Mental Health and Substance Use Co-Occurrence Among Indigenous Peoples: a Scoping Review
- Original Article
- Open access
- Published: 28 July 2023

Cite this article
You have full access to this open access article

- Breanne Hobden ORCID: orcid.org/0000-0002-8489-6152 1 , 2 ,
- Megan Freund 1 , 2 ,
- Jennifer Rumbel 3 , 4 ,
- Todd Heard 1 , 4 , 5 ,
- Robert Davis 1 , 2 ,
- Jia Ying Ooi 1 , 2 ,
- Jamie Newman 6 ,
- Bronwyn Rose 7 ,
- Rob Sanson-Fisher 1 , 2 &
- Jamie Bryant 1 , 2
1643 Accesses
Explore all metrics
This scoping review examined the literature on co-occurring mental health conditions and substance use among Indigenous peoples globally across (i) time, (ii) types of conditions examined, (iii) countries, (iv) research designs, and (v) participants and settings. Medline, Embase, PsycInfo, and Web of Science were searched across all years up until October 2022 for relevant studies. Ninety-four studies were included, with publications demonstrating a slight and gradual increase over time. Depressive disorder and alcohol were the most examined co-occurring conditions. Most studies included Indigenous people from the United States (71%). Ninety-seven percent of the studies used quantitative descriptive designs, and most studies were conducted in Indigenous communities/reservations (35%). This review provides the first comprehensive exploration of research on co-occurring mental health and substance use conditions among Indigenous peoples. The information should be used to guide the development of strategies to improve treatment and prevention.
Similar content being viewed by others

Substance use disorders in Saudi Arabia: a scoping review

Substance Use Disorders Among Forcibly Displaced People: a Narrative Review
Community-based psychosocial substance use disorder interventions in low-and-middle-income countries: a narrative literature review
Avoid common mistakes on your manuscript.
Both between and within countries, Indigenous’ Peoples represent diverse groups with unique perspectives on health and wellbeing. Broadly, Aboriginal and Torres Strait Islander people in Australia view health with the perspective that a holistic and whole-of-life approach is needed to achieve positive health and wellbeing outcomes (Australian Government, 2017 ). This sentiment is echoed by Indigenous groups in the United States (US), Canada, and Aotearoa (New Zealand), where physical health is linked with mental, social, and spiritual wellbeing (Gall et al., 2021 ; Hodge et al., 2009 ; Mark & Lyons, 2010 ). Colonisation continues to impact the health of Indigenous people through ongoing intergenerational trauma and discriminatory systemic policies (Australian Institute of Health & Welfare, 2022 ; O’Neill et al., 2018 ; Te Kōmihana Whai Hua O Aotearoa (New Zealand Productivity Commission), 2022). This impact is apparent through the disproportionate prevalence of mental health (MH) conditions and severity of substance use among Indigenous people. In Australia in 2011, MH conditions and substance use disorders contributed to 23% of the total burden of disease for Aboriginal and Torres Strait Islander people, the largest burden out of any disease group (Australian Institute of Health & Welfare, 2016 ). Similar overrepresentation of MH conditions and substance use has been reported for Maori people in Aotearoa (Ministry of Health New Zealand, 2018 ). Reducing the impact and severity of MH conditions and substance use is important for improving the health and wellbeing of Indigenous people.
While previous research has examined the published literature examining MH conditions or substance use among Indigenous peoples (Kisely et al., 2017 ; Nelson & Wilson, 2017 ), the scope of research examining the co-occurrence of these conditions is less clear. Co-occurring conditions often have an exacerbating and debilitating impact on the health of affected individuals (Leung et al., 2016 ). Co-occurrence is associated with greater severity of MH symptoms, higher quantity of substance use, increased disability or impairment, poorer social functioning, and increased risk of suicide (Burns & Teesson, 2002 ; Leung et al., 2016 ; Quello et al., 2005 ). Co-occurring conditions have also been reported to significantly impact family and carers (Biegel et al., 2007 ; September & Beytell, 2019 ). Considering co-occurring conditions, as opposed to individual conditions, provides a more person-focussed and integrated approach to wellbeing (Mercer et al., 2016 ). Integrated treatment of co-occurring conditions has also demonstrated improved treatment outcomes (Leung et al., 2016 ). Despite this, most research and treatment provision continues to adopt an approach where researchers and clinicians focus on singular conditions (McCartney, 2016 ; Teesson et al., 2014 ).
To the authors’ knowledge, no previous review has systematically examined the literature for co-occurring MH conditions and substance use among Indigenous’ people, nationally or internationally. Scoping reviews allow exploration of the volume and coverage of particular topics to identify gaps, concepts, and key characteristics, as well as informing the feasibility of more detailed systematic reviews (Munn et al., 2018 ). The number of research outputs in an area of research can be considered a proxy for resource and investment in a particular field (Ebadi & Schiffauerova, 2016 ), allowing funding bodies to identify areas where research activity is lacking. Furthermore, examining the scope of the literature, such as location, design, setting, and focus, will allow the identification of research gaps to inform future research and policy directions regarding co-occurring MH conditions and substance use among Indigenous peoples (Munn et al., 2018 ).
To systematically review studies examining co-occurring MH conditions and substance use among Indigenous peoples globally to determine the scope of publications in terms of (i) volume over time, (ii) MH conditions and substance conditions examined, (iii) countries where the research was undertaken, (iv) research designs implemented, and (v) included Indigenous groups and settings.
Methodology is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) scoping review guidelines (Page et al., 2021 ; Tricco et al., 2018 ).
Indigenous Leadership for This Review
This review concept arose through collaboration between Indigenous and non-Indigenous researchers and those working in the health field on an Australian Rotary Health Fellowship to understand the co-occurrence of MH conditions and substance use among Aboriginal and Torres Strait Islander Peoples. Co-authors JR, TH, RD, JN, and BR are Aboriginal members of the team and formed the Aboriginal Advisory Group for this project. In addition to lived experiences, the Aboriginal Advisory Group has expertise in mental health, substance use, and health services. The remaining authors are non-Indigenous. The aims of the review were discussed and revised through ongoing collaborative discussion with the whole research team. Study methodology and interpretation of results were discussed and reviewed by Indigenous and non-Indigenous team members throughout the project.
Search Strategy
A medical librarian was consulted to develop and implement the search strategy. Medline, Embase, PsycInfo, and Web of Science were searched across all years up until 11th October 2022. Key terms included “mental disorders”, “substance related disorders”, “comorbidity” and “Indigenous peoples”. A full list of the search terms used can be found in Appendix 1 . A manual review of the reference lists of included papers was performed to identify any additional articles not identified through the search strategy.
Inclusion and Exclusion Criteria
Studies were included in the review if they:
Focussed on Indigenous peoples. Studies were identified through the use of terms such as “Indigenous”, “First Nations”, “Aboriginal” or referring to the name of a specific Indigenous peoples (e.g. Maori). If the research included both Indigenous and non-Indigenous peoples, comorbidity data needed to be presented separately for the Indigenous cohort or more than 50% of the sample needed to be Indigenous to be included. This criterion was intended to reduce the number of studies that incidentally included Indigenous peoples but did not specifically explore comorbidity among these groups.
Reported on comorbidity across at least one MH condition and one type of substance use. The type of comorbidity examined, and the determination of comorbidities was deliberately broad to enable a more inclusive scoping approach (see Box 1).
Described data-based research, including experimental, quantitative, and qualitative studies.
Box 1 Categorisation of conditions.
Studies were excluded if they:
Exclusively reported on suicide, suicide ideation, suicide attempts, and learning disorders as these are not considered MH conditions.
Exclusively focussed on gambling or gaming addictions as these are not substance-based. Studies which included gambling or gaming addiction and substance addiction were included, but only substance data were extracted.
Focussed on basic sciences (e.g. genetic studies).
Were commentaries, case studies, conference abstracts, theses, or reviews.
Were published in a language other than English.
Article Screening
Paper titles and abstracts were reviewed against the inclusion criteria by three authors (BH, JR, and JYO) and a research assistant. The first 108 papers were independently coded by two researchers (BH and JR or the research assistant) and checked for agreement. There was an 88% agreement rate between coders after initial coding. Discrepancies were discussed until consensus was reached. Following this, JR and the research assistant screened the remaining studies. All excluded studies were cross-checked by JYO at a later date. BH and JYO reviewed the full texts for final inclusion.
Data Extraction
A data extraction template was created using REDCap electronic data capture tools (Harris et al., 2019 ). This was piloted by JB, MF, and JYO with BH making amendments before commencing full data extraction. The following data were extracted from the included studies: author, year, conditions examined and how conditions were assessed (e.g. diagnostic interview), country, Indigenous population group, research design, sample size, and setting. Studies were categorised into experimental, qualitative, or quantitative descriptive research designs. Experimental studies were then coded as randomised-controlled trials, non-randomised controlled trials, interrupted time series, or controlled before and after studies (Cochrane Effective Practice & Organisation of Care, 2017 ). Study setting was categorised based on anticipated settings for MH conditions and substance use research (e.g. general community, Indigenous communities, MH or substance use services, hospitals), with author derived coding for additional settings (e.g. legal settings, such as detention centres). Where multiple papers were derived from one study, data were extracted for each individual paper due to the different combinations of comorbidities examined across papers resulting from large datasets.
Data Analysis
Frequencies and proportions were used to synthesise the extracted data. A linear regression was performed to examine changes in the volume of publications over time, with a p -value of < 0.05 used to indicate significance.
Figure 1 presents the results of the literature search using the PRISMA flow chart. A total of 6049 citations were identified through the search strategy and 4 through searching reference lists, with 4534 articles retained following the removal of duplicates. A total of 3979 articles were excluded at the title and abstract screening stage, and 555 underwent full text review. Ninety-four articles met the inclusion criteria and were included in the review. For brevity, the frequencies of studies are presented in-text without specific references. The Supplementary file ( S1 ), however, provides the detailed data extraction for each included paper.
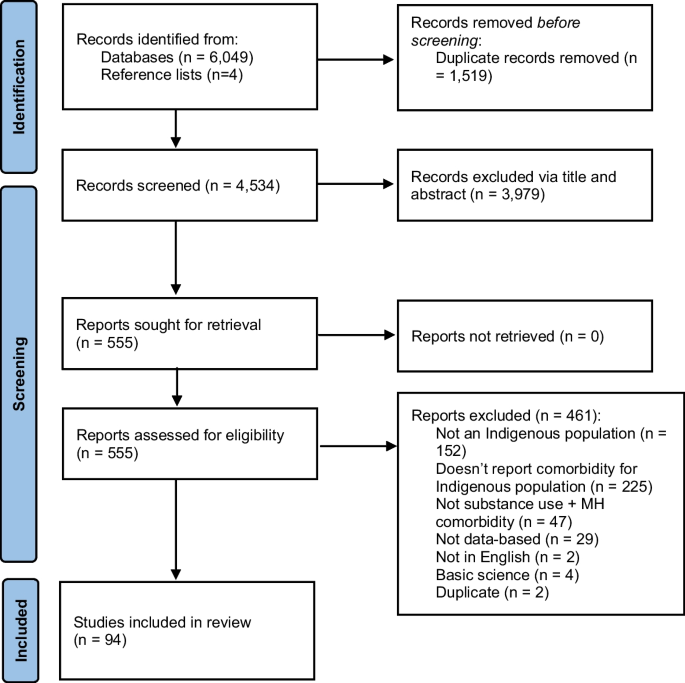
Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow chart
Volume of Publications Over Time
While publications demonstrated a statistically significant increase over time from 1990 to 2022 ( R 2 = 0.26, p -value = 0.003), the volume of publications was low across most years. An average of 2.8 papers were published per year since 1990. From 1990 to 2000, there were an average of 1.3 publications per year ( n = 14 total), which increased from 2001 to 2011 and 2012 to 2022, with an average of 3.4 ( n = 37 total) and 3.8 ( n = 42 total) per year, respectively (see Fig. 2 ).
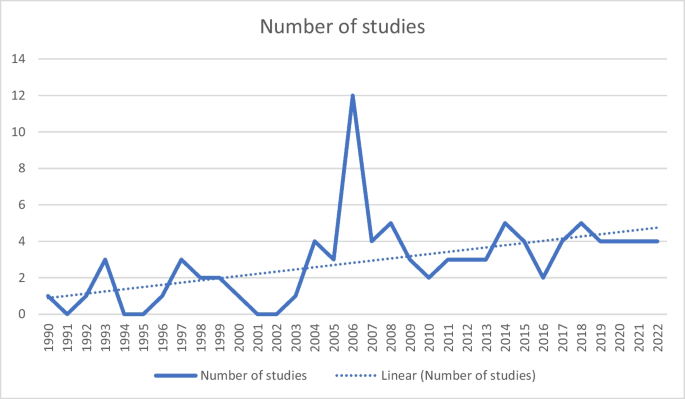
The number of studies examining comorbid mental health conditions with alcohol and other drug use by year
Co-Occurring Conditions Examined
Studies included an average of 2.4 MH condition groupings, and 44 papers examined three or more MH condition groupings. Among these, depressive disorders ( n = 64, 68% of studies) and anxiety disorders ( n = 49, 52%) were the most commonly examined, and eating disorders were the least frequently examined ( n = 6, 6%). MH conditions were primarily measured using diagnostic interviews ( n = 55, 59%), of which 2 studies used validated screening measures in addition to diagnostic interviews. Of the remaining studies, 20 (23%) used validated screening measures, 5 (5%) used non-validated screening measures, and 11 (12%) used medical records. One (1%) study did not report how MH conditions were measured.
For substance use, studies included an average of 1.9 substances, and 25 papers examined three or more substances. Alcohol was the most frequently examined substance ( n = 58, 62% of studies), followed by general substance use or grouping of multiple substances ( n = 45, 48%). Sedatives ( n = 3, 3%), hallucinogens ( n = 3, 3%), and inhalants ( n = 2, 2%) were the least frequently examined substances. Substances were primarily measured using diagnostic interviews ( n = 44, 47%), of which one also used non-validated screening measures. Of the remaining studies, 20 (22%) used standardised screening measures, 13 (14%) used non-validated screening measures, one (1%) study used both validated and non-validated screening measures, 11 (12%) used medical records, and two (2%) used help-seeking to indicate substance use. Three studies did not report how MH conditions were measured.
There were a broad range of co-occurring conditions examined (see Table 1 ). It was also common for papers to group MH or substance use conditions or to consider these in general terms (e.g. reporting on “substance dependence” or “MH conditions”). Alcohol and depression were the most frequently examined co-occurring conditions ( n = 17).
Countries Where the Research Was Undertaken
Most studies were conducted with Indigenous peoples from the US ( n = 67, 71%). Of these, 46 included Native American Indian Peoples, two studies included Indigenous peoples from Alaska, and 12 included both Native American Indian and Alaskan participants. Four studies included Indigenous peoples from the US and Canada, and three studies specifically included Native Hawaiian and other Pacific Islander Peoples. One study included Native American Indian, Alaskan, and Hawaiian people. Fewer studies were conducted in Australia with Aboriginal and Torres Strait Islander people ( n = 13, 14%); Canada among Indigenous Metis and Inuit people ( n = 8, 9%); and Aotearoa of which five included Māori people and one included Pacific Islander people ( n = 6, 6%). While the Pacific Islander groups (i.e. Samoan, Tongan, Cook Islanders) in the latter study are not Indigenous to Aotearoa, they are Indigenous to the Pacific Islands, and therefore, this study was retained. Two studies included Han Chinese people, one study included Malayo-Polynesian Aboriginal people from Taiwan, and one study included Malay people from Malaysia (see Fig. 3 ).
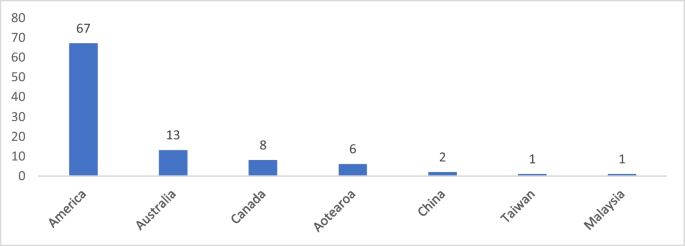
The number of studies examining comorbid mental health and alcohol or other drug use by country. Note: Four studies included Indigenous people from the United States and Canada and have been counted for both countries
Research Designs Implemented
Almost all publications used quantitative descriptive designs ( n = 91, 97%). One study used a mixed method design, including a qualitative phase followed by a randomised controlled trial. One study used a randomised controlled trial design, and one study used a qualitative design. Among the descriptive studies, 79 (87%) used a cross-sectional design, nine (10%) used a longitudinal design, and two (2%) used a cross-sequential design.
Indigenous Sample and Settings
Sixty-nine (73%) of the included studies included only Indigenous participants, while the remaining 25 (27%) included both Indigenous and non-Indigenous people. Only one study had a sample where more than 50% were Indigenous with the outcomes combining both Indigenous and non-Indigenous data (Woodall et al., 2007 ). The remaining studies that included non-Indigenous participants reported the findings separately for the Indigenous participants. The sample ranged from 15 to 16,640 Indigenous participants, with an average of 1387. Most studies were conducted within Indigenous communities/reservations ( n = 33, 35%) or a general/population-based sample ( n = 28, 30%), of which two studies were conducted within the general population and a reservation (see Fig. 4 ).
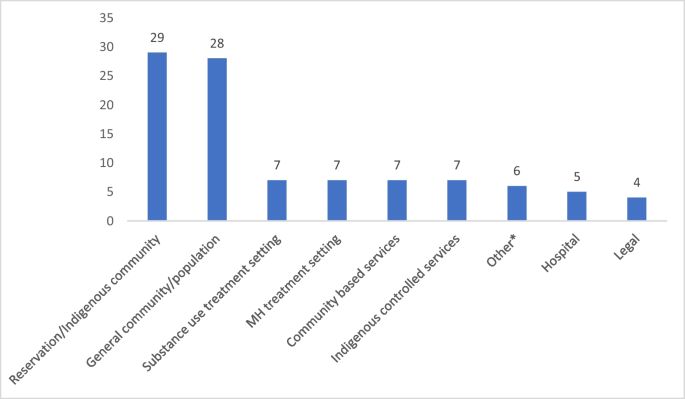
The number of studies examining mental health conditions with alcohol and other drug use by setting. Note: Some studies included multiple settings and have been counted multiple times. *“Other” settings included a homeless community, veteran affairs services, education facilities, and a remote area mental health service database
The number of studies examining co-occurring MH conditions and substance use in Indigenous peoples has increased over time; however, the average number of publications per year was low. This modest increase does not reflect the growth in research outputs in Indigenous health generally in recent decades (Bryant et al., 2022 ; Derrick et al., 2012 ; Kennedy et al., 2022 ), which has been coupled with growing investment and capacity in the MH field for Indigenous peoples in several countries. A recent review of Aboriginal and Torres Strait Islander health in Australia found that 20.5% of all Indigenous health research conducted from 2008 to 2020 was focussed on MH or substance use disorders (Kennedy et al., 2022 ). There was a peak for paper outputs in 2006. These publications reported on studies that were conducted across a range of years, from 1994 to 2004. Furthermore, nine papers published in 2006 reported the outcomes for four individual studies. Although it is difficult to interpret the reasons for the 2006 peak in paper publications, it may reflect researchers’ capacity to publish in a timely manner rather than any policy or funding factors.
Included studies explored a range of comorbidities. It was common for studies to include generalised groupings of MH conditions or substance use. The co-occurrence of depression and alcohol use was the most examined comorbidity, which likely reflects the high prevalence of both of these conditions (GBD 2016 Alcohol Collaborators, 2018 ; Liu et al., 2020 ). There has been limited exploration of substance use with MH conditions such as eating disorders or bipolar disorders. Similarly, MH comorbidities with opioids and stimulants have been limited, although it is likely that these substances have been included in some studies which have explored general substance use. There is significant scope for research exploring several co-occurring MH conditions and substances among Indigenous people, for both prevalence and prevention or treatment strategies. The method of measuring conditions is an important consideration for future research to ensure accuracy in the data provided. While measurement of MH conditions and substance use varied across the studies, this was primarily conducted via diagnostic clinical interviews. This method provides clinical accuracy; however, it may not account for subthreshold symptoms, which have been found to be a significant contributor to burden and disability (Rai et al., 2010 ). The use of validated MH and substance use measures, which allow for exploration of different levels of severity, may therefore be more relevant for understanding comorbidity burden in Indigenous communities rather than via diagnostic interviews.
A substantial majority of the studies were conducted within the US. The output across countries can likely be attributed to variation in research capacity and support. The US was ranked number one for research outputs from 1996 to 2021, far surpassing Canada, Australia, and Aotearoa’s outputs combined (SCImago, 2022 ). In addition, leading US mental health groups have advocated for addressing co-occurring MH conditions and substance use, as well as a need for integrated health systems (Mental Health America, 2017 ; Substance Abuse & Mental Health Services Administration, 2022 ). This review highlights the need for increased research capacity in co-occurring MH conditions and substance use within distinct and unique Indigenous communities in most countries.
Experimental research is important for providing robust evidence for the effectiveness of treatment approaches. However, only two experimental studies (2%) were identified in this review. This finding is similar to a recent review that found only 2.7% of research on Aboriginal and Torres Strait Islander health in Australia used an experimental design (Kennedy et al., 2022 ). Qualitative research was also only utilised in two identified studies. Qualitative research is important for understanding the views and perceptions of Indigenous people (Auger, 2016 ). It allows insight into the factors that contribute to the co-occurrence of MH conditions and substance use and can better inform future research, policy, and practice. Further investment in Indigenous-led qualitative research is needed to allow for Indigenous people’s knowledge and experience to inform future prevention and treatment-focussed research in this field.
Future Directions
There is a need to increase research examining co-occurring MH conditions and substance use to break down the existing silos in research and treatment and promote integrated care for Indigenous peoples. While consideration of international research can provide some guidance on co-occurring MH conditions and substance use, the unique and diverse Indigenous communities within and between countries require localised data to inform healthcare delivery and policy. Despite several quantitative studies within the US, consideration of prevalence is still needed for all countries to inform needs within distinct communities, specific comorbidities, gender, and age groups. This scoping review intended to provide a surface-level understanding of MH conditions and substance use comorbidity among Indigenous people; however, more in-depth exploration of the research in this area should be considered, such as assessing the quality of quantitative studies and the cultural appropriateness of measures examining MH conditions and substance use. Qualitative research is an important avenue for future work, which will allow for a deeper understanding of strategies for prevention and care that are important for local Indigenous communities. This should be followed by robustly designed experiment studies testing the effectiveness of strategies to prevent and manage co-occurring conditions. Ensuring holistic strategies are developed, accounting for the wider social context in which Indigenous people exist, is also important. This includes consideration of systemic racism and the ongoing, pervasive impact of colonisation.
Limitations
For pragmatic reasons, the search for relevant studies was limited to the English language, which resulted in two studies published in other languages being omitted. This may have included studies that have been published in Indigenous languages. While the search strategy was designed to be broad and capture relevant studies, the diversity of Indigenous groups globally, with hundreds of unique tribes, nations, and clans, may have meant that some studies may have been missed. It was also not possible for the title and abstract screening to be conducted independently by two reviewers in parallel due to staffing constraints, and therefore, this was done sequentially. Nevertheless, all papers returned in the search did undergo independent coding by at least two reviewers. One study did not report outcomes separately for Indigenous and non-Indigenous participants, so some non-Indigenous data was included in the results. However, more than half the participants in this study were Indigenous.
Research commitment and expertise in exploring comorbidity prevention and treatment strategies for Indigenous people is needed. This scoping review highlights several gaps in the field of co-occurring MH conditions and substance use among Indigenous peoples. This includes limited research conducted with Indigenous groups outside of the US and a lack of qualitative or experimental research. Further work is needed to understand the extent and impact of comorbidity among Indigenous people. Future studies should be Indigenous-led with locally informed strategies as well as consultation with Indigenous communities.
Data Availability
Extracted data relevant to the study is available in the Supplementary File ( S1 ).
Almeida, O. P., Flicker, L., Fenner, S., Smith, K., Hyde, Z., Atkinson, D., Skeaf, L., Malay, R., & LoGiudice, D. (2014). The Kimberley assessment of depression of older Indigenous Australians: Prevalence of depressive disorders, risk factors and validation of the KICA-dep scale. PLoS ONE, 9 (4), e94983.
Article PubMed PubMed Central Google Scholar
Amu, H., Osei, E., Kofie, P., Owusu, R., Bosoka, S. A., Konlan, K. D., Kim, E., Orish, V. N., Maalman, R.S.-E., & Manu, E. (2021). Prevalence and predictors of depression, anxiety, and stress among adults in Ghana: A community-based cross-sectional study. PLoS ONE, 16 (10), e0258105.
Article CAS PubMed PubMed Central Google Scholar
Auger, M. (2016). Cultural continuity as a determinant of Indigenous peoples’ health: A metasynthesis of qualitative research in Canada and the United States. The International Indigenous Policy Journal , 7 (4). https://doi.org/10.18584/iipj.2016.7.4.3
Australian Government. (2017). National Strategic Framework for Aboriginal and Torres Strait Islander Peoples’ Mental Health and Social and Emotional Wellbeing 2017–2023. https://www.niaa.gov.au/sites/default/files/publications/mhsewb-framework_0.pdf . Accessed 18 July 2023
Australian Institute of Health and Welfare. (2016). Australian burden of disease study: Impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2011. Canberra: AIHW. Australian Government. https://doi.org/10.25816/xd60-4366
Australian Institute of Health and Welfare. (2022). Determinants of health for Indigenous Australians. AIHW, Australian Government. https://www.aihw.gov.au/reports/australias-health/social-determinants-and-indigenous-health . Accessed 18 July 2023
Baxter, J., Kingi, T. K., Tapsell, R., Durie, M., & McGee, M. A. (2006). Prevalence of mental disorders among Maori in Te Rau Hinengaro: The New Zealand mental health survey. Australian and New Zealand Journal of Psychiatry, 40 (10), 914–923. https://doi.org/10.1111/j.1440-1614.2006.01911.x
Article PubMed Google Scholar
Beals, J., Manson, S. M., Whitesell, N. R., Spicer, P., Novins, D. K., & Mitchell, C. M. (2005). Prevalence of DSM-IV disorders and attendant help-seeking in 2 American Indian reservation populations. Archives of General Psychiatry, 62 (1), 99–108.
Beals, J., Novins, D. K., Spicer, P., Whitesell, N. R., Mitchell, C. M., Manson, S. M., Amer Indian Service, U. (2006). Help seeking for substance use problems in two American Indian reservation populations. Psychiatric Services, 57 (4), 512–520. https://doi.org/10.1176/appi.ps.57.4.512
Beals, J., Piasecki, J., Nelson, S., Jones, M., Keane, E., Dauphinais, P., Red Shirt, R., Sack, W. H., & Manson, S. M. (1997). Psychiatric disorder among American Indian adolescents: Prevalence in Northern Plains youth. Journal of the American Academy of Child & Adolescent Psychiatry, 36 (9), 1252–1259. https://doi.org/10.1097/00004583-199709000-00018
Article CAS Google Scholar
Biegel, D. E., Ishler, K. J., Katz, S., & Johnson, P. (2007). Predictors of burden of family caregivers of women with substance use disorders or co-occurring substance and mental disorders. Journal of Social Work Practice in the Addictions, 7 (1–2), 25–49. https://doi.org/10.1300/J160v07n01_03
Article Google Scholar
Bryant, J., Freund, M., Ries, N., Garvey, G., McGhie, A., Zucca, A., Hoberg, H., Passey, M., & Sanson-Fisher, R. (2022). Volume, scope, and consideration of ethical issues in Indigenous cognitive impairment and dementia research: A systematic scoping review of studies published between 2000–2021. Dementia, 21 (8), 2647–2676. https://doi.org/10.1177/14713012221119594
Burns, L., & Teesson, M. (2002). Alcohol use disorders comorbid with anxiety, depression and drug use disorders: Findings from the Australian National Survey of Mental Health and Well Being. Drug and Alcohol Dependence, 68 (3), 299–307.
Cao, L., Burton, V. S., Jr., & Liu, L. (2018). Correlates of illicit drug use among Indigenous peoples in Canada: A test of social support theory. International Journal of Offender Therapy and Comparative Criminology, 62 (14), 4510–4527. https://doi.org/10.1177/0306624x18758853
Charlson, F., Gynther, B., Obrecht, K., Waller, M., & Hunter, E. (2021). Multimorbidity and vulnerability among those living with psychosis in Indigenous populations in Cape York and the Torres Strait. Australian and New Zealand Journal of Psychiatry, 55 (9), 892–902. https://doi.org/10.1177/0004867420984832
Cheng, A. T., Gau, S.-F., Chen, T. H., Chang, J.-C., & Chang, Y.-T. (2004). A 4-year longitudinal study on risk factors for alcoholism. Archives of General Psychiatry, 61 (2), 184–191.
Chisolm, D. J., Mulatu, M. S., & Brown, J. R. (2009). Racial/ethnic disparities in the patterns of co-occurring mental health problems in adolescents in substance abuse treatment. Journal of Substance Abuse Treatment, 37 (2), 203–210. https://doi.org/10.1016/j.jsat.2008.11.005
Cochrane Effective Practice and Organisation of Care. (2017). What study designs should be included in an EPOC review? EPOC resources for review authors . https://epoc.cochrane.org/resources/epoc-resources-review-authors . Accessed 18 July 2023
Condon, J., Robinson, G., Trauer, T., & Nagel, T. (2009). Approach to treatment of mental illness and substance dependence in remote Indigenous communities: Results of a mixed methods study. Australian Journal of Rural Health, 17 (4), 174–182. https://doi.org/10.1111/j.1440-1584.2009.01060.x
Costello, E. J., Farmer, E. M., Angold, A., Burns, B. J., & Erkanli, A. (1997). Psychiatric disorders among American Indian and white youth in Appalachia: The Great Smoky Mountains Study. American Journal of Public Health, 87 (5), 827–832.
Coughlin, L. N., Lin, L. A., Jannausch, M., Ilgen, M. A., & Bonar, E. E. (2021). Methamphetamine use among American Indians and Alaska Natives in the United States. Drug and Alcohol Dependence, 227 , 108921.
Cunningham, J. K., Solomon, T. G. A., Ritchey, J., & Muramoto, M. L. (2022). Dual diagnosis and alcohol/nicotine use disorders: Native American and White hospital patients in 3 States. American Journal of Preventive Medicine, 62 (2), e107–e116.
De Nadai, A. S., Little, T. B., McCabe, S. E., & Schepis, T. S. (2019). Diverse diagnostic profiles associated with prescription opioid use disorder in a nationwide sample: One crisis, multiple needs. Journal of Consulting and Clinical Psychology, 87 (10), 849.
Derrick, G. E., Hayen, A., Chapman, S., Haynes, A. S., Webster, B. M., & Anderson, I. (2012). A bibliometric analysis of research on Indigenous health in Australia, 1972–2008. Australian & New Zealand Journal of Public Health, 36 (3), 269–273.
Deters, P. B., Novins, D. K., Fickenscher, A., & Beals, J. (2006). Trauma and posttraumatic stress disorder symptomatology: Patterns among American Indian adolescents in substance abuse treatment. American Journal of Orthopsychiatry, 76 (3), 335–345. https://doi.org/10.1037/0002-9432.76.3.335
Dharmawardene, V., & Menkes, D. B. (2015). Substance use disorders in New Zealand adults with severe mental illness: Descriptive study of an acute inpatient population. Australasian Psychiatry, 23 (3), 236–240. https://doi.org/10.1177/1039856215586147
Dickerson, D. L., O’Malley, S. S., Canive, J., Thuras, P., & Westermeyer, J. (2009). Nicotine dependence and psychiatric and substance use comorbidities in a sample of American Indian male veterans. Drug and Alcohol Dependence, 99 (1–3), 169–175. https://doi.org/10.1016/j.drugalcdep.2008.07.014
Dillard, D., Jacobsen, C., Ramsey, S., & Manson, S. (2007). Conduct disorder, war zone stress, and war-related posttraumatic stress disorder symptoms in American Indian Vietnam veterans. Journal of Traumatic Stress, 20 (1), 53–62.
Dingwall, K. M., & Cairney, S. (2011). Detecting psychological symptoms related to substance use among Indigenous Australians. Drug and Alcohol Review, 30 (1), 33–39. https://doi.org/10.1111/j.1465-3362.2010.00194.x
Ducci, F., Enoch, M.-A., Funt, S., Virkkunen, M., Albaugh, B., & Goldman, D. (2007). Increased anxiety and other similarities in temperament of alcoholics with and without antisocial personality disorder across three diverse populations. Alcohol, 41 (1), 3–12.
