When you choose to publish with PLOS, your research makes an impact. Make your work accessible to all, without restrictions, and accelerate scientific discovery with options like preprints and published peer review that make your work more Open.
- PLOS Biology
- PLOS Climate
- PLOS Complex Systems
- PLOS Computational Biology
- PLOS Digital Health
- PLOS Genetics
- PLOS Global Public Health
- PLOS Medicine
- PLOS Mental Health
- PLOS Neglected Tropical Diseases
- PLOS Pathogens
- PLOS Sustainability and Transformation
- PLOS Collections
- How to Write Discussions and Conclusions

The discussion section contains the results and outcomes of a study. An effective discussion informs readers what can be learned from your experiment and provides context for the results.

What makes an effective discussion?
When you’re ready to write your discussion, you’ve already introduced the purpose of your study and provided an in-depth description of the methodology. The discussion informs readers about the larger implications of your study based on the results. Highlighting these implications while not overstating the findings can be challenging, especially when you’re submitting to a journal that selects articles based on novelty or potential impact. Regardless of what journal you are submitting to, the discussion section always serves the same purpose: concluding what your study results actually mean.
A successful discussion section puts your findings in context. It should include:
- the results of your research,
- a discussion of related research, and
- a comparison between your results and initial hypothesis.
Tip: Not all journals share the same naming conventions.
You can apply the advice in this article to the conclusion, results or discussion sections of your manuscript.
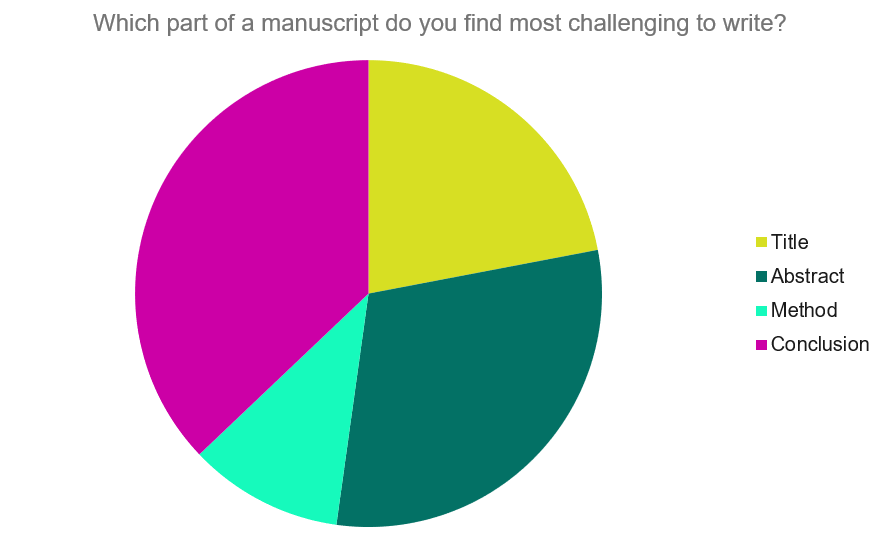
Our Early Career Researcher community tells us that the conclusion is often considered the most difficult aspect of a manuscript to write. To help, this guide provides questions to ask yourself, a basic structure to model your discussion off of and examples from published manuscripts.
Questions to ask yourself:
- Was my hypothesis correct?
- If my hypothesis is partially correct or entirely different, what can be learned from the results?
- How do the conclusions reshape or add onto the existing knowledge in the field? What does previous research say about the topic?
- Why are the results important or relevant to your audience? Do they add further evidence to a scientific consensus or disprove prior studies?
- How can future research build on these observations? What are the key experiments that must be done?
- What is the “take-home” message you want your reader to leave with?
How to structure a discussion
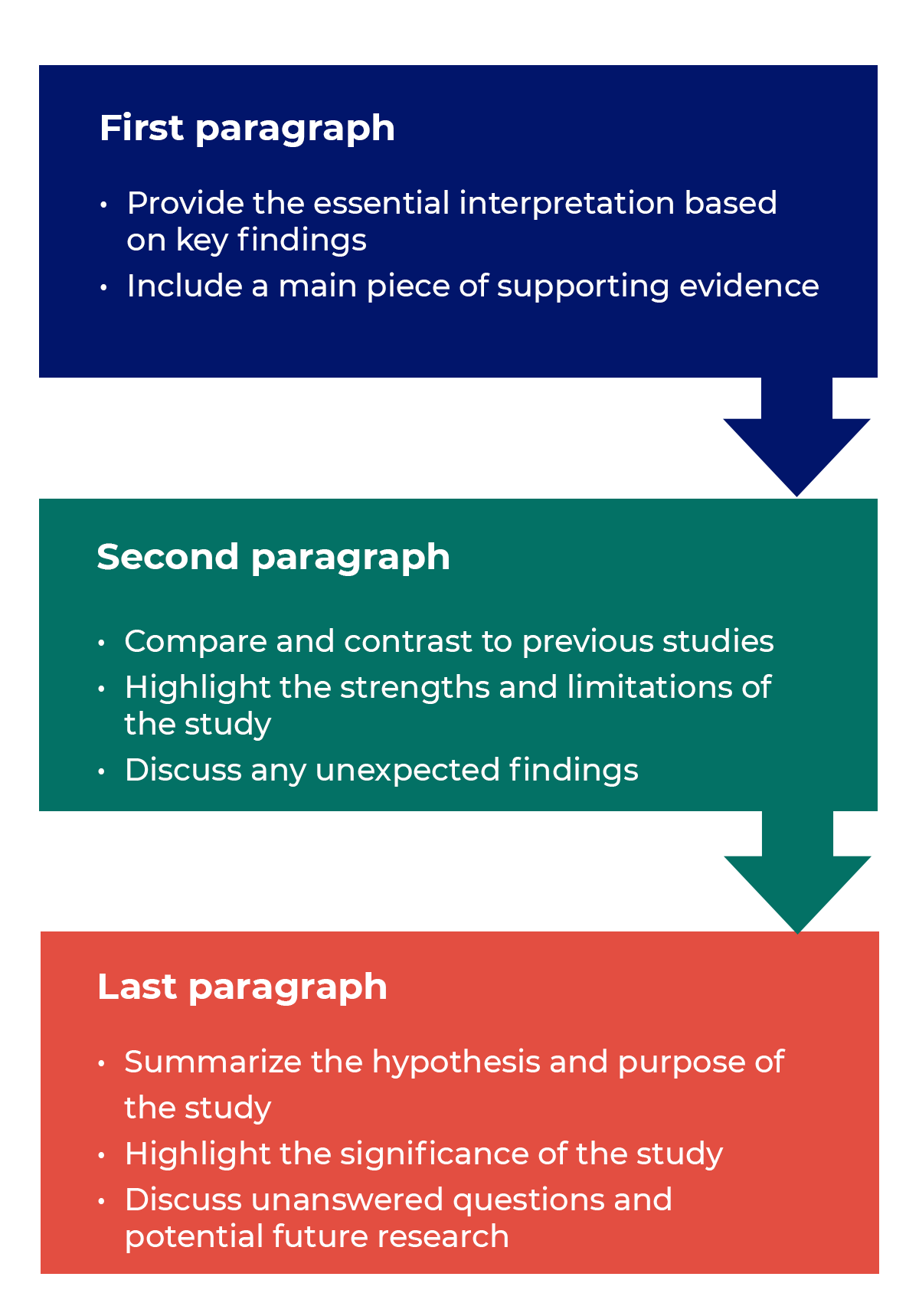
Trying to fit a complete discussion into a single paragraph can add unnecessary stress to the writing process. If possible, you’ll want to give yourself two or three paragraphs to give the reader a comprehensive understanding of your study as a whole. Here’s one way to structure an effective discussion:
Writing Tips
While the above sections can help you brainstorm and structure your discussion, there are many common mistakes that writers revert to when having difficulties with their paper. Writing a discussion can be a delicate balance between summarizing your results, providing proper context for your research and avoiding introducing new information. Remember that your paper should be both confident and honest about the results!

- Read the journal’s guidelines on the discussion and conclusion sections. If possible, learn about the guidelines before writing the discussion to ensure you’re writing to meet their expectations.
- Begin with a clear statement of the principal findings. This will reinforce the main take-away for the reader and set up the rest of the discussion.
- Explain why the outcomes of your study are important to the reader. Discuss the implications of your findings realistically based on previous literature, highlighting both the strengths and limitations of the research.
- State whether the results prove or disprove your hypothesis. If your hypothesis was disproved, what might be the reasons?
- Introduce new or expanded ways to think about the research question. Indicate what next steps can be taken to further pursue any unresolved questions.
- If dealing with a contemporary or ongoing problem, such as climate change, discuss possible consequences if the problem is avoided.
- Be concise. Adding unnecessary detail can distract from the main findings.

Don’t
- Rewrite your abstract. Statements with “we investigated” or “we studied” generally do not belong in the discussion.
- Include new arguments or evidence not previously discussed. Necessary information and evidence should be introduced in the main body of the paper.
- Apologize. Even if your research contains significant limitations, don’t undermine your authority by including statements that doubt your methodology or execution.
- Shy away from speaking on limitations or negative results. Including limitations and negative results will give readers a complete understanding of the presented research. Potential limitations include sources of potential bias, threats to internal or external validity, barriers to implementing an intervention and other issues inherent to the study design.
- Overstate the importance of your findings. Making grand statements about how a study will fully resolve large questions can lead readers to doubt the success of the research.
Snippets of Effective Discussions:
Consumer-based actions to reduce plastic pollution in rivers: A multi-criteria decision analysis approach
Identifying reliable indicators of fitness in polar bears
- How to Write a Great Title
- How to Write an Abstract
- How to Write Your Methods
- How to Report Statistics
- How to Edit Your Work
The contents of the Peer Review Center are also available as a live, interactive training session, complete with slides, talking points, and activities. …
The contents of the Writing Center are also available as a live, interactive training session, complete with slides, talking points, and activities. …
There’s a lot to consider when deciding where to submit your work. Learn how to choose a journal that will help your study reach its audience, while reflecting your values as a researcher…
Get science-backed answers as you write with Paperpal's Research feature
How to Write a Conclusion for Research Papers (with Examples)
The conclusion of a research paper is a crucial section that plays a significant role in the overall impact and effectiveness of your research paper. However, this is also the section that typically receives less attention compared to the introduction and the body of the paper. The conclusion serves to provide a concise summary of the key findings, their significance, their implications, and a sense of closure to the study. Discussing how can the findings be applied in real-world scenarios or inform policy, practice, or decision-making is especially valuable to practitioners and policymakers. The research paper conclusion also provides researchers with clear insights and valuable information for their own work, which they can then build on and contribute to the advancement of knowledge in the field.
The research paper conclusion should explain the significance of your findings within the broader context of your field. It restates how your results contribute to the existing body of knowledge and whether they confirm or challenge existing theories or hypotheses. Also, by identifying unanswered questions or areas requiring further investigation, your awareness of the broader research landscape can be demonstrated.
Remember to tailor the research paper conclusion to the specific needs and interests of your intended audience, which may include researchers, practitioners, policymakers, or a combination of these.
Table of Contents
What is a conclusion in a research paper, summarizing conclusion, editorial conclusion, externalizing conclusion, importance of a good research paper conclusion, how to write a conclusion for your research paper, research paper conclusion examples.
- How to write a research paper conclusion with Paperpal?
Frequently Asked Questions
A conclusion in a research paper is the final section where you summarize and wrap up your research, presenting the key findings and insights derived from your study. The research paper conclusion is not the place to introduce new information or data that was not discussed in the main body of the paper. When working on how to conclude a research paper, remember to stick to summarizing and interpreting existing content. The research paper conclusion serves the following purposes: 1
- Warn readers of the possible consequences of not attending to the problem.
- Recommend specific course(s) of action.
- Restate key ideas to drive home the ultimate point of your research paper.
- Provide a “take-home” message that you want the readers to remember about your study.

Types of conclusions for research papers
In research papers, the conclusion provides closure to the reader. The type of research paper conclusion you choose depends on the nature of your study, your goals, and your target audience. I provide you with three common types of conclusions:
A summarizing conclusion is the most common type of conclusion in research papers. It involves summarizing the main points, reiterating the research question, and restating the significance of the findings. This common type of research paper conclusion is used across different disciplines.
An editorial conclusion is less common but can be used in research papers that are focused on proposing or advocating for a particular viewpoint or policy. It involves presenting a strong editorial or opinion based on the research findings and offering recommendations or calls to action.
An externalizing conclusion is a type of conclusion that extends the research beyond the scope of the paper by suggesting potential future research directions or discussing the broader implications of the findings. This type of conclusion is often used in more theoretical or exploratory research papers.
Align your conclusion’s tone with the rest of your research paper. Start Writing with Paperpal Now!
The conclusion in a research paper serves several important purposes:
- Offers Implications and Recommendations : Your research paper conclusion is an excellent place to discuss the broader implications of your research and suggest potential areas for further study. It’s also an opportunity to offer practical recommendations based on your findings.
- Provides Closure : A good research paper conclusion provides a sense of closure to your paper. It should leave the reader with a feeling that they have reached the end of a well-structured and thought-provoking research project.
- Leaves a Lasting Impression : Writing a well-crafted research paper conclusion leaves a lasting impression on your readers. It’s your final opportunity to leave them with a new idea, a call to action, or a memorable quote.

Writing a strong conclusion for your research paper is essential to leave a lasting impression on your readers. Here’s a step-by-step process to help you create and know what to put in the conclusion of a research paper: 2
- Research Statement : Begin your research paper conclusion by restating your research statement. This reminds the reader of the main point you’ve been trying to prove throughout your paper. Keep it concise and clear.
- Key Points : Summarize the main arguments and key points you’ve made in your paper. Avoid introducing new information in the research paper conclusion. Instead, provide a concise overview of what you’ve discussed in the body of your paper.
- Address the Research Questions : If your research paper is based on specific research questions or hypotheses, briefly address whether you’ve answered them or achieved your research goals. Discuss the significance of your findings in this context.
- Significance : Highlight the importance of your research and its relevance in the broader context. Explain why your findings matter and how they contribute to the existing knowledge in your field.
- Implications : Explore the practical or theoretical implications of your research. How might your findings impact future research, policy, or real-world applications? Consider the “so what?” question.
- Future Research : Offer suggestions for future research in your area. What questions or aspects remain unanswered or warrant further investigation? This shows that your work opens the door for future exploration.
- Closing Thought : Conclude your research paper conclusion with a thought-provoking or memorable statement. This can leave a lasting impression on your readers and wrap up your paper effectively. Avoid introducing new information or arguments here.
- Proofread and Revise : Carefully proofread your conclusion for grammar, spelling, and clarity. Ensure that your ideas flow smoothly and that your conclusion is coherent and well-structured.
Write your research paper conclusion 2x faster with Paperpal. Try it now!
Remember that a well-crafted research paper conclusion is a reflection of the strength of your research and your ability to communicate its significance effectively. It should leave a lasting impression on your readers and tie together all the threads of your paper. Now you know how to start the conclusion of a research paper and what elements to include to make it impactful, let’s look at a research paper conclusion sample.

How to write a research paper conclusion with Paperpal?
A research paper conclusion is not just a summary of your study, but a synthesis of the key findings that ties the research together and places it in a broader context. A research paper conclusion should be concise, typically around one paragraph in length. However, some complex topics may require a longer conclusion to ensure the reader is left with a clear understanding of the study’s significance. Paperpal, an AI writing assistant trusted by over 800,000 academics globally, can help you write a well-structured conclusion for your research paper.
- Sign Up or Log In: Create a new Paperpal account or login with your details.
- Navigate to Features : Once logged in, head over to the features’ side navigation pane. Click on Templates and you’ll find a suite of generative AI features to help you write better, faster.
- Generate an outline: Under Templates, select ‘Outlines’. Choose ‘Research article’ as your document type.
- Select your section: Since you’re focusing on the conclusion, select this section when prompted.
- Choose your field of study: Identifying your field of study allows Paperpal to provide more targeted suggestions, ensuring the relevance of your conclusion to your specific area of research.
- Provide a brief description of your study: Enter details about your research topic and findings. This information helps Paperpal generate a tailored outline that aligns with your paper’s content.
- Generate the conclusion outline: After entering all necessary details, click on ‘generate’. Paperpal will then create a structured outline for your conclusion, to help you start writing and build upon the outline.
- Write your conclusion: Use the generated outline to build your conclusion. The outline serves as a guide, ensuring you cover all critical aspects of a strong conclusion, from summarizing key findings to highlighting the research’s implications.
- Refine and enhance: Paperpal’s ‘Make Academic’ feature can be particularly useful in the final stages. Select any paragraph of your conclusion and use this feature to elevate the academic tone, ensuring your writing is aligned to the academic journal standards.
By following these steps, Paperpal not only simplifies the process of writing a research paper conclusion but also ensures it is impactful, concise, and aligned with academic standards. Sign up with Paperpal today and write your research paper conclusion 2x faster .
The research paper conclusion is a crucial part of your paper as it provides the final opportunity to leave a strong impression on your readers. In the research paper conclusion, summarize the main points of your research paper by restating your research statement, highlighting the most important findings, addressing the research questions or objectives, explaining the broader context of the study, discussing the significance of your findings, providing recommendations if applicable, and emphasizing the takeaway message. The main purpose of the conclusion is to remind the reader of the main point or argument of your paper and to provide a clear and concise summary of the key findings and their implications. All these elements should feature on your list of what to put in the conclusion of a research paper to create a strong final statement for your work.
A strong conclusion is a critical component of a research paper, as it provides an opportunity to wrap up your arguments, reiterate your main points, and leave a lasting impression on your readers. Here are the key elements of a strong research paper conclusion: 1. Conciseness : A research paper conclusion should be concise and to the point. It should not introduce new information or ideas that were not discussed in the body of the paper. 2. Summarization : The research paper conclusion should be comprehensive enough to give the reader a clear understanding of the research’s main contributions. 3 . Relevance : Ensure that the information included in the research paper conclusion is directly relevant to the research paper’s main topic and objectives; avoid unnecessary details. 4 . Connection to the Introduction : A well-structured research paper conclusion often revisits the key points made in the introduction and shows how the research has addressed the initial questions or objectives. 5. Emphasis : Highlight the significance and implications of your research. Why is your study important? What are the broader implications or applications of your findings? 6 . Call to Action : Include a call to action or a recommendation for future research or action based on your findings.
The length of a research paper conclusion can vary depending on several factors, including the overall length of the paper, the complexity of the research, and the specific journal requirements. While there is no strict rule for the length of a conclusion, but it’s generally advisable to keep it relatively short. A typical research paper conclusion might be around 5-10% of the paper’s total length. For example, if your paper is 10 pages long, the conclusion might be roughly half a page to one page in length.
In general, you do not need to include citations in the research paper conclusion. Citations are typically reserved for the body of the paper to support your arguments and provide evidence for your claims. However, there may be some exceptions to this rule: 1. If you are drawing a direct quote or paraphrasing a specific source in your research paper conclusion, you should include a citation to give proper credit to the original author. 2. If your conclusion refers to or discusses specific research, data, or sources that are crucial to the overall argument, citations can be included to reinforce your conclusion’s validity.
The conclusion of a research paper serves several important purposes: 1. Summarize the Key Points 2. Reinforce the Main Argument 3. Provide Closure 4. Offer Insights or Implications 5. Engage the Reader. 6. Reflect on Limitations
Remember that the primary purpose of the research paper conclusion is to leave a lasting impression on the reader, reinforcing the key points and providing closure to your research. It’s often the last part of the paper that the reader will see, so it should be strong and well-crafted.
- Makar, G., Foltz, C., Lendner, M., & Vaccaro, A. R. (2018). How to write effective discussion and conclusion sections. Clinical spine surgery, 31(8), 345-346.
- Bunton, D. (2005). The structure of PhD conclusion chapters. Journal of English for academic purposes , 4 (3), 207-224.
Paperpal is a comprehensive AI writing toolkit that helps students and researchers achieve 2x the writing in half the time. It leverages 21+ years of STM experience and insights from millions of research articles to provide in-depth academic writing, language editing, and submission readiness support to help you write better, faster.
Get accurate academic translations, rewriting support, grammar checks, vocabulary suggestions, and generative AI assistance that delivers human precision at machine speed. Try for free or upgrade to Paperpal Prime starting at US$19 a month to access premium features, including consistency, plagiarism, and 30+ submission readiness checks to help you succeed.
Experience the future of academic writing – Sign up to Paperpal and start writing for free!
Related Reads:
- 5 Reasons for Rejection After Peer Review
- Ethical Research Practices For Research with Human Subjects
7 Ways to Improve Your Academic Writing Process
- Paraphrasing in Academic Writing: Answering Top Author Queries
Preflight For Editorial Desk: The Perfect Hybrid (AI + Human) Assistance Against Compromised Manuscripts
You may also like, measuring academic success: definition & strategies for excellence, phd qualifying exam: tips for success , ai in education: it’s time to change the..., is it ethical to use ai-generated abstracts without..., what are journal guidelines on using generative ai..., quillbot review: features, pricing, and free alternatives, what is an academic paper types and elements , should you use ai tools like chatgpt for..., 9 steps to publish a research paper, what are the different types of research papers.
- USC Libraries
- Research Guides
Organizing Your Social Sciences Research Paper
- 7. The Results
- Purpose of Guide
- Design Flaws to Avoid
- Independent and Dependent Variables
- Glossary of Research Terms
- Reading Research Effectively
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Applying Critical Thinking
- Choosing a Title
- Making an Outline
- Paragraph Development
- Research Process Video Series
- Executive Summary
- The C.A.R.S. Model
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tiertiary Sources
- Scholarly vs. Popular Publications
- Qualitative Methods
- Quantitative Methods
- Insiderness
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Writing Concisely
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Generative AI and Writing
- USC Libraries Tutorials and Other Guides
- Bibliography
The results section is where you report the findings of your study based upon the methodology [or methodologies] you applied to gather information. The results section should state the findings of the research arranged in a logical sequence without bias or interpretation. A section describing results should be particularly detailed if your paper includes data generated from your own research.
Annesley, Thomas M. "Show Your Cards: The Results Section and the Poker Game." Clinical Chemistry 56 (July 2010): 1066-1070.
Importance of a Good Results Section
When formulating the results section, it's important to remember that the results of a study do not prove anything . Findings can only confirm or reject the hypothesis underpinning your study. However, the act of articulating the results helps you to understand the problem from within, to break it into pieces, and to view the research problem from various perspectives.
The page length of this section is set by the amount and types of data to be reported . Be concise. Use non-textual elements appropriately, such as figures and tables, to present findings more effectively. In deciding what data to describe in your results section, you must clearly distinguish information that would normally be included in a research paper from any raw data or other content that could be included as an appendix. In general, raw data that has not been summarized should not be included in the main text of your paper unless requested to do so by your professor.
Avoid providing data that is not critical to answering the research question . The background information you described in the introduction section should provide the reader with any additional context or explanation needed to understand the results. A good strategy is to always re-read the background section of your paper after you have written up your results to ensure that the reader has enough context to understand the results [and, later, how you interpreted the results in the discussion section of your paper that follows].
Bavdekar, Sandeep B. and Sneha Chandak. "Results: Unraveling the Findings." Journal of the Association of Physicians of India 63 (September 2015): 44-46; Brett, Paul. "A Genre Analysis of the Results Section of Sociology Articles." English for Specific Speakers 13 (1994): 47-59; Go to English for Specific Purposes on ScienceDirect;Burton, Neil et al. Doing Your Education Research Project . Los Angeles, CA: SAGE, 2008; Results. The Structure, Format, Content, and Style of a Journal-Style Scientific Paper. Department of Biology. Bates College; Kretchmer, Paul. Twelve Steps to Writing an Effective Results Section. San Francisco Edit; "Reporting Findings." In Making Sense of Social Research Malcolm Williams, editor. (London;: SAGE Publications, 2003) pp. 188-207.
Structure and Writing Style
I. Organization and Approach
For most research papers in the social and behavioral sciences, there are two possible ways of organizing the results . Both approaches are appropriate in how you report your findings, but use only one approach.
- Present a synopsis of the results followed by an explanation of key findings . This approach can be used to highlight important findings. For example, you may have noticed an unusual correlation between two variables during the analysis of your findings. It is appropriate to highlight this finding in the results section. However, speculating as to why this correlation exists and offering a hypothesis about what may be happening belongs in the discussion section of your paper.
- Present a result and then explain it, before presenting the next result then explaining it, and so on, then end with an overall synopsis . This is the preferred approach if you have multiple results of equal significance. It is more common in longer papers because it helps the reader to better understand each finding. In this model, it is helpful to provide a brief conclusion that ties each of the findings together and provides a narrative bridge to the discussion section of the your paper.
NOTE : Just as the literature review should be arranged under conceptual categories rather than systematically describing each source, you should also organize your findings under key themes related to addressing the research problem. This can be done under either format noted above [i.e., a thorough explanation of the key results or a sequential, thematic description and explanation of each finding].
II. Content
In general, the content of your results section should include the following:
- Introductory context for understanding the results by restating the research problem underpinning your study . This is useful in re-orientating the reader's focus back to the research problem after having read a review of the literature and your explanation of the methods used for gathering and analyzing information.
- Inclusion of non-textual elements, such as, figures, charts, photos, maps, tables, etc. to further illustrate key findings, if appropriate . Rather than relying entirely on descriptive text, consider how your findings can be presented visually. This is a helpful way of condensing a lot of data into one place that can then be referred to in the text. Consider referring to appendices if there is a lot of non-textual elements.
- A systematic description of your results, highlighting for the reader observations that are most relevant to the topic under investigation . Not all results that emerge from the methodology used to gather information may be related to answering the " So What? " question. Do not confuse observations with interpretations; observations in this context refers to highlighting important findings you discovered through a process of reviewing prior literature and gathering data.
- The page length of your results section is guided by the amount and types of data to be reported . However, focus on findings that are important and related to addressing the research problem. It is not uncommon to have unanticipated results that are not relevant to answering the research question. This is not to say that you don't acknowledge tangential findings and, in fact, can be referred to as areas for further research in the conclusion of your paper. However, spending time in the results section describing tangential findings clutters your overall results section and distracts the reader.
- A short paragraph that concludes the results section by synthesizing the key findings of the study . Highlight the most important findings you want readers to remember as they transition into the discussion section. This is particularly important if, for example, there are many results to report, the findings are complicated or unanticipated, or they are impactful or actionable in some way [i.e., able to be pursued in a feasible way applied to practice].
NOTE: Always use the past tense when referring to your study's findings. Reference to findings should always be described as having already happened because the method used to gather the information has been completed.
III. Problems to Avoid
When writing the results section, avoid doing the following :
- Discussing or interpreting your results . Save this for the discussion section of your paper, although where appropriate, you should compare or contrast specific results to those found in other studies [e.g., "Similar to the work of Smith [1990], one of the findings of this study is the strong correlation between motivation and academic achievement...."].
- Reporting background information or attempting to explain your findings. This should have been done in your introduction section, but don't panic! Often the results of a study point to the need for additional background information or to explain the topic further, so don't think you did something wrong. Writing up research is rarely a linear process. Always revise your introduction as needed.
- Ignoring negative results . A negative result generally refers to a finding that does not support the underlying assumptions of your study. Do not ignore them. Document these findings and then state in your discussion section why you believe a negative result emerged from your study. Note that negative results, and how you handle them, can give you an opportunity to write a more engaging discussion section, therefore, don't be hesitant to highlight them.
- Including raw data or intermediate calculations . Ask your professor if you need to include any raw data generated by your study, such as transcripts from interviews or data files. If raw data is to be included, place it in an appendix or set of appendices that are referred to in the text.
- Be as factual and concise as possible in reporting your findings . Do not use phrases that are vague or non-specific, such as, "appeared to be greater than other variables..." or "demonstrates promising trends that...." Subjective modifiers should be explained in the discussion section of the paper [i.e., why did one variable appear greater? Or, how does the finding demonstrate a promising trend?].
- Presenting the same data or repeating the same information more than once . If you want to highlight a particular finding, it is appropriate to do so in the results section. However, you should emphasize its significance in relation to addressing the research problem in the discussion section. Do not repeat it in your results section because you can do that in the conclusion of your paper.
- Confusing figures with tables . Be sure to properly label any non-textual elements in your paper. Don't call a chart an illustration or a figure a table. If you are not sure, go here .
Annesley, Thomas M. "Show Your Cards: The Results Section and the Poker Game." Clinical Chemistry 56 (July 2010): 1066-1070; Bavdekar, Sandeep B. and Sneha Chandak. "Results: Unraveling the Findings." Journal of the Association of Physicians of India 63 (September 2015): 44-46; Burton, Neil et al. Doing Your Education Research Project . Los Angeles, CA: SAGE, 2008; Caprette, David R. Writing Research Papers. Experimental Biosciences Resources. Rice University; Hancock, Dawson R. and Bob Algozzine. Doing Case Study Research: A Practical Guide for Beginning Researchers . 2nd ed. New York: Teachers College Press, 2011; Introduction to Nursing Research: Reporting Research Findings. Nursing Research: Open Access Nursing Research and Review Articles. (January 4, 2012); Kretchmer, Paul. Twelve Steps to Writing an Effective Results Section. San Francisco Edit ; Ng, K. H. and W. C. Peh. "Writing the Results." Singapore Medical Journal 49 (2008): 967-968; Reporting Research Findings. Wilder Research, in partnership with the Minnesota Department of Human Services. (February 2009); Results. The Structure, Format, Content, and Style of a Journal-Style Scientific Paper. Department of Biology. Bates College; Schafer, Mickey S. Writing the Results. Thesis Writing in the Sciences. Course Syllabus. University of Florida.
Writing Tip
Why Don't I Just Combine the Results Section with the Discussion Section?
It's not unusual to find articles in scholarly social science journals where the author(s) have combined a description of the findings with a discussion about their significance and implications. You could do this. However, if you are inexperienced writing research papers, consider creating two distinct sections for each section in your paper as a way to better organize your thoughts and, by extension, your paper. Think of the results section as the place where you report what your study found; think of the discussion section as the place where you interpret the information and answer the "So What?" question. As you become more skilled writing research papers, you can consider melding the results of your study with a discussion of its implications.
Driscoll, Dana Lynn and Aleksandra Kasztalska. Writing the Experimental Report: Methods, Results, and Discussion. The Writing Lab and The OWL. Purdue University.
- << Previous: Insiderness
- Next: Using Non-Textual Elements >>
- Last Updated: Apr 24, 2024 10:51 AM
- URL: https://libguides.usc.edu/writingguide
Research Skills
Results, discussion, and conclusion, results/findings.
The Results (or Findings) section follows the Methods and precedes the Discussion section. This is where the authors provide the data collected during their study. That data can sometimes be difficult to understand because it is often quite technical. Do not let this intimidate you; you will discover the significance of the results next.
The Discussion section follows the Results and precedes the Conclusions and Recommendations section. It is here that the authors indicate the significance of their results. They answer the question, “Why did we get the results we did?” This section provides logical explanations for the results from the study. Those explanations are often reached by comparing and contrasting the results to prior studies’ findings, so citations to the studies discussed in the Literature Review generally reappear here. This section also usually discusses the limitations of the study and speculates on what the results say about the problem(s) identified in the research question(s). This section is very important because it is finally moving towards an argument. Since the researchers interpret their results according to theoretical underpinnings in this section, there is more room for difference of opinion. The way the authors interpret their results may be quite different from the way you would interpret them or the way another researcher would interpret them.
Note: Some articles collapse the Discussion and Conclusion sections together under a single heading (usually “Conclusion”). If you don’t see a separate Discussion section, don’t worry. Instead, look in the nearby sections for the types of information described in the paragraph above.
When you first skim an article, it may be useful to go straight to the Conclusion and see if you can figure out what the thesis is since it is usually in this final section. The research gap identified in the introduction indicates what the researchers wanted to look at; what did they claim, ultimately, when they completed their research? What did it show them—and what are they showing us—about the topic? Did they get the results they expected? Why or why not? The thesis is not a sweeping proclamation; rather, it is likely a very reasonable and conditional claim.
Nearly every research article ends by inviting other scholars to continue the work by saying that more research needs to be done on the matter. However, do not mistake this directive for the thesis; it’s a convention. Often, the authors provide specific details about future possible studies that could or should be conducted in order to make more sense of their own study’s conclusions.
- Parts of An Article. Authored by : Kerry Bowers. Provided by : University of Mississippi. Project : WRIT 250 Committee OER Project. License : CC BY-SA: Attribution-ShareAlike

