Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center


Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis

2019, Neurosurgery Clinics of North America
Related Papers
Journal of Neurosurgery: Spine
Steven Glassman
Journal of Orthopaedics and Traumatology
Stavroula Pagkrati
Neurosurgical focus
David Cavanaugh
OBJECTIVE Recently, authors have called into question the utility and complication index of the lateral lumbar interbody fusion procedure at the L4-5 level. Furthermore, the need for direct decompression has also been debated. Here, the authors report the clinical and radiographic outcomes of transpsoas lumbar interbody fusion, relying only on indirect decompression to treat patients with neurogenic claudication secondary to Grade 1 and 2 spondylolisthesis at the L4-5 level. METHODS The authors conducted a retrospective evaluation of 18 consecutive patients with Grade 1 or 2 spondylolisthesis from a prospectively maintained database. All patients underwent a transpsoas approach, followed by posterior percutaneous instrumentation without decompression. The Oswestry Disability Index (ODI) and SF-12 were administered during the clinical evaluations. Radiographic evaluation was also performed. The mean follow-up was 6.2 months. RESULTS Fifteen patients with Grade 1 and 3 patients with G...
Bratislavské lekárske listy
Jana Katuchova
Management of lumbar spondylolisthesis: A retrospective analysis of posterior lumbar interbody fusion versus transforaminal lumbar interbody fusion
Daniel Encarnación-Santos
Background: One of the most frequent etiologies for spinal surgery is unstable lumbar spondylolisthesis (ULS). To decompress affected structures while maintaining or restoring stability through fusion, surgeons utilize a variety of procedures. When paired with interbody fusion, posterior fusion is most applied, resulting in greater fusion rates. The two most popular techniques for implementing spinal fusion are posterior lumbar interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF). As a result, these two procedures have been assessed formally. Methodology: A retrospective analysis of patients who underwent interbody fusion for lumbar stenosis through PLIF and minimally invasive (MI)-TLIF was performed. The patients were followed up for 24 months and fusion rates, Visual Analog Score (VAS), and Oswestry Disability Index (ODI) alongside the MacNab clinical outcome score, were assessed. The Bridwell interbody fusion grading system was used to evaluate fusion rates in computed tomography (CT). Results: Operations were performed in 60 cases where patients suffered from ULS. PLIF was performed on 33 patients (55%) (14 males and 19 females) and 27 patients (45%) (11 males and 16 females) who underwent MI-TLIF. In 87% of our respective cohort, either the L4-5 or the L5-S1 level was operated on. Overall fusion rates were comparable between the two groups; however, the TLIF group improved more in terms of VAS, ODI, and MacNab scores. On average, MI-TLIF surgery was longer and resulted in reduced blood loss. MI-TLIF patients were more mobile than PLIF patients postoperatively. Conclusion: With well-established adequate results in the literature, TLIF offers benefits over other methods used for interbody lumbar fusion in ULS or other diseases of the spine. However, MI-TLIF may procure more advantageous for patients if MI methods are implemented. In this instance, TLIF outperformed PLIF due to shorter operating times, less blood loss, faster ODI recovery, better MacNab scores, and a greater decline in VAS pain ratings.
Nepal Medical College journal : NMCJ
Pramod Devkota
The ideal surgical treatment of spondylolisthesis still remains controversial. There are several methods of treatment and posterior lumbar interbody fusion (PLIF) is one of them. We analyze the results of spondylolisthesis treated by PLIF in term of radiological union, improvement of pre-operative symptoms like back pain, radiating pain and return to normal activities including that of employment, by the review of the medical records. Total of 72 patients, 20 male and 52 female and the age ranges from 15 to 68 years with the mean age being 44.38 years were included in the study. Thirty (41.66%) patients had isthmic spondylolisthesis, 26 (36.12%) had congenital spondylolisthesis, and 16 (22.22%) cases had degenerative spondylolisthesis. There were 38 (52.77%) cases of grade I, 14 (19.44%) cases of grade II and 20 (27.77%) cases of grade III according to the grading criteria of Meyerding. According to the evaluation criteria used by Stauffer and Coventry, 59 patients (81.94%) got good...
Journal of Musculoskeletal Research
Tomoaki Toyone
Fifty consecutive patients with degenerative lumbar spondylolisthesis were treated surgically. The first 17 patients (FU group) underwent decompression with fusion, the second 33 patients (MED group) underwent microendoscopic decompression (MED), and the outcomes following the two surgical methods were compared. The duration of follow-up ranged from 27 to 40 months in the FU group and from 25 to 40 months in the MED group. Clinical outcomes were evaluated with use of the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire. Although statistically not significant, the degrees of improvement in all five functional scores were greater in the MED group than in the FU group. There was no influence of instability before MED to the clinical outcome, and a large percentage of slipping in the neutral position could lead to inadequate improvement in low back pain after MED, but MED is a useful, minimally invasive operation and can lead to a good clinical outcome for degenerativ...
Christopher Shaffrey
OBJECTIVE Lumbar spondylolisthesis is a degenerative condition that can be surgically treated with either open or minimally invasive decompression and instrumented fusion. Minimally invasive surgery (MIS) approaches may shorten recovery, reduce blood loss, and minimize soft-tissue damage with resultant reduced postoperative pain and disability. METHODS The authors queried the national, multicenter Quality Outcomes Database (QOD) registry for patients undergoing posterior lumbar fusion between July 2014 and December 2015 for Grade I degenerative spondylolisthesis. The authors recorded baseline and 12-month patient-reported outcomes (PROs), including Oswestry Disability Index (ODI), EQ-5D, numeric rating scale (NRS)-back pain (NRS-BP), NRS-leg pain (NRS-LP), and satisfaction (North American Spine Society satisfaction questionnaire). Multivariable regression models were fitted for hospital length of stay (LOS), 12-month PROs, and 90-day return to work, after adjusting for an array of p...
Edward Benzel
European Spine Journal
Jean yves Lazennec
RELATED PAPERS
Israel Studies Forum
Jacob Adler
AIP Conference Proceedings
G. Moortgat-pick
Bruce Blumberg
Journal of Korean Endocrine Society
Bong-yun Cha
Pakistan Journal of Biological Sciences
Zainab Batin
Veronika Nečasová
Budsaba Kanoksilapatham
Olga Volkova
Molecular and Cellular Neuroscience
Nicolas Unsain
Biochemical Genetics
naila malkani
Journal of Cereal Science
Boubekeur NADJEMI
J. for Global Business Advancement
Muhammad Mikail Haqimi Bin Abdullah
Jurnal Pengabdian Masyarakat Pesisir
dewi casmiwati
samia samin
Diabetes Care
PMLA/Publications of the Modern Language Association of America
Egi Riandita
Kaliwatu Rafting
Rafting Kaliwatu
European Psychiatry
Lucas Giner
Journal of Sound and Vibration
Mehmet Imregun
Environmental science & technology
Mohamad Sleiman
办理乔治布朗学院毕业证书文凭学位证书 加拿大大学文凭学历认证
Annals of Basic and Medical Sciences
Dahiru Mohammed
Mairton Gomes da Silva
Civil Engineering and Architecture
Ali Akbar Firoozi
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Spondylolisthesis.
Steven Tenny ; Christopher C. Gillis .
Affiliations
Last Update: May 22, 2023 .
- Continuing Education Activity
Spondylolisthesis is a condition that occurs when one vertebral body slips with respect to the adjacent vertebral body causing radicular or mechanical symptoms or pain. It is graded based on the degree of slippage of one vertebral body on the adjacent vertebral body. Any pathological process that can weaken the supports keeping vertebral bodies aligned can allow spondylolisthesis to occur. This activity illustrates the evaluation and management of spondylolisthesis and reviews the role of the interprofessional team in improving care for patients with this condition.
- Describe the pathophysiology of spondylolisthesis.
- Review the workup of a patient with spondylolisthesis.
- Summarize the treatment options for spondylolisthesis.
- Describee the importance of collaboration and communication among the interprofessional team in encouraging weight loss in patients to reduce symptoms and increase the quality of life in those with spondylolisthesis.
