Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- Types of Research Designs Compared | Guide & Examples

Types of Research Designs Compared | Guide & Examples
Published on June 20, 2019 by Shona McCombes . Revised on June 22, 2023.
When you start planning a research project, developing research questions and creating a research design , you will have to make various decisions about the type of research you want to do.
There are many ways to categorize different types of research. The words you use to describe your research depend on your discipline and field. In general, though, the form your research design takes will be shaped by:
- The type of knowledge you aim to produce
- The type of data you will collect and analyze
- The sampling methods , timescale and location of the research
This article takes a look at some common distinctions made between different types of research and outlines the key differences between them.
Table of contents
Types of research aims, types of research data, types of sampling, timescale, and location, other interesting articles.
The first thing to consider is what kind of knowledge your research aims to contribute.
Prevent plagiarism. Run a free check.
The next thing to consider is what type of data you will collect. Each kind of data is associated with a range of specific research methods and procedures.
Finally, you have to consider three closely related questions: how will you select the subjects or participants of the research? When and how often will you collect data from your subjects? And where will the research take place?
Keep in mind that the methods that you choose bring with them different risk factors and types of research bias . Biases aren’t completely avoidable, but can heavily impact the validity and reliability of your findings if left unchecked.
Choosing between all these different research types is part of the process of creating your research design , which determines exactly how your research will be conducted. But the type of research is only the first step: next, you have to make more concrete decisions about your research methods and the details of the study.
Read more about creating a research design
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Normal distribution
- Degrees of freedom
- Null hypothesis
- Discourse analysis
- Control groups
- Mixed methods research
- Non-probability sampling
- Quantitative research
- Ecological validity
Research bias
- Rosenthal effect
- Implicit bias
- Cognitive bias
- Selection bias
- Negativity bias
- Status quo bias
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
McCombes, S. (2023, June 22). Types of Research Designs Compared | Guide & Examples. Scribbr. Retrieved April 9, 2024, from https://www.scribbr.com/methodology/types-of-research/
Is this article helpful?
Shona McCombes
Other students also liked, what is a research design | types, guide & examples, qualitative vs. quantitative research | differences, examples & methods, what is a research methodology | steps & tips, what is your plagiarism score.
Mixed Methods Research: The Case for the Pragmatic Researcher
- First Online: 24 January 2023
Cite this chapter

- Alistair McBeath 3
2108 Accesses
This chapter presents an introduction to mixed methods research and seeks to emphasise that the approach offers more potential to reveal a deeper understanding of life experiences than the use of either qualitative or quantitative research methods on their own. The history and emergence of mixed methods research are described and also its potential to be aligned with the world view of pragmatism. The fundamental design variants of mixed methods research are presented with reference to supporting research examples. The rationale and advantages of mixed methods are discussed as is the importance of its underlying methodological pluralism which favours the inclusive logic of ‘both/and’ as opposed to the dichotomous logic of ‘either/or’. The chapter concludes with a call for more information about mixed methods to be made available to those with a research interest within counselling and psychotherapy allowing them to discover the wonderful possibilities that are offered by mixed methods research.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Bager-Charleson, S., & McBeath, A. G. (2021). Containment, compassion and clarity. Mixed methods research into Supervision during Doctoral research for Psychotherapists and Counselling psychologist. Counselling and Psychotherapy Research . doi: https://doi.org/10.1002/capr.12498 .
Biddle, C., & Schafft, K. A. (2015). Axiology and anomaly in the practice of mixed methods work: Pragmatism, valuation, and the transformative paradigm. Journal of Mixed Methods Research, 9 , 320–334. https://doi.org/10.1177/1558689814533157
Article Google Scholar
Borders, L. D., Wester, K. L., Fickling, M. J., & Adamson, N. A. (2015). Dissertations in CACREP-accredited doctoral programs: An initial investigation. The Journal of Counselor Preparation and Supervision, 7 (3). https://doi.org/10.7729/73.1102
Brannen, J., Dodd, K., Oakley, A., & Storey, P. (1994). Young people, health and family life . Open University Press.
Google Scholar
Braun, V., & Clarke, V. (2019). Reflecting on reflexive thematic analysis. Qualitative Research in Sport, Exercise and Health, 11 (4), 589–597. https://doi.org/10.1080/2159676X.2019.1628806
Brierley, J. A. (2017). The role of a pragmatist paradigm when adopting mixed methods in behavioural accounting research. International Journal of Behavioural Accounting and Finance, 6 (2), 140–154.
Bryman, A. (2006a). Integrating quantitative and qualitative research: How is it done? Qualitative Research, 6 (1), 97–113. https://doi.org/10.1177/1468794106058877
Bryman, A. (2006b). Paradigm Peace and the Implications for Quality. International Journal of Social Research Methodology: Theory & Practice, 9 (2), 111–126. https://doi.org/10.1080/13645570600595280
Cade, R., Gibson, S., Swan, K., & Nelson, K. (2018). A content analysis of counseling outcome research and evaluation (CORE) from 2010 to 2017. Counseling Outcome Research and Evaluation, 9 (1), 5–15. https://doi.org/10.1080/21501378.2017.1413643
Cameron, R. (2011). Mixed methods research: The five P’s framework. The Electronic Journal of Business Research Methods, 9 , 96–108. Retrieved from http://www.ejbrm.com/volume9/issue2/p96
Cameron, R., & Miller, P. (2007) Mixed methods research: Phoenix of the paradigm wars. 21st Annual Australian and New Zealand Academy of Management (ANZAM) Conference, Sydney, December 2007.
Cooper, M., & McLeod, J. (2012). From either/or to both/and: Developing a pluralistic approach to counselling and psychotherapy. European Journal of Psychotherapy and Counselling , 1–13.
Creswell, J., & Plano Clark, V. (2007). Designing and conducting mixed methods research . Sage.
Creswell, J. W. (2003). Research design: Qualitative, quantitative, and mixed methods approaches (2nd ed.). Sage.
Denzin, N. (1978). The research act: A theoretical introduction to sociological methods (2nd ed.). McGraw-Hill.
Etherington, K. (2020). Becoming a narrative inquirer. In S. Bager-Charleson & A. G. McBeath (Eds.), Enjoying research in counselling and psychotherapy (pp. 71–94). Palgrave Macmillan.
Chapter Google Scholar
Fetters, M. D., Curry, L. A., & Creswell, J. W. (2013). Achieving integration in mixed methods designs - Principles and practices. Health Services Research, 48 (6), 2134–2156.
Frost, N., & Bailey-Rodriquez, D. (2020). Doing qualitatively driven mixed methods and pluralistic qualitative research. In S. Bager-Charleson & A. G. McBeath (Eds.), Enjoying research in counselling and psychotherapy (pp. 137–160). Palgrave Macmillan.
Gage, N. L. (1989). The paradigm wars and their aftermath: A “historical” sketch of research on teaching since 1989. Educational Researcher, 18 (7), 4–10. https://doi.org/10.2307/1177163
Greene, J. C., Caracelli, V. J., & Graham, W. F. (1989). Toward a conceptual framework for mixed-method evaluation designs. Educational Evaluation and Policy Analysis, 11 , 255–274. https://doi.org/10.3102/01623737011003255
Grocke, D., Bloch, S., Castle, D., Thompson, G., Newton, R., Stewart, S., & Gold, C. (2014). Group music therapy for severe mental illness: a randomized embedded-experimental mixed methods study. Acta Psychiatrica Scandinavica, 130 (2), 144–153. https://doi.org/10.1111/acps.12224
Article CAS Google Scholar
Hesse-Biber, S. N. (2010). Mixed methods research: Merging theory with practice . The Guilford Press.
Howe, K. R. (1988). Against the quantitative-qualitative incompatibility thesis or Dogmas Die Hard. Educational Researcher, 17 (8), 10–16. https://doi.org/10.2307/1175845
Johnson, R. B., & Onwuegbuzie, A. J. (2004). Mixed methods research: A research paradigm whose time has come. Educational Researcher, 33 , 14–26. https://doi.org/10.3102/0013189X033007014
Johnson, R. B., Onwuegbuzie, A. J., & Turner, L. A. (2007). Toward a definition of mixed methods research. Journal of Mixed Methods Research, 1 , 112–133. https://doi.org/10.1177/1558689806298224
Kaushik, V., & Walsh, C. A. (2019). Pragmatism as a research paradigm and its implications for social work research. Social Sciences, 8 (9), 255. https://doi.org/10.3390/socsci8090255
Lincoln, Y. S., & Guba, E. G. (2000). Paradigmatic controversies, contradictions, and emerging confluences. In N. K. Denzin & Y. S. Lincoln (Eds.), The handbook of qualitative research (2nd ed., pp. 1065–1122). Sage.
Maarouf, H. (2019). Pragmatism as a supportive paradigm for the mixed research approach: Conceptualizing the ontological, epistemological, and axiological stances of pragmatism. International Business Research, 12 (9), 1–12. https://doi.org/10.5539/ibr.v12n9p1
Mahalik, J. R. (2014). Both/and, not either/or: A call for methodological pluralism in research on masculinity. Psychology of Men & Masculinity, 15 (4), 365–368. https://doi.org/10.1037/a0037308
Maxcy, S. J. (2003). Pragmatic threads in mixed method research in the social sciences: The search for multiple modes of inquiry and the end of the philosophy of formalism. In A. Tashakkori & C. Teddlie (Eds.), Handbook of mixed methods in the social and behavioural sciences (pp. 51–89). Sage.
McBeath, A. G. (2019). The motivations of psychotherapists: An in-depth survey. Counselling and Psychotherapy Research, 19 (4), 377–387.
McBeath, A. G., & Bager-Charleson, S. (2022). Views on mixed methods research in counselling and psychotherapy: An online survey of research students and research supervisors (Manuscript submitted for publication). Metanoia Institute.
McBeath, A. G., Bager-Charleson, S., & Abarbanel, A. (2019). Therapists and Academic Writing: “Once upon a time psychotherapy practitioners and researchers were the same people”. European Journal for Qualitative Research in Psychotherapy, 19 , 103–116.
Mertens, D. (2007). Transformative paradigm: Mixed methods and social justice. Journal of Mixed Methods Research, 1 (3), 212–225.
Molina-Azorin, J. F. (2016). Mixed methods research: An opportunity to improve our studies and our research skills. European Journal of Management and Business Economics, 25 , 37–38. https://doi.org/10.1016/j.redeen.2016.05.001
Morgan, D. L. (2007). Paradigms lost and pragmatism regained: Methodological implications of combining qualitative and quantitative methods. Journal of Mixed Methods Research, 1 , 48–76. https://doi.org/10.1177/2345678906292462
Morse, J. M. (1991). Approaches to qualitative-quantitative methodological triangulation. Nursing Research, 40 , 120–123.
Neuman, W. (2014). Social research methods qualitative and quantitative approaches . Pearson.
O’Cathain, A., Murphy, E., & Nicholl, J. (2010). Three techniques for integrating data in mixed methods studies. British Medical Journal, 341 , c4587. Retrieved from https://www.bmj.com/content/341/bmj.c4587
Pietkiewicz, I., & Smith, J. A. (2012). Praktyczny przewodnik interpretacyjnej analizy fenomenologicznej w badaniach jakościowych w psychologii. Czasopismo Psychologiczne, 18 (2), 361–369.
Ponterotto, J. G. (2005). Qualitative research in counseling psychology: A primer on research paradigms and philosophy of science. Journal of Counseling Psychology, 52 (2), 126–136. https://doi.org/10.1037/0022-0167.52.2.126
Reichardt, C. S., & Cook, T. D. (1979). Beyond qualitative versus quantitative methods. In T. D. Cook & C. S. Reichardt (Eds.), Qualitative and quantitative methods in evaluation research (pp. 7–32). Sage.
Stafford, M. R. (2020). Understanding randomised control trial design in counselling and psychotherapy. In G. McBeath (Ed.), S. Bager-Charleson & A (pp. 242–265). Enjoying Research in Counselling and Psychotherapy.
Tashakkori, A., & Teddlie, C. (1998). Mixed methodology: Combining qualitative and quantitative approaches . Sage.
Tashakkori, A., & Teddlie, C. (2003). Handbook of mixed methods in social and behavioral research . Sage.
Williams, R. T. (2020). The paradigm wars: Is MMR really a solution? American Journal of Trade and Policy, 7 (3), 79–84. https://doi.org/10.18034/ajtp.v7i3.507
Download references
Author information
Authors and affiliations.
Metanoia Institute, London, UK
Alistair McBeath
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Alistair McBeath .
Editor information
Editors and affiliations.
Sofie Bager-Charleson
Rights and permissions
Reprints and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
McBeath, A. (2022). Mixed Methods Research: The Case for the Pragmatic Researcher. In: Bager-Charleson, S., McBeath, A. (eds) Supporting Research in Counselling and Psychotherapy . Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-031-13942-0_10
Download citation
DOI : https://doi.org/10.1007/978-3-031-13942-0_10
Published : 24 January 2023
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-031-13941-3
Online ISBN : 978-3-031-13942-0
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Health Serv Res
- v.48(6 Pt 2); 2013 Dec
Achieving Integration in Mixed Methods Designs—Principles and Practices
Michael d fetters.
