Featured Topics
Featured series.
A series of random questions answered by Harvard experts.

Explore the Gazette
Read the latest.

Women rarely die from heart problems, right? Ask Paula.

When will patients see personalized cancer vaccines?
A molecular ‘warhead’ against disease
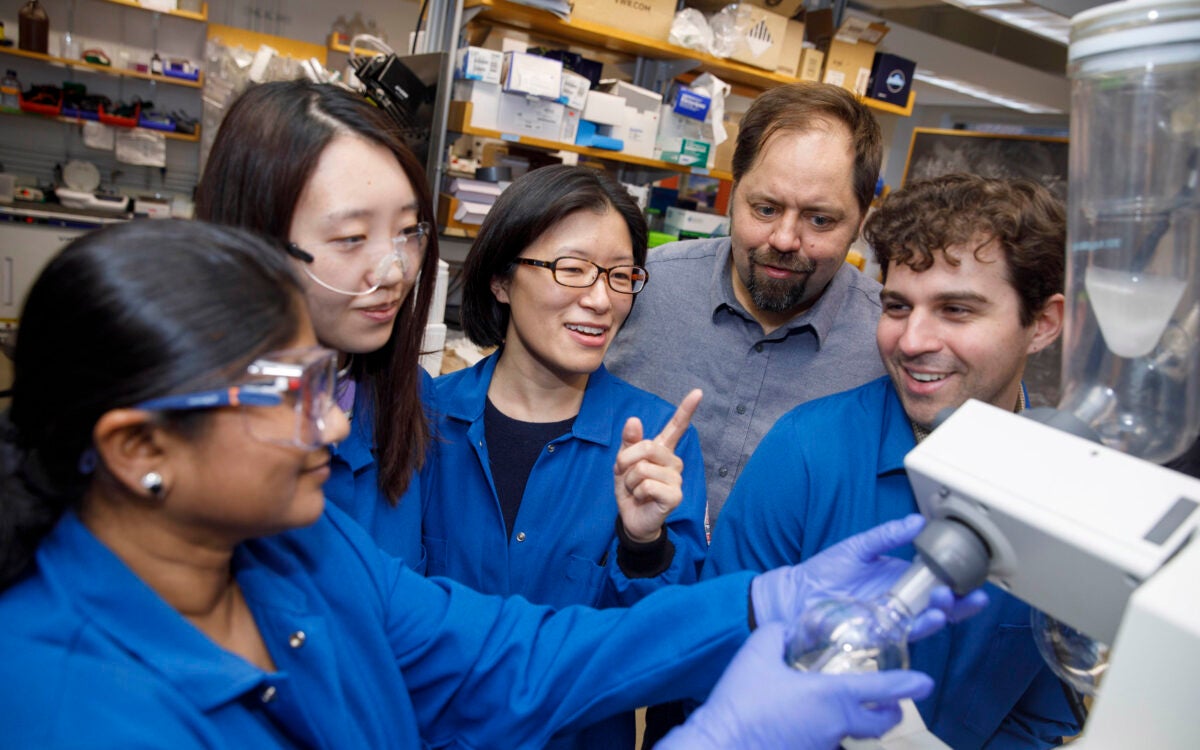
“When my son was diagnosed [with Type 1], I knew nothing about diabetes. I changed my research focus, thinking, as any parent would, ‘What am I going to do about this?’” says Douglas Melton.
Kris Snibbe/Harvard Staff Photographer
Breakthrough within reach for diabetes scientist and patients nearest to his heart
Harvard Correspondent
100 years after discovery of insulin, replacement therapy represents ‘a new kind of medicine,’ says Stem Cell Institute co-director Douglas Melton, whose children inspired his research
When Vertex Pharmaceuticals announced last month that its investigational stem-cell-derived replacement therapy was, in conjunction with immunosuppressive therapy, helping the first patient in a Phase 1/2 clinical trial robustly reproduce his or her own fully differentiated pancreatic islet cells, the cells that produce insulin, the news was hailed as a potential breakthrough for the treatment of Type 1 diabetes. For Harvard Stem Cell Institute Co-Director and Xander University Professor Douglas Melton, whose lab pioneered the science behind the therapy, the trial marked the most recent turning point in a decades-long effort to understand and treat the disease. In a conversation with the Gazette, Melton discussed the science behind the advance, the challenges ahead, and the personal side of his research. The interview was edited for clarity and length.
Douglas Melton
GAZETTE: What is the significance of the Vertex trial?
MELTON: The first major change in the treatment of Type 1 diabetes was probably the discovery of insulin in 1920. Now it’s 100 years later and if this works, it’s going to change the medical treatment for people with diabetes. Instead of injecting insulin, patients will get cells that will be their own insulin factories. It’s a new kind of medicine.
GAZETTE: Would you walk us through the approach?
MELTON: Nearly two decades ago we had the idea that we could use embryonic stem cells to make functional pancreatic islets for diabetics. When we first started, we had to try to figure out how the islets in a person’s pancreas replenished. Blood, for example, is replenished routinely by a blood stem cell. So, if you go give blood at a blood drive, your body makes more blood. But we showed in mice that that is not true for the pancreatic islets. Once they’re removed or killed, the adult body has no capacity to make new ones.
So the first important “a-ha” moment was to demonstrate that there was no capacity in an adult to make new islets. That moved us to another source of new material: stem cells. The next important thing, after we overcame the political issues surrounding the use of embryonic stem cells, was to ask: Can we direct the differentiation of stem cells and make them become beta cells? That problem took much longer than I expected — I told my wife it would take five years, but it took closer to 15. The project benefited enormously from undergraduates, graduate students, and postdocs. None of them were here for 15 years of course, but they all worked on different steps.
GAZETTE: What role did the Harvard Stem Cell Institute play?
MELTON: This work absolutely could not have been done using conventional support from the National Institutes of Health. First of all, NIH grants came with severe restrictions and secondly, a long-term project like this doesn’t easily map to the initial grant support they give for a one- to three-year project. I am forever grateful and feel fortunate to have been at a private institution where philanthropy, through the HSCI, wasn’t just helpful, it made all the difference.
I am exceptionally grateful as well to former Harvard President Larry Summers and Steve Hyman, director of the Stanley Center for Psychiatric Research at the Broad Institute, who supported the creation of the HSCI, which was formed specifically with the idea to explore the potential of pluripotency stem cells for discovering questions about how development works, how cells are made in our body, and hopefully for finding new treatments or cures for disease. This may be one of the first examples where it’s come to fruition. At the time, the use of embryonic stem cells was quite controversial, and Steve and Larry said that this was precisely the kind of science they wanted to support.
GAZETTE: You were fundamental in starting the Department of Stem Cell and Regenerative Biology. Can you tell us about that?
MELTON: David Scadden and I helped start the department, which lives in two Schools: Harvard Medical School and the Faculty of Arts and Science. This speaks to the unusual formation and intention of the department. I’ve talked a lot about diabetes and islets, but think about all the other tissues and diseases that people suffer from. There are faculty and students in the department working on the heart, nerves, muscle, brain, and other tissues — on all aspects of how the development of a cell and a tissue affects who we are and the course of disease. The department is an exciting one because it’s exploring experimental questions such as: How do you regenerate a limb? The department was founded with the idea that not only should you ask and answer questions about nature, but that one can do so with the intention that the results lead to new treatments for disease. It is a kind of applied biology department.
GAZETTE: This pancreatic islet work was patented by Harvard and then licensed to your biotech company, Semma, which was acquired by Vertex. Can you explain how this reflects your personal connection to the research?