Duclos, C. W., Beals, J., Novins, D. K., Martin, C., Jewett, C. S., & Manson, S. M. (1998). Prevalence of common psychiatric disorders among American Indian adolescent detainees. Journal of the American Academy of Child & Adolescent Psychiatry, 37 (8), 866–873.
Duncan, Z., Kippen, R., Sutton, K., Ward, B., Agius, P. A., Quinn, B., & Dietze, P. (2021). Correlates of anxiety and depression in a community cohort of people who smoke methamphetamine. Australian & New Zealand Journal of Psychiatry, 56 (8), 964–973. https://doi.org/10.1177/00048674211048152
Duran, B., Sanders, M., Skipper, B., Waitzkin, H., Malcoe, L. H., Paine, S., & Yager, J. (2004). Prevalence and correlates of mental disorders among Native American women in primary care. American Journal of Public Health, 94 (1), 71–77.
Ebadi, A., & Schiffauerova, A. (2016). How to boost scientific production? A statistical analysis of research funding and other influencing factors. Scientometrics, 106 (3), 1093–1116. https://doi.org/10.1007/s11192-015-1825-x
Ehlers, C. L., Gilder, D. A., Slutske, W. S., Lind, P. A., & Wilhelmsen, K. C. (2008). Externalizing disorders in American Indians: Comorbidity and a genome wide linkage analysis. American Journal of Medical Genetics Part B-Neuropsychiatric Genetics, 147B (6), 690–698. https://doi.org/10.1002/ajmg.b.30666
Ehlers, C. L., Gizer, I. R., Gilder, D. A., & Yehuda, R. (2013). Lifetime history of traumatic events in an American Indian community sample: Heritability and relation to substance dependence, affective disorder, conduct disorder and PTSD. Journal of Psychiatric Research, 47 (2), 155–161.
Emerson, M. A., Moore, R. S., & Caetano, R. (2017). Association between lifetime posttraumatic stress disorder and past year alcohol use disorder among American Indians/Alaska Natives and Non-Hispanic Whites. Alcoholism-Clinical and Experimental Research, 41 (3), 576–584. https://doi.org/10.1111/acer.13322
Federman, E. B., Costello, E. J., Angold, A., Farmer, E. M., & Erkanli, A. (1997). Development of substance use and psychiatric comorbidity in an epidemiologic study of white and American Indian young adolescents the Great Smoky Mountains Study. Drug and Alcohol Dependence, 44 (2–3), 69–78.
Article CAS PubMed Google Scholar
Fisckenscher, A., & Novins, D. (2003). Gender differences and conduct disorder among American Indian adolescents in substance abuse treatment. Journal of Psychoactive Drugs, 35 (1), 79–84. https://doi.org/10.1080/02791072.2003.10399997
Foliaki, S. A., Kokaua, J., Schaaf, D., Tukuitonga, C., Team, N. Z. M. H. S. R. (2006). Twelve-month and lifetime prevalences of mental disorders and treatment contact among Pacific people in Te Rau Hinengaro: The New Zealand Mental Health Survey. Australian & New Zealand Journal of Psychiatry, 40 (10), 924–934.
Gall, A., Anderson, K., Howard, K., Diaz, A., King, A., Willing, E., Connolly, M., Lindsay, D., & Garvey, G. (2021). Wellbeing of Indigenous peoples in Canada, Aotearoa (New Zealand) and the United States: A systematic review. International Journal of Environmental Research and Public Health, 18 (11), 5832. https://doi.org/10.3390/ijerph18115832
GBD 2016 Alcohol Collaborators. (2018). Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study. The Lancet, 392 (10152), 1015–1035.
Gilder, D. A., & Ehlers, C. L. (2012). Depression symptoms associated with cannabis dependence in an adolescent American Indian community sample. The American Journal on Addictions, 21 (6), 536–543.
Gilder, D. A., Lau, P., Corey, L., & Ehlers, C. L. (2008). Factors associated with remission from alcohol dependence in an American Indian community group. American Journal of Psychiatry, 165 (9), 1172–1178.
Gilder, D. A., Lau, P., Dixon, M., Corey, L., Phillips, E., & Ehlers, C. L. (2006). Co-morbidity of select anxiety, affective, and psychotic disorders with cannabis dependence in Southwest California Indians. Journal of Addictive Diseases, 25 (4), 67–79. https://doi.org/10.1300/J069v25n04_07
Gilder, D. A., Stouffer, G. M., Lau, P., & Ehlers, C. L. (2016). Clinical characteristics of alcohol combined with other substance use disorders in an American Indian community sample. Drug and Alcohol Dependence, 161 , 222–229. https://doi.org/10.1016/j.drugalcdep.2016.02.006
Gilder, D. A., Wall, T. L., & Ehlers, C. L. (2004). Comorbidity of select anxiety and affective disorders with alcohol dependence in Southwest California Indians. Alcoholism Clinical and Experimental Research, 28 (12), 1805–1813.
Greenfield, B. L., Sittner, K. J., Forbes, M. K., Walls, M. L., & Whitbeck, L. B. (2017). Conduct disorder and alcohol use disorder trajectories, predictors, and outcomes for indigenous youth. Journal of the American Academy of Child and Adolescent Psychiatry, 56 (2), 133–139. https://doi.org/10.1016/j.jaac.2016.11.009
Gummattira, P., Cowan, K. A., Averill, K. A., Malkina, S., Reilly, E. L., Krajewski, K., Rocha, D., & Averill, P. M. (2010). A comparison between patients diagnosed with bipolar disorder with versus without comorbid substance abuse. Addictive Disorders & Their Treatment, 9 (2), 53–63.
Harris, P., Taylor, R., Minor, B., Elliott, V., Fernandez, M., O’Neal, L., McLeod, L., Delacqua, G., Delacqua, F., Kirby, J., Duda, S., & REDCap Consortium. (2019). The REDCap consortium: Building an international community of software partners. Journal of Biomedical Informatics, 95 (103208). https://doi.org/10.1016/j.jbi.2019.103208
Hartshorn, K. J. S., Whitbeck, L. B., & Prentice, P. (2015). Substance use disorders, comorbidity, and arrest among Indigenous adolescents. Crime & Delinquency, 61 (10), 1311–1332. https://doi.org/10.1177/0011128712466372
Hautala, D., Sittner, K., & Walls, M. (2019). Onset, comorbidity, and predictors of nicotine, alcohol, and marijuana use disorders among North American Indigenous adolescents. Journal of Abnormal Child Psychology, 47 (6), 1025–1038.
He, Q., Yang, L., Shi, S., Gao, J., Tao, M., Zhang, K., Gao, C., Yang, L., Li, K., Shi, J., Wang, G., Liu, L., Zhang, J., Du, B., Jiang, G., Shen, J., Zhang, Z., Liang, W., Sun, J., … Flint, J. (2014). Smoking and major depressive disorder in Chinese women. PloS one, 9 (9), e106287. https://doi.org/10.1371/journal.pone.0106287
Heaton, L. L. (2018). Racial/ethnic differences of justice-involved youth in substance-related problems and services received. American Journal of Orthopsychiatry, 88 (3), 363–375. https://doi.org/10.1037/ort0000312
Heffernan, E., Andersen, K., Davidson, F., & Kinner, S. A. (2015). PTSD among Aboriginal and Torres Strait Islander people in custody in Australia: Prevalence and correlates. Journal of Traumatic Stress, 28 (6), 523–530. https://doi.org/10.1002/jts.22051
Hesselbrock, M. N., Segal, B., & Malcolm, B. P. (2006). Multiple substance dependence and course of alcoholism among Alaska native men and women. Substance Use and Misuse, 41 (5), 729–741. https://doi.org/10.1080/10826080500391803
Hesselbrock, V. M., Segal, B., & Hesselbrock, M. N. (2000). Alcohol dependence among Alaska Natives entering alcoholism treatment: A gender comparison. Journal of Studies on Alcohol, 61 (1), 150–156.
Hodge, D. R., Limb, G. E., & Cross, T. L. (2009). Moving from colonization toward balance and harmony: A Native American perspective on wellness. Social Work, 54 (3), 211–219. https://doi.org/10.1093/sw/54.3.211
Howard, M. O., Walker, R. D., Suchinsky, R. T., & Anderson, B. (1996). Substance-use and psychiatric disorders among American Indian veterans. Substance Use & Misuse, 31 (5), 581–598. https://doi.org/10.3109/10826089609045828
Huang, B., Grant, B. F., Dawson, D. A., Stinson, F. S., Chou, S. P., Saha, T. D., Goldstein, R. B., Smith, S. M., Ruan, W. J., & Pickering, R. P. (2006). Race-ethnicity and the prevalence and co-occurrence of Diagnostic and Statistical Manual of Mental Disorders, alcohol and drug use disorders and Axis I and II disorders: United States, 2001 to 2002. Comprehensive Psychiatry, 47 (4), 252–257.
Hunter, E., Gynther, B., Anderson, C., Onnis, L.-A., Groves, A., & Nelson, J. (2011). Psychosis and its correlates in a remote indigenous population. Australasian Psychiatry : Bulletin of Royal Australian and New Zealand College of Psychiatrists, 19 (5), 434–438. https://doi.org/10.3109/10398562.2011.583068
Kaholokula, J. K., Grandinetti, A., Crabbe, K. M., Chang, H. K., & Kenui, C. K. (1999). Depressive symptoms and cigarette smoking among Native Hawaiians. Asia-Pacific Journal of Public Health, 11 (2), 60–64.
Kennedy, M., Bennett, J., Maidment, S., Chamberlain, C., Booth, K., McGuffog, R., Hobden, B., Whop, L. J., & Bryant, J. (2022). Interrogating the intentions for Aboriginal and Torres Strait Islander health: A narrative review of research outputs since the introduction of Closing the Gap. MJA, 217 (1), 50–57.
PubMed Google Scholar
Kisely, S., Alichniewicz, K. K., Black, E. B., Siskind, D., Spurling, G., & Toombs, M. (2017). The prevalence of depression and anxiety disorders in indigenous people of the Americas: A systematic review and meta-analysis. Journal of Psychiatric Research, 84 , 137–152. https://doi.org/10.1016/j.jpsychires.2016.09.032
Kunitz, S. J., Gabriel, K. R., Levy, J. E., Henderson, E., Lampert, K., McCloskey, J., Quintero, G., Russell, S., & Vince, A. (1999). Alcohol dependence and conduct disorder among Navajo Indians. Journal of Studies on Alcohol, 60 (2), 159–167.
Lacey, C., Cunningham, R., Rijnberg, V., Manuel, J., Clark, M. T. R., Keelan, K., Pitama, S., Huria, T., Lawson, R., & Jordan, J. (2020). Eating disorders in New Zealand: Implications for Maori and health service delivery. International Journal of Eating Disorders, 53 (12), 1974–1982. https://doi.org/10.1002/eat.23372
Lee, K. K., Clough, A. R., Jaragba, M. J., Conigrave, K. M., & Patton, G. C. (2008). Heavy cannabis use and depressive symptoms in three Aboriginal communities in Arnhem Land. Northern Territory. Medical Journal of Australia, 188 (10), 605–608.
Lee, K. S. K., Harrison, K., Mills, K., & Conigrave, K. M. (2014). Needs of Aboriginal Australian women with comorbid mental and alcohol and other drug use disorders. Drug and Alcohol Review, 33 (5), 473–481. https://doi.org/10.1111/dar.12127
Leung, J., Stockings, E., Wong, I., Galasyuk, N., Diminic, S., Leitch, E., Whiteford, H., Degenhardt, L., Ritter, A., & Harris, M. (2016). Co-morbid mental and substance use disorders – a meta-review of treatment effectiveness. NDARC Technical Report No. 336. https://ndarc.med.unsw.edu.au/sites/default/files/ndarc/resources/NDARCTechinicalReport_ComorbidMSDMetaReviewFinal_20170913_0.pdf
Libby, A. M., Orton, H. D., Barth, R. P., Webb, M. B., Burns, B. J., Wood, P., & Spicer, P. (2006). Alcohol, drug, and mental health specialty treatment services and race/ethnicity: A national study of children and families involved with child welfare. American Journal of Public Health, 96 (4), 628–631. https://doi.org/10.2105/ajph.2004.059436
Libby, A. M., Orton, H. D., Novins, D. K., Beals, J., Manson, S. M., & Ai-Superpfp, T. (2005). Childhood physical and sexual abuse and subsequent depressive and anxiety disorders for two American Indian tribes. Psychological Medicine, 35 (3), 329–340. https://doi.org/10.1017/s0033291704003599
Libby, A. M., Orton, H. D., Novins, D. K., Spicer, P., Buchwald, D., Beals, J., Manson, S. M., & Ai-Superpfp, T. (2004). Childhood physical and sexual abuse and subsequent alcohol and drug use disorders in two American-Indian tribes. Journal of studies on alcohol, 65 (1), 74–83. https://doi.org/10.15288/jsa.2004.65.74
Lillie, K. M., Shaw, J., Jansen, K. J., & Garrison, M. M. (2021). Buprenorphine/naloxone for opioid use disorder among Alaska Native and American Indian people. Journal of Addiction Medicine, 15 (4), 297–302. https://doi.org/10.1097/adm.0000000000000757
Liu, Q., He, H., Yang, J., Feng, X., Zhao, F., & Lyu, J. (2020). Changes in the global burden of depression from 1990 to 2017: Findings from the Global Burden of Disease study. Journal of Psychiatric Research, 126 , 134–140. https://doi.org/10.1016/j.jpsychires.2019.08.002
Mark, G. T., & Lyons, A. C. (2010). Maori healers’ views on wellbeing: The importance of mind, body, spirit, family and land. Social Science & Medicine, 70 (11), 1756–1764. https://doi.org/10.1016/j.socscimed.2010.02.001
McCartney, M. (2016). Breaking down the silo walls. BMJ open, 354 (i5199). https://doi.org/10.1136/bmj.i5199
Mellsop, G., Tapsell, R., Holmes, P., & Andreasson, B. B. B. C. D. F. E. F. J. K. K. M. M. M. P. R. S. T. T. (2019). Mental health service users’ progression from illicit drug use to schizophrenia in New Zealand. General Psychiatry, 32 (5), 1–4. https://doi.org/10.1136/gpsych-2019-100088
Mental Health America. (2017). Position statement 16: Addressing the health- related social needs of people with mental health and substance use conditions . https://www.mhanational.org/issues/position-statement-16-addressing-health-related-social-needs-people-mental-health-and#_edn2 . Accessed 17 July 2023
Mercer, S., O’Brien, R., Fitzpatrick, B., Higgins, M., Guthrie, B., Watt, G., & Wyke, S. (2016). The development and optimisation of a primary care-based whole system complex intervention (CARE Plus) for patients with multimorbidity living in areas of high socioeconomic deprivation. Chronic Illness, 12 (3), 165–181.
Ministry of Health New Zealand. (2018). Mental health - Maori Health Statistics . New Zealand Government. https://www.health.govt.nz/our-work/populations/maori-health/tatau-kahukura-maori-health-statistics/nga-mana-hauora-tutohu-health-status-indicators/mental-health . Accessed 18 July 2023
Moghaddam, J. F., Dickerson, D. L., Yoon, G., & Westermeyer, J. (2014). Nicotine dependence and psychiatric and substance use disorder comorbidities among American Indians/Alaska Natives: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence, 144 , 127–133. https://doi.org/10.1016/j.drugalcdep.2014.08.017
Munn, Z., Peters, M. D. J., Stern, C., Tufanaru, C., McArthur, A., & Aromataris, E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18 (1), 143. https://doi.org/10.1186/s12874-018-0611-x
Nadew, G. T., & Tatsioni, T. (2012). Exposure to traumatic events, prevalence of posttraumatic stress disorder and alcohol abuse in Aboriginal communities. Rural and Remote Health, 12 (4), 1–12.
Google Scholar
Nasir, B. F., Ryan, E. G., Black, E. B., Kisely, S., Gill, N. S., Beccaria, G., Kondalsamy-Chennakesavan, S., Nicholson, G. C., & Toombs, M. (2022). The risk of common mental disorders in Indigenous Australians experiencing traumatic life events. BJPsych Open , 8 (1). https://doi.org/10.1192/bjo.2021.1063
Nasir, B. F., Toombs, M. R., Kondalsamy-Chennakesavan, S., Kisely, S., Gill, N. S., Black, E., Hayman, N., Ranmuthugala, G., Beccaria, G., Ostini, R., & Nicholson, G. C. (2018). Common mental disorders among Indigenous people living in regional, remote and metropolitan Australia: A cross-sectional study. BMJ open , 8 (6). https://doi.org/10.1136/bmjopen-2017-020196
Neligh, G., Baron, A. E., Braun, P., & Czarnecki, M. (1990). Panic disorder among American Indians: A descriptive study. American Indian and Alaska Native Mental Health Research , 4 (2), 43–53. https://doi.org/10.5820/aian.0402.1990.43
Nelson, S. E., & Wilson, K. (2017). The mental health of Indigenous peoples in Canada: A critical review of research. Social Science & Medicine, 176 , 93–112. https://doi.org/10.1016/j.socscimed.2017.01.021
Novins, D. K., Fickenscher, A., & Manson, S. M. (2006). American Indian adolescents in substance abuse treatment: Diagnostic status. Journal of Substance Abuse Treatment, 30 (4), 275–284. https://doi.org/10.1016/j.jsat.2005.12.005
O’Neill, L., Fraser, T., Kitchenham, A., & McDonald, V. (2018). Hidden burdens: A review of intergenerational, historical and complex trauma, implications for indigenous families. Journal of Child & Adolescent Trauma, 11 (2), 173–186. https://doi.org/10.1007/s40653-016-0117-9
Onell, T. D. (1992). Feeling worthless - an ethnographic investigation of depression and problem drinking at the Flathead Reservation. Culture Medicine and Psychiatry, 16 (4), 447–469.
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372 , n71. https://doi.org/10.1136/bmj.n71
Pearson, C. R., Kaysen, D., Belcourt, A., Stappenbeck, C. A., Zhou, C., Smartlowit-Briggs, M. L., & Whitefoot, M. P. (2015). Post-traumatic stress disorder and HIV risk behaviors among rural American Indian/Alaska Native women. American Indian and Alaska Native Mental Health Research (online), 22 (3), 1.
Pro, G., Baldwin, J. A., Utter, J., & Haberstroh, S. (2020). Dual mental health diagnoses predict the receipt of medication-assisted opioid treatment: Associations moderated by state Medicaid expansion status, race/ethnicity and gender, and year. Drug and alcohol dependence, 209 , 107952. https://doi.org/10.1016/j.drugalcdep.2020.107952
Quello, S., Brady, K., & Sonne, S. (2005). Mood disorders and substance use disorder: A complex comorbidity. Sci Pract Perspect, 3 (1), 13–21.
Rai, D., Skapinakis, P., Wiles, N., Lewis, G., & Araya, R. (2010). Common mental disorders, subthreshold symptoms and disability: Longitudinal study. British Journal of Psychiatry, 197 (5), 411–412.
Rieckmann, T., McCarty, D., Kovas, A., Spicer, P., Bray, J., Gilbert, S., & Mercer, J. (2012). American Indians with substance use disorders: Treatment needs and comorbid conditions. American Journal of Drug and Alcohol Abuse, 38 (5), 498–504. https://doi.org/10.3109/00952990.2012.694530
Robin, R. W., Long, J. C., Rasmussen, J. K., Albaugh, B., & Goldman, D. (1998). Relationship of binge drinking to alcohol dependence, other psychiatric disorders, and behavioral problems in an American Indian tribe. Alcoholism Clinical and Experimental Research, 22 (2), 518–523.
Sawchuk, C. N., Roy-Byrne, P., Noonan, C., Bogart, A., Goldberg, J., Manson, S. M., & Buchwald, D. (2012). Smokeless Tobacco use and its relation to panic disorder, major depression, and posttraumatic stress disorder in American Indians. Nicotine and Tobacco Research, 14 (9), 1048–1056. https://doi.org/10.1093/ntr/ntr331
Sawchuk, C. N., Roy-Byrne, P., Noonan, C., Bogart, A., Goldberg, J., Manson, S. M., Buchwald, D., Ai-Superpfp, T., & Abelson, B. B. B. B. B. B. B. B. C. C. C. D. D. E. F. F. G. G. G. G. G. J. J. J. K. K. K. K. K. L. (2016). The association of panic disorder, posttraumatic stress disorder, and major depression with smoking in American Indians. Nicotine & Tobacco Research, 18 (3), 259–266. https://doi.org/10.1093/ntr/ntv071
Sawchuk, C. N., Roy-Byrne, P., Noonan, C., Craner, J. R., Goldberg, J., Manson, S., & Buchwald, D. (2017). Panic attacks and panic disorder in the American Indian community. Journal of anxiety disorders, 48 , 6–12.
Schick, M. R., Nalven, T., Thomas, E. D., Weiss, N. H., & Spillane, N. S. (2022). Depression and alcohol use in American Indian adolescents: The influence of family factors. Alcoholism Clinical and Experimental Research, 46 (1), 141–151.
Schütz, C., Choi, F., Jae Song, M., Wesarg, C., Li, K., & Krausz, M. (2019). Living with dual diagnosis and homelessness: Marginalized within a marginalized group. Journal of Dual Diagnosis, 15 (2), 88–94.
SCImago. (2022). SCImago Journal & Country Rank . Scimago Lab. Retrieved 24 Mar from https://www.scimagojr.com/countryrank.php?order=itp&ord=desc
September, U., & Beytell, A.-M. (2019). Family members’ experiences: People with comorbid bipolar and substance use disorder. International Journal of Mental Health and Addiction, 17 (5), 1162–1179. https://doi.org/10.1007/s11469-018-0037-z
Shen, Y.-T., Radford, K., Daylight, G., Cumming, R., Broe, T. G., & Draper, B. (2018). Depression, suicidal behaviour, and mental disorders in older Aboriginal Australians. International Journal of Environmental Research and Public Health, 15 (3), 447.
Smith, S. M., Stinson, F. S., Dawson, D. A., Goldstein, R., Huang, B., & Grant, B. F. (2006). Race/ethnic differences in the prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine, 36 (7), 987–998.
Somervell, P. D., Beals, J., Kinzie, J. D., Boehnlein, J., Leung, P., & Manson, S. M. (1992). Use of the CES-D in an American Indian village. Culture, Medicine and Psychiatry, 16 (4), 503–517.
Subica, A. M., Aitaoto, N., Link, B. G., Yamada, A. M., Henwood, B. F., & Sullivan, G. (2019). Mental health status, need, and unmet need for mental health services among US Pacific Islanders. Psychiatric Services, 70 (7), 578–585. https://doi.org/10.1176/appi.ps.201800455
Substance Abuse and Mental Health Services Administration. (2022). Co-occurring disorders: Diagnoses and integrated treatments . SAMHSA. Retrieved 24 Mar from https://www.samhsa.gov/co-occurring-disorders . Accessed 17 July 2023
Tan, M. C., Thuras, P., Thompson, J., Canive, J., & Westermeyer, J. (2008). Sustained remission from substance use disorder among American Indian veterans. Addictive Disorders and Their Treatment, 7 (2), 53–63. https://doi.org/10.1097/ADT.0b013e31805ea0ad
Te Kōmihana Whai Hua O Aotearoa (New Zealand Productivity Commission). (2022). Colonisation, Racism and Wellbeing . Haemata Limited. https://www.productivity.govt.nz/assets/Documents/NZPC_Colonisation_Racism_Wellbeing_Final.pdf . Accessed 18 July 2023
Teesson, M., Baker, A., Deady, M., Mills, K., Kay-Lambkin, F., Haber, P., Baillie, A., Christensen, H., Birchwood, M., Spring, B., Brady, K. T., Manns, L., & Gournay, K. (2014). Mental health and substance use: Opportunities for innovative prevention and treatment . Mental Health Commission of NSW, Sydney. https://www.nswmentalhealthcommission.com.au/sites/default/files/old/assets/File/NSW%20MHC%20Discussion%20document%20on%20comorbidity%20cover%20page.pdf
Toombs, E., Lund, J., Radford, A., Drebit, M., Bobinski, T., & Mushquash, C. J. (2022). Adverse Childhood Experiences (ACEs) and health histories among clients in a first nations-led treatment for substance use. International journal of mental health and addiction , pp. 1–21. https://doi.org/10.1007/s11469-022-00883-1
Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., Moher, D., Peters, M. D. J., Horsley, T., Weeks, L., Hempel, S., Akl, E. A., Chang, C., McGowan, J., Stewart, L., Hartling, L., Aldcroft, A., Wilson, M. G., Garritty, C., … Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169 (7), 467–473. https://doi.org/10.7326/m18-0850
Verma, R. K., Guen Lin, R. S., Chakravarthy, S., Barua, A., & Kar, N. (2014). Socio-demographic correlates of unipolar major depression among the Malay elderly in Klang Valley, Malaysia an intensive study. International Journal of Pharmacy and Pharmaceutical Sciences, 6 (4), 158–164.
Walls, M., Sittner, K. J., Whitbeck, L. B., Herman, K., Gonzalez, M., Elm, J. H. L., Hautala, D., Dertinger, M., & Hoyt, D. R. (2020). Prevalence of mental disorders from adolescence through early adulthood in American Indian and First Nations communities. International Journal of Mental Health and Addiction . https://doi.org/10.1007/s11469-020-00304-1
Wasserman, G. A., McReynolds, L. S., Schwalbe, C. S., Keating, J. M., & Jones, S. A. (2010). Psychiatric disorder, comorbidity, and suicidal behavior in juvenile justice youth. Criminal Justice and Behavior, 37 (12), 1361–1376.
Westermeyer, J. (1993). Psychiatric disorders among American Indian vs other patients with psychoactive substance use disorders. American Journal on Addictions, 2 (4), 309–314.
Westermeyer, J., & Canive, J. (2013). Posttraumatic stress disorder and its comorbidities among American Indian veterans. Community Mental Health Journal, 49 (6), 704–708. https://doi.org/10.1007/s10597-012-9565-3
Westermeyer, J., Canive, J., Thuras, P., Thompson, J., Crosby, R. D., & Garrard, J. (2009). A comparison of substance use disorder severity and course in American Indian male and female veterans. The American Journal on Addictions, 18 (1), 87–92.
Westermeyer, J., Neider, J., & Westermeyer, M. (1992). Substance use and other psychiatric-disorders among 100 American-Indian patients. Culture Medicine and Psychiatry, 16 (4), 519–529.
Wheeler, A., Robinson, E., & Robinson, G. (2005). Admissions to acute psychiatric inpatient services in Auckland, New Zealand: A demographic and diagnostic review. The New Zealand Medical Journal (Online) , 118 (1226). https://researchspace.auckland.ac.nz/bitstream/handle/2292/4725/16311610.pdf?sequence=1&isAllowed=y
Whitbeck, L., Hoyt, D., Johnson, K., & Chen, X. (2006a). Mental disorders among parents/caretakers of American Indian early adolescents in the Northern Midwest. Social Psychiatry and Psychiatric Epidemiology, 41 (8), 632–640.
Whitbeck, L. B., Johnson, K. D., Hoyt, D. R., & Walls, M. L. (2006c). Prevalence and comorbidity of mental disorders among American Indian children in the Northern Midwest. Journal of Adolescent Health, 39 (3), 427–434. https://doi.org/10.1016/j.jadohealth.2006.01.004
Whitesell, N. R., Beals, J., Mitchell, C. M., Keane, E. M., Spicer, P., & Turner, R. J. (2007). The relationship of cumulative and proximal adversity to onset of substance dependence symptoms in two American Indian communities. Drug and Alcohol Dependence, 91 (2–3), 279–288. https://doi.org/10.1016/j.drugalcdep.2007.06.008
Woodall, W. G., Delaney, H. D., Kunitz, S. J., Westerberg, V. S., & Zhao, H. (2007). A randomized trial of a DWI intervention program for first offenders: Intervention outcomes and interactions with antisocial personality disorder among a primarily American-Indian sample. Alcoholism Clinical and Experimental Research, 31 (6), 974–987.
World Health Organization. (1993). The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. World Health Organization. https://apps.who.int/iris/handle/10665/37108
World Health Organization. (2019). International Statistical Classification of Diseases and related health problems, 11th Revision (ICD-11) . World Health Organization. https://icd.who.int/en
Wu, L.-T., Blazer, D. G., Gersing, K. R., Burchett, B., Swartz, M. S., & Mannelli, P. (2013). Comorbid substance use disorders with other Axis I and II mental disorders among treatment-seeking Asian Americans, Native Hawaiians/Pacific Islanders, and mixed-race people. Journal of Psychiatric Research, 47 (12), 1940–1948. https://doi.org/10.1016/j.jpsychires.2013.08.022
Wu, L.-T., Zhu, H., Mannelli, P., & Swartz, M. S. (2017). Prevalence and correlates of treatment utilization among adults with cannabis use disorder in the United States. Drug and Alcohol Dependence, 177 , 153–162.
Zhu, Z., Huang, H., Chen, H., Hao, W., Ning, K., Zhang, R., Sun, W., Li, B., Jiang, H., Wang, W., Du, J., Zhao, M., Yi, Z., Li, J., Zhu, R., Lu, S., Xie, S., Wang, X., Fu, W., & Gao, C. (2020). Prevalence, demographic, and clinical correlates of comorbid depressive symptoms in Chinese psychiatric patients with alcohol dependence. Frontiers in Psychiatry, 11 , 499. https://doi.org/10.3389/fpsyt.2020.00499
Download references
Acknowledgements
The authors would like to thank Samuel Lawson (research assistant) for assisting with data coding and Angela Smith (librarian) for assisting with the development of the search strategy.
Open Access funding enabled and organized by CAUL and its Member Institutions BH is supported by an Australian Rotary Health Colin Dodds Postdoctoral Fellowship (#1801108). This project did not receive funding.
Author information
Authors and affiliations.
Health Behaviour Research Collaborative, School of Medicine and Public Health, College of Health, Medicine and Wellbeing, University of Newcastle, Callaghan, NSW, 2308, Australia
Breanne Hobden, Megan Freund, Todd Heard, Robert Davis, Jia Ying Ooi, Rob Sanson-Fisher & Jamie Bryant
Equity in Health and Wellbeing Program, Hunter Medical Research Institute, New Lambton Heights, NSW, 2305, Australia
Breanne Hobden, Megan Freund, Robert Davis, Jia Ying Ooi, Rob Sanson-Fisher & Jamie Bryant
Wollotuka Institute, Purai Global Indigenous History Centre, University of Newcastle, Callaghan, Australia
Jennifer Rumbel
Systems Neuroscience Group, Hunter Medical Research Institute, New Lambton Heights, NSW, 2305, Australia
Jennifer Rumbel & Todd Heard
Wiyiliin Ta CAMHS, Hunter New England Local Health District, NSW Health, Newcastle, 2300, Australia
Orange Aboriginal Medical Service, Orange, NSW, 2800, Australia
Jamie Newman
Yimamulinbinkaan Aboriginal Mental Health Service & Social Emotional Wellbeing Workforce Hunter, New England Mental Health Service, Hunter New England Local Health District, NSW Health, Warabrook, 2304, Australia
Bronwyn Rose
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and methodology. Paper coding was performed by Breanne Hobden, Jennifer Rumbel, and Jia Ying Ooi. Data extraction was performed by Breanne Hobden, Megan Freund, Jia Ying Ooi, and Jamie Bryant. Data analysis and synthesis was conducted by Breanne Hobden. The first draft of the manuscript was written by Breanne Hobden. All authors reviewed and commented on iterative versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Breanne Hobden .
Ethics declarations
Ethics approval.
This is a review of available literature; therefore, ethics approval was not required.
Consent to Participate
This is a review of available literature; therefore, consent to participate and consent to publish were not required.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (XLSX 51 KB)
Appendix 1 search strategy.