Family Medicine, University of Michigan, 1018 Fuller St., Ann Arbor, MI 48104-1213
Leslie A Curry
Yale School of Public Health (Health Policy), New Haven, CT
John W Creswell
Educational Psychology, University of Nebraska-Lincoln, Lincoln, NE
Associated Data
Mixed methods research offers powerful tools for investigating complex processes and systems in health and health care. This article describes integration principles and practices at three levels in mixed methods research and provides illustrative examples. Integration at the study design level occurs through three basic mixed method designs—exploratory sequential, explanatory sequential, and convergent—and through four advanced frameworks—multistage, intervention, case study, and participatory. Integration at the methods level occurs through four approaches. In connecting, one database links to the other through sampling. With building, one database informs the data collection approach of the other. When merging, the two databases are brought together for analysis. With embedding, data collection and analysis link at multiple points. Integration at the interpretation and reporting level occurs through narrative, data transformation, and joint display. The fit of integration describes the extent the qualitative and quantitative findings cohere. Understanding these principles and practices of integration can help health services researchers leverage the strengths of mixed methods.
This article examines key integration principles and practices in mixed methods research. It begins with the role of mixed methods in health services research and the rationale for integration. Next, a series of principles describe how integration occurs at the study design level, the method level, and the interpretation and reporting level. After considering the “fit” of integrated qualitative and quantitative data, the article ends with two examples of mixed methods investigations to illustrate integration practices.
Health services research includes investigation of complex, multilevel processes, and systems that may require both quantitative and qualitative forms of data (Creswell, Fetters, and Ivankova 2004 ; Curry et al. 2013 ). The nature of the research question drives the choice of methods. Health services researchers use quantitative methodologies to address research questions about causality, generalizability, or magnitude of effects. Qualitative methodologies are applied to research questions to explore why or how a phenomenon occurs, to develop a theory, or to describe the nature of an individual's experience. Mixed methods research studies draw upon the strengths of both quantitative and qualitative approaches and provides an innovative approach for addressing contemporary issues in health services. As one indication of the growing interest in mixed methods research, the Office of Behavioral and Social Sciences at the National Institutes of Health recently developed for researchers and grant reviewers the first best practices guideline on mixed methods research from the National Institutes of Health (Creswell et al. 2011 ).
Rationale for Integration
The integration of quantitative and qualitative data can dramatically enhance the value of mixed methods research (Bryman 2006 ; Creswell and Plano Clark 2011 ). Several advantages can accrue from integrating the two forms of data. The qualitative data can be used to assess the validity of quantitative findings. Quantitative data can also be used to help generate the qualitative sample or explain findings from the qualitative data. Qualitative inquiry can inform development or refinement of quantitative instruments or interventions, or generate hypotheses in the qualitative component for testing in the quantitative component (O'Cathain, Murphy, and Nicholl 2010 ). Although there are many potential gains from data integration, the extent to which mixed methods studies implement integration remains limited (Bryman 2006 ; Lewin, Glenton, and Oxman 2009 ). Nevertheless, there are specific approaches to integrate qualitative and quantitative research procedures and data (O'Cathain, Murphy, and Nicholl 2010 ; Creswell and Plano Clark 2011 ). These approaches can be implemented at the design, methods, and interpretation and reporting levels of research (see Table Table1 1 ).
Levels of Integration in Mixed Methods Research
Integration at the design level—the conceptualization of a study—can be accomplished through three basic designs and four advanced mixed methods frameworks that incorporate one of the basic designs. Basic designs include (1) exploratory sequential; (2) explanatory sequential; and (3) convergent designs. In sequential designs, the intent is to have one phase of the mixed methods study build on the other, whereas in the convergent designs the intent is to merge the phases in order that the quantitative and qualitative results can be compared.
In an exploratory sequential design , the researcher first collects and analyzes qualitative data, and these findings inform subsequent quantitative data collection (Onwuegbuzie, Bustamante, and Nelson 2010 ). For example, Wallace and colleagues conducted semistructured interviews with medical students, residents, and faculty about computing devices in medical education and used the qualitative data to identify key concepts subsequently measured in an online survey (Wallace, Clark, and White 2012 ).
In an explanatory sequential design , the researcher first collects and analyzes quantitative data, then the findings inform qualitative data collection and analysis (Ivankova, Creswell, and Stick 2006 ). For example, Carr explored the impact of pain on patient outcomes following surgery by conducting initial surveys about anxiety, depression, and pain that were followed by semistructured interviews to explore further these concepts (Carr 2000 ).
In a convergent design (sometimes referred to as a concurrent design), the qualitative and quantitative data are collected and analyzed during a similar timeframe. During this timeframe, an interactive approach may be used where iteratively data collection and analysis drives changes in the data collection procedures. For example, initial quantitative findings may influence the focus and kinds of qualitative data that are being collected or vice versa. For example, in one study Crabtree and colleagues used qualitative findings and quantitative findings iteratively in multiple phases such that the data were interacting to inform the final results (Crabtree et al. 2005 ). In the more common and technically simpler variation, qualitative and quantitative data collection occurs in parallel and analysis for integration begins well after the data collection process has proceeded or has been completed. Frequently, the two forms of data are analyzed separately and then merged. For example, Saint Arnault and colleagues conducted multiple surveys using standardized and culturally adapted instruments as well as ethnographic qualitative interviews to investigate how the illness experience, cultural interpretations, and social structural factors interact to influence help-seeking among Japanese women (Saint Arnault and Fetters 2011 ).
Advanced frameworks encompass adding to one of the three basic designs a larger framework that incorporates the basic design. The larger framework may involve (1) a multistage; (2) an intervention; (3) a case study; or (4) a participatory research framework.
In a multistage mixed methods framework , researchers use multiple stages of data collection that may include various combinations of exploratory sequential, explanatory sequential, and convergent approaches (Nastasi et al. 2007 ). By definition, such investigations will have multiple stages, defined here as three or more stages when there is a sequential component, or two or more stages when there is a convergent component; these differences distinguishes the multistage framework from the basic mixed methods designs. This type of framework may be used in longitudinal studies focused on evaluating the design, implementation, and assessment of a program or intervention. Krumholz and colleagues have used this design in large-scale outcomes research studies (Krumholz, Curry, and Bradley 2011 ). For example, a study by their team examining quality of hospital care for patients after heart attacks consisted of three phases: first, a quantitative analysis of risk-standardized mortality rates for patients with heart attacks to identify high and low performing hospitals; second, a qualitative phase to understand the processes, structures, and organizational environments of a purposeful sample of low and high performers and to generate hypotheses about factors associated with performance; and third, primary data collection through surveys of a nationally representative sample of hospitals to test these hypotheses quantitatively (Curry et al. 2011 ; Bradley et al. 2012 ). Ruffin and colleagues conducted a multistage mixed methods study to develop and test in a randomized controlled trial (RCT) a website to help users choose a screening approach to colorectal cancer. In the first stage, the authors employed a convergent design using focus groups and a survey (Ruffin et al. 2009 ). In the second stage, they developed the website based on multiple qualitative approaches (Fetters et al. 2004 ). In the third stage, the authors tested the website in an RCT to assess its effectiveness (Ruffin, Fetters, and Jimbo 2007 ). The multistage framework is the most general framework among advanced designs. The additional three frameworks frequently involve multiple stages or phases but differ from multistage by having a particular focus.
In an intervention mixed methods framework , the focus is on conducting a mixed methods intervention. Qualitative data are collected primarily to support the development of the intervention, to understand contextual factors during the intervention that could affect the outcome, and/or explain results after the intervention is completed (Creswell et al. 2009 ; Lewin, Glenton, and Oxman 2009 ). For example, Plano Clark and colleagues utilized data from a pretrial qualitative study to inform the design of a trial developed to compare a low dose and high dose behavioral intervention to improve cancer pain management—the trial also included prospective qualitative data collection during the trial (Plano Clark et al. 2013 ). The methodological approach for integrating qualitative data into an intervention pretrial, during the trial, or post-trial is called embedding (see below), and some authors refer to such trials as embedded designs (Creswell et al. 2009 ; Lewin, Glenton, and Oxman 2009 ).
In a case study framework , both qualitative and quantitative data are collected to build a comprehensive understanding of a case, the focus of the study (Yin 1984 ; Stake 1995 ). Case study involves intensive and detailed qualitative and quantitative data collection about the case (Luck, Jackson, and Usher 2006 ). The types of qualitative and quantitative data collected are chosen based on the nature of the case, feasibility issues, and the research question(s). In one mixed methods case study, Luck and colleagues utilized qualitative data from participant observation, semistructured interviews, informal field interviews and journaling, and quantitative data about violent events collected through structured observations to understand why nurses under-report violence in the workplace and describe how they handle it (Luck, Jackson, and Usher 2008 ). Comparative case studies are an extension of this framework and can be formulated in various ways. For example, Crabtree and colleagues used a comparative case approach to examine the delivery of clinical preventive services in family medicine offices (Crabtree et al. 2005 ).
In a participatory framework , the focus is on involving the voices of the targeted population in the research to inform the direction of the research. Often researchers specifically seek to address inequity, health disparities, or a social injustice through empowering marginalized or underrepresented populations. The distinguishing feature of a participatory framework is the strong emphasis on using mixed methods data collection through combinations of basic mixed methods designs or even another advanced design, for example, an intervention framework such as an RCT. Community-based participatory research (CBPR) is a participatory framework that focuses on social, structural, and physical environmental inequities and engages community members, organizational representatives, and researchers in all aspects of the research process (Macaulay et al. 1999 ; Israel et al. 2001 , 2013 ; Minkler and Wallerstein 2008 ). In one CBPR project, Johnson and colleagues used a mixed methods CBPR approach to collaborate with the Somali community to explore how attitudes, perceptions, and cultural practices such as female genital cutting influence their use of reproductive health services—this informed the development of interventional programs to improve culturally competent care (Johnson, Ali, and Shipp 2009 ). A similar variation involving an emerging participatory approach that Mertens refers to as transformative specifically focuses on promoting social justice (Mertens 2009 , 2012 ) and has been used with Laotian refugees (Silka 2009 ).
Creswell and Plano Clark conceptualize integration to occur through linking the methods of data collection and analysis (Creswell et al. 2011 ). Linking occurs in several ways: (1) connecting; (2) building; (3) merging; and (4) embedding (Table (Table2). 2 ). In a single line of inquiry, integration may occur through one or more of these approaches.
Integration through Methods
Integration through connecting occurs when one type of data links with the other through the sampling frame . For example, consider a study with a survey and qualitative interviews. The interview participants are selected from the population of participants who responded to the survey. Connecting can occur through sampling regardless of whether the design is explanatory sequential or convergent. That is, if the baseline survey data are analyzed, and then the participants sampled based on findings from the analysis, then the design is explanatory sequential. In contrast, the design is convergent if the data collection and analyses occur at the same time for the baseline survey and interviews of all or a subsample of the participants of the survey. A key defining factor in sequential or convergent is how the analysis occurs, either through building or merging, respectively.
Integration through building occurs when results from one data collection procedure informs the data collection approach of the other procedure, the latter building on the former. Items for inclusion in a survey are built upon previously collected qualitative data that generate hypotheses or identify constructs or language used by research participants. For example, in a project involving the cultural adaptation of the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey for use in the Arabian Gulf (Hammoud et al. 2012 ), baseline qualitative interviews identified new domains of importance such as gender relations, diet, and interpreter use not found in the existing CAHPS instrument. In addition, phrases participants used during the interviews informed the wording of individual items.
Integration through merging of data occurs when researchers bring the two databases together for analysis and for comparison . Ideally, at the design phase, researchers develop a plan for collecting both forms of data in a way that will be conducive to merging the databases. For example, if quantitative data are collected with an instrument with a series of scales, qualitative data can be collected using parallel or similar questions (Castro et al. 2010 ). Merging typically occurs after the statistical analysis of the numerical data and qualitative analysis of the textual data. For example, in a multistage mixed methods study, Tomoaia-Cortisel and colleagues used multiple sources of existing quantitative and qualitative data as well as newly collected quantitative and qualitative data (Tomoaia-Cortisel et al. 2013 ). The researchers examined the relationship between quality of care according to key patient-centered medical home (PCMH) measures, and quantity of care using a productivity measure. By merging both scores of quality and quantity, with qualitative data from interviews, the authors illuminated the difficulty of achieving highly on both PCMH quality measures and productivity. The authors extended this understanding further by merging staff satisfaction scores and staff interview data to illustrate the greater work complexity but lower satisfaction for staff achieving measures for high-quality care (Tomoaia-Cortisel et al. 2013 ).