MELTON: Semma is named for my two children, Sam and Emma. Both are now adults, and both have Type 1 diabetes. My son was 6 months old when he was diagnosed. And that’s when I changed my research plan. And my daughter, who’s four years older than my son, became diabetic about 10 years later, when she was 14.
When my son was diagnosed, I knew nothing about diabetes and had been working on how frogs develop. I changed my research focus, thinking, as any parent would, “What am I going to do about this?” Again, I come back to the flexibility of Harvard. Nobody said, “Why are you changing your research plan?”
GAZETTE: What’s next?
MELTON: The stem-cell-derived replacement therapy cells that have been put into this first patient were provided with a class of drugs called immunosuppressants, which depress the patient’s immune system. They have to do this because these cells were not taken from that patient, and so they are not recognized as “self.” Without immunosuppressants, they would be rejected. We want to find a way to make cells by genetic engineering that are not recognized as foreign.
I think this is a solvable problem. Why? When a woman has a baby, that baby has two sets of genes. It has genes from the egg, from the mother, which would be recognized as “self,” but it also has genes from the father, which would be “non-self.” Why does the mother’s body not reject the fetus? If we can figure that out, it will help inform our thinking about what genes to change in our stem cell-derived islets so that they could go into any person. This would be relevant not just to diabetes, but to any cells you wanted to transplant for liver or even heart transplants. It could mean no longer having to worry about immunosuppression.
Share this article
You might like.
New book traces how medical establishment’s sexism, focus on men over centuries continues to endanger women’s health, lives

Sooner than you may think, says researcher who recently won Sjöberg Prize for pioneering work in field
Approach attacks errant proteins at their roots
Harvard announces return to required testing
Leading researchers cite strong evidence that testing expands opportunity
For all the other Willie Jacks
‘Reservation Dogs’ star Paulina Alexis offers behind-the-scenes glimpse of hit show, details value of Native representation
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- News & Views
- Published: 11 March 2019
The reconstructed natural history of type 1 diabetes mellitus
- Paolo Pozzilli 1 , 2 &
- Alberto Signore 3
Nature Reviews Endocrinology volume 15 , pages 256–257 ( 2019 ) Cite this article
1226 Accesses
4 Citations
8 Altmetric
Metrics details
- Translational research
The causes of type 1 diabetes mellitus (T1DM) are unclear; however, a general consensus exists that T1DM is a T cell-mediated autoimmune disease characterized by the selective destruction of insulin-secreting β-cells. Now, two imaging mass cytometry studies of human pancreatic tissue illuminate new biology in the pathogenesis of T1DM.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Damond, N. K. et al. A map of human type 1 diabetes progression by imaging mass cytometry. Cell Metab. https://doi.org/10.1016/j.cmet.2018.11.014 (2019).
Article PubMed PubMed Central Google Scholar
Wang, Y. J. et al. Multiplexed in situ imaging mass cytometry analysis of the human endocrine pancreas and immune system in type 1 diabetes. Cell Metab. https://doi.org/10.1016/j.cmet.2019.01.003 (2019).
Gepts, W. Pathologic anatomy of the pancreas in juvenile diabetes mellitus. Diabetes 14 , 619–633 (1965).
Article CAS Google Scholar
Foulis, A. K. & Stewart, J. A. The pancreas in recent-onset type 1 (insulin- dependent) diabetes mellitus: insulin content of islets, insulitis and associated changes in the exocrine acinar tissue. Diabetologia 26 , 456–461 (1984).
Rui, J. et al. B cells that resist immunological attack develop during progression of autoimmune diabetes in NOD mice. Cell Metab. 25 , 727–738 (2017).
Signore, A. et al. Detection of insulitis by pancreatic scintigraphy with 99mTc-labeled IL-2 and MRI in patients with LADA (Action LADA 10). Diabetes Care 38 , 652–658 (2015).
CAS PubMed Google Scholar
Download references
Author information
Authors and affiliations.
Unit of Endocrinology and Diabetes, University Campus Bio-Medico, Rome, Italy
Paolo Pozzilli
Centre of Immunobiology, Blizard Institute, Queen Mary, University of London, London, UK
Nuclear Medicine Unit, Department of Medical-Surgical Sciences and of Translational Medicine, “Sapienza” University of Rome, Rome, Italy
Alberto Signore
You can also search for this author in PubMed Google Scholar
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Correspondence to Paolo Pozzilli .
Ethics declarations
Competing interests.
The authors declare no competing interests.

Rights and permissions
Reprints and permissions
About this article
Cite this article.
Pozzilli, P., Signore, A. The reconstructed natural history of type 1 diabetes mellitus. Nat Rev Endocrinol 15 , 256–257 (2019). https://doi.org/10.1038/s41574-019-0192-8
Download citation
Published : 11 March 2019
Issue Date : May 2019
DOI : https://doi.org/10.1038/s41574-019-0192-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
- Diabetes Care for Children & Young People
Vol:05 | No:01
Children and young people’s diabetes care: Case study
- 12 Jul 2016
This case study demonstrates the physical and psychological difficulties faced by many young people with type 1 diabetes. Over the year following her diagnosis, Max had a deterioration in glycaemic control despite reporting that little had changed in her management. Detailed assessment revealed a number of psychosocial factors that were preventing her from achieving good control. However, working with her multidisciplinary team, she was able to address these issues and improve her blood glucose levels. This article outlines these issues and the action plan that Max and her diabetes team drew up to overcome them.
Share this article + Add to reading list – Remove from reading list ↓ Download pdf
This case study represents the challenges and issues, both physical and psychological, faced by a young person with type 1 diabetes and the support given by her diabetes multidisciplinary team (MDT). Implications for practice are addressed using current evidence-based research. The names of the child and family have been anonymised to protect their identity.
Case study Max (a pseudonym) is a 17-year-old girl who was diagnosed with type 1 diabetes 4 years ago at the age of 13 years. She and her mother were shocked and upset by the diagnosis, and both felt its management would be too great a task to take on by themselves.
Max is an only child and lives with her mother, a single parent. She attends the local state comprehensive school and is popular with her peer group. Her mother was very involved in her care and diabetes management from the onset. Despite this, her diabetes control deteriorated over time ( Table 1 ). In October 2012, her HbA 1c was 56 mmol/mol (7.3%); however, over the next year, this increased to 84 mmol/mol (9.8%) in July 2013. She found it difficult to count the carbohydrate portions in her food and her injections were hurting much more than when she was first diagnosed. She also expressed a fear of hypoglycaemia and of “looking stupid” in front of her friends.
Max and her MDT discussed treatment options to improve her glycaemic control. She refused insulin pump therapy but agreed to a blood glucose monitor and bolus advisor to assist with her regimen of multiple daily insulin injections (MDI). She is now using the bolus advisor confidently and has had regular one-to-one sessions with a psychologist. She is having fewer hypoglycaemic episodes and her HbA 1c has improved; in January 2016 it was 69 mmol/mol (8.5%) and in April 2016 it was 58 mmol/mol (7.5%).
Discussion Diagnosis Max and her mother were extremely shocked and upset by the diagnosis of type 1 diabetes and the potential severity of the condition and intense management required. Both felt it would be too great a task to take on by themselves.
Kübler-Ross and Kessler (2005) suggested that a diagnosis of diabetes is a life-changing event comparable to the experience of loss, and that children and families will often go through the five stages of grief defined by Kübler-Ross (1970) and outlined in Box 1 . They use this as a coping strategy to enable them to eventually acknowledge the condition. However, many families never reach the fifth stage of acceptance and many will fluctuate between the stages.
