Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 20 January 2022

AI in health and medicine
- Pranav Rajpurkar ORCID: orcid.org/0000-0002-8030-3727 1 na1 ,
- Emma Chen 2 na1 ,
- Oishi Banerjee 2 na1 &
- Eric J. Topol ORCID: orcid.org/0000-0002-1478-4729 3
Nature Medicine volume 28 , pages 31–38 ( 2022 ) Cite this article
130k Accesses
557 Citations
620 Altmetric
Metrics details
- Computational biology and bioinformatics
- Medical research
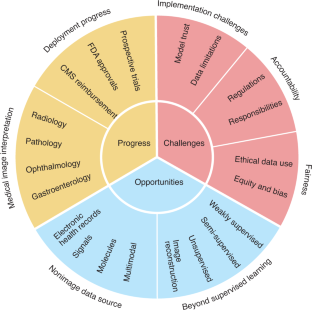
Artificial intelligence (AI) is poised to broadly reshape medicine, potentially improving the experiences of both clinicians and patients. We discuss key findings from a 2-year weekly effort to track and share key developments in medical AI. We cover prospective studies and advances in medical image analysis, which have reduced the gap between research and deployment. We also address several promising avenues for novel medical AI research, including non-image data sources, unconventional problem formulations and human–AI collaboration. Finally, we consider serious technical and ethical challenges in issues spanning from data scarcity to racial bias. As these challenges are addressed, AI’s potential may be realized, making healthcare more accurate, efficient and accessible for patients worldwide.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Gulshan, V. et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. J. Am. Med. Assoc. 316 , 2402–2410 (2016).
Article Google Scholar
Esteva, A. et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature 542 , 115–118 (2017).
Article CAS PubMed PubMed Central Google Scholar
Rajpurkar, P. et al. Deep learning for chest radiograph diagnosis: a retrospective comparison of the CheXNeXt algorithm to practicing radiologists. PLoS Med. 15 , e1002686 (2018).
Article PubMed PubMed Central Google Scholar
Hannun, A. Y. et al. Cardiologist-level arrhythmia detection and classification in ambulatory electrocardiograms using a deep neural network. Nat. Med. 25 , 65–69 (2019).
Wiens, J. et al. Do no harm: a roadmap for responsible machine learning for health care. Nat. Med. 25 , 1337–1340 (2019).
Article CAS PubMed Google Scholar
Kanagasingam, Y. et al. Evaluation of artificial intelligence-based grading of diabetic retinopathy in primary care. JAMA Netw. Open 1 , e182665 (2018).
Beede, E. et al. A human-centered evaluation of a deep learning system deployed in clinics for the detection of diabetic retinopathy. in Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems 1–12 (Association for Computing Machinery, 2020); https://dl.acm.org/doi/abs/10.1145/3313831.3376718
Kiani, A. et al. Impact of a deep learning assistant on the histopathologic classification of liver cancer. NPJ Digit. Med. 3 , 23 (2020).
Lin, H. et al. Diagnostic efficacy and therapeutic decision-making capacity of an artificial intelligence platform for childhood cataracts in eye clinics: a multicentre randomized controlled trial. EClinicalMedicine 9 , 52–59 (2019).
Gong, D. et al. Detection of colorectal adenomas with a real-time computer-aided system (ENDOANGEL): a randomised controlled study. Lancet Gastroenterol. Hepatol. 5 , 352–361 (2020).
Article PubMed Google Scholar
Wang, P. et al. Effect of a deep-learning computer-aided detection system on adenoma detection during colonoscopy (CADe-DB trial): a double-blind randomised study. Lancet Gastroenterol. Hepatol. 5 , 343–351 (2020).
Hollon, T. C. et al. Near real-time intraoperative brain tumor diagnosis using stimulated Raman histology and deep neural networks. Nat. Med. 26 , 52–58 (2020).
Phillips, M. et al. Assessment of accuracy of an artificial intelligence algorithm to detect melanoma in images of skin lesions. JAMA Netw. Open 2 , e1913436 (2019).
Nimri, R. et al. Insulin dose optimization using an automated artificial intelligence-based decision support system in youths with type 1 diabetes. Nat. Med. 26 , 1380–1384 (2020).
Wijnberge, M. et al. Effect of a machine learning-derived early warning system for intraoperative hypotension vs. standard care on depth and duration of intraoperative hypotension during elective noncardiac surgery. J. Am. Med. Assoc. 323 , 1052–1060 (2020).
Wismüller, A. & Stockmaster, L. A prospective randomized clinical trial for measuring radiology study reporting time on Artificial Intelligence-based detection of intracranial hemorrhage in emergent care head CT. in Medical Imaging 2020: Biomedical Applications in Molecular, Structural, and Functional Imaging vol. 11317, 113170M (International Society for Optics and Photonics, 2020).
Liu, X. et al. Reporting guidelines for clinical trial reports for interventions involving artificial intelligence: the CONSORT-AI extension. Br. Med. J. 370 , m3164 (2020).
Rivera, S. C. et al. Guidelines for clinical trial protocols for interventions involving artificial intelligence: the SPIRIT-AI extension. Nat. Med. 26 , 1351–1363 (2020).
Centers for Medicare & Medicaid Services. Medicare Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long-Term Care Hospital Prospective Payment System and Final Policy Changes and Fiscal Year 2021 Rates; Quality Reporting and Medicare and Medicaid Promoting Interoperability Programs Requirements for Eligible Hospitals and Critical Access Hospitals. Fed. Regist. 85 , 58432–59107 (2020).
Benjamens, S., Dhunnoo, P. & Meskó, B. The state of artificial intelligence-based FDA-approved medical devices and algorithms: an online database. NPJ Digit. Med. 3 , 118 (2020).
Wu, N. et al. Deep neural networks improve radiologists’ performance in breast cancer screening. IEEE Trans. Med. Imaging 39 , 1184–1194 (2020).
McKinney, S. M. et al. International evaluation of an AI system for breast cancer screening. Nature 577 , 89–94 (2020).
Ghorbani, A. et al. Deep learning interpretation of echocardiograms. NPJ Digit. Med. 3 , 10 (2020).
Ouyang, D. et al. Video-based AI for beat-to-beat assessment of cardiac function. Nature 580 , 252–256 (2020).
Ardila, D. et al. End-to-end lung cancer screening with three-dimensional deep learning on low-dose chest computed tomography. Nat. Med. 25 , 954–961 (2019).
Huynh, E. et al. Artificial intelligence in radiation oncology. Nat. Rev. Clin. Oncol. 17 , 771–781 (2020).
Huang, P. et al. Prediction of lung cancer risk at follow-up screening with low-dose CT: a training and validation study of a deep learning method. Lancet Digit. Health 1 , e353–e362 (2019).
Kather, J. N. et al. Deep learning can predict microsatellite instability directly from histology in gastrointestinal cancer. Nat. Med. 25 , 1054–1056 (2019).
Jackson, H. W. et al. The single-cell pathology landscape of breast cancer. Nature 578 , 615–620 (2020).
Campanella, G. et al. Clinical-grade computational pathology using weakly supervised deep learning on whole slide images. Nat. Med. 25 , 1301–1309 (2019).
Fu, Y. et al. Pan-cancer computational histopathology reveals mutations, tumor composition and prognosis. Nat. Cancer 1 , 800–810 (2020).
Courtiol, P. et al. Deep learning-based classification of mesothelioma improves prediction of patient outcome. Nat. Med. 25 , 1519–1525 (2019).
Bera, K., Schalper, K. A., Rimm, D. L., Velcheti, V. & Madabhushi, A. Artificial intelligence in digital pathology: new tools for diagnosis and precision oncology. Nat. Rev. Clin. Oncol. 16 , 703–715 (2019).
Zhou, D. et al. Diagnostic evaluation of a deep learning model for optical diagnosis of colorectal cancer. Nat. Commun. 11 , 2961 (2020).
Zhao, S. et al. Magnitude, risk factors, and factors associated with adenoma miss rate of tandem colonoscopy: a systematic review and meta-analysis. Gastroenterology 156 , 1661–1674 (2019).
Freedman, D. et al. Detecting deficient coverage in colonoscopies. IEEE Trans. Med. Imaging 39 , 3451–3462 (2020).
Liu, H. et al. Development and validation of a deep learning system to detect glaucomatous optic neuropathy using fundus photographs. JAMA Ophthalmol. 137 , 1353–1360 (2019).
Milea, D. et al. Artificial intelligence to detect papilledema from ocular fundus photographs. N. Engl. J. Med. 382 , 1687–1695 (2020).
Wolf, R. M., Channa, R., Abramoff, M. D. & Lehmann, H. P. Cost-effectiveness of autonomous point-of-care diabetic retinopathy screening for pediatric patients with diabetes. JAMA Ophthalmol. 138 , 1063–1069 (2020).
Xie, Y. et al. Artificial intelligence for teleophthalmology-based diabetic retinopathy screening in a national programme: an economic analysis modelling study. Lancet Digit. Health 2 , e240–e249 (2020).
Arcadu, F. et al. Deep learning algorithm predicts diabetic retinopathy progression in individual patients. NPJ Digit. Med. 2 , 92 (2019).
Senior, A. W. et al. Improved protein structure prediction using potentials from deep learning. Nature 577 , 706–710 (2020).
Alley, E. C., Khimulya, G., Biswas, S., AlQuraishi, M. & Church, G. M. Unified rational protein engineering with sequence-based deep representation learning. Nat. Methods 16 , 1315–1322 (2019).
Gainza, P. et al. Deciphering interaction fingerprints from protein molecular surfaces using geometric deep learning. Nat. Methods 17 , 184–192 (2020).
Greener, J.G. et al. Deep learning extends de novo protein modelling coverage of genomes using iteratively predicted structural constraints. Nat. Commun. 10 , 3977 (2019).
Chabon, J. J. et al. Integrating genomic features for non-invasive early lung cancer detection. Nature 580 , 245–251 (2020).
Luo, H. et al. Circulating tumor DNA methylation profiles enable early diagnosis, prognosis prediction, and screening for colorectal cancer. Sci. Transl. Med. 12 , eaax7533 (2020).
Cristiano, S. et al. Genome-wide cell-free DNA fragmentation in patients with cancer. Nature 570 , 385–389 (2019).
Gussow, A. B. et al. Machine-learning approach expands the repertoire of anti-CRISPR protein families. Nat. Commun. 11 , 3784 (2020).
Wang, D. et al. Optimized CRISPR guide RNA design for two high-fidelity Cas9 variants by deep learning. Nat. Commun. 10 , 4284 (2019).
Bhattacharyya, R. P. et al. Simultaneous detection of genotype and phenotype enables rapid and accurate antibiotic susceptibility determination. Nat. Med. 25 , 1858–1864 (2019).
Stokes, J. M. et al. A deep learning approach to antibiotic discovery. Cell 181 , 475–483 (2020).
Zhavoronkov, A. et al. Deep learning enables rapid identification of potent DDR1 kinase inhibitors. Nat. Biotechnol. 37 , 1038–1040 (2019).
Lee, J. et al. BioBERT: a pre-trained biomedical language representation model for biomedical text mining. Bioinformatics 36 , 1234–1240 (2020).
CAS PubMed Google Scholar
Zhu, Y., Li, L., Lu, H., Zhou, A. & Qin, X. Extracting drug-drug interactions from texts with BioBERT and multiple entity-aware attentions. J. Biomed. Inform. 106 , 103451 (2020).
Smit, A. et al. CheXbert: Combining automatic labelers and expert annotations for accurate radiology report labeling using BERT. in Proceedings of the 2020 Conference on Empirical Methods in Natural Language Processing 1500–1519 (2020).
Sarker, A., Gonzalez-Hernandez, G., Ruan, Y. & Perrone, J. Machine learning and natural language processing for geolocation-centric monitoring and characterization of opioid-related social media chatter. JAMA Netw. Open 2 , e1914672 (2019).
Claassen, J. et al. Detection of brain activation in unresponsive patients with acute brain injury. N. Engl. J. Med. 380 , 2497–2505 (2019).
Porumb, M., Stranges, S., Pescapè, A. & Pecchia, L. Precision medicine and artificial intelligence: a pilot study on deep learning for hypoglycemic events detection based on ECG. Sci. Rep. 10 , 170 (2020).
Attia, Z. I. et al. An artificial intelligence-enabled ECG algorithm for the identification of patients with atrial fibrillation during sinus rhythm: a retrospective analysis of outcome prediction. Lancet 394 , 861–867 (2019).
Chan, J., Raju, S., Nandakumar, R., Bly, R. & Gollakota, S. Detecting middle ear fluid using smartphones. Sci. Transl. Med. 11 , eaav1102 (2019).
Willett, F. R., Avansino, D. T., Hochberg, L. R., Henderson, J. M. & Shenoy, K. V. High-performance brain-to-text communication via handwriting. Nature 593 , 249–254 (2021).
Green, E. M. et al. Machine learning detection of obstructive hypertrophic cardiomyopathy using a wearable biosensor. NPJ Digit. Med. 2 , 57 (2019).
Thorsen-Meyer, H.-C. et al. Dynamic and explainable machine learning prediction of mortality in patients in the intensive care unit: a retrospective study of high-frequency data in electronic patient records. Lancet Digit. Health 2 , e179–e191 (2020).
Porter, P. et al. A prospective multicentre study testing the diagnostic accuracy of an automated cough sound centred analytic system for the identification of common respiratory disorders in children. Respir. Res. 20 , 81 (2019).
Tomašev, N. et al. A clinically applicable approach to continuous prediction of future acute kidney injury. Nature 572 , 116–119 (2019).
Kehl, K. L. et al. Assessment of deep natural language processing in ascertaining oncologic outcomes from radiology reports. JAMA Oncol. 5 , 1421–1429 (2019).
Huang, S.-C., Pareek, A., Seyyedi, S., Banerjee, I. & Lungren, M. P. Fusion of medical imaging and electronic health records using deep learning: a systematic review and implementation guidelines. NPJ Digit. Med. 3 , 136 (2020).
Wang, C. et al. Quantitating the epigenetic transformation contributing to cholesterol homeostasis using Gaussian process. Nat. Commun. 10 , 5052 (2019).
Li, Y. et al. Inferring multimodal latent topics from electronic health records. Nat. Commun. 11 , 2536 (2020).
Tshitoyan, V. et al. Unsupervised word embeddings capture latent knowledge from materials science literature. Nature 571 , 95–98 (2019).
Li, X. et al. Deep learning enables accurate clustering with batch effect removal in single-cell RNA-seq analysis. Nat. Commun. 11 , 2338 (2020).
Amodio, M. et al. Exploring single-cell data with deep multitasking neural networks. Nat. Methods 16 , 1139–1145 (2019).
Urteaga, I., McKillop, M. & Elhadad, N. Learning endometriosis phenotypes from patient-generated data. NPJ Digit. Med. 3 , 88 (2020).
Brbić, M. et al. MARS: discovering novel cell types across heterogeneous single-cell experiments. Nat. Methods 17 , 1200–1206 (2020).
Seymour, C. W. et al. Derivation, validation, and potential treatment implications of novel clinical phenotypes for sepsis. J. Am. Med. Assoc. 321 , 2003–2017 (2019).
