
Dr Benjamin Jacobs Paediatrics
Rickets: a case study of a young child with vitamin d deficiency.
Rickets , which is often referred to as ‘the English disease’ was thought to be eradicated after the second world war, but recently it has started to make a comeback, with two known cases in the UK of children dying from this preventable disease, which is caused by vitamin D and/or calcium deficiency which prevents proper bone growth in children. It can also lead to heart problems and seizures if not treated.

Rickets case study
Dr Benjamin Jacobs, a leading consultant paediatrician with expertise in rickets, is treating a two-year-old boy who was diagnosed with rickets six months before. The boy’s mother started to notice that his legs were starting to bed outwards, and that they weren’t getting any better. As he was starting to walk, his left foot was bending inwards.
After consulting with Dr Jacobs, the boy was prescribed vitamin D supplements. This has stopped the increased bending of the legs, and caused them to become stronger, and slowly become straighter, though not completely straight yet.
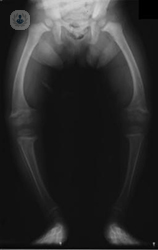
Alongside the bowing of the legs, the boy’s ankle and knee joints also become swollen. Upon consulting x-rays of the boy’s legs, Dr Jacobs is able to see that at the end of the bones, where bone growth and development occurs, the bones don’t appear ‘clean’ and healthy, but rather frayed and ‘rotten’, which is a classical display of rickets.
Rickets and bone strength
Vitamin D deficiency causes the growth plate at the end of the bone to grow irregularly and in a disorganised fashion. The growing part of the bone fails to calcify because of a lack of calcium and phosphate in the blood, this causes the bone to not grow properly, and the bone becomes short and deformed. Vitamin D is necessary for absorption of calcium and phosphate into the bones, to provide the ingredients for the ‘building blocks’ of the body to form.
Due to the malformation of the bones caused by rickets, it can cause the child to suffer with bone pain, and may not be able to walk or run for as long a period of time as other children. They may also suffer with a lack of energy.
Following the treatment of vitamin D supplements, the boy is able to run, jump, and play for much longer periods of time, as the bone pain is reduced.
Prevalence of rickets
Though not all cases are as severe as the boy featured in this case study, the number of cases of mild rickets is creeping up.
Getting enough vitamin D, known as ‘the sunshine vitamin’ is a challenge for many children in the UK. The recommended amount of vitamin D intake per day is 10 micrograms. Around 2 or 3mcg are found in a usual diet, so people are required to either make vitamin D naturally from sunshine, or taking it as a supplement.
During the months of November, December, January, February, and even March in the UK it is difficult to find enough sunshine to naturally create vitamin D, so parents are required to either give their children supplements, or use foods that are artificially fortified with vitamin D.
When do you need vitamin D the most?
Vitamin D is really important at stages when children are growing fast. This includes young babies, children going through growth spurts during puberty, pregnant women, to ensure they get enough vitamin D for their own health and for the health of the baby, and elderly people also often lack vitamin D.
Vitamin D deficiency is also more common in people with darker skin, as the skin doesn’t absorb as much sunshine, and in people who dress modestly and cover their skin with clothes at all times will also find it difficult to absorb enough sunshine to make the necessary vitamin D during the winter months.
Recent discoveries have also found that children on restricted diets, such as those with allergies, who may not be drinking milk or eating fish will lack calcium. So even if the vitamin D levels are good, if they’re not getting enough calcium from their diet.
If you are concerned about rickets, or worried that your child may be lacking in vitamin D, make an appointment with a specialist paediatrician here.

Paediatrics in London
Dr Benjamin Jacobs is one of London's leading paediatricians, and treats children and teenagers of all ages with general paediatric or musculoskeletal problems. Dr Benjamin Jacobs has a special interest in bone diseases, ranging from common disorders such as Vitamin D deficiency and ‘growing pains’, to rare and genetic bone diseases such as osteogenesis, rickets and CRMO. He practises at prominent medical establishments in the capital including the Royal National Ort...

By Dr Benjamin Jacobs Paediatrics
Dr Benjamin Jacobs is one of London's leading paediatricians, and treats children and teenagers of all ages with general paediatric or musculoskeletal problems. Dr Benjamin Jacobs has a special interest in bone diseases, ranging from common disorders such as Vitamin D deficiency and ‘growing pains’, to rare and genetic bone diseases such as osteogenesis, rickets and CRMO. He practises at prominent medical establishments in the capital including the Royal National Orthopaedic Hospital and has published in numerous peer-reviewed journals. Dr Benjamin Jacobs forms an integral part of a number of professional bodies including the Royal College of Paediatrics and Child Health and the Paediatric and Adolescent Bone Group, and won the Humanitarian Award in 1998 for his work at the Hospital for Sick Children in Toronto.
- Related procedures
Expert doctors on this topic
See all (Paediatricians)
Paediatricians Cigna
Paediatricians Bupa
Paediatricians WPA
Paediatricians Vitality
Paediatricians AXA

Dr Benjamin Jacobs
(Let us know you are a Top Doctors patient)
By using the telephone number provided by TOP DOCTORS, you automatically agree to let us use your phone number for statistical and commercial purposes. For further information, read our Privacy Policy
If you can't get in touch, book online
Top Doctors
Cookie settings
You can enable or disable according to the purposes:

- INTRODUCTION
- CASE REPORT
- Acknowledgments:
Photographs of children demonstrating typical features of genu valgus, genu varum, wrist swelling, and rachitic rosary before treatment.
Standard child height-for-age charts, differentiated for girls and boys. The red and blue dots represent observed patient data at baseline.
Height-for-age z-score for children at baseline and at 12-month follow-up, with the median (bar) and interquartile range (capped bars).
X-rays of a 6-year-old girl. ( A ) Pre-treatment X-ray shows severe widening/cupping of the metaphyseal growth plates with sclerosis, hypertrophic growth plates, bowing of the diaphyses, and diffuse osteopenia. ( B–D ) Post-treatment X-rays show a gradual straightening of the diaphysis, reduction in sclerosis at the epiphyses, and normalization of the distance between the distal metaphyses and epiphyses over time.
( A ) Serum 25-hydroxyvitamin D (25(OH)D; blue) values at presentation and at follow-up after 1 year. ( B ) Parathyroid (PTH; red) values at presentation and at follow-up after 1 year. ( C ) Alkaline phosphatase (ALP; green) values at presentaTtion and at follow-up after 1 year. Individual patient values (small circles) are shown, along with median (bar) and interquartile range (capped bars). The dotted horizontal line in ( A ) on the y axis represents the lower limit of normal (50 nmol/L) and the continuous line on y axis represents the upper limit of depletion (30 nmol/L). The continuous lines in ( B ) and ( C ) represent the upper limit of normal range for PTH (65 pg/mL) and ALP (800 UL), respectively. Note that not all children had serum sampling at each follow-up.
Direct normal irradiation in Myanmar. Long-term average of yearly totals. 14
- View raw image
- Download Powerpoint Slide
World Health Organization , 2019 . Nutritional Rickets: A Review of Disease Burden, Causes, Diagnosis, Prevention and Treatment . Geneva, Switzerland: WHO. Available at: https://www.who.int/publications/i/item/9789241516587 . Accessed November 2, 2020.
- Export Citation
Agarwal A , Gulati D , Rath S , Walia M , 2009 . Rickets: a cause of delayed walking in toddlers . Indian J Pediatr 76 : 269 – 272 .
- Search Google Scholar
Pettifor JM , 2004 . Nutritional rickets: deficiency of vitamin D, calcium, or both? Am J Clin Nutr 80 : 1725 – 1729 .
Mendes MM , Hart KH , Botelho PB , Lanham-New SA , 2018 . Vitamin D status in the tropics: is sunlight exposure the main determinant? Nutr Bull 43 : 428 – 434 .
Edidin DV , Levitsky LL , Schey W , Dumbovic N , Campos A , 1980 . Resurgence of nutritional rickets associated with breast-feeding and special dietary practices . Pediatrics 65 : 232 – 235 .
Henderson AH , 1899 . Rickets in India and Burma . Ind Med Gaz 34 : 268 .
Craviari T , Pettifor JM , Thacher TD , Meisner C , Arnaud J , Fischer PR , Rickets Convergence Group , 2008 . Rickets: an overview and future directions, with special reference to Bangladesh: a summary of the Rickets Convergence Group Meeting, Dhaka, 26–27 January 2006 . J Health Popul Nutr 26 : 112 – 121 .
Ahmed S , Goldberg GR , Raqib R , Roy SK , Haque S , Braithwaite VS , Pettifor JM , Prentice A , 2020 . Aetiology of nutritional rickets in rural Bangladeshi children . Bone 136 : 115357 .
Combs GF , Hassan N , Dellagana N , Staab D , Fischer P , Hunt C , Watts J , 2008 . Apparent efficacy of food-based calcium supplementation in preventing rickets in Bangladesh . Biol Trace Elem Res 121 : 193 – 204 .
Balasubramanian K , Rajeswari J , Gulab A , Govil YC , Agarwal AK , Kumar A , Bhatia V , 2003 . Varying role of vitamin D deficiency in the etiology of rickets in young children vs. adolescents in northern India . J Trop Pediatr 49 : 201 – 206 .
Aggarwal V , Seth A , Marwaha RK , Sharma B , Sonkar P , Singh S , Aneja S , 2013 . Management of nutritional rickets in Indian children: a randomized controlled trial . J Trop Pediatr 59 : 127 – 133 .
Chabra T , Tahbildar P , Sharma A , Boruah S , Mahajan R , Raje A , 2016 . Prevalence of skeletal deformity due to nutritional rickets in children between 1 and 18 years in tea garden community . J Clin Orthop Trauma 7 : 86 – 89 .
Streym SV , Højskov CS , Møller UK , Heickendorff L , Vestergaard P , Mosekilde L , Rejnmark L , 2016 . Vitamin D content in human breast milk: a 9-mo follow-up study . Am J Clin Nutr 103 : 107 – 114 .
The World Bank , 2019 . Global Solar Atlas 2.0, Solar Resource Data: Solargis . Available at: https://solargis.com/maps-and-gis-data/download/myanmar . Accessed April 25, 2021.
Qin X , Wang S , Yu M , Zhang L , Li X , Zuo Z , Zhang X , Wang L , 2009 . Child skeletal fluorosis from indoor burning of coal in southwestern China . J Environ Public Health 2009 : 969764 .
Thacher TD , Fischer PR , Singh RJ , Roizen J , Levine MA , 2015 . CYP2R1 mutations impair generation of 25-hydroxyvitamin D and cause an atypical form of vitamin D deficiency . J Clin Endocrinol Metab 100 : E1005 – E1013 .
Related Content
Tacaribe virus, a new agent isolated from artibeus bats and mosquitoes in trinidad, west indies, increase in size of entamoeba hartmanni trophozoites cultured on an enriched medium, two nosological forms of cutaneous leishmaniasis, experimental intrahepatic portal embolism induced by adult schistosoma mansoni, ethanol extracts of various helminths in a complement fixation test for eosinophilic lung (tropical eosinophilia).
%20CFA%20Deadline%20Proof%201.png)
- Previous Article
- Next Article
Case Report: Children with Severe Nutritional Rickets in the Naga Region in Northwest Myanmar, on the border with India
- Download PDF
Rickets is an often-neglected, painful, and disabling childhood condition of impaired bone mineralization. In this case series we describe a cluster of 29 children with severe, painful bone deformities who live in the very remote region of Nagaland in northwest Myanmar. Children were found to have low 25-hydroxyvitamin D, elevated parathyroid hormone, and elevated alkaline phosphatase levels, consistent with nutritional rickets secondary to vitamin D deficiency, calcium deficiency, or a combination of the two. After treatment with vitamin D 3 and calcium carbonate, significant improvement was seen in symptoms, biochemistry, and radiography. This is the first report of nutritional rickets in Myanmar in more than 120 years. Vitamin D and calcium supplementation, and food fortification for pregnant women and young children may be required to prevent this potentially devastating disease.
Rickets is a disabling childhood condition that results from impaired bone mineralization at the growth plates. It is characterized by skeletal deformity, stunted growth, bone pain, and muscle weakness. 1 Untreated rickets can result in failure to thrive, developmental delay, lifelong skeletal deformity, obstructed labor, and osteomalacia. 1 , 2 Vitamin D deficiency and/or calcium deficiency are the most common causes of rickets. 3 Vitamin D deficiency is often the result of insufficient sunlight exposure in combination with inadequate vitamin D intake. Although insufficient sun exposure is not expected in (sub-) tropical countries, it can be caused by particular sociocultural or religious behaviors. 4 In Yangon, the commercial capital of Myanmar, vitamin D insufficiency (< 50 nmol/L) was reported in 49 of 60 (82%) health-care workers (M. W. Aung, personal communication). However, this was attributed to a habit of sun avoidance for aesthetic purposes as a pale skin is considered desirable. Children in rural areas are generally expected to have sufficient sun exposure. Inadequate vitamin D intake can be caused by maternal vitamin D deficiency, exclusive breastfeeding, and a vitamin D–poor diet (vegetarian and/or lack of vitamin D–enriched food). 5 Calcium deficiency is caused predominantly by poor access to dietary products after weaning. We report a cluster of children with severe rickets in Nagaland, northwest Myanmar.
Medical Action Myanmar (MAM) is a medical aid organization that provides basic medical care to 275 villages in Nagaland, a remote mountainous region in the far northwest of Myanmar, on the border with India. In January 2019, MAM mobile medical teams identified 29 children in nine villages in Nanyun township (lat. 27°N) with painful joints, walking difficulties, and knee and wrist joint deformities clinically consistent with rickets ( Figure 1 ).

