This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search

Search menu
Ali M. Communication skills 1: benefits of effective communication for patients. Nursing Times. 2017; 113:(12)18-19
Barber C. Communication, ethics and healthcare assistants. British Journal of Healthcare Assistants. 2016; 10:(7)332-335 https://doi.org/10.12968/bjha.2016.10.7.332
Berlo DK. The process of communication; an introduction to theory and practice.New York (NY): Holt, Rinehart and Winston; 1960
Bramhall E. Effective communication skills in nursing practice. Nurs Stand. 2014; 29:(14)53-59 https://doi.org/10.7748/ns.29.14.53.e9355
Bumb M, Keefe J, Miller L, Overcash J. Breaking bad news: an evidence-based review of communication models for oncology nurses. Clin J Oncol Nurs. 2017; 21:(5)573-580 https://doi.org/10.1188/17.CJON.573-580
Caldwell L, Grobbel CC. The importance of reflective practice in nursing. International Journal of Caring Sciences. 2013; 6:(3)319-326
Communication skills for workplace success employers look for these communication skills. The Balance (online). 2019. http://tinyurl.com/yyx3eeoy (accessed 27 June 2019)
Evans N. Knowledge is power when it comes to coping with a devastating diagnosis. Cancer Nursing Practice. 2017; 16:(10)8-9 https://doi.org/10.7748/cnp.16.10.8.s7
Gibbs G. Learning by doing: a guide to teaching and learning methods.Oxford: Further Education Unit, Oxford Polytechnic; 1988
Gillett A, Hammond A, Martala M. Successful academic writing.Harlow: Pearson Education Limited; 2009
Hanratty B, Lowson E, Holmes L Breaking bad news sensitively: what is important to patients in their last year of life?. BMJ Supportive & Palliative Care. 2012; 2:(1)24-28 https://doi.org/10.1136/bmjspcare-2011-000084
Hemming L. Breaking bad news: a case study on communication in health care. Gastrointestinal Nursing. 2017; 15:(1)43-50 https://doi.org/10.12968/gasn.2017.15.1.43
Macmillan Cancer Support. Cancer clinical nurse specialists (Impact Briefs series). 2014. http://tinyurl.com/yb96z88j (accessed 27 June 2019)
Healthcare professionals: acknowledging emotional reactions in newly-diagnosed patients. 2012. http://www.justgotdiagnosed.com (accessed 27 June 2019)
Oelofsen N. Using reflective practice in frontline nursing. Nurs Times. 2012; 108:(24)22-24
Paterson C, Chapman J. Enhancing skills of critical reflection to evidence learning in professional practice. Phys Ther Sport. 2013; 14:(3)133-138 https://doi.org/10.1016/j.ptsp.2013.03.004
Pincock S. Poor communication lies at heart of NHS complaints, says ombudsman. BMJ. 2004; 328 https://doi.org/10.1136/bmj.328.7430.10-d
Royal College of Nursing. Revalidation requirements: reflection and reflective discussion. 2019. http://tinyurl.com/yy8l68cy (accessed 27 June 2019)
Schildmann J, Cushing A, Doyal L, Vollmann J. Breaking bad news: experiences, views and difficulties of pre-registration house officers. Palliat Med. 2005; 19:(2)93-98 https://doi.org/10.1191/0269216305pm996oa
Shipley SD. Listening: a concept analysis. Nurs Forum. 2010; 45:(2)125-134 https://doi.org/10.1111/j.1744-6198.2010.00174.x
Reflecting on the communication process in health care. Part 1: clinical practice—breaking bad news
Beverley Anderson
Macmillan Uro-oncology Clinical Nurse Specialist, Epsom and St Helier NHS Trust
View articles · Email Beverley
This is the first of a two-part article on the communication process in health care. The interactive process of effective communication is crucial to enabling healthcare organisations to deliver compassionate, high-quality nursing care to patients, in facilitating interactions between the organisation and its employees and between team members. Poor communication can generate negativity; for instance, misperception and misinterpretation of the messages relayed can result in poor understanding, patient dissatisfaction and lead to complaints. Reflection is a highly beneficial tool. In nursing, it enables nurses to examine their practice, identify problems or concerns, and take appropriate action to initiate improvements. This two-part article examines the role of a uro-oncology clinical nurse specialist (UCNS). Ongoing observations and reflections on the UCNS's practice had identified some pertinent issues in the communication process, specifically those relating to clinical practice and the management of practice-related issues and complaints. Part 1 examines the inherent problems in the communication process, with explanation of their pertinence to delivering optimal health care to patients, as demonstrated in four case studies related to breaking bad news to patients and one scenario related to communicating in teams. Part 2 will focus on the management of complaints.
In health care, effective communication is crucial to enabling the delivery of compassionate, high-quality nursing care to patients ( Bramhall, 2014 ) and in facilitating effective interactions between an organisation and its employees ( Barber, 2016 ; Ali, 2017 ). Poor communication can have serious consequences for patients ( Pincock, 2004 ; Barber, 2016 ; Ali, 2017 ). Misperception or misinterpretation of the messages relayed can result in misunderstanding, increased anxiety, patient dissatisfaction and lead to complaints ( McClain, 2012 ; Ali, 2017 ; Bumb et al, 2017 ; Evans, 2017 ; Doyle, 2019 ), which, as evidence has shown, necessitates efficient management to ensure positive outcomes for all stakeholders—patients, health professionals and the healthcare organisation ( Barber, 2016 ; Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ). Complaints and their management will be discussed in Part 2.
Reflection is a highly beneficial tool ( Oelofsen, 2012 ), one that has played a key role in the author's ongoing examination of her practice. In this context, reflection enables a personal insight into the communication process and highlights the inherent challenges of communication and their pertinence to patient care and clinical practice outcomes ( Bramhall, 2014 ). The author, a uro-oncology clinical nurse specialist (UCNS), is required to ensure that appropriate reassurance and support is given to patients following the receipt of a urological cancer diagnosis ( Macmillan Cancer Support, 2014 ; Hemming, 2017 ). Support consists of effective communication, which is vital to ensuring patients are fully informed and understand their condition, prognosis and treatment and, accordingly, can make the appropriate choices and decisions for their relevant needs ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ; Hemming, 2017 ; Doyle, 2019 ).
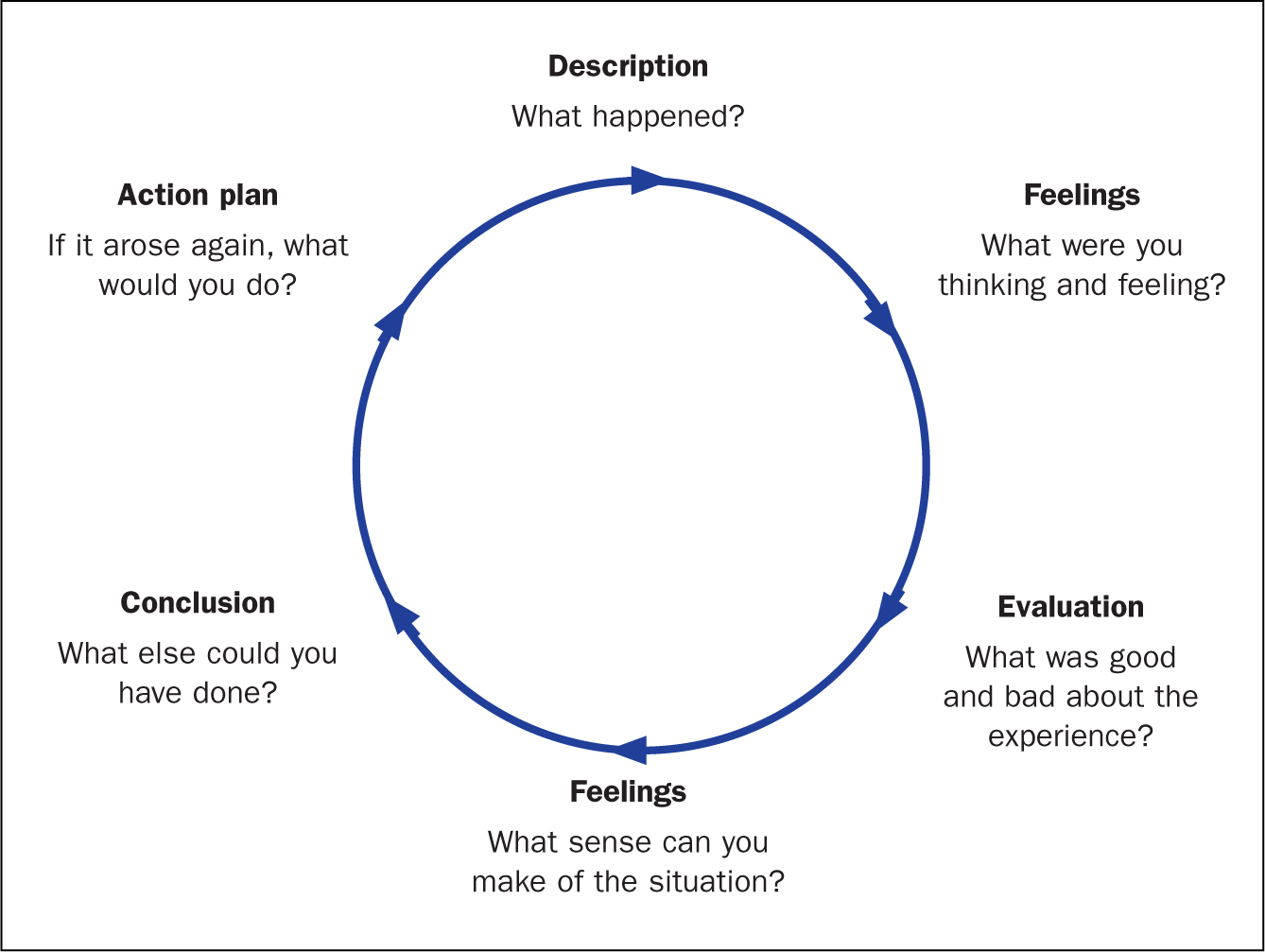
Reflection is a process of exploring and examining ourselves, our perspectives, attributes, experiences, and actions and interactions, which helps us gain insight and see how to move forward ( Gillett et al, 2009:164 ). Reflection is a cycle ( Figure 1 ; Gibbs, 1988 ), which, in nursing, enables the individual to consciously think about an activity or incident, and consider what was positive or challenging and, if appropriate, plan how a similar activity might be enhanced, improved or done differently in the future ( Royal College of Nursing (RCN), 2019 ).
Reflective practice
Reflective practice is the ability to reflect on one's actions and experiences so as to engage in a process of continuous learning ( Oelofsen, 2012 ), while enhancing clinical knowledge and expertise ( Caldwell and Grobbel, 2013 ). A key rationale for reflective practice is that experience alone does not necessarily lead to learning—as depicted by Gibbs' reflective cycle (1988) . Deliberate reflection on experience, emotions, actions and responses is essential to informing the individual's existing knowledge base and in ensuring a higher level of understanding ( Paterson and Chapman, 2013 ). Reflection on practice is a key skill for nurses—it enables them to identify problems and concerns in work situations and in so doing, to make sense of them and to make contextually appropriate changes if they are required ( Oelofsen, 2012 ).
Throughout her nursing career, reflection has been an integral part of the author's ongoing examinations of her practice. The process has enabled numerous opportunities to identify the positive and negative aspects of practice and, accordingly, devise strategies to improve both patient and practice outcomes. Reflection has also been a significant part author's professional development, increasing her nursing knowledge, insight and awareness and, as a result, the author is an intuitive practitioner, who is able to deliver optimal care to her patients.
Communication
Figure 2 provides a visual image of communication—it is both an expressive, message-sending, and a receptive, message-receiving, process ( Berlo, 1960 ; McClain, 2012 ; Evans, 2017 ). This model was originally designed to improve technical communication, but has been widely applied in different fields ( Berlo, 1960 ). Communication is the sharing of information, thoughts and feelings between people through speaking, writing or body language, via phone, email and social media ( Bramhall, 2014 ; Barber, 2016 ; Doyle, 2019 ). Effective communication extends the concept to require that transmitted content is received and understood by someone in the way it was intended.
