Research Projects
The Division of Diabetes Translation (DDT) conducts and supports studies, often in collaboration with partners, to develop and apply sound science to reduce the burden of diabetes and to address the research needs of DDT programs and the diabetes community.
Analyses from various studies, such as LEAD and SEARCH, to help improve diabetes surveillance and guide decision-making.
Research, including the Diabetes Prevention Program Outcome Study (DPPOS), that evaluates the success of diabetes interventions and strategies.
Reviews of the effect of type 2 diabetes-related health policies on various populations, such as the NEXT-D2 study.
Collection of the most recent publications and access to archived ones.
- US Diabetes Surveillance System
- Chronic Kidney Disease Surveillance System
- Vision and Eye Health Surveillance System
- Diabetes State Burden Toolkit
- Diabetes Prevention Impact Toolkit
To receive updates about diabetes topics, enter your email address:
- Diabetes Home
- State, Local, and National Partner Diabetes Programs
- National Diabetes Prevention Program
- Native Diabetes Wellness Program
- Chronic Kidney Disease
- Vision Health Initiative
- Heart Disease and Stroke
- Overweight & Obesity

Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.
A molecular ‘warhead’ against disease

Asking the internet about birth control

‘Harvard Thinking’: Facing death with dignity
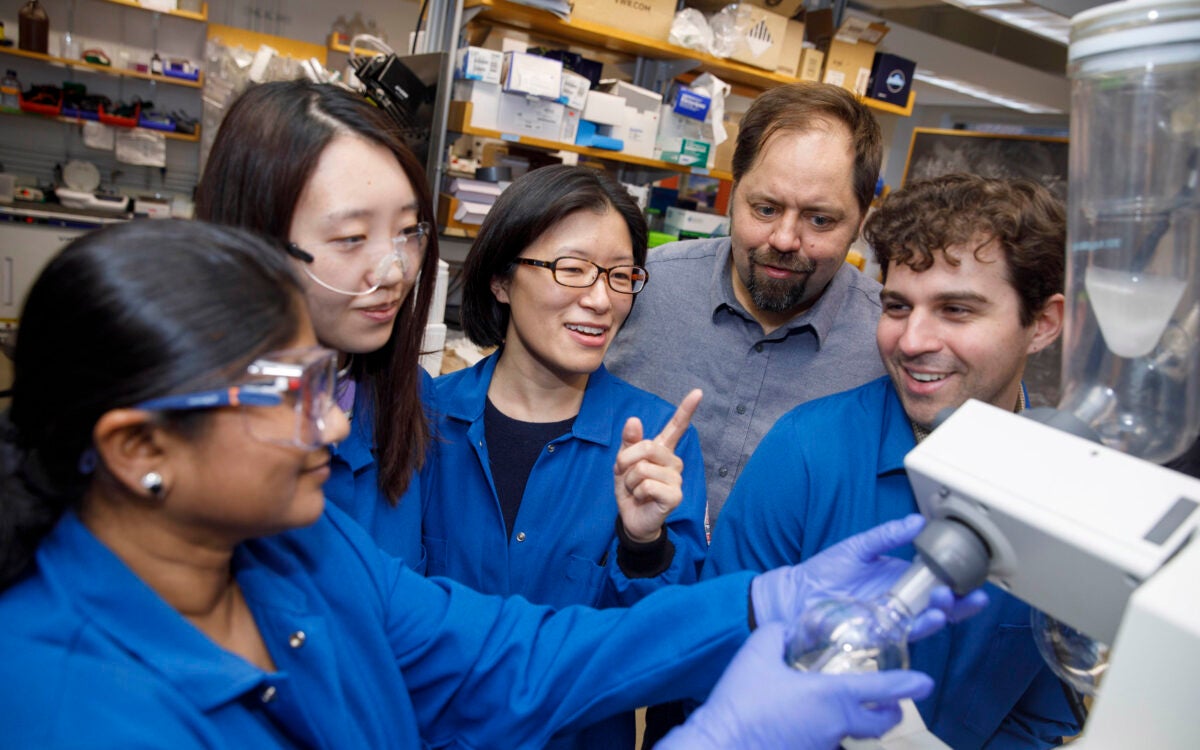
“When my son was diagnosed [with Type 1], I knew nothing about diabetes. I changed my research focus, thinking, as any parent would, ‘What am I going to do about this?’” says Douglas Melton.
Kris Snibbe/Harvard Staff Photographer
Breakthrough within reach for diabetes scientist and patients nearest to his heart
Harvard Correspondent
100 years after discovery of insulin, replacement therapy represents ‘a new kind of medicine,’ says Stem Cell Institute co-director Douglas Melton, whose children inspired his research
When Vertex Pharmaceuticals announced last month that its investigational stem-cell-derived replacement therapy was, in conjunction with immunosuppressive therapy, helping the first patient in a Phase 1/2 clinical trial robustly reproduce his or her own fully differentiated pancreatic islet cells, the cells that produce insulin, the news was hailed as a potential breakthrough for the treatment of Type 1 diabetes. For Harvard Stem Cell Institute Co-Director and Xander University Professor Douglas Melton, whose lab pioneered the science behind the therapy, the trial marked the most recent turning point in a decades-long effort to understand and treat the disease. In a conversation with the Gazette, Melton discussed the science behind the advance, the challenges ahead, and the personal side of his research. The interview was edited for clarity and length.
Douglas Melton
GAZETTE: What is the significance of the Vertex trial?
MELTON: The first major change in the treatment of Type 1 diabetes was probably the discovery of insulin in 1920. Now it’s 100 years later and if this works, it’s going to change the medical treatment for people with diabetes. Instead of injecting insulin, patients will get cells that will be their own insulin factories. It’s a new kind of medicine.
GAZETTE: Would you walk us through the approach?
MELTON: Nearly two decades ago we had the idea that we could use embryonic stem cells to make functional pancreatic islets for diabetics. When we first started, we had to try to figure out how the islets in a person’s pancreas replenished. Blood, for example, is replenished routinely by a blood stem cell. So, if you go give blood at a blood drive, your body makes more blood. But we showed in mice that that is not true for the pancreatic islets. Once they’re removed or killed, the adult body has no capacity to make new ones.
So the first important “a-ha” moment was to demonstrate that there was no capacity in an adult to make new islets. That moved us to another source of new material: stem cells. The next important thing, after we overcame the political issues surrounding the use of embryonic stem cells, was to ask: Can we direct the differentiation of stem cells and make them become beta cells? That problem took much longer than I expected — I told my wife it would take five years, but it took closer to 15. The project benefited enormously from undergraduates, graduate students, and postdocs. None of them were here for 15 years of course, but they all worked on different steps.
GAZETTE: What role did the Harvard Stem Cell Institute play?
MELTON: This work absolutely could not have been done using conventional support from the National Institutes of Health. First of all, NIH grants came with severe restrictions and secondly, a long-term project like this doesn’t easily map to the initial grant support they give for a one- to three-year project. I am forever grateful and feel fortunate to have been at a private institution where philanthropy, through the HSCI, wasn’t just helpful, it made all the difference.