Database: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations and Daily <1946 to October 11, 2022>
Search Strategy:
--------------------------------------------------------------------------------
1 exp Mental Disorders/ (1275030)
2 ((mental or psychologic* or emotional) adj (illness* or condition* or disorder* or health)).ti,ab,kw,kf. (241020)
3 (eating disorder* or anorexi* or bulimi*).ti,ab,kw,kf. (51634)
4 (disorder* adj1 mood).ti,ab,kw,kf. (19263)
5 (depression or depressive or dysthymi*).ti,ab,kw,kf. (404197)
6 (neurotic or neuros?s or psychoneuros?s or psycho-neuros?s).ti,ab,kw,kf. (17018)
7 (bipolar or bi-polar).ti,ab,kw,kf. (65793)
8 affective disorder*.ti,ab,kw,kf. (17230)
9 anxiety.ti,ab,kw,kf. (207161)
10 (panic adj (disorder* or attack*)).ti,ab,kw,kf. (11506)
11 (phobia* or phobic disorder* or arachnophobia* or acrophobi* or claustrophobi*).ti,ab,kw,kf. (10310)
12 (stress adj1 (disorder* or acute)).ti,ab,kw,kf. (40074)
13 (post traumatic stress or posttraumatic stress or PTSD or psycho?trauma* or psychological trauma*).ti,ab,kw,kf. (41549)
14 (obsessive compulsive disorder or obsessive behavio?r* or compulsive behavio?r* or OCD).ti,ab,kw,kf. (16735)
15 (stress adj1 (disorder* or psychological or condition*)).ti,ab,kw,kf. (63542)
16 schizo*.ti,ab,kw,kf. (148918)
17 (paranoid or paranoia).ti,ab,kw,kf. (8448)
18 (psychotic or psychos?s).ti,ab,kw,kf. (73522)
19 (adjustment adj1 (emotional or disorder*)).ti,ab,kw,kf. (2782)
20 (personality adj1 disorder*).ti,ab,kw,kf. (20994)
21 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 (1820924)
22 exp Substance-related disorders/ (284659)
23 ((aerosol* or alcohol* or amphetamin* or barbituat* or benzodiazepin* or buprenorphin* or cannabi* or cocaine* or codeine or crack or crystal or depressant* or ecstasy or fentanyl or GHB or hallucinogen* or heroin* or hydromorphone or hypnotic* or inhalant* or ketamin* or LSD or marihuana* or marijuana* or MDMA or methadone or methamphetamin* or morphine* or narcotic* or nitrous oxide or opiate* or opioid* or opium or oxycodone or painkiller* or pain killer* or PCP or pethidin* or psychedelic* or psychoactive* or psychostimulant* or ritalin or sedative* or solvent* or steroid* or stimulant*) adj3 (abus* or use* or using* or misus* or mis-us* or depend* or addict* or illegal* or illicit* or habit* or intoxica* or in-toxica* or disorder* or condition* or illness*)).ti,ab,kw,kf. (279135)
24 ((drug* or chemical* or substance*) adj3 (abus* or use* or using* or misus* or mis-us* or depend* or addict* or illegal* or illicit* or habit* or intoxica* or in-toxica* or disorder*)).ti,ab,kw,kf. (367349)
25 ((prescription* or prescribed) adj3 (abus* or misus* or mis-us* or depend* or addict*)).ti,ab,kw,kf. (3507)
26 22 or 23 or 24 or 25 (717202)
27 exp Comorbidity/ (114881)
28 (comorbid* or co-morbid* or cooccurr* or co-occurr*).ti,ab,kw,kf. (221037)
29 (multimorbid* or multi-morbid*).ti,ab,kw,kf. (6638)
30 (coexist* or co-exist*).ti,ab,kw,kf. (98036)
31 "Diagnosis, Dual (Psychiatry)"/ (3622)
32 (dual adj2 diagnos*).ti,ab,kw,kf. (2331)
33 27 or 28 or 29 or 30 or 31 or 32 (386202)
34 exp Indians, North American/ or exp Indigenous Canadians/ or American Natives/ or Oceanic Ancestry Group/ (27937)
35 indigenous.ti,ab,kw,kf. (34356)
36 aborigin*.ti,ab,kw,kf. (10310)
37 (first nation or first nations or first people* or native population* or native people*).ti,ab,kw,kf. (4714)
38 torres strait islander*.ti,ab,kw,kf. (1793)
39 australoid race*.ti,ab,kw,kf. (3)
40 maori*.ti,ab,kw,kf. (3622)
41 (pacific islander* or south sea islander* or pacific island american*).ti,ab,kw,kf. (3882)
42 (native* adj1 (hawaiian* or polynesian*)).ti,ab,kw,kf. (1259)
43 ((north america* or american or alaska*) adj2 (native* or indian*)).ti,ab,kw,kf. (13195)
44 (amerind* or american indian*).ti,ab,kw,kf. (9120)
45 eskimo*.ti,ab,kw,kf. (1558)
46 (inuit* or meti or inupiat* or aleut* or yupik or athabaska*).ti,ab,kw,kf. (3200)
47 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 (77476)
48 21 or 26 (2221807)
49 33 and 47 and 48 (555)
50 limit 49 to english language (547)
51 limit 50 to (comment or editorial or letter or news) (4)
52 50 not 51 (543)
Database: Embase <1947 to present>
1 exp mental disease/ (2441346)
2 ((mental or psychologic* or emotional) adj (illness* or condition* or disorder* or health)).ti,ab,kw. (302885)
3 (eating disorder* or anorexi* or bulimi*).ti,ab,kw. (75151)
4 (disorder* adj1 mood).ti,ab,kw. (30170)
5 (depression or depressive or dysthymi*).ti,ab,kw. (582832)
6 (neurotic or neuros?s or psychoneuros?s or psycho-neuros?s).ti,ab,kw. (24209)
7 (bipolar or bi-polar).ti,ab,kw. (99252)
8 affective disorder*.ti,ab,kw. (24768)
9 anxiety.ti,ab,kw. (307605)
10 (panic adj (disorder* or attack*)).ti,ab,kw. (15489)
11 (phobia* or phobic disorder* or arachnophobia* or acrophobi* or claustrophobi*).ti,ab,kw. (15304)
12 (stress adj1 (disorder* or acute)).ti,ab,kw. (50900)
13 (post traumatic stress or posttraumatic stress or PTSD or psycho?trauma* or psychological trauma*).ti,ab,kw. (54307)
14 (obsessive compulsive disorder or obsessive behavio?r* or compulsive behavio?r* or OCD).ti,ab,kw. (24522)
15 (stress adj1 (disorder* or psychological or condition*)).ti,ab,kw. (80289)
16 schizo*.ti,ab,kw. (207220)
17 (paranoid or paranoia).ti,ab,kw. (13769)
18 (psychotic or psychos?s).ti,ab,kw. (112382)
19 (adjustment adj1 (emotional or disorder*)).ti,ab,kw. (4166)
20 (personality adj1 disorder*).ti,ab,kw. (29138)
21 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 (2943948)
22 exp drug dependence/ or substance abuse/ (302956)
23 ((aerosol* or alcohol* or amphetamin* or barbituat* or benzodiazepin* or buprenorphin* or cannabi* or cocaine* or codeine or crack or crystal or depressant* or ecstasy or fentanyl or GHB or hallucinogen* or heroin* or hydromorphone or hypnotic* or inhalant* or ketamin* or LSD or marihuana* or marijuana* or MDMA or methadone or methamphetamin* or morphine* or narcotic* or nitrous oxide or opiate* or opioid* or opium or oxycodone or painkiller* or pain killer* or PCP or pethidin* or psychedelic* or psychoactive* or psychostimulant* or ritalin or sedative* or solvent* or steroid* or stimulant*) adj3 (abus* or use* or using* or misus* or mis-us* or depend* or addict* or illegal* or illicit* or habit* or intoxica* or in-toxica* or disorder* or condition* or illness*)).ti,ab,kw. (396550)
24 ((drug* or chemical* or substance*) adj3 (abus* or use* or using* or misus* or mis-us* or depend* or addict* or illegal* or illicit* or habit* or intoxica* or in-toxica* or disorder*)).ti,ab,kw. (517532)
25 ((prescription* or prescribed) adj3 (abus* or misus* or mis-us* or depend* or addict*)).ti,ab,kw. (5107)
26 22 or 23 or 24 or 25 (949786)
27 comorbidity/ (294387)
28 (comorbid* or co-morbid* or cooccurr* or co-occurr*).ti,ab,kw. (386102)
29 (multimorbid* or multi-morbid*).ti,ab,kw. (8998)
30 (coexist* or co-exist*).ti,ab,kw. (127917)
31 (dual adj2 diagnos*).ti,ab,kw. (3878)
32 27 or 28 or 29 or 30 or 31 (612625)
33 indigenous people/ or alaska native/ or american indian/ or canadian aboriginal/ or first nation/ or indigenous australian/ (29671)
34 indigenous.ti,ab,kw. (42404)
35 aborigin*.ti,ab,kw. (13451)
36 (first nation or first nations or first people* or native population* or native people*).ti,ab,kw. (6139)
37 torres strait islander*.ti,ab,kw. (2352)
38 australoid race*.ti,ab,kw. (9)
39 maori*.ti,ab,kw. (4686)
40 (pacific islander* or south sea islander* or pacific island american*).ti,ab,kw. (5565)
41 (native* adj1 (hawaiian* or polynesian*)).ti,ab,kw. (1569)
42 ((north america* or american or alaska*) adj2 (native* or indian*)).ti,ab,kw. (16645)
43 (amerind* or american indian*).ti,ab,kw. (11735)
44 eskimo*.ti,ab,kw. (1999)
45 (inuit* or meti or inupiat* or aleut* or yupik or athabaska*).ti,ab,kw. (3770)
46 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 (95627)
47 21 or 26 (3490245)
48 32 and 46 and 47 (858)
49 limit 48 to english language (849)
50 limit 49 to (books or chapter or conference abstract or conference paper or "conference review" or editorial or letter or note) (243)
51 49 not 50 (606)
Database: APA PsycInfo <1806 to October 11, 2022>
1 exp mental disorders/ (883496)
2 ((mental or psychologic* or emotional) adj (illness* or condition* or disorder* or health)).ti,ab,id. (296538)
3 (eating disorder* or anorexi* or bulimi*).ti,ab,id. (38535)
4 (disorder* adj1 mood).ti,ab,id. (17434)
5 (depression or depressive or dysthymi*).ti,ab,id. (301849)
6 (neurotic or neuros?s or psychoneuros?s or psycho-neuros?s).ti,ab,id. (27989)
7 (bipolar or bi-polar).ti,ab,id. (41378)
8 affective disorder*.ti,ab,id. (17980)
9 anxiety.ti,ab,id. (204692)
10 (panic adj (disorder* or attack*)).ti,ab,id. (12988)
11 (phobia* or phobic disorder* or arachnophobia* or acrophobi* or claustrophobi*).ti,ab,id. (13848)
12 (stress adj1 (disorder* or acute)).ti,ab,id. (42787)
13 (post traumatic stress or posttraumatic stress or PTSD or psycho?trauma* or psychological trauma*).ti,ab,id. (49364)
14 (obsessive compulsive disorder or obsessive behavio?r* or compulsive behavio?r* or OCD).ti,ab,id. (18248)
15 (stress adj1 (disorder* or psychological or condition*)).ti,ab,id. (46731)
16 schizo*.ti,ab,id. (131738)
17 (paranoid or paranoia).ti,ab,id. (13774)
18 (psychotic or psychos?s).ti,ab,id. (80976)
19 (adjustment adj1 (emotional or disorder*)).ti,ab,id. (4845)
20 (personality adj1 disorder*).ti,ab,id. (33681)
21 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 (1282281)
22 exp "substance use disorder"/ (133011)
23 ((aerosol* or alcohol* or amphetamin* or barbituat* or benzodiazepin* or buprenorphin* or cannabi* or cocaine* or codeine or crack or crystal or depressant* or ecstasy or fentanyl or GHB or hallucinogen* or heroin* or hydromorphone or hypnotic* or inhalant* or ketamin* or LSD or marihuana* or marijuana* or MDMA or methadone or methamphetamin* or morphine* or narcotic* or nitrous oxide or opiate* or opioid* or opium or oxycodone or painkiller* or pain killer* or PCP or pethidin* or psychedelic* or psychoactive* or psychostimulant* or ritalin or sedative* or solvent* or steroid* or stimulant*) adj3 (abus* or use* or using* or misus* or mis-us* or depend* or addict* or illegal* or illicit* or habit* or intoxica* or in-toxica* or disorder* or condition* or illness*)).ti,ab,id. (132642)
24 ((drug* or chemical* or substance*) adj3 (abus* or use* or using* or misus* or mis-us* or depend* or addict* or illegal* or illicit* or habit* or intoxica* or in-toxica* or disorder*)).ti,ab,id. (152314)
25 ((prescription* or prescribed) adj3 (abus* or misus* or mis-us* or depend* or addict*)).ti,ab,id. (2186)
26 22 or 23 or 24 or 25 (258622)
27 comorbidity/ or dual diagnosis/ (35623)
28 (comorbid* or co-morbid* or cooccurr* or co-occurr*).ti,ab,id. (73389)
29 (multimorbid* or multi-morbid*).ti,ab,id. (1223)
30 (coexist* or co-exist*).ti,ab,id. (11539)
31 (dual adj2 diagnos*).ti,ab,id. (3045)
32 27 or 28 or 29 or 30 or 31 (91931)
33 indigenous populations/ or alaska natives/ or american indians/ or inuit/ or exp pacific islanders/ (14098)
34 indigenous.ti,ab,id. (12358)
35 aborigin*.ti,ab,id. (4055)
36 (first nation or first nations or first people* or native population* or native people*).ti,ab,id. (1770)
37 torres strait islander*.ti,ab,id. (512)
38 australoid race*.ti,ab,id. (0)
39 maori*.ti,ab,id. (1427)
40 (pacific islander* or south sea islander* or pacific island american*).ti,ab,id. (1862)
41 (native* adj1 (hawaiian* or polynesian*)).ti,ab,id. (722)
42 ((north america* or american or alaska*) adj2 (native* or indian*)).ti,ab,id. (9578)
43 (amerind* or american indian*).ti,ab,id. (5416)
44 eskimo*.ti,ab,id. (364)
45 (inuit* or meti or inupiat* or aleut* or yupik or athabaska*).ti,ab,id. (633)
46 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 (30108)
47 21 or 26 (1356306)
48 32 and 46 and 47 (343)
49 limit 48 to english language (328)
50 limit 49 to (chapter or "column/opinion" or "comment/reply" or dissertation or editorial or letter) (50)
51 49 not 50 (278)
Web of Science
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Hobden, B., Freund, M., Rumbel, J. et al. Mental Health and Substance Use Co-Occurrence Among Indigenous Peoples: a Scoping Review. Int J Ment Health Addiction (2023). https://doi.org/10.1007/s11469-023-01114-x
Download citation
Accepted : 04 July 2023
Published : 28 July 2023
DOI : https://doi.org/10.1007/s11469-023-01114-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Indigenous health
- Comorbidity
- First Nations people
- Mental health
- Substance use
- Find a journal
- Publish with us
- Track your research
Indigenous People and Qualitative Research - Making It Work
Research output : Contribution to journal › Article › peer-review
Other files and links
- Link to publisher version
Fingerprint
- Procedures Nursing and Health Professions 100%
- Researcher Nursing and Health Professions 100%
- Research Experience Nursing and Health Professions 100%
- Qualitative Research Psychology 100%
- Methodology Psychology 14%
- Qualitative Research Method Psychology 14%
T1 - Indigenous People and Qualitative Research - Making It Work
AU - Roman, Curtis
N2 - Indigenous people currently comprise 26.8 % of the Northern Territory population. The Federal Government has recently embarked on a closing the gap campaign to improve the lives of Indigenous people and to address the disadvantage that exits in the lives of Indigenous people. This paper is designed to provide Indigenous and nonindigenous people working in research with some practical advice on how to improve the research experience for Indigenous people and how to develop culturally appropriate research methodologies. The paper proposes that qualitative research methods are practical, useful, beneficial and culturally appropriate for research on and with Indigenous people. The paper also provides practical advice on how to ensure that Indigenous people are represented in research to ensure that their voices are clearly heard. It is hoped that this paper creates awareness among researchers so that they can use this awareness in their research on Indigenous people. The methodology used to write the paper is based on the author's own research experiences as an Indigenous researcher. In the main, the data used in this paper has been gathered from qualitative research textbooks and from personal experiences in research and based on the author's personal experiences of delivering post graduate research courses on Indigenous research issues. The paper shows that qualitative research methods can be useful, productive and culturally appropriate for Indigenous people and can be used to enrich data and to encourage Indigenous people to participate in research. The paper shows that through qualitative research techniques, Indigenous people are able to express themselves and identify issues themselves, which means that researchers are able to gather more data while at the same time, providing Indigenous research participants with a feeling of cultural safety. This is important for those in the area of Indigenous research as Indigenous people have had a long history of negative research experiences.
AB - Indigenous people currently comprise 26.8 % of the Northern Territory population. The Federal Government has recently embarked on a closing the gap campaign to improve the lives of Indigenous people and to address the disadvantage that exits in the lives of Indigenous people. This paper is designed to provide Indigenous and nonindigenous people working in research with some practical advice on how to improve the research experience for Indigenous people and how to develop culturally appropriate research methodologies. The paper proposes that qualitative research methods are practical, useful, beneficial and culturally appropriate for research on and with Indigenous people. The paper also provides practical advice on how to ensure that Indigenous people are represented in research to ensure that their voices are clearly heard. It is hoped that this paper creates awareness among researchers so that they can use this awareness in their research on Indigenous people. The methodology used to write the paper is based on the author's own research experiences as an Indigenous researcher. In the main, the data used in this paper has been gathered from qualitative research textbooks and from personal experiences in research and based on the author's personal experiences of delivering post graduate research courses on Indigenous research issues. The paper shows that qualitative research methods can be useful, productive and culturally appropriate for Indigenous people and can be used to enrich data and to encourage Indigenous people to participate in research. The paper shows that through qualitative research techniques, Indigenous people are able to express themselves and identify issues themselves, which means that researchers are able to gather more data while at the same time, providing Indigenous research participants with a feeling of cultural safety. This is important for those in the area of Indigenous research as Indigenous people have had a long history of negative research experiences.
UR - http://search.informit.com.au/documentSummary;dn=787614138844049;res=IELAPA
M3 - Article
SN - 1037-3403
JO - Aboriginal and Torres Strait Islander Health Worker Journal
JF - Aboriginal and Torres Strait Islander Health Worker Journal
- Open access
- Published: 13 September 2022
Decolonising qualitative research with respectful, reciprocal, and responsible research practice: a narrative review of the application of Yarning method in qualitative Aboriginal and Torres Strait Islander health research
- Michelle Kennedy 1 , 2 ,
- Raglan Maddox 3 ,
- Kade Booth 1 , 2 ,
- Sian Maidment 1 ,
- Catherine Chamberlain 4 , 5 , 6 &
- Dawn Bessarab 7
International Journal for Equity in Health volume 21 , Article number: 134 ( 2022 ) Cite this article
16k Accesses
25 Citations
19 Altmetric
Metrics details
Indigenous academics have advocated for the use and validity of Indigenous methodologies and methods to centre Indigenous ways of knowing, being and doing in research. Yarning is the most reported Indigenous method used in Aboriginal and Torres Strait Islander qualitative health research. Despite this, there has been no critical analysis of how Yarning methods are applied to research conduct and particularly how they privilege Indigenous peoples.
To investigate how researchers are applying Yarning method to health research and examine the role of Aboriginal and Torres Strait Islander researchers in the Yarning process as reported in health publications.
Narrative review of qualitative studies.
Data sources
Lowitja Institute LitSearch January 2008 to December 2021 to access all literature reporting on Aboriginal and Torres Strait Islander health research in the PubMed database. A subset of extracted data was used for this review to focus on qualitative publications that reported using Yarning methods.
Thematic analysis was conducted using hybrid of inductive and deductive coding. Initial analysis involved independent coding by two authors, with checking by a third member. Once codes were developed and agreed, the remaining publications were coded and checked by a third team member.
Forty-six publications were included for review. Yarning was considered a culturally safe data collection process that privileges Indigenous knowledge systems. Details of the Yarning processes and team positioning were vague. Some publications offered a more comprehensive description of the research team, positioning and demonstrated reflexive practice. Training and experience in both qualitative and Indigenous methods were often not reported. Only 11 publications reported being Aboriginal and/or Torres Strait Islander led. Half the publications reported Aboriginal and Torres Strait Islander involvement in data collection, and 24 reported involvement in analysis. Details regarding the role and involvement of study reference or advisory groups were limited.
Aboriginal and Torres Strait Islander people should be at the forefront of Indigenous research. While Yarning method has been identified as a legitimate research method to decolonising research practice, it must be followed and reported accurately. Researcher reflexivity and positioning, and Aboriginal and Torres Strait Islander ownership, stewardship and custodianship of data collected were significantly under detailed in the publications included in our review. Journals and other establishments should review their processes to ensure necessary details are reported in publications and engage Indigenous Editors and peer reviewers to uphold respectful, reciprocal, responsible and ethical research practice.
Introduction
Indigenous peoples have undertaken research since time immemorial, as evidenced in our continued survival prior to, and post colonisation and contemporary coloniality [ 1 ]. However, Indigenous peoples have long been researched by non-Indigenous peoples as mere objects, without prior consent to the research and commonly without meaningful engagement, or access to the results. In colonised countries, research has been utilised as a tool to dehumanise Indigenous peoples [ 1 ]. In Australia, research was used as a tool to justify Terra Nullius, “no man’s land”, the grounds on which the continent was taken by the crown with no negotiation or treaty offered [ 2 ] to the 500 Aboriginal and Torres Strait Islander nations [ 2 , 3 ] that have lived on this land, now called Australia, for over 60,000 years [ 4 ]. Research such as that conducted by D. J Cunningham (1889) “The Spinal Curvature in an Aboriginal Australia” which reported “…In these particulars the Australian spine resembles somewhat the spine of a Chimpanzee” [ 5 ] was used to de-humanise Aboriginal people, disrupting culture and cultural practice [ 6 ]. Findings were applied to understand the antithetical other and to justify the claim of Australia as uninhabited lands. Further, Darwin used such data to support his theory of evolution, arguing that the “natives” (sic) were the living example of the difference in degree between humans and apes [ 7 ]. Australia was colonised on a racially imperialistic basis which has been embedded through coloniality [ 8 ]. In the words of Linda Tuhiwai Smith:
“This collective memory of imperialism has been perpetuated through the ways in which knowledge about indigenous peoples was collected, classified and then represented in various ways back to the West, and then through the eyes of the West, back to those who have been colonized”. [ 1 ] (p. 30)
In response to the colonial legacy of research and its dirty [ 1 ] reputation among Indigenous people, the use of Indigenous research methodologies and methods to aid in decolonising the research process have been advocated for, and by Indigenous academics domestically and internationally [ 1 , 9 ]. Decolonising approaches recognise that the way of knowing has been historically and institutionally contrived in a Western construct, [ 10 ] and that Indigenous methodologies and methods can be used to shift the research paradigm and privilege Indigenous ways of knowing, being and doing. Indigenous ways of knowing, being and doing are shaped by our relationality. Relationality to each other, our lands, our knowledge systems and our storylines [ 11 ].
Morton Robinson describes;
“Relationality is an inextricable part of our sovereign knowledges, informing our scholarship to produce innovative social research. As a presupposition it shapes ways of knowing, being and doing to be connected is to know, and knowing is embodied in social relations and bloodline to country, determined by ancestors and creator beings that guide who can be a knower and of what knowledges” . [ 11 ]
Relationality shapes Indigenous methodologies, informing the ways in which research is conceptualised, designed, conducted, analysed and disseminated. As such the ways in which Indigenous methodologies are applied will vary depending on the relationality, social and cultural positioning of the researcher and peoples involved. In an example outlining Indigenist Research Methodology, Aboriginal scholar Rigney states:
“Indigenist research is research by Indigenous Australians whose primary informants are Indigenous Australians and whose goals are to serve and inform the Indigenous struggle for self-determination”. [ 12 ] (p. 118)
Research methods are then applied by the researcher to undertake the research, the ‘doing’. An international systematic review by Drawson et al. reported three key components to Indigenous Research Methods:
Researchers must situate themselves and the Indigenous Peoples with whom they are collaborating in the research process
The inclusion of Indigenous Peoples in the research process in a way that is respectful, reciprocal, and decolonizing and preserving of self-determinism, and
Prioritization of Indigenous ways of knowing [ 13 ]
These key components of Indigenous research methods coincide with the established standards for conducting ethical research with Aboriginal and Torres Strait Islander people, such as the National Health and Medical Research Council (NHMRC) Values and Ethics Guideline, [ 14 ] the Australian Institute of Aboriginal and Torres Strait Islander Studies (AIATSIS) Code of Ethics [ 15 ] and the Aboriginal Health and Medical Research Council (AHMRC) Key Principles [ 16 ].
Yarning in Indigenous qualitative research is one method being used in Australia and internationally, [ 17 ] and has been recommended for use in Aboriginal and Torres Strait Islander health research [ 9 ] to privilege Indigenous ontologies [ 18 ]. Yarning has been used in recent research as a way to safely engage with participants to explore research questions relating to the topic of the study. The cultural safety of yarning enables sensitive issues to emerge as it fosters agency among participant(s) including the ability to disclose information at their own discretion [ 14 ]. Yarning is led by the researcher where the participant is encouraged to tell their story from the position of their lived experience. Whilst the research topic yarn does not follow a pre-determined set of questions, it does include a yarning topic guide relating to the research that the researcher is listening for in the story. Yarning does not follow the formal conventions of research interviewing and can weave in and out of the yarning story where the role of the researcher is to listen for cues related to the research topic. Yarning as a research method must also draw on cultural protocols and practices that are relevant to the people’s involved. Yarning draws on relationality through processes of the Social, Work and Research Topic Yarn which can inform either Collaborative Yarning or Therapeutic Yarning as presented in Fig. 1 [ 17 ]. Relationality of the Yarn is paramount to producing rich data [ 19 ]. It is reasonable to expect that Indigenous Standpoint generates deeper relationality, through shared experience and understandings of the Yarn [ 19 ].
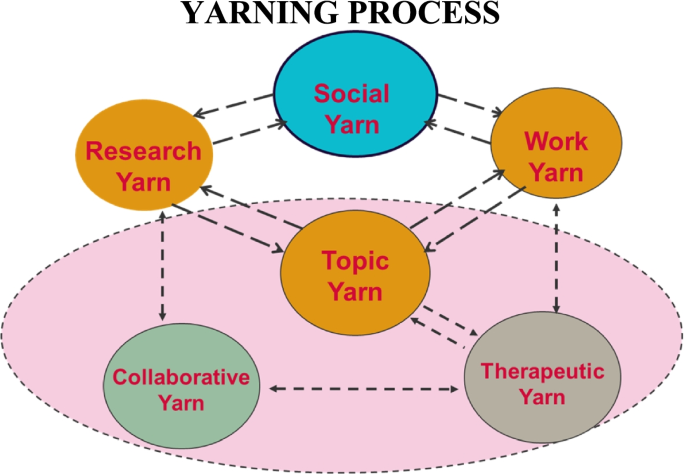
A working depiction of the Yarning Process as developed by Dawn Bessarab
Whilst there appears to be consensus among Indigenous and non-Indigenous scholars on the need for decolonising research approaches and the importance of utilising Indigenous research methodologies and methods, we could not find literature specifically relating to how these are pragmatically applied to the conduct of research. The NHMRC directs researchers to conduct ethical research in line with six core values: Spirit and integrity, Cultural continuity, Equity, Respect, Reciprocity, and Responsibility [ 14 ]. Our Indigenous-led team sought to investigate how researchers are applying Yarning method to ethical health research. We then examined and analysed the Yarning process, including the role of Aboriginal and Torres Strait Islander people as reported in health publications.
Research team
Our lived experiences and coming to understand our relation to the world is complex, dynamic, but fundamentally important, as we recognise that Indigenous peoples ways of knowing, being and doing are relational [ 11 ]. This includes, but is limited to what is known, how it is known; the nature and embodiment of our realities, encapsulating what exists, what is possible, [ 20 ] and how we relate to our respective programs of research.
The majority Indigenous research team is led by a Wiradjuri woman MK with disciplinary training in social science/social work and Indigenous knowledges connected to Wiradjuri, Worimi and Awabakal country. KB is a non-Indigenous researcher, experienced in qualitative health research with a social science background. SM is a Noongar woman with disciplinary training in exercise and sport science and a current medical student. CC is a Palawa woman of the Trawlwoolway clan with training in midwifery, nursing and public health, and experienced in mixed methods research. DB is an Indigenous researcher from the Bard and Yjindabandi nations in Western Australia and is a senior social worker with extensive background and expertise in Aboriginal health research and methodologies specifically yarning. RM is from the Bagumani (Modewa) Clan in Papua New Guinea, with training and experience in public health and epidemiology.
Our research team embodies over 200 years of lived Indigenous experience and over 60 years’ experience conducting qualitative research in Aboriginal and Torres Strait Islander health.
Methodology
This review forms part of a larger project exploring the conduct of Aboriginal and Torres Strait Islander health research, led by an Aboriginal and Torres Strait Islander research team. A primary scoping review was conducted of all Aboriginal and Torres Strait Islander health research published since the establishment of the Closing the Gap campaign [ 21 ]. This parent review included 2,150 articles and is published elsewhere [ 22 ]. When conducting this review, the authors sought to extract information on the reported use of Indigenous research methodologies and found 5% of articles reported using Indigenous methodologies and/or methods. Indigenous methodologies/methods were predominately reported in qualitative papers. This was not published in the parent review.
This review of Yarning aims to answer two research questions:
How are researchers applying the Yarning method in qualitative health research?
What is the role of Aboriginal and Torres Strait Islander researchers in the Yarning process, as reported in health publications?
Design and inclusion criteria
The parent review applied a systematic literature search via the Lowitja Institute website using the search tool Lowitja.search to access all Aboriginal and Torres Strait Islander health literature in the PubMed database. The selected topics in the database were “all” and “Aboriginal and Torres Strait Islander”. Publications were included if they presented original data on Aboriginal and Torres Strait Islander health in Australia and were published between January 2008 and December 2020. The search was updated to include publications until December 2021. Publications that were identified as using qualitative methods for data collection and analysis were assessed. From this, those that reported using Yarning method were included for analysis in this review.
Level of reporting assessment
We assessed the level of reporting in the selected publications using a purpose-built tool to examine Aboriginal and Torres Strait Islander engagement and oversight of the research. The tool was developed as informed by our research questions, ethical research guidelines and an established Aboriginal and Torres Strait Islander quality appraisal tool [ 23 ]. The tool was developed due to the timeframe of included publications, and an acknowledgment of the lack of reporting guidelines for ethical research practice with Indigenous peoples prior to 2019 [ 24 ]. The tool has six categories; (1) Aboriginal and Torres Strait Islander engagement in development of the research, (2) Aboriginal and Torres Strait Islander engagement in data collection, (3) experience of researchers reported, (4) Aboriginal and Torres Strait Islander engagement in the analysis, (5) Aboriginal and Torres Strait Islander specific ethics approval granted, and (6) whether the original method publication was cited. Two authors (MK, KB) independently reviewed each document and ranked each publications level of reporting high (5–6), medium (3–4) or low (0–2). This assessment was not used to exclude studies or inform analysis, but rather it was used for Collaborative Yarning among the authorship team which is reflected in the discussion.
Data analysis
Full text publications were imported into NVivo software for analysis. Three members of the research team who conducted the quality appraisal (KB, MK & SM) engaged in Collaborative Yarning with all authors (MK, RM, KB, SM, CC & DB) to inform the analysis.
Thematic analysis, as outlined by Braun & Clarke, [ 25 ] was used to examine how researchers apply Yarning method in qualitative health research (MK & KB). The initial phase included familiarisation with the data. The team members involved in data coding (KB, SM & MK) have been immersed in the data throughout the primary review, and by reading and sorting each qualitative publication that reported using Yarning methods during the inclusion phase. The senior author DB familiarised the data by reading a sample of publications identified by MK. The sample of papers were selected, including a variety of reporting levels, to inform Collaborative Yarning practice to unpack the different perceptions in reporting of Yarning methods. Further, this approach assisted to ensure consistency between the authorship team, actively facilitating discussion on different points of view. The team members met and engaged in Collaborative Yarning to discuss the data after reading the selected publications on how Yarning was reported, and how it was being analysed according to the research questions.
