- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- Trends in incidence of...
Trends in incidence of total or type 2 diabetes: systematic review
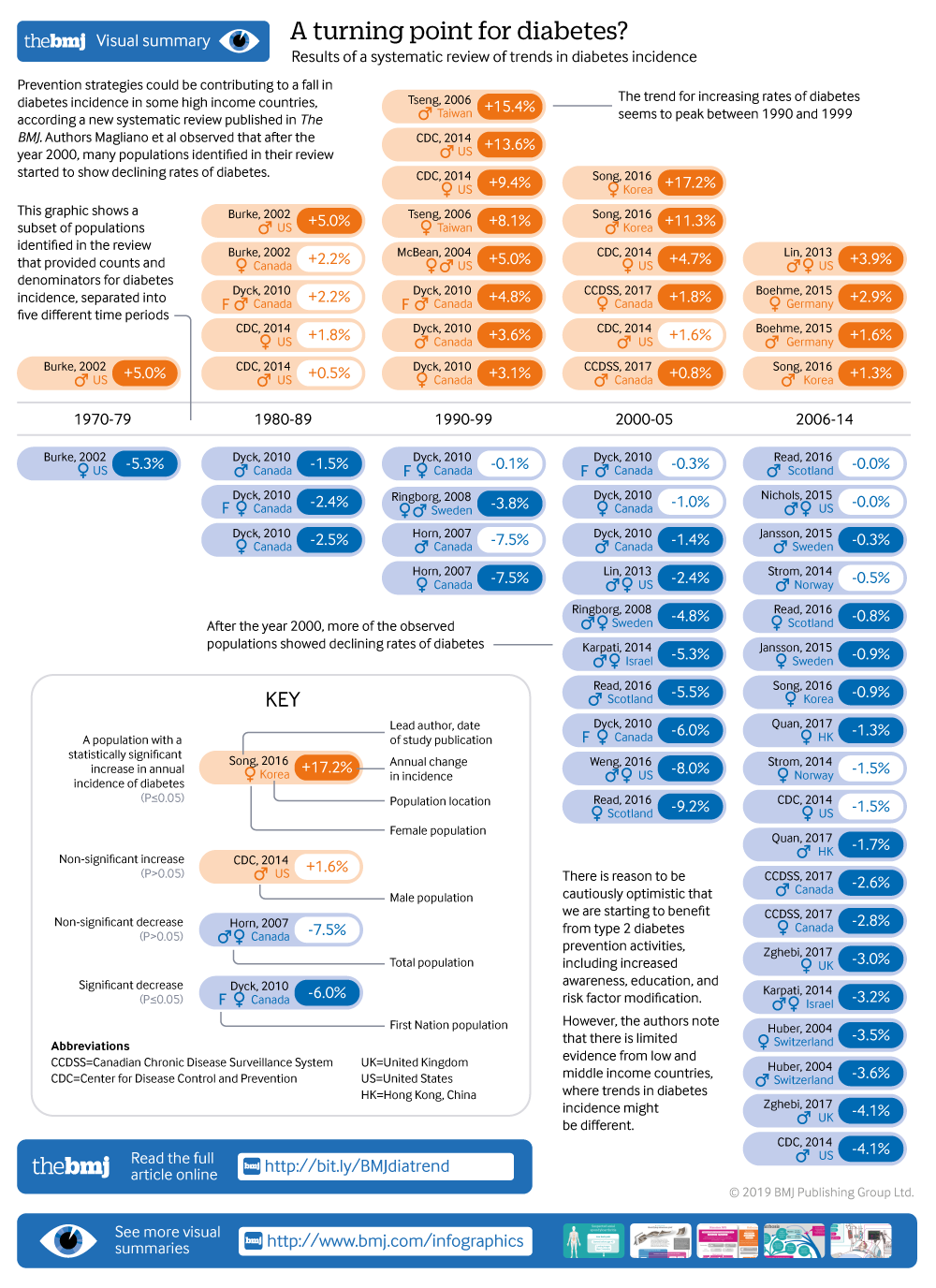
Visual summary available
Showing the turning point in diabetes incidence in 61 populations
Linked editorial
Trends in type 2 diabetes
- Related content
- Peer review
- Rakibul M Islam , postdoctoral research fellow 1 2 ,
- Elizabeth L M Barr , postdoctoral research fellow 1 ,
- Edward W Gregg , chair in diabetes and cardiovascular disease epidemiology 3 4 ,
- Meda E Pavkov , physician scientist 3 ,
- Jessica L Harding , research fellow 3 ,
- Maryam Tabesh , research study coordinator 1 2 ,
- Digsu N Koye , postdoctoral research fellow 1 2 ,
- Jonathan E Shaw , deputy director of Baker Heart and Diabetes Institute 1 2
- 1 Baker Heart and Diabetes Institute, Melbourne, VIC 3004, Australia
- 2 School of Public Health and Preventive Medicine, Monash University, Melbourne, VIC 3004, Australia
- 3 Centres for Diseases Control and Prevention, Division of Diabetes Translation, Atlanta, GA, USA
- 4 School of Public Health, Epidemiology and Biostatistics, Imperial College London, London, UK
- Correspondence to: D J Magliano dianna.magliano{at}baker.edu.au
- Accepted 16 July 2019
Objective To assess what proportions of studies reported increasing, stable, or declining trends in the incidence of diagnosed diabetes.
Design Systematic review of studies reporting trends of diabetes incidence in adults from 1980 to 2017 according to PRISMA guidelines.
Data sources Medline, Embase, CINAHL, and reference lists of relevant publications.
Eligibility criteria Studies of open population based cohorts, diabetes registries, and administrative and health insurance databases on secular trends in the incidence of total diabetes or type 2 diabetes in adults were included. Poisson regression was used to model data by age group and year.
Results Among the 22 833 screened abstracts, 47 studies were included, providing data on 121 separate sex specific or ethnicity specific populations; 42 (89%) of the included studies reported on diagnosed diabetes. In 1960-89, 36% (8/22) of the populations studied had increasing trends in incidence of diabetes, 55% (12/22) had stable trends, and 9% (2/22) had decreasing trends. In 1990-2005, diabetes incidence increased in 66% (33/50) of populations, was stable in 32% (16/50), and decreased in 2% (1/50). In 2006-14, increasing trends were reported in only 33% (11/33) of populations, whereas 30% (10/33) and 36% (12/33) had stable or declining incidence, respectively.
Conclusions The incidence of clinically diagnosed diabetes has continued to rise in only a minority of populations studied since 2006, with over a third of populations having a fall in incidence in this time period. Preventive strategies could have contributed to the fall in diabetes incidence in recent years. Data are limited in low and middle income countries, where trends in diabetes incidence could be different.
Systematic review registration Prospero CRD42018092287.
Introduction
Over the past few decades, the prevalence of diabetes in developed and developing countries has risen substantially, making diabetes a key health priority globally. 1 Examination of trends in total burden of diabetes is an essential part of the monitoring of this health priority area, but, to date, it has consisted primarily of studies looking at diabetes prevalence. 1 2 3 4 5 Prevalence estimates suggest that the diabetes burden is still rising in most countries, and this is often interpreted as evidence of increasing risk in the population. However, selective incidence studies 6 7 and some accompanying risk factor data 8 suggest otherwise. Prevalence can be a crude and misleading metric of the trajectory of an epidemic, because increasing prevalence of a disease might be due to either increasing incidence or to improved survival. Furthermore, prevalence cannot be reliably used to study the effects of changes in population risk factors, because their effects are detected earlier with incidence trends than with prevalence trends, and incidence is not affected by changes in survival.
Incidence measures the proportion of people who develop diabetes over a period of time among the population at risk. It is the appropriate measure of population risk, and a valuable way of assessing whether public health campaigns for diabetes prevention are succeeding. While prevalence can rise simply because mortality falls, incidence of diagnosed diabetes is affected only by the risk of the population and the amount of screening undertaken. Changes in prevalence might be an inadequate guide to the effects of prevention activities, and could lead to the inappropriate rejection of effective interventions. It is only by measuring both incidence and prevalence that a better understanding of the extent of diabetes can be achieved.
Among existing diabetes incidence data, a few studies suggest that diabetes incidence could be falling despite rising or stable prevalence, 6 7 9 but not all data are consistently showing the same trends. For example, studies from England and Wales (1994-98), 10 Portugal (1992-2015), 11 and Canada (1995-2007) 12 are reporting increases in diabetes incidence. To understand what is happening at a global level over time, a systematic approach to review all incidence trend data should be undertaken to study patterns and distributions of incidence trends by time, age, and sex. So far, no systematic reviews have reported on trends in the incidence of diabetes. Therefore, we conducted a systematic review of the literature reporting diabetes incidence trends.
Data sources and searches
We conducted a systematic review in accordance with PRISMA guidelines. 13 We searched Medline, Embase, and CINAHL from January 1980 to December 2017 without language restrictions. The full search strategy is available in supplementary table 1.
Study selection
Inclusion and exclusion criteria.
Eligible studies needed to report diabetes incidence in two or more time periods. Study populations derived from open, population based cohort studies (that is, with ongoing recruitment over time), diabetes registries, or administrative or health insurance databases based mainly or wholly in primary care (electronic medical records, health insurance databases, or health maintenance organisations). We also included serial, cross sectional, population based studies where incidence was defined as a person reporting the development of diabetes in the 12 months before the survey. Studies were required to report on the incidence of either total diabetes or type 2 diabetes. We excluded studies reporting incidence restricted to select groups (eg, people with heart failure) and studies reporting only on children or youth.
Each title and abstract was screened by at least two authors (DJM, JES, DNK, JLH, and MT) and discrepancies were resolved by discussion. We aimed to avoid overlap of populations between studies. Therefore, if national data and regional data were available from the same country over the same time period, we only included the national data. If multiple publications used the same data source, over the same time period, we chose the publication that covered the longest time period.
Outcome measure
Our outcome was diabetes incidence using various methods of diabetes ascertainment including: blood glucose, glycated haemoglobin (HbA1c), linkage to drug treatment or reimbursement registries, clinical diagnosis by physicians, administrative data (ICD codes (international classification of diseases)), or self report. Several studies developed algorithms based on several of these elements to define diabetes. We categorised the definition of diabetes into one of five groups: clinical diagnosis, diabetes treatment, algorithm derived, glycaemia defined (blood glucose or HbA1c, with or without treatment), and self report.
Data extraction and quality of studies
We extracted crude and standardised incidence by year (including counts and denominators) and the reported pattern of the trends (increasing, decreasing, or stable, (that is, no statistically significant change)) in each time period as well as study and population characteristics. Age specific data were also extracted if available. Data reported only in graphs were extracted by DigitizeIt software (European Organisation for Nuclear Research, Germany). We assessed study quality using a modified Newcastle-Ottawa scale for assessing the risk of bias of cohort studies 14 (supplementary material).
Statistical methods
Data were reported as incidence density (per person year) or yearly rates (percentage per year). From every study, we extracted data from every subpopulation reported, such that a study reporting incidence in men and women separately contributed two populations to this analysis. If studies reported two different trends over different time periods, we considered these as two populations. Further, if the study was over 10 years in duration, we treated these as two separate time periods. To avoid double counting, when the data were reported in the total population as well as by sex and ethnic groups, we only included data once and prioritised ethnicity specific data over sex specific data.
We extracted the age specific incidence data reported for every individual calendar year. These data were then categorised into four age bands (<40, 40-54, 55-69, and ≥70), and were plotted against calendar year. In studies where counts and denominators were reported by smaller age groups than we used, we recalculated incidence across our specified larger age groups. If we found multiple age groups within any of our broader age groups, but with insufficient information to combine the data into a new category, only data from one age group were used. To limit overcrowding on plots, if data were available for men, women, and the total population, only total population data were plotted. Data from populations with high diabetes incidence such as Mauritians 15 and First Nation populations from Canada 16 were plotted separately to allow the examination of most of the data more easily on a common scale (supplementary material). Furthermore, studies reporting data before 1991 or populations with fewer than three data points were not plotted. We also categorised studies into European and non-European populations on the basis of the predominant ethnicity of the population in which they were conducted. Studies conducted in Israel, Canada, and the United States were assigned to the European category.
We took two approaches to analyse trends of diabetes incidence over time. Firstly, we allocated the reported trend (increasing, decreasing, or stable (that is, no statistically significant change)) of each population to the mid-point of each study’s observational period, and then assigned this trend into one of five time periods (1960-79, 1980-89, 1990-99, 2000-05, and 2006-14). Where a test of significance of trends was not reported or when a time period was longer than 10 years, we performed Joinpoint trend analyses 17 18 to observe any significant trends in the data (assuming a constant standard deviation). Joinpoint Trend Analysis Software (version 4.5.0.1) uses permutation tests to identify points where linear trends change significantly in direction or in magnitude, and calculates an annual percentage change for each time period identified. In sensitivity analyses we also tested different cut points in the last two time periods.
The second approach was used to more accurately allocate trends to the prespecified time periods. Among the studies that reported raw counts of diabetes cases and denominators, we examined the association between calendar year and incidence, using Poisson models with the log person years as offset. The midpoints of age and calendar period were used as continuous covariates, and the effects of these were taken as linear functions. We analysed each study separately by prespecified time periods, and reported annual percentage change when the number of data points in the time period was at least four. For studies that did not provide raw data but did report a sufficient number of points, we analysed the relation between year and incidence using Joinpoint regression across the time periods specified above and reported annual percentage change. Analyses were conducted with Stata software version 14.0 (Stata Corporation, College Station, TX, USA), and Joinpoint (Joinpoint Desktop Software Version 4.5.0.1). 17 18
Patient and public involvement
No patients or members of the public were involved in setting the research question or the outcome measures for this study. No patients were asked to advise on interpretation or writing up of results. We intend to disseminate this research through press releases and at research meetings.
We found 22 833 unique abstracts from 1 January 1980 to the end of 2017. Among these, 80 described trends of diabetes incidence, of which 47 met all inclusion criteria. Articles describing trends were excluded for the following reasons: duplicated data (n=21), closed cohorts (n=5), populations included youth only (n=1), occupational cohorts (n=2), or no usable data presented (n=4; fig 1 ).

Flowchart of study selection
- Download figure
- Open in new tab
- Download powerpoint
Table 1 and supplementary material table 2 describe the characteristics of the included studies. Only 19% (9/47) of studies were from predominantly non-Europid populations and 4% (2/47) of studies were from low or middle income countries (China 25 and Mauritius 15 ). Administrative datasets, health insurance data, registry data, survey data, and cohort studies accounted for 38% (n=18), 21% (n=10), 19% (n=9), 11% (n=5), and 11% (n=5) of the 47 data sources, respectively. Among the 47 studies, diabetes was defined by a clinical diagnosis, diabetes treatment (via linkage to drug treatment registers), an algorithm, blood glucose, and self report in 28% (n=13), 9% (n=4), 47% (n=22), 11% (n=5), and 6% (n=3) of studies, respectively. Sample sizes of the populations were greater than 10 000 in every year in 85% (n=40) of the studies, and greater than 130 000 per year in 70% (n=33) of the studies. A total of 62% (n=29) of the 47 included studies exclusively reported on type 2 diabetes, and 38% (n=18) reported on total diabetes.
Characteristics of 47 included studies reporting on diabetes incidence trends, by country
- View inline
Summary of patterns of diabetes incidence trends based on analyses reported in publications in 1960-99
Trends of diabetes incidence
Among the 47 studies, 16 provided information on incidence by age group. Of these 16 studies, 14 were plotted in figure 2 , with those from high incidence countries plotted in supplementary figure 1. In these figures, incidence in most studies increased progressively until the mid-2000s in all age groups. Thereafter, most studies showed a stable or decreasing trend, apart from studies in Denmark 26 27 and Germany 31 and in a US health insurance population 9 where the incidence inflected upwards in the later years for some age groups.

Incidence of diabetes over time for populations aged under 40, 40-54, 55-69, and 70 or more, among studies reporting age specific data. Only populations with at least three points were plotted. NHIS=National Health Interview Survey
Using the first approach to analyse trends of diabetes incidence over time, we separated the data into populations based on sex and ethnicity, and allocated a time period to each population, generating 105 populations for analysis. Seventy four and 31 populations were predominantly Europid and non-Europid, respectively. Table 2 and table 3 show the reported trend for each population. Table 4 summarises the findings in table 2 and table 3 , and shows that the proportion of populations reporting increasing trends peaked in 1990-99 and fell progressively in the two later time periods. Between 1960 and 1989, 36% (8/22) of the populations studied had increasing trends in incidence of diabetes, 55% (12/22) had stable trends, and 9% (2/22) had decreasing trends. In 1990-2005, diabetes incidence increased in 66% (33/50) of populations, was stable in 32% (16/50), and decreased in 2% (1/50). In 2006-14, increasing trends were reported in 33% (11/33) of populations, whereas 30% (10/33) and 36% (12/33) had stable or declining incidence, respectively.
Summary of patterns of diabetes incidence trends based on analyses reported in publications in 2000-14
Summary of incidence trends over time of total or type 2 diabetes
Populations that reported a decrease in incidence after 2005 came from the US, 6 9 Israel, 34 Switzerland, 46 Hong Kong, 32 Sweden, 43 and Korea. 36 Populations reporting increasing incidence after 2005 included Portugal, 11 Denmark, 26 27 and Germany, 31 while populations from Canada, 19 Italy, 35 Scotland, 40 Norway, 39 US (non-Hispanic white), 56 and the United Kingdom 50 showed stable incidence. For two studies (16 populations), 16 29 we could not determine a direction of a trend (increasing, decreasing, or stable), because they showed three phases of change with the trend of the middle phase differing from the trend of the first and last phase. Across the total time period, we observed a higher proportion of populations reporting stable or decreasing trends in predominantly Europid than in non-Europid populations (52% v 41%).
Using the second approach to analyse trends of diabetes incidence over time, we modelled 21 studies (62 populations) that reported diabetes counts and denominators specifically within each time period ( table 5 ). The percentage of populations with a decreased or stable incidence was highest in 1980-89 (88%; 7/8), but this proportion was based on only eight populations in three studies. From 1990 onwards, the percentage with decreasing or stable incidence increased progressively, reaching 83% (19/23) of populations in 2006-14. Eight studies (21 populations) that were analysed by Joinpoint had no data on counts or denominators (supplementary table 3). When these data were considered with the data in table 5 , the percentage of populations in 2006-14 with decreasing or stable incidence fell to 70% (19/27), but this proportion was still the highest of all the time periods, whereas the percentage for 1990-99 remained the lowest at 31% (5/16).
Annual percentage change in diabetes incidence in men (M), women (W), or total population (T) among studies that provided counts and denominators, by time period
In a sensitivity analysis, we tested whether our selection of time periods was driving our results. When we defined the final time periods to be 2000-07 and 2008-14, our results were not altered, with 66% (21/32) of the populations in the last time period showing decreasing or stable trends. We also repeated the analysis in table 4 and excluded cohort studies and surveys, and found that the results were not materially altered, with 65% (20/31) of populations in the last time period (from 2006 onwards) showing decreasing or stable incidence of diabetes.
Quality of studies
The median score for study quality was 10 (interquartile range 8-11; supplementary table 4). We repeated the analyses reported in table 4 after excluding studies that had quality scores in the lowest quarter, and observed similar results to the main findings. For example, in 1960-89, 67% (10/15) of populations reported stable or decreasing incidence, while in the final time period, 67% (18/27) of populations reported stable or decreasing incidence of diagnosed diabetes.
Principal findings
In this systematic review of population based studies on diabetes incidence, we show evidence that the incidence of diagnosed diabetes increased in most populations from the 1960s to the early 2000s, after which a pattern emerged of levelling trends in 30% and declining trends in 36% of the reported populations. Although the lack of data for non-Europid populations leaves global trends in incidence unclear, these findings suggest that trends in the diabetes epidemic in some high income countries have turned in a more encouraging direction compared with previous decades. It is important to note that these results apply predominantly to type 2 diabetes, as even though many studies did not accurately define diabetes type, the incidence of type 2 diabetes in adults is an order of magnitude greater than that of type 1 diabetes.
The countries that showed stable or decreasing trends in the last time period were from Europe and east Asia, with no obvious clustering or commonalities. For the countries showing decreasing or stable diabetes trends, if the prevalence data were used to understand the diabetes epidemic in that country, a different message would be obtained. For example, national data from Korea showed that the prevalence of diabetes increased from 2000 to 2010. 59 Similarly in Sweden, the prevalence of pharmacologically treated diabetes increased moderately from 2006 to 2014. 43 In the US, the prevalence of diabetes reached a plateau when incidence began to decrease. However, we lacked incidence data from many areas of the world where the most steady and substantial increases in prevalence have been reported, including the Pacific Islands, Middle East, and south Asia. Large increases in incidence could still be occurring in these areas. The lack of incidence data for much of the world, combined with the common observation of discordance between incidence and prevalence rates where such data exist, both underscore the importance of using incidence data to understand the direction of the diabetes epidemic.
Incidence could be starting to fall for several reasons. Firstly, we might be starting to benefit from prevention activities of type 2 diabetes, including increased awareness, education, and risk factor modification. These activities have involved both targeted prevention among high risk individuals, similar to that conducted in the Diabetes Prevention study 60 and Diabetes Prevention Programme 61 62 in many countries, 63 and less intensive interventions with broader reach such as telephone counselling in the general community. 64 65 67 Secondly, health awareness and education programmes have also been implemented in schools and work places, and many changes to the physical environment, such as the introduction of bike tracks and exercise parks, have occurred. 68 Thirdly, favourable trends in selected risk factors of type 2 diabetes in some countries provide indirect evidence of positive changes to reduce diabetes incidence. Finally, in the US, there is some evidence in recent years of improved diets and related behaviours, which include reductions in intake of sugar sweetened beverages 69 and fat, 70 small declines in overall energy intake, and declines in some food purchases. 8 71
Similar reduction in consumptions of sugar sweetened beverages have occurred in Norway 72 and Australia 73 and fast food intake has decreased in Korea. 74 Some of these changes could be linked to a fall in diabetes incidence. Some places such as Scotland 75 have also had a plateauing of obesity prevalence, but this is not universal. In the US, despite earlier studies suggesting that the rate of increase in obesity might be slowing down, 76 77 more recent data show a small increase. 78 79 While some evidence supports the hypothesis that these prevention activities for type 2 diabetes and an improved environment could trigger sufficient behaviour change to have an effect on diabetes incidence, other data, such as the continuing rising obesity prevalence in the US, 79 casts some doubt over the explanations underpinning our findings on diabetes incidence trends.
Other factors might have also influenced reported diabetes incidence. Only 11% (n=5) of the studies reported here screened for undiagnosed diabetes, and therefore trends could have been influenced by secular changes in diagnostic behaviour. In 1997, the threshold for fasting plasma glucose for diagnosis of diabetes was reduced from 7.8 to 7.0 mmol/L, which could increase diagnosis of new cases of type 2 diabetes. In 2009-10, HbA1c was then introduced as an alternative way to diagnose diabetes. 80 Evidence from some studies suggests that the HbA1c diagnostic threshold detects fewer people with diabetes than do the thresholds for fasting plasma blood glucose, 80 81 potentially leading to a lowering of incidence estimates. However, across multiple studies, prevalence estimates based on fasting plasma glucose only versus HbA1c definitions are similar. 82 Furthermore, because HbA1c can be measured in the non-fasting state (unlike the fasting blood glucose or oral glucose tolerance test), the number of people who actually undergo diagnostic testing could be higher with HbA1c. Nichols and colleagues 56 reported that among seven million insured US adults, despite a shift towards HbA1c as the diagnostic test in 2010, the incidence of diabetes did not change from 2010 to 2011.
Another potential explanation for declining or stable diabetes incidence after the mid-2000s is a reduction in the pool of undiagnosed diabetes 83 through the intensification of diagnostic and screening activities 83 84 and changing diagnostic criteria during the previous decade. 80 Data from Read and colleagues provide some evidence to support this notion. 41
Among the included studies, two studies specifically examined clinical screening patterns in parallel with incidence trends. These studies reported that the proportion of the population screened for diabetes increased over time, and the incidence of diabetes remained stable 56 or fell. 34 While the Karpati study 34 combined data for glucose testing with HbA1c testing, the study by Nichols and colleagues 56 separated the two, and showed that both glucose testing and HbA1c testing increased over time. A third study, in Korea, 36 also noted that the incidence of diabetes decreased in the setting of an increase in the uptake of the national health screening programme. Despite the introduction of HbA1c for diagnosis of diabetes by the World Health Organization, this practice has not been adopted everywhere. For example, neither Scotland nor Hong Kong have introduced the use of HbA1c for screening or diagnosis of diabetes, and studies in these areas showed a levelling of diabetes incidence trends and decreasing trends, respectively.
Our findings appear to contrast with data showing increasing global prevalence of diabetes. 1 3 However, increasing prevalence could be influenced by improved survival of people with diabetes, because this increases the length of time that each individual remains within the diabetes population. As is shown in several studies in this review, 23 41 mortality from diabetes and incidence of diabetes might both be falling but as long as mortality is lower than incidence, prevalence will rise. Therefore, we argue that prevalence alone is an insufficient measure to track the epidemic of diabetes and other non-communicable diseases.
Strengths and weaknesses of this study
A key strength of this work was the systematic approach and robust methodology to describe trends in diagnosed diabetes incidence. We also presented the reported trends allocated to approximate time periods, as well as conducting our own regression within exact time periods. The following limitations should also be considered. Firstly, we did not formally search the grey literature, because a preliminary grey literature search revealed only low quality studies, with inadequate methodological detail to provide confidence in any observed incidence trends, and thus review could be subject to publication bias. Secondly, we were not able to source age or sex specific data on all populations. Thirdly, it was not possible to adjust for different methods of diabetes diagnosis or ascertain trends by different definitions of diabetes. Fourthly, most data sources reported only on clinically diagnosed diabetes and so were subject to influence from diagnostic behaviour and coding practices. Fifthly, study type changed over time, with large administrative datasets becoming more common and cohort studies becoming less common over time. Nevertheless, the size and absence of volunteer bias in administrative datasets likely make them less biased. Finally, data were limited in low and middle income countries.
Conclusions and unanswered questions
This systematic review shows that in most countries for which data are available, the incidence of diagnosed diabetes was rising from the 1990s to the mid-2000s, but has been stable or falling since. Preventive strategies and public health education and awareness campaigns could have contributed to this recent trend. Data are limited in low and middle income countries where trends in diabetes incidence might be different. Improvement of the collection, availability, and analysis of incidence data will be important to effectively monitor the epidemic and guide prevention efforts into the future.
What is already known on this topic
Monitoring of the diabetes epidemic has mainly focused on reporting diabetes prevalence, which continues to rise; however, increasing prevalence is partly driven by improved medical treatment and declining mortality
Studies on diabetes incidence are scarce, but among those that exist, some report a fall or stabilisation of diabetes incidence;
Whether the proportion of studies reporting falling incidence has changed over time is not known
What this study adds
This systematic review of published data reporting diabetes incidence trends over time shows that in most countries with available data, incidence of diabetes (mainly diagnosed diabetes) increased from the 1990s to the mid-2000s, and has been stable or falling since
Preventive strategies and public health education and awareness campaigns could have contributed to this flattening of rates, suggesting that worldwide efforts to curb the diabetes epidemic over the past decade might have been effective
Published data were very limited in low and middle income countries, where trends in diabetes incidence might be different
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention (CDC).
Contributors: MT, DNK, JLH, and RMI are postdoctoral fellows who screened abstracts for selection into the systematic review. JES and DJM also screened abstracts. ELMB applied the quality criteria to the selected articles. RMI extracted data, applied quality criteria to selected articles, and contributed to preparing the manuscript. DJM conceived the project, screened abstracts, extracted the data, analysed the data, and wrote the manuscript. JES, MEP, and EWG conceived the project, edited the manuscript, and provided intellectual input throughout the process. The funder of the study (CDC) was part of the study group and contributed to data collection, data analysis, data interpretation, and writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication. DJM is guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: Funded by the CDC. The researchers were independent from the funders.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: support from the CDC for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Not required because this work was a systematic review.
Data sharing: Data are available from the corresponding author ([email protected]).
The lead author affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Finucane MM ,
- Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose)
- Whiting DR ,
- Guariguata L ,
- International Diabetes Federation
- NCD Risk Factor Collaboration (NCD-RisC)
- Karuranga S ,
- Abraham TM ,
- Pencina KM ,
- Pencina MJ ,
- Slining MM ,
- Kimball ES ,
- Newnham A ,
- de Sousa-Uva M ,
- Antunes L ,
- Johnson JA ,
- Hemmelgarn BR ,
- Liberati A ,
- Tetzlaff J ,
- Altman DG ,
- PRISMA Group
- ↵ Wells G, Shea B, O’connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute, 2014. www.ohri.ca/programs/clinical_epidemiology/oxford.asp Last accessed 14 December 2018.
- Söderberg S ,
- Tuomilehto J ,
- ↵ Joinpoint Regression Program. 4.6.0.0 version. Statistical Methodology and Applications Branch, Surveillance Research Program: National Cancer Institute, 2018. https://surveillance.cancer.gov/joinpoint/ .
- Midthune DN
- ↵ Canadian Chronic Disease Surveillance System. Canadian Chronic Disease Surveillance System 2017. https://www.canada.ca/en/public-health.html
- Blanchard JF ,
- Lipscombe LL ,
- Jacobs-Whyte H ,
- Paradis G ,
- Macaulay AC
- Carstensen B ,
- Kristensen JK ,
- Ottosen P ,
- Borch-Johnsen K ,
- Steering Group of the National Diabetes Register
- Jensen PB ,
- Abouzeid M ,
- Wikström K ,
- Peltonen M ,
- Reunanen A ,
- Klaukka T ,
- Maatela J ,
- Michaelis D ,
- Boehme MW ,
- Buechele G ,
- Frankenhauser-Mannuss J ,
- Vilbergsson S ,
- Sigurdsson G ,
- Sigvaldason H ,
- Hreidarsson AB ,
- Sigfusson N
- Karpati T ,
- Cohen-Stavi CJ ,
- Leibowitz M ,
- Feldman BS ,
- Baviera M ,
- Marzona I ,
- Zimmet PZ ,
- Ruwaard D ,
- Bartelds AI ,
- Hirasing RA ,
- Verkleij H ,
- Birkeland KI ,
- Barnett KN ,
- Ogston SA ,
- Kerssens JJ ,
- McAllister DA ,
- Scottish Diabetes Research Network Epidemiology Group
- Stenström G ,
- Sundkvist G
- Jansson SP ,
- Andersson DK ,
- Svärdsudd K
- Ringborg A ,
- Lindgren P ,
- Martinell M ,
- Stålhammar J
- Schwenkglenks M ,
- Holden SH ,
- Barnett AH ,
- Peters JR ,
- Zghebi SS ,
- Steinke DT ,
- Rutter MK ,
- Emsley RA ,
- Ashcroft DM
- Akushevich I ,
- Kravchenko J ,
- Ukraintseva S ,
- O’Brien P ,
- Centers for Disease Control and Prevention (CDC)
- McBean AM ,
- Gilbertson DT ,
- Narayanan ML ,
- Schraer CD ,
- Bulkow LR ,
- Nichols GA ,
- Schroeder EB ,
- Karter AJ ,
- SUPREME-DM Study Group
- Tabaei BP ,
- Chamany S ,
- Driver CR ,
- Pavkov ME ,
- Hanson RL ,
- Knowler WC ,
- Bennett PH ,
- Krakoff J ,
- Lindström J ,
- Eriksson JG ,
- Finnish Diabetes Prevention Study Group
- Barrett-Connor E ,
- Fowler SE ,
- Diabetes Prevention Program Research Group
- Saaristo T ,
- Moilanen L ,
- Korpi-Hyövälti E ,
- Troughton J ,
- Chatterjee S ,
- Schmittdiel JA ,
- Neugebauer R ,
- Solomon LS ,
- Giles-Corti B ,
- Vernez-Moudon A ,
- Bolt-Evensen K ,
- Brand-Miller JC ,
- ↵ Bromley C, Dowling S, L G. The Scottish Health Survey. Scotland: A National Statistics Publication for Scotland, 2013.
- Carroll MD ,
- Flegal KM ,
- Kruszon-Moran D ,
- Freedman DS ,
- American Diabetes Association
- Lorenzo C ,
- Rasmussen SS ,
- Johansen NB ,
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 23 July 2015
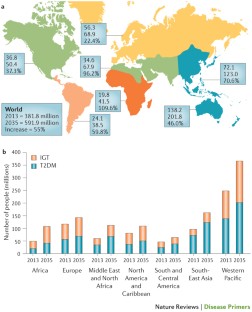
Type 2 diabetes mellitus
- Ralph A. DeFronzo 1 ,
- Ele Ferrannini 2 ,
- Leif Groop 3 ,
- Robert R. Henry 4 ,
- William H. Herman 5 ,
- Jens Juul Holst 6 ,
- Frank B. Hu 7 ,
- C. Ronald Kahn 8 ,
- Itamar Raz 9 ,
- Gerald I. Shulman 10 ,
- Donald C. Simonson 11 ,
- Marcia A. Testa 12 &
- Ram Weiss 13
Nature Reviews Disease Primers volume 1 , Article number: 15019 ( 2015 ) Cite this article
51k Accesses
132 Altmetric
Metrics details
- Diabetes complications
- Type 2 diabetes
Type 2 diabetes mellitus (T2DM) is an expanding global health problem, closely linked to the epidemic of obesity. Individuals with T2DM are at high risk for both microvascular complications (including retinopathy, nephropathy and neuropathy) and macrovascular complications (such as cardiovascular comorbidities), owing to hyperglycaemia and individual components of the insulin resistance (metabolic) syndrome. Environmental factors (for example, obesity, an unhealthy diet and physical inactivity) and genetic factors contribute to the multiple pathophysiological disturbances that are responsible for impaired glucose homeostasis in T2DM. Insulin resistance and impaired insulin secretion remain the core defects in T2DM, but at least six other pathophysiological abnormalities contribute to the dysregulation of glucose metabolism. The multiple pathogenetic disturbances present in T2DM dictate that multiple antidiabetic agents, used in combination, will be required to maintain normoglycaemia. The treatment must not only be effective and safe but also improve the quality of life. Several novel medications are in development, but the greatest need is for agents that enhance insulin sensitivity, halt the progressive pancreatic β-cell failure that is characteristic of T2DM and prevent or reverse the microvascular complications. For an illustrated summary of this Primer, visit: http://go.nature.com/V2eGfN
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 1 digital issues and online access to articles
111,21 € per year
only 111,21 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Double or hybrid diabetes: A systematic review on disease prevalence, characteristics and risk factors