Integration through embedding occurs when data collection and analysis are being linked at multiple points and is especially important in interventional advanced designs, but it can also occur in other designs. Embedding may involve any combination of connecting, building, or merging, but the hallmark is recurrently linking qualitative data collection to quantitative data collection at multiple points. Embedding may occur in the pretrial period, when qualitative (or even a combination of qualitative and quantitative) data can be used in various ways such as clarifying outcome measures, understanding contextual factors that could lead to bias and should be controlled for, or for developing measurement tools to be utilized during the trial. During the trial, qualitative data collection can be used to understand contextual factors that could influence the trial results or provide detailed information about the nature of the experience of subjects. Post-trial qualitative data collection can be used to explain outliers, debrief subjects or researchers about events or experiences that occurred during the trial, or develop hypotheses about changes that might be necessary for widespread implementation outside of a controlled research environment. Such studies require caution to avoid threatening the validity of the trial design. In a site-level controlled trial of a quality improvement approach for implementing evidence-based employment services for patients at specialty mental health clinics, Hamilton and colleagues collected semistructured interview data before, during, and after implementation (Hamilton et al. 2013 ). In another interesting example, Jaen and colleagues used an embedded approach for evaluating practice change in a trial comparing facilitated and self-directed implementation strategies for PCMH. The authors use both embedded quantitative and qualitative evaluation procedures including medical record audit, patient and staff surveys, direct observation, interviews, and text review (Jaen et al. 2010 ).
Method level integration commonly relates to the type of design used in a study. For example, connecting follows naturally in sequential designs, while merging can occur in any design. Embedding generally occurs in an interventional design. Thus, the design sets parameters for what methodological integration choices can be made.
Integration of qualitative and quantitative data at the interpretation and reporting level occurs through three approaches: (1) integrating through narrative; (2) integrating through data transformation; and (3) integrating through joint displays. A variety of strategies have been offered for publishing that incorporate these approaches (Stange, Crabtree, and Miller 2006 ; Creswell and Tashakkori 2007 ).
When integrating through narrative , researchers describe the qualitative and quantitative findings in a single or series of reports. There are three approaches to integration through narrative in research reports. The weaving approach involves writing both qualitative and quantitative findings together on a theme-by-theme or concept-by-concept basis. For example, in their work on vehicle crashes among the elderly, Classen and colleagues used a weaving approach to integrate results from a national crash dataset and perspectives of stakeholders to summarize causative factors of vehicle crashes and develop empirical guidelines for public health interventions (Classen et al. 2007 ). The contiguous approach to integration involves the presentation of findings within a single report, but the qualitative and quantitative findings are reported in different sections. For example, Carr and colleagues reported survey findings in the first half of the results section and the qualitative results about contextual factors in a subsequent part of the report (Carr 2000 ). In their study of a quality improvement approach for implementing evidence-based employment services at specialty mental health clinics, Hamilton and colleagues used this approach but differ by presenting the qualitative results first and the quantitative results second (Hamilton et al. 2013 ). The staged approach to integration often occurs in multistage mixed methods studies when the results of each step are reported in stages as the data are analyzed and published separately. For example, Wilson and colleagues used an intervention mixed methods framework involving a clinical trial of usual care, nicotine gum, and gum plus counseling on smoking cessation (Wilson et al. 1988 ). They also used interviews to find the meaning patients attributed to their stopping smoking (Willms 1991 ). The authors published the papers separately but in the second published paper, the interview paper, they only briefly mention the original clinical trial paper.
Integration through data transformation happens in two steps. First, one type of data must be converted into the other type of data (i.e., qualitative into quantitative or quantitative into qualitative). Second, the transformed data are then integrated with the data that have not been transformed. In qualitative studies, researchers sometimes code the qualitative data and then count the frequency of codes or domains identified, a process known also as content analysis (Krippendorff 2013 ). Data transformation in the mixed methods context refers to transforming the qualitative data into numeric counts and variables using content analysis so that the data can be integrated with a quantitative database. Merging in mixed methods goes beyond content analysis by comparing the transformed qualitative data with a quantitative database. Zickmund and colleagues used qualitatively elicited patient views of self transformed to a numerical variable, and mortality data to conduct hierarchical multivariable logistical modeling (Zickmund et al. 2013 ).
Researchers have used additional variations. Qualitative data can be transformed to quantitative data, then integrated with illustrative examples from the original qualitative dataset. For example, Ruffin and colleagues transformed qualitative responses from focus group data about colorectal cancer (CRC) screening preferences into quantitative variables, and then integrated these findings with representative quotations from three different constituencies (Ruffin et al. 2009 ). Quantitative data can also be transformed into a qualitative format that could be used for comparison with qualitatively accessed data. For example, Pluye and colleagues examined a series of study outcomes with variable strengths of association that were converted into qualitative levels and compared across the studies based on patterns found (Pluye et al. 2005 ).
When integrating through joint displays , researchers integrate the data by bringing the data together through a visual means to draw out new insights beyond the information gained from the separate quantitative and qualitative results. This can occur through organizing related data in a figure, table, matrix, or graph. In their quality improvement study to enhance colorectal cancer screening in practices, Shaw and colleagues collocated a series of qualitatively identified factors with CRC screening rates at baseline and 12 months later (Shaw et al. 2013 ).
When using any of these analytical and representation procedures, a potential question of coherence of the quantitative and qualitative findings may occur. The “fit” of data integration refers to coherence of the quantitative and qualitative findings. The assessment of fit of integration leads to three possible outcomes. Confirmation occurs when the findings from both types of data confirm the results of the other. As the two data sources provide similar conclusions, the results have greater credibility. Expansion occurs when the findings from the two sources of data diverge and expand insights of the phenomenon of interest by addressing different aspects of a single phenomenon or by describing complementary aspects of a central phenomenon of interest. For example, quantitative data may speak to the strength of associations while qualitative data may speak to the nature of those associations. Discordance occurs if the qualitative and quantitative findings are inconsistent, incongruous, contradict, conflict, or disagree with each other. Options for reporting the findings include looking for potential sources of bias, and examining methodological assumptions and procedures. Investigators may handle discordant results in different ways such as gathering additional data, re-analyzing existing databases to resolve differences, seeking explanations from theory, or challenging the validity of the constructs. Further analysis may occur with the existing databases or in follow-up studies. Authors deal with this conundrum by discussing reasons for the conflicting results, identifying potential explanations from theory, and laying out future research options (Pluye et al. 2005 ; Moffatt et al. 2006 ).
Below, two examples of mixed methods illustrate the integration practices. The first study used an exploratory sequential mixed methods design (Curry et al. 2011 ) and the second used a convergent mixed methods design (Meurer et al. 2012 ).
Example 1. Integration in an Exploratory Sequential Mixed Methods Study—The Survival after Acute Myocardial Infarction Study (American College of Cardiology 2013 )
Despite more than a decade of efforts to improve care for patients with acute myocardial infarction (AMI), there remains substantial variation across hospitals in mortality rates for patients with AMI (Krumholz et al. 2009 ; Popescu et al. 2009 ). Yet the vast majority of this variation remains unexplained (Bradley et al. 2012 ), and little is known about how hospitals achieve reductions in risk-standardized mortality rates (RSMRs) for patients with AMI. This study sought to understand diverse and complex aspects of AMI care including hospital structures (e.g., emergency department space), processes (e.g., emergency response protocols, coordination within hospital units), and hospital internal environments (e.g., organizational culture).
Integration through design . An exploratory sequential mixed methods design using both qualitative and quantitative approaches was best suited to gain a comprehensive understanding of how these features may be related to quality of AMI care as reflected in RSMRs. The 4-year investigation aimed to first generate and then empirically test hypotheses concerning hospital-based efforts that may be associated with lower RSMRs (Figure (Figure1 1 ).

Example Illustrating Integration in an Exploratory Sequential Mixed Methods Design from the Survival after Acute Myocardial Infarction Study
Integration through methods . The first phase was a qualitative study of acute care hospitals in the United States (Curry et al. 2011 ). Methodological integration occurred through connecting as the 11 hospitals in the purposeful sample ranked in either the top 5 percent or bottom 5 percent of RSMRs for each of the two most recent years of data (2005–2006, 2006–2007) from the Centers for Medicare & Medicaid Services (CMS). The qualitative data from 158 key staff interviews informed the generation of hypotheses regarding factors potentially associated with better performance (see Table Table3) 3 ) (Curry et al. 2011 ). These hypotheses were used to build an online quantitative survey that was administered in a cross-sectional study of 537 acute care hospitals (91 percent response rate) (Curry et al. 2011 ; Krumholz, Curry, and Bradley 2011 ; Bradley et al. 2012 ).
Examples of How the Qualitative Data Were Used to Build Quantitative Survey Items in the Survival after Acute Myocardial Infarction Study
AMI, acute myocardial infarction; CEO, chief executive officer. Adapted with permission from Bradley, Curry et al., Annals of Internal Medicine , May 1, 2012.
Mixed methods were used to characterize the care practices and processes in higher performing organizations as well as the organizational environment where they were implemented. Figure Figure1 1 illustrates points in the process of integration. In Aim 1, the qualitative component connected with the CMS database in order to identify a positive deviance sample. The investigators conducted a systematic analysis of the qualitative data using a multidisciplinary team. This provided (point 1, Figure 1 ) a rich characterization of prominent themes that distinguished higher-performing from lower-performing hospitals and generated hypotheses regarding factors influencing AMI mortality rates (Curry et al. 2011 ). In Aim 2, the investigators built a 68 item-survey from the qualitative data. Key concepts from the qualitative data (point 2, Figure 1 ) were operationalized as quantitative items for inclusion in a web-based survey in order to test the hypotheses statistically in a nationally representative sample of hospitals (Bradley et al. 2012 ). The authors analyzed the quantitative survey data and then merged the quantitative findings (point 3, Figure 1 ) and qualitative analysis (point 4, Figure 1 ) in a single paper. The merging of the qualitative and quantitative produced a comprehensive, multifaceted description of factors influencing RSMRs as well as the impact of these factors on RSMRs that was presented using a weaving narrative . For example, problem-solving and learning was a prominent theme that differentiated higher-performing from lower-performing hospitals. In higher-performing hospitals, adverse events were perceived as opportunities for learning and improvement, approaches to data feedback were nonpunitive, innovation and creativity were valued and supported, and new ideas were sought. In the multivariable analysis, having an organizational environment where clinicians are encouraged to creatively solve problems was significantly associated with lower RSMRs (0.84 percentage points). Finally, additional analyses of qualitative data examining organizational features related to high-quality discharge planning (point 5, Figure Figure1) 1 ) (Cherlin et al. 2013 ), and examining collaborations with emergency medical services (point 6, Figure Figure1) 1 ) (Landman et al. 2013 ) were also methodologically connected through sampling of high-performing hospitals in the CMS database.
Integration through Interpretation and Reporting . The authors used primarily a staged narrative approach for reporting their results. The process and outcomes of integration of qualitative and quantitative data were primarily described in the quantitative paper (Bradley et al. 2012 ). The qualitative data informed the development of domains and concepts for a quantitative survey. Mapping of all survey items to corresponding concepts from the qualitative findings was reported in a web appendix of the published article. In the presentation of results from the multivariate model, multiple strategies that had significant associations with RSMRs were reported, with a summary of how these strategies corresponded to five of the six domains from the qualitative component. Quantitative and qualitative findings were synthesized through narrative both in the results and discussion using weaving . Key aspects of the organizational environment included effective communication and collaboration among groups, broad staff presence, and expertise. A culture of problem solving and learning were apparent in the qualitative findings and statistically associated with higher RSMRs in the quantitative findings. Regarding fit , the quantitative findings (Bradley et al. 2012 ) primarily confirmed the qualitative findings (Curry et al. 2011 ). Thus, higher performing hospitals were not distinguished by specific practices, but instead by organizational environments that could foster higher quality care. An accompanying editorial (Davidoff 2012 ) discusses the complementary relationship between the qualitative and quantitative findings, highlighting again the respective purposes of each component. The additional qualitative analyses were published separately (Cherlin et al. 2013 ; Landman et al. 2013 ) and illustrate staged approach to reporting through narrative with ample referencing to the previous studies. This example also illustrates expansion of the previously published findings (Stange, Crabtree, and Miller 2006 ).
Example 2. Integration in a Convergent Mixed Methods Study—The Adaptive Designs Accelerating Promising Trials into Treatments (ADAPT-IT) Study
The RCT is considered by many trialists to be the gold standard of evidence. Adaptive clinical trials (ACTs) have been developed as innovative trials with potential benefits over traditional trials. However, controversy remains regarding assumptions made in ACTs and the validity of results (Berry 2011 ). Adaptive designs comprise a spectrum of potential trial design changes (Meurer et al. 2012 ). A simple adaptation involves early trial termination rules based on statistical boundaries (Pocock 1977 ), while a complex adaptation in a dose-finding trial could identify promising treatments for specific subpopulations and tailor enrollment to maximize information gained (Yee et al. 2012 ). The overarching objective of ADAPT-IT is “To illustrate and explore how best to use adaptive clinical trial designs to improve the evaluation of drugs and medical devices and to use mixed methods to characterize and understand the beliefs, opinions, and concerns of key stakeholders during and after the development process”(Meurer et al. 2012 ).