Citation: The American Journal of Tropical Medicine and Hygiene 105, 1; 10.4269/ajtmh.20-1431
- Download Figure
- Download figure as PowerPoint slide
The children had a median age of 6 years (interquartile range [IQR], 5–8 years). Twelve of the 29 children had a first-degree relative included in the case series. All but one patient complained of joint pain and walking difficulty that started at a median age of 3 years (IQR, 2–4 years). Leg deformity (genu valgum, 72%; genu varum, 28%), antalgic gait (86%), and wrist enlargement (75%) were the most common abnormalities. Three patients (10%) were unable to walk. Other deformities included pectus carinatum (62%), rachitic rosary (17%), and teeth abnormalities (31%) ( Table 1 ). Most patients were stunted (27 of 29, 93%) ( Figures 2 and 3 ) and underweight (15 of 21, 71%). Ten of 25 children started walking after 18 months of age. Patients reported a diet composed primarily of rice, grains, and leafy vegetables, without food rich in vitamin D and/or calcium, such as fish, eggs, or milk products. Meat was consumed only rarely, after successful hunting. Fortified food was absent. Children did not avoid sun exposure unless their mobility was severely limited.
Demographic and clinical findings ( N = 29)
IQR = interquartile range.

Serum biochemistry demonstrated a low 25-hydroxyvitamin D (25OHD) level of < 30 nmol/L in 22 of 29 (76%) children, a high parathyroid hormone PTH) level of > 65 pg/mL in 22 of 28 (79%) children, and an elevated alkaline phosphatase (ALP) level of > 800 UL in 28 of 29 children (97%). Fourteen children (48%) had low serum phosphate levels and six (21%) had low serum calcium levels ( Table 2 ). Nonfasted venous blood samples were kept between 2 and 8°C, and were analyzed within 48 hours at a laboratory in Yangon. Serum concentrations of 25OHD and PTH were calculated using an electrochemiluminescence immunoassay (Roche cobas e411 analyzer, Roche Diagnostics International, Rotkreuz ZG, Switzerland).
Biochemical findings at baseline and after treatment with vitamin D 3 and calcium carbonate.
25OHD = 25-hydroxyvitamin D; ALT = alkaline phosphatase; IQR = interquartile range; PTH = parathyroid hormone.
Because of the extreme remoteness of the children’s location, X-ray examination performed at the Township hospital was limited to five children. X-rays illustrated diffuse osteopenia, widening of the metaphyseal growth plates with sclerosis, hypertrophic growth plates, and bowing of the diaphyses ( Figure 4 ).

A diagnosis of nutritional rickets with low 25OHD was made and the children were administered vitamin D 3 (a loading dose of 100,000 IU, followed by 5,000 IU/d for 2 months and then 1,000 IU/d for 10 months) plus calcium carbonate (750 mg/d for children with a bodyweight of 10–19 kg and 1,500 mg/d for children ≥ 20 kg for 2 months, followed by 500 mg/d for all). The children were monitored every 2 to 3 months for 12 months. At 12 months, the children reported improved joint pain and mobility (93% and 96%, respectively). Two of 3 children who could not walk at all before, were able to walk. The third child had malunion and nonunion fractures at an early age and still could not walk. Considerable improvement was seen in biochemistry ( Table 2 and Figure 5 ) and in radiography, in the five children who had undergone serial radiography ( Figure 4 ). There was a significant improvement in height-for-age z-score: from –3.89 at baseline to –3.20 at 12 months (Wilcoxon’s signed rank test, P < 0.0001) ( Figure 3 ).

We describe a cluster of children with rickets who presented with severe, disabling symptoms and skeletal deformities; and low 25OHD, raised PTH, and raised ALP levels consistent with calcipenic rickets. Treatment with vitamin D 3 and calcium carbonate resulted in considerable symptomatic, biochemical, and radiological improvement.
These children are the first reported cases of rickets in Myanmar for 120 years, following only a description of rickets in 19th-century Burma. 6 In the neighboring countries of Bangladesh and India, rickets has been described repeatedly, with varying etiological factors depending on age and geographic location. Rickets in Bangladesh is more common after 2 years of age, and calcium deficiency is thought to be the primary etiological factor in the context of poor vitamin D status. 7 – 9 In north India, dietary calcium deficiency was identified as the cause of rickets among young children (< 10 years), whereas rickets among adolescent girls was caused by vitamin D deficiency. 10 In another study in north India, children (age, 6 months–5 years) with rickets experienced a better response after a combination of vitamin D plus calcium compared with vitamin D or calcium alone, indicating that a combination of vitamin D and calcium deficiency was causing rickets. 11 In the tea plantations of east Assam, northeast India, close to the Naga region in Myanmar, of 16,274 screened children age 1 to 18 years, 44 (0.27%) had skeletal deformities consistent with nutritional rickets. 12 Causative factors of rickets were not reported.
In Myanmar, it is generally assumed that ultraviolet B radiation is adequate to prevent vitamin D deficiency. However, the diet of the people in Naga is based predominantly on rice, grains, and leafy vegetables, and appears to be very low in vitamin D. Pregnant and lactating women in these communities could be vitamin D deficient. Breast milk contains very little vitamin D, and in the absence of vitamin D supplementation, prolonged breastfeeding (median duration, 20 months in this case series) likely contributed to low vitamin D levels in infants. 13 The mountainous Naga region is often shrouded in clouds and sunlight is among the lowest in the country ( Figure 6 ). 14 Naga children do not habitually avoid sun unless their mobility is restricted. As several children reported a late start in walking, limited ultraviolet exposure may have played a contributing factor to vitamin D deficiency. After breastfeeding, the typical diet was low in vitamin D and calcium, and high in phytates. Calcium deficiency could be a causative factor, in combination with vitamin D deficiency or on its own. This could explain the late onset of recognized symptoms, at 3 years of age, after the start of weaning. The age of onset was similar to a study conducted in southeast Bangladesh, where rickets was predominantly the result of a dietary calcium deficiency in the context of a chronically low vitamin D status. 10 However, the serum calcium levels of the Bangladeshi children with active rickets were less than in our cohort, possibly suggesting an alternative etiology. 10

