What is Critical Thinking in Nursing? (With Examples, Importance, & How to Improve)

Successful nursing requires learning several skills used to communicate with patients, families, and healthcare teams. One of the most essential skills nurses must develop is the ability to demonstrate critical thinking. If you are a nurse, perhaps you have asked if there is a way to know how to improve critical thinking in nursing? As you read this article, you will learn what critical thinking in nursing is and why it is important. You will also find 18 simple tips to improve critical thinking in nursing and sample scenarios about how to apply critical thinking in your nursing career.

What is Critical Thinking in Nursing?
4 reasons why critical thinking is so important in nursing, 1. critical thinking skills will help you anticipate and understand changes in your patient’s condition., 2. with strong critical thinking skills, you can make decisions about patient care that is most favorable for the patient and intended outcomes., 3. strong critical thinking skills in nursing can contribute to innovative improvements and professional development., 4. critical thinking skills in nursing contribute to rational decision-making, which improves patient outcomes., what are the 8 important attributes of excellent critical thinking in nursing, 1. the ability to interpret information:, 2. independent thought:, 3. impartiality:, 4. intuition:, 5. problem solving:, 6. flexibility:, 7. perseverance:, 8. integrity:, examples of poor critical thinking vs excellent critical thinking in nursing, 1. scenario: patient/caregiver interactions, poor critical thinking:, excellent critical thinking:, 2. scenario: improving patient care quality, 3. scenario: interdisciplinary collaboration, 4. scenario: precepting nursing students and other nurses, how to improve critical thinking in nursing, 1. demonstrate open-mindedness., 2. practice self-awareness., 3. avoid judgment., 4. eliminate personal biases., 5. do not be afraid to ask questions., 6. find an experienced mentor., 7. join professional nursing organizations., 8. establish a routine of self-reflection., 9. utilize the chain of command., 10. determine the significance of data and decide if it is sufficient for decision-making., 11. volunteer for leadership positions or opportunities., 12. use previous facts and experiences to help develop stronger critical thinking skills in nursing., 13. establish priorities., 14. trust your knowledge and be confident in your abilities., 15. be curious about everything., 16. practice fair-mindedness., 17. learn the value of intellectual humility., 18. never stop learning., 4 consequences of poor critical thinking in nursing, 1. the most significant risk associated with poor critical thinking in nursing is inadequate patient care., 2. failure to recognize changes in patient status:, 3. lack of effective critical thinking in nursing can impact the cost of healthcare., 4. lack of critical thinking skills in nursing can cause a breakdown in communication within the interdisciplinary team., useful resources to improve critical thinking in nursing, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. will lack of critical thinking impact my nursing career, 2. usually, how long does it take for a nurse to improve their critical thinking skills, 3. do all types of nurses require excellent critical thinking skills, 4. how can i assess my critical thinking skills in nursing.
• Ask relevant questions • Justify opinions • Address and evaluate multiple points of view • Explain assumptions and reasons related to your choice of patient care options
5. Can I Be a Nurse If I Cannot Think Critically?

30 Top Nursing Interview Questions & Answers | 2024
- Types of Interview Questions
- Question Themes
- How to Answer
- Common Interview Questions & Answers
Questions to Ask the Employer
Things to do before leaving the interview.
- Interview Prep

Wondering which nursing interview questions you might be asked at your next job interview? You've come to the right place. Read on for the top nursing interview questions and answers to help you nail that next interview.
Types of Nursing Interview Questions
Healthcare employers tend to lean towards asking behavioral-based interview questions.
Behavioral-based questions are about how you acted in a specific situation. The goal is to gauge how you react under different circumstances. It is best to answer these questions with real-life stories and examples.
Popular Online Master of Science in Nursing (MSN) Programs

WGU's award-winning online programs are created to help you succeed while graduating faster and with less debt. WGU is a CCNE accredited, nonprofit university offering nursing bachelor's and master's degrees.
Enrollment: Nationwide
- BSN-to-MSN - Family NP
- BSN-to-MSN - Psychiatric Mental Health NP
- BSN-to-MSN - Nursing Informatics
- RN-to-MSN - Nursing Informatics
- BSN-to-MSN - Nursing Education
- RN-to-MSN - Nursing Education
- RN-to-MSN - Nursing Leadership & Management
- BSN-to-MSN - Nursing Leadership & Management

GCU's College of Nursing and Health Care Professions has a nearly 35-year tradition of preparing students to fill evolving healthcare roles as highly qualified professionals. GCU offers a full spectrum of nursing degrees, from a pre-licensure BSN degree to a Doctor of Nursing Practice (DNP) program.
- MSN - Family NP
- MSN - Adult Gerontology Acute Care NP
- MSN - Nursing Education
- MSN - Health Informatics
- MSN - Public Health Nursing
- MSN - Health Care Quality & Patient Safety
- MBA & MSN - Nursing Leadership in Health Care Systems
- See more GCU nursing programs

As a working RN, you need a flexible, transfer-friendly program to help you save time and money as you take the next step in your nursing career. In our CCNE-accredited4 RN to BSN program, you can transfer in up to 134 credits—which is nearly 75% of program requirements. Your transfer credits can be reviewed in one business day (on average).
Enrollment: FL
- MSN - Psychiatric-Mental Health NP
- MSN - Adult-Gerontology NP - Primary Care
- MSN - Pediatric NP - Primary Care
- MSN - Nursing Leadership & Admin
- See more Rasmussen nursing programs

Enrollment: Nationwide, excluding NY and WA.
- MSN - Women's Health NP
- MSN - Nurse-Midwifery/Women's Health NP
Nursing Interview Question Themes
Most behavioral interview questions asked of nurses are based on the following themes:
- Patient-care
- Adaptability
- Time management
- Communication style
- Motivation and core values
How to Answer Behavioral-Based Questions
When telling stories during interviews, we suggest using the S-T-A-R format - this will ensure your story is direct, concise and to the point. So, what does the acronym S-T-A-R stand for?
A ction-steps
You can learn more about answering interview questions by using the S-T-A-R format by reading our complete guide to nursing interviews.
30 Common Nursing Interview Questions & Answers
- Teamwork questions
- Patient care questions
- Adaptability questions
- Time management questions
- Communication style questions
- Motivation and core values questions
Sample Nurse Interview Questions: Teamwork
Interviewers want to envision how you will fit in with their team and how you work well with various personalities. We suggest telling a story about a time you dealt with a co-worker who had a conflicting personality, a disagreement within your healthcare team, or a challenging patient case involving your team. Always remember to talk about what you learned from the situation and if anything positive came from it.
1. Describe a situation when you had to work closely with a difficult coworker. How did you handle the situation? Were you able to build a relationship with this person?
Never talk badly about anyone during an interview. Explain the situation and why the individual was difficult. Share how you handled the situation. Try to turn anything negative into a positive. What did you learn from the situation? What might you do differently now? What was the “silver lining”? Were you able to talk through your differences? Did you become friends?
Sample answer:
Working closely with difficult coworkers can be challenging, but it is important to remember the patient, their care, and their family is most important. Putting aside differences is essential for all nurses because not everyone is the same. Sometimes this means not discussing specific topics such as religion or politics at work. With that being said, not everyone will become friends in the workplace but working together is key for the successful care of patients.
2. Talk about a conflict within your healthcare team. What was the conflict, and how did you handle it?
Explain the conflict surrounding the situation. Who was involved? What was your role? Did anything positive come from this? What did you learn?
Conflict often occurs in the hospital setting, particularly between new nurses and more seasoned staff, as well as doctors and nurses. At one specific time, there was concern from a parent that a newer nurse was not monitoring a patient’s breathing postoperatively as closely as she would have liked.
I was covering the nurse for lunch and the mother brought her concerns to me. I discussed and validated her concerns. Once the nurse was back from lunch, I spoke with her regarding the mother’s concerns. The nurse was very upset and felt it was not my place to say anything to her regarding this. A parent or patient’s concerns should never be dismissed. I spoke to the nurse educator on the unit to use the opportunity as a teaching moment.
3. Describe a time when you were particularly proud of your healthcare team. What was your role in this situation?
Describe the circumstances and actions step-by-step. What happened to make you feel proud? What was your role? Who was involved? What was the result?
Working in the ICU setting, there are countless moments that make me proud to be a nurse and proud to be part of this amazing community. Watching a patient survive a code, take their first steps on prosthetic legs, or be in the room when a patient I tell is receiving a new heart is the moment we all want to be a part of. Even if I am not delivering the news or caring personally, the information my patient receives directly affects me.
4. Tell me about a time you stepped into a leadership role.
This doesn’t need to be anything official. Think about a time when you stepped up to the plate and took charge of a situation. What was the circumstance? What made you take the lead? Who was involved? Did any opportunities arise from this situation?
I have acted as a charge nurse numerous times in my career. I have had to lead code teams, respond to rapid responses, and make difficult staffing decisions. As a charge nurse I have determined patient assignments to ensure that assignments are fair and equal. Furthermore, I have to ensure that the nurses’ skill set is sufficient for the assignment.
Sample Nurse Interview Questions: Patient Care
Healthcare hiring professionals want to hire nurses who provide excellent patient care. Education is of utmost importance to healthcare employers. We suggest telling stories about times you provided top-notch patient care or went out of your way to educate patients and/or their families.
1. Tell me about a time when a patient’s family was dissatisfied with your care. How did you handle that situation?
Make sure to explain the situation in detail, including both perspectives (the patient’s family and yours). Never talk badly about patients or their families. Take ownership if you indeed did something wrong. Share any positives that came from this - what did you learn? What would you do differently now? How did you turn this into a positive?
I once was floated to a unit that I had never worked in and wasn’t sure where supplies were located. The patient's mother did not recognize me as a regular floor nurse on the unit, which already made the family leery of me from the start of the shift. I continually had to prove myself throughout the day because, as nurses, we all do things slightly differently.
There is not always a wrong way or a right way to do things but in this case, there was a policy to be followed. I followed it, and apparently, my dressing change was slightly different than the previous ones. I communicated regularly with the charge nurse, and she came to check in with the family to address any issues in real time.
2. What approach do you take in communicating with people who do not know medical jargon? Give an example of a time you explained medical terminology to someone who is not medically trained.
Explain step-by-step how you’ve performed in a similar situation. What specific words and terminology did you use? How did you know that the individual understood your explanation?
It is imperative that we use simple words for our patients and families who are not medically trained and utilize a teach-back method to ensure they understand the information that is communicated to them. I once had to explain post-operative care to a family whose child had tonsil surgery. I had to use words such as poop instead of bowel movement. I used Tylenol instead of acetaminophen.
3. Describe a time you provided effective patient or family education.
Tell a story about a time when you knew your patient or family retained your teachings. How did you know that you effectively communicated the piece of education?
After teaching families, I ask them to repeat the information in their own words. Using a teach-back method allows nurses to know if families truly understood the information that was given to them. It is also important to provide the family with written educational material and use other forms of education, such as videos or hands-on, when possible.
I taught a family post-operative spine care after a posterior spinal fusion. The parents were able to properly demonstrate how to transfer their child from the bed to the chair. In doing so, I was able to determine that they had retained the information.
4. Talk about a time a patient or their family was particularly pleased and appreciative of your care.
Tell a story about a family who was happy with your care. What did you do in particular that they were pleased with? How did you know they were happy? What were the results of this situation?
Working in pediatrics can be challenging but also very rewarding. There are times when parents are unable to stay at the bedside 24/7 because of work, other children, or previous commitments.
I was taking care of a 6-month-old twin during a specific shift. The family was unable to be at the bedside because the father had to work, and the mother was at home with the twin sister and the other children. I spent my shift playing with the infant with age-appropriate toys, and when the mother called to check in – I put the phone next to the infant. The mother was able to hear her baby laughing while singing to her. This brought them closer together and the mother to tears. She stated that no other nurse had done that during the hospitalization, and she was eternally grateful.
5. Give an example of a time you had to interact with a hostile patient. How did you handle the situation, and what was the outcome?
Tell a story about a hostile patient and your step-by-step actions. What was the patient doing that was hostile? How did you react? How did you feel? What procedures did you follow to interact with the patient? What was the result of your actions?
Unfortunately, hostile patients often are part of the job. It’s important to remember some of the patients are being hostile because they are in pain, away from family, and in the hospital setting.
T here was a time when a patient refused to take her medication. I tried everything, but she would spit them out at me when she tried to take them. Because of this behavior, I involved my charge nurse, the physician in charge of her care, and the social worker.
After many conversations and phone calls, it was determined the patient was spitting the medication out because she liked it mixed in chocolate pudding. The woman was elderly and suffered from dementia. It was only after speaking with the social worker that we learned of her medication preference. She was not able to communicate with us her wants and needs and this led to hostility.
6. Describe a time you were faced with a patient who chose not to communicate or disclose important information. How did you handle the situation, and what was the outcome?
Tell a story about a patient you worked with in a similar situation. What step-by-step actions did you take to obtain the information from the patient? What were the results of your actions?
A parent once didn’t disclose that the father of the child was not her current boyfriend. This was important as the patient was going to need consent forms signed, and legally, this boyfriend was not able to sign the consent forms. Additionally, there was a man calling the unit, claiming to be the father of the child. Social work and the nurse manager were notified.
Through an open conversation, the mother disclosed the correct identity of the father. While I personally did not discover the information, it is essential to know the resources that are available to you and utilize them to the best of your ability.
Interviewing isn’t easy—for anyone! It’s important to be overly prepared to put your best foot forward during every stage of the process. Nurse.org put together this super helpful workbook packed full of exercises, sample questions, and checklists to help you ace your next interview.

By clicking download, you agree to receive email newsletters and special offers from Nurse.org. You may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.
Your request has been received. Thanks!
Sample Nurse Interview Questions: Adaptability
The nursing profession is one of constant urgency, crisis, and uncertainty. Tell stories of challenges and follow up with key takeaways and learned lessons.
1. Tell me about a time you were under a lot of pressure. What was going on, and how did you get through it?
Tell a story about a time you were stressed and under pressure to perform. Explain the situation and why you felt pressured. Describe step-by-step the actions you took to make it through the situation. What was the result? What did you learn? What might you do differently now?
I was the most senior nurse in the unit by over a decade. I had to handle my patient assignments and act as a resource to the other newer nurses on the unit. I had to make sure my time management was great, as well as my ability to drop everything and help someone else. I had to stay organized; otherwise, I would not have been able to assist others.
2. Describe a time when your facility was undergoing some change. How did that impact you, and how did you adapt?
Talk about a time your facility changed. Maybe they were acquired by another facility. Perhaps they transitioned to a new computer system. Describe the change and the steps you took to adapt to such change.
One healthcare system I worked for switched from paper charting to electronic medical records and computerized charting. This transition was confusing and often overwhelming. I was able to adapt quickly, but unfortunately, some of my coworkers were not able to.
3. Tell me about a time when you didn’t know the answer to something at work. How did you go about finding the information?
Tell a story about a time when you did not know the answer. Explain step-by-step the action you took to find the information. Talk about the result of your actions.
As nurses, there is no way that we can possibly know everything. Knowing where to go for help is the first step. At the beginning of every shift, I identify a nurse that I can use as a resource, such as the charge nurse, nurse educator, or unit resource nurse. This individual is generally someone who is more senior with an advanced skill set.
If I am unable to get the answer from them or they are busy I look at the healthcare systems policy and procedure manager. If there is a concern regarding a medication dosage or interaction, I look to Lexi-Comp.
4. Give me an example of an awkward situation at work. How did you remove yourself from the situation?
Tell a story about an uncomfortable situation. What was the situation, and why did it feel awkward? Explain the steps you took to leave the situation. What were the results of your actions? What did you learn?
I once had a teenage male patient make very inappropriate sexual comments towards me. At first, I ignored them, thinking it was a one-time thing. The second time, I told him that the comments were inappropriate and I did not want him to say those things to me. The third time, I left the patient’s room and went directly to the charge nurse.
I explained the situation and how uncomfortable I was in caring for the patient. She gathered a team to speak to the patient. My assignment was switched for the remainder of the shift.
5. Tell me about a time you failed. How did you deal with this situation?
Share a story about when you experience failure. Talk about your feelings and why you felt that you failed. Discuss anything positive that came from this failure. What did you learn from failing? What might you do differently now?
Failing is one of the worst feelings in the world, either professionally or personally. Working in the ICU setting, patients die. We fail them when this happens. I fail them when this happens.
After every death, there is a debriefing to discuss what went well and what could have been done differently. I took that time to reflect on my participation in the event and if there was something I could have done differently. Failure doesn’t equal weakness. It simply is something that we must improve upon.
Sample Nurse Interview Questions: Time Management
Nurses are masters at multitasking - for example, managing multiple patients and administering medication on time while maintaining detailed notes. Tell stories about your punctuality, ability to meet deadlines, and how you remain organized through it all.
1. Talk about a time you worked in a fast-paced setting. How do you prioritize tasks while maintaining excellent patient care?
Give an example of a time you had to prioritize your tasks quickly. Explain your thought process in detail and why you chose to complete the duties in such an order.
Working in an ICU setting is extremely fast-paced, and it is essential to prioritize your tasks for the day. At the beginning of the shift, I make a to-do list with everything that needs to be accomplished. I put the must-do things at the top of the list and the things I would like to do at the bottom.
Administering medications is placed at the top of the list, and washing a patient’s hair is further down. While I would love to accomplish everything, it just isn’t possible.
2. Describe your experience with a very ill patient who required a lot of your time. How did you manage this patient’s care while ensuring your other patients were adequately cared for?
Talk about the patient’s care and why they needed much of your time. What was the illness, trauma or injury? How did you ensure that this patient received quality care? How did you manage your other patients?
Delegation is key here. Knowing when to ask for help is important. Without identifying resources and asking for help, success is impossible.
3. Talk about a time when you felt overwhelmed with your work or patient load. What did you do?
Give a specific example of a time you were overwhelmed. Explain step-by-step the actions you took to overcome this feeling and to focus on the task at hand.
I asked for help during these situations. Without identifying resources and asking for help, success is impossible.
4. Give an example of an important goal you set for yourself. Did you accomplish that goal? How did you ensure that you accomplished it?
Make sure the goal you share is related to your career. Explain the steps you took to accomplish your goal. What challenges did you face? How did you feel once you accomplished your goal?
I set the goal of earning my pediatric certification and made a list of things that I must do to achieve that. I signed up for the exam and paid the fee, so I had to take it. There was no backing out.
Sample Nurse Interview Questions: Communication Style
It is important to convey your particular communication style and techniques. Tell stories about specific times you either had difficulty communicating or times you communicated well. If you can, walk through your step-by-step thought process and give examples.
1. Give an example of a time when you were able to successfully persuade a patient to agree to something. How did you persuade this person?
Tell a story about a specific time when you had a difficult time getting a patient to agree to something at work. What was the situation, and what did they need to agree to? What specific actions did you take to get them to agree? What was the result?
Ideally, we never want to persuade a patient to do something. We would like the patient to agree to it freely. However, I did bargain with a child that if he ate his breakfast, I would play video games with him afterward. Using a bargaining system worked well to ensure the patient was well nourished.
2. Tell me about a time when you had to rely on written communication to explain yourself to your team or to a patient.
Talk about a time when you successfully relied on written (or typed) communication. What were the circumstances? What was being discussed? How did you ensure success?
Most hospitals utilize a text feature to communicate quickly with the medical team. It is important to be concise and provide all of the important information so that the medical team can determine the best course of action.
3. Talk about a time when you had not communicated well. How did you correct the situation?
No one is perfect; we all have flaws. Discuss a time when you experienced miscommunication at work. What were the circumstances? How did you know you did not communicate well? What did you learn? What were the results?
This often happens when there is a language barrier. I learned that it is always better to ask for an in-person interpreter or utilize computer translation software. This ensures there is no miscommunication of information. Unfortunately, hand gestures and speaking louder don’t always work.
4. Describe a time when you received negative feedback and turned it into something positive.
Discuss a time at work when you received negative feedback. What was the feedback and circumstances surrounding the feedback? Who gave you the negative feedback? How did it make you feel? What did you do as a result of the feedback?
I was once told that I needed to be more social at work and try and bond with my work colleagues. I disagreed with my manager because I felt that we were there to work and take care of our patients, not to make friends. Becoming close friends with coworkers is an added bonus.
While I didn’t become best friends with anyone from the unit, I was able to spend downtime reading and studying to earn additional certifications, which helped me secure better jobs and opportunities in nursing.
Sample Nurse Interview Questions: Motivation and Core Values
These questions are designed to help interviewers understand your motivation and personal values. When answering such questions, you should share motivational stories from your life that convey your core values.
1. What is one professional accomplishment that you are most proud of and why?
Tell a story about one of your most noteworthy accomplishments at work. What was the accomplishment? What steps did you take to achieve it? Who else was involved in this accomplishment? What happened as a result of the accomplishment?
Earning my advanced pediatric certification is something I worked very hard for, and it validates the years I have spent at the bedside.
2. Have you ever felt dissatisfied with your work as a Nurse? What could have been done to make it better?
Most nurses encounter difficulties while working. Talk about a time when you felt dissatisfied with your work. What were the circumstances, and what happened? What was your role? Why did you feel dissatisfied? What would you do differently now? What did you learn?
I once became extremely dissatisfied because I was consistently being given easier assignments and not being given the ICU level of patients. It became frustrating, and while I understood that others needed to learn and gain experience, it quickly left me annoyed with my position, the unit, and the healthcare system.
I sat down and spoke to my nurse manager about my concerns and inquired why it was happening. The nurse manager was not aware of the situation and it was later determined that a few of the charge nurses were giving the sicker patients to their friends and not spreading them out amongst the nurses.
3. Describe a time when you went over and above your job requirements. What motivated you to put forth the extra effort?
Talk about a specific instance when you went out of your way for your job or for a patient. What were the circumstances? Why did you choose to take the action? What did you do? What were the results?
I personally feel like I give 110% to all of my patients every shift, but there was one that I grew especially close with. For some reason, the patient had been dropped off by a family member, and no one had come to see the child for months. It was obvious the patient was missing key developmental milestones and was becoming increasingly lonely and depressed.
I asked to become the primary nurse for the patient, which meant every time I worked, he would be assigned to me. I worked with him over several months to get him potty trained and to improve his vocabulary. I don’t know exactly why I was extra motivated, but at that time in our lives, the patient and I needed each other.
4. Give an example of a mistake you’ve made. How did you handle it?
It is important to admit that you make mistakes and to own up to them. Talk about the specific mistake and why it happened. What was your role in the mistake? How did you know that you made a mistake? Who was involved? What did you learn? What have you done to improve? What were the results?
Mistakes are part of nursing, whether we like to admit to it or not. It’s important to learn from those mistakes and become a better nurse. One mistake that I will never forget is leaving the gastronomy tube unclamped with medication administration.
Because it was unclamped when I opened the port to give the next medication, the last medication, as well as formula, came out. I was unable to clamp it quickly enough, and the medications I had already given were leaking onto the bed.
I had to speak with the medical team and pharmacy to discuss replacing them. I have never forgotten to clamp the gastronomy tube again.
5. What do you find most difficult about being a Nurse? How do you overcome this difficulty?
Be honest and talk about the most difficult component of nursing. Maybe it’s working with a specific patient population. Or acting in a leadership role. Whatever it is to you, always make sure to talk about the steps and actions you’ve taken to cope with the difficulty.
The most difficult aspect of being a nurse is watching a patient die, especially one that I have cared for when they were healthy. Watching the family lose a loved one is heartbreaking. Sometimes I sit in the bathroom and take a moment for myself to cry, to reflect, and to pause to remember the patient. Death is part of our everyday world, and sometimes that is hard to remember.
Interviewing is a two-way street. Often, nurses are so excited and nervous about answering questions well during their interviews that they forget to ask questions to their potential future employers.
After all, how do you know if the job is an excellent fit unless you ask about the details that are important to you?
Most of the time, when you reach the end of your interview, employers will ask interviewees if they have any questions about the position. This is a great opportunity to show that you have done your research on their facility and expected job duties and demonstrate how excited you are about the position.
Depending on time, you may want to consider limiting your questions to two or three questions. Most nursing administrators set aside an allotted amount of time to interview each potential new hire, and you don’t want to be disrespectful of their time.
Many of these questions may also be great to ask after you have the job and work 1:1 with a preceptor or other helpful nurses. Experienced nurses are great resources for questions once you get the job!
Sample Questions To Ask During an Interview: Onboarding
- How long is the training period, and what does it entail?
- How will my training success be measured?
- Will I have orientation days, and what will they entail?
- What advice would you give to a nurse who is just starting on the unit?
- How quickly are you looking to hire someone?
- Who will I be reporting to?
- What shifts are you hiring for: night, day, mid-shift, or alternating?
- Will I be required to work on-call shifts?
Sample Questions To Ask During an Interview: Mentoring
- Will I be assigned a preceptor?
- How will my success as a new hire be measured?
- What is your training process for new hires?
- What advice do you have for a new hire who wants to succeed in this unit?
- How frequently do you perform performance reviews?
Sample Questions To Ask During an Interview: Culture
- Can you explain what the nursing culture is like here?
- Does the nursing staff face any ongoing challenges on the unit? What are the most critical challenges?
- What is the management style of this unit?
- What does an ideal candidate look like for this role?
- How does this nursing environment facilitate collaboration and unity?
Sample Questions To Ask During an Interview: Professional Development
- Are there any professional development opportunities?
- How long do nurses work at the bedside before taking on a charge nurse role?
- Do you offer tuition reimbursement for nurses advancing their education to take on higher-level nursing roles?
- Are nurses encouraged to become certified in their specialties?
- Will I be expected to float to other units? How often will that occur?
Sample Questions for New Nursing Graduates
- Do you offer a new nursing graduate program, how long is it, and what does it entail?
- How are new graduates measured on performance and competency?
- Do new graduates have a mentor? How long do they provide supervision and nursing support?
- What are the most common challenges new grads experience in this unit?
- When will I be eligible to become involved on unit committees?
Other Important Questions You May Want to Ask
You will not have enough time to ask all of these questions during your interview, but you may want to pick one or two to ask if there is any remaining time left.
Otherwise, keep these questions handy for when you have an opportunity to ask them in the future. They may help provide essential information to help you exceed expectations in your new job!
- What electronic medical record (EMR) system does this facility use?
- Describe the patient population on the unit and how many patients will we have at capacity?
- Do you have overtime policies for nurses who want to work extra shifts?
- What are staffing ratios here?
- How does the scheduling process work?
- What are your protocols for dealing with challenging or difficult patients?
Remember to ask what the next steps in the interview process are and express your interest in the position.

Top 10 Cheap, Fast, Online MSN Programs
For example, if the hiring manager says something like, “I am not sure that you have enough critical care experience to take on this position,” you can respond and assure them that you are perfect for the role.
You may want to say something like, “I have always wanted to work in a high-acuity environment. I am extremely dedicated and eager to learn new skills necessary to succeed in this role. I am like a sponge and ready to learn!”
Remember to close the interview on a high note before walking away.
How to Prepare for Your Nursing Interview
1. dress for success.
You don’t get a second chance to make a first impression! In fact, many hiring managers say they know if they are interested in hiring someone within the first five minutes.
It is essential to look professional and air on the more conservative side of style versus wearing bright and flashy clothing. Keep jewelry simple and understated. If it is appropriate to wear a suit, stick to neutral colors such as black, navy, or dark brown shades.
Your goal is to look as professional as possible so the person you are speaking with can focus on the essential skills you will bring to their organization.
2. Practice answering as many interview questions as you can out loud
Many interviewees review interview questions by reading them alone. But that may not help prepare you as well as speaking your answers out loud. In fact, you may find that you aren’t as clear on many of your answers as you thought you were.
Consider enlisting a friend or family member to act as the interviewer and ask you sample questions. Practice answering your questions and focus on ways you can communicate more effectively. Be assertive and don’t ramble. You will know if you are ready if you can answer questions clearly and constantly.
3. Research the institution thoroughly
LinkedIn is a great resource for learning about healthcare facilities and the types of employees who work there. Employers usually appreciate it when candidates show they have basic knowledge about an organization's goals.
The last thing you want is to be asked something about the organization and not have an answer for it.
4. Arrive at least 20 minutes or more before your interview starts
Arrive early enough that you can use the restroom if needed, straighten yourself up, and not feel rushed walking into the interview.
5. Bring a great attitude
Make sure you get plenty of shut-eye the night before your interview and eat a good breakfast. Drink coffee if it helps you perform at your best, but avoid it as it can make you jittery.
But most importantly, smile and bring a positive vibe. You are going to do great!
Phone Interviews
Many employers do an initial phone interview before bringing candidates in to meet face-to-face. This often helps recruiters weed out candidates who aren’t serious about a position and offer additional information to candidates to make sure they really want the job.
Bu phone interviews are just as important as in-person or online interviews.
Here are a few tips to remember:
- Prepare for a phone interview the same way you would for a face-to-face interview. You have no way of predicting what questions will be asked, and it's better to be overly prepared than under-prepared.
- Stand up while you are talking. Standing during a phone interview may help you project your answers more clearly than if you are sitting down.
- Keep your resume and cover letter within reach in case you are asked about them.
- Don’t eat or drink during the phone interview, even though they can’t see you.
- Shower and get ready as if it were a face-to-face interview. You will feel more confident and professional, and it may help you perform better.
Zoom Interview Tips
Ever since the start of the pandemic, Zoom interviews have become exceedingly common. Employers continue to utilize online interviewing because it is often more accessible and convenient for everyone involved.
Preparing for a Zoom interview is similar to preparing for an in-person or phone interview. However, there are several tips you should keep in mind:
1. Dress professionally as if you were going to a face-to-face interview
If you would have worn a suit to an in-person interview, consider wearing it for your Zoom interview. Remember that even though employers usually don’t see your lower half on Zoom, there is a slight chance you may have to stand up or grab something. So no pajama pants!
2. Make sure your background is set up nicely
The interviewer will see your surroundings, so make sure your background is clean and organized. Consider a blank wall so nothing distracts your interviewer from your amazing skills. Also, never have a window behind you because the light can drown you out.
3. Keep it quiet
If you have roommates, let them know you will be on a Zoom interview, and they must stay quiet. If you have pets that have the potential to interrupt your interview, make arrangements for them beforehand. The last thing you want is for your cat to walk right in front of your screen!
4. Set up your Zoom space and practice the day before
If you are new to Zoom, don’t fret! It is a fairly simple platform to use. But it may be a good idea to set yourself up beforehand and practice so there are no surprises.
5. Ensure a good internet connection
No connection, no interview! Ensure that a quality connection is set up early so you don’t have to scramble when you should be starting your interview.
6. Practice with a friend
If you are new to Zoom, you may not be aware of your body language or how you present over video. Consider making a few Zoom calls with friends and family to get comfortable with it and ensure that you have an excellent video presence.
Nursing Behavioral Interview Flash Cards With Answers
Healthcare employers are increasingly asking behavioral questions - this means they want to know exactly how you will perform during different circumstances. They will be asking for you to provide examples of specific scenarios. Sound overwhelming? Don’t fret; Nurse.org has over 50 behavioral interview questions to help you practice. We’ve even included sample answers!