Article CAS Google Scholar
Fries, J. A. et al. Weakly supervised classification of aortic valve malformations using unlabeled cardiac MRI sequences. Nat. Commun. 10 , 3111 (2019).
Jin, L. et al. Deep learning enables structured illumination microscopy with low light levels and enhanced speed. Nat. Commun. 11 , 1934 (2020).
Vishnevskiy, V. et al. Deep variational network for rapid 4D flow MRI reconstruction. Nat. Mach. Intell. 2 , 228–235 (2020).
Masutani, E. M., Bahrami, N. & Hsiao, A. Deep learning single-frame and multiframe super-resolution for cardiac MRI. Radiology 295 , 552–561 (2020).
Rana, A. et al. Use of deep learning to develop and analyze computational hematoxylin and eosin staining of prostate core biopsy images for tumor diagnosis. JAMA Netw. Open 3 , e205111 (2020).
Liu, X. et al. A comparison of deep learning performance against health-care professionals in detecting diseases from medical imaging: a systematic review and meta-analysis. Lancet Digit. Health 1 , e271–e297 (2019).
Chen, P.-H. C. et al. An augmented reality microscope with real-time artificial intelligence integration for cancer diagnosis. Nat. Med. 25 , 1453–1457 (2019).
Patel, B. N. et al. Human–machine partnership with artificial intelligence for chest radiograph diagnosis. NPJ Digit. Med. 2 , 111 (2019).
Sim, Y. et al. Deep convolutional neural network–based software improves radiologist detection of malignant lung nodules on chest radiographs. Radiology 294 , 199–209 (2020).
Park, A. et al. Deep learning–assisted diagnosis of cerebral aneurysms using the HeadXNet model. JAMA Netw. Open 2 , e195600 (2019).
Steiner, D. F. et al. Impact of deep learning assistance on the histopathologic review of lymph nodes for metastatic breast cancer. Am. J. Surg. Pathol. 42 , 1636–1646 (2018).
Jain, A. et al. Development and assessment of an artificial intelligence-based tool for skin condition diagnosis by primary care physicians and nurse practitioners in teledermatology practices. JAMA Netw. Open 4 , e217249 (2021).
Seah, J. C. Y. et al. Effect of a comprehensive deep-learning model on the accuracy of chest x-ray interpretation by radiologists: a retrospective, multireader multicase study. Lancet Digit. Health 3 , e496–e506 (2021).
Rajpurkar, P. et al. CheXaid: deep learning assistance for physician diagnosis of tuberculosis using chest x-rays in patients with HIV. NPJ Digit. Med. 3 , 115 (2020).
Kim, H.-E. et al. Changes in cancer detection and false-positive recall in mammography using artificial intelligence: a retrospective, multireader study. Lancet Digit. Health 2 , e138–e148 (2020).
Tschandl, P. et al. Human–computer collaboration for skin cancer recognition. Nat. Med. 26 , 1229–1234 (2020).
van der Laak, J., Litjens, G. & Ciompi, F. Deep learning in histopathology: the path to the clinic. Nat. Med. 27 , 775–784 (2021).
Willemink, M. J. et al. Preparing medical imaging data for machine learning. Radiology 295 , 4–15 (2020).
Irvin, J. et al. CheXpert: a large chest radiograph dataset with uncertainty labels and expert comparison. in Proceedings of the AAAI Conference on Artificial Intelligence vol. 33, 590–597 (2019).
Kelly, C. J., Karthikesalingam, A., Suleyman, M., Corrado, G. & King, D. Key challenges for delivering clinical impact with artificial intelligence. BMC Med. 17 , 195 (2019).
DeGrave, A. J., Janizek, J. D. & Lee, S.-I. AI for radiographic COVID-19 detection selects shortcuts over signal. Nat. Mach. Intell. 3 , 610–619 (2021).
Cutillo, C. M. et al. Machine intelligence in healthcare: perspectives on trustworthiness, explainability, usability, and transparency. NPJ Digit. Med. 3 , 47 (2020).
Sendak, M. P., Gao, M., Brajer, N. & Balu, S. Presenting machine learning model information to clinical end users with model facts labels. NPJ Digit. Med. 3 , 41 (2020).
Saporta, A. et al. Deep learning saliency maps do not accurately highlight diagnostically relevant regions for medical image interpretation. Preprint at medRxiv https://doi.org/10.1101/2021.02.28.21252634 (2021).
Ehsan, U. et al . The who in explainable AI: how AI background shapes perceptions of AI explanations. Preprint at https://arxiv.org/abs/2107.13509 (2021).
Reyes, M. et al. On the interpretability of artificial intelligence in radiology: Challenges and opportunities. Radio. Artif. Intell. 2 , e190043 (2020).
Liu, C. et al . On the replicability and reproducibility of deep learning in software engineering. Preprint at https://arxiv.org/abs/2006.14244 (2020).
Beam, A. L., Manrai, A. K. & Ghassemi, M. Challenges to the reproducibility of machine learning models in health care. J. Am. Med. Assoc. 323 , 305–306 (2020).
Gerke, S., Babic, B., Evgeniou, T. & Cohen, I. G. The need for a system view to regulate artificial intelligence/machine learning-based software as medical device. NPJ Digit. Med. 3 , 53 (2020).
Lee, C. S. & Lee, A. Y. Clinical applications of continual learning machine learning. Lancet Digit. Health 2 , e279–e281 (2020).
Food and Drug Administration. Proposed Regulatory Framework for Modifications to Artificial Intelligence/Machine Learning (AI/ML)-Based Software as a Medical Device (SaMD): Discussion Paper and Request for Feedback (FDA, 2019).
Morley, J. et al. The debate on the ethics of AI in health care: a reconstruction and critical review. SSRN http://dx.doi.org/10.2139/ssrn.3486518 (2019.
Price, W. N., Gerke, S. & Cohen, I. G. Potential liability for physicians using artificial intelligence. J. Am. Med. Assoc. 322 , 1765–1766 (2019).
Larson, D. B., Magnus, D. C., Lungren, M. P., Shah, N. H. & Langlotz, C. P. Ethics of using and sharing clinical imaging data for artificial intelligence: a proposed framework. Radiology 295 , 675–682 (2020).
Kaissis, G. A., Makowski, M. R., Rückert, D. & Braren, R. F. Secure, privacy-preserving and federated machine learning in medical imaging. Nat. Mach. Intell. 2 , 305–311 (2020).
Larrazabal, A. J., Nieto, N., Peterson, V., Milone, D. H. & Ferrante, E. Gender imbalance in medical imaging datasets produces biased classifiers for computer-aided diagnosis. Proc. Natl Acad. Sci. USA 117 , 12592–12594 (2020).
Vyas, D. A., Eisenstein, L. G. & Jones, D. S. Hidden in plain sight: reconsidering the use of race correction in clinical algorithms. N. Engl. J. Med. 383 , 874–882 (2020).
Obermeyer, Z., Powers, B., Vogeli, C. & Mullainathan, S. Dissecting racial bias in an algorithm used to manage the health of populations. Science 366 , 447–453 (2019).
Cirillo, D. et al. Sex and gender differences and biases in artificial intelligence for biomedicine and healthcare. NPJ Digit. Med. 3 , 81 (2020).
Download references
Acknowledgements
We thank A. Tamkin and N. Phillips for their feedback. E.J.T. receives funding support from US National Institutes of Health grant UL1TR002550.
Author information
These authors contributed equally: Pranav Rajpurkar, Emma Chen, Oishi Banerjee.
Authors and Affiliations
Department of Biomedical Informatics, Harvard University, Cambridge, MA, USA
Pranav Rajpurkar
Department of Computer Science, Stanford University, Stanford, CA, USA
Emma Chen & Oishi Banerjee
Scripps Translational Science Institute, San Diego, CA, USA
Eric J. Topol
You can also search for this author in PubMed Google Scholar
Contributions
P.R. and E.J.T. conceptualized this Review. E.C., O.B. and P.R. were responsible for the design and synthesis of this Review. All authors contributed to writing and editing the manuscript.
Corresponding author
Correspondence to Eric J. Topol .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Medicine thanks Despina Kontos and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Karen O’Leary was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Rajpurkar, P., Chen, E., Banerjee, O. et al. AI in health and medicine. Nat Med 28 , 31–38 (2022). https://doi.org/10.1038/s41591-021-01614-0
Download citation
Received : 23 July 2021
Accepted : 05 November 2021
Published : 20 January 2022
Issue Date : January 2022
DOI : https://doi.org/10.1038/s41591-021-01614-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Development and validation of a machine learning model to predict time to renal replacement therapy in patients with chronic kidney disease.
- Takeshi Nakata
- Hirotaka Shibata
BMC Nephrology (2024)
Individualized estimation of arterial carbon dioxide partial pressure using machine learning in children receiving mechanical ventilation
- Bongjin Lee
- June Dong Park
BMC Pediatrics (2024)
“That’s just Future Medicine” - a qualitative study on users’ experiences of symptom checker apps
- Regina Müller
- Malte Klemmt
- Robert Ranisch
BMC Medical Ethics (2024)
Machine learning in physical activity, sedentary, and sleep behavior research
- Vahid Farrahi
- Mehrdad Rostami
Journal of Activity, Sedentary and Sleep Behaviors (2024)
Physician–machine partnerships boost diagnostic accuracy, but bias persists
Nature Medicine (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Editor's Choice: Self-Managed Abortion Before and After the Dobbs Decision
- Preliminary Communication Aspirin for Metabolic Dysfunction–Associated Steatotic Liver Disease Without Cirrhosis: A Randomized Clinical Trial Tracey G. Simon, MD, MPH; Robert M. Wilechansky, MD; Stefania Stoyanova, BA; et al
Just Published
- Provision of Medications for Self-Managed Abortion Before and After the Dobbs Decision Abigail R. A. Aiken, PhD; et al. Original Investigation online first free access has multimedia Abigail R. A. Aiken, PhD; et al.
- Donor Heart Acceptance and Race and Gender of Patients on the Transplant Waiting List Khadijah Breathett, MD, MS; et al. Original Investigation online first Khadijah Breathett, MD, MS; et al. Editorial
- Vibration-Controlled Transient Elastography Scores and Liver-Related Events in Steatotic Liver Disease Huapeng Lin, PhD; et al. Original Investigation online first Huapeng Lin, PhD; et al. Editorial
- Skin Biopsy Detection of Phosphorylated α-Synuclein in Patients With Synucleinopathies Christopher H. Gibbons, MD, MMSc; et al. Original Investigation online first has active quiz Christopher H. Gibbons, MD, MMSc; et al.
- Partner Plan Choices and Medicare Advantage Enrollment Decisions Among Older Adults Lianlian Lei, PhD; et al. Research Letter online first Lianlian Lei, PhD; et al.
- Impacts of the Supreme Court Decision in FDA v Alliance for Hippocratic Medicine Eve Espey, MD, MPH; et al. Viewpoint online first free access has multimedia Eve Espey, MD, MPH; et al.
- FDA in the Crosshairs of Science, Politics, and Abortion Holly Fernandez Lynch, JD, MBE; et al. Viewpoint online first free access has multimedia Holly Fernandez Lynch, JD, MBE; et al.
- Selective Androgen Receptor Modulators: Transformative or Abuse Potential? Henrik A. Hahamyan, BSE; et al. Viewpoint online first free access Henrik A. Hahamyan, BSE; et al.
- Is Equity Being Traded for Access to Heart Transplant? Paul A. Heidenreich, MD, MS; et al. Editorial online first Paul A. Heidenreich, MD, MS; et al.
- Predicting Liver-Related Outcomes in Steatotic Liver Disease Zobair M. Younossi, MD, MPH Editorial online first Zobair M. Younossi, MD, MPH
- Effect Scores to Characterize Heterogeneity of Treatment Effects Guanbo Wang, PhD; et al. JAMA Guide to Statistics and Methods online first free access Guanbo Wang, PhD; et al.
- Arteriovenous Access for Hemodialysis Charmaine E. Lok, MD, MSc; et al. Review online first has active quiz has multimedia Charmaine E. Lok, MD, MSc; et al.
- Management of Individuals With Diabetes at High Risk of Hypoglycemia Celeste C. Thomas, MD, MS; et al. JAMA Clinical Guidelines Synopsis online first has active quiz Celeste C. Thomas, MD, MS; et al.
- Allergic Rhinitis Jonathan A. Bernstein, MD; et al. Review has active quiz has multimedia Jonathan A. Bernstein, MD; et al.
- Disease-Modifying Drugs for Adult-Onset Rheumatoid Arthritis Maya N. Faison, MD; et al. JAMA Clinical Guidelines Synopsis online first has active quiz Maya N. Faison, MD; et al.
Latest from the USPSTF
- USPSTF Recommendation: Primary Care Interventions to Prevent Child Maltreatment
- USPSTF Recommendation: Screening for Speech and Language Delay and Disorders
- USPSTF Recommendation: Screening and Preventive Interventions for Oral Health in Adults
- 47,955 Views Adverse Events After XBB.1.5-Containing COVID-19 mRNA Vaccines
- 42,904 Views GLP-1 Agonists for Obesity—A New Recipe for Success?
- 34,667 Views Brain Waves Appear to Wash Out Waste During Sleep
- 33,954 Views International Consensus Criteria for Pediatric Sepsis and Septic Shock
- 29,713 Views Effect of Tirzepatide on Maintenance of Weight Reduction
- 22,178 Views Pharmacotherapy and Mortality in Individuals With ADHD
- 21,020 Views Misinformation and the Vaccine Adverse Event Reporting System
- 20,284 Views Long-Term Outcomes of Medical Management vs Bariatric Surgery in Type 2 Diabetes
- 20,229 Views Study Provides Insight Into ME/CFS
- 19,637 Views Meta-Analysis: Exercise as Effective as Therapy for Treating Depression
- 711 Citations Antibody Response to 2-Dose SARS-CoV-2 mRNA Vaccine Series in Solid Organ Transplant Recipients
- 582 Citations Pancreatic Cancer
- 575 Citations Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization
- 570 Citations Updated Guidance on the Reporting of Race and Ethnicity in Medical and Science Journals
- 566 Citations USPSTF Recommendation: Screening for Colorectal Cancer
- 501 Citations Effect of 2 Inactivated SARS-CoV-2 Vaccines on Symptomatic COVID-19 Infection in Adults
- 440 Citations The Leading Causes of Death in the US for 2020
- 437 Citations Association Between IL-6 Antagonists and Mortality Among Patients Hospitalized for COVID-19
- 433 Citations Effect of Intermediate- vs Standard-Dose Anticoagulation on Outcomes of Patients With COVID-19
- 401 Citations Association Between 3 Doses of mRNA COVID-19 Vaccine and Symptomatic Infection Caused by Omicron and Delta Variants
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Doctors’ real terms purchasing power has declined substantially over 15 years, independent analysis confirms
As doctors in England enter their 13th month of industrial action, Adele Waters explores the economic case for increasing their pay, and junior doctors share the details of their earnings and outgoings