Similar to Fereday, [ 26 ] thematic analysis was approached through a hybrid of inductive and deductive coding. As noted in our first research question, the role of Aboriginal and Torres Strait Islander people was a key component to our analysis. Codes were developed deductively from our research questions as we sought to draw out the role of Aboriginal and Torres Strait Islander people in the Yarning process. These codes included: “Aboriginal Involvement”, “Analysis approach”, “Framework Methodology”, and “Yarning Processes”. While these were not necessarily “pre-conceived” by the coders (MK & KB), they were broadly discussed prior to coding in relation to the research questions and were then sought out by the researchers. In conjunction with the initial deductive codes that were drawn out to address parts of the research aims, the coding process was predominantly inductive. Inductive coding was used to examine the integral components of Yarning processes, justification of method and the way that these methods, processes and involvement were being reported. MK & KB independently coded the same three publications before meeting to discuss initial themes. The authors found that overall, coding was similar, with some variations on wording to describe themes. After agreement, MK & KB continued to code a further five of the same publications before meeting again to compare. Any conflicts were discussed until agreement was reached, although disagreements were limited. SM cross checked codes and contributed to discussions of clarity of definitions. MK & KB coded an additional seven publications for comparison, before KB went on to singularly code the remaining publications. SM then reviewed all publications and codes for consistency and agreement to ensure all paper were coded independently and in duplicate.
Search results are outlined in Fig. 2 using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) four-phase flow diagram. The total 2,150 papers in the parent reviewed were screened, an updated search was conducted and found 8 new qualitative research papers. N = 354 papers reported use of qualitative methods, Yarning method was reported in n = 46 papers and were included in analysis.
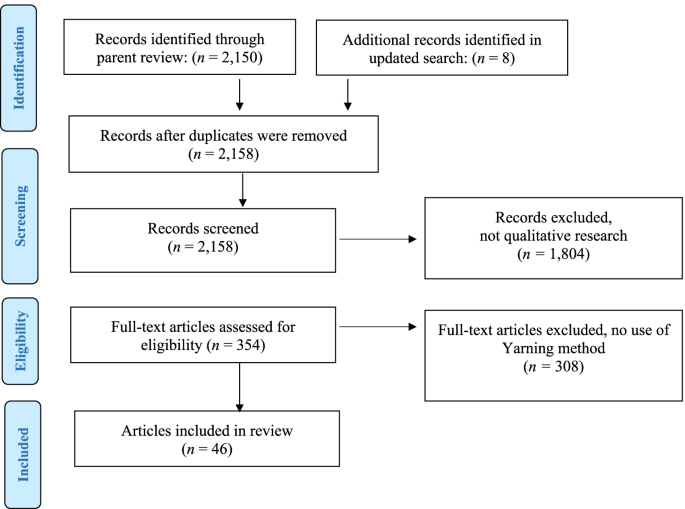
PRISMA Flow diagram of study selection process
Of the 46 included publications, 15 were considered high level reporting across focus area, 19 medium level reporting, and 12 low level reporting. We elaborate on the intricacies of this throughout the result section.
We found that researchers are reporting the application of the Yarning method to qualitative research methodology in a wide variety of ways. Both Aboriginal and non-Aboriginal researchers and research teams are using the method, collecting data and involved in analysis.
The following sections will be presented in a manner that addresses the research questions, by detailing how Yarning is being applied to qualitative health research as reported by the included publications, and what role Aboriginal and Torres Strait Islander play in the research process.
How Yarning is being applied to qualitative health research
Our analysis of the 46 publications showed a variety of reporting on the way that Yarning is applied to Aboriginal and Torres Strait Islander qualitative health research. We begin our critical analysis into this, by first looking at why researchers report using Yarning, followed by how they report using Yarning and how they situate themselves as qualitative researchers and their team in the research process.
Why Yarning?
Reasoning for using Yarning method varied across publications. It was predominantly considered to provide a culturally safe and sensitive data collection process [ 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 ] that privileged Indigenous knowledge systems through connection and relationships [ 27 , 31 ]. Enabling two-way knowledge sharing; [ 27 , 37 , 39 ] using narratives; [ 40 , 41 ] storytelling [ 27 , 28 , 31 , 34 , 37 , 41 , 42 , 43 , 44 , 45 ] and addressing unequal power relationships were most commonly used to justify why Yarning was used, as it is a research process that acknowledges and builds on cultural protocols. One publication stated Yarning was the preferred research method for the older Aboriginal community (see Table 2 , 1.3) [ 46 ].
Yarning was reported to be an Indigenist research practice [ 28 ] that allows for more flexibility than other interviewing approaches [ 27 ]. Yarning method was considered to provide an environment that fosters rapport with participants, open discussion, and allow for participant-led research to co-create knowledge and privilege Indigenous voices.
How Yarning processes are being reported
Details regarding the specifics of the way that Yarning was conducted were often vague. For example, many publications simply stated that Yarning took place, without detail on the settings or the conversations that took place. However, some publications described various components of yarning, such as Therapeutic or Social yarning. For example, “ In this study, social yarning was used at the beginning of conversations with young people to establish a connection not strongly associated with the actual purpose of the yarn.” [ 27 ] (see Table 2 , 2.1).
Most publications reported using audio recording and transcribing to collect data, however, note taking was also reported as a form of data collection [ 27 , 47 ]. Note taking replaced audio recording to reduce potential harm and was deemed culturally safe in some instances. Mostly, it was due to consent not being obtained by participants who preferred note taking. One publication recognised that starting the recorder had the potential to break the flow of the yarn, so continued taking notes instead.
Eleven publications provided their entire interview guide [ 31 , 34 , 39 , 45 , 48 , 49 , 50 , 51 , 52 , 53 , 54 ]. Others provided a sample of example questions, [ 40 , 44 , 55 , 56 , 57 ] while others briefly described areas explored during Yarning [ 27 , 28 , 39 , 43 , 47 , 54 , 58 , 59 , 60 , 61 ]. One publication noted that there was “no set interview guide and that participants were encouraged, with consistent prompts to ‘yarn’ about their experiences with renal service providers” [ 62 ]. Some descriptions were minimal stating guides either had minimal questioning or use of probes [ 42 ] or simply stated that they were semi structured.
Some of the more comprehensive papers provided insight into seating arrangement, reimbursement to participants, and provision of meals. One publication described the seating arrangement as a component to providing a safe environment that allowed the researcher to observe body language and non-verbal cues (see Table 2 , 2.4) [ 27 ]. Eight publications reported reimbursement to participants, which were usually vouchers of between $20 and $50 for their time in participating in the study [ 40 , 49 , 50 , 51 , 52 , 63 , 64 , 65 ]. Five publications reported incorporating a meal within the data collection. [ 32 , 38 , 45 , 63 , 65 ] Study sizes for individual Yarning was reported to include between 4 [ 49 ] and 74 participants [ 28 ] with minimal justification for the choice of numbers. Yarning circles were often applied across community settings with each Yarning circle including between 5–17 participants at each individual circle. All but one [ 66 ] of the publications ( n = 45) reported the sample size.
Publications reported using varied sampling approaches including convenient sampling, [ 41 ] and opportunistic sampling [ 42 ], usually through routine health care [ 27 , 41 , 51 , 58 , 67 ]. However most papers reported purposeful sampling , [ 27 , 28 , 29 , 34 , 39 , 47 , 48 , 55 , 56 , 59 , 60 , 61 , 68 ] including through key community Elders and representatives [ 33 , 50 , 69 ].
Timeframes when conducting Yarning varied significantly from 10-30 min [ 27 ] up to 2.5 h, [ 44 , 55 , 56 ] more generally publications reported 40-60 min. Yarning circles were often reported as generally held at a time and place suitable to the participant [ 58 ] with use of community outdoor settings or participants houses. While Yarning was predominantly used to engage with Aboriginal and Torres Strait Islander people, some Yarning circles included non-Aboriginal participants such as health providers.
Research team positioning
Generally, details regarding the research team positioning were not available in publications (see: Table 1 & supp. 1 ). Exemplar papers described the research team and their positioning and demonstrated reflexivity on how this influences all stages of research (see Table 2 , 3.1). In these instances, authors described their ability to have “deeper” conversations with their participants, and the importance of established relationships in Aboriginal and Torres Strait Islander research. Some publications acknowledged that this contributed to providing a safe and favourable environment for participants.
Training and experience in both qualitative and Indigenous methods were often not reported. Eleven of the publications that reported Aboriginal and/or Torres Strait Islander involvement in data collection also outlined the experience, qualifications and expertise of the interviewer/s (see Table 2 , 3.2) [ 33 , 39 , 40 , 42 , 45 , 50 , 51 , 60 , 64 , 65 , 72 ]. Six of the publications specifically stated that the interviewers had relevant training in conducting qualitative interviews [ 31 , 33 , 45 , 50 , 51 , 72 ]. One publication [ 31 ] specifically detailed that the research team had been trained in Yarning methods with Professor Dawn Bessarab, who validated the method. This was a more comprehensive example of the way training was reported compared to the way training was reported in other publications.
The role of Aboriginal and Torres Strait Islander people in the Yarning process
We sought to detail the role of Aboriginal and Torres Strait Islander people in each stage the research process in publications that use Yarning method. In particular, we examine the role of Aboriginal and Torres Strait Islander people in leading the research, collecting data, analysis, and acting as an advisory to the research.
Aboriginal & Torres Strait Islander led research
Eleven of the forty-seven publications reported Aboriginal and Torres Strait Islander people as having led the research [ 28 , 30 , 32 , 33 , 34 , 40 , 42 , 54 , 64 , 65 , 70 ]. Those that were led by Aboriginal and Torres Strait Islander academics occasionally offered details on the authors and their roles. This was detailed using the authors initials, followed by their Aboriginal status, positioning, and role in the project. However, these details were scarce and difficult to immediately identify within publications. More comprehensive papers reflected on how these factors created an approach that helped centre Aboriginal voices in the research process (see Table 3 , 1.1).
Aboriginal & Torres Strait Islander involvement in data collection
Aboriginal and Torres Strait Islander researchers were reported as responsible for data collection and interviews in only half of the publications [ 71 ]. Some publications provided less detail on data collection involvement than others, and simply noted that the researcher was Aboriginal and therefore culturally safe (see Table 3 , 3.2).
Seven publications reported that interviews were conducted by both Aboriginal and/or Torres Strait Islander and non-Aboriginal and/or Torres Strait Islander researchers, [ 28 , 31 , 39 , 56 , 57 , 59 , 63 ] often citing that one was there to assist the other. One publication identified that there was “no difference in data, in terms of collection or results, was perceived by the non-Indigenous researcher when conducting the interviews.” [ 57 ].
Six publications reported that there was no Aboriginal and/or Torres Strait Islander involvement in data collection and the conducting of Yarning circles [ 29 , 38 , 48 , 49 , 67 ]. Some publications did not expand on this, and simply stated that the data collection was conducted by a non-Aboriginal researcher without further discussion (see Table 3 , 3.3). Others were more reflexive when addressing not having had an Aboriginal and Torres Strait Islander person collect the data. One publication [ 29 ] stated that they attempted to have an Aboriginal and Torres Strait Islander researcher involved, however, due to existing responsibilities of Aboriginal people in the area, they were unsuccessful (see Table 3 , 3.4). This publication then addressed the absence of Aboriginal involvement by detailing the critical part that relationships with the staff at Aboriginal Health Services were to different stages of the project. Another paper stated that the lack of Aboriginal involvement “may have impacted on the richness of interview data” [ 48 ].
Whilst rare, some papers suggested Yarning methods as an effective way to counter the impact of not having an Aboriginal or Torres Strait Islander person collect the data (see Table 3 , 3.5).
Others accounted for the lack of Aboriginal and/or Torres Strait Islander involvement in data collection through using Aboriginal guidance over the project, stating ongoing guidance was sought throughout various stages of the project (see Table 3 , 3.6).
Overall, the absence of Aboriginal and Torres Strait Islander involvement in the collection of data was frequently not addressed by publications. Eighteen publications did not report whether or not there were Aboriginal and/or Torres Strait Islander involvement in data collection [ 28 , 31 , 32 , 34 , 36 , 37 , 41 , 46 , 47 , 52 , 53 , 54 , 58 , 62 , 66 , 69 , 70 , 72 ]. For the most part, these publications did not identify who was responsible for conducting the Yarning circles.
Aboriginal & Torres Strait Islander involvement in analysis
Twenty-four of the 46 publications reported Aboriginal and/or Torres Strait Islander involvement in analysis [ 28 , 29 , 30 , 31 , 32 , 33 , 34 , 39 , 40 , 43 , 45 , 47 , 49 , 50 , 52 , 55 , 56 , 58 , 59 , 60 , 61 , 62 , 64 , 65 ]. Predominately it was simply stated that there were Aboriginal and/or Torres Strait Islander researchers or advisory groups involved in the process, without further elaboration of exactly what the involvement entailed. One paper suggested that Aboriginal and/or Torres Strait Islander investigators helped non-Indigenous researchers to “increase their cultural understandings and read the data differently. ” [ 28 ]. Other publications reported a collaborative analysis revision by experts and Aboriginal and/or Torres Strait Islander coinvestigators (see Table 3 , 4.1). This was deemed efficient in the inclusivity of perspectives that may have not been considered.
Many publications did not report whether or not they had Aboriginal and/or Torres Strait Islander involvement in data analysis. Some of these included publications that used the researchers initials to demonstrate involvement in analysis but did not specify whether they were Aboriginal and/or Torres Strait Islander. Not having Aboriginal and/or Torres Strait Islander involvement in data collection was typically not reflexively addressed.
One publication did report not having Aboriginal and/or Torres Strait Islander involvement in data collection and identified potential issues with this throughout their publication with reflections such as “The challenge for a non-Aboriginal researcher exploring issues within the Aboriginal community is to avoid repeating mistakes of the past.” [ 67 ] Other publications noted (by those who acknowledge it) that Aboriginal and/or Torres Strait Islander advisory, person or group was used to overlook data analysis.
A limited number of publications indicated that participants were offered the opportunity to provide feedback on the findings (see Table 3 , 4.2). It was often reported by simply stating that data was returned to participants for feedback. Some publications elaborated on this, with one suggesting that yarning with participants about the results allowed for them to review and engage with the interpretation of data. Some publications noted that transcripts were not returned to participants, nor were the data validated by participants without further comment.
The few publications that reported using an ‘Indigenous approach’ to analysis were slightly more comprehensive than those that reported grounded theory approach (see Table 3 , 4.3). Overall, details on analysis were often lacking, and were the least comprehensive component of the methodology sections.
“Aboriginal Advisory”
Only twenty-nine of the 46 included publications reported having an Aboriginal and/or Torres Strait Islander advisory, person or group throughout the course of their study [ 27 , 28 , 29 , 31 , 33 , 34 , 36 , 37 , 39 , 40 , 41 , 42 , 43 , 45 , 46 , 47 , 51 , 53 , 54 , 55 , 56 , 59 , 60 , 62 , 63 , 65 , 66 , 67 , 68 ]. Advisory groups were used to oversee the research, analyse data, develop protocols, guide research conduct, identify potential services and recruitment, and develop interview guides. Publications that offered a more comprehensive description of the role of the advisory group gave details on who was involved, such as Elders and community members, and how their guidance was utilised in each stage of the research process (see Table 3 , 5.1). Often, these publications noted that the reference groups held the study team accountable for conducting appropriate and respectful research.
Most publications reported an Aboriginal reference or guiding group, with limited details on who was involved, or what exactly their role entailed (see Table 3 , 5.2). Many of the publications did not mention Aboriginal and/or Torres Strait Islander Advisory until the acknowledgment section of the manuscript. The process of Aboriginal and/or Torres Strait Islander advisory varied across publications, with limited consistency in the level of reporting and who was involved.
This is the first review to critically analyse the use of Yarning method in Aboriginal and Torres Strait Islander health research. Through this, we make recommendations on how systems, including the Academy and other mechanisms such as journals, can better incorporate Aboriginal and Torres Strait Islander ways of knowing, being and doing into systems and processes, to ultimately uphold research integrity.
Although there is a strong and growing evidence-base for Indigenous quantitative methods that have been used by Indigenous scholars with ongoing room for improvement in everyday practice, [ 73 ] researchers using Indigenous methods in health research frequently report using qualitative methods [ 13 ]. Qualitative methods are said to privilege Indigenous voices [ 12 ] and remove power imbalances [ 13 , 18 ]. Yarning method is the most commonly reported Indigenous method applied to Aboriginal and Torres Strait Islander qualitative health research. Despite this, our analysis shows that details regarding how Yarning methods were applied, and the intricacies of Aboriginal and Torres Strait Islander involvement (such as stages, level or type of involvement), were significantly under reported. While part of this may be attributed to limitations in researcher reflexivity, the level of detail required to situate authors positionality, relationality as well as thoroughly describe research processes are not always achievable within the existing parameters of journal and reporting guidelines. We offer our recommendations and improvement opportunities for both researchers, and academic institutions to ensure reporting in publications reflects the need for ethical and reciprocal research with Aboriginal and Torres Strait Islander people, as per the NHMRC Values and Ethics Guideline, [ 14 ] the AIATSIS Code of Ethics [ 15 ] and the AHMRC Key Principles [ 16 ].
The right reasons? Why are researchers using Yarning methods?
In the reviewed publications, Yarning was frequently cited as a way of decolonising research practice. It was considered culturally safe, offer two-way knowledge sharing, built on cultural protocols, and allow participant led research while attempting to better balance and privilege Indigenous voices. Numerous research has validated Yarning as a recommended method to privilege Indigenous ontologies [ 9 , 17 , 18 ]. However, it is not simply enough to report employing an Indigenous method such as Yarning and assume that it is adequate. Yarning is grounded in cultural positioning [ 17 ] and relationality [ 11 ]. Therefore, the application of Yarning will vary based on the context and the researcher (including their social and cultural positioning, and considerations of power and control) and the Aboriginal and Torres Strait Islander community involved. Similarly, Yarning is not simply the means to collect the data. Decolonising research must address the research process as a whole and centre Indigenous worldviews, values and principles [ 1 , 74 ]. This is depicted in Fig. 3 .
Visual representation of the Yarning Process in line with decolonising research practice as depicted by Michelle Kennedy
Reporting positioning, reflexivity and relationality is essential for ethical research
Irrespective of employing a decolonising approach, researcher positioning is well understood as a necessary component to conducting reflexive, ethical and quality research in all qualitative research practice. Researchers are embedded within the research process, and are therefore required to constantly consider their worldview and positionality [ 75 ]. As Kiekelame and Swartz (2019) conclude “the importance of reflexivity and self-reflexivity as a transformative approach in a decolonising process cannot be over emphasised” [ 76 ]. Despite researcher positioning and reflexive practices being at the core of qualitative research and the importance of Aboriginal and Torres Strait Islander led research, we found limited information reported on the research team’s context, including social and cultural positioning and relationality which is a central “presupposition of an Indigenous social research paradigm”; [ 11 ] our belonging to Mob and Country, the connection to the living earth must be recognised and strategically mobilised by Indigenous peoples in developing an Indigenous research agenda.
While some publications articulated social and cultural positioning and relationality of researchers and decolonising research practice, most were silent on these aspects. This silence and subsequent invisibility, often leads to reinscribe racial dominance in theorising, analysing and undertaking research in practice; embedded through the ongoing experience of colonisation and the ingrained nature of coloniality across Australia.
Non-Indigenous authors did not always detail reflective practice or identify their social and cultural positioning. This is in opposition to decolonising research practice which seeks to address Euro-Western dominant paradigms [ 1 , 77 ]. Describing Aboriginal and Torres Strait Islander involvement, researcher reflexivity and positionality, and relationalities are crucial in research, including both qualitative processes and decolonising approaches. This is even more critical when Indigenous methodologies and methods are reportedly being applied by non-Indigenous peoples. Publications that reported using an “Indigenous lens” rarely articulated how this was applied, and how it informed the publication. While this can partially be attributed to structural publishing barriers, such as word count limitations, it is essential for researchers to describe how an Indigenous lens was applied as well as their role and how their perspectives inform the research process. It is not enough to note the application of an “Indigenous lens” but also how they applied this lens, particularly from a non-Indigenous standpoint. Reflecting on how their own practices, world views and experiences impacted and influenced the research outcomes and effectively and accurately represented the voices of participants in the research. Accountability in qualitative research requires the application and description of reflexive research practices in relation to the researcher and the researched. It is not possible for a researcher to completely omit researcher bias. It is therefore imperative to outline the reflexive processes, and how Indigenous peoples informed the research in a comprehensive manner in favour of upholding culturally safe, ethical and best practice qualitative research.
Aboriginal and Torres Strait Islander people should be involved in all stages of the research process
Despite ongoing calls for, and emphasis on the importance of having research to be led by Aboriginal and Torres Strait Islander people, only a quarter of publications self-reported Aboriginal or Torres Strait Islander people as lead researcher. The remaining papers were silent in reporting Aboriginal and/or Torres Strait Islander researcher(s) involvement or were led by non-Indigenous researchers. The transformative nature of Indigenous-led research is well established, [ 1 ] as such we urge all researchers to report leadership of the research in the publication.
Just over half the papers reported Aboriginal and/or Torres Strait Islander people’s involvement in data collection, with limited information provided on qualifications/training or the relationship and cultural expertise to the participants or community engaged in the research. Acknowledging the centrality of following cultural protocols and practices when conducting Yarning method, details on data collection must report this detail when applying the method.
Aboriginal and/or Torres Strait Islander involvement in analysis was seldom detailed, more frequently papers reported advisory groups, increasing cultural understanding, with and oversight as their primary role. Researchers and coders play a pivotal role in the process of thematic analysis [ 78 ]. Detailing Aboriginal and Torres Strait Islander involvement in all levels of the research conduct including the analysis is paramount to accurately representing the voices of those being researched and supporting ethical and cultural safe research. Decolonising research practice must privilege Indigenous knowledges and uphold self-determination and sovereignty which is not excluded from the analysis and reporting process. In line with recent research into Yarning application, [ 19 ] we recognise the need for refinement in the analysis process, and the importance of producing details of method and methodologies used.
As stated by Atkinson et al. [ 19 ] “the more relational the Yarn, the greater the thickness of data, and an Indigenous Standpoint is likely to generate more relationality through shared implicit and explicit understanding for the Yarn”. Our research demonstrates that the relationality of Yarns is not consistently carried beyond the stages of data collection and into analysis, or at least, is not reported on.
We found that at times, Aboriginal research assistants were used to collect the data, but were not involved in the interpretation of the Yarns. To produce ethical, quality research, Aboriginal people should be involved in all stages of the research from conceptualisation to dissemination, including the analysis and interpretation. Understanding and conceptualising data collected from Yarning should involve Indigenous ontologies and standpoints to ensure participants stories are correctly and appropriately reported in the research results.
The role and details of Aboriginal reference/Advisory groups need to be reported
The formation of a community advisory or Aboriginal reference group (CAG/ARG) is important in ensuring governance and efficacy in the research process, as well as upholding Indigenous knowledges, sovereignty, and self-determination. The Aboriginal Health & Medical Research Council ethical guidelines state that Aboriginal and Torres Strait Islander ‘Advisory’ or reference groups must be representative of the group being studied and have knowledge or experience of the research matter and must be engaged throughout the life cycle of the project not just at the development or consultation stage [ 16 ].
While the majority of publications reported having a CAG/ARG that provided oversight to the research process, we found that publications reported limited details on who was involved, and their specific role, particularly regarding analysis, reporting and validation of results. This detail is critical to understanding how the CAG/ARG is both representative of the group being studied and how their Indigenous knowledge, self-determination and sovereignty were upheld in the research process. While some publications offered detailed explanations of who was in the advisory group and what their role was through the research process, others simply stated that the research was overseen or guided by an Aboriginal advisory group. Offering details on the CAG/ARG is crucial, particularly when non-Indigenous researchers are engaging with Indigenous methods, such as Yarning. We question: Who validates that the methods are applied correctly? Is this left to the researcher to self-validate? And where is the research team’s accountability to the Aboriginal and/or Torres Strait Islander community being studied?
Aboriginal and Torres Strait Islander “Advisory” or reference group are critical to ethical research practice, and must not be used to rubber stamp the research process. Research that aims to improve the lives of Aboriginal and Torres Strait Islander peoples must foreground Indigenous knowledges, sovereignty, and self-determination through relationality. Watego asserts “The transdisciplinarity required to effect change requires more than a bringing together of different methodologies—it demands attention to different ways of knowing and being in a relational, rather than hierarchical, manner, recognising the limitations of different knowledge systems as well as their strengths, so that the most appropriate conceptual tools are brought to bear in addressing the grand challenges we face both now and into the future” [ 79 ].
Academic institutions and journals require structural change to account for reporting
As detailed throughout the results and discussion section of this review, authors frequently omitted important details regarding standpoint, positioning, reflexivity, level of Aboriginal and Torres Strait Islander involvement, and explanations of methods. It is reasonable to assume that silence in some of these areas are due to barriers in publishing. Academic journals should cater to the need to report reflexivity and positionality, particularly in relation to Indigenous research, including Aboriginal and Torres Strait Islander research. Many journals have restrictive word counts and journal structures and essential reporting requirements, which create barriers to effectively reporting adequate details that demonstrate best practice, ethical and equitable research. Academic journals and existing structures should require accurate reporting to produce community relevant, scientific excellence in quality and valid qualitative inquiry, that considers and contextualises findings to the local context. Additionally, it is important to move beyond reporting qualitative rigour as simply just a check box exercise. The Qualitative Health Research (QHR) journal recently released an editorial detailing why their review process does not use checklists:
These lists ignore the value of the product of the research: They do not address the originality, the substance, the contribution, and the potential results to the actual topic—which is after all the purpose of the project itself. [ 80 ]
The editorial explains that checklist reviews can undermine the value of qualitative inquiry [ 80 ]. This authorship team suggested that beyond checklists, journals acknowledge Indigenous knowledge systems and seek contribution of Indigenous peer reviewers on the reporting of Indigenous methodologies and methods to uphold the appropriate reporting requirements [ 81 ].
Strengths and limitations
This paper reports a review of publications reporting the use of Yarning method in Aboriginal and Torres Strait Islander health research. Our review was led by an Aboriginal research team including the author of the Yarning as a legitimate research method publication [ 17 ]. Our review provides a critical analysis of Yarning method as applied to qualitative health research and provides guidance to researchers on the future use, and reporting of Yarning method. Whilst Yarning is a culturally safe method that is preferred by Aboriginal and Torres Strait Islander people, non-Indigenous researchers need to consider the significance of relationality, sovereignty, and integrity of the research in the doing through the inclusion of Indigenous leadership at every stage.
Authors note that the Yarning method is applied to other disciplines of research and as such this paper offers limitations to understanding it’s broader application. Some publications in this review also included the use of other Indigenous and/or decolonising methods which were not analysed and out of scope in this review. Further analysis on additional Indigenist methods would be insightful.
Aboriginal and Torres Strait Islander people should be at the forefront of research about them. Coloniality has embedded systemic racism in our societal structures, privileging non-Indigenous peoples and disadvantaging Indigenous peoples. Coloniality perpetuates ideas about Indigeneity which are then formed and validated through social, cultural, and political structures, practices, and beliefs. They play out in our languages, knowledges, academic discourse, personal and social interactions and popular cultures, and other domains that assign and negotiate meanings and values [ 82 ]. Universities and research are not omitted from coloniality, which too, continue to systematically privilege non-Indigenous knowledge systems, methodologies and methods. Despite cutting edge research by Aboriginal and Torres Strait Islander people since time immemorial, the exclusion of Indigenous knowledges, ways of knowing being and doing has a lasting impact that extends to peer review publications processes and policy development. Euro-Western academic hierarchies, “gold standard” reporting do not necessarily allow for, or consider, Indigenous ways of knowing or uphold Indigenous sovereignty and self-determination in the research process. Although Yarning is recognised as a legitimate research method to decolonising research practice, this method must not be used lightly to justify safety and security in research with Aboriginal and Torres Strait Islander people. It must be applied rigorously and reported accurately, describing how the different types of yarning were applied in research, the involvement of Aboriginal and Torres Strait Islander peoples at all levels of the research, and the outcomes. We found that researcher reflexivity and positioning were significantly under detailed as was Aboriginal and Torres Strait Islander ownership, stewardship, custodianship and analysis of data collected in our reviewed publications. Researchers, particularly non-Indigenous led research teams, must only report using an Indigenous method if they are willing to report adequate detail on its application and comprehensive detail on how Aboriginal and Torres Strait Islander peoples were involved in all levels of the research. Journals and other establishments should review their process to allow for these details to be documented in research publications without penalty and acknowledge the critical role of Indigenous Editors and peer reviewers. Only through this, can we uphold respectful, reciprocal, ethical, and responsible research practice.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
Community advisory or Aboriginal reference group
Smith LT. Decolonizing Methodologies: Research and Indigenous Peoples. London: Zed Books; 1999.
Google Scholar
Borch M. Rethinking the origins of terra nullius. Aust Hist Stud. 2001;32(117):222–39.
Article Google Scholar
Vivian A, Halloran MJ. Dynamics of the policy environment and trauma in relations between Aboriginal and Torres Strait Islander peoples and the settler-colonial state. Crit Soc Policy. 2021;1:22.
Clarkson C, Jacobs Z, Marwick B, Fullagar R, Wallis L, Smith M, et al. Human occupation of northern Australia by 65,000 years ago. Nature. 2017;547(7663):306–10.
Article CAS PubMed Google Scholar
Cunningham DJ. The Spinal Curvature in an Aboriginal Australian. Proc R Soc Lond. 1888;45:487–504.
Fraser J. ‘Science, Museums and Collecting the Indigenous Dead in Colonial Australia’ by Paul Turnbull. History of Anthropology Review. 2020. p. 44.
Race CG, Exclusion F. Race For Exclusion. Aust N Z J Sociol. 1986;22(1):3–24.
Huggins J. Black women and women’s liberation. A Reader in feminist knowledge. London: Routledge; 1991.
Smith RL, Devine S, Preston R. Recommended methodologies to determine Australian Indigenous community members’ perceptions of their health needs: a literature review. Aust J Prim Health. 2020;26(2):95–103.
Article PubMed Google Scholar
Sherwood J. Who is not coping with colonization? Laying out the map for decolonization. Australas Psychiatry. 2009;17(Suppl 1):S24–7.
Moreton-Robinson A. Relationality: A Key Presupposition of an Indigenous Social Research Paradigm. Sources and Methods in Indigenous Studies. United Kingdom: Routledge; 2017. p. 69–77.
Rigney LI. Internationalization of an Indigenous Anticolonial Cultural Critique of Research Methodologies: A Guide to Indigenist Research Methodology and Its Principles. Wicazo Sa Rev. 1999;14(2 Emergent Ideas in Native American Studies):109–21.
Drawson AS, Toombs E, Mushquash CJ. Indigenous Research Methods: A Systematic Review. Int Indig Policy J. 2017;8(2):1-25.
National Health and Medical Research Council. Values and ethics: guidelines for ethical conduct in Aboriginal and Torres Strait Islander health research. Canberra: Commonwealth of Australia; 2003. 2003.
AIATSIS. AIATSIS Code of Ethics for Aboriginal and Torres Strait Islander Research. Canberra: ACT; 2020.
AHMRC. Aboriginal Health and Medical Research council Key Principles 2020 V2.0. Surry Hills: Aboriginal Health & Medical Research Council; 2020.
Bessarab D, Ng’andu B. Yarning About Yarning as a Legitimate Method in Indigenous Research. Int J Crit Indig Stud. 2010;3(1):37–50.
Geia LK, Hayes B, Usher K. Yarning/Aboriginal storytelling: towards an understanding of an Indigenous perspective and its implications for research practice. Contemp Nurse. 2013;46(1):13–7.
Atkinson P, Baird M, Adams K. Are you really using Yarning research? Mapping Social and Family Yarning to strengthen Yarning research quality. AlterNative: Int J Indig Peoples. 2021;17(2):191–201.
Martin K. Ways of knowing, ways of being and ways of doing: a theoretical framework and methods for Indigenous research and Indigenist research. J Aust Stud. 2003;765:203-24.
Australian Government. National Partnership Agreement on Closing the Gap in Indigenous Health Outcomes 2009–2013. Canberra: Australian Government; 2008.
Kennedy M, Bennett J, Maidment S, Chamberlain C, Booth K, McGuffog R, et al. Interrogating the intentions for Aboriginal and Torres Strait Islander health: a narrative review of research outputs since the introduction of Closing the Gap. Med J Aust. 2022;217(1):50–7.
Harfield S, Pearson O, Morey K, Kite E, Canuto K, Glover K, et al. Assessing the quality of health research from an Indigenous perspective: the Aboriginal and Torres Strait Islander quality appraisal tool. BMC Med Res Methodol. 2020;20(1):79.