Privacy Policy
- SpringerLink shop
Discussion and Conclusions
Your Discussion and Conclusions sections should answer the question: What do your results mean?
In other words, the majority of the Discussion and Conclusions sections should be an interpretation of your results. You should:
- Discuss your conclusions in order of most to least important.
- Compare your results with those from other studies: Are they consistent? If not, discuss possible reasons for the difference.
- Mention any inconclusive results and explain them as best you can. You may suggest additional experiments needed to clarify your results.
- Briefly describe the limitations of your study to show reviewers and readers that you have considered your experiment’s weaknesses. Many researchers are hesitant to do this as they feel it highlights the weaknesses in their research to the editor and reviewer. However doing this actually makes a positive impression of your paper as it makes it clear that you have an in depth understanding of your topic and can think objectively of your research.
- Discuss what your results may mean for researchers in the same field as you, researchers in other fields, and the general public. How could your findings be applied?
- State how your results extend the findings of previous studies.
- If your findings are preliminary, suggest future studies that need to be carried out.
- At the end of your Discussion and Conclusions sections, state your main conclusions once again .
Back │ Next
- How to Cite
- Language & Lit
- Rhyme & Rhythm
- The Rewrite
- Search Glass
What Is the Difference Between Results and Conclusions in a Scientific Experiment?
Five steps make up most scientific experiments, beginning with the research question. The next step is the formulation of a hypothesis, which is a statement of what you expect your project will show. The procedure is your step-by-step plan for the experiment. The final two steps are the results, or what happens, and, finally, the conclusion, or what the results showed.
The Results
When you record the results of a scientific experiment, you record what happens as you follow your procedure. Results should be raw data that is measurable rather than general observations, and it should relate directly to your research question and hypothesis. For example, if your experiment involves growing plants, the results will be data about one aspect of the plants’ growth, such as how much each plant grows over a particular period of time or which seed sprouts first. The results should also include notations of any variations in the conditions of the experiment, which in this case might be an unexpected overnight freeze or which seed received the most water.
Data Organization
At the end of your experiment’s procedure, you have data that tells what happened, but at this point it is just a collection of facts or numbers. The data needs to be organized before you can understand it, but how you organize the data depends on the factor tested in your experiment. If you entered the data into a chart as you collected it, you may already see a pattern. Another way to organize the data is with a line graph to show change over time, especially temperature changes. In the example of plant growth, a bar graph can illustrate how much each plant grew between measurements.
The Conclusion
After all the data is organized in a form that relates it to your hypothesis, you can interpret it and reach a conclusion about the experiment. The conclusion is simply a report about what you learned based on whether the results agree or disagree with your hypothesis. It usually contains a summary of the actual procedure and makes note of anything unexpected that happened during the experiment. Your conclusion should consider all possible explanations of the data, including any errors you might have made, such as forgetting to water the plants one day. It can also give you a point from which to create further hypotheses relating to the experiment.
No Right or Wrong
The conclusion, which is also sometimes called a discussion or interpretation, is a statement about the experiment’s results. As a report of your data, it can’t be considered wrong even if the results don’t support your hypothesis. You have learned that your hypothesis does not answer your original research question.
- Agriculture Is a Science: Parts of a Science Project
- Vermont EPSCoR Streams Project: Data Analysis Tutorial
Cynthia Gast began writing professionally over 25 years ago in the automotive magazine niche and has also taught preschoolers and elementary grades. She has been a full-time freelance writer since 2008. Gast holds a Bachelor of Arts in history from the University of Illinois.

Organizing Academic Research Papers: 9. The Conclusion
- Purpose of Guide
- Design Flaws to Avoid
- Glossary of Research Terms
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Choosing a Title
- Making an Outline
- Paragraph Development
- Executive Summary
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tertiary Sources
- What Is Scholarly vs. Popular?
- Qualitative Methods
- Quantitative Methods
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Annotated Bibliography
- Dealing with Nervousness
- Using Visual Aids
- Grading Someone Else's Paper
- How to Manage Group Projects
- Multiple Book Review Essay
- Reviewing Collected Essays
- About Informed Consent
- Writing Field Notes
- Writing a Policy Memo
- Writing a Research Proposal
- Acknowledgements
The conclusion is intended to help the reader understand why your research should matter to them after they have finished reading the paper. A conclusion is not merely a summary of your points or a re-statement of your research problem but a synthesis of key points. For most essays, one well-developed paragraph is sufficient for a conclusion, although in some cases, a two-or-three paragraph conclusion may be required.
Importance of a Good Conclusion
A well-written conclusion provides you with several important opportunities to demonstrate your overall understanding of the research problem to the reader. These include:
- Presenting the last word on the issues you raised in your paper . Just as the introduction gives a first impression to your reader, the conclusion offers a chance to leave a lasting impression. Do this, for example, by highlighting key points in your analysis or findings.
- Summarizing your thoughts and conveying the larger implications of your study . The conclusion is an opportunity to succinctly answer the "so what?" question by placing the study within the context of past research about the topic you've investigated.
- Demonstrating the importance of your ideas . Don't be shy. The conclusion offers you a chance to elaborate on the significance of your findings.
- Introducing possible new or expanded ways of thinking about the research problem . This does not refer to introducing new information [which should be avoided], but to offer new insight and creative approaches for framing/contextualizing the research problem based on the results of your study.
Conclusions . The Writing Center. University of North Carolina; Kretchmer, Paul. Twelve Steps to Writing an Effective Conclusion . San Francisco Edit, 2003-2008.
Structure and Writing Style
https://writing.wisc.edu/wp-content/uploads/sites/535/2018/07/conclusions_uwmadison_writingcenter_aug2012.pdf I. General Rules
When writing the conclusion to your paper, follow these general rules:
- State your conclusions in clear, simple language.
- Do not simply reiterate your results or the discussion.
- Indicate opportunities for future research, as long as you haven't already done so in the discussion section of your paper.
The function of your paper's conclusion is to restate the main argument . It reminds the reader of the strengths of your main argument(s) and reiterates the most important evidence supporting those argument(s). Make sure, however, that your conclusion is not simply a repetitive summary of the findings because this reduces the impact of the argument(s) you have developed in your essay.
Consider the following points to help ensure your conclusion is appropriate:
- If the argument or point of your paper is complex, you may need to summarize the argument for your reader.
- If, prior to your conclusion, you have not yet explained the significance of your findings or if you are proceeding inductively, use the end of your paper to describe your main points and explain their significance.
- Move from a detailed to a general level of consideration that returns the topic to the context provided by the introduction or within a new context that emerges from the data.
The conclusion also provides a place for you to persuasively and succinctly restate your research problem, given that the reader has now been presented with all the information about the topic . Depending on the discipline you are writing in, the concluding paragraph may contain your reflections on the evidence presented, or on the essay's central research problem. However, the nature of being introspective about the research you have done will depend on the topic and whether your professor wants you to express your observations in this way.
NOTE : Don't delve into idle speculation. Being introspective means looking within yourself as an author to try and understand an issue more deeply not to guess at possible outcomes.
II. Developing a Compelling Conclusion
Strategies to help you move beyond merely summarizing the key points of your research paper may include any of the following.
- If your essay deals with a contemporary problem, warn readers of the possible consequences of not attending to the problem.
- Recommend a specific course or courses of action.
- Cite a relevant quotation or expert opinion to lend authority to the conclusion you have reached [a good place to look is research from your literature review].
- Restate a key statistic, fact, or visual image to drive home the ultimate point of your paper.
- If your discipline encourages personal reflection, illustrate your concluding point with a relevant narrative drawn from your own life experiences.
- Return to an anecdote, an example, or a quotation that you introduced in your introduction, but add further insight that is derived from the findings of your study; use your interpretation of results to reframe it in new ways.
- Provide a "take-home" message in the form of a strong, succient statement that you want the reader to remember about your study.
III. Problems to Avoid Failure to be concise The conclusion section should be concise and to the point. Conclusions that are too long often have unnecessary detail. The conclusion section is not the place for details about your methodology or results. Although you should give a summary of what was learned from your research, this summary should be relatively brief, since the emphasis in the conclusion is on the implications, evaluations, insights, etc. that you make. Failure to comment on larger, more significant issues In the introduction, your task was to move from general [the field of study] to specific [your research problem]. However, in the conclusion, your task is to move from specific [your research problem] back to general [your field, i.e., how your research contributes new understanding or fills an important gap in the literature]. In other words, the conclusion is where you place your research within a larger context. Failure to reveal problems and negative results Negative aspects of the research process should never be ignored. Problems, drawbacks, and challenges encountered during your study should be included as a way of qualifying your overall conclusions. If you encountered negative results [findings that are validated outside the research context in which they were generated], you must report them in the results section of your paper. In the conclusion, use the negative results as an opportunity to explain how they provide information on which future research can be based. Failure to provide a clear summary of what was learned In order to be able to discuss how your research fits back into your field of study [and possibly the world at large], you need to summarize it briefly and directly. Often this element of your conclusion is only a few sentences long. Failure to match the objectives of your research Often research objectives change while the research is being carried out. This is not a problem unless you forget to go back and refine your original objectives in your introduction, as these changes emerge they must be documented so that they accurately reflect what you were trying to accomplish in your research [not what you thought you might accomplish when you began].
Resist the urge to apologize If you've immersed yourself in studying the research problem, you now know a good deal about it, perhaps even more than your professor! Nevertheless, by the time you have finished writing, you may be having some doubts about what you have produced. Repress those doubts! Don't undermine your authority by saying something like, "This is just one approach to examining this problem; there may be other, much better approaches...."
Concluding Paragraphs. College Writing Center at Meramec. St. Louis Community College; Conclusions . The Writing Center. University of North Carolina; Conclusions . The Writing Lab and The OWL. Purdue University; Freedman, Leora and Jerry Plotnick. Introductions and Conclusions . The Lab Report. University College Writing Centre. University of Toronto; Leibensperger, Summer. Draft Your Conclusion. Academic Center, the University of Houston-Victoria, 2003; Make Your Last Words Count . The Writer’s Handbook. Writing Center. University of Wisconsin, Madison; Tips for Writing a Good Conclusion . Writing@CSU. Colorado State University; Kretchmer, Paul. Twelve Steps to Writing an Effective Conclusion . San Francisco Edit, 2003-2008; Writing Conclusions . Writing Tutorial Services, Center for Innovative Teaching and Learning. Indiana University; Writing: Considering Structure and Organization . Institute for Writing Rhetoric. Dartmouth College.
Writing Tip
Don't Belabor the Obvious!
Avoid phrases like "in conclusion...," "in summary...," or "in closing...." These phrases can be useful, even welcome, in oral presentations. But readers can see by the tell-tale section heading and number of pages remaining to read, when an essay is about to end. You'll irritate your readers if you belabor the obvious.
Another Writing Tip
New Insight, Not New Information!
Don't surprise the reader with new information in your Conclusion that was never referenced anywhere else in the paper. If you have new information to present, add it to the Discussion or other appropriate section of the paper. Note that, although no actual new information is introduced, the conclusion is where you offer your most "original" contributions in the paper; it's where you describe the value of your research, demonstrate your understanding of the material that you’ve presented, and locate your findings within the larger context of scholarship on the topic.
- << Previous: Limitations of the Study
- Next: Appendices >>
- Last Updated: Jul 18, 2023 11:58 AM
- URL: https://library.sacredheart.edu/c.php?g=29803
- QuickSearch
- Library Catalog
- Databases A-Z
- Publication Finder
- Course Reserves
- Citation Linker
- Digital Commons
- Our Website
Research Support
- Ask a Librarian
- Appointments
- Interlibrary Loan (ILL)
- Research Guides
- Databases by Subject
- Citation Help
Using the Library
- Reserve a Group Study Room
- Renew Books
- Honors Study Rooms
- Off-Campus Access
- Library Policies
- Library Technology
User Information
- Grad Students
- Online Students
- COVID-19 Updates
- Staff Directory
- News & Announcements
- Library Newsletter
My Accounts
- Interlibrary Loan
- Staff Site Login
FIND US ON
- Open access
- Published: 19 April 2024
A scoping review of continuous quality improvement in healthcare system: conceptualization, models and tools, barriers and facilitators, and impact
- Aklilu Endalamaw 1 , 2 ,
- Resham B Khatri 1 , 3 ,
- Tesfaye Setegn Mengistu 1 , 2 ,
- Daniel Erku 1 , 4 , 5 ,
- Eskinder Wolka 6 ,
- Anteneh Zewdie 6 &
- Yibeltal Assefa 1
BMC Health Services Research volume 24 , Article number: 487 ( 2024 ) Cite this article
674 Accesses
Metrics details
The growing adoption of continuous quality improvement (CQI) initiatives in healthcare has generated a surge in research interest to gain a deeper understanding of CQI. However, comprehensive evidence regarding the diverse facets of CQI in healthcare has been limited. Our review sought to comprehensively grasp the conceptualization and principles of CQI, explore existing models and tools, analyze barriers and facilitators, and investigate its overall impacts.
This qualitative scoping review was conducted using Arksey and O’Malley’s methodological framework. We searched articles in PubMed, Web of Science, Scopus, and EMBASE databases. In addition, we accessed articles from Google Scholar. We used mixed-method analysis, including qualitative content analysis and quantitative descriptive for quantitative findings to summarize findings and PRISMA extension for scoping reviews (PRISMA-ScR) framework to report the overall works.
A total of 87 articles, which covered 14 CQI models, were included in the review. While 19 tools were used for CQI models and initiatives, Plan-Do-Study/Check-Act cycle was the commonly employed model to understand the CQI implementation process. The main reported purposes of using CQI, as its positive impact, are to improve the structure of the health system (e.g., leadership, health workforce, health technology use, supplies, and costs), enhance healthcare delivery processes and outputs (e.g., care coordination and linkages, satisfaction, accessibility, continuity of care, safety, and efficiency), and improve treatment outcome (reduce morbidity and mortality). The implementation of CQI is not without challenges. There are cultural (i.e., resistance/reluctance to quality-focused culture and fear of blame or punishment), technical, structural (related to organizational structure, processes, and systems), and strategic (inadequate planning and inappropriate goals) related barriers that were commonly reported during the implementation of CQI.
Conclusions
Implementing CQI initiatives necessitates thoroughly comprehending key principles such as teamwork and timeline. To effectively address challenges, it’s crucial to identify obstacles and implement optimal interventions proactively. Healthcare professionals and leaders need to be mentally equipped and cognizant of the significant role CQI initiatives play in achieving purposes for quality of care.
Peer Review reports
Continuous quality improvement (CQI) initiative is a crucial initiative aimed at enhancing quality in the health system that has gradually been adopted in the healthcare industry. In the early 20th century, Shewhart laid the foundation for quality improvement by describing three essential steps for process improvement: specification, production, and inspection [ 1 , 2 ]. Then, Deming expanded Shewhart’s three-step model into ‘plan, do, study/check, and act’ (PDSA or PDCA) cycle, which was applied to management practices in Japan in the 1950s [ 3 ] and was gradually translated into the health system. In 1991, Kuperman applied a CQI approach to healthcare, comprising selecting a process to be improved, assembling a team of expert clinicians that understands the process and the outcomes, determining key steps in the process and expected outcomes, collecting data that measure the key process steps and outcomes, and providing data feedback to the practitioners [ 4 ]. These philosophies have served as the baseline for the foundation of principles for continuous improvement [ 5 ].
Continuous quality improvement fosters a culture of continuous learning, innovation, and improvement. It encourages proactive identification and resolution of problems, promotes employee engagement and empowerment, encourages trust and respect, and aims for better quality of care [ 6 , 7 ]. These characteristics drive the interaction of CQI with other quality improvement projects, such as quality assurance and total quality management [ 8 ]. Quality assurance primarily focuses on identifying deviations or errors through inspections, audits, and formal reviews, often settling for what is considered ‘good enough’, rather than pursuing the highest possible standards [ 9 , 10 ], while total quality management is implemented as the management philosophy and system to improve all aspects of an organization continuously [ 11 ].
Continuous quality improvement has been implemented to provide quality care. However, providing effective healthcare is a complicated and complex task in achieving the desired health outcomes and the overall well-being of individuals and populations. It necessitates tackling issues, including access, patient safety, medical advances, care coordination, patient-centered care, and quality monitoring [ 12 , 13 ], rooted long ago. It is assumed that the history of quality improvement in healthcare started in 1854 when Florence Nightingale introduced quality improvement documentation [ 14 ]. Over the passing decades, Donabedian introduced structure, processes, and outcomes as quality of care components in 1966 [ 15 ]. More comprehensively, the Institute of Medicine in the United States of America (USA) has identified effectiveness, efficiency, equity, patient-centredness, safety, and timeliness as the components of quality of care [ 16 ]. Moreover, quality of care has recently been considered an integral part of universal health coverage (UHC) [ 17 ], which requires initiatives to mobilise essential inputs [ 18 ].
While the overall objective of CQI in health system is to enhance the quality of care, it is important to note that the purposes and principles of CQI can vary across different contexts [ 19 , 20 ]. This variation has sparked growing research interest. For instance, a review of CQI approaches for capacity building addressed its role in health workforce development [ 21 ]. Another systematic review, based on random-controlled design studies, assessed the effectiveness of CQI using training as an intervention and the PDSA model [ 22 ]. As a research gap, the former review was not directly related to the comprehensive elements of quality of care, while the latter focused solely on the impact of training using the PDSA model, among other potential models. Additionally, a review conducted in 2015 aimed to identify barriers and facilitators of CQI in Canadian contexts [ 23 ]. However, all these reviews presented different perspectives and investigated distinct outcomes. This suggests that there is still much to explore in terms of comprehensively understanding the various aspects of CQI initiatives in healthcare.
As a result, we conducted a scoping review to address several aspects of CQI. Scoping reviews serve as a valuable tool for systematically mapping the existing literature on a specific topic. They are instrumental when dealing with heterogeneous or complex bodies of research. Scoping reviews provide a comprehensive overview by summarizing and disseminating findings across multiple studies, even when evidence varies significantly [ 24 ]. In our specific scoping review, we included various types of literature, including systematic reviews, to enhance our understanding of CQI.
This scoping review examined how CQI is conceptualized and measured and investigated models and tools for its application while identifying implementation challenges and facilitators. It also analyzed the purposes and impact of CQI on the health systems, providing valuable insights for enhancing healthcare quality.
Protocol registration and results reporting
Protocol registration for this scoping review was not conducted. Arksey and O’Malley’s methodological framework was utilized to conduct this scoping review [ 25 ]. The scoping review procedures start by defining the research questions, identifying relevant literature, selecting articles, extracting data, and summarizing the results. The review findings are reported using the PRISMA extension for a scoping review (PRISMA-ScR) [ 26 ]. McGowan and colleagues also advised researchers to report findings from scoping reviews using PRISMA-ScR [ 27 ].
Defining the research problems
This review aims to comprehensively explore the conceptualization, models, tools, barriers, facilitators, and impacts of CQI within the healthcare system worldwide. Specifically, we address the following research questions: (1) How has CQI been defined across various contexts? (2) What are the diverse approaches to implementing CQI in healthcare settings? (3) Which tools are commonly employed for CQI implementation ? (4) What barriers hinder and facilitators support successful CQI initiatives? and (5) What effects CQI initiatives have on the overall care quality?
Information source and search strategy
We conducted the search in PubMed, Web of Science, Scopus, and EMBASE databases, and the Google Scholar search engine. The search terms were selected based on three main distinct concepts. One group was CQI-related terms. The second group included terms related to the purpose for which CQI has been implemented, and the third group included processes and impact. These terms were selected based on the Donabedian framework of structure, process, and outcome [ 28 ]. Additionally, the detailed keywords were recruited from the primary health framework, which has described lists of dimensions under process, output, outcome, and health system goals of any intervention for health [ 29 ]. The detailed search strategy is presented in the Supplementary file 1 (Search strategy). The search for articles was initiated on August 12, 2023, and the last search was conducted on September 01, 2023.
Eligibility criteria and article selection
Based on the scoping review’s population, concept, and context frameworks [ 30 ], the population included any patients or clients. Additionally, the concepts explored in the review encompassed definitions, implementation, models, tools, barriers, facilitators, and impacts of CQI. Furthermore, the review considered contexts at any level of health systems. We included articles if they reported results of qualitative or quantitative empirical study, case studies, analytic or descriptive synthesis, any review, and other written documents, were published in peer-reviewed journals, and were designed to address at least one of the identified research questions or one of the identified implementation outcomes or their synonymous taxonomy as described in the search strategy. Based on additional contexts, we included articles published in English without geographic and time limitations. We excluded articles with abstracts only, conference abstracts, letters to editors, commentators, and corrections.
We exported all citations to EndNote x20 to remove duplicates and screen relevant articles. The article selection process includes automatic duplicate removal by using EndNote x20, unmatched title and abstract removal, citation and abstract-only materials removal, and full-text assessment. The article selection process was mainly conducted by the first author (AE) and reported to the team during the weekly meetings. The first author encountered papers that caused confusion regarding whether to include or exclude them and discussed them with the last author (YA). Then, decisions were ultimately made. Whenever disagreements happened, they were resolved by discussion and reconsideration of the review questions in relation to the written documents of the article. Further statistical analysis, such as calculating Kappa, was not performed to determine article inclusion or exclusion.
Data extraction and data items
We extracted first author, publication year, country, settings, health problem, the purpose of the study, study design, types of intervention if applicable, CQI approaches/steps if applicable, CQI tools and procedures if applicable, and main findings using a customized Microsoft Excel form.
Summarizing and reporting the results
The main findings were summarized and described based on the main themes, including concepts under conceptualizing, principles, teams, timelines, models, tools, barriers, facilitators, and impacts of CQI. Results-based convergent synthesis, achieved through mixed-method analysis, involved content analysis to identify the thematic presentation of findings. Additionally, a narrative description was used for quantitative findings, aligning them with the appropriate theme. The authors meticulously reviewed the primary findings from each included material and contextualized these findings concerning the main themes1. This approach provides a comprehensive understanding of complex interventions and health systems, acknowledging quantitative and qualitative evidence.
Search results
A total of 11,251 documents were identified from various databases: SCOPUS ( n = 4,339), PubMed ( n = 2,893), Web of Science ( n = 225), EMBASE ( n = 3,651), and Google Scholar ( n = 143). After removing duplicates ( n = 5,061), 6,190 articles were evaluated by title and abstract. Subsequently, 208 articles were assessed for full-text eligibility. Following the eligibility criteria, 121 articles were excluded, leaving 87 included in the current review (Fig. 1 ).
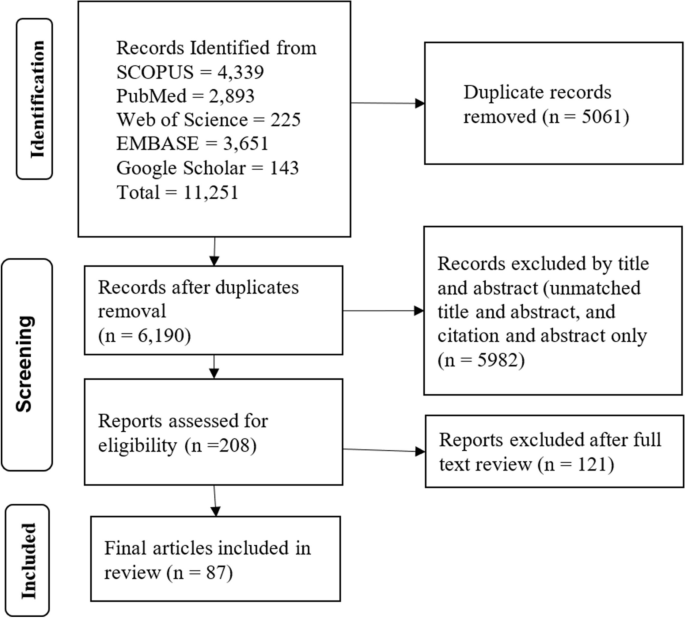
Article selection process
Operationalizing continuous quality improvement
Continuous Quality Improvement (CQI) is operationalized as a cyclic process that requires commitment to implementation, teamwork, time allocation, and celebrating successes and failures.
CQI is a cyclic ongoing process that is followed reflexive, analytical and iterative steps, including identifying gaps, generating data, developing and implementing action plans, evaluating performance, providing feedback to implementers and leaders, and proposing necessary adjustments [ 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 ].
CQI requires committing to the philosophy, involving continuous improvement [ 19 , 38 ], establishing a mission statement [ 37 ], and understanding quality definition [ 19 ].
CQI involves a wide range of patient-oriented measures and performance indicators, specifically satisfying internal and external customers, developing quality assurance, adopting common quality measures, and selecting process measures [ 8 , 19 , 35 , 36 , 37 , 39 , 40 ].
CQI requires celebrating success and failure without personalization, leading each team member to develop error-free attitudes [ 19 ]. Success and failure are related to underlying organizational processes and systems as causes of failure rather than blaming individuals [ 8 ] because CQI is process-focused based on collaborative, data-driven, responsive, rigorous and problem-solving statistical analysis [ 8 , 19 , 38 ]. Furthermore, a gap or failure opens another opportunity for establishing a data-driven learning organization [ 41 ].
CQI cannot be implemented without a CQI team [ 8 , 19 , 37 , 39 , 42 , 43 , 44 , 45 , 46 ]. A CQI team comprises individuals from various disciplines, often comprising a team leader, a subject matter expert (physician or other healthcare provider), a data analyst, a facilitator, frontline staff, and stakeholders [ 39 , 43 , 47 , 48 , 49 ]. It is also important to note that inviting stakeholders or partners as part of the CQI support intervention is crucial [ 19 , 38 , 48 ].
The timeline is another distinct feature of CQI because the results of CQI vary based on the implementation duration of each cycle [ 35 ]. There is no specific time limit for CQI implementation, although there is a general consensus that a cycle of CQI should be relatively short [ 35 ]. For instance, a CQI implementation took 2 months [ 42 ], 4 months [ 50 ], 9 months [ 51 , 52 ], 12 months [ 53 , 54 , 55 ], and one year and 5 months [ 49 ] duration to achieve the desired positive outcome, while bi-weekly [ 47 ] and monthly data reviews and analyses [ 44 , 48 , 56 ], and activities over 3 months [ 57 ] have also resulted in a positive outcome.
Continuous quality improvement models and tools
There have been several models are utilized. The Plan-Do-Study/Check-Act cycle is a stepwise process involving project initiation, situation analysis, root cause identification, solution generation and selection, implementation, result evaluation, standardization, and future planning [ 7 , 36 , 37 , 45 , 47 , 48 , 49 , 50 , 51 , 53 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 ]. The FOCUS-PDCA cycle enhances the PDCA process by adding steps to find and improve a process (F), organize a knowledgeable team (O), clarify the process (C), understand variations (U), and select improvements (S) [ 55 , 71 , 72 , 73 ]. The FADE cycle involves identifying a problem (Focus), understanding it through data analysis (Analyze), devising solutions (Develop), and implementing the plan (Execute) [ 74 ]. The Logic Framework involves brainstorming to identify improvement areas, conducting root cause analysis to develop a problem tree, logically reasoning to create an objective tree, formulating the framework, and executing improvement projects [ 75 ]. Breakthrough series approach requires CQI teams to meet in quarterly collaborative learning sessions, share learning experiences, and continue discussion by telephone and cross-site visits to strengthen learning and idea exchange [ 47 ]. Another CQI model is the Lean approach, which has been conducted with Kaizen principles [ 52 ], 5 S principles, and the Six Sigma model. The 5 S (Sort, Set/Straighten, Shine, Standardize, Sustain) systematically organises and improves the workplace, focusing on sorting, setting order, shining, standardizing, and sustaining the improvement [ 54 , 76 ]. Kaizen principles guide CQI by advocating for continuous improvement, valuing all ideas, solving problems, focusing on practical, low-cost improvements, using data to drive change, acknowledging process defects, reducing variability and waste, recognizing every interaction as a customer-supplier relationship, empowering workers, responding to all ideas, and maintaining a disciplined workplace [ 77 ]. Lean Six Sigma, a CQI model, applies the DMAIC methodology, which involves defining (D) and measuring the problem (M), analyzing root causes (A), improving by finding solutions (I), and controlling by assessing process stability (C) [ 78 , 79 ]. The 5 C-cyclic model (consultation, collection, consideration, collaboration, and celebration), the first CQI framework for volunteer dental services in Aboriginal communities, ensures quality care based on community needs [ 80 ]. One study used meetings involving activities such as reviewing objectives, assigning roles, discussing the agenda, completing tasks, retaining key outputs, planning future steps, and evaluating the meeting’s effectiveness [ 81 ].
Various tools are involved in the implementation or evaluation of CQI initiatives: checklists [ 53 , 82 ], flowcharts [ 81 , 82 , 83 ], cause-and-effect diagrams (fishbone or Ishikawa diagrams) [ 60 , 62 , 79 , 81 , 82 ], fuzzy Pareto diagram [ 82 ], process maps [ 60 ], time series charts [ 48 ], why-why analysis [ 79 ], affinity diagrams and multivoting [ 81 ], and run chart [ 47 , 48 , 51 , 60 , 84 ], and others mentioned in the table (Table 1 ).
Barriers and facilitators of continuous quality improvement implementation
Implementing CQI initiatives is determined by various barriers and facilitators, which can be thematized into four dimensions. These dimensions are cultural, technical, structural, and strategic dimensions.
Continuous quality improvement initiatives face various cultural, strategic, technical, and structural barriers. Cultural dimension barriers involve resistance to change (e.g., not accepting online technology), lack of quality-focused culture, staff reporting apprehensiveness, and fear of blame or punishment [ 36 , 41 , 85 , 86 ]. The technical dimension barriers of CQI can include various factors that hinder the effective implementation and execution of CQI processes [ 36 , 86 , 87 , 88 , 89 ]. Structural dimension barriers of CQI arise from the organization structure, process, and systems that can impede the effective implementation and sustainability of CQI [ 36 , 85 , 86 , 87 , 88 ]. Strategic dimension barriers are, for example, the inability to select proper CQI goals and failure to integrate CQI into organizational planning and goals [ 36 , 85 , 86 , 87 , 88 , 90 ].
Facilitators are also grouped to cultural, structural, technical, and strategic dimensions to provide solutions to CQI barriers. Cultural challenges were addressed by developing a group culture to CQI and other rewards [ 39 , 41 , 80 , 85 , 86 , 87 , 90 , 91 , 92 ]. Technical facilitators are pivotal to improving technical barriers [ 39 , 42 , 53 , 69 , 86 , 90 , 91 ]. Structural-related facilitators are related to improving communication, infrastructure, and systems [ 86 , 92 , 93 ]. Strategic dimension facilitators include strengthening leadership and improving decision-making skills [ 43 , 53 , 67 , 86 , 87 , 92 , 94 , 95 ] (Table 2 ).
Impact of continuous quality improvement
Continuous quality improvement initiatives can significantly impact the quality of healthcare in a wide range of health areas, focusing on improving structure, the health service delivery process and improving client wellbeing and reducing mortality.
Structure components
These are health leadership, financing, workforce, technology, and equipment and supplies. CQI has improved planning, monitoring and evaluation [ 48 , 53 ], and leadership and planning [ 48 ], indicating improvement in leadership perspectives. Implementing CQI in primary health care (PHC) settings has shown potential for maintaining or reducing operation costs [ 67 ]. Findings from another study indicate that the costs associated with implementing CQI interventions per facility ranged from approximately $2,000 to $10,500 per year, with an average cost of approximately $10 to $60 per admitted client [ 57 ]. However, based on model predictions, the average cost savings after implementing CQI were estimated to be $5430 [ 31 ]. CQI can also be applied to health workforce development [ 32 ]. CQI in the institutional system improved medical education [ 66 , 96 , 97 ], human resources management [ 53 ], motivated staffs [ 76 ], and increased staff health awareness [ 69 ], while concerns raised about CQI impartiality, independence, and public accountability [ 96 ]. Regarding health technology, CQI also improved registration and documentation [ 48 , 53 , 98 ]. Furthermore, the CQI initiatives increased cleanliness [ 54 ] and improved logistics, supplies, and equipment [ 48 , 53 , 68 ].
Process and output components
The process component focuses on the activities and actions involved in delivering healthcare services.
Service delivery
CQI interventions improved service delivery [ 53 , 56 , 99 ], particularly a significant 18% increase in the overall quality of service performance [ 48 ], improved patient counselling, adherence to appropriate procedures, and infection prevention [ 48 , 68 ], and optimised workflow [ 52 ].
Coordination and collaboration
CQI initiatives improved coordination and collaboration through collecting and analysing data, onsite technical support, training, supportive supervision [ 53 ] and facilitating linkages between work processes and a quality control group [ 65 ].
Patient satisfaction
The CQI initiatives increased patient satisfaction and improved quality of life by optimizing care quality management, improving the quality of clinical nursing, reducing nursing defects and enhancing the wellbeing of clients [ 54 , 76 , 100 ], although CQI was not associated with changes in adolescent and young adults’ satisfaction [ 51 ].
CQI initiatives reduced medication error reports from 16 to 6 [ 101 ], and it significantly reduced the administration of inappropriate prophylactic antibiotics [ 44 ], decreased errors in inpatient care [ 52 ], decreased the overall episiotomy rate from 44.5 to 33.3% [ 83 ], reduced the overall incidence of unplanned endotracheal extubation [ 102 ], improving appropriate use of computed tomography angiography [ 103 ], and appropriate diagnosis and treatment selection [ 47 ].
Continuity of care
CQI initiatives effectively improve continuity of care by improving client and physician interaction. For instance, provider continuity levels showed a 64% increase [ 55 ]. Modifying electronic medical record templates, scheduling, staff and parental education, standardization of work processes, and birth to 1-year age-specific incentives in post-natal follow-up care increased continuity of care to 74% in 2018 compared to baseline 13% in 2012 [ 84 ].
The CQI initiative yielded enhanced efficiency in the cardiac catheterization laboratory, as evidenced by improved punctuality in procedure starts and increased efficiency in manual sheath-pulls inside [ 78 ].

