An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Spondylolisthesis.
Steven Tenny ; Andrew Hanna ; Christopher C. Gillis .
Affiliations
Last Update: May 22, 2023 .
- Continuing Education Activity
Spondylolisthesis is a condition that occurs when one vertebral body slips with respect to the adjacent vertebral body causing radicular or mechanical symptoms or pain. It is graded based on the degree of slippage of one vertebral body on the adjacent vertebral body. Any pathological process that can weaken the supports keeping vertebral bodies aligned can allow spondylolisthesis to occur. This activity illustrates the evaluation and management of spondylolisthesis and reviews the role of the interprofessional team in improving care for patients with this condition.
- Describe the pathophysiology of spondylolisthesis.
- Review the workup of a patient with spondylolisthesis.
- Summarize the treatment options for spondylolisthesis.
- Describee the importance of collaboration and communication among the interprofessional team in encouraging weight loss in patients to reduce symptoms and increase the quality of life in those with spondylolisthesis.
- Introduction
Spondylolisthesis is the slippage of one vertebral body with respect to the adjacent vertebral body causing mechanical or radicular symptoms or pain. It can be due to congenital, acquired, or idiopathic causes. Spondylolisthesis is graded based on the degree of slippage of one vertebral body on the adjacent vertebral body. [1]
Spondylolisthesis commonly classifies as one of five major etiologies: degenerative, isthmic, traumatic, dysplastic, or pathologic. Degenerative spondylolisthesis occurs from degenerative changes in the spine without any defect in the pars interarticularis. It is usually related to the combined facet joint and disc degeneration leading to instability and forward movement of one vertebral body relative to the adjacent vertebral body. Isthmic spondylolisthesis results from defects in the pars interarticularis. The cause of isthmic spondylolisthesis is undetermined, but a possible etiology includes microtrauma in adolescence related to sports such as wrestling, football, and gymnastics, where repeated lumbar extension occurs. Traumatic spondylolisthesis occurs after fractures of the pars interarticularis or the facet joint structure and is most common after trauma. Dysplastic spondylolisthesis is congenital and secondary to variation in the orientation of the facet joints to an abnormal alignment. In dysplastic spondylolisthesis, the facet joints are more sagittally oriented than the typical coronal orientation. Pathologic spondylolisthesis can be from systemic causes such as bone or connective tissue disorders or a focal process, including infection, neoplasm, or iatrogenic origin. Additional risk factors for spondylolisthesis include a first-degree relative with spondylolisthesis, scoliosis, or occult spina bifida at the S1 level. [1]
- Epidemiology
Spondylolisthesis most commonly occurs in the lower lumbar spine but can also occur in the cervical spine and rarely, except for trauma, in the thoracic spine. Degenerative spondylolisthesis predominately occurs in adults and is more common in females than males with increased risk in the obese. Isthmic spondylolisthesis is more common in the adolescent and young adult population but may go unrecognized until symptoms develop in adulthood. There is a higher prevalence of isthmic spondylolisthesis in males. Dysplastic spondylolisthesis is more common in the pediatric population, with females more commonly affected than males. Current estimates for prevalence are 6 to 7% for isthmic spondylolisthesis by the age of 18 years, and up to 18% of adult patients undergoing MRI of the lumbar spine. Grade I spondylolisthesis accounts for 75% of all cases. Spondylolisthesis most commonly occurs at the L5-S1 level with an anterior translation of the L5 vertebral body on the S1 vertebral body. The L4-5 level is the second most common location for spondylolisthesis.
- Pathophysiology
Any process that can weaken the supports keeping vertebral bodies aligned can allow spondylolisthesis to occur. As one vertebra moves relative to the adjacent vertebrae, local pain can occur from mechanical motion or radicular or myelopathic pain can occur due to compression of the exiting nerve roots or spinal cord, respectively. Pediatric patients are more likely to increase spondylolisthesis grade when going through puberty. Older patients with lower grades I or II spondylolistheses are less likely to progress to higher grades over time.
- History and Physical
Patients typically have intermittent and localized low back pain for lumbar spondylolisthesis and localized neck pain for cervical spondylolisthesis. The pain is exacerbated by flexing and extending at the affected segment, as this can cause mechanic pain from motion. Pain may be exacerbated by direct palpation of the affected segment. Pain can also be radicular in nature as the exiting nerve roots become compressed due to the narrowing of nerve foramina as one vertebra slips on the adjacent vertebrae, the traversing nerve root (root to the level below) can also be impinged through associated lateral recess narrowing, disc protrusion, or central stenosis. Pain can sometimes improve in certain positions such as lying supine. This improvement is due to the instability of the spondylolisthesis that reduces with supine posture, thus relieving the pressure on the bony elements as well as opening the spinal canal or neural foramen. Other symptoms associated with lumbar spondylolisthesis include buttock pain, numbness, or weakness in the leg(s), difficulty walking, and rarely loss of bowel or bladder control.
Anteroposterior and lateral plain films, as well as lateral flexion-extension plain films, are the standard for the initial diagnosis of spondylolisthesis. One is looking for the abnormal alignment of one vertebral body to the next as well as possible motion with flexion and extension, which would indicate instability. In isthmic spondylolisthesis, there may be a pars defect, which is termed the "Scotty dog collar." The "Scotty dog collar" shows a hyperdensity where the collar would be on the cartoon dog, which represents the fracture of the pars interarticularis. Computed tomography (CT) of the spine provides the highest sensitivity and specificity for diagnosing spondylolisthesis. Spondylolisthesis can be better appreciated on sagittal reconstructions as compared to axial CT imaging. MRI of the spine can show associated soft tissue and disc abnormalities, but it is relatively more challenging to appreciate bony detail and a potential pars defect on MRI. [2] [3]
- Treatment / Management
For grade I and II spondylolisthesis, treatment typically begins with conservative therapy, including nonsteroidal anti-inflammatory drugs (NSAIDs), heat, light exercise, traction, bracing, and/or bed rest. Approximately 10% to 15% of younger patients with low-grade spondylolisthesis will fail conservative treatment and need surgical treatment. No definitive standards exist for surgical treatment. Surgical treatment includes a varying combination of decompression, fusion with or without instrumentation, or interbody fusion. Patients with instability are more likely to require operative intervention. Some surgeons recommend a reduction of the spondylolisthesis if able as this not only decreases foraminal narrowing but also can improve spinopelvic sagittal alignment and decrease the risk for further degenerative spinal changes in the future. The reduction can be more difficult and riskier in higher grades and impacted spondylolisthesis. [4] [5] [6] [7] [8] [2] [9] [10]
- Differential Diagnosis
- Degenerative Lumbar Disc Disease
- Lumbar Disc Problems
- Lumbosacral Disc Injuries
- Lumbosacral Discogenic Pain Syndrome
- Lumbosacral Facet Syndrome
- Lumbosacral Radiculopathy
- Lumbosacral Spine Acute Bony Injuries
- Lumbosacral Spondylosis
- Myofascial Pain in Athletes
- Pearls and Other Issues
Meyerding’s classification of spondylolisthesis is the most commonly used grading method. Its basis is on the percentage of anterior translation relative to the adjacent level. Grade I spondylolisthesis is 1 to 25% slippage, grade II is up to 50% slippage, grade III is up to 75% slippage, and grade IV is 76-100% slippage. If there is more than 100% slippage, it is known as spondyloptosis or grade V spondylolisthesis.
Subclasses of isthmic spondylolisthesis are subtype A (stress fractures of the pars), subtype B (elongation of the pars without overt fracture), subtype C (acute fracture of the pars).
Subclasses of pathologic spondylolisthesis are subtype A (systemic causes) and subtype B (focal processes).
- Enhancing Healthcare Team Outcomes
An interprofessional team consisting of a specialty-trained orthopedic nurse, a physical therapist, and an orthopedic surgeon or neurosurgeon will provide the best outcome and long-term care of patients with degenerative spondylolisthesis. Chiropractors may also have involvement, as they may be the first to encounter the condition on X-rays. The treating clinician will decide on the management plan, and then have the other team members engaged - surgical cases with include the nursing staff in pre-, intra-, and post-operative care, and coordinating with PT for rehabilitation. In non-operative cases, the PT will keep the rest of the team informed of progress or lack thereof. The team should encourage weight loss as weight reduction may reduce symptoms and increase the quality of life. Interprofessional collaboration, as above, will drive patient outcomes to their best results. [Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Click here for a simplified version.
- Comment on this article.
Grade II Spondylolisthesis, CT. Lumbar spine sagittal CT of L5-S1 revealing grade II spondylolisthesis. Contributed by C Gillis, MD, and S Tenny, MD
Disclosure: Steven Tenny declares no relevant financial relationships with ineligible companies.
Disclosure: Andrew Hanna declares no relevant financial relationships with ineligible companies.
Disclosure: Christopher Gillis declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Tenny S, Hanna A, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PubMed Links to PubMed
Similar articles in PubMed
- Isthmic Spondylolisthesis. [StatPearls. 2024] Isthmic Spondylolisthesis. Burton MR, Dowling TJ, Mesfin FB. StatPearls. 2024 Jan
- High-grade slippage of the lumbar spine in a rat model of spondylolisthesis: effects of cyclooxygenase-2 inhibitor on its deformity. [Spine (Phila Pa 1976). 2006] High-grade slippage of the lumbar spine in a rat model of spondylolisthesis: effects of cyclooxygenase-2 inhibitor on its deformity. Komatsubara S, Sairyo K, Katoh S, Sakamaki T, Higashino K, Yasui N. Spine (Phila Pa 1976). 2006 Jul 15; 31(16):E528-34.
- [Three vertebral reduction and fixation for revision of lumbar spondylolisthesis]. [Zhongguo Gu Shang. 2014] [Three vertebral reduction and fixation for revision of lumbar spondylolisthesis]. Li CS. Zhongguo Gu Shang. 2014 Sep; 27(9):717-21.
- Review A review of the pathomechanism of forward slippage in pediatric spondylolysis: the Tokushima theory of growth plate slippage. [J Med Invest. 2015] Review A review of the pathomechanism of forward slippage in pediatric spondylolysis: the Tokushima theory of growth plate slippage. Sairyo K, Nagamachi A, Matsuura T, Higashino K, Sakai T, Suzue N, Hamada D, Takata Y, Goto T, Nishisho T, et al. J Med Invest. 2015; 62(1-2):11-8.
- Review Isthmic spondylolisthesis in adults… A review of the current literature. [J Clin Neurosci. 2022] Review Isthmic spondylolisthesis in adults… A review of the current literature. Alomari S, Judy B, Sacino AN, Porras JL, Tang A, Sciubba D, Witham T, Theodore N, Bydon A. J Clin Neurosci. 2022 Jul; 101:124-130. Epub 2022 May 18.
Recent Activity
- Spondylolisthesis - StatPearls Spondylolisthesis - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
What Is Spondylolisthesis?
Spondylolisthesis is a spine condition caused when one vertebra slips over another. This condition's symptoms sometimes mimic those of other back pain conditions.

The complex design of the spinal column is a biological wonder. It comprises 33 bones at birth – some eventually fusing to become 24 bones in most adults – 23 discs and more than 40 muscles and ligaments. The spine is genuinely nature's stage for the human body's performance. And all those bones, discs, muscles and ligaments must work together perfectly for our bodies to function correctly.

Getty Images
Sometimes, the mighty machinery of the spine breaks down. Many spinal conditions can affect a person throughout their lifetime, from simple back pain to spinal tumors . With so many working pieces, plenty can go wrong when the anatomy of the spine isn't quite right.
A spinal condition called spondylolisthesis occurs when one vertebra of the spine slips forward over the one beneath it. This vertebra becomes out of alignment with the rest of the spinal column. The condition appears most commonly at the base of the spine in the low back vertebrae, also known as the lumbar spine.
There are three main types of spondylolisthesis:
- Congenital : appears in the womb, before birth, when a baby's spine doesn't properly form.
- Degenerative : happens over time, usually with advanced age.
- Traumatic : occurs due to direct injury to the spine.
Diagnosis and Symptoms
Spondylolisthesis is graded by diagnosing physicians on a percentage severity scale from 1 and 5, with five being the most severe degree of vertebral slippage. An MRI is typically required to diagnose spondylolisthesis fully and to help rule out other spinal conditions, since its symptoms closely match those experienced by people with other spine issues.
In some people who have spondylolisthesis, especially those with a lower degree of vertebral slippage, the condition may cause no symptoms. However, in those who have a higher vertebral slippage score, or when the slipped vertebra is pressing on a nerve, a variety of symptoms can result, including:
- Back pain that seems to worsen with activity.
- Difficulty standing or walking, especially for long periods.
- Numbness, stiffness or tightness in the muscles of the spine, especially those in the lower back, or tightness in the hamstrings.
- Pain in the low back or buttocks, which may radiate down the legs, and is known as sciatica pain.
Exercise with Spondylolisthesis
Because certain types of activity can make spondylolisthesis symptoms worse for some people, this diagnosis can lead to inactivity. However, it's crucial to note that certain types of regular movement can help relieve the symptoms associated with spondylolisthesis. Moving the body regularly helps to strengthen the spine and core muscles , which ultimately create better support for the spine in the long run.
When the symptoms of spondylolisthesis begin to impair mobility or proper body mechanics, that is when people should evaluate activities for safety. For example, heavy weightlifting, backbends or high-intensity sports that involve running or jumping should likely be avoided because they can make spondylolisthesis worse, which could lead to a condition called spinal stenosis.
There are still plenty of alternative activities a person with spondylolisthesis can engage in that may help provide back pain relief from the condition. These activities include gentler core exercises such as planks, yoga and gentle stretching. The key is to modify activities to reduce stress or strain on an already irritated spine.
Physical Therapy and Treatment Options
If you're unsure of what to do that won't worsen the condition, physical therapy can be a powerful and effective place to start. Under the trained guidance of a physical therapist, many people with spondylolisthesis develop the proper technique to perform exercises that help alleviate their symptoms and allow them the confidence to continue those activities at home.
From physical therapy to specific medications, most spine experts agree that conservative options are effective best places to start for spondylolisthesis treatment. Surgery is only considered when such alternatives fail to provide adequate relief or are ineffective in helping someone with spondylolisthesis return to active living.
As a complex spinal condition, it's always recommended to seek care and treatment for spondylolisthesis by a trained and experienced spine specialist .
The Health Risks of Poor Posture