Article PubMed PubMed Central Google Scholar
Huria T, Palmer SC, Pitama S, Beckert L, Lacey C, Ewen S, et al. Consolidated criteria for strengthening reporting of health research involving indigenous peoples: the CONSIDER statement. BMC Med Res Methodol. 2019;19(1):173.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Fereday J, Muir-Cochrane E. Demonstrating Rigor Using Thematic Analysis: A Hybrid Approach of Inductive and Deductive Coding and Theme Development. Int J Qual Methods. 2006;5(1):80–92.
Hamilton S, Reibel T, Maslen S, Watkins R, Jacinta F, Passmore H, et al. Disability “In-Justice”: The Benefits and Challenges of “Yarning” With Young People Undergoing Diagnostic Assessment for Fetal Alcohol Spectrum Disorder in a Youth Detention Center. Qual Health Res. 2020;30(2):314–27.
Marriott R, Reibel T, Coffin J, Gliddon J, Griffin D, Robinson M, et al. “Our culture, how it is to be us” - Listening to Aboriginal women about on Country urban birthing. Women Birth. 2019;32(5):391–403.
Carlin E, Atkinson D, Marley JV. “Having a Quiet Word”: Yarning with Aboriginal Women in the Pilbara Region of Western Australia about Mental Health and Mental Health Screening during the Perinatal Period. Int J Environ Res Public Health. 2019;16(21):4253.
Article PubMed Central Google Scholar
Butler TL, Anderson K, Condon JR, Garvey G, Brotherton JML, Cunningham J, et al. Indigenous Australian women’s experiences of participation in cervical screening. PLoS One. 2020;15(6):e0234536.
Article CAS PubMed PubMed Central Google Scholar
Cullen P, Mackean T, Worner F, Wellington C, Longbottom H, Coombes J, et al. Trauma and Violence Informed Care Through Decolonising Interagency Partnerships: A Complexity Case Study of Waminda’s Model of Systemic Decolonisation. Int J Environ Res Public Health. 2020;17(20):7363.
Coombes J, Hunter K, Mackean T, Ivers R. The journey of aftercare for Australia’s First Nations families whose child had sustained a burn injury: a qualitative study. BMC Health Serv Res. 2020;20(1):536.
Coombes J, Lukaszyk C, Sherrington C, Keay L, Tiedemann A, Moore R, et al. First Nation Elders’ perspectives on healthy ageing in NSW, Australia. Aust N Z J Public Health. 2018;42(4):361–4.
Durey A, McEvoy S, Swift-Otero V, Taylor K, Katzenellenbogen J, Bessarab D. Improving healthcare for Aboriginal Australians through effective engagement between community and health services. BMC Health Serv Res. 2016;16:224.
Chapman R, Smith T, Martin C. Qualitative exploration of the perceived barriers and enablers to Aboriginal and Torres Strait Islander people accessing healthcare through one Victorian Emergency Department. Contemp Nurse. 2014;48(1):48–58.
Rix EF, Barclay L, Stirling J, Tong A, Wilson S. The perspectives of Aboriginal patients and their health care providers on improving the quality of hemodialysis services: a qualitative study. Hemodial Int. 2015;19(1):80–9.
Meiklejohn JA, Arley BD, Pratt G, Valery PC, Bernardes CM. “We just don’t talk about it”: Aboriginal and Torres Strait Islander peoples’ perceptions of cancer in regional Queensland. Rural Remote Health. 2019;19(2):4789.
PubMed Google Scholar
Parmenter J, Basit T, Nelson A, Crawford E, Kitter B. Chronic disease self-management programs for Aboriginal and Torres Strait Islander people: Factors influencing participation in an urban setting. Health Promot J Austr. 2019.
Kong AC, Sousa MS, Ramjan L, Dickson M, Goulding J, Gwynne K, et al. “Got to build that trust”: the perspectives and experiences of Aboriginal health staff on maternal oral health. Int J Equity Health. 2020;19(1):187.
Canuto K, Towers K, Riessen J, Perry J, Bond S, Ah Chee D, et al. “Anybody can make kids; it takes a real man to look after your kids”: Aboriginal men’s discourse on parenting. PLoS One. 2019;14(11):e0225395.
Lyall V, Guy J, Egert S, Pokino LA, Rogers L, Askew D. “They Were Willing to Work with Me and Not Pressure Me”: A Qualitative Investigation into the Features of Value of a Smoking Cessation in Pregnancy Program for Aboriginal and Torres Strait Islander Women. Int J Environ Res Public Health. 2020;18(1):49.
Bryce S, Scales I, Herron LM, Wigginton B, Lewis M, Lee A, et al. Maitjara Wangkanyi: Insights from an Ethnographic Study of Food Practices of Households in Remote Australian Aboriginal Communities. Int J Environ Res Public Health. 2020;17(21):8109.
Lin IB, Ryder K, Coffin J, Green C, Dalgety E, Scott B, et al. Addressing Disparities in Low Back Pain Care by Developing Culturally Appropriate Information for Aboriginal Australians: “My Back on Track, My Future.” Pain medicine (Malden, Mass). 2017;18(11):2070–80.
Lin I, O’Sullivan P, Coffin J, Mak DB, Toussaint S, Straker L. “I can sit and talk to her”: Aboriginal people, chronic low back pain and healthcare practitioner communication. Aust Fam Physician. 2014;43(5):320–4.
Lukaszyk C, Coombes J, Turner NJ, Hillmann E, Keay L, Tiedemann A, et al. Yarning about fall prevention: community consultation to discuss falls and appropriate approaches to fall prevention with older Aboriginal and Torres Strait Islander people. BMC Public Health. 2017;18(1):77.
Gibson C, Crockett J, Dudgeon P, Bernoth M, Lincoln M. Sharing and valuing older Aboriginal people's voices about social and emotional wellbeing services: a strength-based approach for service providers. Aging Ment Health. 2018;4(3):481-8.
Gonzalez T, Harris R, Williams R, Wadwell R, Barlow-Stewart K, Fleming J, et al. Exploring the barriers preventing Indigenous Australians from accessing cancer genetic counseling. J Genet Couns. 2020;29(4):542–52.
Munro A, Allan J, Shakeshaft A, Breen C. “I just feel comfortable out here, there’s something about the place”: staff and client perceptions of a remote Australian Aboriginal drug and alcohol rehabilitation service. Subst Abuse Treat Prev Policy. 2017;12(1):49.
Seear KH, Lelievre MP, Atkinson DN, Marley JV. “It’s Important to Make Changes.” Insights about Motivators and Enablers of Healthy Lifestyle Modification from Young Aboriginal Men in Western Australia. Int J Environ Res Public Health. 2019;16(6):1063.
Busija L, Cinelli R, Toombs MR, Easton C, Hampton R, Holdsworth K, et al. The Role of Elders in the Wellbeing of a Contemporary Australian Indigenous Community. Gerontologist. 2018.
Deacon-Crouch M, Skinner I, Connelly M, Tucci J. Chronic disease, medications and lifestyle: perceptions from a regional Victorian Aboriginal community. Pharm Pract. 2016;14(3):798.
Meiklejohn JA, Bailie R, Adams J, Garvey G, Bernardes CM, Williamson D, et al. "I'm a Survivor": Aboriginal and Torres Strait Islander Cancer Survivors' Perspectives of Cancer Survivorship. Cancer Nurs. 2018.
Pilkington L, Haigh MM, Durey A, Katzenellenbogen JM, Thompson SC. Perspectives of Aboriginal women on participation in mammographic screening: a step towards improving services. BMC Public Health. 2017;17(1):697.
Murrup-Stewart C, Whyman T, Jobson L, Adams K. "Connection to Culture Is Like a Massive Lifeline": Yarning With Aboriginal Young People About Culture and Social and Emotional Wellbeing. Qual Health Res. 2021;31(10):1833-46.
Lin IB, O’Sullivan PB, Coffin JA, Mak DB, Toussaint S, Straker LM. Disabling chronic low back pain as an iatrogenic disorder: a qualitative study in Aboriginal Australians. BMJ Open. 2013;3(4):e002654.
Lin IB, O’Sullivan PB, Coffin JA, Mak DB, Toussaint S, Straker LM. “I am absolutely shattered”: the impact of chronic low back pain on Australian Aboriginal people. Eur J Pain (London, England). 2012;16(9):1331–41.
Article CAS Google Scholar
Butten K, Johnson NW, Hall KK, Toombs M, King N, O’Grady KF. Impact of oral health on Australian urban Aboriginal and Torres Strait Islander families: a qualitative study. Int J Equity Health. 2019;18(1):34.
Meiklejohn JA, Garvey G, Bailie R, Walpole E, Adams J, Williamson D, et al. Follow-up cancer care: perspectives of Aboriginal and Torres Strait Islander cancer survivors. Support Care Cancer. 2017;25(5):1597–605.
Kendall S, Lighton S, Sherwood J, Baldry E, Sullivan E. Holistic Conceptualizations of Health by Incarcerated Aboriginal Women in New South Wales. Australia Qual Health Res. 2019;29(11):1549–65.
Reibel T, Morrison L, Griffin D, Chapman L, Woods H. Young Aboriginal women’s voices on pregnancy care: factors encouraging antenatal engagement. Women Birth. 2015;28(1):47–53.
Carlin E, Cox Z, Spry E, Monahan C, Marley JV, Atkinson D. "When I got the news": Aboriginal fathers in the Kimberley region yarning about their experience of the antenatal period. Health Promot J Austr. 2020;32:513–22.
Rix EF, Barclay L, Stirling J, Tong A, Wilson S. “Beats the alternative but it messes up your life”: aboriginal people’s experience of haemodialysis in rural Australia. BMJ Open. 2014;4(9):e005945.
Schoen D, Balchin D, Thompson S. Health promotion resources for Aboriginal people: lessons learned from consultation and evaluation of diabetes foot care resources. Health Promot J Austr. 2010;21(1):64–9.
Bovill M, Gruppetta M, Cadet-James Y, Clarke M, Bonevski B, Gould GS. Wula (Voices) of Aboriginal women on barriers to accepting smoking cessation support during pregnancy: Findings from a qualitative study. Women Birth. 2018;31(1):10–6.
Bovill M, Bar-Zeev Y, Gruppetta M, Clarke M, Nicholls K, O’Mara P, et al. Giri-nya-la-nha (talk together) to explore acceptability of targeted smoking cessation resources with Australian Aboriginal women. Public Health. 2019;176:149–58.
Peake RM, Jackson D, Lea J, Usher K. Meaningful Engagement With Aboriginal Communities Using Participatory Action Research to Develop Culturally Appropriate Health Resources. J Transcult Nurs. 2021;32(2):129–36.
Helps C, Barclay L. Aboriginal women in rural Australia; a small study of infant feeding behaviour. Women Birth. 2015;28(2):129–36.
Hamilton SL, Maslen S, Watkins R, Conigrave K, Freeman J, O’Donnell M, et al. ‘That thing in his head’: Aboriginal and non-Aboriginal Australian caregiver responses to neurodevelopmental disability diagnoses. Sociol Health Illn. 2020;42(7):1581–96.
Southcombe A, Cavanagh J, Bartram T. Capacity building in indigenous men’s groups and sheds across Australia. Health Promot Int. 2015;30(3):606–15.
Ryder C, Mackean T, Hunter K, Coombes J, Holland AJA, Ivers R. Yarning up about out-of-pocket healthcare expenditure in burns with Aboriginal families. Aust N Z J Public Health. 2021;45(2):138–42.
Henwood M, Shaw A, Cavanagh J, Bartram T, Marjoribanks T, Kendrick M. Men’s health and communities of practice in Australia. J Health Organ Manag. 2017;31(2):207–22.
Belton S, Kruske S, Jackson Pulver L, Sherwood J, Tune K, Carapetis J, et al. Rheumatic heart disease in pregnancy: How can health services adapt to the needs of Indigenous women? A qualitative study. Aust N Z J Obstet Gynaecol. 2018;58(4):425–31.
Walter MA, C. Indigenous Statistics: A Quantitative Research Methodology. London & New York: Left Coast Pres, Inc; 2013.
Haynes E, Marawili M, Mitchell A, Walker R, Katzenellenbogen J, Bessarab D. “Weaving a Mat That We Can All Sit On”: Qualitative Research Approaches for Productive Dialogue in the Intercultural Space. Int J Environ Res Public Health. 2022;19(6):3654.
Sutton J, Austin Z. Qualitative Research: Data Collection, Analysis, and Management. Can J Hosp Pharm. 2015;68(3):226–31.
PubMed PubMed Central Google Scholar
Keikelame MJ, Swartz L. Decolonising research methodologies: lessons from a qualitative research project, Cape Town, South Africa. Glob Health Action. 2019;12(1):1561175.
Wilson S. Research Is Ceremony: Indigenous Research Methods. Winnipeg, Manitoba: Fernwood Publishing; 2008.
Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual Res Psychol. 2021;18(3):328–52.
Watego C, Whop LJ, Singh D, Mukandi B, Macoun A, Newhouse G, et al. Black to the Future: Making the Case for Indigenist Health Humanities. Int J Environ Res Public Health. 2021;18(16):8704.
Morse J. Why the Qualitative Health Research (QHR) Review Process Does Not Use Checklists. Qual Health Res. 2021;31(5):819–21.
Movono A. Indigenous scholars struggle to be heard in the mainstream. Here’s how journal editors and reviewers can help 2021. Available from: https://theconversation.com/indigenous-scholars-struggle-to-be-heard-in-the-mainstream-heres-how-journal-editors-and-reviewers-can-help-157860 .
Watego CS, Singh D, Macoun A. Partnership for Justice in Health: Scoping Paper on Race, Racism and the Australian Health System. Melbourne: The Lowitja Institute. 2021.
Download references
Acknowledgements
We wish to acknowledge Aboriginal and Torres Strait Islander people as the continuing custodians of the lands on which we live and work. We pay respects to the Awabakal, Worimi, Wurundjeri, Ngunnawal, Whadjuk peoples and their Elders past, present, and emerging.
No funding was received for this study. MK was supported by an NHMCR Early Career Fellowship (No. 1158670) during study period.
Author information
Authors and affiliations.
College of Health Medicine and Wellbeing, The University of Newcastle, Callaghan, NSW, Australia
Michelle Kennedy, Kade Booth & Sian Maidment
Hunter Medical Research Institute, New Lambton Heights, NSW, Australia
Michelle Kennedy & Kade Booth
National Centre for Epidemiology and Public Health, The Australian National University, Canberra ACT, Australia
Raglan Maddox
School of Population and Global Health, Centre for Health Equity, University of Melbourne, Melbourne, VIC, Australia
Catherine Chamberlain
Judith Lumley Centre, School of Nursing and Midwifery, La Trobe University, Melbourne, VIC, Australia
Ngangk Yira Research Centre for Aboriginal Health and Social Equity, Murdoch University, Perth, WA, Australia
Centre for Aboriginal Medical and Dental Health, UWA Medical School, Crawley, WA, Australia
Dawn Bessarab
You can also search for this author in PubMed Google Scholar

Contributions
MK & DB were responsible for study conception and design. MK, KB & SM were responsible for data extraction and analysis. All authors contributed to interpretation of data, as well as the drafting and revision of the manuscript. All authors have viewed and approved the current version for submission.
Authors’ information
See ‘ Research Team ’ within manuscript for relevant authors’ information.
Corresponding author
Correspondence to Michelle Kennedy .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Level of reporting table and scoring system.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kennedy, M., Maddox, R., Booth, K. et al. Decolonising qualitative research with respectful, reciprocal, and responsible research practice: a narrative review of the application of Yarning method in qualitative Aboriginal and Torres Strait Islander health research. Int J Equity Health 21 , 134 (2022). https://doi.org/10.1186/s12939-022-01738-w
Download citation
Received : 10 May 2022
Accepted : 22 August 2022
Published : 13 September 2022
DOI : https://doi.org/10.1186/s12939-022-01738-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Qualitative
- Aboriginal health
- Indigenous methods
- Critical review
- Yarning method
International Journal for Equity in Health
ISSN: 1475-9276
- General enquiries: [email protected]
- Research article
- Open access
- Published: 29 October 2019
What does it mean to conduct participatory research with Indigenous peoples? A lexical review
- Ann Dadich ORCID: orcid.org/0000-0001-5767-1794 1 , 2 ,
- Loretta Moore 3 , 4 &
- Valsamma Eapen 5 , 6 , 7
BMC Public Health volume 19 , Article number: 1388 ( 2019 ) Cite this article
10k Accesses
19 Citations
4 Altmetric
Metrics details
To better understand and promote public health, participatory research with Indigenous peoples represents recommended practice, worldwide. However, due to the different ways such research is referred to, described, and used, it is unclear what might (and might not) warrant the term when collaborating with Indigenous peoples. As such, this article expands conceptual understandings of participatory research with Indigenous peoples, across timelines and regions.
Following a systematic search of 29 academic databases in April 2018, a lexical analysis of the methods sections was conducted, which were sourced from 161 publications across 107 journals.
The active involvement of Indigenous peoples in research that is expressly participatory is limited across all project phases. This might be because the ways in which Indigenous peoples were involved throughout were not reported – however, it might also be because Indigenous peoples were not involved in all project phases. Furthermore, descriptions differ by study location and publication timeframe – notably, studies in the region of the Americas chiefly refer to pandemics, surveyors, and art; and those published in the last two decades have given primacy to artifacts of interest.
Conclusions
Findings from this corpus of data suggest participatory research with Indigenous peoples is not always described across different project phases; furthermore, it differs according to study location and publication timeframe. This offers considerable opportunity to further this important research area via alternative methodologies that award primacy to Indigenous expertise and agency.
Peer Review reports
To redress the power imbalance in research with Indigenous peoples, participatory research represents recommended practice, worldwide [ 1 ]. This recommendation recognizes that, ‘Discrimination against… indigenous peoples… causes and magnifies poverty and ill-health’ [ 2 ]. Conventional, non-participatory approaches have largely failed to address health inequalities, with Indigenous peoples more likely to experience poor health, reduced quality of life, and premature death, relative to their non-Indigenous counterparts. Consider for instance, the ways in which some research approaches, steeped in colonialism, have subjugated Indigenous voices. As Indigenous scholar, Tuhiwai Smith [ 3 ], critiqued:
Research[ers] within late-modern and late-colonial conditions… enter communities armed with goodwill in their front pockets and patents in their back pockets… Research… on indigenous people is still justified by the ends rather than by the means… [Some] researchers… collect… beliefs systems and ideas about healing, about the universe, about relationships and the ways of organizing… The global hunt for new knowledges… brings new threats to indigenous communities… what counts as Western research… (1) allow[s] ‘us’ to characterize and classify societies into categories, (2) condense[s] complex images of other societies through a system of representation, (3) provide[s] a standard model of comparison, and (4) provide[s] criteria of evaluation against which other societies can be ranked… These are the procedures by which indigenous peoples and their societies were coded into the Western system of knowledge [ 3 , original italics].
Research on Indigenous peoples differs from with Indigenous peoples, which requires ‘relational accountability’ [ 4 , 5 ]. At best, research on Indigenous peoples yields findings of reduced validity and reliability [ 6 ]; at worst, it exacerbates the longstanding overrepresentation of Indigenous peoples who experience poor wellbeing [ 7 , 8 ].
Although the value of participatory research with Indigenous peoples is not contested, it has varied understandings [ 9 ]. For instance, Windsor and colleagues [ 10 ] described ‘a 2 × 2 × 2 × 2 factorial design to engineer the most efficient, effective, and scalable version’ of a behavioral-health intervention, which was ‘Grounded in critical consciousness theory, community-based participatory research principles’. In essence, participatory research was used to design a cost-effective intervention for wide-spread use, by ‘ensur[ing]… that research questions and procedures reflect[ed] the needs and priorities of the communities… [to] facilitate[e] uptake’. Yet another approach by Genuis and colleagues [ 11 ] reported on high-school students at a First Nation community school who were trained as co-researchers. Specifically, nine students were ‘recruited as project co-researchers’, incentivized through an ‘offer… [of] credit towards classroom assignments, as well as an opportunity to positively impact their community’. Following ‘5 training sessions with university investigators’, the co-researchers ‘conducted semi-structured… interviews’, which were primarily ‘analys[ed] by university researchers’. These two (of many other) examples demonstrate the different ways in which Indigenous peoples are involved in participatory research. Although variation within most methodologies might be expected [ 12 ], it is unclear what might (and might not) warrant the term when collaborating with Indigenous peoples [ 13 ].
Given increasing interest in such research [ 14 ], this article expands conceptual understandings of participatory research with Indigenous peoples, across timelines and regions. This was achieved via a lexical analysis of the methods sections of 161 publications, identified via a systematic review of academic databases. Aided by the software program – Leximancer – a lexical analysis involves the examination of a corpus of qualitative data to ascertain patterns in the ways in which words – and their associated phrases – travel together [ 15 ]. This is achieved via ranked lists of terms that commonly occur and co-occur, from which a thesaurus is built to delineate salient themes and the concepts, therein. This article commences with an overview of participatory research with Indigenous peoples. It then presents the findings from the aforesaid lexical analysis. The article then concludes with a discussion of key findings, and the associated implications.
Participatory research with indigenous peoples
Participatory research with Indigenous peoples prizes partnership between individuals (and/or the groups they represent) who have a stake in the research, including (but not limited to) Indigenous peoples and researchers [ 6 ]. This partnership involves equal opportunities for engagement between different individuals (and/or the groups they represent) to pursue a common purpose by sharing and generating knowledge [ 16 ]. Accordingly, participatory research can range in scope and form – for instance, it can involve individuals who identify as Indigenous, and/or communities that identify as Indigenous. The latter involves partnerships between an Indigenous community and research agencies, and can range from, ‘being consultative through community-directed to community-controlled, where community groups exercise the highest expression of autonomy over research, assisted by research institutions’ [ 17 ]. Participatory research aims to democratize scholarship and knowledge by: relegating conventional understandings of expertise and evidence; ‘shift… the balance of control towards those being researched’ [ 18 ]; and reposition scholars as participants of a process in which they listen, learn, and offer service [ 19 , 20 , 21 ]. In effect, it is the intersection of skillsets to enhance the translation of the outcomes associated with the partnership into policy and/or practice. While conventional research typically prioritizes professional and institutional interests, disciplinary conventions, and codified-forms of evidence, participatory research with Indigenous peoples prioritizes culture and community [ 19 ].
Although participatory research with Indigenous peoples can range in scope and form, it is premised on some key principles [ 22 , 23 , 24 ]. According to the World Health Organization [ 1 ], both research institutions and Indigenous peoples are to ‘enter into a research relationship as equal partners’, whereby both parties develop a proposal and endorse an agreement – however, the research should only proceed if its focus and processes align with the priorities and needs of Indigenous peoples. This is not to suggest that translating these principles into practice is always straightforward – for instance, Morton Ninomiya and Pollock [ 25 ] described accountability tensions when research teams have a responsibility to ‘the “hands off” community leaders and stakeholders involved in… research and… the “hands on” academic world, full of rules and regulations’. Nevertheless, there are many international exemplars in which such tensions have been respectfully managed with considerable success – consider for instance, a large-scale, community-based participatory research project to address the high-rate of tobacco smoking among Aboriginal and Torres Strait Islander peoples across Australia [ 17 , 26 , 27 ]. The principles espoused by the World Health Organization [ 1 ] were adapted for the purpose of a reporting framework to clearly articulate what each of the seven project phases would involve and how each would be assessed to ultimately democratize the participation of the partners. This and other international studies make a strong public health case for participatory research with Indigenous peoples [ 28 , 29 , 30 , 31 , 32 ].
In addition to being respectful, such research can help to address intractable public health problems, where conventional epidemiological approaches have achieved limited success [ 33 ]. For instance, following their ‘comprehensive literature review’, Bath and Wakerman [ 20 ] found some evidence that participatory approaches are associated with improved health outcomes within Indigenous communities. Similarly, in their systematic review on community development projects in Australian Indigenous communities, Snijder and colleagues [ 34 ] identified two studies that reported statistically significant outcomes. Although there is a dearth of empirically-robust research (as conventionally-defined), available evidence suggests that participatory research with Indigenous peoples holds potential and is worthy of future scholarship.
The aim of this article is to determine what it means to conduct participatory research with Indigenous peoples. Specifically, it examines how such research was described. This was achieved via a lexical analysis of relevant publications. Given the aforesaid aim of this article, all publications that are expressly participatory were considered. Rather than appraise the quality of studies with reference to an established research standard, this approach was deemed appropriate because of the varied understandings of such research with Indigenous peoples [ 9 ]. As such, the aim of this article is not to assess research quality – but rather, to investigate how research that is expressly participatory was described. Details of this lexical review are described as follows.
Search strategies
In April 2018, search strategies were deployed across 29 purposely-selected academic databases to identify all publications on participatory research with Indigenous peoples. Guided by previous research [ 35 ], the search strategies encompassed euphemisms for Indigenous (19 terms) and participatory (12 terms) within the publication title. Although potentially limiting, more inclusive search strategies largely served to identify irrelevant publications. The breadth of these publications might be partly due to multifaceted nature of both Indigeneity and participatory research. As such, a focused search strategy was used. Publications were included in this review if they met all three of the following criteria: (1) it represented a research publication, rather than a letter, a commentary, or an editorial, to ensure the inclusion of empirical research; (2) it did not represent a systematic, narrative, or literature review or meta-analysis, given the limited methodological detail typically reported from the publications that are included within such reviews; and (3) it was published in the English language. Of the 473 publications identified, 161 met these three criteria (see Fig. 1 and Additional file 1 ). This was determined by one author and cross-checked by another for accuracy. Discrepancies in this process were reconciled through consensus. The methods section from each publication was then extracted for a lexical analysis. Collectively sourced from 107 journals, the earliest publication was published in 1970, and the latest, in 2018.
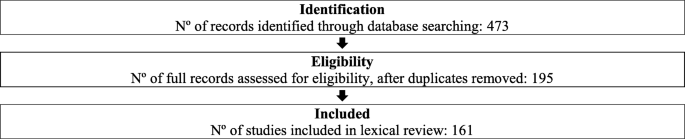
Flow Diagram of Study Selection [adaption of PRISMA, 36 ]
- Lexical analysis
The lexical analysis was aided by Leximancer – data-mining software that uses Bayesian reasoning to detect key concepts and reveal their relationships [ 37 ]. By identifying frequently occurring and co-occurring words, Leximancer visually maps concepts that reflect topics within the text [ 38 ]. The maps convey ‘the main concepts in the text and their relative importance; the strengths of links between concepts (how often they co-occur); and similarities in contexts where links occur’ [ 39 ]. Clusters of concepts within a map – known as themes – suggest contextual similarity [ 40 ]. Themes are color-coded to signify those that are (and are not) important, whereby the ‘most important theme appears in red, and the next hottest in orange, and so on according to the colour wheel’ [ 41 ]. Further detail on Leximancer can be sourced from previous publications [ 42 , 43 ].
For four key reasons, Leximancer was purposely selected to aid this review. First, it can offer a ‘helicopter’ view of a substantial body of qualitative data, illustratively portraying relationships and patterns between representative themes and concepts [ 44 ]. Second, as a form of computer assisted qualitative data analysis software (CAQDAS), it offers a systematic, logical, and an efficient method to ‘text mine’, allowing the researcher to interactively connect themes and concepts with the data. As Hyndman and Pill [ 45 ] noted:
The advantage of Leximancer is that it extracts a populated list from the text document that displays the weighted term classifications and connections between key words. From this list it creates concept maps that illustrate the level of connections between key words in the text being analysed… In other words, the software processes the level of relationship between concepts and the rate at which concepts and the significantly related terms appear close to each other within the text.
Third, unlike alternative approaches when systematically analyzing qualitative data – like the oft-cited use of thematic analysis [ 46 , 47 , 48 ] – Leximancer can help to reveal, and make sense of different findings [ 49 ]. Given its capacity to offer an ‘unsupervised’ view of the data [ 50 ], it can facilitate ‘broader opportunities for interrogating the text’ [ 51 ] by grounding the analysis in the voice of the authors of the data. This is not to suggest the limited value of alternative approaches – but rather, Leximancer can direct researcher attention to the unexpected (as well as what might be expected). As Smith [ 52 ] observed:
The meaning contained within any data set is very much dependent on the way you interpret it. Not only do you need to carefully decide what things to measure, but you need to understand what the analysis method is trying to achieve, and finally, you need to understand what this result actually tells you about your world… the only value to be obtained from textual data is a more accurate understanding of the way the authors of the data viewed some aspect of their world… if we assume that the task is for the analyst to understand the human meanings contained with their text data, the role of software such a Leximancer is… to let the data generate a transparent model which can be interpreted by the analyst, so that this person may efficiently conduct a sense making examination of conceivably vast amounts of text.
Fourth, although Leximancer has been used to systematically review literature in other fields – including (but not limited to) infection control [ 43 ], knowledge management [ 53 ], marketing [ 54 ], nursing [ 55 ], and physical education [ 45 ] – it is yet to be used to ‘text mine’ literature on participatory research with Indigenous peoples. Leximancer was therefore used because it was fit-for-purpose, helping to address the aim of this article and ensure the unexpected would be balanced with the expected.
Leximancer was used in two steps. First, once the methods section from each publication was collated, the ‘discovery’ mode was used to, ‘see what concepts were automatically generated by Leximancer without intervention’ [ 56 ]. Illustrating the automatically-generated relationships within the text, in the first instance, helps to ‘create learning and understanding’ [ 57 ] and identify ways to make sense of these relationships. Second, for comparative value, each publication was associated with two tags. Tagging helps to compare the conceptual content of different data [ 58 ]. To determine whether (and how) study location influences the ways participatory research with Indigenous peoples is described, each publication was tagged according to one of six regional groupings, as defined by the World Health Organization [ 59 ]. To determine whether (and how) time influences the ways participatory research with Indigenous peoples is described, each publication was tagged according to one of four timeframes – namely: ‘Seventies and Eighties’ (given that only one publication was published in 1970); ‘Nineties’; ‘Noughties’; and ‘Tensies’ (reflecting accepted vernacular). Once tagged, and guided by previous research [ 39 ], thirty concepts were profiled within each concept map to avoid diluting the focus of each map. To identify differences between locations and timeframes, the thirty concepts were profiled using the themed discovery setting, ‘Concepts in EACH’, to ‘discover concepts that distinguish… categories from one another’ [ 41 ]. For succinctness, attention is awarded to the word-like concept (rather than pronouns) that is most pertinent to each tag, as indicated by the likelihood percentage. Calculated by Leximancer, the likelihood percentage denotes the proportion of text segments that is shared by a tag concept and another concept, thus providing both directions of conditional probability [ 60 ].
The discovery mode concept map reveals four themes – namely: community , data , health , and change (see Fig. 2 ). These highlight the key clusters of concepts – or topics – represented within the text. Theme position illustrates the relationships between the themes. Consider the prominence of community , which appears in red and overlaps with the less-prominent themes, particularly data . This suggests that when the publications refer to community (and the concepts therein), they are inclined to refer to data (and the concepts therein):
Discovery Mode Concept Map (visible concepts: 100%, theme size: 60%)
The team comprised health services researchers, physicians, Indigenous researchers, social scientists, data analysts, nurses, a community development specialist, and community-based experts and participants such as FNs [First Nations] Elders, health care workers and community members [ 61 ].
Given the focus of this review and the purposeful analysis of the methods sections, the absence of a concept that explicitly denotes participatory , participation , or participate is curious. Although the concept, involved , is evident within the salient theme, community , it is most-likely to be connected to the concept, project . This suggests that when the publications refer to being involved , they are inclined to refer to a project :
As well, in Saskatchewan, Sage, another participant described why she became involved in this PAR project. She said: I joined (this research project) because I know that I’ll get my word out [ 62 ].
Although this finding might appear intuitive, the concept, involved , is dissociated from specific project phases. Consider its distance from intervention , control , survey , conducted , interviews , and analysis . Furthermore, these are distanced from germane concepts like, Indigenous and Aboriginal . This suggests when the publications mention involved , Indigenous , or Aboriginal they are disinclined to refer to intervention , control , survey , conducted , interviews , and analysis . This is not to suggest that the publications do not describe how Indigenous peoples were actively involved in the collection or analysis of data – but rather, the methods, as presented in this corpus of data, suggest the former concepts (and the words within their thesaurus) seldom travel with the latter concepts (and the words within their thesaurus):
The Family Spirit intervention was staffed to provide regular on-site supervision, weekly cross-site conference calls and quarterly site visits. A policy and procedures manual guides implementation of the curriculum and gives home visitors flexibility to address mothers’ and families’ scheduling needs [ 63 ].