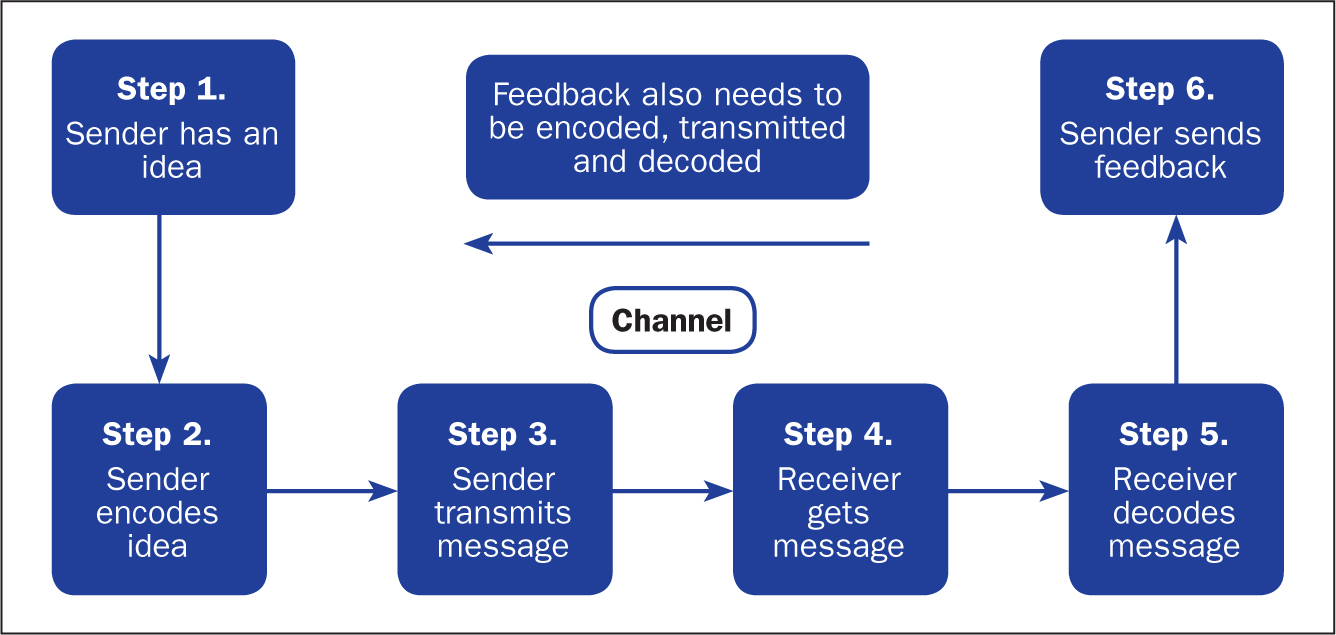
The process is more than just exchanging information. It is about the components/elements of the communication process, ie understanding the emotion and intentions behind the information—the tone of voice, as well as the actual words spoken, hearing, listening, perception, honesty, and ensuring that the messages relayed are correctly interpreted and understood ( Bramhall, 2014 ; Barber, 2016 ; Evans, 2017 ; Doyle, 2019 ). It is about considering emotions, such as shock, anger, fear, anxiety and distress ( Bumb et al, 2017 ; Evans, 2017 ). Language and conceptual barriers may also negatively impact on the efficacy of the communication being relayed.
Challenges of effective communication
The following sections explain the challenges involved in communication—namely, conveying a cancer diagnosis or related bad news.
Tone of voice and words spoken
According to Barber (2016) , when interacting with patients, especially communicating ‘bad news’ to them, both the tone of voice and the actual words spoken are important. The evidence has shown that an empathetic and sensitive tone is conducive to providing appropriate reassurance and in aiding understanding ( McClain, 2012 ; Evans, 2017 ; Hemming, 2017 ). However, an apathetic and insensitive tone will likely evoke fear, anxiety and distress ( Pincock, 2004 ; Ali, 2017 ; Doyle, 2019 ). In terms of the words used, the use of jargon, or highly technical language and words that imply sarcasm and disrespect, can negatively impact on feelings and self-confidence ( Doyle, 2019 ).
Hearing what is being conveyed is an important aspect of effective communication. When interacting with patients it is vital to consider potential barriers such as language (ie, is the subject highly technical or is English not the patient's first language) and emotions (ie shock, anger, fear, anxiety, distress) ( Bumb et al, 2017 ; Evans, 2017 ). A patient may fail to hear crucial information because he or she is distressed during an interaction, or may be unable to fully understand the information being relayed ( Bumb et al, 2017 ). Good communication involves ascertaining what has been heard and understood by the patient, allowing them to express their feelings and concerns, and ensuring these are validated ( Evans, 2017 ).
Listening to the patient
Listening is a deliberate act that requires a conscious commitment from the listener ( Shipley, 2010 ). The key attributes of listening include empathy, silence, attention to both verbal and non-verbal communication, and the ability to be non-judgemental and accepting ( Shipley, 2010 ). Listening is an essential component of effective communication and a crucial element of nursing care ( Shipley, 2010 ; Evans, 2017 ; Doyle, 2019 ). In health care, an inability to fully listen to and appreciate what the patient is saying could result in them feeling that their concerns are not being taken seriously. As observed by the author in practice, effective listening is essential to understanding the patient's concerns.
Perception, interpretation, understanding
Relevant and well-prepared information is key to the patient's perception and interpretation of the messages relayed ( McClain, 2012 ). It is vital to aiding their understanding and to informing their personal choices and decisions. If a patient were to misinterpret the information received, this could likely result in a misunderstanding of the messages being relayed and, consequently, lead to an inability to make clear, informed decisions about their life choices ( McClain, 2012 ; Bramhall, 2014 ).
Fully informing the patient and treating them with honesty, respect and dignity
In making decisions about their life/care, a patient is entitled to all information relevant to their individual situation and needs (including those about the actual and potential risks of treatment and their likely disease trajectory) ( McClain, 2012 ). Information equals empowerment—making a decision based on full information about a prognosis, for example, gives people choices and enables them to put their affairs in order ( Evans, 2017 ). Being honest with a patient not only shows respect for them, their feelings and concerns, it also contributes to preserving the individual's dignity ( Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ). However, as observed in practice, a reluctance on the health professional's part to be totally open and honest with a patient can result in confusion and unnecessary emotional distress.
When reflecting on the efficacy of the communication being relayed, it is important for health professionals to acknowledge the challenges and consider how they may actually or potentially impact on the messages being relayed ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ).
Communication and the uro-oncology clinical nurse specialist
It is devastating for a patient to receive the news that they have cancer ( Bumb et al, 2017 ). Providing a patient with a cancer diagnosis—the ‘breaking of bad news’, defined as any information that adversely and seriously affects an individual's view of his or her future ( Schildmann et al 2005 )—is equally devastating for the professional ( Bumb et al, 2017 ; Hemming, 2017 ). It is thus imperative to ensure the appropriate support is forthcoming following receipt of bad news ( Evans, 2017 ).
Integral to the delivery of bad news is the cancer CNS, in this context, the UCNS, who is acknowledged to be in the ideal position to observe the delivery of bad news (usually by a senior doctor in the urology clinic), and its receipt by patients ( Macmillan Cancer Support, 2014 ; Hemming, 2017 ), and to offer appropriate support afterwards ( Evans, 2017 ). Support includes allocating appropriate time with the patient, and their family, after the clinic appointment to ensure they have understood the discussion regarding the diagnosis, prognosis and treatment options ( Evans, 2017 ; Hemming, 2017 ). In this instance, effective communication, as well as the time required, is usually tailored to each individual patient, allowing trust to be built ( Bumb et al, 2017 ; Evans, 2017 ; Hemming, 2017 ).
In the performance of her role, the UCNS is fully aware of the importance placed on delivering bad news well. She has seen first hand how bad news given in a less than optimal manner can impact on the patient's emotions and their subsequent ability to deal with the results. Hence, her role in ensuring that the appropriate support is forthcoming following the delivery of bad news is imperative. It is important to understand that the delivery of bad news is a delicate task—one that necessitates sensitivity and an appreciation of the subsequent impact of the news on the individual concerned. It should also be acknowledged that while the receipt of bad news is, understandably, difficult for the patient, its delivery is also extremely challenging for the health professional ( Bumb et al, 2017 ).
Communicating bad news
The primary functions of effective communication in this instance are to enhance the patient's experience and to motivate them to take control of their situation ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ; Doyle, 2019 ).
Telling a patient that they have a life-threatening illness such as cancer, or that their prognosis is poor and no further treatment is available to them, is a difficult and uncomfortable task for the health professional ( Bumb et al, 2017 ). It is a task that must be done well nonetheless ( Schildmann, 2005 ). Doing it well is reliant on a number of factors:
- Ensuring communicated information is sensitively delivered ( Hanratty et al 2012 ) to counter the ensuing shock following the patient's receipt of the bad news ( McClain, 2012 )
- Providing information that is clear, concise and tailored to meeting the individual's needs ( Hemming, 2017 )
- Acknowledging and respecting the patient's feelings, concerns and wishes ( Evans 2017 ).
This approach to care is important to empower patients to make the right choices and decisions regarding their life/care, and gives them the chance to ‘put their affairs in order’ ( McClain, 2012 ; Ali, 2017 ; Evans, 2017 ).
Choices and decision-making
Case studies 1 and 2 show the importance of honesty, respect, listening and affording dignity to patients by health professionals, in this case senior doctors and the UCNS. The issue of choice and decision-making is highlighted. It is important to note that, while emphasis is placed on patients receiving all the pertinent information regarding their individual diagnosis and needs ( McClain 2012 ), despite receipt of this information, a patient may still be unable to make a definite decision regarding their care. A patient may even elect not to have any proposed treatment, a decision that some health professionals find difficult to accept, but one that must be respected nevertheless ( Ali, 2017 ; Evans, 2017 ; Hemming, 2017 ).
Case study 1. Giving a poor prognosis and accepting the patient's decision
Jane Green, aged 48, received a devastating cancer diagnosis, with an extremely poor prognosis. It was evident that the news was not what she expected. She had been convinced that she had irritable bowel syndrome and, hence, a cancer diagnosis was quite a shock. Nevertheless, she had, surprisingly, raised a smile with the witty retort: ‘Cancer, you bastard—how dare you get me.’ Mrs Green had been married to her second husband for 3 years. Sadly, her first husband, with whom she had two daughters, aged 17 and 21, had died from a heart attack at the age of 52. His sudden death was hugely upsetting for his daughters; consequently, Mrs Green's relationship with her girls (as she lovingly referred to them) was extremely close. The legacy of having two parents who had died young was not one Mrs Green wished to pass on to her daughters. Her main concern, therefore, was to minimise the inevitable distress that would ensue, following her own imminent death.
In the relatively short time that Mrs Green had to digest the enormity and implications of her diagnosis, she had been adamant that she did not wish to have any life-prolonging interventions, particularly if they could not guarantee a reasonable extension of her life, and whose effects would impact on the time she had left. This decision was driven by previously having observed her mother-in-law's experience of cancer: its management with chemotherapy and the resultant effect on her body and her eventual, painful demise. Mrs Green's memory of this experience was still vivid, and had heightened her fears and anxieties, and reinforced her wish not to undergo similar treatment.
Mrs Green requested a full and honest discussion and explanation from the consultant urologist and the UCNS regarding the diagnosis and its implications. This included the estimated prognosis, treatment interventions and the relevant risks and benefits—specifically, their likely impact on her quality of life. In providing Mrs Green with this information, the consultant and the UCNS had ensured information was clear and concise, empathetic and sensitive to her needs ( Shipley, 2010 ; Hanratty, et al, 2012 ; Evans, 2017 ; Hemming, 2017 ) and, importantly, that her request for honesty was respected. Not disclosing the entire truth can ‘inadvertently create a false sense of hope for a cure and perceptions of a longer life expectancy’ ( Bumb et al, 2017:574 ). Being honest had empowered Mrs Green to come to terms with both the diagnosis and prognosis, to consider the options as well as the risks and benefits. She had a choice between quantity of life and quality of life. Mrs Green elected for quality of life and, accordingly, made decisions that she felt were in her own, and her family's, best interests.
Despite receiving pertinent information and sound advice on why a patient should agree to treatment intervention, they may still elect not to have any treatment ( Ali, 2017 ; Evans, 2017 ; Hemming, 2017 ). This decision, as observed by the UCNS in practice, is difficult for some health professionals to accept. In Mrs Green's case, accepting her decision not to have any treatment was extremely difficult for both the consultant and the UCNS. In an attempt to try to change Mrs Green's mind, the consultant asked the UCNS to speak to her. The UCNS was aware that the consultant's difficulty to accept the decision was compounded by Mrs Green's age (48) and a desire to give her more time. However, the UCNS had listened closely to Mrs Green's wishes and, in view of her disclosure regarding the experience of her mother-in-law's death, her first husband's untimely death, her fear of upsetting her daughters and her evident determination to keep control of her situation, the UCNS felt compelled to respect her decision.
Following the consultant's request, the UCNS spoke to Mrs Green but, on hearing what she had to say regarding her decision not to have more treatment, concluded that she had to respect Mrs Green's decision. She also clarified whether Mrs Green were willing to continue communication with her GP and ensured that the GP was fully updated regarding current events. Mrs Green had thanked the staff for all their support, but did not wish to continue follow-up with the service. The GP assured the UCNS that she would keep a close eye on Mrs Green and her family.
Case study 2. Giving an honest account of disease progression
The following case study explains how a reluctance by health professionals to be totally honest with a patient had inadvertently hampered the individual's ability to make informed decisions regarding his life choices.
Mr Brown, aged 87, had been previously diagnosed and treated for cancer. On his referral to the urology clinic, his disease had progressed to the metastatic stage, which had limited his management options to palliative care.
Since we have established that delivering bad news to a patient is a difficult task ( Bumb et al, 2017 ), it is not surprising that some health professionals fail to be totally honest with the patient for fear of upsetting them. During the consultation, it transpired that Mr Brown had other serious illnesses and was being managed by other clinicians. Seemingly, previous communications with these clinicians had left Mr Brown and his family unenlightened about his prognosis and his future prospects. In hindsight, the family would have appreciated total honesty sooner, since this would have allowed them to make realistic decisions.