What questions are asked in a nursing interview?
- Healthcare hiring managers usually ask behavioral-based interview questions. These questions help provide information about how you may handle specific situations in the workplace and allow you to show your critical thinking skills.
How do I prepare for a nursing interview?
- Preparing for your interview starts well in advance of your actual interview date. Here are a few essential tips to prepare for your nursing interview: Practice as many interview questions as you can, dress professionally, research the institution thoroughly, show up early, bring a great attitude, and relax. You will do great!
What are the four skills of a nursing interview?
- Listening actively and taking notes when appropriate. Asking important questions. Good non-verbal communication - ways to do this include leaning forward slightly, smiling, making good eye contact, and head nodding when appropriate. Answer behavioral questions with examples from your own work experience.
How do you introduce yourself in a nursing interview?
- Start with your name and a brief history of your education and work history. You may want to explain why you chose this career and are so passionate about it. It is also important to talk about why you make a good fit for the position and what your career goals are in the future.

Kathleen Gaines (nee Colduvell) is a nationally published writer turned Pediatric ICU nurse from Philadelphia with over 13 years of ICU experience. She has an extensive ICU background having formerly worked in the CICU and NICU at several major hospitals in the Philadelphia region. After earning her MSN in Education from Loyola University of New Orleans, she currently also teaches for several prominent Universities making sure the next generation is ready for the bedside. As a certified breastfeeding counselor and trauma certified nurse, she is always ready for the next nursing challenge.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. You may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.
The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
Account Management
Log in to manage your policy, generate a certificate of insurance (COI), make a payment, and more.
Log in to your account to update your information or manage your policy.
Download a Certificate of Insurance (COI) to provide to your employer.
Make a Payment
Make a one-time payment, set up autopay, or update your payment information.
Submit a notice of an incident or claim in just minutes.
Topics on this page:
Why Critical Thinking in Nursing Is Important
8 examples of critical thinking in nursing, improving the quality of patient care, the importance of critical thinking in nursing.
Jul 24, 2024
While not every decision is an immediate life-and-death situation, there are hundreds of decisions nurses must make every day that impact patient care in ways small and large.
“Being able to assess situations and make decisions can lead to life-or-death situations,” said nurse anesthetist Aisha Allen . “Critical thinking is a crucial and essential skill for nurses.”
The National League for Nursing Accreditation Commission (NLNAC) defines critical thinking in nursing this way: “the deliberate nonlinear process of collecting, interpreting, analyzing, drawing conclusions about, presenting, and evaluating information that is both factually and belief-based. This is demonstrated in nursing by clinical judgment, which includes ethical, diagnostic, and therapeutic dimensions and research.”
An eight-year study by Johns Hopkins reports that 10% of deaths in the U.S. are due to medical error — the third-highest cause of death in the country.
“Diagnostic errors, medical mistakes, and the absence of safety nets could result in someone’s death,” wrote Dr. Martin Makary , professor of surgery at Johns Hopkins University School of Medicine.
Everyone makes mistakes — even doctors. Nurses applying critical thinking skills can help reduce errors.
“Question everything,” said pediatric nurse practitioner Ersilia Pompilio RN, MSN, PNP . “Especially doctor’s orders.” Nurses often spend more time with patients than doctors and may notice slight changes in conditions that may not be obvious. Resolving these observations with treatment plans can help lead to better care.
Key Nursing Critical Thinking Skills
Some of the most important critical thinking skills nurses use daily include interpretation, analysis, evaluation, inference, explanation, and self-regulation.
- Interpretation: Understanding the meaning of information or events.
- Analysis: Investigating a course of action based on objective and subjective data.
- Evaluation: Assessing the value of information and its credibility.
- Inference: Making logical deductions about the impact of care decisions.
- Explanation: Translating complicated and often complex medical information to patients and families in a way they can understand to make decisions about patient care.
- Self-Regulation: Avoiding the impact of unconscious bias with cognitive awareness.
These skills are used in conjunction with clinical reasoning. Based on training and experience, nurses use these skills and then have to make decisions affecting care.
It’s the ultimate test of a nurse’s ability to gather reliable data and solve complex problems. However, critical thinking goes beyond just solving problems. Critical thinking incorporates questioning and critiquing solutions to find the most effective one. For example, treating immediate symptoms may temporarily solve a problem, but determining the underlying cause of the symptoms is the key to effective long-term health.
Here are some real-life examples of how nurses apply critical thinking on the job every day, as told by nurses themselves.
Example #1: Patient Assessments
“Doing a thorough assessment on your patient can help you detect that something is wrong, even if you’re not quite sure what it is,” said Shantay Carter , registered nurse and co-founder of Women of Integrity . “When you notice the change, you have to use your critical thinking skills to decide what’s the next step. Critical thinking allows you to provide the best and safest care possible.”
Example #2: First Line of Defense
Often, nurses are the first line of defense for patients.
“One example would be a patient that had an accelerated heart rate,” said nurse educator and adult critical care nurse Dr. Jenna Liphart Rhoads . “As a nurse, it was my job to investigate the cause of the heart rate and implement nursing actions to help decrease the heart rate prior to calling the primary care provider.”
Nurses with poor critical thinking skills may fail to detect a patient in stress or deteriorating condition. This can result in what’s called a “ failure to rescue ,” or FTR, which can lead to adverse conditions following a complication that leads to mortality.
Example #3: Patient Interactions
Nurses are the ones taking initial reports or discussing care with patients.
“We maintain relationships with patients between office visits,” said registered nurse, care coordinator, and ambulatory case manager Amelia Roberts . “So, when there is a concern, we are the first name that comes to mind (and get the call).”
“Several times, a parent called after the child had a high temperature, and the call came in after hours,” Roberts said. “Doing a nursing assessment over the phone is a special skill, yet based on the information gathered related to the child’s behavior (and) fluid intake, there were several recommendations I could make.”
Deciding whether it was OK to wait until the morning, page the primary care doctor, or go to the emergency room to be evaluated takes critical thinking.
Example #4: Using Detective Skills
Nurses have to use acute listening skills to discern what patients are really telling them (or not telling them) and whether they are getting the whole story.
“I once had a 5-year-old patient who came in for asthma exacerbation on repeated occasions into my clinic,” said Pompilio. “The mother swore she was giving her child all her medications, but the asthma just kept getting worse.”
Pompilio asked the parent to keep a medication diary.
“It turned out that after a day or so of medication and alleviation in some symptoms, the mother thought the child was getting better and stopped all medications,” she said.
Example #5: Prioritizing
“Critical thinking is present in almost all aspects of nursing, even those that are not in direct action with the patient,” said Rhoads. “During report, nurses decide which patient to see first based on the information gathered, and from there they must prioritize their actions when in a patient’s room. Nurses must be able to scrutinize which medications can be taken together, and which modality would be best to help a patient move from the bed to the chair.”
A critical thinking skill in prioritization is cognitive stacking. Cognitive stacking helps create smooth workflow management to set priorities and help nurses manage their time. It helps establish routines for care while leaving room within schedules for the unplanned events that will inevitably occur. Even experienced nurses can struggle with juggling today’s significant workload, prioritizing responsibilities, and delegating appropriately.
Example #6: Medication & Care Coordination
Another aspect that often falls to nurses is care coordination. A nurse may be the first to notice that a patient is having an issue with medications.
“Based on a report of illness in a patient who has autoimmune challenges, we might recommend that a dose of medicine that interferes with immune response be held until we communicate with their specialty provider,” said Roberts.
Nurses applying critical skills can also help ease treatment concerns for patients.
“We might recommend a patient who gets infusions come in earlier in the day to get routine labs drawn before the infusion to minimize needle sticks and trauma,” Robert said.
Example #7: Critical Decisions
During the middle of an operation, the anesthesia breathing machine Allen was using malfunctioned.
“I had to critically think about whether or not I could fix this machine or abandon that mode of delivering nursing anesthesia care safely,” she said. “I chose to disconnect my patient from the malfunctioning machine and retrieve tools and medications to resume medication administration so that the surgery could go on.”
Nurses are also called on to do rapid assessments of patient conditions and make split-second decisions in the operating room.
“When blood pressure drops, it is my responsibility to decide which medication and how much medication will fix the issue,” Allen said. “I must work alongside the surgeons and the operating room team to determine the best plan of care for that patient’s surgery.”
“On some days, it seems like you are in the movie ‘The Matrix,’” said Pompilio. “There’s lots of chaos happening around you. Your patient might be decompensating. You have to literally stop time and take yourself out of the situation and make a decision.”
Example #8: Fast & Flexible Decisions
Allen said she thinks electronics are great, but she can remember a time when technology failed her.
“The hospital monitor that gives us vitals stopped correlating with real-time values,” she said. “So I had to rely on basic nursing skills to make sure my patient was safe. (Pulse check, visual assessments, etc.)”
In such cases, there may not be enough time to think through every possible outcome. Critical thinking combined with experience gives nurses the ability to think quickly and make the right decisions.
Nurses who think critically are in a position to significantly increase the quality of patient care and avoid adverse outcomes.
“Critical thinking allows you to ensure patient safety,” said Carter. “It’s essential to being a good nurse.”
Nurses must be able to recognize a change in a patient’s condition, conduct independent interventions, anticipate patients and provider needs, and prioritize. Such actions require critical thinking ability and advanced problem-solving skills.
“Nurses are the eyes and ears for patients, and critical thinking allows us to be their advocates,” said Allen.
Image courtesy of iStock.com/ davidf
Last updated on Jul 24, 2024. Originally published on Aug 25, 2021.
- Career Growth
The views expressed in this article are those of the author and do not necessarily reflect those of Berxi™ or Berkshire Hathaway Specialty Insurance Company. This article (subject to change without notice) is for informational purposes only, and does not constitute professional advice. Click here to read our full disclaimer
The product descriptions provided here are only brief summaries and may be changed without notice. The full coverage terms and details, including limitations and exclusions, are contained in the insurance policy. If you have questions about coverage available under our plans, please review the policy or contact us at 833-242-3794 or [email protected] . “20% savings” is based on industry pricing averages.
Berxi™ is a part of Berkshire Hathaway Specialty Insurance ( BHSI ). Insurance products are distributed through Berkshire Hathaway Global Insurance Services, California License # 0K09397. BHSI is part of Berkshire Hathaway’s National Indemnity group of insurance companies, consisting of National Indemnity and its affiliates, which hold financial strength ratings of A++ from AM Best and AA+ from Standard & Poor’s. The rating scales can be found at www.ambest.com and www.standardandpoors.com , respectively.
No warranty, guarantee, or representation, either expressed or implied, is made as to the correctness, accuracy, completeness, adequacy, or sufficiency of any representation or information. Any opinions expressed herein are subject to change without notice.
The information on this web site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment, and does not purport to establish a standard of care under any circumstances. All content, including text, graphics, images and information, contained on or available through this web site is for general information purposes only based upon the information available at the time of presentation, and does not constitute medical, legal, regulatory, compliance, financial, professional, or any other advice.
BHSI makes no representation and assumes no responsibility or liability for the accuracy of information contained on or available through this web site, and such information is subject to change without notice. You are encouraged to consider and confirm any information obtained from or through this web site with other sources, and review all information regarding any medical condition or treatment with your physician or medical care provider. NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING THAT YOU HAVE READ ON OR ACCESSED THROUGH THIS WEB SITE.
BHSI is not a medical organization, and does not recommend, endorse or make any representation about the efficacy, appropriateness or suitability of any specific tests, products, procedures, treatments, services, opinions, health care providers or other information contained on or available through this web site. BHSI IS NOT RESPONSIBLE FOR, AND EXPRESSLY DISCLAIMS ALL LIABILITY FOR, ANY ADVICE, COURSE OF TREATMENT, DIAGNOSIS OR ANY OTHER SERVICES OR PRODUCTS THAT YOU OBTAIN AFTER REVIEWING THIS WEB SITE.
Want Berxi articles delivered straight to your inbox? Sign up for our monthly newsletter below!
" * " indicates required fields
How we use your email address Berxi will not sell or rent your email address to third parties unless otherwise notified. Other than where necessary to administer your insurance policy or where required by law, Berxi will not disclose your email address to third parties. Your email address is required to identify you for access to the Berxi website. You may also receive newsletters, product updates, and communications about quotes and policies.
Paul Dughi is a contributing writer for Berxi, as well as a journalist and freelance writer. He has held executive management positions in the media industry for the past 25 years.
Related Articles

Breaking Bad News to Patients: A Nurse’s Guide to SPIKES
Michael Walton Jul 24, 2024

Delegation in Nursing: Steps, Skills, & Solutions for Creating Balance at Work
Kristy Snyder Jul 24, 2024

The 7 Most Common Nursing Mistakes (And What You Can Do If You Make One)
Paul Dughi Aug 28, 2024

How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
Last updated on August 19th, 2023
Nurses play a critical role in making critical decisions that directly impact patient outcomes in the dynamic field of healthcare. Developing strong critical thinking skills is essential for success in this role.
In this article, we present a comprehensive list of 23 nursing-specific strategies aimed at improving critical thinking and improve the quality of patient care.
24 Strategies to improve critical thinking skills in nursing
You may also want to check out: 15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)
1. Reflective Journaling: Delving into Deeper Understanding
Reflective journaling is a potent tool for nurses to explore their experiences, actions, and decisions.
By regularly pondering over situations and analyzing their thought processes, nurses can identify strengths and areas for improvement.
This practice encourages the conscious development of critical thinking by comparing past experiences with current knowledge and exploring alternative solutions.
After a particularly challenging case, a nurse reflects on their decision-making process, exploring what worked well and what could have been done differently.
2. Meeting with Colleagues: Collaborative Learning for Critical Thinking
Regular interactions with colleagues foster a collaborative learning environment. Sharing experiences, discussing diverse viewpoints, and providing constructive feedback enhance critical thinking skills .
Colleagues’ insights can challenge assumptions and broaden perspectives, ultimately leading to more well-rounded clinical judgments.
A nursing team gathers to discuss a recent complex case, sharing their perspectives, insights, and lessons learned to collectively improve patient care strategies.
3. Concept Mapping: Visualizing Complexity
Concept mapping is an excellent technique to synthesize intricate patient information. By creating visual representations of patient problems and interventions, nurses can identify relationships and patterns that might not be apparent otherwise.
This strategy aids in comprehensive care planning and encourages nurses to think holistically about patient care.
Creating a concept map to connect patient symptoms, diagnostics, and interventions reveals patterns that help the nurse formulate a comprehensive care plan.
4. Socratic Questioning: Digging Deeper into Situations
The art of Socratic questioning involves asking probing questions that lead to deeper understanding.
Applying this technique allows nurses to uncover assumptions, examine inconsistencies, and explore multiple viewpoints.
This approach is especially valuable when reviewing patient history, discussing conditions, and planning care strategies.
When assessing a patient’s deteriorating condition, a nurse asks probing questions to uncover potential underlying causes and prioritize appropriate interventions.
5. Inductive and Deductive Reasoning: From Specifics to Generalizations
Developing skills in both inductive and deductive reasoning equips nurses to analyze situations from different angles.
Inductive reasoning involves drawing conclusions from specific observations, while deductive reasoning starts with general premises to arrive at specific conclusions.
Proficient use of these methods enhances nurses’ ability to make accurate clinical judgments.
When encountering a series of patients with similar symptoms, a nurse uses inductive reasoning to identify a common pattern and deduce potential causes.
6. Distinguishing Statements: Fact, Inference, Judgment, and Opinion
Clear thinking demands the ability to differentiate between statements of fact, inference, judgment, and opinion.
Nurses must critically evaluate information sources, ensuring they rely on evidence-based practice.
This skill safeguards against misinformation and supports informed decision-making.
While reviewing a patient’s history, a nurse differentiates factual medical information from inferences and subjective judgments made by different healthcare professionals.
7. Clarifying Assumptions: Promoting Effective Communication
Recognizing assumptions and clarifying their underlying principles is vital for effective communication. Nurses often hold differing assumptions, which can impact patient care.
By acknowledging these assumptions and encouraging open discussions, nursing teams can collaboratively create care plans that align with patients’ best interests.
Before suggesting a treatment plan, a nurse engages in a conversation with a patient to understand their cultural beliefs and preferences, ensuring assumptions are not made.
8. Clinical Simulations: Learning through Virtual Scenarios
Clinical simulations provide nurses with a risk-free environment to practice decision-making and problem-solving skills.
These virtual scenarios mimic real-life patient situations and allow nurses to test different approaches, assess outcomes, and reflect on their choices.
By engaging in simulations, nurses can refine their critical thinking abilities, learn from mistakes, and gain confidence in their clinical judgment.
Engaging in a simulated scenario where a patient’s condition rapidly changes challenges a nurse’s decision-making skills in a controlled environment.
9. Case Studies and Grand Rounds: Analyzing Complex Cases
Engaging in case studies and participating in grand rounds exposes nurses to complex patient cases that require in-depth analysis.
Working through these scenarios encourages nurses to consider various factors, potential interventions, and their rationale.
Discussing these cases with colleagues and experts fosters collaborative critical thinking and widens the spectrum of possible solutions.
Nurses participate in grand rounds, discussing a challenging case involving multiple medical specialties, encouraging a holistic approach to patient care.
10. Continuing Education and Lifelong Learning: Expanding Knowledge
Staying up-to-date with the latest advancements in nursing and healthcare is crucial for effective critical thinking.
Pursuing continuing education opportunities, attending conferences, and engaging in self-directed learning keeps nurses informed about new research, technologies, and best practices.
This continuous learning enriches their knowledge base, enabling them to approach patient care with a well-rounded perspective.
Attending a nursing conference on the latest advancements in wound care equips a nurse with evidence-based techniques to improve patient outcomes.
11. Debates and Discussions: Encouraging Thoughtful Dialogue
Organizing debates or participating in structured discussions on healthcare topics stimulates critical thinking.
Engaging in debates requires researching and presenting evidence-based arguments, promoting the evaluation of different perspectives.
Nurses can exchange insights, challenge assumptions, and refine their ability to defend their viewpoints logically.
Engaging in a debate on the pros and cons of a new treatment method encourages nurses to critically analyze different viewpoints and strengthen their own understanding.
12. Multidisciplinary Collaboration: Gaining Insights from Various Disciplines
Collaborating with professionals from diverse healthcare disciplines enriches nurses’ critical thinking.
Interacting with doctors, pharmacists, therapists, and other experts allows nurses to benefit from different viewpoints and approaches.
This cross-disciplinary collaboration broadens their understanding and encourages innovative problem-solving.
Collaborating with physical therapists, nutritionists, and pharmacists helps a nurse develop a holistic care plan that addresses all aspects of a patient’s recovery.
13. Ethical Dilemma Analysis: Balancing Patient Autonomy and Best Practice
Ethical dilemmas are common in nursing practice. Analyzing these situations requires nurses to weigh the principles of beneficence, non-maleficence, autonomy, and justice.
By critically examining ethical scenarios, nurses develop the capacity to navigate morally complex situations, prioritize patient welfare, and make ethically sound decisions.
When faced with a patient’s refusal of treatment due to religious beliefs, a nurse evaluates the ethical considerations, respects autonomy, and seeks alternatives.
14. Root Cause Analysis: Investigating Adverse Events
When adverse events occur, performing a root cause analysis helps identify the underlying causes and contributing factors.
Nurses engage in a systematic process of analyzing events, exploring the “5 Whys” technique , and developing strategies to prevent similar occurrences in the future.
This approach cultivates a thorough and analytical approach to problem-solving.
After a medication error, a nurse leads a root cause analysis to identify system failures and implement preventive measures to enhance patient safety.
15. Creative Thinking Exercises: Expanding Solution Repertoire
Encouraging creative thinking through brainstorming sessions or scenario-based exercises widens the range of possible solutions nurses consider.
By thinking outside the box and exploring innovative approaches, nurses develop adaptable problem-solving skills that can be applied to complex patient care challenges.
Brainstorming creative approaches to comfort a distressed pediatric patient empowers a nurse to find innovative methods beyond routine interventions.
16. Journal Clubs: Fostering Evidence-Based Discussion
Participating in journal clubs involves healthcare professionals coming together to dissect recent research articles.
This practice ignites critical thinking by allowing nurses to evaluate study methodologies, scrutinize findings, and consider the implications for their practice.
Engaging in evidence-based discussions not only cultivates a culture of critical inquiry but also reinforces continuous learning.
At the monthly journal club meeting, Nurse Mark engages in a discussion on a recent research article focusing on pain management strategies for post-operative patients.
The group analyzes the study design, scrutinizes the findings, and considers the potential implications for their practice.
During the discussion, Mark raises thought-provoking questions about the study’s methodology and suggests potential applications in their hospital’s patient care protocols.
This active participation in journal clubs not only refines Mark’s critical thinking but also instills evidence-based practices into his nursing approach.
17. Critical Reflection Groups: Collaborative Learning and Analysis
Similarly, establishing critical reflection groups, where nurses meet regularly to discuss experiences, cases, and challenges, fosters collective learning.
These sessions encourage the exchange of diverse perspectives, enriching the analysis process and ultimately enhancing patient care strategies.
Through shared insights and discussions, nurses can refine their clinical reasoning and broaden their problem-solving capabilities.
Nurse Emma actively participates in critical reflection groups in order to broaden her clinical knowledge. During a recent meeting, the group tackled a difficult patient case with complicated symptomatology.
Emma suggests alternative diagnostic pathways based on her own experiences. Emma’s critical thinking skills are honed as a result of the group’s dynamic interaction, which also emphasizes the importance of collaborative decision-making in complex scenarios.
18. Mindfulness and Reflection Practices: Enhancing Self-Awareness
Mindfulness techniques, such as meditation and deep breathing, encourage self-awareness and a clear mind.
Engaging in these practices helps nurses become more attuned to their thoughts and emotions, leading to better self-regulation and improved decision-making during high-pressure situations.
Engaging in mindfulness exercises before a demanding shift helps a nurse maintain focus, manage stress, and make clear-headed decisions.
19. Problem-Based Learning: Applying Knowledge in Real Scenarios
Problem-based learning involves presenting nurses with real-world patient cases and encouraging them to collaboratively solve the problems.
This approach bridges the gap between theoretical knowledge and practical application, fostering critical thinking through active problem-solving.
Working through a simulated patient case challenges nurses to apply theoretical knowledge to practical situations, refining their clinical reasoning.
20. Self-Assessment and Feedback: Evaluating Decision-Making Skills
Regularly assessing one’s own decision-making process and seeking feedback from peers and mentors is essential for improvement.
Reflecting on past decisions, considering alternative approaches, and understanding the rationale behind them contribute to the refinement of critical thinking skills.
A nurse evaluates their performance after a patient’s unexpected complication, seeking feedback from peers and mentors to identify areas for improvement.
21. Cultural Competence Training: Navigating Diverse Perspectives
Cultural competence training enhances critical thinking by enabling nurses to understand the diverse cultural beliefs and practices of patients.
This knowledge is vital for providing patient-centered care, as it encourages nurses to think critically about the unique needs of each individual.
A nurse attends cultural competence training to understand the dietary preferences of a diverse patient population, ensuring respectful and patient-centered care.
22. Active Listening and Empathetic Communication: Gathering Insights
Active listening and empathetic communication with patients and their families enable nurses to gather comprehensive information about their conditions, concerns, and preferences.
This data forms the basis for critical analysis and informed decision-making in patient care.
Through attentive listening, a nurse uncovers a patient’s underlying concerns, leading to an informed care plan that addresses both medical needs and emotional well-being.
23. Mentorship and Preceptorship: Learning from Experienced Professionals
Having a mentor or preceptor provides novice nurses with the opportunity to learn from experienced professionals.
Mentors guide critical thinking by sharing their insights, challenging assumptions, and offering guidance in complex situations. This relationship fosters growth and expertise development.
A novice nurse gains valuable insight from a mentor, who guides them through complex cases, offering real-world wisdom and refining critical thinking skills.
24. Self-Assessment and Feedback: Evaluating Decision-Making Skills
Reflecting on past decisions, considering alternative approaches, and understanding the rationale behind them contribute to the refinement of critical thinking skills .
Nurse Sarah regularly takes time to assess her decision-making skills by reviewing past patient cases. After a challenging case involving conflicting symptoms, she reflects on her initial approach, the outcomes, and what she could have done differently.
She seeks feedback from her senior colleague, who provides insights on alternative diagnostic paths. Sarah’s self-assessment and feedback-seeking process enable her to identify areas for improvement and refine her critical thinking in similar situations.
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
- What is Critical Thinking in Nursing? (Explained W/ Examples)
Enhancing critical thinking skills is an ongoing journey that transforms nursing practice.
Reflective journaling, collaborative learning, concept mapping, Socratic questioning , reasoning techniques, distinguishing statements, and clarifying assumptions all play integral roles in nurturing these skills.
By incorporating these strategies into their daily routines, nurses can improve their critical thinking skills.
Additionally, this will help nurses in navigating the complexities of the healthcare field with confidence, expertise, and the ability to make well-informed decisions that improve patient outcomes.
Comments are closed.
Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.

ANA Nursing Resources Hub
Search Resources Hub

Problem Solving in Nursing: Strategies for Your Staff
4 min read • September, 15 2023
Problem solving is in a nurse manager’s DNA. As leaders, nurse managers solve problems every day on an individual level and with their teams. Effective leaders find innovative solutions to problems and encourage their staff to nurture their own critical thinking skills and see problems as opportunities rather than obstacles.
Health care constantly evolves, so problem solving and ingenuity are skills often used out of necessity. Tackling a problem requires considering multiple options to develop a solution. Problem solving in nursing requires a solid strategy.
Nurse problem solving
Nurse managers face challenges ranging from patient care matters to maintaining staff satisfaction. Encourage your staff to develop problem-solving nursing skills to cultivate new methods of improving patient care and to promote nurse-led innovation .
Critical thinking skills are fostered throughout a nurse’s education, training, and career. These skills help nurses make informed decisions based on facts, data, and evidence to determine the best solution to a problem.
Problem-Solving Examples in Nursing
To solve a problem, begin by identifying it. Then analyze the problem, formulate possible solutions, and determine the best course of action. Remind staff that nurses have been solving problems since Florence Nightingale invented the nurse call system.
Nurses can implement the original nursing process to guide patient care for problem solving in nursing. These steps include:
- Assessment . Use critical thinking skills to brainstorm and gather information.
- Diagnosis . Identify the problem and any triggers or obstacles.
- Planning . Collaborate to formulate the desired outcome based on proven methods and resources.
- Implementation . Carry out the actions identified to resolve the problem.
- Evaluation . Reflect on the results and determine if the issue was resolved.
How to Develop Problem-Solving Strategies
Staff look to nurse managers to solve a problem, even when there’s not always an obvious solution. Leaders focused on problem solving encourage their team to work collaboratively to find an answer. Core leadership skills are a good way to nurture a health care environment that supports sharing concerns and innovation .
Here are some essentials for building a culture of innovation that encourages problem solving:
- Present problems as opportunities instead of obstacles.
- Strive to be a positive role model. Support creative thinking and staff collaboration.
- Encourage feedback and embrace new ideas.
- Respect staff knowledge and abilities.
- Match competencies with specific needs and inspire effective decision-making.
- Offer opportunities for continual learning and career growth.
- Promote research and analysis opportunities.
- Provide support and necessary resources.
- Recognize contributions and reward efforts .

