Patient Safety Incident Reporting [ 19 ], and the Ideal Facility Framework [ 20 ]. Despite the aforementioned governmental obligations, achieving quality in healthcare continues to be a struggle [ 21 ]. This has been evidenced by the reports of litigations experienced by public health hospitals [ 22 ]. A major concern of the National Department of Health is the sudden increase in expenditure related to medico-legal claims. In the 2020/2021 financial year, more than ZAR6.5 billion (US $343,496.02) was awarded in medicolegal claims in the public sector [ 23 ].
Nurses as frontline, street-level bureaucrats in the implementation of the policies related to quality of care and patient safety in healthcare have critical experience of the nurse practice environment, quality of care and patient safety, and their views could contribute to future improvements [ 5 ]. Given existing evidence that the nurse practice environment influences quality of care and patient safety, it is important to understand the current situation. While there are existing policies directing quality of care and patient safety, it is not known how having these policies in place shapes the nurse practice environment, perceived quality of care and patient safety. This article expands on the findings of a previous national study [ 11 ], which demonstrated that the public sector had a more negative nurse practice environment, quality of care and patient safety. To add to the body of knowledge, this study examines the public sector and four hospital levels: central, tertiary, provincial, and district (small, medium, and large) hospitals. Hence this national study sought to examine nurses' perceptions of the practice environment, quality of care and patient safety across four hospital levels within the public health sector of South Africa.
Theoretical framework
This study is based on the theoretical framework of Tvedt et al. [ 24 ], which is a system perspective based on the model of Donabedian and modified by Battles (2006) to show how hospital structures and practice environment features improve quality of care and patient safety [ 24 ]. These outcomes are specifically identified as quality of care, patient safety (work-related outcome measures), and low-frequency adverse events and self-care ability (patient-related outcome measures).
Study context
This study was conducted in all nine provinces of South Africa, namely, Northern Cape, Western Cape, Eastern Cape, Free State, North West, Gauteng, Limpopo, Mpumalanga, and KwaZulu-Natal. South Africa has a two-tier healthcare system, with a public and a private sector [ 18 , 25 ]. The public sector is state-funded and caters to the majority – 71% – of the population [ 19 , 25 ]. The private sector is largely funded through individual contributions to medical aid schemes or health insurance, and serves a minority of the population [ 20 , 25 ]. This study focused on the public sector hospitals as they cater for the majority of the population. There are five categories of hospitals in the public sector, including district, regional, tertiary, central, and specialised hospitals, which are categorised according to the nature and extent of services provided and size [ 26 ]. The first point of entry to the South African health system is through primary healthcare (PHC) facilities, often referred to as clinics. Patients are referred from PHC facilities to district hospitals, regional, tertiary and central hospitals or specialised hospitals [ 26 ]. District hospitals are categorised into small, medium, and large district hospitals. Small district hospitals have between 50 and 150 beds; medium district hospitals have between 150 and 300 beds; and large district hospitals have between 300 and 600 beds [ 26 ]. These hospitals serve a defined population within a health district and support PHC facilities, providing services that include in-patient, ambulatory health services as well as emergency health services [ 26 ]. A regional hospital has between 200 and 800 beds and receives referrals from several district hospitals. Regional hospitals provide health services on a 24-h basis to a defined regional population, limited to provincial boundaries [ 26 ]. A tertiary hospital has between 400 and 800 beds and receives referrals from regional hospitals not limited to provincial boundaries, and also provides specialist level services [ 26 ]. A central hospital has a maximum of 1200 beds, receives patients referred from more than one province, and provides tertiary hospital services; they may also provide national referral services, including conducting research. A central hospital is attached to a medical school as the main teaching platform [ 26 ].
Study design
This study had a cross-sectional descriptive design. The STROBE checklist of items that should be included in reports of cross-sectional studies was used to guide the study and the reporting thereof.
Population and sampling
Multi-phase sampling was applied in the public sector. Purposive sampling was applied to the selection of hospitals in the public sector. A total of 27 hospitals were included by selecting the largest central or tertiary hospital in every province, and the provincial and district hospital in closest proximity to the selected central or tertiary hospital. The district hospitals were further stratified into large ( n = 2), medium ( n = 3), and small ( n = 4) hospitals. Specialist hospitals were excluded. All in-patient medical and surgical units were included. Total population sampling was applied to all categories of nursing staff (registered nurses, community service nurses, enrolled nurses [2-year diploma], and enrolled nursing auxiliaries [1-year certificate]), including temporary staff, in these selected units. Nurses had to have worked in the respective unit for at least three months, and student nurses were excluded. The total sample of participants was as follows: central n = 408; tertiary, n = 254; provincial, n = 401; and district, n = 244 [large n = 81; medium n = 83 and small n = 80]). Data were collected from April 2021 to June 2022. A sample size calculation was performed in g-power using the F-tests as the Test Family and the ANOVA: Fixed effects, special, main effects and interactions as the Statistical test in order to take the structure of the data into account. The parameters were specified as follow: Effect size f as and large (0.4) and medium (0.25), α err prob as 0.05, Power (1-β err prob) as 0.95, Numerator df as 10, Number of groups 6. The total sample sizes calculated were 162 and 400, which is well below the realised sample size of 1307. Total population sampling was used and not a random sample, thus no generalisations are made beyond the study population of nurses from these hospitals.
Instruments
In accordance with the theoretical framework of Tvedt et al., the variables measured included practice environment, quality of care, self-care ability, patient safety, and adverse events [ 24 ] . The practice environment was measured using the Practice Environment Scale of the Nurse Work Index Revised (PES-NWI-R). It consists of 32 questions and is divided into five subscales measuring nurse participation in hospital affairs; nursing foundations for quality of care; nurse manager ability, leadership, and support of nurses; staffing and resource adequacy; and collegial nurse-physician relations. The questions are measured on a Likert scale from 1 to 4, where 1 represents strongly disagree and 4 strongly agree. A mean score of 2.5 or more is indicative of a positive practice environment. This tool was found to be valid and reliable in many countries, including South Africa [ 27 ].
Quality of care was measured using the following question: In general, how would you describe the quality of nursing care delivered to patients on your unit/ward? The question was measured on a Likert scale from 1 to 5, where 1 represented excellent and 5 poor. Self-care ability was measured using one question (How confident are you that your patients and their caregivers can manage their care after discharge?), measured on a Likert scale from 1 to 4, where 1 represented very confident and 5 not at all confident.
Patient safety was measured using the following question: Please give your current practice setting an overall grade on patient safety. This was measured on a Likert scale from 1 to 5, where 1 represented excellent and 5 represented failing. The other eight items came from the Hospital Survey on Patient Safety Culture (HSOPSC) [ 28 ]. They were answered on a Likert scale from 1 to 5, where one represented strongly agree and five strongly disagree.
Finally, adverse events were measured by five questions on a five-point scale, where 1 represented never and 5 represented daily. These questions have been employed in multi-country research in South Africa [ 29 ], Europe [ 30 ], the United States of America [ 31 ], and Asia [ 32 ]. The specific outcomes have also been used in a meta-analysis [ 33 ]. The authors tried to control for response bias and subjectivity by asking neutrally worded questions, using anonymous surveys, ensuring that answer options were not leading, and that the order of the answers was randomised. i.e. the range for the practice environment was 1 = Strongly disagree.
4 = Strongly agree (ascending order), while quality of care and patient safety ranged from 1 = Excellent; 4 = Poor (descending order).
Data collection
Data collection took place between April 2021 and June 2022 after ethics approval and obtaining permission from relevant health departments. A team of trained field workers visited the hospitals to administer a paper-based survey to all of the consenting nurses in the hospitals, according to participation criteria. Upon arrival at each hospital, each unit manager was approached and a discussion was held between researcher, manager and staff regarding permission to do a survey among nurses in the unit. The discussion gave detailed information about the study, including the voluntary nature of participation, with an invitation to participate. The survey forms were given to the participants and they were allowed to complete them at a time convenient to them. The survey was completed anonymously, and participants were requested to return them in a sealed envelope via a sealed box with a post-box split, which was placed in all departments in the participating hospitals. The contents of these boxes were emptied by the researcher at the end of each day and removed a week later upon completion of data collection at the selected hospital.
Quantitative data analysis
Data was analysed using SPSS [ 34 ]. Descriptive statistics were used to analyse the demographic data, and data from each subscale representing the practice environment, quality of care and patient safety. These described frequencies, percentages, means and standard deviations. ANOVA type Hierarchical Linear Modelling (HLM), with p -values for all effects and interactions were calculated to present the differences in nurses’ perceptions of the practice environment, quality of care and patient safety across four hospital levels within the public health sector of South Africa, as the means of the different hospital levels and not the regression coefficients were important in the interpretation of the results. After the ANOVA type HLM, pair wise post-hoc comparisons were done to determine the statistically significant differences between the groups. Additionally, effect sizes were computed to determine which of these differences were important in practice. Where significant p - values lead to generalisations of results, effect sizes only indicate whether the differences in the sample groups were important in practice and are not used for generalisation if the p -values are not significant. Effect sizes were calculated and the magnitude of difference between the groups indicated as 0.2 = small, 0.5 = medium, 0.8 = large. Correlations between aspects of the nurse practice environment, quality of care and patient safety were also explored for the entire sample with 0.1. = small; 0.3 = medium and 0.5 = large relationships. Normality of the data was tested using the Kolmogorov–Smirnov test, but due to the unlikelihood of non-significant p -values in such a large sample size, more significance was ascribed to results from Q-Q plots. The points in the Q-Q plot lies close enough to the straight line to retain the assumption that the data distribution is normal for all variables [ 35 ].
Demographic data
We obtained a 43.1% response rate. As indicated in Table 1 , the majority of the participants were female ( n = 1159; 88.7%), working on a full-time basis ( n = 1158; 89.35%) and in the registered nurse/midwifery category ( n = 593; 45.58%). Most nurses worked in the surgical units ( n = 483; 36.95%), and we received most participation from the central level hospitals ( n = 408; 31.22%).
- Nurse practice environment
The overall practice environment was not considered to be positive (M = 2.46; SD = 0.65), especially with regard to the subscales of nurse participation in hospital affairs (M = 2.22, SD = 0.76), staffing and resource adequacy (M = 2.23; SD = 0.80), and nurse manager ability, leadership, and support of nurses (M = 2.39; SD = 0.81), see Table 2 .
Table 3 provides an overview of responses to items on quality of care, patient safety, and adverse events.
- Quality of care
When asked about their perception of the quality of nursing care delivered to patients in their work setting, a third of participants (38.45%; n = 486) indicated a negative outcome, and more than half of the nurses reported that they lacked confidence in patient or caregiver post-discharge care abilities (52.22%; n = 658).
- Patient safety
As indicated in Table 3 , the overall grade for patient safety was rated as poor or failing by 19.59% ( n = 248) of participants, and 430 participants (35.95%) agreed that there was a high reliance on temporary staff in their hospitals. In addition, more than half of the participants strongly agreed that their mistakes were held against them (64.38%; n = 770), and that there was a lack of support for staff involved in patient safety errors (63.15%; n = 749). Close to half felt that they could not question the decisions or actions of those in authority when related to patient safety issues (42.22%; n = 505).
Adverse events
The subscale on adverse events examined the weekly and daily occurrence of adverse events. At least 21.32% ( n = 252) of the participants experienced complaints weekly or daily, while 9.29% ( n = 108) reported a weekly or daily incidence of hospital-acquired infections, and 7.77% ( n = 93) weekly or daily medication errors.
Table 4 shows several effect sizes between the different levels of hospitals; however, only medium effect sizes will be reported on. Regarding the practice environment, there were medium practical effects between central hospitals and the small district hospitals for nurse participation in hospital affairs ( r = 0.40; p = 0.291), nursing foundations for quality of care ( r = 0.44; p = 0.469), and nurse manager ability, leadership, and support of nurses ( r = 0.45; p = 0.484), where central hospitals reported a more positive perception of these elements. There were also medium practical effects between provincial hospitals and the small district hospitals for nurse participation in hospital affairs ( r = 0.40; p = 0.211) and nursing foundations for quality of care ( r = 0.43; p = 0.398), where provincial hospitals reported a more positive perception of these elements of the practice environment.
Regarding the quality of care, there were medium practical effects with statistical significance between central hospitals and tertiary hospitals ( r = 0.54; p = 0.015) and small district hospitals ( r = 0.51; p = 0.061), where central hospitals reported better quality of care. Regarding patients’ self-care ability, there were medium practical effects between central hospitals and tertiary hospitals ( r = 0.42; p = 0.042) as well as medium district hospitals ( r = 0.41; p = 0.110) and small district hospitals ( r = 0.56; p = 0.007), where central hospitals reported more confidence in patients’ ability to manage their own care after discharge.
Regarding patient safety, there were medium practical effects between central hospitals and tertiary hospitals ( r = 0.45; p = 0.178), and also between medium district hospitals ( r = 0.44; p = 0.399), and small district hospitals ( r = 0.51; p = 0.178), where central hospitals reported higher grades of patient safety. Regarding staff feeling that their mistakes are held against them, there was a medium practical effect between small and medium district hospitals ( r = 0.42; p = 0.681), where small district hospitals reported that mistakes were held against them more often. There was also a medium practical effect between medium and large district hospitals regarding lack of support for staff involved in patient safety errors ( r = 0.44; p = 0.572), where small district hospitals reported less support for staff involved in patient safety errors. Finally, there was a medium practical effect between large and small district hospitals regarding the actions of hospital management showing that patient safety is a top priority ( r = 0.40; p = 0.856), where small district hospitals felt that the actions of hospital management showed that patient safety is a top priority.
Complaints were the only adverse event that had a medium practical effect, these effects being between provincial hospitals and large district hospitals ( r = 0.57; p = 0.056), and large district hospitals and small district hospitals ( r = 0.60; p = 0.114), where large district hospitals had a greater incidence of complaints.
As shown in Table 5 , all practice environment subscales showed medium to large negative correlations with the quality of nursing care delivered ( r = -3.20 to r = -4.28; p = 0.00) and that patients and their caregivers can manage care after discharge ( r = -0.282 to r = -0.327; p = 0.00). When considering the correlations of the practice environment on overall grade of patient safety, the practice environment had a large negative correlation ( r = -0.405; p = 0.00), especially regarding nurse foundations of quality of care ( r = -0.411; p = 0.00). Furthermore, medium negative correlations were noted between overall grade of patient safety and staffing and resources ( r = -0.347; p = 0.00) and nurse management, leadership, and support of nurses ( r = -0.340; p = 0.00), nurse participation ( r = -0.323; p = 0.00) and collegial nurse-physician relationships ( r = -0.299; p = 0.00). This shows that the more that participants agreed with positive statements about the nurse practice environment, the better they rated their quality of care, the more confidence they had in their patients’ post-discharge management, and the better they rated their overall grade on patient safety.
All practice environment items, except for collegial nurse-physician relationships, had medium negative correlations with the AHRQ item that the unit regularly reviews work processes to determine if changes are needed to improve patient safety ( r = -0.221 to r = -0.275; p = 0.00). Furthermore, foundations of quality of care showed a medium negative correlation with staff speaking up when they see something that may negatively impact patient care ( r = -0.226; p = 0.00). Nurse participation ( r = 0.235; p = 0.00), leadership ( r = 0.278; p = 0.00), collegial nurse- physician relationship ( r = 0.200; p = 0.00), and the total practice environment scale ( r = 0.259; p = 0.00) all showed medium positive correlations with the AHRQ item ‘Staff feel like their mistakes are held against them’. All practice environment subscales exhibited medium correlations with the lack of support for staff involved in patient safety errors ( r = 0.239 to r = 0.315; p = 0.00). Foundations of quality of care ( r = -0.222; p = 0.00), leadership, management, and support of nurses ( r = -0.223; p = 0.00), and the overall practice environment scale ( r = -0.219; p = 0.00) had negative medium correlations with discussing ways to prevent errors from happening again. All except the collegial nurse-physician relationship subscale of the practice environment showed medium negative correlations with staff feeling free to question the decisions or actions of those in authority ( r = -0.222 to r = -0.314; p = 0.00). All practice environment subscales had medium correlations with the actions of hospital staff showing that patient safety is a top priority ( r = -0.222 to r = -0.362; p = 0.00). To explain, the more that nurses agreed with positive practice environment items, the more they would agree to positive patient safety (AHRQ) items and the more they would disagree with negative patient safety (AHRQ) items.