Type 2 diabetes mellitus in adults: pathogenesis, prevention and therapy

Novel therapies with precision mechanisms for type 2 diabetes mellitus
DeFronzo, R. A. Banting lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 58 , 773–795 (2009). A classic review of the aetiology of T2DM, with a therapeutic approach based on its pathophysiology.
Article CAS PubMed PubMed Central Google Scholar
Abdul-Ghani, M. A., Tripathy, D. & DeFronzo, R. A. Contributions of β-cell dysfunction and insulin resistance to the pathogenesis of impaired glucose tolerance and impaired fasting glucose. Diabetes Care 29 , 1130–1139 (2006).
Article CAS PubMed Google Scholar
Gerstein, H. C. et al . Annual incidence and relative risk of diabetes in people with various categories of dysglycemia: a systematic overview and meta-analysis of prospective studies. Diabetes Res. Clin. Pract. 78 , 305–312 (2007).
Article PubMed Google Scholar
Hawa, M. I. et al . Adult-onset autoimmune diabetes in Europe is prevalent with a broad clinical phenotype: action LADA 7. Diabetes Care 36 , 908–913 (2013).
Article PubMed PubMed Central Google Scholar
Gardner, D. S. & Tai, E. S. Clinical features and treatment of maturity onset diabetes of the young (MODY). Diabetes. Metab. Syndr. Obes. 5 , 101–108 (2012).
American Diabetes Association. Standards of medical care in diabetes. Diabetes Care 37 , S14–S80 (2014). A comprehensive overview of the standards of medical care published by the ADA.
Article Google Scholar
DeFronzo, R. A. & Abdul-Ghani, M. A. Preservation of β-cell function: the key to diabetes prevention. J. Clin. Endocrinol. Metab. 96 , 2354–2366 (2011).
Ferrannini, E., Gastaldelli, A. & Iozzo, P. Pathophysiology of prediabetes. Med. Clin. North Am. 95 , 327–339 (2011).
Garvey, W. T. et al . Prevention of type 2 diabetes in subjects with prediabetes and metabolic syndrome treated with phentermine and topiramate extended release. Diabetes Care 37 , 912–921 (2014).
Nathan, D. M. et al . Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care 30 , 753–759 (2007).
DeFronzo, R. A. et al . Pioglitazone for diabetes prevention in impaired glucose tolerance. N. Engl. J. Med. 364 , 1104–1115 (2011). A large prospective study demonstrating the efficacy of thiazolidinediones in preventing the progression of IGT to T2DM.
Zinman, B. et al . Low-dose combination therapy with rosiglitazone and metformin to prevent type 2 diabetes mellitus (CANOE trial): a double-blind randomised controlled study. Lancet 376 , 103–111 (2010).
Dansinger, M. L., Tatsioni, A., Wong, J. B., Chung, M. & Balk, E. M. Meta-analysis: the effect of dietary counseling for weight loss. Ann. Intern. Med. 147 , 41–50 (2007).
Purcell, K. et al . The effect of rate of weight loss on long-term weight management: a randomised controlled trial. Lancet Diabetes Endocrinol. 2 , 954–962 (2014).
Ali, M. K., Echouffo-Tcheugui, J. & Williamson, D. F. How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health Aff. (Millwood) 31 , 67–75 (2012).
Tuomilehto, J. et al . Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N. Engl. J. Med. 344 , 1343–1350 (2001).
Inzucchi, S. E. et al . Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 35 , 1364–1379 (2012). ADA position statement on the treatment of T2DM, advocating a stepped care approach starting with metformin.
American Association of Clinical Endocrinologists. AACE Comprehensive Diabetes Algorithm 2013 Consensus Statement. Endocr. Pract. Suppl. 1 , 1–87 (2015). AACE position statement on the treatment of T2DM, advocating initial monotherapy or combination therapy based upon the starting HbA1c, and recommending various antidiabetic medications as initial therapy.
Google Scholar
Pozzilli, P. et al . The A1C and ABCD of glycaemia management in type 2 diabetes: a physician's personalized approach. Diabetes Metab. Res. Rev. 26 , 239–244 (2010). The first published report by key opinion leaders recommending individualized therapy based on the age and body weight of patients, the presence or absence of complications, and duration and aetiology of disease.
International Diabetes Federation. IDF Diabetes Atlas 6th Edition. IDF [online] , (2013).
Hu, F. B. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care 34 , 1249–1257 (2011). An important study emphasizing the role of diet, physical activity and genes — beyond obesity — in the diabetes epidemic that is engulfing Asian countries as they are exposed to westernization.
Chan, J. C. et al . Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 301 , 2129–2140 (2009).
Ley, S. H., Hamdy, O., Mohan, V. & Hu, F. B. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet 383 , 1999–2007 (2014).
Grøntved, A., Rimm, E. B., Willett, W. C., Andersen, L. B. & Hu, F. B. A prospective study of weight training and risk of type 2 diabetes mellitus in men. Arch. Intern. Med. 172 , 1306–1312 (2012).
Grøntved, A. & Hu, F. B. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA 305 , 2448–2455 (2011).
Cappuccio, F. P., D'Elia, L., Strazzullo, P. & Miller, M. A. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 33 , 414–420 (2009).
Pan, A., Schernhammer, E. S., Sun, Q. & Hu, F. B. Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Med. 8 , e1001141 (2011).
Barnett, A. H., Eff, C., Leslie, R. D. & Pyke, D. A. Diabetes in identical twins. A study of 200 pairs. Diabetologia 20 , 87–93 (1981).
Wang, Y. C., McPherson, K., Marsh, T., Gortmaker, S. L. & Brown, M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 378 , 815–825 (2011).
Wang, X. et al . Inflammatory markers and risk of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 36 , 166–175 (2013).
Li, S., Shin, H. J., Ding, E. L. & van Dam, R. M. Adiponectin levels and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA 302 , 179–188 (2009).
Ding, E. L. et al . Sex hormone-binding globulin and risk of type 2 diabetes in women and men. N. Engl. J. Med. 361 , 1152–1163 (2009).
Wang, T. J. et al . Metabolite profiles and the risk of developing diabetes. Nat. Med. 17 , 448–453 (2011).
Esteve, E., Ricart, W. & Fernández-Real, J.-M. Gut microbiota interactions with obesity, insulin resistance and type 2 diabetes: did gut microbiote co-evolve with insulin resistance? Curr. Opin. Clin. Nutr. Metab. Care 14 , 483–490 (2011).
Hu, F. B. et al . Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N. Engl. J. Med. 345 , 790–797 (2001).
Schellenberg, E. S., Dryden, D. M., Vandermeer, B., Ha, C. & Korownyk, C. Lifestyle interventions for patients with and at risk for type 2 diabetes. Ann. Intern. Med. 159 , 543–551 (2013). A comprehensive review of the effectiveness of lifestyle intervention in the treatment of T2DM, emphasizing that, although initially successful, most subjects with diabetes regain the majority of lost weight over the subsequent 3–5 years.
DeFronzo, R. A. Insulin resistance, lipotoxicity, type 2 diabetes and atherosclerosis: the missing links. The Claude Bernard Lecture 2009. Diabetologia 53 , 1270–1287 (2010). A comprehensive review describing the role of excess tissue lipid deposition in the development of insulin resistance, β-cell failure and atherosclerotic cardiovascular disease: that is, lipotoxicity.
Hemminki, K., Li, X., Sundquist, K. & Sundquist, J. Familial risks for type 2 diabetes in Sweden. Diabetes Care 33 , 293–297 (2010).
Groop, L. et al . Metabolic consequences of a family history of NIDDM (the Botnia study): evidence for sex-specific parental effects. Diabetes 45 , 1585–1593 (1996).
Lyssenko, V. et al . Predictors of and longitudinal changes in insulin sensitivity and secretion preceding onset of type 2 diabetes. Diabetes 54 , 166–174 (2005).
Grant, S. F. et al . Variant of transcription factor 7-like 2 ( TCF7L2 ) gene confers risk of type 2 diabetes. Nat. Genet. 38 , 320–323 (2006).
Lyssenko, V. et al . Mechanisms by which common variants in the TCF7L2 gene increase risk of type 2 diabetes. J. Clin. Invest. 117 , 2155–2163 (2007).
Sladek, R. et al . A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature 445 , 881–885 (2007).
Saxena, R. et al . Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science 316 , 1331–1336 (2007).
Morris, A. P. et al . Large-scale association analysis provides insights into the genetic architecture and pathophysiology of type 2 diabetes. Nat. Genet. 44 , 981–990 (2012).
Flannick, J. et al . Loss-of-function mutations in SLC30A8 protect against type 2 diabetes. Nat. Genet. 46 , 357–363 (2014).
Lyssenko, V. et al . Common variant in MTNR1B associated with increased risk of type 2 diabetes and impaired early insulin secretion. Nat. Genet. 41 , 82–88 (2009).
Rosengren, A. H. et al . Overexpression of alpha2A-adrenergic receptors contributes to type 2 diabetes. Science 327 , 217–220 (2010).
Tang, Y. et al . Genotype-based treatment of type 2 diabetes with an α2A-adrenergic receptor antagonist. Sci. Transl Med. 6 , 257ra139 (2014). These paper provides an example in which a genetic finding in an animal model of diabetes has been translated into a drug target in humans, the ADRA2A gene.
De Jesus, D. F. & Kulkarni, R. N. Epigenetic modifiers of islet function and mass. Trends Endocrinol. Metab. 25 , 628–636 (2014).
Ozcan, S. Minireview: microRNA function in pancreatic β cells. Mol. Endocrinol. 28 , 1922–1933 (2014).
Lyssenko, V. et al . Clinical risk factors, DNA variants, and the development of type 2 diabetes. N. Engl. J. Med. 359 , 2220–2232 (2008). This paper presents a genetic explanation for the development of T2DM.
Travers, M. E. et al . Insights into the molecular mechanism for type 2 diabetes susceptibility at the KCNQ1 locus from temporal changes in imprinting status in human islets. Diabetes 62 , 987–992 (2013).
Gulli, G., Ferrannini, E., Stern, M., Haffner, S. & DeFronzo, R. A. The metabolic profile of NIDDM is fully established in glucose-tolerant offspring of two Mexican-American NIDDM parents. Diabetes 41 , 1575–1586 (1992).
Martin, B. C. et al . Role of glucose and insulin resistance in development of type 2 diabetes mellitus: results of a 25-year follow-up study. Lancet 340 , 925–929 (1992).
Ferrannini, E. & Mari, A. β-cell function in type 2 diabetes. Metabolism 63 , 1217–1227 (2014).
Kahn, S. E., Cooper, M. E. & Del Prato, S. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet 383 , 1068–1083 (2014).
Muller, D. C., Elahi, D., Tobin, J. D. & Andres, R. Insulin response during the oral glucose tolerance test: the role of age, sex, body fat and the pattern of fat distribution. Aging (Milano) 8 , 13–21 (1996).
CAS Google Scholar
Nauck, M. A., Vardarli, I., Deacon, C. F., Holst, J. J. & Meier, J. J. Secretion of glucagon-like peptide-1 (GLP-1) in type 2 diabetes: what is up, what is down? Diabetologia 54 , 10–18 (2011).
Madsbad, S. The role of glucagon-like peptide-1 impairment in obesity and potential therapeutic implications. Diabetes Obes. Metab. 16 , 9–21 (2014).
Bays, H., Mandarino, L. & DeFronzo, R. A. Role of the adipocyte, free fatty acids, and ectopic fat in pathogenesis of type 2 diabetes mellitus: peroxisomal proliferator-activated receptor agonists provide a rational therapeutic approach. J. Clin. Endocrinol. Metab. 89 , 463–478 (2004).
Perry, R. J., Samuel, V. T., Petersen, K. F. & Shulman, G. I. The role of hepatic lipids in hepatic insulin resistance and type 2 diabetes. Nature 510 , 84–91 (2014). An excellent review of the specific lipid varieties and the molecular events through which they cause insulin resistance in the liver.
Bensellam, M., Laybutt, D. R. & Jonas, J.-C. The molecular mechanisms of pancreatic β-cell glucotoxicity: recent findings and future research directions. Mol. Cell. Endocrinol. 364 , 1–27 (2012).
Ritzel, R. A., Meier, J. J., Lin, C.-Y., Veldhuis, J. D. & Butler, P. C. Human islet amyloid polypeptide oligomers disrupt cell coupling, induce apoptosis, and impair insulin secretion in isolated human islets. Diabetes 56 , 65–71 (2007).
Collins, S., Pi, J. & Yehuda-Shnaidman, E. Uncoupling and reactive oxygen species (ROS) — a double-edged sword for β-cell function? “Moderation in all things”. Best Pract. Res. Clin. Endocrinol. Metab. 26 , 753–758 (2012).
Cabrera, O. et al . The unique cytoarchitecture of human pancreatic islets has implications for islet cell function. Proc. Natl Acad. Sci. USA 103 , 2334–2339 (2006).
Hodson, D. J. et al . Lipotoxicity disrupts incretin-regulated human β cell connectivity. J. Clin. Invest. 123 , 4182–4194 (2013).
Brandhorst, H., Brandhorst, D., Brendel, M. D., Hering, B. J. & Bretzel, R. G. Assessment of intracellular insulin content during all steps of human islet isolation procedure. Cell Transplant. 7 , 489–495 (1998).
Rahier, J., Guiot, Y., Goebbels, R. M., Sempoux, C. & Henquin, J. C. Pancreatic β-cell mass in European subjects with type 2 diabetes. Diabetes Obes. Metab. 10 (Suppl. 4), 32–42 (2008). A post-mortem study demonstrating a decline in β-cell mass with preservation of α-cell mass in individuals with T2DM.
Marselli, L. et al . Are we overestimating the loss of beta cells in type 2 diabetes? Diabetologia 57 , 362–365 (2014).
Marchetti, P. et al . The endoplasmic reticulum in pancreatic beta cells of type 2 diabetes patients. Diabetologia 50 , 2486–2494 (2007).
Marchetti, P. & Masini, M. Autophagy and the pancreatic beta-cell in human type 2 diabetes. Autophagy 5 , 1055–1056 (2009).
Gupta, D. & Leahy, J. L. Islet amyloid and type 2 diabetes: overproduction or inadequate clearance and detoxification? J. Clin. Invest. 124 , 3292–3294 (2014).
Mezza, T. et al . Insulin resistance alters islet morphology in nondiabetic humans. Diabetes 63 , 994–1007 (2014). This work in human islets describes the impact of insulin resistance on the relative proportion of α-cells and β-cells, and the functional consequences — in terms of insulin and glucagon secretion — of this chronic adaptation.
Deng, S. et al . Structural and functional abnormalities in the islets isolated from type 2 diabetic subjects. Diabetes 53 , 624–632 (2004).
Igoillo-Esteve, M. et al . Palmitate induces a pro-inflammatory response in human pancreatic islets that mimics CCL2 expression by beta cells in type 2 diabetes. Diabetologia 53 , 1395–1405 (2010).
Giacca, A., Xiao, C., Oprescu, A. I., Carpentier, A. C. & Lewis, G. F. Lipid-induced pancreatic β-cell dysfunction: focus on in vivo studies. Am. J. Physiol. Endocrinol. Metab. 300 , E255–E262 (2010).
Halban, P. A. et al . β-cell failure in type 2 diabetes: postulated mechanisms and prospects for prevention and treatment. J. Clin. Endocrinol. Metab. 99 , 1983–1992 (2014).
Ferrannini, E. et al . Natural history and physiological determinants of changes in glucose tolerance in a non-diabetic population: the RISC Study. Diabetologia 54 , 1507–1516 (2011). This longitudinal study of non-diabetic subjects identifies baseline insulin resistance and β-cell dysfunction as predictors of future dysglycaemia.
Michaliszyn, S. F. et al . β-cell function, incretin effect, and incretin hormones in obese youth along the span of glucose tolerance from normal to prediabetes to type 2 diabetes. Diabetes 63 , 3846–3855 (2014).
Mari, A. et al . Mechanisms of the incretin effect in subjects with normal glucose tolerance and patients with type 2 diabetes. PLoS ONE 8 , e73154 (2013).
Holst, J. J., Knop, F. K., Vilsbøll, T., Krarup, T. & Madsbad, S. Loss of incretin effect is a specific, important, and early characteristic of type 2 diabetes. Diabetes Care 34 , S251–S257 (2011).
Camastra, S. et al . Long-term effects of bariatric surgery on meal disposal and β-cell function in diabetic and nondiabetic patients. Diabetes 62 , 3709–3717 (2013).
Ferrannini, E. The stunned β cell: a brief history. Cell Metab. 11 , 349–352 (2010).
Shulman, G. I. et al . Quantitation of muscle glycogen synthesis in normal subjects and subjects with non-insulin-dependent diabetes by 13C nuclear magnetic resonance spectroscopy. N. Engl. J. Med. 322 , 223–228 (1990). This study demonstrated that defects in insulin-stimulated muscle glycogen synthesis was the major factor responsible for whole-body insulin resistance in patients with T2DM.
Groop, L. C. et al . Glucose and free fatty acid metabolism in non-insulin-dependent diabetes mellitus. Evidence for multiple sites of insulin resistance. J. Clin. Invest. 84 , 205–213 (1989).
Guilherme, A., Virbasius, J. V., Puri, V. & Czech, M. P. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nat. Rev. Mol. Cell Biol. 9 , 367–377 (2008).
Gerich, J. E., Meyer, C., Woerle, H. J. & Stumvoll, M. Renal gluconeogenesis: its importance in human glucose homeostasis. Diabetes Care 24 , 382–391 (2001).
Honka, H. et al . Validation of [ 18 F]fluorodeoxyglucose and positron emission tomography (PET) for the measurement of intestinal metabolism in pigs, and evidence of intestinal insulin resistance in patients with morbid obesity. Diabetologia 56 , 893–900 (2013).
Meijer, R. I. et al . Insulin-induced microvascular recruitment in skin and muscle are related and both are associated with whole-body glucose uptake. Microcirculation 19 , 494–500 (2012).
Blázquez, E., Velázquez, E., Hurtado-Carneiro, V. & Ruiz-Albusac, J. M. Insulin in the brain: its pathophysiological implications for states related with central insulin resistance, type 2 diabetes and Alzheimer's disease. Front. Endocrinol. (Lausanne) 5 , 161 (2014).
Kleinridders, A., Ferris, H. A., Cai, W. & Kahn, C. R. Insulin action in brain regulates systemic metabolism and brain function. Diabetes 63 , 2232–2243 (2014).
Kulkarni, R. N. et al . Tissue-specific knockout of the insulin receptor in pancreatic β cells creates an insulin secretory defect similar to that in type 2 diabetes. Cell 96 , 329–339 (1999). An insightful study documenting that β-cell-specific insulin receptor knockout results in markedly impaired insulin secretion and overt diabetes, thereby providing a unifying mechanism whereby insulin resistance explains both the defects in insulin-stimulated tissue glucose uptake and decreased insulin secretion.
Oliveira, J. M., Rebuffat, S. A., Gasa, R. & Gomis, R. Targeting type 2 diabetes: lessons from a knockout model of insulin receptor substrate 2. Can. J. Physiol. Pharmacol. 92 , 613–620 (2014).
Samuel, V. T. & Shulman, G. I. Mechanisms for insulin resistance: common threads and missing links. Cell 148 , 852–871 (2012). An excellent review of the molecular mechanism responsible for insulin resistance in T2DM and obesity.
Magnusson, I., Rothman, D. L., Katz, L. D., Shulman, R. G. & Shulman, G. I. Increased rate of gluconeogenesis in type II diabetes mellitus. A 13C nuclear magnetic resonance study. J. Clin. Invest. 90 , 1323–1327 (1992). This study demonstrated that increased rates of hepatic glucose production in patients with poorly controlled T2DM could entirely be attributed to increased rates of gluconeogenesis.
Matsuda, M. et al . Glucagon dose-response curve for hepatic glucose production and glucose disposal in type 2 diabetic patients and normal individuals. Metabolism 51 , 1111–1119 (2002).
Samuel, V. T. et al . Fasting hyperglycemia is not associated with increased expression of PEPCK or G6Pc in patients with type 2 diabetes. Proc. Natl Acad. Sci. USA 106 , 12121–12126 (2009).
Baron, A. D., Schaeffer, L., Shragg, P. & Kolterman, O. G. Role of hyperglucagonemia in maintenance of increased rates of hepatic glucose output in type II diabetics. Diabetes 36 , 274–283 (1987).
DeFronzo, R. A., Ferrannini, E., Hendler, R., Wahren, J. & Felig, P. Influence of hyperinsulinemia, hyperglycemia, and the route of glucose administration on splanchnic glucose exchange. Proc. Natl Acad. Sci. USA 75 , 5173–5177 (1978).
Ferrannini, E. et al . The disposal of an oral glucose load in patients with non-insulin-dependent diabetes. Metabolism 37 , 79–85 (1988).
DeFronzo, R. A. et al . Characterization of renal glucose reabsorption in response to dapagliflozin in healthy subjects and subjects with type 2 diabetes. Diabetes Care 36 , 3169–3176 (2013).
Barrett, E. J., Wang, H., Upchurch, C. T. & Liu, Z. Insulin regulates its own delivery to skeletal muscle by feed-forward actions on the vasculature. Am. J. Physiol. Endocrinol. Metab. 301 , E252–E263 (2011).
Baron, A. D. Hemodynamic actions of insulin. Am. J. Physiol. 267 , E187–E202 (1994).
CAS PubMed Google Scholar
Krüger, M. et al . Dissection of the insulin signaling pathway via quantitative phosphoproteomics. Proc. Natl Acad. Sci. USA 105 , 2451–2456 (2008).
Cusi, K. et al . Insulin resistance differentially affects the PI 3-kinase- and MAP kinase-mediated signaling in human muscle. J. Clin. Invest. 105 , 311–320 (2000). The first study in humans with T2DM to demonstrate impaired insulin signal transduction through the IRS1–PI3K pathway in muscle, with normal to increased insulin signalling through the MAPK pathway.
Krook, A. et al . Characterization of signal transduction and glucose transport in skeletal muscle from type 2 diabetic patients. Diabetes 49 , 284–292 (2000).
Copps, K. D. & White, M. F. Regulation of insulin sensitivity by serine/threonine phosphorylation of insulin receptor substrate proteins IRS1 and IRS2. Diabetologia 55 , 2565–2582 (2012).
Bouzakri, K. et al . IRS-1 serine phosphorylation and insulin resistance in skeletal muscle from pancreas transplant recipients. Diabetes 55 , 785–791 (2006).
Hiratani, K. et al . Roles of mTOR and JNK in serine phosphorylation, translocation, and degradation of IRS-1. Biochem. Biophys. Res. Commun. 335 , 836–842 (2005).
Krssak, M. et al . Intramyocellular lipid concentrations are correlated with insulin sensitivity in humans: a 1H NMR spectroscopy study. Diabetologia 42 , 113–116 (1999).
Petersen, K. F. et al . Leptin reverses insulin resistance and hepatic steatosis in patients with severe lipodystrophy. J. Clin. Invest. 109 , 1345–1350 (2002).
Petersen, K. F. et al . Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes. Diabetes 54 , 603–608 (2005).
Lara-Castro, C. & Garvey, W. T. Intracellular lipid accumulation in liver and muscle and the insulin resistance syndrome. Endocrinol. Metab. Clin. North Am. 37 , 841–856 (2008).
Yu, C. et al . Mechanism by which fatty acids inhibit insulin activation of insulin receptor substrate-1 (IRS-1)-associated phosphatidylinositol 3-kinase activity in muscle. J. Biol. Chem. 277 , 50230–50236 (2002).
Bezy, O. et al . PKCδ regulates hepatic insulin sensitivity and hepatosteatosis in mice and humans. J. Clin. Invest. 121 , 2504–2517 (2011).
Samuel, V. T. et al . Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease. J. Biol. Chem. 279 , 32345–32353 (2004).
Samuel, V. T. et al . Inhibition of protein kinase Cε prevents hepatic insulin resistance in nonalcoholic fatty liver disease. J. Clin. Invest. 117 , 739–745 (2007).
Choi, C. S. et al . Suppression of diacylglycerol acyltransferase-2 ( DGAT2 ), but not DGAT1 , with antisense oligonucleotides reverses diet-induced hepatic steatosis and insulin resistance. J. Biol. Chem. 282 , 22678–22688 (2007).
Morino, K. et al . Reduced mitochondrial density and increased IRS-1 serine phosphorylation in muscle of insulin-resistant offspring of type 2 diabetic parents. J. Clin. Invest. 115 , 3587–3593 (2005).
Szendroedi, J. et al . Role of diacylglycerol activation of PKCθ in lipid-induced muscle insulin resistance in humans. Proc. Natl Acad. Sci. USA 111 , 9597–9602 (2014).
Larsen, P. J. & Tennagels, N. On ceramides, other sphingolipids and impaired glucose homeostasis. Mol. Metab. 3 , 252–260 (2014).
Turpin, S. M. et al . Obesity-induced CerS6-dependent C16:0 ceramide production promotes weight gain and glucose intolerance. Cell Metab. 20 , 678–686 (2014).
Cantley, J. L. et al . CGI-58 knockdown sequesters diacylglycerols in lipid droplets/ER-preventing diacylglycerol-mediated hepatic insulin resistance. Proc. Natl Acad. Sci. USA 110 , 1869–1874 (2013).
Patti, M.-E. & Corvera, S. The role of mitochondria in the pathogenesis of type 2 diabetes. Endocr. Rev. 31 , 364–395 (2010). Mitochondrial dysfunction as a causative factor in the development of insulin resistance in T2DM is reviewed.
Ritov, V. B. et al . Deficiency of subsarcolemmal mitochondria in obesity and type 2 diabetes. Diabetes 54 , 8–14 (2005).
Petersen, K. F. et al . Mitochondrial dysfunction in the elderly: possible role in insulin resistance. Science 300 , 1140–1142 (2003).
Petersen, K. F., Dufour, S., Befroy, D., Garcia, R. & Shulman, G. I. Impaired mitochondrial activity in the insulin-resistant offspring of patients with type 2 diabetes. N. Engl. J. Med. 350 , 664–671 (2004).
Mogensen, M. et al . Mitochondrial respiration is decreased in skeletal muscle of patients with type 2 diabetes. Diabetes 56 , 1592–1599 (2007).
Petersen, K. F., Dufour, S. & Shulman, G. I. Decreased insulin-stimulated ATP synthesis and phosphate transport in muscle of insulin-resistant offspring of type 2 diabetic parents. PLoS Med. 2 , e233 (2005).
Wang, C.-H., Wang, C.-C., Huang, H.-C. & Wei, Y.-H. Mitochondrial dysfunction leads to impairment of insulin sensitivity and adiponectin secretion in adipocytes. FEBS J. 280 , 1039–1050 (2013).
Rains, J. L. & Jain, S. K. Oxidative stress, insulin signaling, and diabetes. Free Radic. Biol. Med. 50 , 567–575 (2011).
Morino, K. et al . Regulation of mitochondrial biogenesis by lipoprotein lipase in muscle of insulin-resistant offspring of parents with type 2 diabetes. Diabetes 61 , 877–887 (2012).
Romeo, G. R., Lee, J. & Shoelson, S. E. Metabolic syndrome, insulin resistance, and roles of inflammation — mechanisms and therapeutic targets. Arterioscler. Thromb. Vasc. Biol. 32 , 1771–1776 (2012).
Arkan, M. C. et al . IKK-β links inflammation to obesity-induced insulin resistance. Nat. Med. 11 , 191–198 (2005).
De Alvaro, C., Teruel, T., Hernandez, R. & Lorenzo, M. Tumor necrosis factor α produces insulin resistance in skeletal muscle by activation of inhibitor κB kinase in a p38 MAPK-dependent manner. J. Biol. Chem. 279 , 17070–17078 (2004).
Howard, J. K. & Flier, J. S. Attenuation of leptin and insulin signaling by SOCS proteins. Trends Endocrinol. Metab. 17 , 365–371 (2006).
Lebrun, P. & Van Obberghen, E. SOCS proteins causing trouble in insulin action. Acta Physiol. (Oxf.) 192 , 29–36 (2008).
Article CAS Google Scholar
Uysal, K. T., Wiesbrock, S. M. & Hotamisligil, G. S. Functional analysis of tumor necrosis factor (TNF) receptors in TNF-α-mediated insulin resistance in genetic obesity. Endocrinology 139 , 4832–4838 (1998).
Ofei, F., Hurel, S., Newkirk, J., Sopwith, M. & Taylor, R. Effects of an engineered human anti-TNF-α antibody (CDP571) on insulin sensitivity and glycemic control in patients with NIDDM. Diabetes 45 , 881–885 (1996).
Kim, J. K. et al . Prevention of fat-induced insulin resistance by salicylate. J. Clin. Invest. 108 , 437–446 (2001).
Yuan, M. et al . Reversal of obesity- and diet-induced insulin resistance with salicylates or targeted disruption of IKK β. Science 293 , 1673–1677 (2001).
Goldfine, A. B. et al . The effects of salsalate on glycemic control in patients with type 2 diabetes: a randomized trial. Ann. Intern. Med. 152 , 346–357 (2010).
Lumeng, C. N. & Saltiel, A. R. Inflammatory links between obesity and metabolic disease. J. Clin. Invest. 121 , 2111–2117 (2011).
Nishimura, S. et al . CD8 + effector T cells contribute to macrophage recruitment and adipose tissue inflammation in obesity. Nat. Med. 15 , 914–920 (2009).
Feuerer, M. et al . Lean, but not obese, fat is enriched for a unique population of regulatory T cells that affect metabolic parameters. Nat. Med. 15 , 930–939 (2009).
Bertola, A. et al . Identification of adipose tissue dendritic cells correlated with obesity-associated insulin-resistance and inducing Th17 responses in mice and patients. Diabetes 61 , 2238–2247 (2012).
Cai, D. et al . Local and systemic insulin resistance resulting from hepatic activation of IKK-β and NF-κB. Nat. Med. 11 , 183–190 (2005).
Perry, R. J. et al . Hepatic acetyl CoA links adipose tissue inflammation to hepatic insulin resistance and type 2 diabetes. Cell 160 , 745–758 (2015).
Mori, M. A. et al . A systems biology approach identifies inflammatory abnormalities between mouse strains prior to development of metabolic disease. Diabetes 59 , 2960–2971 (2010).
Mauer, J. et al . Myeloid cell-restricted insulin receptor deficiency protects against obesity-induced inflammation and systemic insulin resistance. PLoS Genet. 6 , e1000938 (2010).
Shi, H. et al . TLR4 links innate immunity and fatty acid-induced insulin resistance. J. Clin. Invest. 116 , 3015–3025 (2006).
Ron, D. & Walter, P. Signal integration in the endoplasmic reticulum unfolded protein response. Nat. Rev. Mol. Cell Biol. 8 , 519–529 (2007).
Boden, G. et al . Increase in endoplasmic reticulum stress-related proteins and genes in adipose tissue of obese, insulin-resistant individuals. Diabetes 57 , 2438–2444 (2008).
Eizirik, D. L., Cardozo, A. K. & Cnop, M. The role for endoplasmic reticulum stress in diabetes mellitus. Endocr. Rev. 29 , 42–61 (2008). A comprehensive review of ER stress and the UPR in the development of insulin resistance and obesity.
Gregor, M. F. et al . Endoplasmic reticulum stress is reduced in tissues of obese subjects after weight loss. Diabetes 58 , 693–700 (2009).
Ozawa, K. et al . The endoplasmic reticulum chaperone improves insulin resistance in type 2 diabetes. Diabetes 54 , 657–663 (2005).
Herschkovitz, A. et al . Common inhibitory serine sites phosphorylated by IRS-1 kinases, triggered by insulin and inducers of insulin resistance. J. Biol. Chem. 282 , 18018–18027 (2007).
Boden, G. Endoplasmic reticulum stress: another link between obesity and insulin resistance/inflammation? Diabetes 58 , 518–519 (2009).
Sengupta, S., Peterson, T. R. & Sabatini, D. M. Regulation of the mTOR complex 1 pathway by nutrients, growth factors, and stress. Mol. Cell 40 , 310–322 (2010).
Shah, O. J., Wang, Z. & Hunter, T. Inappropriate activation of the TSC/Rheb/mTOR/S6K cassette induces IRS1/2 depletion, insulin resistance, and cell survival deficiencies. Curr. Biol. 14 , 1650–1656 (2004).
Ozcan, U. et al . Loss of the tuberous sclerosis complex tumor suppressors triggers the unfolded protein response to regulate insulin signaling and apoptosis. Mol. Cell 29 , 541–551 (2008).
Park, S. W. et al . The regulatory subunits of PI3K, p85α and p85β, interact with XBP-1 and increase its nuclear translocation. Nat. Med. 16 , 429–437 (2010).
Stratton, I. M. et al . Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 321 , 405–412 (2000). A seminal UK Prospective Diabetes Study study unequivocally demonstrating that improved glycaemic control reduced the incidence of microvascular, and to a lesser extent, macrovascular complications in patients with T2DM.
Holman, R. R., Paul, S. K., Bethel, M. A., Matthews, D. R. & Neil, H. A. 10-year follow-up of intensive glucose control in type 2 diabetes. N. Engl. J. Med. 359 , 1577–1589 (2008). A long-term follow-up of the UK Prospective Diabetes Study showing that early intensive glycaemic control has a persistent impact on preventing both microvascular and macrovascular complications long after initiation of the intensified antidiabetic regimen has been discontinued: that is, the ‘legacy effect’.
Brownlee, M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes 54 , 1615–1625 (2005). A lucid discussion of the molecular pathways involved in the development of diabetic microvascular complications.
Giacco, F. & Brownlee, M. Oxidative stress and diabetic complications. Circ. Res. 107 , 1058–1070 (2010).
Coutinho, M., Gerstein, H. C., Wang, Y. & Yusuf, S. The relationship between glucose and incident cardiovascular events. A metaregression analysis of published data from 20 studies of 95,783 individuals followed for 12.4 years. Diabetes Care 22 , 233–240 (1999).
Taskinen, M.-R. & Borén, J. New insights into the pathophysiology of dyslipidemia in type 2 diabetes. Atherosclerosis 239 , 483–495 (2015). An up-to-date review of the pathogenesis of diabetic dyslipidaemia and its treatment.
Isomaa, B. et al . Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 24 , 683–689 (2001).
Adler, A. I. et al . Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 321 , 412–419 (2000).
Williams, B. Treating hypertension in patients with diabetes: when to start and how low to go? JAMA 313 , 573–574 (2015). The optimal blood pressure goal in hypertensive patients with T2DM is discussed in light of the controversial results observed in the blood pressure arm of the ACCORD trial.
Lastra, G., Syed, S., Kurukulasuriya, L. R., Manrique, C. & Sowers, J. R. Type 2 diabetes mellitus and hypertension: an update. Endocrinol. Metab. Clin. North Am. 43 , 103–122 (2014).
International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 32 , 1327–1334 (2009).
[No authors listed.] Report of the Expert Committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 20 , 1183–1197 (1997). A reference publication by the ADA on the diagnosis and classification of diabetes mellitus.
Herman, W. H. Diabetes epidemiology: guiding clinical and public health practice: the Kelly West Award Lecture, 2006. Diabetes Care 30 , 1912–1919 (2007). A landmark lecture providing a comprehensive overview of the epidemiology of T2DM and the public health implications for diabetes prevention.
DECODE Study Group, European Diabetes Epidemiology Group. Is the current definition for diabetes relevant to mortality risk from all causes and cardiovascular and noncardiovascular diseases? Diabetes Care 26 , 688–696 (2003).
Engelgau, M. M., Narayan, K. M. & Herman, W. H. Screening for type 2 diabetes. Diabetes Care 23 , 1563–1580 (2000).
LeFevre, M. L. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: U.S. Preventive Services Task Force Recommendation Statement. Ann. Intern. Med. 161 , 587–593 (2014).
Lindström, J. & Tuomilehto, J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care 26 , 725–731 (2003).
Tabaei, B. P. & Herman, W. H. A multivariate logistic regression equation to screen for diabetes: development and validation. Diabetes Care 25 , 1999–2003 (2002).
World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complications. report of a WHO consultation. Part 1: diagnosis and classification of diabetes mellitus (WHO, 1999).
Pan, X. R. et al . Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT Diabetes Study. Diabetes Care 20 , 537–544 (1997).
Knowler, W. C. et al . Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 346 , 393–403 (2002).
Ramachandran, A. et al . The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia 49 , 289–297 (2006).
Chiasson, J.-L. et al . Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial. Lancet 359 , 2072–2077 (2002).
Kawamori, R. et al . Voglibose for prevention of type 2 diabetes mellitus: a randomised, double-blind trial in Japanese individuals with impaired glucose tolerance. Lancet 373 , 1607–1614 (2009).
Knowler, W. C. et al . Prevention of type 2 diabetes with troglitazone in the Diabetes Prevention Program. Diabetes 54 , 1150–1156 (2005).
Gerstein, H. C. et al . Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomised controlled trial. Lancet 368 , 1096–1105 (2006).
Li, G. et al . The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet 371 , 1783–1789 (2008).
Lindström, J. et al . Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet 368 , 1673–1679 (2006).
Knowler, W. C. et al . 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 374 , 1677–1686 (2009). Long-term follow-up of body weight regain and diabetes incidence in patients with IGT in the Diabetes Prevention Program treated with lifestyle heavy, lifestyle light and metformin, showing that gradual weight regain is the norm and that 40–50% of patients with IGT develop diabetes despite successful weight loss.
DeFronzo, R. A., Eldor, R. & Abdul-Ghani, M. Pathophysiologic approach to therapy in patients with newly diagnosed type 2 diabetes. Diabetes Care 36 , S127–S138 (2013). A rational approach to the treatment of T2DM is presented based on its pathophysiology.
Raz, I. et al . Personalized management of hyperglycemia in type 2 diabetes: reflections from a Diabetes Care Editors’ Expert Forum. Diabetes Care 36 , 1779–1788 (2013).
Nakagami, T., Kawahara, R., Hori, S. & Omori, Y. Glycemic control and prevention of retinopathy in Japanese NIDDM patients. A 10-year follow-up study. Diabetes Care 20 , 621–622 (1997).
Lim, E. L. et al . Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 54 , 2506–2514 (2011).
Jazet, I. M. et al . Loss of 50% of excess weight using a very low energy diet improves insulin-stimulated glucose disposal and skeletal muscle insulin signalling in obese insulin-treated type 2 diabetic patients. Diabetologia 51 , 309–319 (2008).
Abdul-Ghani, M. A. et al . Initial combination therapy with metformin, pioglitazone and exenatide is more effective than sequential add-on therapy in subjects with new-onset diabetes. Results from the Efficacy and Durability of Initial Combination Therapy for Type 2 Diabetes (EDICT): a randomized trial. Diabetes Obes. Metab. 17 , 268–275 (2015). This prospective randomized trial using a combination of antidiabetic agents proven to reverse known pathophysiological abnormalities in T2DM demonstrated superiority of glycaemic control compared with the stepped approach of metformin followed by a sulfonylurea and then basal insulin recommended by most national diabetes organizations.
Harrison, L. B., Adams-Huet, B., Raskin, P. & Lingvay, I. β-cell function preservation after 3.5 years of intensive diabetes therapy. Diabetes Care 35 , 1406–1412 (2012).
Gram, J. et al . Pharmacological treatment of the pathogenetic defects in type 2 diabetes: the randomized multicenter South Danish Diabetes Study. Diabetes Care 34 , 27–33 (2011).
DeFronzo, R. A. et al . Combination of empagliflozin and linagliptin as second-line therapy in subjects with type 2 diabetes inadequately controlled on metformin. Diabetes Care 38 , 384–393 (2015).
Weng, J. et al . Effect of intensive insulin therapy on β-cell function and glycaemic control in patients with newly diagnosed type 2 diabetes: a multicentre randomised parallel-group trial. Lancet 371 , 1753–1760 (2008).
Hu, Y. et al . Short-term intensive therapy in newly diagnosed type 2 diabetes partially restores both insulin sensitivity and β-cell function in subjects with long-term remission. Diabetes Care 34 , 1848–1853 (2011). One of several recent studies demonstrating that intensive insulin therapy to correct the decompensated metabolic state in newly diagnosed patients with T2DM can lead to durable glycaemic control without or with a marked reduction in antidiabetic medications.
Xiang, A. H. et al . Effect of pioglitazone on pancreatic β-cell function and diabetes risk in Hispanic women with prior gestational diabetes. Diabetes 55 , 517–522 (2006).
Astrup, A. et al . Safety, tolerability and sustained weight loss over 2 years with the once-daily human GLP-1 analog, liraglutide. Int. J. Obes. (Lond.) 36 , 843–854 (2012).
Cusi, K., Consoli, A. & DeFronzo, R. A. Metabolic effects of metformin on glucose and lactate metabolism in noninsulin-dependent diabetes mellitus. J. Clin. Endocrinol. Metab. 81 , 4059–4067 (1996).
Turner, R. C., Cull, C. A., Frighi, V. & Holman, R. R. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA 281 , 2005–2012 (1999). A landmark UK Prospective Diabetes Study documenting the need for progressive add-on therapies in newly diagnosed patients with T2DM receiving initial therapy with metformin or with a sulfonylurea.
Brown, J. B., Conner, C. & Nichols, G. A. Secondary failure of metformin monotherapy in clinical practice. Diabetes Care 33 , 501–506 (2010).
Kahn, S. E. et al . Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N. Engl. J. Med. 355 , 2427–2443 (2006). A 5-year ADOPT study demonstrating long-term durable HbA1c reduction with rosiglitazone compared with a progressive rise in HbA1c observed with metformin and sulfonylureas, and a more rapid deterioration of glycaemic control with sulfonylureas compared with metformin.
Madiraju, A. K. et al . Metformin suppresses gluconeogenesis by inhibiting mitochondrial glycerophosphate dehydrogenase. Nature 510 , 542–546 (2014).
Ferrannini, E. The target of metformin in type 2 diabetes. N. Engl. J. Med. 371 , 1547–1548 (2014).
[No authors listed.] Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet 352 , 854–865 (1998).
Maedler, K. et al . Sulfonylurea induced β-cell apoptosis in cultured human islets. J. Clin. Endocrinol. Metab. 90 , 501–506 (2005).
Roumie, C. L. et al . Comparative effectiveness of sulfonylurea and metformin monotherapy on cardiovascular events in type 2 diabetes mellitus: a cohort study. Ann. Intern. Med. 157 , 601–610 (2012).
Simpson, S. H., Majumdar, S. R., Tsuyuki, R. T., Eurich, D. T. & Johnson, J. A. Dose–response relation between sulfonylurea drugs and mortality in type 2 diabetes mellitus: a population-based cohort study. CMAJ 174 , 169–174 (2006).
Simpson, S. H. et al . Mortality risk among sulfonylureas: a systematic review and network meta-analysis. Lancet Diabetes Endocrinol. 3 , 43–51 (2015). A review of the published literature that examines the relationship between sulfonylurea therapy and the development of adverse cardiovascular events.
Yki-Järvinen, H. Thiazolidinediones. N. Engl. J. Med. 351 , 1106–1118 (2004).
Eldor, R., DeFronzo, R. A. & Abdul-Ghani, M. In vivo actions of peroxisome proliferator-activated receptors: glycemic control, insulin sensitivity, and insulin secretion. Diabetes Care 36 , S162–S174 (2013). An exhaustive review of the mechanism of action, efficacy and side-effect profile of the thiazolidinedione class of antidiabetic medications.
Miyazaki, Y., He, H., Mandarino, L. J. & DeFronzo, R. A. Rosiglitazone improves downstream insulin receptor signaling in type 2 diabetic patients. Diabetes 52 , 1943–1950 (2003).
Gastaldelli, A. et al . Thiazolidinediones improve β-cell function in type 2 diabetic patients. Am. J. Physiol. Endocrinol. Metab. 292 , E871–E883 (2007).
DeFronzo, R. A. et al . Prevention of diabetes with pioglitazone in ACT NOW: physiologic correlates. Diabetes 62 , 3920–3926 (2013).
Kahn, S. E. et al . Effects of rosiglitazone, glyburide, and metformin on β-cell function and insulin sensitivity in ADOPT. Diabetes 60 , 1552–1560 (2011).
Dormandy, J. A. et al . Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet 366 , 1279–1289 (2005). A large prospective study (PROactive) demonstrating that pioglitazone significantly reduced the second principal end point of myocardial infarction, stroke and cardiovascular death; the primary end point did not reach statistical significance because of the inclusion of peripheral arterial disease and leg revascularization, which is known to be refractory to medical intervention, including statin therapy.
Aronoff, S. et al . Pioglitazone hydrochloride monotherapy improves glycemic control in the treatment of patients with type 2 diabetes: a 6-month randomized placebo-controlled dose-response study. The Pioglitazone 001 Study Group. Diabetes Care 23 , 1605–1611 (2000).
Erdmann, E., Song, E., Spanheimer, R., van Troostenburg de Bruyn, A.-R. & Perez, A. Observational follow-up of the PROactive study: a 6-year update. Diabetes Obes. Metab. 16 , 63–74 (2014).
[No authors listed.] Takeda announces completion of the post-marketing commitment to submit data to the FDA, the EMA and the PMDA for pioglitazone containing medicines including ACTOS. Takeda [online] , (2014).
Levin, D. et al . Pioglitazone and bladder cancer risk: a multipopulation pooled, cumulative exposure analysis. Diabetologia 58 , 493–504 (2015).
Kjems, L. L., Holst, J. J., Vølund, A. & Madsbad, S. The influence of GLP-1 on glucose-stimulated insulin secretion: effects on β-cell sensitivity in type 2 and nondiabetic subjects. Diabetes 52 , 380–386 (2003).
Vilsbøll, T., Krarup, T., Madsbad, S. & Holst, J. J. Defective amplification of the late phase insulin response to glucose by GIP in obese Type II diabetic patients. Diabetologia 45 , 1111–1119 (2002).
Aroda, V. R. et al . Efficacy of GLP-1 receptor agonists and DPP-4 inhibitors: meta-analysis and systematic review. Clin. Ther. 34 , 1247–1258.e22 (2012).
Deacon, C. F. Dipeptidyl peptidase-4 inhibitors in the treatment of type 2 diabetes: a comparative review. Diabetes Obes. Metab. 13 , 7–18 (2011).
Balas, B. et al . The dipeptidyl peptidase IV inhibitor vildagliptin suppresses endogenous glucose production and enhances islet function after single-dose administration in type 2 diabetic patients. J. Clin. Endocrinol. Metab. 92 , 1249–1255 (2007).
Drucker, D. J. Incretin action in the pancreas: potential promise, possible perils, and pathological pitfalls. Diabetes 62 , 3316–3323 (2013). A comprehensive review of the effect of incretin hormones on pancreatic hormone secretion and pathology by one of the world's leading authorities.
White, W. B. et al . Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N. Engl. J. Med. 369 , 1327–1335 (2013).
Scirica, B. M. et al . Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N. Engl. J. Med. 369 , 1317–1326 (2013).
Cervera, A. et al . Mechanism of action of exenatide to reduce postprandial hyperglycemia in type 2 diabetes. Am. J. Physiol. Endocrinol. Metab. 294 , E846–E852 (2008).
Bunck, M. C. et al . Effects of exenatide on measures of β-cell function after 3 years in metformin-treated patients with type 2 diabetes. Diabetes Care 34 , 2041–2047 (2011). A landmark 3-year prospective study demonstrating the marked and durable improvement in β-cell function using the combined hyperglycaemic and euglycaemic insulin clamp techniques following exenatide treatment in patients with T2DM.
Klonoff, D. C. et al . Exenatide effects on diabetes, obesity, cardiovascular risk factors and hepatic biomarkers in patients with type 2 diabetes treated for at least 3 years. Curr. Med. Res. Opin. 24 , 275–286 (2008).
Schwartz, S. & Kohl, B. A. Type 2 diabetes mellitus and the cardiometabolic syndrome: impact of incretin-based therapies. Diabetes Metab. Syndr. Obes. 3 , 227–242 (2010).
Eng, C., Kramer, C. K., Zinman, B. & Retnakaran, R. Glucagon-like peptide-1 receptor agonist and basal insulin combination treatment for the management of type 2 diabetes: a systematic review and meta-analysis. Lancet 384 , 2228–2234 (2014).
Egan, A. G. et al . Pancreatic safety of incretin-based drugs — FDA and EMA assessment. N. Engl. J. Med. 370 , 794–797 (2014).
Van de Laar, F. A. et al . Alpha-glucosidase inhibitors for type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2 , CD003639 (2005).
Esposito, K. et al . Dipeptidyl peptidase-4 inhibitors and HbA1c target of <7% in type 2 diabetes: meta-analysis of randomized controlled trials. Diabetes Obes. Metab. 13 , 594–603 (2011).
Richter, B., Bandeira-Echtler, E., Bergerhoff, K. & Lerch, C. L. Dipeptidyl peptidase-4 (DPP-4) inhibitors for type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2 , CD006739 (2008).
Abdul-Ghani, M. A., Norton, L. & DeFronzo, R. A. Role of sodium-glucose cotransporter 2 (SGLT 2) inhibitors in the treatment of type 2 diabetes. Endocr. Rev. 32 , 515–531 (2011). An excellent review of the mechanism of action, efficacy and safety of the recently approved SGLT2 inhibitor class of antidiabetic medications.
Wright, E. M., Loo, D. D. & Hirayama, B. A. Biology of human sodium glucose transporters. Physiol. Rev. 91 , 733–794 (2011).
Merovci, A. et al . Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J. Clin. Invest. 124 , 509–514 (2014).
Ferrannini, E. et al . Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients. J. Clin. Invest. 124 , 499–508 (2014).
Abdul-Ghani, M. A., DeFronzo, R. A. & Norton, L. Novel hypothesis to explain why SGLT2 inhibitors inhibit only 30–50% of filtered glucose load in humans. Diabetes 62 , 3324–3328 (2013).
Cherney, D. Z. I. et al . Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation 129 , 587–597 (2014).
Holman, R. R. et al . Three-year efficacy of complex insulin regimens in type 2 diabetes. N. Engl. J. Med. 361 , 1736–1747 (2009). A comparison of the efficacy and side-effect profile of commonly used complex insulin regimens for the treatment of patients with T2DM.
Gough, S. C. L. et al . Efficacy and safety of a fixed-ratio combination of insulin degludec and liraglutide (IDegLira) compared with its components given alone: results of a phase 3, open-label, randomised, 26-week, treat-to-target trial in insulin-naive patients with type 2 diabetes. Lancet Diabetes Endocrinol. 2 , 885–893 (2014).
Wilding, J. P. et al . Long-term efficacy of dapagliflozin in patients with type 2 diabetes mellitus receiving high doses of insulin: a randomized trial. Ann. Intern. Med. 156 , 405–415 (2012).
Anderson, M., Powell, J., Campbell, K. M. & Taylor, J. R. Optimal management of type 2 diabetes in patients with increased risk of hypoglycemia. Diabetes Metab. Syndr. Obes. 7 , 85–94 (2014).
PubMed PubMed Central Google Scholar
Schopman, J. E. et al . The incidence of mild and severe hypoglycaemia in patients with type 2 diabetes mellitus treated with sulfonylureas: a systematic review and meta-analysis. Diabetes Metab. Res. Rev. 30 , 11–22 (2014).
Desouza, C., Salazar, H., Cheong, B., Murgo, J. & Fonseca, V. Association of hypoglycemia and cardiac ischemia: a study based on continuous monitoring. Diabetes Care 26 , 1485–1489 (2003).
Gerstein, H. C. et al . Effects of intensive glucose lowering in type 2 diabetes. N. Engl. J. Med. 358 , 2545–2559 (2008). The ORIGIN trial demonstrated that physiological insulin replacement doses (30–40 units per day) in newly diagnosed patients with T2DM could control HbA1c without an increased risk of cardiovascular events; however, the risk of hypoglycaemia was significantly increased, and the study did not examine the effect of higher doses of insulin, which are usually required to normalize glycaemia in more long-standing diabetes, on cardiovascular risk or other potential side effects of insulin therapy.
Cushman, W. C. et al . Effects of intensive blood-pressure control in type 2 diabetes mellitus. N. Engl. J. Med. 362 , 1575–1585 (2010).
James, P. A. et al . 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 311 , 507–520 (2014).
Emdin, C. et al . Association of cardiovascular trial registration with positive study findings: Epidemiological Study of Randomized Trials (ESORT). JAMA Intern. Med. 175 , 304–307 (2015).
Testa, M. A. & Simonson, D. C. Health economic benefits and quality of life during improved glycemic control in patients with type 2 diabetes mellitus: a randomized, controlled, double-blind trial. JAMA 280 , 1490–1496 (1998). This was the first randomized trial to demonstrate that better glucose control improves QOL, cognitive function and general perceived health, and reduces symptom distress and absenteeism from work.
Testa, M. A. & Simonson, D. C. Assesment of quality-of-life outcomes. N. Engl. J. Med. 334 , 835–840 (1996).
Testa, M. A., Simonson, D. C. & Turner, R. R. Valuing quality of life and improvements in glycemic control in people with type 2 diabetes. Diabetes Care 21 , C44–C52 (1998).
Bode, B. W. et al . Patient-reported outcomes following treatment with the human GLP-1 analogue liraglutide or glimepiride in monotherapy: results from a randomized controlled trial in patients with type 2 diabetes. Diabetes Obes. Metab. 12 , 604–612 (2010).
Testa, M. A. et al . Comparative effectiveness of basal-bolus versus premix analog insulin on glycemic variability and patient-centered outcomes during insulin intensification in type 1 and type 2 diabetes: a randomized, controlled, crossover trial. J. Clin. Endocrinol. Metab. 97 , 3504–3514 (2012). This randomized trial demonstrated that patient satisfaction with treatment was more positively affected by improved QOL, reduced glucose variability and better glycaemic control with a basal-bolus regimen than negatively affected by the burden of additional injections.
Cotter, A. P., Durant, N., Agne, A. A. & Cherrington, A. L. Internet interventions to support lifestyle modification for diabetes management: a systematic review of the evidence. J. Diabetes Complications 28 , 243–251 (2014).
Rose, M. et al . The PROMIS Physical Function item bank was calibrated to a standardized metric and shown to improve measurement efficiency. J. Clin. Epidemiol. 67 , 516–526 (2014).
DeFronzo, R. A. & Triplitt, C. Novel agents for T2DM. Diabetes Spectr. 27 , 100–112 (2014). This article presents a more detailed review of novel antidiabetic agents that currently are being investigated in animals and humans for the treatment of T2DM.
Wong, A. K., Howie, J., Petrie, J. R. & Lang, C. C. AMP-activated protein kinase pathway: a potential therapeutic target in cardiometabolic disease. Clin. Sci. (Lond.) 116 , 607–620 (2009).
Agrawal, N. K. & Kant, S. Targeting inflammation in diabetes: newer therapeutic options. World J. Diabetes 5 , 697–710 (2014). Inflammation in insulin target tissues and β-cells is a now well-established pathogenetic abnormality T2DM. This article reviews the mechanism by which inflammation contributes to glucose intolerance in T2DM and potential interventions to suppress inflammation and improve insulin sensitivity and β-cell function.
Poy, M. N. et al . miR-375 maintains normal pancreatic α- and β-cell mass. Proc. Natl Acad. Sci. USA 106 , 5813–5818 (2009).
Burant, C. F. et al . TAK-875 versus placebo or glimepiride in type 2 diabetes mellitus: a phase 2, randomised, double-blind, placebo-controlled trial. Lancet 379 , 1403–1411 (2012).
Assmann, A., Hinault, C. & Kulkarni, R. N. Growth factor control of pancreatic islet regeneration and function. Pediatr. Diabetes 10 , 14–32 (2009).
Vasavada, R. C. et al . Protein kinase C-ζ activation markedly enhances β-cell proliferation: an essential role in growth factor mediated β-cell mitogenesis. Diabetes 56 , 2732–2743 (2007).
Wiederkehr, A. & Wollheim, C. B. Mitochondrial signals drive insulin secretion in the pancreatic β-cell. Mol. Cell. Endocrinol. 353 , 128–137 (2012).
Wang, C. et al . Deficiency of APPL1 in mice impairs glucose-stimulated insulin secretion through inhibition of pancreatic beta cell mitochondrial function. Diabetologia 56 , 1999–2009 (2013).
Sivitz, W. I. & Yorek, M. A. Mitochondrial dysfunction in diabetes: from molecular mechanisms to functional significance and therapeutic opportunities. Antioxid. Redox Signal. 12 , 537–577 (2010).
Li, N., Stojanovski, S. & Maechler, P. Mitochondrial hormesis in pancreatic β cells: does uncoupling protein 2 play a role? Oxid. Med. Cell. Longev. 2012 , 740849 (2012).
Aquilano, K., Baldelli, S., Pagliei, B. & Ciriolo, M. R. Extranuclear localization of SIRT1 and PGC-1α: an insight into possible roles in diseases associated with mitochondrial dysfunction. Curr. Mol. Med. 13 , 140–154 (2013).
Matschinsky, F. M. et al . Glucokinase activators for diabetes therapy: May 2010 status report. Diabetes Care 34 , S236–S243 (2011).
Engel, S. S. Glycemic and lipid effects of the short-acting glucagon receptor antagonist MK-3577 in patients with type 2 diabetes. Diabetes Abstr. 61 , A266 (2012).
Gumbiner, B. Pronounced glucose (G) reduction in poorly controlled T2DM with MB07803, a novel fructose-1, 6-biphosphatase inhibitor (FBPasel) with reduced potential for acid-base disturbance versus the 1st generation FBPasel CS-917. Diabetes Abstr. 58 , LB4 (2009).
Kumashiro, N. et al . Targeting pyruvate carboxylase reduces gluconeogenesis and adiposity and improves insulin resistance. Diabetes 62 , 2183–2194 (2013).
Stark, R. et al . A role for mitochondrial phosphoenolpyruvate carboxykinase (PEPCK-M) in the regulation of hepatic gluconeogenesis. J. Biol. Chem. 289 , 7257–7263 (2014).
Harlan, D. M., Kenyon, N. S., Korsgren, O. & Roep, B. O. Current advances and travails in islet transplantation. Diabetes 58 , 2175–2184 (2009).
Motté, E. et al . Composition and function of macroencapsulated human embryonic stem cell-derived implants: comparison with clinical human islet cell grafts. Am. J. Physiol. Endocrinol. Metab. 307 , E838–E846 (2014).
Pagliuca, F. W. et al . Generation of functional human pancreatic β cells in vitro . Cell 159 , 428–439 (2014).
Blum, B. et al . Reversal of β cell de-differentiation by a small molecule inhibitor of the TGFβ pathway. eLife 3 , e02809 (2014).
Pickup, J. C. Banting Memorial Lecture 2014* Technology and diabetes care: appropriate and personalized. Diabet. Med. 32 , 3–13 (2015).
Peyser, T., Dassau, E., Breton, M. & Skyler, J. S. The artificial pancreas: current status and future prospects in the management of diabetes. Ann. NY Acad. Sci. 1311 , 102–123 (2014). This article presents an up-to-to-date status report on progress with the artificial pancreas (closed-loop system).
Klonoff, D. C. Afrezza inhaled insulin: the fastest-acting FDA-approved insulin on the market has favorable properties. J. Diabetes Sci. Technol. 8 , 1071–1073 (2014).
Eldor, R., Arbit, E., Corcos, A. & Kidron, M. Glucose-reducing effect of the ORMD-0801 oral insulin preparation in patients with uncontrolled type 1 diabetes: a pilot study. PLoS ONE 8 , e59524 (2013).
DeFronzo, R. A. Dissociation between metformin plasma exposure and its glucose-lowering effect: a novel gut-mediated mechanism of action. Diabetes 62 , a281 (2013).
DePaoli, A. M., Higgins, L. S., Henry, R. R., Mantzoros, C. & Dunn, F. L. Can a selective PPARγ modulator improve glycemic control in patients with type 2 diabetes with fewer side effects compared with pioglitazone? Diabetes Care 37 , 1918–1923 (2014).
Colca, J. R., Tanis, S. P., McDonald, W. G. & Kletzien, R. F. Insulin sensitizers in 2013: new insights for the development of novel therapeutic agents to treat metabolic diseases. Expert Opin. Investig. Drugs 23 , 1–7 (2014).
Suh, J. M. et al . Endocrinization of FGF1 produces a neomorphic and potent insulin sensitizer. Nature 513 , 436–439 (2014).
Gaich, G. et al . The effects of LY2405319, an FGF21 analog, in obese human subjects with type 2 diabetes. Cell Metab. 18 , 333–340 (2013).
Jeoung, N. H. & Harris, R. A. Role of pyruvate dehydrogenase kinase 4 in regulation of blood glucose levels. Korean Diabetes J. 34 , 274–283 (2010).
Povel, C. M. et al . Metabolic syndrome model definitions predicting type 2 diabetes and cardiovascular disease. Diabetes Care 36 , 362–368 (2013).
Pacini, G., Mari, A., Fouqueray, P., Bolze, S. & Roden, M. Imeglimin increases glucose-dependent insulin secretion and improves β-cell function in patients with type 2 diabetes. Diabetes Obes. Metab. 17 , 541–545 (2015).
Birch, A. M., Buckett, L. K. & Turnbull, A. V. DGAT1 inhibitors as anti-obesity and anti-diabetic agents. Curr. Opin. Drug Discov. Devel. 13 , 489–496 (2010).
Liu, L. et al . Upregulation of myocellular DGAT1 augments triglyceride synthesis in skeletal muscle and protects against fat-induced insulin resistance. J. Clin. Invest. 117 , 1679–1689 (2007).
Harrima, G., Greenwood, J. & Bhar, S. Acetyl-CoA carboxylase inhibition by NDI-630 inhibits fatty acid synthesis stimulates fatty acid oxidative, reduces body weight, improvise insulin sensitivity, and modulates dyslipidemia in rats. Diabetes Abstr. 62 , A161 (2013).
Tao, H., Zhang, Y., Zeng, X., Shulman, G. I. & Jin, S. Niclosamide ethanolamine-induced mild mitochondrial uncoupling improves diabetic symptoms in mice. Nat. Med. 20 , 1263–1269 (2014).
Perry, R. J. et al . Reversal of hypertriglyceridemia, fatty liver disease, and insulin resistance by a liver-targeted mitochondrial uncoupler. Cell Metab. 18 , 740–748 (2013).
Garvey, W. T. et al . Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): a randomized, placebo-controlled, phase 3 extension study. Am. J. Clin. Nutr. 95 , 297–308 (2012).
Carlsson, L. M. et al . Bariatric surgery and prevention of type 2 diabetes in Swedish obese subjects. N. Engl. J. Med. 367 , 695–704 (2012). The effectiveness and safety of bariatric surgery in the treatment of obesity and T2DM is reviewed in this longest ongoing study on surgical intervention.
Neuschwander-Tetri, B. A. et al . Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebo-controlled trial. Lancet 385 , 956–965 (2014).
Out, C., Groen, A. K. & Brufau, G. Bile acid sequestrants: more than simple resins. Curr. Opin. Lipidol. 23 , 43–55 (2012).
Cellitti, S. A novel GLP-1-FGF21 fusion protein for the treatment of diabetes and obesity. Keystone Symp. Obes. (2014).
Thareja, S., Aggarwal, S., Bhardwaj, T. R. & Kumar, M. Protein tyrosine phosphatase 1B inhibitors: a molecular level legitimate approach for the management of diabetes mellitus. Med. Res. Rev. 32 , 459–517 (2012).
Chakraborty, C., Doss, C. G., Bandyopadhyay, S. & Agoramoorthy, G. Influence of miRNA in insulin signaling pathway and insulin resistance: micro-molecules with a major role in type-2 diabetes. Wiley Interdiscip. Rev. RNA 5 , 697–712 (2014).
Tilg, H. & Moschen, A. R. Microbiota and diabetes: an evolving relationship. Gut 63 , 1513–1521 (2014).
Patel, S. R., Hakim, D., Mason, J. & Hakim, N. The duodenal–jejunal bypass sleeve (EndoBarrier Gastrointestinal Liner) for weight loss and treatment of type 2 diabetes. Surg. Obes. Relat. Dis. 9 , 482–484 (2013).
Bhatt, M. P., Lim, Y.-C. & Ha, K.-S. C-peptide replacement therapy as an emerging strategy for preventing diabetic vasculopathy. Cardiovasc. Res. 104 , 234–244 (2014).
Bhat, M., Pouliot, M., Couture, R. & Vaucher, E. The kallikrein–kinin system in diabetic retinopathy. Prog. Drug Res. 69 , 111–143 (2014).
PubMed Google Scholar
Hajhosseiny, R. et al . Have we reached the limits for the treatment of diabetic nephropathy? Expert Opin. Investig. Drugs 23 , 511–522 (2014).
Williams, M. E. et al . Effects of pyridoxamine in combined phase 2 studies of patients with type 1 and type 2 diabetes and overt nephropathy. Am. J. Nephrol. 27 , 605–614 (2007).
De Zeeuw, D. et al . The endothelin antagonist atrasentan lowers residual albuminuria in patients with type 2 diabetic nephropathy. J. Am. Soc. Nephrol. 25 , 1083–1093 (2014).
Boussageon, R. et al . Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ 343 , d4169 (2011).
Colditz, G. A., Willett, W. C., Rotnitzky, A. & Manson, J. E. Weight gain as a risk factor for clinical diabetes mellitus in women. Ann. Intern. Med. 122 , 481–486 (1995).
Chan, J. M., Rimm, E. B., Colditz, G. A., Stampfer, M. J. & Willett, W. C. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care 17 , 961–969 (1994).
Download references
Acknowledgements
The authors acknowledge grants from: the South Texas Veterans Healthcare System to R.A.D.; the National Institutes of Health (grants R01DK24092 to R.A.D.; DK58845 and P30 DK46200 to F.B.H.; R01 DK-040936, R01 DK-049230, R24 DK-085836, UL1 RR-045935, R01 DK-082659 and R24 DK085610 to G.I.S.; P30 DK036836 to C.R.K. Novo Nordisk Foundation for Basic Metabolic Research and the University of Copenhagen to G.I.S. and C.R.K.; DVA-Merit Review grant and VA San Diego Healthcare System to R.H.; National Institute for Diabetes and Digestive and Kidney Disease (grant P30DK092926) to W.H.; the Swedish Research Council (grants 2010–3490 and 2008–6589) and European Council (grants GA269045) to L.G.; Italian Ministry of University & Research (MIUR 2010329EKE) to E.F.; the Patient-Centered Outcomes Research Institute (PCORI) Program Award (CE1304-6756) to D.C.S. and M.A.T.; NovoNordisk Foundation to the NNF Center for Basic Metabolic Research to J.H. W.H. acknowledges the Michigan Center for Diabetes Translational Research and I.R. thanks R. Sprung for editorial assistance.
Author information
Authors and affiliations.
Diabetes Division, Department of Medicine, University of Texas Health Science Center, South Texas Veterans Health Care System and Texas Diabetes Institute, 701 S. Zarzamoro, San Antonio, 78207, Texas, USA
Ralph A. DeFronzo
CNR Institute of Clinical Physiology, Pisa, Italy
Ele Ferrannini
Department of Clinical Science Malmoe, Diabetes & Endocrinology, Lund University Diabetes Centre, Lund, Sweden
University of California, San Diego, Section of Diabetes, Endocrinology & Metabolism, Center for Metabolic Research, VA San Diego Healthcare System, San Diego, California, USA
Robert R. Henry
University of Michigan, Ann Arbor, Michigan, USA
William H. Herman
University of Copenhagen, Kobenhavn, Denmark
Jens Juul Holst
Department of Nutrition, Harvard T.H. Chan School of Public Health and Department of Epidemiology, Harvard T.H. Chan School of Public Health and Channing Division of Network Medicine, Brigham and Women's Hospital, Harvard Medical School, Boston, Massachusetts, USA
Frank B. Hu
Harvard Medical School and Joslin Diabetes Center, Boston, Massachusetts, USA
C. Ronald Kahn
Division of Internal Medicine, Diabetes Unit, Hadassah Hebrew University Hospital, Jerusalem, Israel
Howard Hughes Medical Institute and the Departments of Internal Medicine and Cellular & Molecular Physiology, Yale University School of Medicine, New Haven, Connecticut, USA
Gerald I. Shulman
Division of Endocrinology, Diabetes and Hypertension, Brigham and Women's Hospital, Harvard Medical School, Boston, Massachusetts, USA
Donald C. Simonson
Department of Biostatistics, Harvard T.H. Chan School of Public Health, Boston, Massachusetts, USA
Marcia A. Testa
Department of Human Metabolism and Nutrition, Braun School of Public Health, Hebrew University, Jerusalem, Israel
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (R.R.H.); Epidemiology (F.B.H.); Mechanisms/pathophysiology (L.C.G., C.R.K., E.F., G.I.S. and R.A.D.); Diagnosis, screening and prevention (W.H.H.); Management (R.A.D.); Quality of life (D.C.S. and M.A.T.); Outlook (I.R., J.J.H. and R.W.); overview of Primer (R.A.D.).
Corresponding author
Correspondence to Ralph A. DeFronzo .
Ethics declarations
Competing interests.
The authors declare the following potential COI: (1) R.A.D.: Research Grant Support - AstraZeneca, Bristol Myers Squibb, Janssen; Speaker's Bureau - AstraZeneca, Novo Nordisk, Advisory Board/Consultant - AstraZeneca, Janssen, Novo Nordisk, Boehringer Ingelheim, Lexicon, Intarcia; (2) E.F.: Research Grant Support - Boehringer Ingelheim, Eli Lilly; Consultant/Speaker Bureau-Boehringer Ingelheim, Eli Lilly, Sanofi, Novo Nordisk, Janssen, AstraZeneca, Takeda, Medtronic, Intarcia; (3) C.R.K. serves as a consultant for Medimmune, Merck, Five Prime Therapeutics, CohBar, Antriabio, and Catabasis; (4) L.G. has no conflict of interest; (5) R.H. has received grant support from Hitachi, Janssen, Eli Lilly, Sanofi-Aventis and Viacyte and is a consultant/advisory board member for Alere, Amgen, AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, Clin Met, Eisai, Elcelyx, Gilead, Intarcia, Isis, Janssen, Merck, Novo Nordisk, Sanofi-Aventis, and Vivus; (6) W.H.H. has no conflict of interest; (7) J.J.H. has received grant support from Novartis and Merck and is a consultant/advisory board member for Glaxo, Smith, Kline, Novo Nordisk, and Zealand Pharmaceuticals; (8) M.A.T. has no conflict of interest; (9) R.W. serves as a consultant for Medtronics and Kamada and is on the speaker's bureau for Medtronics and Novo Nordisk; (10) F.H. has received research support from California Walnut Commission and Metegenics; (11) G.I.S. serves on scientific advisory boards for Merck and Novartis and he has received research grant support from Gilead Pharmaceuticals; (12) D.C.S. has no conflict of interest; (13) I.R. – Advisory Board: Novo Nordisk, Astra Zeneca/BMS, MSD, Eli Lilly, Sanofi, Medscape Cardiology; Consultant: Astra Zeneca/BMS, Insuline; Speaker's Bureau: Eli Lilly, Novo Nordisk, Astra Zeneca/BMS, J&J, Sanofi, MSD, Novartis, Teva; Shareholder: Insuline, Labstyle.
PowerPoint slides
Powerpoint slide for fig. 1, powerpoint slide for fig. 2, powerpoint slide for fig. 3, powerpoint slide for fig. 4, powerpoint slide for fig. 5, powerpoint slide for fig. 6, powerpoint slide for fig. 7, powerpoint slide for fig. 8, rights and permissions.
Reprints and permissions
About this article
Cite this article.
DeFronzo, R., Ferrannini, E., Groop, L. et al. Type 2 diabetes mellitus. Nat Rev Dis Primers 1 , 15019 (2015). https://doi.org/10.1038/nrdp.2015.19
Download citation
Published : 23 July 2015
DOI : https://doi.org/10.1038/nrdp.2015.19
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Prevalence of thyroid dysfunction and associated factors among adult type 2 diabetes mellitus patients, 2000–2022: a systematic review and meta-analysis.
- Rishan Hadgu
- Abebaw Worede
- Sintayehu Ambachew
Systematic Reviews (2024)
Deep learning enables the quantification of browning capacity of human adipose samples
- Pingping Shen
Journal of Big Data (2024)
Targeting aging and age-related diseases with vaccines
- Guang-Hui Liu
Nature Aging (2024)
Long-term health outcomes associated with hydration status
- Natalia I. Dmitrieva
- Manfred Boehm
- Sofia Enhörning
Nature Reviews Nephrology (2024)
Comparative impact of Roux-en-Y gastric bypass, sleeve gastrectomy or diet alone on beta-cell function in insulin-treated type 2 diabetes patients
- Matthias Lannoo
- Caroline Simoens
- Bart Van der Schueren
Scientific Reports (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Diabetes Mellitus Review
- PMID: 27093761
Diabetes mellitus is a group of physiological dysfunctions characterized by hyperglycemia resulting directly from insulin resistance, inadequate insulin secretion, or excessive glucagon secretion. Type 1 diabetes (T1D) is an autoimmune disorder leading to the destruction of pancreatic beta-cells. Type 2 diabetes (T2D), which is much more common, is primarily a problem of progressively impaired glucose regulation due to a combination of dysfunctional pancreatic beta cells and insulin resistance. The purpose of this article is to review the basic science of type 2 diabetes and its complications, and to discuss the most recent treatment guidelines.
PubMed Disclaimer
Similar articles
- Lessons for pediatricians from the diabetes control and complications trial. Malone JI. Malone JI. Pediatr Ann. 1994 Jun;23(6):295-9. doi: 10.3928/0090-4481-19940601-08. Pediatr Ann. 1994. PMID: 8078706 Review. No abstract available.
- A desktop guide to Type 2 diabetes mellitus. European Diabetes Policy Group 1999. [No authors listed] [No authors listed] Diabet Med. 1999 Sep;16(9):716-30. Diabet Med. 1999. PMID: 10510947 No abstract available.
- [Management of diabetics in the outpatient department]. Mimura G, Ishikawa K, Higa S, Futema H. Mimura G, et al. Nihon Rinsho. 1990 Dec;48 Suppl:796-802. Nihon Rinsho. 1990. PMID: 2086959 Japanese. No abstract available.
- A 64-year-old man with adult-onset diabetes. Rubenstein AH. Rubenstein AH. JAMA. 1996 Sep 11;276(10):816-22. JAMA. 1996. PMID: 8769592 No abstract available.
- Treatment of non-insulin-dependent diabetes mellitus and its complications. A state of the art review. Ilarde A, Tuck M. Ilarde A, et al. Drugs Aging. 1994 Jun;4(6):470-91. doi: 10.2165/00002512-199404060-00004. Drugs Aging. 1994. PMID: 8075474 Review.
- Prevalence of nephropathy among diabetic patients in North American region: A systematic review and meta-analysis. Zahra S, Saleem MK, Ejaz KF, Akbar A, Jadoon SK, Hussain S, Ali AI, Ifty M, Jannati SZ, Armin F, Sarker D, Islam DZ, Khandker SS, Khan MS, Alvi S. Zahra S, et al. Medicine (Baltimore). 2024 Sep 20;103(38):e39759. doi: 10.1097/MD.0000000000039759. Medicine (Baltimore). 2024. PMID: 39312314 Free PMC article.
- Macrophage Activation Syndrome in Coinciding Pandemics of Obesity and COVID-19: Worse than Bad. Engin AB, Engin ED, Engin A. Engin AB, et al. Adv Exp Med Biol. 2024;1460:919-954. doi: 10.1007/978-3-031-63657-8_31. Adv Exp Med Biol. 2024. PMID: 39287877 Review.
- Paper integrated microfluidic contact lens for colorimetric glucose detection. Isgor PK, Abbasiasl T, Das R, Istif E, Yener UC, Beker L. Isgor PK, et al. Sens Diagn. 2024 Aug 5;3(10):1743-1748. doi: 10.1039/d4sd00135d. eCollection 2024 Oct 10. Sens Diagn. 2024. PMID: 39247807 Free PMC article.
- Function and expression of N-acetyltransferases 1 and 2 are altered in lymphocytes in type 2 diabetes and obesity. Paz-Rodríguez VA, Herrera-Vargas DJ, Turiján-Espinoza E, Martínez-Leija ME, Rivera-López E, Hernández-González O, Zavala-Reyes D, García-Hernández MH, Vargas-Morales JM, Milán-Segovia RDC, Portales-Pérez DP. Paz-Rodríguez VA, et al. Biochem Biophys Rep. 2024 May 3;38:101716. doi: 10.1016/j.bbrep.2024.101716. eCollection 2024 Jul. Biochem Biophys Rep. 2024. PMID: 38737726 Free PMC article.
- Influence of Diabetes Mellitus and Universal Adhesive Application Mode on the Bond Strength of Composite Resin to Dentine. Attia R, El-Bahrawy E, Shebl E, Rashed A, El-Husseiny F. Attia R, et al. J Clin Exp Dent. 2024 Apr 1;16(4):e416-e425. doi: 10.4317/jced.61328. eCollection 2024 Apr. J Clin Exp Dent. 2024. PMID: 38725826 Free PMC article.
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Ovid Technologies, Inc.
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