- Introduction
Spondylolisthesis is the slippage of one vertebral body with respect to the adjacent vertebral body causing mechanical or radicular symptoms or pain. It can be due to congenital, acquired, or idiopathic causes. Spondylolisthesis is graded based on the degree of slippage of one vertebral body on the adjacent vertebral body. [1]
Spondylolisthesis commonly classifies as one of five major etiologies: degenerative, isthmic, traumatic, dysplastic, or pathologic. Degenerative spondylolisthesis occurs from degenerative changes in the spine without any defect in the pars interarticularis. It is usually related to the combined facet joint and disc degeneration leading to instability and forward movement of one vertebral body relative to the adjacent vertebral body. Isthmic spondylolisthesis results from defects in the pars interarticularis. The cause of isthmic spondylolisthesis is undetermined, but a possible etiology includes microtrauma in adolescence related to sports such as wrestling, football, and gymnastics, where repeated lumbar extension occurs. Traumatic spondylolisthesis occurs after fractures of the pars interarticularis or the facet joint structure and is most common after trauma. Dysplastic spondylolisthesis is congenital and secondary to variation in the orientation of the facet joints to an abnormal alignment. In dysplastic spondylolisthesis, the facet joints are more sagittally oriented than the typical coronal orientation. Pathologic spondylolisthesis can be from systemic causes such as bone or connective tissue disorders or a focal process, including infection, neoplasm, or iatrogenic origin. Additional risk factors for spondylolisthesis include a first-degree relative with spondylolisthesis, scoliosis, or occult spina bifida at the S1 level. [1]
- Epidemiology
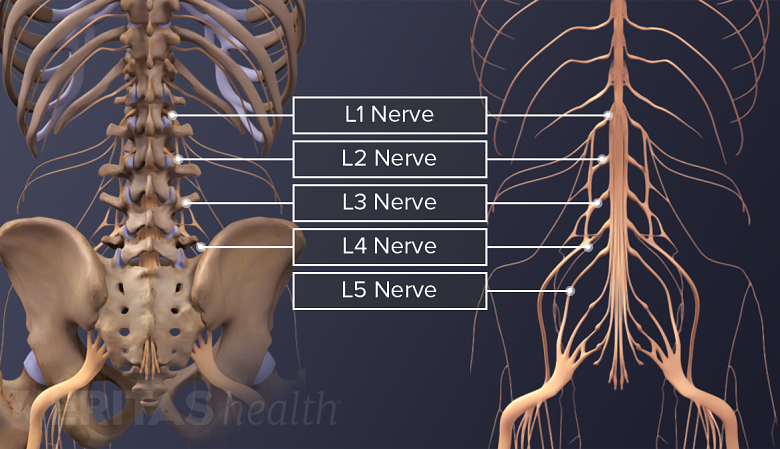
Spondylolisthesis most commonly occurs in the lower lumbar spine but can also occur in the cervical spine and rarely, except for trauma, in the thoracic spine. Degenerative spondylolisthesis predominately occurs in adults and is more common in females than males with increased risk in the obese. Isthmic spondylolisthesis is more common in the adolescent and young adult population but may go unrecognized until symptoms develop in adulthood. There is a higher prevalence of isthmic spondylolisthesis in males. Dysplastic spondylolisthesis is more common in the pediatric population, with females more commonly affected than males. Current estimates for prevalence are 6 to 7% for isthmic spondylolisthesis by the age of 18 years, and up to 18% of adult patients undergoing MRI of the lumbar spine. Grade I spondylolisthesis accounts for 75% of all cases. Spondylolisthesis most commonly occurs at the L5-S1 level with an anterior translation of the L5 vertebral body on the S1 vertebral body. The L4-5 level is the second most common location for spondylolisthesis.
- Pathophysiology
Any process that can weaken the supports keeping vertebral bodies aligned can allow spondylolisthesis to occur. As one vertebra moves relative to the adjacent vertebrae, local pain can occur from mechanical motion or radicular or myelopathic pain can occur due to compression of the exiting nerve roots or spinal cord, respectively. Pediatric patients are more likely to increase spondylolisthesis grade when going through puberty. Older patients with lower grades I or II spondylolistheses are less likely to progress to higher grades over time.
- History and Physical
Patients typically have intermittent and localized low back pain for lumbar spondylolisthesis and localized neck pain for cervical spondylolisthesis. The pain is exacerbated by flexing and extending at the affected segment, as this can cause mechanic pain from motion. Pain may be exacerbated by direct palpation of the affected segment. Pain can also be radicular in nature as the exiting nerve roots become compressed due to the narrowing of nerve foramina as one vertebra slips on the adjacent vertebrae, the traversing nerve root (root to the level below) can also be impinged through associated lateral recess narrowing, disc protrusion, or central stenosis. Pain can sometimes improve in certain positions such as lying supine. This improvement is due to the instability of the spondylolisthesis that reduces with supine posture, thus relieving the pressure on the bony elements as well as opening the spinal canal or neural foramen. Other symptoms associated with lumbar spondylolisthesis include buttock pain, numbness, or weakness in the leg(s), difficulty walking, and rarely loss of bowel or bladder control.
Anteroposterior and lateral plain films, as well as lateral flexion-extension plain films, are the standard for the initial diagnosis of spondylolisthesis. One is looking for the abnormal alignment of one vertebral body to the next as well as possible motion with flexion and extension, which would indicate instability. In isthmic spondylolisthesis, there may be a pars defect, which is termed the "Scotty dog collar." The "Scotty dog collar" shows a hyperdensity where the collar would be on the cartoon dog, which represents the fracture of the pars interarticularis. Computed tomography (CT) of the spine provides the highest sensitivity and specificity for diagnosing spondylolisthesis. Spondylolisthesis can be better appreciated on sagittal reconstructions as compared to axial CT imaging. MRI of the spine can show associated soft tissue and disc abnormalities, but it is relatively more challenging to appreciate bony detail and a potential pars defect on MRI. [2] [3]
- Treatment / Management
For grade I and II spondylolisthesis, treatment typically begins with conservative therapy, including nonsteroidal anti-inflammatory drugs (NSAIDs), heat, light exercise, traction, bracing, and/or bed rest. Approximately 10% to 15% of younger patients with low-grade spondylolisthesis will fail conservative treatment and need surgical treatment. No definitive standards exist for surgical treatment. Surgical treatment includes a varying combination of decompression, fusion with or without instrumentation, or interbody fusion. Patients with instability are more likely to require operative intervention. Some surgeons recommend a reduction of the spondylolisthesis if able as this not only decreases foraminal narrowing but also can improve spinopelvic sagittal alignment and decrease the risk for further degenerative spinal changes in the future. The reduction can be more difficult and riskier in higher grades and impacted spondylolisthesis. [4] [5] [6] [7] [8] [2] [9] [10]
- Differential Diagnosis
- Degenerative Lumbar Disc Disease
- Lumbar Disc Problems
- Lumbosacral Disc Injuries
- Lumbosacral Discogenic Pain Syndrome
- Lumbosacral Facet Syndrome
- Lumbosacral Radiculopathy
- Lumbosacral Spine Acute Bony Injuries
- Lumbosacral Spondylosis
- Myofascial Pain in Athletes
- Pearls and Other Issues
Meyerding’s classification of spondylolisthesis is the most commonly used grading method. Its basis is on the percentage of anterior translation relative to the adjacent level. Grade I spondylolisthesis is 1 to 25% slippage, grade II is up to 50% slippage, grade III is up to 75% slippage, and grade IV is 76-100% slippage. If there is more than 100% slippage, it is known as spondyloptosis or grade V spondylolisthesis.
Subclasses of isthmic spondylolisthesis are subtype A (stress fractures of the pars), subtype B (elongation of the pars without overt fracture), subtype C (acute fracture of the pars).
Subclasses of pathologic spondylolisthesis are subtype A (systemic causes) and subtype B (focal processes).
- Enhancing Healthcare Team Outcomes
An interprofessional team consisting of a specialty-trained orthopedic nurse, a physical therapist, and an orthopedic surgeon or neurosurgeon will provide the best outcome and long-term care of patients with degenerative spondylolisthesis. Chiropractors may also have involvement, as they may be the first to encounter the condition on X-rays. The treating clinician will decide on the management plan, and then have the other team members engaged - surgical cases with include the nursing staff in pre-, intra-, and post-operative care, and coordinating with PT for rehabilitation. In non-operative cases, the PT will keep the rest of the team informed of progress or lack thereof. The team should encourage weight loss as weight reduction may reduce symptoms and increase the quality of life. Interprofessional collaboration, as above, will drive patient outcomes to their best results. [Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Lumbar Spine Sagittal CT of L5-S1, Grade II Spondylolisthesis Contributed by Christopher Gillis, MD, and Steven Tenny, MD
Disclosure: Steven Tenny declares no relevant financial relationships with ineligible companies.
Disclosure: Christopher Gillis declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Tenny S, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PubMed Links to PubMed
Similar articles in PubMed
- Isthmic Spondylolisthesis. [StatPearls. 2024] Isthmic Spondylolisthesis. Burton MR, Dowling TJ, Mesfin FB. StatPearls. 2024 Jan
- High-grade slippage of the lumbar spine in a rat model of spondylolisthesis: effects of cyclooxygenase-2 inhibitor on its deformity. [Spine (Phila Pa 1976). 2006] High-grade slippage of the lumbar spine in a rat model of spondylolisthesis: effects of cyclooxygenase-2 inhibitor on its deformity. Komatsubara S, Sairyo K, Katoh S, Sakamaki T, Higashino K, Yasui N. Spine (Phila Pa 1976). 2006 Jul 15; 31(16):E528-34.
- [Three vertebral reduction and fixation for revision of lumbar spondylolisthesis]. [Zhongguo Gu Shang. 2014] [Three vertebral reduction and fixation for revision of lumbar spondylolisthesis]. Li CS. Zhongguo Gu Shang. 2014 Sep; 27(9):717-21.
- Review A review of the pathomechanism of forward slippage in pediatric spondylolysis: the Tokushima theory of growth plate slippage. [J Med Invest. 2015] Review A review of the pathomechanism of forward slippage in pediatric spondylolysis: the Tokushima theory of growth plate slippage. Sairyo K, Nagamachi A, Matsuura T, Higashino K, Sakai T, Suzue N, Hamada D, Takata Y, Goto T, Nishisho T, et al. J Med Invest. 2015; 62(1-2):11-8.