Overall patient safety correlated positively and strongly with quality of nursing care delivered ( r = 0.563; p = 0.00), with a medium positive correlation with confidence in patients’ and caregivers’ post-discharge management ( r = 0.357; p = 0.00). Overall grade of patient safety also revealed a medium positive correlation with the unit regularly reviewing work processes ( r = 0.258; p = 0.00), staff feeling free to question the actions of those in authority ( r = 0.222; p = 0.00), and the actions of hospital management showing that patient safety is a top priority ( r = 0.372; p = 0.00). Regarding adverse events, overall grade of patient safety showed medium correlations with medication errors ( r = 0.208; p = 0.00) and patient falls ( r = 0.223 p = 0.00). This indicates that, as nurses rated overall patient safety more positively, they would also rate quality of care, confidence in post-discharge management, and positive items on patient safety (AHRQ) better, while at the same time leaning towards a lower incidence of adverse events occurring.
Another strong positive correlation was observed between quality of nursing care, and confidence that patients and their caregivers can manage care after discharge ( r = 0.438; p = 0.00), while medium positive correlations were noted between quality of nursing care and the unit reviewing work processes regularly ( r = 0.273; p = 0.00), staff speaking up if they see something that may negatively impact patient care ( r = 0.209; p = 0.00), staff feeling free to question the actions of those in authority ( r = 0.210; p = 0.00), and the actions of hospital management showing that patient safety is a top priority ( r = 0.305; p = 0.00). Regarding adverse events, quality of nursing care was correlated positively with medication errors ( r = 0.230; p = 0.00), patient falls ( r = 0.237; p = 0.00), and complaints ( r = 0.249; p = 0.00). This shows that the nurses rating the quality of care in their units as more positive would also have more confidence in their patients’ post-discharge management and agree more with positive patient safety items (AHRQ), while indicating a lower incidence of adverse events.
Confidence in post-discharge care and the actions of hospital management showing that patient safety is a top priority were also correlated positively on a medium level ( r = 0.216; p = 0.00). Regarding adverse events, confidence in post-discharge care was correlated positively with patient falls ( r = 0.202; p = 0.00), healthcare-associated infections ( r = 0.206; p = 0.00), and complaints ( r = 0.211; p = 0.00). To explain, this indicates that nurses with a higher rating in confidence in post-discharge management would also have a higher rating of their hospital management’s actions showing that patient safety is a top priority, while also rating the incidence of patient falls, healthcare-associated infections and complaints as occurring less often.
This national study sought to examine nurses' perceptions of the practice environment, quality of care and patient safety across four hospital levels within the public health sector of South Africa. In the participating hospitals we found that there was a negative nurse practice environment, and reports of poor quality of care and patient safety.
The findings on the perceived poor nurse practice environment in the public hospitals is of great concern. The recent South African Human Resources for Health Strategy 2030 advocates for the support of health personnel to deliver quality services [ 36 ]. The findings are worrying given that nurses are the backbone of the health system. A negative practice environment contributes to increased staff turnover and mental health challenges due to a stressful environment [ 37 ]. The challenges of unavailability of resources are common in public hospitals [ 38 ], but when coupled with poor leadership support could worsen the nurse outcomes. The finding on poor participation in hospital affairs indicates a lack of prioritisation of frontline nurses’ voices in hospital affairs; previous studies also found poor involvement of frontline nurses in policy decision making [ 39 , 40 ]. This could also mean that nurse managers may need empowerment on how to be supportive to staff and in improving prioritisation of frontline nurses’ voices in decision making. The implication of poor involvement of staff in hospital affairs usually includes retaliation, lack of a sense of belonging, and demotivation [ 41 ], and it also indicates weak leadership [ 42 ]. System level improvements, including relational leadership focused on prioritising staff involvement in decision making, could improve nursing practice environments in these hospitals [ 43 , 44 , 45 ]. Nurses’ perceptions of a negative practice environment have been reported in the literature. A study in Menoufia University Hospital, Egypt, reported that about 66.3% of nurses had a poor perception of the work environment [ 46 ]. Equally, a rapid review of literature on positive practice environment in the United Kingdom reported that most articles revealed a negative practice environment [ 47 ]. Nurse practice environment scholars concur that improving the nurse practice environment saves resources while building a culture of safety [ 48 ], and that prudent nurse managers should prioritise creating practice environments that are conducive to providing quality nursing care, as well as that managers should take the lead in impacting the elements of a positive practice environment [ 49 ]. In the context of our study, managers could be advocates for resources, nurse inclusion in hospital affairs, and provide strong leadership support.
The finding that almost half of the participating nurses rated the quality of care in their ward as poor is not new. A study in KwaZulu-Natal province in South Africa that explored nurses’ attitudes in providing care to patients revealed that they reported a poor incidence of nursing care to patients and deliberate disregard of essential patient care [ 50 ]. The study also noted that nurses attributed poor quality of nursing care to the attitudes of patients’ relatives or patients themselves, including unsupportive management behaviour. Maphumulo and Bhengu (2019) also report on poor quality of care [ 51 ]. As mentioned earlier, there are existing national policies to support quality and safety. For example, the Office of Health Standards Compliance set standards on quality in health care; additionally, in 2013 there was a nationwide quality improvement initiative called ideal facility [ 52 ]. Such initiatives focused on setting standards to assess each facility regarding compliance with set criteria for quality care in the facilities, started with the PHC clinics [ 53 ] and rolled out to hospital level. These results could mean that hospitals are not adhering to the set standards. Major challenges reported in the South African literature associated with poor quality of patient care include poor infrastructure [ 54 , 55 ], unavailability of medicine [ 56 , 57 ], shortage of staff, increased workload, shift work and long working hours [ 58 , 59 ]. These have contributed to an ongoing cycle of high staff turnover [ 60 ]. In line with international evidence, it would appear that the practice environment is closely linked to the quality of care [ 11 ].
The findings that nurses rated patient safety in their hospitals as poor could be due to their perceived patient safety culture. Evidence suggests that to achieve patient safety, strong leadership and a culture supportive of learning from errors (rather than a punitive approach) are critical ingredients [ 61 ]. In this study nurses reported that they experience a punitive reaction when reporting errors, and that they lacked support from their managers, and this is of great concern. Management response to errors is a critical determinant of patient safety culture; positive reactions to reported errors have been cited to encourage health providers to report them and subsequently improve patient care [ 62 ]. The findings resonate with recent South African studies that also found a poor patient safety culture in public hospitals [ 13 , 16 ]. A punitive reaction to reporting of adverse events remains a global challenge. A qualitative study conducted in South Korea on nurses’ experiences with disclosure of patient safety incidents found that nurses often prefer not to report patient safety incidents [ 63 ] due to the reaction expected from managers. An integrative review of literature from January 2010 to December 2020 using 31 papers revealed that a non-punitive reaction to patient safety incident reporting could improve patient safety and learning from errors [ 64 ]. Such strategies should be adopted in these participating hospitals.
The findings on weekly and daily reported adverse events and complaints resonate with the perceived poor patient safety. The finding that nurses perceived reactions to reported incidents as punitive could mean that more adverse events are not reported, for fear of the management reaction. Adverse events are a critical indicator of patient safety, hence weekly adverse events reported in a hospital should be a major concern. A qualitative study conducted in Palestine on nurses’ experience of the most common medical errors in the intensive care unit and coronary care unit demonstrated that they usually experience events like medication errors, nursing procedure errors, equipment errors, patient monitoring errors, intravenous medication errors, and resuscitation errors [ 65 ]. Similarly, in their study in Ghana Alhassan et al. (2019) noted that the type of errors nurses experience were wrong documentation, wrong intravenous fluid, and blood transfusion [ 66 ]. Furthermore, a study in Tehran, Iran on the types and causes of medication errors from nurses’ viewpoint indicated that about 64.55% of nurses reportedly made medication errors, and approximately 31.4% nearly experienced medication errors [ 67 ]. In the South African context reporting of adverse events remains a challenge, due to similar fear of reporting patient safety incidents, and evidence suggests that health providers often classify adverse events as minor to avoid reporting them [ 68 ]. A need to emphasise a just culture in the nursing environment will improve reporting of adverse events, and learning from these events will further reduce occurrences.
We also observed that when looking at comparison of effect sizes across hospitals, larger hospitals most often revealed better practice environments, quality of care and patient safety outcomes, while small district hospitals had the worst. These findings are not uncommon, as a Korean study also confirmed a strong relationship between practice environment and hospital sizes, concluding that the nurse practice environment varies with hospital size [ 69 ]. A distinct difference in the hospital categories compared is bed capacity, and complexity of conditions treated in each category, with more complex conditions seen in higher levels of hospitals. In the South African context, hospital categories also influence decisions on allocation and prioritisation of resources among the hospital categories, with more resources given to the larger hospitals [ 26 ]. Availability of resources plays a significant role in improving the nursing practice environment [ 70 ], and this is a possible contributor to a negative practice environment in small hospitals, since they often have fewer staff and resources [ 49 ]. We also found that central hospitals reported more confidence in patients’ ability to manage care after discharge than the smaller hospitals did; this could mean that central hospitals have prioritised teaching of their patients, thereby empowering them for post-discharge care. A 2020 study in the United Kingdom also reported that hospital size is a good predictor of efficient discharge processes [ 71 ].
The finding that patient safety in central hospitals was better than in small district hospitals is contrary to the assumption that large hospitals are busy and likely to be attending to complex patient conditions which could make them more prone to errors and unsafe practice [ 72 ]. In our study better safety in tertiary hospitals could be related to the fact that they are operated mostly by specialised health professionals who may be more knowledgeable than those in non-specialised hospitals, and that tertiary hospitals are teaching hospitals, often with ongoing training related to practice [ 26 , 73 ]. In the South African context to our knowledge this is the first study to link nurse practice environment, quality of care and patient safety in four hospital levels, and showing definite differences in nurses’ perceptions at these different levels of care. It followed a quantitative approach, and it would be interesting to further explore the reasons for the perceived practice environment, quality of care and patient safety using qualitative approaches in these hospitals. The findings of this study, specifically the variations in perceived nurse practice environment, quality of care and patient safety across hospital levels, imply an urgent need for mindfulness in resource allocation so as not to compromise care in the smaller hospitals.
The finding of strong correlations between the nurse practice environment, quality of care and patient safety is similar to those of other studies that also emphasised that a negative practice environment is associated with perceived poor quality of care and patient safety [ 48 , 49 , 74 , 75 ]. For our study it implies a need to intentionally improve the nurse practice environment, in order to influence quality of care and patient safety. It also means that quality of care and patient safety policies should deliberately consider the practice environment. This could start by involving nurses in policy development, so they can contribute to hospital affairs and the feasibility of the policies. This will also make them feel included as important role-players in the health system. Patient safety policies could also not focus on reporting of errors but consider system level contributors to errors; such practice will also address the reported challenges of punitive reactions to reported errors.
Limitations and strengths
Since this was a cross-sectional, self-reported survey, one of the limitations could be that the nurses may have had social-desirable bias in their responses, although the authors did try to control for this by asking neutrally worded questions, using anonymous surveys, ensuring that the answer options were not leading and that the order of the answers was randomised. There are several strengths of this study: firstly a contribution to knowledge of a link between nurse practice environment, quality in health care and patient safety in the South African context; often studies investigating these concepts are isolated. An additional strength is that we included a large sample size, representing all nine provinces of South Africa. To our knowledge this is the first study examining nurses' perceptions of the practice environment, quality of care and patient safety across four hospital levels within the public health sector of South Africa.
Recommendations
There are several recommendations from this study which could contribute to improvement to nurse practice environment, quality of care and patient safety. For example, there is a need to improve organisational culture with a focus on empowering leaders on leading compliance to existing policies, and on supportive leadership; this would lead to an improved nurse practice environment, quality of care and patient safety. A specific focus should be placed on support and empowerment of nurses working in more rural and smaller hospitals. Resource allocation to smaller hospitals should be reviewed, considering the added expenditure associated with remote locations and the added challenges in achieving economies of scale. Enabling positive nursing practice environments by means of enhanced nurse participation, non-punitive strategies of enhancing quality of care, leadership championing and better resource auditing will create environments nurses can thrive in, while also maximising patient outcomes in terms of quality of care and patient safety. In addition, there is an urgent need to review existing policies to identify how the nurse practice environment is enhanced or negatively affected by such policies, and intentionally examine and improve the link between nurse practice environment, quality of care and patient safety in the existing policies.
Nurses perceived the practice environment, quality of care and patient safety to be poor across four hospital levels within the public health sector of South Africa. Since there is a strong correlation between nurse practice environment, quality of care and patient safety, there is a need to review the existing policies on quality of care and patient safety and if and to what extent they enhance the nursing practice environment. In addition, strengthening compliance with existing policies that enhance quality of care and patient safety remains important, including the creation of a culture that supports a positive nurse practice environment characterised by manager support, nurse participation in hospital affairs and increased supply of resources, especially in smaller and more rural hospital settings.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Hospital Survey on Patient Safety Culture
National Department of Health
Practice Environment Scale of the Nurse Work Index Revised
Primary healthcare
Universal Health Coverage
World Health Organization. Global Patient Safety Action Plan 2021–2030: Towards eliminating avoidable harm in health care. Geneva: WHO; 2021.
Rispel LC, Blaauw D, Ditlopo P, White J. Human resources for health and universal health coverage: progress, complexities and contestations. South African Health Rev. 2018;2018(1):13–21.
Google Scholar
World Health Organization. Delivering quality health services: a global imperative for universal health coverage. Geneva: World Health Organization, Organisation for Economic and Development & The World Bank; 2018.
Lee SE, Scott LD, Dahinten VS, Vincent C, Lopez KD, Park CG. Safety culture, patient safety, and quality of care outcomes: a literature review. West J Nurs Res. 2019;41(2):279–304.
Article PubMed Google Scholar
Zeleníková R, Jarošová D, Plevová I, Janíková E. Nurses’ perceptions of professional practice environment and its relation to missed nursing care and nurse satisfaction. Int J Environ Res Public Health. 2020;17(11):3805.
Article PubMed PubMed Central Google Scholar
World Health Organization. Quality of care. 2024. https://www.who.int/health-topics/quality-of-care . Accessed 8 May 2024.
Pérez-Francisco DH, Duarte-Clíments G, del Rosario-Melián JM, Gómez-Salgado J, Romero-Martín M, Sánchez-Gómez MB. Influence of workload on primary care nurses’ health and burnout, patients’ safety, and quality of care: Integrative review. Healthcare. 2020;8:12. MDPI; 2020.
Jarrar MT, Al-Bsheish M, Aldhmadi BK, Albaker W, Meri A, Dauwed M, Minai MS. Effect of practice environment on nurse reported quality and patient safety: the mediation role of person-centeredness. Healthcare. 2021;9:1578. MDPI; 2021.
Lucas P, Jesus É, Almeida S, Araújo B. Relationship of the nursing practice environment with the quality of care and patients’ safety in primary health care. BMC Nurs. 2023;22(1):413.
Lake ET, Sanders J, Duan R, Riman KA, Schoenauer KM, Chen Y. A meta-analysis of the associations between the nurse work environment in hospitals and 4 sets of outcomes. Med Care. 2019;57(5):353–61.
Article Google Scholar
Coetzee SK, Klopper HC, Ellis SM, Aiken LH. A tale of two systems—Nurses practice environment, well being, perceived quality of care and patient safety in private and public hospitals in South Africa: A questionnaire survey. Int J Nur Stud. 2013;50(2):162–73.
Bence AF, Coetzee SK, Klopper HC, Ellis SM. The association between the practice environment and selected nurse educator outcomes in public nursing education institutions: A cross-sectional study. Nurse Educ Pract. 2022;58:103261.