Embrace Innovation to Find Solutions
Try this exercise:
Consider an ongoing departmental issue and encourage everyone to participate in brainstorming a solution. The team will:
- Define the problem, including triggers or obstacles.
- Determine methods that worked in the past to resolve similar issues.
- Explore innovative solutions.
- Develop a plan to implement a solution and monitor and evaluate results.
Problems arise unexpectedly in the fast-paced health care environment. Nurses must be able to react using critical thinking and quick decision-making skills to implement practical solutions. By employing problem-solving strategies, nurse leaders and their staff can improve patient outcomes and refine their nursing skills.
Images sourced from Getty Images
Related Resources

Item(s) added to cart
- Nursing School
Critical Thinking Nursing Interview Questions
Critical thinking nursing interview questions feature prominently in any interview. They aren’t supposed to trip you up, but they will do just that if you aren’t ready.
Along with your nursing school application cover letter and your nursing school letter of intent , your nursing school interview questions give you an opportunity to show an admissions board, in your own words, how perfect you are for nursing school.
This article will show you how to take that opportunity and maximally utilize it to your advantage. We will go through what exactly a critical thinking question is, why they are being asked, and what types of responses you can give. Finally, we will cover several sample answers so that you can prepare your own answers for your upcoming interview.
>> Want us to help you get accepted? Schedule a free initial consultation here <<
Article Contents 7 min read
Why are critical thinking questions asked.
While critical thinking questions may relate to aspects of healthcare and nursing, including patient care, working as part of a team, and response to emergencies, they may also deal with dilemmas that have nothing to do with healthcare. For example, you may be faced with a conflict of interest scenario, or an ethical dilemma with a close friend.
Essentially, you’re being tested on your decision-making processes and how you solve problems, whether they are healthcare related or not. Your interviewer is trying to find out if you think logically, quickly, and in ways that provide good solutions in real-world scenarios.
Critical thinking is important to any job, but is of particular importance to nursing. Any healthcare professional deals with immense challenges on a daily basis. These challenges come up with little warning and require clearheaded responses.
Because the question is looking for your decision-making processes, you need to make sure that your responses put those processes in the limelight. Therefore, your answers should focus on the steps of how you made your decision and the why behind those steps: in other words, how you arrived at that response. You should show off how you evaluate situations and respond, but also how you concluded that your response was the most logical course of action.
Even if the question you are asked is hypothetical or situational, as we like to call it, you can definitely use your personal experiences to answer. Make sure to demonstrate non-judgmental attitude and objectivity when making your decision.
With nursing school interview questions, expert responses are required.
Let’s look at a sample critical thinking question and an expert response.
Prompt: Describe the most stressful event of your life. Why was it stressful, and how did you handle the situation?
Example: I\u2019m not saying it was easy, but that organization made things much more straightforward, and it helped to keep my mind calm and disciplined in all that chaos. I learned how to not only balance all of these disparate elements of my life, but that I could use the very act of balancing as a calming influence. "}]">
Nurses often have to deal with hostile patients. Can you recall a time you had to deal with hostility? What did you do and what were the results?
Sample answer:
I was working in a supporting role at a psychiatric institution, and one of the patients was a very angry person. He had a very quick temper and would often be physically violent, in addition to uncooperative or verbally abusive. The nurses said that giving meds felt like playing Russian roulette.
So, I would always make sure that I was around for that patient’s med time, ready to call security if he became violent.
He didn’t like taking his pills, either. One day, I was speaking with him and I discovered that his anger over medication was coming from a lack of understanding; he didn’t fully know what the pills did. So, I talked to his nurse about it, and she went over the reasons for his particular drugs and their side-effects. I also let his physician know about his concerns so that the doctor could have a conversation about it at her next visit in.
Once those issues had been dealt with, medication was much easier to distribute. It didn’t solve all the problems, but it helped make his days a lot smoother.
Critical thinking questions can be daunting and difficult, but they can also show some of your best talents and establish your abilities in a very concrete way. These aren’t abstract. These are demonstrations of actual actions taken. Use these questions to show off your impressive side with a committee.
The focus is the main difference, and with a critical thinking question, that focus is on how you use problem-solving and decision-making in different scenarios. They are to get a sense of how you deal with challenges and obstacles on a day-to-day basis.
Contrast this to more open-ended questions like “Tell us a little bit about yourself,” or “ Why do you want to be a nurse? ”
Fairly compact; you should answer in less than a minute.
Use just enough language to set up the problem you faced, your thought processes on how to deal with those problems, the actions you took, and the outcomes that those actions produced. This can be done in a fairly swift amount of time.
That doesn’t mean you should skimp on detail. While the interviewers don’t need every small thing that happened, they shouldn’t be confused or feel like they’re missing anything. Remember to showcase your abilities – don't brush past them: highlight!
Use mock interviews as part of your nursing school interview preparation to hone your answers for time and detail.
The most important reason is that you will wind up sounding robotic and insincere.
Additionally, the critical thinking questions might be slight variants, so a memorized answer could (or will) end up not quite fitting the question.
Better to memorize scenarios than words so that you can apply those examples to any question that comes up.
You can, and sometimes are directly asked to provide an example of failure.
If an interviewer asks you to describe a time you failed at implementing critical thinking, of course you must supply them with something, and should prepare for such questions in their own right.
Remember that they are looking for your decision-making processes and skills, so the outcome might have been bad, but if your processes were excellent, the interviewer will make note of that. Sometimes even good decisions lead to negative outcomes – sometimes that’s inevitable.
If you failed to apply good critical thinking in a situation, you can highlight what you learned from the experience and how it has improved subsequent actions and decision-making processes.
Failure is only truly failure if no lessons were learned.
You can take a short pause to think, and give yourself enough time to recall an appropriate event or incident. It’s important to research the different types of nursing school interview questions and prepare a relevant story for a variety of scenarios.
While it is unlikely that you will be asked about something that you can’t relate to at all (most of the questions are broad enough to allow some sort of connection) it might happen that you just haven’t had a given experience yet.
You can’t just say, “That’s never happened to me,” and leave it at that.
However, you might want to acknowledge this by saying, “That exact thing has never happened to me, but I have had a similar experience,” and speak of the closest thing you have to what was asked. Perhaps it wasn’t a work or healthcare setting, but maybe something that happened with family members or friends in a social setting, for instance – that will do.
Get as close as you can to the question, acknowledge the discrepancy, and answer to the best of your ability.
Expect anything, because depending on the interview, almost anything can be covered.
Even the type of interview can change, depending on the school. Some will use a traditional panel-style interview, but others will use the multiple mini-interview (MMI) format. If the latter, you might want to learn more about how to prepare for your multiple mini interview .
What exactly is in the interview depends on the school and panel, so be ready for anything.
Want more free tips? Subscribe to our channels for more free and useful content!
Apple Podcasts
Like our blog? Write for us ! >>
Have a question ask our admissions experts below and we'll answer your questions, get started now.
Talk to one of our admissions experts
Our site uses cookies. By using our website, you agree with our cookie policy .
FREE Training Webclass:
How to improve your nursing school interview practice score by 27% , using the proven strategies they don’t want you to know.
- Practice Test
- Fundamentals of Nursing
- Anatomy and Physiology
- Medical and Surgical Nursing
- Perioperative Nursing
- Psychiatric Mental Health Nursing
- Maternal & Child Nursing
- Community Health Nursing
- Pathophysiology
- Nursing Research
- Study Guide and Strategies
- Nursing Videos
- Work for Us!
- Privacy Policy

- Journals and Essays

Thinking Like a Nurse: The Critical Thinking Skills in the Nursing Practice

Thinking how to nurse is thinking like a nurse. Florence Nightingale (1860) wrote on her notes that women who have charge of the other’s health—to which the application of her integrated experiences must teach herself to think how to nurse, a self-learning acquired from “hints”.
Perhaps, Nightingale referred “hints” as the use of critical thinking skills in patient’s care. The ability to think critically was the foundation of nursing practice started from historic times and is becoming one of the key performance indicators for both students and nursing professionals nowadays.
Educational system continues to evolve and progresses heeding to the needs of the society, and parallel to the changing educational structure and methodology. However, Haber (2020) reported that only 75% of employers claim that the students they hire who underwent 12 or more years of formal education lack of critical thinking and problem-solving abilities despite the progress in the educational system.
What is Critical Thinking?
Critical thinking skills, a fundamental skill that plays a pivotal role in our daily survival. In general terms, the skill will not stop in memorization, the process goes beyond connecting the dots from one to concept to another, problem-solving techniques, think creatively, and apply the learned knowledge in new ways (Walden University, 2020). Kaminske (2019), defines critical thinking skills as a domain-specific skill on the ability to solve problems and make effective decisions that require expertise to be applied in a range of situations and scenarios.
In the nursing practice, Critical thinking skill works in assimilation with critical reasoning as a practice-based discipline of decision-making to the health care professionals. Critical thinking is the process of the intentional higher level of thinking to identify patient’s health care needs and appraise evidence-based practice to make choices in the delivery of care.

On the other hand, clinical reasoning as integrated to clinical thinking in application to clinical situation works as a cognitive process to utilized thinking strategies to gather and critically analyze the data concerning the health care needs of the patient, organized the information according to its prioritization, and formulate efficient nursing care plans to improve patient’s outcomes (Berman, et al., 2016).
“Critical thinking is the intellectually disciplined process of actively and skillfully conceptualizing, applying, analyzing, synthesizing, and/or evaluating information gathered from, or generated by, observation, experience, reflection, reasoning, or communication, as a guide to belief and action”, a precise definition presented by Michael Scriven and Richard Paul at the Eighth Annual International Conference on Critical Thinking and Education Reform during the summer of 1987 (Lakhanigam, 2017).
Lakhanigam added the definition published by the Journal of Nursing Education in 2010 that describes critical thinking as the process involving interpretation and analysis of the problem, reasoning to find a solution, applying, and finally evaluation of the outcomes”. Regis College (2020), emphasized the use of deductive reasoning in observation, analyzing information, formulate conclusions, and performing appropriate actions in a self-directed process .
Theories on the Physiology of Thinking
From the ancient theory of “tabula rasa”, as describes in Wikipedia (2020) that humans are born without built-in mental content, and all knowledge is collected by the brain from experiences and perceptions. In this computer age, a neurologist discovered neurological pathways on how to re-program or reformat our brains like computers by analyzing how the brain appears to process, recognize, remember and transfer information at the level of neural circuits, synapses and neurotransmitters. Willis (2012) discussed the brain’s neuroplastic response to stimulation called neuroplasticity. The information is processed in the reflective and cognitive functions of prefrontal cortex wherein learning incorporated into networks of longterm conceptual memory.
Neuroplasticity is greatly affected by stress, boredom and frustration as seen in the neuroimaging scans of students showed that active metabolic states block the processing in the prefrontal cortex. In response to stress, the amygdala as the switching station became hyperactive resulting to switches of input and output away from the prefrontal cortex down to the control of the lower reactive brain, this response is called fight/flight/freeze (act out/zone out). In this situation, the lower brain’s reactive behaviours are in control. This will result in the loss of information access to the prefrontal cortex and new learning is not retained.
Elseways, Knowles (1984) four principles of andragogy of adult learning included (a.) experiences from mistakes that provide the basis for the learning activities; and (b.) the importance of problems and crisis, as adult learning is problem-centred rather than content-oriented; as well as (c.) involvement in the planning and evaluation of learning; and lastly, (d.) that adults are most interested in a subject that is relevant to their job and personal life.
Learning and thinking as applied in a higher-level context, Ausubel’s assimilation theory may recount the theories on critical thinking. In this theory, Ausubel claimed that learning occurs as a result of the interaction between the acquired learning and the cognitive structure in application to practice (Seel, 2012). Moreover, critical analysis and differentiation of interrelationships between concepts called concept mapping refines the knowledge into a more organized, precise, specific, and integrated learning.
In different circumstances, nursing as a professional working in a toxic environment of the sick, pained, hopeless, weak, and dying patients; bullying, queen bee syndrome, and seniority egoism of colleagues; and backbreaking workloads—have reported cases of work-related boredom and stress. The application of the three theories may improve mentoring-learning strategies in meaningful nursing education and training.
Theories on learning acquisition from the collection of information, physiologic processing on cognitive-reflective functions of the brain, concept mapping, and internal/external utilization of knowledge in application to critical thinking are the frameworks of a skilled critical thinker.
Characteristics of a Skilled Critical-Thinker
Health care system can go a long way, achieving a considerable success having employees that possess the ability to think critically thus decreasing errors in clinical judgments. For this purpose, every nurse is required to obtain the characteristics of an excellent skilled critical thinker.
The study of Scheffer and Rubenfeld revealed the common qualities among internationally diverse expert nurses from nine different countries supporting the idea of critical thinking in nursing that encompasses logic and reasoning (Berman, et. Al., 2016), and that includes:
11 Affective Components of a Skilled Critical-Thinker Nurse:
- Perseverance
- Open-mindedness
- Flexibility
- Inquisitiveness
- Intellectual integrity
- Perspective
7 Cognitive Skills of a Skilled Critical-Thinker Nurse:
- Information seeking
- Discriminating
- Transforming knowledge
- Applying standards
- Logical reasoning
Critical Thinking Beyond Exigency and Expediency
Undeniably, nurses with critical thinking ability diversified with effective problem-solving and efficient decision-making skills are the most in-demand and highly valued in the field of the health care industry and academe.
As a nurse striding in the most complicated, stressful and multi-tasking job, you are responsible for making life-changing decisions under the pressure of time and emotions. These reasons as to why critical thinking skills in nursing practice plays a vital role in the care of the patient. Luna (2020), cited seven importance of critical thinking skills in the practice of nursing, such as:
- Nurses’ Critical Thinking Heavily Impacts Patient Care
- It’s Vital to Recognizing Shifts in Patient Status
- It’s Integral to an Honest and Open Exchange of Ideas
- It Allows You to Ensure Patient Safety
- It Helps Nurses Find Quick Fixes and Troubleshooting
- Critical Thinking can Lead to Innovative Improvements
- It Plays a Role in Rational Decision Making
Critical thinking skill is needed in problems identification and implementation of interventions resulting in improved patients outcomes, as well as development in nursing practice by providing new insights on the learned knowledge. Feedback and reflections provide interconnections between nursing research , critical thinking and the nursing practice (Berman, et. Al., 2016).
Critical Thinking Skills: The Mastery, Update and Upgrade
Critical thinking skill is an ability beyond thinking rationally and clearly. It is a process of thinking independently and working at your own feet in formulating own opinions or new theory by utilizing critical analysis on the interrelationship of two or more ideas and delineating conclusions without external control (Wabisabi Learning, 2020).
Modified Wabisabi Learning’s 12 Solid Strategies for Teaching Critical Thinking Skills, and its Application to Nursing Education, Training and Practice:
1. Practice on Eloquence in Question and Answer (Solution Fluency)
Mastery requires ample amount of practice to become highly skilled in critical thinking. Accustom to deliberate open discussions encouraging brainstorming on issues affecting the practice and daily living by using explicit open-ended questions and comprehensive instructions for problem-solving may provide opportunities to apply knowledge into practice as well as encouraging the transfer of ideas between domains (Haber, 2020). Brainstorming is an excellent learning tool to exercise critical thinking (Walden University, 2020) particularly if applied in a situational crisis or a hospital scenario.
2. Create a Foundation
From the theory of back to basic, mastery of low-level skills is a requirement in preparatory to the application of critical thinking skills (Kaminske, 2019).
Learning experiences from theoretical and experiential knowledge are good foundations to start critical thinking. Moreover, practicing thinking skills obtained from theoretical and experiential undertakings improve intellectual ability (Berman, et. al., 2016). Practical understanding and specialization on a particular focus may excel you more in thinking critically. The competence and skills acquired from clinical experience are the most essential learning in developing clinical judgment.
3. Consult the Classics
Nursing theorists and their work are the best examples of consulting the classics. In critical thinking, nurses identify claims based on facts, conclusions, judgment/opinions and evidence-based practice. Exploring nursing theorists and their works are like exploring great minds, acquiring lessons on character motivation, refuting theories or formulating a new theory from existing theory. Case studies and in-depth objective critiques of nursing theories may not only promote critical thinking but act as a leverage to bridge the gap between theory and practice.
4. Create an Environment for Open Communication
During clinical rounds, nurses and/or students with a clinical instructor are engaged into thinking process by providing the opportunity to communicate assessment data, collaborate ideas, formulate nursing care plan, and discuss the various context of the situation from different perspectives (Di Vito-Thomas, 2005).
5. Use Information Fluency
Information fluency is mastering the proper use of information and to the ability to intuitively analyze and interpret it in unearthing knowledge and appropriate facts useful in solving a problem (Wabisabi Learning, 2020).
Knowledge of medical conditions, procedures and its connections to patient’s care are important in building critical thinking. Learning from available resources like medical journals, surfing the internet, and meaningful dialogue with colleagues can increase your medical know-how (Jillings, 2020).
6. Utilize Peer Groups
Peer groups, particularly well experienced and highly skilled colleagues are an excellent source of information, questions, and problem-solving techniques as it expands thinking and viewpoints. It also develops interpersonal skills like teamwork and resolving conflicts (Berman, et. Al., 2016).
7. Try One Sentence of Reflections at a time
Reflections will teach the learner to apply their knowledge, logic and reasoning by explaining themselves in a low-pressure setting. It provides an opportunity to explore situations with a different approach and better solutions for future use (Jillings, 2020).
The mastery of metacognition helps the learner to use reflection in defining clinical experiences and explore ways on how to improve it. Recollecting facts and events in patient’s care may integrate the learner into different concepts by connecting different ideas from one another (Di Vito-Thomas, 2005).
8. Problem-solving with Reasoning
Understanding rationale, the sets of reasons or logical basis for a course of action assist the learners to gain a broad knowledge of the topic and promotes a higher level of understanding. Problem-solving guided by rationale is a technique to the use of deductive and inductive reasoning in the thinking process (Di Vito-Thomas, 2005).
9. Roleplaying and Return Demonstration
Role-playing is a self-directed activity that encourages analytic and creative thinking. It helps the learner to internalize empathy while compromising in portraying a role or another persona creating a wider chance for memory retention.
Practice and repetition of observed procedures during return demonstration creates an avenue for re-thinking ways on how to do a task properly with ease in your own phase as you implement it by yourself.
10. Thinking and Speaking With Sketch (Concept Mapping)
Incorporating a concept with multiple perspectives and connecting complex ideas in a structured way to search for potential solutions. These processes create an abstract concept that encourages logical arguments used in critical thinking (Kaminske, 2019).
Interactive activities such as case study with a panel discussion, observing clinical dynamics during in-depth arguments, making a multidisciplinary joint care plan for patient promotes an environment for critical thinking thus facilitating the development of clinical judgment (Di Vito-Thomas, 2005).
11. Do Some Prioritizing and Decision-making
Make critical thinking as a culture and not just an activity by encouraging decision-making. Prioritizing through analyzing information, applying knowledge, and evaluating a prospected solution are the cornerstones of decision-making. This will allows the learner to apply learned theories to a different scenario by weighing the advantages and disadvantages of different solutions and option in deciding best practices.
12. Correct Misconceptions and Personal Bias
Personal beliefs greatly influence one’s ability to think critically as people always seek out ideas that conform to their own beliefs (Kaminske (2019). Several factors that act as the pitfalls in critical thinking are misconceptions, personal bias, and assumptions—which can bring a learner into a wrong direction. A discussion with colleagues who have mastery in evidence-based practice and conducting more in-depth investigations can give ideas and extends point of view (Jillings, 2020).
Conclusion and Suggestions:
Analytical skills through keen observation, understanding important data, and identifying a pattern of recognition; problem-solving capacity by connecting relationship of phenomena, data interpretation guided by significance and rationale; and use of reflection and evaluation abilities in formulating conclusion are the important factors in clinical judgment and decision-making.
Critical thinking is a learned skill resulted from a rolled-up innate curiosity in the application of strong theoretical and experiential foundations in solving clinical problems that direct to the best care decision, which produce positive patient outcomes and improve patient care services.
In this era of technological advancement where machine replaces almost of everything, critical thinking still plays an important role in the nursing practice. Nurses who can manipulate complex clinical situations with efficient skills on critical/analytical thinking, problem-solving and decision-making are often in the front line to compete for the position with greater autonomy and higher chances for opportunities.
- Nightingale, F. (1860). Notes on Nursing: What it Is, and what it is Not. London: Harrisons & Sons.
- Haber, J. (2020). It’s Time to Get Serious About Teaching Critical Thinking. Inside Higher Ed. Retrieved on 24 October 2020 from https://www.insidehighered.com/views/2020/03/02/teaching-students-think-critically-opinion
- Walden University. (2020). 7 Ways to Teach Critical Thinking in Elementary Education. Retrieved on 24 October 2020 from https://www.waldenu.edu/online-bachelors-programs/bs-in-elementary-education/resource/seven-ways-to-teach-critical-thinking-in-elementary-education
- Kaminske, A.N. (2019). Can We Teach Critical Thinking?. The Learning Scientists. Retrieved on 24 October 2020 from https://www.learningscientists.org/blog/2019/2/28/can-we-teach-critical-thinking#:~:text=beliefs%20(3).-,Can%20we%20teach%20critical%20thinking%3F,happens%20to%20enjoy%20science%20fiction
- Berman, A., Snyder, S.J. & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, Process, and Practice, 10 th New Jersey: Pearson Education, Inc.
- Lakhanigam, S. (2017). Critical Thinking: A Vital Trait for Nurses. Minority Nurse. Retrieved on 24 October 2020 from https://minoritynurse.com/critical-thinking-vital-trait-nurses/
- Regis College (2020). How to Leverage Critical Thinking in Nursing Practice. Retrieved on 24 October 2020 from https://online.regiscollege.edu/blog/how-to-leverage-critical-thinking-in-nursing-practice/
- (2020). Tabula Rasa. Retrieved on 24 October 2020 from https://en.wikipedia.org/wiki/Tabula_rasa
- Willis, J. (2012). A Neurologist Makes the Case for Teaching Teachers About the Brain. George Lucas Educational Foundation. Retrieved on 24 October 2020 from https://www.edutopia.org/blog/neuroscience-higher-ed-judy-willis
- Knowles, M. (1984). The Adult Learner: A Neglected Species, 3 rd Houston, TX: Gulf Publishing.
- Seel, N.M. (2012). Assimilation Theory of Learning. In: Seel N.M. (eds) Encyclopedia of the Sciences of Learning. Springer, Boston, MA. https://doi.org/10.1007/978-1-4419-1428-6_358
- Luna, A. (2020). 7 Reasons Critical Thinking In Nursing Is Important. AMN Healthcare Company. Retrieved on 24 October 2002 from https://www.onwardhealthcare.com/nursing-resources/seven-reasons-critical-thinking-in-nursing-is-important/
- Wabisabi Learning. (2020). 12 Solid Strategies for Teaching Critical Thinking Skills. Retrieved on 24 October 2020 from https://wabisabilearning.com/blogs/critical-thinking/teaching-critical-thinking-skills
- Di Vito-Thomas, P. (2005). Nursing Student Stories on Learning How to Think Like a Nurse. Nurse Educator, 30(3), pp. 133-136.
- Jillings, B. (2020). Critical Thinking in Nursing: Why It’s Important and How to Improve. AMN Healthcare Company. Retrieved on 24 October 2020 from https://www.americanmobile.com/mobile/NZArticle/?articleId=3346
RELATED ARTICLES MORE FROM AUTHOR
Autism: a comprehensive guide to raising and supporting a child with autism, the most common types of eating disorder, 120+ fresh nursing essay topics (with faqs and essay writing tips), nursing personal statement: your voice in writing, the nursing essay: learning how to write, covid-19: the nursing case management approach, leave a reply cancel reply.
Save my name, email, and website in this browser for the next time I comment.
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Nurse leaders as problem-solvers
Addressing lateral and horizontal violence.
Anthony, Michelle R. PhD, RN; Brett, Anne Liners PhD, RN
Michelle R. Anthony is a program coordinator at Columbia (S.C.) VA Health Care System. Anne Liners Brett is doctoral faculty at the University of Phoenix in Tempe, Ariz.
Acknowledgment: The authors acknowledge the support of the University of Phoenix Center for Educational and Instructional Technology Research.
The contents of this article do not represent the views of the US Department of Veterans Affairs or the United States Government.
The authors and planners have disclosed no potential conflicts of interest, financial or otherwise.
For more than 126 additional continuing-education articles related to management topics, go to NursingCenter.com/CE .
Earn CE credit online: Go to http://nursing.ceconnection.com and receive a certificate within minutes .
Read about a qualitative, grounded theory study that looked to gain a deeper understanding of nurse leaders' perceptions of their role in addressing lateral and horizontal violence, and the substantive theory developed from the results.

The issue of lateral and horizontal violence (LHV) has plagued the nursing profession for more than 3 decades, yet solutions remain elusive. The significance of LHV isn't lost on nurse leaders because it creates an unhealthy work environment. Research literature worldwide has continued to report the prevalence of disruptive behaviors experienced by nursing students, novice nurses, and seasoned nurses in the workforce. The World Health Organization, International Council of Nurses, and Public Services International have recognized this issue as a major global public health priority. 1
LHV, also called nurse-on-nurse aggression, disruptive behavior, or incivility, undermines a culture of safety and negatively impacts patient care. 2,3 This experience, known to nurses as “eating their young,” isn't only intimidating and disruptive, it's also costly and demoralizing to the nursing profession and healthcare organizations. 4,5 Although the impact of LHV can be dreadful for both the institution and its staff, little is known about the reasons for these behaviors among nursing professionals. 2
LHV encompasses all acts of meanness, hostility, disruption, discourtesy, backbiting, divisiveness, criticism, lack of unison, verbal or mental abuse, and scapegoating. 6 The sole intent of bullying behaviors is to purposefully humiliate and demean victims. Bullying behaviors also taint healthcare organizations; cause irreparable harm to workplace culture; breakdown team communication; and severely impact the quality of the care provided, thereby jeopardizing patient safety. 7,8 Researchers have reported that acts of LHV are used to demonstrate power, domination, or aggression; for retribution; to control others; and to enhance self-image. 9-12
Previous studies have shown that the frequency of LHV in healthcare organizations is quite severe, with about 90% of new nurses surveyed reporting acts of incivility by their coworkers. 13 Sixty-five percent of nurses in one survey reported witnessing incidents of despicable acts, whereas another 46% of coworkers in the same survey reported the issue as “very serious” and “somewhat serious.” 13
LHV poses a significant challenge for nurse leaders who are legally and morally responsible for providing a safe working environment. 2,6 The purpose of this qualitative, grounded theory study was to gain a deeper understanding of nurse leaders' perceptions of their role in addressing LHV and develop a substantive theory from the results.
Literature review
A paucity of evidence exists in the literature regarding how nurse leaders perceive their role in addressing LHV. 14 Studies have shown that this phenomenon is attributed to heavy workloads, a stressful work environment, and lack of workgroup cohesiveness, as well as organizational factors such as misuse of authority and the lack of organizational policies and procedures for addressing LHV behaviors. 15
In one study, one-third of the nurses reported that they had observed emotional abuse during several of their work shifts. 16 Another study indicated that 30% of survey respondents (n = 2,100) stated LHV occurs weekly. 17 A third study revealed that 25% of participants noted LHV happened monthly, and a fourth study of ED nurses reported that about 27.3% of the nurses had experienced LHV perpetrated by nursing leadership (managers, supervisors, charge nurses, and directors), physicians, or peers in the last 6 months. 18
In a survey completed by members of the Washington State Emergency Nurses Association, 27% of respondents experienced acts of bullying in the past 6 months. 19 Another study reported that 27% to 85% of nurse respondents had experienced some form of uncivil behavior. 20 Other data have shown that those more vulnerable to violent, disruptive, and intimidating behaviors are newly licensed nurses beginning their careers. 21
Although nurse leaders can be perpetrators of LHV, they play an essential role in addressing LHV behaviors and creating a safe work environment. 22 The literature suggests that, in many cases, a lack of awareness and response by nurse leaders adds to the prevalence of LHV. 23 This may be due, in part, to nurse leaders being aligned with the perpetrators who are creating the toxic work environment. 6 The literature suggests that an environment where staff members feel safe to practice results in a culture that decreases burnout and promotes nurse retention and quality outcomes. 24,25
This qualitative, grounded theory study focused on nurse leaders' perception of their role in breaking the cycle of LHV for staff members whom they supervise. Two research questions guided the study: 1. How do nurse leaders perceive their role in addressing LHV among nursing staff members under their supervision? 2. What substantive theory may emerge from the data collected during interviews with nurse leaders?
A grounded theory methodology was used to explore the nurse leader's role in addressing LHV with the intent of developing a substantive theory through the meaningful organization of data themes to provide a framework to address the phenomenon of LHV. Purposive sampling was used to recruit a total of 14 participants for this study from a large healthcare system in the Southeastern US. The participants were chosen because of their experience with LHV and their ability to discuss and reflect on those experiences. Informed consent was obtained before the start of the study, which included explaining the reason for the study and what to expect. In addition, permission was obtained from the Institutional Review Board.
Data collection and analysis
Demographic data collected to describe the sample included gender, age range, number of years holding a management position, supervisory responsibility, and highest degree obtained. (See Table 1 .)

Semistructured, in-depth interviews were the primary mode of data collection. The recorded interviews were conducted face-to-face and lasted about 60 minutes. Data collection continued until saturation was achieved. Data saturation occurred when no new descriptive codes, categories, or themes were emerging from the analyzed data. The interviews were transcribed verbatim and verified through a member check process.
During the data analysis process, themes and patterns were identified. Data from each participant's interview were examined to determine if the responses were aligned with the identified themes. Analysis of the data included coding at increasingly abstract levels and constant comparison. Qualitative software assisted in coding the information and uncovering subtle trends.
Four themes emerged from core categories developed during the qualitative data coding process.
Theme 1: Understanding/addressing LHV . In question one, participants were asked to describe their understanding of LHV. Five subthemes emerged from the data collected with this question. (See Table 2 .)

Theme 2: Experience addressing LHV . In the second question, participants were asked about their experience with addressing incidents of LHV. Six subthemes were identified. (See Table 3 .)

Theme 3: Role perception in addressing LHV . In the third question, participants were asked what they perceive their role to be in addressing LHV. Six subthemes resulted from this question. (See Table 4 .)

Theme 4: Organizational impediment to addressing LHV . In question four, participants were asked to describe the factors within the organization that influence or impede their role in addressing LHV. This question yielded nine subthemes. (See Table 5 .)

Substantive theory
As a result of the themes that emerged from the data, a substantive theory was developed. This is especially important for the nursing profession to develop as a scientifically based practice. Theories help guide research and provide the expansion, generation, and validation of the science of nursing knowledge. 26 The substantive theory will help nurse leaders become more cognizant of the role that effective leadership plays in preventing or intervening in incidents of LHV in the workplace. The analysis revealed that nurse leaders are aware that the quality of patient care and staff well-being can be adversely affected by the impact of LHV.
Data themes were used to formulate the following theory: Nurse leaders address LHV affecting their staff members by solving problems, creating a safe work environment, and reducing institutional barriers that impede addressing LHV in a timely fashion. Nurse leaders perceive their role as a problem-solver, which is a necessary step in advocacy. 27 Problem-solving is a process that contains the elements of decision-making and critical thinking. 28
The theory that emerged from the core categories explicitly focused on the central phenomenon of LHV in the nursing work environment. Figure 1 shows the interrelatedness of the themes to the resultant substantive theory.