Tags: back problems , patients , patient advice , health
Most Popular
Second Opinion

Pregnancy Resource Center

Patient Advice

health disclaimer »
Disclaimer and a note about your health ».
Sign Up for Our 3-Day Guide to Medicare
Confused about Medicare? We can help you understand the different Medicare coverage options available to help you choose the best Medicare coverage for you or a loved one.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
Best hospitals for maternity care update.
Jennifer Winston, Ph.D. and Ben Harder Oct. 24, 2024
Medicare Open Enrollment
Elaine Hinzey Oct. 21, 2024
What Is Medicare Part A?
Elaine K. Howley Oct. 18, 2024
What to Know About Flu Shots
Vanessa Caceres Oct. 18, 2024
Medicare Mental Health Treatment
Payton Sy Oct. 16, 2024

Medicare and Medical Equipment
Elaine K. Howley Oct. 16, 2024

Picking Top Medicare Insurance Companies
Ben Harder and C.J. Trent-Gurbuz Oct. 15, 2024

2025 Medicare Supplement Insurance
Elaine Hinzey and Paul Wynn Oct. 15, 2024

Best Medicare Advantage Insurance 2025
Sarah Shelton Oct. 15, 2024

Best Medicare Part D Companies


- (952) 225-5266
- Conditions & Treatments
- Spondylolisthesis
What is Spondylolisthesis?
Spondylolisthesis comes from the Greek words spondyl, meaning “whorl,” plus olisthesis (dislocation), derived from olisthanein, meaning “to slip, slide, or fall.” Simply put, spondylolisthesis is the displacement, slippage, or subluxation of a vertebra.
Your spinal column is made up of flat, more or less round or ring-shaped bones called vertebrae. They’re stacked up like poker chips and connected by supporting structures, including the intervertebral discs that lie between them.
A misaligned vertebra can compress spinal nerves, causing a kind of pain called radiculopathy, or it can impinge on the spinal cord itself, causing pain and dysfunction known as myelopathy. Spondylolisthesis can occur in the cervical spine, usually at the level of the third and fourth cervical vertebrae or the fourth and fifth cervical vertebrae. Vertebral displacement can also occur in the thoracic spine. But it’s most common in the lumbar spine (the lower back) at the level of the fourth and fifth vertebrae.
Spondylolisthesis is frequently preceded by spondylosis—age-related degeneration of the spine. The term spondylosis is used interchangeably with the term osteoarthritis of the spine .
What Are the Symptoms of Spondylolisthesis?
Spondylolisthesis can cause severe back pain, particularly radiculopathy. Other symptoms are common as well, although not all patients have all symptoms. Your symptoms will depend on the location of the displaced vertebra:
- Pain radiating down the leg (sciatic pain)
- Numbness or weakness of an arm or leg
- Pain that gradually worsens over the day
- Leg pain that shifts from side to side
- An altered gait (a change in your walking pattern) or pain while walking
- Diminished coordination and more frequent falls
Patients with cervical spondylolisthesis tend to have focal neck pain that gets worse when the neck is flexed forward or backward. “Focal” just means that the pain is focused—that is, you can point to the spot where it hurts. The opposite would be a generalized “it hurts all through here” kind of pain.
Patients with lumbar spondylolisthesis tend to have focal lower back pain. Sometimes the pain improves when lying down since that position stabilizes the spine. A displaced lumbar vertebra may also produce sciatic pain in the leg or buttocks, weakness in the legs, or difficulty walking. Walking may intensify the pain.
What Causes Spondylolisthesis?
There are several forms of spondylolisthesis:
- Pathologic: Bony, noncancerous tumors can weaken part of the vertebra called the pars interarticularis. The pars is a segment of the ring of the bone surrounding the spinal cord. Weakened bone can fracture, leaving it untethered and making that segment of the spine unstable.
- Dysplastic: Dysplastic spondylolisthesis is a congenital condition in which the facet joints and other structures are slightly malformed.
- Isthmic: Isthmic spondylolisthesis usually occurs in children and adolescents as a result of a defect, such as a poorly healed fracture, in the pars. This defect makes the vertebra unstable, and over time it can slip forward.
- Degenerative: Spondylolisthesis is often preceded by spondylosis. This condition is characterized by degenerative changes that make a portion of the spine unstable: degeneration of the disc and facet joints, calcification of surrounding ligaments, or spinal stenosis (narrowing of the spinal canal). Degenerative spondylolisthesis is the most common form that we treat at Inspired Spine.
- Traumatic Injury: A strong impact can cause traumatic injury to the spine, and vertebrae can be suddenly forced out of alignment, causing spondylolisthesis. Falls and accidents involving motor vehicles often precede traumatic spondylolisthesis, but any serious accident can precipitate such trauma. In one case, a pilot was injured in this way in the ejector seat of a flight simulator.
Conservative Spondylolisthesis Treatments
If you have spondylolisthesis but have no symptoms, treatment is unnecessary.
If the displacement is causing progressive spinal cord compression, though, you probably do have pain and other symptoms. Unfortunately, myelopathy associated with spondylolisthesis won’t go away on its own. Eventually, a surgical procedure will be necessary to subside the symptoms and pain.
Nonsurgical Spondylolisthesis Treatments
If your condition is causing pain or dysfunction, such as difficulty walking, treatment is needed. Your doctor will probably try conservative measures first—that is, therapies that don’t require a scalpel or heavy-duty prescription drugs.
Cervical collars, traction, physical therapy, and injections are good options for some patients. Many doctors follow a four-pronged approach to the initial management of spondylolisthesis:
Anti-Inflammatory Medication
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as naproxen (Aleve) and ibuprofen (Advil) are great at relieving the pain of spondylolisthesis. Sometimes they’re more effective than muscle relaxants, opioid medications, or short-term oral corticosteroids.
Aerobic Fitness
Aerobic physical activity promotes blood flow to areas of nerve compression in the spine and strengthens muscles and other supporting structures. Walking, swimming, and use of an elliptical machine are suitable aerobic conditioning activities, but the use of a stationary bicycle is especially useful for patients with spondylolisthesis.
Look for a bike in which the pedals are more or less below the seat (like on a real bicycle), rather than choosing a recumbent bike in which the pedals are out in front of you. A more traditional configuration of the seat, pedals, and handlebars shifts your weight toward your upper body. In contrast, a recumbent bike directs your body weight toward the seat, thereby putting pressure on your lumbar spine.
Weight Loss
If you’re overweight or obese, your doctor may recommend that you lose weight. The less body weight the spine must support, the less it will hurt. That theory, of course, doesn’t always pan out in practice. But if you’re overweight, it’s a gamble worth taking, since weight loss produces a wide range of other health benefits unrelated to the spine.
Management of Osteoporosis
Osteoporosis weakens bones, leading to fractures and other problems. To prevent or slow the progression of spondylolisthesis, your doctor will keep a careful eye on your bone mass to ensure that the bones of your spine are as dense, strong, and healthy as possible.
Inspired Spine is Minnesota’s leading spine center. We are a total spine care provider dedicated to relieving chronic back pain with the least invasive treatment possible.
- Degenerative Disc Disease
- Adult Degenerative Scoliosis
- Herniated Discs
- Collapsed Discs
- Facet Joint Syndrome
- Spinal Stenosis
- Thoracic Disc Disease
- Spinal Arthritis
- Spinal Fractures
- Radiculopathy
- Spine Deformities
See Our Treatments
Inspired Spine has developed advanced minimally invasive spinal surgery techniques that allow us to treat even complex spinal conditions without the drawbacks of traditional open back surgery.
Are You a Candidate for MIS Spinal Surgery?
Is neck or back pain restricting your daily activities? For 6 months or more? Have non-surgical treatments failed to help?
“I Live a Whole Different Life.”
Over 1,000 patients have benefited from Inspired Spine MIS Surgeries. See testimonials from just a few.
Spinal Surgery Facts
Not all MIS Spine Surgeries are Created Equal.
MEET OUR SURGEONS
- DOWNLOAD PATIENT GUIDE
- NEWS & BLOG
- PATIENT PORTAL
- FOR MEDICAL PROFESSIONALS
- INSPIRED SPINE SURGCENTER
Copyright © 2024
- Accessibility
- Privacy Policy
- User Agreement
APPOINTMENT
- ALEXANDRIA, MN
- BURNSVILLE, MN
- CROOKSTON, MN
- Inspired Spine Health of KS, PA
- the institute for-minimally invasive spine surge
- EL PASO, TX
- BACK PAIN CAUSES
- WHAT TO EXPECT
- PATIENT FORMS
- INSURANCE COVERAGE
- WHY SEEK A SECOND OPINION BEFORE YOUR SPINE SURGERY?
- FAQS ABOUT MINIMALLY INVASIVE SPINAL SURGERY
- TELEHEALTH SERVICES
- NEWS & BLOG
- COVID-19 UPDATE
- PAY MY BILL
- PATIENT GUIDES
- VIDEO GALLERY
- OUR INNOVATIVE APPROACH
- OUR PROVIDERS
- THE BENEFITS OF MINIMALLY INVASIVE SPINE SURGERY
- PATIENT TESTIMONIALS
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Spondylolisthesis?
Types of spondylolisthesis, frequently asked questions.
Spondylolisthesis is a condition in which a vertebra in the lumbar (lower) spine slips out of normal position, sliding forward (or sometimes backward) relative to the vertebra beneath it. It can be the result of an injury, lower back stress associated with sports, or age-related changes in the spine.
Depending on the extent of movement of the vertebra involved, symptoms can range from none at all to severe pain caused by pressure on a spinal nerve .
Spondylolisthesis usually is diagnosed with an X-ray . Low-grade spondylolisthesis may be relieved with non-invasive measures, while more severe cases may require a surgical procedure.
Hero Images / Digital Vision / Getty Images
The vertebrae are the box-shaped bones stacked on top of each other that make up the spinal column. Each vertebra should be neatly stacked on the one above and below. The spinal column has a normal S-shaped curvature when viewed from the side, but each vertebra should be neatly positioned on top of the vertebra below.
In spondylolisthesis, the vertebrae shift from their normal position. As a result, the condition is often referred to as "slipped vertebrae." Forward slippage is called anterolisthesis and backward slippage is called retrolisthesis .
Most often, this is a very slowly progressive condition with different types that include:
- Isthmic spondylolisthesis: This results from spondylolysis, a condition that leads to small stress fractures (breaks) in the vertebrae. In some cases, the fractures weaken the bone so much that it slips out of place.
- Degenerative spondylolisthesis: Degenerative spondylolisthesis is related to spine changes that tend to occur with age. For example, the discs can start to dry up and become brittle; as this occurs, they shrink and may bulge. Spinal arthritis is another age-related condition. Degenerative spondylolisthesis can cause spinal stenosis , in which the bones narrow and put pressure on the spinal cord.
- Congenital spondylolisthesis: Congenital spondylolisthesis results from abnormal bone formation that is present from birth, leaving the vertebrae vulnerable to slipping.
Less common forms of the condition include:
- Traumatic spondylolisthesis: With this, a spinal fracture or vertebral slipping occurs due to injury.
- Pathological spondylolisthesis: In this case, spondylolisthesis occurs due to another disease, such as osteoporosis , a tumor, or an infection.
- Post-surgical spondylolisthesis: This occurs when spine surgery results in slippage of the vertebrae.
Many people with spondylolisthesis have no obvious symptoms. Sometimes the condition is not discovered until an X-ray is taken for an unrelated injury or condition.
The most common symptom is lower back pain that can radiate to the buttocks and down the backs of the thighs. The symptoms may get worse during activity and subside during rest. Specifically, you may find that symptoms disappear when you bend forward or sit and get worse when you stand or walk.
This is because sitting and bending open up the space where spinal nerves are located, relieving pressure. Other potential symptoms include:
- Muscle spasms
- Tight hamstrings (muscles in the back of the thigh)
- Difficulty walking or standing for a long period of time
- Changes in gait
Severe or high-grade slips may result in pressure on a nearby spinal nerve root, causing tingling, numbness, or weakness in one or both legs.
Children involved in sports such as gymnastics, football, and diving tend to be at an increased risk for isthmic spondylolisthesis. These sports require repeated spinal hyperextension , which can cause a stress fracture of the pars interarticularis in the L5 vertebra.
Unless the hyperextension exercises are stopped to give the bone time to heal, scar tissue can form and prevent the bones from ever healing properly. This can lead to spondylolysis or stress fractures in the pars interarticularis, a condition that commonly leads to spondylolisthesis.
It's possible to be born with spondylolysis or spondylolisthesis, but both conditions can also develop from an injury, a disease, or a tumor.
Genetics may play a role in the risk of spondylolisthesis. There have been higher reports of spondylolisthesis in certain ethnic groups, namely Inuit Eskimos and Black Americans assigned female at birth .
Degenerative spondylolisthesis, the most common type, tends to affect adults over the age of 40. Older age, female gender, being overweight or obese, and conditions that can affect the spine, such as degenerative disc disease (DDD) and osteoarthritis , are thought to be factors that elevate the risk for this condition.
A healthcare professional will first talk to you and/or your child about symptoms, medical history, general health, and any participation in sports or physical activities. Then, they will examine the spine, looking for areas of tenderness or muscle spasms, and assess whether there are problems with gait or posture.
Next, your practitioner may order imaging studies, including:
- X-rays: These help distinguish between spondylolysis and spondylolisthesis. An X-ray taken from the side is also used to assign a grade between I and V, based on the severity of the slippage.
- Computed tomography (CT) scans : These provide greater detail than X-rays and help a healthcare professional prescribe the most appropriate treatment.
- Magnetic resonance imaging (MRI) scans : An MRI focuses on the body's soft tissues and can reveal damage to the intervertebral disks between the vertebrae or compression of spinal nerve roots.
There are five spondylolisthesis grades, each representing an incremental 25% increase of slippage in the vertebra.
Spondylolisthesis is treated according to the grade. For grades I and II, conservative treatments are often sufficient, including nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, physical therapy, home exercises, stretching, and the use of a brace. In physical therapy, core strengthening and stabilization exercises are emphasized.
Over the course of treatment, periodic X-rays may be taken to determine whether the vertebra is changing position.
For high grades or progressive worsening, spinal fusion surgery may be recommended. During this procedure, the affected vertebrae are fused together so that they heal into a single, solid bone.
During the procedure, the surgeon will realign the vertebrae in the lumbar spine. Small pieces of bone—called a bone graft—are then placed into the spaces between the vertebrae to be fused. Over time, the bones grow together, much like when a broken bone heals. Metal screws and rods may be installed to further stabilize the spine and improve the chances of successful fusion.
In some cases, patients with high-grade slippage also have compression of the spinal nerve roots. If this is the case, a procedure known as spinal decompression can help open up the spinal canal and relieve pressure on the nerves.
Spondylolisthesis is a spine condition in which a vertebra slips out of position. This may cause symptoms like low back pain and back stiffness. Young athletes are often at increased risk for spondylolisthesis as overextending the spine—which commonly happens in sports like football and gymnastics—is one of the most common causes of the condition.
To diagnose spondylolisthesis, a healthcare professional will review a person's symptoms and medical history, and they'll use imaging tests like X-rays and CT scans to analyze the spine and determine the severity, or grade, of the problem.
Lower-grade cases of spondylolisthesis typically respond well to conservative treatment like anti-inflammatory medication and physical therapy, while higher-grade cases may require surgery.
In most cases, it's possible to resume activities, including sports, once the condition has been treated. If symptoms reappear after treatment, tell a healthcare provider so that they can determine what strategies are needed to relieve them and restore your quality of life.
Spondylosis is a condition in which there is a stress fracture or weakness in a vertebra. Spondylolisthesis occurs when a vertebra slips out of position. Spondylosis may lead to spondylolisthesis, as a fracture in a vertebra may cause it to slip.
If you have spondylolisthesis, you may qualify for disability insurance if symptoms are severe and greatly impact your quality of life.
Those with spondylolisthesis should avoid movements that put great stress on the spine, such as lifting heavy objects. They should also avoid participating in sports that can lead to overtwisting or overextending the spine, like gymnastics and wrestling, until after treatment.
Cleveland Clinic. Spondylolisthesis .
Cedars Sinai. Spondylolisthesis .
American Academy of Orthopaedic Surgeons. Spondylolysis and spondylolisthesis .
NYU Langone Health. Diagnosing spondylolisthesis in adults .
Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence . J Orthop Translat . 2016;11:39-52. doi:10.1016/j.jot.2016.11.001
Tedyanto EH. Relationship between body mass index and radiological features of spondylolisthesis . International Journal of Science and Research. 2020;9(2):2319-7064. doi:10.21275/SR20215210921
Koslosky E, Gendelberg D. Classification in brief: The Meyerding classification system of spondylolisthesis . Clin Orthop Relat Res . 2020;478(5):1125-1130. doi:10.1097/CORR.0000000000001153
American Academy of Orthopaedic Surgeons. Spinal fusion .
Cleveland Clinic. Spondylolysis .
By Jonathan Cluett, MD Dr. Cluett is board-certified in orthopedic surgery. He served as assistant team physician to Chivas USA (Major League Soccer) and the U.S. national soccer teams.
Spondylolisthesis
Spondylolisthesis is where one of the bones in your spine, called a vertebra, slips forward. It can be painful, but there are treatments that can help.
It may happen anywhere along the spine, but is most common in the lower back.
Check if you have spondylolisthesis
The main symptoms of spondylolisthesis include:
- pain in your lower back, often worse when standing or walking and relieved when sitting or bending forward
- pain spreading to your bottom or thighs
- tight hamstrings (the muscles in the back of your thighs)
- pain, numbness or tingling spreading from your lower back down 1 leg ( sciatica )
Spondylolisthesis does not always cause symptoms.
Spondylolisthesis is not the same as a slipped disc . This is when the tissue between the bones in your spine pushes out.
Non-urgent advice: See a GP if:
- you have lower back pain that does not go away after 3 to 4 weeks
- you have pain in your thighs or bottom that does not go away after 3 to 4 weeks
- you're finding it difficult to walk or stand up straight
- you're worried about the pain or you're struggling to cope
- you have pain, numbness and tingling down 1 leg for more than 3 or 4 weeks
What happens at your GP appointment
If you have symptoms of spondylolisthesis, the GP may examine your back.
They may also ask you to lie down and raise 1 leg straight up in the air. This is painful if you have tight hamstrings or sciatica caused by spondylolisthesis.
The GP may arrange an X-ray to see if a bone in your spine has slipped forward.
You may have other scans, such as an MRI scan , if you have pain, numbness or weakness in your legs.
Treatments for spondylolisthesis
Treatments for spondylolisthesis depend on the symptoms you have and how severe they are.
Common treatments include:
- avoiding activities that make symptoms worse, such as bending, lifting, athletics and gymnastics
- taking anti-inflammatory painkillers such as ibuprofen or stronger painkillers on prescription
- steroid injections in your back to relieve pain, numbness and tingling in your leg
- physiotherapy to strengthen and stretch the muscles in your lower back, tummy and legs
The GP may refer you to a physiotherapist, or you can refer yourself in some areas.
Waiting times for physiotherapy on the NHS can be long. You can also get it privately.
Surgery for spondylolisthesis
The GP may refer you to a specialist for back surgery if other treatments do not work.
Types of surgery include:
- spinal fusion – the slipped bone (vertebra) is joined to the bone below with metal rods, screws and a bone graft
- lumbar decompression – a procedure to relieve pressure on the compressed spinal nerves
The operation is done under general anaesthetic , which means you will not be awake.
Recovery from surgery can take several weeks, but if often improves many of the symptoms of spondylolisthesis.
Talk to your surgeon about the risks and benefits of spinal surgery.
Causes of spondylolisthesis
Spondylolisthesis can:
- happen as you get older – the bones of the spine can weaken with age
- run in families
- be caused by a tiny crack in a bone (stress fracture) – this is more common in athletes and gymnasts
Page last reviewed: 01 June 2022 Next review due: 01 June 2025
Select a Community
- MB 1 Preclinical Medical Students
- MB 2/3 Clinical Medical Students
- ORTHO Orthopaedic Surgery
Are you sure you want to trigger topic in your Anconeus AI algorithm?
You are done for today with this topic.
Would you like to start learning session with this topic items scheduled for future?
Degenerative Spondylolisthesis