Accessibility
CQI initiatives were effective in improving accessibility in terms of increasing service coverage and utilization rate. For instance, screening for cigarettes, nutrition counselling, folate prescription, maternal care, immunization coverage [ 53 , 81 , 104 , 105 ], reducing the percentage of non-attending patients to surgery to 0.9% from the baseline 3.9% [ 43 ], increasing Chlamydia screening rates from 29 to 60% [ 45 ], increasing HIV care continuum coverage [ 51 , 59 , 60 ], increasing in the uptake of postpartum long-acting reversible contraceptive use from 6.9% at the baseline to 25.4% [ 42 ], increasing post-caesarean section prophylaxis from 36 to 89% [ 62 ], a 31% increase of kangaroo care practice [ 50 ], and increased follow-up [ 65 ]. Similarly, the QI intervention increased the quality of antenatal care by 29.3%, correct partograph use by 51.7%, and correct active third-stage labour management, a 19.6% improvement from the baseline, but not significantly associated with improvement in contraceptive service uptake [ 61 ].
Timely access
CQI interventions improved the time care provision [ 52 ], and reduced waiting time [ 62 , 74 , 76 , 106 ]. For instance, the discharge process waiting time in the emergency department decreased from 76 min to 22 min [ 79 ]. It also reduced mean postprocedural length of stay from 2.8 days to 2.0 days [ 31 ].
Acceptability
Acceptability of CQI by healthcare providers was satisfactory. For instance, 88% of the faculty, 64% of the residents, and 82% of the staff believed CQI to be useful in the healthcare clinic [ 107 ].
Outcome components
Morbidity and mortality.
CQI efforts have demonstrated better management outcomes among diabetic patients [ 40 ], patients with oral mucositis [ 71 ], and anaemic patients [ 72 ]. It has also reduced infection rate in post-caesarean Sect. [ 62 ], reduced post-peritoneal dialysis peritonitis [ 49 , 108 ], and prevented pressure ulcers [ 70 ]. It is explained by peritonitis incidence from once every 40.1 patient months at baseline to once every 70.8 patient months after CQI [ 49 ] and a 63% reduction in pressure ulcer prevalence within 2 years from 2008 to 2010 [ 70 ]. Furthermore, CQI initiatives significantly reduced in-hospital deaths [ 31 ] and increased patient survival rates [ 108 ]. Figure 2 displays the overall process of the CQI implementations.
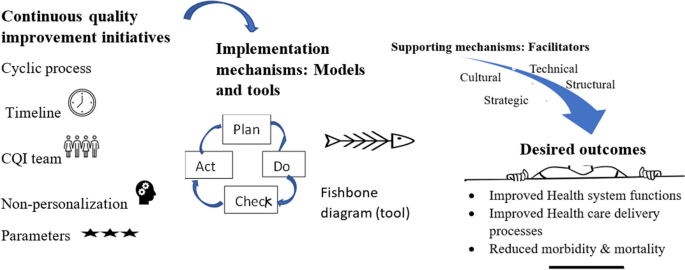
The overall mechanisms of continuous quality improvement implementation
In this review, we examined the fundamental concepts and principles underlying CQI, the factors that either hinder or assist in its successful application and implementation, and the purpose of CQI in enhancing quality of care across various health issues.
Our findings have brought attention to the application and implementation of CQI, emphasizing its underlying concepts and principles, as evident in the existing literature [ 31 , 32 , 33 , 34 , 35 , 36 , 39 , 40 , 43 , 45 , 46 ]. Continuous quality improvement has shared with the principles of continuous improvement, such as a customer-driven focus, effective leadership, active participation of individuals, a process-oriented approach, systematic implementation, emphasis on design improvement and prevention, evidence-based decision-making, and fostering partnership [ 5 ]. Moreover, Deming’s 14 principles laid the foundation for CQI principles [ 109 ]. These principles have been adapted and put into practice in various ways: ten [ 19 ] and five [ 38 ] principles in hospitals, five principles for capacity building [ 38 ], and two principles for medication error prevention [ 41 ]. As a principle, the application of CQI can be process-focused [ 8 , 19 ] or impact-focused [ 38 ]. Impact-focused CQI focuses on achieving specific outcomes or impacts, whereas process-focused CQI prioritizes and improves the underlying processes and systems. These principles complement each other and can be utilized based on the objectives of quality improvement initiatives in healthcare settings. Overall, CQI is an ongoing educational process that requires top management’s involvement, demands coordination across departments, encourages the incorporation of views beyond clinical area, and provides non-judgemental evidence based on objective data [ 110 ].
The current review recognized that it was not easy to implement CQI. It requires reasonable utilization of various models and tools. The application of each tool can be varied based on the studied health problem and the purpose of CQI initiative [ 111 ], varied in context, content, structure, and usability [ 112 ]. Additionally, overcoming the cultural, technical, structural, and strategic-related barriers. These barriers have emerged from clinical staff, managers, and health systems perspectives. Of the cultural obstacles, staff non-involvement, resistance to change, and reluctance to report error were staff-related. In contrast, others, such as the absence of celebration for success and hierarchical and rational culture, may require staff and manager involvement. Staff members may exhibit reluctance in reporting errors due to various cultural factors, including lack of trust, hierarchical structures, fear of retribution, and a blame-oriented culture. These challenges pose obstacles to implementing standardized CQI practices, as observed, for instance, in community pharmacy settings [ 85 ]. The hierarchical culture, characterized by clearly defined levels of power, authority, and decision-making, posed challenges to implementing CQI initiatives in public health [ 41 , 86 ]. Although rational culture, a type of organizational culture, emphasizes logical thinking and rational decision-making, it can also create challenges for CQI implementation [ 41 , 86 ] because hierarchical and rational cultures, which emphasize bureaucratic norms and narrow definitions of achievement, were found to act as barriers to the implementation of CQI [ 86 ]. These could be solved by developing a shared mindset and collective commitment, establishing a shared purpose, developing group norms, and cultivating psychological preparedness among staff, managers, and clients to implement and sustain CQI initiatives. Furthermore, reversing cultural-related barriers necessitates cultural-related solutions: development of a culture and group culture to CQI [ 41 , 86 ], positive comprehensive perception [ 91 ], commitment [ 85 ], involving patients, families, leaders, and staff [ 39 , 92 ], collaborating for a common goal [ 80 , 86 ], effective teamwork [ 86 , 87 ], and rewarding and celebrating successes [ 80 , 90 ].
The technical dimension barriers of CQI can include inadequate capitalization of a project and insufficient support for CQI facilitators and data entry managers [ 36 ], immature electronic medical records or poor information systems [ 36 , 86 ], and the lack of training and skills [ 86 , 87 , 88 ]. These challenges may cause the CQI team to rely on outdated information and technologies. The presence of barriers on the technical dimension may challenge the solid foundation of CQI expertise among staff, the ability to recognize opportunities for improvement, a comprehensive understanding of how services are produced and delivered, and routine use of expertise in daily work. Addressing these technical barriers requires knowledge creation activities (training, seminar, and education) [ 39 , 42 , 53 , 69 , 86 , 90 , 91 ], availability of quality data [ 86 ], reliable information [ 92 ], and a manual-online hybrid reporting system [ 85 ].
Structural dimension barriers of CQI include inadequate communication channels and lack of standardized process, specifically weak physician-to-physician synergies [ 36 ], lack of mechanisms for disseminating knowledge and limited use of communication mechanisms [ 86 ]. Lack of communication mechanism endangers sharing ideas and feedback among CQI teams, leading to misunderstandings, limited participation and misinterpretations, and a lack of learning [ 113 ]. Knowledge translation facilitates the co-production of research, subsequent diffusion of knowledge, and the developing stakeholder’s capacity and skills [ 114 ]. Thus, the absence of a knowledge translation mechanism may cause missed opportunities for learning, inefficient problem-solving, and limited creativity. To overcome these challenges, organizations should establish effective communication and information systems [ 86 , 93 ] and learning systems [ 92 ]. Though CQI and knowledge translation have interacted with each other, it is essential to recognize that they are distinct. CQI focuses on process improvement within health care systems, aiming to optimize existing processes, reduce errors, and enhance efficiency.
In contrast, knowledge translation bridges the gap between research evidence and clinical practice, translating research findings into actionable knowledge for practitioners. While both CQI and knowledge translation aim to enhance health care quality and patient outcomes, they employ different strategies: CQI utilizes tools like Plan-Do-Study-Act cycles and statistical process control, while knowledge translation involves knowledge synthesis and dissemination. Additionally, knowledge translation can also serve as a strategy to enhance CQI. Both concepts share the same principle: continuous improvement is essential for both. Therefore, effective strategies on the structural dimension may build efficient and effective steering councils, information systems, and structures to diffuse learning throughout the organization.
Strategic factors, such as goals, planning, funds, and resources, determine the overall purpose of CQI initiatives. Specific barriers were improper goals and poor planning [ 36 , 86 , 88 ], fragmentation of quality assurance policies [ 87 ], inadequate reinforcement to staff [ 36 , 90 ], time constraints [ 85 , 86 ], resource inadequacy [ 86 ], and work overload [ 86 ]. These barriers can be addressed through strengthening leadership [ 86 , 87 ], CQI-based mentoring [ 94 ], periodic monitoring, supportive supervision and coaching [ 43 , 53 , 87 , 92 , 95 ], participation, empowerment, and accountability [ 67 ], involving all stakeholders in decision-making [ 86 , 87 ], a provider-payer partnership [ 64 ], and compensating staff for after-hours meetings on CQI [ 85 ]. The strategic dimension, characterized by a strategic plan and integrated CQI efforts, is devoted to processes that are central to achieving strategic priorities. Roles and responsibilities are defined in terms of integrated strategic and quality-related goals [ 115 ].
The utmost goal of CQI has been to improve the quality of care, which is usually revealed by structure, process, and outcome. After resolving challenges and effectively using tools and running models, the goal of CQI reflects the ultimate reason and purpose of its implementation. First, effectively implemented CQI initiatives can improve leadership, health financing, health workforce development, health information technology, and availability of supplies as the building blocks of a health system [ 31 , 48 , 53 , 68 , 98 ]. Second, effectively implemented CQI initiatives improved care delivery process (counselling, adherence with standards, coordination, collaboration, and linkages) [ 48 , 53 , 65 , 68 ]. Third, the CQI can improve outputs of healthcare delivery, such as satisfaction, accessibility (timely access, utilization), continuity of care, safety, efficiency, and acceptability [ 52 , 54 , 55 , 76 , 78 ]. Finally, the effectiveness of the CQI initiatives has been tested in enhancing responses related to key aspects of the HIV response, maternal and child health, non-communicable disease control, and others (e.g., surgery and peritonitis). However, it is worth noting that CQI initiative has not always been effective. For instance, CQI using a two- to nine-times audit cycle model through systems assessment tools did not bring significant change to increase syphilis testing performance [ 116 ]. This study was conducted within the context of Aboriginal and Torres Strait Islander people’s primary health care settings. Notably, ‘the clinics may not have consistently prioritized syphilis testing performance in their improvement strategies, as facilitated by the CQI program’ [ 116 ]. Additionally, by applying CQI-based mentoring, uptake of facility-based interventions was not significantly improved, though it was effective in increasing community health worker visits during pregnancy and the postnatal period, knowledge about maternal and child health and exclusive breastfeeding practice, and HIV disclosure status [ 117 ]. The study conducted in South Africa revealed no significant association between the coverage of facility-based interventions and Continuous Quality Improvement (CQI) implementation. This lack of association was attributed to the already high antenatal and postnatal attendance rates in both control and intervention groups at baseline, leaving little room for improvement. Additionally, the coverage of HIV interventions remained consistently high throughout the study period [ 117 ].
Regarding health care and policy implications, CQI has played a vital role in advancing PHC and fostering the realization of UHC goals worldwide. The indicators found in Donabedian’s framework that are positively influenced by CQI efforts are comparable to those included in the PHC performance initiative’s conceptual framework [ 29 , 118 , 119 ]. It is clearly explained that PHC serves as the roadmap to realizing the vision of UHC [ 120 , 121 ]. Given these circumstances, implementing CQI can contribute to the achievement of PHC principles and the objectives of UHC. For instance, by implementing CQI methods, countries have enhanced the accessibility, affordability, and quality of PHC services, leading to better health outcomes for their populations. CQI has facilitated identifying and resolving healthcare gaps and inefficiencies, enabling countries to optimize resource allocation and deliver more effective and patient-centered care. However, it is crucial to recognize that the successful implementation of Continuous Quality Improvement (CQI) necessitates optimizing the duration of each cycle, understanding challenges and barriers that extend beyond the health system and settings, and acknowledging that its effectiveness may be compromised if these challenges are not adequately addressed.
Despite abundant literature, there are still gaps regarding the relationship between CQI and other dimensions within the healthcare system. No studies have examined the impact of CQI initiatives on catastrophic health expenditure, effective service coverage, patient-centredness, comprehensiveness, equity, health security, and responsiveness.
Limitations
In conducting this review, it has some limitations to consider. Firstly, only articles published in English were included, which may introduce the exclusion of relevant non-English articles. Additionally, as this review follows a scoping methodology, the focus is on synthesising available evidence rather than critically evaluating or scoring the quality of the included articles.
Continuous quality improvement is investigated as a continuous and ongoing intervention, where the implementation time can vary across different cycles. The CQI team and implementation timelines were critical elements of CQI in different models. Among the commonly used approaches, the PDSA or PDCA is frequently employed. In most CQI models, a wide range of tools, nineteen tools, are commonly utilized to support the improvement process. Cultural, technical, structural, and strategic barriers and facilitators are significant in implementing CQI initiatives. Implementing the CQI initiative aims to improve health system blocks, enhance health service delivery process and output, and ultimately prevent morbidity and reduce mortality. For future researchers, considering that CQI is context-dependent approach, conducting scale-up implementation research about catastrophic health expenditure, effective service coverage, patient-centredness, comprehensiveness, equity, health security, and responsiveness across various settings and health issues would be valuable.
Availability of data and materials
The data used and/or analyzed during the current study are available in this manuscript and/or the supplementary file.
Shewhart WA, Deming WE. Memoriam: Walter A. Shewhart, 1891–1967. Am Stat. 1967;21(2):39–40.
Article Google Scholar
Shewhart WA. Statistical method from the viewpoint of quality control. New York: Dover; 1986. ISBN 978-0486652320. OCLC 13822053. Reprint. Originally published: Washington, DC: Graduate School of the Department of Agriculture, 1939.
Moen R, editor Foundation and History of the PDSA Cycle. Asian network for quality conference Tokyo. https://www.deming.org/sites/default/files/pdf/2015/PDSA_History_Ron_MoenPdf . 2009.
Kuperman G, James B, Jacobsen J, Gardner RM. Continuous quality improvement applied to medical care: experiences at LDS hospital. Med Decis Making. 1991;11(4suppl):S60–65.
Article CAS PubMed Google Scholar
Singh J, Singh H. Continuous improvement philosophy–literature review and directions. Benchmarking: An International Journal. 2015;22(1):75–119.
Goldstone J. Presidential address: Sony, Porsche, and vascular surgery in the 21st century. J Vasc Surg. 1997;25(2):201–10.
Radawski D. Continuous quality improvement: origins, concepts, problems, and applications. J Physician Assistant Educ. 1999;10(1):12–6.
Shortell SM, O’Brien JL, Carman JM, Foster RW, Hughes E, Boerstler H, et al. Assessing the impact of continuous quality improvement/total quality management: concept versus implementation. Health Serv Res. 1995;30(2):377.
CAS PubMed PubMed Central Google Scholar
Lohr K. Quality of health care: an introduction to critical definitions, concepts, principles, and practicalities. Striving for quality in health care. 1991.
Berwick DM. The clinical process and the quality process. Qual Manage Healthc. 1992;1(1):1–8.
Article CAS Google Scholar
Gift B. On the road to TQM. Food Manage. 1992;27(4):88–9.
CAS PubMed Google Scholar
Greiner A, Knebel E. The core competencies needed for health care professionals. health professions education: A bridge to quality. 2003:45–73.
McCalman J, Bailie R, Bainbridge R, McPhail-Bell K, Percival N, Askew D et al. Continuous quality improvement and comprehensive primary health care: a systems framework to improve service quality and health outcomes. Front Public Health. 2018:6 (76):1–6.
Sheingold BH, Hahn JA. The history of healthcare quality: the first 100 years 1860–1960. Int J Afr Nurs Sci. 2014;1:18–22.
Google Scholar
Donabedian A. Evaluating the quality of medical care. Milbank Q. 1966;44(3):166–206.
Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US). 2001. 2, Improving the 21st-century Health Care System. Available from: https://www.ncbi.nlm.nih.gov/books/NBK222265/ .
Rubinstein A, Barani M, Lopez AS. Quality first for effective universal health coverage in low-income and middle-income countries. Lancet Global Health. 2018;6(11):e1142–1143.
Article PubMed Google Scholar
Agency for Healthcare Reserach and Quality. Quality Improvement and monitoring at your fingertips USA,: Agency for Healthcare Reserach and Quality. 2022. Available from: https://qualityindicators.ahrq.gov/ .
Anderson CA, Cassidy B, Rivenburgh P. Implementing continuous quality improvement (CQI) in hospitals: lessons learned from the International Quality Study. Qual Assur Health Care. 1991;3(3):141–6.
Gardner K, Mazza D. Quality in general practice - definitions and frameworks. Aust Fam Physician. 2012;41(3):151–4.
PubMed Google Scholar
Loper AC, Jensen TM, Farley AB, Morgan JD, Metz AJ. A systematic review of approaches for continuous quality improvement capacity-building. J Public Health Manage Pract. 2022;28(2):E354.
Hill JE, Stephani A-M, Sapple P, Clegg AJ. The effectiveness of continuous quality improvement for developing professional practice and improving health care outcomes: a systematic review. Implement Sci. 2020;15(1):1–14.
Candas B, Jobin G, Dubé C, Tousignant M, Abdeljelil AB, Grenier S, et al. Barriers and facilitators to implementing continuous quality improvement programs in colonoscopy services: a mixed methods systematic review. Endoscopy Int Open. 2016;4(02):E118–133.
Peters MD, Marnie C, Colquhoun H, Garritty CM, Hempel S, Horsley T, et al. Scoping reviews: reinforcing and advancing the methodology and application. Syst Reviews. 2021;10(1):1–6.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
McGowan J, Straus S, Moher D, Langlois EV, O’Brien KK, Horsley T, et al. Reporting scoping reviews—PRISMA ScR extension. J Clin Epidemiol. 2020;123:177–9.
Donabedian A. Explorations in quality assessment and monitoring: the definition of quality and approaches to its assessment. Health Administration Press, Ann Arbor. 1980;1.
World Health Organization. Operational framework for primary health care: transforming vision into action. Geneva: World Health Organization and the United Nations Children’s Fund (UNICEF); 2020 [updated 14 December 2020; cited 2023 Nov Oct 17]. Available from: https://www.who.int/publications/i/item/9789240017832 .
The Joanna Briggs Institute. The Joanna Briggs Institute Reviewers’ Manual :2014 edition. Australia: The Joanna Briggs Institute. 2014:88–91.
Rihal CS, Kamath CC, Holmes DR Jr, Reller MK, Anderson SS, McMurtry EK, et al. Economic and clinical outcomes of a physician-led continuous quality improvement intervention in the delivery of percutaneous coronary intervention. Am J Manag Care. 2006;12(8):445–52.
Ade-Oshifogun JB, Dufelmeier T. Prevention and Management of Do not return notices: a quality improvement process for Supplemental staffing nursing agencies. Nurs Forum. 2012;47(2):106–12.
Rubenstein L, Khodyakov D, Hempel S, Danz M, Salem-Schatz S, Foy R, et al. How can we recognize continuous quality improvement? Int J Qual Health Care. 2014;26(1):6–15.
O’Neill SM, Hempel S, Lim YW, Danz MS, Foy R, Suttorp MJ, et al. Identifying continuous quality improvement publications: what makes an improvement intervention ‘CQI’? BMJ Qual Saf. 2011;20(12):1011–9.
Article PubMed PubMed Central Google Scholar
Sibthorpe B, Gardner K, McAullay D. Furthering the quality agenda in Aboriginal community controlled health services: understanding the relationship between accreditation, continuous quality improvement and national key performance indicator reporting. Aust J Prim Health. 2016;22(4):270–5.
Bennett CL, Crane JM. Quality improvement efforts in oncology: are we ready to begin? Cancer Invest. 2001;19(1):86–95.
VanValkenburgh DA. Implementing continuous quality improvement at the facility level. Adv Ren Replace Ther. 2001;8(2):104–13.
Loper AC, Jensen TM, Farley AB, Morgan JD, Metz AJ. A systematic review of approaches for continuous quality improvement capacity-building. J Public Health Manage Practice. 2022;28(2):E354–361.
Ryan M. Achieving and sustaining quality in healthcare. Front Health Serv Manag. 2004;20(3):3–11.
Nicolucci A, Allotta G, Allegra G, Cordaro G, D’Agati F, Di Benedetto A, et al. Five-year impact of a continuous quality improvement effort implemented by a network of diabetes outpatient clinics. Diabetes Care. 2008;31(1):57–62.
Wakefield BJ, Blegen MA, Uden-Holman T, Vaughn T, Chrischilles E, Wakefield DS. Organizational culture, continuous quality improvement, and medication administration error reporting. Am J Med Qual. 2001;16(4):128–34.
Sori DA, Debelew GT, Degefa LS, Asefa Z. Continuous quality improvement strategy for increasing immediate postpartum long-acting reversible contraceptive use at Jimma University Medical Center, Jimma, Ethiopia. BMJ Open Qual. 2023;12(1):e002051.
Roche B, Robin C, Deleaval PJ, Marti MC. Continuous quality improvement in ambulatory surgery: the non-attending patient. Ambul Surg. 1998;6(2):97–100.
O’Connor JB, Sondhi SS, Mullen KD, McCullough AJ. A continuous quality improvement initiative reduces inappropriate prescribing of prophylactic antibiotics for endoscopic procedures. Am J Gastroenterol. 1999;94(8):2115–21.
Ursu A, Greenberg G, McKee M. Continuous quality improvement methodology: a case study on multidisciplinary collaboration to improve chlamydia screening. Fam Med Community Health. 2019;7(2):e000085.
Quick B, Nordstrom S, Johnson K. Using continuous quality improvement to implement evidence-based medicine. Lippincotts Case Manag. 2006;11(6):305–15 ( quiz 16 – 7 ).
Oyeledun B, Phillips A, Oronsaye F, Alo OD, Shaffer N, Osibo B, et al. The effect of a continuous quality improvement intervention on retention-in-care at 6 months postpartum in a PMTCT Program in Northern Nigeria: results of a cluster randomized controlled study. J Acquir Immune Defic Syndr. 2017;75(Suppl 2):S156–164.
Nyengerai T, Phohole M, Iqaba N, Kinge CW, Gori E, Moyo K, et al. Quality of service and continuous quality improvement in voluntary medical male circumcision programme across four provinces in South Africa: longitudinal and cross-sectional programme data. PLoS ONE. 2021;16(8):e0254850.
Article CAS PubMed PubMed Central Google Scholar
Wang J, Zhang H, Liu J, Zhang K, Yi B, Liu Y, et al. Implementation of a continuous quality improvement program reduces the occurrence of peritonitis in PD. Ren Fail. 2014;36(7):1029–32.
Stikes R, Barbier D. Applying the plan-do-study-act model to increase the use of kangaroo care. J Nurs Manag. 2013;21(1):70–8.
Wagner AD, Mugo C, Bluemer-Miroite S, Mutiti PM, Wamalwa DC, Bukusi D, et al. Continuous quality improvement intervention for adolescent and young adult HIV testing services in Kenya improves HIV knowledge. AIDS. 2017;31(Suppl 3):S243–252.
Le RD, Melanson SE, Santos KS, Paredes JD, Baum JM, Goonan EM, et al. Using lean principles to optimise inpatient phlebotomy services. J Clin Pathol. 2014;67(8):724–30.
Manyazewal T, Mekonnen A, Demelew T, Mengestu S, Abdu Y, Mammo D, et al. Improving immunization capacity in Ethiopia through continuous quality improvement interventions: a prospective quasi-experimental study. Infect Dis Poverty. 2018;7:7.
Kamiya Y, Ishijma H, Hagiwara A, Takahashi S, Ngonyani HAM, Samky E. Evaluating the impact of continuous quality improvement methods at hospitals in Tanzania: a cluster-randomized trial. Int J Qual Health Care. 2017;29(1):32–9.
Kibbe DC, Bentz E, McLaughlin CP. Continuous quality improvement for continuity of care. J Fam Pract. 1993;36(3):304–8.
Adrawa N, Ongiro S, Lotee K, Seret J, Adeke M, Izudi J. Use of a context-specific package to increase sputum smear monitoring among people with pulmonary tuberculosis in Uganda: a quality improvement study. BMJ Open Qual. 2023;12(3):1–6.
Hunt P, Hunter SB, Levan D. Continuous quality improvement in substance abuse treatment facilities: how much does it cost? J Subst Abuse Treat. 2017;77:133–40.
Azadeh A, Ameli M, Alisoltani N, Motevali Haghighi S. A unique fuzzy multi-control approach for continuous quality improvement in a radio therapy department. Qual Quantity. 2016;50(6):2469–93.
Memiah P, Tlale J, Shimabale M, Nzyoka S, Komba P, Sebeza J, et al. Continuous quality improvement (CQI) institutionalization to reach 95:95:95 HIV targets: a multicountry experience from the Global South. BMC Health Serv Res. 2021;21(1):711.
Yapa HM, De Neve JW, Chetty T, Herbst C, Post FA, Jiamsakul A, et al. The impact of continuous quality improvement on coverage of antenatal HIV care tests in rural South Africa: results of a stepped-wedge cluster-randomised controlled implementation trial. PLoS Med. 2020;17(10):e1003150.
Dadi TL, Abebo TA, Yeshitla A, Abera Y, Tadesse D, Tsegaye S, et al. Impact of quality improvement interventions on facility readiness, quality and uptake of maternal and child health services in developing regions of Ethiopia: a secondary analysis of programme data. BMJ Open Qual. 2023;12(4):e002140.
Weinberg M, Fuentes JM, Ruiz AI, Lozano FW, Angel E, Gaitan H, et al. Reducing infections among women undergoing cesarean section in Colombia by means of continuous quality improvement methods. Arch Intern Med. 2001;161(19):2357–65.
Andreoni V, Bilak Y, Bukumira M, Halfer D, Lynch-Stapleton P, Perez C. Project management: putting continuous quality improvement theory into practice. J Nurs Care Qual. 1995;9(3):29–37.
Balfour ME, Zinn TE, Cason K, Fox J, Morales M, Berdeja C, et al. Provider-payer partnerships as an engine for continuous quality improvement. Psychiatric Serv. 2018;69(6):623–5.
Agurto I, Sandoval J, De La Rosa M, Guardado ME. Improving cervical cancer prevention in a developing country. Int J Qual Health Care. 2006;18(2):81–6.
Anderson CI, Basson MD, Ali M, Davis AT, Osmer RL, McLeod MK, et al. Comprehensive multicenter graduate surgical education initiative incorporating entrustable professional activities, continuous quality improvement cycles, and a web-based platform to enhance teaching and learning. J Am Coll Surg. 2018;227(1):64–76.
Benjamin S, Seaman M. Applying continuous quality improvement and human performance technology to primary health care in Bahrain. Health Care Superv. 1998;17(1):62–71.
Byabagambi J, Marks P, Megere H, Karamagi E, Byakika S, Opio A, et al. Improving the quality of voluntary medical male circumcision through use of the continuous quality improvement approach: a pilot in 30 PEPFAR-Supported sites in Uganda. PLoS ONE. 2015;10(7):e0133369.
Hogg S, Roe Y, Mills R. Implementing evidence-based continuous quality improvement strategies in an urban Aboriginal Community Controlled Health Service in South East Queensland: a best practice implementation pilot. JBI Database Syst Rev Implement Rep. 2017;15(1):178–87.
Hopper MB, Morgan S. Continuous quality improvement initiative for pressure ulcer prevention. J Wound Ostomy Cont Nurs. 2014;41(2):178–80.
Ji J, Jiang DD, Xu Z, Yang YQ, Qian KY, Zhang MX. Continuous quality improvement of nutrition management during radiotherapy in patients with nasopharyngeal carcinoma. Nurs Open. 2021;8(6):3261–70.
Chen M, Deng JH, Zhou FD, Wang M, Wang HY. Improving the management of anemia in hemodialysis patients by implementing the continuous quality improvement program. Blood Purif. 2006;24(3):282–6.
Reeves S, Matney K, Crane V. Continuous quality improvement as an ideal in hospital practice. Health Care Superv. 1995;13(4):1–12.
Barton AJ, Danek G, Johns P, Coons M. Improving patient outcomes through CQI: vascular access planning. J Nurs Care Qual. 1998;13(2):77–85.
Buttigieg SC, Gauci D, Dey P. Continuous quality improvement in a Maltese hospital using logical framework analysis. J Health Organ Manag. 2016;30(7):1026–46.
Take N, Byakika S, Tasei H, Yoshikawa T. The effect of 5S-continuous quality improvement-total quality management approach on staff motivation, patients’ waiting time and patient satisfaction with services at hospitals in Uganda. J Public Health Afr. 2015;6(1):486.
PubMed PubMed Central Google Scholar
Jacobson GH, McCoin NS, Lescallette R, Russ S, Slovis CM. Kaizen: a method of process improvement in the emergency department. Acad Emerg Med. 2009;16(12):1341–9.
Agarwal S, Gallo J, Parashar A, Agarwal K, Ellis S, Khot U, et al. Impact of lean six sigma process improvement methodology on cardiac catheterization laboratory efficiency. Catheter Cardiovasc Interv. 2015;85:S119.
Rahul G, Samanta AK, Varaprasad G A Lean Six Sigma approach to reduce overcrowding of patients and improving the discharge process in a super-specialty hospital. In 2020 International Conference on System, Computation, Automation and Networking (ICSCAN) 2020 July 3 (pp. 1-6). IEEE
Patel J, Nattabi B, Long R, Durey A, Naoum S, Kruger E, et al. The 5 C model: A proposed continuous quality improvement framework for volunteer dental services in remote Australian Aboriginal communities. Community Dent Oral Epidemiol. 2023;51(6):1150–8.
Van Acker B, McIntosh G, Gudes M. Continuous quality improvement techniques enhance HMO members’ immunization rates. J Healthc Qual. 1998;20(2):36–41.
Horine PD, Pohjala ED, Luecke RW. Healthcare financial managers and CQI. Healthc Financ Manage. 1993;47(9):34.
Reynolds JL. Reducing the frequency of episiotomies through a continuous quality improvement program. CMAJ. 1995;153(3):275–82.
Bunik M, Galloway K, Maughlin M, Hyman D. First five quality improvement program increases adherence and continuity with well-child care. Pediatr Qual Saf. 2021;6(6):e484.
Boyle TA, MacKinnon NJ, Mahaffey T, Duggan K, Dow N. Challenges of standardized continuous quality improvement programs in community pharmacies: the case of SafetyNET-Rx. Res Social Adm Pharm. 2012;8(6):499–508.
Price A, Schwartz R, Cohen J, Manson H, Scott F. Assessing continuous quality improvement in public health: adapting lessons from healthcare. Healthc Policy. 2017;12(3):34–49.
Gage AD, Gotsadze T, Seid E, Mutasa R, Friedman J. The influence of continuous quality improvement on healthcare quality: a mixed-methods study from Zimbabwe. Soc Sci Med. 2022;298:114831.
Chan YC, Ho SJ. Continuous quality improvement: a survey of American and Canadian healthcare executives. Hosp Health Serv Adm. 1997;42(4):525–44.
Balas EA, Puryear J, Mitchell JA, Barter B. How to structure clinical practice guidelines for continuous quality improvement? J Med Syst. 1994;18(5):289–97.
ElChamaa R, Seely AJE, Jeong D, Kitto S. Barriers and facilitators to the implementation and adoption of a continuous quality improvement program in surgery: a case study. J Contin Educ Health Prof. 2022;42(4):227–35.
Candas B, Jobin G, Dubé C, Tousignant M, Abdeljelil A, Grenier S, et al. Barriers and facilitators to implementing continuous quality improvement programs in colonoscopy services: a mixed methods systematic review. Endoscopy Int Open. 2016;4(2):E118–133.
Brandrud AS, Schreiner A, Hjortdahl P, Helljesen GS, Nyen B, Nelson EC. Three success factors for continual improvement in healthcare: an analysis of the reports of improvement team members. BMJ Qual Saf. 2011;20(3):251–9.
Lee S, Choi KS, Kang HY, Cho W, Chae YM. Assessing the factors influencing continuous quality improvement implementation: experience in Korean hospitals. Int J Qual Health Care. 2002;14(5):383–91.
Horwood C, Butler L, Barker P, Phakathi S, Haskins L, Grant M, et al. A continuous quality improvement intervention to improve the effectiveness of community health workers providing care to mothers and children: a cluster randomised controlled trial in South Africa. Hum Resour Health. 2017;15(1):39.
Hyrkäs K, Lehti K. Continuous quality improvement through team supervision supported by continuous self-monitoring of work and systematic patient feedback. J Nurs Manag. 2003;11(3):177–88.
Akdemir N, Peterson LN, Campbell CM, Scheele F. Evaluation of continuous quality improvement in accreditation for medical education. BMC Med Educ. 2020;20(Suppl 1):308.
Barzansky B, Hunt D, Moineau G, Ahn D, Lai CW, Humphrey H, et al. Continuous quality improvement in an accreditation system for undergraduate medical education: benefits and challenges. Med Teach. 2015;37(11):1032–8.
Gaylis F, Nasseri R, Salmasi A, Anderson C, Mohedin S, Prime R, et al. Implementing continuous quality improvement in an integrated community urology practice: lessons learned. Urology. 2021;153:139–46.
Gaga S, Mqoqi N, Chimatira R, Moko S, Igumbor JO. Continuous quality improvement in HIV and TB services at selected healthcare facilities in South Africa. South Afr J HIV Med. 2021;22(1):1202.
Wang F, Yao D. Application effect of continuous quality improvement measures on patient satisfaction and quality of life in gynecological nursing. Am J Transl Res. 2021;13(6):6391–8.
Lee SB, Lee LL, Yeung RS, Chan J. A continuous quality improvement project to reduce medication error in the emergency department. World J Emerg Med. 2013;4(3):179–82.
Chiang AA, Lee KC, Lee JC, Wei CH. Effectiveness of a continuous quality improvement program aiming to reduce unplanned extubation: a prospective study. Intensive Care Med. 1996;22(11):1269–71.
Chinnaiyan K, Al-Mallah M, Goraya T, Patel S, Kazerooni E, Poopat C, et al. Impact of a continuous quality improvement initiative on appropriate use of coronary CT angiography: results from a multicenter, statewide registry, the advanced cardiovascular imaging consortium (ACIC). J Cardiovasc Comput Tomogr. 2011;5(4):S29–30.
Gibson-Helm M, Rumbold A, Teede H, Ranasinha S, Bailie R, Boyle J. A continuous quality improvement initiative: improving the provision of pregnancy care for Aboriginal and Torres Strait Islander women. BJOG: Int J Obstet Gynecol. 2015;122:400–1.
Bennett IM, Coco A, Anderson J, Horst M, Gambler AS, Barr WB, et al. Improving maternal care with a continuous quality improvement strategy: a report from the interventions to minimize preterm and low birth weight infants through continuous improvement techniques (IMPLICIT) network. J Am Board Fam Med. 2009;22(4):380–6.
Krall SP, Iv CLR, Donahue L. Effect of continuous quality improvement methods on reducing triage to thrombolytic interval for Acute myocardial infarction. Acad Emerg Med. 1995;2(7):603–9.
Swanson TK, Eilers GM. Physician and staff acceptance of continuous quality improvement. Fam Med. 1994;26(9):583–6.
Yu Y, Zhou Y, Wang H, Zhou T, Li Q, Li T, et al. Impact of continuous quality improvement initiatives on clinical outcomes in peritoneal dialysis. Perit Dial Int. 2014;34(Suppl 2):S43–48.
Schiff GD, Goldfield NI. Deming meets Braverman: toward a progressive analysis of the continuous quality improvement paradigm. Int J Health Serv. 1994;24(4):655–73.
American Hospital Association Division of Quality Resources Chicago, IL: The role of hospital leadership in the continuous improvement of patient care quality. American Hospital Association. J Healthc Qual. 1992;14(5):8–14,22.
Scriven M. The Logic and Methodology of checklists [dissertation]. Western Michigan University; 2000.
Hales B, Terblanche M, Fowler R, Sibbald W. Development of medical checklists for improved quality of patient care. Int J Qual Health Care. 2008;20(1):22–30.
Vermeir P, Vandijck D, Degroote S, Peleman R, Verhaeghe R, Mortier E, et al. Communication in healthcare: a narrative review of the literature and practical recommendations. Int J Clin Pract. 2015;69(11):1257–67.
Eljiz K, Greenfield D, Hogden A, Taylor R, Siddiqui N, Agaliotis M, et al. Improving knowledge translation for increased engagement and impact in healthcare. BMJ open Qual. 2020;9(3):e000983.
O’Brien JL, Shortell SM, Hughes EF, Foster RW, Carman JM, Boerstler H, et al. An integrative model for organization-wide quality improvement: lessons from the field. Qual Manage Healthc. 1995;3(4):19–30.
Adily A, Girgis S, D’Este C, Matthews V, Ward JE. Syphilis testing performance in Aboriginal primary health care: exploring impact of continuous quality improvement over time. Aust J Prim Health. 2020;26(2):178–83.
Horwood C, Butler L, Barker P, Phakathi S, Haskins L, Grant M, et al. A continuous quality improvement intervention to improve the effectiveness of community health workers providing care to mothers and children: a cluster randomised controlled trial in South Africa. Hum Resour Health. 2017;15:1–11.
Veillard J, Cowling K, Bitton A, Ratcliffe H, Kimball M, Barkley S, et al. Better measurement for performance improvement in low- and middle-income countries: the primary Health Care Performance Initiative (PHCPI) experience of conceptual framework development and indicator selection. Milbank Q. 2017;95(4):836–83.
Barbazza E, Kringos D, Kruse I, Klazinga NS, Tello JE. Creating performance intelligence for primary health care strengthening in Europe. BMC Health Serv Res. 2019;19(1):1006.
Assefa Y, Hill PS, Gilks CF, Admassu M, Tesfaye D, Van Damme W. Primary health care contributions to universal health coverage. Ethiopia Bull World Health Organ. 2020;98(12):894.
Van Weel C, Kidd MR. Why strengthening primary health care is essential to achieving universal health coverage. CMAJ. 2018;190(15):E463–466.
Download references
Acknowledgements
Not applicable.
The authors received no fund.
Author information
Authors and affiliations.
School of Public Health, The University of Queensland, Brisbane, Australia
Aklilu Endalamaw, Resham B Khatri, Tesfaye Setegn Mengistu, Daniel Erku & Yibeltal Assefa
College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Aklilu Endalamaw & Tesfaye Setegn Mengistu
Health Social Science and Development Research Institute, Kathmandu, Nepal
Resham B Khatri
Centre for Applied Health Economics, School of Medicine, Grifth University, Brisbane, Australia
Daniel Erku
Menzies Health Institute Queensland, Grifth University, Brisbane, Australia
International Institute for Primary Health Care in Ethiopia, Addis Ababa, Ethiopia
Eskinder Wolka & Anteneh Zewdie
You can also search for this author in PubMed Google Scholar
Contributions
AE conceptualized the study, developed the first draft of the manuscript, and managing feedbacks from co-authors. YA conceptualized the study, provided feedback, and supervised the whole processes. RBK provided feedback throughout. TSM provided feedback throughout. DE provided feedback throughout. EW provided feedback throughout. AZ provided feedback throughout. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Aklilu Endalamaw .
Ethics declarations
Ethics approval and consent to participate.
Not applicable because this research is based on publicly available articles.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Endalamaw, A., Khatri, R.B., Mengistu, T.S. et al. A scoping review of continuous quality improvement in healthcare system: conceptualization, models and tools, barriers and facilitators, and impact. BMC Health Serv Res 24 , 487 (2024). https://doi.org/10.1186/s12913-024-10828-0
Download citation
Received : 27 December 2023
Accepted : 05 March 2024
Published : 19 April 2024
DOI : https://doi.org/10.1186/s12913-024-10828-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Continuous quality improvement
- Quality of Care
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
More From Forbes
Ge aerospace reports robust 1q24 results; raise target price.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
(Photo by Jaap Arriens/NurPhoto via Getty Images)
On April 23, 2024, GE Aerospace (NYSE: GE, $161.26, Market Capitalization: $176.5 billion) reported robust 1Q24 results, with a strong beat on EPS versus consensus. It should be noted that as GE Vernova was spun off from GE on April 2, and Vernova remained a part of the consolidated company for 1Q24. The company released consolidated results for General Electric General Electric on 4/23 for 1Q24, while GE Vernova’s results were declared on 4/25. As for GE Aerospace, the company reported strong revenue growth of 15.5% YoY to $8.1 billion in 1Q24, while Profit increased 15.3% YoY to $1.5 billion. Orders of $11.0 billion increased by 34% YoY, with strength in both Commercial Engines & Services and Defense & Propulsion Technologies. GE Aerospace’s adjusted EPS (on a consolidated basis) increased to $0.92 per share in 1Q24, up 46% YoY from $0.63 per share in 1Q23. Due to the upbeat results delivered by the company, the company raised its FY24 outlook, where it expects revenue growth in lower double-digits and expects operating profit in the range of $6.2 and $6.6 billion for the year (earlier $6.0-$6.5 billion). Overall, GE’s results showed a strong operating margin strength in the commercial spares market business, which is likely to persist throughout the year. Following the results, GE stock rose by 8.3% to close at 162.62 on 4/23, indicating a positive reaction from investors.
GE Price Performance and Spin-Off Details
On April 2, General Electric spun-off GE Vernova, and the remaining company was renamed GE Aerospace. GE Vernova is now a standalone company that includes Renewable Energy and Power.
Key Data and Top 5 Shareholders
Valuation and Recommendation
We value GE Aerospace using the 2025e EV/EBITDA methodology. Our intrinsic value of $175.00 (Previously: $142.00) per share for GE Aerospace is based on the 2025e EV/ EBITDA multiple of 21.5x (at a ~9% premium to the multiple of TransDigm Group TransDigm Group and ~16% discount to the multiple of HEICO Corp). Our valuation for GE Aerospace also includes a 6.7% stake in GE Healthcare. We maintain our ‘Hold’ rating on GE Aerospace with an implied upside of 8.5% from the current market price of $161.26 on 4/25. Risks to our target price include slower than expected growth in the Aviation industry, supply chain shortages, decline in quality, and lower-than-expected time on wing improvements on LEAP engines.
GE Aerospace’s profit and revenue gains may persist on strong maintenance and new engine demand, though margins might edge lower as spare demand rises and new engine builds increase. Furthermore, Boeing’s Boeing production problems are expected to lead to a higher mix of spares as they are GE’s largest customer for margin-dilutive new engines. However, supply chain problems continued in the quarter and remained challenging for GE and the industry. GE is the market leader in narrow-body and wide-body engines, with the largest installed base. Reduced durability of new-technology narrow-body engines should keep demand for spares and overhauls on its largest fleet (CFM56) robust as the older fleet is used longer. GE has a strong portfolio in the defense business, powering US destroyers and critical combat helicopters like the Black Hawk and Apache, providing stability to the commercial business.
Samsung Is Giving Away A Free Galaxy S24 In A New Promotion
Google makes a new sale offer to pixel 8 buyers, the best reading glasses plus expert tips from an ophthalmologist.
The Company is expected to deliver revenue growth in the lower double digit range in FY24. GE Aerospace raised its earlier operating profit guidance, expecting between $6.2 and $6.6 billion for the year ($6.0-$6.5 billion earlier). Further, Adjusted EPS is forecasted to be between $3.80 and $4.05 for the year, and Free Cash Flow Flow is expected to be more than $5.0 billion (100% Conversion). Commercial Engines & Services continues to expect revenue growth of mid-to-high teens and increasing operating profit to $6.1 to $6.4 billion, up from the original guidance of $6.0 to $6.3 billion. Defense & Propulsion Technologies predicted revenue growth of mid-single-digits to high-single-digits and operating profit of $1.0 to $1.3 billion. Corporate costs are estimated at ~ $1 billion, including $600 million in expenses and $400 million in eliminations.
GE Aerospace hosted its Investor Day, outlining the company’s strategy. Its financial outlook targets $10 billion in operating profit by 2028, and its capital allocation framework authorizes a $15 billion share buy-back program. The company also raised its dividend to $0.28 per share, initiated on April 5, 2024, a 250% increase
Other Updates
• The Company repurchased ~$1.1 million common shares for $0.1 billion in 1Q24 under the company’s previously authorized $3 billion share repurchase program. The investment in GE HealthCare comprises 30.5 million shares (~ 6.7% ownership interest) on March 31, 2024. During 1Q24, the Company received total proceeds of $2.6 billion from the disposition of 31.1 million shares of GE HealthCare.
• The senior note from AerCap, which has adopted the fair value option and matures in the 4Q25, is still outstanding as of March 31, 2024.
• The Company incurred pre-tax separation costs of $0.4 billion in the quarter, primarily related to employees, establishing standalone functions and IT systems, and professional fees.
• Received an order for F414 engines to power additional KF-21 fighter jets for the Korean Air Force, continuing to build the international business, and finalized testing designs with Sikorsky Innovations for a hybrid electric vertical takeoff and landing demonstrator.
• The Company reached an agreement at the Singapore Airshow with Thai Airways for GEnx-1B engines to power its new widebody fleet of 45 Boeing 787 aircraft. It extended Cebu Pacific’s TrueChoice services agreement for its CFM56 engines. Secured a commitment from easyJet for more than 300 LEAP-1A engines and a services agreement from American Airlines American Airlines for 400 LEAP-1B engines.
• The Company announced plans to invest over $650 million in its manufacturing facilities and supply chain, including $550 million in US and international site upgrades and $100 million in the supply chain. Nearly $450 million will go towards new machines, inspection equipment, building upgrades, and new test cells and safety enhancements at 22 GE Aerospace facilities across 14 states. An additional $100 million will go to supplier partners based in the United States. In addition to the investments announced today, GE Aerospace hires over 1,000 employees for open external positions at its U.S. factories.
• GE Aerospace introduced FLIGHT DECK, the company’s lean operating model, accelerating its next stage of lean progress, ensuring focused execution, and bridging strategy to results.
Financial Overview General Electric
GE (consolidated) posted strong revenue growth of 10.8% YoY to $16.0 billion in 1Q24, compared to $14.5 billion in 1Q23, driven by an increase in all segments and Corporate. Adjusted Sales increased to $15.2 billion from $7.4 billion in 1Q23. Operating Profit (GAAP) was down by 71.3% YoY to $1.9 billion. In comparison, the operating margin was down by 3320 bps YoY to 11.6%, primarily due to a decrease in gains on retained and sold ownership interests of $5.3 billion, primarily related to its GEHC equity position and an increase in separation costs of $0.2 billion. On the other hand, operating profit (Non- GAAP) was up by 75.8% YoY to 1.5 billion from $0.9 billion in 1Q23, with the non-GAAP operating margin increasing by 380 bps YoY to 10.2%. Net income (continuing operations) was $1.5 billion, down by 75% YoY, with EPS (continuing operations) of $1.38, down 75.2% YoY. Net earnings (loss) per share was reported to be lower at $1.39 in 1Q24 against $6.71 in 1Q23; the Adjusted Earnings (loss) per share increased to $0.82 in 1Q24 Vs. $0.27 in 1Q23. Adjusted net income was $906 million, up by 206.1%, with adjusted diluted EPS of $0.82 per share (up 203.7%), which excluded the results from run-off Insurance operations, non-operating benefit income, gains (losses) on purchases and sales of business interests, gains (losses) on equity securities, restructuring costs and separation costs.
GE Aerospace
GE Aerospace’s 1Q24 performance reflects a robust start to FY24, with revenues exhibiting a commendable 15.5% YoY growth to $8.1 billion, compared to $7.0 billion in 1Q23. This growth was primarily driven by pricing, spare parts volume, and increased wide-body and defense deliveries. Further, Commercial Engines & Services revenue rose 16.8% YoY to $6.1 billion in 1Q24, followed by a 17.3% YoY rise in Defense and Propulsion Technologies revenues to $2.3 billion. Commercial Engines and Services revenue increased, primarily due to higher prices, increased commercial spare part shipments, higher services work scopes, and a favorable widebody engine mix. These increases were partially offset by an unfavorable change in the estimated profitability of long-term service agreements of $0.2 billion. Defense and Propulsion Technologies revenues increased, primarily due to 45 more Defense engine unit sales than the prior year and growth in classified development programs and services revenue, partially offset by the Defense engine mix. In 1Q24, for Commercial Engines & Services, orders of $8.3 billion increased 34% YoY, primarily from equipment growth, and revenue was up 16% YoY, with equipment growth outpacing services. In Defense & Propulsion Technologies, orders of $3.0 billion were up 34% YoY with a Defense book-to-bill of 1.1x, and revenue increased by 18% YoY, driven by growth in deliveries, pricing and classified programs. The Segment profit (Non-GAAP) was up 15.3% YoY to $1.5 billion, primarily due to benefits from higher prices and increased commercial spare part shipments. These increases in profit were partially offset by an unfavorable change in the estimated profitability of long-term service agreements of $0.2 billion, additional growth investment, and inflation in the supply chain. Segment margin remained flat YoY. Moreover, Adjusted EPS was up by 46% YoY to $0.92 per share in 1Q24, compared to $0.63 per share in 1Q23. From 2Q24, GE Aerospace will present Commercial Engines & Services and Defense & Propulsion Technologies as reportable segments. As GE Vernova was spun-off from the company, we will discuss GE Vernova’s results separately in the next report on 4/29.
A] GE Aerospace: Post-spin-off of GE Vernova, GE Aerospace operates as a standalone entity comprising GE’s aviation business. The company has become a more focused, simpler, stronger aviation franchise winning in growing aerospace & defense markets. For FY24, GE Aerospace now expects revenue growth in lower double-digits. It expects operating profit in the range of $6.2 and $6.6 billion for the year ($6.0-$6.5 billion earlier), with adjusted EPS of $3.80 - $4.05 and free cash flow greater than $5 billion. Also, the company provided a long-term outlook, where GE expects a high single-digit CAGR from 2025-2028, ~$10 billion of operating income and 100% cash flow conversion by 2028.
EV/EBITDA Valuation: We value GE Aerospace using the 2025e EV/EBITDA methodology. Our intrinsic value of $175.00 (Previously: $142.00) per share for GE Aerospace is based on the 2025e EV/ EBITDA multiple of 21.5x (at a ~9% premium to the multiple of TransDigm Group and ~16% discount to the multiple of HEICO Corp). The increase in our price factors into the company’s robust 1Q24 performance and the outlook for FY24. Our target price also factors in the 6.7 % stake in GE Healthcare (valued at market cap). We have increased our adjusted EBITDA estimate to $9 billion from $8.7 billion earlier. We have assumed net debt and non-controlling interests of $4.3 billion, to arrive at an Equity value of $192.0 billion.
Company Description
Post spin-off, GE Aerospace (NYSE: GE), earlier known as General Electric Co., is a global leader in aerospace propulsion, services, and systems, with an installed base of approximately 44,000 commercial and 26,000 military aircraft engines. With a global team of 52,000 employees, GE Aerospace is inventing the future of flight, lifting people, and safely bringing them home. The company provides jet engines and turboprops for commercial airframes, maintenance, component repair, overhaul services, replacement parts, additive machines and materials, and engineering services. From 2Q24, GE Aerospace will present Commercial Engines & Services and Defense & Propulsion Technologies as reportable segments. For FY23, GE Aerospace reported revenues of $31.8 billion.
- Editorial Standards
- Reprints & Permissions