We acknowledge the limitations inherent to case series study design. Additional limitations of this study include the limited access to radiography, remote laboratory analysis, and lack of a comprehensive dietary assessment. Additional causative factors, such as environmental heavy metals or fluoride exposure, that may have contributed to the clinical syndrome require additional investigation. 15 Furthermore, a genetic abnormality of vitamin D biosynthesis, such as a mutation of 25OHD (CYP2R1), although extremely rare, needs to be excluded, particularly given the apparent clustering within families. 16
During the 12-month follow-up of the 29 children described in our study, an additional 307 children were clinically diagnosed and treated for rickets in Naga, making rickets an important public health problem in this region. Fortifying staple foods with vitamin D, and promoting the intake of indigenous food sources rich in calcium or vitamin D and calcium supplements may be required to prevent this potentially devastating disease.
Calcipenic rickets is an important problem for children in the Naga region. Several factors made these children at risk. First, the local diet appears to be low in vitamin D, potentially leading to maternal deficiency and low vitamin D levels of newborns and breastfed children. Second, the diet also appears to be low in calcium and high in phytates, potentially causing calcium deficiency. Third, breastfeeding is generally prolonged. Fourth, sunlight is relatively low in this region. Treatment with vitamin D and calcium improved symptoms and reversed bone deformities. Further research is urgently required to understand more completely the etiology of this neglected and devastating disease. This understanding can determine the specific interventions required.
We thank all MAM staff in the Naga region—in particular, San Lin Aung, for his hard work, and John Pettifor, for his critical appraisal of the manuscript.
Author Notes
Financial support: This project was supported by the Planet Wheeler Foundation, the DAK Foundation, the Ripple Foundation, and Shindy Skaar. T. L. is supported by a Hamish Ogston Foundation fellowship. This research was funded, in part, by the Wellcome Trust grant number: 220211. For the purpose of Open Access, the author has applied a CCBY public copyright licence to any Author Accepted Manuscript version arising from this submission.
Authors’ addresses: Hein Aung, Medical Action Myanmar, Yangon, Myanmar, E-mail: [email protected] . Kyaw Soe and Thomas Lamb, Myanmar Oxford Clinical Research Unit, Yangon, Myanmar, E-mails: [email protected] and [email protected] . Frank F. Smithuis, Department of Radiology, Amsterdam UMC Imaging Center, Amsterdam, The Netherlands, E-mail: [email protected] . Moe Wint Aung, Department of Endocrinology, Yangon General Hospital, Yangon, Myanmar, E-mail: [email protected] . Frank M. Smithuis, Medical Action Myanmar, Yangon, Myanmar, and Myanmar Oxford Clinical Research Unit, Yangon, Myanmar, E-mail: [email protected] .
American Journal of Tropical Medicine and Hygiene
241 18th Street South, Suite 501
Arlington, VA 22202 USA
© 2022 The American Journal of Tropical Medicine and Hygiene
Access brought to you by:
Powered by: PubFactory
- [66.249.64.20|185.80.151.9]
- 185.80.151.9
Character limit 500 /500
From a Mass to Nutritional Rickets: A Case Study
- Picture of the Month
- Published: 15 November 2023
Cite this article
- Nour Jelalia ORCID: orcid.org/0009-0005-1881-0639 1 ,
- Asma Marzouk 1 ,
- Mohamed Zairi 2 ,
- Ahmed Msakni 2 ,
- Imen Abbes 3 ,
- Syrine Bouslema 3 &
- Asma Bouaziz 1
36 Accesses
Explore all metrics
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Nguyen-Tang EG, Parvex P, Goischke A, Wilhelm-Bals A. Vitamin D deficiency and rickets: screening and treatment, practical aspects for the clinician [Article in French]. Rev Med Suisse. 2019;638:384–9.
Google Scholar
Estrade S, Majorel C, Tahhan N, et al. Severe nutritional rickets in young children: Resurgence of an old disease [Article in French]. Arch Pediatr. 2017;24:737–42.
Article CAS PubMed Google Scholar
Aljalil A, Bouaity B. Brown tumor of the mandible revealing primary hyperparathyroidism: report of a case [Article in French]. Pan Afr Med J. 2014;18:200.
Download references
Author information
Authors and affiliations.
University El Manar, Faculty of Medicine of Tunis, Department of Pediatrics and Neonatology, Yasminette, Ben Arous, Tunisia
Nour Jelalia, Asma Marzouk & Asma Bouaziz
Department of Pediatric Orthopedics, Bechir Hamza Children’s Hospital, Tunis, Tunisia
Mohamed Zairi & Ahmed Msakni
Department of Pathological Anatomy and Cytology, Salah Azaiez Institute, Tunis, Tunisia
Imen Abbes & Syrine Bouslema
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Nour Jelalia .
Ethics declarations
Conflict of interest, additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Jelalia, N., Marzouk, A., Zairi, M. et al. From a Mass to Nutritional Rickets: A Case Study. Indian J Pediatr (2023). https://doi.org/10.1007/s12098-023-04944-8
Download citation
Received : 22 September 2023
Accepted : 09 November 2023
Published : 15 November 2023
DOI : https://doi.org/10.1007/s12098-023-04944-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
- Case Report
- Open access
- Published: 14 May 2009
Nutritional vitamin D deficiency: a case report
- Rachel L Stevens 1 &
- Corey Lyon 1
Cases Journal volume 2 , Article number: 7000 ( 2009 ) Cite this article
12k Accesses
3 Citations
Metrics details
We present a 6-month-old African American male child with a chief complaint of failure to appropriately gain weight despite adequate caloric intake via breastfeeding. While he has met developmental milestones he appears small for age and is diagnosed with failure to thrive after crossing two major growth curve percentiles. After appropriate diagnostic workup, a diagnosis of nutritional vitamin D deficiency (rickets) was reached and supplementation was initiated with ensuing adequate catch-up growth.
Introduction
Rickets is often considered an "old" disease, a nutritional deficiency that has plagued communities for centuries. The re-emergence of vitamin D deficiency in westernized societies is thought to be multifactorial secondary to poor dietary intake, popularization of breastfeeding, and diminished exposure to sunlight. It is the most common metabolic bone disease in the world and is easily treatable as well as preventable with sun exposure and dietary supplementation [ 1 ].
Vitamin D is a prohormone essential for absorption of calcium from the intestines. Its supply stems from two well-known sources: exposure to sunlight and dietary intake, which accounts for less than 10% [ 2 ]. Vitamin D is primarily made in the skin after exposure to UV-B radiation (290 to 315 nm wavelengths) [ 2 ]. In rickets, decreased stores of this prohormone leads to low levels of ionized calcium, which initially stimulates parathyroid hormone release to initiate calcium resorption in the renal tubules (along with loss of phosphorous), and increase 1,25 dihydroxy vitamin D synthesis. A level of 25 hydroxy vitamin D (25-OH D) less than 12.5 nmol/L (5 ng/mL) is suggested for the diagnosis of rickets with a healthy maintenance level of approximately greater than 50 nmol/L (20 ng/mL) [ 1 , 2 ]. It should be noted that newer data suggests a lower limit of 80 nmol/L may be a more acceptable level in adults [ 1 , 2 ].
Case presentation
We present a 6-month-old African American male child with poor interval growth. His mother has noticed that though he is thought to be breastfeeding appropriately, as defined by feeding 4 ounces of pumped breast milk every 2-3 hours, and has been meeting developmental milestones, his weight and height are not as expected. He has been exclusively breastfed and his mother has not introduced solid foods as of yet to his diet.
He was a full term, spontaneous vaginal delivery without complications during the pregnancy or labor. He was in the 50 th percentile for both height and weight at his 2 month visit, but has fallen to below the 3 rd percentile for weight and is at the 3 rd percentile for height. He is on no medications, there are no other siblings with failure to thrive and his mother has no post-partum depression or substance abuse issues. There is no family history of malabsorptive conditions. His mother and father are of normal stature.
His review of systems is negative for emesis, diarrhea, fever, appetite changes, swallowing abnormalities, respiratory symptoms, apnea, repeated acute illnesses, or frequent injuries.
His weight at the four month well child visit was 6477 grams with a length of 63.5 cm increasing to only 6761 grams and a length of 66 cm by his six month well child visit. His vitals signs are otherwise stable. His physical exam is significant for an alert, playful, developmentally appropriate child, small for his age. His head/neck, cardiac, respiratory, gastrointestinal, genitourinary, musculoskeletal and neurological exams were within normal limits.
He is appropriately diagnosed with failure to thrive at this visit based on deviation across two major percentiles on standardized growth curves. His estimated weight needs were calculated to 0.33 kg/month and a follow up visit was established in one month with addition of solid foods and continued breastfeeding with the addition of formula to pumped breast milk for increased caloric intake. His mother was also instructed to keep a strict food diary.
Interval weight gain was not maintained with a weight of 7045 grams at follow up despite adequate caloric intake estimated based on his food diary and formula supplementation. Laboratory studies ordered were complete metabolic profile, thyroid stimulating hormone (TSH), lead level, and complete blood count (CBC). Electrolytes, kidney function, bilirubin, AST, ALT, protein, albumin, TSH, CBC, and lead were all normal. Alkaline phosphatase was elevated at 4280 (on repeat 6310). Normal should be less than 500 IU/L in neonates and 1000 IU/L in children up to age 9. Follow-up labs including gamma glutamyl transferase (which was normal, suggestive of boney resorption) [ 2 ], C reactive protein, T3, free T4, phosphate, parathyroid hormone, and 25-OH D were ordered. Phosphate was low at 2.9 (normal 3.0-4.5) and the vitamin D level was 11 (45-50 ng/mL).
A skeletal survey was ordered showing metaphyseal fraying and cupping of bilateral distal femurs, bilateral proximal and distal tibiae and fibulae, bilateral proximal and distal humeri, bilateral distal radii and ulni and the distal aspects of 2 nd through the 5 th metacarpals most consistent with rickets of the extremities, see radiograph 1 and 2. These classic findings may be paired with a separation of the periosteum from the diaphysis secondary to unmineralized osteoid when evaluating radiographic evidence of rickets [ 1 , 3 ]. Radiographic improvement should manifest within 3 months of appropriate treatment. Underlying malabsorptive conditions or noncompliance should be considered if this is not observed [ 2 ].
The diagnosis of rickets was made and the patient was started on 2000 IU of vitamin D and calcium carbonate 1000 mg daily. He was also started on iron sulfate 22 mg daily and Zinc 20 mg daily as recommended by pediatric endocrinology and nutrition staff. His catch-up growth has lead to a current weight (at 2 years of age) in the 45 th percentile and height in the 30 th percentile (Figure 1 ). Follow up labs (calcium, phosphorous, alkaline phosphatase) should be performed one month after therapy is initiated and again at 3 months along with magnesium, PTH, and 25-OH D [ 1 , 2 ]. Follow up labs in this patient indicated an improvement in vitamin D up to 29 ng/mL with ongoing supplementation continuing.
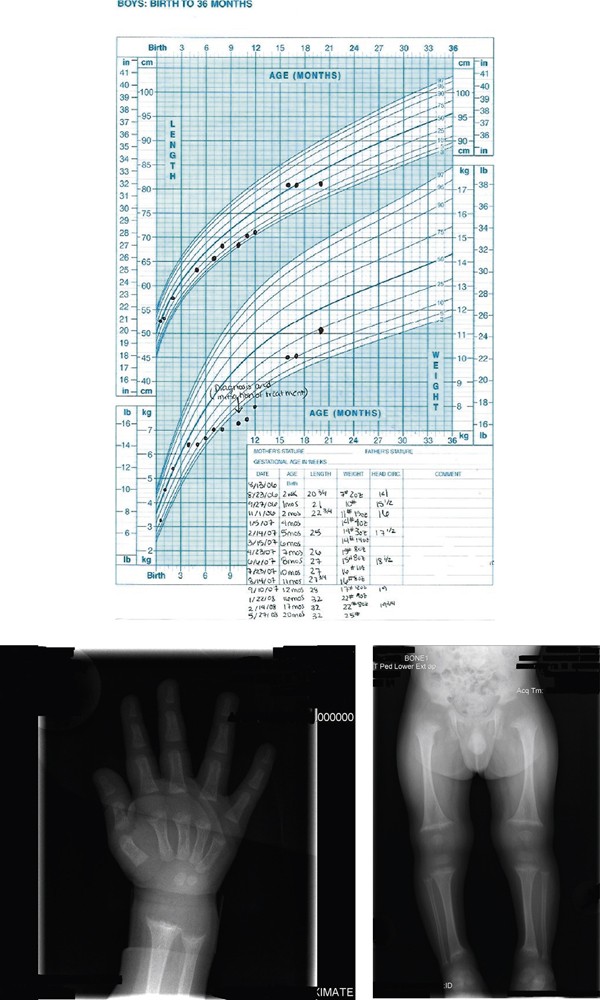
Growth Chart: Growth chart from birth to 20 months showing failure of appropriate growth and then his catch up growth after appropriate treatment . Radiograph Wrist/Hand: Metaphyseal fraying and cupping of distal radius and ulna and the distal aspects of the second through fifth metacarpals. Skeletal survey: Metaphyseal fraying and cupping involving bilateral distal femurs, bilateral proximal and distal tibiae and fibulae, bilateral proximal and distal humeri.
Infants and adolescents are predisposed to rickets secondary to increased flux in body composition and rates of rapid bone growth causing increased need/utilization of calcium and phosphate. Further increased risk is associated with dark-skinned individuals, lack of UV-B exposure, solely breastfed infants and prematurity. Screening should be considered for children with poor growth/development, seizure activity/tetany, and children with chronic malabsorptive states.
It is indisputable that breast milk is the ideal nutrition for infants, however, it only contains 15 - 50 IU/L of vitamin D [ 1 , 2 , 4 ]. There is limited prevalence estimates for vitamin D deficiency rickets in North America and the United Kingdom. Reported and published cases in the United States increased from 65 between 1975 to 1985 to 228 from 1986 to present [ 2 ]. This has led for the American Academy of Pediatrics (AAP) recommendation of vitamin D supplementation in all breast fed infants who do not consume 500 mL/day of vitamin D fortified formula and all non-breastfed infants that do not consume at least 500 mL/day of vitamin D fortified formula. It is recommended this begin in the first days of life and continue through childhood/adolescence [ 2 ]. The 2003 AAP breastfeeding guidelines suggest 200 IU/day to maintain a minimum level of 27.5 nmol/L, however this has been shown insufficient for prevention of all cases of rickets leading to controversy and newer recommendations for 400 IU/day, especially in deeply pigmented breastfed infants [ 2 , 5 ]. Despite appropriate breastfeeding technique and the appropriate amount of breast milk our patient was at risk for vitamin D deficiency secondary to the lack of oral vitamin D supplementation and his ethnicity.
The primary source of vitamin D (sunlight) is dependent on geographic location as well as outdoor exposure. To maintain a low normal level (>27.5 nmol/L) of vitamin D, a fully clothed child would have to spend two hours outside weekly and darker skinned individuals may require exposures up to 6-10 times this amount [ 1 , 2 ]. Sunscreen with an SPF of 15 reduces synthetic capacity by up to 98% [ 2 , 6 ]. The current AAP recommendation (to prevent sunburns and reduce skin cancer risk) is to keep infants less than 6 months of age out of direct sunlight and encourage the use of protective clothing/sunscreen again increasing the risk of vitamin D deficiency in this patient [ 2 ].
Because of this recommendation, management of vitamin D deficiency is via oral vitamin supplementation. Ergocalciferol (plant formulated vitamin D2) or Cholecalciferol (animal formulated vitamin D3) at >5000 IU daily for 2-4 months is suggested for toddlers greater than 12 months of age and up to 10,000 IU in adolescents. In younger infants (1-12 months) 1,000-5000 IU daily has been suggested. In infants <1 month old, 1000 IU daily is recommended [ 2 ]. Once laboratory values have normalized, maintenance of 400 IU per day is suggested [ 1 , 2 ]. If compliance is a concern a one time treatment with high dose oral formulation is appropriate (100,000-600,000 IU) over 1-5 days with a follow up dose in 3 months if necessary [ 2 ]. It is suggested that vitamin D3 may be up to 3 times as potent as D2 and may be preferable, especially when used in bolus form. Some formulations of vitamin D may contain propylene glycol, which is toxic at high doses so caution is advised [ 2 ].
Conclusions
While rickets is a disease that has plagued society for many centuries it is certainly still a significant cause for both skeletal and non-skeletal complications in today's culture. Despite recommendations for supplementation in all breast-fed infants and fortification of multiple household food items, it is still a relatively common nutritional deficiency. Education on proper nutrition during pregnancy and supplementation during breastfeeding is necessary to prevent its growing resurgence. Proper childhood maintenance visits with growth and development screenings are critical for early detection of this easily treatable condition.
Written informed consent was obtained from the patient's mother for publication of this case report and accompanying images of radiographs and growth chart. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
American Academy of Pediatrics
Alanine Aminotransferase
Aspartate Aminotransferase
Complete blood count
Parathyroid hormone
Sun Protection Factor
Thyroid stimulating hormone
Ultra violet-B.
Dimitri P, Bishop N, Rickets : New insights into a re-emerging problem. Curr Op in Ortho. 2007, 18: 486-493. 10.1097/BCO.0b013e3282b97118.
Article Google Scholar
Misra M, Pacaud D, Petryk A, et al: Vitamin D deficiency and its management: review of current knowledge and recommendations. Pediatrics. 2008, 122: 398-417. 10.1542/peds.2007-1894.
Article PubMed Google Scholar
Hickey L, Cross C, Ewald MB: Nutritional rickets: beyond the chief complaint. Ped Emer Care. 2006, 22: 121-123. 10.1097/01.pec.0000199559.96356.3d.
Ward LM, et al: Vitamin D deficiency rickets among children in Canada. CMAJ-JAMC. 2007, 177: 161-166.
Breastfeeding and the Use of Human Milk. Pediatrics. 2005, 115: 496-506. 10.1542/peds.2004-2491.
Hickey L, Gordon CM: Vitamin D Deficiency: new perspective on an old disease. Curr Op in Endo and Diab. 2004, 11: 18-25. 10.1097/00060793-200402000-00006.
Article CAS Google Scholar
Download references
Author information
Authors and affiliations.
Research Family Medicine Residency, Research Medical Center, 6650 Troost Ave, Kansas City, 64131, USA
Rachel L Stevens & Corey Lyon
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Corey Lyon .
Additional information
Competing interests.
The author(s) declare that they have no competing interests.
Authors' contributions
RS provided care for this patient when he presented to her clinic at 6 months of age. RS completed the work-up, researched and initiated the treatment. CL provided assistance with the preparation of the manuscript
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Stevens, R.L., Lyon, C. Nutritional vitamin D deficiency: a case report. Cases Journal 2 , 7000 (2009). https://doi.org/10.1186/1757-1626-2-7000
Download citation
Received : 02 January 2009
Accepted : 03 March 2009
Published : 14 May 2009
DOI : https://doi.org/10.1186/1757-1626-2-7000
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Thyroid Stimulate Hormone
- Nutritional Vitamin
- Adequate Caloric Intake
- Parathyroid Hormone Release
Cases Journal
ISSN: 1757-1626

