How to Write an Article Critique Step-by-Step
Table of contents
- 1 What is an Article Critique Writing?
- 2 How to Critique an Article: The Main Steps
- 3 Article Critique Outline
- 4 Article Critique Formatting
- 5 How to Write a Journal Article Critique
- 6 How to Write a Research Article Critique
- 7 Research Methods in Article Critique Writing
- 8 Tips for writing an Article Critique
Do you know how to critique an article? If not, don’t worry – this guide will walk you through the writing process step-by-step. First, we’ll discuss what a research article critique is and its importance. Then, we’ll outline the key points to consider when critiquing a scientific article. Finally, we’ll provide a step-by-step guide on how to write an article critique including introduction, body and summary. Read more to get the main idea of crafting a critique paper.

What is an Article Critique Writing?
An article critique is a formal analysis and evaluation of a piece of writing. It is often written in response to a particular text but can also be a response to a book, a movie, or any other form of writing. There are many different types of review articles . Before writing an article critique, you should have an idea about each of them.
To start writing a good critique, you must first read the article thoroughly and examine and make sure you understand the article’s purpose. Then, you should outline the article’s key points and discuss how well they are presented. Next, you should offer your comments and opinions on the article, discussing whether you agree or disagree with the author’s points and subject. Finally, concluding your critique with a brief summary of your thoughts on the article would be best. Ensure that the general audience understands your perspective on the piece.
How to Critique an Article: The Main Steps
If you are wondering “what is included in an article critique,” the answer is:
An article critique typically includes the following:
- A brief summary of the article .
- A critical evaluation of the article’s strengths and weaknesses.
- A conclusion.
When critiquing an article, it is essential to critically read the piece and consider the author’s purpose and research strategies that the author chose. Next, provide a brief summary of the text, highlighting the author’s main points and ideas. Critique an article using formal language and relevant literature in the body paragraphs. Finally, describe the thesis statement, main idea, and author’s interpretations in your language using specific examples from the article. It is also vital to discuss the statistical methods used and whether they are appropriate for the research question. Make notes of the points you think need to be discussed, and also do a literature review from where the author ground their research. Offer your perspective on the article and whether it is well-written. Finally, provide background information on the topic if necessary.
When you are reading an article, it is vital to take notes and critique the text to understand it fully and to be able to use the information in it. Here are the main steps for critiquing an article:
- Read the piece thoroughly, taking notes as you go. Ensure you understand the main points and the author’s argument.
- Take a look at the author’s perspective. Is it powerful? Does it back up the author’s point of view?
- Carefully examine the article’s tone. Is it biased? Are you being persuaded by the author in any way?
- Look at the structure. Is it well organized? Does it make sense?
- Consider the writing style. Is it clear? Is it well-written?
- Evaluate the sources the author uses. Are they credible?
- Think about your own opinion. With what do you concur or disagree? Why?

Article Critique Outline
When assigned an article critique, your instructor asks you to read and analyze it and provide feedback. A specific format is typically followed when writing an article critique.
An article critique usually has three sections: an introduction, a body, and a conclusion.
- The introduction of your article critique should have a summary and key points.
- The critique’s main body should thoroughly evaluate the piece, highlighting its strengths and weaknesses, and state your ideas and opinions with supporting evidence.
- The conclusion should restate your research and describe your opinion.
You should provide your analysis rather than simply agreeing or disagreeing with the author. When writing an article review , it is essential to be objective and critical. Describe your perspective on the subject and create an article review summary. Be sure to use proper grammar, spelling, and punctuation, write it in the third person, and cite your sources.
Article Critique Formatting
When writing an article critique, you should follow a few formatting guidelines. The importance of using a proper format is to make your review clear and easy to read.
Make sure to use double spacing throughout your critique. It will make it easy to understand and read for your instructor.
Indent each new paragraph. It will help to separate your critique into different sections visually.
Use headings to organize your critique. Your introduction, body, and conclusion should stand out. It will make it easy for your instructor to follow your thoughts.
Use standard fonts, such as Times New Roman or Arial. It will make your critique easy to read.
Use 12-point font size. It will ensure that your critique is easy to read.
How to Write a Journal Article Critique
When critiquing a journal article, there are a few key points to keep in mind:
- Good critiques should be objective, meaning that the author’s ideas and arguments should be evaluated without personal bias.
- Critiques should be critical, meaning that all aspects of the article should be examined, including the author’s introduction, main ideas, and discussion.
- Critiques should be informative, providing the reader with a clear understanding of the article’s strengths and weaknesses.
When critiquing a research article, evaluating the author’s argument and the evidence they present is important. The author should state their thesis or the main point in the introductory paragraph. You should explain the article’s main ideas and evaluate the evidence critically. In the discussion section, the author should explain the implications of their findings and suggest future research.
It is also essential to keep a critical eye when reading scientific articles. In order to be credible, the scientific article must be based on evidence and previous literature. The author’s argument should be well-supported by data and logical reasoning.
How to Write a Research Article Critique
When you are assigned a research article, the first thing you need to do is read the piece carefully. Make sure you understand the subject matter and the author’s chosen approach. Next, you need to assess the importance of the author’s work. What are the key findings, and how do they contribute to the field of research?
Finally, you need to provide a critical point-by-point analysis of the article. This should include discussing the research questions, the main findings, and the overall impression of the scientific piece. In conclusion, you should state whether the text is good or bad. Read more to get an idea about curating a research article critique. But if you are not confident, you can ask “ write my papers ” and hire a professional to craft a critique paper for you. Explore your options online and get high-quality work quickly.
However, test yourself and use the following tips to write a research article critique that is clear, concise, and properly formatted.
- Take notes while you read the text in its entirety. Right down each point you agree and disagree with.
- Write a thesis statement that concisely and clearly outlines the main points.
- Write a paragraph that introduces the article and provides context for the critique.
- Write a paragraph for each of the following points, summarizing the main points and providing your own analysis:
- The purpose of the study
- The research question or questions
- The methods used
- The outcomes
- The conclusions were drawn by the author(s)
- Mention the strengths and weaknesses of the piece in a separate paragraph.
- Write a conclusion that summarizes your thoughts about the article.
- Free unlimited checks
- All common file formats
- Accurate results
- Intuitive interface
Research Methods in Article Critique Writing
When writing an article critique, it is important to use research methods to support your arguments. There are a variety of research methods that you can use, and each has its strengths and weaknesses. In this text, we will discuss four of the most common research methods used in article critique writing: quantitative research, qualitative research, systematic reviews, and meta-analysis.
Quantitative research is a research method that uses numbers and statistics to analyze data. This type of research is used to test hypotheses or measure a treatment’s effects. Quantitative research is normally considered more reliable than qualitative research because it considers a large amount of information. But, it might be difficult to find enough data to complete it properly.
Qualitative research is a research method that uses words and interviews to analyze data. This type of research is used to understand people’s thoughts and feelings. Qualitative research is usually more reliable than quantitative research because it is less likely to be biased. Though it is more expensive and tedious.
Systematic reviews are a type of research that uses a set of rules to search for and analyze studies on a particular topic. Some think that systematic reviews are more reliable than other research methods because they use a rigorous process to find and analyze studies. However, they can be pricy and long to carry out.
Meta-analysis is a type of research that combines several studies’ results to understand a treatment’s overall effect better. Meta-analysis is generally considered one of the most reliable type of research because it uses data from several approved studies. Conversely, it involves a long and costly process.
Are you still struggling to understand the critique of an article concept? You can contact an online review writing service to get help from skilled writers. You can get custom, and unique article reviews easily.
Tips for writing an Article Critique
It’s crucial to keep in mind that you’re not just sharing your opinion of the content when you write an article critique. Instead, you are providing a critical analysis, looking at its strengths and weaknesses. In order to write a compelling critique, you should follow these tips: Take note carefully of the essential elements as you read it.
- Make sure that you understand the thesis statement.
- Write down your thoughts, including strengths and weaknesses.
- Use evidence from to support your points.
- Create a clear and concise critique, making sure to avoid giving your opinion.
It is important to be clear and concise when creating an article critique. You should avoid giving your opinion and instead focus on providing a critical analysis. You should also use evidence from the article to support your points.
Readers also enjoyed

WHY WAIT? PLACE AN ORDER RIGHT NOW!
Just fill out the form, press the button, and have no worries!
We use cookies to give you the best experience possible. By continuing we’ll assume you board with our cookie policy.
Making sense of research: A guide for critiquing a paper
Affiliation.
- 1 School of Nursing, Griffith University, Meadowbrook, Queensland.
- PMID: 16114192
- DOI: 10.5172/conu.14.1.38
Learning how to critique research articles is one of the fundamental skills of scholarship in any discipline. The range, quantity and quality of publications available today via print, electronic and Internet databases means it has become essential to equip students and practitioners with the prerequisites to judge the integrity and usefulness of published research. Finding, understanding and critiquing quality articles can be a difficult process. This article sets out some helpful indicators to assist the novice to make sense of research.
Publication types
- Data Interpretation, Statistical
- Research Design
- Review Literature as Topic
- All eBooks & Audiobooks
- Academic eBook Collection
- Home Grown eBook Collection
- Off-Campus Access
- Literature Resource Center
- Opposing Viewpoints
- ProQuest Central
- Course Guides
- Citing Sources
- Library Research
- Websites by Topic
- Book-a-Librarian
- Research Tutorials
- Use the Catalog
- Use Databases
- Use Films on Demand
- Use Home Grown eBooks
- Use NC LIVE
- Evaluating Sources
- Primary vs. Secondary
- Scholarly vs. Popular
- Make an Appointment
- Writing Tools
- Annotated Bibliographies
- Summaries, Reviews & Critiques
- Writing Center
Service Alert

Article Summaries, Reviews & Critiques
- Writing an article SUMMARY
- Writing an article REVIEW
Writing an article CRITIQUE
- Citing Sources This link opens in a new window
- About RCC Library
Text: 336-308-8801
Email: [email protected]
Call: 336-633-0204
Schedule: Book-a-Librarian
Like us on Facebook
Links on this guide may go to external web sites not connected with Randolph Community College. Their inclusion is not an endorsement by Randolph Community College and the College is not responsible for the accuracy of their content or the security of their site.
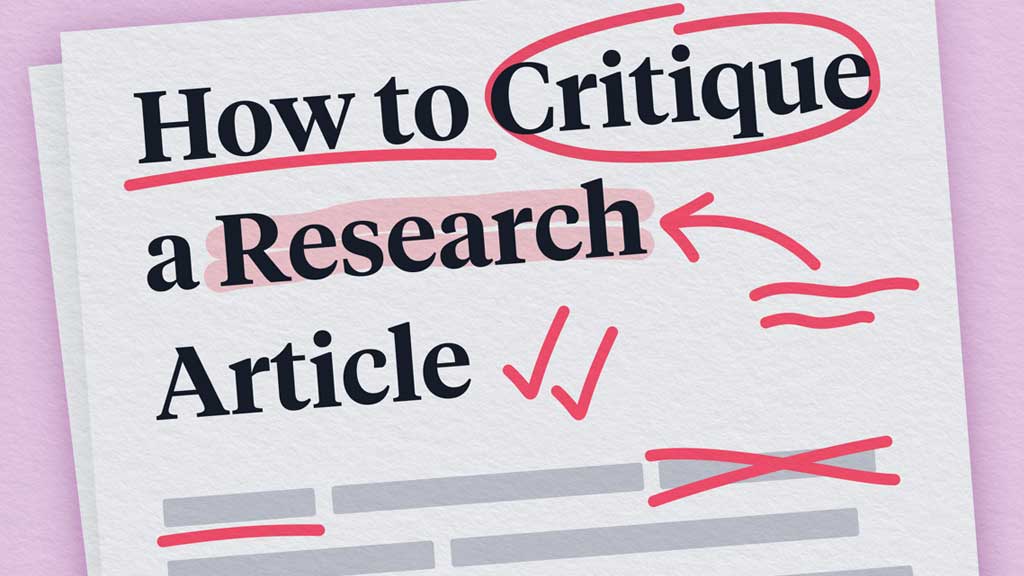
A critique asks you to evaluate an article and the author’s argument. You will need to look critically at what the author is claiming, evaluate the research methods, and look for possible problems with, or applications of, the researcher’s claims.
Introduction
Give an overview of the author’s main points and how the author supports those points. Explain what the author found and describe the process they used to arrive at this conclusion.
Body Paragraphs
Interpret the information from the article:
- Does the author review previous studies? Is current and relevant research used?
- What type of research was used – empirical studies, anecdotal material, or personal observations?
- Was the sample too small to generalize from?
- Was the participant group lacking in diversity (race, gender, age, education, socioeconomic status, etc.)
- For instance, volunteers gathered at a health food store might have different attitudes about nutrition than the population at large.
- How useful does this work seem to you? How does the author suggest the findings could be applied and how do you believe they could be applied?
- How could the study have been improved in your opinion?
- Does the author appear to have any biases (related to gender, race, class, or politics)?
- Is the writing clear and easy to follow? Does the author’s tone add to or detract from the article?
- How useful are the visuals (such as tables, charts, maps, photographs) included, if any? How do they help to illustrate the argument? Are they confusing or hard to read?
- What further research might be conducted on this subject?
Try to synthesize the pieces of your critique to emphasize your own main points about the author’s work, relating the researcher’s work to your own knowledge or to topics being discussed in your course.
From the Center for Academic Excellence (opens in a new window), University of Saint Joseph Connecticut
Additional Resources
All links open in a new window.
Writing an Article Critique (from The University of Arizona Global Campus Writing Center)
How to Critique an Article (from Essaypro.com)
How to Write an Article Critique (from EliteEditing.com.au)
- << Previous: Writing an article REVIEW
- Next: Citing Sources >>
- Last Updated: Mar 15, 2024 9:32 AM
- URL: https://libguides.randolph.edu/summaries
You are using an outdated browser
Unfortunately Ausmed.com does not support your browser. Please upgrade your browser to continue.
How to Critique a Research Article
Published: 01 October 2023
Let's briefly examine some basic pointers on how to perform a literature review.
If you've managed to get your hands on peer-reviewed articles, then you may wonder why it is necessary for you to perform your own article critique. Surely the article will be of good quality if it has made it through the peer-review process?
Unfortunately, this is not always the case.
Publication bias can occur when editors only accept manuscripts that have a bearing on the direction of their own research, or reject manuscripts with negative findings. Additionally, not all peer reviewers have expert knowledge on certain subject matters , which can introduce bias and sometimes a conflict of interest.
Performing your own critical analysis of an article allows you to consider its value to you and to your workplace.
Critical evaluation is defined as a systematic way of considering the truthfulness of a piece of research, its results and how relevant and applicable they are.
How to Critique
It can be a little overwhelming trying to critique an article when you're not sure where to start. Considering the article under the following headings may be of some use:
Title of Study/Research
You may be a better judge of this after reading the article, but the title should succinctly reflect the content of the work, stimulating readers' interest.
Three to six keywords that encapsulate the main topics of the research will have been drawn from the body of the article.
Introduction
This should include:
- Evidence of a literature review that is relevant and recent, critically appraising other works rather than merely describing them
- Background information on the study to orientate the reader to the problem
- Hypothesis or aims of the study
- Rationale for the study that justifies its need, i.e. to explore an un-investigated gap in the literature.

Materials and Methods
Similar to a recipe, the description of materials and methods will allow others to replicate the study elsewhere if needed. It should both contain and justify the exact specifications of selection criteria, sample size, response rate and any statistics used. This will demonstrate how the study is capable of achieving its aims. Things to consider in this section are:
- What sort of sampling technique and size was used?
- What proportion of the eligible sample participated? (e.g. '553 responded to a survey sent to 750 medical technologists'
- Were all eligible groups sampled? (e.g. was the survey sent only in English?)
- What were the strengths and weaknesses of the study?
- Were there threats to the reliability and validity of the study, and were these controlled for?
- Were there any obvious biases?
- If a trial was undertaken, was it randomised, case-controlled, blinded or double-blinded?
Results should be statistically analysed and presented in a way that an average reader of the journal will understand. Graphs and tables should be clear and promote clarity of the text. Consider whether:
- There were any major omissions in the results, which could indicate bias
- Percentages have been used to disguise small sample sizes
- The data generated is consistent with the data collected.
Negative results are just as relevant as research that produces positive results (but, as mentioned previously, may be omitted in publication due to editorial bias).
This should show insight into the meaning and significance of the research findings. It should not introduce any new material but should address how the aims of the study have been met. The discussion should use previous research work and theoretical concepts as the context in which the new study can be interpreted. Any limitations of the study, including bias, should be clearly presented. You will need to evaluate whether the author has clearly interpreted the results of the study, or whether the results could be interpreted another way.
Conclusions
These should be clearly stated and will only be valid if the study was reliable, valid and used a representative sample size. There may also be recommendations for further research.
These should be relevant to the study, be up-to-date, and should provide a comprehensive list of citations within the text.
Final Thoughts
Undertaking a critique of a research article may seem challenging at first, but will help you to evaluate whether the article has relevance to your own practice and workplace. Reading a single article can act as a springboard into researching the topic more widely, and aids in ensuring your nursing practice remains current and is supported by existing literature.
- Marshall, G 2005, ‘Critiquing a Research Article’, Radiography , vol. 11, no. 1, viewed 2 October 2023, https://www.radiographyonline.com/article/S1078-8174(04)00119-1/fulltext
Sarah Vogel View profile
Help and feedback, publications.
Ausmed Education is a Trusted Information Partner of Healthdirect Australia. Verify here .

- Queen's University Library
- Research Guides
How to Critique an Article (Psychology)
- Introduction
Participants
- Is the sample size adequate to find the effect? Are power analyses mentioned?
- Are there equal numbers of males and females?
- Are there a range of socioeconomic strata and ethnicities?
- For this class, is the diagnosis confirmed?
- Where were the participants obtained from, and are they a biased sample?
- If it is an experimental design, was true random assignment done (random number generator)?
- Are the measures widely used in the field?
- Are the measures reliable and valid?
- Are they appropriate for the group or age being studied (i.e. not too difficult or too easy)?
- Are all the measures explained adequately?
- Do the measures seem to have face validity -- that is, do they measure what the authors say the variable of interest is in an adequate fashion?

- Last Updated: Nov 5, 2021 9:46 AM
- Subjects: Psychology
- PRO Courses Guides New Tech Help Pro Expert Videos About wikiHow Pro Upgrade Sign In
- EDIT Edit this Article
- EXPLORE Tech Help Pro About Us Random Article Quizzes Request a New Article Community Dashboard This Or That Game Popular Categories Arts and Entertainment Artwork Books Movies Computers and Electronics Computers Phone Skills Technology Hacks Health Men's Health Mental Health Women's Health Relationships Dating Love Relationship Issues Hobbies and Crafts Crafts Drawing Games Education & Communication Communication Skills Personal Development Studying Personal Care and Style Fashion Hair Care Personal Hygiene Youth Personal Care School Stuff Dating All Categories Arts and Entertainment Finance and Business Home and Garden Relationship Quizzes Cars & Other Vehicles Food and Entertaining Personal Care and Style Sports and Fitness Computers and Electronics Health Pets and Animals Travel Education & Communication Hobbies and Crafts Philosophy and Religion Work World Family Life Holidays and Traditions Relationships Youth
- Browse Articles
- Learn Something New
- Quizzes Hot
- This Or That Game
- Train Your Brain
- Explore More
- Support wikiHow
- About wikiHow
- Log in / Sign up
- Education and Communications
- Critical Reviews
How to Write an Article Review (With Examples)
Last Updated: April 24, 2024 Fact Checked
Preparing to Write Your Review
Writing the article review, sample article reviews, expert q&a.
This article was co-authored by Jake Adams . Jake Adams is an academic tutor and the owner of Simplifi EDU, a Santa Monica, California based online tutoring business offering learning resources and online tutors for academic subjects K-College, SAT & ACT prep, and college admissions applications. With over 14 years of professional tutoring experience, Jake is dedicated to providing his clients the very best online tutoring experience and access to a network of excellent undergraduate and graduate-level tutors from top colleges all over the nation. Jake holds a BS in International Business and Marketing from Pepperdine University. There are 12 references cited in this article, which can be found at the bottom of the page. This article has been fact-checked, ensuring the accuracy of any cited facts and confirming the authority of its sources. This article has been viewed 3,107,156 times.
An article review is both a summary and an evaluation of another writer's article. Teachers often assign article reviews to introduce students to the work of experts in the field. Experts also are often asked to review the work of other professionals. Understanding the main points and arguments of the article is essential for an accurate summation. Logical evaluation of the article's main theme, supporting arguments, and implications for further research is an important element of a review . Here are a few guidelines for writing an article review.
Education specialist Alexander Peterman recommends: "In the case of a review, your objective should be to reflect on the effectiveness of what has already been written, rather than writing to inform your audience about a subject."
Article Review 101
- Read the article very closely, and then take time to reflect on your evaluation. Consider whether the article effectively achieves what it set out to.
- Write out a full article review by completing your intro, summary, evaluation, and conclusion. Don't forget to add a title, too!
- Proofread your review for mistakes (like grammar and usage), while also cutting down on needless information.

- Article reviews present more than just an opinion. You will engage with the text to create a response to the scholarly writer's ideas. You will respond to and use ideas, theories, and research from your studies. Your critique of the article will be based on proof and your own thoughtful reasoning.
- An article review only responds to the author's research. It typically does not provide any new research. However, if you are correcting misleading or otherwise incorrect points, some new data may be presented.
- An article review both summarizes and evaluates the article.

- Summarize the article. Focus on the important points, claims, and information.
- Discuss the positive aspects of the article. Think about what the author does well, good points she makes, and insightful observations.
- Identify contradictions, gaps, and inconsistencies in the text. Determine if there is enough data or research included to support the author's claims. Find any unanswered questions left in the article.

- Make note of words or issues you don't understand and questions you have.
- Look up terms or concepts you are unfamiliar with, so you can fully understand the article. Read about concepts in-depth to make sure you understand their full context.

- Pay careful attention to the meaning of the article. Make sure you fully understand the article. The only way to write a good article review is to understand the article.

- With either method, make an outline of the main points made in the article and the supporting research or arguments. It is strictly a restatement of the main points of the article and does not include your opinions.
- After putting the article in your own words, decide which parts of the article you want to discuss in your review. You can focus on the theoretical approach, the content, the presentation or interpretation of evidence, or the style. You will always discuss the main issues of the article, but you can sometimes also focus on certain aspects. This comes in handy if you want to focus the review towards the content of a course.
- Review the summary outline to eliminate unnecessary items. Erase or cross out the less important arguments or supplemental information. Your revised summary can serve as the basis for the summary you provide at the beginning of your review.

- What does the article set out to do?
- What is the theoretical framework or assumptions?
- Are the central concepts clearly defined?
- How adequate is the evidence?
- How does the article fit into the literature and field?
- Does it advance the knowledge of the subject?
- How clear is the author's writing? Don't: include superficial opinions or your personal reaction. Do: pay attention to your biases, so you can overcome them.

- For example, in MLA , a citation may look like: Duvall, John N. "The (Super)Marketplace of Images: Television as Unmediated Mediation in DeLillo's White Noise ." Arizona Quarterly 50.3 (1994): 127-53. Print. [9] X Trustworthy Source Purdue Online Writing Lab Trusted resource for writing and citation guidelines Go to source

- For example: The article, "Condom use will increase the spread of AIDS," was written by Anthony Zimmerman, a Catholic priest.