Integration through design . One study from the mixed methods evaluation aim of the investigation seeks to describe and compare the beliefs and perspectives of key stakeholders in the clinical trial enterprise about potential ethical advantages and disadvantages of ACT approaches. A mixed methods convergent design was utilized to collect quantitative data through a 22-item ACTs beliefs survey using questions with a 100-point visual analog scale, and qualitative data from unstructured open-response questions on the survey and mini focus group interviews. The scales on the survey instrument assessed beliefs about ethical advantages and disadvantages of adaptive designs from the patient, research, and societal perspectives. The qualitative questions on the survey and in the interview guides elicited why participants feel there are advantages or disadvantages to using adaptive designs. A mixed methods approach was implemented to elucidate participants’ beliefs, to identify the reasoning behind the beliefs expressed, and to integrate the data together to provide the broadest possible understanding. Fifty-three individuals participated from the four stakeholder groups: academic clinicians ( n = 22); academic biostatisticians ( n = 5); consultant biostatisticians ( n = 6); and other stakeholders, including FDA and NIH personnel and patient advocates ( n = 20).
Integration through methods . The quantitative and qualitative data were collected concurrently, and the approach to integration involved merging . With the content of the scales on the survey in mind, the mixed methods team developed the open-ended responses on the survey and interview questions for mini focus groups to parallel visual analog scale (VAS) questions about ethical advantages and disadvantages. By making this choice intentionally during the design, integration through merging would naturally follow. The research team conducted separate analyses of the quantitative and qualitative data in parallel . For the quantitative analytics, the team calculated descriptive statistics, mean scores, and standard deviations across the four stakeholder groups. Box plots of the data by group were developed to allow intra- and intergroup comparisons. For the qualitative analytics, the investigators immersed themselves in the qualitative database, developed a coding scheme, and conducted thematic searches using the codes. Since the items on the VASs and the questions on the qualitative interview guides were developed in tandem, the codes in the coding scheme were similarly developed based on the items on the scales and the interview questions. As additional themes emerged, codes to capture these were added. The methodological procedures facilitated thematic searches of the text database about perceived ethical advantages and disadvantages that could be matched and merged with the scaled data on beliefs about ethical advantages and disadvantages.
Integration through Interpretation and Reporting Procedures . Having organized the quantitative and the qualitative data in a format based on thematic relevance to allow merging , higher order integration interpretation was needed. Two approaches were used. First the results from the quantitative and qualitative data were integrated using a joint display. As illustrated in Figure Figure2, 2 , the left provides the participants’ quantitative ratings of their beliefs about the ethical advantages as derived from the visual analog scales, with the lowest anchor of 0 signifying definitely not agreeing with the statement and the highest anchor of 100 signifying definite agreement with the statement. The right side provides illustrative qualitative data from the free-text responses on the survey and the mini focus groups. Color matching (see online version) of the box plots and text responses was devised to help the team match visually the quantitative and qualitative responses from the constituent groups. Multiple steps in developing the joint display contributed to an interpretation of the data.

Example of Joint Display Illustrating Integration at the Interpretation and Reporting Level from the ADAPT-IT Project—Potential Ethical Advantages for Patients When Using Adaptive Clinical Trial Designs
In the final report, the quantitative data integration uses a narrative approach that describes the quantitative and qualitative results thematically. The specific type of narrative integration is weaving because the results are connected to each other thematically, and the qualitative and quantitative data weave back and forth around similar themes or concepts. The narrative provides intragroup comparisons of the results from the scales about beliefs that are supported by text from the qualitative database. Each of the six sections of the results contain quantitative scores with intergroup comparisons among the four groups studied, that is, academic researchers, academic biostatisticians, consultant biostatisticians, and “other” stakeholders and quotations from each group.
Regarding the fit of the quantitative and qualitative data, the integration resulted in an expansion of understanding. The qualitative comments provided information about the spectrum of opinions about ethical advantages and disadvantages, but the scales in particular were illustrative showing there was polarization of opinion about these issues among two of the constituencies.
This article provides an update on mixed methods designs and principles and practices for achieving integration at the design, methods, and interpretation and reporting levels. Mixed methodology offers a new framework for thinking about health services research with substantial potential to generate unique insights into multifaceted phenomena related to health care quality, access, and delivery. When research questions would benefit from a mixed methods approach, researchers need to make careful choices for integration procedures. Due attention to integration at the design, method, and interpretation and reporting levels can enhance the quality of mixed methods health services research and generate rigorous evidence that matters to patients.
Acknowledgments
Joint Acknowledgment/Disclosure Statement : At the invitation of Helen I. Meissner, Office of Behavioral and Social Sciences Research, an earlier version of this article was presented for the NIH-OBSSR Workshop, “Using Mixed Methods to Optimize Dissemination and Implementation of Health Interventions,” Natcher Conference Center, NIH Campus, Bethesda, MD, May 3, 2012. Beth Ragle assisted with entry of references and formatting. Dr. Fetters acknowledges the other members of the ADAPT-IT project's Mixed Methods team, Laurie J. Legocki, William J. Meurer, and Shirley Frederiksen, for their contributions to the development of Figure 2 .
Disclosures : None.
Disclaimers : None.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
- American College of Cardiology. 2013. “Surviving MI Intiative” [accessed on May 12, 2013]. Available at http://www.cardiosource.org/Science-And-Quality/Quality-Programs/Surviving-MI-Initiative.aspx .
- Berry DA. “Adaptive Clinical Trials: The Promise and the Caution” Journal of Clinical Oncology. 2011; 29 (6):606–9. [ PubMed ] [ Google Scholar ]
- Bradley EH, Curry LA, Spatz ES, Herrin J, Cherlin EJ, Curtis JP, Thompson JW, Ting HH, Wang Y, Krumholz HM. “Hospital Strategies for Reducing Risk-Standardized Mortality Rates in Acute Myocardial Infarction” Annals of Internal Medicine. 2012; 156 (9):618–26. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bryman A. “Integrating Quantitative and Qualitative Research: How Is It Done?” Qualitative Inquiry. 2006; 6 (1):97–113. [ Google Scholar ]
- Carr E. “Exploring the Effect of Postoperative Pain on Patient Outcomes Following Surgery” Acute Pain. 2000; 3 (4):183–93. [ Google Scholar ]
- Castro FG, Kellison JG, Boyd SJ, Kopak A. “A Methodology for Conducting Integrative Mixed Methods Research and Data Analyses” Journal of Mixed Methods Research. 2010; 4 (4):342–60. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cherlin EJ, Curry LA, Thompson JW, Greysen SR, Spatz E, Krumholz HM, Bradley EH. “Features of High Quality Discharge Planning for Patients Following Acute Myocardial Infarction” Journal of General Internal Medicine. 2013; 28 (3):436–43. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Classen S, Lopez ED, Winter S, Awadzi KD, Ferree N, Garvan CW. “Population-Based Health Promotion Perspective for Older Driver Safety: Conceptual Framework to Intervention Plan” Clinical Interventions in Aging. 2007; 2 (4):677–93. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Crabtree BF, Miller WL, Tallia AF, Cohen DJ, DiCicco-Bloom B, McIlvain HE, Aita VA, Scott JG, Gregory PB, Stange KC, McDaniel RR., Jr “Delivery of Clinical Preventive Services in Family Medicine Offices” Annals of Family Medicine. 2005; 3 (5):430–5. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Creswell JW, Fetters MD, Ivankova NV. “Designing a Mixed Methods Study in Primary Care” Annals of Family Medicine. 2004; 2 (1):7–12. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage Publications, Inc; 2011. [ Google Scholar ]
- Creswell JW, Tashakkori A. “Editorial: Developing Publishable Mixed Methods Manuscripts” Journal of Mixed Methods Research. 2007; 1 (107):106–11. [ Google Scholar ]
- Creswell JW, Fetters MD, Plano Clark VL, Morales A. “Mixed Methods Intervention Trials” In: Andrew S, Halcomb E, editors. Mixed Methods Research for Nursing and the Health Sciences. Chichester, West Sussex; Ames, Iowa: Blackwell Publishing; 2009. pp. 161–80. [ Google Scholar ]
- Creswell JW, Klassen AC, Plano Clark VL, Smith KC, Working Group Assistance . Washington, DC: Office of Behavioral and Social Sciences Research (OBSSR), National Institutes of Health (NIH); 2011. “Best Practices for Mixed Methods Research in the Health Sciences” p. 27. H. I. Meissner. [ Google Scholar ]
- Curry LA, Spatz E, Cherlin E, Thompson JW, Berg D, Ting HH, Decker C, Krumholz HM, Bradley EH. “What Distinguishes Top-Performing Hospitals in Acute Myocardial Infarction Mortality Rates? A Qualitative Study” Annals of Internal Medicine. 2011; 154 (6):384–90. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Curry L, Krumholz HM, O'Cathain A, Plano Clark V, Cherlin E, Bradley EH. “Mixed Methods in Biomedical and Health Services Research” Circulation. 2013; 6 (1):119–23. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Davidoff F. “Is Every Defect Really a Treasure?” Annals of Internal Medicine. 2012; 156 (9):664–5. [ PubMed ] [ Google Scholar ]
- Fetters MD, Ivankova NV, Ruffin MT, Creswell JW, Power D. “Developing a Web Site in Primary Care” Family Medicine. 2004; 36 (9):651–9. [ PubMed ] [ Google Scholar ]
- Hamilton A, Cohen A, Glover D, Whelan F, Chemerinski E, McNagny KP, Mullins D, Reist C, Schubert M, Young AS. “Implementation of Evidence-Based Employment Services in Specialty Mental Health: Mixed Methods Research” Health Services Research. 2013; 48 (S2):2224–44. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hammoud MM, Elnashar M, Abdelrahim H, Khidir A, Elliott HAK, Killawi A, Padela AI, Al Khal AL, Bener A, Fetters MD. “Challenges and Opportunities of US and Arab Collaborations in Health Services Research: A Case Study from Qatar” Global Journal of Health Science. 2012; 4 (6):148–59. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Israel BA, Schulz AJ, Parker EA, Becker AB. “Community-Based Participatory Research: Policy Recommendations for Promoting a Partnership Approach in Health Research” Education for Health. 2001; 14 (2):182–97. [ PubMed ] [ Google Scholar ]
- Israel BA, Eng E, Schulz AJ, Parker E. Methods for Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2013. [ Google Scholar ]
- Ivankova NV, Creswell JW, Stick S. “Using Mixed-Methods Sequential Explanatory Design: From Theory to Practice” Field Methods. 2006; 18 (1):3–20. [ Google Scholar ]
- Jaen CR, Crabtree BF, Palmer RF, Ferrer RL, Nutting PA, Miller WL, Stewart EE, Wood R, Davila M, Stange KC. “Methods for Evaluating Practice Change Toward a Patient-Centered Medical Home” Annals of Family Medicine. 2010; 8 (Suppl 1):S9–20. S92. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Johnson CE, Ali SA, Shipp MPL. “Building Comunity-Based Participatory Research Partnerships with a Somali Refugee Community” American Journal of Preventive Medicine. 2009; 37 (6S1):S230–6. [ PubMed ] [ Google Scholar ]
- Krippendorff K. Content Analysis: An Introduction to Its Methodology. 3rd ed. Thousand Oaks, CA: Sage; 2013. [ Google Scholar ]
- Krumholz HM, Curry LA, Bradley EH. “Survival after Acute Myocardial Infarction (SAMI) Study: The Design and Implementation of a Positive Deviance Study” American Heart Journal. 2011; 162 (6):981–7. e9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Krumholz HM, Merrill AR, Schone EM, Schreiner GC, Chen J, Bradley EH, Wang Y, Lin Z, Straube BM, Rapp MT, Normand SL, Drye EE. “Patterns of Hospital Performance in Acute Myocardial Infarction and Heart Failure 30-Day Mortality and Readmission” Circulation. 2009; 2 (5):407–13. [ PubMed ] [ Google Scholar ]
- Landman AB, Spatz ES, Cherlin EJ, Krumholz HM, Bradley EH, Curry LA. “Hospital Collaboration with Emergency Medical Services in the Care of Patients with Acute Myocardial Infarction: Perspectives from Key Hospital Staff” Annals of Emergency Medicine. 2013; 61 (2):185–95. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lewin S, Glenton C, Oxman AD. “Use of Qualitative Methods Alongside Randomised Controlled Trials of Complex Healthcare Interventions: Methodological Study” British Medical Journal. 2009; 339 :b3496. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Luck L, Jackson D, Usher K. “Case Study: A Bridge across the Paradigms” Nursing Inquiry. 2006; 13 (2):103–9. [ PubMed ] [ Google Scholar ]
- Usher K. “Innocent or Culpable? Meanings that Emergency Department Nurses Ascribe to Individual Acts of Violence” Journal of Clinical Nursing. 2008; 17 (8):1071–8. [ PubMed ] [ Google Scholar ]