- Previous Article
- Next Article
Introduction
Definitions of health disparities, health equity, and sdoh, sdoh nomenclatures and contextual factors, review of sdoh and diabetes, linkages across health care and community sectors to address sdoh, article information, social determinants of health and diabetes: a scientific review.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Felicia Hill-Briggs , Nancy E. Adler , Seth A. Berkowitz , Marshall H. Chin , Tiffany L. Gary-Webb , Ana Navas-Acien , Pamela L. Thornton , Debra Haire-Joshu; Social Determinants of Health and Diabetes: A Scientific Review. Diabetes Care 1 January 2021; 44 (1): 258–279. https://doi.org/10.2337/dci20-0053
Download citation file:
- Ris (Zotero)
- Reference Manager
Decades of research have demonstrated that diabetes affects racial and ethnic minority and low-income adult populations in the U.S. disproportionately, with relatively intractable patterns seen in these populations’ higher risk of diabetes and rates of diabetes complications and mortality ( 1 ). With a health care shift toward greater emphasis on population health outcomes and value-based care, social determinants of health (SDOH) have risen to the forefront as essential intervention targets to achieve health equity ( 2 – 4 ). Most recently, the COVID-19 pandemic has highlighted unequal vulnerabilities borne by racial and ethnic minority groups and by disadvantaged communities. In the wake of concurrent pandemic and racial injustice events in the U.S., the American College of Physicians, American Academy of Pediatrics, Society of General Internal Medicine, National Academy of Medicine, and other professional organizations have published statements on SDOH ( 5 – 8 ), and calls to action focus on amelioration of these determinants at individual, organizational, and policy levels ( 9 – 11 ).
In diabetes, understanding and mitigating the impact of SDOH are priorities due to disease prevalence, economic costs, and disproportionate population burden ( 12 – 14 ). In 2013, the American Diabetes Association (ADA) published a scientific statement on socioecological determinants of prediabetes and type 2 diabetes ( 15 ). Toward the goal ofunderstanding and advancing opportunities for health improvement among the population with diabetes through addressing SDOH, ADA convened the current SDOH and diabetes writing committee, prepandemic, to review the literature on 1 ) associations of SDOH with diabetes risk and outcomes and 2 ) impact of interventions targeting amelioration of SDOH on diabetes outcomes. This article begins with an overview of key definitions and SDOH frameworks. The literature review focuses primarily on U.S.-based studies of adults with diabetes and on five SDOH: socioeconomic status (education, income, occupation); neighborhood and physical environment (housing, built environment, toxic environmental exposures); food environment (food insecurity, food access); health care (access, affordability, quality); and social context (social cohesion, social capital, social support). This review concludes with recommendations for linkages across health care and community sectors from national advisory committees, recommendations for diabetes research, and recommendations for research to inform practice.
Table 1 displays definitions of key terms. Differences in diabetes risk and outcomes can result from multiple contributors, including biological, clinical, and nonclinical factors ( 1 ). A substantial body of scientific literature demonstrates the adverse impact of a particular type of difference, health disparities ( 16 ) in diabetes ( 1 , 17 , 18 ). A preponderance of health disparities research in the U.S. has examined disparities by race and ethnicity ( 3 , 19 ). Internationally, the term health equity has traditionally been used to encompass the range of population inequalities resulting from demographic and economic characteristics, and this term is used increasingly in the U.S. ( 20 – 24 ). Addressing healthy equity necessitates an understanding of social and environmental factors that combined account for 50% to 60% of health outcomes ( 22 , 25 ). These social and environmental factors collectively are known as SDOH ( 21 , 26 , 27 ).
Definitions
| Term . | Definition . |
|---|---|
| Health disparities | A particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage. Health disparities adversely affect groups of people who have systematically experienced greater obstacles to health based on their racial or ethnic group; religion; socioeconomic status; sex; age; mental health; cognitive, sensory, or physical disability; sexual orientation or gender identity; geographic location; or other characteristics historically linked to discrimination or exclusion ( ). |
| Health equity | Equity is the absence of avoidable, unfair, or remediable differences among groups of people, whether those groups are defined socially, economically, demographically, or geographically or by other means of stratification. “Health equity” or “equity in health” implies that ideally everyone should have a fair opportunity to attain their full health potential and that no one should be disadvantaged from achieving this potential ( ). |
| Health equity is attainment of the highest level of health for all people. Achieving health equity requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and the elimination of health and health care disparities ( ). | |
| Social determinants of health (SDOH) | The social determinants of health are the conditions in which people are born, grow, live, work, and age. These circumstances are shaped by the distribution of money, power, and resources at global, national, and local levels. The social determinants of health are mostly responsible for health inequities—the unfair and avoidable differences in health status seen within and between countries ( ). |
| Term . | Definition . |
|---|---|
| Health disparities | A particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage. Health disparities adversely affect groups of people who have systematically experienced greater obstacles to health based on their racial or ethnic group; religion; socioeconomic status; sex; age; mental health; cognitive, sensory, or physical disability; sexual orientation or gender identity; geographic location; or other characteristics historically linked to discrimination or exclusion ( ). |
| Health equity | Equity is the absence of avoidable, unfair, or remediable differences among groups of people, whether those groups are defined socially, economically, demographically, or geographically or by other means of stratification. “Health equity” or “equity in health” implies that ideally everyone should have a fair opportunity to attain their full health potential and that no one should be disadvantaged from achieving this potential ( ). |
| Health equity is attainment of the highest level of health for all people. Achieving health equity requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and the elimination of health and health care disparities ( ). | |
| Social determinants of health (SDOH) | The social determinants of health are the conditions in which people are born, grow, live, work, and age. These circumstances are shaped by the distribution of money, power, and resources at global, national, and local levels. The social determinants of health are mostly responsible for health inequities—the unfair and avoidable differences in health status seen within and between countries ( ). |
The writing committee reviewed the following commonly referenced SDOH frameworks for classifications and terminology: the World Health Organization (WHO) Commission on Social Determinants of Health ( 28 ), Healthy People 2020 ( 29 , 30 ), the County Health Rankings Model ( 31 , 32 ), and Kaiser Family Foundation Social Determinants of Health factors ( 33 ).
No single consensus set of factors define SDOH. Nomenclatures used by each framework, for shared SDOH factors, are depicted in Fig. 1 . Common among the frameworks is placement of economic and socioeconomic determinants as foremost. Food SDOH factors (e.g., insecurity and access) are classified as economic stability ( 29 ), neighborhood and built environment ( 29 ), material circumstances ( 28 ), or as an independent category ( 33 ). Housing is classified as material circumstances ( 28 ), economic stability ( 29 ), or neighborhood and built environment ( 33 ). Environmental exposures (i.e., toxins, air pollution, and water quality) are classified as neighborhood and physical environment ( 31 ) or built environment ( 29 ). Social environment is represented as community and societal context ( 29 , 33 ), social cohesion and social capital ( 28 ), or social factors ( 31 ). Health care is a SDOH in the WHO, Healthy People 2020, and County Health Rankings models, with access factors as primary, with or without quality of care factors.