I am exceptionally grateful as well to former Harvard President Larry Summers and Steve Hyman, director of the Stanley Center for Psychiatric Research at the Broad Institute, who supported the creation of the HSCI, which was formed specifically with the idea to explore the potential of pluripotency stem cells for discovering questions about how development works, how cells are made in our body, and hopefully for finding new treatments or cures for disease. This may be one of the first examples where it’s come to fruition. At the time, the use of embryonic stem cells was quite controversial, and Steve and Larry said that this was precisely the kind of science they wanted to support.
GAZETTE: You were fundamental in starting the Department of Stem Cell and Regenerative Biology. Can you tell us about that?
MELTON: David Scadden and I helped start the department, which lives in two Schools: Harvard Medical School and the Faculty of Arts and Science. This speaks to the unusual formation and intention of the department. I’ve talked a lot about diabetes and islets, but think about all the other tissues and diseases that people suffer from. There are faculty and students in the department working on the heart, nerves, muscle, brain, and other tissues — on all aspects of how the development of a cell and a tissue affects who we are and the course of disease. The department is an exciting one because it’s exploring experimental questions such as: How do you regenerate a limb? The department was founded with the idea that not only should you ask and answer questions about nature, but that one can do so with the intention that the results lead to new treatments for disease. It is a kind of applied biology department.
GAZETTE: This pancreatic islet work was patented by Harvard and then licensed to your biotech company, Semma, which was acquired by Vertex. Can you explain how this reflects your personal connection to the research?
MELTON: Semma is named for my two children, Sam and Emma. Both are now adults, and both have Type 1 diabetes. My son was 6 months old when he was diagnosed. And that’s when I changed my research plan. And my daughter, who’s four years older than my son, became diabetic about 10 years later, when she was 14.
When my son was diagnosed, I knew nothing about diabetes and had been working on how frogs develop. I changed my research focus, thinking, as any parent would, “What am I going to do about this?” Again, I come back to the flexibility of Harvard. Nobody said, “Why are you changing your research plan?”
GAZETTE: What’s next?
MELTON: The stem-cell-derived replacement therapy cells that have been put into this first patient were provided with a class of drugs called immunosuppressants, which depress the patient’s immune system. They have to do this because these cells were not taken from that patient, and so they are not recognized as “self.” Without immunosuppressants, they would be rejected. We want to find a way to make cells by genetic engineering that are not recognized as foreign.
I think this is a solvable problem. Why? When a woman has a baby, that baby has two sets of genes. It has genes from the egg, from the mother, which would be recognized as “self,” but it also has genes from the father, which would be “non-self.” Why does the mother’s body not reject the fetus? If we can figure that out, it will help inform our thinking about what genes to change in our stem cell-derived islets so that they could go into any person. This would be relevant not just to diabetes, but to any cells you wanted to transplant for liver or even heart transplants. It could mean no longer having to worry about immunosuppression.
Share this article
You might like.
Approach attacks errant proteins at their roots

Only a fraction of it will come from an expert, researchers say

In podcast episode, a chaplain, a bioethicist, and a doctor talk about end-of-life care
College accepts 1,937 to Class of 2028
Students represent 94 countries, all 50 states
Pushing back on DEI ‘orthodoxy’
Panelists support diversity efforts but worry that current model is too narrow, denying institutions the benefit of other voices, ideas
So what exactly makes Taylor Swift so great?
Experts weigh in on pop superstar's cultural and financial impact as her tours and albums continue to break records.

Curing Diabetes
Our research progress.

Nanotechnology and combined strategies to enhance local immunomodulation for treatment of Type 1 Diabetes
In the quest to enhance the lives of those suffering from T1D, Dr. Diana Velluto, Research Assistant Professor in the Department of Surgery at the Diabetes Research Institute, University of Miami School of Medicine, is making incredible advances. Her work centers on the use of innovative nanotechnology to transform how we approach diabetes treatment.

First-ever Dynamic Analysis of Pancreatic Regeneration in Human T1D
A groundbreaking technique has been established which has allowed scientists from the Diabetes Research Institute (DRI) at the University of Miami Miller School of Medicine to culture live sections of the pancreas for nearly two weeks. The scientists have used the living pancreas sections to chart the first dynamic single-cell map of the regenerative pathways of the pancreas.