Abraham V, Meyer JC, Godman B, Helberg E. Perceptions of managerial staff on the patient safety culture at a tertiary hospital in South Africa. Int J Qual Stud Health Well Being. 2022;17(1):2066252.
Nyelisani M, Makhado L, Luhalima T. A professional nurse’s understanding of quality nursing care in Limpopo province, South Africa. Curationis. 2023;46(1):2322.
Gqaleni TM, Bhengu BR. Analysis of patient safety incident reporting system as an indicator of quality nursing in critical care units in KwaZulu-Natal, South Africa. Health SA Gesondheid. 2020;25(1):1–8.
Abraham V, Meyer J, Godman B, Helberg E. Patient safety culture at the unit level of a tertiary hospital in South Africa: a survey study. J Public Health in Afr. 2023;14:2228.
Mayeng LM, Wolvaardt JE. Patient safety culture in a district hospital in South Africa: An issue of quality. Curationis. 2015;38(1):1–7.
NDoH. Towards quality care for patients: National core standards for health establishments in South Africa. Pretoria: Government Printers; 2011.
NDoH. National guideline for patient safety incident reporting and learning in the public health sector of South Africa. Pretoria: Government Printers; 2022.
NDoH. Ideal hospital realisation and maintenance framework manual. Pretoria: Government Printers; 2018.
Maphumulo WT, Bhengu BR. Challenges of quality improvement in the healthcare of South Africa post-apartheid: A critical review. Curationis. 2019;42(1):1–9.
Aikman N. The crisis within the South African healthcare system: A multifactorial disorder. S Afr J Bioeth Law. 2019;12(2):52–6.
Prinsen L. Medicine and the Law: The leading causes of medicolegal claims and possible solutions. S Afr Med Jo. 2023;113(4):1140–2.
Tvedt C, Sjetne IS, Helgeland J, Bukholm G. An observational study: associations between nurse-reported hospital characteristics and estimated 30-day survival probabilities. BMJ Qual Saf. 2014;23(9):757–64.
Republic of South Africa. National health insurance bill. Pretoria: Government Printers; 2019.
Republic of South Africa. National Health Amendment Act No.12 of 2013. Cape Town: Government Printers; 2013.
Zangaro GA, Jones K. Practice environment scale of the nursing work index: a reliability generalization meta-analysis. West J Nurs Res. 2019;41(11):1658–84.
Blegen MA, Gearhart S, O’Brien R, Sehgal NL, Alldredge BK. AHRQ’s hospital survey on patient safety culture: psychometric analyses. J patient saf. 2009;5:139–44.
Coetzee SK, Klopper HC, Ellis SM, Aiken LH. A tale of two systems—Nurses practice environment, well being, perceived quality of care and patient safety in private and public hospitals in South Africa: A questionnaire survey. Int J Afr Nurs Sci. 2013;50(2):162–73.
Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Sermeus W. Consortium Rc: Nurses’ reports of working conditions and hospital quality of care in 12 countries in Europe. Int J Nurs Stud. 2013;50(2):143–53.
Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, McKee M, Bruyneel L, Rafferty AM, Griffiths P, Moreno-Casbas MT. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. Bmj. 2012;344:e1717.
Liu K, You LM, Chen SX, Hao YT, Zhu XW, Zhang LF, Aiken LH. The relationship between hospital work environment and nurse outcomes in Guangdong, China: a nurse questionnaire survey. J Clin Nurs. 2012;21(9–10):1476–85.
Lake ET, Sanders J, Duan R, Riman KA, Schoenauer KM, Chen Y. A Meta-Analysis of the Associations Between the Nurse Work Environment in Hospitals and 4 Sets of Outcomes. Med Care. 2019;57(5):353–61.
IBM Corp. IBM SPSS statistics for windows. Version 28.0. Armonk: IBM Corp; 2021.
Habibzadeh F. Data Distribution: Normal or Abnormal? J Korean Med Sci. 2024;39(3):e35.
Republic of South Africa. 2030 Human resources for health strategy: Investing in the health workforce for universal health coverage. Pretoria: Government Printers; 2020.
Cranage K, Foster K. Mental health nurses’ experience of challenging workplace situations: a qualitative descriptive study. Int J Ment Health Nurs. 2022;31(3):665–76.
Muthathi IS, Rispel LC. Policy context, coherence and disjuncture in the implementation of the ideal clinic realisation and maintenance programme in the Gauteng and Mpumalanga provinces of South Africa. Health Res Policy Sys. 2020;18(55):1–15.
Muthathi IS, Levin J, Rispel LC. Decision space and participation of primary healthcare facility managers in the Ideal Clinic Realisation and Maintenance programme in two South African provinces. Health Policy Plan. 2020;35(3):302–12.
Taderera BH. Decision space and its contribution to the pursuit of human resources for health reform in local health systems: An exploratory review of literature. Int J Healthcare Manag. 2021;14(3):621–8.
Byers V. The challenges of leading change in health-care delivery from the front-line. J Nurs Manag. 2017;25(6):449–56.
Lotfi Z, Atashzadeh-Shoorideh F, Mohtashami J, Nasiri M. Relationship between ethical leadership and organisational commitment of nurses with perception of patient safety culture. J Nurs Manag. 2018;26(6):726–34.
Al Sabei SD, Labrague LJ, Miner Ross A, Karkada S, Albashayreh A, Al Masroori F, Al Hashmi N. Nursing work environment, turnover intention, job burnout, and quality of care: The moderating role of job satisfaction. J Nurs Scholarsh. 2020;52(1):95–104.
Lake ET, Riman KA, Sloane DM. Improved work environments and staffing lead to less missed nursing care: A panel study. J Nurs Manag. 2020;28(8):2157–65.
Carthon JMB, Hatfield L, Brom H, Houton M, Kelly-Hellyer E, Schlak A, Aiken LH. System-level improvements in work environments lead to lower nurse burnout and higher patient satisfaction. J Nurs Care Qual. 2021;36(1):7–13.
Hegazy AM, Ibrahim MM, Shokry WA. Nurses’ perception of work environment factors and its relation with their work engagement. Egypt J Health Care. 2022;13(1):280–93.
Carvajal B, Hancock A, Lewney K, Hagan K, Jamieson S, Cooke A. A global overview of midwives’ working conditions: A rapid review of literature on positive practice environment. Women and Birth. 2023;37(1):15–20.
Mihdawi M, Al-Amer R, Darwish R, Randall S, Afaneh T. The influence of nursing work environment on patient safety. Workplace health & safety. 2020;68(8):384–90.
Smith S, Lapkin S, Sim J, Halcomb E. Nursing care left undone, practice environment and perceived quality of care in small rural hospitals. J Nurs Manag. 2020;28(8):2166–73.
Haskins J, Phakathi S, Grant M, Horwood C. Attitudes of nurses towards patient care at a rural district hospital in the KwaZulu-Natal province of South Africa. Afr J Nurs Midwifery. 2014;16(1):32–44.
Steinhobel R, Massyn N, Peer N. The Ideal Clinic Programme 2015/16. Durban: Health Systems Trust and South African National Department of Health; 2015.
Jarbandhan D, Pillay P, Mantzaris E. Corruption in healthcare infrastructure public-private partnerships: A South African Case study. Administratio Publica. 2023;31(1):78–97.
Ranchod S, Adams C, Burger R, Carvounes A, Dreyer K, Smith A, Van Biljon C, Stewart J. South Africa’s hospital sector: old divisions and new developments. South Afr Health Rev. 2017;2017(1):101–10.
Magadzire BP, Ward K, Leng HM, Sanders D. Inefficient procurement processes undermine access to medicines in the Western Cape Province of South Africa. S Afr Med J. 2017;107(7):581–4.
Modisakeng C, Matlala M, Godman B, Meyer JC. Medicine shortages and challenges with the procurement process among public sector hospitals in South Africa; findings and implications. BMC Health Serv Res. 2020;20(1):1–10.
Manyisa ZM, van Aswegen EJ. Factors affecting working conditions in public hospitals: A literature review. Int J Afr Nurs Sci. 2017;6:28–38.
Von Holdt K, Murphy M. Public hospitals in South Africa: stressed institutions, disempowered management. In Buhlungu S,Daniel J, Southall R & Lutchman J (editors) State of the Nation: South Africa, Cape Town, HSRC Press; 2007:312–341.
Lumadi TG, Matlala MS. Perceptions of midwives on shortage and retention of staff at a public hospital in Tshwane District. Curationis. 2019;42(1):1–10.
Tenza IS, Attafuah PY, Abor P, Nketiah-Amponsah E, Abuosi AA. Hospital managers’ views on the state of patient safety culture across three regions in Ghana. BMC Health Serv Res. 2022;22(1):1300.
Huang H, Xiao L, Chen Z, Cao S, Zheng S, Zhao Q, Xiao M. A National Study of Patient Safety Culture and Patient Safety Goal in Chinese Hospitals. J Patient Saf. 2022;18(8):e1167.
Kim Y, Lee H. Nurses’ experiences with disclosure of patient safety incidents: a qualitative study. Risk Manag Healthc Pol. 2020;13:453–64.
Woo MWJ, Avery MJ. Nurses’ experiences in voluntary error reporting: an integrative literature review. Int J Nurs Sci. 2021;8(4):453–69.
PubMed PubMed Central Google Scholar
Battat M. Nurses’ experiences of the most common medical errors in the intensive care unit and the coronary care unit: A hermeneutic phenomenological study from Palestine. J Clin Med Img Case Rep. 2022;2(4):1223.
Alhassan RK, Halilu B, Benin SM, Donyor BF, Kuwaru AY, Yipaalanaa D, Nketiah-Amponsah E, Ayanore MA, Abuosi AA, Afaya A. Experiences of frontline nurses with adverse medical events in a regional referral hospital in northern Ghana: A cross-sectional study. Trop Med Health. 2019;47(1):1–10.
Cheragi MA, Manoocheri H, Mohammadnejad E, Ehsani SR. Types and causes of medication errors from nurse’s viewpoint. Iran J Nurs Midwifery Res. 2013;18(3):228.
Zoghby MG, Hoffman D, Mahomed Z. The reporting of adverse events in Johannesburg academic emergency departments. Afr J Emerg Med. 2021;11(1):207–10.
Lee MH, Kim JK. A comparative study on nursing practice environment, professionalism, and job satisfaction according to hospital size. J Korean Acad Nurs Admin. 2013;19(4):470–9.
Rivaz M, Momennasab M, Yektatalab S, Ebadi A. Adequate resources as essential component in the nursing practice environment: A qualitative study. J Clin Diagn Res JCDR. 2017;11(6):IC01.
PubMed Google Scholar
DeVolder R, Serra-Sastre V, Zamora B. Examining the variation across acute trusts in patient delayed discharge. Health Policy. 2020;124(11):1226–32.
Mesman R, Westert GP, Berden BJ, Faber MJ. Why do high-volume hospitals achieve better outcomes? A systematic review about intermediate factors in volume–outcome relationships. Health Policy. 2015;119(8):1055–67.
NDoH. Towards Quality Care for Patients: National Core Standards for Health Establishments in South Africa. Pretoria: Government Printers; 2011.
Malinowska-Lipień I, Micek A, Gabryś T, Kózka M, Gajda K, Gniadek A, Brzostek T, Fletcher J, Squires A. Impact of the work environment on patients’ safety as perceived by nurses in Poland—a cross-sectional study. Int J Environ Res Public Health. 2021;18(22):12057.
Gensimore MM, Maduro RS, Morgan MK, McGee GW, Zimbro KS. The Effect of nurse practice environment on retention and quality of care via burnout, work characteristics, and resilience: a moderated mediation model. JONA J Nursing Adm. 2020;50(10):546–53.
General Assembly of the World Medical Association. World Medical Association Declaration of Helsinki ethical principles for medical research involving human subjects. J Am Coll Dentists. 2014;81(3):14–8.
Download references
Acknowledgements
We would like to thank all the participants of this study; without their participation, this study would not be in existence.
Open access funding provided by North-West University. This work is based on the research supported in part by the National Research Foundation of South Africa (Grant Number 123541). All opinions, findings expressed, and conclusions arrived at, are solely those of the author and are not attributed to the National Research Foundation in any way.
Author information
Authors and affiliations.
School of Nursing Science, Faculty of Health Sciences, North-West University, Potchefstroom, South Africa
Immaculate Sabelile Tenza, Alwiena J. Blignaut & Siedine K. Coetzee
Department of Statistical Consultation, Faculty of Humanities, North-West University, Potchefstroom, South Africa
Suria M. Ellis
You can also search for this author in PubMed Google Scholar
Contributions
IST; AJB; SME and SKC, conceptualised the manuscript. SKC, AJB, and SME analysed the data. IST wrote the original draft of the manuscript. All authors reviewed and edited the manuscript. SKC is a primary investigator, project administrator and a recipient of funding of this study.
Corresponding author
Correspondence to Immaculate Sabelile Tenza .
Ethics declarations
Ethics approval and consent to participate.
This study has been performed following the Declaration of Helsinki [ 76 ] and has obtained ethical approval from the North-West University Health Research Ethics Committee, with ethics number (NWU-00033–19-A1). We also obtained permission to conduct the study from the health authorities and individual public health facilities in the nine provinces of South Africa. All participants were given a detailed information sheet, as well as a verbal explanation of the study. We also informed study participants of the voluntary and confidential nature of participation in the study. All participants signed an informed consent to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Tenza, I.S., Blignaut, A.J., Ellis, S.M. et al. Nurse perceptions of practice environment, quality of care and patient safety across four hospital levels within the public health sector of South Africa. BMC Nurs 23 , 324 (2024). https://doi.org/10.1186/s12912-024-01992-z
Download citation
Received : 15 December 2023
Accepted : 06 May 2024
Published : 13 May 2024
DOI : https://doi.org/10.1186/s12912-024-01992-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- South Africa
- Public hospitals
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- 10 Essential Public Health Services
- Cooperative Agreements, Grants & Partnerships
- Public Health Professional: Programs
- Health Assessment: Index
- Research Summary
- COVID-19 Health Disparities Grant Success Stories Resources
- Communication Resources

Performance Management and Quality Improvement: Definitions and Concepts
At a glance.
In the public health field, many initiatives and organizations focus on improving public health practice, using different terms. This page provides common definitions for public health performance management.
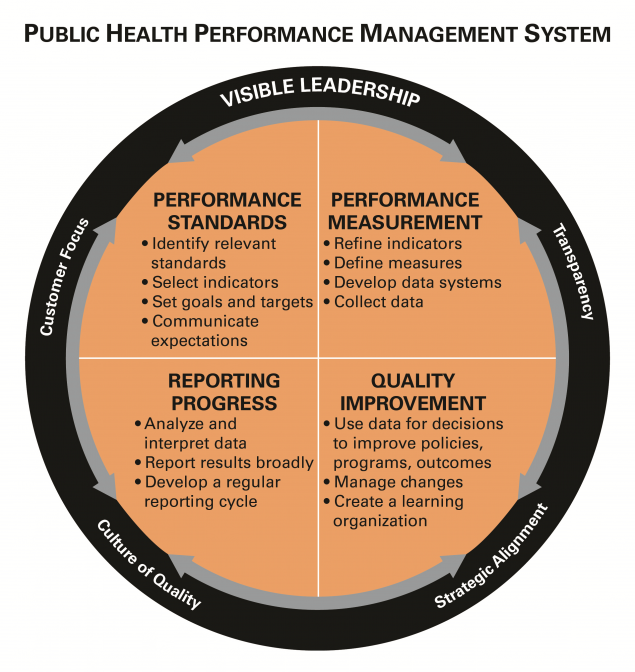
Definitions and concepts
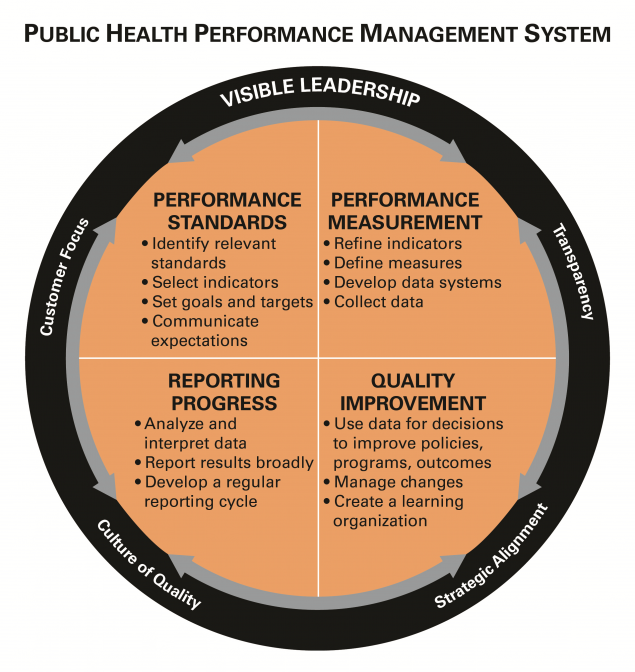
There has been a rapidly growing interest in performance and quality improvement within the public health community, and different names and labels are often used to describe similar concepts or activities. Other sectors, such as industry and hospitals, have embraced a diverse and evolving set of terms but which generally have the same principles at heart (i.e., continuous quality improvement, quality improvement, performance improvement, six sigma, and total quality management).