- Your introduction should only be 10-25% of your review.
- End the introduction with your thesis. Your thesis should address the above issues. For example: Although the author has some good points, his article is biased and contains some misinterpretation of data from others’ analysis of the effectiveness of the condom.

- Use direct quotes from the author sparingly.
- Review the summary you have written. Read over your summary many times to ensure that your words are an accurate description of the author's article.

- Support your critique with evidence from the article or other texts.
- The summary portion is very important for your critique. You must make the author's argument clear in the summary section for your evaluation to make sense.
- Remember, this is not where you say if you liked the article or not. You are assessing the significance and relevance of the article.
- Use a topic sentence and supportive arguments for each opinion. For example, you might address a particular strength in the first sentence of the opinion section, followed by several sentences elaborating on the significance of the point.

- This should only be about 10% of your overall essay.
- For example: This critical review has evaluated the article "Condom use will increase the spread of AIDS" by Anthony Zimmerman. The arguments in the article show the presence of bias, prejudice, argumentative writing without supporting details, and misinformation. These points weaken the author’s arguments and reduce his credibility.

- Make sure you have identified and discussed the 3-4 key issues in the article.

You Might Also Like

- ↑ https://libguides.cmich.edu/writinghelp/articlereview
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4548566/
- ↑ Jake Adams. Academic Tutor & Test Prep Specialist. Expert Interview. 24 July 2020.
- ↑ https://guides.library.queensu.ca/introduction-research/writing/critical
- ↑ https://www.iup.edu/writingcenter/writing-resources/organization-and-structure/creating-an-outline.html
- ↑ https://writing.umn.edu/sws/assets/pdf/quicktips/titles.pdf
- ↑ https://owl.purdue.edu/owl/research_and_citation/mla_style/mla_formatting_and_style_guide/mla_works_cited_periodicals.html
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4548565/
- ↑ https://writingcenter.uconn.edu/wp-content/uploads/sites/593/2014/06/How_to_Summarize_a_Research_Article1.pdf
- ↑ https://www.uis.edu/learning-hub/writing-resources/handouts/learning-hub/how-to-review-a-journal-article
- ↑ https://writingcenter.unc.edu/tips-and-tools/editing-and-proofreading/
About This Article

If you have to write an article review, read through the original article closely, taking notes and highlighting important sections as you read. Next, rewrite the article in your own words, either in a long paragraph or as an outline. Open your article review by citing the article, then write an introduction which states the article’s thesis. Next, summarize the article, followed by your opinion about whether the article was clear, thorough, and useful. Finish with a paragraph that summarizes the main points of the article and your opinions. To learn more about what to include in your personal critique of the article, keep reading the article! Did this summary help you? Yes No
- Send fan mail to authors
Reader Success Stories
Prince Asiedu-Gyan
Apr 22, 2022
Did this article help you?

Sammy James
Sep 12, 2017
Juabin Matey
Aug 30, 2017
Vanita Meghrajani
Jul 21, 2016
Nov 27, 2018

Featured Articles

Trending Articles

Watch Articles

- Terms of Use
- Privacy Policy
- Do Not Sell or Share My Info
- Not Selling Info
wikiHow Tech Help Pro:
Develop the tech skills you need for work and life

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

8.1: What’s a Critique and Why Does it Matter?
- Last updated
- Save as PDF
- Page ID 6510

- Steven D. Krause
- Eastern Michigan University
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
Critiques evaluate and analyze a wide variety of things (texts, images, performances, etc.) based on reasons or criteria. Sometimes, people equate the notion of “critique” to “criticism,” which usually suggests a negative interpretation. These terms are easy to confuse, but I want to be clear that critique and criticize don’t mean the same thing. A negative critique might be said to be “criticism” in the way we often understand the term “to criticize,” but critiques can be positive too.
We’re all familiar with one of the most basic forms of critique: reviews (film reviews, music reviews, art reviews, book reviews, etc.). Critiques in the form of reviews tend to have a fairly simple and particular point: whether or not something is “good” or “bad.”
Academic critiques are similar to the reviews we see in popular sources in that critique writers are trying to make a particular point about whatever it is that they are critiquing. But there are some differences between the sorts of critiques we read in academic sources versus the ones we read in popular sources.
- The subjects of academic critiques tend to be other academic writings and they frequently appear in scholarly journals.
- Academic critiques frequently go further in making an argument beyond a simple assessment of the quality of a particular book, film, performance, or work of art. Academic critique writers will often compare and discuss several works that are similar to each other to make some larger point. In other words, instead of simply commenting on whether something was good or bad, academic critiques tend to explore issues and ideas in ways that are more complicated than merely “good” or “bad.”
The main focus of this chapter is the value of writing critiques as a part of the research writing process. Critiquing writing is important because in order to write a good critique you need to critically read : that is, you need to closely read and understand whatever it is you are critiquing, you need to apply appropriate criteria in order evaluate it, you need to summarize it, and to ultimately make some sort of point about the text you are critiquing.
These skills-- critically and closely reading, summarizing, creating and applying criteria, and then making an evaluation-- are key to The Process of Research Writing, and they should help you as you work through the process of research writing.
In this chapter, I’ve provided a “step-by-step” process for making a critique. I would encourage you to quickly read or skim through this chapter first, and then go back and work through the steps and exercises describe.
Selecting the right text to critique
The first step in writing a critique is selecting a text to critique. For the purposes of this writing exercise, you should check with your teacher for guidelines on what text to pick. If you are doing an annotated bibliography as part of your research project (see chapter 6, “The Annotated Bibliography Exercise”), then you are might find more materials that will work well for this project as you continuously research.
Short and simple newspaper articles, while useful as part of the research process, can be difficult to critique since they don’t have the sort of detail that easily allows for a critical reading. On the other hand, critiquing an entire book is probably a more ambitious task than you are likely to have time or energy for with this exercise. Instead, consider critiquing one of the more fully developed texts you’ve come across in your research: an in-depth examination from a news magazine, a chapter from a scholarly book, a report on a research study or experiment, or an analysis published in an academic journal. These more complex essays usually present more opportunities for issues to critique.
Depending on your teacher’s assignment, the “text” you critique might include something that isn’t in writing: a movie, a music CD, a multimedia presentation, a computer game, a painting, etc. As is the case with more traditional writings, you want to select a text that has enough substance to it so that it stands up to a critical reading.
Exercise 7.1
Pick out at least three different possibilities for texts that you could critique for this exercise. If you’ve already started work on your research and an annotated bibliography for your research topic, you should consider those pieces of research as possibilities. Working alone or in small groups, consider the potential of each text. Here are some questions to think about:
- Does the text provide in-depth information? How long is it? Does it include a “works cited” or bibliography section?
- What is the source of the text? Does it come from an academic, professional, or scholarly publication?
- Does the text advocate a particular position? What is it, and do you agree or disagree with the text?
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Turk J Urol
- v.39(Suppl 1); 2013 Sep
How to write a review article?
In the medical sciences, the importance of review articles is rising. When clinicians want to update their knowledge and generate guidelines about a topic, they frequently use reviews as a starting point. The value of a review is associated with what has been done, what has been found and how these findings are presented. Before asking ‘how,’ the question of ‘why’ is more important when starting to write a review. The main and fundamental purpose of writing a review is to create a readable synthesis of the best resources available in the literature for an important research question or a current area of research. Although the idea of writing a review is attractive, it is important to spend time identifying the important questions. Good review methods are critical because they provide an unbiased point of view for the reader regarding the current literature. There is a consensus that a review should be written in a systematic fashion, a notion that is usually followed. In a systematic review with a focused question, the research methods must be clearly described. A ‘methodological filter’ is the best method for identifying the best working style for a research question, and this method reduces the workload when surveying the literature. An essential part of the review process is differentiating good research from bad and leaning on the results of the better studies. The ideal way to synthesize studies is to perform a meta-analysis. In conclusion, when writing a review, it is best to clearly focus on fixed ideas, to use a procedural and critical approach to the literature and to express your findings in an attractive way.
The importance of review articles in health sciences is increasing day by day. Clinicians frequently benefit from review articles to update their knowledge in their field of specialization, and use these articles as a starting point for formulating guidelines. [ 1 , 2 ] The institutions which provide financial support for further investigations resort to these reviews to reveal the need for these researches. [ 3 ] As is the case with all other researches, the value of a review article is related to what is achieved, what is found, and the way of communicating this information. A few studies have evaluated the quality of review articles. Murlow evaluated 50 review articles published in 1985, and 1986, and revealed that none of them had complied with clear-cut scientific criteria. [ 4 ] In 1996 an international group that analyzed articles, demonstrated the aspects of review articles, and meta-analyses that had not complied with scientific criteria, and elaborated QUOROM (QUality Of Reporting Of Meta-analyses) statement which focused on meta-analyses of randomized controlled studies. [ 5 ] Later on this guideline was updated, and named as PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses). [ 6 ]
Review articles are divided into 2 categories as narrative, and systematic reviews. Narrative reviews are written in an easily readable format, and allow consideration of the subject matter within a large spectrum. However in a systematic review, a very detailed, and comprehensive literature surveying is performed on the selected topic. [ 7 , 8 ] Since it is a result of a more detailed literature surveying with relatively lesser involvement of author’s bias, systematic reviews are considered as gold standard articles. Systematic reviews can be diivded into qualitative, and quantitative reviews. In both of them detailed literature surveying is performed. However in quantitative reviews, study data are collected, and statistically evaluated (ie. meta-analysis). [ 8 ]
Before inquring for the method of preparation of a review article, it is more logical to investigate the motivation behind writing the review article in question. The fundamental rationale of writing a review article is to make a readable synthesis of the best literature sources on an important research inquiry or a topic. This simple definition of a review article contains the following key elements:
- The question(s) to be dealt with
- Methods used to find out, and select the best quality researches so as to respond to these questions.
- To synthetize available, but quite different researches
For the specification of important questions to be answered, number of literature references to be consulted should be more or less determined. Discussions should be conducted with colleagues in the same area of interest, and time should be reserved for the solution of the problem(s). Though starting to write the review article promptly seems to be very alluring, the time you spend for the determination of important issues won’t be a waste of time. [ 9 ]
The PRISMA statement [ 6 ] elaborated to write a well-designed review articles contains a 27-item checklist ( Table 1 ). It will be reasonable to fulfill the requirements of these items during preparation of a review article or a meta-analysis. Thus preparation of a comprehensible article with a high-quality scientific content can be feasible.
PRISMA statement: A 27-item checklist
Contents and format
Important differences exist between systematic, and non-systematic reviews which especially arise from methodologies used in the description of the literature sources. A non-systematic review means use of articles collected for years with the recommendations of your colleagues, while systematic review is based on struggles to search for, and find the best possible researches which will respond to the questions predetermined at the start of the review.
Though a consensus has been reached about the systematic design of the review articles, studies revealed that most of them had not been written in a systematic format. McAlister et al. analyzed review articles in 6 medical journals, and disclosed that in less than one fourth of the review articles, methods of description, evaluation or synthesis of evidence had been provided, one third of them had focused on a clinical topic, and only half of them had provided quantitative data about the extend of the potential benefits. [ 10 ]
Use of proper methodologies in review articles is important in that readers assume an objective attitude towards updated information. We can confront two problems while we are using data from researches in order to answer certain questions. Firstly, we can be prejudiced during selection of research articles or these articles might be biased. To minimize this risk, methodologies used in our reviews should allow us to define, and use researches with minimal degree of bias. The second problem is that, most of the researches have been performed with small sample sizes. In statistical methods in meta-analyses, available researches are combined to increase the statistical power of the study. The problematic aspect of a non-systematic review is that our tendency to give biased responses to the questions, in other words we apt to select the studies with known or favourite results, rather than the best quality investigations among them.
As is the case with many research articles, general format of a systematic review on a single subject includes sections of Introduction, Methods, Results, and Discussion ( Table 2 ).
Structure of a systematic review
Preparation of the review article
Steps, and targets of constructing a good review article are listed in Table 3 . To write a good review article the items in Table 3 should be implemented step by step. [ 11 – 13 ]
Steps of a systematic review
The research question
It might be helpful to divide the research question into components. The most prevalently used format for questions related to the treatment is PICO (P - Patient, Problem or Population; I-Intervention; C-appropriate Comparisons, and O-Outcome measures) procedure. For example In female patients (P) with stress urinary incontinence, comparisons (C) between transobturator, and retropubic midurethral tension-free band surgery (I) as for patients’ satisfaction (O).
Finding Studies
In a systematic review on a focused question, methods of investigation used should be clearly specified.
Ideally, research methods, investigated databases, and key words should be described in the final report. Different databases are used dependent on the topic analyzed. In most of the clinical topics, Medline should be surveyed. However searching through Embase and CINAHL can be also appropriate.
While determining appropriate terms for surveying, PICO elements of the issue to be sought may guide the process. Since in general we are interested in more than one outcome, P, and I can be key elements. In this case we should think about synonyms of P, and I elements, and combine them with a conjunction AND.
One method which might alleviate the workload of surveying process is “methodological filter” which aims to find the best investigation method for each research question. A good example of this method can be found in PubMed interface of Medline. The Clinical Queries tool offers empirically developed filters for five different inquiries as guidelines for etiology, diagnosis, treatment, prognosis or clinical prediction.
Evaluation of the Quality of the Study
As an indispensable component of the review process is to discriminate good, and bad quality researches from each other, and the outcomes should be based on better qualified researches, as far as possible. To achieve this goal you should know the best possible evidence for each type of question The first component of the quality is its general planning/design of the study. General planning/design of a cohort study, a case series or normal study demonstrates variations.
A hierarchy of evidence for different research questions is presented in Table 4 . However this hierarchy is only a first step. After you find good quality research articles, you won’t need to read all the rest of other articles which saves you tons of time. [ 14 ]
Determination of levels of evidence based on the type of the research question
Formulating a Synthesis
Rarely all researches arrive at the same conclusion. In this case a solution should be found. However it is risky to make a decision based on the votes of absolute majority. Indeed, a well-performed large scale study, and a weakly designed one are weighed on the same scale. Therefore, ideally a meta-analysis should be performed to solve apparent differences. Ideally, first of all, one should be focused on the largest, and higher quality study, then other studies should be compared with this basic study.
Conclusions
In conclusion, during writing process of a review article, the procedures to be achieved can be indicated as follows: 1) Get rid of fixed ideas, and obsessions from your head, and view the subject from a large perspective. 2) Research articles in the literature should be approached with a methodological, and critical attitude and 3) finally data should be explained in an attractive way.
How to Critique an Article: Mastering the Article Evaluation Process

Did you know that approximately 4.6 billion pieces of content are produced every day? From news articles and blog posts to scholarly papers and social media updates, the digital landscape is flooded with information at an unprecedented rate. In this age of information overload, honing the skill of articles critique has never been more crucial. Whether you're seeking to bolster your academic prowess, stay well-informed, or improve your writing, mastering the art of article critique is a powerful tool to navigate the vast sea of information and discern the pearls of wisdom.
How to Critique an Article: Short Description
In this article, we will equip you with valuable tips and techniques to become an insightful evaluator of written content. We present a real-life article critique example to guide your learning process and help you develop your unique critique style. Additionally, we explore the key differences between critiquing scientific articles and journals. Whether you're a student, researcher, or avid reader, this guide will empower you to navigate the vast ocean of information with confidence and discernment. Still, have questions? Don't worry! We've got you covered with a helpful FAQ section to address any lingering doubts. Get ready to unleash your analytical prowess and uncover the true potential of every article that comes your way!
What Is an Article Critique: Understanding The Power of Evaluation
An article critique is a valuable skill that involves carefully analyzing and evaluating a written piece, such as a journal article, blog post, or news article. It goes beyond mere summarization and delves into the deeper layers of the content, examining its strengths, weaknesses, and overall effectiveness. Think of it as an engaging conversation with the author, where you provide constructive feedback and insights.
For instance, let's consider a scenario where you're critiquing a research paper on climate change. Instead of simply summarizing the findings, you would scrutinize the methodology, data interpretation, and potential biases, offering thoughtful observations to enrich the discussion. Through the process of writing an article critique, you develop a critical eye, honing your ability to appreciate well-crafted work while also identifying areas for improvement.
In the following sections, our ' write my paper ' experts will uncover valuable tips on and key points on how to write a stellar critique, so let's explore more!
Unveiling the Key Aims of Writing an Article Critique
Writing an article critique serves several essential purposes that go beyond a simple review or summary. When engaging in the art of critique, as when you learn how to write a review article , you embark on a journey of in-depth analysis, sharpening your critical thinking skills and contributing to the academic and intellectual discourse. Primarily, an article critique allows you to:
%20(3).webp)
- Evaluate the Content : By critiquing an article, you delve into its content, structure, and arguments, assessing its credibility and relevance.
- Strengthen Your Critical Thinking : This practice hones your ability to identify strengths and weaknesses in written works, fostering a deeper understanding of complex topics and critical evaluation skills.
- Engage in Scholarly Dialogue : Your critique contributes to the ongoing academic conversation, offering valuable insights and thoughtful observations to the existing body of knowledge.
- Enhance Writing Skills : By analyzing and providing feedback, you develop a keen eye for effective writing techniques, benefiting your own writing endeavors.
- Promote Continuous Learning : Through the writing process, you continually refine your analytical abilities, becoming an avid and astute learner in the pursuit of knowledge.
How to Critique an Article: Steps to Follow
The process of crafting an article critique may seem overwhelming, especially when dealing with intricate academic writing. However, fear not, for it is more straightforward than it appears! To excel in this art, all you require is a clear starting point and the skill to align your critique with the complexities of the content. To help you on your journey, follow these 3 simple steps and unlock the potential to provide insightful evaluations:
%20(4).webp)
Step 1: Read the Article
The first and most crucial step when wondering how to do an article critique is to thoroughly read and absorb its content. As you delve into the written piece, consider these valuable tips from our custom essay writer to make your reading process more effective:
- Take Notes : Keep a notebook or digital document handy while reading. Jot down key points, noteworthy arguments, and any questions or observations that arise.
- Annotate the Text : Underline or highlight significant passages, quotes, or sections that stand out to you. Use different colors to differentiate between positive aspects and areas that may need improvement.
- Consider the Author's Purpose : Reflect on the author's main critical point and the intended audience. Much like an explanatory essay , evaluate how effectively the article conveys its message to the target readership.
Now, let's say you are writing an article critique on climate change. While reading, you come across a compelling quote from a renowned environmental scientist highlighting the urgency of addressing global warming. By taking notes and underlining this impactful quote, you can later incorporate it into your critique as evidence of the article's effectiveness in conveying the severity of the issue.
Step 2: Take Notes/ Make sketches
Once you've thoroughly read the article, it's time to capture your thoughts and observations by taking comprehensive notes or creating sketches. This step plays a crucial role in organizing your critique and ensuring you don't miss any critical points. Here's how to make the most out of this process:
- Highlight Key Arguments : Identify the main arguments presented by the author and highlight them in your notes. This will help you focus on the core ideas that shape the article.
- Record Supporting Evidence : Take note of any evidence, examples, or data the author uses to support their arguments. Assess the credibility and effectiveness of this evidence in bolstering their claims.
- Examine Structure and Flow : Pay attention to the article's structure and how each section flows into the next. Analyze how well the author transitions between ideas and whether the organization enhances or hinders the reader's understanding.
- Create Visual Aids : If you're a visual learner, consider using sketches or diagrams to map out the article's key points and their relationships. Visual representations can aid in better grasping the content's structure and complexities.
Step 3: Format Your Paper
Once you've gathered your notes and insights, it's time to give structure to your article critique. Proper formatting ensures your critique is organized, coherent, and easy to follow. Here are essential tips for formatting an article critique effectively:
- Introduction : Begin with a clear and engaging introduction that provides context for the article you are critiquing. Include the article's title, author's name, publication details, and a brief overview of the main theme or thesis.
- Thesis Statement : Present a strong and concise thesis statement that conveys your overall assessment of the article. Your thesis should reflect whether you found the article compelling, convincing, or in need of improvement.
- Body Paragraphs : Organize your critique into well-structured body paragraphs. Each paragraph should address a specific point or aspect of the article, supported by evidence and examples from your notes.
- Use Evidence : Back up your critique with evidence from the article itself. Quote relevant passages, cite examples, and reference data to strengthen your analysis and demonstrate your understanding of the article's content.
- Conclusion : Conclude your critique by summarizing your main points and reiterating your overall evaluation. Avoid introducing new arguments in the conclusion and instead provide a concise and compelling closing statement.
- Citation Style : If required, adhere to the specific citation style guidelines (e.g., APA, MLA) for in-text citations and the reference list. Properly crediting the original article and any additional sources you use in your critique is essential.
How to Critique a Journal Article: Mastering the Steps
So, you've been assigned the task of critiquing a journal article, and not sure where to start? Worry not, as we've prepared a comprehensive guide with different steps to help you navigate this process with confidence. Journal articles are esteemed sources of scholarly knowledge, and effectively critiquing them requires a systematic approach. Let's dive into the steps to expertly evaluate and analyze a journal article:
Step 1: Understanding the Research Context
Begin by familiarizing yourself with the broader research context in which the journal article is situated. Learn about the field, the topic's significance, and any previous relevant research. This foundational knowledge will provide a valuable backdrop for your journal article critique example.
Step 2: Evaluating the Article's Structure
Assess the article's overall structure and organization. Examine how the introduction sets the stage for the research and how the discussion flows logically from the methodology and results. A well-structured article enhances readability and comprehension.
Step 3: Analyzing the Research Methodology
Dive into the research methodology section, which outlines the approach used to gather and analyze data. Scrutinize the study's design, data collection methods, sample size, and any potential biases or limitations. Understanding the research process will enable you to gauge the article's reliability.
Step 4: Assessing the Data and Results
Examine the presentation of data and results in the article. Are the findings clear and effectively communicated? Look for any discrepancies between the data presented and the interpretations made by the authors.
Step 5: Analyzing the Discussion and Conclusions
Evaluate the discussion section, where the authors interpret their findings and place them in the broader context. Assess the soundness of their conclusions, considering whether they are adequately supported by the data.
Step 6: Considering Ethical Considerations
Reflect on any ethical considerations raised by the research. Assess whether the study respects the rights and privacy of participants and adheres to ethical guidelines.
Step 7: Identifying Strengths and Weaknesses
Identify the article's strengths, such as well-designed experiments, comprehensive, relevant literature reviews, or innovative approaches. Also, pinpoint any weaknesses, like gaps in the research, unclear explanations, or insufficient evidence.
Step 8: Offering Constructive Feedback
Provide constructive feedback to the authors, highlighting both positive aspects and areas for improvement for future research. Suggest ways to enhance the research methods, data analysis, or discussion to bolster its overall quality.
Step 9: Presenting Your Critique
Organize your critique into a well-structured paper, starting with an introduction that outlines the article's context and purpose. Develop a clear and focused thesis statement that conveys your assessment. Support your points with evidence from the article and other credible sources.
By following these steps on how to critique a journal article, you'll be well-equipped to craft a thoughtful and insightful piece, contributing to the scholarly discourse in your field of study!
Got an Article that Needs Some Serious Critiquing?
Don't sweat it! Our critique maestros are armed with wit, wisdom, and a dash of magic to whip that piece into shape.
An Article Critique: Journal Vs. Research
In the realm of academic writing, the terms 'journal article' and 'research paper' are often used interchangeably, which can lead to confusion about their differences. Understanding the distinctions between critiquing a research article and a journal piece is essential. Let's delve into the key characteristics that set apart a journal article from a research paper and explore how the critique process may differ for each:
Publication Scope:
- Journal Article: Presents focused and concise research findings or new insights within a specific subject area.
- Research Paper: Explores a broader range of topics and can cover extensive research on a particular subject.
Format and Structure:
- Journal Article: Follows a standardized format with sections such as abstract, introduction, methodology, results, discussion, and conclusion.
- Research Paper: May not adhere to a specific format and allows flexibility in organizing content based on the research scope.
Depth of Analysis:
- Journal Article: Provides a more concise and targeted analysis of the research topic or findings.
- Research Paper: Offers a more comprehensive and in-depth analysis, often including extensive literature reviews and data analyses.
- Journal Article: Typically shorter in length, ranging from a few pages to around 10-15 pages.
- Research Paper: Tends to be longer, spanning from 20 to several hundred pages, depending on the research complexity.
Publication Type:
- Journal Article: Published in academic journals after undergoing rigorous peer review.
- Research Paper: May be published as a standalone work or as part of a thesis, dissertation, or academic report.
- Journal Article: Targeted at academics, researchers, and professionals within the specific field of study.
- Research Paper: Can cater to a broader audience, including students, researchers, policymakers, and the general public.
- Journal Article: Primarily aimed at sharing new research findings, contributing to academic discourse, and advancing knowledge in the field.
- Research Paper: Focuses on comprehensive exploration and analysis of a research topic, aiming to make a substantial contribution to the body of knowledge.
Appreciating these differences becomes paramount when engaging in the critique of these two forms of scholarly publications, as they each demand a unique approach and thoughtful consideration of their distinctive attributes. And if you find yourself desiring a flawlessly crafted research article critique example, entrusting the task to professional writers is always an excellent option – you can easily order essay that meets your needs.
Article Critique Example
Our collection of essay samples offers a comprehensive and practical illustration of the critique process, granting you access to valuable insights.
Tips on How to Critique an Article
Critiquing an article requires a keen eye, critical thinking, and a thoughtful approach to evaluating its content. To enhance your article critique skills and provide insightful analyses, consider incorporating these five original and practical tips into your process:
1. Analyze the Author's Bias : Be mindful of potential biases in the article, whether they are political, cultural, or personal. Consider how these biases may influence the author's perspective and the presentation of information. Evaluating the presence of bias enables you to discern the objectivity and credibility of the article's arguments.
2. Examine the Supporting Evidence : Scrutinize the quality and relevance of the evidence used to support the article's claims. Look for well-researched data, credible sources, and up-to-date statistics. Assess how effectively the author integrates evidence to build a compelling case for their arguments.
3. Consider the Audience's Perspective : Put yourself in the shoes of the intended audience and assess how well the article communicates its ideas. Consider whether the language, tone, and level of complexity are appropriate for the target readership. A well-tailored article is more likely to engage and resonate with its audience.
4. Investigate the Research Methodology : If the article involves research or empirical data, delve into the methodology used to gather and analyze the information. Evaluate the soundness of the study design, sample size, and data collection methods. Understanding the research process adds depth to your critique.
5. Discuss the Implications and Application : Consider the broader implications of the article's findings or arguments. Discuss how the insights presented in the article could impact the field of study or have practical applications in real-world scenarios. Identifying the potential consequences of the article's content strengthens your critique's depth and relevance.
Wrapping Up
In a nutshell, article critique is an essential skill that helps us grow as critical thinkers and active participants in academia. Embrace the opportunity to analyze and offer constructive feedback, contributing to a brighter future of knowledge and understanding. Remember, each critique is a chance to engage with new ideas and expand our horizons. So, keep honing your critique skills and enjoy the journey of discovery in the world of academic exploration!
Tired of Ordinary Critiques?
Brace yourself for an extraordinary experience! Our critique geniuses are on standby, ready to unleash their extraordinary skills on your article!
What Steps Need to Be Taken in Writing an Article Critique?
What is the recommended length for an article critique.