After fully assessing Mr Brown's case (and in light of this disclosure) the doctor decided to be totally honest with Mr Brown and his family regarding his current situation and the choices available to him. Explanations were empathetic and sensitive to Mr Brown's and his family's feelings ( Hanratty et al, 2012 ; Evans, 2017 ). While the news was not entirely unexpected, Mr Brown and his family appreciated the consultant's candour. In this instance, the consultant had respected Mr Brown's entitlement to total honesty. By receiving all the facts, and the appropriate reassurance and support from the UCNS, Mr Brown could now consider his options and, with his family's support, proceed to put his affairs in order.
Management and treatment of cancer
The management and treatment of cancer is determined by several factors. These include: the grade and stage of the individual's disease—whether the disease is low-grade/low-risk, intermediate-grade/intermediate-risk, or high-grade/high-risk. For some low-grade/low-risk disease, the recommended treatment of choice is surgery alone. However, in certain cases, further review of the staging and histology might reveal features of cancer within the sample that are at a high-risk of local recurrence, necessitating additional treatment intervention, ie chemotherapy or radiotherapy, to minimise this threat.
Following the primary treatment intervention (ie surgery), for low-risk/low-grade disease, the risk of local recurrence is usually low, as is the need for additional treatment intervention (chemotherapy or radiotherapy). Nonetheless, local recurrence is still a possibility. A failure to make the patient aware of this possibility creates a lack of trust and a false sense of hope ( Bumb et al, 2017 ), and evokes unnecessary emotional distress for the patient, their families and carers ( McClain, 2012 ).
As previously explained, the term ‘fully informed’ relates to a patient's entitlement to all information relevant to their situation and needs (including those about the actual and potential risks) ( McClain 2012 ). Informed knowledge is power, thus honesty is imperative ( Evans, 2017 ). The following case studies highlight the consequence of failing to fully inform patients about risks and diagnosis.
Case study 3. Consequences of not being fully informed
Mr White, aged 36, had been diagnosed with a low-grade/low-risk cancer. After the initial diagnosis was explained, Mr White was explicitly told by the doctor that after surgery he would not require any additional treatment. However, a subsequent review of his staging and histology revealed features of cancer within the sample that were at a high risk of local recurrence. Therefore the decision was made to offer Mr White additional treatment with radiotherapy to reduce the risk of recurrence down the line. Understandably, this news and the ensuing emotional impact—fear, anxiety and distress—was significant for Mr White. The author contends that, to avoid inciting these emotions, Mr White should have been fully informed, at the initial diagnosis, of the potential risks that further treatment might be necessary, no matter how unlikely these risks were perceived to be. Having observed the emotional impact on Mr White, and other similar cases in local practice, the author proposed that, when delivering a cancer diagnosis, consideration must be given not only to the physical, but also the emotional/psychological impact of the diagnosis on the individuals concerned and all risks, even those deemed small, discussed.
The following case study illustrates how a lack of honesty can lead to misinterpretation and misunderstanding of the messages relayed ( McClain, 2012 ; Bramhall, 2014 ) and, accordingly, raises questions regarding the patient's care.
Case study 4. Consequences of ‘sugar-coating’ a diagnosis
Mrs Black, aged 78, had been diagnosed with a low-grade/low-risk bladder cancer, for which the recommended treatment is a course of six doses of intravesical chemotherapy (mitomycin). In providing Mrs Black with the diagnosis, the doctor had failed to clarify that the term ‘bladder polyp/wort’ in fact meant cancer. It is evident to the UCNS that the doctor's intention was to reduce the impact of the news for Mrs Black. However, if a cancer diagnosis is not clearly explained at the outset ( Evans, 2017 ), then, as the UCNS's personal observations in practice have shown, the offer of subsequent cancer treatments will raise questions. In a follow-up meeting with the UCNS, Mrs Black queried why she was having a cancer treatment, when a cancer diagnosis had not been clearly given ( Bumb et al, 2017 ). In this instance, Mrs Black's query placed the UCNS in an uncomfortable position, but one in which she ultimately had to be honest in her response.
Despite the physician's good intentions, a lack of honesty or in this case ‘sugar-coating’ the truth was an infringement of Mrs Black's right to receive full and honest information regarding her diagnosis and treatments and impacted her ability to make clear decisions regarding her care ( McClain, 2012 ; Ali, 2017 ; Bumb et al, 2017 ).
Scenario: communicating in teams
In the UCNS's experience, effective communication is crucial when communicating in teams. The UCNS's observations in practice evoked reflection on past experiences of poor communication and its ensuing impact on her feelings, including hurt and, to some extent, a degree of anger.
Seemingly, poor communication is ingrained in all areas of practice and is highly evident in teams ( Doyle, 2019 ). The ability to communicate effectively is essential to team cohesiveness. One of the chief requirement is to facilitate an environment in which individuals can grow and excel, thus good/effective communication is vital. As previously stated, the tone of voice and actual words spoken are important ( Bramhall, 2014 ; Evans, 2017 ; Doyle, 2019 ). A tone that is respectful and conducive to elevating the individual's self-esteem and morale, ultimately increases self-worth and confidence. Conversely, a patronising attitude—a tone of voice and words spoken that imply sarcasm and disrespect—can, and often does, result in hurt feelings and a significant loss of confidence ( Doyle, 2019 ). Some senior professionals clearly believe in a hierarchy of entitlement to respect in the way that individuals communicate with other team members. A patronising tone of voice and words that imply sarcasm and disrespect impact significantly on individual team members' morale, self-esteem, self-worth, confidence and professional standing. This can lead to disharmony within the clinical environment. This could be communication between a consultant and a junior doctor, or a junior doctor and senior nurse, for example.
As health professionals, admittedly, we could all attest to poor communication at some point in our careers. Nevertheless, we have a responsibility to work and communicate effectively with other team members ( Ali, 2017 ; Doyle, 2019 ). The objective here is in facilitating a happy and functional team, one that demonstrates professionalism and competency in providing the care necessary to improving patients' experiences and outcomes ( Ali, 2017 ; Doyle, 2019 ). Securing improvements necessitates the health professional reflecting on their communication skills, acknowledging their limitations and initiating steps to address these ( Barber, 2016 ).
These case studies and scenario provide an insight into the UCNS's observations and reflections on her area of clinical practice and highlight the importance of effective communication. Acknowledgement of the inherent challenges within the communication process are clearly explained, with consideration given to the actual and potential impact in terms of patient, health professionals and clinical practice outcomes ( Oelofsen, 2012 ; RCN, 2019 ).
Communicating effectively is a key interpersonal skill that is fundamental to success in many aspects of life, but seemingly few people, including health professionals, have mastered the skill of truly effective communication. There are evident pitfalls that could lead to patient care being compromised as a result of poor communication between health professionals. The UCNS's role in delivering bad news and supporting patients involves ensuring that patients are adequately informed to enable them to take control of their individual situation and, accordingly, that they are able to make the appropriate choices and decisions for their respective needs. Poor communication within teams can affect patient care and staff morale, and learning how to communicate more effectively is beneficial in terms of improving staff interactions with each other. Essentially, communicating effectively is everyone's responsibility; hence, all health professionals should look at the way they interact and communicate with each other and take the necessary steps to improve this extremely important activity.
- The cancer clinical nurse specialist (CNS) role is pivotal when patients receive bad news. It is crucial not only to the individual's understanding of the diagnosis, prognosis and treatment options, but also to the provision of appropriate support following the bad news and countering the ensuing impact of the news on the patient
- Reflection is a powerful tool, one that enables nurses to examine their practice, identifying salient issues and initiate change/improvements
- Communicating effectively is a key interpersonal skill that is fundamental to success in many aspects of life—few people (in this context health professionals) have mastered the skill of truly effective communication
- Poor communication has implications for the patient, health professional and the health organisation
CPD reflective questions
- Reflection on practice is a key skill for nurses that enables them to identify salient issues and initiate actions to address these. How well do you think you reflect in practice, and does this provide the insight you seek?
- Effective communication is an important interpersonal skill. How well do you communicate with patients and colleagues in your area of practice? Reflect on any situations that you find difficult
- The issue of poor communication within teams and its impact on team members has been highlighted in this article. Have you observed poor communication within your team or within your area of practice? If so, how could this be improved?

How to Write a Nursing Reflective Essay (Guide for Nurse Students)

If you are a nursing or medicine student, you are aware that you will come across or have already come across assignments requiring you to write a nursing reflection essay. At first, such a task always appears challenging, but given the understanding of the steps, things flat out, and you can write reflective essays and get better grades.
Reflective practice is highly encouraged in nursing. Reflection entails making sense of situations, events, actions, and phenomena in the workplace.
As a nursing student, you will be asked to write a reflective essay on your clinical placement, practicum, shadowing experience, shadow health DCE activities, personal nursing philosophy, why you want to become a nurse, nursing program, ethical dilemma, knowledge, skills, and abilities, systems, and processes.
The easiest way to complete the reflective essay assignment is by first determining what reflective writing entails, its significance, its steps, and some of the best tips that form the core of this ultimate guide.
Basics of Reflective Writing in Nursing
Reflective writing is an analytical writing practice where the writer describes a real or imaginary event, scene, phenomenon, occurrence, or memory, including their takeaway. It entails the critical analysis of an experience, including recording how it has impacted you and what you intend to do with the new knowledge or how to act when such an occurrence recurs.
As you document the encounter, you can use first-person pronouns and write subjectively and objectively. This means that you can decide to either use personal experiences alone or support these experiences using citations from scholarly sources.
When writing a reflective essay in nursing, you must recount the events and give critical detail of how the events shaped your knowledge acquisition. Reflection helps nursing students develop skills in self-directed learning, which is directly associated with high motivation and improved quality of care .
In most cases, reflection occurs on what went well and what went wrong. It could be a successful operation, a thank you note from a patient, a patient who regained their health faster, or a new nursing care plan that worked. However, it can also be about adverse events such as death, postoperative complications, death of an infant at birth, dissatisfied patient, medical error, or a failed procedure.
As a nursing student, when you learn to reflect on situations, you grow to become a professional nurse who diligently does their noble duty.
When writing a reflective essay, you begin by setting the scene (explaining what, where, how, and who-the situation), detailing how you felt (emotional state), why it happened (making sense of the situation), critical review and development of insights, a note on what was learned, and strategies to address future recurrence.
Your professor may ask you to write a nursing reflective paper about various topics in your course or your experience working in a group, how you solved a problem, a healthcare issue, or clinical practice. Consider the following example of a reflective statement in nursing; in my clinical practices, I realized I focused more on the technical aspects but failed to explain what it was doing to improve their health. I would like to understand more about listening to patience and their concerns to better care for them.
As you will notice later, these reflective stages are structured into different reflective models and frameworks that we will explore in-depth. So, with the understanding of what comprises reflective writing and its importance in nursing, let's now get solid on the structure.
Related Reading:
- Philosophy of Nursing Example.
- Ideas and topics for nursing capstone or project papers
- How to write a SOAP note paper
- Top nursing debate topics
- Nursing Theories and Theorists.
Structure of a Reflective Essay in Nursing
A reflective essay is an analytical writing piece describing and evaluating encounters or experiences. When asked to write one, you should know that an excellent reflective essay consists of different parts, just like a typical academic essay. It comprises the cover or title page, introduction, body paragraphs, conclusions, and a references page.
The title page contains information about the assignment. If you are writing the reflective essay in APA, include these on the title page:
- Title of the reflective essay
- Course code and name
- Instructors name
- Name of your institution
- Date of submission
When writing in Harvard format, the title or the cover page will consist of the following:
- Title of the essay in title case and the page number (upper right margin),
- Title of the essay in CAPS,
- Name of class or course,
- Name of the instructor,
- Name of your school,
- City and state where your school is located and,
- The date of submission.
Introduction
The introduction begins with an attention grabber or a hook sentence to attract readers' attention. It should then explain the essay's purpose and signpost the ideas that will come later in the essay. The introduction also has a thesis statement at the end of the paragraph- the last sentence. The thesis is concise, clear, and relatable and should reflect your position.
Body Paragraphs
The body paragraphs of a reflective essay can be three or more, depending on the length of the essay. Essentially, the body comprises 80% of the total word count.
The first paragraph is where you describe the situation, including the events, why they occurred, how they occurred, and those involved.
The second paragraph entails your personal feelings or reaction to the situation and how it made you feel.
The third paragraph can include making sense of the situation. You have to think about why things happened the way they did. You should also critically review and develop insights based on the situation. Finally, think of the factors that could have influenced the situation.
The next paragraph should explain how the event or situation will change your practice, approach, decisions, perspective, or perception. This is where you evaluate the experience by detailing the knowledge and skills you took from the experience.
The last body paragraph should entail a critical reflection on the learning opportunities. First, describe the situation and what it made you learn. Next, elaborate on how you intend to make yourself better poised to address such situations.
Mostly, you should structure the body of your essay as per the preferred nursing reflective model.
After everything else falls into place, you need to summarize the information you presented in the essay. Then, finally, restate your thesis and have a call to action to bring a sense of closure to your readers.
Steps for Writing a Nursing Reflection Essay � The Guide
When assigned to write a reflective essay for your nursing class, here are the surefire steps to get you to success.