- Review Spondylolisthesis. [Orthop Rev (Pavia). 2022] Review Spondylolisthesis. Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Orthop Rev (Pavia). 2022; 14(4):36917. Epub 2022 Jul 27.
Recent Activity
- Spondylolisthesis - StatPearls Spondylolisthesis - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Select a Community
- MB 1 Preclinical Medical Students
- MB 2/3 Clinical Medical Students
- ORTHO Orthopaedic Surgery
Are you sure you want to trigger topic in your Anconeus AI algorithm?
You are done for today with this topic.
Would you like to start learning session with this topic items scheduled for future?

Guideline summary review: An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis.
- The North American Spine Society's (NASS) Evidence-Based Clinical Guideline for the Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis features evidence-based recommendations for diagnosing and treating degenerative lumbar spondylolisthesis. The guideline updates the 2008 guideline on this topic and is intended to reflect contemporary treatment concepts for symptomatic degenerative lumbar spondylolisthesis as reflected in the highest quality clinical literature available on this subject as of May 2013. The NASS guideline on this topic is the only guideline on degenerative lumbar spondylolisthesis included in the Agency for Healthcare Research and Quality's National Guideline Clearinghouse (NGC).
- The purpose of this guideline is to provide an evidence-based educational tool to assist spine specialists when making clinical decisions for patients with degenerative lumbar spondylolisthesis. This article provides a brief summary of the evidence-based guideline recommendations for diagnosing and treating patients with this condition.
- A systematic review of clinical studies relevant to degenerative spondylolisthesis was carried out.
- This NASS spondyolisthesis guideline is the product of the Degenerative Lumbar Spondylolisthesis Work Group of NASS' Evidence-Based Guideline Development Committee. The methods used to develop this guideline are detailed in the complete guideline and technical report available on the NASS website. In brief, a multidisciplinary work group of spine care specialists convened to identify clinical questions to address in the guideline. The literature search strategy was developed in consultation with medical librarians. Upon completion of the systematic literature search, evidence relevant to the clinical questions posed in the guideline was reviewed. Work group members used the NASS evidentiary table templates to summarize study conclusions, identify study strengths and weaknesses, and assign levels of evidence. Work group members participated in webcasts and in-person recommendation meetings to update and formulate evidence-based recommendations and incorporate expert opinion when necessary. The draft guidelines were submitted to an internal peer review process and ultimately approved by the NASS Board of Directors. Upon publication, the Degenerative Lumbar Spondylolisthesis guideline was accepted into the NGC and will be updated approximately every 5 years.
- Twenty-seven clinical questions were addressed in this guideline update, including 15 clinical questions from the original guideline and 12 new clinical questions. The respective recommendations were graded by strength of the supporting literature, which was stratified by levels of evidence. Twenty-one new or updated recommendations or consensus statements were issued and 13 recommendations or consensus statements were maintained from the original guideline.
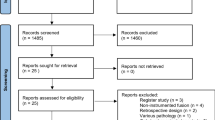
- The clinical guideline was created using the techniques of evidence-based medicine and best available evidence to aid practitioners in the care of patients with degenerative lumbar spondylolisthesis. The entire guideline document, including the evidentiary tables, literature search parameters, literature attrition flow chart, suggestions for future research, and all of the references, is available electronically on the NASS website at https://www.spine.org/Pages/ResearchClinicalCare/QualityImprovement/ClinicalGuidelines.aspx and will remain updated on a timely schedule.
On a scale of 1 to 10, rate how much this article will change your clinical practice?
Will this article lead to more cost-effective healthcare, was this article biased (commercial or personal), what level of evidence do you think this article is.
Please Login to add comment
- Surgery for Degenerative Spondylolisthesis
By: Marco Funiciello, DO, Physiatrist
Peer-Reviewed
Surgery for degenerative spondylolisthesis may be beneficial for select patients with lumbar radicular pain.
About 10% to 15% of individuals seeking treatment for degenerative spondylolisthesis eventually opt for surgical treatment. 1 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
In This Article:
- Degenerative Spondylolisthesis
- Degenerative Spondylolisthesis Symptoms
- Degenerative Spondylolisthesis Treatment
Degenerative Spondylolisthesis Video
Indications for degenerative spondylolisthesis surgery.
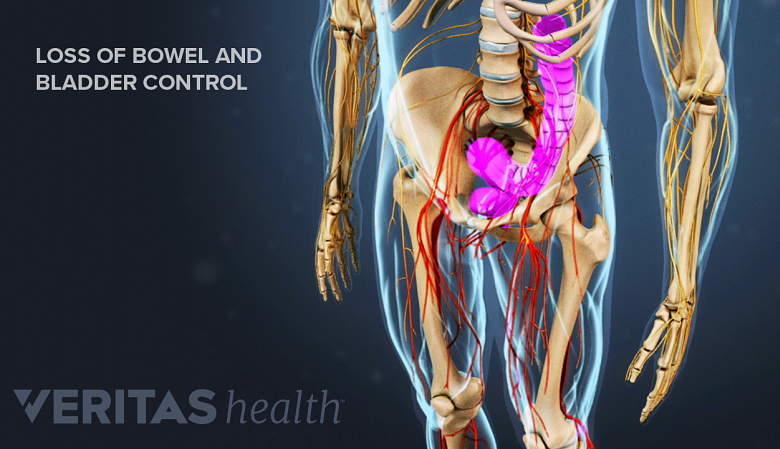
Loss of bowel and bladder control indicates a medical emergency.
Surgery for degenerative spondylolisthesis may be recommended when 2 Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008 Mar;17(3):327-335. doi: 10.1007/s00586-007-0543-3. Epub 2007 Nov 17. PMID: 18026865; PMCID: PMC2270383. :
- A series of nonsurgical treatments have been tried for a minimum of 3 to 6 months with no improvement in symptoms
- There is persistent or recurrent back and/or leg pain or neurogenic claudication
- The quality of life is significantly reduced
- There is progressive neurological deficit (more indicative of a surgical emergency)
- Bladder or bowel symptoms are present (more indicative of a surgical emergency)
See When Back Pain May Be a Medical Emergency
The goals of surgery are to stop progression of neurological deficits by alleviating pressure on nerve roots and the spinal nerves and provide stability to the area.
Success Rates of Surgical Treatment
Research shows that in appropriately selected patients, 66% to 96% of individuals may have successful outcomes, such as decreased pain and increased function, after surgery with a low rate of complications. 3 Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed.; 2016. , 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
Some studies also suggest that long-term improvement in pain and function from surgical treatment is better than nonsurgical treatment, especially in patients with leg pain. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
Types of Surgeries for Degenerative Spondylolisthesis
Your user agent does not support the HTML5 Video element.
A short video showing lumbar laminectomy procedure.
Lumbar laminectomy relieves neural compression by removing the bone compressing the nerve tissue.
Surgery for degenerative spondylolisthesis usually includes two parts, typically done together in one operation 5 Samuel AM, Moore HG, Cunningham ME. Treatment for Degenerative Lumbar Spondylolisthesis: Current Concepts and New Evidence. Curr Rev Musculoskelet Med. 2017 Dec;10(4):521-529. doi: 10.1007/s12178-017-9442-3. PMID: 28994028; PMCID: PMC5685964. , 6 Tenny S, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767/ :
- Spinal decompression (also called a laminectomy), which helps relieve nerve root compression
- Spinal fusion with pedicle screw instrumentation and spinal interbody fusion, which helps improve the stability of the degenerated spinal segment
For single-level, low-grade degenerative spondylolisthesis with only central stenosis (narrowing of the spinal canal) and no foraminal stenosis (narrowing of the intervertebral foramen), decompression alone may provide equivalent outcomes compared to decompression with fusion. 5
The additional step of spinal fusion with instrumentation is recommended to correct the deformity and prevent further progression of the condition. 7 Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Spondylolisthesis. Orthop Rev (Pavia). 2022 Jul 27;14(4):36917. doi: 10.52965/001c.36917. PMID: 35910544; PMCID: PMC9329062.
Interbody fusion may be used when the degree of slippage is higher and greater stability is needed. 7 Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Spondylolisthesis. Orthop Rev (Pavia). 2022 Jul 27;14(4):36917. doi: 10.52965/001c.36917. PMID: 35910544; PMCID: PMC9329062.
Considerations for Specific Interbody Fusion Approaches
The type of fusion depends on the underlying condition, skill, and experience of the surgeon, and the patient’s overall health.
- ALIF and XLIF are typically recommended for the restoration of the disc and foraminal height. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
- TLIF is typically recommended for increasing spinal canal cross-sectional area and relieving nerve compression. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
- XLIF may cause lesser intraoperative blood and muscle damage when compared with TLIF or PLIF . 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009 However, the XLIF procedure may be associated with a risk of transient neurologic deficits. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
- TLIF and PLIF when performed as an open procedure may be associated with a higher risk of adjacent segment disease and subsidence. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
If the patient has undergone previous abdominal surgery, ALIF is usually not recommended. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
Open vs Minimally Invasive Surgery for Spondylolisthesis
Multiple studies have demonstrated that minimally invasive spine surgery yields similar clinical results to traditional open fusion while offering several notable benefits. These benefits include reduced costs, shorter operating times, decreased blood loss, and a shorter hospital stay. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
Due to these benefits, minimally invasive spine surgery may be more helpful for patients requiring a two-level fusion procedure. 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi:10.1016/j.nec.2019.02.009
Potential Risks and Complications of Surgery
Damage to the lumbar spinal nerves is a potential risk of spinal surgery.