Although Max and her mum did accept the diagnosis eventually, at times both of them reverted to the earlier stages of grief. The diabetes MDT supported the family from diagnosis and will continue to support them throughout their time within the paediatric diabetes service, through the transition period with both paediatric and young people’s teams, until discharged to adult diabetes care.
The diabetes MDT was established after the Best Practice Tariff was introduced in 2012. It consists of doctors, nurses, dietitians, a psychologist and a personal assistant. It is well recognised that the MDT needs to work together in close cooperation to achieve good practice, and this can be strengthened by using written protocols, guidelines and targets (Brink, 2010). Logic would suggest that centres with MDTs and the same approaches and treatment regimens would have similar outcomes, yet the Hvidøre Childhood Diabetes Study Group has shown this is not the case (de Beaufort et al, 2013). In terms of glycaemic control, there were notable differences in patient outcomes across 21 diabetes clinics, all of which were committed to MDT-based practice. Although factors such as age, type of insulin regimen and socioeconomic status were shown to have some influence over specific outcomes, they did not explain the apparent differences between these clinics.
Family/social history Max is an only child and lives with her mother, a single parent. East et al (2006) suggested that rapid social change over the past 20 years has seen a marked increase in the number of mother-headed single-parent families. Max attends the local state comprehensive school, where she is generally doing well. She is popular with her peer group. La Greca et al (1995) suggested that peer relationships are important in diabetes management, as children and young people (CYP) may receive considerable emotional support from their friends. However, on occasions, Max’s peer relationships have had a counterproductive effect on her, and she feels she is different from her friends as the only one who has diabetes. This at times affects her self-esteem and impacts her diabetes control.
Max’s mother was very involved in her care and diabetes management from the onset. Anderson and Brackett (2005) suggested that parents typically take on most of the responsibility for management of diabetes when children are young or newly diagnosed.
Deterioration in diabetes control Max’s diabetes control had deteriorated since her diagnosis ( Table 1 ). In October 2012, her HbA 1c was 56 mmol/mol (7.3%), which indicated a good level of diabetes control and a reduced risk of diabetes complications, as suggested by the DCCT (Diabetes Control and Complications Trial; DCCT Research Group, 1994). At her subsequent diabetes clinic appointments up to July 2013, she reported that “nothing had really changed,” except she “didn’t have time to think about her diabetes,” although she felt guilty because she knew she could make herself ill and her mum would get upset. She stated that it was hard counting the carbohydrate portions in her food and her injections were hurting much more than when she was first diagnosed. Her height and weight remained static.
Diabetes care is greatly influenced by psychosocial factors when they obstruct people’s ability to manage their diabetes and achieve good metabolic control. A team-based approach to addressing an individual’s ability to cope is critical (Kent et al, 2010). It is important for healthcare professionals to be aware of how CYP think at the different stages of their development, as their understanding of illness and chronic health conditions is often greater than that of their peers. Jean Piaget (1896–1980) investigated cognitive processes in children, calling them “schemas”. By the time children reach around 12 years of age, they can describe illness in terms of non-functioning or malfunctioning of an internal organ or process. Later in development they can appreciate that a person’s thoughts or feelings can affect the way the body functions, which demonstrates an awareness of psychological factors (Taylor et al, 1999).
Spear (2013) proposed that we can begin to understand how young people with type 1 diabetes think, feel and behave if we consider the cognitive and biological changes that occur during adolescence. Glasper and Richardson (2005) suggested there is now a growing awareness that CYP are able to make their own decisions if given information in an age-appropriate manner. Gillick competence identifies children aged under 16 years as having the capacity to consent to their own treatment if they understand the consequences (NSPCC, 2016).
Butler et al (2007) suggest that adolescence is a time of upheaval when young people have to deal with the influence of peers, school life and developing their own identity, as well as all the physiological changes that occur. Young people with type 1 diabetes have the added responsibility of developing autonomy regarding the self-management of their condition. Hanas (2006) suggests that parents should continue to take part in their child’s diabetes care into adolescence and not hand the responsibility to the young person too early. Snoek and Skinner (2002) suggest that intensive self-management of diabetes is complex and time-consuming, and creates a significant psychosocial burden on children and their families.
There are significant challenges for CYP to engage in effective diabetes self-management. Several of these were identified with Max and her mother:
- Deterioration in diabetes control.
- Difficulty with carbohydrate counting.
- Insulin omission.
- Fear of hypoglycaemia.
- Painful injections.
Action plan An action plan was discussed between Max and the MDT. As she was on an MDI regimen (a long-acting insulin at bedtime and rapid-acting insulin with meals), a bolus advisor/blood glucose monitor was demonstrated and discussed with her and her mum. Max felt she would be able to use this to help eliminate the calculations which, although she was capable of doing them, she often lacked time to do so. With further discussion, Max said she was “scared of getting it wrong and having a hypo”. Insulin pump therapy was discussed but she did not want to “have a device attached to my body because it would remind me all the time that I have diabetes”. Insulin pump therapy is recommended as a treatment option for adults and children over 12 years of age with type 1 diabetes whose HbA 1c levels remain above 69 mmol/mol (8.5%) on MDI therapy despite a high level of care (NICE, 2015a).
The National Service Framework standard 3 (Department of Health, 2001) recommends empowering people with diabetes and encourages them and their carers to gain the knowledge and skills to be partners in decision-making, and giving them more personal control over the day-to-day management of their diabetes, ensuring the best possible quality of life. However, if a diabetes management plan is discussed in partnership with a (Gillick-competent) young person but they elect not to comply with the plan despite full awareness of the implications of their actions, then the diabetes team should support them whilst trying to encourage them to maintain the treatment plan. This can be very difficult and frustrating at times, as a healthcare professional is an advocate for the patient, and promotion of the best interests of the patient is paramount.
Psychology involvement Max was reviewed by the psychologist to assess her psychological health and wellbeing. The psychologist used the Wellbeing in Diabetes questionnaire (available from the Yorkshire and Humber Paediatric Diabetes Network) to assess her and identify an optimal plan of care.
The psychology sessions were focussed on her issues around the following:
- Worry about deterioration in control.
- The consequences of insulin omission.
Max had a series of one-to-one appointments and some joint sessions with the paediatric diabetes specialist nurse and/or dietitian, so this linked into other team members’ specialities.
Carbohydrate counting and use of a bolus advisor The dietitian assessed Max and her mother’s ability to carbohydrate count using a calculator, food diagrams and portion sizes, and both of them were able to demonstrate competency in this task. Garg et al (2008) have shown that the use of automated bolus advisors is safe and effective in reducing postprandial glucose excursions and improving overall glycaemic control. However, this can only be true if the bolus advisor is being used correctly and is confirmed as such by comparing blood glucose and HbA 1c results before and after initiation of the bolus advisor, and observing the patient using the device to ensure it is being used safely and correctly.
Barnard and Parkin (2012) propose that, as long as safety and lifestyle are taken into consideration, advanced technology will benefit CYP, as inaccurate bolus calculation can lead to persistent poor diabetes control. These tools can help with removing the burden of such complex maths and have the potential to significantly improve glycaemic control.