Nomenclatures for shared determinants among four social determinants of health frameworks, the World Health Organization Commission on the Social Determinants of Health, the U.S. Department of Health and Human Services Healthy People 2020, the County Health Rankings Model, and the Kaiser Family Foundation Social Determinants of Health framework.
Each framework posits complex interactions among SDOH factors. WHO additionally maps causal priority among the determinants. For example, the upstream sociopolitical context and resulting socioeconomic position are root cause, structural determinants of health inequities that work through intermediary sets of determinants to cause health inequities. WHO positions the health system as an SDOH that plays a role in mediating impact of intermediary determinants on health outcomes ( 28 ).
SDOH inclusion in this review was determined by representation within one or more existing SDOH frameworks and presence of a sufficient body of literature to demonstrate influence of the determinant on diabetes. The reviewed SDOH are shown in Table 2 . Studies of primarily adult populations are described, and the terms type 2 diabetes mellitus (T2DM), type 1 diabetes mellitus (T1DM), and “diabetes” (indicating either a mixed T2DM and T1DM sample or diabetes case ascertainment methods that do not enable specifying clinical diagnostic type) are used in accordance with the terminology used in the respective studies.
SDOH and component factors included in the diabetes review
| Socioeconomic status . | Neighborhood and physical environment . | Food environment . | Health care . | Social context . |
|---|---|---|---|---|
| Education | Housing | Food security | Access | Social cohesion Social capital Social support |
| Income | Built environment | Food access | Affordability Quality | |
| Occupation | Toxic environmental exposures | Food availability |
| Socioeconomic status . | Neighborhood and physical environment . | Food environment . | Health care . | Social context . |
|---|---|---|---|---|
| Education | Housing | Food security | Access | Social cohesion Social capital Social support |
| Income | Built environment | Food access | Affordability Quality | |
| Occupation | Toxic environmental exposures | Food availability |
Socioeconomic Status and Diabetes
Socioeconomic status (SES) is a multidimensional construct that includes educational, economic, and occupational status ( 34 – 36 ). SES is a consistently strong predictor of disease onset and progression at all levels of SES for many diseases, including diabetes ( 37 ). SES is linked to virtually all of the established SDOH. It is associated with the extent to which individuals and communities can access material resources including health care, housing, transportation, and nutritious food and social resources such as political power, social engagement, and control.
The three components of SES are intercorrelated ( 38 ), but each aspect has unique implications for health. Each component can be assessed at the individual or population level ( 39 ). For example, economic status is often measured by determining a person’s own income. However, it is also assessed by the income of the household in which the person resides and by the income level of the community (e.g., mean household income of the census track in which a person resides) as a proxy for the individual’s household income. Census-level household income also operates as a contextual variable, reflecting the composition and available resources in a defined area.
Educational status can be quantified either in years of schooling or highest degree earned. It may be assessed at the level of the individual (e.g., the person’s own educational attainment), the household (the highest grade completed by anyone in the household), or the community (e.g., percent of high school or college graduates in a census track). Quantity of education does not capture differences in quality of education that may be relevant to SES measurement ( 38 ). Literacy has emerged as a measure of educational quality and as potentially more reflective of SES than years of schooling among African Americans and low-income Whites ( 40 , 41 ). Health literacy, which is directly associated with literacy and is context specific ( 42 – 44 ), and literacy are included as SDOH in Healthy People 2020 ( 29 ).
Occupation is itself multidimensional. It has been measured as employment status (e.g., employed vs. unemployed), stability (e.g., job insecurity), job type (e.g., manual vs. nonmanual, prestige of the occupation), and working conditions (e.g., shift work, number of hours worked, job demands, and control) ( 39 , 45 ). For members of large organizations, occupational hierarchies of job titles capture work conditions as well as qualifications and pay (e.g., civil service grades).
Associations of SES With Diabetes Incidence, Prevalence, and Outcomes
Income, education, and occupation show a graded association with diabetes prevalence and complications across all levels of SES, up to the very top. Those lower on the SES ladder are more likely to develop T2DM, experience more complications, and die sooner than those higher up on the SES ladder ( 46 , 47 ). The higher a person’s income, the greater their educational attainment, and the higher their occupational grade, the less likely they are to develop T2DM or to experience its complications. The gradient is steeper at the bottom, however, and research has focused primarily on those with the lowest levels of income and education.
Prevalence of diabetes increases on a gradient from highest to lowest income ( 48 , 49 ). In data from the National Health Interview Survey (NHIS) covering 2011–2014, Beckles and Chou ( 50 ) found increasing diabetes prevalence at lower levels of income as reflected in the levels of ratio of income to poverty level. Compared with those with high income, the relative percentage difference in prevalence of diabetes for those classified as middle income, near poor, and poor, was 40.0%, 74.1%, and 100.4%, respectively. The difference in diabetes prevalence by income was greater during this time period than it had been in a prior period (1999–2002), pointing to widening disparities in diabetes prevalence associated with income.
At the neighborhood level, differences in diabetes prevalence by census track are attributable to SES ( 51 , 52 ). For example, in a recent study by Kolak et al. ( 52 ), rate of T2DM was found to be significantly higher and concentrated in census tracts characterized by factors including lower incomes, lower high school graduation rates, more single-parent households, and crowded housing. Living in neighborhood census tracts with lower educational attainment, lower annual income, and larger percentage of households receiving Supplemental Nutrition Assistance Program benefits has been associated with higher risk of progression to T2DM among adults with prediabetes ( 53 ).
Gaskin et al. ( 49 ) examined the interaction of individual poverty with neighborhood poverty and found that, compared with nonpoor adults living in nonpoor neighborhoods, poor adults living in nonpoor neighborhoods have increased odds of having diabetes, and poor adults living in poor neighborhoods have twofold higher odds of having diabetes. In addition, a race-poverty-place gradient was observed. Compared with nonpoor Whites in nonpoor neighborhoods, odds of diabetes were highest for poor Whites in poor neighborhoods (odds ratio [OR] 2.51, 95% CI = 1.31–4.81), followed by poor Blacks in poor neighborhoods and nonpoor Blacks in poor neighborhoods (OR 2.45, 95% CI 1.50–4.01, and OR 2.49, 95% CI 1.48–4.19), and finally poor Whites in nonpoor neighborhoods (OR 1.73, 95% CI 1.16–2.57) ( 49 ).
Adults with T2DM who have a family income below the federal poverty level have a twofold higher risk of diabetes-related mortality compared with their counterparts in the highest family income levels ( 54 ). This pattern of diabetes-related mortality has been observed specifically in adults with T1DM as well ( 55 ). A meta-analysis by Bijlsma-Rutte et al. ( 56 ) observed an inverse association between income and HbA 1c levels in people with T2DM, with a pooled mean difference in HbA 1c of 0.20% (95% CI −0.05 to 0.46) between people with low and high income. Low income is associated with a higher risk of experiencing diabetic ketoacidosis among youth and adults with T1DM ( 57 ) and with higher HbA 1c levels, particularly among racial/ethnic minority youth with lower SES ( 58 , 59 ).
Age-adjusted incidence of diagnosed diabetes in adults is associated also with educational level in a stepwise pattern. Diabetes incidence is highest (10.4 per 1,000 persons) for adults with less than a high school education, 7.8 per 1,000 persons for those with a terminal high school education, and 5.3 per 1,000 persons for those with more than a high school education ( 60 ). Diabetes prevalence in the adult U.S. population is similarly inversely associated with educational level in a stepwise pattern. In the U.S., the age-adjusted prevalence of diagnosed diabetes is 12.6% for those with less than a high school education, 9.5% for those with a high school education, and 7.2% for those with more than a high school education ( 61 ). Having a college education or more is associated with the lowest odds of diabetes ( 62 ). Mirroring findings on income, temporal trends in diabetes prevalence at different levels of education show increasing disparities in prevalence associated with educational attainment ( 50 ).
The risk of diabetes-related mortality demonstrates a gradient from lowest to highest education level. Compared with adults with a college degree or higher, having less than high school education is associated with a twofold higher mortality from diabetes (relative hazard 2.05, 95% CI 1.78–2.35) ( 54 ). In adults with T1DM, not having a college degree is associated with a threefold higher mortality from diabetes compared with counterparts with a college degree ( 63 ). Lower educational level is associated with higher HbA 1c , with a meta-analysis ( 56 ) reporting a pooled mean difference in HbA 1c of 0.26% (95% CI, 0.09–0.43) between people with low and high educational levels. Regarding literacy/health literacy as a SDOH, Marciano et al. ( 64 ) conducted a meta-analysis of 61 studies of 18,905 adults with T1DM or T2DM to determine associations of health literacy with several diabetes outcomes and found that higher levels of health literacy were significantly associated with lower HbA 1c levels and better diabetes knowledge, but not with more frequent self-management activities.
Occupation.
Systematic reviews and meta-analyses have examined several aspects of occupation in relation to diabetes risk, although most of this research has been conducted outside of the U.S. Ferrie et al. ( 65 ) conducted a meta-analysis of associations of job insecurity with incident diabetes and found an association of high job insecurity with higher risk of incident diabetes (OR 1.19, 95% CI 1.09–1.30). A meta-analysis by Varanka-Ruuska et al. ( 66 ) found that unemployment was associated with increased odds of both prediabetes (OR 1.58, 95% CI 1.07–2.35) and T2DM (OR 1.72, 95% CI 1.14–2.58). Exposure to shift work is associated with higher risk of diabetes than working normal daytime schedules ( 67 ). A meta-analysis by Kivimäki et al. ( 68 ) reported an association of long work hours (≥55 h per week) as compared with standard work hours (35–40 h per week) with higher incident diabetes in adults with low SES but not in adults with high SES. A U.S. population-based survey on diabetes and occupation found highest prevalence of diabetes among transportation workers and lowest prevalence of diabetes among physicians ( 69 , 70 ).
SES Interventions and Diabetes Outcomes
To date, there is no body of literature describing impact of change in income, change to higher educational status, or different employment/occupational status on diabetes outcomes, although income and wage changes, and job changes and loss, do occur naturalistically. Similarly, no diabetes outcomes have been reported from interventions directly targeting living wages, early childhood education, educational quality, or educational access for poor children and families. Studies have examined diabetes self-management interventions in the setting of low literacy/health literacy, particularly among racial/ethnic minority adults with T2DM and have demonstrated effectiveness of low-literacy adaptions ( 71 ) and health literacy and numeracy tools in improving diabetes knowledge and self-care ( 72 – 74 ). A meta‐analysis of nine intervention trials with 1,874 adults with T2DM found that literacy-sensitive interventions were associated with a small but statistically significant decrease in HbA 1c (–0.18%; 95% CI –0.36 to –0.004) in comparison with usual clinical care ( 75 ) in patients regardless of health literacy status. Literacy-adapted education and tools may need to be combined with more comprehensive evidence-based behavioral self-management intervention approaches to achieve substantive clinical improvements in racial/ethnic minority populations with T2DM and low literacy/health literacy ( 76 , 77 ). In conclusion, despite the long-standing evidence for SES as a key determinant both of diabetes risk and outcomes, systematic investigation of impact on diabetes of change in SES remains a gap in the literature.
Neighborhood and Physical Environment and Diabetes
The neighborhood environment in which one lives has been of major interest as a setting in which to understand contextual and multilevel influences on health ( 78 ). Diez Roux and Mair ( 78 ) have described the role of historical and contemporary residential segregation by race, ethnicity, and SES as the socioeconomic and political context that produced the patterns of unequal resource distribution resulting in neighborhood environments that maintain health inequities. Tung et al. ( 79 ) also discuss the multiple intricacies associated with how race, place, and poverty converge in a dynamic way across various spatial contexts and circumstances to influence health and propose that understanding the intersection of these contextual influences is needed to prevent diabetes inequities. Neighborhood and physical environment factors of housing, built environment, and environmental exposures are reviewed.
Stable housing is a key indicator of economic stability ( 80 ) and a core SDOH ( 80 ). Housing instability refers to a spectrum of situations that can range from living in one’s car, staying with relatives or friends, having trouble paying rent, suffering evictions or frequent moves, paying more than 50% of income in rent, and living in crowded conditions (historically defined as having more than one person per room) to homelessness—the most extreme form of unstable housing ( 81 – 85 ). Homelessness is defined as “lacking a regular nighttime residence or having a primary nighttime residence that is a temporary shelter or other place not designed for sleeping” ( 86 ). As of 2020, the U.S. government reported 567,715 or 17 of 10,000 people in the country are homeless; African Americans accounted for 40% of people experiencing homelessness, while those identifying as Hispanic or Latino comprised 22% of the homeless population ( 87 ). A common theme in conceptual models linking housing instability to poor health is that the instability inherent to the situation makes it difficult to attend to preventive services and self-care ( 83 , 88 – 90 ), leading to worse control of chronic conditions, higher use of acute-care services like emergency departments, and higher likelihood of complications ( 91 – 93 ).
Associations of Housing Instability With Diabetes Incidence, Prevalence, and Outcomes.
The prevalence of diabetes among those with housing instability in the U.S., and whether it differs from that among those without housing instability, is not known. A key limitation for the field is that there is no single, accepted definition of housing instability or a commonly used assessment instrument. Further, because housing instability is more likely to occur among individuals with lower SES—which is independently associated with higher diabetes prevalence—it is unclear whether housing instability is causally related to developing diabetes. One systematic review did not find higher diabetes prevalence than in the general population among persons experiencing homelessness, estimating approximately 8% prevalence in adults who do and do not experience homelessness ( 94 ). A recent study using nationally representative data from individuals seen in community health centers found that approximately 37% of individuals with diabetes reported housing instability. This study also found that individuals with diabetes and housing instability were more likely to self-report having an emergency department visit or hospitalization for their diabetes (adjusted OR 5.17, 95% CI 2.08–12.87) ( 82 ). A cross-sectional study in a single health care system found that housing instability among individuals with diabetes was associated with higher outpatient utilization (incident rate ratio 1.31, 95% CI 1.14–1.51) ( 95 ). Though not specific to diabetes, additional work has linked housing instability to poor health outcomes and reduced health care access ( 91 , 96 – 100 ). A longitudinal study in the Department of Veterans Affairs (VA) health care system found that experiencing homelessness was associated with higher adjusted odds of having an HbA 1c >8.0% and >9.0%. Vijayaraghavan et al. ( 84 ) identified unstable housing as a key barrier to diabetes care among low-income individuals. There was an observed linear decrease in diabetes self-efficacy as housing instability increased (β-coefficient −0.94, 95% CI −1.88 to −0.01, P < 0.01), which was partially mediated by food insecurity. Qualitative work has found that unstable housing makes it more difficult to engage in self-care, follow self-management routines, afford diabetes medications and supplies, and eat healthy foods ( 91 , 92 ). Choice of medication is important, and considerations should include medication cost and the ability to store medication and diabetes care supplies safely. Brooks et al. provide a narrative review of considerations for diabetes treatment among individuals experiencing homelessness ( 101 ).
Housing Instability Interventions and Diabetes Outcomes.
Given its expense, housing is one of the most difficult health-related social needs to intervene upon. Housing intervention studies reporting diabetes outcomes are few; however, there is some high-quality evidence for housing interventions. The Moving To Opportunity for Fair Housing Demonstration Project (MTO), a randomized social experiment conducted through the Department of Housing and Urban Development, in partnership with behavioral scientists and other federal agencies, was designed to determine what impact moving from a high-poverty to a low-poverty census tract would have on multiple outcomes ( 102 , 103 ). In 1994–1998, MTO randomized 4,498 women with children living in public housing within high-poverty census tracts in five cities to one of three study arms. The 1,788 women in the experimental arm received Section 8 vouchers usable only in low-poverty areas (census tracts with <10% of the population below the poverty line) along with counseling and assistance in finding a private rental unit. The 1,312 women in the Section 8 arm received traditional unrestricted vouchers and the usual briefing the local Section 8 program provided. The 1,398 women in the control arm received no vouchers but continued to receive MTO project-based assistance. Those who received vouchers could choose whether to use the vouchers or not. Findings from the follow-up survey in 2008 through 2010 found a 21.6% relative reduction in prevalence of an elevated HbA 1c (>6.5%) in the group that moved to low-poverty census tracts compared with the control group, with an absolute difference of 4.31 percentage points (95% CI −7.82 to −0.80). The low-poverty group also had relative reductions of 13.0% in prevalence of BMI ≥35 and relative reduction of 19.1% in BMI ≥40 kg/m 2 , with absolute differences of 4.61 percentage points (95% CI −8.54 to −0.69) and 3.38 percentage points (95% CI −6.39 to −0.36), respectively ( 102 ). The usual vouchers and control arms did not differ. Other MTO outcomes among the group randomized to low-poverty census tracts included higher housing quality, education, employment, and earnings as well as multiple additional improvements to child and adult health ( 103 ). A 10–15 year follow-up study found substantial and sustained reductions in diabetes prevalence, rates of extreme obesity, and improvement in mental health outcomes among the adults who received vouchers to move to low-poverty neighborhoods and reduction in extreme obesity among the adults who received Section 8 vouchers ( 104 ). While not specific to diabetes, a meta-analysis of randomized trials that provided low-barrier housing support for individuals experiencing homelessness found significant reductions in health care utilization ( 105 ).
Housing interventions may facilitate access to diabetes care. The Collaborative Initiative to End Chronic Homelessness provided adults who were chronically homeless with permanent housing and supportive primary health care and mental health services ( 106 ). Placed persons were more likely to receive evaluation and management services (relative risk [RR] 1.03, 95% CI 1.01–1.04) than unplaced persons ( 107 ). Placed persons were more likely to receive HbA 1c tests (RR 1.10, 95% CI 1.02–1.19) and lipid tests (RR 1.09, 95% CI 1.02–1.17), while for those without baseline diabetes placement was associated with lower risk of new diabetes diagnoses (RR 0.87, 95% CI 0.76–0.99). Keene et al. ( 91 ) suggest the relationship of stable housing to diabetes management is due to its role as a foundation for prioritizing care and allowing for the routinization of diabetes management, critical to disease control. This suggests the benefits of supportive and stable housing may be extended to diabetes care and prevention. A naturalistic qualitative study of the impact of transitioning to rental-assisted housing among low-income, housing-insecure adults with T2DM reported that rental assistance afforded individuals more environmental and financial control over life circumstances, thereby enabling diabetes routines and allocation of financial resources to diabetes care ( 108 ).
Built Environment
The built environment, as defined by the U.S. Centers for Disease Control and Prevention (CDC), includes the physical parts of where people live and work, such as infrastructure, buildings, streets, and open spaces ( 109 ). Here, built environment factors of walkability and greenspace are reviewed.
Associations of Built Environment with Diabetes Incidence, Prevalence, and Outcomes.
A robust literature has demonstrated associations of the built environment with obesity-related outcomes ( 110 – 113 ). However, a smaller body of research has examined associations of the built environment with diabetes specifically. Smalls et al. ( 114 ) reported significant associations of both walking environment (β = −0.040) and neighborhood activities (β = −0.104) with exercise in a southeastern U.S. population with diabetes. A recent U.S. review and meta-analysis by Chandrabose et al. ( 113 ) examined longitudinal studies of the built environment and cardiometabolic health. Results showed strong evidence for impact of walkability on T2DM outcomes, with four of seven studies (57%) showing significant findings in the aggregated analyses using objective and perceived measures of walkability. Although the methods to determine mediation by physical activity in most studies were ineffective to make conclusions, one study tested the indirect effect of walkability on 10-year change in HbA 1c and found a partial mediation effect for self-reported physical activity using structural equation modeling. For other measures of built environment, such as neighborhood recreational facilities or destinations/routes, there was insufficient data to examine the relationship with T2DM outcomes. A larger body of research on built environment and diabetes has been conducted in countries outside of the U.S ( 110 – 112 ). In these studies, neighborhood physical activity (PA) environments, specifically better walkability of neighborhoods and access to greenspace, have been consistently associated with lower risk of T2DM and better outcomes ( 115 , 116 ). Numerous studies have been conducted on walkability measured by macroscale aspects of the neighborhood, including higher population density, land use mix, and aesthetics, to microscale aspects, including sidewalks, street connectivity, and street safety. A review by Bilal et al. ( 115 ) on walkability and diabetes incidence and prevalence found that more walkable neighborhoods are associated with a lower incidence and prevalence of T2DM. Similarly, Twohig-Bennett and Jones ( 117 ) conducted a systematic review and meta-analysis examining the relationship to diabetes outcomes of “high” and “low” exposure to greenspace in neighborhoods (defined as open, undeveloped land with natural vegetation and/or spaces such as parks and tree-lined areas). The meta-analysis, representing 462,220 participants, showed an association of high exposure with reductions in the incidence of T2DM (OR 0.71, 95% CI 0.61–0.85) ( 117 ). After decades of research, many built environment factors related to PA and obesity risk have been identified for consideration in urban planning ( 118 ).
Neighborhood-Level Interventions on the Built Environment and Diabetes Outcomes.
Because it is often not feasible or ethical to randomize neighborhoods to receive certain structural interventions, natural experiment designs are used in which the researcher does not control or withhold intervention allocation to particular areas; rather, natural or predetermined variation in allocation occurs, often as a result of policy intervention ( 119 ). Several review articles of natural experiments summarize the benefits of policy and built environment changes on obesity-related outcomes ( 112 ) and diet and PA outcomes ( 120 , 121 ). The strongest diet-related studies were those that evaluated regulations to the food environment, and the strongest PA-related studies were those that improved infrastructure for active transport. Although this literature does not directly address diabetes outcomes, improvements in obesity and diet and PA behaviors are relevant to populations with diabetes and warrant rigorous evaluation ( 122 ).
Toxic Environmental Exposures
Toxic environmental exposures can be naturally occurring (e.g., arsenic in private wells, radon) or introduced into the environment through human activity (e.g., pollution, synthetic pesticides) ( 123 ). Marginalized communities in the U.S. are disproportionately exposed to environmental agents that have evidence of an association with diabetes, including air pollution, environmental toxicants, and ambient noise ( 124 – 129 ), and subgroups that generate the least pollution have highest exposures ( 130 ).
Factors contributing to inequities in toxic environmental exposures include residential segregation and inequity in goods and services, due in part to systemic racism in environmental regulation and opportunities ( 128 , 130 – 133 ). Explanatory factors are closer proximity of underserved neighborhoods to nearby pollution sources, poor enforcement of regulations, and inadequate response to community complaints ( 134 – 138 ). In rural and suburban communities, including Native American Indian communities, unregulated private wells are a source of water contaminants including arsenic and other metals/metalloids, pesticides, and hazardous chemicals, affecting millions of people ( 139 – 141 ). Both food packaging and fast-food consumption, which can be high in low-income neighborhoods, can expose people to chemicals known to be endocrine disrupters ( 142 – 145 ). Examples include chemicals released from plastic packaging during microwave heating ( 142 ), higher urinary phthalate levels associated with fast food ( 145 ), and higher urinary bisphenol A levels from canned foods ( 146 ). Certain personal care and cosmetic products, which are a source of phthalates and metals (e.g., skin-lightening products, which are high in mercury), are disproportionately marketed to marginalized population subgroups ( 147 ).
Associations of Environmental Risk Factors With Diabetes Incidence, Prevalence, and Outcomes.
In 2011, the National Toxicology Program at the National Institute of Environmental Health Sciences convened an international workshop to evaluate the experimental and epidemiologic evidence on the relationship of environmental chemicals with obesity, diabetes, and metabolic syndrome ( 148 – 150 ). Evidence was deemed strongest for arsenic, with relative risks of diabetes found to range from 1.11 to 10.05 in different studies (median 2.69) at high arsenic exposure levels. More recent systematic reviews and meta-analyses present the growing literature examining multiple groups of chemicals ( 148 , 151 ) or specific groups of chemicals ( 152 – 154 ). Overall, the evidence supports an increased risk of diabetes in populations exposed to environmental chemicals including arsenic, persistent organic pollutants, phthalates, and possibly bisphenol.
In 11 prospective studies of air pollution exposure and incident diabetes in adults, the pooled hazard ratio (HR) (95% CI) per 10 µg/m 3 increment particulate matter of <2.5 µm aerodynamic diameter was 1.10 (1.04–1.17) ( 155 ). Other reviews have reached conclusions consistent with this increased diabetes risk finding ( 156 – 158 ). The epidemiologic evidence is also supported by animal experiments showing that air pollution exposure can increase susceptibility to insulin resistance and T2DM ( 159 – 161 ). These findings highlight that populations more exposed to air pollution are also disproportionately at risk for developing diabetes.
There is epidemiologic and experimental evidence that environmental exposures increase susceptibility to cardiovascular disease (CVD) in people with diabetes. The evidence is extensive for air pollution exposures ( 162 , 163 ). For example, in Medicare patients, a daily increase of 10 µg/m 3 in particulate matter <10 µm of aerodynamic diameter was associated with 2.01% increase in CVD hospitalizations for those with diabetes compared with 0.94% increase among those without diabetes ( 162 ). Short-term increases in air pollution exposure are also related to higher risk of stroke mortality in patients with diabetes compared with those without ( 164 ). In an experimental model, mice with diabetes exposed to diesel exhaust particles showed increased cardiovascular susceptibility compared with mice without diabetes ( 165 ). In natural experiments in human populations, air pollution exposure also resulted in increased vascular reactivity ( 166 ) and inflammation in patients with diabetes compared with those without ( 167 ). In addition to air pollution, some evidence is also available for metals. In the Strong Heart Study of American Indian adults followed since 1989–1991, the risk of CVD associated with higher exposure to arsenic and cadmium was higher among participants with diabetes compared with those without diabetes ( 168 , 169 ). In a clinical trial in patients with a previous myocardial infarction (Trial to Assess Chelation Therapy [TACT]), the beneficial effects of repeated chelation with disodium edetate on cardiovascular outcomes were greater in patients with diabetes ( 170 ).
Environmental Exposures Interventions and Diabetes.
Few studies have evaluated the effect of population-based or clinical interventions related to environmental exposures and diabetes prevention or control. The increased risk of diabetes in populations exposed to environmental chemicals and the increased susceptibility for diabetes complications in individuals with diabetes exposed to air pollution potentially provides an opportunity for prevention and treatment that can be particularly relevant for the most vulnerable populations. For example, a comparison of preterm births among four studies in different countries, before and after the implementation of smoke-free legislation, has shown reductions in diabetes risk (pooled risk change −18.4%, 95% CI −18.8 to −2), although the long-term benefits have not yet been evaluated ( 171 ).
Because individuals generally have limited control over environmental agents, the most effective interventions will be at the population level, through policy and regulation, with a particular focus on protecting marginalized and underserved populations. There is evidence that declines in air pollution levels and metal exposures have contributed to improvements in CVD development ( 172 , 173 ); benefits for diabetes development are pending. Research is also needed to test intermediate strategies at the clinical level, such as exposure screening (e.g., asking about living near highways or using private wells for drinking water) and recommendations to test air or water, reduce known sources of exposure (e.g., minimize packaged foods, avoid heating food in plastic containers, and minimize use of certain cosmetic products), and make home interventions (e.g., install filters for air or water contaminants) ( 174 – 176 ).
Food Environment and Diabetes
The food environment can be defined as the physical presence of food that affects a person’s diet; a person’s proximity to food store locations; the distribution of food stores, food service, and any physical entity by which food may be obtained; or a connected system that allows access to food ( 177 ). It is the “collective physical, economic, policy and sociocultural surroundings, opportunities and conditions that influence people’s food and beverage choices and nutritional status” ( 178 ). It is also referred to as the community food environment (e.g., number, type, location, and accessibility of food outlets such as food stores, markets, or both) and the consumer-level environment (e.g., healthful, affordable foods in stores, markets, or both), which interact to affect food choices and diet quality ( 179 , 180 ). Key dimensions of the food environment include accessibility, availability, affordability, and quality ( 181 – 184 ). These factors, which define the quality of the food environment, are of particular importance in marginalized communities, which may have poor access to supermarkets and healthy foods but abundant access to fast-food outlets and energy-dense foods and are often disproportionately impacted by physical hazards (e.g., vacant houses, traffic, and crime) ( 78 ). At their root, differences in the food environment can be caused by government policies and incentives, and the legacy of such policies as redlining and segregation.
Associations of Food Environment With Diabetes Incidence, Prevalence, and Outcomes
Food access and availability..
Cross-sectional studies have shown associations between food access, availability, geographic characteristics, and T2DM prevalence. Ahern et al. ( 185 ) examined 3,128 counties across the U.S. for food access (assessed as percent of households with no car living more than one mile from a grocery store) and food availability (assessed as number of fast-food restaurants, full-service restaurants, grocery stores, convenience stores, and per capita sales in dollars from local farms made directly to consumers). Higher access to food was associated with lower T2DM rates in metro and nonmetro counties, and higher availability of full-service restaurants and grocery stores and lower availability of fast-food and convenience stores were associated with lower diabetes rates ( 185 ). Haynes-Maslow and Leone ( 186 ) similarly found availability of full-service restaurants to be associated with lower prevalence of diabetes in adults and availability of fast-food restaurants generally to be associated with higher diabetes prevalence. However, the study reported variability in associations among numerous food environment characteristics based on county composition (low poverty/low minority, low poverty/medium minority, high poverty/low minority), highlighting complexities in understanding patterns among variables of county socioeconomic status, demographics, food availability, and diabetes prevalence ( 186 ).
Several observational, longitudinal studies report neighborhood resources in general, and access and availability of the food environment in particular, as associated with diabetes prevalence and incidence ( 187 ). A systematic review by den Braver et al. ( 188 ) found availability of fast-food outlets and convenience stores to be associated with higher T2DM risk/prevalence and perceived healthfulness of the food environment to be associated with lower diabetes risk/prevalence, but no association was found between density of grocery stores and T2DM risk/prevalence. Heterogeneity across the studies prevented the conduct of meta-analyses. Gabreab et al. ( 189 ) examined neighborhood, social, and physical environments and T2DM in 3,700 African Americans through the Jackson Heart Study and found higher density of unfavorable food stores was associated with a 34% higher T2DM incidence after adjusting for individual-level risk factors. In a longitudinal employee cohort, Herrick et al. ( 190 ) found that living in a zip code with higher supermarket density was associated with a reduction in T2DM risk, while zip codes with a higher percentage of poverty and zip codes with higher walkability scores were both associated with higher diabetes risk. Christine et al. ( 191 ) reported long-term exposure to residential environments that offer resources to support healthy diets and PA was associated with a lower incidence of T2DM, although results varied by measurement method.
Studies have also examined both food and PA environments in combination and diabetes risk. Meyer et al. ( 192 ) combined measures of neighborhood food and PA environments and weight-related outcomes ( N = 14,379) of the Coronary Artery Risk Development in Young Adults (CARDIA) study, examining population density–specific (less than vs. greater than 1,750 people per square kilometer) clusters of neighborhood indicators: road connectivity, parks and PA facilities, and food stores/restaurants. In lower–population density areas, higher food and PA resource diversity relative to other clusters was significantly associated with higher diet quality ( 192 ). In higher–population density areas, a cluster with relatively more natural food/specialty stores, fewer convenience stores, and more PA resources was associated with higher diet quality. Neighborhood clusters were inconsistently associated with BMI or insulin resistance and not associated with fast-food consumption, or walking, biking, or running ( 192 ). Tabaei et al. ( 193 ) examined associations of residential socioeconomic, food, and built environments with glycemic control in adults with diabetes ascertained from the New York City A1C Registry from 2007 to 2013. Individuals who lived continuously in the most advantaged residential areas, including greater ratio of healthy food outlets to unhealthy food outlets and residential walkability, achieved increased glycemic control and took less time to achieve glycemic control compared with the individuals who lived continuously in the least advantaged residential areas ( 193 ).
Food Affordability.
Kern et al. ( 194 ) note that it is reasonable to expect that large differences in price between healthy and unhealthy foods would lead to differences in purchasing patterns and resulting diets and that those differences would be more prominent for individuals of lower SES. In a longitudinal study, they examined food affordability and neighborhood price of healthier food relative to unhealthy food and its association with T2DM and insulin resistance. Higher prices of healthy foods relative to unhealthy foods were found to be associated with lower odds of having a high-quality diet; however, there was no association with diabetes incidence or prevalence ( 194 ). More studies are needed in this area.
Food Insecurity.
Food insecurity is defined as not having adequate quantity and quality of food at all times for all household members to have an active, healthy life ( 195 , 196 ). Approximately 20% of diabetes patients report household food insecurity ( 197 ), and food insecurity is a risk factor for poor diabetes management ( 196 ). Researchers have investigated several pathways through which food insecurity may worsen T2DM outcomes ( 198 – 200 ). First, in the nutritional pathway , food insecurity is associated with lower diet quality ( 201 ), which is in turn associated with higher HbA 1c . Food insecurity incentivizes more affordable, energy-dense foods that can directly raise serum glucose (e.g., refined carbohydrates, processed snacks and sweets, sugar-sweetened beverages, etc.) and may lead to greater insulin resistance ( 202 , 203 ). Conversely, low or inconsistent food availability can increase risk of hypoglycemia. Second, via a compensatory pathway , behavioral strategies necessary to cope with the immediate problem of food insecurity can inadvertently undermine T2DM management. For example, financial resources that might otherwise have been used for medications or diabetes care supplies are diverted to meet dietary needs ( 197 , 204 – 206 ). Third, through the psychological pathway , the state of food insecurity, in which meeting basic needs is outside an individual’s control, undermines self-efficacy and increases depressive symptoms and diabetes distress ( 207 – 210 ). Several studies have reported a relationship between food insecurity and adverse diabetes outcomes ( 211 , 212 ), and a review by Barnard et al. ( 213 ) has suggested that food insecurity among patients with and at high risk for T2DM may be particularly toxic because, in addition to issues of accessing sufficient calories overall, the dietary quality of the foods eaten is even more important than for the general population. Several cross-sectional studies report a relationship between food insecurity and T2DM diabetes outcomes ( 214 – 216 ), including poor metabolic control ( 217 , 218 ), experience of severe hypoglycemia in low-income and low-education samples ( 218 ), lower diabetes self-management behavioral adherence and worse glycemic control ( 219 ), and increased outpatient visits but not increased emergency department/inpatient visits ( 95 , 212 ).
Food Environment Interventions and Diabetes
Three studies reported food bank and pantry interventions with food insecure clients with T2DM ( 196 , 220 , 221 ). Seligman et al. ( 196 ) conducted a pilot program in Texas, California, and Ohio with a pre/post design, encompassing provision of diabetes-appropriate food, blood glucose monitoring, self-management support, and primary care referrals. The study resulted in improvements in HbA 1c , fruit and vegetable consumption, self-efficacy, and medication adherence. In a randomized controlled trial of the intervention, Seligman et al. ( 220 ) found improvements in nutritional consumption, food security, and distress but no clinical changes. Palar et al. ( 221 ) found reduction in BMI but not HbA 1c and better nutritional and psychosocial outcomes.
Studies have examined effect of supermarket gain or loss on T2DM outcomes. A study conducted within the setting of the Kaiser Permanente Northern California Diabetes Registry linked clinical measures to metrics from a geographic information system based on participants’ residential addresses ( 115 , 222 , 223 ). Results over 4 years of tracking supermarket change in low-income neighborhoods showed that relative to no change in supermarket presence, supermarket loss was associated with worse HbA 1c trajectories, especially among those with highest HbA 1c . Supermarket gain in neighborhoods was associated with marginally better HbA 1c outcomes, but only for those with near-normal HbA 1c baseline values ( 223 ). In a natural experiment design, the Pittsburgh Hill/Homewood Study on Eating, Shopping, and Health (PHRESH) tested the effects of adding a supermarket, along with other neighborhood investments, on cardiometabolic risk factors among a randomly selected cohort of residents from two low-income, urban, and predominately African American matched neighborhoods ( 222 , 224 ). Results for the intervention neighborhood (receiving the supermarket) showed improved perceived access to healthy food ( 225 ), and the prevalence of diabetes increased less in the neighborhood with the supermarket than in the comparison neighborhood. Since the initiation of the supermarket, many other investments including greenspace, housing, and commercial spaces have been implemented in the intervention neighborhood ( 226 ). Results of these neighborhood investments on measured BMI, blood pressure, HbA 1c , and HDL cholesterol will be forthcoming. In sum, food environment factors of food unavailability, inaccessibility, and insecurity each demonstrate associations with worse diabetes risk and outcomes, and interventions including diabetes-targeted food and self-management care at food banks and pantries and increasing grocery store presence in low-income neighborhoods are few, but collectively they demonstrate the potential to impact diabetes risk, clinical outcomes, and psychosocial outcomes.
Health Care and Diabetes
Health care as a SDOH includes access, affordability, and quality of care factors. In the U.S., these factors are highly correlated with race/ethnicity, SES, and place/geographic region ( 19 ).
Associations of Health Care With Diabetes Incidence, Prevalence, and Outcomes
In population-based studies, having health insurance is the strongest predictor of whether adults with diabetes have access to diabetes screenings and care ( 227 ). Uninsured adults in the U.S. population have a higher likelihood of having undiagnosed diabetes than adults with insurance ( 228 ). Compared with insured adults with diabetes, the uninsured have 60% fewer office visits with a physician, are prescribed 52% fewer medications, and have 168% more emergency department visits ( 229 ). Liese et al. ( 230 ) found that, among adolescents and young adults with T1DM or T2DM, compared with having private insurance, having state or federal health insurance was associated with higher HbA 1c values by 0.68%, and having no insurance was associated with higher HbA 1c by 1.34%. Having insurance has also been found to attenuate associations of financial barriers with higher HbA 1c ( 231 ).
Geographic access to adult and pediatric endocrinologists varies substantially by state and county in the U.S ( 232 ), with disparities in access in many of the geographic regions with highest diabetes prevalence and socioeconomic disadvantage ( 232 , 233 ). Similarly, factors that increase odds of having a diabetes self-management education program in a geographic area include a higher percentage of the population with at least a high school education, a higher percentage of insured individuals, and a lower rate of unemployment ( 234 ). DeVoe et al. ( 235 ) found that among adults with diabetes, having both insurance and a usual source of care, rather than one or the other, conferred the greatest odds of receiving at least minimum diabetes health care. Being uninsured and without a usual source of care was associated with three to five times lower odds of adults receiving an HbA 1c screen, blood pressure check, or access to urgent care when needed ( 235 ). Among adolescents and young adults with diabetes who had state or federal health insurance, not having any usual source of provider (primary care or diabetes specialist) was associated with higher HbA 1c than having a usual source of provider, and HbA 1c was similar whether in primary care or specialist care ( 230 ).
Affordability.
On average, health care costs of people with diabetes are 2.3 times those of people without diabetes ( 229 ). Approximately 14% to 20% of adults with diabetes report reducing or delaying medications due to cost ( 236 – 238 ). Among adults with diabetes who are prescribed insulin, rates may be >25% ( 236 , 239 ). Cost-related or cost-reducing nonadherence (CRN) is associated with income, insured status, and type of insurance. Adults with diabetes with an annual household income of <$50,000 are more likely to engage in CRN than their counterparts with income ≥$50,000, and uninsured adults with diabetes are more likely to engage in CRN than those with insurance ( 236 ). Within a diabetes clinic population of adults with T1DM or T2DM prescribed insulin, odds of CRN were three times higher for those with Medicaid or no insurance compared with those with Medicare ( 239 ). Piette et al. ( 240 ) found differences based on health system model. Compared with VA patients with diabetes, risk of CRN was found to be almost three times higher for privately insured patients and four to eight times higher for patients with Medicare, Medicaid, or no health insurance ( 240 ). Higher financial stress, financial insecurity, and financial barriers are associated with likelihood of CRN ( 231 , 238 ). People with CRN experience poorer diabetes management, higher HbA 1c , and decreased functional status ( 231 , 240 ). Deaths have been reported from insulin CRN among youth and adults with T1DM ( 241 ).
Having insurance is the strongest single predictor of whether adults with diabetes are likely to meet individual quality measures of diabetes care ( 242 ). Sociodemographic disparities in care quality are well documented in national reports and recommendations ( 2 ) and appear to remain consistent over time ( 243 ). In a U.S. population-based study of achievement of a composite diabetes treatment goal from 2005 to 2016, data from 2013 to 2016 showed that non-Hispanic Blacks had lower odds of achieving a composite diabetes quality measure than non-Hispanic Whites (adjusted OR 0.57, 95% CI 0.39–0.83), and women had lower odds than men (adjusted OR 0.60, 95% CI 0.45–0.80), with no improvement in diabetes treatment gaps from prior time periods (2005–2008 and 2009–2012), especially for minorities, women, and younger adults ( 227 ). Within insured settings, disparities have been reported among Blacks as compared with Whites—in measures including dilated eye exam taken; LDL test taken; LDL, blood pressure, or HbA 1c control; and statin therapy ( 244 – 246 ). A study of 21 VA facilities found Blacks with diabetes were more likely than Whites with diabetes to receive care at lower-performing facilities overall, which explained some racial differences in diabetes quality measures ( 246 ).
Health Care Interventions and Diabetes
Community health workers..
Several systematic reviews have concluded that community health worker (CHW) interventions using trained lay workforces are effective for multiple outcomes in underserved African American and Hispanic adults with T2DM and comorbid conditions ( 247 – 250 ). CHWs have been integrated into care delivery ( 251 , 252 ) with reimbursement in some states ( 253 ). Roles of CHWs include patient navigation, appointment scheduling, visit attendance, patient education, home-based monitoring, assessment of social needs and connection with social services, social support, and advocacy ( 252 , 254 ). Reported outcomes include better diabetes knowledge and self-care behaviors, increased quality of life, reduced emergency visits and hospitalizations, reduced costs, and modest improvements in glycemic control ( 247 – 250 , 255 ), using home-based or integrated health team delivery models ( 252 , 256 ). A majority of the CHW interventions designed for adult populations with diabetes have been diabetes-focused in content and goals and have utilized structured curricula ( 254 ); however, one series of studies reported use of a standardized, all-condition CHW intervention and found modest gain in diabetes outcomes along with additional health benefits ( 257 , 258 ).
Organizational Interventions.
Systematic reviews report improvements in quality of diabetes care among racial/ethnic minorities resulting from quality improvement employing health information technology (i.e., patient registries in the electronic health record, computerized decision support for providers, reminders, centralized outreach for diabetes patients overdue for specific services) ( 245 , 259 , 260 ). There is also evidence of effectiveness of self-management interventions delivered directly to underserved patients with diabetes when interventions are designed to overcome barriers. For example, the Centers for Medicare & Medicaid Services (CMS)-sponsored National Diabetes Prevention Program (DPP) Medicaid demonstration found CDC-recognized DPP lifestyle change programs were effective in achieving performance measures among Medicaid recipients in Maryland and Oregon, and additional strategies (i.e., transportation assistance and child care) facilitated the high retention reported over the 12 months of DPP visits ( 261 ). In a series of studies, a problem-based self-management training addressing multiple life barriers to care in low-income and minority populations was adapted for low literacy and prevalent diabetes-related functional limitations (e.g., low vision, physical disability, and mild cognitive impairment) that impede self-management education ( 73 , 262 ). The approach has proven effective in improving clinical outcomes (HbA 1c , blood pressure), self-care behaviors, and self-management knowledge and problem-solving skills in low-income, racial/ethnic minority, and rural populations ( 76 , 263 , 264 ).
Studies have examined the impact of the Affordable Care Act (ACA) on insurance coverage and health care access for patients with diabetes ( 265 ). Analyses of NHIS data from 2009 and 2016 found an increase nationwide of 770,000 more adults with diabetes aged 18 to 64 years with health insurance coverage in 2016, with a significant increase in coverage seen among Whites, Blacks, and Hispanics, people with family income <$35,000, and people across educational attainment strata (less than high school and more than high school) ( 266 ). Among people with diabetes in the lowest income strata, the proportion of income spent on health costs decreased significantly from 6.3% to 4.8% ( 266 ). Other studies found increased access to care, diabetes management, and health status among people with diabetes in Medicaid expansion states as compared with their counterparts in non–Medicaid expansion states ( 267 ); increased rates of diabetes detection and diagnosis among Medicaid patients with undiagnosed diabetes in states with Medicaid expansion ( 268 ); and reduction in cost-related medication nonadherence rates and uninsured rates among people with diabetes following ACA ( 269 ).
Social Context and Diabetes
Several multidimensional factors shape the social environment as a determinant of health ( 270 ), including social capital, social cohesion, and social support ( 28 , 29 ). Social capital is defined as the features of social structures that serve as resources for collective action (e.g., interpersonal trust, reciprocity norms, and mutual aid) ( 271 – 273 ). Bonding social capital refers to trusting and co-operative relations between members of a network who see themselves as being similar in terms of their shared social identity; by contrast, bridging social capital refers to aspects of respect and mutuality between people who do not share social identities (e.g., differing by race/ethnicity, social class, age) ( 274 – 276 ). Racism, discrimination, and inclusion versus exclusion are macro-level social capital factors that impact health ( 28 ).
Social cohesion refers to the extent of connectedness and solidarity among groups in a community ( 271 , 277 ) and has two dimensions: reduction of inequalities and patterns of social exclusion of population subgroups from full participation in society ( 278 ) and strengthening of social relationships and interactions ( 279 – 281 ). Social cohesion actions facilitate the goal of keeping the society united, not only through social relations, community ties, and intergroup harmony but also through reducing bias and discrimination toward economically disadvantaged groups within a society, such as women and ethnic minorities ( 28 ).
Social support describes experiences in individuals’ formal and informal personal relationships as well as their perceptions of those relationships. Categories include emotional support, tangible support, informational support, and companionship ( 282 – 285 ). Social support is theorized to operate by either buffering the effects of poor health or by directly impacting health ( 285 , 286 ).
Associations of Social Context With Diabetes Incidence, Prevalence, and Outcomes
A systematic review by Flôr et al. ( 287 ) concluded that social capital was positively associated with diabetes control among different populations, independent of the quality or quantity of social capital. However, the few studies available and variations among populations and measures limit the ability to draw firm conclusions related to dimensions of social capital and whether the association is the same at the individual or neighborhood level ( 272 , 288 – 290 ). Gebreab et al. ( 189 ), using data from the Jackson Heart Study, examined social cohesion, measured as trust in neighbors, shared values with neighbors, willingness to help neighbors, and extent to which neighbors get along. The study revealed higher neighborhood social cohesion was associated with a 22% lower incidence of T2DM ( 189 ). Studies demonstrating the relationship between social support and diabetes have associated increased social support with better glycemic control and improved quality of life ( 291 – 295 ), while lack of social support has been associated with increased mortality and diabetes-related complications ( 291 ).
A number of studies suggest social cohesion, social capital, and social support may influence—or be influenced by—racism and discrimination ( 296 ). Racism interacts with other social entities, creating a set of dynamic, interdependent components that reinforce each other, sustaining racial inequities and promoting both institutional- and individual-level discrimination across various sectors of society impacting diabetes incidence ( 296 , 297 ). For example, Whitaker et al. ( 298 ) documented associations of major and everyday discrimination experiences with incident diabetes among a diverse sample of 5,310 middle-aged to older adults from the Multi-Ethnic Study of Atherosclerosis. The Black Women’s Health Study found that, when compared with women in the lowest quartile of exposure, those in the highest quartile of exposure to everyday racism had a 31% increased risk of diabetes (HR 1.31, 95% CI 1.20–1.42), and women with the highest exposure to lifetime racism had a 16% increased risk (HR 1.16, 95% CI 1.05–1.27); both associations were mediated by BMI ( 298 , 299 ). Further work is needed to understand the multiple ways that the social environment influences inequities in diabetes outcomes.
Social Context Interventions and Diabetes Outcomes
To our knowledge, there is no empirical research on social capital or social cohesion interventions and impact on diabetes outcomes, but a body of literature has examined effects of social support. The systematic review by Strom and Egede ( 284 ) of 18 observational studies of adults with T2DM found that higher levels of social support were associated with outcomes including better glycemic control, knowledge, treatment adherence, quality of life, diagnosis awareness and acceptance, and stress reduction ( 284 ). Lack of social support has been linked with increased mortality and diabetes-related complications in T2DM ( 291 , 295 ). Strom and Egede’s review of 16 social support intervention studies demonstrated improved diabetes-related outcomes (clinical, psychosocial, and/or self-management behavior change) in adults with T2DM, and improvements in clinical outcomes (HbA 1c , blood pressure, lipids) appeared to be unrelated to the source or delivery (i.e., peer support, couples/spouse, or nurse manager).
With regard to preferences—in a study conducted before the coronavirus disease 2019 pandemic—Sarkar et al. ( 300 ) found that, compared with White adults with diabetes, Hispanics with diabetes preferred telephone-based and group support (including promotoras ), while African Americans demonstrated more variability in their preferences (i.e., telephone, group, internet). Reliance on support from family and community tended to be higher in minority populations, while Whites relied more on media and health care professionals ( 300 ).
International and U.S. national committees have convened to provide guidance on SDOH intervention approaches. These expert committee recommendations are not specific to any disease; rather, they are applicable to all conditions and populations of health inequity. Table 3 displays recommendations from the WHO Commission on Social Determinants of Health ( 27 ), the National Academies of Sciences, Engineering, and Medicine (NASEM) (formerly, Institute of Medicine) Committee on the Recommended Social and Behavioral Domains and Measures for Electronic Health Records ( 80 ), the NASEM Committee on Educating Health Professionals to Address the Social Determinants of Health ( 301 ), and the NASEM Committee on Integrating Social Needs Care into the Delivery of Health Care to Improve the Nation's Health ( 5 ).
SDOH intervention recommendations from international and national (U.S.) committees
| Committee . | Recommended actions . | Description . |
|---|---|---|
| Commission on the Social Determinants of Health, WHO (2008) ( ) | Improve daily living conditions | Put major emphasis on early childhood education and development. Improve living and working conditions. Create social protection policy supportive of all. |
| Tackle the inequitable distribution of power, money, and resources | Create a strong public sector that is committed, capable, and adequately financed. Ensure legitimacy, space, and support for civil society, for an accountable private sector, and for the public to agree to reinvestment in collective action. | |
| Measure and understand the problem and assess the impact of action | Acknowledge there is a problem. Ensure that health inequity is measured. Develop national and global health equity surveillance systems for routine monitoring of health inequity and the social determinants of health. Evaluate the health equity impact of policy and action. Ensure stronger focus on social determinants in public health research. | |
| Committee on Recommended Social and Behavioral Domains and Measures for Electronic Health Records, Institute of Medicine, NASEM (2014) ( ) | Standardize data collection and measurement to facilitate the critical use and exchange of information on social and behavioral determinants of health | Office of the National Coordinator for Health Information Technology and the CMS should include the recommended standardized measures in the certification and meaningful use regulations: Commonly used measures: race and ethnicity, residential address, alcohol use, tobacco use Additional recommended measures: census tract-median income, education, financial resource strain, social connections and social isolation, depression, intimate partner violence, physical activity, stress |
| Committee on Educating Health Professionals to Address the Social Determinants of Health, NASEM (2016) ( ) | Create a learning environment for health professionals to foster community collaborations | Health professional educators should create lifelong learners who appreciate the value of relationships and collaborations for understanding and addressing community-identified needs and for strengthening community assets. |
| Prepare health professionals to take action on SDOH | To prepare health professionals to take action on the social determinants of health in, with, and across communities, health professional and educational associations and organizations at the global, regional, and national levels should apply [frameworks for] partnering with communities to increase the inclusivity and diversity of the health professional student body and faculty. | |
| Integrate SDOH into organizational mission and values | Governments and individual ministries (e.g., signatories of the Rio Declaration), health professional and educational associations and organizations, and community groups should foster an enabling environment that supports and values the integration of the social determinants framework principles into their mission, culture, and work. | |
| Build the evidence base for SDOH learning, intervention, and evaluation approaches | Governments, health professional and educational associations and organizations, and community organizations should use [a social determinants] framework and model to guide and support evaluation research aimed at identifying and illustrating effective approaches for learning about the social determinants of health in and with communities while improving health outcomes, thereby building the evidence base. | |
| Committee on Integrating Social Needs Care Into the Delivery of Health Care to Improve the Nation's Health, NASEM (2019) ( ) | Design health care delivery to integrate social care into health care, guided by the five health care system activities—awareness, adjustment, assistance, alignment, and advocacy | Establish organizational commitment to addressing disparities and health-related social needs. Incorporate strategies for screening and assessing for social risk factors and needs. Incorporate social risk into care decisions using patient-centered care. Establish linkages between health care and social service providers. Include social care workers in team care. Develop infrastructure for care integration, including financing of referral relationships with select social providers. |
| Build a workforce to integrate social care into health care delivery | Social workers and other social care workforces should be providers eligible for reimbursement from payers. Integrate SDOH competencies in medical and health professional credentialing. | |
| Develop a digital infrastructure that is interoperable between health care and social care organizations | Establish ACA-recommended digital infrastructure for social care. The Office of the National Coordinator should support identification of interoperable, secure, platforms for use across health and social care communities. The Federal Health Information Technology Coordinating Committee should facilitate data sharing across domains (e.g., health care, housing, and education). Analytic and technology implementation must have an explicit focus on equity to avoid unintended consequences such as perpetuation or aggravation of discrimination, bias, and marginalization. | |
| Finance the integration of health care and social care | CMS should define and use flexibility in what social care constitutes Medicaid-covered services. Health systems, payers, and governments should consider collective financing to spread risk and create shared returns on investments in social care. Health systems subject to community benefit regulations should comply with those regulations and should align their hospital licensing requirements and public reporting with community benefits regulations and should link their community benefits providing social care. | |
| Fund, conduct, and translate research and evaluation on the effectiveness and implementation of social care practices in health care settings | Federal (e.g., NIH, AHRQ, PCORI) and state agencies, payers, providers, delivery systems, and foundations should contribute to advancing research and evaluation of social care through funding opportunities, researcher support (i.e., cultivate health services, social sciences, and cross-disciplinary researchers), and use of experimental trials, rapid learning cycles, and dissemination of learnings. CMS should fully finance independent state waiver evaluations to ensure robust evaluation of social care and health care integration pilot programs and dissemination. |
| Committee . | Recommended actions . | Description . |
|---|---|---|
| Commission on the Social Determinants of Health, WHO (2008) ( ) | Improve daily living conditions | Put major emphasis on early childhood education and development. Improve living and working conditions. Create social protection policy supportive of all. |
| Tackle the inequitable distribution of power, money, and resources | Create a strong public sector that is committed, capable, and adequately financed. Ensure legitimacy, space, and support for civil society, for an accountable private sector, and for the public to agree to reinvestment in collective action. | |
| Measure and understand the problem and assess the impact of action | Acknowledge there is a problem. Ensure that health inequity is measured. Develop national and global health equity surveillance systems for routine monitoring of health inequity and the social determinants of health. Evaluate the health equity impact of policy and action. Ensure stronger focus on social determinants in public health research. | |
| Committee on Recommended Social and Behavioral Domains and Measures for Electronic Health Records, Institute of Medicine, NASEM (2014) ( ) | Standardize data collection and measurement to facilitate the critical use and exchange of information on social and behavioral determinants of health | Office of the National Coordinator for Health Information Technology and the CMS should include the recommended standardized measures in the certification and meaningful use regulations: Commonly used measures: race and ethnicity, residential address, alcohol use, tobacco use Additional recommended measures: census tract-median income, education, financial resource strain, social connections and social isolation, depression, intimate partner violence, physical activity, stress |
| Committee on Educating Health Professionals to Address the Social Determinants of Health, NASEM (2016) ( ) | Create a learning environment for health professionals to foster community collaborations | Health professional educators should create lifelong learners who appreciate the value of relationships and collaborations for understanding and addressing community-identified needs and for strengthening community assets. |
| Prepare health professionals to take action on SDOH | To prepare health professionals to take action on the social determinants of health in, with, and across communities, health professional and educational associations and organizations at the global, regional, and national levels should apply [frameworks for] partnering with communities to increase the inclusivity and diversity of the health professional student body and faculty. | |
| Integrate SDOH into organizational mission and values | Governments and individual ministries (e.g., signatories of the Rio Declaration), health professional and educational associations and organizations, and community groups should foster an enabling environment that supports and values the integration of the social determinants framework principles into their mission, culture, and work. | |
| Build the evidence base for SDOH learning, intervention, and evaluation approaches | Governments, health professional and educational associations and organizations, and community organizations should use [a social determinants] framework and model to guide and support evaluation research aimed at identifying and illustrating effective approaches for learning about the social determinants of health in and with communities while improving health outcomes, thereby building the evidence base. | |
| Committee on Integrating Social Needs Care Into the Delivery of Health Care to Improve the Nation's Health, NASEM (2019) ( ) | Design health care delivery to integrate social care into health care, guided by the five health care system activities—awareness, adjustment, assistance, alignment, and advocacy | Establish organizational commitment to addressing disparities and health-related social needs. Incorporate strategies for screening and assessing for social risk factors and needs. Incorporate social risk into care decisions using patient-centered care. Establish linkages between health care and social service providers. Include social care workers in team care. Develop infrastructure for care integration, including financing of referral relationships with select social providers. |
| Build a workforce to integrate social care into health care delivery | Social workers and other social care workforces should be providers eligible for reimbursement from payers. Integrate SDOH competencies in medical and health professional credentialing. | |
| Develop a digital infrastructure that is interoperable between health care and social care organizations | Establish ACA-recommended digital infrastructure for social care. The Office of the National Coordinator should support identification of interoperable, secure, platforms for use across health and social care communities. The Federal Health Information Technology Coordinating Committee should facilitate data sharing across domains (e.g., health care, housing, and education). Analytic and technology implementation must have an explicit focus on equity to avoid unintended consequences such as perpetuation or aggravation of discrimination, bias, and marginalization. | |
| Finance the integration of health care and social care | CMS should define and use flexibility in what social care constitutes Medicaid-covered services. Health systems, payers, and governments should consider collective financing to spread risk and create shared returns on investments in social care. Health systems subject to community benefit regulations should comply with those regulations and should align their hospital licensing requirements and public reporting with community benefits regulations and should link their community benefits providing social care. | |
| Fund, conduct, and translate research and evaluation on the effectiveness and implementation of social care practices in health care settings | Federal (e.g., NIH, AHRQ, PCORI) and state agencies, payers, providers, delivery systems, and foundations should contribute to advancing research and evaluation of social care through funding opportunities, researcher support (i.e., cultivate health services, social sciences, and cross-disciplinary researchers), and use of experimental trials, rapid learning cycles, and dissemination of learnings. CMS should fully finance independent state waiver evaluations to ensure robust evaluation of social care and health care integration pilot programs and dissemination. |
AHRQ, Agency for Healthcare Research and Quality; NASEM, National Academies of Sciences, Engineering, and Medicine; NIH, National Institutes of Health; CMS, Centers for Medicare & Medicaid Services; PCORI, Patient-Centered Outcomes Research Institute.
SDOH measures.
The WHO recommendations are unique in their emphasis on root-cause, multisector interventions designed to remove the SDOH as a barrier to health equity. The NASEM recommendations are based in the health care sector and, collectively, focus on integration of SDOH into the health care mission, operations, and financial model. Accountable care organizations, value-based purchasing, and shared savings programs could be intentionally designed to support and incentivize health care systems to address patients’ health-related social needs as a strategy to improve health outcomes ( 5 ). The Accountable Health Communities is one current CMS demonstration project examining impact on health care costs of three models for health care response to SDOH through linkages with community services: awareness (screening for social needs within the health care setting and patient referral to services using an inventory of available local community services), assistance (screening, referral, plus navigation to enable access to and use of community services), and alignment (screening, referral, community service navigation, plus partner alignment using a “backbone” organization for capacity building, data sharing among community and health care partners, and scaling of services) ( 302 ). Many health care systems are utilizing electronic medical records and health information exchanges to capture SDOH data and commercially available SDOH algorithms to identify patients at social risk and trigger service referrals ( 303 ). NASEM provided assessment questions to capture SDOH domains and frequencies for assessment ( 304 ) with evidence of feasibility ( 305 ). In addition, Table 4 displays publicly available resources and tools to aid providers in addressing individual patients’ social needs.
Examples of resources on SDOH available for health care organizations and health care professionals
| Organization . | Resource . |
|---|---|
| Centers for Disease Control and Prevention (CDC) | Tools for Putting Social Determinants of Health Into Action ( ) |
| National Academies of Science, Engineering, and Medicine | Questions for conducting social and behavioral determinant assessment and frequencies for assessing |
| Adler NE, Stead WW. Patients in context—EHR capture of social and behavioral determinants of health. N Engl J Med 2015;372:698–701. | |
| National Institutes of Health (NIH) Division of Extramural Affairs | The Neighborhood Atlas—Free social determinants of health data for all! |
| Kind AJH, Buckingham W. Making neighborhood disadvantage metrics accessible: the neighborhood atlas. N Engl J Med 2018;378:2456–2458. PMCID: PMC6051533 | |
| American Academy of Family Physicians | The EveryONE Project's Neighborhood Navigator Toolkit ( ) |
| American College of Physicians | Addressing Social Determinants to Improve Patient Care and Promote Health Equity: An American College of Physicians Position Paper. DOI: 10.7326/M17-2441 |
| American Medical Association | Podcast: Social determinants of health: What they are and what they aren’t ( ) |
| Nonprofit services | 211: A service of the United Way that continuously identifies links for all “211” health and human services referral services in the U.S. |
| HealthLeads: A nonprofit offering tools, training and resources for integrating SDOH into accountable care | |
| Aunt Bertha: A service that provides links to hundreds of programs serving every U.S. zip code. Free basic use. |
| Organization . | Resource . |
|---|---|
| Centers for Disease Control and Prevention (CDC) | Tools for Putting Social Determinants of Health Into Action ( ) |
| National Academies of Science, Engineering, and Medicine | Questions for conducting social and behavioral determinant assessment and frequencies for assessing |
| Adler NE, Stead WW. Patients in context—EHR capture of social and behavioral determinants of health. N Engl J Med 2015;372:698–701. | |
| National Institutes of Health (NIH) Division of Extramural Affairs | The Neighborhood Atlas—Free social determinants of health data for all! |
| Kind AJH, Buckingham W. Making neighborhood disadvantage metrics accessible: the neighborhood atlas. N Engl J Med 2018;378:2456–2458. PMCID: PMC6051533 | |
| American Academy of Family Physicians | The EveryONE Project's Neighborhood Navigator Toolkit ( ) |
| American College of Physicians | Addressing Social Determinants to Improve Patient Care and Promote Health Equity: An American College of Physicians Position Paper. DOI: 10.7326/M17-2441 |
| American Medical Association | Podcast: Social determinants of health: What they are and what they aren’t ( ) |
| Nonprofit services | 211: A service of the United Way that continuously identifies links for all “211” health and human services referral services in the U.S. |
| HealthLeads: A nonprofit offering tools, training and resources for integrating SDOH into accountable care | |
| Aunt Bertha: A service that provides links to hundreds of programs serving every U.S. zip code. Free basic use. |
There is SDOH evidence supporting associations of SES, neighborhood and physical environment, food environment, health care, and social context with diabetes-related outcomes. Inequities in living and working conditions and the environments in which people reside have a direct impact on biological and behavioral outcomes associated with diabetes prevention and control ( 12 , 48 ). Life-course exposure based on the length of time one spends living in resource-deprived environments—defined by poverty, lack of quality education, or lack of health care—significantly impacts disparities in diabetes risk, diagnosis, and outcomes ( 12 , 48 , 306 ). Although the review reports SDOH intervention studies for aspects of housing, built and food environment, and health care, there appears to be relatively limited U.S.-based research examining impact on diabetes of interventions designed to target education, income, occupation, toxic environmental exposures, social cohesion, and social capital.
In the U.S., integrating social context into health care delivery has become a priority strategy ( 5 – 8 ). A clinical context alone, however, is too narrow to accommodate systemic SDOH influences. Structural and legal interventions are needed to address root causes driving SDOH ( 27 , 307 ). Similarly, additional emphasis is needed on a next generation of research that prioritizes interventions impacting the root causes of diabetes inequities, rather than compensatory interventions assisting the individual to adapt to inequities ( 18 , 308 ). For example, in the U.S., proficient literacy and resulting health literacy are disproportionately low in marginalized populations and communities ( 42 ), with historical sociopolitical root causes. U.S. antiliteracy laws for Blacks, which prohibited Blacks from being taught to read or write, persisted until the 1930s in some states ( 309 , 310 ), and laws prohibiting African Americans from attending public and private schools Whites attended continued until 1954 and 1976, respectively ( 311 ). Although adapting health materials for low-literacy suitability is an effective intervention to compensate for centuries of legal racial discrimination in educational access and quality, a next-generation intervention might target the education sector and implement delivery of high-quality early education to all within both the public and private school systems and with equitable educational funding for sociodemographic populations. Similarly, while partnerships to bring bags of healthy groceries to low-income families living in food deserts are important to compensate for food deserts, a next-generation approach might target historical redlining and zoning policies that are the root cause of absence of supermarkets and fresh food markets in minority and lower-income neighborhoods ( 312 – 314 ).
The review has limitations. First, the undertaking was designed to summarize literature on the range of SDOH identified as having impact on diabetes outcomes. As such, this article describes findings from systematic reviews and meta-analyses as well as more recent published studies on the named SDOH; it was not designed as a primary systematic review of all published research on the topic. Second are limitations of the research itself, including wide variability in measures and definitions used in studies within an SDOH area, making it more difficult to describe outcomes for an SDOH area in a consistent or uniform manner or to report quantitative outcomes derived from meta-analyses. Third, this review was U.S.-focused; conclusions from SDOH research in other countries, which in some instances may utilize more standardly defined SDOH variables (e.g., occupation) are not part of this initial review. Finally, the many complexities of SDOH and their potentially different pathways and impacts on populations are beyond the scope of this initial review and require attention to specificity in designs of future SDOH research in diabetes.
Recommendations for SDOH research in diabetes resulting from this SDOH review are described in Table 5 and include establishing consensus SDOH definitions and metrics, designing studies to examine specificities based on populations, prioritizing next-generation interventions, embedding SDOH context within dissemination and implementation science in diabetes, and training researchers in methodological techniques for future SDOH intervention studies. By addressing these critical elements, there is potential for progress to be realized in achieving greater health equity in diabetes and across health outcomes that are socially determined.
SDOH and diabetes research recommendations
| Research recommendation 1 | Consensus is needed around language and metrics associated with SDOH and diabetes care that move beyond health care and capture the impact of social advantage and disadvantage in population settings. Clarity and consistency in measurement, evaluation, and reporting of progress will allow for appropriate planning of interventions, allocation of resources, and analysis of impact in achieving equity goals. |
| Establish consensus core SDOH definitions and metrics | |
| Research recommendation 2 | Examinations of potential differences in pathways or impacts of SDOH based on characteristics including diabetes type or diagnostic category (e.g., T1DM vs. T2DM, gestational diabetes mellitus, prediabetes), age group (e.g., children and youth, adults, older adults), and different SES (wealthy vs. middle class vs. poor) are needed. In addition, complexities of SDOH pathways and impacts for different racial/ethnic groups, based on historical drivers and policies, warrant elucidation to inform intervention and mitigation strategies. |
| Examine specificities in SDOH pathways and impacts among different populations with diabetes | |
| Research recommendation 3 | Multisector partnerships, comprising academic institutions, government sectors (e.g., housing, education, justice), and public health entities are required in order to design and test observational and intervention studies to better understand and intervene on SDOH as root causes of diabetes disparities. Priorities need to move from compensatory to the next-generation of research that will be larger in scope, addressing foundational causes of disparities (e.g., policy, systems change), and tested over time across sectors. Complex studies, examining the interactive effects of multifaceted systems that influence SDOH, will also transform and move translational efforts toward large-scale solutions that promote equity for all populations and mitigate the influence of SDOH on diabetes outcomes. |
| Prioritize a next generation of research that targets SDOH as the root cause of diabetes inequities | |
| Research recommendation 4 | For clinical research programs, dissemination and implementation methods will shorten the translation gap from discovery to impact of evidence-based interventions by addressing the complexity of integrating and adapting evidence-based practices to real-world community and clinical settings. This will assure all populations benefit from the billions of U.S. tax dollars spent on research to prevent diabetes and to improve diabetes population health. |
| Use dissemination and implementation science to ensure SDOH considerations are embedded within diabetes research and evaluation studies | |
| Research studies must also consider the potential influence of either positive or negative SDOH (e.g., wealth or economic security vs. poverty, food security vs. insecurity, stable vs. unstable housing) on intervention appropriateness and outcomes, on study recruitment and participation, and on study outcomes and conclusions. | |
| Research recommendation 5 | Training on SDOH and their influence on diabetes prevention and treatment is needed. Training priorities include interdisciplinary science, multisector collaboration research approaches, and methods to advance root cause research on SDOH. Additionally, increasing diversity among research workforces, and fostering educational experiences encompassing multisector partners will develop a workforce that is congruent with promoting diabetes health equity. |
| Train researchers in methodologies and experimental techniques for multisector and next generation SDOH intervention studies |
| Research recommendation 1 | Consensus is needed around language and metrics associated with SDOH and diabetes care that move beyond health care and capture the impact of social advantage and disadvantage in population settings. Clarity and consistency in measurement, evaluation, and reporting of progress will allow for appropriate planning of interventions, allocation of resources, and analysis of impact in achieving equity goals. |
| Establish consensus core SDOH definitions and metrics | |
| Research recommendation 2 | Examinations of potential differences in pathways or impacts of SDOH based on characteristics including diabetes type or diagnostic category (e.g., T1DM vs. T2DM, gestational diabetes mellitus, prediabetes), age group (e.g., children and youth, adults, older adults), and different SES (wealthy vs. middle class vs. poor) are needed. In addition, complexities of SDOH pathways and impacts for different racial/ethnic groups, based on historical drivers and policies, warrant elucidation to inform intervention and mitigation strategies. |
| Examine specificities in SDOH pathways and impacts among different populations with diabetes | |
| Research recommendation 3 | Multisector partnerships, comprising academic institutions, government sectors (e.g., housing, education, justice), and public health entities are required in order to design and test observational and intervention studies to better understand and intervene on SDOH as root causes of diabetes disparities. Priorities need to move from compensatory to the next-generation of research that will be larger in scope, addressing foundational causes of disparities (e.g., policy, systems change), and tested over time across sectors. Complex studies, examining the interactive effects of multifaceted systems that influence SDOH, will also transform and move translational efforts toward large-scale solutions that promote equity for all populations and mitigate the influence of SDOH on diabetes outcomes. |
| Prioritize a next generation of research that targets SDOH as the root cause of diabetes inequities | |
| Research recommendation 4 | For clinical research programs, dissemination and implementation methods will shorten the translation gap from discovery to impact of evidence-based interventions by addressing the complexity of integrating and adapting evidence-based practices to real-world community and clinical settings. This will assure all populations benefit from the billions of U.S. tax dollars spent on research to prevent diabetes and to improve diabetes population health. |
| Use dissemination and implementation science to ensure SDOH considerations are embedded within diabetes research and evaluation studies | |
| Research studies must also consider the potential influence of either positive or negative SDOH (e.g., wealth or economic security vs. poverty, food security vs. insecurity, stable vs. unstable housing) on intervention appropriateness and outcomes, on study recruitment and participation, and on study outcomes and conclusions. | |
| Research recommendation 5 | Training on SDOH and their influence on diabetes prevention and treatment is needed. Training priorities include interdisciplinary science, multisector collaboration research approaches, and methods to advance root cause research on SDOH. Additionally, increasing diversity among research workforces, and fostering educational experiences encompassing multisector partners will develop a workforce that is congruent with promoting diabetes health equity. |
| Train researchers in methodologies and experimental techniques for multisector and next generation SDOH intervention studies |
See accompanying articles, pp. 1 , 8 , 11 , and 188 .
Acknowledgments. The authors express appreciation to Malaika I. Hill and Mindy Saraco of the American Diabetes Association; Elizabeth A. Vrany, Johns Hopkins University School of Medicine; and Shelly Johnson, Washington University in St. Louis, for providing technical assistance for this review.
Funding. F.H.-B. is supported in part by the Johns Hopkins Institute for Clinical and Translational Research (ICTR), which is funded in part by grant UL1TR003098 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. F.H.-B. is also supported in part by NIH National Heart, Lung, and Blood Institute (NHLBI) grant T32HL07180. D.H.-J. is supported in part by NIH National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant P30DK092950. M.H.C. is supported in part by NIH and NIDDK grant P30DK092949. T.L.G.-W. is supported in part by NHLBI grant R01HL131531. A.N.-A. is supported in part by National Institute of Environmental Health Sciences grants P42ES010349 and P30ES009089. S.A.B. is supported in part by NIDDK grant K23DK109200.
The findings and conclusion in this report are those of the authors and do not necessarily represent the official position of the Johns Hopkins ICTR, NCATS, NIH, NIDDK, or any other institution mentioned in the article.
Duality of Interest. M.H.C. reports being co-coordinator of the “Bridging the Gap: Reducing Disparities in Diabetes Care National Program Office,” supported by the Merck Foundation, a consultant to the Patient-Centered Outcomes Group, and a member of the Bristol-Myers Squibb Company Health Equity Advisory Board. S.A.B. received personal fees for service on an advisory board about prioritizing food insecurity research topics for the Aspen Institute. T.L.G.-W. received personal fees for service on an advisory board about prioritizing food insecurity research topics for the Aspen Institute. No other potential conflicts of interests relevant to this article were reported.
Author Contributions . F.H.-B. researched data and wrote the manuscript. N.E.A. contributed to writing and reviewing/editing the manuscript. S.A.B. researched data and contributed to writing and reviewing/editing the manuscript. M.H.C. contributed to writing and reviewing/editing the manuscript. T.L.G.-W. researched data and contributed to writing and reviewing/editing the manuscript. A.N.-A. researched data and contributed to writing the manuscript. P.L.T. researched data and contributed to writing and reviewing/editing the manuscript. D.H.-J. researched data and contributed to writing and reviewing/editing the manuscript.
Email alerts
- Social Determinants of Health and Structural Inequities—Root Causes of Diabetes Disparities
- A Lesson From 2020: Public Health Matters for Both COVID-19 and Diabetes
- Metabolic Syndrome and COVID-19 Mortality Among Adult Black Patients in New Orleans
- 2019 Health Care & Education Presidential Address: It’s All About Access!
- Online ISSN 1935-5548
- Print ISSN 0149-5992
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
DIABETES: A LITERATURE REVIEW
- Health and Society 2(02)
- This person is not on ResearchGate, or hasn't claimed this research yet.
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations

- Thomas Reinehr
- ARQ BRAS ENDOCRINOL
- Celma Lúcia Rocha Alves Ferreira
- Márcia Gonçalves Ferreira
- A. Pacheco-Silva

- Denise B Mory
- Elaine Davini
- The Committee of the Japan Diabetes Society on the Diagnostic Criteria of Diabetes Mellitus

- Arthur C. Guyton
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up

Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Journal Proposal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Emerging role of natriuretic peptides in diabetes care: a brief review of pertinent recent literature.

1. Introduction
2. pathophysiology of heart failure in diabetes, 3. natriuretic peptides and their clinical applications in heart failure, 4. natriuretic peptides for hf risk stratification and management in diabetes.
- The St Vincent’s Screening to Prevent Heart Failure (STOP-HF) study involved 1374 participants at HF risk (including those with diabetes), randomized into usual care or BNP screening groups. Those with BNP ≥ 50 pg/mL received echocardiography and collaborative care. The primary outcome showed a lower prevalence of LV dysfunction in the intervention group (5.3% vs. 8.7%) after a mean follow-up period of 4.2 years. Moreover, the incidence of cardiovascular hospitalizations was lower in the intervention group. BNP-based screening reduced the composite endpoint of incident asymptomatic LV dysfunction with or without newly diagnosed HF [ 28 ].
- The NT-proBNP Selected Prevention of Cardiac Events in a Population of Diabetic Patients without a History of Cardiac Disease (PONTIAC) study included 300 patients with T2DM and NT-proBNP > 125 pg/mL but without any history of cardiac disease. Participants were randomized into a control group (receiving usual care) and an intensified group, which received additional cardiac outpatient care for the up-titration of RAAS antagonists and beta-blockers and was followed up for 2 years. Notably, intensified therapy led to a significant reduction in cardiac hospitalizations/deaths compared to the control group (hazard ratio: 0.351; p = 0.044) [ 29 ].
- In the Examination of Cardiovascular Outcomes with Alogliptin versus Standard of Care (EXAMINE) trial, two NT-pro BNP measurements (6 months apart) in patients ( n = 5380) with T2DM effectively identified those at the highest risk of developing symptomatic HF. Patients with persistently high or increasing NT-pro BNP levels at 6 months had a significantly higher risk of CV death or HF compared to those with consistently low levels or initial high levels that declined [ 30 ].
- The Canagliflozin Cardiovascular Assessment Study (CANVAS) involved 4330 participants with T2DM and either CVD or other risk factors for cardiac events. Plasma NT-proBNP concentrations were measured at baseline, year 1, and year 6, and associations between NT-proBNP levels and various cardiovascular, renal, and mortality outcomes were investigated. NT-pro BNP levels ≥ 125 pg/mL predicted incident hospitalization for HF (hazard ratio 5.40; p < 0.001). Furthermore, it was suggested that elevated NT-pro BNP levels could predict a wide range of deleterious cardiovascular and renal outcomes in T2DM, HF death, and all-cause mortality [ 31 ].
- The Thousand and I study assessed the prognostic significance of elevated NT-pro BNP levels in patients ( n = 960) with type 1 DM with preserved LVEF and without known heart disease. During a median follow-up of 6.3 years, 121 participants experienced major cardiovascular events (MACE) and 51 died. Higher NT-pro BNP levels were linked to poorer outcomes, with adjusted hazard ratios for MACE at 1.56 and 4.29 per Loge increase for NT-proBNP [ 32 ].
5. Analytical and Clinical Considerations in Natriuretic Peptide Testing
6. future prospects and conclusions, author contributions, data availability statement, conflicts of interest, abbreviations.
| ARNI | Angiotensin receptor neprilysin inhibitor |
| BNP | B-type natriuretic peptide |
| NT-pro BNP | N-terminal pro-B-type natriuretic peptide |
| RAAS | Renin–angiotensin–aldosterone system |
| SGLT2i | Sodium–glucose cotransporter 2 inhibitor |
| T2DM | Type 2 diabetes mellitus |
- GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2023 , 402 , 203–234. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Pop-Busui, R.; Januzzi, J.L.; Bruemmer, D.; Butalia, S.; Green, J.B.; Horton, W.B.; Knight, C.; Levi, M.; Rasouli, N.; Richardson, C.R. Heart Failure: An Underappreciated Complication of Diabetes. A Consensus Report of the American Diabetes Association. Diabetes Care 2022 , 45 , 1670–1690. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Palazzuoli, A.; Iacoviello, M. Diabetes leading to heart failure and heart failure leading to diabetes: Epidemiological and clinical evidence. Heart Fail. Rev. 2023 , 28 , 585–596. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kannel, W.B.; McGee, D.L. Diabetes and cardiovascular disease. The Framingham study. JAMA 1979 , 241 , 2035–2038. [ Google Scholar ] [ CrossRef ]
- McAllister, D.A.; Read, S.H.; Kerssens, J.; Livingstone, S.; McGurnaghan, S.; Jhund, P.; Petrie, J.; Sattar, N.; Fischbacher, C.; Kristensen, S.L.; et al. Incidence of hospitalization for heart failure and case-fatality among 3.25 million people with and without diabetes mellitus. Circulation 2018 , 138 , 2774–2786. [ Google Scholar ] [ CrossRef ]
- Dunlay, S.M.; Givertz, M.M.; Aguilar, D.; Allen, L.A.; Chan, M.; Desai, A.S.; Deswal, A.; Dickson, V.V.; Kosiborod, M.N.; Lekavich, C.L.; et al. Type 2 Diabetes Mellitus and Heart Failure: A Scientific Statement From the American Heart Association and the Heart Failure Society of America: This statement does not represent an update of the 2017 ACC/AHA/HFSA heart failure guideline update. Circulation 2019 , 140 , e294–e324. [ Google Scholar ] [ CrossRef ]
- Verma, S.; Pandey, A.; Bhatt, D. Forecasting Heart Failure Risk in Diabetes. J. Am. Coll. Cardiol. 2022 , 79 , 2294–2297. [ Google Scholar ] [ CrossRef ]
- Cannistraci, R.; Mazzetti, S.; Mortara, A.; Perseghin, G.; Ciardullo, S. Risk stratification tools for heart failure in the diabetes clinic. Nutr. Metab. Cardiovasc. Dis. 2020 , 30 , 1070–1079. [ Google Scholar ] [ CrossRef ]
- American Diabetes Association Professional Practice Committee. 10. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes—2022. Diabetes Care 2022 , 45 , S144–S174. [ Google Scholar ] [ CrossRef ]
- Bozkurt, B.; Coats, A.J.S.; Tsutsui, H.; Abdelhamid, C.M.; Adamopoulos, S.; Albert, N.; Anker, S.D.; Atherton, J.; Böhm, M.; Butler, J.; et al. Universal definition and classification of heart failure: A report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur. J. Heart Fail. 2021 , 23 , 352–380. [ Google Scholar ]
- Emdin, M.; Vittorini, S.; Passino, C.; Clerico, A. Old and new biomarkers of heart failure. Eur. J. Heart Fail. 2009 , 11 , 331–335. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Schwinger, R.H.G. Pathophysiology of heart failure. Cardiovasc. Diagn. Ther. 2021 , 11 , 263–276. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Elendu, C.; Amaechi, D.C.; Elendu, T.C.; Ashna, M.; Ross-Comptis, J.; Ansong, S.O.; Egbunu, E.O.; Okafor, G.C.; Jingwa, K.A.; Akintunde, A.A.; et al. Heart failure and diabetes: Understanding the bidirectional relationship. Medicine 2023 , 102 , e34906. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Panchal, K.; Lawson, C.; Chandramouli, C.; Lam, C.; Khunti, K.; Zaccardi, F. Diabetes and risk of heart failure in people with and without cardiovascular disease: Systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2023 , 207 , 111054. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sobczak, A.I.S.; Stewart, A.J. Coagulatory Defects in Type-1 and Type-2 Diabetes. Int. J. Mol. Sci. 2019 , 20 , 6345. [ Google Scholar ] [ CrossRef ]
- Nakagawa, Y.; Nishikimi, T.; Kuwahara, K. Atrial and brain natriuretic peptides: Hormones secreted from the heart. Peptides 2019 , 111 , 18–25. [ Google Scholar ] [ CrossRef ]
- de Bold, A.J.; Borenstein, H.B.; Veress, A.T.; Sonnenberg, H. A rapid and potent natriuretic response to intravenous injection of atrial myocardial extract in rats. Life Sci. 1981 , 28 , 89–94. [ Google Scholar ] [ CrossRef ]
- Pandey, K.N. Emerging Roles of Natriuretic Peptides and their Receptors in Pathophysiology of Hypertension and Cardiovascular Regulation. J. Am. Soc. Hypertens. 2008 , 2 , 210–226. [ Google Scholar ] [ CrossRef ]
- Bhatia, V.; Nayyar, P.; Dhindsa, S. Brain natriuretic peptide in diagnosis and treatment of heart failure. J. Postgrad. Med. 2003 , 49 , 182–185. [ Google Scholar ]
- Tanase, D.M.; Radu, S.; Al Shurbaji, S.; Baroi, G.L.; Florida Costea, C.; Turliuc, M.D.; Ouatu, A.; Floria, M. Natriuretic Peptides in Heart Failure with Preserved Left Ventricular Ejection Fraction: From Molecular Evidences to Clinical Implications. Int. J. Mol. Sci. 2019 , 20 , 2629. [ Google Scholar ] [ CrossRef ]
- Cao, Z.; Jia, Y.; Zhu, B. BNP and NT-proBNP as Diagnostic Biomarkers for Cardiac Dysfunction in Both Clinical and Forensic Medicine. Int. J. Mol. Sci. 2019 , 20 , 1820. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022 , 145 , e895–e1032. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sim, D.; Lin, W.; Sindone, A.; Yingchoncharoen, T.; Prameswari, H.S.; Mohd Ghazi, A.; Pin, L.C.; Louis, T.; Aw, T.C.; Michael-Joseph, A.; et al. Asian Pacific Society of Cardiology Consensus Statements on the Diagnosis and Management of Chronic Heart Failure. J. Asian Pac. Soc. Cardiol. 2023 , 2 , e10. [ Google Scholar ] [ CrossRef ]
- Januzzi, J.L., Jr.; Zannad, F.; Anker, S.D.; Butler, J.; Filippatos, G.; Pocock, S.J.; Ferreira, J.P.; Sattar, N.; Verma, S.; Vedin, O.; et al. Prognostic Importance of NT-proBNP and Effect of Empagliflozin in the EMPEROR-Reduced Trial. J. Am. Coll. Cardiol. 2021 , 78 , 1321–1332. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mebazaa, A.; Davison, B.; Chioncel, O.; Cohen-Solal, A.; Diaz, R.; Filippatos, G.; Metra, M.; Ponikowski, P.; Sliwa, K.; Voors, A.A.; et al. Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): A multinational, open-label, randomised, trial. Lancet 2022 , 400 , 1938–1952. [ Google Scholar ] [ CrossRef ]
- Reza, N.; Pellicori, P.; Starling, R.C. REVOLUTION in Heart Failure Care and SELECT Highlights from the European Society of Cardiology-Heart Failure Association Heart Failure & World Congress on Acute Heart Failure 2024. J. Card Fail. 2024 , 30 , 1157–1160. [ Google Scholar ]
- Oktay, A.A.; Paul, T.K.; Koch, C.A.; Lavie, C.J. Diabetes, Cardiomyopathy, and Heart Failure ; Updated 26 September 2023; Feingold, K.R., Anawalt, B., Blackman, M.R., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. Available online: https://www.ncbi.nlm.nih.gov/books/NBK560257/ (accessed on 5 February 2024).
- Ledwidge, M.; Gallagher, J.; Conlon, C.; Tallon, E.; O’Connell, E.; Dawkins, I.; Watson, C.; O’Hanlon, R.; Bermingham, M.; Patle, A.; et al. Natriuretic peptide-based screening and collaborative care for heart failure: The STOP-HF randomized trial. JAMA 2013 , 310 , 66–74. [ Google Scholar ] [ CrossRef ]
- Huelsmann, M.; Neuhold, S.; Resl, M.; Strunk, G.; Brath, H.; Francesconi, C.; Adlbrecht, C.; Prager, R.; Luger, A.; Pacher, R.; et al. PONTIAC (NT-proBNP selected prevention of cardiac events in a population of diabetic patients without a history of cardiac disease): A prospective randomized controlled trial. J. Am. Coll. Cardiol. 2013 , 62 , 1365–1372. [ Google Scholar ] [ CrossRef ]
- Jarolim, P.; White, W.B.; Cannon, C.P.; Gao, Q.; Morrow, D.A. Serial Measurement of Natriuretic Peptides and Cardiovascular Outcomes in Patients with Type 2 Diabetes in the EXAMINE Trial. Diabetes Care 2018 , 41 , 1510–1515. [ Google Scholar ] [ CrossRef ]
- Januzzi, J.L., Jr.; Xu, J.; Li, J.; Shaw, W.; Oh, R.; Pfeifer, M.; Butler, J.; Sattar, N.; Mahaffey, K.W.; Neal, B.; et al. Effects of Canagliflozin on Amino-Terminal Pro-B-Type Natriuretic Peptide: Implications for Cardiovascular Risk Reduction. J. Am. Coll. Cardiol. 2020 , 76 , 2076–2085. [ Google Scholar ] [ CrossRef ]
- Rørth, R.; Jørgensen, P.G.; Andersen, H.U.; Christoffersen, C.; Gøtze, J.P.; Køber, L.; Rossing, P.; Jensen, M.T. Cardiovascular prognostic value of echocardiography and N terminal pro B-type natriuretic peptide in type 1 diabetes: The Thousand & 1 Study. Eur. J. Endocrinol. 2020 , 182 , 481–488. [ Google Scholar ] [ PubMed ]
- American Diabetes Association Professional Practice Committee. 10. Cardiovascular Disease and Risk Management: Standards of Care in Diabetes—2024. Diabetes Care 2024 , 47 , S179–S218. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Marx, N.; Federici, M.; Schütt, K.; Müller-Wieland, D.; Ajjan, R.A.; Antunes, M.J.; Christodorescu, R.M.; Crawford, C.; Di Angelantonio, E.; Eliasson, B. 2023 ESC Guidelines for the management of cardiovascular disease in patients with diabetes. Eur. Heart J. 2023 , 44 , 4043–4140. [ Google Scholar ] [ PubMed ]
- Beavers, C.J. Heart Failure Pharmacotherapy Over the Past 30 Years: Boats Against the Current. J. Card. Fail. 2024 , 30 , 1044–1046. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ramzi, Z.S. N-Terminal Prohormone Brain Natriuretic Peptide as a Prognostic Biomarker for the Risk of Complications in Type 2 Diabetes: A Systematic Review and Meta-Analysis. Lab. Med. 2023 , 54 , 339–351. [ Google Scholar ] [ CrossRef ]
- Segar, M.W.; Patel, K.V.; Hellkamp, A.S.; Vaduganathan, M.; Lokhnygina, Y.; Green, J.B.; Wan, S.H.; Kolkailah, A.A.; Holman, R.R.; Peterson, E.D.; et al. Validation of the WATCH-DM and TRS-HF DM Risk Scores to Predict the Risk of Incident Hospitalization for Heart Failure Among Adults with Type 2 Diabetes: A Multicohort Analysis. J. Am. Heart Assoc. 2022 , 11 , e024094. [ Google Scholar ] [ CrossRef ]
- Patel, K.V.; Segar, M.W.; Klonoff, D.C.; Khan, M.S.; Usman, M.S.; Lam, C.S.P.; Verma, S.; DeFilippis, A.P.; Nasir, K.; Bakker, S.J.L.; et al. Optimal Screening for Predicting and Preventing the Risk of Heart Failure Among Adults with Diabetes Without Atherosclerotic Cardiovascular Disease: A Pooled Cohort Analysis. Circulation 2024 , 149 , 293–304. [ Google Scholar ] [ CrossRef ]
- García de Guadiana-Romualdo, L.; Ramos-Arenas, V.; Campos-Rodríguez, V.; Consuegra-Sánchez, L.; Albaladejo-Otón, M.D. In vitro stability of B-type natriuretic peptide (BNP) in plasma stored under different conditions when measured with the Lumipulse ® assay. Scand. J. Clin. Lab. Investig. 2019 , 79 , 455–458. [ Google Scholar ] [ CrossRef ]
- Revuelta-López, E.; Barallat, J.; Cserkóová, A.; Gálvez-Montón, C.; Jaffe, A.S.; Januzzi, J.L.; Bayes-Genis, A. Pre-analytical considerations in biomarker research: Focus on cardiovascular disease. Clin. Chem. Lab. Med. 2021 , 59 , 1747–1760. [ Google Scholar ] [ CrossRef ]
- Lee, D.J.W.; Aw, T.C. Natriuretic Peptides in Clinical Practice: A Current Review. J. Immunol. Sci. 2023 , 7 , 28–34. [ Google Scholar ] [ CrossRef ]
- Troughton, R.W.; Richards, A.M.; Yandle, T.G.; Frampton, C.M.; Nicholls, M.G. The effects of medications on circulating levels of cardiac natriuretic peptides. Ann. Med. 2007 , 39 , 242–260. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ibrahim, N.; McCarthy, C.P.; Shrestha, S.; Gaggin, H.K.; Mukai, R.; Szymonifka, J.; Apple, F.S.; Burnett, J.C., Jr.; Iyer, S.; Januzzi, J.L., Jr. Effect of Neprilysin Inhibition on Various Natriuretic Peptide Assays. J. Am. Coll. Cardiol. 2019 , 73 , 1273–1284. [ Google Scholar ] [ CrossRef ]
- Ibrahim, N.E.; Januzzi, J.L. Beyond Natriuretic Peptides for Diagnosis and Management of Heart Failure. Clin. Chem. 2017 , 63 , 211–222. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mohana, I.K.; Sai-Babaa, K.S.S.; Iyyapu, R.; Thirumalasetty, S.; Satish, O.S. Advances in congestive heart failure biomarkers. Adv. Clin. Chem. 2023 , 112 , 205–248. [ Google Scholar ]
- Lewsey, S.C.; Breathett, K. Racial and ethnic disparities in heart failure: Current state and future directions. Curr. Opin. Cardiol. 2021 , 36 , 320–328. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Shalmia, T.W.; Jensen, A.S.B.; Goetze, J.P. Cardiac natriuretic peptides. Advances Clin. Chem. 2024 , 122 , 115–139. [ Google Scholar ]
- Commodore-Mensah, Y.; Wang, D.; Jeon, Y.; Foti, K.; McEvoy, J.W.; Coresh, J.; Tang, O.; Echouffo-Tcheugui, J.B.; Christenson, R.; Ndumele, C.E.; et al. Racial and ethnic differences in circulating N-terminal pro-brain-type natriuretic peptide (NT-proBNP) in US adults. Am. J. Prev. Cardiol. 2023 , 15 , 100526. [ Google Scholar ]
- Lam, C.S.; Li, Y.H.; Bayes-Genis, A.; Ariyachaipanich, A.; Sato, N.; Kahale, P.; Cuong, T.M.; Dong, Y.; Li, X.; Zhou, Y. The role of N-terminal pro-B-type natriuretic peptide in prognostic evaluation of heart failure. J. Chin. Med. Assoc. 2019 , 82 , 447–451. [ Google Scholar ] [ CrossRef ]
- Ibrahim, I.; Kuan, W.S.; Frampton, C.; Troughton, R.; Liew, O.W.; Chong, J.P.C.; Chan, S.P.; Tan, L.L.; Lin, W.Q.; Pemberton, C.J.; et al. Superior performance of N-terminal pro brain natriuretic peptide for diagnosis of acute decompensated heart failure in an Asian compared with a Western setting. Eur. J. Heart Fail. 2017 , 19 , 209–217. [ Google Scholar ] [ CrossRef ]
- Tromp, J.; Richards, A.M.; Tay, W.T.; Teng, T.H.K.; Yeo, P.S.D.; Sim, D.; Jaufeerally, F.; Leong, G.; Ong, H.Y.; Ling, L.H.; et al. N-terminal pro-B-type natriuretic peptide and prognosis in Caucasian vs. Asian patients with heart failure. ESC Heart Fail. 2018 , 5 , 279–287. [ Google Scholar ] [ CrossRef ]
- Pascual-Figal, D.; Bayés-Genis, A.; Beltrán-Troncoso, P.; Caravaca-Pérez, P.; Conde-Martel, A.; Crespo-Leiro, M.G.; Delgado, J.F.; Díez, J.; Formiga, F.; Manito, N. Sacubitril-Valsartan, Clinical Benefits and Related Mechanisms of Action in Heart Failure with Reduced Ejection Fraction. A Review. Front. Cardiovasc. Med. 2021 , 11 , 754499. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tsai, M.L.; Lin, Y.; Lin, M.S.; Tsai, T.H.; Yang, N.I.; Wang, C.Y.; Hsieh, I.C.; Hung, M.J.; Chen, T.H. Comparing angiotensin receptor-neprilysin inhibitors with sodium-glucose cotransporter 2 inhibitors for heart failure with diabetes mellitus. Diabetol. Metab. Syndr. 2023 , 15 , 110. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yusuf, S.; Pfeffer, M.A.; Swedberg, K.; Granger, C.B.; Held, P.; McMurray, J.J.; Michelson, E.L.; Olofsson, B.; Ostergren, J.; CHARM Investigators and Committees. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: The CHARM-Preserved Trial. Lancet 2003 , 362 , 777–781. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cleland, J.G.; Tendera, M.; Adamus, J.; Freemantle, N.; Polonski, L.; Taylor, J.; PEP-CHF Investigators. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur. Heart J. 2006 , 27 , 2338–2345. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Carson, P.E.; Anand, I.S.; Win, S.; Rector, T.; Haass, M.; Lopez-Sendon, J.; Miller, A.; Teerlink, J.R.; White, M.; McKelvie, R.S.; et al. The Hospitalization Burden and Post-Hospitalization Mortality Risk in Heart Failure with Preserved Ejection Fraction: Results From the I-PRESERVE Trial (Irbesartan in Heart Failure and Preserved Ejection Fraction). JACC Heart Fail. 2015 , 3 , 429–441. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gronda, E.; Vanoli, E.; Iacoviello, M. The PARAGON-HF trial: The sacubitril/valsartan in heart failure with preserved ejection fraction. Eur. Heart J. Suppl. 2020 , 22 (Suppl. L), L77–L81. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Anker, S.D.; Butler, J.; Filippatos, G.; Ferreira, J.P.; Bocchi, E.; Böhm, M.; Brunner-La Rocca, H.P.; Choi, D.J.; Chopra, V.; Chuquiure-Valenzuela, E.; et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N. Engl. J. Med. 2021 , 385 , 1451–1461. [ Google Scholar ] [ CrossRef ]
- Solomon, S.D.; McMurray, J.J.; Claggett, B.; de Boer, R.A.; DeMets, D.; Hernandez, A.F.; Inzucchi, S.E.; Kosiborod, M.N.; Lam, C.S.; Martinez, F.; et al. Dapagliflozin in heart failure with preserved and mildly reduced ejection fraction. N. Engl. J. Med. 2022 , 387 , 1089–1098. [ Google Scholar ]
- Huelsmann, M.; Neuhold, S.; Strunk, G.; Moertl, D.; Berger, R.; Prager, R.; Abrahamian, H.; Riedl, M.; Pacher, R.; Luger, A.; et al. NT-proBNP has a high negative predictive value to rule-out short-term cardiovascular events in patients with diabetes mellitus. Eur. Heart J. 2008 , 29 , 2259–2264. [ Google Scholar ]
- Walter, E.; Arrigo, M.; Allerstorfer, S.; Marty, P.; Hülsmann, M. Cost-effectiveness of NT-proBNP-supported screening of chronic heart failure in patients with or without type 2 diabetes in Austria and Switzerland. J. Med. Econ. 2023 , 26 , 1287–1300. [ Google Scholar ]
- Spahillari, A.; Jackson, L.; Varrias, D.; Michelhaugh, S.A.; Januzzi, J.L.; Shahideh, B.; Daghfal, D.; Valkov, N.; Murtagh, G.; Das, S. MicroRNAs are associated with cardiac biomarkers, cardiac structure and function and incident outcomes in heart failure. ESC Heart Fail. 2024 , 11 , 1400–1410. [ Google Scholar ]
Click here to enlarge figure
| Cohort Name | Population Studied | Follow-Up (Median) | Major Findings |
|---|---|---|---|
| STOP-HF [ ] | 1374 participants with cardiovascular risk factors. Mean age 64.8 years | 4.2 years | Lower prevalence of LV dysfunction in the BNP-based screening group (5.3% vs. 8.7%). |
| PONTIAC [ ] | 300 patients with T2DM and NT-proBNP > 125 pg/mL but without any history of cardiac disease | 2 years | Intensified therapy led to a significant reduction in cardiac hospitalizations/deaths compared to control (hazard ratio: 0.351; p = 0.044). |
| EXAMINE [ ] | 5380 patients with T2DM and a recent ACS event | 597 days | Two NT-proBNP measurements (6 months apart) identified those at the highest risk of developing HF (p < 0.001). |
| CANVAS [ ] | 4330 patients with T2DM and risk factors for CVD | 5.75 years | Higher baseline NT-proBNP levels in those with investigator-reported HF; canagliflozin reduced serial NT-proBNP levels. |
| Thousand and I [ ] | 960 patients with T1DM | 6.3 years | Increased levels of NT-proBNP associated with worse outcomes (hazard ratio 1.56). |
| Guideline | NP Threshold for Ruling In and Ruling Out HF |
|---|---|
| AHA [ ] | BNP > 35 pg/mL and NT-proBNP > 125 pg/mL to rule in HF in diabetes |
| APSC [ ] | BNP < 35 pg/mL and NT-proBNP < 125 pg/mL to exclude HF |
| ADA [ ] | BNP > 50 pg/mL and NT-proBNP > 125 pg/mL for screening those with diabetes |
| ESC [ ] | BNP > 35 pg/mL and NT-proBNP > 125 pg/mL to identify those with HF |
| Study | Year | Drug Class | NP Level as Selection Criterion | Results |
|---|---|---|---|---|
| CHARM [ ] | 2003 | ARB | Not a criterion | Non-significant to borderline-significant outcomes |
| PEP-CHF [ ] | 2006 | ACEI | Not a criterion | Non-significant to borderline-significant outcomes |
| I-PRESERVE [ ] | 2008 | ARB | Not a criterion | Non-significant to borderline-significant outcomes |
| PARAGON [ ] | 2019 | ARNI | Optional | Borderline-significant outcomes |
| EMPEROR-Preserved [ ] | 2021 | SGLT2i | Absolute | Significant outcomes |
| DELIVER [ ] | 2022 | SGLT2i | Absolute | Significant outcomes |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Tiwari, D.; Aw, T.C. Emerging Role of Natriuretic Peptides in Diabetes Care: A Brief Review of Pertinent Recent Literature. Diagnostics 2024 , 14 , 2251. https://doi.org/10.3390/diagnostics14192251
Tiwari D, Aw TC. Emerging Role of Natriuretic Peptides in Diabetes Care: A Brief Review of Pertinent Recent Literature. Diagnostics . 2024; 14(19):2251. https://doi.org/10.3390/diagnostics14192251
Tiwari, Dipti, and Tar Choon Aw. 2024. "Emerging Role of Natriuretic Peptides in Diabetes Care: A Brief Review of Pertinent Recent Literature" Diagnostics 14, no. 19: 2251. https://doi.org/10.3390/diagnostics14192251
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- View PDF
- Download full issue