RCP members vote to limit physician associate roles amid calls for president to resign
Members and fellows of the Royal College of Physicians have voted to limit the pace and scale of the rollout of physician associates

Effectiveness and safety of drugs for obesity
This review summarises recent evidence on the safety and efficacy of antiobesity medications, to help guide practicing physicians
clinical review

Stroke rehabilitation in adults: summary of updated NICE guidance
This guideline summary covers new and updated recommendations, with a focus on those most relevant to primary care
Type 1 diabetes: Randox removes adverts after claims that it was using fear to sell genetic test
Transgender care: doctors are advised to return to “ordinary best practice”, supporting health can help to boost employment, sixty seconds on . . . pig kidney transplants, why i . . . am a cricket umpire, dry eye disease management, the bmj editorial scholar 2024/2025, latest articles.

Virologist who was fired from research laboratory in Canada over security threat resurfaces in China
Global leaders call for negotiators to push through pandemic accord ahead of may deadline, uk foundation programme: why are some trainees so unhappy with the new allocation system, whooping cough: over 3000 cases reported in czech republic so far this year, government criticised over failure to implement patient safety recommendations, long waits in child mental health are a “ticking time bomb” regulator warns, nhs workforce plan: spending watchdog questions modelling and optimism, gaza: “hospitals should never be battlegrounds,” says who amid raids on al-shifa hospital.

Quality and safety of artificial intelligence generated health information
Assessing robustness to worst case publication bias using a simple subset meta-analysis, 25 year trends in cancer incidence and mortality among adults in the uk, cervical pessary versus vaginal progesterone in women with a singleton pregnancy, comparison of prior authorization across insurers, diagnostic accuracy of magnetically guided capsule endoscopy with a detachable string for detecting oesophagogastric varices in adults with cirrhosis, ultra-processed food exposure and adverse health outcomes, added benefit and revenues of oncology drugs approved by the ema.

New allocation system for foundation training leaves doctors demoralised before they’ve even started work
Maintaining independence in older adults, future roles, responsibilities, and rewards, nhs funding for a secure future, early pprom: women and babies who should not be lost in the system, physician associates in the uk: some fundamental questions that need answers now, we need medical leadership built on trust, women’s health needs beyond sexual, reproductive, and maternal health are missing from the government’s 2024 priorities, information gaps in england’s independent healthcare sector.

Caring is the invisible piece of the stroke recovery puzzle
How to make the most of your ophthalmology placement, premature ovarian insufficiency, even short periods of diabetes remission are linked to lower risk of heart attack and stroke, identification and management of co-infections in people with malaria, suspected acute respiratory infection in over 16s—summary of nice guidance, how common are side effects of treatment to prevent gout flares when starting allopurinol, weights, resistance bands, and rest days are best for tendinopathy, advance and future care planning, using illness trajectories to inform person centred, advance care planning, sustainable practice, sustainable practice: what can i do.

A new BMJ series offers tangible actions clinicians can take to reduce the carbon footprint of healthcare
Why learning to swallow pills is good for patients, parents, and the planet

Swapping liquids to pills can be safer, more cost effective, and is likely to reduce the carbon footprint of prescribing
Patient and planetary harms from high anticholinergic burden medication
Sustainable practice: optimising surgical instrument trays, sustainable practice: sustainable prescribing of iron replacement therapy, sustainable practice: switching to reusable vaginal speculums, bmj medicine, machine learning in the assessment and management of acute gastrointestinal bleeding.

In this narrative review, Nigam and colleagues provide insights into the current state of machine learning applications in acute gastrointestinal bleeding management, highlighting key themes, trends, and future directions
Multimorbidity research: where one size does not fit all

This editorial reviews research on multimoridity by Beaney and colleagues, and explains why timeframes and frequency are important considerations when defining chronic conditions for multimorbidity research
Effectiveness and cost effectiveness of pharmacological thromboprophylaxis for medical inpatients
Effect of timeframes to define long term conditions and sociodemographic factors on prevalence of multimorbidity, association of vaginal oestradiol and rate of breast cancer, adnex risk prediction model for diagnosis of ovarian cancer, current issue.

Large language models and the generation of health disinformation
Medical associates: the introduction of pas, anps, and acps is creating new challenges for doctors on rotational training, switching from disposable to reusable ppe, ultra-processed food exposure and adverse health outcomes: umbrella review of epidemiological meta-analyses, effect of exercise for depression: systematic review and network meta-analysis of randomised controlled trials, added benefit and revenues of oncology drugs approved by the european medicines agency between 1995 and 2020: retrospective cohort study, rosuvastatin versus atorvastatin treatment in adults with coronary artery disease: secondary analysis of the randomised lodestar trial, 25 year trends in cancer incidence and mortality among adults aged 35-69 years in the uk, 1993-2018: retrospective secondary analysis, comparative effectiveness of glp-1 receptor agonists on glycaemic control, body weight, and lipid profile for type 2 diabetes: systematic review and network meta-analysis, latest responses, re: caring is the invisible piece of the stroke recovery puzzle, re: switching from disposable to reusable ppe - papr devices, response to daniel, re: new allocation system for foundation training leaves doctors demoralised before they’ve even started work, from metrics to preferences: reflections on the 2024 foundation programme allocation results, what are your thoughts.

Covid-19: Researcher blows the whistle on data integrity issues in Pfizer’s vaccine trial

Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: systematic review and meta-analysis

Covid-19: Social murder, they wrote—elected, unaccountable, and unrepentant

The illusion of evidence based medicine
Follow us on, content links.
- Collections
- Health in South Asia
- Women’s, children’s & adolescents’ health
- News and views
- BMJ Opinion
- Rapid responses
- Editorial staff
- BMJ in the USA
- BMJ in South Asia
- Submit your paper
- BMA members
- Subscribers
- Advertisers and sponsors
Explore BMJ
- Our company
- BMJ Careers
- BMJ Learning
- BMJ Masterclasses
- BMJ Journals
- BMJ Student
- Academic edition of The BMJ
- BMJ Best Practice
- The BMJ Awards
- Email alerts
- Activate subscription
Information
FDA Publishes Public Update About Oversight of AI-Enabled Healthcare Technologies
The page you recommended will be added to the "what others are reading" feed on "My ACR".
The page you bookmarked will be added to the "my reading list" feed on "My ACR".
The U.S. Food and Drug Administration (FDA) published a paper March 15, to update the public about intra-agency activities to oversee artificial intelligence (AI)-enabled healthcare technologies. The paper summarizes priorities shared across the biologics, drugs and medical devices domains of FDA jurisdiction.
Four general focus areas are discussed: fostering collaboration with stakeholders; developing appropriate regulatory approaches; promoting development of standards and best practices; and supporting research on performance evaluation. Moving forward, the FDA intends to evolve its own regulatory approaches with the continued progression of AI tools.
For more information about various American College of Radiology®(ACR®) AI-specific initiatives, visit the ACR Data Science Institute ®. For more information about FDA oversight and digital health policy, contact Michael Peters , ACR Senior Government Affairs Director.
This paper is in the following e-collection/theme issue:
Published on 25.3.2024 in Vol 26 (2024)
Where Do Oncology Patients Seek and Share Health Information? Survey Study
Authors of this article:

Research Letter
- Eric Freeman 1 , BA ;
- Darshilmukesh Patel 2 , BA ;
- Folasade Odeniyi 1 , MPH, MBA ;
- Mary Pasquinelli 2 , DNP ;
- Shikha Jain 2 , MD
1 College of Medicine, University of Illinois at Chicago, Chicago, IL, United States
2 Department of Medicine, University of Illinois at Chicago, Chicago, IL, United States
Corresponding Author:
Eric Freeman, BA
College of Medicine
University of Illinois at Chicago
1853 West Polk Street
Chicago, IL, 60612
United States
Phone: 1 847 791 0189
Email: [email protected]
Introduction
Social media in health care has many benefits, including the dissemination of health information [ 1 ] and health promotion [ 2 ]. The COVID-19 pandemic has highlighted the benefits of the internet and social media as tools through which individuals can exchange health information. While little is known about oncology patients’ preferences for social media platforms, particularly among minority populations and those in low socioeconomic status communities, some studies have shown its use is linked to the alleviation of patient stress and loneliness, increased feelings of self-efficacy and control of care, and efficient delivery of health information from health practitioners [ 3 ]. The study aims to assess where patients from marginalized communities receive a majority of their health care information by surveying patients in a cancer clinic. This study was conducted at the University of Illinois Chicago, which is a public hospital that mainly serves patients from underresourced communities.
Between March 2021 to June 2021, we administered a 16-item survey ( Multimedia Appendix 1 ) adapted from the National Cancer Institute’s Health Information National Trends Survey (HINTS) [ 4 ] to patients scheduled for an oncology visit at the Outpatient Care Center at UI Health. The survey was administered to 145 patients via email and 161 patients in person. Respondents were asked to identify sources used to self-educate about their diagnosis, preferred information source, social media use and preferences, and demographics. We used chi-square tests to assess associations between categorical variables.
Ethics Approval
This study was approved by the institutional review board at the University of Illinois Chicago and was found to meet the criteria for exemption as defined in the US Department of Health and Human Services Regulations for the Protection of Human Subjects (45 CFR 46.104(d)).
The demographics of our sample can be found in Table 1 . Respondents routinely accessed several forms of health information sources. The top three included their doctor or health care provider (n=274, 89.3%), internet search engines (n=218, 71.2%), and brochures and pamphlets (n=125, 40.7%). However, when directed to choose just one source, 207 (67.4%) chose their doctor or health care provider, while 67 (21.8%) chose internet search engines. The majority of respondents used a smartphone with the internet (n=237, 77.2%), a home desktop or laptop with the internet (n=192, 62.5%), or a tablet with the internet (n=188, 61.2%). However, approximately one-quarter of respondents indicated that they used a mobile phone without internet or a data plan.
We found that the majority of respondents accessed social media in the past year (n=198, 64.7%). Using social media was associated with age ( χ 2 3 =18.7; P <.001) and sex (Fisher P =.001). While respondents primarily used Facebook (n=69, 22.5%), YouTube (n=66, 21.5%), and Instagram (n=25, 8.1%) to receive health information, few shared health information with a medical professional (n=17, 5.5%), and if they did, they primarily used Facebook (n=8, 48.7%).
Principal Findings
Understanding how patients exchange health information is important to ensure access to accurate information and promote engagement with the health care team. We found that a majority of our patients use social media to find health-related information. However, there continues to be an internet access disparity that can limit patients’ ability to improve their health literacy. As social media engagement is linked to positive patient outcomes, using social media interventions can help us improve oncology patients’ illness experience. While both oncology providers and patients are increasingly using social media as a learning and sharing tool [ 5 ], the exact information-seeking behavior of patients with cancer has yet to be fully examined, especially in disadvantaged populations. In the current climate of rampant online medical misinformation, health care workers should find innovative ways to disseminate evidence-based patient-facing information using the platforms most accessed by oncology patients. Our study highlights the need to further explore communication preferences to help develop tailored communication strategies to support underserved patients and their families.