Insulin omission and fear of hypoglycaemia Max also expressed her fear of hypoglycaemia and of “looking stupid” in front of her friends. She admitted to missing some of her injections, especially at school. Wild et al (2007) suggest that a debilitating fear of hypoglycaemia can result in poor adherence to insulin regimens and subsequent poor metabolic control. Crow et al (1998) describe the deliberate omission or reduced administration of insulin, which results in hyperglycaemia and subsequent rapid reduction in body weight. Type 1 diabetes predisposes a person to a high BMI. Adolescent girls and adult women with type 1 diabetes generally have higher BMI values than their peers without the condition (Domargård et al, 1999). Affenito et al (1998) observed that insulin misuse was the most common method of weight control used by young women with type 1 diabetes. However, Max’s weight remained stable and there was no clinical indication that she was missing insulin to lose weight; rather, it was her fear of hypoglycaemia that drove her to omitting insulin at school. With the use of the bolus calculator, she was reassured about her calculations for insulin-to-carbohydrate ratios, but it was reinforced with her that the device would only work efficiently if she used it correctly with each meal.
Painful injections Max also highlighted that her injections were now more painful than when she was first diagnosed, and this was causing her distress each time she had to inject. Injection technique was discussed with her and demonstrated using an injection model, and her injection technique was observed and appeared satisfactory. She was using 5-mm insulin needles and so was switched to 4-mm needles, as recommended by Forum for Injection Technique (2015) guidelines.
Appropriate technique when giving injections is key to optimal blood glucose control; however, evidence suggests that injection technique is often imperfect. Studies by Strauss et al (2002) and Frid et al (2010) revealed disturbing practices in relation to injection technique, with little improvement over the years. Current diabetes guidelines do not include detailed advice on injection technique, and only the guidance on type 2 diabetes in adults (NICE, 2015b) makes any reference to providing education about injectable devices for people with diabetes. However, the older Quality Standard for diabetes in adults (NICE, 2011) recommends a structured programme of education, including injection site selection and care (Diggle, 2014).
Conclusion The issues and concerns this young girl had were identified and addressed by the diabetes MDT. She was assessed by several members of the team, and a credible, evidence-based action plan was put into place to assist her and her mother to manage her diabetes at this difficult time. Max is now using the bolus advisor confidently and having fewer hypoglycaemic episodes, and her HbA 1c has improved. She prefers using the 4-mm injection pen needles, although she remains hesitant when giving injections; she will still not consider insulin pump therapy. Her one-to-one sessions with the psychologist have now ceased, but she is aware she can access a psychologist at clinic on request, or if the MDT assesses that her psychological health has deteriorated.
When a child in a family develops a chronic condition such as type 1 diabetes, effective communication is vitally important to address issues with the family at the earliest stage so that problems can be discussed and, hopefully, resolved before they escalate out of control. Upon reflection, the team could have become more intensely involved at an earlier stage to prevent Max’s diabetes management issues and stop her HbA 1c from reaching such a high level. Furthermore, the new NICE (2015a) guideline has set the target HbA 1c at ≤48 mmol/mol (6.5%), so there is still some work to be done. However, the outcome of this case appears to be favourable at present.
Affenito SG, Rodriguez NR, Backstrand JR et al (1998) Insulin misuse by women with type 1 diabetes mellitus complicated by eating disorders does not favorably change body weight, body composition, or body fat distribution. J Am Diet Assoc 98 : 686–8 Anderson BJ, Brackett J (2005) Diabetes in children. In: Snoek FJ, Skinner TC (eds). Psychology in Diabetes Care (2nd edition). John Wiley & Sons, Chichester Barnard K, Parkin C (2012) Can automated bolus advisors help alleviate the burden of complex maths and lead to optimised diabetes health outcomes? Diabetes Care for Children & Young People 1 : 6–9 Brink SJ (2010) Pediatric and adolescent multidisciplinary diabetes team care. Pediatr Diabetes 11 : 289–91 Butler JM, Skinner M, Gelfand D et al (2007) Maternal parenting style and adjustment in adolescents with type I diabetes. J Pediatr Psychol 32 : 1227–37 Crow SJ, Keel PK, Kendall D (1998) Eating disorders and insulin-dependent diabetes mellitus. Psychosomatics 39 : 233–43 de Beaufort CE, Lange K, Swift PG et al (2013) Metabolic outcomes in young children with type 1 diabetes differ between treatment centers: the Hvidoere Study in Young Children 2009. Pediatr Diabetes 14 : 422–8 Department of Health (2001) National Service Framework: Diabetes . DH, London. Available at: http://bit.ly/18OpAzL (accessed 24.02.16) Diabetes Control and Complications Trial Research Group (1994) Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. J Pediatr 125 : 177–88 Diggle J (2014) Are you FIT for purpose? The importance of getting injection technique right . Journal of Diabetes Nursing 18 : 50–7 Domargård A, Särnblad S, Kroon M et al (1999) Increased prevalence of overweight in adolescent girls with type 1 diabetes mellitus. Acta Paediatr 88 : 1223–8 East L, Jackson D, O’Brien L (2006) Father absence and adolescent development: a review of the literature. J Child Health Care 10 : 283–95 Forum for Injection Technique (2015) The UK Injection Technique Recommendations (3rd edition). Available at: http://bit.ly/1QeZU2E (accessed 24.02.16) Frid A, Hirsch L, Gaspar R et al (2010) The Third Injection Technique Workshop in Athens (TITAN). Diabetes Metab 36 (Suppl 2): 19–29 Garg SK, Bookout TR, McFann KK et al (2008) Improved glycemic control in intensively treated adult subjects with type 1 diabetes using insulin guidance software. Diabetes Technol Ther 10 : 369–75 Glasper EA, Richardson J (2005) A Textbook of Children’s and Young People’s Nursing . Churchill Livingston, London Hanas R (2006) Type 1 Diabetes in Children, Adolescents and Young Adults (3rd edition). Class Publishing, London: 329, 349–50 Kent D, Haas L, Randal D et al (2010) Healthy coping: issues and implications in diabetes education and care. Popul Health Manag 13 : 227–33 Kübler-Ross E (1970) On Death and Dying: What the Dying Have to Teach Doctors, Nurses, Clergy and Their Own Families . Tavistock Publications, London Kübler-Ross E, Kessler D (2005) On Grief and Grieving: Finding the Meaning of Grief Through the Five Stages of Loss . Simon & Schuster UK, London La Greca AM, Auslander WF, Greco P et al (1995) I get by with a little help from my family and friends: adolescents’ support for diabetes care. J Pediatr Psychol 20 : 449–76 NICE (2011) Diabetes in adults (QS6). NICE, London. Available at: www.nice.org.uk/guidance/qs6 (accessed 24.02.16) NICE (2015a) Diabetes (type 1 and type 2) in children and young people: diagnosis and management (NG18). NICE, London. Available at: www.nice.org.uk/guidance/ng18 (accessed 24.02.16) NICE (2015b) Type 2 diabetes in adults: management (NG28). NICE, London. Available at: www.nice.org.uk/guidance/ng28 (accessed 24.02.16) NSPCC (2016) A Child’s Legal Rights: Gillick Competency and Fraser Guidelines . NSPCC, London. Available at: http://bit.ly/1Tj6DcF (accessed 24.02.16) Snoek FJ, Skinner TC (2002) Psychological counselling in problematic diabetes: does it help? Diabet Med 19 : 265–73 Spear LP (2013) Adolescent neurodevelopment. J Adolesc Health 52 (Suppl 2): 7–13 Strauss K, De Gols H, Hannat I et al (2002) A pan-European epidemiologic study of insulin injection technique in patients with diabetes. Practical Diabetes International 19 : 71–76 Taylor J, Müller D, Wattley L, Harris P (1999) The development of children’s understanding. In: Nursing Children: Psychology, Research and Practice . Stanley Thornes, Cheltenham Wild D, von Maltzahn R, Brohan E et al (2007) A critical review of the literature on fear of hypoglycemia in diabetes: implications for diabetes management and patient education. Patient Educ Couns 68 : 10–5
Do youth workers have a role in improving diabetes transition services?