New Discoveries Offer Hope in the Fight Against T1D
In a momentous breakthrough, researchers at the Diabetes Research Institute (DRI) have revealed pivotal revelations that may transform our strategy for averting and postponing the emergence of type 1 diabetes (T1D).

Revolutionizing Transplantation: Re-igniting a New Beacon of Hope in Immunotherapy
Another significant step is being achieved by researchers at the DRI on the lengthy journey to bring islet cell transplantation closer to reality for individuals with type 1 diabetes.

How Do Research Discoveries Translate into Clinical Cures?
Scientific research drives discovery into novel biological pathways that regulate normal bodily functions and can indicate alterations that may play a role in autoimmunity, cancer and other diseases. Understanding of the cells, molecules and genes involved in these pathways can lead to the development of drugs, cell therapies, devices and other technologies that might enable prevention, modification, or reversal of disease. But how do scientists take laboratory findings and translate them into people?

Inside Our Labs: New T1D Therapies
August 2022 – Dr. Giacomo Lanzoni is an Assistant Professor at the Diabetes Research Institute, University of Miami Miller School of Medicine. His research is focused on developing stem cell-based therapies for Type 1 Diabetes. In this disease, insulin-producing pancreatic islet beta cells are lost due to an autoimmune attack.

Inside Our Labs: Islet Transplantation
June 2022 – The Diabetes Research Institute (DRI) at the University of Miami Miller School of Medicine in Miami, Florida first began performing clinical islet transplantation in 1985. Since then, our center has blossomed into one of the largest independent centers worldwide, with 57 transplant recipients totaling 101 islet infusions since the year 2000.

Inside Our Labs: Treg Therapy and other Autoimmune Therapies
May 2022 – Dr. Bayer’s lab focuses on Treg therapy and other autoimmune therapies. The main overarching goal of their current work is to better understand autoimmune-targeted treatments and how it can lead to diabetes reversal or late-stage development treatment. They focus on understanding the mechanisms by which the immune system provides immune regulation to maintain health and prevent disease.
Inside Our Labs: Mechanisms of Islet Transplant Immune Tolerence
April 2022 – Dr. Abdulreda’s DRIF funded project entitled “Mechanisms of Islet Transplant Immune Tolerance” aims to understand immune pathways that contribute to graft rejection or immune tolerance. Currently, islet transplantation requires continual immunosuppressive treatment to reduce the chance of islet graft rejection.

COVID-19, Diabetes and Mesenchymal Stem Cells: Groundbreaking Findings Bring New Hope
February 2022 – At the DRI, we have been studying Mesenchymal Stem Cells and their immunomodulatory properties for more than a decade. These cells can function as potent inhibitors of inflammation, can modulate immunity, and can stimulate Regulatory T cells (Tregs). Intense studies are ongoing at our Institute to use these cells to fend off autoimmunity in type 1 diabetes and to limit progression of diabetes complication.

2020 Long-Term Culture of Human Pancreatic Slices Reveals Regeneration of Insulin-Producing Cells
DRI scientists developed a method allowing for the long-term culture of “pancreatic slices” to study the regeneration of the human pancreas in real time. The results, published Nature Communications, demonstrate for the first time that extended cultures of near-intact human pancreatic tissue retain the ability of the live organ to replenish insulin-producing beta cells. The use of this system as a model to study pancreatic regeneration could have important therapeutic implications for the treatment of diabetes.

2019 Long-Term Islet Transplant Recipients Show Near-Normal Glucose Control
Using continuous glucose monitoring (CGM), DRI scientists show that a small group of islet transplant recipients who were insulin independent for an average of 10 years have blood sugar levels that are similar to those without type 1 diabetes.

2019 Engineered ‘Suicide Genes’ Prevent Tumors in Stem-Cell Derived Beta Cells
For the first time, DRI scientists engineer a stem cell line containing two ‘suicide genes’ that induce cell death in all but the desired insulin-producing cells. This double fail-safe approach, published in Stem Cell Reports , opens the door to advancing cell-replacement therapies for people living with type 1 diabetes.

2018 DRI Launches POSEIDON Study to Assess Impact of Omega-3 and Vitamin D in Type 1 Diabetes
Several scientific reports have suggested that high-dose omega-3 fatty acids and vitamin D may have a beneficial effect on autoimmune conditions, like type 1 diabetes. DRI researchers will formally test the effects of this intervention in children and adults newly diagnosed and in those with longer-standing T1D to evaluate any benefit on reducing inflammation, halting autoimmunity, and increasing insulin sensitivity and secretion.

2018 DRI Scientists Identify Unique Pancreatic Stem Cells
DRI scientists confirm the existence of progenitor cells (pancreatic stem cells) within the large ducts of the human pancreas that can be stimulated to develop into glucose-responsive beta cells. The findings, published in Cell Reports , could pave the way to regenerating a person’s own insulin-producing cells in type 1 diabetes patients.

2017 DRI Scientists Identify New Metabolic “Signature” as Potential Key Biomarker for Type 1 Diabetes Development
Currently, there is no good biomarker to detect whether the immune attack on the beta cells is underway. DRI researchers mapped out the biochemical changes that occur during type 1 diabetes onset, which is important not only for preventing the disease, but also for monitoring the recurrence of immune attack. This first-ever longitudinal study in experimental models was published in the Journal of Proteome Research .