Discussion and implications
The study results have several implications for both the nursing profession and nurse leaders. The nursing profession requires decisive and robust leadership, and the role of the nurse leader is to be a combination of nurturer, investigator, and judge to examine incidents of LHV. 26,29-32 Nurse leaders are responsible for setting the tone and expectations for a safe work environment. This includes modeling the expected ethical behaviors; for example, doing the right things for the right reasons, being collegial toward each other, and being respectful of other's differences. One participant remarked, “This is a different world based on how I was raised. I was raised to be respectful to people.”
In addition, nurse leaders are responsible for enforcing policies created to address disruptive behaviors and working with the administration as soon as an incident occurs. Past research indicates that a healthy and collaborative work environment fosters nurse engagement and patient safety. 25,30 Staff members and patients need a leader to protect them when necessary; thus, the nurse leader needs to “walk the walk” in providing a safe environment for all. Nurse leaders engaged in these kinds of behaviors are providing strong leadership and practicing strong decision-making, thus ensuring the continued robustness of their organizations.
Recommendations and limitations
Future research could replicate this study in a different geographic region to explore the causes of LHV by soliciting the views of nursing students, new graduate nurses, and nurse educators from unionized and nonunionized hospital systems and comparing the results to further understand this phenomenon. Additionally, developing a tool to test the substantive theory could substantiate the nurse leader's role as a problem-solver to address incidence of LHV in the workplace.
The decision to conduct this study in one type of healthcare organization limits the ability to compare the interviewed nurse leaders' experiences with nurse leaders in other healthcare organizations. The experiences of nurses in other healthcare organizations may be different; thus, overall generalizability of the study may be limited.
Say “no” to the status quo
The results of this study support the findings of previous researchers. 23,31,33,34 Accepting the status quo is unacceptable and can cause irreparable harm to organizational well-being if LHV isn't addressed. Collaboration between nurse leaders and administrators is essential to successfully reduce institutional obstacles that prevent the timely handling of LHV incidents. The role of the nurse leader as a problem-solver should be clear, defined, and well supported to seek resolutions to toxic behaviors that are hurting the work environment. But we must remember that creating a policy doesn't equal change. Every employee from the lowest level in the organization to the highest ranks of administration must model civil behaviors.
INSTRUCTIONS Nurse leaders as problem-solvers: Addressing lateral and horizontal violence
Test instructions.
- Read the article. The test for this CE activity is to be taken online at http://nursing.ceconnection.com .
- You'll need to create (it's free!) and login to your personal CE Planner account before taking online tests. Your planner will keep track of all your Lippincott Professional Development online CE activities for you.
- There's only one correct answer for each question. A passing score for this test is 14 correct answers. If you pass, you can print your certificate of earned contact hours and access the answer key. If you fail, you have the option of taking the test again at no additional cost.
- For questions, contact Lippincott Professional Development: 1-800-787-8985 .
- Registration deadline is June 3, 2022 .
PROVIDER ACCREDITATION
Lippincott Professional Development will award 1.5 contact hours for this continuing nursing education activity.
Lippincott Professional Development is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation.
This activity is also provider approved by the California Board of Registered Nursing, Provider Number CEP 11749 for 1.5 contact hours, and the District of Columbia, Georgia, and Florida CE Broker #50-1223.
Payment: The registration fee for this test is $17.95.
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Leadership strategies to promote frontline nursing staff engagement, nurse leader competencies: a toolkit for success, keeping the peace: conflict management strategies for nurse managers, principles for sustaining shared/professional governance in nursing, workplace incivility: nurse leaders as change agents.
MockQuestions
Situational Nursing Mock Interview
To help you prepare for your nursing interview, here are 50 situational nursing interview questions and answer examples.
Situational Nursing was updated by Krista Wenz on May 30th, 2023. Learn more here.
Question 1 of 50
How do you handle being asked to do a nursing task you've never completed before?
How to Answer
1st answer example, 2nd answer example.
Most situational interview questions are best answered using the STAR method which involves thinking about the situation, task, action and result and providing solid and thorough answers. This is not the time to say that you would jump in with both feet. The interviewer is not looking for someone who just jumps when someone says jump, but someone willing to jump with confidence and competence. Your job is to provide an answer that illustrates this difference.
"I really want to be liked and be a contributing member of the team, but I always stop and do a check-in before enthusiastically saying I'll do something I'm not sure about! I know the basics of nursing skills, so if I can look it up in the policy and procedure manual, such as a simple but different dressing change, I am able to do that independently. If it's totally novel, I will ask for supervision when first performing it so that I always work within the scope of my nursing practice."
"If I'm asked to complete a nursing task I've never done before, I will use our hospital's intranet site to read about the procedure and/or watch a video about completing the procedure. If I feel comfortable doing the task after looking up the instructions, I will do so. If the task is complex or very different from something I've done before, and I don't feel competent to do it without supervision, I will ask for help. I would ask either another floor nurse or the charge nurse to review the steps with me and supervise me while I perform the task. That way, I can make sure that I'm learning about a task that I am responsible for completing while ensuring that my patient receives safe care."
Next Question
50 Situational Nursing Interview Questions & Answers
Below is a list of our Situational Nursing interview questions. Click on any interview question to view our answer advice and answer examples. You may view 15 answer examples before our paywall loads. Afterwards, you'll be asked to upgrade to view the rest of our answers.
Table of Contents
- 1. Adaptability Questions
- 2. Communication Questions
- 3. Competency Questions
- 4. Conflict Questions
- 5. Creative Thinking Questions
- 6. Critical Thinking Questions
- 7. Customer Service Questions
- 8. Diligence Questions
- 9. Discovery Questions
- 10. Leadership Questions
- 11. Management Questions
- 12. Operational Questions
- 13. Performance Based Questions
- 14. Problem Solving Questions
- 15. Role-Specific Questions
- 16. Scenario Based Questions
- 17. Situational Questions
- 18. Teamwork Questions
- 19. Tough Questions
Situational questions are asked so the interviewer can gain insight into your thought process, how you problem-solve, and how you communicate in the workplace. Situational nursing questions can include inquiries about drug dosages, procedures, or specific signs and symptoms of a patient and how you would proceed. Additionally, interviewers can ask how you would respond when faced with an ethical dilemma, a challenging colleague, or when abruptly put into a leadership role. While these questions can be challenging, there are a few ways to prepare before your interview. First, think about your interview as having a chat with a friend. They ask you what you would do in a particular situation, and you respond using your knowledge and experience. Additional tips include the following: 1. Make sure you understand the question. If you are unsure how to respond, ask the interviewer to clarify. 2. Use your critical-thinking skills if asked about a situation you have not encountered in your career. 3. Use real-life examples as often as possible. 4. Practice answering these types of questions with a friend or colleague. 5. Be honest with the interviewer. If you are unsure of the answer, let the interviewer know that while you do not know the answer, you will find it after the interview. If you would like more practice questions to review before your interview, we have many great resources at Mockquestions. Here are 50 General Nursing Interview Questions that will help you prepare for many different kinds of nursing interviews. We have specific Behavioral Nursing Interview Questions as well! For more modern virtual nursing interviews, we have HireVue Nursing Interview Questions . Additionally, we have interview questions for a Registered Nurse that will help you better prepare for your interview than just our general nursing questions. Remember to approach your interview as if you are having a professional discussion with a friend. If you have successfully completed nursing school, you can ace your interview! Best of luck!
Adaptability
1. How do you handle being asked to do a nursing task you've never completed before?
Written by Dianne Barnard on March 9th, 2021
Written by Kate Buckley on January 10th, 2023
Communication
2. You are talking with a patient during rounds, and the patient tells you she does not understand what the doctors tell her and she is unsure of what is going on with her health. Tell me how you respond to the patient.
Unfortunately, these types of situations are very common in the healthcare system, as patients are often confused or misinformed about their health. This is particularly true for elderly patients and/or patients without someone present to advocate for them. In this situation, the nurse should take time to help the patient understand what is going on with her health. The interviewer is asking this question to determine if the candidate would take initiative to help the patient; and to effectively answer this question, the candidate should indicate they would explain the medical situation to the patient in layman's terms. A more successful answer to this question would include a specific example from the nurse's career where they helped clarify a diagnosis, procedure, or other medical-related situation when a patient was confused.
Written by Kelly Burlison on June 3rd, 2019
"This type of situation has to be so frightening for a patient, and unfortunately, it happens so often. I would take time to explain the patient's medical condition to them at a level in which they could understand, and I would not leave until I was sure they understood. I have dealt with this many times in my nursing career, but one time in particular sticks out to me. I was caring for a patient who had been admitted after a car accident, and after she had a CT scan on her head, a mass was found on her pituitary gland. The doctors did not think the mass was cancerous, and the patient was told it was likely benign; but unfortunately, she didn't know the meaning of benign. Later, when I went to check on the patient, she was devastated and thought she had brain cancer. Luckily, I was able to help explain the situation to her, just like I would do in the situation with the patient you described to me."
"In the hospital, it can be common for patients to feel confused and scared about their medical condition. Patients may be dealing with pain or poor sleep, which can make it difficult to focus on information from doctors or others in the hospital. Also, regardless of patients' education or socioeconomic status, we can't assume that we know a patient's 'health literacy,' which is their ability to understand health and medical information. So, I have encountered scenarios a lot like this at the bedside. In this case, I would stay in the patient's room and pull up her most recent clinical notes from her primary team and consulting teams. I would explain what their assessments are in simple terms, avoiding healthcare jargon. I would ask the patient if she now feels that she understands her condition and plan. In most cases, just taking the time to explain things in clear terms relieves much of the patient's anxiety."
Anonymous Interview Answers with Professional Feedback
Anonymous Answer

Cindy's Feedback
3. How would you explain a complex task to someone using verbal instructions?
Teaching patients in a way they can understand is an integral part of nursing. Healthcare is increasingly complex, so it makes sense that the instructions can be, as well. This question provides a chance to showcase your talent to take a complicated idea and explain it without losing the integrity of dumbing it down.
"I read once that most newspapers are written at a 5th grade level so that most people can understand the message. I think that today we are inundated with verbal messages and written messages, so what we choose to say should be prime real estate. That means no filler or fluff words for me, and to speak in a way that the patient or family can understand. Nurses are so used to throwing big words and acronyms around, and personally I am mindful not to do that. I break the information down into bite sized pieces and frequently check in with the person to see if they are understanding. I ask them to repeat back what I explained to them. I also watch them closely for non-verbal signs of confusion. I always feel so good when the patient is able to understand my instructions right away!"
"Because we can't know always know a patient's health literacy level, it's important to try to explain concepts about a patient's care in a way that anyone can understand. When I have to explain a complex task, such as how to check your own blood glucose, verbally only, I make sure to use simple terms and avoid healthcare jargon. I 'chunk' the main points so that I'm not explaining too many concepts at once. I speak slowly. And I ask the patient to repeat back the instructions to me, so I can check for understanding."
4. You were recently transferred to another unit and notice a fellow nurse consistently displaying incompetency in their work. How would you proceed?
The interviewer wants to gauge your level of professionalism and ability to handle difficult situations in the workplace. It's essential to approach this question with tact and diplomacy, as you don't want to come across as overly critical or negative toward your colleagues. Instead, focus on how you would approach the situation in a constructive and positive manner, such as subtly offering to help the coworker improve their skills or suggesting additional training opportunities to a supervisor. Ultimately, the goal is to demonstrate your ability to work collaboratively and supportively with your team, even in challenging circumstances. However, while you want to display that you can work well with others, you also want the interviewer to understand that the patient's safety is of utmost importance. If your colleague is incompetent to the level that it compromises patient care, you want to quickly bring it to the attention of a charge nurse.
Written by Krista Wenz on May 29th, 2023
"If I encountered a fellow nurse who I believed was struggling with their duties, I would approach the situation with empathy and understanding. I would first try to understand the root cause of their incompetence - whether it be a lack of training, personal issues, or being overwhelmed. Once I understand the situation better, I would offer my support and assistance in any way I can. This could include providing additional training, offering to help with their workload, or simply being a listening ear if they need to talk. It is essential to prioritize patient safety above all else. If a fellow nurse cannot provide safe and effective care, action must be taken to address the issue. If, after offering my support, I still believe their incompetence is putting patients at risk, I would bring my concerns to a supervisor or manager. Ultimately, my goal would be to approach the situation with kindness and empathy while prioritizing our patients' safety and well-being."
"If I recently transferred to another unit and encountered a coworker exhibiting incompetence, I would first try to assess the situation and determine the extent of their shortcomings. Depending on the severity of the issue, I might consider discussing the matter with my supervisor or seeking guidance from a more experienced colleague. However, I would always approach the situation with tact and sensitivity, recognizing that everyone has strengths and weaknesses and that we all have the potential to learn and improve. My goal would be to ensure the highest standards of patient care are being met and that my colleague is given the resources and support they need to succeed."
5. A coworker left her computer open with sensitive information on the screen. You are the only one in the nurses' station. How would you address this with her?
Patient confidentiality must be honored, and leaving a computer open even to run to the bathroom for a minute risks a serious breach of patient confidentiality. Even though you are the only person in the room, you should not have access to patient information that you have no need to know. Even if you wouldn't say a word to anyone and you are a professional nurse with integrity, you should not be able to see possible protected information on a patient that you are not personally taking care of. Leaving a computer wide open is a serious risk to confidentiality. If you see this, you could gently close the computer so that the screen is not visible and discuss the seriousness of this when your coworker returns. You must protect your license and you should report to supervision. It's uncomfortable to do so, but a nurse always takes the action that protects and advocates for the patient.
"I would immediately close or cover the computer. I would not look at the information, of course. If I wasn't sure where the coworker was or when he or she left, I would be compelled to report it to supervision because someone could have accessed the information. It's a tough call and may cause some coworker tension, but as a nurse, I must do what is best for my nursing license and the patient, and that is to protect the confidentiality of the patient."
"I would lock my coworker's computer without looking at anything on the screen and then let her know that I did so. If I knew for sure that no one looked at her computer screen while she was away, then I would remind her of the importance of locking her computer when she steps away. If I couldn't verify that no one had access to the sensitive information, I would have to let my supervisor know what happened. Potential violations of patient privacy are very serious."
6. Give an example of how you may connect and find common ground with a patient to gain understanding.
All patients are different and come from different backgrounds and life experiences. Sometimes, the patient will have biases and reject you as a competent individual. Learning how to connect and find common ground with a patient quickly can improve patient outcomes. There is always something that you can find in common with someone. It could be the weather, good or bad, a comment on a crossword they are completing, admiration for their turquoise necklace, anything that is authentic and sincere to start to build a bridge or connection. It doesn't have to be a colossal sharing of souls, but just looking quickly for similarities instead of differences can have real impact. Take the time to learn conversational techniques that can elicit conversation and build rapport.
"I try to establish conversational rapport with each patient and humanize our interaction a little bit. I want to be seen as a professional and competent nurse, but also as a warm and caring human being. I don't think idle chitchat is helpful overall, but I do believe an authentic comment about a picture of their dog or maybe a sweater they are wearing can leapfrog into more personalized conversations. I think that it makes people feel seen by the nurse and that helps."
"There are so many ways to connect with a patient during my shift. I think it always starts with identifying myself and my role. It sounds simple, but I always say a variation of 'Good morning, I'm Kate and I'll be your nurse until 7 p.m. today' when I first meet a patient. Over the years, many patients have told me that they feel frustrated or confused when people enter their rooms and just start talking without identifying themselves. Identifying myself to the patient in a friendly way helps to establish trust right away. After that, I may ask them about any drawings done by kids that I see in their room, the sports team they're watching on TV, the sodoku puzzle they're working on, or whatever type of Indiana weather we may be having. Talking about everyday things can help us develop a rapport that will be useful as we need to talk about medications and other aspects of treatment later."

Stephanie's Feedback
7. How do you handle difficult family members who disagree with the care that the patient agreed to?
Patient families can be challenging, and they do not always agree with the patient's decision. Sometimes they will pull you aside and tell you their opinion. As long as the patient is competent to make their own decisions, the best way to deal with these situations is to tell the family that they really need to talk with the patient. You should not be talking about the patient's condition when they are not present, anyway. Remember your license and advocate for your patient's rights.
"I would acknowledge that I understand they want the best for their family member, but explain that I cannot discuss the patient's care with them and that the patient has the right to make their own decision. I would encourage them to discuss their concerns with the patient directly and perhaps ask for a shared meeting with the doctor so their concerns could be addressed. I would definitely report the interaction to my nursing supervisor."
"When a patient is a competent adult who can make their own healthcare decision, I will respectfully direct the patient's family member back to the patient. I will remind the family member that I must respect the patient's privacy. If the patient agrees, I can call the doctor and ask the doctor to come to the patient's room and answer the family member's questions with the patient present."
8. You are caring for a young patient who is being discharged with a prescription for an inhaler. Upon asking the patient if he knows how to use the inhaler, he says, "Yes, I do." Tell me how you proceed.
Although most medications are dispensed with administration instructions at the pharmacy, many patients do not understand how to administer to themselves which results in their misuse. For medications such as beta agonists or corticosteroids which are administered via inhaler, misusing the inhalant device could mean the patient is not getting enough medication to help manage their condition. This is common for all medications which is why it is important for nurses to ensure patients understand how to properly take their medications before discharge. The interviewer is asking this question to determine if the candidate would ensure the understands how to use the inhaler before discharging him, rather than simply taking the patient's word for it. To effectively answer this question, the candidate should describe, in detail, how they would verify that the patient understands how to use the inhaler. A more successful answer to this question would include a specific example from the candidate's nursing career where they helped educate a patient on their medication regimen before discharge or how they developed patient education protocols or materials for their unit or organization.
"Even if the patient was adamant that he knew how to use the inhaler, I would get him to demonstrate how he uses an inhaler, either by using a teaching tool or by simply using an unrelated object to mock up the situation. Inhalers are more difficult to use than most people realize, and so many patients make mistakes when administering their inhaled medications to themselves. But this isn't only limited to inhaled medications, I always make sure my patients understand their medication regimen, and after I go over it with them, I have them demonstrate it to me or repeat it back to me, to ensure they understand. This is something I have always done in my nursing career and will continue to do so before I discharge my patients."
"Even if a patient assures me that he knows how to use his inhaler, I will ask him to demonstrate or explain its use to me. If we have a dose of his inhaler due soon, I will verbally review the steps of using his inhaler, and then I will ask him to show me using it. If he won't be due for a dose of his inhaler before discharge time, I will use the teach-back method, in which I will ask him to verbally 'teach me' to use his inhaler. It's important that patients can administer their medications to themselves upon discharge, and I always make sure to review patients' medications with them and check for understanding before discharge. I had a similar scenario with a patient who was being discharged with a new insulin pen. The patient told me he understood how to load the needle onto the pen, but when I asked him to demonstrate, he wasn't able to do it. We practiced a few times to make sure he understood the entire process, and he then was able to put the pen and needle together prior to discharge."

Chad's Feedback
9. How do you handle situations in which you disagree with a doctor's orders?
Nurses follow doctor's orders, but sometimes there are orders that a nurse feels are not in the patient's best interest. For example, if the doctor orders an antibiotic that the patient remembers she is allergic to, then it's easy for the nurse to tell the doctor that a different alternative is needed. But sometimes, the nurse disagrees with the validity of treatment that the doctor and patient agreed on. It's always helpful to say your dissension for the big stuff. You are more likely to be heard if you are known as a reasonable nurse who strives for excellence in their work ethic. If you have reasonable questions, ask the doctor if you could have several minutes of his time. Organize your thoughts, put your emotions in check, and outline your thoughts and rationales. The best outcome would be that the MD would do the same and it would be a learning moment. There is a chance that the doctor will not be as receptive as you would like and you will not impact the decision, but that should not stop you from advocating for your patient in a plain and reasonable manner.
"Dr. Welby, may I speak with you for a minute, privately? I see that you wrote an order to increase Mrs. Steinway's pain medication. I understand that she is rating her pain as a 10, and that's concerning to me, as well. However, when she takes her pain medication, she gets very tired and then refuses to get out of bed for PT and that has always helped her pain tremendously. Is there anything else we can do to help manage her pain, while still allowing her to have the energy to do the things she enjoys and that help her?"
"If I don't agree with a doctor's order, it's important to advocate for my patient in a respectful way. I once had an experience when taking care of a patient with an acute exacerbation of his heart failure. His doctor ordered a high dose of IV Lasix, and he said he was going to order a Foley catheter to make it easier to get a strict intake and output record for this patient. However, the patient was alert, oriented, and not a fall risk, and per our hospital guidelines, we shouldn't jump straight to using a urinary catheter in this case. The catheter could put the patient at risk of infection and skin breakdown. So, I asked the doctor if I could try using two urinals in the patient's room and providing the patient with education about why it was so important to record his urinary output. I also assured the doctor I would put a reminder sign above the toilet in the patient's room, reiterating the teaching to use the plastic urinal rather than the toilet. The doctor agreed to remove the catheter order, and we were able to accurately record the patient's urinary output without it."
10. How would you change your communication style if the patient's family was having trouble understanding what you were trying to tell them?
Nurses are teachers and instruct patients on difficult concepts and challenging instructions. The efficacy of their instructions is extremely important for optimal patient outcomes. For example, if a patient leaves the hospital or clinic setting without full comprehension of the plan of care then they may return to the hospital or have worsening symptoms or complications. Poor comprehension comes with a high burden of decreased patient outcomes, increased financial ramifications for patient and healthcare system, and decreased patient satisfaction. It is extremely important that the nurse learns to communicate with the patient and family in a way that they understand and can implement.
"I review the instructions before I give them to the patient, and I always make certain that I have written ones for them as well. When I review instructions, I decrease the stimulation in the room and make certain I have there attention, and they are not hungry or tired or something else. I look at their faces when I am talking and sometimes you can see the confusion even if they are saying that they understand. Even when they say they understand, I ask them to either show me or explain back to me what I need them to know. Watching them tells me what I missed, and then I keep instructing in different ways until they can explain it back to me."
"People learn in all sorts of different ways. If a patient's family was having a hard time understanding verbal information I'm giving them verbally, I can provide them with written information or with a picture guide. I can also use a hospital-approved patient education video if there is one relevant to the information I'm providing. Once I've switched to a different style or tool, I would request that the family 'teach back' to me the information I've provided them. Then I can assess their understanding and provide additional information as needed."
11. You are caring for a patient who is three-years-old and the physician has ordered a weight-based medication. When you look at the patient's records, you find the weight is documented in pounds. Explain how you proceed.
Many pediatric medications are weight-based, which means the dosage that the patient will receive depends on their weight. However, for most of these medications, the dosing guidance is listed in kilograms and not pounds, the common unit of weight in the United States. Because of this difference in weight units, medication dosing errors in pediatric patients is very common. The interviewer is asking this question to determine if the candidate is aware of the common issues regarding pediatric weight and medication dosing errors and to determine how they would respond in this situation. To effectively answer this question, the candidate should indicate that they would convert the patient's weight to kilograms in order to determine the correct dosage of the medication for the child. A more successful answer to this question would include an example of when the candidate successfully mitigated such a situation during their nursing career.
"If the child's weight was documented in pounds and I had to administer a weight-based medication, the first thing I would do is convert the weight to kilograms so I could determine the correct dosage of medication. While I have always been aware that pediatric medications were dosed based on kilograms, early in my nursing career, I was busy and distracted and nearly overdosed a child with medication because I had forgotten to convert their weight to kilograms. Luckily, one of my colleagues, who saw me draw up the dose, stopped me, or I would have committed the medical error. Ever since this day, I have always been very cognizant of weight documentation when administering pediatric medication."
"If the physician orders a weight-based medication for a 3-year-old, and the child's weight is documented in pounds, I would convert the weight to kilograms and document the weight in kilograms in the appropriate area of the patient's medical record. That way, the doctor, the pharmacist, myself, and anyone else using the patient's weight to ensure the correct medication dose would be working with the patient's weight in the correct format."
12. A patient on your unit you are caring for has had his peripheral venous catheter in place for approximately 100 hours. The catheter looks normal and the vein is open. Tell me how you proceed with administering more IV medications.
In order to help prevent nosocomial infection, which is an infection a patient acquires while receiving care in a hospital, peripheral catheters should be replaced every 72-96 hours. If not changed, the IV catheter may become infected and cause the patient's hospital length of stay to increase or could even cause death in extreme cases. Although a peripheral catheter may look normal and the vein may be open, it is imperative the catheter be changed. The interviewer is asking this question to determine if the candidate understands the importance of changing peripheral catheters on time in order to prevent infections. To successfully answer this question, the candidate should indicate they would change the catheter, specifically noting that the catheter should have been changed at a maximum of 96 hours.
"This patient's peripheral venous catheter needs to be changed, no matter how good it may look. Unfortunately, you can't see bacteria, and these types of catheters are prone to infection, so they must be changed often. In fact, this patient's IV catheter should have been changed prior, as they shouldn't be inserted more than 96 hours. I typically change my patients' IV catheters every 72 hours, which is at the low-end of the suggested range for changing, just as a precautionary measure. So in this case, I would change this patient's IV catheter before administering anymore medication and change it every 72 hours after that."
"Although I would be glad that the patient's peripheral venous catheter site does not show signs of infection, this site can't be used anymore. It's an infection risk to keep the same peripheral venous catheter in place for over 96 hours. Before administering IV medication to the patient, I would change the site, making sure to place the date and time both on the dressing and in the electronic medical record. Because I may or may not be the patient's nurse it's time to change the IV catheter, I could also write 'change by ___ date at ___ time' on the dressing, to better ensure that the IV catheter would be changed within 96 hours, or sooner if that is unit policy. Changing IV catheters per unit policy is one of the important ways that we as nurses can prevent infections and phlebitis in our patients."
13. You are conducting intake on a patient who was just seen at your facility earlier in the week. After you enter the patient's vital signs, you see their medication list, which was updated earlier in the week. Tell me how you proceed.
Because patient medications can change very quickly, even over a few days, it is important that nurses verify current medications for every patient at the beginning of every patient visit. If a patient's medication list is not verified and accurately updated, they are at risk of being prescribed a new medication that could interfere with one they are taking. If the nurse does not verify and update the patient medication list, the prescribing provider will not be aware of undocumented medications and will not be able to avoid prescribing errors. The interviewer is asking this question to assess whether or not the candidate understands that medication must be reviewed and verified with the patient or a caregiver during each encounter. To effectively answer this question, the candidate should indicate that they would review and verify the medications with the patient. A more successful answer to this question could include an example of how the candidate has dealt with a similar situation in the past, learned from a mistake that was made because they did not verify the medication, or spearheaded a policy change at their facility to ensure medications are verified during each patient visit.
"I would review and verify the patient's medication with them again, even though they were just seen in the facility a few days prior. It is too risky to assume that the patient's medications have not changed, as the provider may prescribe a medication that interferes with something the patient is taking that is not documented. Unfortunately, I had to learn this lesson the hard way early in my career. It was a similar situation, where a patient had just been seen a few days earlier, and I assumed their medication list was the same, so I did not ask about it. The next day, I learned that the patient had a bad reaction due to a medication interaction from something they were taking that wasn't documented and a new medication that was prescribed by the doctor during the appointment the previous day. Luckily, the patient was okay, but after this happened, failing to verify medications was a mistake I only had to make once."
"When when reviewing any kind of intake record with the patient, it's important to read to the patient what is already in our record, rather than just saying 'Has anything changed since your last visit?' We can't assume the patient knows what is written in their electronic medical record, or that everything was documented completely the last time. Therefore, after I entered the patient's vital signs, I say to the patient, 'Okay, now we're going to update your medication list.' I would read the list to the patient to have her confirm each medication/dose and make any changes as needed. Then I would ask if she is on any additional medication."
14. We are work with difficult and uncooperative coworkers, at times. How do you handle uncooperative coworkers?
Nursing is challenging and stressful sometimes. People get cranky, machines break, trays are late, and families are needy. Nurses are human beings and have off days. However, the goal for excellent patient outcomes must take precedence over bad days and bad moods, and the interviewer is looking for a candidate who can weather the storm, hold their own, and get the job done for the patient, without adding stress or chaos to the situation.
"I have learned to work out my emotions first, before I address issues. I take a minute to think things through. Sometimes you only have a minute, but I take it. I ask myself if I was reasonable. Was there anything else going on? Was I clear in my communication as to what I needed? Is this a pattern or is the coworker just having a busy or off day? I assume best intentions and own my part of the interaction before I address it, or do the best I can, but I don't let it wait. Patient care cannot wait, and if it's something clinical that needs done, I figure out how to get it done or get what I need from that worker right then and ask if there is a time when I could speak with them later in more detail. I don't think it benefits anyone to get angry or frustrated, but it doesn't help to not address problems either."
"I generally get along well with most coworkers because I have a calm attitude and I always offer to help my colleagues when I am able. However, everyone can have a bad day, including me. If a coworker seems to be grouchy or having a bad day, I would give them more space than usual while still offering my assistance whenever possible. If I noticed a pattern where a certain coworker always seems to be rude or curt to me, I would probably ask her if I could talk to her privately. Then, I would ask if I have done anything offensive or if there is anything I could do differently to be more helpful to her. I would attempt to take any input my coworker gives and implement it. It may not improve her attitude, but I think it's important to try."
15. How would you handle a coworker who is habitually late, which causes you to leave work late?
This is a management and leadership issue which impacts other staff members' lives and team morale. However, it's worth taking the opportunity to address it with the coworker individually before elevating it to leadership. There is something happening if leadership is not addressing it, as they would be alerted if they were chronically punching or signing in late. It may be that the time clock is a distance walk to the unit, or they stop at the cafeteria on the way for coffee and the result is they are late for their shift. It is not helpful to be passive-aggressive and complain to other staff members. Learn to have the uncomfortable conversation directly, kindly, and professionally with the person or people that need to hear it.
"Laine, can I speak to you privately for a minute? Is something going on? I am a little concerned. This is the third time this week you have been at least 10 minutes late, and it's really affecting me, as I have to leave to get my kids on the bus. I've not mentioned this to leadership. I wanted to talk to you first and ask you to be here on time to relieve me. Will you please do that? I would appreciate that very much."
"After a few instances, I would address this issue with my coworker directly. I would let her know that her coming in late is causing me to be late to take my daughter to school, and the situation can't continue. If it continues after this point, I would bring it up to the charge nurse on my shift."
16. Tell me about a time you were uncomfortable with a colleague. How did you handle the situation?
The interviewer asks about a time when you felt uncomfortable with a colleague to gauge your communication, critical thinking, and problem-solving/conflict-resolution skills. They want to know how you handle difficult situations and whether you can work effectively with others. It's important to be honest about the situation and explain how you approached it in a professional and respectful manner. This shows that you can resolve conflicts and maintain positive working relationships. There are, unfortunately, many ways that a colleague could make their coworkers feel uncomfortable. This can range from making inappropriate comments or jokes, invading personal space, or displaying aggressive or threatening behavior. It's essential to address any behavior that makes you uncomfortable and communicate your boundaries clearly with your colleagues. If that does not solve the problem, the interviewer wants to hear that you would report the situation to a supervisor or HR.
"When I first started at my current job, a colleague made inappropriate comments about my appearance. I found it uncomfortable and unprofessional. I decided to address the situation privately by calmly expressing my discomfort with their behavior and explaining that it was not acceptable. I also made it clear that I expected to be treated with respect and professionalism in the workplace. The colleague apologized and we were able to move forward with a more positive and respectful working relationship. It was important for me to address the issue in a mature and professional manner to ensure a safe and comfortable working environment for everyone involved."
"To be honest, there was only one time in my career when I felt uncomfortable with a colleague. During a team meeting, my colleague made inappropriate comments about my sexuality that made me feel uneasy. I didn't feel comfortable confronting my colleague in front of everyone, so I talked to them privately after the meeting. I approached my peer and calmly explained how their comments made me uncomfortable and why it was inappropriate. My colleague seemed surprised and apologized immediately. They also thanked me for bringing it to their attention and promised to be more mindful in the future. In fact, they apologized for their remarks at the next team meeting, which I appreciated. After that conversation, I felt much better and was able to continue working with my colleague without any further issues. It was definitely a difficult situation, but I'm glad I addressed it directly and respectfully."