There are several potential risks and complications associated with degenerative spondylolisthesis surgery, which are typically the same for any fusion or decompression surgery.
Since degenerative spondylolisthesis is a condition that disproportionately affects older individuals, surgery may present some additional risk in this age group. Surgical risk is more directly related to the overall health of a patient and not his or her absolute age.
Potential risks and complications include:
- Fusion failure (arthrodesis)
- Hardware failure
- Continued pain
- Adjacent segment disease
- Nerve root damage
These complications are usually rare, but increased risks can be seen in certain situations. Conditions that increase the risk of surgery include smoking (or any type of nicotine intake), obesity, multilevel fusions, osteoporosis (thinning of the bones), diabetes, rheumatoid arthritis, or prior failed back surgery.
See Failed Back Surgery Syndrome (FBSS): What It Is and How to Avoid Pain after Surgery
The surgeon must discuss the potential risks, benefits, and alternatives to surgery with the patient before surgical treatment is chosen.
- 1 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi: 10.1016/j.jot.2016.11.001
- 2 Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008 Mar;17(3):327-335. doi: 10.1007/s00586-007-0543-3 . Epub 2007 Nov 17. PMID: 18026865; PMCID: PMC2270383.
- 3 Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed.; 2016.
- 4 Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am. 2019;30(3):353-364. doi: 10.1016/j.nec.2019.02.009
- 5 Samuel AM, Moore HG, Cunningham ME. Treatment for Degenerative Lumbar Spondylolisthesis: Current Concepts and New Evidence. Curr Rev Musculoskelet Med. 2017 Dec;10(4):521-529. doi: 10.1007/s12178-017-9442-3 . PMID: 28994028; PMCID: PMC5685964.
- 6 Tenny S, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767/
- 7 Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Spondylolisthesis. Orthop Rev (Pavia). 2022 Jul 27;14(4):36917. doi: 10.52965/001c.36917 . PMID: 35910544; PMCID: PMC9329062.
Dr. Marco Funiciello is a physiatrist with Princeton Spine and Joint Center. He has a decade of clinical experience caring for spine and muscle conditions with non-surgical treatments.
- Surgery for Degenerative Spondylolisthesis "> Share on Facebook
- Surgery for Degenerative Spondylolisthesis "> Share on Pinterest
- Surgery for Degenerative Spondylolisthesis "> Share on X
- Subscribe to our newsletter
- Print this article
- Surgery for Degenerative Spondylolisthesis &body=https://www.spine-health.com/conditions/spondylolisthesis/surgery-degenerative-spondylolisthesis&subject= Surgery for Degenerative Spondylolisthesis "> Email this article
Editor’s Top Picks
Lumbar laminectomy surgery video, alif (anterior lumbar interbody fusion) video, lumbar spinal fusion surgery, xlif: lumbar spinal fusion, transforaminal lumbar interbody fusion (tlif) back surgery.
Popular Videos

Lower Back Pain Treatment Video

Cervical Disc Replacement Surgery Video

Lumbar Herniated Disc Video

4 Steps to Relieve Sciatica Pain Video
Undergoing a Spinal Fusion?
Learn how bone growth stimulation therapy can help your healing process
Sponsored by Orthofix
Health Information (Sponsored)
- Take the Chronic Pain Quiz
- Suffering from Lumbar Spinal Stenosis? Obtain Long Term Pain Relief
- Learn How Bone Growth Therapy Can Help You
- Learn How Cedars-Sinai's Experts Can Relieve Your Pain
Inclusion Criteria
Recommendation scope, diagnosis and imaging, medical/interventional treatment, surgical treatment, value/cost-effectiveness of spine care.
Diagnosis And Treatment Of Degenerative Lumbar Spondylolisthesis
Recommendations
- What is the role of pharmacological treatment in the management of degenerative lumbar spondylolisthesis?
- What is the role of physical therapy/exercise in the treatment of degenerative lumbar spondylolisthesis?
- What is the role of manipulation in the treatment of degenerative lumbar spondylolisthesis?
- What is the role of ancillary treatments such as bracing, traction, electrical stimulation and transcutaneous electrical stimulation (TENS) in the treatment of degenerative lumbar spondylolisthesis?
- What is the long-term result (four + years) of medical/interventional management of degenerative lumbar spondylolisthesis?
Recommendation Grading
Authoring organization.
North American Spine Society
Publication Month/Year
November 5, 2015
Last Updated Month/Year
July 31, 2023

Document Type
External publication status, country of publication.
Female, Male, Adult, Older adult
Health Care Settings
Ambulatory, Emergency care, Hospital, Operating and recovery room, Outpatient
Intended Users
Physical therapist, chiropractor, nurse, nurse practitioner, physician, physician assistant
Assessment and screening, Diagnosis, Rehabilitation, Management, Treatment
Diseases/Conditions (MeSH)
D013168 - Spondylolisthesis
lumbar spondylolysthesis, Degenerative Lumbar Spondylolisthesis
Grading Table
Emerging innovations for lumbar spondylolisthesis management: a systematic review of active and prospective clinical trials
- Published: 11 November 2022
- Volume 45 , pages 3629–3640, ( 2022 )
Cite this article

- Daniel Jeremiah Harrison 1 , 2 , 3 ,
- Archis R. Bhandarkar 1 , 2 , 3 ,
- Sulaman Durrani 1 , 2 ,
- Cameron Zamanian 1 , 2 ,
- Rohin Singh 4 &
- Mohamad Bydon 1 , 2
956 Accesses
3 Altmetric
Explore all metrics
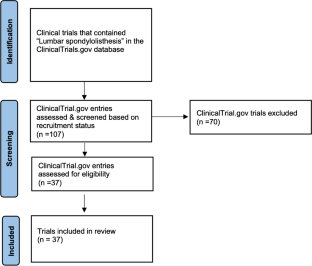
The literature has had some conflicting evidence regarding the effective management of lumbar spondylolisthesis (LS). Herein, we review active and prospective clinical trials to identify the emerging trends for the management of LS. A systematic search was conducted utilizing the NIH Clinical Trials database using the search term “lumbar spondylolisthesis” on February 2, 2022. Currently active and prospective clinical trials for LS were included and analyzed. All statistical analyses were performed on R 4.1.2. We identified 37 clinical trials. Nearly half the trials ( n = 18, 48.6%) include novel technologies; 6 (16.2%) are comparing surgical approaches, of which 4 (67%) include decompression alone versus decompression with instrumented fusion; 6 (16.2%) are evaluating perioperative pain management protocols, of which 3 (50%) include bupivacaine or ropivacaine; 3 (8.1%) are evaluating alternative medicines in LS; 2 (5.4%) are observational studies about the natural history of LS; 1 (2.7%) involves surgical infection prophylaxis; and 1 (2.7%) is evaluating AK1320 microspheres. The 18 trials involving novel technologies include 3D-printed titanium cages ( n = 3, 16.7%), interbody implants ( n = 4, 22.2%), bone graft materials ( n = 4, 22.2%), and miscellaneous intraoperative devices ( n = 7, 38.9%). The top 3 outcomes measured were Oswestry Disability Index ( n = 28, 75.7%), visual analog scale ( n = 21, 56.7%), and postoperative radiographs ( n = 16, 43.2%). Patient-reported outcome measures (PROMs) were included in 34 (91.9%) trials, while 23 (62.2%) trials included lumbar spine imaging. LS can often require a multifaceted approach. Novel technologies and utilization of PROMs appear to be a significant emerging trend in LS management.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Clinical effectiveness of reduction and fusion versus in situ fusion in the management of degenerative lumbar spondylolisthesis: a systematic review and meta-analysis
The comparison of instrumented and non-instrumented fusion in the treatment of lumbar spondylolisthesis: a meta-analysis.
Decompression alone versus decompression with fusion in patients with lumbar spinal stenosis with degenerative spondylolisthesis: a systematic review and meta-analysis
Data availability.
Raw data were generated. Derived data supporting the findings of this study are available from the corresponding author MB on request.