LINDA S. NIELD, M.D., PRASHANT MAHAJAN, M.D., M.P.H., APARNA JOSHI, M.D., AND DEEPAK KAMAT, M.D., PH.D.
Am Fam Physician. 2006;74(4):619-626
See related editorial on page 561.
Patient information: See related handout on rickets , written by the authors of this article.
Author disclosure: Nothing to disclose.
Rickets develops when growing bones fail to mineralize. In most cases, the diagnosis is established with a thorough history and physical examination and confirmed by laboratory evaluation. Nutritional rickets can be caused by inadequate intake of nutrients (vitamin D in particular); however, it is not uncommon in dark-skinned children who have limited sun exposure and in infants who are breastfed exclusively. Vitamin D–dependent rickets, type I results from abnormalities in the gene coding for 25(OH)D 3 -1-α-hydroxylase, and type II results from defective vitamin D receptors. The vitamin D–resistant types are familial hypophosphatemic rickets and hereditary hypophosphatemic rickets with hypercalciuria. Other causes of rickets include renal disease, medications, and malabsorption syndromes. Nutritional rickets is treated by replacing the deficient nutrient. Mothers who breastfeed exclusively need to be informed of the recommendation to give their infants vitamin D supplements beginning in the first two months of life to prevent nutritional rickets. Vitamin D–dependent rickets, type I is treated with vitamin D; management of type II is more challenging. Familial hypophosphatemic rickets is treated with phosphorus and vitamin D, whereas hereditary hypophosphatemic rickets with hypercalciuria is treated with phosphorus alone. Families with inherited rickets may seek genetic counseling. The aim of early diagnosis and treatment is to resolve biochemical derangements and prevent complications such as severe deformities that may require surgical intervention.
Illustrative Case
The mother of a 26-month-old black infant expresses concern that her son is not growing properly. Born at 34 weeks of gestation at 3 lb, 5 oz (1.5 kg), he was exclusively breastfed until 11 months of age. He is a picky eater, is breastfed twice daily, and consumes minimal dairy products.
His examination reveals a weight of 21 lb (9.6 kg; below the fifth percentile for age), height of 72.5 cm (below the fifth percentile), and head circumference of 74.5 cm (50th percentile). Other abnormal findings include frontal bossing, open anterior fontanel, wide wrists, and bowlegs.
Nutritional rickets is suspected and confirmed with laboratory and radiographic evaluations. Levels of serum alkaline phosphatase and parathyroid hormone are elevated, and calcidiol (25[OH]D 3 ) is decreased. Radiographic images of the wrist show fraying and cupping of the distal radius and ulna, as well as bone demineralization. Treatment is initiated with oral solution of ergocalciferol at 4,000 IU per day for six weeks with close monitoring of calcium and phosphorus levels.
Introduction
Rickets is not a disease only of the past, nor is it limited to developing countries. Until recently, vitamin D supplementation for breastfed infants was not advised. 1 , 2 However, multiple case reports 3 – 11 of nutritional rickets in the United States have prompted the recent recommendation by the American Academy of Pediatrics to provide a daily vitamin D supplement for all solely breastfed babies beginning in the first two months of life. 12 In the United States, rickets should be included in the differential diagnosis of children presenting with failure to thrive, developmental delay, and orthopedic abnormalities. Early diagnosis is essential because morbidity can be minimized if children are treated before eight months of age. 7 An extensive literature search of MEDLINE forms the basis of this report, which briefly addresses several causes of rickets with a more in-depth review of nutritional rickets.
Epidemiology
Because rickets is not a reportable disease in the United States, national data are unavailable. Statistics from Connecticut reveal that less than one third of children with rickets between 1986 and 2000 had nutritional deficiencies, whereas the remaining children had underlying disease or genetic factors responsible for the illness. 3 Nutritional rickets is the main type reported outside the United States, followed by vitamin D–dependent, vitamin D–resistant, and renal rickets 13 ( Table 1 4 , 14 – 20 ) .
Unlike developing countries, the United States saw the eradication of nutritional rickets in the 1930s following the discovery that vitamin D possessed antirachitic properties. 21 Today, in the absence of ongoing national surveillance, it is difficult to know how likely it is that a child with rickets will present to the primary care physician’s office. As a result, the true burden of this condition must be estimated. In one study, 22 the prevalence of nutritional rickets was estimated to be nine cases per 1 million children, whereas the Centers for Disease Control and Prevention places this rate at five cases per 1 million children six months to five years of age. 23 Of note, in multiple studies, most affected children were black. 22

Pathogenesis
A disease that occurs during childhood, rickets is the failure of growing bone to mineralize. Many skeletal and radiographic changes can occur ( Table 2 14 , 19 , 24 ) because of the lack of calcified osteoid and the buildup of unossified cartilage. 14 Proper bone formation requires a complex interplay of several organs and chemicals ( Table 3 ) , 25 and vitamin D deserves special mention because any disturbance in its production, absorption, or metabolism is paramount in the development of rickets. Human beings maintain adequate levels of vitamin D by producing it from cholesterol or by absorbing it from ingested food sources. Sunlight is a vital component necessary for the production of vitamin D, which begins in the skin and ends in the kidney, as depicted in Figure 1 . 25
Types of Rickets
Nutritional.
Nutritional rickets results from inadequate sunlight exposure or inadequate intake of dietary vitamin D, calcium, or phosphorus. Although uncommon in the United States, vitamin D deficiency still can occur, particularly when an infant is solely breastfed, is dark skinned, or has limited sunlight exposure. Dark-skinned persons require more sunlight exposure than others to produce the same amount of vitamin D because melanin acts as a neutral filter and absorbs solar radiation. 8 A diet deficient in calcium, 3 such as one dependent on nonfortified milk substitutes, can lead to rickets. 6 , 10 , 23 Nutritional rickets presents in the first two years of life with short stature, gait abnormality, developmental delay, and characteristic findings ( Tables 1 4 , 14 – 20 and 2 14 , 19 , 24 ) . Commonly, infants younger than six months present with hypocalcemic tetany or seizures, whereas older children present with failure to thrive or skeletal deformities. 14
VITAMIN D DEPENDENT
Vitamin D–dependent rickets, type I is secondary to a defect in the gene that codes for the production of renal 25(OH)D 3 –1-α-hydroxylase ( Figure 1 25 ) . Vitamin D–dependent rickets, type II is a rare autosomal disorder caused by mutations in the vitamin D receptor. Type II does not respond to vitamin D treatment; elevated levels of circulating calcitriol differentiate this type from type I.
VITAMIN D RESISTANT
Rickets refractory to vitamin D treatment may be caused by the most common heritable form, known as vitamin D–resistant rickets or familial hypophosphatemic rickets. 15 , 16 Because of mutations of the phosphate-regulating gene on the X chromosome, renal wasting of phosphorus at the proximal tubule level results in hypophosphatemia. 17 Normal levels of calcitriol are found in this disorder.
Hypophosphatemia also can occur secondary to hereditary hypophosphatemic rickets with hypercalciuria, which is believed to result from an isolated defect in renal reabsorption of phosphorus.
OTHER CAUSES
Various medical conditions and medications can cause rickets ( Table 4 ) . 17 , 26 , 27 In rickets secondary to malignancy, the most common pathophysiology is tumor secretion of a renal phosphate–wasting factor and impaired calcitriol production. 17 Rickets caused by renal disease (renal osteodystrophy) is caused by disturbances in calcium and phosphorus regulation and calcitriol production. Malabsorption syndromes such as celiac disease and cystic fibrosis can cause vitamin D deficiency.
Premature infants are at risk of developing rickets from calcium and phosphorus deficiency and side effects of their medications (e.g., loop diuretics, corticosteroids). Other medications associated with the development of rickets include anticonvulsants and antacids. Phenytoin (Dilantin) may cause target organ resistance to calcitriol. 26 Excess oral administration of aluminum-containing antacids can lead to hypophosphatemic rickets caused by the phosphate-binding property of aluminum. 27
MEDICAL HISTORY
The infant’s gestational age, diet, and degree of sunlight exposure should be noted. A detailed dietary history should include specifics of vitamin D and calcium intake. Researchers have suggested an appropriate amount of sunlight exposure for infants (i.e., 30 minutes per week if only in a diaper and two hours per week if fully clothed), 28 but the exact amount needed for a particular child is not known. It helps to know if the child avoids sun exposure completely. A family history of short stature, orthopedic abnormalities, poor dentition, alopecia, and parental consanguinity may signify inherited rickets.
The review of systems should focus on growth and orthopedic concerns and signs and symptoms of hypocalcemia, such as muscle cramps, numbness, paresthesias, tetany, and seizures.
PHYSICAL EXAMINATION
In children with rickets, complete physical and dental examinations should be performed. The entire skeletal system must be palpated to search for tenderness and bony abnormalities ( Table 2 14 , 19 , 24 ) . Bowlegs in the absence of other findings are relatively common in normal children in the first two years of life; rickets should be suspected in older bowlegged children and in cases associated with asymmetry, pain, or progression in severity. Gait disturbances in the ambulatory child and neurologic abnormalities (such as hyperreflexia) in all children should be sought.
LABORATORY AND RADIOGRAPHIC FINDINGS
Laboratory investigation may include serum levels of calcium (total and ionized with serum albumin), phosphorus, alkaline phosphatase, parathyroid hormone, urea nitrogen, creatinine, and calcidiol. Urine studies include urinalysis and levels of urinary calcium and phosphorus. The serum level of calcidiol is indicative of the patient’s overall vitamin D status. 29 Although calcitriol is the active form of vitamin D, it has a short half-life and circulates at a concentration that is 1,000 to 2,000 times less than calcidiol. 29 Depending on the stage of the disease, laboratory values can vary. The most common laboratory findings in nutritional rickets are decreases in serum calcium, serum phosphorus, calcidiol, calcitriol, and urinary calcium. Conversely, parathyroid hormone, alkaline phosphatase, and urinary phosphorus levels are elevated.
An anteroposterior radiograph of rapidly growing skeletal areas, such as the knee or wrist, is most helpful in diagnosing rickets. The skeletal changes caused by rickets usually are most pronounced at the knees, wrists, and anterior rib ends (rachitic rosary) 24 ( Figures 2 through 4 ) . Classic radiographic findings include widening of the distal physis, fraying and widening of the metaphysis, and angular deformities of the arm and leg bones. Bony changes of rickets may be mistaken for other conditions of childhood such as congenital syphilis, osteogenesis imperfecta, or child abuse, 30 and it can be beneficial to consult an experienced children’s radiologist for radiographic interpretation.