is an expert in nursing and healthcare, with a strong background in history, law, and literature. Holding advanced degrees in nursing and public health, his analytical approach and comprehensive knowledge help students navigate complex topics. On EssayPro blog, Adam provides insightful articles on everything from historical analysis to the intricacies of healthcare policies. In his downtime, he enjoys historical documentaries and volunteering at local clinics.

Related Articles
.webp)
- Open access
- Published: 21 May 2024
A modern way to teach and practice manual therapy
- Roger Kerry 1 ,
- Kenneth J. Young ORCID: orcid.org/0000-0001-8837-7977 2 ,
- David W. Evans 3 ,
- Edward Lee 1 , 4 ,
- Vasileios Georgopoulos 1 , 5 ,
- Adam Meakins 6 ,
- Chris McCarthy 7 ,
- Chad Cook 8 ,
- Colette Ridehalgh 9 , 10 ,
- Steven Vogel 11 ,
- Amanda Banton 11 ,
- Cecilia Bergström 12 ,
- Anna Maria Mazzieri 13 ,
- Firas Mourad 14 , 15 &
- Nathan Hutting 16
Chiropractic & Manual Therapies volume 32 , Article number: 17 ( 2024 ) Cite this article
114 Altmetric
Metrics details
Musculoskeletal conditions are the leading contributor to global disability and health burden. Manual therapy (MT) interventions are commonly recommended in clinical guidelines and used in the management of musculoskeletal conditions. Traditional systems of manual therapy (TMT), including physiotherapy, osteopathy, chiropractic, and soft tissue therapy have been built on principles such as clinician-centred assessment , patho-anatomical reasoning, and technique specificity. These historical principles are not supported by current evidence. However, data from clinical trials support the clinical and cost effectiveness of manual therapy as an intervention for musculoskeletal conditions, when used as part of a package of care.
The purpose of this paper is to propose a modern evidence-guided framework for the teaching and practice of MT which avoids reference to and reliance on the outdated principles of TMT. This framework is based on three fundamental humanistic dimensions common in all aspects of healthcare: safety , comfort , and efficiency . These practical elements are contextualised by positive communication , a collaborative context , and person-centred care . The framework facilitates best-practice, reasoning, and communication and is exemplified here with two case studies.
A literature review stimulated by a new method of teaching manual therapy, reflecting contemporary evidence, being trialled at a United Kingdom education institute. A group of experienced, internationally-based academics, clinicians, and researchers from across the spectrum of manual therapy was convened. Perspectives were elicited through reviews of contemporary literature and discussions in an iterative process. Public presentations were made to multidisciplinary groups and feedback was incorporated. Consensus was achieved through repeated discussion of relevant elements.
Conclusions
Manual therapy interventions should include both passive and active, person-empowering interventions such as exercise, education, and lifestyle adaptations. These should be delivered in a contextualised healing environment with a well-developed person-practitioner therapeutic alliance. Teaching manual therapy should follow this model.
Musculoskeletal (MSK) conditions are leading contributors to the burden of global disability and healthcare [ 1 ]. Amongst other interventions, manual therapy (MT) has been recommended for the management of people with MSK conditions in multiple clinical guidelines, for example [ 2 , 3 ].
MT has been described as the deliberate application of externally generated force upon body tissue, typically via the hands, with therapeutic intent [ 4 ]. It includes touch-based interventions such as thrust manipulation, joint mobilisation, soft-tissue mobilisation, and neurodynamic movements [ 5 ]. For people with MSK conditions, this therapeutic intent is usually to reduce pain and improve movement, thus facilitating a return to function and improved quality of life [ 6 ]. Patient perceptions of MT are, however, vague and sit among wider expectations of treatment including education, self-efficacy and the role of exercise, and prognosis [ 7 ].
Although the teaching and practice of MT has invariably changed over time, its foundations arguably remain unaltered and set in biomedical and outdated principles. This paper sets out to review contemporary literature and propose a revised model to inform the teaching and practice of MT.
The aim of this paper is to stimulate debate about the future teaching and practice of manual therapy through the proposal of an evidence-informed re-conceptualised model of manual therapy. The new model dismisses traditional elements of manual therapy which are not supported by research evidence. In place, the model offers a structure based on common humanistic principles of healthcare.
Consenus methodology
We present the literature synthesis and proposed framework as a consensus document to motivate further professional discussion developed through a simple three-stage iterative process over a 5-year period. The consensus methodology was classed as educational development which did not require ethical approval. Stage 1: a change of teaching practice was adopted by some co-authors (VG, RK, EL) on undergraduate and postgraduate Physiotherapy programmes at a UK University in 2018. This was a result of standard institutional teaching practice development which includes consideration of evidence-informed teaching. Stage 2: Input from a broader spectrum of stakeholders was sought, so a group of experienced, internationally-based educators, clinicians, and researchers from across the spectrum of manual therapy was convened. Perspectives were elicited through discussions in an iterative process. Stage 3: Presentations were made by some of the co-authors (VG, RK, SV, KY) to multidisciplinary groups (UK, Europe, North America) and feedback via questions and discussions was incorporated into further co-author discussions on the development of the framework. Consensus was achieved through repeated discussion of relevant elements. Figure 1 summarises the consensus methodology.
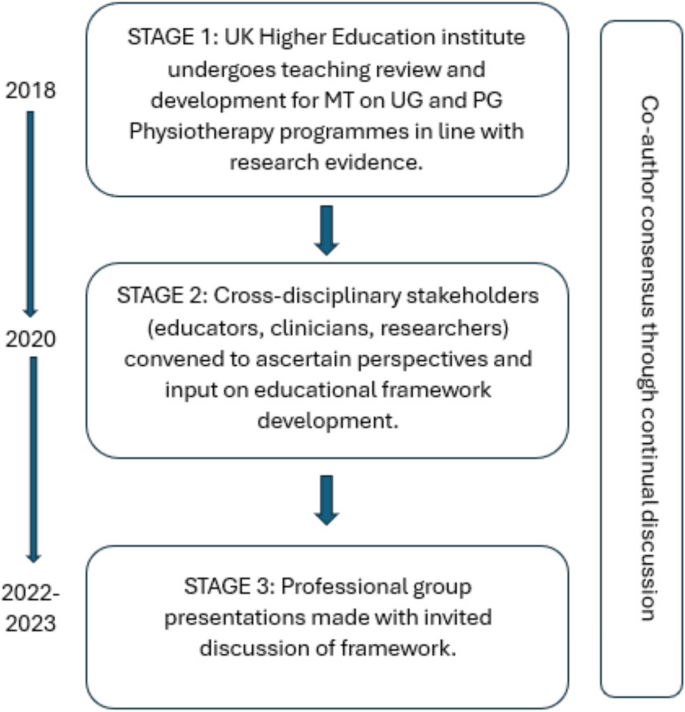
Summary and timeline of iterative consensus process for development of framework (MT: Manual Therapy; UG: Undergraduate; PG: Postgraduate)
Clinical & cost effectiveness of manual therapy
Manual therapy has been suggested to be a valuable part of a multimodal approach to managing MSK pain and disability, for example [ 8 ]. The majority of recent systematic reviews of clinical trials report a beneficial effect of MT for a range of MSK conditions, with at least similar effect sizes to other recommended approaches, for example [ 9 ]. Some systematic reviews report inconclusive findings, for example [ 10 ], and a minority report effects that were no better than comparison or sham treatments, for example [ 11 ].
Potential benefits must always be weighed against potential harms, of course. Mild to moderate adverse events from MT (e.g. mild muscle soreness) are common and generally considered acceptable [ 12 ], whilst serious adverse events are very rare and their risk may be mitigated by good practice [ 13 ]. MT has been reported by people with MSK disorders as a preferential and effective treatment with accepted levels of post-treatment soreness [ 14 ].
MT is considered cost-effective [ 15 ] and the addition of MT to exercise packages has been shown to increase clinical and cost-effectiveness compared to exercise alone in several MSK conditions [ 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 ]. Further, manual therapy has been shown to be less costly and more beneficial than evidence-based advice to stay active [ 24 ].
In summary, MT is considered a useful evidence-based addition to care packages for people experiencing pain and disability associated with MSK conditions. As such, MT continues to be included in national and international clinical guidelines for a range of MSK conditions as part of multimodal care.
Principles of traditional manual therapy (TMT)
Manual therapy has been used within healthcare for centuries [ 4 ] with many branches of MT having appeared (and disappeared) over time [ 25 ]. In developed nations today, MT is most commonly utilised by the formalised professional groups of physiotherapy, osteopathy, chiropractic, as well as groups such as soft tissue therapists. All of these groups have a history that borrows heavily from traditional healers and bone-setters [ 26 ].
Although there are many elements of MT, three principles appear to have become ubiquitous within what we shall now refer to as ‘traditional manual therapy’ (TMT): clinician-centred assessment , patho-anatomical reasoning , and technique specificity [ 27 , 28 , 29 , 30 ]. These principles continue to influence the teaching and practice of manual therapy over recent years, for example [ 31 ].
However, they have become increasingly difficult to defend given a growing volume of empirical evidence to the contrary.
Traditional manual therapy (TMT) principles: origins and problems
Clinician-centred assessment.
TMT has long had an emphasis on what we shall refer to as clinician-centred assessments . Within this, we claim, is an assumption that clinical information is both highly accurate and diagnostically important, for example [ 32 ]. Clinician-centred assessments include, for example, routine imaging, the search for patho-anatomical 'lesions’ and asymmetries, and specialised palpation. Although the focus of this paper is on the ‘hands-on’ examples of client-centred assessment, the notion of imaging is presented below to expose some of the flaws in the underlying belief system for TMT.
The emphasis on clinician-centred assessments has probably been driven, in part, by a desire for objective diagnostic tests which align well with gold-standard imaging. Indeed, since the discovery of x-rays, radiological imaging been used as an assessment for spinal pain – and a justification for using spinal manipulation – particularly in the chiropractic profession [ 33 ]. Contrary to many TMT claims, X-ray imaging is not without risk [ 34 ]. Additionally, until relatively recently (with the advent of magnetic resonance imaging) it was not widely appreciated that patho-anatomical ‘lesions’ believed to explain MSK pain conditions were nearly as common in pain-free individuals as those with pain [ 35 ]. Accordingly, the rates of unnecessary treatments, including surgery, are known to increase when imaging is used routinely [ 36 ]. For patients with non-specific low back pain, for example, imaging does not improve outcomes and risks overdiagnosis and overtreatment [ 37 ]. Hence, despite being objective in nature, the value of imaging for many MSK pain conditions (particularly spinal pain) has reduced drastically with clinical guidelines across the globe recommending against routine imaging for MSK pain of non-traumatic origin [ 38 ]. Even so, the practice of routine imaging continues [ 39 ].
Hands-on interventions are inextricably related to hands-on assessment [ 40 ], and often associated with claims of ‘specialisation’ [ 41 ]. By this we mean where a great level of training and precision are claimed to be necessary for influencing the interpretation of assessment findings, treatment decisions, and/or treatment outcomes. Implicit within this claim is that therapists who are unable to achieve such precision are not able to perform MT to an acceptable level (and thereby are not able to provide benefit to patients).
There are numerous studies that cast doubt over claims of highly specialised palpation skills. Palpation of anatomical landmarks does not reach a clinically acceptable level of validity [ 42 ]. Specialised motion palpation does not appear to be a good method for differentiating people with or without low back pain [ 43 ]. Poor content validity of specialised motion tests have been reported, in line with a lack of acceptable reference standards [ 44 ]. Palpable sensations reported by therapists are unlikely to be due to tissue deformation [ 45 ]. Furthermore, the delivery of interventions based on specialised palpatory findings is no better than non-specialised palpation [ 46 ]. Generally poor reliability of motion palpation skills has been reported, for example [ 47 ] and appear to be independent of clinician experience or training, for example [ 48 ]. Notably, person-centred palpation—for pain and tenderness for example—has slightly higher reliability, but is still fair at best [ 49 ].
This does not mean that palpation is of no use at all though; just that effective manual therapy does not depend upon it. For example, expert therapists can display high levels of interrater reliability during specialised motion palpation [ 50 ]. Focused training can improve the interrater reliability of specialised skills [ 51 ]. However, the validity of the phenomenon remains poor. Given the weight of the evidence and consistency of data over recent decades, we suggest that the role of clinician-centred hands-on assessment is no longer central to contemporary manual therapy.
Patho-anatomical reasoning
The justification for selecting particular MT interventions has historically been based upon the patho-anatomical status of local peripheral tissue [ 52 , 53 , 54 , 55 ]. Patho-anatomical reasoning, we propose, is the framework that links clinician-centred assessments to the desire for highly specific delivery of MT interventionsKey to this is the relationship between a patho-anatomic diagnosis and the assumed mechanisms of action of the intervention employed.
Theories for the mechanisms of action of MT interventions are many. Some of the most prominent include reductions of disc herniations [ 56 ], re-positioning of a bone or joint [ 32 ], removal of intra-articular adhesions [ 57 ], changes in the biomechanical properties of soft tissues [ 58 ], central pain modulation [ 59 ], and biochemical changes [ 60 ]. These theories have been used to justify the choice of certain interventions: a matching of diagnosis (i.e., existence of a lesion) to the effect of treatment takes place. However, most of these mechanistic theories either lack evidence or have been directly contested [ 61 ].
The causal relationship between proposed tissue-based factors such as posture, ergonomic settings, etc. and painful experience has also been disputed [ 62 ]. Although local tissue stiffness has been observed in people with pain, this is typically associated with neuromuscular responses, rather than patho-anatomical changes at local tissue level [ 63 , 64 , 65 , 66 ]. Overall, although some local tissue adaptions have been identified in people with recurrent MSK pain, this is inconsistent and the evidence is currently of low quality [ 67 ] are generally limited to short-term follow-up measures [ 68 ].
Technique specificity
TMT techniques have been taught with an emphasis that a particular direction, ‘grade’ of joint movement, or deformation of tissue at a very specific location in a certain way, is required to achieve a successful treatment outcome.
One problem with a demand for technique specificity in manual therapy is that an intervention does not always result in the intended effect. For example, posteroanterior forces applied during spinal mobilization consistently induce sagittal rotation, as opposed to the assumed posteroanterior translation, for example [ 69 ]. Furthermore, irrespective of the MT intervention chosen, restricting movements to a particular spinal segment is difficult and a regional, non-specific motion is typically induced, for example [ 70 ].
To support technique specificity, comparative data must repeatedly and reproducibly show superiority of outcome from specific MT interventions over non-specific MT, which is consistently not observed [ 71 , 72 , 73 ]. Some studies have demonstrated localised effects of targeted interventions [ 74 ] but there appears to be no difference in outcome related to: the way in which techniques are delivered [ 75 ]; whether technique selection is random or clinician-selected [ 41 ]; or variations in the direction of force or targeted spinal level [ 76 ]. Conversely, there is evidence that non-specific technique application may improve outcomes [ 77 , 78 , 79 ]. Further, sham techniques produce comparable results to specialised approaches [ 11 ].
Passive movement and localised touch have been associated with significant analgesic responses [ 80 ]. These data indicate the presence of an analgesic mechanism. Unfortunately, mechanistic explanation for the therapeutic effects of MT upon pain and disability still remain largely in a ‘black box’ state [ 81 ]. Nevertheless, there are several plausible mechanisms of action to explain the analgesic action of MT interventions, including the activation of modulatory spinal and supraspinal responses [ 82 , 83 , 84 , 85 ]. In support of this, MT interventions have been associated with a variety of neurophysiological responses [ 61 ]. However, it must be acknowledged that these studies provide mechanistic evidence based on association, which is insufficient to make causal claims [ 86 ]. Importantly, none of these neurophysiological responses have been directly related to either the analgesic mechanisms or clinical outcome and may therefore be incidental.
There is evidence that MT does not provide analgesia in injured tissues [ 87 , 88 ]. Conversely, MT has been shown to decrease inflammatory biomarkers [ 89 , 90 , 91 , 92 , 93 ], although these changes have not been evaluated in the longer-term, nor associated with clinical outcomes.
A modern framework for manual therapy
We propose a new direction for the future of MT in which the teaching and practice of this core dimension of MSK care are no longer based on the traditional principles of clinician-centred assessment , patho-anatomical reasoning , and technique specificity .
In doing so, this framework places MT more explicitly as part of person-centred care and appeals to common principles of healthcare, best available evidence, and contemporary theory which avoids unnecessary and over-complicated explanations of observed effects. The framework is simple in terms of implementation and delivery and contextualised by common elements of best practice for healthcare, in line with regulated standard of practice, e.g., [ 94 , 95 , 96 , 97 ]. Our proposal simply illustrates the operationalisation of these common elements through manual therapy.
Too much emphasis has been given to clinician-centred assessments and this should be rebalanced with an increased use of patient-centred assessments, such as a thorough case history, the use of validated patient-reported outcome measures (PROMS), and real-time patient feedback during assessments.
The new framework considers fundamental and humanistic dimensions of touch-based therapies, such as non-specific neuromodulation, communication and sense-making, physical education, and contextual clinical effectiveness. This aligns to contemporary ideas regarding therapeutic alliance and a move towards genuinely holistic healthcare [ 98 , 99 ]. The framework needs to be “open” in order to represent and allow expression of the complexity of the therapeutic encounter. However, to prevent the exploitation of this openness the framework is underpinned by evidence, and any manual therapy approaches without plausible and measurable mechanisms are not supported.
To provide the best care, common healthcare elements such as the safety and comfort of the person seeking help and therapist must be considered, and care should be provided as efficiently as possible. Our framework embraces these dimensions and employs an integration of current evidence. It is transdisciplinary in nature and may be adopted by all MT professions. Figure 1 provides a graphical representation of the framework. It is acknowledged that all components overlap, relate, and influence each. There are two main components: the practical elements on the inside, comprised of safety, comfort, and efficiency, and the conceptual themes on the outer regions, consisting of communication, context, and person-centred care Fig. 2 .
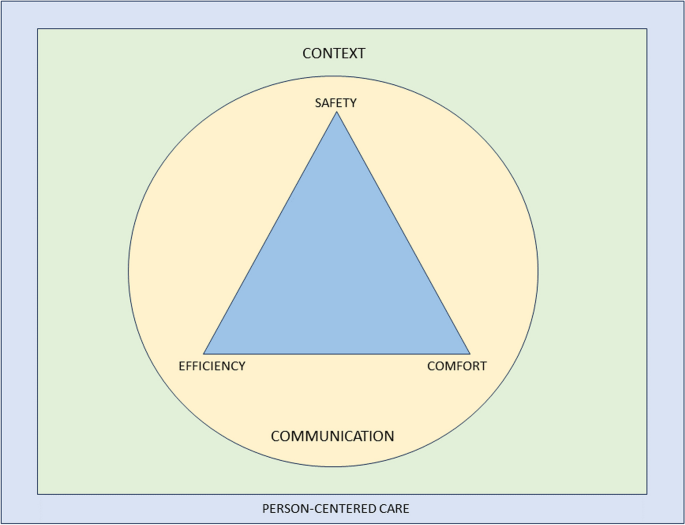
Representation of a modern teaching and practice framework for manual therapy. The image is purposefully designed to be simple, and has been developed primarily to be used as a teaching aid. When displayed in a learning environment, learners and clinicians can quickly refer to the image to check their practice against each element. To keep the image clear, each element of the image is described in detail in the text below”
Practical elements
Safety for people seeking help is a primary concern for all healthcare providers, with the aims to “ prevent and reduce risks, errors and harm that occur to patients [sic] during provision of health care… and to deliver quality essential health services ” [ 100 ]. This, and the notion of safety more generally (including that of the therapist), should be central to way MT is taught and practised.
A fundamentally safe context should be created where there is an absence of any obvious danger or risk of harm to physical or mental health. Consideration should be given to ensuring that communication and consent processes are orientated towards the safety of both the person seeking help and the therapist. The therapist should pay attention to any sense of threat that could be present in the physical, emotional, cognitive and environmental domains of the clinical encounter, and use skilful communication to mitigate anxiety about the assessment or therapeutic process.
Safety should also be considered in the clinical context of the assessment and treatment approach, ensuring that relevant and meaningful safety screenings have been undertaken [ 67 , 101 ]. There remains a need for good, skilful practice and development of manually applied techniques, but this can be achieved without reference to the principles of TMT and without the dogma of a proprietary therapeutic approach.