Abdu WA, Sacks OA, Tosteson ANA, Zhao W, Tosteson TD, Morgan TS, Pearson A, Weinstein JN, Lurie JD (2018) Long-term results of surgery compared with nonoperative treatment for lumbar degenerative spondylolisthesis in the Spine Patient Outcomes Research Trial (SPORT). Spine 43:1619–1630. https://doi.org/10.1097/BRS.0000000000002682
Article PubMed PubMed Central Google Scholar
Beck AW, Simpson AK (2019) High-grade lumbar spondylolisthesis. Neurosurg Clin N Am 30:291–298. https://doi.org/10.1016/j.nec.2019.02.002
Article PubMed Google Scholar
Burton MR, Dowling TJ, Mesfin FB (2022) Isthmic spondylolisthesis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441846/
Butt S, Saifuddin A (2005) The imaging of lumbar spondylolisthesis. Clin Radiol 60:533–546. https://doi.org/10.1016/j.crad.2004.07.013
Article CAS PubMed Google Scholar
Bydon M, Alvi MA, Goyal A (2019) Degenerative lumbar spondylolisthesis: definition, natural history, conservative management, and surgical treatment. Neurosurg Clin N Am 30:299–304. https://doi.org/10.1016/j.nec.2019.02.003
Chan AK, Sharma V, Robinson LC, Mummaneni PV (2019) Summary of guidelines for the treatment of lumbar spondylolisthesis. Neurosurg Clin N Am 30:353–364. https://doi.org/10.1016/j.nec.2019.02.009
Dantas F, Dantas FLR, Botelho RV (2022) Effect of interbody fusion compared with posterolateral fusion on lumbar degenerative spondylolisthesis: a systematic review and meta-analysis. Spine J 22(5):756–768. https://doi.org/10.1016/j.spinee.2021.12.001
Demetriades AK, Park JJ, Tiefenbach J (2022) Is there resource wastage in the research for spinal diseases? An observational analysis of discontinuation and non-publication in randomised controlled trials. Brain Spine 2:100922
Försth P, Ólafsson G, Carlsson T, Frost A, Borgström F, Fritzell P, Öhagen P, Michaëlsson K, Sandén B (2016) A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med 374:1413–1423. https://doi.org/10.1056/NEJMoa1513721
Ghogawala Z, Dziura J, Butler WE, Dai F, Terrin N, Magge SN, Coumans J-VCE, Harrington JF, Amin-Hanjani S, Schwartz JS, Sonntag VKH, Barker FG 2nd, Benzel EC (2016) Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 374:1424–1434. https://doi.org/10.1056/NEJMoa1508788
Kalichman L, Kim DH, Li L, Guermazi A, Berkin V, Hunter DJ (2009) Spondylolysis and spondylolisthesis: prevalence and association with low back pain in the adult community-based population. Spine 34:199–205. https://doi.org/10.1097/BRS.0b013e31818edcfd
Kurd MF (2022) A clinical study to evaluate safety and performance of PEEK-OPTIMA™ HA enhanced interbody cages in the lumbar spine. ClinicalTrials.gov identifier: NCT03928041. https://clinicaltrials.gov/ct2/show/NCT03928041 . Accessed 10 Mar 2022
Prosidyan, Inc (2020) Prospective, multi-center study to assess posterolateral fusion using FIBERGRAFT. ClinicalTrials.gov identifier: NCT03884283. https://clinicaltrials.gov/ct2/show/record/NCT03884283 . Accessed 10 Mar 2022.
Farhadi HF (2021) Single-armed use of ViviGen cellular bone matrix in patients undergoing posterolateral lumbar surgery. ClinicalTrials.gov identifier: NCT04007094. https://clinicaltrials.gov/ct2/show/NCT04007094 . Accessed March 10, 2022.
Barber SM (2020) Clinical effectiveness of pre-operative methadone in single level lateral transpsoas interbody fusions. ClinicalTrials.gov identifier: NCT04112550. https://clinicaltrials.gov/ct2/show/NCT04112550 . Accessed 10 Mar 2022
Kim S (2022) Effectiveness and safety of korean medicine for low back pain or sciatica due to lumbar stenosis/spondylolisthesis. ClinicalTrials.gov identifier: NCT03879447. https://clinicaltrials.gov/ct2/show/NCT03879447 . Accessed 10 Mar 2022
Kalani MA (2022) Return of bowel function after one or two level anterior lumbar interbody fusion with chewing gum. ClinicalTrials.gov identifier: NCT03945461. https://clinicaltrials.gov/ct2/show/NCT03945461 . Accessed 10 Mar 2022
Kovacs FM, Urrútia G, Alarcón JD (2011) Surgery versus conservative treatment for symptomatic lumbar spinal stenosis: a systematic review of randomized controlled trials. Spine 36:E1335–E1351. https://doi.org/10.1097/BRS.0b013e31820c97b1
Labelle H, Mac-Thiong J-M, Roussouly P (2011) Spino-pelvic sagittal balance of spondylolisthesis: a review and classification. Eur Spine J 20(Suppl 5):641–646. https://doi.org/10.1007/s00586-011-1932-1
Martin CR, Gruszczynski AT, Braunsfurth HA, Fallatah SM, O’Neil J, Wai EK (2007) The surgical management of degenerative lumbar spondylolisthesis: a systematic review. Spine 32:1791–1798. https://doi.org/10.1097/BRS.0b013e3180bc219e
Matz PG, Meagher RJ, Lamer T, Tontz WL Jr, Annaswamy TM, Cassidy RC, Cho CH, Dougherty P, Easa JE, Enix DE, Gunnoe BA, Jallo J, Julien TD, Maserati MB, Nucci RC, O’Toole JE, Rosolowski K, Sembrano JN, Villavicencio AT, Witt J-P (2016) Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J 16:439–448. https://doi.org/10.1016/j.spinee.2015.11.055
Metz LN, Deviren V (2007) Low-grade spondylolisthesis. Neurosurg Clin N Am 18:237–248. https://doi.org/10.1016/j.nec.2007.02.010
Naeem K, Nathani KR, Barakzai MD, Khan SA, Rai HH, Mubarak F, Enam SA (2021) Modifications in lumbar facet joint are associated with spondylolisthesis in the degenerative spine diseases: a comparative analysis. Acta Neurochir 163:863–871. https://doi.org/10.1007/s00701-020-04657-3
Weldring T, Smith SMS (2013) Patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs). Health Serv Insights 6:61–68. https://doi.org/10.4137/HSI.S11093
Zanoli G, Strömqvist B, Jönsson B (2001) Visual analog scales for interpretation of back and leg pain intensity in patients operated for degenerative lumbar spine disorders. Spine 26:2375–2380. https://doi.org/10.1097/00007632-200111010-00015
Home - ClinicalTrials.gov. http://clinicaltrials.gov . Accessed 25 Jan 2022
SLIP II registry: spinal laminectomy versus instrumented pedicle screw fusion - full text view - ClinicalTrials.Gov. https://clinicaltrials.gov/ct2/show/NCT03570801?cond=NCT03570801&draw=2&rank=1 . Accessed 10 Mar 2022
Degenerative spondylolisthesis; micro-decompression alone vs decompression plus instrumented fusion - full text view - ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT03469791?cond=NCT03469791&draw=2&rank=1 . Accessed 9 Mar 2022
The NORDSTEN Study - degenerative spondylolisthesis - full text view - ClinicalTrials.Gov. https://clinicaltrials.gov/ct2/show/NCT02051374?cond=NCT02051374&draw=2&rank=1 . Accessed 10 Mar 2022
Decompression vs. fusion for stable degenerative spondylolisthesis. https://clinicaltrials.gov/ct2/show/NCT02348645?cond=NCT02348645&draw=2&rank=1 . Accessed 10 Mar 2022
Comparative study of anterior vs. posterior surgical treatment for lumbar isthmic spondylolisthesis - full text view - ClinicalTrials.Gov. https://clinicaltrials.gov/ct2/show/NCT02564705?cond=NCT02564705&draw=2&rank=1 . Accessed 10 Mar 2022
Smiley face shaped rod technique versus instrumented posteriolateral fusion in treatment of isthmic lumbar spondylolisthesis. https://clinicaltrials.gov/ct2/show/NCT04559399?cond=NCT04559399&draw=2&rank=1 . Accessed 10 Mar 2022
Clinical and radiographic outcomes of TLIF w/3D printed cellular implant. https://clinicaltrials.gov/ct2/show/NCT05023733?cond=NCT05023733&draw=2&rank=1 . Accessed 10 Mar 2022
SPIRA TM -A 3D and HCT/p DBM vs. Medtronic Divergent TM -L/Perimeter TM and Recombinant BMP-2. https://clinicaltrials.gov/ct2/show/NCT04566874?cond=NCT04566874&draw=2&rank=1 . Accessed 10 Mar 2022
Lumbar fusion with Nexxt Spine 3D-printed titanium interbody cages. https://clinicaltrials.gov/ct2/show/NCT03647501?cond=NCT03647501&draw=2&rank=1 . Accessed 10 Mar 2022
Lumbar fusion with the Icotec CF/PEEK Pedicle System in combination with the Icotec CF/PEEK TLIF Cage ETurn TM . https://clinicaltrials.gov/ct2/show/NCT02087267?cond=NCT02087267&draw=2&rank=1 . Accessed 10 Mar 2022
Lumbar interbody implant study. https://clinicaltrials.gov/ct2/show/NCT04418830?cond=NCT04418830&draw=2&rank=1 . Accessed 10 Mar 2022
A clinical study to evaluate safety and performance of PEEK-OPTIMA TM HA enhanced. https://clinicaltrials.gov/ct2/show/NCT04416321?cond=NCT04416321&draw=2&rank=1 . Accessed 10 Mar 2022
Evaluation of NB1 bone graft following lumbar interbody arthrodesis. https://clinicaltrials.gov/ct2/show/NCT03810573?cond=NCT03810573&draw=2&rank=1 . Accessed 10 Mar 2022
TLIF Osteo3 ZP Putty Study (Also Known as the TOP Fusion Study). https://clinicaltrials.gov/ct2/show/NCT05114135?cond=NCT05114135&draw=2&rank=1 . Accessed 10 Mar 2022
Clinical outcomes associated with the use of ViviGen® for the treatment of lumbar degenerative disc disease - full text view - ClinicalTrials.Gov. https://clinicaltrials.gov/ct2/show/NCT03733626?cond=NCT03733626&draw=2&rank=1 . Accessed 10 Mar 2022
Study of nucel for one and two level lumbar interbody fusion. https://clinicaltrials.gov/ct2/show/NCT02808234?cond=NCT02808234&draw=2&rank=1 . Accessed 9 Mar 2022
LimiFlex Clinical Trial for the treatment of degenerative spondylolisthesis with spinal stenosis. https://clinicaltrials.gov/ct2/show/NCT03115983?cond=NCT03115983&draw=2&rank=1 . Accessed 10 Mar 2022
3Spine TLIF real world evidence study - full text view - ClinicalTrials.Gov. https://clinicaltrials.gov/ct2/show/NCT04823858?cond=NCT04823858&draw=2&rank=1 . Accessed 10 Mar 2022