How The Inquirer is reporting the results of Pennsylvania’s 2024 primary election
T hough Tuesday’s presidential primary is a foregone conclusion with former President Donald Trump and President Joe Biden having already secured their parties’ nominations, Pennsylvania voters will still decide nominees for several key state and congressional races.
The Inquirer’s mission in 2024 is what it has always been: to provide the most accurate and up-to-date information as possible. That includes letting you know when a race has been called by The Associated Press; providing the latest vote counts, along with contextual information to help understand those numbers; explaining the vote count as it occurs; and covering any developments that arise.
Here are some key things to know about how we’re reporting the results of the April 23 primary election, that includes primaries for President, U.S. Senate and House, State Attorney General, row offices and state General Assembly seats.
Our results come from the Associated Press and county election offices
The Inquirer’s results page is powered by data from the Associated Press. Those numbers are usually updated right after county election offices, which oversee counting, release new vote totals to its website.
Results for races across the state, including the presidential primary, are compiled by the AP through a combination of methods, including having workers across the state calling in county election results as they come in.
Elections are run by counties, which then report results to the Pennsylvania Department of State throughout the night. The state displays those results on its unofficial election returns page , but that feed often lags behind the real-time vote count in many counties. Philadelphia, for example, reports its vote totals on its own page , which is usually far ahead of the state’s compilation.
We rely on the AP to call winners
To call races, The Inquirer relies primarily on the AP, which has a long track record of accurately declaring winners in even the closest of elections.
Those race calls aren’t a projection of a likely outcome. The AP only declares a winner when it’s clear a candidate has won.
“If our race callers cannot definitively say a candidate has won, we do not engage in speculation,” the AP says in its guide to its process .
The AP said it plans to call the primary winners for these races:
•U.S. Senate
•U.S. House districts
•Attorney General
•Auditor General
•State Senate districts
•State House districts
For the race on the Philadelphia ballot that the AP does not call — the ballot question — The Inquirer will declare a winner only if it is certain of that result, based on on-the-ground reporting of the vote count and reporters’ and editors’ analysis of the voting patterns. When the result is still uncertain, our goal is to report on the results and contextualize them so readers can make sense of the numbers.
It takes time to count votes, which is why the numbers are unofficial until they’re certified three weeks after Election Day
It’s important to remember that race calls are unofficial declarations from news organizations. That doesn’t make them unreliable — the AP was 100% accurate in calling the presidential and congressional races in every state in 2020. It just means the final official result takes time.
Votes always take time to count, which is why Pennsylvania’s vote certification doesn’t occur until 20 days after Election Day.
Pennsylvania has far fewer mail ballots than in 2020, and the vote count should be significantly faster. Most votes cast this election should be counted within a few hours of polls closing. That’s partly because most votes will be cast in person, with those results reported on election night. Elections workers will begin counting mail ballots at 7 a.m., when state law allows them to start, and run their vote counts around the clock until they’re done .
The use of electronic poll books will also speed up the count.
But a small number of votes won’t be counted for days.
There will be a number of paper ballots that have to be manually adjudicated, with county elections boards deciding what to do with them. In the past, for example, officials have had to decide what to do with ballots that voters returned to the wrong county.
There are also always some votes that need to be counted by hand because of issues with the ballots themselves, such as having stray marks or coffee stains on them. There are provisional ballots, too, which counties can’t start counting until Friday.
And overseas and military ballots can arrive up to one week after Election Day if they’re postmarked in time.
We’re reporting the results based on the expected overall totals. No ‘percentage of precincts reporting.’
When we present election results, you’ll see a percentage of expected votes that have been reported. That gives a sense of how far along in the vote count we are.
Those expected vote counts come from the AP, and those estimates change throughout the night. They become more accurate as votes are counted, giving a clearer and clearer picture of how much is left. The numbers will shift, going up or down as the expected vote count is adjusted.
That doesn’t mean something nefarious is going on — it just means the AP is updating its estimate to reflect new information. If the percentage of expected votes counted suddenly goes down, for example, all that means is the AP has increased its estimated vote total.
We use that expected vote number to present each candidate’s vote share. So in the first moments after polls close, if only 1% of the expected votes are in, we won’t say that a candidate has won 50% of the vote so far — that would be misleading. Instead, we’ll tell you the candidate has won 0.5% of the expected vote so far.
One thing you won’t see: the term “precincts reporting.” In the past, when 95% or so of Pennsylvania’s votes were cast in person, knowing how many precincts had reported their in-person results was a handy way of knowing where the count stood. Now that a significant portion of votes are cast by mail, we’re using the expected vote count instead.
Correction: This story was updated to clarify that the AP’s numbers come from county election offices.
©2024 The Philadelphia Inquirer. Visit inquirer.com. Distributed by Tribune Content Agency, LLC.