Read the instructions
The first step after receiving an assignment is to begin reading the instructions. as you read, note what your instructor or professor expects in the paper you will submit for marking.
Reading instructions helps you to get informed on the scope of the paper, word count, number of references and pages, and the formatting style to use.
Besides, you also get to plan your paper with the deadline highlighted in the instructions.
You need to get a conducive environment where you can start writing.
The first step of writing is to brainstorm about situations during your clinical hours when you were shadowing a Nurse Practitioner or one you have read about.
Assess whether the situation or scenario you have thought, encountered, or chosen can help you write a reflective essay that meets the requirements.
Research and Plan
After choosing a scenario, the next step is researching the best reflective model.
You can use your class text, the instructions, the college library, course readings, and online nursing journals to get articles and resources with information about specific reflective models.
Select the best reflective model and take notes on the steps it entails.
As you research, write down notes on how to address your paper based on your selected framework or model of reflection . Additionally, research nursing journal articles with information you can use when critically analyzing a situation.
Plan how you will handle the paper as well. For instance, as you research, develop a thesis statement that grounds your entire paper, then draft an outline on how to develop the thesis.
Write an Outline
Outlining is a crucial aspect of writing. It helps you envision how you will meet the objective of writing a reflective essay. As an essential part of the essay writing process, outlining helps create a good flow of ideas and can come in handy in helping you overcome writer's block. Your outline should comprise the following:
- The hook or attention grabber
- Thesis statement
- Main points of each body paragraph (topic sentence, evidence, examples, illustrations, etc.)
- Conclusion (restated thesis and call-to-action)
With the outline done, you should take a break and resume writing your first draft of the nursing reflection essay. Writing with an outline helps avoid mistakes and also helps you write faster.
Describe the Experience
Once you have identified the relevant experience, begin describing it chronologically.
Describe the experience that prompted you to consider nursing your ideal career goal. Think of this experience's key elements, such as the setting, patient demographics, and significant events that impacted you.
Show how these events changed your perspective on life. Ensure you are as descriptive as possible to paint a clear picture for readers.
Consider the following questions to come up with a good description:
- What happened?
- Was there someone involved? If yes, what part did they play?
- Where did the event take place?
- What actions did you take?
Set the context of this experience by giving relevant background information. Ensure you are objective and pay attention to the facts.
Provide a Reflection
Talk about your feelings and thoughts concerning the particular experience you went through. You have to be honest and open up about your initial expectations and challenges you faced at each stage of the experience. The following questions can help you come up with a good reflection:
- What was I trying to achieve?
- What prompted me to act the way I did?
- Are there any consequences for my actions? If yes, what are they?
- How did I feel about this event as it was happening?
- How did those around me react to it?
- How do I know how those around me felt about it?
Analyze the Experience
Description of an experience is essential, but so is analysis. You have to move beyond the surface and give a critical analysis of your experience.
State your actions, and your overall experience will give insights into your experience. Think of how the experience has impacted your actions, feelings, and thoughts.
Give an Evaluation
Evaluate the skills and knowledge you got from the experience. Show how you can apply these skills and knowledge in your nursing practice. Also, state the actions and interventions you took during the nursing experience.
State whether you achieved the desired outcome and if there are any specific areas that you need to improve on.
Talk about how you built or improved skills like communication, teamwork, and critical thinking.
As you evaluate the experience, identify what you believe to be your strengths and weaknesses in the nursing experience. What have you learned from the experience? State the areas where you excelled and what abilities contributed to your success.
Talk about how those you were with during the clinical experience complimented you. Similarly, acknowledge your weaknesses.
What kind of mistakes did you make, and how did you improve them? Talk about the tasks that drain you most during the experience.
Illustrate Learning
Demonstrate elements of deeper thought and reflection levels. This is a great point to include nursing theories in your reflection essay to support analysis of your experience.
Relate your experiences to the theoretical frameworks you were taught in class. This is effective learning and will demonstrate your ability to apply knowledge to real-life nursing situations.
Doing this will also show that you can effectively deduce different things from observations made during the reflection process.
Ensure you also demonstrate a change in perspective, as this will prove that you learned something from the experience.
Write Your Conclusion
Conclude by summarizing your points and highlighting the lessons learned.
The lessons you reached as part of your reflection should support your overall conclusion.
Also, restate your thesis statement.
Come Up with an Action Plan
Now that you have learned from your reflection develop an action plan for future nursing practice.
This part should contain all the details you have learned and actions needed to improve when faced with a similar situation. Consider the following questions:
- What would I change if faced with a similar situation?
- How can I develop the necessary skills needed to face this situation?
- How can I act differently in a similar situation?
Ensure you identify areas to improve and set realistic goals to enhance your nursing skills. Discuss how you intend to seek additional education, training, or mentorship to address your shortcomings.
Finally, end the essay with a happy note so readers know you learned something from the experiences.
Proofread, Edit, and Polish
After doing your first draft, take a break to relax and get out of the writing mood - it helps you to become objective.
You can then resume reading out loud to yourself, make necessary tweaks, and ensure that every part you include meets the rubric requirements.
Edit for grammar, punctuation, tenses, voice, spelling, and use of language. You should also proofread the essay to adhere to the style, organization, and presentation requirements.
Ensure that all the in-text citations are accounted for in the reference list and are up-to-date. You are good to go when you have an essay that meets all the instructions.
Finally, you can submit the paper for grading.
Writing is not everyone's cup of tea. For that reason, you can hire a nursing reflection essay writer from our website to assist you in crafting a top-grade paper. In addition, we have nursing writers whose forte is writing various nursing papers.
Choosing the suitable Reflective Model or Framework
As you can see above, many reflective models are used for your reflective essay. We have not exhaustively listed and expounded on all of them. Other reflective models and frameworks you can also consider when writing a reflective essay in nursing include:
- Bouds Reflective Model
- Brookfield Reflective Model
- Pender's Health Promotion Model
- Roper Logan and Tierney Model
- Driscoll Reflective Model
- The Johari window model
Note that most nursing instructors will often suggest the models they prefer for you to use in your essay.
For example, in most nursing reflective essays. Whichever the case, readily available information expands on each model to make it easier to write a reflection essay on a specific aspect of nursing education or practice.
Read the assignment rubric and instructions to understand the specific model. If it is unclear, ask for clarification from your instructor early enough.
Tips for Writing a Good Nursing Reflective Essay
As you try to figure out how to write a nursing reflective essay, keep the following tips in mind.
Choose the Right Topic
If the instructions from your professors involve choosing a topic for the reflective essay, you must select one that is meaningful to you.
This will ensure you can easily write and easily develop relevant elements about the topic. Therefore, take time to pick a topic that you find interesting.
As you write, ensure you stay on topic, whether sharing a one-off event or a recurrent story.
Use the Right Tone
A reflective essay is more personal, unlike other types of academic essays. This means you don't need a strict or formal tone.
Since this is about your experiences, use personal pronouns such as I and Me.
Be Vulnerable
You must be extremely vulnerable to learn how to write a reflective essay in nursing.
Be open about your thoughts, feelings, and beliefs about something you went through that sparked an interest in nursing.
It's okay to share mistakes or things you did wrong that eventually led you to this career path.
Choose the Right Focus
A reflection essay is all about narrating your experience during the nursing experience.
While including other people in your experience is okay, please let them not be the center of your reflection.
This is your essay, so you should be the focus of attention.
Keep it Brief
A good nursing reflection essay should be between 300 and 800 consciously written words. Because of this length, you must only write relevant information about your reflection. Refrain from lengthy reflections, as they make it difficult to pass your points across.
Convey Your Information Wisely
Even though a nursing reflection essay is about your personal experiences, it doesn't mean you should reveal everything about yourself. Ask yourself whether something is appropriate before including it in your paper.
Mistakes to Avoid When Writing a Reflection Essay in Nursing
A good reflection essay involves reflecting on your nursing studies and practices throughout school and career to demonstrate your competence. For this reason, there are certain mistakes you should be aware of when writing an essay.
Not including a Personal Story
Like food tastes bland without salt, so does a reflection essay without a personal story. At the center of a reflection essay is You. This means the essay should focus on your personal story that led you to want a nursing career. A lot of times, students miss out on this instead of talking about their story. You need more than just the personal qualities you think will be a great fit for the nursing program; you must also share a story that shows how well you contributed to nursing care.
Failing to Share Your Experience
You will lose points when you fail to include nursing-related experiences in your reflection essay. Mentioning that you want to be a nurse is great, but failing to show specific events that led to the desire will cost you a great point.
Plagiarizing Your Essay
Plagiarism is a serious academic offense because it is considered taking other people's ideas and using them as your own without crediting the author. So, provide relevant citations and references for any ideas that aren't your own. Also, an AI will not write your essay as a human writer would.
Related Readings:
- How to write a student nurse resume with no experience.
- PICOT examples and guides
Sample of a Nursing Reflective Essay
The following is a sample of a nursing Reflective essay using Gibb's Model of Reflection. Use this sample to guide you when writing your own.
Introduction Communication is an important element in healthcare practice as it determines patient satisfaction and treatment outcomes. This essay will focus on reflecting on an experience I went through with a 40-year-old diabetic patient who also had a foot infected with an ulcer. When I approached the patient to sign the consent form, I noticed that he wasn't happy because of the news given to him about his health. I concluded that there must be a communication dilemma. I will reflect on the experience using Gibb's Model of Reflection. Using this model, I will identify and discuss the actions taken to resolve the issue. Description This incident happened a few months ago when I was working as a wound nurse in a Methodist hospital in my hometown. I was part of a care team handling the case of a 40-year-old male patient with diabetes and an infected diabetic foot ulcer. After careful examination, a team comprising various specialists concluded that his leg needed amputation below the knee. After making this decision, the team left, and I was asked to give the patient a consent form to sign. When I came back from retrieving the form, I noticed the patient looked sorrowful because of the news given to him. Feelings As soon as I saw the patient, I knew what he was going through. He perceived the situation to be irreparable, but I wasn't sure whether to console the patient or not. I was powerless and couldn't imagine what he was going through. At the same time, I was startled that the team left without showing any compassion. They could have handled the situation more delicately. I, on the other hand, could have relayed the information better. I wasn't sure whether my approach would be acceptable or appropriate. Evaluation I always go back to that particular situation and wonder whether I could have acted better. The situation helped me better understand the importance of good communication in patient care, particularly in therapeutic care. Before the incident, I didn't acknowledge the role of nurses play in caring for patient's emotional needs. I realized nurses must show compassion and console patients in their low moments. Analysis Most healthcare professionals do not know how to deliver bad news to patients. They find the process extremely challenging and always feel psychologically unprepared. This has a negative impact on patients and could lead to bad health outcomes. Furthermore, how information is relayed could impact a patient's adherence to treatment. Because of these effects, multiple protocols and approaches were developed to help with communicating bad news to patients. One of the approaches that was proposed is emotion-centered. This proposes that a healthcare provider acknowledges how sad the patient is and builds a professional relationship based on empathy and sympathy. Action Plan I now understand the essence of communicating bad news with compassion. The experience allowed me to look closely at different aspects of my professional development that needed more improvement. Thus, I plan to be more empathetic and speak up in support of patient's emotional and psychological well-being, especially when presented with traumatic news about their health. Additionally, I now understand I am not powerless when dealing with a sorrowful patient. I believe I have learned from my experience, and I'm not able to communicate well with patients any more. Conclusion The experience allowed me to value good communication in nursing and the need to incorporate it into daily nurse-patient interaction. Nurses must learn how to deliver bad news and manage patient's sorrow. This has been and will continue to be my biggest priority in patient care. References Street Jr, R. L., Makoul, G., Arora, N. K., & Epstein, R. M. (2009). How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient education and counselling, 74(3), 295-301. Buckman, R. (1992). Breaking bad news: why is it still so difficult? BMJ: British Medical Journal, 304(6842), 886. Ptacek, J. T., & Eberhardt, T. L. (1996). Breaking bad news: a review of the literature. The Journal of the American Medical Association, 276(6), 496-502.
Writing is not everyone's cup of tea. For that reason, you can hire a nursing reflection essay writer from NurseMyGrade to assist you in crafting a top-grade paper. In addition, we have nursing writers whose forte is writing various nursing papers. Just place an order , and we will get back to you ASAP.
Struggling with
Related Articles

How to Create an Effective Poster Presentation (A Nurse Student?s Guide)

Tips and Steps for Writing a Great Community Health Assessment Paper

How to Make a Great Cover Page for an Essay
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.

Writing a Nursing Reflective Essay: Unveiling the 4 Biggest Success Tips for Nurses
Reflective practice is a cornerstone of the nursing profession, empowering nurses to enhance their skills, knowledge, and personal development. Nursing reflective essays serve as a powerful tool for nurses to explore their experiences, emotions, and thoughts surrounding specific incidents or situations encountered in their practice. In this blog post, we will delve into the significance of reflective essays in nursing, understand the reflective process, highlight the benefits of self-reflection for professional growth, and provide valuable tips for writing an impactful nursing reflective essay.