- Degenerative Spondylolisthesis is a common degenerative condition characterized by subluxation of one vertebral body anterior to the adjacent inferior vertebral body with intact pars.
- The condition is most common in females over 40 years of age, at the L4-5 level.
- Diagnosis is made with lateral radiographs. Flexion and extension lateral lumbar radiographs can identify the degree of instability. MRI studies can be helpful for central or foraminal stenosis.
- Treatment is a trial of nonoperative management with NSAIDs and physical therapy. Surgical management is indicated for progressive disabling pain that has failed nonoperative management, and/or progressive neurological deficits.
- ~9% in woman
- more common in African Americans, diabetics, and woman over 40 years of age
- increase in prevalence in women postulated to be due to increased ligamentous laxity related to hormonal changes
- this is different that isthmic spondylolisthesis which is most commonly seen at L5/S1
- sacralization of L5 (transitional L5 vertebrae)
- sagittally oriented facet joints
- facet joint degeneration
- facet joint sagittal orientation
- intervertebral disc degeneration
- ligamentous laxity (possibly from hormonal changes)
- disc degeneration leads to facet capsule degeneration and instability
- microinstability which leads to further degeneration and eventual macroinstability and anterolithesis
- instability is worsening with sagittally oriented facets (congenital) that allow forward subluxation
- caused by slippage, hypertrophy of ligamentum flavum, and encroachment into the spinal canal of osteophytes from facet arthrosis
- a degenerative slip at L4/5 will affect the L4 nerve root as it is compressed in the foramen
- loss of disk height
- osteophytes from posterolateral corner of vertebral body pushing the nerve root up against the inferior surface of the pedicle
- degenerative changes of the superior articular facet and posterior vertebral body
- most common presenting symptom
- usually relieved with rest and sitting
- second most common symptoms
- relieved by sitting
- not relieved by standing in one place (as is vascular claudication)
- may be unilateral or bilateral
- same symptoms found with spinal stenosis
- cauda equina syndrome (very rare)
- best seen with sit to stand exam maneuver
- best seen with heel-walk exam maneuver
- decreased patellar reflex
- weakness to EHL (great toe extension)
- weakness to gluteus medius (hip abduction)
- if pain resolves this is consistent with vascular claudication
- if pain resolves this is consistent with neurogenic claudication (DS)
- commonly found in this patients, and must differentiate this from neurogenic leg pain
- weight bearing lumbar AP, lateral neutral, lateral flexion, lateral extension
- slip is evident on lateral x-ray
- instability defined as 4 mm of translation or 10° of angulation of motion compared to adjacent motion segment
- persistent leg pain that has failed nonoperative modalities
- best study to evaluate impingement of neural elements
- T2 weighted sagittal and axial images best to look for compression of neurologic elements
- useful to identify bony pathology
- helpful in patients in which a MRI is contraindicated (pacemaker)
- most patients can be treated nonoperatively
- activity restriction
- second line of treatment if non-invasive methods fail
- most common is persistent and incapacitating pain that has failed 6 mos. of nonoperative management and epidural steroid injections
- progressive motor deficit
- cauda equina syndrome
- often combined with a posterior lumbar interbody fusion or transforaminal interbody fusion
- new data shows equivalent outcomes using cortical screw fixation verses pedicle screw fixation
- decompression often performed with a PLC perserving unilateral (undercutting) approach
- navigation and MIS techniques are widely used
- ~79% have satisfactory outcomes
- improved fusion rates shown with pedicle screws
- improved outcomes with successful arthrodesis
- smokers should undergo smoking cessation prior to surgery
- usually not indicated due to instability associated with spondylolithesis
- only indicated in medically frail patients who cannot tolerate the increased surgical time of performing a fusion
- ~69% treated with decompression alone are satisfied
- ~ 31% have progressive instability
- reserved for revision cases with pseudoarthrosis
- injury to superior hypogastric plexus can cause retrograde ejaculation
- posterior midline approach
- multiple parasagittal incisions for minimally invasive approaches
- usually done with laminectomy, wide decompression, and foraminotomy
- posterolateral fusion with instrumentation most common
- TLIF/PLIF growing in popularity and may increase fusion rates and decrease risk of postoperative slip progression
- limited role in adults
- in degenerative spondylolisthesis adding an interbody cage increases hospital costs without increasing fusion rates
- lower intraoperative blood loss, smaller skin incision, and decreased pain scores at 1-week post-op
- fusion rates and functional outcomes similar to conventional pedicle screw fixation
- other studies have demonstrated greater screw pullout strength given cortical contact of screw
- mostly described in combination with interbody fusion (PLIF or TLIF)
- trajectory is more cephalad and lateral than traditional screw
- cortical trajectory screws are generally smaller than traditional pedicle screws
- CT scan is more reliable than MRI for identifying failed arthrodesis
- risk of adjacent segment degeneration requiring surgery is about 20-29% at 10 years
- treat with irrigation and debridement (usually hardware can be retained)
- seen with prone positioning due to iliac bolster
- from prone positioning with inappropriate position
- increased intraoperative blood loss
- longer operative time
- number of levels fused
Technique guides are not considered high yield topics for orthopaedic standardized exams including ABOS, EBOT and RC.
- - Adult Isthmic Spondylolisthesis
- - Degenerative Spondylolisthesis
Please Login to add comment
- Virtual Visits Available
- 303-429-6448 Text Us
Spondylolisthesis
Causes, symptoms, treatment, & other resources.
How bad is spondylolisthesis surgery recovery? Let’s review what spondylolisthesis is, and what can be done.
What Is Spondylolisthesis?
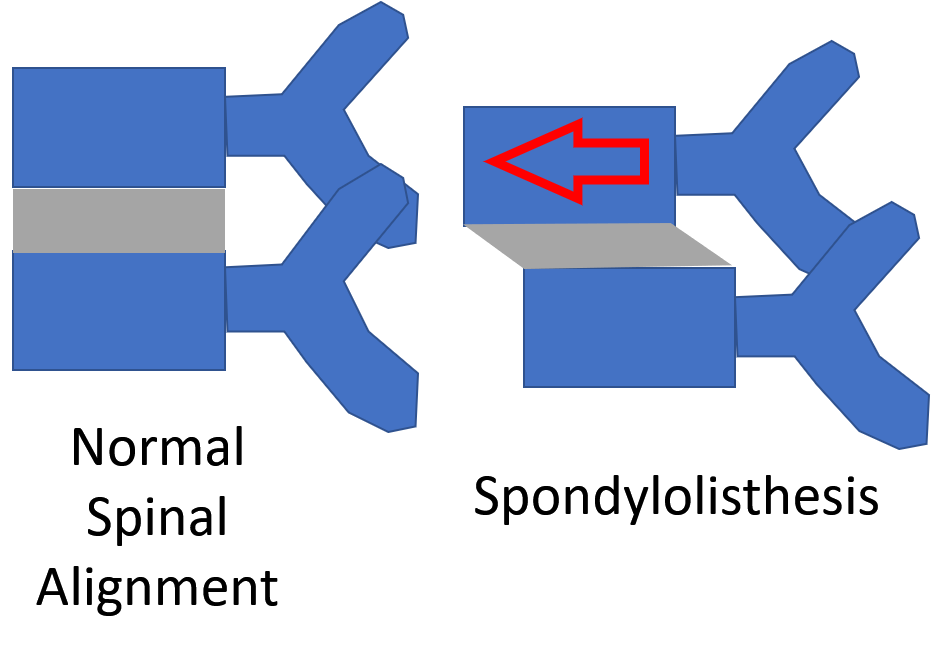
Spondylolisthesis means that one vertebra is slipping forward or backwards on another. This causes the hole where the nerve exits (foramen) to get smaller (also called foraminal stenosis). It also causes more wear and tear on the facet joint which can lead to arthritis or what’s called “facet hypertrophy”.
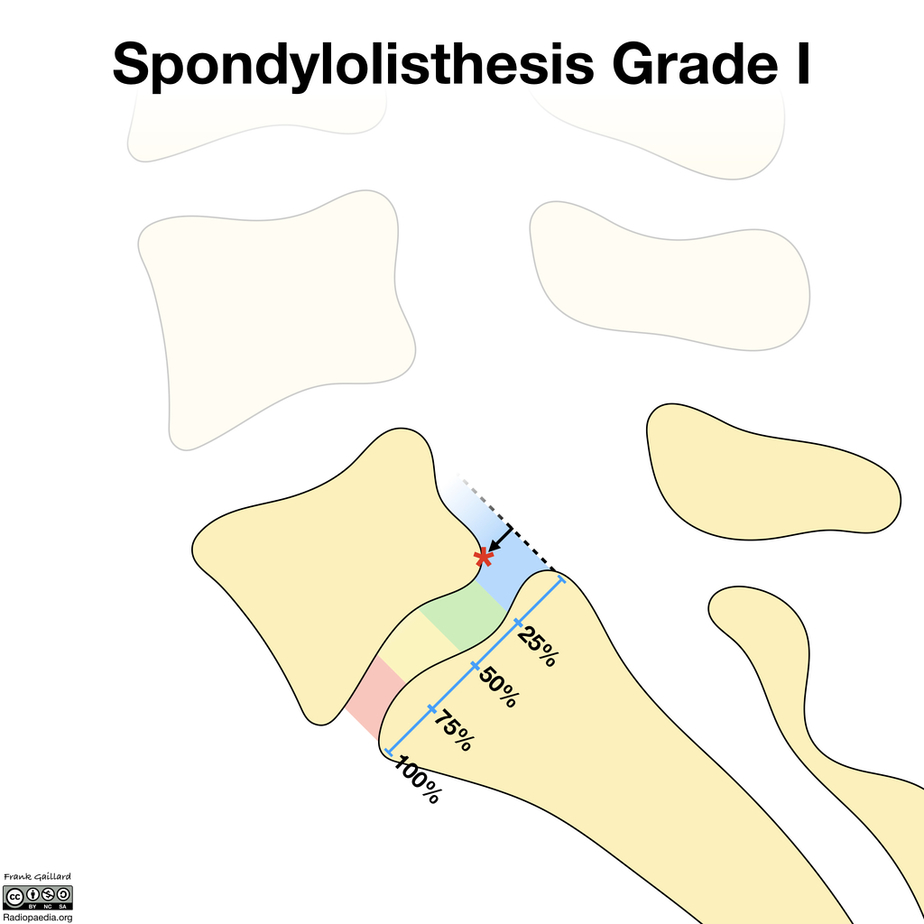
The amount of slippage is graded 1-4, with grade 1 meaning that the one vertebra has slipped up to 25% on the other vertebra. Grade 2 means that one bone has slipped from 25-50% with higher grades indicating more slippage. The vast majority of patients are grade 1 to 2.
What Causes It?
What causes this to happen? Some people are born with bones not properly connected (congenital spondylolisthesis), but most just have wear and tear arthritis which causes one vertebra to begin to shift (degenerative spondylolisthesis). When the bone isn’t connected this is also called spondylolysis and this issue is more common in men while degenerative spondylolisthesis is more common in women (1).
Symptoms of Spondylolisthesis
Spondylolisthesis may not have any symptoms. Some people have it without realizing it. If you do, lower back discomfort is usually the primary symptom. The discomfort might extend down your legs and into your buttocks. You could also get:
- Back stiffness.
- Difficulty walking or standing for lengthy periods of time.
- Pain when bending over.
- Numbness, weakness, or tingling in the foot, hamstrings, calves, knees, and legs.
Big Toe Numbness
Believe it or not, one of those significant issues that can present as numbness stems from the low back. In the lumbar spine, the nerve that exits the spine at the L5 level branches down through the hip, thigh, knee, lower leg, and, yes, all the way into the foot and toes. So a pinched or irritated nerve at that L5 level in the back can create problems, such as pain, numbness, tingling, and so on, anywhere along the nerve branch. So what can irritate the L5 spinal nerve? The list is long, but it includes disc issues, such as herniated…
Knee Buckling
Knees can buckle, causing a sensation of one or both knees giving out that affects nearly 17% of adults. The knees are regarded to be one of the most essential (and biggest) joints in the human body because they play significant roles in basic activities such as walking and sitting. When our knees begin to feel unstable, weak, or begin giving out, it is easy to become stressed since we rely so heavily on them for movement. The knee can become stable from numerous types of injuries. The knee is kept stable by the following structures: Tendons attach the leg muscles…
Leg Feels Disconnected
So what exactly causes the leg to feel disconnected? The hip joint is the connection point between the leg and the rest of the body. The femur in the leg and the acetabulum in the pelvis create the hip joint. So if the left SI joint, for example, in the back and the symphysis pubis joint in the front becomes unstable due to loose supporting ligaments, then the left leg, which is connected between the two joints, is likely to also feel a bit disconnected. Likewise, if the right SI joint were unstable, then the right leg might feel disconnected. How This Patient’s “Disconnected” Leg Was Fixed Despite “leg feels…
Leg Gives Out
Have you ever been walking and your leg gives out? It can be both surprising and alarming What would cause your leg to give out? Can sciatica cause your leg to give out? How do you treat weak legs? Let’s dig in.Weakness in the leg can arise from three principal sources: nerve problems, muscle weakness, and SI joint dysfunction. Weakness in the legs may indicate a significant nerve problem. In many cases, it may be the first indication of a nerve problem. There are three common causes of nerve injury: low back disorders, nerve compression as it descends down into the hip, thigh, and shin and medical conditions such as diabetes…
Lower Back Pain When Sitting
After a long day on your feet sitting down is supposed to be way to relaxing. Unfortunately for some sitting for any length of time can be painful. Most people experience low back pain at some point in their life. The lifetime prevalence of low back pain is 85% (1). Let’s take a deeper look at the different types of pain and causes of low back pain when sitting. Pain can present in many different ways. It can be intermitent or constant. The quality of the low back pain can also vary depending upon the actual source of injury. Common examples include: Sharp and Stabbing, Dull and Aching, Throbbing/ Pulsating, Pins and Needles, Burning, Electrical