2017 Novel Tissue-Engineered Islet Transplant Achieves Insulin Independence
DRI researchers report on the first trial participant to receive an islet transplant within a tissue-engineered scaffold, demonstrating that islets transplanted within this BioHub platform can successfully engraft and achieve insulin independence. The trial tests the omentum as an alternative transplant site. The one-year findings are published in the prestigious New England Journal of Medicine (NEJM) .

2016 Researchers Develop and Test “Biological” DRI BioHub Platform
The DRI develops and tests a bioengineered scaffold to house insulin-producing cells. This biological platform, which uses the recipient’s own plasma combined with thrombin, offers the opportunity to incorporate helper cells, nutrients, and local immune protection. These preclinical experiments are the basis for FDA submission for a Phase I/II clinical trial. The work is featured on the cover of the journal Diabetes .

2016 Novel Protocol Achieves 100 Percent Disease Remission in Experimental Models
DRI’s Dr. Allison Bayer and her team have developed a novel protocol demonstrating that adoptive Regulatory T cell (T reg) therapy can reverse the disease and reset autoimmunity in experimental models, achieving disease remission in 100 percent of the recipients. Importantly, the therapy was directed specifically at halting the destruction of the beta cells while the normal immune responses remained intact.

2015 DRI Researchers Convert Pancreatic Exocrine Cells into Insulin-Producing Endocrine Cells Using a Single Protein, BMP-7
Researchers successfully convert non-insulin producing cells into insulin-producing cells using a single agent, BMP-7 (bone morphogenetic protein-7), which is already clinically approved by the FDA. Their published findings in Diabetes demonstrate for the first time that non-endocrine tissue can be reprogrammed to respond to blood glucose without the use of any genetic manipulation, representing a safer method to increase the supply of islets for transplant into people with T1D.

2014 DRI Pioneers New Encapsulation Technology
DRI researchers demonstrate that their unique cell coating process allows efficient encapsulation of islets without compromising viability and function of the cells. The team’s novel method for “shrink wrapping” each cell had been designed to specifically address what are considered to be the limitations of traditional cell encapsulation strategies. The results of their study earn the cover position in Proceedings of the National Academy of Sciences .


2013 DRI Introduces Plans for BioHub Mini Organ
Scientists unveil their plan for the DRI BioHub, a bioengineered “mini organ” designed to mimic the native pancreas. The platform technology will contain thousands of insulin-producing cells that manage blood sugar levels in real time, plus other components that keep the cells healthy and viable long term. The DRI will focus on three primary areas: the development of a new transplant site; the development of a reliable supply of islets; and the ability to sustain the cells’ function without the need for harsh, systemic anti-rejection drugs.

2012 DRI and Collaborators Use Stem Cells to Eliminate Immunosuppression
Scientists from the Diabetes Research Institute (DRI) University of Miami Miller School of Medicine and DRI Federation center at Xiamen University (China) show that the use of mesenchymal stem cells (MSC) in kidney transplant recipients may replace a powerful anti-rejection drug. The results are published in the Journal of the American Medical Association (JAMA) .

2010 Researchers Identify Master Regulatory Genes in Pancreatic Islets
The DRI’s molecular biology team is the first to identify a disproportionately higher number of genes, called miR-7, in pancreatic islets compared to the non-islet tissue of the organ. These master regulatory genes are also found in fetal endocrine cells during development and play a central role in islet cell development, as well as in maintaining this endocrine function (as opposed to developing into other tissue). The findings are published in BMC Genomics .

2010 Study Shows Recurrence of T1D, Need for Multiple Strategies
Scientists show recurrence of type 1 diabetes may occur in patients after kidney-pancreas transplantation. Despite use of immunosuppression and continuous function of the kidney and exocrine portion of the transplanted pancreas, researchers identified the presence of autoimmune cells known to target insulin-producing cells. This study demonstrates the need to block the immune response to foreign tissue and prevent autoimmunity. The findings are published in Diabetes .

2010 DRI Performs Auto-Islet Transplant after Pancreas Trauma
DRI researchers report on the success of an islet auto-transplant performed after severe trauma. Walter Reed Army Medical Center surgeons remove the damaged pancreas from a soldier wounded in the Middle East. The tissue is sent to DRI where islets are isolated and sent back for transplant into the same patient, preventing diabetes. The findings, published in the New England Journal of Medicine , indicate that islet isolation and auto-transplant in cases of severe abdominal trauma can be performed using a remote processing center.

2008 Researchers Pioneer “Living Window” to Observe Islets in Real Time
DRI researchers develop novel method to monitor healthy islets in a living experimental model. For the first time, researchers can obtain real-time imaging of functioning islets transplanted in the anterior chamber of the eye. The clear “window” allows researchers to witness the islets in the same model over time as nerves and blood vessels develop and immune reactions occur. The work is featured on the cover of Nature Medicine .

2007 Invention Supplies Critical Oxygen, Increases Beta Cell Growth
Scientists at the DRI design and test a new cell culture device that closely mimics the natural oxygen environment, demonstrating a dramatic increase in beta cell development from an embryonic mouse pancreas. The findings were published in the journal Stem Cells .

2006 Discovery Shows that Human and Animal Islets Differ Dramatically
Scientists from the DRI’s islet physiology team discover that the internal structure of a human islet cell is dramatically different from the more often studied rodent islet – a striking finding that argues for the importance of studying human islets if medical research is to benefit people living with diabetes. The findings were published Proceedings of the National Academy of Sciences (PNAS) .

2006 Islet Transplantation Improves Patients’ Quality of Life
A Diabetes Research Institute study shows type 1 diabetes patients’ quality of life and sense of well-being improve following islet transplantation despite having to take harsh anti-rejection drugs. The findings were published in the American Journal of Transplantation .