Limitations
Our study has various limitations. This study was a single clinic, single institution study with a relatively small sample size. Additionally, our patient population was older, which could have influenced preferred social media platforms.
Data Availability
The data sets generated or analyzed during this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
None declared.
Social media survey.
- Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, Hoving C. A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res. Apr 23, 2013;15(4):e85. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Khatri C, Chapman SJ, Glasbey J, Kelly M, Nepogodiev D, Bhangu A, et al. STARSurg Committee. Social media and internet driven study recruitment: evaluating a new model for promoting collaborator engagement and participation. PLoS One. 2015;10(3):e0118899. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Leist AK. Social media use of older adults: a mini-review. Gerontology. 2013;59(4):378-384. [ CrossRef ] [ Medline ]
- National Cancer Institute. Healthcare Information National Trends Survey. 2018. URL: https://hints.cancer.gov/ [accessed 2023-09-12]
- Watson J. Social media use in cancer care. Semin Oncol Nurs. May 2018;34(2):126-131. [ CrossRef ] [ Medline ]
Abbreviations
Edited by A Mavragani; submitted 21.03.22; peer-reviewed by S El kefi, S Hargreavess, K Na; comments to author 17.11.22; revised version received 16.06.23; accepted 04.07.23; published 25.03.24.
©Eric Freeman, Darshilmukesh Patel, Folasade Odeniyi, Mary Pasquinelli, Shikha Jain. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 25.03.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
- Português Br
- Journalist Pass
Medical Research
- AI and Digital Health
- Biotherapeutics
- Clinical Trials
- Discovery Science
- Healthcare Delivery
- Individualized Medicine
- Translational Science

March is Women's History Month, an opportunity to highlight the contributions of women in science and the challenges they face. A career in science and[...]
Latest stories

Signup to receive email notifications
Explore more topics

For Journalists Only Sign up for a Journalist Pass

Mayo Clinic Connect
An online patient support community
[ORGANIZATION OF MEDICAL CARE FOR CHILDREN WITH A NEW CORONAVIRUS INFECTION IN PATIENT CONDITIONS ON THE EXAMPLE OF THE CHILDREN'S CITY CLINICAL HOSPITAL NAMED AFTER Z. A. BASHLYAEVA]
Affiliations.
- 1 Children's City Clinical Hospital named after Z. A. Bashlyaeva of the Moscow City Health Department, 125373, Moscow, Russian Federation.
- 2 Pirogov Russian National Research Medical University, 117997, Moscow, Russian Federation.
- 3 Russian Medical Academy of Continuous Professional Education of the Ministry of Healthcare of the Russian Federation, 125993, Moscow, Russian Federation.
- 4 Pirogov Russian National Research Medical University, 117997, Moscow, Russian Federation, [email protected].
- 5 Research Institute for Healthcare Organization and Medical Management of Moscow Healthcare Department, 115088, Moscow, Russian Federation.
- PMID: 34792888
- DOI: 10.32687/0869-866X-2021-29-s2-1343-1349
The article presents an analysis of the work of the largest children's COVID-19 center in Moscow, organized on the basis of the Children's City Clinical Hospital named after Z. A. Bashlyaeva of the Moscow City Health Department. From March to November 2020 at the COVID-19 Center were hospitalized 2,837 patients with suspected/confirmed diagnosis of COVID-19, in total in 2020 1,876 children with a confirmed diagnosis of COVID-19 were treated, 58 (3%) children were in serious condition in the intensive care unit, of which children 11-18 years old were 25%. At the 2020 neonatal COVID-19 center, 215 newborns were observed with suspected COVID-19 diagnosis. The diagnosis of COVID-19 was confirmed in 18 children, while 8 newborns came from the home of COVID-19. In the Center for rehabilitation, where children aged 0 to 3 years old who were born with very low and extremely low body weight are observed, dispensary observation for children who have undergone COVID-19 is organized. 45 children who were observed fell ill with the new coronavirus infection. There were no deaths among children with COVID-19.
Keywords: COVID-19; COVID-center; children; new coronavirus infection; newborns; treatment.
- COVID-19 Testing*
- Child, Preschool
- Hospitals, Pediatric
- Infant, Newborn
- Retrospective Studies
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
March 25, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Study reveals new details about Argonaute syndromes, a class of neurodevelopmental disorders
by University of Massachusetts Medical School
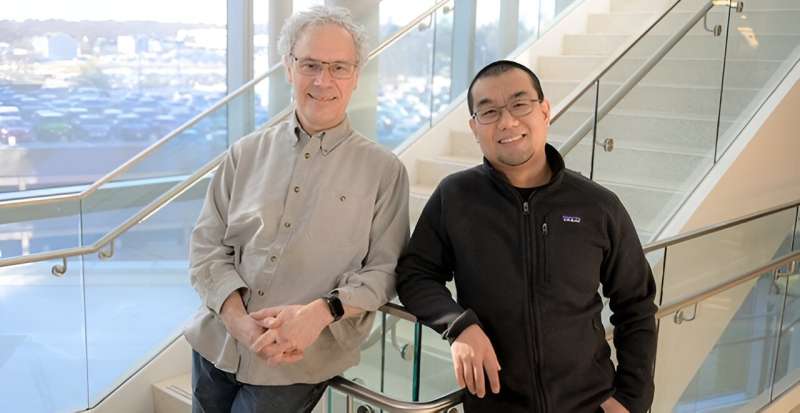
Research by Victor Ambros, Ph.D., provides new insights into a recently identified class of neurodevelopmental disorders called Argonaute syndromes. Dr. Ambros and colleagues believe their Proceedings of the National Academy of Sciences paper will help inform clinical and translational researchers in their pursuit of a treatment for this class of neurodevelopmental and autism-spectrum disorders.
"These findings will help the clinical scientists studying Argonaute syndromes in human cells to test for similar biological mechanisms," said Ambros, the Silverman Chair in Natural Sciences and professor of molecular medicine.
"Much of basic biology is shared between organisms. The power of the C. elegans model is that we can learn something new about basic biology that can then be applied directly to humans and human disease . Our work uncovers potential new aspects of Argonaute function in humans that then can help guide the search for treatments for disease."
A central figure in ribonucleic acid (RNA) biology research, Ambros was the first person to identify and characterize a known microRNA, a class of noncoding RNAs that plays an important role in modulating or regulating gene expression, specifically the process by which genes are silenced or turned off. Today, the discovery of microRNA is recognized as a pioneering step toward understanding that many RNA molecules play a critical role in the complex regulation of genes.
In this new study, Ambros and colleagues show that the RNA silencing complex is globally disrupted by single amino acid changes found in mutations associated with the newly identified Argonaute syndromes. These genetic mutations , studied in the C. elegans model, cause an organism-wide disruption of microRNA levels and messenger RNA translation, impacting hundreds of different genes, some of which are associated with neurodevelopmental disorders.
The Argonaute protein family consists of four proteins in humans, AGO1, AGO2, AGO3 and AGO4. First discovered for their evolutionarily conserved function in stem cells and development, these proteins play a central role in the RNA silencing process. Found in C. elegans, the microscopic worms scientists use to study basic biological processes, as well as humans and all animals, the Argonaute protein family has the same job—inhibit gene expression.
Argonaute proteins are the active part of the RNA-induced silencing complex (RISC), which degrade or cleave messenger RNA (mRNA) strands or inhibit their translation into proteins that would otherwise lead to protein production. The Argonaute protein targets complementary strands and reduces protein production by limiting the amount of mRNA or their translation efficiency found in the cell.
A complex biological molecule, Argonaute proteins have been associated with certain cancers, male infertility and neuronal development disorders. In 2021, a team of researchers led by Amélie Piton, Ph.D., associate professor of genetics and pathophysiology in neurodevelopmental disorders at the Institute of Genetics, Molecular and Cellular Biology in Strasbourg, France, described the first Argonaute related syndrome in humans caused by a mutation in the AGO1gene .
And a team led by Davor Lessel, MD, Ph.D., head of the Institute of Human Genetics at the University Hospital Salzburg, and Hans-Jürgen Kreienkamp, Ph.D., professor of human genetics at University of Hamburg, discovered in 2020 an AGO2-related syndrome , also known Lessel-Kreienkamp or Leskres syndrome.
Argonaute syndromes are extremely rare. To date, only 85 cases of Argonaute syndrome have been found in humans. These syndromes are characterized by a range of intellectual and physical symptoms including problems speaking and understanding language, delayed motor development, frequent seizures and cognitive impairment. Many patients exhibit autism spectrum-like pathologies.
Using C. elegans and CRISPR/Cas 9-mediated genome editing, Ye (Oscar) Duan, Ph.D.'23, a postdoctoral researcher in the Ambros lab and the study co-author, probed four human AGO1 mutations by introducing the same mutations in the worm's AGO1 counterpart. Results showed that mutations that change the function of the AGO1 gene exhibit stronger effects than mutations that completely turn off the AGO1 gene.
Duan explained that these results suggest that the mutant protein competes or interferes with the functions of the other, healthy Argonaute proteins such as AGO2. "This disparity occurs, we think, because in the complete absence of AGO1, the other Argonaute proteins, such as AGO2, step in and pick up the slack. Everything continues to operate normally," said Duan.
"But in the case of these single amino acid changes, the AGO1 protein being produced is aberrant and somehow keeps the RNA silencing process from happening, most likely by sequestering functional components of the microRNA silencing complex."
The result is a cascade of perturbations in global gene expression that impact microRNA levels and messenger RNA translation throughout the organism. Many of the genes impacted, according to Duan, have been linked to neurodevelopmental disorders in humans.
The next step for clinical and translational researchers will be to identify how these mutations are causing the microRNA silencing complex to misfire.
Explore further
Feedback to editors

Study suggests that estrogen may drive nicotine addiction in women
4 hours ago

Study: Black men may be less likely to receive heart transplant than white men, women

Friend or foe: A closer look at the role of health care algorithms in racial and ethnic disparities

CBD products don't ease pain and are potentially harmful, study finds

Research identifies characteristics of cities that would support young people's mental health
5 hours ago

Study with rodents identifies key genes for control of blood pressure and heart rate
6 hours ago

Study finds less obesity in 3- and 4-year-olds after the pandemic

Cancer therapies show promise in combating tuberculosis

New implant and app enable patients to monitor bladder function

Global study could change how children with multiple sclerosis are treated
Related stories.

Molecular 'hub' regulates gene-silencing proteins
Jun 27, 2023

Argonaute proteins help fine-tune gene expression
Oct 28, 2019

A matter of concentration
Sep 17, 2019

Researchers reveal novel role of Argonaute proteins in regulating protein quality control
Mar 25, 2022

Humans no longer have ancient defence mechanism against viruses
Sep 15, 2017

Exploring how Staufen and Argonaute proteins interact with each other
Jul 5, 2022
Recommended for you

Newly discovered beneficial mutation in mitochondrial DNA seems to help Alzheimer's gene carriers live longer
8 hours ago

Research suggests common household chemicals pose threat to brain health
9 hours ago

Mitochondrial DNA fragment losses predict Parkinson's disease before symptoms appear

Scientists identify a key driver of myelin repair
11 hours ago
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Intermittent fasting linked to higher risk of cardiovascular death, research suggests
Intermittent fasting, a diet pattern that involves alternating between periods of fasting and eating, can lower blood pressure and help some people lose weight , past research has indicated.
But an analysis presented Monday at the American Heart Association’s scientific sessions in Chicago challenges the notion that intermittent fasting is good for heart health. Instead, researchers from Shanghai Jiao Tong University School of Medicine in China found that people who restricted food consumption to less than eight hours per day had a 91% higher risk of dying from cardiovascular disease over a median period of eight years, relative to people who ate across 12 to 16 hours.
It’s some of the first research investigating the association between time-restricted eating (a type of intermittent fasting) and the risk of death from cardiovascular disease.
The analysis — which has not yet been peer-reviewed or published in an academic journal — is based on data from the Centers for Disease Control and Prevention’s National Health and Nutrition Examination Survey collected between 2003 and 2018. The researchers analyzed responses from around 20,000 adults who recorded what they ate for at least two days, then looked at who had died from cardiovascular disease after a median follow-up period of eight years.
However, Victor Wenze Zhong, a co-author of the analysis, said it’s too early to make specific recommendations about intermittent fasting based on his research alone.
“Practicing intermittent fasting for a short period such as 3 months may likely lead to benefits on reducing weight and improving cardiometabolic health,” Zhong said via email. But he added that people “should be extremely cautious” about intermittent fasting for longer periods of time, such as years.
Intermittent fasting regimens vary widely. A common schedule is to restrict eating to a period of six to eight hours per day, which can lead people to consume fewer calories, though some eat the same amount in a shorter time. Another popular schedule is the "5:2 diet," which involves eating 500 to 600 calories on two nonconsecutive days of the week but eating normally for the other five.