In the public health field, an array of initiatives has set the stage for attention to improving public health practice, using assorted terms. The Turning Point Collaborative focused on performance management, the National Public Health Performance Standards Program created a framework to assess and improve public health systems, while the US Department of Health and Human Services has provided recommendations on how to achieve quality in healthcare . In 2011, the Public Health Accreditation Board launched a national voluntary accreditation program that catalyzes quality improvement but also acknowledges the importance of performance management within public health agencies. Regardless of the terminology, a common thread has emerged—one that focuses on continuous improvement and operational excellence within public health programs, agencies, and the public health system.
To anchor common thinking, below are links to some of the definitions that are frequently used throughout these pages.
Key definitions
- Riley et al, "Defining Quality Improvement in Public Health", JPHMP, 2010, 16(10), 5-7.
- Public Health Accreditation Board Acronyms and Glossary of Terms, Version 2022 [PDF]
Public Health Gateway
CDC's National Center for State, Tribal, Local, and Territorial Public Health Infrastructure and Workforce helps drive public health forward and helps HDs deliver services to communities.
- Open access
- Published: 09 May 2024
Evaluation of integrated community case management of the common childhood illness program in Gondar city, northwest Ethiopia: a case study evaluation design
- Mekides Geta 1 ,
- Geta Asrade Alemayehu 2 ,
- Wubshet Debebe Negash 2 ,
- Tadele Biresaw Belachew 2 ,
- Chalie Tadie Tsehay 2 &
- Getachew Teshale 2
BMC Pediatrics volume 24 , Article number: 310 ( 2024 ) Cite this article
127 Accesses
Metrics details
Integrated Community Case Management (ICCM) of common childhood illness is one of the global initiatives to reduce mortality among under-five children by two-thirds. It is also implemented in Ethiopia to improve community access and coverage of health services. However, as per our best knowledge the implementation status of integrated community case management in the study area is not well evaluated. Therefore, this study aimed to evaluate the implementation status of the integrated community case management program in Gondar City, Northwest Ethiopia.
A single case study design with mixed methods was employed to evaluate the process of integrated community case management for common childhood illness in Gondar town from March 17 to April 17, 2022. The availability, compliance, and acceptability dimensions of the program implementation were evaluated using 49 indicators. In this evaluation, 484 mothers or caregivers participated in exit interviews; 230 records were reviewed, 21 key informants were interviewed; and 42 observations were included. To identify the predictor variables associated with acceptability, we used a multivariable logistic regression analysis. Statistically significant variables were identified based on the adjusted odds ratio (AOR) with a 95% confidence interval (CI) and p-value. The qualitative data was recorded, transcribed, and translated into English, and thematic analysis was carried out.
The overall implementation of integrated community case management was 81.5%, of which availability (84.2%), compliance (83.1%), and acceptability (75.3%) contributed. Some drugs and medical equipment, like Cotrimoxazole, vitamin K, a timer, and a resuscitation bag, were stocked out. Health care providers complained that lack of refreshment training and continuous supportive supervision was the common challenges that led to a skill gap for effective program delivery. Educational status (primary AOR = 0.27, 95% CI:0.11–0.52), secondary AOR = 0.16, 95% CI:0.07–0.39), and college and above AOR = 0.08, 95% CI:0.07–0.39), prescribed drug availability (AOR = 2.17, 95% CI:1.14–4.10), travel time to the to the ICCM site (AOR = 3.8, 95% CI:1.99–7.35), and waiting time (AOR = 2.80, 95% CI:1.16–6.79) were factors associated with the acceptability of the program by caregivers.
Conclusion and recommendation
The overall implementation status of the integrated community case management program was judged as good. However, there were gaps observed in the assessment, classification, and treatment of diseases. Educational status, availability of the prescribed drugs, waiting time and travel time to integrated community case management sites were factors associated with the program acceptability. Continuous supportive supervision for health facilities, refreshment training for HEW’s to maximize compliance, construction clean water sources for HPs, and conducting longitudinal studies for the future are the forwarded recommendation.
Peer Review reports
Integrated Community Case Management (ICCM) is a critical public health strategy for expanding the coverage of quality child care services [ 1 , 2 ]. It mainly concentrated on curative care and also on the diagnosis, treatment, and referral of children who are ill with infectious diseases [ 3 , 4 ].
Based on the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) recommendations, Ethiopia adopted and implemented a national policy supporting community-based treatment of common childhood illnesses like pneumonia, Diarrhea, uncomplicated malnutrition, malaria and other febrile illness and Amhara region was one the piloted regions in late 2010 [ 5 ]. The Ethiopian primary healthcare units, established at district levels include primary hospitals, health centers (HCs), and health posts (HPs). The HPs are run by Health Extension Workers (HEWs), and they have function of monitoring health programs and disease occurrence, providing health education, essential primary care services, and timely referrals to HCs [ 6 , 7 ]. The Health Extension Program (HEP) uses task shifting and community ownership to provide essential health services at the first level using the health development army and a network of woman volunteers. These groups are organized to promote health and prevent diseases through community participation and empowerment by identifying the salient local bottlenecks which hinder vital maternal, neonatal, and child health service utilization [ 8 , 9 ].
One of the key steps to enhance the clinical case of health extension staff is to encourage better growth and development among under-five children by health extension. Healthy family and neighborhood practices are also encouraged [ 10 , 11 ]. The program also combines immunization, community-based feeding, vitamin A and de-worming with multiple preventive measures [ 12 , 13 ]. Now a days rapidly scaling up of ICCM approach to efficiently manage the most common causes of morbidity and mortality of children under the age of five in an integrated manner at the community level is required [ 14 , 15 ].
Over 5.3 million children are died at a global level in 2018 and most causes (75%) are preventable or treatable diseases such as pneumonia, malaria and diarrhea [ 16 ]. About 99% of the global burden of mortality and morbidity of under-five children which exists in developing countries are due to common childhood diseases such as pneumonia, diarrhea, malaria and malnutrition [ 17 ].
In 2013, the mortality rate of under-five children in Sub-Saharan Africa decreased to 86 deaths per 1000 live birth and estimated to be 25 per 1000live births by 2030. However, it is a huge figure and the trends are not sufficient to reach the target [ 18 ]. About half of global under-five deaths occurred in sub-Saharan Africa. And from the top 26 nations burdened with 80% of the world’s under-five deaths, 19 are in sub-Saharan Africa [ 19 ].
To alleviate the burden, the Ethiopian government tries to deliver basic child care services at the community level by trained health extension workers. The program improves the health of the children not only in Ethiopia but also in some African nations. Despite its proven benefits, the program implementation had several challenges, in particular, non-adherence to the national guidelines among health care workers [ 20 ]. Addressing those challenges could further improve the program performance. Present treatment levels in sub-Saharan Africa are unacceptably poor; only 39% of children receive proper diarrhea treatment, 13% of children with suspected pneumonia receive antibiotics, 13% of children with fever receive a finger/heel stick to screen for malaria [ 21 ].
To improve the program performance, program gaps should be identified through scientific evaluations and stakeholder involvement. This evaluation not only identify gaps but also forward recommendations for the observed gaps. Furthermore, the implementation status of ICCM of common childhood illnesses has not been evaluated in the study area yet. Therefore, this work aimed to evaluate the implementation status of integrated community case management program implementation in Gondar town, northwest Ethiopia. The findings may be used by policy makers, healthcare providers, funders and researchers.
Method and material
Evaluation design and settings.
A single-case study design with concurrent mixed-methods evaluation was conducted in Gondar city, northwest Ethiopia, from March 17 to April 17, 2022. The evaluability assessment was done from December 15–30, 2021. Both qualitative and quantitative data were collected concurrently, analyzed separately, and integrated at the result interpretation phase.
The evaluation area, Gondar City, is located in northwest Ethiopia, 740 km from Addis Ababa, the capital city of the country. It has six sub-cities and thirty-six kebeles (25 urban and 11 rural). In 2019, the estimated total population of the town was 338,646, and 58,519 (17.3%) were under-five children. In the town there are eight public health centers and 14 health posts serving the population. All health posts provide ICCM service for more than 70,852 populations.
Evaluation approach and dimensions
Program stakeholders.
The evaluation followed a formative participatory approach by engaging the potential stakeholders in the program. Prior to the development of the proposal, an extensive discussion was held with the Gondar City Health Department to identify other key stakeholders in the program. Service providers at each health facility (HCs and HPs), caretakers of sick children, the Gondar City Health Office (GCHO), the Amhara Regional Health Bureau (ARHB), the Minister of Health (MoH), and NGOs (IFHP and Save the Children) were considered key stakeholders. During the Evaluability Assessment (EA), the stakeholders were involved in the development of evaluation questions, objectives, indicators, and judgment criteria of the evaluation.
Evaluation dimensions
The availability and acceptability dimensions from the access framework [ 22 ] and compliance dimension from the fidelity framework [ 23 ] were used to evaluate the implementation of ICCM.
Population and samplings
All under-five children and their caregivers attended at the HPs; program implementers (health extension workers, healthcare providers, healthcare managers, PHCU focal persons, MCH coordinators, and other stakeholders); and ICCM records and registries in the health posts of Gondar city administration were included in the evaluation. For quantitative data, the required sample size was proportionally allocated for each health post based on the number of cases served in the recent one month. But the qualitative sample size was determined by data saturation, and the samples were selected purposefully.
The data sources and sample size for the compliance dimension were all administrative records/reports and ICCM registration books (230 documents) in all health posts registered from December 1, 2021, to February 30, 2022 (three months retrospectively) included in the evaluation. The registries were assessed starting from the most recent registration number until the required sample size was obtained for each health post.
The sample size to measure the mothers’/caregivers’ acceptability towards ICCM was calculated by taking prevalence of caregivers’ satisfaction on ICCM program p = 74% from previously similar study [ 24 ] and considering standard error 4% at 95% CI and 10% non- responses, which gave 508. Except those who were seriously ill, all caregivers attending the ICCM sites during data collection were selected and interviewed consecutively.
The availability of required supplies, materials and human resources for the program were assessed in all 14HPs. The data collectors observed the health posts and collected required data by using a resources inventory checklist.
A total of 70 non-participatory patient-provider interactions were also observed. The observations were conducted per each health post and for health posts which have more than one health extension workers one of them were selected randomly. The observation findings were used to triangulate the findings obtained through other data collection techniques. Since people may act accordingly to the standards when they know they are observed for their activities, we discarded the first two observations from analysis. It is one of the strategies to minimize the Hawthorne effect of the study. Finally a total of 42 (3 in each HPs) observations were included in the analysis.
Twenty one key informants (14 HEWs, 3 PHCU focal person, 3 health center heads and one MCH coordinator) were interviewed. These key informants were selected since they are assumed to be best teachers in the program. Besides originally developed key informant interview questions, the data collectors probed them to get more detail and clear information.
Variables and measurement
The availability of resources, including trained healthcare workers, was examined using 17 indicators, with weighted score of 35%. Compliance was used to assess HEWs’ adherence to the ICCM treatment guidelines by observing patient-provider interactions and conducting document reviews. We used 18 indicators and a weighted value of 40%.
Mothers’ /caregivers’/ acceptance of ICCM service was examined using 14 indicators and had a weighted score of 25%. The indicators were developed with a five-point Likert scale (1: strongly disagree, 2: disagree, 3: neutral, 4: agree and 5: strongly agree). The cut off point for this categorization was calculated using the demarcation threshold formula: ( \(\frac{\text{t}\text{o}\text{t}\text{a}\text{l}\, \text{h}\text{i}\text{g}\text{h}\text{e}\text{s}\text{t}\, \text{s}\text{c}\text{o}\text{r}\text{e}-\,\text{t}\text{o}\text{t}\text{a}\text{l}\, \text{l}\text{o}\text{w}\text{e}\text{s}\text{t} \,\text{s}\text{c}\text{o}\text{r}\text{e}}{2}) +total lowest score\) ( 25 – 27 ). Those mothers/caregivers/ who scored above cut point (42) were considered as “satisfied”, otherwise “dissatisfied”. The indicators were adapted from the national ICCM and IMNCI implementation guideline and other related evaluations with the participation of stakeholders. Indicator weight was given by the stakeholders during EA. Indicators score was calculated using the formula \(\left(achieved \,in \%=\frac{indicator \,score \,x \,100}{indicator\, weight} \right)\) [ 26 , 28 ].
The independent variables for the acceptability dimension were socio-demographic and economic variables (age, educational status, marital status, occupation of caregiver, family size, income level, and mode of transport), availability of prescribed drugs, waiting time, travel time to ICCM site, home to home visit, consultation time, appointment, and source of information.
The overall implementation of ICCM was measured by using 49 indicators over the three dimensions: availability (17 indicators), compliance (18 indicators) and acceptability (14 indicators).
Program logic model
Based on the constructed program logic model and trained health care providers, mothers/caregivers received health information and counseling on child feeding; children were assessed, classified, and treated for disease, received follow-up; they were checked for vitamin A; and deworming and immunization status were the expected outputs of the program activities. Improved knowledge of HEWs on ICCM, increased health-seeking behavior, improved quality of health services, increased utilization of services, improved data quality and information use, and improved child health conditions are considered outcomes of the program. Reduction of under-five morbidity and mortality and improving quality of life in the society are the distant outcomes or impacts of the program (Fig. 1 ).
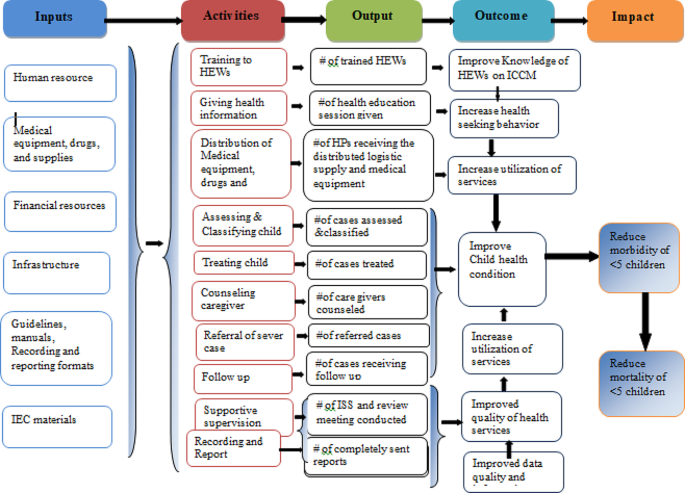
Integrated community case management of childhood illness program logic model in Gondar City in 2022
Data collection tools and procedure
Resource inventory and data extraction checklists were adapted from standard ICCM tool and check lists [ 29 ]. A structured interviewer administered questionnaire was adapted by referring different literatures [ 30 , 31 ] to measure the acceptability of ICCM. The key informant interview (KII) guide was also developed to explore the views of KIs. The interview questionnaire and guide were initially developed in English and translated into the local language (Amharic) and finally back to English to ensure consistency. All the interviews were done in the local language, Amharic.