- Macaulay AC, Commanda LE, Freeman WL, Gibson N, McCabe ML, Robbins CM, Twohig PL. “Participatory Research Maximises Community and Lay Involvement” British Medical Journal. 1999; 319 (7212):774–8. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mertens DM. Transformative Research and Evaluation. New York: The Guilford Press; 2009. [ Google Scholar ]
- Mertens DM. “Transformative Mixed Methods: Addressing Inequities” American Behavioral Scientist. 2012; 56 (6):802–13. [ Google Scholar ]
- Meurer WJ, Lewis RJ, Tagle D, Fetters M, Legocki L, Berry S, Connor J, Durkalski V, Elm J, Zhao W, Frederiksen S, Silbergleit R, Palesch Y, Berry DA, Barsan WG. “An Overview of the Adaptive Designs Accelerating Promising Trials Into Treatments (ADAPT_IT) Project” Annals of Emergency Medicine. 2012; 60 (4):451–7. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Minkler M, Wallerstein N. Community-Based Participatory Research for Health: From Process to Outcomes. San Francisco, CA: Josey-Bass; 2008. [ Google Scholar ]
- Moffatt S, White M, Mackintosh J, Howel D. “Using Quantitative and Qualitative Data in Health Services Research—What Happens When Mixed Methods Findings Conflict?” BMC Health Services Research. 2006; 6 (28):1–10. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nastasi BK, Hitchcock J, Sarkar S, Burkholder G, Varjas K, Jayasena A. “Mixed Methods in Intervention Research: Theory to Adaptation” Journal of Mixed Methods Research. 2007; 1 (2):164–82. [ Google Scholar ]
- O'Cathain A, Murphy E, Nicholl J. “Three Techniques for Integrating Data in Mixed Methods Studies” British Medical Journal. 2010; 341 :c4587. [ PubMed ] [ Google Scholar ]
- Onwuegbuzie AJ, Bustamante RM, Nelson JA. “Mixed Research as a Tool for Developing Quantitative Instruments” Journal of Mixed Methods Research. 2010; 4 (1):56–78. [ Google Scholar ]
- Plano Clark VL, Schumacher K, West C, Edrington J, Dunn LB, Harzstark A, Melisko M, Rabow MW, Swift PS, Miaskowski C. “Practices for Embedding an Interpretive Qualitative Approach within a Randomized Clinical Trial” Journal of Mixed Methods Research. 2013; 7 (3):219–42. [ Google Scholar ]
- Pluye P, Grad RM, Dunikowski LG, Stephenson R. “Impact of Clinical Information-Retrieval Technology on Physicians: A Literature Review of Quantitative, Qualitative and Mixed Methods Studies” International Journal of Medical Informatics. 2005; 74 (9):745–68. [ PubMed ] [ Google Scholar ]
- Pocock SJ. “Group Sequential Methods in the Design and Analysis of Clinical Trials” Biomedics. 1977; 64 (2):191–9. [ Google Scholar ]
- Popescu I, Werner RM, Vaughan-Sarrazin MS, Cram P. “Characteristics and Outcomes of America's Lowest-Performing Hospitals: An Analysis of Acute Myocardial Infarction Hospital Care in the United States” Circulation. 2009; 2 (3):221–7. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ruffin MTI, Fetters MD, Jimbo M. “Preference-Based Electronic Decision Aid to Promote Colorectal Cancer Screening: Results of A Randomized Controlled Trial” Preventive Medicine. 2007; 45 (4):267–73. [ PubMed ] [ Google Scholar ]
- Ruffin MT, Creswell JW, Jimbo M, Fetters MD. “Factors Influencing Choices for Colorectal Cancer Screening among Previously Unscreened African and Caucasion Americans: Findings from a Mixed Methods Investigation” Journal of Community Health. 2009; 34 (2):79–89. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Saint Arnault D, Fetters MD. “RO1 Funding for Mixed Methods Research: Lessons Learned from the “Mixed-Method Analysis of Japanese Depression” Project” Journal of Mixed Methods Research. 2011; 5 (4):309–29. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Scammon DL, Tomoaia-Cotisel A, Day R, Day J, Kim J, Waitzman N, Farrell T, Magill M. “Connecting the Dots and Merging Meaning: Using Mixed Methods to Study Primary Care Delivery Transformation” Health Services Research. 2013; 48 (S2):2181–207. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shaw EK, Ohman-Strickland PA, Piasecki A, Hudson SV, Ferrante JM, McDaniel RR, Jr, Nutting PA, Crabtree BF. “Effects of Facilitated Team Meetings and Learning Collaboratives on Colorectal Cancer Screening Rates in Primary Care Practices: A Cluster Randomized Trial” Annals of Family Medicine. 2013; 11 (3):220–8. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Silka L. “Partnership Ethics” In: Mertens DM, Ginsberg PE, editors. Handbook of Social Research Ethics. Thousand Oaks, CA: Sage; 2009. pp. 337–52. [ Google Scholar ]
- Stake R. The Art of Case Study Research. Thousand Oaks, CA: Sage; 1995. [ Google Scholar ]
- Stange KC, Crabtree BF, Miller WL. “Publishing Multimethod Research” Annals of Family Medicine. 2006; 4 (4):292–4. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wallace S, Clark M, White J. “‘It's On My iPhone’: Attitudes to the Use of Mobile Computing Devices in Medical Education, A Mixed-Methods Study” BMJ Open. 2012; 2 (4) e001099. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Willms DG. “A New Stage, A New Life: Individual Success in Quitting Smoking” Social Science and Medicine. 1991; 33 (12):1365–71. [ PubMed ] [ Google Scholar ]
- Wilson DM, Taylor DW, Gilbert JR, Best JA, Lindsay EA, Willms DG, Singer J. “A Randomized Trial of a Family Physician Intervention for Smoking Cessation” Journal of the American Medical Association. 1988; 260 (11):1570–4. [ PubMed ] [ Google Scholar ]
- Yee D, Haddad T, Albain K, Barker A, Benz C, Boughey J, Buxton M, Chien AJ, DeMichele A, Dilts D, Elias A, Haluska P, Hogarth M, Hu A, Hytlon N, Kaplan HG, Kelloff GG, Khan Q, Lang J, Leyland-Jones B, Liu M, Nanda R, Northfelt D, Olopade OI, Park J, Parker B, Parkinson D, Pearson-White S, Perlmutter J, Pusztai L, Symmans F, Rugo H, Tripathy D, Wallace A, Wholley D, Van't Veer L, Berry DA, Esserman L. “Adaptive Trials in the Neoadjuvant Setting: A Model to Safely Tailor Care While Accelerating Drug Development” Journal of Clinical Oncology. 2012; 30 (36):4584–6. author reply 88–9. [ PubMed ] [ Google Scholar ]
- Yin RK. Case Study Research: Design and Methods. Beverly Hills, CA: Sage; 1984. [ Google Scholar ]
- Zickmund S, Yang S, Mulvey EP, Bost JE, Shinkunas LA, LaBrecque DR. “Predicting Cancer Mortality: Developing a New Cancer Care Variable Using Mixed Methods and the Quasi-Statistical Approach” Health Services Research. 2013; 48 (S2):2208–23. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Open access
- Published: 12 April 2024
Participatory methods used in the evaluation of medical devices: a comparison of focus groups, interviews, and a survey
- Kas Woudstra 1 , 2 ,
- Marcia Tummers 1 ,
- Catharina J. M. Klijn 3 ,
- Lotte Sondag 3 ,
- Floris Schreuder 3 ,
- Rob Reuzel 1 &
- Maroeska Rovers 2
BMC Health Services Research volume 24 , Article number: 462 ( 2024 ) Cite this article
Metrics details
Stakeholder engagement in evaluation of medical devices is crucial for aligning devices with stakeholders’ views, needs, and values. Methods for these engagements have however not been compared to analyse their relative merits for medical device evaluation. Therefore, we systematically compared these three methods in terms of themes, interaction, and time-investment.
We compared focus groups, interviews, and an online survey in a case-study on minimally invasive endoscopy-guided surgery for patients with intracerebral haemorrhage. The focus groups and interviews featured two rounds, one explorative focussing on individual perspectives, and one interactive focussing on the exchange of perspectives between participants. The comparison between methods was made in terms of number and content of themes, how participants interact, and hours invested by all researchers.
The focus groups generated 34 themes, the interviews 58, and the survey 42. Various improvements for the assessment of the surgical procedure were only discussed in the interviews. In focus groups, participants were inclined to emphasise agreement and support, whereas the interviews consisted of questions and answers. The total time investment for researchers of focus groups was 95 h, of interviews 315 h, and survey 81 h.
Conclusions
Within the context of medical device evaluation, interviews appeared to be the most appropriate method for understanding stakeholder views since they provide a scope and depth of information that is not generated by other methods. Focus groups were useful to rapidly bring views together. Surveys enabled a quick exploration. Researchers should account for these methodological differences and select the method that is suitable for their research aim.
Peer Review reports
Medical devices form an intricate part of the healthcare system. Novel medical devices like robots, nano-technologies, and e-health platforms carry the promise of improving healthcare systems [ 1 ]. As medical devices become more pervasive and complex, it is essential to develop and apply these technologies so that they solve the most pressing medical problems in global healthcare systems. Multiple guidelines and regulations exist that stimulate a practice of medical device research and development that is aimed at solving critical health problems [ 2 , 3 , 4 ]. In these documents, one of the recommendations is to actively involve a diverse selection of stakeholders in the research and development process of medical devices. This should lead to better informed decisions during evaluation: aligning devices with the views, needs, and values of stakeholders like medical professionals or patients. This, in turn, can optimise the use of resources spent on research, development, implementation, or use [ 5 ].
There are several methods for stakeholder involvement but these have not been compared against the background of their suitability for medical device evaluation purposes. Studying methods within this context is important, because there are some typical requirements in medical device evaluation. Methods should yield relevant information for research or development choices, preferably foster agreement among stakeholders regarding the future development and implementation of the medical device, and be feasible in terms of resources. By relevant information we mean: any information that helps to understand what features a device should have or how research into a device should be conducted to meet the needs and values of stakeholders. This could involve effectiveness, functionalities, ease of use, affordability, or possible spill overs. By analysing stakeholder needs and practices and making consequent design changes, medical devices can become more valuable [ 6 , 7 ]. Fostering agreement is important to ensure that a device is sufficiently endorsed to make implementation successful. This requires interaction between stakeholders to find common ground [ 8 ]. In entrepreneurial settings where resources are limited and the life-cycle of medical devices is relatively short, development trajectories generally cannot be too long and costly [ 9 ]. Participatory methods can—on the other hand – give insights into development, evaluation, and implementation issues that can occur, and therefore possibly save costs. Due to these unique conditions, it is important to specifically analyse participatory methods in the context of medical device evaluation or development. Some general comparisons of interviews, focus groups, and surveys exist terms of effect on outcomes exist, but these comparisons are not directly applicable to medical devices, nor are they compared all three together [ 10 , 11 , 12 ].
Interviews and focus groups are the most often-used methods in participatory research of medical devices and therefore we compare these in this study [ 13 ]. Surveys are chosen because they are also used in qualitative research and because they methodologically differ on various aspects from interviews and focus groups [ 13 ]. Qualitative surveys offer open text boxes and therefore researchers cannot ask follow-up questions, and there is no direct interaction between researchers and participants. Therefore, we aimed to investigate how focus groups, interviews, and a survey compare in terms of the number of relevant themes they provide, interaction between stakeholders, and time-investment, when conducted in the context of the evaluation of a medical device.
Comparison in one clinical case
We simultaneously employed and compared three participatory methods: focus groups, interviews, and a survey, in an empirical case-study on minimally-invasive endoscopy-guided surgery for patients with intracerebral haemorrhage (ICH). ICH is the deadliest stroke subtype, with a 30-day case fatality of 40%, and of the patients surviving many live with severe disability [ 14 ]. To improve outcome of patients with ICH, an innovative endoscopic device has been developed that has the potential of removing the haemorrhage by minimally-invasive surgery. A systematic review and meta-analysis of randomised trials investigating surgical treatment of ICH showed that minimally-invasive surgery was associated with a reduction in mortality and an increase in good functional outcome, particularly when performed early after symptom onset [ 15 ]. The Dutch Intracerebral haemorrhage Surgery Trial (DIST) pilot study (NCT03608423) has recently demonstrated in 40 patients with ICH that minimally-invasive endoscopy-guided surgery within 8 h of symptom onset using the novel endoscopy-guided approach was feasible, safe, and technically effective for hematoma removal (Sondag, personal communication). At the time of our research, members of our team (CK, LS, FS) were preparing a phase 3 randomised clinical trial to evaluate effectiveness on functional outcome using early minimally-invasive endoscopy-guided surgery in patients with ICH (NCT05460793). Against this background we employed focus groups, interviews, and a survey to elicit [ 1 ] views of stakeholders on the new endoscopic device and (2) the quality of the (received) hospital care for ICH-patients.

