Home — Essay Samples — Nursing & Health — Oncology — Prostate Cancer

Essay Examples on Prostate Cancer
Prostate cancer: practice essentials, background, anatomy, family genetics and associated risks of developing prostate cancer, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
Vitamin D for Human Body
Relevant topics.
- Breast Cancer
- Ovarian Cancer
- Skin Cancer
- Mental Health
- Eating Disorders
- Affordable Care Act
- Healthy Food
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Patient Care & Health Information
- Diseases & Conditions
- Prostate cancer
Learn more about prostate cancer from Mayo Clinic urologist Mitchell Humphreys, M.D.
Hi. I'm Dr. Humphreys, a urologist at Mayo Clinic. In this video, we'll cover the basics of prostate cancer: What is it? Who gets it? The symptoms, diagnosis, and treatment. Whether you're looking for answers about your own health or that of someone you love, we're here to provide you with the best information available. Prostate cancer, unfortunately, is common. It affects one in seven men, making it the second most common cancer among men worldwide. The good news is, is that prostate cancer can be curable, especially when identified and treated early. That is why I and most urologists and medical professionals you talk to encourage men over a certain age to get regular prostate screenings. First, let's talk about what the prostate is and how it functions. The prostate is a small gland that is involved in reproduction and makes some of the essential components in semen. While it is small, it has an important role in reproductive health and can cause voiding or urinary symptoms as men age, as well becoming a source of cancer. Like other kinds of cancer, prostate cancer starts when cells mutate. These small changes in DNA cause the cells to grow faster and live longer than they normally would. As these abnormal cells accumulate, they monopolize resources from normal cells, which can damage surrounding tissue. These cancerous cells can then spread to other parts of the body.
By definition, prostate cancer only affects bodies with male reproductive organs. But in addition, there are some other risk factors that we can monitor. Age is a big one, as prostate cancer is more prevalent in older men, which is why testing is encouraged as men age. For reasons that are unclear, Black men also have a greater risk compared to other races or ethnicities. Being at a higher weight as another possible risk factor. Genetics can also play a role in prostate cancer. A family history of prostate cancer or certain kinds of breast cancer increases the likelihood of being diagnosed with prostate cancer. Well, it's not a guarantee, there are plenty of steps you can take to reduce your risk. A healthy diet and exercise helps your body's overall well-being and can lower your chances of getting prostate cancer.
A big reason to get regular testing is that prostate cancer usually has no presenting symptoms. And when they do show up, it generally indicates a worse stage of cancer. When symptoms do occur, they can include: trouble urinating or decreased force of stream, blood in the urine or semen, bone pain, unexpected weight loss, and unexplained fevers. If you consistently notice any of these symptoms, you should see your doctor right away. How is it diagnosed? There are a variety of ways to detect prostate cancer in both physical exam and from the blood. For starters, there's the DRE, the digital rectal exam. Just like the name suggests, the doctor inserts their finger and your rectum to feel the prostate to detect any abnormalities. You can also get a blood test to look for prostate-specific antigen, or PSA. It is recommended that you have this as well as the physical exam. And if there are any abnormalities, there are additional tests that can be used. If prostate cancer is detected, the next step is figuring out how fast it grows. Fortunately, prostate cancer often doesn't grow very fast. Prostate cancer is graded by a Gleason score, which measures how abnormal or different from normal cells are. There are also other tests to see if the cancer has spread: bone scan, CT scan, MRI, and even specific PET scans. Your doctor will be able to determine which, if any, is appropriate for you.
Treatments are most effective when the cancer is caught early. In fact, immediate treatment isn't always necessary. Keeping an eye on the cancer until it grows bigger is sometimes enough. When cancer is localized only to the prostate, surgery to remove the prostate, or a radical prostatectomy, could be your best option. Radiation is another possibility. With external beam radiation, high-energy beams that deliver photons, target and kill the abnormal cells of the prostate from outside your body. Another treatment is chemotherapy, which uses powerful chemicals, destroy the cancer cells. Cryotherapy, which freezes the cancer cells, or heat, can be used to kill the cancer cells with high-intensity focused ultrasound. Consider that prostate cancer uses male hormone or testosterone as an important factor for growth. In some prostate cancers, it may be beneficial to block that hormone with androgen deprivation therapy, or ADT, which can slow the cancer or even put it in remission. It is generally not curative and usually the cancer will find a way to grow even with the lack of testosterone. Sometimes ADT is used in combination to enhance the treatment success of other therapies, such as with radiation. All of these treatments have side effects of various degrees and have different success rates of treating prostate cancer. It's important that you have a candid discussion with your family and your care team and weigh all that information to make the best choice for you. Support groups for cancer survivors can be helpful in dealing with the stress of the diagnosis and treatments.
As we've seen here, research and scientific advancement has provided us with a host of options for this extremely treatable form of cancer. And with early detection, your chances are even better. While it may not be a thing people want to think about, it's an important part of your health and an expert medical care team can guide you to the solutions that are most tailored for you, your wishes and your body. If you'd like to learn even more about prostate cancer, watch our other related videos or visit mayoclinic.org. We wish you well.
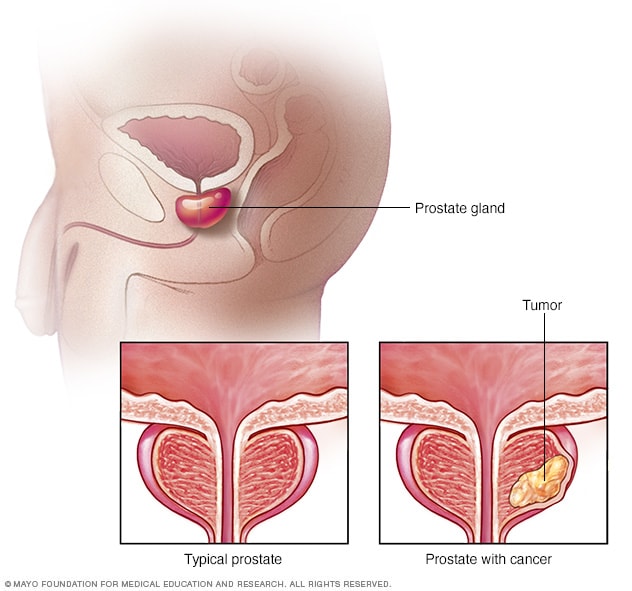
Prostate cancer occurs in the prostate gland. The gland sits just below the bladder in males. It surrounds the top part of the tube that drains urine from the bladder, called the urethra. This illustration shows a healthy prostate gland and a prostate gland with cancer.
Prostate cancer is cancer that occurs in the prostate. The prostate is a small walnut-shaped gland in males that produces the seminal fluid that nourishes and transports sperm.
Prostate cancer is one of the most common types of cancer. Many prostate cancers grow slowly and are confined to the prostate gland, where they may not cause serious harm. However, while some types of prostate cancer grow slowly and may need minimal or even no treatment, other types are aggressive and can spread quickly.
Prostate cancer that's detected early — when it's still confined to the prostate gland — has the best chance for successful treatment.
Products & Services
- A Book: Man Overboard!
- A Book: Mayo Clinic on Healthy Aging
- A Book: Mayo Clinic on Prostate Health
- Assortment of Pill Aids from Mayo Clinic Store
Prostate cancer may cause no signs or symptoms in its early stages.
Prostate cancer that's more advanced may cause signs and symptoms such as:
- Trouble urinating
- Decreased force in the stream of urine
- Blood in the urine
- Blood in the semen
- Losing weight without trying
- Erectile dysfunction
When to see a doctor
Make an appointment with your doctor if you have any persistent signs or symptoms that worry you.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
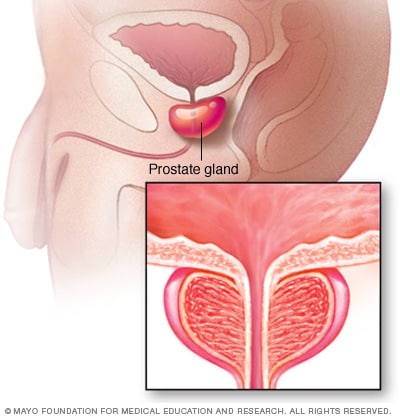
- Prostate gland
The prostate gland is located just below the bladder in men and surrounds the top portion of the tube that drains urine from the bladder (urethra). The prostate's primary function is to produce the fluid that nourishes and transports sperm (seminal fluid).
It's not clear what causes prostate cancer.
Doctors know that prostate cancer begins when cells in the prostate develop changes in their DNA. A cell's DNA contains the instructions that tell a cell what to do. The changes tell the cells to grow and divide more rapidly than normal cells do. The abnormal cells continue living, when other cells would die.
The accumulating abnormal cells form a tumor that can grow to invade nearby tissue. In time, some abnormal cells can break away and spread (metastasize) to other parts of the body.
Risk factors
Factors that can increase your risk of prostate cancer include:
- Older age. Your risk of prostate cancer increases as you age. It's most common after age 50.
- Race. For reasons not yet determined, Black people have a greater risk of prostate cancer than do people of other races. In Black people, prostate cancer is also more likely to be aggressive or advanced.
- Family history. If a blood relative, such as a parent, sibling or child, has been diagnosed with prostate cancer, your risk may be increased. Also, if you have a family history of genes that increase the risk of breast cancer (BRCA1 or BRCA2) or a very strong family history of breast cancer, your risk of prostate cancer may be higher.
- Obesity. People who are obese may have a higher risk of prostate cancer compared with people considered to have a healthy weight, though studies have had mixed results. In obese people, the cancer is more likely to be more aggressive and more likely to return after initial treatment.
Complications
Complications of prostate cancer and its treatments include:
- Cancer that spreads (metastasizes). Prostate cancer can spread to nearby organs, such as your bladder, or travel through your bloodstream or lymphatic system to your bones or other organs. Prostate cancer that spreads to the bones can cause pain and broken bones. Once prostate cancer has spread to other areas of the body, it may still respond to treatment and may be controlled, but it's unlikely to be cured.
- Incontinence. Both prostate cancer and its treatment can cause urinary incontinence. Treatment for incontinence depends on the type you have, how severe it is and the likelihood it will improve over time. Treatment options may include medications, catheters and surgery.
- Erectile dysfunction. Erectile dysfunction can result from prostate cancer or its treatment, including surgery, radiation or hormone treatments. Medications, vacuum devices that assist in achieving erection and surgery are available to treat erectile dysfunction.
More Information
Prostate cancer care at Mayo Clinic
- Prostate cancer metastasis: Where does prostate cancer spread?
You can reduce your risk of prostate cancer if you:
Choose a healthy diet full of fruits and vegetables. Eat a variety of fruits, vegetables and whole grains. Fruits and vegetables contain many vitamins and nutrients that can contribute to your health.
Whether you can prevent prostate cancer through diet has yet to be conclusively proved. But eating a healthy diet with a variety of fruits and vegetables can improve your overall health.
- Choose healthy foods over supplements. No studies have shown that supplements play a role in reducing your risk of prostate cancer. Instead, choose foods that are rich in vitamins and minerals so that you can maintain healthy levels of vitamins in your body.
- Exercise most days of the week. Exercise improves your overall health, helps you maintain your weight and improves your mood. Try to exercise most days of the week. If you're new to exercise, start slow and work your way up to more exercise time each day.
- Maintain a healthy weight. If your current weight is healthy, work to maintain it by choosing a healthy diet and exercising most days of the week. If you need to lose weight, add more exercise and reduce the number of calories you eat each day. Ask your doctor for help creating a plan for healthy weight loss.
Talk to your doctor about increased risk of prostate cancer. If you have a very high risk of prostate cancer, you and your doctor may consider medications or other treatments to reduce the risk. Some studies suggest that taking 5-alpha reductase inhibitors, including finasteride (Propecia, Proscar) and dutasteride (Avodart), may reduce the overall risk of developing prostate cancer. These drugs are used to control prostate gland enlargement and hair loss.
However, some evidence indicates that people taking these medications may have an increased risk of getting a more serious form of prostate cancer (high-grade prostate cancer). If you're concerned about your risk of developing prostate cancer, talk with your doctor.
- Prostate cancer prevention
- Frequent sex: Does it protect against prostate cancer?
- Prostate Cancer Q and A
Living with prostate cancer?
Connect with others like you for support and answers to your questions in the Prostate Cancer support group on Mayo Clinic Connect, a patient community.
Prostate Cancer Discussions

54 Replies Tue, Mar 26, 2024

105 Replies Thu, Mar 28, 2024

18 Replies Sat, Mar 23, 2024
- AskMayoExpert. Prostate cancer (adult). Mayo Clinic; 2018.
- Niederhuber JE, et al., eds. Prostate cancer. In: Abeloff's Clinical Oncology. 6th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed May 29, 2020.
- Partin AW, et al., eds. In: Campbell-Walsh-Wein Urology. 12th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 29, 2020.
- AskMayoExpert. Prostate biopsy (adult). Mayo Clinic; 2019.
- Prostate cancer. National Comprehensive Cancer Network. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed May 29, 2020.
- AskMayoExpert. Radical prostatectomy (adult). Mayo Clinic; 2019.
- Rock CL, et al. American Cancer Society guideline for diet and physical activity for cancer prevention. CA: A Cancer Journal for Clinicians. 2020; doi:10.3322/caac.21591.
- Distress management. National Comprehensive Cancer Network. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed May 29, 2020.
- Thompson RH, et al. Radical prostatectomy for octogenarians: How old is too old? Journal of Urology. 2006; doi:10.1016/j.urology.2006.05.031.
- Choline C-11 injection (prescribing information). Mayo Clinic PET Radiochemistry Facility; 2012. https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=203155. Accessed June 23, 2020.
- Woodrum DA, et al. Targeted prostate biopsy and MR-guided therapy for prostate cancer. Abdominal Radiology. 2016; doi:10.1007/s00261-016-0681-3.
- Agarwal DK, et al. Initial experience with da Vinci single-port robot-assisted radical prostatectomies. European Urology. 2020; doi:10.1016/j.eururo.2019.04.001.
- Gettman MT, et al. Current status of robotics in urologic laparoscopy. European Urology. 2003; doi:10.1016/S0302-2838(02)00579-1.
- Krambeck AE, et al. Radical prostatectomy for prostatic adenocarcinoma: A matched comparison of open retropubic and robot-assisted techniques. BJU International. 2008; doi:10.1111/j.1464-410X.2008.08012.x.
- Warner KJ. Allscripts EPSi. Mayo Clinic. Feb. 4, 2020.
- Digital rectal exam
- Prostate Cancer backgrounder
- Prostate cancer stages
- Prostate cancer: Does PSA level affect prognosis?
- Transrectal biopsy of the prostate
Associated Procedures
- Ablation therapy
- Active surveillance for prostate cancer
- Brachytherapy
- Chemotherapy
- Choline C-11 PET scan
- Cryoablation for cancer
- External beam radiation for prostate cancer
- Prostatectomy
- Proton therapy
- Radiation therapy
News from Mayo Clinic
- Prostate cancer: screening and treatment options Jan. 22, 2024, 11:55 p.m. CDT
- Mayo Clinic Minute: Signs there is a problem with your prostate Nov. 07, 2022, 05:20 p.m. CDT
- Mayo Clinic researchers identify drug resistance factors for advanced prostate cancer Sept. 22, 2022, 02:00 p.m. CDT
- Mayo Clinic Minute: Importance of exercise for men with prostate cancer Sept. 13, 2022, 04:30 p.m. CDT
- Mayo Clinic Minute: Prostate biopsy technique reduces infection risk June 13, 2022, 04:20 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
Skip to Content
- Conquer Cancer
- ASCO Journals
- f Cancer.net on Facebook
- t Cancer.net on Twitter
- q Cancer.net on YouTube
- g Cancer.net on Google
Types of Cancer
- Navigating Cancer Care
- Coping With Cancer
- Research and Advocacy
- Survivorship
Prostate Cancer: Introduction
ON THIS PAGE: You will find some basic information about this disease and the parts of the body it may affect. This is the first page of Cancer.Net’s Guide to Prostate Cancer. Use the menu to see other pages. Think of that menu as a roadmap for this entire guide.
About the prostate
The prostate is a walnut-sized gland located behind the base of the penis, in front of the rectum, and below the bladder. It surrounds the urethra, the tube-like channel that carries urine and semen through the penis. The prostate's main function is to make seminal fluid, the liquid in semen that protects, supports, and helps transport sperm.
The prostate continues to enlarge as people age. This can lead to a condition called benign prostatic hypertrophy (BPH), which is when the urethra becomes blocked. BPH is a common condition associated with growing older, and it has not been associated with a greater risk of having prostate cancer.
About prostate cancer
Cancer begins when healthy cells in the prostate change and grow out of control, forming a tumor. A tumor can be cancerous or benign. A cancerous tumor is malignant, meaning it can grow and spread to other parts of the body. A benign tumor means the tumor can grow but will not spread.
Prostate cancer is somewhat unusual when compared with other types of cancer. This is because many prostate tumors do not spread quickly to other parts of the body. Some prostate cancers grow very slowly and may not cause symptoms or problems for years or ever. Even when prostate cancer has spread to other parts of the body, it often can be managed with treatment for a long time. So people with prostate cancer, and even those with advanced prostate cancer, may live with good health and quality of life for many years. However, if the cancer cannot be well controlled with existing treatments, it can cause symptoms like pain and fatigue and can sometimes lead to death. An important part of managing prostate cancer is watching for growth over time to find out if it is growing slowly or quickly. Based on the pattern of growth, your doctor can decide the best available treatment options and when to give them.
Histology is how cancer cells look under a microscope. The most common histology found in prostate cancer is called adenocarcinoma. Other, less common histologic types, called variants, include neuroendocrine prostate cancer and small cell prostate cancer. These variants tend to be more aggressive, produce much less prostate-specific antigen (PSA), and spread outside the prostate earlier. Read more about neuroendocrine tumors .
About prostate-specific antigen (PSA)
Prostate-specific antigen (PSA) is a protein produced by cells in the prostate gland and released into the bloodstream. PSA levels are measured using a blood test. Although there is no such thing as a “normal PSA” for anyone at any given age, a higher-than-normal level of PSA can be found in people with prostate cancer. Other non-cancerous prostate conditions, such as BPH (see above) or prostatitis can also lead to an elevated PSA level. Prostatitis is the inflammation or infection of the prostate. In addition, some activities like ejaculation can temporarily increase PSA levels. Ejaculations should be avoided before a PSA test to avoid falsely elevated tests. People should discuss with their primary care doctor the pros and cons of PSA testing before using it to screen for prostate cancer. See the Screening section for more information.
Looking for More of an Introduction?
If you would like more of an introduction, explore these related items. Please note that these links will take you to other sections on Cancer.Net:
ASCO Answers Fact Sheet: Read a 1-page fact sheet that offers an introduction to prostate cancer. This free fact sheet is available as a PDF, so it is easy to print.
ASCO Answers Guide: Get this free 52-page booklet that helps you better understand the disease and treatment options. The booklet is available as a PDF, so it is easy to print.
Cancer.Net En Español: Read about prostate cancer in Spanish or read a 1-page ASCO Answers Fact Sheet in Spanish. Infórmase sobre cáncer de próstata en español o una hoja informativa de una página, Respuestas sobre el cáncer .
The next section in this guide is Statistics . It helps explain the number of people who are diagnosed with prostate cancer and general survival rates. Use the menu to choose a different section to read in this guide.
Prostate Cancer Guide
Cancer.Net Guide Prostate Cancer
- Introduction
- Medical Illustrations
- Risk Factors and Prevention
- Symptoms and Signs
- Stages and Grades
- Types of Treatment
- About Clinical Trials
- Latest Research
- Coping with Treatment
- Follow-Up Care
- Questions to Ask the Health Care Team
- Additional Resources
View All Pages
Timely. Trusted. Compassionate.
Comprehensive information for people with cancer, families, and caregivers, from the American Society of Clinical Oncology (ASCO), the voice of the world's oncology professionals.
Find a Cancer Doctor
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Published: 31 July 2018
Landmarks in prostate cancer
- Niranjan J. Sathianathen ORCID: orcid.org/0000-0002-3710-014X 1 , 2 , 3 ,
- Badrinath R. Konety 1 ,
- Juanita Crook 4 ,
- Fred Saad 5 &
- Nathan Lawrentschuk 2 , 3
Nature Reviews Urology volume 15 , pages 627–642 ( 2018 ) Cite this article
6574 Accesses
66 Citations
47 Altmetric
Metrics details
- Cancer screening
- Health care
- Outcomes research
- Prostate cancer
The field of prostate cancer has been the subject of extensive research that has resulted in important discoveries and shaped our appreciation of this disease and its management. Advances in our understanding of the epidemiology, natural history, anatomy, detection, diagnosis, grading, staging, imaging, and management of prostate cancer have changed clinical practice and influenced guideline recommendations. The development of the Gleason score and subsequent modifications enabled accurate prediction of prognosis. Increased anatomical understanding and improved surgical techniques resulted in the development of nerve-sparing surgery for radical prostatectomy. The advent of active surveillance has changed the management of low-risk disease, and chemotherapy and hormonal therapy have improved the outcomes of patients with distant disease. Ongoing research and clinical trials are expected to yield more practice-changing results in the near future.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout

Reproduced from ref. 5 , Springer Nature Limited.
Similar content being viewed by others
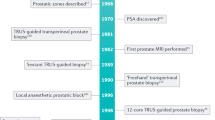
Landmarks in the evolution of prostate biopsy
Martin J. Connor, Michael A. Gorin, … Hashim U. Ahmed

Impact of preoperative prostate magnetic resonance imaging on the surgical management of high-risk prostate cancer
Janet Baack Kukreja, Tharakeswara K. Bathala, … Brian F. Chapin

A critical evaluation of visual proportion of Gleason 4 and maximum cancer core length quantified by histopathologists
Lina Maria Carmona Echeverria, Aiman Haider, … Hayley C. Whitaker
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2015. CA Cancer J. Clin. 65 , 5–29 (2015).
PubMed Google Scholar
Ferlay, J. et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer. 136 , E359–E386 (2015).
CAS PubMed Google Scholar
Tasian, G. E. et al. PSA screening: determinants of primary-care physician practice patterns. Prostate Cancer Prostat. Dis. 15 , 189–194 (2012).
CAS Google Scholar
Shoag, J. et al. Decline in prostate cancer screening by primary care physicians: an analysis of trends in the use of digital rectal examination and prostate specific antigen testing. J. Urol. 196 , 1047–1052 (2016).
Fleshner, K., Carlsson, S. V. & Roobol, M. J. The effect of the USPSTF PSA screening recommendation on prostate cancer incidence patterns in the USA. Nat. Rev. Urol. 14 , 26 (2016).
PubMed PubMed Central Google Scholar
Howard, D. H. Declines in prostate cancer incidence after changes in screening recommendations. Arch. Intern. Med. 172 , 1267–1268 (2012).
Potosky, A. L., Miller, B. A., Albertsen, P. C. & Kramer, B. S. The role of increasing detection in the rising incidence of prostate cancer. JAMA 273 , 548–552 (1995).
Gaylis, F. D. et al. Change in prostate cancer presentation coinciding with USPSTF screening recommendations at a community-based urology practice. Urol. Oncol. 35 , 663.e1–663 (2017).
Google Scholar
Cooperberg, M. R. The new US Preventive Services Task Force “C” draft recommendation for prostate cancer screening. Eur. Urol. 72 , 326–328 (2017).
US Preventive Services Task Force. Draft prostate cancer screening recommendation statement (US Preventive Services, 2017).
Patel, A. R. & Klein, E. A. Risk factors for prostate cancer. Nat. Clin. Practice Urol. 6 , 87 (2009).
Odedina, F. T. et al. Prostate cancer disparities in Black men of African descent: a comparative literature review of prostate cancer burden among Black men in the United States, Caribbean, United Kingdom, and West Africa. Infect. Agent Cancer. 4 (Suppl. 1), S2 (2009).
Steinberg, G. D., Carter, B. S., Beaty, T. H., Childs, B. & Walsh, P. C. Family history and the risk of prostate cancer. Prostate 17 , 337–347 (1990).
Bancroft, E. K. et al. Targeted prostate cancer screening in BRCA1 and BRCA2 mutation carriers: results from the initial screening round of the IMPACT study. Eur. Urol. 66 , 489–499 (2014).
Albertsen, P. C., Hanley, J. A., Gleason, D. F. & Barry, M. J. Competing risk analysis of men aged 55 to 74 years at diagnosis managed conservatively for clinically localized prostate cancer. JAMA 280 , 975–980 (1998).
Albertsen, P. C., Hanley, J. A. & Fine, J. 20-year outcomes following conservative management of clinically localized prostate cancer. JAMA 293 , 2095–2101 (2005).
Johansson, J. E. et al. Natural history of early, localized prostate cancer. JAMA 291 , 2713–2719 (2004).
Pound, C. R. et al. Natural history of progression after PSA elevation following radical prostatectomy. JAMA 281 , 1591–1597 (1999).
Wang, M. C., Valenzuela, L. A., Murphy, G. P. & Chu, T. M. Purification of a human prostate specific antigen. Invest. Urol. 17 , 159–163 (1979).
Stamey, T. A. et al. Prostate-specific antigen as a serum marker for adenocarcinoma of the prostate. N. Engl. J. Med. 317 , 909–916 (1987).
Carter, H. et al. Longitudinal evaluation of prostate-specific antigen levels in men with and without prostate disease. JAMA 267 , 2215–2220 (1992).
CAS PubMed PubMed Central Google Scholar
Carter, H. B. et al. Early detection of prostate cancer: AUA Guideline. J. Urol. 190 , 419–426 (2013).
Wolf, A. M. et al. American Cancer Society guideline for the early detection of prostate cancer: update 2010. CA Cancer J. Clin. 60 , 70–98 (2010).
Cooner, W. H. et al. Prostate cancer detection in a clinical urological practice by ultrasonography, digital rectal examination and prostate specific antigen. J. Urol. 143 , 1146–1152; discussion 52–54 (1990).
Catalona, W. J. et al. Measurement of prostate-specific antigen in serum as a screening test for prostate cancer. N. Engl. J. Med. 324 , 1156–1161 (1991).
Catalona, W. J. et al. Comparison of digital rectal examination and serum prostate specific antigen in the early detection of prostate cancer: results of a multicenter clinical trial of 6,630 men. J. Urol. 151 , 1283–1290 (1994).
Thompson, I. M. et al. Prevalence of prostate cancer among men with a prostate-specific antigen level ≤4.0 ng per milliliter. N. Engl. J. Med. 350 , 2239–2246 (2004).
Mottet, N. et al. EAU-ESTRO-SIOG Guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur. Urol. 71 , 618–629 (2017).
Carroll, P. R. et al. NCCN Guidelines insights: prostate cancer early detection, version 2.2016. J. Natl Compr. Cancer Netw. 14 , 509–519 (2016).
Draisma, G. et al. Lead times and overdetection due to prostate-specific antigen screening: estimates from the European Randomized Study of Screening for Prostate Cancer. J. Natl Cancer Inst. 95 , 868–878 (2003).
Andriole, G. L. et al. Mortality results from a randomized prostate-cancer screening trial. N. Engl. J. Med. 360 , 1310–1319 (2009).
Schroder, F. H. et al. Screening and prostate-cancer mortality in a randomized European study. N. Engl. J. Med. 360 , 1320–1328 (2009).
Moyer, V. A. et al. Screening for prostate cancer: US Preventive Services Task Force recommendation statement. Ann. Intern. Med. 157 , 120–134 (2012).
Jemal, A. et al. Prostate cancer incidence and psa testing patterns in relation to uspstf screening recommendations. JAMA 314 , 2054–2061 (2015).
Bhindi, B. et al. Impact of the US Preventive Services Task Force recommendations against prostate specific antigen screening on prostate biopsy and cancer detection rates. J. Urol. 193 , 1519–1524 (2015).
Weiner, A. B., Matulewicz, R. S., Eggener, S. E. & Schaeffer, E. M. Increasing incidence of metastatic prostate cancer in the United States (2004–2013). Prostate Cancer Prostatic Dis. 19 , 395–397 (2016).
Hu, J. C. et al. Increase in prostate cancer distant metastases at diagnosis in the united states. JAMA Oncol. 3 , 705–707 (2017).
Rezaee, M. E., Ward, C. E., Odom, B. D. & Pollock, M. Prostate cancer screening practices and diagnoses in patients age 50 and older, Southeastern Michigan, pre/post 2012. Prev. Med. 82 , 73–76 (2016).
Bibbins-Domingo, K., Grossman, D. C. & Curry, S. J. The US preventive services task force 2017 draft recommendation statement on screening for prostate cancer: an invitation to review and comment. JAMA 317 , 1949–1950 (2017).
US Preventive Services Task Force et al. Screening for prostate cancer: US Preventive Services Task Force recommendation statement. JAMA 319 , 1901–1913 (2018).
Schroder, F. H. et al. Screening for prostate cancer decreases the risk of developing metastatic disease: findings from the European Randomized Study of Screening for Prostate Cancer (ERSPC). Eur. Urol. 62 , 745–752 (2012).
Schroder, F. H. et al. Screening and prostate cancer mortality: results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet 384 , 2027–2035 (2014).
Martin, R. M. et al. Effect of a low-intensity PSA-based screening intervention on prostate cancer mortality: the cap randomized clinical trial. JAMA 319 , 883–895 (2018).
Thompson, I. M. et al. The influence of finasteride on the development of prostate cancer. N. Engl. J. Med. 349 , 215–224 (2003).
Thompson, I. M. et al. Long-term survival of participants in the prostate cancer prevention trial. N. Engl. J. Med. 369 , 603–610 (2013).
Unger, J. M. et al. Using medicare claims to examine long-term prostate cancer risk of finasteride in the prostate cancer prevention trial. Natl Cancer Inst. https://doi.org/10.1093/jnci/djy035 (2018).
Article Google Scholar
Kramer, B. S. et al. Use of 5-α-reductase inhibitors for prostate cancer chemoprevention: American Society of Clinical Oncology/American Urological Association 2008 Clinical Practice Guideline. J. Clin. Oncol. 27 , 1502–1516 (2009).
Lippman, S. M. et al. Effect of selenium and vitamin E on risk of prostate cancer and other cancers: the Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA 301 , 39–51 (2009).
Klein, E. A. et al. Vitamin E and the risk of prostate cancer: the Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA 306 , 1549–1556 (2011).
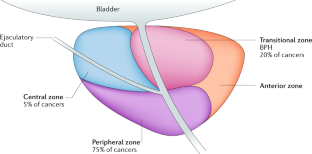
McNeal, J. E. The zonal anatomy of the prostate. Prostate 2 , 35–49 (1981).
Kourambas, J., Angus, D. G., Hosking, P. & Chou, S. T. A histological study of Denonvilliers’ fascia and its relationship to the neurovascular bundle. Br. J. Urol. 82 , 408–410 (1998).
Costello, A. J., Brooks, M. & Cole, O. J. Anatomical studies of the neurovascular bundle and cavernosal nerves. BJU Int. 94 , 1071–1076 (2004).
Walsh, P. C. & Donker, P. J. Impotence following radical prostatectomy: insight into etiology and prevention. J. Urol. 128 , 492–497 (1982).
Walsh, P. C. & Lepor, H. The role of radical prostatectomy in the management of prostatic cancer. Cancer 60 , 526–537 (1987).
Walsh, P. C., Lepor, H. & Eggleston, J. C. Radical prostatectomy with preservation of sexual function: anatomical and pathological considerations. Prostate 4 , 473–485 (1983).
Barringer, B. S. Carcinoma of the prostate. Surg. Gynecol. Obstet. 34 , 168–176 (1922).
Young, H. H. & Davis, D. M. Young’s Practice of Urology (Philadelphia & London, WB Saunders, 1926).
Hodge, K. K., McNeal, J. E. & Stamey, T. A. Ultrasound guided transrectal core biopsies of the palpably abnormal prostate. J. Urol. 142 , 66–70 (1989).
Levine, M. A., Ittman, M., Melamed, J. & Lepor, H. Two consecutive sets of transrectal ultrasound guided sextant biopsies of the prostate for the detection of prostate cancer. J. Urol. 159 , 471–475; discussion 5–6 (1998).
Presti, J. C. et al. Extended peripheral zone biopsy schemes increase cancer detection rates and minimize variance in prostate specific antigen and age related cancer rates: results of a community multi-practice study. J. Urol. 169 , 125–129 (2003).
Siddiqui, M. M. et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 313 , 390–397 (2015).
Chang, D. T. S., Challacombe, B. & Lawrentschuk, N. Transperineal biopsy of the prostate — is this the future? Nat. Rev. Urol. 10 , 690 (2013).
Wright, J. L. & Ellis, W. J. Improved prostate cancer detection with anterior apical prostate biopsies. Urol. Oncol. 24 , 492–495 (2006).
Bott, S. R. et al. Extensive transperineal template biopsies of prostate: modified technique and results. Urology 68 , 1037–1041 (2006).
Hu, Y. et al. A biopsy simulation study to assess the accuracy of several transrectal ultrasonography (TRUS)-biopsy strategies compared with template prostate mapping biopsies in patients who have undergone radical prostatectomy. BJU Int. 110 , 812–820 (2012).
Grummet, J. P. et al. Sepsis and ‘superbugs’: should we favour the transperineal over the transrectal approach for prostate biopsy? BJU Int. 114 , 384–388 (2014).
Kasivisvanathan, V. et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis. N. Engl. J. Med. 378 , 1767–1777 (2018).
Gleason, D. F. Classification of prostatic carcinomas. Cancer Chemother. Rep. 50 , 125–128 (1966).
Gleason, D. in Pathology of the Prostate (ed. Bostwick D.G. ) 83–93 (Churchill Livingstone, 1990).
Humphrey, P. A. Gleason grading and prognostic factors in carcinoma of the prostate. Mod. Pathol. 17 , 292–306 (2004).
Delahunt, B., Miller, J., Srigley, J. R., Evans, A. J. & Samaratunga, H. Gleason grading: past, present and future. Histopathology 60 , 75–86 (2012).
Billis, A., et al. The impact of the 2005 international society of urological pathology consensus conference on standard Gleason grading of prostatic carcinoma in needle biopsies. J. Urol. 180 , 548–552; discussion 52–53 (2008).
Epstein, J. I. et al. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. Am. J. Surg. Pathol. 40 , 244–252 (2016).
Wymenga, L. F., Boomsma, J. H., Groenier, K., Piers, D. A. & Mensink, H. J. Routine bone scans in patients with prostate cancer related to serum prostate-specific antigen and alkaline phosphatase. BJU Int. 88 , 226–230 (2001).
Sanda, M. G. et al. Clinically localized prostate cancer: AUA/ASTRO/SUO guideline. Part I: risk stratification, shared decision making, and care options. J. Urol. https://doi.org/10.1016/j.juro.2017.11.095 (2017).
Article PubMed PubMed Central Google Scholar
Taneja, S. S. Imaging in the diagnosis and management of prostate cancer. Rev. Urol. 6 , 101–113 (2004).
Umbehr, M. H., Muntener, M., Hany, T., Sulser, T. & Bachmann, L. M. The role of 11C-choline and 18F-fluorocholine positron emission tomography (PET) and PET/CT in prostate cancer: a systematic review and meta-analysis. Eur. Urol. 64 , 106–117 (2013).
Afshar-Oromieh, A. et al. The diagnostic value of PET/CT imaging with the 68Ga-labelled PSMA ligand HBED-CC in the diagnosis of recurrent prostate cancer. Eur. J. Nuclear Med. Mol. Imag. 42 , 197–209 (2015).
Eiber, M. et al. Evaluation of hybrid 68Ga-PSMA-ligand PET/CT in 248 patients with biochemical recurrence after radical prostatectomy. J. Nucl. Med. 55 , 668–674 (2015).
Boorjian, S. A., Karnes, R. J., Rangel, L. J., Bergstralh, E. J. & Blute, M. L. Mayo Clinic validation of the D’amico risk group classification for predicting survival following radical prostatectomy. J. Urol. 179 , 1354–1360; discussion 60–61 (2008).
Lee, S. E. et al. Application of the Epstein criteria for prediction of clinically insignificant prostate cancer in Korean men. BJU Int. 105 , 1526–1530 (2010).
D’Amico, A. V. et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 280 , 969–974 (1998).
Partin, A. W. et al. Combination of prostate-specific antigen, clinical stage, and Gleason score to predict pathological stage of localized prostate cancer. A multi-institutional update. JAMA 277 , 1445–1451 (1997).
Kattan, M. W., Eastham, J. A., Stapleton, A. M., Wheeler, T. M. & Scardino, P. T. A preoperative nomogram for disease recurrence following radical prostatectomy for prostate cancer. J. Natl Cancer Inst. 90 , 766–771 (1998).
Kattan, M. W., Wheeler, T. M. & Scardino, P. T. Postoperative nomogram for disease recurrence after radical prostatectomy for prostate cancer. J. Clin. Oncol. 17 , 1499–1507 (1999).
Stephenson, A. J. et al. Preoperative nomogram predicting the 10-year probability of prostate cancer recurrence after radical prostatectomy. J. Natl Cancer Inst. 98 , 715–717 (2006).
Cooperberg, M. R. et al. The University of California, San Francisco Cancer of the Prostate Risk Assessment score: a straightforward and reliable preoperative predictor of disease recurrence after radical prostatectomy. J. Urol. 173 , 1938–1942 (2005).
Cooperberg, M. R., Hilton, J. F. & Carroll, P. R. The CAPRA-S score: a straightforward tool for improved prediction of outcomes after radical prostatectomy. Cancer 117 , 5039–5046 (2011).
Brajtbord, J. S., Leapman, M. S. & Cooperberg, M. R. The CAPRA score at 10 years: contemporary perspectives and analysis of supporting studies. Eur. Urol . 71 , 705–709.
Hricak, H. et al. Prostatic carcinoma: staging by clinical assessment, CT, and MR imaging. Radiology 162 , 331–336 (1987).
Kurhanewicz, J., Swanson, M. G., Nelson, S. J. & Vigneron, D. B. Combined magnetic resonance imaging and spectroscopic imaging approach to molecular imaging of prostate cancer. J. Magnet. Resonance Imag. 16 , 451–463 (2002).
Langer, D. L. et al. Prostate cancer detection with multi-parametric MRI: Logistic regression analysis of quantitative T2, diffusion-weighted imaging, and dynamic contrast-enhanced MRI. J. Magnet. Resonance Imag. 30 , 327–334 (2009).
Tanimoto, A., Nakashima, J., Kohno, H., Shinmoto, H. & Kuribayashi, S. Prostate cancer screening: the clinical value of diffusion-weighted imaging and dynamic MR imaging in combination with T2-weighted imaging. J. Magnet. Resonance Imag. 25 , 146–152 (2007).
Barentsz, J. O. et al. ESUR prostate MR guidelines 2012. Eur. Radiol. 22 , 746–757 (2012).
Vargas, H. A. et al. Updated prostate imaging reporting and data system (PIRADS v2) recommendations for the detection of clinically significant prostate cancer using multiparametric MRI: critical evaluation using whole-mount pathology as standard of reference. Eur. Radiol. 26 , 1606–1612 (2016).
Ahmed, H. U. et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 389 , 815–822 (2017).
Fulgham, P. F. et al. AUA policy statement on the use of multiparametric magnetic resonance imaging in the diagnosis, staging and management of prostate cancer. J. Urol. 198 , 832–838 (2017).
Newschaffer, C. J., Otani, K., McDonald, M. K. & Penberthy, L. T. Causes of death in elderly prostate cancer patients and in a comparison nonprostate cancer cohort. J. Natl Cancer Inst. 92 , 613–621 (2000).
Montie, J. E. & Smith, J. A. Whitmoreisms: memorable quotes from Willet F. Whitmore Jr, M. D. Urology 63 , 207–209 (2004).
Bill-Axelson, A. et al. Radical prostatectomy versus watchful waiting in localized prostate cancer: the Scandinavian prostate cancer group-4 randomized trial. J. Natl Cancer Inst. 100 , 1144–1154 (2008).
Johansson, E. et al. Long-term quality-of-life outcomes after radical prostatectomy or watchful waiting: the Scandinavian Prostate Cancer Group-4 randomised trial. Lancet Oncol. 12 , 891–899 (2011).
Hamdy, F. C. et al. 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N. Engl. J. Med. 375 , 1415–1424 (2016).
Wilt, T. J. et al. Radical prostatectomy versus observation for localized prostate cancer. N. Engl. J. Med. 367 , 203–213 (2012).
Wilt, T. J. et al. Follow-up of prostatectomy versus observation for early prostate cancer. N. Engl. J. Med. 377 , 132–142 (2017).
Choo, R. et al. Feasibility study: watchful waiting for localized low to intermediate grade prostate carcinoma with selective delayed intervention based on prostate specific antigen, histological and/or clinical progression. J. Urol. 167 , 1664–1669 (2002).
Lawrentschuk, N. & Klotz, L. Active surveillance for low-risk prostate cancer: an update. Nat. Rev. Urol. 8 , 312–320 (2011).
Parker, C. Active surveillance: towards a new paradigm in the management of early prostate cancer. Lancet Oncol. 5 , 101–106 (2004).
Klotz, L. et al. Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J. Clin. Oncol. 33 , 272–277 (2015).
Tosoian, J. J. et al. Active surveillance of prostate cancer: use, outcomes, imaging, and diagnostic tools. Am. Soc. Clin. Oncol. 35 , e235–e245 (2016).
Adolfsson, J. Watchful waiting and active surveillance: the current position. BJU Int. 102 , 10–14 (2008).
Young, H. H. The early diagnosis and radical cure of carcinoma of the prostate. Being a study of 40 cases and presentation of a radical operation which was carried out in four cases. 1905. J. Urol. 168 , 914–921 (2002).
Millin T. Retropubic urinary surgery. London: Livingstone 35 , 442 (1947).
Millin, T. Retropubic prostatectomy a new extravesical technique: report on 20 cases. Lancet. 246 , 693–696 (1945).
Walsh, P. C. The discovery of the cavernous nerves and development of nerve sparing radical retropubic prostatectomy. J. Urol. 177 , 1632–1635 (2007).
Saranchuk, J. W. et al. Achieving optimal outcomes after radical prostatectomy. J. Clin. Oncol. 23 , 4146–4151 (2005).
Schuessler, W. W., Kavoussi, L. R., Clayman, R. V. & Vancaille, T. Laparoscopic radical prostatectomy: initial case report. J. Urol. 147 , 246A (1992).
Guillonneau, B. & Vallancien, G. Laparoscopic radical prostatectomy: the Montsouris technique. J. Urol. 163 , 1643–1649 (2000).
Carlucci, J. R., Nabizada-Pace, F. & Samadi, D. B. Robot-assisted laparoscopic radical prostatectomy: technique and outcomes of 700 cases. Int. J. Biomed. Sci. 5 , 201–208 (2009).
Abbou, C. C. et al. Laparoscopic radical prostatectomy with a remote controlled robot. J. Urol. 165 , 1964–1966 (2001).
Menon, M., Hemal, A. K. & VIP Team. Vattikuti Institute prostatectomy: a technique of robotic radical prostatectomy: experience in more than 1000 cases. J. Endourol. 18 , 611–619 (2004).
Yaxley, J. W. et al. Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: early outcomes from a randomised controlled phase 3 study. Lancet 388 , 1057–1066 (2016).
Glickman, L., Godoy, G. & Lepor, H. Changes in continence and erectile function between 2 and 4 years after radical prostatectomy. J. Urol. 181 , 731–735 (2009).
Bagshaw, M. A., Kaplan, H. S. & Sagerman, R. H. Linear accelerator supervoltage radiotherapy. VII. Carcinoma of the prostate. Radiology 85 , 121–129 (1965).
Bolla, M. et al. Duration of androgen suppression in the treatment of prostate cancer. N. Engl. J. Med. 360 , 2516–2527 (2009).
D’Amico, A. V., Chen, M. H., Renshaw, A. A., Loffredo, M. & Kantoff, P. W. Androgen suppression and radiation versus radiation alone for prostate cancer: a randomized trial. JAMA 299 , 289–295 (2008).
Denham, J. W. et al. Short-term androgen deprivation and radiotherapy for locally advanced prostate cancer: results from the Trans-Tasman Radiation Oncology Group 96.01 randomised controlled trial. Lancet Oncol. 6 , 841–850 (2005).
Horwitz, E. M. et al. Ten-year follow-up of radiation therapy oncology group protocol 92-02: a phase III trial of the duration of elective androgen deprivation in locally advanced prostate cancer. J. Clin. Oncol. 26 , 2497–2504 (2008).