Minuteman spinal fusion implant versus surgical decompression for lumbar spinal stenosis. https://clinicaltrials.gov/ct2/show/NCT01455805?cond=NCT01455805&draw=2&rank=1 . Accessed 10 Mar 2022
A pivotal study of the Premia Spine TOPS TM system. https://clinicaltrials.gov/ct2/show/NCT03012776?cond=NCT03012776&draw=2&rank=1 . Accessed 10 Mar 2022
Efficacy and Tolerance Study of B-DYN Versus Conventional Fusion in the Treatment of Lumbar Stenosis on the Degree of Post-operative Functional Incapacity (BDYNCLIN) - Full Text View - ClinicalTrials.Gov. https://clinicaltrials.gov/ct2/show/NCT04407338?cond=NCT04407338&draw=2&rank=1 . Accessed 10 Mar 2022
Liposomal bupivacaine in one-level instrumented posterior spinal fusion. https://clinicaltrials.gov/ct2/show/NCT03745040?cond=NCT03745040&draw=2&rank=1 . Accessed 10 Mar 2022
Randomized control trial of quadratus lumborum block for lumbar spine decompression and fusion surgery. https://clinicaltrials.gov/ct2/show/NCT04447950?cond=NCT04447950&draw=2&rank=1 . Accessed 10 Mar 2022
Peri-incisional drug injection in lumbar spine surgery. https://clinicaltrials.gov/ct2/show/NCT03513445?cond=NCT03513445&draw=2&rank=1 . Accessed 10 Mar 2022
Regional anesthesia in minimally invasive lumbar spine surgery. https://clinicaltrials.gov/ct2/show/NCT05029726?cond=NCT05029726&draw=2&rank=1 . Accessed 10 Mar 2022
Cognitive behavioral therapy (CBT) after lumbar spinal fusion in patients with high pain catastrophizing - full text view - ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT03969602?cond=NCT03969602&draw=1&rank=1 . Accessed 9 Mar 2022
Korean medicine for symptomatic lumbar spinal spondylolisthesis. https://clinicaltrials.gov/ct2/show/NCT03107468?cond=NCT03107468&draw=2&rank=1 . Accessed 10 Mar 2022
Does teicoplanin powder use in lumbar instrumentation surgery reduce surgical site infection. https://clinicaltrials.gov/ct2/show/NCT04341831?cond=NCT04341831&draw=2&rank=1 . Accessed 10 Mar 2022
First-in-human study of AK1320 encapsulated microspheres (AK1320 MS) - full text view - ClinicalTrials.Gov. https://clinicaltrials.gov/ct2/show/NCT04483297?cond=NCT04483297&draw=2&rank=1 . Accessed 10 Mar 2022
The NORDSTEN Studies/The Observational Cohort Study - full text view - ClinicalTrials.Gov. https://clinicaltrials.gov/ct2/show/NCT03562936?cond=NCT03562936&draw=2&rank=1 . Accessed 10 Mar 2022
Instability in the lumbar spine of patients with age related changes and narrowing of the spinal canal (spinal stenosis). https://clinicaltrials.gov/ct2/show/NCT04406987?cond=NCT04406987&draw=2&rank=1 . Accessed 10 Mar 2022
Cho MK, Shohara R, Schissel A, Rennie D (2000) Policies on faculty conflicts of interest at US universities. JAMA 284(17):2203–2208. https://doi.org/10.1001/jama.284.17.2203
Download references
This work was supported by the Charles B. and Ann L. Professorship of Neurosurgery.
Author information
Authors and affiliations.
Mayo Clinic Neuro-Informatics Laboratory, Department of Neurologic Surgery, Mayo Clinic, 200 1St Street SW, Rochester, MN, 55905, USA
Daniel Jeremiah Harrison, Archis R. Bhandarkar, Sulaman Durrani, Cameron Zamanian & Mohamad Bydon
Department of Neurologic Surgery, Mayo Clinic, Rochester, MN, USA
Mayo Clinic Alix School of Medicine, Mayo Clinic, Rochester, MN, USA
Daniel Jeremiah Harrison & Archis R. Bhandarkar
Mayo Clinic Alix School of Medicine, Mayo Clinic, Scottsdale, AZ, USA
Rohin Singh
You can also search for this author in PubMed Google Scholar
Contributions
All the authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Daniel Jeremiah Harrison and Archis R. Bhandarkar. The first draft of the manuscript was written by Daniel Jeremiah Harrison and Archis R. Bhandarkar, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Correspondence to Mohamad Bydon .
Ethics declarations
Ethics approval and consent to participate.
This study did not involve any human or animal subjects and does not require any ethical approval, nor any informed consent.
Human and animal ethics
Not applicable.
Consent for publication
Conflict of interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Harrison, D.J., Bhandarkar, A.R., Durrani, S. et al. Emerging innovations for lumbar spondylolisthesis management: a systematic review of active and prospective clinical trials. Neurosurg Rev 45 , 3629–3640 (2022). https://doi.org/10.1007/s10143-022-01889-y
Download citation
Received : 07 April 2022
Revised : 20 September 2022
Accepted : 25 October 2022
Published : 11 November 2022
Issue Date : December 2022
DOI : https://doi.org/10.1007/s10143-022-01889-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lumbar spondylolisthesis
- Spinal surgery
- Anterolisthesis
- Retrolisthesis
- Find a journal
- Publish with us
- Track your research
- Help & FAQ
Guideline summary review: An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis
- Department of Physical Medicine and Rehabilitation
- Penn State Neuroscience Institute
Research output : Contribution to journal › Review article › peer-review
Background Context The North American Spine Society's (NASS) Evidence-Based Clinical Guideline for the Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis features evidence-based recommendations for diagnosing and treating degenerative lumbar spondylolisthesis. The guideline updates the 2008 guideline on this topic and is intended to reflect contemporary treatment concepts for symptomatic degenerative lumbar spondylolisthesis as reflected in the highest quality clinical literature available on this subject as of May 2013. The NASS guideline on this topic is the only guideline on degenerative lumbar spondylolisthesis included in the Agency for Healthcare Research and Quality's National Guideline Clearinghouse (NGC). Purpose The purpose of this guideline is to provide an evidence-based educational tool to assist spine specialists when making clinical decisions for patients with degenerative lumbar spondylolisthesis. This article provides a brief summary of the evidence-based guideline recommendations for diagnosing and treating patients with this condition. Study Design A systematic review of clinical studies relevant to degenerative spondylolisthesis was carried out. Methods This NASS spondyolisthesis guideline is the product of the Degenerative Lumbar Spondylolisthesis Work Group of NASS' Evidence-Based Guideline Development Committee. The methods used to develop this guideline are detailed in the complete guideline and technical report available on the NASS website. In brief, a multidisciplinary work group of spine care specialists convened to identify clinical questions to address in the guideline. The literature search strategy was developed in consultation with medical librarians. Upon completion of the systematic literature search, evidence relevant to the clinical questions posed in the guideline was reviewed. Work group members used the NASS evidentiary table templates to summarize study conclusions, identify study strengths and weaknesses, and assign levels of evidence. Work group members participated in webcasts and in-person recommendation meetings to update and formulate evidence-based recommendations and incorporate expert opinion when necessary. The draft guidelines were submitted to an internal peer review process and ultimately approved by the NASS Board of Directors. Upon publication, the Degenerative Lumbar Spondylolisthesis guideline was accepted into the NGC and will be updated approximately every 5 years. Results Twenty-seven clinical questions were addressed in this guideline update, including 15 clinical questions from the original guideline and 12 new clinical questions. The respective recommendations were graded by strength of the supporting literature, which was stratified by levels of evidence. Twenty-one new or updated recommendations or consensus statements were issued and 13 recommendations or consensus statements were maintained from the original guideline. Conclusions The clinical guideline was created using the techniques of evidence-based medicine and best available evidence to aid practitioners in the care of patients with degenerative lumbar spondylolisthesis. The entire guideline document, including the evidentiary tables, literature search parameters, literature attrition flow chart, suggestions for future research, and all of the references, is available electronically on the NASS website at https://www.spine.org/Pages/ResearchClinicalCare/QualityImprovement/ClinicalGuidelines.aspx and will remain updated on a timely schedule.
All Science Journal Classification (ASJC) codes
- Orthopedics and Sports Medicine
- Clinical Neurology
Access to Document
- 10.1016/j.spinee.2015.11.055
Other files and links
- Link to publication in Scopus
- Link to the citations in Scopus
Fingerprint
- Spondylolisthesis Medicine & Life Sciences 100%
- Guidelines Medicine & Life Sciences 49%
- Spine Medicine & Life Sciences 26%
- Therapeutics Medicine & Life Sciences 12%
- Consensus Medicine & Life Sciences 6%
- Webcasts Medicine & Life Sciences 5%
- Librarians Medicine & Life Sciences 5%
- Peer Review Medicine & Life Sciences 4%
T1 - Guideline summary review
T2 - An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis
AU - Matz, Paul G.