2005 DRI Develops Safer Method for Turning Stem Cells into Insulin-Producing Cells
Scientists report for the first time that protein technology can be used to promote pancreatic cell differentiation. DRI’s Stem Cell and Molecular Biology teams use this technology to show how stem cells can be progressively educated along the pathway leading to functional beta cells. The findings, published in Diabetes , open a promising new avenue of research that might enable the development of more insulin-producing cells for transplant in the future.

2003 DRI Performs First Successful Islet Transplant in Asia
Espousing its philosophy of global collaboration, the Diabetes Research Institute was asked to send members of its clinical cell transplant team to Shanghai’s First People’s Hospital to assist the Chinese team with both the islet isolation and transplantation efforts. Receiving telephone guidance from the DRI’s senior faculty, the DRI team in China was able to overcome every technical obstacle encountered, despite the formidable distance, technology, and language barriers.

2001 New Islet Transplant Protocol Leads to Insulin Independence
Using a new combination of anti-rejection drugs and improved culture media for islets, the DRI’s cell transplant team performs a series of “islets alone” transplants in study participants with long-standing type 1 diabetes. The recipients are able to discontinue insulin therapy for more than a year following islet transplantation.

1999 DRI Study Results Ignite Global Interest in Islet Transplantation
Using monthly injections of a monoclonal antibody, DRI is the first to show that transplanted islets reverse diabetes in pre-clinical models without the need for any other anti-rejection drug. The recipients remain insulin independent for over one year post-transplant and emerging rejection episodes can be reversed using this antibody. Even after discontinuation of the antibody, many subjects remain off insulin with glucose responsiveness for several months. The results are published in Proceedings of the National Academy of Sciences.

1997 Researchers Identify Cells that Regulate Autoimmunity
The DRI’s immunogenetics team publishes new findings related to insulin production in the thymus and its role in the development of type 1 diabetes. The Nature Genetics paper describes how this type of insulin might play a key role in the immune system’s ability to recognize insulin molecules as “self”. Scientists believe that the amount of thymic insulin might determine either susceptibility to or protection from diabetes.

1995 Islet Transplant Patient Insulin Independent for Five Years
Biopsies show intact, functioning human islet cells in the liver of a patient who was completely insulin independent for five years following an islet transplant.

1990 Organ Transplant Patients Become Insulin Independent After Receiving Islets
Nine patients receive islet cells in conjunction with their multi-organ transplants. This study, published in The Lancet , demonstrates that islets can produce insulin independence in patients who had previously been pancreatectomized.

1988 Invention Expands the Number of Clinical Islet Transplantation Trials
Camillo Ricordi, M.D., develops an automated method for isolating large numbers of islets from a single donor pancreas. This technology leads to expansion of clinical trials in cell therapy for the treatment and cure of type 1 diabetes. The findings were published in the journal Diabetes .

1987 Researchers Discover New Method for Visualizing Islets, Improving Outcomes
DRI’s Rodolfo Alejandro, M.D., identifies a chemical that differentiates islets from non-islet tissue of the pancreas during the isolation process. This zinc-binding substance (dithizone) is absorbed only by islets, giving them a distinctive red color. This discovery enables researchers to optimize the cell separation process for improved clinical outcomes. It was also shown that the use of this substance does not interfere with islet function in vitro or in vivo. The findings were published in Transplantation .

1985 DRI Performs First Clinical Islet Transplants
Based upon results obtained in preclinical transplant models, DRI researchers begin the first human pilot clinical trial in patients with type 1 diabetes. The results of the pioneering study appeared in Advanced Models for the Therapy of Insulin-Dependent Diabetes .

1984 Successful Islet Transplant in Dogs Restores Natural Insulin Production
DRI researchers conduct the first successful transplant of healthy islets into dogs with diabetes, restoring long-term natural insulin-production and normalizing blood sugar levels. Previously, these experiments were only successful in the rodent model. The findings were published in the journal Diabetes .

1978 DRI Develops Gold-Standard Treatment for Pregnant Women with Type 1 Diabetes
Using newly developed self-glucose monitoring and individualized algorithms for intensive insulin therapy, DRI researchers demonstrate that tight blood sugar control in women with type 1 diabetes during pregnancy can result in successful, full-term deliveries with normal birth weights. The study results were published in Diabetes Care .

1975 DRI Researchers Reverse Diabetes in Rodents
Islet cells are successfully transplanted into rats with diabetes, restoring natural insulin production and normalizing blood sugar levels in laboratory animals. The results are published in the journal Diabetes.
back to top
Keep Up With Our Progress Toward A Cure & More
Research & Grants
The ADA’s research strategy is strategic, targeted, and laser focused. We remain dedicated to supporting all of the key aspects of research that have been part of our commitment for decades: funding for early career investigators, fostering the next generation of leaders, and support for investigator-initiated research that generates discoveries to bring us effective new treatments and paths to a cure.

Current Funding Opportunities
Information for Current Grantees
Pathway to Stop Diabetes Program
Grant Management Site
Funded Research
Resources for Researchers
ADA RESEARCH PROGRAMS
ADA has a few different grant initiatives. Calls are broad in scope and encompass basic through clinical research. Significant emphasis will be placed on diabetes clinical research and translation.
Applications will be evaluated on the potential of the research, if successful, to have a major impact on the development, dissemination or implementation of effective interventions or strategies that improve the outcomes for individuals living with diabetes.
American Diabetes Association’s Pathway to Stop Diabetes program is designed to transform diabetes research by attracting innovative scientists, physicians, and researchers through financial support and professional mentorship.
ADA is committed to nurturing the next generation of leaders in diabetes research. Our goal with Postdoctoral Fellowships is to support outstanding researchers in their pursuit of innovative and impactful research projects.
RFA submissions should indicate how the proposed research will have a significant impact on outcomes.