Cgm for children and young people with type 1 diabetes: nice criteria and effects of decision fatigue and alarm fatigue , improving paediatric diabetes in england: areas of focus, delays in accessing continuous glucose monitoring in people with type 1 diabetes, celebrating may ng: the woman behind the obe, fiona campbell awarded an obe for services to paediatric diabetes, diabetes transition: a time to act.

Can the involvement of youth workers improve diabetes care for young people transitioning to adult diabetes services?

The impact of decision fatigue and alarm fatigue in children and young people using continuous glucose monitoring

NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022

NICE guidance urges local trusts to improve processes and advocate for CGM use in children and young people.
Sign up to all DiabetesontheNet journals
- CPD Learning
- Diabetes & Primary Care
- Journal of Diabetes Nursing
- The Diabetic Foot Journal
- Diabetes Digest
Useful information
- Terms and conditions
- Privacy policy
- Editorial policies and ethics

By clicking ‘Subscribe’, you are agreeing that DiabetesontheNet.com are able to email you periodic newsletters. You may unsubscribe from these at any time. Your info is safe with us and we will never sell or trade your details. For information please review our Privacy Policy .
Are you a healthcare professional? This website is for healthcare professionals only. To continue, please confirm that you are a healthcare professional below.
We use cookies responsibly to ensure that we give you the best experience on our website. If you continue without changing your browser settings, we’ll assume that you are happy to receive all cookies on this website. Read about how we use cookies .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Endocrinol Metab
- v.19(Suppl 1); 2015 Apr
Type 1 diabetes mellitus-common cases
Surender kumar.
Department of Endocrinology, Sir Ganga Ram Hospital, New Delhi, India
Tight glycemic control in type 1 diabetes mellitus patients is associated with the risk of hypoglycemia. Diabetic patients are forced to change their lifestyle to adjust to the disease condition and survive it. The best way to manage diabetes would be to develop a therapy, which could adjust to the patient's conditions. Here, I present few cases wherein switching to a long-acting basal insulin analog helped combat recurrent hypoglycemic episodes experienced by the patients.
I NTRODUCTION
Tight glycemic control in type 1 diabetes mellitus (T1DM) patients is not possible because of hypoglycemia. Diabetic patients are forced to change their lifestyle to adjust to the disease condition and survive it. The best way to manage diabetes would be to develop a therapy, which could adjust to the patient's conditions.[ 1 ]
A 6-year-old boy presented with classic features of diabetic ketoacidosis, that is, weight loss and extreme weakness and osmotic features. The fasting blood sugar level was 300 mg/dL, postprandial glucose level was 467 mg/dL and hemoglobin A1c (HbA1c) was 7.2%. He was administered with standard intravenous insulin and fluid, which finally brought down the fasting blood glucose level to around 120 mg/dL. He was administered basal-bolus therapy and was discharged. Patient had two episodes of severe hypoglycemia. His parents were worried due to frequent checking of blood glucose levels many times in a day. The challenge was also to avoid urination in bed at night by the child. Otherwise he would get a common cold. The patient remained unconscious in the middle of the night and was fed up with the frequent monitoring of blood sugar. The patient and the parents had severe anxiety, depression, frustration, and disgust. The parents considered diabetes as a curse on their family. He was informed about degludec/injection tresiba, which is not yet approved in children because of lack of experience. The physician explained to them that there was nothing wrong in administering it and is not contra-indicated in T1DM.[ 2 ] The parents were also explained that insulin degludec may even help the child to convert from four injections to one injection a day, and from very frequent monitoring to once in a day. After reviewing the literature about insulin degludec, the parents were finally convinced about it. The patient was then put from basal-bolus to 2 bolus plus 1 basal and finally degludec at 16 U. Over the period of time, blood sugar level came to normal at around 110 mg/dL-pre meal. The patient was trained very well that if he wanted to reduce the frequency of monitoring of blood sugar level, then he had to follow small frequent meals. This made him felt happy because once the sugar was controlled then small amount of sweets was also given. The techniques resulted in good compliance from the patient. The patient did not report any hypoglycemic event over a period of 3 months. This was a big relief for the patient and his parents. Later parents were told that the child may require basal-bolus therapy. The outcomes of this case study were that in case of T1DM the physician should not be very aggressive except during the first 2 weeks of admission. The physician should also try to convince the parents about line of treatment, and educate both the patients and the child. The dose may be gradually stabilized without being aggressive, and this also prevents frequent episodes of hypoglycemia. Hence, gradual tightening of glycemic control is very important. The doctor should analyze the psyche of the patient and his parents.
A 57-year-old female presented with a 13 year history of diabetes. Due to the failure of oral hypoglycemic agents (OHAs) in controlling her sugar levels, for the last 3 years, she was treated with biphasic insulin aspart 30/70. She was a very frequent flier, a regular swimmer and socially very active, and this led her to have irregular meals. Hence, she often go into frequent hypoglycemia and during the last 6 months the patient's average blood glucose level during fasting were 170 mg/dL and postprandial glucose levels varied from 230 to 280 mg/dL. Even after high sugar levels, she fortunately had normal kidney functions. Patient was able to afford an insulin pump, so she was put on one. With the pump, her blood glucose was in control and patient was happy. However she soon realized the limitation of carrying it everywhere she went. These were the true feelings of a patient who was very active while she was on an insulin pump. The physician, after discussing with the patient, started her on insulin degludec and lifestyle modification, especially the diet component. Patient understood these problems and followed the diet. She followed the dietary modification and over 2 months of time, fasting blood glucose was 110 mg/dL, post meals values were around 180 mg/dL. She had only one episode of minor hypoglycemia which was due to delayed meal. The doctor later reduced degludec from 44 U to 40 U and blood glucose was still improving without any episode of hypoglycemia in the last 3 months. The outcome of this case is that with this therapy and dietary modification, a desired level of blood glucose can be achieved, without hypoglycemic risk.
An 80-year-old retired army officer, staying alone, has type 2 diabetes for the last 12 years and renal function test was normal and patient was on insulin along with other OHAs. Despite this, the patient was getting attacks of hypoglycemia, which scared the patient of unconsciousness and even death. The limiting factors were that the patient was staying alone and was dependent upon an attendant to get injections. During the weekends or holidays, the attendant was not on a regular time, and this led to irregular insulin injections, causing hypoglycemic episode to patient. This patient as well was put on insulin degludec and over a period the dose of degludec was also increased. His HbA1c and fasting blood glucose level improved without any episode of hypoglycemia. The outcomes of this case are that degludec along with dietary modifications gave desired diabetes control without any hypoglycemia.
The main barrier to tight glycemic control is hypoglycemia. This can be adjusted with slight dietary modification without changing the therapy.[ 3 ]
Source of Support: Nil
Conflict of Interest: None declared.
R EFERENCES
Diabetes Type 1 – Evolve Case Study – Flashcards

Unlock all answers in this set
Haven't found what you were looking for, search for samples, answers to your questions and flashcards.