Comfort suggests that both the person seeking help and the therapist are physically and emotionally content during the assessment and therapeutic process. For example, the person seeking help is agreeable with any necessary state of dress (sociocultural difference should be considered); the person is relaxed and untroubled in whatever position they are in, and is adequately supported whether sitting, standing or recumbent during assessment and treatment; the therapist is comfortable with their positioning and posture; any discomfort produced by the therapeutic process is negotiated and agreed. Any physical mobilisation or touch should be applied with respect to the feedback from the person in relation to their comfort, rather than a pre-determined force based on the notion of resistance. This process requires clinical phronesis, sensitivity, responsivity, dexterity, and embodied communication [ 102 ].
The therapeutic process should be undertaken in a well-organised, competent manner aiming to achieve maximum therapeutic benefit with minimum waste of effort, time, or expense. To enhance the efficiency dimension, the assessment and therapeutic process should be an integral part of a holistic educational and/or activity-based approach to the management of the people which might also address psychological, nutritional, or ergonomic aspects of care, while being aware of social determinants to health. Recommendations exist which serve as a useful guide for enhancing care and promoting self-management in an efficient way [ 103 ].
A principle of this new model of MT is that therapists should not lose sight of the goals they develop with the people they help and ensure that there is coherence between their management aims and their techniques. Therapists should aim to support a person’s self-efficacy and use active approaches to empower them in their recovery. The overall number of therapeutic applications should be made in the context of fostering therapeutic alliance and supporting people to make sense of their situation and symptoms. This should be informed by contemporary views of the effects of manual therapy, emphasising a “physical education process” to promote sense-making and self-efficacy in alliance with the people they aim to help.
Clinical interactions need to be reproducible under a person’s own volition, serving to enhance self-empowerment. For example, someone could be taught how to “self-mobilise” if a positive effect is found with a particular therapeutic application. This should be appropriately scaffolded with behavioural change principles and functional contextualism that promote autonomy and self-management, rather than inappropriate reliance on the therapist [ 103 , 104 ].
An important and emergent notion from the proposed model is to question what constitutes indications for MT given that the model excludes traditional factors which would have informed whether manual therapy is indicated or not for a particular person. The response to this sits within the efficiency and safety dimensions: MT can be beneficial as part of a multi-dimensional approach to management across a broad population of people with musculoskeletal dysfunction, with no evidence to suggest any clinician-centered or patho-anatomical finding influences outcomes. The choice of whether or not to include MT as part of a management strategy should therefore be a product of a lack of contraindications and shared-decision making.
This framework aligns with evidence-based propositions that effectiveness and efficiency in assessment, diagnosis, and outcomes are not reliant on the therapist’s skill set of specialised elements of TMT, but rather other factors—for example variations in pain phenotypes [ 5 ].
Conceptual themes
Communication.
Communication is the overriding critical dimension to the whole therapeutic process and should be aimed at addressing peoples’ fundamental needs to make sense of their symptoms and path to recovery. The delivery and uptake of the therapy should therefore be operationalised in a communication process that meaningfully represents shared-decision making and the best possible attempt to contextualise the therapy in positive and evidence-informed explanations of the process and desired effects [ 105 ].
Within a therapeutic encounter, practitioners must give the time to listen to peoples’ accounts and explanations of their symptoms, including their ideas about their cause [ 106 ]. The assessment and diagnostic process should be a shared endeavour, for example, the negotiation of symptom reproduction. This should be done in a manner that facilitates sense-making, and which simultaneously encourages people to move on from unhelpful beliefs about their symptoms [ 107 , 108 ], encouraging understanding of the uncertain nature of pain and injury. Person-centered communication requires attention to what we communicate and how we communicate across the entire clinical interaction including interview, examination, and management planning [ 109 ]. Therapists need to be open, reflective, aware and responsive to verbal and non-verbal cues, and demonstrate a balance between engaging with people (e.g. eye-gaze) and writing/typing notes during the interview [ 110 , 111 , 112 ].
People should be given the opportunity to discuss their understanding of the diagnosis and options for treatment and rehabilitation. The decision-making process is dialogical, in which alternative options to the offered therapy should also be discussed with the comparative risks and benefits of all available management options, including doing nothing [ 113 , 114 ].
The therapist must fully appreciate the potential consequences of touch without consent. Continual dialogue should ensure that all parties are moving towards mutually agreed goals. The context of the therapy should be explicitly communicated to give appropriate context for any particular intervention as part of a holistic, evidence-based approach [ 115 , 116 , 117 ]. Therapists should be aware that their own beliefs can affect the way they communicate with their people; in the same way, a person’s context affects how they communicate what they expect from their treatment [ 107 , 118 , 119 , 120 ]. The construction of contextual healing scenarios which support positive outcomes, whilst minimising nocebic effects, is critical to effective healthcare [ 121 , 122 , 123 ].
There is a growing academic interest in the nature, role, and purpose of social and affective touch, and any re-framing of MT should consider touch as a means of communication to develop and enhance cooperative communications and strengthen the therapeutic relationship [ 124 , 125 , 126 , 127 , 128 , 129 ]. It can be soothing for a person in pain to experience the caring touch of a professional therapist [ 130 ]; on the other hand, probing, diagnostic, and touch can be experienced as alienating [ 131 , 132 , 133 ]. Touch can alter a person’s sense of body ownership and their ability to recognise and process their emotions by modulating interoceptive precision [ 129 , 134 , 135 ], and intentional touch may be perceived differently from casual, unfocussed touch [ 136 , 137 ]. There is also a thesis that touch generates shared understanding and meaning [ 138 , 139 , 140 ]. This wider appreciation of touch should be embedded in modern MT communication.
The contextual quality of a person’s experience of the therapeutic encounter can affect satisfaction and clinical outcomes [ 141 , 142 , 143 , 144 , 145 ]. The context in which therapeutic care takes place should therefore be developed to enhance this experience. There could be very local, practical aspects of the context, such as the type of passive information available in the clinical space, e.g. replacing biomedical and pathological imagery and objects with positive, active artefacts; judicious and thoughtful organisation and use of treatment tables to discourage a sense of passivity and disempowerment; allocating a comfortable space where communication can take place; colour schemes and light sources which facilitate positivity; ensuring consistency through all clinical and administrative staff promoting encouraging and non-nocebic messages. Importantly, the way the therapist dresses influences peoples’ perception of their healthcare experience [ 146 , 147 ], and that in turn should be contextually and culturally sensitive [ 148 , 149 , 150 ].
Beyond the local clinical space is the broader social environment. The undertaking of MT should serve a role in a person’s engagement with their social environment. For example, someone returning home after engaging with their therapist and disseminating positive health messages within their home and social networks; people acting as advocates for self-empowered healthcare. Furthermore, early data have demonstrated that aligning treatment with the beliefs and values of culturally and linguistically diverse communities enhances peoples’ engagement with their healthcare [ 151 ].
Person-centred care
Here we borrow directly from one of the most established and clinically useful definitions of Person-Centered Medicine [ 152 ]:
“(Person-Centered Medicine is) an affordable biomedical and technological advance to be delivered to patients [sic] within a humanistic framework of care that recognises the importance of applying science in a manner that respects the patients [sic] as a whole person and takes full account of [their] values, preferences, aspirations, stories, cultural context, fears, worries and hopes and thus that recognises and responds to [their] emotional, social and spiritual necessities in addition to [their] physical needs” [ 152 ] , p219.
Person-centred care incorporates a person’s perspective as part of the therapeutic process. In practice, therapists need to communicate in a manner that creates adequate conversational space to elicit a person’s agenda (i.e. understanding, impact of pain, concerns, needs, and goals), which guides clinical interactions. This approach encourages greater partnership in management [ 109 , 153 , 154 ].
A roadmap outlining key actions to implement person-centeredness in clinical practice has been outlined in detail elsewhere [ 155 ]. This includes screening for serious pathology, health co-morbidities and psychosocial factors; adopting effective communication; providing positive health education; coaching and supporting people towards active self-management; and facilitating and managing co-care (when needed) [ 154 ].
It is critical and necessary now to make these features explicit and central to the revised model of MT proposed in this paper. We wish to identify common ground across all MT professions in order to achieve a trans-disciplinary understanding of the evidence supporting the use of MT.
We acknowledge that our arguments here are rooted in empiricism and deliberately based on available research data from within the health science disciplines. We also acknowledge that there is a wider debate about future directions in person-centred care arising from the current evolution of the evidence-based health care movement, which has pointed to the need to learn more about peoples’ lived experiences, to redefine the model of the therapeutic relationship. Although beyond the scope of this paper, a full exploration of modern health care provision involves reconsideration of the ethics and legal requirements of communication and shared decision-making [ 156 , 157 , 158 , 159 ]. The authors envision this paper as a stimulus for self-reflection, stakeholder discussions, and ultimately change that can positively impact outcomes for people who seek manual therapy interventions.
Manual therapy has long been part of MSK healthcare and, given that is likely to continue. Current evidence suggests that effectiveness does not rely on the traditional principles historically developed in any of the major manual therapies. Therefore, the continued teaching and practice based on the principles of clinician-centred palpation , patho-anatomical reasoning , and technique specificity are no longer justified and may well even limit the value of MT.
A revised and reconceptualised framework of MT, based on the humanistic domains of safety, comfort and efficiency and underpinned by the dimensions of communication, context and person-centred care will ensure an empowering, biopsychosocial, evidence-informed approach to MSK care. We propose that the future teaching and practice of MT in physiotherapy, osteopathy, chiropractic, and all associated hands-on professions working within the healthcare field should be based on this new framework.
Availability of data and materials
Young C, Argáez C. CADTH Rapid Response Reports. Manual Therapy for Chronic Non-Cancer Back and Neck Pain: A Review of Clinical Effectiveness. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health. Copyright © 2020 Canadian Agency for Drugs and Technologies in Health.; 2020.
Blanpied PR, Gross AR, Elliott JM, Devaney LL, Clewley D, Walton DM, et al. Neck Pain: Revision 2017. J Orthop Sports Phys Ther. 2017;47(7):A1-a83.
Article PubMed Google Scholar
NICE. Low back pain and sciatica in over 16s: assessment and management. NICE guideline [NG59]. 2016.
Pettman E. A history of manipulative therapy. J Man Manip Ther. 2007;15(3):165–74.
Article PubMed PubMed Central Google Scholar
Damian K, Chad C, Kenneth L, David G. Time to evolve: the applicability of pain phenotyping in manual therapy. J Man Manip Ther. 2022;30(2):61–7.
McCarthy CJ. Combined Movement Theory: Rational Mobilization and Manipulation of the Vertebral Column. London, UK: Churchill Livingstone; 2010.
Google Scholar
Subialka JA, Smith K, Signorino JA, Young JL, Rhon DI, Rentmeester C. What do patients referred to physical therapy for a musculoskeletal condition expect? A qualitative assessment. Musculoskel Sci Pract. 2022;59:102543.
Article Google Scholar
Louw A, Nijs J, Puentedura EJ. A clinical perspective on a pain neuroscience education approach to manual therapy. J Man Manip Ther. 2017;25(3):160–8.
Wilhelm M, Cleland J, Carroll A, Marinch M, Imhoff M, Severini N, et al. The combined effects of manual therapy and exercise on pain and related disability for individuals with nonspecific neck pain: A systematic review with meta-analysis. J Man Manip Ther. 2023;31(6):393–407.
Schenk R, Donaldson M, Parent-Nichols J, Wilhelm M, Wright A, Cleland JA. Effectiveness of cervicothoracic and thoracic manual physical therapy in managing upper quarter disorders - a systematic review. J Man Manipulative Therap. 2021:1–10.
Lavazza C, Galli M, Abenavoli A, Maggiani A. Sham treatment effects in manual therapy trials on back pain patients: a systematic review and pairwise meta-analysis. BMJ Open. 2021;11(5):e045106.
Funabashi M, Pohlman KA, Goldsworthy R, Lee A, Tibbles A, Mior S, et al. Beliefs, perceptions and practices of chiropractors and patients about mitigation strategies for benign adverse events after spinal manipulation therapy. Chiropr Man Therap. 2020;28(1):46.
Rushton A, Carlesso LC, Flynn T, Hing WA, Rubinstein SM, Vogel S, et al. International Framework for Examination of the Cervical Region for Potential of Vascular Pathologies of the Neck Prior to Musculoskeletal Intervention: International IFOMPT Cervical Framework. J Orthop Sports Phys Ther. 2022;53(1):7–22.
Thomas M, Thomson OP, Kolubinski DC, Stewart-Lord A. The attitudes and beliefs about manual therapy held by patients experiencing low back pain: a scoping review. Musculoskelet Sci Pract. 2023;65:102752.
Lilje S, van Tulder M, Wykman A, Aboagye E, Persson U. Cost-effectiveness of specialised manual therapy versus orthopaedic care for musculoskeletal disorders: long-term follow-up and health economic model. Ther Adv Musculoskelet Dis. 2023;15:1759720x221147751.
Article CAS PubMed PubMed Central Google Scholar
Abbott JH, Robertson MC, Chapple C, Pinto D, Wright AA, Leon de la Barra S, et al. Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee: a randomized controlled trial. 1: clinical effectiveness. Osteoarthritis Cartilage. 2013;21(4):525–34.
Article CAS PubMed Google Scholar
Bove AM, Smith KJ, Bise CG, Fritz JM, Childs JD, Brennan GP, et al. Exercise, Manual Therapy, and Booster Sessions in Knee Osteoarthritis: Cost-Effectiveness Analysis From a Multicenter Randomized Controlled Trial. Phys Ther. 2018;98(1):16–27.
Leininger B, McDonough C, Evans R, Tosteson T, Tosteson AN, Bronfort G. Cost-effectiveness of spinal manipulative therapy, supervised exercise, and home exercise for older adults with chronic neck pain. Spine J. 2016;16(11):1292–304.
Tsertsvadze A, Clar C, Court R, Clarke A, Mistry H, Sutcliffe P. Cost-effectiveness of manual therapy for the management of musculoskeletal conditions: a systematic review and narrative synthesis of evidence from randomized controlled trials. J Manipulative Physiol Ther. 2014;37(6):343–62.
UK Beam Trial Team. United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: effectiveness of physical treatments for back pain in primary care. BMJ. 2004;329(7479):1377.
Article PubMed Central Google Scholar
UK Beam Trial Team. United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: cost effectiveness of physical treatments for back pain in primary care. BMJ (Clinical research ed). 2004;329(7479):1381.
van Dongen JM, Groeneweg R, Rubinstein SM, Bosmans JE, Oostendorp RA, Ostelo RW, et al. Cost-effectiveness of manual therapy versus physiotherapy in patients with sub-acute and chronic neck pain: a randomised controlled trial. Eur Spine J. 2016;25(7):2087–96.
Woods B, Manca A, Weatherly H, Saramago P, Sideris E, Giannopoulou C, et al. Cost-effectiveness of adjunct non-pharmacological interventions for osteoarthritis of the knee. PLoS ONE. 2017;12(3):e0172749.
Aboagye E, Lilje S, Bengtsson C, Peterson A, Persson U, Skillgate E. Manual therapy versus advice to stay active for nonspecific back and/or neck pain: a cost-effectiveness analysis. Chiropr Man Therap. 2022;30(1):27.
Paris SV. A History of Manipulative Therapy Through the Ages and Up to the Current Controversy in the United States. J Man Manipulative Ther. 2000;8(2):66–77.
MacDonald CW, Osmotherly PG, Parkes R, Rivett DA. The current manipulation debate: historical context to address a broken narrative. J Man Manipulative Therap. 2019;27(1):1–4.
Fryer G. Intervertebral dysfunction: a discussion of the manipulable spinal lesion. J Am Osteopath Assoc. 2003;6(2):64–73.
McCarthy CJ. Spinal manipulative thrust technique using combined movement theory. Man Ther. 2001;6(4):197–204.
Vickers A, Zollman C. ABC of complementary medicine Massage therapies. BMJ (Clinical research ed). 1999;319(7219):1254–7.
Evans DW. Osteopathic principles: More harm than good? Int J Osteopath Med. 2013;16(1):46–53.
Mourad F, Yousif MS, Maselli F, Pellicciari L, Meroni R, Dunning J, et al. Knowledge, beliefs, and attitudes of spinal manipulation: a cross-sectional survey of Italian physiotherapists. Chiropr Man Therap. 2022;30(1):38.
Cyriax JH, Cyriax PJ. Cyriax's Illustrated Manual of Orthopaedic Medicine. 3rd ed: Butterworth-Heinemann; 1996.
Young KJ. Words matter: the prevalence of chiropractic-specific terminology on Australian chiropractors’ websites. Chiropr Man Therap. 2020;28(1):18.
Jenkins HJ, Downie AS, Moore CS, French SD. Current evidence for spinal X-ray use in the chiropractic profession: a narrative review. Chiropr Man Therap. 2018;26:48.
Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811–6.
Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Intern Med. 2013;173(17):1573–81.
Hall AM, Aubrey-Bassler K, Thorne B, Maher CG. Do not routinely offer imaging for uncomplicated low back pain. BMJ (Clinical research ed). 2021;372:n291.
PubMed Google Scholar
Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020;54(2):79.
Hall AM, Scurrey SR, Pike AE, Albury C, Richmond HL, Matthews J, et al. Physician-reported barriers to using evidence-based recommendations for low back pain in clinical practice: a systematic review and synthesis of qualitative studies using the Theoretical Domains Framework. Implement Sci. 2019;14(1):49.
Eriksson L, Ekenberg L, Melander-Wikman A. The concept of palpation of the shoulder – A basic element of physiotherapy practice: A focus group study with physiotherapists. Adv Physiother. 2012;14(4):183–93.
Nim CG, Downie A, O’Neill S, Kawchuk GN, Perle SM, Leboeuf-Yde C. The importance of selecting the correct site to apply spinal manipulation when treating spinal pain: Myth or reality? A systematic review. Sci Rep. 2021;11(1):23415.
Alexander N, Rastelli A, Webb T, Rajendran D. The validity of lumbo-pelvic landmark palpation by manual practitioners: A systematic review. Int J Osteopath Med. 2021;39:10–20.
Leboeuf-Yde C, van Dijk J, Franz C, Hustad SA, Olsen D, Pihl T, et al. Motion palpation findings and self-reported low back pain in a population-based study sample. J Manipulative Physiol Ther. 2002;25(2):80–7.
Najm WI, Seffinger MA, Mishra SI, Dickerson VM, Adams A, Reinsch S, et al. Content validity of manual spinal palpatory exams - A systematic review. BMC Complement Altern Med. 2003;3:1.
Chaudhry H, Schleip R, Ji Z, Bukiet B, Maney M, Findley T. Three-dimensional mathematical model for deformation of human fasciae in manual therapy. J Am Osteopath Assoc. 2008;108(8):379–90.
Gabriel A, Konrad A, Roidl A, Queisser J, Schleip R, Horstmann T, et al. Myofascial Treatment Techniques on the Plantar Surface Influence Functional Performance in the Dorsal Kinetic Chain. J Sports Sci Med. 2022;21(1):13–22.
PubMed PubMed Central Google Scholar
Nolet PS, Yu H, Côté P, Meyer A-L, Kristman VL, Sutton D, et al. Reliability and validity of manual palpation for the assessment of patients with low back pain: a systematic and critical review. Chiropr Man Therap. 2021;29(1):33.
Seffinger MA, Najm WI, Mishra SI, Adams A, Dickerson VM, Murphy LS, et al. Reliability of spinal palpation for diagnosis of back and neck pain: a systematic review of the literature. Spine. 2004;29(19):E413–25.
Beynon AM, Hebert JJ, Walker BF. The interrater reliability of static palpation of the thoracic spine for eliciting tenderness and stiffness to test for a manipulable lesion. Chiropr Man Therap. 2018;26:49.
Petersen EJ, Thurmond SM, Shaw CA, Miller KN, Lee TW, Koborsi JA. Reliability and accuracy of an expert physical therapist as a reference standard for a manual therapy joint mobilization trial. J Man Manip Ther. 2021;29(3):189–95.
Petersen EJ, Thurmond SM, Buchanan SI, Chun DH, Richey AM, Nealon LP. The effect of real-time feedback on learning lumbar spine joint mobilization by entry-level doctor of physical therapy students: a randomized, controlled, crossover trial. J Man Manip Ther. 2020;28(4):201–11.