Jones, C. U. et al. Radiotherapy and short-term androgen deprivation for localized prostate cancer. N. Engl. J. Med. 365 , 107–118 (2011).
Pilepich, M. V. et al. Androgen suppression adjuvant to definitive radiotherapy in prostate carcinoma — long-term results of phase III RTOG 85–31. Int. J. Radiat. Oncol. Biol. Phys. 61 , 1285–1290 (2005).
Roach, M. et al. Short-term neoadjuvant androgen deprivation therapy and external-beam radiotherapy for locally advanced prostate cancer: long-term results of RTOG 8610. J. Clin. Oncol. 26 , 585–591 (2008).
Bolla, M. et al. Improved survival in patients with locally advanced prostate cancer treated with radiotherapy and goserelin. N. Engl. J. Med. 337 , 295–300 (1997).
Pilepich, M. V. et al. Phase III radiation therapy oncology group (RTOG) trial 86–10 of androgen deprivation adjuvant to definitive radiotherapy in locally advanced carcinoma of the prostate. Int. J. Radiat. Oncol. Biol. Phys. 50 , 1243–1252 (2001).
Widmark, A. et al. Endocrine treatment, with or without radiotherapy, in locally advanced prostate cancer (SPCG-7/SFUO-3): an open randomised phase III trial. Lancet 373 , 301–308 (2009).
Warde, P. et al. Combined androgen deprivation therapy and radiation therapy for locally advanced prostate cancer: a randomised, phase 3 trial. Lancet 378 , 2104–2111 (2011).
Zelefsky, M. J., Fuks, Z. & Leibel, S. A. Intensity-modulated radiation therapy for prostate cancer. Semin. Radiat. Oncol. 12 , 229–237 (2002).
Das, S. et al. Comparison of image-guided radiotherapy technologies for prostate cancer. Am. J. Clin. Oncol. 37 , 616–623 (2014).
Wiegel, T. et al. Phase III postoperative adjuvant radiotherapy after radical prostatectomy compared with radical prostatectomy alone in pT3 prostate cancer with postoperative undetectable prostate-specific antigen: ARO 96-02/AUO AP 09/95. J. Clin. Oncol. 27 , 2924–2930 (2009).
Wiegel, T. et al. Adjuvant radiotherapy versus wait-and-see after radical prostatectomy: 10-year follow-up of the ARO 96-02/AUO AP 09/95 trial. Eur. Urol. 66 , 243–250 (2014).
Thompson, I. M. et al. Adjuvant radiotherapy for pathologic T3N0M0 prostate cancer significantly reduces risk of metastases and improves survival: long-term followup of a randomized clinical trial. J. Urol. 181 , 956–962 (2009).
Thompson, I. M. et al. Adjuvant radiotherapy for pathologically advanced prostate cancer: a randomized clinical trial. JAMA 296 , 2329–2335 (2006).
Bolla, M. et al. Postoperative radiotherapy after radical prostatectomy: a randomised controlled trial (EORTC trial 22911). Lancet 366 , 572–578 (2005).
Bolla, M. et al. Postoperative radiotherapy after radical prostatectomy for high-risk prostate cancer: long-term results of a randomised controlled trial (EORTC trial 22911). Lancet 380 , 2018–2027 (2012).
Morris, W. J. et al. Low-dose-rate brachytherapy is superior to dose-escalated EBRT for unfavourable risk prostate cancer: the results of the ASCENDE-RT* randomized control trial. Brachytherapy 14 , S12 (2015).
Stock, R. G., Cahlon, O., Cesaretti, J. A., Kollmeier, M. A. & Stone, N. N. Combined modality treatment in the management of high-risk prostate cancer. Int. J. Radiat. Oncol. Biol. Phys. 59 , 1352–1359 (2004).
Dearnaley, D. et al. Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5-year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol. 17 , 1047–1060 (2016).
Huggins, C., Stevens, R. E. Jr & Hodges, C. V. Studies on prostatic cancer. The effects of castration on advanced carcinoma of the prostate gland. Arch. Surg. 43 , 209–223 (1941).
Huggins, C., Stevens, R. E. Jr & Hodges, C. V. Studies on prostatic cancer. The effect of castration, of oestrogen and of androgen injection on serum phosphatases in metastatic carcinoma of the prostate. Arch. Surg. 43 , 209–223 (1941).
Ahmann, F. R. et al. Zoladex: a sustained-release, monthly luteinizing hormone-releasing hormone analogue for the treatment of advanced prostate cancer. J. Clin. Oncol. 5 , 912–917 (1987).
Goldenberg, S. L. & Bruchovsky, N. Use of cyproterone acetate in prostate cancer. Urol. Clin. North Am. 18 , 111–122 (1991).
Labrie, F. et al. New hormonal therapy in prostatic carcinoma: combined treatment with an LHRH agonist and an antiandrogen. Clin. Invest. Med. 5 , 267–275 (1982).
Crawford, E. D. et al. A controlled trial of leuprolide with and without flutamide in prostatic carcinoma. N. Engl. J. Med. 321 , 419–424 (1989).
Duchesne, G. M. et al. Timing of androgen-deprivation therapy in patients with prostate cancer with a rising PSA (TROG 03.06 and VCOG PR 01–03 [TOAD]): a randomised, multicentre, non-blinded, phase 3 trial. Lancet Oncol. 17 , 727–737 (2016).
Messing, E. M. et al. Immediate hormonal therapy compared with observation after radical prostatectomy and pelvic lymphadenectomy in men with node-positive prostate cancer. N. Engl. J. Med. 341 , 1781–1788 (1999).
Messing, E. M. et al. Immediate versus deferred androgen deprivation treatment in patients with node-positive prostate cancer after radical prostatectomy and pelvic lymphadenectomy. Lancet Oncol. 7 , 472–479 (2006).
Crook, J. M. et al. Intermittent androgen suppression for rising PSA level after radiotherapy. N. Engl. J. Med. 367 , 895–903 (2012).
Hussain, M. et al. Intermittent versus continuous androgen deprivation in prostate cancer. N. Engl. J. Med. 368 , 1314–1325 (2013).
Walker, L. M., Tran, S. & Robinson, J. W. Luteinizing hormone — releasing hormone agonists: a quick reference for prevalence rates of potential adverse effects. Clin. Genitourin. Cancer 11 , 375–384 (2013).
Green, H. J. et al. Quality of life compared during pharmacological treatments and clinical monitoring for non-localized prostate cancer: a randomized controlled trial. BJU Int. 93 , 975–979 (2004).
Rhee, H. et al. Adverse effects of androgen-deprivation therapy in prostate cancer and their management. BJU Int. 115 (Suppl. 5), 3–13 (2015).
Keating, N. L., O’Malley, A. J., Freedland, S. J. & Smith, M. R. Does comorbidity influence the risk of myocardial infarction or diabetes during androgen-deprivation therapy for prostate cancer? Eur. Urol. 64 , 159–166 (2013).
Hamilton, E. J. et al. Structural decay of bone microarchitecture in men with prostate cancer treated with androgen deprivation therapy. J. Clin. Endocrinol. Metab. 95 , E456–463 (2010).
Cornford, P. et al. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part II: treatment of relapsing, metastatic, and castration-resistant prostate cancer. Eur. Urol. 71 , 630–642 (2017).
Berthold, D. R., Sternberg, C. N. & Tannock, I. F. Management of advanced prostate cancer after first-line chemotherapy. J. Clin. Oncol. 23 , 8247–8252 (2005).
Wozniak, A. J. et al. Cyclophosphamide, methotrexate, and 5-fluorouracil in the treatment of metastatic prostate cancer. A Southwest Oncology Group study. Cancer 71 , 3975–3978 (1993).
Sridhar, S. S. et al. Castration-resistant prostate cancer: from new pathophysiology to new treatment. Eur. Urol. 65 , 289–299 (2014).
Petrylak, D. P. et al. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N. Engl. J. Med. 351 , 1513–1520 (2004).
Tannock, I. F. et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N. Engl. J. Med. 351 , 1502–1512 (2004).
Berthold, D. R. et al. Treatment of hormone-refractory prostate cancer with docetaxel or mitoxantrone: relationships between prostate-specific antigen, pain, and quality of life response and survival in the TAX-327 study. Clin. Cancer Res. 14 , 2763–2767 (2008).
de Bono, J. S. et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet 376 , 1147–1154 (2010).
Gravis, G. et al. Androgen-deprivation therapy alone or with docetaxel in non-castrate metastatic prostate cancer (GETUG-AFU 15): a randomised, open-label, phase 3 trial. Lancet Oncol. 14 , 149–158 (2013).
Sweeney, C. J. et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N. Engl. J. Med. 373 , 737–746 (2015).
James, N. D. et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet. 387 , 1163–1177 (2016).
James, N. D. et al. Abiraterone for prostate cancer not previously treated with hormone therapy. N. Engl. J. Med. 377 , 338–351 (2017).
Fizazi, K. et al. LATITUDE: a phase III, double-blind, randomized trial of androgen deprivation therapy with abiraterone acetate plus prednisone or placebos in newly diagnosed high-risk metastatic hormone-naive prostate cancer. J. Clin. Oncol. 35 , LBA3 (2017).
Mohler, J. L. et al. The androgen axis in recurrent prostate cancer. Clin. Cancer Res. 10 , 440–448 (2004).
Kumar, A. et al. Substantial interindividual and limited intraindividual genomic diversity among tumors from men with metastatic prostate cancer. Nat. Med. 22 , 369–378 (2016).
Veldscholte, J. et al. A mutation in the ligand binding domain of the androgen receptor of human LNCaP cells affects steroid binding characteristics and response to anti-androgens. Biochem. Biophys. Res. Commun. 173 , 534–540 (1990).
Pienta, K. J. & Bradley, D. Mechanisms underlying the development of androgen-independent prostate cancer. Clin. Cancer Res. 12 , 1665–1671 (2006).
Antonarakis, E. S. et al. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N. Engl. J. Med. 371 , 1028–1038 (2014).
Guo, Z. et al. A novel androgen receptor splice variant is up-regulated during prostate cancer progression and promotes androgen depletion-resistant growth. Cancer Res. 69 , 2305–2313 (2009).
Beer, T. M. et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N. Engl. J. Med. 371 , 424–433 (2014).
Shore, N. D. et al. Efficacy and safety of enzalutamide versus bicalutamide for patients with metastatic prostate cancer (TERRAIN): a randomised, double-blind, phase 2 study. Lancet Oncol. 17 , 153–163 (2016).
Scher, H. I. et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N. Engl. J. Med. 367 , 1187–1197 (2012).
Ryan, C. J. et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N. Engl. J. Med. 368 , 138–148 (2013).
Ryan, C. J. et al. Abiraterone acetate plus prednisone versus placebo plus prednisone in chemotherapy-naive men with metastatic castration-resistant prostate cancer (COU-AA-302): final overall survival analysis of a randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 16 , 152–160 (2015).
Fizazi, K. et al. Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 13 , 983–992 (2012).
Parker, C. et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N. Engl. J. Med. 369 , 213–223 (2013).
Saad, F. et al. A randomized, placebo-controlled trial of zoledronic acid in patients with hormone-refractory metastatic prostate carcinoma. J. Natl Cancer Inst. 94 , 1458–1468 (2002).
Saad, F. et al. Long-term efficacy of zoledronic acid for the prevention of skeletal complications in patients with metastatic hormone-refractory prostate cancer. J. Natl Cancer Inst. 96 , 879–882 (2004).
Fizazi, K. et al. Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet 377 , 813–822 (2011).
Litwin, M. S. et al. The UCLA Prostate Cancer Index: development, reliability, and validity of a health-related quality of life measure. Med. Care. 36 , 1002–1012 (1998).
Wei, J. T., Dunn, R. L., Litwin, M. S., Sandler, H. M. & Sanda, M. G. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology 56 , 899–905 (2000).
Szymanski, K. M., Wei, J. T., Dunn, R. L. & Sanda, M. G. Development and validation of an abbreviated version of the expanded prostate cancer index composite instrument (epic-26) for measuring health-related quality of life among prostate cancer survivors. Urology 76 , 1245–1250 (2010).
Resnick, M. J. et al. Long-term functional outcomes after treatment for localized prostate cancer. N. Engl. J. Med. 368 , 436–445 (2013).
Feldman, H. A., Goldstein, I., Hatzichristou, D. G., Krane, R. J. & McKinlay, J. B. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J. Urol. 151 , 54–61 (1994).
Kim, E. H. & Andriole, G. L. A simplified prostate cancer grading system. Nat. Rev. Urol. 12 , 601–602 (2015).
Epstein, J. I., Walsh, P. C., Carmichael, M. & Brendler, C. B. Pathologic and clinical findings to predict tumor extent of nonpalpable (stage T1c) prostate cancer. JAMA 271 , 368–374 (1994).
de Bono, J. S. et al. Abiraterone and increased survival in metastatic prostate cancer. N. Engl. J. Med. 364 , 1995–2005 (2011).
Penson, D. F. et al. Enzalutamide versus bicalutamide in castration-resistant prostate cancer: the STRIVE Trial. J. Clin. Oncol. 34 , 2098–2106 (2016).
Kantoff, P. W. et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N. Engl. J. Med. 363 , 411–422 (2010).
Download references
Author information
Authors and affiliations.
Department of Urology, University of Minnesota, Minneapolis, MN, USA
Niranjan J. Sathianathen & Badrinath R. Konety
University of Melbourne, Department of Surgery, Urology Unit and Olivia Newton-John Cancer Research Institute Austin Health, Melbourne, Victoria, Australia
Niranjan J. Sathianathen & Nathan Lawrentschuk
Department of Surgical Oncology, Peter MacCallum Cancer Centre, Melbourne, Victoria, Australia
Department of Radiation Oncology and Developmental Radiotherapeutics, University of British Columbia, Kelowna, British Columbia, Canada
Juanita Crook
Division of Urology, Centre Hospitalier de l’Université de Montreal, University of Montreal, Montreal, Québec, Canada
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Niranjan J. Sathianathen .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary tables 1 and 2, rights and permissions.
Reprints and permissions
About this article
Cite this article.
Sathianathen, N.J., Konety, B.R., Crook, J. et al. Landmarks in prostate cancer. Nat Rev Urol 15 , 627–642 (2018). https://doi.org/10.1038/s41585-018-0060-7
Download citation
Published : 31 July 2018
Issue Date : October 2018
DOI : https://doi.org/10.1038/s41585-018-0060-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
External validation of predictive models of sexual, urinary, bowel and hormonal function after surgery in prostate cancer subjects.
- Matthew A. Borg
- Michael E. O’Callaghan
- Andrew D. Vincent
BMC Urology (2024)
Diagnosis and management of indeterminate testicular lesions
- Stefanie M. Croghan
- Jamil W. Malak
- Niall F. Davis
Nature Reviews Urology (2024)
N6-methyladenosine regulator YTHDF1 represses the CD8 + T cell-mediated antitumor immunity and ferroptosis in prostate cancer via m6A/PD-L1 manner
- Yibing Wang
Apoptosis (2024)
The role of GCNT1 mediated O-glycosylation in aggressive prostate cancer
- Kirsty Hodgson
- Margarita Orozco-Moreno
- Jennifer Munkley
Scientific Reports (2023)
- Martin J. Connor
- Michael A. Gorin
- Hashim U. Ahmed
Nature Reviews Urology (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Cancer newsletter — what matters in cancer research, free to your inbox weekly.
Prostate Cancer Research Results and Study Updates
See Advances in Prostate Cancer Research for an overview of recent findings and progress, plus ongoing projects supported by NCI.
Under a new FDA approval, enzalutamide (Xtandi) can now be used alone, or in combination with leuprolide, to treat people with nonmetastatic prostate cancer that is at high risk of returning after surgery or radiation.
FDA approved enzalutamide (Xtandi) combined with talazoparib (Talzenna) for metastatic castration-resistant prostate cancer with alterations in any of 12 DNA repair genes. The drug combination, which blocks both DNA repair activities and hormones that fuel cancer growth, was more effective than the standard treatment in a large clinical trial.
The Decipher genomic test found high-risk prostate cancer even when conventional tests said the tumors were lower risk. This discrepancy appeared to happen more frequently for African-American men.
Men diagnosed with low-risk prostate cancer are increasingly opting against immediate treatment and choosing active surveillance instead, a new study finds. In fact, rates of active surveillance more than doubled between 2014 and 2021.
Adding darolutamide (Nubeqa) to ADT and docetaxel (Taxotere) can improve how long men with hormone-sensitive metastatic prostate cancer live without causing more side effects, results from the ARASENS trial show.
Many with prostate cancer can safely receive shorter, higher-dose radiation therapy after surgery, a new study has found. The approach, called HYPORT, didn’t harm patients’ quality of life compared with the standard radiation approach, trial finds.
A drug called Lu177-PSMA-617 may be a new option for treating advanced prostate cancer. In a large clinical trial, adding the drug—a type of radiopharmaceutical—to standard treatments improved how long participants lived.
For some men with prostate cancer, a genetic biomarker test called Decipher may help predict if their cancer will spread elsewhere in the body. The test could help determine whether hormone therapy, which can cause distressing side effects, is needed.
FDA’s recent approval of relugolix (Orgovyx) is expected to affect the treatment of men with advanced prostate cancer. A large clinical trial showed that relugolix was more effective at reducing testosterone levels than another common treatment.
FDA has approved olaparib (Lynparza) and rucaparib (Rubraca) to treat some men with metastatic prostate cancer. The PARP inhibitors are approved for men whose cancers have stopped responding to hormone treatment and have specific genetic alterations.
For some men with prostate cancer at high risk of spreading, a large clinical trial shows an imaging method called PSMA PET-CT is more likely to detect metastatic tumors than the standard imaging approach used in many countries.
Testing for prostate cancer with a combined biopsy method led to more accurate diagnosis and prediction of the course of the disease in an NCI study. The method is poised to reduce the risk of prostate cancer overtreatment and undertreatment.
In the Veterans Affairs health care system—where all patients have equal access to care—African American men did not appear to have more-aggressive prostate cancer when diagnosed or a higher death rate from the disease than non-Hispanic white men.
In two large clinical trials, the drugs enzalutamide (Xtandi) and apalutamide (Erleada), respectively, combined with the androgen deprivation therapy, improved the survival of men with metastatic prostate cancer that still responds to hormone-suppressing therapies.
The Prostate Cancer Prevention Trial showed that finasteride can reduce the risk of prostate cancer, but might increase the risk of aggressive disease. NCI’s Howard Parnes talks about subsequent findings and what they mean for men aged 55 and older.
The investigational drug darolutamide can help delay the spread of prostate cancer in some men with the disease, a recent clinical trial shows. In addition, the drug caused fewer side effects than similar prostate cancer drugs.
For African American men, the risk of dying from low-grade prostate cancer is double that of men of other races, a new study has found. But, despite the increase, the risk is still small.
Researchers have found that men with advanced prostate cancer may be more likely than previously thought to develop a more aggressive form of the disease. The subtype, called t-SCNC, was linked with shorter survival than other subtypes.
RESPOND is the largest coordinated study on biological and non-biological factors associated with aggressive prostate cancer in African-American men. The study is an effort to learn why these men disproportionally experience aggressive disease.
In a small clinical trial, researchers compared the efficacy of a much lower dose of the cancer drug abiraterone (Zytiga) taken with a low-fat breakfast with a full dose taken on an empty stomach, as directed on the drug’s label.
In the trial that led to the approval, apalutamide (Erleada) delayed cancer metastasis for men with prostate cancer that is resistant to androgen deprivation therapy.
A new study in mice has revealed a molecular link between a high-fat diet and the growth and spread of prostate cancer. The findings, the study leaders believe, raise the possibility that changes in diet could potentially improve treatment outcomes in some men.
The Food and Drug Administration (FDA) has expanded the approval of abiraterone (Zytiga®) for men with prostate cancer. The agency approved abiraterone, in combination with the steroid prednisone, for men with metastatic prostate cancer that is responsive to hormone-blocking treatments (also known as castration-sensitive) and is at high risk of progressing.
Researchers have identified an emerging subtype of metastatic prostate cancer that is resistant to therapies that block hormones that fuel the disease.
In two large clinical trials, adding the hormone-blocking drug abiraterone to androgen-deprivation therapy (ADT) allowed men with metastatic hormone-sensitive prostate cancer to live longer than men who were treated with ADT alone.
Findings from a new study show testing for two biomarkers in urine may help some men avoid an unnecessary biopsy to detect a suspected prostate cancer.
Long-term results from an NCI-sponsored clinical trial suggest that adding androgen deprivation therapy to radiation therapy can improve survival for some men with recurrent prostate cancer.
Researchers estimate that nearly 12% of men with advanced prostate cancer have inherited mutations in genes that play a role in repairing damaged DNA.
Researchers have identified a potential alternative approach to blocking a key molecular driver of an advanced form of prostate cancer, called androgen-independent or castration-resistant prostate cancer.
Essay: Raising awareness about prostate cancer