Selection procedure participants
We selected participants who are involved in hospital care for ICH and involved in the use of the new endoscopic device. Three stakeholder groups were identified: patients and relatives, healthcare professionals (HCPs), and policy experts. The number of participants that were determined for each method was guided by the concept of information power, which helps to establish how many participants are needed to acquire a reliable dataset [ 16 ]. Patients, relatives, and HCPs were approached by KW, LS and FS. LS and FS had a physician–patient relationship with the invited patients and relatives, or knew patients and relatives because they had participated in a previous studies related to ICH. HCPs were approached via the network of the neurologists involved in this research (CK, LS, FS), which spans over various ICH care institutions across the Netherlands. Policy experts were approached through networks of CK and MR. In the initial invitations, participants were assigned at random to one of the three methods. Participants that were invited for one method were not allowed to participate in other methods, so there were no cross-overs between methods. Subsequently, all potential participants were contacted via e-mail or by phone. After expressing their willingness to participate, they received an information letter and an informed consent form. In these documents, the aim, conditions, practical details, advantages, and disadvantages of participation were explained. All participants were given two weeks to consider participation, and the conditions of participation were again discussed or presented before each interview, focus group, or survey started. All participants gave written or verbal consent on audio tapes. The local certified ethics committee approved the research protocol.
Data collection method 1: focus groups
We organised five 45-min focus groups, all planned on one evening. The first three focus groups were homogeneous: one for patients, one for HCPs, and one for policy experts. These three focus groups were conducted simultaneously. In these sessions, patients and relatives, HCPs, and policy experts convened in their own groups to discuss their views on the intervention with the new endoscopic device and the quality of hospital care. The participants were first placed in homogeneous groups to familiarize and become comfortable with people with a comparable perspective and make participants at ease. They were also placed in these groups to mirror the first round of interviews that was not primarily aimed at interaction but at constructing the different views of participants. The last two focus groups were also planned simultaneously, fifteen minutes after the first three focus groups. In these focus groups the patients and relatives, HCPs, and policy experts who participated in the first round of focus groups were mixed into two heterogeneous groups to discuss findings from the earlier homogeneous focus groups and to discuss how the different perspectives could be brought together. A number of four to twelve participants per focus groups is advised in literature, so we aimed to include six persons in the homogeneous focus groups, and nine persons in the ensuing heterogenous focus groups [ 17 ]. A minimum number of participants for qualitative research has been proposed of 12, so we aimed to include a higher number than that and tried to include a number that was comparable to the interviews [ 18 ]. Each focus group was led by one moderator, who probed for more in-depth answers if needed, and ensured that every participant was able to participate. All moderators were experienced in moderating group discussions and not in any way involved in ICH-care. Two moderators who participated in the first round moderated the second round. We used semi-structured focus groups protocols (see Appendix 1 ). All focus groups were audio-recorded and transcribed verbally. The audio tapes and transcripts were stored in accordance with European data safety requirements [ 19 ]. Due to the COVID-19 pandemic, the focus groups were organised online via a video call platform. The literature on online or ‘synchronous’ focus groups and interviews indicates that there can be some methodological specificalities to online data collection. It might improve the representation of certain groups, e.g. geographically dispersed people and people with disabilities, and it might be easier to generate richer data on sensitive topics. However, visual ques are harder to read [ 20 , 21 , 22 ]. Altogether, online focus groups might therefore be a useful way of data collection, especially for patients with ICH that encounter many mobility issues and social obstacles.
Data collection method 2: interviews
For the interviews, we used fourth-generation evaluation methodology with some minor modifications [ 23 , 24 , 25 ]. All participants were interviewed twice: in the first round they were asked to share their views on the new endoscopic device and the quality of hospital care, and in the second round they were invited to respond to rival claims of other participants. We aimed to include a number that was comparable to the focus groups and above the minimum number of 12 participants that has been proposed [ 18 ]. All interviews were conducted by KW (3 years of interviewing experience). For both interview rounds, a semi-structured interview protocol was used (see Appendix 2 ). All opinions were processed and presented to other participants anonymously. Due to the COVID-19 pandemic, all interviews were taken via a video call platform, or by phone. As described above, online or synchronous data collection has distinctive features and might be a valuable method of data collection. All interviews were audio recorded and transcribed. The audio tapes and transcripts were stored in accordance with European data safety requirements [ 19 ].
Data collection method 3: qualitative survey
The survey started with information about the study, then asked questions about characteristics of the person filling out the survey, including age, gender, education level, profession, and subsequently questions about improvements in the hospital treatment for ICH and the minimally invasive intervention with the new device. Patients and HCPs were asked to list unmet needs of patients and relevant outcome measures. The questions were closed, answer categories limited, but always followed by an opportunity to provide additional information in an open text field. We invited 78 participants, above the number of participants that proposed as a minimum in qualitative research (which is 12) and above the number of participants that is proposed for qualitative surveys (which is 25 to 50) [ 18 , 26 ]. The survey was conducted via Castor, a digital survey platform. The data were stored in accordance with European data safety requirements [ 19 ].
Units of comparison
The three methods were compared on three outcomes: the number of themes, interaction, and the time-investment of the methods, which are described below.
Number and type of themes
The analysis of the number and type of themes was supported by Atlas.ti software (V.9) and performed by one author (KW) to increase consistency. Following the six steps of thematic analysis by Braun and Clarke [ 27 ], the analysis started with reading and coding the transcripts and survey answers. In later phases these codes were arranged and grouped into themes. This process was discussed with MT and RR to check the credibility of the codes and the themes to ensure consistency and minimise a possible bias. We compared the number of themes provided by each method, and determined what themes were constructed in only one of the methods. Counting themes may not be a conventional approach in qualitative research. However, we aim to provide insight into the breadth and thus comprehensiveness of information collected. Because the coding method was consistent along the three methods, we believe counting themes is an adequate unit of comparison.
Interaction
To assess interaction, we performed three analyses to determine: (i) what themes were addressed by multiple stakeholder groups, (ii) which participants interact with each other, and (iii) how participants interact. All these analyses were performed after the data were collected, and supported by Atlas.ti software (V.9). For the first analysis, we calculated the percentage of the themes that was addressed by two or three stakeholder groups in each data-collection method. For example, if both HCPs and policy experts addressed theme X, this theme was marked as ‘shared’, and consequently the percentage of shared themes of the total amount of themes could be calculated. For this comparison, all methods were taken into account, even though participants did not directly interact in surveys. For the other two analyses, we examined how participants interact. To this aim, we adapted coding schemes by Morgan & Hoffman [ 28 ] and Keyton [ 29 ], which can be applied on verbatim transcripts to code how people react. Our main aims for this analysis were to identify how extensive topics were addressed, and to identify whether stakeholders could reach forms of agreement while interacting. The codes as described by Morgan & Hoffman [ 28 ] were most applicable for these aims so we have used their code book, whereas Keyton [ 29 ] more concisely describes how different turns in an interaction can be coded, so we have adapted her coding process. The main change in the coding book that we made, is that we distinguished who interact from the ways how people interact, which was not clearly incorporated in Morgan & Hofmann’s code book (see Appendix 3 ). We coded who the speaker is and to whom this speaker addresses the message, which will be referred to as turn . When a moderator asked a question to participants, or vice versa, this is coded as a ‘moderator-participant’ turn, and when participants ask and answer questions to each other, these are coded as ‘turn between participants’. When a moderator presented views of other participants, and when participants reacted, these were separately coded as a ‘turn between moderator and participant where moderator presents view of others’. Besides turns we also coded how participants interact in the conversation, using the codes ‘question’, ‘answer’, ‘expansion: sharing new aspect of previous topic’, and ‘agreement’, which will be referred to as acts . Acts are mutually exclusive, but multiple acts could be assigned to one turn in a conversation and vice versa, for example when a participant gives an answer to a moderator and directly poses a question the moderator. KW performed the coding process. These analyses were discussed in-depth with MT and RR, to ensure consistency and minimise a possible bias.
Time-investment
We have operationalised time-investment as the absolute number of hours that all the involved researchers and moderators spent on preparing and performing data-collection and analysing the data. We chose not to analyse the investment from the perspective of the participants, because in this paper aims to compare participatory methods from the perspective of the person or organisation conducting them. Time-investment was based on the researchers’ (KW) agenda, supplemented by sources in the literature, to establish the average time that is needed to transcribe a one-hour audio-tape [ 30 , 31 ]. Because the focus groups and interviews were conducted online, travelling time for researchers and moderators was not taken into account. The calculation of time-investment is set out in detail in Appendix 4 .
Researcher characteristics and reflexivity
The research team partially consists of researchers developing qualitative evaluation methods (KW, MT, MR, RR), and partially of neurologists (CK, FS, LS). There was a doctor-patient relationship between FS and some of the participants. RR is an expert on interactive interviews.
Participants
We invited 24 persons for the focus groups of whom 18 participated, 23 for the interviews of whom 17 participated, and 79 for the survey of whom 43 participated (see Table 1 ). In the focus groups, we had equal numbers of patients or relatives, HCPs, and policy makers: 6 participants in each group. The 17 participants in the interviews were patients ( n = 7 and n = 3 in round 1 and 2), HCPs ( n = 8 and n = 6 in round 1 and 2), and policy makers ( n = 2 in both rounds). In the survey, we included 21 patients, 18 HCPs, and 4 policy makers. See Appendix 5 for an overview of the types and number of enrolled participants per data-collection methods that is completed with the total number of invited participants. The majority of interviews lasted an hour, but the duration varied from 30 to 90 min. All focus groups lasted 45 min.
The number of themes varied between the different methods (see Fig. 1 ). In the explorative round 31 themes were constructed. In the interactive round 19 themes were constructed and 16 of these were also discussed in the first round, so 34 themes were constructed in all focus groups. The first interview round generated 58 themes, the second 40, and all themes in the second round of interviews had already been discussed in the first round. The survey generated 42 unique themes. An overview of all the themes generated can be found in Appendix 6 .
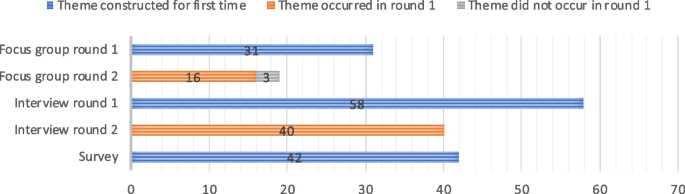
Number of themes constructed in three data collection methods
All methods generated themes about research improvements for the innovation and care experiences in the hospital but there were some unique themes that specifically came up in one of the methods and not in the others. In the focus groups, four themes were constructed that were not generated in the other methods, two of which related to communication between HCPs and patients and relatives. In the interviews 19 themes were generated, that addressed various aspects of the assessment of the new treatment, such as the characteristics of the study population that ideally should undergo the new treatment in a subsequent research phase, and the informed consent procedure of that research phase. In the survey, 9 unique themes were present, ranging from ‘trust in HCPs’ to ‘outcome measure: feasibility’.
Percentage of themes that is addressed by multiple groups of stakeholders
Figure 2 shows that some themes were addressed by multiple stakeholder groups, whereas other themes were mentioned by one stakeholder group only. In the first explorative round of the focus groups, 16 percent of the themes was addressed by two or three stakeholder groups. In the second interactive round the percentage of themes addressed by multiple groups was 35 percent. In the first round of interviews the percentage of themes addressed by multiple groups was 25 percent in the first round and 58 percent in the second round. In the survey, 21 percent of the themes was addressed by multiple stakeholder groups, and these shared themes are all based on the numeric answers. None of the open-text box answers led to themes that were addressed by multiple stakeholders.
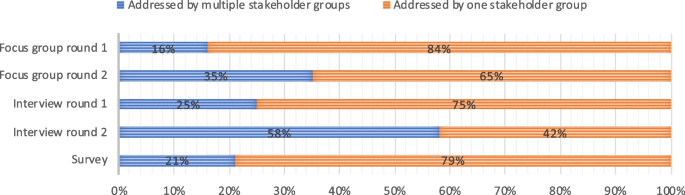
Percentage of themes addressed by multiple stakeholder groups in three data collection methods in round 1 (exploration) and round 2 (reaction)
Which participants interact with each other: turns
Figure 3 depicts which participants interacted with each other. In the first round of the focus group the moderators and participants primarily interacted, whereas in the second interactive round, participants more often interacted directly with each other. In the first interview round, 98% of the turns consisted of direct interaction between participants and the moderator and 2% of the turns consisted of interactions about other participants’ perspectives. In interview round 2, 20% of the turns consisted of direct interaction, and 80% percent of the turns entailed other participants’ opinions. The total number of turns in focus groups round one is 89, in round two 115. The total number of turns in interview round one is 1472 and in round two 894.