- Enter your topic/question
- Receive an explanation
- Ask one question at a time
- Enter a specific assignment topic
- Aim at least 500 characters
- a topic sentence that states the main or controlling idea
- supporting sentences to explain and develop the point you’re making
- evidence from your reading or an example from the subject area that supports your point
- analysis of the implication/significance/impact of the evidence finished off with a critical conclusion you have drawn from the evidence.

- Previous Article
- Next Article
Case Presentation
Case study: a patient with uncontrolled type 2 diabetes and complex comorbidities whose diabetes care is managed by an advanced practice nurse.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Geralyn Spollett; Case Study: A Patient With Uncontrolled Type 2 Diabetes and Complex Comorbidities Whose Diabetes Care Is Managed by an Advanced Practice Nurse. Diabetes Spectr 1 January 2003; 16 (1): 32–36. https://doi.org/10.2337/diaspect.16.1.32
Download citation file:
- Ris (Zotero)
- Reference Manager
The specialized role of nursing in the care and education of people with diabetes has been in existence for more than 30 years. Diabetes education carried out by nurses has moved beyond the hospital bedside into a variety of health care settings. Among the disciplines involved in diabetes education, nursing has played a pivotal role in the diabetes team management concept. This was well illustrated in the Diabetes Control and Complications Trial (DCCT) by the effectiveness of nurse managers in coordinating and delivering diabetes self-management education. These nurse managers not only performed administrative tasks crucial to the outcomes of the DCCT, but also participated directly in patient care. 1
The emergence and subsequent growth of advanced practice in nursing during the past 20 years has expanded the direct care component, incorporating aspects of both nursing and medical care while maintaining the teaching and counseling roles. Both the clinical nurse specialist (CNS) and nurse practitioner (NP) models, when applied to chronic disease management, create enhanced patient-provider relationships in which self-care education and counseling is provided within the context of disease state management. Clement 2 commented in a review of diabetes self-management education issues that unless ongoing management is part of an education program, knowledge may increase but most clinical outcomes only minimally improve. Advanced practice nurses by the very nature of their scope of practice effectively combine both education and management into their delivery of care.
Operating beyond the role of educator, advanced practice nurses holistically assess patients’ needs with the understanding of patients’ primary role in the improvement and maintenance of their own health and wellness. In conducting assessments, advanced practice nurses carefully explore patients’ medical history and perform focused physical exams. At the completion of assessments, advanced practice nurses, in conjunction with patients, identify management goals and determine appropriate plans of care. A review of patients’ self-care management skills and application/adaptation to lifestyle is incorporated in initial histories, physical exams, and plans of care.
Many advanced practice nurses (NPs, CNSs, nurse midwives, and nurse anesthetists) may prescribe and adjust medication through prescriptive authority granted to them by their state nursing regulatory body. Currently, all 50 states have some form of prescriptive authority for advanced practice nurses. 3 The ability to prescribe and adjust medication is a valuable asset in caring for individuals with diabetes. It is a crucial component in the care of people with type 1 diabetes, and it becomes increasingly important in the care of patients with type 2 diabetes who have a constellation of comorbidities, all of which must be managed for successful disease outcomes.
Many studies have documented the effectiveness of advanced practice nurses in managing common primary care issues. 4 NP care has been associated with a high level of satisfaction among health services consumers. In diabetes, the role of advanced practice nurses has significantly contributed to improved outcomes in the management of type 2 diabetes, 5 in specialized diabetes foot care programs, 6 in the management of diabetes in pregnancy, 7 and in the care of pediatric type 1 diabetic patients and their parents. 8 , 9 Furthermore, NPs have also been effective providers of diabetes care among disadvantaged urban African-American patients. 10 Primary management of these patients by NPs led to improved metabolic control regardless of whether weight loss was achieved.
The following case study illustrates the clinical role of advanced practice nurses in the management of a patient with type 2 diabetes.
A.B. is a retired 69-year-old man with a 5-year history of type 2 diabetes. Although he was diagnosed in 1997, he had symptoms indicating hyperglycemia for 2 years before diagnosis. He had fasting blood glucose records indicating values of 118–127 mg/dl, which were described to him as indicative of “borderline diabetes.” He also remembered past episodes of nocturia associated with large pasta meals and Italian pastries. At the time of initial diagnosis, he was advised to lose weight (“at least 10 lb.”), but no further action was taken.
Referred by his family physician to the diabetes specialty clinic, A.B. presents with recent weight gain, suboptimal diabetes control, and foot pain. He has been trying to lose weight and increase his exercise for the past 6 months without success. He had been started on glyburide (Diabeta), 2.5 mg every morning, but had stopped taking it because of dizziness, often accompanied by sweating and a feeling of mild agitation, in the late afternoon.
A.B. also takes atorvastatin (Lipitor), 10 mg daily, for hypercholesterolemia (elevated LDL cholesterol, low HDL cholesterol, and elevated triglycerides). He has tolerated this medication and adheres to the daily schedule. During the past 6 months, he has also taken chromium picolinate, gymnema sylvestre, and a “pancreas elixir” in an attempt to improve his diabetes control. He stopped these supplements when he did not see any positive results.
He does not test his blood glucose levels at home and expresses doubt that this procedure would help him improve his diabetes control. “What would knowing the numbers do for me?,” he asks. “The doctor already knows the sugars are high.”
A.B. states that he has “never been sick a day in my life.” He recently sold his business and has become very active in a variety of volunteer organizations. He lives with his wife of 48 years and has two married children. Although both his mother and father had type 2 diabetes, A.B. has limited knowledge regarding diabetes self-care management and states that he does not understand why he has diabetes since he never eats sugar. In the past, his wife has encouraged him to treat his diabetes with herbal remedies and weight-loss supplements, and she frequently scans the Internet for the latest diabetes remedies.
During the past year, A.B. has gained 22 lb. Since retiring, he has been more physically active, playing golf once a week and gardening, but he has been unable to lose more than 2–3 lb. He has never seen a dietitian and has not been instructed in self-monitoring of blood glucose (SMBG).
A.B.’s diet history reveals excessive carbohydrate intake in the form of bread and pasta. His normal dinners consist of 2 cups of cooked pasta with homemade sauce and three to four slices of Italian bread. During the day, he often has “a slice or two” of bread with butter or olive oil. He also eats eight to ten pieces of fresh fruit per day at meals and as snacks. He prefers chicken and fish, but it is usually served with a tomato or cream sauce accompanied by pasta. His wife has offered to make him plain grilled meats, but he finds them “tasteless.” He drinks 8 oz. of red wine with dinner each evening. He stopped smoking more than 10 years ago, he reports, “when the cost of cigarettes topped a buck-fifty.”
The medical documents that A.B. brings to this appointment indicate that his hemoglobin A 1c (A1C) has never been <8%. His blood pressure has been measured at 150/70, 148/92, and 166/88 mmHg on separate occasions during the past year at the local senior center screening clinic. Although he was told that his blood pressure was “up a little,” he was not aware of the need to keep his blood pressure ≤130/80 mmHg for both cardiovascular and renal health. 11
A.B. has never had a foot exam as part of his primary care exams, nor has he been instructed in preventive foot care. However, his medical records also indicate that he has had no surgeries or hospitalizations, his immunizations are up to date, and, in general, he has been remarkably healthy for many years.