Other than skin cancer, prostate cancer is the most common cancer in men and is the second most common cause of cancer death in the United States.
The American Cancer Society estimates that in 2021 more than 248,000 American men will be diagnosed and more than 34,000 men will die of prostate cancer. Nearly 1 in 8 men will be afflicted by this disease in their lifetime and 1 in 41 men will die of prostate cancer.
Most commonly, prostate cancer manifests as a localized, silent disease, progressing slowly with minimal to no symptoms. Once the disease has spread out of the prostate to adjacent organs, lymph nodes or bones, symptoms become more prevalent. These include pain, urinary problems, neurologic symptoms, and more.
Data have shown that active screening can lead to early diagnosis. Studies with long-term follow-up have demonstrated an approximate 30 percent decrease in prostate cancer mortality when screening is implemented. In fact, the implementation of prostate cancer screening has been one of the main reasons for the decrease in prostate cancer-specific death by more than 50 percent from 1993 to 2017.
Screening for prostate cancer is simple and quick, performed with a digital rectal exam (DRE) assessing prostate size and contour and a blood test for prostate-specific antigen (PSA). PSA is a protein made by cells located in the prostate gland (both normal cells and cancer cells). The risk of being diagnosed with prostate cancer increases as the PSA blood level increases.
The National Comprehensive Cancer Network (NCCN) guidelines recommend that men over the age of 45 should discuss prostate cancer screening with their physicians. For men at increased risk (known family history, known genetic risk factors, or African ancestry) discussion about screening should start even earlier at age 40.
When prostate cancer is diagnosed at an early stage, and is still localized, the cure rate is incredibly high, with a nearly 100 percent five-year cancer-free survival rate. Once prostate cancer is diagnosed, various treatment options are available, ranging from “active surveillance” (frequent monitoring of the disease with no active treatment) to radiation or surgery and other therapeutic options.
Novel scientific discoveries, new treatment options and robust research published in the last decade have led to significant advances in the diagnosis and treatment of this common malignancy.
Despite the continuous increase in the incidence and prevalence of prostate cancer and a constant rising rate of cancer-specific death, not all men actively seek preventive care and undergo screening.
September is Prostate Cancer Awareness Month. During this time, various attempts are made across the country to raise awareness of this highly prevalent cancer and promote screening and early detection.
At Upstate Urology at the Mohawk Valley Health System (MVHS), we are organizing a free screening event at various dates and times throughout the month of September. These events are being scheduled so as to adhere to social distancing guidelines, with individual appointments being made.
It’s important that you don’t put off screenings during this time of COVID, and we encourage all men between the ages of 45-75 to use this opportunity to be screened for prostate cancer.
Visit mvhealthsystem.org/urology for more information.
As a urologist treating prostate cancer patients and as a son of a prostate cancer survivor, I hope our call is answered, and with your help, we will succeed in raising awareness and spreading the word.
Please join our important quest to fight this cancer by reaching out to more men and improving early detection rates.
Dr. Hanan Goldberg, MD, MSc, is assistant professor at SUNY Upstate Medical University and chief of Upstate Urology at the Mohawk Valley Health System (MVHS).
bestessayhelp.com
Prostate Cancer – Essay Sample
Prostate cancer is the second most common type of cancer diagnosed in men around the world today. Despite years of research, little is known as to the exact cause of prostate cancer, making it an area of intense research in medicine today. The pathology of prostate cancer has yielded important information on prevention, diagnosis and treatment methods. It has been understood that diet has much to do with tumor growth, and new research into nutrition is revealing new strategies in prostate cancer prevention. Genetics also play an important factor and must be taken into consideration A number of new treatments for prostate cancer have been successfully implemented. Since prostate cancer is most common in men 50 and older it is for the, as well as for younger men, to be aware of prostate cancer prevention, screening, diagnosis and treatment options. The healthcare physician can play an important role in patient education to help patients know how they can prevent prostate cancer from occurring.
A gland that occurs only in men, the prostate is a small, walnut sized gland associated with the male reproductive system. (Porth, 2011, p.1023). This small organ is prone to a number of diseases, one of which is prostate cancer. While the exact cause of prostate cancer is still unknown, it effects a large number of men, especially in America, making it a great cause of concern for American over the age of 50. While the exact cause of prostate cancer is still unclear, there are several factors that have been linked to its frequency. One is diet. It has been noted that men that have a low consumption of fish oils have have a higher rate of prostate cancer than those with a high consumption of fish oils (Terry et al, 2001, 1766). Dietary fat has also been linked to the occurrence of prostate cancer in men. Dietary fats may alter the production of sex hormones and growth factors, leading to an increased risk for prostate cancer (Porth, 2011, p. 1026). In addition, those who have a diet high in vitamins D and E, selenium, soy, green tea and tomato-rich products (which contain lycopene) typically have a lower occurrence (Porth, 2011, p.1026).
Genetics has also been found to be an important factor in determining who is at risk for prostate cancer. “It has been estimated that men who have an affected first degree relative (e.g., father, brother) and an affected second-degree relative (e.g., grandfather, uncle) have an eightfold increase in risk” (Porth, 2001, p. 1026). It is unclear as to whether this genetic disposition has to do with actual gene defects or with similar patterns in diet and lifestyle.
There are many factors that impact the prognosis of prostate cancer. One is age. Prostate cancer is uncommon in men under the age of 50. In fact, more than 85% of those diagnosed with prostate cancer are older than 65 years of age. Another factor is race. Prostate cancer is most common in men of African American descent (Porth, 2011, p. 1026). Weight can also factor in to the likelihood of a person having prostate cancer due to the fact that it is indicative of a diet high in dietary fats, which has been linked to prostate cancer.
While there is no single way to prevent prostate cancer there are several things that can be done to help reduce the risk of developing it. The most effective preventative treatment is a change in diet. The consumption of fish containing high amounts of fatty acids, such as salmon, herring and mackerel (Terry et al, 2001, p. 1765) has been found in several studies to reduce the risk of prostate cancer (Terry et al, 2001 and Augustsson et al, 2003). However, it is still not clear as to the exact mechanism by wish fish, and fish oil, prevents tumor growth. As Augustsson et al (2003, p.64) reported, the reduced risk of prostate cancer varied between groups that ate fish more than three times per week and groups that simply added marine fatty acid supplements to their diet. Other nutritional factors include ensuring an adequate amount of vitamins D and E are being taken into the body, as well as selenium, soy and green tea. Soy and green tea are consumed in high amounts by Asian populations, all of which have a much lower incidence of prostate cancer than those from cultures from which these foods are typically absent from the diet.
There are currently four main treatment methods for prostate cancer, radiation therapy, surgery, hormonal manipulations and watchful waiting. Chemotherapy has not been proven to be an effective treatment for prostate cancer. They type of treatment that is most appropriate depends upon the grade and stage of growth of the tumor itself. It also depends on the health and age of the individual. Watchful waiting, or expectant therapy, is typically recommended for older men and those who already have other health problems, as long as the tumor is not producing symptoms or expected to grow too quickly (Porth, 2011, p. 1027). Surgery, typically radical prostatectomy, is used to treat prostate cancer by removing the seminal vesicles, prostate and ampullae of the vas deferens. Thanks to new refinements in surgical techniques, including nerve-sparing prostatectomy, in many continence and erectile function has been spared in those undergoing surgery for prostate cancer. Another common treatment for prostate cancer is radiation therapy, in which a small external beam of radiation is focused on the tumor to shrink and kill it. Finally, hormone therapy is also being used as a way to treat prostate cancer. Hormone therapy relies on a variety of techniques to reduce testosterone levels, a hormone which stimulates tumor growth (Porth, 2011, p. 1027).
The road to success is easy with a little help. Let's get your assignment out of the way.
A monthly newsletter from the National Institutes of Health, part of the U.S. Department of Health and Human Services
Search form
Print this issue
Health Capsule
Comparing Side Effects of Prostate Cancer Treatments

Prostate cancer is the most common cancer for men in the United States. Luckily, most men with prostate cancer will still be alive 15 years after diagnosis.
Men with prostate cancer that hasn’t spread outside the gland have several treatment choices. These include surgery, radiation therapy, and active surveillance, where treatment is delayed until a cancer starts to grow.
Men live a similar length of time regardless of the chosen treatment. But it’s been unclear if there were significant differences in the long-term side effects of these treatments. Side effects can include bladder and bowel problems, and difficulty with sexual functioning.
To learn more, researchers followed 2,500 men for 10 years after prostate cancer treatment. As expected, survival rates were similar. But the long-term side effects differed depending on the treatment.
Men who had surgery had a higher risk of leaking urine. But men who had radiation therapy had a higher risk of bowel problems. Certain men had a higher risk of sexual problems soon after surgery. But by 10 years, no significant differences were found between the treatment groups.
“Given the similar survival rates, the choice of treatment for patients may be influenced by the adverse effects of the treatments,” says Dr. Bashir Al Hussein Al Awamlh, of Vanderbilt University, who helped lead the study.
Related Stories

Testing an mRNA Vaccine to Treat Pancreatic Cancer

Stop Smoking Early To Improve Cancer Survival

Advances in Childhood Cancer

Are You Overdue for a Cervical Cancer Screening?
NIH Office of Communications and Public Liaison Building 31, Room 5B52 Bethesda, MD 20892-2094 [email protected] Tel: 301-451-8224
Editor: Harrison Wein, Ph.D. Managing Editor: Tianna Hicklin, Ph.D. Illustrator: Alan Defibaugh
Attention Editors: Reprint our articles and illustrations in your own publication. Our material is not copyrighted. Please acknowledge NIH News in Health as the source and send us a copy.
For more consumer health news and information, visit health.nih.gov .
For wellness toolkits, visit www.nih.gov/wellnesstoolkits .
Ben Stiller's Essay About Prostate Cancer Is Moving But Not Scientific
Senior Reporter, HuffPost

Ben Stiller went public with his prostate cancer diagnosis in an essay on Medium on Tuesday. The comedian was diagnosed in 2014 and has been cancer-free since treatment that year.
He credits a controversial screening test ― the prostate-specific antigen, or PSA, test ― with saving his life:
Taking the PSA test saved my life. Literally. That’s why I am writing this now. There has been a lot of controversy over the test in the last few years. Articles and op-eds on whether it is safe, studies that seem to be interpreted in many different ways, and debates about whether men should take it all. I am not offering a scientific point of view here, just a personal one, based on my experience. The bottom line for me: I was lucky enough to have a doctor who gave me what they call a “baseline” PSA test when I was about 46. I have no history of prostate cancer in my family and I am not in the high-risk group, being neither ― to the best of my knowledge ― of African or Scandinavian ancestry. I had no symptoms.
Counterintuitively, while Stiller believes that he saved his own life by getting a PSA test early, his example goes against medical recommendations that are in place to protect men from unnecessary treatment and serious, potentially life-threatening side effects that can come from treating a cancer that probably won’t kill them.
And that’s the catch: Prostate cancer is often so slow-growing as to never be fatal. The majority of evidence shows that most men with prostate cancer will not die of their disease, regardless of whether they were diagnosed, received treatment or are monitored carefully. Indeed, the five-year survival rate for prostate cancer is almost 100 percent , and the 15-year survival rate is 95 percent.
This means that the 26,000 men who will die from prostate cancer in the U.S. this year likely would not have been helped by routine, asymptomatic PSA screening, explains Dr. Otis Brawley , chief medical officer of the American Cancer Society.
“The harsh truth is that even under the best conditions, with careful screening, some men will still die of prostate cancer,” Brawley said in a statement. “This is why no major health group recommends all men be screened. The PSA test can be useful, but it is not perfect, by a long shot.”
More testing does not mean more lives saved
The prostate produces PSA normally, and levels can become elevated because of a cancerous growth. Increased PSA is the first clue doctors normally have that an asymptomatic patient may have a problem. However, PSA levels can also become elevated because of infection or the natural process of aging ― not cancer.
For this reason, while high PSA readings might lead doctors to find aggressive, spreading cancer, it can also lead to unnecessary surgery or other cancer treatment for a tumor that either doesn’t exist, or is so slow growing that it wouldn’t otherwise be deadly.
Unnecessary surgery and treatment is harmful ― and can even be deadly ― because procedures can introduce medical complications that men may not have otherwise faced if they hadn’t treated the cancer in the first place. These complications can include bowel and urinary incontinence , sexual dysfunction and life-threatening cardiovascular issues.
And just because a man is diagnosed with prostate cancer, that doesn’t necessarily mean he should be treated for it. A study recently published in the New England Journal of Medicine found that almost half of the men who decided to take a “watch and wait” approach to prostate cancer, opting for active surveillance over radiation or surgery, didn’t need any additional treatment over the course of 10 years. This means that they were able to avoid the potentially dangerous side effects of treatment, all the while being secure that they had identified a potential problem and were being proactive about it.
Indeed, this is already happening in the U.S.: About 50 percent of men who get diagnosed with prostate cancer now opt for active monitoring over aggressive treatment.
Why health experts no longer recommend the PSA test
Because the PSA test has a risk of false positives and over-diagnoses (some trials estimate the over-diagnosis rate at 17 to 50 percent ), the U.S. Preventive Services Task Force, a government-backed volunteer group of national medical experts, recommend in 2012 to stop routine PSA testing among asymptomatic men in all age groups.
The Task Force breaks down the benefits and risks of routine screening in asymptomatic men this way:
- Five in 1,000 men will die of prostate cancer without screening, while four in 1,000 men will die of prostate cancer with screening. This means one life out of 1,000 will be saved with screening.
- Prostate cancer screening causes false positives in up to 120 men per 1,000 tested.
- About 110 men in 1,000 will be diagnosed with prostate cancer, and 90 percent of these men will have treatment that could cause serious cardiovascular events, deep venous thrombosis, urinary incontinence, erectile dysfunction and death. The Task Force considers these risks unacceptable, or at least questionable, considering the fact most men with prostate cancer have a tumor that was never going to kill them.
The American Cancer Society, another organization that releases screening guidelines, recommends that men and doctors discuss the known risks and benefits of a PSA test, and then make a decision about screening that best fits in with that man’s life and medical history.
As Stiller notes in his essay, for most average-risk men who decide to get screened, testing will start at age 50 . Men at high risk of developing prostate cancer, like African Americans or men with a father, brother or son who had prostate cancer at an early age, should discuss screening at age 45, while men with more than one first-degree relative with early prostate cancer should talk to their doctor at age 40.
The average age of prostate cancer diagnosis is 66 years old , but early diagnoses like Stiller’s (he was 46 at his first PSA test) make the case for earlier screening for certain men. After all, the younger you are when you get it, the more years you have to lose if the tumor turns out to be aggressive or deadly.
Ben Stiller’s prostate cancer journey
Stiller didn’t fit any of those high risk categories and yet, at age 46, his doctor Bernard Kruger administered a PSA test to establish a “baseline” for Stiller’s normal PSA levels. Kruger continued to monitor Stiller’s PSA levels every six months, and realized that over 18 months, Stiller’s levels kept rising.
Kruger sent Stiller to a urologist, who administered a digital rectal exam and then recommended an MRI scan to see his prostate in more detail. After the MRI came a biopsy to test the tissue for cancer, and they found that Stiller had “mid-range aggressive cancer.”
Stiller decided to get a prostatectomy, which is a surgery to remove all or part of the prostate gland. Since then, the cancer has not returned.
Stiller writes that his treatment might look very different if Kruger had not taken the initiative to screen Stiller early.
If he had waited, as the American Cancer Society recommends, until I was 50, I would not have known I had a growing tumor until two years after I got treated. If he had followed the US Preventive Services Task Force guidelines, I would have never gotten tested at all, and not have known I had cancer until it was way too late to treat successfully.
So should you follow Ben Stiller’s example? Experts weigh in
When asked about prostate cancer patients like Ben Stiller, experts said that his case presents a complex truth about this particular illness: while it’s difficult to convince prostate cancer survivors otherwise, early screening is less likely to save a life than it is to result in serious medical complications that harm people more than the tumor ever would.
“The problem that the medical community has struggled with regarding the PSA test is that for every PSA success story, there’s another man who has been unnecessarily treated as a result of an elevated PSA,” said Dr. Timothy J. Daskivich, a urologic oncologist and director of health services research for the Cedars-Sinai department of surgery in Los Angeles. “These are often men with low-grade cancers (the most common type of prostate cancer in the U.S.) or men with limited life expectancy.”
Stiller’s experience is counter to most medical recommendations about how to screen for prostate cancer, but his story represents a larger trend, according to Dr. Inderbir Gill, chairman of the USC Institute Of Urology at the University of Southern California.
Gill believes that while the 2012 recommendations played an important role in alerting the public to the dangers of overdiagnosis and overtreatment, the field has become much more sophisticated in the past four years.
In fact, Gill said that Stiller’s case is an example of how prostate cancer care has become highly personalized, informed by high-tech testing that involves MRI scans, genomic markers and molecular markers to stratify patients into low, medium and high-risk cases.
Gill said that Stiller’s anecdote is an example of the fact that doctors are having sophisticated conversations with their patients about the risks and benefits of screening, and that treatment has become highly personalized, informed by high-tech testing.
This relies on educating patients about what a PSA level really means. While testing positive for elevated PSA levels used to mean anxiety, fear and medical interventions, now we know that abnormally high levels don’t necessarily mean men should rush to treatment. It could simply mean that men need more monitoring to see if anything worsens over time, as Stiller did.
So what are a doctor and patient to do? Daskivich endorses the ACS’ approach: selectively screen men based on their risk factors, life expectancy and health status. He also agrees with Gill’s assertion that there are now ways to stratify risk so that doctors and patients can choose whether or not to even treat a tumor.
“By doing this, we will target screening and treatment to those who need it, to minimize harms and maximize benefits of screening and treatment,” he concluded.
If Stiller’s story has you wondering about prostate cancer screening, talk to your doctor about the risks and benefits of the PSA test for someone of your age, ethnicity and medical history.
Support HuffPost
Our 2024 coverage needs you, your loyalty means the world to us.
At HuffPost, we believe that everyone needs high-quality journalism, but we understand that not everyone can afford to pay for expensive news subscriptions. That is why we are committed to providing deeply reported, carefully fact-checked news that is freely accessible to everyone.
Whether you come to HuffPost for updates on the 2024 presidential race, hard-hitting investigations into critical issues facing our country today, or trending stories that make you laugh, we appreciate you. The truth is, news costs money to produce, and we are proud that we have never put our stories behind an expensive paywall.
Would you join us to help keep our stories free for all? Your contribution of as little as $2 will go a long way.
As Americans head to the polls in 2024, the very future of our country is at stake. At HuffPost, we believe that a free press is critical to creating well-informed voters. That's why our journalism is free for everyone, even though other newsrooms retreat behind expensive paywalls.
Our journalists will continue to cover the twists and turns during this historic presidential election. With your help, we'll bring you hard-hitting investigations, well-researched analysis and timely takes you can't find elsewhere. Reporting in this current political climate is a responsibility we do not take lightly, and we thank you for your support.
Contribute as little as $2 to keep our news free for all.
Dear HuffPost Reader
Thank you for your past contribution to HuffPost. We are sincerely grateful for readers like you who help us ensure that we can keep our journalism free for everyone.
The stakes are high this year, and our 2024 coverage could use continued support. Would you consider becoming a regular HuffPost contributor?
The stakes are high this year, and our 2024 coverage could use continued support. If circumstances have changed since you last contributed, we hope you’ll consider contributing to HuffPost once more.
Already contributed? Log in to hide these messages.
Before You Go