Lower Back Pain When Standing
When you’re seated, the facet joints in your lower back are in an open and slightly flexed position. When you stand up, these joints compress. If they are painful or have arthritis, you’ll have pain as you stand up because this puts pressure on the painful joints. In addition, if there is any type of movement of one vertebra forward on another (called spondylolisthesis), then this shift will have occurred as you sit. This is called degenerative spondylolisthesis. When you get back up, the vertebrae will come back into position after a few seconds, leading to that awkward “walk it out period” that starts out painful and ends up more normal.
SI Joint Pain
The SI Joint is an important joint in the lower back that can cause pain and dysfunction. Pain is typically one-sided involving the low back and buttock but when severe can radiate down the leg. Each of us has a right and left SI joint. The pelvic ring consists of the two SI Joints and the symphysis pubis. Each is rich in supporting ligaments that provide stability for the joint. SI Joint pain is aggravated by ligament instability and muscle weakness. Physical therapy is the first line of treatment for SI Joint injuries. For best clinical results the stability of the joint and muscle strength must be evaluated and treated…
Tight Hamstrings & Calves
The hamstrings are a group of muscles in the upper leg. They are located on the backside of the upper leg and are comprised of three muscles: biceps femoris, semitendinosus, and semimembranosus. The calf muscles are located on the backside of the lower leg and are comprised of two muscles: the gastrocnemius and soleus. Tight hamstring and calf muscles can be painful, limiting someone mobility. They also make lower extremity muscles more vulnerable to injuries. Tight hamstrings and calves can arise from different sources which include: medication, muscle and tendon injury, overuse, muscle imbalance, dehydration, poor posture, low back injury…
Upper Back Pain Between The Shoulder Blades
Upper back pain between the shoulder blades is also known as interscapular pain. Fifteen percent of the population suffers from chronic upper back pain. Finding the source of interscapular pain can be tricky because the upper back houses many important structures like the heart, the upper lobes of the lung, the cervical spine, the scapulas, and a dozen or so of muscles and nerves.
Weak in Knees
Weakness in the knee can be a symptom of many different knee conditions. Some of the most common causes of weakness in the knee include ligament tears, meniscus tears, and arthritis. Another important but often overlooked cause of knee weakness is irritation or injury of the nerves in the low back. If you are experiencing any type of weakness in your knee for long durations of time (3 weeks), it is important to see a doctor to determine the cause. Some of the most common symptoms of knee weakness include difficulty standing up from a seated position, difficulty walking, climbing or descending stairs…
Can You Become Paralyzed from Spondylolisthesis?
One reason patients decide to embark on spondylolisthesis surgery recovery is that they’re told they could become paralyzed if they don’t have immediate surgery. However, it is very unlikely that you will become paralyzed from a prior spinal abnormality like spondylolisthesis, even if you’re in a car crash. For example, patients with spinal stenosis (where the hole for the spinal cord is too small) are often told that if they sustain significant trauma they may become paralyzed hence they need surgery now. However, research has shown that the risks from the surgery are much greater than any risk of paralysis (2).
Treatment Options for Spondylolisthesis
There are various non-surgical therapies available to help you manage and reduce discomfort. The following are among them:
- Physical therapy. You can increase the strength of the muscles surrounding the afflicted region by exercising in a way that minimizes strain on your back and increases mobility.
- Medication. The pain can be managed by any of a number of over-the-counter pain medications, including Tylenol or anti-inflammatory medicines. A doctor may also subscribe muscle relaxers.
- Epidural steroid injections. For patients suffering significant pain or numbness in the back or legs, an epidural steroid injection can reduce inflammation and relieve pain.
- Platelet-rich plasma injection (more specifically, the Perc-FSU procedure)
When conservative care ends, surgery is often the first thing that is called for. However, this shouldn’t be the case. Why? Let’s dig in.
ACDF Surgery
ACDF stands for “anterior cervical discectomy and fusion.” It is a surgical procedure performed on the neck to relieve pressure on the spinal cord or nerve roots caused by a damaged or degenerated disc. During the procedure, the surgeon removes the damaged disc and replaces it with a bone graft or synthetic implant. Metal plates and screws may be used to hold the vertebrae together during the fusion process. ACDF surgery can help relieve symptoms such as neck pain, numbness, tingling, and weakness in the arms or hands caused by nerve compression in the neck. It is a commonly performed procedure…
Cervical Disc Replacement
Cervical disc arthroplasty (CDA), also known as cervical disc replacement, is a surgical procedure used to treat cervical disc disease. The procedure involves removing the damaged or degenerated intervertebral disc in the cervical spine and replacing it with an artificial disc device. CDA is typically performed for patients with symptomatic cervical disc disease, such as disc herniation, degenerative disc disease, or spinal stenosis. The procedure is intended to relieve symptoms such as neck pain, arm pain, and numbness or tingling in the arms or hands. CDA is considered a less invasive and more motion-preserving alternative to traditional cervical spinal fusion surgery…
Cervical Epidural Steroid Injection
The neck pain started out as a dull ache but steadily progressed. It becomes constant and oftentimes keeps you up at night. Turning your head can send an electrical current down your arm. Rest, medications and physical therapy failed to provide much relief. Your doctor referred you to a pain clinic for a Cervical Epidural steroid injection. The injection was performed at an ambulatory surgical center. Unfortunately, the pain is now worse. What is a Cervical Epidural injection? Are there different types of Cervical Epidural injections? What are…
Cervical Fusion
Cervical Fusion is often recommended when chronic neck pain problems worsen over time. What exactly is it? Cervical Fusion is a major surgery that involves joining one or more of the spinal bones together using screws, bolts, and plates (1). The hardware may be placed in the front (anterior) or the back( posterior) of the Cervical spine. The disc between the spinal bones is often times removed and replaced with a bone graft or a spacer. The neck of composed of 7 boney building blocks that are numbered from 1-7. The letter C is associated with the numbers to designate the Cervical Spine.
Disc Replacement Surgery
The surgeon first accesses the spinal column (for example, in the cervical spine, the surgeon would access the spine through an incision in the front of the neck). From here the surgery is quite aggressive as the disc is scraped and chiseled out of the disc space. Pins are screwed into the vertebrae above and below the disc space that will anchor the space in place as the surgeon works. A tool is inserted into the disc space and used to further separate the upper and lower vertebrae, enlarging the space. The vertebrae surfaces within the disc space are prepared…
L 4/5 Fusion Surgery
Spinal fusion is a major surgery where one or more spinal bones (vertebrae) are fused together using screws, bolts, and or plates. The hardware may be placed in the front (anterior) or the back (posterior) of the spine. The disc between the spinal bones is often times removed and replaced with bone or a spacer. L 4/5 refers to the level of the surgery. There are 5 spinal bones in the low back which are numbered from top to bottom L1, L2, L3, L4, and L5. Sandwiched between each of the spinal bones is a disc. The disc is named for the two spinal bones it is sandwiched between.
L5 S1 Fusion Surgery
Spinal fusion is a major surgery where one or more spinal bones (vertebrae) are fused together using screws, bolts, and or plates. The hardware may be placed in the front (anterior) or the back (posterior) of the spine. The disc between the spinal bones is often times removed and replaced with bone or a spacer. L5 S1 Fusion refers to the level of the surgery. There are 5 spinal bones in the low back which are numbered from top to bottom L1, L2, L3, L4, and L5. Sandwiched between each of the spinal bones is a disc. The disc is named for the two spinal bones it is sandwiched between.
The other day I was evaluating a patient and reviewing the treatment options for their spine condition. After discussing prior treatments, we got to the topic of medications taken for pain relief. She explained that she mainly utilized anti-inflammatory (NSAID) medications and then she told me to hold much she takes and has been for many years…..she takes close to 2 grams (2000 milligrams) on a daily basis which equated to about 9-10 capsules of medication per day. I was shocked, considering she was pre-diabetic and with high blood pressure plus the kicker of it is that her PCP (primary care physician) is ok with this…
Perc-FSU – Trusted Alternative to Spinal Fusion
The Perc-FSU Procedure is an injection-based treatment that utilizes the patients’ own blood platelets to bring stability to the spine without the need for the rods, nuts, bolts, and hardware of fusion surgery. “Perc” stands for percutaneous, and “FSU” stands for “Functional Spinal Unit,” which means that the spine is treated as one functioning unit. Up and down the spine, the discs, facet joints, ligaments, and muscles that assist in stabilizing the spine are treated with image-guided injections of PRP and Platelet Lysate to help bring stability to the spine as a whole. It is the trusted alternative to spinal fusion.
PLIF Surgery
PLIF is a specific type of lumbar fusion surgery. It is an acronym that stands for the Posterior Lumbar Interbody Fusion (1). Posterior refers to the approach used by the surgeon. Posterior refers to the backside of the body vs anterior which refers to the front. Lumbar is the section of the spine involved. The spine is divided into cervical, thoracic, and lumbar. Lumbar is your low back. Interbody fusion refers to a specific type of fusion. For example, in interbody fusion, the disc is surgically removed and a bone graft and spacer is inserted between the spinal bones (vertebral bodies). The inserted bone graft is expected…