1. Understanding Reflective Practice
Reflective practice is a deliberate process that involves critically examining one’s experiences, actions, and responses in various clinical scenarios. It is a cyclical journey that incorporates observation, analysis, and evaluation to gain insights into personal strengths and areas for improvement. Reflective essays provide nurses with a structured platform to document and assess these experiences, enabling them to identify patterns, evaluate their performance, and enhance their practice.
By engaging in reflective practice, nurses are encouraged to think deeply about their actions, decisions, and the impact they have on patient care. It allows them to question their assumptions, biases, and preconceptions, leading to a more comprehensive understanding of the complexities of healthcare delivery. Reflective practice promotes an ongoing process of learning and growth, ensuring that nurses continually strive for excellence in their profession.
2. The Reflective Process
A. description:.
In this initial stage of the reflective process, nurses provide a detailed account of the event or incident they wish to reflect upon. They describe the context, setting, and individuals involved, ensuring a clear understanding of the situation. This description sets the foundation for a thorough reflection.
b. Feelings and Thoughts:
Nurses delve into their emotional and cognitive responses to the event, expressing their initial feelings, thoughts, and reactions. They consider how their emotions may have influenced their actions and decision-making during the incident. This introspection allows nurses to recognize their own biases and explore alternative perspectives.
c. Evaluation:
This stage involves an objective evaluation of the event, considering the outcome, patient outcomes, and the nurse’s own performance. Nurses analyze their actions, identifying strengths and areas for improvement. They reflect on their communication skills, technical proficiency, and adherence to professional standards. This evaluation helps nurses acknowledge their achievements and recognize areas where further development is required.
d. Analysis:
Nurses engage in critical analysis of the event, seeking underlying factors, patterns, and relevant literature or guidelines. They explore the impact of personal beliefs, values, and ethical considerations on their decision-making. They may reference research, best practices, or theoretical frameworks to gain a broader understanding of the situation and identify potential areas for improvement.
e. Conclusion:
In this final stage, nurses summarize their learnings from the reflective process. They outline the key insights gained, identify changes in their understanding or practice, and explore strategies for future improvement. This conclusion serves as a roadmap for personal and professional growth, providing a clear direction for further development and enhancement of nursing practice.
3. Benefits of Nursing Reflective Essays
A. enhancing critical thinking:.
Reflective essays foster critical thinking skills by encouraging nurses to question their actions, assumptions, and the evidence behind their decisions. This process promotes a deeper understanding of the complexities of patient care and encourages evidence-based practice. Nurses develop the ability to analyze situations from multiple perspectives and make informed decisions that prioritize patient safety and well-being.
b. Personal Development:
Nursing reflective essays promote self-awareness, emotional intelligence, and personal growth. Nurses gain a deeper understanding of their own values, beliefs, and biases, which allows them to provide more compassionate and patient-centered care. By reflecting on their experiences, nurses can identify their strengths and weaknesses, reflect on their interpersonal skills, and enhance their ability to empathize and connect with patients and their families.
c. Professional Growth:
Nursing reflective essays provide nurses with a platform to reflect on their professional development, identifying areas for improvement and formulating strategies for advancement. Through self-reflection, nurses can assess their competence in various aspects of nursing practice, such as clinical skills, leadership abilities, and communication. They can set goals for ongoing learning and development, ensuring they keep pace with evolving healthcare practices, technologies, and research.
d. Improved Patient Care:
By engaging in reflective practice, nurses can improve the quality of care provided to their patients. Nursjng reflective essays enable them to identify and rectify errors, enhance communication and teamwork, and ensure patient safety and satisfaction. Nurses gain valuable insights into their own performance, allowing them to make necessary adjustments to their practice to deliver optimal patient outcomes. Reflective practice encourages a proactive approach to addressing challenges and continuously improving the care provided.
4. Tips for Writing a Nursing Reflective Essay
A. select an appropriate incident:.
Choose an incident or situation that had a significant impact on your practice or personal growth. It should be relevant, recent, and conducive to deep reflection. Consider incidents that challenged your assumptions, presented ethical dilemmas, or highlighted areas for improvement.
b. Use a Structured Approach:
Follow a reflective framework, such as the Gibbs’ Reflective Cycle or the Johns Model of Reflection , to guide your nursing reflective essay. This structure will help ensure a comprehensive and organized reflection. Start by describing the incident, explore your feelings and thoughts, evaluate your actions, analyze the situation, and conclude with key learnings and action points.
c. Be Honest and Self-Critical:
Reflect on your actions and decisions with honesty and self-criticism. It is essential to acknowledge any mistakes or areas where you could have performed better. Nursing reflective essays are not meant to place blame but rather to promote growth and improvement. Recognize your strengths and weaknesses and explore strategies to build on them.
d. Connect Theory and Practice:
When researching your nursing reflective essay, explore relevant theories, guidelines, or evidence-based practices that relate to the incident. Consider how these resources could have influenced your actions or outcomes. Integrating theoretical knowledge with practical experience enhances your understanding and enables you to make informed decisions in future situations.
e. Focus on Learning and Growth:
Emphasize the lessons learned from the nursing reflective essay writing process. Identify specific actions or changes you will implement in your future practice to enhance your skills and improve patient care. Nursing reflective essays should demonstrate a commitment to ongoing learning and improvement. Share your plans for continuing professional development, such as attending relevant workshops, seeking mentorship, or engaging in further education.
Nursing reflective essays offer a valuable opportunity for self-reflection and professional growth. By engaging in the reflective process, nurses can gain insights into their actions, emotions, and thoughts, leading to improved critical thinking, personal development, and ultimately, enhanced patient care.
Embracing reflective practice allows nurses to continually evolve and adapt to the ever-changing healthcare landscape, ensuring the provision of high-quality, patient-centered nursing care. Through reflective essays, nurses can unlock their potential, foster empathy and compassion, and become lifelong learners committed to continuous improvement.
Nursing Assignment Help
At Nursing Research Help , we understand the challenges and demands that nursing students face in their academic journey. That’s why we are here to provide comprehensive assignment help services tailored specifically for nursing students. Our team of experienced and qualified professionals is equipped with in-depth knowledge of nursing principles, practices, and theories, ensuring that we deliver top-notch assistance for your assignments. Whether you need help with a nursing reflective essay, case studies, psychology assignments , research papers, or any other academic tasks, our experts are ready to provide you with the support you need.
We offer timely delivery, original and well-researched content, and a commitment to meeting your specific requirements. With our assignment help services, you can focus on honing your practical skills and gaining hands-on experience, knowing that your academic assignments are in capable hands. Trust us to help you achieve academic success and excel in your nursing studies. Contact us today to learn more about how we can assist you in your nursing assignments.
You might also like

Nursingresearchhelp.com is the fastest, easiest and most reliable way to have content written for your website. You’ll be able to post a project and 1000s of freelance writers from across the globe will have instant access to write your content quickly, professionally, and affordably.
QUICK LINKS
- HOW IT WORKS
- OUR SERVICES
- TERMS OF USE

Call/Text: +1 608 912 3884

- Cancer Nursing Practice
- Emergency Nurse
- Evidence-Based Nursing
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- RCN Nursing Awards
- Nursing Live
- Nursing Careers and Job Fairs
- CPD webinars on-demand
- --> Advanced -->

- Clinical articles
- CPD articles
- CPD Quizzes
- Expert advice
- Clinical placements
- Study skills
- Clinical skills
- University life
- Person-centred care
- Career advice
- Revalidation
CPD Previous Next
Effective communication skills in nursing practice, elaine bramhall managing director, consultant and trainer, effective communication matters, manchester, england.
This article highlights the importance of effective communication skills for nurses. It focuses on core communication skills, their definitions and the positive outcomes that result when applied to practice. Effective communication is central to the provision of compassionate, high-quality nursing care. The article aims to refresh and develop existing knowledge and understanding of effective communication skills. Nurses reading this article will be encouraged to develop a more conscious style of communicating with patients and carers, with the aim of improving health outcomes and patient satisfaction.
Nursing Standard . 29, 14, 53-59. doi: 10.7748/ns.29.14.53.e9355
This article has been subject to double blind peer review
Received: 18 July 2014
Accepted: 01 September 2014
communication - communication skills - active listening - non-verbal communication - nurse-patient relations
User not found
Want to read more?
Already have access log in, 3-month trial offer for £5.25/month.
- Unlimited access to all 10 RCNi Journals
- RCNi Learning featuring over 175 modules to easily earn CPD time
- NMC-compliant RCNi Revalidation Portfolio to stay on track with your progress
- Personalised newsletters tailored to your interests
- A customisable dashboard with over 200 topics
Alternatively, you can purchase access to this article for the next seven days. Buy now
Are you a student? Our student subscription has content especially for you. Find out more

09 December 2014 / Vol 29 issue 14
TABLE OF CONTENTS
DIGITAL EDITION
- LATEST ISSUE
- SIGN UP FOR E-ALERT
- WRITE FOR US
- PERMISSIONS
Share article: Effective communication skills in nursing practice
We use cookies on this site to enhance your user experience.
By clicking any link on this page you are giving your consent for us to set cookies.
Using reflection in nursing practice to enhance patient care
Affiliation.
- 1 The Open University, Milton Keynes, England.
- PMID: 37005865
- DOI: 10.7748/ns.2023.e11598
The ability to reflect on, and learn from, practice experiences is essential for nurses when seeking to provide effective person-centred care. This article outlines the various types of reflection that nurses can use, such as reflection-in-action and reflection-on-action. It also details some of the main models of reflection and explains how nurses might develop their skills in reflection to enhance the quality of patient care. The article provides examples of cases and reflective activities to demonstrate how nurses can use reflection in their practice.
Keywords: continuing professional development; education; nursing models and theories; professional; professional issues; reflection.
© 2023 RCN Publishing Company Ltd. All rights reserved. Not to be copied, transmitted or recorded in any way, in whole or part, without prior permission of the publishers.
- Metacognition
- Patient Care*
Communication in Nursing Practice: Gibbs’ Reflective Cycle Essay
Introduction, description, action plan, reflective conclusion.
Communication is a fundamental element in nursing practice. This element can possibly determine patients’ satisfaction and even the outcomes of their treatment (Lotfi et al., 2019). The situation described in the paper will exemplify the potential role of communication, which is why it will serve as a Gibbs Reflective Cycle nursing example. The cycle will help to assess the situation and extract lessons from it.
The model is a widely-recognized and crucial learning instrument, allowing individuals to extract lessons from life experiences. The pattern helps one to consider previous experiences, reevaluate them in the light of new knowledge, and implement the freshly obtained insight to improve future practice (Markkanen et al., 2020). The cycle is composed of six stages (description, feelings, evaluation, analysis, conclusion, and action plan), on which the reflection regarding the personal experience will be based (Markkanen et al., 2020). The paper’s principal objective is to outline a challenging situation from personal practice using Gibbs’ Reflective Cycle. The problematic situation is an encounter with a patient suffering from an infected diabetic foot ulcer and in need of amputation. Overall, the paper aims to critically analyze the situation and transform it into a learning opportunity useful in improving my future practice as a wound care specialist.
The situation concerns a 40-year-old patient with diabetes and an infected foot ulcer who was admitted to the hospital where I was working at the moment. The patient had a long history of diabetes, from which he suffered since he was ten years old. A multidisciplinary team examined the patient and established that he needed an amputation. As I approached the patient to get a consent form, I noticed that he looked upset. Given the described situation, it might be suggested that a communication dilemma here is of ethical character, in particular – it is the delivery of the bad news. By applying the model, the provided Gibbs Reflective Cycle example communication will demonstrate what actions were undertaken to resolve the mentioned dilemma.
The incident that will be analyzed is an outstanding Gibbs Reflective Cycle nursing example, which happened several years ago when I began working as a wound care nurse. A 40-year-old diabetic patient with an infected diabetic foot ulcer was admitted to the hospital. He had a long history of diabetes, suffering from the condition for three decades. A multidisciplinary team examined and communicated with the patient; it was established that he needed a below-knee amputation. The group stated their decision and left, and I had to retrieve the consent form. While retrieving the record, I perceived that the patient looked exceedingly sorrowful and depressed. Nevertheless, I did not know whether I needed to intervene in the situation and left.
Although I worked for many years in nursing before the incident, I became a certified wound care nurse relatively recently before it took place. At the moment, I saw the situation as irreparable, so I was not sure whether I should have tried to console the patient. I felt anxious and, to an extent, powerless when faced with the man’s grief. I thought that words or an empathic response would not be able to mitigate his sadness. Additionally, I was also somewhat startled that the multidisciplinary team did not handle the conversation more delicately and left rather abruptly. Overall, I did not feel confident enough to handle the situation and was unsure whether my intervention would be appropriate.
I frequently returned to the incident, trying to understand what should have been done instead. Retrospectively, I believe that it helped me to reevaluate the role of therapeutic communication in my profession. Prior to the incident, I did not perceive preoccupation with patients’ emotional well-being as my duty as a nurse. I believed that administering medications and treatment, performing tests, recording medical history, educating patients, et cetera, was all that was required of me. Nevertheless, I did not fulfill another vital function in the described situation. To understand that a holistic approach to care presupposes therapeutic communication, I had to experience the case (2). As a nurse, showing empathy and consoling patients is a critical function that is sometimes overlooked. Furthermore, the incident demonstrates a lack of cooperation between the nursing staff and the team since communication was needed to ensure that the emotional impact of amputation on the patient was alleviated.