Zhong said it’s not clear why his research found an association between time-restricted eating and a risk of death from cardiovascular disease. He offered an observation, though: People who limited their eating to fewer than eight hours per day had less lean muscle mass than those who ate for 12 to 16 hours. Low lean muscle mass has been linked to a higher risk of cardiovascular death .
Cardiovascular and nutrition experts who were not involved in the analysis offered several theories about what might explain the results.
Dr. Benjamin Horne, a research professor at Intermountain Health in Salt Lake City, said fasting can increase stress hormones such as cortisol and adrenaline, since the body doesn’t know when to expect food next and goes into survival mode. That added stress may raise the short-term risk of heart problems among vulnerable groups, he said, particularly elderly people or those with chronic health conditions.
Horne’s research has shown that fasting twice a week for four weeks, then once a week for 22 weeks may increase a person’s risk of dying after one year but decrease their 10-year risk of chronic disease.
“In the long term, what it does is reduces those risk factors for heart disease and reduces the risk factors for diabetes and so forth — but in the short term, while you’re actually doing it, your body is in a state where it’s at a higher risk of having problems,” he said.
Even so, Horne added, the analysis “doesn’t change my perspective that there are definite benefits from fasting, but it’s a cautionary tale that we need to be aware that there are definite, potentially major, adverse effects.”
Intermittent fasting gained popularity about a decade ago, when the 5:2 diet was touted as a weight loss strategy in the U.K. In the years to follow, several celebrities espoused the benefits of an eight-hour eating window for weight loss, while some Silicon Valley tech workers believed that extreme periods of fasting boosted productivity . Some studies have also suggested that intermittent fasting might help extend people’s lifespans by warding off disease .
However, a lot of early research on intermittent fasting involved animals. In the last seven years or so, various clinical trials have investigated potential benefits for humans, including for heart health.
“The purpose of intermittent fasting is to cut calories, lose weight,” said Penny Kris-Etherton, emeritus professor of nutritional sciences at Penn State University and a member of the American Heart Association nutrition committee. “It’s really how intermittent fasting is implemented that’s going to explain a lot of the benefits or adverse associations.”
Dr. Francisco Lopez-Jimenez, a cardiologist at Mayo Clinic, said the timing of when people eat may influence the effects they see.
“I haven’t met a single person or patient that has been practicing intermittent fasting by skipping dinner,” he said, noting that people more often skip breakfast, a schedule associated with an increased risk of heart disease and death .
The new research comes with limitations: It relies on people’s memories of what they consumed over a 24-hour period and doesn’t consider the nutritional quality of the food they ate or how many calories they consumed during an eating window.
So some experts found the analysis too narrow.
“It’s a retrospective study looking at two days’ worth of data, and drawing some very big conclusions from a very limited snapshot into a person’s lifestyle habits,” said Dr. Pam Taub, a cardiologist at UC San Diego Health.
Taub said her patients have seen “incredible benefits” from fasting regimens.
“I would continue doing it,” she said. “For people that do intermittent fasting, their individual results speak for themselves. Most people that do intermittent fasting, the reason they continue it is they see a decrease in their weight. They see a decrease in blood pressure. They see an improvement in their LDL cholesterol.”
Kris-Etherton, however, urged caution: “Maybe consider a pause in intermittent fasting until we have more information or until the results of the study can be better explained,” she said.
Aria Bendix is the breaking health reporter for NBC News Digital.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

The use of Big Data Analytics in healthcare
Kornelia batko.
1 Department of Business Informatics, University of Economics in Katowice, Katowice, Poland
Andrzej Ślęzak
2 Department of Biomedical Processes and Systems, Institute of Health and Nutrition Sciences, Częstochowa University of Technology, Częstochowa, Poland
Associated Data
The datasets for this study are available on request to the corresponding author.
The introduction of Big Data Analytics (BDA) in healthcare will allow to use new technologies both in treatment of patients and health management. The paper aims at analyzing the possibilities of using Big Data Analytics in healthcare. The research is based on a critical analysis of the literature, as well as the presentation of selected results of direct research on the use of Big Data Analytics in medical facilities. The direct research was carried out based on research questionnaire and conducted on a sample of 217 medical facilities in Poland. Literature studies have shown that the use of Big Data Analytics can bring many benefits to medical facilities, while direct research has shown that medical facilities in Poland are moving towards data-based healthcare because they use structured and unstructured data, reach for analytics in the administrative, business and clinical area. The research positively confirmed that medical facilities are working on both structural data and unstructured data. The following kinds and sources of data can be distinguished: from databases, transaction data, unstructured content of emails and documents, data from devices and sensors. However, the use of data from social media is lower as in their activity they reach for analytics, not only in the administrative and business but also in the clinical area. It clearly shows that the decisions made in medical facilities are highly data-driven. The results of the study confirm what has been analyzed in the literature that medical facilities are moving towards data-based healthcare, together with its benefits.
Introduction
The main contribution of this paper is to present an analytical overview of using structured and unstructured data (Big Data) analytics in medical facilities in Poland. Medical facilities use both structured and unstructured data in their practice. Structured data has a predetermined schema, it is extensive, freeform, and comes in variety of forms [ 27 ]. In contrast, unstructured data, referred to as Big Data (BD), does not fit into the typical data processing format. Big Data is a massive amount of data sets that cannot be stored, processed, or analyzed using traditional tools. It remains stored but not analyzed. Due to the lack of a well-defined schema, it is difficult to search and analyze such data and, therefore, it requires a specific technology and method to transform it into value [ 20 , 68 ]. Integrating data stored in both structured and unstructured formats can add significant value to an organization [ 27 ]. Organizations must approach unstructured data in a different way. Therefore, the potential is seen in Big Data Analytics (BDA). Big Data Analytics are techniques and tools used to analyze and extract information from Big Data. The results of Big Data analysis can be used to predict the future. They also help in creating trends about the past. When it comes to healthcare, it allows to analyze large datasets from thousands of patients, identifying clusters and correlation between datasets, as well as developing predictive models using data mining techniques [ 60 ].
This paper is the first study to consolidate and characterize the use of Big Data from different perspectives. The first part consists of a brief literature review of studies on Big Data (BD) and Big Data Analytics (BDA), while the second part presents results of direct research aimed at diagnosing the use of big data analyses in medical facilities in Poland.
Healthcare is a complex system with varied stakeholders: patients, doctors, hospitals, pharmaceutical companies and healthcare decision-makers. This sector is also limited by strict rules and regulations. However, worldwide one may observe a departure from the traditional doctor-patient approach. The doctor becomes a partner and the patient is involved in the therapeutic process [ 14 ]. Healthcare is no longer focused solely on the treatment of patients. The priority for decision-makers should be to promote proper health attitudes and prevent diseases that can be avoided [ 81 ]. This became visible and important especially during the Covid-19 pandemic [ 44 ].
The next challenges that healthcare will have to face is the growing number of elderly people and a decline in fertility. Fertility rates in the country are found below the reproductive minimum necessary to keep the population stable [ 10 ]. The reflection of both effects, namely the increase in age and lower fertility rates, are demographic load indicators, which is constantly growing. Forecasts show that providing healthcare in the form it is provided today will become impossible in the next 20 years [ 70 ]. It is especially visible now during the Covid-19 pandemic when healthcare faced quite a challenge related to the analysis of huge data amounts and the need to identify trends and predict the spread of the coronavirus. The pandemic showed it even more that patients should have access to information about their health condition, the possibility of digital analysis of this data and access to reliable medical support online. Health monitoring and cooperation with doctors in order to prevent diseases can actually revolutionize the healthcare system. One of the most important aspects of the change necessary in healthcare is putting the patient in the center of the system.
Technology is not enough to achieve these goals. Therefore, changes should be made not only at the technological level but also in the management and design of complete healthcare processes and what is more, they should affect the business models of service providers. The use of Big Data Analytics is becoming more and more common in enterprises [ 17 , 54 ]. However, medical enterprises still cannot keep up with the information needs of patients, clinicians, administrators and the creator’s policy. The adoption of a Big Data approach would allow the implementation of personalized and precise medicine based on personalized information, delivered in real time and tailored to individual patients.
To achieve this goal, it is necessary to implement systems that will be able to learn quickly about the data generated by people within clinical care and everyday life. This will enable data-driven decision making, receiving better personalized predictions about prognosis and responses to treatments; a deeper understanding of the complex factors and their interactions that influence health at the patient level, the health system and society, enhanced approaches to detecting safety problems with drugs and devices, as well as more effective methods of comparing prevention, diagnostic, and treatment options [ 40 ].
In the literature, there is a lot of research showing what opportunities can be offered to companies by big data analysis and what data can be analyzed. However, there are few studies showing how data analysis in the area of healthcare is performed, what data is used by medical facilities and what analyses and in which areas they carry out. This paper aims to fill this gap by presenting the results of research carried out in medical facilities in Poland. The goal is to analyze the possibilities of using Big Data Analytics in healthcare, especially in Polish conditions. In particular, the paper is aimed at determining what data is processed by medical facilities in Poland, what analyses they perform and in what areas, and how they assess their analytical maturity. In order to achieve this goal, a critical analysis of the literature was performed, and the direct research was based on a research questionnaire conducted on a sample of 217 medical facilities in Poland. It was hypothesized that medical facilities in Poland are working on both structured and unstructured data and moving towards data-based healthcare and its benefits. Examining the maturity of healthcare facilities in the use of Big Data and Big Data Analytics is crucial in determining the potential future benefits that the healthcare sector can gain from Big Data Analytics. There is also a pressing need to predicate whether, in the coming years, healthcare will be able to cope with the threats and challenges it faces.
This paper is divided into eight parts. The first is the introduction which provides background and the general problem statement of this research. In the second part, this paper discusses considerations on use of Big Data and Big Data Analytics in Healthcare, and then, in the third part, it moves on to challenges and potential benefits of using Big Data Analytics in healthcare. The next part involves the explanation of the proposed method. The result of direct research and discussion are presented in the fifth part, while the following part of the paper is the conclusion. The seventh part of the paper presents practical implications. The final section of the paper provides limitations and directions for future research.
Considerations on use Big Data and Big Data Analytics in the healthcare
In recent years one can observe a constantly increasing demand for solutions offering effective analytical tools. This trend is also noticeable in the analysis of large volumes of data (Big Data, BD). Organizations are looking for ways to use the power of Big Data to improve their decision making, competitive advantage or business performance [ 7 , 54 ]. Big Data is considered to offer potential solutions to public and private organizations, however, still not much is known about the outcome of the practical use of Big Data in different types of organizations [ 24 ].
As already mentioned, in recent years, healthcare management worldwide has been changed from a disease-centered model to a patient-centered model, even in value-based healthcare delivery model [ 68 ]. In order to meet the requirements of this model and provide effective patient-centered care, it is necessary to manage and analyze healthcare Big Data.
The issue often raised when it comes to the use of data in healthcare is the appropriate use of Big Data. Healthcare has always generated huge amounts of data and nowadays, the introduction of electronic medical records, as well as the huge amount of data sent by various types of sensors or generated by patients in social media causes data streams to constantly grow. Also, the medical industry generates significant amounts of data, including clinical records, medical images, genomic data and health behaviors. Proper use of the data will allow healthcare organizations to support clinical decision-making, disease surveillance, and public health management. The challenge posed by clinical data processing involves not only the quantity of data but also the difficulty in processing it.
In the literature one can find many different definitions of Big Data. This concept has evolved in recent years, however, it is still not clearly understood. Nevertheless, despite the range and differences in definitions, Big Data can be treated as a: large amount of digital data, large data sets, tool, technology or phenomenon (cultural or technological.
Big Data can be considered as massive and continually generated digital datasets that are produced via interactions with online technologies [ 53 ]. Big Data can be defined as datasets that are of such large sizes that they pose challenges in traditional storage and analysis techniques [ 28 ]. A similar opinion about Big Data was presented by Ohlhorst who sees Big Data as extremely large data sets, possible neither to manage nor to analyze with traditional data processing tools [ 57 ]. In his opinion, the bigger the data set, the more difficult it is to gain any value from it.
In turn, Knapp perceived Big Data as tools, processes and procedures that allow an organization to create, manipulate and manage very large data sets and storage facilities [ 38 ]. From this point of view, Big Data is identified as a tool to gather information from different databases and processes, allowing users to manage large amounts of data.
Similar perception of the term ‘Big Data’ is shown by Carter. According to him, Big Data technologies refer to a new generation of technologies and architectures, designed to economically extract value from very large volumes of a wide variety of data by enabling high velocity capture, discovery and/or analysis [ 13 ].
Jordan combines these two approaches by identifying Big Data as a complex system, as it needs data bases for data to be stored in, programs and tools to be managed, as well as expertise and personnel able to retrieve useful information and visualization to be understood [ 37 ].
Following the definition of Laney for Big Data, it can be state that: it is large amount of data generated in very fast motion and it contains a lot of content [ 43 ]. Such data comes from unstructured sources, such as stream of clicks on the web, social networks (Twitter, blogs, Facebook), video recordings from the shops, recording of calls in a call center, real time information from various kinds of sensors, RFID, GPS devices, mobile phones and other devices that identify and monitor something [ 8 ]. Big Data is a powerful digital data silo, raw, collected with all sorts of sources, unstructured and difficult, or even impossible, to analyze using conventional techniques used so far to relational databases.
While describing Big Data, it cannot be overlooked that the term refers more to a phenomenon than to specific technology. Therefore, instead of defining this phenomenon, trying to describe them, more authors are describing Big Data by giving them characteristics included a collection of V’s related to its nature [ 2 , 3 , 23 , 25 , 58 ]:
- Volume (refers to the amount of data and is one of the biggest challenges in Big Data Analytics),
- Velocity (speed with which new data is generated, the challenge is to be able to manage data effectively and in real time),
- Variety (heterogeneity of data, many different types of healthcare data, the challenge is to derive insights by looking at all available heterogenous data in a holistic manner),
- Variability (inconsistency of data, the challenge is to correct the interpretation of data that can vary significantly depending on the context),
- Veracity (how trustworthy the data is, quality of the data),
- Visualization (ability to interpret data and resulting insights, challenging for Big Data due to its other features as described above).
- Value (the goal of Big Data Analytics is to discover the hidden knowledge from huge amounts of data).
Big Data is defined as an information asset with high volume, velocity, and variety, which requires specific technology and method for its transformation into value [ 21 , 77 ]. Big Data is also a collection of information about high-volume, high volatility or high diversity, requiring new forms of processing in order to support decision-making, discovering new phenomena and process optimization [ 5 , 7 ]. Big Data is too large for traditional data-processing systems and software tools to capture, store, manage and analyze, therefore it requires new technologies [ 28 , 50 , 61 ] to manage (capture, aggregate, process) its volume, velocity and variety [ 9 ].
Undoubtedly, Big Data differs from the data sources used so far by organizations. Therefore, organizations must approach this type of unstructured data in a different way. First of all, organizations must start to see data as flows and not stocks—this entails the need to implement the so-called streaming analytics [ 48 ]. The mentioned features make it necessary to use new IT tools that allow the fullest use of new data [ 58 ]. The Big Data idea, inseparable from the huge increase in data available to various organizations or individuals, creates opportunities for access to valuable analyses, conclusions and enables making more accurate decisions [ 6 , 11 , 59 ].
The Big Data concept is constantly evolving and currently it does not focus on huge amounts of data, but rather on the process of creating value from this data [ 52 ]. Big Data is collected from various sources that have different data properties and are processed by different organizational units, resulting in creation of a Big Data chain [ 36 ]. The aim of the organizations is to manage, process and analyze Big Data. In the healthcare sector, Big Data streams consist of various types of data, namely [ 8 , 51 ]:
- clinical data, i.e. data obtained from electronic medical records, data from hospital information systems, image centers, laboratories, pharmacies and other organizations providing health services, patient generated health data, physician’s free-text notes, genomic data, physiological monitoring data [ 4 ],
- biometric data provided from various types of devices that monitor weight, pressure, glucose level, etc.,
- financial data, constituting a full record of economic operations reflecting the conducted activity,
- data from scientific research activities, i.e. results of research, including drug research, design of medical devices and new methods of treatment,
- data provided by patients, including description of preferences, level of satisfaction, information from systems for self-monitoring of their activity: exercises, sleep, meals consumed, etc.
- data from social media.
These data are provided not only by patients but also by organizations and institutions, as well as by various types of monitoring devices, sensors or instruments [ 16 ]. Data that has been generated so far in the healthcare sector is stored in both paper and digital form. Thus, the essence and the specificity of the process of Big Data analyses means that organizations need to face new technological and organizational challenges [ 67 ]. The healthcare sector has always generated huge amounts of data and this is connected, among others, with the need to store medical records of patients. However, the problem with Big Data in healthcare is not limited to an overwhelming volume but also an unprecedented diversity in terms of types, data formats and speed with which it should be analyzed in order to provide the necessary information on an ongoing basis [ 3 ]. It is also difficult to apply traditional tools and methods for management of unstructured data [ 67 ]. Due to the diversity and quantity of data sources that are growing all the time, advanced analytical tools and technologies, as well as Big Data analysis methods which can meet and exceed the possibilities of managing healthcare data, are needed [ 3 , 68 ].
Therefore, the potential is seen in Big Data analyses, especially in the aspect of improving the quality of medical care, saving lives or reducing costs [ 30 ]. Extracting from this tangle of given association rules, patterns and trends will allow health service providers and other stakeholders in the healthcare sector to offer more accurate and more insightful diagnoses of patients, personalized treatment, monitoring of the patients, preventive medicine, support of medical research and health population, as well as better quality of medical services and patient care while, at the same time, the ability to reduce costs (Fig. 1 ).