Newsroom / News Release
Project ECHO Launches Study on Improving Outcomes for Diabetic Patients with Chronic Conditions
Funds awarded by the patient-centered outcomes research institute .
ALBUQUERQUE, NM – A research team at Project ECHO, part of The University of New Mexico Health Sciences Center, has been approved for a $10.8 million funding award by the Patient-Centered Outcomes Research Institute (PCORI) to study how to help primary care physicians in New Mexico upskill in their treatment of complex diabetes.
In New Mexico, about 12.3% of the adult population has been diagnosed with diabetes; an additional 36.1% of the adult population has “prediabetes,” or blood glucose levels that are higher than normal but not yet high enough to be diagnosed, according to the American Diabetes Association .
In a rural state with a strained health care system, care for these patients often falls to their primary care provider. Adding to the complexity of care, patients with diabetes have an increased risk of high cholesterol, obesity and depression. Furthermore, these patients face higher risks of losing physical or mental function, experiencing other chronic conditions and death.
“We have been using the ECHO Model to improve diabetes care in New Mexico for a decade. This new funding allows us to examine the impact ECHO has on patient outcomes in a large randomized controlled trial,” says Dr. Sanjeev Arora, founder and director of Project ECHO, and co-principal investigator of the PCORI-funded study with Yiliang Zhu, Ph.D.
“There are not enough specialists available to provide timely care to everyone that needs it. We are relying on our primary care providers to fill in the gap, which can be overwhelming. Through telementorship, the ECHO Model enables health care providers to get the specific, actionable knowledge that they need to treat the patients that they are seeing the very next day,” says Raj Shah, Ph.D., project co-lead.
This PCORI-funded research studies a specific intervention: can health care providers who attend ECHO sessions, and learn specialized care for patients with diabetes and multiple chronic conditions, successfully lower blood sugar levels in patients treated at primary care clinics in New Mexico?
“There is a great shortage of endocrinologists in rural New Mexico. By receiving best-practice care right in their hometowns, these patients will be able to improve their health, without the stress and expense of traveling; or the wait times to see a specialist,” says Dr. Matt Bouchonville, endocrinologist and professor of medicine at the UNM Health Sciences Center.
Project ECHO will partner with Presbyterian Medical Services, the state’s largest network of primary care clinics. Providers and care teams from 10 clinics will be selected at random to participate in the ECHO program for 18 months; while providers at 10 other clinics will continue with care as usual. A research team will collect data from both groups—about 7,000 patients—and hopes to see improvements in blood sugar levels as well as co-occurring chronic conditions including high cholesterol, obesity and depression.
The study, ECHO for Diabetes and Multiple Chronic Conditions , was selected through a PCORI Funding Announcement focused on research comparing different approaches to incorporating access to and use of telehealth in primary care to improve outcomes among individuals with multiple chronic conditions, particularly among vulnerable populations.
“This study was selected for PCORI funding for its potential to answer the need for real-world evidence about how best to incorporate telehealth into the primary care of people with multiple chronic conditions and how this may differ among populations at risk for health disparities,” said PCORI Executive Director Nakela L. Cook, M.D., MPH. “We look forward to following the study’s progress and working with Project ECHO to share the results.”
About Project ECHO Founded in 2003, a global not-for-profit organization, headquartered at The University of New Mexico Health Sciences Center. ECHO empowers practitioners in rural and underserved areas to reduce disparities and improve the well-being of people in the communities where they live. ECHO’s low-cost virtual mentoring model addresses some of the world’s greatest challenges in clinical medicine and public health, with a mission to touch 1 billion lives by 2025.
The ECHO Endocrinology Program has been serving New Mexicans since 2014. Local health care providers are invited to join at no cost through iECHO.org
About Presbyterian Medical Services
Presbyterian Medical Services (PMS) is a non-profit health care provider that has been serving the state of New Mexico since its inception in 1969. With a history that dates to 1908, PMS has grown into a comprehensive health care system that offers a wide range of services to meet the diverse needs of New Mexicans. Their services encompass primary care, dental, behavioral health, early childhood education, supportive living, senior programs, among other services operating approximately 100 programs across the state. PMS is dedicated to working collaboratively with community groups, school districts, local providers, hospitals, and governments to develop programs that cater to the needs of the communities they serve, with a particular focus on individuals living at or below the federal poverty level. With over 100 locations across New Mexico, we strive to make accessing quality health care, childhood education and social services possible for everyone. To learn more about PMS and its programs and services, please visit www.pmsnm.org .
Share this story:
Media contact:.
Email Our Media Relations Team [email protected]
Sign Up For Our Newsletters
Return to Newsroom
Media Contact
If you are a member of the news media, use the email button below. Include: your name, press affiliation, phone number, questions or interview request and deadline.
Email Our Media Relations Team
None Available
Related Stories
Echo supports infection control network in africa, ‘every infant matters’ for this mother-daughter nonprofit team , transforming hiv care in native communities , defining a calling: the magic of echo autism.
Talk to us about diabetes
0345 123 2399
customer support
Our diabetes research
Everything we know about diabetes - every drug , device and development has only been possible because of research. And, one day, research will find a cure.
We’re the UK’s leading charitable funder of diabetes research. For 87 years, our research has been behind some of the biggest leaps forward in diabetes care and changed lives for the better.
Today, our scientists are relentlessly pushing for the next treatment breakthrough and speeding up progress towards a cure . Your support allows us to fund it and by listening to you, we deliver research that makes the biggest possible impact.