Perhaps the most explicit reference to participatory research is CBPR (community-based participatory research). Although positioned between community and research , it is in closer proximity to the latter. As such, CBPR , as described within the methods sections, is inclined to travel with words that denote research , rather than be equidistant from words that denote community :
A Community-Based Participatory Research (CBPR) framework was used to develop a qualitative study around young Indigenous people’s sexual health. Our participatory approach… involved a range of strategies to ensure the project was a genuine collaboration between university researchers and Indigenous community members, and in particular that young Indigenous people were actively involved throughout [ 64 ].
Given the publications explicitly focus on participatory approaches with Indigenous peoples, it is encouraging to observe research in close proximity to process , involved , development , design , and partnership . This suggests the methods sections speak of processual or progressive scholarship. In addition to the concept map and the exemplary excerpts, this is supported by the absence of concepts that denote outputs and deliverables:
Key terms and significant issues for data analysis were identified through a collective contribution process by the elders, leaders, knowledge-holders and youths during a subsequent traditional sharing circle. Participants wanted to be sure their needs and dreams were included in the draft findings, so that this research would have an impact on policy level and speak on behalf of them [ 65 ].
Another curious finding is the salience of health as a theme – this is because the search strategy was devoid of the term, health. Furthermore, of the academic databases searched, 15 were not (mental) health-specific. This suggests that wellbeing is a prominent focus in participatory research with Indigenous peoples, as presented in these systematically-identified publications:
People recognize that these diseases are transmitted by insects, which they call shidru (Triatominae, kissing bugs) for Chagas and shirakbina (Anopheles, mosquitoes) for malaria. Local health services consist of an infirmary attended by a nurse, and the nearest healthcare center requires 2 h of travel by river [ 66 ].
As illustrated by the grey spanning tree, health is most-likely to be connected with the concepts, program , based , experiences , education , care , services , and community . The spanning tree portrays, ‘the most-likely connections between concepts (like a road map of highways), but there are other (less-strong) connections between concepts (like backstreets)’ [ 58 ]. This finding is noteworthy for two key reasons. First, these connections speak of initiatives to intercede in, and/or affect wellbeing. This extends to the concept, experiences :
We explained that the data collected at these initial encounters would then inform the semi-structured interviews intended to further explore the young people’s understandings and experiences of health in the hopes that this would lead to a youth-led project [ 67 ].
Second, as per the preceding excerpt, references to these initiatives travel with references to particular cohorts – notably, youth , women , family , students , and children . These demonstrate the research priorities within this corpus of data. Consider the concept, youth , and its proximity to traditional and Aboriginal . This illustrates the connectedness between discourse pertaining to youth and Indigenous peoples and customs:
The focus group began with a welcome, introductions and an Inuk elder ceremonially lighting the qulliq , a traditional oil lamp. Apart from introductory and concluding activities, there were four main segments: understanding violence, coping with violence, preventing violence, and what Inuit youth should know about violence [ 68 , original italics].
Although reference to the aforesaid cohorts is noteworthy, so too is the absence of expressed reference to others. In this regard, the concepts automatically generated by Leximancer did not include references to (or euphemisms for) men, the elderly, infants, people with a disability, or people who identify as lesbian, gay, bisexual, trans, and/or intersex, among others. This is not to suggest the publications ignored these cohorts, but rather, they did not feature prominently in the methods sections of these publications, all of which pertained to participatory research with Indigenous peoples.
In the context of publications that expressly focused on participatory research with Indigenous peoples, there is a curious divide between the themes, data and change . The concept map suggests that discourse pertaining to participants , study , focus , groups , analysis , questions , interviews , intervention , and survey , is not well-connected with that pertaining to practices , values , and culture :
This pedagogy is appropriate for Samoans since they have an oral tradition that values collective decision-making, experiential education, trust building, and interpersonal interactions [ 69 ].
Although it is not the purpose of this article to hypothesize reasons for this divide, this finding does not portray discourse pertaining to conventional demonstrations of research – including the collection and analysis of data – as inextricably connected to that pertaining to cultural values and practices. But rather, they appear disconnected.
The 161 publications reported studies that were conducted across at least 16 nations, with one publication encompassing ‘communities from Siberia to Norway’. These publications represented five (of six) regional groupings, the exception being the Eastern Mediterranean region. Although the concept map is seemingly busy, this was necessary to ensure all five groupings are represented. This helpful comparison suggests study location influences the ways participatory research with Indigenous peoples is described, with variation between studies conducted within the region of the Americas, and those conducted elsewhere (see Fig. 3 ). Studies conducted within this region refer chiefly to the concepts, pandemic (100%), surveyors (100%), and art (100%):

Concept Map tagged by Regional Groupings (visible concepts: 100%, theme size: 60%)
to understand the barriers participants faced and suggested improvements for the pandemic response, the interview questions were based on the aspects of a health sector pandemic response outlined in academic literature [ 70 , Region of the Americas].
Conversely, those conducted within the remaining four regions feature discourse pertaining to: discharge processes (Western Pacific Region: 100%); the young (European Region: 17%); practices (South-East Asia Region: 17%; African Region: 5%); and care (African Region: 5%). These nuances reveal two notable findings. First, there are shared interests among the studies conducted in the South-East Asia and African Regions, with reference to personal, social, and organizational practices:
Hygienic practices common in Kerala are not universally adopted; over a quarter of the households do not systematically boil their drinking water. Their health needs are great [ 71 , South-East Asia Region].
Second, studies conducted in the Western Pacific Region are strongly connected with discourse on non-Indigenous healthcare conventions. These include the admission and release of patients from health services, and the artifacts accrued to codify patient care:
First, client details were hand-written into a service admission book upon intake and discharge. Data collected included: demographics; referral type; and service utilization characteristics [ 72 , Western Pacific Region].
The 161 publications reported studies across the seventies and eighties ( n = 2), the nineties ( n = 6), the noughties ( n = 43), and the tensies ( n = 110). The centrality of the themes, community and people , suggest their salience across the decades (see Fig. 4 ). Although the concept map is heavily populated with concepts, this was necessary to ensure all four periods are represented. However, the likelihood percentages reveal key differences between these periods. Specifically, unlike more recent publications, those published the earliest are most-likely to be associated with discourse regarding children (Seventies and Eighties: 9%) and action (Nineties: 9%) – while those published during the last and current decades are strongly associated with discourse pertaining to surveyors , art (Noughties: 100%), and discharge (Tensies: 100%). These findings reveal a pattern in the ways participatory research with Indigenous peoples are described. While the methods sections of earlier publications present language about particular cohorts and change efforts to address identified issues, those of more recent publications award primacy to artifacts that denote areas of interest, including culture, the terrain, and service-use:

Concept Map tagged by Timeframes (visible concepts: 100%, theme size: 60%)
Hospital representatives reported that they were receiving fewer requests from community health centres for ‘missing’ discharge summaries and that the content of the discharge summaries had improved [ 73 , Tensies].
The importance of participatory research with Indigenous peoples has international recognition. Yet there are discrepancies in the ways such research is conducted and reported. Participatory research with Indigenous peoples can help to improve research quality and optimize the relevance of associated outcomes for Indigenous peoples [ 20 , 34 ]. It is important for researchers to reflect on how they engage with Indigenous peoples, given limited progress to redress longstanding health inequalities [ 74 , 75 ].
The key finding from this lexical review is that publications that explicitly pertain to participatory research with Indigenous peoples do not always demonstrate Indigenous participation across different project phases. For instance, discourse regarding Indigenous peoples is distanced from that regarding the collection and analysis of data, and the reporting of the associated findings. Furthermore, the ways the research is collectively described suggests a disconnect between research and cultural values and practices. Although it is beyond the scope of this review to account for these findings, it is possible that although the studies were participatory, the ways in which Indigenous peoples were involved throughout were not reported – however, it might also be because Indigenous peoples were not involved in all project phases.
An examination of participatory research with Indigenous peoples across regions and decades reveals key differences. For instance, studies conducted within the Americas allude to pandemics, surveyors, and art; while those conducted within the Western Pacific region feature Western healthcare processes – this demonstrates differences in the focus of studies within each region. Over time, there have been considerably more publications reporting participatory research with Indigenous peoples – yet these descriptions have changed over time. While early publications consider particular cohorts of Indigenous peoples and change efforts to address the issues they experience, later publications demonstrate an interest in codified-forms of culture, the terrain, and service-use.
Collectively, these findings suggest that, across the globe and over time, participatory research with Indigenous peoples is understood, conducted, and described in disparate ways. Although disparity can optimize inclusiveness, it can be problematic for (at least) two reasons. First, it potentially dilutes scholarship, stymies the development of innovative solutions, and compromises theory-development – this is because researchers and Indigenous peoples engage with, and among each other without shared understandings. Second, research with Indigenous peoples might be inappropriately labelled as participatory and exacerbate longstanding inequalities [ 7 ].
Although the findings from this lexical review are illustrative, three limitations warrant mention. First, given the disparate ways in which participatory research and Indigenous peoples are described, it is possible that some relevant publications were obscured by the indexing systems used by the academic databases that were searched. Despite the comprehensiveness of each database, the terms that were searched are referred to, and defined in disparate ways. Second, because participatory research with Indigenous peoples is understood in different ways, the accounts reported in the publications could not be verified. Third, Leximancer regulates researchers’ analysis – although this can strengthen qualitative research [ 48 ], the use of alternative approaches, like (but not limited to) thematic analysis [ 45 , 46 , 47 ], might yield different findings.
Despite the aforesaid limitations, the key finding from this lexical review has implications for scholars, practitioners, and Indigenous peoples. For scholars, given the importance of impact, this review would suggest that there is much scope and opportunity to actively engage Indigenous peoples in all research phases to improve public health initiatives and redress longstanding health inequalities. Several methodologies have a demonstrated capacity to enhance engagement – consider for instance, citizen social science [ 76 ] and video reflexive ethnography (VRE, [ 77 , 78 ]). Informed by both crowdsourcing and citizen science, citizen social science involves avocational researchers who examine social phenomena by collecting and analyzing data, disseminating the associated findings, and translating these into practice. In the context of participatory research with Indigenous peoples, citizen social science might involve inviting Indigenous peoples to collect, access, and/or critique practices that influence public health; share insights and experiences; identify knowledges and conditions that shape the translation of preferred practices into different contexts; and co-design resources (sensu lato ) to promote public health outcomes.
VRE purposely harnesses the expertise of individuals who are typically relegated to the position of research subjects – like Indigenous peoples. Specifically, non-academic researchers are invited to collaborate as co-researchers by: featuring in and/or gathering video-recordings; analyzing the recordings; and understanding practices and experiences [ 79 ].
For practitioners, the findings provoke potentially challenging questions about how they conduct research and/or quality improvement exercises, and whether current practices serve to reinforce health inequalities [ 7 ]. For Indigenous peoples, given the seeming importance of their involvement in, and research about healthcare [ 80 ], these findings demonstrate the relative absence of participatory research. This then is a call to Indigenous peoples to hold scholars and practitioners to account by challenging, if not pushing the agenda of academic institutions, health services (sensu lato ), and the governments that fund them.
This lexical review suggests the active involvement of Indigenous peoples in research that is expressly participatory is limited across all project phases. Notwithstanding opportunities to engage Indigenous peoples in a ‘project’, there is limited clarity regarding their involvement in the collection and analysis of data, and the reporting of the findings. This suggests the expertise and skills of Indigenous peoples are not always harnessed. With exceptions [ 11 , 81 ], Indigenous connections to research – as depicted in this corpus of data – was sometimes driven by (non-Indigenous) researchers who ‘invited’ [ 82 ] the participation of Indigenous peoples, who were – at times – at arm’s length of the project phases. As suggested by the previously noted implications, participatory research with Indigenous peoples is everybody’s business. There are opportunities that scholars, practitioners, and Indigenous peoples might pursue if, as per the World Health Organization [ 1 ], ‘Health research involving Indigenous Peoples… [is] to be organized, designed and carried out in a manner that takes account of cultural differences, is based on mutual respect, and is beneficial and acceptable to both… [research institutions] and [Indigenous peoples]’.
Availability of data and materials
Not applicable.
Abbreviations
Computer assisted qualitative data analysis software
Community-based participatory research
First Nation
Video reflexive ethnography
WHO (World Health Organization). Indigenous peoples & participatory health research. Geneva: WHO (World Health Organization); 2003.
Google Scholar
Health of Indigenous peoples [ https://www.who.int/mediacentre/factsheets/fs326/en/ ].
Tuhiwai Smith L. Decolonizing methodologies: research and indigenous peoples, Second edn. London: Zed Books; 2012.
Delbanco T, Berwick DM, Boufford JI, Edgman-Levitan S, Ollenschläger G, Plamping D, Rockefeller RG. Healthcare in a land called PeoplePower: nothing about me without me. Health Expect. 2001;4(3):144–50.
Article CAS PubMed PubMed Central Google Scholar
Wilson S. What is an indigenous research methodology? Can J Nativ Educ. 2001;25(2):175–9.
Cochran PA, Marshall CA, Garcia-Downing C, Kendall E, Cook D, McCubbin L, Gover RM. Indigenous ways of knowing: implications for participatory research and community. Am J Public Health. 2008;98(1):22–7.
Article PubMed PubMed Central Google Scholar
Martin B. Methodology is content: indigenous approaches to research and knowledge. Educ Philos Theory. 2017;49(14):22–7.
Article Google Scholar
Pacheco LS, Hernández-Ontiveros DA, Iniguez-Stevens E, Brodine S, Garfein RS, Santibañez M, Fraga MA. Prevalence and correlates of diabetes and metabolic syndrome in a rural indigenous community in Baja California, Mexico. BMC Public Health. 2018;18(1):1–11.
Article CAS Google Scholar
Faridi Z, Grunbaum JA, Gray BS, Franks A, Simoes EC. Community-based participatory research: necessary next steps. Prev Chronic Dis. 2007;4(3):1–5.
Windsor LC, Benoit E, Smith D, Pinto RM, Kugler KC, Newark community collaborative board (NCCB). Optimizing a community-engaged multi-level group intervention to reduce substance use: an application of the multiphase optimization strategy. Trials. 2018;19(1):1–15.
Genuis SK, Willows N, Alexander first nation, Jardine CG. Partnering with indigenous student co-researchers: improving research processes and outcomes. International Journal of Circumpolar Health. 2015;74(27838):1–9.
Denzin NK, Lincoln YS (eds.): Handbook of qualitative research, third edn. Thousand Oaks, CA: Sage Publications; 2005.
Brunger F, Wall D. “what do they really mean by partnerships?” questioning the unquestionable good in ethics guidelines promoting community engagement in indigenous health research. Qual Health Res. 2016;26(13):1862–77.
Article CAS PubMed Google Scholar
Kovach M: Emerging from the margins: indigenous methodologies. In: Research as resistance: Revisiting critical, Indigenous, and anti-oppressive approaches. Second edn. Edited by Strega S, Brown L. Thousand Oaks, CA: Sage Publications; 2015.
Thompson J, Davis J, Mazerolle L. A systematic method for search term selection in systematic reviews. Res Synth Methods. 2014;5(2):87–97.
Article PubMed Google Scholar
Metro North Hospital and Health Service: Procedure Metro North HHS-wide - Research: Partnership and collaboration. In . Brisbane, QLD: Queensland Government; 2017.
Couzos S, Nicholson AK, Hunt JM, Davey ME, May JK, Bennet PT, Westphal DW, Thomas DP. Talking about the smokes: a large-scale, community-based participatory research project. Med J Aust. 2015;202(10):S13–9.
PubMed Google Scholar
Couzos S, Lea T, Murray R, Culbong M. ‘We are not just participants - we are in charge’: the NACCHO ear trial and the process for aboriginal community-controlled health research. Ethn Health. 2015;10(2):91–111.
Cornwall A, Jewkes R. What is participatory research? Soc Sci Med. 1995;41(12):1667–76.
Bath J, Wakerman J. Impact of community participation in primary health care: what is the evidence? Australian Journal of Primary Health. 2015;21(1):2–8.
Denzin NK, Giardina MD: Introduction: Ethical futures in qualitative research. In: Ethical futures in qualitative research: Decolonizing the politics of knowledge. edn. Edited by Denzin NK, Lincoln YS. Walnut Creek, CA: Left Coast Press; 2007: 9–43.
NHMRC (National Health and Medical Research Council): Ethical conduct in research with Aboriginal and Torres Strait Islander peoples and communities. In . Canberra, ACT: NHMRC (National Health and Medical Research Council); 2018.
FNIGC (First Nations Information Governance Centre): Ownership, control, access and possession (OCAP™): The path to first nations information governance. In . Ottawa, ON: FNIGC (First Nations Information Governance Centre); 2014.
CIHR (Canadian Institutes of Health Research), NSERC (Natural Sciences and Engineering Research Council of Canada), SSHRC (Social Sciences and Humanities Research Council of Canada): Tri-council policy statement: ethical conduct for research involving humans. In . Ottawa, ON: Secretariat on Responsible Conduct of Research; 2014.
Morton Ninomiya ME, Pollock NJ. Reconciling community-based indigenous research and academic practices: knowing principles is not always enough. Soc Sci Med. 2017;172:28–36.
Thomas DP, Briggs VL, Couzos S, Davey ME, Hunt JM, Panaretto KS, van der Sterren AE, Stevens M, Nicholson AK, Borland R. Research methods of talking about the smokes: an international tobacco control policy evaluation project study with aboriginal and Torres Strait islander Australians. Med J Aust. 2015;202(10):S5–S12.
Thomas DP, Davey ME, Briggs VL, Borland R. Talking about the smokes: summary and key findings. Med J Aust. 2015;202(10):S3–4.
Bach M, Jordan S, Hartung S, Santos-Hövener C, Wright MT. Participatory epidemiology: the contribution of participatory research to epidemiology. Emerging Themes in Epidemiology. 2017;14(2):1–15.
Glover M, Kira A, Johnston V, Walker N, Thomas D, Chang AB, Bullen C, Segan CJ, Brown N. A systematic review of barriers and facilitators to participation in randomized controlled trials by indigenous people from New Zealand, Australia, Canada and the United States. Glob Health Promot. 2015;22(1):21–31.
Baum FE. Power and glory: applying participatory action research in public health. Gac Sanit. 2016;30(6):405–7.
Dankwa-Mullan I, Rhee KB, Williams K, Sanchez I, Sy FS, Stinson NJ, Ruffin J. The science of eliminating health disparities: Summary and analysis of the NIH summit recommendations. American Journal of Public Health. 2010;100(Supp. 1):S12–8.
Parker WM, Becker-Benton A. Experiences in conducting participatory communication research for HIV prevention globally: translating critical dialog into action through action media. Front Public Health. 2016;4(28):1–10.
Leung MW, Yen IH, Minkler M. Community based participatory research: a promising approach for increasing epidemiology's relevance in the 21st century. Int J Epidemiol. 2004;33(3):499–508.
Snijder M, Shakeshaft A, Wagemakers A, Stephens A, Calabria B. A systematic review of studies evaluating Australian indigenous community development projects: the extent of community participation, their methodological quality and their outcomes. BMC Public Health. 2015;15(1154):1–16.
Haijes HA, van Thiel GJMW. Participatory methods in pediatric participatory research: a systematic review. Pediatr Res. 2016;79(5):676–83.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Zuell C, Weber RP, Mohler P (eds.): Computer-assisted text analysis for the social sciences. Mannheim, Germany: Center for Surveys, Methods and Analysis (ZUMA); 1989.
Young L, Denize S. Competing interests: the challenge to collaboration in the public sector. Int J Sociol Soc Policy. 2008;28(1/2):46–58.
Hewett DG, Watson BM, Gallois C, Ward M, Leggett BA. Intergroup communication between hospital doctors. Soc Sci Med. 2009;69(12):1732–40.
Hepworth N, Paxton SJ. Pathways to help-seeking in bulimia nervosa and binge eating problems: a concept mapping approach. Int J Eat Disord. 2007;40(6):493–504.
Leximancer: Leximancer manual. In . Brisbane, QLD: Leximancer Pty Ltd; 2011.
Dadich A, Doloswala N. What can organisational theory offer knowledge translation in healthcare? A thematic and lexical analysis. BMC Health Serv Res. 2018;18(351):1–20.
Dadich A, Wyer M: Patient involvement in healthcare-associated infections research: A lexical review. Infect Control Hosp Epidemiol 2018, Epub-ahead-of-print:1–8.
Gapp R, Stewart H, Harwood I, Woods P: Discovering the value in using Leximancer for complex qualitative data analysis. In: British Academy of Management Conference Liverpool; 2013: 1–6.
Hyndman B, Pill S. What’s in a concept? A Leximancer text mining analysis of physical literacy across the international literature. Eur Phys Educ Rev. 2018;24(3):292–313.
Muhlack E, Carter D, Braunack-Mayer A, Morfidis N, Eliott J. Constructions of alcohol consumption by non-problematised middle-aged drinkers: a qualitative systematic review. BMC Public Health. 2018;18(1):1–10.
Mackenzie K, Such E, Norman P, Goyder E. The development, implementation and evaluation of interventions to reduce workplace sitting: a qualitative systematic review and evidence-based operational framework. BMC Public Health. 2018;18(1):1–18.
Brunton G, Thomas J, O’Mara-Eves A, Jamal F, Oliver S, Kavanagh J. Narratives of community engagement: a systematic review-derived conceptual framework for public health interventions. BMC Public Health. 2017;17(1):1–15.
Sotiriadou P, Brouwers J, Le T-A. Choosing a qualitative data analysis tool. Annals of Leisure Research. 2012;17(2):218–34.
Smith AE, Humphreys MS. Evaluation of unsupervised semantic mapping of natural language with Leximancer concept mapping. Behav Res Methods. 2006;38(2):262–79.
Gurd B: Qualitative data analysis – could I use NVivo or Leximancer? In: ANZAM (Australian and New Zealand Academy of Management) Conference. Perth, WA; 2012.
Sense making - The goal of any Leximancer analysis [ https://info.leximancer.com/blogb/2017/3/15/sense-making-the-goal-of-any-leximancer-analysis ].
Ribière V, Walter C. 10 years of KM theory and practices. Knowledge Management Research & Practice. 2013;11:4–9.
Young L, Wilkinson I, Smith A. A scientometric analysis of publications in the journal of business-to-business marketing 1993-2014. J Bus Bus Mark. 2015;22(1–2):111–23.
Bell E, Campbell S, Goldberg LR. Nursing identity and patient-centredness in scholarly health services research: a computational text analysis of PubMed abstracts 1986-2013. BMC Health Serv Res. 2015;15(3):1–16.
CAS Google Scholar
Angus-Leppan T, Benn S, Young L. A sensemaking approach to trade-offs and synergies between human and ecological elements of corporate sustainability. Bus Strateg Environ. 2010;19(4):230–44.
Stewart H, Gapp R. Achieving effective sustainable management: a small-medium enterprise case study. Corp Soc Responsib Environ Manag. 2014;21(1):52–64.
Leximancer: Leximancer user guide: Release 4.5. In . Brisbane, QLD: Leximancer Pty Ltd; 2018.
Definition of regional groupings [ http://www.who.int/healthinfo/global_burden_disease/definition_regions/en/ ].
Understanding displays and outputs [ https://hypermancer.leximancer.com/faq/display_and_output.html# ].
Kyoon-Achan G, Lavoie J, Avery Kinew K, Phillips-Beck W, Ibrahim N, Sinclair S, Katz A. Innovating for transformation in first nations health using community-based participatory research. Qual Health Res. 2018;28(7):1036–49.
McHugh T-LF, Kowalski KC. ‘A new view of body image’: a school-based participatory action research project with young aboriginal women. Action Res. 2004;9(3):220–41.
Mullany B, Barlow A, Neault N, Billy T, Jones T, Tortice I, Lorenzo S, Powers J, Lake K, Reid R, et al. The family spirit trial for American Indian teen mothers and their children: CBPR rationale, design, methods and baseline characteristics. Prev Sci. 2012;13(5):504–18.
Mooney-Somers J, Olsen A, Erick W, Scott R, Akee A, Maher L. Young indigenous Australians’ sexually transmitted infection prevention practices: a community-based participatory research project. J Community Appl Soc Psychol. 2012;22(6):519–32.
Datta R, Khyang NU, Prue Khyang HK, Prue Kheyang HA, Ching Khyang M, Chapola J. Participatory action research and researcher’s responsibilities: an experience with an indigenous community. Int J Soc Res Methodol. 2015;18(6):581–99.
SantoDomingo AF, Castro-Diaz L, Gonzalez-Uribe C. Ecosystem research experience with two indigenous communities of Colombia: the ecohealth calendar as a participatory and innovative methodological tool. EcoHealth. 2016;13(4):687–97.
Roberts EB, Jette SL. Implementing participatory research with an urban American Indian community: lessons learned. Health Educ J. 2016;75(2):158–69.
Morris M. Inuit involvement in developing a participatory action research project on youth, violence prevention, and health promotion. Etudes Inuit Inuit Studies. 2016;40(1):105–25.
Mishra SI, Luce PH, Baquet CR. Increasing pap smear utilization among Samoan women: Results from a community based participatory randomized trial. J Health Care Poor Underserved. 2009;20(Supp. 2):85–101.
Charania NA, Tsuji LJ. A community-based participatory approach and engagement process creates culturally appropriate and community informed pandemic plans after the 2009 H1N1 influenza pandemic: remote and isolated first nations communities of sub-arctic Ontario, Canada. BMC Public Health. 2012;12:268.
Mohindra K, Narayana D, Harikrishnadas C, Anushreedha S, Haddad S. Paniya voices: a participatory poverty and health assessment among a marginalized south Indian tribal population. BMC Public Health. 2010;10(149):1–9.
Munro A, Shakeshaft A, Clifford A. The development of a healing model of care for an indigenous drug and alcohol residential rehabilitation service: a community-based participatory research approach. Health & justice. 2017;5(1):1–12.
Josif C, Barclay L, Bar-Zeev S, Kildea S, Britten M. How participatory action research supported improvements to the postnatal discharge summary system used for remote dwelling aboriginal mothers and infants in the top end of Australia. Action Res. 2012;10(4):387–405.
Universal declaration of human rights [ http://www.ohchr.org/EN/UDHR/Documents/UDHR_Translations/eng.pdf ].
Department of the Prime Minister and Cabinet: Closing the gap prime minister’s report 2018. In . Canberra, ACT: Commonwealth of Australia; 2018.
Dadich A. Citizen social science: a methodology to facilitate and examine workplace learning in continuing interprofessional education. Journal of Interprofessional Care. 2014;28(3):194–9.
Dadich A, Collier A, Hodgins M, Crawford G. Using POSH VRE to examine positive deviance to new public management in healthcare. Qual Health Res. 2018;28(8):1203–16.
Wyer M, Jackson D, Iedema R, Hor SY, Gilbert GL, Jorm C, Hooker C, O'Sullivan MV, Carroll K. Involving patients in understanding hospital infection control using visual methods. J Clin Nurs. 2015;24(11–12):1718–2.
Iedema R, Carroll K, Collier A, Hor S, Mesman J, Wyer M. Video reflexive ethnography in health research and healthcare improvement. Milton Park: Taylor & Francis; 2018.
Book Google Scholar
Ocloo J, Matthews R. From tokenism to empowerment: progressing patient and public involvement in healthcare improvement. BMJ Quality & Safety. 2016;25(8):626–32.
Allen J, Mohatt GV, Rasmus SM, Hazel KL, Thomas L, Lindley S. The tools to understand: community as co-researcher on culture-specific protective factors for Alaska natives. Journal of Prevention & Intervention in the Community. 2006;32(1–2):41–59.
Whitewater S, Reinschmidt KM, Kahn C, Attakai A, Teufel-Shone NI. Flexible roles for American Indian elders in community-based participatory research. Prev Chronic Dis. 2016;13:E72.
Download references
Acknowledgements
No funding was sourced to explicitly support this study.
Author information
Authors and affiliations.
School of Business, Western Sydney University, 169 Macquarie Street, Parramatta, NSW, 2150, Australia
1797 Locked Bag, Western Sydney University, 1797 Locked Bag, Penrith, NSW, 2751, Australia
Autism Spectrum Australia (Aspect), Building 1, Level 2, 14 Aquatic Drive, Frenchs Forest, NSW, 2086, Australia
Loretta Moore
Forestville, NSW, 2087, Australia
Academic Unit of Infant, Child, Adolescent Psychiatry South West Sydney, University of New South Wales, Sydney, Australia
Valsamma Eapen
ICAMHS, L1 MHC, Liverpool Hospital, Elizabeth Street, Liverpool, NSW, 2170, Australia
University of New South Wales Sydney, Sydney, NSW, 2052, Australia
You can also search for this author in PubMed Google Scholar
Contributions
AD conceived, led, and managed the study, devised and deployed the search strategies, prepared the data for analysis, interpreted the data, and led the development of the Methods, Results, and Discussion sections of the manuscript. LM developed the Introduction section of this manuscript, devised and deployed the search strategies, extracted the data, and contributed to the Discussion section of the manuscript. VE reviewed and critiqued the manuscript, offering expertise regarding research with vulnerable populations. All authors read and approved the final manuscript.
Authors’ information
Associate Professor Dadich is a registered psychologist, a full member of the Australian Psychological Society, and a Justice of the Peace in New South Wales. She has accumulated considerable expertise in health service management, notably knowledge translation. This encompasses scholarship on the processes through which different knowledges coalesce to promote quality care. This is demonstrated by her publishing record, which includes over 150 refereed publications; the research grants she has secured; and the awards she has received. A/Prof. Dadich holds editorial appointments with several academic journals, including the Australian Health Review and BMC Health Services Research. She is also the Deputy Director of the Sydney Partnership for Health, Education, Research and Enterprise (SPHERE) Knowledge Translation Strategic Platform; she co-chairs the Australian and New Zealand Academy of Management (ANZAM) Health Management and Organisation (HMO) Conference Stream; and she co-convenes the ANZAM HMO Special Interest Group. Additionally, A/Prof. Dadich supervises doctoral candidates and teaches undergraduate units on change management, innovation, creativity, and organisational behaviour.
Ms Loretta Moore is a Clinical Psychology Registrar at Autism Spectrum Australia (Aspect). Prior to this, she provided research assistance at the Academic Unit of Infant, Child, Adolescent Psychiatry South West Sydney. Professor Valsamma Eapen has expertise in child and adolescent psychiatry, specifically: epidemiology; genetic underpinnings; neurocognitive processes; and clinical presentations of neurodevelopmental disorders. She leads the Early Life Determinants of Health (ELDoH) Clinical Academic Group within the Sydney Partnership for Health, Education, Research and Enterprise (SPHERE) – an Advanced Health Research Translational Centre (AHRTC) approved by the National Health and Medical Research Council (NHMRC).
Corresponding author
Correspondence to Ann Dadich .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Publications that Met all Inclusion Criteria and included the Lexical (DOCX 222 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Dadich, A., Moore, L. & Eapen, V. What does it mean to conduct participatory research with Indigenous peoples? A lexical review. BMC Public Health 19 , 1388 (2019). https://doi.org/10.1186/s12889-019-7494-6
Download citation
Received : 05 November 2018
Accepted : 14 August 2019
Published : 29 October 2019
DOI : https://doi.org/10.1186/s12889-019-7494-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Indigenous research
- Participatory methodologies
- Knowledge translation
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 29 April 2024
Advancing health equity for Indigenous peoples in Canada: development of a patient complexity assessment framework
- Anika Sehgal 1 ,
- Rita Henderson 1 ,
- Adam Murry 2 ,
- Lynden (Lindsay) Crowshoe 1 &
- Cheryl Barnabe 3
BMC Primary Care volume 25 , Article number: 144 ( 2024 ) Cite this article
196 Accesses
8 Altmetric
Metrics details
Indigenous patients often present with complex health needs in clinical settings due to factors rooted in a legacy of colonization. Healthcare systems and providers are not equipped to identify the underlying causes nor enact solutions for this complexity. This study aimed to develop an Indigenous-centered patient complexity assessment framework for urban Indigenous patients in Canada.
A multi-phased approach was used which was initiated with a review of literature surrounding complexity, followed by interviews with Indigenous patients to embed their lived experiences of complexity, and concluded with a modified e-Delphi consensus building process with a panel of 14 healthcare experts within the field of Indigenous health to identify the domains and concepts contributing to health complexity for inclusion in an Indigenous-centered patient complexity assessment framework . This study details the final phase of the research.
A total of 27 concepts spanning 9 domains, including those from biological, social, health literacy, psychological, functioning, healthcare access, adverse life experiences, resilience and culture, and healthcare violence domains were included in the final version of the Indigenous-centered patient complexity assessment framework.