Thoracic Spine Surgery
Thoracic spine surgery is a major surgery aimed at treating injuries in the thoracic spine. Because of the complex anatomy and close proximity to the heart and lungs, there are significant surgical risks and complications. Surgery on the thoracic spine can take hours and may require deflating the lung in order to gain access to the thoracic injury. Recovery can be lengthy depending upon the specific thoracic spine surgery performed. There are several different types of thoracic spine surgery. The specific thoracic spine performed depends upon the underlying thoracic injury and a symptoms of the patient. For example, a thoracic disc herniation…
Transforaminal Lumbar Interbody Fusion (TLIF)
Transforaminal Lumbar Interbody Fusion is a variant of the Posterior Lumbar Interbody Fusion (PLIF) technique described by Cloward in the 1950s. PLIF has been associated with the high incidences of neurological complications, up to 13.6% of permanent neurologic lesions in Barnes’ et al. study, in particular of the traversing nerve root (2,3) This is due to the fact that a great amount of traction on the dural sac is required to implant the interbody fusion devices. Surgeons have transitioned to TLIF in efforts to reduce complication rates. Success rates vary depending on what literature you read and recently all orthopedic surgery literature has come under fire…
Is Surgery for Spondylolisthesis Successful?
There different types of surgeries performed for this condition and each has a different spondylolisthesis surgery recovery pathway. First up is fusion, which means that the doctor uses rods and screws to bolt the spine together. The discs, which are usually mobile shock absorbers, are removed and a bone or a spacer device is inserted in that spot. Another option is decompression surgery without fusion, where the doctor will remove bone, parts of the disc, or ligaments to “open up” the area around the spinal nerves.
If you opt for more aggressive spinal fusion surgery, one major decision you’ll have to make is whether to get fusion and opt for a longer recovery. Meaning the decompression is usually performed, but the surgeon can either fuse or not. The research on which is better shows no difference between decompression with or without fusion (9,10). So why is fusion often added? That’s a great question to which there is no easy answer.
Also, realize that the gold standard in medical research is comparing a surgery against a faked procedure known as a sham operation. No such research exists for spondylolisthesis surgery. Meaning we have no high-level research on whether the surgery is more effective than doing nothing.
What Does Spondylolisthesis Surgery Recovery Look Like?
Your spondylolisthesis surgery recovery will be longer starting with spending more time in the hospital (generally a few days) if you have fusion surgery. Fusion patients also need more narcotics for the first two months compared with decompression alone (11). In a worker’s comp setting, only 30-60% of patients who had the fusion surgery returned to full-time work (12).
What are the Complications of a Lumbar Fusion?
There are a several ways in which fusion surgery can fail and here are the categories:
- Non-union (failure of the bones to heal or grow together)
- Loosening or breakage of the hardware (screws, rods, and connectors)
- Pain caused by the hardware
- ASD (Adjacent segment disease)
First, the level being operated on and fused together with bone can fail to heal and this problem is called a non-union. For procedures that need more bone, like a fusion that is posterior-lateral, the non-union rates can be quite high from 26% to 36% (3, 4). The screws or rods can break or cause pain themselves and both common reasons a second surgery is undertaken after an initial fusion. Overall, a bit more than 1 in 10 patients who have a low back fusion require a second surgery to fix a problem with the first operation (5).
Adjacent segment disease (ASD) means that the spinal levels above or below get degenerated due to excessive force on those areas because of the solid fusion (6). At about 24 months after a back fusion, 12% of patients will get ASD (7). In addition, about 2-4% of the patients will get ASD for every year the patient is active after the fusion, so at 5-years after the first operation, up to 1 in 5 patients will get ASD (8). To understand more, watch my video below:
Can Spondylolisthesis Be Cured without Surgery?
I have a grade 1 degenerative spondylolisthesis, so I’m pretty experienced with this one. Have I had a fusion or decompression surgery? Nope. What did I have done?
As discussed, this problem usually happens because of loose ligaments. There are also arthritic facet joints and pinched nerves and weak muscles. Hence, I had the Perc-FSU (Percutaneous-Functional Spinal Unit) procedure where my own blood platelets were concentrated and injected precisely using x-ray guidance into the ligaments, joints, muscles, and around nerves. This allowed me to get more functional with fewer problems and combined with gains from physical therapy, I no longer throw my back out every time I lean forward. My x-rays also look better, no longer showing that pronounced slippage of L5 on S1. See the video below for information on that procedure:
The upshot? Spondylolisthesis surgery recovery can be rough. That’s why I decided to skip the surgery. Instead, I used Regenexx procedures for spine and cervical conditions . However, if you do need surgery, the research is clear that fusion isn’t required.
Doctors Who Assist with Spondylolisthesis