Jaymie's Feedback
17. Describe how you handle and interact with hostile or aggressive patients.
No matter where you work as a nurse, you will encounter aggressive or hostile patients throughout your career. Patients may become aggressive or hostile due to a medical emergency, intoxication, head injury, or cognitive disorders, to name a few. The interviewer asks you to describe how you handle and interact with hostile or aggressive patients to gain insight into how you handle difficult situations. It's crucial to maintain a calm and professional demeanor when dealing with patients who may be upset or aggressive while still providing the necessary care and attention. This skill is essential in any healthcare setting, and the interviewer wants to ensure you have the necessary experience and qualities to handle the job effectively. Be sure to give specific examples of how you have handled similar situations in the past and demonstrate your ability to remain calm and collected under pressure. You also want to stress how you know when to call for security or outside assistance when needed to protect yourself and your patients.
"My top priority is always safety when dealing with hostile or aggressive patients. I remain calm and composed and try to defuse the situation by listening carefully to the patient's concerns and providing reassurance. I try to determine if the patient is sick or injured or if they are having a mental health crisis so I can call for the appropriate help. If necessary, I may need to involve other healthcare professionals or security personnel to ensure everyone's safety. Regardless of the situation, I treat the patient with respect and empathy and strive to find a solution that meets their needs while maintaining a safe and secure environment for everyone involved."
"Working in the emergency department most of my career, I deal with hostile and aggressive patients daily. First, I always prioritize safety for everyone involved. I remain calm and composed, using a reassuring tone of voice and body language to de-escalate the situation. I listen attentively to their concerns and validate their feelings while setting clear boundaries and expectations for respectful behavior. If needed, I involve other healthcare professionals or security personnel to ensure the safety of everyone involved. My ultimate goal is to provide all patients the best possible care and support, even in difficult situations."
Creative Thinking
18. What are some action steps you could take to alleviate stress in patients in an ER waiting room?
Emergency room waiting rooms are stressful places. After all, everyone in that waiting area is experiencing some kind of emergency and many of them feel their need is just important as anyone else's. Time slows down when someone is frightened, sick, or in pain, so even the shortest wait can get tempers flaring. People who are sick do not have an expansive world view but naturally are narrowly focused on their situation. They may have no ideas of the car crash victims arriving via ambulances through the back but only know that they are waiting. There are a limited number of things that you can do to shorten the wait, but you can humanize the experience by letting them know that they are seen and valued. When they come in, explain the wait time because knowledge is power. Check in with them every so often. Remind the individuals who accompany them where the cafeteria is. There really is nothing you can do to lessen their wait, but you can reduce their frustration by acknowledging their wait time and providing information in a friendly and respectful manner.
"Although it's difficult to face angry and frustrated people, I think it's important to lean in and acknowledge their frustration and give them updates. They are in the ER, so nurses should be checking on them; even just a little bit goes a long way. It is good nursing. I also think it's important to let them know where the comfort stations and cafeteria are located."
"The ER waiting room is usually a stressful place, especially if the ER is busy and the waits will be long. Although some patients and companions will still feel frustrated after I do so, I will make sure to provide as accurate an estimate of their wait time as possible. I will make sure to check in with patients and their companions when I can and update them if their wait time is going to be longer than we originally anticipated. I will allow them to vent their frustrations and let them know I understand that it's stressful. I will also remind the patient's companions where the cafeteria and closest restrooms are."
Critical Thinking
19. You are rounding on your patients on your inpatient unit, and as you enter an elderly woman's room, you find her sitting up and alert. Tell me what steps you take to prevent her from falling between now and the next time you round.
Falls are a common risk for patients who are receiving inpatient care, particularly among the elderly or patients with decreased mobility. Because of this, falls prevention is a common initiative at most hospitals and care facilities. Most nurses are expected to round on their patients hourly, at a minimum, and during these rounds, they are expected to ask their patients about the four P's - Pain, Potty, Positioning, and Possessions. By ensuring the four P's are covered, the nurse is ensuring the patient is comfortable and has everything they need, which will likely prevent them from attempting to get up on their own, hence preventing falls. The interviewer is asking this question to determine if the candidate has an understanding of falls prevention and the four P's of nursing. To effectively answer this question, the candidate should describe how they would check on the patient using the four P's. A more successful answer to this question can include a situation of how the candidate has used the four P's to prevent a patient from falling in their nursing career, how they trained a colleague on the four P's, or even how they implemented a falls prevention program at their facility using the four P's.
"In this situation, I would go through the four P's with the patient to prevent her from attempting to get up and falling between then and the next time I rounded on her. I would first assist her to the restroom then help her relieve any pain she was having. Then, before I left the room, I would ensure she was in a comfortable position and had everything she needed near her. This is something I do with all my patients, even if they seem well enough and able bodied, because failing to do so could mean they may attempt to get up on their own and fall. This is a part of my job as a nurse that I take very seriously because I know how serious patient falls are."
"Early in my nursing career, I had an alert and oriented patient fall when trying to get up himself to use the bathroom. Although the patient didn't sustain any injury, that incident really drove home to me how important it is to work to prevent falls for my patients. Before I leave this patient's room, I will assess to make sure all of her needs are met. Does she need to go to the bathroom? Is she sitting comfortably? Does she have her water, any other needed possessions, and her call light all within easy reach? Does she need any pain medication? Once I have addressed all of these concerns, I will reiterate to the patient to please call if she needs anything, rather than trying to get up herself."
20. You are currently in a patient's room during hourly rounds and although she is not due for another dose of pain medication for two more hours, she is complaining of increased pain. Tell me how you proceed.
The interviewer is asking this question for two reasons - first, to ensure the candidate will not give the patient a dose of pain medication before it is due; and second, to see if the candidate will attempt to lower the patient's pain using other comfort measures. While the administration of pain medication will relieve a patient's pain, it is important that pain medication is administered as directed by the physician, in order to avoid patient overdose or other negative side effects. Although patients may ask for pain medication in advance of their scheduled dose, nurses can help reduce their pain using other comfort measures, such as repositioning, offering heated blankets or warm compresses, helping them stretch, or getting them up for a walk. To effectively answer this question, the candidate should indicate that they would avoid giving the patient their pain medication early and instead use alternative comfort measures to help reduce the patient's pain. A more successful answer to this question would include an example from the candidate's nursing career where they helped a patient manage their pain using comfort measures rather than pain medication.
"Unfortunately, since the patient is not due for their medication for a couple of more hours, I would not be able to administer it to them. But, I would be able to help reduce their pain using other comfort measures. So, instead of simply telling the patient that they could not have any medication, I would work with them to see what I could do to make them comfortable in the meantime. Having many years of experience as a nurse in the emergency department, I have a lot of experience helping patients manage their pain when they do not get the desired relief from pain medications that were administered, and I would be able to draw from this experience to help this patient get relief until their next dose of medication."
"If a patient is not due for their pain medication for two more hours, I would explain to the patient when they can next have their pain medication. I would explore non-medication measures, such as heat, cold, repositioning, massage, or other options. Many patients that I've worked with over the years have found relief with non-medication interventions. During this time, I would also be reassessing the patient to see if any changes have occurred in the patient's condition--for example, if a surgical site looks reddened when it hadn't before, or if a patient was complaining of increased pain in their foot and their pedal pulse was weakened or absent when it had previously been palpable or audible by doppler. If any changes have occurred in the patient's condition, I would contact their doctor and report these changes."
Customer Service
21. Everyone on your unit is busy and you requested that your unit's nursing assistants bathe one of your patients earlier today. The patient has yet to be bathed and she is upset about it. Tell me how you proceed.
Inpatient nursing is very much a team effort, and while nursing assistants and care partners are typically available to assist with tasks such as bathing patients, they are sometimes at capacity and are unable to take on all the requests. In these situations, it is a requirement of all members of the care team, including nurses, to care for the patient, and this includes changing, bathing, or otherwise cleaning them. To effectively answer this question, the candidate should indicate that they would take initiative and bathe the patient rather than allowing the patient to wait even longer and become even more upset. A more successful answer to this question would include a specific example from the candidate's nursing career where they provided similar care for a patient when nursing assistants were unavailable.
"In this situation, it sounds like the nursing assistants are very busy and are unable to get to the request put in for the patient. So, I would cancel the request I previously sent to the nursing assistants and bathe the patient myself. Not only would this help my patient feel more comfortable, it would help my nursing assistant team members out as well because it would be one less thing they would need to do. I know I am a nurse, but I do not feel I am above doing things like changing and bathing patients. To me, these tasks are part of providing adequate care to my patients, and I will always do what is needed."
"If the patient had not yet had her bath, I would apologize and let her know I would help her with her bath right away. Then I would set up the bath and assist my patient. Having the help of a nursing assistant is so useful, but sometimes a nursing assistant gets too busy with other tasks to complete every request. Helping my patient with her bath is a great time to assess her skin and any lines, wounds, or surgical sites. It's also a time I can get to know the patient better, reiterate any teaching we're working on, and find out if there are other needs she has."
22. Tell me a time when you went above and beyond for a patient.
The interviewer wants to gauge your commitment and passion for the nursing profession and learn more about your dedication to providing exceptional patient care. They want to know if you will go above and beyond the call of duty to ensure patients receive the best possible care. By asking this question, they hope to hear a specific example of a time when you went above and beyond for a patient and how it positively impacted their care and overall experience. One example of going above and beyond for a patient would be taking extra time to sit and talk with them, providing emotional support and reassurance during a difficult time. Another example could be staying late to ensure your patient receives the necessary treatment and care, even if it means sacrificing your own personal time. Overall, going above and beyond for patients involves showing empathy, compassion, and a willingness to go the extra mile to ensure their well-being and comfort.
"Last week, I had a patient who was feeling very anxious and nervous about their upcoming surgery. Despite my busy schedule, I took the time to sit with them and listen to their concerns. I reassured them that everything would be alright and answered all of their questions to the best of my ability. I even stayed with them after my shift ended until their family arrived to provide additional support. The patient later wrote a note to the hospital praising the care they received, and it was gratifying to know that I was able to make a positive impact on their experience. To me, it didn't seem like I went above and beyond, but the patient sure thought I did!"
"Recently, one of my patients was feeling very down and missing their dog they hadn't seen in weeks due to being hospitalized. I knew how much their dog meant to them and how it could help lift their spirits, so I went above and beyond my duties and sought permission to bring their dog into the hospital. After obtaining the necessary permissions, I arranged for the patient's dog to visit them in their room. The patient's face lit up with joy, and they were so grateful for the opportunity to see their longtime companion. It was a heartwarming moment, and I was glad to be able to bring some happiness into their day."
23. You are assisting a physician to perform a procedure when you are asked to retrieve a bottle of acetic acid that can be used on the patient. After retrieving the bottle from its normal location, what do you do before passing it to the physician?
The interviewer is asking this question to determine if the candidate would verify that they retrieved the correct chemical before passing it to the physician. This confirmation is important, as the nurse may have accidentally retrieved the incorrect bottle or a bottle containing a different chemical may have been in the place where the requested chemical was typically kept. If either of these were the case, and the incorrect chemical was passed to the physician and used on the patient, significant consequences could occur. Simply verifying that the correct chemical is being passed to the physician could help avoid a serious medical error. To effectively answer this question, the candidate should indicate that they would verify that they have the correct chemical by checking the label on the bottle. A more successful answer to this question would include a specific example from the candidate's nursing career where they avoided a medical error by verifying the name of a chemical or drug that was to be administered to a patient.
"I know exactly what I would do in this situation, as I have been in a situation almost identical to this. Before handing the bottle to the physician, I would read details on the label to verify that I am handing them what they requested. This is similar to a situation I was in a few years ago, while I was working in an oncology office and was assisting a physician with a colposcopy, which requires acetic acid. During the procedure, I went and grabbed the bottle, which I assumed was acetic acid, from where it was normally stored on the shelf; but when I checked the label, I found that it was sulfuric acid, which would have burned the patient if applied. Someone had placed the sulfuric acid in the incorrect location, but since I verified I had the correct chemical, I avoided a medical error."
"In this situation, before I hand the bottle of acetic acid to the physician, I would read the label to make sure that I was actually giving the physician the medication she requested. Although it has not happened to me directly, in my hospital there was a situation where a concentration of heparin was stocked in a location where a different concentration was normally placed, and a nurse administered the incorrect concentration to a patient. During my orientation, this incident was brought up to us as an example of why we always have to verify the name and dose of a medication, even if we take a bottle or bag from its 'usual' place, and it's always stuck with me."
24. You just finished preparing IV medications for a patient, and you thoroughly washed your hands before doing so. As you enter the patient's room with the medication, describe the first thing you do to prevent patient infection.
While hospitalized or receiving outpatient medical treatment, patients are at significant risk of picking up an infection as a consequence of the care they are receiving. Although infection prevention measures in the healthcare industry have greatly improved over the years, the risk still exists and healthcare professionals must be vigilant in order to prevent healthcare-acquired infections. Although it may seem obvious, the simple task of handwashing is the first step in infection prevention. The interviewer is asking this question to determine if the candidate understands the importance of handwashing and is in the habit of washing their hands upon entering a patient's room and/or before administering IV medication. To effectively answer this question, the candidate should explain that the first step they would take to prevent infection would be to wash their hands thoroughly. A more successful answer to this question would include an example of how the candidate has helped train colleagues on handwashing in such situations and/or assisted in the development and implementation of handwashing policies for their nursing unit.
"The first thing I would do to prevent the patient from getting an infection is to wash my hands. There are other actions I would need to take in preventing infection, but handwashing is primary. I have always been an advocate of handwashing, even when many of my colleagues were not. When I found out that my nursing and care partner colleagues on my unit were not following handwashing protocols last year, I worked with my supervisor to develop a training on the importance of proper handwashing, handwashing technique, and infection prevention. After this training, handwashing compliance on my unit improved greatly, and the infection control nurse attributed it to a reduction in secondary infections."
"Upon entering the patient's room, it's very important for me to practice hand hygiene again, either by washing my hands or using the alcohol-based hand sanitizer available outside of the patient's room. Although I washed my hands prior to preparing the patient's IV medication, I have potentially touched other items on my way to the patient's room, and I had to knock on the patient's door and touch the door handle to enter. Hand hygiene is the number one way to prevent patient infections, and I demonstrate good hand hygiene at all times. When our hospital did an audit of nurses' hand hygiene using 'undercover' staff members to score the nurses, I scored a 100%, because I know how important hand hygiene is."
25. Describe a situation where it may be appropriate to use humor in the workplace.
Being sick is not funny business, and someone coming in cracking jokes under dire circumstances may find their humor is rejected. There is a time for humor in healthcare, but it must be mindful. What people think is funny can vary wildly. If humor is used, it should be very mild and universal. It's a good policy to be kind, tolerant, professional, and compassionate with your patients. Certainly, laugh at a child's joke, if appropriate, and acknowledge a patient's attempt to be cheerful, but follow rather than lead with humor and only support, chuckle or smile at anything that would be universally accepted as OK. Some people poke fun at themselves, but sometimes, it's a self-esteem issue so it's best to avoid playing along.
"I am not opposed to a funny nursing meme posted in the office away from patient eyes, but I feel that we should represent the hospital as compassionate, caring and professional individuals. There's a lot of room for smiling, but I personally save the humor for the comedians."
"If it seems it would help a patient to go along with their light-hearted attempts at humor, I will smile or laugh along. I would never laugh at an offensive joke, political humor, or any type of racism or bigotry, but something light like chuckling at a joke a patient makes about the reputation of hospital food can help the patient feel at ease."
26. What kinds of review questions do you ask yourself after dealing with a difficult and challenging patient situation?
All nurses desire to have positive and impactful shifts every day, but this is not a reality. Things happen, situations go awry, and it's important to reflect as an individual or a team and extract the lesson to learn how to be better. It's human nature to rationalize or justify and not face the difficult feelings or emotions of a situation gone bad, but this reflection is extremely important so that it doesn't happen again.
"I really like to go back and review with myself and the team what happened and ways to be better. I think it's important to distance myself a little bit from the emotions and try to review it logically. I think that when emotions run high, intelligence can run low, and we need to talk about situations and responses for what they are without blaming. That isn't helpful and impedes learning."
"I was a part of an initiative at my hospital called 'Dealing With Difficult Patients.' In this initiative, we learned techniques to help us identify possible situations in which patients or visitors were becoming agitated, and how we could diffuse the situation. Then, we gave presentations to help teach this information to our colleagues. In a case where a patient's anger escalated, I would ask myself, 'What early clue did I miss?' In that way, I will be better able to catch and react to a similar early warning sign next time, and I can hopefully help my coworkers be prepared to identify such a warning sign in the future, too."
27. How would you handle someone asking you for medical advice or diagnosis validation outside the workplace?
This is a difficult challenge for nurses who know things and also have a compelling need to serve others. It's easy and ego-boosting to become the resident 'expert', but that can backfire. There is a reason why when people call the ER for advice, the standard answer is to present for an evaluation and advice isn't given over the phone. We live in a litigious society, and you worked hard for your license. Protect it just as hard. What may seem to be benign advice to your neighbor may result in catastrophic consequences. Also, it is best to give advice that points people in the direction of great care, such as writing down all symptoms.
"Mrs. Lokley...I'm so sorry you're not feeling well. Do you need me to help call and schedule the earliest appointment with your PCP? Do you have a little notebook where you can write down all your symptoms? Sometimes people get overwhelmed at the doctor's and forget to tell them important things. I could help you write out your medication list to take to the PCP. Come, let's make that call now and get you an appointment. You seem very worried, so it's wise to be seen."
"If someone in my life asks for medical advice when they are not working, I offer to help them call their doctor's office or their insurance's nurse triage line. I have not encountered someone in my life asking for this type of advice who does not have insurance or an established doctor. However, if someone who doesn't have an established doctor or insurance asked for medical advice, I would offer to help them get to an urgent care clinic or the emergency department."
28. Describe a time when you had to step into a leadership role.
As a nurse, you are used to working as part of a multidisciplinary team but also know how to take charge when necessary. This question assesses your leadership skills and how you handle challenges and tasks that require you to take control. The interviewer wants to hear about when you stepped into a leadership role to understand your ability to lead in a healthcare setting. You can use this opportunity to showcase your skills and demonstrate how you have successfully led a team in the past, highlighting the skills you utilized to accomplish the goals set forth. It is important to be honest and specific in your response, clearly showing your leadership qualities and how they have benefited your patients and colleagues.
"As a nurse, I have had the opportunity to step into a leadership position on a few occasions. One particular experience stands out in my mind. I was working on a busy medical-surgical floor, and the charge nurse had to leave for a family emergency. I was asked to step in and take on some of her responsibilities. At first, I was a bit nervous about taking on such a big role, but I quickly realized that I had the skills and knowledge necessary to be an effective leader. I worked closely with the other nurses on the floor, delegating tasks and ensuring everyone had the support they needed. I also communicated closely with the doctors and other healthcare professionals to ensure our patients received the best possible care. It was a challenging experience, but it was also incredibly rewarding. I learned a lot about myself as a nurse and a leader, and I felt proud to have been able to step up and help out when needed most."
"I vividly remember the first day I stepped into a leadership role as a nurse. A few years ago, my unit was short-staffed, and I was asked to take charge for the day. At first, I was nervous and unsure if I was up for the task, as I only had six months of experience. But as the day progressed, I found myself stepping up to the challenge and taking charge of the situation. I delegated tasks, made critical decisions, and ensured patient care was at the forefront of everything we did. By the end of the shift, I felt proud of myself for rising to the occasion and leading my team through a difficult day. From that day forward, I knew that I had the potential to be a great leader and continue to strive towards that goal."
29. How would you handle a situation in which nursing leadership were to reject an idea you pitched to streamline your job?
It's difficult to be rejected in any way, and it's really difficult when you excitedly share something that you feel will be helpful and it is not received well. If you pitch an idea to a supervisor or leadership team, ask for good feedback and learn their perspective. While it's easy to become defeated and not want to contribute, nursing needs you on the leading edge of thought. Review your idea and your presentation. Revise your pitch, if necessary, and ask for another opportunity to present your idea after further considerations. Consider the real possibility that you may have not presented your idea in a way that resonated with the recipient.
"I know I would feel disappointed, but I would definitely go back and ask for feedback on my idea and be grateful for the feedback. I would ask for feedback from others to see if I presented my idea in a reasonable way. If I still thought it was a great idea, I would review how I explained it, simplify and reorganize the information, and ask for another opportunity to present. I once heard that Walt Disney applied to 302 banks before he got the loan for Disney Land, so I try to remember that success doesn't always happen right away, but it does leave clues. I would want to know what I did right and what I could improve upon and then learn from the rejection."
"If nursing leadership rejected an idea that I thought would really help streamline my job and the job of my coworkers, I would feel disappointed. But, I would try to figure out if something in my pitch was off or missing. I would ask some of my most straightforward coworkers if I could run my presentation by them to see how I could tweak it. I've always worked with people with amazing ideas about how we can make things safer and more efficient, so I know I would get useful feedback from coworkers. Then I would ask leadership when there will be another opportunity to present my updated idea."
Operational
30. You are preparing medication in your unit's med room when you are paged to the nurse's station. You plan to immediately return to the med room, which you can see from the nurse's station. Do you lock the door upon leaving the med room?
While most medication rooms in hospitals and clinical facilities automatically lock when closed with current technology, some do not, and in these cases, it is important that nurses and other clinical professionals keep the medication room secured at all times. Not only does leaving medications unsecured place the facility at significant financial risk, it also places patients and the public at risk as well. If an unauthorized individual enters an unlocked medication room and takes medications, these drugs will not be available to patients who need them and may end up being misused by those who end up receiving them. The interviewer is asking this question to ensure the candidate understands the importance of securing the unit's medications. To effectively answer this question, the candidate should indicate that they would ensure the medication room was secured. A more successful answer to this question would include a specific example from the candidate's nursing career where they were in a similar situation or when they helped develop or implement a new policy for securing medications for their unit.
"Even though I would only going to the nursing station and could see the medication room, I would lock the door behind me. You can't take chances with the medication room, and there is no guarantee that you are only being called away for only a moment. In my nursing career, I've learned that a quick page to the nursing station could mean I am away for a 15-minute period, or even longer. The environment on the nursing unit is too volatile to assume you can visually monitor an unlocked medication room, so it is best to ensure the room is secured at all times. Each time I leave the medication room on my unit, I ensure it is locked, and I will continue to do so no matter where I am working."
"In all of my previous inpatient nurse jobs, the medication room had an automatic lock so that every time the door closed, the med room door locked. I think this is an ideal setup, because the medication room always needs to be locked, even if a nurse thinks he or she will be away for 'just a minute.'. In this scenario, if the med room door doesn't automatically lock when shut, yes, I would lock the door upon leaving, no matter how short of a time I think I will be gone."
Performance Based
31. Your patient, who has just returned from surgery, now has multiple tubes and lines that you did not insert. You need to administer a drug into her central line, but are having a hard time finding this tube. As you are in a rush, tell me how you proceed.
When returning from the operating room, intensive care unit, or other units of the hospital, a patient may have many more tubes and lines inserted into their body than normal, and at times, it may be difficult for a nurse to differentiate the lines. This is especially the case if the nurse is in a rush. In this scenario, the nurse, in order to administer medication into the patient's central line, they should take time to ensure they have the correct tube. Administering the medication into the incorrect line or into a drain is a medical error that could have negative consequences for the patient. The interviewer is asking this question to determine if the candidate would take the time to confirm that they are using the correct tube to administer the medication in the patient's central line. To effectively answer this question, the patient should indicate that they would carefully ensure that they had the correct tube for the central line before administering the medication. A more successful answer to this question would include a specific example from the candidate's nursing career where they were in a similar situation, and they took time to ensure they were administering a medication in the appropriate line.
"I was in a very similar situation a couple of weeks ago when one of our patients returned from the ICU with a number of new tubes and lines that were all scattered around. When I received an order to flush one of the patient's lines, I had to take time to ensure I had the correct tube, as I did not one to mistakenly flush a drain or flush the wrong line. So, in the case of the patient you just described, even though I am in a rush, I would take the time needed to ensure I was pushing the medication into the patient's central line and not a different tube."
"In this scenario, I would need to make sure to identify the central line before doing anything else. Being in a rush, it may make me feel stressed to take this time, but administering the medication through an incorrect line could have big consequences.."
32. You are caring for a patient on your inpatient unit, and after making a call to the physician hospitalist on staff for support, you learn that the patient's medication regimen needs to be changed. Tell me the first steps you take.
While many individuals may believe the first step a nurse should take in this situation would be to give the patient the new drugs that were verbally ordered by the physician, this is not the case. The first step the nurse should take after receiving the verbal order by the physician is to document the medication change in the patient's electronic medical record. Documentation errors are very common among nurses, and these errors include failing to document medications, procedures, and/or nursing actions. Because nurses are extremely busy and often distracted by multiple tasks and demands, it is important for this type of information to be immediately be documented in the patient record. To effectively answer this question, the candidate should indicate that they would document the changes in the patient's medication regimen before administering medications to the patient. A more successful answer to this question would include specific details from a similar situation from the candidate's nursing career where they ensured changes to the patient's care regimen were documented before administering care to the patient.
"I actually dealt with a similar situation last week. It wasn't medications in particular, but I had to call our hospitalist because one of my patient's pulse ox was getting very low, and I was beginning to worry about him. Once the hospitalist learned about the patient's condition, she ordered oxygen for the patient, and the first thing I did was document the verbal order in the patient's medical record. I knew if I didn't document the order immediately, there was a chance I would get busy and forget, which could have detrimental consequences for my patient."
"This is a scenario I encounter all of the time as an inpatient nurse. In my current hospital, we have physician order entry, so the physicians often enter their medication orders themselves. However, there are still times when a physician will need to give a medication order verbally. If the physician gives the order verbally to me over the phone, I will enter the order into the EMR under her name, repeat back the order out loud to verify all of the info is correct, and then sign the order. Then, once pharmacy has verified the order on their end, I will be able to pull the medication from the Pyxis machine in the medication room and take the appropriate steps to administer the medication to the patient."