Surgical intervention may be necessary to repair severe bony abnormalities, but for optimal healing to occur, the metabolic and nutritional imbalances have to be corrected first. 31 Vitamin D and supplements of calcium and phosphorus are used to treat nutritional rickets.
Various vitamin D preparations, dosages (high versus low), dosing schedules (single versus multiple doses), and administration routes (oral or intramuscular) are available ( Table 5 ) . 32 , 33 Ergocalciferol (Calciferol) is a useful medication for infants and children because it can be administered intramuscularly or orally in liquid or capsule form. The capsules can be softened in water and mixed with a palatable food such as applesauce. 34 A single intramuscular or oral dose of various strengths (150,000 to 600,000 IU) of vitamin D in patients as young as three months has been studied and found to be adequate treatment for nutritional rickets. 35 – 37 Hypercalcemia is more likely with oral doses greater than 300,000 IU. 35
Researchers comparing a single intramuscular dose (600,000 IU) of vitamin D to a lower daily oral dosage (2,000 IU) for four weeks found that patients who received the intramuscular dose responded promptly without hypervitaminosis, whereas 40 percent of infants who received the oral dosages had no or minimal response. 38 The physician must determine the best treatment strategy for each patient on a case-by-case basis. For example, if compliance is a major concern, the single intramuscular dose may be more appropriate.
After treatment initiation, all patients will require careful monitoring of serum calcium, phosphorus, alkaline phosphatase, and calcidiol levels and of urine calcium and phosphorus levels. A spot urine calcium to creatinine ratio should be followed to detect hypercalciuria. Adjustments to medications are made to accommodate any abnormal fluctuations in serum or urine values. The earliest biochemical change after treatment initiation is a rise in the level of phosphorus followed by calcium within the first week. Radiographic changes may be evident within a week, and physical examination findings may normalize within six months. No matter which treatment course is chosen, the physician has to closely monitor the child’s progress.
With regard to nutritional rickets, the most important role of the primary care physician is helping parents prevent it. Along with sun protection advice, measures needed to prevent nutritional rickets must be stressed to the child’s caregivers. Besides all exclusively breastfed infants, some older children also may need vitamin D supplementation. Parents should be encouraged to give their children foods that are high in calcium ( Table 6 33 ) .
Because vitamin D–dependent rickets, type I is caused by lack of production of calcitriol, treatment requires the replacement of that active product. The treatment of type II is more complex, 39 and consultation with a children’s nephrologist is advised.
Familial hypophosphatemic rickets is treated with oral phosphorus and calcitriol (Rocaltrol), whereas hereditary hypophosphatemic rickets with hypercalciuria requires replacement of oral phosphorus alone. Investigators stress that treatment begun early in life lessens the disease burden. 40 To ensure early treatment, infants of affected parents must be screened often for hypophosphatemia and increased levels of serum alkaline phosphatase.
Supplementation for breast-fed and bottle fed infants. Vitamin supplements. In: Shelov SP, ed. Caring for Your Baby and Young Child: Birth to Age 5. New York, N.Y.: Bantam Books, 1991:104–5.
Wharton B. Weaning: pathophysiology, practice and policy. In: Walker WA, Watkins JB, eds. Nutrition in Pediatrics: Basic Science and Clinical Applications. 2nd ed. Hamilton, Ontario: B.C. Decker, 1997:433.
DeLucia MC, Mitnick ME, Carpenter TO. Nutritional rickets with normal circulating 25-hydroxyvitamin D: a call for reexamining the role of dietary calcium intake in North American infants. J Clin Endocrinol Metab. 2003;88:3539-45.
Peng LF, Serwint JR. A comparison of breastfed children with nutritional rickets who present during and after the first year of life. Clin Pediatr. 2003;42:711-7.
Biser-Rohrbaugh A, Hadley-Miller N. Vitamin D deficiency in breast-fed toddlers. J Pediatr Orthop. 2001;21:508-11.
Carvalho NF, Kenney RD, Carrington PH, Hall DE. Severe nutritional deficiencies in toddlers resulting from health food milk alternatives. Pediatrics. 2001;107:E46.
Tomashek KM, Nesby S, Scanlon KS, Cogswell ME, Powell KE, Parashar UD, et al. Nutritional rickets in Georgia. Pediatrics. 2001;107:E45.
Kreiter SR, Schwartz RP, Kirkman HN, Charlton PA, Calikoglu AS, Davenport ML. Nutritional rickets in African American breast-fed infants. J Pediatr. 2000;137:153-7.
Fitzpatrick S, Sheard NF, Clark NG, Ritter ML. Vitamin D-deficient rickets: a multifactorial disease. Nutr Rev. 2000;58:218-22.
Shah M, Salhab N, Patterson D, Seikaly MG. Nutritional rickets still afflict children in north Texas. Tex Med. 2000;96:64-8.
Weisberg P, Scanlon KS, Li R, Cogswell ME. Nutritional rickets among children in the United States: review of cases reported between 1986 and 2003. Am J Clin Nutr. 2004;80(6 suppl):1697S-705S.
Gartner LM, Greer FR for the Section on Breastfeeding and Committee on Nutrition. American Academy of Pediatrics. Prevention of rickets and vitamin D deficiency: new guidelines for vitamin D intake. Pediatrics. 2003;111(4 pt 1):908-10.
Abdullah MA, Salhi HS, Bakry LA, Okamoto E, Abomelha AM, Stevens B, et al. Adolescent rickets in Saudi Arabia: a rich and sunny country. J Pediatr Endocrinol Metab. 2002;15:1017-25.
Tolo VT, Wood BP. Torsional and angular conditions in the lower extremity. In: Tolo VT, Wood BP, eds. Pediatric Orthopaedics in Primary Care. Baltimore, Md.: Williams & Wilkins, 1993:258–60.
Chung WT, Niu DM, Lin CY. Clinical aspects of X-linked hypophosphatemic rickets. Acta Paediatr Taiwan. 2002;43:26-34.
Seikaly MG, Baum M. Thiazide diuretics arrest the progression of nephrocalcinosis in children with X-linked hypophosphatemia. Pediatrics. 2001;108:E6.
Brame LA, White KE, Econs MJ. Renal phosphate wasting disorders: clinical features and pathogenesis. Semin Nephrol. 2004;24:39-47.
Al-Khenaizan S, Vitale P. Vitamin D-dependent rickets type II with alopecia: two case reports and review of the literature. Int J Dermatol. 2003;42:682-5.
McWhorter AG, Seale NS. Prevalence of dental abscess in a population of children with vitamin D-resistant rickets. Pediatr Dent. 1991;13:91-6.
Chaussain-Miller C, Sinding C, Wolikow M, Lasfargues JJ, Godeau G, Garabedian M. Dental abnormalities in patients with familial hypophosphatemic vitamin D-resistant rickets: prevention by early treatment with 1-hydroxyvitamin D. J Pediatr. 2003;142:324-31.
Rajakumar K. Vitamin D, cod-liver oil, sunlight and rickets: a historical perspective. Pediatrics. 2003;112:E132-5.
Scanlon KS, ed. Vitamin D expert panel meeting: October 11–12, 2001, Atlanta, Ga. Final report. Accessed April 20, 2006, at: http://www.cdc.gov/nccdphp/dnpa/nutrition/pdf/Vitamin_D_Expert_Panel_Meeting.pdf .
Centers for Disease Control and Prevention. Severe malnutrition among young children—Georgia, January 1997-June 1999. MMWR Morb Mortal Wkly Rep. 2001;50:224-7.
Markowitz RI, Zackai E. A pragmatic approach to the radiologic diagnosis of pediatric syndromes and skeletal dysplasias. Radiol Clin North Am. 2001;39:791-802.
Drezner MK. Rickets and osteomalacia. In: Goldman L, Ausiello DA, eds. Cecil Textbook of Medicine. 22nd ed. Philadelphia, Pa.: Saunders, 2004:1545.
Bringhurst FR, Demay MD, Knonenberg HM. Hormones and disorders of mineral metabolism. In: Larsen PR, Kronenberg HM, Melmed S, Polonsky KS, eds. Williams Textbook of Endocrinology. 10th ed. Philadelphia, Pa.: Saunders, 2003:1346.
Robinson RF, Casavant MJ, Nahata MC, Mahan JD. Metabolic bone disease after chronic antacid administration in an infant. Ann Pharmacother. 2004;38:265-8.
Specker BL, Valanis B, Hertzberg V, Edwards N, Tsang RC. Sunshine exposure and serum 25-hydroxyvitamin D concentrations in exclusively breast-fed infants. J Pediatr. 1985;107:372-6.
Greer FR. Vitamin D deficiency—it’s more than rickets. J Pediatr. 2003;143:422-3.
DeRusso PA, Spevak MR, Schwarz KB. Fractures in biliary atresia misinterpreted as child abuse. Pediatrics. 2003;112(1 pt 1):185-8.
Calmar EA, Vinci RJ. The anatomy and physiology of bone fracture and healing. Clin Ped Emerg Med. 2002;3:85-93.
Khatib R, Alsaek Y, Cakan N, Kamat DM. Nutritional rickets. A case report and review. Consultant Pediatrician. 2005;4:33-9.
National Institutes of Health Consensus Conference. Optimal calcium intake. NIH Consensus Development Panel on Optimal Calcium Intake. JAMA. 1994;272:1942-8.
Pal BR, Shaw NJ. Rickets resurgence in the United Kingdom: improving antenatal management in Asians [Published reply appears in J Pediatr 2001;139:338]. J Pediatr. 2001;139:337-8.
Cesur Y, Caksen H, Gundem A, Kirimi E, Odabas D. Comparison of low and high dose vitamin D treatment in nutritional vitamin D deficiency rickets. J Pediatr Endocrinol Metab. 2003;16:1105-9.
Kutluk G, Cetinkaya F, Basak M. Comparisons of oral calcium, high dose vitamin D and a combination of these in the treatment of nutritional rickets in children. J Trop Pediatr. 2002;48:351-3.
Shah BR, Finberg L. Single-day therapy for nutritional vitamin D-deficiency rickets: a preferred method. J Pediatr. 1994;125:487-90.
Lubani MM, al-Shab TS, al-Saleh QA, Sharda DC, Quattawi SA, Ahmed SA, et al. Vitamin-D-deficiency rickets in Kuwait: the prevalence of a preventable disease. Ann Trop Paediatr. 1989;9:134-9.
Wong GW, Leung SS, Law WY, Cheung NK, Oppenheimer SJ. Oral calcium treatment in vitamin D-dependent rickets type II. J Paediatr Child Health. 1994;30:444-6.
Makitie O, Doria A, Kooh SW, Cole WG, Daneman A, Sochett E. Early treatment improves growth and biochemical and radiographic outcome in X-linked hypophosphatemic rickets. J Clin Endocrinol Metab. 2003;88:3591-7.
Continue Reading
More in afp, more in pubmed.
Copyright © 2006 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
Second Case
Conclusions, acknowledgments, dental complications of rickets in early childhood: case report on 2 young girls.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Tiphaine Davit-Béal , Julie Gabay , Pauline Antoniolli , Jeanne Masle-Farquhar , Maryse Wolikow; Dental Complications of Rickets in Early Childhood: Case Report on 2 Young Girls. Pediatrics April 2014; 133 (4): e1077–e1081. 10.1542/peds.2013-0733
Download citation file:
- Ris (Zotero)
- Reference Manager
Vitamin D is an essential hormone for calcium gut absorption. It is also involved in child growth, cancer prevention, immune system responses, and tooth formation. Due to inadequate vitamin D intake and/or decreased sunlight exposure, vitamin D deficiency has resurfaced in developed countries despite known inexpensive and effective preventive methods. Vitamin D deficiency is a common cause of rickets, a condition that affects bone development in children and that can have serious dental complications. Deficiency during pregnancy can cause enamel hypoplasia of primary teeth. Enamel regeneration is currently impossible; hypoplasia is therefore irreversible, and once affected, teeth are prone to fast caries development. Deficiency during early childhood can affect permanent teeth and ensuing caries can sometimes lead to tooth loss at a young age. Oral manifestations of rickets should be diagnosed early by both physicians and dentists to prevent severe dental complications. This case study presents 2 young girls with rickets in early childhood who suffered from subsequent serious tooth decay.
Vitamin D is an essential prohormone. Once activated by successive hydroxylations in the liver and in the kidney, it binds to the nuclear vitamin D receptor (VDR) and triggers pathways regulating calcium homeostasis, cell proliferation, and cell differentiation. 1 , – 4
Cost-effective preventive methods once eradicated vitamin D deficiency in developed countries, but it has now resurfaced worldwide and has become a major public health issue. Low, moderate, and extreme deficiencies are defined as 25-hydroxyvitamin D levels <50, <25, and <12.5 nmol/L, respectively. Moderate and extreme deficiencies result in impaired bone mineralization and ossification, leading to bone-softening diseases such as rickets, osteomalacia, and osteoporosis. 1 , 3 , 5 Several types of rickets have been described on the basis of etiology, namely nutritional rickets, vitamin D–dependent rickets (VDDR), vitamin D–resistant rickets (VDRR), and hypophosphatemic rickets (HR). 1 General signs of vitamin D deficiency are well known and are easy to detect on physical examination. Hypotonia, hypocalcemia, bone deformations, and lethargy are the most common symptoms. 5
Vitamin D is also required for tooth mineralization. Its deficiency during gestation affects primary teeth, whereas during early childhood it affects permanent teeth. Tooth defects (enamel and/or dentin) depend on the type of rickets. Dental anomalies caused by HR have been well described. 6 , – 10 However, little is known about the dental manifestations of VDDR, VDRR, or nutritional rickets. 11 , – 14 General manifestations make early diagnosis of rickets possible. Physicians should pay particular attention to the 2 highest-risk groups: pregnant women and young children (ie, when crown formation of both primary and permanent teeth occurs). They should refer diagnosed patients to a dentist to prevent major dental complications.
Here we report the oral manifestations of nutritional rickets in 2 young dark-skinned adolescents, both of whom were treated by undergraduate and postgraduate students at the Department of Pediatric Dentistry, Charles Foix Hospital, Paris Descartes University, France. The differential diagnoses with other enamel hypoplasia etiologies are also discussed.
A 12-year-old black girl presented to the Pediatric Dentistry Department with posterior upper right jaw pain that prevented her from sleeping. Clinical and radiographic examinations revealed a deep carious lesion on her permanent upper right first molar. Emergency pulpotomy was performed after irreversible pulpitis was diagnosed. Initial medical history questioning revealed that the girl has been exclusively breastfed from birth to 7 months old, age at which fluoride and vitamine D supplements were introduced. Global oral health assessment showed deep caries on all other 3 permanent first molars as well as round-shaped enamel hypoplasia on the coronal side of both upper and lower incisors ( Fig 1 A–C ). Because radiographic examination confirmed the presence of all permanent teeth including third molars ( Fig 1D ), we decided to extract all permanent first molars and implement orthodontic treatment to correct malpositioned teeth.