Physical Exam
A physical examination reveals the following:
Weight: 178 lb; height: 5′2″; body mass index (BMI): 32.6 kg/m 2
Fasting capillary glucose: 166 mg/dl
Blood pressure: lying, right arm 154/96 mmHg; sitting, right arm 140/90 mmHg
Pulse: 88 bpm; respirations 20 per minute
Eyes: corrective lenses, pupils equal and reactive to light and accommodation, Fundi-clear, no arteriolovenous nicking, no retinopathy
Thyroid: nonpalpable
Lungs: clear to auscultation
Heart: Rate and rhythm regular, no murmurs or gallops
Vascular assessment: no carotid bruits; femoral, popliteal, and dorsalis pedis pulses 2+ bilaterally
Neurological assessment: diminished vibratory sense to the forefoot, absent ankle reflexes, monofilament (5.07 Semmes-Weinstein) felt only above the ankle
Lab Results
Results of laboratory tests (drawn 5 days before the office visit) are as follows:
Glucose (fasting): 178 mg/dl (normal range: 65–109 mg/dl)
Creatinine: 1.0 mg/dl (normal range: 0.5–1.4 mg/dl)
Blood urea nitrogen: 18 mg/dl (normal range: 7–30 mg/dl)
Sodium: 141 mg/dl (normal range: 135–146 mg/dl)
Potassium: 4.3 mg/dl (normal range: 3.5–5.3 mg/dl)
Lipid panel
• Total cholesterol: 162 mg/dl (normal: <200 mg/dl)
• HDL cholesterol: 43 mg/dl (normal: ≥40 mg/dl)
• LDL cholesterol (calculated): 84 mg/dl (normal: <100 mg/dl)
• Triglycerides: 177 mg/dl (normal: <150 mg/dl)
• Cholesterol-to-HDL ratio: 3.8 (normal: <5.0)
AST: 14 IU/l (normal: 0–40 IU/l)
ALT: 19 IU/l (normal: 5–40 IU/l)
Alkaline phosphotase: 56 IU/l (normal: 35–125 IU/l)
A1C: 8.1% (normal: 4–6%)
Urine microalbumin: 45 mg (normal: <30 mg)
Based on A.B.’s medical history, records, physical exam, and lab results, he is assessed as follows:
Uncontrolled type 2 diabetes (A1C >7%)
Obesity (BMI 32.4 kg/m 2 )
Hyperlipidemia (controlled with atorvastatin)
Peripheral neuropathy (distal and symmetrical by exam)
Hypertension (by previous chart data and exam)
Elevated urine microalbumin level
Self-care management/lifestyle deficits
• Limited exercise
• High carbohydrate intake
• No SMBG program
Poor understanding of diabetes
A.B. presented with uncontrolled type 2 diabetes and a complex set of comorbidities, all of which needed treatment. The first task of the NP who provided his care was to select the most pressing health care issues and prioritize his medical care to address them. Although A.B. stated that his need to lose weight was his chief reason for seeking diabetes specialty care, his elevated glucose levels and his hypertension also needed to be addressed at the initial visit.
The patient and his wife agreed that a referral to a dietitian was their first priority. A.B. acknowledged that he had little dietary information to help him achieve weight loss and that his current weight was unhealthy and “embarrassing.” He recognized that his glucose control was affected by large portions of bread and pasta and agreed to start improving dietary control by reducing his portion size by one-third during the week before his dietary consultation. Weight loss would also be an important first step in reducing his blood pressure.
The NP contacted the registered dietitian (RD) by telephone and referred the patient for a medical nutrition therapy assessment with a focus on weight loss and improved diabetes control. A.B.’s appointment was scheduled for the following week. The RD requested that during the intervening week, the patient keep a food journal recording his food intake at meals and snacks. She asked that the patient also try to estimate portion sizes.
Although his physical activity had increased since his retirement, it was fairly sporadic and weather-dependent. After further discussion, he realized that a week or more would often pass without any significant form of exercise and that most of his exercise was seasonal. Whatever weight he had lost during the summer was regained in the winter, when he was again quite sedentary.
A.B.’s wife suggested that the two of them could walk each morning after breakfast. She also felt that a treadmill at home would be the best solution for getting sufficient exercise in inclement weather. After a short discussion about the positive effect exercise can have on glucose control, the patient and his wife agreed to walk 15–20 minutes each day between 9:00 and 10:00 a.m.
A first-line medication for this patient had to be targeted to improving glucose control without contributing to weight gain. Thiazolidinediones (i.e., rosiglitizone [Avandia] or pioglitizone [Actos]) effectively address insulin resistance but have been associated with weight gain. 12 A sulfonylurea or meglitinide (i.e., repaglinide [Prandin]) can reduce postprandial elevations caused by increased carbohydrate intake, but they are also associated with some weight gain. 12 When glyburide was previously prescribed, the patient exhibited signs and symptoms of hypoglycemia (unconfirmed by SMBG). α-Glucosidase inhibitors (i.e., acarbose [Precose]) can help with postprandial hyperglycemia rise by blunting the effect of the entry of carbohydrate-related glucose into the system. However, acarbose requires slow titration, has multiple gastrointestinal (GI) side effects, and reduces A1C by only 0.5–0.9%. 13 Acarbose may be considered as a second-line therapy for A.B. but would not fully address his elevated A1C results. Metformin (Glucophage), which reduces hepatic glucose production and improves insulin resistance, is not associated with hypoglycemia and can lower A1C results by 1%. Although GI side effects can occur, they are usually self-limiting and can be further reduced by slow titration to dose efficacy. 14
After reviewing these options and discussing the need for improved glycemic control, the NP prescribed metformin, 500 mg twice a day. Possible GI side effects and the need to avoid alcohol were of concern to A.B., but he agreed that medication was necessary and that metformin was his best option. The NP advised him to take the medication with food to reduce GI side effects.
The NP also discussed with the patient a titration schedule that increased the dosage to 1,000 mg twice a day over a 4-week period. She wrote out this plan, including a date and time for telephone contact and medication evaluation, and gave it to the patient.
During the visit, A.B. and his wife learned to use a glucose meter that features a simple two-step procedure. The patient agreed to use the meter twice a day, at breakfast and dinner, while the metformin dose was being titrated. He understood the need for glucose readings to guide the choice of medication and to evaluate the effects of his dietary changes, but he felt that it would not be “a forever thing.”
The NP reviewed glycemic goals with the patient and his wife and assisted them in deciding on initial short-term goals for weight loss, exercise, and medication. Glucose monitoring would serve as a guide and assist the patient in modifying his lifestyle.
A.B. drew the line at starting an antihypertensive medication—the angiotensin-converting enzyme (ACE) inhibitor enalapril (Vasotec), 5 mg daily. He stated that one new medication at a time was enough and that “too many medications would make a sick man out of me.” His perception of the state of his health as being represented by the number of medications prescribed for him gave the advanced practice nurse an important insight into the patient’s health belief system. The patient’s wife also believed that a “natural solution” was better than medication for treating blood pressure.
Although the use of an ACE inhibitor was indicated both by the level of hypertension and by the presence of microalbuminuria, the decision to wait until the next office visit to further evaluate the need for antihypertensive medication afforded the patient and his wife time to consider the importance of adding this pharmacotherapy. They were quite willing to read any materials that addressed the prevention of diabetes complications. However, both the patient and his wife voiced a strong desire to focus their energies on changes in food and physical activity. The NP expressed support for their decision. Because A.B. was obese, weight loss would be beneficial for many of his health issues.
Because he has a sedentary lifestyle, is >35 years old, has hypertension and peripheral neuropathy, and is being treated for hypercholestrolemia, the NP performed an electrocardiogram in the office and referred the patient for an exercise tolerance test. 11 In doing this, the NP acknowledged and respected the mutually set goals, but also provided appropriate pre-exercise screening for the patient’s protection and safety.