Healthcare Big Data Analytics applications
(Source: Own elaboration)
The main challenge with Big Data is how to handle such a large amount of information and use it to make data-driven decisions in plenty of areas [ 64 ]. In the context of healthcare data, another major challenge is to adjust big data storage, analysis, presentation of analysis results and inference basing on them in a clinical setting. Data analytics systems implemented in healthcare are designed to describe, integrate and present complex data in an appropriate way so that it can be understood better (Fig. 2 ). This would improve the efficiency of acquiring, storing, analyzing and visualizing big data from healthcare [ 71 ].

Process of Big Data Analytics
The result of data processing with the use of Big Data Analytics is appropriate data storytelling which may contribute to making decisions with both lower risk and data support. This, in turn, can benefit healthcare stakeholders. To take advantage of the potential massive amounts of data in healthcare and to ensure that the right intervention to the right patient is properly timed, personalized, and potentially beneficial to all components of the healthcare system such as the payer, patient, and management, analytics of large datasets must connect communities involved in data analytics and healthcare informatics [ 49 ]. Big Data Analytics can provide insight into clinical data and thus facilitate informed decision-making about the diagnosis and treatment of patients, prevention of diseases or others. Big Data Analytics can also improve the efficiency of healthcare organizations by realizing the data potential [ 3 , 62 ].
Big Data Analytics in medicine and healthcare refers to the integration and analysis of a large amount of complex heterogeneous data, such as various omics (genomics, epigenomics, transcriptomics, proteomics, metabolomics, interactomics, pharmacogenetics, deasomics), biomedical data, talemedicine data (sensors, medical equipment data) and electronic health records data [ 46 , 65 ].
When analyzing the phenomenon of Big Data in the healthcare sector, it should be noted that it can be considered from the point of view of three areas: epidemiological, clinical and business.
From a clinical point of view, the Big Data analysis aims to improve the health and condition of patients, enable long-term predictions about their health status and implementation of appropriate therapeutic procedures. Ultimately, the use of data analysis in medicine is to allow the adaptation of therapy to a specific patient, that is personalized medicine (precision, personalized medicine).
From an epidemiological point of view, it is desirable to obtain an accurate prognosis of morbidity in order to implement preventive programs in advance.
In the business context, Big Data analysis may enable offering personalized packages of commercial services or determining the probability of individual disease and infection occurrence. It is worth noting that Big Data means not only the collection and processing of data but, most of all, the inference and visualization of data necessary to obtain specific business benefits.
In order to introduce new management methods and new solutions in terms of effectiveness and transparency, it becomes necessary to make data more accessible, digital, searchable, as well as analyzed and visualized.
Erickson and Rothberg state that the information and data do not reveal their full value until insights are drawn from them. Data becomes useful when it enhances decision making and decision making is enhanced only when analytical techniques are used and an element of human interaction is applied [ 22 ].
Thus, healthcare has experienced much progress in usage and analysis of data. A large-scale digitalization and transparency in this sector is a key statement of almost all countries governments policies. For centuries, the treatment of patients was based on the judgment of doctors who made treatment decisions. In recent years, however, Evidence-Based Medicine has become more and more important as a result of it being related to the systematic analysis of clinical data and decision-making treatment based on the best available information [ 42 ]. In the healthcare sector, Big Data Analytics is expected to improve the quality of life and reduce operational costs [ 72 , 82 ]. Big Data Analytics enables organizations to improve and increase their understanding of the information contained in data. It also helps identify data that provides insightful insights for current as well as future decisions [ 28 ].
Big Data Analytics refers to technologies that are grounded mostly in data mining: text mining, web mining, process mining, audio and video analytics, statistical analysis, network analytics, social media analytics and web analytics [ 16 , 25 , 31 ]. Different data mining techniques can be applied on heterogeneous healthcare data sets, such as: anomaly detection, clustering, classification, association rules as well as summarization and visualization of those Big Data sets [ 65 ]. Modern data analytics techniques explore and leverage unique data characteristics even from high-speed data streams and sensor data [ 15 , 16 , 31 , 55 ]. Big Data can be used, for example, for better diagnosis in the context of comprehensive patient data, disease prevention and telemedicine (in particular when using real-time alerts for immediate care), monitoring patients at home, preventing unnecessary hospital visits, integrating medical imaging for a wider diagnosis, creating predictive analytics, reducing fraud and improving data security, better strategic planning and increasing patients’ involvement in their own health.
Big Data Analytics in healthcare can be divided into [ 33 , 73 , 74 ]:
- descriptive analytics in healthcare is used to understand past and current healthcare decisions, converting data into useful information for understanding and analyzing healthcare decisions, outcomes and quality, as well as making informed decisions [ 33 ]. It can be used to create reports (i.e. about patients’ hospitalizations, physicians’ performance, utilization management), visualization, customized reports, drill down tables, or running queries on the basis of historical data.
- predictive analytics operates on past performance in an effort to predict the future by examining historical or summarized health data, detecting patterns of relationships in these data, and then extrapolating these relationships to forecast. It can be used to i.e. predict the response of different patient groups to different drugs (dosages) or reactions (clinical trials), anticipate risk and find relationships in health data and detect hidden patterns [ 62 ]. In this way, it is possible to predict the epidemic spread, anticipate service contracts and plan healthcare resources. Predictive analytics is used in proper diagnosis and for appropriate treatments to be given to patients suffering from certain diseases [ 39 ].
- prescriptive analytics—occurs when health problems involve too many choices or alternatives. It uses health and medical knowledge in addition to data or information. Prescriptive analytics is used in many areas of healthcare, including drug prescriptions and treatment alternatives. Personalized medicine and evidence-based medicine are both supported by prescriptive analytics.
- discovery analytics—utilizes knowledge about knowledge to discover new “inventions” like drugs (drug discovery), previously unknown diseases and medical conditions, alternative treatments, etc.
Although the models and tools used in descriptive, predictive, prescriptive, and discovery analytics are different, many applications involve all four of them [ 62 ]. Big Data Analytics in healthcare can help enable personalized medicine by identifying optimal patient-specific treatments. This can influence the improvement of life standards, reduce waste of healthcare resources and save costs of healthcare [ 56 , 63 , 71 ]. The introduction of large data analysis gives new analytical possibilities in terms of scope, flexibility and visualization. Techniques such as data mining (computational pattern discovery process in large data sets) facilitate inductive reasoning and analysis of exploratory data, enabling scientists to identify data patterns that are independent of specific hypotheses. As a result, predictive analysis and real-time analysis becomes possible, making it easier for medical staff to start early treatments and reduce potential morbidity and mortality. In addition, document analysis, statistical modeling, discovering patterns and topics in document collections and data in the EHR, as well as an inductive approach can help identify and discover relationships between health phenomena.
Advanced analytical techniques can be used for a large amount of existing (but not yet analytical) data on patient health and related medical data to achieve a better understanding of the information and results obtained, as well as to design optimal clinical pathways [ 62 ]. Big Data Analytics in healthcare integrates analysis of several scientific areas such as bioinformatics, medical imaging, sensor informatics, medical informatics and health informatics [ 65 ]. Big Data Analytics in healthcare allows to analyze large datasets from thousands of patients, identifying clusters and correlation between datasets, as well as developing predictive models using data mining techniques [ 65 ]. Discussing all the techniques used for Big Data Analytics goes beyond the scope of a single article [ 25 ].
The success of Big Data analysis and its accuracy depend heavily on the tools and techniques used to analyze the ability to provide reliable, up-to-date and meaningful information to various stakeholders [ 12 ]. It is believed that the implementation of big data analytics by healthcare organizations could bring many benefits in the upcoming years, including lowering health care costs, better diagnosis and prediction of diseases and their spread, improving patient care and developing protocols to prevent re-hospitalization, optimizing staff, optimizing equipment, forecasting the need for hospital beds, operating rooms, treatments, and improving the drug supply chain [ 71 ].
Challenges and potential benefits of using Big Data Analytics in healthcare
Modern analytics gives possibilities not only to have insight in historical data, but also to have information necessary to generate insight into what may happen in the future. Even when it comes to prediction of evidence-based actions. The emphasis on reform has prompted payers and suppliers to pursue data analysis to reduce risk, detect fraud, improve efficiency and save lives. Everyone—payers, providers, even patients—are focusing on doing more with fewer resources. Thus, some areas in which enhanced data and analytics can yield the greatest results include various healthcare stakeholders (Table (Table1 1 ).
The use of analytics by various healthcare stakeholders
Source: own elaboration on the basis of [ 19 , 20 ]
Healthcare organizations see the opportunity to grow through investments in Big Data Analytics. In recent years, by collecting medical data of patients, converting them into Big Data and applying appropriate algorithms, reliable information has been generated that helps patients, physicians and stakeholders in the health sector to identify values and opportunities [ 31 ]. It is worth noting that there are many changes and challenges in the structure of the healthcare sector. Digitization and effective use of Big Data in healthcare can bring benefits to every stakeholder in this sector. A single doctor would benefit the same as the entire healthcare system. Potential opportunities to achieve benefits and effects from Big Data in healthcare can be divided into four groups [ 8 ]:
- assessment of diagnoses made by doctors and the manner of treatment of diseases indicated by them based on the decision support system working on Big Data collections,
- detection of more effective, from a medical point of view, and more cost-effective ways to diagnose and treat patients,
- analysis of large volumes of data to reach practical information useful for identifying needs, introducing new health services, preventing and overcoming crises,
- prediction of the incidence of diseases,
- detecting trends that lead to an improvement in health and lifestyle of the society,
- analysis of the human genome for the introduction of personalized treatment.
- doctors’ comparison of current medical cases to cases from the past for better diagnosis and treatment adjustment,
- detection of diseases at earlier stages when they can be more easily and quickly cured,
- detecting epidemiological risks and improving control of pathogenic spots and reaction rates,
- identification of patients who are predicted to have the highest risk of specific, life-threatening diseases by collating data on the history of the most common diseases, in healing people with reports entering insurance companies,
- health management of each patient individually (personalized medicine) and health management of the whole society,
- capturing and analyzing large amounts of data from hospitals and homes in real time, life monitoring devices to monitor safety and predict adverse events,
- analysis of patient profiles to identify people for whom prevention should be applied, lifestyle change or preventive care approach,
- the ability to predict the occurrence of specific diseases or worsening of patients’ results,
- predicting disease progression and its determinants, estimating the risk of complications,
- detecting drug interactions and their side effects.
- supporting work on new drugs and clinical trials thanks to the possibility of analyzing “all data” instead of selecting a test sample,
- the ability to identify patients with specific, biological features that will take part in specialized clinical trials,
- selecting a group of patients for which the tested drug is likely to have the desired effect and no side effects,
- using modeling and predictive analysis to design better drugs and devices.
- reduction of costs and counteracting abuse and counseling practices,
- faster and more effective identification of incorrect or unauthorized financial operations in order to prevent abuse and eliminate errors,
- increase in profitability by detecting patients generating high costs or identifying doctors whose work, procedures and treatment methods cost the most and offering them solutions that reduce the amount of money spent,
- identification of unnecessary medical activities and procedures, e.g. duplicate tests.
According to research conducted by Wang, Kung and Byrd, Big Data Analytics benefits can be classified into five categories: IT infrastructure benefits (reducing system redundancy, avoiding unnecessary IT costs, transferring data quickly among healthcare IT systems, better use of healthcare systems, processing standardization among various healthcare IT systems, reducing IT maintenance costs regarding data storage), operational benefits (improving the quality and accuracy of clinical decisions, processing a large number of health records in seconds, reducing the time of patient travel, immediate access to clinical data to analyze, shortening the time of diagnostic test, reductions in surgery-related hospitalizations, exploring inconceivable new research avenues), organizational benefits (detecting interoperability problems much more quickly than traditional manual methods, improving cross-functional communication and collaboration among administrative staffs, researchers, clinicians and IT staffs, enabling data sharing with other institutions and adding new services, content sources and research partners), managerial benefits (gaining quick insights about changing healthcare trends in the market, providing members of the board and heads of department with sound decision-support information on the daily clinical setting, optimizing business growth-related decisions) and strategic benefits (providing a big picture view of treatment delivery for meeting future need, creating high competitive healthcare services) [ 73 ].
The above specification does not constitute a full list of potential areas of use of Big Data Analysis in healthcare because the possibilities of using analysis are practically unlimited. In addition, advanced analytical tools allow to analyze data from all possible sources and conduct cross-analyses to provide better data insights [ 26 ]. For example, a cross-analysis can refer to a combination of patient characteristics, as well as costs and care results that can help identify the best, in medical terms, and the most cost-effective treatment or treatments and this may allow a better adjustment of the service provider’s offer [ 62 ].
In turn, the analysis of patient profiles (e.g. segmentation and predictive modeling) allows identification of people who should be subject to prophylaxis, prevention or should change their lifestyle [ 8 ]. Shortened list of benefits for Big Data Analytics in healthcare is presented in paper [ 3 ] and consists of: better performance, day-to-day guides, detection of diseases in early stages, making predictive analytics, cost effectiveness, Evidence Based Medicine and effectiveness in patient treatment.
Summarizing, healthcare big data represents a huge potential for the transformation of healthcare: improvement of patients’ results, prediction of outbreaks of epidemics, valuable insights, avoidance of preventable diseases, reduction of the cost of healthcare delivery and improvement of the quality of life in general [ 1 ]. Big Data also generates many challenges such as difficulties in data capture, data storage, data analysis and data visualization [ 15 ]. The main challenges are connected with the issues of: data structure (Big Data should be user-friendly, transparent, and menu-driven but it is fragmented, dispersed, rarely standardized and difficult to aggregate and analyze), security (data security, privacy and sensitivity of healthcare data, there are significant concerns related to confidentiality), data standardization (data is stored in formats that are not compatible with all applications and technologies), storage and transfers (especially costs associated with securing, storing, and transferring unstructured data), managerial skills, such as data governance, lack of appropriate analytical skills and problems with Real-Time Analytics (health care is to be able to utilize Big Data in real time) [ 4 , 34 , 41 ].