Conclusions
The proposed framework outlines critical components that indicate the presence of health complexity among Indigenous patients. The framework serves as a source of reference for healthcare providers to inform their delivery of care with Indigenous patients. This framework will advance scholarship in patient complexity assessment tools through the addition of domains not commonly seen, as well as extending the application of these tools to potentially mitigate racism experienced by underserved populations such as Indigenous peoples.
Peer Review reports
Introduction
Indigenous peoples in Canada include First Nations, Métis , and Inuit peoples, who are the descendants of original inhabitants of the territories claimed in the British North American Act; these peoples now represent 5% of the total country’s population [ 1 , 2 ], exceeding the growth rate of the non-Indigenous population [ 3 ]. Preceding European settlers, Indigenous peoples had established sophisticated self-governing nations reflecting their distinct cultures and diverse languages [ 4 , 5 ]. Prior to European contact, in general, Indigenous peoples had good health buffered by active ways of life and balanced, nutritional diets that promoted longevity [ 6 , 7 , 8 ]. Colonization was an ethnic and cultural genocide with devastating impacts that have persisted until the present-day [ 9 , 10 , 11 ]. Calculated practices and policies such as land displacement, forced removal of children from their communities, and the spread of novel and deadly diseases by European settlers extinguished many Indigenous communities and burdened those who survived [ 12 , 13 , 14 , 15 , 16 , 17 ], undermining their Ways of Being, Doing, and Knowing [ 18 , 19 ]. Ample research has linked the longstanding impacts of colonialism directly to the burden of disease and poverty that is experienced by Indigenous peoples today [ 20 , 21 , 22 ]. The current study seeks to extend beyond profiling such impacts to identify possibilities for orienting healthcare providers (HCPs) to better respond to the resulting health inequities.
Though Canada has now embarked on a journey of reconciliation with Indigenous peoples to acknowledge the past and its present-day impacts [ 23 , 24 ], the consequences of forced assimilation cannot be entirely undone and are most evident within the vast health inequities that exist between Indigenous and non-Indigenous peoples [ 25 , 26 , 27 ]. In addition to significantly lower life expectancies than their non-Indigenous counterparts [ 28 , 29 ], Indigenous peoples are disproportionately burdened by diabetes [ 30 , 31 ], problem substance use [ 32 , 33 ], perinatal health inequities [ 34 ], arthritis [ 35 ], and mental health concerns [ 36 , 37 ] among many other health problems [ 20 , 38 ]. While persistent disparities attributed to historical consequences have shaped the health of many Indigenous peoples [ 39 , 40 ], current healthcare systems continue to amplify these inequities through entrenched and systemic racism, played out in discrimination, unequal treatment, and outright violence towards Indigenous peoples [ 41 , 42 ]. Racism has been described as an “epidemic” within Canadian healthcare systems and a significant contributor to poorer health outcomes by means of stress and harm arising from discriminatory interactions [ 43 , 44 , 45 ]. Racial discrimination is also evident in the foundation of healthcare systems, which operate on a Western biomedical epistemology of health that tends to situate disease within the physical bodies of individual patients [ 46 , 47 , 48 , 49 ], dismissing repercussions of a colonial legacy impacting genetically, culturally, and geographically diverse populations with a shared experience of oppression from colonization [ 50 , 51 ].
With healthcare systems denying Indigenous peoples’ needs and priorities [ 52 , 53 , 54 ], Indigenous patients’ become viewed increasing through the lens of having “complex health needs” [ 55 , 56 ]. Factors that contribute to this “complexity” are rooted in a legacy of colonization yet often go unnoticed in clinical settings, creating discordance between Indigenous patients and their HCP, as well as discordance between Indigenous patients and broader health systems [ 57 , 58 ]. Although there is no universal and agreed-upon definition of patient complexity and/or health complexity (terms often used interchangeably within the literature) core indicators include higher healthcare resource utilization, increased need of support, higher risk of adverse health outcomes, and lower satisfaction with care [ 59 , 60 ]. It is however agreed that patient complexity is not simply co- or multi-morbidity which is marked by the presence of two or more diseases [ 61 ]. While co- and/or multi-morbidity may cause a patient to present as “more” complex than patients with a single disease, as in defying easy resolution to their conditions, it is not the only factor that causes a patient to present as complex [ 61 ].
Patient complexity is deemed to arise from a patient’s socioeconomic status, environmental and mental health factors, along with the coordination of care and medical decision making which can all complicate a patient’s diagnosis and/or course of treatment causing complexity to arise [ 62 , 63 ]. Identified domains of patient complexity include:
“demographics (e.g., age, sex, race, and culture), patient personal characteristics or behavior (e.g., communication, burden of disease, coping strategies, and resilience), socio-economic factors, medical, and mental health (e.g., severity of illness, psychiatric disorders, addiction, cognitive impairment), patient risk of mortality, and healthcare system (e.g., care coordination and healthcare utilization), medical decision-making, and environment (e.g., pollution and neighborhood).” [ 62 ]
While the conceptualization of patient complexity may be novel to the Western biomedical understandings of health, it serves to reaffirm that broader social factors external to individuals and their physical bodies remain largely unexplored in clinical practice [ 64 ].
Given that health inequities across large populations, such as Indigenous peoples, can translate into a higher burden on healthcare systems by way of taxing limited available resources [ 65 ], identifying and acting on patient complexity to improve care may feasibly promote better resource allocation to meet patient needs. Patients with complexity often require interventions that are beyond the scope of typical biomedical care and the training of most HCPs [ 63 ], which is compounded by healthcare systems being ill-equipped to provide HCPs the appropriate resources necessary to care for patients [ 64 ].
Identifying patient complexity is increasingly important, therefore a variety of instruments exist to identify and address patient complexity within different healthcare settings, outpatient or in-patient (including hospitals, treatment centers, and long-term care facilities). Patient complexity assessment tools (PCATs) have emerged as means to aid HCPs in collecting vital information to more effectively deliver care [ 66 , 67 , 68 , 69 ]. PCATs may provide a comprehensive assessment that considers all aspects of a patient’s needs, and they are inclusive of the patient's experience of their own health [ 66 , 67 , 68 , 70 ]. PCATs have been noted to enhance patient engagement, more accurately identify the source of complexity challenging care plans, and allow HCPs to engage in appropriate courses of action (e.g. referrals), to improve the health of a patient with complexity [ 66 , 67 , 68 , 70 ].
PCATs follow two common formats, these being: i) a face-to-face interview between a patient and provider where the provider determines the responses within the PCAT, or ii) for patients to complete in written or digital form on their own in a self-assessment method [ 65 ]. PCATs may be specific to in-patient or outpatient populations, and in the case of some populations such as the elderly, PCATs may be applicable to those outside of healthcare settings too [ 65 , 71 , 72 ]. Though PCATs present great utility in identifying patient needs, sources of their complexity, and their resources, limited longitudinal data supports their utility beyond these. Few studies have investigated associations between a patient’s complexity and their subsequent healthcarerelated costs [ 73 , 74 , 75 ] and impacts on HCPs [ 76 ].
Despite utility for general patient populations, existing PCATs remain inadequate to effectively address the needs of Indigenous patients, as factors most relevant to Indigenous populations often remain under-explored [ 55 ]. HCPs rarely understand the full scope of the contributors of poor health that arise from colonial traumas and the impacts of structural inequities that continue to influence the health of Indigenous peoples [ 50 , 77 ]. Recognizing this gap, the current research aims to identify components that are critical to include in a PCAT developed for use with Indigenous patients. A program of research was undertaken to a) determine the extent to which existing PCATs contain domains for inquiry relevant to the care of Indigenous patients [ 55 ], b) explore the components of health complexity among Indigenous patients and the circumstances that allow it to persist [ 56 ], and c) identify the most effective constructs that characterize these complexities. The present study aims to engage a diverse panel of healthcare experts to reach consensus on which domains, concepts, and items are critical to effectively assess health complexity among Indigenous patients. Concepts are defined as constructs that represent a logical category while items are those which measure something. This work describes the development of an Indigenous-centered patient complexity assessment framework. The framework will then ultimately be used to derive an appropriate PCAT.
Positionality
The first author, AS, is a settler woman who completed this study as part of her PhD research. The second author, RH, is a settler woman and medical anthropologist who works as an assistant professor and primary care models of care scientist. The third author, AM, is a man of Ukrainian, Irish and Apache descent, and works as an assistant professor of Indigenous psychology. The fourth author, LC, is a Piikani First Nation’s man who works as an associate professor, family physician-scholar and assistant dean, and was a co-supervisor for the first author. The last author, CB, is a Métis woman and a mid-career clinician-scientist in rheumatology and health services research who was the primary supervisor for the first author. As a collective, the team was composed of individuals from both Indigenous and non-Indigenous backgrounds. The authors purposefully approached the research to bring forth unique perspectives with a shared commitment to doing research in a ‘good way’ respecting Indigenous research methodologies and remaining conscious of biases and assumptions.
Development of core framework structure and candidate item pool
The framework was developed over the course of four main phases. In the first phase, the core framework structure was identified primarily through review of existing PCATs. In the second phase, the framework was informed by the lived experience of Indigenous patients to embed additional domains relevant to this patient population. In phase three, the framework was refined and categorized logically. Finally, in phase four, the framework was verified with expert consensus. An overview of the phases of this study is presented in Fig. 1 .
Phases of developing Indigenous-centered patient complexity assessment framework
A scoping review was conducted to identify all existing tools and items, and to assess these in terms of the extent to which they are inclusive of social realities that shape Indigenous health [ 55 , 78 ]. The review determined that no existing tools are broadly suitable to the needs of Indigenous patients and that existing concepts within many tools need heavy contextualization in order to effectively assess complexity among Indigenous patients [ 55 ]. To identify additional domains and concepts of complexity, nine urban Indigenous patients (seven females, two males) were recruited to participate in semi-structured relational conversations with AS to explore the factors contributing to health complexity (see Appendix A for interview guide). Participants were from diverse Indigenous backgrounds but resided in [namewithheld] region where this study took place. The interview guide was pre-tested with the research team (RH, AM, LC, and CB) prior to data collection. Interview data was co-coded with an Indigenous health expert to ensure findings would be culturally sensitive and respect the perspectives of Indigenous peoples. Data was further refined with the research team. Adversity arising from material resources and healthcare interactions were identified as sources of health complexity that elicit psychological responses among patients [ 56 ]. Drivers of resilience and other protective factors were also identified that work to prevent health complexity [ 56 ]. A targeted search based on additional factors identified through the patient interviews was conducted to identify pre-existing instruments that assess these additional domains to further populate the candidate item pool.
Refinement and contextualization of framework and candidate item pool
Based on synthesized knowledge from the scoping review and the patient interview study, the third phase of the study outlined here aims to (a) contextualize the most significant emergent concepts to better align with the realities of Indigenous patients; (b) remove redundant items from the pool of candidate items (i.e., concepts and queries for potential inclusion in an Indigenous-focused PCAT); and (c) modify existing items within the concepts in the candidate item pool to better reflect the needs of Indigenous patients. This was done by AS, LC, and CB. Concepts were contextualized (see Table 1 ) by leveraging a constructivist paradigm [ 79 , 80 , 81 ] and building upon the experiences of both LC and CB in their clinical practice with Indigenous patients [ 82 ]. This was an iterative, reflective, and time-intensive process which consisted of five meetings over the course of 4 months to review an item pool of over 300 items.
Redundancy was common within the item pool as several items asked the same questions but with phrasing variations; therefore, these were merged into one item when duplicated. For example, many items asked “what is your age?” or “please indicate your age,” – these were merged into a single item that upheld its core concept to reduce repetition. Existing items were modified as per established recommendations for adaptations of research instruments [ 83 ]; they were also adjusted to keep operational equivalence [ 84 ], which refers to items kept within similar formats to their original state, including the measurement scale that was used originally [ 85 ]. Broader concepts were adjusted to better suit use with an Indigenous population [ 78 , 86 ]. For example, we broadened the concept of income which commonly asked the patient how much money they made annually to include considerations of the extent to which their money may be going to support others in their household.
Modified e-Delphi consensus process
The RAND/UCLA appropriateness method [ 87 ] was chosen to define the domains and concepts and then refine the item pool. Through a modified e-Delphi consensus process [ 88 , 89 , 90 ], concepts were verified to be included in an Indigenous-centered complexity framework along with essential items for collecting information about these concepts. To generate input from diverse perspectives, a purposive panel of HCPs, researchers, and policymakers who work within the field of Indigenous health in Alberta, Canada were identified and invited to participate in this phase. Experts were recruited via email to participate in a 3-round modified e-Delphi consensus process [ 90 ] carried out over the course of 4 weeks (October 3rd – November 1st, 2022) using the Qualtrics platform for electronic surveys in the following order:
Orientation to the modified e-Delphi consensus process
Round #1: voting on concepts
Provide a report summarizing results and free-text responses
Round #2: voting on items
Group discussion
Round #3: voting on items again
Honoraria for experts was not provided therefore only those who felt a commitment towards this work participated. The three rounds progressed attention from identifying concepts, to ranking effectiveness, to discussing and reviewing prioritized items. To launch the e-Delphi consensus process, an introductory orientation meeting was held with the panel of experts to provide an opportunity to ask and address any uncertainties about the process. In Round #1, experts rated each of the overarching concepts based on whether or not they should be included in a tool of this nature, ranking these on a scale of 1 (absolutely not) to 9 (absolutely yes). Free-text fields were provided for each concept for experts to submit any additional feedback on the concepts and their definitions. Concepts would have to achieve a median score ≥ 7 from the panel with no disagreement among experts to be carried forward into the next rounds. Median scores were calculated according to the RAND/UCLA appropriateness method handbook [ 87 ] and disagreement was defined according to the inter-percentile range adjusted for symmetry [ 87 ].
In Round #2, experts were asked to rate each item on a scale of 1 to 9 (as above) based on how effective [ 91 ] the item would be in assessing health complexity with Indigenous patients. Prior to completing responses, expert panel participants were provided via a PDF as an email attachment with the group ratings of concepts from Round #1 as well as the anonymous text feedback from others [ 92 , 93 ]. An added benefit of sharing the collective responses from prior rounds was that experts could consider the subject matter in terms of how their peers made sense of it. As before, free-text fields were provided for experts to submit any additional feedback on the items and their scoring in Round #2. The inclusion of items in the next round also required median scores ≥7 with no disagreement among experts [ 87 ].
Following the completion of Round #2, the experts were invited to a two-hour online video-based group discussion to review concepts and items that were scored lower and to revisit any comments indicating uncertainty or dissension recurring within the free-text fields. This meeting was recorded to track important discussion points and make any final changes or clarifications to the wording and/or scoring of the concepts and items. Changes were made in this group discussion session if the experts indicated consensus amongst themselves, defined as no voiced opposition. The sample of experts consisted of a panel who broadly knew and worked with one another at advanced levels, presuming consensus from no voiced opposition was reasonable. Participants were able to express opposition anonymously by reaching out to the lead author directly.
Following this group session, a report was circulated to all healthcare experts highlighting the summary of suggestions and changes made. A third round of voting was conducted, focused on how effective [ 91 ] the experts considered items would be if included in such a tool, again on a scale of 1 (not at all) to 9 (completely). Experts were provided with free-text fields to enter any final feedback on the items. To be included in the final item pool, items once again required median scores ≥7 with no disagreement [ 87 ].
This study was approved by the University of Calgary's Conjoint Health Research Ethics Board, Certification #REB20–0972. All participants in the modified e-Delphi consensus process provided their consent to participate in this study.
After refinement of the framework and candidate item pool, a total of 3 concepts within the biological and social domains were eliminated as they were deemed irrelevant in the context of Indigenous patient complexity. Cognition was eliminated as it was subject to the HCP's perception of a patient's cognitive capacity and therefore deemed potentially dangerous within the context of complexity among Indigenous patients. Weight was eliminated as it only provides one aspect of an individual’s body composition. Community was eliminated as it was not inclusive of what ‘community’ includes for Indigenous peoples, which was rather captured in a domain that was added. Domains of adverse life experiences, healthcare violence, and resilience and culture were added (see Table 2 ). Items within concepts were also separated if they would be completed by the patient or the HCP, see Appendix B .
The Delphi panel was comprised of n = 14 experts in Round #1, n = 11 experts in Round #2, and n = 10 experts in Round #3. The research team (AS, CB, LC) did not participate in the Delphi panel. There were seven researchers who work in various domains of Indigenous health, three researchers and policymakers in Indigenous health, and four health service providers, including one community health provider, one family physician, one radiation therapist, and one palliative care physician – all of which had extensive experience working with Indigenous patient populations. Of the panel, five members self-identified as Indigenous. A total of n = 3 experts attended the summative group discussion session including a community health researcher, an Indigenous health social scientist, and a family physician. In Round #1, all concepts were agreed upon to be included in the Indigenous-centered patient complexity framework (see Table 3 ).
In Round #2, no items were eliminated and all voting members agreed that these items should be included in the proposed Indigenous-centered complexity framework (see Table 4 ). In the group discussion meeting, items were modified based on wording suggestions and repetitive feedback. One new item was added, which asked whether the patient was a caregiver for someone else for a total of 64 items to be voted on in Round #3. In Round #3, all 64 items met the criteria to be included in the final set of items for an Indigenous-centered PCAT (see Table 4 and Appendix B ).
Within comments in the free-text fields provided and during the group discussion, concerns were raised regarding the feasibility of a tool if it were to include all items, given their length and the lack of item reduction that took place during Rounds #2 and #3. Despite an emphasis on reduction during the group discussion and circulated report to experts, all items met the criteria to be included as part of the final tool, demonstrating their importance in assessing complexity among Indigenous patients and stirring possible need for other strategies to help reduce the burden of length.
Healthcare systems in Canada are set up in ways that tend to dismiss the colonial history and its ongoing impacts on Indigenous peoples’ health [ 94 , 95 ]. Current models of healthcare delivery seldom take into account broader determinants of health that influence Indigenous peoples and their well-being, in turn, further perpetuating health inequities [ 94 , 96 ]. Clinical frameworks can serve as tools to foster a culturally safe environment [ 97 , 98 ], and respectful dialogue [ 99 , 100 ] with Indigenous patients to promote shared decision-making [ 101 , 102 ], honour self-determination in health [ 103 , 104 ], and arrive at mutually agreed-upon management plans that advance good health while simultaneously honouring Indigenous values [ 105 , 106 ]. This study describes the development of a framework tailored for use with Indigenous peoples in clinical settings, with the intention that it may eventually serve as a resource for HCPs to engage critical theoretical domains important to complex patient care. The goal of the framework is to provide a categorization of the dimensions that are encompassed within complexity—providing an understanding of why a patient may be present as “complex” in healthcare settings. By purposefully exploring the aspects that all collectively contribute to complexity observed in patient presentations, this framework aims to help HCPs gain insight into the nature of health complexity among Indigenous patients, ultimately promoting their capacity to navigate and address the challenges that arise with health complexity. As the culmination of a multi-phased approach, findings offer a theoretical structure for key domains of complexity shaping Indigenous patient health. The present study explores the sources of complexity and their presentations among Indigenous patients.
The Truth and Reconciliation Commission (TRC) of Canada has called for HCPs to be educated on the impacts of colonialism on Indigenous health, to promote cultural safety and sensitivity in healthcare interactions [ 23 , 78 , 107 ]. HCPs today may not fully understand or perceive the historical and ongoing drivers of poor health that continue to harm Indigenous patients, presenting with an overall lack of awareness that can impact the effectiveness of healthcare delivery [ 47 , 108 ]. Service innovations that exist at the interface of Indigenous patients and HCPs, such as a patient complexity assessment framework, can be a resource to bridge gaps in understanding contributors to good health for Indigenous patients. This framework could provide comprehensive high-quality care provisions by opening possibilities for addressing social and structural determinants of health within Western biomedical spaces.
For Indigenous peoples, health is inextricably tied to the determinants of health that have arisen from colonization. As outlined in the TRC’s 94 Calls to Action [ 23 ], there are many possibilities within the health sector to support reconciliation with Indigenous peoples [ 109 ]. The findings of this study are aligned with the directions of reconciliation set out by the TRC Calls to Action [ 23 ]. By providing care that is better suited to the needs of Indigenous peoples, we can advance health equity [ 110 , 111 , 112 ] and diminish the impacts of systemic factors that negatively influence the health of Indigenous peoples. Having appropriate resources, such as an Indigenous-centered patient complexity framework, is a means to foment capacity among HCPs to better engage with Indigenous patients, as well as to acknowledge and act on the insidious role of colonization in shaping health outcomes [ 113 , 114 ]. HCPs require the awareness and competencies to effectively address complexity among Indigenous patients [ 107 , 113 , 115 , 116 ]. The patient complexity assessment framework presented here builds evidence for a potential resource aimed at enabling deeper and more meaningful clinical interactions between HCPs and Indigenous patients. It can help to advance cultural safety in clinical settings which refers to having practices rooted in a basic understanding of Indigenous peoples’ beliefs and history while also engaging a process of self-reflection to understand the power differences between the HCP and patient which can impact the process of care and healing [ 117 ]. Not only might the framework provide a lens for HCPs to better discern health determinants stemming from colonization, but it may also enhance the capacity of the HCPs to reconstruct their pathways of care to more effectively address the needs of Indigenous patients. This work supports directions to culturally safe care and leads the way in decolonizing approaches to care.
Strengths and limitations
The framework presented offers HCPs an opportunity to understand the nature and specific origins of the realities that continue to shape the health of Indigenous patients. This knowledge presents an actionable opportunity to shift HCPs’ tendencies to locate blame within the patient for health outcomes to instead locate cause within structural and systemic dynamics arising from inequity as an outcome of colonization. The approach taken to develop this framework is critical and rigorous in how it engages with many disciplines of knowledge, centering Indigenous knowledge throughout the process. The framework holds significant theoretical rigour that provides a strong foundation of knowledge for informing any future PCATs given its multi-phased development and continuous refinement. Furthermore, items developed are highly validated derived from published measures, informed by the lived experiences of Indigenous patients, contextualized to reflect the social realities that shape the health of Indigenous peoples, and reviewed by healthcare experts within the field of Indigenous health.
As noted in the results section, it is limited by the number of items selected to be included in the proposed Indigenous-centered PCAT, risking that such a tool is burdensome to employ in regular clinical practice. Future advancements of this work will employ psychometric methods and experiment with novel delivery approaches in order to reduce the burden of eliciting items and to ensure the tool’s feasibility for use in clinical settings. Considerations of health literacy will also be undertaken in the refinement of the items as many of them may not be easily understood by patients without prior knowledge and/or clear definitions. Within the item pool, there are no items that directly ask about the role of discrimination, racism, stereotyping, and mistrust in perpetuating complexity within the Indigenous patient. While important concepts, the nature of the tool’s employment causes concern to be cautious in alienating the HCPs and creating context that causes discomfort for both the patient and HCP. Likewise, inquiries about systemic inequities may serve to paralyze HCPs, implicitly suggesting that if complexity is caused by structural and institutional factors, HCPs are then incapable of addressing complexity within the Indigenous patient. This is a limitation of the nature of such tools, and future advancements of this research will explore avenues to create safety for such disclosures. A key question remains whether complexity, which is an unobservable construct, exists as a unitary construct or if it represents a collection of correlated facets without a common core [ 118 ]. Future analyses will explore the presence of any dimensions within the framework that reflect a global, underlying construct of complexity [ 118 ]. Another limitation is that both the Indigenous patients who contributed to phase two of this work and the HCPs, policymakers, and researchers who participated in phase four of this work represent the regional area of Alberta, Canada. Future advancements of this work will explore the applicability of such a PCAT outside of this region.
Future steps
While we have presented a framework of Indigenous patient complexity, future steps of this work are aligned with addressing the limitations of this study and will advance the goal of having a PCAT for use in clinical settings. A subsequent PCAT developed from the framework presented here could be used in practice as an initial screening tool to assess new Indigenous patients for complexity or as a longitudinal tool that may be employed across many points throughout the patients’ healthcare journey providing opportunity for comparative analyses to determine changes in complexity. Pilot data will be collected for a factor analysis in a bid to reduce the number of items included in such an Indigenous-centered PCAT [ 119 , 120 , 121 ]. Using the framework presented as a model of data, we will test hypotheses regarding the number of factors, the correlation between those factors, and the relationship of the items to the factors [ 119 , 120 , 121 ]. Factors are larger than items and concepts to allow for refining and rendering a more precise tool. Pilot data will also help to inform the best use of the tool, ensuring Indigenous patient needs are being met.
Through the critical application of the integrated concepts presented within the framework, we put forth a set of recommendations to improve clinical care interactions between HCPs and Indigenous patients, advance cultural safety in healthcare settings, and hold space for Indigenous epistemologies and experiences within social and healthcare structures that continue to systemically disadvantage Indigenous peoples. The framework presented here offers an evolving body of knowledge to enhance capacity to inform HCPs, systems, and policies on how to facilitate better health outcomes with Indigenous peoples. Future research will work to reduce the number of items in such a tool to advance usability within clinical settings.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due privacy considerations but are available from the corresponding author on reasonable request.
Abbreviations
Healthcare providers
Patient complexity assessment tools
Interquartile range
Truth and Reconciliation Commission
Willows ND. Determinants of healthy eating in Aboriginal peoples in Canada: the current state of knowledge and research gaps. Canadian J Public Health/Revue Canad de Sante’e Publ. 2005;1:S32–6.
Google Scholar
Statistics Canada. Dictionary: 2016 census of population. Ottawa: Statistics Canada; 2017.
Statistics Canada. Aboriginal peoples of Canada: a demographic profile, 2006 census. Ottawa: Statistics Canada; 2006.
Khawaja M. Consequences and remedies of Indigenous language loss in Canada. Societies. 2021;11(3):89.
Article Google Scholar
Von Der Porten S. Canadian Indigenous governance literature: a review. AlterNative: An Int J Indigen Peoples. 2012;8(1):1–4.
Gracey M. Historical, cultural, political, and social influences on dietary patterns and nutrition in Australian Aboriginal children. Am J Clin Nutr. 2000;72(5):1361s–7s.
Article CAS PubMed Google Scholar
Lancet T. The past is not the past for Canada's Indigenous peoples. Lancet (London England). 2021;397(10293):2439.
Walde D. Sedentism and pre-contact tribal organization on the northern plains: colonial imposition or Indigenous development? World Archaeol. 2006;38(2):291–310.
Crichlow W. Western colonization as disease: native adoption and cultural genocide. Crit Soc Work. 2002;3(1):1–4.
Neu D. Accounting and accountability relations: colonization, genocide and Canada’s first nations. Account Audit Account J. 2000;13(3):268–88.
Jimenez VM. With good intentions: euro-Canadian and Aboriginal relations in colonial Canada. Can Ethn Stud. 2006;38(2):181.
Leach A. The roots of Aboriginal homelessness in Canada. Parity. 2010;23(9):12–3.
Brown HJ, McPherson G, Peterson R, Newman V, Cranmer B. Our land, our language: connecting dispossession and health equity in an Indigenous context. Canadian J Nurs Res Archiv. 2012;1:44–63.
Bombay A, Matheson K, Anisman H. The intergenerational effects of Indian residential schools: implications for the concept of historical trauma. Transcult psychiat. 2014;51(3):320–38.
De Leeuw S. ‘If anything is to be done with the Indian, we must catch him very young’: colonial constructions of Aboriginal children and the geographies of Indian residential schooling in British Columbia. Canada Child Geograph. 2009;7(2):123–40.
Daschuk JW. Clearing the plains: disease, politics of starvation, and the loss of Aboriginal life. University of Regina Press; 2013.
Book Google Scholar
Osterath B. European diseases left their mark on First Nations' DNA. Nat News. 2016;1–2.
Martin K, Mirraboopa B. Ways of knowing, being and doing: a theoretical framework and methods for Indigenous and indigenist re-search. J Aust Stud. 2003;27(76):203–14.
McGuire–Kishebakabaykwe PD. Exploring resilience and Indigenous ways of knowing. Pimatisiwin. 2010;8(2):117–31.
Adelson N. The embodiment of inequity: health disparities in Aboriginal Canada. Can J Public Health. 2005;96(Suppl 2):S45–61.
Article PubMed PubMed Central Google Scholar
Kendall J. Circles of disadvantage: Aboriginal poverty and underdevelopment in Canada. Am Rev Can Stud. 2001;31(1–2):43–59.
Richmond CA, Ross NA. The determinants of first nation and Inuit health: a critical population health approach. Health place. 2009;15(2):403–11.
Article PubMed Google Scholar
Truth and Reconciliation Commission of Canada. Calls to Action. Truth and Reconciliation Commission of Canada. 2015.
Stanton K. Reconciling reconciliation: differing conceptions of the supreme court of Canada and the Canadian truth and reconciliation commission. J Law Soc Policy. 2017;26:21.
MacDonald C, Steenbeek A. The impact of colonization and western assimilation on health and wellbeing of Canadian Aboriginal people. Int J Reg Local Hist. 2015;10(1):32–46.
Kubik W, Bourassa C, Hampton M. Stolen sisters, second class citizens, poor health: the legacy of colonization in Canada. Human Soc. 2009;33(1–2):18–34.
Kim PJ. Social determinants of health inequities in Indigenous Canadians through a life course approach to colonialism and the residential school system. Health Equity. 2019;3(1):378–81.
Tjepkema M, Bushnik T, Bougie E. Life expectancy of first nations, Métis and Inuit household populations in Canada. Health Rep. 2019;30(12):3–10.
PubMed Google Scholar
King M. Chronic diseases and mortality in Canadian Aboriginal peoples: learning from the knowledge. Prev Chronic Dis. 2011;8(1)
Leung L. Diabetes mellitus and the Aboriginal diabetic initiative in Canada: an update review. J Family Med Prim Care. 2016;5(2):259.
Crowshoe L, Dannenbaum D, Green M, Henderson R, Hayward MN, Toth E. Diabetes Canada clinical practice guidelines expert committee. Type 2 diabetes and Indigenous peoples. Can J Diabet. 2018;42:S296–306.
Jacobs K, Gill K. Substance abuse in an urban Aboriginal population: social, legal and psychological consequences. J Ethn Subst Abus. 2001;1(1):7–25.
Callaghan RC, Cull R, Callaghan RC, Cull R, Vettese LC, Taylor L. A gendered analysis of Canadian Aboriginal individuals admitted to inpatient substance abuse detoxification: a three-year medical chart review. Am J Addict. 2006;15(5):380–6.
Hickey S, Roe Y, Ireland S, Kildea S, Haora P, Gao Y, et al. A call for action that cannot go to voicemail: research activism to urgently improve Indigenous perinatal health and wellbeing. Women Birth. 2021;34(4):303–5.
Barnabe C, Jones CA, Bernatsky S, Peschken CA, Voaklander D, Homik J, et al. Inflammatory arthritis prevalence and health services use in the first nations and non–first nations populations of Alberta. Canada Arthrit care res. 2017;69(4):467–74.
Kirmayer LJ, Brass GM, Tait CL. The mental health of Aboriginal peoples: transformations of identity and community. Can J Psychiat. 2000;45(7):607–16.
Article CAS Google Scholar
Montgomery PB, Hall L, Newton-Mathur D, Forchuk C, Mossey S. Sheltering Aboriginal women with mental illness in Ontario, Canada: being “kicked” and nurtured. J Nurs Care. 2014;3(3):1–6.
Laupland KB, Karmali S, Kirkpatrick AW, Crowshoe L, Hameed SM. Distribution and determinants of critical illness among status Aboriginal Canadians. A population-based assessment. J Crit Care. 2006;21(3):243–7.
Axelsson P, Kukutai T, Kippen R. The field of Indigenous health and the role of colonisation and history. J Popul Res. 2016;33:1–7.
Paradies Y. Colonisation, racism and Indigenous health. J Popul Res. 2016;33(1):83–96.
Paradies Y. Racism and Indigenous health. Oxford Research Encyclopedia of Global Public Health. 2018. p. 1–21.
Fraser SL, Gaulin D, Fraser WD. Dissecting systemic racism: policies, practices and epistemologies creating racialized systems of care for Indigenous peoples. Int J Equity Health. 2021;20:1–5.
Waterworth P, Pescud M, Braham R, Dimmock J, Rosenberg M. Factors influencing the health behaviour of Indigenous Australians: perspectives from support people. PLoS One. 2015;10(11):e0142323.
Turpel-Lafond ME, Johnson H. In plain sight: addressing Indigenous-specific racism and discrimination in BC health care. BC Stud. 2021;5(209):7–17.