Browser does not support script.
- Writing opinion articles
- Latest news
- Video and audio
- LSE News FAQs
Educational damage caused by the pandemic will mean poorer GCSE results for pupils well into the 2030s
Without a raft of equalising policies, the damaging legacy from COVID-19 school closures will be felt by generations of pupils.

The educational damage wrought by the COVID-19 pandemic will impact on children well into the 2030s, with generations of pupils set for the biggest declines in GCSE results for decades.
These are the devastating conclusions of a major new study from LSE, the University of Exeter and the University of Strathclyde. The report predicts that less than four in ten pupils in England in 2030 will achieve a grade 5 or above in English and Mathematics GCSEs – lower than the 45.3 per cent of pupils who achieved this benchmark in 2022/23.
The research, funded by the Nuffield Foundation, is the first to chart how school closures during COVID-19 hindered children’s socio-emotional and cognitive skills at age 5, 11, and 14, and predict how these will impact on future GCSE prospects and later life outcomes.
Socio-emotional skills include the ability to engage in positive social interactions, regulate emotions and maintain attention. Cognitive skills are measured by how well children perform in academic tests, reflecting maths, reading and writing skills.
The research finds that socio-emotional skills are just as important as cognitive skills for young people’s GCSE results. For example, 20 per cent of the best performing pupils in cognitive tests at age 14 but who had average socio-emotional skills fail to go on to attain five good GCSEs including English and Maths. Teenagers with strong socio-emotional skills were much more likely to achieve basic GCSEs.
A gender divide in the importance of different skills emerges in the teenage years. For boys, cognitive skills at age 14 are twice as important as socio-emotional skills in determining future GCSE prospects; for girls the opposite is true, with socio-emotional skills 50 per cent more impactful than cognitive skills.
The analysis uses the latest econometric techniques to develop a model of skill formation, based on just under 19,000 pupils in the Millennium Cohort Study. This was applied to later pupil cohorts to predict how GCSE results will be impacted by disruption from school closures during the pandemic.
Alongside an overall fall in GCSE results, the model points to a significant widening in socio-economic inequalities in GCSE results. The researchers use these results to estimate that the UK’s relative income mobility levels will decline by 12-15 per cent for generations of pupils leaving school over the next decade, a significant drop by international standards.
An international review as part of the work concludes that COVID-19 amplified long-term persistent education gaps across a range of OECD countries including the UK. Compared with most other nations, England’s pandemic response was heavily focused on academic catch-up with less emphasis on socio-emotional skills, extracurricular support, and wellbeing.
The report “A generation at risk: Rebalancing education in the post-pandemic era” was produced by Lee Elliot Major, Professor of Social Mobility at the University of Exeter; Andy Eyles; Professor Steve Machin from the Centre for Economic Performance (CEP) at the London School of Economics; and Esme Lillywhite from the University of Strathclyde. It proposes several low-cost policies with the potential to improve children’s outcomes, including:
- A national programme of trained undergraduate student tutors helping to boost the foundational skills of pupils, and enabling undergraduates to consider a career in teaching.
- Rebalancing Ofsted inspections to explicitly focus on how schools are performing for pupils from under-resourced backgrounds and credit schools excelling when serving under-resourced communities.
- Rebalancing the school calendar to improve teacher wellbeing, prevent holiday hunger, improve pupil prospects and help parents with child-care during the long summer break.
Professor of Social Mobility at the University of Exeter and LSE CEP Associate Professor Elliot Major said : “Without a raft of equalising policies, the damaging legacy from COVID-19 school closures will be felt by generations of pupils well into the next decade. Our review shows that COVID amplified long-term persistent education gaps in England and other countries.
“The policies we propose would rebalance the school system so that it supports all children irrespective of their backgrounds. A particular worry is a group of pupils who are falling significantly behind, likely to be absent from the classroom and to leave school without the basic skills needed to function and flourish in life. The decline in social mobility levels threatens to cast a long shadow over our society.”
LSE CEP Associate Andy Eyles added : “To our knowledge, this is the first time this type of analysis has been used in this way to assess the consequences of the pandemic in England. Our results suggest that to improve child outcomes, much greater emphasis is needed in schools on activities that improve both socio-emotional and cognitive skills.”
Esme Lillywhite from the University of Strathclyde and a research assistant at LSE CEP said: “Compared with most other nations, England’s pandemic response was heavily focused on academic catch-up with less emphasis on socio-emotional skills, extracurricular support, and wellbeing. Much more could be gained by closer international collaboration to learn what approaches have been promising elsewhere.”
Dr Emily Tanner, Programme Head at the Nuffield Foundation said : "The mounting evidence on the long-term impact of learning loss on young people's development shows how important it is for students to develop socio-emotional skills alongside academic learning. The insights from this report on timing and gender provide a useful basis for targeting effective interventions."
Behind the article
The Nuffield Foundation is an independent charitable trust with a mission to advance social well-being. It funds research that informs social policy, primarily in Education, Welfare, and Justice. The Nuffield Foundation is the founder and co-funder of the Nuffield Council on Bioethics, the Ada Lovelace Institute and the Nuffield Family Justice Observatory. The Foundation has funded this project, but the views expressed are those of the authors and not necessarily the Foundation.

- Notices of Funding Opportunities
- NIH RePORTER
- Co-Funding Activities
- BSSR Clinical Trials
- Reports and Publications
- OBSSR-Supported Training
- Online Training Resources
- OBSSR Connector Monthly Newsletter
- The Director’s Voice Blog
- Research Spotlights
- BSSR News and Announcements
- All Upcoming Events and Meetings
- NIH Behavioral and Social Sciences Research Festival
- NIH Matilda White Riley Behavioral and Social Sciences Honors
- OBSSR Director’s Webinar Series
- Mission and History
- BSSR Definition
- BSSR Accomplishments
- Strategic Plan
- NIH Behavioral and Social Sciences Research Coordinating Committee (BSSR-CC)
- Coordination of NIH-wide Initiatives
- Staff Directory