Christopher J. Centeno, MD
Christopher J. Centeno, M.D. is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno is one of the few physicians in the world with extensive experience in the culture expansion of and clinical use of adult bone marrow concentrate to treat orthopedic injuries. His clinic incorporates a variety of revolutionary pain management techniques to bring its broad patient base relief and results. Dr. Centeno treats patients from all over the US who…

John Schultz, MD
John R. Schultz M.D. is a national expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate for orthopedic injuries. He is board certified in Anesthesiology and Pain Medicine and underwent fellowship training in both. Dr. Schultz has extensive experience with same day as well as culture expanded bone marrow concentrate and sees patients at the CSC Broomfield, Colorado Clinic, as well the Regenexx Clinic in Grand Cayman. Dr. Schultz emphasis is on the evaluation and treatment of thoracic and cervical disc, facet, nerve, and ligament injuries including the non-surgical treatment of Craniocervical instability (CCI). Dr. Schultz trained at George Washington School of…

John Pitts, M.D.
Dr. Pitts is originally from Chicago, IL but is a medical graduate of Vanderbilt School of Medicine in Nashville, TN. After Vanderbilt, he completed a residency in Physical Medicine and Rehabilitation (PM&R) at Emory University in Atlanta, GA. The focus of PM&R is the restoration of function and quality of life. In residency, he gained much experience in musculoskeletal medicine, rehabilitation, spine, and sports medicine along with some regenerative medicine. He also gained significant experience in fluoroscopically guided spinal procedures and peripheral injections. However, Dr. Pitts wanted to broaden his skills and treatment options beyond the current typical standards of care.

Jason Markle, D.O.
Post-residency, Dr. Markle was selected to the Interventional Orthopedic Fellowship program at the Centeno-Schultz Clinic. During his fellowship, he gained significant experience in the new field of Interventional Orthopedics and regenerative medicine, honing his skills in advanced injection techniques into the spine and joints treating patients with autologous, bone marrow concentrate and platelet solutions. Dr. Markle then accepted a full-time attending physician position at the Centeno-Schultz Clinic, where he both treats patients and trains Interventional Orthopedics fellows. Dr. Markle is an active member of the Interventional Orthopedic Foundation and serves as a course instructor, where he trains physicians from around the world.