Marcie's Feedback
Problem Solving
33. During your shift in the ER, a patient presents with bruising from a fall. Her male companion answers questions for her, and she barely gives eye contact. What do you do in this situation to get the patient to answer independently?
Sometimes a domestic abuse victim's only connection to help might be a trip to the ER or urgent care. All patients should be screened for abuse whether man, woman, or child. A nurse needs to know the warning signs and learn how to assess and ask effective questions. The nurse needs to learn how to optimize the interview and assessment so that the patient (man, woman, or child) can express themselves in a safe space. In the above scenario, the nurse needs to separate the woman safely from the man, so that she can ask if the woman feels safe and assess her for abuse. It may be difficult to separate the individual from the companion, but it's best they be separated, as the potential abuse victim may not speak openly in front of the abuser.
"I would need to separate the potential abuse victim from the abuser, though I understand that it may be difficult. I could ask him to leave the room for the assessment and if he balked, I would probably take her to the bathroom for a urine sample to ask her questions. I would be careful not to judge or prejudge the situation, but I would do what I needed to do to assess the potential abuse victim thoroughly. I definitely would seek guidance from my shift leadership."
"It's possible that this patient is the victim of abuse. In order to make sure the patient can give honest answers about what caused her injury, I would ask the companion to leave the room so I can complete my assessment. If the companion refuses, I can explain that I need to get a urine sample from the patient and escort the patient to the bathroom so that we can talk privately. If the patient or companion refuses this as well, I would talk to my charge nurse about what other actions I can take."
34. You are caring for a patient on your inpatient unit who is bedridden and unconscious. When the patient came to you, they already had a bedsore. How do you prevent this from happening again?
For patients who are bedridden, bedsores can be a common, but avoidable, problem. If these sores become infected, the consequences for the patients can be severe, especially if they are in a weakened medical state. To prevent bedsores for their patients who are bedridden, nurses should ensure their patients are repositioned at least once every two hours. This repositioning may be completed by a care partner or nursing assistant, but it is ultimately the responsibility of the nurse to ensure their patients are properly cared for. The interviewer is asking this question to ensure the candidate understands it is their responsibility to protect their patients from hazards such as bedsores. To effectively answer this question, the candidate should indicate that they would ensure the patient was repositioned at least every two hours. A more successful answer to this question could include examples of how the candidate has worked with physicians and the physical therapy department to ensure the patient was properly moved, trained care partners or nursing assistants on proper patient repositioning, or helped their colleagues prevent bedsores in similar situations with their patients.
"To prevent additional bedsores, I would ensure the patient was moved and repositioned every two hours, at a minimum. If I am fortunate enough to have the support of a nursing assistant while caring for this patient, I would as for their help, but I would still ensure my patient was being moved, rather than assuming it was being done. I know how serious bedsores can be, and I do everything I can to prevent them. If the patient is unconscious for a long period, I will usually ask the physician if the patient needs an intervention from physical therapy, not only to prevent bedsores but to also prevent muscle atrophy."
"To prevent the bedridden patient from developing additional bedsores, I would work with my team to make sure the patient is turned every two hours. I will document the patient's turning and what position we moved the patient to. If available, I will try to get the patient a specialized hospital bed that uses air to help prevent further pressure ulcers. I would use either pillows or waffle boots to prevent pressure ulcers from forming on heels. I would use a foam dressing or other appropriate material to pad any bony prominences that are in danger of contributing to skin breakdown."
Role-Specific
35. Describe a time when you did not provide the type of patient care you normally would. What could you have done to improve care?
The interviewer is interested in your ability to recognize your shortcomings and that you learn from your mistakes. They want to see that you are self-aware and constantly strive to improve your patient care skills. Discussing a time when you fell short demonstrates your willingness to learn and grow as a healthcare professional. Ultimately, the goal is to provide the best possible care for all patients, and being able to reflect on past experiences is a valuable tool in achieving that goal. Describe a time when you did not provide the care you normally would, the reason why, and what you learned from that experience.
"When I first started working as a nurse, there was a time I didn't provide the type of patient care that I normally would. I felt overwhelmed by the number of patients I had to take care of, and my energy levels were low as I felt like I was getting a cold. As a result, I wasn't as attentive as I could have been. Looking back, I realize I should have taken a break and refueled my energy or called in sick before my shift started, as I was not feeling well. I also could have asked for help from my colleagues or supervisor to ensure that all patients received the care they needed. Being new at the job, I did not want to appear as if I could not handle the work, even if a little under the weather. However, I now realize that I cannot help others unless I take care of myself, and I pay close attention to how I am feeling before each shift."
"I have always strived to maintain a professional demeanor while on duty. However, one time, my personal issues almost got the better of me. I was going through a rough patch in my personal life and was finding it hard to focus on my work. One day, I was assigned to care for a particularly challenging patient. Despite my best efforts, I became increasingly short with them and less patient than I should have been. It was only after a colleague pulled me aside and reminded me of my duty to my patients that I was able to put aside my personal problems and focus on providing the best care possible. It was a valuable lesson that I will never forget and has made me a better nurse. Looking back, I realize I should have taken time to deal with my personal issues outside of work and not let them interfere with my responsibilities. It's important to remember that our patients rely on us to provide the best care possible, and we need to be fully present and focused on their needs."
36. You are caring for a patient on your unit who is now resting well but has tried to get up and fallen multiple times over the past couple of days. As you prepare to leave the patient's room, do you restrain her to prevent her from falling again?
While it may seem like the most rationale step to take in this situation would be to restrain the patient, only current behavior should determine whether a patient should be restrained. The use of restraints can have physical and psychological consequences for the patient, so it is important that nurses and other medical professionals be very careful with their use. In this situation, since the patient is resting well and not agitated, the nurse should avoid using restraints. The interviewer is asking this question to determine if the candidate understands that restraints should be used judiciously, and to effectively answer this question, the candidate should indicate they would not restrain the patient in this situation. A more successful answer this question would include an example from the candidate's nursing career where they chose not to restrain a patient based on current behavior, despite previous history of falls, violence, and/or intentional or unintentional self-harm.
"Since I have been an inpatient nurse for many years, I have dealt with these types of situations many times, and in this situation, I would not restrain the patient. Even though the patient has fallen since she has been admitted, if she is currently resting well and isn't agitated, I would not restrain her. Restraints are very difficult for patients, and I will not use them unless it is absolutely necessary. This reminds me of a patient who I was caring for recently who had been violent and restrained while in the ICU, but when he was transferred to my unit, he was much calmer. The nurse who cared for him the shift prior to mine had kept him restrained, as she was fearful of him, but the patient was now much more lucid and the restraints were stressful to him. Once I took the handoff, I immediately removed the restraints from the patient, and from then on, he was able to relax."
"Restraints should be used as a last resort, as they can be upsetting to patients and their family members, and they may increase the risk of other types of injury, such as skin tears or pressure wounds. I would work with my patient care tech and other nurses to implement other measures, such as frequently rounding on the patient to make sure her elimination needs are met. We could also place a bed or chair alarm underneath the patient to make sure staff are alerted if she tried to get up, and we could place fall alert socks on her feet so that the color indicates to all staff that the patient should not get up by herself."
37. You are caring for a patient and the physician has ordered an IV medication for them. You have collected the medication and the supplies needed to administer the IV. Tell me how you will proceed from this point.
Before starting an IV and administering the medication, in this situation, the nurse should look in the patient's electronic health record and review the physician's medication order to verify they have the correct medication, dosage, and administration duration. This is a safety protocol that is standard in nursing practice to prevent medical errors, as administering the incorrect medication, incorrect dosage, and/or incorrect duration can have dire consequences to the patient. The interviewer is asking this question to assess the candidate's understanding and regular practice for such precautions. To effectively answer this question, the candidate should indicate that they would verify the medication, dosage, and administration duration by reviewing the order in the electronic health record. A more successful answer to this question could include examples of how the candidate prevented a colleague from committing a medical error by reminding them to review this information, helped develop training materials on the matter for their unit, or even helped change protocols to improve compliance and patient outcomes.
"Before I did anything to the patient, I would go to the patient's electronic record and verify the drug name, the dosage, and the administration duration. This is so important because so many times, nurses are busy or get distracted and accidentally grab the wrong medication, dosage, or set the incorrect administration duration. A couple of years ago, we had several new nursing graduates working on my unit, and we had several medical errors related to this issue take place. Because I am so passionate about this issue, I helped my supervisor develop training materials to help remind my colleagues to verify these medication elements before they administer IV drugs. While these materials did not eliminate medication errors, they helped reduce them."
"Before administering the IV medication, I would check the patient's wristband and/or verbally confirm the patient's name and date of birth with the patient. Then I would verify the medication order in the patient's electronic medical record, ensuring that the medication, dose, route, and duration all matched the information that I have."
38. In your inpatient unit, you are caring for a patient who is still weak from surgery. Upon reviewing physician orders, you see the patient is to get up and walk two laps in the hall. Tell me how you would proceed.
The interviewer is attempting to determine if the candidate would assess the patient's ability to participate in physical activity before getting her up to walk around the hall of the inpatient unit. Patient falls is one of the biggest patient safety concerns for hospitals, and it is the onus of the nursing staff to ensure they protect their patients from falls in all situations, even when there is a physician order stating otherwise. To effectively answer this question, the candidate should indicate that they would assess the patient's ability to participate in the physical activity, and if they, in fact, the patient was too weak, they would contact the physician for alternative orders. A more successful answer to this question would include a specific example from the candidate's nursing career where they prevented a patient fall by assessing their ability to participate in physical activity.
"If the patient was still weak from their surgical procedure, I would assess their ability to get up and walk, to ensure they are not at risk for a fall. This is something I deal with often at my current job as an inpatient nurse. Just recently, I was caring for a patient who had been admitted for a serious infection. When the patient seemed to be getting better, the physician ordered that he get up and walk, and he did well the first couple of days. However, on the third day, he was feeling worse, and when it was time for his walk, instead of just getting him up, I assessed his condition and found that getting him up for a walk would put him at risk. Upon calling the physician and updating him on the patient's condition, he came to check on him, and found that the patient needed emergency surgery as the infection had returned. Not only did my diligence prevent the patient from becoming injured, it also helped alert the physician of an emergent issue."
"When I worked on the post-op cardiac unit, we were constantly assessing if patients could safely walk around the unit with just a nurse to support them. Ambulating after surgery is very important to increase strength and decrease the chance of pneumonia, blood clots, and other complications. However, if a patient isn't ready to walk, even with a gait belt or a walker, they could risk falling and sustaining serious injury. In this case, I would assess the patient and see if he can safely walk 2 laps in the hall. If his assessment shows that he can walk 2 laps in the hall, I would walk with him. If the assessment did not show that he could safely do this yet, I would contact the physician, explain the scenario, and request an order for a physical therapist to come to evaluate and work with the patient."
Scenario Based
39. How would you handle a patient that assumes a 'helpless' role, does not do what is necessary for their treatment, and asks you to do certain tasks that they could and should perform for themselves?
A nurse cares about patients, so it's difficult sometimes to recognize when we over function for patients and do not encourage them to be their best. Doing too much for patients is as damaging as doing too little. Nurses need to learn the subtle dance between empathy and advocacy for patients helping themselves. You want to encourage without being demeaning or too harsh, but also push them to do what they can for themselves in every situation possible. A weight lifter doesn't bench press 200 pounds over night but adds weight little by little. Each time a patient swings his own leg out of the bed, or shuffles to the bathroom with the assist of two, wonderful things are building incrementally in his or her body. Sometimes, nurses do things for patients because they are busy and don't have time for the slower patient to do it. Occasionally, on a booming floor this may be necessary, but should be the exception, not the rule.
"Sally, today is bath day and it's a great day to get up and stretch your legs today. No bed bath today. I'll help you up and you can dangle at the edge of the bed while I turn the shower on. It will do you good to get up, and I'll help you so you don't fall, but we are going to try to walk independently to the bathroom today. Does that sound good?"
"When I work with a patient who seems to be acting helpless, I try to use motivational interviewing techniques to help them find a reason for why they might want to participate in their treatment plan. So, we might talk about their trying to get back to their apartment or home, their desire to be able to sit up at their grandchild's wedding, or another goal they want to reach. Then I help them see how taking a walk in the hall or using their incentive spirometer will help them get stronger and more likely to achieve their goal."
40. You have a coworker with a large following on TikTok, who brags constantly about her followers. One day you notice a video of her with one of her patients in the background. What would you do in this situation?
The interviewer asks what you would do if you saw a coworker with a patient visible in a TikTok video because it is imperative to maintain patient privacy and confidentiality. Suppose you were to come across such a video. In that case, the interviewer wants to see if you would immediately bring it to your coworker's attention and advise them to remove it or if you would first inform your supervisor and follow appropriate protocols to protect the patient's privacy. It is crucial to prioritize patient safety and confidentiality in any healthcare setting, and you must be committed to upholding these values. How you respond will give the interviewer insight into your communication, problem-solving, and critical-thinking skills.
Written by Krista Wenz on May 26th, 2023
"As a responsible nurse who takes my job very seriously, I would immediately report the situation to my immediate supervisor. Patient privacy and confidentiality are of the utmost importance in healthcare, and any breach of these principles must be taken seriously. It is important to ensure that all healthcare professionals understand the gravity of protecting patient information and upholding the profession's ethical standards."
"I would be very concerned if I saw a TikTok video featuring my coworker and a patient. It's crucial to prioritize the well-being and privacy of our patients above all else. Patient privacy and confidentiality are critical in this field, and violating them is a serious breach of ethics. I would first speak with my coworker privately to express my concerns and remind them of the importance of maintaining patient privacy. Depending on the severity of the situation, I may also need to report the incident to our supervisor or the hospital's compliance team. Of course, how I proceed also depends on the policies and procedures of my organization."
41. You are caring for a patient on your inpatient unit who is taking a turn for the worse. You decide you need to call the hospitalist physician. Tell me how you will proceed.
Before calling for the assistance of a physician, therapist, or nursing colleague, unless it is a dire emergency, nurses should gather as much pertinent information on the patient as they can so they can effectively and succinctly explain the situation and the needs of the patient. If the nurse does not collect this information in advance of making the call to the physician, the call will likely take additional time as they will have to look the information up and take more of the physician's time. While patients are not typically put at risk in these situations, having the information ready to report during the call assists nurses with building professional relationships with the many professionals the must consult with on a daily basis. The interviewer is asking this question to determine how important the candidate feels it is to collect information before calling the physician. To effectively answer this question, the candidate should indicate that they would collect all pertinent information on the patient, including diagnosis, condition, impression, test results, and vital signs. A more successful answer to this question can include experience from the candidate's nursing career, information the candidate typically relays during such a call, or how the candidate assisted a colleague with such a call.
"This is a very common situation that I find myself in, as I work in the inpatient environment, so I understand that it is important to gather as much information about the patient and the patient's current situation before making the call to the physician. Early in my nursing career, I sometimes would call before I had gathered the necessary information, and when I did so, it was very difficult to communicate the situation to the physician, and sometimes they would become frustrated. Now that I have more experience, I understand the importance of gathering information such as current impression, vital signs, test results, and other pertinent information, so the conversation can be efficient and brief."
"When I call the hospitalist to inform them of a downturn in my patient's condition, I make sure to go over my mental checklist first. Have I gathered all the needed information about the patient's history, current vitals/labs, and changes in condition? If so, I will call, and identify myself and the patient, and then make sure the physician is ready to hear the information I have. One of the first times I needed to call a physician about his patient's change in level of consciousness, I was so anxious that I started talking quickly and forgot to identify myself as the patient's nurse. In trying to get things moving quickly, I actually ended up taking more time than needed, because the physician wasn't clear on who I was. From that point on, I have always taken a breath and made sure to stay calm on calls to physicians."
42. You are alone in an elevator with two nurses from another floor who are talking about a patient. How would you respond?
Interviewers ask situational questions to test interviewees' people skills and their capacity to communicate and find optimal solutions. The answer here doesn't have to be work specific, unless it is apparent as in this question, but it's always a good idea to incorporate appropriate work behaviors in, when possible.
"My grandmother always taught me that when you are silent about questionable things, in a way you are agreeing with them, or people might think that you are. I feel strongly about protecting patient rights, and I would be very uncomfortable in that situation. I think that I would feel compelled to address it right on the spot and very pleasantly say that I don't feel comfortable with the conversation. If they were talking details and gossip, I would address it and definitely report it to supervisors. If it were a casual slip and vague in content, I would definitely report it to the supervisor if anyone else was on the elevator but if not, I would just address them directly."
"I encountered almost this same scenario, except it was two doctors that I recognized by sight but didn't know by name. I would handle this scenario in the same way I handled that situation. In that situation, I calmly said, 'Doctor, please don't discuss patient information in front of a person without a need to know this information.' The doctor nodded and said, 'Thank you,' and the conversation stopped. I think calmly and firmly reminding staff or physicians of a patient's right to privacy is the way to go, most of the time. If for some reason I saw a breach of confidentiality in front of a patient or visitor, I would report it to the unit manager in addition to my reminder to the staff."
43. You are working phone triage for your physician practice when a patient calls asking for advice as he is having chest pains. Tell me what you direct the patient to do.
In this situation there are multiple directions the nurse could give the patient, but in a situation when a patient is having chest pains, the patient should be directed to go to the emergency department. While care can be given at a physician office or urgent care center, a patient with chest pains could be in the midst of a medical crisis which requires the service of an emergency department. The interviewer is asking this question to determine if the candidate understands the clinical significance of chest pains and the fact that the patient needs to be evaluated in the emergency department. To effectively answer this question, the candidate should indicate that they would direct the patient to hang up and immediately go to the emergency department. A more successful answer to this question would include a specific example from the nurse's career where they directed a patient with chest pains to the emergency department.
"If a patient called with complaints of chest pains, I would tell them to go to the emergency department immediately after hanging up. Even though the patient's chest pains may not be from a heart condition, there is a chance that they could be, and an evaluation in an emergency department is necessary. In these situations, it is easy to assume the patient's symptoms or conditions may be caused by an ancillary condition, such as anxiety, but until they are properly evaluated, it is too risky to assume."
"When working phone triage, if a patient calls with chest pain, I would instruct him to go to the emergency department immediately. I would request verbal confirmation that the patient understands my instruction and will go to the emergency department immediately. Chest pain can indicate myocardial infarction, and delay in treatment can lead to heart failure or death. This isn't a time to take a chance that the chest pain might be caused by something else."
Situational
44. How would you handle a patient who is trying to manipulate you in some way or talks about the other shift to you?
This answer appears easy ,but it's not. Being a new nurse sometimes makes people over eager to please and hearing great things about yourself rarely falls on unappreciative ears. You want to help and be sympathetic, but it's not helpful to engage in any conversation that downgrades your coworkers in any way. Sometimes these conversations are subtle and sometimes they are not. The easiest way to circumvent these situations is to enter each room prepared and with a plan for the visit or encounter and perform that task in a professional and kind manner. If the patient begins to complain about another individual, handle it by stating that you're sorry they had the experience and ask if they'd like for you to get the nursing manager to speak to.
"If a patient starts to tell me something, I listen briefly and ask if she would like for me to get my nursing leader. I don't want to shut the patient down if she really had a bad experience, but I don't want to feed into it either and damage their view of my coworker. The best thing I can think of is to hear them out briefly but not agree. I'd say that I'm sorry they had the experience and ask if they would like me to get nursing leadership. Now if it's something horrible, of course I would report it directly, if it was a medical concern. It depends on the situation, but I know not to simply be silent because silence implies consent sometimes, so I would feel the need to say that I hear them, but I'm not the person who has the power to take action on that concern."
"When a patient has a legitimate complaint, I will attempt to rectify their problem myself or bring up their complaint to the charge nurse, the nurse manager, or another person in leadership. However, if a patient seems to be manipulative or complaining to try to start conflict, I usually use reflective listening. So, I reflect their statement back to them neutrally, such as saying, 'I hear you saying you were frustrated that the night shift nurse's aid didn't get you up to the chair at the time you wanted. What are the top 2 priorities I can address during my shift today to make you comfortable?' I don't feed into any negativity about another shift, and I focus on what I can do during my shift If the patient persists in complaining about something that happened earlier, I would offer to bring in my nursing manager."
45. If you have too many things on your to-do list, how to you decide which to do first and which to postpone?
A nurse shift is usually a very busy one, with few unimportant tasks. Taking the time to organize and frontload your day by doing the most important patient tasks first helps free up time later. Sometimes, it is helpful to delegate to others when possible, but it's never an acceptable answer if anything patient-care related is not done because there wasn't time. Future pace your day and sketch out a timeline for each activity. When you follow your plan and you realize at 10 AM that you are still dealing with some problems with your 8 AM task, then the best time to ask for support or help is at 10 AM. At 2 PM, it's too late to gather support and finish the shift completely and correctly.
"At work, I take a couple minutes to sketch out my day and I frontload the more important and difficult tasks in the morning, so I can complete them well. That gives me time to work through the rest of my shift, and if I end up having to ask for help, then the tasks that still need to get done are not the most difficult or important ones. In my personal life, when my to-do list gets too large, I sit down, weed it out, and focus on what moves my life forward and brings meaning and value."
"At the beginning of my shift, I use my shift 'cheat sheet' to help me organize and prioritize my day. This helps me determine which tasks should be done first, based on both how important they are and how long they might take. If tasks take longer than I anticipated, or I run into a situation where a patient's condition takes a downturn, I will need to ask for help. I can delegate tasks like blood glucose tests or a patient bath to a patient care tech. I can also ask my coworkers or the charge nurse to take on a task that only a nurse can do. In an inpatient unit, we have to work as a team to make sure all patient care tasks are completed. I am comfortable asking my colleagues for help because they know I always offer to assist them with tasks when I can."
46. What tools or techniques do you use to remember difficult information or instructions given verbally only?
Situational interview questions are designed to assess candidate competencies in more depth and to avoid rote, standardized answers. The interviewer is looking to observe how you would triage a problem and figure out how to handle it in an optimal way. Situational questions allow the interviewer to showcase unique talents and competencies. Situational interview questions challenge the interviewee to think about situations that they may have never experienced before.
"While I prefer to listen to instructions and have written instructions as well, I have a formula for remembering things verbally. I believe this is a good skill to have as a nurse. First, I listen to understand, and I listen attentively. I give the individual my full attention, particularly if it's new information. After I listen to them, I ask questions for clarity, and then I repeat back what they want me to do. Sometimes, I use imagery or acronyms to remember things when I am getting complicated directions."
"When I am given instructions verbally only, I repeat the information back to the source to ensure I have all of the information correct. Once the physician or other person has confirmed that I have all of the information correct, I break the steps down into sections or 'chunks' in my head, and then I repeat them to myself 5-7 times to ensure they stick. If there's an opportunity, I will also write down the instructions later; however, if there's not an opportunity, my chunking and repeating method works for me."
47. You are nearing the end of your 12-hour shift on your inpatient unit and you are exhausted from caring for eight high-acuity patients. As your colleague arrives to relieve you, tell me how you proceed.
When inter-shift information is involved, nurses must ensure that they properly handover information to their colleagues properly, even if this means they stay late to complete handover paperwork on each of their patients. Failing to properly handover information to the next nurse could have dire consequences to patients, making handovers a vital element of a nurse's set of responsibilities. Many facilities have standardized handover templates for nurses to complete before the end of their shifts, and these templates include elements such as: background, assessments, vitals, and recommendations. While many electronic health record systems pre-populate much of this information, it is imperative the remaining information is completed. The interviewer is asking this question to determine if the candidate understands the importance of completing handovers. To effectively answer this question, the candidate should indicate they would ensure handover information for all patients was completed before departing for the day. A more successful answer to this question would include an example from the candidate's nursing career where they ensured their handovers were completed despite being exhausted or dealing with other confounding factors.
"In this situation, even though I am exhausted, I would complete handover templates for all my patients, if I haven't already. This is especially true because you said the eight patients are high-acuity, which means there is a lot the next nurse needs to know about them. I could never leave my patients without completing handovers, because not only could I not leave my coworker in a bad situation, but I also don't want to put my patients at risk. Last week, I was in a similar situation, where I had been so busy that I didn't have time to complete handovers until my coworker arrived to relieve me. So, I stayed late and completed the templates for all my patients, despite the fact that I was tired and ready to go home."
"At shift change, it's so important to give a concise but thorough report to the oncoming nurse who will be caring for the patients I had during my shift. If these patients were high-acuity, that's all the more reason to make sure no important details are missed. I want to ensure the oncoming nurse has all of the information needed to provide safe care to our patients. I have a brief 'cheat sheet' that I keep for all of my patients throughout the shift. It keeps me on track for all of my patients' orders, vital signs, conditions, and charting. Therefore, regardless of how tired I am at the end of my shift, I have the information necessary to complete a safe handoff to my oncoming colleague or colleagues."
Amanda's Feedback
48. Your coworker forgot to sign off that she gave Tylenol as a PRN before she punched out and calls you from the car. She asks you to initial that it was given so nobody gives it again. What do you do?
It sounds like the right thing to do. After all, you don't want the patient to be given extra Tylenol, but you should never do this. It's illegal and forging the medical record. It's unethical and risks your nursing license. The correct thing to do is to write down the information about the dose and attach a sticky note to the MAR so that there is a visual reminder for the person administering medications. This information should be reported to the shift nurse manager and guidance received. Under no circumstances should the nurse sign off a medication that he or she did not administer.
"Sally, I'm sorry, but I'm not comfortable doing that. Thank you so much for calling and letting me know. I put a sticky note on the chart to remind myself of the time you gave the Tylenol and let Ruthann know, so we can follow her guidance. Call Ruthann tomorrow to figure out what you need to do about not signing that. Have a good night and drive safely!"
"Unfortunately, I can't sign off on a medication that you administered. That would put both of our licenses at risk. Do you have time to come back in and chart it yourself? If not, I will place a sticky note on my nurse cheat sheet to remind me what time you administered the Tylenol. Make sure you check with the manager tomorrow to see how you can chart a late entry. Good night!"
49. Have you ever caught a coworker stealing? If so, how did you handle it? If not, what would you do if you saw a colleague stealing?
Interviewers ask what you would do if you saw a colleague stealing for a few reasons. First, they want to gauge your sense of ethics and integrity. Nurses are held to high standards of moral and ethical conduct, and it is important to ensure the people working in this field meet these standards. Second, they want to see how you would handle a difficult workplace situation. It can be challenging to confront a colleague about unethical behavior, and interviewers want to know that you would handle the situation appropriately and professionally. Ultimately, it is essential to prioritize patient care and safety and to take action if you witness any behavior that could compromise these priorities.
"No, I have never caught a coworker stealing. However, if I witnessed such behavior, I would first approach my colleague privately and confront them about what I had seen. I would explain that stealing is unethical and illegal and that their actions could have serious consequences for both themselves and our workplace. Depending on their response and the hospital's policies, I would escalate the issue to our supervisor or HR department if necessary. As healthcare professionals, we are responsible for acting with integrity and honesty and holding our colleagues accountable when they fall short of these standards."
"Yes, unfortunately, I have witnessed a coworker stealing. When doing my rounds, I walked into a patient's room and saw a nurse's aide quickly put something from the patient's bedside table into their pocket. After checking on my patient, I asked the aide to speak privately with me outside the room. I asked what they put into their pocket, and they said they had not taken anything. I asked to look in their pocket, and they refused. Since I was sure the aide had taken something from the patient, I reported what I saw to the charge nurse. After an investigation, it was discovered the aide had a problem with prescription pills and had taken the patient's medications. Those who work with me understand my values and that I do not condone stealing of any kind."
50. How do you handle ethical or philosophical differences with a patient?
Nurses care for all patients, so they must have emotional mastery and cultural competence. It's difficult sometimes to separate our personal preferences and philosophies from our patients and not superimpose our cultural grid on their choices and feel disapproval. It is unprofessional and not optimal patient care to do so. Nurses must remind themselves when they enter the door to a patient's room that they do not need to know the whole story, and they can never know all the nuances that led to the belief or decision they disagree with. They must lead themselves to treat the individual in front of them as a human being who they are there to help, serve, and not to judge.
"When I feel judgement or disapproval welling up inside me, I do a quick mental inventory and check-in. It doesn't happen often, but I would not be human if I said it never has or will again. I don't know why the person made the choices they made, or what led up to it. I only know that my job is to help them, and I stay focused on that. I've worked with drug addicts and criminals, but my job is to be kind, provide excellent care, and maybe even learn something from them."
"In two of the hospitals I've worked out, I've taken care of prisoners that are recovering from heart surgery. I've never looked up or asked a patient what crime they are in jail for, but some have volunteered this information to me, and it can be momentarily disconcerting to learn that you're taking care of a person who has committed an assault. However, I know that all patients deserve safe and effective care. I can never know anyone's full story, so regardless of the circumstances, I provide my best care to all patients."
About the Author
I began my career in emergency medical services (EMS) over 30 years ago, working as a Firefighter-Paramedic, EMS Captain, Mental Health Technician, ER Technician, EMT and Paramedic Adjunct Instructor, and EMS Educator. During my career, I had the privilege of serving on over one thousand interview panels to help various organizations choose the right candidate for the job. I have created curricula and training materials to prepare candidates for interviews and held mock interview courses for all types of healthcare professionals. My interview experience includes hiring emergency medical technicians, paramedics, firefighters, nurses, medical assistants, home health aides, and physician assistants. As a coach and contributor for MockQuestions, I am excited to help you navigate your upcoming nursing interview. While these situational questions assess your critical thinking and communication skills, interviewers also ask these questions to gain insight into your personality to determine if you will be a good fit with the company culture. Remember to be relaxed and be your authentic self. Best of luck in nailing your interview!
Learn more about Krista Wenz
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Effects of Problem-Based Learning Strategies on Undergraduate Nursing Students’ Self-Evaluation of Their Core Competencies: A Longitudinal Cohort Study
Yen-chiao angel lu.
1 Department of Nursing, Chung Shan Medical University, Taichung 40201, Taiwan
2 Department of Nursing, Chung Shan Medical University Hospital, Taichung 40201, Taiwan
Shu-Hsin Lee
Ming-yi hsu, fen-fen shih, wen-jiuan yen, cheng-yi huang, pei-ching li, ching-yen hung, hsiao-ling chuang, ching-pyng kuo, associated data.
Not applicable.
To respond to patients’ increasing demands and strengthen nursing professionals’ capabilities, nursing students are expected to develop problem-solving skills before they enter the workforce. Problem-based learning (PBL) is expected to provide effective simulation scenarios and realistic clinical conditions to help students achieve those learning goals. This article aims to explore the effects of PBL strategies on nursing students’ self-evaluation of core competencies. This longitudinal cohort survey study evaluated 322 nursing students attending Chung Shan Medical University, Taiwan, in 2013 and 2014, where PBL teaching strategies are used in all four undergraduate years from freshman to senior. Based on their undergraduate academic levels, students were categorized into three groups- one-year PBL exposure, two-year PBL exposure, and three-year exposure. A core competency questionnaire was administered twice to ask participants to self-assess five professional competencies: learning attitude, problem identification, information analysis, execution, and life-long learning. The results showed that students with the longest exposure to PBL (Group 3) had higher self-evaluated scores for all core competencies than the other groups, except for the execution competency. The mean total competency score increased by 0.12 points between the pre-and-test. In addition, the mean score increased significantly more in Group 3 than in Groups 1 and 2. These trends were consistent for the information analysis, execution, and life-long learning competencies. In conclusion, the changes in the self-evaluated scores between groups indicate PBL strategies effectively improve nursing students’ core competencies. The longest exposure group reported higher self-evaluated core competency scores than the other groups, especially for the information analysis, execution, and life-long learning competencies.
1. Introduction
In recent years, improvements in teaching and learning strategies have led to continual expansion of the teaching methods available to educators [ 1 , 2 ]. Additionally, nursing curricula should be designed to prepare nursing students for their future careers. Therefore, nursing educators have emphasized a shift from traditional teaching methods to learner-centered teaching strategies to improve the effectiveness of learning [ 2 , 3 ]. To respond to the increasing demands of patients and strengthen nursing professionals’ capabilities, nurses are expected to develop problem-solving skills [ 4 , 5 ]. However, gaps still exist between the curricula of current nursing education programs and the requirements of clinical practice [ 6 , 7 ]. Moreover, due to the increasing complexity and demands of healthcare, nurses are expected to develop critical thinking skills to assess complex clinical problems [ 8 , 9 ] and provide holistic care [ 10 ]. Thus, it is necessary to adopt new methodologies for nursing education to respond to the rapidly changing medical context and promote key competencies in the areas of problem-solving, critical thinking, and creativity among nurses.
During the process of integrating nursing students into clinical situations, case problems should be based on realistic clinical conditions [ 11 ] and challenge nursing faculty. Therefore, the incorporation of PBL learning provides a strategy to flip the classroom [ 12 ] and can provide effective simulation scenarios and parallel learning experiences.
The problem-based learning (PBL) strategy was developed by the Faculty of Health Sciences of McMaster University in the late 1960s [ 13 ]. The PBL strategy has since been adopted in numerous medical [ 14 , 15 ] and nursing schools [ 16 , 17 ], including in Taiwan [ 18 , 19 , 20 ]. PBL is a student-centered approach that aims to facilitate autonomous and independent learning and seeks to enable students in higher education to apply knowledge, acquire skills, and achieve diverse learning goals [ 21 ]. Compared with nursing students who study traditional education courses, this approach develops self-directed learners, who build capability in terms of critical thinking, leadership, and teamwork [ 21 ]. Therefore, the role of the educator in PBL is entirely considered as a facilitator and to allow learners to seek a variety of potential solutions [ 22 ]. PBL strategies have been designed to promote learner interaction, problem-solving, and learning through teamwork [ 23 ]. Educators develop various learning activities based on actual situations and case problems to encourage autonomous learning [ 23 , 24 ]. Research has shown that PBL teaching strategies can effectively improve students’ scores for curiosity, systematic, analytical, and critical thinking [ 25 ], as well as their leadership, teamwork [ 21 ], and problem-solving abilities [ 26 ].
Despite PBL being widely used in professional healthcare courses, few studies have assessed the effectiveness of PBL using valid instruments or employed longitudinal follow-up to measure the strength of the effects. Furthermore, most related studies were qualitative [ 27 , 28 ], only measured the performance of some abilities [ 3 , 5 , 29 ], or focused on evaluations of student achievements by faculty [ 30 ]. Therefore, this study aimed to evaluate the influence of PBL strategies on students’ self-evaluation of their core competencies over two years among students studying at different grades of the same nursing school in Taiwan.
2.1. Research Design and Subjects
This study adopted a longitudinal survey design to investigate the differences in nursing students’ self-evaluations of their core competencies over two years between grades.
At Chung Shan Medical University, PBL teaching strategies are used in the course design of various nursing modules (from freshman to senior). In September 2013, we recruited freshman to junior class nursing students attending Chung Shan Medical University for this study. In September 2014, these students were advanced to sophomore, junior and senior standing. Overall, a total of 322 nursing students completed the same questionnaire in both 2013 and 2014.
We grouped the students by their undergraduate academic level to study the effect of exposure to the PBL strategy: Group 1 ( n = 106, 2013 as Freshman students, 2014 as Sophomore students) had PBL exposure for 1 year; Group 2 had PBL exposure of 2 years ( n = 111, 2013 as Sophomore students, 2014 as Junior students); and Group 3 had PBL exposure of 3 years ( n = 105, 2013 as Junior students, 2014 as Senior students).
2.2. Measures
Data on the students’ characteristics were collected, including age, gender, and grade level.
A core competencies questionnaire was designed based on a literature review and nursing education principles as a framework. Content validity was performed, and five dimensions were identified: learning attitude, problem identification, information analysis, execution, and life-long learning. The overall content validity index of the instrument was high (overall S-CVI = 0.93) The final instrument includes sixteen items out of twenty-four items originally developed. Individual items related to the five dimensions were provided in Table 1 .
Items analyzed in the questionnaire.
| Dimensions | Number of Items | Items Indicators |
|---|---|---|
| Learning Attitudes | 4 | I like solving problems regarding the group project with team members. I enjoy cooperative learning with team members. When I encounter a problem, I learn to think, understand and analyze the problem first. I have learned to tolerate and respect different opinions. |
| Problem Identification | 2 | I can identify problems from the case scenarios provided. I am familiar with problem-solving techniques. |
| Information Analysis | 3 | It is easy for me to find the appropriate references to meet course objectives. I can evaluate the credibility and reliability of data or information retrieved. I can conclude from the information retrieved. |
| Execution | 3 | I can come up with strategies to solve problems. I can provide safe and competent care when dealing with individual clients. I can apply communication skills to build a trusting nurse-patient relationship. |
| Lifelong Learning | 4 | I can connect academic learning to practical problems. I can apply the knowledge and skills I have learned to clinical practice and my personal life. I think I am a self-directed learner. I often think about how to improve my learning and problem-solving skills. |
“Learning attitude” was defined as students’ tendency to respond a certain way towards PBL learning. Four items were included in the questionnaire to measure students’ learning attitudes. “Problem identification” was students’ ability to identify the key problem to be solved or addressed. Two items were used to assess subjects’ problem-identification skills. “Information analysis” aimed to check students’ ability to inspect and comprehend information collected. Three items were included to evaluate students’ information analysis competency. “Execution” focused on students’ abilities to perform a certain task or complete study goals. Three items were employed to assess students’ execution competency. “Life-long learning” was described as students’ self-initiated and ongoing learning intentions or behaviors. It was measured by 4-item questions.
A five-point Likert scale was adopted for data collection and the responses were rated as follows: 1 = Strongly disagree, 2 = Disagree, 3 = Neutral (neither agree nor disagree), 4 = Agree, and 5 = Strongly agree. A higher score indicates a positive self-evaluation of core competencies.
Students (from freshman to junior classes) were recruited to participate in the survey in September 2013. Those students were tracked to complete the survey in September 2014. Overall, a total of 322 nursing students completed the same questionnaire in both 2013 and 2014.
Each student was asked to self-evaluate their core competencies using the same questionnaire in 2013 and 2014. The Cronbach’s alpha values of internal consistency were 0.944 for the overall scale and 0.772 to 0.866 for each of the five dimensions (learning attitude, 0.772; problem identification, 0.844; information analysis, 0.821, execution, 0.777; life-long learning, 0.866). Therefore, the present study had acceptable internal consistency.
2.3. Data Collection and Analysis
We collected data twice during the research period, as all participants completed the same core competencies questionnaire in both 2013 and 2014. The Institutional Review Board approved this study at the Chung Shan Medical University Hospital (No: CS2-21113), and data were only collected after informed consent had been obtained. All participants signed an informed consent stating that they had the right to withdraw from the study at any time. The data collected were only used for research purposes.
Descriptive statistics including frequencies, percentages, means, and standard deviations were used to assess the distributions of the students’ characteristics and core competencies. Chi-square tests and paired t -tests were used to analyze the differences between groups. Radar charts were plotted to compare the changes in the student’s self-evaluations of their core competencies between groups. To adjust for the interaction between exposure and group, we used generalized estimating equations and statistical methods to predict the changes in the core competencies of each group. The significance level was set at p < 0.05 and all tests were two-tailed. The SPSS for Windows version 20.0 (SPSS Inc., Chicago, IL, USA) was used for data analysis.
Descriptive statistics such as Chi-square tests, paired-sample t -tests, and generalized estimating equations (GEE) were used to analyze data.
3.1. Characteristics of the Nursing Students
A total of 322 nursing students (Group 1 = 106, Group 2 = 111, and Group 3 = 105 students) completed the core competency questionnaire twice, in 2013 and 2014. Though most students were female (81.4%), Chi-square tests confirmed that there was no significant difference ( p = 0.379) in the sex distribution between groups, showing that the distribution of the characteristics was homogenous between groups ( Table 2 ).
Characteristics of the three groups of nursing students (Chi-squared tests).
| Group | Male, (%) | Female, (%) | X | Sig. |
|---|---|---|---|---|
| Group 1 | 22 (37.9) | 84 (31.8) | 1.940 | 0.379 |
| Group 2 | 16 (27.6) | 95 (36.0) | ||
| Group 3 | 20 (34.5) | 85 (32.2) |
3.2. Comparison of the Differences in Students’ Self-Evaluations of Core Competencies between Groups
Pre-and post-tests revealed significant changes (from 2013 to 2014) in the total self-evaluated competency scores of the students in Group 3 ( p < 0.000). Similarly, significant differences were observed for the competencies learning attitude ( p = 0.007), problem identification ( p = 0.0181), information analysis ( p = 0.007), and life-long learning ( p < 0.000) in Group 3. However, the score for the execution competency ( p = 0.086) did not significantly change in Group 3. In Group 2, pre-and post-tests showed the students’ self-evaluation scores for all competencies did not significantly change. In Group 1, students’ self-evaluation scores were only significantly different for the execution ( p = 0.021) and life-long learning competencies ( p = 0.037) in pre-and post-tests ( Table 3 ).
Comparison of the differences in students’ self-evaluations of core competencies between groups. (Paired-samples t -test).
| Variable | Mean | SD | Mean of Difference | SD of Difference | 95% C.I. | -Value | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Learning attitude | |||||||||
| Group 1 pre | 106 | 3.7571 | 0.54167 | ||||||
| post | 106 | 3.6958 | 0.62010 | ||||||
| 0.06132 | 0.69933 | −0.07336 | 0.19600 | 0.903 | 0.369 | ||||
| Group 2 pre | 111 | 3.8333 | 0.67026 | ||||||
| post | 111 | 3.8446 | 0.53625 | ||||||
| −0.01126 | 0.58035 | −0.12043 | 0.09790 | −0.204 | 0.838 | ||||
| Group 3 pre | 105 | 4.0881 | 0.51653 | ||||||
| post | 105 | 3.9286 | 0.57566 | ||||||
| 0.15952 | 0.59860 | 0.04368 | 0.27537 | 2.731 | 0.007 | ||||
| Problem identification | |||||||||
| Group 1 pre | 106 | 3.2783 | 0.77791 | ||||||
| post | 106 | 3.3538 | 0.72692 | ||||||
| −0.07547 | 0.96558 | −0.26143 | 0.11049 | −0.805 | 0.423 | ||||
| Group 2 pre | 111 | 3.4640 | 0.77960 | ||||||
| post | 111 | 3.4955 | 0.69248 | ||||||
| −0.03153 | 0.76062 | −0.17460 | 0.11154 | −0.437 | 0.663 | ||||
| Group 3 pre | 106 | 3.8726 | 0.62129 | ||||||
| post | 106 | 3.6934 | 0.70566 | ||||||
| 0.17925 | 0.76591 | 0.03174 | 0.32675 | 2.409 | 0.018 | ||||
| Information analysis | |||||||||
| Group 1 pre | 106 | 3.6195 | 0.57171 | ||||||
| post | 106 | 3.4874 | 0.70699 | ||||||
| 0.13208 | 0.73848 | −0.01015 | 0.27430 | 1.841 | 0.068 | ||||
| Group 2 pre | 111 | 3.7447 | 0.71627 | ||||||
| post | 111 | 3.7297 | 0.60388 | ||||||
| 0.01502 | 0.62180 | −0.10195 | 0.13198 | 0.254 | 0.800 | ||||
| Group 3 pre | 106 | 4.0220 | 0.54872 | ||||||
| post | 106 | 3.8113 | 0.59986 | ||||||
| 0.21069 | 0.61088 | 0.09304 | 0.32834 | 3.551 | 0.001 | ||||
| Execution | |||||||||
| Group 1 pre | 106 | 3.7233 | 0.66424 | ||||||
| post | 106 | 3.5535 | 0.69142 | ||||||
| 0.16981 | 0.74783 | 0.02579 | 0.31383 | 2.338 | 0.021 | ||||
| Group 2 pre | 111 | 3.8228 | 0.66183 | ||||||
| post | 111 | 3.8048 | 0.63161 | ||||||
| 0.01802 | 0.63220 | −0.10090 | 0.13693 | 0.300 | 0.765 | ||||
| Group 3 pre | 106 | 3.9937 | 0.59269 | ||||||
| post | 106 | 3.8805 | 0.68265 | ||||||
| 0.11321 | 0.67281 | −0.01637 | 0.24278 | 1.732 | 0.086 | ||||
| Life-long learning | |||||||||
| Group 1 pre | 106 | 3.6840 | 0.65946 | ||||||
| post | 106 | 3.5283 | 0.66576 | ||||||
| 0.15566 | 0.75786 | 0.00971 | 0.30161 | 2.115 | 0.037 | ||||
| Group 2 pre | 111 | 3.6847 | 0.75431 | ||||||
| post | 111 | 3.7027 | 0.64975 | ||||||
| −0.01802 | 0.68234 | −0.14637 | 0.11033 | −0.278 | 0.781 | ||||
| Group 3 pre | 106 | 4.0896 | 0.58268 | ||||||
| post | 106 | 3.7901 | 0.75288 | ||||||
| 0.29953 | 0.67119 | 0.17026 | 0.42879 | 4.595 | <0.000 | ||||
| Total scale | |||||||||
| Group 1 pre | 106 | 3.6468 | 0.49657 | ||||||
| post | 106 | 3.5454 | 0.57674 | ||||||
| 0.10142 | 0.61106 | −0.01627 | 0.21910 | 1.709 | 0.090 | ||||
| Group 2 pre | 111 | 3.7314 | 0.63063 | ||||||
| post | 111 | 3.7365 | 0.52928 | ||||||
| −0.00507 | 0.51020 | −0.10104 | 0.09090 | −0.105 | 0.917 | ||||
| Group 3 pre | 105 | 4.0327 | 0.49404 | ||||||
| post | 105 | 3.8304 | 0.58558 | ||||||
| 0.20238 | 0.51206 | 0.10328 | 0.30148 | 4.050 | <0.000 | ||||
Furthermore, we used radar charts to compare the changes in the students’ self-evaluations of their core competencies between groups. The students in group 3 had higher self-evaluation scores for the core competencies than the students in the other groups, except for the execution competency. In Group 1, the most significant change was observed in the competency of execution. The changes in student scores were lowest in Group 2; only the problem identification competency score was significantly higher in Group 2 compared with Group 1 (see Figure 1 ).