- News and Events
A New Model for Studying Social Isolation and Health in People with Serious Mental Illnesses
Researchers have developed a promising new framework for studying the link between social disconnection and poor physical health in people living with serious mental illnesses (SMI). Drawing on published research from animal models and data from the general population, this framework builds on existing social isolation and loneliness models by integrating insights from evolutionary and cognitive theories. This research was supported by the Office of Behavioral and Social Sciences Research and the National Institute of Mental Health.
What were the researchers studying and why?
One of the most challenging aspects of living with SMI is difficulties with social perception, motivation, and social behaviors. These difficulties can lead to social withdrawal and loneliness, outcomes that can contribute to poor heart health and early death. However, researchers have an incomplete understanding of how differences in the brain functions in people living with SMIs impact the connection between their social perception and self-reported, lived experience of social withdrawal, isolation, or loneliness.
How did the researchers conduct the study?
Researchers from Boston University and Harvard Medical School conducted a selective narrative review of studies addressing social withdrawal, isolation, loneliness, and health in SMI.
Their review highlighted evidence indicating differences in brain activity between people experiencing loneliness and those who are not, particularly in regions associated with social cognitive processes. Additionally, neuroimaging studies have shown increased activation in brain areas responsible for risk assessment among lonely individuals.
Furthermore, the researchers discussed findings suggesting that individuals experiencing loneliness, who perceive others negatively and exhibit signs of psychopathology, may misinterpret social cues, leading to social disconnection. Over time, this social disconnection can prompt a defensive response to social situations, further reducing motivation for social interaction.
What did the study results show?
Based on a synthesis of recent findings that indicate a causal relationship between loneliness and nervous system responses in the human body that cause inflammation and reduce immunity, the authors developed a testable model of the psychological and neural mechanisms of social disconnection in SMI. They hypothesize that people living with SMI are more likely to experience high levels of chronic psychological stress and therefore, more likely to experience persistently high levels of physiological inflammation. Stress and inflammation biomarkers can serve as indicators of an unmet need for social connection. Health providers and caregivers could use these indicators to provide social support and connection to those experiencing this need.
What is the potential impact of these findings?
The authors suggest that once their hypothesis has been rigorously tested and verified, new methods to improve health outcomes for people living with SMI may be developed, including potential “just-in-time” digital interventions through mobile devices. The authors also suggest that people living with SMI and experiencing loneliness can receive interventions that address any potential negative beliefs they hold about rejection, thus interrupting the cycle of social isolation.
Citation: Fulford D, Holt DJ. Social Withdrawal, Loneliness, and Health in Schizophrenia: Psychological and Neural Mechanisms . Schizophr Bull. 2023 Sep 7;49(5):1138-1149. doi: 10.1093/schbul/sbad099. PMID: 37419082; PMCID: PMC10483452.
31 Center Drive, Building 31, Room B1C19 Bethesda, MD 20892
Email: [email protected]
Phone: 301-402-1146
NIH Virtual Tour
- Open access
- Published: 18 April 2024
The endothelium: gatekeeper to lung ischemia-reperfusion injury
- Huy Q. Ta 1 ,
- Maniselvan Kuppusamy 2 ,
- Swapnil K. Sonkusare 2 , 3 ,
- Mark E. Roeser 1 &
- Victor E. Laubach 1
Respiratory Research volume 25 , Article number: 172 ( 2024 ) Cite this article
228 Accesses
9 Altmetric
Metrics details
The success of lung transplantation is limited by the high rate of primary graft dysfunction due to ischemia-reperfusion injury (IRI). Lung IRI is characterized by a robust inflammatory response, lung dysfunction, endothelial barrier disruption, oxidative stress, vascular permeability, edema, and neutrophil infiltration. These events are dependent on the health of the endothelium, which is a primary target of IRI that results in pulmonary endothelial barrier dysfunction. Over the past 10 years, research has focused more on the endothelium, which is beginning to unravel the multi-factorial pathogenesis and immunologic mechanisms underlying IRI. Many important proteins, receptors, and signaling pathways that are involved in the pathogenesis of endothelial dysfunction after IR are starting to be identified and targeted as prospective therapies for lung IRI. In this review, we highlight the more significant mediators of IRI-induced endothelial dysfunction discovered over the past decade including the extracellular glycocalyx, endothelial ion channels, purinergic receptors, kinases, and integrins. While there are no definitive clinical therapies currently available to prevent lung IRI, we will discuss potential clinical strategies for targeting the endothelium for the treatment or prevention of IRI. The accruing evidence on the essential role the endothelium plays in lung IRI suggests that promising endothelial-directed treatments may be approaching the clinic soon. The application of therapies targeting the pulmonary endothelium may help to halt this rapid and potentially fatal injury.
Introduction
While lung transplant rates continue to rise annually, the outcomes of lung transplantation are the worst of any solid organ transplant [ 1 ]. Approximately 50% of patients die within 5 years of transplant, and ~ 67% within 10 years, despite progress in lung preservation, surgical management and immuno-suppression therapies [ 2 ]. The success of lung transplantation is limited by a high rate of primary graft dysfunction (PGD) due to ischemia-reperfusion injury (IRI), which is a rapid and complex sterile inflammatory response characterized by dramatic elevations of extracellular adenosine triphosphate (ATP), oxidative stress, robust innate immune responses, rapid and potent release of proinflammatory signals, vascular permeability, edema, and endothelial and epithelial barrier dysfunction after transplant [ 3 , 4 , 5 , 6 ].
Lung IRI not only leads to PGD after transplantation, but IRI is also a risk factor for chronic lung allograft dysfunction, the major cause of mortality in recipients [ 7 , 8 ]. 29% of transplant patients with IRI will die within 90 days, compared to 5% of recipients without [ 9 ]. Furthermore, those transplant patients with IRI and PGD will experience protracted mechanical ventilation and inpatient hospital care, as well as increased risk of multi-organ failure [ 10 ]. Currently no therapeutic agents are clinically available to prevent IRI, and treatment strategies are limited to maintaining function.
The pulmonary endothelium is a primary target of IRI, and a key hallmark of IRI is endothelial cell (EC) dysfunction, which leads to increased pulmonary fluid accumulation (edema), impaired gas exchange, and decreased lung compliance [ 11 ]. IR stimulates the production of proinflammatory chemokines, cytokines, damage-associated molecular patterns (DAMPs), and reactive oxygen species (ROS) from a variety of cells including ECs, resulting in EC swelling and detachment from the basement membrane. This EC-mediated inflammatory response results in increased vascular permeability, which in turn activates innate immune cells and promotes leukocyte adherence and transmigration. Furthermore, these immune cells release additional inflammatory mediators that further damages the endothelium, ultimately leading to lung injury and graft failure. The leukocyte-endothelial interface is regulated by a complex signaling network of proteins, enzymes, receptors, and channels that perform crucial functions in the endothelium. While the mechanisms of lung IRI are not fully understood, a plethora of studies have determined that EC injury plays a critical role, and many of the regulators that influence endothelial dysfunction and IRI have been identified, providing promising therapeutic strategies to prevent IRI (Fig. 1 ). Therefore, in this review, we discuss the impact that the endothelium has on lung IRI, with a focus on the more recent and targetable mediators of EC dysfunction. We also present potential clinical strategies for targeting the endothelium for the treatment of IRI.
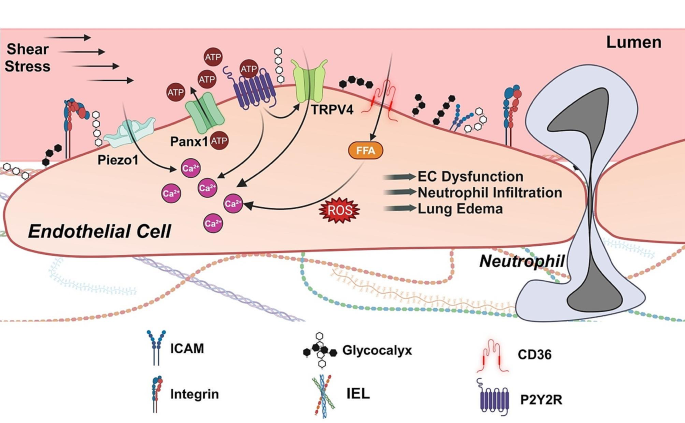
Endothelial events leading to lung IRI . Reperfusion can increase fluid shear stress and activate mechanosensitive Piezo1 channels at the cell membrane. Piezo1 channels are a crucial Ca 2+ entry pathway in endothelial cells. IR also increases extracellular ATP levels in the lung via Panx1 channels. Extracellular ATP can activate purinergic receptors, further increasing cytosolic Ca 2+ levels. ATP activation of purinergic P2Y2 receptors (P2Y2R) leads to increased activity of TRPV4 channels, another mechanically activated Ca 2+ entry pathway on endothelial cell membrane. FFA transporter CD36 elevates cytosolic FFA levels, in turn increasing Ca 2+ influx and ROS production and triggering a cytokine storm. These pro-inflammatory intracellular signaling events dismantle intercellular junctions and promote neutrophil infiltration, increased capillary fluid extravasation, and lung edema formation. Glycocalyx masks the endothelial surface adhesion molecules (ICAM, VCAM, P- and L-selectin) and has a protective effect against IR-mediated deleterious events. Integrins at the cell surface are also involved in increased vascular permeability after IR. IEL, internal elastic lamina; FFA, Free fatty acid; CD36, Cluster of differentiation 36
Endothelium
The vascular endothelium was once believed to be an inactive, stagnant structure. However, it is now appreciated as a highly specialized metabolically active organ that modulates several fundamental physiological, immunological, and synthesizing processes, such as leukocyte extravasation, intravascular clotting, vasomotor tone, inflammation, barrier permeability, production of chemokines, cytokines, growth factors, and ROS, as well as expression of receptors, signaling molecules, and adhesion molecules [ 12 , 13 , 14 , 15 ]. Lining the innermost layer of blood vessels, the vascular endothelium consists of a monolayer of mesenchyme-derived ECs, subcellular extracellular matrix (ECM) proteins, and lumenal glycocalyx. The glycocalyx structure functions as a permeable barrier segregating blood from lung tissue, regulating trafficking of proteins, nutrients, leukocytes, and fluids [ 16 , 17 ]. Furthermore, components within the EC membrane can also modulate intracellular signaling pathways that regulate fundamental biological functions, such as metabolism, gene expression, and cell structure, by sensing changes in fluid shear stress and hemodynamic pressure [ 18 , 19 ].
The integrity of the endothelium is regulated by intercellular junctions (tight junctions and adherens junctions) between neighboring ECs [ 16 ]. These junctions maintain barrier function and modulate signal transduction through interactions with cytoskeletal microtubules and actin microfilaments in response to forces exerted on the endothelium [ 20 ]. Cell surface integrins connect the monolayer of ECs at focal adhesion plaques. Although the integrity of the endothelium depends on both tight and adherens junctions, vascular permeability and subsequent edema develops mainly as a result of dysfunction of tight junctions [ 12 ]. Since interendothelial junctions are also covered by the endothelial glycocalyx, dysfunction of the glycocalyx can also cause leakage [ 21 ].
Given its roles in mechanosensation, secretion, and metabolism, it is not surprising that the endothelium is highly vulnerable to the damaging effects of IR [ 3 ]. Ischemia initiates a proinflammatory response within the endothelium that primes and sensitizes it to additional injury upon reperfusion, where a robust local and systemic inflammatory response extensively damages the integrity of the endothelial barrier through the formation of gaps and expression of transmembrane ion channels. Oxidative stress, ROS, and reactive nitrogen species (RNS) from ECs and transmigrating leukocytes recruited to the endothelium are major contributors to the degradation of the endothelium and EC dysfunction [ 22 ].
Mechanotransduction is the process that translates forces sensed by mechanosensors into biological signaling to modulate gene expression driving a multitude of cellular processes, including cell migration, proliferation, and differentiation. The endothelium converts mechanical forces into biological signals that trigger intracellular signaling pathways through the endothelial surface glycocalyx, activation of ion channels, receptor and nonreceptor kinases, and membrane-associated protein complexes [ 19 ].
The glycocalyx, a negatively charged extracellular layer of proteoglycans, glycoproteins, glycosaminoglycans, heparan sulfate, hyaluronic acid, and syndecans lining the luminal surface of ECs, is highly important in endothelial function, as it plays a role in many physiological processes, such as endothelial barrier function, oxidative stress, and inflammation [ 22 , 23 , 24 , 25 , 26 ]. Accessibility of macromolecules to the EC surface is regulated by the overall charge distribution and structural conformation of the glycocalyx [ 24 , 27 ]. Furthermore, the depth of the glycocalyx masks the interaction of leukocytes and plasma proteins with EC surface adhesion molecules, such as intercellular adhesion molecule 1 (ICAM-1), vascular cell adhesion molecule 1 (VCAM-1), as well as P- and L-Selectin. The presence of extracellular superoxide dismutase in the glycocalyx protects ECs from oxidative stress damage by quenching oxygen radicals and maintaining nitric oxide (NO) bioavailability [ 23 ]. Moreover, the glycocalyx can modulate an inflammatory response by binding or excluding certain cytokines, thereby providing or preventing access to cell surface receptors [ 23 , 28 , 29 ]. Thus, all these physiological functions of the glycocalyx contribute to the health of the endothelium and vascular homeostasis.
Damage to the glycocalyx occurs during IRI and contributes to endothelial dysfunction and barrier disruption [ 30 , 31 , 32 , 33 ]. Under normal conditions, the glycocalyx is continuously turned over, as the rate of synthesis of components of the glycocalyx equals the rate of degradation. However, IR drives the equilibrium towards degradation and shedding, thereby leading to the rapid dismantling of the glycocalyx and obstructing glycocalyx function [ 22 , 23 , 34 ]. In fact, degradation of the glycocalyx may be the earliest form of structural damage after IR [ 35 , 36 ]. By measuring increasing levels of components of the glycocalyx, syndecan-1 and heparan sulfate, in blood at different timepoints from patients undergoing surgery of the ascending aorta with global ischemia or regional ischemia, Rehm and colleagues were the first to present evidence of IRI-mediated endothelial glycocalyx shedding in humans [ 37 ]. Furthermore, higher concentrations of syndecan-1 and heparan sulfate were also observed in coronary effluent from guinea pig hearts exposed to hypoxia-reoxygenation, thereby supporting a role for IRI in the degradation of the glycocalyx [ 38 ]. Sladden et al. showed that the presence of elevated endothelial glycocalyx breakdown products in donor lungs for transplant was associated with poor pulmonary function, reduced acceptability for lung transplant, and PGD in transplant recipients [ 39 ]. Vascular sites with deteriorated glycocalyx are more susceptible to proinflammatory effects [ 22 ].
Loss of the glycocalyx exposes cellular adhesion molecules, thus increasing leukocyte adhesion and vascular permeability with subsequent edema formation. Treatment with hydrocortisone or antithrombin III prior to IR significantly decreased the shedding of glycocalyx constituents, syndecan-1 and heparan sulfate, and inhibited the adhesion of neutrophils, thus protecting the vascular endothelium against IRI [ 40 ]. In addition, Annecke and colleagues demonstrated that protection of the endothelial glycocalyx from IRI was achieved by an inhalational anesthetic gas given before ischemia or during reperfusion [ 41 ]. This group showed that Sevoflurane preconditioning and postconditioning attenuated the release of markers of glycocalyx shedding through the inhibition of lysosomal cathepsin B secretion and preserved the structure of the glycocalyx in guinea pig hearts exposed to IR, thus proposing that Sevoflurane protected the glycocalyx from IR-mediated damage [ 41 ]. In a study comparing patients anesthetized with sevoflurane or propofol during lung resection surgery with one lung ventilation, Kim et al. discovered that the protective effects on the glycocalyx provided by sevoflurane was similar to that supplied by the intravenous anesthetic propofol [ 42 ].
Disruption of the glycocalyx contributes to neutrophil activation and adhesion, a hallmark of IRI. Neutrophils contain proteases, elastase, and proteinase-3 that degrade certain components of the glycocalyx, and the destruction of the endothelial glycocalyx has been associated with increased vascular permeability, leukocyte adhesion, and inflammation in the lungs [ 43 , 44 ]. Pretreatment of guinea pig hearts subjected to 20 min of warm ischemia and 10 min of reperfusion with sevoflurane maintained the endothelium by reducing the shedding of glycocalyx constituents, which masked the adhesion molecules required for neutrophil binding [ 45 ]. Casanova and colleagues were the first to show that sevoflurane preconditioning before IRI preserved the pulmonary glycocalyx by attenuating the expression of inflammatory chemokines (MCP-1, MIP-1, and MIP-2) and leukocyte adhesion molecules (ICAM-1 and VCAM-1) in an in vivo lung autotransplant model [ 35 ]. Using a porcine lung autotransplant model, this group also demonstrated that continuous intravenous administration of lidocaine protected lungs from glycocalyx shedding, as they observed that the effects of IRI (i.e. decreased levels of syndecan-1 and heparan sulfate in lung tissue; elevated glycocalyx markers and adhesion molecules in blood; elevated levels of adhesion molecules and neutrophil activation) were significantly lower in the lidocaine cohort [ 36 ]. Moreover, mice treated with recombinant human vimentin (rhVim) prior to endotoxin exposure had significantly lower histologic acute lung injury scores compared to control mice [ 46 ]. In vitro adhesion and binding assays demonstrated that rhVim protected the vascular endothelium from neutrophil adhesion and infiltration by binding P-selectin and obstructing the interaction between P-selectin and P-selectin glycoprotein ligand-1 [ 46 ]. Although the exact mechanisms underlying glycocalyx destruction are not fully understood, these studies support a significant role for endothelial glycocalyx in IRI.
- Ion channels
Over the past decade, research has been focused on mechanosensitive ion channels, including transient receptor potential (TRP) channels and piezo channels, as potential mediators of IRI. TRP channels are non-selective transmembrane cation channels that regulate Ca 2+ influx and signaling in the pulmonary endothelium, among other cells [ 47 ]. Activated by a number of stimuli, including sheer stress, mechanical stretch, pH, temperature, ROS, extracellular ATP, inflammatory cytokines, and membrane potential changes, the TRP family consists of seven subtypes: TRPC (canonical), TRPV (vanilloid), TRPM (melastatin), TRPML (mucolipin), TRPP (polycystin), TRPA (ankyrin), and TRPN (nitric oxide-mechanoreceptor potential C) [ 4 , 48 , 49 ]. Lung ECs primarily express TRPC, TRPV, TRPM, and TRPP channels.
Evidence from multiple studies demonstrates that a major contributor to lung IRI is the dysregulation of mechanotransduction-mediated TRP channels. Ca 2+ influx through seven members of TRPC subfamily (TRPC1-7) can activate myosin light chain kinase (MLCK), inhibit cAMP generation, and reorganize cytoskeletal structures, resulting in increases in endothelial permeability, endothelial barrier failure, endothelial contraction, and subsequent extravasation of plasma macromolecules and immune cells [ 47 , 48 , 50 , 51 ]. For example, during the early stages of lung IRI, the rise in intracellular Ca 2+ concentration and NADPH oxidase 2 (NOX2)-derived ROS in ECs activates TRPC6, causing cell morphology changes and increasing endothelial leakage, ultimately resulting in pulmonary edema [ 50 , 52 , 53 ]. Stable lung weights and capillary filtration coefficient values from TRPC6 knockout mice before and after IR demonstrated that these mice were protected from IR-induced pulmonary edema [ 52 ]. Here, the specific contribution of TRPC6 to pulmonary oedema was underlined by the fact that lungs from TRPC1- and TRPC4-deficient mice were not protected from increased vascular permeability caused by IR. Furthermore, this study demonstrated that NOX2-generated ROS and phospholipase C-g-generated diacylglycerol precedes TRPC6 activation and IRI [ 52 ].
The TRPV subfamily consists of six members (TRPV1-6), of which TRPV4 is the most researched channel and has been discovered to be a crucial player in the regulation of lung endothelial barrier integrity [ 54 , 55 ]. TRPV4 channels are expressed in many cell types in the lung, including ECs, alveolar epithelial cells, macrophages, and neutrophils [ 56 ], and can be activated by many forces, such as temperature, membrane stretch, oxidative and sheer stress, among others [ 19 ]. Recent studies now indicate that TRPV4 channels on ECs, immune cells, and alveolar epithelial cells mediate acute lung injury [ 57 ]. Studies have described TRPV4 channels being involved in oxidative stress-induced endothelial barrier failure in that H 2 O 2 exposure induces Ca 2+ influx through TRPV4 channels in murine and human lung microvascular ECs in a Fyn-dependent manner, resulting in increased endothelial permeability [ 58 ]. Using the TRPV4 agonist GSK1016790A at doses that induce injury, Villalta and colleagues observed that lung edema (total protein in bronchoalveolar lavage (BAL) fluid and lung wet-to-dry weight ratio) increased in wild-type mice [ 59 ]. Furthermore, TRPV4 activation increased protein levels of the active forms of matrix metalloproteinase 2 (MMP2) and MMP9 along with decreased expression of tissue inhibitor of metalloproteinase 2 (TIMP2), an endogenous MMP inhibitor. This was the first evidence linking the downstream effectors MMP2 and MMP9 to TRPV4-induced increases in lung permeability and edema. These data indicated that TRPV4-mediated Ca 2+ influx elicited the activation of MMP2 and MMP9, which contributed to barrier permeability.
Our group demonstrated that endothelial cell-specific TRPV4 knockout mice as well as inhibition of TRPV4 in wild-type mice with GSK2193874 resulted in attenuation of lung dysfunction and edema following IR as demonstrated by improved oxygenation and compliance, and decreased edema, neutrophil infiltration, and proinflammatory cytokine expression [ 60 ]. This study was the first to demonstrate a role for endothelial TRPV4 in mediating edema after lung IR and highlighted the potential use of TRPV4 inhibitors as a therapeutic strategy to prevent lung IRI. Furthermore, the attenuation of proinflammatory cytokines in endothelial cell-specific TRPV4-deficient mice after IR [ 60 ] suggests that endothelial TRPV4 channels are important mediators of vascular inflammation and endothelial barrier disruption after IR.
The TRPM subfamily is a group of oxidant-activated cation channels that consists of eight members (TRPM1-8), of which TRPM2 is highly expressed in ECs. TRPM2 mediates Ca 2+ entry in response to intracellular ADP-ribose that is generated during oxidative stress [ 61 ]. In human pulmonary artery ECs, H 2 O 2 induces Ca 2+ influx through TRPM2 channels, resulting in increased endothelial permeability [ 62 ]. Conditional knockout of endothelial TRPM2 in mice reduced transmigration and sequestration of neutrophils in lungs following lipopolysaccharide (LPS) challenge [ 63 ]. Although less is known about the role of TRPM2 in lung IRI, Zhong et al. demonstrated a crucial role for TRPM2-mediated ferroptosis in hepatic IRI and that pharmacological inhibition of TRPM2 may provide an effective therapeutic strategy to attenuate hepatic IR injury [ 64 ]. In addition, Khanahmad et al. showed that TRPM2 deficient mice are resistant to renal IRI and that TRPM2 channels are activated by ROS and cyclic adenosine diphosphate ribose (cADPR) generated during renal IRI [ 65 ]. These data suggest that TRPM2 channels in ECs actively mediate endothelial barrier integrity by facilitating Ca 2+ influx by ECs and promoting the transmigration of neutrophils across the endothelium during IRI.
While TRP channels mediate Ca 2+ influx into cells, not all Ca 2+ influx occurs via TRP channels. Discovered in 2010, Piezo channels are non-selective cation channels that open in response to mechanical forces to allow the influx of cations, where PCa > PNa = PK [ 66 ]. Piezo channels respond to stimuli directly (e.g. mechanical stretch, chemical agonists), as well as indirectly (via other channels and upstream signals) [ 67 ]. Humans have two Piezo genes, PIEZO1 and PIEZO2 , and the resulting proteins share approximately 50% amino acid identity. In lungs, Piezo1 channels are highly expressed in pulmonary microvascular ECs as well as alveolar epithelial cells, and Piezo2 channels are highly expressed in airway-innervating sensory neurons [ 68 , 69 ]. Three main signaling pathways have been identified downstream of Piezo1: ATP-purinergic P2X/P2Y receptors [ 70 ], Ca 2+ -dependent calpain signaling [ 71 ], and Ca 2+ -dependent TRPV4 signaling [ 72 ]. These pathways play important roles in cellular function, cell-cell communication, cell cycle progression, proliferation, apoptosis, and angiogenesis.
Endothelial Piezo1 channels have been recently shown to play a role in endothelial barrier integrity. Jiang et al. showed that high tidal volume ventilation produces excessive mechanical stretch that drastically increases the influx of Ca 2+ through endothelial Piezo1 channels, which activates calpain signaling and promotes pulmonary endothelial hyperpermeability and edema as a result of the internalization and breakdown of VE-cadherin junctions [ 73 ]. Friedrich and colleagues used endothelial Piezo1-deficient mice to demonstrate that lung vascular hyperpermeability following increased capillary pressure is the result of Piezo1 activation and the breakdown of lung endothelial adherens junctions (AJs) and opening of paracellular routes [ 69 ]. Furthermore, the endothelial barrier was disrupted through Piezo1-dependent activation of calpain and subsequent proteolysis of VE-cadherin, b-catenin, and p120-catenin. Zhong et al. identified a novel adaptive role of EC-expressed Piezo1 in stabilizing the lung endothelial barrier in response to alveolar stretch [ 69 ]. They demonstrated that activation of Piezo1 channels in ECs elicited calcium signaling and activated calpain which cleaves Src tyrosine kinase, consequentially suppressing Src-mediated VE-cadherin phosphorylation, thereby preventing VE-cadherin internalization from AJs. Tyrosine phosphorylation of adhesion molecules by tyrosine kinases including Src may induce disassembly of catenin-cadherin complexes and microtubules [ 74 , 75 ]. These findings uncovered an adaptive feedback regulation by which alveolar stretch-induced Piezo1 activation in ECs preserves the lung endothelial barrier function. Although the role of Piezo1 in IRI has not been well studied, Guo et al. hypothesized that PIEZO1 may be involved in cerebral ischemia-reperfusion injury through ferroptosis regulation [ 76 ].
Purinergic receptors
During inflammatory injury such as IRI, cell surface pannexin 1 (Panx1) channels rapidly release ATP, a DAMP molecule, into the extracellular space, where the pro-inflammatory actions of extracellular ATP are exerted by members of the purinergic P2 receptor family such as P2X7 and P2Y2 receptors [ 4 , 77 ]. A study by Sugimoto et al. in 2009 was the first to demonstrate a role of extracellular ATP in lung IRI by showing that recipient animals treated with apyrase, which hydrolyzes ATP, resulted in significant attenuation of lung IRI and vascular injury after transplantation [ 78 ]. Our laboratory recently showed that endothelial Panx1 knockout mice, and wild type mice treated with Panx1 inhibitor, are protected against vascular permeability, inflammation, and edema after lung IR, suggesting that endothelial Panx1 and efflux of ATP play important roles in the pathogenesis of lung IRI [ 79 ].
Our laboratory recently used tamoxifen-inducible, endothelial-specific purinergic P2Y2 receptor (P2Y2R), Panx1, and TRPV4 knockout mice in combination with in vivo, ex vivo, and in vitro models of IR to show that lung IR induces endothelial Panx1 channel-mediated efflux of ATP, which then activates endothelial P2Y2R signaling. In turn, this P2Y2R activation stimulated endothelial TRPV4 channel activity, resulting in endothelial barrier disruption, lung edema, leukocyte infiltration, and lung dysfunction after IR [ 80 ]. Our finding that endothelial knockout of P2Y2R reduced the expression of inflammatory cytokines in lungs after IR suggests that the endothelium may also be a source of inflammatory cytokines in lung IRI. Another possibility is that P2Y2R knockout preserves the endothelial barrier after IR, thereby dampening overall inflammation and activation of innate immune cells. This study and those described above suggest that inhibitors of components of the Panx1-P2Y2R-TRPV4 signaling axis on endothelium may be an effective therapeutic strategy to prevent or treat lung IRI via preservation of endothelial barrier function, which supports future studies toward eventual translation of these therapies to human lung transplant patients.
Kinase signaling
Intracellular signaling pathways involving kinases in ECs have been indicated to play critical roles in IRI, where the generation of ROS and rise in intracellular Ca 2+ through Ca 2+ influx from plasma membrane ion channels have been shown to promote endothelial permeability and dysfunction [ 81 , 82 , 83 ]. The Src tyrosine kinase family member Fyn associates with the fatty acid transporter CD36 in the endothelium [ 81 ]. In addition to serving as a membrane anchor for kinase activation, data suggests that CD36 also plays a critical role in Ca 2+ signaling, where loss of CD36 attenuates Ca 2+ influx following thapsigargin-induced store depletion [ 84 ]. CD36 also plays an important role in ROS and Ca 2+ signaling in the lung microvasculature. CD36 gene deficiency led to a significant attenuation of H 2 O 2 -induced Ca 2+ influx and endothelial permeability in vitro as well as protection from lung IRI in vivo [ 85 ]. These findings suggest that loss of CD36 protects against lung IRI, likely due to CD36-mediated changes in H 2 O 2 -induced Ca 2+ influx. Furthermore, the mechanism by which CD36 participates in this process may be by acting as a membrane scaffold for Fyn, allowing for the interactions between Fyn and TRPV4 to facilitate the phosphorylation and activation of TRPV4 in response to oxidative stress. Inhibition of another Src family member, c-Abl, protected against IRI by attenuating oxidative stress-induced endothelial barrier dysfunction and inflammation [ 86 ]. In an ex vivo IR model, lungs from New Zealand White rabbits demonstrated significantly better oxygenation and wet:dry weight ratio following IR and imatinib treatment, which inhibits c-Abl [ 86 ]. Moreover, there was remarkably less total protein in BAL fluid and infiltrating neutrophils in imatinib-treated lungs, and imatinib also abrogated DNA double-strand breaks and p53 upregulation after IR. Together, these data highlight the potential role of Src family kinases as IRI biomarkers and therapeutic targets.
Recent studies reported that p38 mitogen-activated protein kinase (MAPK) plays a role in the development of lung IRI by mediating lung endothelial barrier dysfunction. After treatment with a p38 MAPK inhibitor SB203580, left lungs of rats showed remarkably less alveolar wall thickening and inflammatory cell infiltration in an in vivo lung IRI model [ 87 ]. In addition, p38 MAPK inhibition attenuated total protein levels in BAL fluid and Evans blue dye staining, indicating that SB203580 diminished endothelial leakage after IRI. Furthermore, Western blot and immunofluorescence revealed that inhibition of p38 MAPK partially reversed the IR-induced disruption of the endothelial barrier, as expression of zonula occludens 1 (ZO-1, a key junction protein) and VE-cadherin (a critical endothelial adhesion molecule) were downregulated while ICAM-1 was upregulated [ 87 ]. Furthermore, in an in vitro IR model of lung transplantation, knockdown of p38 MAPK with small interfering RNAs in rat PMVECs reduced oxidative injury associated with inflammation, apoptosis, and cell cycle arrest [ 88 ]. Wang and colleagues demonstrated that the protective effects of p38 MAPK inhibition on IRI were enhanced when c-Jun NH 2 -terminal protein kinase was knockdown in rat PMVECs as well [ 89 ]. These studies suggest that the inhibition of p38 MAPK signaling could mitigate lung IRI-induced endothelial damage.
Sphingosine 1-Phosphate (S1P) is a sphingolipid that acts as a bioactive signal transducer, mediating intra- and extracellular signaling pathways that control endothelial barrier integrity, proliferation, cell survival, and immune cell migration [ 90 ]. ECs are the major source of S1P in the lungs [ 91 ]. Treatment of rat lung recipients with S1P prior to lung transplantation significantly improved oxygenation and lung graft wet:dry ratios compared to control recipients [ 92 ]. Furthermore, S1P treatment prevented neutrophil accumulation, reduced NF-κB-mediated proinflammatory cytokine levels (TNF-α, IL-1β, and MIP-2), and blunted the activation of Akt, p38, and JNK, indicating that S1P abrogated IRI after lung transplantation through the reduction of vascular permeability, neutrophil infiltration, proinflammatory cytokines, and EC apoptosis [ 92 ]. Our group showed that S1P-mediated protection from IRI signaled through the G-protein-coupled receptor, S1P receptor 1 (S1PR1), since a selective S1PR1 agonist, VPC01091, attenuated lung IRI and preserved endothelial barrier in mice [ 93 ]. In addition, our group found that modifying the S1P gradient (higher circulating S1P, lower tissue S1P) through the combination of S1P and sphingosine kinase 2 inhibition during ex vivo lung perfusion (EVLP) significantly improved lung compliance and vascular permeability in a murine lung IRI model [ 94 ]. While S1P and its analogues have been shown to reduce vascular leakage in small and large animal lung injury models [ 92 , 93 , 94 , 95 , 96 ], the clinical application is currently limited by systemic toxicity, as prolonged exposure to S1P agonists worsen vascular leakage and promote fibrosis [ 97 ]. Design of safer analogues with promising preclinical data will be required.
Rho-associated coiled-coil containing protein kinase 1 (ROCK1) is a serine/threonine kinase that is the downstream effector of the small GTPase Rho and negative regulator of endothelial barrier function [ 98 ]. In a rat lung transplant model, flushing the donor lungs with the ROCK1 inhibitor, Y-27632, prevented inflammatory cells from invading the alveolar space and decreased TNF-α levels in BAL fluid, leading to reduced pulmonary edema [ 99 ]. Furthermore, inhibition of ROCK1 by miR-144 mimetics resulted in the downregulation of ROCK1 and downstream target myosin phosphatase-targeting subunit 1 [ 100 ]. These events favor the inactivation of myosin light chain kinase, thereby stabilizing the endothelial barrier and limiting vascular leakage during lung injury. Thus, these data illustrate the important role that ROCK1 plays in the pathogenesis of lung IRI and endothelial barrier disruption.
Integrins, a family of cell surface receptors consisting of 24 members, each containing a single α subunit and single β subunit, regulate cellular proliferation, migration, cytokine secretion, and signaling, and thereby play critical roles in cell growth, apoptosis, inflammation, and endothelial barrier integrity [ 101 , 102 ]. These receptors link the intracellular cytoskeleton with the ECM, and thus transduce external and internal mechanochemical signals across the plasma membrane upon activation after ligand binding [ 101 ]. Several studies have shown that blockade of integrin αVβ5 with inhibitory monoclonal antibodies specifically prevented increases in lung vascular permeability, which has been considered a hallmark of lung injury that is largely responsible for its characteristic pulmonary edema formation. Su et al. demonstrated that both αVβ5 genetic deletion and blocking antibody (ALULA) prevented vascular permeability after IRI in rats [ 103 ]. Furthermore, treatment of donor lungs with ALULA significantly decreased extravascular lung water, neutrophil infiltration and total protein in BAL fluid, and improved arterial oxygenation, suggesting that αVβ5 blockade prevented IRI following transplantation [ 104 ]. Zhang and colleagues examined the role of αVβ5 in IR-induced endothelial cell apoptosis and autophagy and found that αVβ5 inhibition with ALULA reduced cell permeability and cleaved caspase-3 expression after IR [ 105 ]. Moreover, ALULA treatment enhanced endothelial autophagy levels, which was reflected in the increase in LC3-II expression and decrease in p62 levels [ 105 ]. Together, these data indicated that αVβ5 inhibition mitigates IR-induced endothelial cell apoptosis, leading to attenuation of lung IRI.
Current Therapeutics
Considerable research effort has been focused on a better understanding of the molecular mechanisms that cause lung endothelial barrier failure after IR in order to identify therapeutic targets to treat or prevent IRI. One of the endothelial protection methods that is often implemented in many transplantation clinics to reduce lung IRI and improve lung function is the “controlled reperfusion” or regulated reestablishment of blood flow during the early stages of reperfusion, combined with controlled ventilation to prevent hypercapnia [ 106 , 107 ]. Several novel strategies have emerged over the past years which show considerable promise for preservation or reconstitution of endothelial barrier function in vitro and in preclinical trials. However, there are no current therapeutic agents yet clinically available to prevent or treat IRI, and treatment strategies are limited to maintaining lung function (Table 1 ).