The research is based on a critical analysis of the literature, as well as the presentation of selected results of direct research on the use of Big Data Analytics in medical facilities in Poland.
Presented research results are part of a larger questionnaire form on Big Data Analytics. The direct research was based on an interview questionnaire which contained 100 questions with 5-point Likert scale (1—strongly disagree, 2—I rather disagree, 3—I do not agree, nor disagree, 4—I rather agree, 5—I definitely agree) and 4 metrics questions. The study was conducted in December 2018 on a sample of 217 medical facilities (110 private, 107 public). The research was conducted by a specialized market research agency: Center for Research and Expertise of the University of Economics in Katowice.
When it comes to direct research, the selected entities included entities financed from public sources—the National Health Fund (23.5%), and entities operating commercially (11.5%). In the surveyed group of entities, more than a half (64.9%) are hybrid financed, both from public and commercial sources. The diversity of the research sample also applies to the size of the entities, defined by the number of employees. Taking into account proportions of the surveyed entities, it should be noted that in the sector structure, medium-sized (10–50 employees—34% of the sample) and large (51–250 employees—27%) entities dominate. The research was of all-Poland nature, and the entities included in the research sample come from all of the voivodships. The largest group were entities from Łódzkie (32%), Śląskie (18%) and Mazowieckie (18%) voivodships, as these voivodships have the largest number of medical institutions. Other regions of the country were represented by single units. The selection of the research sample was random—layered. As part of medical facilities database, groups of private and public medical facilities have been identified and the ones to which the questionnaire was targeted were drawn from each of these groups. The analyses were performed using the GNU PSPP 0.10.2 software.
The aim of the study was to determine whether medical facilities in Poland use Big Data Analytics and if so, in which areas. Characteristics of the research sample is presented in Table Table2 2 .
Characteristics of the research sample
The research is non-exhaustive due to the incomplete and uneven regional distribution of the samples, overrepresented in three voivodeships (Łódzkie, Mazowieckie and Śląskie). The size of the research sample (217 entities) allows the authors of the paper to formulate specific conclusions on the use of Big Data in the process of its management.
For the purpose of this paper, the following research hypotheses were formulated: (1) medical facilities in Poland are working on both structured and unstructured data (2) medical facilities in Poland are moving towards data-based healthcare and its benefits.
The paper poses the following research questions and statements that coincide with the selected questions from the research questionnaire:
- From what sources do medical facilities obtain data? What types of data are used by the particular organization, whether structured or unstructured, and to what extent?
- From what sources do medical facilities obtain data?
- In which area organizations are using data and analytical systems (clinical or business)?
- Is data analytics performed based on historical data or are predictive analyses also performed?
- Determining whether administrative and medical staff receive complete, accurate and reliable data in a timely manner?
- Determining whether real-time analyses are performed to support the particular organization’s activities.
Results and discussion
On the basis of the literature analysis and research study, a set of questions and statements related to the researched area was formulated. The results from the surveys show that medical facilities use a variety of data sources in their operations. These sources are both structured and unstructured data (Table (Table3 3 ).
Type of data sources used in medical facility (%)
1—strongly disagree, 2—I disagree, 3—I agree or disagree, 4—I rather agree, 5—I strongly agree
According to the data provided by the respondents, considering the first statement made in the questionnaire, almost half of the medical institutions (47.58%) agreed that they rather collect and use structured data (e.g. databases and data warehouses, reports to external entities) and 10.57% entirely agree with this statement. As much as 23.35% of representatives of medical institutions stated “I agree or disagree”. Other medical facilities do not collect and use structured data (7.93%) and 6.17% strongly disagree with the first statement. Also, the median calculated based on the obtained results (median: 4), proves that medical facilities in Poland collect and use structured data (Table (Table4 4 ).
Collection and use of data determined by the size of medical facility (number of employees)
In turn, 28.19% of the medical institutions agreed that they rather collect and use unstructured data and as much as 9.25% entirely agree with this statement. The number of representatives of medical institutions that stated “I agree or disagree” was 27.31%. Other medical facilities do not collect and use structured data (17.18%) and 13.66% strongly disagree with the first statement. In the case of unstructured data the median is 3, which means that the collection and use of this type of data by medical facilities in Poland is lower.
In the further part of the analysis, it was checked whether the size of the medical facility and form of ownership have an impact on whether it analyzes unstructured data (Tables (Tables4 4 and and5). 5 ). In order to find this out, correlation coefficients were calculated.
Collection and use of data determined by the form of ownership of medical facility
Based on the calculations, it can be concluded that there is a small statistically monotonic correlation between the size of the medical facility and its collection and use of structured data (p < 0.001; τ = 0.16). This means that the use of structured data is slightly increasing in larger medical facilities. The size of the medical facility is more important according to use of unstructured data (p < 0.001; τ = 0.23) (Table (Table4 4 .).
To determine whether the form of medical facility ownership affects data collection, the Mann–Whitney U test was used. The calculations show that the form of ownership does not affect what data the organization collects and uses (Table (Table5 5 ).
Detailed information on the sources of from which medical facilities collect and use data is presented in the Table Table6 6 .
Data sources used in medical facility
1—we do not use at all, 5—we use extensively
The questionnaire results show that medical facilities are especially using information published in databases, reports to external units and transaction data, but they also use unstructured data from e-mails, medical devices, sensors, phone calls, audio and video data (Table (Table6). 6 ). Data from social media, RFID and geolocation data are used to a small extent. Similar findings are concluded in the literature studies.
From the analysis of the answers given by the respondents, more than half of the medical facilities have integrated hospital system (HIS) implemented. As much as 43.61% use integrated hospital system and 16.30% use it extensively (Table (Table7). 7 ). 19.38% of exanimated medical facilities do not use it at all. Moreover, most of the examined medical facilities (34.80% use it, 32.16% use extensively) conduct medical documentation in an electronic form, which gives an opportunity to use data analytics. Only 4.85% of medical facilities don’t use it at all.
The use of HIS and electronic documentation in medical facilities (%)
Other problems that needed to be investigated were: whether medical facilities in Poland use data analytics? If so, in what form and in what areas? (Table (Table8). 8 ). The analysis of answers given by the respondents about the potential of data analytics in medical facilities shows that a similar number of medical facilities use data analytics in administration and business (31.72% agreed with the statement no. 5 and 12.33% strongly agreed) as in the clinical area (33.04% agreed with the statement no. 6 and 12.33% strongly agreed). When considering decision-making issues, 35.24% agree with the statement "the organization uses data and analytical systems to support business decisions” and 8.37% of respondents strongly agree. Almost 40.09% agree with the statement that “the organization uses data and analytical systems to support clinical decisions (in the field of diagnostics and therapy)” and 15.42% of respondents strongly agree. Exanimated medical facilities use in their activity analytics based both on historical data (33.48% agree with statement 7 and 12.78% strongly agree) and predictive analytics (33.04% agrees with the statement number 8 and 15.86% strongly agree). Detailed results are presented in Table Table8 8 .
Conditions of using Big Data Analytics in medical facilities (%)
Medical facilities focus on development in the field of data processing, as they confirm that they conduct analytical planning processes systematically and analyze new opportunities for strategic use of analytics in business and clinical activities (38.33% rather agree and 10.57% strongly agree with this statement). The situation is different with real-time data analysis, here, the situation is not so optimistic. Only 28.19% rather agree and 14.10% strongly agree with the statement that real-time analyses are performed to support an organization’s activities.
When considering whether a facility’s performance in the clinical area depends on the form of ownership, it can be concluded that taking the average and the Mann–Whitney U test depends. A higher degree of use of analyses in the clinical area can be observed in public institutions.
Whether a medical facility performs a descriptive or predictive analysis do not depend on the form of ownership (p > 0.05). It can be concluded that when analyzing the mean and median, they are higher in public facilities, than in private ones. What is more, the Mann–Whitney U test shows that these variables are dependent from each other (p < 0.05) (Table (Table9 9 ).
Conditions of using Big Data Analytics in medical facilities determined by the form of ownership of medical facility
When considering whether a facility’s performance in the clinical area depends on its size, it can be concluded that taking the Kendall’s Tau (τ) it depends (p < 0.001; τ = 0.22), and the correlation is weak but statistically important. This means that the use of data and analytical systems to support clinical decisions (in the field of diagnostics and therapy) increases with the increase of size of the medical facility. A similar relationship, but even less powerful, can be found in the use of descriptive and predictive analyses (Table (Table10 10 ).
Conditions of using Big Data Analytics in medical facilities determined by the size of medical facility (number of employees)
Considering the results of research in the area of analytical maturity of medical facilities, 8.81% of medical facilities stated that they are at the first level of maturity, i.e. an organization has developed analytical skills and does not perform analyses. As much as 13.66% of medical facilities confirmed that they have poor analytical skills, while 38.33% of the medical facility has located itself at level 3, meaning that “there is a lot to do in analytics”. On the other hand, 28.19% believe that analytical capabilities are well developed and 6.61% stated that analytics are at the highest level and the analytical capabilities are very well developed. Detailed data is presented in Table Table11. 11 . Average amounts to 3.11 and Median to 3.
Analytical maturity of examined medical facilities (%)
The results of the research have enabled the formulation of following conclusions. Medical facilities in Poland are working on both structured and unstructured data. This data comes from databases, transactions, unstructured content of emails and documents, devices and sensors. However, the use of data from social media is smaller. In their activity, they reach for analytics in the administrative and business, as well as in the clinical area. Also, the decisions made are largely data-driven.
In summary, analysis of the literature that the benefits that medical facilities can get using Big Data Analytics in their activities relate primarily to patients, physicians and medical facilities. It can be confirmed that: patients will be better informed, will receive treatments that will work for them, will have prescribed medications that work for them and not be given unnecessary medications [ 78 ]. Physician roles will likely change to more of a consultant than decision maker. They will advise, warn, and help individual patients and have more time to form positive and lasting relationships with their patients in order to help people. Medical facilities will see changes as well, for example in fewer unnecessary hospitalizations, resulting initially in less revenue, but after the market adjusts, also the accomplishment [ 78 ]. The use of Big Data Analytics can literally revolutionize the way healthcare is practiced for better health and disease reduction.
The analysis of the latest data reveals that data analytics increase the accuracy of diagnoses. Physicians can use predictive algorithms to help them make more accurate diagnoses [ 45 ]. Moreover, it could be helpful in preventive medicine and public health because with early intervention, many diseases can be prevented or ameliorated [ 29 ]. Predictive analytics also allows to identify risk factors for a given patient, and with this knowledge patients will be able to change their lives what, in turn, may contribute to the fact that population disease patterns may dramatically change, resulting in savings in medical costs. Moreover, personalized medicine is the best solution for an individual patient seeking treatment. It can help doctors decide the exact treatments for those individuals. Better diagnoses and more targeted treatments will naturally lead to increases in good outcomes and fewer resources used, including doctors’ time.
The quantitative analysis of the research carried out and presented in this article made it possible to determine whether medical facilities in Poland use Big Data Analytics and if so, in which areas. Thanks to the results obtained it was possible to formulate the following conclusions. Medical facilities are working on both structured and unstructured data, which comes from databases, transactions, unstructured content of emails and documents, devices and sensors. According to analytics, they reach for analytics in the administrative and business, as well as in the clinical area. It clearly showed that the decisions made are largely data-driven. The results of the study confirm what has been analyzed in the literature. Medical facilities are moving towards data-based healthcare and its benefits.
In conclusion, Big Data Analytics has the potential for positive impact and global implications in healthcare. Future research on the use of Big Data in medical facilities will concern the definition of strategies adopted by medical facilities to promote and implement such solutions, as well as the benefits they gain from the use of Big Data analysis and how the perspectives in this area are seen.
Practical implications
This work sought to narrow the gap that exists in analyzing the possibility of using Big Data Analytics in healthcare. Showing how medical facilities in Poland are doing in this respect is an element that is part of global research carried out in this area, including [ 29 , 32 , 60 ].
Limitations and future directions
The research described in this article does not fully exhaust the questions related to the use of Big Data Analytics in Polish healthcare facilities. Only some of the dimensions characterizing the use of data by medical facilities in Poland have been examined. In order to get the full picture, it would be necessary to examine the results of using structured and unstructured data analytics in healthcare. Future research may examine the benefits that medical institutions achieve as a result of the analysis of structured and unstructured data in the clinical and management areas and what limitations they encounter in these areas. For this purpose, it is planned to conduct in-depth interviews with chosen medical facilities in Poland. These facilities could give additional data for empirical analyses based more on their suggestions. Further research should also include medical institutions from beyond the borders of Poland, enabling international comparative analyses.
Future research in the healthcare field has virtually endless possibilities. These regard the use of Big Data Analytics to diagnose specific conditions [ 47 , 66 , 69 , 76 ], propose an approach that can be used in other healthcare applications and create mechanisms to identify “patients like me” [ 75 , 80 ]. Big Data Analytics could also be used for studies related to the spread of pandemics, the efficacy of covid treatment [ 18 , 79 ], or psychology and psychiatry studies, e.g. emotion recognition [ 35 ].
Acknowledgements
We would like to thank those who have touched our science paths.
Authors’ contributions
KB proposed the concept of research and its design. The manuscript was prepared by KB with the consultation of AŚ. AŚ reviewed the manuscript for getting its fine shape. KB prepared the manuscript in the contexts such as definition of intellectual content, literature search, data acquisition, data analysis, and so on. AŚ obtained research funding. Both authors read and approved the final manuscript.
This research was fully funded as statutory activity—subsidy of Ministry of Science and Higher Education granted for Technical University of Czestochowa on maintaining research potential in 2018. Research Number: BS/PB–622/3020/2014/P. Publication fee for the paper was financed by the University of Economics in Katowice.
Availability of data and materials
Declarations.
Not applicable.
The author declares no conflict of interest.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kornelia Batko, Email: [email protected] .
Andrzej Ślęzak, Email: moc.liamg@25kazelsa .