The radar chart comparing the changes in the core competencies.
3.3. Predicted Changes in the Students’Sself-Evaluations of Their Core Competencies
The study questionnaire was administered twice to the same students, in 2013 and 2014. Thus, a GEE model was used to analyze the trends in the changes in the self-evaluated core competency scores between the three groups of nursing students over time. The mean changes in the total core competency scores between groups remained significantly different after controlling for the interaction effect between exposure (i.e., years of exposure to PBL) and group.
We found that the mean self-evaluated total competency score increased by 0.12 points at the post-test compared with the pre-test ( p = 0.038). Moreover, the mean total score (five competencies) for Group 3 significantly increased by 0.286 points compared with Group 1 ( p < 0.000), and the mean score of Group 2 also significantly increased by 0.199 points compared with Group 1 ( p = 0.006; Table 4 ).
Predictions of changes in the students’ self-evaluations of their core competencies (GEE model).
| Dependent Variable | Parameter | S.E. | 95% Wald C.I. | Wald X | -Value | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Learning attitude | Group 3 | 0.223 | 0.0783 | 0.070 | 0.377 | 8.141 | 0.004 |
| Group 2 | 0.159 | 0.0749 | 0.013 | 0.306 | 4.532 | 0.033 | |
| time 2 | 0.063 | 0.0665 | −0.067 | 0.193 | 0.899 | 0.343 | |
| Group 3 × time 2 | 0.084 | 0.0880 | −0.089 | 0.256 | 0.904 | 0.342 | |
| Group 2 × time 2 | −0.084 | 0.0865 | −0.254 | 0.085 | 0.949 | 0.330 | |
| Problem identification | Group 3 | 0.347 | 0.0954 | 0.160 | 0.534 | 13.226 | 0.000 |
| Group 2 | 0.134 | 0.0937 | −0.050 | 0.317 | 2.035 | 0.154 | |
| time 2 | −0.057 | 0.0917 | −0.237 | 0.122 | 0.392 | 0.531 | |
| Group 3 × time 2 | 0.259 | 0.1188 | 0.026 | 0.492 | 4.763 | ||
| Group 2 × time 2 | 0.040 | 0.1167 | −0.189 | 0.269 | 0.116 | ||
| Information analysis | Group 3 | 0.352 | 0.0873 | 0.181 | 0.523 | 16.260 | 0.000 |
| Group 2 | 0.264 | 0.0873 | 0.093 | 0.435 | 9.171 | 0.002 | |
| time 2 | 0.151 | 0.0705 | 0.013 | 0.290 | 4.605 | 0.032 | |
| Group 3 × time 2 | 0.048 | 0.0911 | −0.131 | 0.226 | 0.276 | 0.600 | |
| Group 2 × time 2 | −0.136 | 0.0917 | −0.316 | 0.044 | 2.193 | 0.139 | |
| Execution | Group 3 | 0.294 | 0.0907 | 0.116 | 0.471 | 10.480 | 0.001 |
| Group 2 | 0.253 | 0.0855 | 0.085 | 0.421 | 8.739 | 0.003 | |
| time 2 | 0.175 | 0.0707 | 0.037 | 0.314 | 6.142 | 0.013 | |
| Group 3 × time 2 | −0.024 | 0.0957 | −0.211 | 0.164 | 0.061 | 0.805 | |
| Group 2 × time 2 | −0.160 | 0.0924 | −0.341 | 0.021 | 3.002 | 0.083 | |
| Life-long learning | Group 3 | 0.262 | 0.0943 | 0.077 | 0.446 | 7.697 | 0.006 |
| Group 2 | 0.183 | 0.0863 | 0.014 | 0.352 | 4.506 | 0.034 | |
| time 2 | 0.167 | 0.0724 | 0.025 | 0.309 | 5.339 | 0.021 | |
| Group 3 × time 2 | 0.157 | 0.0971 | −0.033 | 0.347 | 2.609 | 0.106 | |
| Group 2 × time 2 | −0.190 | 0.0969 | −0.379 | 0.000 | 3.824 | 0.051 | |
| Total scale | Group 3 | 0.286 | 0.0766 | 0.136 | 0.436 | 13.902 | 0.000 |
| Group 2 | 0.199 | 0.0719 | 0.058 | 0.340 | 7.683 | 0.006 | |
| time 2 | 0.120 | 0.0580 | 0.006 | 0.234 | 4.291 | 0.038 | |
| Group 3 × time 2 | 0.103 | 0.0774 | −0.049 | 0.254 | 1.758 | 0.185 | |
| Group 2 × time 2 | −0.131 | 0.0755 | −0.278 | 0.017 | 2.993 | 0.084 | |
Note: Group 1: Freshman students in 2013, Sophomore students in 2014. Group 2: Sophomore students in 2013; Junior students in 2014. Group 3: Junior students in 2013; Senior students in 2014.Time 1: 2013 data collection; time 2: 2014 data collection. Reference group: 1 = Group 1; 2 = time 1; 3 = Group 3 × time 1; 4 = Group 2 × time 1.
The students’ mean post-test scores for the competency information analysis, execution, and life-long learning increased by 0.151–0.175 points compared with the pre-test score ( p = 0.013–0.032). In addition, the mean score of Group 3 for these competencies significantly increased by 0.262–0.352 points compared with Group 1 ( p < 0.000–0.006), and the mean score of Group 2 significantly increased by 0.183–0.264 points compared with Group 1 ( p = 0.002–0.034; Table 4 ).
However, after controlling for the interaction of exposure and group, there were no significant differences between the mean pre-and post-test scores for the competencies of learning attitude and problem identification ( p = 0.154–0.343). However, the mean learning attitude score of Group 3 significantly increased by 0.223 points compared with Group 1 ( p = 0.004), and the mean learning attitude score of Group 2 significantly increased by 0.159 points compared with Group 1 ( p = 0.033). However, the mean problem identification competency score was only significantly different between Group 3 compared with Group 1, with an increase of 0.347 points in Group 3 ( p < 0.000; Table 4 ).
4. Discussion
The study aimed to explore the effects of PBL strategies on nursing students’ self-evaluation of core competencies. Nursing educators needed to evaluate the effects of PBL teaching strategies on students. These study results would help nursing educators develop curricula and improve teaching strategies. We found that the students with the longest exposure to PBL (Group 3) had more significant improvements in their self-evaluation scores for all competencies than the shorter exposure groups (groups 1 and 2). Thus, this study demonstrates that nursing students’ self-evaluations of their core competencies improved each grade, which indicates PBL strategies effectively help students build core competencies. The PBL model advocates that a paradigm shift is required in nursing education [ 3 ]. Yet, despite the number of teaching experiences reported to date with PBL, almost no studies in Taiwan have assessed self-evaluations of the core competencies of students educated using this strategy. Most research has focused on the impact of PBL on individual capabilities, including critical thinking [ 29 , 31 ], problem-solving [ 26 ], and metacognitive awareness [ 31 ]. Other studies have focused on learner satisfaction [ 32 , 33 ]. This study found that nursing students studying a PBL curriculum gradually improved their total core competencies as their exposure to PBL increased. Specifically, our study shows that students’ execution and life-long learning competencies were improved by the end of the sophomore year. In addition, the students’ self-evaluations of the learning attitude, problem identification, and information analysis competencies were significantly improved by the end of their junior year. Researchers have indicated that the PBL strategy encourages students to discuss and cooperate to solve problems through self-directed study [ 21 , 28 , 34 ]. Cultivation of these abilities is necessary to accumulate knowledge and, combined with exposure to clinical situations, prepare nursing students to adapt to the reality of the workplace [ 3 , 28 ].
Learning strategies are essential components of a curriculum and could help students to learn more efficiently and effectively [ 13 ]. In addition, new learning strategies should emerge spontaneously to address the increasingly complex clinical environment and rapidly changing clinical patient problems [ 30 , 35 ]. Therefore, PBL strategies are one option [ 10 , 36 ]. Many studies have recently discussed the effectiveness of this learning strategy in health discipline educational programs [ 6 ]. However, how students self-evaluate their development of core competencies in nursing education was poorly understood [ 37 ]. Therefore, more research from the perspective of nursing students’ self-evaluations of their progression in terms of core competencies is necessary to confirm the effectiveness of PBL strategies [ 37 , 38 ]. This study showed that exposure to PBL strategies improved the students’ self-evaluations of their core competencies, and the differences between grades and individual progression between years were significant.
Research has indicated that the strengths of PBL include its ability to promote the integration of knowledge, problem-solving skills, critical thinking skills, group collaboration, and self-autonomous learning [ 13 , 30 , 39 ]. Our students experienced a series of PBL teaching courses and their self-evaluation scores revealed that PBL increased the students’ perceptions of their core competencies. The improvements in the information analysis, execution, and life-long learning competencies were directly proportional to the grade of the students, and hence the duration of their exposure to PBL. However, the scores for the core competencies of learning attitude and problem identification only increased significantly after the junior year, indicating that the PBL teaching strategy could lead to the accumulation of skills, especially in the learning attitude and problem identification competencies. Thus, the results of this study show that PBL teaching provides a strategy that allows students to become self-directed learners and cooperate with other members of a team. The benefits of the PBL teaching strategy were previously demonstrated by students’ responses in three areas of cognitive, emotional, and social skills [ 40 ].
Despite PBL being widely used in professional healthcare courses, few studies have assessed the effectiveness of PBL using specific instruments. Most studies have only assessed outcomes based on qualitative data [ 27 , 28 ], students’ ability to perform a single skill [ 3 , 5 , 41 ], learner satisfaction [ 12 , 42 ], or evaluations by faculty or the academic performance of students [ 30 , 43 ]. The present study used an instrument to assess the effectiveness of PBL by measuring nursing students’ self-evaluation of their competency in five domains: learning attitude, problem identification, information analysis, execution, and life-long learning. Thus, in contrast to other studies that only assessed a single ability or where only faculty evaluation of students’ performance was used, our study represents a more comprehensive program evaluation method that includes both faculty evaluation and students’ self-assessment.
Overall, this study indicates PBL has cumulative effects on core competencies as nursing students progress through their academic years. Therefore, teaching strategies could be designed according to the grade and maturity of students, as well as the sequence of formation of core competencies. PBL teaching strategies can provide students with experience of actual cases and promote deep self-learning and the development of core competencies. Using this approach, nursing students will be able to adapt to the changing clinical environment of the future and solve diverse health problems.
5. Conclusions
This study highlights the ability of PBL strategies to promote the development of core competencies in an undergraduate nursing course. Therefore, PBL appears to have a favorable effect on nursing education. The differences in the self-evaluation scores between groups indicate PBL strategies effectively improve nursing students’ core competencies. The students with the longest exposure to PBL had higher self-evaluation scores than the other groups, especially for competency information analysis, execution, and life-long learning. The difference in progress between groups was most obvious in Group 3, which suggests that a PBL curriculum design has a cumulative effect on students’ development of core competencies.
However, this study only sampled students studying at a single school using the same curriculum and measured the student’s self-evaluations of their core competencies using a single questionnaire. Thus, the results of this study may not be generalizable to other schools or curricula. Consequently, it is necessary to expand this curricular design to other schools and assess a larger sample size to evaluate the effectiveness of PBL teaching strategies and further research is recommended to confirm the reliability and validity of the core competency measurement tool used in this study. A follow-up outcome study will be conducted to examine the long-term effects of PBL on the core competencies of graduates. We believe that extending the time for data collection would enable an analysis of the trajectory of the long-term effects and provide more specific data on the effectiveness of PBL.
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization, S.-H.L., H.-L.C. and C.-P.K.; methodology, S.-H.L., M.-Y.H. and C.-P.K.; investigation, F.-F.S., P.-C.L. and C.-Y.H. (Ching-Yen Hung); writing—original draft, C.-Y.H. (Cheng-Yi Huang) and H.-L.C.; writing—review & editing, Y.-C.A.L.; project administration, Y.-C.A.L. and W.-J.Y. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the Chung Shan Medical University guidelines and approved by the Chung Shan Medical University Hospital Institutional Review Board (No: CS2-21113).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Two Examples of How I Used Critical Thinking to Care for my Patient (Real Life Nursing Stories) | NURSING.com

What are you struggling with in nursing school?
NURSING.com is the BEST place to learn nursing. With over 2,000+ clear, concise, and visual lessons, there is something for you!
Critical Thinking on the Nursing Floor
Critical thinking can seem like such an abstract term that you don’t practically use. However, this could not be farther from the truth. Critical thinking is frequently used in nursing. Let me give you a few examples from my career in which critical thinking helped me take better care of my patient.
The truth is, that as nurses we can’t escape critical thinking . . . I know you hate the word . . . but let me show you how it actually works!
Critical Thinking in Nursing: Example 1
I had a patient that was scheduled to go to get a pacemaker placed at 0900. The physician wanted the patient to get 2 units of blood before going downstairs for the procedure. I administered it per protocol. About 30 minutes after that second unit got started, I noticed his oxygen went from 95% down to 92% down to 90%. I put 2L of O2 on him and it came up to 91%. But it just sort of hung around the low 90s on oxygen.
I stopped. And thought. What the heck is going on?
I looked at his history. Congestive heart failure.
I looked at his intake and output. He was positive 1.5 liters.
I thought about how he’s got extra fluid in general, and because of his CHF, he can’t really pump out the fluid he already has, let alone this additional fluid. Maybe I should listen to his lungs..
His lungs were clear earlier. I heard crackles throughout both lungs.
OK, so he’s got extra fluid that he can’t get out of his body. What do I know that will get rid of extra fluid and make him pee? Maybe some Lasix?
I ran over my thought process with a coworker before calling the doc. They agreed. I called the doc and before I could suggest anything, he said “Give him 20 mg IV Lasix one time, and I’ll put the order in.” CLICK.
I gave the Lasix. He peed like a racehorse (and was NOT happy with me for making that happen!). And he was off of oxygen before he went down to get his pacemaker.
Badda Bing Bada Boom!
Critical Thinking in Nursing: Example 2
My patient just had her right leg amputated above her knee. She was on a Dilaudid PCA and still complaining of awful pain. She maxed it out every time, still saying she was in horrible pain. She told the doctor when he rounded that morning that the meds weren’t doing anything. He added some oral opioids as well and wrote an order that it was okay for me to give both the oral and PCA dosings, with the goal of weaning off PCA.
“How am I going to do that?” I thought. She kept requiring more and more meds and I’m supposed to someone wean her off?
I asked her to describe her pain. She said it felt like nerve pain. Deep burning and tingling. She said the pain meds would just knock her out and she’d sleep for a little while but wake up in even worse pain. She was at the end of her rope.
I thought about nerve pain. I thought about other patients that report similar pain. Diabetics with neuropathy would talk about similar pain… “What did they do for it? ” I thought. Then I remembered that many of my patients with diabetic neuropathy were taking gabapentin daily for pain.
“So if this works for their nerve pain, could it work for a patient who has had an amputation?” I thought.
I called the PA for the surgeon and asked them what they thought about trying something like gabapentin for her pain after I described my patient’s type of pain and thought process.
“That’s a really good idea, Kati. I’ll write for it and we’ll see if we can get her off the opioids sooner. ”
She wrote for it. I gave it. It takes a few days to really kick in and once it did, the patient’s pain and discomfort were significantly reduced. She said to get rid of those other pain meds because they “didn’t do a damn thing,” and to “just give her that nerve pain pill because it’s the only thing that works”.
And that we did!
She was able to work with therapy more because her pain was tolerable and was finally able to get rest.
What the HELL is Critical Thinking . . . and Why Should I Care?
What your nursing professor won’t tell you about critical thinking .
by Ashely Adkins RN BSN
When I started nursing school, I remember thinking, “how in the world am I going to remember all of this information, let alone be able to apply it and critically think?” You are not alone if you feel like your critical thinking skills need a little bit of polishing.
Let’s step back for a moment, and take a walk down memory lane. It was my first semester of nursing school and I was sitting in my Fundamentals of Nursing course. We were learning about vital signs, assessments, labs, etc. Feeling overwhelmed with all of this new information (when are you not overwhelmed in nursing school?), I let my mind wonder to a low place…
Am I really cut out for this? Can I really do this? How can I possibly retain all of this information? Do they really expect me to remember everything AND critically think at the same time?
One of my first-semester nursing professors said something to me that has stuck with me throughout my nursing years. It went a little something like this:
“Critical thinking does not develop overnight . It takes time. You don’t learn to talk overnight or walk overnight. You don’t learn to critically think overnight .”
My professor was absolutely right.
As my journey throughout nursing school, and eventually on to being a “real nurse” continued, my critical thinking skills began to BLOSSOM. With every class, lecture, clinical shift, lab, and simulation, my critical thinking skills grew.
You may ask…how?
Well, let me tell you…
- Questioning
These are the key ingredients to growing your critical thinking skills.
Time. Critical thinking takes time. As I mentioned before, you do not learn how to critically think overnight. It is important to set realistic expectations for yourself both in nursing school and in other aspects of your life.
Exposure. It is next to impossible to critically think if you have never been exposed to something. How would you ever learn to talk if no one ever talked to you? The same thing applies to nursing and critical thinking.
Over time, your exposure to new materials and situations will cause you to think and ask yourself, “why?”
This leads me to my next point. Questioning. Do not be afraid to ask yourself…
“Why is this happening?”
“Why do I take a blood pressure and heart rate before I give a beta-blocker?”
“Why is it important to listen to a patient’s lung sounds before and after they receive a blood transfusion?”
It is important to constantly question yourself. Let your mind process your questions, and discover answers.
Confidence. We always hear the phrase, “confidence is key!” And as cheesy as that phrase may be, it really holds true. So many times, we often times sell ourselves short.
YOU KNOW MORE THAN YOU THINK YOU KNOW.
In case you did not catch it the first time…
Be confident in your knowledge, because trust me, it is there. It may be hiding in one single neuron in the back of your brain, but it is there.
It is impossible to know everything. Even experienced nurses do not know everything.
And if they tell you that they do…they are wrong!
The key to critical thinking is not about knowing everything ; It is about how you respond when you do not know something .
How do you reason through a problem you do not know the answer to? Do you give up? Or do you persevere until you discover the answer?
If you are a nursing student preparing for the NCLEX, you know that the NCLEX loves critical thinking questions. NRSNG has some great tips and advice on critical thinking when it comes to taking the NCLEX .
There are so many pieces to the puzzle when it comes to nursing, and it is normal to feel overwhelmed. The beauty of nursing is when all of those puzzle pieces come together to form a beautiful picture.
That is critical thinking.
Critical thinking is something you’ll do every day as a nurse and honestly, you probably do it in your regular non-nurse life as well. It’s basically stopping, looking at a situation, identifying a solution, and trying it out. Critical thinking in nursing is just that but in a clinical setting.
We’ve written a MASSIVE lesson on Care Plans and Critical Thinking :
Mastering The COPD Nursing Care Plan in Just 10 Minutes!
Renal Failure Pt Care
4 "real world" examples of using clinical judgement to figure out what to do first as a nurse | nursing.com, 12 study tips for how to study for pharmacology in nursing school | nursing.com, similar blog posts.

Critical Thinking and Nursing Care Plans Go Together Like Chicken and Waffles | NURSING.com