Since IRI involves glycocalyx damage, several therapeutics have been investigated, either targeted to the prevention of glycocalyx injury or restoration of the ultrastructure of the endothelium. Sevoflurane is an anesthetic and potent vasodilator that protects the endothelium following IR. Blood from sevoflurane-anesthetized pigs subjected to IRI (induced by a balloon catheter in the thoracic aorta) had low levels of negatively charged heparan sulfate compared to blood from propofol-anesthetized pigs, signifying a healthy glycocalyx [ 108 ]. In an in vivo lung autotransplant model in pigs, sevoflurane pretreatment preserved the pulmonary glycocalyx, reduced serum levels of heparan sulfate and syndecan, and decreased expression of adhesion molecules and chemokines [ 35 ].
A phase I clinical trial demonstrated mortality benefit in acute respiratory distress syndrome treated with interferon-β-1a [ 109 ]. The proposed mechanisms of benefit were modulation of inflammation (possibly neutrophil endothelial interactions) and endothelial barrier function via CD73-mediated dephosphorylation of AMP. While non-randomized, the mortality benefit (24% absolute reduction) in this study suggests that targeting the lung endothelium may hold promise as a viable therapeutic strategy in IRI.
An increase in intracellular calcium not only increases the permeability of ECs, but also contributes to neutrophil activation and EC inflammation. Since calcium influx plays a crucial role in the occurrence and development of lung IRI, blocking calcium influx into ECs may be an effective therapeutic strategy for lung injury. An orally active TRPV4 antagonist, GSK2193874, was effective in inhibiting lung edema induced by heart failure [ 110 ]. Two other TRPV4 inhibitors (GSK2220961, GSK2337429) ameliorated acute lung injury in mice when administered 30 min after exposure to hydrochloric acid or chlorine gas [ 54 ]. When GSK2193874 was administered 20 min before the induction of acute lung injury by acid instillation, key hallmarks of acute lung injury (i.e. lung edema, inflammation, poor gas exchange, lung dysfunction, and neutrophil infiltration) were attenuated in mice [ 111 ]. However, another TRPV4 inhibitor, HC-067047, applied 45 min after lung injury to simulate a clinically more relevant scenario, offered no protection from acute lung injury, suggesting that timing of treatment may be important in the effectiveness of TRPV4 inhibition in preventing IRI [ 111 ]. Blocking TRPV4 (e.g. with GSK2798745) was also proposed as a promising and feasible approach to protecting the alveolo-capillary barrier in lungs of Covid-19 patients [ 112 ]. In the first human clinical trial (NCT03511105), LPS-induced elevation of total protein and neutrophils in BAL fluid from the airway site after application of GSK2798745 was not different in comparison to placebo-treated controls [ 113 , 114 ]. However, the effectiveness of TRPV4 inhibition as a strategy to treat lung IRI after transplantation has not yet been tested. Therefore, although modulating TRPV4 channel activity may be useful as a therapeutic approach for lung IRI, cell type and injury model should be considered in order to establish clinically successful drugs.
Mibefradil and Flunarizine, two T-type Ca 2+ channel blockers, significantly decreased LPS-induced total cell number, protein concentration, and Evans blue dye extravasation in the lung, as well as TNF-α and IL-6 levels in BAL fluid [ 115 ]. In addition, Mibefradil also attenuated pathological alterations in lung tissue of LPS-challenged mice and suppressed the activity of MPO and NF-κB, a central transcription factor regulating gene expression of various inflammatory mediators [ 115 ]. Since influx of inflammatory cells, protein leakage, and cytokine storms are crucial events of IRI, these Ca 2+ channel inhibitors may provide protection against IR injury.
Tyrosine kinase inhibitor imatinib, which was originally developed to inhibit the chronic myelogenous leukemia-causing BCR-Abl fusion protein, has been shown to attenuate pulmonary vascular permeability induced by a broad range of mediators in a clinically relevant murine model of ARDS [ 116 ]. Imatinib also attenuated thrombin and histamine-induced barrier dysfunction in vitro [ 117 ]. Given its multiple sites of action, further mechanistic work is required to progress imatinib as a potential therapy in ARDS. We propose that imatinib may be a therapeutic option to prevent or treat lung IRI, which warrants further investigation.
Autophagy was implicated to be involved in the pathogenesis of lung IRI, as the inhibition of autophagy by 3-methyladenine (3-MA) resulted in reduced edema, oxidative stress, and neutrophil activation in a rat lung IRI model [ 118 ]. Furthermore, Liu et al. demonstrated that 3-MA inhibited apoptosis and enhanced proliferation to protect against IR-induced lung injury in a rat model of orthotopic left lung transplantation [ 119 ]. However, another study showed that promoting autophagy with rapamycin in human pulmonary microvascular endothelial cells and mice ameliorated tight junction damage and cell death, suggesting that autophagy was protective against IRI [ 120 ]. While there seems to be a paucity of research on the role autophagy plays in lung IRI, these studies advocate for more research on whether autophagy preserves or damages the endothelium.
The important, recent development of ex vivo lung perfusion (EVLP) has allowed the use of marginal donor lungs, such as donation after cardiac death (DCD) lungs, to help resolve the shortage of available donor lungs for transplantation. Steen and colleagues developed the “Lund protocol” that utilized a special perfusion solution (Steen solution) aimed directly at preserving the endothelium to reduce edema, and were the first group to successfully transplant DCD lungs [ 121 ]. Furthermore, they were also able to perform transplantations with marginal donor lungs using EVLP and Steen solution [ 122 ]. A group from Toronto modified the perfusion flow, perfusate composition and temperature, and respiratory rate, in the Lund protocol to create the “Toronto protocol” and successfully transplanted 372 EVLP-rehabilitated marginal donor lungs and DCD lungs [ 123 ]. These studies have encouraged the idea that EVLP can be used as a platform for therapeutic treatment to further recondition lungs to prevent primary graft dysfunction. Our group showed that EVLP with Steen solution supplemented with an adenosine A 2A receptor (A2AR) agonist significantly reduced pulmonary edema and interferon-γ and dramatically improved the oxygenation index, suggesting that acute IRI was attenuated in porcine lungs undergoing EVLP with A2AR-supplemented Steen solution [ 124 ]. This combination of EVLP and A2AR agonists has also been demonstrated to recondition DCD lungs for lung transplantation in preclinical murine and porcine models [ 125 , 126 , 127 ]. Furthermore, we determined that adenosine A 2B receptor antagonist treatment during EVLP significantly attenuated lung dysfunction, interleukin-8 production, and vascular permeability in a murine lung IRI model [ 128 ] as well as enabled successful transplantation of porcine DCD lungs [ 129 ]. As mentioned above, the combination of S1P and sphingosine kinase inhibitors during EVLP provided endothelial protection to improve lung function in a murine DCD model [ 94 ]. These studies give support for the use of EVLP in combination with therapies targeted towards the many mediators of IRI (especially to block endothelial barrier dysfunction) to prevent the detrimental effects of lung IRI.
Lung IRI is a complex, rapid and robust inflammatory response marked by lung dysfunction, endothelial barrier disruption, oxidative stress, increased vascular permeability, edema, alveolar damage, and neutrophil infiltration. Two key events during IRI are vascular permeability and neutrophil infiltration, which results in severe edema and neutrophil-mediated injury. Each of these events are connected and dependent on the health of the endothelium, consequently leading to endothelial barrier dysfunction and edema, a principal hallmark of IRI. Although early studies on mechanisms of lung IRI focused on the innate immune responses, more recent studies have focused more on the endothelium, which is beginning to unravel the multi-factorial pathogenesis and immunologic mechanisms underlying IRI. Many important mediators of endothelial dysfunction after IR have now been identified, as reviewed here (Fig. 1). Spanning from the extracellular glycocalyx to ion channels and purinergic receptors to kinases and possibly many others yet to be discovered, these mediators of endothelial barrier integrity and IRI may serve as prospective targets for lung IRI therapy. While there are no definitive clinical therapies currently available, the accumulating evidence on the critical role the endothelial barrier plays in IRI suggests that promising treatments targeting the endothelium may be approaching soon. The ability to halt this rapid and potentially fatal injury could be significantly enhanced through the application of endothelial-directed therapies, as well as combination therapies, where more than one signaling pathway may be targeted.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
Acute respiratory distress syndrome
Adenosine triphosphate
Adherens junctions
Bronchoalveolar lavage
Breakpoint cluster region-Abelson
Damage-associated molecular patterns
Endothelial cell
Ex vivo lung perfusion
Extracellular matrix
Intercellular adhesion molecule 1
Interleukin
- Ischemia-reperfusion injury
Keratinocyte growth factor-2
Monocyte chemotactic protein 1
Macrophage inflammatory protein 1
Macrophage inflammatory protein 2
Matrix metalloproteinase 2
Mitogen-activated protein kinase
NADPH oxidase 2
Nitric oxide
Primary graft dysfunction
Recombinant human vimentin
reactive nitrogen species
Reactive oxygen species
Rho associated coiled-coil containing protein kinase 1
Severe acute respiratory syndrome coronavirus type 2
Sphingosine 1-phosphate
Transient receptor potential
Transient receptor potential canonical
Transient receptor potential melastatin
Transient receptor potential mucolipin
Transient receptor potential nitric oxide-mechanoreceptor potential C
Transient receptor potential polycystin
Transient receptor potential vanilloid
Vascular cell adhesion molecule 1
Chambers DC, Cherikh WS, Harhay MO, Hayes D Jr., Hsich E, Khush KK, et al. The international thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: thirty-sixth adult lung and heart-lung transplantation Report-2019; focus theme: Donor and recipient size match. J Heart Lung Transpl. 2019;38(10):1042–55.
Article Google Scholar
Valapour M, Lehr CJ, Schladt DP, Smith JM, Goff R, Mupfudze TG, et al. Am J Transpl. 2023;23(2 Suppl 1):S379–442. OPTN/SRTR 2021 Annual Data Report: Lung.
Eltzschig HK, Eckle T. Ischemia and reperfusion–from mechanism to translation. Nat Med. 2011;17(11):1391–401.
Article CAS PubMed Google Scholar
Haywood N, Ta HQ, Rotar E, Daneva Z, Sonkusare SK, Laubach VE. Role of the purinergic signaling network in lung ischemia-reperfusion injury. Curr Opin Organ Transpl. 2021;26(2):250–7.
Article CAS Google Scholar
Gelman AE, Fisher AJ, Huang HJ, Baz MA, Shaver CM, Egan TM, et al. Report of the ISHLT Working Group on primary lung graft dysfunction part III: mechanisms: a 2016 Consensus Group Statement of the International Society for Heart and Lung Transplantation. J Heart Lung Transpl. 2017;36(10):1114–20.
Laubach VE, Sharma AK. Mechanisms of lung ischemia-reperfusion injury. Curr Opin Organ Transpl. 2016;21(3):246–52.
Diamond JM, Arcasoy S, Kennedy CC, Eberlein M, Singer JP, Patterson GM, et al. Report of the International Society for Heart and Lung Transplantation Working Group on Primary Lung Graft Dysfunction, part II: epidemiology, risk factors, and outcomes-A 2016 Consensus Group statement of the International Society for Heart and Lung Transplantation. J Heart Lung Transpl. 2017;36(10):1104–13.
Fiser SM, Tribble CG, Long SM, Kaza AK, Kern JA, Jones DR et al. Ischemia-reperfusion injury after lung transplantation increases risk of late bronchiolitis obliterans syndrome. Ann Thorac Surg. 2002;73(4):1041-7; discussion 7–8.
Diamond JM, Lee JC, Kawut SM, Shah RJ, Localio AR, Bellamy SL, et al. Clinical risk factors for primary graft dysfunction after lung transplantation. Am J Respir Crit Care Med. 2013;187(5):527–34.
Article PubMed PubMed Central Google Scholar
Rosenheck J, Pietras C, Cantu E. Early Graft Dysfunction after Lung Transplantation. Curr Pulmonol Rep. 2018;7(4):176–87.
Article CAS PubMed PubMed Central Google Scholar
Rizzo AN, Schmidt EP. The role of the alveolar epithelial glycocalyx in acute respiratory distress syndrome. Am J Physiol Cell Physiol. 2023;324(4):C799–806.
Galley HF, Webster NR. Physiology of the endothelium. Br J Anaesth. 2004;93(1):105–13.
Mehta D, Malik AB. Signaling mechanisms regulating endothelial permeability. Physiol Rev. 2006;86(1):279–367.
Pries AR, Kuebler WM. Normal endothelium. Handb Exp Pharmacol. 2006;176(Pt 1):1–40.
Google Scholar
Millar FR, Summers C, Griffiths MJ, Toshner MR, Proudfoot AG. The pulmonary endothelium in acute respiratory distress syndrome: insights and therapeutic opportunities. Thorax. 2016;71(5):462–73.
Article PubMed Google Scholar
Sukriti S, Tauseef M, Yazbeck P, Mehta D. Mechanisms regulating endothelial permeability. Pulm Circ. 2014;4(4):535–51.
Chatterjee S, Nieman GF, Christie JD, Fisher AB. Shear stress-related mechanosignaling with lung ischemia: lessons from basic research can inform lung transplantation. Am J Physiol Lung Cell Mol Physiol. 2014;307(9):L668–80.
Chatterjee S, Chapman KE, Fisher AB. Lung ischemia: a model for endothelial mechanotransduction. Cell Biochem Biophys. 2008;52(3):125–38.
Goldenberg NM, Kuebler WM. Endothelial cell regulation of pulmonary vascular tone, inflammation, and coagulation. Compr Physiol. 2015;5(2):531–59.
Dudek SM, Garcia JG. Cytoskeletal regulation of pulmonary vascular permeability. J Appl Physiol (1985). 2001;91(4):1487–500.
Benatti MN, Fabro AT, Miranda CH. Endothelial glycocalyx shedding in the acute respiratory distress syndrome after flu syndrome. J Intensive Care. 2020;8:72.
Rubio-Gayosso I, Platts SH, Duling BR. Reactive oxygen species mediate modification of glycocalyx during ischemia-reperfusion injury. Am J Physiol Heart Circ Physiol. 2006;290(6):H2247–56.
Pries AR, Secomb TW, Gaehtgens P. The endothelial surface layer. Pflugers Arch. 2000;440(5):653–66.
Becker BF, Chappell D, Jacob M. Endothelial glycocalyx and coronary vascular permeability: the fringe benefit. Basic Res Cardiol. 2010;105(6):687–701.
Yu H, Kalogeris T, Korthuis RJ. Reactive species-induced microvascular dysfunction in ischemia/reperfusion. Free Radic Biol Med. 2019;135:182–97.
Murphy LS, Wickersham N, McNeil JB, Shaver CM, May AK, Bastarache JA, et al. Endothelial glycocalyx degradation is more severe in patients with non-pulmonary sepsis compared to pulmonary sepsis and associates with risk of ARDS and other organ dysfunction. Ann Intensive Care. 2017;7(1):102.
Curry FE, Adamson RH. Endothelial glycocalyx: permeability barrier and mechanosensor. Ann Biomed Eng. 2012;40(4):828–39.
Broekhuizen LN, Mooij HL, Kastelein JJ, Stroes ES, Vink H, Nieuwdorp M. Endothelial glycocalyx as potential diagnostic and therapeutic target in cardiovascular disease. Curr Opin Lipidol. 2009;20(1):57–62.
Becker BF, Chappell D, Bruegger D, Annecke T, Jacob M. Therapeutic strategies targeting the endothelial glycocalyx: acute deficits, but great potential. Cardiovasc Res. 2010;87(2):300–10.
Brettner F, von Dossow V, Chappell D. The endothelial glycocalyx and perioperative lung injury. Curr Opin Anaesthesiol. 2017;30(1):36–41.
Platts SH, Linden J, Duling BR. Rapid modification of the glycocalyx caused by ischemia-reperfusion is inhibited by adenosine A2A receptor activation. Am J Physiol Heart Circ Physiol. 2003;284(6):H2360–7.
Selim J, Hamzaoui M, Boukhalfa I, Djerada Z, Chevalier L, Piton N, et al. Cardiopulmonary bypass increases endothelial dysfunction after pulmonary ischaemia-reperfusion in an animal model. Eur J Cardiothorac Surg. 2021;59(5):1037–47.
Abassi Z, Armaly Z, Heyman SN. Glycocalyx Degradation in Ischemia-Reperfusion Injury. Am J Pathol. 2020;190(4):752–67.
Mulivor AW, Lipowsky HH. Inflammation- and ischemia-induced shedding of venular glycocalyx. Am J Physiol Heart Circ Physiol. 2004;286(5):H1672–80.
Casanova J, Simon C, Vara E, Sanchez G, Rancan L, Abubakra S, et al. Sevoflurane anesthetic preconditioning protects the lung endothelial glycocalyx from ischemia reperfusion injury in an experimental lung autotransplant model. J Anesth. 2016;30(5):755–62.
Rancan L, Simon C, Sanchez Pedrosa G, Aymonnier K, Shahani PM, Casanova J, et al. Glycocalyx degradation after pulmonary transplantation surgery. Eur Surg Res. 2018;59(3–4):115–25.
Rehm M, Bruegger D, Christ F, Conzen P, Thiel M, Jacob M, et al. Shedding of the endothelial glycocalyx in patients undergoing major vascular surgery with global and regional ischemia. Circulation. 2007;116(17):1896–906.
Annecke T, Fischer J, Hartmann H, Tschoep J, Rehm M, Conzen P, et al. Shedding of the coronary endothelial glycocalyx: effects of hypoxia/reoxygenation vs ischaemia/reperfusion. Br J Anaesth. 2011;107(5):679–86.
Sladden TM, Yerkovich S, Grant M, Zhang F, Liu X, Trotter M, et al. Endothelial glycocalyx shedding predicts Donor Organ acceptability and is Associated with primary graft dysfunction in lung transplant recipients. Transplantation. 2019;103(6):1277–85.
Chappell D, Dorfler N, Jacob M, Rehm M, Welsch U, Conzen P, et al. Glycocalyx protection reduces leukocyte adhesion after ischemia/reperfusion. Shock. 2010;34(2):133–9.
Annecke T, Chappell D, Chen C, Jacob M, Welsch U, Sommerhoff CP, et al. Sevoflurane preserves the endothelial glycocalyx against ischaemia-reperfusion injury. Br J Anaesth. 2010;104(4):414–21.
Kim HJ, Kim E, Baek SH, Kim HY, Kim JY, Park J, et al. Sevoflurane did not show better protective effect on endothelial glycocalyx layer compared to propofol during lung resection surgery with one lung ventilation. J Thorac Dis. 2018;10(3):1468–75.
Schmidt EP, Yang Y, Janssen WJ, Gandjeva A, Perez MJ, Barthel L, et al. The pulmonary endothelial glycocalyx regulates neutrophil adhesion and lung injury during experimental sepsis. Nat Med. 2012;18(8):1217–23.
Naumann DN, Hazeldine J, Midwinter MJ, Hutchings SD, Harrison P. Poor microcirculatory flow dynamics are associated with endothelial cell damage and glycocalyx shedding after traumatic hemorrhagic shock. J Trauma Acute Care Surg. 2018;84(1):81–8.
Chappell D, Heindl B, Jacob M, Annecke T, Chen C, Rehm M, et al. Sevoflurane reduces leukocyte and platelet adhesion after ischemia-reperfusion by protecting the endothelial glycocalyx. Anesthesiology. 2011;115(3):483–91.
Lam FW, Da Q, Guillory B, Cruz MA. Recombinant human vimentin binds to P-Selectin and blocks Neutrophil capture and rolling on platelets and endothelium. J Immunol. 2018;200(5):1718–26.
Pedersen SF, Owsianik G, Nilius B. TRP channels: an overview. Cell Calcium. 2005;38(3–4):233–52.
Uhlig S, Yang Y, Waade J, Wittenberg C, Babendreyer A, Kuebler WM. Differential regulation of lung endothelial permeability in vitro and in situ. Cell Physiol Biochem. 2014;34(1):1–19.
Chen YL, Sonkusare SK. Endothelial TRPV4 channels and vasodilator reactivity. Curr Top Membr. 2020;85:89–117.
Becker LB. New concepts in reactive oxygen species and cardiovascular reperfusion physiology. Cardiovasc Res. 2004;61(3):461–70.
Tiruppathi C, Ahmmed GU, Vogel SM, Malik AB. Ca2 + signaling, TRP channels, and endothelial permeability. Microcirculation. 2006;13(8):693–708.
Weissmann N, Sydykov A, Kalwa H, Storch U, Fuchs B, Mederos y Schnitzler M, et al. Activation of TRPC6 channels is essential for lung ischaemia-reperfusion induced oedema in mice. Nat Commun. 2012;3:649.
Peters SC, Piper HM. Reoxygenation-induced Ca2 + rise is mediated via Ca2 + influx and Ca2 + release from the endoplasmic reticulum in cardiac endothelial cells. Cardiovasc Res. 2007;73(1):164–71.
Balakrishna S, Song W, Achanta S, Doran SF, Liu B, Kaelberer MM, et al. TRPV4 inhibition counteracts edema and inflammation and improves pulmonary function and oxygen saturation in chemically induced acute lung injury. Am J Physiol Lung Cell Mol Physiol. 2014;307(2):L158–72.
Morty RE, Kuebler WM. TRPV4: an exciting new target to promote alveolocapillary barrier function. Am J Physiol Lung Cell Mol Physiol. 2014;307(11):L817–21.
Earley S, Heppner TJ, Nelson MT, Brayden JE. TRPV4 forms a novel Ca2 + signaling complex with ryanodine receptors and BKCa channels. Circ Res. 2005;97(12):1270–9.
Sonkusare SK, Laubach VE. Endothelial TRPV4 channels in lung edema and injury. Curr Top Membr. 2022;89:43–62.
Suresh K, Servinsky L, Reyes J, Baksh S, Undem C, Caterina M, et al. Hydrogen peroxide-induced calcium influx in lung microvascular endothelial cells involves TRPV4. Am J Physiol Lung Cell Mol Physiol. 2015;309(12):L1467–77.
Villalta PC, Rocic P, Townsley MI. Role of MMP2 and MMP9 in TRPV4-induced lung injury. Am J Physiol Lung Cell Mol Physiol. 2014;307(8):L652–9.
Haywood N, Ta HQ, Zhang A, Charles EJ, Rotar E, Noona St, et al. Endothelial transient receptor potential vanilloid 4 channels mediate Lung Ischemia-Reperfusion Injury. Ann Thorac Surg. 2022;113(4):1256–64.
Dietrich A, Steinritz D, Gudermann T. Transient receptor potential (TRP) channels as molecular targets in lung toxicology and associated diseases. Cell Calcium. 2017;67:123–37.
Hecquet CM, Ahmmed GU, Vogel SM, Malik AB. Role of TRPM2 channel in mediating H2O2-induced Ca2 + entry and endothelial hyperpermeability. Circ Res. 2008;102(3):347–55.
Mittal M, Nepal S, Tsukasaki Y, Hecquet CM, Soni D, Rehman J, et al. Neutrophil activation of endothelial cell-expressed TRPM2 mediates Transendothelial Neutrophil Migration and Vascular Injury. Circ Res. 2017;121(9):1081–91.
Zhong C, Yang J, Zhang Y, Fan X, Fan Y, Hua N et al. TRPM2 mediates hepatic ischemia-reperfusion Injury via ca(2+)-Induced mitochondrial lipid peroxidation through increasing ALOX12 expression. Research (Wash D C). 2023;6:0159.
Khanahmad H, Mirbod SM, Karimi F, Kharazinejad E, Owjfard M, Najaflu M, et al. Pathological mechanisms Induced by TRPM2 Ion channels activation in Renal Ischemia-Reperfusion Injury. Mol Biol Rep. 2022;49(11):11071–9.
Zhong M, Komarova Y, Rehman J, Malik AB. Mechanosensing Piezo channels in tissue homeostasis including their role in lungs. Pulm Circ. 2018;8(2):2045894018767393.
Parpaite T, Coste B. Piezo channels. Curr Biol. 2017;27(7):R250–2.
Nonomura K, Woo SH, Chang RB, Gillich A, Qiu Z, Francisco AG, et al. Piezo2 senses airway stretch and mediates lung inflation-induced apnoea. Nature. 2017;541(7636):176–81.
Friedrich EE, Hong Z, Xiong S, Zhong M, Di A, Rehman J, et al. Endothelial cell Piezo1 mediates pressure-induced lung vascular hyperpermeability via disruption of adherens junctions. Proc Natl Acad Sci U S A. 2019;116(26):12980–5.
Wei L, Mousawi F, Li D, Roger S, Li J, Yang X, et al. Adenosine Triphosphate Release and P2 receptor signaling in Piezo1 Channel-Dependent Mechanoregulation. Front Pharmacol. 2019;10:1304.
Suzuki K, Hata S, Kawabata Y, Sorimachi H. Structure, activation, and biology of calpain. Diabetes. 2004;53(Suppl 1):S12–8.
Swain SM, Liddle RA. Piezo1 acts upstream of TRPV4 to induce pathological changes in endothelial cells due to shear stress. J Biol Chem. 2021;296:100171.
Jiang L, Zhang Y, Lu D, Huang T, Yan K, Yang W, et al. Mechanosensitive Piezo1 channel activation promotes ventilator-induced lung injury via disruption of endothelial junctions in ARDS rats. Biochem Biophys Res Commun. 2021;556:79–86.
Gong P, Angelini DJ, Yang S, Xia G, Cross AS, Mann D, et al. TLR4 signaling is coupled to SRC family kinase activation, tyrosine phosphorylation of zonula adherens proteins, and opening of the paracellular pathway in human lung microvascular endothelia. J Biol Chem. 2008;283(19):13437–49.
Vandenbroucke St Amant E, Tauseef M, Vogel SM, Gao XP, Mehta D, Komarova YA, et al. PKCalpha activation of p120-catenin serine 879 phospho-switch disassembles VE-cadherin junctions and disrupts vascular integrity. Circ Res. 2012;111(6):739–49.
Guo XW, Lu Y, Zhang H, Huang JQ, Li YW. PIEZO1 might be involved in cerebral ischemia-reperfusion injury through ferroptosis regulation: a hypothesis. Med Hypotheses. 2021;146:110327.
Di Virgilio F, Sarti AC, Coutinho-Silva R. Purinergic signaling, DAMPs, and inflammation. Am J Physiol Cell Physiol. 2020;318(5):C832–5.
Sugimoto S, Lin X, Lai J, Okazaki M, Das NA, Li W, et al. Apyrase treatment prevents ischemia-reperfusion injury in rat lung isografts. J Thorac Cardiovasc Surg. 2009;138(3):752–9.
Sharma AK, Charles EJ, Zhao Y, Narahari AK, Baderdinni PK, Good ME, et al. Pannexin-1 channels on endothelial cells mediate vascular inflammation during lung ischemia-reperfusion injury. Am J Physiol Lung Cell Mol Physiol. 2018;315(2):L301–12.
Kuppusamy M, Ta HQ, Davenport HN, Bazaz A, Kulshrestha A, Daneva Z, et al. Purinergic P2Y2 receptor-induced activation of endothelial TRPV4 channels mediates lung ischemia-reperfusion injury. Sci Signal. 2023;16(808):eadg1553.
Silverstein RL, Febbraio M. CD36, a scavenger receptor involved in immunity, metabolism, angiogenesis, and behavior. Sci Signal. 2009;2(72):re3.
Villalta PC, Townsley MI. Transient receptor potential channels and regulation of lung endothelial permeability. Pulm Circ. 2013;3(4):802–15.
Sarmiento D, Montorfano I, Cerda O, Caceres M, Becerra A, Cabello-Verrugio C, et al. Increases in reactive oxygen species enhance vascular endothelial cell migration through a mechanism dependent on the transient receptor potential melastatin 4 ion channel. Microvasc Res. 2015;98:187–96.
Kuda O, Jenkins CM, Skinner JR, Moon SH, Su X, Gross RW, et al. CD36 protein is involved in store-operated calcium flux, phospholipase A2 activation, and production of prostaglandin E2. J Biol Chem. 2011;286(20):17785–95.
Suresh K, Servinsky L, Reyes J, Undem C, Zaldumbide J, Rentsendorj O, et al. CD36 mediates H2O2-induced calcium influx in lung microvascular endothelial cells. Am J Physiol Lung Cell Mol Physiol. 2017;312(1):L143–53.
Magruder JT, Grimm JC, Crawford TC, Johnston L, Santhanam L, Stephens RS, et al. Imatinib is Protective Against Ischemia-Reperfusion Injury in an Ex vivo rabbit model of Lung Injury. Ann Thorac Surg. 2018;105(3):950–6.
Wang T, Liu C, Pan LH, Liu Z, Li CL, Lin JY, et al. Inhibition of p38 MAPK mitigates Lung Ischemia Reperfusion Injury by reducing blood-air barrier hyperpermeability. Front Pharmacol. 2020;11:569251.
Tan J, Liu D, Lv X, Wang L, Zhao C, Che Y, et al. MAPK mediates inflammatory response and cell death in rat pulmonary microvascular endothelial cells in an ischemia-reperfusion model of lung transplantation. J Heart Lung Transpl. 2013;32(8):823–31.
Wang J, Tan J, Liu Y, Song L, Li D, Cui X. Amelioration of lung ischemia–reperfusion injury by JNK and p38 small interfering RNAs in rat pulmonary microvascular endothelial cells in an ischemia–reperfusion injury lung transplantation model. Mol Med Rep. 2018;17(1):1228–34.
CAS PubMed Google Scholar
Hla T. Signaling and biological actions of sphingosine 1-phosphate. Pharmacol Res. 2003;47(5):401–7.
Fukuhara S, Simmons S, Kawamura S, Inoue A, Orba Y, Tokudome T, et al. The sphingosine-1-phosphate transporter Spns2 expressed on endothelial cells regulates lymphocyte trafficking in mice. J Clin Invest. 2012;122(4):1416–26.
Okazaki M, Kreisel F, Richardson SB, Kreisel D, Krupnick AS, Patterson GA, et al. Sphingosine 1-phosphate inhibits ischemia reperfusion injury following experimental lung transplantation. Am J Transpl. 2007;7(4):751–8.
Stone ML, Sharma AK, Zhao Y, Charles EJ, Huerter ME, Johnston WF, et al. Sphingosine-1-phosphate receptor 1 agonism attenuates lung ischemia-reperfusion injury. Am J Physiol Lung Cell Mol Physiol. 2015;308(12):L1245–52.
Mehaffey JH, Charles EJ, Narahari AK, Schubert S, Laubach VE, Teman NR, et al. Increasing circulating sphingosine-1-phosphate attenuates lung injury during ex vivo lung perfusion. J Thorac Cardiovasc Surg. 2018;156(2):910–7.
Mathew B, Jacobson JR, Berdyshev E, Huang Y, Sun X, Zhao Y, et al. Role of sphingolipids in murine radiation-induced lung injury: protection by sphingosine 1-phosphate analogs. FASEB J. 2011;25(10):3388–400.
Szczepaniak WS, Zhang Y, Hagerty S, Crow MT, Kesari P, Garcia JG, et al. Sphingosine 1-phosphate rescues canine LPS-induced acute lung injury and alters systemic inflammatory cytokine production in vivo. Transl Res. 2008;152(5):213–24.
Shea BS, Brooks SF, Fontaine BA, Chun J, Luster AD, Tager AM. Prolonged exposure to sphingosine 1-phosphate receptor-1 agonists exacerbates vascular leak, fibrosis, and mortality after lung injury. Am J Respir Cell Mol Biol. 2010;43(6):662–73.
van Nieuw Amerongen GP, Beckers CM, Achekar ID, Zeeman S, Musters RJ, van Hinsbergh VW. Involvement of rho kinase in endothelial barrier maintenance. Arterioscler Thromb Vasc Biol. 2007;27(11):2332–9.
Kohno M, Watanabe M, Goto T, Kamiyama I, Ohtsuka T, Tasaka S, et al. Attenuation of lung ischemia-reperfusion injury by rho-associated kinase inhibition in a rat model of lung transplantation. Ann Thorac Cardiovasc Surg. 2014;20(5):359–64.
Siddiqui MR, Akhtar S, Shahid M, Tauseef M, McDonough K, Shanley TP. Mir-144-mediated inhibition of ROCK1 protects against LPS-induced lung endothelial hyperpermeability. Am J Respir Cell Mol Biol. 2019;61(2):257–65.
Mezu-Ndubuisi OJ, Maheshwari A. The role of integrins in inflammation and angiogenesis. Pediatr Res. 2021;89(7):1619–26.
Lampugnani MG, Resnati M, Dejana E, Marchisio PC. The role of integrins in the maintenance of endothelial monolayer integrity. J Cell Biol. 1991;112(3):479–90.
Su G, Hodnett M, Wu N, Atakilit A, Kosinski C, Godzich M, et al. Integrin alphavbeta5 regulates lung vascular permeability and pulmonary endothelial barrier function. Am J Respir Cell Mol Biol. 2007;36(3):377–86.
Mallavia B, Liu F, Sheppard D, Looney MR. Inhibiting integrin alphavbeta5 reduces Ischemia-Reperfusion Injury in an Orthotopic Lung Transplant Model in mice. Am J Transpl. 2016;16(4):1306–11.
Zhang D, Li C, Song Y, Zhou J, Li Y, Li J, et al. Integrin alphavbeta5 inhibition protects against ischemia-reperfusion-induced lung injury in an autophagy-dependent manner. Am J Physiol Lung Cell Mol Physiol. 2017;313(2):L384–94.
de Perrot M, Liu M, Waddell TK, Keshavjee S. Ischemia-reperfusion-induced lung injury. Am J Respir Crit Care Med. 2003;167(4):490–511.
Mrazkova H, Lischke R, Hodyc D, Herget J. The protective effect of hypercapnia on ischemia-reperfusion injury in lungs. Respir Physiol Neurobiol. 2015;205:42–6.
Annecke T, Rehm M, Bruegger D, Kubitz JC, Kemming GI, Stoeckelhuber M, et al. Ischemia-reperfusion-induced unmeasured anion generation and glycocalyx shedding: sevoflurane versus propofol anesthesia. J Invest Surg. 2012;25(3):162–8.
Bellingan G, Maksimow M, Howell DC, Stotz M, Beale R, Beatty M, et al. The effect of intravenous interferon-beta-1a (FP-1201) on lung CD73 expression and on acute respiratory distress syndrome mortality: an open-label study. Lancet Respir Med. 2014;2(2):98–107.
Thorneloe KS, Cheung M, Bao W, Alsaid H, Lenhard S, Jian MY, et al. An orally active TRPV4 channel blocker prevents and resolves pulmonary edema induced by heart failure. Sci Transl Med. 2012;4(159):159ra48.
Yin J, Michalick L, Tang C, Tabuchi A, Goldenberg N, Dan Q, et al. Role of transient receptor potential vanilloid 4 in Neutrophil activation and Acute Lung Injury. Am J Respir Cell Mol Biol. 2016;54(3):370–83.
Kuebler WM, Jordt SE, Liedtke WB. COVID-19: urgent reconsideration of lung edema as a preventable outcome inhibition of TRPV4 as a promising and feasible approach. SSRN. 2020:3558887.
Goyal N, Skrdla P, Schroyer R, Kumar S, Fernando D, Oughton A, et al. Clinical pharmacokinetics, Safety, and tolerability of a Novel, First-in-class TRPV4 Ion Channel inhibitor, GSK2798745, in healthy and heart failure subjects. Am J Cardiovasc Drugs. 2019;19(3):335–42.
Mole S, Harry A, Fowler A, Hotee S, Warburton J, Waite S, et al. Investigating the effect of TRPV4 inhibition on pulmonary-vascular barrier permeability following segmental endotoxin challenge. Pulm Pharmacol Ther. 2020;64:101977.
Wan L, Wu W, Jiang S, Wan S, Meng D, Wang Z, et al. Mibefradil and Flunarizine, two T-Type Calcium Channel inhibitors, protect mice against Lipopolysaccharide-Induced Acute Lung Injury. Mediators Inflamm. 2020;2020:3691701.
Rizzo AN, Sammani S, Esquinca AE, Jacobson JR, Garcia JG, Letsiou E, et al. Imatinib attenuates inflammation and vascular leak in a clinically relevant two-hit model of acute lung injury. Am J Physiol Lung Cell Mol Physiol. 2015;309(11):L1294–304.
Aman J, van Bezu J, Damanafshan A, Huveneers S, Eringa EC, Vogel SM, et al. Effective treatment of edema and endothelial barrier dysfunction with imatinib. Circulation. 2012;126(23):2728–38.
Zhang J, Wang JS, Zheng ZK, Tang J, Fan K, Guo H, et al. Participation of autophagy in lung ischemia-reperfusion injury in vivo. J Surg Res. 2013;182(2):e79–87.
Liu WC, Chen SB, Liu S, Ling X, Xu QR, Yu BT, et al. Inhibition of mitochondrial autophagy protects donor lungs for lung transplantation against ischaemia-reperfusion injury in rats via the mTOR pathway. J Cell Mol Med. 2019;23(5):3190–201.
Zhang D, Li C, Zhou J, Song Y, Fang X, Ou J, et al. Autophagy protects against ischemia/reperfusion-induced lung injury through alleviating blood-air barrier damage. J Heart Lung Transpl. 2015;34(5):746–55.
Steen S, Sjoberg T, Pierre L, Liao Q, Eriksson L, Algotsson L. Transplantation of lungs from a non-heart-beating donor. Lancet. 2001;357(9259):825–9.
Ingemansson R, Eyjolfsson A, Mared L, Pierre L, Algotsson L, Ekmehag B, et al. Clinical transplantation of initially rejected donor lungs after reconditioning ex vivo. Ann Thorac Surg. 2009;87(1):255–60.
Cypel M, Yeung JC, Donahoe L, Chen M, Zamel R, Hoetzenecker K, et al. Normothermic ex vivo lung perfusion: does the indication impact organ utilization and patient outcomes after transplantation? J Thorac Cardiovasc Surg. 2020;159(1):346–55. e1.
Emaminia A, Lapar DJ, Zhao Y, Steidle JF, Harris DA, Laubach VE, et al. Adenosine A(2)a agonist improves lung function during ex vivo lung perfusion. Ann Thorac Surg. 2011;92(5):1840–6.
Wagner CE, Pope NH, Charles EJ, Huerter ME, Sharma AK, Salmon MD, et al. Ex vivo lung perfusion with adenosine A2A receptor agonist allows prolonged cold preservation of lungs donated after cardiac death. J Thorac Cardiovasc Surg. 2016;151(2):538–45.
Stone ML, Sharma AK, Mas VR, Gehrau RC, Mulloy DP, Zhao Y, et al. Ex vivo Perfusion with Adenosine A2A receptor agonist enhances Rehabilitation of Murine Donor lungs after circulatory death. Transplantation. 2015;99(12):2494–503.
Mulloy DP, Stone ML, Crosby IK, Lapar DJ, Sharma AK, Webb DV, et al. Ex vivo rehabilitation of non-heart-beating donor lungs in preclinical porcine model: delayed perfusion results in superior lung function. J Thorac Cardiovasc Surg. 2012;144(5):1208–15.
Huerter ME, Sharma AK, Zhao Y, Charles EJ, Kron IL, Laubach VE. Attenuation of Pulmonary Ischemia-Reperfusion Injury by Adenosine A2B receptor antagonism. Ann Thorac Surg. 2016;102(2):385–93.
Charles EJ, Mehaffey JH, Sharma AK, Zhao Y, Stoler MH, Isbell JM, et al. Lungs donated after circulatory death and prolonged warm ischemia are transplanted successfully after enhanced ex vivo lung perfusion using adenosine A2B receptor antagonism. J Thorac Cardiovasc Surg. 2017;154(5):1811–20.
Download references
Sources of funding include NIH R01 HL157407, NIH R01 HL142110, and NIH R01 HL146914.
Author information
Authors and affiliations.
Department of Surgery, University of Virginia, P. O. Box 801359, Charlottesville, VA, 22908, USA
Huy Q. Ta, Mark E. Roeser & Victor E. Laubach
Robert M. Berne Cardiovascular Research Center, University of Virginia, Charlottesville, VA, 22908, USA
Maniselvan Kuppusamy & Swapnil K. Sonkusare
Department of Molecular Physiology and Biological Physics, University of Virginia, Charlottesville, VA, 22908, USA
Swapnil K. Sonkusare
You can also search for this author in PubMed Google Scholar
Contributions
HQT drafted the manuscript, VEL and SKS revised the manuscript and provided additional content, MK created Fig. 1 and contributed to specific areas of the manuscript as well as manuscript review, MER revised and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Victor E. Laubach .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ta, H.Q., Kuppusamy, M., Sonkusare, S.K. et al. The endothelium: gatekeeper to lung ischemia-reperfusion injury. Respir Res 25 , 172 (2024). https://doi.org/10.1186/s12931-024-02776-4
Download citation
Received : 09 February 2024
Accepted : 14 March 2024
Published : 18 April 2024
DOI : https://doi.org/10.1186/s12931-024-02776-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Endothelial barrier dysfunction
- Lung transplantation
- Inflammation
- Oxidative stress
Respiratory Research
ISSN: 1465-993X
- General enquiries: [email protected]
Help | Advanced Search
Computer Science > Computation and Language
Title: openelm: an efficient language model family with open-source training and inference framework.
Abstract: The reproducibility and transparency of large language models are crucial for advancing open research, ensuring the trustworthiness of results, and enabling investigations into data and model biases, as well as potential risks. To this end, we release OpenELM, a state-of-the-art open language model. OpenELM uses a layer-wise scaling strategy to efficiently allocate parameters within each layer of the transformer model, leading to enhanced accuracy. For example, with a parameter budget of approximately one billion parameters, OpenELM exhibits a 2.36% improvement in accuracy compared to OLMo while requiring $2\times$ fewer pre-training tokens. Diverging from prior practices that only provide model weights and inference code, and pre-train on private datasets, our release includes the complete framework for training and evaluation of the language model on publicly available datasets, including training logs, multiple checkpoints, and pre-training configurations. We also release code to convert models to MLX library for inference and fine-tuning on Apple devices. This comprehensive release aims to empower and strengthen the open research community, paving the way for future open research endeavors. Our source code along with pre-trained model weights and training recipes is available at \url{ this https URL }. Additionally, \model models can be found on HuggingFace at: \url{ this https URL }.
Submission history
Access paper:.
- Other Formats
References & Citations
- Google Scholar
- Semantic Scholar
BibTeX formatted citation
Bibliographic and Citation Tools
Code, data and media associated with this article, recommenders and search tools.
- Institution
arXivLabs: experimental projects with community collaborators
arXivLabs is a framework that allows collaborators to develop and share new arXiv features directly on our website.
Both individuals and organizations that work with arXivLabs have embraced and accepted our values of openness, community, excellence, and user data privacy. arXiv is committed to these values and only works with partners that adhere to them.
Have an idea for a project that will add value for arXiv's community? Learn more about arXivLabs .