In her role as diabetes educator, the NP taught A.B. and his wife the importance of foot care, demonstrating to the patient his inability to feel the light touch of the monofilament. She explained that the loss of protective sensation from peripheral neuropathy means that he will need to be more vigilant in checking his feet for any skin lesions caused by poorly fitting footwear worn during exercise.
At the conclusion of the visit, the NP assured A.B. that she would share the plan of care they had developed with his primary care physician, collaborating with him and discussing the findings of any diagnostic tests and procedures. She would also work in partnership with the RD to reinforce medical nutrition therapies and improve his glucose control. In this way, the NP would facilitate the continuity of care and keep vital pathways of communication open.
Advanced practice nurses are ideally suited to play an integral role in the education and medical management of people with diabetes. 15 The combination of clinical skills and expertise in teaching and counseling enhances the delivery of care in a manner that is both cost-reducing and effective. Inherent in the role of advanced practice nurses is the understanding of shared responsibility for health care outcomes. This partnering of nurse with patient not only improves care but strengthens the patient’s role as self-manager.
Geralyn Spollett, MSN, C-ANP, CDE, is associate director and an adult nurse practitioner at the Yale Diabetes Center, Department of Endocrinology and Metabolism, at Yale University in New Haven, Conn. She is an associate editor of Diabetes Spectrum.
Note of disclosure: Ms. Spollett has received honoraria for speaking engagements from Novo Nordisk Pharmaceuticals, Inc., and Aventis and has been a paid consultant for Aventis. Both companies produce products and devices for the treatment of diabetes.
Email alerts
- Advanced Practice Care: Advanced Practice Care in Diabetes: Epilogue
- Advanced Practice Care: Advanced Practice Care in Diabetes: Preface
- Online ISSN 1944-7353
- Print ISSN 1040-9165
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account

IMAGES
VIDEO
COMMENTS
smoo793. Preview. Study with Quizlet and memorize flashcards containing terms like What is the mechanism that results in Kussmaul respirations?, To achieve a goal of restoring fluid volume in ketoacidosis, the nurse would expect to implement which intervention?, To restore blood glucose to a normal level during ketoacidosis, what should the ...
PRESENTATION OF CASE. Dr. Max C. Petersen (Medicine): A 34-year-old woman was evaluated in the diabetes clinic of this hospital for hyperglycemia. Eleven years before this presentation, the blood glucose level was 126 mg per deciliter (7.0 mmol per liter) on routine laboratory evaluation, which was performed as part of an annual well visit.
A case report: First presentation of diabetes mellitus type 1 with severe hyperosmolar hyperglycemic state in a 35‐month‐old girl. Clin Case Rep. 2021; 9:e04984. 10.1002/ccr3.4984 [PMC free article] [Google Scholar] Funding information
Registered dietitians (RDs) who have earned the Board Certified-Advanced Diabetes Manager (BC-ADM) credential hold a master's or doctorate degree in a clinically relevant area and have at least 500 hours of recent experience helping with the clinical management of people with diabetes.1 They work in both inpatient and outpatient settings, including diabetes or endocrine-based specialty ...
MELTON: The first major change in the treatment of Type 1 diabetes was probably the discovery of insulin in 1920. Now it's 100 years later and if this works, it's going to change the medical treatment for people with diabetes. Instead of injecting insulin, patients will get cells that will be their own insulin factories.
A 59-year-old woman with type 1 diabetes and a 2-year history of cognitive decline presented with obtundation. There was diffuse, symmetric hypointensity in the brain on T2-weighted images and abno...
Describe the physiologic consequences of diabetes mellitus. Outline the importance of maintaining glycemic control in reducing the risk of diabetic complications. Detail specific clinical applications of insulin therapy to achieve both basal and meal-related glycemic control. Manage a patient's glycemic status by continuously refining the ...
Use your knowledge and apply key concepts to realistic patient care scenarios. HESI Case Studies provide real-world patient care scenarios accompanied by application-based questions and rationales that will help you learn how to manage complex patient conditions and make sound clinical judgments. Questions cover nursing care for patients with a wide variety physiological and psychosocial ...
Metrics. The causes of type 1 diabetes mellitus (T1DM) are unclear; however, a general consensus exists that T1DM is a T cell-mediated autoimmune disease characterized by the selective destruction ...
Diabetes Case Studies: Real Problems, Practical Solutions. Edited by: Boris Draznin, MD, PhD, Cecilia C. Low Wang, MD, FACP, Daniel J. Rubin, MD, MSc, FACE. ... Open the PDF Link PDF for Case 15: Type 1 Diabetes versus LADA in a Patient Misdiagnosed with Type 2 Diabetes in another window. Case 16: Type 1 Diabetes Can Present at Any Age. By
In one trial, captopril slowed the progression of kidney disease in patients with type 1 diabetes and nephropathy without affecting the risk of death from cardiovascular causes. 26 However ...
Type 1 diabetes results from autoimmune destruction of the pancreatic β-cells that produce insulin and can occur at any age. 1 When it occurs in adults, type 1 diabetes can progress to total insulin deficiency at different rates. The slowly progressive form is known as LADA (sometimes called "type 1.5 diabetes").
The patient was diagnosed with type 1 diabetes mellitus supported by a low C peptide level of 43 (370-1470 pmol/L) and an antiglutamic acid decarboxylase (GAD) antibody titre of 4.7 (ref. 0-1.0). ... In the case report presented here, the patient was newly diagnosed with diabetes with a short duration of symptoms of the disease. ...
This case study represents the challenges and issues, both physical and psychological, faced by a young person with type 1 diabetes and the support given by her diabetes multidisciplinary team (MDT). Implications for practice are addressed using current evidence-based research. The names of the child and family have been anonymised to protect ...
Abstract. Tight glycemic control in type 1 diabetes mellitus patients is associated with the risk of hypoglycemia. Diabetic patients are forced to change their lifestyle to adjust to the disease condition and survive it. The best way to manage diabetes would be to develop a therapy, which could adjust to the patient's conditions.
Diabetes Type 1 - Evolve Case Study - Flashcards 🎓 Get access to high-quality and unique 50 000 college essay examples and more than 100 000 flashcards and test answers from around the world! ... The highest risk for the onset of Type 1 diabetes is linked to the presence of certain antigens, so there seems to be a genetic predisposition ...
Known as latent autoimmune diabetes of adulthood (LADA) or type 1.5 diabetes,2 it is a slowly progressive form of type 1 diabetes.3 After months to years, affected individuals become increasingly insulin-dependent. This type of diabetes could be the explanation for W.G.'s symptoms and progression of disease.
HESI Case Study Diabetes Type 1 (2022) 25 terms. Arnold_Chin. Preview. HESI RN Case Study Diabetes Type 1. 26 terms. Luz-Gonzalez-Miller. Preview. USA learns CNA Unit 5 more vocab. Teacher 29 terms. clccambridge. Preview. 222 evaluate outcomes. 10 terms. Sophie_Ridge. Preview. HESI: Case Study: Diabetes Type 1.
In diabetes, the role of advanced practice nurses has significantly contributed to improved outcomes in the management of type 2 diabetes,5 in specialized diabetes foot care programs,6 in the management of diabetes in pregnancy,7 and in the care of pediatric type 1 diabetic patients and their parents.8,9 Furthermore, NPs have also been ...