Patients We Will Never Forget | NURSING.com

Stress Overload Nursing Diagnosis and Care Plan | NURSING.com
Learning Materials
- Business Studies
- Combined Science
- Computer Science
- Engineering
- English Literature
- Environmental Science
- Human Geography
- Macroeconomics
- Microeconomics
- Problem Solving in Nursing Management
Dive deep into the multifaceted world of nursing management with a special focus on problem-solving. This comprehensive guide presents a detailed look at the process, importance, and challenges of problem-solving in nursing management. By highlighting essential skills, neurologically based frameworks, and the relationship with decision-making, it offers both theoretical understanding and practical solutions. Explore real-life case studies, leadership's role, and the link with critical thinking. This is an enriching journey towards developing strategic competencies and achieving effective problem-solving in a vital healthcare sector.
Create learning materials about Problem Solving in Nursing Management with our free learning app!
- Instand access to millions of learning materials
- Flashcards, notes, mock-exams and more
- Everything you need to ace your exams
Millions of flashcards designed to help you ace your studies
- Cell Biology
What do the algorithm-based and intuition-driven approaches to problem-solving in nursing management entail?
What is the first stage of problem solving in nursing practice?
What is problem solving in nursing management and how is it different from decision making?
What is the relationship between critical thinking and problem solving in nursing?
What is the final stage of problem solving in nursing practice?
What is the significance of problem-solving in nursing management?
What are the key skills required for effective problem-solving in nursing management?
How can critical thinking skills be enhanced for effective problem solving in nursing management?
What are the key steps involved in the problem-solving process in nursing management?
What does the neurological framework in nursing management involve?
What is decision making in nursing management?
Review generated flashcards
to start learning or create your own AI flashcards
Start learning or create your own AI flashcards
- Clinical Placement
- Human Anatomy
- Intensive Care Nursing
- Mental Health Nursing
- Nursing Management
- Antimicrobial Stewardship
- Audit Compliance Nursing
- Billing Practices for Hospitals
- Biohazard Management
- Budget Management
- Budget Planning
- Capital Resources
- Care Evaluation
- Clinical Pathways
- Communication Skills
- Crisis Management
- Customer Service in Nursing
- Delegation of Nurses
- Disinfection Techniques
- Emergency Drills
- Emergency Preparedness
- Expense Management
- Financial Management in Nursing
- Fiscal Responsibility
- HIPAA Compliance
- Hazard Identification
- Healthcare Technology
- Hospital Asset Management
- Hospital Contract Negotiation
- Hospital Funding Sources
- Hospital Revenue Cycle
- Hygiene Protocols
- Insurance Relations Hospitals
- Interdisciplinary Team
- Labor Relations
- Nurse Staff Training
- Nursing Data Analysis
- Nursing Grant Writing
- Nursing Scheduling
- Operational Efficiency
- Patient Flow
- Patient Loyalty
- Reimbursement Strategies
- Retention Strategies
- Revenue Generation
- Sanitation Practices
- Staff Development
- Staffing Models
- Staffing in Nursing
- Stakeholder Engagement
- Strategic Planning in Nursing
- Time Management
- Waste Disposal in Hospital
- Worker Safety
- Workforce Planning
- Workplace Harmony
- Nursing Theories
- Types of Nursing
Understanding Problem Solving in Nursing Management
Problem solving in nursing management is a crucial process that you need to grasp as a prospective or current nurse. This involves using a logical, systematic approach to resolving issues encountered in a nursing environment, focusing on maintaining quality patient care .
Problem Solving: This is identifying and overcoming obstacles to achieving a goal. In nursing, this generally revolves around improving patient health outcomes and ensuring efficient healthcare facility operations.
Importance of Problem Solving in Nursing Management
Nursing professionals are constantly faced with intricate issues that require decisive and effective solutions. The ability to implement problem-solving is crucial in maintaining optimal patient care , operational efficiency , and fostering team collaboration.
For instance, suppose a sudden shortage of resources like catheters or syringes is experienced in a healthcare facility. In such a case, the nursing manager will need to swiftly solve the problem either by reallocating resources, timely ordering supplies, or finding a temporary alternative, ensuring the patients' needs are continually met.
Key Skills Required for Problem Solving in Nursing Management
Effective problem-solving in nursing management is anchored on a set of key skills. These abilities equip you to navigate complex situations and formulate impactful solutions. They include:
- Critical Thinking: This is your ability to analyse situations in detail and understand their implications.
- Decisiveness: The readiness to make important decisions swiftly and confidently.
- Communication: Sharing and receiving information clearly and effectively.
- Collaboration: Working effectively as part of a team.
These skills are interconnected. For example, your ability to think critically informs your decisiveness. Your decisions are then made clear to your team through effective communication, and together, through collaboration, the problem is solved.
Common Challenges in Problem Solving in Nursing Management
In your nursing management journey, you will come across multiple challenges when attempting to solve problems. These obstacles might occur due to several factors, such as resource limitations, personnel issues, and complex patient needs .
| Resource Constraints | Shortage of essential medical supplies or understaffing. |
| Personnel Issues | Conflicts among team members or unforeseen absence of staff. |
| Complex | Patients with rare medical conditions that require specialized care. |
While these challenges can be daunting, equipping yourself with robust problem-solving skills will help you navigate these complications and maintain high standards of patient care.
Scrutinising the Problem Solving Process in Nursing Management
Delving deeper into the problem-solving process in nursing management, you get to navigate its intricacies and mechanisms. This exploration can bolster your abilities to resolve complex situations in your nursing career.
Steps involved in the Problem Solving Process
Problem-solving in nursing management is a multifaceted task that often involves several steps. To understand how to tackle issues expertly, you will need a clear understanding of each stage.
Problem-Solving Process: A systematic approach used to address complications and make decisions. In nursing, it’s composed of several steps, each essential to the resolution of issues.
Here are the key steps:
- Identification: In this stage, you recognise the existence of a problem. It is essential to understand the barriers to your goals and spotlight areas that require improvement.
- Definition: You clearly articulate the problem. By understanding its nuances, magnitude, and implications, you can efficiently tailor a solution.
- Analysis: This involves examining the problem closely from different perspectives, which includes understanding the cause and effect, stakeholders involved, and potential impacts.
- Development of Solutions: Here you brainstorm possible solutions. It's essential to contemplate multiple alternatives to ensure the most effective resolution is chosen.
- Decision Making: In this step, you select the best solution based on the gathered information and analysis. Considerations may include effectiveness, resources needed, and potential side effects.
- Implementation: You put the chosen solution into action, carefully monitoring its effectiveness and making necessary adjustments.
- Evaluation: Finally, you assess the outcome. This helps to determine the effectiveness of your solution and informs future problem-solving efforts.
Neurological Framework for Problem Solving in Nursing Management
Many problem-solving methods exist, but one valuable perspective is through understanding the neurological framework in nursing management. This biological approach delves into how your brain processes information and develops solutions.
Neurological Framework: A biological perspective that explains how a nurse's brain processes, analyses, and responds to problems encountered in the nursing environment.
This framework refers to cognitive processes which involve:
- Critical thinking: This involves actively and skillfully conceptualising, applying, analysing, and evaluating information gathered from observation, experience, reflection, or communication.
- Decision making: This is the cognitive process of selecting a course of action from multiple possibilities. It's based on both intuition and logical reasoning.
- Problem-solving: This involves overcoming hurdles and finding a conclusion, and it usually includes decision-making. It involves creativity and critical thinking to arrive at effective solutions.
Role of Creativity in the Problem Solving Process
Nursing management often involves complex and unique problems. To effectively tackle these challenges, it's crucial to breed creativity in the problem-solving process.
Imagine there's a sudden surge in patient intake due to a local health crisis, resulting in a bed shortage. A creative solution might be to convert other non-critical spaces such as conference rooms temporarily into patient monitoring units, thereby managing the surge effectively.
Importance of Team Collaboration in the Problem Solving Process
In a nursing environment, you are not working in isolation. Collaboration is a critical aspect of problem-solving in nursing management, as diverse insights can lead to innovative and effective solutions.
Consider a scenario where there's a need to implement a new system for managing patient records. To effectively solve potential issues in system implementation, you might need input from various team members including nursing staff, IT specialists, and data management experts. Each member's contribution, based on their expertise and perspective, is crucial in charting a comprehensive problem-solving strategy, ensuring the successful implementation and integration of the new system.
Decision Making and Problem Solving in Nursing Management
Decision making and problem-solving are two interconnected aspects in the realm of nursing management. Understanding their correlation and distinctiveness is key to effectively managing issues and improving patient outcomes in a healthcare setting.
The Interplay between Decision Making and Problem Solving
The connection between decision making and problem solving in nursing management is truly significant. In almost every situation where a problem arises, decision making is an inseparable component of the problem-solving process.
Decision Making in Nursing: This involves selecting a course of action from different alternatives. It is the bridge connecting problem analysis with implementing solutions, and it requires evaluation of information, predicaments, and possible outcomes.
Once you have identified and defined a problem, analysed it, and developed potential solutions, the next step involves decision making. This is where you select the most suitable solution among the alternatives.
For instance, if you are dealing with a bed shortage problem in your healthcare facility, some possible solutions could be outsourcing to other healthcare facilities, using other spaces such as conference rooms as makeshift wards, or deploying portable hospital beds.
Each of these solutions has its pros and cons, and it's here that decision-making skills come into play. You'll need to compare and contrast each option, considering factors like cost, time, resources available, and the overall impact on patient care. The chosen solution is then implemented, and the effects are evaluated for future reference.
Distinguishing Decision Making from Problem Solving in Nursing Management
Though inherently connected, problem solving and decision making are distinct processes within nursing management. Where problem-solving is a comprehensive process that entails identifying, analysing, and solving issues, decision making is a component nested within this process, acting as the transition point from analysis to action.
Problem Solving in Nursing: This is a broader process involving the identification of an issue or obstacle, systematic analysis to understand it, devising potential solutions, choosing the most suitable through decision making, implementing it, and finally reviewing the effectiveness of the implemented solution.
Consider a real-life scenario such as medication errors. If these errors are occurring frequently in your healthcare setup, the problem-solving process will involve identifying the issue (increased medication errors), defining and analysing it (finding the root causes, such as miscommunication or system glitches). This would then lead to brainstorming potential solutions, like improved communication systems or enhanced employee training. The decision-making process would then come into play when choosing the best solution to implement.
Techniques for Effective Decision Making in Problem Solving Scenarios
Effective decision making underpins successful problem solving in nursing management. Implementing the right techniques can enhance your decision-making process, thus leading to more effective problem resolution.
Some proven techniques include:
- Pros and Cons Analysis: List the advantages and disadvantages of each solution to help you visualise the impacts of each decision.
- Decision Matrix: Establish criteria and rate potential solutions. The choice with the highest score is then considered the best decision.
- Cost-Benefit Analysis: Determine the financial implication of each decision and compare it to the benefits. Solutions with a high benefit-cost ratio are preferred.
Working collaboratively to brainstorm and analyse solutions promotes critical thinking and creativity, ensuring that the chosen solution maximises the use of resources and improves patient outcomes .
In unavoidable circumstances where decisions have to be made rapidly and with limited information, using intuition, a nurse's experience, and insights combined with analytical thinking can be beneficial. This is where the balanced blend of clinical expertise and effective risk-taking come into play.
Decision making is never static in nursing management. The cyclic nature of the decision-making process, where outcomes of decisions are continually assessed and feedback is used to improve future decision making, showcases its dynamic and iterative nature. This reinforces the vital role decision making plays in the problem-solving process.
Unpacking Examples of Problem Solving in Nursing Management
By exploring various examples and case studies, you gain a practical view of problem-solving in nursing management. These insights can better equip you to tackle real-life challenges in a healthcare setting.
Case Study Analysis of Problem Solving Scenarios
Case studies provide a thorough view of how problem-solving strategies are applied in various nursing management scenarios. Analysing such cases exposes you to diverse methods and solutions and encourages you to think critically and innovatively.
Case Study Analysis: A detailed examination of a particular instance or event to draw conclusions, develop solutions, or learn from the situation.
Let's investigate a case concerning patient waiting times. In a healthcare facility, it is observed that patients often have to wait for prolonged periods to receive care, leading to dissatisfaction and affecting the overall quality of service. The problem-solving steps might look like this:
- Identification and Definition: The problem is identified as long patient waiting times. It is defined as patients waiting more than 45 minutes to receive care.
- Analysis: The cause of the problem is found to be a shortage of nursing staff during peak hours.
- Development of Solutions: Several possible solutions emerge, such as recruiting additional staff, offering overtime to existing staff, or streamlining operational processes to reduce inefficiencies.
- Decision Making: After careful analysis, it is decided to hire additional part-time staff to handle peak hours.
- Implementation: The recruitment process is initiated and new members integrated into the team.
- Evaluation: After a few months, waiting times are reassessed. A significant reduction is observed, confirming the effectiveness of the solution.
Case study analysis provides a rich source of knowledge and transferable insights that can be helpful in similar or entirely different scenarios. Drawing parallels from varying contexts and understanding how solutions are adapted to unique situations helps bolster your problem-solving skills and adaptability in nursing management.
Varied Approaches to Problem Solving in Different Nursing Scenarios
Different nursing scenarios call for diverse problem-solving strategies. Understanding the varying approaches, from algorithm-based to intuition-driven, equips you to manage multidimensional and intricate issues effectively.
Algorithm-based Approach: This involves following a clearly defined set of rules or procedures to solve a problem. It can be applicable in situations with defined parameters and scope, such as diagnosing a health condition based on a specific set of symptoms.
Intuition-driven Approach: This combines a nurse's experience, knowledge, and instinct to solve a problem. It applies to ambiguous scenarios where conventional rules may not be applicable, such as managing a patient's fear or anxiety.
Problem-solving in nursing management is all about adapting to the environment and the situation. The right approach may vary, calling for flexibility, creativity, critical thinking, and a deep understanding of the issue for successful resolution.
Real Life Applications of Problem Solving Strategies in Nursing Management
The real world of nursing is complex and dynamic, and various problem-solving strategies can apply on any given day. To navigate smoothly, you need to understand how the various approaches can be adapted to specific situations.
Consider solving a recurrent communication issue within your nursing team. The algorithmic approach might involve establishing clear communication protocols or using digital tools to streamline interaction. However, the intuition-driven approach might involve informal team-building meetings to foster better personal connections. In this situation, the best solution might be a blend of the two approaches to ensure both procedural clarity and improved team relationships.
The key takeaway here is that there is no "one-size-fits-all" solution in nursing management. Problem-solving requires flexibility, openness, and the ability to judge which strategy will perform best in a particular scenario.
Exploring Nursing Management Problem-Solving Strategies
Problem-solving strategies in nursing management form the backbone of effective healthcare services. By ensuring that nursing personnel can tackle issues with aplomb and proficiency, these strategies contribute significantly to patient satisfaction and positive outcomes.
Development of Strategic Problem-Solving Competencies
The first step towards demystifying problem-solving processes in nursing management is the development of strategic problem-solving competencies. The journey from novice to expert involves honing these skills and integrating them into your practical work.
Strategic Problem-Solving Competencies: These are a set of core skills that facilitate effective problem-solving in nursing management, including critical thinking, innovative thinking, collaboration, adaptability, leadership, and decision-making.
Acquiring these skills involves both academic learning and practical experiences. Gaining theoretical knowledge lays the foundation, while integrating this knowledge within a clinical context enriches and refines these competencies.
- Critical Thinking: This involves analysing situations from multiple perspectives, evaluating different solutions, and making informed decisions.
- Innovative Thinking: Innovative thinking pertains to thinking outside the box, especially when conventional solutions are inadequate.
- Collaboration: In nursing, effective problem-solving often requires collaborative efforts, valuing diverse ideas and working towards common goals.
- Adaptability: Healthcare settings are continually changing, and the ability to swiftly adapt to new situations is crucial.
- Leadership: Good leadership skills facilitate effective management of teams and ensuring that everyone is following the established problem-solving process.
- Decision Making: Ability to implement effective decisions is vital for successful problem solving.
Role of Leadership in Implementing Problem Solving Strategies
The role of leadership in implementing problem-solving strategies must not be understated. Effective leadership not only guides teams through problem-solving processes but also fosters a supportive environment where team members feel safe to contribute ideas and question assumptions.
Leadership in Nursing: This involves guiding, motivating, and supporting nursing staff to deliver quality healthcare services. Also, it encompasses enhancing team cooperation, improving communication, and fostering a culture of continuous learning.
Leadership employs a variety of approaches in implementing problem-solving strategies. Different leadership styles can be applied based on the nature of the problem and the team dynamics. Transformational leadership, for instance, inspires others to exceed their personal goals and work for a collective purpose. On the other hand, participative leadership encourages open discussions and collective decision-making, promoting a more inclusive and democratic problem-solving process.
Leadership is also instrumental in creating an environment that encourages the sharing of problems openly, without fear of judgment, hence facilitating early identification and efficient resolution of issues. By also ensuring that learning opportunities are provided to enhance team problem-solving capabilities, leadership positively influences problem-solving outcomes.
Use of Resources in Problem Solving Strategies
Effective resource utilization is a critical component of successful problem-solving strategies in nursing management. The term 'resources' in this context includes human resources such as nursing staff and doctors, as well as material resources like medical supplies, equipment, and facilities.
Resource Utilisation: This refers to the efficient and effective use of available resources to achieve desired outcomes. In nursing, it involves ensuring that staff, equipment, and supplies are optimally used to deliver quality healthcare services and solve arising problems.
Problem-solving often necessitates the optimal use of available resources. For example, if there is an issue of high patient-to-nurse ratio, one of the possible solutions could be redistributing nursing staff according to workload and patient needs, or hiring additional staff if finances permit.
Every solution should be weighed based on its resource implications. The best solution is often the one that optimally utilises available resources to provide the maximum benefit. For example, while hiring additional staff might solve the problem, it might not be the best solution if the budget is very limited. In such a case, reallocation of existing staff may be a more practical solution.
Similarly, if there is a shortage of a particular supply, then alternatives may need to be sought, or rationing implemented. A critical analysis of such situations is necessary to ensure that the solutions proposed and implemented do not create other problems related to resource allocation and use.
It's also important to remember to continuously evaluate the impact of your solutions on resource utilisation. This will not only help you ensure sustainable use of resources but also contribute to continuous improvement in problem-solving strategies.
Understanding the stages of problem-solving in nursing practice is fundamental to addressing various challenges that arise in the healthcare sector. These problem-solving stages enable you to identify issues, create and implement solutions, and review the outcomes for improvement purposes.
Initial Assessment and Identification: The First Stage of Problem Solving
The initial phase of problem-solving in nursing management involves the assessment and identification of the issue at hand. This stage is critical as the correct identification of the problem lays the foundation for effective solution design and implementation.
Initial Assessment: This is the preliminary evaluation of the situation, leading to the recognition of existing problems. This stage involves observation, questioning, and data gathering to understand the issue better.
This initial step requires keen observation skills and critical thinking. While observation helps in gathering relevant details, critical thinking enables you to scrutinize this information and identify potential problems. You could also use feedback from your team and other relevant stakeholders to gain a comprehensive understanding of the issue.
For instance, suppose you discover unusually high levels of patient discomfort during specific hours. The initial assessment might involve examining patient records during these hours, observing nursing practices in these time frames, and seeking feedback from both patients and nursing staff. This comprehensive approach could potentially reveal the issue, like a shortage of staff during peak hours, leading to delayed or inefficient care.
Formulating Actionable Solutions: The Mid Stages of the Problem-solving Process
Once the problem is identified, the next phase is generating actionable solutions. The validity and effectiveness of these solutions significantly influence the problem-solving process's success, thus necessitating careful deliberation and thorough evaluation.
Actionable Solution: A practical, feasible strategy that can be implemented to resolve the problem. It's typically developed through brainstorming, analysis, and evaluation of various alternatives.
The process of formulating actionable solutions involves brainstorming potential remedies, evaluating these against a set criteria, and choosing the most viable option. Ideally, this should be a collaborative effort involving all relevant stakeholders. Collaborative problem-solving encourages diversity in ideas and promotes inclusivity.
| Careful Analysis | Evaluation Against Set Criteria | Choosing Viable Option |
| Gather as many potential solutions as possible through brainstorming sessions | Evaluate potential solutions based on criteria such as feasibility, efficiency, and impact | The most suitable solution is chosen after careful evaluation |
Innovation is a key driver in formulating actionable solutions. Traditional problem-solving methods might fail in the face of complex or unique problems, necessitating innovative ideas. Remember, the most effective solutions often result from 'thinking outside the box'.
Evaluation and Reflection: The Final Stage of Problem Solving
The final stage of problem-solving is evaluation and reflection. After implementing the chosen solution, it is essential to assess its effectiveness in solving the identified problem. This stage offers an opportunity to learn from the implemented action and make necessary adjustments for future improvement.
Evaluation and Reflection: This stage involves reviewing the implemented solution to assess its effectiveness. Reflection involves learning from the process and experiences to ensure continuous improvement.
To achieve meaningful evaluation and reflection, a systematic approach must be adopted. Begin with the assessment of the effect of the solution on the original problem. Have the waiting times reduced following the staff adjustments? Is there an improved level of patient comfort? These are the kind of questions you need to address.
Following the evaluation, it's crucial to reflect on the entire process. Consider what worked well and what didn't. Reflecting on these experiences offers valuable insights that can be used to improve future problem-solving processes.
Take the earlier example of high levels of patient discomfort due to staff shortage during peak hours. Suppose, after implementing the solution of adjusting staff schedules, you find that there's a significant improvement in patient comfort levels. This shows that your solution worked. However, during reflection, you realise that the process took more time than necessary due to delayed decision-making. For future improvement, you could consider setting specific timelines for each stage of the problem-solving process.
In conclusion, problem-solving is a cyclical process. It doesn't end with implementing a solution; instead, it opens doors for continuous learning and improvement. Adapting to this cycle is key to honing your problem-solving proficiency in nursing management.
Critical Thinking and Problem Solving in Nursing
Problem solving in nursing management is underpinned by the practice of critical thinking. An understanding of the delicate interplay between these two capabilities is central to the enhancement of nursing management and the ultimate delivery of efficient patient care.
The Connection Between Critical Thinking and Problem Solving in Nursing
There is a strong relationship between critical thinking and problem solving in nursing, evidenced by the significant role each plays in the healthcare sector. Critical thinking provides the foundation upon which problem-solving strategies are built.
Critical Thinking: This is the disciplined process of analysing, interpreting, evaluating, and drawing conclusions from varying levels of data, information or experiences. It involves a deeper level of thinking to understand, evaluate and resolve complex issues or situations.
The process of problem-solving often begins with an evaluation of the situation, gathering data, appraising the data, and coming with strategic solutions. By applying critical thinking, you can get a clear understanding of the problem, which helps devise more effective solutions.
For example, in implementing new protocols in a nursing unit, critical thinking may involve evaluating the necessity of the change, the potential effect on the nursing staff’s workflow, and patient care. The ability to think critically facilitates well-informed decisions, thereby enhancing the problem-solving process.
Beyond problem identification and solution generation, critical thinking is also instrumental in the review phase of the problem-solving process. It allows you to reflect on the effectiveness of implemented solutions, the overall process, and areas that could be improved. Therefore, the integration of critical thinking not only enriches problem-solving but also contributes to continuous learning and improvement in nursing management.
Enhancing Critical Thinking for Effective Problem Solving in Nursing Management
Enhancing critical thinking skills in the nursing workforce enriches problem-solving efforts and ultimately results in improved patient outcomes and service delivery. This strengthening could be achieved through several strategies.
Enhancing Critical Thinking: The process of improving critical thinking skills to enhance one's ability to evaluate complex situations effectively and make informed decisions.
Firstly, continuous learning and professional development activities such as workshops, seminars, and online courses can provide essential tools for sharpening critical thinking skills.
Secondly, fostering a culture of open communication and collaborative problem-solving offers great benefits. These platforms facilitate the sharing of diverse perspectives, promoting deep analyses, and enriching the problem-solving process.
Lastly, reflective practice can also positively impact critical thinking abilities. Regular reflection on your practice, experiences, and learnings enables you to identify gaps in your thinking and areas of improvement. It encourages a deeper level of thinking that enriches the problem-solving process.
- Continuous learning and participation in professional development activities.
- Fostering a culture of open communication and collaborative problem-solving.
- Engaging in reflective practice regularly.
Examples of Critical Thinking Leading to Effective Problem Solving
The application of critical thinking skills often results in improved problem-solving outcomes in nursing management. Several instances illustrate this relationship.
For instance, consider a situation where a nursing unit has seen a significant increase in medication errors. The nursing manager applies critical thinking to evaluate the situation, identify potential causes, and devise solutions. Through an in-depth review of pharmaceutical administration procedures, team collaboration, discussion, and data evaluation, the nursing manager identifies the root cause - an overly complicated method of logging medication.
Armed with this information, they innovate a simpler, more effective system. By cutting down on needless complexity, the nursing unit sees a drastic decrease in medication errors. This example shows how the application of critical thinking streamlined a complex process, providing an effective solution to the problem at hand.
Another instance could be changing patient demographics, with more elderly patients requiring care. A nursing manager applies critical thinking to understand the unique needs of these patients and the potential challenges that might arise in catering to these needs. As a result, they develop tailored care plans and training programmes for the nursing staff to better care for elderly patients, resulting in improved patient satisfaction.
These examples highlight how critical thinking can lead to effective problem solving in nursing management, ultimately resulting in better service delivery and patient care. Therefore, enhancing critical thinking should be seen as a vital strategy for improving problem-solving proficiency in nursing management.
Problem Solving in Nursing Management - Key takeaways
- Problem Solving in Nursing Management: It is a thorough process involving the identification, analysis, and (de)cision-making to solve issues in nursing management. It also includes implementation and review of the effectiveness of the solutions.
- Decision Making Techniques: Different techniques such as Pros and Cons Analysis, Decision Matrix, and Cost-Benefit Analysis can enhance the decision-making process in problem-solving scenarios.
- Case Study Analysis: It involves the detailed examination of various scenarios to inform problem-solving strategies and practice.
- Approaches to Problem-Solving: Different approaches may apply in different nursing scenarios, such as the algorithm-based approach for well-defined scenarios and the intuition-driven approach for ambiguous situations.
- Strategic Problem-Solving Competencies: These are essential skills including critical thinking, innovative thinking, collaboration, adaptability, leadership, and decision-making, crucial in effective problem-solving.
- Leadership in Nursing: Leadership plays a key role in guiding, motivating, and supporting nursing staff. It influences the successful implementation of problem-solving strategies.
- Resource Utilisation: Efficient and effective use of available resources, such as nursing staff, equipment, and supplies, is vital in problem-solving in nursing management.
- Stages of Problem Solving in Nursing Practice: The stages include the identification, analysis, and resolution of problems, which are crucial in responding to challenges in the healthcare sector.
Flashcards in Problem Solving in Nursing Management 14
The algorithm-based approach involves following a clear set of rules or procedures to solve a problem, often with defined parameters. The intuition-driven approach combines a nurse's experience, knowledge, and instinct to solve a problem, especially in ambiguous scenarios.
The first stage of problem solving in nursing practice is initial assessment and identification, which involves the evaluation of the situation to recognise existing problems. This stage requires observation, questioning, and data gathering.
Problem solving is a broader process involving the identification of an issue, systematic analysis to understand it, devising potential solutions, choosing the most suitable through decision making, implementing it, and finally reviewing the effectiveness of the implemented solution. Decision making, on the other hand, is a component nested within this process.
Critical thinking provides the foundation for problem-solving strategies in nursing. It involves the disciplined process of analysing, evaluating, and interpreting data, which allows for a clear understanding of the problem and thus the generation of effective solutions. Critical thinking also enriches the problem-solving process by facilitating review and continuous improvement.
The final stage of problem solving in nursing practice is evaluation and reflection, where the effectiveness of the implemented solution is assessed, and learnings are drawn from the process for future improvement.
Problem-solving in nursing management is crucial in maintaining optimal patient care, operational efficiency, and fostering team collaboration by resolving intricate issues with decisive and effective solutions.
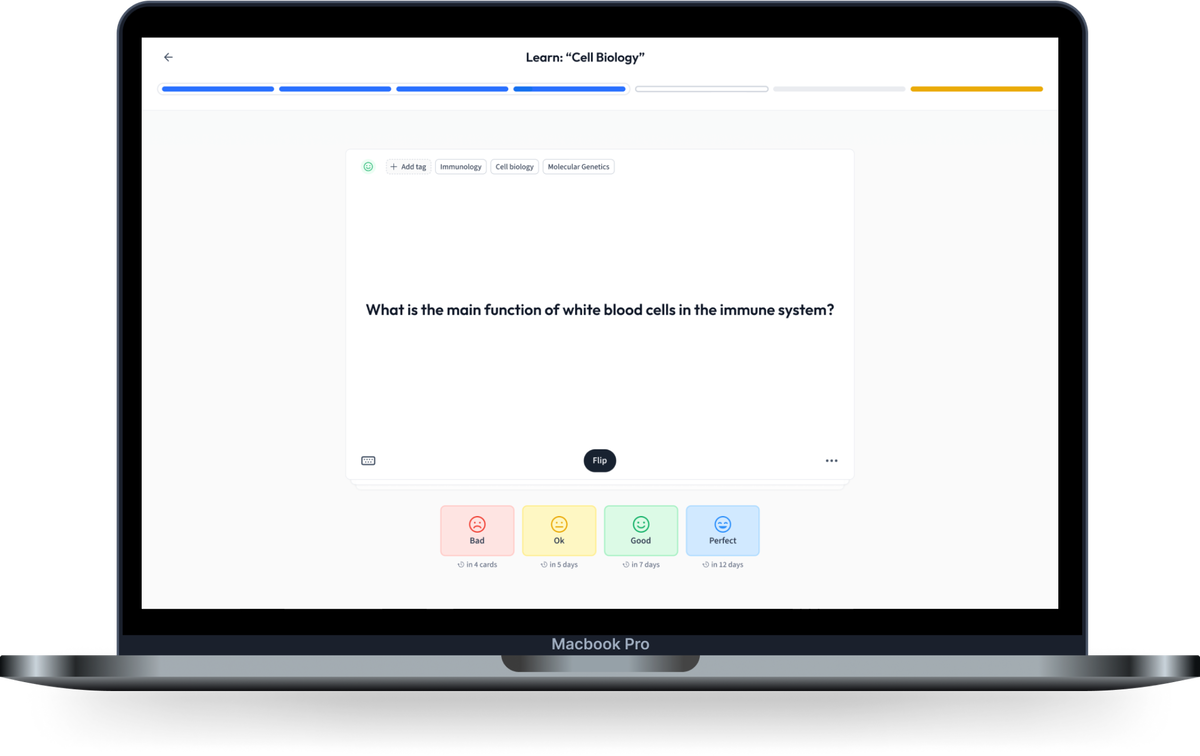
Learn with 14 Problem Solving in Nursing Management flashcards in the free StudySmarter app
We have 14,000 flashcards about Dynamic Landscapes.
Already have an account? Log in
Frequently Asked Questions about Problem Solving in Nursing Management
Test your knowledge with multiple choice flashcards.
Join the StudySmarter App and learn efficiently with millions of flashcards and more!
Keep learning, you are doing great.
Discover learning materials with the free StudySmarter app

About StudySmarter
StudySmarter is a globally recognized educational technology company, offering a holistic learning platform designed for students of all ages and educational levels. Our platform provides learning support for a wide range of subjects, including STEM, Social Sciences, and Languages and also helps students to successfully master various tests and exams worldwide, such as GCSE, A Level, SAT, ACT, Abitur, and more. We offer an extensive library of learning materials, including interactive flashcards, comprehensive textbook solutions, and detailed explanations. The cutting-edge technology and tools we provide help students create their own learning materials. StudySmarter’s content is not only expert-verified but also regularly updated to ensure accuracy and relevance.

StudySmarter Editorial Team
Team Nursing Teachers
- 25 minutes reading time
- Checked by StudySmarter Editorial Team
Study anywhere. Anytime.Across all devices.
Create a free account to save this explanation..
Save explanations to your personalised space and access them anytime, anywhere!
By signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Sign up to highlight and take notes. It’s 100% free.
Join over 22 million students in learning with our StudySmarter App
The first learning app that truly has everything you need to ace your exams in one place
- Flashcards & Quizzes
- AI Study Assistant
- Study Planner
- Smart Note-Taking


COMMENTS
Learn what problem-solving in nursing is, why it is important, and how to improve your skills. This article explains the nursing process and provides examples of problem-solving scenarios in nursing.
They want to see your problem-solving style and get a sense of how you react and respond to the specific challenges nurses tend to face. Asking behavioral and situational questions is a great way for your interviewer to assess your response. STAR: The #1 Strategy for Answering Scenario-Based Nursing Interview Questions
Learn what critical thinking in nursing is and why it is essential for effective patient care. Find 18 tips to improve critical thinking skills and sample scenarios to apply them.
This web page provides 30 common nursing interview questions and answers based on behavioral-based themes. It does not include any problem solving scenarios or questions related to nursing problem solving skills.
Learning to provide safe and quality health care requires technical expertise, the ability to think critically, experience, and clinical judgment. The high-performance expectation of nurses is dependent upon the nurses' continual learning, professional accountability, independent and interdependent decisionmaking, and creative problem-solving abilities.
Learn why critical thinking is essential for nurses and how to improve it with case-based learning, self-reflection, questioning, self-awareness, and a process. Find out how nurses use critical thinking to make decisions, solve problems, and provide excellent care.
Learn how to identify, solve, and reflect on nursing problems using critical-thinking skills. Find out the elements, importance, and ways to improve your critical thinking in nursing practice.
Learn how to apply critical thinking, decision-making, and problem-solving skills in nursing practice. This course covers brainstorming, mapping, prioritizing, multivoting, and 7 steps to problem-solving with examples and exercises.
Key Nursing Critical Thinking Skills. Some of the most important critical thinking skills nurses use daily include interpretation, analysis, evaluation, inference, explanation, and self-regulation. Interpretation: Understanding the meaning of information or events. Analysis: Investigating a course of action based on objective and subjective data.
Learn how to develop strong critical thinking skills for nursing practice with 24 strategies and examples. Explore techniques such as reflective journaling, concept mapping, Socratic questioning, clinical simulations, and more.
Learn how to use the nursing process and critical thinking skills to solve problems in health care. Find examples, tips, and exercises to develop problem-solving strategies for nurses and nurse managers.
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
Learn how to answer critical thinking nursing interview questions and showcase your skills for nursing school admission. Find out what types of questions to expect, why they are asked, and how to prepare with sample answers.
Modified Wabisabi Learning's 12 Solid Strategies for Teaching Critical Thinking Skills, and its Application to Nursing Education, Training and Practice: 1. Practice on Eloquence in Question and Answer (Solution Fluency) Mastery requires ample amount of practice to become highly skilled in critical thinking.
Nurse leaders perceive their role as a problem-solver, which is a necessary step in advocacy. 27 Problem-solving is a process that contains the elements of decision-making and critical thinking. 28. The theory that emerged from the core categories explicitly focused on the central phenomenon of LHV in the nursing work environment.
Step 2: Analyze the Problem. Break down the problem to get an understanding of the problem. Determine how the problem developed. Determine the impact of the problem. Step 3: Develop Solutions. Brainstorm and list all possible solutions that focus on resolving the identified problem. Do not eliminate any possible solutions at this stage.
17. Situational Questions. 18. Teamwork Questions. 19. Tough Questions. Situational questions are asked so the interviewer can gain insight into your thought process, how you problem-solve, and how you communicate in the workplace. Situational nursing questions can include inquiries about drug dosages, procedures, or specific signs and symptoms ...
6 Steps to Replace Clinical Using Case Studies. 1. Watch the intro video as a group. Gather the entire class together and view the intro video. This video lays out the scenario for the given case study and helps them begin to consider the disease process. 2.
To respond to patients' increasing demands and strengthen nursing professionals' capabilities, nursing students are expected to develop problem-solving skills before they enter the workforce. Problem-based learning (PBL) is expected to provide effective simulation scenarios and realistic clinical conditions to help students achieve those ...
Critical thinking can seem like such an abstract term that you don't practically use.However, this could not be farther from the truth. Critical thinking is frequently used in nursing. Let me give you a few examples from my career in which critical thinking helped me take better care of my patient.
A problem-based learning scenario and Kirkpatrick's model for evaluation were used to address incivility and the "reality shock" between what students learn about the practice of nursing and the interactions they may experience in the workplace. ... Solving real nursing problems through problem-based learning.
Dive deep into the multifaceted world of nursing management with a special focus on problem-solving. This comprehensive guide presents a detailed look at the process, importance, and challenges of problem-solving in nursing management. By highlighting essential skills, neurologically based frameworks, and the relationship with decision-making, it offers both theoretical understanding and ...