About our research

Get involved in research

For researchers
Share this page.
© The British Diabetic Association operating as Diabetes UK, a charity registered in England and Wales (no. 215199) and in Scotland (no. SC039136). A company limited by guarantee registered in England and Wales with (no.00339181) and registered office at Wells Lawrence House, 126 Back Church Lane London E1 1FH


City of Hope Research
- Beckman Research Institute
- Arthur Riggs Diabetes & Metabolism Research Institute
- Comprehensive Cancer Center
- Hematologic Malignancies Research Institute
- Translational Genomics Research Institute
- Irell & Manella Graduate School of Biological Sciences
- Shared Resources
- Additional Resources
City of Hope is home to some of the world’s leading research centers and institutes, where our scientists are renowned for breakthrough innovations.
Sharing our state-of-the-art equipment and resources, and the expertise to apply them to meaningful research, are crucial to the pursuit of new treatments and potential cures.
Among the worldwide leaders in administering clinical trials, City of Hope conducts more than 400 studies annually, enrolling more than 6,000 patients.
Research Centers & Institutes
Our insights into gene therapy, recombinant DNA technology, computational medicine, biology and other fields have made us a world leader in creating greater understanding of cancer, HIV/AIDS and other life-threatening diseases.

- Department of Cancer Biology and Molecular Medicine
- Department of Cancer Genetics & Epigenetics
- Department of Comparative Medicine
- Department of Computational and Quantitative Medicine
- Department of Hematologic Malignancies Translational Science
- Department of Immuno-Oncology
- Department of Integrative Translational Sciences
- Department of Molecular Diagnostics and Experimental Therapeutics
- Department of Population Sciences
- Department of Stem Cell Biology and Regenerative Medicine
- Department of Systems Biology
- Center for Cancer and Aging
- Center for Precision Medicine
- Center for RNA Biology and Therapeutics
We offer a broad diabetes and endocrinology program combining groundbreaking research, unique treatments and comprehensive education to help people with diabetes and other endocrine diseases live longer, better lives.
- Department of Diabetes & Cancer Discovery Science
- Department of Diabetes & Cancer Metabolism
- Department of Diabetes Complications & Metabolism
- Department of Diabetes, Endocrinology & Metabolism
- Department of Immunology & Theranostics
- Department of Molecular & Cellular Endocrinology
- Department of Translation Research & Cellular Therapeutics
- The Wanek Family Project for Type 1 Diabetes
Recognizing our team’s accomplishments in cancer research, treatment, patient care, education and prevention, the National Cancer Institute has designated City of Hope as a comprehensive cancer center, the highest designation possible from the NCI.

- Cancer Control and Population Sciences
- Cancer Immunotherapeutics
- Center for Cancer Prevention and Early Detection
- Developmental Cancer Therapeutics
- Hematologic Malignancies
- Molecular and Cellular Biology of Cancer
Our dedicated, multidisciplinary team of health care and research professionals combine innovative research discoveries with superior clinical treatments to improve outcomes for patients with hematologic cancers.

- Cellular Immunotherapy Center
- Center for Gene Therapy
- Center for Stem Cell Transplantation
- Center for Survivorship and Outcomes
- Gehr Family Center for Leukemia Research
- The Judy and Bernard Briskin Center for Multiple Myeloma Research
- Toni Stephenson Lymphoma Center
This alliance provides City of Hope with access to TGen's innovative genomics technologies, helping physicians and researchers move research discoveries into the clinic for the benefit of patients.

Through rigorous coursework and laboratory research, you’ll be training in an academically stimulating, collaborative and diverse environment. The program develops a professionally trained scientist, prepared for a career in academia, medicine or industry.

- Ph.D. in Biological Sciences
- Ph.D. in Translational Medicine
- M.S. in Translational Medicine
- M.S. in Regulatory Affairs
- For Postdoctoral Fellows
- Eugene and Ruth Roberts Summer Student Academy
City of Hope and Beckman Research Institute offer a host of resources meeting researchers’ needs for specialized equipment, services or expert consultation. Sharing state-of-the-art equipment and resources, and the expertise to apply them to meaningful research, are crucial to the pursuit of new treatments and potential cures. They’re key pillars of our status as an NCI-designated Comprehensive Cancer Center.

- Analytical Cytometry
- Analytical Pharmacology
- Biostatistics and Mathematical Oncology
- Chemical GMP Synthesis
- Comprehensive Metabolic Phenotyping
- Design and Fabrication Laboratory
- Drug Discovery and Structural Biology
- Electron Microscopy
- Gene Editing and Viral Vector
- Hematopoietic Tissue Bank
- Immuno-Oncology Core
- Integrative Genomics and Bioinformatics
- Light Microscopy/Digital Imaging
- Mass Spectrometry and Proteomics
- Pathology Research Services
- Population Facing Research
- Small Animal Studies
- Stem Cell Core Facility
By having world-renowned scientists, physicians, and treatment manufacturing facilities working side by side at our main campus, we’re able to quickly turn breakthrough discoveries into experimental treatments. In a given year, City of Hope conducts more than 400 clinical trials enrolling more than 6,000 patients.
Search by name or department to learn more about their research.

Research Events & Seminars
Join us in the pursuit of a cure.
The library furnishes materials and services that support the institution's clinical, scientific and educational mission. It offers an expansive collection of scientific and biomedical journals and online databases, as well as a wide array of other services.
Join one of our forward-thinking, interdisciplinary teams of investigators, renowned researchers and postdoctoral fellows.
When you donate to City of Hope, you’re providing hope, second chances and the power to heal.