IMAGES
VIDEO
COMMENTS
The New England Journal of Medicine (NEJM) is a weekly general medical journal that publishes new medical research and review articles, and editorial opinion on a wide variety of topics of ...
Original Article Mar 13, 2024 Brief Report: Intraventricular CARv3-TEAM-E T Cells in Recurrent Glioblastoma. B.D. Choi and Others DOI: 10.1056/NEJMoa2314390. Perspective Mar 6, 2024 Back to the ...
Health care today is often characterized by mediocre quality, poor safety, and high costs. 1 Though change usually comes slowly, the Covid-19 pandemic has demonstrated that it is possible to rapidly retool our systems if there is a strong enough stimulus. 2 In this article, we examine the future of health care — how it should change over the next 10 years, and the key drivers to enable our ...
A comparison of deep learning performance against health-care professionals in detecting diseases from medical imaging: a systematic review and meta-analysis. Lancet Digit. Health 1 , e271-e297 ...
Art and Images in Psychiatry Artificial Intelligence (AI) Resource Center Best of the JAMA Network Caring for the Critically Ill Patient Clinical Crosswords from JAMA Coronavirus Resource Center Evidence-Based Medicine: An Oral History Fishbein Fellowship Genomics and Precision Health Hypertension JAMA Forum Archive JAMA Network Audio JAMA Network Video JAMA Network Conferences JAMA Surgery ...
PubMed Central (PMC) Home Page. PubMed Central ® (PMC) is a free full-text archive of biomedical and life sciences journal literature at the U.S. National Institutes of Health's National Library of Medicine (NIH/NLM)
Methods and findings. Two independent investigators systematically searched the Medical Literature Analysis and Retrieval System Online (MEDLINE), the Excerpta Medica Database (EMBASE), the Cumulative Index to Nursing and Allied Health Literature (CINAHL+), the Health Management Information Consortium, and the Journal of Research Evaluation from inception until May 2017 for publications that ...
Artificial intelligence in healthcare: transforming the practice of medicine is a review article that explores the current and potential applications of AI in various domains of medicine, such as diagnosis, treatment, research, and education. The article also discusses the challenges and ethical issues of implementing AI in healthcare, and provides some recommendations for future directions ...
Original research studies that can improve decision making in clinical medicine, public health, health care policy, medical education, or biomedical research. Intended for healthcare professionals Our Company Subscribe My Account Login
Journal indexing and metrics. Research Methods in Medicine & Health Sciences is a peer reviewed journal, publishing rigorous research on established "gold standard" methods and new cutting edge research methods in the health sciences and clinical medicine. View full journal description. This journal is a member of the Committee on ...
High impact medical journal. Champion of better research, clinical practice & healthcare policy since 1840. For GPs, hospital doctors, educators, policymakers.
The remainder of this paper is oriented toward the main AI applications. Section 2 includes a description of information processing and algorithm implementation, while Section 3 focuses on disease diagnostics and prediction. Case studies of the prediction of two medical diseases are reported in Section 4.
The concept of ML and its versatile capabilities have been reported to serve the healthcare domain in various ways. Fig. 2 explores the different enablers and quality pillars for helping and caring for healthcare units. The outbreak prediction capability, medical imaging diagnosis, behavioural modifications, records of patient data, etc., are some of the majorly elaborated quality pillars of ...
He received past research support ending in 2020 from the Agency for Healthcare Quality and Research (K08-HS024599). Jon Genuneit is project manager of unrestricted research grants by Danone Nutricia Research on the composition of breast milk to the institutions Ulm University and Leipzig University, both Germany.
The U.S. Food and Drug Administration (FDA) published a paper March 15, to update the public about intra-agency activities to oversee artificial intelligence (AI)-enabled healthcare technologies. The paper summarizes priorities shared across the biologics, drugs and medical devices domains of FDA jurisdiction.
Pregnancy is a time filled with uncertainties, which can be challenging and lead to fear or anxiety for expectant parents. Health monitoring technologies that allow monitoring of the vital signs of both the mother and fetus offer a way to address health-related uncertainties. But are smart health monitoring technologies (SHMTs) actually an effective means to reduce uncertainties during ...
Abstract. Artificial intelligence is to reduce human cognitive functions. It is bringing an approach to healthcare, powdered by increasing the availability of healthcare data and rapid progress of ...
Journal of Medical Internet Research 8245 articles ... JMIR Public Health and Surveillance 1346 articles ... This paper is in the following e-collection/theme issue: Research Letter (23) Demographics of Users, Social & Digital Divide (644) Medicine 2.0 ...
Federal State Budgetary Institution "National Medical and Surgical Center named after N.I. Pirogov" of the Ministry of Health of the Russian Federation. Evgeny Shults. Federal State Autonomous Institution "N.N. Burdenko National Medical Research Centr of Neurosurgery" of the Ministry of Health of the Russian Federation. Mikhail Samsonov
The main health benefits of BD are found in disease prevention, in identifying the main health risk factors and in designing more effective healthcare measures [ 58, 59, 75 ]. BD, in fact, supports the digitization of all medical records by making all data related to each patient's medical history available [ 76 ].
Find the latest medical research news. Medical Research. Overview. Overview; Aging; AI and Digital Health; Biotherapeutics; Cancer; Clinical Trials; Discovery Science; Education; ... Nurturing children's mental health in Puerto Rico. Mayo Clinic Staff. March 18, 2024. Cancer . Assessing breast cancer risk. Mayo Clinic Staff. March 15, 2024 ...
4 Chief Medical Officer of City Clinical Hospital No. 52 of Moscow Healthcare Department, 3 Pekhotnaya Street, Moscow, 123182, Russia. 5 Department of Internal Medicine, Faculty of Additional Professional Education at Federal State Autonomous Educational Institution of Higher Education Pirogov Russian National Research Medical University, 1 ...
Affiliations 1 Children's City Clinical Hospital named after Z. A. Bashlyaeva of the Moscow City Health Department, 125373, Moscow, Russian Federation.; 2 Pirogov Russian National Research Medical University, 117997, Moscow, Russian Federation.; 3 Russian Medical Academy of Continuous Professional Education of the Ministry of Healthcare of the Russian Federation, 125993, Moscow, Russian ...
GTC— NVIDIA today launched more than two dozen new microservices that allow healthcare enterprises worldwide to take advantage of the latest advances in generative AI from anywhere and on any cloud. The new suite of NVIDIA healthcare microservices includes optimized NVIDIA NIM™ AI models and workflows with industry-standard APIs, or application programming interfaces, to serve as building ...
The authors recommend that routine pediatric primary care play a critical role in this life transition to ultimately improve population-level menstrual health. The paper is published in The Lancet ...
Through collaboration with numerous organizations, and powered by millions of volunteers, we fund innovative research, advocate for the public's health and share lifesaving resources. The Dallas-based organization has been a leading source of health information for a century. During 2024 - our Centennial year - we celebrate our rich 100-year ...
Research by Victor Ambros, Ph.D., provides new insights into a recently identified class of neurodevelopmental disorders called Argonaute syndromes. Dr. Ambros and colleagues believe their ...
Earning an MD at Harvard Medical School doesn't end in the classroom or clinic. Students also learn to conduct research that pushes medical science ahead, whether in basic research, clinical or translational science, or the compassionate and just delivery of health care. On March 12, 70 MD ...
Horne's research has shown that fasting twice a week for four weeks, then once a week for 22 weeks may increase a person's risk of dying after one year but decrease their 10-year risk of ...
For the purpose of this paper, the following research hypotheses were formulated: (1) medical facilities in Poland are working on both structured and unstructured data (2) medical facilities in Poland are moving towards data-based healthcare and its benefits. The paper poses the following research questions and statements that coincide with the ...