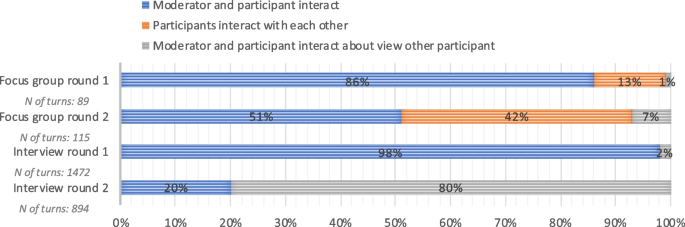
Which participants interact with each other: presented as percentage of total number of interactions
How participants interact: acts
Figure 4 presents how participants and moderators interacted in each of the rounds in the focus groups and interviews. In the first round of the focus groups, 93% of the acts consisted of questions, follow-up questions, answers, and expansions on topics, whereas concrete expressions of agreement (18 percent) and support (8 percent) were more prevalent in the second round. In interview round one, 99% of the acts consisted of questions, follow-up questions, answers, and expansions upon previous answers. In round two this was 98%.
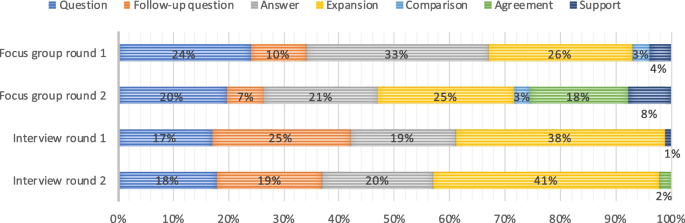
Form of interaction as percentage of total number of interactions
Figure 5 provides insight in the time-investment of each of the methods, operationalised as the number of hours that needs to be worked by all researchers. The preparation, data-collection, and analysis of the focus groups took 26, 15, and 54 h within in an overall time span of seven months. Of these 54 h of analysis, 19 consisted of transcribing interviews. The recruitment of participants for the interviews and setting a date took a preparation time that spanned over 5 months. The interviews took 26 h, 45 and 244 h for preparation, data-collection and analysis in a time span of 5 months and 10 months for the first and second round. Of these 244 h of analysis, 140 were dedicated to transcribing. The survey took 57 h to prepare and was completed over the course of nine months, as all questions had to be carefully integrated, checked, and piloted using a digital survey platform.
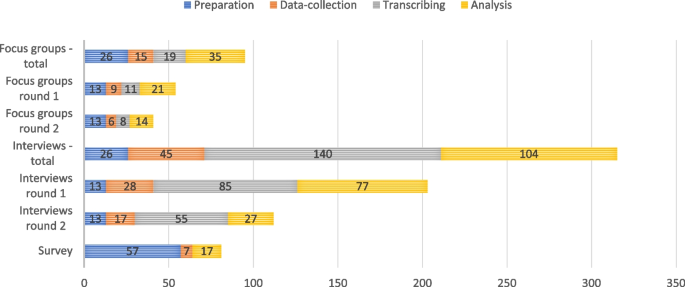
Accumulative number of hours worked by researchers
Summary main findings
This comparison of focus groups, interviews and a survey in an empirical case study on minimally-invasive endoscopy-guided surgery in patients with ICH showed considerable differences in themes, interaction, and time-investment. In the focus groups relatively few themes were discussed, in the survey slightly more themes occurred, and in the interviews the largest number of themes was constructed. Many improvements for the assessment of the minimally invasive procedure were only discussed in the interviews, such as in- and exclusion criteria for the randomised clinical trial. We assume this is due to the extended time that can be dedicated to data collection, so that more detailed topics can be discussed in-depth. In other respects, there were no clear patterns of topics that occurred in specific methods. In terms of interaction, the focus groups where characterised by relatively much agreement and support. In the interviews agreement and support were seldomly expressed: nearly only questions and answers occurred. In terms of time-investment, the survey required the lowest total time investment: a total of 81 h, followed by focus groups with 96 h, and interviews required the highest time investment with a total of 315 h. There were no significant differences in time investment between the two rounds, neither for the focus groups nor for the interviews. The time allocated for preparation, data collection, and analysis was proportional to the number of interviews and focus groups conducted in each round.
Taking these results together, we can conclude that interviews generated the most useful data within the clinical case because they generated the highest number of relevant themes. They did however require a high-time investment. Focus groups appeared to be a technique that can better be employed to generate agreement and support instead of generating many relevant themes. Surveys do not generate the most comprehensive overview of themes, but can be useful if researchers want to map themes in a quick way without asking follow-up questions. It is important to be aware that we analysed these differences in the context of medical device evaluation, where the aim of participatory methods is to inform the research or development process, rather than merely describing stakeholder views.
Comparison literature
Our results are in agreement with other studies that show that focus groups generate fewer themes compared to interviews, and that focus groups are relatively time efficient [ 32 , 33 , 34 ]. Other studies, however, report that focus groups and interviews generate a comparable large number of themes, whereas our results clearly show that interviews generate more themes [ 10 , 35 , 36 , 37 ]. The discrepancy might be explained by the large number of focus groups that were held and the number of participants that participated in these latter studies. Namey et al. [ 35 ] for example assigned 310 participants to 40 focus groups and 40 participants to interviews. Because these authors include such high numbers in focus groups, they also state that focus groups require a lower time-investment. Based on our findings and the findings in the literature, we can assume that with equal inclusion numbers, focus groups take less time at the expense of generating less data.
Strengths and limitations
The major strength of our study is that we compared three participatory methods in one single empirical case study on the development and evaluation of a medical device. With rigorous control of many contextual and methodological factors we can conclude that the differences in the three outcomes of this study are mainly caused by the characteristics of the data collection methods. Another strength is that we have embedded the comparison in an actual participatory assessment of an innovative minimally-invasive surgical treatment, increasing the ecological validity of the results. Patients and their relatives were involved, they interacted with different physicians and policy makers, and the findings were used in later assessments of the new procedure. Therefore, the results of this study are representative for interactions between these groups. The insights have also informed subsequent quantitative studies on the surgical treatment. Albeit our study is focussed on medical device evaluation, it also has consequences for comparisons of qualitative methods in a broader perspective, because we have adopted conventional focus group, interview and survey methodologies. Our results can therefore be compared with those from related studies outside the domain of medical device evaluation. Finally, we performed an analysis of interaction. The analysis of interaction is rarely done, probably because it is laborious. However, this analysis is crucial because interaction between participants and between participants and moderator(s) is one of the primary aims of focus groups and interviews. By showing who interacts with whom and how, we offer insights in the processes of these methods, which can be of use in the selection of one of these methods by others.
Some limitations should also be addressed. First, there are still some variations in the three research designs that could have influenced the outcomes. Different moderators and stakeholders were involved in each method, and their specific characteristics could have affected the results. Using different moderators and participants was a considerate choice, however, since the use of the same moderator or participants in all methods would have influenced the outcomes, as they would have taken their experiences from one activity to the other. Second, a substantial proportion of themes was found in only two or one of the methods, which indicates that none of the methods generated a complete set of data. This implies that the concept of information power might not have been the most suitable technique to determine the number of participants. Saturation might be a better point to close the data collection phase, especially when a diverse range of participants is included, such as in this study. Third, in the survey a relatively low number of participants were enrolled. The data may therefore not be representative of surveys with higher inclusion numbers. Yet, the survey in this study was constructed for qualitative research aims and not intended to produce quantitatively significant results. Fourth, the data of all three methods were collected digitally, because the data-collection was performed during the COVID-19 pandemic. Therefore, the results may not be directly applicable to face-to-face interactions. As work is increasingly being digitalised and organised remotely, it is likely that in the future qualitative data more often are being collected by means of video consulting applications.
Implications
Our results help researchers and innovators to choose a method that is most suitable for their research aim, both in- and outside the domain of medical device evaluation. First we will place the methodological findings in the clinical context in which we worked. Next, we will discuss contextual factors that are relevant for medical device evaluation in general.
As described in the methods section, three methods were compared against the background of the design of a phase 3 randomised clinical trial to evaluate early minimally-invasive endoscopy-guided surgery in patients with ICH (NCT05460793). The clinical results of our research were used to inform different aspects of this randomised clinical trial, such as the selection of relevant outcome variables and the process of acquiring informed consent in this acute intervention trial. The results were also used to see how hospital care for ICH could be improved in general. All methods generated relevant insights in the context of this study, but interviews generated the most comprehensive body of relevant results for the trial and were thus most useful in the specific clinical context.
As described, there are some implications that are relevant for all types of researchers or innovators that want to employ participatory methods. Elucidating needs of stakeholders might especially be relevant in early development stages since they can be translated in the further development and evaluation of a device. It is thus relevant to have a comprehensive, in-depth assessment of these needs and interviews appear to be most appropriate for that aim. If in later stages more specific development issues need to be resolved, stakeholders could be brought together in a small focus group to make a joint decision. Since financial investments are required for participatory evaluations, the question arises whether the benefits live up to these investments. In the literature, stakeholder involvement is generally considered to be beneficial, but an important caveat is that low budgets and small-scale involvements can lead to flawed stakeholder representation and reproducing existing power differences [ 38 ]. We strongly recommend to invest in participatory development and evaluation as this is likely to be highly beneficial, because the perspectives of stakeholders are embedded in the innovation process.
Furthermore, we posit the existence of overarching methodological implications pertinent to participatory research at large, and delineate some considerations. The body of results generated by focus groups was not as comprehensive as in the interviews. This is possibly due to the social dynamic that is at play between participants and the limited time that each individual speaker is talking, which makes expansive questioning by a moderator on all relevant topics hard to realize. This implies that for comprehensively answering a research question, focus groups are not the most suitable method. Nevertheless, topics can be discussed and resolved relatively quickly in a focus group if the participants are more or less on the same page, which implies that focus groups can be a useful decision-making technique. Interviews can best be used for in-depth analyses of different perspectives, to generate much data, and therefore comprehensively answer a research question. Researchers or innovators may shorten the time-investment of interviews by speeding up the analysis, for example by not transcribing full interviews but writing summaries directly after an interview. Surveys might be suitable if researchers or innovators want to carry out a fast exploration of themes, and do not require interaction or an in-depth explication of topics. Qualitative surveys lack the option for inductive questioning, so they are not suitable if researchers want to apply an open research design. Methods presented in this paper could also be combined, or integrated in a stepwise manner in a research of development process. A researcher might first use a survey to explore multiple stakeholders’ wishes, and subsequently arrange a round of interactive focus groups when fast and definite decision needs to be made. An evaluation trajectory of medical devices is hard to plan in advance and unforeseen issues might arise, and these issues might demand specific participatory methods.
Focus groups, interviews, and surveys have clear methodological differences and provide different results within the context of medical device evaluation. Focus groups can best be used to bring views together, but do not enable a comprehensive analysis. Interviews enable an in-depth analysis of stakeholder views and can best be used to comprehensively answer an explorative research question, but are time-intensive. Surveys can be used for a rapid exploration of perspectives. Researchers should account for these methodological differences and select the method that serves their research aim.
Availability of data and materials
No data are available. All relevant data are presented in this study.
Royal College of Surgeons. Future Surg. 2022 [cited 2022 Jul 14]. https://futureofsurgery.rcseng.ac.uk/#start . Accessed 4 April 2024.
Marcus HJ, Bennett A, Chari A, Day T, Hirst A, Hughes-Hallett A, et al. IDEAL-D framework for device innovation. Ann Surg. 2022;275(1):73–9.
Article PubMed Google Scholar
Food and Drug Administration (FDA) Patient Engagement in the Design and Conduct of Medical Device Clinical Studies Guidance for Industry, Food and Drug Administration Staff, and Other Stakeholders. 2022. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-engagement-design-and-conduct-medical-device-clinical-studies . Accessed 4 April 2024.
The European Parliament and the Council of the European Union Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on medical devices, amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and repealing Council Directives 90/385/EEC and 93/42/EEC. http://data.europa.eu/eli/reg/2017/745/oj . Accessed 4 April 2024.
Bitkina OV, Kim HK, Park J. Usability and user experience of medical devices: an overview of the current state, analysis methodologies, and future challenges. Int J Ind Ergon. 2020;76(November 2019):102932. Available from: https://doi.org/10.1016/j.ergon.2020.102932 .
Article Google Scholar
Bitkina OV, Kim HK, Park J. Usability and user experience of medical devices: an overview of the current state, analysis methodologies, and future challenges. Int J Ind Ergon. 2020;76(November 2018):102932. Available from: https://doi.org/10.1016/j.ergon.2020.102932 .
Hansen NB, Dindler C, Halskov K, Iversen OS, Bossen C, Basballe DA, et al. How participatory designworks: mechanisms and effects. ACM International Conference Proceeding Series; 2019. p. 30–41.
Harder MK, Burford G, Hoover E. What is participation? Design leads the way to a cross-disciplinary framework. Des Issues. 2013;29(4):41–58. Available from: www.magno-design.com .