Five trained clinical nurses and one BSC nurse were recruited from Gondar zuria and Wegera district as data collectors and supervisors, respectively. Two days training on the overall purpose of the evaluation and basic data collection procedures were provided prior to data collection. Then, both quantitative and qualitative data were gathered at the same time. The quantitative data were gathered from program documentation, charts of ICCM program visitors and, exit interview. Interviews with 21 KIIs and non-participatory observations of patient-provider interactions were used to acquire qualitative data. Key informant interviews were conducted to investigate the gaps and best practices in the implementation of the ICCM program.
A pretest was conducted to 26 mothers/caregivers/ at Maksegnit health post and appropriate modifications were made based on the pretest results. The data collectors were supervised and principal evaluator examined the completeness and consistency of the data on a daily basis.
Data management and analysis
For analysis, quantitative data were entered into epi-data version 4.6 and exported to Stata 14 software for analysis. Narration and tabular statistics were used to present descriptive statistics. Based on established judgment criteria, the total program implementation was examined and interpreted as a mix of the availability, compliance, and acceptability dimensions. To investigate the factors associated with ICCM acceptance, a binary logistic regression analysis was performed. During bivariable analysis, variables with p-values less than 0.25 were included in multivariable analysis. Finally, variables having a p-value less than 0.05 and an adjusted odds ratio (AOR) with a 95% confidence interval (CI) were judged statistically significant. Qualitative data were collected recorded, transcribed into Amharic, then translated into English and finally coded and thematically analyzed.
Judgment matrix analysis
The weighted values of availability, compliance, and acceptability dimensions were 35, 40, and 25 based on the stakeholder and investigator agreement on each indicator, respectively. The judgment parameters for each dimension and the overall implementation of the program were categorized as poor (< 60%), fair (60–74.9%), good (75-84.9%), and very good (85–100%).
Availability of resources
A total of 26 HEWs were assigned within the fourteen health posts, and 72.7% of them were trained on ICCM to manage common childhood illnesses in under-five children. However, the training was given before four years, and they didn’t get even refreshment training about ICCM. The KII responses also supported that the shortage of HEWs at the HPs was the problem in implementing the program properly.
I am the only HEW in this health post and I have not been trained on ICCM program. So, this may compromise the quality of service and client satisfaction.(25 years old HEW with two years’ experience)
All observed health posts had ICCM registration books, monthly report and referral formats, functional thermometer, weighting scale and MUAC tape meter. However, timer and resuscitation bag was not available in all HPs. Most of the key informant finding showed that, in all HPs there was no shortage of guideline, registration book and recording tool; however, there was no OTP card in some health posts.
“Guideline, ICCM registration book for 2–59 months of age, and other different recording and reporting formats and booklet charts are available since September/2016. However, OTP card is not available in most HPs.”. (A 30 years male health center director)
Only one-fifth (21%) of HPs had a clean water source for drinking and washing of equipment. Most of Key-informant interview findings showed that the availability of infrastructures like water was not available in most HPs. Poor linkage between HPs, HCs, town health department, and local Kebele administer were the reason for unavailability.
Since there is no water for hand washing, or drinking, we obligated to bring water from our home for daily consumptions. This increases the burden for us in our daily activity. (35 years old HEW)
Most medicines, such as anti-malaria drugs with RDT, Quartem, Albendazole, Amoxicillin, vitamin A capsules, ORS, and gloves, were available in all the health posts. Drugs like zinc, paracetamol, TTC eye ointment, and folic acid were available in some HPs. However, cotrimoxazole and vitamin K capsules were stocked-out in all health posts for the last six months. The key informant also revealed that: “Vitamin K was not available starting from the beginning of this program and Cotrimoxazole was not available for the past one year and they told us they would avail it soon but still not availed. Some essential ICCM drugs like anti malaria drugs, De-worming, Amoxicillin, vitamin A capsules, ORS and medical supplies were also not available in HCs regularly.”(28 years’ Female PHCU focal)
The overall availability of resources for ICCM implementation was 84.2% which was good based on our presetting judgment parameter (Table 1 ).
Health extension worker’s compliance
From the 42 patient-provider interactions, we found that 85.7%, 71.4%, 76.2%, and 95.2% of the children were checked for body temperature, weight, general danger signs, and immunization status respectively. Out of total (42) observation, 33(78.6%) of sick children were classified for their nutritional status. During observation time 29 (69.1%) of caregivers were counseled by HEWs on food, fluid and when to return back and 35 (83.3%) of children were appointed for next follow-up visit. Key informant interviews also affirmed that;
“Most of our health extension workers were trained on ICCM program guidelines but still there are problems on assessment classification and treatment of disease based on guidelines and standards this is mainly due to lack refreshment training on the program and lack of continuous supportive supervision from the respective body.” (27years’ Male health center head)
From 10 clients classified as having severe pneumonia cases, all of them were referred to a health center (with pre-referral treatment), and from those 57 pneumonia cases, 50 (87.7%) were treated at the HP with amoxicillin or cotrimoxazole. All children with severe diarrhea, very severe disease, and severe complicated malnutrition cases were referred to health centers with a pre-referral treatment for severe dehydration, very severe febrile disease, and severe complicated malnutrition, respectively. From those with some dehydration and no dehydration cases, (82.4%) and (86.8%) were treated at the HPs for some dehydration (ORS; plan B) and for no dehydration (ORS; plan A), respectively. Moreover, zinc sulfate was prescribed for 63 (90%) of under-five children with some dehydration or no dehydration. From 26 malaria cases and 32 severe uncomplicated malnutrition and moderate acute malnutrition cases, 20 (76.9%) and 25 (78.1%) were treated at the HPs, respectively. Of the total reviewed documents, 56 (93.3%), 66 (94.3%), 38 (84.4%), and 25 (78.1%) of them were given a follow-up date for pneumonia, diarrhea, malaria, and malnutrition, respectively.
Supportive supervision and performance review meetings were conducted only in 10 (71.4%) HPs, but all (100%) HPs sent timely reports to the next supervisory body.
Most of the key informants’ interview findings showed that supportive supervision was not conducted regularly and for all HPs.
I had mentored and supervised by supportive supervision teams who came to our health post at different times from health center, town health office and zonal health department. I received this integrated supervision from town health office irregularly, but every month from catchment health center and last integrated supportive supervision from HC was on January. The problem is the supervision was conducted for all programs.(32 years’ old and nine years experienced female HEW)
Moreover, the result showed that there was poor compliance of HEWs for the program mainly due to weak supportive supervision system of managerial and technical health workers. It was also supported by key informants as:
We conducted supportive supervision and performance review meeting at different time, but still there was not regular and not addressed all HPs. In addition to this the supervision and review meeting was conducted as integration of ICCM program with other services. The other problem is that most of the time we didn’t used checklist during supportive supervision. (Mid 30 years old male HC director)
Based on our observation and ICCM document review, 83.1% of the HEWs were complied with the ICCM guidelines and judged as fair (Table 2 ).
Acceptability of ICCM program
Sociodemographic and obstetric characteristics of participants.
A total of 484 study participants responded to the interviewer-administered questionnaire with a response rate of 95.3%. The mean age of study participants was 30.7 (SD ± 5.5) years. Of the total caregivers, the majority (38.6%) were categorized under the age group of 26–30 years. Among the total respondents, 89.3% were married, and regarding religion, the majorities (84.5%) were Orthodox Christian followers. Regarding educational status, over half of caregivers (52.1%) were illiterate (unable to read or write). Nearly two-thirds of the caregivers (62.6%) were housewives (Table 3 ).
All the caregivers came to the health post on foot, and most of them 418 (86.4%) arrived within one hour. The majority of 452 (93.4%) caregivers responded that the waiting time to get the service was less than 30 min. Caregivers who got the prescribed drugs at the health post were 409 (84.5%). Most of the respondents, 429 (88.6%) and 438 (90.5%), received counseling services on providing extra fluid and feeding for their sick child and were given a follow-up date.
Most 298 (61.6%) of the caregivers were satisfied with the convenience of the working hours of HPs, and more than three-fourths (80.8%) were satisfied with the counseling services they received. Most of the respondents, 366 (75.6%), were satisfied with the appropriateness of waiting time and 431 (89%) with the appropriateness of consultation time. The majority (448 (92.6%) of caregivers were satisfied with the way of communicating with HEWs, and 269 (55.6%) were satisfied with the knowledge and competence of HEWs. Nearly half of the caregivers (240, or 49.6%) were satisfied with the availability of drugs at health posts.
The overall acceptability of the ICCM program was 75.3%, which was judged as good. A low proportion of acceptability was measured on the cleanliness of the health posts, the appropriateness of the waiting area, and the competence and knowledge of the HEWs. On the other hand, high proportion of acceptability was measured on appropriateness of waiting time, way of communication with HEWs, and the availability of drugs (Table 4 ).
Factors associated with acceptability of ICCM program
In the final multivariable logistic regression analysis, educational status of caregivers, availability of prescribed drugs, time to arrive, and waiting time were factors significantly associated with the satisfaction of caregivers with the ICCM program.
Accordingly, the odds of caregivers with primary education, secondary education, and college and above were 73% (AOR = 0.27, 95% CI: 0.11–0.52), 84% (AOR = 0.16, 95% CI: 0.07–0.39), and 92% (AOR = 0.08, 95% CI: 0.07–0.40) less likely to accept the program as compared to mothers or caregivers who were not able to read and write, respectively. The odds of caregivers or mothers who received prescribed drugs were 2.17 times more likely to accept the program as compared to their counters (AOR = 2.17, 95% CI: 1.14–4.10). The odds of caregivers or mothers who waited for services for less than 30 min were 2.8 times more likely to accept the program as compared to those who waited for more than 30 min (AOR = 2.80, 95% CI: 1.16–6.79). Moreover, the odds of caregivers/mothers who traveled an hour or less for service were 3.8 times more likely to accept the ICCM program as compared to their counters (AOR = 3.82, 95% CI:1.99–7.35) (Table 5 ).
Overall ICCM program implementation and judgment
The implementation of the ICCM program in Gondar city administration was measured in terms of availability (84.2%), compliance (83.1%), and acceptability (75.3%) dimensions. In the availability dimension, amoxicillin, antimalarial drugs, albendazole, Vit. A, and ORS were available in all health posts, but only six HPs had Ready-to-Use Therapeutic Feedings, three HPs had ORT Corners, and none of the HPs had functional timers. In all health posts, the health extension workers asked the chief to complain, correctly assessed for pneumonia, diarrhea, malaria, and malnutrition, and sent reports based on the national schedule. However, only 70% of caretakers counseled about food, fluids, and when to return, 66% and 76% of the sick children were checked for anemia and other danger signs, respectively. The acceptability level of the program by caretakers and caretakers’/mothers’ educational status, waiting time to get the service and travel time ICCM sites were the factors affecting its acceptability. The overall ICCM program in Gondar city administration was 81.5% and judged as good (Fig. 2 ).
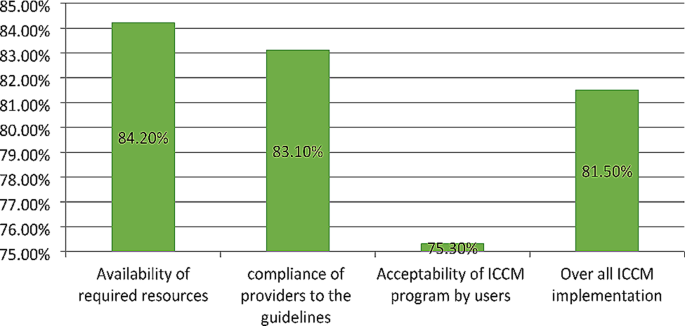
Overall ICCM program implementation and the evaluation dimensions in Gondar city administration, 2022
The implementation status of ICCM was judged by using three dimensions including availability, compliance and acceptability of the program. The judgment cut of points was determined during evaluability assessment (EA) along with the stakeholders. As a result, we found that the overall implementation status of ICCM program was good as per the presetting judgment parameter. Availability of resources for the program implementation, compliance of HEWs to the treatment guideline and acceptability of the program services by users were also judged as good as per the judgment parameter.
This evaluation showed that most medications, equipment and recording and reporting materials available. This finding was comparable with the standard ICCM treatment guide line [ 10 ]. On the other hand trained health care providers, some medications like Zink, Paracetamol and TTC eye ointment, folic acid and syringes were not found in some HPs. However the finding was higher than the study conducted in SNNPR on selected health posts [ 33 ] and a study conducted in Soro district, southern Ethiopia [ 24 ]. The possible reason might be due to low interruption of drugs at town health office or regional health department stores, regular supplies of essential drugs and good supply management and distribution of drug from health centers to health post.
The result of this evaluation showed that only one fourth of health posts had functional ORT Corner which was lower compared to the study conducted in SNNPR [ 34 ]. This might be due poor coverage of functional pipe water in the kebeles and the installation was not set at the beginning of health post construction as reported from one of ICCM program coordinator.
Compliance of HEWs to the treatment guidelines in this evaluation was higher than the study done in southern Ethiopia (65.6%) [ 24 ]. This might be due to availability of essential drugs educational level of HEWs and good utilization of ICCM guideline and chart booklet by HEWs. The observations showed most of the sick children were assessed for danger sign, weight, and temperature respectively. This finding is lower than the study conducted in Rwanda [ 35 ]. This difference might be due to lack of refreshment training and regular supportive supervision for HEWs. This also higher compared to the study done in three regions of Ethiopia indicates that 88%, 92% and 93% of children classified as per standard for Pneumonia, diarrhea and malaria respectively [ 36 ]. The reason for this difference may be due to the presence of medical equipment and supplies including RDT kit for malaria, and good educational level of HEWs.
Moreover most HPs received supportive supervision and performance review meeting was conducted and all of them send reports timely to next level. The finding of this evaluation was lower than the study conducted on implementation evaluation of ICCM program southern Ethiopia [ 24 ] and study done in three regions of Ethiopia (Amhara, Tigray and SNNPR) [ 37 ]. This difference might be due sample size variation.
The overall acceptability of the ICCM program was less than the presetting judgment parameter but slightly higher compared to the study in southern Ethiopia [ 24 ]. This might be due to presence of essential drugs for treating children, reasonable waiting and counseling time provided by HEWs, and smooth communication between HEWs and caregivers. In contrast, this was lower than similar studies conducted in Wakiso district, Uganda [ 38 ]. The reason for this might be due to contextual difference between the two countries, inappropriate waiting area to receive the service and poor cleanness of the HPs in our study area. Low acceptability of caregivers to ICCM service was observed in the appropriateness of waiting area, availability of drugs, cleanness of health post, and competence of HEWs while high level of caregiver’s acceptability was consultation time, counseling service they received, communication with HEWs, treatment given for their sick children and interest to return back for ICCM service.
Caregivers who achieved primary, secondary, and college and above were more likely accept the program services than those who were illiterate. This may more educated mothers know about their child health condition and expect quality service from healthcare providers which is more likely reduce the acceptability of the service. The finding is congruent with a study done on implementation evaluation of ICCM program in southern Ethiopia [ 24 ]. However, inconsistent with a study conducted in wakiso district in Uganda [ 38 ]. The possible reason for this might be due to contextual differences between the two countries. The ICCM program acceptability was high in caregivers who received all prescribed drugs than those did not. Caregivers those waited less than 30 min for service were more accepted ICCM services compared to those more than 30 minutes’ waiting time. This finding is similar compared with the study conducted on implementation evaluation of ICCM program in southern Ethiopia [ 24 ]. In contrary, the result was incongruent with a survey result conducted by Ethiopian public health institute in all regions and two administrative cities of Ethiopia [ 39 ]. This variation might be due to smaller sample size in our study the previous one. Moreover, caregivers who traveled to HPs less than 60 min were more likely accepted the program than who traveled more and the finding was similar with the study finding in Jimma zone [ 40 ].