Brandon T. Money, D.O., M.S.
Dr. Money is an Indiana native who now proudly calls Colorado home. He attended medical school at Kansas City University and then returned to Indiana to complete a Physical Medicine and Rehabilitation residency program at Indiana University, where he was trained on non-surgical methods to improve health and function as well as rehabilitative care following trauma, stroke, spinal cord injury, brain injury, etc. Dr. Money has been following the ideology behind Centeno-Schultz Clinic and Regenexx since he was in medical school, as he believed there had to be a better way to care for patients than the status quo. The human body has incredible healing capabilities…
Other Resources
The Spine Owner’s Manual: How to Avoid Back Pain & Life-Altering Surgery
This e-book from Dr. Chris Centeno focuses on the spine and how it functions within the human musculoskeletal system and the body as a whole. Everything in our bodies works together like a well-tuned symphony to support our well-being, and a strong spine (including all of its component parts, such as spinal nerves, ligaments, muscles, etc.) is critical to complete health.
Using the Regenexx SANS approach, The Spine Owner’s Manual provides a series of tests and clearly defined exercises that you can do on your own to measure and monitor your own spinal health. These musculoskeletal tests will allow you to monitor where your own body might be struggling to maintain proper stability, articulation, symmetry, and neuromuscular function.
Relevant Blog Posts
Back cracking: the truth of what’s actually happening in your body.
Back cracking is a phenomenon that many people experience, often eliciting both curiosity and concern. Whether it’s the satisfying pop from a morning stretch or the deliberate twist during a yoga session, the sound and sensation of cracking your back can be oddly gratifying. But what exactly is happening inside your body when you hear…
Back Fusion
Spinal fusion, also known as back fusion, is a surgical procedure designed to help severe spinal instability that causes severe pain or nerve injuries. It involves permanently connecting two or more vertebrae in your spine to eliminate motion between them. This article will delve into the intricacies of spinal fusion, exploring the reasons behind the…
Understanding the Normal Curvature of the Spine
The human spine, a marvel of engineering, is not a straight column but rather a structure with gentle curves. These natural curves are essential for maintaining balance, allowing flexibility, and absorbing the shock of movement. The spine’s curvature plays a critical role in overall health, influencing posture, mobility, and the function of the nervous system. …
Spinal Anterior Longitudinal Ligament Function
Have you had a neck injury or whiplash trauma? Do you have neck pain, especially when looking up, and you don’t know the cause? Then you may want to learn about the cervical anterior longitudinal ligament (ALL). Anatomy of the Anterior Longitudinal Ligament The ALL is a strong, wide ligament that runs along the front…
Effective Thoracic Herniated Disc Treatment Exercises You Can Do
A thoracic herniated disc occurs when the soft center of a spinal disc in the thoracic area of the spinal region ruptures. This condition can lead to symptoms such as pain, numbness, and weakness in the chest, back, and potentially radiating down the arms, legs or abdomen. Effective thoracic herniated disc treatment often involves a…
The L5 Vertebra: Everything You Need to Know
The spine, consisting of 33 individual bones called vertebrae, is divided into five major regions: cervical (neck), thoracic (upper back), lumbar (lower back), sacral (pelvic region), and coccygeal (tailbone). These vertebrae are separated by intervertebral discs, which act as cushions and allow for flexibility in movement. The lumbar spine, also known as the lower back,…
References:
(1) Osti L, Buda M, Del Buono A. Fatty infiltration of the shoulder: diagnosis and reversibility. Muscles Ligaments Tendons J. 2014;3(4):351–354. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3793342/
(2) Murphy, Donald R et al. “Cervical spondylosis with spinal cord encroachment: should preventive surgery be recommended?.” Chiropractic & osteopathy vol. 17 8. 24 Aug. 2009, doi: 10.1186/1746-1340-17-8
(3) Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991 Jul; 73(6):802-8. https://www.ncbi.nlm.nih.gov/pubmed/2071615/
(4) Tsutsumimoto T, Shimogata M, Yoshimura Y, Misawa H. Union versus nonunion after posterolateral lumbar fusion: a comparison of long-term surgical outcomes in patients with degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(8):1107–1112. doi: 10.1007/s00586-008-0695-9
(5) Greiner-Perth R, Boehm H, Allam Y, Elsaghir H, Franke J. Reoperation rate after instrumented posterior lumbar interbody fusion: a report on 1680 cases. Spine (Phila Pa 1976). 2004 Nov 15;29(22):2516-20. https://www.ncbi.nlm.nih.gov/pubmed/15543064
(6) Saavedra-Pozo FM, Deusdara RA, Benzel EC. Adjacent segment disease perspective and review of the literature. Ochsner J. 2014;14(1):78–83. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3963057/
(7) Zhong ZM1 Deviren V, Tay B, Burch S, Berven SH. Adjacent segment disease after instrumented fusion for adult lumbar spondylolisthesis: Incidence and risk factors. Clin Neurol Neurosurg. 2017 May;156:29-34. doi: 10.1016/j.clineuro.2017.02.020 .
(8) Tobert DG, Antoci V, Patel SP, Saadat E, Bono CM. Adjacent Segment Disease in the Cervical and Lumbar Spine. Clin Spine Surg. 2017 Apr;30(3):94-101. doi: 10.1097/BSD.0000000000000442 .
(9) Försth P, Ólafsson G, Carlsson T, Frost A, Borgström F, Fritzell P, Öhagen P, Michaëlsson K, Sandén B. A Randomized, Controlled Trial of Fusion Surgery for Lumbar Spinal Stenosis. N Engl J Med. 2016 Apr 14;374(15):1413-23. doi: 10.1056/NEJMoa1513721 .
(10) Noorian S, Sorensen K, Cho W. A systematic review of clinical outcomes in surgical treatment of adult isthmic spondylolisthesis. Spine J. 2018 Aug;18(8):1441-1454. doi: 10.1016/j.spinee.2018.04.022 .
(11) Vail D, Azad TD, O’Connell C, Han SS, Veeravagu A, Ratliff JK. Postoperative Opioid Use, Complications, and Costs in Surgical Management of Lumbar Spondylolisthesis. Spine (Phila Pa 1976). 2018;43(15):1080–1088. doi: 10.1097/BRS.0000000000002509
(12) Anderson JT, Haas AR, Percy R, Woods ST, Ahn UM, Ahn NU. Workers’ Compensation, Return to Work, and Lumbar Fusion for Spondylolisthesis. Orthopedics. 2016 Jan-Feb;39(1):e1-8. doi: 10.3928/01477447-20151218-01
If you need stem cell therapy in Denver CO , please gives us a call at 303-429-6448.
Wait! Did you get your free download of The Spine Owner's Manual?
This book is full of tests and exercises to understand what is happening to cause your orthopedic pain.
Ready to get help for your Spondylolisthesis?
- 303-429-6448
- East Of England
- North East & Yorkshire
- 01223 266900 Cambridge Lea Hospital
- 01277 232525 Hartswood Hospital
- 01603 456181 Norwich Hospital
- 01702 462944 Wellesley Hospital
- Clinics and Centres
- 020 8950 9090 Bushey Hospital
- 01582 763 191 Harpenden Hospital
- 020 8551 1100 London East Hospital
- 020 8337 6691 St Anthony's Hospital
- 01753 662241 Thames Valley Hospital
- 020 8901 0330 Elstree Cancer Centre
- 020 8736 4608 Spire Bushey Diagnostic Centre
- 0116 2720888 Leicester Hospital
- 0121 353 2444 Little Aston Hospital
- 0115 937 7800 Nottingham Hospital
- 0121 704 1451 Parkway Hospital
- 01905 350003 South Bank Hospital
- 01905 402 547 The Spire Clinic, Droitwich Spa
- 0114 263 0330 Claremont Hospital
- 01422 324000 Elland Hospital
- 01482 659471 Hull and East Riding Hospital
- 0113 269 3939 Leeds Hospital
- 01977 518518 Methley Park Hospital
- 0191 415 1272 Washington Hospital
- 01924 410 610 Spire Dewsbury Clinic
- 0808 239 6869 Spire Healthcare Harrogate Clinic
- 01482 659 471 Spire Hesslewood Clinic
- 01482 659 471 Spire Lowfield Clinic
- 01925 265 000 Cheshire Hospital
- 01253 394 188 Fylde Coast Hospital
- 0151 733 7123 Liverpool Hospital
- 0161 447 6677 Manchester Hospital
- 0151 648 7000 Murrayfield Hospital Wirral
- 01625 501 150 Regency Hospital Macclesfield
- 0161 447 6700 Spire Kenmore Clinic
- 0161 927 3878 Spire Manchester Clinic Hale
- 0161 447 6888 The OrthTeam Centre
- 01829 289 057 Spire Tarporley Clinic
- 0131 334 0363 Edinburgh Hospitals, Murrayfield and Shawfair Park
- 01634 687 166 Alexandra Hospital
- 01252 850 216 Clare Park Hospital
- 0118 958 7676 Dunedin Hospital
- 01293 785 511 Gatwick Park Hospital
- 02392 456 000 Portsmouth Hospital
- 023 8077 5544 Southampton Hospital
- Tunbridge Wells Hospital
- 01273 828120 Montefiore Hospital
- 0117 980 4000 Bristol Hospital
- 01454 456500 GenesisCare Bristol
- 029 2073 5515 Cardiff Hospital
- 01978 438 478 Yale Hospital
- 01978 291 306 Spire Yale - Chesney Court Outpatient and Diagnostic Centre
- 01745 828 900 Spire Abergele Clinic

Search for hospitals, consultants & treatments
- Conditions >
Spondylolisthesis
Persistent back pain and numbness down your legs may be caused by spondylolisthesis, where one of the bones in your spine has slipped out of position.
By Wallace Health I Medically reviewed by Adrian Roberts. Page last reviewed: October 2018 I Next review due: October 2023
What is spondylolisthesis?
This usually occurs in your lower back but can also occur in your neck or mid to upper back. A slipped vertebra can put pressure on the nerves in your spinal canal, which connect your brain and your body. This can cause pain, pinching, numbness and weakness, usually in your lower back and legs.
Spondylolisthesis is not the same as a slipped disc — a slipped disc refers to one of the fluid-filled cushions between your vertebrae slipping out of position.
Spondylolisthesis is pronounced spohn-di-low-less-THEE-sis. In Greek, spondylos means spine or vertebra and listhesis means movement, sliding or slipping.
Is spondylolisthesis the same as spondylolysis?
Spondylolysis and spondylolisthesis both cause lower back pain but they are not the same condition.
Spondylolysis is caused by a bone defect in your spine, which is usually caused by a stress fracture. It is common in young athletes.
Spondylolisthesis is caused by a vertebra slipping out of place and putting pressure on the vertebra below it as well as the nerves that run through the spinal canal.
However, spondylolysis can cause spondylolisthesis if the stress fracture results in the vertebra slipping.
How to tell if you have spondylolisthesis
Spondylolisthesis is most common in your lower back and might cause these symptoms:
- Lower back pain which may get worse during activity
- Pain, numbness or pins and needles down your legs (these symptoms are known as sciatica )
- Tight hamstrings
- Curvature or bulging of the spine
If you have difficulty walking and feel unsteady on your feet, this may also be a sign.
It's possible to have spondylolisthesis without any of these symptoms.
Talk to your doctor if you’re concerned about symptoms
You can book an appointment with a Spire private GP today.
Book an appointment

Diagnosis and tests for spondylolisthesis
You should see your GP if:
- You have persistent back pain or stiffness
- You have persistent pain in your buttocks or thighs
- Your back curves outwards
Your GP may examine your back, although spondylolisthesis doesn’t usually cause any visible symptoms. They may also examine your limbs to see the amount of movement and pain you have. This may include a straight leg test — this involves lying on your back while your GP holds your foot and gently lifts your leg up while you keep your knee straight.
You may need an X-ray while standing to see if you have a slipped vertebra in your spine or a spinal fracture. If you have numbness, weakness or tingling in your legs, you may also need an MRI scan or CT scan to detect if your slipped vertebra is compressing a nerve.
Causes of spondylolisthesis
There are different causes of spondylolisthesis:
- A birth defect in a vertebra — this can cause the vertebra to slip forward
- A sudden injury, such as a fracture from a car accident
- An infection or tumour that causes a bone abnormality
- Gradual wear and tear of the vertebrae and cartilage ( osteoarthritis ) — this is more common in older people
- Repetitive trauma, such as heavy weight lifting or gymnastics, which causes a defect in your spine to develop
- Spinal stenosis
Types of spondylolisthesis
The three most common types of spondylolisthesis are:
- Congenital spondylolisthesis — a defect in the formation of a baby's spine before birth that increases the risk of a vertebra slipping in later life
- Degenerative spondylolisthesis — the most common type of spondylolisthesis caused by thinning of the vertebral discs (fluid-filled cushions that sit between the vertebrae) as you get older; the discs thin because they lose water and thinner discs increase the chance of a vertebra slipping out of place
- Isthmic spondylolisthesis — caused by spondylolysis ie a defect of the spine usually caused by a stress fracture
Less common types of spondylolisthesis include:
- Pathological spondylolisthesis — caused by a disease (eg osteoporosis) or a tumour
- Post-surgical spondylolisthesis — caused by spinal surgery
- Traumatic spondylolisthesis — caused by an injury to the spine
Who is at risk of spondylolisthesis?
Your risk of developing spondylolisthesis is greater if:
- You are a young athlete — children and teenagers who play sports that stretch the lower spine eg football or gymnastics; spondylolisthesis usually occurs during a growth spurt and is the most common cause of back pain in teenagers
- You are aged over 50 — degenerative spondylolisthesis is more likely as you get older as it is caused by wear and tear of the spine over time, although it also has a genetic component
- You are born with part of your vertebra called the pars interarticularis being thinner than normal — the pars interarticularis connects the facet joints which link a vertebra to the vertebrae above and below it so your spine can function as a unit; a thinner pars interarticularis is more likely to fracture and cause the vertebra to slip
- You have another degenerative spinal condition
Common treatments for spondylolisthesis
The treatment you receive will depend on the severity of your symptoms and how much they are affecting your quality of life. In most cases, your doctor will recommend non-surgical treatments first, such as:
- Anti-inflammatory painkillers eg ibuprofen — if over-the-counter medications are not enough to reduce your pain, your doctor may prescribe stronger painkillers
- Bracing — usually only for children
- Steroid injections to relieve inflammation and pain — this includes:
- Facet joint injections
- Injections around the nerve that is being compressed by the slipped vertebra
- Physiotherapy — targeted daily exercises to stretch and strengthen your abdomen, hamstrings and lower back; this will help reduce your pain and increase your range of motion
- Rest — avoiding activities, such as bending, lifting, athletics and other sports, for a short period of time
These treatments provide temporary relief and during this time, your symptoms may go away on their own.
Your doctor will usually only recommend back surgery if:
- A nerve is compressed
- Non-surgical treatments have not worked
- Your symptoms are persistent and severe
The type of back surgery you have will depend on what type of spondylolisthesis you have. This could be:
- Decompression surgery to remove part of your spine to relieve pressure
- Surgery to fuse the slipped vertebra to the vertebrae next to it using metal rods and screws and a piece of your own bone — this will keep the slipped vertebra in place
- Surgery to remove the vertebral disc between two vertebrae and replace it with a metal cage containing a bone graft — this will hold the vertebrae apart
These are major surgeries and you will need to stay in hospital for up to a week. It will take months for a full recovery.
Surgery usually relieves many spondylolisthesis symptoms, including pain and numbness in the legs. However, there are risks of complications, including:
- Damage to the spinal nerves or spinal cord — this can cause ongoing symptoms of numbness or weakness in the legs and in rare cases, bowel incontinence , urinary incontinence or paralysis
- Deep vein thrombosis (DVT) — a blood clot in one of the deep veins in your leg
- Infection at the surgical site
Your doctor or surgeon will discuss the details of your surgical options and the risks involved before you make a decision.
Will spondylolisthesis come back?
In most cases, pain caused by spondylolisthesis goes away after recovering from spondylolisthesis surgery. Over time, you can return to your normal activities and regain full function and movement.
Spondylolisthesis complications
Spondylolisthesis can cause cauda equina syndrome. At the base of your spinal cord is a collection of nerves called the cauda equina. In cauda equina syndrome, these nerves are compressed, which can cause loss of feeling in your legs and bladder problems. It is a medical emergency. If it is not treated it can cause urinary incontinence and paralysis.
How can I reduce my risk of spondylolisthesis?
- Eat a healthy, balanced diet to maintain strong bones
- Maintain a healthy weight — being overweight or obese puts extra strain on your spine
- Perform regular exercises to strengthen your back and abdomen
Spondylolisthesis outlook
In some cases, spondylolisthesis comes back but this is usually if your first instance of spondylolisthesis was severe ie your vertebra moved considerably out of its normal position.
However, after spondylolisthesis surgery, most people return to normal activities after a recovery period, although your spine will be less flexible.
Frequently asked questions
How do you fix spondylolisthesis?
Spondylolisthesis can be treated without surgery by using anti-inflammatory painkillers, physiotherapy and with rest. In some cases, you may need steroid injections. However, if these treatments are not effective, back surgery may be recommended.
Is spondylolisthesis serious?
Spondylolisthesis can be mild, moderate or severe. Severe cases of spondylolisthesis can be serious as they may lead to cauda equina syndrome, which is a medical emergency — if this condition is not treated it can cause urinary incontinence and paralysis. Even moderate cases, over time, if left untreated, can cause nerve damage if a nerve is compressed. You should therefore see your GP if you are concerned that you have spondylolisthesis as there are effective treatments.
What is the difference between spondylolysis and spondylolisthesis?
Both conditions can cause lower back pain. However, the underlying cause is different. Spondylolisthesis is caused by a bone in your spine (vertebra) slipping out of place, whereas spondylolysis is caused by a defect in your vertebra, which is usually caused by a stress fracture.
Is walking bad for spondylolisthesis?
Walking is not bad for spondylolisthesis as long as it doesn’t worsen your pain. Walking and other exercises that do not bend or strain your back can help strengthen your back and abdominal muscles, which can reduce your pain and improve your range of motion.
Can chiropractic help spondylolisthesis?
A chiropractor can’t fix your spondylolisthesis — they can’t push the slipped vertebra back into place. However, they can improve your range of movement and reduce your pain by focusing on the rest of your spine.
What should you not do with spondylolisthesis?
You should not take part in activities that strain or stretch your back, such as athletics, bending, lifting and football.
Can you become paralyzed from spondylolisthesis?
If a nerve is compressed, over time, spondylolisthesis can cause nerve damage, which may lead to paralysis. In some cases, spondylolisthesis can cause cauda equina syndrome — another spinal condition that is a medical emergency because if it is left untreated there is a high risk of paralysis.
Can you live with spondylolisthesis without surgery?
Yes, in many cases, spondylolisthesis can be effectively treated with non-surgical interventions, such as physiotherapy, resting your back, taking painkillers and/or steroid injections.
How should I sleep with spondylolisthesis?
Sleeping on your back in a reclining position can help reduce the pressure on your spine caused by the slipped vertebra ie sleeping propped up on several pillows.
When should you have surgery for spondylolisthesis?
If you have tried non-surgical treatments for spondylolisthesis (rest, physiotherapy, painkillers and steroid injections) and they have not worked, then surgery may be recommended. Your doctor may also recommend surgery if a nerve is compressed or your symptoms are persistent and severe.
Can you live a normal life after spinal fusion?
After a period of recovery, you can return to your normal activities. However, you will have reduced flexibility in the area of your spine where the vertebrae were fused.
Can spondylolisthesis cause bowel problems?
If spondylolisthesis is causing severe compression of a nerve, this can cause bowel incontinence.
Does spondylolisthesis get worse over time?
This depends on the severity and type of spondylolisthesis you have. Over time, symptoms of mild spondylolisthesis may go away on their own. However, in other cases, symptoms can get worse eg if a nerve is compressed or if you have degenerative spondylolisthesis.
https://www.nhs.uk/conditions/spondylolisthesis/
http://www.britscoliosissoc.org.uk/patient-information/spondylolisthesis
https://orthoinfo.aaos.org/en/diseases--conditions/spondylolysis-and-spondylolisthesis/
https://my.clevelandclinic.org/health/diseases/10302-spondylolisthesis
https://www.webmd.com/back-pain/guide/pain-management-spondylolisthesis
https://patient.info/doctor/spondylolysis-and-spondylolisthesis
https://spinalresearch.com.au/6735-2/
https://www.healthline.com/health/healthy-sleep/best-sleeping-position-for-lower-back-pain
Related topics
Related treatments:
- Back surgery (spinal surgery)
- Facet joint injections
- Physiotherapy from Spire
Related symptoms:
Related conditions:
Spondylolisthesis
What is Spondylolisthesis?
Patient education video.
Types of Spondylolisthesis
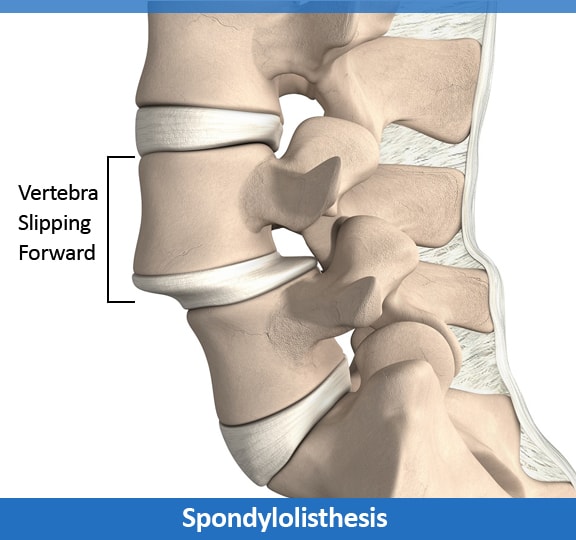
What Are the Signs and Symptoms of Spondylolisthesis?
How is it diagnosed.
- Grade I – Less than 25 percent slippage
- Grade II – Between 25 and 50 percent slippage
- Grade III – Between 50 and 75 percent slippage
- Grade IV – More than 75 percent slippage
- Grade V – The upper vertebral body has slipped all the way off the front of the lower vertebral body. This is a rare situation that is called a spondyloptosis.
How is it Treated?
Surgery & treatment for spondylolisthesis, what are you looking for.