Jet Lag Health Effects/SleepIt Might Increase Cancer Risk
Popular in the community, from our partner, huffpost shopping’s best finds, more in life.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
March 29, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
New research highlights combining prostate MRI with a blood test to avoid unnecessary prostate biopsies
by Brigham and Women’s Hospital

MRI of the prostate, combined with a blood test, can help determine if a prostate lesion is clinically significant cancer, new research suggests
A new meta-analysis by investigators from Brigham and Women's Hospital suggests that doctors and patients can avoid unnecessary prostate biopsies by combining MRI of the prostate findings with prostate-specific antigen (PSA) density.
This new approach to diagnosing clinically significant prostate cancer can decrease patient harm and health care costs of prostate biopsies. Their results are published in JAMA Network Open .
An enlarged prostate or potential prostate cancer is a common issue for older men . There will be approximately 300,000 new cases of prostate cancer in the U.S. this year. But not all those cancers require treatment—or even need to be biopsied.
"In the workup of men suspected of having prostate cancer, prostate MRI findings combined with PSA density measurement can help doctors decide which patients to biopsy ," said senior author Ramin Khorasani, MD, MPH, Radiology Vice Chair for Quality and Safety at Brigham and Women's Hospital and Mass General Brigham and Philip H. Cook Professor of Radiology at Harvard Medical School.
"With this new analysis, we looked to see how MRI can help urologists decide which patients to biopsy and which patients may not need aggressive diagnosis and treatment."
Researchers have known for a long time that not all prostate cancer is dangerous. However, telling which cancers need treatment without a biopsy can be difficult. Biopsies, especially those of the prostate, can be uncomfortable, invasive, and expensive.
To doctors, clinically significant prostate cancer (csPCa) is prostate cancer that has a high chance of threatening a patient's life. They have cells that look more aggressive, or cancer is found outside of the prostate gland.
"Prostate cancer is the second most common cancer in men worldwide, but we need to be able to identify patients who require prostate biopsy while avoiding unnecessary procedures and minimizing the risk of missing clinically significant prostate cancer," Adam Kibel, MD, chair of the Department of Urology and co-author of the study.
"These findings suggest that patient-tailored prostate biopsy decisions based on information from MRI and blood tests could prevent unnecessary procedures while maintaining high sensitivity."
MRI of the prostate can provide some of this information. Still, a biopsy is traditionally needed to determine how aggressive the cancer cells look. This study tested a new approach: combining MRI-based prostate imaging reporting and data system (PI-RADS) scores with prostate-specific antigen (PSA) density to determine which cancers were likely to be clinically significant without including information from a biopsy.
PI-RADS scores the prostate lesion from 1 (highly unlikely to be clinically significant) to 5 (cancer is highly likely to be clinically significant). PSA density (PSAD) is the PSA blood level divided by the prostate's volume (as determined by MRI).
The JAMA Network Open study builds upon previous findings from a similar study using data only obtained at Brigham Women's Hospital, published in the Journal of the American College of Radiology in 2022. That study found that an analysis using PI-RADS and PSAD cutoffs could pinpoint up to 50% of cases in which a biopsy would be unnecessary.
The new study, whose first and second authors are Arya Haj-Mirzaian, MD, MPH, and Kristine S. Burk, MD, did the same analysis on data from 72 previously published studies of men with prostate cancer , including their PI-RADS results, prostate-specific antigen density testing, and determination of clinical significance from a biopsy.
The meta-analysis gave them a dataset of more than 36,000 patients to determine if their earlier findings at BWH held in a more diverse sample set. They found that prostate biopsies may be unnecessary for patients with a PI-RADS under 4 and a PSAD below 0.10 ng/ml 2 . The researchers found that using specific PI-RADS and PSAD cutoffs, doctors could confidently skip 50% of biopsies while only missing 5% of clinically significant cancers, or they could skip 30% and only miss 3%.
"These data give us the confidence to say that in some cases, we can safely follow men with testing rather than aggressively pursue a biopsy in all cases," Kibel said. "By making this information available to physicians and patients, we can help them make a more informed decision about undergoing a biopsy."
The next step in this research is using the analysis to create an easy-to-use patient-level scoring system that urologists can use to evaluate their patient's need for a biopsy.
Explore further
Feedback to editors

Researchers produce grafts that replicate the human ear
Mar 30, 2024

An infamous 'inflammasome'—a rogue protein complex—appears to underlie a rare and disabling autoimmune disorder
Mar 29, 2024

Researchers discover skin biomarkers in infants that predict early development of food allergies

Veterans help provide greater insight into Klinefelter and Jacobs syndromes


High-resolution images reveal similarities in protein structures between Alzheimer's disease and Down syndrome

How blocking a neural receptor responsible for addiction could reduce alcohol use

Study finds few hospitals promoting potentially predatory medical payment products

COVID-19 research: Study reveals new details about potentially deadly inflammation

Enhanced melanoma vaccine offers improved survival for men

How music choices can affect productivity
Related stories.

New test for prostate cancer could help avoid unnecessary biopsies
Oct 6, 2023

Prostate cancer upgrade, downgrade rates in PI-RADS 2.0 versus 2.1
Sep 20, 2023

At the same PSA level, Black men found more likely to have prostate cancer than white men
Nov 6, 2023

Free, easy-to-use tool could reduce unnecessary prostate cancer biopsies
Feb 4, 2022

Mayo Clinic minute: Prostate biopsy technique reduces infection risk
Jun 15, 2022

MRI assisted biopsies more effective at detecting prostate cancers
Aug 13, 2019
Recommended for you

New synapse type discovered through spatial proteomics

Researchers develop AI-based tool paving the way for personalized cancer treatments

Researchers demonstrate technique for identifying single cancer cells in blood for the first time

Private and secure generative AI tool supports operations and research in a cancer center

'Exhausted' immune cells in healthy women could be target for breast cancer prevention
Mar 28, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

Ultrasound applied with MRI may be effective for treating prostate cancer
P recisely delivered ultrasound could be an effective treatment for prostate cancer , with high-frequency sound waves heating and killing off cancer cells, a new study says.
The treatment killed off all prostate cancer cells in 76% of men who underwent a follow-up biopsy one year later, researchers said.
It also cut down on unwanted side effects, such as incontinence and sexual dysfunction.
In the procedure, MRI scans are used to precisely apply ultrasound to a man's prostate cancer, through a small catheter-like device inserted through the urethra.
"This image-guided therapy maximizes our ability to kill cancer cells while minimizing collateral damage to the prostate to achieve the ultimate trifecta in prostate cancer treatment: full local cancer control while maintaining urinary continence and potency," lead researcher Dr. Steven Raman , a professor of radiology, urology and surgery at the David Geffen School of Medicine at UCLA, said in a news release.
For this study, 115 men with prostate cancer were recruited at 13 hospitals in five countries and given the ultrasound treatment, researchers said. The procedure can be performed in an outpatient facility in two or three hours, under general or spinal anesthesia.
Results show that the treatment reduced or eliminated cancer cells, and also shrank men's prostates and reduced their prostate-specific antigen (PSA) levels.
The men treated with ultrasound experienced a 92% decrease in average prostate size within a year, and a healthy decrease in PSA levels at five years. High PSA levels are a warning sign for prostate cancer.
The therapy also produced fewer side effects than other prostate cancer treatments.
After five years, 92% of the men had control over their bladder and 87% had good erectile function. Incontinence and erectile dysfunction are two common side effects of prostate cancer surgery.
Raman believes that ultrasound therapy "represents a revolution in whole-gland treatment for prostate cancer."
"Prostate cancer is the most common form of cancer in men, affecting one in eight men in their lifetime," he said. "We have more research to do, but if validated, (ultrasound) has the potential to change the standard of care for thousands of men."
Researchers are scheduled to present these findings in Salt Lake City at a meeting of the Society of Interventional Radiology, which begins Saturday.
Findings presented at medical meetings should be considered preliminary until published in a peer-reviewed journal.
More information
The California Institute of Technology has more about ultrasound treatment to kill cancer .
Copyright © 2024 HealthDay. All rights reserved.

Help | Advanced Search
Electrical Engineering and Systems Science > Image and Video Processing
Title: benchmarking image transformers for prostate cancer detection from ultrasound data.
Abstract: PURPOSE: Deep learning methods for classifying prostate cancer (PCa) in ultrasound images typically employ convolutional networks (CNNs) to detect cancer in small regions of interest (ROI) along a needle trace region. However, this approach suffers from weak labelling, since the ground-truth histopathology labels do not describe the properties of individual ROIs. Recently, multi-scale approaches have sought to mitigate this issue by combining the context awareness of transformers with a CNN feature extractor to detect cancer from multiple ROIs using multiple-instance learning (MIL). In this work, we present a detailed study of several image transformer architectures for both ROI-scale and multi-scale classification, and a comparison of the performance of CNNs and transformers for ultrasound-based prostate cancer classification. We also design a novel multi-objective learning strategy that combines both ROI and core predictions to further mitigate label noise. METHODS: We evaluate 3 image transformers on ROI-scale cancer classification, then use the strongest model to tune a multi-scale classifier with MIL. We train our MIL models using our novel multi-objective learning strategy and compare our results to existing baselines. RESULTS: We find that for both ROI-scale and multi-scale PCa detection, image transformer backbones lag behind their CNN counterparts. This deficit in performance is even more noticeable for larger models. When using multi-objective learning, we can improve performance of MIL, with a 77.9% AUROC, a sensitivity of 75.9%, and a specificity of 66.3%. CONCLUSION: Convolutional networks are better suited for modelling sparse datasets of prostate ultrasounds, producing more robust features than transformers in PCa detection. Multi-scale methods remain the best architecture for this task, with multi-objective learning presenting an effective way to improve performance.
Submission history
Access paper:.
- HTML (experimental)
- Other Formats
References & Citations
- Google Scholar
- Semantic Scholar
BibTeX formatted citation
Bibliographic and Citation Tools
Code, data and media associated with this article, recommenders and search tools.
- Institution
arXivLabs: experimental projects with community collaborators
arXivLabs is a framework that allows collaborators to develop and share new arXiv features directly on our website.
Both individuals and organizations that work with arXivLabs have embraced and accepted our values of openness, community, excellence, and user data privacy. arXiv is committed to these values and only works with partners that adhere to them.
Have an idea for a project that will add value for arXiv's community? Learn more about arXivLabs .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley-Blackwell Online Open