IMAGES
VIDEO
COMMENTS
The conclusion of a research paper restates the research problem, summarizes your arguments or findings, and discusses the implications. FAQ About us . Our editors ... (you will have presented your in-depth results and discussion already), but do clearly express the answers to the research questions you investigated.
Your results should always be written in the past tense. While the length of this section depends on how much data you collected and analyzed, it should be written as concisely as possible. Only include results that are directly relevant to answering your research questions. Avoid speculative or interpretative words like "appears" or ...
the results of your research, a discussion of related research, and; ... You can apply the advice in this article to the conclusion, results or discussion sections of your manuscript. Our Early Career Researcher community tells us that the conclusion is often considered the most difficult aspect of a manuscript to write. To help, this guide ...
The conclusion in a research paper is the final section, where you need to summarize your research, presenting the key findings and insights derived from your study. ... It restates how your results contribute to the existing body of knowledge and whether they confirm or challenge existing theories or hypotheses. Also, by identifying unanswered ...
The conclusion is intended to help the reader understand why your research should matter to them after they have finished reading the paper. A conclusion is not merely a summary of the main topics covered or a re-statement of your research problem, but a synthesis of key points derived from the findings of your study and, if applicable, where you recommend new areas for future research.
Research Paper Conclusion. Definition: A research paper conclusion is the final section of a research paper that summarizes the key findings, significance, and implications of the research. It is the writer's opportunity to synthesize the information presented in the paper, draw conclusions, and make recommendations for future research or ...
The conclusion is where you describe the consequences of your arguments by justifying to your readers why your arguments matter (Hamilton College, 2014). Derntl (2014) also describes conclusion as the counterpart of the introduction. Using the Hourglass Model (Swales, 1993) as a visual reference, Derntl describes conclusion as the part of the ...
Step 2: Summarize and reflect on your research. Step 3: Make future recommendations. Step 4: Emphasize your contributions to your field. Step 5: Wrap up your thesis or dissertation. Full conclusion example. Conclusion checklist. Other interesting articles. Frequently asked questions about conclusion sections.
For most research papers in the social and behavioral sciences, there are two possible ways of organizing the results. Both approaches are appropriate in how you report your findings, but use only one approach. Present a synopsis of the results followed by an explanation of key findings. This approach can be used to highlight important findings.
The way the authors interpret their results may be quite different from the way you would interpret them or the way another researcher would interpret them. Note: Some articles collapse the Discussion and Conclusion sections together under a single heading (usually "Conclusion"). If you don't see a separate Discussion section, don't worry.
Research Results. Research results refer to the findings and conclusions derived from a systematic investigation or study conducted to answer a specific question or hypothesis. These results are typically presented in a written report or paper and can include various forms of data such as numerical data, qualitative data, statistics, charts, graphs, and visual aids.
Tips to Write the Results Section. Direct the reader to the research data and explain the meaning of the data. Avoid using a repetitive sentence structure to explain a new set of data. Write and highlight important findings in your results. Use the same order as the subheadings of the methods section.
A conclusion is the final paragraph of a research paper and serves to help the reader understand why your research should matter to them. The conclusion of a conclusion should: Restate your topic and why it is important. Restate your thesis/claim. Address opposing viewpoints and explain why readers should align with your position.
Discuss your conclusions in order of most to least important. Compare your results with those from other studies: Are they consistent? If not, discuss possible reasons for the difference. Mention any inconclusive results and explain them as best you can. You may suggest additional experiments needed to clarify your results.
The Conclusion. After all the data is organized in a form that relates it to your hypothesis, you can interpret it and reach a conclusion about the experiment. The conclusion is simply a report about what you learned based on whether the results agree or disagree with your hypothesis. It usually contains a summary of the actual procedure and ...
The way the authors interpret their results may be quite different from the way you would interpret them or the way another researcher would interpret them. Note: Some articles collapse the Discussion and Conclusion sections together under a single heading (usually "Conclusion"). If you don't see a separate Discussion section, don't worry.
The conclusion is intended to help the reader understand why your research should matter to them after they have finished reading the paper. A conclusion is not merely a summary of your points or a re-statement of your research problem but a synthesis of key points. For most essays, one well-developed paragraph is sufficient for a conclusion ...
Results are findings of the study or research, discussion is the relationship between results and literature review while conclusion is the relationship between the study aims/objectives and and ...
The "Results section" is the third most important anatomical structure of IMRAD (Introduction, Method and Material, Result, And Discussion) frameworks, the almost universally accepted framework in many journals in the late nineteenth century. 3 Before using a structured IMRAD format, research findings in scientific papers were presented in ...
Protocol registration and results reporting. Protocol registration for this scoping review was not conducted. Arksey and O'Malley's methodological framework was utilized to conduct this scoping review [].The scoping review procedures start by defining the research questions, identifying relevant literature, selecting articles, extracting data, and summarizing the results.
Conclusion. The Helium network and its token offer a compelling vision for decentralised wireless communication, especially in the IoT domain. By incentivising individuals and businesses to participate in and expand the network, Helium has the potential to revolutionise how devices connect across the globe.
Your results section is where you objectively report all relevant findings and leave them open for interpretation by readers. While you should state whether the findings of statistical tests lend support to your hypotheses, refrain from forming conclusions to your research questions in the results section. Explanation of how statistics tests work
On April 23, 2024, GE Aerospace (NYSE: GE, $161.26, Market Capitalization: $176.5 billion) reported robust 1Q24 results, with a strong beat on EPS versus consensus.
Here are some key things to know about how we're reporting the results of the April 23 primary election, that includes primaries for President, U.S. Senate and House, State Attorney General, row ...
The educational damage wrought by the COVID-19 pandemic will impact on children well into the 2030s, with generations of pupils set for the biggest declines in GCSE results for decades. These are the devastating conclusions of a major new study from LSE, the University of Exeter and the University of Strathclyde. The report predicts that less ...
Researchers have developed a promising new framework for studying the link between social disconnection and poor physical health in people living with serious mental illnesses (SMI). Drawing on published research from animal models and data from the general population, this framework builds on existing social isolation and loneliness models by integrating insights from evolutionary and ...
The success of lung transplantation is limited by the high rate of primary graft dysfunction due to ischemia-reperfusion injury (IRI). Lung IRI is characterized by a robust inflammatory response, lung dysfunction, endothelial barrier disruption, oxidative stress, vascular permeability, edema, and neutrophil infiltration. These events are dependent on the health of the endothelium, which is a ...
The reproducibility and transparency of large language models are crucial for advancing open research, ensuring the trustworthiness of results, and enabling investigations into data and model biases, as well as potential risks. To this end, we release OpenELM, a state-of-the-art open language model. OpenELM uses a layer-wise scaling strategy to efficiently allocate parameters within each layer ...
With planting season upon us, now is the time to dig deeper into agricultural practices and determine what best fits the needs of every operation. Download a copy of the 2023 Research Results book today from the NOFRN site. For more information about the 2023 Research Results book or the NOFRN, please contact Taylor Lexow at 402-245-2222.
A research paper that presents a sustained argument will usually encapsulate this argument in a thesis statement. A research paper designed to present the results of empirical research tends to present a research question that it seeks to answer. It may also include a hypothesis—a prediction that will be confirmed or disproved by your research.