Abbott JH, Flynn TW, Fritz JM, Hing WA, Reid D, Whitman JM. Manual physical assessment of spinal segmental motion: intent and validity. Man Ther. 2009;14(1):36–44.
Bialosky JE, Simon CB, Bishop MD, George SZ. Basis for spinal manipulative therapy: a physical therapist perspective. J Electromyogr Kinesiol. 2012;22(5):643–7.
Henderson CN. The basis for spinal manipulation: chiropractic perspective of indications and theory. J Electromyogr Kinesiol. 2012;22(5):632–42.
Sizer PS Jr, Felstehausen V, Sawyer S, Dornier L, Matthews P, Cook C. Eight critical skill sets required for manual therapy competency: a Delphi study and factor analysis of physical therapy educators of manual therapy. J Allied Health. 2007;36(1):30–40.
Ombregt L. A System of Orthopaedic Medicine: Elsevier; 2013.
Cramer GD, Henderson CN, Little JW, Daley C, Grieve TJ. Zygapophyseal joint adhesions after induced hypomobility. J Manipulative Physiol Ther. 2010;33(7):508–18.
George JW, Tunstall AC, Tepe RE, Skaggs CD. The Effects of Active Release Technique on Hamstring Flexibility: A Pilot Study. J Manipulative Physiol Ther. 2006;29(3):224–7.
Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531–8.
Plaza-Manzano G, Molina-Ortega F, Lomas-Vega R, Martínez-Amat A, Achalandabaso A, Hita-Contreras F. Changes in biochemical markers of pain perception and stress response after spinal manipulation. J Orthop Sports Phys Ther. 2014;44(4):231–9.
Zusman M. Mechanism of mobilization. Physical Therapy Reviews. 2011;16(4):233–6.
De Carvalho DE, de Luca K, Funabashi M, Breen A, Wong AYL, Johansson MS, et al. Association of Exposures to Seated Postures With Immediate Increases in Back Pain: A Systematic Review of Studies With Objectively Measured Sitting Time. J Manipulative Physiol Ther. 2020;43(1):1–12.
Colloca CJ, Keller TS. Stiffness and neuromuscular reflex response of the human spine to posteroanterior manipulative thrusts in patients with low back pain. J Manipulative Physiol Ther. 2001;24(8):489–500.
Colloca CJ, Keller TS, Gunzburg R. Biomechanical and neurophysiological responses to spinal manipulation in patients with lumbar radiculopathy. J Manipulative Physiol Ther. 2004;27(1):1–15.
Reed WR, Long CR, Kawchuk GN, Sozio RS, Pickar JG. Neural Responses to Physical Characteristics of a High-velocity, Low-amplitude Spinal Manipulation: Effect of Thrust Direction. Spine. 2018;43(1):1–9.
Reed WR, Pickar JG, Sozio RS, Liebschner MAK, Little JW, Gudavalli MR. Characteristics of Paraspinal Muscle Spindle Response to Mechanically Assisted Spinal Manipulation: A Preliminary Report. J Manipulative Physiol Ther. 2017;40(6):371–80.
Devecchi V, Rushton AB, Gallina A, Heneghan NR, Falla D. Are neuromuscular adaptations present in people with recurrent spinal pain during a period of remission? a systematic review. PLoS ONE. 2021;16(4):e0249220.
Pagé I, Nougarou F, Lardon A, Descarreaux M. Changes in spinal stiffness with chronic thoracic pain: Correlation with pain and muscle activity. PLoS ONE. 2018;13(12):e0208790.
Lee RY, McGregor AH, Bull AM, Wragg P. Dynamic response of the cervical spine to posteroanterior mobilisation. Clin Biomech (Bristol, Avon). 2005;20(2):228–31.
Ross JK, Bereznick DE, McGill SM. Determining cavitation location during lumbar and thoracic spinal manipulation: is spinal manipulation accurate and specific? Spine. 2004;29(13):1452–7.
Donaldson M, Petersen S, Cook C, Learman K. A Prescriptively Selected Nonthrust Manipulation Versus a Therapist-Selected Nonthrust Manipulation for Treatment of Individuals With Low Back Pain: A Randomized Clinical Trial. J Orthop Sports Phys Ther. 2016;46(4):243–50.
McCarthy CJ, Potter L, Oldham JA. Comparing targeted thrust manipulation with general thrust manipulation in patients with low back pain. A general approach is as effective as a specific one. A randomised controlled trial. BMJ Open Sport Exerc Med. 2019;5(1):e000514.
Sutlive TG, Mabry LM, Easterling EJ, Durbin JD, Hanson SL, Wainner RS, et al. Comparison of short-term response to two spinal manipulation techniques for patients with low back pain in a military beneficiary population. Mil Med. 2009;174(7):750–6.
Tuttle N, Evans K, Sperotto dos Santos Rocha C. Localised manual therapy treatment has a preferential effect on the kinematics of the targeted motion segment. Musculoskelet Sci Pract. 2021;56:102457.
Ali MN, Sethi K, Noohu MM. Comparison of two mobilization techniques in management of chronic non-specific low back pain. J Bodyw Mov Ther. 2019;23(4):918–23.
de Oliveira RF, Costa LOP, Nascimento LP, Rissato LL. Directed vertebral manipulation is not better than generic vertebral manipulation in patients with chronic low back pain: a randomised trial. J Physiother. 2020;66(3):174–9.
Gevers-Montoro C, Provencher B, Northon S, Stedile-Lovatel JP, Ortega de Mues A, Piché M. Chiropractic Spinal Manipulation Prevents Secondary Hyperalgesia Induced by Topical Capsaicin in Healthy Individuals. Front Pain Res (Lausanne, Switzerland). 2021;2:702429.
Provencher B, Northon S, Piché M. Segmental Chiropractic Spinal Manipulation Does not Reduce Pain Amplification and the Associated Pain-Related Brain Activity in a Capsaicin-Heat Pain Model. Front Pain Res (Lausanne, Switzerland). 2021;2:733727.
Watanabe N, Piché M. Editorial: Mechanisms and Effectiveness of Complementary and Alternative Medicine for Pain Management. Front Pain Res (Lausanne, Switzerland). 2022;3:863751.
Muhsen A, Moss P, Gibson W, Walker B, Jacques A, Schug S, et al. The Association Between Conditioned Pain Modulation and Manipulation-induced Analgesia in People With Lateral Epicondylalgia. Clin J Pain. 2019;35(5):435–42.
Howick J, Glasziou P, Aronson JK. Evidence-based mechanistic reasoning. J Roy Soc Med. 2010;103(11):433–41.
Haavik Taylor H, Murphy B. The effects of spinal manipulation on central integration of dual somatosensory input observed after motor training: a crossover study. J Manipulative Physiol Ther. 2010;33(4):261–72.
Haavik-Taylor H, Murphy B. Cervical spine manipulation alters sensorimotor integration: a somatosensory evoked potential study. ClinNeurophysiol. 2007;118(2):391–402.
Ogura T, Tashiro M, Masud M, Watanuki S, Shibuya K, Yamaguchi K, et al. Cerebral metabolic changes in men after chiropractic spinal manipulation for neck pain. Altern Ther Health Med. 2011;17(6):12–7.
Sparks C, Cleland JA, Elliott JM, Zagardo M, Liu WC. Using functional magnetic resonance imaging to determine if cerebral hemodynamic responses to pain change following thoracic spine thrust manipulation in healthy individuals. J Orthop Sports Phys Ther. 2013;43(5):340–8.
Evans DW. How to gain evidence for causation in disease and therapeutic intervention: from Koch’s postulates to counter-counterfactuals. Med Health Care Philos. 2022;25(3):509–21.
Lascurain-Aguirrebeña I, Newham D, Critchley DJ. Mechanism of Action of Spinal Mobilizations: A Systematic Review. Spine. 2016;41(2):159–72.
Parravicini G, Bergna A. Biological effects of direct and indirect manipulation of the fascial system Narrative review. J Bodyw Mov Ther. 2017;21(2):435–45.
Crane JD, Ogborn DI, Cupido C, Melov S, Hubbard A, Bourgeois JM, et al. Massage therapy attenuates inflammatory signaling after exercise-induced muscle damage. Sci Transl Med. 2012;4(119):119ra13.
Degenhardt BF, Darmani NA, Johnson JC, Towns LC, Rhodes DC, Trinh C, et al. Role of osteopathic manipulative treatment in altering pain biomarkers: a pilot study. J Am Osteopath Assoc. 2007;107(9):387–400.
Kovanur-Sampath K, Mani R, Cotter J, Gisselman AS, Tumilty S. Changes in biochemical markers following spinal manipulation-a systematic review and meta-analysis. Musculoskelet Sci Pract. 2017;29:120–31.
Lohman EB, Pacheco GR, Gharibvand L, Daher N, Devore K, Bains G, et al. The immediate effects of cervical spine manipulation on pain and biochemical markers in females with acute non-specific mechanical neck pain: a randomized clinical trial. J Man Manip Ther. 2019;27(4):186–96.
Teodorczyk-Injeyan JA, McGregor M, Triano JJ, Injeyan SH. Elevated Production of Nociceptive CC Chemokines and sE-Selectin in Patients With Low Back Pain and the Effects of Spinal Manipulation: A Nonrandomized Clinical Trial. Clin J Pain. 2018;34(1):68–75.
Council GC. The Code: Standards of conduct, performance and ethics for chiropractors. GCC; 2019.
Council HaCP. Standards of Proficiency - Physiotherapists. HCPC; 2013.
Council GO. Osteopathic Practice Standards. GOC; 2023.
Therapies TCfST. GCMT Code of Practice, Ethics and Proficiency for Professional Associations. GCMT; 2023.
Daluiso-King G, Hebron C. Is the biopsychosocial model in musculoskeletal physiotherapy adequate? An evolutionary concept analysis. Physiotherapy theory and practice. 2020:1–17.
Søndenå P, Dalusio-King G, Hebron C. Conceptualisation of the therapeutic alliance in physiotherapy: is it adequate? Musculoskelet Sci Pract. 2020;46:102131.
World Health Organisation. Patient Safety 2019 [Available from: https://www.who.int/news-room/fact-sheets/detail/patient-safety#:~:text=Patient%20Safety%20is%20a%20health,during%20provision%20of%20health%20care .
Vogel S, Mars T, Keeping S, Barton T, Marlin N, Froud R, et al. Clinical Risk Osteopathy and Management Scientific Report. 2012.
Ekerholt K, Bergland A. Learning and knowing bodies: Norwegian psychomotor physiotherapists’ reflections on embodied knowledge. Physiother Theory Pract. 2019;35(1):57–69.
Hutting N, Johnston V, Staal JB, Heerkens YF. Promoting the Use of Self-management Strategies for People With Persistent Musculoskeletal Disorders: The Role of Physical Therapists. J Orthop Sports Phys Ther. 2019;49(4):212–5.
Kongsted A, Ris I, Kjaer P, Hartvigsen J. Self-management at the core of back pain care: 10 key points for clinicians. Braz J Phys Therap. 2021.
Elwyn G, Durand MA, Song J, Aarts J, Barr PJ, Berger Z, et al. A three-talk model for shared decision making: multistage consultation process. BMJ (Clinical research ed). 2017;359:j4891.
Broom B. The Practice of Whole Person-Centred Healthcare. In: Anjum RL, Copeland S, Rocca E, editors. Rethinking Causality, Complexity and Evidence for the Unique Patient: A CauseHealth Resource for Healthcare Professionals and the Clinical Encounter. Cham: Springer International Publishing; 2020. p. 215–26.
Chapter Google Scholar
Darlow B, Dowell A, Baxter GD, Mathieson F, Perry M, Dean S. The enduring impact of what clinicians say to people with low back pain. Ann Fam Med. 2013;11(6):527–34.
Stewart M, Loftus S. Sticks and Stones: The Impact of Language in Musculoskeletal Rehabilitation. J Orthop Sports Phys Ther. 2018;48(7):519–22.
Lin I, Wiles L, Waller R, Caneiro JP, Nagree Y, Straker L, et al. Patient-centred care: the cornerstone for high-value musculoskeletal pain management. Br J Sports Med. 2020;54(21):1240–2.
Cowell I, O’Sullivan P, O’Sullivan K, Poyton R, McGregor A, Murtagh G. Perceptions of physiotherapists towards the management of non-specific chronic low back pain from a biopsychosocial perspective: A qualitative study. Musculoskelet Sci Pract. 2018;38:113–9.
Edmond SN, Keefe FJ. Validating pain communication: current state of the science. Pain. 2015;156(2):215–9.
O’Keeffe M, Cullinane P, Hurley J, Leahy I, Bunzli S, O’Sullivan PB, et al. What Influences Patient-Therapist Interactions in Musculoskeletal Physical Therapy? Qualitative Systematic Review and Meta-Synthesis. Phys Ther. 2016;96(5):609–22.
Copnell G. Informed consent in physiotherapy practice: it is not what is said but how it is said. Physiotherapy. 2018;104(1):67–71.
Lee A. Bolam’ to “Montgomery” is result of evolutionary change of medical practice towards ’patient-centred care. Postgrad Med J. 2017;93(1095):46–50.
Lewis J, O’Sullivan P. Is it time to reframe how we care for people with non-traumatic musculoskeletal pain? Br J Sports Med. 2018;52(24):1543–4.
Lewis J, Ridehalgh C, Moore A, Hall K. This is the day your life must surely change: Prioritising behavioural change in musculoskeletal practice. Physiotherapy. 2021.
Lewis JS, Stokes EK, Gojanovic B, Gellatly P, Mbada C, Sharma S, et al. Reframing how we care for people with persistent non-traumatic musculoskeletal pain. Suggestions for the rehabilitation community. Physiotherapy. 2021.
Bishop A, Foster NE, Thomas E, Hay EM. How does the self-reported clinical management of patients with low back pain relate to the attitudes and beliefs of health care practitioners? A survey of UK general practitioners and physiotherapists. Pain. 2008;135(1–2):187–95.
Darlow B, Fullen BM, Dean S, Hurley DA, Baxter GD, Dowell A. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review. Eur J Pain (London, England). 2012;16(1):3–17.
Article CAS Google Scholar
Lakke SE, Soer R, Krijnen WP, van der Schans CP, Reneman MF, Geertzen JH. Influence of Physical Therapists’ Kinesiophobic Beliefs on Lifting Capacity in Healthy Adults. Phys Ther. 2015;95(9):1224–33.
Howe LC, Leibowitz KA, Crum AJ. When Your Doctor “Gets It” and “Gets You”: The Critical Role of Competence and Warmth in the Patient-Provider Interaction. Front Psych. 2019;10:475.
Newell D, Lothe LR, Raven TJL. Contextually Aided Recovery (CARe): a scientific theory for innate healing. Chiropr Man Therap. 2017;25:6.
Rossettini G, Camerone EM, Carlino E, Benedetti F, Testa M. Context matters: the psychoneurobiological determinants of placebo, nocebo and context-related effects in physiotherapy. Arch Physiother. 2020;10:11.
Gallace A. Social Touch. In: Olausson H, Wessberg J, Morrison I, McGlone F, editors. Affective Touch and the Neurophysiology of CT Afferents: Springer; 2016.
Gallace A, Spence C. The science of interpersonal touch: an overview. Neurosci Biobehav Rev. 2010;34(2):246–59.
Kelly MA, Nixon L, McClurg C, Scherpbier A, King N, Dornan T. Experience of Touch in Health Care: A Meta-Ethnography Across the Health Care Professions. Qual Health Res. 2018;28(2):200–12.
McGlone F, Cerritelli F, Walker S, Esteves J. The role of gentle touch in perinatal osteopathic manual therapy. Neurosci Biobehav Rev. 2017;72:1–9.
Olausson H, Wessberg J, Morrison I, McGlone F. Affective Touch and the Neurophysiology of CT Afferents: Springer; 2016.
McParlin Z, Cerritelli F, Rossettini G, Friston KJ, Esteves JE. Therapeutic Alliance as Active Inference: The Role of Therapeutic Touch and Biobehavioural Synchrony in Musculoskeletal Care. Front Behav Neurosci. 2022;16:897247.
Meijer LL, Ruis C, van der Smagt MJ, Scherder EJA, Dijkerman HC. Neural basis of affective touch and pain: A novel model suggests possible targets for pain amelioration. J Neuropsychol. 2021.
Allen-Collinson J, Pavey A. Touching moments: phenomenological sociology and the haptic dimension in the lived experience of motor neurone disease. Sociol Health Illn. 2014;36(6):793–806.
Bjorbækmo WS, Mengshoel AM. “A touch of physiotherapy” - the significance and meaning of touch in the practice of physiotherapy. Physiother Theory Pract. 2016;32(1):10–9.
Nummenmaa L, Tuominen L, Dunbar R, Hirvonen J, Manninen S, Arponen E, et al. Social touch modulates endogenous μ-opioid system activity in humans. Neuroimage. 2016;138:242–7.
Calsius J, De Bie J, Hertogen R, Meesen R. Touching the Lived Body in Patients with Medically Unexplained Symptoms. How an Integration of Hands-on Bodywork and Body Awareness in Psychotherapy may Help People with Alexithymia. Front Psychol. 2016;7:253.
Gentsch A, Crucianelli L, Jenkinson P, Fotopoulou A. The touched self: Affective touch and body awareness in health and disease. Affective touch and the neurophysiology of CT afferents Springer; 2016.
Cerritelli F, Chiacchiaretta P, Gambi F, Ferretti A. Effect of Continuous Touch on Brain Functional Connectivity Is Modified by the Operator’s Tactile Attention. Front Hum Neurosci. 2017;11:368.
Tramontano M, Cerritelli F, Piras F, Spanò B, Tamburella F, Piras F, et al. Brain Connectivity Changes after Osteopathic Manipulative Treatment: A Randomized Manual Placebo-Controlled Trial. Brain Sci. 2020;10(12):969.
Øberg GK, Blanchard Y, Obstfelder A. Therapeutic encounters with preterm infants: interaction, posture and movement. Physiother Theory Pract. 2014;30(1):1–5.
Øberg GK, Normann B, Gallagher S. Embodied-enactive clinical reasoning in physical therapy. Physiother Theory Pract. 2015;31(4):244–52.
Consedine S, Standen C, Niven E. Knowing hands converse with an expressive body – An experience of osteopathic touch. Int J Osteopath Med. 2016;19:3–12.
Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39–48.
Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41–8.
Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201–3.
Sherriff B, Clark C, Killingback C, Newell D. Musculoskeletal practitioners’ perceptions of contextual factors that may influence chronic low back pain outcomes: a modified Delphi study. Chiropr Man Therap. 2023;31(1):12.
Sherriff B, Clark C, Killingback C, Newell D. Impact of contextual factors on patient outcomes following conservative low back pain treatment: systematic review. Chiropr Manual Therap. 2022;30(1):20.
Mercer E, Mackay-Lyons M, Conway N, Flynn J, Mercer C. Perceptions of outpatients regarding the attire of physiotherapists. Physiother Can. 2008;60(4):349–57.
Petrilli CM, Mack M, Petrilli JJ, Hickner A, Saint S, Chopra V. Understanding the role of physician attire on patient perceptions: a systematic review of the literature— targeting attire to improve likelihood of rapport (TAILOR) investigators. BMJ Open. 2015;5(1):e006578.
Beach MC, Fitzgerald A, Saha S. White Coat Hype: Branding Physicians With Professional Attire. JAMA Intern Med. 2013;173(6):467–8.
Bearman G, Bryant K, Leekha S, Mayer J, Munoz-Price LS, Murthy R, et al. Healthcare Personnel Attire in Non-Operating-Room Settings. Infect Control Hosp Epidemiol. 2014;35(2):107–21.
Rehman SU, Nietert PJ, Cope DW, Kilpatrick AO. What to wear today? Effect of doctor’s attire on the trust and confidence of patients. Am J Med. 2005;118(11):1279–86.
Brady B, Veljanova I, Schabrun S, Chipchase L. Integrating culturally informed approaches into physiotherapy assessment and treatment of chronic pain: a pilot randomised controlled trial. BMJ Open. 2018;8(7):e021999.
Miles A, Mezzich JE. The care of the patient and the soul of the clinic: person-centered medicine as an emergent model of clinical practice. Int J Person Centred Med. 2012;1(2):207–22.
Cowell I, McGregor A, O’Sullivan P, O’Sullivan K, Poyton R, Schoeb V, et al. How do physiotherapists solicit and explore patients’ concerns in back pain consultations: a conversation analytic approach. Physiother Theory Pract. 2021;37(6):693–709.
Hutting N, Caneiro JP, Ong'wen MO, Miciak M, Roberts LE. Patient-centered care in musculoskeletal practice: key elements to support clinicians to focus on the person. 2021.
Caneiro JP, Roos EM, Barton CJ, O’Sullivan K, Kent P, Lin I, et al. It is time to move beyond “body region silos” to manage musculoskeletal pain: five actions to change clinical practice. Br J Sports Med. 2020;54(8):438–9.
Greenhalgh T, Howick J, Maskrey N, EBM Renaissance Group. Evidence based medicine: a movement in crisis? Brit Med J. 2014;348:g3725.
Greenhalgh T, Snow R, Ryan S, Rees S, Salisbury H. Six ‘biases’ against patients and carers in evidence-based medicine. Bmc Med. 2015;13(1):200.
Loughlin M, Fuller J, Bluhm R, Buetow S, Borgerson K. Theory, experience and practice. J Eval Clin Pract. 2016;22(4):459–65.
Simpson JK, Innes S. Informed consent, duty of disclosure and chiropractic: where are we? Chiropr Man Therap. 2020;28(1):60.
Download references
Acknowledgements
Use of any animal or human data or tissue.
No funding was received for this paper.
Author information
Authors and affiliations.
School of Health Sciences, Queens Medical Centre, University of Nottingham, Nottingham, NG7 2HA, UK
Roger Kerry, Edward Lee & Vasileios Georgopoulos
Allied Health Research Unit, University of Central Lancashire, Preston, PR1 2HE, UK
Kenneth J. Young
Centre of Precision Rehabilitation for Spinal Pain, School of Sport, Exercise and Rehabilitation Sciences, University of Birmingham, Edgbaston, Birmingham, B15 2TT, UK
David W. Evans
Nottingham CityCare Partnership, Bennerley Rd, Nottingham, NG6 8WR, UK
School of Medicine, University of Nottingham, Queens Medical Centre, Nottingham, NG7 2HA, UK
Vasileios Georgopoulos
Department of Orthopaedics, West Herts Hospitals Trust, Watford, WD18 0HB, UK
Adam Meakins
School of Physiotherapy, Manchester Metropolitan University, Manchester, M15 6GX, UK
Chris McCarthy
Department of Orthopaedics, Duke University, 200 Morris Street, Durham, NC, 27701, USA
School of Sport and Health Sciences, University of Brighton, Darley Rd, Eastbourne, BN20 7UR, UK
Colette Ridehalgh
Clinical Neuroscience, Trafford Building, Brighton and Sussex Medical School, University of Sussex, Brighton, BN1 9PX, UK
University College of Osteopathy, 275 Borough High St, London, SE1 1JE, UK
Steven Vogel & Amanda Banton
Department of Clinical Sciences, Obstetrics and Gynecology, Umeå University, S-90187, Umeå, Sweden
Cecilia Bergström
The School of Soft Tissue Therapy, Exmouth, Devon, EX8 1DQ, UK
Anna Maria Mazzieri
Department of health, LUNEX, Differdange, 4671, Luxembourg
Firas Mourad
Luxembourg Health & Sport Sciences Research Institute A.s.b.l., 50, Avenue du Parc des Sports, Differdange, 4671, Luxembourg
Department of Occupation and Health, School of Organization and Development, HAN University of Applied Sciences, Nijmegen, the Netherlands
Nathan Hutting
You can also search for this author in PubMed Google Scholar
Contributions
Concept and research design: RK, KJY, DWE, EL, AM, VG. Data collection: All authors. Data analysis: All authors. Writing and editing of the manuscript: All authors.
Corresponding author
Correspondence to Kenneth J. Young .
Ethics declarations
Ethics approval and consent to participate.
All participants are co-authors. Ethical approval was not necessary.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kerry, R., Young, K.J., Evans, D.W. et al. A modern way to teach and practice manual therapy. Chiropr Man Therap 32 , 17 (2024). https://doi.org/10.1186/s12998-024-00537-0
Download citation
Received : 18 October 2023
Accepted : 17 April 2024
Published : 21 May 2024
DOI : https://doi.org/10.1186/s12998-024-00537-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Manual Therapy
- Evidence-based healthcare
- Person-centred healthcare
- Physiotherapy
- Chiropractic
- Soft-tissue therapy
Chiropractic & Manual Therapies
ISSN: 2045-709X
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 22 May 2024