Strengths and limitations
This evaluation used three evaluation dimensions, mixed method and different data sources that would enhance the reliability and credibility of the findings. However, the study might have limitations like social desirability bias, recall bias and Hawthorne effect.
The implementation of the ICCM program in Gondar city administration was measured in terms of availability (84.2%), compliance (83.1%), and acceptability (75.3%) dimensions. In the availability dimension, amoxicillin, antimalarial drugs, albendazole, Vit. A, and ORS were available in all health posts, but only six HPs had Ready-to-Use Therapeutic Feedings, three HPs had ORT Corners, and none of the HPs had functional timers.
This evaluation assessed the implementation status of the ICCM program, focusing mainly on availability, compliance, and acceptability dimensions. The overall implementation status of the program was judged as good. The availability dimension is compromised due to stock-outs of chloroquine syrup, cotrimoxazole, and vitamin K and the inaccessibility of clean water supply in some health posts. Educational statuses of caregivers, availability of prescribed drugs at the HPs, time to arrive to HPs, and waiting time to receive the service were the factors associated with the acceptability of the ICCM program.
Therefore, continuous supportive supervision for health facilities, and refreshment training for HEW’s to maximize compliance are recommended. Materials and supplies shall be delivered directly to the health centers or health posts to solve the transportation problem. HEWs shall document the assessment findings and the services provided using the registration format to identify their gaps, limitations, and better performances. The health facilities and local administrations should construct clean water sources for health facilities. Furthermore, we recommend for future researchers and program evaluators to conduct longitudinal studies to know the causal relationship of the program interventions and the outcomes.
Data availability
Data will be available upon reasonable request from the corresponding author.
Abbreviations
Ethiopian Demographic and Health Survey
Health Center/Health Facility
Health Extension Program
Health Extension Workers
Health Post
Health Sector Development Plan
Integrated Community Case Management of Common Childhood Illnesses
Information Communication and Education
Integrated Family Health Program
Integrated Management of Neonatal and Childhood Illness
Integrated Supportive Supervision
Maternal and Child Health
Mid Upper Arm Circumference
Non-Government Organization
Oral Rehydration Salts
Outpatient Therapeutic program
Primary health care unit
Rapid Diagnostics Test
Ready to Use Therapeutic Foods
Sever Acute Malnutrition
South Nation Nationalities People Region
United Nations International Child Emergency Fund
World Health Organization
Brenner JL, Barigye C, Maling S, Kabakyenga J, Nettel-Aguirre A, Buchner D, et al. Where there is no doctor: can volunteer community health workers in rural Uganda provide integrated community case management? Afr Health Sci. 2017;17(1):237–46.
Article PubMed PubMed Central Google Scholar
Mubiru D, Byabasheija R, Bwanika JB, Meier JE, Magumba G, Kaggwa FM, et al. Evaluation of integrated community case management in eight districts of Central Uganda. PLoS ONE. 2015;10(8):e0134767.
Samuel S, Arba A. Utilization of integrated community case management service and associated factors among mothers/caregivers who have sick eligible children in southern Ethiopia. Risk Manage Healthc Policy. 2021;14:431.
Article Google Scholar
Kavle JA, Pacqué M, Dalglish S, Mbombeshayi E, Anzolo J, Mirindi J, et al. Strengthening nutrition services within integrated community case management (iCCM) of childhood illnesses in the Democratic Republic of Congo: evidence to guide implementation. Matern Child Nutr. 2019;15:e12725.
Miller NP, Amouzou A, Tafesse M, Hazel E, Legesse H, Degefie T, et al. Integrated community case management of childhood illness in Ethiopia: implementation strength and quality of care. Am J Trop Med Hyg. 2014;91(2):424.
WHO. Annual report 2016: Partnership and policy engagement. World Health Organization, 2017.
Banteyerga H. Ethiopia’s health extension program: improving health through community involvement. MEDICC Rev. 2011;13:46–9.
Article PubMed Google Scholar
Wang H, Tesfaye R, Ramana NV, Chekagn G. CT. Ethiopia health extension program: an institutionalized community approach for universal health coverage. The World Bank; 2016.
Donnelly J. Ethiopia gears up for more major health reforms. Lancet. 2011;377(9781):1907–8.
Legesse H, Degefie T, Hiluf M, Sime K, Tesfaye C, Abebe H, et al. National scale-up of integrated community case management in rural Ethiopia: implementation and early lessons learned. Ethiop Med J. 2014;52(Suppl 3):15–26.
Google Scholar
Miller NP, Amouzou A, Hazel E, Legesse H, Degefie T, Tafesse M et al. Assessment of the impact of quality improvement interventions on the quality of sick child care provided by Health Extension workers in Ethiopia. J Global Health. 2016;6(2).
Oliver K, Young M, Oliphant N, Diaz T, Kim JJNYU. Review of systematic challenges to the scale-up of integrated community case management. Emerging lessons & recommendations from the catalytic initiative (CI/IHSS); 2012.
FMoH E. Health Sector Transformation Plan 2015: https://www.slideshare.net . Accessed 12 Jan 2022.
McGorman L, Marsh DR, Guenther T, Gilroy K, Barat LM, Hammamy D, et al. A health systems approach to integrated community case management of childhood illness: methods and tools. The American Journal of Tropical Medicine and Hygiene. 2012;87(5 Suppl):69.
Young M, Wolfheim C, Marsh DR, Hammamy D. World Health Organization/United Nations Children’s Fund joint statement on integrated community case management: an equity-focused strategy to improve access to essential treatment services for children. The American journal of tropical medicine and hygiene. 2012;87(5 Suppl):6.
Ezbakhe F, Pérez-Foguet A. Child mortality levels and trends. Demographic Research.2020;43:1263-96.
UNICEF, Ending child deaths from pneumonia and diarrhoea. 2016 report: Available at https://data.unicef.org. accessed 13 Jan 2022.
UNITED NATIONS, The Millinium Development Goals Report 2015: Available at https://www.un.org.Accessed 12 Jan 2022
Bent W, Beyene W, Adamu A. Factors Affecting Implementation of Integrated Community Case Management Of Childhood Illness In South West Shoa Zone, Central Ethiopia 2015.
Abdosh B. The quality of hospital services in eastern Ethiopia: Patient’s perspective.The Ethiopian Journal of Health Development. 2006;20(3).
Young M, Wolfheim C, Marsh DR, Hammamy DJTAjotm, hygiene. World Health Organization/United Nations Children’s Fund joint statement on integrated community case management: an equity-focused strategy to improve access to essential treatment services for children.2012;87(5_Suppl):6–10.
Obrist B, Iteba N, Lengeler C, Makemba A, Mshana C, Nathan R, et al. Access to health care in contexts of livelihood insecurity: a framework for analysis and action.PLoS medicine. 2007;4(10):e308.
Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implementation science. 2007;2(1):1–9.
Dunalo S, Tadesse B, Abraham G. Implementation Evaluation of Integrated Community Case Management of Common Childhood Illness (ICCM) Program in Soro Woreda, Hadiya Zone Southern Ethiopia 2017 2017.
Asefa G, Atnafu A, Dellie E, Gebremedhin T, Aschalew AY, Tsehay CT. Health System Responsiveness for HIV/AIDS Treatment and Care Services in Shewarobit, North Shewa Zone, Ethiopia. Patient preference and adherence. 2021;15:581.
Gebremedhin T, Daka DW, Alemayehu YK, Yitbarek K, Debie A. Process evaluation of the community-based newborn care program implementation in Geze Gofa district,south Ethiopia: a case study evaluation design. BMC pregnancy and childbirth. 2019;19(1):1–13.
Pitaloka DS, Rizal A. Patient’s satisfaction in antenatal clinic hospital Universiti Kebangsaan Malaysia. Jurnal Kesihatan Masyarakat (Malaysia). 2006;12(1):1–10.
Teshale G, Debie A, Dellie E, Gebremedhin T. Evaluation of the outpatient therapeutic program for severe acute malnourished children aged 6–59 months implementation in Dehana District, Northern Ethiopia: a mixed-methods evaluation. BMC pediatrics. 2022;22(1):1–13.
Mason E. WHO’s strategy on Integrated Management of Childhood Illness. Bulletin of the World Health Organization. 2006;84(8):595.
Shaw B, Amouzou A, Miller NP, Tafesse M, Bryce J, Surkan PJ. Access to integrated community case management of childhood illnesses services in rural Ethiopia: a qualitative study of the perspectives and experiences of caregivers. Health policy and planning.2016;31(5):656 – 66.
Organization WH. Annual report 2016: Partnership and policy engagement. World Health Organization, 2017.
Berhanu D, Avan B. Community Based Newborn Care Baseline Survey Report Ethiopia,October 2014.
Save the children, Enhancing Ethiopia’s Health Extension Package in the Southern Nations and Nationalities People’s Region (SNNPR) Shebedino and Lanfero Woredas report.Hawassa;. 2012: Avalable at https://ethiopia.savethechildren.net
Kolbe AR, Muggah R, Hutson RA, James L, Puccio M, Trzcinski E, et al. Assessing Needs After the Quake: Preliminary Findings from a Randomized Survey of Port-au-Prince Households. University of Michigan/Small Arms Survey: Available at https://deepbluelibumichedu PDF. 2010.
Teferi E, Teno D, Ali I, Alemu H, Bulto T. Quality and use of IMNCI services at health center under-five clinics after introduction of integrated community-based case management (ICCM) in three regions of Ethiopia. Ethiopian Medical Journal. 2014;52(Suppl 3):91 – 8.
Last 10 Km project, Integrated Community Case Management (iCCM) Survey report in Amhara, SNNP, and Tigray Regions, 2017: Avaialable at https://l10k.jsi.com
Tumuhamye N, Rutebemberwa E, Kwesiga D, Bagonza J, Mukose A. Client satisfaction with integrated community case management program in Wakiso District, Uganda, October 2012: A cross sectional survey. Health scrip org. 2013;2013.
EPHI. Ethiopia service provision assessment plus survey 2014 report: available at http://repository.iifphc.org
Gintamo B. EY, Assefa Y. Implementation Evaluation of IMNCI Program at Public Health Centers of Soro District, Hadiya Zone, Southern Ethiopia,. 2017: Available at https://repository.ju.edu.et
Download references
Acknowledgements
We are very grateful to University of Gondar and Gondar town health office for its welcoming approaches. We would also like to thank all of the study participants of this evaluation for their information and commitment. Our appreciation also goes to the data collectors and supervisors for their unreserved contribution.
No funding is secured for this evaluation study.
Author information
Authors and affiliations.
Metema District Health office, Gondar, Ethiopia
Mekides Geta
Department of Health Systems and Policy, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, P.O. Box 196, Gondar, Ethiopia
Geta Asrade Alemayehu, Wubshet Debebe Negash, Tadele Biresaw Belachew, Chalie Tadie Tsehay & Getachew Teshale
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the preparation of the manuscript. M.G. conceived and designed the evaluation and performed the analysis then T.B.B., W.D.N., G.A.A., C.T.T. and G.T. revised the analysis. G.T. prepared the manuscript and all the authors revised and approved the final manuscript.
Corresponding author
Correspondence to Getachew Teshale .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from Institutional Review Board (IRB) of Institute of Public Health, College of Medicine and Health sciences, University of Gondar (Ref No/IPH/1482/2013). Informed consent was obtained from all subjects and/or their legal guardian(s).
Consent for publication
Not applicable.
Competing interests
All authors declared that they have no competing interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Geta, M., Alemayehu, G.A., Negash, W.D. et al. Evaluation of integrated community case management of the common childhood illness program in Gondar city, northwest Ethiopia: a case study evaluation design. BMC Pediatr 24 , 310 (2024). https://doi.org/10.1186/s12887-024-04785-0
Download citation
Received : 20 February 2024
Accepted : 22 April 2024
Published : 09 May 2024
DOI : https://doi.org/10.1186/s12887-024-04785-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Integrated community case management
BMC Pediatrics
ISSN: 1471-2431
- Submission enquiries: [email protected]
- General enquiries: [email protected]

East African Medical Journal Journal / East African Medical Journal / Vol. 103 No. 4 (2024): UON Supplement / Articles (function() { function async_load(){ var s = document.createElement('script'); s.type = 'text/javascript'; s.async = true; var theUrl = 'https://www.journalquality.info/journalquality/ratings/2405-www-ajol-info-eamj'; s.src = theUrl + ( theUrl.indexOf("?") >= 0 ? "&" : "?") + 'ref=' + encodeURIComponent(window.location.href); var embedder = document.getElementById('jpps-embedder-ajol-eamj'); embedder.parentNode.insertBefore(s, embedder); } if (window.attachEvent) window.attachEvent('onload', async_load); else window.addEventListener('load', async_load, false); })();
Article sidebar, article details, main article content, assessment of health facility access to care, surveillance and response readiness and readiness score for malaria elimination in four counties, kenya, 2023, j.g. murangiri, f.o. odhiambo, r.j. kosgei, a.b. kihara.
Objectives : To determine capacity for; surveillance and response; access to care and readiness score for malaria elimination implementation amongst the sampled health facilities.
Design : A retrospective cross-sectional study that used routinely collected Malaria program data using a District-Level Readiness for Elimination of Malaria Tool (DREAM-IT) tool, adopted by the Ministry of Health and modified to fit the country’s context.
Settings : Four malaria elimination target counties in Kenya namely; Kirinyaga, Nyandarua, Laikipia and Nyeri.
Subject : Healthcare workers in twenty- four sampled health facilities offering outpatient and inpatient malaria services across all levels of care. Interventions : Implementation of malaria elimination strategy in Kenya.
Main outcome measures : Health facility readiness and score in Access to care (Case management), Surveillance and response for malaria elimination implementation.
Results : Most of the study health facilities were government- owned (public) and level 2. Kirinyaga recorded the best performance in case management. Surveillance and response was performed over 50% in Kirinyaga and Nyandarua, and was poorly performed in less than 40% in Nyeri and Laikipia.
Conclusion : In elimination settings, a case-based surveillance system with increased sensitivity and specificity as part of broader strengthening of the passive surveillance systems is key. High-quality and prompt case management that allows testing and treatment of all suspected and confirmed malaria cases respectively should be put in place to reduce transmission, especially in lower-level health facilities where majority of people seek care. More investments in health systems in readiness for malaria elimination implementation in Kenya is required.
AJOL is a Non Profit Organisation that cannot function without donations. AJOL and the millions of African and international researchers who rely on our free services are deeply grateful for your contribution. AJOL is annually audited and was also independently assessed in 2019 by E&Y.
Your donation is guaranteed to directly contribute to Africans sharing their research output with a global readership.
- For annual AJOL Supporter contributions, please view our Supporters page.
Journal Identifiers


Protocol for the Enhanced Management of Multimorbid Patients with Chronic Pulmonary Diseases: Role of Indoor Air Quality
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Alba Gomez-Lopez
- ORCID record for Ebymar Arismendi
- For correspondence: [email protected]
- ORCID record for Isaac Cano
- ORCID record for Ramon Farre
- ORCID record for Carme Hernandez
- ORCID record for Nuria Sanchez-Ruano
- ORCID record for Benigno Sanchez
- ORCID record for Antoni Siso-Almirall
- ORCID record for Emili Vela
- ORCID record for Jose Fermoso
- ORCID record for Josep Roca
- ORCID record for Ruben Gonzalez-Colom
- Info/History
- Supplementary material
- Preview PDF
Introduction: Reducing unplanned hospital admissions in chronic patients at risk is a key area for action due to the high healthcare and societal burden of the phenomenon. The inconclusive results of preventive strategies in patients with chronic respiratory disorders and comorbidities are explainable by multifactorial but actionable factors. The current protocol (January 2024 to December 2025) relies on the hypothesis that intertwined actions in four dimensions: i) management change, ii) personalisation of the interventions based on early detection/treatment of acute episodes and enhanced management of comorbidities, iii) mature digital support, and iv) comprehensive assessment, can effectively overcome most of the limitations shown by previous preventive strategies. Accordingly, the main objective is to implement a novel integrated care preventive service for enhanced management of these patients, as well as to evaluate its potential for value generation. Methods and analysis: At the end of 2024, the specifics of the novel service will be defined through the articulation of its four main components: i) Enhanced lung function testing through oscillometry, ii) Continuous monitoring of indoor air quality as a potential triggering factor, iii) Digital support with an adaptive case management approach, and iv) Predictive modelling for early identification and management of exacerbations. During 2025, the novel service will be assessed using a Quintuple Aim approach. Moreover, the Consolidated Framework for Implementation Research will be applied to assess the implementation. The service components will be articulated through four sequential six-months Plan-Do-Study-Act cycles. Each cycle involves a targeted co-creation process following a mixed-methods approach with the active participation of patients, health professionals, managers, and digital experts. Ethics and dissemination: The Ethics Committee for Human Research at Hospital Clinic de Barcelona approved the protocol on June 29, 2023 (HCB/2023/0126). Before any procedure, all patients in the study must sign an informed consent form. Registration: NCT06421402 . Keywords: COPD, Severe Asthma, Digital Support, Integrated Care, Quintuple Aim, Service Assessment
Competing Interest Statement
Isaac Cano and Josep Roca hold shares of Health Circuit. All other authors declare no conflicts of interest.