Some medical professionals find the process of delivering bad news challenging and feel psychologically unprepared (Van Keer et al., 2019). A lack of skills in this aspect can negatively affect patients: they might undergo extra stress, have lower psychological adjustment, and have worse health outcomes (Biazar et al., 2019; Matthews et al., 2019). Furthermore, the way the news is handled can impact patients’ understanding of the situation and adherence to treatment (Galehdar et al., 2020). Given the adverse effects, multiple protocols and approaches to communicating bad news and dealing with its consequences were developed. This situation is analyzed in detail in a ‘Gibbs Reflective Cycle example essay pdf’ that focuses on these communication challenges in healthcare.
In the patient- and family-centered approach, the process occurs based on the patient’s needs as well as their cultural and religious beliefs (Hagqvist et al., 2020). Upon communicating the information, a medical professional is supposed to assess their understanding and show empathy (Hagqvist et al., 2020). In an emotion-centered approach, a medical professional is supposed to embrace the sadness of the situation and build the patient-medical professional interaction on empathy and sympathy (Hagqvist et al., 2020). Yet, the patient- and family-centered approach seems more effective since excessive empathy can be counter-productive and impede information exchange.
Managing patients’ reactions is the final and particularly vital step in communicating bad news. Nurses are commonly involved in handling emotional responses, which entails several responsibilities:
- Additional emotional support should be given to those who cannot accept the information (Galehdar et al., 2020).
- Nurses can find more related information and share it with patients (Rathnayake et al., 2021).
- Nurses are supposed to improve the situation if bad news has been delivered poorly (Dehghani et al., 2020).
In the case of amputation, heightened emotional attention should be given to the patient, as limb loss is a life-altering procedure. Such patients commonly undergo the five stages of grief (denial, anger, bargaining, depression, and acceptance) and are prone to developing anxiety, depression, and body image issues (Madsen et al., 2023). Hence, upon delivering the news regarding amputation, it is vital to provide a patient with community resources for dealing with emotional and psychological implications.
Currently, I understand more in-depth that delivering and handling the consequences of bad news is an inescapable reality of the nursing profession. The incident allowed me to notice the aspects of my professional development that necessitate more attention and improvement. Hence, I strive to be more empathetic in my clinical practice and not undervalue the role of patient-nurse communication. I attempt to provide psychological and emotional support to patients and console them to the best of my ability and knowledge, especially if a patient has just received traumatic news. Due to the incident, I comprehended better that a patient’s emotional well-being can be dependent on my actions. I also stopped presuming that other medical professionals provide the necessary emotional support. Moreover, I understand that I am not powerless when faced with a patient’s sorrow.
Consequently, I will not neglect the importance of patient-nurse communication for patients’ health outcomes and mental well-being. I will offer hope where it is appropriate and encourage and validate patients’ emotions to help them deal with traumatic information (Font-Jimenez et al., 2019). In the future, I will use verbal and non-verbal communication clues to show that I care and, generally, be more empathetic (Font-Jimenez et al., 2019). I will not prevent my insecurities from fulfilling my nursing duties, nor will I allow the feeling of hopelessness to affect my clinical practice. Furthermore, I will rely on evidence-based approaches to handle bad news effectively and facilitate its delivery to patients.
Additionally, I will be more mindful in my nursing practice. Gibb’s reflective cycle will assist me in attaining this objective. I will continue to apply it to the situations occurring at work in order to think systematically as well as analyze and evaluate them. Furthermore, Gibb’s reflective cycle will enhance my ability to learn from my experience. The model will help me to refine my communication skills and make patient-nurse interactions more intuitive and productive (Markkanen et al., 2020).
The situation allowed me to understand the actual value of therapeutic communication in nursing. Now, I understand the need to exercise it in my clinical practice, which is a realization that I further explored in a ‘Gibbs Reflective Cycle example essay pdf.’ Learning to provide emotional support and manage the consequences of bad news is an essential quality for nurses, influencing health outcomes and satisfaction from a visit. Additionally, I become more conscious of my own emotions and the way they can prevent me from acting in a patient’s best interests. Overall, the proper tactics of delivering bad news and assisting patients in handling them became a higher priority in my clinical practice.
To conclude, this reflection featured an episode from my practice in which I analyzed a communication situation using Gibbs’ Reflective Cycle. It showed that I need to concentrate on my abilities to resolve the communication dilemma of the delivery of bad news. The above discussion also demonstrated how the implementation of an appropriate and significant evidence-based model – Gibbs’ Reflective Cycle – may result in better patient outcomes.
Biazar, G., Delpasand, K., Farzi, F., Sedighinejad, A., Mirmansouri, A., & Atrkarroushan, Z. (2019). Breaking bad news: A valid concern among clinicians . Iranian Journal of Psychiatry, 14 (3), 198–202. Web.
Dehghani, F., Barkhordari-Sharifabad, M., Sedaghati-kasbakhi, M., & Fallahzadeh, H. (2020). Effect of palliative care training on perceived self-efficacy of the nurses . BMC Palliative Care, 19 , 63. Web.
Font-Jimenez, I., Ortega-Sanz, L., Acebedo-Uridales, M. S., Aguaron-Garcia, M. J., & de Molina-Fernández, I. (2019). Nurses’ emotions on care relationship: A qualitative study . Journal of Nursing Management, 28 (8), 2247-2256. Web.
Galehdar, N., Kamran, A., Toulabi, T., & Heydari, H. (2020). Exploring nurses’ experiences of psychological distress during care of patients with COVID-19: A qualitative study . BMC Psychiatry, 20 , 489. Web.
Hagqvist, P., Oikarainen, A., Tuomikoski, A.-M., Juntunen, J., & Mikkonen, K. (2020). Clinical mentors’ experiences of their intercultural communication competence in mentoring culturally and linguistically diverse nursing students: A qualitative study . Nurse Education Today, 87 , 104348. Web.
Lotfi, M., Zamanzadeh, V., Valizadeh, L., & Khajehgoodari, M. (2019). Assessment of nurse–patient communication and patient satisfaction from nursing care . Nursing Open, 6 (3), 1189-1196. Web.
Madsen, R., Larsen, P., Carlsen, A. M. F., & Marcussen, J. (2023). Nursing care and nurses’ understandings of grief and bereavement among patients and families during cancer illness and death – A scoping review . European Journal of Oncology Nursing, 62 , 102260. Web.
Markkanen, P., Välimäki, M., Anttila, M., & Kuuskorpi, M. (2020). A reflective cycle: Understanding challenging situations in a school setting . Educational Research, 62 (1), 46-62. Web.
Matthews, T., Baken, D., Ross, K., Ogilvie, E., & Kent, L. (2019). The experiences of patients and their family members when receiving bad news about cancer: A qualitative meta-synthesis . Psycho-Oncology, 28 (12), 2286-2294. Web.
Rathnayake, S., Dasanayake, D., Maithreepala, S. D., Ekanayake, R., & Basnayake, P. L. (2021). Nurses’ perspectives of taking care of patients with Coronavirus disease 2019: A phenomenological study. PLoS ONE, 16 (9), e0257064
Van Keer, R. L., Deschepper, R., Huyghens, L., & Bilsen, J. (2019). Challenges in delivering bad news in a multi-ethnic intensive care unit: An ethnographic study . Patient Education and Counseling, 102 (12), 2199-2207. Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, January 22). Communication in Nursing Practice: Gibbs' Reflective Cycle. https://ivypanda.com/essays/gibbs-reflective-cycle-essay-essay-examples/
"Communication in Nursing Practice: Gibbs' Reflective Cycle." IvyPanda , 22 Jan. 2024, ivypanda.com/essays/gibbs-reflective-cycle-essay-essay-examples/.
IvyPanda . (2024) 'Communication in Nursing Practice: Gibbs' Reflective Cycle'. 22 January.
IvyPanda . 2024. "Communication in Nursing Practice: Gibbs' Reflective Cycle." January 22, 2024. https://ivypanda.com/essays/gibbs-reflective-cycle-essay-essay-examples/.
1. IvyPanda . "Communication in Nursing Practice: Gibbs' Reflective Cycle." January 22, 2024. https://ivypanda.com/essays/gibbs-reflective-cycle-essay-essay-examples/.
Bibliography
IvyPanda . "Communication in Nursing Practice: Gibbs' Reflective Cycle." January 22, 2024. https://ivypanda.com/essays/gibbs-reflective-cycle-essay-essay-examples/.
- Gibbs' Reflective Cycle in Healthcare
- Gibbs’ Reflective Cycle
- The Cultural Safety Concept: Gibbs' Reflective Cycle
- Inattention in Patient-Nurse Relationships
- Learning Theories of Kolb, Schön, and Gibbs
- Nursing Practicum Based on Gibbs’ Framework
- Gibbs’s Reflective Cycle and Borton’s Model of Reflection
- "The Epic of Gilgamesh" by Ryan Gibbs
- The Topic of Diagnostic Measures
- Medical Ethics of Amputation
- Modern Nurse’s Role: Leadership
- Professional Mentoring in the Context of the Dnp
- Nurse Leader and Abbott Northwestern Hospital
- Mindfulness Meditation Program and Nursing Outcomes
- Issue of Nursing Turnover
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Patient Exp
The Meaning of the Empathetic Nurse–Patient Communication: A Qualitative Study
Atye babaii.
Tarbiat Modares University, Tehran, Iran
Eesa Mohammadi
Afsaneh sadooghiasl.
Nurse–patient communication is the foremost step in providing professional care. Nurses can use effective communication as a simple and powerful tool to create comfort, happiness, and vitality to reduce the patient's grief and suffering. This study aimed to explain the nurses’ perception of empathetic nurse–patient communication. This qualitative study was conducted with a content analysis method in 2020. Seventeen hospital nurses were recruited with maximum variation from the educational hospitals affiliated to Qom University of Medical Sciences, Qom, Iran, and semi-structured interviews were conducted until data saturation was reached. Data analysis was performed using Graneheim and Lundman approach. Nurses establish empathetic communication with patients through three main categories of: (1) having humanistic and unique behaviors with the patients; (2) providing a calm and happy environment for the patients; and (3) reducing the patients’ fear and consolation to them. These findings indicate empathetic communication that is appropriate to the conditions and needs of hospitalized patients. The three main categories were accomplished through 14 subcategories. The finding of this study can help to develop a training framework of empathetic nurse–patient communication and design instruments for measuring it.
Introduction
Nursing communication is a vital element in all nursing areas such as prevention, treatment, rehabilitation, education, and health promotion ( 1 ). The quality of communication between nurse and patient is recognized as an influential factor in improving patients’ care ( 2 ). Luker et al. showed that effective patient care is achieved through effective communication ( 3 ). Also, effective communication can improve patients’ independence and satisfaction ( 4 , 5 ) and protect the patient from adverse health consequences caused by ineffective communication such as medication error ( 6 ). One of the techniques of effective communication with the patient is empathetic communication ( 7 ). Empathy is one of the communication tools that we use to understand others and share our feelings, thoughts, and experience ( 8 ). According to some studies, empathy plays a crucial role in effective nurse–patient communication ( 7 , 9 , 10 ). Therefore, considerable attention has been paid to empathy in nursing, and this concept has firmly embedded in the nursing discourse ( 11 ).
In the social sciences, two empathy theories that explain this critical communication process include the theory of the mind and the theory of simulation ( 12 ). The theory of the mind shows the human ability to attribute mental states, such as desires, intentions, and beliefs, to others to other people using a controlled, thoughtful process ( 13 , 14 ). The theory of simulation reflects the attributions about others’ thoughts and emotions, which are more automatic or reflexive ( 15 ). The theory of simulation refers to our cognitive capacities to simulate and pretend to be in the situation of others ( 13 ). In the nursing profession, also, various theories have been proposed. Peplau emphasizes empathetic relationships with patients at all stages of nurse–patient communication ( 16 ). In the theory of human-to-human relationships, Travelbee states that the empathic nurse can understand another person's distress, identify its source, and predict the behavior that will result from it ( 17 ). Paterson and Zderad's emphasized that the experience of the nurse–patient relationship is interactive and empathetic ( 18 ). In these theories, theorists have theoretically explained the nature, importance, necessity, and elements of relationship between two people or between the nurses and patients based on their and perspective and professional knowledge. However, empathetic communication formed on the values, feels, needs, and special and unique socio-cultural conditions of human beings and cannot be explained solely by these theories ( 19 ). Therefore, if we want to understand the empathetic relationship between the patient and the nurse, we must pay attention to the experiences and perceptions of the main stakeholders in the clinical context, namely the patient and nurse.