Patient Education and Counseling
Review a systematic literature review of diabetes self-management education features to improve diabetes education in women of black african/caribbean and hispanic/latin american ethnicity, practical implications.
- Previous article in issue
- Next article in issue
Cited by (0)
Advertisement
Impact of pesticides exposure and type 2 diabetes risk: a systematic review and meta-analysis
- Published: 09 October 2024
Cite this article

- Yang Chen 1 , 2 ,
- Yaqin Deng 1 , 2 ,
- Minjia Wu 1 , 2 ,
- Peixuan Ma 1 , 2 ,
- Wen Pan 1 , 2 ,
- Weiqi Chen 1 , 2 ,
- Lina Zhao 3 &
- Xiaowei Huang 1 , 2
We conducted a systematic review and meta-analysis of observational studies that assessed the relationship between pesticides exposure and type 2 diabetes. We also examined the presence of heterogeneity and biases across the available studies.
We conducted a comprehensive literature search of peer-reviewed studies published from 2011 to 2023, without language limitations. A random-effects model was employed to calculate the overall odds ratio (OR) and its corresponding 95% confidence interval (CI).
We included 19 studies (n = 12 case-control and n = 7 cross-sectional) for a total of 45,813 participants in our analysis. Our findings revealed a notable correlation between pesticide exposure and type 2 diabetes (non-specific definition) when not limiting pesticide types (OR: 1.19, 95% CI: 1.11–1.28). Subgroup analysis identified associations between pyrethroid (OR: 1.17, 95% CI: 1.05–1.30) and type 2 diabetes, as well as between organochlorine (OR: 1.26, 95% CI: 1.11–1.43) and type 2 diabetes. However, no statistically significant association was observed between herbicide exposure and the onset of type 2 diabetes (OR: 1.26, 95% CI: 0.91–1.75). In the elderly group, pesticide exposure significantly heightened the risk of type 2 diabetes (OR: 1.25, 95% CI: 1.14–1.38), with no statistically significant heterogeneity among studies (I 2 = 14.2%, p = 0.323).
Conclusions
Pesticide (organochlorine and pyrethroid) exposure constitutes a risk factor for type 2 diabetes.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
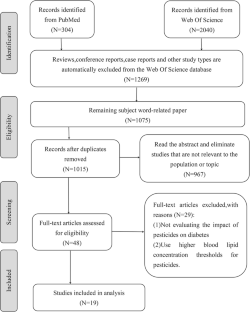
Similar content being viewed by others
Dietary pesticide exposure and non-communicable diseases and mortality: a systematic review of prospective studies among adults
Pesticide exposure and liver cancer: a review.