Clinical Trial
NCT06421402
Funding Statement
The K-HEALTHinAIR project funded this study, Grant Agreement number 101057693, under a European Union Call on Environment and Health (HORIZON-HLTH-2021-ENVHLTH-02). Disclaimer: Views and opinions expressed are, however, those of the authors only and do not necessarily reflect those of the European Union or the European Health and Digital Executive Agency as granting authority. Neither the European Union nor the granting authority can be held responsible.
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
The details of the IRB/oversight body that provided approval or exemption for the research described are given below:
The Ethical Committee for Human Research at Hospital Clinic de Barcelona approved the core study protocol of K-Health in Air on June 29, 2023 (HCB/2023/0126). The study design adheres to data minimisation principles, ensuring that only essential data are collected and utilised. The study will be conducted in compliance with the Helsinki Declaration (Stronghold Version, Brazil, October 2013) and in accordance with the protocol and the relevant legal requirements (Biomedical Research Act 14/2007 of July 3). All patients in the study must sign an informed consent form before any procedure. The participants can withdraw their consent at any time without altering their relationship with their doctor or harming their treatment. The One Beat watch does not hold medical device certification and will be utilized solely for data collection and exploring potential patterns informing exacerbations, not for decision-making within the study. Any future application derived from this research must ensure that the technology aligns with medical device regulations.
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
Data availability does not apply to this article since it describes a protocol rather than presenting study results
View the discussion thread.
Supplementary Material
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
- Addiction Medicine (324)
- Allergy and Immunology (627)
- Anesthesia (163)
- Cardiovascular Medicine (2373)
- Dentistry and Oral Medicine (289)
- Dermatology (206)
- Emergency Medicine (379)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (836)
- Epidemiology (11770)
- Forensic Medicine (10)
- Gastroenterology (702)
- Genetic and Genomic Medicine (3738)
- Geriatric Medicine (350)
- Health Economics (633)
- Health Informatics (2395)
- Health Policy (933)
- Health Systems and Quality Improvement (896)
- Hematology (341)
- HIV/AIDS (782)
- Infectious Diseases (except HIV/AIDS) (13310)
- Intensive Care and Critical Care Medicine (767)
- Medical Education (365)
- Medical Ethics (104)
- Nephrology (398)
- Neurology (3502)
- Nursing (198)
- Nutrition (525)
- Obstetrics and Gynecology (674)
- Occupational and Environmental Health (664)
- Oncology (1823)
- Ophthalmology (537)
- Orthopedics (219)
- Otolaryngology (287)
- Pain Medicine (232)
- Palliative Medicine (66)
- Pathology (446)
- Pediatrics (1033)
- Pharmacology and Therapeutics (426)
- Primary Care Research (420)
- Psychiatry and Clinical Psychology (3175)
- Public and Global Health (6139)
- Radiology and Imaging (1280)
- Rehabilitation Medicine and Physical Therapy (747)
- Respiratory Medicine (826)
- Rheumatology (379)
- Sexual and Reproductive Health (372)
- Sports Medicine (323)
- Surgery (402)
- Toxicology (50)
- Transplantation (172)
- Urology (145)
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Integr Care
- v.22(1); Jan-Mar 2022

Case Management Programs for Improving Integrated Care for Frequent Users of Healthcare Services: An Implementation Analysis
Dr. catherine hudon.
1 Département de médecine de famille et de médecine d’urgence, Université de Sherbrooke, 3001, 12e Avenue Nord, Sherbrooke, QC, Canada
2 Centre de recherche du CHUS, 12e Avenue Nord Porte 6, Sherbrooke, QC, Canada
Maud-Christine Chouinard
3 Faculté des sciences infirmières, Université de Montréal, Pavillon Marguerite-d’Youville, 2375 Chemin de la Côte-Sainte-Catherine, Montreal, QC, Canada
Mathieu Bisson
Astrid brousselle.
4 School of Public Administration, University of Victoria, Public Administration, HSD building, Room A302, Victoria, BC, Canada
Mireille Lambert
5 Centre intégré universitaire de santé et services sociaux du Saguenay–Lac-Saint-Jean, 930 rue Jacques-Cartier E, Chicoutimi, QC, Canada
Alya Danish
Charo rodriguez.
6 Department of Family Medicine, McGill University, 5858, Chemin de la Côte-des-Neiges, Montreal, QC, Canada
Véronique Sabourin
7 Patient partner, CA
Introduction:
Case management programs (CMP) for frequent users of healthcare services presenting complex healthcare needs constitute an effective strategy to improve patient experience of integrated care and to decrease healthcare overuse and cost. This study sought to identify characteristics of these programs, and their implementation contexts, that help to improve patient self-management, experience of integrated care, and healthcare services use.
A mixed methods multiple embedded case study design was conducted, with six CMP implemented in six hospitals of a region of Quebec (Canada).
Within-case analysis describes the structural, environmental, organizational, practitioner, patient, and innovation level characteristics of each CMP and their services integration outcomes based on patient experience, self-management and healthcare services use. Cross-case analysis suggests that the skills, leadership and experience of the case manager, providers’ access to the individualized services plan, consideration of the needs of the patient and family members, their participation in decision-making, and the self-management approach, impact integrated care and healthcare services use.
Conclusion and discussion:
This study underscores the necessity of an experienced, knowledgeable and well-trained case manager with interpersonal skills to optimize CMP implementation such that patients are more proactive in their care and their outcomes improve.
Introduction
Individuals with chronic conditions sometimes have complex healthcare needs, due to mental health comorbidities and/or social vulnerabilities [ 1 ] and become frequent users of healthcare services [ 2 , 3 , 4 ]. Organizing services to improve care for these patients with complex needs is a priority for healthcare systems [ 4 ] and requires an integration of clinical services offered by health and social care professionals, as well as community-based ones [ 5 ]. Models of integrated care such as case management [ 6 ] improve the quality of care, patient satisfaction, access to care, and care transitions [ 7 , 8 ], and reduce the probability of hospitalization, when compared with usual care [ 9 ].
Case management programs (CMP) for frequent users of healthcare services with complex needs constitute an effective strategy to improve patient experience of integrated care and to decrease healthcare overuse and cost [ 10 , 11 , 12 ]. Case management is a dynamic, systematic and collaborative approach used to ensure, coordinate, and integrate care and services for a clientele. The case manager is a key practitioner or navigator (often a nurse or a social worker) who evaluates, plans, implements, coordinates, and prioritizes services based on individuals’ needs, and offers self-management support in close collaboration with health, social and community partners [ 13 ].
A majority of studies have reported the effectiveness of CMP with indicators such as improvement in patient satisfaction and quality of life, and reduction of healthcare services use, ED visits, hospitalization rates, and cost [ 10 , 11 , 12 ]. Although the evidence in support of CMP is strong, there remains a paucity of evidence about the implementation process that lead to these outcomes in local contexts [ 14 ]. The aim of this study was to identify characteristics of CMP, and the contexts where they are implemented, that help to improve patient self-management, experience of integrated care, and healthcare services use.
Methodology
Design of the study.
This was a case study, more specifically a multiple embedded case study with a mixed-methods design [ 15 ]. Such a methodology appears the most appropriate for an implementation analysis in a complex system, and to study cases, with varied contexts, as they evolve over time [ 15 , 16 ]. In addition to allowing for an in-depth analysis of each case, the analysis strategies used in this design help to systematically compare trends observed between cases. It is recommended that four to ten cases be considered [ 17 ] in the multiple case study logic of theoretical replication [ 15 ]. This study included six cases, where each case was the CMP implemented in each hospital. The three different units of analysis that were interwoven to obtain an in depth understanding of each case were: 1) the hospital (organizational ‘macro’ level); 2) the CMP itself for frequent users of services (‘meso’ level) and 3) the individual (‘micro’ level), more particularly patients who are frequent users.
Context of the study
The study was realized in the Saguenay-Lac-Saint-Jean region of Quebec, a province in Canada. This region is the third largest territory in Quebec and has a very low average population density of 2.9 inhabitants per square kilometre. Much of the population is French-speaking and less than 1% are immigrants. Compared to the whole Quebec population, the residents of the Saguenay-Lac-Saint-Jean region have lower educational attainment and experience more mental health conditions [ 18 ]. In the province of Quebec, regions are divided into administrative sectors referred to as County Regional Municipalities (CRM). In the Saguenay subregion, one of these CRM is served by three hospitals, and in the Lac-Saint-Jean subregion, three of these CRM are each served by a hospital.
Case management program
In 2008, the Saguenay-Lac-Saint-Jean health and social services agency mandated the six hospitals of its territory to implement CMP for frequent users of healthcare services. Between 2009 and 2015, six CMP, the cases included in this study, were deployed by stakeholders’ committees made up of a coordinator, managers, services coordinators and case managers. CMP aimed to improve self-management support and integrated care, and decrease ED use, hospitalizations as well as healthcare cost. Case managers (a nurse or a social worker or both in dyad) in each of the six hospitals were recruited and trained to the case management approach. The training enabled the case managers to identify patients with complex care needs, assess their specific needs, and develop the individualized service plans (ISP) to respond to those needs in collaboration with the patient, their relatives and other actors involved in the implementation of the ISP, including nurses, social workers, family physicians, pharmacists, and representatives of community organizations.
In 2015, during the data collection of the study, the government of Quebec reorganized the healthcare system by merging local hospitals into larger regional entities in order to centralize health and social services. This resulted in an effort from a single CMP committee made up of a coordinator, a manager, a performance improvement consultant and case managers to standardize the program offered by the six hospitals. Members of the committee also discussed challenges and facilitators to the implementation of the CMP in this new context, as well as factors at the healthcare system level that could influence the case managers’ work. Criteria for enrolment were standardized, targeting patients with more than six ED visits or three hospitalizations in the previous year. Frequent users were identified electronically through hospital admissions and ED records. The provincial healthcare system reorganization had major impacts on clinical, professional, administrative, management and governance aspects of the healthcare system. For example, there was staff turnover at the case manager and manager level, which affected the implantation of CMP in many cases.
Conceptual framework
Two conceptual frameworks guided this study. First, given that we were interested in the implementation of CMP, we used Chaudoir et al. [ 19 ] which proposes five broad categories of factors to consider when evaluating the implementation of an innovation, namely: 1) structural and environmental-level factors; 2) organizational-level factors; 3) practitioner-level factors; 4) patient–level factors, and 5) innovation-level factors. Second, to examine patient experience of integrated care, the model proposed by the National Collaboration in Integrated Care and Support was used [ 20 ]. It consists of six dimensions of care integration based on patient experience: 1) consideration of patient and family needs, 2) communication with the patient and between practitioners, 3) access to information, 4) patient involvement in decision-making, 5) care planning, and 6) transitions between various professionals.
Participants
Key informants involved in the six CMP and healthcare services used by patients with complex health needs were recruited through purposeful sampling [ 21 ] in each hospital. Patients recruited were frequent users of hospital services, who had six visits to the ED or more, or three hospitalizations or more in the previous year.
Data collection
An implementation analysis strategy [ 22 ] guided the three methods of qualitative data collection and the method of quantitative data collection. While qualitative methods were used to inform self-management and patient experience of integrated care, quantitative data collection methods allowed the measurement of ED services use.
Qualitative data
Individual interviews and focus groups.
Semi-structured individual interviews (n = 56) and focus groups (n = 11) were conducted between December 2014 and May 2018 with 24 patients, 12 case managers and intermediate managers, 8 senior managers, 12 family physicians, 25 community stakeholders and 6 pharmacists, with interview guides, adapted for each type of actor, and addressed the five main categories of factors of the Chaudoir et al. framework of innovation implementation [ 19 ], and the six dimensions of patient experience [ 20 ]. Data saturation was not the goal for each group, but the diversity of actors engaged provided a complete representation of each case [ 23 ]. All individual interviews and focus groups were audio recorded and transcribed verbatim.
Participant observation
A member of the research team performed participant observation during one case management training session, individual case manager activities (n = 6) (e.g. evaluation of targeted patient needs, contacts with patients and their healthcare providers, ISP meetings), and quarterly meetings of the CMP committee of each of the six hospitals (n = 11). The member of the research team was invited to attend all committee meetings and share updates about the research project. These meetings were also an opportunity to consult committee members on how the research project could provide new knowledge that would help them. Data were collected using field notes [ 21 ].
Document analysis
Minutes of the CMP committee meetings were collected as they provided insight into the characteristics of the CMP and the CMP implementation, including challenges and means to overcome them [ 24 ].
Quantitative data
Clinical and administrative data.
Using the hospitals’ Magic Chronique computer software [ 25 ], the number of frequent users of ED was recorded monthly for each hospital beginning in December 2012 (the year preceding the start date of the study) and ending on May 2018. Data quality was controlled using an integrated model of information quality and a series of validation algorithms.
For each case, all qualitative data were analysed together as one data corpus using a deductive (themes based on the conceptual frameworks [ 19 , 20 ] and inductive (themes emerging from the data) thematic analysis [ 26 ]. All data sources were examined to identify characteristics of CMP, and their contexts that can be related (positively or negatively) to the examined outcomes, i.e. patient self-management, experience of integrated care, and healthcare services use. Qualitative data were managed by two authors who used NVivo V.11 server software (QSR International Pty). Other authors, including an experienced patient partner, participated in the analysis. Persistent observation, and methodological and investigator triangulation were used to ensure credibility [ 27 ].
The number of ED frequent users (six visits or more in the previous year) was tabulated for each hospital and represented in one graph to allow for visual comparison.
Integration of qualitative and quantitative data
Qualitative and quantitative results were compared for each case [ 28 ]. Qualitative data was analysed first, quantitative data second, then cross-analyses merged the two corpora of data [ 15 ]. A case history was written for each case ( Table 2 ) to summarize merged data [ 26 ]. To compare the six case records, three analytic techniques used in case study research were used, namely pattern comparison, search for competing explanations and construction of explanations [ 15 ]. Management, data reduction and cross case comparisons were conducted with NVivo V.11 software using matrix queries.
Case management program (CMP) implementation in each setting: case stories.
The study was approved by the ethics committee of the Centre for integrated health and social services of Saguenay-Lac-Saint-Jean (2014–015).
Table 1 provides the descriptive characteristics of each of the six CMP.
Characteristics of the six case management programs.
CMP: case management program; CRM: County regional municipality; ED: Emergency department; ISP: Individual service plan.
Figure 1 illustrates the evolution of the number of ED frequent users during the implementation of the CMP. While the number of frequent users increased considerably in the case A and increased slightly in the case D, an important decrease was observed for the case C and a slight decrease in the case F. These last two cases are considered “success stories”. The cases B and E remain relatively stable.

Number of ED frequent users* for each hospital.
* FU: 6 ED visits or more in the previous year.
Intra-case results
Table 2 merged qualitative and quantitative data to present case stories.