Enhancing clinical skills in pediatric trainees: a comparative study of ChatGPT-assisted and traditional teaching methods
- Hongjun Ba 1 , 2 ,
- Lili zhang 1 &
- Zizheng Yi 1
BMC Medical Education volume 24 , Article number: 558 ( 2024 ) Cite this article
Metrics details
As artificial intelligence (AI) increasingly integrates into medical education, its specific impact on the development of clinical skills among pediatric trainees needs detailed investigation. Pediatric training presents unique challenges which AI tools like ChatGPT may be well-suited to address.
This study evaluates the effectiveness of ChatGPT-assisted instruction versus traditional teaching methods on pediatric trainees’ clinical skills performance.
A cohort of pediatric trainees ( n = 77) was randomly assigned to two groups; one underwent ChatGPT-assisted training, while the other received conventional instruction over a period of two weeks. Performance was assessed using theoretical knowledge exams and Mini-Clinical Evaluation Exercises (Mini-CEX), with particular attention to professional conduct, clinical judgment, patient communication, and overall clinical skills. Trainees’ acceptance and satisfaction with the AI-assisted method were evaluated through a structured survey.
Both groups performed similarly in theoretical exams, indicating no significant difference ( p > 0.05). However, the ChatGPT-assisted group showed a statistically significant improvement in Mini-CEX scores ( p < 0.05), particularly in patient communication and clinical judgment. The AI-teaching approach received positive feedback from the majority of trainees, highlighting the perceived benefits in interactive learning and skill acquisition.
ChatGPT-assisted instruction did not affect theoretical knowledge acquisition but did enhance practical clinical skills among pediatric trainees. The positive reception of the AI-based method suggests that it has the potential to complement and augment traditional training approaches in pediatric education. These promising results warrant further exploration into the broader applications of AI in medical education scenarios.
Peer Review reports
Introduction
The introduction of ChatGPT by OpenAI in November 2022 marked a watershed moment in educational technology, heralded as the third major innovation following Web 2.0’s emergence over a decade earlier [ 1 ] and the rapid expansion of e-learning driven by the COVID-19 pandemic [ 2 ]. In medical education, the integration of state-of-the-art Artificial Intelligence (AI) has been particularly transformative for pediatric clinical skills training—a field where AI is now at the forefront.
Pediatric training, with its intricate blend of extensive medical knowledge and soft skills like empathetic patient interaction, is pivotal for effective child healthcare. The need for swift decision-making, especially in emergency care settings, underscores the specialty’s complexity. Traditional teaching methods often fall short, hindered by logistical challenges and difficulties in providing a standardized training experience. AI tools such as ChatGPT offer a promising solution, with their ability to simulate complex patient interactions and thus improve pediatric trainees’ communication, clinical reasoning, and decision-making skills across diverse scenarios [ 3 , 4 ].
ChatGPT’s consistent, repeatable, and scalable learning experiences represent a significant advancement over traditional constraints, such as resource limitations and standardization challenges [ 5 ], offering a new paradigm for medical training. Its proficiency in providing immediate, personalized feedback could revolutionize the educational journey of pediatric interns. Our study seeks to investigate the full extent of this potential revolution, employing a mixed-methods approach to quantitatively and qualitatively measure the impact of ChatGPT on pediatric trainees’ clinical competencies.
Despite AI’s recognized potential within the academic community, empirical evidence detailing its influence on clinical skills development is limited [ 6 ]. Addressing this gap, our research aims to contribute substantive insights into the efficacy of ChatGPT in enhancing the clinical capabilities of pediatric trainees, establishing a new benchmark for the intersection of AI and medical education.
Participants and methods
Participants.
Our study evaluated the impact of ChatGPT-assisted instruction on the clinical skills of 77 medical interns enrolled in Sun Yat-sen University’s five-year program in 2023. The cohort, consisting of 42 males and 35 females, was randomly allocated into four groups based on practicum rotation, using a computer-generated randomization list. Each group, composed of 3–4 students, was assigned to either the ChatGPT-assisted or traditional teaching group for a two-week pediatric internship rotation. Randomization was stratified by baseline clinical examination scores to ensure group comparability.
Study design
A controlled experimental design was implemented with blind assessment. The interns were randomly assigned to the ChatGPT-assisted group (39 students) or the traditional group (38 students), with no significant differences in gender, age, or baseline clinical examination scores ( p > 0.05). The ChatGPT-assisted group received instruction supplemented with ChatGPT version 4.0, while the traditional group received standard bedside teaching (as depicted in Fig. 1 ). Both groups encountered identical clinical case scenarios involving common pediatric conditions: Kawasaki disease, gastroenteritis, congenital heart disease, nephrotic syndrome, bronchopneumonia, and febrile convulsion. All interns had equal access to the same teaching materials, instructors, and intensity of courses. The core textbook was the 9th edition of “Pediatrics” published by the People’s Medical Publishing House. Ethical approval was obtained from the institutional review board, and informed consent was secured, with special attention to privacy concerns due to the involvement of pediatric patient data.
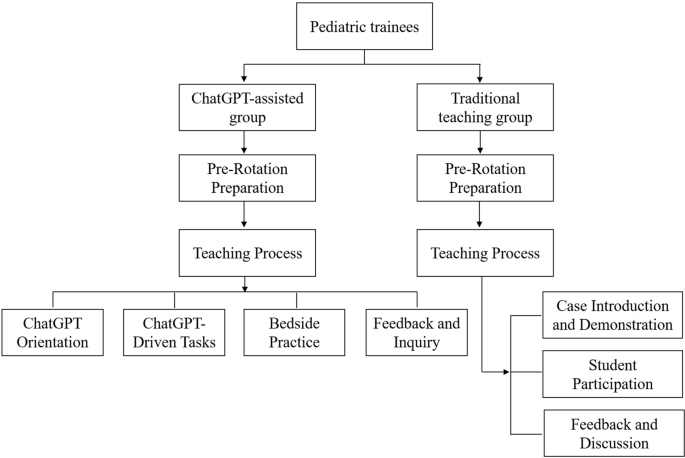
Study design and flow chart
Instructional implementation
Traditional teaching group, pre-rotation preparation.
Instructors designed typical cases representing common pediatric diseases and updated knowledge on the latest diagnostic and therapeutic advancements. They developed multimedia presentations detailing the presentation, diagnostic criteria, and treatment plans for each condition.
Teaching process
The teaching method during the rotation was divided into three stages:
Case introduction and demonstration
Instructors began with a detailed introduction of clinical cases, explaining diagnostic reasoning and emphasizing key aspects of medical history-taking and physical examination techniques.
Student participation
Students then conducted patient interviews and physical assessments independently, with the instructor observing. For pediatric patients, particularly infants, history was provided by the guardians.
Feedback and discussion
At the end of each session, instructors provided personalized feedback on student performance and answered questions, fostering an interactive learning environment.
ChatGPT-assisted teaching group
Educators prepared structured teaching plans focusing on common pediatric diseases and representative cases. The preparation phase involved configuring ChatGPT (version 4.0) settings to align with the educational objectives of the rotation.
The rotation was executed in four consecutive steps:
ChatGPT orientation
Students were familiarized with the functionalities and potential educational applications of ChatGPT version 4.0.
ChatGPT-driven tasks
In our study, ChatGPT version 4.0 was used as a supplementary educational tool within the curriculum. Students engaged with the AI to interactively explore dynamically generated clinical case vignettes based on pediatric medicine. These vignettes encompassed clinical presentations, history taking, physical examinations, diagnostic strategies, differential diagnoses, and treatment protocols, allowing students to query the AI to enhance their understanding of various clinical scenarios.
Students accessed clinical vignettes in both text and video formats, with video particularly effective in demonstrating physical examination techniques and communication strategies with guardians, thereby facilitating a more interactive learning experience.
ChatGPT initially guided students in forming assessments, while educators critically reviewed their work, providing immediate, personalized feedback to ensure proper development of clinical reasoning and decision-making skills. This blend of AI and direct educator involvement aimed to improve learning outcomes by leveraging AI’s scalability alongside expert educators’ insights.
Bedside clinical practice
Students practiced history-taking and physical examinations at the patient’s bedside, with information about infants provided by their guardians.
Feedback and inquiry
Instructors offered feedback on performance and addressed student queries to reinforce learning outcomes.
Assessment methods
The methods used to evaluate the interns’ post-rotation performance included three assessment tools:
Theoretical knowledge exam
Both groups completed the same closed-book exam to test their pediatric theoretical knowledge, ensuring consistency in cognitive understanding assessment.
Mini-CEX assessment
The Mini-CEX has been widely recognized as an effective and reliable method for assessing clinical skills [ 7 , 8 ]. Practical skills were evaluated using the Mini-CEX, which involved students taking histories from parents of pediatric patients and conducting physical examinations on infants, supervised by an instructor. Mini-CEX scoring utilized a nine-point scale with seven criteria, assessing history-taking, physical examination, professionalism, clinical judgment, doctor-patient communication, organizational skills, and overall competence.
History taking
This assessment measures students’ ability to accurately collect patient histories, utilize effective questioning techniques, respond to non-verbal cues, and exhibit respect, empathy, and trust, while addressing patient comfort, dignity, and confidentiality.
Physical examination
This evaluates students on informing patients about examination procedures, conducting examinations in an orderly sequence, adjusting examinations based on patient condition, attending to patient discomfort, and ensuring privacy.
Professionalism
This assesses students’ demonstration of respect, compassion, and empathy, establishment of trust, attention to patient comfort, maintenance of confidentiality, adherence to ethical standards, understanding of legal aspects, and recognition of their professional limits.
Clinical judgment
This includes evaluating students’ selection and execution of appropriate diagnostic tests and their consideration of the risks and benefits of various treatment options.
Doctor-patient communication
This involves explaining test and treatment rationales, obtaining patient consent, educating on disease management, and discussing issues effectively and timely based on disease severity.
Organizational efficiency
This measures how students prioritize based on urgency, handle patient issues efficiently, demonstrate integrative skills, understand the healthcare system, and effectively use resources for optimal service.
Overall competence
This assesses students on judgment, integration, and effectiveness in patient care, evaluating their overall capabilities in caring and efficiency.
The scale ranged from below expectations (1–3 points), meeting expectations (4–6 points), to exceeding expectations (7–9 points). To maintain assessment consistency, all Mini-CEX evaluations were conducted by a single assessor.
ChatGPT method feedback survey
Only for the ChatGPT-assisted group, the educational impact of the ChatGPT teaching method was evaluated post-rotation through a questionnaire. This survey used a self-assessment scale with a Cronbach’s Alpha coefficient of 0.812, confirming its internal consistency and reliability. Assessment items involved active learning engagement, communication skills, empathy, retention of clinical knowledge, and improvement in diagnostic reasoning. Participant satisfaction was categorized as (1) very satisfied, (2) satisfied, (3) neutral, or (4) dissatisfied.
Statistical analysis
Data were analyzed using R software (version 4.2.2) and SPSS (version 26.0). Descriptive statistics were presented as mean ± standard deviation (x ± s), and independent t-tests were performed to compare groups. Categorical data were presented as frequency and percentage (n[%]), with chi-square tests applied where appropriate. A P -value of < 0.05 was considered statistically significant. All assessors of the Mini-CEX were blinded to the group assignments to minimize bias.
Theoretical knowledge exam scores for both groups of trainees
The theoretical knowledge exam revealed comparable results between the two groups, with the ChatGPT-assisted group achieving a mean score of 92.21 ± 2.37, and the traditional teaching group scoring slightly higher at 92.38 ± 2.68. Statistical analysis using an independent t-test showed no significant difference in the exam scores (t = 0.295, p = 0.768), suggesting that both teaching methods similarly supported the trainees’ theoretical learning.
Mini-CEX evaluation results for both groups of trainees
All trainees completed the Mini-CEX evaluation in 38 ± 0.5 min on average, with immediate post-evaluation feedback averaging 5.8 ± 0.6 min per student. The ChatGPT group demonstrated statistically significant improvement in professional conduct, clinical judgment, patient communication, and overall clinical skills compared to the traditional group. A detailed comparison of the CEX scoring for both student groups is presented in Table 1 ; Fig. 2 .
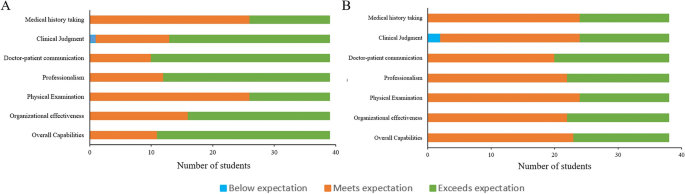
The scale scores of Mini-CEX assessment between the two groups. A : ChatGPT-assisted group; B : Traditional teaching group
Satisfaction survey results of trainees in the ChatGPT-assisted teaching
Feedback from the trainees regarding the ChatGPT-assisted teaching method was overwhelmingly positive. High levels of satisfaction and interest were reported, with no instances of dissatisfaction noted. The summary of these findings, including specific aspects of the teaching method that were rated highly by the students, is detailed in Table 2 .
The integration of ChatGPT into pediatric medical education represents a significant stride in leveraging artificial intelligence (AI) to enhance the learning process. Our findings suggest that while AI does not substantially alter outcomes in theoretical knowledge assessments, it plays a pivotal role in the advancement of clinical competencies.
The parity in theoretical examination scores between the ChatGPT-assisted and traditionally taught groups indicates that foundational medical knowledge can still be effectively acquired through existing educational frameworks. This underscores the potential of ChatGPT as a complementary, rather than a substitutive, educational instrument [ 9 , 10 ].
Mini-CEX evaluations paint a different picture, revealing the ChatGPT group’s superior performance in clinical realms. These competencies are crucial for the comprehensive development of a pediatrician and highlight the value of an interactive learning environment in bridging the gap between theory and practice [ 11 , 12 ].
The unanimous satisfaction with ChatGPT-assisted learning points to AI’s capacity to enhance student engagement. This positive response could be attributed to the personalized and interactive nature of the AI experience, catering to diverse learning styles [ 13 , 14 ]. However, it is critical to consider the potential for overreliance on technology and the need for maintaining an appropriate balance between AI and human interaction in medical training.
The ChatGPT group’s ascendency in clinical skillfulness could be a testament to the repetitive, adaptive learning scenarios proffered by AI technology. ChatGPT’s proficiency in tailoring educational content to individual performance metrics propels a more incisive and efficacious learning journey. Furthermore, the on-site, real-time feedback from evaluators is likely instrumental in consolidating clinical skillsets, echoing findings on the potency of immediate feedback in clinical education [ 15 , 16 ].
The study’s strength lies in its pioneering exploration of ChatGPT in pediatric education and the structured use of Mini-CEX for appraising clinical competencies, but it is not without limitations. The ceiling effect may have masked subtle differences in theoretical knowledge, and our small, single-center cohort limits the generalizability of our findings. The transitory nature of the study precludes assessment of long-term retention, a factor that future research should aim to elucidate [ 17 , 18 ].
Moreover, the ongoing evolution of AI and medical curricula necessitates continuous reevaluation of ChatGPT’s role in education. Future studies should explore multicenter trials, long-term outcomes, and integration strategies within existing curricula to provide deeper insights into AI’s role in medical education. Ethical and practical considerations, including data privacy, resource allocation, and cost, must also be carefully navigated to ensure that AI tools like ChatGPT are implemented responsibly and sustainably.
In conclusion, ChatGPT’s incorporation into pediatric training did not significantly affect the acquisition of theoretical knowledge but did enhance clinical skill development. The high levels of trainee satisfaction suggest that ChatGPT is a valuable adjunct to traditional educational methods, warranting further investigation and thoughtful integration into medical curricula.
Availability of data and materials
All data sets generated for this study were included in the manuscript.
Hollinderbäumer A, Hartz T, Uckert F. Education 2.0 — how has social media and web 2.0 been integrated into medical education? A systematical literature review. GMS Z Med Ausbild. 2013;30(1):Doc14. https://doi.org/10.3205/zma000857 .
Article Google Scholar
Turnbull D, Chugh R, Luck J. Transitioning to E-Learning during the COVID-19 pandemic: how have higher education institutions responded to the challenge? Educ Inf Technol (Dordr). 2021;26(5):6401–19. https://doi.org/10.1007/s10639-021-10633-w .
Bright TJ, Wong A, Dhurjati R, Bristow E, Bastian L, Coeytaux RR, et al. Effect of clinical decision-support systems: a systematic review. Ann Intern Med. 2012;157(1):29–43. https://doi.org/10.7326/0003-4819-157-1-201207030-00450 .
Chan KS, Zary N. Applications and challenges of implementing artificial intelligence in medical education: integrative review. JMIR Med Educ. 2019;5(1):e13930. https://doi.org/10.2196/13930 .
Geoffrey Currie. A conversation with ChatGPT. J Nucl Med Technol. 2023;51(3):255–60. https://doi.org/10.2967/jnmt.123.265864 .
Hossain E, Rana R, Higgins N, Soar J, Barua PD, Pisani AR, et al. Natural language processing in electronic health records in relation to healthcare decision-making: a systematic review. Comput Biol Med. 2023;155:106649. https://doi.org/10.1016/j.compbiomed.2023.106649 .
Mortaz Hejri S, Jalili M, Masoomi R, Shirazi M, Nedjat S, Norcini J. The utility of mini-clinical evaluation Exercise in undergraduate and postgraduate medical education: a BEME review: BEME guide 59. Med Teach. 2020;42(2):125–42. https://doi.org/10.1080/0142159X.2019.1652732 .
Motefakker S, Shirinabadi Farahani A, Nourian M, Nasiri M, Heydari F. The impact of the evaluations made by Mini-CEX on the clinical competency of nursing students. BMC Med Educ. 2022;22(1):634. https://doi.org/10.1186/s12909-022-03667-2 .
Eysenbach G. The role of ChatGPT, generative language models, and artificial intelligence in medical education: a conversation with ChatGPT and a call for papers. JMIR Med Educ. 2023;9:e46885. https://doi.org/10.2196/46885 .
Guo J, Bai L, Yu Z, Zhao Z, Wan B. An AI-application-oriented In-Class teaching evaluation model by using statistical modeling and ensemble learning. Sens (Basel). 2021;21(1):241. https://doi.org/10.3390/s21010241 .
Vishwanathaiah S, Fageeh HN, Khanagar SB, Maganur PC. Artificial Intelligence its uses and application in pediatric dentistry: a review. Biomedicines. 2023;11(3):788. https://doi.org/10.3390/biomedicines11030788 .
Cooper A, Rodman A. AI and Medical Education - A 21st-Century Pandora’s Box. N Engl J Med. 2023;389(5):385–7. https://doi.org/10.1056/NEJMp2304993 .
Arif TB, Munaf U, Ul-Haque I. The future of medical education and research: is ChatGPT a blessing or blight in disguise? Med Educ Online. 2023;28(1):2181052. https://doi.org/10.1080/10872981.2023.2181052 .
Nagi F, Salih R, Alzubaidi M, Shah H, Alam T, Shah Z, et al. Applications of Artificial Intelligence (AI) in medical education: a scoping review. Stud Health Technol Inf. 2023;305:648–51. https://doi.org/10.3233/SHTI230581 .
van de Ridder JM, Stokking KM, McGaghie WC, ten Cate OT. What is feedback in clinical education? Med Educ. 2008;42(2):189–97. https://doi.org/10.1111/j.1365-2923.2007.02973.x .
Wilbur K, BenSmail N, Ahkter S. Student feedback experiences in a cross-border medical education curriculum. Int J Med Educ. 2019;10:98–105. https://doi.org/10.5116/ijme.5ce1.149f .
Morrow E, Zidaru T, Ross F, Mason C, Patel KD, Ream M, et al. Artificial intelligence technologies and compassion in healthcare: a systematic scoping review. Front Psychol. 2023;13:971044. https://doi.org/10.3389/fpsyg.2022.971044 .
Soong TK, Ho CM. Artificial intelligence in medical OSCEs: reflections and future developments. Adv Med Educ Pract. 2021;12:167–73. https://doi.org/10.2147/AMEP.S287926 .
Download references
Acknowledgements
Author information, authors and affiliations.
Department of Pediatric Cardiology, Heart Center, First Affiliated Hospital of Sun Yat-sen University, 58# Zhongshan Road 2, Guangzhou, 510080, China
Hongjun Ba, Lili zhang & Zizheng Yi
Key Laboratory on Assisted Circulation, Ministry of Health, 58# Zhongshan Road 2, Guangzhou, 510080, China
You can also search for this author in PubMed Google Scholar
Contributions
H-JB conceived and designed the ideas for the manuscript. H-JB, L-LZ, and Z-ZY participated in all data collection and processing. H-JB was the major contributors in organizing records and drafting the manuscript. All authors proofread and approved the manuscript.
Corresponding author
Correspondence to Hongjun Ba .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the the Ethics Committee of The First Affiliated Hospital, Sun Yat-sen University, and informed consent was secured, with special attention to privacy concerns due to the involvement of pediatric patient data.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ba, H., zhang, L. & Yi, Z. Enhancing clinical skills in pediatric trainees: a comparative study of ChatGPT-assisted and traditional teaching methods. BMC Med Educ 24 , 558 (2024). https://doi.org/10.1186/s12909-024-05565-1
Download citation
Received : 01 March 2024
Accepted : 16 May 2024
Published : 22 May 2024
DOI : https://doi.org/10.1186/s12909-024-05565-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Pediatric training
- Clinical skills
- Medical education
- AI in healthcare
- Mini-clinical evaluation exercise
- Interactive learning
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Particle Swarm Optimization in 3D Medical Image Registration: A Systematic Review
- Review article
- Published: 25 May 2024
Cite this article