Prostate cancer and supportive care: a systematic review and qualitative synthesis of men's experiences and unmet needs
A.j.l. king.
1 Centre for Academic Primary Care, School of Social and Community Medicine, University of Bristol, Bristol, UK
T.H.M. Moore
C. paterson.
2 Urology, Bristol Urological Institute Southmead Hospital, Bristol, UK
A.L. Huntley
Prostate cancer is the second most common cancer in men worldwide, accounting for an estimated 1.1 million new cases diagnosed in 2012 ( www.globocan.iarc.fr ). Currently, there is a lack of specific guidance on supportive care for men with prostate cancer. This article describes a qualitative systematic review and synthesis examining men's experience of and need for supportive care. Seven databases were searched; 20 journal articles were identified and critically appraised. A thematic synthesis was conducted in which descriptive themes were drawn out of the data. These were peer support, support from partner, online support, cancer specialist nurse support, self‐care, communication with health professionals, unmet needs (emotional support, information needs, support for treatment‐induced side effects of incontinence and erectile dysfunction) and men's suggestions for improved delivery of supportive care. This was followed by the development of overarching analytic themes which were: uncertainty, reframing, and the timing of receiving treatment, information and support. Our results show that the most valued form of support men experienced following diagnosis was one‐to‐one peer support and support from partners. This review highlights the need for improved access to cancer specialist nurses throughout the care pathway, individually tailored supportive care and psychosexual support for treatment side effects.
Introduction
Prostate cancer is the second most common cancer in men worldwide, accounting for an estimated 1.1 million new cases diagnosed in 2012 (Globocan, 2012 ). This figure has been rising due to increased use of Prostate Specific Antigen (PSA) testing (Ferlay et al . 2008 ). Men with prostate cancer are likely to have a long illness pathway, and as well as the individual burden to patients, this also represents a burden on healthcare resources. One way of managing this is to provide good supportive care for men which ‘helps the patient and their family to cope with cancer and treatment of it … helps the patient to maximise the benefits of treatment and to live as well as possible with the effects of the disease’ (NICE 2008 ). Supportive care will ideally involve strong elements of self‐care, in order to encourage independence in managing symptoms and side effects (Cockle‐Hearne & Faithfull 2010 ). However, the available guidance on supportive care and self‐management tends to be generic to all cancer patients (NCSI 2013 ).
A recent survey in seven European countries and involving over 1000 men found that 81% of the respondents had some unmet supportive care needs (Cockle‐Hearne et al . 2013 ). These findings echoes earlier surveys in Australia and the UK showing that the areas of greatest need were for psychological distress, sexuality‐related issues and managing of enduring lower urinary tract symptoms (Steginga et al . 2001 ; Ream et al . 2008 ). Other studies highlight the need for the provision of information to patients and carers throughout the disease pathway (Gulavita et al . 2000 ; Sinfield et al . 2009 ). The psychological distress that many men with prostate cancer experience is not always assessed or managed well. A study from Germany looked at adjustment to disease and suggested that up to 20% of patients might benefit from mental health support following prostatectomy (Kohler et al . 2014 ). Research also reveals that post‐treatment care from nurses had a significant positive impact on health outcomes (Cockle‐Hearne et al . 2013 ).
Surveys of unmet need make a case for improving supportive care but an important step is to clarify men's experiences of support using qualitative research methods. Many qualitative studies have been carried out looking at men's experiences of prostate cancer and the impact of the disease on their sense of masculinity (Gray et al . 2002 ; Arrington 2003 ; Maliski et al . 2008 ) but less has been written about men's experiences of supportive care provision. The ideal study design for bringing these data together and creating an overview of men's experiences and needs is to conduct a qualitative systematic review and synthesis.
The parent search strategy was devised and run in Medline and Medline in process ( Appendix 1 ). Modified search strategies based on this search were run in Embase, Psych Info, CINAHL, British Nursing Index, IBSS and Sociological Abstracts. All searches were run from inception to July 2013.
Inclusion and exclusion criteria
Inclusion criteria for full‐text articles were: qualitative studies that included men with a diagnosis of prostate cancer who were undergoing or had undergone any type of standard treatment (including active surveillance) that explored their needs for, attitude toward or experience of supportive care. These qualitative studies included ethnographic and observational studies, involving interviews and focus groups with men with prostate cancer. Two of the studies were longitudinal surveys that included qualitative data. Exclusion criteria were men at risk from prostate cancer, and men in end of life care.
References were screened by title and abstract by two reviewers and differences were resolved by discussion with a third person if necessary, and full articles were obtained that met the above criteria. The reference list of papers retrieved as full text were hand searched and key authors contacted.
Data extraction and synthesis
A thematic synthesis of the evidence in the qualitative papers was conducted, taking an interpretive approach. The reviewers adopted a ‘thematic synthesis’ approach (Thomas & Harden 2008 ). ‘Descriptive themes’ were drawn out of the data followed by the development of ‘analytic themes’ identified by the reviewers. The identification of themes was partly driven by the research question and partly grounded in the data. Data were extracted independently by at least two reviewers using customised forms and any discrepancies were resolved by discussion. All papers were reviewed by AJLK and additional reviewers including co‐authors, members of the advisory group and patients with prostate cancer from a local support group. All included papers were critically appraised independently by two reviewers using the Critical Appraisal Skills Programme quality appraisal tool as an integral part of the systematic review (CASP 2014 ). Disagreements around critical appraisal were resolved by discussion between the reviewers.
Findings were organised into ‘first‐order constructs’ (the verbatim views and experiences of research participants) and ‘second‐order constructs’ (the interpretations of the authors). Patient quotes (‘first‐order constructs’) provide a significant voice of patient experience of supportive care in the analysis and discussion of the secondary qualitative data derived from the review papers. A framework was constructed in Excel with columns for first‐ and second‐order constructs and a row for each article. Members of the research team met to identify and agree consensus on descriptive themes emerging across papers, incorporating all the first‐ and second‐order constructs. The themes were summarised and mapped to show which articles had contributed to each theme. The development of descriptive themes remained very close to the constructs in the primary studies. Overarching analytic themes were subsequently identified, enabling synthesis of themes across studies and the development of new ideas.
The searches yielded 1684 articles excluding duplicates ( Appendix 2 ). Twenty papers describing 20 individual qualitative studies were included in the synthesis, all published between 2004 and 2013 in Europe, the USA, Canada, Australia and the UK (Matsunaga & Gotay 2004 ; Boehmer & Babayan 2005 ; Broom 2005 ; Wallace & Storms 2007 ; Tarrant et al . 2008 ; Milne et al . 2008 ; Oliffe et al . 2009 ; Ream et al . 2009 ; Nanton et al . 2009 ; Ervik et al . 2010 ; O'Brien et al . 2010 ; Walsh & Hegarty 2010 ; Carter et al . 2011 ; Nanton & Dale 2011 ; O'Brien et al . 2011 ; Chambers et al . 2012 ; Galbraith et al . 2012 ; O'Shaughnessy et al . 2013 ; Rivers et al . 2012 ; Thomas 2013 ). Dual critical appraisal revealed that the papers were generally of good quality and none were excluded due to poor quality overall (see Appendix 3 ). Negative scoring on reflexivity and ethical considerations were not sufficient to warrant rejection of individual papers. If the papers had scored poorly on the other criteria, the reviewers would then have conducted a sensitivity analysis (Dixon‐Woods et al . 2007 ). The study characteristics are included in Table 1 .
Study characteristics of review studies
AC: African‐Caribbean; AA: African‐American; A: Asian; W: White; L: Latino; O: Other.
Twelve descriptive themes emerged across the papers. They fall into three groups: (1) prostate cancer patients' experience of supportive care; (2) their accounts of unmet needs; and (3) their suggestions about how to improve supportive care. Table 2 lists the papers that contributed to each of the 12 themes. The reviewers then developed three overarching themes that cut across the 12 descriptive themes. These were uncertainty, reframing and timing.
Reviewers' themes
Authors: (1) Matsunaga and Gotay 2004 ; (2) Boehmer and Babayan 2005 ; (3) Broom 2005 ; (4) Wallace and Storms 2007 ; (5) Tarrant et al . 2008 ; (6) Milne et al . 2008 ; (7) Oliffe et al . 2009 ; (8) Ream et al . 2009 ; (9) Nanton et al . 2009 ; (10) Ervik et al . 2010 ; (11) O'Brien et al . 2010 ; (12) Walsh and Hegarty 2010 ; (13) Carter et al . 2011 ; (14) Nanton and Dale 2011 ; (15) O'Brien et al . 2011 ; (16) Chambers et al . 2012 ; (17) Galbraith et al . 2012 ; (18) O'Shaughnessy et al . 2013 ; (19) Rivers et al . 2012 ; (20) Thomas 2013 .
Prostate cancer patients' experience of supportive care
There were seven themes in this group: peer support, support from church communities, trusted other support, online support, communication with health professionals, the role of the prostate cancer specialist nurse and self‐care. The analysis revealed that men's experience of supportive care was predominantly provided and influenced by informal networks of peer support or ‘trusted others’, and that formal support from health professionals was lacking.
Peer support
This was the most frequent theme to emerge, discussed in 10 of the 20 papers (Table 3 ). Peer support took different forms: support groups led by peers or by health professionals, and one‐to‐one peer support. Men were generally proactive in accessing this kind of support. Three papers described referral or signposting by health professionals (Table 3 ). Wallace and Storms ( 2007 ) describe that one study in which participant was told of support services by his urologist. The other papers referred mainly to one‐to‐one informal peer support found within patients' friendship networks, families, work colleagues, church group or leisure clubs.
I was fortunate in that I knew two or three men who had prostate cancer, so I found it very helpful to talk to them. ( Wallace & Storms 2007 : participant quotation)
Types of peer support
Men's experience of peer support lifted them out of a sense of isolation and enabled them to talk about their illness experience, share information and exchange tips and ideas on dealing with treatment side effects. The reciprocal nature of talking and sharing was experienced as empowering. Galbraith et al . ( 2012 ) describes how it provided a sense of meaning in men's experience of the disease. However, he does not distinguish between informal one‐to‐one support or group support. Matsunaga and Gotay ( 2004 ) highlight the importance of reciprocity in such support. This had a positive effect on helping men to adjust to their diagnosis.
Many participants desired to help others who had been diagnosed and treated for prostate cancer as a way to provide meaningful outcome from their challenges with prostate cancer and its treatment. ( Galbraith et al . 2012 : author quotation) Once you go through the procedure, you feel like you could be of assistance, especially about the operation and what to expect. ( Matsunaga & Gotay 2004 : participant quotation)
The value of peer support was evident at all stages of prostate cancer with diagnosis, treatment decision making and advanced disease being three critical times.
[diagnosis was] such an emotional thing that I needed to be with people who had gone through this or were going through it. ( Wallace & Storms 2007 : participant quotation) Participants felt that the ideal support programme should be made available immediately after diagnosis so that they could literally ‘walk out of the urologist's office and begin to discuss options'. The participants were most interested in meeting with other men with the disease, not a physician or a nurse. ( Wallace & Storms 2007 : author quotation) I finally found a fellow around the corner from me and he came over to my house. We had coffee; we got to be pretty good friends and he kind of sold me on the laparoscopic. ( Milne et al . 2008 : participant quotation)
Being in a mixed group with men at different stages of prostate cancer helped men confront and accept disease progression:
For me, who was newly diagnosed in the middle of treatment, to people who had been diagnosed for 15 or 16 years … it may have been confronting but I didn't find it so because they seemed to be able to cope with it and that was reassuring. ( Chambers et al . 2012 : participant quotation)
Carter's study focuses on men with advanced disease in which men were looking for information rather than emotional support. However, not all men found it useful, and some men stopped going when they felt they were no longer learning new information (Carter et al . 2011 ).
Support accessed within a church community
Two papers referred specifically to peer support accessed through their local church. One paper reports the experience of African‐Caribbean men in the UK (Nanton & Dale 2011 ) and another focuses on African‐American men in the USA (Rivers et al . 2012 ). They recount how participants attended church services more frequently and became more involved in church activities after diagnosis. Their church community facilitated access to other men with prostate cancer from whom patients could get information on diagnosis and treatment. This networking helped some men to ‘find their voice’ and become advocates for others:
… there's been several men within my church and in my community that has … (prostate cancer) … when I found out that he was goin’ through it, I went up … we sat down and talked about it and so it's … it's made me somewhat of an advocate. ( Rivers et al . 2012 : participant quotation)
Support from a partner or ‘trusted other’
Wives, partners, friends and families were described as significant sources of support by men in six papers (Matsunaga & Gotay 2004 ; Boehmer & Babayan 2005 ; Ervik et al . 2010 ; Walsh & Hegarty 2010 ; O'Shaughnessy et al . 2013 ; Rivers et al . 2012 ). Boehmer and Babayan ( 2005 ) coined the phrase ‘trusted other’ in recognition that other key individuals, apart from a spouse, may fulfill this role. Ambivalence was expressed about how much to disclose to close family. Men recognised that family members have their own emotional reactions to cope with. For some men the need to retain their ‘normal’ lifestyle despite their diagnosis was paramount.
… and our son, he doesn't say much, he doesn't show a lot of feelings, but our daughter had a hard time … I don't know maybe men are more tough in such cases … now I have a more open attitude towards illness and that sort of question. Earlier in life, I had a much more tough attitude. … ( Ervik et al . 2010 : participant quotation) I mean I only told my wife and nobody else from the day I was informed … So my lifestyle didn't change one iota … because we didn't want to upset them. We could handle it. ( Walsh & Hegarty 2010 : participant quotation)
Ervik et al . ( 2010 ) stresses the importance of support from spouses but several papers highlight the need for spouses to also receive support. For example, concern was raised about spouses' ongoing ability to adequately care for and support them during and after treatment (Boehmer & Babayan 2005 ; Rivers et al . 2012 ):
Some of the women expressed feeling overwhelmed by the caretaker role. … Some feared how this were to change their relationship, were they cast in the nurse role. ( Boehmer & Babayan 2005 : author quotation)
Online support
The internet was cited as a source of information by men in five studies ( Boehmer & Babayan 2005 ; Wallace & Storms 2007 ; Milne et al . 2008 ; Carter et al . 2011 ; Rivers et al . 2012 ). Milne highlights the need for nurses to guide patients to reliable information sources. One article focuses on the experience of men using online support groups in Australia (Broom 2005 ). Men described how engaging with others online as opposed to face‐to‐face reduced their inhibition; they valued the anonymity in accessing and receiving support and information.
Some men don't want to be face to face. Maybe they're frightened of it … maybe they're scared of being ridiculed … maybe they're a bit anxious about having the problem and not wanting to share it. I think that's men for you. ( Broom 2005 : participant quotation)
Some men took a passive role, observing how others responded to prostate cancer and how they were coping without divulging their own experience. Some men found that the online medium enabled them to distance themselves from their disease.
Communication with health professionals
Several papers describe patients' difficulties in talking to health professionals about important issues early on post diagnosis, when many appeared not to have a clear understanding of PSA testing or what a biopsy is.
I think GPs should make a point of saying what it is about and why it's being done at a particular time. ( Walsh & Hegarty 2010 : participant quotation)
Walsh and Hegarty ( 2010 ) highlight that several men in her study did not feel that their general practitioner (GP) had communicated adequately on what the PSA test was and its significance.
So he came up to me and said he was going to do blood tests the next day. Now no one ever told me not even my GP that the blood test was called a PSA. ( Walsh & Hegarty 2010 : participant quotation)
When looking back at their diagnostic appointment (given in some cases by a hospital consultant, a GP or sometimes by specialist nurses) patients singled out that this was not handled with sufficient sensitivity (Wallace & Storms 2007 ; Nanton & Dale 2011 ). Communication difficulties also continued long term after treatments (Ervik et al . 2010 ; Thomas 2013 ).
Men also reported poor communication with health professionals about the potential severity and duration of side effects of treatment, so patients felt unclear about what to expect (Ream et al . 2009 ; Thomas 2013 ), USA (Galbraith et al . 2012 ), Norway (Ervik et al . 2010 ) and Australia (Broom 2005 ).
Three reasons for this difficulty in communication emerged across papers. First, patients felt unable to talk about changes in sexual function, because for the most part, they were not asked about this at an appropriate time or in a suitable context.
Men can be reluctant to volunteer information on erectile function but generally respond with relief when the question is asked. ( Milne et al . 2008 : author quotation)
Second, men said that they could not easily discuss psychological issues with health professionals owing partly to their experience of a lack of continuity of care.
I think if you saw the same person each time you would probably build up a rapport with that person. But seeing a stranger every time you're thinking ‘oh my God I'm not going to walk in there and start talking about my sex life with someone I've never seen in my life before …. I think I glossed over it [the psychological impact]. ( O'Brien et al . 2011 : participant quotation) It was quite a shock when you go there and it's somebody else … I don't think I spoke about my psychological problems. ( O'Brien et al . 2011 : participant quotation)
Third, men felt that there was a lack of empathy shown by health professionals, leaving then feeling depersonalised.
Cavalier attitudes expressed by the treatment team were disquieting … We were treated liked test subjects, not equals. ( Galbraith et al . 2012 : participant quotation)
This prevalent finding may be summed up by Ervik et al . ( 2010 ) who describe what he calls the ‘ silence of the healthcare system ’. This patient is referring to his follow‐up appointment with a physician:
It is never really time for it … he was not that good with words. ( Ervik et al . 2010 : participant quotation)
Thomas's ( 2013 ) article suggests that participants perceived GPs to be more empathetic than urologists:
In marked contrast to the perception of the urologists, most participants were satisfied with the role of their general practitioner in the prostate cancer journey. The local GPs … were thought to be empathetic to the experiences of the participants. ( Thomas 2013 : author quotation)
Experience of a cancer specialist nurse
Men who had received care from a cancer specialist nurse reported a positive experience of enabling them to discuss non‐medical aspects of their illness (Tarrant et al . 2008 ; Ream et al . 2009 ). This was exemplified by the way nurses communicated the diagnosis (Ream et al . 2009 ) and could act as patient advocates by accessing appropriate care and support. Another key element of the specialist nurse role was in terms of long‐term and ongoing care (O'Shaughnessy et al . 2013 ), and the fact that contact could be initiated by the patient.
… men with prostate cancer would utilize the services of a specialist prostate cancer nurse at all stages of the prostate cancer journey. ( O'Shaughnessy et al . 2013 : author quotation)
Key stages when men valued specialist nurse input was around treatment decision making and treatment choice after initial hormone therapy has failed (O'Shaughnessy et al . 2013 ). Specialist nurses sometimes arranged or referred patients to support groups (Tarrant et al . 2008 ) and played a role in helping men reframe their illness experience in a positive way, enabling better adaptation and coping skills.
She's the link, the liaison and to me the liaison officer, or whatever you want to call it … the surgeon, the consultant is very important but only at a specific time. The one you are relying on most is the (prostate cancer specialist nurse). ( Ream et al . 2009 : participant quotation) It worried me to death..I felt I had to ring (the specialist nurse) … I was asking myself questions I couldn't answer … after I spoke to her I felt a lot better. Oh, I can ring (the specialist nurse) up any time I want to. ( Tarrant et al . 2008 : participant quotation)
Tarrant states that patients who saw a specialist nurse were more likely to have received written information and clear explanations about their tests, treatment options and sources of support (Tarrant et al . 2008 ).
Self‐care
Self‐care is discussed in nine of the papers. Several authors discuss the empowerment and sense of control that comes from self‐care and making lifestyle changes such as diet and exercise.
[By] taking an active part in their own health management [through making changes in their diet and/or exercise] men were taking control of their illness. ( Nanton et al . 2009 : author quotation)
This was particularly true for men with advanced hormone‐resistant cancer who were most likely to have changed their diet and lifestyle (O'Shaughnessy et al . 2013 ).
For the last four years, … eating better, exercising more … and living life more fully. ( O'Shaughnessy et al . 2013 : participant quotation)
Other aspects of self‐care include taking an ‘active problem solving approach’ to illness by, for example, joining a support group (Nanton et al . 2009 ), returning to work or seeking out social and emotional support from family, friendship and faith networks (Rivers et al . 2012 ; Nanton & Dale 2011 ).
Self‐care is particularly important for prostate cancer patients who are under active surveillance. They tried to combine ‘ living a normal life ’ with ‘ doing something extra ’, using strategies similar to men at other stages of disease and treatment such as making dietary or lifestyle changes, and engaging with their partner, family and friends (Oliffe et al . 2009 ; O'Shaughnessy et al . 2013 ). The authors emphasise the significance of men's wives and partners in helping men to make lifestyle changes.
Patients' accounts of unmet supportive care needs
There were three themes in this group: need for emotional support, need for support to deal with treatment side effects, in particular changes in sexual function and urinary incontinence, and need for information. A major concern is the difficulty that men experienced in actually broaching sensitive subjects with health professionals (Milne et al . 2008 ; Ream et al . 2009 ; Ervik et al . 2010 ; Galbraith et al . 2012 ; Thomas 2013 ).
Need for emotional support
Men described their long‐term need for emotional or psychological support, beginning at diagnosis and continuing through treatment into survivorship (Oliffe et al . 2009 ; Ream et al . 2009 ; Ervik et al . 2010 ; O'Brien et al . 2010 ; Galbraith et al . 2012 ; O'Shaughnessy et al . 2013 ; Thomas 2013 ). They felt that there was a lack of understanding by health professionals in primary and secondary care of the emotional impact of prostate cancer particularly in the longer term (Matsunaga & Gotay 2004 ; Boehmer & Babayan 2005 ; Oliffe et al . 2009 ; O'Brien et al . 2010 ; Thomas 2013 ). O'Shaughnessy et al . ( 2013 ) define ‘psychosocial’ needs as men's fears around treatment, anxiety and depression, changes in sexuality, masculinity and relationships. O'Shaughnessy et al . ( 2013 ) and Boehmer and Babayan ( 2005 ) highlight that men's distress and need for psychological support is especially evident when they are first diagnosed and Boehmer and Babayan refer to a later peak of distress if their cancer reoccurs.
The estrangement of men from ‘softer’ psychosocial healthcare services was especially evident in how few ideas or recommendations were offered by the study participants when directly asked about what services and how services might best support them. ( Oliffe et al . 2009 : author quotation)
Carter et al . ( 2011 ) highlight the need for psychological support to be ongoing. O'Brien et al . ( 2010 ) and Galbraith et al . ( 2012 ) talk about the need for support through the psycho‐emotional responses to survivorship.
Participants strongly expressed the need for the health care team to acknowledge their experiences of uncertainty, anger, and grief or loss. ( Galbraith et al . 2012 : author quotation)
Need for support to deal with treatment side effects – changes in sexual function and urinary incontinence
Several of the papers highlighted the need for emotional and psychological support for treatment side effects, primarily urinary incontinence and erectile dysfunction.
The follow‐ups (at the hospital) … have been more concerned with the physical side of things, not the mental side of it … there could have been more emphasis on (that). ( O'Brien et al . 2011 : participant quotation)
O'Brien et al . ( 2011 ) highlight that assessment of psychosexual needs has to take place throughout the follow‐up period, not only at the time of initial treatment, particularly because ‘patients may take time to identify that they have a need for psychosexual support’. O'Brien points out that there may be a role for GPs in assessing wider psychosexual needs and signposting where to get help, and to include patients' partners in this. Galbraith suggests that specialist nurses are in a key position to offer support for men's relational and emotional needs.
Men in several studies expressed a need for information on the severity and duration of incontinence and erectile dysfunction side effects, as well as practical support (Milne et al . 2008 ; Walsh & Hegarty 2010 ; Carter et al . 2011 ; Nanton & Dale 2011 ; O'Brien et al . 2011 ; Thomas 2013 ). Men said they lacked help and support in dealing with these. Difficult reactions to surgery were common:
If I had known what was gonna happen, they'd never have done it … They must have cut muscles and everything. And I'll tell you, your sex life is gone. … I should have been filled in. ( Carter et al . 2011 : participant quotation) Immediately postoperatively the question of impotence doesn't really come into your head … I think it's only later on that you have to … face up psychologically to how you handle that … There's not a lot of counselling form either the primary care or the hospital in terms of the psychological aspect. ( O'Brien et al . 2010 : participant quotation)
Need for information
Information can help empower patients to feel more in control of their disease through increased understanding.
Acquiring knowledge allows patients to be in control because it increases their level of understanding'. He highlights the importance of acquiring first‐hand knowledge from other men with prostate cancer. ( Milne et al . 2008 )
Across the articles, men reported receiving information about prostate cancer and its treatment from a variety of sources including oncologists, urologists, nurses, GPs, cancer charities, the internet, friends and family members. A major and valued source of information is through peer networks (Matsunaga & Gotay 2004 ; Wallace & Storms 2007 ; Milne et al . 2008 ; Walsh & Hegarty 2010 ).
In relation to information from health professionals, there were two issues: content and timing. In Matsunaga and Gotay's ( 2004 ) study, men said that physicians did not give them enough information about treatment options and assumed they understood more than they really did. In three studies (Wallace & Storms 2007 ; Tarrant et al . 2008 ; Nanton et al . 2009 ), men expressed a need for information after diagnosis on what the PSA test was and what changes in it meant, and on appropriateness of treatment and treatment options. Timing was sometimes felt to be inappropriate, e.g. when they received information on treatment side effects, it was often too little too late. As a result, men felt unprepared for the severity and duration of these side effects (Milne et al . 2008 ; Carter et al . 2011 ; Nanton & Dale 2011 ). One study participant highlighted that it is hard to absorb information directly upon diagnosis:
No you can't absorb it and that's in a way one little criticism of (the specialist) nurse … ‘you've got prostate cancer’ … and she carts you off into a tiny little cubicle of a room..and I don't know what the hell she said because … that was too soon. … I was in a state of numbness..at that point and so I don't really know what she was trying to achieve. ( Tarrant et al . 2008 : participant quote) .
The importance of including both men and their partners in information provision on treatment and side effects was highlighted by Rivers et al . ( 2012 ) and O'Shaughnessy et al . ( 2013 ). The ‘need for information’ theme highlights the lack of communication between patients and health professionals particularly in relation to who communicates it, and at what point in the care pathway.
Men's suggestions for improved delivery of supportive care
There were two themes in this group: need for information and need for more time with a specialist cancer nurse (to provide practical, emotional and psychological support). Suggestions were forthcoming from the men themselves, across many articles, as to priority areas for targeting improvements. In terms of information, they suggested making more disease‐related information available at or shortly after diagnosis (Tarrant et al . 2008 ). They also suggested that assistance be provided in interpreting the information (Matsunaga & Gotay 2004 ).
Another suggestion was to make more contact time available with a cancer specialist nurse, particularly after diagnosis and after active treatment (Tarrant et al . 2008 ). Emotional and psychological support for both patients and their partners was flagged up as an important area for improvement (Wallace & Storms 2007 ; Carter et al . 2011 ). Ervik et al . ( 2010 ) stated that when asked directly, half of the men in his study would consider organised counselling if this were an option.
Overarching themes
The reviewers developed overarching analytic themes that cut across the 12 descriptive themes within the papers: uncertainty, reframing and timing of support.
Uncertainty
Men's experience of the prostate cancer pathway was full of uncertainty and anxiety (Milne et al . 2008 ; Oliffe et al . 2009 ; Nanton et al . 2009 ; Ervik et al . 2010 ; O'Brien et al . 2010 ; Walsh & Hegarty 2010 ; Carter et al . 2011 ; Nanton & Dale 2011 ; Galbraith et al . 2012 ; O'Shaughnessy et al . 2013 ; Rivers et al . 2012 ; Thomas 2013 ). Uncertainty was associated with a perceived lack of information provision linked to treatment options and outcomes, about the extent and severity of treatment side effects, and likely prognosis. Uncertainty was particularly pronounced in men under active surveillance (Oliffe et al . 2009 ) particularly around the time leading up to PSA testing, and for those with advanced or recurrent disease (Nanton et al . 2009 ). Even the care pathway seemed to be uncertain for some men who did not fully understand the link between their illness experience and the process of care, for example, not knowing when events in their care were going to take place and who was responsible for particular aspects of their care (Nanton et al . 2009 ).
The theme of ‘reframing’ arises as a means of coping with uncertainty. The term ‘reframing’ was used in two of the articles (Nanton et al . 2009 ; Thomas 2013 ), but the concept was relevant across many more. Galbraith's description of men adapting to a ‘new normal’ is conceptually similar. Reframing can be a positive way whereby patients dealing with uncertainty about a prostate cancer prognosis determine a positive reconstruction of the situation, thus giving mental shape to an uncertain future. Reframing can also help allay unrealistic hopes to return to a pre‐treatment level of functioning (Galbraith et al . 2012 ).
Over half the participants found a new appreciation for living in the ‘Now’ and expressed an appreciation of the love and support of those close to them. There was a re‐evaluation as to what was really important in the lives of a number of these men. ( Thomas 2013 : author quotation)
A participant in this study felt that his diagnosis had given him the opportunity to reframe his sense of his sexuality and of being a gay man.
The process of reappraisal and reframing was evident across all patient groups including older men and whose with advanced disease, although it was harder for patients with metastatic disease (Nanton et al . 2009 ). Reframing can be facilitated by support from an individual or a group. For example, the specialist nurse can play a role in the process:
[the nurse] was instrumental in making me feel positive about everything rather than feeling negative … instead of ‘dying of cancer’ you are ‘living with it. ( Ream et al . 2009 : participant quotation)
Reframing also took place during patients’ experience of a peer support group by using the information they had gained through their illness experience to help others in the group.
… through participation in support group activities for example, anxiety over their own situation was displaced … by the process of doing something useful. … men demonstrated the possibility of a positive response in the face of an uncertain future. ( Matsunaga & Gotay 2004 : author quotation)
Timing of support
A trajectory becomes evident in the included studies, from early information needs to later psychological needs, and ongoing support for psychosexual needs. Many articles portray men as relatively uninformed about prostate cancer before and after their diagnosis, and even post‐treatment in some cases (Wallace & Storms 2007 ; Walsh & Hegarty 2010 ; Nanton & Dale 2011 ). A key time for information provision is between testing and diagnosis and before a consultant appointment. Men reported failing to gain a good understanding of treatment and side effects, their severity and longevity. Information at this stage would help patients to realistically appraise or ‘reframe’ their experience and put plans in place to effectively deal with the consequences of treatment. Diagnosis is inevitably a difficult time and for some men their psychological support needs begin here. It can be difficult to retain information given out at this stage (Thomas 2013 ).
The provision of supportive care must be carefully targeted in terms of its content and the timing of delivery. Men experienced uncertainty, lack of information and poor communication with their medical team about the nature of diagnostic tests, the extent of treatment side effects and the likely progression of the disease. Communication with their medical team about these issues was limited and difficult. This was ameliorated if a specialist nurse was in the team. Some of the uncertainty experienced by men reflected inherent problems in treating prostate cancer, such as the uncertainty around disease progression and clinical equipoise around treatments.
There appears to be a strong link between patients' need for information and individual levels of uncertainty. Information to ameliorate uncertainty and its consequent anxiety was not forthcoming, and men reported a lack of information about any support that might be available. Men received most of their information and support from peer groups or individuals but not all managed to access these resources.
Uncertainty as a theme has emerged in previous studies of prostate cancer patients where it has been shown to ‘adversely influence patients' and their spouses’ quality of life (Bailey et al . 2007 ; Shaha et al . 2008 ). Some men deal with uncertainty by focusing their attention on their work life or engaging in self‐care strategies, such as using complementary medicines (Bailey et al . 2007 ). Uncertainty also emerges as a theme in the literature of health and illness more widely. Mishel ( 1990 ) defines uncertainty as ‘ the inability to determine the meaning of illness‐related events. It is a cognitive state created when the individual cannot adequately structure or categorize an illness because of insufficient cues ’. Mishel proposes that managing uncertainty is critical to adapting to illness and that people cognitively process events linked to illness and construct meaning from them. Uncertainty is reappraised over time; it may not be resolved but may become part of people's reality (Mishel 1990 ; Bailey et al . 2007 ). Open discussion between patients and health professionals in a one‐to‐one or group setting may facilitate this process. This theme highlights the need for individual assessment of levels of uncertainty and coping in patients, in order for health professionals to identify areas of need, support and information for patients and families.
Reframing is one possible way of supporting men with prostate cancer around uncertainty. There is a link between reframing and self‐care in that some men in the studies (Milne et al . 2008 ; O'Shaughnessy et al . 2013 ) who felt an overwhelming need to regain control of their lives by returning to pre‐operative activities, and a need to develop a renewed sense of self. The wider literature on prostate cancer also discusses peoples' experience of reframing their illness experience (Lepore & Helgeson 1998 ; Bailey et al . 2007 ). In discussing the reframing process, Bailey et al . ( 2007 ) refers to cognitive reframing, which helps men as ‘ they attempt to incorporate the experience of prostate cancer and watchful waiting in to their life structure ’. Bailey highlights the importance of positive appraisal of the disease in order to enhance quality of life and stresses the ways in which nurses can help men with prostate cancer with this process. This review reveals that men can experience reframing of their illness experience directly for themselves or be encouraged to do this by health professionals in a more formal context (referred to in the wider literature as cognitive reframing (Bailey et al . 2007 ).
Information on the process of care, the timing of events and treatment and responsibility for care has also been highlighted as an unmet need (Nanton et al . 2009 ). To facilitate the delivery and retention of information, the presence of a partner or ‘trusted other’ at the appointment could be encouraged; information could be given in written form and reinforced at subsequent appointments along the disease pathway, for example by a specialist nurse (Tarrant et al . 2008 ). While some men need specialised support such as psycho‐sexual counseling, for many men peer support meets their needs.
Strengths and limitations to the study
The strengths of this study are that it is to our knowledge the first qualitative review and synthesis to be conducted on the experience of, and need for supportive care for men with prostate cancer in the literature and uses rigorous systematic review and qualitative synthesis methodology. Thematic synthesis was chosen as it addresses questions of intervention need, appropriateness and acceptability.
A limitation of this review was that articles focusing specifically on diagnosis and treatment decision making were excluded from this review. The included review papers were predominantly from North America so the authors' findings may not be universally applicable. The overall quality of the papers was good and contributed significantly to the discussion on prostate cancer and supportive care. The review identifies that there are few papers on the experience of men from minority ethnic groups, single men and gay men, highlighting a need for future research with these populations.
Conclusions
The review concludes that the most valued form of support men with prostate cancer experience is one‐to‐one peer support and support from partners. The review also shows that men perceive support groups to have two different roles, that of information giving (particularly when health professional led) and emotional sharing (peer led). Some men indicated the need following diagnosis to be referred by health professionals to one‐to‐one peer support, or to local support groups. This review also highlights the need for improved access to cancer specialist nurses throughout the care pathway, individually tailored supportive care and psychosexual support for treatment side effects.
Implications for Practice
There is a need for more timely and accurate information and resources to help manage daily living impacted by treatment side effects. For some men, this may translate into a need for access to psychosexual and specialist support.
Positive experiences with health professionals were considered to improve health outcomes. The practice implications of this study's findings are the need to improve access to cancer specialist nurses at key points in men's disease progression and care pathway.
Men in the included studies indicated a need for individually tailored care packages based on needs and changing needs.
There is also a need for healthcare professionals to acknowledge patients' uncertainty, and emotional responses in dealing with prostate cancer.
Health professionals also need to encourage self‐care of patients with prostate cancer and their partners, and to provide information and support to encourage this.
In view of the significant role played by partners, there is a need for health professionals to acknowledge the ‘care burden’ on partners/significant others and provide access to support.
Acknowledgements
The authors would like to acknowledge the role and work of the research advisory group (David Gillatt, John Graham, Alice Malpass and Bristol Prospect members: Malcolm Gamlin, Richard Firth, Geoff Perkins and Paul Williams). This study was supported by a NIHR RFPB grant (National Institute of Health Research, Research for Patient Benefit).
Biographies
Anna J.L. King is a research associate in the Centre of Academic Primary Care, School of Social and Community Medicine, University of Bristol. Her research interests lie in patient experience of health services, evaluation of health and social care, and involving patients in research.
Maggie Evans is a research fellow at the Centre of Academic Primary Care, School of Social and Community Medicine, University of Bristol. She specialises in qualitative work with a research focus on the supportive care needs of patients with cancer.
Theresa H.M. Moore is a research associate in the School of Social and Community Medicine, University of Bristol. Her experience lies in systematic reviews of interventions for treating or preventing disease.
Charlotte Paterson is an honorary senior research fellow, an experienced general practitioner and is currently training in acupuncture and Chinese medicine. Charlotte has a keen interest in methodology and experience of both qualitative and quantitative methods, including qualitative synthesis using meta‐ethnography.
Debbie Sharp is professor of Primary Health Care in the Centre of Academic Primary Care in the University of Bristol. She has had a long‐standing research interest in Complementary and Alternative Medicine, obtaining grant funding from a wide variety of sources and supervising higher degrees in this area.
Raj Persad is director of Oncology Studies at The Bristol Urological Institute and honorary professor at UWE. He is senior consultant urological surgeon in Bristol at North Bristol NHS Trust and a senior clinical lecturer at the University of Bristol. He is also honorary professor of Medicine at Pittsburgh University, USA, and member of the National Prostate Cancer Audit Clinical Reference Group.
Alyson Huntley is a research fellow in the Centre of Academic Primary care in the University of Bristol. She is an experienced systematic reviewer, and her research interests lie in the relationship of primary health care and the reduction of unscheduled secondary care, and supportive care interventions for patients with cancer.
Appendix 1 Medline Search Strategy run J uly 2013
Appendix 2 prisma flow chart of review.