Cross-case results
Tables 3 , ,4, 4 , ,5 5 present the cross-case results. The outcomes (see the legend) are identified according to the five categories of Chaudoir et al. framework.
Structural, environmental, and organizational characteristics influencing integrated care, self-management and health services use for each case.
ISP: Individualized services plan.
Practitioner and patient characteristics influencing integrated care, self-management and health services use for each case.
CT: care trajectory; ED: emergency department.
Characteristics of the innovation (the CMP) influencing integrated care, self-management and health services use for each case.
Legend for Tables 3 , ,4 4 and 5 5
Outcomes associated with each CMP characteristic
- 1.1 Consideration of patient and family needs
- 1.2 Communication with the patient and between practitioners
- 1.3 Access to information
- 1.4 Patient involvement in decision-making
- 1.5 Care planning
- 1.6 Transitions between various health professionals and practitioners
- 2 Self-management
- 3 Health services use
In the tables, the arrows represent an increase (↑), a decrease (↓), or an effect on another outcome (→), while the + and – signs represent contextual factors having a positive or negative impact on the implantation of CMPs.
Cross-Case Synthesis
The skills, leadership and experience of the case manager seem to be the characteristics of the CMP that have the most positive influence on patient experience of integrated care, self-management and healthcare services use. The case manager’s leadership was critical in both successful cases (C and F), i.e. where we observed a decrease of ED visits. Their coordination, communication and networking skills improved integrated care by facilitating collaboration among professionals and also the transitions between health services, for which information access was a key. These improvements were also observed when the case manager was experienced, well-known in his/her workplace (C and F) and located near the providers (cases D, E, F).
Regarding the other characteristics of the CMP, four stand out from our cross-case analysis: 1) the individualized services plan (all cases), 2) patient and family needs assessment (all cases), 3) patient and family participation in decision-making (all cases), and 4) the self-management approach (cases C, D and F).
Our results suggest that where staff turnover and thus, health care team instability, was present due to organizational issues and the health system reorganization (cases B, D and E), negative impacts on care integration, especially regarding communication and care transitions, were observed. However, when case managers were well supported by their managers (cases B, E and F), they had the opportunity to create more personalized care trajectories. Therefore, patient transition through care pathways was optimized and their use of services was more appropriate. Reassurance of patients by their case manager appears to be particularly important for those with anxiety as it seems to have contributed to a reduction in their ED visits.
This study underscores the necessity of an experienced, knowledgeable, and well-trained case manager with strong interpersonal skills to optimize CMP implementation such that patients are more proactive in their care and their outcomes improve. These qualities improve care coordination which is one of the main components of CMP [ 30 , 31 ]. Similarly, Ross et al. pointed out that the case manager skills such as ability to develop good interpersonal relationships, problem-solving, negotiation and brokerage, prescribing qualifications play a key role to facilitate CMP implementation and improve outcomes [ 32 ]. Case manager training could include a focus on these skills. Indeed, a qualitative systematic review by Joo et al. revealed that insufficient training was a barrier to the case manager’s role [ 33 ]. Likewise, our results also underscored the importance of adequate training, but also that it can be challenging to ensure such training when there is a high turnover of case managers. Hong et al. provide a potential solution to this by suggesting that all care team members receive training, in order to build a relationship of trust with the patient [ 31 ].
To improve integrated care, although coordination by a skilled case manager is the core of case management, self-management support is important for CMP as a whole [ 14 , 34 , 35 ]. Self-management support seeks to improve patients’ knowledge and awareness of their care plan, self-efficacy, sense of control over their condition, and motivation to take more responsibility for their health [ 36 , 37 ]. To effectively provide this support, case managers should adopt an approach that is relevant, meaningful and centred on patient needs [ 32 ]. When the patient and caregiver manage the patient’s care adequately, their use of healthcare services is more appropriate and reduced rates of readmission are observed [ 38 ]. Furthermore, encouraging patients and their families to participate in decisions regarding the ISP better meets patient needs, promotes patient and family involvement in patient care and leads to fewer ED visits [ 35 , 39 , 40 ].
It could be argued that in-depth descriptions of the six CMP settings studied would be helpful to judge whether the results of this study are transferable to similar healthcare system settings [ 41 ]. However, given that the six CMP are heterogenous in terms of the populations they serve, their urban and rural environments, their size, the types of providers, among other key features (see Table 1 ), this aspect increases the theoretical transferability of the results. That said, this study’s findings should be considered in light of some limitations that could be addressed in future research. First, only one source of quantitative data (ED visits) was used to measure CMP efficacy. Second, the qualitative data did not provide much insight into the factors linked to the ‘patient’ category of outcomes outlined in the Chaudoir et al. conceptual framework. Third, the qualitative results are relevant to many contextual factors in the other five categories of outcomes, but only those regarding the outcomes of interest (i.e., patient experience of integrated care and integrated care) are reported. Fourth, the case managers’ activities were not measured and evaluated. To further increase the credibility of the results, survey studies could be conducted with validated questionnaires that assess the impact of CMP on patients and the results could be triangulated with those presented herein. Finally, exploring system or organization level outcomes could complete the picture of the impact of CMP on frequent users’ health outcomes.
Studying CMP as they unfold is crucial to building the knowledge base regarding the components of CMP and the roll-out required to improve integrated care. This study is one of few that explore the implementation of CMP for frequent users of ED services in hospital settings. Additional implementation studies conducted in differing contexts or healthcare systems would be useful to confirm and further enrich the findings. In this regard, Malebranche et al. recently suggested that further research was needed to better understand the advantages and disadvantages of implementing case management as primary care program versus predominantly ED or hospital-based one [ 42 ]. Teper et al.’s systematic review of CMP implementation in primary care settings identified common facilitators and barriers of CMP implementation in hospital settings including case managers’ skills, training, and relationship building and team communication practices [ 43 ]. In a systematic mixed studies review on the barriers of CMP implementation for people with dementia in community-based primary health care, Khanassov et al. also reported the importance of communication between case managers and other professionals and services [ 44 ]. Identifying contextual barriers to CMP implementation can help to select more effective implementation strategies resulting in increased positive outcomes [ 44 , 45 ].
Based on the results of the study, recommendations can be made to senior and intermediate managers and clinicians for the planning and implementation of CMP. Senior managers should ensure ongoing support for the implementation of CMP and information sharing among health professionals. They should ensure stability in the health and social care teams, especially to maintain an experienced case manager. They also have a responsibility to promote the culture of a person-centred approach, i.e. one that encourages the consideration of patients’ needs and shared decision-making. Intermediate managers should facilitate the skills, leadership and experience of the case manager, as well as his/her proximity to providers. They will need to focus on the case manager’s skills during the hiring process and provide quality training in case management with frequent users. In addition, intermediate managers should foster professional development by, for example, allowing time for the case manager to participate in a community of practice or co-development activities. Clinicians must consider the needs of patients and their families when implementing the CMP. They should also provide support to patients and encourage their autonomy and involve them and their families in decision-making.
This study underscores the necessity of an experienced, knowledgeable and well-trained case manager with interpersonal skills to optimize CMP implementation such that patients are more proactive in their care and their outcomes improve. Providers’ access to the individualized services plan, consideration of the needs of the patient and family members, their participation in decision-making, and the self-management approach, also impact patient experience of integrated care, self-management and services use.
Acknowledgements
We would like to thank the following intermediate and senior managers (Myriam-Nicole Bilodeau, Martine Couture, Julie Labbé, Jean Morneau, Sylvie Massé, Mélanie Paradis, Caroline Savard and Marc Villeneuve), patient partners (Claude Spence, Gilles Gauthier), and clinicians (Marie-Ève Bergeron, Marc Bolduc, Audrey Corneau, Sylvain Gagnon, Julie Godbout and Cécilia Ruiz) who participated in the governance of this study and made valuable contributions. We also thank Paula L. Bush, PhD, for her substantive and editorial comments and revisions to a previous version of this manuscript.
Adelaide Belo, Senior Consultant – Internal Medicine, Coordinator of Integrated Care Team – Unidade Local de Saúde do Litoral Alentejano – Portugal and President of the Portuguese Association for Integrated Care -PAFIC.
One anonymous reviewer.
Competing Interests
The authors have no competing interests to declare.

IMAGES
VIDEO
COMMENTS
1. Introduction. The Patient Safety and Quality Improvement (QI) movements in healthcare have been slow to achieve momentum in improving outcomes [].Braithwaite et al. (2018) estimate that in healthcare organisations, nearly two-thirds of initiatives experience implementation failure [].Changes in healthcare tend to be project-based with whole system change, which acknowledges the ...
A hospital-based healthcare quality management system model was released to healthcare organizations across the globe in April 2016. It was developed by a team of practitioners from the ASQ Healthcare Quality and Improvement Committee (HQIC), representing the Society's Healthcare and Quality Management Divisions. The model provides a conceptual framework for healthcare leaders and quality ...
The studies provide practical examples of efforts to improve performance on various aspects of patients' experience of health care as measured by the CAHPS surveys. Each case study presents a short overview of the steps an organization took in its quality improvement initiative, followed by a more detailed description of specific actions ...
Then, repeated citations, dissertations and case studies were deleted. Via reading of the title and abstract, the remaining articles were narrowed down by relevance. Only peer-reviewed academic and practice articles that focus on total quality management, implementation, CSFs health care and nursing were selected.
Impact Case Studies. AHRQ's evidence-based tools and resources are used by organizations nationwide to improve the quality, safety, effectiveness, and efficiency of health care. The Agency's Impact Case Studies highlight these successes, describing the use and impact of AHRQ-funded tools by State and Federal policy makers, health systems ...
Healthcare Quality Management: A Case Study Approach is the first comprehensive case-based text combining essential quality management knowledge with real-world scenarios. With in-depth healthcare quality management case studies, tools, activities, and discussion questions, the text helps build the competencies needed to succeed in quality ...
Within healthcare there is no universally accepted definition of 'quality', but those commonly used pick up on this multi-dimensionality. The following popular definition, from the US Institute of Medicine and also used by the World Health Organization, describes quality as 'the degree to which health services for individuals and populations increase the likelihood of desired health ...
Healthcare Quality Management: A Case Study Approach is the first comprehensive case-based text combining essential quality management knowledge with real-world scenarios. With in-depth healthcare quality management case studies, tools, activities, and discussion questions, the text helps build the competencies needed to succeed in quality management.Written in an easy-to-read style, Part One ...
In accordance with Key Driver 3: Optimize health information systems to extract data and support use of evidence in practice, the case study discusses how the practice used its electronic health record to develop a registry and identify and engage patients, as called for by Key Driver 5: Engage with patients and families in evidence-based care ...
Background: Quality management systems are essential in hospitals, but evidence shows a real literature gap on the sustainable implementation of quality. Purpose: This study aimed to explore and identify enablers towards sustainable quality management in hospitals. Research design and Study Sample: Interviews were conducted with 23 healthcare ...
A Health Care Organization (HCO) is a complex organization by nature owing to the intangible outcome of service and a blend of diverse professional personnel. Quality management in healthcare is a critical requirement in health sector. The principles of quality have been implicit in health care. However, quality is not a physical attribute service.
Integrated approach to healthcare quality management: A case study. November 2006. The TQM Journal 18 (6) DOI: 10.1108/09544780610707093. Authors: Prasanta Kumar Dey. Aston University. Seetharaman ...
It is noteworthy the strong impact on the healthcare sector, considering the large number of case studies published, which are focused on hospitals and improving medical procedures [4, 5]. In healthcare, it is crucial the use of quality management systems for ensuring efficiency because the commission of errors may seriously harm patients.
The International Organization for Standardization (ISO) standard ISO 8402:1994 defines total quality management (TQM) as "A management approach of an organisation centred on quality, based on the participation of all its members and aiming at long term success through customer satisfaction and benefits to all members of the organisation and society." 1 TQM has gained extensive prominence ...
Total Quality Management (TQM) is an evolving management philosophy which has recently been introduced to the health care industry. TQM requires the use of a continuous process improvement methodology for delivered services. It was implemented at Charleston VAMC's Dental Service as a study to determine its effectiveness at the grassroots level.
The keywords used in the search are TQM, total quality management, implementation, critical success factors, health care and nursing. As presented in Figure 1, a search of Science Direct, MEDLINE, EBSCO, CINAHL and PubMed yielded 2133, 6341, 1867, 7 and 474 articles, respectively. Then, repeated citations, dissertations and case studies were ...
The major contribution of this study is to advance the understanding of the interactions among the different dimensions of place on Q&PS improvement. For example, findings indicate that some of the characteristics of the physical infrastructure of the hospital have a negative impact on the quality of care provided and/or significantly limit the ...
Originality/value - The paper shows that quality improvement in healthcare services is a complex and multi‐dimensional task. Although various quality management tools are routinely deployed for identifying quality issues in health care delivery and corrective measures are taken for superior performance, there is an absence of an integrated approach, which can identify and analyze issues ...
Nursing homes face serious, ongoing patient safety challenges. This qualitative data analysis identified challenges and facilitators that are experienced by nursing home leaders in Norway as they manage the dual responsibilities of Health, Safety and Environment (HSE) and Quality and Patient Safety (QPS). The analysis identified four themes - temporal capacity, relational capacity ...
According to Teresa Whitacre, of international consulting firm ASQ, proper quality management also boosts a company's profitability. "Total quality management allows the company to look at their management system as a whole entity — not just an output of the quality department," she says. "Total quality means the organisation looks at ...
Healthcare Quality Management: A Case Study Approach is the first comprehensive case-based text combining essential quality management knowledge with real-world scenarios. With in-depth healthcare quality management case studies, tools, activities, and discussion questions, the text helps build the competencies needed to succeed in quality ...
Theoretical framework. This study is based on the theoretical framework of Tvedt et al. [], which is a system perspective based on the model of Donabedian and modified by Battles (2006) to show how hospital structures and practice environment features improve quality of care and patient safety [].These outcomes are specifically identified as quality of care, patient safety (work-related ...
Other sectors, such as industry and hospitals, have embraced a diverse and evolving set of terms but which generally have the same principles at heart (i.e., continuous quality improvement, quality improvement, performance improvement, six sigma, and total quality management). In the public health field, an array of initiatives has set the ...
The "Chronic disease management programme (PROLANIS) in Indonesia: case study" details the impact of PROLANIS on improving quality of care and controlling costs, showcasing how strategic purchasing arrangements can enhance health care delivery for chronic diseases on a national scale.
A Case Study of a Successful Quality Improvement Intervention Denise D. Quigley, Shelley H. Wiseman, and Donna O. Farley WR-848-AHRQ . August 2011 . Prepared for the Agency for Healthcare Research and Quality . This product is part of the RAND Health working paper series. RAND working papers are intended . to share researchers' latest findings
Integrated Community Case Management (ICCM) is a critical public health strategy for expanding the coverage of quality child care services [1, 2].It mainly concentrated on curative care and also on the diagnosis, treatment, and referral of children who are ill with infectious diseases [3, 4].Based on the World Health Organization (WHO) and the United Nations Children's Fund (UNICEF ...
CM is "a collaborative process of assessment, planning, facilitation, care coordination, evaluation, and advocacy for options and services to meet an individual's and family's comprehensive health needs through communication and available resources to promote quality, cost-effective outcomes" (Case Management Society of America, 2017). ...
High-quality and prompt case management that allows testing and treatment of all suspected and confirmed malaria cases respectively should be put in place to reduce transmission, especially in lower-level health facilities where majority of people seek care. ... Results: Most of the study health facilities were government- owned (public) and ...
Introduction: Reducing unplanned hospital admissions in chronic patients at risk is a key area for action due to the high healthcare and societal burden of the phenomenon. The inconclusive results of preventive strategies in patients with chronic respiratory disorders and comorbidities are explainable by multifactorial but actionable factors. The current protocol (January 2024 to December 2025 ...
Case management programs (CMP) for frequent users of healthcare services with complex needs constitute an effective strategy to improve patient experience of integrated care and to decrease healthcare overuse and cost [10,11,12]. Case management is a dynamic, systematic and collaborative approach used to ensure, coordinate, and integrate care ...