Pesticide exposure and diabetes mellitus in a semi-urban Nepali population: a cross-sectional study
H. Sun, P. Saeedi, S. Karuranga et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diab. Res. Clin. Pract. 183 , 109119 (2022). https://doi.org/10.1016/j.diabres.2021.109119
Article Google Scholar
E. Standl, K. Khunti, T.B. Hansen et al. The global epidemics of diabetes in the 21st century: current situation and perspectives. Eur. J. Prev. Cardiol. 26 , 7–14 (2019). https://doi.org/10.1177/2047487319881021
Article PubMed Google Scholar
D.M.F. Ingrosso, M. Primavera, S. Samvelyan et al. Stress and diabetes mellitus: pathogenetic mechanisms and clinical outcome. Horm. Res. Paediatr. 96 , 34–43 (2023). https://doi.org/10.1159/000522431
Article CAS PubMed Google Scholar
J. Juan, H. Yang, Prevalence, prevention, and lifestyle intervention of gestational diabetes mellitus in China. Int. J. Environ. Res. Public Health 17 , 9517 (2020). https://doi.org/10.3390/ijerph17249517
Article PubMed PubMed Central Google Scholar
J.W.J. Beulens, M.G.M. Pinho, T.C. Abreu et al. Environmental risk factors of type 2 diabetes-an exposome approach. Diabetologia 65 , 263–274 (2022). https://doi.org/10.1007/s00125-021-05618-w
L. Lind, S. Salihovic, P.M. Lind, Mixtures of environmental contaminants and diabetes. Sci. Total Environ. 859 , 159993 (2023). https://doi.org/10.1016/j.scitotenv.2022.159993
J. Zhang, W. Song, Y. Sun et al. Changes in glucose metabolism and mRNA expression of IRS-2 in rats exposed to phoxim and the protective effects of vitamin E. Toxicol. Res. 7 , 201–210 (2017). https://doi.org/10.1039/c7tx00243b
Article CAS Google Scholar
M. Czajka, M. Matysiak-Kucharek, B. Jodłowska-Jędrych et al. Organophosphorus pesticides can influence the development of obesity and type 2 diabetes with concomitant metabolic changes. Environ. Res. 178 , 108685 (2019). https://doi.org/10.1016/j.envres.2019.108685
C.M. Park, K.T. Kim, D.Y. Rhyu, Exposure to a low concentration of mixed organochlorine pesticides impairs glucose metabolism and mitochondrial function in L6 myotubes and zebrafish. J. Hazard Mater. 414 , 125437 (2021). https://doi.org/10.1016/j.jhazmat.2021.125437
H. Lee, Y. Gao, E. Ko et al. Nonmonotonic response of type 2 diabetes by low concentration organochlorine pesticide mixture: findings from multi-omics in zebrafish. J. Hazard Mater. 416 , 125956 (2021). https://doi.org/10.1016/j.jhazmat.2021.125956
S. Tyagi, B.K. Mishra, T. Sharma et al. Level of organochlorine pesticide in prediabetic and newly diagnosed diabetes mellitus patients with varying degree of glucose intolerance and insulin resistance among north Indian population. Diab. Metab. J. 45 , 558–568 (2021). https://doi.org/10.4093/dmj.2020.0093
X. Guo, H. Wang, Q. Song et al. Association between exposure to organophosphorus pesticides and the risk of diabetes among US adults: cross-sectional findings from the national health and nutrition examination survey. Chemosphere 301 , 134471 (2022). https://doi.org/10.1016/j.chemosphere.2022.134471
G. Velmurugan, K. Swaminathan, S. Mohanraj et al. Association of co-accumulation of arsenic and organophosphate insecticides with diabetes and atherosclerosis in a rural agricultural community: KMCH-NNCD-I study. Acta Diabetol. 57 , 1159–1168 (2020). https://doi.org/10.1007/s00592-020-01516-6
J.Á. Hernández-Mariano, M.C. Baltazar-Reyes, E. Salazar-Martínez et al. Exposure to the pesticide DDT and risk of diabetes and hypertension: systematic review and meta-analysis of prospective studies. Int. J. Hyg. Environ. Health 239 , 113865 (2022). https://doi.org/10.1016/j.ijheh.2021.113865
X. Yao, S. Geng, L. Zhu et al. Environmental pollutants exposure and gestational diabetes mellitus: Evidence from epidemiological and experimental studies. Chemosphere 332 , 138866 (2023). https://doi.org/10.1016/j.chemosphere.2023.138866
F. Cao, Z. Li, Q. He et al. Occurrence, spatial distribution, source, and ecological risk assessment of organochlorine pesticides in Dongting Lake, China. Environ. Sci. Pollut. Res. Int. 28 , 30841–30857 (2021). https://doi.org/10.1007/s11356-021-12743-x
F. Deng, J. Sun, R. Dou et al. Contamination of pyrethroids in agricultural soils from the Yangtze River Delta, China. Sci. Total Environ. 731 , 139181 (2020). https://doi.org/10.1016/j.scitotenv.2020.139181
H. Lamat, M.P. Sauvant-Rochat, I. Tauveron et al. Metabolic syndrome and pesticides: a systematic review and meta-analysis. Environ. Pollut. 305 , 119288 (2022). https://doi.org/10.1016/j.envpol.2022.119288
P.A. Modesti, G. Reboldi, F.P. Cappuccio et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS ONE 11 , e0147601 (2016). https://doi.org/10.1371/journal.pone.0147601
Article CAS PubMed PubMed Central Google Scholar
T.B. Huedo-Medina, J. Sánchez-Meca, F. Marín-Martínez et al. Assessing heterogeneity in meta-analysis: q statistic or I2 index? Psychol. Methods 11 , 193–206 (2006). https://doi.org/10.1037/1082-989X.11.2.193
Q. Jing, J. Liu, A. Chen et al. The spatial-temporal chemical footprint of pesticides in China from 1999 to 2018. Environ. Sci. Pollut. Res. Int. 29 , 75539–75549 (2022). https://doi.org/10.1007/s11356-022-20602-6
Q. Zhu, Y. Yang, Y. Zhong et al. Synthesis, insecticidal activity, resistance, photodegradation and toxicity of pyrethroids (A review). Chemosphere 254 , 126779 (2020). https://doi.org/10.1016/j.chemosphere.2020.126779
W. Tang, D. Wang, J. Wang et al. Pyrethroid pesticide residues in the global environment: an overview. Chemosphere 191 , 990–1007 (2018). https://doi.org/10.1016/j.chemosphere.2017.10.115
E. Evangelou, G. Ntritsos, M. Chondrogiorgi et al. Exposure to pesticides and diabetes: a systematic review and meta-analysis. Environ. Int. 91 , 60–68 (2016). https://doi.org/10.1016/j.envint.2016.02.013
M. Tudi, H. Daniel Ruan, L. Wang et al. Agriculture development, pesticide application and its impact on the environment. Int. J. Environ. Res. Public Health 18 , 1112 (2021). https://doi.org/10.3390/ijerph18031112
R.M. Gutgesell, E.E. Tsakiridis, S. Jamshed et al. Impact of pesticide exposure on adipose tissue development and function. Biochem. J. 477 , 2639–2653 (2020). https://doi.org/10.1042/BCJ20200324
E. Ko, M. Choi, S. Shin, Bottom-line mechanism of organochlorine pesticides on mitochondria dysfunction linked with type 2 diabetes. J. Hazard Mater. 393 , 122400 (2020). https://doi.org/10.1016/j.jhazmat.2020.122400
N. Tawar, B.D. Banerjee, S.V. Madhu et al. Association of organochlorine pesticides with genetic markers of endoplasmic reticulum stress in type 2 diabetes mellitus: a case-control study among the North-Indian population. Front. Endocrinol. 13 , 841463 (2022). https://doi.org/10.3389/fendo.2022.841463
J. Shi, D. Wei, C. Ma et al. Combined effects of organochlorine pesticides on type 2 diabetes mellitus: Insights from endocrine disrupting effects of hormones. Environ. Pollut. 341 , 122867 (2024). https://doi.org/10.1016/j.envpol.2023.122867
S. Shrestha, C.G. Parks, D.M. Umbach et al. Use of permethrin and other pyrethroids and mortality in the Agricultural Health Study. Occup. Environ. Med. 79 , 664–672 (2022). https://doi.org/10.1136/oemed-2021-108156
S. Shrestha, D.M. Umbach, L.E. Beane Freeman et al. Occupational pesticide use and self-reported olfactory impairment in US farmers. Occup. Environ. Med. oemed-2020-106818 (2020). https://doi.org/10.1136/oemed-2020-106818
Y. Wei, W. Liu, J. Liu, Environmentally relevant exposure to cypermethrin aggravates diet-induced diabetic symptoms in mice: the interaction between environmental chemicals and diet. Environ. Int. 178 , 108090 (2023). https://doi.org/10.1016/j.envint.2023.108090
J. Verma, A.K. Rai, N.K. Satija, Autophagy perturbation upon acute pyrethroid treatment impacts adipogenic commitment of mesenchymal stem cells. Pestic. Biochem. Physiol. 195 , 105566 (2023). https://doi.org/10.1016/j.pestbp.2023.105566
J. Wang, Y. Zhu, X. Cai et al. Abnormal glucose regulation in pyrethroid pesticide factory workers. Chemosphere 82 , 1080–1082 (2011). https://doi.org/10.1016/j.chemosphere.2010.10.065
R. Airaksinen, P. Rantakokko, J.G. Eriksson et al. Association between type 2 diabetes and exposure to persistent organic pollutants. Diab. Care 34 , 1972–1979 (2011). https://doi.org/10.2337/dc10-2303
C.J. Everett, O.M. Thompson, C.E. Dismuke, Exposure to DDT and diabetic nephropathy among Mexican Americans in the 1999-2004 national health and nutrition examination survey. Environ. Pollut. 222 , 132–137 (2017). https://doi.org/10.1016/j.envpol.2016.12.069
B.A. Grice, R.G. Nelson, D.E. Williams et al. Associations between persistent organic pollutants, type 2 diabetes, diabetic nephropathy and mortality. Occup. Environ. Med. 74 , 521–527 (2017). https://doi.org/10.1136/oemed-2016-103948
L.A. Henríquez-Hernández, O.P. Luzardo, P.F. Valerón et al. Persistent organic pollutants and risk of diabetes and obesity on healthy adults: results from a cross-sectional study in Spain. Sci. Total Environ. 607-608 , 1096–1102 (2017). https://doi.org/10.1016/j.scitotenv.2017.07.075
C. Juntarawijit, Y. Juntarawijit, Association between diabetes and pesticides: a case-control study among Thai farmers. Environ. Health Prev. Med. 23 , 3 (2018). https://doi.org/10.1186/s12199-018-0692-5
G. Zong, D. Valvi, B. Coull et al. Persistent organic pollutants and risk of type 2 diabetes: a prospective investigation among middle-aged women in Nurses’ Health Study II. Environ. Int. 114 , 334–342 (2018). https://doi.org/10.1016/j.envint.2017.12.010
E.C. Meek, D.D. Jones, J.A. Crow et al. Association of serum levels of p,p′-dichlorodiphenyldichloroethylene (DDE) with type 2 diabetes in African American and caucasian adult men from agricultural (Delta) and non-agricultural (non-Delta) regions of Mississippi. J. Toxicol. Environ. Health A 82 , 387–400 (2019). https://doi.org/10.1080/15287394.2019.1610678
A. Tornevi, J. Sommar, P. Rantakokko et al. Chlorinated persistent organic pollutants and type 2 diabetes-A population-based study with pre- and post-diagnostic plasma samples. Environ. Res. 174 , 35–45 (2019). https://doi.org/10.1016/j.envres.2019.04.017
K. Wolf, B.W.C. Bongaerts, A. Schneider et al. Persistent organic pollutants and the incidence of type 2 diabetes in the CARLA and KORA cohort studies. Environ. Int. 129 , 221–228 (2019). https://doi.org/10.1016/j.envint.2019.05.030
Z. Sharafi, M.H. Ehrampoush, A. Salehi-Abargouei et al. Investigation of the association between pesticide exposure and the prevalence of type 2 diabetes in Shahedieh population in Yazd. Environ. Sci. Pollut. Res. Int. 28 , 43394–43401 (2021). https://doi.org/10.1007/s11356-021-13821-w
D. Charles, V. Berg, T.H. Nøst et al. Longitudinal changes in concentrations of persistent organic pollutants (1986-2016) and their associations with type 2 diabetes mellitus. Environ. Res. 204 , 112129 (2022). https://doi.org/10.1016/j.envres.2021.112129
J. Huang, L. Hu, J. Yang, Dietary magnesium intake ameliorates the association between household pesticide exposure and type 2 diabetes: data from NHANES, 2007-2018. Front. Nutr. 9 , 903493 (2022). https://doi.org/10.3389/fnut.2022.903493
C. Jia, S. Zhang, X. Cheng et al. Association between serum pyrethroid insecticide levels and incident type 2 diabetes risk: a nested case-control study in Dongfeng-Tongji cohort. Eur. J. Epidemiol. 37 , 959–970 (2022). https://doi.org/10.1007/s10654-022-00906-0
R. Liang, L. Yu, W. Liu et al. Associations of bifenthrin exposure with glucose homeostasis and type 2 diabetes mellitus in a general Chinese population: roles of protein carbonylation. Environ. Pollut. 315 , 120352 (2022). https://doi.org/10.1016/j.envpol.2022.120352
C. Jia, S. Zhang, X. Cheng et al. Circulating organochlorine pesticide levels, genetic predisposition and the risk of incident type 2 diabetes. Environ. Pollut. 337 , 122541 (2023). https://doi.org/10.1016/j.envpol.2023.122541
M. Wang, M. Zhou, Q. Tan et al. Triazine herbicides exposure, natural immunoglobulin M antibodies, and fasting plasma glucose changes: association and mediation analyses in general Chinese urban adults. Environ. Pollut. 330 , 121833 (2023). https://doi.org/10.1016/j.envpol.2023.121833
D. Wei, L. Wang, Q. Xu et al. Exposure to herbicides mixtures in relation to type 2 diabetes mellitus among Chinese rural population: results from different statistical models. Ecotoxicol. Environ. Saf. 261 , 115109 (2023). https://doi.org/10.1016/j.ecoenv.2023.115109
M.Z. Zhao, D. Wei, L. Wang, et al. The interaction of inflammation and exposure to pyrethroids is associated with impaired fasting glucose and type 2 diabetes. Exposure And Health, 16 (4), 1–13 (2023). https://doi.org/10.1007/s12403-023-00602-8
Download references
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 21966010) and Advance Innovation Teams and Xinghu Scholars Program of Guangxi Medical University.
Author information
Authors and affiliations.
Department of Toxicology, School of Public Health, Guangxi Key Laboratory of Environment and Health Research, Guangxi Medical University, Nanning, China
Yang Chen, Yaqin Deng, Minjia Wu, Peixuan Ma, Wen Pan, Weiqi Chen & Xiaowei Huang
Guangxi Colleges and Universities Key Laboratory of Prevention and Control of Highly Prevalent Diseases, Guangxi Medical University, Nanning, China
School of Public Health, Wuhan University, Wuhan, China
You can also search for this author in PubMed Google Scholar
Contributions
Yang Chen: Conceptualization, Data curation, Formal analysis, Methodology, Writing—original draft, Writing—review & editing. Yaqin Deng: Conceptualization, Data curation, Writing —original draft. Minjia Wu: Formal analysis, Methodology.Peixuan Ma: Formal analysis, Methodology.Wen Pan: Validation.Weiqi Chen: Validation.Lina Zhao: Writing—review & editing. Xiaowei Huang: Conceptualization, Funding acquisition, Methodology, Supervision, Writing—review & editing.
Corresponding author
Correspondence to Xiaowei Huang .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary materials, rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Chen, Y., Deng, Y., Wu, M. et al. Impact of pesticides exposure and type 2 diabetes risk: a systematic review and meta-analysis. Endocrine (2024). https://doi.org/10.1007/s12020-024-04067-w
Download citation
Received : 14 July 2024
Accepted : 03 October 2024
Published : 09 October 2024
DOI : https://doi.org/10.1007/s12020-024-04067-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Type 2 diabetes
- Pyrethroid pesticides
- Organochlorine
- Systematic review
- Meta-analysis
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 10 October 2024
Examining noncommunicable diseases using satellite imagery: a systematic literature review
- Elizabeth J. Folkmann 1 ,
- M. Courtney Hughes 2 ,
- Uzma Amzad Khan 3 &
- Mahdi Vaezi 4
BMC Public Health volume 24 , Article number: 2774 ( 2024 ) Cite this article
Metrics details
Introduction
Noncommunicable diseases (NCDs) are the leading cause of morbidity and mortality worldwide, accounting for 74% of deaths annually. Satellite imagery provides previously unattainable data about factors related to NCDs that overcome limitations of traditional, non-satellite-derived environmental data, such as subjectivity and requirements of a smaller geographic area of focus. This systematic literature review determined how satellite imagery has been used to address the top NCDs in the world, including cardiovascular diseases, cancers, chronic respiratory diseases, and diabetes.
A literature search was performed using PubMed (including MEDLINE), CINAHL, Web of Science, Science Direct, Green FILE, and Engineering Village for articles published through June 6, 2023. Quantitative, qualitative, and mixed-methods peer-reviewed studies about satellite imagery in the context of the top NCDs (cancer, cardiovascular disease, chronic respiratory disease, and diabetes) were included. Articles were assessed for quality using the criteria from the Oxford Centre for Evidence-Based Medicine.
A total of 43 studies were included, including 5 prospective comparative cohort trials, 22 retrospective cohort studies, and 16 cross-sectional studies. Country economies of the included studies were 72% high-income, 16% upper-middle-income, 9% lower-middle-income, and 0% low-income. One study was global. 93% of the studies found an association between the satellite data and NCD outcome(s). A variety of methods were used to extract satellite data, with the main methods being using publicly available algorithms (79.1%), preprocessing techniques (34.9%), external resource tools (30.2%) and publicly available models (13.9%). All four NCD types examined appeared in at least 20% of the studies.
Researchers have demonstrated they can successfully use satellite imagery data to investigate the world’s top NCDs. However, given the rapid increase in satellite technology and artificial intelligence, much of satellite imagery used to address NCDs remains largely untapped. In particular, with most existing studies focusing on high-income countries, future research should use satellite data, to overcome limitations of traditional data, from lower-income countries which have a greater burden of morbidity and mortality from NCDs. Furthermore, creating and refining effective methods to extract and process satellite data may facilitate satellite data’s use among scientists studying NCDs worldwide.
Peer Review reports
Noncommunicable diseases (NCDs) account for 74% of global deaths annually, with cardiovascular diseases, cancers, chronic respiratory diseases, and diabetes responsible for over 80% of premature NCD mortalities [ 1 ]. NCDs are not limited to older adults, with 17 million deaths before age 70, predominantly in low- and middle-income countries [ 1 ]. In the United States, direct health costs related to NCDs exceed $1 trillion annually [ 2 ]. Unhealthy behaviors like smoking, poor diet, and physical inactivity increase NCD susceptibility [ 3 ]. The third largest underlying risk factor of chronic disease (after high blood pressure and tobacco usage) is air pollution, an environmental risk factor most often increasing the risk for three of the top four NCDs - cardiovascular disease, cancers, and chronic respiratory diseases [ 4 ].
Achieving the World Health Organization Sustainable Development Goal Target 3.4 of reducing premature NCD mortality by one-third by 2030 [ 5 ] is challenging, with most countries making minimal progress [ 6 ]. Identifying geographic locations with populations most at risk for NCDs is one step toward directing prevention-related policies and programs to achieve this goal [ 7 ]. Satellite technologies offer tools to help identify at-risk geographic locations that overcome limitations of traditional, non-satellite-derived environmental data (e.g., surveys and ground monitoring stations) such as subjectivity and being limited to smaller geographic areas. Satellite data is open source, available on a global scale, and has four resolutions: temporal, spatial, radiometric and spectral [ 8 ]. With over 400 Earth observation satellites orbiting our planet [ 9 ], satellite imagery data, often coupled with artificial intelligence (AI), has shown great promise in advancing areas of research outside of healthcare, such as earth science [ 10 ] and economics [ 11 ], and within health sciences, particularly in infectious disease [ 12 , 13 , 14 ]. While satellite data helps mitigate the problem of traditional environmental data availability, it presents new challenges in understanding what satellite data to use and how to interpret the data. Fortunately, publicly available algorithms, tools, and tutorials exist to help scientists extract, process, and interpret satellite data. Satellite imagery has been less commonly used for analyzing and managing NCDs [ 15 ].
Traditional (non-satellite-derived) environmental measurements have been successfully used in research in the form of surveys (e.g., light at night (LAN), greenspace) and ground monitoring stations (e.g., air pollution), both of which have limitations [ 8 ]. Survey data can be subjective and non-uniform, while ground monitoring station data is limited to areas within a close proximity to a station, most often a developed urban area [ 8 ]. Satellite data has been found to overcome these limitations by its being open source, available on a global scale, and having four resolutions: temporal, spatial, radiometric and spectral [ 8 ].
Satellite data is derived from remote sensors located on satellites. The amount of energy reflected, absorbed, or transmitted by any item on Earth creates a “spectral fingerprint.” Remote sensors can detect a number (specific to the type of remote sensor and called its spectral resolution) of spectral bands, which allows items to be identified by their spectral fingerprint [ 16 , 17 ]. There are two types of sensors: passive sensors (e.g., radiometers and spectrometers operating in the visible, infrared, thermal infrared and microwave electromagnetic spectrum) that measure land and sea physical attributes (e.g., temperature, vegetation properties, aerosol properties, cloud properties) and active sensors (e.g., radar sensors, altimeters operating in the microwave band of the electromagnetic spectrum) that measure vertical profiles of land and sea attributes (e.g., forest structure, ice, aerosols). Satellites have specific orbits and sensor designs that dictate resolution [ 16 ]. How well a remote sensor can distinguish between small differences in energy is called its radiometric resolution, which is the amount of information in each pixel (e.g., 8 bit resolution that can store up to 256 values). Higher resolution means more detail, though this also requires more processing power. Spatial resolution is defined as the size of each pixel. For example, to see buildings you would need 10 m (m) spatial resolution, which represents a 10 m by 10 m square on the ground. Neighborhoods need 20 m spatial resolution, which represents a 20 m by 20 m square on the ground, while regional needs 1 km (km), which represents 1 km by 1 km square on the ground (national: 10 m, continent: 30 km and global: 110 km) [ 16 ]. Spectral resolution is defined by both the number of bands and how narrow the bands are. For example, 3–10 bands is referred to as multispectral, whereas hundreds or thousands of bans are hyperspectral. Temporal resolution is defined as the time it takes the satellite to complete one iteration of its orbit, which is dependent on its orbit, its swath, width and the specific sensor (e.g., Moderate Resolution Imaging Spectroradiometer (MODIS) on NASA’s Terra and Aqua satellite’s temporal resolution is 1–2 days) [ 16 ].
We aimed to provide the first systematic literature review focusing on how environmental factors data collected from satellite imagery has been used to examine risk, incidence, prevalence, or mortality related to an NCD, both methodologically and technically. This review can illuminate resources and methods for using emerging satellite imagery technologies to capture and analyze comprehensive data that can inform NCD prevention and control interventions and policies. By integrating satellite-derived data with ground-based monitoring systems, scientists and policymakers can better understand the risk and distribution of NCDs, allocate resources more effectively, and implement targeted strategies to lessen NCD burden.
This systematic review was registered at PROSPERO (CRD42023433472). We followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines [ 18 ].
Data sources
We conducted a systematic review of literature related to satellite imagery and the top 4 NCDs (cardiovascular diseases, cancers, chronic respiratory diseases, and diabetes) in the world through June 6, 2023. We did not restrict our search to any start date. To gather relevant studies, we searched PubMed (including MEDLINE), CINAHL, Web of Science, Science Direct, Green FILE, and Engineering Village databases. See Additional file 1 for keyword search strings.
Study selection
First, we removed duplicate studies. Next, at least two study authors independently assessed the remaining abstracts based on predetermined inclusion criteria of needing to examine the top four NCDs in the world using satellite imagery. We considered all quantitative, qualitative, and mixed method study designs written in English. Then 2 study authors independently evaluated the full-text articles for inclusion, with discrepancies resolved through discussion. Studies that were not about one or more NCDs, not about satellite imagery, or review articles were excluded. Another way to describe our inclusion criteria is using the PECO (Population, Exposure, Comparator, Outcomes) framework recommended for exploring associations of environmental and other exposures with health outcomes [ 19 ]. Table 1 presents the inclusion and exclusion criteria.
Data extraction
At least two study authors independently extracted information for each study that met the inclusion criteria, including the study aim, disease, geographic level, year of data collection, methods, tools and resources, data extracted from images, measures, results, and findings. The authors discussed and resolved any discrepancies in the extracted data. We assessed the quality of the evidence for each study using the criteria from the Oxford Centre for Evidence-Based Medicine [ 20 ]. The quality of each study was independently graded by two study authors, with any discrepancies resolved through discussion. Following is a description of the quality ratings: 1 for properly powered randomized clinical trials, 2 for well-designed controlled trials without randomization and prospective comparative cohort trials, 3 for case-control studies and retrospective cohort studies, 4 for case series with or without intervention and cross-sectional studies, and 5 for case reports or opinions of respected authorities.
We conducted a qualitative synthesis of satellite data by determining if an association (statistically significant relationship) was found between the satellite data and each study’s dependent variable (e.g., NCD outcome) and explored the authors’ statements about the value of using satellite data. We also recorded statements that included wording about satellite data such as “overcame the problem,” “great tool,” and “enhanced.” We used a spreadsheet so that at least two authors could track these associations and statements and used codes to categorize aspects about the value of satellite imagery for examining NCD outcomes for each article. Our analysis also included all authors reviewing the frequency of the findings and the wording of the statements. Based on this analysis, the authors developed themes about the value of satellite imagery for examining NCDs.
We identified 1,495 articles from our database searches. After applying inclusion and exclusion criteria, 43 studies were selected for inclusion and 1,452 were excluded (Fig. 1 ). Table 2 includes details, quality assessment, and study authors’ statements about satellite value for all the reviewed studies and Table 3 presents the study characteristics, analysis, and data synthesis.
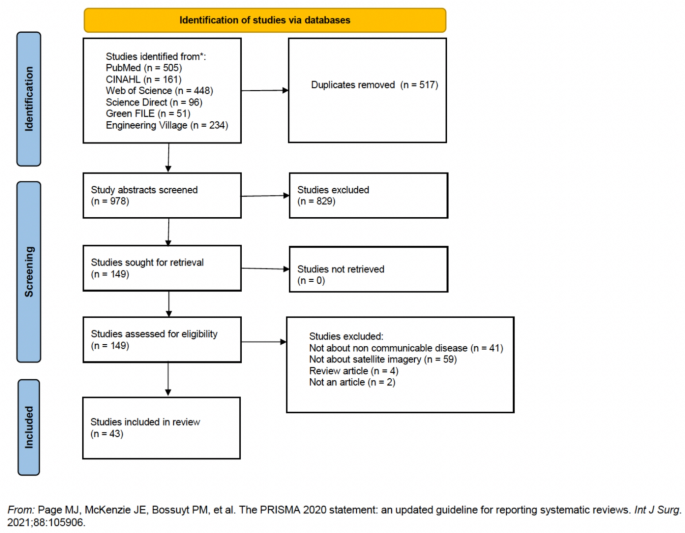
PRISMA flow diagram
The study publication dates spanned over 15 years, 2008–2023, with more than half published within the 5 years before our study search end date. Overall, 70% of the studies were from high-income countries, with over half of those from the United States. The remaining studies were from middle-income countries, and none were from low-income countries. The majority of studies (66%) used satellite data examined at the city, census tract or census block, or county level. About half of the study designs were retrospective cohort and about one-third were cross-sectional. The 12% of studies that fit in the most rigorous study design category for this review (had prospective study designs) all focused on cancer. There were no randomized control trials or case reports. Regarding disease outcomes examined, prevalence was an outcome in over half of the studies (53.5%), incidence in about 30% of the studies, mortality in just under 20%, and disease risk in just under 5% (Table 2 ).
30% of the studies used satellite images from MODIS [ 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 ], an instrument located on NASA’s Aura, Terra, and Aqua satellites, and 16% used unspecified instruments located on NASA’s Landsat satellites [ 24 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ]. The other major satellite image source was the United States Space Force’s Department of Meteorological Satellite Program (DMSP) [ 46 , 47 , 48 , 49 , 50 , 51 , 52 ], with images used in 21% of the studies. MODIS and Landsat were primarily used to extract air pollution and greenspace data, while DMSP was primarily used to detect LAN. Greenspace was the most frequently extracted data, with nearly half of the studies examining this feature. The next most frequently extracted data was air pollution, appearing in 37.2% of the studies (Table 3 ).
All 4 major NCDs examined—cardiovascular disease, cancers, chronic respiratory disease, and diabetes—appeared in at least 20% of the studies, with chronic respiratory diseases and cancers each appearing in about 40%. Cardiovascular disease, chronic respiratory disease, and diabetes studies heavily used greenspace and air pollution data. All studies using LAN examined cancer outcomes [ 46 , 47 , 48 , 49 , 50 , 51 , 52 ], with 4 of the 7 specific to breast cancer [ 46 , 47 , 50 , 51 ]. DMSP data was from 1996 to 97 and was used as a baseline for determining LAN in 6 [ 47 , 48 , 49 , 50 , 51 , 52 ] of the 7 articles [ 46 , 47 , 48 , 49 , 50 , 51 , 52 ]. Approximately one-third of the cancer studies included air pollution data [ 23 , 25 , 29 , 35 , 53 , 54 ], while less than one-fifth included greenspace data [ 27 , 53 , 55 ] (Table 3 ). Air pollution was the primary data extracted for chronic respiratory disease, closely followed by greenspace. We found the reverse with the studies on cardiovascular disease; greenspace was the primary data extracted, closely followed by air pollution. Greenspace was the primary data extracted for diabetes studies (Fig. 2 ).
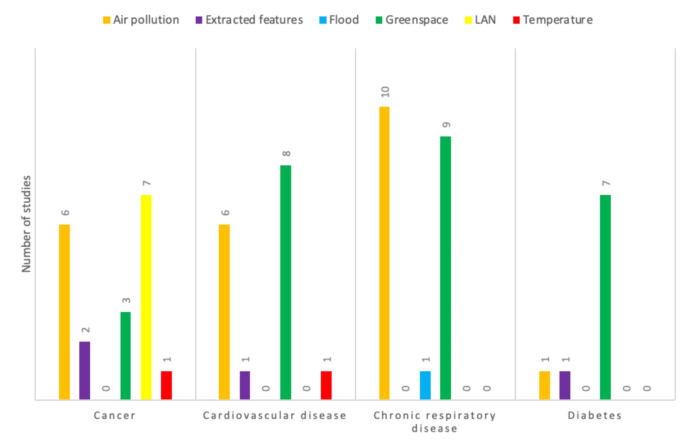
The number of studies of each type of satellite data for each noncommunicable disease. “LAN” is “light at night” and refers to ambient light exposure at night. “Extracted features” refers to features extracted using machine learning to inform a machine learning model. “Air pollution” refers to aerosol optic depth measures, particle matter in air with diameter less than 2.5 micrometers, particle matter in air with diameter less than 10 micrometers, “Flood” refers to changes in land and water surface due to rainfall. “Greenspace” refers to normalized difference vegetation index (NDVI), enhanced vegetation index (EVI), photosynthetic vegetation (PV), and soil adjusted vegetation index (SAVI). “Temperature” refers to the land surface temperature (LST) and surface urban heat island (SUHI)
The majority of the articles (60%) used data from earlier than 5 years from the publication date and matched health data year(s) to satellite data year(s). Of the 10 articles [ 26 , 37 , 41 , 45 , 47 , 48 , 49 , 50 , 51 , 52 ] using data from earlier than 10 years from the publication date, 6 used data from DMSP [ 47 , 48 , 49 , 50 , 51 , 52 ], and 3 used data from LandSat [ 37 , 41 , 45 ]. All but 3 articles [ 39 , 48 , 49 ] in the review found associations between the satellite data and NCD outcomes of risk, incidence, prevalence, or mortality. For example, Fan and colleagues [ 38 ] found a positive association between neighborhood greenness and COPD prevalence using the NDVI based on satellite imagery. Two of the studies that found no association used LAN and cancer [ 48 , 49 ]; however, both found that LAN was a valid representation of circadian rhythm disruption. The third article found no association between greenspace in early life and insulin resistance in adolescence [ 39 ] (Table 2 ).
All data extracted in the studies in this review were related to a previously known disease risk factor. That is, no studies introduced a new disease risk factor that had not been established in prior research. Additionally, the majority of the studies included covariates such as sociodemographic factors like age and income level or health-related factors like body mass index (BMI) and smoking. Most studies focused on one type of satellite data, such as greenspace. However, 9% of the studies [ 22 , 24 , 28 , 37 , 38 , 40 , 44 , 53 , 56 ] examined multiple environmental factors extracted from satellites, such as greenspace and air pollution, in studying the incidence [ 28 , 44 ], prevalence [ 22 , 24 , 37 , 38 , 40 , 56 ], and mortality [ 28 , 53 ] of NCDs. Two articles used a type of AI, convolutional neural networks (CNN), to extract numerical features from satellite imaging. One article [ 57 ] used a CNN with t-SNE (t-distributed Stochastic Neighbor Embedding) to verify the capacity of the neural network to extract relevant features related to cancer prevalence. The other article [ 58 ] used a visual geometry group fast convolution neural network (VGG-CNN-F), a network previously described by Chatfield and colleagues [ 59 ] with elastic net regression to prevent overfitting of the model to training data and minimize mean cross-validation error in a study examining obesity prevalence.
All articles used satellite data extracted based on geolocation(s) specific to the population of interest’s location (versus using data from a convenience sample based on data availability) using one or two of a variety of methods (Table 3 ). Existing publicly available algorithms were the primary method for satellite data extraction, with such algorithms used for analyzing 85% of greenspace data (primarily the normalized difference vegetation index, or NDVI) and 50% of air pollution data (such as the multi-angle Implementation of Atmospheric Correction (MAIAC) and deriving aerosol optical depth (AOD) with geographically weighted regression (GWR), primarily for particulate matter 2.5, or PM2.5). Two articles used the Jenk’s Natural Break method algorithm to classify LAN data [ 46 , 47 ]. Image preprocessing methods performed on raw satellite image data to prepare it for further data processing were referenced in just under half of the studies. Examples of image preprocessing are LAN data transformed into radiance [ 49 , 50 , 52 ] or determining image inclusion according to criteria such as 10% or less cloud cover. Image preprocessing calibration, gauging the data with a standard scale, was used in two articles [ 50 , 60 ]. One article calibrated LAN with satellite sensor data to provide average daily radiance [ 50 ] and another calibrated satellite air pollution data with ground data using a land-use regression model [ 60 ]. One-quarter of the studies referenced external resource tools that extract data from satellite images, such as ArcGIS, MERRA-2, NASA’s Giovanni tool, and the Sentinel Application Platform [ 26 , 28 , 29 , 46 , 47 , 51 , 52 , 53 , 56 ]. Five articles used models, three of which were specific to chemistry: WRF-Chem [ 28 ], GEOS-chem [ 30 ], and an unspecified global chemical transport model [ 54 ]. Yuan and colleagues [ 54 ] also used the radiation transfer model and the differential absorption spectroscopy inversion technique. Qu and colleagues [ 31 ] used a spatial-statistical model with the NDVI to derive an estimate of residential greenness, and Qazi and colleagues [ 42 ] used a model for supervised classification. The “satellite data extraction method(s)” section in Table 3 shows the breakdown of satellite data extraction methods used in the studies.
The vast majority (90%) of studies found an association between their dependent variable and the satellite-derived data [ 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 40 , 42 , 43 , 44 , 45 , 46 , 47 , 50 , 51 , 52 , 53 , 55 , 56 , 57 , 58 , 60 , 61 , 62 , 63 , 64 , 65 ] (Table 2 ). For example, both Bauer and colleagues [ 46 ] and Kloog and colleagues [ 47 ] found breast cancer incidence was associated with high LAN exposure. Fan and colleagues [ 38 ] found a significant positive association between COPD prevalence and greenness (NDVI). Another 2% of studies [ 39 ] found value in satellite data but no association with their dependent variable [ 39 ]. In this article, Jimenez and colleagues [ 39 ] found that NDVI is the most widely used satellite-derived indicator of green space and can be used as a longitudinal exposure measure. Furthermore, 58% of the articles stated that satellite data overcomes the difficulties present in research when geographic areas do not have environmental data or the available ground data is sparse [ 21 , 22 , 23 , 24 , 25 , 26 , 28 , 30 , 32 , 33 , 34 , 35 , 36 , 38 , 39 , 42 , 44 , 51 , 53 , 55 , 57 , 58 , 63 , 64 , 65 ]. For example, Prud’homme [ 30 ] (2013) and Yitshak [ 64 ] (2015) specifically noted the limitation of ground data for air pollution, proximity to monitoring stations, and sparse spatial data, which can be overcome by using satellite data. The final two columns of Table 2 shows if the dependent variable and satellite-derived data were related and any claims stated by the study authors about the value of using satellite data. We found two themes regarding the value of using satellite imagery to examine risk, incidence, prevalence, and mortality related to NCDs. The first theme was that satellite data overcomes problems of sparse or missing spatial and temporal data. Traditional environmental data (non-satellite data) is limited by the range of each sensor and the completeness of data. Satellite data complements traditional data and extends the availability of environmental spatial and temporal data to a global scale. The following representative quote illustrates such sentiments:
In particular, we have clearly shown that, thanks to data availability and big data technologies, it is now possible to jointly study heterogenous data, such as health care and air pollution information extracted from satellites. This provides an unprecedented opportunity to improve our understanding of phenomena by extracting unseen temporal and spatial correlations [ 36 ]. Use of satellite images has become a great tool for epidemiology because with this technological advance we can determine the environment in which transmission occurs, the distribution of the disease and its evolution over time [ 44 ].
The second theme was the ability of open-source satellite data to enable studies to be extrapolated to other areas. Traditional data sources are specific to a distinct geographic area, whereas satellite data often allows for (spatial and temporal) data to be available globally. The following representative quote illustrates such sentiments:
The results of studies like ours could be extrapolated to other cities, given that the use of Sentinel 3 satellite images lies within the reach of the entire scientific community, and their use for determining land surface temperature (LST) and surface urban heat island (SUHI) is straight forward [ 53 ]. Our findings will have important public health implications for policy makers when they are planning the size, shape, density and accessibility of surrounding green spaces in living areas [ 38 ].
Satellite imagery has been used in a variety of ways to address NCDs. A key finding of this review is that nearly all studies found an association between at least one type of satellite data and one NCD. Most of the studies used existing publicly available algorithms to extract data from images. Furthermore, a couple of studies [ 57 , 58 ] attempted to harness the power of AI to see beyond predetermined features.
Over half of the studies analyzed satellite data based on geolocation(s) specific to the research population of interest’s location at the city, census tract, or census block level. One reason the authors may have chosen these geographic levels could be because sociodemographic and health-related data, types of data that have been integral to NCD studies [ 3 ], is often available at these levels [ 3 , 66 ]. Furthermore, by adding satellite data at these geographic levels, study authors may have been able to fill gaps in environmental factors when using ground data alone, such as in Allen and colleagues’ [ 35 ] examination of air pollution in the city of Ulaanbaatar, Mongolia. Just one article used satellite data globally; it replicated previous studies that either excluded areas without ground monitoring or were limited by “coarse spatial resolution” [ 23 ].
Over 80% of premature deaths caused by NCD occur in lower-income countries [ 1 ], yet just one-quarter of the studies in our review were from lower-income countries. Satellites orbiting the Earth capture data from across the globe, including areas without robust healthcare data collection, such as lower-income countries [ 8 ]. Using satellite data for these countries could better enable disease surveillance, tracking health trends and risk factors, and informed healthcare decision-making [ 15 , 67 ]. One potential strategy for using satellite data in lower-income countries is identifying trends between certain satellite-derived data and health outcomes in similar countries or regions that have health data available and extrapolating those trends to the lower-income country of focus. A similar method has been succeesfully used with satellite imagery data in the field of economics [ 68 ]. However, a limiting factor for using satellite imagery for health is a lack of proper tools, knowledge, and skills in collecting and analyzing satellite data among researchers, engineers, and government employees [ 69 ]. This is particularly problematic in lower-income countries with fewer educational resources to train people [ 69 , 70 ]. One potential solution to address the lack of training is to use the publicly available governmental and university-based tutorial programs and resources designed to make satellite data easier to use [ 69 , 70 , 71 , 72 ]. Additional file 2 presents resources to help researchers, scientists, and policymakers understand, find, and use satellite imagery data.
Most reviewed articles discussed how satellite data is an asset to NCD research by providing open-access environmental data that surmounts the constraints of ground-based data collection methods and availability. However, it is important that investigators consider tradeoffs between levels of spatial, temporal, and spectral resolution when choosing their satellite remote sensing data sources [ 15 ]. Researchers can use guidance from organizations such as NASA [ 73 , 74 ] and the European Space Agency [ 75 , 76 ] to help determine the optimal scale of data needed for their research. For example, MODIS (on Terra, Aura, Aqua, and Sentinel 1a satellites) is an instrument that produces moderate-resolution images, while Sentinel 2 and 3 instruments produce high-resolution images. The choice between using MODIS or Sentinel 2 or Sentinel 3 would depend on the investigator team’s resources (e.g., computing processing power and available investigator hours) and the data needs (e.g., general greenspace in a city versus specific greenspace by city block) for their research questions.
While satellite imagery has existed for over a half-century [ 77 ], not until recently did scientists have a method to process the vast amounts of data amassed by observing our planet from space [ 78 , 79 ]. AI can quickly and efficiently extract meaningful patterns, trends, and insights from satellite images. Most articles in this review (95%) examined previously known environmental factors (e.g., air pollution, LAN) using satellite image data. The paucity of studies employing AI to analyze satellite image data for NCD research–just two studies in this review–is notable given that other fields (e.g., waste management [ 80 , 81 ], agriculture [ 82 , 83 ], urban planning [ 82 , 84 ], and defense [ 82 , 85 ]) have more readily adopted AI methods to process satellite image data. Within health sciences, satellite imagery coupled with AI has been used to study patterns in infectious diseases [ 12 , 13 , 71 ]. With 241 in-orbit Earth observation satellites registered with the United Nations and that number growing [ 86 ], there is an opportunity to expand the use of AI and satellite data to monitor and analyze NCD risk for informing policy and programmatic decisions to improve noncommunicable disease outcomes.
Several studies used existing algorithms to measure satellite data. These algorithms allowed the researchers to avoid developing a new measure and better enabled comparisons between studies. We recommend that researchers continue testing these existing algorithms and develop and test new algorithms to measure satellite data to help facilitate future satellite imagery-based NCD research. Such algorithms could be constructed by researchers or generated using AI and validated through research studies. The existence of previously validated algorithms may help epidemiologists and other individuals focused on studying NCD conduct more robust satellite data-based studies and avoid the need to create and study the properties of a new measure.
Our study deviated from the original protocol in a few ways. First, due to the quantitative nature of the studies, we ended up using the assessment of quality from the Oxford Centre for Evidence-Based Medicine instead of the Mixed Methods Appraisal Tool. Second, we focused on the top four NCDs in the world because the World Health Organization highlights these four diseases as the deadliest diseases [ 1 ]. Third, we added more technical engineering and environmental databases to our literature search to ensure we captured as many articles as possible that fit our search criteria.
This review has some limitations. First, it was limited in scope to peer-reviewed literature; thus, it could be missing case reports and other grey literature contributions. Second, there is a risk of publication bias in a review of published studies. Third, due to the heterogeneity of the research methods across studies, we did not perform a meta-analysis to quantitatively examine how satellite imagery has been used to address the top NCDs in the world. This limits the depth of the analysis that could be achieved through more rigorous statistical exploration. Fourth, given that most studies are from developed regions, findings are skewed toward higher-income countries. Future studies should explore ways to include more diverse geographical inputs to research using satellite imagery in examining noncommunicable diseases.
Conclusions
Overall, this systematic review found satellite data to be an asset to NCD research. However, given the recent proliferation of satellites and the emerging capabilities of AI, using satellite imagery data to address the global health threat of NCDs has barely scratched the surface, particularly for locations most vulnerable to NCDs, such as low- and middle-income countries. Scientists and policymakers worldwide should take concerted and collaborative action to keep pace with the advancement of satellite imagery to produce better data-driven health outcomes.
Data availability
Data is provided within the manuscript or supplementary information files.
Abbreviations
Artificial intelligence
Aerosol Optical Depth
Body Mass Index
Convolutional Neural Networks
Department of Meteorological Satellite Program
Geographically weighted regression
Light at night
Multi-angle Implementation of Atmospheric Correction
Moderate Resolution Imaging Spectroradiometer
National Aeronautics and Space Administration
- Noncommunicable disease
Normalized Difference Vegetation Index
Particulate matter 2.5
Preferred Reporting Items for Systematic Reviews and Meta-analyses
t-distributed Stochastic Neighbor Embedding
World Health Organization. Noncommunicable Diseases. 2022. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
Waters H, Graf M. The Costs of Chronic Disease in the U.S.. Milken Institute; 2018 Aug [cited 2023 Sep 20]. https://milkeninstitute.org/sites/default/files/reports-pdf/ChronicDiseases-HighRes-FINAL_2.pdf
Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. 2023 [cited 2023 Aug 26]. PLACES: Local Data for Better Health. https://www.cdc.gov/places/index.html
World health Organization. Environmental risk factors and NCDs. [cited 2024 Mar 21]. https://www.who.int/teams/noncommunicable-diseases/integrated-support/environmental-risk-factors-and-ncds
World Health Organization W health statistics. The Global Health Observatory. 2023. WHO Indicator Data: Global Health Observatory. https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/sdg-target-3.4-noncommunicable-diseases-and-mental-health#:~:text=Indicator Groups-,SDG Target 3.4 %7C Noncommunicable diseases and mental health%3A By 2030,mental health and well%2Dbeing
Watkins DA, Msemburi WT, Pickersgill SJ, Kawakatsu Y, Gheorghe A, Dain K, et al. NCD countdown 2030: efficient pathways and strategic investments to accelerate progress towards the sustainable development goal target 3.4 in low-income and middle-income countries. Lancet. 2022;399(10331):1266–78.
Article Google Scholar
World Health Organization. Global NCD Compact 2020–2030. [cited 2023 Aug 9]. https://www.who.int/initiatives/global-noncommunicable-diseases-compact-2020-2030/achievements
NASA Earth Science Data Systems. What is Remote Sensing? | Earthdata. 2019 [cited 2024 Mar 21]. https://www.earthdata.nasa.gov/learn/backgrounders/remote-sensing
World Economic Forum. 2020 [cited 2023 Aug 29]. Who owns our orbit: Just how many satellites are there in space? https://www.weforum.org/agenda/2020/10/visualizing-easrth-satellites-sapce-spacex/
Barnard PL, Vitousek S. Earth science looks to outer space. Nat Geosci. 2023;16(2):108–9.
Article CAS Google Scholar
Yeh C, Perez A, Driscoll A, Azzari G, Tang Z, Lobell D, et al. Using publicly available satellite imagery and deep learning to understand economic well-being in Africa. Nat Commun. 2020;11(1):2583.
Article CAS PubMed PubMed Central Google Scholar
Amoroso N, Cilli R, Maggipinto T, Monaco A, Tangaro S, Bellotti R. Satellite data and machine learning reveal a significant correlation between NO2 and COVID-19 mortality. Environ Res. 2022;204:111970.
Article CAS PubMed Google Scholar
Desai AN, Kraemer MU, Bhatia S, Cori A, Nouvellet P, Herringer M, et al. Real-time epidemic forecasting: challenges and opportunities. Health Secur. 2019;17(4):268–75.
Article PubMed PubMed Central Google Scholar
Rogers DJ, Randolph SE, Snow RW, Hay SI. Satellite imagery in the study and forecast of malaria. Nature. 2002;415(6872):710–5.
Jia P, Stein A, James P, Brownson RC, Wu T, Xiao Q, et al. Earth Observation: investigating Noncommunicable diseases from Space. Annu Rev Public Health. 2019;40(1):85–104.
Article PubMed Google Scholar
Earthdata | Earthdata. [cited 2022 Nov 8]. https://www.earthdata.nasa.gov/
ESA - Eduspace EN - Home. - What is remote sensing?. 2010 [cited 2024 Jan 25]. https://www.esa.int/SPECIALS/Eduspace_EN/SEMF9R3Z2OF_0.html#:~:text=Remote sensing is a way of collecting and,data being in direct contact with the object
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Morgan RL, Whaley P, Thayer KA, Schünemann HJ. Identifying the PECO: a framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ Int. 2018;121(Pt 1):1027.
Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A et al. OCEBM Levels of Evidence. Centre for Evidence-Based Medicine (CEBM), University of Oxford. 2021.
Chan CC, Chuang KJ, Chen WJ, Chang WT, Lee CT, Peng CM. Increasing cardiopulmonary emergency visits by long-range transported Asian dust storms in Taiwan. Environ Res. 2008;106(3):393–400.
De Roos AJ, Kenyon CC, Yen YT, Moore K, Melly S, Hubbard RA, et al. Does living near Trees and other Vegetation affect the contemporaneous odds of Asthma Exacerbation among Pediatric Asthma patients? J Urban Health. 2022;99(3):533–48.
Evans J, Van Donkelaar A, Martin RV, Burnett R, Rainham DG, Birkett NJ, et al. Estimates of global mortality attributable to particulate air pollution using satellite imagery. Environ Res. 2013;120:33–42.
Gao J, Liu J, Xu R, Pandey S, Vankayala Siva VSKS, Yu D. Environmental Pollution Analysis and Impact Study—A Case Study for the Salton Sea in California. Atmosphere. 2022;13(6):914.
Garzon-Chavez DR, Quentin E, Harrison SL, Parisi AV, Butler HJ, Downs NJ. The geospatial relationship of pterygium and senile cataract with ambient solar ultraviolet in tropical Ecuador. Photochem Photobiol Sci. 2018;17(8):1075–83.
Higgs G, Sterling DA, Aryal S, Vemulapalli A, Priftis KN, Sifakis NI. Aerosol Optical Depth as a measure of Particulate exposure using Imputed Censored Data, and relationship with Childhood Asthma Hospital Admissions for 2004 in Athens, Greece. Environ Health Insights. 2015;9s1:EHI.S15665.
James P, Hart JE, Banay RF, Laden F. Exposure to greenness and mortality in a nationwide prospective cohort study of women. Environ Health Perspect. 2016;124(9):1344–52.
Nguyen HD, Azzi M, White S, Salter D, Trieu T, Morgan G, et al. The summer 2019–2020 wildfires in East Coast Australia and their impacts on Air Quality and Health in New South Wales, Australia. Int J Environ Res Public Health. 2021;18(7):3538.
Prabhu V, Shridhar V, Choudhary A. Investigation of the source, morphology, and trace elements associated with atmospheric PM10 and human health risks due to inhalation of carcinogenic elements at Dehradun, an Indo-Himalayan city. SN Appl Sci. 2019;1(5):429.
Prud’homme G, Dobbin NA, Sun L, Burnett RT, Martin RV, Davidson A, et al. Comparison of remote sensing and fixed-site monitoring approaches for examining air pollution and health in a national study population. Atmos Environ. 2013;80:161–71.
Qu Y, Yang B, Lin S, Bloom MS, Nie Z, Ou Y, et al. Associations of greenness with gestational diabetes mellitus: the Guangdong Registry of congenital heart Disease (GRCHD) study. Environ Pollut. 2020;266:115127.
Ramesh B, Jagger MA, Zaitchik BF, Kolivras KN, Swarup S, Yang B, et al. Estimating changes in emergency department visits associated with floods caused by Tropical Storm Imelda using satellite observations and syndromic surveillance. Health Place. 2022;74:102757.
Stowell JD, Geng G, Saikawa E, Chang HH, Fu J, Yang CE, et al. Associations of wildfire smoke PM2.5 exposure with cardiorespiratory events in Colorado 2011–2014. Environ Int. 2019;133:105151.
Zhang D, Bai K, Zhou Y, Shi R, Ren H. Estimating ground-level concentrations of Multiple Air Pollutants and their Health impacts in the Huaihe River Basin in China. Int J Environ Res Public Health. 2019;16(4):579.
Allen RW, Gombojav E, Barkhasragchaa B, Byambaa T, Lkhasuren O, Amram O, et al. An assessment of air pollution and its attributable mortality in Ulaanbaatar, Mongolia. Air Qual Atmos Health. 2013;6(1):137–50.
Dagliati A, Marinoni A, Cerra C, Decata P, Chiovato L, Gamba P, et al. Integration of administrative, clinical, and Environmental Data to support the management of type 2 diabetes Mellitus: from satellites to Clinical Care. J Diabetes Sci Technol. 2016;10(1):19–26.
Eldeirawi K, Kunzweiler C, Zenk S, Finn P, Nyenhuis S, Rosenberg N, et al. Associations of urban greenness with asthma and respiratory symptoms in Mexican American children. Ann Allergy Asthma Immunol. 2019;122(3):289–95.
Fan J, Guo Y, Cao Z, Cong S, Wang N, Lin H, et al. Neighborhood greenness associated with chronic obstructive pulmonary disease: a nationwide cross-sectional study in China. Environ Int. 2020;144:106042.
Jimenez MP, Oken E, Gold DR, Luttmann-Gibson H, Requia WJ, Rifas-Shiman SL, et al. Early life exposure to green space and insulin resistance: an assessment from infancy to early adolescence. Environ Int. 2020;142:105849.
Klompmaker JO, Laden F, Browning MHEM, Dominici F, Ogletree SS, Rigolon A, et al. Associations of parks, greenness, and blue space with cardiovascular and respiratory disease hospitalization in the US Medicare cohort. Environ Pollut. 2022;312:120046.
Lambert KA, Lodge C, Lowe AJ, Prendergast LA, Thomas PS, Bennett CM, et al. Pollen exposure at birth and adolescent lung function, and modification by residential greenness. Allergy. 2019;74(10):1977–84.
Qazi S, Iqbal J, Khan JA. Assessment of the health impact of paper mulberry (Broussonetia papyrifera L.), an invasive plant species in Islamabad, Pakistan. Geospatial Health. 2019 Nov 12 [cited 2023 Jul 12];14(2). https://geospatialhealth.net/index.php/gh/article/view/727
Silveira IHD, Junger WL. Green spaces and mortality due to cardiovascular diseases in the city of Rio De Janeiro. Rev Saúde Pública. 2018;52:49.
Vargas-Cuentas NI, Roman-Gonzalez A, Mantari AA, Muñoz LA. Chagas disease study using satellite image processing: a Bolivian case. Acta Astronaut. 2018;144:216–24.
Walker BB, Brinkmann ST, Große T, Kremer D, Schuurman N, Hystad P, et al. Neighborhood Greenspace and Socioeconomic Risk are Associated with Diabetes Risk at the Sub-neighborhood Scale: results from the prospective Urban and Rural Epidemiology (PURE) Study. J Urban Health. 2022;99(3):506–18.
Bauer SE, Wagner SE, Burch J, Bayakly R, Vena JE. A case-referent study: light at night and breast cancer risk in Georgia. Int J Health Geogr. 2013;12(1):23.
Kloog I, Haim A, Stevens RG, Barchana M, Portnov BA. Light at night co-distributes with incident breast but not Lung Cancer in the Female Population of Israel. Chronobiol Int. 2008;25(1):65–81.
Medgyesi DN, Trabert B, Fisher JA, Xiao Q, James P, White AJ, et al. Outdoor light at night and risk of endometrial cancer in the NIH-AARP diet and health study. Cancer Causes Control. 2023;34(2):181–7.
Park Y, Ramirez Y, Xiao Q, Liao LM, Jones GS, McGlynn KA. Outdoor light at night and risk of liver cancer in the NIH-AARP diet and health study. Cancer Causes Control. 2022;33(9):1215–8.
Portnov BA, Stevens RG, Samociuk H, Wakefield D, Gregorio DI. Light at night and breast cancer incidence in Connecticut: an ecological study of age group effects. Sci Total Environ. 2016;572:1020–4.
Xiao Q, James P, Breheny P, Jia P, Park Y, Zhang D, et al. Outdoor light at night and postmenopausal breast cancer risk in the NIH-AARP diet and health study. Int J Cancer. 2020;147(9):2363–72.
Xiao Q, Jones RR, James P, Stolzenberg-Solomon RZ. Light at night and risk of pancreatic Cancer in the NIH-AARP Diet and Health Study. Cancer Res. 2021;81(6):1616–22.
Hidalgo-García D, Arco-Díaz J. Spatiotemporal analysis of the surface urban heat island (SUHI), air pollution and disease pattern: an applied study on the city of Granada (Spain). Environ Sci Pollut Res. 2023;30(20):57617–37.
Yuan Q, Shen H, Li T, Li Z, Li S, Jiang Y, et al. Deep learning in environmental remote sensing: achievements and challenges. Remote Sens Environ. 2020;241:111716.
Upegui E, Viel JF. GeoEye Imagery and Lidar Technology for small-area Population Estimation: an epidemiological viewpoint. Photogramm Eng Remote Sens. 2012;78(7):693–702.
Liu Y, Zhao B, Cheng Y, Zhao T, Zhang A, Cheng S, et al. Does the quality of street greenspace matter? Examining the associations between multiple greenspace exposures and chronic health conditions of urban residents in a rapidly urbanising Chinese city. Environ Res. 2023;222:115344.
Bibault JE, Bassenne M, Ren H, Xing L. Deep learning prediction of Cancer Prevalence from Satellite Imagery. Cancers. 2020;12(12):3844.
Maharana A, Nsoesie EO. Use of Deep Learning to Examine the Association of the built Environment with Prevalence of Neighborhood adult obesity. JAMA Netw Open. 2018;1(4):e181535.
Chatfield K, Simonyan K, Vedaldi A, Zisserman A. Return of the Devil in the Details: Delving Deep into Convolutional Nets. arXiv; 2014 [cited 2023 Sep 14]. http://arxiv.org/abs/1405.3531
Kim Y, Bak SH, Kwon SO, Kim H, Kim WJ, Lee CY. Association between Long-Term exposure to PM2.5 and lung imaging phenotype in CODA Cohort. Atmosphere. 2021;12(2):282.
Brown SC, Lombard J, Wang K, Byrne MM, Toro M, Plater-Zyberk E, et al. Neighborhood Greenness and Chronic Health conditions in Medicare Beneficiaries. Am J Prev Med. 2016;51(1):78–89.
Gariepy G, Kaufman JS, Blair A, Kestens Y, Schmitz N. Place and health in diabetes: the neighbourhood environment and risk of depression in adults with type 2 diabetes. Diabet Med. 2015;32(7):944–50.
Wang K, Lombard J, Rundek T, Dong C, Gutierrez CM, Byrne MM, et al. Relationship of Neighborhood Greenness to Heart Disease in 249 405 US Medicare Beneficiaries. J Am Heart Assoc. 2019;8(6):e010258.
Yitshak Sade M, Novack V, Ifergane G, Horev A, Kloog I. Air Pollution and ischemic stroke among young adults. Stroke. 2015;46(12):3348–53.
Yuan Y, Wu Y, Zhao H, Ren J, Su W, Kou Y, et al. Tropospheric formaldehyde levels infer ambient formaldehyde-induced brain diseases and global burden in China, 2013–2019. Sci Total Environ. 2023;883:163553.
Bureau UC. Census.gov. [cited 2023 Aug 26]. Census.gov. https://www.census.gov/en.html
Schwalbe N, Wahl B. Artificial intelligence and the future of global health. Lancet. 2020;395(10236):1579–86.
Lehnert P, Niederberger M, Backes-Gellner U, Bettinger E. T Jaworski editor 2023 Proxying economic activity with daytime satellite imagery: filling data gaps across time and space. PNAS Nexus 2 4 pgad099.
Rolf E, Proctor J, Carleton T, Bolliger I, Shankar V, Ishihara M, et al. A generalizable and accessible approach to machine learning with global satellite imagery. Nat Commun. 2021;12(1):4392.
Malekzadeh A, Michels K, Wolfman C, Anand N, Sturke R. Strengthening research capacity in LMICs to address the global NCD burden. Glob Health Action. 2020;13(1):1846904.
Canadian Space Agency, Canadian Space A. 2018 [cited 2023 Aug 11]. How satellites help you stay healthy. https://www.asc-csa.gc.ca/eng/satellites/everyday-lives/how-satellites-help-you-stay-healthy.asp
mosaiks.org. 2023 [cited 2023 Aug 11]. mosaiks.org. https://www.mosaiks.org
National Oceanic and Atmospheric Administration. GOES-R Algorithm Theoretical Basis Documents. 2023 [cited 2023 Dec 3]. https://www.star.nesdis.noaa.gov/goesr/documentation_ATBDs.php
NASA. Worldview. [cited 2023 Sep 17]. https://worldview.earthdata.nasa.gov/
Earth Online. [cited 2023 Sep 17]. https://earth.esa.int/eogateway/
EUMETSAT. EUMETSAT | Monitoring the weather and climate from space | EUMETSAT. [cited 2023 Sep 17]. https://www.eumetsat.int/
Gettelman A, Geer AJ, Forbes RM, Carmichael GR, Feingold G, Posselt DJ, et al. The future of Earth system prediction: advances in model-data fusion. Sci Adv. 2022;8(14):eabn3488.
Chen CP, Zhang CY. Data-intensive applications, challenges, techniques and technologies: a survey on Big Data. Inf Sci. 2014;275:314–47.
Kotawadekar R. 9 - Satellite data: big data extraction and analysis. In: Binu D, Rajakumar BR, editors. Artificial Intelligence in Data Mining. Academic Press; 2021 [cited 2023 Aug 26]. pp. 177–97. https://www.sciencedirect.com/science/article/pii/B9780128206010000082
Abu Qdais H, Shatnawi N. Assessing and predicting landfill surface temperature using remote sensing and an artificial neural network. Int J Remote Sens. 2019;40(24):9556–71.
Baghanam AH, Vakili AT, Nourani V, Dąbrowska D, Soltysiak M. AI-based ensemble modeling of landfill leakage employing a lysimeter, climatic data and transfer learning. J Hydrol. 2022;612:128243.
Tahir A, Munawar HS, Akram J, Adil M, Ali S, Kouzani AZ, et al. Automatic target detection from Satellite Imagery using machine learning. Sensors. 2022;22(3):1147.
Tariq A, Siddiqui S, Sharifi A, Shah SHIA. Impact of spatio-temporal land surface temperature on cropping pattern and land use and land cover changes using satellite imagery, Hafizabad District, Punjab, Province of Pakistan. Arab J Geosci. 2022;15(11):1045.
Jiang H, Peng M, Zhong Y, Xie H, Hao Z, Lin J, et al. A Survey on Deep Learning-based change detection from high-resolution remote sensing images. Remote Sens. 2022;14(7):1552.
Bistron M, Piotrowski Z. Artificial Intelligence Applications in Military systems and their influence on sense of security of citizens. Electronics. 2021;10(7):871.
United Nations Register of Objects. Launched into Outer Space. [cited 2023 Aug 29]. https://www.unoosa.org/oosa/en/spaceobjectregister/index.html
Download references
Acknowledgements
The authors would like to thank Lei Hua for his review of the manuscript.
The authors received no external financial support for the research, authorship, and/or publication of this article.
Author information
Authors and affiliations.
Shirley Ryan AbilityLab, 355 East Erie Street, Chicago, IL, 60611, USA
Elizabeth J. Folkmann
School of Health Studies, College of Health and Human Sciences, Northern Illinois University, 209 Wirtz Hall, DeKalb, IL, 60115, USA
M. Courtney Hughes
College of Business, Northern Illinois University, 328 Barsema Hall, DeKalb, IL, USA
Uzma Amzad Khan
College of Engineering and Engineering Technology, Northern Illinois University, 590 Garden Road, DeKalb, IL, USA
Mahdi Vaezi
You can also search for this author in PubMed Google Scholar
Contributions
Review conception and design: MV, MCH, EF, UK. Search strategy and literature search: EF, UK. Study coding, selection, and data extraction: EF, UK. Review and interpretation: EF, MCH. Drafting of manuscript: EF, MCH. Critical revision: EF, MCH, MV. All authors read and approved the final manuscript.
Corresponding author
Correspondence to M. Courtney Hughes .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Folkmann, E.J., Hughes, M.C., Khan, U.A. et al. Examining noncommunicable diseases using satellite imagery: a systematic literature review. BMC Public Health 24 , 2774 (2024). https://doi.org/10.1186/s12889-024-20316-z
Download citation
Received : 03 December 2023
Accepted : 07 October 2024
Published : 10 October 2024
DOI : https://doi.org/10.1186/s12889-024-20316-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Geospatial Epidemiology
- Chronic disease
- Population Health
- Satellite Imagery
- Systematic review
- Heart Disease
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Endocrinol (Lausanne)
- PMC11457016
Whole body vibration therapy and diabetes type 2: a systematic review and meta-analysis
Juan fabregat-fernández.
1 Department of Nursing, University of Extremadura, Plasencia, Spain
Vicente Rodríguez-Pérez
2 Department of Nursing and Physiotherapy, Universidad de Salamanca, Salamanca, Spain
Rocío Llamas-Ramos
3 Institute of Biomedical Research of Salamanca (IBSAL), Salamanca, Spain
Ana Felicitas López-Rodríguez
4 Department of Nursing and Physiotherapy, Faculty of Nursing and Physiotherapy, Universidad de León, León, Spain
María Cortés-Rodríguez
5 Department of Statistics, Universidad de Salamanca, Salamanca, Spain
Inés Llamas-Ramos
6 University Hospital of Salamanca, Salamanca, Spain
Adérito Ricardo Duarte Seixas, Escola Superior de Saúde Fernando Pessoa, Portugal
Associated Data
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Vibration platforms have demonstrated systemic effects generated by the use of mechanical vibrations, which are similar to those of any physical activity. The effect that whole body vibration (WBV) generates on the organism could be recommended in Diabetes Mellitus 2 (DM 2) patients.
To systematically review and meta-analyze the available evidence on the effects of WBV on glycemic control in patients with DM 2
Material and methods
Exhaustive bibliographic searches were carried out until October 2023 in different biomedical portals and databases: Public Medline (PubMed), Scientific Electronic Library Online (SciELO), VHL Regional Portal, Cochrane Central and Latin American and Caribbean Literature in Health Sciences (LILACS). Randomized clinical trials based on the effects of Whole Body Vibration on glycosylated hemoglobin levels, with control group and participants were non-insulin dependent were the inclusion criteria. Two reviewers extracted data independently. A third reviewer was available for discrepancies.
Six articles with 223 participants met the criteria and were included in the systematic review; only four of them met the criteria to be part of the meta-analysis. This meta-analysis reveals a positive and significant effect size (μ ê=0.5731), indicating a substantial difference between the groups studied. Although there is some variability between studies (heterogeneity of 30.05%), the overall direction of the effects is consistent. These findings conclusively suggest the presence of a significant influence of the variable evaluated, underscoring the robustness and consistency of the relationship observed in the literature reviewed.
There are no conclusive results due to the lack of data for some variables, which prevents comparison; but WBV may be an effective therapy to improve glycemic control in DM 2 patients. More studies with more patients and longer follow-up are needed.
1. Introduction
Worldwide, 537 million people suffer from diabetes and this data will be increased up to 643 million by 2030 and 783 by 2045; in our country (Spain) the incidence of Diabetes Mellitus type 2 (DM 2) is estimated at 1 in 7 people, equivalent to 10.3% of the population (around 5.1 million adults). This situation generates a great impact on society, as well as concern among health professionals due to its high and ever-increasing prevalence, not to mention the high cost to the health system which could reach USD 966 billion dollars, which represents an increase of 316% over the last 15 years; raising awareness among these people is the key to combating this problem ( 1 ).
Several disciplines have made contributions to the current knowledge about DM 2; however, despite the passage of time, the fundamental pillars in the treatment of a diabetic person are based on diet and exercise, especially in DM 2. In addition, the physical disabilities and comorbidity present in most people with DM 2 are challenges to adherence to physical activity ( 2 ).
Due to the research during the last decades, the etiology, pathophysiological mechanisms, diagnosis and treatment of DM 2 are better understood. Traditionally, vibration exposure has been considered detrimental for causing harm in humans. However, several studies have shown beneficial effects of the application of whole-body vibration (WBV) with low frequencies, low amplitudes and short exposure times ( 3 , 4 ) as a novel treatment for DM 2 patients ( 5 ).
The application of WBV has been associated with favorable changes in hormone levels, strength, power, muscle mass, muscle electrical activity, jumping ability, balance, psycho-physical health and activation at the cortical level, among others ( 6 ). Nevertheless, the effects of WBV on DM 2 are less well known.
Various systematic reviews have evaluated the impact of WBV on glycemic control in patients with DM 2. The results obtained are contradictory. While some studies, conducted in 2016 ( 7 ) and 2019 ( 8 ), suggest a slight improvement in glucose and HbA1c levels, another systematic review published in 2018 ( 9 ) questions the strength of this evidence, pointing out a low methodological quality in the included studies.
Nowadays most WBV studies published are focused on the level of neuromuscular dysfunction ( 10 ) and the muscular system. Muscles are known to react to vibration by contracting and stretching automatically. Vibration produces a muscle contraction reflex, called the tonic vibratory reflex ( 11 – 13 ). This reflex has been related to decreased pain threshold, increased blood circulation ( 14 ) increased hormone secretion, activation of the Golgi tendon organ and inhibition of antagonist muscles ( 4 , 15 – 17 ).
The physiological modifications observed with WBV are analogous to those of any physical activity, having been described in addition to acute changes, chronic adaptations. Adaptation to physical exercise is what determines the positive changes that appear in our organism when performing any sport. The WBV effectiveness could be explained by the fact that, while with training work is performed on a certain number of tissues, with the use of mechanical vibrations the whole body is subjected to vibration, obtaining beneficial effects at a systemic level (16-118-19).
To summarize the current evidence, our objective was to perform a systematic review and meta-analysis of the effects of WBV intervention on blood glucose levels and glycosylated hemoglobin (HbA1c) levels in people with DM 2.
2. Materials and methods
2.1. systematic literature research.
An exhaustive literature search including randomized and controlled clinical trials obtained from the different biomedical portals and existing databases, from January 2019 to October 2023: Public Medline (PubMed), Scientific Electronic Library Online (SciELO), VHL Regional Portal, Cochrane Central Register of Controlled Trials (Cochrane CENTRAL) and Latin American and Caribbean Literature in Health Sciences (LILACS) has been conducted. Search terms included were Type 2 Diabetes Mellitus , physical exercise , whole body vibration and glycosylated hemoglobin or HbA1c .
The databases were searched using Boolean operators such as: “AND” and “OR”. Keywords have been combined with connectors in order to find valid articles for the aim of the present work. The “OR” connector has been used by joining the words that mean almost the same thing “exercise” and “Exercise on vibrating platforms”, and the “AND” connector has been used in order to give greater sensitivity and specificity to the search. No filters have been used and searches were made in “all fields” and “all index” ( Table 1 ).
Table 1
Search strategy.
| DATABASE | SEARCH STRATEGY |
|---|---|
| ((((“diabetes mellitus, type 2”[MeSH Terms] OR “type 2 diabetes mellitus”[All Fields]) AND (“exercise”[MeSH Terms] OR “exercise”[All Fields] OR (“physical”[All Fields] AND “exercise”[All Fields]) OR “physical exercise”[All Fields])) OR ((“exercise”[MeSH Terms] OR “exercise”[All Fields] OR “exercises”[All Fields] OR “exercise therapy”[MeSH Terms] OR (“exercise”[All Fields] AND “therapy”[All Fields]) OR “exercise therapy”[All Fields] OR “exercising”[All Fields] OR “exercise s”[All Fields] OR “exercised”[All Fields] OR “exerciser”[All Fields] OR “exercisers”[All Fields]) AND (“vibrate”[All Fields] OR “vibrated”[All Fields] OR “vibrates”[All Fields] OR “vibrating”[All Fields] OR “vibration”[MeSH Terms] OR “vibration”[All Fields] OR “vibrations”[All Fields] OR “vibrational”[All Fields] OR “vibrator”[All Fields] OR “vibrators”[All Fields]) AND (“platform”[All Fields] OR “platform s”[All Fields] OR “platforms”[All Fields]))) AND ((“whole”[All Fields] OR “wholeness”[All Fields] OR “wholes”[All Fields]) AND (“human body”[MeSH Terms] OR (“human”[All Fields] AND “body”[All Fields]) OR “human body”[All Fields] OR “body”[All Fields]) AND (“vibrate”[All Fields] OR “vibrated”[All Fields] OR “vibrates”[All Fields] OR “vibrating”[All Fields] OR “vibration”[MeSH Terms] OR “vibration”[All Fields] OR “vibrations”[All Fields] OR “vibrational”[All Fields] OR “vibrator”[All Fields] OR “vibrators”[All Fields])) AND (“glycosylated haemoglobin”[All Fields] OR “glycated hemoglobin”[MeSH Terms] OR (“glycated”[All Fields] AND “hemoglobin”[All Fields]) OR “glycated hemoglobin”[All Fields] OR (“glycosylated”[All Fields] AND “hemoglobin”[All Fields]) OR “glycosylated hemoglobin”[All Fields])) OR (“glycated hemoglobin”[MeSH Terms] OR (“glycated”[All Fields] AND “hemoglobin”[All Fields]) OR “glycated hemoglobin”[All Fields] OR “hba1c”[All Fields] OR “hba1cs”[All Fields]) | |
| (Type 2 Diabetes Mellitus) AND (physical exercise) OR (whole body vibration) | |
| (Type 2 Diabetes Mellitus) AND (whole body vibration) (Type 2 Diabetes Mellitus) AND (physical exercise OR whole body vibration) | |
| (Type 2 Diabetes Mellitus) AND (physical exercise OR exercise on vibrating platforms) AND (whole body vibration) AND (glycosylated hemoglobin OR HbA1c) | |
| (Type 2 Diabetes Mellitus) AND (whole body vibration) (Type 2 Diabetes Mellitus) AND (physical exercise OR whole body vibration) (whole body vibration) AND (glycosylated hemoglobin OR HbA1c) |
PICO strategy has been followed as follows:
- POPULATIONS: diabetes type 2 patients
- INTERVENTIONS: whole body vibration therapy
- COMPARISONS: control groups
- OUTCOMES: fasting blood glucose, glycosylated hemoglobin
2.2. Selection criteria
Randomized controlled trials were considered eligible if they met inclusion criteria such as addressing the effects of WBV on glycosylated hemoglobin levels, the WBV intervention had to be at least 8 weeks, at least one control group did not perform WBV, and participants were non-insulin dependent. Exclusion criteria were studies in which individuals had a reported diabetic complication (neuropathy, retinopathy or diabetic peripheral nephropathy), animal studies and studies with insufficient description of WBV. Besides, a manual search was carried out based on the references of the selected articles as well as the references of other articles not included because they are a different type of study than the one selected in the present review.
2.3. Screening, selection and data extraction
Two independent reviewers in a first step carried out the bibliographic research and after that, examined the titles and abstracts of all studies identified through the search strategies. Studies that did not meet the inclusion criteria, based on titles or abstracts, were discarded. The two reviewers analyzed the full text of the remaining studies in a second review independently. If there is any disagreement a third reviewer was available to solve it.
Reviewers independently extracted data from the studies that met the inclusion criteria using a standardized data extraction form. Data extracted were: authors; year of publication; type of platform used; number of individuals forming the study sample; WBV parameters and intervention outcomes; mean and standard deviation of results.
2.4. Assessment of methodological quality and risk of bias
The physiotherapy evidence database (PEDro) scale was used to evaluate the methodological quality and the risk of bias of the randomized clinical trials included. This is a useful tool for assessing trial quality and the total score of this scale is 10 points. Punctuation more than 6 points is considered as a high-quality clinical trial. Sample selection, randomization, blinding (both participants and therapists), initial homogeneity and statistical analysis (intention to treat and comparisons) are included in this scale ( 20 ).
The quality of the included studies was scored by 2 investigators using the PEDro scale. The investigators rated the studies independently scoring from 0 to 10. If there is any disagreement a third reviewer was available to solve it.
Besides, the Van Heuvelen et al. ( 21 ) guidelines has been followed to report the quality of WBV studies. These guidelines encourage the authors to provide a detailed description of the WBV protocol applied (type of platform, frequency and amplitude of vibration, acceleration), the exposure parameters such as the duration and number of sessions as well as the total duration of the training program and the mode of application. In addition, the characteristics of the participants (demographic data, inclusion and exclusion criteria) should be presented. randomization and the existence of control groups should also be controlled, together with a presentation of the results and analysis of the data with statistical methods. finally, the existence of adverse effects and the existence or not of adherence, the interpretation of the results and the recommendations for clinical practice should be presented.
Besides, to test the quality of the meta-analysis the analysis implemented Random Effect Model using Jamovi software ( 22 ).
The Random-Effect Model : The analysis was carried out using the standardized mean difference as the outcome measure. A random-effects model was fitted to the data. The amount of heterogeneity (i.e., tau²), was estimated using the restricted maximum-likelihood estimator ( 23 ). In addition to the estimate of tau², the Q-test for heterogeneity ( 24 ) and the I² statistic are reported. In case any amount of heterogeneity is detected (i.e., tau² > 0, regardless of the results of the Q-test), a prediction interval for the true outcomes is also provided. Studentized residuals and Cook’s distances are used to examine whether studies may be outliers and/or influential in the context of the model. Studies with a studentized residual larger than the 100 x (1 - 0.05/(2 X k))th percentile of a standard normal distribution are considered potential outliers (i.e., using a Bonferroni correction with two-sided alpha = 0.05 for k studies included in the meta-analysis). Studies with a Cook’s distance larger than the median plus six times the interquartile range of the Cook’s distances are considered to be influential. The rank correlation test and the regression test, using the standard error of the observed outcomes as predictor, are used to check for funnel plot asymmetry.
3.1. Study selection
After the initial search, 735 potential studies were found to evaluate its possible inclusion in the systematic review. 131 manuscripts were removed as duplicates. The first screening by title and abstract reduced the sample to 174. A carefully full- text read of these files was made by reviewers and finally 6 records were included in the systematic review and 4 in the meta-analysis due the lack of some values in the two studies removed, which avoid comparisons. Figure 1 shows the Prisma flowchart of the study selection.