Appendix 3 Critical Appraisal Skills Programme (CASP) evaluation of included studies
King A.J.L., Evans M., Moore T.H.M., Paterson C., Sharp D., Persad R. & Huntley A.L. (2015) European Journal of Cancer Care 24 , 618–634 Prostate cancer and supportive care: a systematic review and qualitative synthesis of men's experiences and unmet needs [ PMC free article ] [ PubMed ] [ Google Scholar ]
National Institute of Health Research grant, Research for Patient Benefit (RFPB code: PB‐PG ‐111‐26018)
- Arrington M. (2003) ‘I don't want to be an artificial man’: narrative reconstruction of sexuality among prostate cancer survivors . Sexuality and Culture 7 , 30–58. [ Google Scholar ]
- Bailey D.E., Wallace M. & Mishel M.H. (2007) Watching, waiting and uncertainty in prostate cancer . Journal of Clinical Nursing 16 , 734–741. [ PubMed ] [ Google Scholar ]
- Boehmer U. & Babayan R.K. (2005) A pilot study to determine support during the pre‐treatment phase of early prostate cancer . Psycho‐Oncology 14 , 442–449. [ PubMed ] [ Google Scholar ]
- Broom A. (2005) The eMale. Prostate cancer, masculinity and online support as a challenge to medical expertise . Journal of Sociology 41 , 87–104. [ Google Scholar ]
- Carter R., Bryant‐Lukosius D., DiCenso A., Blythe J. & Neville A.J. (2011) The supportive care needs of men with advanced prostate cancer . Oncology Nursing Forum 38 , 189–198. [ PubMed ] [ Google Scholar ]
- CASP (2014) Critical Appraisal Skills Programme . Available at: www.brookes.ac.uk/services/upgrade/study‐skills/critical‐appraisal.html . Accessed October 2014.
- Chambers S.K., Foley E., Galt E., Ferguson M. & Clutton S. (2012) Mindfulness groups for men with advanced prostate cancer: a pilot study to assess feasibility and effectiveness and the role of peer support . Supportive Care in Cancer 20 , 1183–1192. [ PubMed ] [ Google Scholar ]
- Cockle‐Hearne J. & Faithfull S. (2010) Self‐management for men surviving prostate cancer: a review of behavioural and psychosocial interventions to understand what strategies can work, for whom and in what circumstances . Psycho‐Oncology 19 , 909–922. [ PubMed ] [ Google Scholar ]
- Cockle‐Hearne J., Charnay‐Sonnek F., Denis L., Fairbanks H.E., Kelly D., Kav S., Leonard K., Muilekom E., van Fernandez‐Ortega P., Jensen B.T. & Faithfull S. (2013) The impact of supportive nursing care on the needs of men with prostate cancer: a study across seven European countries . British Journal of Cancer 109 , 2121–2130. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dixon‐Woods M., Sutton A., Shaw R., Miller T., Smith J., Young B. et al (2007) Appraising qualitative research for inclusion in systematic reviews: a quantitative and qualitative comparison of three methods . Journal of Health Services Research and Policy 12 , 42–47. [ PubMed ] [ Google Scholar ]
- Ervik B., Nordoy T. & Asplund K. (2010) Hit by waves – living with local advanced or localised prostate cancer treated with endocrine therapy or under active surveillance . Cancer Nursing 33 , 382–389. [ PubMed ] [ Google Scholar ]
- Ferlay J., Parkin D.M. & Steliarova‐Foucher E. (2008) Estimates of cancer incidence and mortality in Europe in 2008 . European Journal of Cancer 46 , 765–781. [ PubMed ] [ Google Scholar ]
- Galbraith M., Hays L. & Tanner T. (2012) What men say about surviving prostate cancer: complexities represented in a decade of comments . Clinical Journal of Oncology Nursing 16 , 65–72. [ PubMed ] [ Google Scholar ]
- Globocan . (2012) Globocan World Cancer Statistics . Available at: http://globocan.iarc.fr/Pages‐fact‐sheets‐cancer.aspx . Accessed October 2014.
- Gray R.E., Fitch M.I., Fergus K.D., Mykhalovskiy E. & Church K. (2002) Hegemonic masculinity and the experience of prostate cancer: a narrative approach . Journal of Aging and Identity 7 , 43–62. [ Google Scholar ]
- Gulavita S., Sinnott C., Setliff A.E. & Sellick S.M. (2000) Short report: what do men with prostate cancer want to know? Canadian Family Physician 46 , 1769–1771. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kohler N., Friedrich M., Gansera L., Holze S., Thiel R., Roth S., Rebmann U., Stolzenburg J.U., Truss M.C., Fahlenkamp D., Scholz H.‐J. & Brahler E. (2014) Psychological distress and adjustment to disease in patients before and after radical prostatectomy. Results of a prospective multi‐centre study . European Journal of Cancer Care , 23 , 795–802. doi: 10.1111/ecc.12186 . [ PubMed ] [ Google Scholar ]
- Lepore S.J. & Helgeson V.S. (1998) Social constraints, intrusive thoughts, and mental health after prostate cancer . Journal of Social and Clinical Psychology 17 , 89–106. [ Google Scholar ]
- Maliski S.L., Rivera S., Connor S., Lopez G. & Litwin M.S. (2008) Renegotiating masculine identity after prostate cancer treatment . Qualitative Health Research 18 , 1609–1620. [ PubMed ] [ Google Scholar ]
- Matsunaga D.S. & Gotay C.C. (2004) Characteristics contributing to an enduring prostate cancer support group in an Asian and Pacific islander community . Journal of Psychosocial Oncology 22 , 1–29. [ Google Scholar ]
- Milne J., Spiers J.A. & Moore K.N. (2008) Men's experiences following laparoscopic radical prostatectomy: a qualitative descriptive study . International Journal of Nursing Studies 45 , 765–774. [ PubMed ] [ Google Scholar ]
- Mishel M.H. (1990) Reconceptualization of the uncertainty in illness theory . Image–the Journal of Nursing Scholarship 22 , 256–262. [ PubMed ] [ Google Scholar ]
- Nanton V. & Dale J. (2011) It don't make sense to worry too much’: the experience of prostate cancer in African‐Caribbean men in the UK . European Journal of Cancer Care 20 , 62–71. [ PubMed ] [ Google Scholar ]
- Nanton V., Docherty A., Meystre C. & Dale J. (2009) Finding a pathway: information and uncertainty along the prostate cancer patient journey . British Journal of Health Psychology 14 , 437–458. [ PubMed ] [ Google Scholar ]
- NCSI (2013) Living with and Beyond Cancer: Taking Action to Improve Outcomes . NHS National Cancer Survivorship Initiative. Available at: http://www.ncsi.org.uk/wp‐content/uploads/Living‐with‐and‐beyond‐2013.pdf
- NICE (2008) Guidelines on Supportive and Palliative Care in Cancer Services . Available at: http://www.nice.org.uk/nicemedia/live/10893/28820/28820.pdf
- O'Brien R., Rose P., Campbell C., Weller D., Neal R.D., Wilkinson C., McIntosh H. & Watson E. (2010) Experiences of follow‐up after treatment in patients with prostate cancer: a qualitative study . BJU International 106 , 998–1003. [ PubMed ] [ Google Scholar ]
- O'Brien R., Rose P., Campbell C., Weller D. & Watson E. (2011) I wish I'd told them’: a qualitative study examining the unmet psychosexual needs of prostate cancer patients during follow‐up after treatment . Patient Education and Counselling 84 , 200–207. [ PubMed ] [ Google Scholar ]
- Oliffe J.L., Davison J., Pickles T. & Mroz L. (2009) The self‐management of uncertainty among men undertaking active surveillance for low‐risk prostate cancer . Qualitative Health Research 19 , 432–443. [ PubMed ] [ Google Scholar ]
- O'Shaughnessy P.K., Laws T.A. & Ester man A.J. (2013) The Prostate Cancer Journey. Results of an online survey of men and their partners . Cancer Nursing 1 , 1–12. [ PubMed ] [ Google Scholar ]
- Ream E., Quennell A., Fincham L., Faithfull S., Khoo V., Wilson‐Barnett J. & Richardson A. (2008) Supportive care needs of men living with prostate cancer in England: a survey . British Journal of Cancer 98 , 1903–1909. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ream E., Wilson‐Barnett J., Faithfull S., Fincham L., Khoo V. & Richardson A. (2009) Working patterns and perceived contribution of prostate cancer clinical nurse specialists: a mixed method investigation . International Journal of Nursing Studies 46 , 1345–1354. [ PubMed ] [ Google Scholar ]
- Rivers B., August E.M., Quin G.P., Gwede C.K., Pow‐Sang J.M., Green B.L. & Jacobsen P.B. (2012) Understanding the Psychosocial Issues of African American Couples Surviving Prostate Cancer . Journal of Cancer Education 27 , 546–558. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shaha M., Cox C., Talman K. & Kelly D. (2008) Uncertainty in breast, prostate and colorectal cancer: implications for supportive care . Journal of Nursing Scholarship 40 , 60–67. [ PubMed ] [ Google Scholar ]
- Sinfield P., Baker R., Camosso‐Stefinovic J., Colman A.M., Tarrant C., Mellon J.K., Steward W., Kockelbergh R. & Agarwal S. (2009) Men and carers’ experience of care for prostate cancer: a narrative literature review . Health Expectations: An International Journal of Public Participation in Health Care and Health Policy 12 , 301–312. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Steginga S.K., Occhipinti S., Dunn J., Gardiner R.A., Heathcote P. & Yaxley J. (2001) The supportive care needs of men with prostate cancer . Psycho‐Oncology 10 , 66–75. [ PubMed ] [ Google Scholar ]
- Tarrant C., Sinfield P., Agarwal S. & Baker R. (2008) Is seeing a specialist nurse associated with positive experiences of care? The role and value of specialist nurses in prostate cancer care . BMC Health Services Research 8 , 65. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Thomas C. (2013) The experiences of gay and bisexual men diagnosed with prostate cancer: results from an online focus group . European Journal of Cancer Care 22 , 522–529. [ PubMed ] [ Google Scholar ]
- Thomas J. & Harden A. (2008) Methods for the thematic synthesis of qualitative research in systematic reviews . BMC Medical Research Methodology 8 , 45 Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2478656/ [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wallace M. & Storms S. (2007) The needs of men with prostate cancer: results of a focus group study . Applied Nursing Research 20 , 181–187. [ PubMed ] [ Google Scholar ]
- Walsh E. & Hegarty J. (2010) Men's experiences of radical prostatectomy as treatment for prostate cancer . European Journal of Oncology Nursing 14 , 125–133. [ PubMed ] [ Google Scholar ]
- Share full article
Advertisement
Supported by
Guest Essay
Heavy Lies the Crown