A, Intraoral photograph showing slight defects on upper and lower incisors (arrows). B, Upper jaw. Note the severe decay on the first permanent molars and the presence of the second left primary molar. C, Lower jaw. Note the severe decay on the first permanent molars and the eruption of the second permanent right molar. D, Panoramic radiograph showing deep lesions on the first permanent molars.
An 11-year-old black girl from Cameroon was referred to the clinic by her dentist on suspicion of amelogenesis imperfecta. No similar concerns had been raised for other family members. Her health record was illegible, but her father stated that she had been treated for nutritional vitamin D deficiency with vitamin D supplements (cholecalciferol, vitamin D 3 ) since the age of 4 years. Her general development was otherwise normal. Clinical examination revealed severe enamel hypoplasia of incisors, canines, and permanent first molars. Premolars seemed to be intact or only slightly affected, whereas the primary lower right second molar (her single remaining primary tooth) presented enamel defects similar to those on the permanent first molars ( Fig 2 A–C ). Panoramic radiographic examination showed healthy lower second premolars and permanent second and third molars ( Fig 2D ). Anterior teeth were restored with dental composite materials, and permanent first molars were extracted.

A, Intraoral photograph showing severe defects on upper and lower incisors and canines and slight defects on the first upper bicuspid (arrows). B, Upper jaw. Note the severe enamel hypoplasia on the first permanent molars, whereas the bicuspids are only lightly (first biscuspid) or not (second biscuspid) affected. C, Lower jaw. Note that the second primary right molar is as severely affected as the first permanent molars. Only the bicuspids appear to be healthy. D, Panoramic radiograph showing healthy second and third permanent molars.
Unlike its general complications, little is known about dental complications of rickets. Crown mineralization of primary teeth occurs from gestation to 12 months of age, as indicated in Table 1 , and that of permanent teeth extends from birth to 8 years of age, except for third molars as shown in Table 2 . The chronological onset of crown mineralization is tooth-group dependent. Consequently, systemic diseases or intoxications at a given period can affect various teeth differently. For example, if a chronic disease occurs in newborns, the end-stage primary tooth crown formation and the initial mineralization of permanent first molars and incisors are affected. Likewise, a similar incidence at age 3 years disrupts the mineralization of the cervical third of permanent first molars, incisors, and canines; the coronal half of first premolars; and the coronal third of second premolars. Permanent second molars may be spared. Note that these data are based on normal gestational age and are subject to slight individual variations.
Crown Mineralization of Primary Teeth
Adapted from ref 15 .
Crown Mineralization of Permanent Teeth
The first patient was not provided with vitamin D supplements from birth to 7 months of age, when crown mineralization of permanent first molars and central and lateral incisors begins. 15 In the anterior region, only incisors displayed half-moon–shaped enamel defects. Hypoplasia affected only a reduced surface, and decay did not extend to smooth surfaces. Because the extent of dental defects is correlated with vitamin D deficiency, one can deduce that deficiency was minimal. In the posterior region, crown destruction was such that severely decayed teeth required extraction. Anomalies on the occlusal surfaces of molars make them caries sensitive, and early interception of the caries process could have therefore prevented the extractions.
The second patient suffered from more severe vitamin D deficiency. Indeed, rickets occurred throughout the first 4 years, and cholecalciferol supplementation only began at age 4 years. Tooth lesions were more extensive and mostly affected the whole crown surface of permanent central incisors and first molars. Moreover, half of the crowns of the upper lateral incisors and canines and cusps of first premolars were also affected. Given that the crown of the primary second molars mineralizes from the sixth month in utero to 10 to 12 months after birth, 15 this deficiency may have been already present during gestation. We were unable to assess exactly when the deficiency began because the other primary teeth had already exfoliated.
Dental manifestations of nutritional rickets must be differentiated from those of hereditary VDDR, VDRR, and HR. There are 2 types (types 1A and 1B) of VDDR that are caused by mutations in the CYP27B1 and CYP2R1 genes, respectively. Both affect vitamin D-25 hydroxylation. Oral manifestations described by Zambrano et al 11 in a 10-year-old patient were yellowish to brownish, markedly hypoplastic enamel; large pulp chambers; and short roots in all permanent teeth, as well as periodontal disease.
There are also 2 types (types 2A and 2B) of VDRR. Their etiologies are different: type 2A results from mutations in the VDR, whereas type 2B results from a normal VDR but abnormal proteins inferring with VDR ligands. Both present similar general phenotypes. Two studies 12 , 13 have described dental anomalies in humans, that is, abnormal pulp chambers and thin dentin, as did Descroix et al 14 in VDR-ablated mice.
HR encompasses various hereditary defects, including the following: an autosomal-dominant form (ADHR) caused by mutation in the FGF23 gene; autosomal-recessive forms (ARHR1 and ARHR2) caused by mutations in the DMP1 and ENPP1 genes, respectively; an X-linked recessive form caused by mutation in the CLCN5 gene; and an X-linked dominant form (XLHR) due to mutation in the PHEX gene. The oral impact of the last form has been well described: enlarged pulp chambers, prominent horns extending to the dentin-enamel junction, thinner enamel, and spontaneous infectious abscesses. 6 , – 10
Differential diagnosis of rickets with inherited anomalies such as amelogenesis imperfecta and dentinogenesis imperfecta was uncomplicated: in the present 2 cases, some teeth remained intact, whereas inherited anomalies affected all primary and permanent teeth. 16 Other vitamin deficiencies (eg, hypovitaminosis A, C, and E) were also explored because they are all responsible for enamel hypoplasia but lead to different clinical signs. Additionally, mineral deficiencies including phosphorus and calcium deficiencies (which affect enamel and dentine formation) and magnesium deficiency (which causes enamel hypoplasia, dentine mineralization disorders, and pulp calcifications) were explored. Other possible etiologies of enamel hypoplasia, such as premature birth; celiac, renal, and congenital heart diseases; and childhood diseases such as rubella, measles, chicken pox, scarlet fever, and cytomegalovirus infections were ruled out. Endocrine pathologies such as hypothyroidism, hypoparathyroidism, pseudohypoparathyroidism, and other systemic disorders were also screened for. 17 , 18
Enamel defects increase the incidence of dental caries. Pediatricians, physicians, and dentists should diagnose dental manifestations of rickets early to prevent decay progression. Ideally, a first dental visit at 12 months of age enables parents to gauge the importance of oral health, feeding, and annual dental checkups. 19 If parents fail to bring their children at that young age, a first visit at age 3 is essential; all primary teeth should have erupted by then. A checkup at 6 to 7 years of age allows the dentist to check for enamel hypoplasia or caries on permanent first molars and incisors. Finally, the American Academy of Pediatrics recommends vitamin D supplements for all age groups. 20 Recent guidelines from the Institute of Medicine and the Endocrine Society offer additional preventive strategies. 21 , 22
hypophosphatemic rickets
vitamin D–dependent rickets
vitamin D receptor
vitamin D–resistant rickets
Dr Davit-Béal conceptualized the case report, determined patient treatment options, supervised all clinical steps, and drafted the initial manuscript; Dr Gabay carried out the orthodontic treatment on 1 of the 2 patients and reviewed the final manuscript; Dr Antoniolli carried out the restorative treatment of 1 patient’s anterior teeth and reviewed the final manuscript; Ms Masle-Farquhar critically reviewed the manuscript; Dr Wolikow coordinated and supervised all treatments and reviewed the final manuscript; and all authors approved the final manuscript as submitted.
FUNDING: No external funding.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
We thank our colleagues from the Departments of Pediatric Dentistry and Orthodontics (Charles Foix Hospital) for their help in data collection and extend our thanks to Dr Florence Chemla (Dentistry Department Head, Charles Foix Hospital) and Dr Louis Maman (Dean of Paris Descartes University Dental School).
Competing Interests
Advertising Disclaimer »
Citing articles via
Email alerts.

Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account

Citation, DOI, disclosures and case data
At the time the case was submitted for publication Ian Bickle had the following disclosures:
- 4ways diagostics, I work for this out sourcing company during non NHS hours (ongoing)
These were assessed during peer review and were determined to not be relevant to the changes that were made.
Presentation
Hypocalcemia and low vitamin D in an infant.
Patient Data
Cupping and fraying of the radial and ulna metaphyses bilaterally.
Case Discussion
Classical appearances of infantile rickets with consistent correlating blood results.
1 public playlist includes this case
- Rotherham teaching set 15 by Ian Bickle ◉
Related Radiopaedia articles
- Rickets (mnemonic)
Promoted articles (advertising)
How to use cases.
You can use Radiopaedia cases in a variety of ways to help you learn and teach.
- Add cases to playlists
- Share cases with the diagnosis hidden
- Use images in presentations
- Use them in multiple choice question
Creating your own cases is easy.
- Case creation learning pathway
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers

Two cases of rickets presenting with poor growth, hypotonia, and respiratory problems
- PMID: 25443772
- DOI: 10.1179/2295333714Y.0000000103
Rickets is a rare disease in developed countries. In children, it is a disease which affects growing bone. Depending on the severity, it can present with a wide variety of symptoms. Because it is such a rare disease in developed countries, symptoms suggesting rickets are often not easily recognized. This can cause a delay in diagnosing and treating rickets. Often unnecessary and sometimes invasive investigations are performed. First leading clues to rickets on physical examination are poor growth, especially length, thickening of wrists, bow legs, and craniotabes. At further examination, special attention should be paid to osteopenia and cupping and fraying at the metaphyses on X-rays. Laboratory results suggestive for rickets are elevated alkaline phosphatase and disturbances in calcium and phosphate homeostasis. In this report, we present two cases presenting with poor growth, severe pain, and respiratory problems secondary to calcipenic rickets.
Keywords: Failure to thrive,; Osteopenia,; Poor growth; Rickets,; Vitamin D,.
Publication types
- Case Reports
- Alkaline Phosphatase / blood
- Bone Density Conservation Agents / administration & dosage
- Bone Diseases, Metabolic* / diagnostic imaging
- Bone Diseases, Metabolic* / etiology
- Calcium / blood
- Calcium / therapeutic use
- Failure to Thrive / etiology*
- Hydroxycholecalciferols / administration & dosage*
- Muscle Hypotonia / etiology*
- Phosphates / blood
- Phosphates / therapeutic use
- Radiography
- Respiratory Insufficiency / etiology*
- Rickets* / blood
- Rickets* / diagnosis
- Rickets* / drug therapy
- Rickets* / etiology
- Rickets* / physiopathology
- Treatment Outcome
- Vitamin D* / blood
- Vitamin D* / therapeutic use
- Bone Density Conservation Agents
- Hydroxycholecalciferols
- Alkaline Phosphatase
- alfacalcidol
O.J. Simpson, football star turned celebrity murder defendant, dead at 76
- Medium Text
Get weekly news and analysis on the U.S. elections and how it matters to the world with the newsletter On the Campaign Trail. Sign up here.
Reporting by Will Dunham in Washington; additional reporting by Brendan O'Brien in Chicago; Editing by Bill Trott, Diane Craft and Neil Fullick
Our Standards: The Thomson Reuters Trust Principles. New Tab , opens new tab

World Chevron

Kremlin says any new 'colonial' U.S. aid to Ukraine won't change frontline situation
The Kremlin said on Thursday that any new U.S. military aid for Ukraine would not change the situation at the front where Kyiv's forces were in a poor position and cast such aid as part of a "colonial" policy which enriched the United States.

A Ukrainian attack on a military airfield in Russian-occupied Crimea on Wednesday seriously damaged four missile launchers, three radar stations and other equipment, Ukraine's military spy agency said on Thursday.
- Skip to main content
- Keyboard shortcuts for audio player
O.J. Simpson, football legend acquitted of notorious killings, dies at 76

Russell Lewis

Becky Sullivan

Emma Bowman

O.J. Simpson, pictured in September 2008 in Las Vegas, died Wednesday, according to a statement from his family. Isaac Brekken/Getty Images hide caption
O.J. Simpson, pictured in September 2008 in Las Vegas, died Wednesday, according to a statement from his family.
The football great Orenthal James Simpson, known as O.J., who was accused and ultimately acquitted in the killings of his ex-wife and her friend, has died. Simpson was 76.
In a post on X , his family said he died on Wednesday. He "succumbed to his battle with cancer," and was surrounded by his children and grandchildren.
Simpson was a cultural icon who starred on the football field and in movies and commercials. That legacy was forever eclipsed after he made headlines in 1994 for another reason when he was accused of killing his ex-wife, Nicole Brown Simpson, and her friend Ronald Goldman. In 1995, jurors determined he was not guilty in the stabbing deaths. No one else was ever charged. Dubbed the "trial of the century," the nationally televised proceedings captivated the country with a verdict that reverberated across the U.S. with debates about police misconduct, race, celebrity and domestic abuse.
On April 10th, our father, Orenthal James Simpson, succumbed to his battle with cancer. He was surrounded by his children and grandchildren. During this time of transition, his family asks that you please respect their wishes for privacy and grace. -The Simpson Family — O.J. Simpson (@TheRealOJ32) April 11, 2024
O.J. Simpson first found fame on the football field. Once a kid who wore leg braces until age 5 after developing rickets, Simpson went on to become one of the greatest running backs of all time. He played at the University of Southern California (USC) in the late 1960s. The powerful tailback danced, dashed and dazzled on the field, propelling the Trojans to a national championship in 1967. He won the Heisman trophy, as college football's best player, in 1968.
After graduating from USC, he played 11 seasons in the NFL; nine of them with the Buffalo Bills, and two seasons with the San Francisco 49ers. Known as "The Juice," he collected four rushing titles, played in five Pro Bowls and, in 1973, became the first running back to break the 2,000-yard rushing mark.
During and after his pro career ended in 1979, he starred in TV commercials, mostly notably as a pitchman for Hertz as he rushed through airports for the rental car company. He also later appeared in several shows and movies, including The Naked Gun and the TV miniseries Roots , as producers seized on his fame and likeability.

O.J. Simpson, accompanied by his parents, his son, Jason, and Ralph Wilson, owner of the Buffalo Bills, is inducted into the Wall of Fame in Rich Stadium on Sept. 14, 1980. Ross Lewis/Getty Images hide caption
O.J. Simpson, accompanied by his parents, his son, Jason, and Ralph Wilson, owner of the Buffalo Bills, is inducted into the Wall of Fame in Rich Stadium on Sept. 14, 1980.
In 1994, the bodies of his ex-wife, Nicole Brown Simpson, and her friend, Ronald Goldman, were found stabbed outside her home in Los Angeles. Not long after, Simpson was arrested and his subsequent "low-speed" white Bronco car chase on L.A. freeways was televised nationwide; some 95 million people tuned into the chase coverage. In 1995, a criminal jury determined he was not guilty of committing the killings.
The most famous moment of the months-long trial was when a prosecutor asked OJ to try on the gloves believed to belong to the killer. In a dramatic showing, Simpson struggled to pull on the snug pair.
Defense lawyer Johnnie Cochrane seized on this, delivering the most famous line of the whole spectacle in his closing arguments: "If it doesn't fit, you must acquit."

On June 17, 1994, Los Angeles police "chased" a white Ford Bronco carrying O.J. Simpson and driven at low speed by Al Cowlings on a freeway in Los Angeles. Joseph R. Villarin/AP hide caption
On June 17, 1994, Los Angeles police "chased" a white Ford Bronco carrying O.J. Simpson and driven at low speed by Al Cowlings on a freeway in Los Angeles.
Prosecutors Marcia Clark, William Hodgman and Christopher Darden came to the trial with strong evidence linking Simpson to the killings, including DNA tests, the right hand of a pair of blood-stained gloves that were found at his home, and his history of spousal abuse.
Simpson's legal team of prominent criminal defense lawyers, including Johnnie Cochran and Alan Dershowitz, F. Lee Bailey and Robert Kardashian, successfully made the case to the jury that there was reasonable doubt. It cast the LAPD as racist and corrupt, arguing that it had tampered with forensic evidence at a shoddy crime scene.
When the mixed-race jury announced the not guilty verdict, public reaction seen in media coverage largely fell along racial lines, showing Black people celebrating and white people shocked by his acquittal.
Those TV clips didn't tell the full story, says Camille Charles, a professor of Africana Studies at the University of Pennsylvania. It wasn't that Black Americans all thought he was innocent, she says.

The Los Angeles Riots, 25 Years On
When la erupted in anger: a look back at the rodney king riots.

The Two-Way
O.j. simpson released from prison.
"Black people were more conflicted than was really ever shown in the media," Charles says. But, she says, "Black folks had had such a bad experience with the criminal justice system that they rooted for him as a Black man who actually had the resources to mount a proper defense."
The trial took place three years after the acquittal of four LAPD officers in the beating of Rodney King had inflamed the deep distrust among Black people and police.
But, as a wealthy celebrity who married a white woman, Simpson was "never seen as a staunch proponent of the African American community," says Darnell Hunt, a professor of sociology and African American studies at UCLA, and as a result, didn't engender overwhelming sympathy among African Americans during his trial.
Two years later, a different civil jury determined he was liable in the deaths and ordered him to pay $33 million to the families of Brown and Goldman.
Simpson continued to maintain his innocence in media interviews.
That wasn't his last tangle with legal trouble. In 2007, he led a group of men to a Las Vegas hotel room to confront some sports memorabilia dealers. Several people brought guns with them, and Simpson was later convicted of armed robbery. He served almost a decade in a Nevada prison and was released on parole in 2017 .
The public's fascination with O.J. Simpson never waned. He was the subject of numerous documentaries about the killings and his life.
- O.J. Simpson
2024 - Supercharging social protection systems with anticipatory cash: Case study on Fiji’s Anticipatory Action Framework

This paper explains how, through close collaboration with the Fijian Government and other relevant stakeholders, WFP has developed a first-of-its-kind system where 100 percent of WFP’s anticipatory cash assistance will be channelled through the country’s existing social protection infrastructure. By building on the country’s disaster risk management capacities and leveraging the Government’s existing social protection infrastructure, the initiative promotes local ownership—firmly placing the Fijian Government and people in the driver’s seat of proactive disaster mitigation.
Christoph Baade and Osborne Sibande, 2024, Supercharging social protection systems with anticipatory cash: Case study on Fiji’s Anticipatory Action Framework
Publications
Integrating anticipatory action and social protection.
2023 Anticipatory Action Activations

Scaling up anticipatory actions for food security: Anticipatory Action Year in Focus 2022
Advanced search
Advertisement
Supported by
For Filmmakers, O.J. Simpson’s Trial Was a Powerful Case Study
In 2016, both an FX mini-series and an ESPN documentary re-examined the polarizing criminal accusations against Simpson and the nation’s divided conversation about race.
- Share full article