Zakery A, Saremi MS. Knowledge and intellectual capital in internationalizing SMEs, case study in technology-based health companies. J Intellect Cap. 2021;22(2):219–42.
Guest G, Namey E, McKenna K. How many focus groups are enough? Building an evidence base for nonprobability sample sizes. Field Methods. 2017;29(1):3–22.
van Velthoven MH, Wang W, Wu Q, Li Y, Scherpbier RW, Du X, et al. Comparison of text messaging data collection vs face-to-face interviews for public health surveys: a cluster randomized crossover study of care-seeking for childhood pneumonia and diarrhoea in rural China. J Glob Health. 2018;8(1):010802.
Vadi MG, Malkin MR, Lenart J, Stier GR, Gatling JW, Applegate RL. Comparison of web-based and face-to-face interviews for application to an anesthesiology training program: a pilot study. Int J Med Educ. 2016;7:102–8.
Article PubMed PubMed Central Google Scholar
Woudstra K, Reuzel R, Rovers M, Tummers M. An overview of stakeholders, methods, topics, and challenges in participatory approaches used in the development of medical devices: a scoping review. Int J Health Policy Manag. 2022;(Article in). Available from: https://www.ijhpm.com/article_4317.html .
van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. 2010;9(2):167–76. Available from: https://doi.org/10.1016/S1474-4422(09)70340-0 .
Sondag L, Schreuder FHBM, Boogaarts HD, Rovers MM, Vandertop WP, Dammers R, et al. Neurosurgical intervention for supratentorial intracerebral hemorrhage. Ann Neurol. 2020;88(2):239–50. Available from: https://doi.org/10.1002/ana.25732 .
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–60.
Carlsen B, Glenton C. What about N? A methodological study of sample-size reporting in focus group studies. BMC Med Res Methodol. 2011;11(26):1–10.
Google Scholar
Boddy CR. Sample size for qualitative interviews. Qual Mark Res Int J. 2003;2015(19):426–32.
The European Parliament and The Council of The European Union. Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation) (Text with EEA relevance). http://data.europa.eu/eli/reg/2016/679/oj . Accessed 4 April 2024.
Greenspan SB, Gordon KL, Whitcomb SA, Lauterbach AA. Use of video conferencing to facilitate focus groups for qualitative data collection. Am J Qual Res. 2021;5(1):85–93.
Keemink JR, Sharp RJ, Dargan AK, Forder JE. Reflections on the use of synchronous online focus groups in social care research. Int J Qual Methods. 2022;1:21.
Thunberg S, Arnell L. Pioneering the use of technologies in qualitative research–a research review of the use of digital interviews. Int J Soc Res Methodol. 2022;25(6):757–68.
Reuzel R. Interactive technology assessment of paediatric cochlear implantation. Poiesis Praxis. 2004;2(2–3):119–37.
Guba EG, Lincoln YS. Fourth generation evaluation. Newbury Park: SAGE Publications Inc.; 1992.
Moret-Hartman M, Reuzel R, Grin J, Kramers C, van der Wilt GJ. Strengthening evaluation through interactive problem structuring: a case study of hospital care after attempted suicide. Evaluation. 2011;17(1):37–52.
Tran VT, Porcher R, Tran VC, Ravaud P. Predicting data saturation in qualitative surveys with mathematical models from ecological research. J Clin Epidemiol. 2017;82:71–78.e2. Available from: https://www.sciencedirect.com/science/article/pii/S0895435616305431 .
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Morgan DL, Hoffman K. A system for coding the interaction in focus groups and dyadic interviews. Qual Rep. 2018;23(3):519–31.
Keyton J. Interaction Process Analysis (IPA). In: Brauner E, Boos M, Kolbe M, editors. The Cambridge Handbook of Group Interaction Analysis. Cambridge: Cambridge University Press; 2018. p. 441–50.
Chapter Google Scholar
Dearnley C. A reflection on the use of semi-structured interviews. Nurse Res. 2005;13(1):19–28.
Stuckey H. The first step in data analysis: transcribing and managing qualitative research data. J Soc Health Diabetes. 2014;02(01):6–8.
Woolley K, Edwards KL, Glazebrook C. Focus group or individual interviews for exploring children’s health behaviour: the example of physical activity. Adv Pediatr Res. 2018;05(02):1–10.
Rat AC, Pouchot J, Guillemin F, Baumann M, Retel-Rude N, Spitz E, et al. Content of quality-of-life instruments is affected by item-generation methods. Int J Qual Health Care. 2007;19(6):390–8.
Fern EF. The use of focus groups for idea generation: the effects of group size, acquaintanceship, and moderator on response quantity and quality. J Mark Res. 1982;19(1):1.
Namey E, Guest G, McKenna K, Chen M. Evaluating bang for the buck: a cost-effectiveness comparison between individual interviews and focus groups based on thematic saturation levels. Am J Eval. 2016;37(3):425–40.
Griffin A, Hauser JR. The voice of the customer. Mark Sci. 1993;12(1):1–27.
Coenen M, Stamm TA, Stucki G, Cieza A. Individual interviews and focus groups in patients with rheumatoid arthritis: a comparison of two qualitative methods. Qual Life Res. 2012;21(2):359–70.
Anggraeni M, Gupta J, Verrest HJLM. Cost and value of stakeholders participation: a systematic literature review. Environ Sci Policy. 2019;101:364–73.
Download references
Acknowledgements
We wish to express our gratitude to Leon Bijlmakers and Anke Oerlemans for their valuable help in guiding the focus groups.
This work was sponsored by a Vici fund by the Nederlandse organisatie voor gezondheidsonderzoek en zorginnovatie (ZonMw) (grant number 91818617). CK and LS are supported by the Netherlands Cardiovascular Research Initiative, which is supported by the Dutch Heart Foundation, CVON2015-01: CONTRAST and the support of the Brain Foundation Netherlands (HA2015.01.06). CK is supported by ZonMw (ASPASIA grant, 015008048). FS is supported by the Dutch Heart Foundation (senior clinical scientist grant, T2019T060).
Author information
Authors and affiliations.
Department of Health Evidence, Radboudumc, Nijmegen, Netherlands
Kas Woudstra, Marcia Tummers & Rob Reuzel
Department of Operating Rooms, Radboudumc, Nijmegen, Netherlands
Kas Woudstra & Maroeska Rovers
Department of Neurology, Donders Institute for Brain, Cognition, and Behavior, Radboudumc, Nijmegen, Netherlands
Catharina J. M. Klijn, Lotte Sondag & Floris Schreuder
You can also search for this author in PubMed Google Scholar
Contributions
KW, RR, MR, MT contributed to the conception and design. KW, CK, LS, RR and MT contributed to the acquisition, analysis and interpretation of data. KW, RR, MR, MT, CK, LS and FS have been drafting the manuscript. MR has obtained funding.
Corresponding author
Correspondence to Kas Woudstra .
Ethics declarations
Ethics approval and consent to participate.
Our study was approved by the local certified ethics committee METC Oost-Nederland (WMO) file number: 2021–6055. All methods included in this study are performed in accordance with the declaration of Helsinki. All participants gave written or verbal informed consent on a recorded audio file prior to enrolment in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., supplementary material 4., supplementary material 5., supplementary material 6., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Woudstra, K., Tummers, M., Klijn, C.J.M. et al. Participatory methods used in the evaluation of medical devices: a comparison of focus groups, interviews, and a survey. BMC Health Serv Res 24 , 462 (2024). https://doi.org/10.1186/s12913-024-10887-3
Download citation
Received : 08 March 2023
Accepted : 21 March 2024
Published : 12 April 2024
DOI : https://doi.org/10.1186/s12913-024-10887-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Qualitative methods
- Stakeholder involvement
- Medical devices
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Mixed methods research combines elements of quantitative research and qualitative research in order to answer your research question. Mixed methods can help you gain a more complete picture than a standalone quantitative or qualitative study, as it integrates benefits of both methods. Mixed methods research is often used in the behavioral ...
The above view of multimethod research is also in line with the explanations given in the renowned Sage Handbook of Mixed Methods in Social & Behavioral Research (Taskakkori and Teddie 2010a, b), which describes multi-method studies as studies involving multiple types of qualitative research (e.g., case studies and ethnographic studies) or ...
Combining methods in social scientific research has recently gained momentum through a research strand called Mixed Methods Research (MMR). This approach, which explicitly aims to offer a framework for combining methods, has rapidly spread through the social and behavioural sciences, and this article offers an analysis of the approach from a field theoretical perspective. After a brief outline ...
Quantitative dominant [or quantitatively driven] mixed methods research is the type of mixed research in which one relies on a quantitative, postpositivist view of the research process, while concurrently recognizing that the addition of qualitative data and approaches are likely to benefit most research projects. (p.
You can also create a mixed methods research design that has elements of both. Descriptive research vs experimental research. Descriptive research gathers data without controlling any variables, while experimental research manipulates and controls variables to determine cause and effect.
Mixed‐methods research, or multi‐strategy designs, 1 can be defined as 'the collection, analysis and integration of both qualitative and quantitative data in a single study': 2 semi‐structured interviews and workplace measures (e.g. attendance data) might be undertaken concurrently to gain a multifaceted perspective on a particular ...
MMCSR. "A mixed methods case study design is a type of mixed methods study in which the quantitative and qualitative data collection, results, and integration are used to provide in-depth evidence for a case(s) or develop cases for comparative analysis" (Creswell & Plano Clarke, 2018, p.116).
Introduction. Mixed methods research burst onto the scene around the beginning of the second millennium. After decades of intense dispute between those who preferred the qualitative perspective and their quantitative counterparts—with both sides having grown deeply entrenched in their respective views—a complementary approach promising the possibility of integration had finally been proposed.
This research is in the intersection between mixed method and case study research (Plano Clark et al., 2018; Walton et al., 2019). According to Plano Clark et al., a mixed method case study is "a ...
Abstract. This chapter presents an introduction to mixed methods research and seeks to emphasise that the approach offers more potential to reveal a deeper understanding of life experiences than the use of either qualitative or quantitative research methods on their own. The history and emergence of mixed methods research are described and also ...
Mixed methods can be understood as a methodology.Alternatively, mixed methods can be seen as one of three overall "approaches" to research (alongside qualitative or quantitative approaches), within which we might identify a more specific methodology for a particular study such as case study, phenomenology, or grounded theory (any of these can be done using mixed methods).
Typically, case study research (CSR) is associated with a qualitative approach. However, the increased use of mixed methods to address complex research prob- lems provides an opportunity to ...
The four major types of mixed methods designs are the Triangulation Design, the Embedded Design, the Explanatory Design, and the Exploratory Design. The following sections provide an overview of each of these designs: their use, procedures, common variants, and challenges. Choosing a Mixed Methods Design- -59.
Mixed methods single case research (MMSCR) is research in which single case experimental and qualitative case study methodologies, and their accompanying sets of methods and techniques, are integrated to answer research questions that concern a single case. This article discusses the historical roots and the distinct nature of MMSCR, the kinds ...
His research interests, scholarship, and teaching are in research methodology—namely, general research design and mixed methods research. His recent empirical work uses mixed methods research. Michael D. Fetters (MD, Ohio State University, MPH, University of North Carolina, Chapel Hill, MA, Michigan State University) is a family medicine ...
1 BACKGROUND. An increasing number of researchers are interested in combining qualitative and quantitative research in a systematic review. Various names have been given to designate this type of review such as mixed methods systematic review, 1-3 mixed methods research synthesis, 4 mixed studies review, 5 mixed methods-mixed research synthesis, 6 multi-method review, 7 multi-sources review, 8 ...
Approach to integration at conceptual level Guetterman and Fetters (2018) propose two primary designs to the integration of case study with mixed methods: (1) (2) a case study-mixed-methods design ...
mixed methods [6]. Nowadays, mixed methods are utilized in different fields and disciplines ranging from psychology to health and education as well. However, it is not required to nec-essarily be recognized as mixed-method and can be re-mained unknown. Therefore, researchers can promote the gained benefits of the applications of the mixed methods
However, the adoption of a mixed method case study research design has failed to keep pace with the growth of DBA research in the UK and commentary as to the value, application, and implications of adopting a case study research design and mixed methods is currently lacking. ... or look for similarities and differences between cases. Since the ...
This article examines key integration principles and practices in mixed methods research. It begins with the role of mixed methods in health services research and the rationale for integration. Next, a series of principles describe how integration occurs at the study design level, the method level, and the interpretation and reporting level.
Mixed methods is usually contrasted with the exclusive use of either qualitative or quantitative methods alone, but a case study could be based on qualitative or quantitative or mixed methods ...
The major strength of our study is that we compared three participatory methods in one single empirical case study on the development and evaluation of a medical device. With rigorous control of many contextual and methodological factors we can conclude that the differences in the three outcomes of this study are mainly caused by the ...
As far as multiple case studies go, that implies the systematic comparison of several different cases. As others have pointed out, you are essentially using a mixed methods research design as the ...