AU - Meagher, R. J.
AU - Lamer, Tim
AU - Tontz, William L.
AU - Annaswamy, Thiru M.
AU - Cassidy, R. Carter
AU - Cho, Charles H.
AU - Dougherty, Paul
AU - Easa, John E.
AU - Enix, Dennis E.
AU - Gunnoe, Bryan A.
AU - Jallo, Jack
AU - Julien, Terrence D.
AU - Maserati, Matthew B.
AU - Nucci, Robert C.
AU - O'Toole, John E.
AU - Rosolowski, Karie
AU - Sembrano, Jonathan N.
AU - Villavicencio, Alan T.
AU - Witt, Jens Peter
N1 - Publisher Copyright: © 2016 Elsevier Inc. All rights reserved.
PY - 2016/3/1
Y1 - 2016/3/1
N2 - Background Context The North American Spine Society's (NASS) Evidence-Based Clinical Guideline for the Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis features evidence-based recommendations for diagnosing and treating degenerative lumbar spondylolisthesis. The guideline updates the 2008 guideline on this topic and is intended to reflect contemporary treatment concepts for symptomatic degenerative lumbar spondylolisthesis as reflected in the highest quality clinical literature available on this subject as of May 2013. The NASS guideline on this topic is the only guideline on degenerative lumbar spondylolisthesis included in the Agency for Healthcare Research and Quality's National Guideline Clearinghouse (NGC). Purpose The purpose of this guideline is to provide an evidence-based educational tool to assist spine specialists when making clinical decisions for patients with degenerative lumbar spondylolisthesis. This article provides a brief summary of the evidence-based guideline recommendations for diagnosing and treating patients with this condition. Study Design A systematic review of clinical studies relevant to degenerative spondylolisthesis was carried out. Methods This NASS spondyolisthesis guideline is the product of the Degenerative Lumbar Spondylolisthesis Work Group of NASS' Evidence-Based Guideline Development Committee. The methods used to develop this guideline are detailed in the complete guideline and technical report available on the NASS website. In brief, a multidisciplinary work group of spine care specialists convened to identify clinical questions to address in the guideline. The literature search strategy was developed in consultation with medical librarians. Upon completion of the systematic literature search, evidence relevant to the clinical questions posed in the guideline was reviewed. Work group members used the NASS evidentiary table templates to summarize study conclusions, identify study strengths and weaknesses, and assign levels of evidence. Work group members participated in webcasts and in-person recommendation meetings to update and formulate evidence-based recommendations and incorporate expert opinion when necessary. The draft guidelines were submitted to an internal peer review process and ultimately approved by the NASS Board of Directors. Upon publication, the Degenerative Lumbar Spondylolisthesis guideline was accepted into the NGC and will be updated approximately every 5 years. Results Twenty-seven clinical questions were addressed in this guideline update, including 15 clinical questions from the original guideline and 12 new clinical questions. The respective recommendations were graded by strength of the supporting literature, which was stratified by levels of evidence. Twenty-one new or updated recommendations or consensus statements were issued and 13 recommendations or consensus statements were maintained from the original guideline. Conclusions The clinical guideline was created using the techniques of evidence-based medicine and best available evidence to aid practitioners in the care of patients with degenerative lumbar spondylolisthesis. The entire guideline document, including the evidentiary tables, literature search parameters, literature attrition flow chart, suggestions for future research, and all of the references, is available electronically on the NASS website at https://www.spine.org/Pages/ResearchClinicalCare/QualityImprovement/ClinicalGuidelines.aspx and will remain updated on a timely schedule.
AB - Background Context The North American Spine Society's (NASS) Evidence-Based Clinical Guideline for the Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis features evidence-based recommendations for diagnosing and treating degenerative lumbar spondylolisthesis. The guideline updates the 2008 guideline on this topic and is intended to reflect contemporary treatment concepts for symptomatic degenerative lumbar spondylolisthesis as reflected in the highest quality clinical literature available on this subject as of May 2013. The NASS guideline on this topic is the only guideline on degenerative lumbar spondylolisthesis included in the Agency for Healthcare Research and Quality's National Guideline Clearinghouse (NGC). Purpose The purpose of this guideline is to provide an evidence-based educational tool to assist spine specialists when making clinical decisions for patients with degenerative lumbar spondylolisthesis. This article provides a brief summary of the evidence-based guideline recommendations for diagnosing and treating patients with this condition. Study Design A systematic review of clinical studies relevant to degenerative spondylolisthesis was carried out. Methods This NASS spondyolisthesis guideline is the product of the Degenerative Lumbar Spondylolisthesis Work Group of NASS' Evidence-Based Guideline Development Committee. The methods used to develop this guideline are detailed in the complete guideline and technical report available on the NASS website. In brief, a multidisciplinary work group of spine care specialists convened to identify clinical questions to address in the guideline. The literature search strategy was developed in consultation with medical librarians. Upon completion of the systematic literature search, evidence relevant to the clinical questions posed in the guideline was reviewed. Work group members used the NASS evidentiary table templates to summarize study conclusions, identify study strengths and weaknesses, and assign levels of evidence. Work group members participated in webcasts and in-person recommendation meetings to update and formulate evidence-based recommendations and incorporate expert opinion when necessary. The draft guidelines were submitted to an internal peer review process and ultimately approved by the NASS Board of Directors. Upon publication, the Degenerative Lumbar Spondylolisthesis guideline was accepted into the NGC and will be updated approximately every 5 years. Results Twenty-seven clinical questions were addressed in this guideline update, including 15 clinical questions from the original guideline and 12 new clinical questions. The respective recommendations were graded by strength of the supporting literature, which was stratified by levels of evidence. Twenty-one new or updated recommendations or consensus statements were issued and 13 recommendations or consensus statements were maintained from the original guideline. Conclusions The clinical guideline was created using the techniques of evidence-based medicine and best available evidence to aid practitioners in the care of patients with degenerative lumbar spondylolisthesis. The entire guideline document, including the evidentiary tables, literature search parameters, literature attrition flow chart, suggestions for future research, and all of the references, is available electronically on the NASS website at https://www.spine.org/Pages/ResearchClinicalCare/QualityImprovement/ClinicalGuidelines.aspx and will remain updated on a timely schedule.
UR - http://www.scopus.com/inward/record.url?scp=84963565257&partnerID=8YFLogxK
UR - http://www.scopus.com/inward/citedby.url?scp=84963565257&partnerID=8YFLogxK
U2 - 10.1016/j.spinee.2015.11.055
DO - 10.1016/j.spinee.2015.11.055
M3 - Review article
C2 - 26681351
AN - SCOPUS:84963565257
SN - 1529-9430
JO - Spine Journal
JF - Spine Journal
Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of adult isthmic spondylolisthesis
Affiliations.
- 1 Ahwatukee Sports & Spine, 4530 E. Muirwood Dr, Ste. 110, Phoenix, AZ 85048-7693, USA. Electronic address: [email protected].
- 2 Department of Neurosurgery, Medical College of Wisconsin, 8701 W Watertown Plank Rd, Milwaukee, WI 53226, USA.
- 3 Cleveland Clinic Center for Spine Health, 9500 Euclid Ave, Cleveland, OH 44195, USA.
- 4 University of Michigan, 1500 E Medical Center Dr, Ann Arbor, MI 48109, USA.
- 5 Department of Orthopedic Surgery, New York University School of Medicine, 550 1st Avenue, New York, NY 10016, USA.
- 6 University of Kansas Medical Center, 3901 Rainbow Blvd # 5013, Kansas City, KS 66103, USA.
- 7 The CORE Institute, 18444 N 25th Ave, Phoenix, AZ 85023, USA.
- 8 Neurological Monitoring Associates, LLC, 333 W Brown Deer Rd, Milwaukee, WI 53217, USA.
- 9 Norton Leatherman Spine Center, Department of Orthopaedic Surgery, University of Louisville, 210 E Gray St, Louisville, KY 40202, USA.
- 10 Denver Spine, 7800 E. Orchard Road, Greenwood Village, CO 80111, USA.
- 11 Department of Neurological Surgery, University of Wisconsin, 20 S Park St, Madison, WI 53715, USA.
- 12 Department of Neurosurgery, Tufts Medical Center, 800 Washington St, Boston, MA 02111, USA.
- 13 Department of Neurosurgery, Trakya University Faculty of Medicine, Edirne, Turkey 22030.
- 14 Center for Diagnostic Imaging, 5775 Wayzata Blvd, Saint Louis Park, MN 55416, USA.
- 15 Department of Neurosurgery, University of Michigan, 1500 E Medical Center Dr, Ann Arbor, MI 48109, USA.
- 16 North American Spine Society, 7075 Veterans Blvd, Willowbrook, IL 60527, USA.
- 17 Spine and Pain Medicine, 655 Shrewsbury Ave, Shrewsbury, NJ 07702, USA.
- 18 Cumberland Brain & Spine, 5655 Frist Blvd, Hermitage, TN 37076, USA.