Kitching GT, Firestone M, Schei B, Wolfe S, Bourgeois C, O’Campo P, et al. Unmet health needs and discrimination by healthcare providers among an Indigenous population in Toronto. Canada Canad J Public Health. 2020;111:40–9.
Eni R, Phillips-Beck W, Achan GK, Lavoie JG, Kinew KA, Katz A. Decolonizing health in Canada: a Manitoba first nation perspective. Int J Equity Health. 2021;20(1):1–2.
National Collaborating Centre for Indigenous Health. Access to health services as a social determinant of First Nations, Inuit and Métis health. 2019. Available from: https://www.nccih.ca/docs/determinants/FS-AccessHealthServicesSDOH-2019-EN.pdf .
Hewa S, Hetherington RW. Specialists without spirit: limitations of the mechanistic biomedical model. Theor Med. 1995;16:129–39.
West-McGruer K. There’s ‘consent’ and then there’s consent: Mobilising Māori and Indigenous research ethics to problematise the western biomedical model. J Sociol. 2020;56(2):184–96.
Phillips-Beck W, Eni R, Lavoie JG, Avery Kinew K, Kyoon Achan G, Katz A. Confronting racism within the Canadian healthcare system: systemic exclusion of first nations from quality and consistent care. Int J Environ Res Public Health. 2020;17(22):8343.
Anderson W. The colonial medicine of settler states: comparing histories of Indigenous health. Health Hist. 2007;9(2):144–54.
Davy C, Harfield S, McArthur A, Munn Z, Brown A. Access to primary health care services for Indigenous peoples: a framework synthesis. Int J Equity Health. 2016;15:1–9.
Nguyen NH, Subhan FB, Williams K, Chan CB. Barriers and mitigating strategies to healthcare access in Indigenous communities of Canada: a narrative review. Healthcare. 2020;8(2):112.
Hole RD, Evans M, Berg LD, Bottorff JL, Dingwall C, Alexis C, et al. Visibility and voice: Aboriginal people experience culturally safe and unsafe health care. Qual Health Res. 2015;25(12):1662–74.
Sehgal A, Barnabe C, Crowshoe L. Patient complexity assessment tools containing inquiry domains important for Indigenous patient care: a scoping review. PLoS One. 2022;17(8):e0273841.
Article CAS PubMed PubMed Central Google Scholar
Sehgal A, Scott S, Murry A, Henderson R, Barnabe C, Crowshoe L. Exploring health complexity with urban Indigenous peoples for healthcare equity: a qualitative study. BMJ Open. 2023;13(10):1–9.
Knibb-Lamouche J. Culture as a social determinant of health. In: Commissioned paper prepared for the institute on medicine, roundtable on the promotion of health equity and the elimination of health disparities. 2012.
Smylie J, Firestone M. The health of Indigenous peoples. Social Determ Health Canad Perspect. 2016;6:434–69.
Peek CJ, Baird MA, Coleman E. Primary care for patient complexity, not only disease. Famil Syst Health. 2009;27(4):287.
Loeb DF, Bayliss EA, Candrian C, deGruy FV, Binswanger IA. Primary care providers’ experiences caring for complex patients in primary care: a qualitative study. BMC Fam Pract. 2016;17(1):1–9.
Ben-Menahem S, Sialm A, Hachfeld A, Rauch A, von Krogh G, Furrer H. How do healthcare providers construe patient complexity? A qualitative study of multimorbidity in HIV outpatient clinical practice. BMJ Open. 2021;11(11):e051013.
Nicolaus S, Crelier B, Donzé JD, Aubert CE. Definition of patient complexity in adults: a narrative review. J Multimorbid Comorbid. 2022;17(12):26335565221081288.
Mount JK, Massanari RM, Teachman J. Patient care complexity as perceived by primary care physicians. Famil Syst Health. 2015;33(2):137.
Webster F, Rice K, Bhattacharyya O, Katz J, Oosenbrug E, Upshur R. The mismeasurement of complexity: provider narratives of patients with complex needs in primary care settings. Int J Equity Health. 2019;18(1):1–8.
Kaneko H, Hanamoto A, Yamamoto-Kataoka S, Kataoka Y, Aoki T, Shirai K, et al. Evaluation of complexity measurement tools for correlations with health-related outcomes, health care costs and impacts on healthcare providers: a scoping review. Int J Environ Res Public Health. 2022;19(23):16113.
Bodenheimer T, Berry-Millett R. Care management of patients with complex health care needs. Policy. 2009;1(6):1–6.
Latour CH, Huyse FJ, De Vos R, Stalman WA. A method to provide integrated care for complex medically ill patients: the INTERMED. Nurs Health Sci. 2007;9(2):150–7.
Pratt R, Hibberd C, Cameron IM, Maxwell M. The patient centered assessment method (PCAM): integrating the social dimensions of health into primary care. J Comorbid. 2015;5(1):110–9.
Schaink AK, Kuluski K, Lyons RF, Fortin M, Jadad AR, Upshur R, et al. A scoping review and thematic classification of patient complexity: offering a unifying framework. J comorbid. 2012;2(1):1–9.
De Jonge P, Huyse FJ, Slaets JP, Söllner W, Stiefel FC. Operationalization of biopsychosocial case complexity in general health care: the INTERMED project. Austral New Zealand J Psychiat. 2005;39(9):795–9.
Reuben DB, Keeler E, Seeman TE, Sewall A, Hirsch SH, Guralnik JM. Development of a method to identify seniors at high risk for high hospital utilization. Med Care. 2002;1:782–93.
Wallace E, McDowell R, Bennett K, Fahey T, Smith SM. External validation of the probability of repeated admission (Pra) risk prediction tool in older community-dwelling people attending general practice: a prospective cohort study. BMJ Open. 2016;6(11):e012336.
Wild B, Heider D, Maatouk I, Slaets J, König HH, Niehoff D, et al. Significance and costs of complex biopsychosocial health care needs in elderly people: results of a population-based study. Psychosom Med. 2014;76(7):497–502.
Pacala JT, Boult C, Boult L. Predictive validity of a questionnaire that identifies older persons at risk for hospital admission. J Am Geriatr Soc. 1995;43(4):374–7.
Peters LL, Burgerhof JG, Boter H, Wild B, Buskens E, Slaets JP. Predictive validity of a frailty measure (GFI) and a case complexity measure (IM-E-SA) on healthcare costs in an elderly population. J Psychosom Res. 2015;79(5):404–11.
Yoshida S, Matsushima M, Wakabayashi H, Mutai R, Sugiyama Y, Yodoshi T, et al. Correlation of patient complexity with the burden for health-related professions, and differences in the burden between the professions at a Japanese regional hospital: a prospective cohort study. BMJ Open. 2019;9(2):e025176.
Horrill T, McMillan DE, Schultz AS, Thompson G. Understanding access to healthcare among Indigenous peoples: a comparative analysis of biomedical and postcolonial perspectives. Nurs Inq. 2018;25(3):e12237.
Crowshoe LL, Henderson R, Jacklin K, Calam B, Walker L, Green ME. Educating for equity care framework: addressing social barriers of Indigenous patients with type 2 diabetes. Can Fam Phys. 2019;65(1):25–33.
Adom D, Yeboah A, Ankrah AK. Constructivism philosophical paradigm: implication for research, teaching and learning. Global j arts human soc sci. 2016;4(10):1–9.
Lee CJ. Reconsidering constructivism in qualitative research. Educ Philos Theory. 2012;44(4):403–12.
Kamal SS. Research paradigm and the philosophical foundations of a qualitative study. PEOPLE. Int J Soc Sci. 2019;4(3):1386–94.
Burns M, Bally J, Burles M, Holtslander L, Peacock S. Constructivist grounded theory or interpretive phenomenology? Methodological choices within specific study contexts. Int J Qual Methods. 2022;7(21):16094069221077758.
Gjersing L, Caplehorn JR, Clausen T. Cross-cultural adaptation of research instruments: language, setting, time and statistical considerations. BMC Med Res Methodol. 2010;10:1.
Reichenheim ME, Moraes CL. Operationalizing the cross-cultural adaptation of epidemological measurement instruments. Rev Saude Publica. 2007;41:665–73.
Herdman M, Fox-Rushby J, Badia X. A model of equivalence in the cultural adaptation of HRQoL instruments: the universalist approach. Qual Life Res. 1998;7:323–35.
Cook DA, Beckman TJ. Current concepts in validity and reliability for psychometric instruments: theory and application. Am J Med. 2006;119(2):166–e7.
Fitch K, Bernstein SJ, Aguilar MD, Burnand B, LaCalle JR, Lazaro P, et al. The RAND/UCLA appropriateness method user’s manual. Santa Monica: RAND Corporation; 2001.
Donohoe H, Stellefson M, Tennant B. Advantages and limitations of the e-Delphi technique: implications for health education researchers. Am J Health Educ. 2012;43(1):38–46.
Rowe G, Wright G, Bolger F. Delphi: a reevaluation of research and theory. Technol Forecast Soc Chang. 1991;39(3):235–51.
Hsu CC, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval. 2007;12(1):10.
Health Quality Council of Alberta. The Alberta Quality Matrix for Health. 2005. Available from: https://hqca.ca/wp-content/uploads/2021/12/HQCA_11x8_5_Matrix.pdf .
Vernon W. The Delphi technique: a review. Int J Ther Rehabil. 2009;16(2):69–76.
Humphrey-Murto S, Varpio L, Wood TJ, Gonsalves C, Ufholz LA, Mascioli K, et al. The use of the Delphi and other consensus group methods in medical education research: a review. Acad Med. 2017;92(10):1491–8.
Boyer Y. Healing racism in Canadian health care. CMAJ. 2017;189(46):E1408–9.
Burnett K, Sanders C, Halperin D, Halperin S. Indigenous peoples, settler colonialism, and access to health care in rural and northern Ontario. Health Place. 2020;1(66):102445.
Kolahdooz F, Nader F, Yi KJ, Sharma S. Understanding the social determinants of health among Indigenous Canadians: priorities for health promotion policies and actions. Glob Health Act. 2015;8(1):27968.
Nguyen HT. Patient centred care: cultural safety in Indigenous health. Aust Fam Phys. 2008;37(12).
Greenwood M, Lindsay N, King J, Loewen D. Ethical spaces and places: Indigenous cultural safety in British Columbia health care. AlterNative. 2017;13(3):179–89.
Hovey RB, Delormier T, McComber AM, Lévesque L, Martin D. Enhancing Indigenous health promotion research through two-eyed seeing: a hermeneutic relational process. Qual Health Res. 2017;27(9):1278–87.
Maar M, Yeates K, Barron M, Hua D, Liu P, Lum-Kwong MM, et al. I-RREACH: an engagement and assessment tool for improving implementation readiness of researchers, organizations and communities in complex interventions. Implement Sci. 2015;10(1):1–3.
Groot G, Waldron T, Barreno L, Cochran D, Carr T. Trust and world view in shared decision making with Indigenous patients: a realist synthesis. J Eval Clin Pract. 2020;26(2):503–14.
Jull J, Giles A, Boyer Y, Lodge M, Stacey D. Shared decision making with Aboriginal women facing health decisions: a qualitative study identifying needs, supports, and barriers. AlterNative: An Int J Indigen Peoples. 2015;11(4):401–16.
Auger M, Howell T, Gomes T. Moving toward holistic wellness, empowerment and self-determination for indigenous peoples in Canada: can traditional Indigenous health care practices increase ownership over health and health care decisions? Can J Public Health. 2016;107:e393–8.
Black K, McBean E. Increased Indigenous participation in environmental decision-making: a policy analysis for the improvement of Indigenous health. Int Indigen Policy J. 2016;7(4).
Allen L, Hatala A, Ijaz S, Courchene ED, Bushie EB. Indigenous-led health care partnerships in Canada. Cmaj. 2020;192(9):E208–16.
Dwyer JM, Lavoie J, O’Donnell K, Marlina U, Sullivan P. Contracting for Indigenous health care: towards mutual accountability. Aust J Public Adm. 2011;70(1):34–46.
Towle A, Godolphin W, Alexander T. Doctor–patient communications in the Aboriginal community: towards the development of educational programs. Patient Educ Couns. 2006;62(3):340–6.
Anderson MJ, Smylie JK. Health systems performance measurement systems in Canada: how well do they perform in first nations, Inuit, and Métis contexts? Pimatisiwin. 2009;7(1):99.
PubMed PubMed Central Google Scholar
McNally M, Martin D. First nations, Inuit and Métis health: considerations for Canadian health leaders in the wake of the truth and reconciliation Commission of Canada report. Healthc Manage Forum. 2017;30(2):117–22.
Browne AJ, Varcoe C. Critical cultural perspectives and health care involving Aboriginal peoples. Contemp Nurse. 2006;22(2):155–68.
Tookenay VF. Improving the health status of Aboriginal people in Canada: new directions, new responsibilities. CMAJ. Can Med Assoc J. 1996;155(11):1581.
CAS Google Scholar
Beavis AS, Hojjati A, Kassam A, Choudhury D, Fraser M, Masching R, et al. What all students in healthcare training programs should learn to increase health equity: perspectives on postcolonialism and the health of Aboriginal peoples in Canada. BMC Medic Educ. 2015;15(1):1–11.
Kerrigan V, Lewis N, Cass A, Hefler M, Ralph AP. “How can I do more?” cultural awareness training for hospital-based healthcare providers working with high Aboriginal caseload. BMC Medic Educ. 2020;20:1–11.
Wilson AM, Kelly J, Jones M, O’Donnell K, Wilson S, Tonkin E, et al. Working together in Aboriginal health: a framework to guide health professional practice. BMC Health Serv Res. 2020;20(1):1–11.
Wilson D, de la Ronde S, Brascoupé S, Apale AN, Barney L, Guthrie B, et al. Health professionals working with first nations, Inuit, and Métis consensus guideline. J Obstet Gynaecol Can. 2013;35(6):S1–4.
Macaulay AC. Improving Aboriginal health: how can health care professionals contribute? Can Fam Phys. 2009;55(4):334–6.
Royal College of Physicians and Surgeons of Canada. Indigenous values, health and principles statement. The Indigenous Health Advisory Committee and the Office of Health Policy and Communications. 2013. Available from: http://www.royalcollege.ca/portal/page/portal/rc/common/documents/policy/indigenous_health_values_principles_report_e.pdf .
Morin AJ, Arens AK, Tran A, Caci H. Exploring sources of construct-relevant multidimensionality in psychiatric measurement: a tutorial and illustration using the composite scale of Morningness. Int J Methods Psychiatr Res. 2016;25(4):277–88.
Orçan F. Exploratory and confirmatory factor analysis: which one to use first? J Measure Evaluat Educ Psychol. 2018;9(4):414–21.
Thompson B. Exploratory and confirmatory factor analysis: understanding concepts and applications. Washington DC: American Psychological Association; 2004.
Hurley AE, Scandura TA, Schriesheim CA, Brannick MT, Seers A, Vandenberg RJ, et al. Exploratory and confirmatory factor analysis: guidelines, issues, and alternatives. J Organ Behav. 1997;1:667–83.
Download references
Acknowledgements
None to report.
Author information
Authors and affiliations.
Department of Family Medicine, Cumming School of Medicine, University of Calgary, 3330 Hospital Dr NW, Calgary, AB, T2N 4N1, Canada
Anika Sehgal, Rita Henderson & Lynden (Lindsay) Crowshoe
Department of Psychology, University of Calgary, 2500 University Dr NW, Calgary, AB, T2N 1N4, Canada
Department of Medicine, Cumming School of Medicine, University of Calgary, 3330 Hospital Dr NW, Calgary, AB, T2N 4N1, Canada
Cheryl Barnabe
You can also search for this author in PubMed Google Scholar
Contributions
AS, CB, and LC led the conception, design, data analysis, interpretation, and writing of this manuscript. AM and RH supported equally to the interpretation and writing of this manuscript.
Corresponding author
Correspondence to Anika Sehgal .
Ethics declarations
Ethical approval and consent to participation.
This study was approved by the University of Calgary’s Conjoint Health Research Ethics Board, Certification #REB20–0972. The study was carried out according to the Declaration of Helsinki. All participants in the modified e-Delphi consensus process provided implied informed consent to participate in this study.
Consent to publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sehgal, A., Henderson, R., Murry, A. et al. Advancing health equity for Indigenous peoples in Canada: development of a patient complexity assessment framework. BMC Prim. Care 25 , 144 (2024). https://doi.org/10.1186/s12875-024-02362-z
Download citation
Received : 27 May 2023
Accepted : 03 April 2024
Published : 29 April 2024
DOI : https://doi.org/10.1186/s12875-024-02362-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health equity
- Social determinants of health
- Health care disparities
- Health economics
- Primary care
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
- Directories
- Scholarly Articles
- Books & Dissertations
- Indigenous Languages
- Indigenous Research Methods
- Organizations & More
- Start Your Research
- Research Guides
- University of Washington Libraries
- Library Guides
- UW Libraries
- Indigenous Studies
Indigenous Studies: Indigenous Research Methods
"To reclaim research is to take control of our lives and our lands to benefit us in issues of importance for our self-determination. It is to liberate and emancipate by decolonisation and privileging the voices, experiences and lives of Aboriginal people and Aboriginal lands so that research frameworks are reflective of this. To reframe research is to focus on matters of importance as we identify these. It is to respect our ways and honour our rights and social mores as essential processes, through which we live, act and learn."
Selected eBooks

Key Principles
From: Russell-Mundine, Gabrielle. “ Reflexivity in Indigenous Research: Reframing and Decolonising Research? ” Journal of Hospitality and Tourism Management , vol. 19, no. 1, 2012, pp. 85–90.
Indigenous researchers have identified some of the key principles that research by, or with, Indigenous peoples should incorporate. That is, such research should:
- empower Indigenous peoples
- aim to decolonise and reframe research
- be critical and liberationist recognising social, political and historical contexts
- have political integrity
- privilege Indigenous voices
- recognise and represent the diversity of cultures, voices and experiences
- allow Indigenous peoples to set the agenda
- focus on matters of importance to Indigenous peoples
- use core structures of Aboriginal world-views
- integrate cultural protocols, social mores and behaviours into methodology
- integrate Indigenous ways of knowledge creation.
Key Questions for the Indigenous Researcher
From: Tuhiwai Smith, Linda, " Kaupapa Maori Research ." In Battiste, Marie Ann. Reclaiming Indigenous Voice and Vision . UBC Press, 2000.
- What research do we want done?
- Whom is it for?
- What difference will it make?
- Who will carry it out?
- How do we want the research done?
- How will we know it is worthwhile?
- Who will own the research?
- Who will benefit?
Decolonizing Knowledge
2013 conversation with Professor Linda Tuhiwai Smith, author of Decolonizing Methodologies: Research and Indigenous Peoples .
Selected Articles
- "Indigenous Epistemologies and Education: Self-Determination, Anthropology, and Human Rights." Special issue: Anthropology & Education Quarterly, Vol. 36, No. 1 (2005).
- Datta, Ranjan. “Decolonizing Both Researcher and Research and Its Effectiveness in Indigenous Research.” Research Ethics Review, vol. 14, no. 2, 2018, pp. 1–24.
- Drawson, Alexandra S, et al. “Indigenous Research Methods: A Systematic Review.” International Indigenous Policy Journal, vol. 8, no. 2, 2017.
- Thambinathan, Vivetha, and Kinsella, Elizabeth Anne. “Decolonizing Methodologies in Qualitative Research: Creating Spaces for Transformative Praxis.” International Journal of Qualitative Methods, vol. 20, 2021, pp. 1-9.
"Indigenous peoples are used to being studied by outsiders; indeed, many of the basic disciplines of knowledge are implicated in studying the Other and creating expert knowledge. More recently, however, indigenous researchers have been active in seeking ways to disrupt the “history of exploitation, suspicion, misunderstanding, and prejudice” of indigenous peoples in order to develop methodologies and approaches to research that privilege indigenous knowledges, voices, experiences, reflections, and analyses of their social, material, and spiritual conditions. . .
Indigenist research also includes a critique of the “rules of practice regarding research, the way research projects are funded, and the development of strategies that address community concerns about the assumptions, ethics, purposes, procedures, and outcomes of research. These strategies often have led to innovative research questions, new methodologies, new research relationships, deep analyses of the researcher in context, and analyses, interpretations, and the making of meanings that have been enriched by indigenous concepts and language. . .
Research, like schooling, once the tool of colonization and oppression, is very gradually coming to be seen as a potential means to reclaim languages, histories, and knowledge, to find solutions to the negative impacts of colonialism and to give voice to an alternative way of knowing and of being."
Additional Resources
- Toolbox of Research Principles in an Aboriginal Context: Ethics, Respect, Fairness, Reciprocity, Collaboration and Culture
- Indigenous Knowledges Research (University of Melbourne Library)
- Indigenous Research & Knowledges in North America (University of Colorado Libraries)
- Indigenous Research Methodologies (University of British Columbia)
Sources for quotes:
Karen Martin, "Ways of knowing, ways of being, and ways of doing: Developing a theoretical framework and methods for Indigenous re-search and indigenist research." Australian Institute of Aboriginal and Torres Strait Islander Studies conference, The Power of Knowledge and the Resonance of Tradition, 2001. Cited in Karina L. Walters, et al., ""Indigenist" Collaborative Research Efforts in Native American Communities" In Stiffman, Arlene Rubin. The Field Research Survival Guide . Oxford University Press, 2009.
Tuhiwai Smith, Linda." On tricky ground: Researching the Native in the age of uncertainty." In Luttrell, Wendy. Qualitative Educational Research: Readings in Reflexive Methodology and Transformative Practice . Routledge, 2010.
- << Previous: Indigenous Languages
- Next: Organizations & More >>
- Last Updated: Oct 23, 2023 4:34 PM
- URL: https://guides.lib.uw.edu/research/indigenous-studies
Skip to Content
Other ways to search:
- Events Calendar
Tai Koester: Building on Undergraduate Training to Lead Research in Political Ecology and Indigenous Geographies

I am a Masters student in the School of Geography, Development and Environment at the University of Arizona working with Dr. Andrew Curley. My research draws from political ecology and Indigenous geographies to study environmental politics in the US West and examines how the energy transition is shaping the political and economic futures of Native Nations. My Masters research is focused on the Northern Cheyenne Tribe, a federally-recognized tribe, whose reservation is located in southeastern Montana. This is coal country, part of the Powder River Basin, the most productive coalfields in the US. The Northern Cheyenne Reservation is surrounded by large coal strip mines on three sides and is 20 miles from the Colstrip Generating Station, once one of the largest coal-fired power stations in the US. In this remote region, coal extraction represents a reliable source of income for tribal members. However, coal’s future is uncertain, and the Colstrip Generating Station has closed half of its units that produce electricity. Against this backdrop, the Tribe is exploring options for developing its own tribally-owned utility based on renewable energy production, which has the potential to reduce the Tribe’s dependence on external electricity providers (e.g. costs for heating in winter are extremely high) and could employ tribal members.
My research is grounded in qualitative methods involving interviews with tribal government officials, economic development experts, coal miners and plant operators, and renewable energy developers, among others. These interviews are supplemented by participant observation at regional energy events and conferences focused on the energy transition. My preliminary findings suggest that the energy transition seems likely to reinforce existing inequalities. The same power companies that own coal infrastructure are developing renewables that will compete with the Tribe’s own ambitions. Furthermore, existing paternalistic bureaucracy that structures the relationship tribal nations have with the federal government presents roadblocks that make it very difficult to pursue economic development in general. For example, the Northern Cheyenne must negotiate with the Bureau of Indian Affairs, a federal agency, in addition to any energy developers before constructing solar on tribal trust lands, while private energy developers operating off-reservation face no comparable obstacles.
My research at Arizona builds off the research and experiences I had as an undergraduate in the Department of Geography at CU-Boulder. Under the guidance of Dr. Joe Bryan, I completed my honors thesis on the role of US public lands and historical mapping in the dispossession of Indigenous peoples, which together have gone on to shape the terrain upon which present-day Indigenous campaigns to protect southeast Utah’s Bears Ears region must struggle. This area was made famous in part by the Trump administration’s rollback of federal protections, centering on its status as a National Monument. Bears Ears, like all public lands, was mapped and managed to facilitate extraction and settlement at the direct expense of Indigenous people and the land itself, putting Indigenous claims of authority over the landscape at a significant disadvantage to the those made by white settlers and miners.
Moving forward, I hope to continue to pursue engaged research that examines the tangled legacies of colonialism and resource extraction on Native Nations in the US. I owe much of where I am to the faculty and peers I had at CU-Boulder.

Personal tools
Skip to content. | Skip to navigation

- Legal Developments
The Civil Rights Project / Proyecto Derechos Civiles 8370 Math Sciences, Box 951521 Los Angeles, CA 90095-1521 [email protected]
- Copyright Policy
- Accessibility
Copyright © 2010 UC Regents

IMAGES
VIDEO
COMMENTS
This study explores how principles of Indigenous research methodologies informed research relationships with Indigenous communities, particularly through the dis-semination phase of research. We conducted an Indigenous qualitative content anal-ysis of 79 peer-reviewed articles published from January 1996 to June 2018,
Researchers must ensure that research involving Indigenous peoples is premised on respecting the self-determination of communities and is carried out with collaboration and engagement between researchers and participants. While respecting self-determination, ethical research with Indigenous communities endeavors to integrate community cultural ...
Furthermore, in their qualitative study of Indigenous Peoples' perspectives on and recommendations for conducting public health research in their communities, a group of Ontario researchers reveal potential points of discomfort and friction, including the perception of a project as "overwhelming and disjointed," general research fatigue ...
Using simple binary quantitative tools and qualitative approach to research and application of Indigenous research methods and critical pedagogy as analytical lens, the study found that the implementation of Philippine policies on the rights to Education, specifically the IPRA of 1997, is more of a tokenism rather than a complete transformation ...
Among a sample of 472 Indigenous high school students, juxtaposed with 15,884 non-Indigenous students from the same 54 schools, we investigated variation in motivation and engagement from school ...
This review will consider studies that involve Indigenous peoples' positive experiences with culturally safe health care from any study setting. Studies that present relevant qualitative findings including descriptions, examples, or stories about how a health care provider enacted cultural safety from Indigenous perspectives will be considered.
Increasingly research involving Indigenous people is being undertaken by Indigenous researchers, ... Two qualitative Indigenous research methods, sharing circles and Anishnaabe symbol-based reflection, will be discussed. ... It is important that the research studies that advance these efforts be disseminated widely, from Web-based community ...
Identification of the existing literature. We used an 'integrative review' methodology, a well-established method to systematically review and produce qualitative syntheses from the existing literature. 13 We summarised principles, existing recommendations and strategies for community engagement with Indigenous peoples in Canada, the USA, Australia and New Zealand, in order to generate a ...
Qualitative research was also only utilised in two identified studies. Qualitative research is important for understanding the views and perceptions of Indigenous people (Auger, 2016). It allows insight into the factors that contribute to the co-occurrence of MH conditions and substance use and can better inform future research, policy, and ...
International Review of Qualitative Research 6(4):559-577 ... Indigenous peoples are engaging in research. ... and collaborative analysis of data with Indigenous researchers, this study ...
This paper is designed to provide Indigenous and nonindigenous people working in research with some practical advice on how to improve the research experience for Indigenous people and how to develop culturally appropriate research methodologies. The paper proposes that qualitative research methods are practical, useful, beneficial and ...
Indigenous academics have advocated for the use and validity of Indigenous methodologies and methods to centre Indigenous ways of knowing, being and doing in research. Yarning is the most reported Indigenous method used in Aboriginal and Torres Strait Islander qualitative health research. Despite this, there has been no critical analysis of how Yarning methods are applied to research conduct ...
This paper presents an examination of research on Indigenous people and information and communications technology by surveying the landscape of existing studies. A literature review of the relevant 166 publications worldwide from 1995 to 2013 inclusive was performed, and bibliometrics were applied to identify the trends of research in terms of ...
Introduction. Indigenous peoples bear a disproportionate burden of disease and have poorer health outcomes as compared to non-Indigenous populations within Canada [Citation 1].Indigenous peoples face challenges during medical visits that include bias, microaggressions, provider turnover, and a lack of understanding of Indigenous health beliefs [Citation 2-4].
A scoping study was conducted of all relevant peer-reviewed literature and public-facing Indigenous research ethical guidelines from First Nations, Metis, and Inuit communities and organizations in Canada. A total of 20 different Indigenous research ethics boards, frameworks, and protocols were identified.
A Community-Based Participatory Research (CBPR) framework was used to develop a qualitative study around young Indigenous people's sexual health. Our participatory approach… involved a range of strategies to ensure the project was a genuine collaboration between university researchers and Indigenous community members, and in particular that ...
The paper proposes that qualitative research methods are practical, useful, beneficial and culturally appropriate for research on and with Indigenous people. The paper also provides practical advice on how to ensure that Indigenous people are represented in research to ensure that their voices are clearly heard.
Beginning with the American Indian Civil Rights ("Red Power") Movement of the 1970s, Indigenous people in the United States pursued social justice and self-determination with explicit interest in reclaiming or revitalizing traditional—usually framed as prereservation or even precontact—culture and spirituality (Nagel, 1996).With the increasing presence of Indigenous faculty and ...
During the first half of the 20th century the research was about indigenous communities, and by the end of the 20th century research began to document research produced by and with indigenous peoples. Thus, the qualitative research agenda put forward at the end of the 20th century by native researchers was one in which indigenous communities ...
Background Indigenous patients often present with complex health needs in clinical settings due to factors rooted in a legacy of colonization. Healthcare systems and providers are not equipped to identify the underlying causes nor enact solutions for this complexity. This study aimed to develop an Indigenous-centered patient complexity assessment framework for urban Indigenous patients in ...
More recently, however, indigenous researchers have been active in seeking ways to disrupt the "history of exploitation, suspicion, misunderstanding, and prejudice" of indigenous peoples in order to develop methodologies and approaches to research that privilege indigenous knowledges, voices, experiences, reflections, and analyses of their ...
Historically, health research involving Indigenous peoples has been fraught with problems, including researchers not addressing Indigenous research priorities and then subsequently often failing to utilize culturally appropriate methods. Given this historical precedence, some Indigenous populations may be reluctant to participate in research projects. In response to these concerns, the ...
These are the focal considerations of Margaret Kovach's study, which offers guidance to those conducting research in the academy using Indigenous methodologies. Kovach includes topics such as Indigenous epistemologies, decolonizing theory, story as method, situating self and culture, Indigenous methods, protocol, meaning-making, and ethics.
Study design. A qualitative descriptive study design was used to investigate participants' perceptions about the value of NBIs. Qualitative research is appropriate when the focus is describing and understanding people's "insider" perspective of a phenomenon in a real-life context [Citation 18].
The research was undertaken in Aotearoa New Zealand (NZ), a country known for its diverse and multicultural population of approximately 5 million people. Māori are the indigenous people of Aotearoa NZ, accounting for 16.5% of the population, with European (70.2%), Asian (15.1%), and people with Pacific Island backgrounds (8.1%) constituting ...
My research draws from political ecology and Indigenous geographies to study environmental politics in the US West and examines how the energy transition is shaping the political and economic futures of Native Nations. ... My research is grounded in qualitative methods involving interviews with tribal government officials, economic development ...
I pinpoint three elements to consider when research-ing Indigenous peoples and being non-Indigenous: reflection, reciprocity, and heterogene-ity. The first two are common characteristics of qualitative research. Heterogeneity refers to how Indigenous peoples (and others) form subgroups and are unique individuals and that speaking of Sámi as ...
Two new studies of California teachers show we are far from reaching our goals of racial equality in the state. The first study uses a mix of qualitative and quantitative data collected over the course of one year from system leaders in teacher preparation, pre-service teachers, in-service teachers, and former teachers to better understand current policies and practices that may be ...
DOI: 10.1111/1756-185X.15186 Corpus ID: 269634316; The impact of gout flare triggers: A qualitative interview study of people with gout. @article{Rennie2024TheIO, title={The impact of gout flare triggers: A qualitative interview study of people with gout.}, author={Julia Rennie and Mike Frecklington and Belinda Ihaka and Nicola Dalbeth and Sarah Stewart}, journal={International journal of ...
Interviewing people with life-limiting illness for the purposes of research is always challenging. There has been much consideration of whether, in the advanced stages of illness, it is appropriate to take up people's limited time with research (Barnett, 2001; Gysels et al., 2008).Discussing experiences of palliative and end of life care and decision-making can be difficult for participants ...