Avoid Spinal Fusion
Disc / Facet Replacement

Robotic Spine Surgery
Stem Cell Regeneration

Minimally Invasive Surgery

Spine Rehabilitation
Join Our Youtube Channel
- GP practice services
- Health advice
- Health research
- Medical professionals
Health topics
Advice and clinical information on a wide variety of healthcare topics.
All health topics
Latest features
Allergies, blood & immune system
Bones, joints and muscles
Brain and nerves
Chest and lungs
Children's health
Cosmetic surgery
Digestive health
Ear, nose and throat
General health & lifestyle
Heart health and blood vessels
Kidney & urinary tract
Men's health
Mental health
Oral and dental care
Senior health
Sexual health
Signs and symptoms
Skin, nail and hair health
Travel and vaccinations
Treatment and medication
Women's health
Healthy living
Expert insight and opinion on nutrition, physical and mental health.
Exercise and physical activity
Healthy eating
Healthy relationships
Managing harmful habits
Mental wellbeing
Relaxation and sleep
Managing conditions
From ACE inhibitors for high blood pressure, to steroids for eczema, find out what options are available, how they work and the possible side effects.
Featured conditions
ADHD in children
Crohn's disease
Endometriosis
Fibromyalgia
Gastroenteritis
Irritable bowel syndrome
Polycystic ovary syndrome
Scarlet fever
Tonsillitis
Vaginal thrush
Health conditions A-Z
Medicine information
Information and fact sheets for patients and professionals. Find out side effects, medicine names, dosages and uses.
All medicines A-Z
Allergy medicines
Analgesics and pain medication
Anti-inflammatory medicines
Breathing treatment and respiratory care
Cancer treatment and drugs
Contraceptive medicines
Diabetes medicines
ENT and mouth care
Eye care medicine
Gastrointestinal treatment
Genitourinary medicine
Heart disease treatment and prevention
Hormonal imbalance treatment
Hormone deficiency treatment
Immunosuppressive drugs
Infection treatment medicine
Kidney conditions treatments
Muscle, bone and joint pain treatment
Nausea medicine and vomiting treatment
Nervous system drugs
Reproductive health
Skin conditions treatments
Substance abuse treatment
Vaccines and immunisation
Vitamin and mineral supplements
Tests & investigations
Information and guidance about tests and an easy, fast and accurate symptom checker.
About tests & investigations
Symptom checker
Blood tests
BMI calculator
Pregnancy due date calculator
General signs and symptoms
Patient health questionnaire
Generalised anxiety disorder assessment
Medical professional hub
Information and tools written by clinicians for medical professionals, and training resources provided by FourteenFish.
Content for medical professionals
FourteenFish training
- Professional articles
Evidence-based professional reference pages authored by our clinical team for the use of medical professionals.
View all professional articles A-Z
Actinic keratosis
Bronchiolitis
Molluscum contagiosum
Obesity in adults
Osmolality, osmolarity, and fluid homeostasis
Recurrent abdominal pain in children
Medical tools and resources
Clinical tools for medical professional use.
All medical tools and resources
Isabel DDx Companion professional symptom checker
Spondylolisthesis and spondylolysis
Peer reviewed by Dr Laurence Knott Last updated by Dr Colin Tidy, MRCGP Last updated 20 Nov 2021
Meets Patient’s editorial guidelines
- Download Download Article PDF has been downloaded
- Share via email
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Cervical spondylosis article more useful, or one of our other health articles .
In this article :
What is spondylolisthesis, spondylolisthesis vs spondylolysis.
- Who gets spondylolisthesis and spondylolysis? (Epidemiology)
Spondylolisthesis causes (aetiology)
- Types of spondylolisthesis
- Presentation
Differential diagnosis
Investigations.
- Spondylolisthesis treatment and management
Complications of surgical repair
Spondylolisthesis prognosis.
Continue reading below
Spondylolisthesis is the movement of one vertebra relative to the others in either the anterior or posterior direction due to instability. Degenerative spondylolisthesis is a common pathology, often causing lumbar canal stenosis 1 .
Anatomy of the vertebrae
The vertebrae can be divided into three portions:
Centrum - involved in weight bearing. This is the body of the vertebra and is formed of cancellous bone.
Dorsal arch - surrounds and protects the spinal cord. It carries the upper and lower facet joints of each vertebra which articulate with the facet joints of the vertebra above and below, respectively. The part of the vertebral arch between them is the thinnest part and is called the pars interarticularis, or the isthmus.
Posterior aspect - protrudes and can be palpated on the lower back.
Lumbar vertebra 1 inferior surface
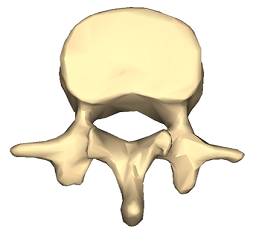
Lumbar vertebra 1 anterior surface
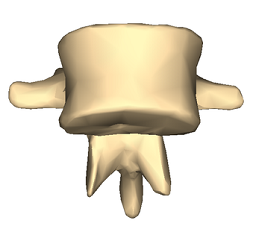
Images by Anatomography, via Wikimedia Commons . Click here to see a lumbar vertebra 1 close-up superior surface animation.
Spondylolysis and spondylolisthesis are separate conditions, although spondylolysis often precedes spondylolisthesis.
Spondylolysis is a bony defect (commonly due to a stress fracture but it may be a congenital defect) in the pars interarticularis of the vertebral arch, separating the dorsum of the vertebra from the centrum. It may occur unilaterally or bilaterally. It most commonly affects the fifth lumbar vertebra and may cause back pain.
Spondylolisthesis refers to the anterior slippage of one vertebra over another (or the fifth vertebra over the sacrum). There are five forms:
Isthmic : the most common form, usually acquired in adolescence as a consequence of spondylolysis but often unnoticed until adulthood.
Degenerative : developing in older adults as a result of facet joint osteoarthritis and bone remodelling.
Traumatic (rare): resulting from fractures of the neural arch.
Pathologic : from metastases or metabolic bone disease.
Dysplastic : (rare): congenital, resulting from malformation of the pars.
Spondylosis is a general term for degenerative osteoarthritic changes in the spine. It involves dehydration of the intervertebral discs with consequent narrowing of the intervertebral spaces. There may be changes in the facet joints with osteophyte formation and this may put pressure on the nerve roots, causing motor and sensory disturbance.
Who gets spondylolisthesis and spondylolysis? (Epidemiology) 2
Spondylolysis is a common diagnosis with a high prevalence in children and adolescents complaining of low back pain.
There is an increased risk of spondylolysis in young athletes like gymnasts, presumably due to impact-related stress fractures . However most cases are low-grade. At-risk activities include gymnastics, diving, tennis, cricket, weightlifting, football and rugby.
Isthmic spondylolisthesis affects around 5% of the population but is more common in young athletes. 60-80% of people with spondylolysis have associated spondylolisthesis 3 4 .
The majority of cases of spondylolysis and spondylolisthesis affect L5 and most of the remainder affect L4.
Degenerative spondylolisthesis is more common in older people, particularly women.
Traumatic, metastatic and dysplastic spondylolistheses are relatively rare.
Many cases of spondylolisthesis are asymptomatic.
Spondylolisthesis commonly occurs due to a fracture or defect in the pars interarticularis, the narrowest part of the posterior vertebral arch between the upper and lower facet joints. When this is breached, the upper facet joint may no longer be able to hold the vertebra in place against the downward force of body weight and forward/downward slippage occurs.
Risk factors that increase the risk of spondylolysis developing into spondylolisthesis include 5 :
Female gender.
Presence of spina bifida or spina bifida occulta .
Vertebral wedging.
Hyperlordosis.
Positive family history.
Certain high-impact sports, as evidenced by increased rates in athletes and gymnasts 3 .
Types of spondylolisthesis 2
Stable or unstable.
Asymptomatic or symptomatic.
Graded according to degree of slippage; the Meyerding classification is based on the ratio of the overhanging part of the superior vertical body to the anterio-posterior length of the inferior vertebral body:
Grade I: 0-25%.
Grade II: 26-50%.
Grade III: 51-75%.
Grade IV: 76-100%.
Grade V (spondyloptosis): >100%.
Graded according to type; the Wiltse classification (1976):
Type I: dysplastic (congenital).
Type II: isthmic: secondary to a lesion involving the pars interarticularis:
Subtype A: secondary to stress fracture.
Subtype B: result of multiple healed stress fractures resulting in an elongated pars.
Subtype C: acute pars fracture (rare).
Type III: degenerative.
Type IV: post-traumatic: fracture in a region other than the pars.
Type V: pathological: diffuse or local disease.
Type VI: iatrogenic.
Presentation 4
Spondylolysis symptoms.
Most cases of spondylolysis are asymptomatic and identified incidentally.
It may present with low back pain provoked by lumbar extension, paraspinal spasm and tight hamstrings.
It frequently does not show on X-ray. It is important to consider it in the differential diagnosis of back pain, as its identification can prevent progression and avoid the potential need for aggressive intervention.
Spondylolisthesis symptoms
Presentation varies slightly by type although common spondylolisthesis symptoms include exercise-related back pain, radiating to the lower thighs, which tends to be eased by rest, particularly in positions of spinal flexion.
Isthmic spondylolisthesis
Most patients are asymptomatic, even with progressing slippage.
Symptoms often begin around the adolescent growth spurt.
Back pain - worse with activity (particularly back extension) - this may come on acutely or insidiously.
Pain may flare with sudden or trivial activities and is relieved by resting.
Pain is worse with higher grades of disease.
Pain may radiate to buttocks or thighs
There are usually no neurological features with lower grades of slippage but radicular pain becomes common with larger slips. Pain below the knee due to nerve root compression or disc herniation would suggest more severe slippage. High degrees of spondylolisthesis may present with neurogenic claudication or even cauda equina impingement.
Tightened hamstrings are very common
There may be enhanced lordosis and a waddling gait with shortened step length.
There may be gluteal muscular wasting.
Degenerative spondylolisthesis
Pain is aching in nature and insidious in onset.
Pain is in the low back and posterior thighs.
Neurogenic claudication may be present with lower-extremity symptoms worsening with exercise.
Symptoms are often chronic and progressive, sometimes with periods of remission.
If lumbar stenosis is also present, reflexes may be diminished.
Dysplastic spondylolisthesis
Presentation and physical findings are similar to isthmic spondylolisthesis but with a greater likelihood of neurological compromise.
Traumatic spondylolisthesis
Patients will have experienced acute trauma and are likely to have significant pain.
Severe slips may cause cauda equina compression with bladder and bowel dysfunction, radicular symptoms or neurogenic claudication.
Physical findings are as for the other types.
Pathological spondylolisthesis
Symptoms may be insidious in onset and associated with radicular pain.
Other causes of back pain need to be ruled out - eg:
Osteoarthritis .
Ankylosing spondylitis .
Mechanical lower back pain .
Spinal cord lesion.
Multiple myeloma .
Vertebral compression fracture .
Lumbar disc prolapse.
Discitis/other spinal disc problems .
Blood tests - looking for infection, myeloma, hypercalcaemia/hypocalcaemia.
Lateral spinal X-rays - will show spondylolisthesis. These are best performed in the position of maximal pain.
Oblique spinal X-rays - may (but will often not) detect spondylolysis.
Radionuclide scintigraphy and CT may help in cases of spondylolysis in distinguishing progressing lesions of the pars from stable lesions.
MRI is often performed perioperatively to look at relationships between the bony and neurological structures in the compromised area.
Spondylolisthesis treatment and management 1 2 4
The goal of treatment is to relieve pain, stabilise the spinal segment and stop or reverse the slippage. Patients need to be evaluated for the presence of instability, as if there is an unstable segment early surgery will be needed.
Depending on the severity of the spondylolysis and symptoms associated it may be treated either conservatively or surgically, both of which have shown significant success.
Conservative treatments such as bracing and decreased activity have been shown to be most effective with patients who have early diagnosis and treatment. Low-intensity pulsed ultrasound in addition to conservative treatment appears to achieve a higher rate of bony union. Surgery may be required if conservative treatment, for at least six months, failed to give sustained pain relief for the activities of daily living.
For degenerative spondylolisthesis, surgery is indicated mainly for perceived functional impairment. Improvement in neurological symptoms is one of the main treatment objectives. For this, it is useful to perform radicular decompression. The most frequent technique is direct posterior decompression.
Conservative treatment
Complete bed rest for 2-3 days can be helpful in relieving pain, particularly in spondylolysis, although longer periods are likely to be counterproductive. Patients should try to sleep on their side as much as possible, with a pillow between the knees.
Activity modification to prevent further injury. This may mean avoidance of activities if there is >25% slippage.
Analgesia - eg, paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs), codeine phosphate.
Steroid and local anaesthetic injections are sometimes used around compressed nerve roots or even into the fracture area of the pars for diagnostic purposes.
Bracing: a brace or corset may be recommended for a pars interarticularis fracture which is likely to heal. Bracing with exercise may be beneficial for patients with mild or even more severe degrees of slippage.
Physiotherapy: this includes massage, ultrasound, bracing, mobilisation, biomechanical correction, hydrotherapy, exercises for flexibility, strength and core stability and a gradual return to activity programme.
More than 80% of children treated non-surgically will have full resolution of symptoms.
A meta-analysis of observation studies suggested that around 80% of all patients treated non-operatively would have a successful clinical outcome after one year. Lesions diagnosed at the acute stage and unilateral lesions were the best subgroups 6 .
Surgical treatment
If there is evidence of progression or if conservative measures are ineffective then surgical therapy may be offered. This depends also on degree and aetiology.
Surgical intervention involves a prolonged rehabilitation period so it is generally not considered until conservative treatments have failed. An exception would be in the case of significant instability or neurological compromise and in high-grade slips.
Surgical therapy involves fusing the affected vertebra with a neighbouring normally aligned vertebra (both anteriorly and posteriorly). The intervertebral disc is usually also removed, as it is inevitably damaged. The slipped vertebra may be realigned.
Whilst most surgeons agree that decompression of the nerves is of benefit to patients, the benefit of realigning slipped vertebrae is uncertain. For example, when the spondylolisthesis is very gradual in onset, or in cases of congenital spondylolisthesis, compensatory changes in the spine and musculature occur so that realignment may increase the possibility of further injury.
There is good evidence that surgical treatment of symptomatic spondylolisthesis is significantly superior to non-surgical management in the presence of 7 :
Significant neurological deficit.
Failed response to conservative therapy.
Instability with neurological symptoms.
Degree of subluxation of III or more.
Unremitting pain affecting quality of life.
A large systematic review concluded that reduction of displacement carried benefits over fusion alone, although a large retrospective review showed high complication rates, particularly for older patients with more severe disease 8 9 10 11 .
Fusion techniques can be associated with neurological complications in older patients with degenerative spondylolisthesis, but in adolescent patients outcomes are good 9 .
Surgery is commonly complicated by pseudoarthrosis (non-union) which may result in chronic pain years down the line.
In the case of spondylolysis, if surgery is offered it would involve pinning the defect. However, most cases are managed conservatively.
Implant failure.
Pseudoarthrosis (failure of bone healing leading to a 'false joint').
Poor alignment of the fusion.
Neurological damage: foot drop, spinal cord compression . Chronic nerve injury/inflammation: neuropathic pain can persist in the face of apparent surgical success, possibly due to permanent changes in the nerves or a deregulation of pain control mechanisms.
Spondylolisthesis is generally a benign condition; however, it runs a chronic course and is therefore a cause of much morbidity and disability. In degenerative spondylolisthesis this will relate in part to the progress and prognosis of the underlying changes.
Dr Mary Lowth is an author or the original author of this leaflet.
Further reading and references
- Guigui P, Ferrero E ; Surgical treatment of degenerative spondylolisthesis. Orthop Traumatol Surg Res. 2017 Feb;103(1S):S11-S20. doi: 10.1016/j.otsr.2016.06.022. Epub 2016 Dec 30.
- Gagnet P, Kern K, Andrews K, et al ; Spondylolysis and spondylolisthesis: A review of the literature. J Orthop. 2018 Mar 17;15(2):404-407. doi: 10.1016/j.jor.2018.03.008. eCollection 2018 Jun.
- Toueg CW, Mac-Thiong JM, Grimard G, et al ; Prevalence of spondylolisthesis in a population of gymnasts. Stud Health Technol Inform. 2010;158:132-7.
- Syrmou E, Tsitsopoulos PP, Marinopoulos D, et al ; Spondylolysis: a review and reappraisal. Hippokratia. 2010 Jan;14(1):17-21.
- Sadiq S, Meir A, Hughes SP ; Surgical management of spondylolisthesis overview of literature. Neurol India. 2005 Dec;53(4):506-11.
- Klein G, Mehlman CT, McCarty M ; Nonoperative treatment of spondylolysis and grade I spondylolisthesis in children and young adults: a meta-analysis of observational studies. J Pediatr Orthop. 2009 Mar;29(2):146-56. doi: 10.1097/BPO.0b013e3181977fc5.
- Alfieri A, Gazzeri R, Prell J, et al ; The current management of lumbar spondylolisthesis. J Neurosurg Sci. 2013 Jun;57(2):103-13.
- Weinstein JN, Lurie JD, Tosteson TD, et al ; Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009 Jun;91(6):1295-304. doi: 10.2106/JBJS.H.00913.
- Sansur CA, Reames DL, Smith JS, et al ; Morbidity and mortality in the surgical treatment of 10,242 adults with spondylolisthesis. J Neurosurg Spine. 2010 Nov;13(5):589-93. doi: 10.3171/2010.5.SPINE09529.
- Kasliwal MK, Smith JS, Kanter A, et al ; Management of high-grade spondylolisthesis. Neurosurg Clin N Am. 2013 Apr;24(2):275-91. doi: 10.1016/j.nec.2012.12.002. Epub 2013 Feb 21.
- Longo UG, Loppini M, Romeo G, et al ; Evidence-based surgical management of spondylolisthesis: reduction or arthrodesis in situ. J Bone Joint Surg Am. 2014 Jan 1;96(1):53-8. doi: 10.2106/JBJS.L.01012.
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 19 Nov 2026
20 nov 2021 | latest version.
Last updated by
Peer reviewed by

Are you protected against flu?
See if you are eligible for a free NHS flu jab today.

Feeling unwell?
Assess your symptoms online for free

IMAGES
VIDEO
COMMENTS
Thoracic spondylosis is a condition that affects the middle of your spine and causes pain, stiffness, and nerve compression. Learn about the causes, symptoms, diagnosis, and treatment options for ...
Spondylolysis is a stress fracture in the vertebrae of the lower back, while spondylolisthesis is when the fractured vertebra slips forward. Learn about the causes, symptoms, diagnosis, and treatment of these conditions that affect children and adolescents.
Spondylolisthesis is a condition in which a vertebra slips out of place and puts pressure on a nerve. Learn about the types, grades, diagnosis, and treatment options for this spine problem.
Thoracic spondylosis is a degenerative condition of the mid back that can cause pain, stiffness, tingling and numbness. Learn about the causes, risk factors, symptoms and treatment options from Centeno Schultz, a clinic that specializes in regenerative medicine.
Spondylolisthesis is the slippage of one vertebral body with respect to the adjacent vertebral body causing mechanical or radicular symptoms or pain. It can be due to congenital, acquired, or idiopathic causes. ... in the thoracic spine. Degenerative spondylolisthesis predominately occurs in adults and is more common in females than males with ...
Spondylolisthesis is a spine condition caused when one vertebra slips over another. This condition's symptoms sometimes mimic those of other back pain conditions.
Slippage of one spinal vertebra over another is spondylolisthesis.; Spondylolisthesis occurs in different grades and can be either congenital or acquired. Spondylolisthesis can cause symptoms by irritation of nervous tissue, either within the nearby spinal cord or of the adjacent spinal nerves.; Radiology imaging is used to confirm the diagnosis of spondylolisthesis.
Spondylolisthesis is a condition where a vertebra slips forward or backward in relation to the next vertebra, causing lower back pain and nerve compression. Learn about the types, risk factors, diagnosis, and treatment options for spondylolisthesis, including surgery and physical therapy.
Spondylolisthesis can cause severe back pain, particularly radiculopathy. Other symptoms are common as well, although not all patients have all symptoms. Your symptoms will depend on the location of the displaced vertebra: Pain radiating down the leg (sciatic pain) Numbness or weakness of an arm or leg; Pain that gradually worsens over the day
Isthmic spondylolisthesis: This results from spondylolysis, a condition that leads to small stress fractures (breaks) in the vertebrae.In some cases, the fractures weaken the bone so much that it slips out of place. Degenerative spondylolisthesis: Degenerative spondylolisthesis is related to spine changes that tend to occur with age.For example, the discs can start to dry up and become brittle ...
Spondylolisthesis is a condition where one of the bones in your spine, called a vertebra, slips forward. It can cause lower back pain, sciatica, tight hamstrings and other symptoms. Learn about the causes, diagnosis and treatments of spondylolisthesis.
Learn about degenerative spondylolisthesis, a common condition of vertebral subluxation with intact pars, most common at L4-5 level. Find out the epidemiology, etiology, classification, presentation, imaging, and treatment options.
Spondylolisthesis is a spinal condition that affects the lower vertebrae (spinal bones). This disease causes one of the lower vertebrae to slip forward onto the bone directly beneath it.
Symptoms of Spondylolisthesis. Spondylolisthesis may not have any symptoms. Some people have it without realizing it. If you do, lower back discomfort is usually the primary symptom. ... The spine is divided into cervical, thoracic, and lumbar. Lumbar is your low back. Interbody fusion refers to a specific type of fusion. For example, in ...
Spondylolisthesis is a condition where a vertebra slips forward onto the vertebra below, causing nerve compression and back pain. Learn about the causes, symptoms and treatment options for spondylolisthesis, and how it differs from anterolisthesis and other related conditions.
Spondylolisthesis is a condition where a vertebra slips out of position and puts pressure on the nerves in your spine. Learn about the types, causes, diagnosis and treatment options for this condition, and what to avoid if you have it.
Spondylolisthesis is a condition where one vertebra slips forward over the vertebra below it, causing back pain and nerve compression. Learn about the causes, symptoms, diagnosis and treatment options for this spine condition from Spine Connection.
Spondylolysis is a bony defect in the vertebra that may lead to spondylolisthesis, the slippage of one vertebra over another. Learn about the types, risk factors, diagnosis and management of these conditions that affect the lower back.