Some studies have discussed empathetic nurse–patient communication. Pehrson et al., based on the experiences of cancer ward nurses, introduced a model of empathetic communication with the patients. This model's strategies included recognizing or eliciting a patient's empathic opportunity, working toward a shared understanding of the patient's emotion/experience, empathically responding to the emotion/experience, and facilitating coping and connecting to social support ( 7 ). Wu, based on the experience of psychotherapists, describes ten practices of nurses in establishing empathetic communication with patients as follows: partaking in the clients’ feelings or thoughts, offering comfort, sharing the same experiences as clients, formulating the gist of clients’ problematic experiences, formulating the upshot of clients’ problematic experiences, offering an empathic diagnosis, offering a candidate a method for solving the reported problem, elaborating on clients’ emotional experiences, making a positive assessment of the client's action toward solving their problems and displaying downgraded epistemic access to clients’ problematic experiences ( 20 ). Tyner, based on the experiences of dying patients and their families, commented that the nonverbal behaviors of empathetic communication with the cancer patients included using facial expressions to convey a message that we understand the patient's concerns, intentional sitting and facing the patient to create a feeling of interest, bodily movements to show understanding and hand gestures to establish proper humility and sensitivity ( 21 ). Raudonis, based on the experiences of hospice nurses, argues that an empathic relationship means acknowledging patients as valuable individuals regardless of their physical diagnoses and have a friendly relationship with them ( 22 ).
These studies have described the empathetic nurse–patient communication in different settings, statuses, and stakeholders as various forms and meanings. According to our search, no study in Iran has examined the meaning of empathetic nurse–patient communication. As shown, the way of empathetic communication is different in different cultures. Therefore, Iranian nurses cannot fully use the patterns of other cultures to communicate empathetically. Also, non-Iranian nurses will be challenged if they want to have empathetic communication with Iranian patients according to their cultural patterns. Therefore, this study was conducted to clarify empathetic communication with the patient based on the experiences of Iranian nurses.
Qualitative content analysis is a systematic method to analyse qualitative data ( 23 ). Content analysis is used for condensing and abstracting a large amount of textual data ( 23 ) and direct extraction of participants’ messages without imposing a researcher's opinion ( 24 ) to gain new insights into the study phenomenon. Therefore, according to the question of the study, “what's the meaning of empathetic nurse–patient communication?” we chose the qualitative content analysis approach.
Setting and Participants
The setting was hospitals affiliated to Qom University of Medical Sciences, Iran. Seventeen nurses were purposefully selected and entered the study. Inclusion criteria included having at least 2 years of nursing experience, having at least a bachelor's degree, having direct communication with the patients, and having informed consent to participate in the study. As shown in Table 1 , we select the participants that have the most diversity in terms of gender (male or female), education levels (from bachelor to PhD degree), job positions (nurses, head nurse), workplaces (internal ward, surgical ward, intensive care unit, and emergency department), and work experiences (from three to 23 years).
Table 1.
Characteristics of Study Participants.
Data Collection
In the qualitative analysis methods, the extracted data are based on the perception and daily experience of the participants ( 25 ). From March to September 2020, we used face-to-face interviews to extract nurses’ experiences from empathetic communication with the patient. The first author conducted the Persian language interviews in a convenient and quiet place in the hospitals. In the two interviews, some ambiguities did not allow for deep extraction of the data. Therefore, the participants were reinterviewed. Each interview lasted for 40–90 min. At the beginning of the interview, the nurses’ trust was gained using the adequate description of their confidentiality and preserving the interviews and audio files. Text notes were immediately reviewed and completed to ensure an accurate record of the participants’ experiences. Interview questions were: “In day-to-day care of patients, please describe your experiences about communication with the patient,” “Please describe your successful experiences of communicating with the patient,” and “How do you try to make your relationship with your patients happy?” Then, probing questions were also used to clarification or elicit further details during the interviews: “Can you explain more?”, “What does it mean?” or “Give an example, please.” Also, the field notes over the interaction of nurse(s) were recorded. The interviews continued until the saturation of the data. It means that no additional data are being found whereby the researcher can develop a new category ( 26 ). The categories seemed saturated regarding their properties and dimensions after the 15th interview. However, two additional interviews were conducted to ensure no new data emerged and no new conceptual code emerged. The research team and the external reviewer made the decision about achieved data saturation by continuous review along with data collection.
Data Analysis
All interviews were recorded with the permission of the participants. After each interview, the content was transcribed with Microsoft Office Word software and analyzed by Graneheim and Lundman ( 27 ). In the first step, each interview was transcribed word by word. In the second step, each interview's text was read several times word by word, sentence-to-sentence, and paragraph-to-paragraph to obtain a sense of the whole. In the third step, the meaning units of each interview transcript were identified and coded. The first author analyzed the total data, while the second and third authors analyzed half of the textual data. Three authors then compared the codes and revised minor disagreements after discussion. In the fourth step, codes are grouped into subcategories according to their conceptual similarities and differences. In the fifth step, subcategories compared with each other and the latent data content identified and presented as the main categories. The final three categories were examined by all authors to ensure a clear difference between the main categories and subcategories and fit the data within each category. Also, all the codes, subcategories, and main categories were given to one of the faculty members outside the research team. He separately reviewed and confirmed the appropriateness of data analysis. Parts of the audiotape were translated from Persian into English by an independent translator blind to the study to check for consistent translation. An example of the process of category formation is shown in Table 2 .
Table 2.
An Example of the Process of Categories Formation.
Trustworthiness
Lincoln and Guba criteria, including credibility, transferability, dependability, and confirmability, were used ( 28 ). The credibility was established by allocating enough time for each interview and member check-in the interview and data analysis stages. Also, two research supervisors checked the quality of interviews, coding, and categories to reach a consensus. Dependability was accomplished by long-term engagement with participants and the constant comparative method. In this way, the initial codes were examined and compared several times, and the repeated codes were analyzed and categorized. For dependability, all stages of the study were reported in detail. For confirmability, codes and categories were reviewed and approved by a faculty member outside the research team. Finally, transferability was established through maximum variation sampling.
Data analysis led to three main categories and 14 subcategories ( Table 3 ). According to the findings of this study, nurses establish empathetic communication with patients through three main categories of: (1) having humanistic and unique behaviors with the patients; (2) providing a calm and happy environment for the patients; and (3) reducing the patients’ fear and consolation to them.
Table 3.
The Products of Data Analysis in This Study.
Having Humanistic and Unique Behaviors with the Patients
Nurses’ quotes showed that they have humanistic and individual behaviors with the patient. Friendly behavior, the unique way of dealing with each patient, maintaining patients’ dignity, considering the patient's beliefs and culture, and paying attention to changing patient behavior indicate nurses’ humanistic and unique relationship with patients.
A male nurse said, “ When patients feel that all their needs have been met and respected, they trust us more … This creates a stronger relationship between the patient and us ” (P4).
A female nurse said, “ It is not possible to communicate with all patients in the same way … Patients have different cultures and beliefs … In my first encounter with the patient, I tried to understand his cultures and beliefs so that I can have a good relationship with him/her ” (P17).
Friendly Behavior with Patients
Most participants stated that they put themselves in the patients’ shoes to understand their needs and establish close and friendly communication. They indicated that they spoke to patients with humility, in a pleasant and sincere tone, and answered patients’ questions in a kind and straightforward language.
A female head nurse commented, “ I try to use simple words to get closer to the patient, and if the patient asks me a question about the treatment process, I am not indifferent. Modestly, with openness and a good tone, I make the patient's mood a little better ” (P2).
A female nurse described, “When the nurse is agitated, the patient becomes agitated too … I tell the novice nurse that if you want to have an empathetic relationship with the patient, you must speak to them friendly with humility, and sincere tone” (P16).
The Unique Way of Dealing with Each Patient
Participants believed that each patient had their personality, and nurses should not have the same stereotypical behavior in empathetic communication with the patients. Instead, they should establish a unique communication based on the personality and interests of the patients.
In this regard, a male nurse said, “ I do not treat all patients in the same way. By my understanding of each patient's personality, I communicate with them. I talk to some of them very seriously, and I communicate with some patients with jokes and laughter ” (P15).
Maintaining Patients’ Dignity
Some participants stated that using appropriate words, introducing oneself at the beginning of communication, explaining and informing the patient about interventions, respecting patient decisions, and avoiding sarcasm make the patient feel good about nurses and softens communication.
A female nurse commented, “ One of my colleagues uses harsh words with the patients, which causes arguing. However, I talk to the patients very respectfully. When I enter the room… I introduce myself. I call them with friendly words, like “dear mom” I teach them with simple and soft expressions, so when I am a shift nurse, the patients are delighted and in a good mood ” (P9).
A female nurse said, “ Nurses who talk to a polite patient are less likely to argue with the patient, and the patient is more likely to follow their treatment recommendations ” (P3).
Considering the Patients’ Beliefs and Culture
Most participants believed that effective and uplifting communication with patients required communication according to patients’ culture, language, preferences, or religious beliefs. Because if you ignore the patient's beliefs and culture, who have lived with that for many years, they suddenly become very anxious, and the communication continues to be disrupted.
A male nurse stated, “ I give patients clothes, prayer books, or poems, consistent with religious and cultural beliefs. I care for the dying patient as much as possible according to the patient's beliefs. I allow the family to be present at the bedside and prepare them for the patient's death according to the family's preferences and beliefs. In this way, they will communicate more with me, and they will have more peace and joy ” (P1).
A female head nurse commented, “ After heart surgery, a patient insisted on having a radio … he said that if I did not have a radio, I would be stressed … I gave him a radio … he calmed down after I gave him the radio and I was able to communicate well To have with him ” (P10).
Paying Attention to Changing Patients’ Behavior
Participants in this study believed that when we pay attention to the patient's appearance and behaviors and give him feedback about changes in these issues, the patient realizes that he is important for the nurse and feels closer with the nurse.
A male head nurse said, “ Some nurses work like a robot without paying attention to the patient's nonverbal reactions, But I try to act differently. For example, when I do IV Cath and see the patient is scared, I try to talk to distract her ” (P8).
Providing a Calm and Happy Environment for the Patients
Clinical nurses establish empathetic nurse–patient communication by creating a pleasant atmosphere, using jokes, providing conditions for family meetings, and being neat and happy.
A female head nurse expressed, “ In a pleasant and happy environment, patients feel more relaxed and more inclined to communicate” (P10).
A female nurse described, “ Agitated people are not focused and do not have the patience to communicate with others … Sometimes, providing a pleasant atmosphere allows the patient to calm down and communicate with them ” (P3).
Creating a Pleasant Environment
Participants stated that the strange and noisy environment of the ward causes patient anxiety and impedes proper communication with nurses. They emphasized that providing a pleasant smell, adequate ventilation, reducing annoying noises, and providing an environment according to patients’ habits, tastes, and beliefs can help to establish empathetic communication.
A female nurse described, “ Sometimes the patient may be agitated by loud noises or unpleasant room odors. Before doing anything, I pay attention to what disturbs my patients. I prepare the environment as much as possible to the patient's habits and tastes so that I can calm the patient down and be able to communicate with him easily ” (P16).
A female nurse commented, “ I went to the patient who had just been admitted to talking to him about his illness, the patient was constantly moving around the bed, and he was not paying attention to me … I found that the patient is bothered by the hospital pillow … After his wife brought his pillow, the patient calmed down, and I was able to have a good relationship with him. ” (P7).
Using Jokes
Participants stated that joking with patients, using funny sentences, encouraging patients to define happy memories, and, if possible, celebrating on different occasions had a significant effect on establishing close communication with patients.
A male nurse commented, “ A young woman was hospitalized with quadriplegia, which despite injecting many painkillers, she did not calm down and expressed pain. I went to her and started joking… I danced funny and made the patient laugh so much that he got tired of laughing a lot and slept painlessly until morning ” (P13).
A male nurse described, “By turning the patient away from grief using funny sentences, you can have an effective relationship with the patient ” (P1).
Providing Conditions for Family Meetings
Most of the participants stated that loneliness and being in an unfamiliar environment cause nostalgia and discomfort to patients, and in such cases, patients are reluctant to communicate. The nurses had experienced that a family member's presence calms the patient and creates more favorable conditions for the patient to communicate.
A female nurse said, “ They are much calmer when a family member is with the patient, and it is easier to communicate with them ” (P17).
Being Neat and Happy
Most of the participants stated that most patients were reluctant to communicate with sloppy and untidy nurses. They emphasized that a nurse at the patient's bedside with clean clothes, beautiful appearance, smiling face, and pleasant smell can lead to empathetic communication.
A male nurse said, “ When I look neat and talk to the patient with a smile, the patient communicates in a better mood ” (P4).
Reducing the Patients’ Fear and Consolation to Them
Participants showed that stress, anxiety, pain, and suffering are the barriers to empathetic nurse–patient communication. Participants argued that by giving hope, using distraction, spirituality, and normalizing new circumstances, they provided the conditions for empathetic communication.
A male nurse commented, “ Existence of numerous medical types of equipment and unfamiliar environment leads to patients’ fear and anxiety …. Patients’ fear makes them distrust us and have no desire to communicate ” (P6).
A male nurse described, “ Patients with pain or stress avoid communication … By turning on the TV or encouraging them to listen to music, I distract them from their pain and anxiety so that I can give them the training they need” (P5).
Giving Hope to Patients
Sometimes the condition of the disease causes the patient to feel frustrated. The frustrated patient is reluctant to communicate. Participants stated that they give patients hope for a better future by talking about the transience of periods of suffering and showing successful people with similar conditions.
A female head nurse said, “ I told a patient who had deformed appearance due to burns not to be disappointed that cosmetic surgery could alleviate your problem, and despite these changes, you can have good days in the future ” (P10).