- Lucia Ballerini ORCID: orcid.org/0000-0002-1956-4012 1
Medical image registration seeks to find an optimal spatial transformation that best aligns the underlying anatomical structures. These problems usually require the optimization of a similarity metric. Swarm Intelligence techniques are very effective and efficient optimization methods. This systematic review focuses on 3D medical image registration using Particle Swarm Optimization.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Swarm Intelligence Algorithms for Medical Image Registration: A Comparative Study
Feature and intensity based medical image registration using particle swarm optimization.

Improved Particle Swarm Optimization algorithm applied to rigid registration in medical images
Hill DLG, Batchelor PG, Holden M, Hawkes DJ (2001) Medical image registration. Phys Med Biol 46(3):1. https://doi.org/10.1088/0031-9155/46/3/201
Article Google Scholar
Kennedy J, Eberhart R (1995) Particle swarm optimization. In: Proceedings of ICNN’95—International Conference on Neural Networks, 4:1942–19484 . https://doi.org/10.1109/ICNN.1995.488968
Rundo L, Tangherloni A, Militello C, Gilardi MC, Mauri G (2017) Multimodal medical image registration using particle swarm optimization: A review. In: 2016 IEEE Symposium Series on Computational Intelligence, SSCI 2016. IEEE Inc., Athens. https://doi.org/10.1109/SSCI.2016.7850261
Saiti E, Theoharis T (2020) An application independent review of multimodal 3D registration methods. Comput Graph (Pergamon) 91:153–178. https://doi.org/10.1016/j.cag.2020.07.012
Maintz JBA, Viergever MA (1998) A survey of medical image registration. Med Image Anal 2(1):1–36. https://doi.org/10.1016/S1361-8415(01)80026-8
Zitová B, Flusser J (2003) Image registration methods: a survey. Image Vis Comput 21(11):977–1000. https://doi.org/10.1016/S0262-8856(03)00137-9
Nayak J, Swapnarekha H, Naik B, Dhiman G, Vimal S (2022) 25 years of particle swarm optimization: flourishing voyage of two decades. Arch Comput Methods Eng. https://doi.org/10.1007/s11831-022-09849-x
Gad AG (2022) Particle swarm optimization algorithm and its applications: a systematic review. Arch Comput Methods Eng 29:2531–2561. https://doi.org/10.1007/s11831-021-09694-4
Article MathSciNet Google Scholar
Brereton P, Kitchenham BA, Budgen D, Turner M, Khalil M (2007) Lessons from applying the systematic literature review process within the software engineering domain. J Syst Softw 80:571–583. https://doi.org/10.1016/j.jss.2006.07.009
Talbi H, Batouche M (2004) Hybrid particle swarm with differential evolution for multimodal image registration 3:1567–1572. https://doi.org/10.1109/icit.2004.1490800
Wachowiak MP, Smolíková R, Zheng Y, Zurada JM, Elmaghraby AS (2004) An approach to multimodal biomedical image registration utilizing particle swarm optimization. IEEE Trans Evol Comput 8:289–301. https://doi.org/10.1109/TEVC.2004.826068
Li H, Lin Y, Wang A (2008) An medical image registration approach using improved Hausdorff distance combined with particle swarm optimization 5:428–432. https://doi.org/10.1109/ICNC.2008.444
Chen YW, Mimori A (2009) Hybrid particle swarm optimization for medical image registration. In: 5th International Conference on Natural Computation, ICNC 2009, vol. 6, pp. 26–30. https://doi.org/10.1109/ICNC.2009.699
Chen YW, Mimori A, Lin CL (2009) Hybrid particle swarm optimization for 3-D image registration. In: Proceedings—International Conference on Image Processing, ICIP. IEEE Computer Society, Cairo, Egypt, pp. 1753–1756. https://doi.org/10.1109/ICIP.2009.5414613
Li H, Yu Z, Wang A (2010) Medical image registration based on JS measure and niche chaotic mutation quantum-behaved particle swarm optimization. https://doi.org/10.1109/WICOM.2010.5601015
Zhang J, Huo P, Teng J (2010) Multi-resolution medical image registration based on generalized mutual information 3:1244–1247. https://doi.org/10.1109/CISP.2010.5647264
Bao Y, Sun J (2011) Image registration with a modified quantum-behaved particle swarm optimization, pp. 202–206. https://doi.org/10.1109/DCABES.2011.51
Zhou D, Sun J, Lai CH, Xu W, Lee X (2011) An improved quantum-behaved particle swarm optimization and its application to medical image registration. Int J Comput Math 88:1208–1223. https://doi.org/10.1080/00207160.2010.499934
Ayatollahi F, Shokouhi SB, Ayatollahi A (2012) A new hybrid particle swarm optimization for multimodal brain image registration. J Biomed Sci Eng 05:153–161. https://doi.org/10.4236/jbise.2012.54020
Lin CL, Mimori A, Chen YW (2012) Hybrid particle swarm optimization and its application to multimodal 3D medical image registration. Comput Intell Neurosci. https://doi.org/10.1155/2012/561406
Kang X, Armand M, Otake Y, Yau WP, Cheung PYS, Hu Y, Taylor RH (2014) Robustness and accuracy of feature-based single image 2-D-3-D registration without correspondences for image-guided intervention. IEEE Trans Biomed Eng 61:149–161. https://doi.org/10.1109/TBME.2013.2278619
Schwab L, Schmitt M, Wanka R (2015) Multimodal medical image registration using particle swarm optimization with influence of the data’s initial orientation. In: 2015 IEEE Conference on Computational Intelligence in Bioinformatics and Computational Biology, (CIBCB 2015). IEEE Inc., Niagara Falls, pp. 1–8. https://doi.org/10.1109/CIBCB.2015.7300314
Wang C, Goatman KA, MacGillivray T, Beveridge E, Koutraki Y, Boardman J, Stirrat C, Sparrow S, Moore E, Paraky R, Alam S, Dweck M, Chin C, Gray C, Newby D, Semple S (2015) Automatic multi-parametric mr registration method using mutual information based on adaptive asymmetric k-means binning. In: Proceedings - International Symposium on Biomedical Imaging, vol. 2015-July. IEEE Computer Society, Brooklyn, pp. 1089–1092. https://doi.org/10.1109/ISBI.2015.7164061
Hui L, Zhijun Z (2015) 3D multi-modality medical image registration based on quantum-behaved particle swarm optimization algorithm. In: Proceedings—14th International Symposium on Distributed Computing and Applications for Business, Engineering and Science, DCABES 2015. Institute of Electrical and Electronics Engineers Inc., Guiyang, pp. 312–315. https://doi.org/10.1109/DCABES.2015.85
Manoj S, Ranjitha S, Suresh HN (2016) Hybrid BAT-PSO optimization techniques for image registration. In: International Conference on Electrical, Electronics, and Optimization Techniques, ICEEOT 2016. Institute of Electrical and Electronics Engineers Inc., Chennai, pp. 3590–3596. https://doi.org/10.1109/ICEEOT.2016.7755375
Hering J, Wolf I, Maier-Hein KH (2016) Multi-objective memetic search for robust motion and distortion correction in diffusion MRI. IEEE Trans Med Imaging 35:2280–2291. https://doi.org/10.1109/TMI.2016.2557580
Li M, Huang Q, Li W, Li J (2017) CT to ultrasound registration for non-invasive kinematic analysis of knee joints. In: 4th International Conference on Systems and Informatics (ICSAI 2017), Hangzhou, pp. 1197–1202. https://doi.org/10.1109/ICSAI.2017.8248467
Zaman A, Ko SY (2018) Improving the accuracy of 2d-3d registration of femur bone for bone fracture reduction robot using particle swarm optimization. In: GECCO 2018 Companion—Proceedings of the 2018 Genetic and Evolutionary Computation Conference Companion. Association for Computing Machinery, Inc, Kyoto, Japan, pp. 101–102. https://doi.org/10.1145/3205651.3205718
Wang C, Goatman KA, Boardman JP, Beveridge EL, Newby DE, Semple SI (2019) Distance oriented particle swarm optimizer for brain image registration. IEEE Access 7:56016–56027. https://doi.org/10.1109/ACCESS.2019.2907769
Hernandez-Matas C, Zabulis X, Argyros AA (2020) REMPE: registration of retinal images through eye modelling and pose estimation. IEEE J Biomed Health Inform 24(12):3362–3373. https://doi.org/10.1109/JBHI.2020.2984483
Liu J, Li X, Shen S, Jiang X, Chen W, Li Z (2021) Research on panoramic stitching algorithm of lateral cranial sequence images in dental multifunctional cone beam computed tomography. Sensors 21:1–19. https://doi.org/10.3390/s21062200
Yoon S, Yoon CH, Lee D (2021) Topological recovery for non-rigid 2d/3d registration of coronary artery models. Comput Methods Programs Biomed. https://doi.org/10.1016/j.cmpb.2020.105922
Shao L, Yang S, Fu T, Lin Y, Geng H, Ai D, Fan J, Song H, Zhang T, Yang J (2022) Augmented reality calibration using feature triangulation iteration-based registration for surgical navigation. Comput Biol Med. https://doi.org/10.1016/j.compbiomed.2022.105826
West J, Fitzpatrick JM, Wang MY, Dawant BM, Maurer CR Jr, Kessler RM, Maciunas RJ, Barillot C, Lemoine D, Collignon A et al (1997) Comparison and evaluation of retrospective intermodality brain image registration techniques. J Comput Assist Tomogr 21(4):554–568. https://doi.org/10.1097/00004728-199707000-00007
RIRE dataset. https://www.insight-journal.org/rire/index.php . Accessed on Feb 2023
The whole brain atlas. http://www.med.harvard.edu/AANLIB/home.html . Accessed on Feb 2023
Kwan RK-S, Evans AC, Pike GB (1999) MRI simulation-based evaluation of image-processing and classification methods. IEEE Trans Med Imaging 18(11):1085–1097. https://doi.org/10.1109/42.816072
BrainWeb dataset. https://brainweb.bic.mni.mcgill.ca . Accessed on Feb 2023
Jain AK, Mustafa T, Zhou Y, Burdette C, Chirikjian GS, Fichtinger G (2005) FTRAC–a robust fluoroscope tracking fiducial. Med Phys 32(10):3185–3198. https://doi.org/10.1118/1.2047782
NLM-NIH visible human project. https://www.nlm.nih.gov/research/visible/ visible_human.html . Accessed on Feb 2023
Yumin D, Li Z (2014) Quantum behaved particle swarm optimization algorithm based on artificial fish swarm. Math Probl Eng 2014:592682. https://doi.org/10.1155/2014/592682
Fitzpatrick JM, West JB (2001) The distribution of target registration error in rigid-body point-based registration. IEEE Trans Med Imaging 20(9):917–927. https://doi.org/10.1109/42.952729
Download references
Author information
Authors and affiliations.
University for Foreigners of Perugia, Perugia, 06123, Italy
Lucia Ballerini
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Lucia Ballerini .
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Ballerini, L. Particle Swarm Optimization in 3D Medical Image Registration: A Systematic Review. Arch Computat Methods Eng (2024). https://doi.org/10.1007/s11831-024-10139-x
Download citation
Received : 14 March 2023
Accepted : 24 April 2024
Published : 25 May 2024
DOI : https://doi.org/10.1007/s11831-024-10139-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- Contribution of hospital pharmacists to sustainable healthcare: a systematic review
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0009-0001-5789-5939 Maria Pitard 1 ,
- Ninon Rouvière 1 ,
- http://orcid.org/0000-0001-5191-0977 Géraldine Leguelinel-Blache 1 , 2 ,
- http://orcid.org/0000-0003-3942-5172 Virginie Chasseigne 1 , 2
- 1 Department of Pharmacy , Nimes University Hospital, University of Montpellier , Nimes , France
- 2 Institute Desbrest of Epidemiology and Public Health, INSERM , University of Montpellier , Montpellier , France
- Correspondence to Dr Maria Pitard, Department of Pharmacy, CHU Nimes, Nimes, Gard, France; maria.pitard{at}gmail.com
Background With a global annual carbon footprint of the healthcare sector of 2 gigatons of CO 2 e, healthcare systems must contribute to the fight against climate change. Hospital pharmacists could be key players in ecological transition due to their role in managing healthcare products. The aim of this study was to summarise the evidence on interventions implemented in healthcare facilities involving pharmacists to improve the environmental footprint of healthcare.
Methods This systematic review was conducted following PRISMA 2020 guidelines. The Medline, Web of Science and ScienceDirect databases were searched for studies published between 2013 and 2023. To be eligible for inclusion, studies had to include hospital pharmacists and present contributions aimed at reducing the environmental footprint of healthcare in healthcare facilities. Outcomes were the description of the contribution, the methods used and the stages of healthcare product lifecycle analysed. A Mixed Methods Appraisal Tool was used to assess the risk of bias for each study.
Results Seventeen studies were included. Pharmacists played a leading role in 15 (88%) and had a supporting role in the others. The healthcare products targeted were medicines (59%), medical devices (12%) or both (29%). The stages of the healthcare product cycle addressed by the contributions were elimination (71%), dispensing (35%), procurement and supply (35%), production (29%), and prescription (24%). Only two studies used life cycle assessment and only one assessed all three pillars of sustainability. Two studies had good methodological quality while the rest had at least one element of uncertainty.
Conclusion This review confirms the central role of the pharmacist and the importance of a multidisciplinary approach in implementing eco-responsible actions. It could be useful to hospitals and other teams wanting to improve sustainable actions and it emphasises the importance of collaborating with pharmacists when planning sustainable initiatives. Future eco-responsible initiatives must use robust reproducible methods.
Trial registration PROSPERO #CRD42023406835
- PHARMACY SERVICE, HOSPITAL
- PHARMACEUTICAL PREPARATIONS
- Drug Compounding
- MEDICATION SYSTEMS, HOSPITAL
- STERILIZATION
- PUBLIC HEALTH
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
https://doi.org/10.1136/ejhpharm-2024-004098
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
The healthcare system contributes to climate change and paradoxically contributes to the deterioration in the health of the population.
It is now possible to incorporate sustainable development into healthcare and to decarbonise healthcare systems.
No review has assessed pharmacist contributions to greener healthcare.
WHAT THIS STUDY ADDS
The methods used to measure the environmental impacts of an action are still heterogeneous, and the reference method (life cycle assessment) is insufficiently implemented.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This literature review provides an overview of eco-responsible hospital contributions conducted by hospital pharmacists.
The temperature of the Earth’s atmosphere has risen by approximately 1°C since the late 19th century. 1 The impacts of climate change on our society and human health have been extensively studied for many years. In 2019 the New England Journal of Medicine described the major health risks, demonstrating, for example, that air quality can potentially affect cardiovascular diseases, asthma exacerbations and respiratory illnesses. 2 Paradoxically, although they care for people, healthcare systems contribute to global warming. 3 To achieve the goal of limiting the temperature increase to 1.5°C above the pre-industrial levels set by the 2015 Paris Agreement, all stakeholders have a role to play. 4 Healthcare systems must participate in the global fight against climate change and engage in sustainable development (SD) initiatives. SD was described as a “development that meets the needs of the present without compromising the ability of future generations to meet their own needs” by Gro Harlem Brundtland, the Norwegian Prime Minister in 1987. 5 Healthcare professionals are gradually taking initiatives to reduce the environmental footprint of healthcare. In France, hospital pharmacists are responsible for healthcare products (HP) (medication and sterile medical devices) from supply to distribution in healthcare units. This cross-functional role positions them as potential key players in SD within healthcare facilities. Despite the emergence of studies evaluating the environmental impact of various actions within healthcare facilities, no reviews have specifically explored the contributions of pharmacists to assess their environmental footprint or the knowledge of healthcare professionals and patients on the subject. To address this gap, our systematic review sought to explore the involvement of hospital pharmacists in SD strategies by answering the following questions: (1) What is the role of hospital pharmacists in SD? (2) Who do they interact with, and how? (3) What methods do they use? and (4) Which stages of the lifecycle of HP are analysed? We thus identified and summarised articles on hospital pharmacists’ contribution to assess the environmental impacts of healthcare.
Sustainable development (SD)
SD is defined as economically efficient, socially equitable, and ecologically SD. These three foundational pillars of SD are conventionally represented by three spheres (social, economic and environmental) that intersect, with sustainability positioned at the intersection of the three. The simultaneous consideration of these three components is an essential prerequisite for the concept of sustainability.
Life cycle assessment (LCA)
Life cycle assessment is the most advanced tool for assessing environmental impact of products or services. This standardised approach (ISO 14040 standard) allows for the measurement of quantifiable effects of products or services on the environment. It analyses and quantifies the physical flows of material and energy associated with human activities throughout the life cycle of products. LCA is a multi-criteria approach as it provides results on various environmental impacts (up to 18 impacts including climate change, water resource depletion, etc). However, by evaluating only the environmental footprint of a product or service, LCA does not take into account the remaining two pillars of SD (economic and social).
Protocol and registration
This systematic review was conducted in accordance with the 2020 PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines 6 (see online supplemental file 1 ) and the protocol was registered on PROSPERO (ID number CRD42023406835). 7
Supplemental material
Eligibility criteria.
Eligible studies included research published between 1 January 2013 and 1 January 2023. The inclusion and non-inclusion criteria are summarised in table 1 .
- View inline
Inclusion and non-inclusion criteria
Search strategy
Three databases were searched (Medline, Web of Science and ScienceDirect). The complete list of search terms is shown in table 2 and the search strategy is detailed in online supplemental file 2 . Apart from the terms “hospital pharmacy” and “hospital pharmacist(s)”, which were sought in the full text, all other terms were only sought in the article title. Studies deemed relevant from manual searches of the reference lists of selected articles were also retained.
Search terms used
Study selection
Using inclusion and exclusion criteria, two authors (MP, VC) independently selected relevant articles based on title and abstract readings and subsequently analysed them. In case of disagreement, the opinion of a third author (GL) was considered.
Risk of bias assessment
The same methodology was used for assessing the methodological quality of the included studies. The methodological quality of the included studies was evaluated using the 2018 version of the Mixed Methods Appraisal Tool (MMAT) due to the different study methodologies. 8 Each study was assessed according to seven items depending on the study design (non-randomised quantitative, descriptive quantitative, or mixed method), classed as ‘yes’, ‘no’, or ‘can’t tell’. The algorithm employed to assist in selecting the category of criteria is shown in online supplemental file 3 . No quality score was calculated because the MMAT developers advise against calculating an overall score from the ratings of each criterion. Additionally, it is not recommended to exclude studies solely based on low methodological quality.
Data collection and data items
Two authors (MP, VC) independently extracted data including the year, country, research question/objective, targeted HP (medication, sterile medical devices), description of the contributions, the pharmacist’s role (lead or support), type of participant, outcomes measured and the stage of the pharmaceutical process targeted (purchasing/procurement, prescription, preparation/pharmaceutical compounding, dispensing/distribution of care services, elimination). The results of all selected articles were summarised in two Excel spreadsheets. These different tables are available in the results section. Missing data were specified in the tables.
A total of 829 articles were found from the initial database search, of which 121 were duplicates. After removal of 618 articles that were not relevant and a further 11 which could not be retrieved, 79 articles were assessed, with 69 deemed ineligible mostly due to the absence of a pharmacist (n=48). With the seven studies found by the manual search of reference lists, 17 articles were included in this review. The search process is shown in figure 1 .
- Download figure
- Open in new tab
- Download powerpoint
Summary of the the search process.
Study characteristics
Study characteristics are summarised in online supplemental table 1 . All 17 included studies described contributions taking place in a healthcare facility. Only one study was carried out in the central sterilisation unit, 9 while the other studies assessed the hospital pharmacy, the operating room, and/or other care departments. The studies were primarily based in Europe and North America: France (n=4), USA (n=4), Ethiopia (n=2), Saudi Arabia (n=2), and one each from England, Italy, Netherlands, Brazil, and Spain. For 10 studies (59%) the contribution involved a team composed exclusively of pharmacy personnel (pharmaceutical team). 10–19 The remaining studies (41%) involved medical (healthcare professionals) 18 20–25 or mixed multidisciplinary teams (healthcare professionals and professionals from other fields such as a sustainability engineer). The study by Rouvière et al 9 was the only one involving a mixed multidisciplinary team.
Description of contributions
The description of contributions is summarised in online supplemental table 2 .
Studies highlighted the contribution of hospital pharmacists to the SD across various stages of the HP cycle. Some studies were interventional, 9 11 18 20–22 24 25 where pharmacists directly or indirectly implemented actions aimed at reducing the environmental impact of care. Others were observational studies 10 12 13 19 led by pharmaceutical research teams, reflecting the practices of healthcare professionals or patients. Some studies used several methods concurrently. Most studies (53%) included a survey in their contributions. 9 10 12 13 15–17 19 20 This could involve a questionnaire asking healthcare professionals or patients about waste management 15 16 19 or assessing the social pillar of SD through staff satisfaction. 20 The description of the questionnaires used in the articles is shown in online supplemental file 5 .
The second most commonly targeted contribution was waste collection. Seven studies (41%) documented the waste generated 18 21 23 24 and/or weighed it. 9 20 22
Four studies (24%) used quality management techniques to help develop and implement their contribution. 11 18 21 25 Lin et al 18 and Abbasi et al 25 employed the ‘lean management’ technique and Furukawa et al 21 used the ‘Lean Six Sigma’ technique. Toerper et al 11 employed a computer simulation technique to develop the optimal production schedule. Four studies (24%) used theoretical and practical training in addition to other methods to improve their study outcomes. 9 11 21 24 Only two studies (12%) used LCA, which is currently the most advanced tool for assessing the environmental impact of a contribution. Rouvière et al 9 conducted their own LCA to quantify the environmental impacts of their actions whereas Leraut et al 14 used LCA results published in the literature.
The role of the pharmacist was identified in each study. In 15 studies (88%) pharmacists were defined as the pilot, directly implementing or executing the action. 9–21 24 25 In the remaining studies, 22 23 pharmacists played a supporting role in the contribution and the implementation did not directly depend on them.
Regarding the HP distribution circuit, the majority of contributions focused on the disposal phase of HP (71%). 9 10 13 15–17 19–24 Six studies (35%) evaluated the purchasing and procurement stages of HP 9 10 12 13 17 20 and six studies (35%) addressed the dispensing and distribution stages of HP to healthcare units. 10 13 14 17 21 24 Five studies (29%) involved the preparation of medications (pharmaceutical compounding) within the production units of the hospital pharmacy, 10 11 17 18 25 or the operating room. 23 Finally, four studies (24%) focused on medical prescription. 10 13 17 21
Risk of bias in the studies
The bias risk analysis for each study is shown in online supplemental file 4 . Two of the non-randomised quantitative studies were judged as being of good quality. 9 20 The remaining studies received at least one ‘Can’t tell’ response and were therefore considered of lower quality. The maximum number of ‘Can't tell’ responses obtained per article was two (n=4). 10 21 22
Only one study received a ‘no’ response, 11 which was the response to the question ‘Are the confounders accounted for in the design and analysis?’ in the quantitative non-randomised studies category.
The questions that received the most ‘Can't tell’ responses were: ‘Are there complete outcome data?’ and ‘Are the confounders accounted for in the design and analysis?’ for quantitative non-randomised studies; ‘Is the risk of non-response bias low?’ for quantitative descriptive studies; and ‘Are divergences and inconsistencies between quantitative and qualitative results adequately addressed?’ for mixed methods studies.
Results of interventions
Online supplemental table 1 summarises the outcomes measured in the studies. These criteria included environmental impact measurements (expressed in kgCO2e, weight of waste), economic impacts, and any other relevant qualitative results.
Regarding the primary outcome of environmental impact, only one study calculated the impact of its interventions on the environment. 9
Among the studies that evaluated the number or weight of waste through their research, 100% showed a reduction in waste generated after the interventions. 9 11 18 20–22 24 25 Six studies conducted different assessments to highlight the extent of HP waste and its economic impact or sought to identify pharmaceutical waste management practices. By assessing the disposal practices of healthcare professionals and/or patients, Mohammed et al, 15 Gidey et al 16 and Al-Shareef et al 19 showed that methods of healthcare product disposal were varied, including open-air incineration, 15 household waste, 19 with a small portion being returned to the pharmacy (1.7%). 19 Gidey et al found that 60.7% of surveyed patients had received no information about HP disposal methods, 16 while Al-Shareef et al reported that preferred methods for teaching good disposal practices included social networks (16.72%), mobile applications (14.17%) and hospital pharmacists (13.91%). 19 The engagement of healthcare professionals in SD was assessed by Giraud et al 12 and Singleton et al. 13 Giraud et al focused on HP procurement procedures by pharmacists and reported that 90% of HP suppliers considered themselves to be significantly or very significantly engaged, with 40% of sustainable purchasing criteria being integrated into the overall rating by at least one buyer. Singleton et al explored the engagement of hospital pharmacists in the NHS carbon reduction policy and highlighted the main barriers to incorporating SD into their practice, such as a lack of professional training and the absence of environmental guidelines. 13
Two studies described SD actions that could be initiated by pharmacists. Bekker et al identified 14 actions in ‘developed countries’ 10 and Alhomoud identified 21 actions in the Gulf countries. 17
Only one study simultaneously evaluated the three pillars of SD. 20 In this study the social pillar was assessed by three different means: calculation of the difference in equipment preparation time; analysis of musculoskeletal disorder factors; and surgeon satisfaction survey regarding the implementation of the custom pack.
Nine studies (53%) measured the economic effects of their intervention. 9 11 15 18 20 22–25 For eight studies it was an economic gain 11 15 18 20 22–25 and for one study it was an additional economic cost. 20
The economic impact analysis of interventions has most often been conducted based on the price of HP saved through the implementation of the intervention, notably using the bottom-up micro-costing methodology based on unitary costs from a hospital perspective (89%). 9 11 15 18 20 23–25
The economic impact was also analysed by calculating the average monthly savings in the segregation of healthcare waste, considering prices from the contract with the company responsible for hospital waste removal (11%). 22
The main findings of this systematic review have been summarised in a graphical abstract shown in online supplemental file 6 . Seventeen studies describing contributions to reduce the environmental footprint of healthcare involving hospital pharmacists were included in this review. In the majority, the pharmacist had a leading role (88%) and they were integrated into a pharmaceutical team (59%), a multidisciplinary medical team (35%) or a mixed multidisciplinary team (6%). These results demonstrate the central and cross-disciplinary role of hospital pharmacists in the field of SD. The only study that implemented a mixed multidisciplinary team was also the only study to have used LCA, the reference method for calculating the environmental impacts of actions. 9 The other methodologies used to reduce the environmental footprint of healthcare included surveys, waste collection and/or weighing, quality management methods and theoretical and practical training. Waste collection was the most commonly used method (41%) but, in most studies, no environmental impact results were extracted from these data beyond reduction in the mass of waste generated. Some studies presented methodological uncertainties (eg, non-response bias, incomplete effect data) leading to studies that were less reproducible and less robust. Furthermore, since most of the included studies were qualitative, it is difficult to draw conclusions about the actual impact of the contributions. Finally, the study by Rouvière et al 9 demonstrated significant environmental impacts by involving both medical and non-medical personnel (sustainability engineer) using the reference methodology and presenting good methodological quality. Although LCA is the reference methodology, this literature review shows that LCA is rarely applied in healthcare. It is a rigorous methodology that requires human resources, theoretical and practical training, and specific software. This demanding methodology would benefit from a designated team member, such as a pharmacist, with the knowledge and skills in this field to carry out these studies.
Furthermore, only one study investigated all three pillars of SD. 20 The social pillar is often neglected in favour of the ecological and economic pillars, but to meet the definition of SD, this third aspect must be assessed and taken into account. The aim of the social aspect is to ensure a quality of work life for practitioners and caregivers throughout the care process, while also satisfying all users. This pillar can be assessed through satisfaction surveys; Mouarbes et al evaluated the social pillar by analysing musculoskeletal disorder factors and conducting satisfaction surveys in staff. 20
Regarding the economic pillar, only nine studies examined the economic impact of interventions. 9 11 15 18 20 23–25 These studies focused on the prices of HP, demonstrating the savings achieved through the reduction of pharmaceutical waste or changes in care practices. Indeed, the ‘micro-costing’ approach is the most precise method for estimating the actual cost of a healthcare intervention in a healthcare facility. However, in this approach, the estimated costs reflect the state of practice at a particular healthcare facility. On the other hand, the additional costs related to personnel generated by data collection or the implementation of actions were not assessed and can vary the economic impact of an action. Conversely, potential time saving-related economic gains were not reported in the studies. It would be interesting to integrate the costs of healthcare personnel into economic studies of interventions.
Despite the heterogeneous results of the contributions, this literature review shows that the actions already cover all the key stages of the HP circuit. The disposal of HP was addressed in almost all studies, indicating that the amount of waste generated by healthcare facilities is a significant concern and waste-related actions were generally the first initiatives taken. However, some studies took place in developing countries, making it challenging to compare the results with those of developed countries with different regulations, for example, regarding HP disposal. Few contributions have been described concerning the purchase, procurement and stock management of HP. As shown by Giraud et al , implementing sustainable actions at this stage of the HP circuit requires commitment from suppliers, healthcare facilities and governments to update regulations. 12 Although suppliers claim to be committed to sustainable policies (with 90% of criteria being considered important or very important by the suppliers), the practical implementation of these results needs further evaluation. Thus, mandatory questionnaires for suppliers, specifically targeting HP, to incorporate environmental rating in procurement contracts seem necessary to initiate a sustainable approach. Regarding the dispensing and distribution of HP in healthcare units, the studies were mainly descriptive and applied to specific services, making the reproducibility of these contributions more challenging. 24 Contributions targeting the pharmaceutical prescription stage highlighted the importance of consolidating prescriptions for patients requiring specific preparations or medications to minimise waste. However, no study has explored the potential role of the pharmacist in the concept of eco-directed prescribing. It is conceivable that, in the coming years, pharmacists could raise awareness among prescribers about the environmental impact of prescribed medications and medical devices in their role as clinical pharmacists. However, this role would require transparency from suppliers regarding the environmental impact of their pharmaceutical products, as well as the mobilisation of governments to update regulations, especially in terms of marketing authorisations or CE marking access.
Regarding the pharmaceutical compounding stage, the included studies focused on optimising pharmaceutical compounding to limit dose wastage. These studies applied quality management methods initially designed for the automotive industry. These methods, aimed at improving the quality and efficiency of work processes, seem relevant for optimising production processes.
In parallel, several studies showed a lack of environmental knowledge, indicating a deficiency in practitioner training. 13 16 19 Pharmacists could contribute to the theoretical and practical environmental training of future healthcare professionals by integrating directly into health studies curricula. They could also participate in the theoretical and practical training of their colleagues, encouraging good practices in pharmaceutical waste disposal, for example.
The locations targeted by the contributions were mostly the hospital pharmacy or the operating room (94% of included studies). Only one study included the sterile processing department by implementing the recycling of defective metallic medical devices ineligible for repair. 9 The sterilisation unit is a significant consumer of water (washers, autoclaves, air conditioning circuit in the controlled atmosphere area), electricity (washers, autoclaves) and plastics (sterile packaging), concentrating numerous environmental challenges. As this service is not always under the responsibility of the pharmacist, particularly in France, it may explain the low number of studies included in our research. Nonetheless, the study by McGain et al, who calculated the environmental impact of extinguishing inactive autoclaves, optimising loads or implementing automatic standby mode in this unit, reported a reduction of 79 tons of CO 2 per year. 26
This study has several limitations to be considered. The low number of articles identified in this review may be due to the lack of explicit mention of the pharmacist’s role in the studies, despite their participation, or to differences in pharmaceutical responsibilities between countries. To overcome this limitation, the reference lists of included publications were manually searched, which is why some articles were only found through manual searches. However, numerous studies can be found in the grey literature but we did not search the grey literature sources because of the sometimes lower methodological quality and difficult access to these studies. Studies focusing on medications (88%) were more numerous than those on medical devices (41%). This imbalance may be related to the fact that the management of medical devices is not necessarily the responsibility of the pharmacist in all countries. Finally, some reports may have been missed despite our broad search strategy and new studies may have been published since our last search and will continue to emerge.
The topic of SD is not currently mentioned in the French Public Health Code regarding the missions of the hospital pharmacy and hospital pharmacists. However, the 2010 version of the hospital pharmacy reference framework already stated that hospital pharmacists should take SD into account and integrate its challenges. 27 This role involves economic management concepts (eg, procurement policy), social responsibility and environmental responsibility.
This systematic literature review is the first to specifically address the role of hospital pharmacists in SD contributions within healthcare institutions. It serves as a starting point to enable hospital pharmacists to engage in the development, implementation and monitoring of SD actions. It demonstrates that, through their cross-functional role and expertise, hospital pharmacists are major players in the ecological transition of healthcare institutions and can actively contribute to the shift towards low carbon healthcare systems. This review could also signal to hospital managers that pharmacists ought to be involved in SD. Based on this review, the first step for a hospital pharmacist wishing to implement SD actions would be creating or participating in a sustainable multidisciplinary working group including various professional profiles. The actions implemented should be monitored using before-and-after indicators and LCAs should be undertaken to obtain robust results. Social and economic pillars should be integrated into the methodology as early as possible to assess all three pillars of SD. Any action initiated could begin with theoretical training for healthcare professionals to provide them with the necessary knowledge. Moreover, further studies are still required to evaluate the feasibility and environmental impact of interventions in sterilisation or chemotherapy production units. Other studies are also required to assess the role and environmental impact of the clinical pharmacist—for example, e-prescribing, raising awareness during pharmaceutical interviews and the impact of pharmaceutical interventions on healthcare facility effluents.
This systematic review shows that there is limited research published on the role of pharmacists in interventions to reduce the environmental impact of healthcare, and that most of the existing studies do not use the standard method (LCA) to quantify their impacts. The results of the studies were heterogeneous but cover all stages of the healthcare product cycle, which nonetheless confirms the central role of the pharmacist and the importance of a multidisciplinary approach in implementing eco-responsible actions. Future studies should systematically quantify the environmental impacts of their interventions and describe the role of each participant to improve the robustness of results and enhance replicability.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
- ↵ Rapport de synthèse AR6: Changement climatique 2023 — GIEC , 2023 . Available : https://www.ipcc.ch/report/sixth-assessment-report-cycle/ [Accessed 5 Oct 2023 ].
- ↵ Health Care Without Harm. L’empreinte climatique du secteur de la santé , 2019 . Available : https://healthcareclimateaction.org/sites/default/files/2021-11/French_HealthCaresClimateFootprint_091619_web.pdf [Accessed 5 Oct 2023 ].
- United Nations Climate Change (CCNUCC)
- ARE O fédéral du développement territorial
- McKenzie JE ,
- Bossuyt PM , et al
- Chasseigne V
- National Collaborating Centre for Methods and Tools
- Rouvière N ,
- Auger F , et al
- Gardarsdottir H ,
- Egberts A , et al
- Toerper MF ,
- Veltri MA ,
- Hamrock E , et al
- Giraud J-S ,
- Hamidou F ,
- Hassani Y , et al
- Singleton JA ,
- Boissinot L ,
- Mohammed SA ,
- Kahissay MH ,
- Birhanu AH ,
- Tsadik AG , et al
- Ivey MF , et al
- Al-Shareef F ,
- El-Asrar SA ,
- Al-Bakr L , et al
- Mouarbes D ,
- Garde E , et al
- Furukawa P de O ,
- Pedreira M da L
- Mosquera M ,
- Andrés-Prado MJ ,
- Rodríguez-Caravaca G , et al
- Barbariol F ,
- Lucchese F , et al
- Enten G , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
- Data supplement 3
- Data supplement 4
- Data supplement 5
- Data supplement 6
- Data supplement 7
- Data supplement 8
EAHP Statement 2: Selection, Procurement and Distribution. EAHP Statement 3: Production and Compounding. EAHP Statement 4: Clinical Pharmacy Services. EAHP Statement 6: Education and Research.
Contributors MP wrote the main manuscript and prepared figure 1, tables 1 and 2 and supplementary tables 1 and 2. GL resolved disagreements in the article selection. VC and NR reviewed the manuscript. All authors read and approved the final manuscript.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Watch CBS News
We may receive commissions from some links to products on this page. Promotions are subject to availability and retailer terms.
5 tips for safe online shopping
By Jake Safane
Edited By Angelica Leicht
May 28, 2024 / 10:10 AM EDT / CBS News