By Tina Brown
Ms. Brown is the author of “The Diana Chronicles” and “The Palace Papers.”
I was in London last week when the febrile madness of Where Is Kate? was blowing up social media, and the Curious Mystery of the Doctored Mother’s Day Photograph consumed every news outlet and dinner table conversation.
After The Associated Press issued a kill notification on the botched photoshopped image of a suspiciously glossy Princess of Wales surrounded by her beaming progeny, there was a typical outburst of tabloid pomposity questioning whether Kensington Palace could ever be considered a trusted source of news.
Huh? When was the last time any tabloid considered the palace a trusted source of news? As the editor of Vanity Fair in 1985, I wrote a piece revealing that Prince Charles and Princess Diana were having awful marital fights. The palace roundly denied it, and the royal couple denied it in a television interview , confirming in my mind — correctly, as it turned out — that it was all true.
But this time, the volume and tenor of the gossip was off the charts. In all the raucous, salacious and often cruel rumormongering about Catherine, almost no one considered that behind the scenes something tragic was unfolding. When social media shrieked that there would be a very somber press announcement on Friday, royal-watchers assumed it would be from King Charles, who is battling an unspecified cancer .
But then the bombshell: Catherine announced in a video message that she, too, had cancer. After which there has rightly been a wave of cosmic shame about what this gracious public servant has been made to endure.
Catherine’s explanation of her cancer diagnosis was composed and moving, her face strained but brave. Filmed on a bench against a glimpse of spring daffodils, here was an ill woman trying to cope with a shocking diagnosis and painful medical treatment while shielding her young, worried children from the vultures of modern media.
I am told the turmoil behind the scenes has been intense, resulting in what has felt like a series of baffling press screw-ups. We hear often of Prince Harry’s hatred of the press . If possible, Prince William — while concealing it better — hates the press even more. His bloody-minded determination to stick to his grandmother Queen Elizabeth’s script of “never complain, never explain” is magical thinking in the era of the social media maelstrom, creating a vacuum filled by rumor and deranged conspiracy theories.
The almost simultaneous news of Charles’s cancer has put William and Catherine in frightening proximity to ascending the throne just when they had hoped for a span of years to parent their children out of the public eye. The prospect of it, I am told, is causing them intense anxiety.
Help from other family members is scant, aside from the redoubtable Princess Anne , Charles’s sister, and the good-egg Gaiety Girl Queen Camilla. The slimmed-down monarchy that Charles always promoted is suddenly looking very lean indeed. The combination of the Harry and Meghan clown show in Montecito, Calif.; the fusillades from Harry’s memoir, “ Spare ”; and the disgrace of Prince Andrew — who has little social contact with anyone except his horse — have put William and Catherine under unmanageable pressure.
Catherine is the most popular member of the royal family after William. The future of the monarchy hangs by a thread, and that thread is her.
It may not be a popular thought, but in many ways I blame the predicament and weakness of the monarchy today on Queen Elizabeth. It’s possible that future generations will see her as the Ruth Bader Ginsburg of the British monarchy. She stayed too long, and by doing so, left behind a legacy that may be the opposite of what she wanted.
The time for Elizabeth II to step down was not long after her Diamond Jubilee in 2012, the year I have come to think of as peak London, when Britain dazzlingly hosted the Olympics. Elizabeth II had embarked on a triumphantly healing visit for the first time to the Republic of Ireland in 2011 , Charles proved he was a settled married man at last to Camilla, Harry was a national hero after two military tours of Afghanistan, and William and Kate Middleton had recently tied the knot at Westminster Abbey in a blaze of national good will.
It would have been such a gift to her heirs if at that glorious moment Elizabeth II had stepped aside, as Margrethe II, the queen of Denmark, did in January 2024. After 52 years on the throne, she announced her abdication in her New Year’s address with the elegant explanation that “the time takes its toll.”
Instead, Elizabeth II stayed on some 10 years — to the end. Apparently to honor her oath to serve “my whole life, whether it be long or short,” but actually because she loved her job. She had seen how bored and marginalized the Queen Mother felt when, widowed young by George VI and deprived of power dinners with heads of state or the inside scoop from her husband’s tête-à-têtes with the prime minister, she was relegated to boring rounds of cutting ribbons in those huge feathery hats . No, Elizabeth II loved the world of politics and power as much as she did breeding horses and tramping the heather of her Balmoral estate.
But her 70-year reign has left a pileup of heirs infantilized by too little to do and trapped by a dusty structure that should have been reformed decades ago.
Charles, full of prescient ideas, inventive concepts of philanthropy and imaginative plans of how to modernize the monarchy, saw his hopes and dreams curdle as he waited and waited to put them into action. The beleaguered flexitarian was allowed to marry the woman he loved only when he was 56 years old. Even with the best prognosis for his cancer, he has been left with a rueful rump of a reign. His sad-sack motto was always “just my luck,” but that has never seemed more true than now.
And William, instead of taking over the Duchy of Cornwall estates in his early 30s and creating a space for the popular Harry to develop a strong portfolio of his own, ended up in a rivalrous relationship with his younger brother that exploded irretrievably when Meghan Markle entered the scene. A less hidebound palace might have come up with a more creative way to solve the Sussex imbroglio.
The fascination of the crown will always be the tension between a venerable institution and the human beings who are trapped inside it. Isn’t it just too cruel to expect modern mortals to live and love and parent in such a blisteringly unforgiving media gaze?
Catherine is battling more — much more — than cancer. A tidal wave of premature responsibility is crashing in her and William’s direction. Frozen, unready and with Catherine now seriously unwell, the Prince and Princess of Wales await the awesome burden of the crown.
Tina Brown is the author of “The Diana Chronicles” and “The Palace Papers.”
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
I Hope You All Feel Terrible Now
How the internet—and Stephen Colbert—hounded Kate Middleton into revealing her diagnosis

Updated at 4:04 p.m ET on March 22, 2024
For many years, the most-complained-about cover of the British satirical magazine Private Eye was the one it published in the week after the death of Diana, Princess of Wales, in 1997. At the time, many people in Britain were loudly revolted by the tabloid newspapers that had hounded Diana after her divorce from Charles, and by the paparazzi whose quest for profitable pictures of the princess ended in an underpass in Paris.
Under the headline “Media to Blame,” the Eye cover carried a photograph of a crowd outside Buckingham Palace, with three speech bubbles. The first was: “The papers are a disgrace.” The next two said: “Yeah, I couldn’t get one anywhere” and “Borrow mine, it’s got a picture of the car.” People were furious. Sacks of angry, defensive mail arrived for days afterward, and several outlets withdrew the magazine from sale. (I am an Eye contributor, and these events have passed into office legend.) But with the benefit of hindsight, the implication was accurate: Intruding on the private lives of the royals is close to a British tradition. We Britons might have the occasional fit of remorse, but that doesn’t stop us. And now, because of the internet, everyone else can join in too.
Read: Just asking questions about Kate Middleton
That cover instantly sprang to mind when, earlier today, the current Princess of Wales announced that she has cancer. In a video recorded on Wednesday in Windsor, the former Kate Middleton outlined her diagnosis in order to put an end to weeks of speculation, largely incubated online but amplified and echoed by mainstream media outlets, about the state of her health and marriage.
Kate has effectively been bullied into this statement, because the alternative—a wildfire of gossip and conspiracy theories—was worse. So please, let’s not immediately switch into maudlin recriminations about how this happened. It happened because people felt they had the right to know Kate’s private medical information. The culprits may include three staff members at the London hospital that treated her, who have been accused of accessing her medical records, perhaps driven by the same curiosity that has lit up my WhatsApp inbox for weeks. Everyone hates the tabloid papers, until they become them.
In her statement, Kate said that after her abdominal surgery earlier in the year, which the press was told at the time was “planned”—a word designed to minimize its seriousness—later tests revealed an unspecified cancer. She is now undergoing “preventative chemotherapy,” but has not revealed the progression of the disease, or her exact prognosis. “I am well,” she said, promising that she is getting stronger every day. “I hope you will understand that as a family, we now need some time, space and privacy while I complete my treatment.”
This news will surely make many people feel bad. The massive online guessing game about the reasons for Kate’s invisibility seems far less fun now. Stephen Colbert’s “spilling the tea” monologue , which declared open season on the princess’s marriage, should probably be quietly interred somewhere. The sad simplicity of today’s statement, filmed on a bench with Kate in casual jeans and a striped sweater, certainly gave me pause. She mentioned the difficulty of having to “process” the news, as well as explaining her condition to her three young children in terms they could understand. The reference to the importance of “having William by my side” was pointed, given how much of the speculation has gleefully dwelt on the possibility that she was leaving him or vice versa.
Read: The eternal scrutiny of Kate Middleton
However, the statement also reveals that the online commentators who suggested that the royal household was keeping something from the public weren’t entirely wrong. Kate’s condition was described as noncancerous when her break from public life was announced in late January . The updated diagnosis appears to have been delivered in February, around the time her husband, Prince William, abruptly pulled out of speaking at a memorial service for the former king of Greece. Today’s statement represents a failure of Kensington Palace to control the narrative: first, by publishing a photograph of Kate and her children that was so obviously edited that photo agencies retracted it, and second, by giving its implicit permission for the publication of a grainy video of the couple shopping in Windsor over the weekend. Neither of those decisions quenched the inferno raging online—in fact, they fed it.
Some will say that Kate has finally done what she should have done much earlier: directly address the rumors in an official video, rather than drip-feed images that raised more questions than they answered. King Charles III has taken a different approach to his own (also unspecified) cancer, allowing footage to be filmed of him working from home. But then again, Kate has cancer at 42, is having chemo, and has three young children. Do you really have it in you to grade her media strategy and find it wanting?
Ironically, Britain’s tabloid papers have shown remarkable restraint; as I wrote earlier this month , they declined to publish the first paparazzi pictures of Kate taken after her withdrawal from public life. They have weighted their decisions toward respect and dignity—more so than the Meghan stans, royal tea-spillers, and KateGate theorists, who have generated such an unstoppable wave of interest in this story that its final destination was a woman with cancer being forced to reveal her diagnosis. If you ever wanted proof that the “mainstream media” are less powerful than ever before, this video of Kate Middleton sitting on a bench is it.

IMAGES
VIDEO
COMMENTS
Family Genetics and Associated Risks of Developing Prostate Cancer. Prostate cancer is the most common cancer in men, and occurs in the male reproductive system (Williams, 2013). Few known and many unknown risk factors are related to prostate cancer, including family history, age and diet (Zatzkin, 2013.) Prostate cancer has many unclear and ...
Treating Metastatic Prostate Cancer If prostate cancer is diagnosed after it has spread beyond the prostate and its immediate environs or if the cancer returns after surgery or radiation, treatment with hormone therapy to lower testosterone levels is typically initiated. Because prostate cancer growth is fueled by testosterone,
Symptoms. Prostate cancer may cause no signs or symptoms in its early stages. Prostate cancer that's more advanced may cause signs and symptoms such as: Trouble urinating. Decreased force in the stream of urine. Blood in the urine. Blood in the semen.
Prostate cancer overall has a strong five-year survival rate, thanks in part to these treatment methods. If the cancer hasn't spread to other parts of the body, the chance of recovery is about 99%.
Cancer begins when healthy cells in the prostate change and grow out of control, forming a tumor. A tumor can be cancerous or benign. A cancerous tumor is malignant, meaning it can grow and spread to other parts of the body. A benign tumor means the tumor can grow but will not spread. Prostate cancer is somewhat unusual when compared with other ...
Worldwide, prostate cancer is the most commonly diagnosed male malignancy and the fifth leading cause of cancer death in men.[1][2] This amounted to 1,414,249 newly diagnosed cases and 375,000 deaths worldwide yearly from this disease in 2020.[1][2][3][4][5] Globally, prostate cancer is the most commonly diagnosed malignancy in more than fifty percent of countries (112 of 185).[6]
Five papers reported men's perceptions of the causes of prostate cancer. 15-19 Prostate cancer was seen as a common terminal disease caused by ageing; men likened it to a machine wearing out with use. 17 20 Some men also named diet, environment and genetics as causes 20; others identified healthy behaviour as reducing the likelihood of ...
The management of prostate cancer continues to evolve rapidly, with substantial advances being made in understanding the genomic landscape and biology underpinning both primary and metastatic prostate cancer. Similarly, the emergence of more sensitive imaging methods has improved diagnostic and staging accuracy and refined surveillance strategies. These advances have introduced personalised ...
1. Introduction. Prostate cancer affects middle-aged men between the ages of 45 and 60 and is the highest cause of cancer-associated mortalities in Western countries [].Many men with prostate cancer are diagnosed by prostate biopsy and analysis, prostate-specific antigen (PSA) testing, digital rectal examination, magnetic resonance imaging (MRI), or health screening.
Age, race, and family history are the strongest established risk factors for prostate cancer 11.On the basis of SEER data, the age-adjusted incidence per 100,000 men in 2014 was 218.3 for 50-64 ...
Show abstract. ... Prostate cancer is the most common cancer among men, and is the second-leading cause of cancer deaths in men in the United States [1]. Treatment methods include hormone therapy ...
Abstract. Prostate Cancer is a disease in which there is an uncontrolled growth of cells that lines the ducts of the prostate gland. The abnormal cells can spread throughout the prostate and nearby organs, such as the seminal vesicles. If not caught early they can spread (metastasized) to other organs of the body through the lymph or blood stream.
The Prostate Cancer Prevention Trial showed that finasteride can reduce the risk of prostate cancer, but might increase the risk of aggressive disease. NCI's Howard Parnes talks about subsequent findings and what they mean for men aged 55 and older. Darolutamide Delays the Spread of Some Prostate Cancers.
Essay: Raising awareness about prostate cancer. Other than skin cancer, prostate cancer is the most common cancer in men and is the second most common cause of cancer death in the United States ...
Cancer of the prostate, a common form of cancer, is a disease in which cancer (malignant) cells are found in the prostate. The prostate is on the male sex glands, and is located just below the bladder and in front of the rectum. The size of the prostate is about the size of a walnut. It surrounds the part of the urethra, the tube that carries ...
Prostate cancer refers to the malignant growth of glandular cells located in the prostate. At the age of 85, a man is said to have a 1 in 5 chances of developing prostate cancer sometime in their life. Unfortunately Prostate cancer is a disease that does not give any warning signs when it is. 4196 Words. 17 Pages.
Prostate Cancer - Essay Sample. Abstract. Prostate cancer is the second most common type of cancer diagnosed in men around the world today. Despite years of research, little is known as to the exact cause of prostate cancer, making it an area of intense research in medicine today. The pathology of prostate cancer has yielded important ...
Prostrate Cancer. Prostate cancer is the cancer of the prostate glands. Prostate gland is a small walnut sized organ and an important part of a man's reproductive system. It is one of the most common forms of cancer in men aged above 75 years. The incidence of prostate cancer in men younger than the age of 40 is very rare.
Guest Essay. Not Everything We Call Cancer Should Be Called Cancer. Aug. 30, 2023 ... A long-term study of 1,800 men with low- or very low-risk prostate cancer begun in 1995 found that within the ...
Prostate cancer is the most common cancer for men in the United States. Luckily, most men with prostate cancer will still be alive 15 years after diagnosis. Men with prostate cancer that hasn't spread outside the gland have several treatment choices. These include surgery, radiation therapy, and active surveillance, where treatment is delayed ...
As Stiller notes in his essay, for most average-risk men who decide to get screened, testing will start at age 50.Men at high risk of developing prostate cancer, like African Americans or men with a father, brother or son who had prostate cancer at an early age, should discuss screening at age 45, while men with more than one first-degree relative with early prostate cancer should talk to ...
An enlarged prostate or potential prostate cancer is a common issue for older men. There will be approximately 300,000 new cases of prostate cancer in the U.S. this year.
Prostate cancer is the most common form of cancer that affects British men, with about 52,000 cases annually, according to Cancer Research UK senior science engagement manager Rupal Mistry.
452 Words. 2 Pages. Open Document. One of the most common cancers to be diagnosed in men, prostate cancer has a good prognosis when diagnosed early. Approximately 2.8 million men in the United States have prostate cancer. Raising awareness for this type of cancer is key in being able to detect this cancer early and saving more lives.
For this study, 115 men with prostate cancer were recruited at 13 hospitals in five countries and given the ultrasound treatment, researchers said. The procedure can be performed in an outpatient ...
PURPOSE: Deep learning methods for classifying prostate cancer (PCa) in ultrasound images typically employ convolutional networks (CNNs) to detect cancer in small regions of interest (ROI) along a needle trace region. However, this approach suffers from weak labelling, since the ground-truth histopathology labels do not describe the properties of individual ROIs. Recently, multi-scale ...
All papers were reviewed by AJLK and additional reviewers including co‐authors, members of the advisory group and patients with prostate cancer from a local support group. All included papers were critically appraised independently by two reviewers using the Critical Appraisal Skills Programme quality appraisal tool as an integral part of the ...
Ms. Brown is the author of "The Diana Chronicles" and "The Palace Papers." I was in London last week when the febrile madness of Where Is Kate? was blowing up social media, and the Curious ...
The first was: "The papers are a disgrace." The next two said: "Yeah, I couldn't get one anywhere" and "Borrow mine, it's got a picture of the car." People were furious.
Prostate cancer is the most prevalent nonskin cancer among men in the United States and is the second leading cause of cancer death in men. While prostate cancer is most regularly diagnosed in men at the age of 65 years and older, the occurrence can begin at 50. One in 6 men will be diagnosed with prostate cancer during their lifetime.