A female nurse commented, “ I went to teach a diabetic patient about her self-care… she did not listen to me at all … she said that if you cut off my toe, I could not return to normal life … … I asked a patient who had previously had her toe amputated due to diabetes to explain her lifestyle after the operation. When the patient realized that she could return to a normal life after the operation, she listened to me ” (P11).
Using Distraction to Reduce Patients’ Stress and Suffering
Fear, anxiety, and suffering from illness interfere with the positive communication of patients. In this regard, participants stated that using thought destruction methods such as watching TV, reading books, asking deviant questions, or involving patients in self-care can promote empathetic nurse–patient communication.
A male nurse expressed, “ There was a child in the ward. At first, he did not look at us or talk at all … he was scared. I took a latex glove and made a doll, and talked in a funny cartoon character. I brought him a piece of paper. He painted for me. We played like this, and we all laughed, and then he trusted me and answered the questions ” (P6).
Using Spirituality to Reduce Patients’ Pain and Stress
Participants in the study believed that in addition to distraction techniques, focusing on spirituality could reduce patients’ suffering and create an empathetic nurse–patient relationship.
A female nurse said, “One of the patients who had just been diagnosed with cancer was very upset and crying. I explained to him that God loves the patients very much because of the pain and suffering they endure. I told him to pray and ask God for help and hope. After that, the patient's mood improved” (P14).
Normalization of new Conditions
The presence of patients in new conditions, especially the presence of various medical equipment connected to the patient, can increase the patient's stress, and this stress is a barrier to effective communication with patients. Most participants in the study stated that normalization of new conditions using methods such as explaining patient-connected equipment, providing an opportunity for sick children to touch medical equipment, and showing a film of postoperative conditions could reduce the patient's stress as a barrier to empathetic communication.
A female head nurse commented, “ In the ICU, a child was scared and anxious because of seeing the types of equipment and did not allow us to take care of him… I helped him to touch the equipment that was connected to him… this reduced his stress, and I was able to take care of him ” (P12).
A male nurse commented, “ my patient regained consciousness and opened her eyes … she was very agitated … I explained to her where she is, what happened to her and why she is here … with my explanations, the patient calmed down, and she did not fight with the ventilator. ” (P13).
This study showed that nurses try to establish empathetic nurse–patient communication by having humanistic and unique behaviors with the patient, providing a calm and happy environment for the patient, and reducing the patient's fear and consolation to them.
Finfgeld-Connett, argues that having intimate relationships with the patients requires listening, providing information, encouraging close associates to express their concerns, ensuring that they look after themselves, helping them cope with difficult situations, and sharing personal thoughts and feelings openly and honestly ( 29 ). Raudonis also showed that an empathic relationship means acknowledging patients as valuable individuals regardless of their physical diagnoses and have a friendly relationship with them ( 22 ). Unlike the current study, Finfgeld-Connett and Raudonis do not mention providing a happy environment for more effective communication. According to the findings of this study, providing a calm and happy environment for the patient can be effective in establishing effective empathetic nurse–patient communication. Some studies highlighted that physical environmental factors such as adequate lighting, a quiet environment, and providing pen and paper can support the patients in communication to be more involved in conversations ( 30 – 32 ). However, the difference between the findings of our study and these studies is that in these studies, the environment is considered more as a physical environment. None of these studies mentioned the use of techniques to create a happy environment with the patient. According to the findings of our study, nurses can provide a happy environment for the patients using jokes, providing conditions for family meetings, and being neat and happy. Our study participants believed that these techniques could establish effective nurse–patient communication by creating a sense of coherence between them and reducing patients’ depression and anxiety.
Lukmanulhakim showed that effective communication with the patient requires the nurse's eye contact, quick response to the patient's needs, clarity of speech, comprehensible language, active listening, and friendly treatment of the patient ( 33 ). The findings of the Lukmanulhakim study focus more on the principles of proper message delivery, and reducing the patient's fear and consolation to them has been neglected. Papadantonaki commented that effective communication requires understanding patient experiences and understanding what concerns the patient ( 34 ). However, she did not explain how to alleviate the patient's concerns.
Some studies have described ways to reduce patients’ fear and anxiety. Appukuttan found that dental anxiety can be managed by psychotherapeutic interventions such as muscle relaxation, relaxation breathing, imagery, hypnosis, acupuncture, distraction, and positive reinforcement ( 35 ). Croke suggested aromatherapy, acupuncture, music, therapy dogs, visitation, education, and virtual reality as ways to help reduce preoperative patient anxiety ( 36 ). According to the findings of our study, using some strategies such as giving hope, building trust, using distraction, using spirituality, and normalizing new circumstances, nurses can reduce patients’ fears and thus establish empathetic communication with them. In our study, unlike the above two studies, the use of spiritual care has been introduced as one of the basic strategies to reduce patients’ fears. This can be related to the high importance of spirituality among the Iranian people. Scott et al. believe that trust and hope are the outcomes of an effective relationship with the patients ( 37 ). However, according to the findings of our study, giving hope to patients and establishing trust with them are the main elements of empathetic communication with the patient. In line with the findings of our study, Rutherford emphasized that trust, as one of the nursing's intangible assets, is an essential component of the establishment of meaningful relationships with patients ( 38 ).
Wu introduced four types of empathy as namely cognitive empathy, affective empathy, sharing empathy, and nurturant empathy ( 39 ). Connett states that an intimate nurse–patient relationship requires listening, providing information, encouraging close associates to express their concerns, ensuring that they look after themselves, helping them cope with difficult situations, and sharing personal thoughts and feelings openly and honestly ( 29 ). Also, Hashim emphasized that effective nurse–patient communication requires understanding the patient's perspective entails exploring the patient's feelings, ideas, concerns, and experience regarding the impact of the illness ( 40 ). These studies have focused on interacting to identify patients’ feelings, concerns, and needs. However, they did not explain how to identify the patients’ feelings, concerns, and needs. Our study showed that in interacting with patients, nurses should respect patients’ beliefs and culture, maintain their dignity, and have friendly relations with them so that patients trust them and express their real feelings, needs and concerns. There is a limitation in this study. The nurses were interviewed while they were under a lot of stress due to the Covid-19 crisis. This can affect the quality of the interviews.
The findings of our study are similar to other studies in terms of having unique relationships with patients and reducing their fears and concerns in empathetic nurse–patient communication. However, it is unique in features such as friendly behavior with patients, maintaining patients’ dignity, providing a happy environment, and using spirituality to reduce patients’ pain and stress. The framework developed in this study for empathetic nurse–patient communication can be used to design a context-based tool instead of existing theory-based tools to measure the empathetic relationship. The characteristics mentioned in this article for the empathetic nurse–patient communication can be used as an educational framework for nursing students and nurses to improve their relationship with the patient.
Acknowledgments
The authors would like to thank the Research Administration of Tarbiat Modares Universityand all patients who participated in the study.
Authors’ Contribution: A.B, E.M, A.S contributed to study design and conceptualization. A.B, E.M, A.S contributed to data collection. A.B, E.M, A.S contributed to data analysis and interpretation. A.B, E.M, A.S contributed to manuscript writing. E.M, A.S contributed to study supervision.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research Council of the Tarbiat Modares University financially supported the study.
Ethical Approval: Ethical approval to report this case was obtained from Research Committee of Tarbiat Modares University (Ethical code: IR.MODARES.REC.1397.234).
ORCID iDs: Atye Babaii https://orcid.org/0000-0001-8941-2455
Afsaneh Sadooghiasl https://orcid.org/0000-0002-4756-2428
Statement of Human and Animal Rights: All procedures in this study were conducted in accordance with the Research Committee of Tarbiat Modares University (Ethical code: IR.MODARES.REC.1397.234) approved protocols.
Statement of Informed Consent: Verbal informed consent was obtained from the patient(s) for their anonymized information to be published in this article.

IMAGES
VIDEO
COMMENTS
Introduction. Communication skills are taught to nurses in the educational environment and are an important part of educational programs, but there are many concerns about communication weaknesses and lack of communication skills. 1 Some nursing experts believe that appropriate communication skills are the cornerstone of all nursing care activities, 2 resulting in improved patient care and ...
Critical Reflection Of Communication Skills Relevant To Selected Clinical Scenario Nursing Essay. In 2006, a patient named Robin became pregnant. In the 5th month of pregnancy, the patient began having trouble with diarrhoea and then developed a severe infection in her upper respiratory system. Ro...
Reflection is a highly beneficial tool (Oelofsen, 2012), one that has played a key role in the author's ongoing examination of her practice. In this context, reflection enables a personal insight into the communication process and highlights the inherent challenges of communication and their pertinence to patient care and clinical practice outcomes (Bramhall, 2014).
Communication Skills in Nursing | Reflection. This essay will present a reflective account of communication skills in practice whist undertaking assessment and history taking of two Intensive Care patients with a similar condition. It will endeavour to explore all aspects of non verbal and verbal communication styles and reflect upon these ...
Nurses engage in compassionate, supportive, professional relationships with their clients as part of the "art of nursing." [1] This chapter will review the nurse-client relationship, therapeutic communication, and motivational interviewing. It will also introduce teletherapy and telehealth.
Sample of a Nursing Reflective Essay . The following is a sample of a nursing Reflective essay using Gibb's Model of Reflection. Use this sample to guide you when writing your own. Introduction . Communication is an important element in healthcare practice as it determines patient satisfaction and treatment outcomes.
This nursing reflective essay guide provides a comprehensive overview of the reflective writing process for nursing students + examples and outlines. ... Reflective writing in nursing is a practical tool to foster critical thinking, improve communication skills, and promote professional development. Not only does it contribute to academic ...
1.1. Background. Based on Peplau's model of interpersonal relationships by (), which is the most widely held theory in the mental health nursing community, many authors have based their models on person‐centred mental health nursing (Barker & Buchanan‐Barker, 2010; O'Brien, 2001; Scanlon, 2006).All of them identify the therapeutic relationship as the foundation of nursing practice and the ...
3. Benefits of Nursing Reflective Essays a. Enhancing Critical Thinking: Reflective essays foster critical thinking skills by encouraging nurses to question their actions, assumptions, and the evidence behind their decisions. This process promotes a deeper understanding of the complexities of patient care and encourages evidence-based practice.
1. Introduction. Physicians have a challenging task in tailoring communication with patients to their needs, perspectives and contexts [1].This challenge involves life-long learning and development right from the start of medical training [2].Communication must be taught practically, but the learning of skills cannot be limited to mimicking defined behaviours.
This article highlights the importance of effective communication skills for nurses. It focuses on core communication skills, their definitions and the positive outcomes that result when applied to practice. Effective communication is central to the provision of compassionate, high-quality nursing care. The article aims to refresh and develop ...
The aim of this study was to determine the effect of reflection on nurse-patient communication skills of nurses working in emergency departments. Methods: This interventional study was conducted ...
The ability to reflect on, and learn from, practice experiences is essential for nurses when seeking to provide effective person-centred care. This article outlines the various types of reflection that nurses can use, such as reflection-in-action and reflection-on-action. It also details some of the main models of reflection and explains how ...
Strong communication skills are essential to provide safe, quality, patient-centered care. Nurses develop therapeutic relationships with patients and family members each day to ensure that health care concerns and needs are addressed. If communication breaks down, information exchange stops and needs go unidentified. Nurses optimize communication channels with patients and families by ...
Communication is a vital part of the nurse's role. Theorists such as Peplau (1952), Rogers (1970) and King (1971) all emphasise therapeutic communication as a primary part of nursing and a major focus of nursing practice. Long (1992) further suggests that communication contains many components including presence, listening, perception, caring ...
Communication is a fundamental element in nursing practice. This element can possibly determine patients' satisfaction and even the outcomes of their treatment (Lotfi et al., 2019). The situation described in the paper will exemplify the potential role of communication, which is why it will serve as a Gibbs Reflective Cycle nursing example.
6.89.2 reflection on learning that informs professional development and practice In the Standards of proficiency for nursing associates (2018) reflection is linked to being an accountable practitioner (platform 1) and the need for ongoing continuous development. It is also included in working in teams (platform 4) with the need to act as
Development of communication skills is always an ongoing and ever-changing process, which all student nurses go through and continue with into qualified
Nurses can use effective communication as a simple and powerful tool to create comfort, happiness, and vitality to reduce the patient's grief and suffering. This study aimed to explain the nurses' perception of empathetic nurse-patient communication. This qualitative study was conducted with a content analysis method in 2020.
Communication Skills Reflection: Patient Interaction. Info: 4283 words (17 pages) Nursing Essay Published: 11th Feb 2020. ... Importance Of Communication Of Nurses Nursing Essay. Communication involves the exchange of messages and is a process which all individuals participate in. Whether it is through spoken word, written word, non-verbal ...
This essay will present a reflective account of communication skills in practice whist undertaking assessment and history taking of two Intensive Care patients with a similar condition. It will endeavour to explore all aspects of non verbal and verbal communication styles and reflect upon these areas using Gibbs reflective cycle (1988).
Self Reflection on Communication in Nursing. AMITA KHOWAJA. Introduction. Reflection is an organized and a planned way to think positively and make better decisions. Reflection allow person to learn from their mistakes and past experiences. This is more applicable to form the fundamentals of healing and therapeutic process in health care field.