Study selection.
3.2. Study characteristics
The sample analyzed in the articles reviewed ranged from 24 to 50 subjects, the mean of the sample being 37.1 patients. The selected articles show that 33.33% of the reviewed studies show the existence of a statistically significant decrease in glycosylated haemoglobin (HbA1c) after exposure to vibratory exercise ( 25 – 27 ). While for the remaining 66.66% ( 28 , 29 ) there is no statistically significant decrease in HbA1c. Fasting blood glucose (FBG), however, decreased in 66.66% of the studies analyzed ( 25 – 27 , 29 ), after the use of WBV, while for 33.33% ( 25 , 30 ) there was no significant decrease.
There are basically 2 types of vibration platforms: vertical platforms or oscillating platforms. Vertical platforms vibrate in a predominantly vertical direction, moving vertically under both feet at the same time. Oscillating platforms vibrate around a horizontal axis, resulting in a simultaneous and symmetrical movement of both sides of the body during exposure ( 31 , 32 ). The most commonly used platform in several studies ( 25 , 26 , 28 ), was the oscillating platform, obtaining positive results with respect to HbA1c and white blood cells (WBC). However, the use of the vertical platform ( 27 ), also concluded with positive effects on HbA1c and WBC results.
The duration of the intervention in the studies analyzed was between 8 ( 29 ) and 12 weeks ( 25 – 28 , 30 ), with a mean of 11.33 weeks. Regarding the rest time between exercises applied in the interventions, it is located in an average of 34 seconds for those that reflect rest time between exercises ( 25 – 27 ). The other authors do not reflect rest time between exercises ( 28 , 30 ). Most researchers propose an exercise frequency of 3 times per week, except Michels et al. ( 30 ) who carried out the intervention with 7 days of vibratory exercises. No study reports on possible adverse effects during the period of vibration work.
In Table 2 , the main results of these articles were showed.
Table 2
Study characteristic of the selected articles.
| AUTHOR | OBJECTIVE | PLATFORM | SAMPLE | INTERVENTION | RESULTS | CONCLUSIONS |
|---|---|---|---|---|---|---|
| ( ) | To identify beneficial changes for the health of people with DM 2 at WBV. | Fitvibe Excel (Vertical) | n = 36 WBVG (n=17) CG (usual physical activity) (n=19) | f 30Hz-2mm: 1 Wk. f 40Hz-4mm: 5-12 Wk. 3 x/Wk; 12 Wk 60sec VE/20 sec rest 12 min/session | ↓ (p > 0,05) in FBG, HbA1c, insulin level and insulin sensitivity in both groups. | WBV may be an effective method to control some of the deleterious outcomes of DM 2 only in the most severe cases. No adverse effects. |
| ( ) | To determine the applicability and effectiveness of WBV to improve functional capacity and quality of life in subjects with DM 2. | Physio Wave 700 (Oscillating) | n = 39 WBVG (n=19) CG (n=20) | f 12, 14 and 16Hz- 4mm 3 x/Wk; 12Wk. 30-45-60 sec VE (↑ progressive)/30 sec rest 8-16 min/session | ↓ (p < 0,05) HbA1c and FBG WBVG CG ↓ HbA1C and FBG | ↓ Glycaemia level in a VE session. No adverse effects. |
| ( ) | To test the feasibility, safety and effectiveness of a 12-wk WBV intervention on glycemic control, lipid-related cardiovascular risk factors and functional capacity among DM 2 patients in a primary care context. | Physio Wave 700 (Oscillating) | n = 50 WBVG (n= 25) CG (n=25) | f 12, 14 and 16 Hz - 4mm 3 x/Wk; 12Wk. 30-45-60 sec VE (↑ progressive)/30 sec rest 10 min/session | ↓ (p < 0,05) HbA1c and FBG WBVG and CG | VE is feasible, safe and effective in improving glycemic profile. No adverse effects. |
| ( ) | nfluence of AE and vibration on glucose metabolism parameters in people with DM 2. | Vibrogym Professional (Oscillating) | n = 40 WBVG (n=14) Flexibility training group (8 static exercises)(n=13) Strength training group (8 stations in weight machines) (n=13) | f 30Hz-2mm: de la 1-9 Wk. f 35Hz-2mm: 10-12 Wk 3 x/Wk; 12Wk 30 sec EV/no rest 20 min/session | ↓ (p < 0,05) in FBG for all groups. HbA1c ↓ (p > 0,05) in WBVG. ↑ HbA1c for other groups. | VE can be an effective and time-efficient tool for improving glycemic control in people with DM 2, although no significant data were obtained. No adverse effects. |
| ( ) | Comparing how AE and WBV affect glycemic control in DM 2. | Star Sport-Taiwan (Oscillant) | n 30 AEG (n=10) WBVG (n=10) CG (n=10) | f= 30Hz-2 mm 3 x/Wk; 8 Wk 60 sec EV/60 sec rest 16 min/session (1-3 week) 20 min/session (4-6 week) 24min/session (7-8 week) | No effect for FBG for HbA1c. ↓ higher for AE and WBV than CG | Insignificant results due the sample size. WBV could be an option for DM 2 patients with obesity or those who cannot implement active physical activity No adverse effects. |
| ( ) | To evaluate the effect of whole-body vibration at 28 Hz on glycemic control and other metabolic parameters in adults with DM 2. | SmartWalk (Vertical) | n = 22 WBVG (n= 11) CG (n=12) | f 28 Hz mm (no data) 7 x/Wk; 12Wk. 20-30 min/session No rest | HbA1c ↓ (p < 0,05) in WBVG FBG increase in both groups but there are no significant changes | Daily use of the vibration platform for 12 weeks improved HbA1c in adults with DM 2. |
n, Sample size; WBV, whole body vibration; WBVG, whole body vibration group; CG, Control Group; DM 2, Diabetes mellitus type 2; FBG, fasting blood glucose; AEG, aerobic exercise group; Wk, week; Hz, Hertz; VE, vibration exercise; HbA1c, Glycosylated Hemoglobin; f, Frequency; AE, aerobic exercise; mm, millimeters; min, minutes.
Manimmanakorn ( 25 ) implemented a research with 36 patients with DM 2 divided into two groups. The WBV group performed for 3 times per week, 2 sets of 6 one-minute vibrating squats for 12 weeks and the control group performed their usual physical activity. These six positions were “(a) a deep squat position (knee angle 90o), (b) high squat position (knee angle 125o), (c) high squat position (with raised heels), (d) slight knee flexion 1 (holding hand straps with shoulder flexion), (e) slight knee flexion 2 (holding hand straps with shoulder abduction) and (f) slight knee flexion 3 (holding hand straps with elbow flexion)”. It was established a progression to 40 Hz and 4mm. They found no significant differences in HbA1c or FBG, concluding that WBV did not improve glycemic indices.
Alfonso-Rosa ( 26 ) published an article with 19 subjects with DM 2 exposed to a training based on 8 static and dynamic exercises with an elastic band (warm-up exercise: squat, up and down once with each foot, lunge, heel lift, squat, squat with weight changes, squats held with elastic bands, squat with elastic bands and side with elastic bands) on a vibrating platform at different frequencies (12, 14 and 16 Hz) while the control group continued with their usual activity. After 12 weeks it can be concluded that WBV produces an acute decrease in plasma levels, and the application of WBV at low frequencies is shown to be an effective and safe technique for the co-treatment and management of DM 2.
In this line, Del Pozo Cruz et al. ( 27 ) carried out a study with 50 subjects diagnosed with DM 2 were studied to test the feasibility, safety and efficacy of a whole body vibration intervention for 12 weeks in a primary health care setting performing 8 exercises in Physio Wave 700 oscillating platform (lunge, step up and down, squat, calf raises, left and right pivot, shoulder abduction with elastic bands, shoulder abduction with elastic bands while squatting, arm swinging with elastic bands) and the control group followed standard care. They establish a progression from 30 seconds for exercises and 30 seconds rest during the first month, while during the second and third months the exercise duration increased to 45-60 seconds and 30 seconds of rest and 2 more Hz each 4 weeks. They found a reduction in HbA1c and FGB compared to the control group concluding that the application of WBV in primary care is feasible, safe and effective in improving the glycemic profile.
Besides, Baum et al. ( 28 ) conducted another investigation with 40 non-insulin-dependent adult patients divided into 3 groups analyzed during 12 weeks of training with 3 training sessions per week. One group followed the WVB training with 30 Hz and 2mm from 1 to 9 week and 35 Hz the last weeks, the second, the strength group did the leg extension, seated leg flexion, leg press, seated calf raise, lat pulley, horizontal chest press, butterfly, and rowing exercises (1 set the first 6 weeks and 2 sets the last weeks) and the third group, flexibility group (control group) implemented 8 static exercises (the same progression was done increasing from 1 to 2 sets the last weeks). The main findings were that FBG remained unchanged after training and HbA1c tended to decrease below baseline in the vibration training group, while they increased in the other two intervention groups. Besides, the glucose tolerance improvement in WBV and strength groups. The authors concluded that these results suggest that vibration exercise may be an effective and low time-consuming tool to control glycemic control in patients with DM 2.
Behboudi et al. ( 29 ) selected a sample, 30 diabetic males, who followed a vibration exercise during 8–12-minute sessions of standing and semi-sitting positions at a frequency of 30 Hz and an amplitude of 2 mm, for 8 weeks three times a week. The aerobic exercise implemented 3 walking sessions a week and control group continued their routine activities. They detected no significant differences in HbA1c concentrations or fasting WBC between the conventional aerobic exercise groups and those subjected to vibration.
Finally, Michels et al. ( 30 ) investigated 22 adults with DM 2 who were taking oral antidiabetic agents were divided into 2 groups to submit one of them to 12-weeks intervention of WBV and control group received tips on how to change their lifestyle. After 12 weeks of intervention, they found a significant reduction in HbA1c in the WBV group, but no significant differences in FGB between groups.
3.3. Methodological quality and risk of bias
PEDro scale shows the quality of the randomized clinical trials. In this review, three articles showed high quality with 6, 7 and 9 points. Nevertheless, low methodological quality was shown in the other three articles with scores of 4, 5 and 5 points. In Table 3 , the PEDro Scale assessment of the six selected articles is presented. Given the variability of the data presented in each manuscript and the lack of data for comparison with the other articles in the review, two manuscripts were removed from the meta-analysis.
Table 3
PEDro score of the randomized clinical trials selected.
| AUTHOR | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | SCORE |
|---|---|---|---|---|---|---|---|---|---|---|---|
| ( ) | Yes | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | 9/10 |
| ( ) | Yes | No | Yes | No | No | No | No | Yes | Yes | Yes | 5/10 |
| ( ) | Yes | No | Yes | No | No | No | No | Yes | Yes | Yes | 5/10 |
| ( ) | Yes | No | Yes | No | No | No | Yes | Yes | Yes | Yes | 7/10 |
| ( ) | Yes | No | Yes | No | No | No | Yes | No | Yes | No | 4/10 |
| ( ) | Yes | No | Yes | No | No | No | Yes | Yes | Yes | Yes | 6/10 |
3.3.1. Quality of studies
Considering Van Heuvelen guidelines most of the articles have not adhered to these lines, so the results should be interpreted with caution ( Table 4 ).
Table 4
Van Heuvelen et al. guidelines.
| ITEM | Manimmanakorn et al. ( ) | Alfonso-Rosa et al. ( ) | Del Pozo-Cruz et al. ( ) | Baum et al. ( ) | Behboudi et al. ( ) | Michels et al. ( ) | |
|---|---|---|---|---|---|---|---|
| Device specifications | Yes | Yes | Yes | Yes | Yes | Yes | |
| Platform constructions | No | No | No | No | No | No | |
| Type of vibration | Yes | Yes | Yes | Yes | No | No | |
| Vibration parameters | Yes | Yes | Yes | Yes | Yes | Yes | |
| Parameters verification | No | No | No | No | No | No | |
| Side-alternating vibrations: accelerometer location | No | No | No | No | No | No | |
| Frequency and magnitude: constant or modulated | Modulated | Modulated | Modulated | Constant | Modulated | Constant | |
| Posture/body position | Yes | Yes | No | Yes | Yes | Yes | |
| Feet position | Partly | Yes | No | Yes | No | Yes | |
| Feet skidding prevention | No | No | No | No | No | No | |
| Head vibration transmission prevention | No | No | No | No | No | No | |
| Handrail | No | No | No | No | No | No | |
| Hands position | Partly | Partly | No | Partly | No | No | |
| Body parts subjected to vibration | Yes | Yes | Yes | Yes | Yes | Yes | |
| General exercise parameters | Yes | Yes | Yes | Yes | No | Yes | |
| Setting of sessions | Yes | Yes | No | No | No | No | |
| Trainer | No | No | No | Yes | No | No | |
| Previous instructions | Yes | Yes | Yes | No | No | No | |
| Preparatory exercises | No | No | Yes | No | Yes | No | |
| Subjects’ footwear | No | No | No | No | No | No | |
| Control intervention | Yes | Yes | Yes | Yes | Yes | Yes | |
| Time of outcome measurement | Yes | Yes | Yes | Yes | Yes | Yes | |
| General characteristics | Yes | Yes | Yes | Yes | Yes | Yes | |
| Previous experience | No | No | No | No | No | No | |
| Acute, short-term or long-term effects | Acute | Acute | Acute | Acute | Yes | Acute |
3.3.2. Random-effect model
A total of k=4 studies were included in the analysis. The observed standardized mean differences ranged from 0.2582 to 1.3338, with most estimates being positive (100%). The estimated average standardized mean difference based on the random-effects model was \hat{\mu} = 0.5895 (95% CI: 0.1782 to 1.0008). Therefore, the average outcome differed significantly from zero (z= 2.8088, p = 0.0050). According to the Q-test, there was no significant amount of heterogeneity in the true outcomes (Q ( 3 ) = 4.2890, p = 0.2319, tau² = 0.0436, I² = 24.6411%). A 95% prediction interval for the true outcomes is given by 0.0092 to 1.1698. Hence, even though there may be some heterogeneity, the true outcomes of the studies are generally in the same direction as the estimated average outcome. An examination of the studentized residuals revealed that none of the studies had a value larger than ± 2.4977 and hence there was no indication of outliers in the context of this model. According to the Cook’s distances, none of the studies could be considered to be overly influential. Neither the rank correlation nor the regression test indicated any funnel plot asymmetry (p = 0.3333 and p = 0.1512, respectively). The funnel plot asymmetry was not assessed because there are less than 10 articles ( Tables 5 , 6 , Figure 2 ).
Table 5
Random-effects model.
| Random-Effects Model (k = 4) | ||||||
|---|---|---|---|---|---|---|
| Estimate | se | Z | p | CI Lower Bound | CI Upper Bound | |
| 0.589 | 0.210 | 2.81 | 0.005 | 0.178 | 1.001 | |
Table 6
Heterogeneity statistics.
| Heterogeneity Statistics | |||||||
|---|---|---|---|---|---|---|---|
| Tau | Tau | I | H | R | df | Q | p |
| 0.0436 M (SE = 0.1438) | 24.64% | 1.327 | 3.000 | 4.289 | 0.232 | ||

Forest plot.
4. Discussion
Whole body vibration is a simple, safe and effective non-pharmacological measure to reduce HbA1c and plasma glucose levels in patients with DM 2 whose physical condition prevents conventional aerobic exercise ( 33 ).
Regarding the pharmacological drugs for the treatment of DM 2, they do not inherently exhibit the ability to maintain sustained glycemic control over a prolonged period ( 34 ). In addition, adverse effects such as gastroenteritis, hypoglycemia and weight gain, among others, are undesirable manifestations associated with the use of orally administered pharmacological agents in patients with DM 2. These side effects lead to a decrease in adherence to pharmacological treatment by patients diagnosed with DM2 ( 35 , 36 ). For that reason, moderate-intensity aerobic physical exercise is recognized as an effective non-pharmacological approach to reducing blood glucose levels for people whose physical condition allows it to be performed. However, WBV could be a physical exercise option to reduce blood glucose and HbA1c levels for those who cannot perform aerobic exercise ( 26 – 29 ).
Regular physical exercise increases glucose uptake in activated muscle, which induces increased insulin sensitivity in diabetics. Regular WBV training has been shown to generate muscle adaptation similar to resistance exercise training ( 37 ). Thus, regular WBV training may help diabetic patients to control glucose metabolism ( 25 ).
WBV does not require a specific physical condition, nor prior supervision and may help in physical exercise adherence for patients with DM 2. Moreover, it has demonstrated its efficacy in animal ( 38 – 40 ) and human ( 16 , 41 , 42 ) studies. Some of the participants who underwent the WBV intervention showed a statistically significant reduction in HbA1c levels compared to those who did not receive the intervention.
Some studies ( 26 , 27 , 30 ) point out, it seems that 12 weeks of WBV intervention is sufficient for a statistically significant improvement in both WBC and HbA1c in people with DM 2 compared to those who did not undergo any intervention. This data is similar to those found in another meta-analysis ( 7 ) in which the sample was subjected to aerobic training for 12 weeks, achieving a reduction in HbA1c. On the other hand, authors stated that there is no significant differences in HbA1c concentrations or fasting WBC between the conventional aerobic exercise groups and those subjected to vibration ( 29 ).
However, there is no clear consensus on what the most beneficial parameters for these patients should be. Studies with longer duration and parameters of frequency, intensity and duration should be investigated in the future in order to adapt this therapy to patients with type 2 diabetes.
In this period, Baum et al. ( 28 ) and Manimmanakorn ( 25 ), using a step-up frequency of 30-40Hz, did not show a significant reduction in HbA1c which was only revealed after post-hoc dichotomization. However, Alfonso-Rosa ( 26 ) and Del Pozo-Cruz et al. ( 27 ), using a lower frequency, also of progressive increase (12-16Hz), did show a significant reduction in both HbA1c and WBC. These data coincide with another study ( 31 ), where an increase in the effects was demonstrated in relation to the progressive increase in frequency. The gradual increase in frequency may be the reason for the difference in the results. Therefore, it seems that a low frequency with progressive increase and the number of weeks of intervention play a determining role in obtaining a beneficial effect. On the other hand, Michels et al. ( 30 ), using a constant frequency of 28 Hz, showed a reduction in HbA1c and WBC. Behboudi et al. ( 29 ) using a constant high frequency of 30 Hz for a shorter number of weeks showed no significant differences in HbA1c or fasting glucose, but concentration was higher in the control group.
During exposure, the vibration of the vertical platform moves vertically under both feet at the same time, producing a simultaneous symmetrical movement of both sides of the body, whereas the oscillating platform generates an asymmetrical perturbation of the legs. Vertical platforms work at higher frequencies (between 30 and 50 Hz) than oscillating platforms (between 5 and 30 Hz). In addition, vertical platforms have shown greater chronic effects on strength training and oscillating platforms greater acute effects ( 31 ). However, the limited scientific literature on the use of these platforms in diabetes makes it difficult to determine which is the best choice. Regarding the type of platform used, different studies ( 26 , 28 ) have carried out an intervention using an oscillating type of platform, obtaining positive results with respect to HbA1c and WBC, as in the study by Lythgo et al. ( 43 ). However, in one of the studies ( 25 ), using the same type of platform, they did not obtain positive results for HbA1c, but did obtain positive results for WBC.
On the other hand, two of the studies ( 27 , 30 ) used a vertical type of vibrating platform and found positive effects on HbA1c and WBC results. These data agree with what was announced by another study ( 32 ) where they determined that vibration transmission was higher during vertical vibration compared to oscillating vibration. This could indicate that the type of platform alone is not determinant to assess its effectiveness, more conclusive studies are needed to evaluate the different vibratory devices in people with DM 2.
HbA1C is one of the most determinant parameters in the diagnosis and long-term control of DM. According to the American Diabetes Association (ADA) ( 44 ), an HbA1c > 6.5% is considered a diagnostic criterion for DM, while values < 7.0% HbA1c determine good blood glucose control in the last four months ( 45 , 46 ). Unfortunately, most of the studies using the HbA1chave performed short-term follow-ups, which prevents us from knowing the physiological effects in the long term,
Based on the information offered by the ADA ( 44 ), which considers that maintaining HbA1c levels below 7% acts as a protective factor, helping to manage glycemic imbalance and evaluate the risk of developing, Manimmanakorn ( 25 ) found a slight reduction in HbA1c, after 12 weeks of intervention in subjects with values above 8% using a post hoc dichotomization; in contrast, in a previous study, in which intervention exercises were applied for 8 weeks, no significant improvement in HbA1c was observed ( 47 ).
In relation to the control group, no significant changes in HbA1c levels were observed, according to the data provided by Manimmanakorn ( 25 ). On the other hand, Baum et al. compared the WBV group with a strength and flexibility group. After the vibration intervention, a reduction in HbA1c levels was found in both groups, although not reaching statistical significance ( 28 ). However, other authors, such as Alfonso-Rosa ( 16 ), Del Pozo-Cruz et al. ( 27 ) and Behboudi et al. ( 29 ) indicated that a conventional exercise program resulted in a decrease in HbA1c levels after the intervention period.
These data are in line with those provided by other studies ( 48 ), which show how a conventional training program reduces HbA1c levels.
The WBV guidelines reported by Van Heuvelen et al. ( 21 ) are essential to improve reproducibility and transparency in WBV studies, and their adherence allows for proper assessment of the efficacy and safety of WBV interventions. Follow them ensures that the necessary criteria for robust and replicable research are met. In this sense, all the authors of the selected articles ( 25 – 30 ) have reported the frequency of the intervention, as well as the amplitude, except for Michels et al. ( 30 ), the duration and frequency of the sessions and the total duration of the program, which was established at 12 weeks, except for Behboudi et al. ( 29 ) who applied 8 weeks. The application of the therapy, the results, the statistical analysis and the absence of adverse effects in all the selected articles were described. However, adherence has been variable, with 4 losses reported by Manimmanakorn et al. ( 25 ), 11 by Alonso-Rosa et al. ( 26 ) and del Pozo-Cruz et al. ( 27 ), and 2 by Michels et al. ( 30 ); only Baum et al. ( 28 ) and Behboudi et al. ( 29 ) did not report any losses. The recommendations for clinical practice and future lines of research recommend stratifying patients in the sampling according to the degree of severity of diabetes based on HbA1c or the duration of the disease ( 25 ) and analyzing cost effectiveness ( 27 ) as well as including more patients and longer follow-up ( 30 ) and optimizing frequency, amplitude, and duration of vibration exercises ( 28 ).
Finally, there is no consensus with the conclusions: WBV is applicable, safe and effective in reducing HbA1C and basal blood glucose level ( 26 – 28 , 30 ), while for others ( 25 ) there was no change in FBS or HbA1c, nor for Behboudi et al. ( 29 ) who proposed that insignificant results of the present study can be attributed to the small number of samples and improper time and intensity of exercise. However, whole body vibration can be considered as a better way to exercise in a shorter time for majority of diabetic patients who suffer from obesity and unwillingness to join active physical activities. Because of these results, the effect size of these interventions is small and the clinical implications, although they appear to be promising, should be interpreted with caution.
The review has several limitations. the review was not registered; however, all steps were taken to ensure the reliability, transparency and thoroughness of the process and data. Only full-text registries have been considered; the number of experimental clinical trials using WBV in these pathologies is small and some of the studies do not provide all the data on the variables used like disease duration or some outcomes which prevent the effect comparisons. One of the selected articles has not been submitted a per-review process, therefore, the results obtained in this manuscript should be treated with caution and most of them did not follow the quality guidelines and recommendations exposed by Van Heuvelen ( 21 ). In addition, the sample size has been very diverse and small; there is not a standard protocol or parameters to achieve the best effectiveness of this therapy although most of them agree with a frequency of three times a week for 12 weeks, and the follow-up of the studies has been only focused on the short-term effects of WBV. In addition, it should be noted that the treatments received by the patients of the selected studies were not composed only of WBV treatment, so that the sum of the effects of the prescribed pharmacological treatment and lifestyle may have contributed to the positive effects obtained.
Nevertheless, the clinical implications are promising, being a safe therapy with no adverse effects that can be used in this population as a complement to other therapies or as an alternative for patients who are unable to perform physical activity. In future lines of research larger samples should be recruited as well as similar measurements, platforms and long term follow up to be able to better determine the clinical effects of the use of WBV.
5. Conclusion
The habitual use of vibration platforms with a frequency of 14-16 Hz for 12 weeks is reflected in the literature. These results are encouraging and suggest that WBV may be an effective therapy to improve glycemic control in patients with DM 2. The addition of Whole Body Vibration therapy as a complement for exercise programs could be effective in sedentary people and could be a useful tool for clinicians. However, further studies with more patients and longer follow-up are needed to confirm these findings.
Acknowledgments
To our colleagues who have made this possible.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. University of Salamanca funded this manuscript. This publication is financed by the Ministry of Science, Innovation and Universities.

Data availability statement
Author contributions.
JF-F: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. VR-P: Conceptualization, Funding acquisition, Methodology, Project administration, Writing – original draft, Writing – review & editing. RL-R: Conceptualization, Funding acquisition, Methodology, Project administration, Writing – original draft, Writing – review & editing. AL-R: Investigation, Methodology, Writing – review & editing. MC-R: Data curation, Formal analysis, Writing – review & editing. IL-R: Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing, Project administration.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.

COMMENTS
This web page is a literature review of type 2 diabetes management and health literacy, not related to diabetes melitus topic font. It does not contain any information about font styles or formats for diabetes education materials.
Arora T, Taheri S. Sleep optimization and diabetes control: a review of the literature. Diabetes Ther. 2015 Dec; 6 ((4)):425-68. [PMC free article] [Google Scholar] 88. Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Bixler EO. Insomnia with objective short sleep duration is associated with type 2 diabetes: a population-based study.
1. Introduction. Diabetes Mellitus (DM) commonly referred to as diabetes, is a chronic disease that affects how the body turns food into energy .It is one of the top 10 causes of death worldwide causing 4 million deaths in 2017 , .According to a report by the International Diabetes Federation (IDF) , the total number of adults (20-79 years) with diabetes in 2045 will be 629 million from 425 ...
This review article explores the molecular mechanism, pathophysiology, and pharmacology of diabetes mellitus, a metabolic disease characterized by high blood glucose levels. It covers the types, complications, risk factors, diagnosis, and treatment of diabetes mellitus, as well as the role of oxidative stress and insulin resistance.
Introduction. Diabetes mellitus (DM), as a growing epidemic of bipolar disorder, affects near 5.6% of the world's population ().Its global prevalence was about 8% in 2011 and is predicted to rise to 10% by 2030 ().Likewise, its prevalence in China also increased rapidly from 0.67% in 1980 to 10.4% in 2013 ().Therefore, DM is a contributing factor to morbidity and mortality.
The best evidence for a link between diabetes mellitus and breast cancer comes from a systematic review of six prospective cohort studies and more than 150,000 women, in which the hazard ratio (HR ...
Objective: The purpose of this literature review was to identify educational approaches addressing low health literacy for people with type 2 diabetes. Low health literacy can lead to poor management of diabetes, low engagement with health care providers, increased hospitalization rates, and higher health care costs.
This study systematically reviewed studies reporting trends of diabetes incidence in adults from 1980 to 2017. It found that diabetes incidence has increased, stabilised, or declined in different populations and time periods, suggesting that prevention strategies could have contributed to the fall in diabetes incidence in recent years.
This is a literature review aiming to overview, summarise and discuss the role and effect of patient empowerment, self-management education and lifestyle modification in the management of people with DM. ... Kelly JT, et al. Effectiveness of group-based self-management education for individuals with Type 2 diabetes: A systematic review with ...
Type 2 diabetes mellitus (T2DM) is an expanding global health problem, closely linked to the epidemic of obesity. Individuals with T2DM are at high risk for both microvascular complications ...
Methods: The literature search (MEDLINE and Web of Science) identified prospective studies (cohorts or trials) that associated dietary patterns with diabetes incidence in nondiabetic and apparently healthy participants. We summarized evidence by meta-analyses and distinguished different methodologic approaches.
Diabetes mellitus is a group of physiological dysfunctions characterized by hyperglycemia resulting directly from insulin resistance, inadequate insulin secretion, or excessive glucagon secretion. ... The purpose of this article is to review the basic science of type 2 diabetes and its complications, and to discuss the most recent treatment ...
Based on this phenomenon, a literature review was prepared to highlight effectiveness of DSME on T2DM. Design and Methods. ... Descriptive, retrospective chart review: 100 participants: 8: Effect of diabetes self-management education (DSME) on glycated hemoglobin (HbA1c) level among patients with T2DM: Systematic review and meta-analysis of ...
The systematic review widely focused on diabetes and the developments in nutrition and diets required to prevent or control all types of diabetes. Diabetes is characterized by high blood sugar ...
This article reviews the literature on how social and environmental factors affect diabetes risk and outcomes in the U.S. It also provides recommendations for addressing SDOH and health disparities in diabetes care and research.
Type 2 diabetes mellitus is emerging as a new clinical problem within pediatric practice. Recent reports indicate an increasing prevalence of type 2 diabetes mellitus in children and adolescents ...
Diabetes mellitus is a chronic disease characterized by high glucose levels (hyperglycemia) due to metabolic disorders that prevent patients from producing sufficient amounts of insulin. ... Based on this phenomenon, a literature review was prepared to highlight effectiveness of DSME on T2DM. Design and Methods. The collection and review of ...
Diabetes mellitus is a global health challenge associated with alarming rates of morbidity and mortality. As of 2021, the worldwide count of diabetes patients reached a staggering 529 million; this figure is projected to escalate exponentially to over 1.3 billion by 2050 [].In addition to its pervasive prevalence, diabetes poses a significant threat to affected individuals with respect to ...
This systematic literature review aims to identify diabetes self-management education (DSME) features to improve diabetes education for Black African/Caribbean and Hispanic/Latin American women with Type 2 diabetes mellitus. Methods.
Introduction. Diabetes mellitus (DM) is probably one of the oldest diseases known to man. It was first reported in Egyptian manuscript about 3000 years ago. 1 In 1936, the distinction between type 1 and type 2 DM was clearly made. 2 Type 2 DM was first described as a component of metabolic syndrome in 1988. 3 Type 2 DM (formerly known as non-insulin dependent DM) is the most common form of DM ...
Objective We conducted a systematic review and meta-analysis of observational studies that assessed the relationship between pesticides exposure and type 2 diabetes. We also examined the presence of heterogeneity and biases across the available studies. Methods We conducted a comprehensive literature search of peer-reviewed studies published from 2011 to 2023, without language limitations. A ...
This systematic literature review determined how satellite imagery has been used to address the top NCDs in the world, including cardiovascular diseases, cancers, chronic respiratory diseases, and diabetes. A literature search was performed using PubMed (including MEDLINE), CINAHL, Web of Science, Science Direct, Green FILE, and Engineering ...
However, the limited scientific literature on the use of these platforms in diabetes makes it difficult to determine which is the best choice. Regarding the type of platform used, different studies ( 26 , 28 ) have carried out an intervention using an oscillating type of platform, obtaining positive results with respect to HbA1c and WBC, as in ...