By Emmanuel Morgan
More than 20 years after the O.J. Simpson trial, long after the headlines had faded and the news cycle had moved on to other scandals, the polarizing saga was thrust back into the national conversation thanks to two very different projects.
“ The People v. O.J. Simpson: American Crime Story ,” an FX mini-series directed by Ryan Murphy, won nine Emmys in 2016. That year’s “ O.J.: Made in America, ” a nearly eight-hour film for ESPN, won the Academy Award for best documentary feature.
“It was a story that combined everything that obsesses the American people,” the legal analyst Jeffrey Toobin said the day after Simpson died at 76 . Toobin’s 1996 book, “The Run of His Life: The People v. O.J. Simpson,” inspired the FX series.
Toobin said the Simpson odyssey captivated the country’s psyche. There was love, violence, sports and Hollywood. Even a fugitive on the run.
Simpson had been a star football player , winning the Heisman Trophy in college and the Most Valuable Player Award in the N.F.L. But for many people, his athletic highlights are overshadowed by a highway chase involving a white Ford Bronco and murder charges in the 1994 deaths of his ex-wife Nicole Brown Simpson and her friend Ronald L. Goldman.
As Americans followed the nine-month trial, their perception of the criminal case against Simpson, a prominent Black athlete who became an actor and a pitchman , was often split along racial lines. Simpson was acquitted in the criminal case and was later found liable for the deaths in a civil trial .
“I think the reason it still feels so raw is that it still feels like it’s today,” said Larry Karaszewski, a screenwriter for the FX mini-series. “A lot of times people think we’re at this post-racial moment, but it keeps coming back.”
Karaszewski said that like during Simpson’s trial, race was at the forefront of the national conversation when “The People v. O.J. Simpson” was being produced, during the rise of the Black Lives Matter movement after the fatal shooting of Trayvon Martin by a neighborhood watchman in 2012.
The mini-series focused on the Simpson trial, treating him as a secondary character while highlighting other key players in the courtroom , like Marcia Clark, the lead prosecutor, and Johnnie Cochran, one of Simpson’s prominent defense lawyers.
In contrast, ESPN’s documentary, an installment of the sports network’s “30 for 30” series, traced Simpson’s biography and contextualized it through the sports and socioeconomic history of the Los Angeles region. Its director, Ezra Edelman, has said he thought it was important to take that wider view.
“I was interested in the 30 years before the murders, the city, race and identity, and the juxtaposition with O.J.’s story,” he told The New York Times in 2016 . “This is a big American studies paper. This touches on everything in our culture.”
Through an ESPN spokeswoman, Edelman declined to comment after Simpson’s death. Several of the documentary’s producers did not respond to requests for comment.
Karaszewski said the distance from the trial allowed viewers of the FX series to watch the case with fresh eyes, without the emotional response to the verdict. And he and Toobin agreed that it also presented the saga and its characters — including Robert Kardashian, a defense lawyer whose family’s fame grew after the case — to new audiences.
“For those of us who lived through it, it brought it back up,” Toobin said, “but it introduced a whole generation of people who had no firsthand experience with the story.”
Emmanuel Morgan reports on sports, pop culture and entertainment. More about Emmanuel Morgan
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
Case Study: How Aggressively Should a Bank Pursue AI?
- Thomas H. Davenport
- George Westerman

A Malaysia-based CEO weighs the risks and potential benefits of turning a traditional bank into an AI-first institution.
Siti Rahman, the CEO of Malaysia-based NVF Bank, faces a pivotal decision. Her head of AI innovation, a recent recruit from Google, has a bold plan. It requires a substantial investment but aims to transform the traditional bank into an AI-first institution, substantially reducing head count and the number of branches. The bank’s CFO worries they are chasing the next hype cycle and cautions against valuing efficiency above all else. Siti must weigh the bank’s mixed history with AI, the resistance to losing the human touch in banking services, and the risks of falling behind in technology against the need for a prudent, incremental approach to innovation.
Two experts offer advice: Noemie Ellezam-Danielo, the chief digital and AI strategy at Société Générale, and Sastry Durvasula, the chief information and client services officer at TIAA.
Siti Rahman, the CEO of Malaysia-headquartered NVF Bank, hurried through the corridors of the university’s computer engineering department. She had directed her driver to the wrong building—thinking of her usual talent-recruitment appearances in the finance department—and now she was running late. As she approached the room, she could hear her head of AI innovation, Michael Lim, who had joined NVF from Google 18 months earlier, breaking the ice with the students. “You know, NVF used to stand for Never Very Fast,” he said to a few giggles. “But the bank is crawling into the 21st century.”
- Thomas H. Davenport is the President’s Distinguished Professor of Information Technology and Management at Babson College, a visiting scholar at the MIT Initiative on the Digital Economy, and a senior adviser to Deloitte’s AI practice. He is a coauthor of All-in on AI: How Smart Companies Win Big with Artificial Intelligence (Harvard Business Review Press, 2023).
- George Westerman is a senior lecturer at MIT Sloan School of Management and a coauthor of Leading Digital (HBR Press, 2014).
Partner Center

IMAGES
VIDEO
COMMENTS
Case presentation. A 19-month-old male child was referred to the general paediatric department by his family physician as a highly suspected case of severe rickets. The child was born at term by an emergency caesarean due to multiple previous caesarean deliveries with a birth weight of 3.23 kg and length of 51 cm, within the 90th centile range.
Prevalence of rickets . Though not all cases are as severe as the boy featured in this case study, the number of cases of mild rickets is creeping up. Getting enough vitamin D, known as 'the sunshine vitamin' is a challenge for many children in the UK. The recommended amount of vitamin D intake per day is 10 micrograms.
2. Epidemiology. Rickets is still a common disease worldwide. Despite a global estimate of rickets, incidence is limited because of the paucity of basic data such as vitamin D dietary intake, especially among children in non-industrialized countries, and recent reports indicate an increase in its prevalence [2,6].Nutritional rickets remains the most common type globally, representing the most ...
Abstract. Rickets is an often-neglected, painful, and disabling childhood condition of impaired bone mineralization. In this case series we describe a cluster of 29 children with severe, painful bone deformities who live in the very remote region of Nagaland in northwest Myanmar. Children were found to have low 25-hydroxyvitamin D, elevated parathyroid hormone, and elevated alkaline ...
The reported prevalence of nutritional rickets varies among countries. A study on a tea farm population in India in 2016 involving 16 274 children aged 1 to 18 years old reported 2.7 cases of nutritional rickets per 1000 children [14]. ... In addition, she had inadequate dietary intake of calcium and vitamin D, which led her to develop rickets ...
Idiopathic hypophosphatemic rickets has been described recently in children who are fed with an amino acid-based elemental formula, especially Neocate formula products. 61 A retrospective study of 51 children who were evaluated for fractures or rickets were found to have unexplained hypophosphatemia. 61 Most of the children were suffering ...
DEPARTMENT Case Study-Primary Care Rickets: Not Just a Disease Caused by Vitamin D Deficiency Lauren Head Zauche, BSN, RN KEY WORDS Case study, hypophosphatemia, rickets CASE PRESENTATION
Here, we describe the first case of VDDR3 in Brazil due to the previously identified gain-of-function mutation in the CYP3A4 gene that leads to an increased inactivation of vitamin D metabolites and rickets. Individuals who carry this heterozygous mutation have the same clinical and biochemical features as children with nutritional vitamin D deficiency, which makes it important to consider ...
Nutritional rickets is defined as a defect in the mineralization of newly formed pre-osseous tissue due to vitamin D deficiency [].The radiological signs in severe cases are diffuse bone demineralization with multiple erosions [].The appearance of a tumor due to secondary hyperparathyroidism has not been described in the medical literature.
It is indisputable that breast milk is the ideal nutrition for infants, however, it only contains 15 - 50 IU/L of vitamin D [ 1, 2, 4 ]. There is limited prevalence estimates for vitamin D deficiency rickets in North America and the United Kingdom. Reported and published cases in the United States increased from 65 between 1975 to 1985 to 228 ...
AJ, a 2-year-old African-American male, was referred to a nutrition and gastroenterology clinic with the diagnosis of rickets and iron deficiency anemia, ... This case study illustrates the potential problems of giving children vegan diets without proper food choices and supplementation. Recommended articles. References (0)
1. Introduction. Rickets is a metabolic condition in infants and children resulting from a deficiency in vitamin D (blood serum 25-hydroxyvitamin D3), which typically manifests between three and 18 months of age (Pettifor, 2004).Because vitamin D affects the biological regulation of calcium and phosphorus, a deficiency will cause abnormalities in bone and tooth formation and mineralization ...
In one study, 22 the prevalence of nutritional rickets was estimated to be nine cases ... Vitale P. Vitamin D-dependent rickets type II with alopecia: two case reports and review of the literature
ISSN #2168-8184. A 19-month-old boy presented to the general pediatric clinic with delayed development and multiple nutritional deficiencies, after being exclusively breastfed up to the age of nine months without vitamin D supplementation. Upon examination, imaging studies, and lab tests, the patient was diagnosed with nutritional rickets.
Rickets is a rare disease in developed countries. In children, it is a disease which affects growing bone. Depending on the severity, it can present with a wide variety of symptoms. Because it is such a rare disease in developed countries, symptoms suggesting rickets are often not easily recognized.
ABSTRACT. Objective: Early diagnosis and immediate treatment of hypophosphatemic rickets is of utmost importance as it may prevent subsequent sequelae. This report aims at warning pediatricians to consider the presence of the disease. Case description: Description of the metabolic profile, creatinine clearance, nutritional status, weight and ...
Deficiency during early childhood can affect permanent teeth and ensuing caries can sometimes lead to tooth loss at a young age. Oral manifestations of rickets should be diagnosed early by both physicians and dentists to prevent severe dental complications. This case study presents 2 young girls with rickets in early childhood who...
As a population-based incidence study over 40 years, this report provides better information regarding the incidence and temporal trends of diagnosed nutritional rickets than previous studies. Unlike other case series, this study had the advantage of a defined population (ie, denominator), and, consequently, we could determine the actual ...
In this paper we describe a differentially diagnosed case of vitamin D deficiency rickets in a 3-year ± 12-month-old child dating to the 19th century from rural upstate New York. Our analysis reveals that the child likely presented with rickets as a crawling infant and may have suffered subsequent bouts as they learned to walk.
Bickle I, Rickets. Case study, Radiopaedia.org (Accessed on 16 Apr 2024) https://doi.org/10.53347/rID-187512
Laboratory results suggestive for rickets are elevated alkaline phosphatase and disturbances in calcium and phosphate homeostasis. In this report, we present two cases presenting with poor growth, severe pain, and respiratory problems secondary to calcipenic rickets. Keywords: Failure to thrive,; Osteopenia,; Poor growth; Rickets,; Vitamin D,.
www.aes.com
The recent paper describes an unnamed hunter who contracted CJD after regular consumption of venison from deer infected with Chronic Wasting Disease. "In 2022, a 72-year-old man with a history ...
O.J. Simpson, the American football star and actor who was sensationally acquitted in 1995 of murdering his former wife in what U.S. media dubbed the "trial of the century", has died at the age of 76.
O.J. Simpson first found fame on the football field. Once a kid who wore leg braces until age 5 after developing rickets, Simpson went on to become one of the greatest running backs of all time.
Rickets occurs exclusively in children, whereas adults develop osteomalacia after the epiphyseal plate fusion.[1] ... A study revealed 89% of the patients with rickets had no or ... Al-Faqeeh DH. Severe rickets in a young girl caused by celiac disease: the tragedy of delayed diagnosis: a case report. BMC Res Notes. 2014 Oct 08; 7:701. [PMC free ...
This case study provides a technical overview of the collaborative process through which the World Food Programme (WFP) and the Fijian Government set up innovative structures to provide cash assistance ahead of anticipated cyclones. This paper explains how, through close collaboration with the Fijian Government and other relevant stakeholders ...
Toobin's 1996 book, "The Run of His Life: The People v. O.J. Simpson," inspired the FX series. Toobin said the Simpson odyssey captivated the country's psyche. There was love, violence ...
The main exposure of interest was clinically defined rickets at baseline, which was systematically collected as present or not on the trial baseline case report form. A clinical diagnosis of rickets was made by trained study clinicians at study enrolment by the presence of swelling of wrists and ankles, bowed legs, rachitic rosary, craniotabes ...
Anuj Shrestha. Summary. Siti Rahman, the CEO of Malaysia-based NVF Bank, faces a pivotal decision. Her head of AI innovation, a recent recruit from Google, has a bold plan. It requires a ...