- 19 OrthoIndy, 8450 Northwest Blvd, Indianapolis, IN 46278, USA.
- 20 Rockford Health Physicians, 2350 N Rockton Ave, Rockford, IL 61103, USA.
- 21 Department of Orthopaedic Surgery, University of Tennessee-Campbell Clinic, 1400 S Germantown Rd, Germantown, TN 38138, USA.
- PMID: 27592807
- DOI: 10.1016/j.spinee.2016.08.034
Background context: The North American Spine Society's (NASS) Evidence-Based Clinical Guideline for the Diagnosis and Treatment of Adult Isthmic Spondylolisthesis features evidence-based recommendations for diagnosing and treating adult patients with isthmic spondylolisthesis. The guideline is intended to reflect contemporary treatment concepts for symptomatic isthmic spondylolisthesis as reflected in the highest quality clinical literature available on this subject as of June 2013. NASS' guideline on this topic is the only guideline on adult isthmic spondylolisthesis accepted in the Agency for Healthcare Research and Quality's National Guideline Clearinghouse.
Purpose: The purpose of the guideline is to provide an evidence-based educational tool to assist spine specialists when making clinical decisions for adult patients with isthmic spondylolisthesis. This article provides a brief summary of the evidence-based guideline recommendations for diagnosing and treating patients with this condition.
Study design: This is a guideline summary review.
Methods: This guideline is the product of the Adult Isthmic Spondylolisthesis Work Group of NASS' Evidence-Based Clinical Guideline Development Committee. The methods used to develop this guideline are detailed in the complete guideline and technical report available on the NASS website. In brief, a multidisciplinary work group of spine care specialists convened to identify clinical questionsto address in the guideline. The literature search strategy was developed in consultation with medical librarians. Upon completion of the systematic literature search, evidence relevant to the clinical questions posed in the guideline was reviewed. Work group members utilized NASS evidentiary table templates to summarize study conclusions, identify study strengths and weaknesses, and assign levels of evidence. Work group members participated in webcasts and in-person recommendation meetings to update and formulate evidence-based recommendations and incorporate expert opinion when necessary. The draft guidelines were submitted to an internal peer review process and ultimately approved by the NASS Board of Directors. Upon publication, the Adult Isthmic Spondylolisthesis guideline was accepted into the National Guideline Clearinghouse and will be updated approximately every 5 years.
Results: Thirty-one clinical questions were addressed, and the answers are summarized in this article. The respective recommendations were graded according to the levels of evidence of the supporting literature.
Conclusions: The evidence-based clinical guideline has been created using techniques of evidence-based medicine and best available evidence to aid practitioners in the diagnosis and treatment of adult patients with isthmic spondylolisthesis. The entire guideline document, including the evidentiary tables, literature search parameters, literature attrition flowchart, suggestions for future research, and all of the references, is available electronically on the NASS website at https://www.spine.org/ResearchClinicalCare/QualityImprovement/ClinicalGuidelines.aspx and will remain updated on a timely schedule.
Keywords: Adult spondylolisthesis; Clinical practice guideline; Clinical practice recommendations; Evidence-based guideline; Isthmic spondylolisthesis; Spondylolisthesis; Spondylolytic spondylolisthesis.
Copyright © 2016 Elsevier Inc. All rights reserved.
Publication types
- Evidence-Based Medicine / methods*
- Evidence-Based Medicine / standards
- Neurosurgery / organization & administration
- Practice Guidelines as Topic*
- Societies, Medical
- Spondylolisthesis / diagnosis*
- Spondylolisthesis / therapy
- United States

IMAGES
VIDEO
COMMENTS
Abstract. Degenerative lumbar spondylolisthesis is a common cause of low back pain, affecting about 11.5% of the United States population. Patients with symptomatic lumbar spondylolisthesis may first be treated with conservative management strategies including, but not limited to, non-narcotic and narcotic pain medications, epidural steroid ...
Furthermore, 74.1% of the surgery patients noted major improvement in their symptoms, whereas only 24.1% of the nonsurgical treatment patients noted similar improvement. Therefore, SPORT provides Level I evidence that surgery is effective at treating degenerative lumbar spondylolisthesis.
The North American Spine Society's (NASS) Evidence-Based Clinical Guideline for the Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis features evidence-based recommendations for diagnosing and treating degenerative lumbar spondylolisthesis. The guideline updates the 2008 guideline on this topic and is intended to reflect contemporary treatment concepts for symptomatic ...
Summary of Guidelines for t h e Tre a t m e n t o f L u m b a r Spondylolisthesis Andrew K. Chan, MD*, Viraj Sharma, Leslie C. Robinson, MD, PharmD, MBA, Praveen V. Mummaneni, MD KEYWORDS Degenerative lumbar spondylolisthesis Spinal laminectomy Spinal fusion Spinal decompression Clinical guidelines Interbody Minimally invasive surgery KEY ...
Degenerative lumbar spondylolisthesis is a common cause of low back pain, affecting about 11.5% of the United States population. Patients with symptomatic lumbar spondylolisthesis may first be ...
DOI: 10.1016/j.nec.2019.02.009 Corpus ID: 153310378; Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. @article{Chan2019SummaryOG, title={Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis.}, author={Andrew K. Chan and Viraj Sharma and Leslie C. Robinson and Praveen V. Mummaneni}, journal={Neurosurgery clinics of North America}, year={2019}, volume={30 3 ...
treatment concepts for symptomatic degenerative lumbar spondylolisthesis as reflected in the highest quality clinical literature available on this subject as of May 2013. The NASS guideline on this topic is the only guideline on degenerative lumbar spondylolisthesis included in the Agency for Health-
The guideline updates the 2008 guideline on this topic and is intended to reflect contemporary treatment concepts for symptomatic degenerative lumbar spondylolisthesis as reflected in the highest quality clinical literature available on this subject as of May 2013.
Degenerative lumbar spondylolisthesis is a common cause of low back pain, affecting about 11.5% of the United States population. Patients with symptomatic lumbar spondylolisthesis may first be treated with conservative management strategies including, but not limited to, non-narcotic and narcotic pain medications, epidural steroid injections, transforaminal injections, and physical therapy ...
Other symptoms associated with lumbar spondylolisthesis include buttock pain, numbness, or weakness in the leg(s), difficulty walking, and rarely loss of bowel or bladder control. ... Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of adult isthmic spondylolisthesis. Spine J. 2016 Dec; 16 (12):1478 ...
The clinical guidelines published by the North American Spine Society (NASS) in 2014 for the diagnosis and treatment of degenerative spondylolisthesis indicate that conservative treatment should be similar to the treatment used in degenerative lumbar stenosis . Conservative management includes activity restriction, pain relief with the use of ...
The guideline updates the 2008 guideline on this topic and is intended to reflect contemporary treatment concepts for symptomatic degenerative lumbar spondylolisthesis as reflected in the highest quality clinical literature available on this subject as of May 2013.
Degenerative lumbar spondylolisthesis is a common cause of low back pain, affecting about 11.5% of the United States population. Patients with symptomatic lumbar spondylolisthesis may first be treated with conservative management strategies including, but not limited to, non-narcotic and narcotic pain medications, epidural steroid injections, transforaminal injections, and physical therapy ...
Surgery for Degenerative Spondylolisthesis. Surgery for degenerative spondylolisthesis may be beneficial for select patients with lumbar radicular pain. About 10% to 15% of individuals seeking treatment for degenerative spondylolisthesis eventually opt for surgical treatment. 1 Wang YXJ, Káplár Z, Deng M, Leung JCS.
Background context: The North American Spine Society's (NASS) Evidence Based Clinical Guideline for the Diagnosis and Treatment of Low Back Pain features evidence-based recommendations for diagnosing and treating adult patients with nonspecific low back pain. The guideline is intended to reflect contemporary treatment concepts for nonspecific low back pain as reflected in the highest quality ...
Background Context. The North American Spine Society's (NASS) Evidence-Based Clinical Guideline for the Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis features evidence-based recommendations for diagnosing and treating degenerative lumbar spondylolisthesis. The guideline updates the 2008 guideline on this topic and is intended to reflect contemporary treatment concepts for ...
There is insufficient evidence to make a recommendation for or against the use of indirect surgical 7 decompression for the treatment of patients with symptomatic spinal stenosis associated with low 8 grade degenerative lumbar spondylolisthesis whose symptoms have been recalcitrant to a trial of medical/interventional treatment.
A systematic search was conducted utilizing the NIH Clinical Trials database using the search term "lumbar spondylolisthesis" on February 2, 2022. Currently active and prospective clinical trials for LS were included and analyzed. ... Mummaneni PV (2019) Summary of guidelines for the treatment of lumbar spondylolisthesis. Neurosurg Clin N ...
Background Context The North American Spine Society's (NASS) Evidence-Based Clinical Guideline for the Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis features evidence-based recommendations for diagnosing and treating degenerative lumbar spondylolisthesis. The guideline updates the 2008 guideline on this topic and is intended ...
Background context: The North American Spine Society's (NASS) Evidence-Based Clinical Guideline for the Diagnosis and Treatment of Adult Isthmic Spondylolisthesis features evidence-based recommendations for diagnosing and treating adult patients with isthmic spondylolisthesis. The guideline is intended to reflect contemporary treatment concepts for symptomatic isthmic spondylolisthesis as ...