In the first quarter of 2024 alone, U.S. retail e-commerce sales totaled nearly $300 billion, according to the U.S. Census Bureau . But as popular as online shopping has become, there are also increasing risks to consider, as cybercriminals are constantly looking for ways to steal money and conduct identity theft.
In 2023, the FBI's Internet Crime Complaint Center received a 10% increase in complaints from the American public, totaling 880,418, with potential losses of over $12.5 billion, a 22% increase from the year prior. But while there are a range of cybercrimes to worry about when shopping online, there are also ways to reduce the risks.
And that starts with using a combination of common sense practices and technology. Here's what you should know.
Find out how LifeLock can help protect your identity online now .
Consider the following five tips for safer online shopping:
Do your research
Part of the fun of online shopping is discovering new products from new retailers, but you want to keep your guard up if you're buying from a site you're not familiar with. One safe online shopping tip from the National Council on Aging is to review the Better Business Bureau (BBB) listings for these online companies. If an e-commerce site was set up to scam people, for instance, then you might see a lot of BBB complaints.
Sometimes online shopping involves buying from accounts through social media sites. In that case, you might take steps like seeing if they have verified profiles, as well as reading customer reviews.
Find out how LifeLock helps you fight back against online identity theft .
Review site security features
You should also review site security features, such as checking to see whether a website starts with https, which means the site encrypts information, explains the Federal Trade Commission (FTC).
But even if you think you know the site, you should still look for this information, as well as a padlock icon next to the URL, which serves as another security indicator. That's because you might have made a mistake, like typing one wrong letter, that leads to a phishing site. These types of sites look legitimate but have been set up to commit credit card theft or identity theft .
Be careful what you click on
One of the biggest dangers of online shopping is that you'll fall victim to a phishing attack, which typically starts with an email claiming to be from a retailer or shipping company about your order. When you click on the link, though, the email takes you to a site that asks you to input information, like your bank or credit card numbers, which goes directly to cybercriminals, for example.
So, it's important to be careful about any links you click on, not only through email but also other channels, like social media platforms and pop-up ads. If you're not sure of the validity, try going directly to the source. For example, instead of following the link in an email about your supposed Amazon order, go directly to your Amazon account from your web browser to check the status of that order.
That said, accidents happen, and it can be hard to always know what's safe or not. In turn, it can be helpful to have backup. Using a service like LifeLock can improve your online shopping privacy while also giving you the protections you may need in case you do become a victim of identity theft or credit card theft. For example, LifeLock Ultimate Plus memberships provide up to $1 million in stolen funds reimbursement.
Another way to reduce the risks of online shopping is to use a reputable virtual private network (VPN) provider for browsing online, especially if you're using a public Wi-Fi network.
As the National Cybersecurity Alliance explains , public networks, like those at cafes or airports, aren't very secure. If using these networks while online shopping, it's possible that a bad actor would be able to digitally see you input your credit card information, for example, and that could enable them to use that data themselves. But connecting via a VPN can help you gain more privacy if you need to complete an order while out.
Here too, LifeLock can help, as memberships come with VPN access.
Consider your payment method
When it's time to complete your order, think twice about how you pay for the purchase.
One way to reduce the risks of online shopping is to pay by credit card, as the FTC suggests. That's because you have the right to dispute credit card charges, and you might face less liability for fraudulent purchases compared to some other payment methods.
If you want to go a step further, you can use a virtual credit card number, which many credit card companies offer. That way, if the virtual card number gets exposed, at least your main credit card number can remain unknown. Virtual credit cards can also have lower spending limits, which can limit the fallout of a breach.
Lastly, be mindful of situations where an online store asks for a specific, niche payment method and won't accept others. Asking for payment using gift cards or wire transfers is a red flag that means you shouldn't go through with the transaction, according to the FBI's Portland, Oregon field office .
The bottom line
Online shopping can be fun, but it also can be risky. To reduce the chances of financial fallout due to issues like online shopping scams or data breaches, it helps to follow these best practices. It can also help to use safer online shopping technology and identity monitoring services in conjunction, like those from LifeLock.
More from CBS News

Is a short-term CD or long-term CD better to open this June?

How much should you spend on long-term care insurance? What experts say

3 reasons to open a high-yield savings account this June

Some Gen Z credit card users are maxed out: 5 debt relief options to consider

IMAGES
VIDEO
COMMENTS
Before you start writing, you will need to take some steps to get ready for your critique: Choose an article that meets the criteria outlined by your instructor. Read the article to get an understanding of the main idea. Read the article again with a critical eye. As you read, take note of the following: What are the credentials of the author/s?
In this text, we will discuss four of the most common research methods used in article critique writing: quantitative research, qualitative research, systematic reviews, and meta-analysis. Quantitative research is a research method that uses numbers and statistics to analyze data. This type of research is used to test hypotheses or measure a ...
through the literature review, the theoretical framework, the research question, the methodology section, the data analysis, and the findings (Ryan-Wenger, 1992). Literature review The primary purpose of the literature review is to define or develop the research question while also identifying an appropriate method of data collection (Burns and
CRITIQUING RESEARCH ARTICLES . When critiquing research articles, it is useful to ask yourself questions about the purpose of each component of the article, and whether it achieves that purpose. THE TITLE . The title should be descriptive enough to give you a clear idea about what the research deals with. Ask yourself:
Three common types of review articles submitted to CMEJ. Often associated with Cochrane Reviews, this type of review aims to answer a narrowly focused question and uses a predetermined structured method to search, screen, select, appraise and summarize findings. Tang KS, Cheng DL, Mi E, Greenberg PB.
2. Benefits of Review Articles to the Author. Analysing literature gives an overview of the "WHs": WHat has been reported in a particular field or topic, WHo the key writers are, WHat are the prevailing theories and hypotheses, WHat questions are being asked (and answered), and WHat methods and methodologies are appropriate and useful [].For new or aspiring researchers in a particular ...
Learning how to critique research articles is one of the fundamental skills of scholarship in any discipline. The range, quantity and quality of publications available today via print, electronic and Internet databases means it has become essential to equip students and practitioners with the prerequisites to judge the integrity and usefulness of published research.
of the article and the supporting points that the article uses. o 3 Read the article again. To write a thorough article critique you must have thorough knowledge of the article. Reading it more than once helps to ensure that you haven't missed any important details. o 4 Consider the credentials of the author. Does the author of the article
The first step is to critique and appraise the research evidence. Through critiquing and appraising the research evidence, dialog with colleagues, and changing practice based on evidence, NPs can improve patient outcomes ( Dale, 2005) and successfully translate research into evidence-based practice in today's ever-changing health care ...
A critique asks you to evaluate an article and the author's argument. You will need to look critically at what the author is claiming, evaluate the research methods, and look for possible problems with, or applications of, the researcher's claims. Introduction. Give an overview of the author's main points and how the author supports those ...
summarize the article/book's main claim, goals, methods, and findings show how the article/book supports its claims indicate the main position or claim that your review will make in response to the article develop your critique in relation to aspects of the article/book, offering thoughtful, well supported proof for your claim(s)
Undertaking a critique of a research article may seem challenging at first, but will help you to evaluate whether the article has relevance to your own practice and workplace. Reading a single article can act as a springboard into researching the topic more widely, and aids in ensuring your nursing practice remains current and is supported by existing literature.
Speaking of the purpose, composing an article critique, you have to describe the main ideas of the author. Provide a brief description of why it is important in your specific context. Next, remember to mention all the interesting aspects that help to reveal the value of the article. Finally, talk about the author's intention and vision ...
1. Use these guidelines to critique your selected research article to be included in your research proposal. You do not need to address all the questions indicated in this guideline, and only include the questions that apply. 2. Prepare your report as a paper with appropriate headings and use APA format 5th edition.
As mentioned previously, there are a number of existing guidelines for literature reviews. Depending on the methodology needed to achieve the purpose of the review, all types can be helpful and appropriate to reach a specific goal (for examples, please see Table 1).These approaches can be qualitative, quantitative, or have a mixed design depending on the phase of the review.
Are there a range of socioeconomic strata and ethnicities? For this class, is the diagnosis confirmed? Where were the participants obtained from, and are they a biased sample? If it is an experimental design, was true random assignment done (random number generator)? Measures. Are the measures widely used in the field?
3. Identify the article. Start your review by referring to the title and author of the article, the title of the journal, and the year of publication in the first paragraph. For example: The article, "Condom use will increase the spread of AIDS," was written by Anthony Zimmerman, a Catholic priest.
Critiques evaluate and analyze a wide variety of things (texts, images, performances, etc.) based on reasons or criteria. Sometimes, people equate the notion of "critique" to "criticism," which usually suggests a negative interpretation. These terms are easy to confuse, but I want to be clear that critique and criticize don't mean the ...
Before inquring for the method of preparation of a review article, it is more logical to investigate the motivation behind writing the review article in question. The fundamental rationale of writing a review article is to make a readable synthesis of the best literature sources on an important research inquiry or a topic. This simple ...
The description of the research method should include a rationale for why it was chosen. Step 2. Ask yourself whether the method used makes sense in answering the research questions. Most basically, research questions which seek to understand a phenomenon may be best answered with qualitative methods such as case studies or narrative approaches.
Step 9: Presenting Your Critique. Organize your critique into a well-structured paper, starting with an introduction that outlines the article's context and purpose. Develop a clear and focused thesis statement that conveys your assessment. Support your points with evidence from the article and other credible sources.
Study design. The critical review method described by Grant and Booth (Citation 2009) was used, which is appropriate for the assessment of research quality, and is used for literature analysis to inform research and practice.This type of review goes beyond the mapping and description of scoping or rapid reviews, to include "analysis and conceptual innovation" (Grant & Booth, Citation 2009 ...
If you meant that you want to create a methods section in a review article that you are writing, i.e., to describe the methodology you followed to review the literature and write your review article, you can simply introduce a section detailing this. In this section, you would typically start by mentioning how you formulated the research problem.
The need for a new review on masks was highlighted by a widely publicized polarization in scientific opinion. The masks section of a 2023 Cochrane review of non-pharmaceutical interventions was—controversially—limited to randomized controlled trials (RCTs).It was interpreted by the press and by some but not all of its own authors to mean that "masks don't work" and "mask mandates ...
A literature review stimulated by a new method of teaching manual therapy, reflecting contemporary evidence, being trialled at a United Kingdom education institute. A group of experienced, internationally-based academics, clinicians, and researchers from across the spectrum of manual therapy was convened. Perspectives were elicited through ...
The positive reception of the AI-based method suggests that it has the potential to complement and augment traditional training approaches in pediatric education. These promising results warrant further exploration into the broader applications of AI in medical education scenarios. ... a BEME review: BEME guide 59. Med Teach. 2020;42(2):125 ...
Medical image registration seeks to find an optimal spatial transformation that best aligns the underlying anatomical structures. These problems usually require the optimization of a similarity metric. Swarm Intelligence techniques are very effective and efficient optimization methods. This systematic review focuses on 3D medical image registration using Particle Swarm Optimization.
Fatigue limit assessment methodologies based on the thermography technique are comprehensively studied in this work. Three fundamental indicators pertaining to temperature increase, intrinsic energy dissipation, and thermodynamic entropy are discussed in sequence. The main train of thought of thermo-based research is outlined. The main objective of this paper is, on the one hand, to describe ...
Methods This systematic review was conducted following PRISMA 2020 guidelines. The Medline, Web of Science and ScienceDirect databases were searched for studies published between 2013 and 2023. To be eligible for inclusion, studies had to include hospital pharmacists and present contributions aimed at reducing the environmental footprint of healthcare in healthcare facilities.
Consider your payment method. When it's time to complete your order, think twice about how you pay for the purchase. One way to reduce the risks of online shopping is to pay by credit card, as the ...