IMAGES
COMMENTS
Research Projects. Print. The Division of Diabetes Translation (DDT) conducts and supports studies, often in collaboration with partners, to develop and apply sound science to reduce the burden of diabetes and to address the research needs of DDT programs and the diabetes community.
I. Introduction. Diabetes mellitus, a metabolic disease defined by elevated fasting blood glucose levels due to insufficient insulin production, has reached epidemic proportions worldwide (World Health Organization, 2020).Type 1 and type 2 diabetes (T1D and T2D, respectively) make up the majority of diabetes cases with T1D characterized by autoimmune destruction of the insulin-producing ...
Changing our Future Through Research. The ADA is committed to innovation and breakthrough research that will improve the lives of all people living with diabetes. ADA Research: Science. Progress. Hope. ADA research provides critical funding for diabetes research. With 100% of donations directed to research, our goal is to ensure adequate ...
by pivoting to a targeted research strategy that allowed us to fund critical new grants, including the rapidly deployed funding of 10 research projects focused on the impact of diabetes on COVID-19, as well as the impact of COVID-19 on diabetes and its complications. The scientists awarded funding will allow us to better understand the biological
Recent Advances. ADA-funded researchers use the money from their awards to conduct critical diabetes research. In time, they publish their findings in order to inform fellow scientists of their results, which ensures that others will build upon their work. Ultimately, this cycle drives advances to prevent diabetes and to help people burdened by it.
It has been argued that research funders currently prioritize research designs that favour controlled studies at the expense of ignoring complexity in health interventions. 41 Further, in the case of diabetes, research projects are generally expected to generate evidence of clinical impact over a relatively short time period of 6‐18 months ...
The chronic complications of type 2 diabetes are a major cause of mortality and disability worldwide [ 1, 2 ]. Clinical research is the main way to gain knowledge about long-term diabetic complications and reduce the burden of diabetes. This allows for designing effective programs for screening and follow-up and fine-targeted therapeutic ...
For Harvard Stem Cell Institute Co-Director and Xander University Professor Douglas Melton, whose lab pioneered the science behind the therapy, the trial marked the most recent turning point in a decades-long effort to understand and treat the disease. In a conversation with the Gazette, Melton discussed the science behind the advance, the ...
The ADA is committed to continuing progress in the fight against type 2 diabetes by funding research, including support for potential new treatments, a better understating of genetic factors, addressing disparities, and more. For specific examples of projects currently funded by the ADA, see below. Greg J. Morton, PhD.
The research could lead to a better availability of beta cells for future research purposes. Type 1 and type 2 diabetes results when beta cells in the pancreas fail to produce enough insulin, the ...
June 2022 - The Diabetes Research Institute (DRI) at the University of Miami Miller School of Medicine in Miami, Florida first began performing clinical islet transplantation in 1985. ... April 2022 - Dr. Abdulreda's DRIF funded project entitled "Mechanisms of Islet Transplant Immune Tolerance" aims to understand immune pathways that ...
With increasing aging of the population and urbanization of lifestyle, the global prevalence of diabetes is expected to rise from 8.4% in 2017 to nearly 10% by 2045 ().Almost half of patients with diabetes (44%) are >65 years of age, with a prevalence that peaks (22%) at the age-group of 75-79 years ().In older people, diabetes is a disabling disease as a result of vascular complications ...
American Diabetes Association's Pathway to Stop Diabetes program is designed to transform diabetes research by attracting innovative scientists, physicians, and researchers through financial support and professional mentorship. ADA is committed to nurturing the next generation of leaders in diabetes research. Our goal with Postdoctoral ...
Our research projects. We fund world-class diabetes research. At any one time, we have around 120 diabetes research projects making discoveries across the UK. Each of these research projects is only possible thanks to the generous support of our members, donors and local groups. Every research project is reviewed by experts and approved by our ...
ADA research grants focused on innovative projects with high impact and helped researchers establish collaborative networks to move their innovations into the hands of people living with diabetes. "Research at the ADA is the engine that drives clinical advances by catapulting them into practice. 2023 has brought many prominent achievements.
A research team at Project ECHO, part of The University of New Mexico Health Sciences Center, has been approved for a $10.8 million funding award by the Patient-Centered Outcomes Research Institute (PCORI) to study how to help primary care physicians in New Mexico upskill in their treatment of complex diabetes.
Everything we know about diabetes - every drug, device and development has only been possible because of research. And, one day, research will find a cure. We're the UK's leading charitable funder of diabetes research. For 87 years, our research has been behind some of the biggest leaps forward in diabetes care and changed lives for the better.
Project goals include working with people with diabetes to improve control of the disease and reduce complications (tertiary prevention), increasing awareness of risk factors for diabetes and encouraging people at high risk to be screened (secondary prevention), and fostering an environment (physical and social) that supports greater health and ...
Project Power. Know Diabetes by Heart™ ... ADA research provides critical funding for diabetes research so we can support innovative scientific discovery. Find out more. The Scientific Sessions The ADA's annual Scientific Sessions is the world's largest diabetes meeting, featuring nearly 3,000 unique research presentations on the latest ...
If you have questions about any aspect of our research, we're here to provide answers. 626-256-4673. City of Hope is a leader in cancer translational research, integrating basic science, clinical research and patient care. Learn more about current research.
The U.S. government is launching an ambitious high-throughput research program for healthcare as part of the Advanced Research Projects Agency for Health (ARPA-H). 76 This initiative is designed along the lines ... Infrastructure needs for diabetes research in India should support deep dive physiological and molecular mechanistic research with ...